Agent of social change
gotc22w
gotc22w
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
INSIDE<br />
Leaders <strong>of</strong> general practice<br />
A closer look at the GP15 award winners<br />
Doctor–patient boundaries<br />
Maintaining ethical relationships<br />
Nutrition and older patients<br />
The healthy weight range and older people<br />
ISSUE 10, OCTOBER 2015<br />
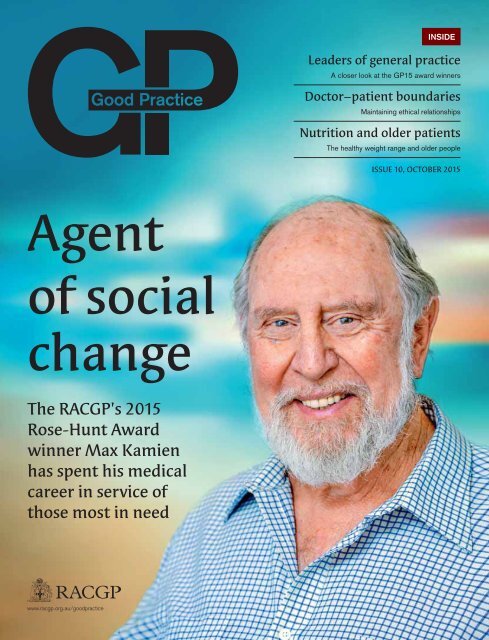
<strong>Agent</strong><br />
<strong>of</strong> <strong>social</strong><br />
<strong>change</strong><br />
The RACGP’s 2015<br />
Rose-Hunt Award<br />
winner Max Kamien<br />
has spent his medical<br />
career in service <strong>of</strong><br />
those most in need<br />
www.racgp.org.au/goodpractice
Contents<br />
Issue 10 – October 2015<br />
04<br />
Your College<br />
RACGP news and events for October.<br />
06<br />
Rose-Hunt Award<br />
<strong>Agent</strong> <strong>of</strong> <strong>social</strong> <strong>change</strong><br />
Emeritus Pr<strong>of</strong>essor Max Kamien’s<br />
career in general practice has allowed<br />
him to advocate for some <strong>of</strong> the world’s<br />
most vulnerable populations.<br />
10<br />
GP <strong>of</strong> the Year<br />
Comprehensive approach<br />
The holistic and collaborative<br />
nature <strong>of</strong> general practice suits<br />
Dr Kean-Seng Lim’s methods <strong>of</strong><br />
delivering healthcare.<br />
06<br />
18<br />
General Practice <strong>of</strong> the Year<br />
Progressive practice<br />
GPs at Western Australia’s Collie River<br />
Valley Medical Centre believe general<br />
practices can evolve to best meet the<br />
needs <strong>of</strong> their patients.<br />
20<br />
Brian Williams Award<br />
Rural pathway<br />
A close relationship with the local<br />
community is one <strong>of</strong> many reasons<br />
Dr Ken Wanguhu loves rural<br />
general practice.<br />
22<br />
Conference for General Practice<br />
Full list <strong>of</strong> award winners from GP15.<br />
12<br />
General Practice Supervisor<br />
<strong>of</strong> the Year<br />
Leading the way<br />
Medical educator Dr Cathy Milligan hopes<br />
registrars at her rural practice can develop<br />
an extensive range <strong>of</strong> skills.<br />
14<br />
General Practice Registrar <strong>of</strong> the Year<br />
Support system<br />
Dr Ashlea Broomfi eld has dedicated<br />
much <strong>of</strong> her time in general practice to<br />
advocating for her fellow registrars.<br />
16<br />
Rural Registrar <strong>of</strong> the Year<br />
One <strong>of</strong> the team<br />
Dr Hannah Visser believes the GP is one<br />
<strong>of</strong> many links in the chain <strong>of</strong> Aboriginal<br />
and Torres Strait Islander health.<br />
10<br />
14<br />
23<br />
Ethics in General Practice<br />
Boundary crossings<br />
Maintaining appropriate doctor–patient<br />
boundaries.<br />
24<br />
Nutrition<br />
BMI and older people<br />
Does the healthy weight range<br />
apply to older patients?<br />
26<br />
Financial Planning<br />
Value <strong>of</strong> trusts<br />
In the fi rst <strong>of</strong> a new series <strong>of</strong> columns,<br />
fi nancial planner Terry McMaster examines<br />
the advantages structuring a general<br />
practice business as a trust.<br />
12 18<br />
Published by<br />
The Royal Australian College<br />
<strong>of</strong> General Practitioners<br />
100 Wellington Parade<br />
East Melbourne<br />
Victoria 3002<br />
T 03 8699 0414<br />
E goodpractice@racgp.org.au<br />
W www.racgp.org.au/goodpractice<br />
ABN 34 000 223 807<br />
ISSN 1837-7769<br />
Editor: Paul Hayes<br />
Writer: Bevan Wang<br />
Graphic Designer: Beverly Jongue<br />
Production Coordinator:<br />
Beverley Gutierrez<br />
Publications Manager: Jenni Stiffe<br />
Advertising enquiries<br />
Kate Marie:<br />
T 0414 517 122<br />
E kate.marie@racgp.org.au<br />
Editorial notes<br />
© The Royal Australian College <strong>of</strong> General Practitioners<br />
2015. Unless otherwise indicated, copyright <strong>of</strong> all images<br />
is vested in the RACGP. Requests for permission to reprint<br />
articles must be made to the editor. The views contained<br />
herein are not necessarily the views <strong>of</strong> the RACGP, its<br />
council, its members or its staff. The content <strong>of</strong> any<br />
advertising or promotional material contained within Good<br />
Practice is not necessarily endorsed by the publisher.<br />
We recognise the traditional custodians <strong>of</strong> the land and<br />
sea on which we work and live.<br />
Cover image Jeremy McCready<br />
Good Practice is printed on PEFC certifi ed paper,<br />
meaning that it originates from forests that are<br />
managed sustainably. PEFC is the Programme for<br />
the Endorsement <strong>of</strong> Forest Certifi cation schemes.<br />
PEFC is an international certifi cation programme<br />
promoting sustainable forest management which<br />
assures consumers that a forest product can be<br />
tracked from a certifi ed, managed forest through<br />
all steps <strong>of</strong> processing and production in the<br />
supply chain by a Chain <strong>of</strong> Custody process.<br />
Reprinted from Good Practice Issue 10, October 2015<br />
3
YOUR COLLEGE<br />
Benjamin Whittaker:<br />
‘I General-ly Practice good study habits! #punny’<br />
Student<br />
winners<br />
Jessie Ling:<br />
‘A cool day in the <strong>of</strong>fi ce #Antarctica #retrieval’<br />
Danielle Todd:<br />
‘GP fi ts into my life like it<br />
fi ts into my handbag’<br />
Lawrence Ling: ‘My daily medicines!’<br />
The successful entrants into the RACGP’s<br />
‘Win a trip to GP15’ Facebook competition<br />
included one general practice registrar and<br />
four medical students from around Australia,<br />
all <strong>of</strong> whome won their way to last month’s<br />
Conference for General Practice in Melbourne.<br />
The prize package for Jessie Ling<br />
(Tasmania), Katie Drewett (Queensland),<br />
Danielle Todd (Victoria), Lawrence Ling<br />
(Queensland) and Benjamin Whittaker<br />
(South Australia) included return fl ights to<br />
Melbourne, four nights’ accommodation and<br />
entry to GP15.<br />
The Facebook competition allowed<br />
participants to post a photo and accompanying<br />
caption in answer to the question, ‘How does<br />
general practice fi t into your daily life?’. The<br />
RACGP was overwhelmed by the positive<br />
response to the competition, with the number<br />
and quality <strong>of</strong> entries surpassing expectations.<br />
Visit the RACGP’s Facebook page<br />
(www.facebook.com/TheRACGP) to view<br />
the full gallery <strong>of</strong> entries.<br />
Katie Drewett: ‘The best <strong>of</strong> both worlds! #jugglingact’<br />
Management <strong>of</strong> moderate acute pain<br />
and the role <strong>of</strong> combination analgesia<br />
This learning activity explores the assessment and<br />
management <strong>of</strong> acute pain in general practice, and<br />
discusses the role <strong>of</strong> combination analgesia.<br />
To access the learning program go to gplearning.racgp.org.au<br />
and sign in with your current RACGP username and password.<br />
This educational program was funded with an educational grant from Aspen Australia 2<br />
4 Reprinted from Good Practice Issue 10, October 2015
September 2015<br />
Vision for general<br />
practice and a sustainable<br />
healthcare system<br />
Images Jessie Ling; Danielle Todd; Lawrence Ling; Katie Drewett; Benjamin Whittaker<br />
New vision<br />
The RACGP’s Vision for general<br />
practice and a sustainable<br />
health system (the Vision) was<br />
<strong>of</strong>fi cially released by President<br />
Frank R Jones at last month’s<br />
Conference for General Practice in Melbourne.<br />
The Vision outlines the RACGP’s plans to better<br />
support the delivery <strong>of</strong> quality, sustainable and effective<br />
primary healthcare, designed to meet the needs <strong>of</strong><br />
Australia’s patients, GPs and governments.<br />
‘When the right system is in place to look after<br />
people in the community, serious conditions such as<br />
heart disease and diabetes can be prevented and<br />
the severity <strong>of</strong> illnesses can also be reduced through<br />
improved management,’ Dr Jones said.<br />
Much <strong>of</strong> the direction <strong>of</strong> the Vision was shaped<br />
by RACGP member feedback, which proved vital to<br />
its development.<br />
‘Our new funding model has been developed by<br />
grassroots GPs who know what the issues are and<br />
what needs to <strong>change</strong> to make a system better for their<br />
patients,’ Dr Jones said. ‘The current funding model for<br />
primary healthcare is not focused on the patient.<br />
‘Our new model will deliver quality, patient-focused<br />
care that will reap long-term benefi ts for communities.’<br />
Visit www.racgp.org.au/vision for more information.<br />
www.racgp.org.au Healthy Pr<strong>of</strong>ession.<br />
17908 RACGP Vision for general practice and a sustainable health system.in d 1<br />
Expert Committee chairs<br />
President Dr Frank R Jones announced the new chairs <strong>of</strong> the RACGP<br />
Expert Committees (RECs) at last month’s Conference for General<br />
Practice in Melbourne:<br />
• Dr Nathan Pinskier – eHealth and Practice Systems<br />
• Dr Beres Wenck – GP Advocacy and Funding<br />
• Dr Kay Atkinson – Pre-Fellowship Education<br />
• Dr Janice Bell – Post-Fellowship Education<br />
• Dr Evan Ackermann – Quality Care<br />
• Pr<strong>of</strong> Tania Winzenberg – Research<br />
• Dr Mike Civil – Standards for General Practices<br />
RECs provide Council with information and advice on general practice<br />
issues and oversee the implementation <strong>of</strong> initiatives developed in<br />
accordance with the RACGP’s strategic plan.<br />
‘Each elected chair has been chosen for their strong community and<br />
pr<strong>of</strong>essional networks across the health sector, as well as their ability to<br />
monitor trends and recommend suitable innovations into RACGP programs<br />
and to provide critical advice to the RACGP Council,’ Dr Jones said.<br />
‘The chairs represent and refl ect a deep knowledge <strong>of</strong> general practice.’<br />
Visit www.racgp.org.au/yourracgp/organisation/committees/racgpexpert-committees<br />
for more informa tion.<br />
Healthy Australia.<br />
RACGP events calendar<br />
October 2015<br />
NSW<br />
CPR course for GPs<br />
Wednesday 7 October,<br />
7.00–9.00 pm, RACGP<br />
House, North Sydney<br />
Contact 02 9886 4700 or<br />
nswact.events@racgp.org.au<br />
VIC<br />
Career speednetworking<br />
event<br />
Saturday 17 October,<br />
12.30–4.00 pm, RACGP<br />
House, East Melbourne<br />
Contact 03 8699 0488 or<br />
vic.events@racgp.org.au<br />
VIC<br />
Perform CPR –<br />
a workshop for GPs<br />
Tuesday 20 October,<br />
6.00–8.00 pm, RACGP<br />
House, East Melbourne<br />
Contact 03 8699 0483 or<br />
vic.qicpd@racgp.org.au<br />
NSW<br />
Embracing<br />
boundaries series<br />
Wednesday 21 October,<br />
4.00–9.30 pm, Harbourview<br />
Queens Wharf, Newcastle<br />
Contact 02 9886 4700 or<br />
nswact.events@racgp.org.au<br />
NSW<br />
CPR course for GPs<br />
Wednesday 21 October,<br />
4.00–6.00 pm, Harbourview<br />
Queens Wharf, Newcastle<br />
Contact 02 9886 4700 or<br />
nswact.events@racgp.org.au<br />
NSW<br />
CEMP intermediate<br />
workshop<br />
Friday 23 October,<br />
8.30 am – 5.00 pm, Sydney<br />
Boulevard Hotel, Sydney<br />
Contact 02 9886 4710 or<br />
nswact.cemp@racgp.org.au<br />
WA<br />
Emergency skills<br />
training ALM<br />
Saturday 24 October,<br />
8.30 am – 5.00 pm,<br />
College House, Perth<br />
Contact 08 9489 9555 or<br />
rachel.patterson@racgp.org.au<br />
NSW<br />
CEMP advanced<br />
workshop<br />
Saturday–Sunday 24–25<br />
October, 8.30 am – 5.00 pm,<br />
Sydney Boulevard Hotel,<br />
Sydney<br />
Contact 02 9886 4710 or<br />
nswact.cemp@racgp.org.au<br />
QLD<br />
CEMP advanced<br />
workshop<br />
Saturday–Sunday<br />
31 October – 1 November,<br />
8.30 am – 5.00 pm,<br />
Queensland University <strong>of</strong><br />
Technology, Brisbane<br />
Contact 07 3456 8944 or<br />
janet.lindsay@racgp.org.au<br />
For further RACGP events please visit<br />
www.racgp.org.au/education/courses/racgpevents<br />
Reprinted from Good Practice Issue 10, October 2015<br />
5
XXXXX SE-HUNT XXXXXX AWARD ROSE-HUNT AWARD ROSE-HUNT AWARD ROSE-HUNT AWARD ROSE-HUNT AWARD ROSE-HUNT AWARD ROSE-HUNT AWARD ROSE-HUNT AW<br />
Universal<br />
practitioner<br />
BEVAN WANG<br />
Emeritus Pr<strong>of</strong>essor Max Kamien’s<br />
career in general practice has allowed<br />
him to advocate for some <strong>of</strong> the<br />
world’s most vulnerable populations.<br />
The Rose-Hunt<br />
Award<br />
The Rose-Hunt Award is the RACGP’s<br />
highest accolade.<br />
The award was a gift to the<br />
RACGP from the UK’s Royal College<br />
<strong>of</strong> General Practitioners (RCGP) in<br />
commemoration <strong>of</strong> two <strong>of</strong> the RCGP’s<br />
founding members, Dr Fraser Rose<br />
and Lord Hunt <strong>of</strong> Fawley (the fi rst<br />
Honorary Secretary).<br />
The Rose-Hunt Award is given to<br />
an RACGP Fellow or member who, in<br />
the opinion <strong>of</strong> Council, has rendered<br />
outstanding service in the promotion <strong>of</strong><br />
the objects <strong>of</strong> the RACGP by individual<br />
patient care, organisation, education,<br />
research or any other means.<br />
Outstanding service may be over<br />
a period <strong>of</strong> 10 years or a substantial<br />
and signifi cant contribution to general<br />
practice over a shorter period.<br />
The inaugural Rose-Hunt Award<br />
was presented to one <strong>of</strong> the RACGP’s<br />
founding fathers, Dr William Arnold<br />
Conolly, in October 1974.<br />
6 Reprinted from Good Practice Issue 10, October 2015<br />
Certain Australians will likely always<br />
be synonymous with their pr<strong>of</strong>ession<br />
– Don Bradman and cricket, Banjo<br />
Paterson and poetry, Cate Blanchett<br />
and acting. When people think about<br />
who is associated with general practice,<br />
especially in Western Australia, few<br />
could look past Emeritus Pr<strong>of</strong>essor Max<br />
Kamien, an RACGP Life Fellow who<br />
has dedicated more than fi ve decades to<br />
Australian and international medicine.<br />
Dr Kamien’s lifelong devotion to<br />
the general practice pr<strong>of</strong>ession, and<br />
his passion for medical education and<br />
Aboriginal and Torres Strait Islander<br />
health are just some <strong>of</strong> the reasons<br />
he was awarded the RACGP’s 2015<br />
Rose-Hunt Award. But this accolade<br />
was far from his fi rst.<br />
Dr Kamien was presented with the<br />
Australian and New Zealand Association<br />
<strong>of</strong> Medical Education Award for<br />
Research in 1995, the Louis Ariotti<br />
Award for Rural Health Research in<br />
2000, named a Western Australian<br />
Citizen <strong>of</strong> the Year in 1998, made a<br />
Member in the Order <strong>of</strong> Australia for<br />
his services to medicine, particularly in<br />
medical education, Aboriginal health<br />
