INNOVATION & TECHNOLOGY ON SHOW AT HOSPIMedica ...
INNOVATION & TECHNOLOGY ON SHOW AT HOSPIMedica ...
INNOVATION & TECHNOLOGY ON SHOW AT HOSPIMedica ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
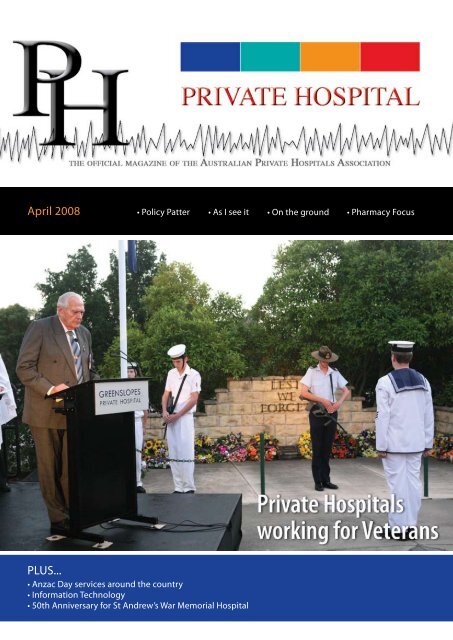
April 2008 • Policy Patter<br />
PLUS...<br />
• Anzac Day services around the country<br />
• Information Technology<br />
• 50th Anniversary for St Andrew’s War Memorial Hospital<br />
• As I see it • On the ground<br />
• Pharmacy Focus
2<br />
Private Hospital - April 2008
Private Hospital - April 2008<br />
3
DIAM<strong>ON</strong>D SP<strong>ON</strong>SOR<br />
APHA Major Sponsors<br />
Private Hospital is published bi-monthly, six times a year<br />
(February, April, June, August, October and December)<br />
as a joint undertaking between the Australian Private<br />
Hospitals Association Ltd (ACN 008 623 809) and the<br />
Australian Publishing Resource Service Pty Ltd<br />
(ACN 082 824 397).<br />
APHA Office: Level 3, 11 National Circuit, Barton ACT 2600.<br />
Postal Address: PO Box 7426,<br />
Canberra BC ACT 2610, Australia.<br />
Phone: (02) 6273 9000. Fax: (02) 6273 7000.<br />
E-mail: info@apha.org.au Website: www.apha.org.au<br />
Executive Director: Michael Roff<br />
Director Policy and Research: Paul Mackey<br />
John Amery .. Mater Misericordiae Hospital T’ville<br />
Steve Atkins ............................. Healthe Care Australia<br />
Dr Peter Catts ... Ind. Private Hospitals of Australia<br />
Dr Leon Clark .................. Sydney Adventist Hospital<br />
Andrew Currie ............ Vimy House Private Hospital<br />
Christine Gee ................... Toowong Private Hospital<br />
Pat Grier .......................................... Ramsay Health Care<br />
Robynne Kent .................... Canossa Private Hospital<br />
Alan Kinkade ............................... Epworth HealthCare<br />
Claire Michalanney ............. Sportsmed SA Hospital<br />
Aaxis Pacific<br />
HAL Leasing Services<br />
Health Super Pty Ltd<br />
APRS Pty Ltd: Level 6, 38 Currie Street, Adelaide SA 5001.<br />
Postal Address: GPO Box 1746, Adelaide SA 5001, Australia.<br />
Phone: (08) 8113 9200. Fax: (08) 8113 9201.<br />
E-mail: aprs@aprs.com.au Website: www.aprs.com.au<br />
Material in Private Hospital is protected under the<br />
Commonwealth Copyright Act 1968. No material may<br />
be reproduced in part or in whole without the written<br />
consent from the copyright holders (APHA).<br />
Private Hospital welcomes submissions and a diversity<br />
of opinion on hospital-related issues and will publish<br />
views that are not necessarily the policy of the APHA.<br />
All material must be relevant, cogent, submitted to the<br />
APHA N<strong>AT</strong>I<strong>ON</strong>AL BOARD<br />
Australian<br />
Private Hospitals<br />
Association<br />
Public Affairs Manager and Editor: Lisa Ramshaw<br />
Member Services Manager: Goran Josifovski<br />
Moira Munro .................................................. Perth Clinic<br />
Craig McNally .............................. Ramsay Health Care<br />
Richard Royle ................................ UnitingCare Health<br />
Daniel Sims ................................... Ramsay Health Care<br />
Mark Stephens ................. Chesterville Day Hospital<br />
Ben Thynne .............................. Healthe Care Australia<br />
George Toemoe ....................................... St Luke’s Care<br />
Stephen Walker .......................... St Andrews Hospital<br />
Amanda Quealy ........................................ Hobart Clinic<br />
PL<strong>AT</strong>INUM ASSOCI<strong>AT</strong>E MEMBERS<br />
3M Healthcare<br />
Active Partners in Health Solutions<br />
Anaesthesia Systems<br />
B. Braun Australia Pty Ltd<br />
Blake Dawson<br />
Cardinal Health<br />
Charity Life<br />
Clear Outcomes Pty Ltd<br />
Communio Pty Ltd<br />
Commercial Flooring Australia<br />
Coregas<br />
Daylabels Pty Ltd T/a Daydots<br />
Ebsworth & Ebsworth Lawyers<br />
Fresenius Medical Care South East Asia Pty Ltd<br />
GE Healthcare<br />
Global Mark<br />
Health Industry Plan<br />
Adesse<br />
Australian Health Services Alliance<br />
Boyd Health Management<br />
Department of Veteran’s Affairs<br />
Energy Impact Pty Ltd<br />
Healthcare Management Advisors Pty Ltd<br />
Herring Health & Management Services Pty Ltd<br />
Home Nurses<br />
John Randall & Associates<br />
NAB Health<br />
Thomson Adsett Architects<br />
GOLD ASSOCI<strong>AT</strong>E MEMBERS<br />
ASSOCI<strong>AT</strong>E MEMBERS<br />
Healthsolve Pty Ltd<br />
Intrinsix Pty Ltd<br />
Johnson & Johnson Medical Pty Ltd<br />
Knight Frank Valuations<br />
Medtronic Australasia Pty Ltd<br />
Menette Pty Ltd<br />
Olympus<br />
Pay Global<br />
Regal Health Services<br />
SAI Global<br />
Schiavello Hospital Solutions Pty Ltd<br />
Stargate Consulting Group<br />
Terumo Corporation<br />
The College of Nursing<br />
The PayOffice Group<br />
Thinc Projects<br />
Medicraft Australia Pty Ltd<br />
Merrill Lynch<br />
Noarlunga Health Services<br />
Novartis Consumer Health Australasia<br />
Origin Healthcare<br />
Queensland X-Ray<br />
Thiess Health<br />
Transport Accident Commission<br />
APHA and accompanied by a stamped<br />
self-addressed envelope, otherwise received<br />
electronically at lisa.ramshaw@apha.org.au<br />
Electronic images must be to print standard - 300 dpi<br />
or higher. Please retain duplicates of all hard copy<br />
text and illustrative materials. The APHA does not<br />
accept responsibility for damage to, or loss of,<br />
material submitted.<br />
Neither the APHA, APRS or their servants and agents<br />
accept liability, including liability for negligence, arising<br />
from the information contained in Private Hospital.
Regulars<br />
18 Michael Roff - As I see it<br />
If you are really sick, go to a Private<br />
Hospital…<br />
26 Christine Gee’s Quality in Focus<br />
Australian Commission on<br />
Safety and Quality in Health Care<br />
36 Paul Mackey’s Policy Patter<br />
Private Hospitals providing good value<br />
for Veterans<br />
40 Moira Munro - Mental Health Forum<br />
Veterans and Mental Health<br />
58 Pharmacy Focus with Michael Ryan<br />
Measuring the performance of the<br />
Drug Committee<br />
62 Membership Matters with Goran Josifovski<br />
Delivering value to members<br />
82 On the ground<br />
Gail Rice - Social welfare worker and Veterans<br />
Liaison Officer<br />
77<br />
Features<br />
Contents<br />
12 Anzac Day Services<br />
Anzac Day at Private Hospitals around Australia<br />
14 Department of Veteran Affairs and<br />
Private Hospitals<br />
22 Information Technology in the<br />
Health Sector<br />
Interview with George Toemoe<br />
32 Queensland Governor returns to hospital<br />
she helped build<br />
38 Revised Medical Technology Code<br />
of Conduct<br />
66 EMU at the San<br />
75 One Life, a Second Chance<br />
79 Book Review – Community Pharmacy<br />
44<br />
10 - Veterans<br />
Feature<br />
Private Hospitals have<br />
a long tradition of<br />
helping Veterans<br />
7
8<br />
Private Hospital - April 2008 PH
Editors Letter<br />
Welcome to the April edition of Private Hospital magazine!<br />
This month, to coincide with Anzac Day and the 90th birthday of the<br />
Repatriation Commission, we celebrate the excellent services so many<br />
private hospitals around the country provide for veterans.<br />
The Repatriation Commission was<br />
established on 8 April 1918 to support the<br />
thousands of veterans, many of them sick<br />
and wounded, returning home from the<br />
battlefields of the First World War.<br />
Through the Second World War and<br />
subsequent wars and conflicts, Australia’s<br />
repatriation system has evolved to meet<br />
the needs of servicemen and women and<br />
their families.<br />
Two APHA member hospitals, Greenslopes<br />
and Hollywood, were initially repatriation<br />
hospitals and have provided services<br />
to Australia’s veterans for many years,<br />
where other members have only become<br />
Department of Veterans Affairs’ Tier 1or<br />
Tier 2 hospitals in recent times.<br />
Veterans are heavy users of the private<br />
system and are becoming increasingly<br />
older. DVA’s statistical unit have forecast<br />
that their numbers will decline by almost<br />
a half over the next decade. They are a<br />
group with some of the more difficult<br />
conditions and yet, private facilities do not<br />
shirk from the responsibility of treating<br />
these important citizens. APHA hospitals<br />
that have a contract with DVA are treating<br />
a wide variety of medical patients, not just<br />
surgical ones.<br />
DVA and APHA members are working<br />
together on a number of projects<br />
including: pay for performance initiatives,<br />
supported discharge programs, data<br />
analysis to make the system work better<br />
and transition care.<br />
No matter which facility veterans choose or<br />
what their health needs are, our member<br />
hospitals are committed to providing the<br />
best possible service and honouring the<br />
Private Hospital - April 2008<br />
Editors Letter<br />
sacrifices these men and women made for<br />
our country.<br />
This is my first issue as Private Hospital’s<br />
editor and it represents a new approach<br />
for the magazine. Just as this issue is<br />
themed around veterans, our June edition<br />
will be themed around an area that has<br />
received much press lately, our healthcare<br />
workforce. We will investigate the Rudd<br />
Government’s plan to bring nurses back<br />
into the workforce and get an idea of what<br />
is happening in private hospitals around<br />
the country.<br />
If you would like to feature an innovative<br />
workforce program at your hospital or<br />
would like to provide feedback on anything<br />
you read in this issue, please contact me<br />
at APHA.<br />
I’d also like to say thank you to everyone<br />
who has made me so welcome at APHA.<br />
I look forward to getting to know more of<br />
you over the coming months and working<br />
together to promote the private hospital<br />
industry.<br />
Lisa Ramshaw<br />
Editor<br />
Lisa.Ramshaw@apha.org.au<br />
9
10<br />
Feature: Veteran Community<br />
A Long Tradition of Helping our Nation’s Veterans<br />
While Hollywood Private Hospital is now a modern, state-of-the-art private<br />
health care facility, it has a proud history that dates back to the Second<br />
World War.<br />
Hollywood was originally built during World War II by the Commonwealth<br />
Government and opened in 1942 as the 500-bed Australian General Hospital<br />
(also known as 110 Military Hospital) and provided care for service men<br />
and women.<br />
Under an agreement with the Department of<br />
Veterans’ Affairs, Hollywood has continued to<br />
be the principal provider of inpatient hospital<br />
services for veterans in Western Australia. Over<br />
the past 12 months Hollywood has provided<br />
over 10,000 inpatient services for veterans and<br />
over 5,000 day case services for veterans.<br />
Although there are no longer any veterans<br />
of ‘the great war’ alive in Western Australia,<br />
Hollywood still sees many of the thousands<br />
of World War II veterans as well as veterans of<br />
the Korea War, the Vietnam War, the Malayan<br />
Emergency, Gulf War 1 and 2, the war on terror,<br />
and the many peacekeeping missions, both<br />
past and current.<br />
The vast majority of Australia’s ex-service<br />
personnel are World War II veterans, and most<br />
of these are now in their 80s. As well as the<br />
health problems normally associated with<br />
ageing, many of the veterans carry health scars<br />
from their service days. It is difficult to say<br />
which of the ailments normally associated<br />
with older age can be directly attributed to<br />
war service.<br />
There are a few obvious ones of course. Many<br />
of Australia’s servicemen carry ‘shrapnel’<br />
- pieces of metal resulting from fragmented<br />
bullets or from other sources. Hearing is an<br />
enormous problem for artillery men (and<br />
indeed infantry who were in close proximity to<br />
the firing of the heavy guns). Many of Australia’s<br />
ex-service people are afflicted with joint<br />
problems, resulting from traumas of battle.<br />
Tobacco was issued as part of ‘ration packs’ to<br />
all of our service personnel. Many young men<br />
and women started smoking as a result of this,<br />
and continued the habit for many years, often<br />
for the rest of their lives. The adverse health<br />
effects of tobacco were not as well known at<br />
that time as they are now - the tobacco was<br />
provided as a well-intentioned treat and a<br />
little luxury.<br />
The link between cardiovascular disease and<br />
tobacco smoking is well known. Cardiovascular<br />
disease can take the form of heart disease,<br />
with an increased propensity for myocardial<br />
infarction (heart attack) and cardiac failure. It<br />
may also affect the blood supply in the brain,<br />
causing stroke, or in the peripheral circulation<br />
causing difficulty walking, or even leg<br />
ulceration which ultimately may result<br />
in amputation.<br />
Smokers have a higher incidence of cancers of<br />
all kinds, particularly lung, stomach and bowel.<br />
Chronic lung disease is a common condition in<br />
the ex-service community. This is partly related<br />
to smoking, but also the effect of inhalation of<br />
dust, gas, fumes and chemicals. People with<br />
chronic obstructive pulmonary disease typically<br />
have shortness of breath, and persistent cough<br />
and phlegm.<br />
They are prone to recurrent infections,<br />
including bronchitis and pneumonia.<br />
Many service men and women contracted<br />
tuberculosis during their service years. This was<br />
particularly rife in the prisoner of war camps.<br />
Tuberculosis was notoriously difficult to treat,<br />
Private Hospital - April 2008<br />
though presently we have excellent drugs to<br />
treat this condition.<br />
As well as the health problems normally<br />
associated with ageing, many of the veterans<br />
carry health scars from their service days.<br />
One specific material which has caused<br />
damage to the lungs of service personnel<br />
has been asbestos. Asbestos was used as a<br />
cheap and easy to use building material for<br />
many years prior to the health risks becoming<br />
known. Asbestos was used for insulating and<br />
protective lagging in much of the defence<br />
force equipment, such as around pipes and in<br />
the hulls of navy ships, aircraft and personnel<br />
carriers and assault vehicles.<br />
While asbestos is most notoriously associated<br />
with an aggressive type of cancer called<br />
mesothelioma, it can also cause chronic fibrosis<br />
in lungs and plaques in the pleura (the lining of<br />
the lungs). This can lead to gradually worsening<br />
breathlessness and in some cases, ultimately,<br />
respiratory failure.
While many service men and women were<br />
exposed to atrocities which are beyond the<br />
imagination of most people, the condition of<br />
Post-traumatic Stress Disorder (or PTSD) was<br />
not formally recognised by the Department of<br />
Veterans’ Affairs until the early 1980s.<br />
Many of the WWII veterans returned from war<br />
zones or internment camps with significant<br />
psychological conditions. These were variously<br />
called ‘war fatigue’, ‘asthenia’, ‘shell shock’ or<br />
‘battle fatigue’. At the time many people just<br />
got on with their lives, but were never able to<br />
access adequate treatment programs which<br />
addressed their problem. Many of these men<br />
and women carried the scars of their condition<br />
for the remainder of their lives.<br />
The Vietnam War was something different.<br />
It was clear that many of the servicemen<br />
and women returning home from Vietnam<br />
had severe psychological issues. These took<br />
the form of vivid nightmares, flashbacks to<br />
traumatic events, severe and incapacitating<br />
anxiety and difficulty returning to mainstream<br />
living in the ‘lucky country’.<br />
The Vietnam War also saw the introduction of<br />
widespread environmental use of defoliants<br />
and other poisonous chemicals, with<br />
widespread, accidental exposure of the troops<br />
and the introduction of the term ‘friendly fire’.<br />
The PTSD program which is conducted in<br />
The Hollywood Clinic, on-site at Hollywood<br />
Private Hospital, is a program that endeavours<br />
to provide PTSD sufferers with insight about<br />
their condition, and offers strategies to manage<br />
some of the worse features, including the<br />
associated use of alcohol and other drugs.<br />
While the program does not profess to be<br />
curative, to date there have around 300<br />
Vietnam Veterans who have gained significant<br />
benefit from the program.<br />
One of the most helpful aspects of Hollywood’s<br />
PTSD program has been the insight the<br />
participants have been able to gain into<br />
the condition.<br />
The program recognises that every individual’s<br />
trauma and their reaction to it is unique. Many<br />
sufferers of PTSD have never spoken about<br />
their pain or the destructive nature of their<br />
stress, and some have harboured a long held<br />
belief that they are the only one with<br />
a problem.<br />
To be in a group of people who have shared<br />
similar traumatic experiences and have suffered<br />
from similar disabling symptoms for many<br />
years has been very healing for many of these<br />
men. There is also mounting evidence that the<br />
children of Vietnam Veterans have a number of<br />
health issues.<br />
There are claims that they experience a higher<br />
rate of congenital abnormalities, ranging from<br />
the very trivial to the very severe. The program<br />
recognises that every individual’s trauma and<br />
their reaction to it is unique.<br />
There would also appear to be a higher<br />
overall death rate from suicide and accidents<br />
in the children of Vietnam Veterans than in a<br />
comparable general population whose parents<br />
Private Hospital - April 2008<br />
Feature: Veteran Community<br />
were not involved in the war. The reasons for<br />
this are unknown, however many theories have<br />
been put forward. At this stage there are no<br />
studies into the health of the grandchildren<br />
of Vietnam Veterans.<br />
With over 60 years of experience in treating<br />
veteran and war widow patients, Hollywood<br />
Private Hospital takes much pride in their<br />
reputation as being the best equipped to<br />
anticipate and meet the needs of these very<br />
special Australians.<br />
By Dr Margaret Sturdy, Director of Medical<br />
Services, Hollywood Hospital<br />
11<br />
The art therapy component of PTSD treatment at Hollywood
12<br />
Feature: Veteran Community<br />
Anzac Day at Private Hospitals around Australia<br />
Members of the Shortland sub branch will<br />
officiate at Hunter Valley Private Hospital’s<br />
annual Anzac Day service. The service usually<br />
has 20 to 30 people in attendance with a<br />
bugler who plays the last post and reveille and<br />
they serve a morning tea with Anzac biscuits<br />
afterwards.<br />
The Sunshine Coast Private Hospital will<br />
be marking Anzac Day with a service in the<br />
Hospital Chapel at 10 am. The service will be for<br />
patients, staff and visitors to the hospital.<br />
Westmead Rehabilitation Centre will again<br />
hold an Anzac Day Ceremony on 24th of April<br />
at 11.00. This ceremony will be conducted by<br />
Vietnam Veterans from St. Marys Outpost, and<br />
is open to patients and visitors. A BBQ lunch<br />
will follow.<br />
Last year was the first year an Anzac Day<br />
Ceremony was held at Westmead Rehabilitation<br />
Centre and patients who had served in the<br />
Armed Forces took part in the ceremony.<br />
Feedback received from patients, visitors and<br />
staff was very positive and the BBQ lunch that<br />
followed was very well received.<br />
Greenslopes Private Hospital will once again<br />
host their annual Anzac Day dawn service.<br />
The service begins at 5.30am in the ANZAC<br />
memorial located adjacent to the Chapel and<br />
is open to the general community, patients<br />
and staff. The Dawn Service is followed by<br />
the traditional gunfire breakfast. Attendance<br />
continues to grow each year with more than<br />
1500 people expected to attend.<br />
Tamara Private Hospital (RHC) will have the<br />
local RSL Branch hold their annual pilgrimage<br />
for ANZAC service on Sunday 20th April in<br />
the Remembrance garden within the hospital<br />
courtyard at 2.00 pm.<br />
Canossa Private Hospital in Brisbane will be<br />
holding a ceremony in their garden near the<br />
flag pole on Anzac Day. Before the ceremony<br />
begins, a breakfast is held for veterans and their<br />
families. Then the veterans do a short march to<br />
the flag pole before the ceremony commences<br />
with one of the local Catholic priests presiding<br />
over the Anzac Day service. Canossa provides<br />
Rehabilitation, Oncology, General Medicine,<br />
Palliative Care and Interim Care for Veterans<br />
and has a very strong focus on the needs of<br />
Veterans and their families.<br />
Private Hospital - April 2008<br />
John Flynn Private Hospital on Queensland’s<br />
Gold Coast will once again hold their Anzac<br />
Day service conducted by the hospital’s<br />
Chaplains.<br />
Baringa Private Hospital has a Remembrance<br />
Garden in the courtyard of their hospital and<br />
holds a small service for patients on Anzac Day<br />
at 9am every year.<br />
Donvale Rehabilitation Hospital will have its<br />
annual Anzac Day ceremony with the local<br />
Doncaster RSL on Monday 21 April 2008 at<br />
10.30am. This will be the 10th service with the<br />
local RSL, since we had a flagpole and plaque<br />
erected in the hospital grounds in 1999.
