ERADICATION OF GUINEA WORM DISEASE
1VIcLdr
1VIcLdr
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>ERADICATION</strong> <strong>OF</strong><br />
<strong>GUINEA</strong> <strong>WORM</strong> <strong>DISEASE</strong><br />
Case Statement
Since The Carter Center began leading global Guinea worm disease eradication efforts in 1986 together with<br />
endemic countries and the World Health Organization, as well as other trusted partners such as UNICEF, the<br />
campaign has reduced the number of cases 99.99 percent, from 3.5 million cases annually in Africa and Asia to<br />
22 cases in 2015.<br />
Guinea worm eradication is drawing ever closer to the finish line. The campaign demonstrates what remarkable<br />
change can occur with full engagement — from national ministries of health and each individual in affected<br />
villages — even though there is no drug to cure Guinea worm disease or a vaccine to prevent it.<br />
Each country that triumphs over Guinea worm disease serves as a reminder to the world that the greatest<br />
challenges can be overcome with hard work, political commitment, and support of the international community.<br />
However, success in global eradication will require stronger commitment of the four endemic countries fighting<br />
the remaining cases, as well as of international partners in this public health initiative.<br />
Everyone has a stake in these efforts. The entire world stands to gain from the eradication of Guinea worm disease,<br />
not only because an age-old affliction will have been wiped off the surface of the planet, but also as proof that<br />
eradication can be achieved with willpower, political involvement, local perseverance, and financial investment.<br />
It was done with smallpox, and we can do it again.<br />
We urge development partners — governments, foundations, and corporations — to generously contribute financial<br />
support in a united demonstration that, together, we can ensure the eradication of Guinea worm disease by 2020.<br />
With best wishes,<br />
Jimmy Carter<br />
Former U.S. President<br />
Co-founder, The Carter Center<br />
Margaret Chan<br />
Director-General<br />
World Health Organization<br />
Boys with Guinea worm disease receive treatment at a case containment center in South Sudan.<br />
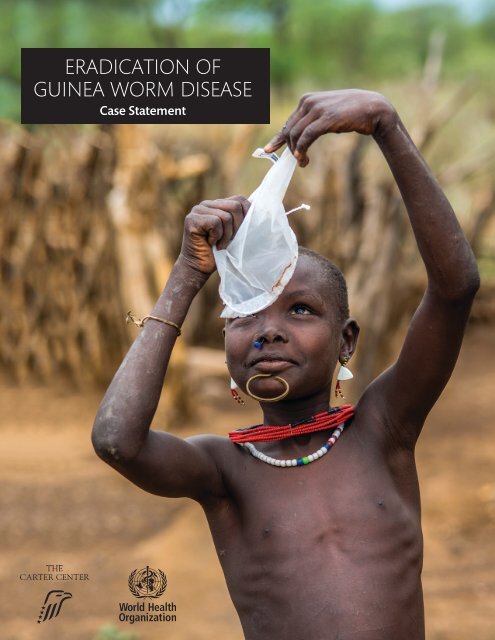
On the cover: A South Sudanese boy examines a cloth filter. Filtration of drinking water prevents Guinea worm disease.
