aagbi
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
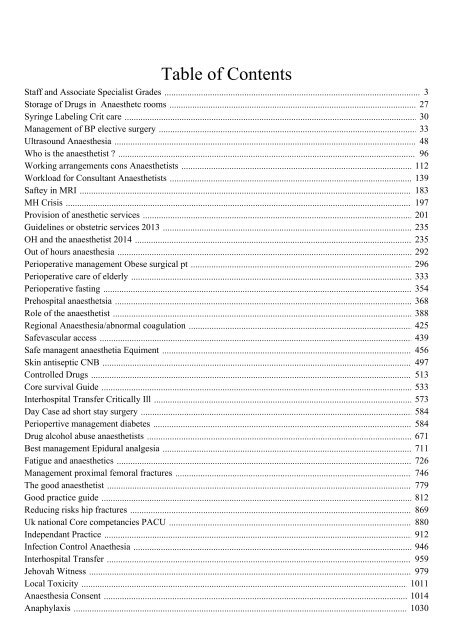
Staff and Associate Specialist Grades<br />
Storage of Drugs in Anaesthetc rooms<br />
Syringe Labeling Crit care<br />
Management of BP elective surgery<br />
Ultrasound Anaesthesia<br />
Who is the anaesthetist ?<br />
Working arrangements cons Anaesthetists<br />
Workload for Consultant Anaesthetists<br />
Saftey in MRI<br />
MH Crisis<br />
Provision of anesthetic services<br />
Guidelines or obstetric services 2013<br />
OH and the anaesthetist 2014<br />
Out of hours anaesthesia<br />
Perioperative management Obese surgical pt<br />
Perioperative care of elderly<br />
Perioperative fasting<br />
Prehospital anaesthetsia<br />
Role of the anaesthetist<br />
Regional Anaesthesia/abnormal coagulation<br />
Safevascular access<br />
Safe managent anaesthetia Equiment<br />
Skin antiseptic CNB<br />
Controlled Drugs<br />
Core survival Guide<br />
Interhospital Transfer Critically Ill<br />
Day Case ad short stay surgery<br />
Periopertive management diabetes<br />
Drug alcohol abuse anaesthetists<br />
Best management Epidural analgesia<br />
Fatigue and anaesthetics<br />
Management proximal femoral fractures<br />
The good anaesthetist<br />
Good practice guide<br />
Reducing risks hip fractures<br />
Uk national Core competancies PACU<br />
Independant Practice<br />
Infection Control Anaethesia<br />
Interhospital Transfer<br />
Jehovah Witness<br />
Local Toxicity<br />
Anaesthesia Consent<br />
Anaphylaxis<br />
Table of Contents<br />
3<br />
27<br />
30<br />
33<br />
48<br />
96<br />
112<br />
139<br />
183<br />
197<br />
201<br />
235<br />
235<br />
292<br />
296<br />
333<br />
354<br />
368<br />
388<br />
425<br />
439<br />
456<br />
497<br />
513<br />
533<br />
573<br />
584<br />
584<br />
671<br />
711<br />
726<br />
746<br />
779<br />
812<br />
869<br />
880<br />
912<br />
946<br />
959<br />
979<br />
1011<br />
1014<br />
1030
Blood components and alternatives<br />
Anaesthesia Team<br />
Anaphylaxis management<br />
Arterial blood sampling and hypoglyceamic brain injury<br />
Asistance for the anaesthetist<br />
Age and the anaesthetist<br />
Safe transfer Brain INjury<br />
Care of critically Ill child<br />
Catastrophes in anaesthesia<br />
Blood transfusion<br />
Checking anaesthetic equipement<br />
Private billing<br />
1032<br />
1090<br />
1112<br />
1155<br />
1169<br />
1185<br />
1204<br />
1228<br />
1244<br />
1276<br />
1299<br />
1319
Staff and Associate<br />
Specialist Grades<br />
2008<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland,<br />
21 Portland Place, London W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org September 2008<br />
1
MEMBERSHIP OF THE WORKING PARTY<br />
Dr Leslie Gemmell<br />
Dr Ramana Alladi<br />
Dr Michael Wee<br />
Dr Kate Bullen<br />
Dr Andy Lim<br />
Dr Anthea Mowat<br />
Chairman, Honorary Secretary Elect, AAGBI<br />
Chairman of SAS Committee and Council Member, AAGBI<br />
Vice President, AAGBI<br />
Deputy Chairman, BMA<br />
Chairman of SAS Committee and Council Member,<br />
Royal College of Anaesthetists<br />
Member, Staff and Associate Specialists Committee, AAGBI<br />
BMA Staff and Associate Specialists Conference Chair<br />
Ex Officio<br />
Dr David Whitaker<br />
Dr Richard Birks<br />
Dr Iain Wilson<br />
Dr William Harrop-Griffiths<br />
Dr Ian Johnston<br />
Dr David Bogod<br />
President<br />
President Elect<br />
Honorary Treasurer<br />
Honorary Secretary<br />
Honorary Membership Secretary<br />
Editor-in-Chief, Anaesthesia<br />
Acknowledgement<br />
The Working Party is grateful to Dr Christine Robison for her advice and comments.<br />
© Copyright of the Association of Anaesthetists of Great Britain and Ireland.<br />
No part of this book may be reproduced without the written permission of the AAGBI.<br />
2
CONTENTS<br />
Section 1 Introduction 4<br />
Section 2 Recommendations 5<br />
Section 3 The grades 6-10<br />
Section 4 Model SAS charter 11-12<br />
Section 5 AAGBI and the SAS anaesthetist 13-14<br />
Section 6 The SAS contract 15-18<br />
Section 7 References and useful websites 19<br />
Appendix 1 20<br />
Appendix 2 21<br />
3
1. Introduction<br />
The number of Staff and Associate Specialist (SAS) doctors employed in the National Health Service<br />
has grown rapidly in the last few years, during which there have been changes in government policy<br />
that include the introduction of revised terms and conditions of service for both Staff Grades and<br />
Associate Specialists. The Royal College of Anaesthetists (RCoA) has published advice on appointments<br />
procedures for these grades. The number of SAS doctors has increased further since the restructuring<br />
of medical careers within the Modernising Medical Careers (MMC) process, in particular producing a<br />
marked increase in the appointment of Trust Grade doctors.<br />
The 1990 NHS and Community Care Act allowed the establishment of NHS Foundation Trusts with the<br />
freedom to offer new staff, including doctors other than those in the training grades, contracts under<br />
their own terms and conditions of service. The national ceiling on Staff Grade numbers was formally<br />
removed in 1997, and employing authorities and Trusts were made responsible for individual Staff<br />
Grade appointments.<br />
The Association of Anaesthetists of Great Britain and Ireland (AAGBI) has produced two guideline<br />
documents, the last being published in 1998, offering recommendations and advice to Non-Consultant<br />
Career Grade Doctors (NCCGs). Since then, there have been significant changes to the grades. The<br />
generic name ‘Non-Consultant Career Grade’ (NCCG) has been replaced by ‘Staff and Associate<br />
Specialist’ (SAS) grade. This appears not to include other grades such as Clinical Assistant, Trust Grade<br />
and Hospital Practitioner. However, the Working Party wishes to include all grades considered in<br />
earlier guidance.<br />
The AAGBI established its SAS Committee in 2002 and the RCoA held elections for the first two SAS<br />
council members in the same year.<br />
This edition replaces existing advice contained in the 1992 and 1998 AAGBI publications. The advice is<br />
intended for doctors in the various grades and for Clinical Directors of Departments of Anaesthesia.<br />
4
2. Recommendations<br />
The AAGBI strongly recommends that all appointments are made to the nationally recognised grades<br />
of Staff Grade or Associate Specialist.<br />
The AAGBI does not recommend non-standard grades and other non-training grades with variable<br />
terms and conditions of service.<br />
All grades are clinically responsible to a named consultant and should not be put in the position<br />
of taking ultimate clinical responsibility for the care of patients. There should be an established<br />
mechanism for any eligible Staff Grade doctor to be promoted to the post of Associate Specialist.<br />
Consultants responsible for SAS doctors should ensure that professional support is available. Every<br />
doctor should have a nominated consultant as a mentor.<br />
The AAGBI supports the RCoA in advising that all SAS appointees should have a postgraduate<br />
qualification. The applicant should have undergone suitable training and should have gained sufficient<br />
relevant clinical experience to fulfill the requirements in the job plan.<br />
Suitably experienced SAS doctors who are involved in supervising trainees are encouraged to apply to<br />
be entered in the RCoA’s ‘Approved to Teach’ list, with the support of the College Tutor.<br />
An SAS doctor’s contract should include time for pre-operative and postoperative visits. Provision in<br />
the job plan must be made for activities such as audit, research, appraisal and continuing professional<br />
development (CPD) activities.<br />
The AAGBI recommends a minimum weekly commitment to anaesthesia of three notional half days or<br />
equivalent, including at least two clinical sessions, with adequate time for all supporting professional<br />
activities.<br />
SAS doctors who have job plans involving emergency work must maintain the appropriate skills.<br />
All SAS doctors should have an annual appraisal that should inform job planning.<br />
All SAS doctors should, as a part of their job plan, spend time working with a consultant.<br />
Provision for adequate study and professional leave must be made to all SAS doctors. Funding must<br />
be available for these activities.<br />
All SAS doctors should have representation at departmental level and be allowed to attend departmental<br />
and directorate meetings. There should be representation on the Local Negotiating Committee at Trust/<br />
Board level, and they should be included in the Trust/Board negotiations.<br />
5
3. The grades<br />
Associate Specialist [1-6]<br />
The Associate Specialist grade was introduced in 1981; it was a development of the Medical Assistant<br />
grade. It is a permanent career grade of limited clinical responsibility. Since 1991 an inclusive<br />
professional contract, similar to that of the pre-2003 NHS Consultant Contract, has been in place, with<br />
discretionary points replacing the performance supplement in 1996. Associate Specialists are employed<br />
on contracts based on 11 notional half days per week, in which one notional half day is equivalent<br />
to a minimum of 3.5 hours worked flexibly. Associate Specialists are senior hospital doctors who are<br />
clinically responsible to a named consultant and who should not therefore be put in the position of<br />
taking ultimate responsibility for care of patients. Associate Specialists are subject to the European<br />
Working Time Directive (WTD), which limits time worked to a maximum of 48 hours per week on<br />
average. Associate Specialists are senior hospital doctors and should therefore occupy a senior position<br />
on the on-call rota.<br />
A medical practitioner appointed to the Associate Specialist grade should have served a minimum of four<br />
years in a Specialist Registrar post or Staff Grade post, at least two of which have been in the appropriate<br />
specialty. Equivalent service is acceptable with the agreement of the relevant College Regional Adviser<br />
and Regional Postgraduate Dean. The doctor should have completed 10 years’ medical work, either as<br />
a continuous period or in aggregate, that is acceptable by the General Medical Council (GMC) for full,<br />
limited or temporary - but not provisional - registration. Possession of a higher qualification, e.g. the<br />
FRCA, is desirable but not mandatory.<br />
Associate Specialist posts are often personal appointments established for those doctors committed<br />
to a career in the hospital service who are unable to complete higher professional training or who,<br />
on completion of higher professional training, are unable or do not wish to accept the full clinical<br />
responsibility of a consultant appointment.<br />
In certain circumstances in England and Wales, Trusts may advertise for and recruit Associate Specialists<br />
directly. However, an Associate Specialist post should only be established when it is in the best interests<br />
of the service. A job description for the post should be drawn up with the advice of a representative of<br />
the RCoA. The Central Consultants and Specialists Committee (CCSC) of the British Medical Association<br />
(BMA) has produced a model workload document for Associate Specialists, which was endorsed by<br />
the newly formed Staff and Associate Specialists Committee of the BMA. Associate Specialists have the<br />
option of whole time, maximum part-time or part-time contracts and, although they have the right to<br />
undertake private practice, they may encounter difficulties when claiming reimbursement from private<br />
health care providers.<br />
When job planning, it is worth noting paragraph 26 of the current Terms and Conditions: National Health<br />
Service Hospital Medical and Dental Staff and Doctors in Public Health Medicine and the Community<br />
Health Service (England and Wales), Terms and Conditions of Service September 2002 Version 2 – 1<br />
December 2002, Version 3 – 10 January 2003, Version 4 – 6 February 2004, Version 5 – 17 February<br />
2005, Version 6 – 1 June 2005, Version 7 – 1 March 2007, and Version 8 – 30 July 2007.<br />
6
Associate Specialists should ensure that their workload, including on-call, is reviewed annually.<br />
Consideration should be given not only to the frequency of on-call but also to the intensity of the work.<br />
Particular care should be taken to ensure that the problems previously encountered by trainees are not<br />
merely transferred to the SAS grades.<br />
In any consideration of a career grade appointment, the following factors should be taken into account:<br />
• The need to develop a consultant-based service<br />
• Overall consultant responsibility for patient care<br />
• Consultant cover both in and out of hours in anaesthesia and, where necessary,<br />
in related subspecialties;<br />
• Provision for the teaching of junior doctors and the supervision of both junior<br />
and career grade medical staff<br />
The appointment committee for new Associate Specialist appointments normally comprises, as a<br />
minimum:<br />
• A senior manager<br />
• A consultant from the Trust/Board in the relevant specialty<br />
• An external senior hospital doctor nominated by the RCoA<br />
Guidance for personal regrading from Staff Grade to Associate Specialist is available on the BMA<br />
website: http://www.bma.org.uk/ap.nsf/content/home<br />
Staff Grade [7,8]<br />
The Staff Grade was introduced in 1988 to meet service requirements, and a national ceiling on<br />
numbers that limited the number of Staff Grades to 10% of the total number of consultants was<br />
removed in 1997 when the current Staff Grade contract was introduced (except in Scotland). A<br />
significant number remain on the pre-1997 contract. Whilst Staff Grade doctors are regarded as senior<br />
hospital doctors, it is important to remember that they are in a non-training career grade. As such, they<br />
exercise an intermediate level of clinical responsibility as delegated by the consultant to whom they<br />
are responsible.<br />
A full time Staff Grade contract is for 10 sessions, all of which are superannuable. Staff Grade doctors<br />
are paid at the same sessional rate for work done during working hours or out-of-hours. A session<br />
is four hours, and WTD regulations limit work to an average of 48 hours per week. The duration of<br />
sessions outside normal working hours may vary subject to local Trust negotiation.<br />
It is recommended that doctors (including those in non-standard posts) transfer to the new terms of<br />
service unless it is clearly disadvantageous to do so. Non-standard contracts do not afford the same<br />
protection as nationally agreed terms of service. The BMA has established LNCs in Trusts and Health<br />
Boards to represent doctors of all grades.<br />
7
When drawing up job descriptions for a Staff Grade, employing authorities have complete flexibility,<br />
after consultation with the responsible consultant, with regard to the deployment, location and<br />
rostering of the available sessions. Currently, the RCoA recommends that those SAS doctors without<br />
a postgraduate qualification should not work in isolated areas unsupervised.<br />
A Staff Grade is normally accountable to a named consultant, normally the Clinical Director but,<br />
on a day-to-day basis, to the duty consultant. A model job description is available from the BMA.<br />
The formal requirements for entry to the Staff Grade are:<br />
• full registration with the GMC<br />
• either a minimum of three years’ full time hospital service at Senior House<br />
Officer (SHO) or higher grade, including adequate experience in the relevant specialty;<br />
or equivalent experience<br />
This requirement may be waived if, in the opinion of the College assessor, the applicant has undertaken<br />
suitable training and has gained sufficient relevant experience to fulfil the requirements of the<br />
job plan.<br />
It is recommended that the job plan be approved by the RCoA Regional Education Advisor before the<br />
post is advertised.<br />
The Advisory Appointments Committee in England normally comprises, as a minimum, the following<br />
people:<br />
• A lay Chairman appointed by the Trust/Board<br />
• A consultant anaesthetist from outside the Trust/Board, approved by the Royal College<br />
• A consultant anaesthetist (usually the Clinical Director) from the Trust/Board<br />
The composition of the panel may be different in the devolved nations. After ratification of the<br />
appointment by the Trust, there is normally a probationary period of one year at the end of which<br />
time, subject to approval, the post becomes permanent and subject to standard terms of notice. The<br />
AAGBI strongly disapproves of annually renewable contracts. All Staff Grades should ensure that their<br />
workload, including on-call commitments, is reviewed annually. Consideration should be given not<br />
only to the frequency of on-call but also to the intensity of that work.<br />
Guidance for personal regrading from Staff Grade to Associate Specialist is available on the BMA<br />
website.<br />
Hospital Practitioner [9]<br />
A doctor appointed to this grade has to be a principal in general practice and must have been fully<br />
registered for at least four years. The numbers in this grade are diminishing, probably as a result of<br />
clinical governance considerations, the difficulties of appraisal in dual specialties, the increasing<br />
workload of General Practitioners and the decrease in the number of anaesthetists who have undergone<br />
a substantial period of training before entering general practice.<br />
8
Appointment is limited to those principals who have at least two years’ whole-time (or equivalent parttime)<br />
experience in anaesthesia. Although a postgraduate qualification is not a specific requirement for<br />
the grade, the AAGBI supports the RCoA recommendation that possession of an FRCA or equivalent<br />
is desirable.<br />
Appointment is renewable after one year, subject to confirmation, until the incumbent reaches<br />
retirement age or ceases to be a principal in general practice. This grade is responsible to a named<br />
consultant, and the AAGBI recommends a minimum of two clinical sessions with appropriate time for<br />
pre-operative visits and postoperative care, i.e. three notional half days per week.<br />
Thirty days’ study leave within each three-year period should be included in the contract, and hospital<br />
practitioners would normally be expected to participate in clinical audit and departmental meetings.<br />
Departments of Anaesthesia and College Tutors must encourage Trusts to support applications from<br />
this grade to participate in CPD.<br />
Clinical Assistants (part-time medical officers) [10]<br />
The AAGBI strongly recommends that no further Clinical Assistant appointments be made and that Staff<br />
Grade posts with nationally agreed terms and conditions of service be created in the future when the<br />
need arises. When General Practitioners wish to continue clinical sessions, the Hospital Practitioner<br />
grade would be a more appropriate appointment. It is essential that College Tutors, postgraduate deans<br />
and Trust managers support the need for CPD by clinical assistants, both for the benefit of the individual<br />
and as an intrinsic requirement of good practice, clinical governance and risk management.<br />
Non-standard grades<br />
Many Trusts have created new grades of doctors with non-standard terms and conditions of service to<br />
circumvent manpower planning mechanisms controlling the proportion of SAS doctors within trusts<br />
and also as a result of resource pressures. Such irregular posts are not protected by national terms and<br />
conditions of service, and the BMA has campaigned for many years against their creation. The AAGBI<br />
supports this view.<br />
These non-standard appointments have a number of titles, including Trust Grade doctor, Trust Specialist,<br />
Staff Specialist, Clinical Fellow and Clinical Specialist. The contracts usually incorporate out-of-hours<br />
work at a rate of remuneration defined by the Trust and often permit the use of fixed-term contracts.<br />
The revised terms and conditions of service for Staff Grades and the ability to appoint Associate<br />
Specialists directly have made such posts unnecessary. The AAGBI strongly recommends that<br />
employers use this opportunity to offer existing non-standard grade doctors of the appropriate level<br />
the option to transfer to the new terms and conditions of service. Those doctors who fail to meet the<br />
standards set down in this advice should be offered the opportunity to undergo further training. If, in<br />
exceptional circumstances, a Trust or Department of Anaesthesia deems such a non-standard post to<br />
be necessary, it is recommended that potential applicants obtain advice from the BMA, the AAGBI or<br />
the College tutor.<br />
9
4. Model SAS Charter<br />
The NHS employer should aim to provide a working environment that recognises both the diversity of<br />
SAS doctors and the major contribution that they make to patient care. The NHS employer should realise<br />
that the SAS doctors need both support and resources to develop personally and professionally. The<br />
NHS employer should be committed to ensuring that the role of the SAS doctor is fully acknowledged<br />
and respected by management, colleagues and patients. In order to deliver these aspirations, the<br />
following recommendations are made.<br />
Each Trust should work towards every SAS doctor having the following:<br />
• An appropriate contract of employment incorporating national terms and conditions<br />
• An appropriate agreed job plan. This may only be changed by mutual agreement<br />
between the SAS doctor and the Clinical Director/Lead in accordance with agreed local<br />
procedures for appraisal and job plan review<br />
• An adequate daytime session allocation with separate and identifiable time allocated<br />
for administration, education, audit and teaching commitments, etc. This should not<br />
be any less favourable than the time allotted to consultants undertaking similar<br />
clinical duties<br />
• Access to office accommodation and a computer in each directorate in which<br />
SAS doctors are employed. This should include access to email and suitable storage<br />
facilities for confidential work, related papers, books, etc<br />
• Adequate support and time allocation to allow SAS doctors to participate fully<br />
in the employer’s appraisal process, including access to appraisal training and the<br />
necessary CPD and study leave requirements, which are a natural consequence<br />
of appraisal<br />
• Adequate and fully funded study leave<br />
• All permanent SAS doctors should be members of the Medical Staff Committee/Hospital<br />
Medical Board and should be invited to attend meetings<br />
• There should be SAS representation on the LNC<br />
• The employer should agree a mechanism or adopt BMA recommendations for regrading<br />
from Staff Grade to Associate Specialist<br />
• Access to a fair and appropriate mechanism for the award of optional points for<br />
Staff Grades and discretionary points for Associate Specialists. The BMA recommend<br />
a minimum number of discretionary points/optional points (available at a rate of 0.35<br />
points per year per eligible candidate) that should be awarded. The points should be<br />
awarded for work and contributions over and above that normally expected for a doctor<br />
in the SAS grade. Guidance on completion of the application form is available on the<br />
BMA website<br />
• SAS doctors should have equal access to the benefits of the Improving Working Lives<br />
initiative [12]<br />
• All SAS doctors should be members of the directorate and should be invited to attend<br />
directorate and departmental meetings<br />
10
5. The AAGBI and the SAS anaesthetist<br />
The SAS Committee (SASC) of AAGBI<br />
The AAGBI SASC was established in 2002. The remit of the committee is to:<br />
• Represent the interests of SAS members of the AAGBI<br />
• Advise the AAGBI Council on matters relating to SAS doctors<br />
• Promote the aims and benefits of the AAGBI to SAS doctors<br />
• Encourage the professional development of SAS doctors<br />
• Ensure effective collaboration with the SAS committee of the RCoA,<br />
other Royal Colleges and professional bodies<br />
The Committee is structured as follows:<br />
• Members of the Executive of the AAGBI<br />
• Elected members of the Council as nominated by Council<br />
• A representative of RCoA SAS Committee<br />
• Five SAS representatives co-opted by the Council on the recommendation<br />
of the SAS committee<br />
SAS doctors and teaching<br />
The College, supported by the AAGBI, recognises that SAS anaesthetists have a valuable role to play in<br />
teaching. To be a teacher, possession of an FRCA is not a prerequisite but, like consultants, SAS doctors<br />
must fulfill the RCoA’s CPD requirements. This is essential for those clinical areas in which they have<br />
clinical and on-call responsibilities.<br />
The RCoA encourages College Tutors to identify those SAS anaesthetists with aptitude and to<br />
nominate them to the local School of Anaesthesia, specifying the areas in which they have appropriate<br />
expertise.<br />
SAS doctors who are Fellows or Members of the RCoA and who have been accepted by their School<br />
of Anaesthesia as teachers may, if they wish, ask for their name to be recorded with the College as<br />
‘Approved to Teach’. This list is available on the RCoA website [13].<br />
The specific areas in which SAS doctors teach are best identified at local level, but may include<br />
specialist operating lists in which an individual has expertise.<br />
SAS anaesthetists who teach trainees must have the opportunity to acquire the skills of a competent<br />
teacher.<br />
When being taught by a SAS doctor, trainees must at all times have unimpeded access to consultants<br />
for advice.<br />
11
6. The SAS contract<br />
What is the contract?<br />
A contract is a set of statements governing the agreement between you and your employer. It covers<br />
what work you agree to perform, what facilities your employer agrees to make available for you to<br />
do this work, and what your employer agrees to reward you for your work. It must be both fair and<br />
compatible with the law. Associate Specialists have the option of a whole-time or maximum part-time<br />
contract or may be employed on a part-time basis.<br />
The contract is not a single document. It has several components:<br />
• The statement of particulars (called the contract)<br />
• The terms and conditions of service<br />
• The job plan<br />
The contract<br />
This is usually a document that states your job title, your employing organisation, further details and is<br />
signed by both you and your employer. Standard contracts are negotiated nationally and should not be<br />
varied locally, except when individual circumstances demand changes that are mutually agreed.<br />
The terms and conditions of service<br />
This is a set of rules describing in more detail how the contract operates. The rules are congruent with<br />
the statement of particulars. Employers do not usually circulate these except on request but they can<br />
be found on the web. They are negotiated nationally and should not be varied locally except where<br />
a collective agreement has been reached with the LNC for medical and dental staff in your Trust.<br />
Examples of such agreements might be to vary the provisions of additional programmed activities in<br />
the case of significant private practice, to confirm arrangements for fee-paying services or to agree<br />
appropriate places for supporting professional activities.<br />
The job plan<br />
This is your personal and detailed agreement about your work. The job plan is congruent with the terms<br />
and conditions of service. It will describe the purpose of your job, your work timetable, your objectives<br />
and the supporting resources that should be allocated to help you achieve them. It should include any<br />
other personal agreements about the way you work.<br />
Job plan annual review<br />
The job plan of every SAS doctor (including the work programme) should be subject to an annual<br />
review. This annual review should provide an opportunity for the SAS doctor and the named consultant<br />
to discuss any problems that may have arisen in the preceding year and to agree any changes that need<br />
to be made to meet new circumstances or changed service priorities. It is likely that, in many cases, job<br />
plans will need to be amended only occasionally and even then will be subject to minimal alteration.<br />
12
Where the SAS doctor and the named consultant are unable to reach agreement on the content of<br />
the job plan, either initially or at an annual review, local procedures that provide for the resolution of<br />
grievances or differences relating to an individual practitioner’s duties should be followed.<br />
Preparing for a job plan meeting: keeping a diary and collecting data<br />
It is crucial in preparing for the job planning meeting that you have accurate information about the<br />
job you currently do. This is particularly important if you are going to argue that your work justifies a<br />
revision of the plan. There is no real alternative to collecting this data via a diary of your activity.<br />
For the most part, your work is likely to follow a regular pattern from week to week and should be<br />
relatively easy to assess. There will undoubtedly be exceptions for SAS doctors who do not have such<br />
a regular pattern and, in those circumstances, a more detailed assessment will be necessary. The<br />
assessment will then need to be made over a longer period. Note in particular that your workload is<br />
likely to be higher when you have colleagues on annual leave. Think about this when you complete<br />
your diary.<br />
For many SAS doctors, the most difficult task will be to assess the amount of time spent doing actual<br />
work whilst on-call because this may well vary from night to night or there may be a concerted period<br />
of on-call, for instance during one week in five. There may therefore need to be an assessment of on-call<br />
work over a longer period.<br />
Include in the diary all the work you do, from when you arrive at work each day until the time you<br />
leave. Travelling time is included between sites and where extra time is taken to get to a site different<br />
to your normal one. All work you do when on-call should also be included, such as telephone advice,<br />
travelling to and from work and waiting to begin work. SAS doctors, like most other professionals,<br />
would expect to be contactable during their lunch breaks and to take such breaks flexibly. Where this<br />
happens, it is reasonable to count such breaks as part of working time.<br />
Fixed commitments<br />
For the SAS doctor on a whole-time (or maximum part-time for an Associate Specialist) contract,<br />
between five and seven notional half-days, depending on specialty, should normally be allocated as<br />
fixed commitments in the work programme. For Associate Specialists on other part-time contracts, at<br />
least half of the notional half-days should normally be allocated to fixed commitments. The number<br />
of fixed commitments may be varied with the agreement of the Associate Specialist and their Clinical<br />
Director/Lead. A fixed commitment, e.g. an out-patient clinic or operating list, is a commitment that an<br />
Associate Specialist must fulfill, except by agreement with their named consultant or in an emergency.<br />
Examples of job plans are given in Appendix 1<br />
Waiting List Initiative lists: SAS doctors should be allowed, with the agreement of the department, to<br />
undertake waiting list initiative lists provided appropriate consultant cover is made available.<br />
13
Work diaries should take note of all aspects of work done. This will comprise:-<br />
• Direct clinical care of patients, including all patient-related administration such<br />
as telephone calls, letters, reviewing results, etc.<br />
• Activities to support professional development and CME including audit, training,<br />
research and other similar non-clinical activities<br />
• Agreed additional NHS responsibilities and agreed external duties<br />
Working time is divided into four components:<br />
1. Direct Clinical Care (DCC)<br />
2. Supporting Professional activities (SPA)<br />
3. Additional NHS responsibilities<br />
4. External duties<br />
Examples of DCCs, SPAs, additional NHS responsibilities and external duties can be<br />
found in the AAGBI document giving guidance for the new consultant contract [14] There are example<br />
job plans given in Appendix 1.<br />
Study leave/audit<br />
There should be opportunities for further training and participation in regular CPD in line with the<br />
recommendations of the RCoA.<br />
Appropriate funding and paid time off must be made available by the trust in accordance with national<br />
agreements.<br />
All SAS doctors should take part in regular departmental and hospital-wide audit/clinical governance<br />
and it is recommended that this is formally included in the job plan.<br />
Named consultant<br />
Since the inception of the NHS, it has been a requirement that every patient’s care is undertaken<br />
either by a consultant or by a trainee or SAS doctor under the supervision of a named consultant. All<br />
departments should have an agreed and recognised system in which a ‘named’ consultant is identified<br />
and recorded for every patient. This will be the person to whom SAS doctor should turn to for advice<br />
or help with a case. It should be clear to the SAS doctor how the local system operates and named<br />
individuals should be able to provide or arrange for immediate advice or direct assistance as required.<br />
The exact local implementation of supervision arrangements for individual SAS doctor will depend<br />
upon a number of factors, not the least of which will be the knowledge, skills and experience of the<br />
individual. Clearly, when a senior Associate Specialist is working in an area with which he or she is<br />
very familiar, the requirement for contact and discussion about individual cases will be uncommon.<br />
In contrast, it may be appropriate for a recently appointed Staff Grade doctor to be more closely<br />
supervised. For further details, please refer to the AAGBI SAS Handbook.<br />
14
Discretionary points and optional points<br />
Performance supplements for Associate Specialists introduced in 1991 have been replaced by<br />
Discretionary Points. Associate Specialists and Staff Grades on the maximum salary scale are eligible for<br />
the award of points: discretionary points for Associate Specialists and optional points for staff grades.<br />
These are consolidated payments made in addition to the maximum salary scale at the discretion of<br />
the employer. They are not seniority payments, nor are they automatic annual increments. They are<br />
superannuable.<br />
The award of points is for work and contributions over and above that normally expected of a doctor<br />
of that grade. Key criteria are clinical expertise and service to patients but account should be taken of<br />
overall workload and its intensity.<br />
It is important that Trusts/Boards set up local award panels in accordance with national guidelines and<br />
that they encourage SAS doctors to apply for these awards. All SAS doctors who are eligible to apply<br />
should make a personal submission each year. The consultants responsible for the work of SAS doctors<br />
may be required to give written recommendations.<br />
There are no absolute requirements to Trusts/Boards to award such discretionary/optional points, but<br />
the BMA recommendation is that a total of 0.35 points be awarded per eligible Associate Specialist per<br />
year and 0.35 points per eligible Staff Grade per year.<br />
15
7. References<br />
1. HSG (91)18: The associate specialist grade: terms and conditions of services. November 1991.<br />
2. DHSS PM (81) 16 recommended form of contract for associate specialists. 1981.<br />
3. NHS Management Executive guidelines relating to terms and conditions of service for doctors in<br />
the associate specialist grade HSG (91) 18. November 1991.<br />
4. Delegation of procedures for appointment to the associate specialist in medical specialties as<br />
announced by the Executive EL (91) 150. November 1991.<br />
5. Arrangements for the payment of Discretionary points to associate specialists AL (MD) 7/95.<br />
1995.<br />
6. NHS executive document on working draft to develop a quality framework for HCHS medical<br />
and dental staffing Annex 2 EL (97) 25. 1995.<br />
7. Advance Letter (MD) 4/97: Terms and Conditions of Service for the Staff Grade. NHS Executive<br />
July 1997.<br />
8. Staff grade DHSS circular giving guidance on arrangements for the employment of hospital<br />
medical and dental staff on the then new staff grade HC (88) 58 and annexes. 1998.<br />
9. In 1979 the Department of Health and Social Security issued guidelines setting out<br />
arrangements for the employment of hospital practitioners HC 7916. The NHS Executive issued<br />
summary guidance amending these arrangements HSG (93) 50. 1993.<br />
10. Guidance relating to conditions of service for clinical assistants was issued by the Department<br />
of Health and Social Security DA (86) 11. 1986.<br />
11. Advance Letter (MD) 05/02 regarding appraisal for NCCGs.<br />
12. http://www.dh.gov.uk/en/Managingyourorganisation/Humanresourcesandtraining/<br />
Modelemployer/Improvingworkinglives/index.htm<br />
13. http://www.rcoa.ac.uk/docs/SAS-teach.pdf<br />
14. http://www.<strong>aagbi</strong>.org/publications/guidelines/docs/jobplanning05.pdf<br />
16
Useful websites<br />
The Association of Anaesthetists of Great Britain and Ireland www.<strong>aagbi</strong>.org<br />
The Royal College of Anaesthetists www.rcoa.ac.uk<br />
British Medical Association (SAS Contract) www.bma.org.uk/sascontract<br />
Department of Health www.dh.gov.uk<br />
General Medical Council www.gmc-uk.org<br />
NHS www.nhs.uk<br />
Sick Doctors Trust www.sick-doctors-trust.co.uk<br />
17
APPENDIX 1<br />
Job plans<br />
Example of an 11 notional half day Associate Specialist job plan with out of hours emergency cover.<br />
5 clinical sessions, 3 of which are fixed (1 being special interest list)<br />
2 for pre-operative and postoperative visits<br />
1 for CPD/Audit<br />
2 for out of hours cover (1 night per week; and 1 in 5 full weekends or 2 in 5 split weekends)<br />
1 NHD with no clinical work<br />
Example of 12 session Staff Grade post with out of hours cover<br />
3 clinical theatre sessions (one of which is always accompanied)<br />
2 clinical emergency sessions (often ITU cover)<br />
1 session to attend teaching programme (1 week in 3, other week doing emergency cover)<br />
1 session for pre-operative and postoperative visits<br />
1 session for CPD/Audit admin<br />
4 sessions for one night per week of out of hours cover<br />
Example of 10 session Staff Grade post with no out of hours emergency cover and additional<br />
management duties<br />
6 clinical theatre sessions (1 of which is accompanied)<br />
2 sessions for pre-operative and postoperative visits<br />
1 session for CPD/audit<br />
1 session for admin duties (departmental rota/leave co-ordination)<br />
Example of an 11 notional half day Associate Specialist job plan with no out of hours emergency<br />
cover, but with special interest, e.g. chronic pain work<br />
4 clinical theatre sessions<br />
2.5 sessions for chronic pain team (2 clinical and 1 administration)<br />
1 session for admin duties (departmental leave/rota co-ordination)<br />
1 session for CPD/ audit<br />
1.5 sessions for pre-operative and postoperative visits<br />
Example of a 6 session/notional half day (part time) contract<br />
4 clinical theatre sessions<br />
1 session for CPD/Audit/Administration<br />
1 session for pre-operative and postoperative visits<br />
18
APPENDIX 2<br />
Update on the new SAS grade contract<br />
Negotiations on a new national (UK-wide) contract for SAS doctors and dentists began in May 2005.<br />
An agreement was reached with NHS Employers in 2006. The contract was ratified, with some<br />
amendments, by the Government in December 2007, following which SAS grades were balloted, and<br />
voted to accept the contract.<br />
Specialty Doctor<br />
The new contract is offered on an optional basis from 1 April 2008 to doctors / dentists currently in the<br />
following grades:<br />
• Staff Grades<br />
• Associate Specialists<br />
• Senior Clinical Medical Officers<br />
• Clinical Medical Officers<br />
• Non-GP Clinical Assistants<br />
• Non-GP Hospital Practitioners<br />
The new grade of Specialty Doctor will replace the Staff Grade and will be offered by employers from<br />
1 April 2008, so there will be no new appointments to the above grades after that date.<br />
Associate Specialist grade closure<br />
The old Associate Specialist (AS) grade will be closed with effect from 1 April 2008. There is a new<br />
Associate Specialist grade with similar structure to the Specialty Doctor. Current Associate Specialists<br />
will have the option to express an interest in switching to this new Associate Specialist grade. As no<br />
new appointments will be made to Associate Specialist level, the only other route to enter the grade<br />
will be to regrade from eligible Staff Grades, Specialty Doctors or Clinical Assistants, but applications<br />
will only be possible until 31 March 2009, and after that time new applications for regrading will not<br />
be accepted. This will mean that, from 1 April 2009, both the old and new Associate Specialist grades<br />
are closed.<br />
New contract is optional for current SAS grades<br />
Work has begun on implementation and employers will write to all current SAS doctors asking for<br />
expressions of interest in switching to the contract. SAS grades will have 12 weeks from receipt of<br />
the letter from employers to express an interest in the new contract. This does not commit doctors to<br />
accepting the new contract but guarantees back pay to 1 April 2008 once a job plan has been agreed.<br />
Written offers of an agreed job plan need to be accepted within 21 days (28 days in Scotland).<br />
• Current SAS doctors must consider whether they would like to apply for the new contract.<br />
Consideration of individual circumstances will be essential.<br />
• If expressing an interest, it is advisable to begin a diary planning exercise to inform<br />
job planning discussions. This should last for a minimum of six weeks, or one rota cycle,<br />
though a longer period of time would be helpful.<br />
19
• Staff Grades eligible to apply to regrade to the Associate Specialist grade should do so<br />
as soon as possible, as applications will not be accepted after 31 March 2009<br />
• Regrading applications started before 1 April 2008 will be to the old Associate Specialist<br />
contract, with the option then of moving to the new Association Specialist contract.<br />
• Successful applications started on or after 1 April 2008 will be direct to the new Associate<br />
Specialist contract.<br />
• Should it not prove possible to agree a job plan, there is a mediation procedure available.<br />
• If mediation fails, there is an appeals process.<br />
• The BMA SASC is producing further guidance to assist in assimilation.<br />
Programmed Activities (PA)<br />
The new contract for both new Associate Specialist and Specialty Doctor grades are time based, with<br />
each unit of time being a four-hour Programmed Activity (PA). Before signing the contract, you should<br />
have an agreed job plan. The minimum unit of time used in job planning should be 0.5 PA. The contract<br />
for current SAS grades moving to the new contract should be based on a robust diary exercise. Contracts<br />
can be for up to 12 PAs but PAs over 10 are not obligatory, and may not be permanent. Up to 10 PAs<br />
are superannuable.<br />
A full time contract is one with 10 PAs, most of the work being Direct Clinical Care (DCC) with a<br />
minimum of one PA for Supporting Professional Activities (SPA). SAS doctors who currently have more<br />
than one notional half day or session for SPA-type activity should continue to receive this. The minimum<br />
of 1 PA is absolute, and will also apply to part-time staff, i.e. it is not pro-rata. Some SAS grades may<br />
also be eligible to have additional PAs for additional NHS responsibilities or for external duties.<br />
Direct Clinical Care<br />
This is any work to do with care of individual patients, such as:<br />
• Emergency duties: including emergency work carried out during or arising from on-call<br />
(including phone call advice)<br />
• Operating sessions: including pre-and post-operative care<br />
• Ward rounds<br />
• Outpatient clinics<br />
• Clinical diagnostic work<br />
• Other patient treatment, e.g. intensive care work<br />
• Public health duties<br />
• Multi-disciplinary meetings about direct patient care<br />
• Administration related to patient care, e.g. referrals, notes, dictation, correspondence<br />
• Travel: to and from home for on-call work; and between hospitals for elective work<br />
Other areas to be considered are starting work earlier, planning operating list including scheduling<br />
order, prioritising difficult cases, mortality and morbidity meetings if presenting specific patients,<br />
handling complaints.<br />
20
Supporting Professional Activities<br />
There should be a minimum of one SPA in the job plan, though as the SAS doctor becomes more senior<br />
and experienced, it is likely that this will need to be increased, as evidenced by work diary<br />
• Training, e.g. teaching trainees, medical students, paramedical staff or ancillary staff<br />
• Teaching: lectures or seminars whether local, regional or national<br />
• Continuing Professional Development: all activity such as attending professional meetings,<br />
departmental CPD sessions and reading journals<br />
• Audit<br />
• Job planning<br />
• Appraisal<br />
• Research<br />
• Clinical management, including rota co-ordination<br />
• Local clinical governance activity<br />
• Local representational activities<br />
Additional NHS responsibilities<br />
There may be activities that cannot be covered within the time set, which should be recognised as<br />
additional NHS responsibilities. It may be appropriate to replace some DDC PAs to enable this work to<br />
be carried out. Examples include<br />
• Audit lead<br />
• Clinical Governance lead<br />
• Subspecialty or project lead<br />
• Clinical management: Clinical Director, other official Trust management role including<br />
LNC, rota management or Lead Clinician<br />
External duties<br />
This involves activities which are for the greater good of the NHS. The Department of Health recognises<br />
the value of, and has given support for, such activities. If these duties are regular, allowance for them<br />
should be given within the job plan.<br />
Examples include:<br />
• Work for General Medical Council or other national bodies<br />
• College tutor<br />
• NHS disciplinary procedures<br />
• Regional Advisor, deputy, Programme Director<br />
• Trade Union duties, e.g. BMA<br />
• Royal College, Specialist Associations, e.g. AAGBI, Specialist Society work<br />
• University roles<br />
• Work for other NHS bodies, e.g. Healthcare Commission<br />
• Acting as an external member of appointment panels<br />
21
On call supplement<br />
There is a supplement for on-call work, payable as a percentage of the basic salary with the percentage<br />
being dependent on the frequency of the on-call. This will not be payable for a shift pattern. It is payable<br />
for on-call work irrespective of the intensity of the duty.<br />
The supplement is 6% of basic salary for rotas with an on-call frequency equal to or more frequent than<br />
1 in 4, 4% for rotas with frequency less than 1 in 4 or equal to 1 in 8, and 2% for rotas with a frequency<br />
of less than 1 in 8.<br />
This payment is added to basic salary and is superannuable.<br />
Out of Hours work (OOH)<br />
Work actually carried out as Out of Hours work (OOH), as demonstrated by diary exercise, will be<br />
payable at an enhanced rate whereby the rate of pay will be time and a third for a four-hour block of<br />
time actually worked. Alternatively, SAS grades may prefer to consider an OOH PA as a three-hour<br />
block of time of time actually worked, payable as a four-hour PA. OOH work is work done between<br />
19:00 and 07:00 on weeknights and all work at weekends and on public holidays. Where OOH work<br />
is included within the 10-session job plan this will be superannuable. If it forms part of additional PAs<br />
above the basic 10 PAs it will not be superannuable.<br />
Regular OOH worked should be part of the job plan, whether elective or emergency. If the actual<br />
number of OOH hours worked is variable, it can be averaged on a weekly basis for the purposes of job<br />
planning, by using the diary exercise to look at total number of OOH hours actually worked during the<br />
diary period, and dividing by the number of weeks for which the diary was kept. Thus it can then be<br />
designated as a specific amount of DCC time.<br />
It is possible for job plans to include regular elective work to be done in OOH time for specialty doctors,<br />
but this does not apply to associate specialists.<br />
Optional and discretionary points<br />
These awards will no longer exist in the new contract, but will continue to be available for those SAS<br />
doctors who choose to remain in their old contracts.<br />
BMA members can access assistance from the BMA for job planning, for mediation and for appeals.<br />
22
23
21 Portland Place, London W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
Storage of Drugs in<br />
Anaesthetic Rooms<br />
Guidance on best practice from<br />
the RCoA and AAGBI
Storage of Drugs in Anaesthetic<br />
Rooms<br />
1<br />
Guidance on best practice from the RCoA and AAGBI<br />
The Royal College of Anaesthetists (RCoA) and Association of Anaesthetists of Great Britain and Ireland (AAGBI) recognise<br />
that secure drug storage makes an important contribution to patient safety, and the safety of the public, but patient safety must<br />
always be the priority. The RCoA and AAGBI support a system of standard operating procedures (SOPs) that makes patient safety<br />
paramount, and recognises that even short delays in accessing drugs may result in an adverse patient outcome. All drugs and<br />
medicines § need to be stored safely. The Royal Pharmaceutical Society (RPS) recognises that there are special requirements for<br />
the storage of drugs in operating theatre departments, and recommends that there should be a system of Standard Operating<br />
Procedures (SOPs) covering each of the activities concerned with medicines use to ensure the safety and security of medicines<br />
stored and used in operating departments. 1<br />
A particular situation not mentioned in the RPS document is that anaesthetic rooms, which function as a form of ‘annexe’ to the<br />
main operating theatre, are usually a place in which drugs and fluids are stored. During the conduct of an anaesthetic and surgery<br />
the anaesthetic room may temporarily and intermittently be unoccupied when the patient is in theatre. Care Quality Commission<br />
(CQC) inspectors have in recent months identified a need for guidance as to whether the storage of drugs and fluids in unlocked<br />
cupboards in temporarily unoccupied anaesthetic rooms is acceptable.<br />
The Health and Social Care Act 2008 2 demands that patients and healthcare staff be protected ‘against the risks associated with<br />
the unsafe use and management of medicines by means of the making of appropriate arrangements for the obtaining, recording,<br />
handling, using, safe keeping, dispensing, safe administration and disposal of medicines’.<br />
There is clear guidance on the storage of Controlled Drugs such as morphine, cocaine, and fentanyl in this setting, 3 but there is<br />
currently no specific advice on best practice for the storage of non-controlled drugs and fluids in anaesthetic rooms. The Royal<br />
College of Anaesthetists (RCoA) and the Association of Anaesthetists of Great Britain and Ireland (AAGBI) convened a working<br />
party to address this issue. This document is the report of the working party.<br />
Guidance<br />
1 Patient safety must be the paramount consideration. Immediate access to a variety of drugs can sometimes be essential, such<br />
that even short delays in drug availability can make a difference to patient outcome.<br />
2 It is not possible to provide a definitive list of ‘emergency drugs’ that should be immediately available at all times, as these<br />
vary depending on patient condition and the surgical procedures being performed. There are few drugs commonly stored in<br />
anaesthetic room drug cupboards that will not be needed urgently on occasion.<br />
3 Local SOPs should exist for the safe storage of drugs (both controlled and non-controlled medicines) and fluids in operating<br />
theatre departments. These should be adequately risk-assessed and agreed by pharmacists, anaesthetists, nurses, operating<br />
department practitioners and ratified by the organisations medicines management committee. The Accountable Officer for<br />
medicines within the organisation should endorse these. 4<br />
4 Decisions about drug security in anaesthetic rooms must reflect a balance between patient safety, staff protection and security.<br />
We understand that this may mean that in defined circumstances, drug cupboards (excluding those containing Controlled<br />
Drugs) may remain unlocked when the anaesthetic room is temporarily unoccupied and the operating theatre is in use.<br />
5 Even if anaesthetic room drug cupboards cannot, in the interests of patient safety, be locked during surgical procedures,<br />
practices can be followed that may minimise medicines security risks, e.g. drugs and fluids prepared in advance for procedures<br />
can be kept in closed cupboards.<br />
6 An unoccupied anaesthetic room should ideally remain visible at all times to those in the operating theatre, usually through<br />
windows in the door.<br />
7 Anaesthetic room drug cupboards must be locked when the operating theatre is unoccupied.<br />
§<br />
For the purposes of this paper the terms drugs, medicines and fluids are used interchangeably.<br />
<br />
In this guidance, the term ‘drug cupboard’ includes all forms of drug and fluid storage, including refrigerators.
Storage of Drugs in Anaesthetic<br />
Rooms<br />
2<br />
Guidance on best practice from the RCoA and AAGBI<br />
8 It is common practice to prepare a selection of ‘emergency drugs’ that should be immediately available during the course of<br />
an anaesthetic. These will often accompany the patient from the anaesthetic room into the operating theatre but, if this is not<br />
possible, they should be stored in the anaesthetic room in a manner that maintains their immediate availability. They should be<br />
adequately labelled, and disposed of appropriately if not used.<br />
9 Certain rarely-used emergency drugs may be stored in a central location, serving the entire theatre suite, e.g. dantrolene and<br />
intralipid. Local SOPs should be compliant with relevant legislation and should ensure that the locations of these drugs are<br />
conspicuously signposted.<br />
10 We support the use of effective access control systems for all routes that allow entry into operating departments, limiting access<br />
to only those with legitimate reasons for access.<br />
References<br />
1 The safe and secure handling of medicines: a team approach. RPSGB, London 2005 (http://bit.ly/1R893Hc).<br />
2 The Health and Social Care Act 2008 (Regulated Activities) Regulations 2014 (http://bit.ly/1Zr5Lny).<br />
3 Controlled Drugs (Supervision of management and use) Regulations 2013: Information about the Regulations. DH, London 2013 (http://bit.ly/1R88CNa).<br />
4 Patient Safety Alert (NHS/PSA/D/2014/005). Stage Three: Directive: Improving medication error incident reporting and learning, 20 March 2014.<br />
MHRA and NHSE, London (http://bit.ly/1Zr6h4T).<br />
The RCoA and AAGBI would like to thank the following organisations for providing beneficial comment on this document:<br />
The Royal Pharmaceutical Society (RPS)<br />
The Association for Perioperative Practice (AfPP)<br />
The College of Operating Department Practitioners (CODP)<br />
The Association of Physicians’ Assistants (APA)<br />
The Care Quality Commission (CQC)<br />
Members of the Working Party<br />
Dr Richard Marks, Vice-President, Royal College of Anaesthetists (Chairman)<br />
Dr William Harrop-Griffiths, Council Member, Royal College of Anaesthetists<br />
Mr Mike Zeiderman, National Professional Advisor for Surgical Specialities, CQC<br />
Dr David Selwyn, Chair of Clinical Director Network<br />
Dr Kathleen Ferguson, Council Member AAGBI, Representative of SALG<br />
Ms Katharina Floss, Critical Care Pharmacist, John Radcliffe Hospital<br />
June 2016<br />
Latest review date June 2019<br />
© The Royal College of Anaesthetists (RCoA) and Association of Anaesthetists of Great Britain and Ireland (AAGBI) 2016<br />
Churchill House, 35 Red Lion Square, London WC1R 4SG<br />
020 7092 1500 standards@rcoa.ac.uk www.rcoa.ac.uk
SYRINGE LABELLING IN CRITICAL CARE AREAS<br />
REVIEW 2014 (updated November 2016)<br />
Since the new standard for syringe labelling was introduced in May 2003 1 , it has become apparent that a number of changes<br />
need to be made. These changes are to bring the standard in line with the change from British Approved Names (BANs) to<br />
recommended International Non-Propriety Names (rINNs) 2 , and also to bring the standard in line with the Australian/New Zealand<br />
Standard 3 and ISO Standard 4 which have superseded it. The changes are as follows:<br />
• BANs to rINNs<br />
Examples of these affecting anaesthetic drugs are:<br />
• Thiopentone to Thiopental<br />
• Lignocaine to Lidocaine<br />
• Glycopyrrolate to Glycopyrronium<br />
• Drug concentrations<br />
These were all shown on the original document as ‘mg/ml’. Correct concentrations should be used. For example:<br />
• Fentanyl micrograms/ml<br />
• Lidocaine %<br />
• Insulin units/ml<br />
• ‘Adrenaline’ is to be used, not ‘Epinephrine’ (similarly ‘Noradrenaline’, not ‘Norepinephrine’).<br />
• Suxamethonium and Adrenaline<br />
All lettering to be black with the exception of the labels for Suxamethonium and Adrenaline which shall be printed against the<br />
background colour as bold reverse plate letters within a black bar running from edge to edge of the upper half of the label, the<br />
rest of which shall display the coloured background.<br />
• Antagonists<br />
To denote a drug of opposite action, 1mm wide diagonal stripes of the designated colour, alternating with a 1 mm wide white<br />
stripe is used. The stripes should run from lower left to upper right at approximately 45 degrees. The striping should be<br />
omitted behind and below the drug name. Protamine, as an antagonist of Heparin, should be a white label with black stripes.<br />
• Anti-emetics<br />
The syringe label for this group of drugs should have the background colour Salmon 156, which is shared by the major<br />
tranquillisers.<br />
• Combinations of drugs<br />
Drugs which are supplied ready mixed in the ampoule should have a syringe label which denotes the drug name of one of the<br />
two drugs against the appropriate background in the upper half of the label, and the drug name of the second drug against the<br />
appropriate background in the lower half. For example:<br />
• Glycopyrronium and neostigmine<br />
• Lidocaine % and Adrenaline<br />
An exception to this is the label for Propofol with user-addition of Lidocaine. This label should read ‘Propofol/lidocaine’ with<br />
‘mg/ml’ for Propofol against the induction agent background (yellow).<br />
Note to users: The colours are only a guide. All syringes containing drugs must be labelled. It is important to check the drug<br />
ampoule and correctly label the syringe with the correctly texted label. Blank coloured labels are a potential source of confusion<br />
and should not be used.<br />
Dr Tim Meek<br />
Chairman Safety Committee<br />
Association of Anaesthetists of Great Britain and Ireland<br />
1<br />
References<br />
Syringe labelling in critical care areas. RCoA Bulletin 19;May 2003:953.<br />
2<br />
Changes in names of certain medicinal substances. Chief Medical Officer, Chief Nursing Officer and Chief Pharmaceutical Officer.<br />
DoH;17 March 2004:PL/CMO2004/1.<br />
3<br />
User-applied labels for use on syringes containing drugs used during anaesthesia. Australian/New Zealand Standard;4375:1996.<br />
4 Geneva, ISO, 2008. ISO 26825:2008, Anaesthetic and respiratory equipment - User-applied labels for syringes containing drugs<br />
used during anaesthesia - Colours, design and performance.
Propofol<br />
.............................mg/ml.<br />
Induction agents<br />
Ketamine<br />
.............................mg/ml.<br />
Diazepam<br />
..........................mg/ml.<br />
Hypnotics<br />
Midazolam<br />
..........................mg/ml.<br />
.............................mg/ml.<br />
Neuromuscular blocking drugs<br />
Vecuronium<br />
.............................mg/ml.<br />
Neuromuscular blocking drug antagonist<br />
Neostigmine<br />
...............micrograms/ml.<br />
Morphine<br />
.............................mg/ml.<br />
Opioids<br />
Fentanyl<br />
................micrograms/ml.<br />
Opioid antagonist<br />
Naloxone<br />
...............micrograms/ml.<br />
Vasopressors<br />
Hypotensive agent<br />
...............micrograms/ml.<br />
Ephedrine<br />
.............................mg/ml.<br />
Labetalol<br />
..............................mg/ml.<br />
Atropine<br />
..............micrograms/ml.<br />
Anticholinergic agents<br />
Glycopyrronium<br />
.............micrograms/ml.<br />
Lidocaine<br />
...............................%.<br />
Local anaesthetics<br />
Bupivacaine<br />
...............................%.<br />
Anti-emetics<br />
Ondansetron<br />
...................mg/ml.<br />
Heparin<br />
...................units/ml.<br />
Miscellaneous<br />
Protamine<br />
...................mg/ml.<br />
Further information is available from the manufacturer or the following websites: www.astm.org and www.csa.ca<br />
Please note that colours are only a guide and the correct Pantone colour code numbers are listed on the reverse of this sheet. It<br />
is still important to check the drug ampoule and correctly label the syringe containing the drug with the correctly texted label.
STANDARD BACKGROUND COLOURS FOR USER-APPLIED<br />
SYRINGE DRUG LABELS<br />
Drug class Examples Pantone ® colour (uncoated)<br />
Anti-emetics Metoclopramide, Ondansetron Pantone ® 156 (salmon)<br />
Induction agents<br />
Thiopental, etomidate, ketamine,<br />
propofol<br />
Yellow<br />
Hypnotics Diazepam, lorazepam, midazolam Pantone ® 151 (orange)<br />
Hypnotic antagonists<br />
Depolarising neuromuscular<br />
blocking drugs<br />
Non-depolarising neuromuscular<br />
blocking drugs<br />
Neuromuscular blocking drug<br />
antagonists<br />
Flumazenil<br />
Suxamethonium<br />
Atracurium, Vecuronium<br />
Neostigmine<br />
Pantone ® 151 (orange with white<br />
diagonal stripes)<br />
Pantone ® 805 (fluorescent or warm<br />
red lettering out of black above, red<br />
below)<br />
Pantone ® 805 (fluorescent or warm<br />
red)<br />
Pantone ® (fluorescent or warm red)<br />
with white diagonal stripes<br />
Opioids Morphine, fentanyl, remifentanil Pantone ® 297 (blue)<br />
Opioid antagonists<br />
Naloxone<br />
Pantone ® 297 (blue) with white<br />
diagonal stripes<br />
Major tranquilizers Droperidol, chlorpromazine Pantone ® 156 (salmon)<br />
Vasopressors<br />
Hypotensive agents<br />
Adrenaline, ephedrine,<br />
phenylephrine<br />
Nitroprusside, nitroclycerine,<br />
phentolamine<br />
Pantone ® 256 (violet) (Adrenaline<br />
is violet out of black above, violet<br />
below)<br />
Pantone ® 256 (violet) with white<br />
diagonal stripes<br />
Local anaesthetics Lidocaine, bupivacaine Pantone ® 401 (grey)<br />
Anticholinergic agents Atropine, glycopyrronium Pantone ® 367 (green)<br />
Other agents<br />
Oxytocin, heparin, protamine,<br />
antibiotics<br />
Pantone ® transparent white<br />
(Protamine is Pantone ® transparent<br />
white with black diagonal stripes)<br />
The examples shown are representative, not restrictive. See Pantone ® Colour Formula Guide. Pantone ® is<br />
a registered trademark of Pantone, Inc.
The measurement of adult blood pressure<br />
and management of hypertension before<br />
elective surgery 2016<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
British Hypertension Society<br />
March 2016
This guideline was originally published in Anaesthesia. If you wish to refer to this<br />
guideline, please use the following reference:<br />
Association of Anaesthetists of Great Britain and Ireland. The measurement of adult<br />
blood pressure and management of hypertension before elective surgery 2016.<br />
Anaesthesia 2016; 71: 326-337.<br />
This guideline can be viewed online via the following URL:<br />
http://onlinelibrary.wiley.com/doi/10.1111/anae.13348/full
Anaesthesia 2016, 71, 326–337<br />
Guidelines<br />
doi:10.1111/anae.13348<br />
The measurement of adult blood pressure and management of<br />
hypertension before elective surgery<br />
Joint Guidelines from the Association of Anaesthetists of Great Britain and Ireland and the<br />
British Hypertension Society<br />
A. Hartle, 1 T. McCormack, 2 J. Carlisle, 3 S. Anderson, 4 A. Pichel, 5 N. Beckett, 6 T. Woodcock 7 and<br />
A. Heagerty 8<br />
1 Consultant, Departments of Anaesthesia and Intensive Care, St Mary’s Hospital, London, UK, and co-Chair,<br />
Working Party on behalf of the AAGBI<br />
2 General Practitioner, Whitby Group Practice, Spring Vale Medical Centre, Whitby, UK, Honorary Reader, Hull York<br />
Medical School, UK, and co-Chair, Working Party, on behalf of the British Hypertension Society<br />
3 Consultant, Departments of Anaesthesia, Peri-operative Medicine and Intensive Care, Torbay Hospital, Torquay, UK<br />
4 Clinical Lecturer, Institute of Cardiovascular Sciences, University of Manchester, Manchester, UK and British<br />
Hypertension Society<br />
5 Consultant, Department of Anaesthesia, Manchester Royal Infirmary, Manchester, UK<br />
6 Consultant, Department of Ageing and Health, Guys’ and St Thomas’ Hospital, London, UK and British<br />
Hypertension Society<br />
7 Independent Consultant Anaesthetist, Hampshire, UK<br />
8 Professor, Department of Medicine, University of Manchester, Manchester, UK, and British Hypertension Society<br />
Summary<br />
This guideline aims to ensure that patients admitted to hospital for elective surgery are known to have blood pressures<br />
below 160 mmHg systolic and 100 mmHg diastolic in primary care. The objective for primary care is to fulfil this criterion<br />
before referral to secondary care for elective surgery. The objective for secondary care is to avoid spurious hypertensive<br />
measurements. Secondary care should not attempt to diagnose hypertension in patients who are normotensive in<br />
primary care. Patients who present to pre-operative assessment clinics without documented primary care blood pressures<br />
should proceed to elective surgery if clinic blood pressures are below 180 mmHg systolic and 110 mmHg diastolic.<br />
.................................................................................................................................................................<br />
This is a consensus document produced by members of a Working Party established by the Association of Anaesthetists<br />
of Great Britain and Ireland (AAGBI) and the British Hypertension Society (BHS). It has been seen and approved by<br />
the AAGBI Board of Directors and the BHS Executive. It is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives<br />
4.0 International License. Date of review: 2020.<br />
Accepted: 16 November 2015<br />
.................................................................................................................................................................<br />
Re-use of this article is permitted in accordance with the Creative Commons Deed, Attribution 2.5, which does not<br />
permit commercial exploitation.<br />
326 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland.<br />
This is an open access article under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs License, which permits use and<br />
distribution in any medium, provided the original work is properly cited, the use is non-commercial and no modifications or adaptations are made.
Management of hypertension before elective surgery guidelines Anaesthesia 2016, 71, 326–337<br />
Recommendations<br />
•<br />
General practitioners should refer patients for elective<br />
surgery with mean blood pressures in primary<br />
care in the past 12 months less than 160 mmHg<br />
systolic and less than 100 mmHg diastolic.<br />
• Secondary care should accept referrals that document<br />
blood pressures below 160 mmHg systolic and<br />
below 100 mmHg diastolic in the past 12 months.<br />
• Pre-operative assessment clinics need not measure<br />
the blood pressure of patients being prepared for<br />
elective surgery whose systolic and diastolic blood<br />
pressures are documented below 160/100 mmHg in<br />
the referral letter from primary care.<br />
• General practitioners should refer hypertensive<br />
patients for elective surgery after the blood pressure<br />
readings are less than 160 mmHg systolic and less<br />
than 100 mmHg diastolic. Patients may be referred<br />
for elective surgery if they remain hypertensive<br />
despite optimal antihypertensive treatment or if<br />
they decline antihypertensive treatment.<br />
• Surgeons should ask general practitioners to supply<br />
primary care blood pressure readings from the last<br />
12 months if they are undocumented in the referral<br />
letter.<br />
• Pre-operative assessment staff should measure the<br />
blood pressure of patients who attend clinic without<br />
evidence of blood pressures less than<br />
160 mmHg systolic and 100 mmHg diastolic being<br />
documented by primary care in the preceding<br />
12 months. (We detail the recommended method<br />
for measuring non-invasive blood pressure accurately,<br />
although the diagnosis of hypertension is<br />
made in primary care.)<br />
• Elective surgery should proceed for patients who<br />
attend the pre-operative assessment clinic without<br />
documentation of normotension in primary care if<br />
their blood pressure is less than 180 mmHg systolic<br />
and 110 mmHg diastolic when measured in clinic.<br />
The disparity between the blood pressure thresholds<br />
for primary care (160/100 mmHg) and secondary<br />
care (180/110 mmHg) allows for a number of factors.<br />
Blood pressure reduction in primary care is based on<br />
good evidence that the rates of cardiovascular morbidity,<br />
in particular stroke, are reduced over years and<br />
decades. There is no evidence that peri-operative blood<br />
pressure reduction affects rates of cardiovascular events<br />
beyond that expected in a month in primary care.<br />
Blood pressure measurements might be more accurate<br />
in primary care than secondary care, due to a less<br />
stressful environment and a more practised technique.<br />
What other guideline statements are available on<br />
this topic?<br />
There is detailed evidence-based guidance on the diagnosis<br />
and treatment of hypertension in the community<br />
from, for example, the National Institute for Health<br />
and Care Excellence [1]. There is little guidance on a<br />
‘safe’ blood pressure for planned anaesthesia and surgery.<br />
Why was this guideline developed?<br />
There is no national guideline for the measurement,<br />
diagnosis or management of raised blood pressure<br />
before planned surgery. There is little evidence that<br />
raised pre-operative blood pressure affects postoperative<br />
outcomes. Local guidelines vary from area to area.<br />
Hypertension is a common reason to cancel or postpone<br />
surgery. In our sprint audit, 1–3% of elective<br />
patients had further investigations precipitated by<br />
blood pressure measurement, of whom half had their<br />
surgery postponed. Across the UK this would equate<br />
to ~100 concerned and inconvenienced patients each<br />
day, with associated costs to the NHS and the national<br />
economy [2, 3].<br />
This guideline is the first collaboration between<br />
the AAGBI and the British Hypertension Society; these<br />
two organisations have very different perspectives.<br />
Members of the British Hypertension Society are concerned<br />
with the long-term reduction in rates of cardiovascular<br />
disease, particularly strokes. Anaesthetists are<br />
more focused on immediate complications, in the perioperative<br />
period. This guideline aims to prevent the<br />
diagnosis of hypertension being the reason that<br />
planned surgery is cancelled or delayed. As such, it<br />
should also be of interest to hospital managers and<br />
commissioners of hospital care.<br />
How does this statement differ from existing<br />
guidelines?<br />
This guideline serves, therefore, not to advise on treatment<br />
of hypertension, but rather to produce a com-<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland. 327
Anaesthesia 2016, 71, 326–337<br />
Management of hypertension before elective surgery guidelines<br />
mon terminology in diagnosis and referral, explaining<br />
the impact of anaesthesia on blood pressure and vice<br />
versa to the wider, non-anaesthetic community. At the<br />
same time, it will review current best practice on the<br />
measurement, diagnosis and treatment of hypertension.<br />
Why does this statement differ from existing<br />
guidelines?<br />
Pre-operative blood pressure management involves<br />
many specialties and professions: primary care, general<br />
medicine, cardiology, endocrinology, pre-operative<br />
assessment clinics and, of course, both anaesthetists<br />
and surgeons. This list is not exhaustive. This guideline<br />
should be a useful summary for all those clinicians<br />
and for patients. The guidance takes into account not<br />
just the best clinical evidence, but the particular pattern<br />
of referral for treatment within the NHS in all<br />
four countries of the UK.<br />
Introduction<br />
The National Institute for Health and Care Excellence<br />
(NICE) has described hypertension as ‘one of the most<br />
important preventable causes of premature morbidity<br />
and mortality in the UK’ [1]. The Association of<br />
Anaesthetists of Great Britain and Ireland (AAGBI),<br />
together with the British Hypertension Society, felt<br />
there was a need for a nationally agreed policy statement<br />
on how to deal with raised blood pressure in the<br />
pre-operative period. We have based this statement on<br />
a consensus view with the backing of graded evidence,<br />
where such evidence is available.<br />
Hypertension is almost always asymptomatic and<br />
it is diagnosed following screening in general practice.<br />
Managing hypertension pre-operatively is a complex<br />
matter of balancing the risks of anaesthesia, treatment<br />
and delay for the individual patient. Most cases of<br />
hypertension are primary, i.e. with no other medical<br />
cause. For the remainder, the cause for hypertension<br />
may be associated with the reason for the proposed<br />
operation.<br />
Cancellations and postponements of planned surgical<br />
procedures have been a major and long-standing<br />
problem for healthcare worldwide. The quantifiable<br />
loss of resource is pitted against unquantifiable and<br />
significant psychological, social and financial implications<br />
of postponement for patients and their families.<br />
Although guidelines exist for the treatment of elevated<br />
blood pressure, there remains a paucity of literature<br />
and accepted guidelines for the peri-operative<br />
evaluation and care of the patient with hypertension<br />
who undergoes non-cardiac surgery [4]. Of particular<br />
importance is defining the patients most vulnerable<br />
to complications and the indications for immediate<br />
and rapid antihypertensive treatment and/or postponement<br />
of surgery to reduce these risks pre-operatively,<br />
intra-operatively and postoperatively. Perioperative<br />
hypertension often occurs in conjunction<br />
with sympathetic nociceptive stimulation during the<br />
induction of anaesthesia, during surgery and with<br />
acute pain in the early postoperative period. Hypertension<br />
may also accompany hypothermia, hypoxia or<br />
intravascular volume overload from excessive intraoperative<br />
fluid therapy, particularly in the ensuing<br />
24–48 h as fluid is mobilised from the extravascular<br />
space [4–6].<br />
There are no nationally agreed guidelines for the<br />
diagnosis or management of raised blood pressure<br />
before elective surgery. The evidence regarding the<br />
effect of raised pre-operative blood pressure is very<br />
limited. Local guidelines do exist but vary from area to<br />
area. Both the AAGBI and the British Hypertension<br />
Society recognised the need for a national guideline<br />
and consensus statement to address the various issues<br />
of concern. We have limited our deliberations to a<br />
specific scope. Only the period before planned surgery<br />
is covered. Blood pressures which may cause an immediate<br />
risk to health are specified, rather than those that<br />
may cause risk over the long-term. The best method of<br />
taking accurate blood pressure measurements is examined.<br />
We considered how long blood pressure should<br />
be controlled before surgery is undertaken. Communication<br />
between different hospital departments, primary<br />
care and the patient are of importance. We hope that<br />
by providing national guidance the chances of a<br />
patient receiving conflicting advice will be minimised.<br />
Scope<br />
This guideline is aimed at adults presenting for<br />
planned surgery. The following groups of patients are<br />
specifically not studied, although many of the general<br />
points covered in the guideline may apply.<br />
328 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland.
Management of hypertension before elective surgery guidelines Anaesthesia 2016, 71, 326–337<br />
Emergency/urgent surgery<br />
By definition, these patients have no or very limited<br />
time for investigation, treatment or postponement.<br />
Such surgery must almost always proceed, but all those<br />
involved, including the patient, must be aware of any<br />
associated increased risk.<br />
Obstetrics<br />
Most cases of hypertension in pregnancy will be<br />
directly related to the pregnancy (although with an<br />
ageing obstetric population with higher rates of obesity,<br />
this may be less so). The monitoring and treatment<br />
of blood pressure is a specific and integral part<br />
of obstetric care, regardless of the need for surgery,<br />
and even for ‘elective’ Caesarean section there may be<br />
very limited opportunity for delay.<br />
Paediatrics<br />
Childhood hypertension is relatively uncommon, and<br />
its epidemiology and natural history is relatively<br />
unclear and there are no definitive trials on screening.<br />
Thus, its diagnosis and management, including preoperatively,<br />
is a specialist area beyond the scope of the<br />
general guidance in this publication.<br />
Cardiac surgery<br />
Peri-operative hypertension commonly complicates<br />
surgery for congenital and acquired cardiac disease.<br />
Management will be affected by many other factors<br />
including the planned procedure, the use or not of cardiopulmonary<br />
bypass and the other indications for<br />
vaso- and cardio-active medication. We have thus considered<br />
it to be a specialist area beyond the scope of<br />
the general guidance in this publication.<br />
Surgery for blood pressure management<br />
This includes surgery for phaeochromocytoma and<br />
bariatric surgery; we have excluded this from our guidance<br />
for similar reasons to that of cardiac surgery.<br />
Methods<br />
We formed a Working Party consisting of four members<br />
from each society who were academics and clinicians<br />
with varied interests, including vascular<br />
anaesthesia, cardiology, elderly care medicine and general<br />
practice. We agreed on the scope of the guideline,<br />
and then carried out a systematic review with the quality<br />
of evidence described using the Grading of Recommendations<br />
Assessment, Development and Evaluation<br />
(GRADE) approach [7, 8]. The GRADE approach considers<br />
the quality of a body of evidence as high, moderate,<br />
low or very low. To achieve a full consensus<br />
document was important. Therefore, we consulted 20<br />
general practitioners, including those with a specialist<br />
interest in cardiovascular medicine, as well as senior<br />
academics. A consultation guideline was then made<br />
available to members of both societies for comment.<br />
We specifically asked for and received comments from<br />
the patient group, Blood Pressure UK. The comments<br />
and responses have been made available online. The<br />
Council and Executive of the respective societies were<br />
given the task of final approval.<br />
Blood pressure, hypertension and<br />
anaesthesia<br />
The anaesthetist has two broad considerations in the<br />
hypertensive patient who presents for surgery. One is<br />
to be cognisant of the effect of chronic hypertension<br />
on the individual’s peri-operative and long-term cardiovascular<br />
risk. The other is to consider whether the<br />
blood pressure measured in the primary care setting is<br />
associated with adverse peri-operative events and to<br />
decide whether this should be reduced before surgery.<br />
The association between hypertension and perioperative<br />
harm was first reported in the 1950s [9, 10].<br />
Systolic blood pressures in excess of 170 mmHg and<br />
diastolic blood pressures in excess of 110 mmHg were<br />
associated with complications such as myocardial<br />
ischaemia [11]. Hypertension was the second-most<br />
common factor associated with postoperative morbidity<br />
[12]. In 2003, Weksler et al. published a ‘quasi’-<br />
randomised controlled study of 989 treated hypertensive<br />
patients who had diastolic blood pressures<br />
between 110 and 130 mmHg measured in the anaesthetic<br />
room [13]. In one group, surgery proceeded<br />
after intranasal nifedipine, and in the other group, surgery<br />
was delayed while further antihypertensive treatment<br />
was pursued in hospital. During the first three<br />
postoperative days, the rates of neurological and cardiovascular<br />
complications were similar. One might<br />
conclude that there was no difference in an infrequent<br />
outcome, or that the study had insufficient power to<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland. 329
Anaesthesia 2016, 71, 326–337<br />
Management of hypertension before elective surgery guidelines<br />
detect a small difference (see section below, treatment<br />
for hypertension: extension of evidence from the community<br />
to the peri-operative period).<br />
The association of hypertension with cardiovascular<br />
disease is established, but there is no clear evidence<br />
that patients with stage 1 or 2 hypertension (Table 1)<br />
without evidence of target organ damage have<br />
increased peri-operative cardiovascular risk [14].<br />
Patients with stage 3 or 4 hypertension, who are more<br />
likely to have target organ damage, have not been subjected<br />
to rigorous randomised controlled trials of perioperative<br />
interventions. There is evidence that hypertension<br />
with target organ damage is associated with a<br />
small increased incidence of peri-operative major<br />
adverse cardiovascular events [4]. It is not known<br />
whether or not reducing blood pressure in these<br />
patients during a postponement of planned surgery<br />
would reduce this rate of events; there is sparse evidence<br />
to guide a decision. Any decision should take<br />
into account factors other than blood pressure, namely:<br />
age; comorbidity; functional capacity (i.e. functional<br />
status and reserve); and the urgency and indication for<br />
surgery (see section below, ‘The treatment of cardiovascular<br />
risk, not hypertension’). The latest guidelines<br />
published by the National Institute for Health and<br />
Care Excellence (NICE), in conjunction with the British<br />
Hypertension Society, recognise the importance of<br />
target organ damage in the management of hypertension<br />
by targeting a lower threshold for further medical<br />
intervention [1]. Whether or not these thresholds and<br />
targets should be rigorously applied in the peri-operative<br />
setting is not clear.<br />
Patients with hypertension (controlled or uncontrolled)<br />
demonstrate a more labile haemodynamic profile<br />
than their non-hypertensive counterparts [5]. The<br />
induction of anaesthesia and airway instrumentation<br />
can lead to a pronounced increase in sympathetic activation,<br />
which may lead to a significant increase in<br />
Table 1 Categorisation of the stages of hypertension.<br />
Category<br />
Systolic blood<br />
pressure; mmHg<br />
Diastolic blood<br />
pressure; mmHg<br />
Stage 1 140–159 90–99<br />
Stage 2 160–179 100–109<br />
Stage 3 180–209 110–119<br />
Stage 4 ≥ 210 ≥ 120<br />
blood pressure and heart rate. A reduction in systemic<br />
vascular resistance soon after the induction of anaesthesia<br />
commonly leads to varying degrees of hypotension.<br />
Reduction in vascular resistance is multifactorial<br />
and may be secondary to loss of the baroreceptor<br />
reflex control, central neuraxial blockade, and direct<br />
effects of anaesthetic agents. The effect on vascular<br />
tone will be exaggerated by ‘deep’ or excessive anaesthesia<br />
and in patients who are fluid-depleted. This,<br />
and the often exaggerated haemodynamic response to<br />
surgery, pain and emergence from anaesthesia, have<br />
also been described as being more common in the<br />
hypertensive population [6]. Some researchers have<br />
demonstrated an association between pre-operative<br />
hypertension and relatively minor physiological<br />
derangements such as intra-operative hypotension,<br />
hypertension and arrhythmia, but studies have not<br />
conclusively demonstrated that fluctuations in haemodynamic<br />
variables cause clinically significant harm<br />
[15]. Larger studies to investigate differences between<br />
untreated hypertensive patients and those treated (successfully<br />
and unsuccessfully) have not demonstrated<br />
increased rates of peri-operative cardiovascular events.<br />
However, these findings may not be applicable to current<br />
practice, as many of these studies were conducted<br />
in the late 1970s [16].<br />
This appreciation of labile haemodynamics in<br />
hypertensive patients has led to a number of anaesthetic<br />
techniques designed to achieve a more stable<br />
haemodynamic profile during surgery. These techniques<br />
include co-induction, invasive arterial monitoring<br />
with titrated or prophylactic vasopressor therapy,<br />
depth-of-anaesthesia monitoring, beta-blockers and the<br />
optimisation of stroke volume with intravascular fluid<br />
therapy. The omission of antihypertensive drugs, such<br />
as angiotensin-converting enzyme inhibitors and<br />
receptor blockers, combined with the careful reintroduction<br />
of these drugs after surgery, is commonplace<br />
and appears to be associated with fewer significant<br />
peri-operative haemodynamic fluctuations [17].<br />
The introduction of peri-operative beta-blockade for<br />
high cardiac-risk patients increases postoperative mortality,<br />
secondary to hypotension and stroke, albeit with<br />
less cardiac injury, as demonstrated in the POISE-1<br />
study [18]. The anaesthetist should be aware that sudden<br />
withdrawal of certain antihypertensive agents such<br />
330 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland.
Management of hypertension before elective surgery guidelines Anaesthesia 2016, 71, 326–337<br />
as clonidine, alpha-methyldopa and beta-blockers can<br />
be associated with adverse events. Withdrawal of<br />
beta-blockers may also be associated with myocardial<br />
ischaemia that is often silent in the peri-operative period<br />
and easily missed without continuous ECG monitoring<br />
and serial serum troponin measurements.<br />
Best practice: the measurement of<br />
blood pressure<br />
Blood pressure should be measured in primary care<br />
before non-urgent surgical referral (Fig. 1). Surgical<br />
outpatients should arrange for primary care to supply<br />
blood pressure readings if these have not been<br />
documented in the referral letter. Blood pressure<br />
should be measured by pre-operative assessment<br />
clinics in patients who attend the clinic without documented<br />
blood pressure readings from the last<br />
12 months. The measurement should follow the<br />
principles mandated for primary care (see below)<br />
[1]. Blood pressures less than 180 mmHg systolic<br />
and 110 mmHg diastolic in secondary care should<br />
not preclude elective surgery, although the patient<br />
Elective surgical referral appropriate<br />
No<br />
Measure blood pressure up to<br />
three times<br />
Mean<br />
SBP < 160 mmHg<br />
AND<br />
DBP < 100 mmHg<br />
in past year?<br />
Yes<br />
Refer<br />
Lowest SBP < 140 mmHg<br />
AND the lowest DBP <<br />
90 mmHg?<br />
Yes<br />
Refer<br />
No<br />
Lowest SBP < 160 mmHg<br />
AND the lowest DBP <<br />
100 mmHg?<br />
Yes<br />
Refer*<br />
No<br />
ABPM or HBPM<br />
Mean ‘out of office’<br />
SBP < 150 mmHg AND<br />
the mean DBP < 95<br />
mmHg?<br />
Yes<br />
Refer*<br />
No<br />
Treat until ‘clinic’ SBP < 160 mmHg<br />
AND DBP < 100 mmHg<br />
Refer*<br />
Figure 1 Primary care blood pressure assessment of patients before referral for elective surgery. *Investigations and<br />
treatment should continue to achieve blood pressures < 140/90 mmHg. ABPM and HBPM, ambulatory and home<br />
blood pressure measurement; DBP and SBP, diastolic and systolic blood pressure.<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland. 331
Anaesthesia 2016, 71, 326–337<br />
Management of hypertension before elective surgery guidelines<br />
should be asked to attend their general practice for<br />
the concurrent determination of whether primary<br />
care hypertension is present.<br />
The setting in which blood pressure is measured<br />
should be relaxed and temperate in a standardised<br />
environment with current calibrated equipment. The<br />
seated patient should have their supported arm outstretched<br />
for at least one minute before the initial<br />
reading. The pulse rate and rhythm should be<br />
recorded before the blood pressure is measured by a<br />
validated device. Automated sphygmomanometers<br />
(www.bhsoc.org/bp-monitors) are inaccurate when the<br />
pulse is irregular, when the blood pressure should be<br />
measured by auscultation over the brachial artery during<br />
manual deflation of an arm cuff.<br />
Blood pressure should be measured in both arms<br />
in patients scheduled for vascular or renal surgery. If<br />
the difference between arms in systolic pressure is<br />
greater than 20 mmHg, repeat the measurements; subsequently,<br />
measure from the arm with the higher<br />
blood pressure.<br />
The patient is normotensive if the blood pressure<br />
measurement is less than 140/90 mmHg. If the first<br />
measurement is equal to or higher than 140/<br />
90 mmHg, the blood pressure should be measured<br />
twice more, with each reading at least one minute<br />
apart. The lower of the last two readings is recorded as<br />
the blood pressure; if it is less than 140/90 mmHg the<br />
patient is normotensive.<br />
If the reading is between 140/90 mmHg and 179/<br />
109 mmHg, the patient may have stage 1 or 2 hypertension.<br />
In primary care, the patient would be offered<br />
ambulatory (ABPM) or home blood pressure monitoring<br />
(HBPM) to establish their true blood pressure<br />
(GRADE 1B). If the reading is equal to or higher than<br />
180/110 mmHg in primary care, the patient may have<br />
severe hypertension and would be considered for<br />
immediate treatment.<br />
Best practice: the diagnosis of<br />
hypertension<br />
General practitioners should establish whether blood<br />
pressure has been measured and managed in all adults<br />
before non-urgent surgical referrals. A blood pressure<br />
measurement taken within the preceding 12 months<br />
should be detailed in the referral letter.<br />
The diagnosis of hypertension in patients<br />
referred for investigation of surgical disease that are<br />
not treated for hypertension and who have not had<br />
a blood pressure measurement in the preceding<br />
12 months follows the same process as any other<br />
primary care patient. We recommend that the practice<br />
instigates ambulatory or home blood pressure<br />
measurements before non-urgent referrals if the standard<br />
blood pressure is equal to or greater than 160/<br />
100 mmHg. If the patient’s ABPM/HBPM blood<br />
pressure is equal to or greater than 150/95 mmHg<br />
(or equal to or greater than 135/85 mmHg with target<br />
organ damage), the patient is diagnosed as having<br />
hypertension; treatment should be discussed and<br />
commenced using the NICE/BHS CG127 algorithm<br />
[19]. This process can take place at the same time<br />
as urgent surgical referral, but a reduction in blood<br />
pressure to less than 160/100 mmHg should precede<br />
non-urgent surgical referral. The referral letter<br />
should document that an informed discussion has<br />
taken place with patients who decline treatment, or<br />
detail that all appropriate attempts have been made<br />
to reduce blood pressure for patients with persistent<br />
hypertension, which might have included specialist<br />
investigations.<br />
Surgical outpatients should request that general<br />
practitioners forward primary care blood pressure<br />
measurements if these have not been documented in<br />
the referral letter. Pre-operative assessment clinics<br />
should measure the blood pressures of patients who<br />
present without documentation of primary care blood<br />
pressures. If the blood pressure is raised above<br />
180 mmHg systolic or 110 mmHg diastolic, the patient<br />
should return to their general practice for primary care<br />
assessment and management of their blood pressure,<br />
as detailed above (Fig. 2). If the blood pressure is<br />
above 140 mmHg systolic or 90 mmHg diastolic, but<br />
below 180 mmHg systolic and below 110 mmHg diastolic,<br />
the GP should be informed, but elective surgery<br />
should not be postponed.<br />
Best practice: the treatment of<br />
hypertension<br />
This section summarises the recommendations for primary<br />
care following the diagnosis of hypertension.<br />
There is good evidence (GRADE 1A) for the treatment<br />
332 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland.
Management of hypertension before elective surgery guidelines Anaesthesia 2016, 71, 326–337<br />
Surgeon receives referral<br />
No<br />
Documented<br />
SBP < 160 mmHg<br />
AND<br />
DBP < 100 mmHg<br />
in past year?<br />
Yes<br />
Proceed<br />
Request measurements from GP<br />
Lowest SBP < 160 mmHg<br />
AND the lowest DBP <<br />
100 mmHg?<br />
Yes<br />
Proceed<br />
No<br />
Measure blood pressure up to<br />
three times<br />
Lowest SBP < 180 mmHg<br />
AND the lowest DBP <<br />
110 mmHg?<br />
Yes<br />
Proceed*<br />
No<br />
Refer back to GP*<br />
Figure 2 Secondary care blood pressure assessment of patients after referral for elective surgery. *The GP should be<br />
informed of blood pressure readings in excess of 140 mmHg systolic or 90 mmHg diastolic, so that the diagnosis of<br />
hypertension can be refuted or confirmed and investigated and treated as necessary. DBP and SBP, diastolic and systolic<br />
blood pressure.<br />
of hypertension with one or more of the following:<br />
diuretics (thiazide, chlorthalidone and indapamide);<br />
beta-blockers; calcium channel-blockers (CCB); angiotensin<br />
converting enzyme (ACE) inhibitors, or an<br />
angiotensin-2 receptor blocker (ARB) [1]. In the<br />
future, the threshold for treating high blood pressure<br />
might change to cardiovascular risk (see below, the<br />
treatment of cardiovascular risk, not hypertension).<br />
Step 1 treatment<br />
Patients aged less than 55 years should be offered an<br />
ACE inhibitor, or a low-cost ARB. If an ACE inhibitor<br />
is prescribed but is not tolerated (for example,<br />
because of cough), offer a low-cost ARB. Angiotensin-converting<br />
enzyme inhibitors and ARBs are not<br />
recommended in women of childbearing potential.<br />
An ACE inhibitor should not be combined with<br />
an ARB.<br />
Patients aged over 55 years and Black patients of<br />
African or Caribbean family origin of any age should<br />
be offered a CCB. If a CCB is not suitable, for example<br />
because of oedema or intolerance, or if there is evidence<br />
of heart failure or a high risk of heart failure, a<br />
thiazide-like diuretic should be offered.<br />
If diuretic treatment is to be initiated or changed,<br />
offer a thiazide-like diuretic, such as chlorthalidone<br />
(12.5–25.0 mg once daily), or indapamide (1.5 mg<br />
modified-release once daily or 2.5 mg once daily), in<br />
preference to a conventional thiazide diuretic such as<br />
bendroflumethiazide or hydrochlorothiazide.<br />
For patients who are already having treatment<br />
with bendroflumethiazide or hydrochlorothiazide<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland. 333
Anaesthesia 2016, 71, 326–337<br />
Management of hypertension before elective surgery guidelines<br />
and whose blood pressure is stable and well controlled,<br />
treatment with the bendroflumethiazide or<br />
hydrochlorothiazide should be continued.<br />
Beta-blockers are not a preferred initial therapy<br />
for hypertension. However, beta-blockers may be<br />
considered in younger patients, particularly those<br />
with an intolerance or contraindication to ACE inhibitors<br />
and ARBs, or women of childbearing potential<br />
or patients with evidence of increased sympathetic<br />
drive. If beta-blockers are started and a second drug<br />
is required, add a CCB rather than a thiazide-like<br />
diuretic to reduce the person’s risk of developing<br />
diabetes.<br />
Step 2 treatment<br />
If blood pressure is not controlled by Step 1 treatment,<br />
use a CCB in combination with either an ACE inhibitor<br />
or an ARB.<br />
If a CCB is not suitable for Step 2 treatment, for<br />
example because of oedema or intolerance, or if there<br />
is evidence of heart failure or a high risk of heart failure,<br />
offer a thiazide-like diuretic.<br />
For Black patients of African or Caribbean family<br />
origin, consider an ARB in preference to an ACE inhibitor,<br />
in combination with a CCB.<br />
Step 3 treatment<br />
Before considering Step 3 treatment, check that drugs<br />
from Step 2 have been prescribed at optimal doses, or<br />
at the maximum tolerated doses. If treatment with<br />
three drugs is required, the combination of ACE inhibitor<br />
or ARB, CCB and thiazide-like diuretic should be<br />
used.<br />
Step 4 treatment<br />
If resistant blood pressure exceeds 140/90 mmHg in<br />
clinic after treatment with the optimal or highest-tolerated<br />
doses of an ACE inhibitor, or an ARB plus a<br />
CCB, with a diuretic; adding a fourth antihypertensive<br />
drug and expert advice should be considered.<br />
Further diuretic therapy with low-dose spironolactone<br />
(25 mg once daily) should be considered if the<br />
serum potassium concentration < 4.6 mmol.l<br />
1 . Caution<br />
is required in patients with reduced estimated<br />
glomerular filtration rates because of an increased risk<br />
of hyperkalaemia. Increasing the dose of thiazide-like<br />
diuretics should be considered if the serum potassium<br />
concentration > 4.5 mmol.l<br />
1 .<br />
Serum sodium and potassium concentrations and<br />
renal function should be checked within 1 month of<br />
increasing diuretic dose, and repeated as required<br />
thereafter. If further diuretic therapy for resistant<br />
hypertension at Step 4 is not tolerated, or is contraindicated<br />
or ineffective, consider an alpha-blocker<br />
or beta-blocker. If blood pressure remains uncontrolled<br />
with the optimal or maximum tolerated doses of four<br />
drugs, expert advice should be sought if it has not yet<br />
been obtained.<br />
As recently as 2008, the HYVET study demonstrated<br />
the clinical benefits of treating hypertension in<br />
people aged ≥ 80 years, while health economic analysis<br />
has confirmed the cost effectiveness of this strategy [1,<br />
20]. As a result, NICE now recommends that patients<br />
aged ≥ 80 years should be offered treatment only if<br />
they have stage 2 hypertension. The 2011 Hypertension<br />
Guideline also recommends that the decision to<br />
treat should be based on standing blood pressure, and<br />
should take into account the presence of co-morbidities<br />
such as dementia. The guideline also makes a distinction<br />
between initiating treatment in the over-80s<br />
and continuing long-term and well-tolerated treatment<br />
when patients reach this age. In other words, patients<br />
who were started on treatment when younger should<br />
not have their current therapy back-titrated when they<br />
celebrate their 80th birthday.<br />
The treatment of cardiovascular risk,<br />
not hypertension<br />
It is likely that treatment for hypertension will no<br />
longer be based upon blood pressure [21]. This is a<br />
surprising statement; the diagnosis of hypertension<br />
that merits treatment has – until recently – been based<br />
on patients’ blood pressure, irrespective of other cardiovascular<br />
risk factors, despite the NICE guidance<br />
recognising their importance [1]. This practice conflicts<br />
with the treatment of hypercholesterolaemia,<br />
which is not based on the cholesterol concentration<br />
alone, but instead on the composite 5- or 10-year risk<br />
of: stroke; myocardial infarction; heart failure; cardiovascular<br />
morbidity; or death, ascribed to these diagnoses.<br />
The magnitude by which cardiovascular disease<br />
is reduced by treatment for both hypercholesterolaemia<br />
334 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland.
Management of hypertension before elective surgery guidelines Anaesthesia 2016, 71, 326–337<br />
and hypertension is dependent on the composite cardiovascular<br />
risk, not the concentration of cholesterol<br />
or the blood pressure. Anaesthetists should gauge their<br />
concern for a hypertensive patient by the calculated<br />
five-year rate of cardiovascular events, not by the<br />
blood pressure measurement per se.<br />
Hypertension is common; this is responsible for<br />
the well-publicised reduction in population rates of<br />
stroke by antihypertensive treatment. The absolute<br />
effect of treatment for the individual, even over a fiveyear<br />
period, is smaller than many anaesthetists might<br />
realise. Table 2 presents the effect of five-year antihypertensive<br />
treatment for cardiovascular risk in a population<br />
quartered by the five-year rate of any<br />
cardiovascular event. Planned major surgery temporarily<br />
increases mortality. For instance, planned open<br />
repair of abdominal aortic aneurysm increases mortality<br />
in the first postoperative month ten times, whereas<br />
endovascular repair increases mortality four times. If<br />
cardiovascular events are similarly increased by major<br />
planned surgery, one would anticipate that the preoperative<br />
antihypertensive treatment of cardiovascular<br />
risk would have a proportionately greater absolute<br />
effect on the rates of events while their risk remains<br />
elevated. Table 3 illustrates the absolute effect of established<br />
antihypertensive treatment in the month following<br />
a planned operation in patients from Table 2,<br />
assuming two scenarios: that the operation does not<br />
affect the rates of cardiovascular events; and that the<br />
operation increases the rates of cardiovascular events<br />
six times.<br />
This guideline has outlined that blood pressure<br />
before planned non-urgent surgery is measured in primary<br />
care, where the diagnosis of hypertension is<br />
Table 2 The effect of antihypertensive treatment on the five-year rates of events (per 1000) in a population quartered<br />
on the basis of the untreated cardiovascular five-year risk: lowest quartile (< 11% risk); next quartile (11–15%<br />
risk); next quartile (15–21% risk); highest quartile (> 21% risk).<br />
Any event Stroke CHD Heart failure<br />
No<br />
Quartile of risk treatment Treatment No treatment Treatment No treatment Treatment No treatment Treatment<br />
Highest quartile<br />
Event rates 270/1000 232/1000 70/1000 58/1000 63/1000 53/1000 47/1000 34/1000<br />
Event reduction 38/1000 12/1000 10/1000 13/1000<br />
Second quartile<br />
Event rates 180/1000 156/1000 49/1000 40/1000 42/1000 36/1000 27/1000 23/1000<br />
Event reduction 24/1000 9/1000 6/1000 4/1000<br />
Third quartile<br />
Event rates 120/1000 100/1000 36/1000 29/1000 33/1000 28/1000 15/1000 13/1000<br />
Event reduction 20/1000 7/1000 5/1000 2/1000<br />
Lowest quartile<br />
Event rates 60/1000 46/1000 17/1000 11/1000 17/1000 14/1000 6/1000 5/1000<br />
Event reduction 14/1000 6/1000 3/1000 1/1000<br />
CHD, coronary heart disease.<br />
Table 3 The absolute reduction in event rates per 1000 patients per month by antihypertensive treatment, assuming<br />
that the control rate is unaffected by surgery (‘same’) or increased, in this example sixfold (‘9 6’).<br />
Any event Stroke CHD Heart failure<br />
Quartile of risk Same 3 6 Same 3 6 Same 3 6 Same 3 6<br />
Highest quartile 0.6 3.8 0.2 1.2 0.2 1 0.2 1.3<br />
Next quartile 0.4 2.4 0.2 0.9* 0.1 0.6 0.1 0.4<br />
Next quartile 0.3 1.8 0.1 0.7 0.1 0.6 0.0 0.2<br />
Lowest quartile 0.2 1.2 0.1 0.6 0.1 0.3 0.0 0.1<br />
*The ‘0.2’ was rounded up from a value near 0.15, which is why this value 9 6 is 0.9, not 1.2.<br />
CHD, coronary heart disease.<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland. 335
Anaesthesia 2016, 71, 326–337<br />
made, and treatment is managed. The lifelong risk of<br />
mortality and morbidity may be unaffected by postponing<br />
surgery for the assessment of cardiovascular<br />
risk by primary care and possible antihypertensive<br />
treatment [22]. For instance, clinicians might like to<br />
consider the uncertainty in how long it takes for cardiovascular<br />
risk to fall with antihypertensive medication<br />
(as opposed to how long it takes for blood<br />
pressure to fall), and the 1% relative increase in cardiovascular<br />
risk that accompanies each postponed<br />
month, due to the patient ageing. Clinicians might also<br />
consider that patients who smoke or who have hypercholesterolaemia<br />
are not subjected to the summary cancellations<br />
justified by blood pressure readings. A<br />
further consideration is the absence of a scale of<br />
enthusiasm for postponing surgery that matches the<br />
continuum of cardiovascular risk, which would result<br />
in older smoking hypercholesterolaemic normotensive<br />
men having surgery postponed more frequently than<br />
younger hypertensive women who do not have any<br />
other cardiovascular risk factors.<br />
Communication<br />
Pre-operative assessment clinics should inform general<br />
practitioners when they measure raised blood pressures<br />
in patients who have not had readings taken in primary<br />
care in the preceding 12 months. The letter<br />
should request that the general practitioner determine<br />
whether the patient has hypertension in primary care.<br />
The letter should also state whether or not surgery will<br />
proceed without a diagnosis of hypertension being<br />
made or treatment commenced.<br />
Appendix 1 is an example of a letter explaining<br />
that surgery will not proceed until the diagnosis of<br />
hypertension has been excluded or confirmed, and in<br />
the latter case treated with the patient’s consent. It is<br />
important that the patient has a copy and is instructed<br />
to make an appointment at their surgery with a nurse<br />
or a doctor and to take the letter with them. The language<br />
used should seek cooperative management<br />
rather than demand action. In the first instance, the<br />
GP will need to establish that the blood pressure is<br />
high and this is not a white coat effect. It must be<br />
clearly stated how to re-establish the procedural pathway<br />
when the blood pressure has been shown to be<br />
satisfactory, treated or not.<br />
Management of hypertension before elective surgery guidelines<br />
References<br />
1. National Institute for Health and Care Excellence. Hypertension:<br />
Clinical management of primary hypertension in adults.<br />
2011 NICE Clinical Guideline CG127. http://www.nice.org.uk/<br />
guidance/cg127 (accessed 15/01/2015).<br />
2. Cook TM, Woodall N, Frerk C. Fourth National Audit Project.<br />
Major complications of airway management in the UK: results<br />
of the Fourth National Audit Project of the Royal College of<br />
Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia.<br />
British Journal of Anaesthesia 2011; 106: 617–31.<br />
3. Cook TM, Andrade J, Bogod DG, et al. The 5th National Audit<br />
Project (NAP5) on accidental awareness during general anaesthesia:<br />
patient experiences, human factors, sedation, consent<br />
and medicolegal issues. Anaesthesia 2014; 69: 1102–16.<br />
4. Howell SJ, Sear JW, Foex P. Hypertension, hypertensive heart<br />
disease and perioperative cardiac risk. British Journal of<br />
Anaesthesia 2004; 92: 57–83.<br />
5. Longnecker DE. Alpine anesthesia: can pretreatment with<br />
clonidine decrease the peaks and valleys? Anesthesiology<br />
1987; 67: 1–2.<br />
6. Prys-Roberts C, Greene LT, Meloche R, Foex P. Studies of<br />
anaesthesia in relation to hypertension II. Haemodynamic<br />
consequences of induction and endotracheal intubation.<br />
British Journal of Anaesthesia 1971; 43: 531–47.<br />
7. Guyatt GH, Oxman AD, Kunz R, et al. Going from evidence to<br />
recommendations. British Medical Journal 2008; 336: 1049–<br />
51.<br />
8. Guyatt GH, Oxman AD, Vist G, et al. for the GRADE Working<br />
Group. Rating quality of evidence and strength of recommendations<br />
GRADE: an emerging consensus on rating quality of<br />
evidence and strength of recommendations. British Medical<br />
Journal 2008; 336: 924–6.<br />
9. Smithwick RH, Thompson JE. Splanchnicectomy for essential<br />
hypertension; results in 1,266 cases. Journal of the American<br />
Medical Association 1953; 152: 1501–4.<br />
10. Thompson JE, Smithwick RH. Surgical measures in hypertension.<br />
Geriatrics 1953; 8: 611–9.<br />
11. Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial<br />
index of cardiac risk in noncardiac surgical procedures. New<br />
England Journal of Medicine 1977; 297: 845–50.<br />
12. Khuri SF, Daley J, Henderson W, et al. The National Veterans<br />
Administration surgical risk study: risk adjustment for the<br />
comparative assessment of the quality of surgical care. Journal<br />
of the American College of Surgeons 1995; 180: 519–31.<br />
13. Weksler N, Klein M, Szendro G, et al. The dilemma of immediate<br />
preoperative hypertension: to treat and operate, or to<br />
postpone surgery? Journal of Clinical Anesthesia 2003; 15:<br />
179–83.<br />
14. Hanada S, Kawakami H, Goto T, et al. Hypertension and anesthesia.<br />
Current Opinion in Anaesthesiology 2006; 19: 315–9.<br />
15. Chung F, Mezei G, Tong D. Pre-existing medical conditions as<br />
predictors of adverse events in day case surgery. British Journal<br />
of Anaesthesia 1999; 83: 262–70.<br />
16. Goldman L, Caldera DL. Risks of general anesthesia and elective<br />
operation in the hypertensive patient. Anesthesiology<br />
1979; 50: 285–92.<br />
17. Comfere T, Sprung J, Kumar MM, et al. Angiotensin system<br />
inhibitors in a general surgical population. Anesthesia and<br />
Analgesia 2005; 100: 636–44.<br />
18. Devereaux PJ, Yang H, Yusuf S, et al. Effects of extended<br />
release metoprolol succinate in patients undergoing non-cardiac<br />
surgery (POISE trial): a randomised controlled trial. Lancet<br />
2008; 371: 1839–47.<br />
336 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland.