and rural medicine, in 1999, and was<br />
Dr Kamien became one <strong>of</strong> the oldest<br />
doctors to work on polar expeditions<br />
when he started at the age <strong>of</strong> 70.<br />
a Western Australian fi nalist in the<br />
Australian <strong>of</strong> the Year Awards in 2009.<br />
But receiving the Rose-Hunt, the<br />
RACGP’s highest honour for a career<br />
in general practice, holds a special<br />
place for Dr Kamien.<br />
‘When one is in his 80th year, the time<br />
for recognition <strong>of</strong> any achievements has<br />
usually long passed, so the Rose-Hunt<br />
Award was completely unexpected. It is<br />
nice that someone thinks highly enough<br />
<strong>of</strong> me to go to the considerable trouble<br />
<strong>of</strong> putting in a nomination for me,’ he<br />
told Good Practice. ‘I put a fair bit <strong>of</strong><br />
effort into whatever I do, but I don’t<br />
expect to get any recognition for it.’<br />
Dr Kamien’s involvement with the<br />
RACGP began when he sat on the<br />
Western Australia Faculty Board from<br />
1977–88. He later became the Western<br />
Australia state archivist, Corlis Fellow<br />
and Provost and is now Chair <strong>of</strong> the<br />
National Archives Committee.<br />
‘I was fairly late to the RACGP. I<br />
was 40 years old before I joined,’ he<br />
said. ‘As I got older, I put my hand up<br />
and said that I would be interested in<br />
being the state archivist because I had<br />
an interest in medical history. Then<br />
they were searching around for a wise<br />
Images Max Kamien
old man to be the Provost, so I said I would<br />
do that as well.<br />
‘I have really enjoyed working with the<br />
Western Australia Faculty, particularly the staff<br />
members. I go in fairly regularly just to remind<br />
them <strong>of</strong> what a good job they are doing.’<br />
Early beginnings<br />
Dr Kamien grew up in Perth during the<br />
Second World War and was accepted into the<br />
academically-selective Perth Modern School<br />
during his secondary years. Despite the lack<br />
<strong>of</strong> a medical school in his home state, he<br />
remained determined to pursue his dream <strong>of</strong><br />
a career in medicine.<br />
‘Because Western Australia did not have a<br />
medical school, those who wanted to study<br />
medicine had to move to South Australia,’<br />
Dr Kamien said. ‘When I fi nished my fourth<br />
year <strong>of</strong> medical school in Adelaide, the<br />
Western Australian medical school had just<br />
begun so I transferred back to Perth.<br />
‘Those were the golden days <strong>of</strong> the<br />
medical school. There were more teachers<br />
than there were students, which enabled<br />
me to form really close relationships with<br />
many <strong>of</strong> those teachers. And I still maintain<br />
relationships with many who are still with us.’<br />
Dr Kamien graduated from medical school<br />
in 1960 and completed his residency at<br />
Fremantle Hospital and Melbourne’s Royal<br />
Children’s Hospital. He then embarked<br />
on three years <strong>of</strong> travelling and practising<br />
medicine in some <strong>of</strong> the more far-fl ung<br />
corners <strong>of</strong> the world.<br />
‘I went to Papua New Guinea for a year,<br />
worked as a volunteer locum for the Save the<br />
Children Fund in South Korea and Jordan,<br />
and I had a stint with the Red Cross in Nepal,<br />
working with Tibetan refugees.’<br />
It was during this time <strong>of</strong> international travel<br />
that Dr Kamien met his future wife, Jackie.<br />
‘I was in Israel administering anaesthetics<br />
in a hospital when I decided I needed to<br />
learn Hebrew in order to converse with my<br />
patients,’ he said.<br />
‘I was at the bottom <strong>of</strong> the class in<br />
the language school and the teacher put<br />
me with the lady who was the top <strong>of</strong> the<br />
class. We ended up getting married and<br />
she has been teaching me and our three<br />
children ever since.’<br />
When his travels ended, Dr Kamien settled<br />
in the UK with the intention <strong>of</strong> training and<br />
working towards becoming a physician.<br />
‘I couldn’t get a job because, at the time,<br />
my travels made me seem quite unreliable,’<br />
he said. ‘Eventually, I got a job in child<br />
psychiatry. After that I got very good jobs and<br />
I had a really good time learning in England.<br />
‘I ended up completing diplomas <strong>of</strong><br />
psychological medicine and child health and<br />
was one <strong>of</strong> 50 candidates from a fi eld <strong>of</strong> 750<br />
who passed the Royal College <strong>of</strong> Physicians<br />
<strong>of</strong> London exam. It was the only exam that<br />
I ever topped.’<br />
While Dr Kamien was working in<br />
gastroenterology at the Royal Postgraduate<br />
Hospital in London in 1969, a psychiatric<br />
research position in the New South Wales<br />
town <strong>of</strong> Bourke became available. A remote<br />
town with a large Aboriginal population<br />
situated approximately nine hours north-west<br />
<strong>of</strong> Sydney, Bourke is where Dr Kamien kickstarted<br />
his Australian general practice career.<br />
‘The very fi rst day that I was in Bourke,<br />
I went to the Bourke Aboriginal Reserve<br />
where the fi rst child that I saw had<br />
kwashiorkor, a protein-defi ciency disease,’<br />
he said. ‘Gradually, I became the GP for the<br />
Aboriginal community.<br />
‘I could see that just being their doctor was<br />
really not enough. I wanted to do more and<br />
I came up with the idea <strong>of</strong> being a doctor who<br />
was also an agent <strong>of</strong> <strong>social</strong> <strong>change</strong>.’<br />
General practice advocacy<br />
Dr Kamien has been credited as a pioneer<br />
who introduced a number <strong>of</strong> different<br />
services to the people <strong>of</strong> Bourke, including<br />
inexpensive housing and various types <strong>of</strong><br />
specialist care. When he fi rst arrived in<br />
Bourke, Dr Kamien found that up to quarter<br />
<strong>of</strong> the Aboriginal children had trachoma, a<br />
bacterial infection <strong>of</strong> the eye.<br />
‘I went to Sydney looking for an architect<br />
interested in low-cost housing with hot<br />
water and protection from fl ies. I was also<br />
looking for an eye doctor and I found Fred<br />
Hollows,’ he said. ‘He came up to Bourke<br />
several months later and it was in a little<br />
place called Enngonia, 100 km from Bourke,<br />
that he thought up the idea <strong>of</strong> a National<br />
Trachoma Campaign.<br />
‘This morphed into a worldwide organisation<br />
[the Fred Hollows Foundation] that has<br />
reduced blindness in over a million people.<br />
The saying “from little things big things grow”<br />
could not be truer than when applied to the<br />
Fred Hollows Foundation.’<br />
Dr Kamien believes GPs’ advocacy role<br />
should extend beyond the walls <strong>of</strong> the<br />
practice and encourages more young doctors<br />
to get involved with health initiatives in<br />
their community.<br />
‘One <strong>of</strong> the ways I thought about getting<br />
rid <strong>of</strong> infective skin disease among the<br />
Aboriginal population in Bourke was to get<br />
the kids into a chlorinated swimming pool,’ he<br />
said. ‘But Aboriginal kids back then did not<br />
go to the swimming pools because they felt<br />
discriminated against.<br />
‘So I decided to start a water polo<br />
association for Aboriginal kids and they then<br />
went to the swimming pool. I really thought<br />
this is one direction that general practice<br />
ought to explore.’<br />
Dr Kamien left Bourke after 3.5 years<br />
to be with his ill mother in Perth. He soon<br />
got his fi rst taste <strong>of</strong> academia when he was<br />
appointed a senior lecturer in medicine at the<br />
University <strong>of</strong> Western Australia. >><br />
Dr Kamien met his wife, Jackie, while working in a hospital in Israel early in his healthcare career.<br />
Reprinted from Good Practice Issue 10, October 2015<br />
7
XXXXX SE-HUNT XXXXXX AWARD ROSE-HUNT AWARD ROSE-HUNT AWARD ROSE-HUNT AWARD ROSE-HUNT AWARD ROSE-HUNT AWARD ROSE-HUNT AWARD ROSE-HUNT AW<br />
Dr Kamien’s history <strong>of</strong> advocating for disadvantaged populations throughout his career has seen him help people in various corners <strong>of</strong> the world, including testing for and treating<br />
malaria in Papua New Guinea (left) and working with Tibetan refugees in Nepal (right).<br />
>> ‘In comparison with Bourke,<br />
teaching hospital medicine was pretty<br />
tame,’ he said.<br />
‘It was predictable because you had 15<br />
beds. Five were people with diabetes, fi ve<br />
had alcohol problems, four were waiting for<br />
aged care accommodation and, once every<br />
three months, there would be a patient that<br />
required real diagnostic acumen.’<br />
Medical education<br />
Growing up in Perth, Dr Kamien aspired<br />
to be a secondary school teacher who<br />
specialised in English, physics and tennis.<br />
His own educators, however, encouraged<br />
him to pursue other career objectives.<br />
‘My teachers took me aside and told<br />
me that they didn’t think I’d do very well<br />
as a teacher because I would have a lot <strong>of</strong><br />
trouble with the educational department,<br />
and vice versa,’ he explained. ‘I saw a<br />
vocational guidance counsellor and he put<br />
me through a whole lot <strong>of</strong> tests and told<br />
me I was totally unsuited for medicine, but<br />
engineering was my forte.<br />
‘I ended up going against his advice and<br />
enrolled in medicine – and probably saved<br />
Western Australia from a few tragedies as<br />
a result <strong>of</strong> collapsing bridges.’<br />
Despite choosing medicine over his<br />
initial aspirations <strong>of</strong> the classroom,<br />
medical education has always been a<br />
signifi cant aspect <strong>of</strong> Dr Kamien’s career<br />
and it remains something about which he<br />
is deeply passionate. He believes more<br />
medical training should be conducted<br />
in general practice, where it can benefi t<br />
patients and students.<br />
‘I just enjoy medical education. No one<br />
had to tell me to do it and I enjoyed that<br />
8 Reprinted from Good Practice Issue 10, October 2015<br />
sort <strong>of</strong> relationship,’ he said. ‘I was aware<br />
that since most medicine occurs in general<br />
practice that is where some more medical<br />
education should take place.’<br />
Dr Kamien was appointed Chair<br />
<strong>of</strong> General Practice and Head <strong>of</strong> the<br />
Department <strong>of</strong> Community Practice at the<br />
University <strong>of</strong> Western Australia in 1976.<br />
‘In those days general practice was<br />
not accorded the status <strong>of</strong> an academic<br />
discipline. Community practice was to<br />
be the new university-based discipline.<br />
It was to include general practice, <strong>social</strong><br />
medicine, epidemiology, the sociology<br />
<strong>of</strong> medicine and medical anthropology,<br />
and so on,’ he explained. ‘It was sort<br />
<strong>of</strong> a catch-all and I thought that would<br />
really suit me.<br />
‘I saw it as an extension <strong>of</strong> my<br />
explorations into the doctor as an agent<br />
<strong>of</strong> <strong>social</strong> <strong>change</strong>.’<br />
Dr Kamien’s much-anticipated<br />
Report <strong>of</strong> the ministerial inquiry into the<br />
recruitment and retention <strong>of</strong> country<br />
doctors in Western Australia (also known<br />
as the Kamien Report) was published in<br />
1987 and played a major role in policies<br />
around general practice in WA’s rural and<br />
remote communities.<br />
‘The report found that a student’s<br />
chances <strong>of</strong> getting into medical school<br />
from a rural high school were close<br />
to nil, and the chances <strong>of</strong> getting in<br />
as an Aboriginal person were nil,’<br />
Dr Kamien said. ‘My recommendations<br />
for affi rmative entry <strong>of</strong> such students to<br />
medical schools were widely resisted. But<br />
they have been proven to be right and<br />
the action <strong>of</strong> taking people [into medical<br />
school] has produced excellent doctors,<br />
many <strong>of</strong> whom have gone into rural<br />
medicine and taken up leadership roles.’<br />
Personal pursuits<br />
While many people choose to slow down<br />
past the age <strong>of</strong> 65, Dr Kamien was 70<br />
when he became one <strong>of</strong> the oldest doctors<br />
to have worked as a medical <strong>of</strong>fi cer on<br />
polar expedition boats in both the Arctic<br />
and Antarctic, something he went on to do<br />
on seven occasions.<br />
‘I have always been interested in polar<br />
exploration and that is sort <strong>of</strong> a retirement<br />
thing that I took up,’ he said. ‘Most <strong>of</strong> the<br />
medical people who go on these boats<br />
are young doctors training in emergency<br />
medicine, but most <strong>of</strong> the passengers are<br />
closer to my age and they don’t always<br />
form a relationship with the young doctors.’<br />
Another <strong>of</strong> Dr Kamien’s long-held<br />
interest lies in writing. His literary pursuits<br />
fi rst began when he became the editor<br />
<strong>of</strong> the University <strong>of</strong> Western Australia’s<br />
medical student magazine, The Refl ex. He<br />
has published more than 200 academic<br />
papers and 400 commentaries over the<br />
course <strong>of</strong> his career and continues to write<br />
for Australian Doctor.<br />
‘I write a lot about the things I do<br />
and see because I need a level <strong>of</strong><br />
self-deprecating humour to sustain me,’<br />
Dr Kamien said. ‘Good general practice<br />
is a hard discipline. I enjoy the long-term<br />
relationships with patients and families. I<br />
also enjoy the lateral thinking that is <strong>of</strong>ten<br />
needed to help them solve their problems.<br />
‘I tell medical students and young<br />
doctors that medicine is a serious business,<br />
but it can also be a lot <strong>of</strong> fun. If there was a<br />
second life, I would do it again.’<br />
Images Max Kamien
The good GP never stops learning.<br />
Royal Australian College <strong>of</strong> General Practitioners<br />
racgp.org.au
GP OF THE YEAR GP OF THE YEAR GP OF THE YEAR GP OF THE YEAR GP OF THE YEAR GP OF THE YEAR GP OF THE YEAR GP OF THE YEAR GP OF THE YEAR GP OF THE<br />
Comprehensive<br />
PAUL HAYES<br />
The holistic and<br />
collaborative nature <strong>of</strong><br />
general practice suits<br />
Dr Kean-Seng Lim’s<br />
methods <strong>of</strong> delivering<br />
healthcare.<br />
10 Reprinted from Good Practice Issue 10, October 2015<br />
Following two years in the hospital system,<br />
Sydney’s Dr Kean-Seng Lim, the recipient<br />
<strong>of</strong> the RACGP’s 2015 GP <strong>of</strong> the Year<br />
Award, came to the conclusion that the<br />
patient and healthcare diversity <strong>of</strong> general<br />