ABOUT <strong>GUINEA</strong><br />
<strong>WORM</strong> <strong>DISEASE</strong><br />
Guinea worm disease is an affliction of<br />
2011<br />
poverty, debilitating residents of remote<br />
COTE GHANA<br />
D’IVOIRE 2015<br />
and marginalized communities in sub-<br />
2013<br />
Saharan Africa. A painful and incapacitating<br />
TOGO BENIN 2009<br />
waterborne disease, it negatively affects health,<br />
2011<br />
agricultural productivity, school attendance, and<br />
overall quality of life in the communities where<br />
it is found. 1 Guinea worm disease is caused by<br />
the parasitic worm Dracunculus medinensis, which<br />
infects people who drink water from stagnant<br />
sources containing microscopic infective larvae<br />
harbored by tiny copepods (“water fleas”). During<br />
the yearlong incubation period, individuals do<br />
not know they are infected and become unwitting<br />
carriers of the parasite until the adult female worms,<br />
measuring up to one meter in length, emerge. An<br />
emerging worm causes a blister on the victim’s skin,<br />
accompanied by a severe burning sensation and<br />
pain, followed by an open lesion with a protruding<br />
Guinea worm. When a patient cools the wound in<br />
a stagnant water source, the worm releases hundreds<br />
1989<br />
1990<br />
of thousands of larvae, which are readily ingested<br />
1991<br />
by copepods, contaminating the water source and<br />
1992<br />
continuing the transmission cycle.<br />
There is no drug to cure Guinea worm<br />
disease or vaccine to prevent it, humans do<br />
not develop immunity to the disease, and<br />
there is no known wild animal reservoir from<br />
which the disease can return to humans once<br />
transmission is interrupted. However, disease<br />
transmission can be prevented. The Carter<br />
Center — in partnership with the national Guinea<br />
worm eradication programs of the ministries of<br />
health of affected countries, the World Health<br />
Organization (WHO), and strategic partners such<br />
as the Centers for Disease Control and Prevention<br />
and UNICEF — have pioneered community-based<br />
responses to prevent transmission, and ultimately<br />
eradicate Guinea worm disease by 2020.<br />
MAURITANIA<br />
2009 MALI<br />
NIGER<br />
5<br />
CHAD SUDAN<br />
SENEGAL<br />
2013<br />
9<br />
YEMEN<br />
2002<br />
2004<br />
2004<br />
BURKINA FASO<br />
NIGERIA<br />
CENTRAL AFRICAN<br />
2013 REPUBLIC SOUTH ETHIOPIA<br />
2007 SUDAN 3<br />
CAMEROON<br />
5<br />
2007<br />
UGANDA<br />
2009 KENYA<br />
1994<br />
1993<br />
1994<br />
1995<br />
1996<br />
1997<br />
1998<br />
1999<br />
2000<br />
2001<br />
2002<br />
2003<br />
2004<br />
2005<br />
2006<br />
2007<br />
2008<br />
2009<br />
2010<br />
2011<br />
2012<br />
2013<br />
2014<br />
2015<br />
77,863<br />
78,557<br />
164,977<br />
129,852<br />
96,293<br />
75,223<br />
63,718<br />
54,638<br />
32,193<br />
16,026<br />
10,674<br />
25,217<br />
9,585<br />
4,619<br />
3,190<br />
1,797<br />
1,058<br />
542<br />
148<br />
126<br />
22<br />
152,814<br />
229,773<br />
374,202<br />
543,585<br />
623,579<br />
PAKISTAN<br />
1996<br />
Progress on Guinea<br />
worm eradication since<br />
1986, by country<br />
Year Certified by<br />
WHO as Free of<br />
Guinea Worm Disease<br />
Year Guinea Worm<br />
Transmission Halted<br />
Cases Remaining<br />
at End of 2015<br />
(provisional count)<br />
Annual number of cases of Guinea worm disease worldwide since 1989<br />
892,055<br />
INDIA<br />
2000<br />
3
Because Guinea worm is a<br />
waterborne disease, water<br />
filtration can prevent its spread.<br />
THE NEEDS<br />
In 1986, an estimated 3.5 million cases of the disease<br />
could be found in 21 countries in Africa and Asia,<br />
where 120 million residents were at risk of the<br />
infection. 2 Since then, cases have been reduced by<br />
more than 99.9 percent. At the end of 2015, there<br />
were only 22 cases in 20 villages in four countries:<br />
South Sudan, Ethiopia, Mali, and Chad. To date, the<br />
World Health Organization has certified 15 formerly<br />
endemic countries and 183 other countries and<br />
territories and areas as free of Guinea worm disease.<br />
Guinea worm is poised to be the second human<br />
disease and the first parasitic disease ever<br />
eradicated. The Carter Center and its partners assist<br />
the national Guinea worm eradication programs to<br />
halt transmission of the disease through:<br />
Education: Communities learn about the disease<br />