Management of hypertension before elective surgery guidelines Anaesthesia 2016, 71, 326–337<br />
19. Hypertension Pathyways. http://pathways.nice.org.uk/pathways/<br />
hypertension#path=view%3A/pathways/hypertension/diagnosisand-assessment-of-hypertension.xml&content=view-index<br />
(accessed<br />
16/01/2015).<br />
20. Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension<br />
in patients 80 years of age or older. New England<br />
Journal of Medicine 2008; 358: 1958–60.<br />
21. Sundstr€om J, Arima H, Woodward M, et al. on behalf of the<br />
Blood Pressure Lowering Treatment Trialists’ Collaboration.<br />
Blood pressure-lowering treatment based on cardiovascular<br />
risk: a meta-analysis of individual patient data. Lancet 2014;<br />
384: 591–8.<br />
22. Carlisle JB. Too much blood pressure? Anaesthesia 2015; 70:<br />
773–8.<br />
Appendix 1<br />
Example of letter to general practitioner from pre-assessment clinic following measurement of raised blood pressure<br />
in patients who have not had readings taken in primary care in the preceding 12 months.<br />
Dear Doctor<br />
Unfortunately, the procedure for Mr/Ms ...................... has been postponed because their blood pressure was<br />
found to be 182/114 in their pre-operative assessment. It was measured several times following the AAGBI/BHS guidelines.<br />
The guidelines suggest a blood pressure level higher than 180/110 is unsuitable for elective anaesthesia.<br />
We have asked the patient to make an appointment at their surgery for further assessment of their blood pressure. We<br />
would be grateful if you could verify that this is the true blood pressure level and not a white coat effect and treat appropriately<br />
if the patient has hypertension.<br />
We will be pleased to accept the patient back for surgery if their clinical blood pressure is below 160/100. Please<br />
ask the patient to contact ........................... and inform us of their current blood pressure and what medication,<br />
if any, was required to achieve this.<br />
Many thanks in anticipation of your help with this matter<br />
The following GPs were consulted about this letter:<br />
Dr Chris Arden, Dr Ivan Benett, Dr Mark Davis, Dr Richard Falk, Prof David Fitzmaurice, Prof Ahmet Fuat, Dr<br />
Napa Gopi, Dr Kathryn Griffith, Dr Rosie Heath, Prof Richard Hobbs, Dr Paul Johnson Prof Richard McManus, Dr<br />
Jonathan Morrell, Dr Washik Parkar, Dr Neil Paul, Dr Jon Pittard, Dr Peter Savill, Dr Jonathan Shribman, Dr Harjit<br />
Singh, Dr Heather Wetherell.<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland. 337
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
in<br />
s<br />
ca<br />
Ultrasound in Anaesthesia and Intensive Care:<br />
A Guide to Training<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
The Royal College of Anaesthetists<br />
The Intensive Care Society<br />
July 2011
Membership of the working party<br />
(Details correct at the start of the working party process)<br />
Dr N M Denny<br />
Dr K Fox<br />
Dr C Gillbe<br />
Dr A W Harrop-Griffiths<br />
Dr M Jones<br />
Dr N Love<br />
Dr P MacNaughton<br />
Dr R McWilliams<br />
Dr B Nicholls<br />
Dr P Nightingale<br />
Dr J Pilcher<br />
Dr S Price<br />
Mr J Sloan<br />
Dr S Ward<br />
AAGBI (Chair)<br />
British Society of Echocardiography<br />
AAGBI<br />
AAGBI<br />
Society for Acute Medicine<br />
Group of Anaesthetists in Training<br />
Intensive Care Society<br />
Royal College of Radiologists<br />
Regional Anaesthesia (UK)<br />
Royal College of Anaesthetists<br />
British Medical Ultrasound Society<br />
Intensive Care Society and British Society of<br />
Echocardiography<br />
College of Emergency Medicine<br />
British Pain Society<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
Website: www.<strong>aagbi</strong>.org<br />
The Royal College of Anaesthetists<br />
Churchill House, 35 Red Lion Square, London, WC1R 4SG<br />
Tel: 020 7092 1500<br />
Fax: 020 7092 1730<br />
Email: info@rcoa.ac.uk<br />
Website: www.rcoa.ac.uk<br />
The Intensive Care Society<br />
Churchill House, 35 Red Lion Square, London, WC1R 4SG<br />
Tel: 020 7280 4350<br />
Fax: 020 7280 4369<br />
Email: info@ics.ac.uk<br />
Website: www.ics.ac.uk<br />
1
Contents<br />
1. Introduction 3<br />
2. Clinical governance and ultrasound 10<br />
3. Recommended essential ultrasound knowledge and skills 11<br />
4. Regional anaesthesia and pain medicine 15<br />
5. Vascular procedures 21<br />
6. Thoracic ultrasound 25<br />
7. Abdominal ultrasound 30<br />
8. Echocardiography 34<br />
9. References 40<br />
Appendix 1 – RCoA DOPS form 43<br />
To be reviewed in 2016<br />
© The Association of Anaesthetists of Great Britain & Ireland, The Royal College of<br />
Anaesthetists and The Intensive Care Society 2011<br />
2
1. Introduction<br />
This document presents a goal for the delivery of training of procedures using<br />
ultrasound in anaesthesia and critical care. The document not only sets out a<br />
practice-based curriculum for those who already hold a Certificate of Completion of<br />
Training (CCT) but also describes how the trainee might organise their own training<br />
within the Royal College of Anaesthetists’ (RCoA’s) CCT curriculum or Out-of-<br />
Programme Training (OOPT) to match these aspirations.<br />
Over the last 10 years, ultrasound has developed into an indispensable tool in<br />
anaesthesia and intensive care. The combination of National Institute of Health<br />
and Clinical Excellence (NICE) guidance for central venous access [1] and the<br />
availability of small, portable, ‘point of care’ machines has led to the introduction<br />
and increasingly widespread use of ultrasound in clinical practice. More recently,<br />
further NICE guidance on the use of ultrasound for epidurals [2] and regional<br />
anaesthesia [3] has ensured that ultrasound is now deeply embedded within<br />
anaesthetic practice. Other uses now include: thoracic scanning for diagnosis and<br />
treatment of pleural effusions and pneumothoraces; abdominal scanning (Focused<br />
Assessment with Sonography in Trauma - FAST) looking for intra-abdominal<br />
fluid; and focused transthoracic echocardiography in non-traumatic resuscitation<br />
(Focused Echocardiography in Emergency Life support – FEEL).<br />
The widespread introduction of ultrasound has brought with it many concerns<br />
relating to competency and training. Ultrasound is not new to medicine but its<br />
use in anaesthesia is. With the greater availability of machines and an increasing<br />
number of clinical indications, it is important to remember that there is a<br />
requirement for employing hospitals to ensure that clinicians are competent in<br />
the use of any equipment used by an employee [4]. Ultrasound has a distinct<br />
learning curve and trainee usage is characterised by common novice behaviour and<br />
mistakes [5,6].<br />
The aim of this document is to produce a set of broad guidelines for current trainees<br />
and those who completed their formal training programmes before the introduction<br />
of ultrasound. Whilst the core knowledge and skills required to perform ultrasound<br />
are identical in both groups, it is recognised that the competencies will be gained<br />
in different ways. These can be termed the ‘trainee-based College programme<br />
pathway’ and the ‘practice pathway’ for non-trainees.<br />
Recommendations for the use of ultrasound for non–radiologists have been<br />
published by the Royal College of Radiologists (2005) [7], the European Federation<br />
of Societies for Ultrasound in Medicine and Biology (EFSUMB) [8] and the College<br />
of Emergency Medicine (CEM) [9]. The importance of these recommendations is<br />
that they specify both a training syllabus and requirements that should be met by an<br />
individual using ultrasound.<br />
3
Training should consist of both theoretical and practical aspects, and be modular<br />
in nature, allowing trainees to acquire different levels of competency depending<br />
upon the practical skills needed, with competency assessment and multidisciplinary<br />
training. The levels of training have been broadly divided into three (Levels 1, 2<br />
and 3), the boundaries of which are not precise and are difficult to define and, as<br />
such, should be seen as a guide to different levels of competence and experience.<br />
It is important to realise that an appropriate level of training in ultrasound is one<br />
that allows for the provision of a safe and effective ultrasound service. This may be<br />
purely diagnostic, predominately interventional or a clinically-focused service.<br />
Equivalent training and experience: the ‘Grandfather Clause’<br />
This working party recognises that many practitioners have received ad hoc<br />
training and have learned ultrasound techniques ‘on the job’. While this pathway<br />
is not prospectively supported, it is recognised that for many such individuals their<br />
knowledge and experience makes them entirely appropriate practitioners and<br />
teachers of others. Furthermore, clinicians from specialties other than anaesthesia<br />
or intensive care medicine may hold equivalent qualifications or training. The<br />
recognition and awarding of an equivalent qualification to one achievable by<br />
a structured training programme is termed a ‘Grandfather Clause’. Failure to<br />
recognise such individuals is likely to lead to a loss of training opportunities for<br />
others, and loss of enthusiasm by the individual. In general, the working party<br />
therefore encourages individuals to seek recognition rather than making this process<br />
obstructive.<br />
The following should be included in any application for recognition under these<br />
circumstances:<br />
• A description of the approximate number of scans performed and any<br />
relevant training experience obtained, e.g. sabbatical or work<br />
placements.<br />
• A description of the current job plan outlining the role ultrasound<br />
plays and the typical range of scanning techniques used with<br />
representative frequencies.<br />
• Confirmation that the individual is in a permanent UK NHS non-training<br />
post of Staff Grade, Associate Specialist, Specialty Doctor or Consultant,<br />
including any UK recognised qualifications of training, e.g. FRCA.<br />
• A declaration from the Service Director, Governance Lead or Ultrasound<br />
Lead confirming substantial experience in ultrasound and ongoing use in<br />
clinical practice.<br />
• Any equivalent training or recognition awarded by other specialties, e.g.<br />
CEM Level 1 and 2 ultrasound, British Society of Echocardiography (BSE)<br />
certification, or similar.<br />
• Any further information demonstrating experience and knowledge of<br />
ultrasound, e.g. developing a service.<br />
4
There is at present no specific body to award such ‘Grandfather’ status, but with the<br />
increased development of ultrasound groups within hospitals to monitor the use and<br />
training of non-radiology ultrasound, these groups may fulfil this role. In awarding<br />
equivalence of training, clinicians need to ensure they keep up to date with<br />
developments in ultrasound and, where feasible, obtain appropriate qualifications<br />
in their sphere of practice. The status of ‘Grandfather’ will need to be agreed by<br />
the head of that individual’s department and the head of Clinical Governance.<br />
This ‘Grandfather Clause’ should be withdrawn in the future when robust training<br />
capacity exists.<br />
Training levels<br />
The concept of levels of training is a way of standardising training requirements<br />
across specialties. These levels are a guide to training and do not necessarily<br />
correspond to individual College recommendations and curriculum needs, e.g. CEM<br />
Level 1 is the standard of knowledge and practice that Emergency Medicine doctors<br />
should have in the future. This is also the case in anaesthesia and intensive care,<br />
where the use of ultrasound is not routinely practised or taught in all departments.<br />
Currently, it is likely that only a few trainees in anaesthesia or intensive care will<br />
be trained to be a Level 1 practitioner in all the aspects of ultrasound applicable to<br />
their clinical practice. Therefore, although Level 1 is the desired level of training for<br />
all trainees, it is at present too comprehensive to be achievable within the current<br />
RCoA curriculum.<br />
Level 1 – core training<br />
This is the expected standard of knowledge and practice that anaesthetic and<br />
intensive care consultants should have in the future and that should be achievable<br />
during normal postgraduate specialist training.<br />
Level 1 practice may be defined by the following generic competencies:<br />
• Ability to perform common examinations and interventions safely and<br />
accurately.<br />
• Ability to recognise normal and abnormal anatomy and pathology.<br />
• Ability to use ultrasound in real time to guide common invasive<br />
procedures (Level 1 specific to anaesthesia and intensive care).<br />
• Ability to recognise when referral for a second opinion is indicated.<br />
• Ability to understand the benefits of ultrasound imaging and its value and<br />
relationship to other imaging modalities used in anaesthesia and<br />
intensive care, e.g. x-ray.<br />
In the future, Level 1 will be considered to be core and fundamental to the practice<br />
of anaesthesia and intensive care, and the components therefore considered<br />
essential parts of a specialist training programme. At present there is no restriction<br />
on the training that can be achieved within an anaesthetic and intensive care<br />
training programme, and it may be common to find individuals who have Level 1<br />
5
training in certain areas and Level 2 training in others at the time of completion of<br />
training and award of a CCT.<br />
Level 2 – extended training<br />
This is a more advanced level of practice and can be considered extended.<br />
This would be the expected level of practice for those with a special interest in<br />
ultrasound. A Level 2 practitioner would have the following abilities:<br />
• Significant experience of Level 1 practice, e.g. >12 months.<br />
• Ability to perform the complete range of examinations in the area of practice.<br />
• Ability to recognise significant pathology within the relevant organ system.<br />
• Ability to use ultrasound to guide the full range of procedures in the particular<br />
area of practice.<br />
• Ability to act as mentor and trainer for Level 1 practitioners.<br />
• Ability to accept referrals from Level 1 practitioners.<br />
Level 2 practice is likely to require a period of additional training and experience<br />
beyond that obtained during normal postgraduate specialist training and the RCoA’s<br />
requirements for a CCT. A modular nature of practice is proposed such that an<br />
individual may be a Level 2 practitioner in one area of ultrasound practice, e.g.<br />
vascular access, and Level 1 in another, e.g. regional anaesthesia.<br />
Level 3 – advanced training<br />
This is an advanced level of practice and is equivalent to a consultant<br />
radiologist with a special interest in ultrasound or a cardiologist specialising in<br />
echocardiography. A Level 3 practitioner will be able to accept referrals from Level<br />
2 practitioners and perform specialised examinations. They are involved in all areas<br />
of ultrasound training and may undertake research within the field of ultrasound.<br />
This level of practice is unlikely to be relevant to the majority of those practising<br />
anaesthesia and intensive care.<br />
Training<br />
Although the training pathway may differ between established specialists and<br />
trainees, the core content of the programme will be the same. The outcomes should<br />
also be the same for anaesthetists and others undertaking similar procedures.<br />
Theoretical training<br />
Preliminary theoretical training should cover relevant anatomy, the physics of<br />
ultrasound, levels and sophistication of equipment, image recording and reporting,<br />
artefacts and the relevance of other imaging. This element of training may be<br />
delivered by existing national courses, local ‘in-house’ courses or by the use of<br />
e-learning modules.<br />
Practical training<br />
Practical training should include both training with phantoms and models before<br />
6
using ultrasound in a clinical situation. Practical experience should be gained<br />
under the guidance of a named supervisor trained in ultrasound. Practical training<br />
should focus on demonstrating competence rather than performance of an arbitrary<br />
number of procedures undertaken. However, to ensure optimal training and timely<br />
acquisition of the required competencies, practical training should involve frequent<br />
supervised examinations. In all cases involving a patient, an explanation of the<br />
technique and consent must be obtained before initiating a practical procedure; this<br />
is even more important in a training situation. A logbook of all training cases should<br />
be kept and ideally should include a number of more detailed case studies. The<br />
ability to store ultrasound images (still and video) for later review is an invaluable<br />
part of training and is essential in certain areas such as echocardiography. The<br />
trainee should ensure that all examinations performed during training are logged.<br />
Examinations should concentrate on the core areas of practice. A competency<br />
assessment sheet should be completed for each area of practice during the course<br />
of training, as it will help to determine in which area(s) the trainee can practise<br />
independently.<br />
Generic training<br />
Training pathways<br />
The training pathway will differ between those who are established anaesthetists<br />
with no previous ultrasound experience, those who have been practising ultrasound<br />
without formal competency assessment, those who have achieved formal<br />
competency in other modules, and specialist trainees in anaesthetics.<br />
Clinical practice pathway<br />
For established anaesthetists, with no previous experience of ultrasound, practical<br />
training will depend upon exposure to it and should be based on a combination<br />
of in-house and external courses. A basic skills and knowledge course (outlined<br />
below) is mandatory before practising on patients. All departments need to develop<br />
a training programme that is appropriate for them, but the following strategies are<br />
useful.<br />
1. Complete basic knowledge and skills course; consider e-learning<br />
modules or web-based courses.<br />
2. Attendance at a dedicated ‘hands-on’ ultrasound course.<br />
3. Practise of normal scanning on colleagues or volunteers.<br />
4. Use of web-based courses and textbooks.<br />
5. Use ultrasound on patients, with their consent, under supervision by a<br />
recognised trainer.<br />
6. Use of commercially available or ‘home-made’ phantoms or meat<br />
products to practise ultrasound-guided needle co-ordination.<br />
7. Clinical practice should be supervised by a Level 2 practitioner or a<br />
Level 1 practitioner with at least 12 months’ experience.<br />
In addition to the suggested competency assessments described below, clinicians<br />
7
should keep a logbook of cases that may include some key images. This could<br />
form part of an overall ultrasound portfolio that would include documentation<br />
of theoretical and practical training and assessments, any related self-audit and<br />
relevant Continuous Professional Development (CPD) teaching. Ideally, those<br />
clinicians already practising without formal competency review should, for the<br />
purposes of appraisal and good clinical governance, seek some form of recognition,<br />
e.g. a letter from a recognised Level 2 practitioner or radiologist confirming their<br />
competency.<br />
Trainee pathway<br />
Although ultrasound is yet to be formally incorporated into the RCoA curriculum, it<br />
is being increasingly taught by ultrasound enthusiasts during trainees’ subspecialty<br />
attachments. Much of the core learning can be self-driven through a variety of<br />
educational media, or possibly by linking to one of the university courses with<br />
Consortium for the Approval of Sonographic Education (CASE) approval [10].<br />
Practical training should ideally be on a weekly basis and overseen by a named<br />
supervisor. A logbook of all training cases should be kept and ideally should include<br />
a number of more detailed case studies.<br />
1. Basic knowledge/skills course (vide supra).<br />
2. Practical training should be overseen by a clinical supervisor at least Level 1.<br />
3. If practical training is not possible in the current training scheme, the trainee<br />
should consider applying through the Deanery for OOPT or Out-of-Programme<br />
Experience (OOPE) [11].<br />
It is envisaged that all anaesthetists using ultrasound need to know and have the<br />
basic skills and competencies outlined in this section. Thereafter, trainees will<br />
follow the training curriculum, and everyone else will follow a clinically based<br />
pathway.<br />
Trainers<br />
Level 1 training should be delivered by a Level 2 practitioner or a Level 1<br />
practitioner with at least 12 months’ experience. The modular nature of training<br />
allows trainers to be competent to train in a focused area of practice, e.g. vascular<br />
access, without needing to be proficient in all areas of ultrasound practice. To<br />
become a Level 2 practitioner, the appropriate level of experience and competence<br />
must be demonstrated by completion of a logbook. A Level 2 practitioner will need<br />
to undertake frequent examinations commensurate with their area of practice. In<br />
addition, an existing Level 2 practitioner will need to confirm that they have the<br />
required competencies. Although there is no formal recognition or certification of<br />
‘level of training’, it is beholden upon the individual clinician to act responsibly and<br />
meet the competencies necessary for the level of personal practice and revalidation<br />
in the area of expertise. These can be enhanced by personal CPD and completion<br />
and maintenance of a current log book. For trainees, assessment will be under the<br />
auspices of their respective Colleges and approved trainers. For all others, it will be<br />
8
up to individual departments to train and assess competencies using this document<br />
as a guide, the use of either individual hospitals’ assessment tools or College-based<br />
assessment tools are to be encouraged. Overall training will be achieved by a<br />
combination of CPD recognised external courses as well as ‘in-house’ training.<br />
Basic skills and knowledge training<br />
All clinicians should be familiar with some basic concepts and practicalities before<br />
placing an ultrasound probe on a patient with the intention of either making a<br />
diagnosis or performing a practical procedure. Ultrasound is different to other<br />
commonly used imaging modalities and as such an understanding of the basic<br />
physics is mandatory. The production of sound waves and their interaction with<br />
tissues is determined and limited by the laws of physics. Knowledge of these<br />
principles enables a clinician to optimise the image with respect to the ultrasound<br />
frequency, probe design, focus and gain. The resulting image is formed from<br />
reflection of the ultrasound waves from multiple tissue interfaces. This reflection<br />
is dependent on the angle of the ultrasound beam, the ultrasound frequency used<br />
and tissue characteristics, which will be weaker at increasing depths. Accurate<br />
interpretation of the image is made with a knowledge of the ultrasound appearances<br />
of the different tissue seen, e.g. veins and arteries, nerves, muscle, bone and pleura,<br />
and the common artefacts encountered. Interpretation of any ultrasound image is<br />
dependent on a thorough and detailed knowledge of the anatomy of the area of<br />
interest. It is important to understand that when using ultrasound, you ‘only see<br />
what you know’: the structures are not labelled and may appear different from<br />
individual to individual.<br />
A variety of ultrasound machines is now available to clinicians, including small<br />
hand-held (pocket-size) devices, laptops and cart-based machines. These machines<br />
will have a variety of probes (hockey stick, linear, curvilinear and phased array)<br />
and preset imaging modalities (harmonic imaging, multibeam function, trapezoid<br />
display and 3D volume rendering). All this can lead to total confusion for an<br />
ultrasound novice; familiarity with the machine and its capabilities before use is<br />
vital.<br />
Theoretical training<br />
Theoretical training and assessment should be undertaken before using ultrasound<br />
in clinical situations, but sometimes this may go hand in hand with supervised<br />
clinical training. Preliminary theoretical training should cover relevant anatomy,<br />
the physics of ultrasound, machine familiarisation, image recording and reporting,<br />
artefacts and the relevance of other imaging modalities to ultrasound. This element<br />
of training may be delivered ‘in-house’ (using ‘Level 1 plus 12 months’ and Level<br />
2 practitioners: anaesthetists, radiologists, ultrasonographers, cardiac physiologists,<br />
cardiologists or medical physicists), and by distance learning or web-based<br />
packages. The identity of who delivers this training is not as important as the<br />
assessment of the individuals to ensure that they have understood and can apply<br />
this knowledge to clinical practice.<br />
9
2. Clinical governance and ultrasound<br />
Keeping records<br />
Logbook data of patients treated during training should be recorded in accordance<br />
with RCoA standards. It is recommended that electronic recordings of ultrasound<br />
examinations and anaesthetic or therapeutic interventions are made and<br />
retained during training. It is recommended that hospitals develop the routine<br />
electronic recording of all ultrasound examinations and anaesthetic or therapeutic<br />
interventions. Even after completing training in ultrasound-based skills, it is<br />
recommended that logbook data are continually recorded.<br />
Audit<br />
The success or failure of ultrasound-based interventions and complications of<br />
these interventions should be recorded to inform audit, appraisal and revalidation<br />
processes. When learning a new skill, cumulative sum control chart (CUSUM)<br />
analysis of success has been shown to be useful in the evaluation of ability and<br />
the need for supervision [12-14]. Even after training, a failure rate in excess of<br />
commonly accepted norms should cause the practitioner to seek advice and, if<br />
appropriate, remedial training.<br />
Maintenance of skills<br />
All manual skills need to be maintained, and it is recommended that after a break<br />
in the performance of an ultrasound-based intervention, the practitioner should<br />
be aware that their practical skills may have deteriorated. The individual has the<br />
responsibility to ensure that their skills are adequately maintained and should seek<br />
supervision where necessary. Having reached Level 1 competency, clinicians will<br />
need to maintain their ultrasound skills, minimising the time between successive<br />
examinations. The number of scans preformed should be commensurate with their<br />
area and level of practice. It is recommended that CPD time is directed towards<br />
ultrasound, either through educational meetings, self audit, or case reviews with a<br />
mentor.<br />
Clinical governance standards [15]<br />
It is the responsibility of individual hospitals to establish clinical governance<br />
processes that will determine the experience and training appropriate for the<br />
unsupervised performance of ultrasound-based examinations or interventions.<br />
Practitioners should make themselves aware of these processes and should only<br />
practise within local clinical governance guidelines. It is recommended that within<br />
each department a designated consultant or permanent member of staff competent<br />
at Level 2 or 3 should oversee ultrasound training and be responsible for basic<br />
training and competency assessment. These activities should form part of their job<br />
plan, and time should be allocated within the job plan for the proper fulfilment of<br />
these duties.<br />
10
3. Recommended essential ultrasound<br />
knowledge and skills<br />
Basics of ultrasound<br />
Basic components of an ultrasound machine.<br />
Types of transducers and production of ultrasound with an emphasis on operator<br />
controlled variables.<br />
Use of ultrasound controls – ‘knobology’.<br />
An understanding of the frequencies used in medical ultrasound and the effect<br />
on image quality and penetration.<br />
The interaction of ultrasound with tissue including biological effects.<br />
Understanding of hyperechoic, hypo-echoic and anechoic and how it relates to<br />
tissues, structures and formation of the image.<br />
Sonographic appearance of tissues, muscle, blood vessels, nerves, tendons, etc.<br />
The safety of ultrasound and of ultrasound contrast agents.<br />
The basic principles of real time and Doppler ultrasound including colour flow<br />
and power Doppler.<br />
The recognition and explanation of common artefacts.<br />
The storage and recording of still and video images, and integration with Picture<br />
Archiving and Communication Systems (PACS).<br />
Administration<br />
Image recording, storing and filing.<br />
Reporting of images.<br />
Medicolegal aspects – outlining the responsibility to practise within specific<br />
levels of competence and the requirement for training.<br />
Understanding of sterility, health and safety, and machine cleaning.<br />
Value and role of departmental and hospital protocols and guidelines.<br />
Resource implication of ultrasound use.<br />
Interpersonal and communications skills<br />
Patient preparation and information.<br />
Sensitive and effective communication with patient and family regarding<br />
ultrasound findings.<br />
Explanation of findings and the complexities of ultrasound techniques in terms<br />
that the patient can understand.<br />
Development of team leadership and management skills in developing and<br />
maintaining an ultrasound service.<br />
Needling techniques<br />
Understanding of terminology of planes of view, e.g. transverse, longitudinal.<br />
Understanding of terminology of needle insertion: in-plane and out-of-plane.<br />
Relationship of needle gauge, angle of insertion, depth and needle visibility.<br />
Limitation of out-of-plane needle insertion with regard to visibility of needle tip.<br />
11
Limitation of in-plane technique: beam width, parallelism.<br />
The use and limitations of needle guides and ultrasound visible needles.<br />
Knowledge of common causes of failure to see the needle during placement.<br />
Practical<br />
Demonstration of knowledge of equipment selection (probe) and settings.<br />
Ergonomic position of patient and equipment.<br />
Pre-scan technique or understanding of benefits.<br />
Correct application of gel and probe contact with skin.<br />
Applications of probe cover, sheath or condom.<br />
Correct orientation of probe with screen image.<br />
Successful identification of the target within phantom or patient.<br />
Adjustment of resolution to improve image of structures.<br />
Correct use of depth and sector width controls to optimise structures being<br />
observed.<br />
Understanding of how to adjust the gain to optimise image quality and<br />
consistency.<br />
Demonstration of knowledge of the relevance of the angle of insonation to<br />
visibility of relevant structures (anisotropy).<br />
Correct use of focus or multiple focal zones to optimise image.<br />
Use of Doppler, including continuous wave and pulsed wave Doppler.<br />
Demonstration of the understanding of the longitudinal (long axis) and transverse<br />
(short axis) planes of view.<br />
Ability to store images.<br />
Cleaning the probe and machine before storing or use on another patient.<br />
Needling<br />
Demonstration of understanding of the term ‘in-plane’ approach by placing<br />
needle under the long axis of the ultrasound probe.<br />
Demonstration of understanding of the term ‘out-of-plane’ approach by placing<br />
needle at 90°to the long axis of the ultrasound probe.<br />
Precise control of the probe and needle with minimal unintentional movement.<br />
Demonstration of techniques to maximise the visibility of the needle,<br />
parallelism, rotation, tissue movement and hydro-dissection.<br />
Positioning of the needle within a vascular structure using both in-plane and outof-plane<br />
technique in a phantom or clinical situation.<br />
Demonstration of correct and appropriate spread of fluid or local anaesthetic<br />
around a nerve in either a phantom model or clinical situation.<br />
Following completion of basic theoretical and practical training, some form of<br />
assessment of knowledge and practical skills should be completed. This can be<br />
achieved by either multiple-choice questions (MCQs) for the theoretical knowledge<br />
and formal Direct Observation of Procedural Skills (DOPS) or other ‘in house’<br />
(individual hospital) assessment. In any case, some form of documentation should<br />
be filed within an individual’s appraisal record or logbook. In an ideal situation, this<br />
12
initial assessment of practical skills should be performed on a phantom or model,<br />
but clinical needs will dictate whether this is the case or if the initial assessment<br />
should be done in a clinical situation. The following table of competencies, and<br />
all others provided in this document, should be assessed using some form of<br />
assessment such as DOPS. The current RCoA DOPS form is provided in Appendix<br />
1.<br />
13
Basic ultrasound competencies<br />
1 Demonstration of knowledge of the equipment and probe selection<br />
2 Ergonomic positioning of self, patient, ultrasound machine and equipment<br />
3 Correct use of gel and probe contact<br />
4 Application of probe cover, sheath or condom to protect probe from<br />
contamination<br />
5 Correct orientation of probe with screen image<br />
6 Ergonomic probe handling and movement<br />
7 Successful identification of target structure within phantom, model or<br />
patient<br />
8 Adjustment of resolution to improve image of structures being imaged<br />
9 Correct use of depth control to optimise structures being visualised<br />
10 Understanding of how to adjust the gain to optimise image quality and<br />
consistency<br />
11 Demonstration of knowledge of the relevance of the angle of insonation to<br />
visibility of relevant structures (anisotropy)<br />
12 Correct use of focus or multiple focal zones to optimise image<br />
13 Demonstration of use of Doppler for identification of vessels and the use<br />
of M mode, continuous wave Doppler and pulsed wave Doppler where<br />
appropriate<br />
13 Demonstration of the understanding of the longitudinal (long axis) and<br />
transverse (short axis) planes of view<br />
14 Demonstration of understanding of the term ‘in-plane’ approach by<br />
placing needle under the long axis of the ultrasound probe<br />
15 Demonstration of understanding of the term ‘out-of-plane’ approach by<br />
placing the needle under middle of the probe at right angles to the long<br />
axis of the probe<br />
16 Precise control of the probe and needle with minimal unintentional<br />
movement<br />
17 Ability to save and store images transfer to PACS or transfer to encrypted<br />
memory stick<br />
18 Cleaning of probe and machine after use to minimise transfer of infection;<br />
storage of probe and machine to minimise damage<br />
14
4. Regional anaesthesia and pain medicine<br />
Over the last five years, ultrasound has revitalised and rejuvenated interest in<br />
regional anaesthesia amongst anaesthetists in general and trainees in particular. The<br />
availability of portable, high-resolution machines driven by NICE guidance on the<br />
insertion of central venous catheters [1] has made it possible for most anaesthetists<br />
to have easy access to a machine. Ultrasound allows direct observation of target<br />
nerves and their surrounding structures, recognition of anatomical variance,<br />
real-time guidance of the needle and direct observation of the spread of local<br />
anaesthetic around the nerve. This is something that established techniques<br />
(peripheral nerve stimulation or paraesthesia) cannot achieve, and improved<br />
success rates, decreased volumes of local anaesthetic solutions, decreased<br />
incidence of side effects and improved patient comfort have all been demonstrated<br />
when using ultrasound.<br />
Ultrasound-guided regional anaesthesia (UGRA) as a technique is rapidly gaining<br />
momentum as shown by the increasing numbers of publications and advertised<br />
workshops. A recent NICE interventional procedure guidance [3] supports the use<br />
of ultrasound guidance in regional anaesthesia, stating “that clinicians wishing to<br />
perform this procedure should be experienced in regional nerve blocks and trained<br />
in ultrasound guided techniques”. This has been supported by American Society<br />
of Regional Anesthesia and Pain Medicine (ASRA) and the European Society of<br />
Regional Anaesthesia and Pain Therapy (ESRA) Joint Committee recommendations<br />
for education and training in ultrasound guided regional anaesthesia [16]. NICE has<br />
also produced guidance on the use of ultrasound and epidural catheterisation [2].<br />
The natural progression from regional anaesthesia to pain medicine has seen the<br />
growing popularity of the use of ultrasound in modern pain management [17-19].<br />
Ultimately, it will be up to practitioners themselves to satisfy not only clinical<br />
governance directives but also the rigours of appraisal and revalidation. This will<br />
almost certainly require the keeping of logbooks and competency curves. As time<br />
passes, more people will have completed their ultrasound training as part of basic<br />
anaesthetic training and the prospect of a more robust certification process can be<br />
realised as part of accreditation.<br />
15
Curriculum for regional anaesthesia<br />
Basic knowledge and skills<br />
See pages 12-15.<br />
Practice<br />
Level 1 practice<br />
Superficial cervical plexus block<br />
Interscalene brachial plexus block<br />
Supraclavicular block<br />
Infraclavicular block<br />
Suprascapular block<br />
Axillary brachial plexus block<br />
Blockade of the terminal peripheral nerves of the arm<br />
Rectus sheath block<br />
Ilio-inguinal / iliohypogastric block<br />
Transversus abdominis plane (TAP) block<br />
Fascia iliaca block<br />
Femoral nerve block<br />
Obturator nerve block<br />
Saphenous nerve block<br />
Lateral cutaneous nerve of thigh block<br />
Sciatic (trans-gluteal, sub-gluteal, anterior or mid-thigh) nerve block<br />
Popliteal sciatic nerve block<br />
Ankle block<br />
Blockade of the terminal peripheral nerves of the leg<br />
Epidural – assessment of spinal level, epidural depth and direction<br />
Caudal<br />
Catheter techniques<br />
Level 2 practice<br />
Lumbar plexus block<br />
Deep cervical plexus block (cervical nerve root)<br />
Paravertebral block / intercostal nerve block<br />
Real-time ultrasound-guided epidural puncture and spinal anaesthesia<br />
Anatomy<br />
Level 1 anatomy<br />
Detailed knowledge of relevant sectional anatomy:<br />
Brachial plexus<br />
Lumbosacral plexus<br />
Terminal peripheral nerves of the arm and hand<br />
16
Terminal peripheral nerves of the abdomen<br />
Terminal peripheral nerves of the leg and foot<br />
Level 2 anatomy<br />
Additional knowledge of sectional anatomy:<br />
Brachial plexus<br />
Interscalene region<br />
Supraclavicular region<br />
Axillary region<br />
Lumbosacral plexus<br />
Posterior abdominal wall, lumbar plexus and psoas muscle<br />
Femoral triangle and anterior thigh, including obturator nerve and<br />
saphenous nerve<br />
Buttock and upper thigh<br />
Popliteal fossa<br />
Ankle and foot<br />
Chest and anterior abdominal wall<br />
Rib and intercostal space<br />
Anterior abdominal wall: rectus sheath; internal and external oblique; and<br />
transversus abdominis<br />
Inguinal region<br />
Spine<br />
Cervical spine, facet joints, cervical roots<br />
Thoracic spine, facet joints and paravertebral space<br />
Lumbar spine, facet joints, spinous process, intraspinous space and<br />
intralaminar space<br />
Cervical, thoracic , lumbar and caudal epidural space<br />
Sacrum and sacral hiatus<br />
Pathology<br />
Regional anaesthesia is primarily the practical performance of standard techniques<br />
with the sole purpose of anaesthesia and analgesia for surgery and postoperative<br />
pain control. Specific associated pathologies, e.g. venous thrombosis and thyroid<br />
cysts, are not deliberately sought but may be noticed or detected by some<br />
clinicians.<br />
Level 1 pathology<br />
Understanding of the common anatomical variations of the brachial and<br />
lumbosacral plexuses.<br />
Level 2 pathology<br />
Knowledge of the common associated pathologies that may be seen with respect to<br />
peripheral nerves and the surrounding structures.<br />
17
Pain<br />
Specific and additional knowledge will be needed for the practice of pain medicine.<br />
Competencies<br />
The technical skills needed to perform any form of UGRA and pain medicine<br />
technique are the same independent of the overall level of training. The ability<br />
to see the nerve, control needle passage and observe the needle/nerve interface<br />
whilst injecting local anaesthetic are core to performing any block. The level of<br />
training is dependent on the technique used: some of these are easily learned with<br />
few complications (Level 1: axillary); others require improved scanning skills and<br />
knowledge (Level 2: paravertebral). The individual levels are arbitrary distinctions<br />
between those that will be required for CCT and those that can be achieved within<br />
a comprehensive training programme, and the distinctions should be viewed as<br />
guidance only. Level 1 training is deliberately minimalistic so that all trainees<br />
can achieve this level of training irrespective of the hospitals visited within their<br />
rotations.<br />
Level 1 competencies<br />
Patient<br />
Performance of gentle ultrasound examinations, provide appropriate sedation.<br />
Demonstration of proper patient selection.<br />
Use of appropriate monitoring to Association of Anaesthetists of Great Britain &<br />
Ireland (AAGBI) standards.<br />
Demonstration of proper nerve location techniques.<br />
Performance of effective and safe nerve block techniques.<br />
Ultrasound knowledge<br />
Understanding of general principles of ultrasound physics.<br />
Understanding of benefits and limitations of UGRA techniques.<br />
Understanding of the differences between in-plane and out-of-plane needling<br />
techniques and their indications and limitations<br />
Understanding of key artefacts and pitfalls of UGRA.<br />
Development of an intimate knowledge of the 2D ultrasound anatomy of the<br />
major neurovascular structures of the upper and lower extremities.<br />
Understanding of common anatomical variations associated with the<br />
neurovascular and musculoskeletal structures of the upper and lower<br />
extremities.<br />
Understanding of the clinical applications and uses of colour Doppler in UGRA.<br />
Understanding of and be able to use ultrasound equipment.<br />
Demonstration of knowledge of sterility, infection control and equipment<br />
cleaning.<br />
Establishment of familiarity with the scientific literature pertaining to UGRA.<br />
Demonstration of knowledge and learning of commonly used UGRA techniques.<br />
18
Interpersonal and communications skills<br />
Sensitive and effective communication with patients and families.<br />
Providing explanation of the procedure in terms that the patient can understand,<br />
outlining the benefits, risks and complications.<br />
Demonstration of effective communication with anaesthetic colleagues,<br />
operating departmental practitioners (ODPs) and supporting nursing and<br />
ancillary staff.<br />
Level 2<br />
Professionalism and learning<br />
Development of the skill to manage a regional anaesthetic service effectively.<br />
Understanding of the costs relating to ultrasound regional anaesthetic service.<br />
Remaining open to constructive criticism.<br />
Awareness of the increasing literature relating to UGRA and its value.<br />
Partaking in research and audit of UGRA practice.<br />
19
Assessment checklist – regional anaesthesia<br />
Demonstration of appropriate attitude and professional manner<br />
Explanation of procedure, risks and complications to patient as appropriate<br />
Checking patient’s details and entering them into record and machine as<br />
appropriate<br />
Confirmation of indication and checking of any supportive imaging<br />
Positioning of patient and machine ergonomically<br />
Selection of appropriate probe and optimisation of machine settings<br />
Identification of nerve or plexus using a preliminary scan<br />
Optimisation of the image by adjustment of gain, depth and focus<br />
Demonstration of good needling technique with maintenance of the needle tip<br />
within the scan plane at all times<br />
Confirmation of position of needle with respect to nerve<br />
Identification of spread of local anaesthetic perineurally, NOT intravascular<br />
Demonstration of spread of local anaesthetic around the nerve or nerves<br />
Performance of technique safely and effectively<br />
Attention to sterility with respect to procedure, patient and machine<br />
Adequate documentation and storage of images and scans as appropriate<br />
Provision of information to patient and reporting of findings where appropriate<br />
Identification of whether a further scan or alternative imaging is indicated<br />
Cleaning of equipment and storage to minimise damage<br />
20
5. Vascular procedures<br />
The use of ultrasound to guide vascular access is associated with a higher firstpass<br />
success and a reduced rate of complications. This led NICE to recommend<br />
that ultrasound guidance be the preferred method for insertion of central venous<br />
catheters (CVC) into the internal jugular vein and that ultrasound should be<br />
considered in most clinical circumstance where CVC insertion is necessary, either<br />
electively or in an emergency [1]. Following this guidance, the use of ultrasound<br />
to guide CVC placement has increased markedly in recent years as clinicians have<br />
realised its benefits in terms of ensuring the success of placement while minimising<br />
the risk of complications [20]. Many experienced clinicians now use ultrasound<br />
successfully to guide all CVC placements regardless of site or urgency such that it<br />
is becoming a standard of care. However, the safe use of ultrasound to guide CVC<br />
placement requires appropriate training and experience to achieve competence.<br />
Some clinicians limit the use of ultrasound to confirm anatomy while they continue<br />
to perform a standard landmark technique when inserting the CVC. This approach<br />
is not recommended, as it does not allow the full benefits of ultrasound guidance<br />
to be realised. It is recommended that when ultrasound is used to assist CVC<br />
placement, it should be used to guide needle placement into the vein in real time.<br />
There is a number of other areas of practice relevant to anaesthesia and intensive<br />
care in which vascular ultrasound may have a useful clinical role. These include the<br />
use of ultrasound to diagnose venous thrombosis, dynamic imaging of the inferior<br />
vena cava to assess circulating volume status and specialist applications such as<br />
transcranial Doppler. These are considered advanced areas of practice within<br />
anaesthesia and intensive care medicine in which clinicians with a special interest<br />
in ultrasound may wish to gain the necessary competencies.<br />
21
Curriculum for vascular procedures<br />
Basic knowledge and skills<br />
See pages 12-15.<br />
Practice<br />
Level 1 practice<br />
Cannulation of internal jugular vein<br />
Cannulation of femoral vessels: vein and artery<br />
Cannulation of peripheral veins and arteries<br />
Insertion of peripheral inserted central catheter<br />
Level 2 practice<br />
Cannulation of axillary and subclavian vein<br />
Assessment and diagnosis of venous thrombosis (upper and lower limb)<br />
Assessment of volume status from dynamic ultrasound imaging of inferior<br />
vena cava (see section on abdominal ultrasound)<br />
Level 3 practice<br />
Specialist vascular examinations, e.g. transcranial Doppler, renal artery<br />
Doppler<br />
Anatomy<br />
Level 1 anatomy<br />
Vascular access<br />
Cross-sectional and ultrasonographic anatomy of:<br />
• Neck (carotid artery and jugular vein)<br />
• Femoral vessels<br />
• Upper limb vessels<br />
• Common anatomical variations<br />
Level 2 anatomy<br />
Axillary and subclavian vessels<br />
Venous thrombosis<br />
Vascular sectional and ultrasound anatomy of the arms and legs including<br />
common anatomical variants<br />
Pathology<br />
Level 1 pathology<br />
Recognition of thrombosis and haematoma in major vessels, e.g. internal jugular<br />
and femoral veins.<br />
22
Level 2 pathology<br />
Ultrasonic appearance of peripheral venous thrombosis.<br />
Competencies<br />
Level 1 competencies<br />
Identification of vein and artery in transverse and longitudinal scan.<br />
Differentiation of the appearance of arteries and veins with 2D ultrasound.<br />
Use of colour flow Doppler.<br />
Identification of common anatomical variations.<br />
Preparation of equipment to maintain sterility during ultrasound-guided<br />
cannulation.<br />
Undertaking of ultrasound-guided cannulation in real time maintaining<br />
sterility.<br />
Identification of needle tip with transverse and longitudinal views.<br />
Identification of guide wire within vessel.<br />
Insertion of appropriate sized cannula into vessel to correct length and secure<br />
fixation.<br />
Level 2 competencies<br />
Identification of deep veins in leg: common femoral, femoral and popliteal<br />
veins.<br />
Assessment of lumen of veins in terms of diameter, echogenicity and<br />
compressibility.<br />
Use of continuous wave Doppler to demonstrate arterial and venous<br />
waveforms.<br />
Use of colour flow and pulsed wave Doppler to demonstrate patency of flow<br />
with phasic variation with respiration and augmentation of flow following<br />
distal compression.<br />
Sequential scanning to demonstrate patency of common femoral, femoral<br />
into lower thigh and popliteal veins.<br />
Identification of common pathology: venous thrombosis, haematoma.<br />
Identification and assessment of external iliac veins.<br />
Identification and assessment of upper limb veins.<br />
23
Assessment checklist – vascular procedures<br />
Demonstration of appropriate attitude and professional manner<br />
Explanation of procedure, risks and complications to patient as appropriate<br />
Checking patient’s details/entry into machine as appropriate<br />
Confirmation of indication and checking of any supportive imaging<br />
Positioning of patient and machine ergonomically<br />
Selection of appropriate probe and optimisation of machine settings<br />
Identification of the vein and artery in transverse and longitudinal scan<br />
Confirmation of patency and absence of thrombus or haematoma by compression,<br />
Doppler<br />
Undertaking of ultrasound guided cannulation in real time maintaining sterility<br />
Identification of needle tip using in-plane or out-of-plane technique<br />
Identification of guide wire within vein<br />
Insertion of appropriate sized cannula into vessel to correct length and secure<br />
Performance of technique safely and effectively<br />
Attention to sterility with respect to procedure, patient and machine<br />
Adequate documentation and storage of images and scans as appropriate<br />
Provision of information to patient and reporting of findings where appropriate<br />
Identification of whether a further scan or alternative imaging is indicated<br />
Cleaning of equipment and storage to minimise damage<br />
24
6. Thoracic ultrasound<br />
The use of point of care ultrasound for assessing and treating thoracic pathology<br />
in the intensive care environment has increased significantly in the last decade.<br />
Not only can it answer queries arising from standard chest radiographs, e.g.<br />
distinguishing effusion from consolidation from collapse, it can also be used to<br />
make primary diagnoses such as pneumothorax and pulmonary oedema or the<br />
interstitial syndrome. As well as a diagnostic tool, ultrasound is increasingly used to<br />
guide invasive procedures relating to the thorax, namely diagnostic thoracocentesis,<br />
chest drain insertion, pleural biopsy and percutaneous tracheostomy [21]. There<br />
is now an increased focus on the use of ultrasound to guide chest drain insertion<br />
for pleural fluid as a result of a rapid response report by the National Patient Safety<br />
Agency in 2008 [22], with subsequent guidelines issued by the British Thoracic<br />
Society [23-27].<br />
As a technique, thoracic ultrasound is relatively straightforward to perform.<br />
However, it fosters a large number of acoustic artefacts. Some of these can aid and<br />
some can hinder diagnosis. Appropriate training is therefore mandatory in order<br />
to avoid serious interpretation errors. Level 1 training in thoracic ultrasound is not<br />
mandatory for the CCT in Anaesthetics and is not part of the RCoA curriculum.<br />
25
Curriculum for thoracic ultrasound<br />
Basic knowledge and skills<br />
See pages 12–15.<br />
Practice<br />
Level 1 practice<br />
Systematic examination of the normal thorax<br />
Assessment and diagnosis of pleural effusions<br />
Ultrasound guided thoracocentesis and chest drain insertion<br />
Use of ultrasound to diagnose pneumothorax<br />
Level 2 practice<br />
Assessment and diagnosis of pleural pathology<br />
Assessment and diagnosis of lung pathology<br />
Assessment of diaphragmatic function<br />
Ultrasound guided pleural and lung biopsy<br />
Ultrasound guided percutaneous tracheostomy and cricthyroidotomy<br />
Identification of the cricoid cartilage and extrathoracic tracheal rings<br />
Knowledge of the appearance of normal thyroid versus goitre and Doppler<br />
assessment of vascularity<br />
Anatomy<br />
Level 1 anatomy<br />
Detailed knowledge of relevant sectional anatomy<br />
Right and left hemidiaphragm<br />
Chest wall layers<br />
Ribs and intercostal spaces<br />
Surface anatomy of pleural reflections<br />
Heart<br />
Liver, spleen and kidneys<br />
Thyroid<br />
Level 2 anatomy<br />
Additional knowledge of sectional anatomy<br />
Supraclavicular region<br />
Anterior and superior mediastinum<br />
Laryngeal cartilages and extrathoracic trachea<br />
Thyroid<br />
26
Pathology<br />
Level 1 pathology<br />
Pleural effusion<br />
Pleural thickening<br />
Pneumothorax<br />
Consolidated lung<br />
Atelectasis<br />
Level 2 pathology<br />
Interstitial thickening<br />
Pulmonary mass/abscess<br />
Paralysed diaphragm<br />
Mediastinal and pleural masses<br />
Multinodular goitre<br />
Competencies<br />
Level 1 competencies<br />
Performance of systematic examination of thorax identifying normal structures<br />
including diaphragm, liver and spleen.<br />
Identification of ultrasound appearances of normal aerated lung including:<br />
• Diaphragmatic movement<br />
• Pleural line and gliding sign<br />
• Normal aerated lung (including A-lines and B-lines artefacts).<br />
Recognition of pleural fluid:<br />
• Appearances suggesting transudate, exudate and loculation<br />
• Assessment of size of effusion<br />
• Differentiation between pleural thickening and effusion<br />
• Distinguishing small or loculated pleural fluid from pleural thickening.<br />
Recognition of consolidated lung:<br />
• Distinguishing atelectasis from consolidation: with and without air<br />
bronchograms<br />
• Recognition of signs of pneumothorax including lung point sign and<br />
appearance on M-mode.<br />
Recognition of heart, liver and spleen.<br />
Performance of ultrasound-guided (direct and indirect) thoracocentesis.<br />
Performance of ultrasound-guided chest drain insertion and identification of<br />
when to use a direct or indirect approach.<br />
Level 2 competencies<br />
Differentiation between consolidated lung, abscess and pulmonary mass.<br />
Differentiation of types of pleural thickening, e.g. pleural masses and plaques.<br />
Use of colour/power Doppler to help distinguish between pleural and<br />
lung pathologies.<br />
27
Familiarity with the altered artefact patterns seen with pulmonary oedema<br />
and interstitial syndrome.<br />
Identification of the cricoid cartilage and extrathoracic tracheal rings.<br />
Knowledge of the appearance of normal thyroid versus goitre and Doppler<br />
assessment of vascularity.<br />
Performance of ultrasound-guided percutaneous tracheostomy or<br />
cricothyrotomy.<br />
28
Assessment checklist – thoracic ultrasound<br />
Demonstration of appropriate attitude and professional manner<br />
Explanation of procedure, risks and complications to patient as appropriate<br />
Checking patient’s details/entry into machine as appropriate<br />
Confirmation of indication and check any supportive imaging<br />
Positioning of patient and machine ergonomically<br />
Selection of appropriate probe and optimisation of machine settings<br />
Correct identification of normal lung, pleural line and movement<br />
Demonstration of pleural sliding in 2D and M mode<br />
Identification of normal diaphragm, liver and spleen<br />
Identification of pleural effusion<br />
Differentiation of pleural effusion from intra-abdominal fluid (ascites)<br />
Description of appearances of transudate and exudate<br />
Demonstration of how volume of effusion may be estimated<br />
Use of ultrasound to identify appropriate site for drainage of effusion<br />
Demonstration of ultrasound guided thoracocentesis<br />
Identification of consolidation<br />
Identification of atelectasis<br />
Recognition of signs of pneumothorax including lung point sign, appearance in M<br />
mode<br />
Demonstration of ultrasound guided chest drain insertion<br />
Performance of technique safely and effectively<br />
Attention to sterility with respect to procedure, patient and machine<br />
Adequate documentation and storage of images and scans as appropriate<br />
Informing patient and reporting findings where appropriate<br />
Identification of whether a further scan or alternative imaging is indicated<br />
Cleaning of equipment and storage to minimise damage<br />
29
7. Abdominal ultrasound<br />
The ability to detect free intraperitoneal fluid, assess the aortic diameter, assess<br />
the inferior vena cava (IVC), and measure bladder volume is extremely valuable.<br />
The finding of free fluid may have significance for patient management, especially<br />
following trauma. The purpose of ultrasound in the initial assessment of abdominal<br />
trauma is solely to document the presence of free intra-peritoneal fluid. In the<br />
context of abdominal trauma this is assumed to be blood. There is no attempt<br />
to identify specific organ injuries as ultrasound is not accurate in the early<br />
assessment of solid or hollow viscus injury. When abdominal scanning techniques<br />
are combined with basic cardiac scanning, the combination is known as ACES<br />
(Abdominal and Cardiac Evaluation with Sonography in shock). Fluid assessment<br />
is also known as FAST (Focused Assessment with Sonography in Trauma) if in a<br />
trauma setting. If one adds assessment of the upper pleura for pneumothorax, this is<br />
known as EFAST (Extended FAST) [28,29]. Level 1 training in abdominal ultrasound<br />
is not mandatory for a CCT in Anaesthetics and is not part of the RCoA curriculum.<br />
30
Curriculum for abdominal ultrasound<br />
Basic knowledge and skills<br />
See pages 12–15.<br />
Practice<br />
Level 1 practice<br />
Detection of free intraperitoneal fluid<br />
Assessment of the abdominal aorta<br />
Assessment of the IVC including filling pressures<br />
Bladder volume assessment<br />
Level 2 practice<br />
Assessment of the gall bladder<br />
Assessment of the kidneys<br />
Level 3 practice<br />
Comprehensive abdominal scanning<br />
Anatomy<br />
Level 1 anatomy<br />
Aorta and IVC<br />
Liver<br />
Morrison pouch and right costophrenic pleural recess / splenorenal recess<br />
and left costophrenic pleural recess<br />
Rectovesical, vesico-uterine and recto-uterine pouches<br />
Bladder<br />
Level 2 anatomy<br />
Kidney<br />
Liver (detailed)<br />
Spleen<br />
Pathology<br />
Level 1 pathology<br />
Intraperitoneal and pleural fluid<br />
Aortic aneurysm and rupture<br />
IVC collapse greater than 50%<br />
Pneumothorax<br />
31
Level 2 pathology<br />
Biliary disease including common bile duct obstruction, gallstones,<br />
gallbladder wall thickening and oedema, common bile duct dilatation.<br />
Mesenteric ischaemia.<br />
Renal parenchymal disease, hydronephrosis, renal stones, renal tract<br />
obstruction.<br />
Competencies<br />
Level 1 competencies<br />
Recognition of what is normal and abnormal in standard abdominal views.<br />
Identification of the aorta and IVC in transverse and longitudinal sections.<br />
Recognition of the main features of the aorta, and know how to measure it, i.e.<br />
antero-posterior diameter, outer anterior to outer posterior layer, distinction from<br />
the IVC.<br />
Ability to carry out scanning in three planes.<br />
Ability to use the machine to determine bladder volume.<br />
Recognition of a catheter balloon within the bladder.<br />
Knowledge of when to repeat the scan, and the value of repeat scans.<br />
Level 2 competencies<br />
Ability to assess the kidneys and recognise hydronephrosis.<br />
Knowledge of how to image the gall bladder and measure wall thickness.<br />
Assessment of the common bile duct for dilatation.<br />
Assessment of the superior mesenteric artery for patency and flow.<br />
Application of these findings to the clinical context appropriately.<br />
32
Assessment checklist – abdominal ultrasound<br />
Demonstration of appropriate attitude and professional manner<br />
Explanation of procedure, risks and complications to patient as appropriate<br />
Checking patient’s details/entry into machine as appropriate<br />
Confirmation of indication and checking any supportive imaging<br />
Positioning of patient and machine ergonomically<br />
Selection of appropriate probe and optimising machine settings: gain, depth and<br />
focus<br />
Demonstration of Morrison’s pouch and right costo-phrenic pleural recess<br />
Demonstration of the spleno-renal interface and left costo-phrenic pleural recess<br />
Identification of the bladder<br />
Demonstration of potential fluid in the pelvis<br />
Demonstration of pericardial views and cardiac motion<br />
Application of examination in an Advanced Life Support (ALS) setting<br />
Demonstration of the pleural space and can identify fluid<br />
Performance of technique safely and effectively<br />
Attention to sterility with respect to procedure, patient and machine<br />
Adequate documentation and storage of images and scans as appropriate<br />
Informing patient and reporting of findings where appropriate<br />
Identification of whether a further scan or alternative imaging is indicated<br />
Cleaning of equipment and storage to minimise damage<br />
33
8. Echocardiography<br />
The application of echocardiography (transthoracic and transoesophageal<br />
echocardiography – TTE and TOE) in the critical care arena has been well<br />
recognised for some time, expanding beyond cardiothoracic critical care to include<br />
diagnosis and monitoring on the general intensive care unit (ICU) [30]. When<br />
dealing with critically ill patients, two clinical scenarios need to be considered,<br />
which may be regarded as corresponding to Level 1 and Level 2 proficiency.<br />
Level 1<br />
In the peri-resuscitation setting, relatively simple information obtained using TTE<br />
may profoundly affect patient management. Here, a basic focused scan may be<br />
appropriate, which when performed during active resuscitation must be strictly<br />
ALS-compliant [31]. There is accumulating evidence in the literature that this can<br />
be achieved with appropriate training of novice practitioners [32, 33]. Several<br />
courses exist to train the novice practitioner to this level, including FEEL-UK, which<br />
is endorsed by the British Society of Echocardiography (BSE) and supported by the<br />
Resuscitation Council (UK) [34, 35]. Beyond peri-resuscitation echocardiography,<br />
the requirements for practitioners in different specialties begin to diverge.<br />
Practitioners already proficient in peri-resuscitation echocardiography may wish<br />
to develop their skills for use in trauma, emergency medicine or critical care,<br />
depending upon their base specialty [36], may do additional training to achieve<br />
accreditation in echocardiography (Level 2 – see below). For these and others<br />
keen to extend their skills, courses and training programmes such as FAST, FATE<br />
(Focused Assessment by Transthoracic Echo), CAUSE (Cardiac Arrest Ultra-Sound<br />
Examination) and FUSE (Focused Ultrasound and Echocardiography) provide a<br />
framework within which to achieve this in the UK [37- 40].<br />
Level 2<br />
As defined elsewhere, Level 2 training includes the ability to perform the<br />
complete range of echocardiographic examinations, recognise almost all cardiac<br />
pathology and to use echocardiography to guide interventional procedures. In<br />
the critically ill patient, Level 2 echocardiography can provide information about<br />
cardiac function and the causes of inadequate cardiac output, guide therapeutic<br />
interventions and monitor the effects of any treatment instigated [41- 43]. This<br />
may be focused or comprehensive, and require TTE or TOE depending upon the<br />
clinical question being asked. This level of practice is equivalent to accreditation in<br />
echocardiography, i.e. the most basic level at which a practitioner is judged to be<br />
capable of independent practice [35]. Echocardiography training is not mandatory<br />
for a CCT in Anaesthetics or General Internal Medicine, and is not part of the RCoA<br />
or Royal College of Physicians (RCP) curriculum.<br />
34
Curriculum for echocardiography<br />
Basic knowledge and skills<br />
See pages 12-15.<br />
Practice<br />
Level 1 practice<br />
Performance of a basic echocardiography examination of a normal heart.<br />
Assessment and diagnosis of significant cardiac pathology including severe left<br />
ventricular dysfunction, right ventricular dysfunction (massive pulmonary<br />
embolus), pericardial effusion and tamponade, and hypovolaemia.<br />
Performance of an ALS compliant examination when indicated.<br />
Level 2 practice<br />
Performance of focused or comprehensive echocardiography examinations in all<br />
relevant situations (emergency care, peri-operative and intensive care, high<br />
dependency unit and coronary care unit) as appropriate for the patient and<br />
clinical scenario.<br />
Recognition of almost all cardiac pathologies.<br />
Use of echocardiography to guide interventional procedures and monitor and<br />
assess the effects of interventions and therapies.<br />
Anatomy<br />
Level 1 anatomy<br />
Basic anatomy of the heart, coronary arteries and great vessels.<br />
Coronary anatomy and correlation with myocardial territories supplied (2D<br />
views).<br />
Left and right ventricular anatomy and correlation with 2D views.<br />
Basic heart valve anatomy and correlation with 2D views.<br />
IVC anatomy and correlation with 2D views.<br />
Normal changes in IVC dimensions in response to spontaneous respiration and<br />
ventilation.<br />
Basic anatomy of the pericardium and normal pericardial space, including<br />
differentiation from pleural space.<br />
Pathology<br />
Level 1 pathology<br />
Dilated left ventricle<br />
Grossly underfilled left ventricle<br />
Significantly impaired left ventricular systolic function<br />
Severe wall motion abnormalities<br />
35
Significant right ventricular dilatation<br />
Features of pulmonary hypertension and massive acute pulmonary<br />
embolism<br />
Features of significant hypovolaemia<br />
Fixed, dilated IVC and its causes<br />
Differentiation of pericardial collection and tamponade<br />
Competencies<br />
Level 1 competencies<br />
Demonstration of the four basic echocardiography scan planes:<br />
• Parasternal long axis view<br />
• Parasternal short axis view including aortic valve, mitral valve and papillary<br />
muscles<br />
• Apical 4-chamber view<br />
• Subcostal view<br />
Recognition of normal cardiac structures and important landmarks in all four<br />
scan plane: left atrium, right atrium, inter-atrial septum, left ventricle, right<br />
ventricle, inter-ventricular septum, aortic valve, ascending aorta, mitral valve,<br />
tricuspid valve, inferior vena cava, descending aorta, pericardium.<br />
Understanding of and performance of measurements of global systolic function:<br />
eyeballing, MAPSE (mitral annular plane systolic excursion), TAPSE (tricuspid<br />
annular plane systolic excursion), fractional shortening and ejection fraction<br />
using Simpson’s rule.<br />
Recognition of a dilated left ventricle.<br />
Recognition of a severely underfilled left ventricle, and differentiate from severe<br />
left ventricular hypertrophy.<br />
Differentiation of normal from significantly impaired left ventricular systolic<br />
function and severe wall motion abnormalities.<br />
Differentiation of normal from significantly impaired left ventricular systolic<br />
function.<br />
Recognition of features of pulmonary hypertension.<br />
Recognition of a significantly dilated right ventricle.<br />
Recognition of significant right ventricular dysfunction.<br />
Recognition of features of acute, massive pulmonary embolism.<br />
Recognition of features of pulmonary hypertension.<br />
Recognition of features of significant hypovolaemia.<br />
Recognition of a fixed, dilated IVC.<br />
Identification of a pericardial collection.<br />
Differentiation of between pleural and pericardial collection.<br />
Identification of right ventricular diastolic collapse.<br />
Identification of swinging heart.<br />
36
Technique of pericardiocentesis, including echo-guidance.<br />
Ability to differentiate asystole from fine ventricular fibrillation.<br />
Ability to differentiate pulseless electrical activity (PEA) from pseudo-PEA.<br />
ALS peri-resuscitation competencies<br />
Knowledge of current ALS algorithm and when to apply FEEL.<br />
Ability to follow the steps required to perform FEEL during cardiopulmonary<br />
resuscitation in an ALS complaint manner.<br />
Ability to follow the steps required if an inadequate echocardiography window<br />
is not obtained.<br />
Ability to obtain cardiac images within 10 s.<br />
Ability to interpret images in the context of a cardiac arrest scenario.<br />
Ability to communicate findings clearly to resuscitation team leader.<br />
37
Assessment checklist – echocardiography<br />
Demonstration of appropriate attitude and professional manner<br />
Explanation of procedure, risks and complications to patient as appropriate<br />
Checking patient’s details/entry into record as appropriate<br />
Confirmation of indication and check any supportive imaging<br />
Positioning of patient and machine ergonomically<br />
Selection of appropriate probe and optimising machine settings<br />
Demonstration of all four standard views:<br />
• Parasternal long axis<br />
• Parasternal short axis<br />
• Apical four chamber<br />
• Sub-costal<br />
Recognition of normal cardiac structures and landmarks in all four major scan<br />
planes<br />
Left ventricle – recognition of dilated or grossly under filled left ventricle and<br />
normal from significantly impaired function<br />
Right ventricle – recognition of significant right ventricular dilatation and features<br />
of acute pulmonary hypertension<br />
Inferior vena cava (IVC) – recognition of signs of significant hypovolaemia and<br />
detection of a fixed dilated IVC<br />
Pericardium – recognition of a pericardial collection, distinguishing this from<br />
pleural effusion, recognition of right ventricular collapse and a ‘swinging heart’<br />
Performance of trans-thoracic ECHO in compliance with an ALS-algorithm<br />
Performance of technique safely and effectively<br />
Attention to sterility with respect to procedure, patient and machine<br />
Adequate documentation and storage of images and scans as appropriate<br />
Informing patient and reporting findings where appropriate<br />
Identification of whether a further scan or alternative imaging is indicated<br />
Cleaning of equipment and storage to minimise damage<br />
38
Level 2 accreditation<br />
A proportion of trainees may wish to extend their echocardiographic skills further<br />
to be competent to perform a comprehensive or focused study either on the ICU, or<br />
during general anaesthesia of the high-risk patient. Before 2010 the only accredited<br />
examination for transthoracic echocardiography in the UK was the ‘Accreditation<br />
in Adult Echocardiography’, administered and awarded by the BSE and for<br />
transoesophageal echocardiography, the ‘ACTA/BSE TOE accreditation’. However,<br />
the BSE has been working together with key stakeholders and has now introduced<br />
an accreditation specifically for critical care. The development of this accreditation<br />
is analogous to those that were developed for cardiothoracic anaesthetists wishing<br />
to obtain TOE accreditation. As with other areas outlined in this document, Level<br />
2 practice in echocardiography is likely to require a period of additional training<br />
and experience beyond that obtained during normal postgraduate specialist training<br />
[44].<br />
39
9. References<br />
1. National Institute for Health and Clinical Excellence. Guidance on the use of<br />
ultrasound locating devices for placing central venous catheters. http://www.<br />
nice.org.uk/nicemedia/pdf/Ultrasound_49_GUIDANCE.pdf (accessed 17/11/10).<br />
2. National Institute for Health and Clinical Excellence IPG 249 Ultrasound<br />
guided catheterisation of the epidural space: Full guidance. http://guidance.<br />
nice.org.uk/IPG249/Guidance/pdf/English (accessed 17/11/10).<br />
3. National Institute for Health and Clinical Excellence. IPG 285 Ultrasoundguide<br />
regional nerve block: guidance. http://guidance.nice.org.uk/IPG285/<br />
NICEGuidance/pdf/English (accessed 17/11/10).<br />
4. Huang SJ, McLean AS. Do we need a critical care ultrasound certification<br />
program? Implications from an Australian medical-legal perspective. Critical<br />
Care 2010; 14: 313.<br />
5. Sites BD, Gallagher JD, Cravero J, Lundberg J, Bilke GT. The learning curve<br />
associated with a simulated ultrasound – guided interventional task by<br />
inexperienced anesthesia residents. Regional Anesthesia and Pain Medicine<br />
2004; 29: 544-8.<br />
6. Sites BD, Spence BC, Gallagher JD, Wiley CW, Bertrand ML, Bilke GT.<br />
Characterizing novice behaviour associated with learning ultrasound-guided<br />
peripheral regional anesthesia. Regional Anesthesia and Pain Medicine 2007;<br />
32: 107-15.<br />
7. Royal College of Radiologists. Ultrasound Training Recommendations for<br />
Medical and Surgical Specialties http://www.rcr.ac.uk/publications.aspx?PageID<br />
=310&PublicationID=209 (accessed 17/11/10).<br />
8. The European Federation of Societies for Ultrasound in Medicine and Biology.<br />
Guidelines and Recommendations. Minimal training for practice of medical<br />
ultrasound in Europe 2006. http://www.efsumb.org/guidelines/guidelines01.asp.<br />
9. The College of Emergency Medicine. Medical Training Initiative. http://www.<br />
collemergencymed.ac.uk/Training-Exams/Medical%20Training%20Initiative/<br />
default.asp accessed 17/11/10).<br />
10. Consortium for the Accreditation of Sonographic Education. Consortium for<br />
the Accreditation of Sonographic Education (CASE). http://www.case-uk.org (<br />
accessed 17/11/10).<br />
11. Medical Specialty Training (England). The Gold Guide. http://www.mmc.nhs.uk/<br />
pdf/Gold%20Guide%20--2009.pdf (accessed 17/11/10).<br />
12. De Oliveria Filho GR. The construction of learning curves for basic skills<br />
in anaesthetic procedures: an application for the cumulative sum method.<br />
Anesthesia and Analgesia 2002; 95(2): 411-6.<br />
13. De Oliveria Filho GR, Helayel PE, da Concelcao DB, Garzel IS, Pavel P,<br />
Ceccon MS. Learning curves and mathematical models for interventional<br />
ultrasound basic skills. Anesthesia and Analgesia 2008; 106: 568-73.<br />
14. Ali D, Rhodes S. Cusum Charts: A tool for assessing competency. Anaesthesia<br />
2009; 64: 1385-6.<br />
40
15. The British Medical Ultrasound Society. Ultrasound Clinical Governance.<br />
www.bmus.org/ policies-guides/ClinicalGovernanceInUltrasound-061108.pdf<br />
(accessed 17/11/10).<br />
16. Sites BD, Chan VW, Neal JM, et al. The American Society of Regional<br />
Anesthesia and Pain Medicine and the European Society of Regional<br />
Anaesthesia and Pain Therapy joint committee recommendations for education<br />
and training in ultrasound-guided regional anesthesia. Regional Anesthesia and<br />
Pain Medicine 2009; 34: 40-6.<br />
17. Curatolo M, Eichenberger U. Ultrasound-guided blocks for the treatment of<br />
chronic pain. Techniques in Regional Anesthesia & Pain Management 2007;<br />
11: 95-102.<br />
18. Gofeld M. Ultrasonography in pain medicine: a critical review. Pain Practitioner<br />
2008; 8: 226-40.<br />
19. Peng PWH, Narouze S. Ultrasound-guided interventional procedures in pain<br />
medicine: a review of anatomy, sonoanatomy and procedures. Regional<br />
Anesthesia and Pain Medicine 2009; 34: 458-78.<br />
20. Karakistos D, Labropoulous N, De Groot E, et al. Real-time ultrasound guided<br />
catheterization of the internal jugular vein: a prospective comparison with the<br />
landmark technique in critical care patients. Critical Care 2006; 10: R162.<br />
21. Lichtenstein A. Whole body Ultrasonography in the Critically Ill, 1 st edition.<br />
Heidelberg: Springer, 2010: 99-209.<br />
22. National Patient Safety Agency. Chest drains: risks associated with the insertion<br />
of chest drains. http://www.npsa.nhs.uk/nrls/alerts-and-directives/rapidrr/risksof-chest-drain-insertion<br />
(accessed 17/11/10).<br />
23. Havelock T, Teoh R, Laws D, Gleeson F. Pleural procedures and thoracic<br />
ultrasound: British Thoracic Society pleural disease guideline 2010. Thorax<br />
2010; 65: i61-76.<br />
24. Bouhemad B, Zhang M, Lu Q, Rouby J-J. Clinical review: bedside ultrasound in<br />
critical care practice. Critical Care 2007; 11: 205.<br />
25. Koh D-M, Burke S, Davies N, Padley S. Transthoracic US of the chest: clinical<br />
uses and application. Radiographics 2002; 22: e1.<br />
26. Lichtenstein DA, Menu Y. A bedside ultrasound sign ruling out pneumothorax<br />
in the critically ill. Lung sliding. Chest 1995; 108: 1345-8.<br />
27. Lichtenstein D, Meziere G, Biderman P, Gepner A, Barre O. The comet-tail<br />
artifact: an ultrasound sign of alveolar-interstitial syndrome. American Journal of<br />
Respiratory Critical Care Medicine. 1997; 156: 1640-1646.<br />
28. Yoshii H, Sato M, Yamamoto S, et al. Usefulness and limitations of<br />
ultrasonography in the intial evaluation of blunt abdominal trauma. Journal of<br />
Trauma 1998; 45: 45-50.<br />
29. Branney SW, Wolfe RE, Moore FE, et al. Quantitative sensitivity of ultrasound in<br />
detecting free intraperitoneal fluid. Journal of Trauma 1995; 39: 375-80.<br />
30. Cholley BP, Viellard-Baron A, Mebazza A. Echocardiography in the ICU: time<br />
for widespread use! Intensive Care Medicine 2006; 32: 9-10.<br />
31. Resuscitation Council (UK). Resuscitation guidelines 2010 p67. http://www.<br />
resus.org.uk/pages/guide.htm (accessed 17/11/10).<br />
41
32. Niendorff D, Rassias A, Palac R, et al. Rapid cardiac ultrasound of inpatients<br />
suffering PEA arrest performed by non expert sonographers. Resuscitation 2005;<br />
67: 81-7.<br />
33. Breitkreutz R, Walcher F, Seegar F. Focused echocardiographic evaluation in<br />
resuscitation management: concept of an advanced life support-conformed<br />
algorithm. Critical Care Medicine 2007; 35: S150-161.<br />
34. Breitkreutz R, Uddin S, Steiger H, et al. Focused echocardiography entry level:<br />
new concept of a 1-day training course. Minerva Anestesiologica 2009; 75:<br />
285-92.<br />
35. Price S, Ilper H, Uddin S, et al., Peri-resuscitation echocardiography: Training<br />
the novice practitioner. Resuscitation 2010; 81: 1534-9.<br />
36. Neri L, Storti E, Lichtenstein D. Toward an ultrasound curriculum for critical<br />
care medicine. Critical Care Medicine 2007; 35: S290-304.<br />
37. Rose JS. Ultrasound in abdominal trauma. Emergency Medicine Clinics North<br />
America 2004; 22: 581-99, vii.<br />
38. Jensen MB, Sloth E, Larsen KM, Schmidt MB. Transthoracic echocardiography<br />
for cardiopulmonary monitoring in intensive care. European Journal of<br />
Anaesthesiology 2004; 21: 700-7.<br />
39. Hernandez C, Shuler K, Hannan H, et al. C.A.U.S.E.: Cardiac arrest ultra-sound<br />
exam – a better approach to managing patients in primary non-arrhythmogenic<br />
cardiac arrest. Resuscitation 2008; 76: 198-206.<br />
40. Morris C, Bennett S, Burn S , Russell C, Jarman R, Swanevelder J.<br />
Echocardiography in the intensive care unit: current position, future directions.<br />
Journal of Intensive Care Society 2010; 11: 90-7.<br />
41. Orme RM, Oram MP, McKinstry CE. Impact of echocardiology on patient<br />
management in the intensive care unit: an audit of district general hospital<br />
practice. British Journal of Anaesthesia 2009; 102: 340-4.<br />
42. Price S, Via G, Sloth E, et al. Echocardiography practice, training and<br />
accreditation in the intensive care: document for the World Interactive Network<br />
Focused on Critical Ultrasound (WINFOCUS). Cardiovascular Ultrasound 2008;<br />
6: 49.<br />
43. ACC/AHA ASE 2003 guideline update for the clinical application of<br />
echocardiography: summary article. Circulation 2003; 108: 1146.<br />
44. British Society of Echocardiography. Accreditation in Adult Critical Care. http://<br />
www.bsecho.org/index.php?option=content&task=category§ionid=13&id=<br />
31&Itemid=57 chocardiography [Information Pack] (accessed 17/11/10).<br />
42
Appendix 1 RCoA Direct Observation of Procedural Skills [DOPS]<br />
Assessment Form<br />
Please complete the question using a cross (x). Please use black ink and CAPITAL LETTERS<br />
Trainee’s surname<br />
Trainee’s forename(s)<br />
GMC number<br />
GMC NUMBER MUST BE COMPLETED<br />
Observation<br />
Code number<br />
Observed by<br />
GMC number<br />
Date<br />
GMC NUMBER MUST BE COMPLETED<br />
Assessment:<br />
Practice was satisfactory<br />
Assessor’s Signature<br />
Practice was unsatisfactory<br />
Assessors Signature<br />
If the performance was judged to be unsatisfactory, you must tick the boxes on the reverse of<br />
this form to indicate which areas of performance you judged to be unsatisfactory.<br />
Example of good practice were:<br />
Areas of practice requiring improvement were:<br />
Further learning and experience should focus on:<br />
43
If you have rated the performance unsatisfactory please indicate which elements were unsatisfactory:<br />
Did not understand the indications and contraindications to the<br />
procedure.<br />
Did not properly explain the procedure to the patient.<br />
Does not understand the relevant anatomy.<br />
Failed to prepare properly for the procedure.<br />
Did not communicate appropriately with the patient or staff.<br />
Aseptic precautions were inadequate.<br />
Did not perform the technical aspects of the procedure correctly.<br />
Failed to adapt to unexpected problems in the procedure.<br />
Failed to demonstrate adequate skill and practical fluency.<br />
Was unable to properly complete the procedure.<br />
Did not properly complete relevant documentation.<br />
Did not issue clear post-procedure instructions to patient and/or<br />
staff.<br />
Did not maintain an appropriate professional demeanor.<br />
44
intensive care<br />
society<br />
care when it matters
DITION<br />
WHO IS THE<br />
ANAESTHETIST?<br />
FIFTH EDITION 2013<br />
www.<strong>aagbi</strong>.org/<br />
professionals/trainees
GROUP OF ANAESTHETISTS IN TRAINING<br />
GAT (Group of Anaesthetists in Training) is the trainee body of the Association of<br />
Anaesthetists of Great Britain and Ireland (AAGBI) through which anaesthetists are<br />
represented at a national level. All trainee members of the Association are automatically<br />
members of GAT and currently account for about a third of the membership of the AAGBI.<br />
Approximately 70% of all anaesthetic trainees in the UK are members of GAT.<br />
The elected GAT Committee has representatives at all levels of training from within<br />
the UK and Ireland. The committee aims to represent the views and perspectives of<br />
anaesthetic trainees throughout the UK and Ireland. The GAT Committee also has links<br />
with anaesthesia training bodies around the world. We strive to maintain transparency and<br />
accuracy, allowing trainees to make their own informed opinions on issues that will affect<br />
them as professionals both at the current time and in their future career.<br />
Information is relayed back through the GAT website (www.<strong>aagbi</strong>.org/professionals/<br />
trainees) and Trainee Network Leads who are in all schools of anaesthesia nationwide.<br />
A comprehensive list of current Trainee Network Leads is available on the GAT website.<br />
ASSOCIATION OF ANAESTHETISTS<br />
OF GREAT BRITAIN AND IRELAND<br />
The Association of Anaesthetists of Great Britain and Ireland (AAGBI) represents the<br />
medical and political views of over 10,000 anaesthetists in the UK and the Republic of<br />
Ireland. Through its overseas membership it has close contact with anaesthetists in many<br />
other countries. The AAGBI is run by the Council who are elected from the membership for<br />
a term of four years. The Executive Officers are elected from within the Council.<br />
The AAGBI has a broad constitution that enables it to promote and advance education,<br />
safety and research in anaesthesia, as well as the professional aspects of the specialty<br />
and the welfare of individual anaesthetists. The AAGBI has been responsible for initiating<br />
or promoting many major developments in British and Irish anaesthesia, and continues to<br />
thrive. It issues and revises guidelines and advice, and encourages and supports specialist<br />
societies. The AAGBI continues to raise the profile and enhance the image of anaesthetists<br />
to the public.<br />
2 WHO IS THE ANAESTHETIST?
THE ROYAL COLLEGE OF ANAESTHETISTS<br />
The Royal College of Anaesthetists (RCoA) is the professional body responsible for the<br />
specialty of anaesthesia throughout the United Kingdom. Its principal responsibility is to<br />
ensure the quality of patient care through the maintenance of standards in anaesthesia,<br />
pain medicine and critical care. The College’s activities include:<br />
• Setting standards of clinical care<br />
• Establishing standards for the training of anaesthetists and those practicing critical<br />
care and/or acute and chronic pain medicine<br />
• Setting and running examinations<br />
• Continued medical education of all anaesthetists.<br />
Every hospital with anaesthetists in training has a College Tutor who can give advice on<br />
training. Information is relayed to members via the RCoA website (www.rcoa.ac.uk) and in<br />
the bi-monthly College Bulletin.<br />
THE COLLEGE OF ANAESTHETISTS OF IRELAND<br />
The College of Anaesthetists of Ireland exists to promote best practice in the fields of<br />
anaesthesia, intensive care and pain medicine through its training, examination and<br />
educational programmes. The College is responsible for setting training standards and for<br />
the organisation, supervision and counselling of doctors in training in Ireland.<br />
WHO IS THE ANAESTHETIST? 3
CONTENTS<br />
Who should read this? 05<br />
Introduction 05<br />
Where can you find an anaesthetist? 05<br />
Operating theatre work 06<br />
Anaesthetic subspecialties 07<br />
Academia and research 09<br />
Training and exams 10<br />
Less than full time training 12<br />
How can I find out more? 13<br />
Useful contacts 14<br />
ACKNOWLEDGEMENTS<br />
The GAT Committee wishes to thank Dr Jonathan Price, Dr Nicholas Love<br />
and Dr Richard Paul for revising and editing this fifth edition.<br />
© Copyright of the Association of Anaesthetists of Great Britain & Ireland.<br />
4 WHO IS THE ANAESTHETIST?
WHO SHOULD READ THIS?<br />
This guide is designed for medical students and foundation<br />
doctors who are considering a career in anaesthesia. Historically,<br />
junior doctors were able to spend several years sampling different<br />
specialties before making their career choices but this is now<br />
increasingly difficult. Foundation doctors have to make tough<br />
decisions about their future careers, sometimes with limited<br />
knowledge and experience of the possibilities.<br />
We hope to explain what a career in anaesthesia entails and explore some of the aptitudes<br />
and skills required. We hope that this will allow you to make a more informed choice and<br />
so start on a successful, enjoyable and rewarding career.<br />
INTRODUCTION<br />
Anaesthetists encounter a wide range of patients and specialties. We are one of<br />
the largest hospital departments and work in a variety of settings. Our core activity is<br />
providing anaesthesia for surgery but this straddles ages and pathologies. It is a very<br />
different challenge to anaesthetise a healthy two-year old for day surgery compared with<br />
a frail elderly patient for an emergency laparotomy. We are evolving into peri-operative<br />
physicians, responsible for assessment and optimisation pre-operatively, ensuring optimal<br />
operative conditions and providing peri-operative support to surgical teams.<br />
Our training programme encourages anaesthetists to generate an in-depth understanding<br />
of basic science, physiology and pharmacology. We learn how to apply these principles to<br />
the broad landscape of clinical practice within the hospital, spanning medical and surgical<br />
specialities. This knowledge is married to the development of expert practical skills and a<br />
patient centred approach, allowing us to manage the large spectrum of patients requiring<br />
anaesthetic services. In one day you may go from seeing outpatients in a chronic pain<br />
clinic to performing an awake fibreoptic intubation for impending airway compromise, or<br />
resuscitating patients with polytrauma in the emergency department.<br />
WHERE CAN YOU FIND AN ANAESTHETIST?<br />
Anaesthetists work in nearly all departments of the hospital and some even work outside of<br />
the hospital too. Our natural habitat is the operating theatre but you will also find us on the<br />
wards, in pre-assessment or chronic pain clinics, on the labour ward, in radiology suites<br />
and in critical care. Anaesthetists work in a wide variety of roles ranging from pre-hospital<br />
care to teaching and research. Broad clinical exposure and strong interest in patient safety<br />
often leads consultant anaesthetists to develop leadership roles within the hospital. It is<br />
not uncommon to find anaesthetists in the senior management team of a hospital or trust.<br />
As multifaceted professionals with a wide range of transferrable skills, no two anaesthetists<br />
are quite the same. A career in anaesthesia enables you to mould yourself to fit a plethora<br />
of different jobs. You may wish to work in a teaching or district general hospital, you may<br />
wish to pursue a particular clinical subspecialty or research interest – all of these options<br />
are available.<br />
WHO IS THE ANAESTHETIST? 5
OPERATING THEATRE WORK<br />
Safe care of patients in theatre starts with a thorough pre-operative assessment, either<br />
in the clinic or on the ward. This allows the operating team to make decisions on the<br />
appropriateness of the proposed procedure and if any additional resources may be<br />
required, such as a postoperative intensive care bed.<br />
Pre-assessment enables the anaesthetist to establish a rapport with the patient and to<br />
identify any potential anaesthetic difficulties or pre-existing medical conditions. Some<br />
patients will require further investigation and optimisation pre-operatively and this may<br />
involve anaesthetic-led advanced physiology testing or expert advice from other medical<br />
specialties.<br />
Having ascertained the necessary information, it is possible to quantify the risks of surgery<br />
and therefore formulate an appropriate management plan to provide the safest possible<br />
care. This may be very straightforward for healthy individuals having minor operations but<br />
can be extremely complex for unwell patients undergoing major surgery. Anaesthetists are<br />
responsible for explaining such risks to a patient and outlining the proposed management<br />
plan.<br />
The choice of anaesthetic management for a particular case is often not clear cut and there<br />
may be a number of possible options available to safely facilitate surgery. For example,<br />
repairing a broken ankle can be appropriately performed under general anaesthesia,<br />
targeted nerve blocks, a spinal injection or a combination of these. The final choice of<br />
technique is determined by patient factors, surgical factors and anaesthetic factors but is<br />
an agreement between the patient, their anaesthetist and the surgical team.<br />
6 WHO IS THE ANAESTHETIST?
In theatre, the anaesthetist becomes the patient’s carer and safety is paramount.<br />
Control of the patient’s airway, breathing and circulation are of particular importance.<br />
Close attention is paid to the patient’s condition during surgery and the anaesthetic<br />
tailored to each individual. Complex operations may require invasive monitoring such<br />
as transoesophageal echocardiography to monitor real time cardiac function, invasive<br />
arterial blood pressures or whole blood clotting effectiveness with thromboelastography.<br />
At the end of the procedure, the anaesthetist is responsible for ensuring full recovery from<br />
anaesthesia in a safe environment and ensuring adequate analgesia.<br />
Not all patients need to be asleep for their surgery and anaesthetists are skilled at using<br />
regional nerve block techniques to anaesthetise discrete regions of the body. Local<br />
anaesthetic is deposited around major nerves or plexuses with the aid of ultrasound or<br />
nerve stimulators to produce numbness or analgesia. Regional techniques are commonly<br />
used for day-stay patients or those considered high risk for general anaesthesia. Some<br />
patients may have surgery performed under local anaesthesia alone.<br />
Anaesthetists are responsible for planning and facilitating effective and safe postoperative<br />
care. This may require postoperative ventilation on the intensive care unit, topping up an<br />
epidural or planning discharge medications for a day case patient.<br />
ANAESTHETIC SUBSPECIALTIES<br />
The majority of anaesthetists are responsible for a wide variety of theatre cases so their<br />
working week may range from quick turnover day cases for fit people to major complex<br />
vascular surgery in sick elderly patients. Along with this, many anaesthetists have one or<br />
more subspecialty interests, which further enhances the breadth of their clinical work.<br />
Intensive care medicine<br />
Intensive care medicine (ICM) treats the most critically ill patients in the hospital. An ICM<br />
doctor can provide advanced organ support and is responsible for coordinating the care<br />
of patients on the intensive care unit. ICM is high-tech, lifesaving care that interacts with<br />
all other areas of the hospital. At present most UK intensive care doctors come from an<br />
anaesthetic background, although some are physicians or surgeons.<br />
Intensivists are experts at recognising and managing organ system failures. Anaesthetists<br />
have a detailed knowledge of physiology and a comprehensive understanding of<br />
pharmacology and monitoring techniques so are perfectly suited to work in a critical care<br />
environment. A good intensive care doctor also needs excellent communication skills, a<br />
firm grasp of ethical principles and an ability to manage people and resources. Effective<br />
and sensitive communication with families is essential in times of extreme stress associated<br />
with critical illness.<br />
Training to become an intensive care doctor has changed recently with the foundation of<br />
the Faculty of Intensive Care Medicine in 2012. It is now possible to train purely in ICM (from<br />
ST3 onwards) or ‘dual train’ in conjunction with another speciality, such as anaesthesia,<br />
although this takes longer. More details are available on the Faculty of Intensive Care<br />
Medicine website (www.ficm.ac.uk). Anaesthetic skills will always remain essential and the<br />
WHO IS THE ANAESTHETIST? 7
majority of currently advertised consultant posts in the UK are for anaesthetists with allied<br />
intensive care qualifications.<br />
Resuscitation and trauma<br />
Anaesthetists are core members of the hospital trauma team, involved in the initial<br />
resuscitation of trauma victims in the emergency department and their ongoing care in<br />
the operating theatre. Some work outside the hospital in pre-hospital emergency teams<br />
to treat trauma victims on the roadside. Specific training programmes for anaesthetists or<br />
emergency medicine trainees interested in a career in pre-hospital medicine are currently<br />
being introduced. More information can be found on the Intercollegiate Board for Training<br />
in Pre-hospital Emergency Medicine website (www.ibtphem.org.uk).<br />
Obstetrics<br />
Two thirds of women giving birth in the UK will come across an anaesthetist in some<br />
capacity and most delivery suites have dedicated anaesthetic cover. We assess women in<br />
antenatal clinics to discuss methods of pain relief, anticipated anaesthetic problems or any<br />
other special requirements. Anaesthetists are responsible for performing labour epidurals<br />
to provide pain relief, as well as anaesthesia for surgical procedures such as caesarean<br />
section. The presence of anaesthetists in the delivery suite has been accompanied by<br />
a marked reduction in morbidity and mortality for both mother and baby. Obstetric<br />
anaesthetists are integral to obstetric high dependency units for mothers with significant<br />
co-morbid disease or for those who have experienced serious complications around<br />
childbirth.<br />
Paediatric anaesthesia<br />
Paediatric anaesthetists do not need to have trained as paediatricians or passed exams<br />
set by the Royal College of Paediatrics and Child Health. Paediatric anaesthetists gather<br />
their skills and knowledge through specific placements during their generic anaesthetic<br />
training, alongside at least one additional year of anaesthesia for children. Most hospitals<br />
will provide anaesthetic services for children to some extent but those under the age of one<br />
are normally treated in a specialist centre.<br />
Cardiac and thoracic anaesthesia<br />
Much like a paediatric anaesthetist, a cardiac anaesthetist is not first required to train as<br />
a cardiac surgeon or cardiologist. All trainees are exposed to cardiothoracic anaesthesia<br />
but to pursue a career it may be necessary to do additional years of specialist training<br />
in the UK or abroad. Many cardiothoracic anaesthetists in the UK practise mainly adult<br />
cardiac anaesthesia but some combine this with thoracic anaesthesia or paediatric cardiac<br />
anaesthesia.<br />
8 WHO IS THE ANAESTHETIST?
Pain medicine<br />
Pain medicine describes the management of patients with acute, chronic and cancer<br />
pain using physical, pharmacological, interventional and psychological techniques in a<br />
multidisciplinary setting. The Faculty of Pain Medicine comes under the umbrella of the<br />
Royal College of Anaesthetists. All anaesthetic trainees complete basic and intermediate<br />
training in pain medicine but to become a pain specialist requires additional units to be<br />
completed.<br />
Acute pain management is a core skill of all anaesthetists. Techniques ranging from simple<br />
oral analgesics to epidurals and infusions of peri-neural local anaesthetic may be utilised<br />
to manage pain. Anaesthetist-led pain teams conduct ward rounds to identify and aid<br />
treatment of complex acute pain problems.<br />
Pain medicine is a distinct and very different specialty to anything else in anaesthesia.<br />
Chronic pain conditions affect a large number of people and there is a great demand for<br />
pain management services. Pain specialists are experts in invasive treatment techniques<br />
such as nerve blocks, injection procedures and implantation of pain-relieving devices. They<br />
play a central role in multidisciplinary pain management programmes, working closely with<br />
psychologists and physiotherapists.<br />
Regional anaesthesia<br />
This involves anaesthetising parts of the body using targeted injections of local anaesthetic<br />
drugs. Regional anaesthesia may be used in conjunction with a general anaesthetic (for<br />
example, in shoulder surgery) or as a sole technique, particularly in sick patients where a<br />
general anaesthetic may be very risky. Regional anaesthesia is common in day surgery<br />
because it allows patients to walk as soon as possible after their operation. Recent<br />
advances in ultrasound technology have encouraged the utilisation of such techniques<br />
and are drawing more anaesthetists to specialise in this area.<br />
ACADEMIA AND RESEARCH<br />
Anaesthetists already have deep roots in scientific knowledge through studying for the<br />
Fellowship of the Royal College of Anaesthetists (FRCA) and their clinical application of<br />
science. Building on these foundations, anaesthetic trainees are well positioned to be<br />
involved in research focused on the improvement of patient care.<br />
Opportunities exist for anaesthetists who wish to make a career of primarily academic work.<br />
A limited number of Academic Clinical Fellow (ACF) in Anaesthesia posts are available at<br />
ST3 level or it is possible to take time out of training to study for a higher degree such as an<br />
MD or PhD. The National Institute of Academic Anaesthesia was established in 2008 and<br />
is committed to the academic advancement of trainees whether they are purely clinically<br />
orientated or future physician-scientists.<br />
WHO IS THE ANAESTHETIST? 9
TRAINING AND EXAMS<br />
Entry to basic training requires graduation from medical school and successful completion<br />
of two years of foundation training (or the equivalent). The training programme consists<br />
of four phases:<br />
Basic level<br />
Intermediate level<br />
Higher level<br />
Advanced level<br />
Core training (2 or 3 years) or ACCS (3 years)<br />
(2 years)<br />
(2 years)<br />
(1 year)<br />
There are two routes into anaesthesia - the direct route through Core Training or the<br />
Acute Care Common Stem (ACCS) route. Core Training is two years in duration (in Wales<br />
this is extended to three years) and is focused purely on anaesthesia and intensive care<br />
medicine. ACCS is a three-year training programme to enable a broader exposure to acute<br />
hospital specialties. The first two years of ACCS are spent rotating through emergency<br />
medicine, general medicine, anaesthesia and intensive care. The third year is spent<br />
providing training that will ensure the trainee meets the minimum requirements for entry<br />
into specialty training in their parent specialty. So for anaesthetic ACCS trainees this third<br />
year will be the equivalent of the second Core Training year. More information is available<br />
on the ACCS National Training website (www.accsuk.org.uk).<br />
The whole anaesthesia programme is normally seven years for trainees taking the Core<br />
anaesthesia route, or eight years for those following the ACCS route. On completion of<br />
the training programme, the GMC awards a Certificate of Completion of Training (CCT) or<br />
Certificate of Eligibility for Specialist Registration [Combined Programmes] (CESR[CP])<br />
which then allows the holder to apply for a consultant post. More information is available at<br />
http://www.rcoa.ac.uk/careers-training/training-anaesthesia/the-cct-vs-cesrcp.<br />
Basic level training (CT1-2)<br />
This is normally two years in duration and concentrates on foundations of anaesthetic<br />
practice and basic anaesthesia. Before a novice anaesthetic trainee can work without<br />
direct supervision they must pass the structured Initial Assessment of Competency which<br />
normally happens after about three months. Basic training includes three months of ICM<br />
and exposure to obstetric anaesthesia but the remainder is dedicated towards general<br />
anaesthesia and passing the Primary FRCA exam. Trainees who enter through the ACCS<br />
route complete their basic level training in three years.<br />
Satisfactory annual assessment, appropriate workplace-based assessments and success<br />
in the Primary FRCA are required to progress to ST3. Application for ST3 posts is a<br />
competitive process.<br />
Intermediate level training (ST3-4)<br />
Intermediate training lasts two years and introduces specialist areas of anaesthesia<br />
including cardiothoracic and neuroanaesthesia. Trainees must pass the Final FRCA<br />
examination to be allowed to progress on to higher training.<br />
10 WHO IS THE ANAESTHETIST?
Higher level training (ST5-6)<br />
Higher level training lasts two years, of which least one year is spent on general duties.<br />
Some flexibility is possible to incorporate the special interests of an individual. Trainees<br />
must complete the essential units of training and may also choose to do one or more<br />
of the optional units. Higher level and advanced level training can be delivered flexibly<br />
depending on individual schools of anaesthesia. For example, a trainee could begin<br />
higher level training in ST5, undertake advanced level in ST6 and finish higher training in<br />
ST7. It is possible to arrange out-of-programme experience or training (OOPE or OOPT)<br />
at this stage. This may include studying for a PhD, anaesthesia in the third world or a<br />
specialist fellowship.<br />
Advanced level training (ST7)<br />
Advanced level training is aimed at preparing you for being a consultant. Trainees may<br />
choose to specialise in paediatric, cardiothoracic or neuroanaesthesia if they aspire to<br />
work in a tertiary referral centre. In preparation for becoming a consultant, learning is<br />
focussed on building expertise in specific areas of practice and greater exposure to the<br />
professional competencies such as leadership, team working and management.<br />
Training in Ireland<br />
The structure and nomenclature of anaesthetic training in Ireland changed in 2012.<br />
Specialist Anaesthesia Training (SAT) in Ireland now takes six years and is based in<br />
hospitals accredited by the College of Anaesthetists of Ireland.<br />
The structure of training is similar to that in the UK; two years of basic training are followed<br />
by three years of sub-speciality training with a final advanced year to finish. At present both<br />
old and new schemes are running in tandem and we would recommend consulting the<br />
College of Anaesthetists of Ireland website for detailed information (www.anaesthesia.ie).<br />
The Committee of Anaesthetic Trainees (CAT) provide trainee representation and support<br />
(cat@coa.ie).<br />
WHO IS THE ANAESTHETIST? 11
LESS THAN FULL TIME TRAINING<br />
If you are considering training less than full time (LTFT) it is likely that you have other<br />
commitments or areas of your life to which you need to devote time, whilst also trying to<br />
get the most out of your training. Anaesthesia has a long tradition of supporting doctors<br />
who wish to train LTFT and of all hospital specialities is second only to paediatrics for<br />
numbers of part-time trainees. LTFT training programmes in anaesthesia have dedicated<br />
programme directors and are usually well organised, and most departments will have had<br />
experience of LTFT trainees. The sessional nature of anaesthesia facilitates a satisfying<br />
career without too much family disruption, compared with working LTFT in other specialties<br />
which may require dropping clinics and cross-cover of inpatients by colleagues in your<br />
absence. There is a comprehensive guide to LTFT available to download from the AAGBI<br />
website.<br />
12 WHO IS THE ANAESTHETIST?
HOW CAN I FIND OUT MORE?<br />
If you have been inspired to join us on the exciting and rewarding career path of anaesthesia<br />
then it is time to do some homework!<br />
Exposure to anaesthesia can be limited as a medical student and most people will want<br />
to know more about the speciality before applying for a job. How best to go about doing<br />
this depends on what stage you are at in your medical career. Undergraduates can<br />
consider doing a special study module or elective in anaesthesia to gain more exposure.<br />
Departments around the world are usually very willing to take students.<br />
Limited numbers of four-month anaesthesia or intensive care posts are available on<br />
foundation programmes. These are often highly sought after as they offer great experience<br />
and learning opportunities with close consultant supervision. If you are applying for<br />
foundation jobs and considering a career in anaesthesia then these offer a brilliant<br />
opportunity to gain exposure to anaesthetists and their work. Current foundation doctors<br />
can organise ‘taster weeks’ in specialties in which they may be interested, so why not<br />
consider anaesthesia or critical care?<br />
Anaesthetists are involved all over the hospital so whether you are a student or a foundation<br />
doctor you are sure to come across them, wherever you are working. We are a friendly<br />
profession so will not mind being approached by an inquisitive and interested potential<br />
colleague! Talk to anaesthetic trainees as well the consultants, as they will tell you what<br />
training is really like and how they secured their training rotation.<br />
Information about a career in anaesthesia, the training and exams involved is available<br />
online. We have included a list of useful contacts towards the end of this document. If<br />
you want to discuss your aspirations then find out who the College Tutor for anaesthesia<br />
is in your hospital and arrange to meet them. These are consultants who also represent<br />
the Royal College of Anaesthetists and will have up-to-date advice on training and how to<br />
apply for jobs.<br />
Regional and national careers fairs offer the opportunity to talk to doctors from a wide<br />
range of specialties in one room and offer advice from clinicians based beyond your local<br />
hospital.<br />
Anaesthesia is a great career. Entry to training is competitive and the exams do require<br />
hard work but it is worth it in the end. The more experience you can get and the more you<br />
can find out before you apply, the better choice you will be making for yourself and the<br />
more likely you will be to secure a job.<br />
WHO IS THE ANAESTHETIST? 13
USEFUL CONTACTS<br />
Group of Anaesthetists in Training (GAT)<br />
c/o The Association of Anaesthetists of Great Britain and Ireland<br />
21 Portland Place, London W1B 1PY<br />
Tel: 020 7631 1650<br />
Email: gat@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org/professionals/trainees<br />
Association of Anaesthetists of Great Britain and Ireland (AAGBI)<br />
21 Portland Place, London W1B 1PY<br />
Tel: 020 7631 1650<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org<br />
