Understand Together
2hrnrQx
2hrnrQx
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
vol. 10 | issue 8 | WINTEr 2016<br />
staff magazine of the IRISH HEALTH SERVICE<br />
<strong>Understand</strong><br />
<strong>Together</strong><br />
Dementia<br />
campaign<br />
Values in<br />
Action<br />
features general news you section lifestyle
Welcome to the<br />
latest edition of<br />
Health Matters<br />
I don’t think any reader will fail to be<br />
moved to tears when they read the story<br />
of Tom Fahy, a young baby diagnosed<br />
with Edwards Syndrome in pregnancy<br />
and lived just 11 days. His parents have<br />
bravely shared their experiences and the<br />
support they received from the staff at<br />
the Coombe maternity hospital during<br />
the heartbreaking time.<br />
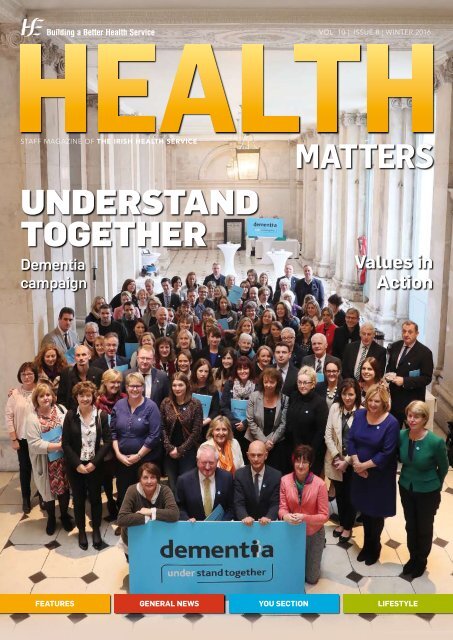
Our cover story for this edition is the<br />
Dementia <strong>Understand</strong> <strong>Together</strong>, a new<br />
campaign to increase awareness of<br />
dementia.<br />
It is an amazing public support,<br />
awareness and information campaign<br />
aimed at inspiring people from all<br />
sections of society to stand together<br />
with the 55,000 Irish people living<br />
with dementia. Nearly every one of<br />
us knows somebody who is directly<br />
affected by dementia.<br />
Another groundbreaking development<br />
we are highlighting is the Values in<br />
Action project which kicked off in the<br />
Midwest recently with 180 volunteers.<br />
Staff were introduced to nine behaviours<br />
that reflect the HSE values of care,<br />
compassion, trust and learning and it is<br />
hoped that these influential individuals<br />
or ‘champions’ will spread the<br />
behaviours to colleagues and put them<br />
into action on the ground.<br />
The project is based on the belief<br />
that real and sustainable culture<br />
change can be shaped by ordinary staff<br />
members across the country. Well done<br />
to all involved.<br />
As ever, we welcome your ideas and<br />
feedback on the magazine.<br />
A sincere thanks to all those who have<br />
sent in contributions to this edition and<br />
I hope you find plenty of interesting<br />
reading in it.<br />
Joanne Weston<br />
Joanne Weston,<br />
Editor<br />
Contents<br />
You Section<br />
06 STAND TOGETHER<br />
New campaign launched to increase<br />
awareness of dementia<br />
08 I QUIT FOR GOOD<br />
One man’s journey to quitting for good<br />
10 SUPPORT FOR PARENTS<br />
Parents of little Tom Fahy share their<br />
heart-breaking experience<br />
12 TALLAGHT NURSE MAKES HISTORY<br />
Helen becomes first Irish Inherited<br />
Cardiac Conditions Clinical Nurse<br />
Specialist<br />
13 SERVICE USER ENGAGEMENT<br />
Interview with Liam Hennessy, new<br />
Head of Service User Engagement in<br />
Mental Health<br />
14 STAFF ACHIEVEMENTS<br />
Staff achievements from around the<br />
country<br />
15 LIMERICK BOOST FOR PIETA HOUSE<br />
Limerick people step out for Pieta House<br />
16 NO ORDINARY SWIMMING CLUB<br />
Mary Arrigan-Langan remembers 35<br />
years of Octopus<br />
17 QUADRULPLETS JOIN TWINS AND<br />
TRIPLETS<br />
Newborn history at University Maternity<br />
Hospital Limerick<br />
18 STAFF UPDATE<br />
Quick updates from around the country<br />
19 CROKE PARK SHOWDOWN<br />
Trainee nurses go head to head at the<br />
All- Ireland Senior Camogie Final<br />
20 BENCHES UNVEILED<br />
Cherry Orchard Hospital teams up with<br />
Irish Prison Service<br />
Features<br />
21 VALUES IN ACTION<br />
Making our values a visible part of our<br />
everyday actions<br />
24 BREASTFEEDING<br />
New expanded services for parents at<br />
www.breastfeeding.ie<br />
26 ACTIVITY-BASED FUNDING<br />
The money follows the patient in new<br />
system<br />
28 NATIONAL OFFICE OF CLINICAL AUDIT<br />
Aiming to improve patient outcomes<br />
29 HSELIVE<br />
New multi-channel information service<br />
to answer your health services<br />
questions<br />
30 COMMUNITY INTERVENTION TEAMS<br />
Service reducing unnecessary hospital<br />
stays<br />
31 STAFF SURVEY<br />
Thanks for giving us your time and<br />
views<br />
32 FRONT LINE OWNERSHIP<br />
Valuing staff knowledge and creativity<br />
34 INDIVIDUAL HEALTH IDENTIFIER<br />
A patient safety initiative<br />
36 INNOVATION SHOWCASE<br />
Exhibition showcases technologies that<br />
will revolutionise healthcare<br />
<br />
This magazine is produced by the<br />
HSE Communications Division<br />
Publishers: Celtic Media Group<br />
www.celticmediagroup.ie<br />
Feedback: Send your feedback to<br />
healthmatters@hse.ie, joanne.weston@hse.ie<br />
Healthy Weight<br />
New policy and action plan
HEALTH MATTERS winter 2016<br />
38 QUALITY AND SAFETY COMMITTEE<br />
The care we provide<br />
39 HBS LOOK TO THE FUTURE<br />
Significant success achieved in first<br />
three years<br />
40 COMMUNICATING CLEARLY<br />
New tools to assist staff in how to<br />
speak to patients and colleagues<br />
42 SCHWARTZ ROUNDS<br />
Staff given opportunity to reflect on<br />
emotional aspect of their work<br />
44 SINGLE ASSESSMENT TOOL<br />
Ensuring older people receive<br />
appropriate care and support<br />
46 CHILDREN FIRST<br />
Promoting the safety and wellbeing of<br />
children<br />
46 AGEING WELL<br />
Overwhelming response to St Finbarr’s<br />
Ageing Well group<br />
47 LINN DARA AWARD<br />
Building is ‘welcoming and reassuring’<br />
48 HEALTH AND SAFETY<br />
Thousands of incidents reported<br />
49 NALOXONE USE<br />
How to save a life<br />
50 HOME SHARING<br />
The alternative to traditional respite<br />
services<br />
51 COPD SERVICES<br />
New outreach clinics in Cork<br />
52 MEDICAL CARDS<br />
Three-year plan outlined<br />
52 LITTLE GOES A LONG WAY<br />
Promotion of public health campaigns<br />
24<br />
63<br />
66<br />
77<br />
17<br />
winter 2016 | health matters |
67<br />
Get the<br />
flu vaccine<br />
Contents<br />
55<br />
59<br />
News<br />
53 TRAINING THE TRAINERS<br />
Organ donation and transplant staff<br />
undertake new course<br />
53 DRUGS AND ALCOHOL HELPLINE<br />
Email support service available<br />
54 INJURY UNITS<br />
Positive feedback from patients<br />
55 DA VINCI ROBOT<br />
State-of-the-art technology comes to<br />
Limerick theatre room<br />
56 #HELLOMYNAMEIS IN TULLAMORE<br />
1,000 staff sign up to campaign<br />
57 VIRTUAL DEMENTIA TOUR<br />
Tour offers unique insight<br />
58 HEALTHY IRELAND SURVEY<br />
One in four people still smoke<br />
59 SAFEGUARDING OLDER PEOPLE<br />
Seminar takes place as part of joint<br />
initiative<br />
59 EMERGENCY EXERCISE<br />
HSE staff volunteer in Dublin Airport<br />
exercise<br />
60 FLU VACCINE<br />
‘Jab helps keep me alive’<br />
61 BABY BOX IN LIMERICK<br />
Initiative to reduce incidence of infant<br />
mortality<br />
62 SEXUAL HEALTH PROMOTION<br />
Concludes first year as a national<br />
programme<br />
63 MEDICAL CAREERS DAY<br />
Building your future<br />
63 INTERCULTURAL HEALTH AWARD<br />
Pilot project one of six finalists<br />
64 PSYCHOACTIVE DRUGS<br />
Use in Ireland continues to rise<br />
73<br />
64 INNOVATIVE WEBINAR<br />
QI Talktime launched<br />
65 BALLAGHDERG GARDEN<br />
Revamp at Special Needs preschool<br />
65 WE MUST WORK TOGETHER<br />
Connecting for Life Donegal conference<br />
66 UNDER THE WEATHER<br />
Treating common complaints with<br />
common sense<br />
67 PREMATURE BABIES LEAFLET<br />
New booklet and online information<br />
Lifestyle<br />
68 OPTIMISING POWER IN WORK<br />
New awareness campaign teaches energy<br />
69 NEW GALWAY HOSPITAL WEBSITE<br />
Site launched in early September to<br />
highlight accessible walking routes<br />
70 LEARNING HOW TO GET ACTIVE<br />
46 HSE staff complete the Irish Heart<br />
Foundation Active@Work training<br />
| health matters | winter 2016
online<br />
Sites we like<br />
www.ehealthireland.ie<br />
60<br />
www.irishprematurebabies.com<br />
HEALTH MATTERS winter 2016<br />
www.understandtogether.ie<br />
71 ACTIVE AT WORK AWARDS<br />
18 HSE workplace earn plaudits<br />
for their efforts<br />
72 ACTIVE IN WINTER<br />
Top tips for getting enough exercise<br />
through the cold winter months<br />
73 ST FINBARR’S GET WALKING<br />
Staff lunchtime walking groups proving<br />
a huge success<br />
74 FOOD ALLERGENS<br />
The Environmental Health Service<br />
protecting the public from this very real<br />
food safety risk<br />
76 REDUCE PORTION SIZES<br />
Parents urged to give children childsized<br />
portions<br />
77 REDUCING THE BURDEN<br />
OF OBESITY<br />
New policy and action plan aims to<br />
reverse obesity trends<br />
78 FIRST DRIVE<br />
We check out the Citroen Grand<br />
C4 Picasso<br />
www.undertheweather.ie<br />
winter 2016 | health matters |
You<br />
Section<br />
<strong>Understand</strong> <strong>Together</strong><br />
campaign to tACKLE<br />
DEMENTIA STIGMA<br />
ementia <strong>Understand</strong> <strong>Together</strong>,<br />
a new campaign to increase<br />
awareness of dementia, was<br />
D<br />
launched on Monday, October<br />
24th at City Hall in Dublin. It is<br />
a public support, awareness and information<br />
campaign aimed at inspiring people from all<br />
sections of society to stand together with<br />
the 55,000 Irish people living with dementia.<br />
The ultimate aim is to create an Ireland that<br />
embraces and includes people living with<br />
dementia, one which displays solidarity with<br />
them and their loved ones.<br />
<strong>Understand</strong> <strong>Together</strong> is led by the HSE<br />
working with The Alzheimer Society of Ireland<br />
and Genio and a coalition of over 30 partners<br />
from business, academic, health and voluntary<br />
and community sectors. The campaign is funded<br />
by the State and The Atlantic Philanthropies.<br />
Any one of us can develop<br />
dementia...<br />
The launch was attended by over 100 people<br />
representing all parts of Irish society showing<br />
their support for building more inclusive and<br />
understanding communities for people with<br />
dementia and their loved ones.<br />
Professor Brian Lawlor, Trinity College Dublin<br />
and chair of the campaign steering group, said,<br />
“Each year over 4,000 people develop dementia<br />
in Ireland - over 11 people a day. All are living<br />
with a brain condition that deeply affects their<br />
lives and the lives of people who love and<br />
care for them.” Research undertaken for the<br />
campaign shows that fear and stigma surround<br />
dementia, resulting in unnecessary loneliness<br />
and isolation for people living with dementia<br />
and for their families. It can also result in delays<br />
in seeking help and diagnosis with people<br />
missing out on available supports and services<br />
as a result. These services and supports can<br />
allow people to live well with dementia for<br />
many years while maintaining their dignity and<br />
quality of life.”<br />
Ronan Smith, who is living with dementia<br />
and is a member of the campaign steering<br />
group, said, “Life doesn’t end when dementia<br />
begins. People with dementia can and do<br />
live meaningful, active lives for many years.<br />
Diagnosis doesn’t mean we immediately lose our<br />
skills and abilities, our need to belong and share<br />
or, above all, our sense of dignity. Respecting<br />
the diversity of the dementia experience and the<br />
individuality of people who are living with it is a<br />
vital step in recognising that the person is a lot<br />
more than the condition.”<br />
everyone can play a part by<br />
understanding more<br />
ONE in two Irish people know or have known<br />
someone with dementia. Despite this, only 1 in<br />
4 people feel they have a good understanding<br />
of what dementia is and what it isn’t. This<br />
campaign, as part of the National Dementia<br />
Strategy, aims to build understanding using<br />
existing projects to promote greater openness<br />
about dementia.<br />
Dementia not only deeply impacts individuals<br />
with the conditioni but also the lives of their<br />
loved ones. Those caring for loved ones with<br />
dementia often experience loneliness and<br />
isolation. Margot McCambridge, who cared for<br />
her husband and is a member of the campaign<br />
steering group, said, “The caring experience is<br />
complicated. It can be rewarding. It can also<br />
be hugely difficult at times. Support is needed<br />
for the carers as much as for the person with<br />
dementia. If the carer is supported, this in itself<br />
supports the person with dementia.”<br />
Dr Stephanie O’ Keeffe, National Director of<br />
Health & Wellbeing, HSE, commented, “The<br />
HSE is proud to be working with the many<br />
organisations and partners who stand with us<br />
today, and look forward to adding to our support<br />
network as the campaign builds over the<br />
coming years.<br />
“Building and sustaining compassionate<br />
MORE INFORMATION<br />
Find out more about the campaign at<br />
www.understandtogether.ie<br />
If you would like to get involved in the<br />
campaign please contact:<br />
Nicola Donnelly, National Dementia Campaign<br />
Manager, HSE Communications Division,<br />
Dr Steevens’ Hospital, Dublin D08 W2A8,<br />
01-6352478 /087-0985529.<br />
Email: nicola.donnelly1@hse.ie<br />
www.hse.ie/dementia<br />
communities supportive of people with<br />
dementia and carers is a challenge which<br />
many key organisations can play a part. We<br />
know from evidence that maintaining social<br />
and community ties is an important element<br />
in helping people live well with dementia and<br />
in helping to support their loved ones. This<br />
campaign seeks to create a collaborative model<br />
in which those already engaged in dementia<br />
specific activities can link with others and<br />
organisations from diverse sectors can work<br />
towards greater understanding of dementia and<br />
inclusion of those affected by it.”<br />
<strong>Understand</strong> <strong>Together</strong> is one of six key<br />
elements of the National Dementia Strategy<br />
and is jointly overseen by the HSE’s Health<br />
and Wellbeing Division, and the HSE’s National<br />
Dementia Office in Services for Older People,<br />
Social Care Division. It involves the development<br />
of radio, print, out of home, digital and television<br />
campaigns alongside the development of a<br />
partnership network comprising local and<br />
| health matters | winter 2016
FAR LEFT: Dr Ronan Glynn, Specialist Registrar in<br />
Public Helath (left) with Mary Manning, General<br />
Manager, National Dementia Office and Professor<br />
Brian Lawlor, Chair of the Campaign Steering<br />
Group (right), pictured at the launch of Dementia<br />
‘<strong>Understand</strong> <strong>Together</strong>’ campaign held in City Hall,<br />
Dublin. Photo: robbie reynolds<br />
TOP LEFT: Michelle Barrett, Caroline Kennedy,<br />
Margaret Moran, Rosie Jones, Delia Roche and<br />
Hilda Archbold at the Carlow Day Centre. Photo:<br />
Pat Moore<br />
TOP RIGHT: Dr Stephanie O’Keeffe, National<br />
Director, HSE Health and Wellbeing.<br />
LEFT: Watermans Lodge, Dementia-specific<br />
Respite/ Day Centre, Ballina/ Killaloe, Co Tipperary.<br />
Back row left to right: Sean Heaney, bus driver’<br />
Marika Peek, volunteer; Eilish Long, administrator;<br />
Katherine Creamer, carer; Ann Fleming, cook;<br />
Adrian Ryan, carer; Elaine Shields, carer; Nicola<br />
Dooley, community employed carer. Front left to<br />
right: Margaret Larkin, Eileen Flannery, Nuala Foley,<br />
Mera Irwin. PHOTOGRAPHY: DERMOT LYNCH<br />
national organisations and groups aimed at<br />
creating better community environments<br />
that actively embrace people with dementia<br />
and their loved ones. The campaign will also<br />
communicate information about dementia<br />
- what it is, who gets it and things people can<br />
do to reduce their risks of developing dementia.<br />
Alongside this information campaign the<br />
campaign will be promoting simple everyday<br />
things that businesses, organisations and<br />
individuals can do to show their support for<br />
people living with dementia and those caring<br />
for loved ones.<br />
working together to promote<br />
understanding of dementia<br />
UNDERSTAND <strong>Together</strong> is a collaborative<br />
campaign that has been developed with<br />
partners, including ASI and Genio.<br />
Tina Leonard, Head of Advocacy & Public<br />
Affairs with the Alzheimer Society of Ireland<br />
(ASI) said, “Each day, we hear of stigma and<br />
isolation from people with dementia and<br />
carers. When people realise that dementia<br />
affects so many in our communities, when<br />
people realise that calling for a chat can make<br />
a world of difference and when people realise<br />
that being ill isn’t shameful, we’ll have a better<br />
society for all.”<br />
Madeline Clarke, Executive Director, Genio,<br />
said, “Through the HSE and Genio Dementia<br />
Programme, innovative projects across the<br />
country are developing personalised ways of<br />
supporting people with dementia to remain<br />
living at home for as long as possible. A<br />
supportive and well informed community<br />
is an essential component to this. Genio is<br />
delighted to be involved in the <strong>Understand</strong><br />
<strong>Together</strong> campaign which will not only<br />
increase knowledge of dementia but also<br />
encourage everyone to become actively<br />
involved in supporting people with dementia<br />
in their community.”<br />
This partnership approach is fundamental<br />
to ensuring that people across all sections of<br />
Irish society are inspired to become involved in<br />
building more inclusive communities for people<br />
with dementia and their loved ones. To date, over<br />
30 businesses and organisations have pledged<br />
their support for the campaign. These include<br />
transport providers Irish Rail, Bus Eireann and<br />
Dublin Bus; financial institutions Bank of Ireland,<br />
Ulster Bank and the Irish League of Credit<br />
Unions; An Post; the IFA; IBEC and ISME. Other<br />
partners include Boots, the Irish Pharmaceutical<br />
Union, the ICGP and the Law Society of Ireland,<br />
as well as a wide range of voluntary and<br />
community organisations including ALONE, Age<br />
Friendly Ireland and Active Retirement Ireland.<br />
<strong>Together</strong> with the campaign, these organisations<br />
hope to promote greater awareness of dementia<br />
and greater inclusion of people affected by the<br />
condition in communities across Ireland.<br />
To find out more:<br />
www.understandtogether.ie<br />
winter 2016 | health matters |
You<br />
Section<br />
Jimmy is 10 years smokefree<br />
200,000 cigarettes<br />
iona Boyle, Smoking Cessation<br />
Advisor, Donegal Community<br />
recently caught up with Jimmy<br />
F<br />
Kavanagh, a former client of the<br />
Smoking Cessation Programme,<br />
for a cuppa as he celebrated 10 years since he<br />
quit smoking which means, for him, that he has<br />
not smoked around 200,000 cigarettes.<br />
Jimmy had made several attempts to quit<br />
smoking and had managed some success - once<br />
for two years and once for three years. On both<br />
occasions, he relapsed while out watching<br />
football in the pub. He confided this week that he<br />
probably smoked up to 60 cigarettes per day and<br />
not the 30 to 40 that he reported at the time.<br />
He used to get up in the middle of the night<br />
to smoke and would normally have had seven<br />
cigarettes taken before starting work in the<br />
morning. He had been smoking for around 30<br />
years and his health was his main reason for<br />
quitting as he was having chest infections.<br />
As is very common, Jimmy’s main concern<br />
about quitting was fear of failure. At the time,<br />
Fiona explained that most clients had this as<br />
their main concern, and that even if you stop<br />
smoking for a short period of time, the chances<br />
are that you will learn something that will<br />
help you on your next attempt. Additionally,<br />
the majority of people make between 5 and 10<br />
quit attempts before they become successful<br />
especially if they are doing it by themselves.<br />
Once motivated to quit ,success is more likely<br />
if appropriate treatments are used ie Champix<br />
tablets, patches, mist etc. and if Smoking<br />
Cessation Services are used also.<br />
Jimmy’s Carbon Monoxide level (breath test)<br />
at his initial appointment was 18ppm in the<br />
breath and 3.2pc in the blood. Normal is 2ppm<br />
in the breath and
etter off<br />
to be –the hardest part was getting the<br />
thinking right<br />
• Try not to think of it as a sacrifice and that<br />
you are giving something up – it’s more<br />
about taking something back as it’s the<br />
biggest favour you’ll ever do for yourself<br />
• Seeing Fiona every few weeks helped<br />
because you knew there was someone<br />
rooting for you and you didn’t want to let<br />
them down. Having the Carbon Monoxide<br />
test each visit also helped to keep you going<br />
Recently, Jimmy was interviewed by Shaun<br />
Doherty on Highland Radio about his achievement<br />
which got a great response on air and as a result<br />
a local woman contacted Jimmy the day after<br />
the radio interview to say that she was inspired<br />
by it. This lady has now quit and is out walking<br />
each day and is keeping in contact with Jimmy by<br />
Facebook. It shows that though quitting smoking<br />
can be difficult, the more support that a person<br />
can get from the people around them and trained<br />
professionals, the more likely they are to quit.<br />
If this story has inspired you to think about<br />
quitting smoking and if you would like free<br />
confidential support at one of the 13 clinics<br />
throughout Donegal then please contact either<br />
Fiona Boyle on 087-2514790 or Catherine<br />
Coleman on 086-0492465. You are 10 times<br />
more likely to quit smoking if you use this service.<br />
Thanks again to Jimmy for allowing his story to<br />
be told.<br />
We Can Quit – Women Supporting Women to kick the habit<br />
The Irish Cancer Society’s ‘We Can Quit’<br />
programme, featured in the summer issue of<br />
Health Matters, is continuing to attract women<br />
in Cork and Dublin who are determined to quit<br />
smoking.<br />
‘We Can Quit’ is a free, community based 12-<br />
week support programme for women who want<br />
to quit smoking. It offers women the opportunity<br />
to develop skills, build confidence and share<br />
experiences with each other in a friendly and<br />
supportive group environment, where everyone<br />
understands what they are going through.<br />
The programme also offers free nicotine<br />
replacement therapy (NRT), a weekly smoking<br />
cessation group and one to one support.<br />
This year will see courses in a total of 10<br />
locations being completed by the end of<br />
this year, with extra locations being added<br />
next year. Over the course of 2015 and<br />
2016, the programme has had a total of 248<br />
women participate in courses in Fettercairn,<br />
Blakestown, Swords, Coolock, Kilmore, Rialto<br />
& Bluebell in Dublin and Mallow, Mayfield and<br />
Ballyphehane/Togher in Cork.<br />
Deciding to quit smoking is no easy feat, as<br />
Carolyn Roche from Tallaght knows only too<br />
well. Carolyn previously tried to stop smoking<br />
on two other occasions. This time, Carolyn was<br />
determined to quit and went along to her local<br />
‘We Can Quit’ programme at Fettercairn in July<br />
of this year. Since then Carolyn has managed<br />
to battle through the highs and lows and is still<br />
off the cigarettes. In fact, Carolyn went on to<br />
be an ambassador at the Tallaght Health and<br />
Wellbeing Week.<br />
Speaking about the programme, Carolyn<br />
said, “I heard about the programme at the<br />
Community Centre in Tallaght where I volunteer<br />
and at the time I was smoking two packs of<br />
cigarettes a day. It was my third time trying to<br />
give up and the first two times I had continued<br />
smoking even with the nicotine patches on me.”<br />
“I was determined to do it this time and I<br />
took it one hour at a time. I thought of the fact<br />
that when anyone gets on an airplane to go<br />
anywhere, they can’t smoke for hours at a time<br />
and that’s a good way to approach it. If I can do<br />
without them when I’m flying somewhere, I can<br />
do it all of the time.<br />
“The course was brilliant, especially the<br />
facilitator Imelda. I was given as much support<br />
and time as I needed and she often took me to<br />
the side and explained things one to one. All of<br />
the women in the group supported each other<br />
and afterwards we started a Facebook group<br />
and we still meet up for coffee and a chat.<br />
“My last cigarette was on May 22nd, so I’m<br />
almost five months off the cigarettes now and I<br />
am delighted with myself. I haven’t had an easy<br />
time recently and was in<br />
hospital for a while, but I<br />
didn’t go back on the cigarettes, even though<br />
at times I was tempted. I keep thinking of that<br />
plane, and I just take it one hour at a time.”<br />
2017 HSE / ‘We Can Quit’<br />
Training<br />
The We Can Quit Programme uses a<br />
co-facilitation model between community<br />
workers and HSE practitioners who are<br />
working with women and families at CHO<br />
area level.<br />
In order to run more courses, the Irish<br />
Cancer Society is urging HSE practitioners,<br />
working at CHO level in Cork and South<br />
Dublin who think this programme would be<br />
relevant to their work, to contact them.<br />
For anyone interested in taking part in HSE<br />
and Irish Cancer Society facilitator training in<br />
the new year, please contact Rachel Burke at<br />
rburke@irishcancer.ie or 01-2316669, or visit<br />
the webpage at www.cancer.ie/we-can-quit<br />
for more information on courses.<br />
Carolyn Roche (centre), with Lavinia Coti and Aisling McGeady at the ‘We Can Quit’ graduation<br />
ceremony in Tallaght. Photo: Andres Poveda Photography<br />
winter 2016 | health matters |
You<br />
Section<br />
Support for parents<br />
Tom’s<br />
Journey<br />
The parents of little Tom Fahy, who was diagnosed<br />
with Edwards Syndrome in Pregnancy, share their<br />
heart-breaking experience with Perinatal Palliative<br />
Care and bereavement standards<br />
n Monday, July 27th, our world<br />
changed forever. Our baby was<br />
diagnosed with Trisomy 18 at<br />
O<br />
the 20-week scan. We were<br />
numb. I remember lying there<br />
hearing the words but almost zoning out<br />
thinking this cannot be happening to us. We<br />
hadn’t planned on finding out the sex of the<br />
baby but Terry asked. The sonographer told us<br />
our baby was a boy.<br />
In the car on the way home, it was so hard to<br />
reconcile the fact that I could feel him moving<br />
yet we were told he was going to die. Our first<br />
instinct was to give this little guy a name. We<br />
decided to call him Tom. By naming him, as<br />
parents we hoped we would give him a strong<br />
sense of belonging. For us, his life started<br />
that day because we knew he would have a<br />
very short life if any outside of the womb.<br />
After we had gotten over the initial shock,<br />
we very quickly realised that we had two<br />
choices: we could spend Tom’s life feeling<br />
sad and miserable or we could celebrate it. I<br />
didn’t want Tom to feel the sadness. We had<br />
an overwhelming desire to breathe as much<br />
love and life into him while he was with us.<br />
It was very much a feeling that this little guy<br />
isn’t going to be around for a long time so<br />
we are going to show him a good time. We<br />
wanted him to feel an overwhelming sense of<br />
love and happiness.<br />
Tom was born on October 30th 2015 and<br />
to everyone’s amazement he lived for 11<br />
wonderful days.<br />
From the moment we got Tom’s diagnosis<br />
till the day he passed away and still to this<br />
day, the staff in the Coombe have been<br />
incredible to us.<br />
We were treated with incredible dignity and<br />
compassion by every staff member we came<br />
into contact with whether they were medical,<br />
administrative, support or auxiliary staff.<br />
There is a strong compassionate ethos that is<br />
almost innate in all of them.<br />
Everyone we met was always up to speed,<br />
from our obstetrician, to the bereavement<br />
midwife, paediatricians, neonatal nurses and<br />
beyond. It was very evident to us that there is<br />
excellent communication behind the scenes<br />
which is incredibly important and reassuring<br />
for parents like us.<br />
The care Tom and I received, both in<br />
pregnancy and beyond, was amazing. Our<br />
obstetrician Dr Michael O’Connell gave us<br />
an enormous sense of security. We knew<br />
we were in safe hands. This took a lot of<br />
the worry off us and allowed us to focus on<br />
the present and be present with Tom. Dr<br />
O’Connell and his colleague whom we saw<br />
while Dr O’Connell was away had the perfect<br />
balance of practicality and compassion. The<br />
neonatal nurses looked after Tom so well. I<br />
stayed awake with Tom for the first 72 hours<br />
of his life and I always looked forward to<br />
seeing the nurses coming in to feed him every<br />
three hours. They always came in with a smile<br />
on their face.<br />
The paediatricians known to us in pregnancy<br />
and present at Tom’s birth treated him with<br />
the utmost concern and dignity.<br />
The emotional support we received from<br />
the bereavement midwife was phenomenal.<br />
She was very much our “life support”. She<br />
was with us every step of our journey and at<br />
our lowest points she carried us through. It<br />
is testament to her and the care we received<br />
from her that our first instinct was to ring her<br />
when Tom died. To lose your baby in your<br />
arms is indescribable but to hear her voice on<br />
the other end of the phone gave us strength.<br />
She continues to give us that strength.<br />
We never felt rushed at any of our<br />
appointments or scans. We were encouraged<br />
from the beginning to embrace our time with<br />
Tom and start memory-making. The foetal<br />
medicine doctor and her midwife manager<br />
always made sure we had plenty of time at<br />
our scans. They got plenty of clear screen<br />
shots and photos of Tom.<br />
The bereavement midwife introduced us<br />
When Tom was born<br />
and the subsequent<br />
days we spent with him in<br />
the hospital were magical.<br />
It was as if time had stopped<br />
and we were living in a<br />
bubble. We were cared for<br />
as a family unit throughout<br />
to the idea of the memory box early on and<br />
she made sure we left the hospital with our<br />
memory box full of keepsakes from Tom’s<br />
time in the hospital, such as locks of his hair<br />
and his footprints. It was incredible to have<br />
people like the bereavement midwife and<br />
the chaplains looking after us because of<br />
their previous experiences they simply knew<br />
10 | health matters | winter 2016
Little Tom Fahy,<br />
pictured during<br />
his very short life,<br />
during which time he<br />
brought immense joy<br />
to his loving parents.<br />
what to do. They put us in contact with the<br />
charity “Now I Lay Me Down To Sleep”. Thanks<br />
to our wonderful photographer we have a<br />
picture of our three boys together, one of our<br />
most treasured possessions. Tom’s name is<br />
also in the book of remembrance which we<br />
are encouraged to visit in the Coombe on<br />
his anniversary each year and we attended<br />
and will continue to attend the annual<br />
remembrance service.<br />
We never felt we were alone on this journey.<br />
The staff helped make an extremely difficult<br />
time an incredibly special time. When Tom<br />
was born and the subsequent days we spent<br />
with him in the hospital were magical. It was<br />
as if time had stopped and we were living in<br />
a bubble. We were cared for as a family unit<br />
throughout. The three of us stayed together<br />
day and night on a ward away from all the<br />
normal healthy crying babies. We looked<br />
forward to our daily visits from doctors,<br />
nurses, the bereavement midwife with her<br />
boundless energy and positivity, the chaplains<br />
and the paediatricians. They very much<br />
became Tom’s second family.<br />
When we left the hospital with Tom, the<br />
Coombe were very much still involved and<br />
put us in contact with an array of community<br />
supports and agencies that supported us<br />
to have Tom at home for the short but very<br />
precious six days.<br />
When we read the National Standards for<br />
Bereavement Care Following Pregnancy Loss<br />
and Perinatal Death, we wondered what was<br />
new about them as we received all and more<br />
than the recommendations outlined.<br />
At their launch, we realised that the care<br />
and support we received in the Coombe was<br />
not standard practice throughout hospitals in<br />
Ireland. We were shocked.<br />
At the launch, we were introduced to the<br />
Minister of Health who went out of his way to<br />
meet with us bereaved parents. We found him<br />
to be very compassionate and were delighted<br />
when he told us that he had already begun<br />
the recruitment of bereavement midwives<br />
nationally and that they would be in post by<br />
the end of the year. It is wonderful to see that<br />
the Minister recognises the need for such vital<br />
support for bereaved parents nationally and<br />
that your postcode should not determine the<br />
care you receive especially when you are at<br />
your most vulnerable.<br />
The staff in the Coombe played such an<br />
important role in Tom’s life. They cared for us<br />
and supported us. They shared our journey.<br />
more information<br />
For more information about the HSE National<br />
Standards for Bereavement Care:<br />
www.hse.ie/bereavementcare<br />
winter 2016 | health matters | 11
You<br />
Section<br />
Tallaght Nurse Makes History<br />
in Inherited Cardiac Conditions<br />
elen Connaughton, a nurse<br />
working at Tallaght Hospital,<br />
has become the first Clinical<br />
H<br />
Nurse Specialist in Ireland in<br />
the area of Inherited Cardiac<br />
Conditions. Her success marks an important<br />
milestone for cardiology and nursing services<br />
nationally and in Tallaght Hospital.<br />
As the first Irish Clinical Nurse Specialist<br />
in this field, Helen is now a national leader in<br />
this area and demonstrates the investment<br />
and advancements that have taken place in<br />
cardiac services at Tallaght Hospital. Helen<br />
was a Clinical Nurse Manager in the Cardiac<br />
Risk in the Young (CRY) unit for eight years.<br />
The CRYP unit aims to provide<br />
comprehensive specialist evaluation of those<br />
diagnosed with or at risk from inherited<br />
cardiac conditions, including<br />
families who have lost<br />
someone to sudden<br />
cardiac death. It<br />
was developed as a<br />
collaboration between<br />
Tallaght Hospital, St<br />
James’s Hospital, St<br />
Vincent’s University<br />
Hospital and Trinity<br />
College Dublin<br />
Helen Connaughton (left) and (above) Helen with some of her colleagues at Tallaght Hospital.<br />
and is located at Tallaght Hospital.<br />
Helen’s post was initially funded by The<br />
Patches Trust, and for the last five years she<br />
has been funded by the charity Cardiac Risk<br />
in the Young (CRY Ireland), who fund much of<br />
the activity at the CRYP Unit.<br />
“It is a great honour to achieve this success<br />
and to be part of this great leap forward<br />
for cardiac services in Ireland,” she said. “I<br />
want to thank all my family and friends who<br />
supported me over the years. I am looking<br />
forward to continuing to bring my developed<br />
skills and experiences to the service of<br />
patients who may be suffering with cardiac<br />
diseases at Tallaght Hospital. The Hospital,<br />
the charities and my colleagues have provided<br />
great support to me over the years and I am<br />
delighted to be part of a team that is doing so<br />
much good for our patients.”<br />
Hilary Daly, Director of Nursing at Tallaght<br />
Hospital, added, “We are all delighted with<br />
Helen’s success. Tallaght Hospital has a<br />
strong ethos of ‘People caring for people’<br />
and Helen achieving this professional<br />
accreditation enables us to put this ethos<br />
into place all the more clearly, in the area of<br />
cardiac services. Helen’s additional expertise<br />
now as a clinical nurse specialist is a huge<br />
asset for the great work that takes place in<br />
the unit.”<br />
nursing graduates<br />
The success of the BSc General Nursing four-year programme in CUH is largely attributed to the ongoing support of students by dedicated preceptors, CNMs<br />
and the Nurse Practice Development Unit during their clinical placements. During their programme, BSc Nursing students have been given the opportunity to<br />
work in a variety of clinical settings within the CUH group to enable them to acquire the skills necessary to practice nursing. The Clinical Placement Co-ordinators<br />
are delighted to announce that all the new graduates have been offered employment in CUH and wish the newly qualified BSc 2012 General Nurses every good<br />
wish and success in their future careers.<br />
12 | health matters | winter 2016
Service-user engagement<br />
a voice for<br />
the patient<br />
s a former service user<br />
himself, the new HSE Head<br />
of Service User Engagement<br />
A<br />
in the Mental Health Division<br />
is only too aware of the value<br />
of involving patients and their family in the<br />
formation of policy and plans.<br />
Liam Hennessy took up his role in<br />
February of this year and is already making<br />
strides in his three-year plan.<br />
The former teacher, senior civil servant,<br />
management consultant and inspector in<br />
the Mental Health Commission revealed<br />
that his office is well on its way to putting<br />
in place the structures needed to bring<br />
about the change needed across the<br />
country.<br />
“The purpose of my job and my role is<br />
to ensure that over the next year that<br />
structures are put in place to deliver<br />
the best healthcare possible. When I say<br />
the structures, I mean the area leads in<br />
particular who will be placed in each of the<br />
Community Health Organisations (CHOs).<br />
Their role will be to gather together the<br />
views of service users and family members<br />
in say Donegal, Roscommon or Kerry and<br />
relay those views to local management<br />
with a view to improving the services based<br />
on those experiences,” said Liam.<br />
The interview process has been<br />
completed and it is hoped to have the nine<br />
leads to be in place in each CHO by the end<br />
of January or the beginning of February.<br />
One main criteria was that each applicant<br />
had to have had experience either as a<br />
service user themselves or as a family<br />
member or carer of a service user.<br />
“Like I do on a national basis, locally they<br />
will reflect the views and experiences<br />
in local services, but they will also have<br />
power and influence in the process. For<br />
the first time ever as part of the senior<br />
management team responsible for making<br />
policy for mental health, there will be<br />
a service user representative in there<br />
with equal standing and equal status,”<br />
explained Liam.<br />
His office was created as the result of<br />
recommendations of a reference group put<br />
together by the HSE.<br />
“I think it was one of the rare times that a<br />
report’s recommendations were all acepted<br />
It will be a challenge<br />
for the new leads to<br />
get around the fact that they<br />
have equal status around<br />
the table that seats many<br />
experienced health service<br />
executives and clinicians.<br />
But they’ll also be expected<br />
to contribute where they<br />
have relevant expertise<br />
and the implementation wasn’t just kicked<br />
down the line, it was made a priority,” he<br />
said.<br />
He acknowledged that the ‘proof will<br />
be in the pudding’ as to whether the new<br />
structures are effective in bringing about<br />
change.<br />
“It will be a challenge for the new leads<br />
to get around the fact that they have equal<br />
status around the table that seats many<br />
experienced health service executives and<br />
clinicians. But they will also be expected<br />
to contribute where they have relevant<br />
expertise. The proof will be in the pudding<br />
as to whether the positions establish the<br />
credibility they deserve,” said Liam.<br />
He added that he envisaged that the<br />
nine leads would establish a tight network<br />
between themselves so they could help<br />
each other out with any problems that<br />
might pop up.<br />
He underlined the need to involve the<br />
experiences of service users and their<br />
families in improving the services.<br />
“Families have not been treated well in<br />
the past, in many cases. Some doctors<br />
have chosen to invoke the veil of patient<br />
confidentiality to avoid talking to family<br />
members about their loved one’s case.<br />
And there have been times where that has<br />
led to major tragedies, simply because<br />
the family were unaware that the person<br />
in question had been engaging with the<br />
mental health services and unaware of the<br />
problems they were going through.<br />
“But I have met with the Minister for<br />
Mental Health Helen McEntee on a number<br />
of occasions and I can see that it has<br />
become a big political issue and one that<br />
people are demanding answers to.”<br />
He said there have been previous<br />
attempts to implement change in the<br />
policy-making in recent years but that<br />
those efforts were not as successful as<br />
they might have been.<br />
His office has employed a full-time action<br />