Greenslopes: Providing for the Veteran Community<br />
Since taking over Greenslopes Hospital in 1995, Ramsay Health Care has<br />
enjoyed providing the veteran community with great private health care.<br />
There have been a great number of changes in that time including the<br />
significant expansion and upgrade of the facilities and services. The hospital<br />
has committed to ensuring it continues to provide excellent services to the<br />
veteran community as well as grow to become Queensland’s finest and most<br />
comprehensive private hospital.<br />
In July 2006, Greenslopes Private Hospital’s<br />
exclusive contract with the Department of<br />
Veterans’ Affairs ended and the veteran market<br />
was opened up to other private hospitals.<br />
Greenslopes Private Hospital Chief Executive<br />
Officer, Associate Professor Jill Watts said that<br />
through this change, GPS has continued to<br />
position itself as the number one choice for<br />
veterans and war widows in Queensland.<br />
“We have enjoyed providing the veteran<br />
community with first class health care for more<br />
than 60 years and we are committed to doing<br />
so well into the future,” Assoc Prof Watts said.<br />
“We continue to welcome feedback from our<br />
patients on how we can improve our service.<br />
This helps us to implement new initiatives and<br />
work harder to ensure we are meeting the<br />
needs of both veterans and private patients.”<br />
The hospital has always invested in ensuring its<br />
facilities and services are second to none and<br />
that we have grown to be Australia’s largest<br />
private hospital.<br />
In 2005 The Gallipoli Research Foundation was<br />
established at Greenslopes Private Hospital<br />
and will endure as a tribute to the Australian<br />
veteran community. The Foundation’s vision<br />
Private Hospital - April 2008<br />
Feature: Veteran Community<br />
is to become an internationally renowned<br />
centre of excellence in health and medical<br />
research, improving future health standards<br />
for the Australian community. In doing so, the<br />
Foundation will provide a lasting legacy to<br />
the veteran and war widow community, and<br />
the wider Australian community. The Gallipoli<br />
Research Foundation continues to receive<br />
outstanding support from the veteran and war<br />
widow community, and the wider community.<br />
By Frances McChlery, Marketing Manager,<br />
Greenslopes<br />
13
14<br />
Feature: Veteran Community<br />
Department of Veterans’ Affairs and Private Hospitals:<br />
Working Together for the Benefit of Veterans<br />
The Department of Veterans’ Affairs (DVA) work closely with most APHA<br />
member hospitals and have developed good partnerships in order to provide<br />
the level of care veterans’ need. There are a number of recent initiatives by<br />
DVA that all contracted hospitals should be aware. DVA have provided Private<br />
Hospital with information on these programs.<br />
The Enhanced Discharge Planning<br />
Initiative<br />
The Department of Veterans’ Affairs (DVA) aims<br />
to work with providers so that veterans receive<br />
quality health care and support services that<br />
will assist them to maintain their independence<br />
and remain living at home. It is recognised<br />
that an admission to hospital, particularly for<br />
the aged and frail, can have an adverse effect<br />
on overall health and wellbeing, from effects<br />
such as delirium, de-conditioning, loss of<br />
confidence, increased risk of falls and possible<br />
premature entry into residential aged care.<br />
A fundamental aspect of DVA’s contractual<br />
arrangements for the provision of hospital<br />
services is effective discharge planning in<br />
accordance with best practice. DVA has<br />
however recognised that some members of the<br />
ageing veteran population require additional<br />
support following discharge from hospital to<br />
ensure that there is a seamless transfer of care<br />
from the hospital to community setting.<br />
The Enhanced Discharge Planning Initiative<br />
is designed to facilitate this by providing for<br />
services over and above the standard discharge<br />
planning requirements contained in the Tier 1<br />
Services Agreements. The service will involve<br />
the hospital supporting the transfer of care<br />
back to community based services in the two<br />
week period post discharge, and in particular,<br />
strengthening communication with General<br />
Practitioners (GPs).<br />
The initiative is targeted at those veterans<br />
with complex health care needs, in particular<br />
those with chronic medical conditions, who on<br />
discharge from hospital are at risk of adverse<br />
health outcomes which might result in an<br />
unplanned or preventable re-admission. It is<br />
expected that in addition to chronic medical<br />
conditions, those at most risk would also have<br />
a combination of the following:<br />
• Previous pattern of unplanned re-admissions<br />
to hospital;<br />
• Loss of functionality, mobility problems, risk<br />
of falls;<br />
• Complex medications or a change in<br />
medication regime;<br />
• Live alone or with a carer unable to provide<br />
the care needed post discharge;<br />
• Advanced age together with multiple<br />
co-morbidities;<br />
• Risk of poor nutrition post discharge; and<br />
• Other risk factors identified during the<br />
episode of care.<br />
The Enhanced Discharge Planning service is<br />
only intended to be provided to those veterans<br />
most at risk following identification of that risk<br />
during their hospitalisation. Accordingly, there<br />
are a number of categories of patients that<br />
DVA would not expect to be targeted, such as<br />
same day or short stay patients; those being<br />
discharged to residential aged care; or where<br />
the standard discharge plan can be effected<br />
without additional intervention by the hospital.<br />
Tier 1 Private Hospitals are encouraged to<br />
establish Enhanced Discharge Planning services<br />
for their high risk veteran patients. Services<br />
commenced at some hospitals from 1 October<br />
2007 and continue to be rolled out nationally.<br />
Should your hospital wish to find out more<br />
about this initiative please contact your DVA<br />
Contract Manager for further information.<br />
Transportation Issues in Discharge<br />
Planning<br />
One aspect of discharge planning that often<br />
can be neglected is transport for the veteran<br />
upon discharge. This is an important element<br />
in ensuring that the discharge from hospital is<br />
made as effective and painless as possible, and<br />
is one that can seriously impact upon the DVA<br />
patient’s wellbeing and overall impression of<br />
the hospital.<br />
There have been cases where patients have<br />
been discharged without due recognition of<br />
their clinical needs for travel, and also where<br />
they have been discharged in inappropriate<br />
clothing, for instance in their night attire.<br />
This is clearly not an acceptable standard of<br />
dress on discharge. In a recent instance a war<br />
widow was discharged in her dressing gown<br />
Private Hospital - April 2008<br />
and, as well, was left by the driver at an airport<br />
to fend for themselves, with no assistance,<br />
thus compounding the problem. While these<br />
incidents are the exception, they often generate<br />
adverse exposure for the facility (by the patient<br />
or their family) which must then be rectified.<br />
Discharge planners and other staff at hospitals<br />
are reminded of the need to ensure that all<br />
aspects of discharge are managed well, not<br />
just the clinical treatment. If hospital staff have<br />
any questions regarding transport they should<br />
contact Veterans’ Transport Services on<br />
1300 550 455 or their DVA contract manager.<br />
Discharge Planning Seminars<br />
The DVA Provider Partnering (PP) team is<br />
coordinating a series of seminars nationally<br />
for Veteran Liaison Officers (VLOs) and private<br />
and public hospital staff involved in discharge<br />
planning for the veteran community. The first<br />
seminar organised by PP was held in Sydney<br />
in August 2007, and since then two other<br />
successful days have been held.<br />
Brisbane Seminar<br />
The Brisbane seminar in this series which<br />
featured information about the range of DVA<br />
services available to veterans post-discharge<br />
and how to access them, was held at the Sebel<br />
and Citigate Hotel in Brisbane on 13 December<br />
2007. As with previous seminars held it was<br />
well supported, with participants coming from<br />
29 private and 13 public, metropolitan and<br />
regional hospitals.<br />
Adelaide Seminar<br />
The most recent discharge planning seminar<br />
was held at the Mecure Grosvenor Hotel in<br />
Adelaide on 6 March 2008. This seminar also<br />
attracted an excellent number of participants,<br />
including a large contingent from rural and<br />
remote locations which was pleasing to see<br />
given that many travelled long distances to<br />
attend. In Adelaide, the majority of participants<br />
(50) worked in public hospitals, while 30 came<br />
from private hospitals.
Seminar Programs<br />
Both seminars featured presentations on a<br />
range of DVA primary and community health<br />
care services including:<br />
• Medical and Allied Health Services;<br />
• Veterans’ Home Care;<br />
• Community Nursing;<br />
• Veterans’ Transport Services;<br />
• Rehabilitation Appliances Program;<br />
• Medication Management; and<br />
• Veterans’ and Veterans’ Families Counselling<br />
Service.<br />
In Brisbane: DVA was pleased to welcome as a<br />
presenter, Ms Valerie Howells from St Andrews<br />
War Memorial Hospital, Brisbane who delivered<br />
a presentation on the discharge planning<br />
model used at St Andrews.<br />
An addition to the Brisbane program was<br />
an interactive session focussing on the roles<br />
of general practitioners and community<br />
nurses in the discharge planning process and<br />
highlighting the importance of hospital staff<br />
sending a discharge summary to the veteran’s<br />
local medical officer and referring doctor. The<br />
DVA Health Medical and Community Nursing<br />
Advisers facilitated this session.<br />
In Adelaide: Ms Stella Goodall from Noarlunga<br />
Health Services delivered a presentation on<br />
the discharge planning model and associated<br />
services used at Noarlunga. As with previous<br />
seminars, DVA is pleased that hospitals and<br />
their staff are willing to be involved in these<br />
seminars to share their discharge planning<br />
models with their peers.<br />
In addition, the Adelaide seminar featured<br />
details on DVA mental health initiatives,<br />
while the final session was also an interactive<br />
session facilitated by a DVA staff member.<br />
At this session, participants were presented<br />
with a scenario and asked to provide their<br />
ideas on the possible issues that needed to<br />
be addressed before and during the discharge<br />
process for a veteran patient.<br />
“ A fundamental aspect of DVA’s contractual arrangements for the<br />
provision of hospital services is effective discharge planning in<br />
accordance with best practice.”<br />
Take home information<br />
A printed program booklet was given to all<br />
participants at each seminar to keep as a<br />
reference tool along with other useful resources<br />
including a handy Discharge Planning Checklist.<br />
Feedback<br />
Forum participants from both Brisbane and<br />
Adelaide provided positive feedback including<br />
comments that they would use the program<br />
booklet as an education tool at their facility<br />
and that, prior to the seminar, they had been<br />
unaware of some DVA services available to<br />
veterans. Participants also made suggestions for<br />
improvement and these are being incorporated<br />
into future seminars.<br />
Future Seminars<br />
The next seminar is scheduled for Perth in<br />
August and invitations will be sent to hospitals<br />
in Western Australia closer to that date. From<br />
the responses received to date to this seminar<br />
again looks like being well attended. A further<br />
seminar is planned for Hobart later this year<br />
(tentatively scheduled for November) and the<br />
PP team will be advising all hospitals in this<br />
state of details as they are known. We look<br />
forward to seeing you at one of these seminars.<br />
If you have any questions about the discharge<br />
planning seminars please contact the team at:<br />
providerpartnering@dva.gov.au.<br />
Quality Reports<br />
Hospitals involved in veteran partnering<br />
arrangements are required to submit sixmonthly<br />
Quality Reports to the Department of<br />
Veterans’ Affairs (DVA). These reports provide<br />
the Department with valuable information<br />
on hospital benchmarking, new activities and<br />
initiatives, veteran concerns, and emerging<br />
trends in the treatment of veteran patients.<br />
Requirements for Quality Reporting are detailed<br />
in the Hospital Services Agreements, under<br />
Clause 11.5. Reports for each six monthly<br />
period are to be submitted to the Department<br />
Private Hospital - April 2008<br />
Feature: Veteran Community<br />
within 90 business days of the end of the<br />
period. e.g. the January-June report is to be<br />
submitted 90 business days after 30 June.<br />
15<br />
Hospitals should take particular note of Clause<br />
11.5.2(b) concerning the inclusion of veteran<br />
complaints in Quality Reports, and Clause<br />
16.9.1, regarding the development of<br />
a complaints handling mechanism for Entitled<br />
Persons. The provision of this information is<br />
vital in allowing DVA to assist in addressing<br />
veteran concerns.<br />
Quality Reporting templates are available<br />
on the Hospital Resources page of the DVA<br />
website. Where information is provided via<br />
ACHS comparative reports, the template<br />
may be customised to avoid duplicating<br />
information.<br />
www.dva.gov.au/health/hospital/resources.htm<br />
Any queries in relation to Quality Reporting should<br />
be directed to your DVA contract manager.<br />
Medications for Veterans in<br />
Private Hospitals<br />
The Department of Veterans’ Affairs (DVA)<br />
funds the majority of medication required for<br />
veteran patients attending private hospitals<br />
through the Repatriation Pharmaceutical<br />
Benefits Scheme (RPBS). The only medication<br />
not funded through the RPBS is that provided<br />
on an ‘imprest’ or similar basis as detailed in the<br />
contractual arrangements.<br />
The RPBS is a flexible pharmaceutical benefits<br />
scheme ensuring that optimal pharmaceutical<br />
treatment is delivered to veterans particularly<br />
those needing treatment in hospital.<br />
It is recognised that hospital medication<br />
treatment can be significantly different from<br />
the usual treatment needed in the community<br />
setting. The RPBS has the ability to approve<br />
a range of non-PBS listed medications, when<br />
clinically appropriate, through the prior<br />
approval process.
16<br />
Feature: Veteran Community<br />
The Veterans’ Affairs Pharmaceutical Advisory<br />
Centre (VAPAC) provides expert pharmacy<br />
advice as well as a prior approval process on a<br />
24/7 basis. Pharmacists answer all calls and can<br />
quickly provide necessary funding approval to<br />
prescribers who call. In addition information on<br />
veteran’s eligibility and treatment card types<br />
can also be provided.<br />
Pharmacists who service private hospitals<br />
are invited to call VAPAC to clarify any issues<br />
regarding RPBS authority prescriptions,<br />
patient entitlements and other pharmacy<br />
related matters.<br />
VAPAC’s phone number is 1800 552 580.<br />
Introduction of a Item Number M153<br />
A new item number, M153, has been<br />
introduced to improve the claiming process<br />
for surgically implanted prostheses items not<br />
listed on the Department of Health and Ageing<br />
(DoHA) Prostheses Schedule.<br />
The use of prosthetic items that have not yet<br />
been considered for listing by the Prostheses<br />
and Devices Committee still requires prior<br />
financial authorisation from the Department<br />
of Veterans’ Affairs (DVA) and this process has<br />
not changed.<br />
Where case-by-case approval has been given<br />
by DVA for a non-listed prosthesis, claims for<br />
payment at invoice cost should now be made<br />
using item number M153. A supply charge is<br />
not payable for non-listed prostheses.<br />
While copies of supplier invoices are not<br />
required, DVA does reserve the right to view<br />
relevant invoices as part of our post-payment<br />
monitoring regime.<br />
Online In Hospital Claiming (IHC)<br />
for DVA<br />
Online In Hospital Claiming (IHC) was<br />
successfully implemented by the Department<br />
of Veterans’ Affairs (DVA) on 1 May 2007.<br />
IHC is an extension to Medicare Australia’s (MA)<br />
online claiming solutions, and offers a secure<br />
connection between private hospitals, MA, DVA<br />
and Private Health Funds.<br />
IHC is a result of a collaborative project<br />
between DVA, MA and Private Health Funds<br />
and enables paperless claiming for DVA private<br />
hospital providers. Private hospitals now have<br />
access to DVA, MA and health funds in one<br />
product. At this time DVA can only accept IHC<br />
claims from private hospitals.<br />
The IHC function enables private hospitals to<br />
submit electronic claims to DVA and health<br />
funds. The claims can be submitted 24 hours<br />
a day, seven days a week without the need<br />
for accompanying documentation - saving<br />
time and resulting in faster payments! (note:<br />
paperwork must be retained by hospitals for<br />
audit purposes).<br />
Participating private hospitals are now able<br />
to check the progress of their hospital claims<br />
assessments and request processing reports<br />
regarding these claims. A further feature of<br />
IHC is the ability for hospitals to automate<br />
account reconciliation through remittance<br />
advice statements which detail the payment<br />
of hospital claims. The submission of Hospital<br />
Casemix Protocol (HCP data) to DVA and health<br />
funds is also facilitated by IHC.<br />
Private hospitals may verify veterans’ details<br />
using the Online Veteran Verification function.<br />
This function checks that the veteran’s details<br />
are correct, and that the veteran is known<br />
to DVA and can be used prior to submitting<br />
claims for payment. If the veteran’s details are<br />
incorrect providers should correct the details<br />
before submitting claims. This process only<br />
verifies that the veteran is known to DVA.<br />
Hospitals will still be required to ensure the<br />
veteran has appropriate eligibility and seek<br />
prior financial approval where required.<br />
Further information is available from the<br />
Medicare Australia eBusiness Service Centre<br />
on 1800 700 199 or visit Medicare Australia’s<br />
website:<br />
http://www.medicareaustralia.gov.au/<br />
providers/online_initiatives/index.shtml<br />
HCP Data Reminder<br />
Submission of HCP Data to DVA<br />
In accordance with Clause 10.6.1 of your<br />
hospital’s arrangements with the Department<br />
of Veterans’ Affairs (DVA), Hospital Casemix<br />
Protocol (HCP) data must be submitted on<br />
a monthly basis. Data should be submitted<br />
via secure file transfer before the end of the<br />
following month e.g.: March 2008 data by the<br />
end of April 2008 etc.<br />
Help for HCP data queries<br />
Queries related to HCP data processes can<br />
be sent to the following email addresses, but<br />
keep in mind these are not to be used for<br />
submission of data:<br />
Victoria<br />
Western Australia<br />
Tasmania PDataSth@dva.gov.au<br />
South Australia<br />
Northern Territory<br />
Private Hospital - April 2008<br />
New South Wales<br />
Queensland HCPDataNth@dva.gov.au<br />
Australian Capital Territory<br />
You can continue to contact DVA by phone on<br />
1300 131 945.<br />
New National Phone Number for<br />
Providers<br />
The Department of Veterans’ Affairs (DVA) has<br />
introduced a new national 1300 telephone<br />
number for health providers from 1 November<br />
2007. A corresponding Freecall 1800 telephone<br />
number was introduced for health providers in<br />
regional areas.<br />
The new number for provider enquiries is:<br />
Metro callers: 1300 550 457<br />
Non-metro callers: 1800 550 457<br />
When dialling the provider-specific telephone<br />
number, providers will be presented with a<br />
number of automated voice prompts. Providers<br />
will respond to the prompts by using the<br />
numbers on their telephone keypad. Once<br />
their enquiry type has been selected from<br />
the available options, providers will then be<br />
directed to the DVA staff member who has<br />
the knowledge and skills to handle that<br />
particular enquiry.<br />
The general enquiries number of 133 254<br />
should only be used by veterans calling DVA<br />
- all health care providers should use the new<br />
numbers 1300 550 457 or 1800 550 457.<br />
PHacts<br />
The Department of Veterans’ Affairs has recently<br />
developed a newsletter, PHacts, to inform<br />
private hospitals of topical information, and<br />
address common issues that many hospitals<br />
may encounter. The first edition came out in<br />
October 2007, and is produced by the Provider<br />
Partnering section within Primary Health in<br />
DVA. The newsletter is a quarterly production,<br />
with expected distribution dates being late<br />
March, late July and late November each year.<br />
The newsletter is sent electronically to all<br />
private hospitals, either individually or to the<br />
relevant corporate group for the attention<br />
of the CEO or Contract Manager but is also<br />
available on the DVA website at:<br />
http://www.dva.gov.au/health/hospital/index.htm<br />
Hard copies are also distributed to delegates<br />
attending APHA conferences, and to interested<br />
participants at discharge planning seminars<br />
coordinated by DVA.