The Royal College of Anaesthetists (RCoA)<br />
Churchill House, 35 Red Lion Square, London WC1R 4SG<br />
Email: training@rcoa.ac.uk<br />
www.rcoa.ac.uk<br />
The College of Anaesthetists of Ireland<br />
22 Merrion Square North, Dublin 2, Ireland<br />
Tel: +353 1 2650600<br />
Email: info@coa.ie<br />
www.anaesthesia.ie<br />
Committee of Anaesthesia Trainees (CAT)<br />
c/o The College of Anaesthetists of Ireland<br />
22 Merrion Square North, Dublin 2, Ireland<br />
Email: cat@coa.ie<br />
www.anaesthesia.ie/index.php/training/committee-of-annaesthetist-trainees<br />
The Faculty of Intensive Care Medicine<br />
Churchill House, 35 Red Lion Square, London WC1R 4SG<br />
Email: ficm@rcoa.ac.uk<br />
www.ficm.ac.uk<br />
Faculty of Pain Medicine of The Royal College of Anaesthetists<br />
Churchill House, 35 Red Lion Square, London WC1R 4SG<br />
Email: fpm@rcoa.ac.uk<br />
www.fpm.ac.uk<br />
NHS Careers<br />
www.nhscareers.nhs.uk<br />
14 WHO IS THE ANAESTHETIST?
WHO IS THE ANAESTHETIST? 15
Group of Anaesthetists in Training (GAT)<br />
c/o The Association of Anaesthetists of Great Britain and Ireland,<br />
21 Portland Place, London W1B 1PY<br />
Tel: 020 7631 1650 Fax: 020 7631 4352 Email: gat@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org/professionals/trainees
Working Arrangements for Consultant Anaesthetists<br />
in the United Kingdom<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org March 2011
Membership of the working party<br />
Contents<br />
Dr Paul Clyburn<br />
Dr Kathleen Ferguson<br />
Dr Ian Geraghty<br />
Dr William Harrop-Griffiths<br />
Dr Robert Harwood<br />
Dr Peter Maguire<br />
Dr Mark Porter<br />
Dr Elizabeth Shewry<br />
Professor Robert Sneyd<br />
AAGBI Council Member<br />
AAGBI Council Member<br />
RCoA Representative<br />
Chair, AAGBI Council Member<br />
BMA Representative<br />
BMA Representative<br />
BMA Representative<br />
GAT Representative<br />
AAGBI Council Member<br />
1. Introduction 4<br />
2. Principles of the 2003 consultant contract 5<br />
3. DCC PAs and their calculation 7<br />
4. SPAs and their justification 11<br />
5. WTR – rest and work patterns 15<br />
6. Leave of all sorts 18<br />
7. On-call 23<br />
8. Part-time and flexible working 28<br />
9. Job planning 31<br />
This guideline has been seen and approved by the Council of the AAGBI.<br />
10. Changes to job plans when services are reconfigured 35<br />
11. Academic contracts 37<br />
12. Differences in the devolved nations 41<br />
13. The pre-2003 contract 45<br />
14. Starting out as a consultant 47<br />
15. References 50<br />
© The Association of Anaesthetists of Great Britain & Ireland 2011<br />
2 3
1. Introduction<br />
The Association of Anaesthetists of Great Britain & Ireland (AAGBI) receives<br />
a number of queries every year from members that relate specifically<br />
to working arrangements. Although not a trade union, the AAGBI has a<br />
responsibility to support and advise its members and it therefore responds to<br />
the majority of these queries. Although we refer some more detailed queries<br />
to the trade unions that represent doctors in the UK (the British Medical<br />
Association – BMA – and Hospital Consultants and Specialists Association<br />
– HCSA), many questions about working arrangements have common<br />
themes. Council of the AAGBI established a working party to consider<br />
questions and problems relating to working arrangements for consultants, and<br />
charged it with producing a concise guide for AAGBI members. Including<br />
representatives from the BMA, the Royal College of Anaesthetists (RCoA) and<br />
the Group of Anaesthetists in Training (GAT), the working party has produced<br />
this report. We plan to update the guidance as necessary, and we would<br />
welcome comments and suggestions from members about future editions of<br />
this document.<br />
It is important to note that the AAGBI cannot arbitrate on or resolve disputes<br />
between consultants and their employers. This guidance is not a definitive<br />
document; it offers the opinion of the AAGBI on some common contractual<br />
issues. Consultants who fail to reach agreement with their clinical managers<br />
on the details of contracts, job plans, working arrangements, terms and<br />
conditions should follow mediation and appeals processes within their<br />
hospitals and should consider seeking the support of their Local Negotiating<br />
Committee (LNC). The AAGBI advises those anaesthetists who are not<br />
members of the armed forces to become members of a trade union that<br />
can offer them formal support in resolving disagreements about contractual<br />
matters.<br />
2. Principles of the 2003 consultant contract<br />
A contract is nothing more than an enforceable agreement that regulates<br />
the relationship between two parties. In this case, the two parties are the<br />
employer and employee, or consultant and their employing health authority,<br />
NHS Trust or Board. In short, it describes what one agrees to do, what one<br />
gets paid for doing it, and a mechanism for enforcing the agreement at law.<br />
The contract thus comprises the agreement between a consultant and<br />
his/her employer, and is described through the national model contract,<br />
the statement of particulars (the letter sent on appointment), the terms and<br />
conditions of service and the consultant’s individual job plan.<br />
The new consultant contracts were negotiated in order to address changes<br />
in the way the NHS and consultants had been working over the preceding<br />
few years and to prepare for future developments. Consultant job planning<br />
had been introduced in 1991 but too often remained just a discussion about<br />
the weekly timetable rather than developing into the intended conversations<br />
about a consultant’s duties, objectives and responsibilities, and the allocation<br />
of time and other supporting resources to achieve these. From a consultant’s<br />
point of view, job planning did not provide tools that were successfully able<br />
to control the growing workload of consultants due to both patient demand<br />
and the increasing burden of out-of-hours work.<br />
The overall principle was that of accountability and mutual respect for both<br />
parties. The profession accepted a time-sensitive contract, in which there is a<br />
simple and direct relationship between the amount of time spent working and<br />
the payment for this work. The relationship did not go so far as to introduce<br />
‘clocking in and clocking out’ – it is accepted that the assessment of time<br />
spent working should be brought to job planning meetings to discuss the<br />
prospective allocations of time, rather than consultants’ being paid by the<br />
hour like many other grades of staff in the NHS. However, it did allow a<br />
consultant to control his/her workload by demonstrating the time spent on<br />
it, and where this workload was excessive, expect either a reduction in the<br />
workload or extra payments.<br />
In return, the contract contained better tools to co-ordinate consultants’ work<br />
with that of his/her hospital or employer, and the needs of his/her local health<br />
economy, through the use of job planning and objective setting. Consultants<br />
would now be expected to be able to account for the time spent on activities<br />
and objectives, whether clinical or other, and the outcomes achieved during<br />
that time, at the job planning meeting and in the appraisal meeting.<br />
4 5
The practical changes were that a closer time-sensitivity came in through<br />
organising work into PAs (programmed activities); payments for work done<br />
while on-call were introduced, along with availability allowances for being<br />
on-call. An ‘overtime rate’ was introduced, with PAs being four hours in<br />
length except during premium time when they are three hours. Overall<br />
salary levels increased and new higher levels were introduced, along with<br />
a threshold system to require the consultant to fulfill basic engagement with<br />
the contract in order to access these higher levels. The ‘10% rule’ reducing<br />
salary when one did significant amounts of private practice was replaced by<br />
a requirement to offer an extra paid PA to the NHS before engaging in private<br />
practice if one wished to progress through the pay thresholds, a requirement<br />
that most anaesthetists found was fulfilled through the new recognition of the<br />
excessive work they had undertaken under the old contract.<br />
Working time was divided for all into direct clinical care – DCC (and patientrelated<br />
administration was recognised for the first time in this category)<br />
- and supporting professional activities (SPA), with some consultants also<br />
undertaking additional NHS responsibilities or external duties. The contract<br />
defined a typical balance – so doctors employed in the consultant grade<br />
should, unless otherwise agreed, spend the 10 programmed activities<br />
of a whole time contract balanced between 7.5 DCC PAs and 2.5 SPAs.<br />
This balance was designed to emphasise the importance of consultants’<br />
undertaking quality assurance and quality improvement.<br />
The consultant’s job plan should contain objectives, and describe the<br />
supporting resources that the employer will provide in order to achieve these<br />
objectives. The contractual commitment is to do one’s best to achieve the<br />
objectives, and discussion on this point should form a central part of the job<br />
plan review.<br />
A new system of mediation and appeal was introduced in order to deal<br />
with those circumstances in which there was a failure to agree the job plan<br />
between the consultant and their employer.<br />
Consultants who did not wish to transfer to the new contracts were able to<br />
remain on the old contract (except in Wales – see section 12), accepting<br />
lower salaries but keeping what was seen as less managerial control over<br />
their working lives.<br />
3. DCC PAs and their calculation<br />
Direct clinical care programmed activities describe the portion of a<br />
consultant’s working week devoted to the delivery of patient care; for an<br />
anaesthetist this is usually individual patient care. Employers are keen to<br />
maximise the proportion of a consultant’s work week devoted to patient<br />
care, sometimes believing such PAs to be of greater worth; it should be<br />
remembered that the 2003 consultant contract rightly places equal value on<br />
both DCC and SPA PAs. The terms and conditions of service for the 2003<br />
consultant contract defines direct clinical care activities as:<br />
• Emergency duties, including emergency work carried out during or arising<br />
from on-call<br />
• Operating sessions, including pre-operative and postoperative care<br />
• Ward rounds<br />
• Outpatient clinic work<br />
• Clinical diagnostic work<br />
• Other patient treatment<br />
• Multidisciplinary meetings about direct patient care<br />
• Administration directly related to the above (including but not limited to<br />
referrals and notes)<br />
• Assessing patients in pre-assessment clinics and as ward referrals<br />
• Checking equipment before use<br />
• Drawing up and checking drugs before use<br />
• Transfer of patient within and between hospitals<br />
• WHO checklists<br />
• Time spent checking/searching for beds for patients<br />
• Time spent at end of list waiting/ensuring full and stable recovery from<br />
anaesthesia<br />
• Clinic letters<br />
• Telephone contact regarding patient care (outside of DCC period of duty)<br />
• Travel time between hospital sites<br />
• Travel time to and from hospital when on-call (from the time of first contact to<br />
arrival back at home)<br />
It may be that other work may reasonably be included as DCC time. Such work<br />
might include:<br />
• Planning, discussing or reviewing the management of complex cases<br />
• Planning surgical lists, managing list throughput<br />
• Theatre floor troubleshooting or postoperative recovery unit based work or<br />
supervision<br />
• Special request pre-operative patient assessment<br />
• The entire period spent within the hospital, whether actively working or not,<br />
while providing resident on-call cover<br />
Finally, the whole approach was supported by the introduction of a new<br />
clinical excellence award (CEA) scheme, extending the scope of the old<br />
distinction award and discretionary points schemes so that the majority of<br />
consultants should be able to progress to an award through application.<br />
6 7
Direct clinical care time may be made up of time worked in standard time<br />
and time worked in premium time. Standard time is defined as the period<br />
from 07:00 h – 19:00 h Monday to Friday, excluding Bank Holidays. Premium<br />
time is any work outside of that period, including weekend and Bank Holiday<br />
working at any time of day. A standard time PA is 4 h in duration; a PA<br />
worked in premium time is 3 h in duration.<br />
Traditional methods of calculating the number of DCCs in an individual<br />
job plan, such as allocating a PA tariff based on the number of half-day lists<br />
worked, are useful rules of thumb but may not properly represent the total<br />
number of PAs worked. Changes to anaesthetist’s working patterns – sameday<br />
patient admission with corresponding earlier start times, all-day and<br />
long-day operating sessions together with decreased trainee presence for outof-hours<br />
work – may have substantially altered the time associated with each<br />
clinical commitment. In financially straitened times it is particularly important<br />
that anaesthetists can demonstrate to employers the full extent of their clinical<br />
activity.<br />
First, record time spent on predictable emergency work during the reference<br />
period, note when the work was done (to note standard or premium time PAs).<br />
Add up the total time spent on predictable emergency work for both standard<br />
and premium time during the reference period. Divide each by the number<br />
of weeks in the reference period to create weekly averages (values W and Y<br />
below). Divide each value again by 4 or 3, as appropriate, to convert to PAs to<br />
reflect work undertaken in standard or premium time (values X and Z, below).<br />
Add together both the PA values (X and Z, below); call the sum value ‘A’.<br />
However, notwithstanding these caveats, many departments do find tariff<br />
systems convenient, allowing changes to sessions and work patterns without<br />
extensive recalculations of the hours worked. A commonly used tariff might<br />
be for an inpatient operating list (a standard ‘session’ of 4 h anaesthesia<br />
and operating time) to represent a standard 1.25 DCC PAs, including preoperative<br />
and postoperative visits, machine and equipment checks, and<br />
drawing up drugs. Extending this value to other sessions such as a day surgery<br />
list, critical care session, obstetric anaesthetic session or outpatient session<br />
such as chronic pain or pre-assessment should be undertaken with caution.<br />
When using tariffs, care should be taken to ensure that the PA tariff allocated<br />
to a particular session is an accurate reflection of the total time spent.<br />
A diary record of some sort is invaluable in demonstrating to an employer<br />
the range and duration of work that an individual consultant undertakes. An<br />
ongoing diary of work activity is accurate, is individually specific and can<br />
accommodate the normal workload variation between working weeks for a<br />
consultant anaesthetist. There are several electronic diary systems available,<br />
both commercial and freely available. An appropriate diary system must be<br />
capable of recording the time spent on different work activities and should<br />
deliver information acceptable to both parties in a job plan discussion.<br />
Alternatively, paper based diaries may be preferred. In this case, consultants<br />
should decide on a reference period of several weeks reflective of their<br />
normal working pattern.<br />
Figure 1: Calculating the PAs spent on predictable emergency work – for<br />
explanation see text.<br />
Repeat the process for unpredictable emergency work; call that sum value ‘B’.<br />
Record the time spent on patient administration (clinic letters, results,<br />
multidisciplinary team meetings) during the reference period; note when the<br />
work was done (to note standard or premium time PAs). Add up the total time<br />
spent on patient administration for both standard and premium time during the<br />
reference period. Divide each by the number of weeks in the reference period<br />
as before to create weekly averages (values S and U, overleaf). Divide each<br />
value again by 4 or 3, as appropriate, to convert to PAs to reflect whether work<br />
8 9
was undertaken in standard or premium time (values T and V, below). Add<br />
together both the PA values (T and V, below); call the sum value ‘C’.<br />
4. SPAs and their justification<br />
Supporting professional activities are the activities that underpin direct<br />
clinical care in one’s own practice and in that of other consultants. They<br />
can be defined for example as participation in training, medical education,<br />
continuing professional development, formal teaching, audit, job planning,<br />
appraisal, research, clinical management and local clinical governance<br />
activities, but it may be more helpful to think of them as activities that are<br />
essential to quality assurance and quality improvement. Clinical practice<br />
is the largest part of the need for employing consultants but all practice,<br />
whether individual or in a team, will atrophy or fail to develop if not<br />
examined in a rigorous manner and the need for change and development<br />
considered.<br />
Figure 2: Calculating the PAs spent on patient administration – for<br />
explanation see text.<br />
Repeat once more for non-emergency clinical work in the reference period<br />
(clinics, rounds, patient assessment, anaesthesia and operating etc). Call this<br />
value ‘D’.<br />
Add A + B + C + D; this gives a value for average DCC PAs worked over the<br />
reference period. Please note: unpredictable emergency work averaging over<br />
2 PAs per week should trigger a job plan review with a view to decreasing the<br />
requirement for such work. It is useful to agree the method and standard of<br />
diary evidence that may be required before any job planning meeting.<br />
Accurate diary monitoring is important in job planning (see page 31)<br />
and is particularly useful if agreement between a consultant and his/her<br />
clinical manager cannot be reached, and a mediation and appeal process is<br />
embarked upon. In fact, experience has suggested that if no diary data are<br />
presented, an appeal is likely to fail.<br />
The model contract states that [1]:<br />
“Subject to the provisions for recognising emergency work arising from<br />
on-call rotas below, the schedule in your Job Plan will typically include an<br />
average of 7.5 Programmed Activities for Direct Clinical Care duties and<br />
2.5 Programmed Activities for Supporting Professional Activities. Where<br />
your agreed level of duties in relation to supporting professional activities,<br />
additional responsibilities and other duties is significantly greater or lower<br />
than 2.5 programmed activities there will be local agreement as to the<br />
appropriate balance between activities. Part-time consultants need to devote<br />
proportionately more of their time to Supporting Professional Activities. This<br />
should be agreed on an individual basis. Refer to the guidance on part time<br />
and flexible working for further information.<br />
“The precise balance will be agreed as part of Job Plan reviews and may<br />
vary to take account of circumstances where the agreed level of duties in<br />
relation to Supporting Professional Activities, Additional NHS Responsibilities<br />
and External Duties is significantly greater or lower than 2.5 Programmed<br />
Activities.”<br />
The meaning of this is clear. The consultant grade is characterised by a<br />
consultant agreeing this balance in his/her job plan, although there is scope<br />
to accept something different where appropriate – and agreed. You are<br />
strongly advised not to accept fewer SPAs in your job plan unless you are<br />
content with the reduced ability to work on quality assurance and quality<br />
improvement, and you should discuss it with a colleague or mentor if you<br />
are considering this. If your employer is not persuaded by your arguments on<br />
this, collect evidence and consider delaying agreement on your job plan until<br />
10 11
further discussion and negotiation have been exhausted before going towards<br />
mediation and appeal.<br />
It appears that some NHS employers do not understand the value of SPAs<br />
and believe that different specialties require different amounts of SPA time<br />
to underpin safe and effective performance. In particular, there seems to<br />
be a belief that the time of consultant anaesthetists is better spent giving<br />
anaesthetics and that anaesthetists have little need for SPAs. The AAGBI<br />
refutes these suggestions and supports the 2003 contract in recommending<br />
that the job plans of consultant anaesthetists should typically include<br />
2.5 SPAs. Although SPAs might not be seen by some Trusts to be directly<br />
productive, this argument ignores the need for quality assurance and<br />
quality improvement through all the listed SPA activities. Not only is it<br />
a strict requirement for Trusts to undertake these activities, e.g. Clinical<br />
Negligence Scheme for Trusts (CNST) compliance, compliance with the<br />
recommendations of national audits, and clinical audit of innovative<br />
techniques, it is also essential for services to change and develop with time.<br />
Consultants hold the prime responsibility for doing this, and the link through<br />
learning about a new technique, planning its introduction and auditing the<br />
results is as valid for consultant anaesthetists as for anyone else. Productivity<br />
is about the efficient and effective generation of desired outcomes, with<br />
services continually improving, not simply carrying on doing what we did last<br />
year and the year before. Continuous improvement requires consultants to<br />
undertake continual reflection and change management.<br />
Supporting professional activities are not as easy to count as patients on<br />
a theatre list, but they can and should be accounted for. The commitment<br />
for someone with 2.5 SPAs in their job plan is to undertake this amount<br />
on average over a representative period, not to do exactly that, no more<br />
and no less, each week. You should expect to undertake some SPAs in a<br />
fixed fashion, e.g. clinical audit meetings, committee meetings, weekly<br />
Continuing Professional Development (CPD) and journal clubs, and some<br />
in a more flexible fashion, e.g. writing a new clinical guideline, undertaking<br />
an audit, reviewing a proposed policy, mandatory training, dealing with<br />
correspondence and teaching at undergraduate and postgraduate level. It is<br />
reasonable for your clinical manager to expect some record of the time spent<br />
on these activities in aggregate so as to ensure that the prescribed balance of<br />
activities is being delivered. After all, a typical consultant anaesthetist is paid<br />
about 20% of his/her pay slip income for these 2.5 SPAs in his/her job plan.<br />
This is also where job planning objectives come in. By agreeing objectives<br />
and working towards them, one can take to the job plan review or the<br />
appraisal meeting a record of the outcomes achieved during SPA time. This<br />
is not only valuable to keep track of one’s own professional development but<br />
also to demonstrate effective use of this time.<br />
It cannot be over-emphasised how important it is to place yourself in a<br />
position to be able to answer cogently when asked what you spend your SPA<br />
time on and what you have achieved during that time.<br />
It is sometimes argued that consultant anaesthetists need less SPA time<br />
than consultants in other specialties. This is wrong. Even though consultant<br />
anaesthetists tend to work in larger teams and departments than many other<br />
consultants, the breadth of scope of anaesthesia practice means that there<br />
need to be lead clinicians with specific responsibilities in a wider range of<br />
areas. A clinical director should maintain a list of departmental leads and<br />
responsibilities [2] and consultants could not only ensure that their name<br />
appears on that list in several places but also that they are active in those<br />
areas and can demonstrate what they have achieved over the past year.<br />
Box 2 (below) contains some suggestions for important roles and activities<br />
within a typical department of anaesthesia.<br />
• Clinical Director<br />
• Chairman of the Department<br />
• SAS Mentor<br />
• Revalidation Advisor and Coordinator<br />
• Appraisal Lead<br />
• Rota-writer<br />
• Job Planning Lead<br />
• Productive Operating Theatre Lead<br />
• On-call Rota-writer and Trouble-<br />
Shooter<br />
• College Tutor and Deputy<br />
• Trainee Rota-writer<br />
• Local Induction Lead<br />
• Clinical Governance Lead<br />
• Risk Management Lead<br />
• Clinical Governance Links for<br />
Subspecialty Areas<br />
• Audit Coordinator<br />
• Safety Lead<br />
• NICE Guideline Lead<br />
• Complaints Lead<br />
• Guideline Development and<br />
Monitoring<br />
• Critical Incident and Serious<br />
Untoward Incident Investigator<br />
• Blood Transfusion Lead<br />
• Infection Lead<br />
• Pharmacy Link<br />
• Equipment Lead<br />
• Medical Devices Training Lead<br />
• Health Informatics Lead<br />
• Procurement Lead<br />
• Airway Lead<br />
• Cell Salvage Lead<br />
• Resuscitation Lead<br />
• Sedation Lead<br />
• Pre-assessment Lead<br />
• Subspecialty Area Leads<br />
• Educational Supervisors<br />
• Programme Directors<br />
• Trainee Mentors<br />
• Acute Pain Lead<br />
• Library Monitor<br />
• Student Work Experience Lead<br />
• Research Lead<br />
• CPD Lead<br />
• Allergy Testing Lead<br />
12 13
For most consultants, the majority of SPA time is not spent on service<br />
objectives in pursuit of the employer’s goals, but is spent on personal<br />
development objectives and other activities that contribute to appraisal<br />
and revalidation. A heavy managerial responsibility should be agreed as<br />
an additional NHS duty, not as SPA time. The Academy of Medical Royal<br />
Colleges has stated that consultants need a minimum of 1.5 SPAs per week<br />
on average to undertake the activities that will lead to personal revalidation,<br />
and more to undertake any duties or responsibilities in management, any<br />
teaching or training or research, and they emphasise that all consultants must<br />
engage in service development and clinical governance activities [3]. All this<br />
applies to consultant anaesthetists as much as anyone else.<br />
Time and place is important when thinking about SPAs. The spectrum might<br />
run from a Trust in which complete freedom exists to undertake SPA work<br />
whenever and wherever one likes, to a Trust in which one is expected to sit<br />
at a specific desk for 10 h every Wednesday. Neither is particularly supported<br />
by the terms and conditions of service, and neither is necessarily appropriate,<br />
but some principles are important:<br />
• If you undertake clinical work during SPA time, which may be<br />
appropriate from time to time, then you have a right to have that SPA<br />
time returned to you.<br />
• If you agree to be in a specific place at a specific time, then your<br />
employer must provide proper supporting resources. A chair might<br />
be sufficient for attending a clinical audit meeting, but for individual<br />
governance work then a desk, computer, office and solitude are<br />
as likely to be important.<br />
• If you take time back one week, put it in the next.<br />
• Be reasonable and repay the trust that someone places in you.<br />
Supporting professional activities are a vital part of consultant practice.<br />
Think as carefully about planning and delivering your SPAs as you do about<br />
your clinical work and all is likely to be well. The AAGBI believes that the<br />
outcome of the time spent on SPA is more important than the number of<br />
minutes spent per week, but consultants should be prepared to deliver – and<br />
to show that they deliver – on the time agreed within their job plans.<br />
5. WTR – rest and work patterns<br />
The Working Time Regulations (WTR) is British and Irish health and safety<br />
legislation that has applied to consultants and other career grade doctors<br />
since 1998 – often incorrectly called the Eurpoean Working Time Directive<br />
(EWTD). The application of WTR to junior doctors has been on a phased<br />
basis, but applied in full – a 48-h maximum average working week – from<br />
August 2009. A very small number of specific junior doctor rotas have<br />
received derogation to have a 52-h working week until 2011. The reason<br />
that WTR impacts so significantly on healthcare services is as a result of two<br />
European Court of Justice (ECJ – Europe’s highest court) rulings (SiMAP and<br />
Jaeger) on working time while on healthcare premises. These rulings have<br />
effectively ended the longstanding practice of on-call duties and made shift<br />
working the norm for doctors resident in hospitals. Box 3 (below) illustrates<br />
these rulings.<br />
SiMAP ruling (2000)<br />
This defined all time when a doctor is required to be present on site as<br />
actual working hours for the purposes of work and rest calculations.<br />
Jaeger ruling (2003)<br />
This confirmed that this was the case even if the doctor is allowed to sleep<br />
when their services are not required.<br />
In April 2010 the European Commission announced its work plans during<br />
the European Parliamentary Session, which would include collation of data<br />
in relation to the actual implementation of the WTR across EU member<br />
states, its actual impact on health services and, most importantly, plans to<br />
renegotiate the Directive by the end of 2010. However, in practice, even<br />
if a new EWTD is agreed at the end of 2010, there will be at least a 2 – 3<br />
year period before any change to employment law is actually enshrined in<br />
individual member state law.<br />
The elected membership of the current European Parliament has moved<br />
significantly towards the right politically following elections during 2009. This<br />
is likely to alter the views of Parliament as a whole on many social issues,<br />
including WTR.<br />
14 15
The European Commission, after consulting European social partners, has<br />
issued opinions on the WTR derogations for the UK underlining that the<br />
average weekly working time for doctors in training may not exceed 52h,<br />
including on-call at the work place, and that the temporary extension will last<br />
until 31 July 2011 [4].<br />
The European Trade Union Confederation recently called upon the European<br />
Commission to pursue infringement proceedings against member states not<br />
adhering to the current WTR rules, including the ECJ rulings. The Commission<br />
has signalled its intention to delay any infringement proceedings for most<br />
countries in order to give individual member states further time to comply<br />
with the rulings but has commenced proceedings against Greece and Ireland,<br />
which on paper have poor track records of implementing WTR within their<br />
healthcare sectors.<br />
‘Hot’ weeks in ICU<br />
Over recent years, especially in intensive care units (ICUs), it has become<br />
customary for consultants to have ‘hot’ or very busy weeks on duty. These<br />
hot weeks allow improved continuity of patient care. This is acceptable<br />
under WTR since guidance specifies that the average 48-h working week is<br />
calculated over a 26-week reference period. The single area that may not be<br />
averaged is the rest period; therefore, ICUs should be staffed to ensure that<br />
all doctors working there have an 11-h rest period in a given 24-h period.<br />
Although consultants can derogate from many aspects of the WTR, they may<br />
not derogate from the requirement to have an 11-h rest period (see Box 4,<br />
below). Those with responsibility for agreeing the job plans of consultant<br />
intensivists should be aware of this. Some ICU rotas provide for a ‘warm<br />
week’ in which a consultant acts as a backup to allow the first-on consultant<br />
to take the rest period if necessary.<br />
Indemnity<br />
The three main UK Medical Defence Organisations (MDOs) and the NHS<br />
Litigation Authority (NHSLA) have confirmed that doctors are indemnified<br />
when working in excess of a 48-h working week. The main exclusion from<br />
this indemnity cover would be wilful neglect or negligence by any doctor<br />
working in contravention of the General Medical Council guidance – ‘Good<br />
Medical Practice’ [5]. A doctor working as a locum (even via an agency)<br />
solely within the NHS will remain covered by the NHS Litigation Authority<br />
(NHSLA). The AAGBI advises that all doctors work responsibly, be mindful of<br />
not working excessive hours or treating patients when tired, and recommends<br />
that AAGBI members should be members of one of the MDOs. While not<br />
mandatory, it is prudent to notify your MDO if you voluntarily opt out of<br />
the WTR maximal working week, advising them of the actual hours you are<br />
working. This should be done in advance of working prolonged hours.<br />
Members should note that NHSLA cover applies to work in the NHS but does<br />
not include all matters that can include representation at coroner’s courts,<br />
disciplinary cover and professional guidance on an individual basis – thus the<br />
recommendation to be an MDO member.<br />
Private practice and the WTR<br />
Question:<br />
Answer:<br />
Question:<br />
Do the WTR apply to private practice?<br />
The WTR only apply to employed work. However, there is<br />
a legal requirement for doctors not to present for work in an<br />
unfit condition.<br />
Can I do private work during my compensatory rest period?<br />
May consultants derogate from the average weekly working hours rules in<br />
the WTR?<br />
The answer is yes – but with two provisos:<br />
1) That they should not be obliged to do so by their employers<br />
2) That they may not derogate from the requirement for 11-h continuous<br />
rest period within any 24-h period<br />
Answer:<br />
This is not recommended, as problems with patient care<br />
might be ascribed to your being unfit for work because of<br />
fatigue.<br />
16 17
6. Leave of all sorts<br />
Annual leave<br />
Consultants are entitled to six weeks’ annual leave. In England, consultants<br />
are allowed an additional two days called statutory days (‘stat’ days).<br />
Consultants in Northern Ireland have an additional two Bank Holidays<br />
(St Patrick’s Day and Orangemen’s Day). Consultants in Scotland and Wales<br />
have to make do with only the six weeks. In England and Northern Ireland,<br />
consultants on the 2003 contract and in post for seven years or more have<br />
an addition two days’ annual leave. While there is no standard definition<br />
of a leave week, it is sensible and fair that this is commensurate with an<br />
individual’s working week. Thus, someone who works three days per week<br />
should expect to calculate leave entitlement on the basis of 6 x 3 (plus any<br />
additional) days, i.e. 18 (plus any additional) days and take leave of 18 (plus<br />
any additional) working days only. This should be defined in local leave<br />
policies and be fairly and equitably applied.<br />
Calculating annual leave<br />
Six weeks’ leave can be 42 days, 30 working days or six weeks’ worth of<br />
clinical sessions. Departments have different ways of calculating leave, but<br />
leave calculations can still be the source of much unhappiness. Consultants<br />
should agree a mechanism for ensuring fairness in leave taking. The AAGBI<br />
thinks that it may sometimes be unfair to employers to take leave primarily<br />
on days that would otherwise include NHS clinical activity. In an extreme<br />
example, a consultant’s working week could be compressed into two long<br />
clinical activity days. If the consultant were to take just these two days off<br />
in each of 21 weeks, they would have taken 42 days’ leave but would have<br />
avoided clinical work for five months. This is evidently unfair. The AAGBI<br />
suggests that leave periods should in general contain the same proportion of<br />
DCC and SPA time as is in the consultant’s job plan.<br />
Another way of achieving fairness to employee and employer is to calculate<br />
consultant leave in terms of clinical sessions missed. Calculated in this way,<br />
a consultant who has six weeks’ annual leave and who does six operating<br />
lists per week would be allowed to miss 36 lists per year. Additional<br />
days’ leave can be calculated as proportions of a week. For instance, if a<br />
consultant is entitled to six weeks and four days’ leave, this equals 6.8 weeks<br />
in decimal notation. If they do six lists per week, this comes to 6 x 6.8 =<br />
40.8 sessions. The kind Leave Monitor will round this up to 41 sessions. The<br />
punctilious Leave Monitor will allow 41 sessions’ leave in four out of every<br />
five years but only 40 sessions in the fifth year.<br />
It is worth noting that some employers are taking an increasingly<br />
unsympathetic view of consultants who seek special leave (see page 21) to<br />
perform duties for the wider NHS, such as work for the AAGBI, RCoA or<br />
BMA. As a result, some consultants are being forced to take annual leave to<br />
fulfil these valuable duties. If this is the case, and if such dates tend to fall<br />
on days when a consultant would normally be committed to direct clinical<br />
care, it is hoped that the Leave Monitor and Clinical Director will take a<br />
lenient approach and relax the approach suggested in the box above. It is<br />
also worth noting that consultants who maintain a meticulous and continuous<br />
year-round work diary will have a record of how many DCC PAs they have<br />
delivered for their Trusts. This may inform discussions and negotiations about<br />
leave, as it will provide an accurate record of what work has actually been<br />
done rather than a calculation of what should have been done.<br />
The annual leave year usually begins at the anniversary of commencement<br />
of the consultant contract but some employers have a standard leave year<br />
for all employers, e.g. 1st April, which should be specified in the contract.<br />
Consultants on a substantive contract may carry over up to five days of<br />
untaken annual leave, although more may be carried over by special<br />
arrangement. Consultants who are not able to take all of their annual leave<br />
or to carry it over may be paid in lieu if this is in line with local agreements.<br />
Consultants must seek formal permission to take leave. Up to two days’<br />
leave may be taken with notification but without formal permission. Many<br />
departments set leave rules that allow the continuation of clinical service.<br />
These often include a minimum booking period, e.g. at least six weeks in<br />
advance of the leave to be taken, and a maximum number of consultants who<br />
can be away at the same time. All Trusts will have an agreed leave policy,<br />
which should be referred to.<br />
Sickness during annual leave<br />
If a consultant falls sick during annual leave and produces a statement to that<br />
effect, he/she will be regarded as having been on sick leave from the date of<br />
the statement. Self-certification can cover up to seven days’ sickness.<br />
Public holidays<br />
A consultant is entitled to 10 days’ public holidays or days in lieu thereof,<br />
which consists in England of eight public or Bank Holidays plus two ‘statutory<br />
days’, and in Northern Ireland 10 public or Bank Holidays. Some Northern<br />
Irish employers add these two additional days to annual leave entitlement.<br />
A consultant who works or is on-call on a Bank Holiday is entitled to a<br />
leave day in lieu. A common problem encountered is when a consultant<br />
requests a day in lieu because they were on-call on the night before a Bank<br />
18 19
Holiday, and was therefore on-call for the period from midnight to the time<br />
of consultant on-call handover. The terms and conditions of service for<br />
consultants are clear: if a consultant is disturbed by work between midnight<br />
and 09.00 h of a Bank Holiday, that consultant is entitled to a leave day in<br />
lieu. In the old (pre-2003) contract, consultants on-call the night before a<br />
Bank Holiday were entitled to a lieu day whether or not they were working in<br />
the hospital or disturbed by calls after midnight.<br />
Study and professional leave<br />
The distinction between professional leave and study leave can be confusing<br />
as the terms may be used interchangeably. Study leave is essentially to enable<br />
a consultant to participate in continued professional development (CPD) and<br />
may include:<br />
• Study, usually but not exclusively or necessarily on a course or<br />
programme<br />
• Research<br />
• Teaching<br />
• Examining and taking examinations<br />
• Visiting and attending professional conferences<br />
• Approved postgraduate purposes<br />
• Working with colleagues in order to acquire new knowledge or skills<br />
The recommended standard for consultants is leave with pay and expenses<br />
within a maximum of 30 days (including non-clinical and non-duty days<br />
falling within the period) in any three-year period. Leave will normally be<br />
granted to the maximum extent and all reasonable expenses should be<br />
met regardless of the employer’s financial constraints. The Department of<br />
Health has clearly stated that professional leave is an allowance based on<br />
an individual’s needs to attend to duties that are important for the broader<br />
benefits of the NHS and necessitates the consultant being away from their<br />
base of employment. Such duties can be recognised as ‘external duty’ PA<br />
rather than as professional leave. Any grant of leave is subject to the need to<br />
maintain NHS services.<br />
What’s the difference between study leave and professional leave?<br />
A good guide to the usual difference is:<br />
Study leave is when you are a registrant at a meeting and your employer<br />
should pay for you to attend it.<br />
Professional leave is when you are part of the faculty at a meeting.<br />
Where a consultant is employed by more than one NHS organisation, leave<br />
must be approved by all these organisations. During study leave with pay, the<br />
consultant should not undertake any remunerative work without the special<br />
permission of the leave granting authority. Unlike supporting activity, study<br />
leave facilitates absence for several days or even weeks at a stretch, where<br />
necessary. Therefore, study leave is a means of achieving professional activity<br />
goals in addition to (not in place of) SPA time.<br />
Special leave with or without pay<br />
The provisions of Section 3 of the terms and conditions of service will still<br />
apply. This leave is granted without formal restriction and some consultants<br />
find it useful in working for medical Royal Colleges or professional<br />
associations.<br />
Can my employers cancel my study, professional or special leave if it is<br />
within my allocation of 30 days per three years?<br />
Yes, they can. Your employers can cancel this leave if not to do so would<br />
impair clinical activity in the hospital. However, employers should make<br />
every reasonable effort to avoid cancelling this leave.<br />
Sabbaticals<br />
A consultant may apply for sabbatical leave according to existing<br />
arrangements. Proposals for sabbatical leave should be made before annual<br />
appraisal and considered in the annual job plan review. The contract in Wales<br />
has provision for consultants to seek a paid sabbatical for up to three months<br />
in order to pursue activity away from normal duties that will subsequently<br />
benefit patient care.<br />
Sick leave<br />
A consultant is entitled to sick leave with pay where they are absent from<br />
work due to illness, injury or other disability. If unable to work for more than<br />
three days, a self-certificate can be submitted for up to the first seven days of<br />
sickness. For longer absences, another medical practitioner should provide<br />
regular medical certificates. The employer is entitled to ask for more frequent<br />
certificates and to assessment by its own appointed medical practitioner.<br />
Entitlement to paid sick leave relates to the duration of NHS service. This may<br />
be extended at the employer’s discretion. Your employer will have a policy<br />
that will determine whom you should tell if you have to take sick leave.<br />
However, as a senior professional within the organisation, it would be right to<br />
tell those people in the area in which you were to be working that day.<br />
20 21
Maternity leave, domestic, personal and care relief<br />
The regulations relating to these different forms of leave are determined by<br />
local employers on the basis of the NHS terms & conditions. Consultants<br />
should check with their employing hospitals.<br />
7. On-call<br />
Emergency work is an important aspect of the clinical duties of consultant<br />
anaesthetists and intensivists. Indeed, it could be argued that all anaesthetists<br />
and intensivists should have emergency work of some sort included in their<br />
job plan. For the large majority of consultants, this will be provided within<br />
the on-call service for their employing hospital. For the minority who do not<br />
do on-call, emergency work can be conducted in the form of trauma lists,<br />
daytime or evening emergency lists, covering the Accident & Emergency<br />
Department during weekday hours or other activities likely to bring the<br />
consultant into contact with emergency work.<br />
The 2003 consultant contract includes payment of an on-call availability<br />
supplement that takes into account the frequency and intensity of the on-call<br />
duties (see table).<br />
The work of consultant anaesthetists and intensivists is almost always in<br />
intensity Category A. It is worth noting that this supplement does not include<br />
payment for work conducted; it is simply for availability. The predictable<br />
amount of work involved in doing on-call work should be included in the<br />
DCC PAs within the consultant’s job plan, taking into account that most,<br />
if not all, of this work is conducted in premium time, i.e. at weekends and<br />
between 19.00 h and 07.00 h on weekdays. If there is doubt about the<br />
amount of work performed during on-call duties, a diary monitoring exercise<br />
that covers at least one full on-call cycle should be conducted. The results of<br />
such an exercise can be used to inform the job planning process.<br />
Compensatory rest after on-call<br />
Consultants are subject to the provisions of the WTR, and therefore cannot<br />
be expected to fulfil a work pattern that does not include 11 consecutive<br />
hours of rest per day. Therefore, predictably onerous on-call duties that almost<br />
always involve work at night should lead to a consideration of whether the<br />
consultant should have clinical duties allocated during the daytime before<br />
22 23
a night on-call or the day after a night on-call. If a consultant is required<br />
to work during a night on-call, he/she is entitled to compensatory rest the<br />
following day. Indeed, patient safety considerations will often mean that it<br />
would be foolish to continue to work after a busy on-call night or period of<br />
duty. If a consultant is scheduled to be working in the operating theatre on<br />
the day after a night on-call that proves to be very busy, the consultant can<br />
demand compensatory rest and miss the lists. In doing so, the consultant<br />
should take into account any risks to safe patient care that this might involve.<br />
In turn, the Clinical Manager of the department of anaesthesia (Clinical<br />
Director, CD) should make every effort to ensure that tired consultants are not<br />
expected to work after onerous nights on-call. A question that is commonly<br />
asked is whether, having missed a list through compensatory rest after a night<br />
on-call, the consultant can be expected to do an additional list to make up<br />
for the list that was missed. The answer is no. Job plans should be designed<br />
such that predictably busy nights on-call are not scheduled before a day of<br />
clinical duties, or indeed SPA activity. In this way, compensatory rest can be<br />
built into consultants’ job plans without compromising service, safe patient<br />
care or CPD activities. A consultant should think carefully before conducting<br />
other clinical activities during an identified period of compensatory rest after<br />
on-call duties.<br />
Question:<br />
Answer:<br />
Caveat No 1:<br />
Caveat No 2:<br />
If I have a very busy night on-call and miss an NHS list the<br />
next day because I am taking compensatory rest, do I have<br />
to pay that list back?<br />
No, you do not have to pay the list back in any way.<br />
Consultants’ job plans should be designed such that NHS<br />
duties are not scheduled in the day after predictably busy<br />
nights on-call.<br />
Consultants should not deliberately arrange their on-call<br />
duties so as to place them the night before NHS duties.<br />
Coming off the on-call rota<br />
Almost all consultant anaesthetists and intensivists are appointed to job plans<br />
that include on-call duties. During their working life, some consultants seek<br />
to relinquish their on-call duties for a variety of reasons that include illness,<br />
increasing age, and family or other domestic or professional commitments. If<br />
a consultant wishes to drop his/her on-call duties, he/she should discuss this<br />
with his/her CD. If the reason relates to stress or illness, assessment by the<br />
Occupational Health Department (OH) is appropriate. If OH recommends<br />
that the consultant be removed from the on-call rota for health reasons,<br />
employers should make every effort to make this possible. Consultants<br />
should note that if they are released from on-call duties for health reasons,<br />
they should think carefully before making themselves responsible for the<br />
emergency cover of any patients out-of-hours. This might occur if the<br />
consultant anaesthetises a private patient who stays overnight in a private<br />
hospital. Under such circumstances, the consultant might wish to ensure that<br />
another consultant is on call for this patient and that there exists a written<br />
agreement confirming this.<br />
The AAGBI has recommended that “there should be a review of on-call<br />
responsibilities for anaesthetists over 55 years of age” [6]. Consultants have<br />
no right to drop on-call duties at a set age, as this would be contrary to UK<br />
age discrimination legislation, but CDs should consider reasonable requests<br />
to discuss on-call duties from older members of the department. Small<br />
departments may find allowing a consultant to come off the on-call rota<br />
very difficult because of the increase in on-call frequency for the remaining<br />
consultants. Larger departments will find it easier to allow people to leave the<br />
on-call rota but should be wary of creating a rule that consultants over a set<br />
age should not do on-call, first because this may be contrary to the provisions<br />
of age discrimination legislation and second, as the demographics of the<br />
consultant body may mean that a large group of consultants of a similar age<br />
may all demand to come off the on-call rota at roughly the same time at some<br />
point in the future, and this may severely compromise service provision.<br />
Some CDs ask consultants coming off the on-call rota to take on additional<br />
duties such as additional weekday lists or regular out-of-hours emergency<br />
commitments such as evening or weekend trauma lists. Such arrangements<br />
should be individually negotiated. No consultant has the right to come off<br />
the on-call rota other than for health reasons. No CD has the right to demand<br />
additional work to compensate for coming off the on-call rota. Contracts can<br />
only be changed by mutual consent from employer and employee. Clinical<br />
Directors should take reasonable steps to cooperate with consultants who<br />
wish to come off the on-call rota for family reasons; Human Resources<br />
Departments are useful points of contact when discussing the rights and<br />
responsibilities of employers and employees in such matters. Again,<br />
negotiation lies at the heart of such arrangements, and it is usually possible<br />
to reach equitable agreements without formal referral to Human Resources or<br />
senior managers. Where agreements cannot be reached, the BMA’s Industrial<br />
Relations Officers (IROs) can be an invaluable source of support and advice.<br />
24 25
Changes to the frequency of on-call<br />
Changes in the number of consultants in the department, in the number of<br />
active consultants in the on-call rota and in the number or nature of on-call<br />
rotas provided by the department may produce changes in the frequency<br />
of on-call duties. Consultants have a responsibility to help the department<br />
fulfil its service commitments safely and effectively, but changes to a<br />
consultant’s job plan and contract should only be made by mutual agreement<br />
after negotiation. If changes to the frequency of on-call affect the on-call<br />
availability supplement or number of DCCs paid for predictable work during<br />
on-call periods, these should be reflected in the pay of consultants.<br />
Consultant residency on-call<br />
Consultants are not obliged to provide a resident on-call service. The 2003<br />
contract states that “a consultant will only be resident during an on-call<br />
period by mutual agreement” [1]. However, changes in trainee numbers and<br />
working hours, and service reconfiguration within a hospital may mean that<br />
consultant residency in out-of-hours periods in the form of shift working or<br />
residency on-call may form part of a possible solution to service demands.<br />
In these circumstances, the AAGBI recommends that the consultants<br />
negotiate with their employers and in doing so make sure that adequate<br />
recognition is made in their job plans and in their pay for the additional<br />
work and inconvenience that such changes will involve. The LNC should<br />
be involved in such a change; the BMA’s IROs can offer invaluable support<br />
in negotiations. Consultants should not commit to such a change without a<br />
formal written agreement that includes the opportunity to review and change<br />
the arrangements after a period of their implementation. Some departments<br />
consider responding to requests for consultants to do shift work or become<br />
resident on-call by making them a requirement of recently appointed<br />
consultants but not of established consultants in a department. The AAGBI<br />
joins the BMA in arguing against such practice; it risks dividing the consultant<br />
body and creating potential tensions that will not be conducive to safe and<br />
effective patient care.<br />
trainee as a last resort. If undertaking work of this kind, the consultant should<br />
ensure that they possess all the necessary competencies required for the role.<br />
For example, some trainee roles require training in safe patient transfer, and<br />
consultants working in some subspecialties not requiring these skills may not<br />
have current training. If a consultant agrees to do this, a written agreement<br />
is highly desirable before the start of any resident work. Local Negotiating<br />
Committees should be encouraged to prepare pro forma agreements to<br />
facilitate these negotiations. The BMA provides a model agreement for LNCs<br />
to use in such circumstances. If the agreement includes payment for the<br />
consultant under these circumstances, the rate of pay should reflect the grade<br />
of the doctor doing the work, not the grade of doctor being replaced, i.e. the<br />
consultant should be paid to do this work as a consultant, not as a trainee.<br />
Covering trainee absence on-call<br />
A consultant has a duty to deputise for absent consultant colleagues so far<br />
as is practicable, but this does not include joining trainee on-call rotas.<br />
However, consultants do have a professional obligation to ensure that<br />
emergency clinical services offered to patients are undertaken safely and<br />
effectively. When faced with a situation in which a trainee scheduled to work<br />
an overnight shift is unavailable because of illness or rota failure, consultants<br />
have a responsibility to work with managers to obtain a locum. Sometimes,<br />
this is not possible and the consultant may have to work in the place of the<br />
26 27
8. Part-time and flexible working<br />
The Department of Health has stated that the current consultant contract<br />
should provide the necessary flexibility for those who wish to work either<br />
part-time or flexibly in nature. Part-time contracts may be offered between<br />
one and nine PAs. For appointments after January 2004, where the request<br />
to work part-time is in order to undertake private practice, the contract<br />
should not normally be for more than 6 PAs. Those with reasons other than<br />
private practice, but who may wish to undertake some private work, can be<br />
appointed to a contract of more than 6 PAs. Part-time consultants wishing<br />
to undertake remunerated clinical work in their non-NHS time would be<br />
expected to offer up to one extra PA on top of their normal working week.<br />
Transitional arrangements from the old contract will require accurate diary<br />
evidence to permit the transfer from notional half days (3.5 h) to programmed<br />
activities (4 h). Any increase in workload can only occur by mutual<br />
agreement and the award of extra PAs. The division of PAs between DCC and<br />
SPA is roughly pro rata but it is acknowledged that part-time consultants need<br />
the same opportunity to maintain their skills through CPD. Proportionally,<br />
more of the PA time should be directed towards SPAs. Part-time consultants<br />
will not carry the same clinical load as full time consultants. Recommended<br />
numbers of SPAs for part-time contracts are shown in the box below.<br />
Total number of PAs<br />
Number of SPAs<br />
2 or less 0.5<br />
2.5 – 3.5 1.0<br />
4.0 – 5.5 1.5<br />
6.0 – 7.5 2.0<br />
8.0 or more 2.5<br />
Apart from the PAs, a part-time consultant should have no other NHS<br />
commitments during the working week. Participation in an on-call rota will<br />
receive remuneration with the same supplement as a full-time consultant on<br />
that rota. Part-time consultants may undertake on-call either at a reduced<br />
frequency – for example at a 90% frequency for a consultant working a 9 PA<br />
job plan – or at the same frequency as full time colleagues. If the consultant<br />
works on-call at a 90% frequency, the on-call supplement is calculated as<br />
a percentage of 9 PAs. If they work on-call at the same frequency as other<br />
full-time colleagues, the on-call supplement is calculated as a percentage of<br />
a full-time, 10 PA salary. If the consultant undertakes an on-call duty on a day<br />
that they do not normally work, then time off in lieu or additional payment<br />
will be agreed.<br />
Flexible training adds time within the training grade. This may make it<br />
difficult for people who have undergone flexible training to reach the top<br />
of the consultant pay scale. Where necessary, they will have their progress<br />
through the thresholds adjusted so that they will reach the threshold they<br />
would have reached if in training on a full-time basis.<br />
The contract allows for flexibility in timing and location of consultants PAs.<br />
Employers have a duty to make reasonable attempts to accommodate this.<br />
The employee has a right to return to a regular pattern of work after a period<br />
of flexible working. Examples of flexible work patterns include job-sharing,<br />
annualised hours contracts, flexi-time and term-time working. Annualisation<br />
allows employees to vary their weekly commitment, for example, during<br />
school holidays, making the time up in term time.<br />
Annualised working<br />
Although the 2003 contract offers little detail to guide CDs and consultants<br />
in devising and agreeing annualised contracts, it does make provision for<br />
them. There are a number of ways that a job plan can be annualised, but<br />
anaesthesia lends itself to such manipulations, as clinical care is readily<br />
divisible into operating lists and clinics. The important principles are as<br />
follows:<br />
• Consultants should work an agreed annual total of PAs instead of the<br />
same number each week.<br />
• The arrangement must be compatible with best practice in job planning<br />
for consultants.<br />
• The arrangement must be agreed, as it would be for any job plan.<br />
• The number of PAs to be worked in a year is usually the product of<br />
the number of PAs per week in a base job plan multiplied by the<br />
number of weeks in a year. For a 10 PA job plan, this would be 520 PAs.<br />
• Consultants do not work 52 weeks per year, so reasonable allowance<br />
must be made for Bank Holidays, annual leave, study and professional<br />
leave, sick leave, maternity leave, special leave, etc. The usual range<br />
of working weeks used in annualised working calculations is 40 – 42<br />
weeks per year.<br />
We will provide one sample calculation as an example. Dr HG is a<br />
consultant anaesthetist whose outside activities include heavy commitments<br />
to the RCoA, AAGBI, NICE and ACCEA. He wishes to annualise his contract<br />
28 29
to give him the flexibility to attend a large number of meetings. His base<br />
contract is for 10 PAs, and comprises 5.5 operating lists per week, 2.5 SPA<br />
and 0.5 PA for predictable emergency work on-call.<br />
He and his CD agree that his annual leave (6 weeks and 4 days) and Bank<br />
Holidays together will amount to 8 weeks per year, his study/professional<br />
leave will be 2 weeks per year and that his special leave allowance on top<br />
of this, given his level of national activity, shall be an additional 1 week. This<br />
means that the number of lists he will be expected to do will be 41 x 5.5 =<br />
223 lists per year. He is allowed to work this fully flexibly given that he gives<br />
at least 6 weeks’ notice of times of the week that he is available to work. He<br />
agrees with his CD that he will also work his 41 x 2.5 = 102 SPAs flexibly<br />
and will agree verifiable outcomes for this SPA time. They agree that if sick<br />
leave is taken during periods of annual leave, time will be given back using<br />
a formula of 6 sessions per week’s sick leave. Both Dr HG and his CD are<br />
happy with this arrangement.<br />
Annualised contracts are not the perfect solution for everyone, and a<br />
department of anaesthesia would not wish too many of its consultants to work<br />
in a fully flexible fashion. The AAGBI recommends that those consultants<br />
working annualised contracts make it clear when they plan to take their<br />
allocated annual leave in order to avoid any arguments if sick leave is taken<br />
in non-working weeks, as sick leave taken during annual leave should be<br />
‘paid back’, but sick leave during non-working periods that are not annual<br />
leave need not be.<br />
9. Job planning<br />
Job planning is the process by which the aims and requirements of employer<br />
organisations are translated into agreements detailing how individual<br />
consultants will contribute to the delivery of those aims. All employing Trusts<br />
want DCC and SPA activity aligned to the Trust’s needs; job planning is the<br />
mechanism to ensure this. It allows Trusts to obtain maximum value from<br />
DCC and SPA sessions. There are some minor differences in the devolved<br />
countries. Country-specific information can be found in detail within the<br />
terms and conditions of service for the country in which you are employed.<br />
Job planning takes place at least annually and is a prospective process. All<br />
consultants, whether or not they are employed under the 2003 consultant<br />
contract arrangements, are obliged to undergo annual job plan reviews.<br />
Job planning is a partnership process; job plans may not be imposed – the<br />
agreement of both parties is required. Job planning is a separate process<br />
to appraisal although outputs from the job plan review will inform the<br />
appraisal mechanism. Should there be significant change to a consultant’s<br />
commitments, then an interim job plan review can be requested at any stage.<br />
There is extensive guidance describing job planning and how to undertake<br />
it. Unhappily, although the requirement for consultant job plans has existed<br />
since 1991, job planning can still be a poorly conducted process: the process<br />
may focus simply on the development of a timetable or be seen as an<br />
opportunity to reduce PAs. At its heart, job planning is really about objectives<br />
and the SPAs that help deliver them. The process is intended as a partnership<br />
activity that delivers benefit for both consultant and employer. It allows<br />
consultants the opportunity to lead on service development both in quality<br />
and productivity and to identify the resources needed to deliver objectives.<br />
Employers are afforded the ability to extract the added value that consultants<br />
bring. Both parties benefit from clarity about commitments.<br />
Preparation for job plan review is essential. Some supporting information will<br />
be required; a work diary is invaluable, where possible supported by activity<br />
data, comparative workload and/or ideal workload data. Consultants must<br />
have an appreciation of the process itself. It is helpful to have read some of<br />
the available guidance ahead of the review meeting. Similarly, it is advisable<br />
for consultants to consider what they need from the review and where they<br />
might be challenged.<br />
The process is based on agreement; job plans are not imposed. A draft job<br />
plan should be prepared by the Clinical Manager – this forms the basis of<br />
30 31
discussion at the review meeting. More than one meeting may be required.<br />
Both parties may be assisted at the meeting(s) – the Clinical Manager by a<br />
General Manager and the consultant by a colleague or advisor.<br />
The job plan review should be systematic. Trusts may be keen to focus on<br />
elective work; it is more appropriate to give early consideration according<br />
to clinical priority or on areas where agreement may be more difficult.<br />
Emergency work should be the first priority – time spent dealing with<br />
predictable on-call work should be reviewed first followed by unpredictable<br />
on-call. On-call activity should be averaged over a 1 – 8 week reference<br />
period. Contentious areas may be, for example, work undertaken in premium<br />
time, SPA allocation or Additional PAs and fee-paying services. Although<br />
consultants cannot be required to undertake planned work in premium time,<br />
there is an increasing need for consultant presence; it may be helpful to<br />
consider a local agreement. Similarly, it should be borne in mind that SPAs<br />
are not an automatic entitlement – they need to be justified and accounted<br />
for with agreed outputs in objective setting.<br />
After discussion the job plan is signed off as agreed by both parties. If<br />
agreement has not been possible consultants may use the mediation and<br />
appeal process.<br />
Mediation and appeal<br />
The mediation and appeal process is part of the 2003 consultant contract<br />
process to help resolve disputes over job plans and pay progression. It<br />
is not designed for use in other settings, for example disagreements over<br />
CEAs. Although consultants on the pre-2003 contract are required to<br />
undergo annual job planning, their contractual arrangements do not include<br />
mediation and appeal.<br />
Mediation and appeal are incremental processes. Mediation, a less formal<br />
process, is tried first, before moving on to appeal where necessary. When<br />
a job plan or pay progression cannot be agreed either the consultant or the<br />
Clinical Manager may refer the matter, in writing, to the Trust’s Medical<br />
Director within two weeks of the disagreement. The referral will describe<br />
their view of the matter, and the other party will be invited to respond in<br />
writing. It is recommended that all areas of dispute be brought to mediation<br />
in case they need to be formally considered at some later stage by an Appeal<br />
Panel. The Medical Director will convene a meeting between the Clinical<br />
Manager, the consultant and him/herself within four weeks of receipt of the<br />
referral. Agreement between parties is sought at the meeting; if this is not<br />
possible then the Medical Director will decide the matter and will inform all<br />
parties in writing.<br />
If the consultant is still not satisfied, then he/she may lodge an appeal in<br />
writing, outlining the basis of the appeal, to the Chief Executive within two<br />
weeks of the outcome of mediation. The Chief Executive will convene an<br />
Appeal Panel that should meet within four weeks of receipt of notification<br />
of appeal. An Appeal Panel consists of three members, none of whom<br />
should have been involved with the case previously. The panel is chaired<br />
by a nominee of the Trust, often a senior non-executive director. The second<br />
member is nominated by the consultant. The third member is chosen from a<br />
list held by the Strategic Health Authority of approved independent appeal<br />
panellists. Such members may either be from BMA/BDA backgrounds or have<br />
managerial backgrounds, often within Human Resources. Either party can<br />
object to the third member suggested and a new member will be appointed.<br />
The 2003 consultant contract specifies that the Appeal Panel will be arranged<br />
by the Chief Executive to meet within four weeks of the written request from<br />
the consultant. Although delay is undesirable, in reality, given the difficulty in<br />
arranging the attendance of consultants and other senior NHS personnel, the<br />
four-week timescale may be subject to some slippage. When delay occurs the<br />
appellant should not normally be penalised; any contested payments should<br />
be backdated to at least the date on which the appeal was lodged.<br />
Both parties make written submissions ahead of a hearing, and copies<br />
are sent to all panellists and to the other party. At the hearing, at which<br />
the consultant may be represented but not by a legal representative, both<br />
parties present their case to the panel. Expert advice may be required by the<br />
employer, the consultant or the panel. Panel members may ask questions of<br />
both parties and of the expert advisor(s). The appeal hearing lasts no more<br />
than one day. The Appeal Panel makes its judgement within two weeks of the<br />
hearing, notifying both the Trust Board and the consultant in writing. The Trust<br />
is not obliged to accept the panel’s recommendations but would normally be<br />
expected to do so.<br />
32 33
Job planning is by agreement, not decree: what to do if you cannot reach<br />
agreement<br />
CD and consultant fail to agree<br />
2 weeks<br />
Inform Medical Director (MD)<br />
4 weeks<br />
MD, CD and consultant have mediation meeting<br />
2 weeks<br />
Consultant appeals to Chief Executive (CE)<br />
4 weeks<br />
CE convenes Appeal Panel<br />
Appeal Panel meets and makes judgement<br />
10. Changes to job plan when services are<br />
reconfigured<br />
Clinical and other services will change with time and so will your job<br />
plan. The usual principle applies – all changes should be agreed changes.<br />
Furthermore, both parties should act reasonably, especially when considering<br />
changing the job plan to fit in with changes in local service provision.<br />
However, from time to time the employer will need to change a consultant’s<br />
job plan to fit in with service changes, to reconfigure services, cut costs or<br />
introduce new technologies.<br />
When facing such a situation, and particularly if it seems likely to involve<br />
a change to one’s own job plan, it would be important to think about the<br />
potential changes and whether one is dissatisfied with them. For example,<br />
would it substantially change the nature of the service that one provides?<br />
Would it involve more or inconvenient travelling? Would it have an impact<br />
on the ability to meet commitments, for example through having on-call<br />
responsibility for a hospital that is further away? You should seek to discuss<br />
such questions with your clinical manager at the earliest opportunity.<br />
Nevertheless, at some point you may be faced with a change to your job plan<br />
that is prompted or required by a reconfiguration and with which you are<br />
unhappy. You should seek personal advice from a trade union representative<br />
as soon as possible, either through the LNC or the BMA. The normal<br />
processes of mediation and appeal are important but in this case there will<br />
be other factors that will affect the judgment that an arbitrator will make on<br />
the disagreement. A consultant would usually be badly advised to seek to<br />
obstruct changes by attempting to veto changes to their job plan when, for<br />
example, a hospital closes or reconfigures its services.<br />
Agreeing or disagreeing with changes<br />
Contractual changes should be by agreement unless an employer is prepared<br />
to give notice of a change. You should know the circumstances under which<br />
you give your agreement and what rights and support you have if you do not<br />
wish to agree. Giving one’s agreement to a job plan change can be tacit as<br />
well as explicit. Most changes to job plans over the years are implicit, and an<br />
important function of job planning meetings is to codify such changes so that<br />
there is an explicit written understanding; but a change need not be written to<br />
be a contract variation. So, where an employer imposes a unilateral change<br />
to a job plan, for example the timing or location of an operating list, and the<br />
consultant carries on working without complaint, they will be treated by the<br />
34 35
law as having agreed to that change. It is a common misconception that one<br />
can preserve one’s rights through refusing to sign a document; it is not the<br />
failure to sign, but the employee’s conduct, that is important.<br />
Should you want to disagree, if you have not already done so, now is the<br />
time to seek professional advice. You should also look for information on job<br />
planning that may be available from the RCoA, AAGBI or BMA websites.<br />
Any unilateral imposition of contractual changes may result in a claim for<br />
breach of contract, or a resignation and then claim for constructive dismissal.<br />
Except where intractable disputes arise or the business needs reorganisation,<br />
Trusts are very unlikely to do this – in the vast majority of cases you will be<br />
able to address problems through negotiation.<br />
11. Academic contracts<br />
This section illustrates principles for job planning in a post where the basic<br />
week is roughly 50:50 divided between NHS and university. Clearly, other<br />
arrangements are possible and may be explored using similar principles.<br />
The basic week<br />
The basic working week comprises 10 PAs. Regardless of whether academic<br />
posts are fully funded by the university (some senior staff and some<br />
Foundation Chairs) or co-funded by the NHS, the principles are the same.<br />
In addition, the split of this 10 for planning purposes should be regarded as<br />
about five to be planned with the university and about five to be planned<br />
with the NHS – and, if you are a university employee, agreed with the<br />
university. All basic contracts comprise 10 PAs and there is no obligation on<br />
either the employer to offer or the employee to accept contracts >10 PAs.<br />
Accordingly, all advertised jobs should include a base 10 PA job plan.<br />
Five PAs for the university<br />
This may be for research, teaching or management as agreed with your line<br />
manager. Typically, for Research Excellence Framework (REF)-returned,<br />
research-active staff, the major activity will be research. None of this time<br />
is to be used for NHS management or other NHS clinical or non-clinical<br />
activities.<br />
Five PAs for the NHS<br />
This comprises a mix of SPA time and DCC. The vigour with which the NHS<br />
partner pursues clinical work from university-employed clinical academics<br />
inevitably reflects their underpinning funding. If the clinical time is universityfunded,<br />
then the NHS partner may reasonably take a ‘light touch’ approach.<br />
Conversely, where the five PAs are NHS-funded (by recharge), then they may<br />
have higher expectations in terms of clinical work delivery.<br />
SPA time<br />
Mindful of personal development, CPD requirements and the increasing<br />
burden to be expected with revalidation, this will never be
elated and other specialty activities outside the Trust. This may include roles<br />
in medical Royal Colleges, specialist societies, regional and national NHS<br />
bodies, etc. This may, with agreement, be properly included in SPA time and<br />
where such agreed activities are extensive then the allowance of SPA time<br />
may be more than 2.5.<br />
Clinical work (DCC)<br />
This includes clinics, operating lists, ward-rounds as well as patient related<br />
paper work and meetings. This must be agreed with the NHS partner. Note<br />
that in order for clinical work to attract PAs over and above the basic week, a<br />
clear and agreed account must be given for first five PAs for the NHS.<br />
Additional PAs for the university<br />
The university may offer additional academic time to clinical academic staff.<br />
This additional academic time is discretionary and you may decline it if you<br />
wish.<br />
Additional PAs for the NHS<br />
By agreement with the NHS and with the approval of your university line<br />
manager, you may work additional PAs to a maximum of 12. On-call is<br />
typically paid for in this part of the contract. Clinical work such as clinics<br />
will only attract additional PAs if the basic 5 PAs for the NHS are clearly<br />
described and justified.<br />
Special activities for the NHS<br />
Special roles for the NHS such as research work, Network Lead, R & D<br />
Director, Clinical Manager, clinical governance, etc may be described in SPA<br />
time. It may be appropriate to include these as additional SPAs for the NHS<br />
provided that the underpinning description of the basic NHS commitment<br />
is convincing and overall commitment is not impacting on academic<br />
performance.<br />
Actual contract<br />
In practice almost all staff employed under the 2003 consultant contract opt<br />
to agree additional activity. Where this is to be offered an alternate shadow<br />
job plan will also be prepared illustrating how an agreed longer working<br />
week might be structured. Typically, a job plan will comprise the university<br />
sessions (paid for and managed by the university) and NHS sessions paid by<br />
the university, managed (with joint appraisal and job plan agreement, see<br />
overleaf) by the NHS partner and recharged at cost to the NHS partner by the<br />
university.<br />
University sessions<br />
A typical academic contract will contain about five university sessions in the<br />
basic 10; there are therefore about 20 h that the staff member should work<br />
in an actively managed process against agreed the university activities, e.g.<br />
management, teaching and research.<br />
NHS time<br />
NHS time will comprise a mixture of DCC PAs and SPAs. The NHS part of the<br />
job plan must include a proportion of SPA time. It is important that the NHS<br />
proportion of the job plan contains an adequate amount of SPA time in order<br />
to give the clinical academic sufficient time to address the non-clinical part of<br />
their NHS role and to ensure that this does not spill over into the Universityfunded<br />
academic time. The following table indicates a typical DCC/SPA split.<br />
This provision of SPA time should be regarded as a minimum and where the<br />
post holder undertakes significant SPA activity for the NHS partner a greater<br />
allocation may be appropriate.<br />
NHS PAs DCC PAs SPAs<br />
(total including on-call)<br />
6 4 2<br />
5 3.5 1.5<br />
4 2.75 1.25<br />
Total contract<br />
The clinical academic consultant contract is a single contract, not two halfcontracts,<br />
and it is ultimately accountable in its entirety to the university line<br />
manager and the employing university, although the active management of<br />
the clinical proportion of the job plan is typically delegated by agreement<br />
to a clinical manager within the NHS partner. The total job plan should not<br />
exceed 12 PAs.<br />
Job planning, appraisal and accountability<br />
NHS pay progression rules require that individuals complete a job planning<br />
process and appraisal every year in order to be eligible for pay progression<br />
and CEAs. Universities endorse and apply this principle. Appraisal of the<br />
university staff with three or more NHS PAs in their job plan should be joint<br />
appraisal (this means three people in one room at the same time, not separate<br />
NHS and University appraisals). The job plan (final version as signed by the<br />
NHS line manager) must be agreed with the university line manager and a<br />
copy lodged with the university HR section (and updated every year).<br />
38 39
Implementation guidance<br />
Individual NHS partners have developed detailed implementation guidance<br />
and this can usefully be applied to the university staff.<br />
Management responsibilities<br />
The university staff may (with the prior agreement of their university line<br />
manager) adopt management roles within NHS partner organisations. Such<br />
roles may be reimbursed by the NHS partner using varied mechanisms.<br />
Typically this involves substitution of management for clinical activity<br />
(without additional payment) or additional payment without allocation<br />
of time or some combination of the two. All NHS management activities<br />
whether paid or unpaid must be accommodated within the proportion of the<br />
job plan allocated to NHS activities. University time is not to be used for NHS<br />
management activities.<br />
Teaching<br />
The nature and quantity of teaching undertaken by clinical academics must<br />
be prospectively and transparently agreed and unequivocally located within<br />
the job plan. Typically, the university clinical academic staff will undertake<br />
some teaching within their actively managed university sessions and will not<br />
receive additional payment for this. Where (by prior agreement) teaching<br />
takes place during the NHS proportion of their contract, it may take place<br />
as an SPA (without additional payments), by substitution for fixed clinical<br />
commitments (without additional payment) or as additional contracted<br />
activity which must be included in the job plan and the total job plan must<br />
not exceed 12 PAs. It is not acceptable for university staff to solicit or receive<br />
supplementary payment for teaching (via NHS partners) and expect or be<br />
expected to deliver this within their contracted university time.<br />
Annualised contracts and additional leave<br />
Some NHS clinicians operate annualised contracts wherein the total<br />
quantum of work for the year is agreed and delivered flexibly (again by prior<br />
agreement). In some cases working weeks beyond 12 PAs are recognised<br />
by 12 PA contracts with additional annual leave. Such arrangements for the<br />
university clinical academic staff should be regarded as exceptional and<br />
should in all cases be prospectively approved by the university.<br />
Universities recognise that clinical academics are hard working, versatile<br />
individuals and expect that contractual arrangements may reasonably be<br />
operated with considerable flexibility. A key principle is transparency,<br />
accountability and continual clarity about time allocation and the proper<br />
relation between NHS and the university duties.<br />
12. Differences in the devolved nations<br />
The 2004 contract in Northern Ireland<br />
By 2010 over 98% of consultants had transferred to work on this contract,<br />
which closely mirrors the 2003 English contract. Despite some years having<br />
passed since the introduction of this contract, many consultants continue to<br />
work to retrospective job plans – Trusts do not appear to have caught up with<br />
prospective job planning. The two main reasons advanced for this are Trust<br />
and NHS reorganisation and lack of medical managerial manpower or time.<br />
It is likely that there will be major change, as the Northern Ireland Health<br />
Service is under severe financial strain and faces further financial cutbacks.<br />
A 2009 moratorium on study leave funding was lifted in some Trusts in 2010<br />
but there is a requirement for annual savings of over £100 million in the<br />
coming years, and there are suggestions that medical staff posts may remain<br />
vacant to save money.<br />
The 2004 Northern Ireland consultant contract has four main elements:<br />
• Direct Clinical Care (DCC)<br />
• Supporting Professional Activities (SPA)<br />
• Additional HPSS (Health and Personal Social Services) Responsibilities<br />
• External Duties<br />
The recommended norm is for a 7.5 DCC to 2.5 SPA split in contractual<br />
obligations. In recent times and associated with budgetary restrictions,<br />
consultant SPA has come under very severe downward pressure with a<br />
suggestion from DHSSPSNI (Department of Health, Social Services and<br />
Public Safety of Northern Ireland) to Trusts that 1.5 SPA should be ‘core’<br />
with all other SPA ‘earned on an individual basis’. Both the BMA and AAGBI<br />
continue to recommend a 2.5 SPA allocation per consultant. In case of<br />
dispute it is essential that each consultant has a detailed and accurate diary<br />
outlining the actual work that they are doing should they need to follow the<br />
contract dispute processes of Facilitation (called Mediation in England) and<br />
thence Appeal.<br />
There were moves from Trusts to assign Additional HPSS responsibilities and<br />
External Duties to a new category of leave – ‘special leave’. However, this<br />
work is outlined specifically in the terms and conditions of service and advice<br />
should be taken from BMA / HCSA on the appropriate time to be included<br />
within a negotiated and agreed job plan.<br />
40 41
Each individual consultant anaesthetist should seek prospective job<br />
plans for the year ahead and retain copy documentation of all contact /<br />
communications seeking job planning.<br />
The latest rates of pay can be found on the BMA website [7].<br />
Take home pay is determined by considering the following:<br />
• Basic salary<br />
• Any additional Programmed Activities<br />
• On Call Allowance / Intensity Supplement<br />
• CEAs / Discretionary Points<br />
• Additional allowances – such as travelling expenses<br />
Since 2007 Northern Ireland has had five Trusts. Each Trust should have<br />
an active LNC that engages with Trust management in negotiating local<br />
contractual arrangements. Issues that are under Trust control include<br />
payments for waiting list initiatives, resident consultant shift working out of<br />
hours and relocation allowances for consultant anaesthetists affected by acute<br />
service reconfigurations. In anaesthesia, resident shift working out of hours is<br />
increasingly likely and contact should be made with the local LNC to ensure<br />
the position and views of anaesthetists are properly represented.<br />
The consultant contract in Wales<br />
Unlike the contract in England, the Welsh contract is an amendment to the<br />
original consultant contract and any points not covered in the amendment<br />
are unchanged from the original contract [8]. The amendment document<br />
is therefore much briefer than the necessarily more comprehensive English<br />
contract. However, many of the principles are the same, though it is<br />
important to appreciate that some of the points in the rest of this guide do not<br />
apply to consultants working in Wales.<br />
The main amendments that are different from the English contract include:<br />
• A basic 37.5-h working week (10 sessions of variable length).<br />
• Typically, 7 DCC and 3 SPA sessions. Increasingly, Health Boards<br />
(formerly NHS Trusts) are appointing new consultants on 8 DCC and 2<br />
SPA and there is pressure on existing consultants to come in line unless<br />
they can demonstrate extra activity to justify the third SPA.<br />
• The first 3 h per week (in place of 3.75 h) of work as part of on-call<br />
(based on an average over 6 months) is counted as 1 session of DCC.<br />
Time worked over this is counted towards additional 3.75-h sessions.<br />
• Provision that 1 SPA may take place at home in the evening<br />
(recognising the work by some consultants at home), allowing<br />
uncontracted free time during the day.<br />
• No requirement to provide an additional session of time to the NHS in<br />
order to acquire the right to undertake private practice.<br />
• Additional sessions for routine work are entirely voluntary with no<br />
requirement for compulsory weekend or evening work.<br />
• Extra sessions requested by the Health Board are voluntary and locally<br />
negotiated for time and payment.<br />
• In exceptional circumstances, resident on-call is remunerated at three<br />
times the sessional payment with an agreed compensatory rest period<br />
the following day.<br />
• Commitment award scheme replaced discretionary points awarded<br />
with progress depending on satisfactory job planning (though<br />
expected to be universally awarded). This ensures continued pay<br />
progression throughout a consultant’s career. National Excellence<br />
Awards are currently the same as in England.<br />
• Recognition of different patterns of work intensity, particularly later in<br />
consultant’s career.<br />
• There is good provision for part-time and academic working through<br />
open, individualised job planning.<br />
• A sabbatical scheme of up to three months of paid leave to undertake<br />
activities away from normal duties that will subsequently benefit patient<br />
care. The application and award of sabbatical leave is made locally.<br />
• Flexibility and professionalism is encouraged as much as possible<br />
within the contract.<br />
• In the event of a job-planning dispute, an initial conciliation procedure<br />
followed, if necessary, by a balanced appeals procedure that is binding<br />
on the Trust and the consultant.<br />
The consultant contract in Scotland<br />
The Scottish model contract remains broadly similar to that in England<br />
although three amendments have been made with respect to maternity<br />
arrangements, flexible working and redundancy payments. Transitional<br />
arrangements, salary scale and the pay progression timescales are similar<br />
to those in England and an updated version of these may be accessed in<br />
the NHS circular PCS(DD)2007/11. Also explicit in the circular are the<br />
arrangements for payment of waiting list initiative work. They are: three times<br />
the hourly rate at point 20 on the seniority scale or, alternatively, twice the<br />
rate of pay with time off in lieu or standard rate plus twice the time off in lieu.<br />
Premium time exists between the 20.00 and 08.00 h as opposed to the 19.00<br />
42 43
and 07.00 h in England. In addition to this, non-emergency work may be<br />
programmed on a Saturday between 09.00 and 13.00 h, although this work<br />
is at premium rate and not standard.<br />
As in England, the need for NHS employers to squeeze SPA time is evident<br />
in the current advertisement of consultant posts with less than 2.5 PAs<br />
identified for SPA in a 10 PA contract. The BMA (Scotland) and Academies<br />
of the Royal Colleges in Scotland have reached a level of understanding<br />
with the Management Steering Group (a self-appointed advisory group<br />
to the Scottish Executive Health Department) whereby all new posts will<br />
be advertised with time explicit for essential CPD. All other SPA must be<br />
agreed during the job planning process. This places accurate diary evidence<br />
as a priority for any consultant within NHS Scotland. All newly appointed<br />
consultants are advised to keep accurate diaries and to request a job plan<br />
review no later than three months after appointment if they feel their work<br />
balance is inappropriate.<br />
Mediation and appeals for the job planning process are handled in a similar<br />
manner to England although the Divisional Chief Executive has a role in<br />
Scotland and the appeal panel make-up differs slightly.<br />
The Merit Award and Discretionary Points system (SACDA – the Scottish<br />
Advisory Committee on Discretionary Awards) has been replaced by<br />
SACCLEA (the Scottish Advisory Committee on Clinical Leadership and<br />
Excellence Awards). Details of the new system are uncertain at the time of<br />
publication.<br />
Local Negotiating Committee involvement remains crucial for the following<br />
issues where national arrangements do not exist: prospective cover<br />
included, re-imbursement for consultants resident on-call, and provision for<br />
leave for forms of leave not otherwise specified.<br />
13. The pre-2003 contract<br />
This section is primarily intended for those clinicians with responsibility for<br />
management, leadership and job planning of consultant anaesthetists still on<br />
the pre-2003 contract. It is assumed that holders of these contracts are fully<br />
aware of the merits of both contracts and have elected to remain on the old<br />
contract. It is not the remit of this document to advise on that choice. This<br />
contract is not available to any consultant appointed since November 2003<br />
or to those who have changed to the 2003 contract.<br />
Types of contract<br />
This contract, initially agreed in 1979, describes units of work in terms of<br />
notional half days (NHDs) worked flexibly. Each NHD lasts 3.5 h. There is<br />
no premium for work in unsociable hours although there is provision for<br />
intensity payments. There are two main types of this contract for those who<br />
work full-time: whole-time and maximum part-time. Holders of both have a<br />
contractual commitment to devote substantially the whole of their working<br />
time to NHS activities with a minimum of 10 NHDs. There is also provision<br />
in this contract for part-time working in which there is no expectation that the<br />
post-holder will devote substantially the whole of their professional time to<br />
the NHS. Part-time contracts may range from one to nine NHDs.<br />
Holders of whole-time contracts are limited to earning not more than 10<br />
per cent of their gross NHS earnings in private practice and are required to<br />
make an annual declaration confirming this. Holders of maximum part-time<br />
contracts are not subject to any restriction on their private practice income<br />
but forfeit 1/11th of their NHS salary. There is also an effect on accrual of<br />
pension benefits in that holders of maximum part-time contracts will be<br />
credited with 10/11ths of a year’s service for each year worked in pension<br />
calculations.<br />
Travel arrangements<br />
Maximum part-time contract holders may count up to 30 min per journey<br />
each way for travel between home or place of private practice and their NHS<br />
place of work.<br />
Job planning<br />
All consultants should expect to have annual job planning meetings and<br />
reviews in which both fixed and flexible work is defined. The same principles<br />
apply to job planning and appraisal for those on the pre-2003 contract as to<br />
those on the 2003 contract. Fixed commitments will largely be clinical work<br />
and times and locations of each NHD should be determined and agreed,<br />
44 45
although NHDs may be flexible in time, location and type of activity. There<br />
is no difference in the number of fixed NHDs expected of full-timers and<br />
maximum part-timers. Normally this is between 5 and 7.<br />
Non-fixed or flexible work describes that work covered in 2003 contract as<br />
SPAs as well as on-call and other irregular or unscheduled work necessarily<br />
undertaken. Evidence of activity and output would be expected. There is no<br />
reason why a consultant anaesthetist on the pre-2003 contract would need<br />
any less time for those activities that underpin their professional knowledge<br />
and skills. However, there may be an argument that those who spend<br />
substantial amounts of time working in private practice should devote some<br />
of their own time to supporting their professionalism and revalidation.<br />
Additional NHDs<br />
Consultants may be contracted for additional NHDs for clinical or nonclinical<br />
work, normally up to a maximum of two NHDs. These are temporary<br />
and non-pensionable activities that are remunerated at 1/11th of the full time<br />
salary.<br />
Question:<br />
Answer:<br />
If you are on the old contract, does it mean that you do<br />
not have to undergo an annual job planning process and<br />
do not have to account for activities performed in paid<br />
non-clinical NHDs (notional half-days)?<br />
The answers are definitely ‘no’ and ‘no’ respectively.<br />
14. Starting out as a consultant<br />
Obtaining a consultant job is just the beginning; it is really just the start of<br />
even more hard work. Whilst new consultant anaesthetists must focus on<br />
their clinical workload, the other roles of a consultant must not be forgotten.<br />
With the likely introduction of revalidation, ongoing proof must be provided<br />
that time has been spent on continuing professional development. There are<br />
also a number of pitfalls to avoid. It is important not to take on every new role<br />
offered to you when starting as a consultant. The majority of new consultants<br />
are undoubtedly eager to get involved with their department but it is also<br />
possible to be swamped. It is worth taking time to decide what your priorities<br />
are and if necessary delaying these decisions until you are aware of the likely<br />
workload. Courses are run to help with ‘saying no’; the ability to say ‘no’ can<br />
greatly improve your working and personal lives.<br />
Continuing Professional Development<br />
Ongoing learning as CPD does not end on achieving a consultant post.<br />
The Trust employing a doctor expects that they will achieve adequate and<br />
appropriate CPD each year. Guidance from the RCoA and Medical Education<br />
(England) will be taken into account in this process; for example, the RCoA<br />
gives advice on how much CPD is provided per activity and which activities<br />
are appropriate. Details of this and the number of CPD points you are<br />
expected to achieve per year are available at from the College’s website.<br />
These CPD points may be acquired by attending a mixture of departmental,<br />
regional, national or international meetings as well as attending and teaching<br />
on courses. Suitable educational activities not awarded CPD points by the<br />
College may, however, be accepted by both the Trust and the individual to<br />
contribute to professional development. Trusts are encouraged to provide<br />
adequate study leave; if you have difficulties with your study leave allowance,<br />
you should consider contacting the BMA. A detailed portfolio or personal<br />
folder including certification should be kept of all activities to assist with the<br />
appraisal process. As well as speciality specific training, you will be expected<br />
to attend Trust mandatory training in areas such as child protection and<br />
manual handling.<br />
Supporting Professional Activity<br />
The 2003 consultant contract specifies that posts should typically contain 7.5<br />
DCCs and 2.5 SPAs per week. With the current financial climate, SPA time<br />
is under scrutiny to ensure that it is being used effectively. If 1.5 SPAs per<br />
week is considered sufficient to maintain revalidation purposes, qualification<br />
for or maintain of the additional SPA may be based on evidence of activity.<br />
This may vary from service improvement projects, formalised teaching, to<br />
46 47
eing the departmental lead in a variety of different areas, e.g. paediatrics.<br />
Some new consultants may be happy to start with 1.5 SPAs but it should be<br />
noted that 2.5 SPAs are recommended by the AAGBI and other professional<br />
bodies for all consultants, including those newly appointed. Should a<br />
smaller number of SPAs be agreed, there must be opportunity for this to<br />
increase as non-clinical workload changes. Anaesthetic departments may<br />
pool their 2.5 SPAs per consultant, allotting more to those fulfilling a higher<br />
non-clinical workload. Maintaining a diary of how SPA time is spent allows<br />
the department to justify the ongoing allocation of such non-clinical time.<br />
Some Trusts may insist on a fixed SPA session or being on site for at least<br />
one of these; this is something that may need to be negotiated with your CD.<br />
Regardless of the number of SPAs decided upon, a formal meeting should<br />
be arranged at six months to reassess and adjust the number of sessions if<br />
required.<br />
senior mentors to junior consultants; the AAGBI supports this. Even if there<br />
is no formal system within your department, you will usually find useful and<br />
sympathetic help and support if you need it. If you wish to seek help outside<br />
of your department, the AAGBI, RCoA and BMA offer support schemes. The<br />
AAGBI supports the BMA Doctors for Doctors scheme, where support can be<br />
found 24/7 for any welfare issue on 0845 920 0169. The AAGBI recognises<br />
the importance of supporting members and the AAGBI Welfare Committee has<br />
been established to help support all members, including those experiencing<br />
problems during this difficult time of transition. Further information can be<br />
found on the AAGBI’s website (www.<strong>aagbi</strong>.org) and a Welfare Resource Pack<br />
is also available to download. For more practical career advice or less urgent<br />
advice from the AAGBI, email wellbeing@<strong>aagbi</strong>.org.<br />
Job planning and development<br />
It is important to discuss, finalise and agree your job plan as soon as possible<br />
after the consultant interview process. You must ensure that your job plan<br />
when appointed matches the job plan advertised. A small alteration here<br />
may lead to a dramatic change in your job or in your work-life balance. It<br />
may be possible to adapt a job plan before starting work or even during the<br />
appointment process. Recently appointed consultants should ensure that<br />
their job plans do not involve a degree of professional isolation by scheduling<br />
work primarily in locations away from main operating theatre suites. The<br />
ready support and availability of experienced consultants can be valuable<br />
in the first few months and years of consultancy. Job plans should continue<br />
to evolve during your time as a consultant and it is important to meet with<br />
your CD to review and update your plan on a regular basis, e.g. at least once<br />
a year. You should sit down at the beginning of your new post and agree<br />
with your CD what is expected of you and your clinical commitments. It<br />
is better to find out exactly what is expected of you at the beginning of the<br />
job. Ongoing diary monitoring of your job will help inform future job plan<br />
discussions; in particular, the clinical burden may be either more or less than<br />
expected when the job plan was instituted. A consultant post may be held for<br />
30 years so this ongoing review process of your job plan is important to keep<br />
you motivated and utilise your skills fully.<br />
Where to get help<br />
Consultants of any age may need help, but it is likely that those starting out<br />
on their consultant careers will need more support and advice than those in<br />
mid-career. Some hospitals have a Young Consultants Group that promotes<br />
the discussion of common issues. Some departments of anaesthesia allocate<br />
48 49
15. References<br />
1) British Medical Association: Consultant’s terms and conditions 2009.<br />
http://www.bma.org.uk/employmentandcontracts/<br />
employmentcontracts/consultantscontracts/<br />
consultantcontractdocuments.jsp (accessed 10/1/11)<br />
2) Association of Anaesthetists of Great Britain & Ireland: Archive of past<br />
issues of Anaesthesia News.<br />
http://www.<strong>aagbi</strong>.org/publications/anaesthesia_news/2009.htm<br />
(Page 11 of September issue) (accessed 10/1/11)<br />
3) Academy of Medical Royal Colleges: Statements Archive.<br />
http://www.aomrc.org.uk/publications/statements/111.html<br />
(Statement of 8th February 2010) (accessed 10/1/11)<br />
4) European Commission: Employment, Social Affairs and Inclusion –<br />
Labour Law.<br />
http://ec.europa.eu/social/main.jsp?langId=en&catId=157&newsId=603<br />
&furtherNews=yes (accessed 10/1/11)<br />
5) General Medical Council: Good Medical Practice (2006).<br />
http://www.gmc-uk.org/guidance/good_medical_practice.asp<br />
(accessed 10/1/11)<br />
6) Association of Anaesthetists of Great Britain & Ireland: Guideline –<br />
Fatigue and Anaesthetists (2004).<br />
http://www.<strong>aagbi</strong>.org/publications/guidelines.htm#f (accessed 10/1/11)<br />
7) British Medical Association: Current Pay Levels – Doctors Pay<br />
Supplement October 2010.<br />
http://www.bma.org.uk/employmentandcontracts/pay/doctorspaysupp.jsp<br />
(accessed 10/1/11)<br />
8) NHS Wales: Amendment to the National Consultant Contract in Wales.<br />
http://www.wales.nhs.uk/sites3/docmetadata.cfm?orgid=433&id=32473<br />
(accessed 10/1/11)<br />
50 51
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
Workload for Consultant Anaesthetists in Ireland<br />
Guidance on the 2008 (Connaughton) Contract<br />
and Job Planning for Consultant Anaesthetists in Ireland<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org April 2010
Membership of Working Party<br />
Dr Michael Staunton <br />
Dr Kevin Bailey <br />
Dr Anne Bergin <br />
Dr David Honan <br />
Dr John Kennedy <br />
Dr Avine Lydon <br />
Dr Geraldine Maloney <br />
Dr John McAdoo <br />
Dr Carlos McDowell <br />
Dr Stephen Mannion <br />
Dr Ellen O’Sullivan <br />
Dr Rory Page <br />
Chairperson, Member of Irish Standing Committee<br />
Member, Irish Standing Committee<br />
Member, Irish Standing Committee<br />
Member, Irish Standing Committee<br />
Member, Irish Standing Committee<br />
Member, Irish Standing Committee<br />
Hon. Secretary, Irish Standing Committee<br />
Member, Irish Standing Committee<br />
Member, Irish Standing Committee<br />
Member, Irish Standing Committee<br />
Member, Irish Standing Committee<br />
Convenor, Irish Standing Committee<br />
The Irish Standing Committee wishes to sincerely thank Mr Donal Duffy,<br />
Assistant Secretary General, Irish Hospital Consultants Association, for his<br />
helpful advice regarding this document.<br />
1
Contents<br />
1. Key points 3<br />
2. Introduction 4<br />
3. Overview of the consultant contract 5<br />
4. Consultant contract types and regulation of private practice 9<br />
5. Consultant work schedule 14<br />
6. Clinical directors and clinical directorates 19<br />
7. Academic consultants 22<br />
8. Locum and temporary consultants 23<br />
9. The European Working Time Directive 26<br />
References 29<br />
Appendices 33<br />
© Copyright of The Association of Anaesthetists of Great Britain & Ireland.<br />
No part of this book may be reproduced without the written permission of the<br />
AAGBI.<br />
2
1. Key points<br />
• The consultant contract is an agreement between an individual<br />
consultant anaesthetist and his or her employer.<br />
• The 2008 (Connaughton) Consultant Contract contains many important<br />
differences from the 1997 (Buckley) Consultant Contract.<br />
• The Irish Standing Committee of the AAGBI advises that all consultants<br />
are members of both a medical representative organisation and a<br />
medical defence organisation.<br />
• Each consultant anaesthetist who has signed the 2008 contract must<br />
agree a consultant work schedule and a ratio of public to private<br />
practice with his or her employer.<br />
• All consultant anaesthetists who have signed the 2008 contract should<br />
fully honour their 37-hour scheduled weekly commitment.<br />
• The increase in weekly working hours under the 2008 contract should<br />
include an increase in both clinical and non-clinical activities.<br />
• As previously recommended by the AAGBI, approximately 25% of total<br />
weekly working hours should be devoted to non-clinical activities.<br />
• Failure to devote adequate time to non-clinical activities may adversely<br />
affect the maintenance of professional competence and the quality of<br />
patient care.<br />
• Consultant anaesthetists within a department of anaesthesia may have<br />
different clinical and non-clinical activities.<br />
• Consultant anaesthetists with additional non-clinical responsibilities,<br />
e.g. chairperson or secretary of department, clinical director, should<br />
have a reduction in working hours devoted to clinical activities.<br />
• The consultant work schedule should be supported by a robust diary<br />
exercise.<br />
• If workload changes, a change in the consultant work schedule may be<br />
required.<br />
• The measurement of the ratio of public to private practice may not<br />
adequately capture many clinical activities which are regularly<br />
performed by consultant anaesthetists.<br />
• Consultant anaesthetists should consider maintaining their own records<br />
of their public and private clinical activity.<br />
• All changes in working patterns as a result of the European Working<br />
Time Directive (EWTD) should be carefully evaluated for their effects on<br />
the safety of patients and staff.<br />
3
2. Introduction<br />
The 2008 (Connaughton) Consultant Contract<br />
The Irish Standing Committee of the Association of Anaesthetists of Great<br />
Britain and Ireland (AAGBI) produced a guideline in 1992 and a supplement<br />
in 1993 to advise members on the 1991 Irish Consultant Contract. The<br />
Irish Consultant Contract was subsequently revised in 1997 and in 2008.<br />
The 2008 (Connaughton) Consultant Contract contains many important<br />
differences from the 1997 (Buckley) Consultant Contract. Therefore, the<br />
Irish Standing Committee considered it appropriate to review and update its<br />
previous guidance.<br />
This new guideline will give members a broad overview of the principles of<br />
the 2008 contract together with specific advice appropriate for consultant<br />
anaesthetists. The objective of this guideline is to enable consultant<br />
anaesthetists and, thus, their patients, to adapt to and benefit from the 2008<br />
contract.<br />
Professional advice on your contract<br />
The Irish Standing Committee advises that you maintain membership of a<br />
medical representative organisation, e.g. the Irish Medical Organisation<br />
(IMO) or the Irish Hospital Consultants Association (IHCA). Both of these<br />
organisations recommend that new consultants have their contracts reviewed<br />
by them before signing. In addition, both organisations provide advice to<br />
consultants regarding the local interpretation of their contracts.<br />
The Irish Standing Committee and the Health Service Executive (HSE)<br />
both advise that you take out supplementary membership of a defence<br />
organisation or insurer of your choice, so that you have adequate cover for<br />
matters not covered by the Clinical Indemnity Scheme, e.g. representation at<br />
disciplinary and fitness to practise hearings or Good Samaritan acts outside<br />
the jurisdiction of the Republic of Ireland (Section A, Part 27).<br />
At the time of writing, at least 85% of consultants in the Republic of Ireland<br />
have signed the 2008 (Connaughton) Consultant Contract. However, it is<br />
important to note that many aspects of the contract are the subject of ongoing<br />
negotiations between the HSE and the medical representative organisations.<br />
4
3. Overview of the consultant contract<br />
Definition<br />
A contract is a set of statements governing the agreement between you<br />
and your employer: what work you agree to perform; what facilities your<br />
employer agrees to make available for you to do this work; and what your<br />
employer agrees to reward you with for your work.<br />
Components<br />
The consultant contract is not a single document. It has several components,<br />
all of which should be given to each consultant:<br />
• Terms and conditions<br />
• Appendices<br />
• Correspondence exchanged between the parties as set out at Appendix<br />
VII of the contract<br />
• HSE Letter of Approval<br />
• Job description<br />
This section will outline the main features of the 2008 (Connaughton)<br />
Consultant Contract. Where appropriate, differences between this contract<br />
and the previous, 1997 (Buckley) Consultant Contract will be highlighted.<br />
Throughout this guideline, the 2008 (Connaughton) Consultant Contract will<br />
be referred to as ‘the 2008 contract’ or ‘the contract’.<br />
Most important differences<br />
The most important differences between the 2008 contract and the previous<br />
contract are as follows:<br />
• Reporting relationship<br />
• Clinical directors and clinical directorates<br />
• Consultant teams<br />
• Increased total hours of work per week<br />
• Longer normal working day<br />
• Structured on-site attendance at weekends and on public holidays<br />
• Re-introduction of a ‘public-only’ contract<br />
• Regulation of private practice<br />
5
Terms and conditions<br />
Appointment and tenure<br />
The qualifications required for the consultant post are set out in the HSE<br />
Letter of Approval which is attached at Appendix 1 of the contract. The HSE<br />
has published revised consultant qualifications with effect from 16 March<br />
2009. These qualifications are given in Appendix 1 of this guideline. It<br />
should be noted that the only special interests that are specified are those in<br />
paediatric anaesthesia, intensive care medicine and pain medicine.<br />
Reporting relationship<br />
The contract states that the consultant’s “reporting relationship” and<br />
“accountability for the discharge of his/her contract” is to “the Chief<br />
Executive Officer/General Manager/Master of the hospital (or other<br />
employing institution) through his/her Clinical Director (where such is in<br />
place).” The contract also states that the hospital network manager “may<br />
require the consultant to report to him/her from time to time.”<br />
The previous contract did not specifically refer to a ‘reporting relationship’<br />
or ‘accountability’, but did state that the consultant was responsible for<br />
“producing a realistic agreed schedule,” “agreeing with management the<br />
details of the service levels and mix to be provided” and “supplying to his<br />
employing authority such information…as is necessary and reasonable to<br />
establish that he is fulfilling his contractual commitment.”<br />
6
Hours of work<br />
The most important differences between the 1997 and 2008 contracts are<br />
summarised below.<br />
Total number of<br />
hours per week<br />
Total number<br />
of sessions per<br />
week<br />
Types of<br />
sessions<br />
Definition of<br />
normal working<br />
day<br />
Total duration<br />
of shift<br />
Splitting of shift<br />
Weekend<br />
sessions<br />
1997 (Buckley) Contract 2008 (Connaughton)<br />
Contract<br />
33 37<br />
11 (= 33 notional hours per<br />
week)<br />
“Mix of fixed and flexible<br />
sessions, the ratio of which<br />
will vary depending on<br />
specialty”<br />
“During the hours normally<br />
worked within the Monday to<br />
Friday working week”<br />
No reference to total duration<br />
of shift<br />
No reference to splitting of<br />
shift<br />
No<br />
No reference to<br />
sessions<br />
No reference to fixed<br />
or flexible sessions<br />
Between 8am and<br />
8pm Monday to<br />
Friday<br />
“The Consultant will<br />
not be obliged to<br />
work more than 8<br />
hours in any one day.”<br />
“This will be<br />
structured as a single<br />
continuous episode.”<br />
Yes<br />
(see below)<br />
In addition to the above 37-hour commitment per week:<br />
• The consultant may be required to participate in an on-call roster.<br />
• The consultant rostered on-call may be required to provide a “structured<br />
commitment on-site of up to 5 hours on a Saturday and/or 5 hours<br />
overtime on a Sunday and/or 5 hours on a public holiday.”<br />
The structured on-site attendance at weekends and on public holidays will<br />
be subject to premium payments of time-and-a-half on Saturdays and doubletime<br />
on Sundays and public holidays. Consultants who have onerous on-call<br />
rosters (1:4 or more frequent) “shall not be expected to deliver the upper end<br />
of this requirement as determined by the Clinical Director.”<br />
7
If a consultant remains in the hospital longer than the structured 5-hour<br />
commitment or is required to re-attend the hospital later in the day, he/she<br />
may claim C Factor (Call-Out) Payments for this additional working time.<br />
The contract states that, where there is local agreement to implement<br />
different work patterns (including any arrangements providing for up to<br />
24/7 hour working), the involvement of any individual consultant in any<br />
such arrangement(s) “shall be subject to his/her agreement.” Appendix VII<br />
(‘Correspondence between the parties’) states that any issues regarding<br />
such local agreements will be referred to the Contract Implementation<br />
Group, a committee comprising representatives of the HSE and the medical<br />
organisations.<br />
Consultant teams<br />
The contract states that the consultant will “generally work as part of a<br />
Consultant team.” The purpose of such teams is “to ensure Consultant<br />
provided services to patients on a frequent and continuing basis.”<br />
The previous contract briefly mentioned the concept of a clinical directorate<br />
being led by a member of its ‘consultant team’. The majority of consultant<br />
anaesthetists in the Republic of Ireland already work as part of a consultant<br />
team with regard to rostering arrangements and delivery of the clinical<br />
service.<br />
On-call commitment of consultants who work on multiple hospital<br />
sites<br />
The contract does not contain guidance regarding the on-call commitment<br />
of consultants who work on multiple hospital sites. Nonetheless, it seems<br />
reasonable that the on-call commitment should reflect the sessional<br />
commitment, e.g. if a consultant has 50% of his sessions in hospital A<br />
and 50% of his sessions in hospital B, and has an on-call commitment on<br />
both sites, 50% of his/her on-call commitment should be in each hospital;<br />
further, his/her on-call commitment in each hospital should be 50% that of<br />
consultants with all their sessions in that hospital. Such arrangements should<br />
be locally discussed and agreed by the departments of anaesthesia on these<br />
hospital sites.<br />
8
4. Consultant contract types and regulation of<br />
private practice<br />
Consultant contract types<br />
A consultant holding contract type A (a ‘public-only’ contract) may not<br />
engage in privately remunerated professional medical practice.<br />
Consultant contract types B, B* and C<br />
Consultants holding contract types B, B* and C may engage in privately<br />
remunerated professional medical practice.<br />
Several types of practice, e.g. preparation of reports relating to insurance<br />
claims or for the courts, are not regarded as private practice (see Section A,<br />
part 21).<br />
The most important differences between these contract types are summarised<br />
on the next page.<br />
9
Consultants<br />
eligible<br />
to hold<br />
contract<br />
Type A Type B Type B* Type C<br />
New<br />
consultants,<br />
category 1<br />
consultants,<br />
category 2<br />
consultants<br />
New<br />
consultants,<br />
category 1<br />
consultants,<br />
category 2<br />
consultants<br />
10<br />
Category 2<br />
consultants<br />
Location of private practice<br />
Public No Yes Yes Yes<br />
hospital(s)<br />
Co-located No Yes Yes Yes<br />
private<br />
hospital(s)<br />
Outside No No Yes Yes<br />
public<br />
hospital(s)<br />
Regulation of private practice<br />
Volume<br />
of public<br />
practice<br />
Volume<br />
of private<br />
practice in<br />
locations 1<br />
and 2<br />
Must fully<br />
discharge<br />
standard 37-<br />
hour weekly<br />
commitment<br />
Must fully<br />
discharge<br />
standard 37-<br />
hour weekly<br />
commitment<br />
None Not > 20%<br />
(not > 30%<br />
for existing<br />
consultants if<br />
this is agreed,<br />
see below)<br />
Must fully<br />
discharge<br />
standard 37-<br />
hour weekly<br />
commitment<br />
Not > 20%<br />
(not > 30%<br />
for existing<br />
consultants if<br />
this is agreed,<br />
see below)<br />
New<br />
consultants<br />
Must fully<br />
discharge<br />
standard 37-<br />
hour weekly<br />
commitment<br />
Not > 20%<br />
(not > 30%<br />
for existing<br />
consultants if<br />
this is agreed,<br />
see below)<br />
Change in contract type<br />
Consultants may apply to change contract type to type A, B or C at fiveyearly<br />
intervals. Consultants who previously held a category 1 or category<br />
2 contract may, 2 years after accepting the 2008 contract, and thereafter<br />
at 5 yearly intervals, apply to transfer to contract type B*. Applicants must<br />
demonstrate “that the change in Contract Type is consistent with the public<br />
interest and that there is a demonstrable benefit to the public health system.”<br />
Where a new or replacement post is designated as type C, the applicant<br />
organisation must satisfy a number of criteria, including the following:
• “A clear indication as to why the post requirements cannot be met<br />
through a Type A or B arrangement.”<br />
• “A clear demonstration as to the added patient, service and public<br />
system benefits and values to be achieved through establishment of the<br />
post as a Type C rather than a Type A or B position.”<br />
The total number of consultants holding category 2, type B* and type C<br />
contracts will be subject to an upper limit of such posts within the system.<br />
Appendix VII (‘Correspondence between the parties’) suggests that this upper<br />
limit will be in the order of approximately 700 posts.<br />
Regulation of private practice<br />
Regulation of private practice for consultants who have type B, B* or C<br />
contracts<br />
For consultants who have type B, B* or C contracts, the contract states:<br />
• The volume of private practice in the public hospital(s) and co-located<br />
private hospital(s) may not exceed 20% of the consultant’s clinical<br />
workload in any of his/her clinical activities, including inpatient,<br />
day-patient and outpatient. Appendix VII (‘Correspondence between<br />
the parties’) states that “Serving consultants whose public to private ratio<br />
in 2006 was greater than 20% will be permitted to retain this higher<br />
ratio, subject to an overriding maximum ratio of 70:30.” However, data<br />
regarding the public to private ratio of individual consultant anaesthetists<br />
were not collected in 2006 and, therefore, cannot be used to determine<br />
their permitted public to private ratio under the new contract.<br />
• The volume of practice shall refer to patient throughput adjusted for<br />
complexity through the medium of the case mix system.<br />
• The 80:20 ratio of public to private practice will be implemented<br />
through the clinical directorate structure. The employer has full<br />
authority to take all necessary steps to ensure that for each element of a<br />
consultant’s practice; he/she shall not exceed the agreed ratio.<br />
• The consultant will be advised on a timely basis if his or her practice<br />
is in excess of the 80:20 ratio of public to private practice in any of his<br />
or her clinical activities. An initial period of six months will be allowed<br />
to bring practice back into line but if within a further period of 3 months<br />
the appropriate ratio is not established, he/she will be required to remit<br />
private practice fees in excess of this ratio to the research and study fund<br />
under the control of the clinical director.<br />
• The clinical director may exercise some discretion in dealing with the<br />
implementation of the ratio either for an individual or a group of<br />
11
consultants once the overall ratio in relation to the particular clinical<br />
activity is satisfied.<br />
• The implementation of the 80:20 ratio of public to private practice shall<br />
be the subject of audit, including audit by the Department of Health and<br />
Children.<br />
Measurement of the ratio of public to private practice<br />
Each hospital inpatient is admitted under the care of a single primary<br />
consultant, e.g. a consultant physician, surgeon, paediatrician or obstetrician.<br />
This primary consultant bears overall responsibility for the patient’s<br />
management throughout his or her hospital stay. A patient may require<br />
the services of other, secondary consultants, e.g. consultant radiologists,<br />
consultant pathologists or consultant anaesthetists. However, he or she will<br />
not be under the care of a single consultant radiologist, consultant pathologist<br />
or consultant anaesthetist. For example, a patient who has several surgical<br />
procedures and is admitted to an intensive care unit may be cared for by<br />
many consultant anaesthetists during his or her hospital stay.<br />
The Casemix System/Hospital In-Patient Enquiry (HIPE) Scheme will be<br />
used to provide monthly reports of each consultant anaesthetist’s ratio of<br />
public to private practice on a casemix adjusted basis. Data will be provided<br />
separately for inpatients and day cases. All consultant encounters in a case<br />
will be recorded and reported. However, the measurement of a consultant<br />
anaesthetist’s ratio of public to private practice is predominantly based<br />
on his or her direct provision of anaesthesia in the operating theatre. This<br />
measurement may not adequately capture the many other clinical activities<br />
that are regularly performed by consultant anaesthetists and are given in<br />
Appendix 2 of this guideline.<br />
Therefore, the measurement of a consultant anaesthetist’s ratio of public to<br />
private practice may not accurately reflect either the number of patients for<br />
whom he or she has cared or the ratio of ‘public patients’ to ‘private patients’.<br />
Consultant anaesthetists should consider maintaining their own records of<br />
their public and private clinical activity. These records should include the<br />
number of patients and the duration of patient care. If consultants detect any<br />
inaccuracies in the measurement of their ratio of public to private practice,<br />
these should be brought to the attention of hospital management.<br />
Control by consultant anaesthetists over their ratio of public to private<br />
practice<br />
Most consultant anaesthetists have no control over their ratio of public to<br />
private practice. With the exception of consultants with a special interest<br />
12
in pain medicine, they are not primary consultants and are not involved in<br />
the scheduling of patients for elective surgery. They also have no control<br />
over the number of patients with private health insurance who require<br />
urgent admission to hospital and subsequently require the services of an<br />
anaesthetist, e.g. patients who require urgent surgery, patients who require<br />
obstetric care or patients who require admission to an intensive care unit.<br />
The Irish Standing Committee believes that it is not rational to attempt to<br />
control the ratio of public to private practice for patients who require urgent<br />
hospital admission.<br />
Measurement of the ratio of public to private practice for consultants<br />
who work on multiple hospital sites<br />
At present, a consultant anaesthetist who works on multiple hospital sites has<br />
his/her ratio of public to private practice measured and reported separately<br />
for each hospital site. The Irish Standing Committee believes that, as a<br />
consultant anaesthetist’s post represents a single appointment, his/her ratio of<br />
public to private practice from multiple hospital sites should be aggregated<br />
and reported as a single ratio.<br />
Regulation of private practice for consultants who remain on the 1997<br />
(Buckley) Consultant Contract<br />
According to the previous contract, a consultant holding a category 1<br />
contract was permitted to engage in private practice only on the site of<br />
the public hospital(s) (‘on-site’ only). A consultant holding a category 2<br />
contract was permitted to engage in private practice on the site of the public<br />
hospital(s) and outside the public hospital (‘on-site’ and ‘off-site’).<br />
With regard to ‘on-site’ private practice, the previous contract stated “a<br />
consultant’s overall proportion of private to public patients should reflect<br />
the ratio of public to private stay beds designated under the 1991 Health<br />
(Amendment) Act, which requires that all public hospital beds be classified as<br />
public, private or non-designated.” This act does not stipulate any particular<br />
ratio of public to private beds. However, the Department of Health has<br />
determined that the ratio of public to private beds in public hospitals should<br />
be 80:20 (the so-called ‘80/20 split’).<br />
13
5. Consultant work schedule<br />