researcher who will track all the work<br />
done there and track what has worked and<br />
what hasn’t for learning and information<br />
purposes.<br />
“From a qualitative perspective, we will<br />
be able to measure the progress of the<br />
structures by compiling case studies of<br />
good practice and using that to learn how<br />
best to do our work,” he explained.<br />
But for Liam, success in his role will<br />
ultimately come when having a service user<br />
representative at a seat around the table is<br />
accepted as the norm.<br />
“I want it to be no big deal, just part of the<br />
fabric of our policy-making, and that people<br />
will simply say, ‘sure, that’s just the way we<br />
do things around here.”<br />
CONTACT<br />
You can contact Liam’s oiffice by email at:<br />
mhengage@hse.ie<br />
winter 2016 | health matters | 13
You<br />
Section<br />
NAS band celebrate 10 years<br />
n 2006, a small group of<br />
interested people working in<br />
the National Ambulance met to<br />
I<br />
consider setting up a band. Fast<br />
forward 10 years, and the NAS<br />
Pipes and Drum band are going from strength<br />
to strength.<br />
“The idea of setting up a band came about<br />
in 2006 when we saw our colleagues in Co.<br />
Cork had a band made up of serving and<br />
retired Paramedics, Advanced Paramedics,<br />
Emergency Medical Technicians and<br />
Emergency Medical Controllers,” explained<br />
Drum Sergeant Stephen Wilson.<br />
“We were also aware of our colleagues<br />
in the Dublin Fire Brigade Pipe Band, both<br />
bands were a real inspiration to us and the<br />
fact that internationally there were very few<br />
Emergency Medical Services pipebands.”<br />
The band has been invited to ceremonies all<br />
over Ireland and also further afield, one such<br />
invitation was to New York to take part in the<br />
St Patrick’s Day parade alongside emergency<br />
services colleagues FDNY EMS Pipes &<br />
Drums. While in New York the band was also<br />
invited to play in New York’s state capital<br />
Albany at a reception hosted by the New York<br />
State Governor Andrew S Cuomo and also<br />
took part in three other parades.<br />
Pipe Major Brian O’Reilly said, “We have<br />
come a long way from our first outing in the<br />
Monasterevin St Patrick’s Day Parade to<br />
marching down New York’s 5th Avenue in the<br />
World’s largest St Patrick’s Day Parade.<br />
“A couple of my most memorable<br />
moments with the band include performing<br />
with Andre Rieu and his famous orchestra at<br />
the O2 arena in 2012 and playing a lament at<br />
the World Trade Centre Memorial in 2013,”<br />
said Brian.<br />
“But my proudest moment as Pipe Major<br />
was when we represented the Ambulance<br />
Service and marched down Dublin’s O’Connell<br />
Street in the 1916 Centenary parade at Easter<br />
this year.”<br />
He added, “It has been a long hard slog to<br />
get the band to where it is today and there<br />
have been many members of the Ambulance<br />
Service Pipes & Drums who have come and<br />
gone over the last ten years, but we now<br />
have a great bunch of people in the band who<br />
are very committed to keeping the National<br />
Ambulance Service Pipes &Drums going from<br />
strength to strength.<br />
staff perform some amazing feats of cycling and running<br />
After cycling for 78 hours and 31 minutes, four Meath-based<br />
paramedics took an incredible sixth place in the gruelling 2,150km<br />
Race Around Ireland.<br />
The ‘Flatliners’ team consisting of Fergal Murray, Phil Gargan,<br />
Brendan Harte and Marc Tighe, Paramedics and Advanced<br />
Paramedics from the National Ambulance Service, stationed in the<br />
Navan and Trim area, managed to complete one of the toughest<br />
challenges that a cyclist can face and earn their sixth place finish<br />
in the four man team section.<br />
Meanwhile, Wicklow nurse Lillian Deegan became the first<br />
Irishwoman to run the 2,900km Wild Atlantic Way from Derry to<br />
Kinsale in Co Cork.<br />
Lillian battled through wind, rain and occasionally blistering heat<br />
during her 47-day run through nine counties.<br />
The nurse ran alongside Tom Reynolds from Co Louth who<br />
completed the run in just over 34 days.<br />
The pair raised more than €12,000 for Pieta House and the<br />
charity Billy’s World Ireland.<br />
Lillian said, “I’m delighted to be finished. In the early stage,<br />
I thought injury was going to take me out. But I soldiered on as they<br />
say. I will eat now like a horse for a long time, just to refuel and let<br />
the body recover.”<br />
14 | health matters | winter 2016
Limerick boost for Pieta House<br />
huge turnout at 5k<br />
EMBERS of the public have<br />
joined UL Hospitals Group<br />
staff in promoting a healthy<br />
M<br />
lifestyle and raising awareness<br />
for Pieta House.<br />
Over 200 people took part in the annual<br />
5k Run/Walk around Dooradoyle/Raheen, an<br />
increase on the numbers who participated last<br />
year. In so doing, they raised almost €5,000 for<br />
suicide prevention and counselling services in<br />
the MidWest.<br />
UL Hospitals’ Healthy Ireland Implementation<br />
Plan 2016-2019 identifies 60 priority actions do<br />
just that for the almost 380,000 people it serves<br />
and the 3,300 staff it employs in Limerick, Clare<br />
and Tipperary.<br />
“We were delighted to have such a great<br />
turnout from staff, including retired members<br />
of staff, and from members of the public in<br />
supporting the event. Physical health and<br />
positive mental health are in so many ways<br />
interlinked and we were delighted to be able to<br />
support such a deserving cause in Pieta House,”<br />
said Hugh Brady, Executive Lead, Health and<br />
Wellbeing, UL Hospitals Group.<br />
The run/walk was chipped and timed, with<br />
each participant receiving a Healthy Ireland<br />
t-shirt and, on completion, a medal. Trophies<br />
were awarded to the first three men and women<br />
home, to the first walker home, and to the first<br />
male and female members of staff to finish the<br />
line having completed an eight-week training<br />
programme, From Couch to 5k.<br />
“The event got great support from athletic<br />
clubs around the region and the times posted<br />
by Mike Carmody (An Bru AC) and Lisa Griffin<br />
(Dooneen AC) would rival anything we have seen<br />
in Rio over the last few days,” said Laura Tobin,<br />
Project Lead, Healthy Ireland, UL Hospitals.<br />
“But of course, the true object of the event<br />
was to get runners and walkers of all abilities<br />
involved. Walking is a great form of aerobic<br />
exercise and it was great to see so many<br />
participate on the night.”<br />
Another 5k run took place around Nenagh<br />
Hospital back in August and was part of the<br />
wider effort to promote Healthy Ireland in the<br />
region, explained Fiona Steed, Physiotherapy<br />
Manager, Nenagh Hospital and Site Lead in<br />
Nenagh for Healthy Ireland. “When we started<br />
out two months ago, our main aim was to get<br />
as many people active as possible, particularly<br />
people not used to exercise. We were delighted<br />
that 25 people completed the Nenagh run,<br />
donating €10 each to such a deserving cause in<br />
Pieta House.”<br />
“Of these, 10 were members of staff who<br />
participated in a training programme we ran.<br />
These staff had never run a 5k before but<br />
after completing the eight weeks, they were<br />
delighted to be able to run every stride of the<br />
5k. These first-timers are immensely proud of<br />
themselves and rightly so. Indeed, they have<br />
set up a What’s App group with the intention of<br />
continuing their training. This is what Healthy<br />
Ireland is all about.”<br />
“The dedication of staff to put in weeks of<br />
training and the hard yards on the night was<br />
great to see,” said UL Hospitals CEO Colette<br />
Cowan, who herself completed the course.<br />
Ms Cowan paid tribute to the 5k Run/Walk<br />
Organising Committee - Hugh Brady, Laura<br />
Tobin, Seamus Hourigan and Michelle Ryan –<br />
and also to the work of Pieta House, represented<br />
by Marian Long.<br />
TOP: Colette Cowan, CEO UL Hospitals Group<br />
presented 1st prize to Michael Carmody, Annacotty,<br />
2nd prize to Peter Madden, Borrisoleigh and 3rd<br />
prize to Derek Casey, Caherline at the UL Hospitals<br />
Group 5k Run/Walk in the presence of Marian Long,<br />
Administration Manager, Pieta House. Picture by<br />
Dave Gaynor<br />
MIDDLE: 5k prize winners are presented with the<br />
prizes by Colette Cowan and Marian Long.<br />
BOTTOM: Competitors setting off on the UL<br />
Hospitals Group 5k Run/Walk from the University<br />
Hospital Limerick in aid of Pieta House. Picture by<br />
Dave Gaynor<br />
winter 2016 | health matters | 15
You<br />
Section<br />
No ordinary swimming club<br />
lives transformed<br />
or almost 35 years, Mary Arrigan-<br />
Langan has been transforming<br />
F<br />
the lives of people with physical<br />
disabilities through the Octopus<br />
Swimming Club.<br />
Octopus is no ordinary swimming club. It<br />
operates using the Halliwick concept, which<br />
allows people with disabilities, such as<br />
amputees, head injury, spinal cord injury, stroke,<br />
spina-bifida, cerebral palsy, multiple sclerosis,<br />
visual impairment, to become “water free” or<br />
independence in the water.<br />
And as she nears retirement from her fulltime<br />
career as a Clinical Nurse Specialist in<br />
Osteoporosis in Merlin Park, Galway, there’s<br />
no sign of her pulling back from her amazing<br />
volunteer work.<br />
It was this work with the Octopus club that<br />
earned Mary, from Renmore in Co Galway, the<br />
Pride of Ireland award last year.<br />
Mary, the daughter of the late Paddy Arrigan, a<br />
former Irish and All-Army swimming champion<br />
who dominated backstroke events in the 1950s,<br />
breaking records and representing Ireland – was<br />
first introduced to the Halliwick concept when<br />
nursing in England in the 1970s.<br />
The technique means no buoyancy aids are<br />
used to help disabled swimmers. The volunteer<br />
helpers aid those with a disability until they<br />
can become comfortable and, in a lot of<br />
cases, independent in the water. This is done<br />
by developing breathing control, balance and<br />
relaxation techniques.<br />
“I get a great thrill and a sense of achievement<br />
when I see the swimmers progressing. I have an<br />
instinct to hold people with severe disabilities<br />
in my hands. If somebody comes to me with<br />
a severe stroke or an amputated leg, I see the<br />
potential in them,” said Mary.<br />
“If someone is stuck in a wheelchair all day, it is<br />
great to see their reaction when you put them in<br />
the water and see their body move and be free.<br />
And when somebody is completely relaxed, they<br />
can float and eventually they can move and swim.<br />
“Somebody might only be able to wiggle and<br />
arm but, to me, they are swimming.”<br />
Initially, she had intended to do physiotherapy,<br />
specialising in hydrotherapy, but when she<br />
saw the Halliwick method in operation she<br />
immediately knew this was what she wanted<br />
to do. “I like helping people to reach their full<br />
potential,” she says.<br />
When she returned to Ireland in 1981, she<br />
got the opportunity to study the Halliwick<br />
method and then worked tirelessly to set up the<br />
Octopus Swimming Club, the first of its kind in<br />
the country.<br />
At first, she received a lukewarm reception<br />
from the several organisations she approached;<br />
that was until she contacted Ernie Boucher of<br />
the Irish Wheelchair Association. “He said they<br />
would be very interested and asked did we<br />
need a bus. It was such a boost to get that first<br />
positive response,” she revealed.<br />
More than 34 years on, the club is still going<br />
from strength to strength, and its committee<br />
members are mainly made up of people with a<br />
physical disability.<br />
“It is their club,” Mary explained.<br />
She revealed that the club brings a number<br />
of major benefits to members, including social<br />
interaction, a chance to get some exercise and<br />
keep healthy, and respite for family members<br />
and carers.<br />
“We don’t claim to be remedial, what we do<br />
won’t replace physiotherapy. But the swimming<br />
brings so many other benefits that last long<br />
beyond the swimming class. People gain<br />
confidence and a great sense of achievement<br />
and independence,” said Mary.<br />
Mary also earned another plaudit recently. She<br />
was given the award for Promoting Bone Health<br />
in Ireland, with particular interest in disabilities,<br />
at the Annual Osteoporosis Conference.<br />
When she leaves the HSE early next year, she<br />
revealed that she will be able to give more time<br />
over to her volunteer work and also plans to<br />
gather all of her father’s writings together as<br />
part of a project for her whole family.<br />
“I have plenty of plans for my retirement.<br />
There’s still lots to do,” she added.<br />
Mary Arrigan-Langan with members of Octopus<br />
Swimming Club on their Monday night swim in<br />
Kilcornan. Back row - semi circle: Helen O’Connor<br />
(green hat), Joanne Stapleton (red hat), Oliver Kane,<br />
Phil Flatley (blue & white hat), Eva Anselm (blue<br />
& white hat) Shane O’Connor (yellow hat), Bridie<br />
Giles (black hat), Dylan O’Boyle (yellow hat). Front<br />
- semi circle: Michael Howley (blue hat), Niko Lascar<br />
(red hat), Tony Cunningham (no hat), founder of<br />
Octopus Swimming Club, Mary Arrigan-Langan<br />
(blue top). Centre: Sammy Fleming.<br />
16 | health matters | winter 2016
Unique set of visitors to UMHL<br />
Quadruplets join<br />
twins and triplets<br />
he Neonatal Unit at University<br />
Maternity Hospital Limerick<br />
is a busy place at any time of<br />
T<br />
year and has been especially<br />
so in recent weeks with the<br />
arrival in quick succession of quadruplets,<br />
triplets and twins.<br />
Photographer PJ Corbett - who specialises<br />
in newborn portraiture - is a regular visitor<br />
to the unit and was on hand to capture<br />
the moment when the unique 4-3-2-1<br />
combination of premature newborns was<br />
brought together for a photo. It is the firsttime<br />
the Limerick unit has had the privilege<br />
of caring for a set of quads, triplets, twins<br />
and singletons all at the same time.<br />
Lisa Fenton from Caherconlish, Co<br />
Limerick, made a little bit of history when<br />
on October 5th she gave birth to the first<br />
set of quadruplets born in Limerick in 50<br />
years. Other quads from the Mid-West born<br />
in the intervening years had been delivered<br />
in the major Dublin maternity units. Babies<br />
Alexander, Ashley, Maxwell and Kayla are<br />
the first children born to Lisa and her partner<br />
Wayne Downey and were delivered at UMHL<br />
by Prof Amanda Cotter and her team. The<br />
quads have been doing very well in Neonatal<br />
Unit ever since.<br />
Triplets Dáire, Liam and Aisling Cussen<br />
were born on October 27th to parents Olive<br />
and William and will soon be strong enough<br />
to go home to Raheen, Limerick.<br />
Twins Ashton and Leo Mulcahy were born<br />
on October 13th to mum Lydia O’Doherty and<br />
dad Calum Mulcahy, from Annacotty.<br />
And representing the 12 tiny singletons<br />
currently being looked after in the Neonatal<br />
Unit in PJ’s photo is little Maggie Roche from<br />
Charleville, Co Cork, born to mum Mairead<br />
and dad Kieran on October 26th.<br />
Neonatal at UMHL is one of the busiest<br />
such specialised units in the country, with<br />
close to 700 admissions every year. There<br />
are now approximately 4,700 births at<br />
UMHL annually.<br />
The Neonatal Unit at UMHL has 19 cots<br />
but often caters for more babies.It provides<br />
neonatal intensive care, high dependency<br />
and special care to premature and sick<br />
babies of the Mid-West, from 23 weeks of<br />
gestation upwards.<br />
“We have had the pleasure of looking after<br />
quadruplets, triplets, twins and singletons in<br />
the Neonatal Units at various times over the<br />
years but not as far as any of us are aware all<br />
at the same time in Limerick. It is a special<br />
occasion for all of the team working here and<br />
it is a time of great joy for us as well as their<br />
parents,” said Consultant Neonatologist, Dr<br />
Roy Philip.<br />
The team involved in caring for these babies<br />
includes four consultant neonatologists:<br />
Dr Roy Philip; Dr Niazy Al Assaf; Dr Con<br />
Sreenan and Dr Anne Doolan; along with<br />
48 neonatal nurses and midwives under<br />
the clinical leadership of Margo Dunworth,<br />
Deirdre O’Connell and Marie Carroll;<br />
ward attendants; healthcare assistants;<br />
physiotherapists; radiography; laboratory and<br />
clerical staff and others.<br />
According to Clinical Nurse Manager<br />
Marie Carroll: “It was amazing to get all<br />
10 babies together for a special photo. We<br />
are very grateful to PJ, who left his studio<br />
in Adare without hesitation to come in and<br />
take the photo. He clearly is a very talented<br />
photographer to manage to get such a<br />
beautiful image of so many babies at once!<br />
PJ also comes in to us every year to take<br />
photos of Santa with the babies and the<br />
parents in the Neonatal Unit. Christmas has<br />
come early for some families this year. All 10<br />
of them are doing well and should hopefully<br />
be back at home with their families before<br />
December 25th.”<br />
winter 2016 | health matters | 17
You<br />
Section<br />
Change of career<br />
clients ‘cry<br />
with delight’<br />
dental nurse has<br />
branched out<br />
into the world<br />
A<br />
of medical<br />
tattooing,<br />
transforming the lives of many<br />
of her patients.<br />
“To see a client actually cry<br />
with delight when they look in the<br />
mirror and see something there which<br />
they have probably not had before or lost at<br />
some stage due to illness or injury is priceless<br />
and totally fulfilling,” explained Kristen Carroll.<br />
Kristen joined the HSE in 1996 as a dental<br />
nurse. Although she enjoyed her job, she said<br />
that the turning point for came when she<br />
turned 40 a few years ago.<br />
“I felt I needed to re evaluate my working life.<br />
The realisation I had more than 25 more years<br />
of work left in me I needed a new challenge so<br />
looked at where that would lie.”<br />
“I looked into things I would like to learn,<br />
work at and most importantly enjoy giving<br />
to people and recalled seeing a permanent<br />
make-up brow procedure being done some<br />
years ago. I recall thinking it looked like a<br />
really nice job, it brought a lot of happiness<br />
to the person who had it as they had suffered<br />
from alopecia so their new brows changed<br />
their life, literally!<br />
“I did my research and discovered that<br />
outside of the make-up part, there was<br />
a medical aspect to SPMU<br />
(semi-permanent make-up)<br />
- areola/nipple restoration for<br />
ladies who have had breast<br />
reconstruction post cancer,<br />
needling and camouflage for<br />
burn scars and restoration of<br />
symmetry in cleft lip. I knew<br />
then this was for me.”<br />
After earning a diploma of<br />
excellence in SPMU, she decided to get<br />
some qualifications in the medical field<br />
awhere my heart truly lies so completed<br />
her training in areola/nipple restoration with<br />
needling for scars.<br />
She plans to train further in the medical<br />
field in scar camouflage so she can deliver<br />
complete treatments to clients and<br />
patients in both cosmetic and medical<br />
tattoo. She was shortlisted amongst the<br />
top six SPMU technicians in the UK for<br />
Best Technician in May.<br />
Kristen recently treated ladies who<br />
were referred to her by Beaumont breast<br />
clinic for free as part of breast cancer<br />
awareness month .<br />
“I am looking forward to working closely<br />
with them in the future as they try to work<br />
through their waiting list for areola, which I<br />
understand is years long. I’m also working<br />
closely with Alopecia Ireland providing a<br />
service at manageable cost for any of their<br />
kerry to calais<br />
In October 2016, over 700 refugees began<br />
their journey from the Calais camp to<br />
accommodation centres across France. A<br />
humanitarian mission from Kerry to Calais<br />
was set up by locals in Killarney and Dingle<br />
to bring clothes, blankets and suitcases to<br />
prepare those in the camp for the move.<br />
5,000 refugees lived in the makeshift<br />
camp called ‘The Jungle’ in Calais; of that<br />
number, 1022 were minors.<br />
Killarney Community Hospitals were very<br />
much involved in this initiative, requesting<br />
donations and providing the mission with<br />
30 large black bags of clothing, footwear<br />
and bedding which were collected by the<br />
Kerry to Calais volunteers.<br />
Three full vans set off to Calais in<br />
October, along €1,800 to purchase food<br />
and essentials. This trip was filmed by<br />
K-Town media, and was aired on the Irish<br />
TV channel on the evening of November<br />
2nd 2016.<br />
All the staff in the Killarney Community<br />
Hospitals were delighted to have taken<br />
part in this important mission.<br />
members who contact me,” she said.<br />
She still works in HSE dental as a nurse on a<br />
part-time basis and sees clients for cosmetic<br />
tattoo the other part of my week.<br />
“The biggest difference being in dental is not<br />
everyone is happy to see you, even on a good<br />
day. In my current role, everybody is happy to<br />
be here and delighted when I finish my work.”<br />
For more information, see her website at<br />
www.dermartcosmetictattoo.ie<br />
Dental nurse Kristen Carroll, who has branched out<br />
into semi-permanent make-up.<br />
endoscopy unit opens in Roscommon University hospital<br />
Minister for Health Simon Harris pictured at the official opening of the New Endoscopy unit at Roscommon University Hospital with Senator Frank Feighan;<br />
Maurice Power, CEO Saolta University Health Care Group; Dr John Killeen, Chairman, Board of Saolta University Health Care Group; Liam McMullin, Consultant<br />
Surgeon, RUH; Elaine Prendergast, General Manager, RUH and Ursula Morgan, Director of Nursing, RUH. Photo: Joe Travers.<br />
18 | health matters | winter 2016
nursing<br />
pals<br />
face off<br />
in croke<br />
park<br />
wo University Hospital<br />
Waterford trainee nurses took<br />
centre stage at Croke Park in<br />
T<br />
September as they lined up in<br />
opposition with each other in the<br />
All-Ireland Senior Camogie final.<br />
Julianne Malone was the victor on the day<br />
with her Kilkenny side, seeing off the brave<br />
attempts of colleague Laura Treacy’s Cork.<br />
Julianne and Laura are both final year<br />
nursing students at the Waterford Institute<br />
of Technology. They have undertaken their<br />
nursing training for the past three years<br />
together in the same class. They just started<br />
a placement in University Hospital Waterford<br />
(UHW) before the final but insisted on<br />
maintaining their level of training and playing,<br />
recognising the benefits to their academic life.<br />
21-year-old Julianne, from Mullinavat Club,<br />
represented Kilkenny at full forward. She has<br />
been playing Camogie since she was eight<br />
years old with her club. In March of this year,<br />
she debuted as a senior playing in a National<br />
League match. Previous to this, she has played<br />
on the county under-16 and under-14 and<br />
minor teams. Julianne’s most memorable<br />
moment was winning the National League final<br />
earlier this year, beating Galway in Semple<br />
Stadium in Thurles, scoring 1-2.<br />
On the other side, playing since she was<br />
seven years old, 21-year-old Laura, from<br />
Killeagh Club, represented Cork on full back<br />
line. Laura has been on the senior panel since<br />
she was sixteen years old, with this being<br />
her third Senior All Ireland Camogie final. In<br />
2015, she also received a Camogie All Star<br />
Nomination. Laura’s most memorable moment<br />
was winning her first ever Senior All Ireland<br />
title in 2014.<br />
Speaking about the prospect of playing<br />
against her colleague and friend in the final,<br />
Julianne said: ‘‘I have spent my last three<br />
years with Laura at the Waterford Institute of<br />
Technology. We are now undertaking our final<br />
year of training; from now until Christmas<br />
we will be studying for our finals and then<br />
from January 2017, we will both commence<br />
our final 36 weeks internship placement in<br />
I am just so excited<br />
and a little nervous<br />
too about Sunday. It will<br />
be strange playing against<br />
Laura, we are both quite<br />
competitive<br />
University Hospital Waterford.<br />
“We both love the same work and the same<br />
sport and we are now going to compete<br />
at the Senior Camogie Final. I am just<br />
so excited and a little nervous too about<br />
Sunday. It will be strange playing against<br />
Laura, we are both quite competitive. I just<br />
hope we both have a great game and do our<br />
clubs and counties proud.”<br />
Laura added: “Words can’t even describe my<br />
feelings right now. After lots of hard training I<br />
can’t wait to get out there and play on Sunday.<br />
I am very excited to share this moment with<br />
Julianne - even if we are going to play for two<br />
different counties. May the best team win!’’<br />
University Hospital Waterford, Director<br />
of Nursing, Claire Tully, said: “This is such<br />
an unusual situation, two of our students<br />
competing at the Senior Camogie Final<br />
representing two different counties. As the<br />
Director of Nursing I am very proud to see that<br />
it is possible to combine both work and sport at<br />
such high levels. It is a testament to the hard<br />
work that the girls put in both on and off the<br />
pitch. I was delighted to watch the match and<br />
on behalf of the University Hospital Waterford.”<br />
TOP: Laura Treacy and Julianne Malone dressed in<br />
their respective county colours ahead of their All-<br />
Ireland Senior Camogie final showdown at Croke<br />
Park. ABOVE: The pair in their nursing whites at<br />
University Hospital Waterford.<br />
winter 2016 | health matters | 19
You<br />
Section<br />
Prisoners collaborate at Cherry Orchard<br />
benches unveiled<br />
herry Orchard Hospital<br />
occupational therapists Liz<br />
Carey and Linda Penny recently<br />
C<br />
completed a collaborative project<br />
in conjunction with the Irish Prison<br />
Services for the construction of six attractive<br />
outdoor wooden benches on the Cherry Orchard<br />
Hospital campus.<br />
Cherry Orchard Hospital in Ballyfermot,<br />
Dublin 10 is now a residential home for older<br />
people and for young adults with physical and<br />
sensory disabilities.<br />
The campus is spread out, with a large number<br />
of residential units and many other services on<br />
site. New recent construction on the site saw the<br />
opening of a Child and Adolescent Mental Health<br />
Services facility for in and outpatient services.<br />
There are ongoing plans to expand services<br />
on site further. Many older Cherry Orchard<br />
Hospital residents fondly recall that prior to the<br />
construction of the hospital; the 74-acre plot<br />
was a combination of farm land, cherry blossom<br />
trees and fruit trees. A wide variety of mature<br />
deciduous trees still grow around the campus<br />
and each spring everyone particularly enjoys<br />
the emerging blooms of the beautiful cherry<br />
blossom trees.<br />
The Occupational Therapy Department in<br />
Cherry Orchard hospital has been in existence<br />
for many years and continues to strive to help<br />
residents to do the things that they need and<br />
want to do in everyday life. OT aims to enable<br />
residents to achieve maximum independence<br />
and quality of life, and to develop and maintain a<br />
meaningful lifestyle.<br />
A need was identified to assist with residents,<br />
family members and friends when they were<br />
walking or using a wheelchair on the widespread<br />
campus. There were no wheelchair accessible<br />
outdoor benches available that could be used<br />
if they got tired, weak, or simply wanted to sit<br />
and chat.<br />
The Irish Prison Services places a strong<br />
emphasis on the provision of vocational training<br />
activities, including carpentry and joinery, for<br />
prisoners and have workshops with courses<br />
externally accredited by City and Guilds. Fergal<br />
Black, Irish Prison Services Director of Care and<br />
Rehabilitation, formerly the HSE Local Health<br />
Manager in Dublin West, agreed to collaborate<br />
with the Occupational Therapy Department<br />
regarding the provision of benches for the<br />
campus after initial contact was made by<br />
Director of Nursing Fiona Cleary.<br />
The OTs were delighted to be of assistance,<br />
as they focus on the holistic person-centred<br />
service that promotes the well being and rights<br />
of the individual, family and carer whilst Liz and<br />
Linda outlined and recommended the specified<br />
measurements for six outdoor benches to be<br />
made to National Disability Authority standards<br />
in order to ensure they are accessible to<br />
everyone. They advised they also needed to take<br />
into account the surrounding paths, grass and<br />
other walkways.<br />
“In deciding on the location for the benches,<br />
it was deceptively difficult to choose spots that<br />
were accessible, pleasant and sociable,” said<br />
Linda. “In certain spots around this city campus,<br />
the Dublin Mountains are visible, peeking<br />
through units and we were keen to capture this<br />
glimpse of nature. In this regard the Maintenance<br />
Department were invaluable and very patient!”<br />
The Maintenance Department also gave input<br />
on the benches and while they were specified to<br />
be functional, durable and safe for public use,<br />
the OTs particularly emphasised the needs of<br />
wheelchair users on campus during this process.<br />
The design and installation were key in ensuring<br />
that they could access the benches themselves<br />
or sit beside a loved one in comfort and safety.<br />
The project involved various departments from<br />
the campus along its journey including Social<br />
Work, Residents Advocacy Group, Maintenance,<br />
Quality Assurance Committee and others.<br />
“We think this is a good opportunity to highlight<br />
the positive work of all involved on the campus<br />
as it brought a good sense of community<br />
involvement and spirit. The new benches<br />
are placed strategically around campus and<br />
residents and staff tell us they offer a great<br />
opportunity to sit near trees, and engage in<br />
conversation or simply enjoy the view of the<br />
Dublin Mountains,” said Liz.<br />
Linda also explained, “As occupational<br />
therapists we were uniquely placed to provide<br />
the skills necessary to ensure that function and<br />
form merged together in a simple, yet incredibly<br />
effective project.”<br />
Tony Harris, Mountjoy Prison Campus<br />
Assistant Governor, said, “The trainees in the<br />
workshops in Castlerea put great effort into the<br />
benches, especially when they heard who the<br />
recipients would be. The benches are a credit to<br />
the trainees and the staff of Castlerea prison,<br />
and highlights all the positive outcomes that can<br />
be achieved within the prison for the benefit of<br />
the community.”<br />
LEFT:<br />
At the bench on<br />
the Cherry Orchard<br />
campus were back<br />
row l-r: Dr Seamus<br />
O’Dea, Cherry Orchard<br />
Hospital Medical<br />
Superintendent; Joe<br />
Hernon, Cloverhill<br />
Assistant Governor; and<br />
Sean Coen, Castlerea<br />
Industrial Manager.<br />
Front row l-r: Bill Maher,<br />
Cherry Orchard Hospital<br />
Residents Advocacy<br />
group member; John<br />
Flavin, Castlerea<br />
Assistant Governor;<br />
Liz Carey, Senior<br />
Occupational Therapist;<br />
and Linda Penny, Senior<br />
Occupational Therapist.<br />
20 | health matters | winter 2016
Feature<br />
Reflecting our values of care,<br />
compassion, trust and learning<br />
putting values into action<br />
Health service staff at the Values in Action event in Limerick in October.<br />
Health service leaders made a big decision<br />
earlier this year to actively develop a culture<br />
where our values become a way of life and a<br />
visible part of our everyday actions in the<br />
Health Services in the Mid-West .<br />
Bringing our values of care, compassion,<br />
trust and learning to life in the health<br />
services is key to providing better workplaces<br />
for staff and delivering better experiences for<br />
patients and the people who use our services.<br />
A peer to peer approach to this culture change<br />
has begun and we call it Values in Action.<br />
There has been a hugely positive reaction to<br />
Values in Action since it kicked off in the Mid-<br />
West with a two-day workshop in October, for<br />
180 staff and voluntary partners.<br />
HSE Director General Tony O’Brien said: ‘<br />
‘We know that everyday thousands of health<br />
service staff around Ireland live our values<br />
of care, compassion, trust and learning.<br />
Sometimes this is very visible, sometimes it<br />
is not. Values in Action is about shaping our<br />
culture around these values, so that they are<br />
evident every day in every workplace. Values in<br />
Action has translated our values from words<br />
into behaviours (or actions) that we can all<br />
demonstrate. Through Values in Action we<br />
can create a better working environment for<br />
our staff and deliver better experiences to<br />
our patients and service users. This is about<br />
ensuring more and more of us put our values<br />
at the heart of our everyday work.’’<br />
Improving the Culture in the Health Services<br />
Values in Action is based on nine behaviours<br />
that reflect our values combined with a ground<br />
up approach to spreading change. It’s about<br />
all of us, irrespective of role or grade working<br />
together to change our workplaces for the<br />
better. The project focuses on behaviours<br />
which are visible and clearly understood.<br />
We all know what instinctively is meant by<br />
them and everyone can adopt them. We learn<br />
our behaviours by copying those around us.<br />
Values in Action is based on the belief that real<br />
sustainable culture change is shaped by the<br />
behaviours of influential individuals at all levels<br />
across the organisation.<br />
Nine behaviours<br />
The Values in Action team developed nine<br />
behaviours that reflect the three dimensions in<br />
our working lives – us as individuals, working<br />
with colleagues and how we treat patients.<br />
Staff at the workshop were introduced<br />
to the nine behaviours which reflect the<br />
HSE values of care, compassion, trust and<br />
learning. The nine behaviours are practical,<br />
very do-able and cost nothing and will<br />
make a positive difference to patients,<br />
service users and staff.<br />
The 9 behaviours were focus-tested with<br />
staff and patients. They are informed by a<br />
comprehensive review of national and local<br />
patient and staff policies and procedures,<br />
staff and patient/service user feedback, direct<br />
engagements with staff and service users and<br />
patient/service user feedback.<br />
Our Champions<br />
The kick off event which took place in<br />
Limerick in October was for staff who had been<br />
identified as ‘champions’. They were nominated<br />
by at least four of their colleagues and peers in<br />
an anonymous survey as the ‘helpful, wellinformed<br />
and motivating’ people working in the<br />
health service in the Mid-West.<br />
winter 2016 | health matters | 21
Reflecting our values of care,<br />
compassion, trust and learning<br />
putting values into action<br />
Staff at the workshop....Values in Action is based on the belief that real sustainable culture change is shaped by the behaviours of influential<br />
individuals at all levels across the organisation.<br />
These influential individuals are creating a<br />
bottom-up, grassroots movement that will<br />
spread through their peers and colleagues.<br />
Each person drew up a personal plan for what<br />
they are doing to spread the behaviours. They<br />
are looking at and implementing ways to put<br />
the behaviours into practice in workplaces<br />
throughout the Mid-West. They are also looking<br />
at ways to capture stories about the impact the<br />
behaviours are having on staff and patients.<br />
Next steps<br />
The champions are now playing a key role in<br />
actively developing a culture where the values<br />
of care, compassion, trust and learning become<br />
a way of life for all who work in the health<br />
services in the Mid West . Importantly other<br />
people can copy and practice these behaviours;<br />
shaping new ‘norms’ and creating a culture we<br />
can all be proud of.<br />
Leadership for Change<br />
Describing how she fully supports Values<br />
in Action, Colette Cowan, CEO UL Hospitals<br />
Group said: “I am delighted to be partnering<br />
with Bernard Gloster and his team from the Mid<br />
West Community Healthcare, and our national<br />
colleagues, to start an important journey<br />
working together to make the culture in the<br />
health services in the Mid-West one which we<br />
can all be very proud of. I am incredibly proud<br />
of what we have already achieved in the UL<br />
Hospital Group – we have wonderful staff and<br />
a huge programme of development underway<br />
that is going to make our Hospital Group one<br />
of the best in the country. That is why I decided<br />
to make UL Hospital Group the first hospital<br />
group in the country to take on Values in Action.<br />
Primarily because it’s all about people – it’s<br />
based on human behaviour, and whether we like<br />
it or not that is the essence of what the health<br />
services are all about – people, working with<br />
other people, to care for people. ‘’<br />
Bernard Gloster, Chief Officer, Mid-West<br />
Community Healthcare Values in Action said:<br />
‘’What’s unique about this project is the 180<br />
people who are involved as champions – they<br />
weren’t picked by managers. They were picked<br />
by their peers and that says something about<br />
them – they are the people who can lead and<br />
influence change. This project really appealed<br />
to me – it’s based on human behaviour and<br />
our 9 behaviours which are simple, practical,<br />
straightforward and very do-able. They are a<br />
guide for us all on how to be the best version of<br />
ourselves – for ourselves as individuals, for our<br />
colleagues and for our patients.”<br />
The next steps<br />
Health service staff in the Mid-west are now<br />
being asked to get to know and to practice<br />
the nine behaviours. This is about using the<br />
language of these behaviours in interactions with<br />
colleagues and the people who use our services.<br />
It’s about talking to colleagues about the<br />
importance of spreading culture in a way that<br />
will make the health services a better place to<br />
work and giving patients/service users a better<br />
experience. It’s about sharing stories where the<br />
behaviours are being seen and talking about<br />
their positive impact.<br />
If you’re based in the Mid-West then get to<br />
know your champions who attended the twoday<br />
workshop and support them. Highlight it<br />
when your colleagues or the people in your<br />
teams demonstrate these behaviours and call<br />
it out when you see opposite ones. Talk to your<br />
champions; empower and endorse their work<br />
as leaders of culture change so that they know<br />
they have your support. Culture change is a<br />
long-term goal and there will be ups and downs<br />
on the journey but ultimately we are all trying<br />
to improve our workplaces and deliver better<br />
health service experiences to those we serve.<br />
The Values in Action Team<br />
The Values in Action Project Team is made up<br />
of staff from across UL Hospitals Group and Mid<br />
West Community Health Organisation supported<br />
by colleagues from National Communications,<br />
HR, Quality and Patient Safety and the<br />
Programme for Health Service Improvement.<br />
more information<br />
Follow us on Twitter @HSEValues<br />
or see hse.ie/valuesinaction<br />
22 | health matters | winter 2016
INDIVIDUAL<br />
Am I putting<br />
myself in other<br />
people’s shoes?<br />
Am I aware that my<br />
actions can impact<br />
on how patients feel?<br />
Am I aware of my<br />
own stress and how<br />
I deal with it?<br />
Am I being fair to my colleagues? Can I see the<br />
challenges that others have and would I change<br />
my attitude or what I do as a result?<br />
Am I aware of how I am heard and seen?<br />
Am I a good example?<br />
Am I dealing with stress appropriately, for<br />
myself and others? Should I ask for help or<br />
support? Am I doing things that can help<br />
relieve stress at work?<br />
Seeing things from other perspectives and<br />
understanding other peoples role/situation is key<br />
to being able to work effectively with others.<br />
We all have a role to play in the care of our<br />
patients/service users. How can we work together<br />
to solve the problem?<br />
Acknowledge the<br />
work of your<br />
COLLEAGUE<br />
Patients never forget how you make them feel.<br />
We need to be aware that patients are observing<br />
our actions and conversations can be heard by<br />
others. Tensions between staff affect the patient’s<br />