and how to prevent it. For example,<br />
people learn never to enter a source<br />
of drinking water if a Guinea worm is<br />
emerging, never to allow anyone else<br />
in the community with an emerging<br />
Guinea worm to do so, and to report<br />
anyone with Guinea worm.<br />
Surveillance: A comprehensive<br />
community-based surveillance<br />
network aims to detect and report<br />
cases of Guinea worm disease<br />
promptly (before or within 24 hours<br />
of worm emergence).<br />
Case containment: Individual<br />
cases are promptly managed<br />
(contained) to prevent infected<br />
people from contaminating sources of<br />
drinking water.<br />
Water treatment: Contaminated, stagnant<br />
sources of drinking water are treated with Abate ®<br />
(temephos), a safe chemical larvicide donated by<br />
BASF Corporation.<br />
Water filtration: Community members are taught to<br />
filter all unsafe drinking water to sieve out copepods<br />
and prevent infection. Cloth filters and pipe filters<br />
are donated by Vestergaard.<br />
As the lead agency over the last 30 years of the<br />
global Guinea worm eradication campaign, The<br />
Carter Center has raised $332.9 million in financial<br />
and in-kind contributions. Sources of support are<br />
illustrated in the chart below.<br />
An estimated $214 million is needed between 2015<br />
and 2020 to fully eradicate Guinea worm disease<br />
and to certify that the disease has been eradicated.<br />
As with any eradication campaign, the last cases<br />
will be the most expensive, but the ultimate reward<br />
is a world free of Guinea worm disease for future<br />
generations.<br />
Contributions and pledges for Guinea worm<br />
eradication by donor type, 1986–2014<br />
4%<br />
13%<br />
41%<br />
4%<br />
FPO<br />
38%<br />
Foundations<br />
Governments<br />
Organizations<br />
Corporations<br />
Individuals<br />
4
THE INTERVENTIONS<br />
The campaign will be successful when all<br />
countries are certified as free of Guinea worm<br />
disease. The following phases outline the work<br />
remaining to reach that goal. Ministries of health,<br />
national Guinea worm eradication programs and<br />
governments of affected countries are key partners<br />
in these efforts.<br />
Phase 1 Interruption of transmission in<br />
remaining endemic countries, led by endemic<br />
countries with support from The Carter<br />
Center: 2016<br />
• Ensure 100 percent coverage of active<br />
surveillance in remaining endemic areas,<br />
including regular case searches, investigation,<br />
documentation and response (within 24 hours) of<br />
rumored cases of Guinea worm disease.<br />
• Maintain surveillance and response capacity in<br />
areas of endemic countries where transmission<br />
has already been stopped.<br />
• Continue health education and mobilization,<br />
including distribution of cloth and pipe water<br />
filters, application of Abate larvicide to treat<br />
contaminated sources of drinking water, provision<br />
of safe drinking water, and promotion of cash<br />
rewards for reporting cases.<br />
• Conduct ongoing advocacy at national and<br />
international levels for continued support and<br />
funding to reach eradication.<br />
• Maintain cross-border surveillance and response<br />
capacity to prevent importation of cases and<br />
ensure that eradication status is maintained in all<br />
countries that have already been certified as free<br />
of Guinea worm disease. (WHO)<br />
Because many families in South Sudan, such as this child and her parents,<br />
move from place to place to care for their cattle, disease surveillance must<br />
cover a wide geographical area.<br />
Phase 2 Pre-certification, led by<br />
concerned countries with support<br />
from The Carter Center and WHO:<br />
2016–2019<br />
• Continue active surveillance in last<br />
group of endemic areas and immediate<br />
reporting and investigation of rumored<br />
cases. (The Carter Center)<br />
• Conduct ongoing advocacy at<br />
national and international levels for<br />
continued support and funding to<br />
reach eradication. (The Carter Center<br />
and WHO)<br />
• Facilitate external assessments to<br />
verify national claim that transmission has been<br />
interrupted. (WHO)<br />
• Implement a global reward for Guinea worm disease<br />
cases. (WHO)<br />
• Maintain cross-border surveillance and response<br />
capacity to prevent importation of cases and ensure<br />
