03-PX-Anabolic-FSH
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
J Bone Miner Metab (2000) 18:2–8<br />
Review article<br />
© Springer-Verlag 2000<br />
The pancreas: A storehouse of protein anabolic factors<br />
and bone/calcium metabolism-regulating factors<br />
Yoshito Takaoka 1 and Toshiyuki Yoneda 2<br />
1<br />
Emeritus Professor of Nagasaki University, Nagasaki, Japan<br />
2<br />
Department of Biochemistry, Osaka University Faculty of Dentistry, 1-8 Yamadaoka, Suita 565-0871, Japan<br />
Key words: pancreas, salivary glands, protein anabolism,<br />
bone/calcium metabolism, elastase<br />
Classical pancreas extract<br />
Salivary glands/pancreas compensation theory<br />
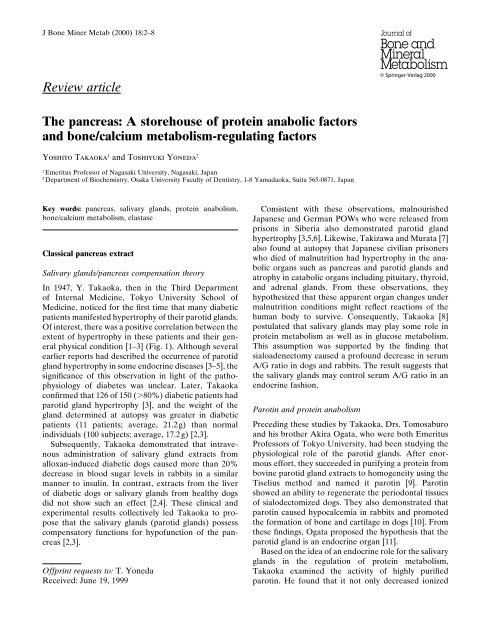
In 1947, Y. Takaoka, then in the Third Department<br />
of Internal Medicine, Tokyo University School of<br />
Medicine, noticed for the first time that many diabetic<br />
patients manifested hypertrophy of their parotid glands.<br />
Of interest, there was a positive correlation between the<br />
extent of hypertrophy in these patients and their general<br />
physical condition [1–3] (Fig. 1). Although several<br />
earlier reports had described the occurrence of parotid<br />
gland hypertrophy in some endocrine diseases [3–5], the<br />
significance of this observation in light of the pathophysiology<br />
of diabetes was unclear. Later, Takaoka<br />
confirmed that 126 of 150 (80%) diabetic patients had<br />
parotid gland hypertrophy [3], and the weight of the<br />
gland determined at autopsy was greater in diabetic<br />
patients (11 patients; average, 21.2g) than normal<br />
individuals (100 subjects; average, 17.2g) [2,3].<br />
Subsequently, Takaoka demonstrated that intravenous<br />
administration of salivary gland extracts from<br />
alloxan-induced diabetic dogs caused more than 20%<br />
decrease in blood sugar levels in rabbits in a similar<br />
manner to insulin. In contrast, extracts from the liver<br />
of diabetic dogs or salivary glands from healthy dogs<br />
did not show such an effect [2,4]. These clinical and<br />
experimental results collectively led Takaoka to propose<br />
that the salivary glands (parotid glands) possess<br />
compensatory functions for hypofunction of the pancreas<br />
[2,3].<br />
Offprint requests to: T. Yoneda<br />
Received: June 19, 1999<br />
Consistent with these observations, malnourished<br />
Japanese and German POWs who were released from<br />
prisons in Siberia also demonstrated parotid gland<br />
hypertrophy [3,5,6]. Likewise, Takizawa and Murata [7]<br />
also found at autopsy that Japanese civilian prisoners<br />
who died of malnutrition had hypertrophy in the anabolic<br />
organs such as pancreas and parotid glands and<br />
atrophy in catabolic organs including pituitary, thyroid,<br />
and adrenal glands. From these observations, they<br />
hypothesized that these apparent organ changes under<br />
malnutrition conditions might reflect reactions of the<br />
human body to survive. Consequently, Takaoka [8]<br />
postulated that salivary glands may play some role in<br />
protein metabolism as well as in glucose metabolism.<br />
This assumption was supported by the finding that<br />
sialoadenectomy caused a profound decrease in serum<br />
A/G ratio in dogs and rabbits. The result suggests that<br />
the salivary glands may control serum A/G ratio in an<br />
endocrine fashion.<br />
Parotin and protein anabolism<br />
Preceding these studies by Takaoka, Drs. Tomosaburo<br />
and his brother Akira Ogata, who were both Emeritus<br />
Professors of Tokyo University, had been studying the<br />
physiological role of the parotid glands. After enormous<br />
effort, they succeeded in purifying a protein from<br />
bovine parotid gland extracts to homogeneity using the<br />
Tiselius method and named it parotin [9]. Parotin<br />
showed an ability to regenerate the periodontal tissues<br />
of sialodectomized dogs. They also demonstrated that<br />
parotin caused hypocalcemia in rabbits and promoted<br />
the formation of bone and cartilage in dogs [10]. From<br />
these findings, Ogata proposed the hypothesis that the<br />