Introduction<br />
A ‘consultant work schedule’ or ‘practice plan’ is a detailed description of<br />
the duties and responsibilities of a consultant and of the facilities required to<br />
carry them out.<br />
In the previous contract, the 33-hour working week was divided into 11<br />
sessions. Each session had a duration of 3 hours. A session could be fixed<br />
or flexible. A fixed session involved work that had to be performed at a<br />
particular time and in a particular place, because it required the presence of<br />
other members of staff and/or other resources, e.g. outpatient clinics, theatre<br />
sessions, ward rounds, investigative and treatment sessions. A flexible session<br />
involved work that could be performed more flexibly as regards time and<br />
location, e.g. teaching, minor ward rounds, reporting, research, meetings,<br />
hospital management and medical audit. The contract stated that “A<br />
consultant’s commitment shall comprise a mix of fixed and flexible sessions,<br />
the ratio of which will vary depending on specialty.”<br />
The 2008 contract does not refer to sessions and does not refer to fixed or<br />
flexible commitments. Therefore, it gives less guidance than the previous<br />
contract regarding the type of work that may be performed as part of the<br />
scheduled weekly commitment. Unlike the 2003 consultant contract in<br />
the United Kingdom, it gives no guidance regarding the proportion of total<br />
working hours that should be devoted to clinical activities (Direct Clinical<br />
Care) and non-clinical activities (Supporting Professional Activity). Appendix<br />
III of the contract contains a sample consultant work schedule, but the<br />
range of clinical and non-clinical activities is very limited and some of the<br />
clinical activities are undertaken by only a few consultant anaesthetists, e.g.<br />
OPD. This section will outline the features of the contract that are relevant<br />
to the consultant work schedule and give recommendations regarding the<br />
formulation of work schedules for individual consultant anaesthetists.<br />
Working greater than or less than 37 hours per week<br />
The contract states: “If the time worked consistently and significantly varies<br />
from the scheduled commitment, there will be a review of the commitment<br />
to ensure that the Consultant is not working regularly in excess of or less<br />
than the 37 hour weekly commitment. Where the commitment is being<br />
unavoidably exceeded for reasons of a temporary nature, local arrangements<br />
will be made to compensate the Consultant concerned.”<br />
14
Non-clinical duties<br />
The contract explicitly mentions the following non-clinical duties of<br />
consultants:<br />
• Medical education and training (Section A, part 1; Section A, part 14).<br />
This may, with the agreement of the employer, include a structured<br />
and scheduled commitment to a medical/dental school or a training<br />
body for postgraduate medical education and training (Section A, part<br />
14)<br />
• Research (Section A, part 1; Section A, part 14)<br />
• Maintenance of professional competence (Section A, part 11)<br />
• Clinical audit (Section A, part 12)<br />
• Proactive risk management (Section A, part 12)<br />
• Formal review of “the execution of the Clinical Directorate Service Plan<br />
with the Clinical Director/Employer.” This should occur “periodically, at<br />
the request of the Consultant or Clinical Director/Employer.” (Section A,<br />
part 12)<br />
• Participation in the “development and operation of the Clinical<br />
Directorate structure and in such management or representative<br />
structures as are in place or being developed.” (Section A, part 12)<br />
• Ensuring, “in consultation with the Clinical Director, that appropriate<br />
medical cover is available at all times.” (Section A, part 12). This would<br />
obviously include the appropriate rostering of consultant anaesthetists<br />
and anaesthetic trainees for daytime and on-call clinical duties<br />
• Participation in “selection processes for non-Consultant Hospital Doctors<br />
and other staff as appropriate.” (Section A, part 12)<br />
Maintenance of professional competence and clinical<br />
governance<br />
The Medical Practitioners Act 2007 places a statutory obligation on all<br />
registered medical practitioners to maintain their professional competence<br />
and cooperate with any professional competence scheme developed,<br />
established or operated by the Medical Council. The Act also places<br />
an obligation on the HSE or other employer to facilitate these activities.<br />
Professional competence schemes will be delivered by the postgraduate<br />
training bodies.<br />
The College of Anaesthetists of Ireland is accredited by the Medical<br />
Council to operate a continuing medical education (CME) credit system<br />
for anaesthetists. CME activity is classified into the following categories: (i)<br />
15
internal activities, (ii) external activities, (iii) personal activities, (iv) research<br />
and (v) postgraduate examining, training and supervision (see Appendix<br />
3). At least 50 CME credits must be obtained annually, of which at least 10<br />
credits must be in the internal category and at least 20 credits must be in the<br />
external category. The College of Anaesthetists of Ireland also recommends<br />
that an individual specialist working in a typical hospital and participating<br />
in the emergency on-call rota should have up to date knowledge of and<br />
proficiency in the list of ‘core topics’ in anaesthesia agreed by the Union of<br />
European Medical Specialists (UEMS). Consultants should aim to cover all<br />
topics relevant to their practice once during a three year cycle.<br />
It is likely that a professional competence scheme for anaesthetists will<br />
include activities other than CME, such as peer review, multi-source<br />
feedback and clinical audit. The report of the Commission on Patient<br />
Safety and Quality Assurance recommends that all healthcare professionals<br />
be involved in clinical governance activities, such as the establishment<br />
and implementation of evidence-based standards and guidelines, clinical<br />
audit, adverse event reporting and participation in CME and competency<br />
revalidation programmes. It is essential that all consultant anaesthetists are<br />
given adequate time and resources to maintain their professional competence<br />
and be actively involved in clinical governance activities.<br />
Performance monitoring<br />
The contract contains several references to monitoring of a consultant’s<br />
performance:<br />
• “Both the Consultant and the Employer shall co-operate in giving effect<br />
to such arrangements as are put into place to verify the delivery of the<br />
Consultant’s contractual commitments.” (Section A, part 4)<br />
• “The scope of this post is as set out in the HSE letter of approval for this<br />
position at Appendix 1 and the Job Description as issued<br />
by the Employer. These describe the Consultant’s service commitments,<br />
accountabilities and specific duties…The Consultant’s annual Clinical<br />
Directorate Service Plan will detail how these are to be implemented<br />
and will be validated by a series of performance monitoring<br />
arrangements.” (Section A, part 9)<br />
• Standard duties and responsibilities include: “To participate in and<br />
facilitate production of all data/information required to validate delivery<br />
of duties and functions and inform planning and management of service<br />
delivery.” (Section A, part 12)<br />
16
As noted on page 16, the previous contract contained several similar<br />
references.<br />
Resources<br />
The contract states that it is the responsibility of the employer to provide<br />
adequate resources: “The determination of the range, volume and type of<br />
services to be provided and responsibility for the provision of same within<br />
available resources rests with the Employer. Services not provided as a<br />
consequence of a resource limit are the responsibility of the Employer and<br />
not the Consultant.” (Section A, part 4)<br />
The resources that may be required for consultant anaesthetists to perform<br />
their duties have been previously outlined by the AAGBI and are given in<br />
Appendix 4 of this guideline.<br />
Advocacy<br />
The core principles of the contract include “recognition of the Consultant’s<br />
role as an advocate.” However, the consultant also has a “responsibility, in<br />
the first instance, to express any concerns within the employment context.”<br />
(Section A, part 1)<br />
Later, the contract states that “In the first instance…advocacy should take<br />
place within the employment context through the relevant Clinical Director<br />
or other line manager.” The contract also states that “Information given to<br />
the public should be expressed in clear and factual terms. It must never<br />
cause unnecessary public concern or personal distress, nor should it raise<br />
unrealistic expectations.” (Section A, part 16)<br />
17
Recommendations<br />
• The consultant contract is an agreement between an individual<br />
consultant anaesthetist and his or her employer.<br />
• Each consultant anaesthetist who has signed the 2008 contract must<br />
agree a consultant work schedule and a ratio of public to private<br />
practice with his or her employer.<br />
• The clinical activities of consultant anaesthetists are given in Appendix 2<br />
of this guideline.<br />
• The non-clinical activities of consultant anaesthetists are given in<br />
Appendix 3 of this guideline.<br />
• All consultant anaesthetists who have signed the 2008 contract should<br />
fully honour their 37-hour scheduled weekly commitment.<br />
• The increase in weekly working hours under the 2008 contract should<br />
include an increase in both clinical and non-clinical activities.<br />
• As previously recommended by the AAGBI, approximately 25% of total<br />
weekly working hours should be devoted to non-clinical activities.<br />
• Failure to devote adequate time to non-clinical activities may adversely<br />
affect the maintenance of professional competence and the quality of<br />
patient care.<br />
• Consultant anaesthetists within a department of anaesthesia may have<br />
different clinical and non-clinical activities.<br />
• Consultant anaesthetists with additional non-clinical responsibilities,<br />
e.g. chairperson or secretary of department, clinical director, should<br />
have a reduction in working hours devoted to clinical activities.<br />
• The consultant work schedule should be supported by a robust diary<br />
exercise.<br />
• A work diary does not have to be kept permanently. However, it is<br />
important that it is representative of the usual hours worked.<br />
• If workload changes, a change in the consultant work schedule may be<br />
required.<br />
18
6. Clinical directors and clinical directorates<br />
Details of the appointment and profile of a clinical director are contained in<br />
Appendix IV of the contract.<br />
Appointment of clinical directors<br />
The post of clinical director is appointed by the employer. Applications are<br />
invited from all eligible consultants within the clinical directorate and all<br />
applicants are interviewed. Alternatively, the body of consultants within the<br />
directorate may nominate a candidate. Appointment is initially for two years.<br />
Clinical director profile<br />
A clinical director may cover one speciality area or a range of specialities.<br />
Each directorate is headed by a clinical director, generally supported by<br />
a nurse manager and a business manager. Each member of staff in the<br />
directorate has a reporting relationship, through his/her line manager, to the<br />
clinical director. Each consultant who has signed the 2008 contract reports to<br />
the clinical director. Clinical directors in a HSE hospital report to the hospital<br />
manager or the hospital network manager. Clinical directors in a voluntary<br />
hospital or agency report to the chief executive of the hospital or agency.<br />
Clinical directorates<br />
The contract does not give any guidance on the size of clinical directorates.<br />
Since the contract was agreed, the HSE has maintained that “Clinical<br />
Directorates must be large enough to justify support by business managers…<br />
In practice, this means that Clinical Directorates shall be based on a<br />
minimum of 30-60 whole time consultant posts.” The clinical directors who<br />
have been appointed appear to have areas of responsibility similar to those of<br />
medical directors in the United Kingdom.<br />
The role and responsibilities of clinical directors and the size and functioning<br />
of clinical directorates will undoubtedly undergo considerable evolution in<br />
the next few years.<br />
A consultant anaesthetist applying for the post of clinical director should:<br />
• Review and understand the principal duties and responsibilities of a<br />
clinical director.<br />
19
• Consider his/her need for additional training and/or support, either<br />
before or after taking up the post of clinical director.<br />
• Discuss the application with his/her lead clinician.<br />
• Discuss the availability of supporting resources with the relevant hospital<br />
or network manager(s). These resources may include accommodation,<br />
staffing, administrative time and additional training and/or support.<br />
• Discuss the functioning of the post and the important current issues with<br />
the existing clinical director (if present).<br />
The discussions with the lead clinician, local manager(s) and the existing<br />
post-holder should include consideration of the necessity to reduce clinical<br />
commitments and the effect of this reduction on clinical skills, the clinical<br />
service and the requirement for locum cover. This is particularly important in<br />
a small department or subspecialty group.<br />
Relationship between clinical directors and departments of<br />
anaesthesia<br />
The relationship between clinical directors and individual clinical specialties<br />
is not specifically discussed in the contract. However, the Irish Standing<br />
Committee believes that departments of anaesthesia should ensure the<br />
following:<br />
• Each department of anaesthesia has a nominated lead clinician.<br />
• Each department of anaesthesia considers the nomination of consultants<br />
with responsibility for anaesthetic subspecialties.<br />
• Arrangements for communication with the clinical director are locally<br />
discussed and agreed.<br />
• The clinical service is compliant with the standards set by the relevant<br />
professional bodies.<br />
Relationship between clinical directors and consultants<br />
who remain on the 1997 (Buckley) Consultant Contract<br />
Consultants who remain on the 1997 (Buckley) Consultant Contract do not<br />
have a “reporting relationship” and “accountability for the discharge of his/<br />
her contract” to a clinical director. However, as discussed above, they are<br />
responsible for “producing a realistic agreed schedule,” “agreeing with<br />
management the details of the service levels and mix to be provided” and<br />
“supplying to his employing authority such information…as is necessary and<br />
reasonable to establish that he is fulfilling his contractual commitment.”<br />
20
The 1997 (Buckley) Consultant Contract contains the following statements<br />
regarding involvement of consultants in management and the role of clinical<br />
directors and clinical directorates:<br />
“Consultants need to be involved in the management process. This<br />
involvement commences with the consultant’s responsibility to manage<br />
his/her own practice and will involve co-operation with colleagues and<br />
other health professionals, at department, unit, hospital or hospital group<br />
level, extending to involvement in the management of the hospital/hospital<br />
grouping through direct membership or representation on the hospital<br />
Executive Management Board.” (Consultant contract Section 7.1 and<br />
memorandum of agreement Section 6.6.1)<br />
“The recent experience of the pilot projects in a number of hospitals confirms<br />
that the concept of a distinct unit, grouping the clinical functions together<br />
under the leadership of a selected consultant (e.g. a Clinical Directorate<br />
model), represents an effective model to facilitate participation of Hospital<br />
Consultants in the management process.” (Consultant contract Section 7.2<br />
and memorandum of agreement Section 6.6.2)<br />
21
7. Academic consultants<br />
All terms of the contract also apply to the holders of academic consultant<br />
posts that have been approved by the HSE/Higher Education Authority. These<br />
posts are joint appointments between universities or the Royal College of<br />
Surgeons in Ireland and the HSE. In general, the posts are structured to ensure<br />
a minimum 50% commitment to the academic institution, but this ratio may<br />
vary with the agreement of the employers and the academic consultant.<br />
22
8. Locum and temporary consultants<br />
Definitions<br />
A locum consultant post is defined as a consultant post that is occupied in a<br />
non-permanent capacity by someone other than the legal post holder. The<br />
locum acts in place of this post holder during, for example, annual or sick<br />
leave.<br />
A temporary consultant post is defined as a consultant post for the interval<br />
between a permanent post becoming vacant and it being filled on a<br />
permanent basis, or for the interval between a permanent post having been<br />
approved by the HSE and it being filled on a permanent basis.<br />
Requirement for locum cover<br />
The Irish Standing Committee recognises that consultant locum cover is<br />
necessary in many circumstances, e.g. to cover annual leave, study leave,<br />
sick leave or maternity leave. The requirement for locum cover may increase<br />
in the future because of the decreased working hours of anaesthetic trainees<br />
as a result of the EWTD. The Irish Standing Committee believes that the<br />
use of locum and temporary consultant anaesthetists should be minimised<br />
and, where possible, these posts should be filled by permanent consultant<br />
anaesthetists.<br />
Recruitment and selection of locum and temporary<br />
consultants<br />
The HSE has published a revised procedure for recruitment and selection<br />
of locum and temporary consultants, with effect from 07 May 2009. This<br />
document states that the same qualifications apply to all permanent,<br />
temporary and locum consultant appointments.An accompanying circular<br />
(HSE HR Circular 014/2009) draws particular attention to the provision that<br />
“an individual applicant who is not qualified for appointment as a Medical<br />
Consultant on a permanent basis may not be appointed to a temporary or<br />
locum position. New appointments to temporary or locum consultant posts<br />
require that the appointee be registered on the Specialist division of the<br />
register of Medical Practitioners maintained by the Medical Council.” This<br />
advice differs from that of the Medical Council which has suggested that<br />
entry in the specialist register may not be required for short-term locum<br />
appointments. The Medical Council newsletter in June 2009 contains the<br />
23
following statements: (i) “Trainee specialist registration only permits the<br />
practice of medicine within the clinical site/health service setting stated on<br />
a doctor’s Certificate of Registration or in the clinics/health service settings<br />
associated with the training post. Trainees should therefore not fill locum<br />
consultant appointments of more than three months’ duration. A trainee<br />
specialist, in the final year of their training, can act up at consultant grade<br />
in that specialty for a period of up to three months.” (ii) “The Council has<br />
expressed particular concern about any medical practitioner, who is not in<br />
the Specialist Division, taking up a locum Consultant appointment of more<br />
than three months’ duration. Entry in the Specialist Division is the most<br />
reliable indication of a doctor’s suitability to practise at a consultant grade.”<br />
Many existing locum and temporary consultant anaesthetists do not have<br />
their names entered in the Register of Medical Specialists in the division<br />
of anaesthesia. The Irish Standing Committee believes that all permanent,<br />
temporary and locum consultant anaesthetists should have the appropriate<br />
knowledge, skills and attitudes to enable them to safely fulfil their role. In<br />
addition, all temporary and locum consultants should have the appropriate<br />
qualifications for appointment on a permanent basis. However, these new<br />
rules will make it more difficult to appoint appropriate candidates to locum<br />
or temporary posts. This may affect the delivery of anaesthesia services,<br />
especially in smaller hospitals which are more dependent on locum and<br />
temporary consultant staff.<br />
Protection of Employees (Fixed-Term Work) Act 2003<br />
This Act implements Directive No.1999/70/EC of 28 June 1999 of the<br />
Council of the European Communities. The purpose of the Act is to improve<br />
the quality of fixed-term work by applying the principle of non-discrimination<br />
and provides a framework to prevent abuse through successive fixed-term<br />
contracts.<br />
While the Act specifically excludes persons such as defence force personnel,<br />
trainee Gardaí and trainee nurses, there is no specific part of the Act relating<br />
to either fully qualified medical staff or doctors-in-training.<br />
“A fixed term employee is a person with a contract of employment entered<br />
into directly with an employer where the end of the contract of employment<br />
concerned is determined by an objective condition such as arriving at a<br />
specific date, completing a specific task or the occurrence of a specific<br />
event.”<br />
24
A contract that contravenes Section 9(1) or 9(2) of the Act is deemed to be<br />
a contract of indefinite duration (Section 9(3)). The terms and conditions of<br />
this contract, except tenure, should be the same as the fixed-term contract<br />
at the time of the breach of the Act. Broadly speaking Sections 9(1) and 9(2)<br />
distinguish between those employed before and after 14 July 2003. The<br />
employer is in breach of Section 9(2) if the aggregate duration of contracts<br />
exceeds four years.<br />
The legal situation is less clear for medical employees. In two recent<br />
cases brought to the Labour Court by NCHDs in Psychiatry (FTC/07/6<br />
DETERMINATION NO. FTD081 and PTW/05/13 DETERMINATION NO.<br />
FTD064), the Court found in favour of the complainants and awarded them<br />
contracts of indefinite duration. However, a case taken by a temporary<br />
consultant orthopaedic surgeon was rejected (FTC 05/4 DETERMINATION<br />
NO. FTD081).<br />
The Irish Standing Committee recommends that independent legal advice on<br />
employment law be sought should members have queries regarding this area.<br />
25
9. The European Working Time Directive<br />
The EWTD is health and safety legislation that is designed to protect you<br />
from being exploited by your employer. From August 2004, the Directive<br />
has applied to all hospital doctors (European Working Time Directive - IMO<br />
AGM 2005 Briefing). The EWTD was originally issued in 1993 (Directive<br />
93/104/EC) and excluded the activities of doctors in training from its<br />
application in relation to key provisions regarding working hours. It was<br />
amended in 2000 (Directive 2000/34/EC) to reverse this exclusion and<br />
provide for a phased reduction of working hours (average 58 hours per week<br />
by August 2004, average 56 hours per week by August 2007 and average 48<br />
hours per week by August 2009). A consolidating Directive was published<br />
in 2003 (Directive 2003/88/EC) which replaced the previous version of the<br />
EWTD and took effect on 02 August 2004. The EWTD has been transposed<br />
into Irish law by means of the Organisation of Working Time Act, 1997, and<br />
the European Communities (Organisation of Working Time) (Activities of<br />
Doctors in Training) Regulations 2004 (S.I. No. 494 of 2004).<br />
Although the EWTD applies to consultants as well as doctors-in-training,<br />
the original Directive (Directive 93/104/EC) stated that member states<br />
may derogate from its requirements when, “on account of the specific<br />
characteristics of the activity concerned, the duration of the working<br />
time is not measured and/or predetermined or can be determined by the<br />
workers themselves…particularly in the case of…managing executives or<br />
other persons with autonomous decision-taking powers.” The Organisation<br />
of Working Time Act, 1997, states that the requirements of the Directive<br />
shall not apply to “a person the duration of whose working time (saving<br />
any minimum period of such time that is stipulated by the employer) is<br />
determined by himself or herself, whether or not provision for the making<br />
of such determination by that person is made by his or her contract of<br />
employment.” It can be argued that this derogation would apply to the<br />
working arrangements of hospital consultants.<br />
The requirements of the EWTD are as follows:<br />
26
Maximum weekly working<br />
time:<br />
Minimum reference period:<br />
Maximum reference period:<br />
Reference period may<br />
include:<br />
Reference period may not<br />
include:<br />
48 hours, averaged over a reference<br />
period<br />
None<br />
6 months<br />
Study leave<br />
Course leave<br />
Exam leave<br />
Interview leave<br />
Annual leave<br />
Sick leave<br />
Maternity leave<br />
Adoptive leave<br />
Daily breaks: At least 15 minutes every 4 hours 30<br />
minutes<br />
or<br />
At least 30 minutes every 6 hours<br />
Daily rest:<br />
At least 11 hours every 24 hours<br />
Weekly/fortnightly rest: At least 35 hours rest (11 hour rest period<br />
followed by 24 hours rest) once a week or<br />
twice a fortnight<br />
or<br />
At least 59 hours rest (11 hour rest period<br />
followed by 48 hours rest) once a fortnight<br />
Compensatory rest must be given to a doctor who has not been granted his<br />
or her daily break, daily rest or weekly/fortnightly rest; it must be equivalent<br />
to the break or rest which the doctor has not had; and it must be taken before<br />
the doctor begins his or her next period of work.<br />
The 2008 contract states that the consultant should “ensure in consultation<br />
with the Clinical Director that appropriate medical cover is available at all<br />
times having due regard to the implementation of the European Working<br />
Time Directive as it relates to doctors in training.” (Section A, Part 12)<br />
However, the joint Royal College of Anaesthetists and Royal College<br />
of Surgeons of England document, ‘WTD - Implications and Practical<br />
Suggestions to Achieve Compliance’ (2009) states: “A 1:8 rota is the<br />
minimum to be able to include prospective cover and adequate training.<br />
A 1:10 rota allows for more flexibility and training opportunities but it is<br />
acknowledged that many of the smaller specialties will be unable to achieve<br />
this.” The Royal College of Physicians document, ‘Designing safer rotas<br />
27
for junior doctors in the 48-hour week’ (2006) states: “A ‘cell’ of 10 junior<br />
doctors is necessary for any post that provides 24-hour cover, plus specialty<br />
work and training during weekdays.” The final report of the Irish National<br />
Implementation Group (2008) states: “As NCHD (Non-Consultant Hospital<br />
Doctor) rosters are currently structured, any roster of 10 doctors or less is<br />
unlikely to comply with the EWTD either from the viewpoint of hours worked<br />
or availing of rest periods. In particular it will not be possible to achieve<br />
compliance in smaller acute units many of whom currently have duty roster<br />
cells consisting of 3-6 doctors.”<br />
Therefore, the EWTD can only be implemented when each on-call rota<br />
contains at least eight to ten anaesthetic trainees. Many smaller hospitals<br />
do not have an adequate number of trainees to achieve this. Attempts<br />
to implement the directive with a smaller number of trainees may cause<br />
unacceptable decreases in the level and safety of anaesthetic service delivery<br />
and the quality of anaesthetic training.<br />
It has been suggested that the two key measures to support EWTD<br />
implementation are cross-cover and reductions in layered/tiered on-call.<br />
These measures are usually not appropriate for anaesthesia and intensive care<br />
services, for the following reasons: (i) trainees in other disciplines do not have<br />
the knowledge or skills to provide anaesthesia services; and (ii) reductions<br />
in the number of anaesthetic trainees on-call are often impractical because<br />
of the necessity to cover multiple clinical areas and the short response time<br />
required for many anaesthetic interventions.<br />
Any decrease in the working hours and/or experience of anaesthetic trainees<br />
has the potential to increase the workload of consultant staff. If this occurs,<br />
changes in consultant work schedules or the appointment of additional<br />
consultant anaesthetists may be required.<br />
All changes in working patterns as a result of the EWTD should be carefully<br />
evaluated for their effects on the safety of patients and staff.<br />
28
References<br />
Irish Standing Committee of the Association of Anaesthetists of Great<br />
Britain and Ireland<br />
• Irish Standing Committee of The Association of Anaesthetists of Great<br />
Britain and Ireland. Workload for Consultant Anaesthetists in Ireland.<br />
London: AAGBI, 1992.<br />
• Irish Standing Committee of the Association of Anaesthetists of Great<br />
Britain and Ireland. Workload for Consultant Anaesthetists in Ireland.<br />
Supplement 1993. London: AAGBI, 1993.<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
• The Association of Anaesthetists of Great Britain and Ireland. Guidance<br />
on The 2003 (New) Contract and Job Planning for Consultant<br />
Anaesthetists. London: AAGBI, 2005.<br />
Health Service Executive<br />
• Health Service Executive. Revised Consultant Qualifications. 16<br />
March 2009. http://hsenet.hse.ie/HSE_Central/Human_Resources/<br />
SServices/Recruitment/Consultants/Revised_Consultants_Qualifications.<br />
pdf (accessed 28/02/2010).<br />
• Health Service Executive. Procedures for the Regulation of Consultant<br />
Appointments. 31 March 2008. http://hsenet.hse.ie/HSE_Central/<br />
Human_Resources/SServices/Recruitment/Consultants/Procedures_<br />
for_the_Regulation_of_Consultant_Appointments.pdf (accessed<br />
28/02/2010).<br />
• Health Service Executive. HR Circular 014/2009. 07 May 2009.<br />
Revised Procedural Arrangements for Appointment of<br />
Medical Consultants. http://hsenet.hse.ie/Intranet/Working_in_the_<br />
HSE/HR_Documents/HR_Circulars/?importUrl=http://localhost:82/eng/<br />
staff/HR/HR_Circulars/HSE_HR_Circular_014_2009_re_Revised_<br />
Procedural_Arrangements_for_Appointment_of_Medical_Consultants.<br />
pdf (accessed 28/02/2010).<br />
• Health Service Executive. Procedures for the Recruitment and Selection<br />
of Locum and Temporary Consultants. 07 May 2009. http://hsenet.<br />
hse.ie/HSE_Central/Human_Resources/SServices/Recruitment/<br />
Consultants/Procedure_for_Recruitment_and_Selection_of_Locum_and_<br />
Temporary_Consultants.pdf (accessed 28/02/2010).<br />
29
Medical Council<br />
• Medical Council. Guide to Professional Conduct and Ethics for<br />
Registered Medical Practitioners. 2009. http://www.medicalcouncil.<br />
ie/Professional-Standards/Professional-Conduct-Ethics/The-Guide-to-<br />
Professional-Conduct-and-Ethics-for-Registered-Medical-Practitioners-<br />
7th-Edition-2009-.pdf (accessed 28/02/2010).<br />
Measurement of the ratio of public to private practice<br />
• Health Service Executive. Consultant Contract 2008 – Measurement<br />
of Public:Private Mix. http://www.hse.ie/eng/staff/HR/tandc/Consultant_<br />
Contract_2008_-_Measurement_of_Public_Private_Mix.pdf (accessed<br />
28/02/2010).<br />
• Health Service Executive. Public and private patients in public hospitals.<br />
Guidance to health service management on the treatment of public<br />
and private patients. 16 September 2009. http://www.hse.ie/eng/staff/<br />
HR/tandc/Public_and_private_patients_in_Public_hospitals_-_Guidance_<br />
to_health_service_management_on_the_treatment_of_public_and_<br />
private_patients_16th_September_2009_.pdf (accessed 28/02/2010)<br />
Maintenance of professional competence and clinical governance<br />
• Medical Council. Performance in Practice. Maintenance of Professional<br />
Standards. 2006.<br />
• Royal College of Anaesthetists and The Association of Anaesthetists<br />
of Great Britain and Ireland. Good practice. A guide for departments<br />
of anaesthesia, critical care and pain management. 2006. http://www.<br />
rcoa.ac.uk/docs/goodpractice(oct2006).pdf (accessed 28/02/2010).<br />
• Part 11. Maintenance of Professional Competence. In: Medical<br />
Practitioners Act 2007. http://www.dohc.ie/publications/pdf/medical_<br />
practitioners_act_2007.pdf (accessed 28/02/2010).<br />
• Dept. of Health and Children. Building a Culture of Patient Safety.<br />
Report of the Commission on Patient Safety and Quality Assurance.<br />
July 2008. http://www.dohc.ie/publications/pdf/en_patientsafety.pdf<br />
(accessed 28/02/2010).<br />
Clinical directors and clinical directorates<br />
• Health Service Executive. Appointment of Clinical Directors throughout<br />
the Health Service. August 2008.<br />
• Irish Hospital Consultants Association. Position Paper on Clinical<br />
30
Governance. August 2008.<br />
Locum and temporary consultants<br />
• Medical Council. Locum Cover. In: Medical Council Newsletter. June<br />
2009. http://medicalcouncil.newsweaver.co.uk/<br />
MedicalCouncil/1l5v9mc7ii4 (accessed 28/02/2010).<br />
• Moffatt J. Employment Law (Law Society of Ireland Manual). Oxford:<br />
Oxford University Press, 2006.<br />
• The Labour Court. Synopsis of Fixed-Term Work Determinations made<br />
by the Labour Court in 2005, 2006, 2007 and 2008. http://www.<br />
labourcourt.ie/Labour/Information.nsf/8e26b9bae107240c80256a4900<br />
5962ca/8b2a95b62cc57321802571b6004afafb?OpenDocument<br />
(accessed 28/02/2010).<br />
European Working Time Directive<br />
• The Organisation of Working Time Act, 1997. http://www.oireachtas.ie/<br />
documents/bills28/acts/1997/a2097.pdf (accessed 28/02/2010).<br />
• The European Communities (Organisation of Working Time) (Activities<br />
of Doctors in Training) Regulations 2004 (S.I. No. 494 of 2004). http://<br />
www.dohc.ie/legislation/statutory_instruments/pdf/si20040494.<br />
pdf?direct=1 (accessed 28/02/2010)<br />
• Dept. of Health and Children. Guidance on the implementation of the<br />
European Working Time Directive. July 2004. http://www.dohc.ie/issues/<br />
european_working_time_directive/guidance.pdf (accessed 28/02/2010).<br />
• Irish Medical Organisation. European Working Time Directive - IMO<br />
AGM 2005 Briefing. http://www.imo.ie/IMOPage_2_574.aspx (accessed<br />
28/02/2010).<br />
• Royal College of Physicians. Designing safer rotas for junior<br />
doctors in the 48-hour week. 2006. http://bookshop.rcplondon.<br />
ac.uk/contents/779336a5-b884-4b5f-8c23-efd75d123868.pdf (accessed<br />
28/02/2010).<br />
• National Implementation Group (NIG). European Working Time<br />
Directive & Non Consultant Hospital Doctors – Final Report. December<br />
2008. http://www.dohc.ie/publications/pdf/NIG_Report_Dec08.pdf<br />
(accessed 28/02/2010).<br />
• Health Service Executive. European Working Time Directive<br />
Implementation. Guidance to health service management on the<br />
implementation of the EWTD and related Labour Court<br />
Recommendation. 26 June 2009.<br />
• Health Service Executive. European Working Time Directive<br />
31
Implementation. Guidance to health service management on the EWTD<br />
and use of compensatory rest. 09 September 2009.<br />
• College of Anaesthetists of Ireland. The European Working Time<br />
Directive and Specialist Training in Anaesthesia, Intensive Care and Pain<br />
Medicine. 26 June 2009.<br />
• Royal College of Anaesthetists and Royal College of Surgeons of<br />
England. WTD - Implications and Practical Suggestions to Achieve<br />
Compliance. 2009. http://www.rcoa.ac.uk/docs/rcs-rcoa_report.pdf<br />
(accessed 28/02/2010).<br />
32
Appendix 1. Qualifications for the post of<br />
consultant anaesthetist<br />
The HSE has specified that the following qualifications are required for<br />
appointment to the post of consultant anaesthetist:<br />
Consultant anaesthetist<br />
Registration as a specialist in the Specialist Division of the Register of<br />
Medical Practitioners maintained by the Medical Council in lreland in the<br />
specialty of anaesthesia.<br />
Consultant paediatric anaesthetist<br />
Registration as a specialist in the Specialist Division of the Register of<br />
Medical Practitioners maintained by the Medical Council in lreland in the<br />
specialty of anaesthesia<br />
and<br />
Two years’ postgraduate training and experience in paediatric anaesthesia.<br />
Consultant anaesthetist with a special interest in paediatric<br />
anaesthesia<br />
Registration as a specialist in the Specialist Division of the Register of<br />
Medical Practitioners maintained by the Medical Council in lreland in the<br />
specialty of anaesthesia<br />
and<br />
One year’s postgraduate training and experience in paediatric anaesthesia.<br />
Consultant anaesthetist with a special interest in pain<br />
medicine<br />
Registration as a specialist in the Specialist Division of the Register of<br />
Medical Practitioners maintained by the Medical Council in lreland in the<br />
specialty of anaesthesia<br />
and<br />
One year’s postgraduate training and experience in pain medicine.<br />
33
Consultant anaesthetist with a special interest in intensive<br />
care medicine<br />
Registration as a specialist in the Specialist Division of the Register of<br />
Medical Practitioners maintained by the Medical Council in lreland in the<br />
specialty of anaesthesia<br />
and<br />
One year postgraduate training and experience in intensive care medicine<br />
and possession of the Diploma in Intensive Care Medicine or its equivalent.<br />
The qualifications required for a post are set out in the Health Service<br />
Executive’s Letter of Approval which is attached at appendix 1 of the<br />
contract.<br />
34
Appendix 2. Clinical activities of consultant<br />
anaesthetists<br />
The clinical activities of consultant anaesthetists may include but are not<br />
limited to the following:<br />
• Provision of anaesthesia in the operating theatre<br />
• Provision of anaesthesia in locations other than the operating theatre,<br />
e.g. intensive care unit, coronary care unit, emergency department,<br />
radiology department<br />
• Pre-operative assessment in hospital wards, day surgery units and preoperative<br />
assessment clinics<br />
• Post-operative care<br />
• Acute pain management, including acute pain management ward<br />
rounds<br />
• Chronic pain management, including chronic pain management ward<br />
rounds and outpatient clinics and chronic pain interventional<br />
procedures<br />
• Obstetric anaesthesia, e.g. epidural analgesia for labour<br />
• Intensive care medicine, including the assessment and management of<br />
patients who may need intensive care in locations other than the<br />
intensive care unit, e.g. hospital wards, coronary care unit, emergency<br />
department, radiology department<br />
• Resuscitation<br />
• Venous access<br />
• Transfer of patients within the hospital and between hospitals.<br />
• Supervison of the clinical work of anaesthetic trainees<br />
• Handover, e.g. in the obstetric unit or in the intensive care unit<br />
• Administration related to patient care, e.g. documentation,<br />
correspondence<br />
35
Appendix 3. Non-clinical Activities of Consultant<br />
Anaesthetists<br />
The non-clinical activities of consultant anaesthetists may include but are not<br />
limited to the following:<br />
Administration<br />
• Chairperson of committee or department<br />
• Secretary of committee or department<br />
• Lead clinician in anaesthetic sub-speciality<br />
• Clinical Director<br />
• College Tutor<br />
• Medical Student Tutor<br />
• Membership of committee<br />
• Attendance at multidisciplinary meetings<br />
• Attendance at morbidity and mortality meetings<br />
• Organisation of theatre rota<br />
• Organisation of on-call rota<br />
• Organisation of meetings<br />
• Organisation of courses<br />
• Clinical governance activity<br />
• Organisation of orientation sessions<br />
• Writing of clinical protocols and guidelines<br />
• Audit<br />
• Research<br />
• Managing equipment and drugs in the local theatre environment, e.g.<br />
maintenance, supply, reporting, compliance with standards<br />
• Clinical management, e.g. examination of consultant anaesthetist<br />
workload and requirements, preparation of application forms and job<br />
specifications for new consultant anaesthetist posts<br />
• Recruitment of hospital staff, including anaesthetic trainees, e.g.<br />
advertising, short listing, interviewing and selection<br />
• External duties, e.g. Chairperson, Secretary or membership of national<br />
committee, Director of training programme, examining in Primary<br />
and Final FCARCSI exams, acting as an external member of an advisory<br />
appointments committee<br />
• Job planning<br />
• Appraisal<br />
36
Teaching<br />
• Medical students<br />
• Trainees in Anaesthesia<br />
• Other trainees<br />
• Nursing staff<br />
• Regional or national meetings<br />
• Courses, e.g. ACLS, ATLS, APLS/PALS, exam preparation courses,<br />
workshops<br />
Continuing professional development (College of<br />
Anaesthetists of Ireland classification)<br />
Internal activities<br />
• Audit meetings, hospital lectures, journal clubs, critical incident<br />
meetings, grand rounds, appraisal training, morbidity & mortality<br />
meetings<br />
• Hospital lectures<br />
• Attending another consultant’s session within the base hospital<br />
• Internet lectures - non-interactive, watched with colleagues<br />
External activities<br />
• Attendance at CARCSI meetings<br />
• Attendance at accredited international meetings<br />
• Attendance at accredited national meetings<br />
• Attending another consultant’s session outside the base hospital<br />
• Training courses, e.g. ATLS, APLS, ACLS<br />
• Video conference teaching with live interaction<br />
Personal activities<br />
• Independent study<br />
• Distance learning<br />
• Computer assisted learning<br />
• Watching educational video without colleague interaction<br />
• MCQs in medical journal<br />
37
Research<br />
• Research meetings<br />
• Presentation of research findings<br />
• Publication in recognised medical journal<br />
• Publication of chapter or book<br />
Postgraduate examining, training and supervision<br />
• College or university examinations<br />
• Trainer in ATLS, ACLS, APLS, etc.<br />
• Preparation of a lecture<br />
• Conducting tutorial<br />
38
Appendix 4. Supporting resources<br />
The resources which may be required for consultant anaesthetists to perform<br />
their duties have been previously outlined by the AAGBI and may include<br />
but are not limited to the following:<br />
Staffing support<br />
• Adequate staffing levels within department, to allow absence on<br />
Continuing Professional Development activities and other leave<br />
• Resident trainee staff to cover on-call work<br />
• Trained anaesthetic assistance, with adequate orientation for new or<br />
temporary staff<br />
• Specialist nursing support, e.g. in pain management, pre-assessment<br />
• Secretarial support<br />
• Technical and information technology support<br />
• Managerial support<br />
• Audit support staff<br />
•<br />
Accommodation<br />
• Office accommodation. The office should be located in a site which is<br />
accessible during the normal working day<br />
• Office space for supporting staff, e.g. allied health professionals in pain<br />
service<br />
• Secretarial office(s)<br />
• Common room<br />
• Teaching space<br />
• Clinic space as required for pre-assessment, pain clinics or other<br />
outpatient work<br />
• Availability of intensive care unit/high dependency unit<br />
• Appropriate space within all theatre areas for changing, rest and<br />
refreshment<br />
• 24 hour staffed recovery room<br />
Equipment<br />
• Up to date anaesthetic machines, monitors and other equipment, which<br />
comply with published standards and which are regularly serviced<br />
• A dedicated computer for each consultant with access to an appropriate<br />
range of programmes and email/internet connection. Software should be<br />
up to date<br />
39
• Access to confidential telephone and fax facilities<br />
• Access to equipment allowing suitable delivery of teaching, e.g.<br />
projectors, flip charts<br />
• Adequate secure storage space, both for paperwork and personal<br />
belongings<br />
• Secure locker space in theatre<br />
• A constant supply of all sizes of theatre clothing and footwear<br />
Other<br />
• Funding for study leave<br />
• Timely access to a full range of supporting services, such as laboratory<br />
services, radiology<br />
• Time allowed for administrative meetings within working hours.<br />
• Access to up to date library services<br />
• Car or bicycle parking, particularly out of hours, should provide for<br />
personal safety as well as protecting the vehicle<br />
40
41
42
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
AAGBI SAFETY GUIDELINE<br />
UPDATE<br />
Safety in Magnetic Resonance Units:<br />
An update<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org July 2010
This update was originally published in Anaesthesia. If you<br />
wish to refer to this update, please use the following reference:<br />
Association of Anaesthetists of Great Britain and Ireland. Safety<br />
in magnetic resonance units: an update. Anaesthesia 2010; 65:<br />
766-70.<br />
This update should be read in conjunction with the Association’s<br />
guideline, Provision of Anaesthetic Services in Magnetic<br />
Resonance Units.
GUIDELINES<br />
Safety in magnetic resonance units:<br />
an update<br />
Association of Anaesthetists of Great Britain and Ireland<br />
Membership of the Working Party: PA Farling; Chairman; PA<br />
Flynn; G Darwent; J De Wilde; D Grainger; S King; ME McBrien;<br />
DK Menon; JP Ridgway; M Sury; J Thornton; SR Wilson.<br />
This is a consensus document produced by expert members of a Working Party<br />
established by the Association of Anaesthetists of Great Britain and Ireland<br />
(AAGBI). It updates and replaces previous guidance published in 2002, and has<br />
been seen and approved by the Council of the AAGBI.<br />
Summary<br />
The number of anaesthetists who are involved in magnetic resonance<br />
(MR) units is increasing. Magnetic resonance systems are becoming more<br />
powerful and interventional procedures are now possible. This paper<br />
updates information relating to safety terminology, occupational exposure,<br />
reactions to gadolinium-based contrast agents and the risk of nephrogenic<br />
systemic fibrosis. Magnetic resonance examinations of patients with<br />
pacemakers are still generally contra-indicated but have been carried out<br />
in specialist centres under strictly controlled conditions. As availability of<br />
MR increases, so the education of anaesthetists, who are occasionally<br />
required to provide a service, must be considered.<br />
Anaesthesia in MR units was first described in the 1980s. Guidelines on<br />
the provision of anaesthetic services in MR units were published by the<br />
Association of Anaesthetists of Great Britain and Ireland (AAGBI) in 2002<br />
Re-use of this article is permitted in accordance with the Creative Commons Deed,<br />
Attribution 2.5, which does not permit commercial exploitation.<br />
Ó 2010 The Authors<br />
Journal compilation Ó 2010 The Association of Anaesthetists of Great Britain and Ireland 1
Safety in magnetic resonance units<br />
.....................................................................................................................................<br />
[1]. Since then, the number of hospitals with MR units, and hence the<br />
number of patients requiring anaesthesia for MR, has increased. While the<br />
issues relating to setting up anaesthetic services in MR have not changed,<br />
there have been a number of developments that warrant this update:<br />
1 Safety terminology and guidelines have changed.<br />
2 MR systems utilise higher magnetic-field strengths and more open<br />
designs are available.<br />
3 Interventional and intra-operative MR are now routine in some<br />
centres.<br />
4 Mobile MR scanners are increasingly used to reduce waiting lists.<br />
5 Although still generally contra-indicated, some patients with pacemakers<br />
have been scanned under strictly controlled conditions in specialist<br />
centres.<br />
6 ‘MR safe’ medical implants are now being produced.<br />
7 New equipment is now available for use in MR.<br />
8 Out-of-hours availability of MR investigations has increased.<br />
9 Reports of allergic reactions to MR contrast media have increased.<br />
10 Gadolinium based contrast agents (Gd-CAs) are associated with a<br />
varying degree of risk of nephrogenic systemic fibrosis in patients with<br />
impaired renal function.<br />
Safety guidelines and legislation<br />
In 2007 the Medicines and Healthcare products Regulatory Agency<br />
(MHRA) updated safety guidance as a Device Bulletin [2]. Three terms are<br />
now to be used as standard in an attempt to remove any ambiguity caused by<br />
the old MR compatible system. These terms are MR conditional, MR safe and<br />
MR unsafe. MR conditional refers to an item that has been demonstrated to<br />
pose no known hazards in a specified MR environment with specified<br />
conditions of use. Many items in the MR environment will now be marked<br />
as MR conditional, and the conditions under which they can be safely used<br />
must accompany the device. This change of terminology has come about<br />
because of reports of injuries and problems with MR compatible equipment<br />
[3]. Conditions that define the specified MR environment include main<br />
magnetic field strength, spatial magnetic field gradient, dB ⁄ dt (time rate of<br />
change of the magnetic field), radio frequency (RF) field strength, and<br />
specific absorption rate. Additional conditions, including specific configurations<br />
of the item of equipment, may be required.<br />
Ó 2010 The Authors<br />
2 Journal compilation Ó 2010 The Association of Anaesthetists of Great Britain and Ireland
Safety in magnetic resonance units<br />
.....................................................................................................................................<br />
Equipment is designated as MR safe if it presents no safety hazard to<br />
patients or personnel when it is taken into the MR examination room,<br />
provided that instructions concerning its use are correctly followed. This<br />
does not, however, guarantee that it will function normally and not<br />
interfere with the correct operation of the MR imaging equipment, with<br />
degradation of image quality.<br />
New equipment, such as infusion pumps [4], warming mattresses and<br />
temperature probes are now available. It is important to understand the<br />
manufacturers’ instructions of all equipment that is brought into the vicinity<br />
of the MR scanner.<br />
It should be recognised that the supervising MR radiographer is<br />
responsible operationally for MR safety within the controlled area and<br />
that anaesthetic staff should defer to him/her in relation to MR safety<br />
matters, in particular control of access of staff and equipment into the<br />
controlled area. Where staff are given access codes or swipe-card access<br />
to the controlled area, they should not be shared with others, nor<br />
should they provide access to others unless specifically authorised to<br />
do so.<br />
Inspired oxygen concentration<br />
The use of 100% O 2 during anaesthesia should be reported to the reporting<br />
radiologist as this can produce an artefact in the form of an abnormally high<br />
signal in cerebrospinal fluid (CSF) spaces in the T2 weighted fluid<br />
attenuated inversion recovery (FLAIR) sequence.<br />
Acoustic noise<br />
The time-varying magnetic field gradients produce audible noise within the<br />
magnet interior. Since the guidelines were published by the AAGBI, the<br />
Control of Noise at Work Regulations have been updated [5]. This<br />
document introduced lower exposure limit values and action values in the<br />
working environment. When the noise level exceeds 80 dB (A), it is<br />
recommended that staff and others remaining in the scanning room should<br />
wear ear protection.<br />
Other documents have been published by the Health Protection Agency<br />
relating to patient exposure guidance [6] and static field guidance [7]. The<br />
website of the British Association of MR Radiographers (BAMRR)<br />
remains an excellent resource for safety issues and provides links to many<br />
useful safety sites [8].<br />
Ó 2010 The Authors<br />
Journal compilation Ó 2010 The Association of Anaesthetists of Great Britain and Ireland 3
Safety in magnetic resonance units<br />
.....................................................................................................................................<br />
New MR systems<br />
At the end of 2006, it was estimated that there were approximately 500<br />
fixed MR scanners involved in human imaging, installed at some 350 sites<br />
across the UK [6]. The SI unit of magnetic field strength or magnetic flux<br />
density is the Tesla (T) and initially, most clinical MR systems were 0.5, 1.0<br />
or 1.5 T. In 1992 there were two MR units in Northern Ireland. Today<br />
there are 16, of which, one is a 3-T system. Other regions will have<br />
experienced a similar expansion but, since the withdrawal of funding from<br />
MagNET, up-to-date information for the UK is difficult to obtain.<br />
Magnets operating at 3 T appeared in the early 1990s and by 2007 it was<br />
estimated that 35 units had installed 3-T systems [5]. The benefits of the<br />
higher field strength systems include improved image quality and higher<br />
spatial resolution. While it is claimed that 3-T scans are quicker, more<br />
efficient and require less Gd-CAs, practically these statements are<br />
debatable. It is the responsibility of the equipment manufacturers to<br />
indicate the field strength at which their equipment is MR safe or MR<br />
conditional. It should not be automatically assumed that equipment that is<br />
MR conditional at 1.5 T remains MR conditional at 3 T. A smaller<br />
number of ultra-high field MR systems are in use in research institutions<br />
world wide and these produce static fields in the range 4.7–9.4 T [6].<br />
Anaesthetists may wish to be aware of the potential implications of<br />
replacing a 1.5-T system by a 3-T system. In a magnetic field strength<br />
survey of a 1.5-T system all spot measurements taken at 1 m above the<br />
floor level were found to be below the 0.5-mT safety limit. A similar<br />
survey for a 3-T system indicated that there were areas outside the magnet<br />
room where levels exceeded the safety limit. Barriers and warning notices,<br />
which indicate the risk of pacemaker malfunction, should be in place to<br />
prevent inadvertent public access.<br />
Open systems<br />
The horizontal-bore cylindrical type of scanner is still the commonest, but<br />
technology constantly changes and magnets are available with wider bores,<br />
which are less claustrophobic. More open scanners have been developed<br />
and units now exist that allow the patient to stand upright thus reducing the<br />
feeling of claustrophobia. In a conventional MR system operating at 1.5 T,<br />
because of its more closed design, it is less likely that radiological and<br />
anaesthetic staff would be exposed to significant static and time varying<br />
fields.<br />
Ó 2010 The Authors<br />
4 Journal compilation Ó 2010 The Association of Anaesthetists of Great Britain and Ireland
Safety in magnetic resonance units<br />
.....................................................................................................................................<br />
Interventional procedures and intra-operative MR<br />
Advances in technology mean MR image-guided surgery is now possible,<br />
providing the surgeon with dynamic high-resolution images during<br />
intricate stereotactic neurosurgery. Various MR systems have been<br />
configured for this application, including ‘doughnut’ shaped magnets<br />
permitting surgery with real-time concurrent imaging, and portable systems<br />
set up to allow easy and rapid interchange between scanning and surgery.<br />
All the hazards associated with diagnostic MR also apply to interventional<br />
procedures. There are additional risks from patient repositioning, contamination<br />
of the sterile field, and the proximity of ferromagnetic surgical<br />
instruments, including scalpels, to the magnetic field. Incorporating MR<br />
technology into the operating room provides new challenges [9].<br />
Occupational exposure<br />
It is difficult to measure occupational exposure to the various electro<br />
magnetic fields in MR units routinely. Personal dosimeters have been<br />
developed but are not, as yet, widely available. Some studies have suggested<br />
that staff members can be exposed to higher than recommended levels of<br />
time-varying gradient fields [10, 11]. In 2004, the European Union adopted<br />
a directive restricting occupational exposure to electromagnetic fields,<br />
including those used in MR. Some of the exposure limits threatened to<br />
impact on the current use and future development of MR technology.<br />
Known adverse effects are adequately addressed in the international standard<br />
governing the manufacture of MR systems. Initially, unable to influence the<br />
regulatory agencies, the MR community began to lobby both the UK and<br />
European Parliaments. Implementation of the directive has been delayed<br />
until 30 April 2012 to allow a permanent solution to be found. However,<br />
the timescale is short given the political and scientific complexities of the<br />
issue. A range of possible outcomes is explored in a report for the Institute of<br />
Physics [12]. Each option has advantages and disadvantages, and a great deal<br />
of detailed discussion and negotiation will be needed over the next 2 years to<br />
ensure satisfactory resolution of the problem.<br />
Pacemakers and medical implants<br />
The MHRA safety guidance [2] still specifies that pacemakers are an<br />
absolute contraindication to MR and it therefore remains the mantra of<br />
Ó 2010 The Authors<br />
Journal compilation Ó 2010 The Association of Anaesthetists of Great Britain and Ireland 5
Safety in magnetic resonance units<br />
.....................................................................................................................................<br />
radiology departments that any individual with a pacemaker should not<br />
enter the MR unit. This is due to the concern that the magnet<br />
field strengths in excess of 0.5 mT (5 Gauss) could cause a fatal<br />
malfunction of the pacemaker. Sudden deaths have been reported in<br />
patients with pacemakers during or shortly after MR investigations [13, 14].<br />
However, both pacemaker and MR technology are continually developing<br />
and there are times when MR is needed to provide valuable clinical<br />
information in patients with pacemakers. There have been a small number<br />
of cases when a patient with a non-compatible pacemaker has required MR<br />
imaging.<br />
Approximately two million Europeans have implanted pacemakers, but<br />
these patients are strongly discouraged from receiving MRI scans.<br />
According to estimates, 50–75% of patients world-wide with implanted<br />
cardiac devices are expected to need a MR scan during the lifetime of their<br />
device [15]. Editorials in the American and European literature concluded<br />
that the risk:benefit ratio for patients with pacemakers undergoing MR has<br />
shifted towards safety, if guidelines are followed [16, 17]. Discussion in the<br />
correspondence sections has been generated [18]. In summary, the presence<br />
of a permanent pacemaker no longer represents a strict contra-indication to<br />
MR in carefully selected clinical circumstances provided that specific<br />
strategies are followed [19].<br />
MR compatible pacemakers are now available and have been implanted<br />
in some patients. One pacemaker manufacturer has received a Conformité<br />
Européenne (CE) Mark for its second-generation MR safe pacing system.<br />
However, approval has not yet been forthcoming from the Food and Drug<br />
Administration in the USA [20].<br />
Programmable shunts<br />
The pressure setting of programmable hydrocephalus shunts may be<br />
unintentionally changed by the magnetic field leading to over- or underdrainage<br />
of CSF. If these patients are to undergo an MR examination, a<br />
programmer and a trained clinician should be available to verify the correct<br />
setting and to reprogram the device, if required, immediately following the<br />
MR procedure. Advice must be given to the patient on how to recognise<br />
over- and under-drainage and whom to contact should these conditions<br />
develop [2].<br />
Ó 2010 The Authors<br />
6 Journal compilation Ó 2010 The Association of Anaesthetists of Great Britain and Ireland
Safety in magnetic resonance units<br />
.....................................................................................................................................<br />
Neurostimulators<br />
A wide variety of neurostimulators are now in use. Concerns about MR<br />
safety relate to the RF and gradient fields that may interfere with the<br />
operation of these devices or cause thermal injury. It is recommended that<br />
patients implanted with neurostimulators should not undergo MR.<br />
However, some manufacturers are suggesting that MR examinations of<br />
specific devices may be safe if strict guidelines relating to scanning<br />
parameters, in particular to RF exposure, are followed [2].<br />
Out-of-hours MR imaging<br />
There are many indications for urgent MR imaging, but they can be<br />
grouped into two main areas: suspected spinal cord or cauda equina<br />
compression; and investigation of acute neurological conditions. Hospital<br />
trusts have faced litigation when treatment has been delayed due to lack of<br />
24-h MR availability. Patients in intensive care units (ICUs) who require<br />
urgent MR will need to be accompanied by anaesthetic staff. Intensive care<br />
patients have additional sources of hazard including central lines and<br />
intracranial pressure transducers [21]. Screening checklists have been<br />
adapted for use in intensive care. It should be remembered that the ultimate<br />
operational responsibility for safety issues remains with an appropriately<br />
trained MR Authorised Person (usually the supervising radiographer) and<br />
the MR radiologist [2].<br />
Training<br />
Training requirements for any staff entering the MR unit are detailed by<br />
the MHRA [2]. The responsibility for safety training lies with the MR<br />
Responsible Person who may be the clinical director, head of department,<br />
clinical scientist or MR superintendent radiographer. The unit’s MR Safety<br />
Advisor should provide technical advice. The wide range of staff from<br />
differing disciplines who need access to the MR environment have been<br />
designated into categories. Anaesthetists fall into MHRA category B; that is,<br />
they may be present with a patient in the MR controlled area during<br />
scanning. They should be aware of safety aspects related to the main static<br />
magnetic fields, RF fields, gradient magnetic fields and electrical safety of<br />
equipment. They must understand the significance of the MR controlled<br />
area and the inner MR controlled area. They should be familiar with<br />
emergency procedures arising from causes other than equipment failure and<br />
Ó 2010 The Authors<br />
Journal compilation Ó 2010 The Association of Anaesthetists of Great Britain and Ireland 7
Safety in magnetic resonance units<br />
.....................................................................................................................................<br />
should be aware of the need to evacuate the patient from the inner<br />
controlled area in order to deal with emergency resuscitation. Training also<br />
includes an understanding of the projectile effect and the influence of the<br />
magnetic field upon medical implants, prostheses and personal effects.<br />
Anaesthetists should understand the consequences of quenching of superconducting<br />
magnets, and be aware of the recommendations on exposure to<br />
MR and the need for ear protection.<br />
How can these training requirements be met? The potential for<br />
e-learning should be considered. The Royal College of Anaesthetists<br />
includes the physics of MRI in its basic science syllabus [22]. Trainees who<br />
have completed an e-learning module and attended an elective MR list<br />
would then be certified as suitable to accompany ICU patients for MR<br />
imaging. Regular reviews of training status as well as updates and refresher<br />
courses will be required. Hospitals will wish to apply local rules regarding<br />
consultant supervision of anaesthetic trainees in MR units.<br />
Contrast reactions<br />
Gadolinium-based contrast agents are used in MR for demonstration of<br />
vascular structures or to improve contrast resolution of tissues. In<br />
comparison with other radiological contrast agents, Gd-CAs are relatively<br />
safe with a high therapeutic ratio and low incidence of anaphylaxis<br />
(approximately 1:100 000). The side-effects of Gd-CAs are generally mild<br />
and include headache, nausea and vomiting, local burning, skin wheals<br />
(2%), itching, sweating, facial swelling and thrombophlebitis [23]. More<br />
severe reactions have occurred and radiology staff should be familiar with<br />
guidelines related to the management of suspected anaphylaxis [24].<br />
Nephrogenic systemic fibrosis<br />
There has been recent attention to reports that patients with renal failure are<br />
at risk of developing a rare, potentially life-threatening condition with<br />
Gd-CAs called nephrogenic systemic fibrosis or nephrogenic fibrosing<br />
dermopathy (NSF ⁄ NFD). The glomerular filtration rate (GFR) should be<br />
estimated in all patients with kidney disease to identify those at risk of<br />
developing NSF ⁄ NSD. If the GFR is estimated at less than 30 ml.min )1<br />
per 1.73 m )2 , the risk of Gd-CAs should be balanced against benefit, and a<br />
minimal dose of Gd-CAs only administered if an unenhanced scan proves<br />
Ó 2010 The Authors<br />
8 Journal compilation Ó 2010 The Association of Anaesthetists of Great Britain and Ireland
Safety in magnetic resonance units<br />
.....................................................................................................................................<br />
insufficient [25]. The Gd-CA should not be administered again for at least<br />
7 days. Current evidence suggests that contrast agents may be classified as<br />
high-risk, e.g. gadopentelic acid, medium-risk, e.g. gadobenic acid, and<br />
low-risk e.g. gadoteridol [26]. The use of high-risk agents is contraindicated<br />
in neonates and during the peri-operative period in patients<br />
undergoing liver transplantation. The Gd-Cas are not recommended in<br />
pregnancy unless absolutely necessary.<br />
Conclusions<br />
While some safety terminology has altered, the basic recommendations<br />
for provision of anaesthetic services in MR units have remained the<br />
same since first published in 2002 [1]. Anaesthetists who are involved<br />
with 3-T systems, open scanners or interventional and intra-operative<br />
procedures should remain acquainted with the constantly changing<br />
recommendations relating to occupational exposure. They should take all<br />
practical steps to minimise the risk from exposure. MR examinations of<br />
patients with pacemakers are no longer absolutely contra-indicated but<br />
may be carried out under strictly controlled conditions in exceptional<br />
cases. Increased requirements for MR imaging in intensive care and<br />
postoperative patients have increased the need for repeated training. The<br />
employment of e-learning modules may facilitate such training. There<br />
has been an increase in the number of allergic reactions to Gd-CAs and<br />
it is recognised that patients with renal failure are at risk of developing<br />
NSF.<br />
References<br />
1 Association of Anaesthetists of Great Britain and Ireland. Provision of Anaesthetic<br />
Services in Magnetic Resonance Units. The Association of Anaesthetists of Great<br />
Britain and Ireland, 2002. http://www.<strong>aagbi</strong>.org/publications/guidelines/docs/<br />
mri02.pdf (accessed 08/12/2009).<br />
2 Device Bulletin Safety Guidelines for Magnetic Resonance Imaging Equipment<br />
in Clinical Use DB2007(03) December 2007 http://www.mhra.gov.uk/<br />
Publications/Safetyguidance/DeviceBulletins/CON2033018 (accessed 08/12/<br />
2009).<br />
3 Farling PA, McBrien ME, Winder RJ. Magnetic resonance compatible<br />
equipment: read the small print! Anaesthesia 2003; 58: 86.<br />
Ó 2010 The Authors<br />
Journal compilation Ó 2010 The Association of Anaesthetists of Great Britain and Ireland 9
Safety in magnetic resonance units<br />
.....................................................................................................................................<br />
4 Bradley PG, Harding SG, Reape-Moore K, Abeygunaratne R, Menon DK.<br />
Evaluation of infusion pump performance in a magnetic resonance environment.<br />
European Journal of Anaesthesiology 2004; 21: 729–33.<br />
5 The Control of Noise at Work Regulations 2005. Statutory instrument<br />
2005 N0.1643 http://www.opsi.gov.uk/si/si2005/20051643.htm (accessed<br />
02/02/2010).<br />
6 Protection of patients and volunteers undergoing MRI procedures. Advice from<br />
the Health Protection Agency. ISBN: 978-0-85951-623-5 http://<br />
www.hpa.org.uk/web/HPAwebFile/HPAweb_C/1222673275524 (accessed<br />
8/12/2009).<br />
7 Static Magnetic Fields. Health Protection Agency. 2008 http://www.hpa.<br />
org.uk/web/HPAwebFile/HPAweb_C/1211184025757 (accessed 9/12/2009).<br />
8 British Society of MR Radiographers http://www.bamrr.org/content.aspx?<br />
Group=links&Page=links (accessed 08/04/2010).<br />
9 Bergese SD, Puente EG. Anesthesia in the intra-operative MRI Environment.<br />
Neurosurgery Clinics of North America 2009; 20: 155–62.<br />
10 Vecchia P, Matthes R, Ziegelberger G, et al. (editors). Exposure to high frequency<br />
electromagnetic fields, biological effects and health consequences<br />
(100 kHz-300 GHz). International Commission on Non-Ionizing Radiation<br />
Protection, 2008. http://www.icnirp.de/documents/RFReview.pdf (accessed<br />
09/12/2009).<br />
11 Bradley JK, Nyekiova M, Price DL, Lopez LD, Crawley T. Occupational<br />
exposure to static and time-varying gradient magnetic fields in MR units. Journal<br />
of Magnetic Resonance Imaging 2007; 26: 1204–9.<br />
12 Keevil S, MRI and the Physical Agents (EMF) Directive. Reproduced by<br />
permission of the Institute of Physics. 2008. http://www.iop.org/activity/<br />
policy/Publications/file_32151.pdf (accessed 08/12/2009).<br />
13 Ferris NJ, Kavnoudias H, Thiel C, Stuckey S. The 2005 Australian MRI safety<br />
survey. American Journal of Roentgenology 2007; 188: 1388–94.<br />
14 Bartsch CH, Irnich W, Risse M, Weller G. Unexpected sudden death of<br />
pacemaker patients during or shortly after magnetic resonance imaging (MRI).<br />
In XIX Congress of International Academy of Legal Medicine. Milan, Italy, 2003; 3–6.<br />
Abstract No 114.<br />
15 Kalin R, Stanton MS. Current clinical issues for MRI scanning of<br />
pacemaker and defibrillator patients. Pacing and Clinical Electrophysiolgy 2005; 28:<br />
326–8.<br />
16 Martin ET, Coman JA, Shellock FG, et al. Magnetic resonance imaging and<br />
cardiac pacemaker safety at 1.5 Tesla. Journal of the American College of Cardiology<br />
2004; 43: 1315–24.<br />
17 Martin ET. Can cardiac pacemakers and magnetic resonance imaging co-exist?<br />
European Heart Journal 2005; 26: 325–7.<br />
Ó 2010 The Authors<br />
10 Journal compilation Ó 2010 The Association of Anaesthetists of Great Britain and Ireland
Safety in magnetic resonance units<br />
.....................................................................................................................................<br />
18 Gimbel JR, Wilkoff BL, Kanal E, Rozner MA. Safe, sensible sagacious:<br />
resposible scanning of pacemaker patients. European Heart Journal 2005; 26:<br />
1683–91.<br />
19 Shellock FG. MR Imaging and electronically activated devices. Radiology 2001;<br />
219: 294.<br />
20 Press Release. http://wwwp.medtronic.com/Newsroom/NewsRelease<br />
Details.do?itemId=1245340154210&lang=en_US (accessed 29/01/2010).<br />
21 Newcombe VF, Hawkes RC, Harding SG, et al. Potential heating caused by<br />
intraparenchymal intracranial pressure transducers in a 3-tesla magnetic resonance<br />
imaging system using a body radiofrequency resonator: assessment of the<br />
Codman MicroSensor Transducer. Journal of Neurosurgery 2008; 109: 159–64.<br />
22 Royal College of Anaesthetists http://www.rcoa.ac.uk/docs/eLA-Curriculum.<br />
pdf (accessed 29/01/2010).<br />
23 Li A, Wong CS, Lee CM, Au Yeung MC. Acute adverse reactions to magnetic<br />
resonance contrast media – gadolinium chelates. British Journal of Radiology 2006;<br />
79: 368–71.<br />
24 Harper NJN, Dixon T, Dugue P, et al. Guidelines: suspected anaphylactic<br />
reactions associated with anaesthesia. Anaesthesia 2009; 64: 199–211.<br />
25 Shellock FG, Spinazzi A. MRI safety update 2008: part 1, MRI contrast agents<br />
and nephrogenic systemic fibrosis. American Journal of Roentgenology 2008; 191:<br />
1129–39.<br />
26 Drug Safety Update 2010; 3: 3–5 http://www.mhra.gov.uk/Publications/<br />
Safetyguidance/DrugSafetyUpdate/CON068297 (accessed 15/02/2010).<br />
Ó 2010 The Authors<br />
Journal compilation Ó 2010 The Association of Anaesthetists of Great Britain and Ireland 11
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
Malignant Hyperthermia Crisis<br />
AAGBI Safety Guideline<br />
Successful management of malignant hyperthermia depends upon early diagnosis and treatment;<br />
onset can be within minutes of induction or may be insidious. The standard operating<br />
procedure below is intended to ease the burden of managing this rare but life threatening emergency.<br />
1<br />
Recognition<br />
2<br />
Immediate<br />
management<br />
• Unexplained increase in ETCO2 AND<br />
• Unexplained tachycardia AND<br />
• Unexplained increase in oxygen requirement<br />
(Previous uneventful anaesthesia does not rule out MH)<br />
• Temperature changes are a late sign<br />
• STOP all trigger agents<br />
• CALL FOR HELP. Allocate specific tasks (action plan in MH kit)<br />
• Install clean breathing system and HYPERVENTILATE with 100% O2 high flow<br />
• Maintain anaesthesia with intravenous agent<br />
• ABANDON/FINISH surgery as soon as possible<br />
• Muscle relaxation with non-depolarising neuromuscular blocking drug<br />
3<br />
Monitoring<br />
& treatment<br />
• Give dantrolene<br />
• Initiate active cooling avoiding<br />
vasoconstriction<br />
• TREAT:<br />
• Hyperkalaemia: calcium<br />
chloride, glucose/insulin, NaHCO3¯<br />
• Arrhythmias:<br />
magnesium/amiodarone/metoprolol<br />
AVOID calcium channel blockers -<br />
interaction with dantrolene<br />
• Metabolic acidosis: hyperventilate,<br />
NaHCO3¯<br />
• Myoglobinaemia: forced alkaline<br />
diuresis (mannitol/furosemide +<br />
NaHCO3¯); may require renal<br />
replacement therapy later<br />
• DIC: FFP, cryoprecipitiate, platelets<br />
• Check plasma CK as soon as able<br />
DANTROLENE<br />
2.5mg/kg immediate iv bolus.<br />
Repeat 1mg/kg boluses as required<br />
to max 10mg/kg<br />
For a 70kg adult<br />
• Initial bolus: 9 vials dantrolene<br />
20mg (each vial mixed with 60ml<br />
sterile water)<br />
• Further boluses of 4 vials<br />
dantrolene 20mg repeated up to<br />
7 times.<br />
Continuous monitoring<br />
Core & peripheral temperature<br />
ETCO2<br />
SpO2<br />
ECG<br />
Invasive blood pressure<br />
CVP<br />
Repeated bloods<br />
ABG<br />
U&Es (potassium)<br />
FBC (haematocrit/platelets)<br />
Coagulation<br />
4<br />
Follow-up<br />
• Continue monitoring on ICU, repeat dantrolene as necessary<br />
• Monitor for acute kidney injury and compartment syndrome<br />
• Repeat CK<br />
• Consider alternative diagnoses (sepsis, phaeochromocytoma, thyroid storm, myopathy)<br />
• Counsel patient & family members<br />
• Refer to MH unit (see contact details below)<br />
The UK MH Investigation Unit, Academic Unit of Anaesthesia, Clinical Sciences Building, Leeds Teaching Hospitals NHS Trust,<br />
Leeds LS9 7TF. Direct line: 0113 206 5270. Fax: 0113 206 4140. Emergency Hotline: 07947 609601 (usually available outside<br />
office hours). Alternatively, contact Prof P Hopkins, Dr E Watkins or Dr P Gupta through hospital switchboard: 0113 243 3144.<br />
Your nearest MH kit is stored<br />
This guideline is not a standard of medical care. The ultimate judgement with regard to a particular clinical procedure or treatment plan must be made<br />
by the clinician in the light of the clinical data presented and the diagnostic and treatment options available.<br />
© The Association of Anaesthetists of Great Britain & Ireland 2011
Recommended Contents of Malignant Hyperthermia Management Kit<br />
(Ideally contained in designated and labelled compartments, e.g. drawers of a trolley)<br />
AAGBI Safety Guideline<br />
Storing together the majority of items required to manage malignant hyperthermia will reduce time spent gathering<br />
equipment and hence expedite initiation of successful treatment.<br />
Compartment 1: dantrolene<br />
• 100 mls vial of sterile water for injection x 12<br />
• 12 vials of dantrolene (20 mg per vial) (sufficient for an initial 2.5mg/kg dose<br />
plus 2 repeat 1mg doses in an average adult)<br />
• 10 x 50ml syringes<br />
• Guideline for management of crisis and task allocations<br />
• Details of location of reserve dantrolene supplies<br />
Compartment 2: treatment<br />
• Calcium chloride 10%<br />
• Sodium bicarbonate (50ml 8.4% syringe)<br />
• Amiodarone 300mg<br />
• β blocker<br />
• Glucose (20%)<br />
• 50ml propofol vials/prefilled syringes for TIVA<br />
Compartment 3: investigation/monitoring<br />
• Blood bottles<br />
• ABG<br />
• FBC<br />
• Coagulation<br />
• Biochem<br />
• Urine sample bottles<br />
• Group & save<br />
• Arterial cannulae and transducer sets<br />
• CVC and transducer sets<br />
Along with part-filled forms labelled ‘MH crisis’<br />
and numbered; 1 st , 2 nd , 3 rd<br />
To include CK and urinary myoglobin assay<br />
Fridge pack<br />
• 2 litres of cold sodium chloride 0.9% for IV administration<br />
• Short-acting insulin<br />
© The Association of Anaesthetists of Great Britain & Ireland 2011
Recommended Contents of Malignant Hyperthermia Management Kit<br />
(Ideally contained in designated and labelled compartments, e.g. drawers of a trolley)<br />
AAGBI Safety Guideline<br />
Storing together the majority of items required to manage malignant hyperthermia will reduce time spent gathering<br />
equipment and hence expedite initiation of successful treatment.<br />
Compartment 1: dantrolene<br />
• 100 mls vial of sterile water for injection x 12<br />
• 12 vials of dantrolene (20 mg per vial) (sufficient for an initial 2.5mg/kg dose<br />
plus 2 repeat 1mg doses in an average adult)<br />
• 10 x 50ml syringes<br />
• Guideline for management of crisis and task allocations<br />
• Details of location of reserve dantrolene supplies<br />
Compartment 2: treatment<br />
• Calcium chloride 10%<br />
• Sodium bicarbonate (50ml 8.4% syringe)<br />
• Amiodarone 300mg<br />
• β blocker<br />
• Glucose (20%)<br />
• 50ml propofol vials/prefilled syringes for TIVA<br />
Compartment 3: investigation/monitoring<br />
• Blood bottles<br />
• ABG<br />
• FBC<br />
• Coagulation<br />
• Biochem<br />
• Urine sample bottles<br />
• Group & save<br />
• Arterial cannulae and transducer sets<br />
• CVC and transducer sets<br />
Along with part-filled forms labelled ‘MH crisis’<br />
and numbered; 1 st , 2 nd , 3 rd<br />
To include CK and urinary myoglobin assay<br />
Fridge pack<br />
• 2 litres of cold sodium chloride 0.9% for IV administration<br />
• Short-acting insulin<br />
© The Association of Anaesthetists of Great Britain & Ireland 2011
Malignant Hyperthermia Crisis Task Allocations<br />
AAGBI Safety Guideline<br />
The successful management of a malignant hyperthermia crisis requires multiple simultaneous<br />
treatment actions. This is made far easier through effective teamwork and specific task allocation.<br />
1 st anaesthetist - commence immediate management (on guideline sheet)<br />
The anaesthetist diagnosing MH or the most senior anaesthetist responding should assume the role of<br />
clinical leader once immediate management actions have been undertaken and avoid becoming focused<br />
on a single task.<br />
2 nd anaesthetist - resuscitation<br />
• Ensure dantrolene is given in correct dose (2.5mg/kg initially then 1mg/kg every 10-15min)<br />
• Commence TIVA<br />
• Management of hyperkalaemia<br />
• Management of arrhythmias<br />
• Management of acidosis<br />
• Renal protection (forced alkaline diuresis)<br />
1 st anaesthetic nurse/ODP<br />
• Collect MH kit<br />
• Collect cold saline & insulin<br />
• Set up lines (arterial/CVC)<br />
• Runner for resuscitation drugs/equipment<br />
2 nd anaesthetic nurse/ODP (ideally two people)<br />
• Draw up dantrolene as requested by anaesthetist in charge of resuscitation<br />
3 rd anaesthetist - lines/investigations<br />
• Site arterial line<br />
• Send bloods for<br />
o ABG – repeated (approx every 30 min initially)<br />
o U&Es<br />
o CK<br />
o FBC<br />
o Coagulation screen<br />
o Cross match<br />
• Central venous access<br />
• Urinary myoglobin<br />
• Monitor core and peripheral temperatures<br />
Surgical team<br />
• Catheterise<br />
• Complete/abandon surgery as soon as feasible<br />
• Undertake cooling manoeuvres<br />
Adapted from the Malignant Hyperthermia Australia and New Zealand (MHANZ) MH Resource Kit with permission
PROVISION OF ANAESTHETIC SERVICES<br />
IN MAGNETIC RESONANCE UNITS<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland,<br />
9 Bedford square, London WC1B 3RE, UK<br />
Telephone: 020 7631 1650, Fax: 020 7631 4352<br />
E-mail: info@<strong>aagbi</strong>.org Website: www.<strong>aagbi</strong>.org May 2002
Membership of the Working Party<br />
Dr Peter Farling<br />
Dr Kate Bullen<br />
Dr Juliet Britton<br />
Ms Gail Darwent<br />
Dr Janet DeWilde<br />
Mrs Sharon Giles<br />
Prof Paul Goddard<br />
Dr Susan King<br />
Dr Michael McBrien<br />
Mrs Pat McDonald<br />
Prof David Menon<br />
Dr John Ridgway<br />
Dr Michael Sury<br />
Dr Sally Wilson<br />
Ex-Officio<br />
Professor Leo Strunin<br />
Dr David Wilkinson<br />
Dr Robert Buckland<br />
Dr Michael Ward<br />
Professor Michael Harmer<br />
Chairman of Working Party<br />
Council member<br />
British Society of Neuroradiologists<br />
British Association of MR Radiographers<br />
MagNET<br />
Department of Health<br />
British Institute of Radiology<br />
Royal College of Radiologists<br />
Consultant Anaesthetist<br />
Medical Devices Agency<br />
Professor of Anaesthesia<br />
Medical Physics<br />
Consultant Anaesthestist<br />
Consultant Anaesthestist<br />
President<br />
Honorary Treasurer<br />
Honorary Secretary<br />
Honorary Membership Secretary<br />
Editor, Anaesthesia<br />
To be reviewed by 2007
Contents<br />
Page<br />
Section I Summary 1<br />
Section II Introduction 2<br />
Section III Planning 3<br />
Section IV Equipment 5<br />
Section V Personnel 7<br />
Section VI Health and safety 8<br />
Section VII Risk management 11<br />
Section VIII Appendix 1 – planning implications 12<br />
Section IX Appendix 2 – glossary 13<br />
Section X References 18<br />
Section XI Further reading 19
Section I: Summary<br />
1. The continuous presence of a strong magnetic field, and restricted access to the patient,<br />
means that the provision of anaesthesia within MR units presents unique problems.<br />
2 Whenever a new MR unit is planned, the possibility of managing sedated or<br />
anaesthetised patients should be considered.<br />
3. In the planning process, adequate space should be made available for the provision of<br />
anaesthesia services.<br />
4. A nominated consultant anaesthetist should be responsible for anaesthesia services in<br />
MR units.<br />
5. The level of assistance for the anaesthetist must be equal to that expected in the<br />
operating theatre environment.<br />
6. Immediate access from the scanning room to the anaesthetic preparation/ resuscitation<br />
area is essential as in the event of an emergency, the patient must be removed from the<br />
magnetic field without delay.<br />
7. Anaesthetic equipment that is used in the scanning room should be MR compatible.<br />
8. The monitoring of patients in MR units during anaesthesia, sedation and recovery must<br />
comply with minimum monitoring standards.<br />
9. It is essential that a remote monitoring facility is available to allow the anaesthetic team<br />
to remain outside the scanning room once the patient’s condition is stable.<br />
10. Only authorised personnel, who have received appropriate training and are fully<br />
conversant with the local protocols, are allowed to enter the controlled area<br />
unsupervised.<br />
11. Resources should be provided to minimise the risk of personal exposure to strong<br />
magnetic fields and noise levels.<br />
1
Section II: Introduction<br />
Magnetic resonance imaging (MRI) is now a routine investigation for many<br />
conditions. The continuous presence of a strong magnetic field, and restricted<br />
access to the patient, means that the provision of anaesthesia within MR units<br />
presents unique problems. Some patients, e.g. children and adults with movement<br />
and learning disorders or claustrophobia, are unable to lie still during the MR<br />
scan and consequently sedation or general anaesthesia is required. Patients<br />
requiring general anaesthesia are often difficult to manage e.g. rare paediatric<br />
syndromes and critical care patients.<br />
At the end of 2001 in Great Britain and Ireland there were approximately 3.9 MR<br />
units per million head of population while the average ratio throughout the rest of<br />
Europe was approximately 5.5 MR units per million. In order to reduce waiting<br />
lists for MR scans, there is a need for investment in new and replacement MR<br />
systems. Some of these may be located in hospitals that currently do not provide<br />
anaesthesia for MR examinations.<br />
This document aims to assist anaesthetists in the planning and provision of<br />
anaesthesia services in new and existing MR units. When planning for a MR<br />
service, radiologists, radiographers, referring clinicians and managers also need to<br />
be aware of the problems associated with the provision of anaesthetic care in MR<br />
units. When introducing a new MR service, it is important that funding is<br />
identified to cover the cost of anaesthetic equipment and associated personnel<br />
who are essential to the provision of anaesthetic care. This will be additional to<br />
the MR equipment costs. (see Appendix 1).<br />
Section III: Planning<br />
Whenever a new MR unit is planned, the possibility of managing sedated or<br />
anaesthetised patients should be considered. This will have specific staffing and<br />
equipment implications as well as significant effects on capital and revenue costs.<br />
Building<br />
NHS Estates have published guidelines relating to accommodation for MR units [1-3].<br />
Input from an anaesthetist, early in the planning process, will ensure that adequate<br />
space is made available for the provision of anaesthesia services. While<br />
recognising that space is at a premium, the unit should be designed to allow<br />
patients to follow a logical progression through each area, with the appropriate<br />
level of privacy.<br />
The MR unit should contain a Controlled Area that contains the 0.5mT (5 gauss)<br />
magnetic field contour. Only Authorised Personnel should have free access to the<br />
controlled area to which there should be strict control of access via self-locking doors.<br />
Consideration of the requirements to provide adequate space for an anaesthesia<br />
service should occur during the design of the following areas:<br />
• Reception area<br />
• Waiting area and changing facilities<br />
• Anaesthesia preparation/ resuscitation room<br />
• Scanner room i.e. the MR examination room or Inner Controlled Area<br />
• Control room<br />
• Recovery area<br />
The preparation area must be large enough to accommodate patients who arrive<br />
on a bed. Adequate space must be available for transfer of patients onto the<br />
scanning table. Anaesthesia should be induced on tables or trolleys with the<br />
facility to tilt the patient head-down. This may require transfer to a MR<br />
compatible trolley after the induction of anaesthesia.<br />
It should be possible to observe patients from an area remote from the MR<br />
examination room e.g. through a window from the control room, where the<br />
radiographers operate the MR system. Once the patient’s condition is stable in the<br />
scanner, the anaesthetist may choose to observe the patient and monitors from the<br />
control room.<br />
2<br />
3
There must be immediate access from the MR examination room to the anaesthetic<br />
preparation/ resuscitation area as it is essential that, in the event of an emergency,<br />
the patient be removed from the magnetic field without delay. Ferromagnetic<br />
equipment including oxygen cylinders, defibrillators or laryngoscopes must never<br />
enter the MR examination room because of the strong magnetic field.<br />
Piped gases and suction will be required in the anaesthetic room, the MR<br />
examination room and the recovery area [4]. Adequate gas scavenging systems<br />
will also be necessary. The installation of facilities such as piped gases is easiest<br />
and least costly during the initial construction of the unit.<br />
While it is recommended that the MR suite should be an integral part of a<br />
radiology department [1], all MR units must be self-sufficient in terms of dealing<br />
with emergency situations including cardiopulmonary resuscitation, anaphylaxis<br />
and difficult airway management. This has staffing, training and equipment<br />
implications. There should be an emergency call system in the MR examination<br />
room and telephones in the anaesthetic room and recovery areas.<br />
Function<br />
A meeting between MR staff and potential users of the unit should be convened at<br />
an early stage in the operational planning process. While this will indicate the<br />
probable case mix of adult and paediatric cases, it should be remembered that this<br />
is only accurate at the time of discussion. Experience has shown that there is<br />
potential for change after the scanner opens. It will also alert staff to problems<br />
associated with specific situations, for example, providing day case anaesthesia or<br />
sedation, the management and transfer of critically ill patients from intensive care<br />
units or children with difficult cardiorespiratory conditions. Children and their<br />
parents attending for a routine examination should be kept separate from critically<br />
ill patients.<br />
Costs<br />
The capital cost of MR compatible anaesthetic machines and monitoring<br />
equipment should be considered when planning the funding of new units. The<br />
revenue consequences of capital investment must be budgeted for and these<br />
include staffing costs, day ward facilities, consumables and service contracts for<br />
equipment. (see Appendix 1).<br />
Section IV: Equipment<br />
All equipment to be used within the scanning room should be passed and clearly<br />
labelled as either ‘MR safe’ or ‘MR compatible’. Equipment is designated as MR<br />
safe if it presents no safety hazard to patients or personnel when it is taken into<br />
the MR scanning room, provided that instructions concerning its use are correctly<br />
followed. This does not, however, guarantee that it will function normally and not<br />
interfere with the correct operation of the MR imaging equipment, with<br />
degradation of image quality. Equipment that is designated as MR compatible is<br />
MR safe, functions normally in the MR environment, and does not interfere with<br />
the correct operation of the MR imaging equipment providing instructions<br />
concerning its proper use are correctly followed.<br />
Clearly, all anaesthetic equipment that is used in the inner controlled area should<br />
be MR compatible but equipment that is only used in anaesthetic rooms and<br />
recovery areas need not be MR compatible.<br />
It is vitally important that MR compatible equipment is easily distinguishable from<br />
standard equipment. The hazards associated with using the wrong equipment include<br />
the projectile effect [5], burns [6] and malfunction [7] e.g. non-MR compatible<br />
syringe drivers may deliver drugs incorrectly with significant effects on patient safety.<br />
The initial designation of MR compatible equipment is the responsibility of the<br />
Responsible Person, but the day-to-day supervision of equipment entering the<br />
inner controlled area is the responsibility of the radiographer in charge of the MR<br />
session.<br />
It is the responsibility of the equipment manufacturer to indicate the field strength<br />
to which their equipment is compatible. To date, most clinical MR scanners have<br />
had a field strength of 1.5Tesla (T) or lower. Recent technological developments<br />
mean that 3T MR scanners will become clinically available in the near future. It<br />
should not be automatically assumed that equipment that was MR compatible or<br />
MR safe at 1.5T, remains compatible or safe at 3T.<br />
Monitors<br />
The monitoring of patients during anaesthesia, sedation and recovery must adhere<br />
to previously published standards [8]. Suppliers of MR scanners may provide<br />
basic monitoring devices as part of the system. These include ECG and<br />
respiration monitors and are provided to facilitate the timing of certain types of<br />
image acquisition. It is recommended that separate anaesthetic monitoring<br />
equipment is available. Early MR compatible monitors may not include some<br />
parameters that are now considered essential e.g. inspired oxygen concentration<br />
and anaesthetic agent monitoring. These monitors will require replacement or<br />
upgrading to meet current recommended standards.<br />
4<br />
5
MR compatible pulse oximeters must use fibreoptic cabling to avoid burns and<br />
special ECG electrodes and cables are required. Padding should be placed between<br />
cables and the patient’s skin and the avoidance of loops in cables within the scanner<br />
is essential. The responsibility for safe placement of monitoring devices and leads<br />
should be clearly and explicitly allocated.<br />
It is essential that a remote monitoring facility is available to allow the anaesthetic<br />
team to remain outside the scanning room once the patient’s condition is stable,<br />
should they wish to do so. This will require the provision of waveguides between<br />
the scanner and control rooms.<br />
The MR environment will cause specific problems with ECG, capnography and<br />
temperature monitoring. Aortic blood flow in a magnetic field generates currents<br />
that result in significant artefact in the ST-T region of the ECG complex, and<br />
monitoring of ischaemia may present significant challenges. There may be a delay<br />
of up to 20 seconds in obtaining the capnograph signal due to the length of the<br />
sampling tubing. While investigational devices allow temperature monitoring, clinical<br />
monitors are only just beginning to provide this facility. The development of<br />
improved monitoring modalities will alter the achievable standard of clinical<br />
monitoring in MR.<br />
The need for acoustic protection during MR imaging will necessitate the use of<br />
ear-plugs or ear defenders, and make audible alarms inappropriate. Clear visible<br />
alarms should be provided on all monitors when the attending anaesthetist is in<br />
the MR examination room with the patient. Anaesthetists remaining in the control<br />
room should have an unobstructed view of the remote monitor, anaesthetic<br />
machine and patient.<br />
Anaesthetic machine<br />
A MR compatible anaesthetic machine should be located within the scanning<br />
room. Only MR compatible vaporisers and gas cylinders must be used on<br />
anaesthetic machines within the scanner room. Any attempt to replace these with<br />
standard equipment will be extremely dangerous and is likely to cause a serious<br />
accident [9].<br />
Section V: Personnel<br />
A nominated consultant anaesthetist should be responsible for anaesthesia services<br />
in MR units. As well as suitably trained anaesthetists, the anaesthetic team will<br />
include nurses, operating department practitioners and technical support. The level<br />
of assistance for the anaesthetist must be equal to that expected in the operating<br />
theatre environment [10]. The potential to encounter unusual cases exists [11]<br />
and good communication between anaesthetic and radiological staff is vital.<br />
All staff entering the MR unit must be aware of the local rules of that unit, which<br />
may be different to those at other MR installations. It is essential that there is a<br />
clear protocol that defines roles and responsibilities of all staff in the event of an<br />
anaesthetic emergency or resuscitation. All staff must be fully aware of this<br />
protocol e.g. the emergency medical resuscitation team should know not to enter<br />
the inner controlled area. Protocols must take account of the possibility of the MR<br />
unit being used outside routine working periods. Individual staff should be<br />
designated to be responsible for regular checking and maintenance of anaesthetic<br />
and resuscitation equipment.<br />
All unauthorised staff entering the controlled area must first be medically screened,<br />
and must be under the supervision of an authorised person for the whole time that<br />
they remain in the controlled area. If their duties require them to enter the inner<br />
controlled area on a regular basis, they should undergo training and be aware of<br />
the local rules of that unit appropriate to their duties. Only authorised personnel,<br />
who have received specific training and are fully conversant with the local safety<br />
rules, are allowed to enter the controlled area unsupervised.<br />
6<br />
7
Section VI: Health and safety<br />
Patient safety<br />
Patient safety is a paramount consideration. Screening procedures to determine<br />
specific contraindications to MR examination are the responsibility of the radiologist<br />
and radiographer. The anaesthesia team should facilitate the adherence to strict<br />
protocols to prevent untoward events. This is particularly important in unusual<br />
situations e.g. critical care patients. Websites are available that indicate the<br />
compatibility of implanted devices [12].<br />
The most commonly used intravenous contrast agent is dimeglumine gadopentetate<br />
(gadolinium DTPA). While there is an extremely low incidence of side effects, a<br />
severe anaphylactoid reaction has been reported [13]. Other side effects include<br />
nausea, vomiting and pain at injection. The recommended dosage is 0.2 ml.kg -1<br />
body weight.<br />
Staff safety<br />
All staff entering the controlled area will be subject to the same safety screening<br />
procedures as the patients. The occupational hazards to which anaesthetists and<br />
their assistants may be subjected include exposure to:<br />
• an intense magnetic field<br />
• acoustic noise<br />
• unscavenged anaesthetic gases<br />
• possible hypoxia if quenching of a superconducting magnet occurs<br />
Magnetic fields<br />
The magnetic fields produced by MR scanners consist of:<br />
• strong static magnetic field<br />
• fast switching magnetic fields - gradient magnetic fields<br />
• pulsed radiofrequency fields.<br />
The switched gradient and radiofrequency fields are only present within or in the<br />
immediate vicinity of the magnet. The static magnetic field extends well beyond<br />
the confines of the magnet. The strength of this stray field depends on the<br />
configuration and shielding of the magnet, and falls rapidly as the distance from the<br />
magnet increases. Actively-shielded magnets are associated with more compact<br />
fringe fields. However, the sharp fall in magnetic field strength with distance<br />
implies a steep field gradient in the immediate vicinity of the magnet, which<br />
substantially increases forces on ferromagnetic objects that are inadvertently<br />
brought close to the magnet.<br />
All those in close proximity to MR scanners may be at risk of injury from<br />
unrestrained objects exposed to intense static magnetic fields, the projectile effect.<br />
All staff should be fully aware of the implications of the projectile effect so that<br />
such items are not taken into the examination room [5]. There is further potential<br />
risk from the static magnetic field on any implanted ferromagnetic objects. These<br />
devices may move or malfunction if exposed to a magnetic field, with potentially<br />
fatal consequences, e.g. pacemakers, some aneurysm clips. The MR unit should<br />
have a policy for screening all individuals for the presence of such metallic implants<br />
and all anaesthetic staff should ensure that they are fully conversant with these<br />
requirements.<br />
Sudden movement of the human body within intense static magnetic fields may<br />
cause very weak electrical currents to be induced in tissues causing symptoms such<br />
as nausea and vertigo from extraneous excitation of the semicircular canals of the<br />
inner ear or flashing lights by effects on the retina. However, there is currently no<br />
scientific evidence for a cumulative harmful effect of intense static magnetic field<br />
exposure on the human body.<br />
Current recommendations for ‘safe’ levels of long term exposure to static magnetic<br />
fields of healthcare personnel are a time-weighted average of 200mT over any 8-<br />
hour period and should not be exceeded. This advice may change therefore<br />
personnel should refer to current edition of the MDA recomendations. [14].<br />
Those who work in close proximity to MR scanners should be made aware of<br />
these safety levels. Risks may be small, but the current lack of evidence to<br />
suggest a harmful effect of cumulative magnetic field exposure does not exclude<br />
such a finding being made in the future. Individual workers should be provided<br />
with the resources to minimise the risk of personal exposure to magnetic fields as<br />
far as is reasonably achievable.<br />
Acoustic noise<br />
Significant levels of acoustic noise are produced during MR imaging due to the<br />
vibration of the switched gradient coils. The magnitude of the noise depends on<br />
the MR sequence and the strength of the magnet used. The trend towards higher<br />
strength magnets and stronger and faster switching gradient fields indicates that<br />
noise levels produced within MR scanners are likely to increase.<br />
Noise at work regulations require employers to take actions to reduce noise<br />
exposure of employees when it is at or above 85dBA (average daily exposure) [15].<br />
Some MR sequences produce noise levels above these safety levels. Individual<br />
MR units must undertake their own measurements and risk assessments.<br />
Remaining at a remote location, e.g. in the control room while the scan is taking<br />
place, will limit risks from noise exposure. Ear protectors should be provided if<br />
staff remain within the examination room during the scan. All patients,<br />
anaesthetised or non-anaesthetised, should be given ear protectors.<br />
8<br />
9
Scavenging of anaesthetic gases<br />
The use of volatile anaesthetic agents and nitrous oxide in MR units must comply<br />
with the Control of Substances Hazardous to Health (COSHH) regulations [16].<br />
MR compatible scavenging systems for use in the MR examination room are<br />
available.<br />
Quenching of superconducting magnets<br />
Quenching may occur due to a system fault or as a deliberate action to shutdown<br />
the magnetic field. There should be no hazard from this procedure provided that<br />
venting of the cryogens to the outside is adequate. There is a potentially lethal<br />
hazard due to asphyxiation in oxygen-deficient atmospheres, if there is rapid<br />
evaporation and escape of the liquid helium that surrounds and cools the<br />
superconducting solenoid. Oxygen sensors should be located in the scanning<br />
room and relayed to the control room to warn of the possible hypoxic effect of<br />
escaped helium. Anaesthetists working in MR should be familiar with the<br />
emergency procedures in the event of a quench being necessary.<br />
Occupational hazards for female staff of childbearing age<br />
For pregnant female staff working within MR scanning rooms, there are the<br />
additional concerns of exposure of the fetus to magnetic fields, acoustic noise and<br />
unscavenged anaesthetic gases. The current guidelines in the UK from the MDA<br />
state that, until further evidence is available, it is prudent not to scan patients in<br />
the first trimester of pregnancy [14]. In the case of female staff in the first<br />
trimester of pregnancy, the MDA guidelines state that ‘it might be prudent to give<br />
them the option of whether or not to enter the inner controlled area during the<br />
first 3 months of their pregnancy’. Female staff of childbearing age working in the<br />
MR environment should be made aware of:<br />
• potentially harmful effects of excessive acoustic noise on the developing fetus<br />
• COSHH regulations in respect to anaesthetic gas exposure<br />
• MDA guidelines in respect to magnetic field exposure.<br />
Section VII: Risk management<br />
The nominated consultant anaesthetist should ensure that anaesthetic staff are<br />
familiar with the anaesthetic machine and monitoring equipment which are often<br />
of a non-standard configuration. All staff entering the MR unit, including anaesthetic<br />
personnel, should have received training from the responsible person or their<br />
designated deputy, usually the superintendent radiographer. Participation in such<br />
training must be recorded and regular updates should be available annually.<br />
Training should involve familiarisation with sections of the local rules of the MR<br />
department which are appropiate to the individual role, and should include:<br />
• Access to hazard notices and safety bulletins relating to MR Safety<br />
• Personal safety i.e. removal of all metal objects and credit cards<br />
• Information relating to safety issues of implants both passive and active<br />
• The screening procedure and contraindications to MR<br />
• Safe placement of monitors and radiofrequency (RF) coil leads<br />
• Cardiac arrest procedure, siting of emergency equipment and emergency drugs<br />
• Fire procedure<br />
• Quench procedure<br />
10<br />
11
Section VIII: Appendix 1<br />
Planning considerations and cost implications for the inclusion of an anaesthesia<br />
service into a new or existing MR installation.<br />
Building<br />
The building plans should include the following (in addition to what is considered<br />
as standard for an MR installation):<br />
1. Adequate access to the MR unit (including ITU beds) may require modification<br />
of corridors and doorways. Alternative access may be required for beds to<br />
avoid passing through the waiting area.<br />
2. Anaesthetic induction and recovery area(s) of sufficient size to accommodate<br />
predicted patient throughput. Consideration of whether more than one patient<br />
is likely to be in induction and/or recovery at any one time. Induction and<br />
recovery should be separate areas.<br />
3. Provision of sufficient storage (including drug fridge) for consumables and<br />
anaesthetic machine when not in use.<br />
4. Installation of piped gases, suction and scavenging units in each of MR<br />
examination room, induction and recovery areas.<br />
5. Provision of RF waveguides for piped gases, suction and monitoring<br />
equipment. This normally needs to be specified at the time of MR equipment<br />
specification as the RF screened room is often included in the tender process<br />
for the MR equipment.<br />
6. Provision of emergency call system and telephone in induction and recovery areas.<br />
Purchase of Capital Equipment<br />
The following additional capital equipment must be purchased:<br />
1. MR compatible monitoring equipment to comply with minimum monitoring<br />
standards.<br />
2. MR compatible anaesthetic machine, vaporisers and ventilator.<br />
3. Standard anaesthetic machine, suction and monitoring equipment for<br />
induction/recovery area.<br />
Revenue Cost Implications<br />
1. Staffing - anaesthetist, anaesthetic assistant, technician, nurses.<br />
2. Provision of day-case recovery facilities.<br />
3. Consumables.<br />
4. Service contract for anaesthetic and monitoring equipment - usually 8-10% of<br />
purchase price per annum.<br />
Section IX: Appendix 2<br />
Glossary of Terms<br />
Authorised Personnel/Person. In the context of the MR safety guidelines,<br />
authorised personnel are able to access the controlled area without supervision.<br />
They must have received appropriate training in MR safety and should be<br />
conversant with the local safety rules of the MR unit appropriate to their duties. In<br />
particular, they should be able to implement the emergency procedures contained<br />
within the local rules. All authorised personnel should have been medically<br />
screened prior to first being given access to the MR unit. They should be<br />
sufficiently competent to supervise non-authorised personnel, patients and visitors<br />
who may require access to the controlled area.<br />
Controlled Area. The controlled area wholly contains the 0.5mT magnetic field<br />
contour. Self-locking doors with coded locks control access to the controlled area.<br />
Only authorised personnel have unsupervised access to the Controlled Area. All<br />
patients, visitors and non-authorised staff should be medically screened before<br />
entering the controlled area.<br />
Cryogens. Cryogens are liquid coolants that are used by superconducting magnets<br />
to keep the magnet coil windings at a superconducting temperature. Liquid<br />
helium is the cryogen used in modern superconducting MR systems, although<br />
older systems also used liquid nitrogen as a secondary coolant to help reduce the<br />
rate at which liquid helium boils off. Rapid boil-off of the cryogen is<br />
accompanied by a loss of superconductivity and is known as a quench.<br />
Fringe field. The fringe field is the magnetic field that exists outside the external<br />
housing of the MR system’s magnet. It decreases with distance from the centre of<br />
the magnet. There are two important safety considerations. First is the position at<br />
which the fringe field decreases to a value below 0.5mT. Persons fitted with<br />
cardiac pacemakers should not be allowed to enter fields above this value. Second<br />
is the rate at which the fringe field increases in close proximity to the magnet as<br />
this determines the force on ferromagnetic objects which causes the projectile<br />
effect. Magnetic shielding is used to make the fringe more compact. In addition to<br />
presenting a safety hazard, the fringe field may also damage items such as wrist<br />
watches, mobile phones and will erase the information stored on credit cards.<br />
Gadolinium DTPA (dimeglumine gadopentetate). This is the most commonly used<br />
MR contrast agent. It reduces the T1 and T2 of tissues (see MRI) with which it<br />
comes in contact. This produces an increase in signal of T1-weighted images, and<br />
a reduction in signal on T2-weighted images. It is most commonly used as a contrast<br />
medium to identify tumours and also in Contrast-enhanced MR angiography.<br />
12<br />
13
Gauss (G) see Tesla. Gauss is a unit of magnetic field strength (the correct term<br />
is magnetic flux density). It has been mostly superseded by the SI Unit, Tesla. 1<br />
Gauss = 0.1 milliTesla (mT). 1 Tesla = 10,000 Gauss. The cardiac pacemaker field<br />
contour is often referred to as the 5 Gauss line.<br />
Gradient magnetic fields. The technique of magnetic resonance imaging uses<br />
magnetic field gradients to localise and encode the MR signals with spatial<br />
information to generate an image. The gradient fields are superimposed onto the<br />
static field but are only switched on for short periods (typically just a few<br />
milliseconds). The fast switching of the gradient fields generates rapidly varying<br />
magnetic fields. This may cause interference on the patient’s electrocardiogram<br />
and, on higher performance MR systems, may cause peripheral nerve stimulation.<br />
The electromagnet coils that generate the switched gradient fields vibrate,<br />
generating acoustic noise, which is often in excess of 100dB. Hearing protection<br />
should always be provided to patients whether conscious or unconscious.<br />
Inner Controlled Area. The Inner Controlled Area is a term which is often used<br />
to describe the MR Examination room which contains the MR system magnet.<br />
The attractive force of the fringe field is at its greatest in this room presenting a<br />
significant projectile hazard. The Inner Controlled Area is always contained<br />
within the Controlled Area.<br />
Magnetic shielding. Magnetic shielding is used to reduce the extent and strength<br />
of the fringe field. There are two main types of magnetic shielding. Passive<br />
shielding uses several tons of steel to constrict the magnetic field. It can be<br />
immediately surrounding the magnet or distributed around the walls of the room.<br />
Active Shielding uses a secondary set of superconducting magnet coils that<br />
reduce the fringe field outside the magnet housing. For active shielding and<br />
passive self-shielding, the attractive forces increase rapidly close to the magnet.<br />
For room shielding (or if no shielding is used), attractive forces are significant<br />
throughout the MR examination room.<br />
MR Examination Room. The MR examination room contains the MR system’s<br />
magnet and is where the fringe field is at its strongest, thus presenting a projectile<br />
hazard. It is often referred to in safety guidelines and local safety rules as the<br />
Inner Controlled Area.<br />
MRI. Magnetic Resonance Imaging (MRI) is the process of acquiring images<br />
using the principle of Nuclear Magnetic Resonance (NMR). Hydrogen nuclei are<br />
caused to resonate by applying a radiofrequency magnetic field in the presence of<br />
a strong static magnetic field. The hydrogen nuclei emit a radiofrequency signal<br />
which is spatially encoded by using magnetic field gradients to form images<br />
which represent anatomical slices within the body. The signals mainly emanate<br />
from both lipid and water-based tissue, and depend on both NMR properties of<br />
the tissue and the acquisition parameters of the MR system set by the operator.<br />
MRI is able to generate a wide range of soft tissue contrast, making it suitable for<br />
a wide range of conditions and diseases. Two common parameters that dictate the<br />
properties of signal evoked from different tissues are the T1 and T2 time<br />
constants, which describe the characteristics of MR signal obtained. MRI<br />
sequence parameters can be chosen to elicit T1 or T2 contrast.<br />
MRS. Magnetic Resonance Spectroscopy (MRS) is the process of acquiring<br />
spectroscopic data using the principle of Nuclear Magnetic Resonance. The MR<br />
spectra obtained reveals the proportion in which many important chemical species<br />
are present in tissue. Localised MR Spectroscopy allows MR spectra to be<br />
obtained from small volumes of tissue in vivo. It can be combined with MRI to<br />
provide both anatomical and metabolic information and is developing as an<br />
important diagnostic tool.<br />
MR safe. Equipment is designated as MR safe if it presents no safety hazard to<br />
patients or personnel when it is taken into the MR examination room, provided<br />
that instructions concerning its use are correctly followed. This does not, however,<br />
guarantee that it will function normally and not interfere with the correct<br />
operation of the MR imaging equipment, with degradation of image quality.<br />
MR compatible. Equipment that is designated as MR compatible is MR safe,<br />
functions normally in the MR environment, and does not interfere with the correct<br />
operation of the MR imaging equipment providing instructions concerning its<br />
proper use are correctly followed.<br />
mT (milliTesla). See Tesla.<br />
Projectile hazard/effect. The magnetic fringe field exerts an attractive force on<br />
any ferromagnetic object that is brought into the vicinity of the magnet. Massive<br />
objects, such as gas cylinders and patient trolleys, and smaller objects with sharp<br />
edges, such as scissors or tools, will accelerate rapidly towards the magnet and<br />
may cause serious injury to staff or patients. The MR system itself may also be<br />
damaged. All personnel entering the Inner Controlled Area must first be screened<br />
for such objects.<br />
Quenching. Quenching refers to the rapid, almost explosive, boil-off of liquid<br />
helium and the accompanying loss of superconductivity. The magnetic field is lost<br />
and a large volume of helium gas is generated and should normally be vented to<br />
the outside atmosphere through a quench pipe. If this pipe were to fracture it<br />
would present a potentially lethal hazard caused by the rapid build-up of helium<br />
gas in the MR examination room, leading to asphyxiation. Quenches can be<br />
14<br />
15
spontaneous, usually occurring when the magnet is being powered up or down<br />
during installation or services, or can be deliberately activated in an emergency,<br />
such as fire.<br />
Radiofrequency (RF) Coil. Radiofrequency (RF) coils are used to detect the RF<br />
signals emitted from the patient. The main RF coil of the system is known as the<br />
Body Coil and is typically located inside the covers within the bore of the magnet.<br />
This coil is also used to transmit the pulsed radiofrequency field. Additional<br />
specialised coils (often known as Surface Coils) may be used to improve the<br />
sensitivity of signal detection from a particular body area. The cables from these<br />
coils must be carefully placed so that they are not in contact with either the<br />
patient or monitoring cables as this can cause RF heating.<br />
Responsible Person. In the context of MRI services, the chief executive or<br />
general manager of the organisation has the ultimate responsibility to ensure that<br />
the MR safety guidelines are implemented. This responsibility is normally<br />
delegated to a specified responsible person who may be the clinical director or<br />
superintendent radiographer in charge of the department in which the MR<br />
equipment is located.<br />
RF heating. The radiofrequency pulses used in MRI deposit energy into the<br />
patient’s tissues, and therefore have a heating effect. The level of power deposition<br />
is strictly controlled, and is calculated per kilogram of tissue for each scan (see<br />
SAR). Metal implants, monitoring transducers and cables may preferentially take<br />
up the RF power, resulting in excessive RF heating, causing burns to the patients<br />
skin. To avoid this risk, only MR compatible monitoring equipment should be<br />
used in the MR environment. Care should be taken when placing RF coil cables<br />
and monitoring cables to ensure that no loops are formed and that they are not in<br />
close contact with each other or the patient’s skin.<br />
RF shielding. Radiofrequency (RF) shielding has a two-fold purpose. Firstly, the<br />
radiofrequency pulses used by the MR system should not interfere with<br />
equipment outside the MR examination room. Secondly, radio signals and other<br />
electromagnetic interference in the external environment should be prevented<br />
from interfering with the MR signal detection. RF shielding is achieved by<br />
making the MR Examination room an RF screened room.<br />
RF screened room. The radiofrequency (RF) screened room (also known as an<br />
RF cabin) provides RF shielding for the MR system. It consists of cladding made<br />
of thin copper or aluminium sheet that forms the inner surface of the walls,<br />
ceiling and floor of the MR examination room. The door (copper clad with leaf<br />
spring edges) and window (copper gauze sheet) of this room form an integral part<br />
of the RF screen. The door must therefore be closed when the MR system is<br />
operating and the screen must not be broken by passing electrical conducting<br />
materials through it. Medical gas supplies and sample tubes for monitoring<br />
equipment must be made of non-conducting material and must be passed through<br />
specially-designed waveguides supplied with the RF screened room to maintain<br />
the integrity of the screen. Cables that carry signals or power must either be<br />
fibreoptic, or must pass through special electrical low pass filters supplied with<br />
the RF screened room.<br />
SAR. The Specific Absorption Rate (SAR) is a measure of the RF power deposited<br />
into the patient, calculated per kilogram of tissue. The patient’s body weight is<br />
entered into the MR system at the start of the examination, and the SAR is calculated<br />
before each scan is commenced. The SAR is strictly limited by the MR system<br />
manufacturer according to national or international guidelines. Higher values of<br />
SAR may lead to core body temperature rises of up to 1 o C, and there is an increased<br />
likelihood of RF heating of transducer cables.<br />
T1-weighted image and T2-weighted image. The MR signal emitted by biological<br />
tissue has an amplitude, which depends both on the properties of the tissue and<br />
upon the timing parameters of the particular MR acquisition pulse sequence used.<br />
The two most important properties are the T1-relaxation and T2-relaxation. The<br />
pulse sequence parameters can be chosen either to emphasise signal differences<br />
which are primarily dependent upon either T1 relaxation, or T2 relaxation,<br />
resulting in images which have soft tissue contrast which is described as either<br />
T1-weighted or T2-weighted respectively. Both types of image are normally<br />
acquired as they provide complimentary diagnostic information.<br />
Tesla (T). Tesla is the SI unit of magnetic field strength (the correct term for field<br />
strength is magnetic flux density). The cardiac pacemaker field contour is often<br />
referred to as the 0.5 milliTesla (mT) line. Typical nominal field strengths of<br />
commercial MR systems are 0.5, 1.0 and 1.5 Tesla. More recently, higher field<br />
strength (e.g. 3.0T) systems are becoming commercially available. MR spectroscopy<br />
is normally performed at higher field strengths up to 7.0 Tesla.<br />
Waveguide. A waveguide is a hollow tube made of brass that forms a conduit<br />
through the wall of the RF screened room without breaking its integrity. Waveguides<br />
are typically 2.5-5.0cm in diameter with the length, dependent on the diameter,<br />
calculated to prevent the passage of radiofrequency interference. It allows nonelectrically<br />
conducting pipes, sample tubes and fibreoptic cables to be passed into<br />
the MR examination room for patient monitoring, and gas and drug delivery purposes.<br />
16<br />
17
Section X: References<br />
1. Health Building Note 6 Supplement 1. Accommodation for magnetic<br />
resonance imaging. NHS Estates 1994, London, HMSO. ISBN<br />
0113217307<br />
2. Health Guidance Note Magnetic Resonance Imaging. NHS Estates,<br />
London, HMSO. ISBN 0113220510.<br />
3. Facilities for Diagnostic Imaging and Interventional Radiology. NHS<br />
Estates 2001, London, HMSO. ISBN 0-11-322000-0.<br />
4. Immediate Postoperative Care. Association of Anaesthetists of Great Britain<br />
and Ireland, 1993.<br />
5. MDA Publication. ‘MRI static magnetic field safety considerations – the<br />
projectile effect caused by the influence of the static magnetic field of<br />
magnetic imaging systems’ 1998.<br />
6. Dempsey MF, Condon B. Thermal injuries associated with MRI. Clinical<br />
Radiology 2001; 56: 457-65.<br />
7. MacIntyre PA, Sury MR. Is propofol infusion better than inhalational<br />
anaesthesia for paediatric MRI? Anaesthesia 1996; 51: 517.<br />
8. Recommendations for Standards of Monitoring during Anaesthesia and<br />
Recovery. Association of Anaesthetists of Great Britain and Ireland, 2000.<br />
9. Chaljub G et al. Projectile cylinder accidents resulting from the presence of<br />
ferromagnetic nitrous oxide or oxygen tanks in the MR suite. American<br />
Journal of Radiology 2001; 177: 27-30.<br />
10. The Anaesthesia Team. Association of Anaesthetists of Great Britain and<br />
Ireland, 1998<br />
11. Andrzejowski J, Mundy J. Anaesthesia for MRI angiography in a patient<br />
with Williams syndrome. Anaesthesia 2000; 55: 97-8.<br />
12. http://www.mrisafety.com<br />
13. Weiss KL. Severe anaphylactoid reaction after i.v. Gd-DTPA. Magnetic<br />
Resonance Imaging. 1990; 8: 817-8.<br />
14. The Medical Devices Agency. Guidelines for Magnetic Resonance Diagnostic<br />
Equipment in Clinical Use with Particular References to Safety. London:<br />
HMSO, 1993. To be revised 2002<br />
15. Health and Safety Executive. Noise at Work Regulations. London: HMSO,<br />
1990.<br />
16. Health Service Advisory Committee. Anaesthetic Agents: Controlling<br />
Exposure Under COSHH London: HMSO, 1995.<br />
Section XI: Further Reading<br />
Keengwe IN, Hegde S, Dearlove O, Wilson B, Yates RW, Sharples A. Structured<br />
sedation programme for magnetic resonance imaging examination in children.<br />
Anaesthesia 1999; 54: 1069-72.<br />
Laurence AS. Sedation, safety and MRI. The British Journal of Radiology 2000;<br />
73: 575-7.<br />
McBrien ME, Winder J, Smyth L. Anaesthesia for magnetic resonance imaging: a<br />
survey of current practice in the UK and Ireland. Anaesthesia 2000; 55: 737-43.<br />
Menon DK, Peden CJ, Hall AS, Sargentoni J, Whitwam JG. Magnetic resonance<br />
for the anaesthetist. Part 1: physical principles, applications, safety aspects.<br />
Anaesthesia 1992; 47: 240-55.<br />
Morton G, Gildersleve C. Noise in the MRI scanner. Anaesthesia 2000; 55: 1213.<br />
NRPB Board statement on restrictions on human exposure to static and time<br />
varying electromagnetic fields and radiation. Documents NRPB 1993; 4: (5)<br />
ISBN 0859513661.<br />
Peden CJ, Menon DK, Hall AS, Sargentoni J, Whitwam JG. Magnetic resonance<br />
for the anaesthetist. Part II: anaesthesia and monitoring in MR units. Anaesthesia<br />
1992; 47: 508-17.<br />
Practical MR Safety Considerations for Physicians, Physicists and Technologists.<br />
Editor Emanual Kanal. 2001 RSNA Course Syllabus.<br />
Rafferty C, Burke AM, Cossar DF, Farling PA. Laryngeal mask and magnetic<br />
resonance imaging. Anaesthesia 1990; 45: 590-1.<br />
Sury MRJ, Hatch DJ, Deeley T, Dicks-Mireaux C, Chong WK. Development of a<br />
nurse-led sedation service for paediatric magnetic resonance imaging. Lancet<br />
1999; 353: 311-12.<br />
Zorab JSM. A general anaesthesia service for magnetic resonance imaging.<br />
European Journal of Anaesthesiology 1995; 12: 387-95.<br />
Zorab JSM, Young AER, Brown PN. Anaesthesia for children and infants<br />
undergoing magnetic resonance imaging: a prospective study. European Journal<br />
of Anaesthesiology 1996; 13: 400-3.<br />
18<br />
19
Designed by Green Sheep Graphics<br />
Hamilton House, Mabledon Place, London, WC1H 9BB<br />
tel: 020 7554 8545 fax: 020 7554 8544 email: the.pen@greensheep.co.uk
Association of Anaesthetists of Great Britain & Ireland<br />
Needlestick Working Party Report<br />
Council of the Association of Anaesthetists of Great Britain & Ireland (AAGBI) established a<br />
Working Party on Needlestick Injuries in December 2007. Its initial membership was:<br />
Dr Andrew Hartle (Chair)<br />
Dr Steve Yentis<br />
Dr Stuart White<br />
Dr Mark Hearn<br />
Dr Dominic Bell<br />
Dr Daniel Sokol<br />
Ms Kim Sunley<br />
Dr Andy Lim<br />
Ms Janette Roberts<br />
AAGBI Council<br />
AAGBI Council<br />
Consultant Anaesthetist, Brighton<br />
GAT Representative<br />
Intensive Care Society<br />
Lecturer in Medical Ethics & Law<br />
Royal College of Nursing<br />
Royal College of Anaesthetists<br />
Patient Liaison Group<br />
The Working Party was to consider the testing of patients for Blood Borne Viruses (BBV) after<br />
needlestick and other occupational injuries, especially in the light of recent legislative change<br />
(Human Tissue Act 2004 [HTA] and Mental Capacity Act 2005 [MCA]), and the withdrawal of<br />
previous guidance from the General Medical Council (GMC).<br />
The legal ‘limbo’ surrounding the testing of patients who lacked capacity, and who had been<br />
the source of a needlestick or other occupational injury had been described in detail in Stuart<br />
White’s editorial in Anaesthesia (Needlestuck. Anaesthesia 2007; 62: 1199-201). Initial<br />
guidance from the GMC had been that testing of such patients could take place in exceptional<br />
circumstances. The introduction of HTA and MCA had led to that guidance being withdrawn,<br />
and advice from Medical Indemnity organisations was now that such testing without the<br />
patient’s consent was unlawful. This now meant that Healthcare professionals who sustained<br />
occupational exposure were unable to know the viral status of the source when making<br />
decisions about the initiation or discontinuation of post exposure prophylaxis (PEP).