practice made it the specialty for him.<br />
‘After doing a variety <strong>of</strong> hospital<br />
rotations, including paediatrics, psychiatry,<br />
general medicine and surgery, I decided<br />
that general practice was where I really<br />
wanted to be,’ he told Good Practice.<br />
‘I found hospitals to be very “partialist”<br />
environments that didn’t always take<br />
a holistic view <strong>of</strong> patients and<br />
their health or their <strong>social</strong><br />
nature. The focus was on<br />
the single illness that the<br />
patient came in with.<br />
‘General practice is<br />
where you have the<br />
greatest capacity to<br />
make a difference to<br />
someone’s life. We<br />
are seeing patients<br />
not just for a single<br />
episode, but on multiple occasions<br />
throughout their life.’<br />
Dr Lim received his medical degree<br />
from the University <strong>of</strong> Sydney in 1991<br />
before undertaking his residency in the<br />
Hunter Region <strong>of</strong> New South Wales.<br />
He has worked at the Mt Druitt Medical<br />
Centre in the western suburbs <strong>of</strong> Sydney<br />
for the past 20 years, where he is able<br />
to <strong>of</strong>fer the holistic, collaborative care<br />
that has appealed to him since his<br />
days as an intern.<br />
‘I have a keen interest in the evolution<br />
<strong>of</strong> the general practice model and our<br />
practice has been strongly infl uenced by<br />
the RACGP’s 2012 paper on the general<br />
practice <strong>of</strong> the future [A quality general<br />
practice <strong>of</strong> the future],’ he said. ‘I am<br />
supported in my day-to-day work by our<br />
practice team <strong>of</strong> doctors, admin staff,<br />
practice nurse, pharmacist, dietitian,<br />
exercise physiologist and psychologist,<br />
who all play an integral role in helping me<br />
provide what I like to think <strong>of</strong> as more<br />
comprehensive care for our patients.<br />
‘A good team allows us to be better<br />
doctors and adds to the joy <strong>of</strong> the<br />
work we do.’<br />
Changing environment<br />
Dr Lim’s primary special interests are<br />
nutrition and lifestyle, subjects that have<br />
driven signifi cant areas <strong>of</strong> his work outside<br />
<strong>of</strong> the consulting room.<br />
‘That interest is what has led to my<br />
involvement with the SALSA [Students<br />
As Lifestyle Activists] program, which<br />
was established about 11 years ago,’<br />
he said. ‘The SALSA program is<br />
a peer-led education program<br />
where we train<br />
Images Kean-Seng Lim; AMA
approach<br />
Year 10 students to be peer leaders, to take<br />
on the role <strong>of</strong> educating Year 8 students in<br />
the context <strong>of</strong> having lessons embedded into<br />
their PDHPE [Personal Development, Health<br />
and Physical Education] curriculum.<br />
‘The purpose <strong>of</strong> the program is to<br />
encourage behavioural <strong>change</strong> in the way <strong>of</strong><br />
improvement in diet, improvement in lifestyle<br />
and reduction in poor health behaviour, such<br />
as screen time, junk food, consumption <strong>of</strong><br />
juices and s<strong>of</strong>t drinks.’<br />
SALSA has now grown from a single<br />
participating school to more than 20. The<br />
idea for the program came about after<br />
Dr Lim and other GPs in Mount Druitt,<br />
following several years <strong>of</strong> treating overweight<br />
and obesity in general practice, came to<br />
understand the relative limitations <strong>of</strong> short<br />
sessions with patients.<br />
‘We realised that managing obesity<br />
and other lifestyle problems was very<br />
diffi cult in the context <strong>of</strong> day-to-day<br />
consultation, and we have much diffi culty<br />
addressing wider issue <strong>of</strong> the obesogenic<br />
environment,’ he said.<br />
‘The SALSA program gives us the<br />
opportunity to intervene at a wider cultural<br />
level, and by this I’m referring to actual<br />
school culture. Having a peer-led education<br />
model, you not only infl uence the leaders<br />
and each peer group, but as those peer<br />
leaders in Year 10 go on to become Year 11<br />
and Year 12 students they actually start to<br />
infl uence the whole school culture.<br />
‘Culture in any organisation, in my<br />
mind, is paramount when it comes to<br />
sustaining any sort <strong>of</strong> <strong>change</strong>. So we really<br />
have the ambition <strong>of</strong> nothing less than<br />
changing society.’<br />
Dr Lim sees the model presented by the<br />
SALSA program as a more organic way<br />
<strong>of</strong> getting a positive nutrition and lifestyle<br />
message across.<br />
‘The model <strong>of</strong> healthcare is very interesting<br />
and works in a whole lot <strong>of</strong> subtle ways,<br />
including the fact that a lot <strong>of</strong> the teachings<br />
do not have to be made directly through the<br />
lessons themselves, but can actually be a<br />
<strong>change</strong> <strong>of</strong> infl uence by role-modelling by<br />
the students, who are peer leaders, and the<br />
infl uences they have on their peers and<br />
their family.<br />
‘The next stage from here is to move<br />
on to infl uencing the broader school<br />
community by going to the parents, the<br />
grandparents and others who are part <strong>of</strong><br />
that extended community.’<br />
Future <strong>of</strong> general practice<br />
Training the next generation <strong>of</strong> GPs through<br />
medical education plays a signifi cant role in<br />
Dr Lim’s career. He is a general practice<br />
supervisor with the Western Sydney GP<br />
training organisation WentWest, and a guest<br />
lecturer at the University <strong>of</strong> Western Sydney<br />
School <strong>of</strong> Medicine.<br />
‘I have been training general practice<br />
registrars and medical students for many<br />
years now. It is part <strong>of</strong> what I see as an<br />
important role for GPs,’ he said.<br />
A good team allows us to<br />
be better doctors and adds to<br />
the joy <strong>of</strong> the work we do<br />
‘Part <strong>of</strong> my belief is that GPs have a<br />
responsibility to leave the system better than<br />
when we entered it and part <strong>of</strong> that involves<br />
training the new generation <strong>of</strong> doctors, from<br />
medical students through to registrars.’<br />
Beyond the people who will populate<br />
it, Dr Lim believes much <strong>of</strong> the future<br />
<strong>of</strong> the general practice pr<strong>of</strong>ession lies in<br />
the digital world.<br />
‘eHealth has certainly been one <strong>of</strong><br />
my other big interests, pretty much right<br />
from the beginning <strong>of</strong> my general practice<br />
career,’ he said. ‘Information management<br />
and information technology is a real game<br />
<strong>change</strong>r when it comes to what we can do<br />
in general practice.’<br />
Dr Lim feels the availability <strong>of</strong> these<br />
new tools will allow GPs to better serve<br />
an ever-growing patient population.<br />
Dr Lim’s wife Sonia is also a GP. ‘When I am having<br />
trouble I always ask myself, “What would Sonia do?”,’<br />
he said.<br />
‘More and more <strong>of</strong> the work we do<br />
in general practice is chronic disease<br />
management, and more <strong>of</strong> the patients<br />
we see are suffering from more complex<br />
diseases and the interactions <strong>of</strong> those<br />
conditions,’ he said.<br />
‘In the general practice <strong>of</strong> the future<br />
we will be doing more proactive<br />
population-based care, which is the sort<br />
<strong>of</strong> work that’s very diffi cult to do without<br />
having very good data on your patient<br />
population and management.<br />
‘So information management and<br />
technology – eHealth technology and<br />
health informatics – is vital for what we will<br />
need to be doing in general practice now<br />
and into the future.’<br />
When refl ecting on his present position<br />
in the industry, namely the RACGP’s GP <strong>of</strong><br />
the Year, Dr Lim shies away from individual<br />
praise, preferring to see the award as the<br />
culmination <strong>of</strong> the work he has done with<br />
many GPs and healthcare pr<strong>of</strong>essionals in<br />
what is a very collaborative pr<strong>of</strong>ession.<br />
‘I’m going to steal from Michael<br />
Crampton – the GP <strong>of</strong> the Year Award<br />
winner from last year – in that I see it as<br />
accepting an award on behalf <strong>of</strong> all <strong>of</strong> the<br />
good work done by so many others that<br />
doesn’t get recognised,’ he said. ‘It is<br />
very nice to be recognised and I am very<br />
grateful to the RACGP.<br />
‘I hope that it will make me a better<br />
doctor.’<br />
Reprinted from Good Practice Issue 10, October 2015<br />
11
XXXXX PERVISOR XXXXXX OF THE YEAR SUPERVISOR OF THE YEAR SUPERVISOR OF THE YEAR SUPERVISOR OF THE YEAR SUPERVISOR OF THE YEAR SUPERVISOR OF THE YEAR SU<br />
Leading<br />
the way<br />
PAUL HAYES<br />
Medical educator Dr Cathy Milligan<br />
hopes registrars at her rural practice<br />
can develop an extensive range <strong>of</strong> skills.<br />
For Western Australia’s Dr Cathy Milligan,<br />
quality medical education can provide almost<br />
as much for the supervisor as it does for the<br />
general practice registrar. As the recipient<br />
<strong>of</strong> the RACGP’s 2015 General Practice<br />
Supervisor <strong>of</strong> the Year Award, Dr Milligan<br />
certainly understands the two-way nature <strong>of</strong><br />
the learning process.<br />
‘Registrars are good with the protocols<br />
and practices and they keep you on your<br />
toes,’ she told Good Practice. ‘They will<br />
<strong>of</strong>ten ask about things you haven’t thought<br />
about for a while, so we can add to that<br />
knowledge together or we can go away and<br />
do our own research.<br />
‘That is a really positive aspect <strong>of</strong> the<br />
relationship – bouncing <strong>of</strong>f each other, both<br />
sides bringing different skill sets.’<br />
Medical educator<br />
A GP and director at Margaret River Surgery,<br />
Dr Milligan has been based in the south-west<br />
<strong>of</strong> WA for the last 19 years. After obtaining<br />
her medical degree from the University <strong>of</strong><br />
12 Reprinted from Good Practice Issue 10, October 2015<br />
Western Australia, she undertook several<br />
different rotations as a junior doctor in major<br />
hospitals in and around Perth, followed<br />
by a year <strong>of</strong> anaesthetics training in the<br />
UK, before starting a career in Australian<br />
general practice.<br />
‘I work as a procedural GP, involving family<br />
practice, plus obstetrics, anaesthetics and<br />
emergency medicine, as well as women’s<br />
health,’ she said.<br />
Medical education has been part <strong>of</strong><br />
Dr Milligan’s career ever since she started<br />
in Margaret River Surgery, with the practice<br />
taking medical students and general<br />
practice registrars as long as she has<br />
worked there. The ability to train and work<br />
with eager young doctors helps Dr Milligan<br />
stay energised and up-to-date in her<br />
work as a rural GP.<br />
‘It’s nice to be in touch with the next<br />
generation <strong>of</strong> doctors coming through<br />
because they bring a freshness and a quality,<br />
and you get to understand how they work<br />
and think,’ she said. ‘Plus, they are always<br />
fresh from the major hospitals so they’re<br />
pretty sharp with their protocols.<br />
‘We [GPs] can share our experience<br />
and it’s really nice to watch the registrars<br />
use their existing skills that blossom in the<br />
environment down here in Margaret River,<br />
which is different from the tertiary hospitals.’<br />
According to Dr Milligan, that different<br />
environment provided by a rural healthcare<br />
setting, in which patients <strong>of</strong>ten prefer to have<br />
their needs met locally rather than having<br />
to travel to see a specialist, provides the<br />
general practice registrars at Margaret River<br />
Surgery the opportunity to develop a broad<br />
variety <strong>of</strong> skills.<br />
‘Because Margaret River is more in a<br />
rural and remote setting, we have limited<br />
specialist support. We are it in a town with a<br />
population <strong>of</strong> about 8000–9000 people,’ she<br />
said. ‘Of course, our specialist colleagues<br />
are on the phone down the road and we can<br />
always contact them for help and advice,<br />
but we largely work on our own and I think<br />
that develops a special skill set <strong>of</strong> crisper<br />
Image Western Australian General Practice Education and Training
judgement, deciding whether you can help<br />
this person or whether you need to transport<br />
them elsewhere.’<br />
While Dr Milligan does acknowledge those<br />
decisions, coupled with patients’ desires to<br />
avoid travel, can place some pressure on young<br />
doctors, she believes the independence helps<br />
to build their confi dence and is ultimately very<br />
benefi cial for their training.<br />
‘They have to be fairly confi dent and be able<br />
to work autonomously,’ she said. ‘Although<br />
they are supervised, the supervisor is not<br />
always on site with them. That said, they are<br />
always supported.’<br />
With a total <strong>of</strong> 12 GPs <strong>of</strong>fering services<br />
including obstetrics, anaesthetics, minor<br />
treatment room procedures, women’s and<br />
men’s health, mental health, palliative care,<br />
geriatric care, immunisations, diabetes<br />
education, and more, general practice registrars<br />
who come to Margaret River Surgery have<br />
access to a wealth <strong>of</strong> experience.<br />
‘As a group practice we can help the<br />
registrars with all <strong>of</strong> our different expertise,<br />
so I think it’s a great experience for them,’<br />
Dr Milligan said.<br />
Special interests <strong>of</strong> obstetrics, anaesthetics,<br />
women’s health and emergency medicine<br />
have proven extremely valuable in Dr Milligan’s<br />
rural healthcare setting. Another <strong>of</strong> her<br />
special interests, however, tends to stand out<br />
from the rest.<br />
Dr Milligan is a keen pilot and her love <strong>of</strong><br />
aviation was one <strong>of</strong> the key motivators behind<br />
her obtaining her qualifi cation as an aviation<br />
medical examiner.<br />
Like any good<br />
relationship, you get more<br />
out <strong>of</strong> being a supervisor<br />
than you put in<br />
‘That involves a study course which<br />
heightens your awareness <strong>of</strong> the special<br />
medical issues in the cockpit and in aviation<br />
generally. CASA [Civil Aviation Safety<br />
Authority] licences you to examine commercial<br />
and general aviation pilots,’ she said.<br />
‘It’s not my core business, but I’d probably<br />
do a couple each month. Of course, the<br />
consultations are extremely long, mainly<br />