A Focus on Veterans – It’s All in the Family<br />
When Anna Shepherd’s grandfather left Australian shores for World War I, it is<br />
certain he never thought that his actions would have such a profound effect on<br />
his granddaughter years later.<br />
Anna leads Regal Health Services, a home<br />
health service in Sydney that cares for many<br />
whose lives have been altered by war. Anna’s<br />
mother, Patricia R Shepherd established Regal<br />
Health Services in 1966 after training and<br />
practising as a RN at Concord Repatriation<br />
Hospital for many years. She had two goals:<br />
firstly a commitment to the highest standard<br />
of care for patients who have the right to live<br />
with dignity, quality of life and independence<br />
in their own home and to provide a service<br />
that supports Community Nurses by providing<br />
a workplace that respects their need to be<br />
recognised and supported to provide the<br />
best care.<br />
Regal Health continues today as a service<br />
to veterans and others in the community.<br />
“As the grand daughter of a soldier who<br />
served in both World War I and World War II I<br />
feel privileged to lead a home health service<br />
that cares for so many whose lives have been<br />
impacted by war,” says Anna. “I had three uncles<br />
who served in World War II who have shared<br />
with me their many experiences of war and<br />
wisdoms passed down through generations.<br />
I am grateful for the many sacrifices our war<br />
veterans have made that allow us our freedom<br />
today.”<br />
Anna says, “Supported by a committed team,<br />
I aim to ensure that Regal Health Services is<br />
acknowledged as a service of excellence in<br />
home healthcare throughout Australia for the<br />
benefit of our clients. I believe that a team<br />
that is comprised of like minded professionals<br />
produces excellent results in terms of service<br />
delivery and job satisfaction. My aim is to<br />
do whatever it takes to acknowledge and<br />
support my team empowering them to achieve<br />
excellence for the benefit of our patients.”<br />
To that end, Anna has established an award<br />
in her mother’s name for community nursing.<br />
The Patricia R. Shepherd award for community<br />
nursing is an annual award granted to a<br />
community nurse who is nominated by peers,<br />
patients and the management staff.<br />
As a leader Regal Health also provides two<br />
scholarships that are open to all Community<br />
Nurses across all sectors each year. The first is<br />
for wound management in community nursing<br />
and provides the winner a $2,000 scholarship<br />
towards education, research and/or conference<br />
participation for wound management. The<br />
second award allows the winning community<br />
nurse to attend and present an abstract at<br />
the biennial Joanna Briggs Colloquium and<br />
International Nursing Conference which in<br />
2008 will be held in Cordoba, Spain.<br />
The investment in her staff pays off, insists<br />
Anna. “We were the first private nursing service<br />
in Australia to achieve ACHS accreditation in<br />
1994. And of course, we have excellent clinical<br />
outcomes. We achieve higher than the DVA’s<br />
benchmarks for wound healing.”<br />
Veterans’ Health to be Examined<br />
The Centre for Military and Veterans’ Health<br />
(CMVH) has been contracted by the Australian<br />
Defence Force to conduct a survey into the<br />
health of ADF personnel who have deployed<br />
on operations. They will compare the health<br />
of those deployed to East Timor and/or<br />
Bougainville with the health of those who<br />
did not deploy to these locations. More than<br />
12,000 Defence personnel are being invited to<br />
take part.<br />
The study will contribute to increasing the<br />
knowledge about Service-related health<br />
and ill health. It may also assist the ADF in<br />
developing the most appropriate supportive<br />
and protective measures against future<br />
health threats.<br />
Private Hospital - April 2008<br />
Feature: Veteran Community<br />
17<br />
“ As the grand daughter of a<br />
soldier who served in both<br />
World War I and World War II<br />
I feel privileged to lead a home<br />
health service that cares for<br />
so many whose lives have<br />
been impacted by war,” says<br />
Anna. “I had three uncles who<br />
served in World War II who<br />
have shared with me their<br />
many experiences of war and<br />
wisdoms passed down through<br />
generations. I am grateful for<br />
the many sacrifices our war<br />
veterans have made that allow<br />
us our freedom today.”<br />
CMVH is a University of Queensland led<br />
consortia, with University of Adelaide and the<br />
Charles Darwin University, supported by the<br />
Department of Defence and the Department<br />
of Veterans’ Affairs, as an Australian<br />
Government initiative.<br />
More information about the study is available<br />
at www.uq.edu.au/dhsp.
18<br />
as it see it... with Michael Roff<br />
If you are really sick, go to a Private Hospital…<br />
This issue of Private Hospital is part of APHA’s contribution to the celebration<br />
of the 90th year of the Australian repatriation system.<br />
Private hospitals have for many years been<br />
working in partnership with Department of<br />
Veterans Affairs (DVA) providing high quality<br />
hospital services for the veteran community.<br />
There is no doubt that many of these are<br />
the oldest and sickest patients, once again<br />
deflating the myth that “if you are really sick,<br />
you go to a public hospital.”<br />
Of course, veterans are also treated in the<br />
public hospital sector. However, the latest<br />
figures available from the Australian Institute<br />
for Health and Welfare indicate that 186,000<br />
DVA patients are treated annually in private<br />
hospitals, compared to just 135,000 in the<br />
(much larger) public hospital system.<br />
This poses two questions; firstly, why would the<br />
private hospital contribution to the provision<br />
of care to veterans be much higher than public<br />
hospitals, and secondly, are there any lessons<br />
from the DVA experience that could be applied<br />
more broadly to the provision of hospital<br />
services?<br />
In answer to the first question, a large part of<br />
the reason could be related to relative cost.<br />
That is, DVA negotiates with State Governments<br />
for veterans to be treated in public hospitals on<br />
a cost-recovery basis with the Commonwealth<br />
picking up 100% of the cost. In private<br />
hospitals, DVA undertakes a national tender<br />
for services. So how do the outcomes of these<br />
processes compare?<br />
According to evidence given by DVA to a<br />
parliamentary committee in 2006;<br />
“the work we have done basically suggests that<br />
we pay significantly lower prices in the private<br />
sector than we do in the public sector.”<br />
And, when talking about the negotiated<br />
arrangements with private hospitals;<br />
“The premise when we first went into those<br />
arrangements was that we had to be able to<br />
demonstrate that they were lower than the cost<br />
of the equivalent services in the public sector. We<br />
can certainly do that.”<br />
DVA subsequently confirmed the cost<br />
differential between public and private<br />
hospitals could be up to 20%.<br />
So the demonstrated efficiency of the private<br />
sector is a major reason the majority of<br />
veterans are treated in private hospitals. But<br />
what does this mean for the rest of the hospital<br />
system beyond just treating veterans?<br />
The Commonwealth Government has been<br />
trumpeting its injection of funding to “blitz”<br />
elective surgery waiting lists. Indeed, $150<br />
million has been allocated across the states<br />
in 2008 to treat additional patients. When this<br />
policy was announced during the election<br />
campaign, we were told that States would be<br />
encouraged to use this funding to contract<br />
with private hospitals because the ALP<br />
believed the capacity of the private sector<br />
should be harnessed.<br />
Well there can’t have been too much<br />
encouragement. Victoria recently announced<br />
how it was dividing up an instalment of $27.11<br />
million provided under that program. Of this<br />
amount, only $1.58 million is being spent on a<br />
“Private Patient Initiative” to treat 470 patients.<br />
It is interesting to note that, on the figures<br />
released, the average cost per additional<br />
elective surgery patient to be treated in<br />
Victorian public hospitals is $4783. This<br />
compares with the Victorian cost per casemix<br />
adjusted separation (including depreciation) of<br />
$3785. The average cost per patient treated in<br />
a private hospital under this scheme is $3361.<br />
Looking at these numbers, I could make the<br />
bold assertion that private hospitals in Victoria<br />
are 30% more efficient than their public<br />
counterparts and the Government could have<br />
saved $7 million if it contracted all of this<br />
elective surgery work to the private sector.<br />
Of course, I can’t do this because we don’t<br />
know what procedures are being performed<br />
so we can’t make a valid comparison.<br />
And although the States have agreed to a<br />
performance reporting framework imposed by<br />
the Commonwealth in return for the funding,<br />
there will be no requirement to report on types<br />
of procedures undertaken so cost comparisons<br />
can be made across states or between sectors<br />
– so much for transparency.<br />
Which brings me to another point. We have<br />
just seen the annual gnashing of teeth from<br />
the usual suspects, including the States, in<br />
relation to health fund premium increases<br />
which averaged 4.99% this year. Once again,<br />
Private Hospital - April 2008<br />
“ The real question for private<br />
hospitals, health funds, the<br />
public system, governments<br />
and patients, is how long can<br />
we sustain the current system<br />
before something cracks?”<br />
this is cited as evidence that “the 30% rebate<br />
is not working” and “costs are out of control” in<br />
the private sector.<br />
Let’s look at the facts which highlight a<br />
breathtaking case of double standards. In the<br />
2003-2008 Australian Health Care Agreement,<br />
the States were guaranteed indexation over the<br />
previous agreement of 17% in real terms. That<br />
is, over the five-year period they would receive<br />
funding increases to run public hospitals of<br />
17% over and above the rate of inflation!<br />
This means they have received increased<br />
funding of 31.1% over the course of the<br />
agreement. And we hear claims, becoming<br />
more strident each day, that this amount is<br />
simply not enough to cover the increased cost<br />
of providing hospital services.<br />
Over the same period, health fund premiums<br />
have increased 30.6% - and this supposedly<br />
means costs are out of control!<br />
But of course the increases in health fund<br />
premiums do not flow through in full to private<br />
hospitals. Perhaps this is an indication that<br />
neither state governments nor health insurers<br />
are particularly good judges of the level of<br />
cost increases being experienced by private<br />
hospitals at the coalface of care delivery.<br />
So for now, let’s forget about arguments over<br />
which sector is more efficient or is better able<br />
to control rapidly rising costs (and we can<br />
because the facts speak for themselves). The<br />
real question for private hospitals, health funds,<br />
the public system, governments and patients,<br />
is how long can we sustain the current system<br />
before something cracks?
20<br />
Sydney Convention & Exhibition Centre, 13 – 15 May 2008<br />
<strong>INNOV<strong>AT</strong>I<strong>ON</strong></strong> & <strong>TECHNOLOGY</strong> <strong>ON</strong> <strong>SHOW</strong> <strong>AT</strong><br />
<strong>HOSPIMedica</strong> AUSTRALIA<br />
With <strong>HOSPIMedica</strong> AUSTRALIA 2008<br />
just around the corner, hospital and<br />
healthcare professionals from all<br />
over Australia and New Zealand are<br />
planning their trips to Sydney!<br />
<strong>HOSPIMedica</strong> AUSTRALIA will be the<br />
ultimate destination for those wishing to<br />
explore the most comprehensive showcase of<br />
technology, equipment, products and services<br />
for the hospital, diagnostic, pharmaceutical,<br />
medical and rehabilitation industries ever<br />
staged in Australia.<br />
There’s no conference or workshop here - just<br />
an unrivaled opportunity to take a look at the<br />
1000’s of products and equipment on show<br />
from over 190 exhibitors, representing some<br />
16 countries - 60 of which have never<br />
exhibited in Australia before!<br />
The event, to be held over three days, offers<br />
a long awaited chance for the trade visitors<br />
to get close to the cutting edge of medical<br />
innovation, from simple products to high-tech<br />
systems, all under one roof.<br />
Not to be missed exhibits include the NEW<br />
Teletom range of power booms – part<br />
of Berchtold’s new Supersuite Custom<br />
Surgical Environments Solutions. Developed<br />
via extensive consultation with surgeons,<br />
operating theatre nurses, biomedical<br />
engineers and many other parties involved<br />
with the theatre preparation and set up,<br />
you’ll be amazed at its ease of operation<br />
in theatre.<br />
Internationally successful EBOS Group will<br />
be launching the NEW VORTEX Macerator<br />
and as the newly appointed Australian agent<br />
for Eschmann, they’ll have a range of their<br />
world-renown operating tables on show.<br />
Siemens will showcase the latest technology<br />
in diagnostic imaging and medical laboratory<br />
systems, whilst Gallay will present all their key<br />
products and feature an endoscope drying<br />
cabinet that’s fresh to the market.<br />
Also look out for the new Patented Model<br />
Nursing Bed from MAXI-CARE - this new<br />
model lifts up and down in a straight<br />
motion which means easier transfers. And<br />
you shouldn’t miss the latest in Biomedical<br />
Equipment from newcomer Nison either.<br />
Visitors will also see exciting displays from the<br />
likes of Gubbemed International, Invacare,<br />
Lumenis, Meiko, Miele Professional, Philips<br />
Medical Systems, Tuta Health, Unique Care,<br />
Visiomed Group, Welch Allyn, AIS Healthcare,<br />
Austco, Bioclone, Bremed, Caraleen, Stern,<br />
C&A Scientific, DB Health and others.<br />
From the big stuff such as the latest DHS<br />
Emergency power-lift stretchers and<br />
loading system to the small including the<br />
all-new Clearview Laryngeal Mask from<br />
Ultimate, <strong>HOSPIMedica</strong> AUSTRALIA will have<br />
something for everyone.<br />
And you’ll save money with over<br />
18 specialised medical consumable<br />
manufacturers and suppliers competing for<br />
your business!<br />
The website, www.hospimedica-australia.com<br />
features a comprehensive preview of exhibit<br />
content that is being updated daily.<br />
A large number of international exhibitors<br />
are also utilising their involvement in the<br />
event to source local distributors and this too<br />
is indicated in listings where applicable.<br />
It just doesn’t get any better than this.<br />
All under one roof, for three days, but only<br />
every two years!<br />
<strong>HOSPIMedica</strong> AUSTRALIA is part of the ‘med by series’ of medical<br />
trade fairs organised throughout the world, including MEDICA,<br />
the world’s largest medical trade fair held annually in Germany.<br />
Private Hospital - April 2008<br />
ORGANISE YOUR FREE TRADE<br />
ENTRY NOW<br />
You can organise trade ID badges in<br />
advance! To gain free trade entry visit<br />
www.hospimedica-australia.com and<br />
complete the on-line trade application<br />
form or simply do it on arrival.<br />
WHERE?<br />
Hall 3, Sydney Convention &<br />
Exhibition Centre, Darling Harbour<br />
WHEN?<br />
Tuesday 13 May 2008<br />
10.00am-6.00pm<br />
Wednesday 14 May 2008<br />
10.00am - 6.00pm<br />
Thursday 15 May 2008<br />
10.00am - 6.00pm<br />
NEED TO KNOW MORE?<br />
For full details including exhibitor<br />
listing, exhibit previews, trade entry<br />
applications, special discounted travel<br />
and accommodation packages and<br />
how to get to the event, visit<br />
www.hospimedica-australia.com
Private Hospital - April 2008<br />
21
22<br />
Interview - George Toemoe<br />
Information Technology in the health sector<br />
In our first interview for 2008, Private Hospital magazine talks to George<br />
Toemoe, CEO of St. Luke’s Care in Sydney and APHA National Board member<br />
about Information Technology in the health sector.<br />
Private Hospital magazine:<br />
How do you think private hospitals generally<br />
are placed in the industry regarding their<br />
information technology systems?<br />
George Toemoe:<br />
First can I say, my focus in commenting on<br />
IT and Health Sector will be from a hospital<br />
clinical information perspective mainly as<br />
general administration systems such as<br />
admissions, billing, coding and financial<br />
information systems have been in place for<br />
over a decade and implemented in most<br />
private hospitals.<br />
Prior to joining the health care sector in 1997,<br />
I had worked in a number of other industries<br />
such as manufacturing, high technology,<br />
finance, mining, waterfront and local<br />
government.<br />
IT systems in these industries in my view were<br />
generally well in advance of systems in health<br />
care sector and particularly in the non back<br />
office applications. However this gap has<br />
significantly narrowed with the progressive<br />
implementation of clinical IT applications over<br />
recent years.<br />
PH magazine:<br />
How are advances in IT impacting on the<br />
health sector? What are the main benefits/<br />
pitfalls/obstacles?<br />
GT:<br />
IT advances in the health care sector are<br />
helping to deliver better health care and<br />
outcomes and these will only improve as<br />
implementation becomes more intensified.<br />
That is, implementations to date have been<br />
concentrated mainly in a few major health<br />
care providers and not across the board.<br />
The benefits of implementing clinical IT are:<br />
• Web, Internet and e-commerce capabilities<br />
including offsite access and clinical planning<br />
by clinicians and other authorised personnel.<br />
• Clinical pathway development and<br />
management including resource and program<br />
scheduling, orders for pharmacy, radiology,<br />
pathology and allied health tests and<br />
procedures.<br />
• Highlighting of overdue tasks including orders<br />
such as pathology and imaging.<br />
• Electronic receipt of order results including<br />
variances and adverse results.<br />
• Warnings for pharmaceutical items ordered<br />
such as drug to drug, drug to age, drug to<br />
allergy and drug to tissue.<br />
• On-line reports and graphs including those<br />
for vital signs such as temperature, blood<br />
pressure and heart beat.<br />
• On-line dictation of clinical notes.<br />
• Data entry and access at the bed side using<br />
wireless application protocols for either<br />
hand-held or trolley based computers.<br />
Private Hospital - April 2008<br />
• Applicability to nursing home and home<br />
care clients.<br />
• Interfaces to existing patient management,<br />
billing and financial software applications.<br />
• Faster coding and therefore transmission<br />
of data to health funds for reimbursement<br />
purposes and therefore improved cash flow.<br />
• Automated discharge notes once again<br />
shortening a perennial bottle neck of having<br />
to wait until busy clinicians could address this<br />
task which is a necessary prelude to coding.<br />
• Multiple user access to records by approved<br />
users rather than one user at a time which is<br />
the case with paper records.