that eradication status is maintained in all countries<br />
that have already been certified as free of Guinea<br />
worm disease. 3 (WHO)<br />
Phase 3 Certification, led by WHO: 2016–2020<br />
• Continue dissemination of information about<br />
rewards for Guinea worm disease cases.<br />
• Assist countries in preparing report for the<br />
International Commission for Certification of<br />
Dracunculiaisis Eradication (ICCDE).<br />
• Certify eight countries remaining, based on ICCDE<br />
assessment: Chad, Ethiopia, Mali, South Sudan,<br />
Kenya, Sudan, Angola, and Democratic Republic of<br />
the Congo.<br />
An Ethiopian<br />
community<br />
learns how to<br />
prevent Guinea<br />
worm disease.<br />
5
The extraction of<br />
a Guinea worm<br />
is a slow and<br />
painful process<br />
that can take up<br />
to two weeks<br />
or more for a<br />
single worm; if a<br />
worm is coaxed<br />
out forcefully, it<br />
can break and<br />
cause infection<br />
or permanent<br />
disability.<br />
6<br />
A health worker in Mali applies the<br />
safe larvicide Abate to a pond where<br />
people get their drinking water.<br />
SOCIAL AND ECONOMIC CASE<br />
FOR <strong>ERADICATION</strong><br />
The burden of Guinea worm disease on individuals,<br />
communities, and societies extends beyond<br />
physical suffering to significant economic and<br />
social consequences, hampering development and<br />
perpetuating a cycle of poverty and disease. 4 Due<br />
to its significant economic burden, Guinea worm<br />
disease is both a symptom of and contributor to<br />
poverty. The disease burden impacts adults and<br />
children alike, resulting in decreased agricultural<br />
and household productivity, as well as impinging<br />
on children’s school attendance.<br />
The economic burden on poor rural communities<br />
is particularly severe and aggravated by the<br />
seasonality of transmission, which coincides with<br />
peak agricultural activities. Agricultural laborers<br />
infected with Guinea worm disease are unable to<br />
harvest and farm crops (average duration of Guinea<br />
worm disability is eight weeks), affecting income<br />
and nutrition for families and the wider community. 5<br />
Additionally, children may be forced to take on<br />
work of their sick family members in the fields or<br />
in the home, causing absences at school. Children’s<br />
malnourishment or their own emerging Guinea<br />
worms that disable them from walking to school can<br />
further exacerbate the impact of the disease.<br />
The effort to eradicate Guinea worm disease is<br />
considered one of the most cost-effective health<br />
interventions available. Over 80 million cases have<br />
been averted since The Carter Center began working<br />
on the campaign in 1986, resulting in improved<br />
health status (including childcare and immunization<br />
coverage), agricultural productivity, and school<br />
attendance for millions of people in some of the most<br />
remote areas of the world at an estimated financial<br />
cost of $3.47 per case averted. Through communitybased<br />
health education, filtration of drinking water,<br />
application of Abate, and prompt detection of<br />
cases, Guinea worm disease can be affordably and<br />
effectively prevented.<br />
However, the costs per case of treatment and<br />
containment do increase toward the end of each<br />
national campaign and the end of the global<br />
campaign for the following reasons:<br />
Long incubation: The one-year-long incubation<br />
period makes it impossible to pre-identify infected<br />
carriers of the disease and ascertain who will develop<br />
infection. An extensive and intensive surveillance<br />
system must be maintained for at least one year<br />
beyond the report of the last indigenous case.<br />
Thus, the surveillance footprint of Guinea worm<br />
eradication programs must not only be maintained<br />
but must encompass all places where infected persons<br />
may be when they develop the disease.<br />
Prompt detection and containment: Interrupting<br />
transmission requires intensified operations during<br />
the last phase of each national eradication effort<br />
in order to detect all cases within 24 hours of<br />
worm emergence, to manage all patients promptly<br />
by case containment and to prevent transmission<br />
effectively, through treatment of contaminated<br />
sources of drinking water and ongoing community<br />
education about the need to consistently filter all<br />
drinking water.