parotid gland is an endocrine organ [11].<br />
Based on the idea of an endocrine role for the salivary<br />
glands in the regulation of protein metabolism,<br />
Takaoka examined the activity of highly purified<br />
parotin. He found that it not only decreased ionized
Y. Takaoka and T. Yoneda: Pancreas: a storehouse of factors 3<br />
Fig. 1. Hypertrophy of the parotid<br />
glands in diabetic patients. Left, 60-<br />
year-old woman; right, 68-year-old<br />
man [6]<br />
blood calcium, total amino acids, and total protein but<br />
also increased blood A/G ratio and leukocyte number<br />
in rabbits. These findings suggest that parotin had an<br />
action equivalent to a growth hormone. From these<br />
results together with other data that are not described<br />
here, Takaoka suggested that the primary physiological<br />
action of parotin might be associated with stimulation<br />
of protein anabolism and, possibly, oxidative phosphorylation<br />
[12].<br />
Because parotin was shown to decrease urinary creatine<br />
in rabbits, an attempt was made to administer<br />
parotin to patients with progressive muscular dystrophy<br />
(PMD) that was characterized by creatinuria. Although<br />
parotin was not effective in patients with Duchenne and<br />
limb girdle-type PMD (the first and second most severe<br />
types of PMD, respectively), it unexpectedly and dramatically<br />
cured one patient with refractory myasthenia<br />
gravis (MG) and later three MG patients who also<br />
exhibited creatinuria [3,13].<br />
Pancreas extract (<strong>PX</strong>)<br />
According to his parotid gland–pancreas compensation<br />
theory [2], Takaoka began in 1952 to attempt to isolate<br />
a more potent protein anabolic hormone-like factor<br />
than parotin from pancreas (hereinafter called <strong>PX</strong>, for<br />
pancreas extract) [6,14,15] for treating PMD. Since<br />
then, 46 scientists have collaborated in this project<br />
(until 1998), innovated diverse techniques to purify <strong>PX</strong>,<br />
and made invaluable contributions to advance this<br />
study. In the early stages of <strong>PX</strong> purification, <strong>PX</strong> activity<br />
was monitored for its capacity to decrease ionized blood<br />
calcium, blood urea nitrogen (BUN), total protein, and<br />
amino acids and to increase white blood cell number in<br />
rabbits. These time-consuming and cumbersome studies<br />
were primarily conducted by Takaoka, then professor<br />
and Chairman of the First Department of Internal<br />
Medicine at Nagasaki University Schools of Medicine,<br />
and his collaborators in the Third Department of<br />
Internal Medicine at Tokyo University School of<br />
Medicine [1,2,8]. Initial problems in <strong>PX</strong> purification<br />
were overcome after they introduced acetone powder<br />
of porcine pancreas for purification. The <strong>PX</strong> prepared<br />
using this method showed several intriguing effects. In<br />
1964, an inpatient with severe MG (a 26-year-old<br />
woman) at Nagasaki University Hospital who had been<br />
unable to move for almost 4 years was cautiously given<br />
intramuscular injections of <strong>PX</strong> that had powerful activity<br />
to decrease BUN and Ca 2 . The patient exhibited<br />
marked improvement in her performance in response to<br />
<strong>PX</strong> within a week [16] and became able to return to her<br />
home only 1 month later. Being encouraged by this<br />
case, six additional MG patients were treated with <strong>PX</strong><br />
and all showed remarkable recovery from their disease.<br />
Furthermore, a patient (a 37-year-old woman) with<br />
facioscapulohumeral (<strong>FSH</strong>) PMD who volunteered<br />
to be treated with <strong>PX</strong> also demonstrated notable responses<br />
to <strong>PX</strong> (Fig. 2) [17–19]. In this case, it was noted<br />
that the patient not only became able to raise her legs<br />
but also gained weight. In fact, Takaoka noticed that the
4 Y. Takaoka and T. Yoneda: Pancreas: a storehouse of factors<br />
Fig. 2. Effects of pancreas extract<br />
(<strong>PX</strong>) on facioscapulohumeral<br />