perceptions and their own vulnerabilities.<br />
Ask your colleagues<br />
how you could<br />
Recognising when you are under too much stress<br />
is important as it can have an effect on your<br />
health and wellbeing and on others around you.<br />
Seeking support from a trusted source or doing<br />
things to relieve stress can help.<br />
Challenge<br />
toxic<br />
VIA_behav_all_bigboards.indd 1 18/10/2016 17:05<br />
colleagues<br />
help them<br />
attitudes<br />
Always say thanks and acknowledge the<br />
efforts of team members and colleagues. Treat<br />
everybody as equal, regardless of hierarchy or<br />
role within the organisation<br />
Ask how you can help or offer advice to try<br />
to guide the way. Share your knowledge and<br />
experience with others.<br />
Challenge toxic negativity, defeatism and<br />
cynicism. Address unacceptable behaviours<br />
(abuse, hostility, etc.) where a person is not<br />
being treated with respect<br />
Be supportive of colleagues and tell them when<br />
they are doing a good job. Say thanks. Don’t<br />
be judgemental; a ‘blame culture’ has no place<br />
here. We are all here to make the patient care<br />
experiences better.<br />
PATIENT<br />
Offer a colleague who’s under pressure time to<br />
listen, some advice or a helping hand. We trust<br />
each other to do the right thing. Work together as<br />
a team. Ask yourself ‘Did I say or do something<br />
today to help a colleague.<br />
Do not accept that we can never change or<br />
improve, intervene. Don’t be a bystander when you<br />
see unacceptable behaviours which are contrary to<br />
our values. Acknowledge difficulties, bring balance<br />
to discussions.<br />
Use my name<br />
and/or your<br />
Keep patients<br />
informed – explain<br />
Do an<br />
extra, kind<br />
VIA_behav_all_bigboards.indd 2 18/10/2016 17:05<br />
name the now and the next thing<br />
Introduce yourself and outline your role –<br />
similar to #hellomynameis. Human-to-Human:<br />
turn towards the patient, make eye contact,<br />
smile, low and calm tone of voice<br />
Give information to the patient/service user on<br />
what you are doing now and what the next step<br />
will be. Reduce uncertainty as much as you can.<br />
Explain the known and unknowns in no rush.<br />
Provide small acts of kindness. The small,<br />
unexpected ‘extra thing’ is very human<br />
and powerful<br />
The Values The first in Action few second’s team interaction developed between nine behaviours a that Sharing reflect information the three with dimensions the patient reduces in our working their lives – Very us as often individuals, the small, working unexpected with ‘extra colleagues mile’ and<br />
how patient we treat and patients. a staff member The behaviours sets the tone were of the informed by vulnerability a comprehensive and gives review them a of sense national of control. and local patient and creates staff an policies enormous and sense procedures, of caring. staff and<br />
patient/service whole interaction. user See feedback, the whole person, direct engagements not just with Use staff language and that service the patient/service users and patient/service user will user Small feedback acts of and kindness tested build with trust staff and and respect patients. for<br />
the problem, not just their number. Make the<br />
patient feel as if he/she is unique, the only one.<br />
understand and invite them to ask questions.<br />
Provide a dignified, safe space for your interaction.<br />
staff. You are proud to work for an organisation<br />
that demonstrates such kindness.<br />
winter 2016 | health matters | 23
Feature<br />
Breastfeeding support<br />
Live webchat<br />
service opens<br />
e have recently expanded<br />
our on-line breastfeeding<br />
supports on our website<br />
W<br />
www.breastfeeding.ie to assist<br />
mothers and mothers-to-be.<br />
If you are working with clients who may be<br />
thinking of becoming pregnant or who are<br />
pregnant or if you or a family member are<br />
pregnant you can get support and information<br />
on www.breastfeeding.ie The new supports<br />
include an extended Ask our Expert service with<br />
a live Webchat service provided by International<br />
Board Certified Lactation Consultants (IBCLCs),<br />
a new HSE Breastfeeding Facebook page,<br />
and breastfeeding support videos featuring<br />
health care professionals and parents of<br />
breastfeeding babies.<br />
www.breastfeeding.ie provides answers to<br />
many of the common questions Mums have,<br />
whether they are thinking about breastfeeding,<br />
just getting started or are well on their way<br />
with a growing baby. For those Mums who have<br />
a specific query, there is also the option to email<br />
your question to a Lactation Consultant via the<br />
Ask our Expert service or through Webchat.<br />
The newly launched HSE Breastfeeding<br />
Facebook page provides a community of<br />
support for mothers to join where they can<br />
receive information and tips from the Ask our<br />
Expert Lactation Consultants. The new Irish<br />
breastfeeding videos on www.breastfeeding.ie<br />
provide guidance for mothers on topics such as<br />
positioning and attaching baby; expressing milk<br />
and what to expect in the early days. The focus<br />
is on assisting mothers with information and<br />
enabling them to overcome challenges they<br />
may be experiencing.<br />
Our on-line support is non-judgemental,<br />
respecting mother’s decisions and<br />
encouraging and supporting them. The<br />
website directs mothers to local health<br />
services and breastfeeding support groups, of<br />
which there are over 260 across the country.<br />
All contact details and times are on www.<br />
breastfeeding.ie/Support-search/. Some of<br />
being these groups are facilitated by hospital<br />
and community Lactation Consultants<br />
(IBCLCs), Public Health Nurses, while others<br />
are organised by trained breastfeeding<br />
support volunteers all who are, or have, been<br />
breastfeeding mums. They are a great source<br />
of information, support and friendships. Our<br />
aim is that the new supports will reach more<br />
mothers and improve access to user friendly<br />
breastfeeding help and information.<br />
In Ireland, 57pc of mothers are breastfeeding<br />
their babies on discharge from maternity<br />
hospitals (HSE, 2016). In the first few days<br />
and weeks at home, mothers may experience<br />
challenges which often prompt them to stop<br />
breastfeeding sooner than they planned.<br />
Breastfeeding support is provided by maternity<br />
services by public health nurses, and voluntary<br />
breastfeeding organisations in the community.<br />
Minister Marcella Corcoran Kennedy, speaking<br />
at the launch of 2016 National Breastfeeding<br />
Week, said: “I breastfed my own children,<br />
and I know that there can be challenges in<br />
the early days. Having somewhere to go for<br />
practical information and support is important<br />
for helping all mothers. As time went on, I<br />
found breastfeeding very rewarding and so<br />
convenient. It is important that we all support<br />
breastfeeding as the normal and healthy way<br />
to feed babies, whether through giving practical<br />
support to mothers or ensuring that mothers<br />
are welcome to breastfeed whenever and<br />
wherever they and their babies need.”<br />
Dr Stephanie O’Keeffe, Director of Health<br />
and Wellbeing said: “The evidence in relation<br />
to breastfeeding and health is now stronger<br />
than ever and the potential for improved health<br />
outcomes for women and children in Ireland<br />
is substantial. We are working to promote,<br />
support and protect breastfeeding. We want to<br />
encourage more mothers to start breastfeeding,<br />
and to breastfeed for longer. The on-line service<br />
on www.breastfeeding.ie is part of the range<br />
of the supports available to provide practical<br />
information and support<br />
to help mothers to<br />
breastfeed their<br />
babies.<br />
“The HSE<br />
website www.<br />
breastfeeding.ie<br />
provides answers<br />
to the common<br />
questions mums<br />
have whether they<br />
are thinking about<br />
breastfeeding, just<br />
getting started or<br />
well on their way<br />
with a growing<br />
baby,” said Siobhan<br />
24 | health matters | winter 2016
Hourigan, National Breastfeeding Co-ordinator.<br />
For those mums who have a specific query,<br />
there is also the option to email your question<br />
to a Lactation Consultant via the Ask our<br />
Expert service or through Webchat. The new<br />
HSE Breastfeeding Facebook page provides<br />
a community of support for mothers to join<br />
with input and information from the Ask our<br />
Expert Lactation Consultants. The new Irish<br />
breastfeeding videos on breastfeeding.ie provide<br />
guidance for mothers on topics like positioning<br />
and attaching baby; expressing milk and what<br />
to expect in the early days.<br />
MORE INFORMATION<br />
For more information and LIVECHAT:<br />
www.breastfeeding.ie<br />
ABOVE: Minister of State Marcella Corcoran<br />
Kennedy TD launches National Breastfeeding<br />
Week with baby Sam. Photo: Robbie Reynolds<br />
Photography.<br />
LEFT: Frances Plunkett, HSE Digital Communications<br />
and an expectant mum, supporting the new Ask Our<br />
Expert online chat service.<br />
Parents share<br />
their stories<br />
Mum Bernadette Martyn, Mullingar, Co<br />
Westmeath, who features on the new videos,<br />
gives encouragement to other mothers in the<br />
early weeks. Bernadette says: “The first two to<br />
three weeks were tough but I was determined<br />
to keep with it. A friend of mine gave me<br />
advice, she said ‘don’t give up on your<br />
toughest day’. So I kept with it and it literally<br />
changed overnight, one day it got better and<br />
then the following week, it was like oh gosh -<br />
It went into place really quickly then. Especially<br />
with the other two kids, it’s really handy that I<br />
can just pick him up and feed him when I need<br />
to, and I can put him back down again.”<br />
Mum Lesley Kavanagh, also from Mullingar,<br />
agrees: “There was a lot of cluster feeding<br />
which I now know is completely normal.<br />
Check their nappies, wet and dirty nappies, as<br />
long as there are lots of them, then they are<br />
perfect. It (breastfeeding) is such a brilliant<br />
thing it makes life so much easier.”<br />
Breastfeeding mums Bernadette, Leslie and<br />
Ciara O’Hara describe how they appreciated<br />
the help and encouragement they got at their<br />
local breastfeeding support group. Ciara says<br />
“I just loved the breastfeeding support group,<br />
everybody is so welcoming, everybody is so<br />
friendly. It was so lovely being able to chat to<br />
people, at the time I wasn’t so comfortable<br />
feeding in public so it was a great way of<br />
getting used to feeding in public. It was lovely<br />
having her around other babies.”<br />
The suite of videos also includes videos of<br />
Irish dads sharing their experiences, tips and<br />
supports. Dads Joe and Noel talk about how<br />
their practical help and support helps mum<br />
when breastfeeding. “Definitely go ahead and<br />
encourage her to breastfeed as much as you<br />
can and support her with it. It really worked<br />
for us.”<br />
Noel describes the importance of<br />
breastfeeding for his children’s health.<br />
“I was very happy, very supportive<br />
of (mum) to breastfeed. I think<br />
they (the children) are all<br />
probably a lot healthier<br />
for it, their immune<br />
systems are<br />
strong,”<br />
he said.<br />
winter 2016 | health matters | 25
ACTIVITY-BASED FUNDING<br />
MONEY FOLLOWS THE PATIENT<br />
UNDER NEW SYSTEM<br />
Activity-Based Funding (ABF) is transforming<br />
the way our healthcare services are funded,<br />
bringing with it significant improvements in<br />
levels of efficiency.<br />
ABF means that hospitals are paid for the<br />
actual quantity and care they deliver to patients,<br />
thereby enabling the hospitals to see clearly the<br />
link between money and the work they do.<br />
Maureen Cronin, Assistant Chief Financial<br />
Officer and Head of Acute Hospital Finance<br />
(ABF) and the Healthcare Pricing Office,<br />
explained that the traditional way healthcare<br />
was funded, either on the community side or in<br />
hospitals, was with a block grant.<br />
“That means that in a year, a hospital might<br />
have got €100m in funding but you didn’t have<br />
an explicit link between the work they were<br />
producing and the money they were attracting,”<br />
she said.<br />
The first time ABF was utilised by the HSE<br />
was in 2011 with the advent of the Fair Deal.<br />
“At that time, we had about a billion euro<br />
and 118 public units, as well as a lot of<br />
private providers too. But we didn’t know in<br />
the public unit with 30 beds whether or not<br />
they had 12 clients or 30 clients in the unit<br />
in a particular month. So we couldn’t link the<br />
product or the production at that unit with<br />
the money they were spending. There was no<br />
link,” she explained.<br />
“So, in a way, that is a disincentive for people.<br />
They were getting the same amount of money<br />
whether they have the 12 clients or the full 30,<br />
while the local hospital could be overflowing<br />
with people in leading care and they weren’t<br />
able to move them on. Now most people would<br />
be very professional and would not do that but<br />
that was what was possible under the block<br />
grant system.”<br />
Since the Fair Deal went live on billing on<br />
January 1st 2012, there has been a marked shift<br />
in behaviour from nursing homes.<br />
“There’s no doubt that has changed<br />
behaviour. People in the public hospital system<br />
have told me that units are much more keen<br />
to take the patients because if they don’t<br />
have full occupancy, then they don’t get<br />
their full funding.”<br />
What Maureen and her team did under<br />
the new scheme was create a link<br />
between the number of beds and the<br />
number of clients being treated with the<br />
money for the first time.<br />
“If a unit had a €105 million budget<br />
then we would take that €105m off<br />
them and divide it by the number of<br />
beds they had, say 30, and say ‘well<br />
that is what it is costing you that per<br />
week per client’. We said will give<br />
you back that €105m but only on<br />
the basis that every month you<br />
had to have 30 clients in the<br />
beds,” said Maureen.<br />
“At national level, that gave us for the first<br />
time visibility. For that billion, we literally had<br />
a list of 23,000 people who we could see their<br />
name and photograph and see what we were<br />
getting for our money.”<br />
But bringing ABF to the acute hospital setting<br />
is a much more complex process, with Maureen<br />
describing it as ‘Fair Deal on speed’.<br />
“Fair Deal is a very simple model. We have<br />
in simple terms a bed in a unit and we have<br />
a person in it. That is the product is being<br />
produced. There’s no product differentiation,”<br />
she said.<br />
“You have to decide what the equivalent of the<br />
product is in the hospital setting. In hospitals,<br />
we have about 16,000 possible diagnoses<br />
and 8,000 possible procedures which we<br />
classify under the Classification of Diseases 10<br />
Australian Modified (ICD10-AM).<br />
“Because you couldn’t work with that huge<br />
number, we use a grouper and that groups<br />
those different procedures and diagnoses into<br />
diagnosis-related groups (DRGs). The DRG<br />
is the product. We have 7/800 products for<br />
inpatients and about 350 or 400 for day cases.<br />
Whereas we have loosely 1000 products in the<br />
hospital settings, we have just one in the Fair<br />
Deal, highlighting the huge challenge of bringing<br />
ABF to the hospitals.”<br />
The foundation stones of the system have<br />
been laid since the 1990s when Brian Donovan<br />
and his team started collecting the cost data<br />
from the hospitals since then. Deirdre Murphy<br />
and her team provide the other vital cog in the<br />
ABF system – the classification system.<br />
“You need the same concept as the ‘€105<br />
million for the 30 beds’ from the Fair Deal for<br />
the hospitals. You need to be able to say, what<br />
is the cost of doing this work, and how do you<br />
measure how many products you are producing.<br />
“There are two systems basically. Deirdre<br />
and her team running the classification system,<br />
which people would know as the HIPE clinical<br />
coding system, and Brian and his team have<br />
been conducting the cost collection for many<br />
years. What we do then is join the two of them,<br />
and that effectively becomes the cost of each of<br />
our products.”<br />
There are statisticians and very elaborate<br />
statistical models that allow them to merge<br />
those two very large data sets. There are 1.6<br />
million discharges a year in the hospital system<br />
26 | health matters | winter 2016
The ABF team: Deirdre Murphy, Joe Sheeky, Maureen Cronin and Brian Donovan.<br />
and all diagnoses, all procedures are grouped<br />
into those products.<br />
“The 1.6 million has to be merged with the<br />
money,” explained Maureen.<br />
Brian said that, for example, they get all the<br />
costing data for treating Alzheimer’s patients<br />
and then set the average.<br />
“Efficient hospitals end up getting more money<br />
and inefficient hospitals get less,” he explained.<br />
“We have relative values for each DRG. The<br />
average case costs €5,000 and each DRG is<br />
given a weighting relative to the average case.<br />
An ICU case could have relative value of 28 and<br />
a normal birth would be 0.6. We weight each of<br />
the DRGs depending on how many resources<br />
they consume and we pay then based on that.<br />
“In the old way when we were measuring<br />
activity based on discharges, then an ingrown<br />
toenail measured the same as a head<br />
transplant. It didn’t make any sense. You had to<br />
acknowledge the complexity of the cases.<br />
“If one hospital gets funding of €100m but<br />
overruns by €1m, then under the previous<br />
system, they were doing badly. Another hospital<br />
could have received funding of €100m too and<br />
managed to come in €1m under budget and<br />
looked good. You could have even looked at<br />
the under-budget hospital, seen that they had<br />
performed 20,000 procedures and thought that<br />
they were doing even better.<br />
“But that hospital could have dealt with<br />
20,000 ingrown toenails while the other<br />
hospital dealt with 10,000 head transplants. So<br />
when you weight them, the first hospital is doing<br />
much better. ABF now can show us that the<br />
over-budget hospital was far more efficient.”<br />
The challenge now for the Healthcare Pricing<br />
Office, under Maureen’s leadership, is to get<br />
good enough data to be able to implement<br />
ABF fully.<br />
“First of all, the costs that we are producing,<br />
we know they are wrong, because hospitals<br />
don’t have good enough systems in place to<br />
capture all the things that we would like them<br />
to capture. We first need to refine and get our<br />
costs better,” said Maureen.<br />
This year Brian and his team will be<br />
implementing across the country new patient<br />
level costing (PLC) software to capture data<br />
from all the feeder systems such as labs,<br />
radiology and theatre.<br />
“The PLC is basically like a hotel bill for your<br />
stay in hospital. It will show how many days you<br />
spent in it, what tests you had, all that would be<br />
on your bill,” said Brian.<br />
Maureen explained: “We need to put a greater<br />
worth on clinical coders. During the recession,<br />
many coders were taken out not replaced.<br />
Clinical coding didn’t take centre stage due to<br />
the pressures people were under. Now we have<br />
the National Office for Clinical Audit and the<br />
clinical programmes looking more at clinical<br />
coding and telling clinicians, ‘this is your data,<br />
your staff is putting it in, make sure it is good’.<br />
For example, if somebody has a catastrophic<br />
stroke but a coder is brand new or the clinical<br />
notes are appalling and it is coded as a minor<br />
stroke, we might pay out €1,900 instead of the<br />
€23,000 is actually cost to treat.”<br />
Deirdre said a coder’s job is to open a patient<br />
file every day and extract the information as<br />
given by the clinician.<br />
“They will give us that picture of the activity<br />
in the hospital and play a critical role in giving<br />
us the 1.6 million pictures - some simple, some<br />
complex – and helping to identify and group<br />
those. It is a massive role and they are vital to<br />
the hospital.”<br />
FURTHER information<br />
For further information: www.hpo.ie<br />
winter 2016 | health matters | 27
Feature<br />
National review of clinical care<br />
national office<br />
of clinical audit<br />
ational clinical audit is a cyclical<br />
process that aims to improve<br />
patient care and outcomes by<br />
N<br />
systematic, structured review and<br />
evaluation of clinical care against<br />
explicit clinical standards on a national basis.<br />
The aim of the National Office of Clinical<br />
Audit (NOCA), established in 2012, is to provide<br />
a national measure of inputs, process and<br />
outcomes of care provided against national and<br />
international best practice standards. National<br />
audit data can also provide a repository of<br />
reliable data for service planning, strategic<br />
development and research.<br />
NOCA is based on the campus of the Royal<br />
College of Surgeons (RCSI) and is funded by the<br />
HSE Quality Improvement Division (HSE QID).<br />
The team is led by Collette Tully, Executive<br />
Director and Ken Mealy, Clinical Director.<br />
Each audit is managed by an Audit<br />
Coordinator and Clinical Lead, with<br />
governance provided by a National Clinical<br />
Audit Governance Committee and the NOCA<br />
Governance Board. Each audit is also supported<br />
by a Statistician and Information Manager.<br />
National audits are well established<br />
internationally including HQIP in England, ISD<br />
Scotland, the Swedish National Audit Office<br />
and the Australian Orthopaedic Association,<br />
National Joint Replacement Registry.<br />
National audit reports identify areas of<br />
excellence as well as concern and include key<br />
findings and recommendations to improve our<br />
healthcare system.<br />
NOCA currently manages the following<br />
national audits:<br />
• Irish National Orthopaedic Register (INOR)<br />
was established in 2013 to improve and<br />
maintain the quality of care for individuals<br />
receiving joint replacement surgery in Ireland.<br />
The register will collect information from<br />
all elective hospitals in Ireland undertaking<br />
joint replacement surgery and will support<br />
early detection of implant performance and<br />
improve the efficiency of the recall and review<br />
process. The register is currently live in South<br />
Infirmary Victoria University Hospital, Cork and<br />
will be implemented across all public elective<br />
orthopaedic hospitals by 2019, with private<br />
hospitals to follow.<br />
• Irish Hip Fracture Database (IHFD) is<br />
live in all 16 hip fracture trauma receiving<br />
hospitals across Ireland. Every year in Ireland,<br />
over 3,000 people are hospitalised with a hip<br />
fracture. International evidence has shown<br />
that care standards, audit and feedback can<br />
drive measurable improvements in hip fracture<br />
outcomes. Quality of hip fracture care is<br />
assessed against the six standards in the British<br />
Orthopaedic Association (BOA) and British<br />
Geriatrics Society (BGS), 2007 ‘Blue Book’: Care<br />
of patients with fragility fracture.<br />
• Major Trauma Audit (MTA) is live in all 26<br />
trauma receiving hospitals across Ireland. Major<br />
trauma is recognised as the leading cause<br />
of death and disability in older children and<br />
adults of 44 years and younger. MTA uses the<br />
internationally recognised the Trauma Audit and<br />
Research Network (TARN) methodology. This<br />
audit assesses the quality of care against clinical<br />
guidelines from National Institute of Clinical<br />
Excellence and system level KPIs.<br />
• Irish National Intensive Care Unit Audit<br />
(INICUA) measures the quality of care in ICU by<br />
benchmarking outcomes to the internationally<br />
recognised standards of the Intensive Care<br />
National Audit & Research Centre (ICNARC) in<br />
the UK. The National ICU audit is currently live<br />
in five public hospitals and seven units – Mater<br />
Hospital Beaumont Hospital, Tallaght Hospital,<br />
Lourdes Hospital, Drogheda and UH Limerick. It<br />
will be implemented across all public ICU units<br />
by 2019.<br />
• National Audit of Hospital Mortality (NAHM)<br />
is live in 44 acute hospitals across Ireland.<br />
NAHM explores hospital mortality patterns and<br />
produces a standardised mortality ratio (SMR).<br />
The SMR compares the observed to the expected<br />
number of deaths within diagnostic groupings in<br />
a hospital setting adjusting for factors that may<br />
influence their outcome such as age, admission<br />
source and type, pre-existing illness etc. SMRs<br />
are only one indicator of quality of care. Hospitals<br />
have access to reports via the NQAIS NAHM tool<br />
that supports the national audit.<br />
NOCA also provides assisted governance for<br />
the National Perinatal Epidemiology Centre<br />
(NPEC) who conduct the following audits:<br />
• Severe Maternal Morbidity<br />
• NPEC Perinatal Mortality<br />
• Planned Home Births<br />
There will be three NOCA audit national<br />
reports published by the end of 2016. The Irish<br />
Hip Fracture Database National Report 2015<br />
was launched recently at the 5th National Hip<br />
Fracture Conference.<br />
The Major Trauma Audit National Report<br />
2014- 2015 is the inaugural report for this<br />
audit and will be launched December 8th at the<br />
National Patient Safety/Clinical Effectiveness<br />
Conference.The inaugural National Audit of<br />
Hospital Mortality Report will be launched on<br />
December 15th.<br />
All reports will be available via the NOCA<br />
website www.noca.ie/publications<br />
more information<br />
If you have any queries, please contact us on<br />
014028577, auditinfo@noca.ie or Tweet us<br />
@noca_irl<br />
28 | health matters | winter 2016
Introducing @HSELive<br />
‘Hello, we’re the health<br />
service. How can we help?’<br />
ABOVE: Geraldine Charman, HSELive; ABOVE LEFT: Lorcan Power, Communications; Lorraine<br />
Reaburn, HSELive and Sarah Kelly HSELive; BELOW LEFT: Geraldine Charman and Geraldine<br />
McCarville, HSELive<br />
We know that it’s not always easy for our<br />
service users and clients to know where<br />
to turn to for guidance or support when<br />
navigating the healthcare system. They find it<br />
confusing and have many questions about our<br />
health system, often during times of emotional<br />
distress when they or their loved ones are ill.<br />
As well as this, public expectations have<br />
changed in recent years and are constantly<br />
changing in this digital age. People expect<br />
to be able to engage with an organisation<br />
directly – to ask questions, get consistent<br />
responses, and support in a timely manner.<br />
Think about your car or house insurance,<br />
even your hairdresser or dentist will send you<br />
text reminders.<br />
The ways in which the public chooses<br />
to engage directly with organisations<br />
has widened. More people are now using<br />
LiveChat, social media and email to interact<br />
with organisations to ask questions, find<br />
information or solve problems. Globally and in<br />
Ireland, phone / voice is the fastest reducing<br />
medium of communication as more and more<br />
people turn to digital channels.<br />
This is why we are launching @HSELive<br />
– a new multi-channel information service to<br />
answer questions and be a guide to the Irish<br />
health system. The purpose of this change is<br />
to deliver an improved responsive customer<br />
service platform with staff who can provide<br />
consistent responses, to the public across<br />
phone, email, Livechat on HSE.ie and via<br />
social media.<br />
The service has been designed with the end<br />
user at the heart of the service, to provide<br />
information and signposting on health and<br />
health services for the public on a channel of<br />
their choosing.<br />
In addition to significantly enhancing the<br />
public face of health services, this digital<br />
transformation also, importantly, gives us an<br />
opportunity to use data to drive improvement.<br />
Every contact with @HSELive signals that the<br />
public are experiencing a problem somewhere<br />
in the health system. The new customer<br />
relationship management tool and data<br />
systems will enable us to focus our energies<br />
on fixing the root cause of the contact or<br />
problem, ultimately using public feedback to<br />
drive improvements, thereby ensuring better<br />
health service experiences to those we serve.<br />
HSELive will bring a renewed focus on<br />
customer service in information provision in<br />
the health services in-line with our values of<br />
care and compassion.<br />
Speaking about the launch of @HSELive,<br />
Geraldine Charman, @HSELive Team Leader<br />
said, “We are looking forward to being able to<br />
deliver an improved service to more peope in<br />
the way they want the service delivered. The<br />
@HSELive team has really embraced these<br />
huge changes and has welcomed the new<br />
technologies, which is fantastic.”<br />
Here’s all the ways you can talk to us<br />
Callsave 1850 24 1850<br />
Livechat on HSE.ie<br />
Tweet us @HSELive<br />
Email hselive@hse.ie<br />
We’re here Monday – Friday 8am to 8pm,<br />
Saturday 10am to 5pm.<br />
winter 2016 | health matters | 29
specialist team providing integrated community care<br />
service helps reduce<br />
unnecessary hospital stays<br />
A key principle of our health service is to provide<br />
patients with the most appropriate care and<br />
service in the most appropriate location provided<br />
by the appropriate health care professionals.<br />
Patients should not have to attend hospital<br />
unnecessarily with all the added stresses and<br />
possible complications that such attendances<br />
involve for them and their families.<br />
A Community Intervention Team (CIT) is a<br />
specialist, nurse-led health professional team<br />
which provides a rapid and integrated response<br />
to a patient with an acute episode of illness who<br />
requires enhanced services/acute intervention<br />
for a defined short period of time. This may be<br />
provided at home, in a residential setting or in<br />
the community as deemed appropriate, thereby<br />
avoiding acute hospital attendance or admission,<br />
or facilitating early discharge.<br />
The CIT, through its fast-tracked provision<br />
of services enhances the overall primary care<br />
system, providing access to nursing and home care<br />
support, usually from 8am to 10pm, seven days<br />
per week. It is available to all patients regardless<br />
of eligibility once they meet the referral criteria.<br />
Referrals are accepted from hospitals, GPs and<br />
other community sources and each person’s<br />
referral is assessed to ensure it meets the criteria<br />
for safe care in the person’s home or in a CIT clinic.<br />
These clinic locations are more convenient<br />
for patients compared with attending an acute<br />
hospital setting. The CIT works in partnership with<br />
the referring clinician and agrees a plan of care for<br />
the patient .<br />
The range of services currently provided by<br />
CITs include:<br />
• Administration of IV antibiotics<br />
• Wound dressings<br />
• Acute anticoagulation management<br />
• Urinary related care (urinary catheter care and<br />
patient education)<br />
• Ostomy Care<br />
• Medication Management<br />
• Enhanced Nurse Monitoring<br />
• Care of patients with respiratory illness<br />
• Male/ female urethral/ supra-pubic<br />
catheterisation<br />
• Palliative care/ end of life care<br />
• Diabetic care and blood sugar monitoring<br />
• Central venous catheter care<br />
• Chemotherapy Pump disconnection<br />
• Physiotherapy and Occupational Therapy<br />
services (Louth)<br />
Key to the service are the working relationships<br />
with both hospital based and community based<br />
health professionals, as all are working together to<br />
support and care for patients living at home with<br />
chronic diseases.<br />
GPs may refer to CIT for interventions such as<br />
subcutaneous fluid administration.<br />
One such case is a lady in her 80s living at home<br />
with carers in South Dublin. She has a medical<br />
diagnosis of Parathyroid adenoma with high<br />
calcium levels and a past medical history of CVA<br />
(stroke). She previously had multiple admissions<br />
to hospital for treatment for dehydration and high<br />
calcium levels, (3 admissions of approximately<br />
10 days each in a 3 month period). In December<br />
2015 her GP referred her to the local CIT for the<br />
administration of subcutaneous fluids twice weekly<br />
to maintain hydration and decrease calcium levels.<br />
CIT has been visiting this lady in her own home,<br />
as requested, twice weekly and administering<br />
fluids as prescribed, usually a litre of normal<br />
saline over 24 hours. Since the GP referral to<br />
the CIT in December 2015, this lady has had<br />
no hospital admissions for dehydration or high<br />
calcium to date (patient has given permission to<br />
document her treatment .<br />
Another example of this collaborative working<br />
relationship is where a patient is referred to CIT<br />
from an Emergency Department with a minor soft<br />
tissue injury sustained after a fall. In this case,<br />
when the CIT nurse assesses the patient on a<br />
home visit, she may note that while previously this<br />
patient had been independent with care at home,<br />
the patient may now require community services<br />
and a Geriatrician review.<br />
The CIT works closely with PHN services, and<br />
may transfer care to the PHN when an acute issue<br />
has been resolved and the patient has ongoing<br />
needs or where the CIT accepted a referral for a<br />
nursing service during out of hours. The PHN may<br />
refer to CIT following discussion with the patient’s<br />
GP, where there is a new acute need or if a patient<br />
requires a service out of hours which the PHN<br />
service cannot provide.<br />
An example is where a PHN visits an elderly<br />
patient for a planned leg ulcer dressing and<br />
determines that the patient is acutely unwell<br />
but does not require hospital care. The PHN may<br />
contact the GP in relation to the need for a home<br />
visit and referral to CIT.<br />
Referrals for administration of home IV<br />
antibiotics (Outpatient Parenteral Antimicrobial<br />
Therapy) (OPAT) are made by hospital consultants<br />
with input from the local Infectious Diseases<br />
30 | health matters | winter 2016
Contact Details for CIT<br />
Dublin South – 01-4987100,<br />
Fax 01-4987132<br />
Dublin North – 01-7044444,<br />
Fax 01-7044497<br />
Meath/Kildare – 01-4276000,<br />
Fax 01-4276099<br />
Louth – 042-9364210,<br />
Fax 042-9389864<br />
Sligo – 01-4688279, Fax 01-6865153<br />
Galway – 01-4270000, Fax 01-4276099<br />
Limerick – 061-483660/483679,<br />
Fax 061-483902<br />
North Tipperary – 067-46472,<br />
Fax 067-46490<br />
Clare – 065-6863260,<br />
Fax 065-6863262<br />
Carlow/Kilkenny, Wicklow, Waterford/<br />
South Tipperary – 0818-300030,<br />
Fax 059-9133968,<br />
Ereferrals available in this area<br />
Cork – 1890-837427, Fax 021-4840093<br />
To discuss the clinical details of<br />
a patient you should phone the<br />
relevant CIT and fax the referral to<br />
the appropriate number outlined<br />
above. Please note that you must<br />
await confirmation of acceptance of<br />
referral by CIT.<br />
In the event of you experiencing<br />
any service difficulties please call<br />
the CIT/OPAT Management Control<br />
Centre at 01 4276000 which provides<br />
a national co-ordination role for<br />
these services.<br />
specialist or Clinical Microbiologist.<br />
This helps to ensure that patients are suitable<br />
for treatment at home and that they are receiving<br />
the appropriate antibiotic treatment. It is assumed<br />
that each day on the OPAT programme equates<br />
to a bed day saved as the patient would otherwise<br />
have remained in hospital. This programme saved<br />
26,307 bed days in 2015 (17,031 on the nurse<br />
administered service HOPAT, and 9,276 where the<br />
antibiotic is compounded in a device and patients<br />
taught to self administer SOPAT). This equates to<br />
72 beds each day.<br />
The OPAT programme has developed a<br />
protocol for the management of cellulitis in the<br />
community including appropriate oral antibiotics/<br />
criteria for prescription of IV antibiotics by the GP<br />
if indicated/ criteria for referral to hospital. This<br />
IV service is currently available for GP referrals<br />
for patients living in Dublin, Kildare, Wicklow,<br />
Louth and Meath. Plans are underway to roll out<br />
to the other CIT teams.<br />
The CIT is a valuable acute nursing service<br />
that can rapidly respond to acute nursing care<br />
needs in the community. It provides a very<br />
patient centred service within the primary care<br />
framework and audits have reported high levels<br />
of patient satisfaction.<br />
Thanks for participating in the Health<br />
Sector National Staff Survey 2016<br />
Thank you for your response to the<br />
2016 Health Sector National Staff<br />
Survey, Your Opinion Counts.<br />
The survey ran for just over<br />
five weeks from Wednesday,<br />
September 28th until Friday,<br />
October 28th and staff<br />
participated from all parts of<br />
the country.<br />
More than 19,000 completed<br />
surveys were received.<br />
The purpose of the Survey was to<br />
access current staff opinions in order to<br />
identify opportunities for improvement which<br />
will help build a better health service for all.<br />
Rosarii Mannion, National Director of Human<br />
Resources, expressed her appreciation to all<br />
of the staff who participated<br />
“Thank you for your participation and<br />
sincerity. Your feedback is an invaluable tool<br />
for the success of the health sector. It is very<br />
much valued. Staff who have good workplace<br />
experiences deliver better care to patients.”<br />
Libby Kinneen, HR Lead on Staff<br />
Engagement, said there were many positive<br />
aspects about the way the Survey was carried<br />
out this year.<br />
“We tried to do something different this<br />
time. We wanted the Survey to be a vehicle<br />
for staff engagement. Therefore we tried to<br />
get as many people to participate as possible.<br />
“We were assisted by 200 staff around the<br />
country who acted as Survey Champions<br />
encouraging colleagues to complete the<br />
questionnaire. Our Survey Champions were<br />
the human face of the Survey and helped to<br />
explain what it was about and why we were<br />
doing it by holding briefings and meetings<br />
around the country.<br />
“In addition we received a lot of feedback<br />
from staff which will be very useful in<br />
informing the 2017 Survey process.”<br />
What’s Next?<br />
Ipsos MRBI has the completed surveys and<br />
has been compiling the results. An overview<br />
of the results is due to be presented to the<br />
HSE Leadership Team this month (December)<br />
and a Communication to all staff will follow<br />
outlining the main findings.<br />
The need for systematic follow up in the<br />
period following staff surveys has been<br />
identified as a very important part of the<br />
whole process.<br />
With this in mind, we plan to hold a series of<br />
workshops across the health sector including<br />
Hospital Groups and Community Health<br />
Organisations in the week beginning January<br />
23rd next.<br />
In the spirit of staff engagement these<br />
workshops will be attended by a<br />
proportional representation of<br />
staff who will plan actions for<br />
their area to address issues<br />
which have been identified in<br />
the Survey.<br />
The workshops will provide<br />
opportunities for staff at<br />
all levels to get involved in<br />
actions which will ensure local<br />
ownership.<br />
Look out for opportunities to give<br />
expressions of interest to participate in<br />
a workshop in your area.<br />
Thanks again for your valued participation!<br />
We on the Project Team really appreciate<br />
your participation and the effort you made to<br />
make time to do the Survey.<br />
Your feedback will help to make the Health<br />
Sector a better place to work.<br />
FURTHER INFORMATION<br />
Further information please contact:<br />
nationalhr@hse.ie<br />
winter 2016 | health matters | 31
Feature<br />
Valuing staff knowledge and creativity<br />
HEARING<br />
STAFF VOICES<br />
hey say there’s nothing as<br />
powerful as being heard and<br />
University Hospital Kerry (UHK)<br />
T<br />
have taken this message to heart<br />
- from sharing their ideas for<br />
quality improvement at staff listening sessions<br />
to acting on those same ideas using an approach<br />
called Front Line Ownership.<br />
In 2015, 69 staff from all disciplines in<br />
University Hospital Kerry participated in<br />
listening sessions designed and facilitated<br />
by the Quality Improvement Division. Before<br />
beginning this work, the Executive Management<br />
Board (EMB) agreed to support and act on the<br />