because we ex<strong>change</strong> stories regarding our<br />
incredible fl ying feats – some <strong>of</strong> which may<br />
even have an element <strong>of</strong> truth.’<br />
Best advice<br />
As a long-time general practice supervisor,<br />
Dr Milligan understands the fact that some<br />
GPs may be somewhat hesitant to take on<br />
the responsibilities that come with the role.<br />
But her advice to anyone considering<br />
becoming a supervisor is simple.<br />
‘Don’t hesitate – it’s a great job,’ she<br />
said. ‘People might feel overwhelmed by<br />
the thought <strong>of</strong> the commitment, but once<br />
you’ve settled into it that time commitment<br />
is nothing huge.<br />
‘The registrars will be an asset to your<br />
practice. The patients like the young ones and<br />
they’re very understanding <strong>of</strong> the fact that<br />
they are training registrars.<br />
‘And like any good relationship, you will get<br />
more out <strong>of</strong> it than you put in.’<br />
Dr Milligan described being named the<br />
RACGP’s 2015 Supervisor <strong>of</strong> the Year as a<br />
‘surprise’, but she is extremely happy to have<br />
had her work acknowledged in such a way.<br />
‘I haven’t really come to terms with it yet,’<br />
she said. ‘It’s an honour to be recognised for<br />
the work I’m doing. There are lots <strong>of</strong> other<br />
doctors out there who are equally deserving,<br />
but I am grateful that this was my year to be<br />
voted. I’m very proud.’<br />
AUSTRALIA’S LEADING<br />
PRIMARY CARE EVENT<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
GPCE<br />
13 – 15 Nov 2015<br />
Melbourne Convention<br />
& Exhibition Centre<br />
MELBOURNE GENERAL<br />
PRACTITIONER CONFERENCE<br />
& EXHIBITION<br />
Early Bird Rates Available for a Limited Time<br />
REGISTER AT GPCE.COM.AU<br />
melbourne.<br />
Reprinted from Good Practice Issue 10, October 2015<br />
13
REGISTRAR OF THE YEAR REGISTRAR OF THE YEAR REGISTRAR OF THE YEAR REGISTRAR OF THE YEAR REGISTRAR OF THE YEAR REGISTRAR OF THE YEAR REGISTRA<br />
Support system<br />
PAUL HAYES<br />
Dr Ashlea Broomfield<br />
has dedicated<br />
much <strong>of</strong> her time in<br />
general practice to<br />
advocating for fellow<br />
registrars.<br />
Dr Broomfi eld said the<br />
General Practice Registrar<br />
<strong>of</strong> the Year Award represents<br />
all <strong>of</strong> the healthcare pr<strong>of</strong>essionals<br />
who have helped inspire<br />
her career.<br />
14 Reprinted ed<br />
from Good dP<br />
Practice eI<br />
Issue su<br />
10, October r2<br />
2015<br />
They say the good GP never stops<br />
learning. For Dr Ashlea Broomfi eld,<br />
recipient <strong>of</strong> the RACGP’s 2015<br />
General Practice Registrar <strong>of</strong> the Year<br />
Award, it was an early learning experience<br />
that saw her embrace general practice<br />
after considering physician training as a<br />
hospital-based specialist.<br />
‘When I fi rst went into medicine I wanted<br />
to do general practice. That was my ideal,’<br />
she told Good Practice. ‘But then I got a<br />
little bit carried away with the interest in<br />
the specialties and the hype and glamour<br />
associated with being a hospital-based<br />
specialist in a particular fi eld. For a little<br />
while there I moved away from wanting<br />
to do general practice until I started<br />
doing my clinical year and experienced<br />
general practice.<br />
‘I noticed the difference between<br />
the trainees in specialty/hospital-based<br />
or FRACP [Fellowship <strong>of</strong> the Royal<br />
Australasian College Physicians] programs<br />
and the general practice trainees.<br />
‘I also did a PGPPP [Prevocational<br />
General Practice Placements Program]<br />
placement and realised that general<br />
practice was well supported, with good<br />
education and a lot <strong>of</strong> autonomy, and<br />
you’re treated like an equal team member<br />
in the general practice environment. So I<br />
decided to go back down that route.’<br />
In training<br />
Following medical studies at the University<br />
<strong>of</strong> New South Wales (UNSW) in Sydney,<br />
Dr Broomfi eld moved to C<strong>of</strong>fs Harbour on<br />
the NSW north coast to attend the UNSW<br />
Rural Clinical School (RCS).<br />
What was supposed to<br />
be a one-year stint in<br />
C<strong>of</strong>fs Harbour turned<br />
into a more<br />
permanent move after Dr Broomfi eld’s<br />
positive experiences at the C<strong>of</strong>fs Harbour<br />
Hospital and the RCS.<br />
From there, Dr Broomfi eld’s efforts in<br />
training and working on behalf <strong>of</strong> other<br />
registrars started to develop.<br />
‘I got on the GP training program<br />
with North Coast GP Training [NCGPT]<br />
and worked in Grafton, Woolgoolga and<br />
Toormina in NSW. Within the fi rst couple<br />
<strong>of</strong> months <strong>of</strong> being a registrar I was<br />
asked to be the Registrar Liaison Offi cer<br />
[RLO] with NCGPT,’ she said. ‘I have<br />
now been working as an RLO for more<br />
than 12 months.’<br />
This RLO position with NCGPT sees<br />
Dr Broomfi eld work closely with doctors<br />
in training from all over Australia.<br />
‘Part <strong>of</strong> our role is to liaise with any<br />
registrars who are having issues in their<br />
practices and then advocate for them to<br />
their training provider or their practice,’<br />
she said. ‘They come to us with a<br />
variety <strong>of</strong> issues.’<br />
According to Dr Broomfi eld, some<br />
<strong>of</strong> those issues include remuneration,<br />
teaching methods, patient load,<br />
communication within their practice,<br />
personal issues, contracts, exam support<br />
and preparation, and more.<br />
‘We have a varied role which <strong>change</strong>s<br />
throughout the year depending on the<br />
needs <strong>of</strong> the registrars,’ she said. ‘There’s<br />
a lot to learn initially, but after that it’s a<br />
role that’s nice to do because you’ve got<br />
a lot <strong>of</strong> people across the country who<br />
experience the same issues and it is good<br />
to be able to help them out by utilising the<br />
network <strong>of</strong> RLOs.’<br />
Dr Broomfi eld was also named Chair<br />
<strong>of</strong> the General Practice Registrar Medical<br />
Educator Network (GPRMEN) earlier this<br />
year. A sub-committee <strong>of</strong> General Practice<br />
Registrars Australia, GPRMEN is designed<br />
to help registrars with a passion to teach,<br />
supporting them in their roles within<br />
training providers.<br />
‘The GPRMEN is a committee that<br />
basically aims to promote positions as<br />
registered medical educators [RMEs]<br />
to general practice training providers and<br />
Image Ashlea Broomfi eld
make sure that’s ongoing. Then to<br />
support RMEs through a variety <strong>of</strong> different<br />
ways – networking, educational events<br />
and general support with each other,’<br />
Dr Broomfi eld said.<br />
Online support<br />
Her role as GPRMEN Chair also allows<br />
Dr Broomfi eld to further another <strong>of</strong> her<br />
interests in general practice, helping registrars<br />
and experienced GPs in the process.<br />
‘At the moment I am trying to move<br />
the GPRMEN a bit more onto online and<br />
<strong>social</strong> media platforms. Lots <strong>of</strong> medical<br />
educators are disconnected all over<br />
Australia so I’m trying to get them together<br />
so they can connect, interact and share<br />
resources,’ she said.<br />
‘We also had a slot at the recent General<br />
Practice Training and Education Conference,<br />
where we talked about how best the<br />
GPRMEN network can support RMEs and<br />
new medical educators in their positions in<br />
terms <strong>of</strong> what they need for education and<br />
what the network might be able to do in<br />
regards to helping them.’<br />
An active <strong>social</strong> media participant,<br />
Dr Broomfi eld understands the potential<br />
advantages this ever-evolving medium <strong>of</strong>fers<br />
healthcare pr<strong>of</strong>essionals, particularly those in<br />
more isolated settings.<br />
‘A lot <strong>of</strong> GPs across Australia might work<br />
in solo practices or practices with only a few<br />
GPs. Or they might fi nd that extra-curricular<br />
work they’ve got to do before or after work<br />
means they are just consulting in their own<br />
room then leaving for the day, which can<br />
be quite isolating,’ she said. ‘Social media<br />
provides a platform to get involved with other<br />
GPs and talk about issues related to the<br />
workplace or wellbeing, and to get support<br />
from other doctors.<br />
‘It also allows you to see any new or<br />
updated information, as well as a variety <strong>of</strong><br />
different information options.<br />
‘Lots <strong>of</strong> GPs have varied levels <strong>of</strong> special<br />
interest and varying degrees <strong>of</strong> expertise in<br />
different areas, so in interactive forums where<br />
you can discuss cases you get a lot <strong>of</strong> input<br />
from people who are experts in their fi eld and<br />
get up-to-date information on assessment,<br />
diagnosis and management.’<br />
Dr Broomfi eld’s digital expertise has also<br />
been put to use in her role at NCGPT, where<br />
she helped develop an online resource for<br />
fellow registrars.<br />
‘As part <strong>of</strong> my role as an RLO at NCGPT<br />
I was asked to be involved in setting up<br />
the resource area on their online learning<br />
platform, so I used all the resources I already<br />
had stored on my own computer to update<br />
them,’ she said. ‘All <strong>of</strong> those resources were<br />
uploaded to the “Resources for registrars”<br />
section <strong>of</strong> NCGPT’s online learning platform.’<br />
Dr Broomfi eld is honoured, if admittedly<br />
a little surprised, to be named the RACGP’s<br />
2015 General Practice Registrar <strong>of</strong> the Year.<br />
‘I am very humbled to win the award and<br />
was very honoured by the people from my<br />
regional training provider who put forward the<br />
nomination for me,’ she said.<br />
‘There are so many doctors and registrars<br />
out there who do so much for their community<br />
and medicine in general, and for education<br />
and the promotion <strong>of</strong> general practice. I’m<br />
inspired by other people around me and that’s<br />
why I do a lot <strong>of</strong> the work I do, because <strong>of</strong><br />
so many inspirational people I’ve seen in<br />
general practice.<br />
‘It’s so nice to be given this award but, at<br />
the same time, there’s so many other people<br />
out there who are doing so much good work.<br />
I wish I could give the award to all those<br />
people as well.’<br />
As an RACGP member<br />
You can SAVE TIME AND MONEY on your next car purchase<br />
1 RESEARCH<br />
Decide on a vehicle to purchase by using the internet, talking to people<br />
and, most <strong>of</strong> all, feel free to give us a call for some independent advice.<br />
2 TEST-DRIVE<br />
Pop down to your local dealer and take your chosen car for a test drive or<br />
contact us to find out how we can arrange a test-drive for you at your home<br />
or <strong>of</strong>fice.<br />
3<br />
MBA<br />
CAR ASSIST NATIONAL TENDER AND VEHICLE FINANCE OPTIONS<br />
Relax and let us take care <strong>of</strong> the rest. Using our unique national tendering<br />
process, we will invite multiple dealers to compete for your business. Our buying<br />
power and trade contacts will ensure that the new car price and trade-in value<br />
will save you precious time and money. Tailored finance options available.<br />
4 ORDER<br />
Takes around 10 minutes by phone. MBA Car Assist will order the vehicle on<br />
your behalf from the winning dealer on the tender.<br />
5 DELIVERY<br />
You will be kept up to date as to estimated delivery times and at your<br />
convenience, your new vehicle will be delivered to your home or work with a<br />
full tank <strong>of</strong> fuel.<br />
6<br />
CORPORATE<br />
BENEFITS PROGRAM*<br />
Many <strong>of</strong> our car suppliers <strong>of</strong>fer special Corporate Benefits which can include<br />
free servicing for up to 5 years, courtesy cars and much more.<br />
* Corporate Program applies to Mercedes-Benz, Audi, BMW and Lexus vehicles.<br />
Contact MBA Car Assist for more information.<br />
1. MBA Car Assist is a subsidiary <strong>of</strong> MBA Pty Ltd.<br />
2. MBA CarAssist tenders out certain brands <strong>of</strong> vehicles.<br />
3. Other brands <strong>of</strong> vehicles are setup through a preferred dealership network.<br />
4. This can <strong>change</strong> at any stage.<br />
For access to these great savings, please call Member Benefits Australia on 1300 119 493 or email info@mbabenefits.com.au<br />
Reprinted from Good Practice Issue 10, October 2015<br />
15
RURAL RESGISTRAR OF THE YEAR RURAL RESGISTRAR OF THE YEAR RURAL RESGISTRAR OF THE YEAR RURAL RESGISTRAR OF THE YEAR RURAL RESGISTRAR OF THE<br />
One <strong>of</strong> the team<br />
PAUL HAYES<br />
16 Reprinted from Good Practice Issue 10, October 2015<br />
Dr Hannah Visser believes the GP is one <strong>of</strong> many<br />
links in the chain <strong>of</strong> Aboriginal and Torres Strait<br />
Islander health.<br />
Dr Hannah Visser, the RACGP’s 2015<br />
Rural Registrar <strong>of</strong> the Year, was exposed to<br />
rural healthcare from a very early age when<br />
she was growing up.<br />
‘My mum is a rural GP back in Germany,<br />
so I grew up with an old school practice<br />
on the ground fl oor and we lived on top <strong>of</strong><br />
it. My mum is a 24/7 GP,’ Dr Visser told<br />
Good Practice.<br />
As a result, rural general practice has<br />
always been Dr Visser’s goal throughout<br />
her healthcare career.<br />
‘You are a part <strong>of</strong> the whole community<br />
and it’s about continuity <strong>of</strong> care,’ she said.<br />
‘The care you provide is broader because<br />
access to some resources is more diffi cult<br />
in the rural setting, so you have to provide<br />
more services. You make more clinical<br />
decisions and usually treat the patient there<br />
and then.’<br />
After completing her medical studies in<br />
Germany, Dr Visser lived and worked in<br />
several places before settling in her current<br />
location in the Northern Rivers region on<br />
the north coast <strong>of</strong> New South Wales.<br />
‘I did my university studies in Germany<br />
and during this time did a lot <strong>of</strong> travelling.<br />
I fi rst went to Sydney for my internship in<br />
2004 and then spent six months in South<br />
Africa, working in a township hospital,<br />
before coming to Australia again in 2006,’<br />
she said.<br />
‘When I came back to Australia I went to<br />
the Sunshine Coast [Queensland] and did a<br />
year at Nambour Hospital.<br />
‘Then I moved to Melbourne for a year,<br />
then to Newcastle for a year, then back to<br />
Melbourne. I then moved up to the north<br />
coast <strong>of</strong> NSW three years ago and have<br />
been there ever since.’