progressive muscular dystrophy<br />
(<strong>FSH</strong> PMD) patient (37 years<br />
old). Left upper panel, 7 months<br />
after treatment. Left lower panel,<br />
before treatment. Right upper<br />
panel, 10 months after treatment.<br />
Right lower panel, 8 months after<br />
treatment. Note that the patient<br />
became able to raise her legs and<br />
also significantly gained weight<br />
after <strong>PX</strong> treatment [18]<br />
Fig. 3. Effects of <strong>PX</strong> on forced swimming<br />
test. Mice (ddy, male, 20–30 g)<br />
were treated with either NaCl or <strong>PX</strong><br />
(3mg/kg, ip, 90 min before test). Mice<br />
administered with <strong>PX</strong> could swim<br />
significantly longer than control mice.<br />
Numbers in parentheses indicate number<br />
of mice studied [14]<br />
majority of patients who were treated with <strong>PX</strong> showed<br />
an increase in their appetite.<br />
The calcium-lowering action of <strong>PX</strong> was another<br />
beneficial effect. In one case of synovial sarcoma of the<br />
knee joint associated with hypercalcemia, <strong>PX</strong> decreased<br />
calcium in a manner similar to salmon calcitonin [6].<br />
This biological property of <strong>PX</strong> suggested that <strong>PX</strong> might<br />
play a role in regulating bone/calcium metabolism.<br />
Consistent with these clinical results, <strong>PX</strong> was shown<br />
to prolong the survival of dystrophic mice [17], extend<br />
forced swimming time in mice (Fig. 3) [14], and increase<br />
RNA synthesis in cultured cells [20]. Histochemical<br />
study also revealed an increased RNA synthesis around<br />
the nuclei of skeletal muscles in rats [18].<br />
In 1967, a new technique of parotin purification from<br />
bovine parotid glands was established. This parotin was<br />
named MP parotin. Of interest, immunohistochemical<br />
studies using 125 I-labeled anti-MP-parotin antibodies<br />
revealed much stronger expression of the protein in<br />
Langerhans’ islets in the pancreas than in the parotid<br />
gland, suggesting the presence of an MP-patotin-like<br />
substance in pancreas [21]. Takaoka, therefore, applied<br />
this new technique for <strong>PX</strong> purification and observed<br />
that the <strong>PX</strong> prepared using this technique had more<br />
consistent and potent effects on serum ionized calcium<br />
than <strong>PX</strong> prepared by the old technique. Takaoka then<br />
began to collaborate with Suzuki and Yoneda in the<br />
Department of Biochemistry at Osaka University
Y. Takaoka and T. Yoneda: Pancreas: a storehouse of factors 5<br />
Faculty of Dentistry early in 1981. They decided to<br />
focus on the calcium-lowering action of <strong>PX</strong> based on<br />
this observation and established an in vitro bioassay<br />
that assesses the capacity of <strong>PX</strong> to inhibit parathyroid<br />
hormone- (PTH-) stimulated bone resorption in organ<br />
cultures of 45 Ca-labeled fetal rat long bones [22]. Introduction<br />
of this assay markedly facilitated purifying the<br />
calcium-lowering activity of <strong>PX</strong>. Moreover, Kikkawa<br />
independently found that this newly prepared <strong>PX</strong><br />
promoted migration of corneal epithelial cells in a<br />
similar manner to epidermal growth factor in vitro<br />
(unpublished observation).<br />
New generation <strong>PX</strong><br />
Potential role of pancreas in bone/calcium metabolism<br />
At the present time, it is widely recognized that bone,<br />
intestine, and kidney are the organs that maintain calcium<br />
homeostasis by regulating bone/calcium metabolism<br />
in cooperation with PTH, 1,25-dihydroxyvitamin<br />
D 3 (1,25-D 3 ), and calcitonin (CT). However, the observations<br />
described earlier suggest that the pancreas<br />
could be another organ that influences bone/calcium<br />
metabolism. There are several lines of evidence suggesting<br />
that pancreas may be involved in the regulation<br />
of bone/calcium metabolism [23–29]. With this background<br />
information, we attempted to identify a molecule<br />
that plays a role in the regulation of bone/calcium<br />