• Improved efficiency as opposed to the<br />
perennial “in transit or lost paper record”.<br />
• Further improved efficiency for clinical staff<br />
in having information available at their finger<br />
tips rather than having to go looking for<br />
information eg pathology results, clinical<br />
records. A survey sometime ago indicated<br />
that a nurse on average walked 14 kms per<br />
shift, a great deal of which was looking for<br />
records and results.<br />
• Further quality of care improvement and<br />
increased clinician and nursing availability<br />
and care with administrative and manual tasks<br />
being computerised.<br />
These benefits result not only in cost savings<br />
but higher quality of care due to significantly<br />
reduced risks of missing clinical pathways<br />
items and also proving more time to that<br />
scarce resource called nursing and<br />
providing care.<br />
The main pitfalls, which can be minimised by<br />
good planning and resource allocation are:<br />
• An under estimation of the time required for<br />
training and implementation.<br />
• An under estimation of the cost involved and<br />
the resources required.<br />
• The non identification of a champion to<br />
deliver the systems.<br />
• Fear by those that do not have good<br />
computing skills and particularly<br />
contemporary ‘point and click’ skills.<br />
• Not supported by senior management.<br />
• Insufficient review of the different solutions<br />
available including user review and testing<br />
and therefore the potential selection of the<br />
wrong solution.<br />
• Inflexibility of the selected solution to be<br />
adapted to existing and preferred work<br />
pattens.<br />
• Insufficient resolution hardware (ie quality<br />
of screen images)<br />
• Insufficient hardware capacity and speed.<br />
The obstacles tend to be:<br />
• A complete misconstruing of the privacy<br />
argument.<br />
• Workforce experience and age.<br />
• The need to allocate some existing<br />
operational resources to project<br />
implementation and the general aversion<br />
of some operational managers to such<br />
a concept.<br />
• The considered non-necessity to use such<br />
systems for simple and short term/day only<br />
type procedures.<br />
PH Magazine:<br />
How is IT helping to streamline processes<br />
in hospital administration?<br />
GT:<br />
This has generally been answered in the<br />
previous point of which examples are discharge<br />
note automation, procedure coding, health<br />
fund data transmission, faster cash receipts<br />
reduced nursing diversions on matters such<br />
as looking for records and results, elimination<br />
of lost and in transit records, multiple user<br />
access and most importantly significantly<br />
improved quality and risk management.<br />
PH Magazine:<br />
Are paper-based systems becoming obsolete?<br />
GT:<br />
Yes except for mainly medico legal reasons or<br />
where hardware resolution insufficient.<br />
The implementation of clinical IT is similar to<br />
experiences in local government where paper<br />
documents and records such as development<br />
applications are now electronically and<br />
simultaneously handled by a number of staff<br />
eg town planners, health and building<br />
surveyors, engineers.<br />
PH Magazine:<br />
How are advances in IT impacting on risk<br />
management?<br />
GT:<br />
In summary, errors and omissions are<br />
significantly reduced and/or eliminated by<br />
the “poor human brain” which is essentially a<br />
computer itself by not being overloaded with<br />
trying to remember tasks carried out, tasks<br />
required and results and prioritisation of these.<br />
Implementation of clinical IT by improving<br />
quality and risk management will also have<br />
Private Hospital - April 2008<br />
Interview - George Toemoe<br />
a positive impact on relevant insurance<br />
premiums such as medical malpractice<br />
insurance.<br />
But most importantly much better patient<br />
care and outcomes.<br />
PH Magazine:<br />
Are advances it IT allowing for more<br />
in-home care?<br />
23<br />
GT:<br />
Yes to the extent that access to clinical<br />
pathways, records, results and the on-line<br />
updating of records and results can be carried<br />
out remotely. Resource management can<br />
also be improved and in St Luke’s case simple<br />
care manager type software has provided<br />
significantly improved community homecare.<br />
PH Magazine:<br />
Is there a resistance to change amongst health<br />
care professionals?<br />
GT:<br />
Yes but only generally to a fairly minor extent.<br />
The reasons in question are:<br />
one being privacy and flexibility of these<br />
selected systems to be adapted to existing<br />
and two, preferred work practices and the<br />
assumption that existing and preferred<br />
practices are appropriate.<br />
PH Magazine:<br />
Has re-training been a problem?<br />
GT:<br />
Yes for those who have little or no experience<br />
with computers, especially with point and click<br />
type applications. The potential complexity of<br />
such applications is much higher than with the<br />
older character based systems. Many people<br />
become quite concerned when exposed to<br />
complexity with sub-optimal time to be trained<br />
and fully understand.
24<br />
Healthcare and medical workers demand<br />
ethical workplaces<br />
In a warning sign to the country’s healthcare and medical employers, staff<br />
within their sector are the most likely to believe that good company ethics<br />
would highly improve their current workplace (31%) according to a new survey.<br />
The SEEK Satisfaction and Motivation survey<br />
also revealed that across all industry sectors,<br />
medical professionals were the most likely to<br />
hold hours of work (51%), the people they work<br />
with (45%) and the workplace environment<br />
(48%) as extremely important when looking for<br />
a new job.<br />
Commenting on the findings, SEEK Sales<br />
Director Joe Powell said:<br />
“In an industry that often has to make tough<br />
ethical decisions it’s not surprising to see that<br />
employees within the healthcare and medical<br />
sector want to work for companies that behave<br />
in an ethical way and expect their staff to do<br />
the same.”<br />
In another interesting discovery, nearly half of<br />
respondents (49%) only intend on staying with<br />
their current employer for a year or less, while<br />
18% plan to stay on for three months or less.<br />
“Healthcare and medical employers need to<br />
think about the demand for ethical workplaces<br />
and take these requirements into consideration<br />
if they hope to retain and attract staff,” he said.<br />
“The added check or difficulty that the<br />
healthcare and medical profession has is that<br />
unethical behaviour in their field often creates<br />
negative publicity that stays in the minds of<br />
potential future employees for a long time to<br />
come. It is far better to avoid these situations<br />
by creating an ethically sound workplace and a<br />
positive reputation, than try to overcome these<br />
barriers in the future,” he said.<br />
Other interesting findings for the healthcare<br />
and medical sector include:<br />
• 34% of respondents rated the ‘company<br />
reputation’ as extremely important when<br />
looking for a new job, exceeding the industry<br />
average of 27%,<br />
NPS RADAR reviews released<br />
Two new drugs are reviewed in the April edition of NPS RADAR, an<br />
independent drug bulletin from National Prescribing Service Limited (NPS).<br />
The drugs are fentanyl lozenges (Actiq), an<br />
oromucosal formulation for the control of<br />
breakthrough cancer pain, and paliperidone<br />
(Invega) for people with schizophrenia.<br />
Both drugs became available on the PBS from<br />
1 April 2008.<br />
NPS RADAR notes that fentanyl lozenges are<br />
only to be used by people who are stabilised<br />
on regular opioid therapy for their underlying<br />
persistent cancer pain. Fentanyl lozenges may<br />
be prescribed on the PBS when escalating<br />
doses of morphine for the control<br />
of breakthrough pain causes intolerable<br />
adverse effects.<br />
NPS CEO Dr Lynn Weekes asked doctors and<br />
pharmacists to be aware of three important<br />
safety issues with the use of fentanyl lozenges.<br />
• Do not use fentanyl lozenges in<br />
opioid-naïve patients, as this increases the<br />
risk of respiratory depression.<br />
• Instruct patients and carers on the correct use,<br />
storage and disposal of fentanyl lozenges to<br />
help prevent accidental or deliberate misuse.<br />
• Intact or partially used lozenges can be fatal<br />
if consumed by a child, so it’s imperative to<br />
keep them out of sight and reach of children.<br />
Any lozenge that remains on the handle<br />
needs to be dissolved under hot running<br />
water and must not be discarded whole.<br />
Paliperidone is the major active metabolite of<br />
risperidone. In its review, NPS RADAR states<br />
that the clinical response to paliperidone is<br />
Private Hospital - April 2008<br />
• The people they work with (24%), benefits<br />
and conditions (12%) and training and<br />
development opportunities (12%) are the top<br />
three things employees love about their job,<br />
• 42% of respondents are unhappy or very<br />
unhappy in their current job,<br />
• The top three hates in their current job are<br />
their stress level (25%), the lack of feedback/<br />
appreciation they receive (21%) and the<br />
quality of overall management (20%),<br />
• Openness and honesty (77%), the ability<br />
to follow up words with actions (73%) and<br />
support of their team (67%) are the most<br />
respected leadership attributes for this group.<br />
likely to be similar to risperidone, but there are<br />
no comparative data.<br />
The April print edition includes an update<br />
on the extended PBS listing for pioglitazone<br />
(Actos) in the treatment of type 2 diabetes<br />
and the review of varenicline (Champix) for<br />
smoking cessation which was published on the<br />
website www.npsradar.org.au in January.<br />
This edition also carries brief reviews of<br />
methylphenidate (Ritalin LA), a second<br />
long-acting formulation PBS listed for attention<br />
deficit hyperactivity disorder; smaller syringe<br />
volume influenza vaccine PBS listed for children<br />
aged 6–35 months; and terbinafine cream and<br />
tablets for fungal infections in Aboriginal and<br />
Torres Strait Islander peoples.
Private Hospital - April 2008<br />
25
26<br />
quality in focus...<br />
with Christine Gee<br />
Australian Commission on<br />
Safety and Quality in Health Care<br />
Christine Gee reports on current activity underway within the national<br />
safety and quality agenda that is being developed and implemented by<br />
the Australian Commission on Safety and Quality in Health Care (ACSQHC).<br />
National Measurement and Reporting<br />
of Safety and Quality Indicators<br />
At their meeting on 24 July 2007, Health<br />
Ministers agreed to “ask the Australian<br />
Commission on Safety and Quality in Health Care<br />
to develop a reporting framework for private<br />
hospitals that is comparable to the reporting<br />
framework for public hospitals, and for general<br />
practice.”<br />
Leaving aside the fact that at present there is no<br />
agreed national reporting framework for public<br />
hospitals, the ACSQHC Private Hospital Sector<br />
Committee (PHSC) has undertaken<br />
the task of identifying an appropriate suite<br />
of indicators for private hospitals to report that it<br />
can recommend to the ACSQHC. In pursuing this<br />
activity, the PHSC has sought input and advice<br />
from the APHA Safety and Quality Committee.<br />
In the box below, I have provided a visual<br />
illustration of the two-way process of providing<br />
private hospital input into the national safety<br />
and quality agenda and the implementation<br />
of this agenda nationally. At each point I have<br />
noted the quantum of private hospital expertise<br />
Australian Health Ministers’ Conference (no<br />
direct private hospital expertise)<br />
Australian Health Ministers Advisory Council<br />
(no direct private hospital expertise)<br />
Australian Commission on Safety and Quality<br />
in Health Care (1 of 10 with Private<br />
Hospital expertise)<br />
ACSQHC Private Hospital Sector Committee<br />
(5 of 9 with private hospital expertise)<br />
APHA Safety and Quality Committee (9 of 9<br />
with private hospital expertise)<br />
Private hospitals<br />
available to inform the development and<br />
implementation of the national agenda.<br />
At the invitation of the Minister for Health and<br />
Ageing, APHA Executive Director Michael Roff<br />
recently attended part of the first meeting<br />
of the new Health and Hospitals Reform<br />
Commission (H&HRC). This session related to<br />
the development of indicators for a national<br />
reporting framework. At the meeting, the H&HRC<br />
confirmed that it would look to the ACSQHC to<br />
develop the indicators for private hospitals.<br />
The H&HRC is working to a very tight deadline<br />
and therefore the development of indicators to<br />
be reported by private hospitals has necessarily<br />
been accelerated by the PHSC and the APHA<br />
Safety and Quality Committee. I will report<br />
on the development of these indicators in<br />
a future column.<br />
National Charter of Patient Rights<br />
As I have outlined in an earlier column, the<br />
work of the ACSQHC is guided by nine priority<br />
programs, one of which is the National Charter<br />
of Patient Rights. During February-March, the<br />
ACSQHC circulated a draft version of the Charter<br />
together with a Consultation paper. The APHA<br />
Safety and Quality Committee provided a<br />
submission to the ACSQHC on the Consultation<br />
paper and the draft Charter (members interested<br />
in a copy of the submission should contact Paul<br />
Mackey at APHA).<br />
One of the central concerns of the APHA Safety<br />
and Quality Committee is that in their present<br />
form, the draft Charter and Principles do not<br />
strike an appropriate balance between the<br />
roles, rights and responsibilities of patients<br />
and providers.<br />
In APHA’s view, the Charter currently omits an<br />
important aspect of a consumer’s interaction<br />
with the health system, their responsibilities,<br />
which is a significant shortcoming. APHA has<br />
recommended to the ACSQHC that the notion<br />
of Responsibilities be added to the Charter<br />
and that a separate set of Principles should be<br />
developed that articulate the responsibilities<br />
expected of health consumers. APHA believes<br />
Private Hospital - April 2008<br />
that this is an important issue as arguably health<br />
care services can only be provided safely when<br />
it is accepted by the Patient/Consumer that they<br />
have responsibilities as well as rights.<br />
While two patient responsibilities are identified<br />
in the draft Principles, these are included, almost<br />
as an afterthought, under the consumer’s right<br />
to Information. The APHA Safety and Quality<br />
Committee believes that greater clarity, for all<br />
parties, would be provided by the inclusion<br />
of a separate set of Principles around the<br />
responsibilities of consumers. These could<br />
include, for example:<br />
• To provide to the best of their knowledge and<br />
ability, accurate and complete information<br />
about past and present illness, medication,<br />
treatments, relevant family history and other<br />
matters relating to their health<br />
• To communicate whether or not they clearly<br />
comprehend the care provided<br />
• To follow the instructions about care provided<br />
by the health care provider and to report any<br />
changes in their condition in a timely manner<br />
• To acknowledge the consequences of their<br />
actions if they refuse treatment or do not follow<br />
the recommended instructions<br />
• To be considerate of the rights or other<br />
patients/consumers and health care workers<br />
• To accept and comply with a policy of zero<br />
tolerance of aggression towards staff and<br />
understand that unacceptable behaviour may<br />
delay or negate receiving treatment<br />
• To adhere to relevant legislative and facility<br />
requirements regarding the safety and security<br />
of those who use the facility<br />
• Health service users should make complaints<br />
in a respectful and honest manner and provide<br />
truthful and accurate information when making<br />
a complaint.<br />
I welcome your feedback on this column and on<br />
any matters relating to quality and safety and<br />
the Australian Commission on Safety and Quality<br />
in Health Care. I can be contacted via the APHA<br />
Secretariat – paul.mackey@apha.org.au
Private Hospital - April 2008<br />
27
Advertorial<br />
Access the latest equipment with an operating lease<br />
One of the greatest challenges to providing exceptional health care is giving health care professionals<br />
access to the most up-to-date and advanced technologies. Diagnostic and treatment equipment is<br />
continually being improved and refined, and medical staff are rightly demanding the very best tools<br />
available so they can deliver more effective health outcomes for patients. However, new technologies<br />
come at a cost, and keeping up to date is difficult even for the most rigorously run organisations.<br />
Operating leases provide a mechanism for<br />
private hospitals to always have the best and<br />
very latest equipment. An operating lease<br />
is particularly well suited to equipment that<br />
becomes relatively obsolete quickly. Continuing<br />
improvements in medical equipment means<br />
there is nearly always something better coming<br />
onto the market – devices that deliver a clearer<br />
image, a faster process or greater accuracy.<br />
So, what does a responsible hospital manager<br />
or financial controller do? Buy now and<br />
put current technology to use or wait for<br />
the next generation of equipment due out<br />
soon? An operating lease solves the dilemma<br />
– your hospital or surgery can have the<br />
latest equipment now, and when the next<br />
improvement is available, simply upgrade.<br />
Hospitals can constantly be at the leading<br />
edge without having the bother and expense<br />
of equipment ownership.<br />
As Hal Leasing’s CEO Raylee Carruthers puts it<br />
“patients benefit when hospitals use advanced<br />
technology, not when they own technology.”<br />
For most modern hospitals, there is little point<br />
in owning and being stuck with equipment<br />
that will be quickly superseded. Out of date<br />
technology is not consistent with the high<br />
standards of care and treatment that both<br />
patients and doctors have come to expect from<br />
the private hospital sector.<br />
Private hospitals generally have greater<br />
autonomy and flexibility in financial matters<br />
than their public counterparts, and so can use<br />
a greater variety of funding mechanisms to<br />
achieve their goals. Operating leases are<br />
a highly effective option for many classes<br />
of equipment.<br />
An operating lease is a rental agreement. In<br />
simple terms it works like this: you source the<br />
equipment you want, the finance company<br />
buys it, you then rent the equipment from the<br />
finance company. At the end of the term of<br />
the lease you simply return the equipment to<br />
the finance company.<br />
The greatest advantage of an operating lease<br />
is the ability to upgrade to newer equipment<br />
at any time during the rental period. But there<br />
are other significant benefits:<br />
• Payments are agreed up front and are not<br />
impacted by changing interest rates, aiding<br />
predictable cash flow<br />
• The overall cost is often less expensive<br />
than owning and disposing of purchased<br />
equipment<br />
• The entire rental payment is usually 100%<br />
tax deductible<br />
• The equipment is generally off balance sheet<br />
• An operating lease does not impact a bank<br />
line of credit<br />
• The residual risk is carried by the finance<br />
company<br />
• There is no need to arrange the sale or<br />
disposal of obsolete equipment<br />
“Not all operating leases are the same” warns<br />
Raylee Carruthers. “Buried in the detail of<br />
some agreements are special clauses designed<br />
to lock you in for additional rental periods,<br />
or clauses that penalise heavily if the original<br />
packaging or peripherals are not returned with<br />
the equipment at the end of the rental period.<br />
Be careful to read the fine print thoroughly<br />
so that you are not caught out.” Hal Leasing,<br />
a leader in this type of funding arrangement,<br />
has worked hard to develop lease agreements<br />
that are commercially sensible and expressed in<br />
plain language.<br />
Raylee also recommends asking your finance<br />
provider about a Master Rental Agreement<br />
with a pre-approved spending limit. A<br />
revolving facility like this allows you to rent<br />
equipment worth a few hundred dollars along<br />
with multi-million dollar equipment on a single<br />
agreement. Simply add additional items to the<br />
lease as the need arises without the need to<br />
reapply for finance.<br />
“An important factor to consider when<br />
choosing a supplier of an operating lease is<br />
the stability of the finance provider” suggests<br />
Hal Leasing’s Chief Financial Officer, Matthew<br />
Sykes. “You don’t want to be caught in<br />
a situation where the owner of the rental<br />
equipment, the finance company, is being<br />
pursued by creditors looking to sell all assets”.<br />
As in all transactions, some amount of due<br />
diligence is wise before committing to<br />
a contract.<br />
Operating leases offer an effective alternate<br />
source of finance to traditional sources, one<br />
that is increasingly becoming popular within<br />
many industries where technology is advancing<br />
rapidly. Rental arrangements sit alongside<br />
and complement other financing options; talk<br />
with your finance provider or adviser about<br />
designing the best funding solution for your<br />
organisation.
30<br />
Robotic surgery introduced at St John of God<br />
Hospital, Subiaco<br />
St John of God Hospital, Subiaco is the first hospital in Western Australia and<br />
within the St John of God Health Care group to offer robotic surgery.<br />
The minimally invasive da Vinci Robot is used<br />
for radical prostatectomy and other delicate<br />
surgery. The hospital’s Chief Executive Officer,<br />
Dr Shane Kelly, spear-headed the campaign to<br />
obtain a surgical robot for Western Australia.<br />
“We are extremely excited about the<br />
possibilities the da Vinci robot offers our<br />
surgeons, patients and the health care industry<br />
in general,” Dr Kelly said.<br />
Patients benefit from less post operative<br />
pain, less scarring, quicker recovery time, less<br />
blood loss and therefore lower chance of cross<br />
infection.<br />
The hospital’s urologists and gynae-oncologists<br />
will use the robot, which offers surgeons the<br />
benefit of a 10x magnified 3D view of the<br />
anatomy and removes the fine tremor of a<br />
surgeon’s hand. Large hand movements can<br />
be scaled down to miniature, fully ‘wristed’<br />
instruments allowing superior dexterity.<br />
Dr Kelly said currently one in every two radical<br />
prostatectomies in the USA is performed<br />
robotically and figures already show Australia<br />
mirroring this growth, indicating that the<br />
da Vinci prostatectomy will become the<br />
standard of care in Australia in the not so<br />
distant future.<br />
“In addition to urological procedures,<br />
the da Vinci Robot will also be available<br />
APHA Speaking Opportunities<br />
APHA has been represented at several<br />
conferences in the past few months.<br />
APHA President Christine Gee spoke at a<br />
Health Focus Forum at Minter Ellison on 15<br />
February 2008. The Forum brought together<br />
Minter Ellison partners, special counsel and<br />
senior associates from the firm’s Health and<br />
Ageing Industry Group and experts in the<br />
health industry. Christine profiled the Private<br />
Hospital industry; the role played by APHA and<br />
canvassed the key challenges facing the sector.<br />
Public and private oncology hospital<br />
representatives from China visited Canberra on<br />
21 February and Paul Mackey, APHA Director of<br />
Policy and Research participated in a briefing<br />
for them on the Australian health system. Paul<br />
explained the role of the private sector in the<br />
provision of cancer services at the briefing at<br />
the Department of Health and Ageing.<br />
Dr Leon Clark, APHA Board member and CEO<br />
of Sydney Adventist Hospital, spoke at the<br />
Financial Review 10th Annual Health Congress<br />
on 28 February. Dr Clark took part in a CEO<br />
forum which looked at a needs audit for 2025<br />
and also presented a paper on private hospitals’<br />
viewpoints on restructuring private health<br />
insurance in Australia.<br />
The Tasmanian Association for Quality in<br />
Health Care Seminar was held on 13 March and<br />
APHA President Christine Gee’s presentation<br />
focused on the work of the APHA and APHA<br />
Quality and Safety Committee, particularly in<br />
terms of coordinating and supporting both<br />
the Australian Commission on Safety and<br />
Private Hospital - April 2008<br />
for gynaecological surgeries such as<br />
hysterectomies, and for some thoracic<br />
operations,” Dr Kelly said.<br />
Already some 1,800 da Vinci procedures have<br />
been carried out in Australia at four hospitals<br />
in Melbourne, Sydney and Adelaide.<br />
Quality in Health Care / Private Hospital Sector<br />
Committee in progressing and translating the<br />
national agenda. She also gave an overview of<br />
the feedback to the Accreditation Alternative<br />
Model Review and emphasised the need<br />
for there to be transparent ‘rules’ (reporting,<br />
assessment etc) across public and private and<br />
the need for partnerships rather than after<br />
thoughts. Christine also chaired a panel session<br />
on Bringing Public and Private together for the<br />
Health of Everyone at the seminar.<br />
Christine Gee also took part in a panel discussion<br />
at the Chronic Disease Management conference<br />
in Sydney on 1 April 2008. The panel looked at<br />
components required of the key stakeholders<br />
to move forward on the government’s chronic<br />
disease management mandate.