Images Hannah Visser<br />
That fi nal move to the north coast <strong>of</strong> NSW<br />
saw Dr Visser take a position at the Bulgarr<br />
Ngaru Medical Aboriginal Corporation Casino<br />
Clinic, an Aboriginal medical service (AMS)<br />
that <strong>of</strong>fers medical and dental services,<br />
chronic disease management, mental health<br />
services and health education programs<br />
covering substance use, sexual health and<br />
lifestyle management.<br />
‘My biggest passion is working with the<br />
communities with limited or no access to<br />
services. That has always been my main<br />
interest,’ Dr Visser said. ‘After being in the<br />
hospital system for most <strong>of</strong> my other time<br />
in healthcare I found myself wanting to do<br />
Aboriginal health, and now that I am doing<br />
it I will never do anything else.’<br />
Team approach<br />
Dr Visser’s time at Bulgarr Ngaru Casino<br />
has helped her develop a new approach to<br />
healthcare, one in which the GP is one <strong>of</strong><br />
several people involved in its delivery.<br />
‘I have been here mostly full-time for the<br />
past 2.5 years and I have really had great<br />
access to the community. They have been<br />
very welcoming <strong>of</strong> me and I really enjoy<br />
working as part <strong>of</strong> a team,’ she said. ‘Working<br />
in Aboriginal health services is different than<br />
working as a mainstream GP; you can <strong>of</strong>ten<br />
be in situations where you might be the GP<br />
but you’re not calling the shots.<br />
‘The team <strong>of</strong> Aboriginal health workers<br />
will help you with cultural things or an<br />
understanding <strong>of</strong> what’s going on with the<br />
situation <strong>of</strong> people’s lives in the community,<br />
which helps you make your treatment plan or<br />
approach people differently.<br />
Above: Dr Visser and her family have settled into life<br />
on the north coast <strong>of</strong> NSW. Left: Dr Visser appreciates<br />
the support <strong>of</strong> many people in the delivery <strong>of</strong> Aboriginal<br />
and Torres Strait Islander health services.<br />
‘Basically, service delivery is just a<br />
bit different because you’re guided by<br />
your team members.’<br />
Dr Visser has used her expanded<br />
knowledge base about the role <strong>of</strong> the GP in<br />
Aboriginal and Torres Strait Islander health to<br />
help other registrars working at AMSs.<br />
‘I recently gave a talk to registrars at North<br />
Coast GP Training – we have a meeting with<br />
all the new registrars working in AMSs in<br />
the region – and I said, “It’s not about your<br />
agenda, it’s really about the agenda <strong>of</strong> other<br />
people around you”.<br />
‘You try to work your health message<br />
around that and make it work and see what<br />
the best chance is that it’s actually been<br />
taken up or followed,’ she said.<br />
In Aboriginal and Torres<br />
Strait Islander health you<br />
are <strong>of</strong>ten more than a<br />
doctor – you are also a<br />
liaison <strong>of</strong>ficer, <strong>social</strong> worker<br />
and advocate<br />
Dr Visser’s international background has<br />
also proven to be something <strong>of</strong> a benefi t<br />
when communicating with Aboriginal and<br />
Torres Strait Islander patients.<br />
‘Cultural understanding is very, very<br />
important in the Aboriginal health setting,’<br />
she said. ‘I’ve always thought, with my<br />
German background, I could just ask very<br />
straightforward questions – tell me about<br />
this or that – because obviously I don’t<br />
know the history that well. So I could still<br />
get very interesting stories and cultural<br />
background explained to me.’<br />
That ability to develop a clearer cultural<br />
understanding has allowed Dr Visser to<br />
tailor her healthcare approach accordingly,<br />
<strong>of</strong>fering Aboriginal and Torres Strait<br />
Islander patients services that are more<br />
appropriate to their needs and desires.<br />
‘Aboriginal and Torres Strait Islander<br />
peoples have a different understanding <strong>of</strong><br />
health, or <strong>of</strong>ten different priorities,’ she<br />
said. ‘For example, if they have to go to a<br />
funeral today, you need to discharge them<br />
from the hospital, or they are not going to<br />
the hospital even if you think, as a doctor,<br />
they really do have to. So you have to kind<br />
<strong>of</strong> negotiate plans around that.<br />
‘It’s very important to give Aboriginal<br />
and Torres Strait Islander patients the<br />
choice to decide what they think would<br />
work best for them. I think a lot <strong>of</strong> it is<br />
about empowerment.’<br />
Broader scope<br />
Research is another <strong>of</strong> Dr Visser’s<br />
healthcare passions outside <strong>of</strong> the<br />
consulting room. She is currently<br />
undertaking a project on population health<br />
with the University Centre for Rural Health,<br />
working with and teaching students<br />
from the Sydney University, Western<br />
Sydney University and the University <strong>of</strong><br />
Wollongong, with her work funded by the<br />
Department <strong>of</strong> Health.<br />
‘I’m doing an academic term at the<br />
moment, which is 1–1.5 days <strong>of</strong> research<br />
and another day <strong>of</strong> teaching per week,’<br />
she said. ‘Working in the Aboriginal<br />
community got me to realise about<br />
population health. We can treat little things<br />
and give antibiotics and we can do this and<br />
do that, but there is also the broader aspect<br />
<strong>of</strong> what’s behind it. That’s what led me to<br />
have some ideas about research projects we<br />
can do to <strong>change</strong> policies and practice and<br />
improve the health <strong>of</strong> the people.’<br />
Dr Visser loves the holistic yet constantly<br />
varied nature <strong>of</strong> her role as a rural registrar,<br />
particularly working with Aboriginal and<br />
Torres Strait Islander peoples.<br />
‘I think it’s nice to see different<br />
generations and have the continuity <strong>of</strong><br />
care <strong>of</strong> rural general practice,’ she said.<br />
‘And with Aboriginal health, you do more<br />
than just the doctor role; you are a liaison<br />
<strong>of</strong>fi cer and <strong>social</strong> worker and advocate. You<br />
have a few roles.’<br />
Regardless <strong>of</strong> the specifi cs, Dr Visser<br />
recommends that those considering<br />
working in an Aboriginal and Torres Strait<br />
Islander community never lose sight <strong>of</strong><br />
the fact their a pproach to healthcare must<br />
remain fl exible.<br />
‘You have to be very open and able to<br />
be guided by the community and what their<br />
needs are, and broaden your skills as much<br />
as possible,’ she said.<br />
Being named the winner <strong>of</strong> the RACGP’s<br />
2015 Rural Registrar <strong>of</strong> the Year Award is<br />
a lot to take in for the usually reserved<br />
Dr Visser, but being recognised by others in<br />
her pr<strong>of</strong>ession means a lot to her.<br />
‘I really appreciate it,’ she said. ‘It’s an<br />
appreciation and recognition <strong>of</strong> the work<br />
that I do and my compassion towards the<br />
community that I work in, and the research<br />
that I’m doing.’<br />
Reprinted from Good Practice Issue 10, October 2015<br />
17
GENERAL XXXXX XXXXXX PRACITCE OF THE YEAR GENERAL PRACTICE OF THE YEAR GENERAL PRACITCE OF THE YEAR GENERAL PRACTICE OF THE YEAR GENERAL PRACITCE OF THE<br />
Progressive practice<br />
BEVAN WANG<br />
GPs at Western<br />
Australia’s Collie<br />
River Valley Medical<br />
Centre believe<br />
general practices<br />
can evolve to best<br />
meet the needs <strong>of</strong><br />
their patients.<br />
Please note: Collie River Medical Centre was also<br />
pr<strong>of</strong>i led in the August 2015 issue <strong>of</strong> Good Practice.<br />
Teaching is a central feature <strong>of</strong> the Collie River<br />
Medical Centre healthcare philosophy.<br />
18 Reprinted from Good Practice Issue 10, October 2015<br />
Australia’s population demographic has<br />
<strong>change</strong>d signifi cantly in the last two<br />
decades and general practice has been<br />
working to keep up.<br />
Western Australian GP Dr Peter<br />
Wutchak, practice principal at Collie River<br />
Valley Medical Centre, believes it is crucial<br />
that individual practices are able to develop<br />
and cater to the requirements <strong>of</strong> their<br />
patient population.<br />
‘General practice has really evolved quite<br />
a lot because we are looking to meet the<br />
needs <strong>of</strong> our community,’ Dr Wutchak told<br />
Good Practice. ‘GPs are now more involved<br />
with chronic health initiatives through things<br />
like general practice management plans,<br />
mental health plans and other health checks.<br />
‘It means that we are involved with the<br />
acute side <strong>of</strong> a patient’s care, but we can<br />
also put preventive steps in place to stop<br />
negative health outcomes from occurring.’<br />
Collie is a mostly industrial town<br />
approximately two hours south <strong>of</strong> Perth with<br />
a population <strong>of</strong> around 7000. Collie River<br />
Valley Medical Centre has been providing<br />
holistic general practice care ever since it<br />
fi rst opened its doors in 1998.<br />
‘We are quite balanced with our patient<br />
demographic,’ Dr Wutchak said. ‘We have<br />
young children and families, some <strong>of</strong> whom<br />
are associated with the main industries<br />
<strong>of</strong> the town. We also have a fairly even<br />
demographic, right through to the elderly<br />
people who are usually retired miners and<br />
their families, who have lived in the town all<br />
<strong>of</strong> their lives.’<br />
Collie River Valley Medical Centre’s<br />
dedication to and involvement with its<br />
community, as well as its commitment to<br />
medical education, are just some <strong>of</strong> the<br />
reasons it was named the RACGP’s 2015<br />
General Practice <strong>of</strong> the Year.<br />
‘We are extremely pleased to have won<br />
the award,’ Dr Wutchak said. ‘The entire<br />
staff has been energised by this recognition<br />
for what we feel was some pretty hard work<br />
over the last 5–10 years.<br />
‘We defi nitely see it as a team effort,<br />
from the receptionists through to all <strong>of</strong> the<br />
nurses and doctors who have been part<br />
<strong>of</strong> the practice.’<br />
Community engagement<br />
Collie River Valley Medical Centre’s key role<br />
in the occupational health and safety <strong>of</strong> its<br />
community is one <strong>of</strong> many ways it has grown<br />
according to patient needs.<br />
‘In an industrial town, it is almost impossible<br />
to divorce from occupational health,’<br />
Dr Wutchak said. ‘We decided to expand<br />
into this area because there was always a<br />
need for injured workers to get treated and<br />
they don’t necessarily want to have to travel<br />
away from home to get that treatment.<br />
‘We built on what was already a strong<br />
relationship with local industries to make it<br />
more encompassing, to allow for companies<br />
to have one point <strong>of</strong> call for their medical<br />
needs. So the workers are well supported,<br />
no matter what they come in with.’<br />
In addition to primary care, the practice is<br />
also involved with the emergency department<br />
at the Collie District Hospital.<br />
‘We provide 24/7 coverage. One <strong>of</strong> our<br />
doctors is available at all times to attend<br />
to any emergency department problem,’<br />
Dr Wutchak said.<br />
‘The emergency department is staffed<br />
by nurses who have had training in an<br />
emergency setting and we support them in<br />
all aspects <strong>of</strong> that.<br />
‘We like it when we have a good<br />
relationship between our practice and the<br />
emergency department because it makes<br />
everyone’s job easier. Also, patients can<br />
get quality services in a timely fashion and<br />
everyone involved feels like they are on<br />
the same page.’<br />
Dr Wutchak believes that he and fellow<br />
practice principal Dr Jan Van Vollenstee<br />
have helped the practice remain engaged<br />
with the Collie community, something<br />
for which he has consistently strived<br />
throughout his career.<br />
‘The practice’s engagement with the<br />
town is incredibly important to us,’ he said.<br />
‘If you take a more alo<strong>of</strong> approach, where<br />
you basically set up a general practice clinic<br />
and expect the patients to come and receive<br />
whatever service you are prepared to deliver,<br />
then you are going to be limited.<br />
‘If you really want to provide an allencompassing,<br />
strong general practice<br />
Image Western Australian General Practice Education and Training
service in a rural community, you need to<br />
engage with the community and with the town.’<br />
Staff members from Collie River Valley<br />
Medical Centre can <strong>of</strong>ten be found at school<br />
functions, local workplaces, sports grounds<br />
and other community events to further enhance<br />
this relationship.<br />
‘Over the last three years we’ve had a stand<br />
at the local agricultural show where we promote<br />
skin cancer checks, which we do for free.<br />
We also take names and arrange follow-up<br />
calls,’ Dr Wutchak said. ‘We are showing that<br />
we want to get involved with the community<br />
and that we feel like we are actually part <strong>of</strong><br />
the community.<br />
‘The benefi t <strong>of</strong> doing that is that the patients<br />
see you as more than just a doctors’ clinic.<br />
They see you as the health resource for the<br />
community, a business that has a real fi nger<br />
on the pulse, particularly in regards to the<br />
health <strong>of</strong> the town.’<br />
