Ch15: Human Papillomaviruses and Papillary Oral Lesions
Ch15: Human Papillomaviruses and Papillary Oral Lesions
Ch15: Human Papillomaviruses and Papillary Oral Lesions
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
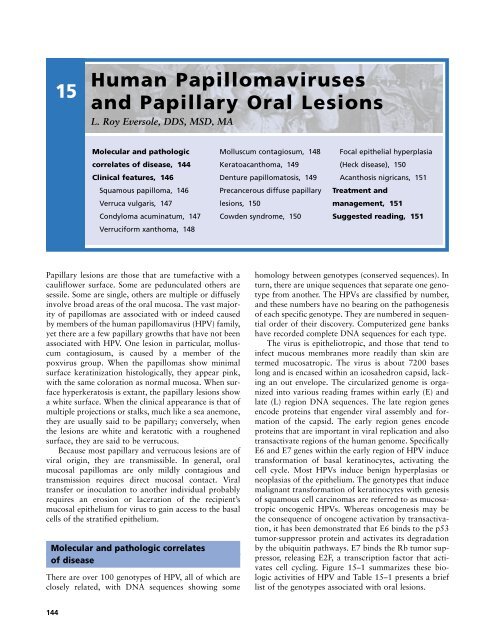
15<strong>Human</strong> <strong>Papillomaviruses</strong><strong>and</strong> <strong>Papillary</strong> <strong>Oral</strong> <strong>Lesions</strong>L. Roy Eversole, DDS, MSD, MAMolecular <strong>and</strong> pathologiccorrelates of disease, 144Clinical features, 146Squamous papilloma, 146Verruca vulgaris, 147Condyloma acuminatum, 147Verruciform xanthoma, 148Molluscum contagiosum, 148Keratoacanthoma, 149Denture papillomatosis, 149Precancerous diffuse papillarylesions, 150Cowden syndrome, 150Focal epithelial hyperplasia(Heck disease), 150Acanthosis nigricans, 151Treatment <strong>and</strong>management, 151Suggested reading, 151<strong>Papillary</strong> lesions are those that are tumefactive with acauliflower surface. Some are pedunculated others aresessile. Some are single, others are multiple or diffuselyinvolve broad areas of the oral mucosa. The vast majorityof papillomas are associated with or indeed causedby members of the human papillomavirus (HPV) family,yet there are a few papillary growths that have not beenassociated with HPV. One lesion in particular, molluscumcontagiosum, is caused by a member of thepoxvirus group. When the papillomas show minimalsurface keratinization histologically, they appear pink,with the same coloration as normal mucosa. When surfacehyperkeratosis is extant, the papillary lesions showa white surface. When the clinical appearance is that ofmultiple projections or stalks, much like a sea anemone,they are usually said to be papillary; conversely, whenthe lesions are white <strong>and</strong> keratotic with a roughenedsurface, they are said to be verrucous.Because most papillary <strong>and</strong> verrucous lesions are ofviral origin, they are transmissible. In general, oralmucosal papillomas are only mildly contagious <strong>and</strong>transmission requires direct mucosal contact. Viraltransfer or inoculation to another individual probablyrequires an erosion or laceration of the recipient’smucosal epithelium for virus to gain access to the basalcells of the stratified epithelium.Molecular <strong>and</strong> pathologic correlatesof diseaseThere are over 100 genotypes of HPV, all of which areclosely related, with DNA sequences showing somehomology between genotypes (conserved sequences). Inturn, there are unique sequences that separate one genotypefrom another. The HPVs are classified by number,<strong>and</strong> these numbers have no bearing on the pathogenesisof each specific genotype. They are numbered in sequentialorder of their discovery. Computerized gene bankshave recorded complete DNA sequences for each type.The virus is epitheliotropic, <strong>and</strong> those that tend toinfect mucous membranes more readily than skin aretermed mucosatropic. The virus is about 7200 baseslong <strong>and</strong> is encased within an icosahedron capsid, lackingan out envelope. The circularized genome is organizedinto various reading frames within early (E) <strong>and</strong>late (L) region DNA sequences. The late region genesencode proteins that engender viral assembly <strong>and</strong> formationof the capsid. The early region genes encodeproteins that are important in viral replication <strong>and</strong> alsotransactivate regions of the human genome. SpecificallyE6 <strong>and</strong> E7 genes within the early region of HPV inducetransformation of basal keratinocytes, activating thecell cycle. Most HPVs induce benign