top three suggestions for improvement.<br />
The key feedback from staff at these<br />
sessions was:<br />
“Helping make a difference in the lives of<br />
those who use our services and working<br />
collaboratively with our colleagues are the<br />
greatest positives of our work. Please ensure<br />
we have sufficient staff to do our jobs safely<br />
and well.<br />
Help us to continue to learn so that we can<br />
continue to improve service delivery. Help us<br />
Principles of Front Line Ownership<br />
• Go slow to go fast<br />
• Invite the unusual suspects<br />
• Work with those who want to work with you<br />
• Participation is voluntary<br />
• Nothing about me without me<br />
• Change can spread bottom up, top down,<br />
and sideways<br />
• Make the invisible visible<br />
• Act your way into a new way of thinking<br />
commit to a culture of mutual respect, kindness<br />
and compassion.<br />
To improve services, improve<br />
communication - keep us informed, listen to<br />
us and value our opinion.<br />
Ask us - we can help reduce waste and<br />
improve processes. Introduce flexible working.<br />
Happy staff - happy patients. And finally<br />
recognise the work of staff - say thank you and<br />
acknowledge us when we do a job well.”<br />
In a follow on action planning session<br />
with staff and management which included<br />
engagement with patients, staff formed five<br />
teams: Communication, Culture, Flexible<br />
Working, Waste and Training and Education.<br />
Using a Front Line Ownership approach,<br />
Dr Michael Gardam and Leah Gitterman,<br />
Ignite Consulting, coached approximately<br />
50 staff members during three on-site visits<br />
and through regular coaching calls on these<br />
themes. A member of EMB acted as a sponsor<br />
for each of the group to raise issues at board<br />
level if required. The Quality Manager who<br />
was also a member of the EMB provided<br />
coaching and leadership support locally. Four<br />
HSE staff shadowed this work to sustain and<br />
spread the learning.<br />
FLO is an internationally recognised and<br />
successful quality improvement approach<br />
which encourages staff to acknowledge their<br />
own capacity and potential to improve service<br />
delivery and make creative sustainable changes.<br />
Some challenges included having time to meet<br />
together. One group utilised ‘What’s App’ and<br />
Twitter to communicate regularly. The methods<br />
used to communicate and engage with other<br />
hospital staff included informal get togethers,<br />
canteen focused events, and conversations<br />
with staff. Coaching via teleconferencing was<br />
more feasible than videoconferencing due to IT<br />
restrictions and access.<br />
32 | health matters | winter 2016
So what happened?<br />
The Communications team introduced the<br />
‘Hello My Name’ is initiative, completed<br />
a social network mapping exercise and<br />
established a UHK choir ‘The Frontliners’!<br />
The Waste team established a pilot for<br />
recycling in theatre and outpatients, provided<br />
recycling awareness training for staff,<br />
introduced patient menu cards to reduce<br />
food waste by introducing portion sizes (also<br />
meeting HIQA Nutrition standards).<br />
The Culture group introduced ‘Happy<br />
Mondays’ and social events to improve staff<br />
culture, held a free staff draw with prizes from<br />
local businesses, improved car parking, raised<br />
awareness of staff uniform policy- clerical<br />
staff now have a standard uniform and staff<br />
outdoor seating area provided.<br />
The Training, Education and Flexible working<br />
time completed a review of mandatory<br />
training and flexible working was agreed; with<br />
staff self rostering systems in place in most of<br />
the wards.<br />
Today the teams continue to work on new<br />
ideas and with new and original members.<br />
Majella Daly, worked as the Quality Manager<br />
in Kerry at the time and she described the<br />
experience (see right).<br />
ABOVE: Pictured at the sessions were Grainne<br />
Rohan, CNM2, Emir Murphy, Speech and<br />
Language, Majella Daly, Quality Manager and<br />
Amanda Brolly, Intensive Care Nurse.<br />
BELOW: Staff celebrating the success of the work in<br />
University Hospital Kerry.<br />
more information<br />
Further information please contact:<br />
Maureen Flynn, Director of Nursing and<br />
Midwifery, Quality Improvement Division,<br />
Lead Governance and Staff Engagement for<br />
Quality maureena.flynn@hse.ie 01-6352344<br />
Juanita Guidera, Quality Improvement<br />
Division, Lead Staff Engagement juanita.<br />
guidera@hse.ie 087-06423 08<br />
Majella Daly, Interim Primary Care Manager<br />
Majella.Daly@hse.ie<br />
For more information,<br />
see www.qualityimprovement.ie<br />
in brief with<br />
majella daly<br />
#hellomynameis Majella Daly. I worked as<br />
Quality Manager in UHK and was the local coordinator<br />
for the front line ownership initiative<br />
in the hospital.<br />
The hospital has almost 300 beds and over<br />
1000 staff delivering services across wide<br />
range of specialities such as maternity services,<br />
orthopaedics, oncology, palliative care, acute<br />
medicine as well as a very busy Emergency<br />
department and outpatient services. So you<br />
can imagine the span and scope of issues and<br />
problem facing staff and patients. This is why I<br />
feel we are really benefiting from being part of<br />
the frontline ownership initiative.<br />
Firstly the staff listening session held in<br />
May/June 2015 offered staff the opportunity<br />
to identify first-hand what their main issues<br />
of concern was. The National QID team<br />
supported this work, provided the final report<br />
and worked with myself and staff to prioritise<br />
the top five issues to address. My role was to<br />
encourage staff to continue their engagement<br />
after the listening session to actually sign up to<br />
join working groups to progress improvements<br />
in the five themes and keep FLO on the<br />
Management team agenda. The role of the<br />
local co-coordinator is key in moving into the<br />
stage of improvement as otherwise we could<br />
fail to walk the talk!<br />
Support staff, management and different<br />
professions were keen to become engaged<br />
in making changes. They signed up to join<br />
working groups and attended training in<br />
Frontline ownership methods - to be honest<br />
staff and I weren’t really sure what Frontline<br />
ownership and liberating structures methods<br />
were all about but we adopted an open mind<br />
and ‘suck it and see’ approach!<br />
We were still learning and having fun! For<br />
me I had to unlearn some of my traditional<br />
QI methods such as PDSA as Frontline<br />
ownership and liberating structures is more<br />
about listening helping staff you work with<br />
think in a different way, ask questions, drill<br />
down to find out why and then come up with<br />
solutions together which staff can try. It’s okay<br />
to fail with the solutions, you just learn, and<br />
try a different approach.<br />
The liberating structure tools provide<br />
different ways to ask the questions, seek the<br />
solutions but most importantly allow staff<br />
themselves to come up with those solutions<br />
and own the implementation of them. So it<br />
has been liberating for me in my role! I no<br />
longer feel I have to be the doer/come up<br />
with the solutions; staff can do this themselves<br />
with the techniques- they’re the best people<br />
to do it. We’ve even started involving some of<br />
our volunteers in the hospital. I believe this<br />
approach will build a sustainable approach to<br />
QI in the hospital now and in the longer term.<br />
winter 2016 | health matters | 33
A Patient Safety Initiative<br />
Introducing the Individual<br />
Health Identifier<br />
– your own “digital key”<br />
When you visit a healthcare practitioner, you<br />
embark upon a journey. This may be a brief trip<br />
to the GP for some advice and perhaps a medical<br />
prescription or it might turn into a lengthier<br />
journey with referrals to different parts of the<br />
healthcare system.<br />
Whoever your healthcare practitioner is, and in<br />
whatever setting you are seen, one of the most<br />
important things in order to deliver the right care<br />
at the right time is that you, as the patient, are<br />
uniquely identified.<br />
This is the key function of the new Individual<br />
Health Identifier (IHI). Your IHI is generated by the<br />
HSE using information about you as set out in the<br />
Health Identifiers Act 2014. This information will<br />
include your name, address, date of birth, etc. The<br />
IHI will not hold any of your health information<br />
and should not be confused with an electronic<br />
health record (EHR) which would gather all of<br />
your health records into one file; the IHI is there<br />
to identify you.<br />
Existing information systems in the Irish health<br />
and social care services need the IHI to help them<br />
identify you as a unique individual. At some stage<br />
future IT connectivity and new developments, for<br />
example the proposed Electronic Health Record<br />
(EHR), will rely upon the IHI as the cornerstone<br />
for unique and safe identification of patients.<br />
This means the risks of information not following<br />
you from your GP to the hospital, will be greatly<br />
reduced; the chances of using the wrong patient<br />
record, delivering the wrong care, prescribing<br />
the wrong medicine or performing the wrong<br />
procedure will be minimised.<br />
The development of the new IHI required<br />
legislation to protect everyone’s data and ensure<br />
the security of the system. The Health Identifiers<br />
Act 2014 was the first step in the creation of an<br />
IHI for Ireland and describes exactly what the<br />
IHI record for every person who uses the health<br />
services is allowed to contain.<br />
The HSE has been given the job of building<br />
and operating the IHI Register of unique health<br />
identifiers that will be used across health and<br />
social care services in the State. Personal data<br />
will be held safely and securely in the IHI Register<br />
and only used within the health and social care<br />
system to accurately identify you, using data such<br />
as your name, date of birth, mother’s maiden<br />
name, etc.<br />
The IHI record itself contains no medical data,<br />
just personal data to uniquely identify you as an<br />
individual. IHI records will be created, stored and<br />
used with the utmost confidentiality and security.<br />
Your individual personal data is private and will<br />
not be shared with anybody outside of the health<br />
and social care system. IHI records will only be<br />
seen by the relevant healthcare staff at the point<br />
of patient care.<br />
An IHI will be generated and assigned<br />
automatically to your existing health and social<br />
care records. In time, the IHI will be connected to<br />
the Maternity and Newborn Clinical Management<br />
Systems (MN-CMS) which will allow for the<br />
IHI to be generated at birth. The IHI number<br />
will be used in the background to identify you<br />
34 | health matters | winter 2016
and enable healthcare systems to identify your<br />
unique records so that we can provide healthcare<br />
services to you at the right time, giving safe and<br />
timely treatment. You will never need to know or<br />
have your IHI to access services as it is just an<br />
identifier within the health and social services<br />
(but it can be provided upon written request to<br />
the IHI Business Service). The IHI programme is<br />
committed to keeping your information safe and<br />
secure and an IHI Privacy Impact Assessment<br />
was opened to public consultation earlier in<br />
2016 (the results of which can be seen on www.<br />
ehealthireland.ie/Strategic-Programmes/IHI/).<br />
As the IHI is implemented in existing and new<br />
healthcare information technology systems<br />
across Ireland’s health and social care services in<br />
the coming years, it will allow you to be identified<br />
uniquely and will increase patient safety benefits.<br />
What does this mean for me, as a health service<br />
staff member?<br />
At the point where a patient registers with<br />
a health or social care provider, the IHI will<br />
become a key process for patient identification.<br />
Patient administration systems will be tailored<br />
to incorporate automatic look-up of the IHI for<br />
each new or return patient who presents to<br />
your service. In the event that a patient is not<br />
automatically allocated an IHI, this will not<br />
prevent their access to health or social care<br />
services. The IHI Business Service will process<br />
the new request in the background to generate a<br />
unique IHI for that patient.<br />
It will take several years for the IHI to be<br />
fully implemented in Ireland. There are many<br />
thousands of points where patients connect with<br />
health and social care services and the IHI Project<br />
will be implemented in each location over the<br />
course of time. Each site will be supported to<br />
identify and communicate with staff that need to<br />
use the IHI number for their patients. Initial pilot<br />
sites will start in both community and hospital<br />
based locations through 2016 / 2017 and, building<br />
upon the experience from these pilots, the rollout<br />
will continue in a managed way across the<br />
entire health and social care system. Already<br />
most European countries, along with Australia,<br />
Singapore and the United States, are benefitting<br />
from this system and we can learn from their<br />
experiences, of how best to introduce the IHI for<br />
maximum patient safety benefits.<br />
As the IHI implementation spreads across the<br />
Irish health and social care system, staff will<br />
begin to see IHI numbers appearing on patient<br />
records or correspondence between healthcare<br />
providers. The subsequent implementation of<br />
the IHI in existing national systems such as<br />
HealthLink / eReferrals, National Integrated<br />
Medical Imaging System (NIMIS) and the National<br />
Laboratory Information System (MedLIS) will<br />
spread the use of the IHI across the services.<br />
Local systems such as GP practice management<br />
systems and hospital patient administration<br />
systems will be added on a continual basis as<br />
we work through the phased roll-out. The IHI<br />
is a cornerstone of the eHealth strategy across<br />
public (both statutory and voluntary), and private<br />
health and social care services. With each phase<br />
of the roll-out careful consideration will be<br />
given to existing work practices of health<br />
service staff who are involved in patient<br />
identification, in order to minimise<br />
any extra workload.<br />
In most cases, the IHI will<br />
be automatically added to<br />
patient records without<br />
requiring much, if any,<br />
intervention from staff. The<br />
pilot approach adopted by<br />
the IHI Project will ensure<br />
that staff training materials<br />
are offered wherever needed.<br />
We are embarking on<br />
a programme of work<br />
that is estimated could<br />
take several years to<br />
be fully embedded<br />
in every health and<br />
social care service.<br />
We are taking<br />
a programmed<br />
approach and adding<br />
locations continually.<br />
We look forward to<br />
working with staff, GPs,<br />
and key agencies to<br />
build the IT platform<br />
FURTHER information<br />
that will improve the safety of our services.<br />
From our patient’s perspective the IHI will be<br />
transparent, working away in the background<br />
to assure health and social care staff that our<br />
patients are correctly and uniquely identified. Our<br />
patients will not need to know their IHI any more<br />
than they need to know other internal health<br />
service reference numbers such as their Medical<br />
Record Number (MRN). However as mentioned<br />
earlier, anyone can apply in writing to get a copy<br />
of their IHI number, the IHI Business Service will<br />
gladly provide an individual with their IHI.<br />
The IHI is a key to the success of safe,<br />
integrated health and social care for tomorrow<br />
and the future. We will keep you updated on new<br />
pilot programmes and progress over the coming<br />
months and years.<br />
Further information, including YouTube video is available at:<br />
www.ehealthireland.ie/Strategic-Programmes/IHI/<br />
winter 2016 | health matters | 35
HSE and e-HEALTH IRELAND<br />
HEALTH TECHNOLOGY<br />
IMPROVING CARE FOR PATIENTS<br />
The HSE and eHealth Ireland recently<br />
showcased the current innovations in Health<br />
as well as innovations from the future in Trinity<br />
Science Gallery in Dublin.<br />
This two day event was part of the eHealth<br />
Innovation week which started with a Hackathon<br />
to deliver solutions for patients with Bi-Polar<br />
disorder. This event was the first of its kind, and<br />
featured a host of health innovation exhibitions,<br />
demonstrations, presentations and devices which<br />
can enable innovations in healthcare today and<br />
into the future.<br />
Speaking at the event, Tony O’Brien, Director<br />
General of the HSE, said, “This event provides<br />
a timely opportunity for the HSE and eHealth<br />
Ireland to showcase the innovations currently<br />
being developed and delivered within the<br />
Health Service and the innovations that will<br />
be available to us in the future with the help of<br />
digital technologies. These innovations are part<br />
of building a better healthcare service for the<br />
patients we serve now and into the future.”<br />
The EH2030 exhibition included exhibits<br />
from suppliers, SMEs, start-ups and a new<br />
HSE initiative -the QIC Programme - which<br />
encourages clinically led innovation. This<br />
is an eHealth Ireland led internal innovation<br />
programme, facilitating the ability to deliver<br />
disruptive technologies and innovative platforms<br />
capable of transforming the Irish healthcare<br />
system by 2020.<br />
Richard Corbridge, HSE Chief Information<br />
Officer, said, “Disruption in digital health is here.<br />
Digital Health is a driving force in healthcare<br />
reform. Mobile technologies and elements<br />
like Internet of Things solutions will be the<br />
dominant platforms to access and create<br />
digital information. Research suggests that<br />
83pc of businesses will be digital by 2020 we<br />
need to work with SME’s and the public to be<br />
ABOVE: Richard Corbridge, Chief Information<br />
Officer , HSE (left) and Tony O’Brien, HSE Director<br />
General, pictured together experiencing the virtual<br />
Reality headsets during the HSE / eHealth Ireland<br />
Innovation Showcase held in the Science Gallery,<br />
Trinity College Dublin. Pic. Robbie Reynolds.<br />
technology bringing assisted living into the 21st century<br />
When people hear the words ‘assisted living’,<br />
chances are they will think of the traditional<br />
pendant alarm that can be worn around the neck.<br />
If you or someone in your family wears one of<br />
these devices, there is a good chance that Tunstall<br />
Emergency Response is the company monitoring<br />
the device and any alerts it sends out.<br />
“We are the largest provider of ‘telecare’ services<br />
in Ireland,” explains Tunstall MD James Doyle.<br />
“We have a 24/7 monitoring centre, which fields<br />
about 450,000 calls per annum – so we’re very<br />
experienced in this area.<br />
“The traditional assisted living device would be<br />
the pendant alarm that people are familiar with<br />
– but the technology is evolving all the time, and<br />
new innovations can really benefit the people we<br />
help care for.”<br />
Tunstall has recently joined forces with another<br />
Irish company, Motech Group, to provide a nextgeneration<br />
assisted living experience – through a<br />
device called the CareClip, designed by Motech.<br />
The CareClip is a matchbox-sized device, worn by<br />
the user. This is supported by a secure web portal<br />
and a mobile app that provide the family member<br />
and/or carer with instant, accurate data as to their<br />
loved one’s wellbeing.<br />
The CareClip has two-way communications<br />
to allow for instant contact from a person in a<br />
response centre, a family member or carer. The<br />
family member and/or carer can use the app to<br />
assure themselves of their loved one’s safety and<br />
wellbeing at any time.<br />
“The CareClip uses the most innovative and<br />
secure technologies available,” says Paul Flavin,<br />
CEO of Motech.<br />
“Traditionally an ‘assisted living’ monitoring<br />
service would be restricted to the home or<br />
residential care unit, due to the technology<br />
available. Motech wanted to extend this level of<br />
service and support, to allow people get the same<br />
reassurance 24/7 – wherever they are,”<br />
he explained.<br />
James from Tunstall continues: “We get<br />
approached on a regular basis by companies who<br />
have new pieces of technology. Motech’s CareClip<br />
36 | health matters | winter 2016
innovative and agile in our projects to provide the<br />
appropriate healthcare that citizens need.<br />
“This is the first time that a Health Innovation<br />
Week has been hosted in the EU. The Health<br />
Innovation Showcase is part of the Health<br />
Innovation Week currently being hosted in Dublin.<br />
The HSE and eHealth Ireland welcome this global<br />
event to Ireland and see it as an important step on<br />
the path towards building a better health service.”<br />
To learn more about the events of the Health<br />
Innovation Showcase or Health Innovation Week<br />
visit www.eh2030.com.<br />
Epilepsy and<br />
technology<br />
– Bridging the Gap<br />
Taking the care of an individual from<br />
the hospital into the community is not a<br />
new concept. However, the sharing of the<br />
most relevant and up to date information<br />
between tertiary and primary care has<br />
often been delayed and fragmented,<br />
requiring the way in which we communicate<br />
relevant information to change.<br />
The electronic patient record (EPR) was<br />
designed to share all relevant patient<br />
information between members of the<br />
multi-disciplinery team both in the hospital<br />
and the community setting at the touch of a<br />
button, in an effort to enhance patient care.<br />
The opportunity and necessity to use<br />
healthcare data/information intelligently<br />
has never been greater.<br />
The technology is now available to<br />
healthcare professionals<br />
to allow the delivery of<br />
a variety of epilepsy<br />
services to multiple sites<br />
to include maternity care.<br />
The use of the EPR<br />
in maternity services has<br />
enhanced the sharing<br />
of information between<br />
obstetrics, primary care,<br />
neurology services and<br />
the patient.<br />
The information gathered<br />
on the EPR is readily available<br />
allowing the various clinicians on site<br />
to make prompt informed decisions in<br />
caring for the woman with epilepsy. The<br />
woman with epilepsy is then more likely<br />
to have a greater awareness of her own<br />
condition, thus allowing her an influence<br />
into her care.<br />
is the best device that we’ve seen. It does exactly<br />
what we would want it to do.” The CareClip works<br />
while a person is at home and also while they are<br />
out and about, therefore allowing both physical and<br />
social interaction with the community.<br />
“This is achieved by combining the best mobile<br />
communications with GPS satellite technology and<br />
rigorous adherence to data security and privacy.<br />
The CareClip allows the wearer to send an alert<br />
if in need of assistance, and it provides automatic<br />
fall detection. It also allows for highly accurate<br />
location identification in the event of an alert – it<br />
will display where the person is instantly (accurate<br />
to within 5m).<br />
The CareClip will even alert if the wearer is out of<br />
a ‘safe zone’ or entering a ‘non-safe zone’, giving an<br />
increased level of reassurance and independence.<br />
James says: “Motech’s device has been<br />
comprehensively field-trialled, and its ability to<br />
roam across all the different networks is one<br />
aspect that we’re particularly delighted with. We’ve<br />
taken it to known black spots, where there is very<br />
poor phone signal coverage, and it has worked<br />
every time.”<br />
The CareClip has two-way communications<br />
to allow for instant contact from a person in a<br />
response centre, a family member or carer.<br />
The family member and/or carer can use the<br />
app to assure themselves of their loved one’s<br />
safety and wellbeing at any time. Both James<br />
and Paul explain that what the CareClip really<br />
offers is peace of mind to families, carers and<br />
wearers themselves.<br />
“Technology can never be a panacea,” says<br />
James, “but technology such as this can be<br />
an enabler – it’s an enabler for promoting<br />
independence and hopefully giving increased<br />
quality of life to both the wearer and their family<br />
or carer.”<br />
FURTHER INFORMATION<br />
To find out more call 1850 247 999 or<br />
go to www.tunstallemergencyresponse.ie<br />
winter 2016 | health matters | 37
NEW QUALITY<br />
AND SAFETY GUIDES<br />
QUALITY and Safety Committees perform<br />
an essential role in our health services by<br />
providing a forum to consider, monitor and<br />
improve the quality and safety of care we<br />
provide, said the HSE National Director for<br />
Quality Improvement, Dr Philip Crowley.<br />
“The committees provide much needed<br />
space to stand back and consider the quality<br />
and safety of care we provide, to monitor this<br />
on a routine basis, and to provide respectful<br />
challenge and act to improve care,” he said.<br />
“To help this process the National Quality<br />
Improvement Division has just updated<br />
guidance and produced templates for HSE staff<br />
who are looking to establish and review Quality<br />
and Safety Committees.<br />
This guidance forms part of a toolkit to<br />
support staff in applying the Framework for<br />
Improving Quality in our Health Service which<br />
was published by the HSE recently.<br />
Quality and Safety Committees address<br />
issues like:<br />
• How do you know what good care is?<br />
• How do you know you are getting better?<br />
• Do you have the appropriate measures?<br />
• Have you confidence in the relevant data?<br />
• Do you know where you stand relative to<br />
the best?<br />
• How do you demonstrate that you are a<br />
learning organisation?<br />
• How do you keep in touch with the front line<br />
reality of service delivery?<br />
• How do you ensure you hear the voices of<br />
patients, families, service users and frontline?<br />
“The guidance and templates are provided<br />
ready for adaptation to the specific context of<br />
each of our services.<br />
These include acute services, mental health,<br />
primary care, social care, health and wellbeing<br />
and the national ambulance service and are<br />
valuable tools for all of us to continue in improving<br />
the care that we deliver,” said Dr Crowley.<br />
more information<br />
The Quality and Safety Guidance is available<br />
to download at www.qualityimprovement.ie<br />
Please contact Karen Reynolds at karen.<br />
reynolds@hse.ie or 086 8394929 for more<br />
information or any questions about the Quality<br />
and Safety Committee Guidance document.<br />
38 | health matters | winter 2016
Claimsure claims system<br />
efficiency and<br />
accuracy boosted<br />
he deployment of Claimsure, a<br />
private health insurance claims<br />
management system, across<br />
T<br />
the acute public hospital sector<br />
is having a positive impact on<br />
the efficiency and accuracy of private health<br />
insurance claims management. Claimsure<br />
has been successfully implemented in all<br />
hospitals by HBS Finance - Income Reporting<br />
and the Office of the Chief Information Officer<br />
in partnership with Claimsure Slainte Ireland<br />
and local hospital resources.<br />
There are 48 public acute statutory and<br />
voluntary hospitals in Ireland which generate<br />
almost €640m worth of income from<br />
privately insured patients. In 99% of cases<br />
hospitals have a direct payment agreement<br />
between Private Insurers / Occupational<br />
Health Schemes and the Hospitals.<br />
Prior to 2012, the majority of hospitals had<br />
their own way of managing this process, so<br />
there were no national standards or national<br />
claims management systems in place.<br />
With the introduction of Claimsure, the<br />
HSE is now in a stronger position when<br />
negotiating changes in business terms at a<br />
high level. There is now national visibility<br />
and hospital uniformity when reporting<br />
on the level / status of private insurance<br />
debt. The direct pay agreement allows<br />
the hospital to directly bill the Private<br />
Insurers on the patient’s behalf and seek<br />
reimbursement from Insurers via Claimsure.<br />
Claimsure now electronically manages<br />
all aspects of a hospital’s claim from<br />
patient admission to discharge, including<br />
e-submissions to health insurance providers.<br />
It replaces the existing paper processing of<br />
claims and integrates with the Hospital’s<br />
admissions systems, patient billing systems<br />
and any external 3rd party consultant<br />
billing services. Patients can electronically<br />
sign insurance forms via an e-pad or tablet<br />
device. Consultants can access an electronic<br />
secure list of their claims via their HSE<br />
approved device, and can electronically sign<br />
appropriate claims.<br />
Claimsure has enhanced claims reporting<br />
at both hospital and national level, increased<br />
efficiencies in claims handling and query<br />
management. Most notably it has enabled<br />
the HSE to agree a significant Memo of<br />
<strong>Understand</strong>ing with the VHI which was<br />
introduced in November 2015 by way of a<br />
Heads of Agreement and adopted fully from<br />
March 1st 2016.<br />
A significant project to provide a national<br />
centralised reporting facility based on<br />
Claimsure is under development by HBS<br />
Finance - Income Reporting. This initiative<br />
will allow for further streamlining and<br />
standardisation of national reporting and is<br />
due for completion by the end of Q4 2016.<br />
HBS ON THE ROAD TO SUCCESS<br />
Health Business Services, the business division of the HSE,<br />
has achieved significant success in its first three years of<br />
operation, Tony O’Brien, Director General of the Health Service,<br />
acknowledged recently.<br />
Mr O’Brien, who is also Chair of the HBS Governance Committee,<br />
was speaking at a senior management forum for HBS leaders in<br />
Castletown House, Co Kildare.<br />
He said HBS was a central part of improving and reforming the<br />
health service.<br />
“There has been significant success in the first three years which<br />
demanded great effort, huge hard work and tremendous cooperation,”<br />
he added.<br />
“The theme and focus for the event centred around the<br />
development of a new Strategy for HBS for the next two years<br />
(2017-2019). The development of the Strategy was discussed in a<br />
series of workshop sessions and feedback discussions.<br />
Director of Health Business Services, Jane Carolan said the<br />
engagement was very successful helping to shape and inform the<br />
approach for progressing the HBS global business services model.<br />
“I am confident that HBS is delivering a world class model for<br />
shared services and that we will see more and more success in<br />
terms of the new Strategy of 2017-2019,” Ms Carolan said.<br />
HBS Management Team with Tony O’Brien, Director General.<br />
winter 2016 | health matters | 39
Feature<br />
Fewer errors and better outcomes<br />
Communicating<br />
ommunicating is something<br />
that happens every day in the<br />
health services. How well we<br />
C<br />
communicate is determined not<br />
by how well we say things but by<br />
how well we are understood.<br />
Research has shown that there are fewer<br />
errors and better treatment outcomes when<br />
there is good communication between patients<br />
and their healthcare providers, and when<br />
patients are fully informed and educated about<br />
their treatment and medication (World Health<br />
Organisation 2012).<br />
How we choose to communicate also<br />
influences our relationships with colleagues<br />
and impacts on the experience of our patients<br />
and service users when they interact with the<br />
health service.<br />
Patients and service users expect us to be<br />
clear when we give them information about<br />
their health. When we explain things clearly and<br />
with care and compassion, people have more<br />
confidence and trust in us, take our advice,<br />
and follow medical guidance. They are better<br />
informed and more likely to ask us questions so<br />
that they can take better care of their health.<br />
“39pc of Irish people ask that healthcare<br />
professionals use more understandable<br />
language and less medical jargon” (National<br />
Adult Literacy Agency, 2015).<br />
The HSE Communications Division supports<br />
effective and consistent communications by<br />
everyone who works in our health and social care<br />
services. On that basis, the Communications<br />
Division is developing a suite of tools for all staff<br />
to assist in effective communications. These are<br />
aimed at supporting HSE staff in communicating<br />
more clearly with service<br />
users and their families<br />
and with colleagues.<br />
Kirsten Connolly,<br />
Deputy Director of<br />
Communications, said,<br />
“We want to assist<br />
staff in thinking<br />
about how they<br />
present information in a way that ensures they<br />
are fully understood. This in turn ensures that<br />
patients, clients and the public in general can<br />
make informed choices, access appropriate<br />
services and take better care of their or their<br />
families, health. We also want to support<br />
staff in reflecting the values of the Health<br />
Service, particularly care and compassion, in<br />
how we all communicate. Through our daily<br />
interactions, we have an opportunity to shape<br />
the kind of communication culture we want in<br />
the health service.”<br />
The Communications Division team has<br />
developed a practical guide to encourage the<br />
use of plain language – using both the written<br />
and spoken word. Quite simply we wanted to<br />
give everyone a succinct and informative guide<br />
to how we communicate in the HSE. We set<br />
out the language and norms we use to ensure<br />
we communicate clearly and are understood.<br />
In a very practical way, this guide has been<br />
developed to support everyone in the health<br />
service adopt plain language in their work<br />
environment. The guide is aimed at all staff and<br />
is applicable for our daily interaction with adult<br />
service users and colleagues.<br />
To develop the Communicating Clearly Guide,<br />
we brought together the larger communications<br />
team and explored what plain language really<br />
means in various contexts and settings in health.<br />
We shared examples of where plain language<br />
worked really well and identified what was<br />
distinctive about the use of language in these<br />
instances. All of this was underpinned by a<br />
key principle; that we reflect our values in<br />
language we all use.<br />
The project team created this guide as<br />
the first in a suite of plain language tools to<br />
be developed over the coming months. The<br />
team was made up of Kirsten Connolly, Deputy<br />
Director of Communications; Norma Deasy,<br />
Campaigns Manager; Ann McLoone, Deputy<br />
Head of Press; Sarah Woods, Communications<br />
Manager, NOSP; Sandra Eaton, Deputy Head of<br />
Digital; Sheila Caulfield, Client Director Health<br />
and Wellbeing; Ross Cullen, Communications<br />
Manager, CHO2; Ciara McWeeney, Office of the<br />
Chief Officer, CHO6.<br />
Entitled ‘Communicating Clearly with<br />
Patients and Service Users’, the guide outlines<br />
how patients and service users ask us to be<br />
clear when we give them information about<br />
their health. It stresses that “clear and<br />
compassionate communication makes for better<br />
outcomes and a better experience for the people<br />
in our care”.<br />
40 | health matters | winter 2016
Clearly<br />
To achieve clarity we have taken an accessible<br />
and simple approach.<br />
The pointers we provide are:<br />
We introduce ourselves by saying:<br />
“Hello, my name is...”<br />
We speak clearly and with empathy:<br />
“How can I help you?”<br />
We put ourselves in our patients and service<br />
users’ shoes when talking to them:<br />
“Is there anything else you need to know?”<br />
We use plain language to explain complex terms:<br />
“Let me explain....”<br />
We listen to what they have to say and respond<br />
kindly:<br />
“I am here to help you understand everything.”<br />
We give contact details for more information:<br />
“In case you want more information...”<br />
To support staff in “writing so that those we<br />
care for can understand our letters and advice,”<br />
we provide further pointers:<br />
• We use clear language and everyday words<br />
• We write it as we would say it, using plain<br />
language<br />
• We avoid using jargon, abbreviations and<br />
acronyms<br />
• We use a font that is easy to read, such as<br />
Helvetica or Arial<br />
• We clearly explain the purpose of our letters<br />
and documents<br />
• We ask non medical staff to check that our<br />
letters and documents are easy to understand<br />
• We use ‘I’, ‘we’ and ‘you’ to personalise our<br />
letters and documents<br />
• We use short sentences and paragraphs<br />
• We give our contact details so that the reader<br />
can contact us for more information.<br />
Over the coming weeks, we will be distributing<br />
hard copies of ‘Communicating Clearly with<br />
Patients and Service Users’ guidelines, which<br />
encourages us all to communicate clearly and<br />
show empathy when talking and writing<br />
to our patients, clients and service<br />
users. These guiding principles, which<br />
have been endorsed by the HSE’s<br />
Leadership team, are designed to<br />
make us all stop and think on how we<br />
communicate. They will assist us to be<br />
more compassionate with our spoken<br />
and written word. They encourage us to<br />
use a clear, narrative and plain language<br />
that is suitable and easy to understand,<br />
and to focus our communications on<br />
the needs of those with whom we are<br />
communicating. Give them a try and see if<br />
it makes a difference in your day.<br />
further information<br />
See www.hse.ie/communicatingclearly<br />
Hard copies available to order from<br />
www.healthpromotion.ie<br />
winter 2016 | health matters | 41
Feature<br />
s you walk in the door of the<br />
Blackrock Hospice, you are<br />
welcomed warmly by Andrea,<br />
A<br />
the soothing scent of essential<br />
oils and the calm that permeates<br />
the building. Then you look left and the choice<br />
of books from ‘Saying Goodbye to Daddy’ to<br />
‘Finding a way through when someone close<br />
has died’ reminds you why people come here.<br />
In Galway, when you enter the spacious<br />
atrium, motivational messages catch your eye,<br />
there are people everywhere and instinctively<br />
you feel that each person has a purpose<br />
– some are waiting for news over a cup of tea,<br />
others on a mission to attend appointments<br />
or visiting loved ones. The one connecting<br />
point for these two diverse settings is that the<br />
staff in each look after people at their most<br />
vulnerable, hear intimate thoughts and share<br />
their time with patients what are often their<br />
greatest joys and sorrows.<br />
In healthcare, there is great privilege in<br />
this work yet when we help families hold<br />
it together, who holds us? Who cares for<br />
the carers?<br />
The Quality Improvement Division<br />
in conjunction with the Point of Care<br />
Foundation (PoCF), is currently working<br />
with Our Lady’s Hospice & Care Services<br />
- Blackrock Hospice and University Hospital<br />
Galway to test the introduction of Schwartz<br />
Rounds in an Irish context.<br />
What are Schwartz Rounds?<br />
Schwartz Rounds are monthly meetings for<br />
all staff working in a health care organisation.<br />
The Rounds provide an opportunity for staff to<br />
reflect on the emotional aspects of their work.<br />
The focus is on the human dimension of care.<br />
Each round is based on the story of a<br />
particular patient or a theme and is briefly<br />
presented by 3 or 4 members of staff.<br />
This is followed by a facilitated discussion<br />
which involves the wider audience and is an<br />
opportunity to listen, share and support.<br />
Schwartz Rounds provide a framework which<br />
helps to improve staff wellbeing, resilience<br />
and support which ultimately has an impact on<br />
improved patient centred care.<br />
What are staff saying in Ireland about<br />
Schwartz Rounds so far?<br />
The feedback from staff so far has been<br />
really positive – staff are telling us:<br />
ENCOURAGES INSIGHT<br />
“Amazing insight into other professional’s<br />
experiences”<br />
“Felt glad that multidisciplinary from cleaner<br />
to consultant was emphasised”<br />
“These rounds help break down barriers<br />
between all the different members of the<br />
hospital staff ...”<br />
“Takes time out to my day to see the patients<br />
on my waiting list but is a good way to focus on<br />