Procedural practice<br />
While Dr Wutchak’s time at Collie River Medical<br />
Centre originally started as a general practice<br />
registrar, the affi nity he developed for the<br />
town and practice has seen him stay on for a<br />
further 17 years.<br />
‘I did my advanced general practice term<br />
in Narrogin [WA] for my procedural skills,<br />
obstetrics and anaesthetics, and felt that I had<br />
the skills needed to be a rural GP,’ he said.<br />
‘I really wanted to be at Collie River Valley<br />
Medical Centre because it was somewhere<br />
I could still practise my procedural skills,<br />
as well as the general practice that such a<br />
vibrant town needs.’<br />
Medical education now takes up a large<br />
part <strong>of</strong> Dr Wutchak’s role at the practice.<br />
He sees this as one <strong>of</strong> the most important<br />
aspects in his career.<br />
‘I have found that training has helped me<br />
to be a much better doctor,’ he explained.<br />
‘The ability to understand my knowledge and<br />
skills, plus the ability to then impart that on to<br />
someone else, has helped me to grow.<br />
‘Teaching really helps in that it keeps<br />
you current and dynamic because it helps<br />
to bring fresh and enthusiastic people into<br />
your practice. If you keep an open mind,<br />
your ability to develop as individual clinicians<br />
and teachers will help the practice to<br />
grow as a whole.’<br />
Procedural work has been at the heart<br />
<strong>of</strong> Collie River Valley Medical Centre since<br />
it fi rst opened, providing the community<br />
with obstetrics, anaesthetics and minor<br />
surgery procedures.<br />
‘A community like Collie is too small to<br />
get access to regular visiting specialists,’<br />
Dr Wutchak said. ‘Most <strong>of</strong> our patients will<br />
have to travel for any procedural skills if we<br />
don’t provide them.<br />
‘Collie, like many rural communities<br />
in Australia, relies on its local practitioners<br />
to provide those skills that people in the<br />
community need.’<br />
Dr Wutchak encourages general practice<br />
registrars and medical students to consider<br />
taking on a procedural skill, especially if they<br />
are thinking <strong>of</strong> moving to a rural or remote<br />
part <strong>of</strong> Australia.<br />
‘We really need to be encouraging the next<br />
generation <strong>of</strong> GPs to take up at least one skill<br />
because most <strong>of</strong> the communities that don’t<br />
have easy access to specialist services or a<br />
hospital need it,’ he said.<br />
‘We certainly give our registrars the<br />
opportunities to take on procedural skills<br />
if they are interested. We want to get the<br />
registrars who leave our practice to have<br />
some degree <strong>of</strong> experience with minor<br />
procedures because that’s what rural general<br />
practice is about.’<br />
Reprinted from Good Practice Issue 10, October 2015<br />
19
XXXXX IAN WILLIAMS XXXXXX AWARD BRIAN WILLIAMS AWARD BRIAN WILLIAMS AWARD BRIAN WILLIAMS AWARD BRIAN WILLIAMS AWARD BRIAN WILLIAMS AWARD BRIA<br />
Rural<br />
pathway<br />
BEVAN WANG<br />
A close relationship<br />
with the local<br />
community is one<br />
<strong>of</strong> many reasons<br />
South Australia’s<br />
Dr Ken Wanguhu<br />
loves rural general<br />
practice.<br />
Dr Wanguhu was surprised and fl attered to<br />
receive the 2015 Brian Williams Award.<br />
20 Reprinted from Good Practice Issue 10, October 2015<br />
The RACGP’s National Rural Faculty<br />
(NRF) commemorates the work <strong>of</strong> the<br />
late Dr Brian Williams, a long-time rural<br />
advocate and former Director <strong>of</strong> the WA<br />
Centre for Remote and Rural Medicine, by<br />
recognising an outstanding rural GP whose<br />
mentoring and support enables other<br />
rural GPs to dedicate themselves to their<br />
patients, family and communities.<br />
South Australia’s Dr Ken Wanguhu<br />
was surprised when he was named the<br />
2015 recipient <strong>of</strong> award.<br />
‘I can’t get over it,’ he told Good<br />
Practice. ‘I would like to know who<br />
nominated me because it is very, very<br />
fl attering. I did not expect it and I am a bit<br />
overwhelmed, to be honest.’<br />
Growing up in Kenya, Dr Wanguhu’s<br />
altruistic nature meant he was <strong>of</strong>ten looking<br />
to help those in need, and he always knew<br />
he wanted to be involved in medicine and<br />
practise as a doctor.<br />
‘It is one <strong>of</strong> those things that I always<br />
wanted to pursue since I was a child<br />
because I always thought medicine and<br />
health were interesting,’ he said. ‘I looked at<br />
the doctors around me when I was growing<br />
up and I just really admired all the work that<br />
they did and I wanted to help people.<br />
‘The doctors in my village were an<br />
important part <strong>of</strong> the community and we<br />
looked up to them.’<br />
After trying his hand at a number <strong>of</strong><br />
specialities areas – anaesthetics, obstetrics,<br />
surgery and emergency medicine –<br />
Dr Wanguhu decided he did not want to<br />
commit to a single area <strong>of</strong> medicine.<br />
‘When I tried all these specialities<br />
I realised that it was not something that<br />
I wanted to do for the rest <strong>of</strong> my life,’ he<br />
said. ‘Nothing really made me think that<br />
I could do this or that particular speciality<br />
because I always wanted to do something<br />
more substantial and more holistic.<br />
‘The reason I got into general practice<br />
is because I can do a little bit <strong>of</strong> everything<br />
and there are fewer restrictions around<br />
that. I choose what I want to specialise in<br />
and work towards that.’<br />
Community care<br />
After practising medicine in South Africa,<br />
Somalia and Kenya, Dr Wanguhu took the<br />
opportunity to move to the South Australian<br />
town <strong>of</strong> Waikerie, two hours north-east<br />
<strong>of</strong> Adelaide. Waikerie is a small rural<br />
community in the SA’s Riverland region with<br />
an estimated population <strong>of</strong> 1635.<br />
‘I immigrated to South Australia from<br />
South Africa for family reasons. After<br />
getting married, I wanted to bring up a<br />
family in a safer environment with fewer<br />
risks, particularly for personal security and<br />
health. Australia provided a most suitable<br />
place for that,’ Dr Wanguhu said. ‘I also<br />
wanted to work where I would be able to do<br />
procedural work because I was interested<br />
in that, and I also wanted somewhere<br />
that I could call home and become part<br />
<strong>of</strong> the community.<br />
‘I came out to Waikerie almost 15<br />
years ago without knowing much about<br />
the community or the place. There was<br />
an attractive job opportunity available that<br />
I was interested in. Needless to say, it<br />
Images Ken Wanguhu
Clockwise from below left: Dr Wanguhu has been a member <strong>of</strong> the NRF executive board as Rural Censor since 2013;<br />
his passion for medical education sees Dr Wanguhu consult with medical schools in various locations, including Papua New<br />
Guinea; the Wanguhu family has become part <strong>of</strong> the community in the SA town <strong>of</strong> Waikerie.<br />
worked well all round. Since then, the Waikerie<br />
folks have looked after us and been really<br />
good with us coming into the community.’<br />
Much <strong>of</strong> Dr Wanguhu’s attraction to rural<br />
Australia was due to the ability to practice<br />
holistic medicine in communities where it<br />
was most needed.<br />
‘Rural general practice allows you to do<br />
a great range <strong>of</strong> things that you would not<br />
always be able to do in metropolitan regions,’<br />
he said. ‘For example, I get to be involved<br />
with obstetrics because I can form great<br />
relationships with the patient before she’s<br />
pregnant, know her family and friends, assess<br />
her when she’s in labour and put in the<br />
epidural, and either attend the delivery or do the<br />
c-section if there are any complications. Then I<br />
get to look after the baby.<br />
‘I have patients I delivered who are now<br />
14 or 15 and I am looking forward to being able<br />
to deliver their babies down the track.<br />
‘It is just an absolute privilege to be able<br />
to go on that journey with the patients and<br />
the community.’<br />
Dr Wanguhu fi rst got involved with<br />
the RACGP as an international medical<br />
graduate (IMG) and became the NRF<br />
Rural Censor in 2013.<br />
‘The NRF has always been a big part<br />
<strong>of</strong> my pr<strong>of</strong>essional life because, like me,<br />
a lot <strong>of</strong> IMGs are in areas <strong>of</strong> need which<br />
are generally rural, so the NRF has a<br />
big membership <strong>of</strong> IMGs,’ he said. ‘The<br />
NRF was probably the fi rst faculty that<br />
realised it needed an IMG representative<br />
and I was approached as one <strong>of</strong> the early<br />
representatives.’<br />
Dr Wanguhu believes it is important for<br />
GPs to take a leading role in helping to<br />
determine Australia’s healthcare policies.<br />
‘The thing is that doctors <strong>of</strong>ten hate<br />
politics. We just want to take care <strong>of</strong> our<br />
patients and move on,’ he said. ‘But what<br />
some people may not realise is that you don’t<br />
decide what you are going to be paid or<br />
have any say as to what is going to happen<br />
in your pr<strong>of</strong>ession, whether it is training or<br />
location <strong>of</strong> students and resources, without<br />
touching on politics.<br />
‘You shouldn’t leave these things solely to<br />
the politicians because you need to inform<br />
politics to base its decisions on the people<br />
who actually live in the community and work<br />
in the fi eld and know what it is all about.’<br />
Imparting knowledge<br />
Dr Wanguhu’s interest in medical education<br />
began when he was studying for his RACGP<br />
Fellowship exam and realised that resources<br />
for IMGs like himself were somewhat limited.<br />
‘When I came to Australia, there was very<br />
little in the way <strong>of</strong> support for IMGs sitting<br />
the Fellowship exams, which are crucially<br />
important for IMGs,’ he said. ‘After I got<br />
my Fellowship I thought about it and really<br />
wanted to do something to help the people<br />
who are coming into the country.<br />
‘I had always enjoyed teaching, well before<br />
I came out to Australia, but being able to help<br />
my fellow IMGs was probably what prompted<br />
me to really step up my efforts and is what I<br />
am most enthusiastic about.’<br />
According to Dr Wanguhu, properly<br />
equipping GPs with procedural skills<br />
necessary to best help their community is<br />
one <strong>of</strong> the signifi cant challenges for rural and<br />
remote general practice in Australia.<br />
‘There really are a lot <strong>of</strong> things that we are<br />
asking <strong>of</strong> these procedural GPs when they<br />
come to rural general practice because the<br />
range is just so wide,’ he said. ‘It is important<br />
that we have the systems in place for medical<br />
students who want to practice procedural<br />
skills and who want to move out into country<br />
areas to do that work.<br />
‘You need procedures such as obstetrics<br />
in the community because it is hard for a<br />
pregnant woman to have to travel hours to get<br />
the medical help she needs.’<br />
Educating and empowering the next<br />
generation <strong>of</strong> GPs is especially important<br />
to Dr Wanguhu.<br />
‘To all the medical students and general<br />
practice registrars, I tell them that they cannot<br />
get a more fulfi lling job,’ he said.<br />
‘It is amazing because if they have the right<br />
mentor they will almost always come out <strong>of</strong><br />
the experience saying that’s what they want<br />
to do. There is nothing better than to be<br />
immersed in rural general practice, to really<br />
get into it then decide if it is for you.<br />
‘It is a great feeling to be able to give these<br />
students a chance and a taste <strong>of</strong> rural general<br />
practice, and to really build them up to take<br />
over from us when we retire.<br />
‘And, as we strive to educate, equip and<br />
encourage our pr<strong>of</strong>ession, it is important that<br />
we tie this to the family relationships that<br />
count the most for all <strong>of</strong> us.<br />
‘I have found that the supportive<br />
environments in which that is practised<br />
mean that rural general practice, which by<br />
its very nature is rigorous and demanding <strong>of</strong><br />
time and energy, provides a unique comfort<br />
for the family.<br />
‘Rural general practice provides a real<br />
sense <strong>of</strong> everyone being in it together.’<br />
Reprinted from Good Practice Issue 10, October 2015<br />
21
GP15 AWARD WINNERS GP15 AWARD WINNERS GP15 AWARD WINNERS GP15<br />
RACGP Academic Session Awards 2015<br />
Rose-Hunt Award<br />
Emeritus Pr<strong>of</strong>essor Max Kamien,<br />
Western Australia<br />
Honorary Fellowship<br />
Dr Frank Moloney, New South Wales<br />
Mr Neil Greenaway, Victoria<br />
National Faculty <strong>of</strong> Aboriginal and<br />
Torres Strait Islander Health<br />
‘Standing Strong Together’ Award<br />
Ms Sue Pinckham and Dr Liz Marles,<br />
Bungee Bidgel Aboriginal Health Clinic,<br />
New South Wales<br />
National Rural Faculty (NRF) Medical<br />
Undergraduate Student Bursary Award<br />
Ms Maureen Krasn<strong>of</strong>f, Western Australia<br />
Brian Williams Award – NRF<br />
Dr Ken Wanguhu, South Australia<br />
Monty Kent-Hughes Memorial Medal<br />
Dr Daniel Edge, South Australia<br />
(2014.2 examination cycle)<br />
Dr Meredith Stewart, Western Australia<br />
(2015.1 examination cycle)<br />
RACGP Foundation Research Awards<br />
• RACGP/MDA National Best General<br />
Practice Research Article in Australian<br />