hyperplasias orneoplasias of the epithelium. The genotypes that inducemalignant transformation of keratinocytes with genesisof squamous cell carcinomas are referred to as mucosatropiconcogenic HPVs. Whereas oncogenesis may bethe consequence of oncogene activation by transactivation,it has been demonstrated that E6 binds to the p53tumor-suppressor protein <strong>and</strong> activates its degradationby the ubiquitin pathways. E7 binds the Rb tumor suppressor,releasing E2F, a transcription factor that activatescell cycling. Figure 15–1 summarizes these biologicactivities of HPV <strong>and</strong> Table 15–1 presents a brieflist of the genotypes associated with oral lesions.144
HUMAN PAPILLOMAVIRUSES AND PAPILLARY ORAL LESIONS 145Binds p53Binds pRbHPV 16E6 oncoproteinE7 oncoproteinExpressionE2 E6 E7 LInhibitionTruncated E2 cannotinhibit expressionof E6, E7Host DNAIntegration at E2Host DNAHPV 16E6 oncoproteinE7 oncoproteinBinds p53Binds pRbE2FUbiquitin enzymatic lysisLoss of cell cycle inhibitionRelease of E2Ffrom RbE2FTranscription or cell cycle activationHost DNAFigure 15–1 Schematic diagram showing human papillomavirus(HPV) infection of keratinocytes leading toeither benign or malignant neoplasias.Molecular methods can be used in lesional tissue todemonstrate the presence of virus. Viral presence doesnot prove causation. Since normal mucosa is oftenfound to harbor viral DNA, it is conceivable that thevirus is merely a passenger. Basic cell biology studieshave shown, however, that E6 <strong>and</strong> E7 sequences transfectedinto human keratinocytes induces transformationinto papillomas (HPV 6, 11) or carcinomas (HPV 16,18). The footprints of the virus are detected by the sensitivemethod of polymerase chain reaction (PCR), <strong>and</strong>RNA transcripts can be detected by reverse transcriptasePCR. Only rarely do immunohistochemical markersfor HPV capsid antigens stain positive in papillomasthat have been shown to contain DNA or RNA. In anycase, it is now well documented which genotypes areassociated with specific histopathologically definedpapillomas. HPV 2, 4, 6, <strong>and</strong> 11 are associated with <strong>and</strong>cause the benign warts of oral mucosa <strong>and</strong> vermilionepithelia; the role of HPV 16, 18 <strong>and</strong> other oncogenicTable 15–1<strong>Lesions</strong>Lesion<strong>Human</strong> Papillomavirus <strong>and</strong> <strong>Oral</strong> <strong>Papillary</strong> or VerrucousAssociated HPV GenotypesVerruca vulgaris 2, 4Squamous papilloma 6, 11Condyloma acuminatum 6, 11Focal epithelial hyperplasia 13, 32Squamous cell carcinoma 16, 18, 31, 33, 35Proliferative verrucous leukoplakia 6, 11, 16Verrucous carcinoma 2, 6, 11, 16Verruciform xanthomaNoneMolluscum contagiosumNone, poxvirusDenture papillary hyperplasiaNoneKeratoacanthomaNone
146 CHAPTER 15the upper layers, the nuclei are swollen, a cytopathiceffect of HPV termed koilocytosis. The histology of proliferativeverrucous leukoplakia <strong>and</strong> carcinomas is discussedin the chapter on precancerous <strong>and</strong> cancerouslesions (see Chapter 20).Pedunculated Sessile VerrucousFigure 15–2lesions.Histologic configurations in papillary <strong>and</strong> verrucousgenotypes in the pathogenesis of oral carcinoma isequivocal. The association for upper aerodigestive tractepithelium is not as convincing as for genital tractmucosa, in which HPV oncogenic viruses are identifiablein over 95% of lesional tissues. Since HPV DNA,RNA, or protein has been identified in some oral squamouscell carcinomas, specific HPV genotypes may be acausal cofactor in some patients, particularly in thoseindividuals who have no evident risk