caring for ourselves”<br />
Schwartz Rounds<br />
who cares<br />
Reaffirms values<br />
“Brings caring and kindness back into the<br />
workforce”<br />
“Helps us remember why we are in a caring<br />
profession”<br />
positive feeling<br />
“Feel-good factor - positive effect overall”<br />
“Incredibly moving and human”<br />
“Stunning - made me very proud to work<br />
with such compassionate, sincere and expert<br />
people”<br />
“Well worth taking the time to attend despite<br />
a very busy schedule”<br />
HIGHLIGHTING IMPORTANT ISSUES<br />
“Highlighted other issues like open<br />
disclosure”<br />
“Very positive and potent reinforcement<br />
of how an individual can impact on patient<br />
care through non-clinical means - smiles,<br />
compassion, greetings”<br />
“Very thought-provoking about what we do<br />
well and when things go wrong”<br />
For more information about Schwartz<br />
Rounds, please see<br />
www.qualityimprovement.ie<br />
A mentor’s experience of<br />
Schwartz Rounds by Nicki<br />
Power, Schwartz Round<br />
Mentor<br />
I have facilitated, mentored and evaluated<br />
more information<br />
If you have any queries about Schwartz<br />
Rounds, please contact:<br />
Maureen Flynn, QID Lead Governance and<br />
Staff Engagement for Quality, maureena.<br />
flynn@hse.ie 01-6352344 or<br />
Juanita Guidera, QID Lead Staff Engagement<br />
juanita.guidera@hse.ie 087-0642308.<br />
Useful Resources<br />
www.qualityimprovement.ie<br />
http://www.theschwartzcenter.org<br />
http://www.pointofcarefoundation.org.<br />
uk/schwartz-rounds/<br />
http://www.kingsfund.org.uk/publications/<br />
schwartz-center-rounds-pilot-evaluation<br />
Schwartz Rounds since 2014 in the UK,<br />
working both within the National Health<br />
Service and with the Point of Care Foundation,<br />
who have supported the development of the<br />
Schwartz Round pilot in Ireland. For me, the<br />
power of Rounds is that they advocate for<br />
vulnerability as a strength, and see bravery<br />
in the emotions we display and acknowledge<br />
the positive impact of our human connections<br />
in a professional context. I have heard a<br />
choke in the throat of a ‘tough’ consultant as<br />
they talk about the guilt of making a mistake,<br />
seen tears in the eyes of audience members<br />
connecting to their own unforgotten patients<br />
and also, heard the silence of an audience<br />
engaged completely in listening to the story of<br />
a colleague, a human being.<br />
Before coming to Ireland to mentor the<br />
42 | health matters | winter 2016
for the carers?<br />
staff at Blackrock Hospice and University<br />
Hospital Galway, I had not considered that<br />
storytelling is innate in Irish culture and<br />
how this might impact on Schwartz Rounds.<br />
As an emigrant, resident in the UK, my<br />
cultural identity is obvious as soon as I speak<br />
– I am Irish. People often ask me why I’m<br />
passionate about Schwartz Rounds. I used to<br />
absentmindedly say that I have always liked<br />
stories and hearing people share their unique<br />
perspectives, but I had not linked this to my<br />
cultural heritage until now.<br />
Ireland offers a unique context in which<br />
to apply this model of staff support – one<br />
where storytelling is already valued and<br />
culturally relevant.<br />
A Schwartz Round at<br />
University Hospital Galway<br />
The reception at University Hospital Galway<br />
invites all those who enter to take care of<br />
themselves before caring for others. This<br />
is communicated through art work which<br />
invites visitors and professionals to reflect<br />
on the toll of caring. It sent a message to me<br />
that the organisation was already engaged<br />
in caring about its staff. The Schwartz Round<br />
I attended, entitled “Behind Closed Doors”,<br />
gave staff from the intensive care unit an<br />
opportunity to share their experience of<br />
treating patients and caring for families in a<br />
high pressure and critical environment where<br />
outcomes routinely involve life or death.<br />
The openness of the audience discussion<br />
struck me immediately. Staff members not<br />
only shared their work related experiences,<br />
but connected to their personal lives. People<br />
spoke about the palliative care of their parents<br />
and the critical care of their children by other<br />
caring professionals. One woman said: “they<br />
carried myself”, referring to the emotional<br />
support she received from healthcare staff.<br />
This short statement has stayed with me<br />
since. There are few jobs where training<br />
equips staff with practical skills but the<br />
demands of the role go far beyond completing<br />
tasks and being effective in the job. Wherever<br />
we work in healthcare, from facilities provision<br />
to wards or therapy rooms, we work with<br />
people who are distressed.<br />
The staff spoke about the needing to be kind<br />
to each other and to themselves. They spoke<br />
about the difficult power of knowing too much<br />
from a professional point of view and having<br />
to find a common language with families to<br />
communicate caring in these most difficult<br />
of circumstances. They also shared their<br />
vulnerabilities through expressing feelings of<br />
helplessness; when the helping profession<br />
cannot help, when death is imminent or when<br />
pain cannot be cured.<br />
A Schwartz Round at<br />
Blackrock Hospice<br />
Blackrock Hospice is tucked away on a<br />
back lane, a light-filled care setting which<br />
offers respite from the City as well as<br />
from life-limiting illness. Here, I felt the<br />
community of staff, cover had been arranged<br />
so that as many staff as possible could<br />
attend the Schwartz Round. The theme was<br />
“What a patient taught me” and four staff<br />
shared their learning from patients for the<br />
benefit of the audience.<br />
The depth of the audience discussion was<br />
what struck me here. Staff spoke about the<br />
times when words fail, when only silence<br />
will suffice to acknowledge the needs of<br />
the patient. Courage was needed by staff<br />
to trust that at times the patient knows<br />
best. A senior colleague said: “don’t just do<br />
something, stand there”. By inverting this<br />
common saying the power of being with a<br />
patient or family member, without the need to<br />
act was recognised. This message, heard by<br />
all staff present communicates the value of<br />
a supportive culture which acknowledges the<br />
human moments of care.<br />
The staff present were able to recognise<br />
their personal limitations as professionals, in<br />
that death cannot be prevented but a ‘good’<br />
death is a privilege for the staff to facilitate<br />
for the families and people who cross the<br />
threshold of the hospice. As well as the<br />
challenge of absorbing strong emotions in the<br />
work, the positives of patient care surfaced,<br />
a nurse spoke about feeling renewed and<br />
energised through her work.<br />
TOP: The Schwartz Rounds facilitators in Galway<br />
pictured in front of some of the artwork there.<br />
winter 2016 | health matters | 43
Feature<br />
Single Assessment Tool<br />
technology helps<br />
assess care needs<br />
ssessing the health and social<br />
care needs of older people is<br />
key to ensuring they receive the<br />
A<br />
appropriate care and support. A<br />
new IT-based assessment beinig<br />
introduced in our health services is enabling staff<br />
to better assess and better plan beople’s care.<br />
Health professionals are now using the<br />
‘Single Assessment Tool’ (SAT) to carry out<br />
comprehensive geriatric assessment of older<br />
people who apply for support under either<br />
the Home Care Package (HCP) Scheme or<br />
the Nursing Home Support Scheme (NHSS),<br />
also known as ‘A Fair Deal’. Using SAT, the<br />
assessment process is the same for everyone,<br />
regardless of where they live or who carries<br />
out the assessment, ensuring it is fair and<br />
equitable. The system is secure, user-friendly,<br />
person-centred, intuitive and informs more<br />
comprehensive care and service planning.<br />
Better care planning<br />
Trained assessors in hospital and community<br />
settings are now using computer Tablets with<br />
specially designed software, SAT Information<br />
System – SATIS, to gather all of the necessary<br />
information from the older person.<br />
There are 20 different sections in the<br />
assessment e.g. functional performance,<br />
cognition/mental health, social life, clinical<br />
issues etc., all of which must be completed.<br />
Each section has a number of questions with a<br />
drop down menu of ‘codes’, one of which must<br />
be selected, as well as options to add additional<br />
information to capture a fuller account of the<br />
person’s holistic needs.<br />
When completed, the system automatically<br />
generates a number of reports which can<br />
be used to determine areas of risk, potential<br />
for improvement, current health status, and<br />
prioritisation of service need e.g. risk of adverse<br />
outcomes such as falls, pressure ulcers and<br />
increasing frailty. This detail enables staff to<br />
develop a care plan that is tailored for the<br />
older person in consultation with their family<br />
representative. The SAT, which will replace<br />
the current paper based ‘Common Summary<br />
Assessment Report’ (CSAR), adds significant<br />
value as all the relevant health and wellbeing<br />
information about the older person is gathered in<br />
one assessment process, rather than through a<br />
battery of individual tests.<br />
SAT also enables staff involved in the older<br />
Ciara Blair, OT and<br />
trained SAT assessor,<br />
with Colette Murphy,<br />
patient at Tallaght<br />
Hospital.<br />
person’s care to easily exchange relevant<br />
information (with the older person’s consent) as it<br />
securely stored electronically.<br />
Specially designed software<br />
The SATIS software enables the use of the<br />
interRAI (International Resident Assessment<br />
Instrument) Home Care assessments that<br />
are designed to assess older people at<br />
home, in hospital or other community-based<br />
settings. interRAI is a world renowned non<br />
profit organisation that provides royalty-free<br />
licenses of its assessment instruments to<br />
help improve the quality of life of vulnerable<br />
persons - www.interrai.org<br />
The SAT is currently being introduced on a<br />
phased basis but the results to date are positive.<br />
Dr. Natalie Vereker, Specialist in Services for<br />
Older People and SAT Project Manager said,<br />
“The SAT is new to the Irish health system but<br />
we know its potential and are already seeing the<br />
opportunities for better use of the information<br />
gathered about older people’s care needs.<br />
The system is intuitive and along with enabling<br />
a comprehensive care needs assessment, it also<br />
identifies opportunities for improvement as well<br />
potential areas of decline.<br />
The SAT will not only benefit older people and<br />
their clinicians but the wider health system as it<br />
has enormous potential to facilitate the delivery<br />
of targeted services, quality initiatives and future<br />
service planning.”<br />
Phased implementation<br />
Since May 2016, Beaumont Hospital,<br />
Tallaght Hospital and University Hospital<br />
Galway have started a trial implementation<br />
of SAT. Multidisciplinary staff in each hospital<br />
were nominated to become SAT assessors<br />
and were trained to use the HSE tablet device<br />
and software.<br />
They also completed the SAT Education and<br />
Development Programme with mixed methods<br />
of training and support involving four days<br />
classroom-based training, practice assessments<br />
with direct feedback, one to one support as<br />
needed and eLearning modules leading to a<br />
mandatory competency evaluation.<br />
Professor Shaun O’Keeffe, Consultant<br />
Geriatrician, University Hospital Galway said,<br />
“The approach for assessing older persons has<br />
now been standardised for clients entering our<br />
services. The introduction of the SAT is a change<br />
in how assessments are completed but this has<br />
been worthwhile. We now have a comprehensive<br />
SAT assessment which will ensure services<br />
for clients are allocated in a fair and equitable<br />
manner based on their care needs.”<br />
44 | health matters | winter 2016
Members of the<br />
SAT National<br />
Implementation<br />
Team<br />
SAT assessments are completed by the<br />
assessors with older people in the hospitals<br />
and are then available to all staff who<br />
are directly involved with the care of the<br />
person with onward referrals being made<br />
as appropriate. These assessments are<br />
also considered by members of the Local<br />
Placement Forum who make a determination<br />
about entry into long term care based on the<br />
older persons wishes and assessed need.<br />
Integrated care<br />
THE implementation of SAT also promotes and<br />
facilitates the continuity and integration of care<br />
between acute and community sectors. In line<br />
with their nearby hospital colleagues, staff in the<br />
community areas of Dublin North, Galway and<br />
Dublin South West are also implementing SAT.<br />
Following an evaluation of the implementation<br />
process in these locations, SAT will then be<br />
implemented nationally on a phased basis<br />
throughout 2017.<br />
JJ O’Kane, Manager of Services for Older<br />
People, Galway CHO 2, “I am looking forward<br />
to the roll out of SAT in the community.<br />
This comprehensive assessment will bring<br />
consistency to the way older people are<br />
assessed for Home Care Services and will<br />
assist us in decision making when allocating and<br />
prioritising services.”<br />
Michael Fitzgerald, HSE Head of Operations<br />
and Service Improvement for Older Persons<br />
Services and Chair of the SAT Project Team said,<br />
“It is best practice nationally and internationally<br />
to advocate for a standardised care needs<br />
assessment. Implementing this project is<br />
a substantial undertaking but in striving to<br />
continuously improve our services we know that<br />
the SAT technology will better support us to<br />
ensure the most appropriate care in the most<br />
appropriate setting for older people.<br />
“We look forward to rolling this out further and<br />
working with the acute and community sites<br />
coming on stream throughout 2017.”<br />
more information<br />
Further information about SAT is available<br />
from: www.hse.ie/SingleAssessmentTool<br />
or email the SAT National Office, Single.<br />
AssessmentTool@hse.ie<br />
patient given due recognition<br />
Trained SAT assessor<br />
Ciara Blair, Senior<br />
Occupational Therapist<br />
in Tallaght Hospital, one<br />
of the SAT Pilot Sites,<br />
shares her experiences<br />
of the new tool<br />
The Single Assessment Tool is new to Ireland<br />
but has been used internationally for over 20<br />
years. The SAT is a much more detailed and<br />
comprehensive assessment tool than the<br />
paper-based CSAR. It captures information,<br />
not just about medical diagnosis, medication<br />
and a broad overview of care required to look<br />
after the patient but more specifics about<br />
personal activities of daily living eg bathing,<br />
dressing, toileting, functional transfers,<br />
eating etc and medication management,<br />
transportation, pressure ulcer risks and<br />
managing household related tasks. It also<br />
acknowledges the importance of a patient’s<br />
mental health and mood.<br />
The SAT system also automatically<br />
generates clinical alerts that trigger<br />
the assessor to ensure further in depth<br />
assessments may need to be done, for<br />
example on cognition, and provides guidance<br />
to the assessor on evidence-based care<br />
planning. The assessment covers in greater<br />
detail information about the patient’s abilities<br />
and capabilities as well as things they need<br />
assistance with.<br />
It also gives the person being assessed a<br />
‘voice’ and recognition as a vital person in<br />
the process of organising long term care<br />
for them by seeking their opinion about how<br />
they are coping, managing and feeling. This<br />
fits in well with our approach in Tallaght<br />
hospital of ‘people caring for people’ so we<br />
are delighted to be one of the first places to<br />
use the SAT system.<br />
We have been using the SAT system for<br />
a number of months and, as with anything<br />
new, it has taken staff some time to get used<br />
to the SAT assessor approaching them for<br />
information with a computer tablet in their<br />
hand instead of a paper based assessment.<br />
Ward staff have said they prefer the SAT<br />
system as they are consulted in completing<br />
the person’s assessment and it has taken<br />
extra paperwork tasks away from them,<br />
such as the CSAR. It does take a little<br />
longer for the SAT assessor to complete<br />
the assessment than the CSAR would<br />
have taken. However, the benefits of such<br />
a comprehensive assessment for the older<br />
person is a far greater advantage to them and<br />
our organisation in the longer term.<br />
winter 2016 | health matters | 45
Feature<br />
Children First:<br />
Guidelines for<br />
child protection<br />
hildren First: National<br />
Guidance for the Protection<br />
and Welfare of Children,<br />
C<br />
(2011) is currently being<br />
reviewed to reflect the pending<br />
implementation of the Children First Act 2015<br />
which is scheduled for January 2017. The most<br />
critical message in the revised Guidance and<br />
Legislation is that we are all responsible; we<br />
are all required to act and we are all required<br />
to report to the Child and Family Agency any<br />
concern we have which suggests that a child<br />
has been harmed or may be at risk.<br />
What is Children First?<br />
Children First aims to promote the safety<br />
and wellbeing of children. It is intended to<br />
assist people in identifying and reporting child<br />
abuse and neglect, and to deal effectively with<br />
concerns.<br />
It states what organisations such as the HSE<br />
need to do to keep children safe, and what<br />
different bodies, and the general public should<br />
do if they are concerned about a child’s safety<br />
and welfare. The Children First Act 2015 places<br />
a number of statutory obligations on specific<br />
groups of professionals, such as health and<br />
social care staff providing services to children.<br />
These obligations extend to mandatory<br />
reporting and mandatory assisting when the<br />
Children First Act 2015<br />
is fully enacted from<br />
January 2017.<br />
Children First<br />
National Office<br />
A Children First<br />
National Office has<br />
been established and<br />
is staffed by a Director<br />
and fifteen training<br />
and development officers nationwide. Their<br />
role is to support the Community Healthcare<br />
Organisations (CHO’s); Hospital Groups (HG’s)<br />
and regional and national services in achieving<br />
full compliance with Children First. In addition,<br />
there is a National Oversight Committee<br />
supported by Divisional and local area<br />
committees to progress the programme of work.<br />
Child Protection and Welfare<br />
Policy 2016<br />
The HSE has developed a Child Protection<br />
and Welfare Policy to assist staff in<br />
understanding the corporate responsibility<br />
of the HSE and the individual responsibility<br />
of each staff member as to their role and<br />
responsibilities. The policy also addresses<br />
the legal frame work for child protection in<br />
Ireland and the legislative protections for any<br />
individual reporting a child<br />
protection or welfare concern<br />
in good faith and in the best<br />
interests of a child.<br />
Resources<br />
The Children First National<br />
Office has produced the<br />
following resources to assist<br />
staff:<br />
• Child Protection and Welfare<br />
Policy, 2016 (leaflets, a briefing<br />
paper and presentations)<br />
• A foundation e-learning programme called<br />
“An Introduction to Children First” available on<br />
www.HSELanD.ie. This e-learning programme<br />
is mandatory for all staff and is in line with the<br />
HSE Child Protection and Welfare Policy, 2016<br />
• The HSE Children First website www.<br />
hse.ie/childrenfirst which has a number<br />
of resources to support HSE staff and<br />
HSE funded organisations in meeting their<br />
responsibilities under Children First<br />
• A generic e-learning programme is<br />
available at http://childrenfirst.hseland.ie/ for<br />
interested people/ bodies/organisations with<br />
an interest in this critical area.<br />
The Children First National Office welcomes<br />
comments or queries at childrenfirst@hse.ie<br />
Record numbers participate in Ageing Well group<br />
Recently, the Primary and Community<br />
Care Occupational Therapy Department,<br />
based in St Finbarr’s Hospital, Douglas Road,<br />
Cork, started an eight-week Ageing Well<br />
group in the local community.<br />
The need for the group arose as part of the<br />
Cork Integrated Falls Service.<br />
One of the strands of this service<br />
is a community strand which includes<br />
developing opportunities to stay healthy and<br />
well as we age..<br />
Record numbers contacted the department<br />
to book a place on the course and, due to<br />
demand, the group is now booked out for<br />
2017 already.<br />
Topics covered included maintaining<br />
physical and mental wellbeing, energy<br />
conservation, safety around the home and<br />
Some of the group participants on their outing.<br />
dealing with finances.<br />
The group was run in the local library in<br />
Ballyphehane, Tory Top Library and it was an<br />
ideal location in the middle of the community<br />
for people to be able to access.<br />
The group had an outing on November 8th<br />
to put some of the principles discussed over<br />
the weeks into practice and excessive wind<br />
and rain did not stop them from enjoying<br />
the occasion.<br />
46 | health matters | winter 2016
linn dara gives warm welcome<br />
ailed for providing a welcoming<br />
and reassuring domestic<br />
ambience, the Linn Dara Child<br />
H<br />
and Adolescent Mental Health<br />
Inpatient Unit won the Best<br />
Universal Design at RIAI Annual Awards.<br />
The unit for children and adolescents with<br />
acute mental health illness opened recently on<br />
the Cherry Orchard Campus. It provides mental<br />
health services for children and adolescents<br />
up to 17 years in Dublin and Mid-Leinster. This<br />
is an in-patient building for acutely ill patients<br />
who reside here for up to six weeks. It includes<br />
a school, a gym hall and an apartment for<br />
family use.<br />
For many of the children and adolescents, this<br />
is the first time spent away from family. The<br />
building plan stems from the brief and wraps<br />
around secure courtyards. The courtyards share<br />
a curvy wall faced with ceramics designed by<br />
artist Diane Jamesion of birds and leaves and<br />
trees. The courtyards are not enormous, but<br />
large enough for play, or to sun yourself on the<br />
grass, or site under the covered ‘shed’ area.<br />
There are two wards, Hazel and Rowan,<br />
and the artwork picks up these themes in the<br />
wardrobe doors and the glass screens. The<br />
bedrooms are grouped around a small planted<br />
courtyard, with the coloured staff bases always<br />
in view. The staff base is round and blue (or<br />
green). The top glows gently, so at night you can<br />
keep it in view if you wish. All residents have a<br />
single room and ensuite bathroom.<br />
There is a small wardrobe and a worktop<br />
for a dressing table or to work. One wall is<br />
painted with white ‘blackboard’ paint – you can<br />
draw on it, and then wipe it down. There is a<br />
large cushioned chill out area nearby, and a<br />
worktop with computer access for games or<br />
for homework if you need company, or you can<br />
move away and sit in a recess beside the planted<br />
courtyard, or go into your room.<br />
There are a variety of living rooms, large and<br />
small, well-furnished and homely, with coloured<br />
carpets or flooring. The living rooms all get<br />
sunshine at some time during the day and<br />
several have direct access to the courtyard. It<br />
all allows for a variety of activities and gives the<br />
staff plenty of options for therapy.<br />
The essential supervision of activities<br />
is achieved within a complex plan in a<br />
subtle manner. It avoids an over stimulated<br />
environment and allows the residents privacy<br />
as well.<br />
At the front entrance there is a waiting area<br />
and office – it is bright and light, a bit quirky, you<br />
can see in and out. It leads to a coffee/meeting<br />
area with a view to planting outside and to the<br />
artworks on the wall. It is calm and spacious.<br />
Beyond the entrance is the school. The<br />
residents leave their unit and make a short<br />
journey across the hall, past the outdoor ball<br />
area and into school. Going to school is normal<br />
and can even be a pleasurable distraction. There<br />
are several classrooms, an art room with access<br />
to the garden and a view of the mature trees on<br />
the campus, a small home economics room and<br />
the occupational therapy room. There is also a<br />
large, bright gym/activities/playroom which the<br />
staff find useful for all kinds of activities.<br />
The staff offices and meeting rooms are<br />
upstairs. There is a small apartment for family<br />
stayovers where required.<br />
Externally, the building elevation is broken into<br />
a number of smaller blocks with large coloured<br />
blocks at the corners. Double volume spaces at<br />
these nodes ensure both wards (two different<br />
orientations) receive sunlight, cross ventilation<br />
and the spaces provide variety in a building of<br />
small domestic sized rooms. Contrasting shapes<br />
and colour reduces scale and adds interest.<br />
Colours were selected to visually compliment<br />
Linn Dara’s outpatient building nearby.<br />
The gardens are landscaped and it is in<br />
harmony with the remainder of the grounds of<br />
Cherry Orchard which is characterised by large<br />
mature trees, brick walls and more recent low<br />
level planting.<br />
“Dealing with mental health issues is tough<br />
when you are very young. The intention is that<br />
this building is welcoming and reassuring and<br />
homely and allows the staff to treat and care for<br />
the residents in a safe and robust environment,”<br />
said one of the staff members.<br />
The project team consisted for: HSE Estates<br />
Dorota Nieznanska, Pat Fogarty; Linn Dara<br />
CAMHS – Brendan Doody and his team.<br />
The design team was: Wejchert Architects;<br />
Varming Consulting Engineers; Civil & Structural<br />
Engineers - O’Connor Sutton Cronin; Quantity<br />
Surveyors - Mulcahy McDonagh and Partners.<br />
The coffee/meeting room at Linn Dara.<br />
winter 2016 | health matters | 47
Feature<br />
thousands of incidents reported<br />
id you know that several<br />
thousand employee health<br />
and wellbeing incidents are<br />
D<br />
reported through the HSE’s<br />
incident reporting system<br />
(National Incident Management System<br />
- NIMS) every three months?<br />
Little is said about the success stories,<br />
about how the application of simple controls<br />
and a dedication by managers and their staff<br />
to the preservation of employee health and<br />
wellbeing can, and does, save people from<br />
horrors such as that described above.<br />
You are the HSE’s most important asset in<br />
the delivery of high quality health and social<br />
services and the HSE has a strong desire<br />
to safeguard your health and wellbeing. In<br />
order to support you in the implementation<br />
of your Safety Management Programme<br />
(SMP), the National Health and Safety<br />
Function is pleased to launch the following<br />
National Occupational Safety and Health<br />
Policies and Guidelines:<br />
HSE Policy on Statutory<br />
Occupational Safety &<br />
Health Training<br />
Training is a key component of the HSE’s<br />
health and safety management programme.<br />
This document sets out policy and<br />
provides advice and guidance on statutory<br />
Occupational Safety and Health (OSH)<br />
Training, i.e. training that is either explicitly<br />
required in legislation or deemed by the<br />
organisation to be necessary to ensure, so<br />
far as is reasonably practicable, the safety,<br />
health and welfare at work of employees<br />
and others.<br />
In summary:<br />
1. The policy applies to all employees and<br />
others working in the HSE<br />
2. A systematic training needs assessment<br />
must be carried out locally, underpinned by<br />
risk assessment<br />
3. Employees should be facilitated in<br />
attending statutory occupational safety<br />
and health training - Statutory Training is<br />
Mandatory for the identified employees<br />
4. Employees must attend statutory OSH<br />
training<br />
5. Records of statutory training required and<br />
attended must be kept at each management<br />
level<br />
HSE Policy on the Prevention<br />
of Sharps Injuries<br />
More than one million sharps injuries are<br />
estimated to occur in the European Union<br />
each year. This document sets out policy and<br />
provides advice and guidance on the sharps<br />
risks and their management.<br />
In summary:<br />
• This policy applies to all employees<br />
and others working in the HSE including<br />
temporary employees, agency employees,<br />
students, volunteers, contractors and any<br />
employees contracted to provide services for<br />
the HSE<br />
• The HSE acknowledges the risk of<br />
exposure to sharps in the workplace<br />
• The HSE is committed to eliminating or<br />
reducing the risk of exposure<br />
• All hazards associated with exposure to<br />
blood and bodily fluids from sharps injuries<br />
must be identified, the risks assessed, control<br />
measures identified and implemented<br />
Guideline on the Safe<br />
Handling and Use of<br />
Cytotoxic Drugs<br />
Cytotoxic drugs are a group of medicines<br />
that contain chemicals which are toxic to<br />
cells. Their toxicity means that they can<br />
present significant risks to those who handle<br />
them and Occupational exposure can occur<br />
when control measures are inadequate. This<br />
document provides advice and guidance<br />
on the management of risks presented by<br />
cytotoxic drugs.<br />
In summary:<br />
• The document applies to all employees<br />
working in hospital departments where work<br />
activities may involve risk of occupational<br />
exposure<br />
• The HSE undertakes to ensure the<br />
protection of employees from the risks related<br />
to exposure to cytotoxic drugs<br />
The guideline does not deal with patient<br />
care, except in the context of workplace<br />
health and safety<br />
Further information can be found on the<br />
National Health and Safety Function website<br />
or through our helpdesk<br />
more information<br />
Log your health and safety request at:<br />
http://www.hse.ie/safetyandwellbeing.<br />
Alternatively contact the National Health &<br />
Safety Helpdesk on 1850 420 420 between<br />
10.30 and 12pm and 2pm and 3.30pm Monday<br />
to Friday.<br />
Launch of new tobacco-free implementation guide<br />
Health service staff from a variety of<br />
backgrounds, as well as delegates from<br />
Malta and members from the International<br />
ENSH-Global Network for Tobacco Free<br />
Healthcare Services attended a recent<br />
‘Tobacco Free Health Service Programme<br />
Conference’ organised by the HSE’s Tobacco<br />
Free Ireland Programme.<br />
The conference also saw the formal launch<br />
of the new tobacco-free implementation<br />
guide ‘How to Implement HSE Tobacco<br />
Free Campus Policy’. This document aims<br />
to support the implementation and ongoing<br />
management of Tobacco Free Campus policy.<br />
The implementation guide was developed<br />
using the updated ENSH-Global Network<br />
for Tobacco Free Health Care Services<br />
Standards 2015. For more go to www.hse.<br />
ie/tobaccocontrol<br />
Pictured are (l-r) Dr Fenton Howell, National Tobacco Control Advisor, Department of Health; Dr<br />
Stephanie O’Keeffe, National Director, Health and Wellbeing; Martina Blake, National Lead Tobacco-<br />
Free Ireland Programme; and Mirian Gunning, HSE Senior HPO for Tobacco. Photo: Paul Connor<br />
48 | health matters | winter 2016
Naloxone Demonstration Project<br />
how to save a life<br />
he HSE has published an<br />
evaluation report on the<br />
Naloxone Demonstration<br />
T<br />
Project which has been running<br />
for 18 months in a number of<br />
sites across the country. Naloxone blocks<br />
or reverses the effects of opioid overdose<br />
including extreme drowsiness, slowed<br />
breathing, or loss of consciousness. It is<br />
used to treat a narcotic overdose in an<br />
emergency situation.<br />
The most recently published data on<br />
overdose mortality rates in Europe is<br />
estimated at 18.3 deaths per million<br />
population aged 15–64. The highest rates are<br />
reported in Estonia (113 per million), Sweden<br />
(93 per million) and Ireland (71 per million).<br />
In 2014, the World Health Organisation<br />
recommended that countries expand naloxone<br />
access (opioid antidote) to people likely to<br />
witness an overdose in their community, such<br />
as friends, family members, partners of people<br />
who use drugs, and social workers. In most<br />
countries, naloxone is accessible only through<br />
hospitals and ambulance crews.<br />
In 2015 the HSE followed that WHO<br />
recommendation with the development<br />
of a demonstration project to introduce<br />
naloxone into local communities. The HSE<br />
commissioned an external review of the<br />
Naloxone Demonstration Project and the<br />
Minister for State Catherine Byrne launched<br />
the evaluation of the report on International<br />
Overdose Awareness Day.<br />
“I’m glad to have the opportunity to raise<br />
awareness of overdose and to speak about<br />
reducing the stigma of drug-related death. I<br />
very much want to recognise and acknowledge<br />
the grief felt by families and friends whose<br />
loved ones have died or been badly injured as<br />
a result of overdose. The number of drugrelated<br />
deaths in Ireland is a matter of serious<br />
concern to me, and this project is an important<br />
element in the Government’s efforts to tackle<br />
the issue,” said Minister Byrne.<br />
Denis O’Driscoll, Chief Pharmacist for<br />
HSE Addiction Services, said, “Overdose<br />
awareness and training has been developed<br />
and made available to drug users, their peers<br />
and families. Training in the use of naloxone<br />
is available nationally to drug users, their<br />
peers and their families and is available to all<br />
staff working in statutory and community/<br />
voluntary Addiction Services. To date we<br />
have trained over 600 people in the use of<br />
naloxone and we look forward to rolling out<br />
more training in 2107 as we work to expand<br />
the service.”<br />
At the launch Melanie Froud, Crosscare<br />
homeless services staff member who availed<br />
of the training, described her experience of<br />
using naloxone while a client of her service<br />
was overdosing. It brings into sharp focus<br />
the value of having naloxone available for<br />
when it is needed. “The main thing was<br />
seeing someone who was unresponsive<br />
and fading in front of me, thinking they<br />
were gone, then regaining consciousness,<br />
breathing and moving.”<br />
Project Partners include: Ana Liffey Drugs<br />
Project, Merchant’s Quay Ireland, Uisce, Novas,<br />
McGarry House, National Family Support<br />
Network, Crosscare, National Ambulance<br />
Service and SafetyNet<br />
For the report please log on to: www.hse.<br />
ie/eng/services/publications/SocialInclusion/<br />
addiction/Naloxonedemoproject.pdf<br />
Naloxone Project Photo Exhibition<br />
To mark International Overdose<br />
Awareness Day and the completion of<br />
the Evaluation Report, our Drug Services<br />
held a photographic exhibition in Temple<br />
Bar, focusing on family members, drug<br />
workers and partner agencies to highlight<br />
the importance of Naloxone. Tim Bingham,<br />
a dedicated Drug Service staff member<br />
took some very evocative photos of family<br />
members who had lost a loved one, others<br />
who were supporting a loved one with<br />
an opioid addiction, drugs workers and<br />
voluntary agencies. All of the photos can be<br />
seen on www.drugs.ie/naloxone<br />
winter 2016 | health matters | 49
Feature<br />
Alternative option to respite<br />
the Home<br />
away from home<br />
ome Sharing in intellectual<br />
disability (ID) services has<br />
been an alternative option to<br />
H<br />
the traditional residential and<br />
respite care offered to people<br />
with intellectual disability and their families<br />
for many years.<br />
The Home Sharing model of support is<br />
divided into three categories:<br />
• ‘Short Breaks’ families - A Home Sharing<br />
family in the community offers a placement<br />
in their home to a person with intellectual<br />
disability for short breaks and cares for that<br />
person as a member of their family.<br />
• ‘Contract’ families - ‘Contract Families’<br />
are specialist carers from within the<br />
approved Home Sharing families who provide<br />
short breaks to children and adults with<br />
more complex and more challenging needs.<br />
• ‘Shared living’ families - A ‘Shared Living’<br />
family provides full-time care in their home<br />
to a person with intellectual disability<br />
similar to a fostering placement. The shared<br />
living family makes their home available to a<br />
person with intellectual disability on a fulltime<br />
basis as a member of their family.<br />
Home Sharing has been developed and<br />
fostered by the National Home-sharing<br />
and Short-breaks Network (NHSN) which<br />
was established to promote uniformity and<br />
high standards amongst disability service<br />
providers throughout Ireland.<br />
In line with the programme of reform<br />
within disability services, the HSE’s<br />
Social Care Division committed to further<br />
developing Home Sharing as a personcentred<br />
and community inclusive type of<br />
support. A National Expert Group including<br />
healthcare professionals, representatives<br />
from the HSE, TUSLA, Federation of<br />
Voluntary Bodies, CEOs from the nonstatutory<br />
sector service providers and<br />
members from the National Home-sharing<br />
and Short-breaks Network (NHSN) was<br />
established to review the service. Their<br />
report, ‘Home Sharing in Intellectual<br />
Disability Services in Ireland’ (HSE, 2016),<br />
has recently been published and, as set out<br />
here, provides for the future development<br />
and the safe governance and management<br />
of Home Sharing.<br />
Home Sharing – a positive<br />
option<br />
It is held internationally, nationally and<br />
indeed from the experience of intellectual<br />
disability service providers in Ireland that<br />
there are many advantages to Home Sharing.<br />
Dr Donal Fitzsimons, HSE National Disability<br />
Specialist and Chairperson of the National<br />
Expert Group spoke about the report findings,<br />
“Home Sharing strives to empower people<br />
with intellectual disability to have dignifying<br />
relationships and to be included meaningfully<br />
in the life of their communities.<br />
The uniqueness of Home Sharing is that<br />
families provide support from their own<br />
homes. People with intellectual disability<br />
enjoy the opportunity of developing<br />
new relationships and being part of new<br />
communities whilst enjoying a short break or<br />
full time support.”<br />
Families are also advising service providers<br />
that one of the supports they need to enable<br />
them to continue to care for their family<br />
member at home is short breaks. Short<br />
breaks give families a break from their role<br />
as carers and it also provides their family<br />
member with an opportunity to be with<br />
others while benefiting from new experiences.<br />
Families have also reported that close<br />
SIUN’s STORY<br />
Siun is a 16- year-old girl who has cerebral<br />
palsy, a profound intellectual and physical<br />
disability. Siun is extremely medically frail.<br />
Attendance at school is sporadic due to poor<br />
health and frequent hospitalisations. Siun<br />
requires 24- hour care and receives all her<br />
nutrition through a peg tube. Her natural<br />
family are overwhelmed and exhausted<br />
with this relentless cycle of caring for their<br />
daughter. A Home Sharing family provides<br />
two overnight breaks per week to Siun. Her<br />
natural family have described this support as<br />
a ‘lifeline to them’. Significant training was<br />
provided to the Home Sharing family by the<br />
clinical nurse specialist with the support of<br />
the paediatric hospital. Regular contact is<br />
maintained with the Home Sharing family<br />
by the clinical nurse manager and the social<br />
work team leader.<br />
and trusting relationships have developed<br />
between them as carers, their family<br />
members and their Home Sharing families.<br />
Challenges to be addressed<br />
While recognising the advantages of<br />
Home Sharing for people with intellectual<br />
disability, there are strategic and<br />
operational challenges in the delivery of this<br />
model of support within an Irish context. A<br />
legal framework for the regulation of Home<br />