At the first meeting held on 9 th May 2008 it was agreed that there were three strands to the<br />
WP’s remit:<br />
• Establish what changes were possible to the current legal situation and make<br />
recommendations.<br />
• Identify mechanisms by which change could be effected.<br />
• Identify ways by which public support for such change could be achieved, including<br />
identifying other stakeholders.<br />
The WP discussed the apparent variability of response to the current situation. In some units<br />
patients were never tested after occupational injury, but in others testing may still be<br />
performed, either with or without the agreement of next of kin. This creates a ‘postcode<br />
lottery’ in the management of occupational injuries, and also places healthcare workers at risk<br />
of legal, disciplinary or regulatory action. Such inconsistency in management is not<br />
acceptable.<br />
After some discussion, the following possible changes were agreed, roughly in order of most to<br />
least restrictive, and possibly in ascending order of likely public acceptability:<br />
• Blanket testing of all patients.<br />
• Testing of all patients who become the source of a needlestick/infective injury.<br />
• ‘Presumed Consent’ for testing unless prior evidence of objection.<br />
• The previous status quo, i.e. testing only after an individual risk/benefit analysis (to<br />
include psychological as well as physical risk).<br />
• Testing with the consent of next of kin.<br />
• No testing without specific consent from the patient.<br />
Members of the WP agreed to analyse each of these options, before making recommendations<br />
to Council. Those analyses are attached.<br />
The WP agreed that, before the situation of testing arose, first priorities for all stakeholders<br />
should be:<br />
• Prevention/preventative technology<br />
• Improved (confidential) reporting<br />
• De-stigmatisation
Three principle methods of achieving a change in the law were identified:<br />
1. A change in the law (Statutory Instrument, amendment, primary legislation)<br />
2. An elaboration of existing law<br />
3. A test case<br />
In order to establish public support, which will be vital for any change, the following themes<br />
were explored:<br />
• Exploring broader benefits and harms to -<br />
o Individual patients<br />
o Individual healthcare staff<br />
o Employers<br />
o Society<br />
• The virtuous/responsible patient<br />
• Comparisons with zero tolerance to violence<br />
• Reciprocity<br />
Other stakeholders included:<br />
• British Association of Operating Department Practitioners<br />
• Unison<br />
• Unite<br />
• Chartered Society of Physiotherapists<br />
• Association of Occupational Health<br />
• NHSE (including medical Directors)<br />
• Patients Association<br />
• Terrence Higgins Trust<br />
• GMC<br />
• NHSLA<br />
• MPS/MDU/MDDUS<br />
• BMA<br />
• Court of Protection<br />
• Office of Official Solicitor<br />
• Health and Safety Executive<br />
• Department of Health<br />
• Human Tissue Authority
Methods to estimate/establish public support included:<br />
• Properly conducted patient/lay person research<br />
• Public opinion poll<br />
• Letters/editorial in other journals<br />
• Parliamentary spokesmen (especially for Trade Unions)<br />
• BBC Online Poll<br />
• Online Downing Street petition<br />
• The general and medical press<br />
The Working Party met again in June 2008, when initial drafts of the analyses were considered.<br />
At a subsequent meeting in February 2009, the WP was joined by Veronica English of the BMA<br />
Ethics Department. The RCN was represented on that occasion by Janice Gabriel, and David<br />
Whitaker (Immediate Past President, AAGBI) was also present.<br />
VE explained that the BMA had met with Lord Warner at the Department of Health.<br />
Amendment(s) of the Human Tissue Act would probably not help clarify the current legal<br />
limbo, as serum (ie not containing cells) was stored and tested for blood borne viruses (BBV),<br />
so the HTA was not engaged.<br />
The BMA would prefer not to stretch a best interests argument, although this might be possible<br />
by changes to the Mental Capacity Act’s code of conduct.<br />
After much discussion the WP narrowed its recommended options to Council as being:<br />
1. All patients who were the source of an occupational injury should be tested for BBV.<br />
This would be the greatest infringement of Human Rights and would need primary<br />
legislation, but would be fair as all patients would be treated the same. An analogy<br />
might be drawn with compulsory testing for alcohol and drugs following a Road Traffic<br />
Accident. There was an impression that this was what lay people thought happened<br />
anyway.<br />
2. The restoration of the previous position whereby the merits of a particular case were<br />
assessed and the decision to test or not could then be justified. This was the BMA’s<br />
preferred option. Trusts could produce policies to ensure fairness, transparency and<br />
accountability.
3. Testing could take place with the consent of next-of-kin or other delegated decision<br />
makers.<br />
Recommendations as to how the necessary legal change could be effected would depend on<br />
meetings between the BMA and the DoH.<br />
AH met with officials from the Department of Health on 15 th May 2009. They were very<br />
interested in the WP’s work, particularly the bringing together of a ‘coalition’ involving such a<br />
wide range of Health Care Workers, and the ethical analyses done by the WP. The<br />
designation of an affected Health Care Worker as ‘patient 2’ was particularly compelling.<br />
There was no doubt that DoH supports some change in the legal position, but was similarly<br />
unsure of which proposal to advocate, or how best to bring this about. Legislation runs serious<br />
risks of having unforeseen consequences, and is dependent on the political cycle.<br />
AH was invited to join the DoH Stakeholder Group, which met in July 2009. DoH legal<br />
advice was Option 1 would be unlikely to be helpful, as individuals who had had blood taken<br />
without consent after road traffic accidents could still withhold consent for its testing, although<br />
they would then be guilty of the offence of “refusing to give a sample”.<br />
In November 2009 the Department of Health published Legal issues relevant to nonheartbeating<br />
organ donation, which clearly endorses an expanded interpretation of best<br />
interests with specific regard to virological testing using the assent of the next of kin. This<br />
interpretation of legislation may be a basis on which to move forward.<br />
[http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidan<br />
ce/DH_108825]<br />
Current position<br />
The WP has now fulfilled its first two objectives (determining whether the legal situation<br />
should be changed, recommending what that change should be). The legal position remains<br />
complicated and will need amendments to the Mental Capacity Act and/or its Code of<br />
Conduct. This will require parliamentary time and political will.
Recommendations<br />
The WP recommends:<br />
1. That AAGBI Council should adopt as policy that the necessary legislative<br />
change is effected at least to restore the previous position to allow individual<br />
cases to be judged on their merits and testing of patients for Blood Borne<br />
Viruses performed after occupational exposure when justified.<br />
2. Council should consider whether to pursue legislative change that would allow<br />
a. Processing of a blood sample taken for any other purpose in the event of<br />
a patient refusal, and<br />
b. presumed consent for testing where the patient lacks capacity and is<br />
unlikely to regain this within a set timeframe, (e.g. 6-12 hours)<br />
3. Pending such legislative change, Council should support the model of next of<br />
kin assent pending the above resolution and for presumed consent where no<br />
next of kin have been identified within the above timeframe of 6-12 hours.<br />
4. Any legislative/policy change should accommodate the principle of reciprocity.<br />
The decision to test should be based on defined, objective principles and avoid<br />
arbitrary or varying decision-making. Logical and defensible solutions already<br />
exist and are currently being applied in some units.<br />
5. Council should approve a revision of its current guidance on ‘Blood Borne<br />
Viruses and the Anaesthetist’. In particular this should focus on the<br />
implications of an occupational injury, post exposure prophylaxis and follow<br />
and the subsequent employment. [Note: a WP on ‘Occupational Health and the<br />
Anaesthetist’ has been established with Dr Paul Clyburn as chair.]<br />
6. Council should consider a survey of members to establish the frequency of<br />
occupational exposure, particularly when the source patient is unable or refuses<br />
to consent to testing [Note: a paper has been accepted for the September 2010<br />
edition of Anaesthesia which describes an anonymised postal survey of current<br />
practice in ICUs in England. This has an accompanying editorial by AH]<br />
June 2010
Appendices:<br />
1. Needlestuck<br />
2. Analysis of benefits and harms of blanket testing<br />
3. Analysis of Presumed Consent<br />
4. Analysis of non-consensual testing<br />
5. Analysis of Status Quo<br />
6. Analysis of Next of Kin Assent/Consent<br />
7. Patient perspectives
Anaesthesia, 2007, 62, pages 1199–1201<br />
.....................................................................................................................................................................................................................<br />
Editorial<br />
Needlestuck<br />
Enacted on the 15th November, 2004,<br />
and fully enforced on the 1st September,<br />
2006, the Human Tissue Act 2004<br />
(HTA) [1] is the UK government’s<br />
woefully impenetrable attempt to clarify<br />
the statutory law in England and Wales<br />
with regard to the use and storage of<br />
human tissue, organs and bodies. The<br />
HTA repeals the Human Tissue Act<br />
1961, the Anatomy Act 1984, and the<br />
Human Organ Transplants Act 1989.<br />
In response to public concern over<br />
the organ retention scandals at Alder<br />
Hey Hospital [2] and the Bristol Royal<br />
Infirmary [3], and the findings of the<br />
Isaacs Inquiry [4], the government hurriedly<br />
introduced a consultation document,<br />
Human Bodies, Human Voices [5],<br />
in July 2002, leading to the introduction<br />
of the Human Tissue Bill, in December<br />
2003.<br />
In line with much recent legislation,<br />
consent was proposed as a fundamental<br />
protection for patients, such that virtually<br />
all tissue taken from humans could<br />
only be used or stored having obtained<br />
appropriate consent (from the patient<br />
if alive, from the parents of children,<br />
or premortem if the patient was now<br />
dead), under penalty of fine or imprisonment.<br />
Some ramifications of the Bill<br />
were immediately apparent, and elicited<br />
considerable debate among, and opposition<br />
from, the research, legal [6–8]<br />
and transplant communities, especially<br />
pertaining to anatomy demonstration,<br />
research using human tissue [9, 10],<br />
tissue databanking [11], genetic research<br />
[12] and organ transplantation [13, 14].<br />
Less apparent, unfortunately, were<br />
some of the ramifications relating to<br />
everyday clinical practice. One scenario<br />
in particular has given rise to concern<br />
about the protection of healthcare professionals<br />
in the event of a needlestick<br />
injury.<br />
Accidental blood and body fluid<br />
exposure is a daily risk for health care<br />
workers, with an incidence of approximately<br />
1–5 per 100 person-years [15].<br />
Up to 40% of patients with HIV are<br />
unaware of their status when they<br />
are admitted to intensive care [16].<br />
Needlestick injuries account for<br />
approximately 80% of exposures, are<br />
more common with more complex<br />
procedures, and can lead to infection<br />
with HIV, and hepatitis B, C and ⁄ or D<br />
[17]. Seroconversion rates are low for<br />
HIV (0.3%) and HCV (0.5%), but much<br />
higher for HBV (18–30%) [18]. A<br />
number of postexposure prophylaxis<br />
(PEP) guidelines are available for HIV<br />
[19], HBV and HCV [20]. In the case of<br />
HIV, PEP should ideally be commenced<br />
within an hour of exposure,<br />
and continued at least until the HIV<br />
status of the source patient is confirmed.<br />
Delays in source patient HIV testing can<br />
expose health care workers to inappropriate<br />
continuation of PEP administration<br />
of drugs with significant side-effect<br />
profiles.<br />
However, there is considerable confusion<br />
surrounding the issue of consent<br />
when testing a source patient for HIV<br />
(or other blood-borne viruses). No<br />
specific statute exists, and so the legality<br />
of testing lies in the common law.<br />
Testing involves physical contact with a<br />
patient, and therefore the patient’s<br />
consent is required. Their consent is<br />
legally valid if they are appropriately<br />
informed (about the nature and purpose<br />
of the test, and the risks and consequences<br />
of testing), competent to<br />
decide (that is, they understand the<br />
information presented to them, remember<br />
it, and use it to decide whether or<br />
not to have the test), and give consent<br />
voluntarily [21]. Competent adult patients<br />
can consent to, or refuse, testing for<br />
any reason, or for no reason at all. At<br />
present, no-one may give consent on<br />
behalf of an incompetent patient (for<br />
example, an unconscious patient in the<br />
intensive care unit). Under the common<br />
law in England and Wales, the<br />
HIV testing of an unconscious patient is<br />
legal if it is necessary and in the patient’s<br />
best interests (for example, to establish<br />
their HIV status for the purposes of<br />
treatment).<br />
Therefore, in theory at least, a doctor<br />
may not test a source patient for HIV<br />
for the benefit of an injured healthcare<br />
worker either if the patient refuses a<br />
test, or if the patient is incompetent<br />
⁄ unconscious.<br />
However, this is not the advice<br />
offered in professional guidelines,<br />
namely the General Medical Council’s<br />
Serious Communicable Diseases guidelines<br />
of 1997 [22] (the British Medical Association<br />
and Department of Health defer<br />
to the GMC in their own advice). The<br />
GMC advises that ‘You must obtain<br />
consent from patients before testing for<br />
a serious communicable disease’ (s.4),<br />
and ‘you may test unconscious patients<br />
for serious communicable diseases,<br />
without their prior consent, where<br />
testing would be in their immediate<br />
clinical interests’ (s.7), in line with the<br />
common law. However, the GMC then<br />
advise that ‘you may test an existing<br />
blood sample, taken for other purposes’<br />
if the patient has refused testing or is<br />
unable to consent, and the doctor has<br />
good reason to believe the patient may<br />
have a communicable disease for which<br />
prophylaxis is available, and an experienced<br />
colleague has been consulted, and<br />
the patient is unlikely to regain capacity<br />
within 48 h (s.8 + s.9), which course of<br />
action may not be in line with the<br />
common law, even if the patient is<br />
informed of the non-consensual test at<br />
the earliest opportunity (s.10).<br />
The advice states that ‘you must<br />
therefore be prepared to justify your<br />
decision (to test non-consensually)’ if a<br />
complaint is made to the doctor’s<br />
employer or the GMC, or if challenged<br />
in court, but justification could prove<br />
difficult. Several arguments might be<br />
used. Firstly, the ‘best interests’ argument:<br />
the patient was tested because<br />
his ⁄ her symptoms were unexplained<br />
and possibly attributable to HIV ⁄<br />
HBV ⁄ HCV, requiring diagnosis and<br />
Ó 2007 The Author<br />
Journal compilation Ó 2007 The Association of Anaesthetists of Great Britain and Ireland 1199
Editorial Anaesthesia, 2007, 62, pages 1199–1201<br />
.....................................................................................................................................................................................................................<br />
treatment. This would require a high<br />
standard of circumstantial medical evidence<br />
suggesting this to be the case.<br />
Second, the ‘good egg’ argument: the<br />
unconscious patient is assumed to be a<br />
kind person, who would consent to<br />
testing if s ⁄ he were competent, and<br />
therefore, have his best interests served<br />
through not subjecting the injured<br />
healthcare worker to either the anxiety<br />
of not knowing the patient’s HIV status,<br />
or the side-effects of PEP. Finally, the<br />
‘rights’ argument: that the healthcare<br />
worker’s right to discover the patient’s<br />
HIV status (possibly with reference to<br />
Articles 2 and 3 of the Human Rights<br />
Act 1998 (HRA) [23]) is more pressing<br />
than the patient’s right to not be tested<br />
(possibly protected by Articles 2, 3 and<br />
8 of the HRA).<br />
In practice, such justification is yet to<br />
be tested in a UK court [24], and is now<br />
unlikely to be, as the GMC has recently<br />
rescinded paragraphs 8–11 of Serious<br />
communicable diseases, in light of the<br />
Human Tissue Act 2004 and the Mental<br />
Capacity Act 2005.<br />
According to the HTA, appropriate<br />
consent from living patients is legally<br />
required [1(1)(d) + (f)] for storage and<br />
use of human tissue (which includes<br />
blood for HIV testing) for the purpose<br />
inter alia of obtaining scientific or<br />
medical information about a living or<br />
deceased person which may be relevant<br />
to any other person [Schedule 1, s.1(4)].<br />
Storage and use of tissue from patients<br />
who lack capacity (i.e. many intensive<br />
care patients) is unlawful (s.6), unless<br />
allowed by the Secretary of State, in this<br />
instance according to the Human Tissue<br />
Act 2004 (Persons Who Lack Capacity<br />
to Consent and Transplants) Regulations<br />
2006 [25]. The Regulations allow<br />
for non-consensual storage and use of<br />
tissue to ‘obtain scientific or medical<br />
information about a living … person<br />
which may be relevant to another’ (i.e.<br />
an HIV test after needlestick injury),<br />
provided inter alia that the nominated<br />
doctor taking the blood does so in ‘what<br />
s ⁄ he reasonably believes to be in the<br />
best interests of the person lacking<br />
capacity from whose body the material<br />
came’. So again, blood may only be<br />
taken if the intent is to benefit the<br />
patient, and not the healthcare worker.<br />
The Mental Capacity Act 2005 [26]<br />
(MCA) is no more helpful in terms of<br />
the non-consensual testing of patients<br />
who lack legal capacity. From October<br />
2007, patients over 16 years of age must<br />
be assumed to have capacity unless they<br />
are found to lack capacity. Any decision<br />
to test a patient without capacity for<br />
HIV must continue to be made in the<br />
patient’s best interests, if there is no<br />
other way to establish his ⁄ her HIV<br />
status. Although it will remain the case<br />
that the doctor will usually decide (s ⁄ he<br />
must be able to justify that decision in<br />
court), any decision must be made in<br />
the patient’s best interests (i.e. not the<br />
interests of the healthcare worker sustaining<br />
a needlestick injury). Interestingly,<br />
a properly appointed donee of an<br />
Lasting Power of Attorney, or a courtappointed<br />
deputy, may give proxy<br />
consent for blood testing, but again<br />
they must do so in the patient’s best<br />
interests. In addition, a patient may, in<br />
theory, consent to or refuse HIV testing<br />
by means of an advanced directive.<br />
Effectively, therefore, the combined<br />
effects of the HTA and MCA have<br />
firmly closed the backdoor to testing<br />
afforded by the GMC’s previous guidelines,<br />
and threatened doctors with<br />
imprisonment if they test patients for<br />
HIV non-consensually.<br />
This problem was foreseen during<br />
the passage of the Mental Capacity Bill,<br />
but an attempt by the British Medical<br />
Association to amend the Bill to allow<br />
non-consensual HIV testing to ‘avert<br />
the death of, or serious illness in,<br />
another person’ was withdrawn, after<br />
assurances from the government that<br />
this circumstance would be clarified in<br />
the Code of Practice accompanying the<br />
Act [27]. Predictably it wasn’t – there is<br />
no reference to HIV testing in all 302<br />
pages of the Code of Practice [28].<br />
Section 6 of the Code deals with the<br />
protections that the Act offers for<br />
healthcare workers (amongst others),<br />
but repeats the maxim that any intervention<br />
must be in the patient’s best<br />
interests.<br />
In an attempt to clarify the law in<br />
relation to HIV testing, I contacted<br />
both the HTA and the Court of<br />
Protection (the latter via the Public<br />
Guardianship Office). Both agencies<br />
were very helpful. After consultation,<br />
the HTA sent me the following statement<br />
for publication:<br />
‘The HTA are aware of the complex<br />
issues this situation generates. The HTA<br />
are currently part of discussions on this<br />
issue being led by the Department of<br />
Health, BMA and other organisations in<br />
relevant sectors. The general status of<br />
the situation is that this issue is still<br />
under discussion and the regulations are<br />
still being drafted. Therefore, at present<br />
it is difficult for the HTA to comment<br />
further on this area. We are waiting<br />
further clarification from the Department<br />
of Health at which point we will<br />
be in a position to move forward on this<br />
area of work. Please keep checking the<br />
HTA and relevant websites in the sector<br />
for any news on this issue’.<br />
The Public Guardianship Office referred<br />
me to the Human Tissue Branch<br />
of the Department of Health, who<br />
concurred with the above analysis of<br />
the problem, and stated by letter: ‘We<br />
are actively considering this complex<br />
issue and have – as the HTA advised<br />
you – been in discussion with a number<br />
of interested bodies. We hope to be in a<br />
position during the summer to consult<br />
on new proposals for addressing some of<br />
the concerns expressed’.<br />
To summarise, anaesthetists must<br />
beware: in the event of a needlestick<br />
injury to a healthworker, blood may<br />
only be drawn from an unconscious<br />
patient for the purposes of communicable<br />
virus detection, provided that to<br />
do so would be in the best interests of<br />
the patient.<br />
The medical and nursing professions,<br />
in partnership with the Department of<br />
Health and the Courts, would be well<br />
advised to strenuously seek an expeditious<br />
solution to this impasse to optimise<br />
the postexposure treatment of<br />
healthcare workers after needlestick<br />
injuries.<br />
Acknowledgements<br />
I would like to thank the Human Tissue<br />
Authority, Public Guardianship Office<br />
and Department of Health for their<br />
prompt assistance, as well as Dr Steve<br />
Yentis for initially raising the issue. An<br />
interesting discussion of the ethics surrounding<br />
these issues can be found on<br />
Ó 2007 The Author<br />
1200 Journal compilation Ó 2007 The Association of Anaesthetists of Great Britain and Ireland
Anaesthesia, 2007, 62, pages 1199–1201<br />
Editorial<br />
.....................................................................................................................................................................................................................<br />
Radio 4’s Inside the Ethics Committee,<br />
broadcast 12th September, 2007 [29].<br />
Stuart M. White<br />
Consultant in Anaesthesia<br />
Brighton Anaesthesia Research Forum,<br />
Brighton and Sussex University<br />
Healthcare NHS Trust<br />
Eastern Road<br />
Brighton, East Sussex, BN2 5BE,<br />
UK<br />
E-mail: igasbest@hotmail.com<br />
References<br />
1 HMSO. The Human Tissue Act,<br />
2004. http://www.opsi.gov.uk/acts/<br />
acts2004/20040030.htm [accessed 10<br />
October 2007].<br />
2 Redfern M. The Royal Liverpool<br />
Children’s Enquiry. January 2001.<br />
http://www.rlcinquiry.org.uk/<br />
download/index.htm [accessed 10<br />
October 2007].<br />
3 Kennedy I. The Bristol Royal Infirmary<br />
Inquiry. Final Report. July 2001.<br />
http://www.bristol-inquiry.org.uk/<br />
final_report/index.htm [accessed 10<br />
October 2007].<br />
4 HM Inspector of Anatomy. The<br />
Investigation of events that followed<br />
the death of Cyril Mark Isaacs. May<br />
2003. http://www.doh.gov.uk/cmo/<br />
isaacsreport/ [accessed 10 October<br />
2007].<br />
5 Department of Health. Human Bodies,<br />
Human Choices. The Law on<br />
Human Organs and Tissue in England<br />
and Wales. A Consultation Report.<br />
July, 2002. http://www.doh.gov.uk/<br />
tissue/humanbodieschoices.pdf<br />
[accessed 10 October 2007].<br />
6 Liddell K, Hall A. Beyond Bristol and<br />
Alder Hey: the future regulation of<br />
human tissue. Medical Law Review<br />
2005; 13: 170–223.<br />
7 McHale J. The Human Tissue Act<br />
2004: innovative legislation – fundamentally<br />
flawed or missed opportunity?<br />
Liverpool Law Review 2005; 26:<br />
169–88.<br />
8 Mavroforou A, Giannoukas A, Michalodimitrakis<br />
E. Consent for organ<br />
and tissue retention in British law in<br />
the light of the Human Tissue Act<br />
2004. Medicine and Law 2006; 25: 427–<br />
34.<br />
9 Furness PN. The Human Tissue Act.<br />
British Medical Journal 2006; 333: 512.<br />
10 Editorial. Effective implementation of<br />
the Human Tissue Act. Lancet 2006;<br />
368: 891.<br />
11 Underwood JC. The impact on<br />
histopathology practice of new human<br />
tissue regulation in the UK. Histopathology<br />
2006; 49: 221–8.<br />
12 Lucassen A, Kaye J. Genetic testing<br />
without consent: the implications of<br />
the new Human Tissue Act 2004.<br />
Journal of Medical Ethics 2006; 32: 690–<br />
2.<br />
13 Bell MD. The UK Human Tissue Act<br />
and consent: surrendering a fundamental<br />
principle to transplantation<br />
needs? Journal of Medical Ethics 2006;<br />
32: 283–6.<br />
14 Bell MD. Emergency medicine, organ<br />
donation and the Human Tissue Act.<br />
Emergency Medicine Journal 2006; 23:<br />
824–7.<br />
15 Elder A, Paterson C. Sharps injuries in<br />
UK health care: a review of injury<br />
rates, viral transmission and potential<br />
efficacy of safety devices. Occupational<br />
Medicine 2006; 56: 566–74.<br />
16 Huang L, Quartin A, Jones D, Havlir<br />
DV. Current concepts: intensive care<br />
of patients with HIV Infection. New<br />
England Journal of Medicine 2006; 355:<br />
173–81.<br />
17 Health Protection Agency. Eye of the<br />
Needle. Surveillance of significant<br />
occupational exposure to bloodborne<br />
viruses in healthcare workers. January<br />
2005. http://www.hpa.org.uk/<br />
infections/topics_az/bbv/pdf/eye_<br />
of_the_needle.pdf [accessed 10<br />
October 2007].<br />
18 Rapiti E, Prüss-Üstün A, Hutin Y.<br />
Assessing the Burden of Disease from<br />
Sharps Injuries to Health-Care Workers at<br />
National and Local Levels. Geneva:<br />
World Health Organization, 2005.<br />
http://www.who.int/quantifying_<br />
ehimpacts/global/7sharps.pdf<br />
[accessed 10 October 2007].<br />
19 UK Chief Medical Officer’s Expert<br />
Advisory Group on AIDS. HIV postexposure<br />
prophylaxis. http://<br />
www.dh.gov.uk/assetRoot/04/08/<br />
36/40/04083640.pdf [accessed 10<br />
October 2007].<br />
20 Puro V, Cicalini S, De Carli G, et al.<br />
European recommendations for the<br />
management of healthcare workers<br />
occupationally exposed to hepatitis B<br />
virus and hepatitis C virus. Euro<br />
Surveillance 2005; 10: 260–4.<br />
21 Consent. In: White SM, Baldwin TJ.<br />
Legal and Ethical Issues in Critical Care<br />
and Perioperative Medicine. Cambridge:<br />
Cambridge University Press, 2004:<br />
49–71.<br />
22 General Medical Council. Serious<br />
communicable diseases. October<br />
1997. http://www.gmc-uk.org/<br />
guidance/current/library/serious_<br />
communicable_diseases.asp [accessed<br />
10 October 2007].<br />
23 White SM, Baldwin TJ. The Human<br />
Rights Act, 1998: implications for<br />
anaesthesia and intensive care. Anaesthesia<br />
2002; 57: 882–8.<br />
24 Halpern SD. HIV testing without<br />
consent in critically ill patients. Journal<br />
of the American Medical Association 2005;<br />
294: 734–7.<br />
25 Human Tissue Act 2004 (Persons<br />
Who Lack Capacity to Consent and<br />
Transplants) Regulations : SI no.<br />
1659. 1. http://www.opsi.gov.uk/<br />
SI/si2006/20061659.htm [accessed 10<br />
October 2007].<br />
26 White SM, Baldwin TJ. The Mental<br />
Capacity Act, 2005. Implications for<br />
anaesthesia and intensive care. Anaesthesia<br />
2006; 61: 381–9.<br />
27 Mental Capacity Bill. Hansard,<br />
1st February 2005, 194. http://www.<br />
publications.parliament.uk/pa/<br />
ld200405/ldhansrd/vo050201/text/<br />
50201-27.htm#50201–27_spnew1<br />
[accessed 10 October 2007].<br />
28 Department for Constitutional Affairs.<br />
Mental Capacity Act 2005. Code of<br />
Practice. http://www.dca.gov.uk/<br />
legal-policy/mental-capacity/mca-cp.<br />
pdf [accessed 10 October 2007].<br />
29 British Broadcasting Corporation.<br />
Inside the Ethics Committee. Can an<br />
unconscious patient be tested for<br />
HIV without his consent? Broadcast<br />
12th September 2007. http://<br />
www.bbc.co.uk/radio4/science/<br />
ethicscommittee_s3_tr3.shtml<br />
[accessed 10 October 2007].<br />
Ó 2007 The Author<br />
Journal compilation Ó 2007 The Association of Anaesthetists of Great Britain and Ireland 1201
Analysis of Benefits and Harms of Compulsory testing<br />
Patient Practitioner Team Trust Public<br />
Benefits<br />
Harms<br />
Fair – all patients<br />
treated the same<br />
Possible early<br />
diagnosis and Rx<br />
Autonomy overridden<br />
- coercion<br />
Small risk from<br />
procedure<br />
False<br />
positives/negatives<br />
Certainty of need<br />
for Rx<br />
Better informed<br />
decision<br />
Feels “valued”<br />
More likely to<br />
report?<br />
Uncertainty of –ve<br />
result<br />
False -ve<br />
Team morale<br />
Feel “valued”<br />
Les likely to have<br />
absence due to stress<br />
May be less risk<br />
averse<br />
More likely to report<br />
Additional procedure -<br />
> additional exposure<br />
May become less<br />
careful<br />
Practicality Additional storage of samples<br />
Cost of testing, staff time<br />
How to deal with results – confidentiality for patient and practitioner<br />
Simplified Process<br />
Primary medical/dental care?<br />
Better Staff Morale<br />
More focused Rx may reduce<br />
costs<br />
Reduced absence<br />
Senior Mgt do not have to<br />
spend time on individual<br />
cases<br />
Legal clarity<br />
Improved Occupational<br />
Health<br />
Resistance from<br />
GUM/Virology<br />
Happier valued workforce<br />
Enhance Recruitment<br />
retention<br />
Better prevalence<br />
information<br />
“right Thing to do”<br />
HCPs may less risk averse<br />
Potential Distrust of<br />
doctors/NHS<br />
Costs of testing/treatment<br />
Potential Compensation to<br />
patient/practitioner
OPTION 3 – PRESUMED CONSENT.<br />
‘Presumed consent’, in the context of blood borne virus testing, assumes that consent has<br />
been given for blood testing unless the patient has specifically refused testing. There is no legal<br />
precedent for presumed consent in the United Kingdom.<br />
Several commentators have decried the very notion of presumption, declaring that<br />
‘presumed consent’ is equivalent to ‘no consent at all’ and that the presumption of consent<br />
affords the patient little protection against what would otherwise be legally considered a battery.<br />
Presumption places no duty on the doctor to ascertain whether the patient might indeed be<br />
capable of giving consent (as should happen according to the Mental Capacity Act 2005), or to<br />
provide information to the patient about the risks and benefits of BBV testing, or to assess<br />
whether there is any voluntariness on the part of the patient to agree to what is proposed. In<br />
addition, vulnerable groups (children, mentally incompetent adults) may not be in a position to<br />
raise an objection. As such, presumed consent is contrary to the increasing emphasis placed on<br />
patient autonomy by UK legislators, through consent.<br />
Nevertheless, 4 arguments might be used to support the introduction of presumed consent<br />
for BBV testing:<br />
1) Public support. Overwhelming public support, through informed public debate, could<br />
consolidate an ethical mandate for presumed consent in this specific instance.<br />
2) Social contract. Doctors and nurses will continue to provide healthcare for patients, on the<br />
understanding that consent will be presumed for BBV testing should a needlestick injury<br />
occur and there is a genuine risk of inoculation (with safeguards similar to the GMC’s<br />
withdrawn advice).<br />
3) ‘Soft’ presumed consent ie presumed consent only with the confirmative assent of relatives or<br />
close acquaintances.<br />
4) Organ donation. The government have recently indicated at least an interest in presumed<br />
consent with regards organ donation. Applied to BBV testing, this would mean that<br />
individuals would have to specifically ‘opt out’ of testing, probably by indicating in written<br />
form that they would not want to be tested. There is a danger that by setting a new legal<br />
context in the case of BBVs, that a precedent of presumed consent could be extended to<br />
organ donation.
AAGBI Needlestick Injuries Working Party<br />
Daniel K. Sokol<br />
Option: non-consensual testing of patients (on an existing or specifically taken sample) in<br />
the event of a needlestick injury for the benefit of the injured healthcare professional.<br />
This option is currently unlawful in England and Wales if the testing is not in the<br />
patient’s best interests.<br />
Several arguments can be presented in favour of the option:<br />
1. The clinical, social and psychological benefits to the healthcare professional outweigh<br />
the relatively minor infringement of autonomy associated with testing a sample.<br />
2. In the case of unconscious patients, it is probable that the vast majority would not<br />
object to the test, given the absence of pain, the virtually non-existent clinical risks of<br />
the testing and the obvious benefits to the healthcare professional.<br />
3. The injured worker’s colleagues who form part of the medical team may be reassured<br />
by a) knowing their colleague’s state of infection, b) knowing that their colleague is<br />
aware of his or her state of infection and c) knowing that testing is a lawful option in<br />
the eventuality of sustaining a needlestick injury themselves.<br />
4. In light of the incidence of needlestick injuries and the distress potentially caused by<br />
ignorance of one’s disease status, allowing such testing is likely to boost staff morale,<br />
reduce ‘burnout’ in the profession generally and may help retain staff. This should<br />
benefit patients generally.<br />
5. This option, which emphasises the autonomy and welfare of the healthcare<br />
professional, may aid recruitment into high-risk specialties or, at least, will not<br />
contribute to a fall in recruitment.<br />
6. Reciprocity – one may argue that patients have certain duties towards the healthcare<br />
professionals who are putting themselves at risk to help them (e.g. the duty not to be<br />
physically or verbally abusive), as long as these duties are not too onerous. Allowing<br />
oneself to be tested for HIV and hepatitis, even if only for the benefit of the<br />
healthcare workers, may constitute a patient’s duty and should be enforced.<br />
There are also arguments against the option:<br />
1. Non-consensual testing may violate the autonomy of those who either explicitly refuse<br />
to be tested or, if unconscious, who would have refused to be tested.<br />
2. Is it really practicable or indeed desirable to obtain a sample from a conscious patient<br />
who does not wish to be tested? One less coercive option, then, would be to permit nonconsensual<br />
testing on unconscious patients only (except when it is known that the patient<br />
would not have wanted to be tested, e.g. in an advance directive or through a Lasting
Power of Attorney) while requiring some form of consent for conscious patients. If the<br />
patient is conscious but incapacitous, we could suggest that testing is permitted on an<br />
existing sample only.<br />
3. If testing is compulsory, patients in need of medical treatment may be reluctant to seek<br />
treatment for fear of being tested against their will (albeit only in the rare eventuality of a<br />
needlestick injury). This could have adverse effects on the patients’ health and have<br />
negative cost implications to the National Health Service. This represents another reason<br />
for preferring the non-mandatory option mentioned above.<br />
A number of questions remain. If the test is performed against a competent patient’s will,<br />
should the information obtained be offered to the patient? Should it be recorded in the<br />
patient’s notes? If the patient was unconscious when the test was performed, when, how<br />
and what should he or she be told?
AAGBI NEEDLESTICK INJURIES WORKING PARTY<br />
OPTIONS FOR CHANGE<br />
OPTION 5 – MAINTAIN STATUS QUO.<br />
A competently made refusal of BBV testing by a patient prohibits a doctor from testing that<br />
patient’s blood for BBVs in the event of a needlestick injury to a third party.<br />
The effect of Mental Capacity Act 2005 and the Human Tissue Act 2004 on the non-consensual<br />
testing for BBVs after needlestick injuries involving patients without capacity has been to countermand<br />
the advice (now withdrawn) of the GMC (Serious Communicable Diseases guidelines, 1997) with<br />
regard to this eventuality. Statute now demands that in the event of a needlestick injury to a<br />
healthworker, blood may only be drawn from a patient who lacks legal capacity for the purposes of<br />
BBV detection, provided that to do so would be in the best interests of the patient.<br />
If BBV testing is prohibited, the injured third party must wait for 3-6 months before secondary<br />
testing to confirm seroconversion, taking appropriate post-exposure prophylaxis (PEP) in the interim<br />
exposing themselves to both the side-effects of PEP drugs, and associated psychological stress.<br />
The prevention of needlestick injuries remains of primary importance. Nevertheless, injuries are<br />
likely to still occur. Pragmatically, such injuries are rare; furthermore, needlestick injuries from a<br />
known patient who is permanently unable to consent are likely to be extremely rare. Nevertheless, a<br />
situation involving an untestable patient is likely to arise, and it is morally untenable that the ‘right’ to<br />
treatment of the injured party should defer to any ‘right’ of an incompetent patient not to have a BBV<br />
test, particularly if a more minimally invasive test can be used and appropriate safeguards regarding<br />
confidentiality are observed.<br />
Possible solutions include:<br />
1) Covert, non-consensual testing – which is against the law;<br />
2) Testing secondary to reassessment of a patient’s BBV risk, in which case testing would (probably)<br />
be in the patient’s best interests<br />
3) Non-consensual testing to provoke a legal test case. This is a high-risk strategy that could lead to<br />
imprisonment, but could stimulate a thus far intransigent government into introducing secondary<br />
legislation<br />
4) Lobbying government to introduce secondary legislation, or MPs to introduce a Private Member’s<br />
Bill<br />
5) Increasing awareness among patients of how to assert their choice under existing legislation, for<br />
example, via a Lasting Power of Attorney or Advance Decision.
Needle-stick injury and HIV testing of the incompetent adult<br />
– the status of assent of the next-of-kin<br />
MD Dominic Bell<br />
The precise status of the next-of-kin in the healthcare management of the incompetent<br />
adult remains ill-defined within the UK or indeed any jurisdiction. The Mental<br />
Health Act 1959 removed any authority under English law and although the Mental<br />
Capacity Act has extended ‘power-of-attorney’ to medical and personal welfare<br />
matters, this will predictably be limited numerically and in the nature of the<br />
undertakings. Responsibility continues to rest therefore with medical staff acting in<br />
the ‘best interests’ of the patient, 1 but directives from both government and the<br />
professional bodies specify the involvement of the next-of-kin in decision-making. 2 3<br />
Furthermore, since ‘best interests’ are not limited to ‘best medical interests’, but<br />
incorporate ‘the patient’s wishes and beliefs when competent, their general well-being<br />
and their spiritual and religious welfare’, 2 3 it appears essential to consult the next-ofkin<br />
to determine their interpretation of these factors.<br />
Despite this somewhat ambivalent position and additional conflict with the duty of<br />
confidentiality, it is routine practice therefore within critical care to engage the next of<br />
kin not only to update them on condition, prognosis and plans, but to ensure their<br />
understanding of and assent to interventions such as surgery, tracheostomy, or blood<br />
transfusion, using Consent Form 4 in certain circumstances.<br />
The responsibility of the next of kin is particularly increased in decision-making on<br />
maintenance, escalation, or withdrawal of life-sustaining medical treatment [LSMT]<br />
when the prognosis and longer-term benefits are doubtful, and the next of kin are<br />
asked to express a view on what they believe the patient would have wanted in such<br />
circumstances, knowing their values and beliefs. This principle is extended further<br />
Appendix6 1
when asking for the family’s position as to whether the patient would have favoured<br />
organ donation when active support is to be withdrawn following a consensus on<br />
futility. The overwhelming benefit of organ donation falls to a third party and it can<br />
be seen that with reference to non heart beating donation, further undertakings are<br />
necessary to ensure that the transplanted organs are at optimal viability and safety,<br />
including serological testing for HIV and other transmissible diseases prior to death,<br />
an intervention endorsed by the Intensive Care Society. 4<br />
The arguments for this<br />
approach are that it is in no one’s interests to embark on the process of retrieval and to<br />
subsequently discover the presence of transmissible disease, or to delay the<br />
transplantation of vulnerable organs whilst awaiting the results of such tests or indeed<br />
tissue typing, taken after death. 5<br />
In this scenario the next of kin are provided with full information as to all the facets of<br />
organ donation, including the above aspects, in line with previous government<br />
directives on provision of information for valid consent, 6 and give assent on that<br />
basis.<br />
The proposal to adopt this approach for serological testing after needlestick injury is<br />
not therefore radical. The historical stigmata associated either with testing or a<br />
positive result have been largely eliminated through legislation and government<br />
directives, as well as the advances in medical therapy such as HAART. The key<br />
principles essential to make this approach ethically defensible would be provision of<br />
full information on what the test involves and the implications of a positive result, full<br />
information on the physical and mental health implications for the relevant healthcare<br />
practitioner of either knowing or not knowing a test result, choice as to how the test<br />
result is recorded and ultimately provided to the patient if and when they should<br />
Appendix6 2
egain capacity, and the absence of coercion. By considering standards in other<br />
settings, it would appear essential to provide a written booklet on the above aspects<br />
and for the interview to be carried out jointly by senior practitioners from intensive<br />
care and genitourinary medicine. [This strategy has been defined and carried out<br />
within the critical care environment of the General Infirmary at Leeds over the last 18<br />
months].<br />
Legal, political and professional implications of these proposals<br />
The above strategy would arguably not require any change in legislation since the<br />
Human Tissue Act does not specifically prohibit serological testing but simply<br />
dictates that any intervention be in the patient’s ‘best interests’. For the protection of<br />
the involved health care practitioners, it would however clearly be helpful for<br />
government to endorse an expanded interpretation of ‘best interests’ to include<br />
‘values and beliefs’ as well as purely medical best interests, and the role of the next of<br />
kin in determining those best interests for the individual patient. If such endorsement<br />
were not to be forthcoming, it should be apparent that non heart beating organ<br />
donation could no longer be considered viable, since the process is critically<br />
dependent on a parallel expanded interpretation of best interests and the assent of the<br />
next of kin. With such endorsement however, it would then fall to the health-care<br />
professions to explicitly define process as above to ensure provision of all essential<br />
information and avoid any consideration of coercion.<br />
1<br />
2<br />
3<br />
4<br />
5<br />
6<br />
Re F (Mental Patient: Sterilisation) [1990] 2 AC 1 (HL)<br />
Department of Health. Good Practice in Consent. HSC 2001/023<br />
GMC. Seeking patients' consent: the ethical considerations. GMC November 1998<br />
Ridley S, Bonner S, Bray K, et al. UK guidance for non-heart beating donation. Br J Anaesth<br />
2005; 95:592-595<br />
Bell MDD. Non-heartbeating organ donation – clinical process and fundamental issues Br J<br />
Anaesth 2005; 94: 474-78<br />
Isaacs Report. Department of Health. London May 2003<br />
Appendix6 3
Needle-stick Injuries from a Patients Perspective<br />
The options considered at the meeting of /May 9 th with regard to the testing of<br />
patients who have been the source of needle stick injuries were discussed with a broad<br />
range of people i.e.: Yorkshire Cancer Network, Members of the Membership Council<br />
of the local Trust, Members of Cancer Connections, general members of the public<br />
with the ages ranging from late teens to 70s.<br />
There was a general concern that NHS staff (considered in the widest terms) could be<br />
left in a vulnerable situation, emotionally and psychologically should there be a<br />
needle stick injury, with no recourse to testing if there is no permission given by the<br />
source of the possible infection. They did not believe that it should be an occupational<br />
hazard that should be accepted. The general opinion was that all staff had the right to<br />
work in a safe environment and that their rights were every bit as important as the<br />
patients.<br />
There was an overwhelming belief that there should be effective training in place for<br />
all staff on how to deal with equipment that could cause a needle-stick injury and how<br />
to dispose of it correctly; also that the correct equipment for disposal should be a top<br />
priority for all Trusts regardless of costs. There was also a belief that the training<br />
should be updated regularly so that standards of care were maintained. It was also felt<br />
that all Trust should be aware of the safest equipment on the market and encourage<br />
staff to use it, thereby having an environment of good practice. There was a wish<br />
expresses that an environment of openness operates within the NHS so that staff felt<br />
that they would be well supported if a needle-stick injury occurred.<br />
All six options were presented to the individuals questioned. There was a range of<br />
responses as to how the case for needle stick testing should take place,<br />
A) Probably most felt that there should that there should be blanket testing, that a<br />
form should be signed when admitted to hospital for any procedure. Even<br />
when it was pointed out that certain patients might not present them-selves for
treatment if it was understood that a sample of body fluids needed to be taken<br />
(for fear of needles). The question was asked if a mouth swab would allow the<br />
range of tests needed to confirm a blood borne disease thereby circumventing<br />
the need to take blood.<br />
B) The next most made response was, all patients should sign a form that should<br />
they be the source of a needle-stick injury they would be prepared to be tested.<br />
It was stressed in both response a / b that the consent forms should be<br />
explained very clearly to all. Not one person spoken to said that they would<br />
refuse consent for testing for them selves or for a relative should that relative<br />
be unable to give permission due to their medical condition.<br />
C) When asked what should happen if an accident occurred when a patient was<br />
unconscious with no person present to give permission for testing to take<br />
place, the general response was that a test should go ahead with a full<br />
explanation given, either to the relatives when they arrive or the patient when<br />
conscious again. Should the relatives be present then they should have a clear<br />
picture drawn of the situation and be asked for permission to test.<br />
D) There was a general resistance to the idea of presumed consent for both<br />
competent and incompetent patients. What was strongly expressed was the<br />
feeling that the treatment throughout a needle-stick injury incident should be<br />
sensitively managed for patient and professional so that it would have the best<br />
outcome for all concerned.<br />
It should be appreciated the general public do not have the detailed knowledge of the<br />
medical ethics that are being considered by the committee. The responses recorded<br />
are their reactions to the six changes to be considered.<br />
Everyone without exception was concerned for the safety of NHS staff, they were<br />
concerned for the cost implications if staff were off sick and if other NHS personnel<br />
did not declare a possible infection and go on to infect other colleagues or patients.<br />
It was recognised by all that there will always be unreasonable people what ever<br />
changes take place and some felt that if they did not co-operate with NHS personnel<br />
then treatment could be refused.
OAA / AAGBI Guidelines for<br />
Obstetric Anaesthetic Services 2013<br />
3<br />
Published by<br />
Association of Anaesthetists of Great Britain & Ireland<br />
Obstetric Anaesthetists’ Association<br />
June 2013
Membership of the working party<br />
Dr Felicity Plaat<br />
Dr David Bogod<br />
Dr Valerie Bythell<br />
Dr Mary Mushambi<br />
Dr Paul Clyburn<br />
Dr Nuala Lucas<br />
Dr Ian Johnston<br />
Dr Sarah Gibb<br />
Dr Iftikhar Parvez<br />
Dr Anne Thornberry<br />
AAGBI, Chair of working party<br />
OAA, President<br />
AAGBI<br />
OAA<br />
AAGBI<br />
OAA<br />
AAGBI<br />
AAGBI, GAT representative<br />
AAGBI, SAS representative<br />
RCoA representative<br />
Association of Anaesthetists of Great Britain & Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
Website: www.<strong>aagbi</strong>.org<br />
Obstetric Anaesthetists’ Association<br />
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 8883<br />
Fax: 020 7631 4352<br />
Email: secretariat@oaa-anaes.ac.uk<br />
Website: www.oaa-anaes.ac.uk<br />
© The Association of Anaesthetists of Great Britain & Ireland and the Obstetric Anaesthetists’ Association 2013.
Contents<br />
1. Key recommendations 2<br />
2. Introduction 3<br />
3. Staffing 4<br />
4. Services and standards 8<br />
5. Training and education 17<br />
6. The labour ward team 20<br />
7. Support services, equipment, facilities and accommodation 23<br />
8. The future 27<br />
9. List of recommended guidelines 28<br />
10. References 30<br />
This is a consensus document produced by expert members of a Working Party established by the<br />
Association of Anaesthetists of Great Britain and Ireland (AAGBI) and the Obstetric Anaesthetists’<br />
Association (OAA). It updates and replaces previous guidance published in May 2005. It has been<br />
seen and approved by the AAGBI Council and the OAA Committee.<br />
• What other guideline statements are available on this topic?<br />
The Royal College of Obstetricians & Gynaecologists have produced guidelines on the provision<br />
of maternity services:<br />
1. High quality women’s health care: A proposal for change. RCOG press, London, 2011.<br />
2. Safer childbirth: Minimum standards for the organization and delivery of care in labour. RCOG<br />
press, London, 2007.<br />
• Why was this guideline developed?<br />
The original guideline published in 1998 was developed to ensure that obstetric patients received<br />
the same standards of anaesthetic care as those recommended for the general surgical<br />
population.<br />
• How and why does this statement differ from existing guidelines?<br />
This guideline concentrates on the roles and activities of the obstetric anaesthetist within the<br />
multidisciplinary team required to deliver safe maternity care. The major changes compared with<br />
the 2005 version include a section on maternity critical care and the recommendation for<br />
increased dedicated consultant anaesthetic sessions.<br />
The need to define anaesthetic services in maternity in 2013 reflect the expanding role of the<br />
anaesthetist as peri-partum physician in caring for an increasingly challenging patient population<br />
in a rapidly changing health service.<br />
Date of review: 2018<br />
1
1. Key recommendations<br />
1. A duty anaesthetist must be immediately available for emergency work on the delivery suite<br />
24 hours a day.<br />
2. There must be a nominated consultant in charge of obstetric anaesthesia with time allocated<br />
for this role.<br />
3. There should be a clear line of communication from the duty anaesthetist to the supervising<br />
consultant at all times.<br />
4. The workload of the obstetric anaesthetist continues to increase. As a basic minimum there<br />
must be 12 consultant sessions per week to cover emergency work on delivery suite.<br />
5. Scheduled obstetric anaesthetic activities (e.g. elective caesarean section lists, clinic) require<br />
additional consultant sessions over and above the 12 for emergency cover.<br />
6. Women should have antenatal access to evidence based information about the availability<br />
and provision of all types of analgesia and anaesthesia. This information should be provided<br />
or at least ratified by the department of obstetric anaesthesia.<br />
7. There should be an agreed system whereby the anaesthetist is given sufficient advance<br />
notice of all potentially high-risk patients.<br />
8. When a 24-hour epidural service is offered, the time from the anaesthetist’s being informed<br />
that a woman is requesting an epidural and ready to receive one until attending the mother<br />
should not normally exceed 30 minutes. This period should only exceed one hour in<br />
exceptional circumstances. Responses times should be regularly audited and if the above<br />
standards are missed frequently, consideration should be given to alteration of staffing<br />
arrangements.<br />
9. Provision should be made for those who cover the delivery suite on-call, but do not have<br />
regular sessions there, to spend time on the delivery suite in a supernumerary capacity with<br />
one of the regular obstetric anaesthetic consultants.<br />
10. There must be separate provision of staffing and resources to enable elective work to run<br />
independently of emergency work, in particular to prevent delays to both emergency and<br />
elective procedures and provision of analgesia in labour.<br />
11. The person assisting the anaesthetist must have no other conflicting duties, must be trained<br />
to a nationally recognised standard and must work regularly and frequently in the obstetric<br />
unit.<br />
12. The training undergone by staff and the facilities provided in the maternity recovery unit must<br />
be of the same standard as for general recovery, as defined in current, published guidelines.<br />
13. Appropriate facilities should be available for the antenatal and peripartum management of the<br />
sick obstetric patient as defined in the document Providing Equity of Critical and Maternity<br />
Care for the Critically Ill Pregnant or Recently Pregnant Patient.<br />
2
2. Introduction<br />
This is the third version of the joint Association of Great Britain and Ireland/Obstetric Anaesthetists’<br />
Association (AAGBI/OAA) guidelines [1, 2]. A major change from the last revision in 2005 is the<br />
inclusion of a section on critical care in maternity. This reflects the belated recognition of this<br />
increasingly important area of obstetrics [3]. The number of women requiring advanced levels of care<br />
is set to increase as the trend towards an older obstetric population with increasing morbidities and<br />
levels of obesity shows no sign of abating. As a result, obstetric anaesthetists will continue to be<br />
required to take on the role of peripartum physician (paralleling a growing enthusiasm for that of perioperative<br />
physician in non-obstetric practice [4]). This will inevitably mean involvement in training of<br />
staff caring for high-risk parturients and adoption of management roles to develop and maintain<br />
critical care facilities.<br />
These guidelines recommend a further increase in the minimum number of weekly anaesthetic<br />
consultant sessions to 12 in order to provide delivery suite cover plus further sessions for scheduled<br />
work (caesarean section lists/clinic, etc). This arises from three developments. Firstly, recent surveys<br />
have confirmed that the workload of obstetric anaesthetists is increasingly onerous and complex [5,<br />
6]. Secondly, the presence of the obstetric consultant on the delivery suite is now mandatory, with the<br />
number of hours per week determined by the number of deliveries [7]; this must be reflected in<br />
anaesthetic input. Thirdly, the Clinical Negligence Scheme for Trusts has circulated a draft standard<br />
that elective work should be independently staffed in order that it can run uninterrupted by<br />
emergencies. This is expected to be adopted as a full standard in due course.<br />
On-call rooms are disappearing from many maternity units despite the well-described benefits of<br />
enabling periods of proper rest during night-time working [8]. Even when working to a shift-based rota,<br />
the most common pattern for trainees, fatigue is more likely to affect performance and thus patient<br />
safety at night. Even short periods of sleep can help mitigate these effects and we have therefore<br />
recommended that appropriate facilities be made available.<br />
Effective teamworking is crucial to maternity care as highlighted in a recent report on safety in<br />
maternity services [9]. Obstetric anaesthetists play a pivotal role in the team itself and in delivering<br />
training in teamworking. This is reflected in our recommendations for anaesthetic representation on all<br />
maternity committees.<br />
As noted in the previous version of these guidelines, we realise that our recommendations potentially<br />
have major financial and organisational implications. However, they are based on consideration of the<br />
safety of the women who deliver in our units and their babies. We have therefore stressed yet again<br />
that consideration should be given to amalgamating units that are too small to support the costs of<br />
providing these services.<br />
3
3. Staffing<br />
Anaesthetists are involved in the care of over 60% of pregnant women. The Audit Commission found<br />
a wide variability of anaesthetic staffing on labour wards [10] and a recent survey confirms this [6].<br />
Previous recommendations concerning anaesthetic staffing were based on delivery rates. Busy units<br />
were defined somewhat arbitrarily as those with > 5000 deliveries per year, an epidural rate > 35%<br />
and a caesarean section rate > 25%, tertiary referral centres and/or centres with a high proportion of<br />
high-risk cases. It was proposed that there should one consultant session per 500 deliveries with at<br />
least 10 sessions for units with over 3000 deliveries [2]. However, there are several problems with the<br />
use of such definitions [11]. The use of crude delivery rates:<br />
• Does not take into account the huge variation in casemix that exists between units<br />
• Does not take into account the impact of changing obstetric demographics (increased maternal<br />
co-morbidities such as obesity, increased maternal age, increased assisted conception,<br />
increasing immigrant population)<br />
• Does not take account of the impact of the changes to training in anaesthesia (in particular the<br />
effect of the European Working Time Regulations on training, associated paperwork and reduced<br />
trainee numbers)<br />
• Does not reflect the increased demand for the delivery of additional anaesthetic services such as<br />
anaesthetic clinics, maternity high dependency units (HDUs) and support for interventional<br />
radiology, etc<br />
• Does not take into account changes in obstetric practice, such as increasing rates of caesarean<br />
section, trial of instrumental delivery, cervical cerclage and repair of complex tears, all of which<br />
increase theatre workload<br />
The calculation of consultant sessions will need to take into account the volume of clinical work, the<br />
contribution by consultants towards administration and other non-clinical activities, and the numbers<br />
and experience of trainees. It is essential that the contribution made by non-consultant career-grade<br />
anaesthetists is included.<br />
It is the unanimous opinion of this Working Party that a move towards obstetric anaesthetic services’<br />
being fully consultant delivered is both desirable and inevitable. Obstetricians have already set this<br />
as an objective and are in the process of working towards it [12]. Ultimately, obstetric consultant<br />
sessions devoted to emergency and elective obstetric activities should be matched by anaesthetic<br />
consultant sessions.<br />
4
Recommendations<br />
Medical staff<br />
The term ‘duty anaesthetist’ denotes an anaesthetist who has been assessed as competent to<br />
undertake duties on the delivery suite under a specified degree of supervision.<br />
The duty anaesthetist should be immediately* available to attend the obstetric unit 24 hours per day,<br />
and must therefore have no other responsibilities outside obstetrics. In all units offering a 24-hour<br />
epidural service, the duty anaesthetist must be resident on site.<br />
If the duty anaesthetist is not a consultant, consultant support and on-call availability is essential 24<br />
hours per day and a clear line of communication from the duty anaesthetist to the on-call consultant is<br />
essential at all times. If the duty anaesthetist is a consultant, the workload of the unit may dictate a<br />
need for additional manpower in order to deliver a safe service, and contact details of a back-up<br />
anaesthetist should be immediately available at all times.<br />
The name of the on-call consultant must be prominently displayed at all times. The names of all<br />
consultants who cover labour ward, and their contact numbers, should be readily available.<br />
The duty anaesthetist should not be responsible for planned maternity work such as elective<br />
caesarean section lists, anaesthetic antenatal clinics, etc. Such activities should be able to continue<br />
uninterrupted in the face of non-elective activities (e.g. emergency caesarean section, requests for<br />
regional analgesia in labour).<br />
In consultant-led obstetric units where anaesthetic care is not primarily consultant-delivered, there<br />
should be a minimum of 12 consultant anaesthetic sessions (direct clinical care) per week to cover<br />
non-elective activity (i.e. a minimum of two sessions per working day, taking account of leave). Where<br />
there is a high turnover of trainees (i.e. a three-month interval or more frequent), a third evening<br />
session may be necessary in order to train and supervise trainees adequately.<br />
In addition, there must be further consultant sessions for direct clinical care, to cover elective<br />
caesarean section lists and anaesthetic clinics.<br />
There must be a nominated lead obstetric anaesthetist who has an active role in leading and<br />
managing services, with this adequately recognised in their job plan.<br />
*Immediately available – able to attend within 5 min or less of being summoned, except in exceptional circumstances.<br />
5
Induction<br />
All trainee and non-trainee anaesthetists, regardless of prior experience in obstetric anaesthesia,<br />
should receive a formal induction to the obstetric anaesthetic unit before commencing duties. This<br />
ideally should include:<br />
• Information regarding the obstetric anaesthetic clinical supervisor and, if relevant, the educational<br />
supervisor for their attachment<br />
• A physical tour of the delivery suite, obstetric theatres, learning environment and any other<br />
relevant areas<br />
• Equipment:<br />
o A demonstration of relevant equipment, e.g. anaesthetic machine, epidural infusion devices<br />
o Location of the difficult airway trolley and its contents, including subglottic airway equipment<br />
o Depending on the stage of training/prior experience, location of other equipment such as<br />
blood storage fridge, rapid infusor device, cell salvage<br />
• Resuscitation:<br />
o Location of the cardiac arrest trolley with demonstration of the defibrillator and any other<br />
equipment if unfamiliar<br />
o Location of lipid emulsion<br />
o Use of the resuscitaire and location of equipment required for neonatal resuscitation<br />
• A clear description of:<br />
o Local arrangements for handover and contacting senior staff<br />
o Local arrangements for contacting the obstetric anaesthetist in an emergency and for a<br />
category-1 emergency caesarean section<br />
o The trainee/non-trainees’ responsibilities whilst covering the delivery suite<br />
• The location of local guidelines for obstetric anaesthesia.<br />
Handover<br />
Time for formal handover between shifts must be built into the timetable. The shift pattern of different<br />
professional groups should be compatible, e.g. anaesthetic and obstetric shifts should start/finish at<br />
the same times to allow multidisciplinary handover.<br />
Anaesthetists not in training<br />
A survey has shown that associate specialist/staff grade/specialty doctors contribute to the provision<br />
of obstetric anaesthetic services in 61% of units in the UK [6].<br />
All non-trainee anaesthetists who undertake anaesthetic duties on the delivery suite should have<br />
successfully completed the Initial Assessment of Competence in Obstetric Anaesthesia (IACOA) and<br />
have been deemed by the consultant in charge of obstetric services to be competent to perform their<br />
duties in accordance with OAA and Royal College of Anaesthetists (RCoA) guidelines. The doctors<br />
must work regularly on the delivery suite and must also regularly undertake non-obstetric anaesthetic<br />
work to ensure maintenance of a broad range of anaesthetic skills. Non-trainee anaesthetists who are<br />
6
appointed directly from other countries may not be familiar with the protocols in the UK. The following<br />
recommendations are to ensure that they are safe and are supported in the new working<br />
environment:<br />
1. There should be a defined period of directly supervised obstetric sessions. The duration of<br />
supervision will depend on individual circumstances and should be mutually agreed<br />
2. The anaesthetist must have successfully completed the IACOA before being allowed to work<br />
unsupervised.<br />
Theatre staffing<br />
Many units still use midwifery staff to assist in the operating theatre and this has an impact on<br />
midwifery staff on the labour ward. Strategic Health Authorities and Health Boards have been urged to<br />
make significant progress in replacing midwifery staff in the scrub/instrument role [13].<br />
Staffing for theatre recovery and anaesthetic assistance<br />
Parturients requiring anaesthesia have the right to the same standards of peri-operative care as any<br />
other surgical patient, including anaesthetic assistance. Training must be to the standards defined for<br />
the care of the general surgical patient [14].<br />
If the person assisting the anaesthetist is a nurse or midwife, they must have current and effective<br />
registration, and must have been appropriately trained and been assessed as having achieved the<br />
required core competencies [15]. They must be experienced and should assist the anaesthetist on<br />
labour ward on a regular basis in order to maintain competence. The team providing care for women<br />
undergoing obstetric operations must include a dedicated anaesthetic assistant for each patient in an<br />
operating theatre. The assistant should have no other duties in the operating suite concurrently.<br />
Newly recruited assistants should undergo a period of induction before working on the maternity unit.<br />
The training undergone by staff in recovery, whether they are midwives, nurses or Operating<br />
Department Practitioners, must also be of the same standard as that required for general recovery<br />
facilities [16]. Midwives with no additional training are not equipped to recover patients following<br />
anaesthesia. Staff should work in a general theatre recovery unit on a regular basis to ensure<br />
competence is maintained.<br />
All staff must be given regular access to continuing professional development and complete all<br />
mandatory training as frequently as required.<br />
7
4. Services and standards<br />
In consultant-led, as opposed to midwifery-led, units, anaesthetic services should be available to all<br />
women. The exact nature and availability of the services offered should be clear both to women<br />
choosing to book in a particular unit and to commissioning bodies.<br />
Antenatal services<br />
Information for mothers<br />
Up-to-date, locally relevant information about the services offered should be available for mothers in a<br />
range of formats appropriate to their needs (e.g. written, electronic, audio with translations), including<br />
as a minimum:<br />
• Analgesia for labour: benefits (including efficacy); risks; and availability of all options offered<br />
• Anaesthesia for caesarean section: benefits; risks; relative merits of all options offered<br />
• All women should be asked if they would be prepared to receive blood in the case of<br />
haemorrhage and this should be documented in the notes.<br />
Information should be given to mothers in a timely way – usually antenatally – that is relevant to them.<br />
Anaesthetists must have central role in the development of all information about pain relief and<br />
anaesthesia. All mothers should be given and encouraged to read information about analgesia for<br />
labour and anaesthesia for caesarean section, as the need for these choices is unpredictable and<br />
may arise in an emergency.<br />
Antenatal assessment and multidisciplinary planning<br />
Timely antenatal anaesthetic assessment services should be provided for women who:<br />
• Might present difficulties should anaesthesia or regional analgesia be required<br />
• Are at high risk of obstetric complications<br />
• Have a body mass index (BMI) greater than 40 kg.m -2 at booking [17]<br />
• Have had previous difficulties with, or complications of, regional or general anaesthesia<br />
• Have significant medical conditions.<br />
Locally agreed referral criteria should be in place. Sample guidelines regarding referral to anaesthetic<br />
services and supporting information are available from the OAA [18].<br />
Reviewing women antenatally allows for communication between obstetric anaesthetists,<br />
obstetricians and other specialists as required, and enables planning for the safe provision of<br />
anaesthesia for high-risk women.<br />
8
Peripartum care<br />
Pre-operative assessment of women scheduled to deliver by caesarean section<br />
Before admission, women should receive information about anaesthesia, relevant investigations<br />
should be undertaken and arrangements made for pre-operative preparation (fasting, antacid therapy<br />
and any other medication that should be given or withheld). This pre-operative assessment and<br />
preparation may be led by midwifery or other appropriate staff, but an anaesthetist must be available<br />
to provide advice and, if necessary, to review patients during this process. The process for such preassessment<br />
services must include anaesthetic input and review.<br />
Women should be assessed by an anaesthetist before their operation, and the plan for the<br />
anaesthetic and informed consent to the anaesthetic confirmed (this may be done verbally – see<br />
below).<br />
Fasting guidelines are discussed below.<br />
Informed consent<br />
Information for mothers about labour analgesia and obstetric anaesthesia is available in a variety of<br />
languages and formats to aid the process of informed consent [19]. The principles of consent for<br />
anaesthesia or analgesia are set out in national guidelines [20]; it is not usually considered necessary<br />
to obtain written consent. Brief details of the discussion that has taken place, and of risks that the<br />
patient has been informed about should be recorded.<br />
Regional analgesia for labour<br />
Regional analgesia is the most effective form of labour analgesia [21]. Regional analgesia should be<br />
available 24 hours per day, seven days per week, to all women delivering in consultant-led obstetric<br />
units. Local guidelines should be developed covering the initiation, maintenance and management of<br />
complications of regional analgesia for labour, based on current national guidelines and/or best<br />
evidence [22].<br />
Time to attend a request for analgesia<br />
Requests for analgesia should be met as soon as possible. The time taken for the anaesthetist to<br />
attend requests for analgesia, and from request for analgesia to achieving analgesia, should be<br />
audited regularly: at least once a year in smaller units and more frequently in larger units. The time<br />
from request for analgesia to the anaesthetist’s attending should not exceed 30 minutes. The RCoA<br />
suggests unit audit standards for the proportion of women attended by anaesthetist within 30 minutes<br />
of requesting epidural analgesia in labour [23].<br />
9
Aseptic technique<br />
It is mandatory to prepare the skin before performing central neuraxial block, and to use full aseptic<br />
precautions to reduce the risk of infective complications. Antiseptic solutions are neurotoxic, hence it<br />
is necessary to develop a systematic process for avoiding accidental injection or contamination of<br />
neuraxial injectate with antiseptic solution. A local policy should be in place taking into account these<br />
factors. Antiseptic solution should not be poured into receptacles on the sterile field that is to be used<br />
for regional blockade [24, 25].<br />
Initiation and maintenance of analgesia<br />
The anaesthetist should be immediately available for review of women and management of initial<br />
complications such as hypotension for at least 20 minutes after administration of the initial dose of<br />
regional analgesic. Local guidelines should address the management of initial complications.<br />
Continuing availability of an anaesthetist for review of women receiving regional analgesia is required<br />
throughout its duration.<br />
Monitoring and care of women receiving regional analgesia in labour<br />
Midwives caring for women receiving regional analgesia for labour should have been trained and<br />
deemed competent to do so by a local mechanism. Competence to care for women with epidural<br />
analgesia should be re-certified annually as a minimum. The specific recommendations set out in<br />
current national guidance should be followed [22].<br />
The workload of the midwife assigned to a woman with a epidural in labour should be such that care<br />
of that woman is not compromised as specified by local guidelines. The anaesthetist must be satisfied<br />
with the level of care available.<br />
Ambulation of mothers following initiation of epidural analgesia<br />
Many delivery units encourage mothers who choose regional analgesia to ambulate. If ambulation is<br />
facilitated, a specific guideline should exist outlining the process in place for assessing whether<br />
women are able to ambulate safely. Falls, slips and trips occurring in women mobilising during<br />
epidural analgesia should be reported via local incident reporting systems and audited.<br />
Post-delivery care following regional analgesia in labour<br />
Removal of the epidural catheter and its integrity should be documented. Return of motor power<br />
should be monitored by continuing observations of motor power until full recovery is present. Women<br />
should be advised not to get out of bed unaccompanied in the first instance. Postnatal falls in women<br />
who have had epidural or regional analgesia for labour should be reported via local incident<br />
monitoring systems, and monitored.<br />
10
Intravenous patient-controlled opioid analgesia in labour<br />
Intravenous patient-controlled analgesia (PCA) may be offered as an alternative to regional analgesia.<br />
Recently, the use of remifentanil PCA has increased [26]. There have been serious safety incidents<br />
associated with the use of remifentanil PCA in labour [27]. Strict adherence to locally developed<br />
guidelines [28], careful monitoring of the mother and baby, and the constant presence of a member of<br />
staff who is trained and competent to monitor maternal respiration are the minimum that is necessary<br />
to ensure that this technique is safe.<br />
Caesarean section<br />
Many aspects of preparation and anaesthesia for caesarean section have been comprehensively<br />
reviewed in the clinical guidelines on caesarean section produced by the National Institute for Health<br />
and Clinical Excellence (NICE) [29]. Some of the more important standards or aspects not covered<br />
are dealt with in this section.<br />
Classification of urgency of caesarean section<br />
Existing national guidelines should be followed regarding classification of urgency of caesarean<br />
section:<br />
1. Immediate threat to the life of the woman or fetus<br />
2. Maternal or fetal compromise which is not immediately life-threatening<br />
3. No maternal or fetal compromise but needs early delivery<br />
4. Delivery timed to suit woman or staff.<br />
The following audit categories have been suggested:<br />
• ≥ 90% category-1 caesarean sections should have a decision-to-delivery interval ≤ 30 min<br />
• ≥ 90% category-2 caesarean sections should have a decision-to-delivery interval ≤ 75 min [23].<br />
However, regardless of the classification, each case must be judged and managed on its own merits<br />
with delivery achieved as quickly as it is safely possible to do.<br />
Pre- operative preparation<br />
Before elective surgery, standard adult fasting guidelines should be adhered to [30]. Women waiting<br />
for planned surgery should not be subjected to long periods of starvation and/or fluid deprivation (they<br />
should be encouraged to drink clear fluids up until two hours pre-operatively). This should be audited<br />
and monitored.<br />
Choice of anaesthesia<br />
The choice of anaesthesia for caesarean section rests with the competent mother. Information for<br />
mothers is available in a variety of formats via the OAA website and should be used to help women<br />
choose. Units should audit the type of anaesthesia used continuously, and monitor the results<br />
annually against the RCoA’s proposed audit standards (Table 1) [23].<br />
11
Table 1 Suggested audit standards for use of regional anaesthesia for caesarean section (CS) [23].<br />
Category 1 2-3 4<br />
Proportion of CS* under regional anaesthesia > 50% > 85% > 95%<br />
Presence of birth partners<br />
Obstetrics stands alone in permitting members of the public (usually the birth partner) to accompany<br />
patients during an operation. Inviting members of the public into the operating theatre environment<br />
carries risks. These should be managed by ensuring that the purpose of the birth partner’s presence<br />
is clear to all concerned, and that the birth partner agrees to follow certain codes of behaviour, which<br />
should be set out in a local guideline and ideally clarified in a written information leaflet. The local<br />
guideline should identify the member of staff responsible for looking after birth partners if they require<br />
care or assistance unexpectedly during the operation.<br />
Any particular needs that the birth partner has should be considered, and organised (if necessary)<br />
antenatally. For example, partners with a raised BMI may require special seating.<br />
Whilst most obstetric units encourage birth partners to support women during operations under<br />
regional anaesthesia, few encourage their presence during general anaesthesia. This may be<br />
distressing for both women and their partners, and policies should be clear. Safety of the woman and<br />
her baby must be paramount. Development of antenatal information for birth partners would help to<br />
address this issue and is encouraged.<br />
Elective caesarean section lists<br />
Women delivering by planned caesarean section should have their operations performed as part of a<br />
scheduled list, resourced separately from the general workload of the delivery unit. A separately run<br />
list requires a full theatre team and should include a consultant obstetrician and a consultant<br />
anaesthetist. The list should be managed in the same way and to the same standards as other<br />
elective surgery lists. This may not be cost effective in units with a low elective workload (e.g. one or<br />
fewer elective caesareans per weekday or approximately 250 planned operations per year) but for all<br />
other units, separate resources should be allocated.<br />
Elective caesarean sections should neither interfere with delivery unit work nor be interrupted by<br />
emergencies. Such interruptions and delays (to both the scheduled and the emergency workload)<br />
should be audited and monitored, and any necessary action taken to correct recurrence.<br />
Postoperative analgesia<br />
Intrathecal or epidural diamorphine or morphine can provide adequate analgesia after caesarean<br />
section without the addition of intravenous PCA opioid. The administration of parenteral opioids to<br />
women who have received neuraxial opioids is discouraged as it increases the risk of respiratory<br />
12
depression. In the absence of contra-indications, women should be prescribed regular oral analgesia<br />
postoperatively. Pain scores on movement and sedation scores should be kept for all women<br />
postoperatively, and additional analgesia should be offered without delay when required.<br />
Recovery care<br />
Local guidelines (based on relevant national standards) for standards of care in recovery should be<br />
regularly updated, audited and monitored.<br />
The following are recommendations of the AAGBI [16]:<br />
• No fewer than two members of staff (of whom at least one must be a registered practitioner)<br />
should be present when there is a patient in recovery who does not fulfil the criteria for discharge<br />
to the ward<br />
• All registered practitioners should be appropriately trained in accordance with the standards and<br />
competencies detailed in the UK National Core Competencies for Post-anaesthesia Care [31].<br />
All women leaving obstetric recovery areas should continue to receive appropriate post-operative<br />
care. Staff caring for post-operative patients on post-natal wards must be trained to do so, and should<br />
carry out post-surgical care as set out in local guidelines.<br />
There should be a ratio of two recovery beds to one operating theatre [31]. It should be noted that<br />
more space is required per bed area for obstetric theatre recovery, compared with general postoperative<br />
recovery areas. This is because there is a need to accommodate birth partners, cots etc as<br />
well as the patient in the same area.<br />
To ensure privacy and dignity are maintained and that infection risk is reduced there should be<br />
adequate space between beds, and the facility to have private conversations with mothers and to<br />
conduct physical examinations (for example to check vaginal blood loss) [29].<br />
Postnatal care<br />
Following operative delivery, women need continuing care [29]. Any woman who has received<br />
neuraxial opioids should have respiratory rate, pain and sedation scores monitored for a period<br />
appropriate to the clinical situation.<br />
Women who have received anaesthetic care (whether analgesia for labour or anaesthesia) should be<br />
followed up routinely to obtain feedback and exclude complications. With early discharge following<br />
delivery, it may be logistically impossible to achieve this, and significant complications may not<br />
become manifest until after women have been discharged. Therefore, all women who have received<br />
regional analgesia or anaesthesia should receive written information about when and how to seek<br />
help if complications should arise; this is particularly important for women who are discharged within<br />
13
24 hours of their procedure. Patients who have suffered significant complications (for example<br />
awareness under general anaesthesia, accidental dural puncture) should be offered follow-up<br />
outpatient review with a consultant anaesthetist in the postnatal period [23].<br />
Resuscitation team<br />
A team trained in advanced resuscitation of the pregnant woman should be available to all women in<br />
obstetric units, and their skills should include the ability to carry out a peri-mortem caesarean section.<br />
A system for calling and admitting the team urgently to the delivery unit should be in place. Regular<br />
team training drills should be held.<br />
Risk management<br />
Units are expected to participate in relevant national audits, e.g. the Confidential Enquiries into<br />
Maternal Deaths, the OAA’s National Obstetric Anaesthetic Database (NOAD), the UK Obstetric<br />
Surveillance System (UKOSS), national incident reporting to the Medicines and Healthcare products<br />
Regulatory Agency (MHRA) and other relevant bodies, local incident reporting and risk management.<br />
Quality improvement, involving continuous monitoring of activity and outcomes to facilitate continuous<br />
quality improvement, using appropriate formats, should be practised. The RCoA publishes a list of<br />
relevant audits of obstetric anaesthesia services, which should be used to audit these standards [23].<br />
Local safety procedures such as syringe labelling, double checking or both should be developed to<br />
reduce the risk of wrong-route and other drug and infusion errors – and there should be adherence to<br />
national standards in all locations, including in delivery rooms.<br />
Local anaesthetic solutions intended for epidural infusion should be stored separately from<br />
intravenous infusion solutions, in a locked cupboard or other safe area, to minimise the risk of<br />
accidental intravenous administration of such drugs [32].<br />
Maternal critical care<br />
Maternity critical care is an important emerging area for obstetric anaesthetists that poses significant<br />
organisational and clinical challenges. Compared with other areas of acute medicine, there is a<br />
paucity of published evidence on which to base guidance.<br />
Timely recognition of the sick parturient is key to ensuring a good outcome and reducing maternal<br />
morbidity and mortality. Maternity services should implement NICE guidance on the recognition and<br />
response to acute illness in adults in hospital [33]. Although these guidelines do not specifically<br />
include the sick parturient, they provide a clear strategy for the delivery of care in this area.<br />
Physiological observations should be recorded on admission for all women admitted to maternity<br />
units, including midwifery-led units. A graded response strategy for patients identified as being at risk<br />
14
of clinical deterioration, as recommended by the Maternity Critical Care Working Party [3], should be<br />
agreed and delivered locally.<br />
It is widely recognised that the quality of evidence for track-and-trigger systems in any area of<br />
medicine is limited. Such systems allowing a graded medical response can be based on aggregate<br />
scoring of physiological parameters (where points are allocated according to the degree of<br />
derangement of physiological variables, and then combined into a composite score). Alternatively,<br />
multiple parameter systems can be used (in which constituent criteria are not assigned a score but<br />
instead trigger when combinations of criteria are met). Both systems have inherent advantages and<br />
disadvantages. The recently published National Early Warning Score is an aggregate system but<br />
specifically excludes the obstetric population [34].<br />
Whether an aggregate or multiple parameter system is used, the response should consist of the<br />
following three levels:<br />
• Low-score group: increased frequency of observations and the midwife in charge alerted<br />
• Medium-score group: urgent call to team with primary medical responsibility for the patient, plus a<br />
simultaneous call to personnel with core competences for acute illness<br />
• High-score group: emergency call to a team with critical care competences and a maternity team.<br />
There should be an immediate response.<br />
The Department of Health has defined a chain of response for the hospital team involved in the care<br />
of the acutely ill patient in hospital (Fig. 1) [34]. This can be adapted for use in the maternity setting.<br />
Non-clinical<br />
Staff<br />
→ Recorder → Recogniser →<br />
Primary<br />
Responder<br />
→<br />
Secondary<br />
Responder<br />
→<br />
Tertiary<br />
Responder<br />
(Critical Care)<br />
Communication and handover<br />
Figure 1 Chain of response for acutely ill patients in hospital. Redrawn from [34].<br />
Staffing<br />
Where level-2 care (see below) is provided in the maternity unit, staff appropriately trained to provide<br />
HDU care should be available 24 hours a day. The midwife/nurse-to-patient ratio must be at least one<br />
midwife/nurse to two patients or one-to-one if care is provided in individual rooms. Midwives working<br />
in this setting should have additional training that equips them with the necessary critical care<br />
competences that have been clearly set out [3].<br />
There should be a named consultant anaesthetist and obstetrician responsible for all level-2 patients,<br />
24 hours a day.<br />
15
High dependency care (level-2 adult critical care)<br />
Since 2007, the obstetric population has been included in the Intensive Care Society (ICS) definitions<br />
of levels of care in the adult population (Table 2) [35].<br />
Table 2 Levels of care as defined by the ICS [35].<br />
Level 0 Patients whose needs can be met by normal ward care<br />
Level 1<br />
Patients at risk of deterioration, needing a higher level of observation or those recently<br />
relocated from higher levels of care<br />
Level 2<br />
Patients requiring invasive monitoring/intervention that includes support for a single<br />
failing organ (excluding advanced respiratory support i.e. mechanical ventilation)<br />
Level 3<br />
Patients requiring advanced respiratory support alone or basic respiratory support in<br />
addition to support of one or more additional organs<br />
All units that care for high-risk patients must be able to access level-2 (HDU care) on site. Level-2<br />
care may be provided within the maternity unit or within a hospital’s general adult critical care unit.<br />
Level-2 care should be delivered to the same standard regardless of the setting.<br />
Larger obstetric units should have a designated consultant (usually an anaesthetist) with relevant<br />
skills who is responsible for delivery of obstetric HDU care. This lead person should ensure that local<br />
standards are developed for identifying women who require critical care, based on existing national<br />
standards [35].<br />
In smaller units, the lead obstetric anaesthetist should ensure that local standards exist.<br />
Intensive care (level-3 adult critical care)<br />
Some patients on the maternity HDU (level 2) may progress to requiring level-3 critical care (ICU).<br />
Delays in the transfer of critically ill obstetric patients to the ICU can significantly increase the mortality<br />
rate. Therefore it is essential that every unit has clear pathways in place to facilitate transfer. There<br />
should be close co-operation between the maternity HDU and the ICU teams at an early stage, with<br />
consultant-to-consultant referral and early involvement of the ICU consultant. Formal, documented<br />
local arrangements should exist for support and input from other disciplines (cardiology, respiratory<br />
medicine and allied professionals) when required.<br />
Escalation protocols should be in place for women requiring level-3 critical care.<br />
All patients must be able to access level-3 critical care if required; units without such provision on site<br />
must have an arrangement with a nominated level-3 ICU and an agreed policy for the stabilisation<br />
and safe transfer of patients to this unit when required.<br />
16
5. Training and education<br />
Each obstetric anaesthetic unit should have a consultant with overall responsibility for the training and<br />
education of trainee and non-trainee anaesthetists. They should be supported locally by trainers,<br />
educational supervisors, College Tutors and Regional Advisors, and programmed activity time should<br />
be allocated for work relating to this responsibility. Trainers must fulfil the RCoA [36] and General<br />
Medical Council (GMC) criteria [37] and can include consultants, SAS doctors and senior trainees.<br />
It is expected that in the future, the service is likely to be consultant-delivered; however, in the interim,<br />
rotas should be designed to maximise training opportunities including, for example, an extended<br />
working day for consultants [38].<br />
Although a 24-hour obstetric anaesthetic consultant presence is the ideal, trainees also need to learn<br />
to work without direct supervision and should develop their skills and confidence accordingly, without<br />
compromising patient safety.<br />
Induction<br />
All trainee and non-trainee anaesthetists, regardless of prior experience in obstetric anaesthesia,<br />
should receive a formal induction to the obstetric anaesthetic unit before commencing duties there<br />
(see Section 3).<br />
Levels of training<br />
• A training programme appropriate to the educational opportunities offered by the unit should be in<br />
place as documented in the RCoA 2010 Curriculum [36]<br />
• Basic training for core trainees: this should consist of an absolute minimum of 20 directly<br />
supervised sessions within a four-month period, during which time the trainee should achieve the<br />
core clinical learning outcomes. It is recommended that at least half of these sessions are<br />
supervised by a consultant obstetric anaesthetist<br />
• Intermediate training for ST3/4 trainees: obstetric anaesthesia is one of the essential units of<br />
intermediate level training. There should be a dedicated block of training over a 4-12 week period<br />
and this should include 20 sessions as a minimum in order that all core clinical learning outcomes<br />
can be completed. It would be anticipated that for most trainees, this would require several more<br />
sessions than the 20 recommended<br />
• Higher training: the majority of ST5/6/7 trainees will be expected to complete this level which is<br />
required for any consultant covering delivery suite out of hours. It can be delivered in nonspecialist<br />
units. Local arrangements should be in place to ensure that all the required learning<br />
outcomes can be completed<br />
• Advanced training for ST6/7 trainees: this should be undertaken by those trainees wishing to<br />
develop a sub-specialty interest in obstetric anaesthesia and/or undertake daytime sessions in<br />
obstetric anaesthesia, and those who are likely to go on to work in an obstetric tertiary referral<br />
17
centre. This level of training can only be delivered in centres that allow the trainee the opportunity<br />
to develop the skills required to manage the delivery suite and undertake complex obstetric cases<br />
whilst building and consolidating knowledge of obstetric anaesthesia, obstetrics and neonatology<br />
• Less than full-time (LTFT) trainees: at each level of training, LTFT trainees should be given an<br />
appropriate period of training in obstetric anaesthesia, proportionate to the percentage of whole<br />
time equivalent worked.<br />
Assessment<br />
Completion of the IACOA is mandatory for all core trainees before being allowed to work in an<br />
obstetric unit without direct supervision. Achieving the IACOA, however, does not signal the<br />
completion of the basic level unit of training in obstetric anaesthesia.<br />
Supervision<br />
All trainees should be supervised directly by a trainer present on delivery suite until the IACOA is<br />
completed. In addition, a joint OAA/ RCoA survey in 2010 [5] recommended that:<br />
• The IACOA should be used in conjunction with a local system of review that satisfies local clinical<br />
governance arrangements before a trainee works without immediate supervision<br />
• No trainee who feels unprepared to start obstetric on-call (regardless of completion of IACOA)<br />
should be expected to join the on-call rota unless directly supervised. Departments should make<br />
provision for this eventuality where rotas are written a long time in advance<br />
• All trainees who have completed their basic obstetric training should have some opportunity to<br />
cover the labour ward without immediate supervision, so that they are confident to take on this<br />
responsibility once they are appointed to an ST3 post.<br />
The first two of the above recommendations should also apply to non-trainee anaesthetists. All trainee<br />
and non-trainee anaesthetists working without direct supervision on delivery suite must have a named<br />
supervising consultant and both parties must be happy with the level of supervision available. In<br />
addition, they must know how to contact the supervising consultant in the event of an emergency.<br />
Simulation<br />
Simulation-based educational techniques can be used to assist all anaesthetists to develop the skills<br />
and attributes required to work safely and efficiently within the multidisciplinary obstetric team,<br />
including:<br />
• Technical skill development using part-task simulators e.g. epidural, cricothyroidotomy [39]<br />
• Reinforcement of emergency drills e.g. failed intubation [40]<br />
• Teaching and assessing clinical skills when clinical opportunities are limited e.g. general<br />
anaesthesia for caesarean section<br />
• Maternal and neonatal resuscitation [40]<br />
• Teamwork training emphasising non-technical skills [9]<br />
18
• Skills and drills training: anaesthetists should help organise and participate in regular<br />
multidisciplinary drills covering delivery suite emergencies such as major obstetric haemorrhage,<br />
maternal collapse and failed intubation [41]. These drills should be followed by debriefing and<br />
feedback so that lessons can be learned at both an individual and a systems level.<br />
Continuing professional development<br />
All anaesthetists involved in the delivery of obstetric anaesthetic services should undertake<br />
appropriate continuing professional development activities in line with revalidation guidelines.<br />
19
6. The labour ward team<br />
Maternity care is delivered by teams rather than individuals. Effective teamwork can increase safety;<br />
poor teamwork can have the opposite effect [9]. A report on safety standards in the maternity services<br />
identified the following problems:<br />
• Differing goals of midwives and doctors with regard to the care of women<br />
• Poor leadership and management<br />
• Difficulties with communication between healthcare professionals during emergencies and shift<br />
changes<br />
It is essential that obstetric anaesthetists should establish clear lines of communication with other<br />
professionals such as intensivists, neurologists, cardiologists, haematologists, other physicians,<br />
surgeons, radiologists, outreach nurses, physiotherapists and pharmacists.<br />
Team briefing and a safety checklist should be used routinely to facilitate good communication and<br />
teamworking and reduce adverse incidents [42].<br />
Checklists and team briefing<br />
Pre-operative checklists and team briefing procedures should be used, both for elective and<br />
emergency obstetric operations. Nationally-developed obstetric modifications of the standard format<br />
exist and should be used or adapted for local use. In extreme emergencies, the procedure may be<br />
truncated, but it must be borne in mind that these are the most error-prone situations. Use of the<br />
checklist should be audited.<br />
Anaesthetists and midwives<br />
‘Midwifery-led care’ refers to all cases in which the lead professional for the case is a midwife rather<br />
than an obstetrician. This type of care may be delivered in a variety of units. If regional analgesia is<br />
required, the anaesthetist may be the only medically-qualified person involved with the<br />
labour/delivery.<br />
It is recommended that the following criteria should be met whenever a hospital or maternity unit is<br />
proposing that anaesthetists should work directly with midwives who are acting as lead providers of<br />
obstetric care:<br />
• There should be a consultant-led obstetric service on site<br />
• There must be guidelines in place for the management of regional analgesia that have been<br />
agreed by anaesthetists, midwives and obstetricians. Midwives practising independently but<br />
intending to make use of a regional analgesia service must agree to follow the guidelines of the<br />
unit where they deliver their clients<br />
20
• The midwife caring for a woman with an epidural must be trained in its management to a standard<br />
acceptable to the anaesthetist responsible for the service, must undergo regular refresher<br />
training, and must be managing regional analgesia on a regular basis<br />
• The midwife must allow the anaesthetist access to any woman considering regional analgesia<br />
who wishes to discuss pain relief options<br />
• If the anaesthetist feels that an obstetric opinion is necessary, he/she should consult the midwife<br />
in the first instance. However, if necessary, the anaesthetist may consult directly with the<br />
obstetricians, but should inform the midwife that this is his/her intention<br />
• All decisions regarding regional analgesia must rest with the anaesthetist.<br />
Anaesthetists and obstetricians<br />
• Anaesthetists should encourage and facilitate consultation in the antepartum period by making<br />
themselves available when antenatal clinics are in progress and by ensuring clear lines of referral.<br />
A system for the antenatal assessment of high-risk mothers should be in place with 24-hour<br />
access to the information on the delivery suite<br />
• Good communication on the delivery suite is vital in order to minimise last-minute referral and the<br />
hasty decision-making that often ensues. Anaesthetists should make themselves known to<br />
obstetricians who should, in turn, keep them informed of developing problems. Anaesthetists’<br />
attendance at obstetric ward rounds is to be encouraged in order to be kept well informed of the<br />
labour ward caseloads and casemix<br />
• There should be formal arrangements in place and protected time for multidisciplinary handover<br />
at the beginning and end of each shift<br />
• Anaesthetists should be involved in planning decisions that affect the delivery of maternity<br />
services. Anaesthesia should be represented on any committee that has relevance to anaesthetic<br />
services on the labour ward such as the labour suite working party, obstetric directorate and risk<br />
management forum.<br />
Communication and classification of urgency<br />
Whilst this section applies primarily to delivery by caesarean section, many of the items also apply in<br />
principle to trial of operative vaginal delivery in the operating theatre. Standard classification of the<br />
urgency of caesarean section as described in Section 4.6 should be used for caesarean section and<br />
this classification should be considered for operative vaginal delivery. It is recognised that this grading<br />
artificially categorises cases when in reality there is a continuum of risk, and that within a grade, some<br />
cases may require delivery more urgently than others. Each case must be graded and managed<br />
individually.<br />
The situation may change after the decision to deliver has been made, and the classification should<br />
be re-assessed following transfer to theatre by the responsible obstetrician, and kept under review<br />
whilst anaesthesia is established.<br />
21
Communicating both the planned procedure and its grade of urgency with the entire theatre team, as<br />
soon as the decision to deliver is taken, is vital, and a process for doing this should be covered by<br />
local guidelines. In addition, the anaesthetist responsible for the anaesthetic should be informed of<br />
both the indication for the procedure and its urgency by the operating obstetrician in person whenever<br />
possible.<br />
Transferring patients to theatre may lead to delays, and measures to reduce such delays should be<br />
covered by local guidelines.<br />
Other professionals and roles<br />
Neonatal resuscitation<br />
Units differ as to their policies about the involvement of the anaesthetist in neonatal resuscitation.<br />
Where they are given a role, anaesthetists should work with the neonatal team to ensure that<br />
appropriate training is delivered and maintained.<br />
Maternity care assistants<br />
The role of maternity care assistants (MCAs) is to complement and not to substitute for midwives. In<br />
some units they may be involved in monitoring and recording routine observations, or in assisting with<br />
epidural placement or in theatre. Appropriate training must be provided if they are to adopt these<br />
roles.<br />
Support personnel<br />
Increasing activity on the labour ward that requires information input, admissions and clerical duties<br />
demonstrate the need for a ward clerk or receptionist to be available at all times. Housekeeping,<br />
portering and maintenance teams need to be accessible on site because of the high turnover bed<br />
occupancy, high technology environment and emergency service provision.<br />
22
7. Support services, equipment, facilities and accommodation<br />
For the efficient functioning of the obstetric anaesthetic service, the following support services,<br />
equipment, facilities and accommodation are essential. The standards of equipment and monitoring<br />
must be the same as that of non-obstetric anaesthetic service.<br />
Support services<br />
A supply of O rhesus-negative blood should be immediately (within five minutes) available to the<br />
delivery suite at all times for emergency use. Grouping can be performed in about 10 minutes [42]<br />
and group-specific blood should be delivered within 20 minutes of request. Standard issue of crossmatched<br />
blood may take approximately 45 minutes [43] although some patients without antibodies<br />
may be eligible for electronic issue which can be much quicker: if the laboratory is in receipt of two<br />
‘group & save’ samples taken on separate occasions they may be able to issue cross-matched blood<br />
as rapidly as group-specific [44].<br />
In order to ensure that blood can be made available within the time frames stipulated, the transfusion<br />
laboratory should ideally be situated on the same site as the maternity unit.<br />
Due to changes in transfusion practice, apart from packed red cells, blood products such as fresh<br />
frozen plasma (FFP), cryoprecipitate and platelets are now required earlier in the management of<br />
haemorrhage. As part of the response to a major obstetric haemorrhage call, the laboratory should<br />
make FFP available as rapidly as possible, enabling an approximate 1:1 ratio of red cells:FFP if<br />
deemed appropriate [44]. Platelets are not stored by all laboratories. If a significant delay is<br />
anticipated, the delivery suite should be notified in advance. The use of fibrinogen and prothrombin<br />
complex concentrates should be considered early [45].<br />
Haematology and biochemistry services must be able to provide rapid analysis of blood and other<br />
body fluids. However, near-patient testing (see below) will guide blood and product replacement far<br />
more quickly than standard laboratory tests and should be utilised whenever possible.<br />
There must be rapid availability of diagnostic radiological services. In tertiary referral centres, 24-hour<br />
access to interventional radiology services is highly recommended.<br />
Medical physics technicians are required to maintain, repair and calibrate anaesthetic machines,<br />
monitoring and infusion equipment.<br />
Physiotherapy services should be available 24 hours a day, 365 days a year for patients requiring<br />
critical care.<br />
23
Hotel services must provide suitable on-call facilities including housekeeping for resident and nonresident<br />
anaesthetic staff. Refreshments must be available throughout the 24-hour period.<br />
There must be adequate secretarial support for the antenatal anaesthetic assessment clinic and other<br />
duties of the consultant obstetric anaesthetist: teaching; research; audit; study; appraisal activities;<br />
and other administrative work.<br />
Equipment<br />
Units should purchase appropriate equipment to enable safe delivery of neuraxial analgesia and<br />
anaesthesia with regard to any relevant national or international safety guidance. It is mandatory that<br />
local obstetric anaesthetists are involved in purchasing decisions involving equipment for neuraxial<br />
analgesia and anaesthesia. Epidural infusion sets should conform to standards for colour-coding and<br />
should be labelled.<br />
A blood warmer allowing the transfusion of blood and fluids as well as warm air blankets must be<br />
available. A Level 1® or equivalent rapid infusion device should be available for the management of<br />