factors.Microscopically the benign verrucae <strong>and</strong> papillomasshow exophytic, finger-like projections of stratifiedsquamous epithelium, showing wide variations in thethickness of the keratin layer, which is usually parakeratinized(Figure 15–2). Verrucous lesions tend to haveacute “churchspire” projections, whereas papillarylesions tend to have rounded surface projections. Thecells of the spinous layer show normal cytology, yet inClinical featuresThe specific types of solitary papillary lesions that occurin the oral cavity include the common squamous papilloma,verruca vulgaris, condyloma acuminatum, verruciformxanthoma, molluscum contagiosum, <strong>and</strong> keratoacanthoma.Condylomas may also occur in crops ofmultiple papillomas, either clustered or widely separated.Denture papillomatosis, proliferative verrucous leukoplakia,verrucous carcinoma, <strong>and</strong> papillary exophyticsquamous cell carcinoma are diffuse sessile lesions.Squamous papillomaThe squamous papilloma is the most common benignepithelial neoplasm of oral epithelium. It may occuranywhere in the mouth with a predilection for the ventraltongue <strong>and</strong> frenum area, palate, <strong>and</strong> mucosal surfaceof the lips. Nonkeratinized lesions appear coralpink; if keratinized, they are white (Figure 15–3). Somehave a cauliflower surface whereas others have discreteACBFigure 15–3 Squamous papilloma. A, Clinical appearance; B, grossspecimen showing finger-like projections; C, microscopic appearance ofpapilloma.
HUMAN PAPILLOMAVIRUSES AND PAPILLARY ORAL LESIONS 147finger-like projections. They may be pedunculated orsessile in configuration. Papillomas are typically single,yet occasionally, more than one may occur. They occurat any age <strong>and</strong> are frequently seen in children <strong>and</strong> adolescents.There is no clearly defined mode of transmission,most occurring spontaneously. The solitary simplesquamous papilloma has not been considered to be asexually transmitted lesion, <strong>and</strong> when these lesionsoccur in children, sexual abuse is not to be suspected.Verruca vulgarisThe common skin wart may be seen on the vermilionborder, or less often, in the oral cavity. This type of oralwart is the least common <strong>and</strong> may occur at any age,being more frequent in children <strong>and</strong> adolescents. In themouth, verruca vulgaris has a tendency to arise most frequentlyon the keratinized surfaces of the gingiva <strong>and</strong>palate. Verrucae are sessile, oval, <strong>and</strong> white, owing tothe thickened keratin layer on the surface (Figure 15–4).In children with warts on their fingers, autoinoculationmay occur to the lips in those with a thumb-suckinghabit. Rarely, there may be more than one lesion present.ACondyloma acuminatumSexually transmitted warts tend to occur in multiples yetmay be single lesions. They are usually broad-based <strong>and</strong>sessile. They occur in both sexes but are more common inhomosexual males. Although oral condylomas can occuron any mucosal surface, they are more commonly foundon the lips, commissure region, <strong>and</strong> gingiva. When multiple,they tend to arrange themselves into regional clusters,although some cases are widely distributed throughoutthe oral mucosa, particularly in humanBACFigure 15–4 Verruca vulgaris. A, Clinical appearance of keratoticlesion on the lip; B, microscopic appearance; C, DNA in situ hybridizationshowing HPV-2 positivity in most keratinocyte nuclei.BFigure 15–5 Condylomas. A, Clinical appearance of multiple confluent<strong>and</strong> clustered condylomas; B, microscopic appearance showing papillaryprojections.