metabolism in the pancreas.<br />
Effects of <strong>PX</strong> on blood calcium levels and<br />
bone resorption<br />
We showed that systemic administration of <strong>PX</strong> that<br />
was prepared according to the methods described by<br />
Takaoka et al. [2] reproducibly decreased blood ionized<br />
calcium levels in normal rabbit and mice. <strong>PX</strong> also<br />
inhibited bone resorption, which was stimulated by<br />
PTH, interleukin-1α, and 1,25-D 3 [30] in organ cultures<br />
of fetal rat long bones. Inhibition of bone resorption<br />
by <strong>PX</strong> was caused by inhibition of osteoclast formation<br />
[30]. These data confirmed Takaoka’s previous<br />
data.<br />
Partial purification of <strong>PX</strong> by anion exchange, followed<br />
by size exclusion column chromatography<br />
Acetone powder of porcine pancreas was processed<br />
through a DE-52 anion exchange column and subsequently<br />
Sephacryl S-200 HR columns. Fractions eluted<br />
between 25 and 43 KDa demonstrated an activity that<br />
promoted DNA synthesis in MG-63 human osteoblastic<br />
osteosarcoma cells and inhibited 1,25-D 3 -stimulated<br />
bone resorption. This partially purified <strong>PX</strong> was approximately<br />
200 times more potent than crude <strong>PX</strong> in hypocalcemic<br />
activity in normal mice.<br />
Effects of partially purified <strong>PX</strong> on cancer-associated<br />
hypercalcemia<br />
<strong>PX</strong> was tested in nude mice bearing a human squamous<br />
cell carcinoma (MH-85) [31] that causes hypercalcemia<br />
with no bone metastases and cachexia with anorexia<br />
and also increases osteoclastic bone resorption [32].<br />
In these tumor-bearing nude mice, <strong>PX</strong> prevented the<br />
progression of hypercalcemia and inhibited osteoclastic<br />
bone resorption [33]. Moreover, <strong>PX</strong> inhibited<br />
osteoclast-like cell formation and bone resorption that<br />
had been stimulated by conditioned medium of MH-85<br />
cells. Interestingly, <strong>PX</strong> increased food intake, decreased<br />
weight loss, and prevented the development of cachexia<br />
[33]. Eventually, <strong>PX</strong> profoundly prolonged survival of<br />
MH-85-tumor-bearing nude mice [33]. Takaoka also<br />
found that <strong>PX</strong> prolonged the survival of irradiated mice<br />
(unpublished observation). Thus, <strong>PX</strong> may potentially<br />
be a beneficial agent for hypercalcemia and cachexia<br />
associated with malignancy.<br />
Purification of <strong>PX</strong> to homogeneity<br />
<strong>PX</strong> was purified to homogeneity by successive steps<br />
including anion exchange chromatography on DE-52,<br />
isoelectric focusing on Miniphor, and reverse-phase<br />
HPLC on a C 18 column. The purified material was<br />
eluted as a single protein peak at 50% acetonitrile in<br />
0.1% trifluoroacetic acid on the C 18 column and showed<br />
promotion of DNA synthesis in MG-63 cells and inhibition<br />
of 1,25-D 3 -stumulated bone resorption. Silver<br />
staining on SDS-PAGE demonstrated that this protein<br />
peak migrated as a single band at approximately<br />
28 KDa. Amino acid sequence analysis of the 28-KDa<br />
protein revealed 32 amino acids from the N-terminus<br />
that had 92% homology with human elastase III B [34]<br />
as previously reported [35].<br />
Effects of recombinant human elastase IIIB (rhEIIIB)<br />
on bone resorption and blood calcium levels<br />
RhEIIIB markedly inhibited 1,25-D 3 -stimulated bone<br />
resorption and pit formation by isolated osteoclasts.<br />
These effects were blocked by polyclonal antibodies to<br />
rhEIIIB. RhEIIIB also decreased blood ionized calcium<br />
levels, which were increased by local administration<br />
of interleukin-1 in normal mice [34]. These results<br />
clearly demonstrate that the bone/calcium metabolismregulating<br />
activity of <strong>PX</strong> is accounted for by elastase<br />
IIIB, and thus, <strong>PX</strong> is distinct from known bone/calciumregulating<br />
hormones and cytokines such as CT, amylin,<br />
glucagon, and transforming growth factor-β.