major haemorrhage.<br />
A difficult intubation trolley with a variety of laryngoscopes, laryngeal mask airways and tracheal tubes<br />
should be available. Second generation supraglottic airway devices that give some protection from<br />
gastric contents [45] and other aids for airway management must be available in theatre. There<br />
should be 24-hour access to a fibreoptic ’scope [46].<br />
The maximum weight that the operating table can support must be known and alternative provision<br />
made for women who exceed this. The operating table should be able to support a weight of at least<br />
160 kg. Other equipment to facilitate the care of obese parturients such as weighing scales,<br />
wheelchairs, equipment to assist with the transfer of patients between beds, equipment to assist with<br />
ramping in order to optimise head and neck position for laryngoscopy, and appropriate ward beds<br />
should be readily available [47].<br />
Cell salvage equipment (and personnel trained it its use) should be available at all times for<br />
emergency and elective caesarean sections in units that deliver women who decline to have blood<br />
transfusion [48].<br />
There must be equipment such as HemoCue® or blood gas analyser to enable bedside estimation of<br />
haemoglobin concentration.<br />
It is strongly recommended that there should be equipment to enable bedside estimation of<br />
coagulation such as thromboelastography (TEG) or thromboelastometry (ROTEM) [43].<br />
24
Equipment for PCA must be available for postoperative pain relief. Ultrasound machines should be<br />
available for the use of ultrasound-guided central venous pressure lines insertion and transversus<br />
abdominis plane (TAP) blocks, and to assist with central neuraxial blocks in obese patients.<br />
Accurate clocks should be available in all delivery rooms and theatres.<br />
Resuscitation equipment including a defibrillator should be readily available on the delivery suite and<br />
should be checked regularly.<br />
Facilities<br />
The delivery suite rooms must be equipped with monitoring equipment for the measurement of noninvasive<br />
blood pressure. There should also be readily available equipment for monitoring ECG,<br />
oxygen saturation, temperature and invasive haemodynamic monitoring if required. All delivery rooms<br />
must have oxygen, suction equipment and access to resuscitation equipment. Delivery suite rooms<br />
must have active scavenging of inhalational analgesics to comply with Control of Substances<br />
Hazardous to Health (COSHH) guidelines on anaesthetic gas pollution [49].<br />
There must be easy and safe access to the delivery suite from the main hospital at all times of the<br />
day.<br />
There should be at least one fully-equipped obstetric theatre within the delivery suite. Where this is<br />
not possible, a lift that can be commandeered for the rapid transfer of women to theatre must be<br />
available. The number of operating theatres required should depend on the number of deliveries and<br />
operative risk profile of the women delivering in the unit.<br />
Obstetric theatres should be equipped and staffed to the same standards as other operating theatres.<br />
[13, 49]. The standard of monitoring in the obstetric theatre must allow the conduct of safe<br />
anaesthesia for surgery. The same standards of monitoring apply whenever an anaesthetist is<br />
responsible for anaesthesia, whether general, regional or local [50].<br />
Adequate post-anaesthesia care facilities, including the ability to monitor systemic blood pressure,<br />
ECG, oxygen saturation and capnography, must be available within the delivery suite theatre<br />
complex. The layout/lighting should conform to established standards; however, it must be<br />
appreciated that obstetric recovery spaces need to be much larger than required for standard adult<br />
recovery [16, 51].<br />
There should be readily available ‘eclampsia boxes’ containing all necessary equipment and a<br />
protocol for eclampsia [52].<br />
25
Lipid emulsion, dantrolene and sugammadex may all be useful in anaesthetic emergencies. These<br />
should be immediately available on the delivery suite and location of these drugs should be clearly<br />
identified. Local anaesthetic and opioid solutions intended for epidural use should be available and<br />
stored separately from intravenous fluids to minimise the risk of accidental intravenous administration<br />
of such fluids.<br />
All units that care for high-risk patients should be able to access level-2 HDU care on site (see<br />
Section 4).<br />
Accommodation<br />
All consultant obstetric units should include dedicated office space for the sole use of the anaesthesia<br />
team on the delivery suite, or close enough for the resident anaesthetist to be able to work there<br />
between cases. This space should have adequate information technology facilities for both trainee<br />
and trained staff to be able to deal with emails, complete mandatory online training, access journals<br />
and search engines via the internet, complete portfolios and enter audit-related data. Local<br />
multidisciplinary evidence-based guidelines must be available in the office. The office space, facilities<br />
and furniture should comply with the standards recommended by AAGBI guidelines [53].<br />
A library of specialist reference books/journals should be available. There should be a separate<br />
anaesthetic consultants’ office available to allow teaching, assessment and appraisal, that complies<br />
with AAGBI guidelines [53].<br />
A communal rest-room in the delivery suite should be provided to enable staff of all specialities to<br />
meet. A seminar room(s) must be available for training, teaching and multidisciplinary meetings.<br />
We strongly support the provision of an on-call room containing a bed as there is good evidence that<br />
even short periods of sleep improve performance during nightshift work (regardless of the length of<br />
the shift) [8, 54].<br />
Where a consultant is required to be resident, appropriate on-call accommodation should be provided<br />
[55].<br />
26
8. The future<br />
The delivery of healthcare constantly needs to evolve to meet the challenges of a changing population<br />
and deliver high-quality care; obstetric anaesthesia is no exception to this.<br />
Changes in healthcare encompass both organisational and clinical aspects. Developments that the<br />
Working Party supports include:<br />
• An aspiration to develop a 24-hour consultant-delivered anaesthesia service in the maternity unit,<br />
with the instigation of twilight and weekend sessions as an initial step<br />
• An expanded role of the obstetric anaesthetist as a ‘peripartum physician’ – in particular, more<br />
antenatal involvement in the management of women with high-risk/complicated pregnancies<br />
• Developing relationships between the maternity team and other specialities in the hospital setting,<br />
e.g. medical specialities such as cardiology, with maternity units receiving support from a named<br />
cardiologist<br />
• More extensive use of near-patient testing in the maternity unit<br />
• Development of safe and effective alternatives to regional analgesia in labour<br />
• Outcome-based research on the impact of intrapartum analgesia and anaesthesia on mother and<br />
baby<br />
• Further research into increased levels of anaesthetic safety<br />
• Development of enhanced recovery programmes in obstetrics<br />
• Confirmation at Department of Health level of the uninterrupted continuation of the Confidential<br />
Enquiries into maternal death and morbidity with more timely and frequent reports<br />
• Promoting equitable provision of anaesthetic services by ensuring anaesthetic representation on<br />
commissioning bodies.<br />
27
9. List of recommended guidelines<br />
Departments should have written guidelines, setting out local standards of care (based on national<br />
standards where these exist), including as a minimum the following (listed alphabetically):<br />
• Analgesia post-caesarean section (including TAP blocks)<br />
• Antacid prophylaxis for labour and delivery<br />
• Antibiotic and thromboprophylaxis for caesarean section<br />
• Awareness under general anaesthesia<br />
• Cell salvage<br />
• Conditions requiring antenatal referral to the anaesthetist<br />
• Fasting before elective and emergency obstetric procedures<br />
• General anaesthesia for caesarean section<br />
• Guideline development<br />
• HDU admission and discharge criteria<br />
• High BMI (> 40 kg.m -2 )<br />
• Intrauterine fetal resuscitation<br />
• Intravenous opioid PCA (Including remifentanil PCA if available locally)<br />
• Management of major haemorrhage (including trigger phrase to activate major haemorrhage<br />
transfusion protocol)<br />
• Management of pre-eclampsia and eclampsia<br />
• Modified Obstetric Early Warning Score use<br />
• Oral intake during labour<br />
• Provision of information to patients including:<br />
o Anaesthesia for caesarean section (general and regional)<br />
o Pain management in labour<br />
• Regional anaesthesia including:<br />
o Hypotension during regional block<br />
o Management of failed or inadequate regional block<br />
o Management of high regional block<br />
o Management of accidental dural puncture<br />
o Management of epidural haematoma<br />
o Management of post-dural puncture headache<br />
o Management of regional techniques in patients receiving thromboprophylaxis<br />
o Regional blocks for labour analgesia<br />
o Regional blocks for surgery<br />
• Recovery following general and regional anaesthesia<br />
• Resuscitation of the pregnant patient<br />
• Staffing levels<br />
• Skills and drills training.<br />
28
The following national guidelines should be displayed or be immediately available in all locations<br />
where obstetric anaesthesia is delivered:<br />
• Adult resuscitation guidelines [Resuscitation Council (UK)]<br />
• Anaesthetic machine checklist [AAGBI]<br />
• Management of:<br />
o Anaphylaxis [AAGBI and/or Resuscitation Council (UK)]<br />
o Failed intubation [to be produced by Dififcult Airway Society/OAA]<br />
o Malignant hyperthermia [AAGBI]<br />
o Neonatal life support [Resuscitation Council (UK)]<br />
o Peri-arrest arrhythmias [Resuscitation Council (UK)]<br />
o Severe local anaesthetic toxicity [AAGBI]<br />
29
10. References<br />
1. Association of Anaesthetists of Great Britain & Ireland and Obstetric Anaesthetists’ Association.<br />
Guidelines for Obstetric Anaesthesia Services. London: AAGBI, 1998.<br />
2. Association of Anaesthetists of Great Britain & Ireland and Obstetric Anaesthetists’ Association.<br />
Guidelines for Obstetric Anaesthetic Services 2. London: AAGBI, 2005.<br />
3. Maternity Critical Care Working Group. Providing Equity of Critical and Maternity Care for the<br />
Critically Ill Pregnant or Recently Pregnant Woman. London: Royal College of Anaesthetists, 2011.<br />
4. Grocott MPW, Pearce RM. Perioperative medicine: the future of anaesthesia? British Journal of<br />
Anaesthesia 2012; 108: 723-6.<br />
5. Obstetric Anaesthetists’ Association. Joint RCoA-OAA obstetric anaesthetic training survey 2010.<br />
http://www.oaa-anaes.ac.uk/content.asp?ContentID=452 (accessed 26/04/2013).<br />
6. Obstetric Anaesthetists’ Association. OAA-AAGBI workload survey. http://www.oaaanaes.ac.uk/content.asp?ContentID=467<br />
(accessed 19/03/2013).<br />
7. Royal College of Obstetricians and Gynaecologists, Royal College of Anaesthetists, Royal College<br />
of midwives, Royal College Paediatrics and Child Health. Safer Childbirth: Minimum Standards for<br />
the Organization and Delivery of Care in Labour. London: RCOG Press, 2007.<br />
8. Association of Anaesthetists of Great Britain & Ireland. Fatigue and Anaesthetists. London: AAGBI,<br />
2004.<br />
9. The King’s Fund. Safe Births: Everybody’s Business. London: The King’s Fund, 2008.<br />
10. Audit Commission. Anaesthesia under Examination: the Efficiency and Effectiveness of<br />
Anaesthesia and Pain Relief Services in England and Wales. Oxford: Audit Commission, 1997.<br />
11. Yentis SM, Robinson PN. Definitions in obstetric anaesthesia: how should we measure anaesthetic<br />
workload and what is ‘epidural rate’? Anaesthesia 1999; 54: 958–62.<br />
12. Royal College of Obstetricians and Gynaecologists. High Quality Women’s Health Care: a Proposal<br />
for Change. London: RCOG Press, 2011.<br />
13. College of Operating Department Practitioners. Staffing of obstetric theatres – a consensus<br />
statement. http://www.codp.org.uk/documents/Staffing%20of%20Obstetric%20Theatres.pdf<br />
(accessed 19/03/2013).<br />
14. Association of Anaesthetists of Great Britain & Ireland. The Anaesthesia Team 3. London: AAGBI,<br />
2010.<br />
15. NHS Education for Scotland. Core competencies for anaesthetic assistants 2011<br />
www.nes.scotland.nhs.uk/media/4239/anaesthetic_core_competencies_2011.pdf (accessed<br />
19/03/2013).<br />
16. Association of Anaesthetists of Great Britain & Ireland. Immediate Post-anaesthesia Recovery<br />
2013. Anaesthesia 2013; 68: 288-97.<br />
17. RCOG/CMACE. Joint Guideline Management of women with obesity in pregnancy. London:<br />
RCOG/CMACE, 2010.<br />
18. Obstetric Anaesthetists’ Association. Referral to anaesthetists. http://www.oaaanaes.ac.uk/content.asp?ContentID=339<br />
(accessed 19/03/2013).<br />
30
19. Obstetric Anaesthetists’ Association. Information for mothers. http://www.oaaanaes.ac.uk/content.asp?ContentID=83<br />
(accessed 19/03/2013).<br />
20. Association of Anaesthetists of Great Britain & Ireland. Consent for Anaesthesia 2. London: AAGBI,<br />
2006.<br />
21. Jones L, Othman M, Dowswell T, et al. Pain management for women in labour: an overview of<br />
systematic reviews. http://www.thecochranelibrary.com/details/file/1598141/CD009234.html<br />
(accessed 19/03/2013).<br />
22. National Institute for Health and Clinical Excellence. NICE Clinical Guideline 55. Intrapartum Care.<br />
London: NICE, 2007. [being updated]<br />
23. Royal College of Anaesthetists. Raising the Standard: a Compendium of Audit Recipes. 3 rd Edition<br />
2012. London: RCoA, 2012.<br />
24. Royal College of Anaesthetists. NAP3 National Audit of Major Complications of Central Neuraxial<br />
Block in the United Kingdom, p75. London: RCoA, 2009.<br />
25. Scott M, Stones J, Pane N. Antiseptic solutions for central neuraxial blockade: which concentration<br />
of chlorhexidine in alcohol should we use? British Journal of Anaesthesia 2009; 103: 456-57.<br />
26. Hinova A, Fernando R. Remifentanil for labor analgesia. Anesthesia and Analgesia 2009; 109:<br />
1925-29.<br />
27. Muchatula NA, Kinsella SM. Remifentanil for labour analgesia: time to draw breath? Anaesthesia<br />
2013; 68: 227- 35.<br />
28. Obstetric Anaesthetists’ Association. Remifentanil. http://www.oaaanaes.ac.uk/content.asp?ContentID=333<br />
(accessed 26/03/13).<br />
29. National Institute for Health and Clinical Excellence. Caesarean section clinical guidelines CG132.<br />
http://www.nice.org.uk/CG132 (accessed 26/03/2013).<br />
30. Association of Anaesthetists of Great Britain & Ireland. Preoperative Assessment and Patient<br />
Preparation. The Role of the Anaesthetist 2. London: AAGBI, 2010.<br />
31. Association of Anaesthetists of Great Britain & Ireland. UK National Core Competencies for Post-<br />
Anaesthesia Care. London: AAGBI, 2013.<br />
32. The Royal College of Anaesthetists. NAP3 full report. www.rcoa.ac.uk/document-store/nap3-fullreport<br />
(accessed 26/03/2013).<br />
33. National Institute for Health and Clinical Excellence. Acutely ill patients in hospital clinical<br />
guidelines CG50. http://guidance.nice.org.uk/CG50 (accessed 26/03/2013).<br />
34. Royal College of Physicians. National Early Warning Scores (NEWS).<br />
http://www.rcplondon.ac.uk/sites/default/files/documents/national-early-warning-scorestandardising-assessment-acute-illness-severity-nhs.pdf<br />
(accessed 26/03/2013).<br />
35. Intensive Care Society. Levels of Critical care for Adult Patients. London: ICS, 2009.<br />
36. Royal College of Anaesthetists. Curriculum for a CCT in Anaesthetics, 2 nd edn, London: RCoA,<br />
2010.<br />
37. General Medical Council. The Trainee Doctor. London: GMC, 2011.<br />
31
38. Royal College of Anaesthetists. Working Time Directive 2009 and shift working: ways forward for<br />
anaesthetic services, training, doctor and patient safety. https://www.rcoa.ac.uk/system/files/TRG-<br />
WTR-Shift-Working.pdf (accessed 10/04/2013).<br />
39. Uppal V, Kearns RJ, McGrady EM. Evaluation of the M43B Lumbar Puncture Simulator II as a<br />
training tool for identification of the epidural space and lumbar puncture. Anaesthesia 2011; 66:<br />
493-6.<br />
40. Pratt S. Simulation in obstetric anaesthesia, Anesthesia and Analgesia 2012; 114: 186-90.<br />
41. NHS Litigation Authority. Clinical Negligence Scheme for Trusts, maternity clinical risk<br />
management standards.<br />
http://www.nhsla.com/safety/Documents/Central%20Manchester%20University%20Hospitlas%20N<br />
HS%20Foundation%20Trust%20-%20February%202012%20-%20Maternity.pdf (accessed<br />
10/04/2013).<br />
42. Haynes AB, Weiser TG, Berry WR, et al. The safe surgery saves lives study group. A surgical<br />
safety checklist to reduce morbidity and mortality in a global population. New England Journal of<br />
Medicine 2009; 360:491-9.<br />
43. Association of Anaesthetists of Great Britain &Ireland. Blood Transfusion and the Anaesthetist.<br />
Management of Massive Haemorrhage. London: AAGBI, 2010.<br />
44. Medicines and Healthcare Products Regulatory Agency. MHRA guidance on electronic issue.<br />
http://www.mhra.gov.uk/home/groups/is-insp/documents/websiteresources/con081801.pdf<br />
(accessed 10/04/2013).<br />
45. Sambasivan CN, Schreiber MA. Emerging therapies in traumatic haemorrhage control. Current<br />
Opinion in Critical Care 2009; 15: 560–8.<br />
46. The Royal College of Anaesthetists. NAP4 full report. http://www.rcoa.ac.uk/system/files/CSQ-<br />
NAP4-Full.pdf (accessed 10/04/2013).<br />
47. Association of Anaesthetists of Great Britain & Ireland. Peri-Operative Management of the Morbidly<br />
Obese Patient. London: AAGBI, 2007.<br />
48. Catling SJ, Freites O, Krishnan S, Gibbs R. Clinical experience with cell salvage in obstetrics: 4<br />
cases from one UK centre. International Journal of Obstetric Anesthesia 2002; 11: 128-34.<br />
49. Health and Safety Executive. EH40/96. Occupational exposure limits 1996. London: HMSO, 1996.<br />
50. Association of Anaesthetists of Great Britain & Ireland. Recommendations for Standards of<br />
Monitoring During Anaesthesia and Recovery. London: AAGBI, 2007.<br />
51. NHS Estates. Revised schedules of accommodation. London: NHS, 2002.<br />
52. Thompson S, Neal S, Clark V. Clinical risk management in obstetrics: eclampsia drills. Quality and<br />
Safety in Health Care 2004; 13:127–129.<br />
53. Association of Anaesthetists of Great Britain & Ireland. Department of Anaesthesia – secretariat<br />
and accommodation guidelines. London: AAGBI, 1992.<br />
54. Department of Health and Social Security. Anaesthetic Service Accommodation in District General<br />
Hospitals. A Design Guide. London: DHSS, 1971.<br />
55. Department of Health and Social Security. Secretarial and Support Services for Hospital Medical<br />
and Dental Staff. Report of a Departmental Working Party. London: DHSS, 1987.<br />
32
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
Occupational Health and the Anaesthetist 2014<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650 Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org October 2014
Membership of the working party<br />
(details correct at the start of the working party process)<br />
Contents<br />
Dr P Clyburn<br />
Dr A Hartle<br />
Dr F Plaat<br />
Dr N Redfern<br />
Dr I Walker<br />
Dr E Anderson<br />
Dr A Docherty<br />
Dr C Shannon<br />
Dr J Hartley<br />
Chair and Immediate Past Honorary Treasurer, AAGBI<br />
President, AAGBI<br />
Honorary Membership Secretary, AAGBI<br />
Honorary Membership Secretary Elect, AAGBI<br />
Vice President, AAGBI<br />
GAT Representative, AAGBI<br />
GAT Representative, AAGBI<br />
RCoA Representative<br />
Occupational Health Representative<br />
1. Summary of recommendations 3-5<br />
2. Introduction – the role of occupational health 6<br />
3. Occupational health and the sick doctor 7-8<br />
4. Wellbeing 9-12<br />
5. Health protection and management of workplace risk and hazard<br />
a. Blood borne viruses 13-16<br />
b. Respiratory infections 17-19<br />
c. Manual handling and back care 20-22<br />
d. Pregnancy 23-26<br />
6. Advice on fitness to work 27-28<br />
This guideline has been seen and approved by the AAGBI Board<br />
The working party acknowledges the assistance from Dr E Davies<br />
and Prof J Harrison.<br />
7. Managing chronic conditions, including arrangements for return to work 29-32<br />
8. Referral to regulatory authorities 33-34<br />
9. References 35-37<br />
10. Appendix 1 38<br />
This is a consensus document produced by expert members of a Working Party<br />
established by the Association of Anaesthetists of Great Britain and Ireland (AAGBI).<br />
© The Association of Anaesthetists of Great Britain & Ireland 2014<br />
Date of review: 2018<br />
1
• What other guideline statements are available on this topic?<br />
There is lot of information on occupational health for doctors. This guidance is<br />
targeted specifically at anaesthetists and signposts much of the broader<br />
available information.<br />
• Why was this guideline developed?<br />
This original guideline on Blood Borne Viruses (1992 and revised 1996) is<br />
updated and extended to cover other occupational health issues relevant to<br />
anaesthetists.<br />
• How and why does this statement differ from existing guidelines?<br />
Much of the information in this guideline is new and has not been previously<br />
covered.<br />
1. Summary<br />
• The consultant occupational health physician’s role is wide-ranging and encompasses<br />
health protection in the workplace, wellbeing, fitness for work, and support for staff with<br />
chronic conditions. They may also have a role in assisting remediation when a doctor is<br />
referred to the regulatory authority or professional assessment.<br />
• Doctors sometimes fail to recognise the role of the occupational health physician,<br />
believing them to be an arm of management.<br />
• Sick doctors may be reluctant to seek help and, as a result, self-treat, seek help from<br />
colleagues bypassing the usual channels, or delay seeking appropriate help and<br />
treatment.<br />
• Staff wellbeing is important to the quality of the delivery of patient care, staff retention<br />
and engagement. Wellbeing is achieved by promoting a healthy lifestyle, providing good<br />
working arrangements and environment, encouraging positive working relationships,<br />
and effective support.<br />
• Hospitals owe a duty of care to employees, and are required to provide prevention,<br />
protection and post-exposure care. This includes the provision of personal protective<br />
equipment and training in its use. Healthcare workers have professional responsibilities<br />
and duties as employees to take up this training and use the equipment provided.<br />
• Blood borne viruses are carried in the blood without necessarily causing symptoms in<br />
the infected person. The most prevalent and important blood borne viruses are hepatitis<br />
B, C and HIV.<br />
• Blood borne viruses may be transmitted by needlestick injuries or by direct contact with<br />
broken skin or mucus membranes. The risk of transmission from a deep penetrating<br />
inoculation with a hollow needle is 1:3 for hepatitis B, 1:30 for hepatitis C and 1:300 for<br />
HIV. Approximately 25% of reported high-risk injuries occur in the operating theatre or<br />
intensive care unit.<br />
• Pre-employment screening for transmissible diseases including tuberculosis and<br />
hepatitis B is mandatory for all healthcare workers. Healthcare workers, who perform<br />
exposure prone procedures, are required to have HIV and hepatitis C tests. Anaesthetists<br />
are not deemed to undertake exposure prone procedures and so may be offered these<br />
tests, but are not obliged to undergo them.<br />
• Anaesthetists who have, or think they might have, any serious condition including a<br />
blood borne virus must consult a suitably qualified colleague and ask for and follow<br />
advice about investigations, treatment and changes to their practice that are considered<br />
necessary.<br />
• Occupational exposure to blood borne viruses is inevitable. Immediate first aid (washing<br />
with soap and water, or irrigation) must be performed and then urgent assistance sought<br />
2<br />
3
from the occupational health department or the emergency department within an hour<br />
of the exposure. Post-exposure prophylaxis for HIV for should be started within an hour<br />
of exposure. Follow-up for hepatitis C must continue for at least 12 months or longer as<br />
sero conversion may be delayed.<br />
• Patients who are the source of exposure should be asked to consent to testing for a<br />
blood borne virus. The decision to start post-exposure prophylaxis should be based on<br />
a risk assessment of the exposure, and should never wait until patient testing has been<br />
done. Post-exposure prophylaxis for hepatitis B and C is not available.<br />
• Respiratory infections are an occupational hazard and anaesthetists should take<br />
appropriate measures to protect themselves. These include immunisation, use of<br />
personal protective equipment – masks, gloves and aprons/gowns, and good hand<br />
hygiene.<br />
• Infections that can cause severe illness if acquired include influenza, SARS, novel<br />
coronavirus or tuberculosis. When managing patients who may have such infections,<br />
doctors should seek and follow guidance from infection prevention and control team,<br />
occupational health and/or health and safety teams.<br />
• The consultant occupational health physician has a central role in advising and<br />
supporting doctors with chronic illness and/or disability.<br />
• Following a period of sick leave, the consultant occupational health physician will work<br />
closely with the relevant manager to design a return to work package consistent with<br />
good employment practice and the Trust’s attendance management policy. He or she<br />
will monitor the individual doctor’s progress, and suggest modifications when needed.<br />
• If an individual has a disability in the terms of the Disability Section of the Equality Act<br />
2010, he or she may be entitled to ‘reasonable adjustment’ under the Act. The consultant<br />
occupational health physician will advise on this, and work closely with the employee’s<br />
manager to re-design the job and to modify equipment such that the individual can work.<br />
• The consultant occupational health physician can advise on referral to the General<br />
Medical Council or Medical Council of Ireland. If remediation is needed, the consultant<br />
occupational health physician’s advice about the timing and nature of the remedial<br />
package should be sought and followed.<br />
• Work-related musculoskeletal disorders, including manual handling injuries, are the<br />
most common type of occupational ill health in the UK accounting for approximately<br />
40% of all sickness absence in the NHS.<br />
• Anaesthetists should receive training in the principles of safe manual handling, and a<br />
Patslide® or Hover Matt® employed whenever possible.<br />
• Environmental factors may present risks to the pregnant mother and the developing<br />
fetus during a normal pregnancy. Specific hazards include heavy physical work,<br />
prolonged standing, long working hours and night shift work, exposure to chemicals<br />
such as anaesthetic agents and to ionising radiation. A number of infections, including<br />
cytomegalovirus, hepatitis A and B, HIV, listeria, parvovirus, rubella, toxoplasma, and<br />
chickenpox are known to be a potential risk to the fetus or neonate and therefore<br />
exposure to these should be avoided.<br />
• The pregnant worker must inform the employer as soon as the pregnancy is known<br />
as employers are required to carry out a risk assessment to decide how best to limit<br />
exposure to hazards including infection and radiation.<br />
• The occupational health physician has a responsibility to the employer to advise on<br />
fitness for work and ‘reasonable adjustment’, and a responsibility to the individual to<br />
advise on the natural history of the illness and potential effects on work, and to be their<br />
advocate.<br />
• Departments should have a defined and transparent process for referring a doctor to<br />
the occupational health physician. This should include guidance on the background<br />
information required and the importance of fully involving the doctor in the referral.<br />
4<br />
5
2. Introduction – the role of occupational health<br />
3. Occupational health and the sick doctor<br />
Consultant occupational health physicians advise both the individual doctor and the<br />
organisation on the relationship between health and work. This includes the management<br />
of any underlying illness within the workplace, and the effect work has on health. They also<br />
have a lead role in ensuring that doctors receive appropriate healthcare support at work as<br />
part of the management of health and wellbeing. The occupational health service should<br />
ensure that factors such as working patterns and professional relationships are addressed<br />
by organisations and by individuals [1].<br />
The occupational health physician’s role is wide-ranging and encompasses:<br />
• Health protection and management of workplace risk and hazard including:<br />
■<br />
Ergonomics and working hours<br />
■ Biological chemical physical hazards such as chemical risks, blood borne<br />
viruses and ionising radiation<br />
■<br />
Psychosocial – behaviour, teamwork, stress and organisational culture<br />
• Wellbeing: Good health, good work, good relationships, good support<br />
• Advice on fitness for work<br />
• Managing chronic conditions<br />
■<br />
■<br />
Regular review of employees with chronic conditions to promote work ability<br />
Management of ‘return to work’ arrangements following a period of ill health<br />
■ Advice on legal protections (e.g. ‘reasonable adjustment’ [2]) for those with<br />
disabilities<br />
■<br />
Advice on early retirement on the grounds of ill health<br />
• Advising the General Medical Council/Medical Council of Ireland and the National<br />
Clinical Assessment Service in the UK<br />
• Role in planning and managing remediation<br />
The occupational health physician’s practice is governed by a set of ethical standards that<br />
describe how issues of privacy and confidentiality about employees are managed [3]. Medical<br />
practitioners sometimes fail to understand the role of the occupational health department,<br />
believing it to be an arm of management. Doctors can be reluctant to seek advice from the<br />
consultant occupational health physician, partly because of the potential impact of health<br />
problems on future careers [1]. Doctors’ professional culture, ways of working and their<br />
behaviour as patients, present particular challenges to the occupational health department.<br />
Organisations should recognise this and provide appropriate resources and facilities to<br />
support doctors in accessing occupational health services.<br />
Sick doctors may be reluctant to seek help [4]. Those with chronic diseases describe<br />
guilt about letting colleagues and patients down, and many come to work even when<br />
unwell (presenteeism). They describe concerns about being stigmatised [5], worries about<br />
confidentiality and loss of control [6] and a feeling of shame, of letting themselves down by<br />
not meeting their own high personal standards, especially if they have a psychiatric illness.<br />
Particular concerns amongst trainees are that they may lose the respect of others by showing<br />
vulnerability, and that disclosing a mental illness may threaten their career and job prospects<br />
[3]. As a result, doctors may self-treat or seek help from colleagues without going through<br />
proper channels; they may not seek help until the condition has become severe [7].<br />
The literature on doctors’ health focuses on mental ill health and substance abuse. Depression<br />
is said to be as common or more prevalent [5] in physicians as in the general population,<br />
although occurring later in life. However, the risk of suicide is greater [8]. Drug misuse is a<br />
problem in the medical profession [9], particularly among trainee and non-consultant grade<br />
doctors [10] and may begin as a coping strategy to manage psychological or stress-related<br />
illness. Indeed, bipolar illness and substance abuse are the main health reasons that doctors<br />
appear before regulators [1].<br />
All employers, including the NHS, have a duty of care to its staff. The NHS Constitution for<br />
England [11] states that all staff are entitled to a healthy working environment and commits<br />
the NHS to providing support and opportunities to enable them to maintain their health,<br />
wellbeing and safety wherever they work. There is a requirement for NHS occupational<br />
health services to meet national quality standards [12, 13], to employ consultant occupational<br />
health physicians [1], and for a doctor who has a health issue to seek and follow the advice<br />
of the relevant specialist, i.e. a doctor on the specialist register.<br />
The report of the working group on the health of health professionals, Invisible Patients<br />
[5], proposed that a group of health professionals (GPs, occupational health physicians<br />
and psychiatrists) should be developed with enhanced skills to treat their colleagues. It<br />
proposed that this group should refer on to a small number of specialist services to manage<br />
6<br />
7
those whose complex problems cannot be dealt with locally and may adversely affect the<br />
quality of care. This training is now underway in the UK, through the Royal Colleges of<br />
General Practice and Psychiatry, the Faculty of Occupational Medicine and the Association<br />
of National Health Service Occupational Physicians. In time, every hospital should have<br />
immediate access to a consultant occupational health physician with these enhanced skills.<br />
4. Wellbeing<br />
NHS organisations that pay attention to the wellbeing of staff deliver higher quality of care,<br />
make better use of resources, have lower patient mortality and have more satisfied patients<br />
[14]. Staff engagement and retention is also better [5]. Good health includes healthy eating,<br />
exercise and sensible drinking; wellbeing encompasses physical, social/relational and<br />
psychological aspects. Components of a healthy workplace include effective leadership/<br />
management, positive working relationships, competence and environmental mastery, a<br />
sense of purpose, personal growth and aspiration and rewards, competent performance and<br />
security [15].<br />
Addressing the health and wellbeing of doctors involves many stakeholders. Until recently,<br />
the medical profession had adopted a medical model that focussed on treating the impaired<br />
physician at a distance from the workplace rather than a preventive biopsychosocial model<br />
that is grounded in a positive work-life balance and centred on work arrangements [1].<br />
A practical organisational model for delivering wellbeing, developed by Business in the<br />
Community (BITC) takes an integrated, holistic and strategic approach and outlines action<br />
that can be taken by both employers and employees to create a healthy workplace [16]. It<br />
identifies four main areas for organisations to focus on:<br />
• ‘good health’ is concerned with physical and mental health, including the social<br />
determinants of health<br />
• ‘good work’ addresses the work environment and work arrangements<br />
• ‘good relationships’ focuses on managers and their ability to promote health and<br />
wellbeing through implementation of best practices and good interpersonal skills<br />
• ‘good support’ ensures that there are high quality support services, such as<br />
occupational health or counselling services to support staff.<br />
Good health<br />
A good occupational health service should offer advice to employees on healthy lifestyle<br />
choices and encourage the organisation to adopt policies that provide and develop a healthy<br />
workplace. Several organisations provide information on aspects of wellbeing with advice on<br />
sensible eating, maintaining hydration, time management, work-life balance and ‘workplace<br />
wellness interventions’ including, advice on stopping smoking, how to access counselling,<br />
‘burnout’ and ‘peer support’, examples include: British Medical Association website wellbeing<br />
page [17]; Peninsula University Medical School [18].<br />
8<br />
9
Good work<br />
Now that the implementation of the European Working Time Regulations [19] has reduced<br />
the hours worked to an average of 48 hours per week or less , workload and shift work are<br />
important considerations. Perception of workload is a function of the job demands and the<br />
attendant time pressures [20]. Job demands in anaesthesia are both physical and mental.<br />
Perception of workload is also affected by sleep loss and fatigue, which may result from<br />
working shifts or from stressful working conditions. For short shift cycles, it is thought to<br />
be better to maintain daytime rhythms by taking naps somewhere quiet and dark, paying<br />
attention to the timing and content of meals and using stimulants such as caffeine. Even<br />
long-term night shift workers have disrupted circadian rhythms, which means that they work<br />
during their low period and try to sleep when alert [21]. Organisations should make efforts<br />
to provide convenient quiet accommodation for those on night shifts to take naps, and offer<br />
regular meal breaks. The occupational health department can provide advice and support<br />
to the organisation about out-of-hours facilities and working arrangements for shift workers.<br />
Stress levels are reduced by the higher levels of social support and role clarity provided by<br />
working in good teams [22]. Working with less defined teams and continually having to forge<br />
new working relationships are both associated with increased stress. This should be taken<br />
into account in planning rotas, particularly for colleagues who are new to the organisation<br />
or who are returning to work, e.g. from maternity leave or following illness. The consultant<br />
occupational health physician may act as an advocate for the employee by providing advice<br />
to management in such circumstances.<br />
Shift work, dysfunctional teams, and poor communication can increase vulnerability to<br />
mental health problems, as can interpersonal conflict, low levels of support and the feeling of<br />
being poorly managed. Conversely, good relationships with colleagues and supervisors, high<br />
levels of job satisfaction and a feeling of accomplishment can be protective. Staff shortages,<br />
funding cuts, inadequate space, equipment and administrative back-up, and poor peer and<br />
supervisory support also drive up stress levels [5].<br />
Evidence suggests that the healthcare environment can be inherently more challenging than<br />
that in other non-health sectors. The current organisation, culture and volume of work in<br />
healthcare can combine to make health professionals vulnerable to unhealthy lifestyles. The<br />
way work is structured and organised – at a personal and organisational level – seems<br />
to have a much greater influence on the risk of developing a mental health problem than<br />
dealing with sick and dying patients and their relatives.<br />
The occupational health department can provide advice on the sorts of interventions that<br />
might be helpful in addressing poor working relationships and difficult team dynamics.<br />
The use of organisational psychologists and of coaching and mentoring can be useful in<br />
managing such situations.<br />
10<br />
Good relationships<br />
According to the BITC model [16], good relationships – at work and at home – provide the<br />
‘social capital’ that individuals need to maintain good mental health and engagement. Key<br />
relationships at work are with line managers and team colleagues. It has been shown that<br />
the principal cause of workplace stress is ‘the boss’ [23], and support from managers is<br />
important for wellbeing. The General Medical Council (GMC) recognises this, stating that:<br />
‘You must support colleagues who have problems with their performance or health’ [24].<br />
Medical managers need to understand how good relationships at work can promote health<br />
and wellbeing and that the support of individuals with health problems can reduce the impact<br />
of illness by reducing levels of anxiety [25]. An open, accountable and supportive workplace<br />
culture in which any concerns can be raised without fear of reprisals reduces harassment<br />
and bullying, enhances quality of care and boosts recruitment and retention [5].<br />
Other recognised work-related stressors include: role-based stress (role ambiguity and<br />
work role conflict); conflicting demands between work and home life; relationship problems;<br />
career development factors (job insecurity, under or over promotion, and thwarted ambition);<br />
and organisational structures and culture. These need to be managed to achieve good work.<br />
The occupational health department may provide training to managers and others in promoting<br />
good working relationships. They may have access to organisational psychologists and<br />
other experts in this field.<br />
Good support<br />
Good occupational health support and counselling is essential to safeguard doctors’ health<br />
and wellbeing. Key criteria for a bespoke occupational health service for doctors include [1]:<br />
1. The services must be led by a consultant occupational health physician<br />
2. The consultants should be experienced in assessing and managing the doctor who is<br />
also a patient. This is not without challenges, as doctors often do not accept the patient<br />
role readily. There are many reasons for this: some relate to issues described earlier<br />
and others are concerned with beliefs and behaviours about illness, role conflict when<br />
with colleagues and perceived loss of control [26]<br />
3. Medical managers (clinical and medical directors, chiefs of service, lead clinicians)<br />
must be trained in how to make appropriate referrals to occupational health and how to<br />
conduct the pre-referral conversation with the referee. There should be transparency of<br />
process and an appreciation of the ethics of practice<br />
4. The service should be part of a larger support network. Many services have singlehanded<br />
consultants who would benefit from being able to discuss difficult cases, and<br />
the opportunity to use mentorship<br />
11
5. There should be arrangements in place for onward referral to appropriate treatment<br />
specialists. Confidentiality of the doctor-patient must be preserved, so arrangements<br />
for such treatment would normally be to a different trust, hospital or health board and<br />
may be in a different locality. It is helpful to develop links with local liaison psychiatrists<br />
and/or psychiatrists specialising in substance abuse<br />
6. There should be links with the postgraduate deanery. This can help to facilitate<br />
interventions for trainee doctors when local solutions cannot be identified. It can also<br />
provide opportunities to influence deanery practice and to build up relationships with<br />
trainers in other specialties. Training in managing the trainee in difficulty is a GMC<br />
requirement and occupational medicine input is often greatly appreciated.<br />
Many telephone helplines have been established. A practitioner health programme has been<br />
established in London to provide off-site help for doctors with health problems [27], and<br />
similar service models exist elsewhere in the UK. This programme is similar to programmes<br />
in the United States. A strength of such help facilities is that they are external to employing<br />
health trusts, thus ensuring actual and perceived confidentiality of care. On the other hand,<br />
the remoteness of such services means that they are unable to satisfactorily address<br />
workplace issues. This means that strategic and operational health and wellbeing issues for<br />
doctors have not been addressed.<br />
5. Health protection and management of workplace risk and hazard<br />
5a. Blood borne viruses<br />
Blood borne viruses (BBVs) are, by definition, viruses carried in the blood without necessarily<br />
causing symptoms in the infected person. The most prevalent and important BBVs are<br />
hepatitis B, C and HIV. Blood borne viruses represent a risk to patients and healthcare<br />
workers alike. Hospitals owe a duty of care to both groups, which may be summarised as:<br />
• Prevention<br />
• Protection<br />
• Post-exposure care<br />
The AAGBI first issued separate guidance about HIV/AIDS in 1988. This is now incorporated<br />
into more generic guidance on occupational health.<br />
Prevalence of hepatitis B [28]:<br />
■<br />
A total of 4756 cases of viral hepatitis from England and Wales were notified to the<br />
Health Protection Agency in 2008. Of these, 1592 (about 33%) were caused by hepatitis<br />
B; and the number of new reports of hepatitis B is increasing each year<br />
■<br />
■<br />
The prevalence of people with antibodies to hepatitis B core antigen (anti-HBc) — a<br />
marker of current or previous infection (sero prevalence) — is 1–2% in the UK. In parts<br />
of China and South Korea, the sero prevalence is 96%<br />
Worldwide, approximately 350 million people have chronic hepatitis B<br />
o<br />
o<br />
The highest rates of chronic hepatitis B (up to 20% of the population) are seen<br />
in South Asia, East Asia, and sub-Saharan Africa<br />
In the UK, the prevalence of positivity to hepatitis B surface antigen (HBsAg) is<br />
highest in those people who were born in countries with endemic infection.<br />
Several thousand people with chronic hepatitis B are estimated to come to<br />
the UK each year from endemic areas, but often they do not present until the<br />
disease is advanced or they become pregnant<br />
Prevalence of hepatitis C [28]<br />
■<br />
■<br />
In the UK, this is estimated to be between 250,000 and 600,000, i.e. around 0.5% of the<br />
population carry the virus, most unknowingly<br />
The incidence of hepatitis C is believed to have peaked at about 15,000 per year in<br />
the late 1980s, when injected drug use was particularly common, the virus had not been<br />
identified, and needle exchange programmes did not exist<br />
12<br />
13
14<br />
o<br />
o<br />
o<br />
The present day true incidence of hepatitis C is not known<br />
Between 1992 and 2007 there were 62,238 laboratory-confirmed cases<br />
reported to the Health Protection Agency<br />
In 2007 there were 7540 cases confirmed. This was an increase of 12% from<br />
the previous year<br />
■ Worldwide, hepatitis C is a major health problem, with an estimated 170 million people –<br />
3% of the global population – infected. In some parts of Europe, Egypt, Japan, and the<br />
Indian subcontinent, the prevalence is as high as 3–5%<br />
Prevalence of HIV [28]<br />
■<br />
■<br />
By the end of 2011, an estimated 96,000 people were living with HIV in the UK,<br />
approximately one quarter of whom were undiagnosed and unaware of their infection<br />
This is an increase from the 91,500 people estimated to have been living with HIV by<br />
the end of 2010. The estimated prevalence of HIV in 2011 was 1.5 per 1000 population<br />
of all ages: 2.1 per 1000 men and 1.0 per 1000 women<br />
Since the late 1990s, following work related exposure, at least 17 healthcare workers have<br />
contracted hepatitis C and there have been five documented cases of HIV transmission.<br />
Methods and risks of transmission<br />
Blood borne viruses may be transmitted by the percutaneous route (needlestick injuries) or<br />
by direct mucocutaneous contact (broken skin or mucus membranes). Risks are highest<br />
with a deep penetrating inoculation with a hollow needle where there is visible contamination<br />
with blood. For such injuries, the risk of transmission is 1:3 for hepatitis B, 1:30 for hepatitis<br />
C and 1:300 for HIV. Approximately 25% of reported high-risk injuries occur in the operating<br />
theatre or intensive care unit.<br />
Prevention<br />
Screening for staff<br />
Transmission of hepatitis B and C from infected healthcare workers to patients is well<br />
documented. The risk of such transmission for HIV is very much less, and the Department<br />
of Health undertook a consultation in 2012 on whether to allow HIV positive healthcare<br />
workers to undertake exposure prone procedures (EPP), subject to strict health supervision.<br />
In August 2013, it announced that such new arrangements will come into effect in April 2014.<br />
Pre-employment screening for transmissible disease is mandatory for all healthcare workers<br />
and includes (for example) tuberculosis and hepatitis B. Since March 2007, in England<br />
(at later in other devolved nations), any new healthcare workers who will perform EPP, or<br />
existing workers who are new to EPP, are additionally required to have HIV and hepatitis C<br />
tests.<br />
Anaesthetists are not deemed to undertake EPP and so may be offered these tests but are<br />
not obliged to undergo them. Anaesthetic departments should liaise with their occupational<br />
health department to ensure that the work of anaesthetists is correctly classified. Schools<br />
of anaesthesia should liaise with the various hospitals to which trainees rotate to minimise<br />
the number of pre-employment screens needed. This is particularly an issue where trainees<br />
undertake many attachments of short duration. Consideration should be given to trainees<br />
having either a lead employer for the whole of training, or a ‘health passport’ which would be<br />
accepted by all hospitals within a school. These measures will save much time and cost for<br />
individual hospitals, and minimise delays before new trainees may start work.<br />
Where indicated, these tests will be carried out by the occupational health department with<br />
appropriate advice, information and consent. The results of tests must be communicated<br />
with due regard to the anaesthetist’s confidentiality; emails to lead clinicians or College<br />
tutors, or results being left in pigeonholes would not meet the requirements for confidentiality<br />
laid down by the Faculty of Occupational Medicine or the GMC.<br />
As with any other serious condition, anaesthetists who have, or think they might have, a<br />
BBV must consult a suitably qualified colleague [24] and ask for and follow advice about<br />
investigations, treatment and changes to their practice that are considered necessary. They<br />
must not rely on self-assessment of the risk they pose to patients [24].<br />
Screening for patients<br />
Routine screening of all patients for BBVs has not been considered practical, effective or<br />
affordable. Patients may be offered screening in some high-risk environments, such as<br />
renal dialysis units, but care cannot be contingent on accepting such screening. Ante-natal<br />
screening for hepatitis B, HIV, syphilis and rubella susceptibility is offered, with a 97% uptake<br />
in 2011 in England [29].<br />
Protection<br />
All hospitals owe a responsibility to employees to reduce the risks of employment, which<br />
arises from numerous pieces of employment law legislation. This includes the provision of<br />
personal protective equipment and training in its use. Healthcare workers have professional<br />
responsibilities and duties as employees to take up this training and use the equipment<br />
provided. Failure to do this may absolve employers of their responsibility in the event of<br />
occupational exposure and harm.<br />
15
European Directive 2010/32/EU specifically applies to the healthcare setting in the public<br />
and private sector and brings together obligations to minimise the risk of harm from sharps<br />
injury. Part of the directive mandates the provision of medical devices with safety-engineered<br />
protection mechanisms. Concerns have been raised by some anaesthetists that some<br />
devices are more difficult to use and may make failure more likely. Anaesthetists must<br />
balance any safety benefit to the user against potential harm to the patient.<br />
Post-exposure care<br />
Occupational exposure to BBVs is inevitable, although some injuries in theatre and ICU<br />
are judged to be preventable. As well as being trained and provided with the equipment to<br />
minimise harm, all staff must be trained in the management of such injury.<br />
Immediate first aid (washing with soap and water, or irrigation) must be performed and<br />
then urgent assistance sought from the occupational health department or the emergency<br />
department – this should be within an hour of the exposure.<br />
Post-exposure prophylaxis (PEP) for HIV for should be started within an hour of exposure.<br />
The decision to start PEP should be based on a risk assessment of the exposure, and should<br />
never wait until patient testing has been done. PEP for hepatitis B and C is not available.<br />
Patients who are the source of exposure should be asked to consent to testing for BBVs.<br />
They should receive appropriate counselling, and are under no obligation to agree (although<br />
most do). Patients must not be approached by the healthcare worker affected. Anaesthetised<br />
patients must be allowed to recover from the anaesthetic before being approached.<br />
Testing of patients who lack capacity (sedated on ICU for example) remains controversial.<br />
Most authorities believe that such testing, while probably ethical, would not be lawful under<br />
the Mental Capacity Act 2005, or Adults with Incapacity Act (Scotland) 2000, although this<br />
has yet to be tested in court.<br />
Healthcare workers exposed to BBVs must now also be considered to be patients of the<br />
occupational health department and must be given time to attend for follow-up. This followup<br />
will allow for consideration of continuing or stopping PEP for HIV in the light of any patient<br />
results and counselling about personal safer sex practice and other matters. Follow-up<br />
for hepatitis C must continue for at least 12 months or longer as sero conversion may be<br />
delayed, the virus may be cleared, and treatment with interferon considered. Follow-up<br />
for trainees rotating between hospitals is particularly challenging. Only 22% of high-risk<br />
hepatitis C exposures are followed up correctly [30].<br />
16<br />
5b. Respiratory infections<br />
Anaesthetists, as specialists in airway management, frequently come into contact with<br />
respiratory secretions of patients, and hence respiratory infections are an occupational<br />
hazard. This was brought into sharp focus during the SARS outbreak in Toronto, Canada,<br />
in 2003 when four anaesthetists/intensivists were infected [31]. The experience of SARS<br />
also highlighted the need for more rigorous infection control within anaesthetic practice. This<br />
section outlines the measures that anaesthetists should take to protect themselves and their<br />
patients from respiratory infections.<br />
Background<br />
All healthcare workers are at risk from acquiring infections from patients and need to take<br />
appropriate measures to protect themselves. Healthcare organisations have a duty to provide<br />
appropriate personal protective equipment and to train employees to use them appropriately<br />
and effectively (Health and Safety at Work Act 1974). Anaesthetists are at particular risk<br />
of acquiring infections from the respiratory tracts of their patients; rhinovirus has been<br />
documented as a commonly acquired infection in anaesthetists [32]. While most would<br />
consider this to be a minor infection of little consequence, patients who have respiratory<br />
infections do not present with a known diagnosis. Such patients may have infections that<br />
can cause severe illness if acquired and these include: influenza, SARS, novel coronavirus,<br />
and tuberculosis.<br />
When patients are being managed in the acute phase of an unknown respiratory infection,<br />
a standard approach is needed to ensure that the anaesthetist is protected effectively from<br />
all possible types of respiratory infection. This section provides general advice; please also<br />
consult your local infection prevention and control policies. When a diagnosis is made, or,<br />
in exceptional circumstances, such as a pandemic influenza year or an outbreak of SARS,<br />
more specific infection prevention and control advice and action is required. This guidance<br />
would be superseded by more specific guidance in those circumstances.<br />
Prevention<br />
There are three key measures that individual anaesthetists can take to prevent the acquisition<br />
of respiratory infections from patients [33, 34]:<br />
• Immunisation<br />
• Personal protective equipment (PPE) – masks, gloves and aprons/gowns<br />
• Hand hygiene<br />
Other important measures include the use of filters on respiratory equipment to protect<br />
machines from becoming contaminated and prevent efflux of infectious particles into the<br />
environment around the respiratory equipment. Each critical care unit should also have<br />
17
access to a negative pressure isolation room, which ensures that highly infectious patients<br />
with air-borne infections can be isolated effectively through controlled ventilation of the<br />
facility. More detailed discussion of these measures is outwith the remit of this section.<br />
For more information on engineering controls and ventilation please see Health Technical<br />
Memorandum 03-01 [35]. Information on appropriate filters for ventilators can be accessed<br />
via the ventilator manufacturers.<br />
AGPs include: bronchoscopy; sputum induction; tracheal intubation; post-mortem procedures<br />
involving high speed devices; cardio-pulmonary resuscitation; high frequency oscillating<br />
ventilation; non-invasive ventilation. This list is not exhaustive, local risk assessment may<br />
identify additional procedures for which AGP precautions are indicated. For an illustration<br />
of how to use and remove PPE follow this link – http://www.england.nhs.uk/ourwork/eprr/id<br />
(accessed 31/08/2014).<br />
Immunisation<br />
Each year the World Health Organisation monitors the influenza viruses in circulation and<br />
makes recommendations for the strain types that are to be included in the vaccine for the<br />
following winter season. Due to the changing nature of influenza viruses, immunisation is<br />
required on an annual basis. Immunisation against influenza is recommended annually for<br />
healthcare workers to protect them and to prevent spread of influenza within the healthcare<br />
setting. Occupational health departments will usually provide healthcare workers with<br />
ample opportunities to take up the flu vaccine in early autumn [36]. Immunisation against<br />
tuberculosis is also recommended for healthcare workers who are likely to have contact with<br />
patients or clinical materials [37].<br />
Personal protective equipment<br />
PPE should be used to minimise the risk of infection in the healthcare worker. The level of<br />
PPE used should be appropriate for the risk. Respiratory infections such as influenza are<br />
transmitted by large particle droplets. When assessing patients with respiratory infections<br />
of unknown cause, droplet precautions should be used. Staff should wear a fluid repellent<br />
surgical mask; a visor should also be used if there is a risk of splash onto mucous membranes.<br />
In addition to masks +/- visors, gloves and aprons/gowns should also be worn.<br />
Hand hygiene<br />
Hand hygiene remains the most important infection control measure to protect healthcare<br />
workers and patients from infections. Clean hands may be decontaminated using alcohol<br />
gel between patient contact; soap and water hand washing remains important if hands are<br />
visibly dirty or contaminated. See Appendix 1 for hand hygiene methods.<br />
Post-exposure protection<br />
If appropriate PPE is not worn and the staff member is not vaccinated when undertaking<br />
assessments and/or AGPs on a patient who is subsequently found to have influenza,<br />
prophylaxis with oseltamivir may be offered [39]. Consult your local occupational health<br />
physician and Infection Prevention and Control team for further advice. For cases of<br />
tuberculosis, contact tracing and follow-up would routinely occur following the identification<br />
of a case. Prevention of exposure by use of PPE and hand hygiene, and appropriate<br />
immunisation are far more effective than any post-exposure measures. For SARS and other<br />
novel coronaviruses there are no post-exposure treatments available.<br />
If aerosol-generating procedures (AGP) are being undertaken, such as intubation, it is<br />
recommended that a filtering face piece (FFP3) mask be used, in addition to eye protection,<br />
gloves and a gown. A FFP3 device is a mask that provides the wearer with a high level<br />
of protection against droplet carried infections and fine aerosols. These masks fit snugly<br />
around the face so that air cannot pass around the mask, only through the filter. For effective<br />
use, the wearer must be ‘fit tested’ to ensure that the mask fits properly and provides the<br />
necessary protection. This is a requirement under Health and Safety Executive (HSE)<br />
guidance [38]. It is imperative that healthcare workers are fit tested for the use of an FFP3<br />
mask as one design of mask may fit an individual better than another. Anaesthetists should<br />
know which make of FFP3 masks fits them and how to obtain them within their healthcare<br />
organisation. Information regarding local arrangements for FFP3 mask fit testing can be<br />
obtained from your local infection prevention and control team, occupational health and/or<br />
health and safety teams.<br />
18<br />
19
5c. Manual handling and back care<br />
Manual Handling is defined as: "...any transporting or supporting of a load (including the<br />
lifting, putting down, pushing, pulling, carrying or moving thereof) by hand or bodily force."<br />
Work-related musculoskeletal disorders, including manual handling injuries, are the most<br />
common type of occupational ill health in the UK. Back pain and other musculoskeletal<br />
disorders account for approximately 40% of all sickness absence in the NHS, resulting in a<br />
cost in the region of £400 million each year [40].<br />
The HSE is the national independent watchdog for work-related health, safety and illness.<br />
The organisation is an independent regulator and acts in the public interest to reduce workrelated<br />
death and serious injury across Great Britain’s workplaces. All employers have a<br />
legal responsibility to ensure the health and safety at work of their staff, and this includes<br />
the prevention of accidents and work related ill health such as musculoskeletal disorders,<br />
back pain and upper limb disorders. There is a legal requirement for employers to consult<br />
employees on health and safety matters, as well as union appointed safety representatives.<br />
Numerical guidelines for lifting and lowering:<br />
The manual lifting of people was condemned as unsafe practice in 1996.<br />
Thus the principles of safe manual handling are:<br />
• Avoid manual lifting<br />
• Assess the patient/load and environment and plan the move<br />
• Ensure the task is within your capabilities<br />
• Get close to the patient/load<br />
• Face the direction of movement, avoid twisting<br />
• Flex or bend your knees<br />
• Keep your back upright, avoid stooping<br />
• Ensure your feet are apart, one foot in front of the other (walk stance)<br />
• Ensure a secure hand grip<br />
• Use the commands ‘ready, steady, move’, numbers can be confusing as some may<br />
move on ‘three’ and some on the unspoken ‘four’<br />
When starting in a new hospital environment, staff should receive an induction, including the<br />
manual handling procedures in place and the location of suitable equipment.<br />
In anaesthesia, we commonly participate in the lateral transfer of patients from bed to trolley<br />
or operating table. Where possible the patient should be encouraged to move independently,<br />
shuffling sideways from one surface to another, with or without the use of a Patslide® to<br />
assist with the transfer.<br />
If the patient is unable to move independently, a Patslide® or Hover Matt® technique may be<br />
used. For the dependent patient, four handlers are required, and more if the patient is obese.<br />
The technique is as follows:<br />
• Tilt the patient towards the far side to insert the Patslide®, partially under the slide<br />
sheets, and extending across to the receiving surface<br />
• Bring receiving surface as close as possible and apply brakes<br />
• Adjust heights so that the receiving surface is slightly lower<br />
[from Manual Handling at Work: A Brief Guide – HSE; Contains public sector information<br />
published by the Health and Safety Executive and licensed under the Open Government<br />
Licence v1.0, http://www.hse.gov.uk/pubns/indg143.pdf (accessed 31/08/2014)]<br />
20<br />
• Two handlers take hold of the pull straps<br />
• A third handler is required to support the head on the pillow, and a fourth for the feet<br />
21
• One handler to co-ordinate with a ‘ready, steady, slide’ command<br />
• The two handlers, holding onto the pull straps, transfer their weight from their front leg<br />
to their back leg, and slide the patient half way across the surfaces and then repeat to<br />
pull the patient fully across onto the receiving surface and its slide sheet<br />
When using a Hover Matt®, one handler must ensure that the air-supply coupling remains<br />
intact throughout the manoeuvre and that the air-supply remains turned on.<br />
5d. Pregnancy<br />
Workforce implications of pregnancy<br />
The number of female anaesthetists likely to be working when pregnant is increasing<br />
year on year. Women make up over 30% of consultant workforce and female trainees are<br />
approximately double this percentage. Approximately a quarter of consultants are aged 30<br />
to 39 years with nearly all trainees being below the age of 40 years.<br />
More information<br />
NHS Employers<br />
National Back Exchange<br />
Health and Safety Executive<br />
Backcare charity website<br />
Society of Diagnostic Medical Sonography<br />
Royal College of Nursing<br />
www.nhsemployers.org/backinwork<br />
www.nationalbackexchange.org<br />
www.hse.gov.uk/msd<br />
www.backcare.org.uk<br />
www.sdms.org/msi<br />
www.rcn.org.uk<br />
Anaesthetists work in an environment where exposure to chemicals such as anaesthetic<br />
agents and ionising radiation are common. There is an increasing reliance on complex<br />
imaging techniques such as CT and MRI in medical diagnostics and anaesthesia is frequently<br />
required to facilitate this. The nature of the work can be physically demanding and, although<br />
hours of work have been reduced for trainees over the past few years, most trainees work<br />
an increasing proportion of their time at night, with the introduction of shift working patterns.<br />
Some of the consultant workforce has opted out of European Working Times legislation and<br />
may still work in excess of 48 hours per week. The effects of these environmental factors<br />
present risks to the pregnant mother and the developing fetus during a normal pregnancy<br />
when the mother is well. Those with pregnancy-related complications would need more<br />
individual consideration from their occupational health physician.<br />
Evidence on the effects of working in anaesthesia while pregnant tends to be based on<br />
observational studies.<br />
The Royal College of Physicians in conjunction with NHS Plus, published a national<br />
guidance document for occupational health professionals containing evidence-based advice<br />
for working women during pregnancy and for their employers [41]. The document focuses<br />
on a number of specific hazards including lifting/manual handling and heavy physical work,<br />
prolonged standing, long working hours and shift work, including night shifts. There is<br />
insufficient evidence to suggest that pregnant workers should completely avoid lifting and<br />
handling or prolonged standing.<br />
Adverse fetal outcomes include spontaneous miscarriage, stillbirth, low birth weight and preterm<br />
delivery. The UK has one of the highest rates of pre-term delivery in Europe. Adverse<br />
maternal outcomes relate to musculoskeletal problems, gestational hypertension including<br />
PET, and pre-term early rupture of membranes with subsequent infection.<br />
22<br />
23
Associated risks to the fetus<br />
1. Physically demanding work, particularly lifting<br />
Manual workers including healthcare workers have a significantly higher risk of:<br />
• Intrauterine growth retardation<br />
• Pre-term birth<br />
• PET and hypertension (Relative Risk = 1.6)<br />
Recommendation: moderate risk - employers should reduce risk of exposure where<br />
possible.<br />
2. Long hours (more that 40 h/week)<br />
Low to moderate risk of:<br />
• Pre-term delivery<br />
• Spontaneous miscarriage<br />
• Perinatal mortality<br />
Recommendation: Working hours should be reduced to below 40 h/week, especially in<br />
late pregnancy.<br />
3. Prolonged standing – more than 3 h per day<br />
• Pre-term birth – small risk<br />
Recommendation: try to reduce standing to < 3 h/day.<br />
4. Shift work/night work<br />
• Pre-term birth<br />
Conflicting evidence. Insufficient to make recommendation about risk of shift or night work.<br />
Specific areas<br />
Anaesthetic drugs<br />
Exposure to high levels of volatile anaesthetic agents, particularly halogenated hydrocarbons<br />
and nitrous oxide is associated with a risk of spontaneous abortion and pre-term labour. The<br />
most significant risk of teratogenesis occurs during the first eight weeks of pregnancy, and<br />
may occur before the woman is aware that she is pregnant. Most of the experimental work<br />
was done in the 1970s when active scavenging systems were not in routine use. It is likely<br />
that with modern low flow anaesthetic machines, active scavenging and the prevalence of<br />
non-volatile based anaesthetic techniques, there is a very low risk of adverse outcomes.<br />
However, it is the employer’s responsibility to ensure pregnant workers and those planning<br />
pregnancy should be made aware of the potential risks and not work in environments where<br />
there is no active scavenging.<br />
The risks to the pregnant anaesthetist can be minimised by the use of well-designed<br />
anaesthetic equipment, modern anaesthetic techniques (e.g. TIVA), and high standards<br />
in scavenging and ventilation. However, in some areas, control measures cannot be as<br />
effectively applied and it can be predicted that exposure may be increased in paediatric,<br />
dental and, to some extent, in obstetric anaesthesia.<br />
Employers have an obligation to ensure that environments are adequately ventilated,<br />
scavenging systems are present and that they are well maintained and monitored (at least<br />
once per year). They should comply with regulations BS6834 1987. Employers must comply<br />
with occupational exposure standards, introduced in 1996, for nitrous oxide, halothane,<br />
isoflurane and enflurane.<br />
The Department of Health recommends a minimum supply of air of 0.65m3.s -1 in anaesthetic<br />
rooms. In theatre and recovery areas, ventilation to allow 15 air changes per hour should<br />
be provided, and where new ventilation is being installed, extract points should be located<br />
near to the head of the recovery bed. In dentistry and midwifery, where Entonox is in use,<br />
ventilation should allow five changes of air per hour.<br />
Risks to mother<br />
Manual handling has significant implications to the health of the pregnant worker (and the<br />
fetus), particularly when associated with long periods of standing and/or walking. Hormonal<br />
changes during pregnancy affect the ligaments and joint laxity, thereby increasing the risks<br />
of injury during manual handling tasks. As pregnancy progresses, and in particular during the<br />
last three months, it becomes difficult to achieve and maintain good posture and this further<br />
reduces manual handling capability. Care should also be taken by postnatal women who<br />
may handle loads, particularly in the three months following childbirth.<br />
24<br />
Active scavenging systems should meet Department of Health standards and the presence<br />
of a visual flow indicator is essential. Awareness of techniques to minimise atmospheric<br />
pollution (e.g. use of closed circuits, introduction of nitrous oxide when the patient is<br />
connected to the breathing system, and capping off circuits at the end of each operation) to<br />
avoid spill in the environment should be encouraged.<br />
Infections<br />
A number of infections are known to be a potential risk to the fetus or neonate and therefore<br />
exposure should be avoided. These include: cytomegalovirus, hepatitis A and B, HIV, listeria,<br />
25
parvovirus, rubella, toxoplasma, and chickenpox. This list is not exhaustive and the advice<br />
should be to take appropriate precautions and avoid unnecessary exposure to any infection.<br />
Ionising radiation<br />
Exposure to high levels of ionising radiation may result in abnormal organogenesis in the<br />
developing fetus resulting in spontaneous miscarriage. Other risks include reduction in<br />
mental capacity due to disruption in development of a normal CNS, and the development of<br />
childhood cancers especially leukaemia. The highest risk to the fetus is in the first trimester<br />
and the risk diminishes in later pregnancy.<br />
The risks of these adverse events are related to total dose of radiation, so working in<br />
environments where the dose of radiation per patient is high, e.g. CT or angiography, should<br />
be avoided.<br />
Typical occupational exposure for an x-ray worker would be 1 to 6 mSV per year and pregnant<br />
workers should be exposed to no more that 1 mSv during the pregnancy. At this level of<br />
exposure, there is no evidence to show any significant risk of radiation effects to the fetus.<br />
When working in x-ray environments, the anaesthetist should wear a lead gown that wraps<br />
around the abdomen, and sit behind lead shielding: good practice whether pregnant or not.<br />
Non-ionising radiation:<br />
MRI - The safety of MRI with respect to the fetus has not been established. The concerns<br />
for the fetus include teratogenesis and acoustic nerve damage. The studies so far indicate<br />
no increased fetal adverse outcome; however, because of the lack of evidence of long-term<br />
effects of MRI on the fetus, it is advisable not to remain in the scan room.<br />
Ultrasound - Pregnant staff working with diagnostic ultrasound do not need to alter their<br />
working practice.<br />
Risk assessment<br />
The pregnant worker must inform the employer as soon as the pregnancy is known and<br />
employers should carry out a risk assessment to decide how best to limit exposure to<br />
hazards including infection and radiation. The assessment should establish what doses of<br />
radiation are likely to be received and what can be done to reduce the risk to the baby. This<br />
may include restricting time in the environment or being reallocated to non-x-ray lists for the<br />
duration of the pregnancy.<br />
6. Advice on fitness to work<br />
Organisations should have systems and policies in place to promote fitness to work and<br />
support work attendance. A good work attendance policy recognises that there may be<br />
occasions when staff are unable to work because of ill health and should describe how<br />
managers, and working with human resources and occupational health, can facilitate an<br />
appropriate and supported return to work. The occupational health assessment will focus on:<br />
• Assisting with return to work following sick leave<br />
• Defining the doctor’s capability in a good environment<br />
o<br />
o<br />
What can/can’t he or she do?<br />
What support does he or she need?<br />
• Enabling the doctor to tackle challenging situations<br />
• Encouraging the doctor to develop robust attitudes to his or her health and wellbeing<br />
The consultant occupational health physician should identify any work-related factors in the<br />
illness and the interventions in working arrangements or the work environment necessary to<br />
minimise the impact of the illness. The occupational health physician has a responsibility to<br />
the employer to advise on fitness for work and ‘reasonable adjustment’, and a responsibility<br />
to the individual to advise on the natural history of the illness and potential effects on work,<br />
and to be their advocate.<br />
Self-referral<br />
It is possible for a practitioner to self-refer to an occupational health physician. This might be<br />
helpful in planning a return to work after illness, to consider the natural history of a disease<br />
and its likely impact on their future career, or to access counselling. Where an employing<br />
organisation does not have a consultant occupational health physician who has enhanced<br />
skills in managing doctors’ illness, it may be valuable to seek an opinion from an expert.<br />
Referring a practitioner to the consultant occupational health physician<br />
Ill health does not always present in a straightforward manner. When a practitioner is in<br />
difficulty, it is often useful to refer them to the occupational health physician, even if only to<br />
rule out illness as a cause of the problem. Becoming ill, recognising there is a problem and<br />
reporting illness can happen at different times, sometimes several months or years apart.<br />
Remember, whenever possible, to copy the practitioner into correspondence. As a general<br />
rule, it is always better to work with the practitioner rather than to have discussions and make<br />
decisions about the practitioner. The doctor-patient is the expert on his or her own illness.<br />
26<br />
27
When making a referral to the occupational health physician it is important to provide all the<br />
necessary background information. The National Clinical Assessment Service provides a<br />
checklist [7].<br />
7. Managing chronic conditions, including arrangements for return to work<br />
The White Paper, Trust Assurance and Safety [42], recognises that the increasing complexity<br />
of modern clinical practice has added to the pressures health professionals face in their<br />
working lives. It proposes that there should be greater support for those with any kind of<br />
health problem, to help them maintain their own health and wellbeing and make it easier for<br />
them to seek appropriate advice or treatment should they become ill. Health professionals<br />
should expect appropriate safeguards to maintain their confidentiality from both clinicians<br />
and managers and so may need to receive treatment outside their local area.<br />
Doctors have the same range of illnesses as others of a similar age, including psychiatric<br />
illness, diabetes, epilepsy, inflammatory bowel disease, arthritis and multiple sclerosis.<br />
The top three causes of sickness absence among NHS employees are: musculoskeletal<br />
disorders; mental ill health (including stress, depression and anxiety); and skin problems.<br />
Musculoskeletal disorders account for almost half of sick leave taken (45%) by NHS<br />
employees. Allergic reactions to gloves and drugs and the need for frequent hand washing<br />
as part of infection control measures may cause occupationally acquired dermatitis.<br />
Coping with chronic physical illness includes managing the illness itself, the effects of<br />
treatment and the psychological sequelae. It takes an average of two years for a doctor who<br />
has a long-term condition to get fully back on track. Doctors who do well are those who learn<br />
to recognise symptoms, use support appropriately and value what they can do rather than<br />
grieve over what they can no longer do.<br />
Developing a good working relationship with the occupational health physician can be an<br />
important part of managing work with a chronic illness. Trust develops as the occupational<br />
health physician demonstrates a robust approach to confidentiality, and gets the right balance<br />
between support and challenge, showing respect to the individual and telling the truth about<br />
the effects of the illness on work. The doctor-patient and the occupational health physician<br />
can then identify and meet the needs of senior clinicians such as the clinical director and the<br />
service. Topic areas the doctor might usefully discuss with the occupational health physician<br />
include:<br />
• Discussing difficulties identified by others<br />
• Confidentiality<br />
• Managing others' curiosity/hostility<br />
• Taking sick leave<br />
• Referral? To whom? By whom?<br />
• Return to work – planning<br />
28<br />
29
• On-going surveillance<br />
• Monitoring progress<br />
• Assessments – (especially for trainees, e.g. ARCP)<br />
• Change of job description or role? Specialty change (for trainees)?<br />
Following a period of sick leave, the occupational health physician will work closely with<br />
the relevant manager to design a return to work package consistent with good employment<br />
practice and the trust's attendance management policy. He or she will monitor the individual<br />
doctor’s progress, and suggest modifications when needed. Further practical advice about<br />
returning to work can be found in:<br />
• The AAGBI’s Welfare Resource Pack at: http://www.<strong>aagbi</strong>.org/sites/default/files<br />
welfare_resource_pack_2008_0.pdf<br />
• The Academy of Medical Royal Colleges has advice at: http://www.aomrc.org.uk<br />
doc_details/9486-return-to-practice-guidance<br />
• The Royal College of Anaesthetists at http://www.rcoa.ac.uk/system/files/PUB<br />
ReturnToWork2012.pdf<br />
notice the signs and whom they should notify. It would be expected that such colleagues<br />
receive training on managing the situation.<br />
Employment Rights Act<br />
If an individual has a disability in the terms of the Disability Section of the Equality Act<br />
2010, he or she may be entitled to ‘reasonable adjustment’ under the Act. The consultant<br />
occupational health physician will advise on this, and work closely with the employee’s<br />
manager to re-design the job and to modify equipment such that the individual can work.<br />
The occupational health physician will be able to advise on ‘access to work’ schemes, which<br />
sometimes fund equipment.<br />
A person has a disability under the Act if he has ‘a physical or mental impairment which has a<br />
substantial (defined as more than ‘trivial’) and long-term adverse effect on his ability to carry<br />
out normal day-to-day activities.’ The effect of an impairment is long-term if:<br />
• It has lasted at least 12 months<br />
• The period for which it lasts is likely to be at least 12 months; or<br />
• It is likely to last for the rest of the life of the person affected<br />
Useful articles article include:<br />
• Anaesthesia News, May 2010, pages 12-13. Returning to work following a major<br />
illness: http://www.<strong>aagbi</strong>.org/sites/default/files/may2010-1.pdf<br />
• Anaesthesia News, Oct 2011, pages 8-9. Returning to work in a wheelchair:<br />
http:/www.<strong>aagbi</strong>.org/sites/default/files/October ANews Final_0.pdf<br />
• RCoA Bulletin, Mar 2011, pages 26-28. Returning to work - as a disabled<br />
anaesthetist: http://www.rcoa.ac.uk/system/files/CSQ-Bulletin66.pdf<br />
Security planning/safety net<br />
It is sometimes helpful for the responsible manager to develop a signed agreement with a<br />
practitioner who has a relapsing illness. Exemplar templates are provided on the National<br />
Clinical Assessment Service (NCAS) website [7]. The agreement might identify early warning<br />
signs (e.g. specific thoughts, feelings or behaviours) that the practitioner notices when he<br />
is becoming unwell, and the actions the practitioner will take to ensure he gets appropriate<br />
help and support. The practitioner can also identify any unwanted extra work-related stress<br />
that can contribute to the problem and ways in which they, and the wider department, can<br />
manage and limit these.<br />
A similar plan describing the actions that close colleagues will take if a practitioner becomes<br />
ill can also be useful. This covers what might happen as a result of the condition, who should<br />
If the effect is likely to recur, it is treated as continuing, even if it does not currently have<br />
a substantial adverse effect on a person’s ability to carry out normal day-to-day activities.<br />
Thus, it is not the condition itself, but the impact it has on the individual’s ability to carry out<br />
full daily duties that constitutes the disability.<br />
Examples of steps which an employer may have to take in relation to a disabled person in<br />
order to comply with the Equality Act include:<br />
• Making adjustments to premises<br />
• Allocating some of the disabled person’s duties to another person<br />
• Transferring him or her to fill an existing vacancy<br />
• Altering his or her working hours<br />
• Assigning him or her to a different place of work<br />
• Allowing him or her to be absent during working hours for rehabilitation, assessment<br />
or treatment<br />
• Giving him or her, or arranging for him or her to be given, training<br />
• Acquiring or modifying equipment<br />
30<br />
31
• modifying instructions or reference manuals<br />
• modifying procedures for testing or assessment<br />
Example:<br />
A staff grade anaesthetist who develops back pain might have his job plan altered so he<br />
works in a theatre environment where portering staff are on hand to lift patients, has the<br />
equipment in his workplace assessed by the occupational health department and is provided<br />
with a chair that is suitable for his needs.<br />
A consultant anaesthetist with a depressive illness may temporarily come off the on-call<br />
rota and have sufficient time made available in his working week to attend psychotherapy<br />
sessions. He might stop working with a surgeon with whom he does not have a good working<br />
relationship. Alternatively, the organisation may address the difficulties in communication<br />
with the surgeon and wider team, perhaps with the support of the occupational health service<br />
or an external organisational psychologist.<br />
8. Referral to regulatory authorities<br />
The consultant occupational health physician can also advise on referral to the GMC or<br />
Medical Council of Ireland.<br />
In some circumstances, referral to the GMC may be considered, for instance when substance<br />
abuse forms part of the picture or the practitioner appears not to be following the appropriate<br />
medical advice. The doctor’s consent must be sought but if it is not provided, the treating<br />
doctor must notify the health professional of his/her intention to alert the regulator. The facts<br />
regarding a person's health and management of the condition may be relevant in determining<br />
whether, and if so how, s/he is able or unable to meet the regulator’s standards. However,<br />
the detail of the diagnosis is not required for concluding whether or not a person's fitness to<br />
practise is impaired.<br />
Policy statement from the GMC on the meaning of fitness to practise<br />
The GMC does not need to be involved merely because a doctor is unwell, even if<br />
the illness is serious. However, a doctor’s fitness to practise is brought into question<br />
if it appears that the doctor has a serious medical condition (including an addiction to<br />
drugs or alcohol) AND the doctor does not appear to be following the appropriate<br />
medical advice about modifying his or her practice. Referral will then be necessary to<br />
minimise the risks to patients [5].<br />
It is important not to confuse fitness for work with being ‘fit to practice’.<br />
Role in NCAS/GMC<br />
When a practitioner is referred to the NCAS or to the GMC, it is sometimes relevant to make<br />
an assessment of the practitioner’s health. A recent survey carried out by the revalidation<br />
support team found that around 25% of concerns about practice are related to health. NCAS<br />
has a small team of experienced occupational health physicians whose responsibilities<br />
include advising on whether the doctor has any underlying ill health or disability that could<br />
affect practice, and on whether the practitioner is currently well enough to undergo a formal<br />
assessment.<br />
Role in planning and managing remediation<br />
If remediation is needed, the consultant occupational health physician’s advice about<br />
the timing and nature of the remedial package should be sought and followed. It is not<br />
appropriate to add further stress to a doctor with a health difficulty by making unrealistic<br />
demands or imposing unrealistic timescales.<br />
32<br />
33
It takes about two years for a trainee who has been ill to get back to full achievement. It is<br />
important to:<br />
• Get well first<br />
• Only make career moves when the trainee is moving to something better and not<br />
away from something bad<br />
9. References<br />
1. Harrison J. Orchestrating the health and wellbeing of doctors. Occupational Health [at<br />
Work] 2011; 8/1; 14-17.<br />
2. Disability Discrimination Acts 1995 and 2005.<br />
3. Harling C, Hunt S, eds. Guidance on Ethics for Occupational Physicians. 6th edn.<br />
London: Faculty of Occupational Medicine, 2006.<br />
4. Silvester S, Allen H, Withey C, Morgan M, Holland W. The provision of medical services<br />
to sick doctors. A conspiracy of friendliness? London: Nuffield Provincial Hospitals<br />
Trust, 1994. http://www.nuffieldtrust.org.uk/publications/provision-medical-servicessick-doctors-conspiracy-friendliness<br />
(accessed 31/08/2014)<br />
5. Invisible Patients: Report of the Working Group on the health of health professionals.<br />
London: Department of Health, 2010.<br />
6. Mental Health and Ill Health in Doctors. London: Department of Health, 2008.<br />
7. Handling concerns about practitioners’ health: A guide for managers. National Clinical<br />
Assessment Service 2011. http://www.ncas.nhs.uk/resources/handling-healthconcerns/<br />
(accessed 31/08/2014).<br />
8. Harrison J. Doctors’ health and fitness to practise: the need for a bespoke model of<br />
assessment. Occupational Medicine 2008; 58: 323–7.<br />
9. Practitioner Health Programme. http://www.php.nhs.uk (accessed 31/08/2014).<br />
10. Ghodse H, Galea S. Misuse of drugs and alcohol. In: Cox J, King J, Hutchinson A,<br />
McAvoy P, eds. Understanding Doctors’ Performance. Oxford: Radcliffe Publishing,<br />
2006.<br />
11. The NHS Constitution for England. London: Department of Health, 2009.<br />
https://www.gov.uk/government/publications/the-nhs-constitution-for-england<br />
(accessed 31/08/2014)<br />
12. Launch of SEQOHS: new UK accreditation system for occupational health services.<br />
http://www.fom.ac.uk/general-news/launch-of-seqohs-new-uk-accreditation-systemfor-occupational-health-services<br />
(accessed 31/08/2014).<br />
13. SEQOHS – NHS Health at work. http://www.nhshealthatwork.co.uk/seqohs.asp<br />
(accessed 31/08/2014).<br />
14. West M, Dawson J, Admasachew L, Topakas A. NHS Staff Management and Health<br />
Service Quality. London: Department of Health, 2011. https://www.gov.uk/government/<br />
publications/nhs-staff-management-and-health-service-quality (accessed 31/08/2014)<br />
15. Employee Well-Being: Taking Engagement and Performance to the Next Level.<br />
New York: Towers Watson, 2010. http://www.towerswatson.com/en-CA/Insights/IC-<br />
Types/Ad-hoc-Point-of-View/2010/Employee-Well-Being-Taking-Engagement-and-<br />
Performance-to-the-Next-Level (accessed 31/08/2014).<br />
34<br />
35
16. The Workwell model: an integrated strategic approach. London: Business in the<br />
Community. http://www.bitc.org.uk/programmes/workwell/workwell-model (accessed<br />
31/08/2014).<br />
17. British Medical Association. Doctors’ well-being. http://bma.org.uk/practical-support-atwork/doctors-well-being<br />
(accessed 31/08/2014).<br />
18. Well-being and general survival tips for doctors. Plymouth: South West Peninsula<br />
Postgraduate Medical Education, 2013. http://www.peninsuladeanery.nhs.uk/files/File/<br />
careers/Advice_Centre/Well_Being/Wellbeing_survival_guide_updated_Oct13.pdf<br />
(accessed 31/08/2014).<br />
19. Directive 2003/88/EC of the European Parliament and of the Council of 4 November<br />
2003 concerning certain aspects of the organisation of working time. http://goo.gl/<br />
oHaG4 (accessed 31/08/2014).<br />
20. Smith L. Workload, sleep loss and shift work. In: Cox J, King J, Hutchinson A, McAvoy P,<br />
eds. Understanding Doctors’ Performance. Oxford: Radcliffe Publishing, 2006.<br />
21. Arendt J. Shift work: coping with the biological clock. Occupational Medicine 2010; 60:<br />
10-20.<br />
22. West M, Borrill C. The influence of team working. In: Cox J, King J, Hutchinson A,<br />
McAvoy P eds. Understanding Doctors’ Performance. Oxford: Radcliffe Publishing,<br />
2006.<br />
23. Firth-Cozens J. Leadership and the quality of healthcare. In: Cox J, King J, Hutchinson<br />
A, McAvoy P eds. Understanding Doctors’ Performance. Oxford: Radcliffe Publishing,<br />
2006.<br />
24. Good Medical Practice 2013. London: General Medical Council, 2013. http://www.gmcuk.org/guidance/good_medical_practice.asp<br />
(accessed 31/08/2014).<br />
25. Firth-Cozens J. A perspective on stress and depression. In: Cox J, King J, Hutchinson<br />
A, McAvoy P eds. Understanding Doctors’ Performance. Oxford: Radcliffe Publishing,<br />
2006.<br />
26. Harrison J and Sterland J. The impact of health on performance. In: Cox J, King J,<br />
Hutchinson A, McAvoy P eds. Understanding Doctors’ Performance. Oxford: Radcliffe<br />
Publishing, 2006.<br />
27. Godwin N. Where can sick doctors turn? Occupational Health [at Work] 2011; 7/6: 11–15.<br />
28. Bloodborne Viruses (BBVs) and Occupational Exposure. Public Health England<br />
http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZBloodborneViruses<br />
AndOccupationalExposure/ (accessed 31/08/2014).<br />
29. National Antenatal Infections Screening Monitoring (NAISM). Public Health England.<br />
http://www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1245581538007<br />
(accessed 31/08/2014).<br />
30. Williams S, Libotte V, Ramsey M. Compliance with follow-up after occupational exposure<br />
to hepatitis C. Occupational Medicine 2007; 57: 596–8.<br />
31. Kamming D, Gardam M, Chung F. Anaesthesia and SARS. British Journal of<br />
Anaesthesia. 2003: 90; 715–8.<br />
32. Sepkowitz KA. Occupationally acquired infections in healthcare workers. Part II. Annals<br />
of Internal Medicine 1996; 125; 917–28.<br />
33. Pandemic Influenza: Guidance for infection control in critical care. London: Department<br />
of Health; 2008. http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@<br />
dh/@en/documents/digitalasset/dh_084179.pdf (accessed 31/08/2014).<br />
34. Pandemic (H1N1) 2009 Influenza: A summary of guidance for infection control in<br />
healthcare settings. London: Department of Health; 2008. http://www.dh.gov.uk/<br />
prod_consum_dh/groups/dh_digitalassets/@dh/@en/@ps/documents/digitalasset/<br />
dh_110899.pdf (accessed 31/08/2014)<br />
35. Heating and ventilation systems. London: TSO; 2007. https://www.gov.uk/government/<br />
uploads/system/uploads/attachment_data/file/144029/HTM_03-01_Part_A.pdf<br />
(accessed 31/08/2014).<br />
36. Influenza: the green book, chapter 19. In: Immunisation against infectious disease.<br />
London: Department of Health, September 2013. http://media.dh.gov.uk/network/211/<br />
files/2012/07/Green-Book-Chapter-19-v4_71.pdf (accessed 31/08/2014).<br />
37. Tuberculosis: the green book, chapter 32. In: Immunisation against infectious disease.<br />
London: Department of Health, July 2011. http://media.dh.gov.uk/network/211/<br />
files/2012/07/chap-32-dh_128356.pdf (accessed 31/08/2014).<br />
38. Respiratory protective equipment at work: A practical guide. London: Health and Safety,<br />
Executive reprint with amendments, 2012.<br />
39. TA158 – Oseltamivir, amantadine (review) and zanamavir for the prophylaxis of<br />
influenza. London: NICE; 2008. http://guidance.nice.org.uk/TA158/Guidance/pdf/<br />
English (accessed 31/08/2014).<br />
40. Manual Handling. http://www.nhsemployers.org/~/media/Employers/Publications/<br />
Manual%20handling.pdf (accessed 31/08/2014).<br />
41. Physical and shift work in pregnancy: occupational aspects of management.<br />
London: Royal College of Physicians; 2009. http://www.rcplondon.ac.uk/sites/<br />
default/files/physical-and-shift-work-in-pregnancy-national-guideline-full-text.pdf<br />
(accessed 31/08/2014).<br />
42. Trust, Assurance and Safety – The Regulation of Health Professionals in the 21st<br />
Century. London: TSO; 2007. http://www.official-documents.gov.uk/document/<br />
cm70/7013/7013.pdf (accessed 31/08/2014).<br />
36<br />
37
Appendix 1<br />
Acknowledgement: Dr Jo Hargreaves, Public Health Wales Microbiology Cardiff for hand hygiene<br />
illustration.<br />
38<br />
39
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
Out of Hours Activity<br />
(Anaesthesia)<br />
Guiding Principles and Recommendations<br />
JOINT POSITION STATEMENT<br />
Association of Anaesthetists of Great Britain and Ireland<br />
and<br />
Royal College of Anaesthetists<br />
October 2014<br />
1
Definitions<br />
The times that can be considered to be “out of hours” (OOH) may be defined contractually or by reference to<br />
published national standards. In the current Consultant Contracts for England and Wales, OOH is defined by<br />
the concept of “premium time”, i.e. that which is outside of 07.00 h – 19.00 h on non-Bank Holiday weekdays.<br />
Current and future contract negotiations may change the periods covered by “premium time”. The National<br />
Confidential Enquiry into Patient Outcome and Death (NCEPOD) defines OOH as: “any time outside 08.00 to<br />
17.59 on weekdays, and any time on a Saturday or Sunday”. We will simply define OOH work as that done<br />
outside of the normal working week.<br />
Emergency work<br />
Anaesthetic services delivered OOH are key to the provision of emergency care. Anaesthetists will<br />
reasonably be expected to provide OOH cover for cases that come under the NCEPOD Classification of<br />
Intervention as being “Immediate” or “Urgent”. Following clinical assessment, those cases classified as being<br />
“Expedited” or “Elective” need not be done OOH. Immediate or urgent cases should be prioritised over<br />
routine / elective care at all times.<br />
Drivers for increased OOH activity<br />
The NHS has always operated a 7 day service for patients requiring emergency admissions and surgery.<br />
There is current pressure towards a “7-day NHS” based on the information that some patients admitted to<br />
hospitals at the weekend have worse outcomes compared with those admitted during the working week. It<br />
seems likely that more consultants will be required to be present in hospitals at the weekend, along with<br />
support services. In some units it may be inevitable that the increased workload combined with sicker<br />
patients with increased co-morbidity will require Consultant Anaesthetists to be in-hospital providing resident<br />
shifts during part of the OOH period. The AAGBI and RCOA support measures to improve patient safety and<br />
quality of care but note that this will have a significant impact on Anaesthesia workforce. It has been<br />
suggested that with increased support services, it would be safe to perform elective operating lists at the<br />
weekend, and the principle of elective work OOH in the form of ‘Waiting List Initiatives’ is well established.<br />
Standards and operating procedures developed to make patient care as safe as possible during normal<br />
working hours would be maintained for any elective care taking place out of hours. This should not be seen<br />
as a solution to the failure to carry out this work successfully in normal hours during the week. An increasing<br />
emergency workload and pressure on beds will increase the demand for daily trauma and emergency lists to<br />
expedite surgery and speed patient throughput. Extending planned surgery throughout the week could<br />
enable existing operating theatres to be used for more hours than at present, although it must be noted that<br />
over 70% of theatre running costs relate to staff, drugs and disposables (information available on line from<br />
Information Services Division, NHS Scotland).<br />
The risks of OOH working<br />
Different risks are posed by OOH working in the evening and overnight to working daytimes at weekends.<br />
There are physiological differences between working during the day, and in the evenings or at night and<br />
these differences cannot be fully mitigated. This must be taken into consideration when OOH working is<br />
considered 1 . Studies have shown that human beings do not adapt despite prolonged exposure to night<br />
work 2 . Working in the evening or night especially after having worked during the day may lead to significant<br />
fatigue, as may work at weekends after a full working week 3 . A further factor in fatigue experienced by<br />
anaesthetists is sleep disturbance caused by shifts and irregular patterns of work. Fatigue is associated with<br />
an increased incidence of critical incidents and thus has a direct impact on patient safety 4 . There are<br />
significant additional risks in OOH working that should be mitigated by limiting night-time work to that which<br />
is clinically necessary and adjusting working patterns and arrangements to minimise fatigue. Onsite facilities<br />
that help mitigate the effects of fatigue, such as the timely availability of healthy foods and appropriate areas<br />
for rest, are important to the delivery of safe OOH care.<br />
Patient considerations<br />
Patients should receive appropriate treatment to national standards of care from competent and fit–for-work<br />
clinicians in a timely fashion. However, there must be a balance between the need for speed with which<br />
urgent and expedited surgery is performed in order to minimise the pain and anxiety, and the need to<br />
maintain standards of safety if the provision of OOH is increased. Patient safety must always be prioritised<br />
over patient convenience.<br />
2
Considerations for anaesthetists<br />
The implementation of the Working Time Regulations (WTR) means that trainees no longer work excessive<br />
hours, although the shift patterns worked by the substantial majority do lead to fatigue 2 . Decreases in trainee<br />
hours and overall numbers as well as an increasingly elderly population with greater co-morbidities mean<br />
that career grade doctors, i.e. Consultants and Specialty Doctors, are doing an increasing proportion of OOH<br />
work. As career grade doctors can derogate from WTR, there is a risk that pressure may be exerted to<br />
increase both the amount of work performed and the proportion of work that is done OOH, and the current<br />
government has signalled its intention to look again at the application of WTR to trainees 5 . The ability to<br />
recover from sleep deprivation deteriorates with age, and particular attention should be paid to the impact of<br />
excessive or irregular working hours on the older anaesthetist. It is essential that all anaesthetists are aware<br />
of the potential impact of fatigue on their cognitive ability and ensure they are well rested before treating<br />
patients 3 . Careful planning is required so that patient risk is not increased as a result of fatigue. Specialties<br />
that conduct larger proportions of their clinical activity OOH may experience problems in recruitment and<br />
retention.<br />
Principles and recommendations<br />
Emergency OOH work has always been a fundamental part of the work of anaesthetists. OOH services<br />
should be planned carefully in order to deliver high quality patient care. The extension of planned and<br />
elective clinical activities into periods outside of the normal working week carries with it patient safety risks<br />
and must only happen with careful planning. The provision, capacity and quality of support services must be<br />
provided to the same degree as those in normal working hours, making due allowance for human factors.<br />
Extended work should not drain resources from other clinical areas<br />
The conduct of planned OOH operating sessions is a matter for local discussion and agreement. The AAGBI<br />
and RCoA are agreed that the following issues must be considered:<br />
• Planned OOH sessions during which expedited or elective cases are performed must have the same<br />
levels of pre and post-operative ward staffing, consultant supervision and training, diagnostic and<br />
laboratory services, support services and critical care facilities as sessions done during working<br />
hours.<br />
• Start and finish times of elective operating sessions that extend into OOH periods must take into<br />
account human performance factors.<br />
• In the interests of providing the highest quality service to patients, appropriate compensatory rest<br />
must be taken particularly after a prolonged duty period and rest should be taken at the earliest<br />
possible opportunity.<br />
• Theatre sessions should be fully staffed with cover for contracted breaks. If sessions extend beyond<br />
normal working hours, there should be provision for additional support and breaks.<br />
• Anaesthetists should only provide cover for elective surgery for more than 12 hours in any 24-hour<br />
period in exceptional circumstances. Travel times should be taken into consideration.<br />
• Only immediate or urgent procedures should be conducted at night (after 21.00hrs).<br />
• Special consideration should be given to the very young, the very old and the clinically unstable<br />
patient who should be operated on during the day where possible.<br />
• There must always be sufficient backup and additional facilities to deal with any life or limb<br />
threatening emergency without delay.<br />
• Recovery units should be scheduled to be sufficiently staffed so that all elective cases admitted may<br />
be fully recovered and transferred to the ward without interfering with the urgent/emergency<br />
workload.<br />
• Anaesthesia and surgery should not commence unless all the necessary arrangements are in place<br />
for the complete perioperative patient care pathway.<br />
• Audit of the outcome and productivity of OOH operating sessions must be conducted and compared<br />
with comparable sessions done within normal working hours.<br />
• Extending elective/expedited surgery into OOH periods will demand more financial and human<br />
resources if patient safety is to be maintained. Clinical Directors of Departments of Anaesthesia must<br />
work with clinical governance systems within hospitals to ensure that patient safety is put first and is<br />
not compromised.<br />
3
Members of the working party:<br />
Dr Kathleen Ferguson (Chair), Dr Ramana Alladi, Dr Les Gemmell, Dr William Harrop-Griffiths, Dr Richard<br />
Griffiths, Dr Barry Nichols, Dr Anna-Maria Rollin,Dr Caroline Wilson, Dr David Whitaker<br />
Contributions were received from:<br />
Dr Andrew Hartle, Dr Peter McGuire, Dr Felicity Plaat, Dr Samantha Shinde, Dr Sean Tighe, Dr Isabeau<br />
Walker<br />
The Joint Position Statement was reviewed by the Council of AAGBI and RCoA prior to publication.<br />
References<br />
1. Folkard S,Tucker P. Shift work, safety and productivity Occupational Medicine 2003; 53; 95‐101.<br />
2. Howard SK, Rosekind MR et al. Fatigue in anaesthesia. Anesthesiology 2002; 97; 1281‐1294.<br />
3. Fatigue and Anaesthetists 2014.<br />
http://www.<strong>aagbi</strong>.org/sites/default/files/Fatigue%20Guideline%20web.pdf<br />
4. Lockley SW, Barger LK, Ayas NT, Rothschild JM, Czeisler CA, Landrigan CP. Effects of health care<br />
provider work hours and sleep deprivation on safety and performance. Joint Commission Journal on<br />
Quality and Patient Safety 2007; 33: 7-18.<br />
5. https://www.gov.uk/government/news/more-flexibility-for-nhs-doctors-under-european-working-timedirective<br />
accessed September 2014<br />
4
Peri-operative management<br />
of the obese surgical patient 2015<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
Society for Obesity and Bariatric Anaesthesia<br />
March 2015
This guideline was originally published in Anaesthesia. If you wish to refer<br />
to this guideline, please use the following reference:<br />
Association of Anaesthetists of Great Britain and Ireland. Peri-operative<br />
management of the obese surgical patient 2015. Anaesthesia 2015, 70,<br />
pages 859–876.<br />
This guideline can be viewed online via the following URL:<br />
http://onlinelibrary.wiley.com/enhanced/doi/10.1111/anae.13101/<br />
© The Association of Anaesthetists of Great Britain & Ireland
Guidelines<br />
Peri-operative management of the obese<br />
surgical patient 2015<br />
Association of Anaesthetists of Great Britain and<br />
Ireland<br />
Society for Obesity and Bariatric Anaesthesia<br />
Members of the Working Party: C. E. Nightingale, 1<br />
M. P. Margarson, 1 E. Shearer, 1 J. W. Redman, 1<br />
D. N. Lucas, 2 J. M. Cousins, 1 W. T. A. Fox, 1 N. J. Kennedy, 1<br />
P. J. Venn, 3 M. Skues, 4 D. Gabbott, 5 U. Misra, 2<br />
J. J. Pandit, 7 M.T. Popat 6 and R. Griffiths (Chair) 7<br />
1 Society for Obesity and Bariatric Anaesthesia, 2 Obstetric Anaesthetists’<br />
Association, 3 Royal College of Anaesthetists, 4 British Association of Day<br />
Surgery, 5 Resuscitation Council (UK), 6 Difficult Airway Society, 7<br />
Association of Anaesthetists of Great Britain & Ireland<br />
Summary<br />
Guidelines are presented for the organisational and clinical peri-operative<br />
management of anaesthesia and surgery for patients who are obese,<br />
along with a summary of the problems that obesity may cause peri-<br />
This is an open access article under the terms of the Creative Commons<br />
Attribution-NonCommercial-NoDerivs License, which permits use and<br />
distribution in any medium, provided the original work is properly<br />
cited, the use is non-commercial and no modifications or adaptations<br />
are made.<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
1
operatively. The advice presented is based on previously published<br />
advice, clinical studies and expert opinion.<br />
....................................................................................................<br />
This is a consensus document produced by expert members of a Working<br />
Party established by the Association of Anaesthetists of Great Britain and<br />
Ireland and the Society for Obesity and Bariatric Anaesthesia. It has been<br />
seen and approved by the elected Board/Council of both organisations.<br />
All AAGBI guidelines are reviewed to ensure relevance/accuracy and are<br />
