Tuberculosis 1. Epidemiology of mycobacterium tuberculosis
Tuberculosis 1. Epidemiology of mycobacterium tuberculosis
Tuberculosis 1. Epidemiology of mycobacterium tuberculosis
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
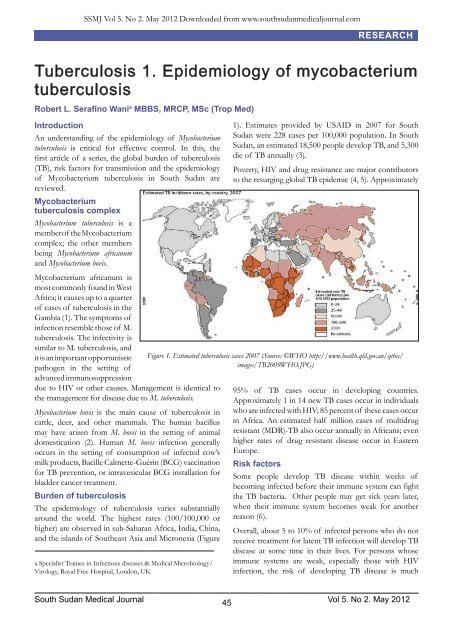
SSMJ Vol 5. No 2. May 2012 Downloaded from www.southsudanmedicaljournal.comRESEARCH<strong>Tuberculosis</strong> <strong>1.</strong> <strong>Epidemiology</strong> <strong>of</strong> <strong>mycobacterium</strong><strong>tuberculosis</strong>Robert L. Serafino Wani a MBBS, MRCP, MSc (Trop Med)IntroductionAn understanding <strong>of</strong> the epidemiology <strong>of</strong> Mycobacterium<strong>tuberculosis</strong> is critical for effective control. In this, thefirst article <strong>of</strong> a series, the global burden <strong>of</strong> <strong>tuberculosis</strong>(TB), risk factors for transmission and the epidemiology<strong>of</strong> Mycobacterium <strong>tuberculosis</strong> in South Sudan arereviewed.Mycobacterium<strong>tuberculosis</strong> complexMycobacterium <strong>tuberculosis</strong> is amember <strong>of</strong> the Mycobacteriumcomplex; the other membersbeing Mycobacterium africanumand Mycobacterium bovis.1). Estimates provided by USAID in 2007 for SouthSudan were 228 cases per 100,000 population. In SouthSudan, an estimated 18,500 people develop TB, and 5,300die <strong>of</strong> TB annually (3).Poverty, HIV and drug resistance are major contributorsto the resurging global TB epidemic (4, 5). ApproximatelyMycobacterium africanum ismost commonly found in WestAfrica; it causes up to a quarter<strong>of</strong> cases <strong>of</strong> <strong>tuberculosis</strong> in theGambia (1). The symptoms <strong>of</strong>infection resemble those <strong>of</strong> M.<strong>tuberculosis</strong>. The infectivity issimilar to M. <strong>tuberculosis</strong>, andit is an important opportunisticpathogen in the setting <strong>of</strong>advanced immunosuppressiondue to HIV or other causes. Management is identical tothe management for disease due to M. <strong>tuberculosis</strong>.Mycobacterium bovis is the main cause <strong>of</strong> <strong>tuberculosis</strong> incattle, deer, and other mammals. The human bacillusmay have arisen from M. bovis in the setting <strong>of</strong> animaldomestication (2). Human M. bovis infection generallyoccurs in the setting <strong>of</strong> consumption <strong>of</strong> infected cow’smilk products, Bacille Calmette-Guérin (BCG) vaccinationfor TB prevention, or intravesicular BCG installation forbladder cancer treatment.Burden <strong>of</strong> <strong>tuberculosis</strong>The epidemiology <strong>of</strong> <strong>tuberculosis</strong> varies substantiallyaround the world. The highest rates (100/100,000 orhigher) are observed in sub-Saharan Africa, India, China,and the islands <strong>of</strong> Southeast Asia and Micronesia (Figurea Specialist Trainee in Infectious diseases & Medical Microbiology/Virology, Royal Free Hospital, London, UKFigure <strong>1.</strong> Estimated <strong>tuberculosis</strong> cases 2007 (Source: ©WHO http://www.health.qld.gov.au/qtbcc/images/TB2009WHO.JPG)95% <strong>of</strong> TB cases occur in developing countries.Approximately 1 in 14 new TB cases occur in individualswho are infected with HIV; 85 percent <strong>of</strong> these cases occurin Africa. An estimated half million cases <strong>of</strong> multidrugresistant (MDR)-TB also occur annually in Africans; evenhigher rates <strong>of</strong> drug resistant disease occur in EasternEurope.Risk factorsSome people develop TB disease within weeks <strong>of</strong>becoming infected before their immune system can fightthe TB bacteria. Other people may get sick years later,when their immune system becomes weak for anotherreason (6).Overall, about 5 to 10% <strong>of</strong> infected persons who do notreceive treatment for latent TB infection will develop TBdisease at some time in their lives. For persons whoseimmune systems are weak, especially those with HIVinfection, the risk <strong>of</strong> developing TB disease is muchSouth Sudan Medical Journal Vol 5. No 2. May 201245