6 Y. Takaoka and T. Yoneda: Pancreas: a storehouse of factors<br />
Table 1. Effects of pancreas extract (<strong>PX</strong>) on bone/calcium<br />
metabolism<br />
In vitro<br />
Stimulates proliferation and differentiation of<br />
osteoblast-like cells<br />
Increases bone nodule formation<br />
Inhibits osteoclastic bone resorption<br />
Decreases osteoclast formation<br />
In vivo<br />
Decreases serum calcium in normal mice<br />
Inhibits bone resorption<br />
Stimulates bone formation<br />
In tumor-bearing mice with hypercalcemia:<br />
Reverses calcium levels<br />
Promotes appetite<br />
Decrease loss of body weight<br />
Prolongs survival<br />
Effects of rhEIIIB on bone formation in vitro and in<br />
vivo<br />
We have recently found that repeated subcutaneous<br />
injections of rhEIIIB on mouse calvariae induced new<br />
bone formation and that treatment of fetal rat calvarial<br />
cells with rhEIIIB increased bone nodule formation in<br />
vitro (manuscript in preparation).<br />
The effects of <strong>PX</strong> on bone/calcium metabolism are<br />
summarized in Table 1.<br />
in turn modulates the proliferation, differentiation, and<br />
function of osteoblasts and osteoclasts.<br />
Some elastases, such as endogenous vascular elastase<br />
[44], are reported to have a homology with adipsin, of<br />
which expression is correlated with the differentiation of<br />
adipocytes [45]. It is notable that adipocytes differentiate<br />
from mesenchymal stem cells, which also differentiate<br />
into osteoblasts [46]. Thus, adipsin might be involved in<br />
the regulation of differentiation of osteoblasts as well as<br />
adipocytes. If this is the case, elastase might also play a<br />
role in osteoblastic differentiation as well.<br />
Recently, a unique cell-surface receptor that mediates<br />
responses of platelets to a serine protease thrombin<br />
has been identified [47]. This receptor, which has seven<br />
transmembrane-spanning structures, is activated by<br />
proteolytic cleavage of the N-terminus at its tethered<br />
end by thrombin. It thus is called protease-activated<br />
receptor. Of note, expression of thrombin receptors has<br />
recently been found in bone [48]. Moreover, thrombin is<br />
shown to stimulate bone resorption and elicit a variety<br />
of cellular responses in osteoblasts [47]. Because the<br />
osteotropic activity of <strong>PX</strong> is at least in part accounted<br />
for by elastase IIIB, which also belongs to the serine<br />
protease family, it is plausible to speculate that osteoblasts<br />
and osteoclasts might possess receptors that<br />
are activated by elastase IIIB. <strong>PX</strong> might exhibit its<br />
biological effects through these receptors.<br />
Mechanisms of EIIIB effects on bone/calcium<br />
metabolism<br />
Mechanisms by which EIIIB affects bone/calcium metabolism<br />
are unknown at the present time. The enzyme<br />
catalytic activity may be essential for exertion of its<br />
inhibitory effect on bone resorption because protease<br />
inhibitors markedly impaired bone resorption-inhibiting<br />
activity (unpublished observation). On the other<br />
hand, Tomomura et al. [36–38], who independently<br />
identified a calcium-lowering molecule named caldecrin<br />
that is homologous to elastase IV in rat pancreas, reported<br />
that a protease inhibitor (PMSF) did not diminish<br />
the activity. Thus, the requirement of enzyme<br />
catalytic activity of elastase for osteotropic activity is yet<br />
to be elucidated.<br />
Elastase-like serine proteases have recently been<br />
found to generate soluble mature form of transforming<br />
growth factor-α (TGF-α) by cleavage of two alanine/<br />
valine sequences located at positions 38–39 and 88–89 in<br />
membrane-bound pro-TGF-α (39–41). Furthermore, it<br />
has also been described that elastase releases extracellular<br />
matrix-bound TGF-β 1 [42] and basic fibroblast<br />
growth factor [43]. Thus, elastases may cleave or release<br />
membrane-anchored or matrix-bound cytokines and<br />
growth factors and increase the local concentrations of<br />