148 CHAPTER 15cavity; however, they are relatively rare (Figure 15–6).They have a unique histology in which the papillaryprojections of the epithelium overlie connective tissuefronds that are populated by foam-cell histiocytes.Unlike cutaneous xanthomas, there has not been a correlationwith hyperlipoproteinemia. Verruciform xanthomaoccurs anywhere in the oral mucosa, being morecommon on the gingiva <strong>and</strong> buccal mucosa, where it isusually of normal mucosal coloration.AMolluscum contagiosumCaused by a large virus of the poxvirus group, molluscumcontagiosum (MC) is an uncommon lesion of theoral mucosa since the tropism of the virus is primarilycutaneous. In the head <strong>and</strong> neck area, the lesions areusually seen on the facial skin <strong>and</strong> around the lips. Theclassic wart of molluscum is a crateriform papule, asmall normal colored skin nodule with a depressed centralpit (Figure 15–7). When present, MC lesions tend tobe multiple. Molluscum contagiosum is most often seenBFigure 15–6 Verruciform xanthoma. A, Sessile lesion of the gingiva ina bone marrow transplant patient; B, Photomicrograph showing bubblyfoam or xanthoma cells in the connective tissue papillae betweenepithelial cells.Aimmunodeficiency virus (HIV)-infected patients (seeChapter 14). Most are coral pink in color, have a wartyappearance, but are slightly keratinized (Figure 15–5).These lesions of the oral mucosa are often transmitted byoral, genital, <strong>and</strong> anal sex. Multiple papillary lesions in achild should arouse suspicion of sexual abuse, warrantinginvestigation of persons in contact with that child.Verruciform xanthomaAn association between verruciform xanthoma <strong>and</strong>HPV has not been substantiated. These lesions clinicallyresemble the other papillomas that frequent the oralBFigure 15–7 Molluscum contagiosum. A, Multiple facial skin lesions inan HIV-positive subject; B, molluscum bodies representing huge viralinclusions in keratinocytes.
HUMAN PAPILLOMAVIRUSES AND PAPILLARY ORAL LESIONS 149on the trunk, <strong>and</strong> when they are located on the face, itis usually an indication that the patient is immunocompromised,particularly as a consequence of HIV infection<strong>and</strong> subsequent immunosuppression. The virus isonly mildly contagious, requiring prolonged skin-toskincontact for transmission.KeratoacanthomaKeratoacanthoma (KA) is usually encountered on thefacial skin <strong>and</strong> lips yet can also arise, albeit rarely, in themouth. An association with HPV is not well established.Clinically they are characterized by a tumefaction withround, mounded borders that surround a central core ofhard keratinized material that may appear pale yellowor brown. The brown appearance is caused by extrinsicpigments that become incorporated with the excessivekeratin. Intraoral KAs are generally nonpigmented. Theperipheral mounded borders show an abrupt transitioninto normal skin or mucosa, both clinically <strong>and</strong> histologically(Figure 15–8). Since these warts can be large,they may cause the clinician to suspect carcinoma.Although the clinical appearance can be confusing, thesymmetrical nature, oval or round configuration, <strong>and</strong>keratotic core are indicative of KA. If left untreated,most KAs spontaneously regress.ing C<strong>and</strong>ida infection, the papillary surface may be whiteor red (pseudomembranous <strong>and</strong> erythematous forms ofc<strong>and</strong>idiasis). This condition is known as denture papillomatosisor papillary inflammatory hyperplasia <strong>and</strong> representsa hyperplastic reaction. The papillary pavementmay extend from the vibrating line posteriorly to the incisivepapilla anteroposteriorly <strong>and</strong> laterally across thepalatal vault without extention onto the edentulous alveolarridges. This is an important clinical feature, since thedifferential diagnosis for diffuse papillary lesions includesproliferative verrucous leukoplakia, verrucous carcinoma,<strong>and</strong> papillary exophytic squamous cell carcinoma,all of which tend to occur in the vestibule, yet frequentlyextend onto edentulous alveolar ridges.Precancerous diffuse papillary lesionsProliferative verrucous leukoplakia, verrucous carcinoma,<strong>and</strong> the papillary, exophytic variant of squamousDenture papillomatosisUnderlying maxillary dentures one may encounter diffusepapillary projections. These proliferations are found evenmore commonly with dentures that afford negative pressuresor are ill-fitting. Clinically, the entire hard palatalvault has the appearance of a mushroom garden withcoalescing small polyps (Figure 15–9). The individualpolyps are easily separated with a dental explorer. Theyare not hyperkeratotic, <strong>and</strong> for this reason their colorationis that of normal mucosa. If there is a complicat-AFigure 15–8Keratoacanthoma of the lip.BFigure 15–9 Denture inflammatory papillary hyperplasia (papillomatosis).A, Clinical appearance of palatal lesions found under an olddenture; B, microscopic appearance of diffuse papillary projections.