Sharing in Ireland is required to underpin<br />
the governance and management of the<br />
service. As Home Sharing has developed<br />
‘piecemeal’ over the years, additional<br />
resources should also be allocated to<br />
the monitoring, management and further<br />
development of Home Sharing nationally.<br />
Dr Fitzsimons said, “Notwithstanding<br />
these challenges, the National Expert<br />
Group advocate for statutory recognition<br />
of Home Sharing and its continued<br />
development as a model of support.<br />
It requires a commitment and further<br />
investment by the HSE and Government<br />
departments for it to continue and for<br />
its future development. This report<br />
provides the blueprint for resolving these<br />
challenges.”<br />
50 | health matters | winter 2016
Making a difference<br />
copd services<br />
ercy University Hospital<br />
(MUH) COPD Outreach Service<br />
is a Cork city based service<br />
M<br />
that aids in the early discharge<br />
of patients who present<br />
with an “exacerbation of COPD” to Mercy<br />
University Hospital.<br />
Once a patient is discharged and meets<br />
certain criteria, the COPD Outreach Team will<br />
perform home visits to patients. International<br />
best practice guidelines suggest that such<br />
a ‘hospital at home’ programme is a safe,<br />
effective and efficient approach to the<br />
treatment of patients with COPD.<br />
One patient explained the benefits they got<br />
from the service, saying, “No-one wants to<br />
stay in hospital, the COPD Outreach Team<br />
helped me to get discharged from hospital<br />
earlier than usual – I am delighted with this. I<br />
have also learnt so much about my condition<br />
and how to manage it better.”<br />
The team consists of Consultant Respiratory<br />
Physician Dr David Curran; Clinical<br />
Nurse Specialist Una Lehane; and Senior<br />
Physiotherapist - Ciara Hanrahan.<br />
Main aims<br />
The main aims of the COPD Outreach<br />
programme are to:<br />
• Aid in the early supported discharge of<br />
patients<br />
• Optimise patient care in the comfort of their<br />
own home<br />
• Reduce the number of admissions and<br />
re-admissions related to COPD<br />
How it works<br />
All patients admitted to Mercy University<br />
hospital with an exacerbation of COPD are<br />
assessed by the COPD Outreach Team<br />
regarding suitability for inclusion in the<br />
programme. The service involves a member<br />
of the COPD Outreach Team visiting a<br />
patient’s home. Depending on the patient’s<br />
length of stay in hospital, a patient will<br />
receive between two to four visits over the<br />
two-week period following discharge.<br />
A visit from one of the COPD Outreach<br />
Team members entails:<br />
• Advice and education on management of<br />
COPD<br />
• Vital signs check<br />
• Spirometry (breathing test)<br />
• Smoking cessation advice<br />
• Provision of a home exercise programme<br />
• Education regarding airway clearance<br />
techniques.<br />
Both outreach and in-reach access is now<br />
offered as part of the COPD Outreach service.<br />
This is available to GPs and their patients<br />
who are known to the service. If possible a<br />
member of the COPD Outreach Team can<br />
offer support in relation to the patients COPD<br />
and help to determine the optimal treatment<br />
for the patient at that time.<br />
The hospital-at-home service provided<br />
by the COPD Outreach Team appears to be<br />
making a positive impact on the patient’s<br />
journey through MUH. The journey is<br />
becoming more seamless and the feedback<br />
from our patients is overwhelmingly positive.<br />
The outreach service has also lead to a<br />
reduction in the average length of hospital<br />
stay for a patient with a COPD exacerbation,<br />
thus easing pressure on bed capacity.<br />
Overview<br />
Chronic obstructive pulmonary disease<br />
(COPD) is a common progressive disease<br />
of the lungs characterised by airflow<br />
obstruction. COPD is a major cause of<br />
morbidity and mortality for patients in this<br />
country. At least 1,500 patients die each<br />
year of this disease and over 15,000 patients<br />
are admitted to hospital with COPD.<br />
Tobacco smoking is the most important<br />
risk factor for the development of COPD.<br />
Other factors that may contribute to the<br />
development of COPD include: genetic<br />
predisposition especially in individuals with<br />
α1-Antitrypsin Deficiency, occupational dust<br />
and fume exposure, exposure to outdoor and<br />
indoor air pollution including tobacco smoke,<br />
recurrent childhood respiratory infections<br />
and bronchial hyper responsiveness.<br />
A person with COPD may present with<br />
chronic cough, sputum production and<br />
shortness of breath. Patients with severe<br />
disease may suffer frequent exacerbations<br />
requiring medical attendance, potential<br />
hospitalisation and severe disruption of their<br />
quality-of-life. An exacerbation is typified<br />
by deterioration in a patient’s symptoms<br />
resulting in an increased cough, sputum<br />
production and shortness of breath.<br />
The establishment of the National<br />
Clinical Programme for COPD, within the<br />
Clinical Strategy and Programmes Division,<br />
facilitates an improvement in the care of<br />
people at risk of, and those who have COPD.<br />
In 2012, the COPD Outreach service was<br />
rolled out in 12 centres throughout the<br />
country as part of this National Clinical<br />
Care Programme.<br />
winter 2016 | health matters | 51
Feature<br />
Medical Card plan<br />
priorities<br />
set out<br />
he HSE National Medical Card Unit<br />
recently published its Strategic<br />
Plan 2016-2018.<br />
T<br />
Anne Marie Hoey, Assistant<br />
National Director PCRS outlined<br />
the work undertaken to develop the plan.<br />
“The development of our three-year strategic<br />
plan was a key recommendation of the Medical<br />
Card Process Review undertaken by the HSE in<br />
2014. In developing the plan, we engaged with a<br />
wide range of customers, staff and stakeholders,”<br />
she said.<br />
“We held a public consultation process on our<br />
five key priorities set out in the strategic plan.<br />
Between March 21st 2016 and April 6th 2016,<br />
more than 200 individuals and organisations<br />
responded to us with submissions providing<br />
valuable input to the completion of the Strategic<br />
Plan.” The feedback from two major customer<br />
surveys, with over 2,000 respondents, also<br />
provided valuable insights and key contributions to<br />
the development of our Strategy.<br />
“We are extremely conscious of our responsibility<br />
to provide an excellent public service to individuals<br />
and families throughout the country who require<br />
eligibility under the General Medical Services<br />
(GMS) and the Community Drugs Schemes<br />
to enable them to access GP care, medicines,<br />
dental and optical services. On September<br />
1st 2016, the number of people with Medical<br />
Card eligibility was 1,709,957. In addition<br />
460,427 people had GP Visit Card eligibility,”<br />
said Anne Marie.<br />
“Our mission is to deliver a first-class<br />
service in a consistent, transparent and<br />
compassionate way to everyone that<br />
engages with us. With the dedication and<br />
commitment of our staff, applications and reviews<br />
of eligibility will be processed in a timely manner<br />
and any engagement with our customers and<br />
stakeholders will be open, respectful and trusting.<br />
“I want to acknowledge the preparation,<br />
planning, and analysis involved in bringing this<br />
strategy to fruition. With the determination and<br />
support of the managers and other colleagues<br />
within the National Medical Card Unit, I am<br />
confident that the implementation of the priorities<br />
in this Strategic Plan will position the National<br />
Medical Card Unit at the forefront of quality<br />
service delivery.”<br />
more information<br />
The National Medical Card Unit Strategic Plan<br />
2016-2018 can be downloaded from<br />
www.hse.ie/publications<br />
National Medical Card Unit Strategic Plan<br />
2016-2018 - Five strategic priorities<br />
A little goes a<br />
long way…<br />
HBS Procurement has partnered with<br />
Health and Wellbeing division supported<br />
by HBS Communications to assist in the<br />
successful promotion of public health<br />
campaigns.<br />
Jane Carolan, Director of HBS, said she<br />
was delighted with the success of this<br />
pilot and the reaction it has received. “This<br />
initiative is a prime example of the synergies<br />
that exist between Health Business Services<br />
and its customers and the mutual benefits<br />
that can be realised by working together.<br />
Brian Long, Head of Logistics and<br />
Inventory Management, said, “With over<br />
30 trucks on the road each day, we saw a<br />
great opportunity to have campaign artwork<br />
displayed on the sides of our vehicles.”<br />
The Logistics and Inventory Management<br />
function of HBS Procurement currently<br />
operates a fleet of HSE delivery vehicles<br />
daily between the National Distribution<br />
Centre in Tullamore to Limerick, Sligo,<br />
Brian Long, Head of Logistics and Inventory Management; Finn Ryan, HBS Business Relationship<br />
Manager; Jane Carolan, Director of Health Business Services; Dr Stephanie O’Keeffe, National Director<br />
of Health and Wellbeing. Photo: Brian Gavin Press 22<br />
Letterkenny, Cherry Orchard and Naas, with<br />
plans to extend to Tralee, Cork, Wexford,<br />
Drogheda and Galway.<br />
For this pilot, artwork from the Little<br />
Things Mental Health and the Under The<br />
Weather campaigns were chosen to feature<br />
on selected vehicles which are well placed<br />
to further enhance delivery of HSE campaign<br />
messages in an innovative approach.<br />
Speaking of this initiative Dr Stephanie<br />
O’Keeffe, National Director Health and<br />
Wellbeing said, “This initiative is about taking<br />
the Healthy Ireland agenda to the highways<br />
and byways of Ireland, in collaboration with<br />
HBS and National Communications, to<br />
improve the impact of our campaigns and to<br />
realise more from our collective investments<br />
and assets.”<br />
52 | health matters | winter 2016
General<br />
News<br />
odti delivers training course<br />
FORTY-FIVE staff working in the field of<br />
Organ Donation and Transplant services<br />
throughout Ireland including Transplant<br />
Surgeons, Anaesthetists, ICU leads and<br />
consultants, and organ donor nurse<br />
managers, recently came together in Dublin<br />
to undertake the internationally recognised<br />
Intermediate Training Course in Transplant<br />
Procurement Management.<br />
The course was presented by Transplant<br />
Procurement Management (TPM), a formal<br />
training initiative based in Barcelona which<br />
has been working with international experts<br />
from around the world to provide training in<br />
transplant procurement management for over<br />
25 years.<br />
The course was organised by HSE Organ<br />
Donation Transplant Ireland and welcoming<br />
the TPM delegation and course participants,<br />
Professor Jim Egan CEO ODTI said, “There are<br />
two key pillars to developing organ donation<br />
in Ireland, namely training and having key<br />
personnel on the ground to work and support<br />
donors, families and recipients.<br />
“Irish people are very supportive of organ<br />
donation and our very simple but important<br />
message is that organ donations save lives.<br />
“Since April 2015 Organ Donation and<br />
Transplant Ireland (ODTI), HSE, has taken the<br />
lead in enhancing the infrastructure in place<br />
to improve organ donation and transplantation<br />
rates for Ireland.”<br />
Opening the course Dr Jeanne Moriarty, Dean<br />
of the Joint Faculty of Intensive Care Medicine<br />
of Ireland, added, “We can make great progress<br />
in organ donation in the Irish Healthcare<br />
Network by applying a nationally recognised<br />
process around organ donation that involves the<br />
identification of the potential donor, discussions<br />
with families and donor management.<br />
“As a training body the Faculty of Intensive<br />
Care Medicine is working towards making this<br />
course in Transplant Procurement Management<br />
mandatory for all our trainees.”<br />
In 2015, a total of 266 people received a<br />
life-saving organ transplant in Ireland, 81<br />
families donated the organs of their loved<br />
ones and 33 people donated their kidney to a<br />
family member.<br />
Nuria Masuou, Ignation Martin Loeches, Jeanne<br />
Moriarty, Jim Egan, Lars Nolke, Catherine<br />
Motherway and Alan Gaffney attending the Train<br />
for Trainers seminar at Castleknock Hotel in Dublin.<br />
HSE Drugs and Alcohol Helpline and Email Support Service<br />
The Drugs and Alcohol Helpline and Email<br />
Support Service, deals with questions or concerns<br />
from the public related to drugs or alcohol use<br />
and provides information and support in relation<br />
to these substances and their effects. The<br />
Helpline also directs people to support services<br />
that are available if needed.<br />
Aileen Dooley, Manager of the Helpline<br />
explained the service they provide. “We offer<br />
non-directive support, information, guidance<br />
and referral to anyone with a question or<br />
concern related to drug or alcohol use. We<br />
receive a diverse range of queries and provide an<br />
opportunity to explore a concern in confidence<br />
with onward referral when necessary. The<br />
Helpline and email support service are run and<br />
funded by the HSE and are accessible throughout<br />
the Republic of Ireland for free.<br />
“Our Helpline staff aim to support callers and<br />
people emailing to talk about their situation,<br />
explore their feelings and how their lives are<br />
being impacted by alcohol/drug use. We facilitate<br />
service users to explore what their options are<br />
and to consider their own personal needs. We<br />
offer information, guidance and support. To date<br />
we have dealt with over 75,000 calls and emails.”<br />
What should a member of the<br />
public expect from contacting<br />
the helpline?<br />
Those who contact the helpline can expect<br />
to be listened to by a professional staff; to<br />
be supported; to have their unique position<br />
considered and to be offered space to explore<br />
how they want to proceed.<br />
Helpline staff are trained to listen in a nonjudgemental<br />
way to what each service user has<br />
to say and offers the space to identify what they<br />
want from the call/email. Staff support callers<br />
and as appropriate offer information to help.<br />
Is the service confidential?<br />
Calls and emails are anonymous and<br />
confidential. The service does not retain any<br />
identifying information on callers or those<br />
who email.<br />
Aileen describes some of the calls and emails<br />
they receive to the service.<br />
“Lately we have been receiving an increasing<br />
number of calls and emails about alcohol. We<br />
dealt with 349 calls and emails about alcohol in<br />
2013; 471 in 2014; 516 in 2015 and as of early<br />
November 2016, we already have dealt with<br />
542 people concerned about alcohol. People are<br />
starting to think about their alcohol consumption.<br />
“We also receive calls from people who are<br />
worried about someone else close to them and<br />
want to know how they can help the situation.<br />
Where appropriate, people are given information<br />
on services and supports such as self-help<br />
supports, counselling, support groups, residential<br />
programmes etc.”<br />
Who contacts the Helpline?<br />
We regularly receive calls/emails from people<br />
with a concern in relation to themselves, but also<br />
many contacts are from family, partners, friends,<br />
professionals and students doing research.<br />
Those working within the health services can<br />
avail of the service also, either to discuss their<br />
own drinking or that of clients or family members.<br />
The service is confidential and free to all.<br />
Ways to contact us:<br />
Freephone: 1800 459 459<br />
Email: helpline@hse.ie<br />
www.hse.ie/go/drugshivhelpline<br />
www.facebook.com/drugsalcoholandhivhelpline<br />
winter 2016 | health matters | 53
General<br />
News<br />
Patients impressed with service IN<br />
Injury Units across the country<br />
As part of an ongoing Injury Units public<br />
awareness campaign, we recently sought<br />
feedback from patients who had attended<br />
an Injury Unit for treatment and care. The<br />
main purpose of the survey was to help<br />
guide our public communications on Injury<br />
Units by finding out what patients knew<br />
about the services provided by Injury Units,<br />
where they were getting this information<br />
from, if they wanted to find out more<br />
information and how they would like to<br />
receive information in the future.<br />
Following on from the public views and<br />
feedback gathered from the initial Injury<br />
Units Advertising campaign on Facebook<br />
, the patient survey went one step further<br />
to seek feedback from the patients who<br />
had used or engaged with the Injury Unit<br />
services directly.<br />
900 surveys were distributed to 10 Injury<br />
Units in Bantry, Mallow, Cork, Nenagh,<br />
Ennis, Limerick, Dundalk, Monaghan,<br />
Dublin and Roscommon. 586 completed<br />
surveys were returned by mid September<br />
representing an extremely high response<br />
rate of 65pc.<br />
For 46pc of respondents it was their<br />
first visit to the Injury Unit while 54pc had<br />
previously availed of the services there.<br />
75pc of respondents (435) stated they were<br />
attending as a patient, 10pc said they were<br />
there with an adult patient while 15pc were<br />
attending with a child.<br />
48pc of respondents had been referred<br />
to the Injury Unit by their GP while 52pc<br />
presented directly. 34pc of patients stated<br />
they incurred their injury while playing<br />
sports, 30pc said the injury happened<br />
at home with a further 36pc stating the<br />
injury happened elsewhere such as a work,<br />
outside, because of a fall etc.<br />
When asked how they heard about the<br />
Injury Units most respondents selected<br />
friends and family 44pc and the GP 49pc as<br />
the source of the information. 65pc stated<br />
they would like to know more about the<br />
injury unit and when asked to select the<br />
way in which they would like to receive this<br />
information 23pc mentioned HSE website,<br />
Social Media 24pc, Local Radio 25pc Local<br />
Newspaper 24pc and 26pc leaflet.<br />
pcWhen asked to rate the Injury Unit<br />
Service on a scale of 1-5 from very poorexcellent,<br />
70pc of respondents (403)<br />
selected Excellent, 25pc Very good( 141)<br />
and 5pc good.<br />
The survey also invited patients to<br />
leave a comment and this is where it<br />
got really interesting. Over a quarter of<br />
respondents chose to write a comment.<br />
While some comments were very similar<br />
to the Facebook comments about service<br />
access and availability, the majority of<br />
the comments focused on the quality<br />
and timely care provided by caring and<br />
compassionate staff working in the Injury<br />
Units. These are some of the comments<br />
received;<br />
Staff are lovely and very short wait time”<br />
“Excellent service long may it continue”<br />
“5 Star”<br />
“Everybody is very nice to me Thank You”<br />
“Met with lovely friendly smile from<br />
receptionist”<br />
“Thanks for always putting me back<br />
together”<br />
Superb service to have in our area brilliant<br />
staff and care”<br />
“Impeccable service given to all by staff,<br />
the premises are spotless”<br />
“We are so fortunate to have this service”<br />
“You can’t get better than that”<br />
“We were in and out of the hospital in one<br />
hour excellent service”<br />
Nurses extremely understanding, helpful,<br />
also reception lady extremely friendly<br />
Great Care very clean unit staff very<br />
professional<br />
I was treated with respect and concern<br />
While the survey feedback will help<br />
us to shape the Injury Unit Campaign<br />
for 2016/17, it has also provided us with<br />
some really great insights into patient’s<br />
appreciation for the service that Injury<br />
Units provide and the gratitude that<br />
patients have to the staff who work in<br />
these Units across the country.<br />
MORE INFORMATION<br />
For further information on the Injury Units visit<br />
www.hse.ie/injuryunits<br />
The Injury Unit Public Awareness campaign will<br />
continue throughout 2016/17. The campaign is<br />
sponsored by the HSE Acute Hospitals Division<br />
and the Emergency Medicine Programme<br />
54 | health matters | winter 2016
Da Vinci brings cutting-edge<br />
technology to midwest<br />
A state-of-the-art art Da Vinci Xi robotic<br />
surgical platform has been installed in<br />
Operating Theatre 7 at University Hospital<br />
Limerick, the first such installation in Ireland.<br />
A similar system was recently installed at<br />
The Royal Marsden Hospital and at Guy’s<br />
Hospital, London.<br />
Since its installation, the team involved have<br />
pioneered robotic colorectal and urologic<br />
surgery in Ireland. Some 25 robotic assisted<br />
cases have been conducted in University<br />
Hospital Limerick. These include surgery for<br />
colon and rectal cancer, inflammatory bowel<br />
disease and cancer of the kidney. On average<br />
at least three cases are now conducted<br />
weekly in University Hospital Limerick.<br />
Robotic surgery represents the highest<br />
international standard of surgery worldwide.<br />
It is the most advanced form of “key hole”<br />
or “laparoscopic” surgery. Until recently,<br />
patients wishing to avail of this type of<br />
surgery had to travel to private health<br />
institutes, or leave Ireland. The introduction of<br />
the robotic surgical program in the UHL Group<br />
has meant the highest international standard<br />
of care is, for the first time, available to all<br />
patients in the Midwest.<br />
Already the teams involved have seen their<br />
patients recover faster and with minimal postoperative<br />
discomfort.<br />
“Following major surgery for colon or rectal<br />
cancer, recovery in three to four days was<br />
the exception rather than the rule. With<br />
robotic surgery we have seen this reversed,<br />
and now this kind of recovery is becoming the<br />
rule rather than the exception,” said Prof J<br />
Calvin Coffey, Colorectal Surgeon, University<br />
Hospital Limerick and Professor of Surgery,<br />
UHL and the University of Limerick.<br />
During robotic operations the surgeon is<br />
seated at a consol and operates the robotic<br />
instruments. The level of control, accuracy<br />
and versatility these provide is unsurpassed<br />
and approaches that possible with the human<br />
hand. The program for robotic surgery<br />
is funded by the HSE, the Mid-Western<br />
Development Trust, and the Graduate Entry<br />
Medical School at the University of Limerick.<br />
The surgeons involved include Professor J<br />
Calvin Coffey (colorectal surgeon), Subhasis<br />
Giri, (urologist) and by Colin Peirce (colorectal<br />
surgeon), who recently completed his training<br />
at the Cleveland clinic. The programme<br />
initially focused on bowel and kidney cancers,<br />
but as it expands, cancers in other areas of the<br />
body including the ovary, uterus, head, neck<br />
and endocrine glands will also be treated.<br />
ABOVE: Subhasis Giri, Consultant Urology Surgeon<br />
with the Da Vinci Xi; TOP: The Da Vinci Xi Team:<br />
Fiona Darmody, Dara Walsh, Technical Support,<br />
UHL , Dr Peter O’Leary, Subhasis Giri, Consultant<br />
Urology Surgeon ,ULHG , Greg Hilton, Prof J Calvin<br />
Coffey, Consultant Colorectal Surgeon, ULHG, Dr.<br />
Seosamh O’Riain, Maura Tully, CNM2, Prof Michael<br />
Larvin, UL, Ursula Morby, Dr Patrick Dillon, Kevin<br />
Hickey, Consultant Gynaecology Surgeon, ULHG.<br />
winter 2016 | health matters | 55
General<br />
News<br />
Tullamore hospital staff<br />
give initiative a very big hello<br />
Midland Regional Hospital Tullamore<br />
(MRHT) launched the ‘Hello My Name<br />
Is’ campaign with more than 1,000 staff<br />
signing up. This patient-centered initiative<br />
encourages staff and healthcare workers<br />
to introduce themselves to both patients<br />
and staff.<br />
The campaign was founded by the late<br />
Kate Granger, a doctor from the UK who<br />
was diagnosed with terminal cancer and the<br />
campaign has become a resounding success<br />
worldwide with the initiative being introduced<br />
in hospitals in Ireland, UK and USA.<br />
Last March, Katherine Kenny (Director<br />
of Nursing), Mary Jane Burke, (Assistant<br />
Director of Nursing) and Claire Foley, (Nurse<br />
Practice Development) from Midland Regional<br />
Hospital Tullamore were fortunate enough<br />
to meet with Dr Kate Granger at the HSE<br />
Masterclass in Communication where Dr Kate<br />
Granger was speaking. They were struck by<br />
her emotional story, her unrelenting passion,<br />
and the simplicity of the concept that they<br />
felt compelled to introduce the initiative into<br />
the hospital.<br />
Director of Nursing at MRHT, Katherine<br />
Kenny, is one of the leaders and champions<br />
behind the campaign. Speaking at the launch,<br />
she said: “Personal interaction between<br />
patients and staff is the basis for an effective<br />
therapeutic relationship. The simple act of<br />
introducing yourself to a patient instantly<br />
creates a rapport and allows the patient, and<br />
indeed their families, to be more at ease.<br />
“Since meeting with Kate Granger last<br />
March, we have been determined to<br />
continue her important legacy and bring<br />
her story to the attention of our team.<br />
Indeed, I am delighted to say that more<br />
than 1,000 of our staff have pledged their<br />
support to the campaign.”<br />
The MRHT hellomynameis committee have<br />
been preparing to launch ‘Hello my name<br />
is’ since March this year. This has included<br />
assigning campaign champions from all<br />
disciplines across the hospital, and creating<br />
new name badges for all staff to include the<br />
‘Hello my name is’ logo. The name badges<br />
were kindly sponsored by Friends of the<br />
Hospital, Tullamore. The launch proved very<br />
successful with over 450 staff members<br />
attending on the day to have their photo taken<br />
to display in the hospital foyer where there<br />
was a great positive atmosphere. All staff<br />
who pledged to this patient-centred initiative<br />
were entered into a raffle for sponsored<br />
prizes from local businesses. This launch<br />
comes in the aftermath of Kate Granger’s<br />
untimely passing in July and staff will ensure<br />
her legacy lives on in Midland Regional<br />
Hospital Tullamore.<br />
ABOVE: (l-r) Mary Jane Burke, Assistant Director<br />
of Nursing; Orlagh Claffey, General Manager;<br />
Katherine Kenny, Director of Nursing; Sean<br />
Johnston, Clinical Director. BELOW: (l-r) Trish Fox,<br />
Senior Radiographer; Claire Foley, Nurse Practice<br />
Development; Paula Duignan, ED Shift Leader;<br />
Katherine Kenny, Director of Nursing; Mary Jane<br />
Burke, Asst Director of Nursing; Orlagh Claffey,<br />
General Manager at the #hellomynameis launch.<br />
56 | health matters | winter 2016
virtual dementia tour<br />
offers unique insight<br />
A unique interactive training experience aimed<br />
at bringing greater understanding and empathy<br />
for people living with dementia is being piloted<br />
by HSE Donegal.<br />
With the support of the Nursing and Midwifery<br />
Planning and Development Unit (NMPDU) and<br />
the cross border partnership (CAWT), the Virtual<br />
Dementia Tour® mobile simulated training was<br />
at St Conal’s Campus, Letterkenny, for two days<br />
in October. It was an exciting opportunity for the<br />
HSE as it will be the first time this type of mobile<br />
simulated training was delivered in Ireland.<br />
International evidence suggests simulated<br />
training in this field is effective and engages<br />
managers, clinical professionals, carers, family<br />
and friends with the experience of what it is<br />
like not only to live with dementia, but to also<br />
sense it. In addition, this type of training helps<br />
us to understand what we need to change in<br />
order to improve the quality of care that will<br />
support families to keep their loved ones at<br />
home longer. The Virtual Dementia Tour® mobile<br />
simulated training will be delivered to a total of<br />
72 healthcare personnel and family carers from<br />
across the entire range of hospital, community<br />
and voluntary services.<br />
The Virtual Dementia Tour® saw health and<br />
social care staff and family carers undergo<br />
specialised training designed not just to show<br />
people what it is like to live with dementia, but<br />
to actually experience it for themselves. As<br />
part of the experience participants wear items<br />
such as gloves, glasses and headphones so<br />
that their vision, touch, sound and pain sensors<br />
are impacted in a similar way to someone with<br />
dementia. This enables participants to gain a<br />
closer appreciation of the physical and mental<br />
challenges facing those with dementia.<br />
One of the organisers responsible for bringing<br />
the initiative to Donegal, Dr Randal Parlour,<br />
Assistant Director NMPD, commented: “Our key<br />
objective, within this process, was to develop an<br />
infrastructure that will fundamentally support<br />
both staff and carers to increase their awareness<br />
around dementia. Following independent<br />
evaluation, we anticipate that this training will<br />
also have real potential with other public service<br />
staff such as An Garda Síochána, Irish Fire<br />
Services etc.”<br />
He added: “Ultimately we anticipate this<br />
initiative will complement measures within the<br />
Irish National Dementia Strategy designed to<br />
promote person-centred practice, raise public<br />
awareness, address stigma, and promote the<br />
inclusion and involvement in society of those<br />
with dementia.”<br />
Edel O’Doherty, Chief Officer of CAWT,<br />
outlined the cross border partnership’s support<br />
saying: “CAWT’s role is to foster and develop<br />
practical cross border health and social care<br />
activity and is delighted to support this cross<br />
border initiative.<br />
“We know the increase in the number of<br />
people with dementia in the coming years will<br />
be significant. This training is timely in enabling<br />
health and social care services staff to reflect<br />
on and improve the care they currently provide.<br />
“We also hope that this initiative will be a<br />
valuable training experience for the carers of<br />
those with dementia.”<br />
At the unit are, from left, Dr Randal Parlour,<br />
Assistant Director NMPD, Martina Conway, Sadie<br />
Toye, Iris Alcrorn, Frank Morrison, Anne Gallen,<br />
Tom McBride, Grace Kelly, Dympna Wynne,<br />
Michelle Baldrick, Pat McDaid, Catriona McIntyre,<br />
Tina Gardiner, Elizabeth Breslin and Sadie Bergin,<br />
CAWT. Photo Clive Wasson.<br />
healthy IrelAND plan will support staff and patients<br />
As part of the delivery of the Saolta Healthy<br />
Ireland Implementation Plan 2015-2017, the<br />
Saolta Hospital Group has developed a new<br />
resource to support the health and wellbeing<br />
of staff and patients and build capacity to<br />
implement health and wellbeing activity.<br />
It is hoped that the Saolta Health and<br />
Wellbeing Training Plan will contribute<br />
to the three goals of the national Healthy<br />
Ireland Implementation Plan of improving<br />
staff health and wellbeing, reducing the<br />
burden of chronic disease and reforming the<br />
health services.<br />
The plan offers a wide range of staff<br />
supports for physical and mental health. It<br />
provides many health and wellbeing training<br />
opportunities for staff within the hospital<br />
group and in the community.<br />
The plan also lists a range of health and<br />
wellbeing services available for patients.<br />
This section in particular will be helpful<br />
to staff in identifying health and wellbeing<br />
supports for patients.<br />
Staff from the National Health and Wellbeing Division, with HSE National Health and Wellbeing Director,<br />
Dr Stephanie O’Keefe and Saolta Group Health and Wellbeing Lead, Greg Conlon.<br />
winter 2016 | health matters | 57
General<br />
News<br />
one in four people still smoke<br />
Almost a quarter of Irish people are<br />
still smokers, while close to a fifth of the<br />
population is exposed to second-hand smoke<br />
on a daily basis, according to the second<br />
annual Healthy Ireland Survey.<br />
The survey of 7,500 people aged 15 and over<br />
living in Ireland gives an up-to-date picture<br />
of the health of the nation and reports on<br />
many lifestyle behaviours such as smoking,<br />
alcohol consumption, physical activity, diet<br />
and mental health. A number of new topics<br />
have been included in this year’s survey,<br />
which examine additional aspects of health<br />
behaviours and issues such as multiple risk<br />
factors and knowledge and attitudes about<br />
health behaviours.<br />
Some new findings in this<br />
year’s survey results include:<br />
• While 90pc of respondents know that<br />
alcohol is a risk factor for liver disease, only<br />
27pc of women are aware of the increased<br />
risk of developing breast cancer as a result of<br />
heavy drinking.<br />
• The majority (55pc) of men who drink<br />
consume six or more standard drinks<br />
(“binge drink”) on a typical drinking occasion<br />
while fewer than 1 in 5 (18pc) women drink<br />
to this level.<br />
• Fewer than 1 in 10 women takes a folic<br />
acid supplement with just 18pc of women<br />
aged 25 to 34 doing so.<br />
• 18pc of the population in Ireland is exposed<br />
to second-hand smoke on a daily basis.<br />
• While only 54pc of people living in<br />
Ireland said they would be willing to live<br />
with somebody with a mental health<br />
problem, 83pc of people said they would<br />
be willing to carry on a relationship with a<br />
friend who developed a<br />
mental health problem.<br />
• People spend 6<br />
hours and 36 minutes<br />
sitting on an average<br />
day and while men<br />
generally spend longer<br />
sitting than women,<br />
younger women spend<br />
more time sitting than men of<br />
the same age.<br />
• Most people (63pc) would like to be more<br />
physically active although many say that time<br />
pressure due to work or caring is a barrier<br />
Speaking at the launch, Minister Marcella<br />
Corcoran Kennedy welcomed publication of<br />
the Report. “The new findings in the second<br />
Healthy Ireland Survey add very useful<br />
evidence about key lifestyle issues affecting<br />
people living in Ireland.<br />
Despite seeing some very positive results in<br />
this Survey, some groups still have a risk of<br />
poor health due to lifestyle behaviours.<br />
“These results will help us in the<br />
Department of Health, as well as in other<br />
Departments and agencies, to focus actions<br />
to promote and improve health and wellbeing<br />
by targeting at-risk groups and those<br />
experiencing health inequalities.<br />
“The Government has made a very clear and<br />
unambiguous commitment to implementing<br />
Healthy Ireland, especially in the recent<br />
Budget, with €5m specifically allocated to<br />
kick starting cross-sectoral engagement, and<br />
I look forward to focusing on specific actions<br />
and initiatives in the coming months.”<br />
The Healthy Ireland Survey showed that<br />
of the four types of unhealthy behaviours<br />
under consideration, the most<br />
common was that almost threequarters<br />
(73pc) of the population<br />
eat fewer than five portions of<br />
fruit and vegetables daily.<br />
Between a fifth and a third of the<br />
population have each of the other<br />
three behaviours – binge drinking<br />
(28pc), sedentary behaviour (26pc) and<br />
smoking (23pc).<br />
Some of the other important<br />
findings include:<br />
• 84pc of people living in Ireland say their<br />
health is very good or good although 28pc<br />
indicate that they have a long-standing illness<br />
or health condition.<br />
• 23% of the population are current<br />
smokers.<br />
• Three in five eat snacks every day with<br />
42pc of the population eating 6 or more<br />
portions daily.<br />
• Just 27pc eat five portions of fruit and<br />
vegetables daily.<br />
• 14pc consume sugar sweetened drinks<br />
daily, rising to 22pc of those aged 15 to 24.<br />
• 37pc of drinkers indicate that they drink six<br />
or more standard drinks (“binge drinking”) on<br />
a typical drinking occasion.<br />
• While 19pc of people living in Ireland<br />
smoke on a daily basis, recruitment of new<br />
smokers continues at a high rate with 20pc of<br />
those aged under 25 currently smoking.<br />
• 67pc of men and 39pc of women aged<br />
under 25 binge drink on a typical drinking<br />
occasion.<br />
• Approximately half of the people living in<br />
Ireland have had some experience of people<br />
with mental health issues.<br />
Search for new digital health technologies at NDRC<br />
Medimorpho Micro Blood Lab was selected<br />
as winner of the digital health technologies<br />
pre-accelerator at NDRC. Led by founder<br />
Joseph O’Brien, Medimorpho is a GSM enabled<br />
small, portable blood lab.<br />
Run in partnership with e-Health Ireland,<br />
the aim of the pre-accelerator was to bring<br />
together health and technology experts<br />
to find digital solutions to healthcare<br />
challenges. Thirteen entrepreneurs won a<br />
place on the programme, based in NDRC,<br />
with ideas that ranged from digital diagnostic<br />
tools to assistive technology.<br />
The idea owners were linked with over<br />
100 volunteers with backgrounds in health<br />
and technology.<br />
The HealthTech pre accelerator is<br />
sponsored by eir Business and Bank of Ireland.<br />
Gary Leyden, Commerical Director, NDRC; Joe O’Brien, Director, Medi Morpho; and Richard<br />
Corbridge, Chief Information Officer, HSE. Photo: Shane O’Neill Photography.<br />
58 | health matters | winter 2016
Safeguarding Older People<br />
in Residential Services<br />
A seminar on safeguarding older people in<br />
residential services took place in September.<br />
Hosted as a joint initiative between the HSE and<br />
Nursing Homes Ireland, the aim was to build<br />
on previous safeguarding training which was<br />
collaboratively delivered to staff in residential<br />
care settings for older people.<br />
Minister for Mental Health and Older People,<br />
Helen McEntee TD, opened the seminar<br />
and highlighted the role that everyone has<br />
to play in safeguarding, both as individuals<br />
and collectively. The Minister reiterated that<br />
the rights of vulnerable persons to live full<br />
and meaningful lives in safe and supportive<br />
environments must always be upheld.<br />
Michael Fitzgerald, Head of Head of<br />
Operations and Service Improvement for Older<br />
People addressed attendees and spoke about<br />
their crucial role in promoting the principles<br />
that prevent abuse. Mr Fitzgerald said, “Today’s<br />
seminar is about promoting knowledge of what<br />
constitutes good care and what helps to prevent<br />
abuse and/or neglect. It demonstrates how we<br />
can all learn from each other and support each<br />
other in promoting a positive culture and in<br />
combating abuse.”<br />
A new ‘Train the Trainer’ initiative for non-HSE<br />
sector nursing homes was launched at the<br />
seminar; an important development in ensuring<br />
that a consistent safeguarding message is<br />
delivered and in providing a foundation for the<br />
future delivery of safeguarding training to staff.<br />
Mr Fitzgerald welcomed the initiative<br />
reiterating that Safeguarding is everyone’s<br />
responsibility, regardless of their role in<br />
the service, “This collaborative approach<br />
ensures that the information being delivered<br />
to HSE and non HSE staff through the<br />
training is the same regardless of the<br />
setting; whether it be residential or day care,<br />
community care, in disability services or in<br />
services for older people.”<br />
Since the publication of the HSE’s<br />
‘Safeguarding Vulnerable Persons at Risk of<br />
Abuse – National Policy and Procedures,’ in<br />
2014, a number of structures and resources<br />
have been put in place including 9 Safeguarding<br />
and Protections Teams have been established,<br />
one in each Community Healthcare Organisation<br />
(CHO); a National Safeguarding Office has been<br />
created to implement the Policy, a National<br />
Safeguarding Committee has been established<br />
and Safeguarding and Protection Committees<br />
have been established in CHOs. Also, a<br />
standardised safeguarding training programme<br />
has been developed for all staff with a target of<br />
8,000 staff to be trained by year end.<br />
hse volunteer sTAFF JOIN DUBLIN AIRPORT<br />
AUTHORITY IN EMERGENCY EXERCISE<br />
The HSE was involved in an Emergency<br />
Exercise with Dublin Airport recently.<br />
Members of the Department of Public<br />
Health and the Ambulance Service were<br />
involved in the exercise, which focused on a<br />
public health incident originating on board an<br />
incoming aircraft.<br />
In conjunction with the activity in Dublin<br />
Airport, two other exercises were undertaken.<br />
The Mater Hospital tested its response to<br />
the airport incident by conducting a table top<br />
exercise in relation to the National Isolation Unit.<br />
Seconly, in conjunction with the airport<br />