National Health and Hospitals Reform Commission:<br />
A Blueprint for Reform<br />
In August 2007, in the lead up to the 2007 Federal Election, the Labor party<br />
announced that a Rudd Labor government would ‘undertake one of the most<br />
significant reforms of Australia’s health and hospital system since Federation’.<br />
As part of this announcement, Labor committed to the establishment of a<br />
National Health and Hospitals Reform Commission within 100 days of the<br />
election.<br />
On 25 February 2008, Federal Cabinet approved<br />
the establishment of the National Health and<br />
Hospitals Reform Commission and the Prime<br />
Minister and the Minister for Health announced<br />
the membership of the Commission to the<br />
public. The Commission, which has been<br />
directed by Cabinet to develop a long-term<br />
health reform plan for a modern Australia, has<br />
been tasked to provide an interim report by the<br />
end of 2008 and a final plan in mid-2009.<br />
The Commission is chaired by Dr Christine<br />
Bennett, chief medical officer for private health<br />
insurer MBF, and includes nine other experts<br />
from both sides of the political fence.<br />
The Commission will provide a blueprint for<br />
tackling future challenges in the Australian<br />
health system including:<br />
• The rapidly increasing burden of chronic<br />
disease;<br />
• The ageing of the population;<br />
• Rising health costs; and<br />
• Inefficiencies exacerbated by cost shifting and<br />
the blame game.<br />
The Commission will focus on health financing,<br />
maximising a productive relationship between<br />
public and private sectors, and improving<br />
rural health. It will also advise the Government<br />
on the key aspects of the framework for the<br />
next health care agreements between the<br />
Commonwealth and the States and Territories.<br />
The other nine members of the commission<br />
are:<br />
• Rob Knowles, former Victorian Liberal Health<br />
Minister and current chair of the Mental<br />
Health Council of Australia;<br />
• Geoff Gallop, former Premier of Western<br />
Australia and current Professor and Director<br />
of the Graduate School of Government at the<br />
University of Sydney;<br />
• Mukesh Haikerwal, Melbourne GP and<br />
immediate past-President of the AMA;<br />
• Stephen Duckett, health economist and<br />
former Secretary of the Commonwealth<br />
Department of Health. He is currently<br />
Executive Director of the Reform and<br />
Development Division of Queensland Health;<br />
Private Hospital - April 2008<br />
31<br />
• Ron Penny, Emeritus Professor of Medicine,<br />
University of NSW and is one of Australia’s<br />
leading immunologists and a well known expert<br />
in chronic disease management and care;<br />
• Sabina Knight, a remote area nurse, is<br />
currently Senior Lecturer at the Centre for<br />
Remote Health. She has worked extensively<br />
in remote health including in Indigenous<br />
Communities;<br />
• Sharon Willcox, Director of consulting firm<br />
Health Policy Solutions. Prior to this Dr Wilcox<br />
had 20 years experience in public health<br />
policy in Victoria, New South Wales and in the<br />
Commonwealth;<br />
• Justin Beilby, Executive Dean of the University<br />
of Adelaide’s Medical School and a GP for 20<br />
years who has practiced in urban, rural and<br />
remote practices; and<br />
• Mary Ann O’Loughlin, Director, The Allen<br />
Consulting Group. She was a senior Social<br />
Policy Advisor to Prime Minister Keating,<br />
and has held a number of Senior executive<br />
positions in the Commonwealth<br />
Public Service.<br />
Medical Industry Association of Australia<br />
changes name to Medical Technology Association<br />
of Australia<br />
The Medical Industry Association of Australia<br />
(MIAA) has changed its name to Medical<br />
Technology Association of Australia (MTAA) to<br />
better reflect the association’s membership and<br />
its role in the healthcare system.<br />
“Our members supply approximately 90%<br />
of the non-pharmaceutical products used in<br />
the diagnosis and treatment of disease and<br />
disability in Australia and our new name better<br />
reflects this key function” said Anne Trimmer,<br />
MTAA CEO.<br />
The range of medical technology is diverse<br />
with products ranging from familiar items such<br />
as syringes and wound dressings, through<br />
to high-technology implanted devices such<br />
as pacemakers, defibrillators, hip and other<br />
orthopaedic implants. Products also include<br />
hospital/surgical equipment, diagnostic<br />
imaging equipment such as ultrasounds<br />
and magnetic resonance imaging machines,<br />
as well as diagnostic (pathology) tests that<br />
detect disease. Members also play a vital role<br />
in providing healthcare professionals with<br />
essential education and training to ensure safe<br />
and effective use of medical technology.<br />
“Medical technology has an essential role in<br />
managing the health of Australians and is relied<br />
upon to alleviate pain, injury and handicap.<br />
Our new name will better assist us position<br />
ourselves in the health environment to ensure<br />
Australian patients have equity and access to<br />
the most appropriate medical technology” Ms<br />
Trimmer concluded.
32<br />
Queensland Governor Returns to the Hospital<br />
She Helped Build to Launch its 50th Anniversary<br />
Celebrations<br />
Governor of Queensland, Quentin Bryce, could hardly have imagined 50 years<br />
ago, as she launched the first door knock appeal in Brisbane to raise money to<br />
build a new hospital, that she would be invited to launch the venue’s jubilee<br />
celebrations in 2008.<br />
St Andrew’s War Memorial Hospital in Spring<br />
Hill this year marks its 50th Anniversary and<br />
launched its celebrations with a special service<br />
on Tuesday, March 4, at St Andrew’s Uniting<br />
Church in Brisbane.<br />
The Governor opened the proceedings and<br />
unveiled a plaque commemorating the<br />
Hospital’s 50th anniversary. She reminisced<br />
about marching the streets of Brisbane as a<br />
University of Queensland student all those<br />
years ago, raising funds for the original<br />
hospital building.<br />
Ms Bryce explained that she had attended<br />
Moreton Bay College as a child, which was<br />
at the time a Presbyterian school, the same<br />
church (now known as the Uniting Church)<br />
that was behind the founding of St Andrew’s.<br />
In her first year studying social work at UQ, she<br />
helped raise funds for what has now become<br />
one of Brisbane’s most medically influential<br />
private hospitals.<br />
“I remember door knocking in Auchenflower,”<br />
she muses, “as it was particularly hot that day<br />
and those hills are very, very steep!”<br />
However all that walking helped towards the<br />
foundation of a great new hospital that is a<br />
living memorial to the men and women of the<br />
armed forces who fought in the world wars,<br />
and subsequent wars after that.<br />
The doors of St Andrew’s opened on May<br />
17, 1958 as a small 84 bed hospital. It is<br />
now undergoing a massive $73 million<br />
redevelopment that will allow it to take 260<br />
inpatients and will boast the most modern<br />
and up to date facilities.<br />
The hospital, which now comes under the<br />
umbrella of UnitingCare Health, has played<br />
an enormous part in the medical history of<br />
Brisbane and indeed has featured heavily in<br />
the life the Governor’s family too.<br />
Her sister Diane was one of the first nurses to<br />
train at the hospital and went on to become<br />
the head theatre nurse. The Governor has also<br />
used the hospital for herself and all her family<br />
when hospital care has been required and<br />
explains: “My daughter was at St Andrew’s for<br />
treatment only last Christmas and received<br />
wonderful care and attention.”<br />
Ms Bryce says her involvement with St<br />
Andrew’s was her first “grass roots experience”<br />
of community activity and helped shape her<br />
future. “The foundation of the hospital was a<br />
remarkable endeavour,” she says. “It was driven<br />
by marvellous doctors and supported by so<br />
many in the church and the community.”<br />
Private Hospital - April 2008
Private Hospital - April 2008<br />
33
34<br />
Private Hospital - April 2008
Private Hospital - April 2008<br />
35
36<br />
policy patter...<br />
with Paul Mackey<br />
Private hospitals providing good<br />
value for Veterans<br />
A recent report from the Australian Institute of Health and Welfare (AIHW)<br />
highlights Veterans’ use of health services.<br />
This report uses linked aged care and<br />
Department of Veterans’ Affairs (DVA)<br />
administrative data to examine patterns<br />
of use of DVA-funded hospital, medical<br />
and allied health services by DVA Gold<br />
Cardholders aged 70 years and over living in<br />
permanent residential aged care (RAC), and<br />
compares these patterns with those of Gold<br />
Cardholders of the same age and sex living in<br />
Health service use of DVA Gold Card Holders, 2002-03 and 2003-04<br />
Services received during<br />
the year<br />
GP Services<br />
% using<br />
$ per patient (mean)<br />
Specialist services<br />
% using<br />
$ per patient (mean)<br />
RPBS<br />
% using<br />
$ per patient<br />
Hospitals<br />
% using<br />
$ per patient per year all<br />
hospitals (mean)<br />
$ per patient per year public<br />
hospitals* (mean)<br />
$ per patient per year private<br />
hospitals (mean)<br />
the community. DVA Gold Card holders living<br />
permanently in residential aged care comprise<br />
around 10% of all DVA Gold Card holders.<br />
Analysis in the report concentrates on use of<br />
health services during 2002-03 with additional<br />
data on use in 2001-02 and 2002-03. Datasets<br />
used in compiling the report are:<br />
• Hospital use (private and public)<br />
Living in RAC Living in the Community<br />
94.4%<br />
$605<br />
46.2%<br />
$435<br />
91.3%<br />
$1,281<br />
37.6%<br />
$8,753<br />
$8,234<br />
$7,005<br />
97.3%<br />
$492<br />
77.5%<br />
$463<br />
94.8%<br />
$1,316<br />
45.6%<br />
$8,538<br />
$8,262<br />
$6,694<br />
Source: Australian Institute of Health and Welfare, Veterans’ Use of Health Services, 2008, p.xi<br />
[Note that utilisation and cost data were not available for public hospitals in Western Australia and the Northern Territory].<br />
Ramsay Health Care Extends UK Platform<br />
Ramsay Health Care Limited has extended its<br />
reach in the UK market, agreeing to acquire<br />
the BMI Nottingham Hospital from General<br />
Healthcare Group. The BMI Nottingham<br />
Hospital is a private acute care hospital<br />
offering a wide range of services notably in<br />
orthopaedics, general surgery, urology and<br />
plastic surgery. It has 41 registered beds, two<br />
theatres and 13 consulting rooms. Ramsay<br />
Managing Director Pat Grier said: “The BMI<br />
Private Hospital - April 2008<br />
• General practitioner (including local medical<br />
officer) consultations<br />
• Medical specialist consultations<br />
• Pharmaceutical use under the Repatriation<br />
Pharmaceutical Benefits Scheme<br />
Key points of interest from the report include:<br />
• The report indicates that private hospitals<br />
provide services to DVA Gold Card Holders<br />
at a lower average cost than public<br />
hospitals. In the case of veterans living in<br />
the community, private hospitals provided<br />
services at an average cost per patient per<br />
year that was 23% lower than public hospitals.<br />
In the case of patients living permanently in<br />
RAC, private hospitals provided services to<br />
DVA Gold Card Holders at an average cost per<br />
patient per year that was 18% lower than in<br />
public hospitals;<br />
• Across all age groups, 46% of DVA Gold Card<br />
holders living in the community and 38% of<br />
Gold Card holders living in RAC used hospital<br />
services at some stage during 2002-03;<br />
• More DVA Gold Card holders living in the<br />
community used private hospitals (34%) than<br />
public hospitals (19%) while a slightly higher<br />
proportion of Gold Card holders living in<br />
RAC used public hospitals (24%) than private<br />
hospitals (20%).<br />
The table below provides an overview of the<br />
use and per patient cost of health services used<br />
by DVA Gold Card holders in 2002-03 (hospital<br />
services and RPBS) and 2003-04 (GP and<br />
specialist services).<br />
The full report is available from: http://www.<br />
aihw.gov.au/publications/index.cfm/title/10390<br />
Nottingham Hospital is a quality hospital and a<br />
valuable addition to Ramsay UK’s portfolio.”
38<br />
Department of Veterans’ Affairs and Private<br />
Hospitals: Working Together for the Benefit<br />
of Veterans<br />
The Medical Technology Association of Australia (together with its New<br />
Zealand sister association, MIANZ) has had a Code of Practice since September<br />
2001. The Code was substantially revised in 2005, and with the Code now<br />
nearing the end of its second year of operation it has again been reviewed<br />
with the 3rd edition of the Code to be put to members for adoption in the<br />
first part of 2008.<br />
The launch of the 3rd edition of the Code this<br />
year will be followed by an extensive education<br />
program, both with industry and with the<br />
healthcare sector with whom industry works<br />
very closely to ensure all stakeholders have<br />
a clear understanding of the Code and its<br />
implications.<br />
There is a high level of public scrutiny<br />
of industry behaviour (which has been<br />
highlighted more recently in articles in The Age<br />
newspaper about company relationships with<br />
the Royal Prince Alfred Hospital in Melbourne)<br />
and MTAA takes the maintenance of integrity<br />
seriously.<br />
The elements of the Code that hospitals and<br />
healthcare professionals need to be aware of<br />
are focused on:<br />
• Claims and endorsements in advertising<br />
material<br />
• Provision of product training and education<br />
by industry<br />
• Sponsorship of, and grants for, third party<br />
educational conferences<br />
• Hospitality for healthcare professionals<br />
• Consultancy arrangements with healthcare<br />
professionals.<br />
Claims and endorsements in<br />
advertising material<br />
As very few products are marketed directly<br />
to consumers, most advertising material<br />
is directed to healthcare professionals. A<br />
company must be able to substantiate a claim<br />
that it makes in an advertisement. It may<br />
only make claims that are consistent with the<br />
intended purpose of the product as listed<br />
with the regulator (the Therapeutic Goods<br />
Administration). It is also not permitted to<br />
use the name or photograph of a healthcare<br />
professional without consent or in a way that<br />
is contrary to the ethical guidelines of the<br />
relevant professional association.<br />
Provision of product training and<br />
education by industry<br />
One of the characteristics of medical<br />
technologies is that further research and<br />
development on a product is often as the result<br />
of feedback from the clinicians who use the<br />
products, thereby creating a very symbiotic<br />
relationship between industry and clinicians.<br />
Companies provide considerable training in<br />
their products to ensure that clinicians are<br />
able to make best use of them. The Code<br />
acknowledges the need for this type of training<br />
and sets out the guidelines within which it<br />
may occur. In general, the training must be<br />
conducted in appropriate training facilities<br />
and any hospitality provided to the healthcare<br />
professional must be modest in value and<br />
subordinate in time and focus. A company may<br />
pay for reasonable travel and accommodation<br />
costs incurred in attending the training.<br />
Sponsorship of, and grants for, third<br />
party educational conferences<br />
One of the most vexed areas is sponsorship<br />
of attendance at professional conferences in<br />
Australia and overseas. There is benefit to a<br />
company in having a healthcare professional<br />
present at a conference on his or her<br />
experience with a procedure or product.<br />
There is also a broader educative benefit<br />
to the healthcare sector in attendance at<br />
a conference by a healthcare professional<br />
or trainee. However in order to ensure<br />
transparency in the relationship between the<br />
healthcare professional and a company, the<br />
Code does not permit direct payment to a<br />
healthcare professional of the costs of travel<br />
and attendance.<br />
Private Hospital - April 2008<br />
The Code permits the payment of a grant or<br />
sponsorship to the organiser of the conference<br />
(usually a professional association or training<br />
institution) to enable funding of attendance,<br />
provided the conference organiser selects the<br />
recipient. Alternatively a company may make a<br />
grant to an educational institution for medical<br />
education which may be applied by that<br />
institution in meeting the cost of a healthcare<br />
professional to attend an educational<br />
conference.<br />
Hospitality for healthcare<br />
professionals<br />
The Code permits companies to provide<br />
hospitality to healthcare professionals in<br />
limited circumstances - by sponsorship of<br />
hospitality at a third party conference and by<br />
provision of hospitality as a subsidiary part of<br />
product training. The key requirements are that<br />
the hospitality is subordinate in time and value<br />
to the overall proceedings.<br />
Consultancy arrangements with<br />
healthcare professionals<br />
For reasons mentioned earlier, there is a very
“ One of the most vexed areas is sponsorship of attendance at<br />
professional conferences in Australia and overseas. There is<br />
benefit to a company in having a healthcare professional<br />
present at a conference on his or her experience with a<br />
procedure or product.“<br />
close and ongoing working relationship<br />
between medical technology companies and<br />
healthcare professionals. It is common for<br />
companies to retain a healthcare professional<br />
on contract as a consultant to provide advice,<br />
research or consulting services, or to serve on<br />
an advisory board. The Code permits such an<br />
arrangement provided that any compensation<br />
is consistent with fair market value for the<br />
services provided, selection is based on the<br />
qualifications and expertise of the consultant<br />
and not on volume or value of business<br />
generated, and the arrangements are<br />
well-documented.<br />
The Code is a voluntary Code and while<br />
binding on members of MTAA and MIANZ<br />
is advisory only for non-member medical<br />
Private Hospital - April 2008<br />
39<br />
technology companies. MTAA would like to see<br />
all companies working in the industry adhere<br />
to its principles for the benefit of all. The Code<br />
includes a comprehensive complaints process<br />
- a complaint may be brought by a range of<br />
interested persons, including a healthcare<br />
professional.<br />
MTAA will be writing to private hospitals<br />
over the next few months to provide further<br />
information about the Code and will also be<br />
providing training on the code to industry. If<br />
you would like more information on the Code<br />
please feel free to contact MTAA.<br />
by Anne Trimmer<br />
Chief Executive Officer, Medical Technology<br />
Association of Australia
40<br />
mental health forum...<br />
Veterans and Mental Health<br />
with Moira Munro<br />
In keeping with the theme of the April issue of Private Hospital, my column<br />
focuses on veterans and mental health.<br />
It is estimated by the Department of Veterans’<br />
Affairs (DVA) that some 40,000 veterans receive<br />
compensation for a mental health condition<br />
and the Department recognises mental health<br />
as “a significant component of the health care<br />
requirements of the veteran community.”<br />
Current estimates indicate that around 22%<br />
of the DVA treatment population receive some<br />
form of mental health treatment within any<br />
given year, which is higher than the population<br />
at large. This mental health treatment is<br />
provided in a variety of settings, including<br />
private hospitals.<br />
A number of private hospitals have developed<br />
treatment programs specifically to meet the<br />
mental health needs of veterans, including:<br />
• Post Traumatic Stress Disorder (PTSD)<br />
• Anger Management<br />
• Alcohol and Drug Treatment and<br />
Rehabilitation<br />
In private mental health facilities, treatment<br />
programs for each of these conditions are<br />
designed around the needs of the individual<br />
veteran and are provided by multi-disciplinary<br />
teams.<br />
Post Traumatic Stress Disorder<br />
Combat or war-related PTSD has a profound<br />
effect on the health and quality of life of<br />
Veterans, Peacekeepers and Defence personnel<br />
and their families. This disorder can stem from<br />
a wide variety of military experiences. While<br />
feelings of stress in response to trauma may<br />
be regarded as normal, PTSD is characterised<br />
by the intensity of the feelings, how long they<br />
last, how an individual behaves in response to<br />
these feelings and the presence of particular<br />
symptoms such as:<br />
• intrusive thoughts recalling the traumatic<br />
event;<br />
• flashbacks and nightmares;<br />
• depression and anxiety;<br />
• being easily startled;<br />
• irritability and being quick to anger.<br />
PTSD can lead to relationship difficulties,<br />
substance abuse and a decline in physical as<br />
well as emotional health.<br />
Programs developed by private mental health<br />
facilities to treat combat-related PTSD are<br />
tailored around the individual needs of the<br />
veteran and a specialist multidisciplinary<br />
program team is assembled to provide a<br />
complete treatment program for individual<br />
veterans and their partners, including:<br />
• Comprehensive assessment<br />
• Primary treatment sessions, including group<br />
and individual therapy sessions<br />
• Review and subsequent treatment sessions<br />
are held following the completion of the<br />
primary treatment sessions and may be held<br />