these molecules in the bone microenvironment, which<br />
Concluding summary<br />
In this review article, we have described diverse effects<br />
of pancreatic factor <strong>PX</strong>, including long-standing large<br />
bodies of work by Takaoka, who has been characterizing<br />
<strong>PX</strong> over the last half-century. Although the precise<br />
molecular mechanisms by which <strong>PX</strong> shows these diverse<br />
effects are unclear, it is likely that <strong>PX</strong> has protein<br />
anabolic effects that evidently cured some patients with<br />
PMD and MG. Whatever the mechanisms are, these<br />
data of Takaoka strongly suggest that the pancreas is<br />
the organ that participates in the regulation of protein<br />
metabolism. His data also suggest that the pancreas<br />
contains yet unknown additional protein anabolic factors<br />
that are involved in controlling BUN, total protein,<br />
and white blood cell count. Further studies are required<br />
for identifying these factors.<br />
Very little has been studied about the role of the<br />
pancreas in the regulation of bone and calcium metabolism<br />
to date. Progress of state-of-the-art techniques for<br />
protein purification and molecular biology has enabled<br />
us to demonstrate that pancreas produces a molecule<br />
that modulates bone/calcium metabolism. This molecule<br />
turns out to be elastase IIIB, which belongs to the<br />
serine protease family. These results suggest that the<br />
pancreas as well as bone, kidney, and intestine also
Y. Takaoka and T. Yoneda: Pancreas: a storehouse of factors 7<br />
plays a role in regulating bone/calcium metabolism. It is<br />
expected that the study of <strong>PX</strong> deepens our insights into<br />
bone biology and calcium metabolism and, it is hoped,<br />
will lead to the development of alternative interventions<br />
for the treatment of metabolic bone diseases such<br />
as osteoporosis.<br />
The pancreas is, therefore, a storehouse of a variety<br />
of previously unappreciated molecules that regulate not<br />
only protein metabolism but also bone/calcium metabolism.<br />
Pursuit of further molecular characterization of<br />
the pancreas is eagerly awaited.<br />
Acknowledgments. The authors are very grateful to all<br />
the collaborators who devoted their invaluable efforts<br />
to <strong>PX</strong> study during the past 50 years. We greatly regret<br />
that not all the names of these researchers can be listed<br />
here. We wish to note that the <strong>PX</strong> study could not have<br />
been accomplished without these people. The authors<br />
also thank Miss Mie Masuda for her excellent secretarial<br />
assistance.<br />
References<br />
1. Takaoka Y, Kosaka K (1948) Studies on the hormonal secretion<br />
of the salivary gland (in Japanese). Rinshoiho 2:87–96<br />
2. Takaoka Y, Yamaguchi T, Yamada N, Kosaka K (1954) Der<br />
hormonale Einfluss der Parotisdruesen auf den Kohlenhydrat und<br />
Eiweiss-stoffwechsel. Klin Wochenschr 32:369–375<br />
3. Takaoka Y (1955) Influence of the salivary gland on the various<br />
kinds of the metabolism (in Japanese). Hormone Rinsyo 3:957–<br />
988<br />
4. Takaoka Y, Ozaka K, Yakawa S (1950) Hypertrophy of parotid<br />
glands in diabetes mellitus and internal secretion of salivary<br />
glands. Jpn Med J 3:199–2<strong>03</strong><br />
5. Takaoka Y, Yamaguchi T, Kosaka K (1952) Relation of the<br />
parotid gland to serum protein and malnutrition. Tohoku J Exp<br />
Med 57:9–15<br />
6. Takaoka Y (1980) A novel protein anabolic hormone in pancreas<br />
(in Japanese). Nihonijishinpo 2951:15–20<br />
7. Murata K, Takizawa E (1947) Histopathological observations of<br />
endocrine organs in malnutrition syndrome (in Japanese). J Jpn<br />
Soc Pathol 36:9–10<br />
8. Takaoka Y (1952) Proposal of a new protein anabolic hormone<br />
from pancreas (in Japanese). Nihon Rinsho 10:515–522<br />
9. Ogata T (1943) Studies on endocrine role of salivary glands in the<br />
Department of Pathology, Tokyo University (in Japanese).<br />