RESEARCHSSMJ Vol 5. No 2. May 2012 Downloaded from www.southsudanmedicaljournal.comhigher than for those with normal immune systems.Generally, persons at high risk for developing TB diseasefall into two categories (7):<strong>1.</strong> Persons who have been recently infected with TBbacteria.2. Persons with medical conditions that weaken theimmune system.<strong>1.</strong> Persons who have been recently infected with TBbacteriaThese include:• Persons who have close contacts with a person withinfectious TB disease.• Persons who have immigrated from areas <strong>of</strong> theworld with high rates <strong>of</strong> TB.• Children less than 5 years <strong>of</strong> age who have a positiveTB test.• Persons from groups with high rates <strong>of</strong> TBtransmission, such as homeless persons, injectiondrug users, and persons with HIV infection.• Persons who work or reside with people who are athigh risk <strong>of</strong> TB in facilities or institutions such ashospitals, homeless shelters, correctional facilities,nursing homes and residential homes for those withHIV.2. Persons with medical conditions that weaken theimmune systemBabies and young children <strong>of</strong>ten have weak immunesystems. Other people can have weak immune systemsespecially those with any <strong>of</strong> these conditions:• HIV infection.• Substance abuse.• Silicosis (8).• Diabetes mellitus.• Severe kidney disease.• Low body weight.• Organ transplants.• Head and neck cancer.• Medical treatments such as corticosteroids or organtransplant.• Specialized treatment for rheumatoid arthritis orCohn’s disease.In South Sudan although the exact incidence <strong>of</strong> HIV/AIDS among TB cases is not known, HIV prevalenceappears to be on the rise. Data from limited populationsurveys show HIV prevalence rates range between 1 and8 percent among the general population, with higher rates(up to 25 percent) found in border towns. Multidrugresistant(MDR) TB cases account for around <strong>1.</strong>9 percent<strong>of</strong> new cases and usually occurs among defaulters andrelapse cases.The TB epidemic is an outgrowth <strong>of</strong> a long-standingwar, which has resulted in poverty, malnutrition, and alarge number <strong>of</strong> displaced populations and refugees.Destruction <strong>of</strong> health infrastructure, lack <strong>of</strong> microscopicservices, and displacement or lack <strong>of</strong> health personnelhave also contributed to the epidemic (3).References:<strong>1.</strong> deJong BC, Antonio M, Gagneux S. Mycobacteriumafricanum: review <strong>of</strong> an important cause <strong>of</strong> human<strong>tuberculosis</strong> in West Africa. PLoS Negl Trop Dis 2010;4:e744.2. Cole ST, Brosch R, Parkhill J, et al. Deciphering the biology<strong>of</strong> Mycobacterium <strong>tuberculosis</strong> from the complete genomesequence. Nature 1998; 393:537.3. USAID Health: Infectious Diseases, <strong>Tuberculosis</strong>,Countries, Sudan. Available on line at: http://www.usaid.gov/our_work/global_health/id/<strong>tuberculosis</strong>/countries/africa/ssudan_pr<strong>of</strong>ile.html4. Corbett EL, Marston B, Churchyard GJ, De Cock KM.<strong>Tuberculosis</strong> in sub-Saharan Africa: opportunities,challenges, and change in the era <strong>of</strong> antiretroviral treatment.Lancet 2006; 367:926.5. Wright A, Zignol M, Van Deun A, et al. <strong>Epidemiology</strong><strong>of</strong> anti<strong>tuberculosis</strong> drug resistance 2002-07: an updatedanalysis <strong>of</strong> the Global Project on Anti-<strong>Tuberculosis</strong> DrugResistance Surveillance. Lancet 2009 Apr 15.6. Centers for Disease Control and Prevention. TB Basicfacts. CDC/TB/Basic TB Facts. Available on line at http://www.cdc.gov/tb/topic/basics/default.htm7. Centers for Disease Control and Prevention. TB Basicfacts. CDC/TB/Basic TB Facts/Risk Factors. Available online at http://www.cdc.gov/tb/topic/basics/risk.htm8. Huaux F. New developments in the understanding <strong>of</strong>immunology in silicosis. Current Opinion in Allergy & ClinicalImmunology: 2007: 7 (2):168-173.South Sudan Medical Journal 46Vol 5. No 2. May 2012