Family Physician (AFP) Award:<br />
Ms Jessica Orchard, New South Wales<br />
• RACGP Family Medical Care Education<br />
and Research (FMCER) Grant:<br />
Dr Penelope Burns, New South Wales<br />
• RACGP Rex Walpole Travelling<br />
Fellowship: Dr Louise Stone,<br />
Australian Capital Territory<br />
• RACGP Family Medical Care Education<br />
and Research (FMCER) Grant and<br />
RACGP PWH Grieve Memorial Award:<br />
Associate Pr<strong>of</strong>essor Clare Heal,<br />
Queensland<br />
• HCF Research Foundation/RACGP<br />
Research Grant 2015:<br />
Associate Pr<strong>of</strong>essor Paresh Dawda,<br />
New South Wales; Associate Pr<strong>of</strong>essor<br />
Christopher Pearce, Victoria<br />
• RACGP/Diabetes Australia<br />
Research Grant: Associate Pr<strong>of</strong>essor<br />
Peter Schattner, Victoria<br />
• Therapeutic Guidelines<br />
Limited/RACGP Research Grant:<br />
Pr<strong>of</strong>essor Danielle Mazza, Victoria<br />
General Practitioner <strong>of</strong> the Year Award<br />
Dr Kean-Seng Lim, New South Wales<br />
General Practice Supervisor <strong>of</strong><br />
the Year Award<br />
Dr Cathryn Milligan, Western Australia<br />
General Practice Registrar <strong>of</strong><br />
the Year Award<br />
Dr Ashlea Broomfi eld, New South Wales<br />
Rural Registrar <strong>of</strong> the Year Award<br />
Dr Hannah Visser, New South Wales<br />
General Practice <strong>of</strong> the Year Award<br />
Collie River Valley Medical Centre,<br />
Western Australia<br />
Join your colleagues and celebrate at<br />
the HESTA Primary Health Care Awards<br />
Tuesday 10 November 2015, Plaza Ballroom, Melbourne<br />
Tickets on sale now at hestaawards.com.au<br />
Discounted price for group bookings.<br />
$<br />
30,000 in prizes to be won! * *Proudly<br />
Follow us:<br />
@HESTAPHCawards<br />
/HESTAPrimaryHealthCareAwards<br />
TICKETS<br />
ON SALE<br />
NOW<br />
sponsored by:<br />
Proudly presented by:<br />
hestaawards.com.au<br />
Issued by H.E.S.T. Australia Ltd ABN 66 006 818 695 AFSL No. 235249 Trustee <strong>of</strong> Health Employees<br />
Superannuation Trust Australia (HESTA) ABN 64 971 749 321. Terms and conditions apply.<br />
See phcawards.com.au for details<br />
22 Reprinted from Good Practice Issue 10, October 2015
ETHICS IN GENERAL PRACTICE<br />
Boundary crossings<br />
SARA BIRD<br />
Maintaining<br />
appropriate<br />
doctor–patient<br />
boundaries.<br />
Doctor–patient<br />
boundaries<br />
According to Good medical practice: A<br />
code <strong>of</strong> conduct for doctors in Australia<br />
(the Code), ‘patients trust their doctors<br />
because they believe that, in addition to<br />
being competent, their doctor will not<br />
take advantage <strong>of</strong> them and will display<br />
qualities such as integrity, truthfulness,<br />
dependability and compassion’.<br />
Section 8.2 <strong>of</strong> the Code states: 4<br />
pr<strong>of</strong>essional boundaries are<br />
integral to a good doctor–patient<br />
relationship. They promote good<br />
care for patients and protect<br />
both parties. Good medical<br />
practice involves:<br />
• maintaining pr<strong>of</strong>essional boundaries<br />
• never using your pr<strong>of</strong>essional<br />
position to establish or pursue<br />
a sexual, exploitative or other<br />
inappropriate relationship with<br />
anybody under your care. This<br />
includes those close to the<br />
patient, such as their carer,<br />
guardian or spouse or the parent<br />
<strong>of</strong> a child patient<br />
• avoiding expressing your<br />
personal beliefs to your patients<br />
in ways that exploit their<br />
vulnerability or that are likely to<br />
cause them distress.<br />
This article is provided by MDA National. They<br />
recommend that you contact your indemnity<br />
provider if you need specifi c advice in relation<br />
to your insurance policy.<br />
What would you do if one <strong>of</strong> your patients said<br />
they could not afford the medications you have<br />
prescribed to treat their acute illness? Would<br />
reaching into your pocket for the $30 to pay for<br />
their prescriptions be an inappropriate boundary<br />
crossing in the doctor–patient relationship?<br />
This case was discussed by a leading US<br />
family physician and researcher in 2013<br />
when he found himself reprimanded for<br />
‘unpr<strong>of</strong>essional boundary crossing behaviour’. 1<br />
What ethical and pr<strong>of</strong>essional concerns arise<br />
in this type <strong>of</strong> situation?<br />
Boundaries<br />
Pr<strong>of</strong>essional boundaries defi ne the expected<br />
and accepted physical, psychological and <strong>social</strong><br />
limits <strong>of</strong> the relationship between a doctor and<br />
their patient. At times, it can be diffi cult to<br />
defi ne these boundaries.<br />
Transgressions include boundary ‘crossings’,<br />
which are departures from usual pr<strong>of</strong>essional<br />
practice that are not exploitative and can be<br />
supportive <strong>of</strong> the therapy. On occasion, a<br />
boundary may be consciously crossed with the<br />
intention <strong>of</strong> assisting a patient’s management.<br />
Boundary ‘violations’, on the other hand, are<br />
transgressions that are harmful, or potentially<br />
harmful, to the patient and their therapy.<br />
The distinction between ‘crossings’ and<br />
‘violations’ involves judgement about whether,<br />
and to what degree, a patient has been<br />
exploited and/or coerced, and the harm<br />
caused to the patient and their relationship<br />
with the doctor.<br />
Boundary violations are unethical because<br />
they exploit the doctor–patient relationship,<br />
undermine the trust patients and the<br />
community have in doctors, and can cause<br />
pr<strong>of</strong>ound psychological harm to patients and<br />
compromise their ongoing clinical care.<br />
Balancing benefits and risks<br />
Many highlight the ‘slippery slope’ concept in<br />
boundary dilemmas. 2 While this model may<br />
assist in grasping boundary violations, it does<br />
not provide a good understanding <strong>of</strong> the larger<br />
area <strong>of</strong> boundary crossings. The slippery<br />
slope model maintains that crossings are likely<br />
to lead to violations and stresses vigilance<br />
in managing these interactions, preferably<br />
by refraining from a boundary crossing in<br />
the fi rst place.<br />
The US family physician was concerned<br />
that strict interpretation and application <strong>of</strong><br />
boundaries can discourage doctors from caring<br />
for and about patients, and risks encouraging<br />
detached, arm’s length, uncaring relationships.<br />
Strict rule-based decision making in<br />
boundary dilemmas, combined with the<br />
slippery slope model, can confuse doctors<br />
and discourage boundary crossings that are<br />
benefi cial to patients.<br />
A graded risk model for boundary dilemmas<br />
provides a framework for ethical decision<br />
making, outlining elements to consider before<br />
crossing a boundary:<br />
1. The potential harm to the patient and the<br />
doctor–patient relationship.<br />
2. The potential benefi t to the patient and the<br />
doctor–patient relationship.<br />
3. The presence, absence or degree <strong>of</strong><br />
coercive and exploitative elements in the<br />
boundary crossing.<br />
4. The doctor’s motives and intentions.<br />
5. The doctor’s aspiration to pr<strong>of</strong>essional<br />
ideals.<br />
6. The context <strong>of</strong> the boundary crossing.<br />
Doctors are encouraged to be alert to<br />
situations in which boundaries may be crossed,<br />
and to have a framework and strategy to<br />
manage such situations. This may include<br />
discussing it with a colleague or other adviser.<br />
Balancing pr<strong>of</strong>essional boundaries and your<br />
duty to make the care <strong>of</strong> patients your fi rst<br />
concern can be complex. But caring for and<br />
about patients and establishing meaningful<br />
therapeutic relationships is at the heart <strong>of</strong><br />
healing and our pr<strong>of</strong>essional satisfaction.<br />
Fears about crossing boundaries may<br />
inadvertently inhibit the care we provide.<br />
Considering the likely benefi t or harm by using<br />
a graded risk model can assist in maintaining<br />
our pr<strong>of</strong>essional responsibilities and values.<br />
References<br />
1. Schiff G, Gordon D. Crossing Boundaries – Violation or<br />
Obligation? JAMA 2013;310(2):1233–34.<br />
2. Galletly CA. Crossing pr<strong>of</strong>essional boundaries<br />
in medicine: the slippery slope to patient sexual<br />
exploitation. Med J Aust 2004;181:380–83.<br />
3. Martinez R. A model for boundary dilemmas: ethical<br />
decision-making in the patient-pr<strong>of</strong>essional relationship.<br />
Ethical Human Sci Serv 2000;2(1):43–61.<br />
4. Medical Board <strong>of</strong> Australia. Good medical practice: A<br />
code <strong>of</strong> conduct for doctors in Australia. Available at<br />
www.medicalboard.gov.au/Codes-Guidelines-Policies/<br />
Code-<strong>of</strong>-conduct.aspx<br />
Reprinted from Good Practice Issue 10, October 2015<br />
23
NUTRITION<br />
BMI and older people<br />
JANE WINTER<br />
Does the healthy<br />
weight range apply to<br />
older patients?<br />
Jane Winter is an accredited practising dietitian<br />
currently undertaking a PhD at Deakin University.<br />
Her area <strong>of</strong> study is malnutrition in community-based<br />
elderly people, identifying nutritional risk in the<br />
primary care setting for this population. Jane is also<br />
Medical Affairs Manager at Nestlé Health Science.<br />
References<br />
1. Morley JE. Anorexia <strong>of</strong> aging: physiologic and<br />
pathologic. Am J Clin Nut 1997;66(4):760–73.<br />
2. Vivanti AP, McDonald CK, Palmer MA, Sinnott M.<br />
Malnutrition associated with increased risk <strong>of</strong> frail<br />
mechanical falls among older people presenting to<br />
an emergency department. Emerg Med Australas<br />
2009;21(5):386–94.<br />
3. Guo JJ, Yang H, Qian H, Huang L, Guo Z, Tang<br />
T. The effects <strong>of</strong> different nutritional measurements<br />
on delayed wound healing after hip fracture in the<br />
elderly. J Surg Res 2010;159(1):503–08.<br />
4. Feldblum I, German L, Bilenko N, et al. Nutritional<br />
risk and health care use before and after an<br />
acute hospitalization among the elderly. Nutrition<br />
2009;25(4):415–20.<br />
5. Payette H, Coulombe C, Boutier V, Gray-Donald<br />
K. Nutrition risk factors for institutionalization in a<br />
free-living functionally dependent elderly population.<br />
J Clin Epidemiol 2000;53(6):579–87.<br />
6. Winter JE, MacInnis RJ, Wattanapenpaiboon<br />
N, Nowson CA. BMI and all-cause mortality in<br />
older adults: a meta-analysis. Am J Clin Nutr<br />
2014;99(4):875–90.<br />
7. Coin A, Veronese N, De Rui M, et al. Nutritional<br />
predictors <strong>of</strong> cognitive impairment severity in<br />
demented elderly patients: the key role <strong>of</strong> BMI. J<br />
Nutr Health Aging 2012;16(6):553–56.<br />
8. Heber D, Ingles S, Ashley JM, Maxwell MH, Lyons<br />
RF, Elash<strong>of</strong>f RM. Clinical detection <strong>of</strong> sarcopenic<br />
obesity by bioelectrical impedance analysis. Am J<br />
Clin Nutr 1996;64(3 Suppl):472S–77S.<br />
9. Kohara K. Sarcopenic obesity in aging population:<br />
current status and future directions for research.<br />
Endocrine 2014;45(1):15–25.<br />
10. Murphy RA, Patel KV, Kritchevsky SB, et al.<br />
Weight <strong>change</strong>, body composition, and risk <strong>of</strong><br />
mobility disability and mortality in older adults: a<br />
population-based cohort study. J Am Geriatr Soc<br />
2014;62(8):1476–83.<br />
11. Somes GW, Kritchevsky SB, Shorr RI, Pahor<br />
M, Applegate WB. Body mass index, weight<br />
<strong>change</strong>, and death in older adults: the systolic<br />
hypertension in the elderly program. Am J Epidemiol<br />
2002;156(2):132–28.<br />
12. Flanagan D, Fisher T, Murray M, et al. Managing<br />
undernutrition in the elderly - prevention is better<br />
than cure. Aust Fam Physician 2012;41(9):695–99.<br />
Most healthcare pr<strong>of</strong>essionals are likely aware<br />
that the World Health Organization (WHO)<br />
defi nes the healthy weight range as a body<br />
mass index (BMI) <strong>of</strong> 18.5–24.9 kg/m 2 , but is<br />
this appropriate for older people?<br />
This range was determined from studies<br />
that primarily focused on younger people<br />
and there has been ongoing debate about its<br />
suitability for older people, generally considered<br />
to be those aged older than 65.<br />
Older people face unique nutritional issues<br />
resulting in a greater risk <strong>of</strong> under-nutrition<br />
rather than over-nutrition. These issues include<br />
physiological <strong>change</strong>s associated with ageing<br />
(the anorexia <strong>of</strong> ageing), chronic disease,<br />
polypharmacy and psycho<strong>social</strong> <strong>change</strong>s. 1<br />
Under-nutrition has serious consequences,<br />
such as increased risk <strong>of</strong> falls and fractures, 2<br />
poor wound-healing, 3 increased risk <strong>of</strong><br />
hospitalisation (with greater length <strong>of</strong> stay) 4 and<br />
entry to residential aged care. 5 However, undernutrition<br />
<strong>of</strong>ten goes unrecognised and using<br />
the healthy weight range to assess appropriate<br />
body weight may be misleading in older people.<br />
BMI analysis<br />
Although healthcare pr<strong>of</strong>essionals <strong>of</strong>ten use<br />
a higher BMI range as the more appropriate<br />
reference for older people, there has been<br />
much debate in the area. To answer this<br />
question, the Dietitians Association <strong>of</strong> Australia<br />
conducted a meta-analysis <strong>of</strong> 32 studies <strong>of</strong><br />
community-living populations aged 65 years or<br />
older, including nearly 200,000 individuals. 6<br />