Ikaishuho 425:831–837<br />
10. Ogata A, Ito Y, Nozaki N, Ogata T, Ishii Z (1944) On the parotid<br />
gland hormone (in Japanese). Med Biol (Tokyo) 5:253–257<br />
11. Ito Y (1960) Parotin: a salivary gland hormone. Ann NY Acad Sci<br />
85:228–312<br />
12. Takaoka Y, Yamaguchi T, Yamada N, Ishikawa T, Yuasa K,<br />
Ninomiya H (1956) Der Einfluss der Parotisdrusen auf den<br />
Stoffwechsel III. Mitteilung Die foerdernde Wirkung des Parotins<br />
auf Eiweissaufbau und Citronensaeurecyclus. Z Ges Exp Med<br />
127:2<strong>03</strong>–212<br />
13. Takaoka Y, Uono M, Ninomiya H, Yoshikawa M, Yamada N,<br />
Ishikawa T (1955) Der hormonale Einfluss der Parotisdrusen auf<br />
den Eiweissstoffwechsel. II. Mitteilung. Parotinbehandlung gegen<br />
Myasthenia gravis. Klin Wochenschr 33:156–160<br />
14. Takaoka Y, Hiwaki C, Ozawa H, Ichinose M, Otsubo Y, Shikaya<br />
T, Kikutani M, Yuasa A, Yamamoto K, Ando K (1966) A pancreatic<br />
protein anabolic extract. Proposal of a protein anabolic<br />
extract fron pancreas. I. Preliminary report. Acta Med<br />
Nagasakiensia 10:51–57<br />
15. Takaoka Y, Yokouchi H, Hiwaki C (1967) Isolation of protein<br />
anabolic factor from mammalian pancreatic tissue. Recent Adv<br />
Gastroenterol (Proce 3rd World Congress Gastroenterol) 4:348–<br />
349<br />
16. Takaoka Y, Takamori M, Ichinose M, Shikiya T, Igawa N,<br />
Kikutani M, Yamamoto K (1969) Hypocalcemic action of a pancreatic<br />
factor and its clinical significance on the myasthenic<br />
patients. Acta Med Nagasakiensia 13:28–35<br />
17. Takaoka Y, Takamori M, Ichinose M, Tujihata M, Mori M,<br />
Eguchi K, Mori T, Mori K, Hazama R, Ezaki K (1977) A protein<br />
anabolic factor from porcine pancreas and its effects on mice<br />
and patients with progressive muscular dystrophy. IRCS 5:1<strong>03</strong>–<br />
105<br />
18. Takaoka Y, Hazama R (1980b) Perspective of therapeutic agents<br />
for progressive muscular dystrophy (in Japanese). Saishinigaku<br />
35:999–1007<br />
19. Takaoka Y, Takamori M (1981) A pancreatic protein anabolic<br />
factor and progressive muscular dystrophy. Excerpta Med Int<br />
Congr Ser 548:356<br />
20. Takaoka Y, Takamori M, Ichinose M, Mori K, Eguchi K,<br />
Kikutani M (1974) Isolation of the blood calcium and urea reducing<br />
factor from mammalian pancreas and its activating effect on<br />
RNA synthesis in cultured cells. IRCS (Lond) 2:1577<br />
21. Iwasaki I, Horie H, Tamaru J, Ide G, Aonuma A (1981)<br />
Pathohistological study on the effects of parotid gland extracts<br />
(parotin and its subunit) on mesenchymal tissues (in Japanese).<br />
Symp Salivary Grand 22:9–14<br />
22. Raisz LG (1965) Bone resorption in tissue culture. Factors<br />
influencing the response to parathyroid hormone. J Clin Invest<br />
44:1<strong>03</strong>–116<br />
23. Lee S, Clark SA, Gill RK, Christakos S (1994) 1,25-<br />
Dihydroxyvitamine D 3 and pancreatic β-cell function: vitamin D<br />
receptors, gene expression, and insulin secretion. Endocrinology<br />
134:1602–1610<br />
24. Steinberg W, Tenner S (1994) Acute pancreatitis. N Engl J Med<br />
330:1198–1210<br />
25. Hauser CJ, Kamrath RO, Sparks J, Shoemaker WC (1983) Calcium<br />
homeostasis in patients with acute pancreatitis. Surgery<br />
(St Louis) 94:830–835<br />
26. Weir GC, Lesser PB, Drop LJ, Fischer JE, Warshaw AL (1975)<br />
The hypercalcemia of acute pancreatitis. Ann Intern Med 83:185–<br />
189<br />
27. Noguchi A, Eren M, Tsang RC (1980) Parathyroid hormone in<br />
hypocalcemic infants of diabetic mothers. J Pediatr 97:112–114<br />
28. Rosai J (1968) Carcinoma of the pancreas simulating giant cell<br />
tumor of bone; electron microscopic evidence of its acinal cell<br />
origin. Cancer (Phila) 22:333–344<br />
29. Newbound MJ, Benbow EW, Sene A, Yong M, Taylor TV (1992)<br />
Adenocarcinoma of the pancreas with osteoclast-like giant cells; a<br />
case report with immunocytochemistry. Pancreas 7:611–615<br />
30. Yoneda T, Takaoka Y, Alsina MM, Garcia J, Mundy GR (1991a)<br />
Porcine pancreas extract decreases blood-ionized calcium in mice<br />