at 6, 12 and 24 month intervals to reinforce<br />
the skills and strategies learnt during the<br />
program with the aim of enhancing recovery<br />
and preventing relapse.<br />
Importantly, this latter phase of treatment<br />
will often include partner-specific sessions<br />
which provide:<br />
• Education around PTSD<br />
• The development of coping skills<br />
• A focus on personal needs<br />
Programs developed by private mental health<br />
facilities to treat PTSD are accredited by the<br />
Australian Centre for Post-traumatic Mental<br />
Health. (http://www.ncptsd.unimelb.edu.au/).<br />
Anger Management programs<br />
Programs are developed by private mental<br />
health facilities to assist veterans to better<br />
manage their feelings of anger and aggression<br />
and to enable improved quality of life for<br />
themselves and their families. Through these<br />
programs, key issues are targeted to facilitate<br />
recovery, including:<br />
• Understanding anger and aggression<br />
• Physical health<br />
• Depression and anxiety<br />
• Relationship difficulties<br />
• Anger management<br />
• Assertion skills<br />
• Relapse prevention<br />
Alcohol and Drug Treatment and<br />
Rehabilitation programs<br />
In recognition that substance abuse disorders<br />
Private Hospital - April 2008<br />
“ Current estimates indicate<br />
that around 22% of the DVA<br />
treatment population receive<br />
some form of mental health<br />
treatment within any given<br />
year, which is higher than the<br />
population at large.”<br />
are increasingly common among veterans<br />
and Defence personnel, private hospitals have<br />
developed treatment programs specifically<br />
tailored to meet the needs of Veterans and<br />
their families. Left untreated, these conditions<br />
can have a severe impact on the health and<br />
quality of life of the individual veteran and<br />
their family.<br />
Following a comprehensive assessment which<br />
identifies individual needs and suitability<br />
to participate in the program, the veteran<br />
undertakes the detoxification component of<br />
the program, usually on an inpatient basis. The<br />
veteran is generally discharged from hospital<br />
prior to commencing the group and individual<br />
therapy sessions, after which a follow up<br />
session is provided at 3 months to reinforce the<br />
skills and strategies learnt during the program<br />
with the aim of enhancing recovery and<br />
preventing relapse. Partner-specific sessions<br />
are also incorporated into the program which<br />
focuses on alcohol and drug education; and<br />
relationship education.<br />
I welcome your feedback on this column and<br />
any matters relating to private mental health<br />
services. I can be contacted at<br />
moiram@perthclinic.com.au
42<br />
Ramsay Managing Director Pat Grier Announces<br />
Retirement, Chris Rex to Become New MD<br />
The Board of Ramsay Health Care announced at the end of February that<br />
Managing Director and CEO Pat Grier intends to retire at the end of the current<br />
financial year and that Chris Rex, currently Chief Operating Officer, has been<br />
appointed Managing Director and CEO, effective 1 July 2008.<br />
Ramsay Chairman Paul Ramsay said Mr Grier’s<br />
contract was due to be renewed at the end of<br />
June and that Mr Grier had advised the Board<br />
that he had made a decision to retire then,<br />
after 13 years as Managing Director. Mr Grier<br />
will remain on the Board as a non-executive<br />
Director assisting the Company with its<br />
aim to expand its offshore business in the<br />
coming years.<br />
“After 20 years with Ramsay, Pat has decided<br />
it is the right time to retire and the Board<br />
respects his decision,” Mr Ramsay said. “Under<br />
Pat’s leadership, Ramsay Health Care has grown<br />
profitably from a relatively small, privatelyowned<br />
operation to the country’s largest<br />
provider of private hospital services, with over<br />
100 hospitals and 8,000 beds across Australia,<br />
the UK and Indonesia and more than 20,000<br />
employees.<br />
“Pat has been the architect of the company’s<br />
special culture known as “The Ramsay<br />
Way” which is central to the success of our<br />
organisation. Under his stewardship and<br />
guidance, Ramsay Health Care has become a<br />
well-respected leader in the private hospital<br />
industry in Australia and I thank him for that. I<br />
really believe Chris will make an excellent CEO<br />
and I look forward to working with him in his<br />
new role from the 1st July” Mr Ramsay said.<br />
Mr Ramsay said Mr Rex – who will also be<br />
appointed as a Director to the Ramsay Board<br />
– was an excellent choice to succeed Mr<br />
Grier. “In his 13 years with Ramsay, Chris<br />
has played an important role in building<br />
Ramsay’s management expertise and has<br />
been instrumental in setting Ramsay’s growth<br />
strategy including the company’s transforming<br />
acquisition of Affinity Hospitals and, more<br />
recently, our first major offshore acquisition<br />
Capio UK.<br />
“Working closely with Pat and the Ramsay<br />
executive committee, Chris has played a key<br />
Private Hospital - April 2008<br />
role in developing the Company’s excellent<br />
record in hospital management. His ability to<br />
run hospitals efficiently and effectively is widely<br />
acknowledged,” Mr Ramsay said.<br />
Commenting on his decision to retire, Mr Grier<br />
said: “This has been a tough decision but I<br />
feel that it is the right time for me to retire.<br />
Ramsay is in terrific shape. We have a wellplanned<br />
growth strategy to create a world class<br />
company and Chris is the right person to lead<br />
the company through this exciting new growth<br />
phase,” Mr Grier said.<br />
Mr Rex said: “It has been a wonderful<br />
opportunity and experience working with Pat.<br />
He leaves the Company well positioned for<br />
growth and I look forward to working with the<br />
Board and the management team as we head<br />
into our next phase of growth.”<br />
Chris Rex, Paul Ramsay and Pat Grier of Ramsay Health Care
Private Hospital - April 2008<br />
43
44<br />
Catholic Health<br />
Appoints New<br />
CEO<br />
Mr Martin Laverty will commence as the<br />
new CEO of Catholic Health Australia from<br />
May 2008. The appointment reaffirms CHA’s<br />
commitment to working with the Australian<br />
and state governments to improve the<br />
capacity of the Australian health and aged<br />
care systems to better meet the needs of<br />
disadvantaged Australians.<br />
Private Health<br />
Insurance<br />
Ombudsman<br />
Ms Samantha Gavel was appointed to<br />
the position of Private Health Insurance<br />
Ombudsman in late March 2008. She<br />
originally joined the staff of the Ombudsman<br />
in 1997 and has held a number of positions<br />
within the office. As Private Health<br />
Insurance Ombudsman, she is responsible<br />
for high level advice to government about<br />
issues affecting consumers in relation to<br />
private health insurance. Recent initiatives<br />
completed by the Office include the<br />
development of the consumer website<br />
www.privatehealth.gov.au and significant<br />
changes to the Office’s corporate<br />
governance arrangements.<br />
Ms Samantha Gavel<br />
New Haemovigilance Report<br />
The National Blood Authority (NBA) has released the Initial Haemovigilance<br />
Report 2008. This report has been developed by the NBA in conjunction with<br />
the NBA Haemovigilance Project Working Group and it provides a national<br />
perspective on transfusion incidents and adverse events reported in a number<br />
of States over the past 3-5 years.<br />
The report indicates that the broad types<br />
of transfusion risks in Australia are similar to<br />
those of other countries that report transfusion<br />
adverse events, such as the United Kingdom,<br />
New Zealand, Sweden and Canada.<br />
Specifically, the data in the report shows<br />
that there is minimal risk of infection from<br />
the provision of blood and blood products<br />
in Australia, as there were no reports of HIV,<br />
hepatitis B or hepatitis C in the data collected<br />
for this project. However, consistent with<br />
international experience, the data show<br />
that patient harm resulting from reactions<br />
and near misses is occurring in Australian<br />
hospitals. Across the various reporting periods<br />
from which the data were drawn, more than<br />
600 transfusion-related incidents, errors and<br />
reactions were reported.<br />
Of these:<br />
• There were 134 instances of patient<br />
misidentification, mislabelling, wrong blood in<br />
tube or near misses reported. If unrecognised<br />
prior to transfusion, these errors can lead to<br />
patients receiving the wrong blood, which<br />
may result in severe morbidity or mortality.<br />
• There were 172 prescription and dispensing<br />
errors reported. Typically, they included<br />
ordering or providing the wrong blood<br />
component or delivering an out-ofspecification<br />
component.<br />
• There were 30 reports of incorrect blood<br />
component transfused. This human error<br />
is a major cause of patient morbidity and<br />
mortality.<br />
• There were 67 reports over five years of<br />
ABO incompatibility. However, there are no<br />
published, consolidated data on the aetiology,<br />
morbidity or mortality associated with these<br />
events.<br />
• There were 26 reports of haemolytic<br />
transfusion reactions, and eight reports of<br />
transfusion-transmitted infections, none of<br />
which were viral.<br />
• There were 59 reports of allergic reactions and<br />
eight reports of anaphylaxis.<br />
• There were 106 reports of febrile<br />
Private Hospital - April 2008<br />
non-haemolytic transfusion reactions.<br />
• There were five reports of transfusion-related<br />
acute lung injury, which is known to be underrecognised<br />
and under-reported, including<br />
when compared to suspected cases reported<br />
to the ARCBS for investigation.<br />
• There were nine reports of circulatory<br />
overload as a result of over-transfusion. A<br />
number of deaths have occurred in Australia<br />
and internationally as a result of overtransfusion.<br />
• Twenty-seven percent (219/810) of events<br />
extracted from AIMS involved labile<br />
components transfused overnight between<br />
the hours of 22:00 and 0:700.<br />
• Two transfusion-related deaths were reported.<br />
The report found that the majority of the<br />
transfusion and adverse events resulted from<br />
human error. The report proposes a number<br />
of key issues for future system improvement,<br />
including:<br />
• The establishment of ongoing haemovigilance<br />
framework to underpin improvements to the<br />
quality and safety of transfusions in Australia;<br />
• Improvements in the consistency of recording<br />
and reporting of transfusion-related adverse<br />
events;<br />
• A focus on procedural training and process<br />
improvement which should lead to<br />
transfusion only when absolutely necessary.<br />
The report is available from: http://www.nba.<br />
gov.au/haemovigilance/index.html
Advertorial
48<br />
Drowning – 1000 a year either die or<br />
are hospitalised<br />
An average of 370 people die and 618 were<br />
hospitalised each year over a five-year<br />
reporting period, according to a new report by<br />
the Australian Institute of Health and Welfare<br />
(AIHW). The report, Deaths and hospitalisations<br />
due to drowning, Australia 1999-00 to 2003-04,<br />
shows that around one-third of all drowning<br />
deaths occurred in natural bodies of water<br />
such as beaches, lakes, the open sea, rivers<br />
and streams, while 10% of deaths occurred<br />
in swimming pools and 10% were boat or<br />
watercraft related.<br />
‘The dangers of swimming pools for very<br />
young children are readily apparent in the<br />
data we have analysed for this report’, said<br />
Renate Kreisfeld of the Institute’s National Injury<br />
Surveillance Unit based at Flinders University in<br />
Adelaide. “The highest death rates for swimming<br />
pool drowning was in the 0-4 year age”.<br />
Coroners’ data showed that by far the most<br />
important factor identified for young children<br />
and death by drowning in swimming pools<br />
was the lack of adequate supervision. Various<br />
aspects of pool fencing and gates were also<br />
commonly identified as contributing factors.<br />
Over the period covered by the report, around<br />
20 deaths a year were the result of drowning<br />
in bathtubs, with 47 hospitalisations for near<br />
drownings.<br />
Private Hospital - April 2008<br />
In such cases, epilepsy, other seizure disorders,<br />
and inadequate or non-existent supervision<br />
were factors commonly identified by coroners.<br />
Alcohol intoxication was also mentioned<br />
frequently in case documents.<br />
Approximately 37 drowning deaths and<br />
65 hospitalisations per year were watercraft<br />
related. These incidents often occurred while<br />
the person was engaged in a leisure activity.<br />
An annual average of 56 drowning deaths and<br />
39 hospitalisations were due to intentional<br />
self-harm.
Private Hospital - April 2008<br />
Nearly two thirds of<br />
Australians die from<br />
heart disease or cancer<br />
The leading underlying cause of death for all Australians<br />
was Ischaemic heart diseases, contributing to 18% of<br />
all male deaths and 17% of all female deaths registered<br />
in 2006, according to figures released in March by the<br />
Australian Bureau of Statistics (ABS).<br />
Ischaemic heart diseases (includes angina, blocked arteries of the heart<br />
and heart attacks) have been the leading cause of death in Australia<br />
over the last 10 years, however the proportion of deaths attributed to<br />
Ischaemic heart diseases has declined from 23% in 1997 to 17% in 2006.<br />
Cardiovascular disease was responsible for the deaths of 45,670<br />
Australians in 2006. It includes diseases such as ischaemic heart<br />
diseases, heart failure aneurysms, heart valve disorders, hypertension,<br />
haemorrhages and strokes and represents 34% of the 133, 739 deaths<br />
registered in Australia in 2006 (down from 41% in 1997).<br />
Cancer was the underlying cause of death for 39,753 registered deaths<br />
in Australia. This is a 12% increase since 1997, when 35,363 people died<br />
from cancer. In 2006, cancer accounted for 30% of all registered deaths<br />
compared with 27% in 1997. Lung cancer is the most prevalent type of<br />
cancer death, with 7,348 Australians dying of the disease in 2006.<br />
Prostate cancer was the underlying cause of 4.3% of all male deaths, with<br />
2,952 deaths registered in 2006. The median age at death for prostate<br />
cancer is 80.4 years. Breast cancer was the underlying cause of all female<br />
deaths with 2,643 (4%) women dying of this disease in 2006. The female<br />
media age at death for breast cancer is 68.3 years, which is 14.9 years<br />
lower than the median age for all female deaths (83.3 years).<br />
Deaths due to Dementia and Alzheimer’s disease have risen by 99% since<br />
1997. Dementia and Alzheimer’s disease is Australia’s 4th leading cause of<br />
death (up from 8th in 1997) with 6,543 deaths registered in 2006<br />
More details are available in Causes of Death, Australia which is available<br />
free of charge when downloaded from the ABS website on<br />
www.abs.gov.au<br />
New Secretary General<br />
for the AMA<br />
The Executive Council of the Federal AMA appointed Mr Francis<br />
Sullivan as Secretary General of the Federal AMA in February. Mr<br />
Sullivan was CEO of Catholic Health Australia for the past 14 years.<br />
51
Advertorial
54<br />
Latest Data from PHIAC<br />
The Private Health Insurance Administration<br />
Council (PHIAC) has released data on private<br />
health insurance membership and utilisation<br />
and benefits paid for insured patients in private<br />
hospitals and day hospitals in the December<br />
quarter 2007. The key features are:<br />
Membership<br />
The proportion of the population covered<br />
by private health insurance has increased to<br />
44.4% of the population and 9,391,000 people<br />
are now insured, an increase of 99,280 people<br />
since the September quarter and an increase<br />
of 392,000 people compared to the December<br />
quarter 2006.<br />
Private Hospitals<br />
Compared to the December quarter 2006:<br />
• Insured episodes increased by 4.5% to<br />
481,247 episodes<br />
• Insured days increased by 3.2% to<br />
1,313,978 days<br />
• Total Benefits increased by 10.2% to<br />
$1.06 billion<br />
• Average Benefit per episode increased by<br />
5.4% to $2,214<br />
• Average benefit per day increased by 7.0%<br />
to $810.75<br />
Day Hospitals<br />
Compared to the December quarter 2006:<br />
• Insured episodes increased by 12.3% to<br />
94,295 episodes<br />
• Total benefits increased by 16% to<br />
$53,755 million<br />
• Average benefit per day increased by<br />
3.7% to $570<br />
Hospital substitute treatment<br />
Compared to the September Quarter 2007:<br />
• Insured episodes fell by 26% to 2917 episodes<br />
• Total benefits paid also fell, by 2.7% to $0.71<br />
million<br />
Private Hospital - April 2008<br />
Chronic Disease Management Programs<br />
(CDMP)<br />
Compared to the September quarter 2007:<br />
• 2,214 CDMP were provided in the December<br />
quarter, an increase of 78% on the previous<br />
quarter<br />
• Total benefits paid increased by 68% to $0.9<br />
million<br />
Medical benefits<br />
Compared to the December quarter 2006:<br />
• Total benefits paid for medical services<br />
increased by 13.8% to $291.16 million<br />
Prostheses benefits<br />
Compared to the December quarter 2006:<br />
• Benefits paid for prostheses increased by<br />
11% to $242.8 million<br />
The full PHIAC reports are available from:<br />
http://www.phiac.gov.au/statistics/<br />
membershipcoverage/index.htm
Vote on proposed MBF merger to take place<br />
on 12 May 2008<br />
MBF Australia Limited (MBF) is just that little bit closer to merging with BUPA<br />
Australia after the Federal Court of Australia approved the release of an<br />
Information Memorandum about the proposal to merge the two companies.<br />
The Information Memorandum will provide eligible contributors with full details<br />
of the $2.41 billion offer from BUPA Australia to combine the businesses of the<br />
MBF Group and the BUPA Australia Group and instructions on how to vote.<br />
The MBF Board recommended the proposal to<br />
combine the two businesses to MBF Council and<br />
MBF Contributors back in December 2007.<br />
The Information Memorandum will be<br />
accompanied by an Allocation Form that will<br />
set out an estimate of the cash entitlement<br />
eligible contributors will receive if the proposal is<br />
approved and implemented. The cash entitlement<br />
will be based on tenure and type of policy.<br />
MBF Chairman, Mr John Conde, said the<br />
combined group will retain the iconic MBF brand.<br />
“MBF is strong in Queensland, New South Wales<br />
and Tasmania while BUPA Australia’s brands<br />
HBA and Mutual Community – are strong in<br />
Victoria and South Australia.<br />
“Together, the two businesses will create a<br />
competitive private health insurer with a national<br />
footprint.”<br />
Mr Conde said the Board of the combined group<br />
would comprise six directors, three each from<br />
MBF and BUPA. MBF Managing Director and<br />
Chief Executive Officer, Eric Dodd, would become<br />
managing director of the combined group to<br />
guide the implementation of the merger before<br />
Private Hospital - April 2008<br />
making the transition to a non-executive<br />
board role.<br />
55<br />
Mr Dodd said the merger was a significant step in<br />
the consolidation of the private health insurance<br />
industry at a time when rationalisation has never<br />
been more essential. “Bringing together MBF and<br />
BUPA Australia Health’s brands will create a strong<br />
and competitive health insurance group with<br />
national reach. This is something MBF has wanted<br />
to achieve for a long time.”<br />
The ACCC has said it will not oppose the merger.
56<br />
Health Privacy – Everything You Wanted to Know<br />
Five new information sheets and seven new Frequently Asked Questions<br />
(FAQs) related to health privacy have been released by the Office of the<br />
Privacy Commissioner.<br />
The new information sheets are intended to<br />
assist private sector health service providers<br />
in fulfilling a range of obligations under the<br />
Privacy Act 1988 relating to use, disclosure and<br />
individual access to health information.<br />
The information sheets address key health<br />
privacy issues which stakeholders in the private<br />
healthcare sector have raised as needing<br />
further clarification or guidance.<br />
The information sheets have a one-page<br />
snapshot of ‘Key Messages’ on the front page to<br />
assist busy providers on the relevant issues. This<br />
is followed by a more detailed explanation for<br />
providers, practice managers and peak bodies<br />
who seek further information and practical<br />
examples. Several of the examples provided<br />
draw on real (de-identified) cases that have<br />
been investigated by the Office of the Privacy<br />
Commissioner.<br />
The titles of the information sheets are:<br />
• Denial of access to health information due<br />
to serious threat to life or health<br />
• Fees for access to health information under<br />
the Privacy Act<br />
• Use and disclosure of health information for<br />
management, funding and monitoring of a<br />
health service<br />
• Disclosure of health information and impaired<br />
capacity<br />
• Sharing health information to provide a health<br />
service<br />
The seven new FAQs cover similar issues to<br />
the five new information sheets. The new<br />
FAQs are primarily designed to provide brief,<br />
user-friendly guidance to health consumers.<br />
It is hoped that the FAQs will promote greater<br />
understanding of privacy rights and raise<br />
awareness of information-handling practices<br />
in the health sector.<br />
Copies of both the information sheets and the<br />
FAQs can be printed from the website,<br />
www.privacy.gov.au. Additional copies can<br />
be mailed on request by calling the Office of<br />
the Privacy Commissioner’s Office Enquiries<br />
Line on 1300 363 992.