150 CHAPTER 15AFigure 15–10syndrome.Diffuse papillary lesions of the gingiva in the Cowdencell carcinoma are diffuse verrucous <strong>and</strong> papillary lesionsof the oral mucous membranes. These entities are HPVassociated<strong>and</strong> are discussed in detail in Chapter 20.Cowden syndromeMultiple hamartomas are encountered in this syndrome,which is a multisystem disease. The importance in recognizingthe oral manifestations of Cowden syndrome is toexplore for the other manifestations, since some of thehamartomatous lesions can progress to cancer. The diseaseis inherited as an autosomal dominant trait. Cutaneouspapules are seen around the nose <strong>and</strong> lips <strong>and</strong> alsoon the palmar surfaces, most represent hair follicle hamartomas(trichilemmomas). The patients develop goiters,thyroid adenomas, <strong>and</strong> fibrocystic disease of the breast,<strong>and</strong> some manifest hamartomatous intestinal polyps. Asmentioned previously, carcinomas can develop in thebreast <strong>and</strong> thyroid. The oral lesions are diffuse sessilepapillomas that have the appearance of a cobblestonestreet (Figure 15–10). Histologically they are benign papillary<strong>and</strong> papular proliferations of epithlium, supportedby fibrous cores. No viral association has been discovered.BFigure 15–11 Focal epithelial hyperplasia. A, Multiple lip nodules;B, mitosoid bodies in spinous cells.Focal epithelial hyperplasia (Heck disease)Caused by HPV 13 <strong>and</strong> 32, focal epithelial hyperplasiais an infection confined to oral mucosa (ie, there are nogenital or cutaneous foci of involvement). The lesionsoccur in children <strong>and</strong> young adults <strong>and</strong> are more commonin central <strong>and</strong> south America than in other areas,yet the disease has a worldwide distribution. Similarinfections can occur in HIV-infected subjects. Thelesions appear on the mucosal surfaces of the upper <strong>and</strong>Figure 15–12 Diffuse papillary lesions in acanthosis nigricans showingan absence of pigmentation.
HUMAN PAPILLOMAVIRUSES AND PAPILLARY ORAL LESIONS 151lower lips, commissures, <strong>and</strong> buccal mucosa. They aremultiple, measure from 3 mm to 10 mm, <strong>and</strong> aresmooth dome-shaped papules that lack a pebbly surface(Figure 15–11). The lesions persist for many monthsthen spontaneously resolve with no treatment.Acanthosis nigricansThere are two forms of acanthosis nigricans, a benignform <strong>and</strong> a malignant form. The malignant form isassociated with an internal malignancy, usually in thegastrointestinal tract, whereas the benign form fails toshow any such association. Acanthosis nigricans occurson the skin <strong>and</strong> may also affect the lips <strong>and</strong> oralmucosa. The papillary lesions are diffuse <strong>and</strong> sessilewith a cobblestone or pebbly appearance (Figure15–12). They are pigmented pale gray, a clinical findingattributable to basilar melanosis in the papillary epithelium.Once the diagnosis has been made, a workup forinternal malignancy is indicated.Treatment <strong>and</strong> managementSingle papillomas, verruca, <strong>and</strong> condylomas aretreated by local excision or laser ablation. Their focalappearance is classic; however, microscopic examinationis recommended since some forms of early squamouscancer may present as papillomas. If laser ablationis to be performed, it is recommended that theexophytic lesion be laser excised <strong>and</strong> submitted forbiopsy, followed by direct ablation of the lateral <strong>and</strong>deep margins. Since these lesions are superficial <strong>and</strong>exophytic, deep excision is not necessary. However, ifsquamous cell carcinoma is strongly considered in thedifferential diagnosis, an incisional biopsy should beperformed prior to treatment.The colonization of oral mucosa, particularly inimmunocompromised patients, by condylomas is a managementdilemma. Multiple