and inhibits osteoclast formation and bone resorption in culture.<br />
FEBS Lett 278:171–174<br />
31. Yoneda T, Nishikawa N, Nishimura R, Kato I, Sakuda M (1989)<br />
Three cases of squamous cancer associated with leukocytosis,<br />
hypercalcemia or both. Oral Surg Oral Med Oral Pathol 68:604–<br />
611<br />
32. Yoneda T, Aufdemorte TB, Nishimura R, Nishikawa N, Sakuda<br />
M, Alsina MM, Chavez JB, Mundy GR (1991) Occurrence of<br />
hypercalcemia and leukocytosis with cachexia in a human squamous<br />
cell of the maxilla in athymic nude mice: a novel experimental<br />
model of 3 concomitant paraneoplastic syndromes. J Clin<br />
Oncol 9:468–477<br />
33. Yoneda T, Takaoka Y, Boyce BF, Scott L, Mundy GR (1994)<br />
Extract of porcine pancreas prevent progression of hypercalcemia
8 Y. Takaoka and T. Yoneda: Pancreas: a storehouse of factors<br />
and cachexia and prolong survival in nude mice bearing a human<br />
squamous carcinoma. Cancer Res 54:2509–2513<br />
34. Izbicka E, Yoneda T, Takaoka Y, Horn D, Williams PJ, Mundy<br />
GR (1996) Identification of a novel bone/calcium metabolismregulating<br />
factor in porcine pancreas. J Biol Chem 271:23230–<br />
23234<br />
35. Tani T, Ohsumi J, Mita K, Takiguchi Y (1988) Identification of a<br />
novel class of elastase III, by cDNA and genomic gene cloning.<br />
J Biol Chem 263:1231–1239<br />
36. Tomomura A, Fukushige T, Noda T, Noikura T, Saheki T (1992)<br />
Serum calcium-decreasing factor (caldecrin) from porcine pancreas<br />
has proteolytic activity which has no clear connection with<br />
the calcium decrease. FEBS Lett 301:277–281<br />
37. Tomomura A, Tomomura M, Fukushige T, Akiyama M, Kubota<br />
N, Kumaki N, Nishii Y, Noikura T, Saheki T (1995) Molecular<br />
cloning and expression of serum calcium-decreasing factor<br />
(caldecrin). J Biol Chem 270:3<strong>03</strong>15–3<strong>03</strong>21<br />
38. Tomomura A, Akiyama M, Itoh H, Yoshino I, Tomomura M,<br />
Nishii Y, Noikura T, Saheki T (1996) Molecular cloning and<br />
expression of human caldecrin. FEBS Lett 386:26–28<br />
39. Massague J (1990) Transforming growth factor-α: a model for<br />
membrane-anchored growth factors. J Biol Chem 15:21393–21396<br />
40. Cappelluti E, Strom SC, Harris RE (1993) Potential role of two<br />
novel elastase-like enzymes in processing pro-transforming<br />
growth factor-α. Biochemistry 32:551–560<br />
41. Baselga J, Mendelsohn J, Kim Y-M, Pandiella A (1996)<br />
Autocrine regulation of membrane transforming growth factor-α<br />
cleavage. J Biol Chem 271:3279–3284<br />
42. Taipale J, Lohi J, Saarinen, Kovanen PT, Keski-Oja J (1995)<br />
Human mast cell chymase and leukocyte elastase release latent<br />
transforming growth factor β-1 from the extracellular matrix of<br />
cultured human epithelial and endothelial cells. J Biol Chem<br />
270:4689–4696<br />
43. Thompson K, Rabinovitch M (1996) Exogenous leukocyte and<br />
endogenous elastases can mediate mitogenic activity in pulmonary<br />
artery smooth muscle cells by release of extracellular matrixbound<br />
basic fibroblast growth factor. J Cell Physiol 166:495–<br />
505<br />
44. Zhu L, Wingle D, Hinek A, Kobayashi J, Ye C, Zuker M, Dodo<br />
H, Keeley FW, Ravinovitch M (1994) The endogenous vascular<br />
elastase that governs development and progression of<br />
monocrotaline-induced pulmonary hypertension in rats is a novel<br />
enzyme related to the serine proteinase adipsin. J Clin Invest<br />
94:1163–1171<br />
45. Cook KS, Min HY, Johnson D, Chaplinsky RJ, Flier JS, Hunt CR,<br />
Spiegelman BM (1987) Adipsin: a circulating serine protease<br />
homologue secreted by adipose tissue and sciatic nerve. Science<br />
237:402–405<br />
46. Bianco P, Robey PG (1999) Diseases of bone and stromal cell<br />
lineage. J Bone Miner Res 14:336–341<br />
47. Grand RJA, Turnell AS, Grabham PW (1996) Cellular consequences<br />
of thrombin-receptor activation. Biochem J 313:353–<br />
368<br />
48. Abraham LA, Jenkins AL, Stone SR, Mackie EJ (1998) Expression<br />
of the thrombin receptor in developing bone and associated<br />
tissues. J Bone Miner Res 13:818–827