58<br />
pharmacy focus....<br />
with Michael Ryan<br />
Measuring the performance of the Drug Committee<br />
The potential of the multi-disciplinary drug and therapeutics committee (DTC)<br />
is too often not realised and as a consequence medicines are not used as safely,<br />
efficaciously and cost-effectively as possible in hospitals.<br />
A DTC potentially can have a significant impact<br />
on medicine use outcomes – clinically and<br />
financially 1 . Unfortunately the DTC for many<br />
hospitals is underutilised or underperforms.<br />
For many, it is a necessarily evil – a committee<br />
created to meet perceived ACHS requirements,<br />
or to deal with a ‘rag-bag’ of medicines or<br />
pharmacy-related issues.<br />
Individual DTCs have attempted to measure<br />
their performance but there is little in the<br />
literature documenting the processes or the<br />
success of these activities.<br />
The following is suggested as one approach<br />
to providing a mechanism to prove the value<br />
(or otherwise) of the DTC. The approach is<br />
based on my experience in an acute care<br />
private hospital.<br />
Process for measuring DTC performance<br />
This includes:<br />
1. developing objectives for the DTC;<br />
2. developing a strategy to achieve these<br />
objectives;<br />
3. developing an action plan to implement the<br />
strategy;<br />
4. developing a process to monitoring the<br />
progress of the action plan; and<br />
5. measuring the success of the DTC in<br />
achieving its objectives.<br />
Space restrictions limit the number of examples<br />
of putting this approach into action which can<br />
be given here. Additional examples can be<br />
supplied on request. Examples include:<br />
Examples of objectives to:<br />
1. increase the safety,<br />
2. maintain (or reduce) the cost, and<br />
3. increase the quality of medicine use in the<br />
private hospital<br />
• safety as measured by the number and<br />
severity of medicine-related incidents;<br />
• costs as measured by total cost of all<br />
medication per patient bed day or total<br />
cost of care of key diagnosis related groups<br />
(DRGs);<br />
• quality as measured by compliance with<br />
best practice guidelines for key medicines.<br />
The DTC may set objectives such as:<br />
1. reduce the number of medicine-related<br />
incidents reported via the Incident Reporting<br />
System by 25% over the next 12 months;<br />
2. reduce the total cost of medicines per<br />
patient bed day or as a percentage of<br />
hospital revenue, to previous financial year’s<br />
level; OR reduce the total cost of care of<br />
patients for those diagnosis related group<br />
(DRGs) which impact most heavily of total<br />
medicine costs for the hospital;<br />
3. compare the use of high risk or high cost<br />
drugs with peer reviewed guidelines using a<br />
drug use evaluation process.<br />
Examples of strategies to achieve safety, cost<br />
and quality objectives:<br />
1. develop and / or regularly review the policies<br />
and procedures to achieve safe, rational and<br />
cost-effective medicine use;<br />
2. review the medicines which are distributed<br />
via imprest and those delivered by dispensed<br />
prescription to ensure that the top 80% (by<br />
total annual expenditure) in each category is<br />
supplied at the least cost to the hospital;<br />
3. identify the medicines which have the<br />
greatest potential to cause adverse events or<br />
to be inappropriately used (e.g. over-use of<br />
antibiotics for which there is a history in the<br />
hospital of the development of resistance).<br />
Examples of actions to implement strategies<br />
related to safety, cost and quality (organised<br />
as a 12 month action plan):<br />
1. review and update three medicine-related<br />
policies and procedures at each DTC meeting<br />
to ensure that all remain current and<br />
appropriate to the Hospital’s needs;<br />
2. review the imprest and dispensed<br />
prescription charges reports twice yearly<br />
to identify if medicines can be supplied at<br />
less cost using an alternative distribution<br />
method;<br />
3. conduct a drug use evaluation of high risk<br />
or high cost or targeted medicines and<br />
compare usage with peer reviews and DTC<br />
approved guidelines, and take action as<br />
appropriate.<br />
Private Hospital - April 2008<br />
“ The following is suggested as<br />
one approach to providing a<br />
mechanism to prove the value<br />
(or otherwise) of the DTC.<br />
The approach is based on my<br />
experience in an acute care<br />
private hospital.”<br />
Monitoring the effectiveness of the DTC<br />
At the end of the 12 month period, the<br />
secretary of the DTC should report on the level<br />
of achievement (complete, partial, none) of the<br />
objectives as each is quantifiable.<br />
In summary<br />
Adapting an approach such as this allows the<br />
DTC to:<br />
• set measurable objectives through a<br />
multi-disciplinary committee related to<br />
the medicine-related issues of greatest<br />
importance to the hospital;<br />
• measure the DTC’s progress in achieving these<br />
on a 12 monthly basis; and<br />
• assess the DTC’s performance in contributing<br />
to safe, cost-effective and quality use of<br />
medicines.<br />
Reference:<br />
1<br />
An EL, Day RO, Brien J. Improving decision<br />
outcomes of drug and therapeutics<br />
committees. J Pharm Pract Research 2003; 33<br />
(1): 65-7.<br />
Michael Ryan, BPharm, FSHP, MBA<br />
Director, PharmConsult<br />
PharmConsult is Australia’s pre-eminent<br />
hospital pharmacy consultancy advising<br />
hospitals on the operational, financial,<br />
professional, service, and legislative issues<br />
associated with hospital pharmacy services.<br />
Telephone: 03 9813 0580<br />
Email: m.ryan@pharmconsult.com.au
MABEL – Improving the working life of Doctors<br />
MABEL (Medicine in Australia: Balancing<br />
Employment and Life) is a major new national<br />
longitudinal survey of doctors, funded by the<br />
NHMRC. Policies about the medical workforce<br />
and how to alleviate shortages of doctors<br />
need to be based on evidence about doctors’<br />
own views, preferences, and work and family<br />
circumstances. Without such evidence, policies<br />
may be insensitive to the realities of medical<br />
practice and less likely to be effective. MABEL is<br />
More talk, more action required<br />
in treatment of type 2 diabetes<br />
The National Prescribing Service Limited (NPS) is advising health professionals<br />
to be more aggressive in their management of patients with type 2 diabetes.<br />
The latest education program for NPS – ‘Early<br />
use of insulin and oral antidiabetic drugs’<br />
– focuses on appropriate drug therapies, earlier<br />
introduction of insulin, lifestyle interventions<br />
and the close relationship between type 2<br />
diabetes and cardiovascular events.<br />
NPS spokeswoman Judith Mackson said a<br />
plethora of recent information surrounding<br />
the risks of thiazolidinedione (glitazone)<br />
use, the need for more pro-active medical<br />
management of diabetes and patient<br />
resistance to introducing insulin had created<br />
concern and uncertainty among some health<br />
professionals about how to escalate treatment<br />
once control is no longer achieved with one or<br />
two oral agents.<br />
“When dietary changes, adequate regular<br />
exercise and oral agents are failing to control<br />
blood glucose levels, it can be challenging<br />
for health professionals to know which drug<br />
therapy will be suitable for their patients,” Ms<br />
Mackson said. NPS still recommends metformin<br />
as first-line therapy in most cases – either alone<br />
or in combination with other<br />
oral drugs.<br />
“When oral therapy is no longer working<br />
effectively, early introduction of insulin is<br />
optimal for reducing diabetes-related<br />
micro-vascular complications and maximising<br />
overall health. However, convincing patients<br />
the first survey that will provide such rigorous<br />
evidence in Australia. The longitudinal nature<br />
of the survey will enable changes in doctors’<br />
views and circumstances to be followed<br />
up over time. The survey gives doctors the<br />
opportunity to provide information about what<br />
it is like working in medicine and how this<br />
interacts with their personal life. Invite letters<br />
for the first wave of the survey will be posted<br />
to a stratified random sample of doctors in May<br />
Private Hospital - April 2008<br />
to start administering insulin is another matter<br />
entirely,” Ms Mackson added. “A major thrust of<br />
this NPS program is advising GPs, pharmacists,<br />
nurses and other health professionals on how<br />
to initiate insulin simply and safely, as well<br />
as specific counselling points to overcome<br />
common patient barriers. Our recommendation<br />
is to introduce night-time basal insulin with<br />
existing combination drug therapy – they<br />
should not be mutually exclusive.”<br />
The program also examines current evidence<br />
and controversies around the benefits and<br />
harms of glitazones, particularly as they relate<br />
to patients with existing heart failure or<br />
ischaemic heart disease and those at high risk.<br />
NPS Facilitators, based in divisions of general<br />
practice around Australia, will conduct<br />
educational visits and group discussions with<br />
a range of health professional groups over<br />
coming months. Additionally, GPs, pharmacists,<br />
nurses and diabetes educators can participate<br />
in a clinical audit and case study, which will<br />
contribute to their continuing professional<br />
development (CPD) points.<br />
To obtain a copy of NPS News or for more<br />
information on the NPS education program,<br />
‘Early use of insulin and oral antidiabetic drugs’,<br />
visit the website www.nps.org.au.<br />
2008. Doctors can also register to take part in<br />
MABEL by going to www.mabel.org.au.<br />
The survey is being led by Professor Anthony<br />
Scott at the Melbourne Institute of Applied<br />
Economic and Social Research (University of<br />
Melbourne) in collaboration with the Faculty<br />
of Medicine, Nursing and Health Sciences at<br />
Monash University, and is supported by a Policy<br />
Reference Group comprising professional<br />
organisations and governments.
62<br />
membership matters... with Goran Josifovski<br />
Delivering Value to Members<br />
With the recent changes in Government and health policy, future consolidation<br />
of the health insurance landscape, and changes to APHA’s constitution and<br />
structure, 2008 is shaping up to be an extremely busy year. The Association’s<br />
commitment to understanding and delivering value to members is particularly<br />
important, moving into the rest of this year and beyond.<br />
APHA Potential New Services –<br />
Web Survey<br />
A survey of senior managers offered to all<br />
APHA member hospitals was recently carried<br />
out and completed via email. A 29% response<br />
rate has provided the APHA with honest and<br />
constructive feedback which will serve as a<br />
guide to our new service undertakings in the<br />
future. The challenge for APHA is to balance<br />
these opportunities with the Association’s<br />
ability to deliver the right services, in order to<br />
ensure maximum benefit to all members.<br />
A number of multiple choice and open<br />
text questions were asked in relation to<br />
APHA developing new services, particularly<br />
focused on educative forums, workshops and<br />
benchmarking activities.<br />
When asked to list the three key issues that<br />
APHA should cover in any educative forums<br />
or workshops, a vast majority listed issues<br />
related to Health funds, Workforce, Safety &<br />
Quality and changes to the IR, legal and policy<br />
environment.<br />
It is perhaps a gauge of the current landscape<br />
that 51% of respondents included contracting,<br />
funding and negotiating with health funds in<br />
their top three issues. This was closely followed<br />
by recruitment and retention strategies and<br />
staffing innovations, which was listed as a key<br />
issue by 37% of respondents. Workshops on<br />
implementing safety and quality initiatives<br />
were also a popular topic highlighted by<br />
respondents.<br />
Members indicated that workshops or<br />
educative forums should be run a maximum<br />
of four times per year and that a fee for service<br />
model would be acceptable depending on<br />
the type of workshop or educative forum<br />
being run.<br />
APHA will look to implement at least one<br />
stream of educative forums or workshops<br />
regularly, on one of the above issues, over the<br />
next 24 months. We will also look to run these<br />
workshops in partnership with a recognised<br />
training provider, where applicable.<br />
At present, a large number of APHA member<br />
hospitals carry out benchmarking actions<br />
on various operations. According to the<br />
survey results, 98% of respondents utilize<br />
benchmarking tools, with 30% developing<br />
their own internal benchmarks. The remainder<br />
of respondents’ utilise external tools of which<br />
Press Gainey (21% of respondents), NHCDC<br />
(17% of respondents) and QPS (11%) are the<br />
most popular.<br />
Qualitative data collected pointed to a number<br />
of barriers which may cause difficulties in<br />
implementing these benchmarking tools.<br />
They include:<br />
- Complexity of the industry (Not for profit vs.<br />
for profit)<br />
- Being able to compare hospitals with similar<br />
case mix and structure<br />
- Getting buy in from a majority so that initial<br />
data is not skewed and/or obvious as to<br />
who has submitted it. Establishment of peer<br />
groups may assist with this issue.<br />
- Keeping cost below $1,000 per module/per<br />
annum<br />
- May require a seed funding investment by<br />
APHA to develop and trial benchmarking<br />
product.<br />
I believe that APHA should continue to assess<br />
the validity of offering benchmarking services<br />
to members; however it is important that we<br />
can confidently navigate around the above<br />
challenges in the first instance.<br />
Member Services Audit<br />
Whilst looking to add new services,<br />
APHA is also keen to ensure that current<br />
members understand and utilise the various<br />
communication services we already provide.<br />
To this background, a review of member<br />
entitlements is underway at present, with<br />
a view to ensuring each hospital employee<br />
on our database is communicated with via<br />
our weekly news, information papers series<br />
(quarterly), member only bulletins, Private<br />
Hospital Magazine (bi-Monthly) and web access<br />
to our member only portal. If you have any<br />
Private Hospital - April 2008<br />
“ I believe that APHA should<br />
continue to assess the validity<br />
of offering benchmarking<br />
services to members; however<br />
it is important that we can<br />
confidently navigate around<br />
the ... challenges in the first<br />
instance.”<br />
questions regarding current member services,<br />
please contact me on 02 6273 9000 or<br />
goranj@apha.org.au.<br />
National Congress<br />
With various changes in the Private Hospital<br />
sector on the horizon the APHA National<br />
Congress and APHA/Baxter Awards should<br />
already be a fixture in your calendars for 2008.<br />
The aptly themed congress “Private Hospitals:<br />
2020” will look to shed light on what the<br />
future holds for our industry. The congress will<br />
run from 26th-28th October at the Adelaide<br />
Convention Centre with topics covering<br />
workforce issues, safety and quality, future of<br />
private hospitals and leadership in healthcare.<br />
The congress will conclude with a motivational<br />
speaker, ensuring each delegate takes<br />
something away from the congress. For more<br />
information on the APHA National congress<br />
please visit www.apha.org.au.<br />
With so much on the cards, I am confident<br />
that 2008 will be a challenging, and hopefully<br />
rewarding year for APHA and our members.
Private Hospital - April 2008<br />
63
Advertorial
66<br />
An ‘EMU’ up and running at Sydney Adventist Hospital<br />
Sick or injured people, particularly the aged, are united by one wish<br />
– the quickest access to competent assessment, diagnosis, stabilisation<br />
and treatment.<br />
Now thanks to a new multi million dollar<br />
dedicated Emergency Medical Unit (EMU),<br />
part of the soon to be redesigned Emergency<br />
Care Department at Sydney Adventist Hospital,<br />
residents on Sydney’s Upper North Shore will<br />
have it.<br />
The Emergency Care Department currently<br />
treats more than 20,000 patients a year, has<br />
24 beds, and is staffed by over 20 emergency<br />
doctors, and dozens of nurses, allied health<br />
professionals and administrative staff.<br />
Since it opened in 1996 the EC has seen a<br />
dramatic rise in the number of aged patients.<br />
Between 2003 - 2007 the proportion of patients<br />
aged 55 and over admitted to the Hospital<br />
via Emergency Care has risen from 63% of<br />
all admissions to just under 70%. Similarly<br />
the proportion of patients aged 75 years and<br />
over has risen from 38% to almost 44% of<br />
admissions.<br />
Planning ahead to meet the challenges of<br />
helping more patients with a complex range of<br />
medical conditions, Sydney Adventist Hospital<br />
(the San’s) new dedicated Emergency Medical<br />
Unit is a key part of the expansion and redesign<br />
of the busy Emergency Care Department.<br />
The San’s Emergency Care Department is a<br />
critical facility supporting the 160,000 yearly<br />
admissions, the 500 visiting medical officers<br />
and the 2000 staff of the largest single campus<br />
not for profit private hospital in NSW.<br />
Dr Greg McDonald, Emergency Care Director<br />
says the additional 9 bed EMU, is the result of a<br />
thorough assessment of how different patients<br />
have different needs and different ‘journeys<br />
of care’ when they arrive at emergency.<br />
The redesign will speed up access to triage,<br />
medical consultation, diagnosis, treatment and<br />
discharge or admission.<br />
“Experience here at the San, and Australiawide<br />
and international research, has taught us<br />
that a well designed space that allows us to<br />
allocate patients to certain areas based on their<br />
condition and their needs, maximises the care<br />
we can give, and it maximises the number of<br />
patients we can help in the fastest time” said<br />
Dr McDonald.<br />
“And when you’re unwell, that’s what<br />
important.”<br />
“An addition to our existing 24 emergency<br />
care beds, the 9 bed Emergency Medical Unit<br />
is a dedicated space where we will care for<br />
patients who will be discharged or admitted<br />
into the main hospital within a 23 hour period,<br />
after initial assessment, tests and treatment.<br />
These patients don’t need or want to be<br />
where patients with more complex needs are<br />
being cared for. Medical and nursing care and<br />
efficiency will be maximised.”<br />
“No matter why you attend Emergency Care<br />
- chest pain, gastroenteritis, fractures, wounds<br />
or infections - you want to know that we will<br />
care for you as quickly and as effectively as<br />
we can. Having separate dedicated triage,<br />
Jill Watts to head Ramsay UK<br />
Ramsay Health Care has announced the appointment<br />
of Associate Professor Jill Watts to the position of<br />
CEO of Ramsay Health Care UK. Jill is currently CEO<br />
of Greenslopes Private Hospital in Brisbane and has<br />
more than 30 years experience in healthcare both as a<br />
practitioner and as a senior executive.<br />
Jill grew up in London, where she started her<br />
healthcare career, before relocating to Australia<br />
in 1981. She has been at Greenslopes since 2001<br />
and prior to this role held executive positions<br />
at other private hospitals in Australia. As well as<br />
Private Hospital - April 2008<br />
emergency medical unit, resuscitation, trauma<br />
area, fast track and aged care observation<br />
areas is all about us recognising that we have<br />
a diverse population and an increasingly busy<br />
Emergency Care department, but that our<br />
prime concern is to provide the best care we<br />
can for every one of our patients”.<br />
“It is two years ago since we started detailed<br />
discussion and planning on this and other<br />
initiatives, including a new computerised<br />
patient medical record system and extra<br />
emergency care physicians,” said Dr McDonald.<br />
The San’s aim is to constantly make sure we<br />
are at the pinnacle of best practice for our<br />
patients….We want to see them, assess them,<br />
treat them and send them either home or to an<br />
inpatient ward, as quickly as we can.<br />
The Unit is expected to open by Spring 2008.<br />
holding a Masters in Business Administration and<br />
postgraduate qualifications in Health Administration<br />
and Information Systems, Jill also has professional<br />
qualifications as a Registered Nurse and Midwife.<br />
Jill replaces David Hillier, who has decided to move<br />
back to France after accepting a role as Managing<br />
Director of a hospital group based in Paris.<br />
With 30 hospitals and day surgery facilities plus two<br />
neuro rehabilitation homes Ramsay Health Care UK is<br />
one of the largest providers of independent hospital<br />
services in England.