updated or archived when necessary. Date of review: 2020.<br />
Accepted: 10 March 2015<br />
• What other guidelines and statements are available on this topic?<br />
The first Association of Anaesthetists of Great Britain and Ireland<br />
(AAGBI) guidelines on the peri-operative management of the obese<br />
patient were published in 2007 [1]. In 2012, a consensus statement<br />
on anaesthesia for patients with morbid obesity was published by the<br />
Society for Obesity and Bariatric Anaesthesia (SOBA) [2]. The Centre<br />
for Maternal and Child Enquiries (CMACE) and the Royal College<br />
of Obstetricians and Gynaecologists (RCOG) have published joint<br />
guidance on management of women with obesity in pregnancy [3].<br />
•<br />
Why were these guidelines developed?<br />
There is an increased recognition that obese patients present a different<br />
set of challenges and require specific peri-operative care compared<br />
with non-obese patients. These guidelines are intended to<br />
inform anaesthetists about best practice management of obese surgical<br />
patients throughout the peri-operative period, as members of a<br />
multidisciplinary team.<br />
•<br />
How does this statement differ from existing guidelines?<br />
These guidelines include new material on several topics including pharmacology,<br />
positioning and sleep-disordered breathing. The advent of bariatric<br />
(weight treatment) surgery has produced a subgroup of<br />
anaesthetists with more specific experience in the management of obese<br />
patients. The Society for Obesity and Bariatric Anaesthesia was set up in<br />
2009 to share the knowledge gained from bariatric anaesthesia to improve<br />
the anaesthetic care of obese patients in general. This experience forms the<br />
basis of these guidelines.<br />
2 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Recommendations<br />
1 Every hospital should nominate an anaesthetic lead for obesity.<br />
2 Operating lists should include the patients’ weight and body mass<br />
index (BMI).<br />
3 Experienced anaesthetic and surgical staff should manage obese<br />
patients.<br />
4 Additional specialised equipment is necessary.<br />
5 Central obesity and metabolic syndrome should be identified as risk<br />
factors.<br />
6 Sleep-disordered breathing and its consequences should always be<br />
considered in the obese.<br />
7 Anaesthetising the patient in the operating theatre should be considered.<br />
8 Regional anaesthesia is recommended as desirable but is often technically<br />
difficult and may be impossible to achieve.<br />
9 A robust airway strategy must be planned and discussed, as desaturation<br />
occurs quickly in the obese patient and airway management<br />
can be difficult.<br />
10 Use of the ramped or sitting position is recommended as an aid to<br />
induction and recovery.<br />
11 Drug dosing should generally be based upon lean body weight and<br />
titrated to effect, rather than dosed to total body weight.<br />
12 Caution is required with the use of long-acting opioids and sedatives.<br />
13 Neuromuscular monitoring should always be used whenever neuromuscular<br />
blocking drugs are used.<br />
14 Depth of anaesthesia monitoring should be considered, especially<br />
when total intravenous anaesthesia is used in conjunction with neuromuscular<br />
blocking drugs.<br />
15 Appropriate prophylaxis against venous thromboembolism (VTE)<br />
and early mobilisation are recommended since the incidence of<br />
venous thromboembolism is increased in the obese.<br />
16 Postoperative intensive care support should be considered, but is<br />
determined more by co-morbidities and surgery than by obesity per<br />
se.<br />
Introduction<br />
The World Health Organization (WHO) uses a class system to define<br />
obesity (Table 1). Statistics for 2013 from the UK, Health and Social Care<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
3
Table 1 World Health Organization classification of obesity [4].<br />
Body mass index;<br />
kg.m 2<br />
Classification<br />
< 18.5 Underweight<br />
18.5–24.9 Normal<br />
25.0–29.9 Overweight<br />
30.0–34.9 Obese 1<br />
35.0–39.9 Obese 2<br />
> 40.0 Obese 3 (previously ‘morbid obesity’)<br />
Information Centre show that in adults, 24% of men and 25% of women<br />
are classified as obese and over 3% have class-3 obesity [5]. For an average<br />
UK district general hospital serving an adult population of 200 000, this<br />
equates to 52 000 obese and over 6000 class-3 obese patients [6].<br />
Obese patients are more likely to present to hospital because they are<br />
more prone to concomitant disease. Between 2001–2002 and 2011–2012,<br />
there was an eleven-fold increase in the number of patients (from 1019<br />
to 11 736) of all ages admitted to NHS hospitals with a primary diagnosis<br />
of obesity (Fig. 1) [6]. In 2007, the UK Government’s Foresight Report<br />
predicted that 50% of the UK population would be clinically obese by<br />
2050, costing the NHS an extra £45.5 billion (€61.5 billion; $70.1 billion)<br />
per year, but even this may be an underestimate [7].<br />
This consensus guidance is a synthesis of expert opinion, current<br />
practice and literature review, designed to replace the 2007 edition [1]<br />
and act as a guide to the delivery of safe anaesthesia to this clinically<br />
demanding group.<br />
Pathophysiology of obesity<br />
Fat distribution (patient shape)<br />
Not all fat within the body is identical. Unlike peripherally deposited<br />
fat, intra-abdominal fat is highly metabolically active and is known to<br />
be a contributor to several disease states [8]. Patients with centrally distributed<br />
or ‘visceral’ fat are at greater peri-operative risk than those with<br />
peripherally distributed fat, and are far more likely to exhibit the metabolic<br />
syndrome, which consists of central obesity, hypertension, insulin<br />
resistance and hypercholesterolemia [9, 10].<br />
Central obesity can be defined as a waist circumference greater than<br />
88 cm in a woman and 102 cm in a man; or a waist-to-height ratio<br />
greater than 0.55 [10, 11].<br />
4 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
35<br />
30<br />
25<br />
Prevalance (%)<br />
20<br />
15<br />
10<br />
5<br />
0<br />
Figure 1 Adult trends in obesity (BMI ≥ 30 kg.m 2 ) in the UK male (○)<br />
and female (●) population, showing three-yearly averages. Redrawn<br />
from Health Survey England 2013 data (see http://www.hscic.gov.uk/<br />
catalogue/PUB16077) accessed 10/03/2015).<br />
People who exhibit central, or visceral, obesity are often male and<br />
can be described as ‘apple shaped’, while those with a predominantly<br />
peripheral fat distribution are more likely to be female and are described<br />
as ‘pear shaped’.<br />
Respiratory system<br />
Obesity results in reduced functional residual capacity (FRC), significant<br />
atelectasis and shunting in dependent lung regions [12], but resting metabolic<br />
rate, work of breathing and minute oxygen demand are increased.<br />
This combination means that, following the cessation of breathing, arterial<br />
oxygen levels decrease rapidly.<br />
Wheeze in the obese may be due to airway closure rather than<br />
asthma: 50% of patients diagnosed with asthma ‘recover’ with weight<br />
loss [13]. Formal assessment of the effectiveness of bronchodilator therapy<br />
may be useful in differentiating the two conditions [14].<br />
Sleep-disordered breathing<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
5
Sleep-disordered breathing describes the spectrum of conditions ranging<br />
from obstructive sleep apnoea (OSA) through obesity hypoventilation<br />
syndrome (OHS). Each of these conditions has a spectrum of severity,<br />
described according to the number and severity of oxygen desaturations<br />
occurring every hour and their impact upon the patient [15].<br />
Severe OSA occurs in 10–20% of patients with BMI > 35 kg.m 2<br />
and is often undiagnosed. Overall, a diagnosis of OSA is associated with<br />
a greater than doubling of the incidence of postoperative desaturation,<br />
respiratory failure, postoperative cardiac events and ICU admission [16].<br />
The presence of multiple and prolonged oxygen desaturations increases<br />
the sensitivity to opioid-induced respiratory depression [17]. However, if<br />
identified pre-operatively and treated appropriately with continuous<br />
positive airway pressure (CPAP), the risk of complications is much<br />
reduced [18].<br />
Increasing severity of OSA is associated with older age, cardiovascular<br />
disease secondary to heart strain, and the development of left ventricular<br />
dysfunction. It is also associated with a difficult airway and<br />
laryngoscopy. If untreated, OSA may progress to obesity hypoventilation<br />
syndrome, a triad of obesity (BMI > 35 kg.m 2 ), sleep-disordered<br />
breathing (usually OSA) and daytime hypercapnia (pCO 2 > 6 kPa) [19].<br />
The combination of chronic hypoxaemia and hypercapnia make this<br />
subgroup particularly susceptible to the effects of anaesthetic agents and<br />
opioids, which may precipitate acute and chronic hypoventilation and<br />
respiratory arrest in the early postoperative period [20].<br />
Formal diagnosis of sleep-disordered breathing is with polysomnography,<br />
but in the majority of cases, diagnosis can be made by overnight<br />
oximetry testing at home [21]. Nocturnal CPAP is the usual treatment<br />
in patients with significant degrees of OSA, but around 50% of patients<br />
are poorly compliant with CPAP therapy and thus will not obtain benefit,<br />
usually because of problems with the fitting of the mask. Seeking<br />
information on compliance during pre-operative assessment is advised.<br />
Cardiovascular system<br />
Obesity leads to increased blood pressure, cardiac output and cardiac<br />
workload. People with untreated OSA may have associated pulmonary<br />
hypertension and heart failure [15].<br />
There is an increased incidence of arrhythmias, predominantly secondary<br />
to sino-atrial node dysfunction and fatty infiltration of the conducting<br />
system. This results in a relative risk of 1.5 for atrial fibrillation<br />
[22], and a markedly increased risk of sudden cardiac death [23]. There<br />
6 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
is an increased incidence of prolonged QT interval with increasing BMI<br />
[24], and therefore a potential increased risk with drugs such as ondansetron<br />
[25].<br />
Ischaemic heart disease and heart failure are more prevalent in the<br />
obese population, with heart failure the predominant risk factor for<br />
postoperative complications [26].<br />
Thrombosis<br />
Obesity is a prothrombotic state and is associated with increased<br />
morbidity and mortality from thrombotic disorders such as myocardial<br />
infarction, stroke and VTE [27]. The postoperative incidence of<br />
VTE may be 10 times higher in obese women compared with their<br />
healthy-weight counterparts [28]. Previous VTE is an independent<br />
risk factor for patients having gastric bypass surgery [29]. A<br />
hypercoagulable state may extend beyond two weeks, warranting<br />
extended postoperative VTE prophylaxis depending on the type of<br />
surgery and the patient’s BMI [30].<br />
Diabetes<br />
Obesity is strongly associated with increased insulin resistance [31].<br />
Poor glycaemic control in the peri-operative period is associated with<br />
increased morbidity, and good glycaemic control is recommended [32].<br />
Gastric bypass surgery causes a unique neurohumeral response,<br />
resulting in a rapid, dramatic reduction in insulin requirement, starting<br />
immediately after surgery. In this cohort of patients, cautious<br />
postoperative reintroduction of diabetic medication and frequent blood<br />
sugar monitoring are essential [33].<br />
Pharmacology<br />
Body composition<br />
There are a number of terms used to describe the weight of a patient;<br />
the four most useful are shown in Table 2.<br />
Drug dosing<br />
There is limited information on the effect of obesity on the pharmacology<br />
of commonly used anaesthetic drugs. Much of the excess weight is<br />
fat, which has a relatively low blood flow. While lipophilic drugs will<br />
have a larger volume of distribution than hydrophilic ones, the current<br />
evidence indicates that changes in volume of distribution in the obese<br />
are drug-specific, so generalisations are difficult [37]. For most anaes-<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
7
Table 2 The four most useful terms for describing patients’ weight.<br />
Total body<br />
weight (TBW)<br />
Ideal body<br />
weight (IBW)<br />
The actual weight of the patient<br />
What the patient should weigh<br />
with a normal ratio of lean to fat mass.<br />
Varies with age, and is usually<br />
approximated to a function of<br />
height and sex:<br />
IBW (kg) ¼ height (cm) x (where x<br />
¼ 105 in females and 100 in malesÞ<br />
Lean body<br />
weight (LBW)<br />
The patient’s weight excluding fat. Many of the<br />
formulae for calculating lean body weight are<br />
complex but one of the most widely used is that<br />
of Janmahasatian et al. [34]:<br />
LBW (kg) ¼<br />
LBW (kg) ¼<br />
9270 TBW (kg)<br />
6680 þð216 BMI (kg.m 2 ÞÞ ðmenÞ<br />
9270 TBW (kg)<br />
8780 þð244 BMI (kg.m 2 ÞÞ ðwomenÞ<br />
Regardless of total body weight, lean body weight<br />
rarely exceeds 100 kg in men and 70 kg in women<br />
(Fig. 2) [35]<br />
Adjusted body<br />
weight (ABW)<br />
Takes into account the fact that obese individuals<br />
have increased lean body mass and an increased<br />
volume of distribution for drugs. It is calculated<br />
by adding 40% of the excess weight to the IBW [36]:<br />
ABW (kg) = IBW (kg) + 0.4 (TBW (kg) IBW (kg))<br />
thetic agents, dosing to total body weight is rarely appropriate and<br />
increases the risk of relative overdose. Fortunately, most anaesthetic<br />
agents are dosed to affect, e.g. loss of eyelash reflex, nerve stimulator<br />
response or relief of pain. Given the paucity of information, the recommendation,<br />
based on current practice amongst experts in bariatric<br />
8 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Figure 2 Relationship between total body weight and body mass index<br />
(BMI), showing how lean body mass effectively plateaus despite increasing<br />
BMI. A male of height 190 cm and ideal body weight (IBW) is indicated,<br />
demonstrating how IBW includes a normal 15% fat mass.<br />
anaesthesia, is that lean or adjusted body weight are used as the scalars<br />
for calculating initial anaesthetic drug doses rather than total body<br />
weight (Table 3).<br />
The fifth National Audit (NAP5) into accidental awareness under<br />
anaesthesia (AAGA) included a disproportionate number of obese<br />
patients who suffered AAGA. Half of the incidents of awareness occurred<br />
during the induction of anaesthesia and neuromuscular blocking drugs<br />
were used in 93% of these cases [38]. In the obese patient, after a bolus of<br />
anaesthetic induction agent, anaesthesia will occur before redistribution<br />
from the central compartment, and the induction dose required to produce<br />
unconsciousness correlates well with lean body weight [39]. However,<br />
more rapid redistribution of induction agents into the larger fat mass<br />
means that patients wake up more quickly than non-obese patients after a<br />
single bolus dose. With induction agents, a dose based on total body<br />
weight will last longer than one calculated using lean or adjusted body<br />
weight but is likely to result in significant hypotension. It is likely that in<br />
the cases of AAGA found in NAP5, small doses of induction agent based<br />
on lean or adjusted body weight were not quickly followed by the introduction<br />
of maintenance anaesthesia, thus raising the risk of AAGA. Thio-<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
9
Table 3 Suggested initial dosing scalars for commonly used anaesthetic<br />
drugs for healthy obese adults (notwithstanding the fact that titration to<br />
a suitable endpoint may be necessary).<br />
Lean body weight*<br />
Adjusted body weight*<br />
Propofol (induction)<br />
Propofol (infusion; see text)<br />
Thiopental<br />
Antibiotics<br />
Fentanyl<br />
Low molecular weight heparin<br />
Rocuronium<br />
Alfentanil<br />
Atracurium<br />
Neostigmine (maximum 5 mg)<br />
Vecuronium Sugammadex †<br />
Morphine<br />
Paracetamol<br />
Bupivacaine<br />
Lidocaine<br />
*See Table 1 for definitions/calculations.<br />
† See product literature.<br />
pental is associated with a greater risk of awareness than propofol. It is<br />
strongly recommended that additional induction agent be given if there is<br />
a delay in commencing effective maintenance anaesthesia after induction.<br />
Hydrophilic drugs such as neuromuscular blocking drugs are distributed<br />
primarily in the central compartment and lean body weight<br />
is a suitable dosing scalar. A dose of rocuronium based on total body<br />
weight does not significantly shorten the onset time, but will markedly<br />
increase the duration of action [40]. However, due to increased<br />
plasma cholinesterase activity, total body weight is appropriate for<br />
suxamethonium. Doses of neostigmine and sugammadex are related to<br />
the timing and total dose of neuromuscular blocking drugs to be<br />
reversed and can usually be titrated to effect.<br />
For opioids, the clinical effect is poorly related to the plasma concentration<br />
[41]. Dosing using lean body weight is therefore a sensible<br />
starting point until the patient is awake and titration to effect is possible.<br />
For target controlled infusions (TCI) of propofol, the Marsh and<br />
Schnider formulae become unreliable for patients weighing over 140–<br />
150 kg [40]. Because of this, none of the commercially available pumps<br />
allow input of weights above 150 kg using the Marsh model, or BMI<br />
> 35 kg.m 2 (female) and 42 kg.m 2 (male) using the Schnider model.<br />
There is a lack of evidence as to the best weight scalar to use with TCI<br />
10 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
techniques, and when used with neuromuscular blocking drugs,<br />
awareness is a significant potential risk. In these situations, some form<br />
of depth of anaesthesia monitoring is strongly recommended [42].<br />
Pre-operative preparation<br />
General considerations<br />
The vast majority of obese patients presenting for surgery are relatively<br />
healthy and their peri-operative risk is similar to that of patients of normal<br />
weight. The patients at high risk of peri-operative complications are<br />
those with central obesity and metabolic syndrome, rather than those<br />
with isolated extreme obesity [10].<br />
Particular attention should be focused on screening patients for<br />
sleep-disordered breathing and those at particularly high risk of VTE. A<br />
clear pathway for referral for specialist sleep studies should be identified.<br />
The Obesity Surgery Mortality Risk Stratification score (OS-MRS)<br />
(Table 4) has been validated for patients undergoing gastric bypass surgery<br />
to identify the risk factors associated with mortality [43]. It<br />
includes features of metabolic syndrome and sleep-disordered breathing.<br />
Although only validated for bariatric surgical patients, it may be applicable<br />
to obese patients undergoing non-bariatric operations. Patients who<br />
Table 4 The Obesity Surgery Mortality Risk Stratification score: (a) risk<br />
factors; (b) risk of mortality [43].<br />
Risk factor<br />
Score<br />
(a)<br />
BMI > 50 kg.m 2 1<br />
Male 1<br />
Age > 45 years 1<br />
Hypertension 1<br />
Risk factors for pulmonary embolism: 1<br />
Previous venous thromboembolism<br />
Vena caval filter<br />
Hypoventilation (sleep-disordered breathing)<br />
Pulmonary hypertension<br />
Risk of mortality<br />
(b)<br />
Class A: 0-1 points 0.2–0.3%<br />
Class B: 2–3 points 1.1–1.5%<br />
Class C: 4–5 points 2.4–3.0%<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
11
score 4–5 on the OS-MRS are more likely to require closer postoperative<br />
monitoring.<br />
All patients should have their height and weight recorded and BMI<br />
calculated, and these should both be recorded on the operating list to<br />
inform the teams that additional time, equipment and preparation may<br />
be needed. There may be an advantage in estimating lean and adjusted<br />
body weight and recording these in the patient’s records to aid the calculation<br />
of drug doses.<br />
Diagnostic testing should be based on the need to evaluate co-morbidity<br />
and the complexity of surgery, rather than merely as a result of<br />
the presence of obesity.<br />
In bariatric surgery, it is routine to initiate a pre-operative ‘liver<br />
shrinking’ diet to reduce the size of the liver and make access to the<br />
stomach technically easier. There is evidence that 2–6 weeks of intense<br />
pre-operative dieting can improve respiratory function and facilitate laparoscopic<br />
surgery, and may be worth considering in the higher risk<br />
patients [44].<br />
Pre-operative discussion can promote smoking cessation, clarify the<br />
importance of thromboprophylaxis and early mobilisation, plan the<br />
management of medication before admission and remind relevant<br />
patients to bring their own CPAP machine into hospital.<br />
Respiratory assessment<br />
Clinical evaluation of the respiratory system and exercise tolerance<br />
should identify functional limitations and guide further assessment. It is<br />
helpful to assess patients’ arterial saturation in the pre-assessment clinic.<br />
Spirometry is also often useful.<br />
The following features may indicate the presence of significant<br />
underlying respiratory disease and should prompt consideration of preoperative<br />
arterial blood gas analysis [45]:<br />
Arterial saturation < 95% on air<br />
Forced vital capacity < 3 l or forced expiratory volume in 1 s < 1.5 l<br />
• Respiratory wheeze at rest<br />
• Serum bicarbonate concentration > 27 mmol.l 1<br />
An arterial PCO 2 > 6 kPa indicates a degree of respiratory failure<br />
and consequently the likelihood of increased anaesthetic risk.<br />
It is essential to screen for sleep-disordered breathing. Of the several<br />
screening tools available, the STOP-BANG questionnaire (Table 5)<br />
is the best validated in obese patients. It is easy to calculate and has<br />
12 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Table 5 The STOP-BANG screening questionnaire for obstructive sleep<br />
apnoea (adapted with permission [46, 47]. One point is scored for each<br />
positive feature; a score ≥ 5 is a significant risk.<br />
Snoring<br />
Do you snore loudly (louder than talking or heard<br />
through a closed door?)<br />
Tired<br />
Do you often feel tired, fatigued or sleepy during the<br />
daytime? Do you fall asleep in the daytime?<br />
Observed<br />
Has anyone observed you stop breathing or choking or<br />
gasping during your sleep?<br />
Blood Pressure Do you have, or are you being treated for, high<br />
blood pressure?<br />
BMI BMI > 35 kg.m 2<br />
Age<br />
Age > 50 years<br />
Neck<br />
Circumference (measured around Adam’s apple) > 43 cm<br />
(17 in) for males, > 41 cm (16 in) for females<br />
Gender<br />
Male<br />
shown good correlation with the severity of postoperative apnoeas. A<br />
STOP-BANG score of 5 or greater indicates the possibility of significant<br />
sleep-disordered breathing and should prompt referral to a sleep<br />
physician if time allows [46, 47]. Even in the presence of a low STOP-<br />
BANG score, a history of marked exertional dyspnoea, morning headaches<br />
and ECG evidence of right atrial hypertrophy may indicate the<br />
presence of sleep-disordered breathing and should also prompt referral<br />
for assessment.<br />
Patients with undiagnosed OSA, or those unable to tolerate CPAP,<br />
are at the highest risk of peri-operative respiratory and cardiovascular<br />
morbidity [48], while patients fully compliant with CPAP (usually<br />
indicated by symptomatic benefit) are at lower risk of peri-operative<br />
events. In general, patients with adequately treated sleep-disordered<br />
breathing do not have problems requiring high dependency care and<br />
may even be suitable for day surgery [49] (see below).<br />
Airway assessment<br />
Obesity is associated with a 30% greater chance of difficult/failed intubation,<br />
although predictors for difficult laryngoscopy are the same as for<br />
the non-obese [50]. A large neck circumference is a useful additional<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
13
indicator and when greater than 60 cm, is associated with a 35% probability<br />
of difficult laryngoscopy [51].<br />
Bag-mask ventilation is also known to be more difficult in the obese<br />
[52, 53]. Beards in particular can cause problems with bag-mask ventilation<br />
and are quite common in the obese male population. If time allows,<br />
it is recommended that all facial hair should be removed pre-operatively,<br />
or at the very least clipped short.<br />
Cardiovascular assessment<br />
Obese patients should be assessed in the same way as any other patient<br />
group. Features of the metabolic syndrome should be actively identified<br />
as there is a strong association with cardiac morbidity [54]. Assessment<br />
of exercise tolerance can be a valuable tool. The requirement for specific<br />
cardiac investigations should be based on: the degree of exercise tolerance;<br />
the presence of additional co-morbidity; and the site and extent of<br />
the anticipated surgery.<br />
Cardiopulmonary exercise testing (CPET) may predict those at high<br />
risk of postoperative complications and increased length of stay [55, 56].<br />
Standard CPET equipment may not be suitable and recumbent bikes are<br />
available for heavier patients.<br />
Planning postoperative care<br />
The planned postoperative management of most obese patients should<br />
resemble the enhanced recovery programmes of many surgical specialities.<br />
Obesity alone is not a clinical indication for high-dependency postoperative<br />
care. Factors that warrant consideration for a level-2 or -3 setting<br />
include the following:<br />
Pre-existing co-morbidities<br />
Indicated high risk (e.g. OS-MRS 4-5 or limited functional capacity)<br />
Surgical procedure<br />
• Untreated OSA plus a requirement for postoperative parenteral opioids<br />
• Local factors including the skill mix of ward staff<br />
An important consideration for all patients is the degree and site of<br />
surgery. If longer acting opioids (e.g. morphine) are necessary, then<br />
these patients will require closer monitoring, specifically watching for<br />
developing hypercapnia, and level-2 care may be indicated [57].<br />
14 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Intra-operative care<br />
Preparation of patients<br />
Patients’ dignity is important, so suitably sized theatre gowns and disposable<br />
underwear should be available. Antacid and analgesic premedication<br />
should be considered. As previously mentioned, it may be<br />
appropriate to ask male patients with beards to shave/trim them before<br />
surgery.<br />
Preparation of staff<br />
The specific peri-operative requirements of the obese patient should be<br />
included in the pre-operative team brief of the WHO surgical checklist<br />
to ensure the presence of appropriate equipment, including suitable<br />
operating tables, beds and trolleys (see below).<br />
Extra time should be allowed for positioning the obese patient and<br />
performing anaesthesia. Anaesthetists should recognise when additional<br />
personnel (another trained anaesthetist or additional operating department<br />
practitioners) are needed.<br />
The seniority of both the anaesthetist and the surgeon should be considered.<br />
Patients with an OS-MRS score > 3 should be discussed with a<br />
consultant, and those with a score of 4–5 should be anaesthetised by an<br />
anaesthetist experienced in the management of such patients. An experienced<br />
surgeon will reduce operative time and this will help to limit perioperative<br />
morbidity.<br />
Regional anaesthesia<br />
Where possible, regional anaesthesia is preferred to general anaesthesia,<br />
although a plan for airway management is still mandatory [58]. There is<br />
a higher risk of failure of regional techniques in the obese, and appropriate<br />
patient counselling/consent is advised. [59] If sedation is required<br />
during regional anaesthesia, this should be kept to the minimum. Specific<br />
equipment such as extra-long spinal or epidural needles should be<br />
available and ultrasound might be a useful adjunct [60].<br />
There are advantages to the patient (comfort) and practitioner (success<br />
rates) in using the sitting position for neuraxial techniques, and it<br />
may be helpful to tilt the bed towards the operator so the patient naturally<br />
leans forward [61]. To reduce epidural catheter migration, it is recommended<br />
that at least 5 cm catheter should be left in the epidural<br />
space [62].<br />
It is safer to calculate local anaesthetic drug dose using lean body<br />
weight. Despite the potential reduction in neuraxial volume due to<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
15
adipose tissue, standard doses of local anaesthetic are recommended for<br />
central neuraxial blockade [63].<br />
The anaesthetist should be aware that hypotension following neuraxial<br />
anaesthesia may be more problematic in the obese as they are less<br />
tolerant of lying flat or in the Trendelenberg position.<br />
Induction of general anaesthesia<br />
Easily reversible drugs, with fast onset and offset, are the agents of<br />
choice for obese patients.<br />
Anaesthetising the patient in the operating theatre has the advantages<br />
of avoiding the problems associated with transporting an obese anaesthetised<br />
patient, and will also reduce the risk of arterial desaturation<br />
and AAGA associated with disconnection of the breathing system during<br />
transfer [38, 64]. In addition, the patient can position him/herself<br />
on the operating table and can help identify pressure points for protection.<br />
There were a number of learning points from the fourth National<br />
Audit Project (NAP4) which looked at airway complications that are<br />
pertinent to the airway management of the obese patient [65]:<br />
• There was often a lack of recognition and planning for potential airway<br />
problems<br />
• As a result of the reduced safe apnoea time, when airway complications<br />
occurred, they did so rapidly and potentially catastrophically<br />
•<br />
There was evidence that rescue techniques such as supraglottic airway<br />
devices and emergency cricothyroidotomy had an increased failure<br />
rate<br />
•<br />
Adverse events occurred more frequently in obese patients when anaesthetised<br />
by inexperienced staff<br />
Since the work of spontaneous breathing is increased in the obese<br />
patient, tracheal intubation with controlled ventilation is the airway<br />
management technique of choice. Use of supraglottic airway devices as<br />
the primary airway device should be reserved for highly selected patients<br />
undergoing short procedures and, where the patient can be kept headup<br />
during surgery. The upper airway should be accessible at all times<br />
and there must be a plan for tracheal intubation if required.<br />
During induction of anaesthesia, the patient should be positioned in<br />
a ramped position with the tragus of the ear level with the sternum, and<br />
the arms away from the chest (Fig. 3). This will improve lung mechanics,<br />
thereby assisting oxygenation and ventilation and as a result, maxi-<br />
16 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Figure 3 Ramping position for obese patients. Note the tragus of the<br />
ear level with the sternum.<br />
mising the safe apnoea time. The addition of positive end-expiratory<br />
pressure (PEEP) may further facilitate pre-oxygenation [66]. Minimising<br />
the time from induction to intubation will reduce the risk of oxygen desaturation<br />
should bag-mask ventilation prove difficult. It has been demonstrated<br />
that ramping improves the view at laryngoscopy in the obese<br />
patient and this is therefore the recommended default position during<br />
induction in all obese patients [67]. Any difficulty with/failure of direct<br />
laryngoscopy should be promptly managed in accordance with the Difficult<br />
Airway Society guidelines [68].<br />
Suxamethonium-associated fasciculations increase oxygen consumption<br />
and have been shown to shorten the safe apnoea time [69]; consequently,<br />
it is unlikely to wear off before profound hypoxia occurs, and so<br />
may not be the drug of choice for obese patients [70]. With the advent of<br />
sugammadex, aminosteroids could instead be considered the neuromuscular<br />
blocking drugs of choice. The use of rocuronium can minimise the<br />
apnoea time from cessation of spontaneous ventilation to control of ventilation<br />
via a secure airway if bag-mask ventilation is difficult. The dose of<br />
sugammadex for emergency reversal should be pre-calculated and be<br />
immediately available for preparation if required [71].<br />
Ideal body weight should be used to size tracheal tubes and to calculate<br />
tidal volume during controlled ventilation. Tracheal diameter<br />
reduces slightly with increasing BMI [72]. During controlled ventilation,<br />
no particular mode of controlled ventilation has been proven to be<br />
superior; however, greater tidal volumes for a given peak pressure can<br />
often be achieved using pressure-controlled, rather than volume-con-<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
17
trolled, ventilation. The addition of sufficient PEEP and recruitment<br />
manoeuvres will reduce intra- and postoperative atelectasis [73]. For<br />
laparoscopic surgery, flexion of the patient’s trunk, i.e. a slight sitting<br />
position, allows increased abdominal excursion and slightly lower airway<br />
pressures [74].<br />
As intravenous access is often difficult in the obese, it is prudent to<br />
site two intravenous cannulae while in theatre. Ultrasound may prove<br />
useful to help locate peripheral veins but consideration should be given<br />
to unusual sites for intravenous access such as the upper arm and anterior<br />
chest wall. Central venous access should only be used if peripheral<br />
access is impossible, or if specifically indicated.<br />
The ‘SDB-safe’ anaesthetic<br />
A simple and safe principle is to assume that all obese patients have<br />
some degree of sleep-disordered breathing (whether formally tested or<br />
not) and to modify the anaesthetic technique accordingly. Useful<br />
peri-operative strategies therefore include the following:<br />
Avoidance of general anaesthesia and sedatives where possible<br />
Use of short acting agents<br />
•<br />
Use of depth of anaesthesia monitoring techniques to limit anaesthetic<br />
load, particularly when neuromuscular blocking drugs and/or<br />
a total intravenous anaesthetic technique are utilised<br />
•<br />
Use of neuromuscular monitoring to maintain a level of block compatible<br />
with surgery and to ensure complete reversal of block before<br />
waking the patient<br />
• Maximal use of local anaesthetic and multimodal opioid-sparing<br />
analgesia<br />
Maintaining the head–up position throughout recovery<br />
• Monitoring of oxygen saturations until mobile postoperatively<br />
If long-acting opioids are required and the patient is not stabilised<br />
on CPAP pre-operatively, then the use of level-2 care is recommended.<br />
Maintenance of anaesthesia<br />
There is limited evidence at present to favour either TCI of propofol or<br />
volatile agents for maintenance of anaesthesia in the obese. However,<br />
due to the increased risk of AAGA in the obese, it is important that<br />
maintenance is commenced promptly after induction of anaesthesia<br />
[38]. Fat-insoluble volatile agents such as desflurane or sevoflurane have<br />
a faster onset and offset than isoflurane. There is evidence of faster<br />
18 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
eturn of airway reflexes with desflurane compared with sevoflurane in<br />
the obese [75].<br />
Multimodal analgesia techniques, including local anaesthesia, enable<br />
opioid sparing and are strongly recommended.<br />
Emergence from anaesthesia<br />
Both NAP4 and NAP5 showed a high incidence of problems during extubation<br />
in the obese. An extubation plan must therefore be in place in<br />
accordance with the Difficult Airway Society extubation guidelines [76].<br />
Reversal of neuromuscular blockade should be guided by a nerve<br />
stimulator. The aim is to restore motor capacity before waking the<br />
patient [38]. Patients should have return of their airway reflexes and be<br />
breathing with good tidal volumes before tracheal extubation, which<br />
should be performed with the patient awake and in the sitting position.<br />
In those patients with confirmed OSA, the insertion of a nasopharyngeal<br />
airway before waking helps mitigate the partial airway obstruction<br />
that is commonly seen during emergence from anaesthesia.<br />
Postoperative care<br />
Immediate post-anaesthesia care<br />
Full monitoring should be maintained in the post-anaesthesia care unit<br />
(PACU). The patient should be managed in the sitting position or with a<br />
45° head-up tilt.<br />
Oxygen therapy should be applied to maintain pre-operative levels<br />
of arterial oxygen saturation and should be continued until the patient<br />
is mobile postoperatively. If the patient was using CPAP therapy at<br />
home, it should be reinstated on return to the ward or even in the<br />
PACU if oxygen saturation levels cannot be maintained by the use of<br />
inhaled oxygen alone [57]. If supplemental oxygen is necessary, this can<br />
either be given via the patient’s CPAP machine or via nasal specula<br />
under the CPAP mask.<br />
Before discharge from the PACU, all obese patients should be<br />
observed whilst unstimulated for signs of hypoventilation, specifically<br />
episodes of apnoea or hypopnoea with associated oxygen desaturation,<br />
which will warrant an extended period of monitoring in the PACU.<br />
Ongoing hypoventilation will require anaesthetic assessment to establish<br />
the need for further respiratory support and level-2 care.<br />
The patient is safe to return to the ward only when:<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
19
Routine discharge criteria are met<br />
•<br />
or apnoea for at least one hour<br />
•<br />
The respiratory rate is normal and there are no periods of hypopnea<br />
The arterial oxygen saturation returns to the pre-operative values<br />
with or without oxygen supplementation<br />
Analgesia and ward care<br />
An enhanced recovery protocol is essential [77]. Early mobilisation is<br />
vital and most patients should be out of bed on the day of surgery. If<br />
possible, restricting the patient with a urinary catheter, intravenous infusions<br />
or other devices should be avoided. Calf compression devices can<br />
be disconnected for mobilisation.<br />
The intramuscular route of drug administration is to be avoided<br />
owing to unpredictable pharmacokinetics.<br />
The use of patient-controlled analgesia (PCA) systems needs careful<br />
consideration because of the increased risk of respiratory depression in<br />
those with undiagnosed sleep-disordered breathing. In those patients<br />
with suspected or poorly treated sleep-disordered breathing, increased<br />
postoperative monitoring in a level-2 unit is recommended if PCA is<br />
required.<br />
Subarachnoid block with an opioid adjunct is a useful technique<br />
resulting in reduced postoperative opioid requirements. Epidural infusions<br />
are associated with reduced postoperative mobility and may be<br />
counterproductive.<br />
In the ward, oxygen therapy should be continued until baseline<br />
arterial oxygen saturations are achieved, and pulse oximetry should continue<br />
until oxygen saturations remain at baseline without supplemental<br />
oxygen and parenteral opioids are no longer required.<br />
Postoperative tachycardia may be the only sign of a postoperative<br />
complication and should not be ignored (see below).<br />
Thromboprophylaxis<br />
Obesity per se is a risk factor for VTE and it is recommended that all<br />
obese patients, undergoing all but minor surgery, should receive VTE<br />
prophylaxis. Guidelines for postsurgical VTE prophylaxis were published<br />
by the National Institute for Health and Care Excellence in 2010<br />
[78]. Strategies to reduce the risk of VTE include: early postoperative<br />
mobilisation; mechanical compression devices; thromboembolic device<br />
(TED) stockings; anticoagulant drugs; and vena caval filters. There is<br />
20 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Table 6 Dosing schedule for thromboprophylaxis [80].<br />
Enoxaparin<br />
Dalteparin<br />
Tinzaparin<br />
< 50 kg 50–100 kg 100–150 kg > 150 kg<br />
20 mg once 40 mg once 40 mg twice 60 mg twice<br />
daily<br />
daily<br />
daily<br />
daily<br />
2500 units 5000 units 5000 units 7500 units<br />
once daily once daily twice daily twice daily<br />
3500 units 4500 units 4500 units 6750 units<br />
once daily once daily twice daily twice daily<br />
currently limited evidence to support the use of TEDs in obesity, but if<br />
used, it is essential that they be fitted correctly to avoid vascular occlusion.<br />
Current evidence does not support the routine use of venal caval<br />
filters in the obese population [79].<br />
The mainstay of VTE prophylaxis in obesity is pharmacological, with<br />
the criteria for pharmacological prophylaxis including: prolonged immobilisation;<br />
total theatre time > 90 min; age > 60 years; BMI > 30 kg.m 2 ; cancer;<br />
dehydration; and a family history of VTE.<br />
Oral agents such as rivaroxiban and dabigatran are licensed for<br />
VTE prophylaxis following orthopaedic surgery, but there is limited evidence<br />
for their use in obesity. At present, dose adjustment for oral<br />
agents is not recommended for the obese.<br />
There is evidence regarding dose adjustments for low molecular<br />
weight heparins in obesity. The Haemostasis, Anticoagulation and<br />
Thrombosis (HAT) Committee published the dosing schedule reproduced<br />
in Table 6 in April 2010 [80].<br />
Rhabdomyolysis<br />
A rare but serious complication in the obese patient is rhabdomyolysis.<br />
Apart from obesity, pre-disposing risk factors include hypotension,<br />
immobility, prolonged operative procedures and dehydration.<br />
Rhabdomyolysis should be considered if the patient has postoperative<br />
deep tissue pain, classically in the buttocks. Serum creatinine kinase<br />
concentration should be measured promptly, and if rising, aggressive<br />
fluid resuscitation, diuretics and urinary alkalinisation may be required<br />
to prevent further acute kidney injury [81].<br />
Special circumstances<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
21
Sedation<br />
Pre-operative evaluation for patients undergoing sedation should be<br />
similar to those having general anaesthesia. Patients with sleep-disordered<br />
breathing are likely to have airway obstruction with even minimal<br />
sedation. Obese patients are not suitable for solo operator-sedator procedures<br />
[82].<br />
Emergency surgery<br />
It is particularly important that obese patients requiring emergency surgery<br />
are managed by an anaesthetist experienced in the care of the<br />
obese, along with an experienced surgeon in order to minimise the<br />
operative time and the risk of complications [83]. Postoperative level-2<br />
nursing care is far more likely to be required owing to the much higher<br />
risk from emergency surgery complications.<br />
Obese patients can look deceptively well and abdominal examination<br />
can be notoriously difficult. Tachycardia, the new onset of abdominal<br />
pain or unexplained fever may be the only signs of intra-abdominal<br />
sepsis and should be an indication for measuring arterial blood gases<br />
and serum lactate.<br />
Day surgery<br />
It is acceptable for obese patients to undergo surgery as a day case if:<br />
the management would not be modified if they were admitted as an<br />
inpatient; and being treated as a day case will not alter the peri-operative<br />
risk.<br />
The exclusion of obese patients from the advantages that day surgery<br />
may offer should not be made on the basis of weight alone. There<br />
is an increased risk of anaesthetic-related complications in obese<br />
patients in the day surgery environment, but these tend to occur on<br />
induction of anaesthesia, intra-operatively or in the early recovery phase<br />
[84]. Obesity has no influence on the rate of unanticipated admission,<br />
postoperative complications, readmission or other unplanned contact<br />
with health professionals after home discharge [85].<br />
Current guidelines advocate automatic acceptance of patients with<br />
BMI < 40 kg.m 2 [86, 87]. A casenote review should be carried out by<br />
an anaesthetist to determine whether individualised discussion and<br />
assessment may be required before the day of surgery for those with comorbidities<br />
or BMI > 40 kg.m 2 .<br />
22 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
A review and meta-analysis by the Society for Ambulatory Anesthesia<br />
provides useful advice on day surgery for patients with sleep-disordered<br />
breathing [49]. Patients with a known diagnosis of OSA can be considered<br />
for day surgery: if they have, and are able to use, a CPAP device after discharge;<br />
if any co-morbid conditions are optimised; and if postoperative<br />
pain relief can be provided predominantly by non-opioid analgesics.<br />
Laparoscopic cholecystectomy and laparoscopic gastric banding are<br />
increasingly being performed as a day-case procedure [88–90].<br />
Obstetrics<br />
Maternal obesity is recognised as one of the most commonly occurring<br />
risk factors seen in obstetrics, with outcomes for both mother and baby<br />
poorer than in the general population [3].<br />
The CMACE report and the Obstetric Anaesthetists’ Association<br />
have made a number of recommendations regarding the care of obese<br />
pregnant women [91, 92]. Obese women have an increased risk of comorbidity<br />
during pregnancy, in particular gestational diabetes and preeclampsia<br />
[93, 94]. Obesity and pregnancy are both significant risk factors<br />
for the development of VTE in pregnancy.<br />
Compared with a non-obese parturient, an obese woman is more<br />
likely to have her labour induced and require instrumental delivery [95,<br />
96]. There is an increased risk of operative and postoperative complications,<br />
including increased rates of postpartum haemorrhage, prolonged<br />
operative times, and infective complications such as endometritis and<br />
wound infection [97].<br />
Fetal outcomes in obese pregnant women are poorer compared with<br />
the general population, with stillbirth rates in women with a BMI<br />
> 35 kg.m 2 twice as high as the national stillbirth rate. There is an<br />
increased risk of preterm delivery in pregnant obese women [98].<br />
In addition, babies born to obese mothers are at increased risk of<br />
shoulder dystocia, brachial plexus lesions, fractured clavicle and congenital<br />
birth defects such as neural tube defects [99].<br />
Specific anaesthetic considerations are similar to those in the nonobstetric<br />
obese patient:<br />
Obese patients are particularly vulnerable to aortocaval compression<br />
• Vascular access may be more difficult and should be established<br />
early in labour in a woman with a BMI > 40 kg.m 2 [3]<br />
•<br />
The provision of general anaesthesia and central neuraxial blockade<br />
is associated with increased difficulties [100–102]. This can lead to<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
23
an increased decision-to-delivery interval in women who require a<br />
category-1 or -2 caesarean section.<br />
The obese obstetric patient is particularly at risk of VTE and conversely,<br />
postpartum haemorrhage. The recommended dosing of anticoagulants<br />
is generally higher for pregnant women; the Royal College of<br />
Obstetricians and Gynaecologists’ Green-top Guideline provides current<br />
recommendations [103].<br />
Critical care<br />
Outcomes of obese patients in critical care remain controversial. In several<br />
recent studies, obesity was not associated with increased mortality;<br />
however, it was associated with a prolonged requirement for mechanical<br />
ventilation, tracheostomy and prolonged length of stay in a critical care<br />
unit [104, 105].<br />
Airway interventions in the obese are associated with an increased<br />
risk of hypoxia and complications and should only be undertaken by<br />
appropriately skilled personnel. Many would advocate an early tracheostomy<br />
if long-term airway management is anticipated. Custom-made tracheostomy<br />
tubes with an adjustable flange may be required to ensure an<br />
adequate length to reach the trachea. Tracheostomies are usually performed<br />
in the intensive care unit using a percutaneous approach, but<br />
surgical placement may be considered, depending on the experience of<br />
the available medical staff.<br />
For mechanical ventilation, ideal body weight is used to calculate<br />
the initial recommended tidal volume of 5–7 ml.kg 1 , ensuring the peak<br />
inspiratory pressure remains < 35 cmH 2 O [106].<br />
Enteral absorption of drugs is not altered in the morbidly obese. However,<br />
owing to the altered pharmacokinetics, monitoring of serum levels is<br />
considered more important in this group of patients to ensure that drug<br />
levels remain within the therapeutic range [37].<br />
Prophylaxis against VTE is vitally important for the morbidly obese<br />
patient in critical care and should follow the guidelines given above.<br />
All critically ill patients are prone to develop protein malnutrition as a<br />
result of metabolic stress and despite having excess fat stores, the morbidly<br />
obese are no different. However, there is some evidence suggesting that<br />
hypocaloric feeding regimens can achieve adequate nitrogen balance with<br />
more favourable outcomes [107].<br />
Early aggressive rehabilitation and physiotherapy should be undertaken<br />
as soon as is possible to encourage early mobilisation. Increased<br />
24 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
numbers of staff are needed to roll these patients to prevent formation<br />
of pressure sores.<br />
Cardiopulmonary resuscitation<br />
Morbid obesity presents additional problems during resuscitation. There<br />
may be delays caused by difficulties in placement of defibrillator pads,<br />
establishment of vascular access or securing an effective airway. Physical<br />
and biological factors related to obesity may affect the quality of chest<br />
compressions delivered, the efficacy of administered vasoactive drugs or<br />
the efficacy of defibrillator shocks applied, because none of these measures<br />
are standardised to a patient’s BMI. The American Heart Association<br />
has concluded that no alterations to resuscitation have been shown<br />
to affect outcome [108].<br />
Inspiratory airway pressures will be higher than normal, and<br />
excessive leak with supraglottic airway devices may mean that chest<br />
compressions will have to be paused to enable ventilation (i.e. a standard<br />
30:2 compression-ventilation ratio). The high airway pressures<br />
that can occur during resuscitation of very obese patients may impair<br />
coronary perfusion pressure and ultimately reduce the chance of survival<br />
[109].<br />
Chest compressions will be difficult to perform in many patients,<br />
simply because of suboptimal positioning of rescuers. A step or platform<br />
may be required, or compressions can be performed from the patients’<br />
head end. Recommended defibrillation energies remain unaltered in the<br />
morbidly obese, though there is evidence that the thoracic impedance is<br />
higher [110]. If defibrillation remains unsuccessful, the defibrillator pads<br />
should be repositioned and the shock energy increased to the maximum<br />
setting.<br />
If intravenous access is difficult, the intraosseous route for drug<br />
delivery is recommended. The upper humerus is a well-established point<br />
of access, and drug delivery during resuscitation is effective via this<br />
route. Standard doses of adrenaline and amiodarone should be used.<br />
Patients with adjustable gastric bands in situ<br />
Laparoscopic adjustable gastric banding is a recognised treatment for<br />
obesity. However, patients with a gastric band in situ are at increased<br />
risk of pulmonary aspiration during general anaesthesia owing to<br />
oesophageal dysmotility and dilatation above the band. The dilatation<br />
may persist following band deflation. There are case reports of regurgitation<br />
of food even after prolonged fasting and a tracheal tube is recom-<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
25
mended in all patients who have a gastric band [111, 112]. Current<br />
advice is not to deflate the band before surgery; however, depending on<br />
the extent and type of surgery, a decision to deflate the band may be<br />
made on an individual basis. Discussion with the bariatric surgical team<br />
is advised.<br />
An important side note is that patients with gastric bands in situ<br />
who present with sudden onset of dysphagia or upper abdominal pain<br />
should be considered as having a band slippage until proved otherwise.<br />
This is a surgical emergency and should be treated by immediate deflation<br />
of the gastric band and referral to a competent general surgeon.<br />
Delay in deflating the band can lead to gastric infarction and perforation.<br />
For the management of other bariatric surgical emergencies, readers<br />
are referred to the American Society for Metabolic and Bariatric Surgery<br />
website (see below).<br />
Resources<br />
Equipment<br />
A 2011 review of incidents related to obesity reported to the National<br />
Patient Safety Agency highlighted that many of these involved inadequate<br />
provision of suitable equipment. This is a clinical governance issue<br />
and hospitals need to invest in appropriate equipment to assist in the<br />
safe management of obese patients. A suggested but not exhaustive list<br />
of equipment to be considered is given in Table 7 [113].<br />
An ‘obesity pack’ is useful; this can include specialised documentation,<br />
the SOBA single-sheet guidelines (see below) and smaller items of<br />
equipment plus a list of where the larger items are located.<br />
Staff<br />
All units managing obese surgical patients must have the ability to escalate<br />
care appropriately in the event of acute deterioration of patients.<br />
It is recommended that a single person in the anaesthetic department<br />
be nominated as the obesity lead. It would be his/her responsibility<br />
to ensure that equipment and training are up to standard and could<br />
act as a point of contact for advice.<br />
Theatre teams should have training in managing obese patients,<br />
which can be provided either internally or externally. In hospitals where<br />
there is a bariatric service, all staff should periodically observe practice<br />
in this area. Specific training on moving the morbidly obese patient<br />
should be provided.<br />
26 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Table 7 Equipment for managing obese surgical patients.<br />
Ward equipment<br />
Specialised electrically operated beds that can raise a patient to standing<br />
without the need for manual handling with<br />
pressure-relieving mattresses<br />
Suitable bathrooms with floor-mounted toilets, suitable commodes<br />
Large blood pressure measuring cuffs<br />
Extra-large gowns<br />
Suitably sized compression stockings and intermittent compression devices<br />
Larger chairs, wheelchairs and trolleys, all marked with the maximal<br />
recommended weight<br />
Scales capable of weighing up to 300 kg<br />
On-site blood gas analysis<br />
Continuous positive airway pressure or high-flow oxygen delivery device for<br />
the post-anaesthesia care unit<br />
Patient hoist or other moving device (may be shared with other<br />
departments)<br />
Theatre equipment<br />
Bariatric operating table, able to incorporate armboards and table<br />
extensions, attachments for positioning such as leg<br />
supports for the lithotomy position, and shoulder and foot supports<br />
Gel pads and padding for pressure points<br />
Wide Velcro strapping to secure the patient to the operating table<br />
Ramping device/pillows<br />
Raised step for the anaesthetist<br />
Large tourniquets<br />
Readily available difficult airway equipment<br />
Anaesthetic ventilator capable of positive end-expiratory pressure and<br />
pressure modalities<br />
Portable ultrasound machine<br />
Hover-mattress or slide sheet<br />
Long spinal and epidural needles<br />
Long arterial lines if femoral access is necessary<br />
Neuromuscular blockade monitor<br />
Depth of anaesthesia monitoring to minimise residual sedation<br />
In ideal circumstances, all anaesthetic trainees should complete a<br />
module in bariatric anaesthesia to gain insight and hands-on experience<br />
in the management of the morbidly obese surgical patient.<br />
The SOBA single-sheet guide<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
27
This is designed as an aide memoire to be laminated and left in the<br />
anaesthetic room for reference when required. It is available on the<br />
SOBA website and updated every six months as new evidence becomes<br />
available (see www.sobauk.com).<br />
Useful websites<br />
The Society for Obesity and Bariatric Anaesthesia UK: www.sobauk.com.<br />
British Obesity Surgery Patient Association: www.bospauk.org.<br />
British Obesity and Metabolic Surgery Society: www.bomss.org.uk.<br />
American Society for Metabolic and Bariatric Surgery: www.asmbs.org.<br />
References<br />
1. Association of Anaesthetists of Great Britain and Ireland. Peri-operative Management<br />
of the Morbidly Obese Patient. London: Association of Anaesthetists of<br />
Great Britain and Ireland, 2007.<br />
2. Bellamy MC, Margarson MP. Designing intelligent anesthesia for a changing patient<br />
demographic: a consensus statement to provide guidance for specialist and nonspecialist<br />
anesthetists written by members of and endorsed by the Society for<br />
Obesity and Bariatric Anaesthesia (SOBA). Perioperative Medicine 2013; 2: 12.<br />
3. Modder J, Fitzsimons KJ. CMACE/RCOG Joint Guideline: Management of Women<br />
with Obesity in Pregnancy. London: Centre for Maternal and Child Enquiries and<br />
the Royal College of Obstetricians and Gynaecologists, 2010.<br />
4. Public Health England. Measurement of Obesity. 2014. http://www.noo.org.uk/<br />
NOO_about_obesity/measurement (accessed 08/01/2015).<br />
5. Health and Social Care Information Centre. Statistics on Obesity, Physical Activity<br />
and Diet: England, 2013. Leeds: Health and Social Care Information Centre, 2013.<br />
6. National Obesity Forum. State of the nation’s waistline – obesity in the UK:<br />
analysis and expectations. 2014. http://www.nationalobesityforum.org.uk/<br />
media/PDFs/StateOfTheNationsWaistlineObesityintheUKAnalysisandExpectations.<br />
pdf (accessed 08/01/2015).<br />
7. Kopelman P, Jebb SA, Butland B. Executive summary: foresight ‘‘Tackling Obesities:<br />
Future Choices’’ project. Obesity Reviews 2007; 8 (Suppl. 1): vi–ix.<br />
8. Kissebah AH. Intra-abdominal fat: is it a major factor in developing diabetes and<br />
coronary artery disease? Diabetes Research and Clinical Practice 1996; 30(Suppl.<br />
1): S25–S30.<br />
9. Ball J, McAnulty G. Ignoring our evolution: the ‘pandemic’ of over-nutrition. Not<br />
simply a metabolic syndrome? Anaesthesia 2014; 69: 203–7.<br />
10. Glance LG, Wissler R, Mukamel DB, et al. Perioperative outcomes among patients<br />
with the modified metabolic syndrome who are undergoing noncardiac surgery.<br />
Anesthesiology 2010; 113: 859–72.<br />
28 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
11. Schneider HJ, Glaesmer H, Klotsche J, et al. Accuracy of anthropometric indicators<br />
of obesity to predict cardiovascular risk. Journal of Clinical Endocrinology and<br />
Metabolism 2007; 92: 589–94.<br />
12. Pelosi P, Croci M, Ravagnan I, et al. The effects of body mass on lung volumes,<br />
respiratory mechanics, and gas exchange during general anesthesia. Anesthesia<br />
and Analgesia 1998; 87: 654–60.<br />
13. Sikka N, Wegienka G, Havstad S, Genaw J. Respiratory medication prescriptions<br />
before and after bariatric surgery. Annals of Allergy, Asthma and Immunology<br />
2010; 104: 326–30.<br />
14. Schachter LM. Obesity is a risk for asthma and wheeze but not airway hyperresponsiveness.<br />
Thorax 2001; 56:4–8.<br />
15. Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in<br />
sleep: update of the 2007 AASM manual for the scoring of sleep and associated<br />
events. Journal of Clinical Sleep Medicine 2012; 8: 597–619.<br />
16. Mutter TC, Chateau D, Moffatt M, et al. A matched cohort study of post-operative<br />
outcomes in obstructive sleep apnea. Anesthesiology 2014; 121: 707–18.<br />
17. Doufas AG, Tian L, Padrez KA, et al. Experimental pain and opioid analgesia in<br />
volunteers at high risk for obstructive sleep apnea. PLoS ONE 2013; 8:<br />
e54807.<br />
18. Weingarten T, Flores A. Obstructive sleep apnoea and perioperative complications<br />
in bariatric patients. British Journal of Anaesthesia 2010; 106: 273–3.<br />
19. Mokhlesi B. Obesity hypoventilation syndrome: a state of the art review. Respiratory<br />
Care 2010; 55: 1347–62.<br />
20. Leykin Y, Brodsky JB. Controversies in the Anesthetic Management of the Obese<br />
Surgical Patient. New York: Springer, 2012.<br />
21. Chung F, Liao P, Elsaid H, Islam S, Shapiro CM, Sun Y. Oxygen desaturation index<br />
from nocturnal oximetry. Anesthesia and Analgesia 2012; 114: 993–1000.<br />
22. Wanahita N, Messerli FH, Bangalore S, Gami AS, Somers VK, Steinberg JS.<br />
Atrial fibrillation and obesity – results of a meta-analysis. American Heart<br />
Journal 2008; 155: 310–5.<br />
23. Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Mamun Al A, Bonneux L.<br />
Obesity in adulthood and its consequences for life expectancy: a life-table analysis.<br />
Annals of Internal Medicine 2003; 138: 24–32.<br />
24. Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor,<br />
paradox, and impact of weight loss. Journal of the American College of Cardiology<br />
2009; 53: 1925–32.<br />
25. Medicines and Healthcare products Regulatory Agency. Ondansetron for intravenous<br />
use: dose-dependent QT interval prolongation – new posology. 2013.<br />
http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON296402<br />
(accessed 08/01/2015).<br />
26. Hernandez AF, Whellan DJ, Stroud S, Sun JL, O’Connor CM, Jollis JG. Outcomes in<br />
heart failure patients after major noncardiac surgery. Journal of the American College<br />
of Cardiology 2004; 44: 1446–53.<br />
27. Blokhin IO, Lentz SR. Mechanisms of thrombosis in obesity. Current Opinion in<br />
Hematology 2013; 20: 437–44.<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
29
28. Parkin L, Sweetland S, Balkwill A, et al. Body mass index, surgery, and risk of<br />
venous thromboembolism in middle-aged women: a cohort study. Circulation<br />
2012; 125: 1897–904.<br />
29. Demaria EJ, Portenier D, Wolfe L. Obesity surgery mortality risk score: proposal<br />
for a clinically useful score to predict mortality risk in patients undergoing gastric<br />
bypass. Surgery for Obesity and Related Diseases 2007; 3: 134–40.<br />
30. Magee CJ, Barry J, Javed S, Macadam R, Kerrigan D. Extended thromboprophylaxis<br />
reduces incidence of postoperative venous thromboembolism in laparoscopic<br />
bariatric surgery. Surgery for Obesity and Related Diseases 2010; 6:<br />
322–5.<br />
31. Tasali E, Ip MSM. Obstructive sleep apnea and metabolic syndrome: alterations in<br />
glucose metabolism and inflammation. Proceedings of the American Thoracic<br />
Society 2008; 5: 207–17.<br />
32. Frisch A, Chandra P, Smiley D, et al. Prevalence and clinical outcome of hyperglycemia<br />
in the perioperative period in noncardiac surgery. Diabetes Care 2010; 33:<br />
1783–8.<br />
33. Guidone C. Mechanisms of recovery from type 2 diabetes after malabsorptive bariatric<br />
surgery. Diabetes 2006; 55: 2025–31.<br />
34. Janmahasatian S, Duffull SB, Ash S, Ward LC, Byrne NM, Green B. Quantification<br />
of lean body weight. Clinical Pharmacokinetics 2005; 44: 1051–65.<br />
35. Ingrande J, Lemmens HJM. Dose adjustment of anaesthetics in the morbidly<br />
obese. British Journal of Anaesthesia 2010; 105(Suppl. 1): i16–23.<br />
36. Gepts E. Pharmacokinetic concepts for TCI anaesthesia. Anaesthesia 1998; 53<br />
(Suppl. 1): 4–12.<br />
37. Hanley MJ, Abernethy DR, Greenblatt DJ. Effect of obesity on the pharmacokinetics<br />
of drugs in humans. Clinical Pharmacokinetics 2010; 49: 71–87.<br />
38. Pandit JJ, Andrade J, Bogod DG, et al. The 5th National Audit Project (NAP5) on<br />
accidental awareness during general anaesthesia: protocol, methods and analysis<br />
of data. Anaesthesia 2014; 69: 1078–88.<br />
39. Ingrande J, Brodsky JB, Lemmens HJM. Lean body weight scalar for the anesthetic<br />
induction dose of propofol in morbidly obese subjects. Anesthesia and Analgesia<br />
2011; 113: 57–62.<br />
40. Leykin Y, Pellis T, Lucca M, Lomangino G, Marzano B, Gullo A. The pharmacodynamic<br />
effects of rocuronium when dosed according to real body weight or ideal<br />
body weight in morbidly obese patients. Anesthesia and Analgesia 2004; 99:<br />
1086–9.<br />
41. Hammoud HA, Aymard G, Lechat P, Boccheciampe N, Riou B, Aubrun F. Relationships<br />
between plasma concentrations of morphine, morphine-3-glucuronide,<br />
morphine-6-glucuronide, and intravenous morphine titration outcomes in the<br />
postoperative period. Fundamental and Clinical Pharmacology 2011; 25: 518–<br />
27.<br />
42. Absalom AR, Mani V, De Smet T, Struys MMRF. Pharmacokinetic models for propofol-defining<br />
and illuminating the devil in the detail. British Journal of Anaesthesia<br />
2009; 103: 26–37.<br />
43. Demaria EJ, Murr M, Byrne TK, et al. Validation of the Obesity Surgery Mortality Risk<br />
score in a multicenter study proves it stratifies mortality risk in patients undergoing<br />
gastric bypass for morbid obesity. Annals of Surgery 2007; 246: 578–84.<br />
30 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
44. Edholm D, Kullberg J, Haenni A, et al. Preoperative 4-week low-calorie diet<br />
reduces liver volume and intrahepatic fat, and facilitates laparoscopic gastric<br />
bypass in morbidly obese. Obesity Surgery 2011; 21: 345–50.<br />
45. Mandal S, Hart N. Respiratory complications of obesity. Clinical Medicine 2012;<br />
12: 75–8.<br />
46. Chung F, Subramanyam R, Liao P, Sasaki E, Shapiro C, Sun Y. High STOP-BANG<br />
score indicates a high probability of obstructive sleep apnoea. British Journal of<br />
Anaesthesia 2012; 108: 768–75.<br />
47. Chung F, Yang Y, Liao P. Predictive performance of the STOP-BANG score for identifying<br />
obstructive sleep apnea in obese patients. Obesity Surgery 2013; 23:<br />
2050–7.<br />
48. Hallowell PT, Stellato TA, Petrozzi MC, et al. Eliminating respiratory intensive care<br />
unit stay after gastric bypass surgery. Surgery 2007; 142: 608–12.<br />
49. Joshi GP, Ankichetty SP, Gan TJ, Chung F. Society for Ambulatory Anesthesia consensus<br />
statement on preoperative selection of adult patients with obstructive<br />
sleep apnea scheduled for ambulatory surgery. Anesthesia and Analgesia. 2012;<br />
115: 1060–8.<br />
50. Lundstrøm LH, Møller AM, Rosenstock C, Astrup G, Wetterslev J. High body mass<br />
index is a weak predictor for difficult and failed tracheal intubation: a cohort<br />
study of 91,332 consecutive patients scheduled for direct laryngoscopy registered<br />
in the Danish Anesthesia Database. Anesthesiology 2009; 110: 266–74.<br />
51. Brodsky JB, Lemmens HJM, Brock-Utne JG, Vierra M, Saidman LJ. Morbid obesity<br />
and tracheal intubation. Anesthesia and Analgesia 2002; 94: 732–6.<br />
52. Kheterpal S, Martin L, Shanks AM, Tremper KK. Predictions and outcomes of<br />
impossible mask ventilation: a review of 50,000 anesthetics. Anesthesiology<br />
2009; 110: 891–7.<br />
53. Langeron O, Masso E, Huraux C, et al. Prediction of difficult mask ventilation.<br />
Anesthesiology 2000; 92: 1229–36.<br />
54. Apovian CM, Gokce N. Obesity and cardiovascular disease. Circulation 2012; 125:<br />
1178–82.<br />
55. McCullough PA, Gallagher MJ, Dejong AT, et al. Cardiorespiratory fitness and<br />
short-term complications after bariatric surgery. Chest 2006; 130: 517–25.<br />
56. Hennis PJ, Meale PM, Hurst RA, et al. Cardiopulmonary exercise testing predicts<br />
postoperative outcome in patients undergoing gastric bypass surgery. British Journal<br />
of Anaesthesia 2012; 109: 566–71.<br />
57. Practice guidelines for the perioperative management of patients with<br />
obstructive sleep apnea: an updated report by the American Society of<br />
Anesthesiologists Task Force on Perioperative Management of patients with<br />
obstructive sleep apnea. Anesthesiology 2014; 120: 268–86.<br />
58. Nielsen KC, Guller U, Steele SM, Klein SM, Greengrass RA, Pietrobon R. Influence<br />
of obesity on surgical regional anesthesia in the ambulatory setting: an analysis<br />
of 9,038 blocks. Anesthesiology 2005; 102: 181–7.<br />
59. Ingrande J, Brodsky JB, Lemmens HJ. Regional anesthesia and obesity. Current<br />
Opinion in Anesthesiology 2009; 22: 683–6.<br />
60. Balki M, Lee Y, Halpern S, Carvalho CA. Ultrasound imaging of the lumbar spine<br />
in the transverse plane: the correlation between estimated and actual depth to<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
31
the epidural space in obese parturients. Anesthesia and Analgesia 2009; 108:<br />
1876–81.<br />
61. Hamza J, Smida M, Benhamou D, Cohen SE. Parturient’s posture during epidural<br />
puncture affects the distance from the skin to epidural space. Journal of Clinical<br />
Anesthesia 1995; 7: 1–4.<br />
62. Afshan G, Chohan U, Khan FA, Chaudhry N, Khan ZE, Khan AA. Appropriate length<br />
of epidural catheter in the epidural space for postoperative analgesia: evaluation<br />
by epidurography. Anaesthesia 2011; 66: 913–8.<br />
63. Carvalho B, Collins J, Drover DR, Atkinson Ralls L, Riley ET. ED(50) and ED(95) of<br />
intrathecal bupivacaine in morbidly obese patients undergoing cesarean delivery.<br />
Anesthesiology 2011; 114: 529–35.<br />
64. Broom MA, Slater J, Ure DS. An observational study of practice during transfer<br />
of patients from anaesthetic room to operating theatre. Anaesthesia<br />
2006; 61: 943–5.<br />
65. Cook TM, Woodall N, Frerk C, on behalf of the Fourth National Audit Project.<br />
Major complications of airway management in the UK: results of the Fourth<br />
National Audit Project of the Royal College of Anaesthetists and the Difficult Airway<br />
Society. Part 1: Anaesthesia. British Journal of Anaesthesia 2011; 106: 617–<br />
31.<br />
66. Gander S, Frascarolo P, Suter M, Spahn DR, Magnusson L. Positive end-expiratory<br />
pressure during induction of general anesthesia increases duration of nonhypoxic<br />
apnea in morbidly obese patients. Anesthesia and Analgesia 2005; 100: 580–4.<br />
67. Collins JS, Lemmens HJM, Brodsky JB, Brock-Utne JG, Levitan RM. Laryngoscopy<br />
and morbid obesity: a comparison of the ‘‘sniff’’ and ‘‘ramped’’ positions. Obesity<br />
Surgery 2004; 14: 1171–5.<br />
68. Henderson JJ, Popat MT, Latto IP, Pearce AC. Difficult Airway Society guidelines for<br />
management of the unanticipated difficult intubation. Anaesthesia 2004; 59:<br />
675–94.<br />
69. Taha SK, El-Khatib MF, Baraka AS, et al. Effect of suxamethonium vs rocuronium<br />
on onset of oxygen desaturation during apnoea following rapid sequence induction.<br />
Anaesthesia 2010; 65: 358–61.<br />
70. Benumof JL, Dagg R, Benumof R. Critical hemoglobin desaturation will occur<br />
before return to an unparalyzed state following 1 mg/kg intravenous succinylcholine.<br />
Anesthesiology 1997; 87: 979–82.<br />
71. Bisschops MMA, Holleman C, Huitink JM. Can sugammadex save a patient in a<br />
simulated ‘cannot intubate, cannot ventilate’ situation? Anaesthesia 2010; 65:<br />
936–41.<br />
72. D’Anza B, Knight J, Greene JS. Does body mass index predict tracheal airway size?<br />
Laryngoscope 2014; http://onlinelibrary.wiley.com/doi/10.1002/lary.24943/full<br />
(accessed 04/03/2015).<br />
73. Santesson J. Oxygen transport and venous admixture in the extremely obese.<br />
Influence of anaesthesia and artificial ventilation with and without positive endexpiratory<br />
pressure. Acta Anaesthesiologica Scandinavica 1976; 20: 387–94.<br />
74. Mulier JPJ, Dillemans B, Cauwenberge S. Impact of the patient’s body position on<br />
the intraabdominal workspace during laparoscopic surgery. Surgical Endoscopy<br />
2010; 24: 1398–402.<br />
32 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
75. McKay RE, Malhotra A, Cakmakkaya OS, Hall KT, McKay WR, Apfel CC. Effect of<br />
increased body mass index and anaesthetic duration on recovery of protective<br />
airway reflexes after sevoflurane vs desflurane. British Journal of Anaesthesia<br />
2010; 104: 175–82.<br />
76. Extubation algorithm. Difficult Airway Society. 2011. http://www.das.uk.com/content/das-extubation-guidelines<br />
(accessed 24/02/2014).<br />
77. Awad S, Carter S, Purkayastha S, et al. Enhanced recovery after bariatric surgery<br />
(ERABS): clinical outcomes from a tertiary referral bariatric centre. Obesity Surgery<br />
2014; 24: 753–8.<br />
78. Venous Thromboembolism Prevention Quality Standard. National Institute for Health<br />
and care Excellence (NICE), 2010. https://www.nice.org.uk/guidance/qs3 (accessed<br />
24/02/2015).<br />
79. Rowland S, Dharmarajah B, Moore H, et al. Inferior vena cava filters for prevention<br />
of venous thromboembolism in obese patients undergoing bariatric surgery.<br />
Annals of Surgery 2015; 261: 35–45.<br />
80. Haematology, Anticoagulation and Thrombosis Committee. Medicines Q&As,<br />
2010. http://vteprevention-nhsengland.org.uk/images/Thromboprophylaxis%<br />
20and%20extreme%20weight.doc (accessed 14/10/2014).<br />
81. Wool DB, Lemmens HJM, Brodsky JB, Solomon H, Chong KP, Morton JM. Intraoperative<br />
fluid replacement and postoperative creatine phosphokinase levels in laparoscopic<br />
bariatric patients. Obesity Surgery 2010; 20: 698–701.<br />
82. Academy of Medical Royal Colleges. Safe Sedation Practice for Healthcare Procedures.<br />
Standards and Guidance. London: Academy of Medical Royal Colleges,<br />
2013.<br />
83. National Confidential Enquiry into Perioperative Outcome and Death. Peri-operative<br />
Care: Knowing the Risk. London: NCEPOD, 2011. www.ncepod.org.uk/<br />
2011poc.htm (accessed 08/01/2015).<br />
84. Chung F, Mezei G, Tong D. Pre-existing medical conditions as predictors of<br />
adverse events in day-case surgery. British Journal of Anaesthesia 1999; 83:<br />
262–70.<br />
85. Davies KE, Houghton K, Montgomery JE. Obesity and day-case surgery. Anaesthesia<br />
2001; 56: 1112–5.<br />
86. Verma R, Alladi R, Jackson I, et al. Day case and short stay surgery: 2. Anaesthesia<br />
2011; 66: 417–434.<br />
87. Jones K, Montgomery J. Pushing the patient boundaries. In: Smith I, McWhinnie D,<br />
Jackson I, eds. Day Case Surgery. Oxford: Oxford University Press, 2012: 327–34.<br />
88. Watkins BM, Ahroni JH, Michaelson R, et al. Laparoscopic adjustable gastric banding<br />
in an ambulatory surgery center. Surgery for Obesity and Related Diseases<br />
2008; 4: S56–62.<br />
89. Dunsire MF, Patel AG, Awad N. Laparoscopic gastric banding for morbid obesity in<br />
the day surgical setting. Journal of One-Day Surgery 2007; 17.3: A19.<br />
90. Cobourn C, Mumford D, Chapman MA, Wells L. Laparoscopic gastric banding is<br />
safe in outpatient surgical centers. Obesity Surgery 2010; 20: 415–22.<br />
91. Centre for Maternal and Child Enquiries (CMACE). Maternal Obesity in the UK:<br />
Findings from a National Project. London: CMACE, 2010.<br />
92. Obstetric Anaesthetists’ Association. Advice to OAA Members from the OAA Committee:<br />
Re: CMACE Report ‘Maternal obesity in the UK: findings from a national<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
33
project’ (2010). 2011. http://www.oaa-anaes.ac.uk/assets/_managed/editor/<br />
File/CMACE/OAA_response_to_obesity_report.pdf (accessed 08/01/2015).<br />
93. Callaway LK, Prins JB, Chang AM, McIntyre HD. The prevalence and impact of<br />
overweight and obesity in an Australian obstetric population. Medical Journal of<br />
Australia 2006; 184: 56–9.<br />
94. Duckitt K, Harrington D. Risk factors for pre-eclampsia at antenatal booking: systematic<br />
review of controlled studies. British Medical Journal 2005; 330: 565.<br />
95. Vahratian A, Zhang J, Troendle JF, Savitz DA, Siega-Riz AM. Maternal prepregnancy<br />
overweight and obesity and the pattern of labor progression in term nulliparous<br />
women. Obstetrics and Gynecology 2004; 104: 943–51.<br />
96. Chu SY, Kim SY, Schmid CH, et al. Maternal obesity and risk of cesarean delivery:<br />
a meta-analysis. Obesity Reviews 2007; 8: 385–94.<br />
97. Myles TD, Gooch J, Santolaya J. Obesity as an independent risk factor for infectious<br />
morbidity in patients who undergo cesarean delivery. Obstetrics and Gynecology<br />
2002; 100: 959–64.<br />
98. Cnattingius S, Villamor E, Johansson S, et al. Maternal obesity and risk of preterm<br />
delivery. Journal of the American Medical Association 2013; 309: 2362–70.<br />
99. Blomberg M. Maternal obesity, mode of delivery, and neonatal outcome. Obstetrics<br />
and Gynecology 2013; 122: 50–5.<br />
100. Bamgbade OA, Khalaf WM, Ajai O, Sharma R, Chidambaram V, Madhavan G.<br />
Obstetric anaesthesia outcome in obese and non-obese parturients undergoing<br />
caesarean delivery: an observational study. International Journal of Obstetric<br />
Anesthesia 2009; 18: 221–5.<br />
101. Hood DD, Dewan DM. Anesthetic and obstetric outcome in morbidly obese parturients.<br />
Anesthesiology 1993; 79: 1210–8.<br />
102. Perlow JH, Morgan MA. Massive maternal obesity and perioperative cesarean<br />
morbidity. American Journal of Obstetrics and Gynecology 1994; 170: 560–5.<br />
103. Royal College of Obstetricians and Gynaecologists. Reducing the Risk of Thrombosis<br />
and Embolism During Pregnancy and the Puerperium. 2009. https://<br />
www.rcog.org.uk/globalassets/documents/guidelines/gtg37areducingriskthrombosis.pdf<br />
(accessed 08/01/2015).<br />
104. Kumar G, Majumdar T, Jacobs ER, et al. Outcomes of morbidly obese patients<br />
receiving invasive mechanical ventilation: a nationwide analysis. Chest 2013;<br />
144: 48–54.<br />
105. Akinnusi ME, Pineda LA, El Solh AA. Effect of obesity on intensive care morbidity<br />
and mortality: a meta-analysis. Critical Care Medicine 2008; 36: 151–8.<br />
106. Ventilation with lower tidal volumes as compared with traditional tidal volumes<br />
for acute lung injury and the acute respiratory distress syndrome. The Acute<br />
Respiratory Distress Syndrome Network. New England Journal of Medicine 2000;<br />
342: 1301–8.<br />
107. Dickerson RN. Hypocaloric, high-protein nutrition therapy for critically ill patients<br />
with obesity. Nutrition in Clinical Practice 2014; 29: 786–91.<br />
108. Vanden Hoek TL, Morrison LJ, Shuster M, et al. Part 12: cardiac arrest in special situations:<br />
2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation<br />
and Emergency Cardiovascular Care. Circulation 2010; 122: S829–61.<br />
34 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
AAGBI SAFETY GUIDELINE<br />
Peri-operative Care of the Elderly 2014<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650 Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org January 2014
This guideline was originally published in Anaesthesia. If you wish to refer<br />
to this guideline, please use the following reference:<br />
Association of Anaesthetists of Great Britain and Ireland. Peri-operative<br />
care of the elderly 2014. Anaesthesia 2014; 69 s1: pages 81-98.<br />
This guideline can be viewed online via the following URL:<br />
http://onlinelibrary.wiley.com/doi/10.1111/anae.12524/abstract<br />
© The Association of Anaesthetists of Great Britain & Ireland 2014
Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
Guidelines<br />
doi:10.1111/anae.12524<br />
Peri-operative care of the elderly 2014<br />
Association of Anaesthetists of Great Britain and Ireland<br />
Membership of the working party: R. Griffiths, F. Beech, 1 A. Brown, J. Dhesi, 2 I. Foo, 3 J. Goodall, 4<br />
W. Harrop-Griffiths, J. Jameson, 5 N. Love, K. Pappenheim and S. White<br />
1 College of Emergency Medicine<br />
2 British Geriatrics Society<br />
3 Age Anaesthesia Association<br />
4 Intensive Care Society<br />
5 Royal College of Surgeons<br />
Summary<br />
1 Increasing numbers of elderly patients are undergoing an increasing variety of surgical procedures.<br />
2 There is an age-related decline in physiological reserve, which may be compounded by illness, cognitive decline,<br />
frailty and polypharmacy.<br />
3 Compared with younger surgical patients, the elderly are at relatively higher risk of mortality and morbidity after<br />
elective and (especially) emergency surgery.<br />
4 Multidisciplinary care improves outcomes for elderly surgical patients. Protocol-driven integrated pathways guide<br />
care effectively, but must be individualised to suit each patient. The AAGBI strongly supports an expanded role<br />
for senior geriatricians in coordinating peri-operative care for the elderly, with input from senior anaesthetists<br />
(consultants/associate specialists) and surgeons.<br />
5 The aims of peri-operative care are to treat elderly patients in a timely, dignified manner, and to optimise rehabilitation<br />
by avoiding postoperative complications. Effective peri-operative care improves the likelihood of very<br />
elderly surgical patients returning to their same pre-morbid place of residence, and maintains the continuity of<br />
their community care when in hospital.<br />
6 Postoperative delirium is common, but underdiagnosed, in elderly surgical patients, and delays rehabilitation.<br />
Multimodal intervention strategies are recommended for preventing postoperative delirium.<br />
7 Peri-operative pain is common, but underappreciated, in elderly surgical patients, particularly if they are cognitively<br />
impaired. Anaesthetists should administer opioid-sparing analgesia where possible, and follow published<br />
guidance on the management of pain in older people.<br />
8 Elderly patients should be assumed to have the mental capacity to make decisions about their treatment. Good<br />
communication is essential to this process. If they clearly lack that capacity, proxy information should be sought<br />
to determine what treatment, if any, is in the patient’s best interests.<br />
9 Anaesthetists must not ration surgical or critical care on the basis of age, but must be involved in discussions<br />
about the utility of surgery and/or resuscitation.<br />
10 The evidence base informing peri-operative care for the elderly remains poor. Anaesthetists are strongly encouraged<br />
to become involved in national audit projects and outcomes research specifically involving elderly surgical patients.<br />
© 2013 The Association of Anaesthetists of Great Britain and Ireland 81
Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
Griffiths et al. | Guidelines: Peri-operative care of the elderly<br />
This is a consensus document produced by expert members of a Working Party established by the Association of<br />
Anaesthetists of Great Britain and Ireland (AAGBI). It has been seen and approved by the AAGBI Board.<br />
Accepted: 25 October 2013<br />
• What other guideline statements are available on<br />
this topic?<br />
This guideline updates the 2001 AAGBI guideline<br />
Anaesthesia and Peri-operative Care of the<br />
Elderly [1]. Other guidelines informing the perioperative<br />
care of the elderly include those published<br />
by the British Geriatric Society [2] and the<br />
American College of Surgeons/American Geriatrics<br />
Society [3]. The Royal College of Surgeons has<br />
published guidelines concerning emergency surgery<br />
[4] and surgery for high-risk patients [5], and the<br />
College of Emergency Medicine has produced<br />
guidelines concerning older people with urgent and<br />
emergency care needs [6], all of which are relevant<br />
to the peri-operative care of the elderly.<br />
• Why was this guideline was developed?<br />
This guideline was developed to update the 2001<br />
AAGBI guideline in light of the National Confidential<br />
Enquiry into Patient Outcome and Death’s<br />
(NCEPOD’s) 2010 report Elective and Emergency<br />
Surgery in the Elderly: An Age Old Problem [7],<br />
which, taken together with the Francis Report [8]<br />
and the Parliamentary and Health Service Ombudsman’s<br />
2011 report Care and Compassion? [9],<br />
indicates that peri-operative care of the elderly<br />
surgical patient is fragmented and managed poorly,<br />
resulting in potentially avoidable morbidity and<br />
mortality.<br />
• How does this statement differ from existing guidelines?<br />
This guideline is intended specifically to inform anaesthetists<br />
about best-practice management of the<br />
older surgical patient throughout the peri-operative<br />
period, as members of a multidisciplinary team. It<br />
updates the only previous specific professional<br />
guidance in this area [1].<br />
• Why does this statement differ from existing guidelines?<br />
This guideline is specific to the role of anaesthesia<br />
within the multidisciplinary peri-operative care<br />
given to elderly surgical patients. Other relevant<br />
guidelines are either specialty-specific [4–6], disease-specific<br />
(for example, hip fracture [10]) or<br />
specific to only pre-operative assessment [3]. In<br />
common with other guidelines, this guideline<br />
reviews current evidence regarding best-practice<br />
anaesthesia, but also recommends best-practice in<br />
the numerous circumstances where evidence is controversial<br />
or incomplete, based on expert consensus<br />
opinion.<br />
In light of the 1999 NCEPOD report Extremes of Age<br />
[11], the AAGBI developed its guideline Anaesthesia<br />
and Perioperative Care of the Elderly [1], which provided<br />
a framework for the management of patients<br />
aged over 80 years undergoing elective and emergency<br />
surgery. In 2001, when the guideline was published,<br />
~6% of the population were aged over 75 years, and<br />
accounted for ~18% of surgical procedures performed.<br />
In 2010, the NCEPOD report Elective and Emergency<br />
Surgery in the Elderly: An Age Old Problem found that<br />
the care of elderly surgical patients had not improved<br />
significantly in the intervening decade [7]. Moreover,<br />
numerous reports have been published since (including<br />
the Francis Report [8] and Health Service Ombudsman’s<br />
report Care and Compassion? [9]) that suggest<br />
that a culture of inadequate, disjointed and unsympathetic<br />
healthcare exists for elderly inpatients in the<br />
UK. This has contributed to the excess of expensive<br />
mortality and morbidity experienced postoperatively<br />
by older patients, and is of concern, given the rapidly<br />
changing demography of the population. Currently,<br />
~8% of the population are now aged over 75 years and<br />
account for ~23% of surgical procedures performed<br />
(Fig. 1), but by 2025, ~10% of the population will be<br />
aged over 75 years, which is likely to increase the economic<br />
and clinical burdens on the National Health<br />
Service, unless the effectiveness and efficiency of surgical<br />
care can be rapidly and significantly improved for<br />
this vulnerable patient group [12].<br />
82 © 2013 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: Peri-operative care of the elderly Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
In comparison with younger patients, older people<br />
undergoing elective and (particularly) emergency surgery<br />
are at higher risk of adverse postoperative outcomes,<br />
resulting from combinations of age-related<br />
physiological decline, multiple co-morbidity, polypharmacy,<br />
cognitive dysfunction and geriatric syndromes,<br />
including frailty. The provision of continuous, coherent,<br />
quality care to elderly patients with complex needs<br />
is difficult, but best achieved by a multidisciplinary<br />
approach involving primary care, emergency medicine,<br />
geriatricians, anaesthetists, intensivists, surgeons – and<br />
patients. The Working Party includes representation<br />
from all of these groups.<br />
To reflect modern terminology, the concept of<br />
chronological age defining ‘older’ has been abandoned.<br />
Instead, the Working Party’s recommendations are<br />
intended to guide the provision of high-quality anaesthesia<br />
input for older people during each phase of<br />
their surgical journey. Supporting evidence for this<br />
advice is reviewed in the same Anaesthesia supplement<br />
in which this guideline is published.<br />
Pathophysiology of ageing<br />
Physiological decline is a feature of normal ageing and<br />
takes place in all organ systems at a rate of ~1% function<br />
per year after 40 years of age. Fundamentally,<br />
Figure 1 Population aged 90 years and over in England<br />
and Wales 1981–2012. Graph reproduced from<br />
the Office for National Statistics (see http://www.ons.<br />
gov.uk/ons/rel/mortality-ageing/estimates-of-the-veryold–including-centenarians-/2002-2012/stbevo2012.<br />
html?format=print under the Open Government<br />
Licence v2.0).<br />
there is a reduction in organ reserve, which limits the<br />
physiological response to stressors, including acute<br />
illness, anaesthesia and surgery. Functional decline of<br />
the cardiovascular, respiratory, renal, central nervous,<br />
haematological/immunological and musculoskeletal<br />
systems is of greatest concern peri-operatively, and<br />
may influence outcome from elective or emergency<br />
surgery.<br />
Cardiorespiratory systems<br />
The inevitable physiological changes that occur in<br />
the ageing cardiovascular system are associated with<br />
changes in the autonomic nervous system, resulting<br />
in reduced cardiac responsiveness to stress [13]. A<br />
reduction in the responsiveness of beta-receptors<br />
renders the older patient effectively ‘beta-blocked’,<br />
which limits the ability to increase cardiac output<br />
and to respond to fluid losses. Cardiac output is further<br />
limited by age-related reductions in cardiac<br />
compliance. Baroreceptor dysfunction and reduced<br />
responsiveness to angiotensin II further limit the<br />
response to hypovolaemia. These factors may be<br />
compounded by co-morbid myocardial ischaemia<br />
related to atherosclerosis, and consequent cardiac<br />
polypharmacy.<br />
Lung function declines with age due to loss of<br />
both lung and chest wall compliance, and oxygen diffusion<br />
capacity [13], more so if the patient has been a<br />
smoker. The closing volume increases, and ventilation/<br />
perfusion mismatch increases during tidal breathing<br />
when supine.<br />
Together with an age-related decline in oxidative<br />
capacity, cardiopulmonary changes contribute to a<br />
decline in both oxygen uptake and oxygen delivery<br />
with age, rendering the patient at greater risk of perioperative<br />
(myocardial and cerebral) ischaemia, resulting<br />
in poorer outcome.<br />
Renal system<br />
There is considerable variation in the decline of renal<br />
function with age, related to the nephrotoxic effects of<br />
co-morbidities (hypertension, diabetes) and drugs (particularly<br />
non-steroidal anti-inflammatory drugs and<br />
ACE inhibitors) [14]. Renal function affects the pharmacokinetics<br />
and pharmacodynamics of anaesthetic<br />
drugs, and therefore should be assessed routinely<br />
© 2013 The Association of Anaesthetists of Great Britain and Ireland 83
Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
Griffiths et al. | Guidelines: Peri-operative care of the elderly<br />
before elective or emergency surgery in elderly patients<br />
[15].<br />
Central nervous system<br />
Age-related decline in cerebral and cerebrovascular<br />
function contributes to the relatively high prevalence<br />
of postoperative delirium and cognitive dysfunction<br />
experienced by elderly patients, which delays discharge<br />
and ongoing functional recovery [16].<br />
Haematological/immunological systems<br />
Anaemia is common in the elderly (~10%), particularly<br />
within the surgical population, and of often unexplained<br />
aetiology possibly related to erythropoietin<br />
resistance and stem-cell ageing [17]. ‘Immunosenescence’<br />
describes the multifactorial deterioration of the<br />
immune system with age that reduces the capacity to<br />
counter infection and heal wounds, and may contribute<br />
to the development of inflammation-mediated<br />
organ dysfunction [18].<br />
Musculoskeletal system<br />
There is a general decline in muscle volume and function<br />
that, together with arthritic and osteoporotic skeletal<br />
changes, increases the likelihood of fragility<br />
fracture requiring orthopaedic surgery, and of impaired<br />
rehabilitation after all types of surgery. Immobility<br />
contributes to a greater prevalence of thromboembolism<br />
and pressure necrosis [19].<br />
The surgical pathway<br />
The peri-operative period is a continuum of inpatient<br />
care that follows outpatient diagnosis and precedes<br />
community rehabilitation after surgery, regardless of<br />
whether the patient is admitted for elective, urgent or<br />
emergency surgery. Rather than recommend management<br />
according to the urgency of surgery, the Working<br />
Party has considered clinical and organisational<br />
themes that are important throughout the peri-operative<br />
journey, and has placed particular emphasis on<br />
interventions that improve the poorer outcomes associated<br />
with emergency surgery.<br />
In all cases, the Working Party recommends that:<br />
• Continuity of care is best provided by the reciprocal<br />
flow of information between patients, their<br />
relatives/carers, and primary and secondary care<br />
services [20];<br />
• Patients who have conditions that may require<br />
future surgery, such as abdominal aortic aneurysm,<br />
should be given written information about symptoms<br />
and signs that require urgent review, and how<br />
to access this review;<br />
• Where possible, treatment plans based on discussion<br />
between patients and senior doctors must be clearly<br />
documented in the patient’s notes in advance of hospital<br />
admission. This discussion should include proposed<br />
management of expected complications;<br />
• Assessment and optimisation must start as early as<br />
possible, but will need to be tailored to the time<br />
available pre-operatively (longer for elective surgery,<br />
shorter for emergency surgery);<br />
• Opportunities to optimise the patient’s pathophysiological<br />
condition must not be missed before surgery.<br />
This may involve fluid resuscitation before emergency<br />
surgery or the pharmacological manipulation<br />
of chronic co-morbidities before elective surgery.<br />
Pre-operative care<br />
The role of the emergency services<br />
Ambulance personnel should be aware of age-related<br />
changes in the physiology of older patients, and appreciate<br />
how these might affect their interpretation of<br />
resuscitation protocols. For example, occult haemorrhage<br />
may not be recognised in the absence of reactive<br />
tachycardia.<br />
Ambulance personnel are frequently able to assess<br />
the need for surgery and warn emergency departments<br />
in advance of arrival.<br />
Priorities during ambulance transport include:<br />
• Analgesia: An assessment should always be<br />
recorded of pain intensity in the conscious patient,<br />
regardless of cognitive impairment. Titrated<br />
intravenous opioids are effective, but their dose and<br />
time of administration must be recorded in writing<br />
and communicated to emergency department personnel,<br />
to minimise secondary overdosage. Alternative<br />
analgesia includes (fracture) immobilisation,<br />
Entonox and paracetamol. Non-steroidal antiinflammatory<br />
drugs should be avoided until renal<br />
function is ascertained [15];<br />
84 © 2013 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: Peri-operative care of the elderly Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
• Fluid resuscitation: Hypovolaemia may result from<br />
haemorrhage, intestinal obstruction, inadequate<br />
dietary intake or diuretic medication, and can be difficult<br />
to assess. Intravenous access should be established,<br />
but the benefits of fluid resuscitation must be<br />
measured against the risks of fluid overload;<br />
• Warming: Older patients may be hypothermic,<br />
related to body habitus (thin and frail), reduced<br />
temperature homeostasis and environmental factors<br />
(for example, immobility after a fall in a cool<br />
room). Core (tympanic) temperature should<br />
be measured at the scene, and active warming<br />
measures employed to normalise this to ~37 °C<br />
[21];<br />
• History taking: Ambulance personnel are often able<br />
to speak to relatives/carers, who may not travel to<br />
the hospital. Personnel should attempt to record<br />
details of pre-morbid physical and cognitive status,<br />
drug therapy and next-of-kin.<br />
The role of the emergency department<br />
Multidisciplinary assessment and treatment should be<br />
available around the clock for all elderly surgical<br />
patients, preferably in a distinct area of the emergency<br />
department, with the aim of time-limited onward discharge<br />
to more individually appropriate care. The College<br />
of Emergency Medicine recommends that “given<br />
the frequent presence of complex co-morbidities in these<br />
individuals and their degree of need, early assessment<br />
and resuscitation should commence and continue in the<br />
ambulance and emergency departments. Rapid access to<br />
geriatricians, anaesthetists, intensivists and surgeons is<br />
essential to develop an early plan of intervention and<br />
provide targeted management of existing co-morbidities<br />
to decrease intra-operative and post-operative complications.<br />
Early senior decision making is also essential to<br />
provide the appropriate palliative care for people who<br />
are dying who would not benefit from invasive management”<br />
[6].<br />
Pre-operative assessment<br />
Pre-operative assessment in older people enables:<br />
• Risk-stratification, informing doctors, patients and<br />
their relatives/carers about the risks and benefits of<br />
having, or not having, surgery;<br />
• Proactive identification and optimisation of modifiable<br />
risk factors, improving the likelihood of a successful<br />
surgical outcome [3].<br />
‘Peri-operative risk’ defines the likelihood of an<br />
adverse outcome resulting from surgery and/or anaesthesia,<br />
and represents the sum of risk related to both<br />
the surgical procedure and the patient’s pre-morbid<br />
age and pathophysiological condition. Pre-operative<br />
assessment is more resource-efficient when targeted<br />
towards patients with higher peri-operative risk.<br />
• Risk related to the surgical procedure: Observational<br />
data can be used to estimate the risk of adverse<br />
outcome after a range of surgical procedure, but<br />
are subject to operator and institution-specific variation<br />
[4]. Adverse outcomes are much more likely<br />
after emergency, rather than elective, surgery in<br />
older people [22]. Procedural risk may be reduced<br />
by using new surgical techniques, adapting perioperative<br />
pathways to include high dependency/<br />
intensive care, or by performing a less invasive<br />
operation in the first instance to permit patient stabilisation<br />
before definitive surgery [23];<br />
• Risk related to the patient [24]: Age-related physiological<br />
decline, multi-morbidity and frailty are<br />
independently associated with increased perioperative<br />
risk. Pre-operative assessment of the<br />
higher-risk elderly patient, involving a structured<br />
multifactorial approach [25], therefore, should be<br />
undertaken by both a senior geriatrician and a<br />
senior anaesthetist with specific subspecialty training<br />
in geriatrics (depending on resources and time<br />
available).<br />
The Working Party recommends that the components<br />
listed in Table 1 represent the minimum criteria for<br />
adequate pre-operative geriatric assessment specific to<br />
anaesthesia [3, 26–28]. Geriatricians and allied health<br />
professionals properly assess other domains, such as<br />
social circumstances, within a comprehensive geriatric<br />
pre-operative assessment.<br />
Pre-operative optimisation of the older surgical<br />
patient<br />
It is insufficient to undertake comprehensive assessment<br />
of the older surgical patient without also attempting to<br />
© 2013 The Association of Anaesthetists of Great Britain and Ireland 85
Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
Griffiths et al. | Guidelines: Peri-operative care of the elderly<br />
improve his/her pre-operative health status. The benefits<br />
of pre-operative optimisation, however, must be balanced<br />
against the risks of delaying surgery to achieve<br />
these. For instance, pre-operative delay before hip fracture<br />
surgery and emergency laparotomy is associated<br />
with poorer postoperative outcome, suggesting that<br />
optimisation and surgery should take place simultaneously<br />
rather than consecutively [23].<br />
Pre-optimisation should focus on reducing the risk<br />
of postoperative complications, namely:<br />
• Organ-specific morbidity: Numerous guidelines are<br />
available concerning the peri-operative management<br />
of important co-morbidities, including diabetes,<br />
cardiorespiratory disease and anaemia.<br />
However, these should be tailored to suit the older<br />
patient, and may require more than one guideline,<br />
or conflicting guidance, to be taken into account,<br />
along with any adverse effects relating to overinvestigation<br />
or extending polypharmacy;<br />
• Ischaemia: Age and disease-related declines in<br />
physiological reserve render the older patient at<br />
risk of organ-specific and generalised ischaemia.<br />
The brain and heart have an absolute requirement<br />
for oxygen, with peri-operative ischaemia increasing<br />
the likelihood of cardiac and cerebral dysfunction.<br />
Intervention, therefore, should aim to reduce<br />
oxygen uptake (analgesia, thermoregulation, antibiotics)<br />
and improve oxygen delivery (oxygen, fluids,<br />
medication review, avoidance of hypotension and<br />
severe anaemia);<br />
• Postoperative cognitive disorders (postoperative delirium<br />
(POD) and postoperative cognitive decline<br />
(POCD) [16]: The process of identifying and reducing<br />
the risk of POD/POCD should begin pre-operatively.<br />
Patients are at higher risk of POD/POCD if<br />
Table 1 Minimum components of pre-operative geriatric assessment specific to anaesthesia.<br />
Domain Items to be assessed Appropriate assessment tools<br />
Medical<br />
Co-morbidity/severity:<br />
● Cardiovascular<br />
Vital signs, ECG, shuttle, CPET<br />
● Respiratory<br />
S p O 2 , (pulmonary function tests)<br />
● Haematological<br />
Full blood count<br />
● Renal<br />
Urea and electrolytes, estimated glomerular filtration rate<br />
● Nutritional<br />
Weight, body mass index, albumin (liver function tests)<br />
● Musculoskeletal<br />
Assessment of potential nerve block insertion sites<br />
Previous anaesthesia<br />
Enquiry after (age-related) problems<br />
Anaesthesia-specific<br />
Airway assessment, dentition<br />
Alcohol intake<br />
CAGE questionnaire for alcoholism<br />
(Pain intensity)<br />
(Visual analogue pain score)<br />
Presenting pathology<br />
Radiological<br />
Medication<br />
Medication review<br />
Anticoagulant therapy<br />
Relevant allergies<br />
NSQIP pre-operative assessment<br />
Coagulation screen<br />
Cognitive<br />
Functional capacity<br />
Use of functional aids<br />
Risk score<br />
Mental capacity<br />
Decision-making capacity<br />
Communication<br />
Risk factors for<br />
postoperative delirium<br />
Gait and balance<br />
Mobility<br />
Visual<br />
Hearing<br />
Mobility<br />
Dentures<br />
Pathology-specific<br />
Frailty<br />
Ask ‘Have you or (your carer) noticed a change in your memory?’,<br />
Abbreviated mental test score<br />
Vision, hearing, speech<br />
NSQIP pre-operative assessment<br />
6-metre walk<br />
Walks unaided/with stick/with frame/does not walk<br />
Housebound? (yes/no)<br />
Glasses<br />
Hearing aids<br />
Walking stick, frame, wheelchair<br />
e.g. Nottingham Hip Fracture Score<br />
NSQIP pre-operative assessment<br />
CPET, cardiopulmonary exercise test; NSQIP, National Surgical Quality Improvement Program.<br />
86 © 2013 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: Peri-operative care of the elderly Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
they are very old, frail, cognitively impaired, or<br />
have cardio-/cerebrovascular disease and multimorbidity/polypharmacy.<br />
Early recognition should be<br />
communicated throughout the multidisciplinary<br />
care team, and facilitates multimodal interventions<br />
aimed at reducing the prevalence, severity and/or<br />
duration of POD;<br />
• Malnutrition: Oral nutrition and supplementation<br />
counteract the effects of poor appetite and illness.<br />
For example, iron, vitamin B 12 and folate supplementation<br />
provided for subclinical nutritional anaemia<br />
at least 28 days before elective orthopaedic<br />
surgery reduces postoperative morbidity and mortality<br />
[29, 30]. Prolonged pre-operative fasting<br />
should be avoided (excepting possibly where there<br />
is intra-abdominal pathology) [31];<br />
• Functional decline: Although currently there is<br />
insufficient evidence to support its use conclusively<br />
as standard practice, anaesthetists should be aware<br />
of their role in ‘prehabilitation’, that is, maintaining<br />
or enhancing an older patient’s functional reserve<br />
to facilitate postoperative rehabilitation and discharge<br />
back into the community. This is a multimodal<br />
process that involves effective<br />
multidisciplinary communication about potential<br />
risk factors for postoperative morbidity, patient<br />
information and encouragement, enhanced recovery<br />
protocols, fluid therapy and avoidance of<br />
ischaemia, analgesia, thermoregulation, selection of<br />
the most appropriate anaesthetic technique,<br />
employment of postoperative care bundles, appropriate<br />
postoperative care planning, and avoidance<br />
of certain medications.<br />
Decision-making<br />
Pre-operative assessment allows for some determination<br />
of the risk to a patient of undergoing a particular<br />
intervention compared with the intended benefits. Risk<br />
scores (such as the Nottingham Hip Fracture Score<br />
[32]) are useful, but are derived from heterogeneous<br />
observational data, and often require positive or negative<br />
adjustment according to the individual patient.<br />
Furthermore, there may be a disparity between what<br />
doctors and patients view as ‘risk’ or ‘acceptable risk’.<br />
Therefore, the manner and circumstances in which<br />
risk is communicated are important. In law, the standard<br />
of information is ‘that which a reasonable patient<br />
in the patient’s circumstances might want to know’<br />
[33]. In practice, this may include information about<br />
the nature, purpose, (short-term and long-term) risks<br />
and benefits of a specific procedure, an alternative procedure,<br />
or no procedure at all (conservative therapy).<br />
For older patients, the Working Party recommends<br />
that information should be provided specifically about<br />
how an intervention might affect the quantity or quality<br />
of a patient’s remaining life; a pre-operative risk<br />
calculator is available for this purpose [24].<br />
All staff involved in the care of older people undergoing<br />
surgery should be aware of their duties under the<br />
Mental Capacity Act 2005 [34], and in relation to professional<br />
guidance about ‘best interests’ determinations<br />
if an older patient lacks the mental capacity to make<br />
decisions [35–37]. Consultants should make decisions<br />
in relation to patients without capacity, after taking<br />
into account the expectations and known wishes of the<br />
patient, his/her relatives and/or carers.<br />
If a patient is critically unwell, then decisions<br />
about the degree and appropriateness of intervention<br />
will need to be made, requiring input from senior surgeons,<br />
anaesthetists, intensivists, geriatricians and relatives/carers.<br />
Management of expectation is important,<br />
and the provision and intensity of postoperative support,<br />
and end-of-life care should be discussed preoperatively.<br />
High-risk surgery should not be carried out without<br />
a pre-operative commitment to appropriate postoperative<br />
care. Once the decision to operate has been<br />
made, appropriately experienced senior personnel<br />
should be available at all times of day to anaesthetise<br />
and operate on the patient, and organise appropriate<br />
postoperative care.<br />
The nature of surgery<br />
The Working Party strongly advocates senior multidisciplinary<br />
communication about the nature of surgical<br />
intervention before and during surgery. Anaesthetists<br />
must ask their surgical colleagues exactly what procedure<br />
is proposed and whether this is appropriate for<br />
the pathophysiological status of the patient, to plan<br />
anaesthesia accordingly. This may involve consideration,<br />
for example, of the type of access proposed<br />
(minimal access vs open approach), whether ‘damage<br />
© 2013 The Association of Anaesthetists of Great Britain and Ireland 87
Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
control’ surgery (e.g. stenting, defunctioning colostomy)<br />
[38] should be used in the first instance to allow<br />
further patient stabilisation, or whether palliative surgery<br />
is/becomes more appropriate.<br />
Intra-operative management<br />
Older people should expect the same level of dignity<br />
and anaesthesia care as younger adult patients [33].<br />
Additional time may be required to allow older people<br />
to prepare themselves for surgery. Functional aids<br />
(glasses, hearing aids, dentures) should remain in place<br />
until just before the induction of anaesthesia.<br />
Pre-operative checklist<br />
The Working Party recommends use of a specific checklist<br />
by anaesthetists caring for patients over the age of<br />
75 years (Table 2). It includes two sections that should<br />
be completed after the WHO Surgical Safety Checklist<br />
[39] ‘sign in’, before induction of anaesthesia, and ‘time<br />