Isolation and marginalization of affected<br />
communities: The dearth of public health<br />
infrastructure in Guinea worm endemic areas requires<br />
establishment and operation of case containment<br />
centers where patients with cases voluntarily<br />
admit themselves for health care and prevention<br />
of transmission. In addition, the last communities<br />
affected by Guinea worm disease are frequently the<br />
most marginalized by local society and distrustful<br />
of government programs and anyone of authority<br />
outside their communities. This often results in<br />
community reluctance to cooperate and likelihood to<br />
hide cases or withhold information about population<br />
movements or sources of drinking water, thus<br />
increasing the chances of missing cases. Community<br />
mobilization and trust are therefore essential.<br />
SUCCESS STORY: HUBEIDA IDDIRISU<br />
Above: In Ghana in 2007, volunteer Sulley Zakaria visits Hubeida Iddirisu at home to treat her three painful wounds where Guinea<br />
worms are emerging from her body. Right: Six years later Hubeida is a smiling teenager, and no one in her family, village, or country is<br />
at risk of the parasitic disease.<br />
In 2007, 11-year-old Hubeida Iddirisu faced<br />
long days of pain as three Guinea worms<br />
began to emerge from blisters on her body.<br />
Hubeida was the victim of a particularly severe<br />
Guinea worm disease outbreak in her town of<br />
Savelugu, Ghana.<br />
“I probably caught the worms when<br />
accepting a drink from a neighbor during my<br />
rounds of charcoal selling,” she said.<br />
Every day for two weeks, a volunteer<br />
came to Hubeida’s home to extract the<br />
worms. Often people suffer from more<br />
than one worm at a time, as Hubeida did,<br />
and the incapacitating wounds caused by<br />
the worms typically take up to two months<br />
to heal. While the worms were emerging,<br />
Hubeida was unable to attend school, handle<br />
her household tasks, or work at her afterschool<br />
job.<br />
During the outbreak, the Ghana Guinea<br />
Worm Eradication Program, assisted by The<br />
Carter Center and its partners, stepped up<br />
efforts to halt the disease in Savelugu by<br />
providing all households with cloth filters to<br />
strain out the Guinea worm larvae in drinking<br />
water. Community members with emerging<br />
worms were told not to enter sources of<br />
drinking water, such as the local dam, because<br />
doing so would allow the worms to release<br />
larvae into the water and continue the<br />
parasite’s life cycle. Stagnant ponds were also<br />
treated with a safe larvicide.<br />
One year later, Hubeida was free of Guinea<br />
worm disease. She was able to carry out her<br />
daily chores as well as her job selling charcoal<br />
to help support her family and pay for school<br />
fees.<br />
Today, Hubeida Iddirisu is a smiling young<br />
woman, and she has never had another<br />
Guinea worm. Ghana saw its last case of the<br />
disease in 2010 and was certified as free of<br />
Guinea worm disease in 2015.<br />
7
Guinea worm eradication campaign<br />
funding requirements, 2015–2020<br />
CALL TO ACTION<br />
Global eradication of Guinea worm disease requires<br />
unrelenting daily acts of courage by field workers in<br />
the four remaining endemic countries to break the<br />
transmission cycle. In spite of numerous challenges<br />
(including, but not limited to, insecurity and difficult<br />
access to endemic areas), the national Guinea worm<br />