The Baxters<br />
The APHA seeks to stimulate, encourage and recognise the pursuit and<br />
achievement of excellence among its members. Peer recognition provides<br />
an impetus for further achievement; improves the image of the organisation<br />
and its members, both within the health care sector and across the broader<br />
community; increases morale and aids in the continuing endeavour towards<br />
improving quality outcomes for patients.<br />
The APHA/Baxter Awards have been running since 1988 and aim<br />
to recognise private hospitals and individuals that have made an<br />
outstanding contribution to patient treatment and care, as well as<br />
the management of hospital facilities.<br />
Baxter Healthcare has supported the awards since their inception and<br />
continues to see the benefit of highlighting excellence in the private<br />
hospital industry. Their commitment to the awards is synonymous, hence<br />
the awards are known as the Baxters.<br />
This year the Baxters will recognise achievement in three categories:<br />
The Baxters<br />
• Clinical Excellence – quality of care and patient outcomes<br />
• Ambulatory Care Award – acute, day surgery, psychiatric or<br />
rehabilitation<br />
• Community Involvement Award – work with/in local broader<br />
community<br />
APHA encourages you to enter these awards. The awards information<br />
brochure has been sent out to each member hospital via email, but if<br />
you have not received yours, please contact Member Services Manager,<br />
Goran Josifovski on 02 6273 9000 or by email goranj@apha.org.au<br />
The closing date is 30 July 2008.<br />
67
68<br />
Annual licence renewal period for nurses begins<br />
Queensland Nursing Council’s (QNC) annual licence<br />
renewal period for 2008 has begun. Between 1 April<br />
and 30 June 2008, almost 60,000 nurses and midwives<br />
in Queensland must renew their licence to continue<br />
practicing in Queensland.<br />
QNC encourages any nurses who haven’t renewed online before to<br />
give it a go. Online renewal is quick, easy and secure.<br />
• With online renewal it typically take less than ten minutes<br />
to complete—just have your credit card, nurse ID and web<br />
password handy.<br />
• With online renewal all that is involved is a few key strokes and mouse<br />
clicks—no postage or travelling necessary.<br />
• With online renewal all your details are secured with digital<br />
encryption—and you don’t have to worry about your form being lost<br />
in the mail.<br />
Joseph Ransfield was the first to renew this year, when he completed<br />
his renewal online at 12:15 am 1 April, shortly after an evening shift at<br />
Bamaga Hospital, Cape York. Joseph was very surprised that he was the<br />
first nurse in Queensland to renew his licence and said that usually he<br />
is the type of person that leaves everything to the last minute.<br />
Joseph said he found online renewal quick and easy, “Online renewal is<br />
so straight forward. You can’t go wrong.” He said he would recommend<br />
online renewal to other nurses, “You can renew your licence when you<br />
want to, anytime at all. I was just winding down at home after work.”<br />
To renew online, visit www.qnc.qld.gov.au and select “renew your<br />
annual licence” towards the bottom of the screen. Complete the<br />
easy-to-follow instructions and licences will be posted in the mail.<br />
Alternatively licence renewal can be completed either by post or<br />
in person.<br />
To ensure your application for licence renewal is approved in time,<br />
QNC asks that you apply for renewal before 1 June 2007, as this is the<br />
peak time for processing.<br />
To find out more, contact the renewal team today on 07 3223 5188<br />
(for Qld callers outside Brisbane 1300 139 993)<br />
QNC is the regulatory body for nursing and midwifery in Queensland.<br />
Its mission is to ensure the people of Queensland receive safe and<br />
competent nursing and midwifery care by setting the standards for<br />
nursing and midwifery education, practice, licensing and conduct.<br />
“ Online renewal is so straight<br />
forward. You can’t go wrong.”<br />
- Joseph Ransfield<br />
Private Hospital - April 2008
Private Hospital - April 2008<br />
69
70<br />
Courses and<br />
Conferences<br />
The 5th Annual Future of the PBS Summit<br />
will be held on the 6th and 7th of May 2008<br />
at the Radisson Plaza Hotel in Sydney. This<br />
national conference will bring together<br />
senior industry leaders to discuss the future<br />
and sustainability of the PBS in the dynamic<br />
healthcare environment. More information<br />
can be found at www.informa.com.au<br />
Operating Theatre Protocols is one of<br />
many courses organised by the Medical<br />
Technology Association of Australia<br />
(MTAA). This full day course will be held<br />
on 3 June in Sydney and will provide<br />
an assessed overview of the Australian<br />
College of Operating Room Nurses (ACORN)<br />
Standards for visitors to the peri-operative<br />
environment. Past operating theatre<br />
registered nurses (within the last two years)<br />
may apply for recognised prior learning<br />
pending a successful pre-assessment. For<br />
more information see www.mtaa.org.au<br />
The 8th Annual Adverse Events<br />
Management Conference will encourage<br />
an industry wide cooperative approach<br />
to enhancing patient safety and quality,<br />
23-24 June 2008 at the Rendezvous Hotel,<br />
Melbourne. To register visit<br />
www.iir.com.au/adverse<br />
The Amora Hotel Jamison in Sydney will<br />
host the 7th Annual Health Insurance<br />
Summit on 28 & 29 July 2008. For more<br />
information see<br />
www.informa.com.au/HealthInsurance<br />
Founding CEO leaves NEHTA<br />
Dr Ian Reinecke, the founding Chief Executive Officer<br />
of the National E-Health Transition Authority, left NEHTA on 4 April 2008.<br />
Dr Reinecke was responsible for establishing<br />
NEHTA as a company in 2005 and the<br />
subsequent development of a work program<br />
that now involves more than 150 staff working<br />
on a range of complex e-health projects.<br />
Chair of the NEHTA Board Dr Tony Sherbon<br />
thanked Dr Reinecke for his leadership of<br />
NEHTA. “Following funding support from<br />
COAG, Dr Reinecke has negotiated the<br />
contract to establish unique health identifiers<br />
for all Australians as well as their health care<br />
providers.<br />
“This project is now well underway and Dr<br />
Reinecke’s efforts will prove<br />
to be of great benefit in the near future to<br />
millions of Australians.<br />
“Dr Reinecke has also overseen negotiations<br />
for Australia to join the world’s most significant<br />
Private Hospital - April 2008<br />
alliance for the international coordination<br />
of clinical terminology development. This<br />
development has significantly accelerated<br />
the development of information standards<br />
throughout Australia.<br />
“Under Dr Reinecke’s leadership NEHTA has<br />
taken the evolution of e-health in Australia to<br />
a new level where much of its work is ready<br />
for implementation to improve the quality of<br />
electronic health information for clinicians and<br />
consumers,” Dr Sherbon said.<br />
Andrew Howard will act as Interim CEO<br />
of NEHTA while an international search<br />
is conducted to recruit Dr Reinecke’s<br />
replacement. Mr Howard is currently the Chief<br />
Information Officer of the Victorian Department<br />
of Human Services.<br />
Upcoming Safety and Quality<br />
Workshops<br />
Following on from last year’s successful<br />
series of workshops on the National Inpatient<br />
Medication Chart (NIMC), APHA is planning to<br />
conduct a series of workshops for our members<br />
during 2008 focussing on key Safety and<br />
Quality issues.<br />
The next series of APHA member workshops<br />
will cover Credentialling and Defining the<br />
Scope of Clinical Practice. As was the case<br />
with the NIMC workshops, the Credentialling<br />
workshops will be facilitated by experts who<br />
will cover a range of relevant issues, including:<br />
• an overview of the Credentialling and<br />
Defining the Scope of Practice Standard,<br />
(which was developed by the former<br />
Australian Council on Safety and Quality in<br />
Health Care)<br />
• how to implement the Standard with a<br />
particular focus on defining the scope of<br />
clinical practice<br />
• highlighting problems and identifying<br />
solutions, for example around:<br />
- delineation of particular specialities<br />
- performance management<br />
- insurance<br />
- appeals processes<br />
• particular challenges/difficulties faced by<br />
smaller facilities, especially those without an<br />
employed Director of Medical Services and<br />
how these issues may be addressed.<br />
An important feature of the 2008 workshops<br />
is the identification of issues around the<br />
implementation of the Credentialling Standard<br />
in private hospitals that can be fed back to the<br />
Australian Commission on Safety and Quality in<br />
Health Care to inform current and future work<br />
being undertaken on the Standard.<br />
Members will be advised of the dates and<br />
places for the workshops in the near future.
Private Hospital - April 2008<br />
71
Advertorial
One Life, A Second Chance<br />
One Life, A Second Chance, a healthy lifestyle program, has recently been<br />
launched to members from health organisations across Australia. This program<br />
has been produced by Heart Support Australia in a user friendly, DVD format,<br />
and is narrated by Mr. Peter Harvey of Channel Nine fame.<br />
Tony Arvidsson developed this program as a<br />
result of a heart event he experienced many<br />
years ago. At the time there were few resources<br />
available which led him to undertake his own<br />
research into heart disease, risk factors and<br />
lifestyle changes. The program is a result of this<br />
endeavour and he is living proof it works.<br />
For the past 10 years, Tony has presented this<br />
program to patients at the HeartStart cardiac<br />
rehabilitation and Disease Prevention program,<br />
working closely with health professionals in the<br />
region to ensure the program meets the needs<br />
of patients.<br />
As a director of Heart Support Australia,<br />
Tony could see the need for this program to<br />
be rolled out on a national level and gifted<br />
the program to the organisation. This will<br />
enable the program to be utilised in cardiac<br />
rehabilitation units, hospitals and clinics across<br />
the country as well as assist people in rural and<br />
remote areas who have little or no access to<br />
cardiac rehabilitation.<br />
Speaking at the launch was Mr Alan Cooper,<br />
CEO of the Friendly Society Private Hospital,<br />
Bundaberg who said, “Patients who have<br />
suffered an adverse cardiac event are often<br />
bewildered as to what action to take. One Life,<br />
A Second Chance is a helpful DVD to assist<br />
them back on the road to recovery.<br />
“This Self Management tool is not only<br />
invaluable for the patient but is an essential<br />
inclusion in the aids for professional staff who<br />
guide these patients to better health,” Mr<br />
Cooper added.<br />
More information about the One Life, A Second<br />
Chance program can be found at<br />
www.heartnet.org.au.<br />
Private Hospital - April 2008<br />
“ Patients who have suffered<br />
an adverse cardiac event are<br />
often bewildered as to what<br />
action to take. One Life, A<br />
Second Chance is a helpful<br />
DVD to assist them back on<br />
the road to recovery.“<br />
75
More brain research suggests “use it or lose it”<br />
Queensland Brain Institute (QBI)<br />
scientists have found another<br />
important clue to why nerve cells die<br />
in neurodegenerative diseases, based<br />
on studies of the developing brain.<br />
Neuroscientists at The University<br />
of Queensland have just published<br />
findings, which add more weight to<br />
the “use it or lose it” model for<br />
brain function.<br />
QBI’s Dr Elizabeth Coulson said a baby’s brain<br />
generates roughly double the number of<br />
nerve cells it needs to function; with those<br />
cells that receive both chemical and electrical<br />
stimuli surviving, and the remaining cells<br />
dying. In research published in the “Journal of<br />
Neuroscience”, Dr Coulson and her colleagues<br />
have identified a crucial step in the cell-death<br />
process.<br />
“It appears that if a cell is not appropriately<br />
stimulated by other cells, it self-destructs,”<br />
Dr Coulson said. This self-destruct process<br />
is also known to be an important factor in<br />
stroke, Alzheimer’s and motor neuron diseases,<br />
leading to the loss of essential nerve cells<br />
from the adult brain. “We know that a lack of<br />
both chemical and electrical stimuli causes<br />
the cells to self-destruct,” Dr Coulson said.<br />
“But we believe that nerve cells will survive if<br />
appropriate electrical stimuli are produced<br />
to block the self-destruct process that we<br />
have identified.”<br />
The researchers’ next step is to test whether<br />
dying cells receiving only electrical stimulation<br />
can be rescued.<br />
More than three years’ research has gone into<br />
understanding these crucial factors regulating<br />
nerve cell survival, but it is a major step in the<br />
long process of discovery needed to combat<br />
neurodegeneration.<br />
QBI Director, Professor Perry Bartlett said<br />
the research is an extremely exciting finding<br />
because it also provides the missing piece of<br />
information as to how the brain likely keeps<br />
alive the new neurons it generates in some<br />
brain areas as an adult.<br />
“Combining this with our knowledge of how<br />
to stimulate new neurons in the brain of adults<br />
following to disease processes such as stroke,<br />
it provides new mechanisms for the treatment<br />
of a variety of diseases from depression to<br />
dementia,” he said.<br />
Commonwealth Chief Nursing<br />
and Midwifery Officer<br />
The Australian Government has announced<br />
it will establish a new position of<br />
Commonwealth Chief Nursing and Midwifery<br />
Officer (CNMO) in recognition of the vital role<br />
nurses play in our health system.<br />
With more than 200,000 nurses across the<br />
country, working in hospitals, clinics, aged<br />
care facilities and schools, nurses are a vital<br />
part of our health system. This new leadership<br />
role comes in response to strong demand<br />
from the nursing profession.<br />
The CNMO will:<br />
• work towards building and strengthening<br />
the nursing profession as a career of choice;<br />
• play a key role in developing a strategic and<br />
collaborative approach to national nursing<br />
policy across all jurisdictions;<br />
• provide advice on key Government<br />
commitments, including the plan to bring<br />
10,000 nurses into the health and aged<br />
care sectors through a combination of cash<br />
incentives and new graduate places; and<br />
• participate in the development of a primary<br />
care strategy and midwifery review.<br />
It is hoped that the new CNMO will be<br />
appointed by April 2008<br />
77
Book Review<br />
- Community Pharmacy: symptoms, diagnosis and treatment<br />
Authors: Rutter and Newby<br />
Imprint: Churchill Livingstone<br />
269 pages. Price $99.00 (inc GST)<br />
Reviewed by: Ian DeBoos, community pharmacist and qualified practising market<br />
researcher, Hawthorn East, Vic.<br />
In recent years there has been an increased<br />
demand on pharmacists and other non medical<br />
practitioners for advice as a result of some<br />
drug deregulation and the publics’ reluctance<br />
to seek medical advice for seemingly simple<br />
ailments. Therefore, for example, community<br />
pharmacy is often the publics’ first step in<br />
gaining advice on a range of complaints.<br />
This book aims to provide the pharmacist (and<br />
other non medical practitioners) with a greater<br />
and deeper knowledge on a range of minor<br />
complaints so a practitioner may be better able<br />
to distinguish more minor complaints from<br />
more grave scenarios.<br />
The book includes chapters on: the<br />
respiratory system, ophthalmology, otic<br />
conditions, women’s health, gastroenterology,<br />
dermatology, musculoskeletal conditions,<br />
paediatrics, and information on a range of<br />
situations. These situations include motion<br />
sickness, emergency hormone contraception,<br />
nicotine replacement therapy and weight loss.<br />
The layout of each chapter covers basic<br />
anatomy, an understanding of the anatomical<br />
location of major structures, a discussion on<br />
the various common conditions relevant to<br />
the chapter, summary tables and algorithms<br />
to assist the reader to arrive at a differential<br />
diagnosis. It also suggests trigger points for<br />
referral and a list of Australian OTC medications<br />
suitable for treatment. At the end of each<br />
chapter there are a set of self assessment<br />
questions and case histories to test the reader’s<br />
comprehension of the chapter. Throughout<br />
the text, photographs assist the reader in<br />
identifying common conditions and diagrams<br />
summarise the relevant information.<br />
Each book chapter has different coloured<br />
tabs to enable the text to be used as a quick<br />
reference guide but the book could equally be<br />
used for study purposes.<br />
Private Hospital - April 2008<br />
Book Review<br />
“ This book aims to provide<br />
the pharmacist (and other<br />
non medical practitioners)<br />
with a greater and deeper<br />
knowledge on a range<br />
of minor complaints so a<br />
practitioner may be better<br />
able to distinguish more<br />
minor complaints from<br />
more grave scenarios. “<br />
79<br />
The text provides a very good summary of<br />
the more common health conditions that<br />
present in the community. It is easy to follow<br />
and the tables and algorithms are very useful<br />
in assisting a differential diagnosis. However<br />
community pharmacists and other non medical<br />
practitioners often conduct consultations<br />
in circumstances which are not completely<br />
private for the consumer. This limits the<br />
practitioner to a quick and sometimes cursory<br />
visual check of the patient. Common skin<br />
conditions and infestations must account<br />
for many OTC consultations. These are often<br />
difficult to diagnose and the text could be<br />
further enhanced with more photographs of<br />
these type of conditions.<br />
Overall this text as it stands is a valuable<br />
addition to an OTC practitioner’s library of<br />
reference texts and is highly recommended<br />
for those who want to refresh or update their<br />
knowledge.
80<br />
Private Hospital - April 2008
Private Hospital - April 2008<br />
81
82<br />
on the ground...<br />
... with Gail Rice<br />
What is your current job and how long<br />
have you been there?<br />
I am social welfare worker and Veterans Liaison<br />
Officer (VLO) at Canossa Private Hospital in<br />
Oxley, QLD. I have worked at Canossa for<br />
the past 4 ½ years. For most of that time,<br />
I have been the VLO. I have always had a<br />
particular interest in working with the veteran<br />
community.<br />
What is your background for your job?<br />
My father was a WWII veteran and after his<br />
death when I was 12, my mother became (and<br />
still is) a DVA war widow. We were supported<br />
by Legacy and DVA. My welfare studies 30<br />
“ Introducing veterans to each<br />
other is a great example of<br />
how a simple gesture can<br />
make the world of difference.<br />
Canossa will maintain its<br />
commitment to the veteran<br />
community, and I intend to<br />
enhance the standing of our<br />
veterans with all local service<br />
providers by way of advocacy<br />
and respect.”<br />
years ago were funded by DVA. I am now in<br />
the privileged position of applying my welfare<br />
skills and knowledge directly to the veteran<br />
community.<br />
What is Canossa’s commitment to<br />
working with veterans?<br />
Patients with DVA Gold Cards are admitted to<br />
all of our wards – palliative care, rehabilitation,<br />
general medical and oncology. We also hold a<br />
contract with DVA to provide interim care for<br />
veterans and war widows who need care while<br />
waiting for residential aged care. Whilst some<br />
interim care patients are offered placement<br />
soon after admission, some are with us for<br />
several months. This allows us to form a close<br />
bond with the patient and their families.<br />
What are your main responsibilities<br />
at VLO?<br />
I am advised of all DVA patients on admission,<br />
and make myself known to them. Many have<br />
no specific veteran-related needs, so my<br />
involvement may simply be supportive visits.<br />
Others benefit from substantial interventions.<br />
Typical involvement could entail:<br />
• Discharge planning. The best outcomes start<br />
with discharge planning from the time of<br />
admission. This involves a team approach of<br />
assessing patient’s needs and linking them<br />
with services in the community such as<br />
Private Hospital - April 2008<br />
community nursing, meal provision, domestic<br />
assistance etc. A thorough knowledge of<br />
services available and how to access them<br />
is essential for discharge to be effective and<br />
successful.<br />
• Residential aged care. Not all of our veterans<br />
and war widows are able to return home, so<br />
assistance to our patients and their family<br />
through the maze of information, paperwork<br />
etc is provided. Networking with the aged<br />
care facilities ensures optimal assistance to<br />
the patient.<br />
• DVA entitlements. This assessment can be<br />
of benefit to the veteran, as many have<br />
entitlements of which they are unaware. We<br />
have excellent relationships with local RSL<br />
sub-branches who will come to the hospital<br />
to provide advocacy and assistance.<br />
• Psychological support. Veterans (and their<br />
families) often have issues that are best met<br />
by veteran-specific services. Thus, referrals to<br />
the Veterans’ & Veterans’ Families Counselling<br />
Service, Veterans Home Care, Repatriation<br />
Transport Scheme, Legacy, War Widows<br />
Association are regularly made.<br />
What is the best part of your job?<br />
I find the most satisfying part of being a VLO<br />
is the positive response from veterans, war<br />
widows and their family. Without fail, veterans<br />
appreciate that there is someone interested<br />
in them. The veteran community is made up<br />
of a cross section of the community who has<br />
a common thread in their lives – ie service<br />
to their country. Ex- P.O.W.s, those with war<br />
related disabilities, recent widows, the socially<br />
isolated, Vietnam vets with specific needs – all<br />
appreciate the opportunity to interact with<br />
someone who cares about their welfare.<br />
Thoughts for the future?<br />
Introducing veterans to each other is a great<br />
example of how a simple gesture can make<br />
the world of difference. Canossa will maintain<br />
its commitment to the veteran community,<br />
and I intend to enhance the standing of our<br />
veterans with all local service providers by way<br />
of advocacy and respect.
PH Private Hospital - April 2008<br />
83
84<br />
Private Hospital - April 2008