WOW February 2017
Granisetron Transdermal System
Granisetron Transdermal System
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Page 4 Volume 17; Issue 2<br />
Granisetron Transdermal System for the Prevention of Chemotherapy-Induced<br />
Nausea and Vomiting<br />
(continued from page 3)<br />
etc. Safety and efficacy has not been established in pediatric patients.<br />
3,6<br />
Granisetron transdermal patch was recently added to the formulary<br />
at the Johns Hopkins Hospital with restrictions. It is restricted<br />
to oncology inpatients who have not responded to or are intolerant<br />
to at least 2 different agents (one of which must be a 5-HT3<br />
antagonist) with optimized dosing and frequency each for at least<br />
24 hours, or who respond to 5HT‐3 antagonists but are unable to<br />
transition from IV to PO antiemetics.<br />
References<br />
1. Basch E, Prestrud AA, Hesketh PJ, et al; American Society of Clinical<br />
Oncology. Antiemetics: American Society of Clinical Oncology<br />
clinical practice guideline update. J Clin Oncol 2011;29:4189-98.<br />
2. Granisetron [monograph]. In: LexiComp Online [online database].<br />
Hudson, OH: Lexi-Comp. Accessed December 2016.<br />
3. Food and Drug Administration. SANCUSO (Granisetron Transdermal<br />
System) prescribing information (September 2015). http://<br />
w w w . a c c e s s d a t a . f d a . g o v / d r u g s a t f d a _ d o c s /<br />
label/2015/022198s003lbl.pdf . Accessed December 2016.<br />
4. National Comprehensive Cancer Network (NCCN) Clinical Practice<br />
Guidelines in Oncology. Antiemesis (updated 2016). https://<br />
www.nccn.org/professionals/physician_gls/pdf/antiemesis.pdf<br />
Accessed December 2016.<br />
5. Boccia, R.V., Gordan, L.N., Clark, G. et al. Efficacy and tolerability<br />
of transdermal granisetron for the control of chemotherapy-induced<br />
nausea and vomiting associated with moderately and highly emetogenic<br />
multi-day chemotherapy: a randomized, double-blind, phase III<br />
study. Support Care Cancer 2011; 19:1609-17.<br />
6. Chabner B, A., Thompson E. C. Management of Adverse Effects of<br />
Cancer Therapy. Merck Manual Professional Version. https://<br />
www.merckmanuals.com/professional/hematology-and-oncology/<br />
principles-of-cancer-therapy/management-of-adverse-effects-ofcancer-therapy.<br />
Access January <strong>2017</strong>.<br />
NINJAs in the Children’s Center<br />
Bethany Sharpless, PharmD, PGY2 Pediatric Pharmacy Resident<br />
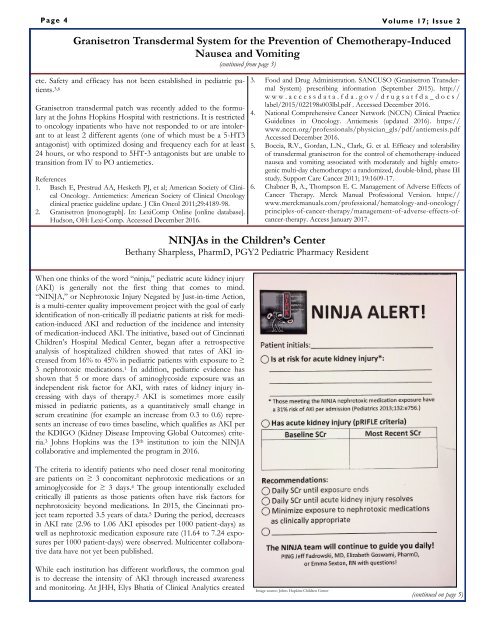
When one thinks of the word “ninja,” pediatric acute kidney injury<br />
(AKI) is generally not the first thing that comes to mind.<br />
“NINJA,” or Nephrotoxic Injury Negated by Just-in-time Action,<br />
is a multi-center quality improvement project with the goal of early<br />
identification of non-critically ill pediatric patients at risk for medication-induced<br />
AKI and reduction of the incidence and intensity<br />
of medication-induced AKI. The initiative, based out of Cincinnati<br />
Children’s Hospital Medical Center, began after a retrospective<br />
analysis of hospitalized children showed that rates of AKI increased<br />
from 16% to 45% in pediatric patients with exposure to ≥<br />
3 nephrotoxic medications. 1 In addition, pediatric evidence has<br />
shown that 5 or more days of aminoglycoside exposure was an<br />
independent risk factor for AKI, with rates of kidney injury increasing<br />
with days of therapy. 2 AKI is sometimes more easily<br />
missed in pediatric patients, as a quantitatively small change in<br />
serum creatinine (for example an increase from 0.3 to 0.6) represents<br />
an increase of two times baseline, which qualifies as AKI per<br />
the KDIGO (Kidney Disease Improving Global Outcomes) criteria.<br />
3 Johns Hopkins was the 13 th institution to join the NINJA<br />
collaborative and implemented the program in 2016.<br />
The criteria to identify patients who need closer renal monitoring<br />
are patients on ≥ 3 concomitant nephrotoxic medications or an<br />
aminoglycoside for ≥ 3 days. 4 The group intentionally excluded<br />
critically ill patients as those patients often have risk factors for<br />
nephrotoxicity beyond medications. In 2015, the Cincinnati project<br />
team reported 3.5 years of data. 5 During the period, decreases<br />
in AKI rate (2.96 to 1.06 AKI episodes per 1000 patient-days) as<br />
well as nephrotoxic medication exposure rate (11.64 to 7.24 exposures<br />
per 1000 patient-days) were observed. Multicenter collaborative<br />
data have not yet been published.<br />
While each institution has different workflows, the common goal<br />
is to decrease the intensity of AKI through increased awareness<br />
and monitoring. At JHH, Elys Bhatia of Clinical Analytics created<br />
Image source: Johns Hopkins Children Center<br />
(continued on page 5)