eradication programs, assisted by The Carter Center<br />
and WHO, continue to deliver on their goals,<br />
steadily reducing cases, stopping transmission in<br />
endemic villages, and ensuring optimal surveillance<br />
and reporting. Continued perseverance and adequate<br />
funding will certainly ensure victory.<br />
Once transmission has been stopped globally, no<br />
further interventions or monitoring will be needed<br />
beyond the three-year-long precertification of<br />
eradication stage required by WHO. 6 The impact of<br />
success without a vaccine or curative drug will extend<br />
to validate the principle of disease eradication, the<br />
potential of community-based engagement and health<br />
education, and provide an example of a successful<br />
$156.97 million remaining<br />
$55.95 million confirmed<br />
$212.92 million total funding needed<br />
program for a neglected tropical disease. The legacy<br />
of the established health infrastructure and networks<br />
created to fight Guinea worm disease will include<br />
community-based surveillance and health education<br />
delivery systems ready to deliver other essential<br />
interventions. 7 Eradication will accrue economic<br />
returns forever by benefiting the health, agricultural<br />
productivity, and school attendance among some of<br />
the world’s poorest people.<br />
Join the global campaign. Your support is essential<br />
to maintaining momentum in the final push to<br />
eradicate Guinea worm disease.<br />
1 Cairncross S, Muller R, Zagaria N (2002). Dracunculiasis (Guinea worm disease)<br />
and the eradication initiative. Clin Microbiol Rev 15:223-246.<br />
2 Watts SJ. (1987) Dracunculiaisis in Africa in 1986: Its Geographic Extent,<br />
Incidence and At-Risk Population. American Journal of Tropical Medicine and<br />
Hygiene. 37(1): 119-125.<br />
3 See: http://apps.who.int/dracunculiasis/dradata/html/report_Countries_i1.html<br />
4 Levine R, What Works Working Group (2007): Case 11: reducing Guinea worm<br />
in Asia and sub-Saharan Africa. In Case studies in global health: millions saved.<br />
Sudbury (Massachusetts): Jones & Bartlett Learning.<br />
5 Kim A, Tandon A, and Ruiz-Tiben E. (1997). Cost-Benefit Analysis of the<br />
Global Dracunculiasis Eradication Campaign (GDEC) Policy Research Working<br />
Paper, No 1835. The World Bank. Available on: http://www.cartercenter.org/<br />
documents/2101.pdf<br />
6 WHO, Dracunculiasis Fact Sheet. May 2015. Available on: http://www.who.int/<br />
mediacentre/factsheets/fs359/en/<br />
7 Callahan K, Bolton B, Hopkins DR, Ruiz-Tiben E, Withers PC, et al. (2013)<br />
Contributions of the Guinea Worm Eradication Campaign toward Achievement<br />
of the Millennium Development Goals. PLoS Negl Trop Dis 7 (5): e2160. Doi<br />
:10.1371/journal.pntd.0002160. Available on: http://www.cartercenter.org/<br />
resources/pdfs/news/health_publications/guinea_worm/plos-contributions-of-gweradication-toward-achievement-of-MDG.pdf<br />
For more details on how to support the<br />
Guinea worm eradication campaign,<br />
please contact:<br />
Nicole Kruse, nicole.kruse@cartercenter.org<br />
Kate Braband, kate.braband@cartercenter.org<br />
Chris Maddock, maddockc@who.int<br />
For the most up-to-date information, including<br />
a link to the current case count, go to<br />
www.cartercenter.org/guinea-worm.<br />
One Copenhill<br />
453 Freedom Parkway<br />
Atlanta, GA 30307<br />
www.cartercenter.org<br />
Avenue Appia 20<br />
1211 Geneva 27<br />
Switzerland<br />
www.who.int