The results showed the lowest mortality risk<br />
was at a BMI <strong>of</strong> 24–31 kg/m 2 (compared with<br />
a reference BMI <strong>of</strong> 23 kg/m 2 ). A BMI <strong>of</strong><br />
21–22 kg/m 2 was associated with a 12%<br />
increase in mortality risk, with the risk starting<br />
to increase at a BMI <strong>of</strong> less than 23 kg/m 2 .<br />
Other studies in older populations have<br />
shown that a low BMI in older people is<br />
associated with other poor health outcomes.<br />
For example, a BMI <strong>of</strong> less than 25 kg/m 2<br />
has been associated with the development <strong>of</strong><br />
dementia and severity <strong>of</strong> cognitive impairment<br />
in those with dementia. 7<br />
Using BMI as an indicator <strong>of</strong> nutritional status<br />
in older people is further complicated by the<br />
age-related <strong>change</strong>s in body composition. With<br />
increasing age, muscle mass declines and the<br />
proportion <strong>of</strong> body fat increases with a <strong>change</strong><br />
in fat distribution. This shift in body composition<br />
gives rise to the problem <strong>of</strong> sarcopenic<br />
obesity, a term used to defi ne excess body<br />
fat in combination with reduced lean mass. 8<br />
Sarcopenic obesity has been associated<br />
with more signifi cant functional decline than<br />
simple obesity. 9<br />
Given the altered relationship between BMI<br />
and mortality with older age, weight <strong>change</strong><br />
is likely to be a more relevant indicator <strong>of</strong><br />
nutritional risk in older people. A loss <strong>of</strong> 5%<br />
in one year (especially if unintentional) is<br />
considered to be signifi cant and associated with<br />
greater disability and mortality. 10 Studies have<br />
shown that even in the presence <strong>of</strong> low or high<br />
BMI, weight stability is associated with reduced<br />
mortality risk. 11<br />
Identifying nutritional risk<br />
Although identifying under-nutrition in older<br />
people is not as easy as simply recording<br />
BMI, the general practice setting is ideally<br />
suited to the early detection <strong>of</strong> nutritional risk,<br />
when intervention and improvement may be<br />
more effective. A 2012 article in Australian<br />
Family Physician (AFP) included the following<br />
recommendations: 12<br />
• Routinely screen for nutritional risk. A short<br />
screening tool such as the mini nutritional<br />
assessment short form (MNA-SF) can<br />
easily be incorporated into the 75-and-older<br />
health assessment.<br />
• Monitor weight, looking for unintentional<br />
<strong>change</strong>s in weight.<br />
• Weight loss should only be recommended<br />
if function is compromised due to<br />
excess weight.<br />
• Review dietary restrictions, such as low-fat<br />
diets, to determine appropriateness.<br />
• Encourage physical activity.<br />
• Refer patients with complex needs to an<br />
accredited practising dietitian for a full<br />
assessment.<br />
Monitoring older patients for signs <strong>of</strong> nutritional<br />
decline and intervening with medical, dietary<br />
and/or <strong>social</strong> supports can improve quality<br />
<strong>of</strong> life and reduce the risk or impact <strong>of</strong> other<br />
comorbidities. Interventions for this population<br />
should not necessarily be based on the<br />
standard healthy weight range – a more<br />
appropriate range for older people may be a<br />
BMI <strong>of</strong> closer to 23–30 kg/m 2 .<br />
24 Reprinted from Good Practice Issue 10, October 2015
TRIENNIUM UPDATE<br />
Have you completed this triennium’s<br />
Quality Improvement (QI) requirement?<br />
What is Quality Improvement?<br />
Quality Improvement (QI) is the process where an opportunity<br />
to <strong>change</strong> practices occurs as a result <strong>of</strong> learning.<br />
Pr<strong>of</strong>essional advice and a growing body <strong>of</strong> evidence<br />
demonstrate quality improvement activities lead to positive<br />
<strong>change</strong> in practices, particularly when involving a whole<br />
practice team approach.<br />
How to meet your QI requirement?<br />
1. Complete a QI activity<br />
2. Participate in a pre-approved QI activity delivered<br />
by an Accredited Activity Provider<br />
3. Identify a Category 1 activity you have already done,<br />
reflect on how you applied the education to your practice<br />
and complete a ‘Quality Improvement Reflection’ form.<br />
130<br />
points<br />
2<br />
CATEGORY 1<br />
activities<br />
including 1<br />
QI activity<br />
1<br />
CPR<br />
Examples <strong>of</strong> QI<br />
Evidence Based Medicine Journal Club<br />
Supervised Clinical Attachment (SCA)<br />
GP Research<br />
Clinical Audit<br />
Plan, Do, Study, Act (PDSA)<br />
Small Group Learning<br />
Royal Australian College <strong>of</strong> General Practitioners
FINANCIAL PLANNING<br />
Value<br />
<strong>of</strong> trusts<br />
TERRY MCMASTER<br />
Structuring the<br />
business as a trust can<br />
<strong>of</strong>fer a general practice<br />
several advantages.<br />
Helpful resources<br />
Australian Securities and<br />
Investments Commission – Your<br />
business structure (http://asic.gov.<br />
au/for-business/your-business/<br />
your-business-structure)<br />
Taxpayers Australia – Business<br />
structures: choosing the right<br />
business structure (www.taxpayer.<br />
com.au/KnowledgeBase/10185/<br />
Small-Business-Tax-Super/<br />
Business_structures#Trusts)<br />
Australian Government:<br />
Business – Key aspects<br />
<strong>of</strong> a trust (www.business.<br />
gov.au/business-topics/<br />
business-structures-and-types/<br />
business-structures/trust/<br />
Pages/default.aspx)<br />
Australian Tax Office –<br />
Assessing the risk: allocation <strong>of</strong><br />
pr<strong>of</strong>i ts within pr<strong>of</strong>essional fi rms<br />
(www.ato.gov.au/business/<br />
starting-your-own-business/<br />
in-detail/pr<strong>of</strong>essional-fi rms/<br />
Assessing-the-risk--allocation-<strong>of</strong>pr<strong>of</strong>i<br />
ts-within-pr<strong>of</strong>essional-fi rms)<br />
Terry McMaster is the founder and principal<br />
director <strong>of</strong> McMasters’ Accountants, Solicitors,<br />
Financial Planners. He has worked exclusively<br />
with medical practices for more than 20 years<br />
and holds degrees in law and commerce from<br />
Melbourne University.<br />
The best tax planning is not schematic or<br />
transaction-based. It’s easy, inexpensive and<br />
won’t raise the eyebrows <strong>of</strong> the Australian Tax<br />
Offi ce (ATO). We are talking about trusts.<br />
Trusts are one <strong>of</strong> many ways in which you<br />
can run a practice and they stack up very<br />
well against the alternatives: companies,<br />
individuals (sole trader) and partnerships.<br />
Two types <strong>of</strong> trusts are particularly well<br />
suited for use in general practice.<br />
Personal services income trusts<br />
Smaller practices that don’t engage other fee<br />
earners, and which don’t have signifi cant plant<br />
and equipment, are generally best served by<br />
a personal services income (PSI) trust. This<br />
type <strong>of</strong> trust doesn’t allow fl exible income<br />
distributions and requires all medical income<br />
to go to the GP who generated it.<br />
The PSI trust helps shield the GP from<br />
negligent acts or omissions by other GPs,<br />
takes advantage <strong>of</strong> the concessional car<br />
fringe benefi ts tax rules and facilitates the<br />
genuine employment <strong>of</strong> related persons.<br />
The PSI trust also gets GPs out <strong>of</strong> the<br />
pay-as-you-go withholding tax cycle and<br />
streamlines their accounting, since there is<br />
no need to make sure the trust ‘breaks even’<br />
every year in the same way a company does.<br />
Business trusts<br />
Business trusts <strong>of</strong>fer a number <strong>of</strong> tax<br />
advantages. Practices that engage other<br />
fee earners, or have signifi cant plant and<br />
equipment and meet the ATO’s defi nition <strong>of</strong> a<br />
business, would reap the most benefi ts from<br />
using a business trust.<br />
A business trust is usually a garden-variety<br />
family trust, but multiple-owner practices may<br />
use a unit or hybrid trust. Business trusts<br />
allow fl exible income distributions because<br />
medical income does not have to go to the<br />
GP who generated it.<br />
The ATO accepts business trusts provided<br />
the defi nition <strong>of</strong> a business is met and one <strong>of</strong><br />
three additional tests is satisfi ed: the fi rst test<br />
says the business trust will be accepted if the<br />
average rate <strong>of</strong> tax paid on medical income is<br />
at least 30% (equal to the company tax rate),<br />
the second test says the amount distributed<br />
to the owner-GP must be at least equal<br />
to the amount paid to the most highly<br />
remunerated non-owner-GP, and the third<br />
test says the amount distributed to the<br />
owner GP must be at least 50% <strong>of</strong> their<br />
patient billings.<br />
The fact the ATO has decreed that only one<br />
<strong>of</strong> these test needs to be met makes it easier<br />
for doctors to comply with the rules. The<br />
three new tests apply in the fi nancial year<br />
ending 30 June 2016 (this tax year).<br />
A business trust will allow doctors who were<br />
paying average tax rates <strong>of</strong> more than 30%<br />
to lower their average rate by distributing to<br />
lower tax rate benefi ciaries.<br />
Business trusts don’t just reduce tax,<br />
however; they can make service trusts<br />
redundant, reducing complexity, costs and<br />
accountants’ fees. Business trusts work even<br />
if there are no tax advantages.<br />
How to make the <strong>change</strong><br />
Changing a practice from a company,<br />
individual or partnership structure to a<br />
trust-based setup is usually relatively simple,<br />
but owner-GPs would be well advised to<br />
seek some guidance before they make any<br />
such <strong>change</strong>s (refer to breakout for more<br />
information).<br />
Capital gains tax has to be considered, but<br />
this will likely not be an issue since general<br />
practice goodwill values are low and various<br />
tax concessions apply under the Federal<br />
Government’s small business tax concessions<br />
regime. The ATO’s public rulings accept<br />
that a practice can <strong>change</strong> to a trust-based<br />
structure without breaching the anti-taxavoidance<br />
rules.<br />
ATO opinion<br />
The last few years have seen the ATO<br />
conduct a wide-ranging review <strong>of</strong> the basis<br />
<strong>of</strong> taxing pr<strong>of</strong>essional practice income, which<br />
included some medical practice audits. The<br />
ATO subsequently released guidelines,<br />
Assessing the risk: allocation <strong>of</strong> pr<strong>of</strong>i ts within<br />
pr<strong>of</strong>essional fi rms, in 2014.<br />
These guidelines apply to all pr<strong>of</strong>essionals,<br />
not just GPs, include the three business tests<br />
noted above and confi rm that the familiar<br />
public rulings for doctors’ incomes still apply.<br />
The guidelines’ most important public<br />
ruling for GPs is ‘IT 2369’ (dated 20 June<br />
1991). This ruling was negotiated by the<br />
Australian Medical Association (AMA) and<br />
sets out the ATO’s rule <strong>of</strong> thumb that a<br />
general practice is a business if it has at least<br />
as many non-owner material fee earners<br />
as it has owners on an equivalent full-time<br />
basis. ‘Fee earners’ includes practitioners<br />
other than doctors.<br />
PSI and business trusts continue to be<br />
accepted by the ATO, but doctors with<br />
business trusts must ensure they meet one<br />
<strong>of</strong> the three tests set out above before they<br />
lodge their 2016 tax returns.<br />
26 Reprinted from Good Practice Issue 10, October 2015
14-15 NOVEMBER<br />
MANLY BEACH | SYDNEY | SEMINAR<br />
Dr Catriona Ooi<br />
Sexual Health Physician,<br />
Clinical Lead <strong>of</strong> the<br />
Western Sydney Sexual<br />
Health Centre and<br />
Senior Lecturer with<br />
the University <strong>of</strong> Sydney<br />
Medical School.<br />
Associate Pr<strong>of</strong>essor<br />
Paul Middleton<br />
Emergency physician,<br />
Fellow <strong>of</strong> the Australasian<br />
College for Emergency<br />
Medicine (ACEM) and<br />
Chair <strong>of</strong> the Australian<br />
Resuscitation Council NSW.<br />
DAY<br />
EVENT<br />
FEATURED SPEAKERS<br />
Active<br />
Learning<br />
Modules<br />
ALS AND CPR<br />
TRAINING AVAILABLE<br />
TRAINING GRANT APPROVED<br />
FOR RURAL GPs DOING ALS<br />
RURAL EMERGENCIES<br />
GP CARDIOLOGY<br />
WOMEN’S HEALTH<br />
For full agenda and registration details<br />
www.ruraldoctorseminar.com.au<br />
Sponsors<br />
Complete the active learning<br />
module (ALM) and earn 40<br />
Category 1 QI&CPD points
16<br />
GP16<br />
The RACGP<br />
Conference<br />
for General<br />
Practice<br />
29 Sep –1 Oct 2016<br />
Perth, Australia<br />
Perth Convention and Exhibition Centre<br />
The RACGP National Conference,<br />
GP16 is the highlight event <strong>of</strong><br />
the general practice calendar.<br />
To be held in Perth, the heartbeat<br />
<strong>of</strong> Australia’s largest state and a<br />
premier destination, the conference<br />
<strong>of</strong>fers both local and international<br />
delegates a unique Australian<br />
experience.<br />
The GP16 program will focus on:<br />
Public health, Chronic conditions,<br />
GP education, Models <strong>of</strong> business,<br />
Rural general practice and<br />
Aboriginal and Torres Strait<br />
Islander health.<br />
Clinical, Digital,<br />
Leadership<br />
Clinical, Digital,<br />
Leadership<br />
Clinical, Digital,<br />
Leadership<br />
Royal Australian College <strong>of</strong> General Practitioners<br />
gp16.com.au