Terugbetalingssystemen voor geneesmiddelen ... - Pharma
Terugbetalingssystemen voor geneesmiddelen ... - Pharma
Terugbetalingssystemen voor geneesmiddelen ... - Pharma
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
10 Drug Reimbursement Systems KCE Reports 147<br />
The required strength of the relationship between the advice and the decision is a<br />
political decision. Countries can choose to consider all socially relevant criteria in the<br />
appraisal process, including the health care sector related and the non-health care<br />
sector related criteria, in which case there is no reason to make a distinction between<br />
the appraisal and decision making phase. Countries can also choose to give discretionary<br />
power to the minister responsible for drug reimbursement decisions.<br />
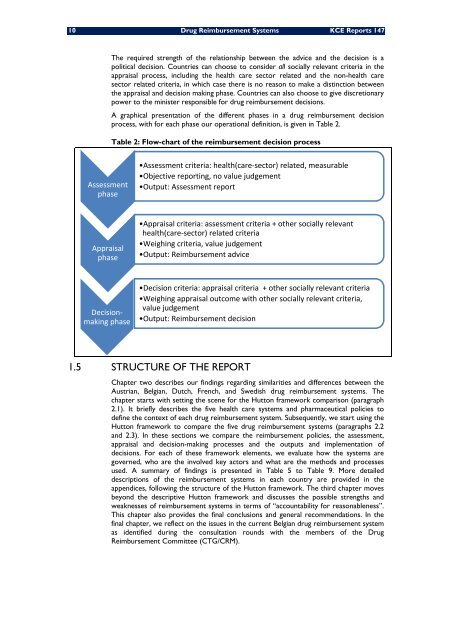
A graphical presentation of the different phases in a drug reimbursement decision<br />
process, with for each phase our operational definition, is given in Table 2.<br />
Table 2: Flow-chart of the reimbursement decision process<br />
Assessment<br />
phase<br />
•Assessment criteria: health(care‐sector) related, measurable<br />
•Objective reporting, no value judgement<br />
•Output: Assessment report<br />
Appraisal<br />
phase<br />
•Appraisal criteria: assessment criteria + other socially relevant<br />
health(care‐sector) related criteria<br />
•Weighing criteria, value judgement<br />
•Output: Reimbursement advice<br />
Decisionmaking<br />
phase<br />
•Decision criteria: appraisal criteria + other socially relevant criteria<br />
•Weighing appraisal outcome with other socially relevant criteria,<br />
value judgement<br />
•Output: Reimbursement decision<br />
1.5 STRUCTURE OF THE REPORT<br />
Chapter two describes our findings regarding similarities and differences between the<br />
Austrian, Belgian, Dutch, French, and Swedish drug reimbursement systems. The<br />
chapter starts with setting the scene for the Hutton framework comparison (paragraph<br />
2.1). It briefly describes the five health care systems and pharmaceutical policies to<br />
define the context of each drug reimbursement system. Subsequently, we start using the<br />
Hutton framework to compare the five drug reimbursement systems (paragraphs 2.2<br />
and 2.3). In these sections we compare the reimbursement policies, the assessment,<br />
appraisal and decision-making processes and the outputs and implementation of<br />
decisions. For each of these framework elements, we evaluate how the systems are<br />
governed, who are the involved key actors and what are the methods and processes<br />
used. A summary of findings is presented in Table 5 to Table 9. More detailed<br />
descriptions of the reimbursement systems in each country are provided in the<br />
appendices, following the structure of the Hutton framework. The third chapter moves<br />
beyond the descriptive Hutton framework and discusses the possible strengths and<br />
weaknesses of reimbursement systems in terms of “accountability for reasonableness”.<br />
This chapter also provides the final conclusions and general recommendations. In the<br />
final chapter, we reflect on the issues in the current Belgian drug reimbursement system<br />
as identified during the consultation rounds with the members of the Drug<br />
Reimbursement Committee (CTG/CRM).