exercise, the Voluntary Emergency Services of<br />
Order of Malta, Irish Red Cross and St John’s<br />
Ambulance conducted a mobilisation exercise<br />
to examine their response capabilities in support<br />
of the HSE.<br />
A large number of HSE staff and volunteers<br />
were involved on the night as participants in a<br />
number of locations. A lot of learning was taken<br />
from the exercises, which were coordinated by<br />
the Emergency Management Office.<br />
ABOVE:National Ambulance Service take part in<br />
the Emergency Exercise at Dublin Airport.<br />
RIGHT: HSE staff in action during the Emergency<br />
Exercise.<br />
winter 2016 | health matters | 59
General<br />
News<br />
‘flu jab helped keep me alive’<br />
The flu vaccine service has ‘helped keep<br />
people like me alive and healthy’, said<br />
RTE correspondent Tommie Gorman<br />
as he launched the annual campaign in<br />
Community Health Organisation (CHO)<br />
Area1 Cavan, Donegal, Leitrim, Monaghan<br />
& Sligo). Tommie was joined in An Clochar,<br />
Health Campus, Ballyshannon by HSE staff<br />
and representatives from various agencies<br />
associated with the HSE.<br />
“For several years, the flu vaccine service<br />
has helped to keep people like me alive<br />
and healthy. I have what’s described as<br />
a chronic illness and I am one of the<br />
many people who are strongly advised<br />
to get the flu vaccine jab. So for obvious<br />
reasons I am delighted to be involved in the<br />
launch of this energetic campaign in our<br />
region. Seeing is believing - at the launch,<br />
here in Ballyshannon, I’m availing of the<br />
opportunity to get my injection.”<br />
Flu can be a very serious and sometimes<br />
deadly disease, with potentially 1,000 flu<br />
related deaths in Ireland during a severe<br />
flu season. Flu is very infectious and can<br />
cause potentially serious illnesses especially<br />
for older people, those who have a chronic<br />
illness, those with weakened immune<br />
systems and pregnant women. Seasonal<br />
flu vaccine can be given at any stage of<br />
pregnancy and also protects the baby. The flu<br />
vaccine cannot give you the flu as it does not<br />
contain any live flu virus and all those at risk<br />
should get vaccinated as soon as possible this<br />
year to make sure that they are protected.<br />
The following groups of at-risk people<br />
should be vaccinated against seasonal<br />
influenza:<br />
• Everyone aged 65 years and over<br />
• Anyone over six months of age with a long<br />
term illness requiring regular medical followup<br />
such as chronic lung disease, chronic<br />
heart disease, diabetes or those with lower<br />
immunity due to disease or treatment<br />
• Pregnant women<br />
• Residents of nursing homes and other<br />
residential care services<br />
• Healthcare workers<br />
The HSE provides the flu vaccine free of<br />
charge for all those in the at-risk groups.<br />
The vaccine and consultation are free<br />
for those with a Medical Card or GP Visit<br />
Card. Those without a Medical Card or GP<br />
Visit Card will be charged a consultation<br />
fee. Those aged 18 years or older in the at<br />
risk groups may attend either their GP or<br />
pharmacist for vaccination and those under<br />
18 years should attend their GP.<br />
“This is the first year we have had a CHO1<br />
wide flu vaccine campaign and I would like<br />
to take this opportunity today to highlight<br />
the importance of increasing the uptake of<br />
the flu vaccine among the at risk groups<br />
and among my colleagues in CHO1. The<br />
flu vaccine is a safe, effective way to help<br />
prevent flu infection, avoid hospitalisation<br />
and reduce flu related deaths and illnesses.<br />
Therefore I urge all those in the at risk<br />
groups to avail of the flu vaccine,” said John<br />
Hayes. Chief Officer, CHO1.<br />
Dr Louise Doherty, Specialist in Public<br />
Health Medicine, spoke at the launch, stating,<br />
“It is important that all those working in<br />
frontline healthcare including doctors, nurses,<br />
therapists and carers protect themselves<br />
from getting the flu and also to prevent<br />
spreading the flu to vulnerable patients. Older<br />
and at risk patients may not get sufficient<br />
protection from the vaccine themselves,<br />
so people who care for them need to be<br />
vaccinated. The flu vaccine is available<br />
free to healthcare workers from their local<br />
Occupational Health Department and in their<br />
workplace from nurse peer vaccinators.”<br />
Delegates at the launch were entertained<br />
by the Markievicz Minstrels, a choir consisting<br />
of HSE Sligo/Leitrim staff who sang a<br />
song especially for the occasion about the<br />
importance of getting the flu vaccine. A<br />
series of posters and fliers were unveiled<br />
targeting the at risk groups and conveying<br />
the message to get vaccinated. These<br />
posters will be displayed in HSE facilities<br />
throughout CHO1. The HSE’s Occupational<br />
Health Service also provided a clinic at the<br />
launch where those attending could avail of<br />
the vaccine.<br />
rugby stars do the right thing<br />
Members of the Connacht rugby squad joined staff from the Saolta University Health Care Group and<br />
HSE to launch the Group’s flu vaccine campaign at University Hospital Galway. This year, the Saolta Group<br />
and the HSE are particularly requesting health care workers to get the vaccine to protect themselves, their<br />
families and their patients. (l-r) James Cooney, Connacht Rugby player getting his flu vaccine from Teresa<br />
Canniffe, CNM 2, Occupational Health Department with fellow teammates Sean O’Brien and Rory Parata.<br />
peer vaccinators<br />
The Peer Vaccination Programme<br />
is a National programme to allow<br />
Nurse Peer Vaccinators to vaccinate<br />
their fellow staff with influenza<br />
vaccine during the influenza season.<br />
The purpose of the programme is<br />
to improve the uptake of seasonal<br />
influenza vaccine among staff, by<br />
making it easier for staff to receive<br />
the vaccine.<br />
Peer Vaccinators would also be seen<br />
as Influenza vaccine champions in<br />
their areas of work. These Nurse Peer<br />
Vaccinators have been provided with<br />
training under a medication protocol,<br />
which is being produced nationally.<br />
A total of four Peer Vaccinators were<br />
trained in St Finbarr’s Hospital, Cork<br />
and seven clinics have been planned in<br />
varying departments on site, to cater<br />
for night staff and day staff. The first<br />
of the Peer Vaccinator Clinics got off<br />
to a great start with a fantastic local<br />
response seen, where a total of 27<br />
staff received the vaccine.<br />
60 | health matters | winter 2016
Baby Box<br />
Project<br />
aims to<br />
reduce<br />
incidence<br />
of infant<br />
mortality<br />
UNIVERSITY Maternity Hospital Limerick<br />
(UMHL) launched a major initiative aimed at<br />
reducing the incidence of infant mortality and<br />
raising awareness through educating parents<br />
on how to care for newborns.<br />
The Baby Box programme – a national first<br />
- will see mothers who complete e-learning<br />
modules provided with a free baby box for<br />
their infant to sleep in. The online education<br />
element is inclusive and accessible; easy<br />
to follow and available in 17 languages,<br />
reflecting the growing diversity of Irish<br />
maternity hospitals. Women booking in at<br />
ante-natal clinics will be given details on<br />
how to sign up for the e-learning at the Baby<br />
Box University.<br />
Sudden Infant Death Syndrome (SIDS), also<br />
known as cot death, is the sudden unexpected<br />
death of an apparently well infant and for<br />
which there is no explanation. About nine out<br />
of 10 cases occur in the first six months of<br />
life, with a greater risk for premature and lowbirth-weight<br />
babies.<br />
The use of Baby Boxes has been credited<br />
with helping reduce infant mortality rates in<br />
Finland, where they have been in use for over<br />
75 years. The tradition has contributed to<br />
reducing the infant mortality rate in Finland<br />
from 65 infant deaths per 1,000 births in 1938<br />
to 2.26 per 1,000 births in 2015. Ireland’s<br />
infant mortality rate is 3.7 per 1,000 births.<br />
Other countries, including the UK,<br />
Canada and USA, have begun to introduce<br />
this concept to their families. UMHL—in<br />
partnership with The Baby Box Co. - is the<br />
first Irish maternity hospital to embrace<br />
the idea. New mothers in Limerick will<br />
be presented with a Baby Box, containing<br />
clothing and other goods as well as<br />
educational materials.<br />
The Baby Boxes, which are made from a<br />
durable cardboard, can be used as a baby’s<br />
bed for up to the first eight months of their<br />
life. Replacing the need for the traditional<br />
Moses basket or cot, it is thought the small<br />
size of the Baby Box prevents babies from<br />
rolling onto their tummies, which experts<br />
think can contribute to SIDS.<br />
The Baby Boxes come with a firm foam<br />
mattress, waterproof mattress cover, cotton<br />
sheet - and education materials with advice<br />
from healthcare professionals in the Mid-<br />
West on reducing risks to baby, improving<br />
parental bonding and making the transition<br />
to parenthood. The theme chosen for the<br />
Limerick initiative is ‘Celebrating Life,<br />
Celebrating Family’.<br />
“The Baby Box programme is a proactive<br />
approach to improving the health and<br />
safety of the newborn child and parents.<br />
We are combining tradition with current<br />
technology and supporting the newborn<br />
child’s family with online educational<br />
material covering a broad range of<br />
essential topics on ante and postnatal<br />
care,”said Dr Mendinaro Imcha, Consultant<br />
Gynaecologist/Obstetrician, UMHL.<br />
Margaret Gleeson, Chief Director of<br />
Nursing and Midwifery, UL Hospitals<br />
Group, said education was a central<br />
element of the project, arising from which<br />
up to 5,000 boxes would be distributed to<br />
the families of babies born at UMHL over<br />
the year of the programme.<br />
“The Baby Boxes designed by one of our<br />
patients are a thing of beauty. Then there<br />
is the invaluable education element of<br />
the initiative which makes it truly patientcentred,”<br />
said Ms Gleeson.<br />
“That education involves brief video<br />
tutorials delivered by local healthcare<br />
professionals addressing the most common<br />
concerns of parents with newborn babies.<br />
A number of these videos were made in our<br />
hospital with our specialists. We think all of<br />
our staff here at UMHL are stars and they<br />
were delighted - along with their colleagues<br />
in public health nursing and community and<br />
primary care - to make videos advising new<br />
parents in critical areas like breastfeeding,<br />
nutrition, perinatal mental health, neonatal<br />
resuscitation, postnatal community support,<br />
postnatal checkup, immunisation, VTE and<br />
sepsis,” added Ms Gleeson.<br />
The Limerick Baby Box has been designed<br />
by Tipperary-based tattoo artist and<br />
expectant mum Karen Smith.<br />
“The whole meaning behind the design is<br />
rebirth. I thought the butterfly was the perfect<br />
symbol for the Baby Box. It is a symbolic<br />
creature in many cultures. It sometimes<br />
represents Beauty itself, or metamorphosis,<br />
and at other times the transitory nature of<br />
happiness and indeed all of life. They lend<br />
themselves to all manner of colourful and<br />
fanciful adaptations, in our case our beautiful<br />
Baby Box,” said Karen.<br />
Jennifer Clary, the CEO of The Baby Box<br />
Co., which is supplying UMHL with the Baby<br />
Boxes and Baby Box University memberships<br />
for participating parents said: “We are<br />
delighted to expand the Baby Box programme<br />
to Ireland and look forward to an impactful<br />
collaboration here at University Maternity<br />
Hospital Limerick.”<br />
winter 2016 | health matters | 61
General<br />
News<br />
Programme in Sexual Health<br />
Promotion off to flying start!<br />
By Moira Germaine and Martin Grogan Health<br />
Promotion & Improvement Officers, HSE South<br />
The Foundation Programme in Sexual<br />
Health Promotion (FPSHP) is concluding<br />
its first year as a national programme<br />
under the aegis of the National Sexual<br />
Health Strategy. The 2016 target of<br />
100 participants has been dramatically<br />
exceeded with 184 completing the training<br />
and a healthy waiting list established for<br />
the 2017 courses.<br />
Originating in HSE South in 2009, the 10-<br />
day FPSHP was developed as a response<br />
to the need for sexual health training that<br />
not only addressed knowledge but also the<br />
comfort levels of participants in addressing<br />
a topic that has historically been taboo.<br />
This approach was taken on foot of a review<br />
of national and international literature,<br />
which revealed that two major blocks to<br />
the promotion of sexual health were the<br />
discomfort of professionals in addressing<br />
the subject and the conscious and<br />
unconscious impact of professionals’ own<br />
attitudes and values in dealing with their<br />
clients. As a result, the FPSHP programme<br />
takes a broad, holistic approach to sexual<br />
health and utilises the principles of adult<br />
learning and experiential methodology to<br />
increase participants’ knowledge, skills<br />
and self awareness. In addition, because<br />
training is only one facet of capacity<br />
building, participants and their organisations<br />
are offered on-going support in order<br />
to implement sexual health promotion<br />
activities within their organisation.<br />
In 2013, an external evaluation of the<br />
FPSHP - funded by Sexual Health & Crisis<br />
Pregnancy Programme and carried out by<br />
the School of Nursing and Midwifery, Trinity<br />
College Dublin - assessed the programme<br />
favourably for its capacity building impact<br />
on participants.. It was on the basis of this<br />
that the FPSHP was then adopted as a<br />
national programme. Following a pilot in<br />
Galway in 2015, the FPSHP was expanded<br />
out of HSE South and is now being delivered<br />
in 10 different locations throughout Ireland.<br />
This work will continue in 2017 with a<br />
further three locations being added to the<br />
training list.<br />
Participants on the FPSHP come from<br />
the Health, Education, Community and<br />
Youthwork sectors and the range of<br />
professions represented is vast including<br />
doctors, nurses, psychologists, occupational<br />
therapists, social workers, social care<br />
workers, teachers, lecturers, counsellors,<br />
people working in the areas of substance<br />
misuse, homelessness, mental health,<br />
intellectual disability and Acquired Brain<br />
Injury. Eligibility for inclusion is simply<br />
dependent on the person’s capacity to<br />
integrate sexual health promotion into their<br />
core work and their personal compatibility<br />
with the learning style of the programme;<br />
both of these are established during a<br />
20-minute interview with each prospective<br />
participant before places are allocated on<br />
the course. Priority is given to personnel<br />
working with the most disadvantaged and<br />
those whose employers have identified an<br />
organisational goal in relation to sexual<br />
health promotion. All groups include a range<br />
of agencies and disciplines to promote<br />
networking and cross- sectoral working.<br />
Anyone interested in further detail on<br />
the Foundation Programme in Sexual<br />
Health Promotion should contact Martin<br />
Grogan- Acting FPSHP Co-ordinator martin.<br />
grogan@hse.ie<br />
The group of staff in Athlone who completed<br />
the Foundation Programme in Sexual Health<br />
Promotion (FPSHP).<br />
What past participants have to say<br />
Participation in the FPSHP in 2012 was the perfect foundation<br />
on which to build a tailor-made programme for our service<br />
users. It also gave me the confidence to facilitate the sessions<br />
and eased any concerns I may have had in covering somewhat<br />
delicate issues in relation to sexual health.<br />
Carol Kelly, Keyworker with Aspect (Autism Services)<br />
In the course of my work with Mental Health Ireland, I have<br />
used the skills and knowledge I acquired in the FPSHP on a<br />
regular basis. Many mental health problems or issues are, in<br />
fact, based in fears around sexual identity and sexual health.<br />
The course has enabled me to explore these very sensitive<br />
issues because I feel confident and grounded in this area<br />
following the course.<br />
Linda Thorpe, Development Officer, Mental Health Ireland<br />
I loved the FPSHP. It opened my eyes that sexuality is from<br />
birth to death, and that all persons, regardless of gender, age,<br />
health and disability, are entitled to explore their sexuality. As a<br />
midwife, it increased my confidence to talk to new parents about<br />
sexuality; as a parent to young children it reinforced my belief<br />
that communication about sexuality can begin in the early years.<br />
I would highly recommend this course.<br />
Claire Bulfin, Midwife, Waterford Regional Hospital<br />
62 | health matters | winter 2016
South East<br />
intercultural<br />
healthcare<br />
project<br />
shortlisted for<br />
national award<br />
An intercultural health pilot project for<br />
the South East based in Waterford and<br />
South Tipperary was one of six finalists<br />
for the overall Health Management<br />
Institute of Ireland, Leaders Awards,<br />
which were presented at a ceremony in<br />
Dublin recently.<br />
The aim of Social Inclusion in<br />
HSE South East is to “support the<br />
development and implementation of<br />
appropriate initiatives that enhance<br />
healthcare delivery to ensure equitable<br />
health outcomes for vulnerable<br />
Minority communities” and this<br />
particular project was highlighted as a<br />
prime example.<br />
The HSE’s Social Inclusion Services,<br />
working in partnership with the<br />
Integration and Support Unit (ISU),<br />
the HSE’s Primary Care Leads, Health<br />
Promotion, Primary Care Social Work,<br />
Tulsa, Mental Health, Homeless and<br />
Substance Misuse Services, sought to<br />
enhance health information and access<br />
to services for vulnerable members of<br />
new communities.<br />
Aileen Colley, Chief Officer of the Area<br />
5 Community Healthcare Organisation,<br />
congratulated all those involved in<br />
the Waterford based healthcare pilot<br />
project and said it was a model for<br />
how things could be done in other<br />
communities around the country.<br />
In illustrating the co-operation<br />
between the HSE and the ISU, Anne<br />
Nolan, Manager of the ISU said,<br />
“The HSE and the ISU initiated a<br />
pilot phase in 2014/15, in which we<br />
focused on the health outcomes of<br />
asylum seekers living in the five ‘direct<br />
provision’ centres in the South East,<br />
four are based in Waterford and one in<br />
South Tipperary. Key areas of health<br />
concerns were identified through the<br />
ISU’s work and research. Namely,<br />
these were sexual and mental health.<br />
Thereafter, a training programme was<br />
designed and delivered to up-skill<br />
‘Peer Community Knowledge Workers’<br />
(CKWs) resident in the South East and<br />
who had lived in direct provision and/or<br />
were members of vulnerable minority<br />
groups. Information sessions were<br />
delivered to staff in health and social<br />
care settings.”<br />
Medical Careers Day<br />
Almost all of the attendees who gave<br />
feedback on the most recent Medical<br />
Careers Day felt the day was beneficial and<br />
would recommend the event to others.<br />
Over 300 medical students and interns<br />
attended the fourth annual Medical<br />
Careers Day “Building Your Future”<br />
with the view to learning more about<br />
postgraduate training opportunities in<br />
Ireland.<br />
Held at the Royal Hospital Kilmainham,<br />
Dublin, the focus of the day was to provide<br />
practical information about postgraduate<br />
training structures in Ireland and specific<br />
information about specialty training.<br />
Over 95pc of the attendees felt that<br />
The Minister for Health Simon Harris<br />
attended the event, and described it<br />
as “not only a great opportunity for<br />
networking with peers, it enables<br />
participants to explore different career<br />
paths through the medical profession”.<br />
Minister Harris also officially launched<br />
the NDTP Strategic Plan for the period<br />
2016-2020. This is the first strategic plan<br />
for the unit since the three functions of<br />
medical education and training, medical<br />
workforce planning and the consultant<br />
post approval process were centralised<br />
in NDTP in November 2014. NDTP has a<br />
statutory remit outlined in the Health Act<br />
2004 and the Medical Practitioners Act<br />
2007. For more information on NDTP go to<br />
www.hse.ie/doctors<br />
the presentations, walks and workshops<br />
provided relating to working and training in<br />
13 broad specialty areas were appropriate<br />
and relevant to their needs.<br />
Some 90pc of those in attendance felt<br />
that the information provided by the<br />
postgraduate training bodies was useful.<br />
Feedback received from attendees will be<br />
incorporated into the planning for the next<br />
Careers Day, to be held in September 2017.<br />
TOP: Prof Eilis McGovern, Director National<br />
Doctors Training and Planning (NDTP) with some<br />
of the attendees at the 4th Medical Careers Day.<br />
BELOW: Prof McGovern with Minister for Health<br />
Simon Harris.<br />
chance to explore new career path<br />
winter 2016 | health matters | 63
General<br />
News<br />
Irish use of psychoactive<br />
drugs continues to rise<br />
A new information campaign aimed at<br />
students has been developed by the Union of<br />
Students of Ireland in partnership with Drugs.<br />
ie and the HSE. The information campaign<br />
focuses on harm reduction and is aimed at<br />
young adults and students who use new<br />
psychoactive substances (NPS).<br />
New Psychoactive Substances’ (NPS) are<br />
designed to mimic established illicit drugs<br />
such as cannabis, cocaine, methamphetamine,<br />
MDMA and LSD. Manufacturers of these<br />
substances develop new chemicals at an<br />
alarming rate to replace those that are banned<br />
in order to stay ahead of the law.<br />
As the availability of new substances<br />
has increased, so have the serious harms<br />
associated with their use particularly acute<br />
poisonings sometimes resulting in death.<br />
These substances also cause other unwanted<br />
physical and psychological side effects. The<br />
increase in these substances and the wide<br />
variation in strength and purity requires a<br />
strong public health response.<br />
The use of psychoactive drugs in Ireland<br />
among the 15-24 year age group is the highest<br />
in Europe (22pc lifetime use). Data suggests<br />
that the purity or potency of most illicit<br />
substances is increasing and that the market<br />
for substances is becoming more varied<br />
and accessible. This phase of the campaign<br />
focuses on two specific drugs MDMA (ecstasy)<br />
and Ketamine (K); this is the first step of an<br />
ongoing campaign to provide harm reduction<br />
information for students. Two posters have<br />
been designed along with Facebook ads and a<br />
social media campaign to give harm reduction<br />
advice and information on accessing support.<br />
Dr Eamon Keenan HSE National Clinical<br />
Lead for Addiction services, added, “The HSE<br />
is partnering with the Union of Students in<br />
Ireland to target students and young people<br />
with an appropriate Harm Reduction message.<br />
Harm Reduction refers to policies, programmes<br />
and practices that aim to reduce the adverse<br />
health, social and economic consequences of<br />
the use of legal and illegal psychoactive drugs.<br />
“Harm reduction benefits people who use<br />
drugs, their families and the community. It is<br />
always safer not to use illegal drugs and we<br />
advise people not to use, however we have<br />
a duty to reduce harm and protect young<br />
peoples’ health.<br />
The key messages that we need to get to<br />
people is to Stay Safe and to be aware of the<br />
strength of the drugs they are taking.”<br />
MORE INFORMATION<br />
There is information, support and help<br />
available through www.drugs.ie or the<br />
Drugs Helpline HSE Drug/Alcohol helpline<br />
Freephone: 1800 459 459 9.30 - 5.30 Monday<br />
– Friday or Email support: helpline@hse.ie<br />
innovative webinar launched to improve quality of services<br />
A new and innovative web based seminar, or webinar – QI Talktime<br />
- has been launched for everyone with an interest in improving the<br />
quality of services we deliver.<br />
The one-hour webinar will be hosted by an exciting mix of local,<br />
national and international speakers and will be held every three weeks<br />
from November 2016, explained Roisin Breen, QI Talktime lead from<br />
the HSE Quality Improvement Division.<br />
“The webinars are open to everyone across our health and social care<br />
services and will provide a forum to share learning and experiences<br />
of service redesign and improvement. They will also be a great way of<br />
connecting with others interested in Quality Improvement (QI)”.<br />
“It’s free and easy to join, all you need is an internet connection. We<br />
would encourage people to get together in their workplace and log<br />
on as a group to help in building your own local QI networks. However,<br />
people can of course join individually as well.”<br />
All links to the webinars will be available on the HSE QI web page of<br />
the HSE website and archived talks will also be available after they<br />
have taken place. Check out the web page to see the range of topics,<br />
speakers and dates.<br />
Please contact Roisin (roisin.breen@hse.ie) who will be happy to help<br />
with any queries and follow QI Talktime on twitter for regular updates<br />
on @QITalktime<br />
64 | health matters | winter 2016
special needs preschool<br />
gets a garden revamp<br />
The Ballaghderg HSE special needs preschool<br />
provides a service for children with moderate<br />
to severe intellectual disabilities and complex<br />
care needs in the Letterkenny area.<br />
The service strives to provide a holistic and<br />
therapeutic environment for the children<br />
in partnership with families and the early<br />
intervention team where each child learns<br />
to develop and grow through play in a<br />
specialised setting.<br />
Over the past five months Fintan<br />
Houston volunteered to lead the project to<br />
revamp the sensory garden with the help<br />
of local volunteers and sponsorship from<br />
local businesses.<br />
The garden was reopened by Fintan<br />
recently and all those involved including<br />
families and friends were invited to celebrate<br />
this special occasion.<br />
Speaking at opening, Catherine Kelly, HSE<br />
Clinical Nurse Manager at Ballaghderg, was<br />
full of praise for the effort given.<br />
“The HSE intellectual disability services<br />
would like to take this opportunity to thank<br />
Fintan Houston and all the volunteers who<br />
kindly gave up their free time to redecorate<br />
and clean up the garden area,” she said.<br />
“We would also like to express our gratitude<br />
for all donations received from local sponsors,<br />
which funded the cost of visual images, new<br />
plants, an all-weather proof wheelchair<br />
accessible swing and to the St Conal’s Garden<br />
Centre team who designed a bird man that<br />
attracts birds into the garden area. The<br />
sensory garden has many benefits for the<br />
preschool children from stimulating their<br />
senses to providing a safe and calming place<br />
where they can learn about their environment<br />
and have endless hours of fun and enjoyment.<br />
Commenting on the re-vamped garden,<br />
Eugene McElroy HSE Donegal Intellectual<br />
Disabilities Business Manager said, “The<br />
garden is an important element of service<br />
provision and the works carried out on the<br />
garden will enhance the experience of children<br />
attending the Preschool.”<br />
BELOW: Fintan Houston cuts the ribbon at the<br />
opening of the HSE Ballaghderg Special Needs<br />
Preschool Garden after its revamp with front, from<br />
left, Veronica Kilpatrick, Senior Human Capital<br />
Specalist Optum United Health Services; Malachey<br />
Dunleavy, Eunan Carol, Sarah Jane O’Connor,<br />
Optum Engagement Team; Catherine Kelly HSE<br />
Clinical Nurse Manager; Orson Sterritt, Optum<br />
Engagement Team; John Burke; and Laura<br />
Campbell, Optum Engagement Team.<br />
Photo: Clive Wasson.<br />
We must work together, conference told<br />
A large crowd attended the Connecting For life Donegal<br />
Conference organised by Donegal County Council held in Buncrana<br />
recently. The aim of the conference was to build connections and<br />
share good practice in suicide prevention. Connecting for Life<br />
Donegal is a countywide suicide prevention action plan which<br />
calls on individuals and organisations to work together to realise<br />
‘a county where fewer lives are lost through suicide and where<br />
communities and individuals are empowered to improve their<br />
mental health and wellbeing’.<br />
The audience heard the personal story of Emma Lawrence who<br />
spoke movingly about her own experiences and the help she received<br />
from the HSE, Child and Family Mental Health service when she<br />
struggled with her mental health as a teenager.<br />
Anne Sheridan, Suicide Resource Officer with the HSE outlined and<br />
complimented the good work being done by numerous organisations<br />
and groups. “We need to keep working together year on year - the<br />
HSE, the County Council, schools, youth, community and voluntary<br />
organisations and groups as every single organisation has an<br />
important part to play in reducing deaths by suicide.”<br />
Other speakers outlined the issue of suicide among the Traveller<br />
Community, individuals struggling with debt, the burden of alcohol<br />
and a new Crisis Suicide Assessment Nursing service working<br />
alongside GPs. Finally, Dr Kevin Malone, UCD complimented Donegal<br />
on leading the way in suicide prevention at a local level and said that<br />
the cumulative grief resulting from suicide deaths and road traffic<br />
accidents was an issue which should be considered.<br />
winter 2016 | health matters | 65
General<br />
News<br />
5,000 people die in Europe<br />
from bugs that are resistant<br />
to antibiotics and someone<br />
2<br />
somewhere in the world dies<br />
every 10 minutes because<br />
antibiotics don’t work, the HSE Clinical Lead<br />
for the Prevention of Healthcare-associated<br />
Infection, Dr Robert Cunney has warned.<br />
“Antibiotics are a precious resource that<br />
saved millions of lives. They are very specifc<br />
drugs designed to kill bacteria. However<br />
using antibiotics when they are not needed<br />
eg for viral infections is a waste of time and<br />
money, puts your health at risk, and makes<br />
it more difficult to fight against infections<br />
in the future. Using antibiotics needlessly<br />
allows bugs that cause infections to build up<br />
resistance against antibiotics and renders<br />
them useless over time. Most infections<br />
children and adults get are caused by<br />
viruses and will get better by themselves ,”<br />
said he said.<br />
“Very few new types of antibiotic are being<br />
developed, which means that we must make<br />
sure that the ones we have remain effective<br />
against infections for the sake of our own<br />
health and future generations. If somebody<br />
develops an infection that antibiotics can’t<br />
kill because it has built up resistance to the<br />
treatment then that person will become<br />
very unwell and may die. This person could<br />
have been cured if the infection had not<br />
become resistant to antibiotics. Examples of<br />
antibiotic resistant infections include MRSA<br />
and C.difficile.<br />
“The more antibiotic prescriptions a person<br />
receives, the higher the likelihood that the<br />
antibiotics won’t work the next time they get<br />
an infection due to the infection developing<br />
resistance to the antibiotics. Antibiotic<br />
consumption is falling in most European<br />
countries but not in Ireland although there<br />
have been improvements in hospitals and<br />
certain age groups in the community.”<br />
The HSE, in partnership with the Irish<br />
College of General Practioners and the<br />
Irish Pharmacy Union, has developed a new<br />
website which gives practical, common sense<br />
advice and information on dealing with many<br />
common illnesses like colds, flu, earaches,<br />
sore throats, tummy bugs and rashes.<br />
www.undertheweather.ie provides the<br />
sound advice that we all need to give us the<br />
confidence and skill we need to take care of<br />
ourselves and our families at home without<br />
resorting to antibiotics, according to the HSE<br />
National Director for Quality Improvement, Dr<br />
Philip Crowley.<br />
“The website tells you how long common<br />
illnesses should last, what to expect,<br />
and what you can do to cope with, and<br />
recover from, these illnesses. The site<br />
includes a series of videos featuring GPs<br />
and pharmacists who offer their expertise<br />
on dealing with these common illnesses,<br />
under the<br />
weather<br />
practical remedies, and advice on when to<br />
seek help from either a pharmacist or a<br />
doctor,” he said.<br />
Dr Nuala O Connor, ICGP lead advisor on<br />
antibiotics, said research has shown that a<br />
lot of people still believe that antibiotics can<br />
help to treat common illnesses, like colds, flu,<br />
earaches, tummy bugs and rashes. We know<br />
in fact that antibiotics are useless against<br />
most of these infections, which are caused by<br />
viruses, and antibiotics don’t work on viruses.<br />
“Learning how to manage common illnesses<br />
with confidence and common sense is a great<br />
life skill and improves our understanding of<br />
when we need antibiotics and when we don’t.<br />
It’s something that we learn from our parents,<br />
friends, doctors, from our own experience and,<br />
more and more, from the internet. Under the<br />
Weather has been developed in response to<br />
this, to support the public in accessing trusted<br />
and reliable health information, developed by<br />
the HSE with expert knowledge and advice<br />
from GPs and pharmacists,” she said.<br />
“The Under the Weather campaign is about<br />
ensuring that we only use antibiotics when<br />
we really need them. Using antibiotics when<br />
they’re not necessary creates stronger, more<br />
resistant infections that can make us very ill.<br />
“Antibiotic resistance is a global health<br />
threat, and one that is being tackled on a<br />
range of fronts, in Ireland and internationally.<br />
We need to ensure that we preserve<br />
antibiotics for when they are really needed<br />
– for everything else, your common cold<br />
and nasty cough - the best advice is on<br />
undertheweather.ie.”<br />
more information<br />
www.undertheweather.ie<br />
Get advice and get better<br />
66 | health matters | winter 2016
support for parents<br />
of preterm babies<br />
A new booklet and on-line information on<br />
breastfeeding for parents of premature babies<br />
has been launched at the National Maternity<br />
Hospital for World Prematurity Day. The day<br />
aims to raise awareness of the issues facing<br />
babies born prematurely and highlights supports<br />
for parents of premature babies<br />
A number of organisations have come together<br />
to develop the information resources for<br />
parents - the HSE, the Association of Lactation<br />
Consultants in Ireland, Irish Premature Babies,<br />
the National Maternity Hospital and Our Lady’s<br />
Children’s Hospital, Crumlin.<br />
Breast milk is vital for premature babies to help<br />
them grow and develop and to prevent infections<br />
and illness.<br />
Speaking at the launch, Master of the National<br />
Maternity Hospital, Dr Rhona Mahony said, ‘Our<br />
babies that are born preterm are particularly<br />
vulnerable. Breast milk is not only nutrition for<br />
premature babies, every drop of breast milk<br />
is protecting your baby’s health. Everything<br />
that we can do to support parents of preterm<br />
babies is important. This practical information<br />
launched today is part of the range of supports<br />
to help mothers.”<br />
Elaine McGovern gave a mum’s perspective,<br />
noting, “So many emotions hit you when you have<br />
a baby that’s born early. You can feel helpless so<br />
it is really good to know that there is something<br />
that you can do as a mother to protect your<br />
baby’s health, by giving breast milk to your baby.”<br />
Irish Premature Babies is a charity dedicated<br />
to supporting parents of preterm babies. Their<br />
website is www.irishprematurebabies.com<br />
“Each year over 4,500 pre-term babies are<br />
born in Ireland, every 116 minutes a pre-term<br />
baby is born, in one of Ireland’s maternity<br />
units. Irish Premature Babies delivers front line<br />
services to families and support the work of<br />
the neonatal intensive care units around Ireland<br />
by providing vital equipment towards the care<br />
of pre-term babies,” said Allison Molloy of Irish<br />
Premature Babies.<br />
National Breastfeeding Co-ordinator Siobhan<br />
Hourigan said, “Mother’s own milk makes such<br />
a difference to premature babies. We want to<br />
support and help mums to provide breast milk for<br />
their babies. The booklet and online information<br />
and videos www.breastfeeding,ie talks parents<br />
through this and gives step by step tips and<br />
photos on expressing milk, kangaroo care, and<br />
lots more’.<br />
MORE INFORMATION<br />
For further information log on to the HSE<br />
website www.breastfeeding.ie/Getting-<br />
Started/Premature-or-ill-baby/<br />
Caitriona Garde and baby Grace attending the<br />
launch at the National Maternity Hospital for World<br />
Prematurity Day. Grace was born at just 30 weeks<br />
and breastfed until she was just over a year.<br />
New Dedicated Paediatric Area opens in UHG<br />
The newly developed dedicated paediatric area<br />
within the emergency department at University<br />
Hospital Galway opened its doors to paediatric<br />
patients in June, reducing wait times and<br />
improving patient flow.<br />
The new paediatric area was reconfigured<br />
from an existing space to facilitate the<br />
development and will accommodate all<br />
paediatric patients from 0 – 16 years of age<br />
and will cater for both medical and surgical<br />
patients. The emergency department<br />
at University Hospital Galway sees<br />
approximately 17,000 paediatric patients<br />
per annum, this accounts for approximately<br />
20-25pc of all presentations to the ED. The<br />
new paediatric ED comprises of 6 cubicles,<br />
2 isolation rooms, a separate waiting area<br />
from the adult waiting area and a separate<br />
access door into the paediatric ED. It is fully<br />
compliant with the national HSE charter<br />
ensuring complete audio-visual separation<br />
from the adult ED area. Children will no<br />
longer have to share the same waiting area as<br />
adults. The separate area is compliant with<br />
the Children First hospital policy, ensuring the<br />
safety and privacy for all paediatric patients<br />
presenting to the department.<br />
Dr Ethel Ryan, Clinical Director for Women’s<br />
and Children’s Directorate & Consultant<br />
Paediatrician, UHG stated, “The new paediatric<br />
ED area benefits the paediatric patients and<br />
their families by providing a safe and secure<br />
environment for them to be reviewed in, with<br />
complete separation from the adult area. This<br />
new area provides them with full privacy and<br />
safety as per the National Children First Policy.<br />
With the increased number of clinical cubicles,<br />
paediatric patients will be seen quicker which<br />
improves patient flow through the department<br />
and reduces their waiting time to be seen.”<br />
winter 2016 | health matters | 67
Lifestyle<br />
The public sector has a target to improve its energy efficiency by 33pc by 2020 and the HSE is well on<br />
its way to achieving this ambitious target. As part of its energy efficiency programme the National Health<br />
Sustainability Office (NHSO), in partnership with the Office of Public Works (OPW), is currently running a<br />
staff energy awareness campaign called Optimising Power at Work which will rolling out in twenty sites<br />
over 2016 and 2017. The initiative aims to change staff behaviour towards energy use and reduce the<br />
amount of energy we use in our buildings. Cathryn Buckley, Office Coordinator in the National Health<br />
Sustainability Office looks at simple ways that you can save energy at home and at work.<br />
Energy Efficiency at<br />
home and<br />
in work<br />
nergy is essential to nearly all<br />
aspects of our daily lives - but<br />
we rarely stop to think about<br />
E<br />
how or why we use it. As the<br />
darker evenings approach and<br />
the weather gets cooler we can all do our<br />
part to avoid wasting energy. This will save<br />
money and also benefit our health and the<br />
environment. Every change no matter how<br />
small can make a difference.<br />
The World Health Organisation supports<br />
the argument that the burning of fossil fuels<br />
and the emission of Green House Gases is<br />