widespread excisions arepainful during the healing phase <strong>and</strong> even after excision,multiple recurrences are common. <strong>Human</strong> immunodeficiencyvirus-infected patients placed on antiretrovirals<strong>and</strong> proteinase inhibitors <strong>and</strong> other multiple drugregimens have been shown to undergo regression oftheir oral warts in some cases. If the patient does notshow a favorable response to anti-HIV drug interventions,laser ablation should be considered.Proliferative verrucous leukoplakia, verrucous carcinoma,<strong>and</strong> the papillary variant of squamous cell carcinomahave been discussed in more detail in Chapter 20.These three premalignant <strong>and</strong> malignant papillarygrowths are treated by surgical excision with wide mar-gins. Even though complete excision is accomplishedwith microscopically confirmed clear margins, all ofthese HPV-associated tumors have a tendency to recur,<strong>and</strong> some become more histologically advanced witheach recurrence. Sometimes, radiation therapy is combinedwith surgical removal. Chemotherapy has notbeen found to be effective.Suggested readingCarlos R, Sedano HO. Multifocal papilloma virus epithelialhyperplasia. <strong>Oral</strong> Surg <strong>Oral</strong> Med <strong>Oral</strong> Pathol 1994;77:631–5.Eversole LR, Laipis PJ. <strong>Oral</strong> squamous papillomas: detectionof HPV DNA by in situ hybridization. <strong>Oral</strong> Surg <strong>Oral</strong>Med <strong>Oral</strong> Pathol 1988;65:545–50.Eversole LR, Laipis PJ, Merrell P, Choi E. Demonstration ofhuman papillomavirus DNA in oral condyloma acuminatum.J <strong>Oral</strong> Pathol 1987;16:266–72.Flaitz CM, Hicks MJ. Molecular piracy: the viral link to carcinogenesis.<strong>Oral</strong> Oncol 1998;34:448–53.Garlick JA, Taichman LB. <strong>Human</strong> papillomavirus infection ofthe oral mucosa. Am J Dermatopathol 1991;13:386–95.Green TL, Eversole LR, Leider AS. <strong>Oral</strong> <strong>and</strong> labial verruca vulgaris:clinical, histologic, <strong>and</strong> immunohistochemical evaluation.<strong>Oral</strong> Surg <strong>Oral</strong> Med <strong>Oral</strong> Pathol 1986;62:410–6Koch WM, Lango M, Sewell D, et al. Head <strong>and</strong> neck cancerin nonsmokers: a distinct clinical <strong>and</strong> molecular entity.Laryngoscope 1999;109:1544–51.Mignogna MD, Lo Muzio L, Ruocco V, Bucci E. Early diagnosisof multiple hamartoma <strong>and</strong> neoplasia syndrome(Cowden disease). The role of the dentist. <strong>Oral</strong> Surg <strong>Oral</strong>Med <strong>Oral</strong> Pathol <strong>Oral</strong> Radiol Endod 1995;79:295–9.Miller CS, White DK. <strong>Human</strong> papillomavirus expression in oralmucosa, premalignant conditions, <strong>and</strong> squamous cell carcinoma:a retrospective review of the literature. <strong>Oral</strong> Surg<strong>Oral</strong> Med <strong>Oral</strong> Pathol <strong>Oral</strong> Radiol Endod 1996;82:57–68.Mostafa KA, Takata T, Ogawa I, et al. Verruciform xanthomaof the oral mucosa: a clinicopathological study withimmunohistochemical findings relating to pathogenesis. VirchowsArch A Pathol Anat Histopathol 1993;423:243–8.Nelen M, Padberg GW, Peeters EA, et al. Localization of thegene for Cowden disease to chromosome 10q22-23. NatGenet 1996;13:114–6.Porter S, Cawson R, Scully C, Eveson J. Multiple hamartomasyndrome presenting with oral lesions. <strong>Oral</strong> Surg <strong>Oral</strong>Med <strong>Oral</strong> Pathol <strong>Oral</strong> Radiol Endod 1996;82:295–301.Praetorius F. HPV-associated diseases of oral mucosa. ClinDermatol 1997;15:399–413.Ramirez-Amador V, Esquivel-Pedraza L, Caballero-MendozaE, et al. <strong>Oral</strong> manifestations as a hallmark of malignantacanthosis nigricans. J <strong>Oral</strong> Pathol Med 1999;28:278–81.Viraben R, Aquilina C, Brousset P, Bazex J. Focal epithelialhyperplasia (Heck disease) associated with AIDS. Dermatology1996;193:261–2.