not only detrimental to the environment but<br />
also to people’s health. For example, policies<br />
supporting cleaner transport, energy-efficient<br />
buildings and better waste management reduce<br />
emissions of CO2 and pollutants, contributing to<br />
the mitigation of climate change. These policies<br />
also reduce key sources of air pollution leading<br />
to improved cardiovascular and respiratory<br />
health of the population. Policies encouraging<br />
sustainable transport can promote physical<br />
activity by encouraging low carbon modes of<br />
transport such as cycling and walking.<br />
Remember these three easy steps to avoid<br />
wasting energy - plug out equipment, switch off<br />
lights and only use what you really need.<br />
Top tips for saving energy<br />
at home<br />
• Turn down your thermostat - if yours is above<br />
20ºC turn it down as lowering your thermostat<br />
by just 1ºC will knock 10pc off your heating bill.<br />
• Turn the lights off when leaving a room or<br />
when there is enough daylight.<br />
• Switch appliances off rather than leaving<br />
them on standby - this will save up to 20pc of<br />
your appliances’ energy use.<br />
• Take a shower rather than a bath - a typical<br />
shower uses only one fifth of the energy of a<br />
bath.<br />
• Use energy efficient light bulbs – they use<br />
80pc less electricity than<br />
ordinary bulbs to produce<br />
comparable light and they last<br />
eight times as long.<br />
• Buy A-Rated appliances<br />
when possible - all appliances<br />
now need an energy label so<br />
check them for one.<br />
• Insulate your attic and<br />
walls – this could save you 30-<br />
40pc on your home heating<br />
bill. SEAI provides grants for<br />
upgrading your insulation<br />
through the Better Energy<br />
Homes scheme.<br />
• Replace your boiler and<br />
improve heating controls<br />
- the Better Energy Homes scheme will also<br />
grant aid for high efficiency boilers and heating<br />
control improvements.<br />
For more information on saving energy<br />
in your home and the grants available<br />
for energy improvements check out the<br />
Sustainable Energy Authority of Irelands<br />
website www.seai.ie.<br />
Top tips for saving energy<br />
at work<br />
• Switch off computers and non-essential<br />
equipment each evening, at weekends, and<br />
before holidays - this will save up to 20pc of your<br />
appliances’ energy use compared to leaving<br />
them on standby.<br />
• Activate the power saving functions on<br />
computers, printers and photocopiers /fax<br />
machines.<br />
• Report any dripping taps, leaking pipes or<br />
broken toilets – saving water also saves energy.<br />
• Keep it on the screen – only print when<br />
necessary which saves paper and energy.<br />
• Ensure windows and outside doors are kept<br />
closed when the heating or air conditioning is on.<br />
• Use the stairs instead of the lift and if<br />
you can, consider walking, cycling or public<br />
transport when travelling to work – this saves<br />
energy and is also good for your health.<br />
More information on sustainability in the<br />
Health Service, including energy efficiency,<br />
water conservation, waste prevention and<br />
sustainable transport, is available at www.hse.<br />
ie/sustainability or you can contact the National<br />
Health Sustainability Office – nhso@hse.ie<br />
National Health Sustainability Office<br />
www.hse.ie/sustainability<br />
Useful links<br />
www.hse.ie/sustainability<br />
www.opw.ie<br />
www.seai.ie<br />
www.seai.ie/Grants/Better_energy_homes/<br />
68 | health matters | winter 2016
www.HospitalWalks.com<br />
Get Up!<br />
Get Out!<br />
Get Active!<br />
F you were offered a daily pill<br />
that could reduce your risk of<br />
Type 2 diabetes, cancer, heart<br />
I<br />
disease and stroke, give you a<br />
healthy dose of vitamin D, help<br />
you lose weight, tone up and increase your<br />
stamina, would you take it? The answer is<br />
sure to be “yes” but before you search for this<br />
new wonder drug, here is the best bit: the<br />
benefits are all yours with a brisk daily walk.<br />
Even if you are physically inactive now, just 30<br />
minutes of brisk walking five days a week is<br />
enough to lower your risk of suffering an early<br />
death by up to 30pc.<br />
A new website was launched in early<br />
September to highlight accessible walking<br />
routes for staff, visitors and patients in<br />
Galway City Hospitals.<br />
By changing the work environment to<br />
include accessible walking routes, we can<br />
help to raise awareness of the many benefits<br />
of physical activity to one’s health and<br />
wellbeing. Walking is a great way for nonexercisers<br />
to begin an activity programme, as<br />
it is free, accessible and we already know how<br />
to do it.<br />
This is the reason Health Promotion and<br />
Improvement and the Saolta University<br />
Health Care Group identified and highlighted<br />
various internal and external accessible<br />
walking routes on both hospital sites in<br />
Galway City, on the grounds of GUH and<br />
Merlin Park University hospitals.<br />
In early September, to coincide with the<br />
hospital step challenge for staff and ‘Culture<br />
Night’, a new website was launched called<br />
www.HospitalWalks.com These hospital<br />
walks are coloured coded and measured in<br />
relation to step count, distance in kms and<br />
duration-walking at a modest pace.<br />
The website clearly highlights interactive<br />
maps, slide shows and photos of all the<br />
routes, to ensure clarity and accessibility<br />
for all. The website also contains links to<br />
Get Ireland Active, Get Ireland Walking and<br />
other relevant websites to support staff,<br />
patients and visitors to become more active,<br />
more often.<br />
It is hoped that the website and promotional<br />
material will support all hospital staff,<br />
patients and visitors to avail of opportunities<br />
at work and while visiting the hospitals to<br />
integrate more physical activity into their<br />
daily routine by engaging in short physical<br />
activity walks.<br />
The walks in Merlin Park University Hospital<br />
were names after central figures in the<br />
hospital’s history such as:<br />
Dr Noel Browne – the Minister for Health<br />
who built this hospital as a TB sanatorium.<br />
Dr Norman White – the architect who<br />
was keen that every patient would get to<br />
see every tree and shrub and hence he<br />
incorporated wonderful views of nature into<br />
the design plans.<br />
The Waithman’s – the Waithmans were the<br />
owners of the property (estate) which was<br />
taken over by compulsory acquisition in order<br />
By changing the<br />
work environment<br />
to include accessible<br />
walking routes, we can<br />
help to raise awareness<br />
of the many benefits of<br />
physical activity to one’s<br />
health and wellbeing<br />
to build a sanatorium and they were very<br />
upset at the time but felt if they could save<br />
one life it would be worth it.<br />
The Hitchcock walk—Dr Hitchcock worked<br />
in MPUH and wrote the book ‘TB or not TB’<br />
The Kneafsey Walk—Dr Kneafsey was a<br />
revolutionary Cardio-thoracic surgeon at<br />
MPUH.<br />
Staff can now set their own activity goals<br />
and begin to indulge in some of these short<br />
walks early in the morning or at lunch time<br />
in the hospital grounds or indeed by simply<br />
getting off the bus early and walking the rest<br />
of the way to work. They will begin to reap<br />
the many health benefits of being active on a<br />
personal level but also enjoy the many social<br />
benefits. Taking part in a lunch time walking<br />
group is a great way to support people to stay<br />
motivated and reach their goals.<br />
For more information, contact Paul.gillen@<br />
hse.ie or Pamela.normoyle@hse.ie.<br />
winter 2016 | health matters | 69
Lifestyle<br />
Awards for Healthy Eating and<br />
Active@Work<br />
o far this year, a total of 46<br />
staff completed the Irish Heart<br />
Foundation Active@Work<br />
S<br />
training day as part of the HSE’s<br />
commitment to improving staff<br />
health and wellbeing guided by Healthy Ireland<br />
in the Health Services implementation plan<br />
2015-2017.<br />
The implementation plan recognises the<br />
role that our staff have in being positive role<br />
models and champions within the workplace.<br />
Staff from all over the country and from<br />
various health care and administrative<br />
disciplines attended various training days<br />
with one common goal - to seek support<br />
and guidance on how to get their staff more<br />
motivated to be active at work.<br />
The course covers the current guidelines<br />
for physical activity, key benefits, barriers<br />
and motivators.<br />
It lists and describes a range of workplace<br />
programmes offered by the Irish Heart<br />
Foundation, including the Step and Walk<br />
Challenge, development of Sli na Slainte<br />
walking routes for workplaces. The course also<br />
presents a number of case studies on how to<br />
implement the Active@Work programme and<br />
recognises success, facilitated through the<br />
annual IHF workplace Awards.<br />
The Irish Heart Foundation Workplace<br />
Awards recognises those who have achieved<br />
key markers in healthy eating and physical<br />
activity in the workplaces.<br />
Emer Smyth, Head of Health Promotion and<br />
Improvement with responsibility for Physical<br />
Activity Programmes nationally, said, “The<br />
HSE’s high level strategic priority to improve<br />
Slí na Sláinte Routes give Nexus staff path to health<br />
The weather was glorious for the launch of six Slí na Slainte Routes<br />
from the Nexus Building, Ballycoolin Dublin 15. The Nexus Building<br />
is home to 180 HSE and TUSLA staff working in Primary Care,<br />
Environmental Health, Health Promotion as well as Children and<br />
Family services and others.<br />
The Health and Wellbeing Committee compromises of<br />
representatives from each department within the building. The<br />
energetic committee have organised several initiatives to date<br />
including lunchtime Pilates, a Book Club, Operation Transformation,<br />
Zumba as well as social events.<br />
Laura Molloy, chair of the group, said, “We were delighted to work<br />
with the Irish Heart Foundation in setting up this initiative. Having six<br />
mapped, measured routes from the building ranging from 330m to<br />
5.8km gives staff of all abilities a choice for lunchtime walks and jogs”.<br />
Slí na Sláinte, meaning ‘Path to Health’, is an innovative scheme<br />
developed by the Irish Heart Foundation and supported by the HSE<br />
and the Irish Sports Council, to encourage people of all ages and<br />
abilities to walk for leisure and good health.<br />
Slí na Sláinte Walking Routes are mapped, measured routes which<br />
use attractive signage at kilometre intervals on established walking<br />
routes to help walkers identify the distance they walk. For more<br />
information see www.irishheart.ie<br />
Staff at the Nexus Building get ready to walk, jog or run at the launch of the<br />
new Sli na Slainte routes.<br />
70 | health matters | winter 2016
staff health and wellbeing along with the<br />
opportunity to train staff in promoting physical<br />
activity in the workplace can only help provide<br />
more opportunities for staff to live more<br />
healthy and active lives.”<br />
At this year’s awards ceremony, staff from<br />
Cavan General Hospital and the Royal Victoria<br />
Eye and Ear Hospital received both awards<br />
- a huge achievement.<br />
For further information on the Active@Work<br />
training day, you can contact Tara Curran in the<br />
Irish Heart Foundation by email at tcurran@<br />
irishheart.ie<br />
FAR LEFT: (l-r) John Healy, TV Maitre’D and Irish<br />
Heart Foundation Ambassador; Dr Kate McGarry,<br />
President, Irish Heart Foundation; Ann Gillick and<br />
Yvonne Doran, Royal Victoria Eye & Ear Hospital,<br />
Dublin 2 who achieved Silver (Active@Work) and<br />
Gold (Healthy Eating) and Marcella Corcoran<br />
Kennedy, Minister for Health Promotion.<br />
TOP OF PAGE: (l-r) John Healy, TV Maitre’D<br />
& Irish Heart Foundation Ambassador; Dr Kate<br />
McGarry, President, Irish Heart Foundation; Jacinta<br />
McAree-Murphy, Paula Gallagher and Peggy<br />
Plunkett, Cavan General Hospital who achieved<br />
Gold (Active@Work) and Silver (Healthy Eating)<br />
Awards with Marcella Corcoran Kennedy, Minister<br />
for Health Promotion.<br />
LEFT: (l-r) John Healy, Irish Heart Foundation<br />
Ambassador; Dr Kate McGarry, President, Irish<br />
Heart Foundation; Liz Timony, Yvonne Collins<br />
and Mary Cullivan, Our Lady’s Hospital, Navan,<br />
Co Meath, who achieved the Bronze Award in<br />
both categories, with Marcella Corcoran Kennedy,<br />
Minister for Health Promotion.<br />
winter 2016 | health matters | 71
Lifestyle<br />
Enjoy this winter by<br />
being physically active<br />
ith the dark evenings and the<br />
worsening weather conditions,<br />
winter can sometimes pose<br />
W<br />
a challenge to even the most<br />
discerning physically active<br />
HSE worker. However, with our reasonable<br />
climate there are no excuses for not being<br />
active during the winter season. Colm<br />
Casey, Physical Activity Co-ordinator,<br />
shares some tips.<br />
Move more<br />
I AM often asked, “What is the best type of<br />
exercise?” The answer is simply, “The one<br />
you do and like.”<br />
Try and find ways to move more daily.<br />
Do your best to accumulate 10,000<br />
steps per day. Use a simple pedometer or<br />
download a pedometer application from<br />
your Smartphone and you will find yourself<br />
looking for opportunities to walk more.<br />
You will probably start talking the stairs<br />
instead of the lift.<br />
You may perhaps park the furthest distance<br />
from the door instead of driving around the<br />
car park for ten minutes before work looking<br />
to park as close as possible to the door.<br />
If possible leave your car at home or a<br />
distance from your worksite and commute<br />
actively. Walk around your estate, park or<br />
garden when you get home in the evenings or<br />
nab a friend and take an hour to catch up.<br />
Home gym<br />
For those who simply can’t get out, you<br />
could also set up a home or office gym by<br />
buying some inexpensive equipment such as<br />
kettlebells or exercise bands and design a<br />
simple exercise circuit. There are numerous<br />
workout sessions for every type of physical<br />
activity on Youtube.<br />
There are a large number of HSE work sites<br />
now offering exercise classes during lunch<br />
and straight after work.<br />
Local gym<br />
You could join a local gym or fitness studio<br />
and avail of the wide range of classes<br />
available in the community. For some gyms,<br />
you don’t have to be a member, you can just<br />
sign up for one of their classes.<br />
Your gear<br />
Try and select the correct training gear. The<br />
breathability and waterproofing of training<br />
gear has come a long way and can make the<br />
harshest conditions bearable. You can pretty<br />
much participate in any sport all year long<br />
by choosing the correct gear and dressing<br />
appropriately. Normally in winter, you should<br />
be looking for gear that covers the whole<br />
body and keeps you warm, dry and allows<br />
perspiration to evaporate.<br />
Layering is the best advice for being active<br />
outdoors. Maybe start by wearing a couple of<br />
layers and as you get warmer, you can peel<br />
the top layer off.<br />
The best and most comfortable materials<br />
for breathability are polyester, goretex or<br />
merino wool. Surfers are able to withstand<br />
the winter north Atlantic swells and stay in<br />
the water for hours at 6 degrees so anything<br />
on land can be possible.<br />
Be safe, be seen<br />
No matter where you live - rural or urban<br />
- you should wear high visible and reflective<br />
garments that can reflect from the front,<br />
sides and behind while exercising outdoors.<br />
You must be visible. There are bike lights<br />
as powerful as car lights on the market<br />
today and make it possible to cycle at<br />
night. Head torch or lamps can be used by<br />
runners, joggers and walkers for lighting in<br />
rural areas on and off road. It’s about being<br />
prepared properly.<br />
CHOOSE THE RIGHT ACTIVITY<br />
FOR YOU<br />
Ideally, you should try and fit in a quick<br />
session before work, during lunch or straight<br />
after work if you like being active during<br />
daylight hours. You should aim for a minimum<br />
of 30 minutes of exercise per day, a minimum<br />
of five days a week.<br />
The key thing is to exercise at the right<br />
intensity. Intensity is how hard a person<br />
works to do a specific exercise. You should<br />
be working out at a moderate to vigorous<br />
intensity.<br />
more information<br />
For more information visit<br />
www.getirelandactive.ie<br />
or follow us on Facebook and Twitter<br />
72 | health matters | winter 2016
St Finbarr’s a hive of activity<br />
Management at St Finbarr’s Hospital<br />
Campus (SFHC) in Cork have been working<br />
closely with staff from the Department<br />
of Public Health and Health Promotion/<br />
Improvement (Health and Wellbeing division)<br />
to improve staff Health and Wellbeing on its<br />
campus for the last three years.<br />
SFHC is located in the heart of Cork City with<br />
a total complement of over 1000 HSE staff.<br />
Since 2014, a small staff Health and Wellbeing<br />
group have been working closely to implement<br />
some important staff Health and Wellbeing<br />
initiatives aimed particularly at reducing<br />
sedentary behaviour of staff that have largely<br />
‘desk-based sitting jobs’ in raising awareness<br />
of the dangers to our health of pro-longed<br />
occupational sitting and the importance of<br />
keeping active at work.<br />
In 2014, an audit and staff survey of the<br />
walkability of the campus was undertaken by<br />
the local Deptartment of Public Health and a<br />
re-vamped “Walkways to Health” 1km walking<br />
path, with new signage and stencil footprints<br />
marking the route, was officially promoted<br />
and launched to staff. It was felt that it was<br />
important to maximise walkability on site for<br />
staff, patrons and residents and to promote<br />
staff walking as a worksite wellness initiative.<br />
Staff lunchtime walking groups were<br />
established during months of June and Sept/<br />
Oct this year. A follow-up staff survey was<br />
conducted in June where 55pc of staff who<br />
took the survey stated that they had used the<br />
“Walkways to Health” route before, with 42pc<br />
stating that they used it at lunch time. Staff<br />
were asked about what further improvements<br />
could be made to the walking route and these<br />
are being addressed.<br />
A communal staff bike scheme is the latest<br />
ABOVE: The staff lunchtime walking group from St Finbarr’s Hospital in Cork. BELOW RIGHT: Launching<br />
the SFHC Staff Bike Scheme was Ruth Bullough of Cycle Sense. BOTTOM OF PAGE: Staff at St Finbarr’s in<br />
Cork get walking during their lunch break.<br />
health and wellbeing initiative that was<br />
launched in September. The purpose is to<br />
replace some car-based trips during the working<br />
day around the city, with trips made by bicycle,<br />
thus reducing traffic congestion and emissions<br />
while simultaneously contributing to improved<br />
staff health and wellbeing. SFHC staff can now<br />
avail of a bicycle for short term use during the<br />
working day should they wish to go for a cycle<br />
at lunchtime or leave the car and cycle to that<br />
meeting in the city. Depending on uptake, more<br />
bikes will be purchased for staff use.<br />
As of March of this year, St Finbarr’s staff<br />
can now avail of an outdoor gym during<br />
lunchtime hours weekdays only between<br />
12.30pm and 2pm.<br />
Finally, the campus has an active staff choir<br />
that has been meeting every Wednesday at<br />
lunchtime for a number of years. Joining a staff<br />
choir is a great way to meet other staff and<br />
contribute to your sense of wellbeing.<br />
winter 2016 | health matters | 73
Lifestyle<br />
HSE earn first conviction<br />
Battling allergens<br />
The Environmental Health Service protecting<br />
the public from this very real food safety risk<br />
he HSE Environmental Health<br />
Service (EHS) recently secured<br />
a conviction against a food<br />
T<br />
business in Galway as a result of<br />
a customer having had a severe<br />
allergic reaction. It was the first legal case of its<br />
kind taken in Ireland and is an example of how<br />
important the regulatory work of the EHS is<br />
with regard to food safety and the protection of<br />
public health.<br />
what is a food allergy?<br />
A food allergy is an abnormal, exaggerated<br />
bodily reaction to certain foods. While the<br />
body’s immune system is designed to protect<br />
against outside invaders, like viruses and<br />
bacteria, sometimes it produces antibodies in<br />
response to something that is normally not<br />
harmful at all, causing an immediate reaction in<br />
a susceptible person.<br />
Most allergies are just annoying with symptoms<br />
such as itchy/ watery eyes, sneezing, and a<br />
runny nose but other allergic reactions such as<br />
anaphylaxis can be more serious and can cause<br />
severe illness and even death. Anaphylaxis is<br />
life-threatening and occurs immediately when<br />
an allergic trigger causes histamines and other<br />
chemicals to be released from various tissues<br />
throughout the body. Dangerous symptoms like<br />
narrowed airways and difficulty breathing, shock,<br />
sudden drop in blood pressure, swelling of the<br />
face or tongue, vomiting or diarrhoea, chest pain<br />
and heart palpitations, slurred speech, loss of<br />
consciousness and death can result.<br />
Incidents<br />
A number of incidents have been reported in<br />
recent years in relation to food allergies. In 2013,<br />
a teenage girl, out for a meal with her family<br />
in Dublin accidentally ate a nut-based sauce<br />
and suffered a severe anaphylactic reaction<br />
within minutes. Not having immediate access<br />
to an EpiPen she tragically died. More recently,<br />
in October this year a pharmacist in Dublin<br />
intervened when a 17-year-old girl presented<br />
suffering from a severe nut allergy.<br />
Displaying characteristic symptoms of<br />
anaphylactic shock including a rash and<br />
swollen lips, pharmacy staff immediately<br />
called an ambulance and administered<br />
two adrenaline pens before the girl was<br />
hospitalised. On this occasion, it is believed<br />
that a chocolate milk drink led to her<br />
allergic reaction.<br />
In the UK recently the owner of an Indian<br />
restaurant was jailed for six years after he<br />
was found guilty of manslaughter following<br />
the death of a customer with a peanut<br />
allergy. Prosecution lawyers said the owner<br />
had replaced almond powder with cheaper<br />
groundnut mix, made from peanuts, to cut<br />
costs. The customer who had informed the<br />
74 | health matters | winter 2016
curry house of his allergy, had ordered a meal<br />
with no nuts but later was found dead in his<br />
bathroom after eating the takeaway. The Court<br />
heard how the owner of the restaurant took a<br />
“reckless and cavalier attitude to risk” and “put<br />
profit before safety”.<br />
legal responsibilities of food<br />
industry<br />
Up to recent times in Ireland the law in this area<br />
meant that those running food businesses when<br />
asked by a customer only had to give verbal<br />
information on any allergic ingredients that may<br />
be in a dish.<br />
New legislation with more specific<br />
requirements on the provision of food information<br />
to the consumer was implemented in 2014.This<br />
legislation applies to both packaged foods and<br />
unwrapped foods/dishes. There are 14 specific<br />
allergens listed and if these are used in preparing<br />
or producing food in the premises they must be<br />
declared. The manner in which this information<br />
has to be provided is proscribed in the law to<br />
ensure that it is clear and understandable for the<br />
consumer. The 14 allergens are:<br />
Cereals containing gluten, Crustaceans e.g.<br />
crab, lobster, crayfish, prawn, shrimp etc.,<br />
Eggs, Fish, Soybeans, Milk (including lactose),<br />
Celery and celeriac, Mustard, Sesame Seeds,<br />
Sulphur dioxide and sulphites, Peanuts, Tree<br />
nuts (including almonds, hazelnuts, walnuts,<br />
cashews, pecans, Brazil nuts, pistachios and<br />
macadamia nuts), Molluscs, Lupin. There is a<br />
responsibility on all food businesses to comply<br />
with this legislation; some have adapted<br />
menus and display boards to do this, while<br />
others display an ‘allergens folder’. The HSE<br />
Environmental Health Service enforces this<br />
legislation routinely in conjunction with other<br />
statutory food safety inspections.<br />
First Prosecution<br />
In September, the Environmental Health Service<br />
received a complaint relating to an adverse<br />
reaction suffered by a customer of a Chinese<br />
restaurant and take-away in Galway. The<br />
customer had ordered a dish in person at the<br />
counter and had specified on two occasions that<br />
she wanted it be ‘nut free’ due to an allergy.<br />
Within minutes of eating her take-away meal<br />
of chicken and prawn chow mein at home, the<br />
customer developed an anaphylactic reaction.<br />
Fortunately an EpiPen was to hand and, following<br />
discharge from the local A&E Department, there<br />
was no long term health damage. Subsequent<br />
analysis of the food by the Public Analysts<br />
Laboratory in Galway showed it contained very<br />
high levels of peanut.<br />
Due to the potential seriousness of the<br />
situation, a prosecution was taken by the<br />
Environmental Health Service.<br />
After hearing evidence, the Galway District<br />
Court judge found the business operator guilty.<br />
He was fined €300 with costs awarded to the<br />
HSE of €750. In her concluding remarks, the<br />
judge praised the customer and advised that “she<br />
had done the state some service” for highlighting<br />
the matter.<br />
Speaking after the hearing, Dave Molloy,<br />
Assistant National Director for Environmental<br />
Health, said “The successful outcome of this case<br />
brings with it valuable lessons for all concernedthe<br />
real risk to public health posed by food<br />
allergens, the symptoms of an allergic reaction,<br />
the need for immediate action if someone<br />
presents with those symptoms and the need<br />
for those known to suffer from severe allergic<br />
reactions to carry an EpiPen.<br />
“For the EHS the lesson learnt is the continued<br />
need to work with food business operators to<br />
inform and educate them on the risks of food<br />
allergens and their legal and moral obligation<br />
to provide accurate and correct consumer<br />
information. In the 45,000 food businesses<br />
that it supervises, the EHS endeavours to work<br />
with industry to build compliance with the law<br />
and recognises that the vast majority of food<br />
businesses in Ireland demonstrate a commitment<br />
to food safety, but where the law is breached the<br />
EHS will continue to protect public health up to<br />
and including the application of legal sanctions<br />
where appropriate.”<br />
Images kindly provided by the Food Safety<br />
Authority of Ireland.<br />
winter 2016 | health matters | 75
Lifestyle<br />
Parents<br />
urged<br />
to give<br />
children<br />
child-sized<br />
portions<br />
Bigger portions of healthy food also<br />
contributing to obesity problems<br />
afefood, in partnership with<br />
the HSE, has recently ran an<br />
awareness campaign recently<br />
S<br />
on child-sized portions.<br />
Portion size was identified as<br />
a key issue in preventing children becoming<br />
overweight and we are urging parents<br />
to give children child-sized portions. The<br />
message is clear that how much children<br />
eat as well as what they eat is very<br />
important. Recent studies¹ have found that<br />
children aged over two ate up to 40pc more<br />
food when bigger portion sizes were made<br />
available to them.<br />
Dr Cliodhna Foley-Nolan, Director, Human<br />
Health and Nutrition, safefood said: “It’s<br />
well established that for adults, we eat<br />
more food and consume more calories<br />
when we’re given bigger portions and we<br />
now recognise that this goes for children<br />
as well.<br />
“There has also been a significant increase<br />
in food portion sizes over the past 20 years,<br />
this all contributes to more of our children<br />
nowadays carrying excess weight.<br />
“What’s also interesting is that young<br />
children up to the age of two have good<br />
appetite control and only eat what they<br />
need, but older children lose this ability to<br />
know when they’re full.”<br />
Research has shown that food portion<br />
sizes have significantly increased over the<br />
past 20 years, particularly among baked<br />
foods like scones, croissants and danishes<br />
as well as takeaway foods; some takeaway<br />
food portion sizes are now 180pc bigger<br />
compared to the late 1990s.<br />
Margaret<br />
O’Neill, HSE’s<br />
National<br />
Dietetic<br />
Advisor said,<br />
“As a parent<br />
myself and a<br />
dietitian, I know<br />
how important food is for growth and<br />
development in children. However, it is<br />
the quality of the food we provide our<br />
children that is key. Infants and children are<br />
not small adults and they need different<br />
nutrients than we do as they are growing.<br />
We need to look at the amounts we are<br />
serving children and give them appropriate<br />
portion sizes of nutritious food for their<br />
age. A teenage boy requires very different<br />
portion sizes to a five-year-old.<br />
Tips on reducing portion sizes for kids<br />
• Kids need child-sized portions, not adult ones. So<br />
give them small portions of food on their plates to<br />
start with. If they want more, then give it to them.<br />
• If they say they’re hungry after a meal, offer them<br />
something nutritious like fruit.<br />
• Try to avoid having fatty and sugary snack foods<br />
freely available between and after meals.<br />
• For smaller kids, use plates and cutlery that<br />
match their size, not yours.<br />
“The food pyramid is a useful guide for<br />
children aged five years and upwards.<br />
The HSE and safefood have published a<br />
very useful guide for health professionals<br />
to assist parents and guardians in<br />
communicating with their children about<br />
body weight.”<br />
See www.healthpromotion.ie/<br />
Submitted by the HSE’s Healthy Eating<br />
and Active Living programme.<br />
• Don’t pressure children to eat all the food on<br />
their plate and allow them to stop when they say<br />
‘I’ve had enough’.<br />
• Remember the proportions of food you offer<br />
during the day. They should be roughly one-third<br />
fruit and veg; one-third starchy foods like bread<br />
and potatoes; one-third dairy like milk, cheese and<br />
yogurt and one-third protein like meat and fish.<br />
• Keep treats at a realistic level – a little and not<br />
every day.<br />
76 | health matters | winter 2016
Plan to improve<br />
Ireland’s health<br />
and reduce the<br />
burden of obesity<br />
new policy and action plan<br />
aims to reverse obesity<br />
trends, prevent health<br />
A<br />
complications and reduce the<br />
overall burden for individuals,<br />
families, the health system and the wider<br />
society and economy.<br />
Minister for Health, Simon Harris, together<br />
with the Minister for Children and Youth Affairs,<br />
Dr Katherine Zappone TD, and Minister of<br />
State for Health Promotion, Marcella Corcoran<br />
Kennedy TD recently launched A Healthy<br />
Weight for Ireland - Obesity Policy and Action<br />
Plan 2016- 202 and Healthy Lifestyles – A<br />
Consultation with Children and Young People.<br />
In recent years, levels of overweight and<br />
obesity have increased dramatically with 60pc<br />
of adults and one in four children in Ireland<br />
either overweight or obese.<br />
It is estimated that the cost to society in<br />
Ireland of adult obesity exceeds €1 billion per<br />
annum.<br />
Overweight and obesity are significant risk<br />
factors for many chronic diseases.<br />
The links between obesity and heart disease,<br />
cancers, Type 2 diabetes, mental health issues,<br />
respiratory problems and musculoskeletal<br />
conditions are well established.<br />
The ministers announced a range of actions<br />
which would be undertaken over the coming<br />
years to address the growing concerns about<br />
overweight and obesity.<br />
These include:<br />
• New national Healthy Eating Guidelines<br />
• Calorie Posting Legislation<br />
• Development of a Nutrition Policy<br />
• A new clinical Lead for Obesity will be<br />
appointed in the HSE<br />
• Prioritisation of Obesity services in the HSE<br />
service plans for 2017 and subsequent years<br />
• Support for introduction of a Sugar Levy<br />
to encourage a reduction in the rates of<br />
consumption of sugar-sweetened beverages<br />
• Working with key stakeholders to develop<br />
a voluntary industry Code of Practice for food<br />
advertising, promotion and marketing<br />
• ‘Whole of school’ approaches to healthy<br />
lifestyles with the Department Education and<br />
Skills<br />
• Development of guidelines in relation to the<br />
built environment<br />
• Agreement on food reformulation targets<br />
with the food industry and establishment<br />
of a forum for engagement with industry on<br />
best practice initiatives towards a healthy<br />
food environment.<br />
Welcoming the launch, Sarah O’Brien, HSE<br />
National Lead, Healthy Eating and Active<br />
Living programme said, “The launch of the<br />
plan is most welcome and many of the actions<br />
will be implemented by the HSE.<br />
“We look forward to co-operating with<br />
colleagues in the Department of Health and<br />
other partners who are equally concerned<br />
about Ireland’s growing weight problem.<br />
“The accompanying report on the<br />
consultation on ‘Healthy Lifestyles with<br />
Children and Young People’ gives us insights<br />
into the views of children and teenagers<br />
and how they think society should tackle<br />
healthy lifestyles.”<br />
Minister Marcella Corcoran Kennedy; Margaret<br />
O’Neill, HSE National Dietetic Advisor; Minister<br />
Simon Harris; and Sarah O’Brien, HSE National<br />
Lead, Healthy Eating and Active Living Programme<br />
pictured at the launch. Photo: Conor McCabe.<br />
winter 2016 | health matters | 77
Lifestyle<br />
CITROEN GRAND<br />
C4 PICASSO<br />
First<br />
Drive!<br />
FACTS AT A GLANCE<br />
Citroen Grand C4 Picasso Flair<br />
BlueHDi 150<br />
Engine: 2.0-litre, four-cylinder turbodiesel<br />
producing 148bhp<br />
Transmission: Six-speed automatic<br />
Performance: 0-62mph in 10.1 seconds,<br />
top speed 129mph<br />
Economy: 64.2mpg combined<br />
Emissions: 115g/km<br />
WHAT’S NEW?<br />
Only a particularly keen eye would be able to<br />
tell the difference between the new Grand C4<br />
Picasso and the second-generation model that<br />
arrived in 2013. Its exterior retains the familiar<br />
shape of the old car, but features a number of<br />
subtle tweaks that help keep it looking fresh<br />
and up-to-date.<br />
As you would expect from a car designed<br />
purely for carting vast numbers of children to<br />
and from school and sports practice, the new<br />
Picasso can be specified with a raft of active<br />
safety systems. These include Speed Limit<br />
Sign Recognition, and Active Land Departure<br />
Warning to name but a few.<br />
LOOKS AND IMAGE<br />
Generally speaking, large MPVs aren’t<br />
the best looking cars on the road. However,<br />
Citroen seems to have this area nailed - the<br />
Grand C4 Picasso is definitely one of the<br />
better-looking people movers currently<br />
available on the market.<br />
A suite of very subtle updates that would<br />
be difficult to notice on their own make<br />
an appearance on the new car. Changes<br />
include a redesigned front end, 3D-effect<br />
rear lights, rear chevrons finished in gloss<br />
black with chrome surrounds and new 18-<br />
inch alloy wheels.<br />
<strong>Together</strong>, these add up to an end product<br />
that is a marked improvement over the<br />
older car. At the end of the day, an MPV is<br />
never really going to be considered a cool<br />
car, even one as attractive as the Grand C4<br />
Picasso. That said, cars like this will always<br />
place function over form. The added bonus<br />
with the big Citroen is that you don’t have to<br />
compromise too much in the form department<br />
if you’ve got a load of children to ferry around.<br />
SPACE AND PRACTICALITY<br />
This is the Grand C4 Picasso’s piece de<br />
resistance. A seven-seat layout means you’ll<br />
be popular with other parents on the school<br />
run, and should help prevent any squabbles<br />
from breaking out on longer journeys with<br />
the family.<br />
The middle row of seats can fold down flat<br />
to increase boot space, and can also slide<br />
back and forth to allow for more legroom in<br />
the third row. The two third row seats fold<br />
down into the boot floor, allowing for 645<br />
litres of storage space in the boot when the<br />
second row of seats are in their forwardmost<br />
position.<br />
Another handy feature that has been<br />
introduced is a hands-free tailgate. Simply<br />
wave your foot underneath the rear bumper<br />
and the boot will pop open, meaning you can<br />
load the car up easily even when your hands<br />
are full.<br />
BEHIND THE WHEEL<br />
The Grand C4 Picasso isn’t exactly a small<br />
car, although it masks its size rather well.<br />
Thanks to plenty of forward visibility out of the<br />
large windscreen and a raised driving position,<br />
you don’t really feel like you’re behind the<br />
wheel of a big people mover.<br />
To drive, the Picasso is very manageable.<br />
At low speeds, the steering is quick enough<br />
to allow you to manoeuvre into tighter<br />
parking spaces, and features like a rear<br />
parking camera mean you shouldn’t bump<br />
into any obstructions.<br />
Out on the open road, you’re afforded a<br />
generous view of the road ahead. The seats<br />
are comfortable, supportive and easily<br />
adjustable – although depending on your body<br />
frame, the driving position might be a tad<br />
awkward. The steering wheel is quite far away,<br />
while the pedals are right under your feet.<br />
There is a fair amount of wind noise at<br />
motorway speeds, owing largely to the boxy<br />
shape of the car, and the 18-inch alloys fitted<br />
to our test car also created a fair amount of<br />
tyre roar. For the most part, the four-cylinder<br />
diesel engine is unobtrusive and refined,<br />
although it does create a bit of a racket under<br />
heavy acceleration.<br />
Any lumps and bumps on the surface of the<br />
road are dealt with by the Citroen’s supple<br />
suspension set-up, although this does lead to<br />
a dash of body roll through the corners.<br />
VALUE FOR MONEY<br />
In terms of bang for your buck, the Grand<br />
C4 Picasso in Flair trim makes a good case<br />
for itself. It comes with a wealth of handy<br />
features as standard, including the new<br />
3D Citroen Nav system. This incorporates<br />
mapping data from TomTom that can be<br />
displayed through either the seven-inch<br />
touchscreen in the middle of the dash, or the<br />
12-inch display on the upper dash.<br />
Other features include front and rear<br />
parking sensors, cruise control, dual-zone air<br />
conditioning, DAB radio and Bluetooth and<br />
USB connectivity. Mirror Link and Car Play -<br />
which are included as standard - help to make<br />
connecting your smartphone that much easier.<br />
WHO WOULD BUY ONE?<br />
This is a car that will largely appeal to buyers<br />
with young children. It will tackle the school<br />
run with ease, and thanks to an economical<br />
diesel engine, it won’t be too expensive to keep<br />
topped up with fuel either.<br />
78 | health matters | winter 2016
Win a two night Bed & Breakfast in one of our Luxury Rooms, with private Balcony<br />
overlooking the River Liffey, with Dinner & a Bottle of Prosecco on one evening in<br />
our RiverBank Restaurant.<br />
The four star Court Yard Hotel, steeped in history, built on the original site where<br />
Arthur Guinness created his brewing empire, and situated in the colourful heritage<br />
town of Leixlip Co. Kildare. A region blessed with some of Ireland’s most spectacular<br />
scenery, the hotel has been meticulously restored and refurbished and offers old<br />
world charm, beautiful original stone work with contemporary design.<br />
The Court Yard Hotel has long been appreciated for its romantic and picturesque<br />
setting. The property combines a stunning location, contemporary accommodation,<br />
unique atmosphere and sumptuous dining to create the perfect getaway in Kildare.<br />
Your home from home, tucked away and nestled on the banks of the River Liffey.<br />
<br />
<br />
<br />
<br />
Email your answer to competition@celticmediagroup.com with ‘Court Yard Hotel’ as the subject,<br />
along with your name, address and contact number. Competition deadline is Sunday February 19th 2017.<br />
T&C’s vouCher valid for 12 monThs from daTe winner is announCed. subjeCT To availabiliTy. seleCTed daTes exCluded.
The Health Service Executive would like to<br />
wish all service users and staff a...<br />
...especially those who find themselves<br />
ill and in hospital over the festive period,<br />
and the staff taking care of them.