out’ criteria, before surgical incision.<br />
Temperature control<br />
The importance of body temperature is often underestimated<br />
in the elderly. Peri-operative hypothermia is<br />
common, and associated with adverse outcomes that<br />
include postoperative delirium, cardiac dysfunction,<br />
prolonged hospital stay and poor wound healing [7, 40].<br />
Elderly patients are at increased risk of hypothermia<br />
in the peri-operative period, and are more difficult<br />
to rewarm once hypothermic. Therefore, measures to<br />
maintain temperature, including regular assessment<br />
(tympanic pre- and postoperatively, tympanic/pharyngeal/oesophageal<br />
intra-operatively) and treatment<br />
(forced air warming, fluid warming) should be available<br />
peri-operatively [41], including during transport to and<br />
from theatres, and in the postoperative recovery area.<br />
Griffiths et al. | Guidelines: Peri-operative care of the elderly<br />
Monitoring<br />
The patient should be monitored during anaesthesia<br />
according to AAGBI guidelines [42]. Additional monitoring<br />
is not used as frequently as it should be, given<br />
the greater peri-operative risk of morbidity and mortality<br />
in this patient population [7]. The Working<br />
Party recommends that anaesthetists routinely consider<br />
use of the following monitoring devices for the elderly,<br />
particularly during major or emergency surgery:<br />
• Intra-arterial blood pressure monitoring: Currently,<br />
there is no internationally agreed definition of<br />
hypotension [43]; however, the ‘least bad’ definition<br />
is a fall in systolic blood pressure of more<br />
than 20% from pre-induction baseline, and the<br />
Working Party recommends that this is a suitable<br />
limit. Ideally, intra-arterial cannulation and transduction<br />
should commence before induction of<br />
anaesthesia, to diagnose, treat and therefore prevent<br />
the significant hypotension that can occur at<br />
this time in elderly patients. Beat-to-beat monitoring<br />
also reduces the incidence of hypotensive episodes<br />
occurring between non-invasive blood<br />
pressure measurements, and facilitates near-patient<br />
testing (haemoglobin concentration, blood glucose,<br />
arterial blood gases).<br />
• Central venous pressure: There is a poor relationship<br />
between central venous pressure and blood<br />
volume, as well as poor correlation in response to a<br />
fluid challenge, particularly in elderly patients with<br />
poorly compliant ventricles and vasculature [44],<br />
potentially resulting in fluid overload. Central<br />
venous catheterisation may provide an additional<br />
route of venous access after complex surgery when<br />
vasoactive drug support or parenteral nutrition is<br />
necessary, but must be balanced against the com-<br />
Table 2 Recommended pre-operative amendments to WHO Surgical Safety Checklist for all patients aged over<br />
75 years.<br />
Sign in: before induction of anaesthesia<br />
Have vital signs been recorded (heart rate, blood pressure,<br />
heart rhythm, S p O 2 , temperature)?<br />
Is the patient’s resuscitation status known?<br />
Does the patient have dentures?<br />
Does the patient have any pre-operative pressure sores?<br />
Has the site of any nerve block been confirmed and marked?<br />
Time out: before surgical incision<br />
Have possible areas of pressure damage been padded?<br />
What is the patient’s haemoglobin concentration?<br />
What is the patient’s eGFR?<br />
eGFR, estimated glomerular filtration rate<br />
88 © 2013 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: Peri-operative care of the elderly Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
plications of such access, including insertion<br />
trauma and infection;<br />
• Cardiac output monitoring: Although NICE guidelines<br />
recommend that oesophageal Doppler monitoring<br />
‘should be considered for use in patients<br />
undergoing major or high-risk surgery’, there is<br />
limited evidence in the elderly and, especially, in<br />
emergency surgery [45]. Cardiac output monitoring<br />
using Doppler directed at the aorta (e.g. oesophageal<br />
Doppler/USCOM) may be less accurate in the<br />
elderly, as flow through a poorly compliant aorta<br />
may overestimate cardiac output, and result in insufficient<br />
fluid resuscitation [46, 47]. Use of other<br />
cardiac output monitoring technologies may also be<br />
problematic; therefore, intra-arterial blood pressure<br />
monitoring should be considered earlier in elderly<br />
unwell patients. Regardless of monitoring used, fluid<br />
therapy should be administered with great care and<br />
in divided boluses to allow assessment of response;<br />
• Cerebral oxygen saturation: If episodes of cerebral<br />
oxygen desaturation (> 15%) are indicative of cerebral<br />
ischaemia, then monitoring and early intervention<br />
(systolic BP < 10% fall from baseline, S p O 2<br />
> 95%) may reduce the prevalence of POD/POCD<br />
[48], although further research is needed to confirm<br />
this;<br />
• Bispectral Index Monitors (BIS) or entropy monitors<br />
should be used to guide depth of anaesthesia and<br />
sedation. The doses of anaesthetic agents required to<br />
induce and maintain general anaesthesia [49] and<br />
sedation [50] decrease with increasing age, and failure<br />
to adjust doses (which is common) can result in<br />
relative overdose and prolonged, significant hypotension<br />
[51]. Depth of anaesthesia monitors are recommended<br />
as an option by NICE “during any type<br />
of general anaesthesia in patients at higher risk of<br />
adverse outcomes. This includes … patients at higher<br />
risk of excessively deep anaesthesia” [52]. If depth-ofanaesthesia<br />
monitors are unavailable, a Lerou nomogram<br />
(see Appendix 1) should be used to calculate<br />
the dose of inhalational anaesthesia according to<br />
age-adjusted MAC values [49]. Age-adjustment algorithms<br />
are built into the software of most new generation<br />
anaesthetic machines, and are routinely used<br />
for TIVA. A ‘triple low’ of low BIS and hypotension<br />
despite low inspired inhalational agent concentration<br />
is associated with higher mortality and prolonged<br />
inpatient stay [53].<br />
• Peripheral nerve stimulation: Pharmacokinetic and<br />
pharmacodynamic changes in the elderly can result<br />
in unpredictably prolonged neuromuscular blockade,<br />
suggesting that neuromuscular function monitoring<br />
should be used routinely for patients administered<br />
neuromuscular blocking agents [54, 55].<br />
Fluid and electrolyte management<br />
Fluid and electrolyte therapy is challenging in older<br />
surgical patients. Pathophysiological changes in elderly<br />
patients reduce homeostatic compensation for blood/<br />
fluid loss, but also for boluses of administered intravenous<br />
fluids. Prolonged pre-operative fasting should be<br />
avoided, with clear fluids normally allowed up to 2 h<br />
before surgery to avoid dehydration. High-risk patients<br />
undergoing major surgery appear to benefit from<br />
‘restrictive’ fluid therapy that avoids hypovolaemia by<br />
administering enough fluid to replace pre- plus intraoperative<br />
losses [7, 11, 56]. Neither GIFTASUP [57]<br />
nor NICE [58] guidance is specific tofluid therapy in<br />
older patients.<br />
Blood transfusion<br />
Pre-operative and postoperative anaemia are common<br />
in the older surgical patient, and are associated with<br />
myocardial ischaemia, falls, poor wound healing and<br />
rehabilitation. However, there is a lack of evidence<br />
specific to the elderly surgical population about when<br />
and how much to transfuse to optimise haemoglobin<br />
concentration without incurring transfusion-related<br />
complications.<br />
Observational data suggest that patients aged<br />
> 65 years have higher mortality after major noncardiac<br />
surgery if there is ‘substantial’ operative blood<br />
loss or they have a pre-operative haematocrit < 24%,<br />
but lower mortality if pre-operative haematocrit is 30–<br />
36%, and operative blood loss is < 500 ml [59]. It is<br />
hoped that peri-operative transfusion requirements in<br />
elderly patients are addressed by the forthcoming<br />
NICE guidelines, due to be published in May 2015.<br />
Positioning<br />
Positioning of the patient on the operating table must<br />
be sympathetic to his/her musculoskeletal condition,<br />
© 2013 The Association of Anaesthetists of Great Britain and Ireland 89
Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
Griffiths et al. | Guidelines: Peri-operative care of the elderly<br />
and take into account, for example, kyphoscoliosis,<br />
arthritic joints and fixed flexion deformities. Functional<br />
splints should not be removed, if practicable.<br />
Older patients are at higher risk of (preventable)<br />
peripheral nerve injuries during prolonged surgery,<br />
including the ulnar nerve when supine, the common<br />
peroneal nerve in lithotomy, the dependent radial<br />
nerve in the lateral position and the brachial plexus<br />
after prolonged periods of lateral neck flexion. Lower<br />
limb compartment syndrome can result from the<br />
lithotomy position, or prolonged intra-abdominal<br />
insufflation or pelvic surgery. The Working Party recommends<br />
that probable sites of nerve injury are comprehensively<br />
padded before the start of surgery, and<br />
assessed routinely every 30 min throughout surgery.<br />
Elderly skin can be friable. Care should be taken<br />
when transferring the patient between his/her bed and<br />
the operating table, and when removing adherent<br />
items from the patient, for example, diathermy pads,<br />
tape holding the eyelids closed and surgical dressings.<br />
Similarly, friable skin is more prone to thermal damage,<br />
hence care should be taken with contact warming<br />
devices. Hair should not be removed with a razor.<br />
Reduced skin depth and vascularity, together with<br />
reduced muscle mass, predispose the older patient to<br />
(preventable) tissue pressure necrosis, usually over<br />
bony protuberances, such as the heel. Prolonged hypotension<br />
may contribute to the development of pressure<br />
necrosis. ‘Pressure sores’ interfere with functional<br />
recovery, may be complicated by infection and pain,<br />
and contribute to delayed discharge.<br />
Positioning, together with appropriate fluid therapy<br />
and antithrombotic measures, reduces the risk of<br />
peri-operative thrombo-embolism in the elderly [19].<br />
Type of anaesthesia<br />
The choice of anaesthesia – regional or general –<br />
appears to be of less importance than how sympathetically<br />
it is administered with regard to the patient’s<br />
pathophysiological status. Observational studies and<br />
meta-analyses do not reliably show any significant difference<br />
in outcome between regional and general<br />
anaesthesia, but this may be because the outcomes<br />
measured are not specifically related to anaesthesia<br />
(e.g. 30-day mortality, length of stay [22, 24] or<br />
because regional anaesthesia is seldom administered<br />
without sedation. The choice of technique, therefore,<br />
should be made according to the individual patient.<br />
Intuitively, sympathetically administered regional<br />
anaesthesia, particularly with minimal/no sedation,<br />
would appear to offer some benefit in terms of avoiding<br />
short-term morbidities, including hypotension,<br />
delirium, cardiorespiratory complications and the need<br />
for opioid analgesia [60–62]. However, patients with<br />
cognitive dysfunction may not be able to comply with<br />
regional anaesthesia without heavy sedation, negating<br />
the benefits of avoiding the postoperative cognitive<br />
effects of general anaesthesia [63].<br />
Age-related alterations in the pharmacokinetic and<br />
pharmacodynamic profiles of all anaesthetic agents<br />
render the older patient sensitive to relative overdose,<br />
resulting in myocardial depression, reduced blood<br />
pressure homeostasis and delayed recovery [64]. Particular<br />
care should be taken with hypnotic agents: the<br />
dose required to induce anaesthesia is lower, and the<br />
onset time longer [55]. Depth of anaesthesia monitoring<br />
is recommended.<br />
End-of-surgery checklist<br />
The Working Party recommends use of a specific<br />
checklist by anaesthetists caring for patients over the<br />
age of 75 years (Table 3) undergoing major and/or<br />
emergency surgery. It should be completed after the<br />
WHO Surgical Safety Checklist [39] ‘sign out’, before<br />
the patient leaves the operating theatre for the recovery<br />
area.<br />
The Working Party supports the routine use of a<br />
specific end-of-surgery bundle for older patients<br />
undergoing emergency laparotomy (Table 4) [5].<br />
Table 3 Recommended postoperative amendments to<br />
WHO Surgical Safety Checklist for all patients aged<br />
over 75 years.<br />
Sign out: before patient leaves the operating theatre<br />
What is the patient’s core temperature?<br />
What is the patient’s haemoglobin concentration?<br />
Have age-adjusted and renal function-adjusted doses<br />
of postoperative analgesia been prescribed?<br />
Has a postoperative fluid plan been prescribed?<br />
Can the patient be returned safely to a general care<br />
ward?<br />
90 © 2013 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: Peri-operative care of the elderly Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
Postoperative care<br />
Definitions of levels of postoperative care are shown in<br />
Table 5 [5]. It is recommended that all patients with a<br />
predicted peri-operative mortality of more than 10%<br />
should be admitted to a level 2 or 3 critical care facility<br />
[5]. However, the Working Party recognises that,<br />
although access to critical care should not discriminate<br />
on the basis of age, there is a chronic mismatch<br />
between the number of beds needed to satisfy the 10%<br />
recommendation and the actual number of beds available,<br />
with no imminent prospect of the number of<br />
beds increasing significantly in the UK. Pragmatically,<br />
therefore, the Working Party recommends that anaesthetists<br />
routinely risk assess older patients towards the<br />
end of surgery with regard to the level of postoperative<br />
care they require, discharging patients into critical care<br />
facilities if this is likely to reduce morbidity or mortality<br />
significantly, or if identifiable organ support is<br />
required.<br />
Anaesthetists are instrumental in reducing the<br />
need for, or required duration of, postoperative care,<br />
through appropriate intra-operative management of<br />
anaesthetic drug administration, blood pressure,<br />
Table 4 Summary of end-of-surgery bundle for older<br />
patients undergoing emergency laparotomy.<br />
Towards the end of surgery<br />
1. Risk score (P-POSSUM) to decide on final patient<br />
destination (ward/high dependency/intensive care)<br />
2. Measure lactate or base deficit<br />
3. Assess fluid requirements<br />
4. Assess reverse neuromuscular blockade<br />
5. Assess temperature<br />
Table 5 Levels of postoperative care.<br />
Level Description Patient characteristics<br />
0 Ward Basic observations<br />
1 Enhanced ward At risk of deterioration, more<br />
frequent observations, basic<br />
resuscitation<br />
2 High dependency Needs detailed observation,<br />
intervention or single organ<br />
support<br />
3 Intensive care Multiple organ support,<br />
complexity<br />
patient temperature, fluid therapy and analgesia.<br />
Despite optimum management, however, patient<br />
pathophysiology may demand critical care admission.<br />
If this cannot be provided immediately, then<br />
postoperative care should be provided in the postoperative<br />
care unit (PACU), to a critical care standard<br />
and by suitably experienced personnel. The<br />
Working Party supports the discontinuation of an<br />
operating list (if appropriate) if anaesthetic personnel<br />
are required to provide such care in PACU,<br />
until such time as the patient can be transferred for<br />
definitive critical care.<br />
Assessment of fitness for discharge from PACU is<br />
the decision of the responsible anaesthetist, and should<br />
take into consideration the patient’s vital signs, temperature,<br />
urine output, pain and cognitive status. Good<br />
documented communication is essential to ensure the<br />
continuation of appropriate postoperative care.<br />
The elements of good peri-operative care continue<br />
into the postoperative period, and are aimed at avoiding<br />
complications and re-enabling the patient. These<br />
include analgesia, maintenance of core temperature,<br />
fluid therapy and pressure care. Basic monitoring<br />
should be continued upon return to the ward, with all<br />
hospitals ensuring employment of Modified Early<br />
Warning Scores and provision of Critical Care Outreach<br />
teams [65].<br />
Pain management<br />
Inadequate analgesia for elderly surgical patients contributes<br />
to postoperative morbidity, including delirium<br />
[66], cardiorespiratory complications [67] and failure<br />
to mobilise [68]. Despite the general acknowledgement<br />
of this fact, postoperative pain is poorly assessed [69]<br />
and treated [70] in the elderly, particularly in patients<br />
who are cognitively impaired [69, 71]. Older people<br />
may also be more reluctant to acknowledge and report<br />
pain.<br />
The 2007 British Pain Society/British Geriatrics<br />
Society guidelines include an algorithm for pain assessment<br />
in older people of all cognitive abilities (Appendix<br />
2) [69].<br />
The use of peri-operative analgesia protocols is<br />
recommended, and improves patient satisfaction [72],<br />
but must be individualised for each patient, to take<br />
into account, for example, his/her chronic pain status,<br />
© 2013 The Association of Anaesthetists of Great Britain and Ireland 91
Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
Griffiths et al. | Guidelines: Peri-operative care of the elderly<br />
frailty, pain assessment, concurrent medication, renal<br />
function and cognitive impairment [73, 74].<br />
Multimodal analgesia is not restricted to pharmacological<br />
agents, and may involve, for example, postural<br />
support, pressure care and patient warming. Nerve<br />
blockade is effective, if not always reliable [64]. Paracetamol<br />
is safe and should be considered first-line therapy.<br />
Non-steroidal anti-inflammatory drugs should be<br />
used with caution if paracetamol is ineffective, and at<br />
their lowest doses and for the shortest duration, with<br />
proton pump inhibitor gastric protection and routine<br />
monitoring for gastric and renal damage.<br />
Morphine is effective, but should be administered<br />
(for moderate or severe pain) cautiously, particularly<br />
to patients with poor renal or respiratory function,<br />
and the cognitively impaired; consideration should be<br />
given to the co-administration of laxatives and antiemetics,<br />
as required.<br />
Anaesthetists should be familiar with which medications<br />
are potentially inappropriate for use in older<br />
patients according to Beers Criteria [75].<br />
Postoperative delirium and postoperative<br />
cognitive dysfunction<br />
The process of identifying and reducing the risk of<br />
POD/POCD should continue postoperatively [16].<br />
Recovery room delirium is a strong predictor for postoperative<br />
delirium [76], and so the recovery area is an<br />
appropriate area for delirium testing [77]. High-quality<br />
peri-operative care reduces the incidence of delirium<br />
[78]. NICE recommend that DSM-IV (Diagnostic and<br />
Statistical Manual of Mental Disorders) criteria or<br />
short-CAM (confusion assessment method) are used<br />
to diagnose delirium [16]. Drugs that precipitate delirium,<br />
and that should therefore be avoided if possible<br />
in patients at risk, include benzodiazepines, opioids,<br />
antihistamines (including cyclizine) [79], atropine [80],<br />
sedative hypnotics and corticosteroids [75].<br />
Nutrition<br />
Nutrition should be continued from the pre-operative<br />
period or instigated early after surgery to improve<br />
wound healing and recovery; supplementation may be<br />
required. Anaesthetists can facilitate enteral nutrition<br />
by delivering age-appropriate anaesthesia and appropriate<br />
fluid therapy, avoiding reliance on postoperative<br />
opioid analgesia, and preventing postoperative nausea.<br />
Enteral nutrition improves outcome compared with<br />
parenteral nutrition in the elderly [81].<br />
Re-enablement after surgery<br />
‘Re-enablement’ describes patients’ return to their preoperative<br />
level of function, and extends beyond remobilisation<br />
or rehabilitation. Anaesthetists contribute<br />
peri-operative components to the multidisciplinary<br />
process of a patient’s re-enablement by providing<br />
appropriate care, important elements of which have<br />
been repeatedly emphasised above: age-appropriate<br />
anaesthesia; fluid therapy; thermoregulation; analgesia;<br />
communication; and risk assessment.<br />
Ethicolegal issues<br />
A stark conclusion common to many recent reports is<br />
that hospital care disregards the dignity of older<br />
patients [7–9]. This may contribute to poor continuity<br />
of care and outcome and is symptomatic of a lowquality<br />
culture of healthcare provision. Professional<br />
leadership is required to reverse these attitudes, and<br />
anaesthetists, as peri-operative physicians, are ideally<br />
suited to managing such a change. The Working Party<br />
strongly recommends that a consultant anaesthetist<br />
within each NHS Trust is appointed Lead Clinician for<br />
Geriatric Anaesthesia, and is encouraged to act as an<br />
‘older person’s champion’ within the operating department,<br />
responsible for improving the dignity and quality<br />
of care received by older patients undergoing<br />
surgery.<br />
Issues concerning mental capacity and decisionmaking<br />
are discussed above. These are also of importance<br />
in discussing end-of-life care with patients or<br />
their relatives/carers, when further intervention is considered<br />
either futile or high-risk to the extent that<br />
resuscitation wishes need to be considered [33]. The<br />
Working Party recommends that all anaesthetists<br />
familiarise themselves with professional guidance about<br />
end-of-life care [36, 82], and, if in doubt about their<br />
professional and legal obligations, contact their hospital’s<br />
legal representative for advice.<br />
Research and Audit<br />
A recurring theme in guidelines (including this document),<br />
reports, systematic reviews and meta-analyses of<br />
92 © 2013 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: Peri-operative care of the elderly Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
peri-operative care for elderly patients concerns the lack<br />
of specific evidence on which to provide high-quality<br />
care [22], most being extrapolated from research involving<br />
younger surgical patients. This does not preclude the<br />
benefit of formulating guidelines with the aim of<br />
informing improvements in treatment where there is<br />
diversity in practice and outcome [83]. However, the<br />
Working Party strongly recommends that the evidence<br />
base for peri-operative care of the elderly is improved,<br />
and urgently. Randomised, controlled trials, although<br />
important, are of less relevance to assessment of<br />
multimodal interventions for elderly patients, and<br />
before-and-after interventional studies and observational<br />
studies may yield at least as much information.<br />
To this end, the Working Party recommends that<br />
anaesthetists:<br />
• Participate in national audit initiatives, including,<br />
for example, the National Emergency Laparotomy<br />
Audit [23] and the National Hip Fracture Database<br />
[10], to ensure the accuracy and completeness of<br />
submitted data;<br />
• Develop and assess the performance of quality<br />
improvement metrics for elderly patients [84, 85];<br />
• Undertake continuous quality improvement, as outlined<br />
in Raising the Standard: a Compendium of<br />
Audit Recipes [86] (especially sections 1.7, 1.10, 2.7,<br />
3.4, 4.1-4.4, 4.7, 4.9, 11.3–11.6) and seek to adapt<br />
these specifically for elderly patients.<br />
Resources for training<br />
The Working Party recommends that the frail elderly<br />
are anaesthetised only by a senior anaesthetist with<br />
appropriate training and expertise in geriatric anaesthesia.<br />
However, given the anticipated increases in the<br />
number of elderly patient expected to require surgery<br />
in future, the Working Party recognises that the current<br />
pool of ‘geriatric’ anaesthetists is insufficient to<br />
fulfil this recommendation. The Working Party, therefore,<br />
strongly recommends that geriatric anaesthesia is<br />
specifically taught as a training module to anaesthetists<br />
in training, and that peri-operative care of the elderly<br />
surgical patient is included within the training<br />
curricula of UK and Irish medical schools, the Royal<br />
Colleges of Anaesthetists, Surgeons and Physicians<br />
[87] and the College of Anaesthetists of Ireland.<br />
Additional resources for doctors,<br />
patients and carers<br />
A number of documents are available that describe<br />
what elderly patients are entitled to expect from their<br />
inpatient care, and inform doctors about how to provide<br />
dignified, quality care for elderly surgical patients.<br />
These include:<br />
1 The Royal College of Surgeons document Access<br />
All Ages. Assessing the Impact of Age on Access to<br />
Surgical Treatment makes recommendations about<br />
how to improve access for older people who need<br />
surgery by promoting age equality [88];<br />
2 The Department of Health’s National Service<br />
Framework for Older People sets quality standards<br />
for health and social care, ensuring that older people<br />
are treated with respect and fairness [89];<br />
3 The Centre for Policy on ageing’s Ageism and Age<br />
Discrimination in Secondary Health Care in the<br />
United Kingdom found that age discrimination in<br />
UK hospitals was rare after the introduction of the<br />
National Service Framework, but that further work<br />
needed to be done educating staff about ageism<br />
[90];<br />
4 The NHS Confederation’s Delivering Dignity.<br />
Securing Dignity in Care for Older People in Hospitals<br />
and Care Homes sets out recommendations<br />
on how to tackle the underlying causes of poor<br />
care of the elderly in hospitals and in care [91];<br />
5 House of Lords and House of Commons Joint<br />
Committee on Human Rights has examined how<br />
the principles of The Human Rights of Older People<br />
in Healthcare might be applied to ensure that<br />
older people in hospital are treated with greater<br />
dignity and respect [92];<br />
6 The Patients Association report Listen to Patients,<br />
Speak up for Change urges hospital staff, patients<br />
and carers to bring poor NHS care to the attention<br />
of senior hospital managers, the Department<br />
of Health and government [93];<br />
7 The King’s Fund has emphasised the importance<br />
of maintaining the continuity of care when hospital<br />
inpatients are admitted from, and discharged<br />
back to, the community, in Continuity of<br />
Care for Older Hospital Patients. A Call for<br />
Action [20].<br />
© 2013 The Association of Anaesthetists of Great Britain and Ireland 93
Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
Acknowledgements<br />
The working party acknowledges the assistance of Dr.<br />
John Carlisle, Torbay Hospital, and Dr. Andrew Klein,<br />
Papworth Hospital.<br />
Competing interests<br />
RG chaired the AAGBI Hip Fracture Guidelines<br />
Working Party, was a member of the NICE guideline<br />
development group for CG124, and founded the Hip<br />
Fracture Perioperative Network; he is also Honorary<br />
Secretary of the AAGBI. SW is a member of the<br />
AAGBI Hip Fracture Guidelines Working Party,<br />
advised NICE during development of CG124, is a<br />
Council member of the Age Anaesthesia Association<br />
(whom he represents at the NHFD), is national<br />
research coordinator for the Hip Fracture Perioperative<br />
Network, and is an Editor of Anaesthesia. IF has lectured<br />
on geriatric anaesthesia on behalf of Baxter<br />
Healthcare. No other external funding or competing<br />
interests declared.<br />
References<br />
1. Association of Anaesthetists of Great Britain and Ireland.<br />
Anaesthesia and peri-operative care of the elderly. 2001.<br />
http://www.<strong>aagbi</strong>.org/sites/default/files/careelderly01.pdf<br />
(accessed 05/10/2013).<br />
2. Dhesi J. British Geriatrics Society Good Practice Guide: perioperative<br />
care for older patients undergoing surgery. 2013.<br />
http://www.bgs.org.uk/index.php/topresources/publicationfi<br />
nd/goodpractice/2402-bpg-pops (accessed 05/10/2013).<br />
3. American College of Surgeons National Surgical Quality<br />
Improvement Program/American Geriatrics Society. Optimal<br />
pre-operative assessment of the geriatric surgical patient.<br />
http://site.acsnsqip.org/wp-content/uploads/2011/12/ACS-N<br />
SQIP-AGS-Geriatric-2012-Guidelines.pdf (accessed 05/10/<br />
2013).<br />
4. Royal College of Surgeons of England. Emergency surgery.<br />
Standards for unscheduled surgical care. 2011. http://www.<br />
rcseng.ac.uk/publications/docs/emergency-surgery-standardsfor-unscheduled-care/@@download/pdffile/rcs_emergency_su<br />
rgery_2011_web.pdf (accessed 05/10/2013).<br />
5. Royal College of Surgeons of England and the Department of<br />
Health. The higher risk general surgical patient. Towards<br />
improved care for a forgotten group. 2011. http://www.<br />
rcseng.ac.uk/publications/docs/higher-risk-surgical-patient/@<br />
@download/pdffile/higher_risk_surgical_patient_2011_web.<br />
pdf (accessed 05/10/2013).<br />
6. College of Emergency Medicine. ‘The Silver Book’: quality care<br />
for older people with urgent and emergency care needs.<br />
2012. http://secure.collemergencymed.ac.uk/code/document.asp?ID=6440<br />
(accessed 05/10/2013).<br />
7. National Confidential Enquiry into Patient Outcome and Death.<br />
Elective and Emergency Surgery in the Elderly: An Age Old<br />
Problem. 2010. http://www.ncepod.org.uk/2010report3/<br />
downloads/EESE_fullReport.pdf (accessed 05/10/2013).<br />
Griffiths et al. | Guidelines: Peri-operative care of the elderly<br />
8. Francis R. Report of the Mid Staffordshire NHS Foundation<br />
Trust Public Inquiry. http://www.midstaffspublicinquiry.com/<br />
report (accessed 05/10/2013).<br />
9. Parliamentary and Health Service Ombudsman. Care and compassion?<br />
Report of the Health Service Ombudsman on ten<br />
investigations into NHS care of older people. 2011. http://<br />
www.ombudsman.org.uk/__data/assets/pdf_file/0016/7216<br />
/Care-and-Compassion-PHSO-0114web.pdf (accessed 05/10/<br />
2013).<br />
10. Association of Anaesthetists of Great Britain and Ireland. Management<br />
of proximal femoral fractures 2011. Anaesthesia<br />
2012; 67: 85–98.<br />
11. National Confidential Enquiry into Patient Outcome and Death.<br />
Extremes of age. 1999. http://www.ncepod.org.uk/pdf/<br />
1999/99full.pdf#search=‘enquiry’ (accessed 05/10/2013).<br />
12. Keays R. The ageing patient – sans everything? Anaesthesia<br />
2014; 69(Suppl. 1); 3–7.<br />
13. Corcoran TB, Hillyard S. Cardiopulmonary aspects of anaesthesia<br />
for the elderly. Best Practice and Research Clinical Anaesthesiology<br />
2011; 25: 329–54.<br />
14. Presta P, Lucisano G, Fuiano L, Fuiano G. The kidney and the<br />
elderly: why does the risk increase? International Urology<br />
and Nephrology 2012; 44: 625–32.<br />
15. National Institute for Health and Care Excellence. CG169.<br />
Acute kidney injury. Prevention, detection and management<br />
of acute kidney injury up to the point of renal replacement<br />
therapy. 2013. http://www.nice.org.uk/nicemedia/live/<br />
14258/65058/65058.pdf (accessed 05/10/2013).<br />
16. Strøm C, Rasmussen LS, Sieber FE. Should general anaesthesia<br />
be avoided in the elderly? Anaesthesia 2014; 69(Suppl. 1);<br />
35–44.<br />
17. Merchant AA, Roy CN. Not so benign haematology: anaemia<br />
of the elderly. British Journal of Haematology 2012; 156:<br />
173–85.<br />
18. Panda A, Arjona A, Sapey E, et al. Human innate immunosenescence:<br />
causes and consequences for immunity in old age.<br />
Trends in Immunology 2009; 30: 325–33.<br />
19. National Institute for Health and Care Excellence. CG 92.<br />
Venous thromboembolism: reducing the risk of venous thromboembolism<br />
(deep vein thrombosis and pulmonary<br />
embolism) in patients admitted to hospital. 2010.<br />
http://www.nice.org.uk/nicemedia/live/12695/47920/479<br />
20.pdf (accessed 05/10/2013).<br />
20. Cornwell J, Levenson R, Sonola L, Poteliakhoff E. Continuity of<br />
care for older hospital patients. A call for action. http://www.<br />
kingsfund.org.uk/sites/files/kf/field/field_publication_file/co<br />
ntinuity-of-care-for-older-hospital-patients-mar-2012.pdf (accessed<br />
05/10/2013).<br />
21. Sessler DI. Temperature monitoring and peri-operative thermoregulation.<br />
Anesthesiology 2008; 109: 318–38.<br />
22. Peden CJ, Grocott MPW. National Research Strategies: what<br />
outcomes are important in peri-operative elderly care? Anaesthesia<br />
2014; 69(Suppl. 1): 61–69.<br />
23. Stoneham M, Murray D, Foss N. Emergency surgery: the big<br />
three – abdominal aortic aneurysm, laparotomy and hip fracture.<br />
Anaesthesia 2014; 69(Suppl. 1): 70–80.<br />
24. Carlisle JB. Pre-operative co-morbidity and postoperative survival<br />
in the elderly: beyond one lunar orbit. Anaesthesia<br />
2014; 69(Suppl. 1): 17–25.<br />
25. Partridge J, Harari D, Martin F, Dhesi J. The impact of preoperative<br />
comprehensive geriatric assessment on postoperative<br />
outcomes in older patients undergoing scheduled surgery: a<br />
systematic review. Anaesthesia 2014; 69(Suppl. 1): 8–16.<br />
94 © 2013 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: Peri-operative care of the elderly Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
26. Martin F. Comprehensive assessment of the frail older patient.<br />
http://www.bgs.org.uk/index.php/topresources/publicationfind/goodpractice/195-gpgcgassessment<br />
(accessed 05/10/<br />
2013).<br />
27. Association of Anaesthetists of Great Britain and Ireland. Preoperative<br />
assessment and patient preparation. The Role of<br />
the Anaesthetist. 2010. http://www.<strong>aagbi</strong>.org/sites/default/<br />
files/preop2010.pdf (accessed 05/10/2013).<br />
28. National Institute for Health and Care Excellence. CG 3. Preoperative<br />
tests. The use of routine preoperative tests for elective<br />
surgery. 2003. http://www.nice.org.uk/nicemedia/pdf/<br />
cg3niceguideline.pdf (accessed 05/10/2013).<br />
29. Kozek-Langenecker SA, Afshari A, Albaladejo P, et al. Management<br />
of severe perioperative bleeding: guidelines from the<br />
European Society of Anaesthesiology. European Journal of<br />
Anaesthesiology 2013; 30: 270–382.<br />
30. Goodnough LT, Maniatis A, Earnshaw P, et al. Detection, evaluation,<br />
and management of preoperative anaemia in the elective<br />
orthopaedic surgical patient: NATA guidelines. British<br />
Journal of Anaesthesia 2011; 106: 13–22.<br />
31. Smith I, Kranke P, Murat I, et al. Perioperative fasting in<br />
adults and children: guidelines from the European Society of<br />
Anaesthesiology. European Journal of Anaesthesiology 2011;<br />
28: 556–69.<br />
32. Moppett IK, Parker M, Griffiths R, Bowers T, White SM, Moran<br />
CG. Nottingham Hip fracture score: longitudinal and multiassessment.<br />
British Journal of Anaesthesia 2012; 109: 546–<br />
50.<br />
33. White SM. Legal and ethical aspects of anaesthesia for the<br />
elderly. Anaesthesia 2014; 69(Suppl. 1): 45–53.<br />
34. White SM, Baldwin TJ. The Mental Capacity Act, 2005. Implications<br />
for anaesthesia and intensive care. Anaesthesia 2006;<br />
61: 381–9.<br />
35. General Medical Council. Consent: patients and doctors making<br />
decisions together. 2008. http://www.gmc-uk.org/static/documents/content/GMC_Consent_0513_Revised.pdf<br />
(accessed<br />
05/10/2013).<br />
36. General Medical Council. Treatment and care towards the end<br />
of life. 2010. http://www.gmc-uk.org/static/documents/content/End_of_life_9_May_2013.pdf<br />
(accessed 05/10/2013).<br />
37. Association of Anaesthetists of Great Britain and Ireland.<br />
Consent for anaesthesia. 2006. http://www.<strong>aagbi</strong>.org/sites/<br />
default/files/consent06.pdf (accessed 05/10/2013).<br />
38. Subramanian A, Balentine C, Palacio CH, Sansgiry S, Berger<br />
DH, Awad SS. Outcomes of damage-control celiotomy in<br />
elderly nontrauma patients with intra-abdominal catastrophes.<br />
American Journal of Surgery 2010; 200: 783–8.<br />
39. Haynes AB, Weiser TG, Berry WR, et al. A surgical safety<br />
checklist to reduce morbidity and mortality in a global population.<br />
New England Journal of Medicine 2009; 360: 491–9.<br />
40. Reynolds L, Beckman J, Kurz A. Peri-operative complications<br />
of hypothermia. Best Practice and Research, Clinical Anaesthesiology<br />
2008; 22: 645–57.<br />
41. National Institute for Health and Care Excellence. CG 65. Inadvertent<br />
perioperative hypothermia. 2008. http://www.<br />
nice.org.uk/nicemedia/live/11962/40432/40432.pdf (accessed<br />
05/10/2013).<br />
42. Association of Anaesthetists of Great Britain and Ireland. Recommendations<br />
for standards of monitoring during anaesthesia<br />
and recovery, 4th edn. 2007. http://www.<strong>aagbi</strong>.org/<br />
sites/default/files/standardsofmonitoring07.pdf (accessed<br />
05/10/2013).<br />
43. Walsh M, Devereaux PJ, Garg AX, et al. Relationship between<br />
intraoperative mean arterial pressure and clinical outcomes<br />
after noncardiac surgery: toward an empirical definition of<br />
hypotension. Anesthesiology 2013; 119: 507–15.<br />
44. Marik PE, Baram M, Vahid B. Does central venous pressure<br />
predict fluid responsiveness? A systematic review of the<br />
literature and the tale of seven mares. Chest 2008; 134:<br />
172–8.<br />
45. National Institute of Health and Care Excellence. MTG 3. CardioQ-<br />
ODM oesophageal Doppler monitor. 2011. http://www.nice.org.<br />
uk/nicemedia/live/13312/52624/52624.pdf (accessed 05/10/<br />
2013).<br />
46. Ghosh S, Arthur B, Klein AA. NICE guidance on CardioQTM<br />
oesophageal Doppler monitoring. Anaesthesia 2012; 66:<br />
1081–3.<br />
47. Morris C. Oesophageal Doppler monitoring, doubt and equipoise:<br />
evidence based medicine means change. Anaesthesia<br />
2013; 68: 684–8.<br />
48. Ballard C, Jones E, Gauge N, et al. Optimised anaesthesia to<br />
reduce post operative cognitive decline (POCD) in older<br />
patients undergoing elective surgery, a randomised controlled<br />
trial. PLoS One 2012; 7: e37410.<br />
49. Lerou JG. Nomogram to estimate age-related MAC. British<br />
Journal of Anaesthesia 2004; 93: 288–91.<br />
50. Sieber FE, Gottshalk A, Zakriya KJ, Mears SC, Lee H. General<br />
anesthesia occurs frequently in elderly patients during propofol-based<br />
sedation and spinal anesthesia. Journal of Clinical<br />
Anesthesia 2010; 22: 179–83.<br />
51. Ekstein M, Gavish D, Ezri T, Weinbroum AA. Monitored anaesthesia<br />
care in the elderly: guidelines and recommendations.<br />
Drugs and Aging 2008; 25: 477–500.<br />
52. National Institute for Health and Care Excellence. DG 6. Depth<br />
of anaesthesia monitors – Bispectral Index (BIS), E-Entropy<br />
and Narcotrend-Compact M. http://publications.nice.org.uk/<br />
depth-of-anaesthesia-monitors-bispectral-index-bis-e-entropy-and-narcotrend-compact-m-dg6/outcomes#clinical-effectiveness<br />
(accessed 05/10/2013).<br />
53. Sessler DI, Sigl JC, Kelley SD, et al. Hospital stay and mortality<br />
are increased in patients having a ‘‘triple low’’ of low blood<br />
pressure, low bispectral index, and low minimum alveolar<br />
concentration of volatile anesthesia. Anesthesiology 2012;<br />
116: 1195–203.<br />
54. Pietraszewski P, Gaszynski T. Residual neuromuscular block in<br />
elderly patients after surgical procedures under general<br />
anaesthesia with rocuronium. Anaesthesiology Intensive Therapy<br />
2013; 45: 77–81.<br />
55. Steinmetz J, Rasmussen LS. The elderly and general anaesthesia.<br />
Minerva Anestesiologica 2010; 76: 745–52.<br />
56. Doherty M, Buggy DJ. Intraoperative fluids: how much is too<br />
much? British Journal of Anaesthesia 2012; 109: 69–79.<br />
57. Powell-Tuck J, Gosling P, Lobo DN, et al. British consensus<br />
Guidelines on Intravenous Fluid Therapy for Adult Surgical<br />
Patients (GIFTASUP). 2011. http://www.bapen.org.uk/pdfs/<br />
bapen_pubs/giftasup.pdf (accessed 05/10/2013).<br />
58. National Institute for Health and Care Excellence. Intravenous<br />
fluid therapy in adults in hospital. (Draft for consultation).<br />
2013. http://www.nice.org.uk/nicemedia/live/13298/63879/<br />
63879.pdf (accessed 05.10/2013).<br />
59. Wu WC, Smith TS, Henderson WG, et al. Operative blood<br />
loss, blood transfusion, and 30-day mortality in older<br />
patients after major noncardiac surgery. Annals of Surgery<br />
2010; 252: 11–7.<br />
60. Parker MJ, Handoll HH, Griffiths R. Anaesthesia for hip fracture<br />
surgery in adults. Cochrane Database of Systematic Reviews<br />
2004; 4: CD000521.<br />
© 2013 The Association of Anaesthetists of Great Britain and Ireland 95
Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
Griffiths et al. | Guidelines: Peri-operative care of the elderly<br />
61. Neuman MD, Silber JH, Elkassabany NM, Ludwig JM, Fleisher<br />
LA. Comparative effectiveness of regional versus general<br />
anesthesia for hip fracture surgery in adults. Anesthesiology<br />
2012; 117: 72–92.<br />
62. Memtsoudis SG, Sun X, Chiu YL, et al. Perioperative comparative<br />
effectiveness of anesthetic technique in orthopedic<br />
patients. Anesthesiology 2013; 118: 1046–58.<br />
63. Tsui BC, Wagner A, Finucane B. Regional anaesthesia in the<br />
elderly: a clinical guide. Drugs and Aging 2004; 21: 895–<br />
910.<br />
64. Kruijt Spanjer MR, Bakker NA, Absalom AR. Pharmacology in<br />
the elderly and newer anaesthesia drugs. Best Practice and<br />
Research: Clinical Anaesthesiology 2011; 25: 355–65.<br />
65. National Institute for Health and Care Excellence. CG 50.<br />
Acutely ill patients in hospital. 2007. http://www.nice.org.<br />
uk/nicemedia/pdf/CG50FullGuidance.pdf (accessed 05/10/<br />
2013).<br />
66. Vaurio LE, Sands LP, Wang Y, Mullen EA, Leung JM. Postoperative<br />
delirium: the importance of pain and pain management.<br />
Anesthesia and Analgesia 2006; 102: 1267–73.<br />
67. Sieber FE, Barnett SR. Preventing postoperative complications<br />
in the elderly. Anesthesiology Clinics 2011; 29: 83–97.<br />
68. Aubrun F. Management of postoperative analgesia in elderly<br />
patients. Regional Anaesthesia and Pain Medicine 2005; 30:<br />
369–79.<br />
69. Royal College of Physicians, British Geriatrics Society and<br />
British Pain Society. The Assessment of Pain in Older People:<br />
National Guidelines. Concise Guidance to Good Practice<br />
Series, No. 8. London: RCP, 2007. http://britishpainsociety.<br />
org/book_pain_older_people.pdf (accessed 05/10/2013).<br />
70. Falzone E, Hoffmann C, Keita H. Postoperative analgesia in<br />
elderly patients. Drugs and Aging 2013; 30: 81–90.<br />
71. Abdulla A, Adams N, Bone M, et al. on behalf of the British<br />
Geriatrics Society Guidance on the management of pain in<br />
older people. Age and Ageing 2013; 42(Suppl. 1): i1–42.<br />
72. Sauaia A, Min SJ, Leber C, et al. Postoperative pain management<br />
in elderly patients: correlation between adherence to<br />
treatment guidelines and patient satisfaction. Journal of the<br />
American Geriatrics Society 2005; 53: 274–82.<br />
73. McLachlan AJ, Bath S, Naganathan V, et al. Clinical pharmacology<br />
of analgesic medicines in older people: impact of frailty<br />
and cognitive impairment. British Journal of Clinical Pharmacology<br />
2011; 71: 351–64.<br />
74. Schofield P. The assessment and management of peri-operative<br />
pain in older people. Anaesthesia 2014; 69(Suppl. 1):<br />
54–60.<br />
75. American Geriatrics Society 2012 Beers Criteria Update<br />
Expert Panel. American Geriatrics Society updated Beers Criteria<br />
for potentially inappropriate medication use in older<br />
adults. Journal of the American Geriatrics Society 2012; 60:<br />
616–31.<br />
76. Radtke FM, Franck M, MacGuill M, et al. Duration of fluid fasting<br />
and choice of analgesic are modifiable factors for early<br />
postoperative delirium. European Journal of Anaesthesiology<br />
2010; 27: 411–6.<br />
77. Dodds C, Foo I, Jones K, Kumar Singh S, Waldman C. Perioperative<br />
care of elderly patients – an urgent need for<br />
change: a consensus statement to provide guidance for specialist<br />
and non-specialist anaesthetists. Perioperative Medicine<br />
2013; 2: 6–11.<br />
78. National Institute for Health and Care Excellence. CG 103.<br />
Delirium: diagnosis, prevention and treatment. 2010. http://<br />
www.nice.org.uk/nicemedia/live/13060/49908/49908.pdf<br />
(accessed 05/10/2013).<br />
79. Clegg A, Young JB. Which medications to avoid in people at<br />
risk of delirium: a systematic review. Age and Ageing 2011;<br />
40: 23–9.<br />
80. Chew ML, Mulsant BH, Pollock BG, et al. Anticholinergic<br />
activity of 107 medications commonly used by older<br />
adults. Journal of the American Geriatrics Society 2008; 56:<br />
1333–41.<br />
81. Wheble GA, Knight WR, Khan OA. Enteral vs total parenteral<br />
nutrition following major upper gastrointestinal surgery. International<br />
Journal of Surgery 2012; 10: 194–7.<br />
82. Gemmell L, McBrien ME, Heyburn G, et al. on behalf of the<br />
Association of Anaesthetists of Great Britain and Ireland. Do<br />
Not Attempt Resuscitation (DNAR) decisions in the perioperative<br />
period. 2009. http://www.<strong>aagbi</strong>.org/sites/default/files/<br />
dnar_09_0.pdf (accessed 05/10/2013).<br />
83. Smith AF. Creating guidelines and treating patients when<br />
there are no trials or systematic reviews. European Journal of<br />
Anaesthesiology 2013; 30: 383–5.<br />
84. Peden CJ. Emergency surgery in the elderly patient: a quality<br />
improvement approach. Anaesthesia 2011; 66: 440–5.<br />
85. McGory ML, Kao KK, Shekelle PG, et al. Developing quality<br />
indicators for elderly surgical patients. Annals of Surgery<br />
2009; 250: 338–47.<br />
86. Royal College of Anaesthetists. Raising the Standard: a compendium<br />
of audit recipes, 3rd edn. 2012. http://www.rcoa.<br />
ac.uk/system/files/CSQ-ARB-2012.pdf (accessed 05/10/<br />
2013).<br />
87. Wilkinson K, Wilson H. Should physicians routinely be involved<br />
in the care of elderly surgical patients? British Medical Journal<br />
2011; 342: d1070.<br />
88. The Royal College of Surgeons. Access all ages. Assessing the<br />
impactofageonaccess to surgicaltreatment. 2012.http://www.<br />
rcseng.ac.uk/publications/docs/access-all-ages/@@down<br />
load/pdffile/access_all_ages.pdf(accessed05/10/2013).<br />
89. Department of Health. National Service Framework for older<br />
people. London: Department of Health, 2001. www.dh.gov.<br />
uk/assetRoot/04/07/12/83/04071283.pdf (accessed 05/<br />
10/2013).<br />
90. Centre for policy on ageing. Ageism and age discrimination in<br />
secondary health care in the United Kingdom. 2009. http://<br />
www.cpa.org.uk/information/reviews/CPA-ageism_and_age_<br />
discrimination_in_secondary_health_care-report.pdf (accessed<br />
05/10/2013).<br />
91. NHS Confederation. Delivering dignity. Securing dignity in care<br />
for older people in hospitals and care homes. 2012. http://<br />
www.nhsconfed.org/Documents/dignity.pdf (accessed 05/<br />
10/2013).<br />
92. House of Lords and House of Commons Joint Committee on<br />
Human Rights. The human rights of older people in healthcare.<br />
2007. http://www.publications.parliament.uk/pa/jt200607/<br />
jtselect/jtrights/156/156i.pdf (accessed 05/10/2013).<br />
93. The Patients Association. Listen to patients, Speak up for<br />
change. 2010. http://www.patients-association.com/Portals/<br />
0/Public/Files/Research%20Publications/Listen%20to%20pati<br />
ents,%20Speak%20up%20for%20change.pdf<br />
96 © 2013 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: Peri-operative care of the elderly Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
Appendix 1<br />
Lerou nomogram [49] relating age, total MAC expressed in MAC units, and end-expired concentrations of volatile<br />
agent and nitrous oxide. A result is found by drawing two straight lines. Example (dotted lines): if the measured<br />
end-expired concentrations of sevoflurane and nitrous oxide are 1.8% and 67% (at 1 atm), respectively, then the total<br />
age-related MAC is 1.3 in a 3-year-old. Reverse example: a total MAC of 1.3 in a 3-year-old, when using sevoflurane<br />
and nitrous oxide 67% in oxygen, requires an end-expired sevoflurane concentration of 1.8%. © 2004 Oxford University<br />
Press. Reproduced with permission [49].<br />
© 2013 The Association of Anaesthetists of Great Britain and Ireland 97
Anaesthesia 2014, 69 (Suppl. 1), 81–98<br />
Griffiths et al. | Guidelines: Peri-operative care of the elderly<br />
Appendix 2<br />
Royal College of Physicians/British Pain Society/British Geriatric Society. Algorithm for the assessment of pain in<br />
older people (Copyright © 2007 Royal College of Physicians. Reproduced with permission) [70].<br />
98 © 2013 The Association of Anaesthetists of Great Britain and Ireland
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
GUIDELINES<br />
Perioperative fasting in adults and children: guidelines from<br />
the European Society of Anaesthesiology<br />
Ian Smith, Peter Kranke, Isabelle Murat, Andrew Smith, Geraldine O’Sullivan, Eldar Søreide, Claudia Spies<br />
and Bas in’t Veld<br />
This guideline aims to provide an overview of the present<br />
knowledge on aspects of perioperative fasting with assessment<br />
of the quality of the evidence. A systematic search was<br />
conducted in electronic databases to identify trials published<br />
between 1950 and late 2009 concerned with preoperative<br />
fasting, early resumption of oral intake and the effects of oral<br />
carbohydrate mixtures on gastric emptying and postoperative<br />
recovery. One study on preoperative fasting which had not been<br />
included in previous reviews and a further 13 studies<br />
published since the most recent review were identified.<br />
The searches also identified 20 potentially relevant studies<br />
of oral carbohydrates and 53 on early resumption of oral<br />
intake. Publications were classified in terms of their<br />
evidence level, scientific validity and clinical relevance. The<br />
Scottish Intercollegiate Guidelines Network scoring system for<br />
assessing level of evidence and grade of recommendations was<br />
used. The key recommendations are that adults and children<br />
should be encouraged to drink clear fluids up to 2 h before<br />
elective surgery (including caesarean section) and all but one<br />
member of the guidelines group consider that tea or coffee with<br />
milk added (up to about one fifth of the total volume) are still clear<br />
fluids. Solid food should be prohibited for 6 h before elective<br />
surgery in adults and children, although patients should not<br />
have their operation cancelled or delayed just because they are<br />
chewing gum, sucking a boiled sweet or smoking immediately<br />
prior to induction of anaesthesia. These recommendations also<br />
apply to patients with obesity, gastro-oesophageal reflux and<br />
diabetes and pregnant women not in labour. There is insufficient<br />
evidence to recommend the routine use of antacids,<br />
metoclopramide or H 2 -receptor antagonists before elective<br />
surgery in non-obstetric patients, but an H 2 -receptor antagonist<br />
should be given before elective caesarean section, with an<br />
intravenous H 2 -receptor antagonist given prior to emergency<br />
1<br />
caesarean section, supplemented with 30 ml of 0.3 mol l<br />
sodium citrate if general anaesthesia is planned. Infants should<br />
be fed before elective surgery. Breast milk is safe up to 4 h and<br />
other milks up to 6 h. Thereafter, clear fluids should be given as in<br />
adults. The guidelines also consider the safety and possible<br />
benefits of preoperative carbohydrates and offer advice on the<br />
postoperative resumption of oral intake.<br />
Eur J Anaesthesiol 2011;28:556–569<br />
Published online 28 June 2011<br />
Why were these guidelines produced?<br />
Widespread consultation suggested that guidelines on perioperative fasting would be useful to European Society of<br />
Anaesthesiology (ESA) members.<br />
Our guideline aims to provide an overview of the present knowledge on perioperative fasting with assessment of the<br />
quality of the evidence in order to allow anaesthesiologists all over Europe to integrate this knowledge in their daily<br />
care of patients.<br />
What is similar to previous guidelines?<br />
The ESA guidelines endorse a 2-h fasting interval for clear fluids and a 6-h interval for solids.<br />
What is different from previous guidelines?<br />
The ESA guidelines:<br />
are recent and include several studies published since previous guidelines;<br />
increase the emphasis on encouraging patients not to avoid fluids for any longer than is necessary;<br />
offer practical, pragmatic advice on chewing gum, smoking and drinks containing milk;<br />
consider the safety and possible benefits of preoperative carbohydrates;<br />
offer advice on the postoperative resumption of oral intake.<br />
From the University Hospital of North Staffordshire, Stoke-on-Trent, UK (IS), University Hospitals of Würzburg, Würzburg, Germany (PK), Armand Trousseau Hospital, Paris,<br />
France (IM), Royal Lancaster Infirmary, School of Health and Medicine, Lancaster University, Lancaster (AS), Guy’s and St Thomas’ NHS Foundation Trust, London (GOS),<br />
UK, Department of Anaesthesia and Intensive Care, Stavanger University Hospital, Stavanger, Norway (ES), Department of Anaesthesiology and Intensive Care Medicine,<br />
Charité – Universitätsmedizin Berlin, Berlin, Germany (CS) and Department of Anesthesiology and Pain Medicine, Haaglanden Medical Centre, The Hague, The<br />
Netherlands (BV)<br />
Correspondence to Dr Ian Smith, Directorate of Anaesthesia, University Hospital of North Staffordshire, Newcastle Road, Stoke-on-Trent, Staffordshire ST4 6QG, UK<br />
Tel: +44 1782 553054; e-mail: damsmith@btinternet.com<br />
0265-0215 ß 2011 Copyright European Society of Anaesthesiology DOI:10.1097/EJA.0b013e3283495ba1<br />
Copyright © European Society of Anaesthesiology. Unauthorized reproduction of this article is prohibited.
Perioperative fasting in adults and children 557<br />
1. Summary of recommendations<br />
Evidence<br />
Recommendation<br />
Fasting in adults and children<br />
Adults and children should be encouraged to drink clear fluids (including water,<br />
1þþ<br />
A<br />
pulp-free juice and tea or coffee without milk) up to 2 h before elective surgery<br />
(including caesarean section)<br />
All but one member of the guidelines group consider that tea or coffee with milk added<br />
(up to about one fifth of the total volume) are still clear fluids<br />
Solid food should be prohibited for 6 h before elective surgery in adults and children 1þ A<br />
Patients with obesity, gastro-oesophageal reflux and diabetes and pregnant women<br />
2 D<br />
not in labour can safely follow all of the above guidelines<br />
However, these factors may alter their overall anaesthetic management<br />
Patients should not have their operation cancelled or delayed just because they are<br />
1 B<br />
chewing gum, sucking a boiled sweet or smoking immediately prior to induction<br />
of anaesthesia<br />
The above is based solely on effects on gastric emptying and nicotine intake (including smoking,<br />
nicotine gum and patches) should be discouraged before elective surgery<br />
Fasting in infants<br />
Infants should be fed before elective surgery. Breast milk is safe up to 4 h and<br />
1þþ<br />
A<br />
other milks up to 6 h. Thereafter, clear fluids should be given as in adults<br />
Prokinetic and other pharmacological interventions<br />
There is insufficient evidence of clinical benefit to recommend the routine use of<br />
1þþ<br />
A<br />
antacids, metoclopramide or H 2 -receptor antagonists before elective surgery in<br />
non-obstetric patients<br />
An H 2 -receptor antagonist should be given the night before, and on the morning of,<br />
1þþ<br />
A<br />
elective caesarean section<br />
The guidelines group recognises that most of the evidence relates to surrogate measures,<br />
such as changes in gastric volume and pH, rather than a clear impact on mortality<br />
An intravenous H 2 -receptor antagonist should be given prior to emergency caesarean<br />
1þþ<br />
A<br />
section; this should be supplemented with 30 ml of 0.3 mol l S1 sodium citrate<br />
if general anaesthesia is planned<br />
The guidelines group recognises that most of the evidence relates to surrogate measures,<br />
such as changes in gastric volume and pH, rather than a clear impact on mortality<br />
Oral carbohydrates<br />
It is safe for patients (including diabetics) to drink carbohydrate-rich drinks up to<br />
1þþ<br />
A<br />
2 h before elective surgery<br />
The evidence for safety is derived from studies of products specifically developed for perioperative<br />
use (predominantly maltodextrins); not all carbohydrates are necessarily safe<br />
Drinking carbohydrate-rich fluids before elective surgery improves subjective<br />
1þþ<br />
A<br />
well being, reduces thirst and hunger and reduces postoperative insulin resistance<br />
To date, there is little clear evidence to show reductions in length of postoperative stay and mortality<br />
Fasting in obstetric patients<br />
Women should be allowed clear fluids (as defined above) as they desire in labour 1þþ A<br />
Solid food should be discouraged during active labour 1þ A<br />
The guidelines group recognise that it may be impractical to stop all women from eating during labour,<br />
especially low-risk women. Consideration should be given to easily digestible, low-residue foods<br />
Postoperative resumption of fluids<br />
Adults and children should be allowed to resume drinking as soon as they wish after<br />
elective surgery. However, fluid intake should not be insisted upon before allowing<br />
discharge from a day or ambulatory surgery facility<br />
1þþ<br />
A<br />
, recommended best practice based on the clinical experience of the guidelines development group.<br />
2. Purpose and development of the guideline<br />
The European Society of Anaesthesiology (ESA) is<br />
committed to the production of high-quality, evidencebased<br />
clinical guidelines. After the formation of the<br />
Guidelines Committee in 2008, a prioritisation exercise<br />
suggested that guidelines on perioperative fasting<br />
would be useful to ESA members and a task force was<br />
established in June 2009 to produce this guideline. The<br />
chairpersons of the relevant subcommittees (Evidencebased<br />
Practice and Quality Improvement, Ambulatory<br />
Anaesthesia, Obstetric Anaesthesia, Paediatric Anaesthesia<br />
and Anaesthesia for the Elderly) of the ESA Scientific<br />
Committee were asked to nominate an ESA member<br />
with expertise in their field to join the task force. Further<br />
experts were co-opted onto the task force as required.<br />
Several European national anaesthesiology societies have<br />
already produced recommendations for aspects of perioperative<br />
fasting. Our guideline aims to provide an overview<br />
of the present knowledge on the subject with<br />
assessment of the quality of the evidence in order to<br />
allow anaesthesiologists all over Europe to integrate –<br />
wherever possible – this knowledge in their daily care<br />
of patients.<br />
Evidence to support the recommendations was obtained<br />
as follows. A systematic search was conducted by<br />
European Journal of Anaesthesiology 2011, Vol 28 No 8<br />
Copyright © European Society of Anaesthesiology. Unauthorized reproduction of this article is prohibited.
558 Guidelines<br />
members of Cochrane Anaesthesia Review Group of<br />
the electronic databases Ovid, MEDLINE and Embase<br />
to identify trials published between 1950 and late 2009<br />
concerned with preoperative fasting, early resumption of<br />
oral intake and the effects of oral carbohydrate mixtures<br />
on gastric emptying and postoperative recovery. A total<br />
of 3714 abstracts from MEDLINE and 3660 from Embase<br />
were identified from the search. After elimination<br />
of duplicates, irrelevant studies, non-clinical trials and<br />
studies with a non-clinical outcome, one study on<br />
preoperative fasting which had not been included in<br />
previous reviews 1–4 and a further 13 studies published<br />
since the most recent review 4 were identified. The<br />
searches also identified 20 potentially relevant studies<br />
of oral carbohydrates and 53 on early resumption of oral<br />
intake.<br />
These publications were classified in terms of their<br />
evidence level, scientific validity and clinical relevance.<br />
We used the Scottish Intercollegiate Guidelines Network<br />
(SIGN) scoring system for assessing level of evidence and<br />
grade of recommendations (Fig. 1). 5 Highest priority<br />
was given to meta-analyses of randomised, controlled<br />
clinical trials. In reaching consensus, particular emphasis<br />
was placed on the level of evidence, ethical aspects,<br />
patient preferences, clinical relevance, risk/benefit ratios<br />
and degree of applicability. For example, a pragmatic<br />
solution to an acceptable amount of milk in tea or<br />
coffee was agreed based on the unpublished experience<br />
accumulated by several members of the group over<br />
many years.<br />
These guidelines have undergone the following review<br />
process. The final draft was reviewed by members of<br />
the relevant Subcommittees of the ESA’s Scientific<br />
Committee who were not involved in the initial preparation<br />
of the guideline. It was posted on the on ESA<br />
website for 4 weeks and all ESA members, individual and<br />
national, were contacted by electronic mail to invite them<br />
to comment on the draft. It was also sent to the International<br />
Association for Ambulatory Surgery (IAAS) for<br />
information and comment. All those who commented<br />
are listed in the ‘Acknowledgements’ section below.<br />
Comments were collated by the chair of the guideline<br />
task force and the guideline amended as appropriate.<br />
The final manuscript was approved by the Guidelines<br />
Committee and Board of the ESA before submission for<br />
publication in the European Journal of Anaesthesiology.<br />
These guidelines are produced as a service to ESA<br />
members and other anaesthesiologists and healthcare<br />
staff in Europe. The ESA recognises that practice and<br />
opinion varies in different European countries. Despite<br />
the availability of the same scientific information, the way<br />
in which healthcare services are organised may result in<br />
different practices in the various European countries.<br />
Thus, it is not always possible to produce guidelines<br />
which will be both appropriate and relevant for every<br />
European nation. Although national societies and<br />
individuals are free to use the guidelines, modified as<br />
necessary for local and national practice contexts, they are<br />
under no obligation to do so. Further, the potential legal<br />
implications may be a point of concern. 6 It cannot be<br />
emphasised enough that guidelines may not be appropriate<br />
for all clinical situations. The decision whether or<br />
not to follow a recommendation from a guideline must be<br />
made by the responsible physician on an individual basis,<br />
taking into account the specific conditions of the patient<br />
and the available resources. Therefore, deviations from<br />
guidelines for specific reasons should remain possible and<br />
can certainly not be interpreted as a base for negligence<br />
claims. However, we hope that these guidelines will<br />
both assist anaesthesiologists throughout Europe to<br />
bring research evidence to bear on their clinical practice<br />
and also provide support to colleagues and healthcare<br />
funders in making changes and improvements necessary<br />
to enhance patient care.<br />
Differences from existing guidelines<br />
Although there is little new evidence relating to fasting<br />
for fluids and solids, the current guidelines review more<br />
recent literature than any of the existing guidelines.<br />
In addition, the American Society of Anesthesiology<br />
(ASA) guidelines on the subject 7 were published in<br />
1999 and contain little on preoperative carbohydrate,<br />
whereas the UK Royal College of Nursing guidelines 4<br />
deal with the safety aspect of preoperative carbohydrate,<br />
but not possible benefits. In these current guidelines,<br />
we have also tried to address practical problems such as<br />
chewing gum.<br />
3. Fasting<br />
3.1. Fluids<br />
Recommendation<br />
Adults and children should be encouraged to drink clear<br />
fluids (including water, pulp-free juice and tea or coffee<br />
without milk) up to 2 h before elective surgery (including<br />
caesarean section) (evidence level 1þþ, recommendation<br />
grade A).<br />
All but one member of the guidelines group consider that tea or<br />
coffee with milk added (up to about one fifth of the total volume)<br />
are still clear fluids.<br />
Rationale<br />
Since the landmark work of Maltby et al. 8 in 1986, a large<br />
body of evidence has been accumulated to show that<br />
the oral intake of clear fluids up to 2 h before an elective<br />
operation is safe. 3,9,10 Many countries have, therefore,<br />
changed their fasting guidelines, allowing most patients<br />
take clear fluids (water, clear juices and coffee or tea<br />
without milk) up to 2 h before elective surgery. 11<br />
In addition to the liberalising of fasting guidelines, the<br />
emphasis is now changing, with the realisation that<br />
European Journal of Anaesthesiology 2011, Vol 28 No 8<br />
Copyright © European Society of Anaesthesiology. Unauthorized reproduction of this article is prohibited.
Perioperative fasting in adults and children 559<br />
Fig. 1<br />
Key to evidence statements and grades of recommendations<br />
1 ++<br />
1 +<br />
1<br />
High-quality meta-analyses, systematic reviews of RCTs, or RCTs with a very low risk of bias<br />
Well conducted meta-analyses, systematic reviews, or RCTs with a low risk of bias<br />
Meta-analyses, systematic reviews, or RCTs with a high risk of bias<br />
2 ++<br />
High-quality systematic reviews of case–control or cohort studies<br />
2 +<br />
Well conducted case–control or cohort studies with a low risk of confounding or bias and a moderate<br />
probability that the relationship is causal<br />
2 -<br />
3<br />
4<br />
Case–control or cohort studies with a high risk of confounding or bias and a significant risk that the<br />
relationship is not causal<br />
Non-analytic studies, e.g. case reports, case series<br />
Expert opinion<br />
Grades of recommendation<br />
Note: the grade of recommendation relates to the strength of the evidence on which the recommendation is<br />
based. It does not refect the clinical importance of the recommendation.<br />
A<br />
At least one meta-analysis, systematic review, or RCT rated as 1 ++,<br />
and directly applicable to the target population; or<br />
a body of evidence consisting principally of studies rated as 1 +,<br />
directly applicable to the target population, and demonstrating overall consistency of results<br />
B<br />
A body of evidence including studies rated as 2 ++,<br />
directly applicable to the target population, and demonstrating overall consistency of results; or<br />
extrapolated evidence from studies rated as 1 ++ or 1 +<br />
C<br />
A body of evidence including studies rated as 2 +,<br />
directly applicable to the target population, and demonstrating overall consistency of results; or<br />
extrapolated evidence from studies rated as 2 ++<br />
D<br />
Evidence level 3 or 4; or<br />
extrapolated evidence from studies rated as 2 +<br />
Ḡood practice points<br />
√<br />
Recommended best practice based on the clinical experience of the guideline development group<br />
Scottish Intercollegiate Guidelines Network (SIGN) grading system. RCT, randomised controlled trial. 5<br />
prolonged fasting is an inappropriate way to prepare<br />
for the stress of surgery. Abstaining from fluids for<br />
a prolonged period prior to surgery is detrimental for<br />
patients, especially the elderly and small children. Rather<br />
than ensuring a minimal fasting interval has been<br />
achieved, it is important to encourage patients to keep<br />
drinking up until 2 h before surgery in order to reduce<br />
their discomfort and improve their well being.<br />
3.1.1. Milk in tea or coffee<br />
Milk in large quantities curdles in the stomach and acts<br />
like a solid, but smaller quantities are handled like other<br />
European Journal of Anaesthesiology 2011, Vol 28 No 8<br />
Copyright © European Society of Anaesthesiology. Unauthorized reproduction of this article is prohibited.
560 Guidelines<br />
liquids and are safe. There is anecdotal evidence<br />
(including from some members of this group) that when<br />
milk is allowed to be added to tea or coffee consumed<br />
before elective surgery, regurgitation and aspiration are<br />
no more likely to occur, but no randomised studies<br />
have looked specifically at the safety of this practice.<br />
Some studies of preoperative tea and coffee 12–14 did<br />
allow milk to be added if desired (R. Maltby, personal<br />
communication), but this is not recorded in the published<br />
text and the number of such patients was small. Unpublished<br />
work has shown that adding small quantities of<br />
milk (from a 12 ml single-portion pot) to a model stomach<br />
caused no restriction in emptying, but that adding three<br />
or more measures caused clumping (R. Maltby, personal<br />
communication). However, the model comprised a glass<br />
vessel with a fixed burette tap as an outlet and, therefore,<br />
did not mimic either a sphincter which can relax or the<br />
effects of churning from muscle contractions.<br />
The lack of evidence from human studies and the<br />
uncertainty in defining and controlling a safe amount<br />
of milk, means that most guidelines only advocate black<br />
tea or coffee. Although this may appear a safe approach,<br />
some patients would rather have nothing at all if they are<br />
denied milk in their morning cup of tea or coffee. With<br />
one exception, the guidelines group considered that tea<br />
or coffee with a modest amount of milk added (up to<br />
about one fifth of the total volume) should still be<br />
considered as clear fluids and, therefore, safe up to<br />
2 h before the induction of anaesthesia. Drinks made<br />
predominantly from milk, however, should be treated<br />
as solids.<br />
3.2. Solid food<br />
Recommendation<br />
Solid food should be prohibited for 6 h before elective<br />
surgery in adults and children (evidence level 1þ, recommendation<br />
grade A).<br />
Rationale<br />
No recent studies have attempted to define a minimal safe<br />
period for preoperative fasting for solid food. One previous<br />
study found no increase in gastric volume after a light<br />
breakfast of tea and buttered toast consumed 2–4 h before<br />
elective surgery, 15 but the presence of residual solids in the<br />
stomach at induction of anaesthesia could not be ruled out<br />
by the methodology used. It remains common practice to<br />
avoid solid food for at least 6 h before elective surgery.<br />
Most patients will accept this if they are permitted to<br />
drink until closer to their surgery. There is no clear benefit<br />
to reducing the fasting time for solids below 6 h.<br />
3.3. Chewing gum, sweets and smoking<br />
Recommendation<br />
Patients should not have their operation cancelled or<br />
delayed just because they are chewing gum, sucking a<br />
boiled sweet or smoking immediately prior to induction<br />
of anaesthesia<br />
The above is based solely on effects on gastric emptying and<br />
nicotine intake (including smoking, nicotine gum and patches)<br />
should be discouraged before elective surgery.<br />
Rationale<br />
There is ongoing debate on how to deal with patients<br />
chewing gum in the immediate preoperative period and<br />
what constitutes a safe fasting interval. There are only<br />
three (partly) randomised controlled studies concerning<br />
the intake of chewing gum during the perioperative<br />
fasting period.<br />
In one comparison of 77 patients, 16 16 did not chew<br />
any kind of gum, 15 patients were allowed to chew<br />
gum until transfer to the operating room and 46 were<br />
allowed to chew gum as long as they wished, even until<br />
the time of anaesthesia induction. The last group was not<br />
allocated by means of randomisation. Both gastric fluid<br />
volume as well as pH did not differ significantly among<br />
the three groups.<br />
Another study compared 46 children between 5 and<br />
17 years old who were allowed to chew either sugar-free<br />
or sugared gum up to 30 min before transfer to the<br />
operating room. Both the sugar-free and sugared gum<br />
chewers had significantly higher gastric fluid volume and<br />
pH than the control group who did not chew any gum. 17<br />
Søreide et al. 18 compared 106 female patients scheduled<br />
for elective gynaecologic surgery. They were either<br />
smokers or non-smokers and were allowed to chew<br />
nicotine-containing chewing gum or nothing (smokers)<br />
or sugar-free gum or nothing (non-smokers), respectively.<br />
Up to one chewing gum per hour was given until<br />
transportation to the operating room. The non-smoking<br />
chewers as well as the smokers (chewing or not) had<br />
significantly higher gastric fluid volume than the nonsmokers<br />
who did not chew gum. As far as gastric pH<br />
values are concerned, the levels were higher in both<br />
non-smoking groups than in both smoking groups.<br />
No case of aspiration or other complication during anaesthesia<br />
induction was reported. Although the differences<br />
in pH and gastric volumes were statistically significant,<br />
the authors did not believe the difference (30 versus<br />
20 ml) was clinically significant (E. Søreide, personal<br />
communication).<br />
3.4. Patients with delayed gastric emptying<br />
Recommendation<br />
Patients with obesity, gastro-oesophageal reflux and<br />
diabetes and pregnant women not in labour can safely<br />
follow all of the above guidelines (evidence level 2 ,<br />
recommendation grade D).<br />
These factors may, however, alter their overall anaesthetic<br />
management.<br />
European Journal of Anaesthesiology 2011, Vol 28 No 8<br />
Copyright © European Society of Anaesthesiology. Unauthorized reproduction of this article is prohibited.
Perioperative fasting in adults and children 561<br />
Rationale<br />
A great number of factors can potentially delay gastric<br />
emptying. These include obesity, gastro-oesophageal<br />
reflux and diabetes. Studies of preoperative fasting have<br />
not evaluated these groups of patients adequately enough<br />
to provide definitive evidence. However, the evidence<br />
which does exist suggests that limitation of gastric<br />
emptying is, at most, mild and that these patients can<br />
follow the same guidelines as healthy adults. This advice<br />
also applies to pregnant women who are not in labour.<br />
Opioid analgesia can also delay gastric emptying, but<br />
again there is insufficient evidence to make any<br />
recommendation. However, patients who have recently<br />
taken sufficient opioids to have a significant effect on<br />
gastric emptying are unlikely to be undergoing elective<br />
surgery often.<br />
4. Medications<br />
Recommendation<br />
There is insufficient evidence of clinical benefit to<br />
recommend the routine use of antacids, metoclopramide<br />
or H 2 -receptor antagonists before elective surgery in nonobstetric<br />
patients (evidence level 1þþ, recommendation<br />
grade A).<br />
Rationale<br />
4.1. Prokinetic medications<br />
In contrast to the prevalence of the perioperative use<br />
of prokinetics, there is limited evidence to support<br />
the prophylactic use of these agents to reduce the risk<br />
of perioperative aspiration of gastric contents.<br />
There are single studies that investigate the effect of<br />
prokinetics on gastric pH and gastric fluid volume during<br />
anaesthesia induction. Iqbal et al. 19 compared 75 women<br />
undergoing caesarean section under general anaesthesia.<br />
Twenty-five women were administered both an<br />
H 2 -antagonist (ranitidine) with a prokinetic drug (metoclopramide),<br />
whereas 25 women served as a placebo<br />
control group (another 25 patients received only ranitidine).<br />
The combination of the two drugs was significantly<br />
more effective in increasing the pH and reducing the<br />
gastric fluid volume than placebo. 19<br />
Hong 20 investigated the effect of ranitidine and metoclopramide<br />
versus placebo. Forty patients scheduled for<br />
laparoscopic gynaecological surgery were administered<br />
either 50 mg ranitidine with 10 mg metoclopramide<br />
intravenously (n ¼ 20) or the same volume of isotonic<br />
saline in the control group. Gastric fluid volume was<br />
significantly higher in the placebo group, as was the<br />
gastric pH in the treatment group. 20<br />
Bala et al. 21 compared the combination of ranitidine–<br />
erythromycin with ranitidine–metoclopramide. Forty<br />
ASA I or II patients were given either erythromycin<br />
250 mg and ranitidine 150 mg or ranitidine 150 mg and<br />
metoclopramide 10 mg orally 60–90 min before induction<br />
of anaesthesia. There was no significant difference in<br />
either gastric pH or fluid volume. 21<br />
So far, valid studies that investigate the effect of<br />
preoperatively administered metoclopramide alone on<br />
gastric pH and gastric fluid volume are lacking, although<br />
metoclopramide significantly improves gastric emptying<br />
in cardiac surgery patients 18 h postoperatively compared<br />
with placebo. 22<br />
So far, there is insufficient evidence that preoperatively<br />
administered metoclopramide alone improves clinical<br />
outcome, reduces gastric fluid volume or increases<br />
gastric pH.<br />
4.2. Histamine H 2 -antagonists and proton pump<br />
inhibitors<br />
The mechanisms of action of H 2 -antagonists and<br />
proton pump inhibitors (PPIs) differ. The former block<br />
H 2 -receptors on the stomach’s parietal cells, thereby<br />
inhibiting the stimulatory effects of histamine on gastric<br />
acid secretion; the latter block the enzyme system<br />
of hydrogen/potassium ATPase (H þ /K þ ATPase), the<br />
‘proton pump’ of the gastric parietal cell, such that the<br />
stimulatory actions of histamine, gastrin and acetylcholine<br />
are inhibited. Both have been applied with the<br />
aim of decreasing the risk of deleterious effects resulting<br />
from a potential acid aspiration syndrome.<br />
A recent meta-analysis 23 comparing these medications<br />
to therapeutic targets suggests that pre-medication<br />
with ranitidine is more effective than PPIs in reducing<br />
the volume of gastric secretions (by an average of<br />
0.22 ml kg 1 , 95% confidence interval 0.04–0.41) and<br />
increasing gastric pH (by an average of 0.85 pH units,<br />
95% confidence interval 1.14–0.28). These conclusions<br />
could be drawn based on nine randomised controlled<br />
trials, of which seven were suitable for meta-analysis. In<br />
these trials a total of 223 patients received ranitidine,<br />
which was the sole H 2 -blocker used in the included trials,<br />
and 222 patients received different PPIs (omeprazole,<br />
lansoprazole, pantoprazole and rabeprazole). Overall, the<br />
size of the trials is rather small. Further, heterogeneity<br />
could also be detected with respect to preoperative fasting<br />
time, route of administration, repeat administration<br />
and the specific PPIs used. It is interesting to note<br />
that patients in the trials received ranitidine at doses<br />
equivalent to, or less than, the daily recommended dose<br />
for the maintenance of peptic ulcer disease, whereas<br />
patients received PPIs at doses higher than those recommended<br />
for this purpose.<br />
It is not clear how long the potential protective effect<br />
on gastric volume or pH lasts. It is also unclear whether<br />
these observed effects can be extrapolated to patient<br />
populations with a higher risk of aspiration, as all the<br />
included trials appeared to be in patients at very low<br />
risk of aspiration and the observed parameters were used<br />
European Journal of Anaesthesiology 2011, Vol 28 No 8<br />
Copyright © European Society of Anaesthesiology. Unauthorized reproduction of this article is prohibited.
562 Guidelines<br />
as a surrogate for the ‘true outcome’, that is, mortality or<br />
adult respiratory distress syndrome following gastric<br />
aspiration, which could not be evaluated.<br />
5. Preoperative carbohydrates: gastric<br />
emptying and potential benefits<br />
Recommendation<br />
It is safe for patients (including diabetics) to drink carbohydrate-rich<br />
drinks up to 2 h before elective surgery<br />
(evidence level 1þþ, recommendation grade A).<br />
The evidence for safety is derived from studies of<br />
products specifically developed for perioperative use<br />
(predominantly maltodextrins); not all carbohydrates<br />
are necessarily safe.<br />
Rationale<br />
Studies in animal models of severe stress, such as haemorrhage<br />
and endotoxaemia, showed that several key systems<br />
involved in the stress responses were markedly impaired<br />
even if the animal had been fasted for a brief period before<br />
the onset of a given stress. These key systems included<br />
fluid homeostasis, stress hormone release, aspects of<br />
metabolism, muscle function and gut integrity. 24 If these<br />
models were fasted for as long as 24 h, there was also a<br />
difference in survival. This indicates that the metabolic<br />
change caused by a recent meal (as opposed to fasting)<br />
and the loss of glycogen occurring even after a brief fast is<br />
sufficient to alter the stress response.<br />
Allowing patients to drink clear fluids up to 2 h prior to<br />
surgery is not likely to produce any major change in<br />
metabolism, as these drinks usually do not contain sufficient<br />
energy. The best known method for changing<br />
metabolism from the overnight fasted state to that of a<br />
fed state is the use of carbohydrates. The key change<br />
required to be achieved is a prompt insulin response,<br />
preferably to an extent similar to that observed after<br />
intake of a meal.<br />
In the first instance, intravenous glucose has been<br />
proposed and used for this purpose. The insulin response<br />
to glucose infusions is determined by the rate of delivery<br />
of glucose in a dose-dependent manner. Infusion of<br />
glucose (and insulin) has been shown to induce an<br />
insulin response to levels of about 60 mUml<br />
1 , 25 reduce<br />
postoperative insulin resistance 26 and retain substrate<br />
oxidation. This is important because postoperative<br />
insulin resistance and hyperglycaemia are associated with<br />
an impaired outcome after surgery. 27 Preoperative oral<br />
carbohydrate loading in humans also reduces postoperative<br />
insulin resistance. Dietary interventions, therefore,<br />
represent a promising and attractive therapeutic strategy<br />
to optimise postprandial glycaemia. Thus far, interventions<br />
with respect to the preoperative addition of<br />
carbohydrates have focused on safety, metabolic effects,<br />
personal perioperative well being and postoperative<br />
length of stay.<br />
5.1. Carbohydrates versus clear liquids or intravenous<br />
infusion<br />
Taniguchi et al. 28 investigated the safety and effectiveness<br />
of oral rehydration as compared with intravenous<br />
rehydration prior to general anaesthesia. Fifty patients<br />
were randomised to either 1000 ml of oral rehydration<br />
solution or 1000 ml of an intravenous electrolyte solution.<br />
Volume of gastric contents, as measured directly after<br />
induction, was significantly lower in the oral rehydration<br />
group.<br />
Kaska et al. 29 performed a randomised controlled trial<br />
comparing preoperative fasting with preoperative<br />
preparation with either oral or intravenous intake of<br />
carbohydrates, minerals and water. 29 Oral intake shortly<br />
before surgery did not increase gastric residual volume<br />
and was not associated with any risk.<br />
In the study by Nygren et al., 30 gastric emptying of a<br />
carbohydrate-rich drink was investigated before elective<br />
surgery and in a control situation. Patients served as<br />
their own control pre and postoperatively. Despite the<br />
increased anxiety experienced by patients before surgery,<br />
gastric emptying did not differ between the experimental<br />
and control situations.<br />
Jarvela et al. 31 investigated the effect of a preoperative<br />
oral carbohydrate drink versus overnight fasting on perioperative<br />
insulin requirements in 101 non-diabetic<br />
patients undergoing elective coronary artery bypass grafting.<br />
According to their findings, it is safe to allow cardiac<br />
surgery patients to drink clear fluids up to 2 h before<br />
induction of anaesthesia, because gastric emptying of the<br />
drink was almost total and no aspiration occurred.<br />
Breuer et al. 32 studied the effects of preoperative oral<br />
carbohydrate administration on gastric fluid volume.<br />
Before surgery, 188 ASA physical status III–IV patients<br />
undergoing elective cardiac surgery were randomised to<br />
receive a clear 12.5% carbohydrate drink, flavoured water<br />
(placebo), or to fast overnight (control). Carbohydrates<br />
and placebo were treated in double-blind format and<br />
patients received 800 ml of the corresponding beverage<br />
in the evening and 400 ml 2 h before surgery. Ingested<br />
liquids did not cause increased gastric fluid volume or<br />
other adverse events.<br />
In these five randomised studies, there was no evidence<br />
of an increased gastric volume after ingesting carbohydrates.<br />
Care should be taken in extrapolating this<br />
evidence beyond those specific carbohydrates which<br />
have been studied; not all oral carbohydrates will necessarily<br />
behave similarly.<br />
5.2. Diabetic patients versus healthy individuals<br />
Investigators have been reluctant to give diabetic<br />
patients oral carbohydrates because of the unknown<br />
effects on preoperative glycaemia and gastric emptying.<br />
Gustafsson et al. 33 investigated the effect of preoperative<br />
European Journal of Anaesthesiology 2011, Vol 28 No 8<br />
Copyright © European Society of Anaesthesiology. Unauthorized reproduction of this article is prohibited.
Perioperative fasting in adults and children 563<br />
oral carbohydrate loading in type 2 diabetic patients.<br />
Twenty-five patients with type 2 diabetes and 10 healthy<br />
controls were studied. A carbohydrate-rich drink (400 ml,<br />
12.5%) was given with paracetamol 1.5 g for determination<br />
of gastric emptying. Patients with type<br />
2 diabetes showed no signs of delayed gastric emptying,<br />
suggesting that a carbohydrate-rich drink may be safely<br />
administrated 180 min before anaesthesia without risk of<br />
hyperglycaemia or aspiration preoperatively.<br />
On the basis of this limited evidence, diabetes (of<br />
either type) should not be seen as a contraindication to<br />
preoperative oral carbohydrates.<br />
5.3. New formulas for preoperative drinks<br />
Beverages containing either amino acids (glutamine)<br />
or peptides (soy peptides) have been studied with regard<br />
to their safety. 34,35 Glutamine (15 g) with carbohydrate<br />
in 300–400 ml of water seems to be safe to give 3 h<br />
preoperatively in healthy volunteers based on stomach<br />
emptying time. A drink containing soy peptide given to<br />
patients admitted for elective bowel resections has been<br />
shown to be safe. There was no difference in gastric<br />
emptying time between the carbohydrate group (12.5 g<br />
per 100 ml carbohydrate drink) and carbohydrate/peptide<br />
group (12.5 g per 100 ml carbohydrate and 3.5 g per 100 ml<br />
of hydrolysed soy protein). 35 More research is necessary<br />
to determine the effects of clear liquids with amino acid<br />
or hydrolysed protein in metabolic response and insulin<br />
sensitivity after surgery.<br />
5.4. Carbohydrates, metabolic response and<br />
postoperative discomfort<br />
Recommendation<br />
Drinking carbohydrate-rich fluids before elective surgery<br />
improves subjective well being, reduces thirst and hunger<br />
and reduces postoperative insulin resistance (evidence<br />
level 1þþ, recommendation grade A).<br />
Rationale<br />
In postoperative patients in need of intensive care,<br />
studies have shown that, when glucose is controlled by<br />
intensive insulin therapy, mortality and morbidity can be<br />
reduced. 27 In addition, data suggest that postoperative<br />
discomfort can be reduced when patients are given a<br />
carbohydrate-rich beverage preoperatively.<br />
In a placebo-controlled randomised trial of 252 patients<br />
undergoing elective gastrointestinal surgery, it was shown<br />
that the intake of carbohydrate-rich clear fluid until<br />
2 h before the operation led to less thirst, restlessness,<br />
weakness and concentration problems as compared<br />
to placebo. 36 Two small placebo-controlled double-blind<br />
studies in 15 37 and 14 38 patients, respectively, undergoing<br />
hip surgery, showed that the intake of a carbohydrate-rich<br />
clear fluid until 2 h before the operation<br />
reduced insulin resistance on days 1 and 3. 37,38 Another<br />
study of 14 patients displayed less reduced insulin<br />
sensitivity after colorectal surgery following preoperative<br />
oral carbohydrate administration as compared with<br />
patients who were operated on after an overnight fast. 39<br />
A recently published study in patients undergoing open<br />
colorectal surgery also showed reduced postoperative<br />
insulin resistance after preoperative oral carbohydrates,<br />
as well as reduced thirst and hunger. 40 However, a preoperative<br />
oral carbohydrate drink did not reduce postoperative<br />
insulin resistance or postoperative nausea and<br />
vomiting in an investigation of 101 non-diabetic patients<br />
undergoing elective coronary artery bypass grafting. 31<br />
In a randomised study in 65 patients undergoing<br />
major abdominal surgery, carbohydrates contributed to<br />
the maintenance of muscle mass. 41 In two randomised<br />
trials in 86 42 and 172 patients 43 undergoing laparoscopic<br />
cholecystectomy, there was either no effect 42 or only a<br />
reduction in postoperative nausea and vomiting. 43 Faria<br />
et al. 44 showed improved glucose metabolism and<br />
organic response in 21 female patients participating in<br />
a randomised controlled trial and undergoing laparoscopic<br />
cholecystectomy.<br />
Helminen et al. 45 studied 210 patients, undergoing<br />
gastrointestinal surgery, randomly assigned to fasting,<br />
intravenous or oral carbohydrates. Intravenous glucose<br />
infusion did not decrease the sense of thirst and hunger as<br />
effectively as in the oral intake group, but it did alleviate<br />
the feelings of weakness and tiredness.<br />
Taniguchi et al. 28 investigated 50 patients randomised to<br />
either 1000 ml of oral rehydration solution or 1000 ml of<br />
an intravenous electrolyte solution. Patients’ satisfaction<br />
favoured oral rehydration as they experienced less<br />
feelings of hunger, less occurrence of dry mouth and less<br />
restriction of movement. Similar subjective benefits were<br />
observed in a recent small study of gynaecological<br />
patients. 46<br />
Kaska et al. 29 performed a randomised controlled trial<br />
comparing preoperative fasting with preoperative preparation<br />
with either oral or intravenous intake of carbohydrates,<br />
minerals and water. Consumption of the mix of<br />
water, minerals and carbohydrates offered some protection<br />
against surgical trauma in terms of metabolic status,<br />
cardiac function and psychosomatic status.<br />
Breuer et al. 32 studied the effects of preoperative oral<br />
carbohydrate administration on postoperative insulin<br />
resistance, preoperative discomfort and variables of organ<br />
dysfunction in 188 ASA physical status III–IV patients<br />
undergoing elective cardiac surgery, including those<br />
with non-insulin-dependent type-2 diabetes mellitus.<br />
Carbohydrates and placebo were administered in doubleblind<br />
format and patients received 800 ml of the corresponding<br />
beverage in the evening and 400 ml 2 h before<br />
surgery. Blood glucose levels and insulin requirements<br />
did not differ between the groups. Patients receiving<br />
European Journal of Anaesthesiology 2011, Vol 28 No 8<br />
Copyright © European Society of Anaesthesiology. Unauthorized reproduction of this article is prohibited.
564 Guidelines<br />
carbohydrate and placebo were less thirsty compared with<br />
controls. The carbohydrate group, however, required<br />
less intraoperative inotropic support after initiation of<br />
cardiopulmonary bypass weaning (P < 0.05). 32<br />
One study of 36 patients undergoing colorectal surgery<br />
has demonstrated a reduction in median length of stay<br />
associated with oral carbohydrate therapy. 47 A retrospective<br />
analysis of three small prospective randomised<br />
trials (one matched-control study), primarily investigating<br />
postoperative insulin resistance, 24 showed that<br />
although the studies were too small to show a significant<br />
reduction in length of stay individually, the combined<br />
effect was a significant reduction of about 20%. 24 This<br />
was confirmed in the randomised trial of Yuill et al. 41 in<br />
2005 in 72 patients undergoing elective abdominal<br />
surgery. However, the recently published randomised<br />
trial of Mathur et al. 48 in 142 patients undergoing<br />
colorectal surgery or liver resection did not confirm these<br />
results.<br />
6. Perioperative fasting in children and<br />
infants<br />
Recommendations<br />
Children should be encouraged to drink clear fluids<br />
(including water, pulp-free juice and tea or coffee without<br />
milk) up to 2 h before elective surgery (evidence level<br />
1þþ, recommendation grade A).<br />
All but one member of the guidelines group consider that tea or<br />
coffee with milk added (up to about one fifth of the total volume)<br />
are still clear fluids.<br />
Infants should be fed before elective surgery. Breast milk<br />
is safe up to 4 h and other milks up to 6 h. Thereafter,<br />
clear fluids should be given as in adults (evidence level<br />
1þþ, recommendation grade A).<br />
Rationale<br />
The recommendations are based on reviews and<br />
guidelines published in the late 1990s and more<br />
recently. 2–4,7,11,49–52 Fasting is aimed at decreasing the<br />
risk of pulmonary aspiration, but the incidence of this<br />
complication is very low in recent series and, although the<br />
risk of aspiration appears to be slightly greater in children<br />
than in adults, 53 the difference is less than that previously<br />
reported. All recent surveys indicate the relatively<br />
good outcome of this event in the paediatric population<br />
compared with previous series.<br />
There is a lot of evidence that clear fluids can be given<br />
up to 2 h prior to surgery in neonates, infants and<br />
children. In neonates and infants, gastric emptying of<br />
clear fluids follows first-order kinetics as in older children<br />
and adults. 54 Allowing clear fluids prior to surgery<br />
improves comfort of the child and the parents, decreases<br />
thirst and decreases the risk of preoperative dehydration<br />
in young infants. 55 The volume of fluids permitted in the<br />
preoperative period does not appear to impact on the<br />
intragastric volume or pH of children. 2 This also applies<br />
to overweight and obese children. 56<br />
6.1. Breast milk and infant formula<br />
Fasting time for breast milk and infant formula is slightly<br />
more controversial. It was demonstrated more than<br />
25 years ago that the gastric emptying of 110–200 ml<br />
of human milk was 82 11% after 2 h in neonates<br />
and infants of less than 1 year of age, 84 21% after<br />
whey-hydrosylated formula, 74 19% after whey-predominant<br />
formula, 61 17% after casein-predominant<br />
formula and 45 19% after cow’s milk. 57 Thus, human<br />
milk and whey-predominant formula emptied faster than<br />
casein-predominant formula and cow’s milk. Two other<br />
studies performed before anaesthesia also demonstrated<br />
that breast milk empties from the stomach faster than<br />
most formulas in infants and both require more than 2 h<br />
to ensure complete gastric emptying. 54,58 According<br />
to these data, the American guidelines recommended<br />
4 h fasting time for breast milk and 6 h for infant formula<br />
and non-human milk. 7 These recommendations were<br />
also endorsed by the Royal College of Nursing that<br />
considered there was insufficient evidence to change<br />
contemporary best practice (i.e. breast milk up to 4 h<br />
and formula and cows’ milk up to 6 h). 4 Scandinavian<br />
guidelines recommended 4 h fasting for breast milk but<br />
also for formula milk in infants of less than 6 months<br />
of age. 3 Thus, it is recommended to finish breast feeding<br />
4 h before anaesthesia and to stop infant formula 4–6 h<br />
prior to anaesthesia depending on the age and on local<br />
considerations. Both cow’s milk and powdered milk are<br />
considered as solid food.<br />
6.2. Solid food<br />
Recommendations for fasting of solid food in children do<br />
not differ from those proposed for healthy adults. There<br />
is no evidence against these recommendations.<br />
6.3. Trauma<br />
Data on fasting in injured children are minimal. One<br />
study suggested that the volume of gastric contents may<br />
depend on the nature of the trauma, but gastric content<br />
was not related to the length of fasting. 59 Gastric volume<br />
was better linked to the interval between the last<br />
meal and the trauma. Thus, the injured child should<br />
be considered as a patient with a full stomach. However,<br />
an increasing number of minor surgical procedures are<br />
done under sedation in the emergency department. The<br />
available literature does not provide sufficient evidence<br />
to conclude that pre-procedure fasting results in a<br />
decreased incidence of adverse outcomes in children<br />
undergoing either moderate or deep sedation. 60,61<br />
6.4. Postoperative fluids<br />
Oral fluid intake is usually allowed within the first 3<br />
postoperative hours in most paediatric patients. Early<br />
European Journal of Anaesthesiology 2011, Vol 28 No 8<br />
Copyright © European Society of Anaesthesiology. Unauthorized reproduction of this article is prohibited.
Perioperative fasting in adults and children 565<br />
oral fluid intake was previously required in most<br />
institutions before discharging the patient from hospital.<br />
This view was challenged, as it has been reported that<br />
withholding oral fluids postoperatively from children<br />
undergoing day surgery reduces the incidence of vomiting.<br />
62,63 However, the most recent study did not find that<br />
postoperative fasting reduces the incidence of vomiting<br />
after general anaesthesia in children when compared<br />
with a liberal regimen. 64 Thus, it seems reasonable to<br />
let children eat and drink according to their own desires,<br />
but not to insist on oral intake before discharge.<br />
7. Fasting in obstetric patients<br />
Recommendations<br />
Women in labour should be allowed clear fluids (as<br />
defined above) as they desire. (evidence level 1þþ,<br />
recommendation grade A).<br />
Solid food should be discouraged during active labour<br />
(evidence level 1þ, recommendation grade A).<br />
Pregnant women, including obese individuals, can<br />
consume clear liquids until up to 2 h prior to surgery<br />
(under regional or general anaesthesia) (evidence level<br />
2 , recommendation grade D).<br />
An H 2 -receptor antagonist should be given the night<br />
before, and on the morning of, elective caesarean section<br />
(evidence level 1þþ, recommendation grade A).<br />
An intravenous H 2 -receptor antagonist should be given<br />
prior to emergency caesarean section; this should be<br />
supplemented with 30 ml of 0.3 mol l<br />
1 sodium citrate<br />
if general anaesthesia is planned (evidence level 1þþ,<br />
recommendation grade A).<br />
The guidelines group recognises that most of the evidence<br />
relates to surrogate measures, such as changes in gastric<br />
volume and pH, rather than a clear impact on mortality.<br />
Rationale<br />
7.1. Oral intake during labour<br />
Surgery during labour is usually unplanned, and when it<br />
occurs the degree of emergency can range from minimal to<br />
surgery that is life saving for either mother or baby. Against<br />
this background, logic dictates that all mothers should be<br />
starved during labour. However, it is often argued that<br />
allowing mothers to eat and drink during labour will<br />
prevent ketosis and dehydration and, thereby, improve<br />
obstetric outcome. There is currently wide variation in<br />
practice with respect to eating during labour in Europe.<br />
However, it has now been shown that although eating a<br />
light diet during labour will prevent ketosis, it will also<br />
increase gastric volume, 65 whereas when isotonic ‘sport<br />
drinks’ are consumed during labour, 66 ketosis can be<br />
eliminated without an increase in intragastric volume.<br />
A recent randomised controlled study evaluated the<br />
effect of food intake during labour on obstetric outcome.<br />
Low-risk nulliparous women in labour (n ¼ 2443) were<br />
randomised to either an ‘eating’ or a ‘water only’ group.<br />
The results were analysed by intention to treat. No<br />
significant difference was found in the normal vaginal<br />
delivery rate; the instrumental vaginal delivery rate;<br />
the caesarean section rate; the duration of labour; or<br />
the incidence of vomiting. 67<br />
Maternal death from aspiration of regurgitated gastric<br />
content is now extremely rare, and its decline probably<br />
owes more to the widespread use of regional anaesthesia<br />
for operative obstetrics than to fasting policies. In view of<br />
the predominant use of regional techniques on most<br />
delivery units, rigid fasting policies are arguably no longer<br />
appropriate during labour and mothers should, therefore,<br />
be allowed to alleviate thirst during labour by consuming<br />
ice chips and clear fluids (isotonic sports drinks, fruit<br />
juices, tea and coffee, etc).<br />
As eating confers no benefit to obstetric outcome, women<br />
should be discouraged from eating solid food during<br />
labour. However, in view of the almost negligible incidence<br />
of deaths from aspiration, low-risk women could<br />
consume low-residue foods (such as biscuits, toast or<br />
cereals) during labour. In addition, when deciding<br />
whether or not women should eat during labour, the<br />
use of parenteral opioids should also be considered<br />
because of their profound delay on the rate of gastric<br />
emptying. Units who perform a significant volume of<br />
their emergency obstetric surgery under general anaesthesia<br />
should probably not allow women in labour to eat.<br />
In high-risk pregnancies, it remains appropriate to not eat<br />
during labour and to achieve hydration by limited<br />
volumes of oral clear fluids or by the intravenous route.<br />
7.2. Preparation for caesarean section<br />
7.2.1. Preoperative fasting in elective obstetric surgery<br />
Evidence suggests that pregnant women, including obese<br />
individuals, can consume clear liquids until up to 2 h prior<br />
to surgery (under regional or general anaesthesia) 68,69<br />
(evidence level 1þ, recommendation A).<br />
7.2.2. Recommended drug regimens in detail<br />
7.2.2.1. Elective obstetric surgery All mothers should<br />
be actively encouraged to have regional anaesthesia for<br />
an elective caesarean section.<br />
An H 2 -receptor antagonist (e.g. 150 mg ranitidine) or a<br />
PPI (e.g. omeprazole 40 mg) should be given at bedtime<br />
and again 60–90 min before the induction of anaesthesia.<br />
The administration of oral metoclopramide 10 mg at the<br />
same time as the H 2 -receptor antagonist or PPI should<br />
also be considered.<br />
7.2.2.2. Emergency obstetric surgery under regional<br />
anaesthesia Intravenous H 2 -antagonist (e.g. ranitidine<br />
50 mg) at time of decision for surgery. In high-risk women<br />
European Journal of Anaesthesiology 2011, Vol 28 No 8<br />
Copyright © European Society of Anaesthesiology. Unauthorized reproduction of this article is prohibited.
566 Guidelines<br />
the use of oral H 2 -antagonists (ranitidine 150 mg), at<br />
regular intervals during labour, should be considered.<br />
7.2.2.3. Emergency obstetric surgery under general<br />
anaesthesia Intravenous H 2 -antagonist and oral antacid<br />
(e.g. 30 ml sodium citrate 0.3 mol l<br />
1 ) prior to induction<br />
of anaesthesia.<br />
7.3. Eating and drinking after caesarean section<br />
The beneficial effects of early postoperative feeding<br />
have been clearly demonstrated in colorectal surgery.<br />
Traditionally, eating and drinking after caesarean section<br />
was not encouraged, food and fluid were usually withheld<br />
for the first 12–24 h after surgery, after which fluids were<br />
slowly introduced, with food being allowed once bowel<br />
sounds had been heard or flatus was passed. A Cochrane<br />
review published in 2002 (the review included six articles<br />
published between 1993 and 2001) concluded that there<br />
was no evidence to justify restricting oral fluids or food<br />
following uncomplicated caesarean section. 70<br />
More recent studies have indicated that clear fluids,<br />
commenced between 30 min and 2 h after caesarean<br />
section, are well tolerated and result in women requiring<br />
less intravenous fluids, earlier ambulation and earlier<br />
breast-feeding. Earlier solid intake appears to cause<br />
more nausea which tends to be self-limiting. 71–73 Current<br />
evidence, therefore, suggests that early oral hydration<br />
following caesarean section is well tolerated and should<br />
perhaps be encouraged. Solid foods should be introduced<br />
more cautiously.<br />
7.4. Effects of pregnancy on gastric function<br />
Gastro-oesophageal reflux, resulting in heartburn, is a<br />
common complication of late pregnancy. Pregnancy<br />
compromises the integrity of the lower oesophageal<br />
sphincter as a result of an alteration in the anatomical<br />
relationship of the oesophagus to the diaphragm and<br />
stomach, an increase in intragastric pressure and the<br />
relaxing effect of progesterone on smooth muscle. A<br />
pregnant woman at term, requiring anaesthesia, should,<br />
therefore, be regarded as having an incompetent lower<br />
oesophageal sphincter. These physiological changes are<br />
less 48 h after delivery. 74<br />
Gastric acid secretion is essentially unchanged during<br />
pregnancy. 75 Pregnancy does not significantly alter the<br />
rate of gastric emptying. 76 Gastric emptying is normal in<br />
early labour, but becomes delayed as labour advances. 77<br />
Parenteral opioids significantly delay gastric emptying<br />
during labour, as do bolus doses of epidural and intrathecal<br />
opioids. 78–80 Continuous epidural infusion of lowdose<br />
local anaesthetic with fentanyl does not appear to<br />
delay gastric emptying until the total dose of fentanyl<br />
exceeds 100 mg. 68<br />
Gastric emptying is not delayed in either obese or nonobese<br />
parturients at term who ingest 300 ml water after<br />
an overnight fast. 69,81 Lewis and Crawford 82 noted that<br />
in patients undergoing elective caesarean section, a meal<br />
of both tea (volume unknown) and toast 2–4 h preoperatively<br />
resulted in an increased gastric volume and<br />
a decreased gastric pH when compared with a control<br />
group of patients. Particulate material was aspirated from<br />
the stomachs of two of the 11 patients who consumed<br />
both tea and toast. Consumption of tea without toast<br />
resulted in an increase in gastric volume, but it did not<br />
alter gastric pH.<br />
7.5. Pharmacological prophylaxis against acid<br />
pulmonary aspiration in obstetrics<br />
The risk of failed intubation is three to 11 times greater<br />
in pregnant patients than in non-pregnant patients. 83<br />
Airway oedema, breast enlargement, obesity and the<br />
high rate of emergency surgery, all contribute to the risk<br />
of failed intubation in pregnant women. Aspiration<br />
pneumonitis is often associated with difficult or failed<br />
intubation during the induction of general anaesthesia.<br />
Pregnant women undergoing caesarean section or other<br />
surgical procedures (both elective and emergency)<br />
should, therefore, receive antacid prophylaxis.<br />
7.5.1. H 2 -receptor antagonists<br />
H 2 -receptor antagonists block histamine receptors on the<br />
oxyntic cell and, thus, decrease gastric acid production.<br />
This results in a slight reduction in gastric volume in the<br />
fasting patient. When given intravenously, an H 2 -receptor<br />
antagonist begins to take effect in as little as 30 min,<br />
but 60–90 min are required for maximal effect. After oral<br />
administration, gastric pH is greater than 2.5 in approximately<br />
60% of patients at 60 min and in 90% at 90 min.<br />
Most studies have evaluated the administration of 50–<br />
100 mg of ranitidine administered intravenously or intramuscularly<br />
or 150 mg administered orally. 84–86 These<br />
studies have noted that the administration of ranitidine<br />
results in a gastric pH greater than 2.5 within 1 h.<br />
Therapeutic concentrations of ranitidine are sustained<br />
for approximately 8 h.<br />
7.5.2. Proton pump inhibitors<br />
Omeprazole (20–40 mg orally) and lansoprazole (15–<br />
30 mg orally) inhibit the hydrogen ion pump on the gastric<br />
surface of the oxyntic cell. 87,88 For elective surgery, the<br />
efficacy of prophylaxis when using a PPI is similar to that<br />
achieved with an H 2 -receptor antagonist. For emergency<br />
caesarean section, studies have shown that H 2 -receptor<br />
antagonists and PPIs, administered intravenously, are<br />
equally effective adjuncts to 0.3 mol l<br />
1 sodium citrate<br />
for reducing gastric acidity and volume.<br />
A recent meta-analysis on the effect of PPIs and<br />
H 2 -antagonists (studies included both obstetric and<br />
non-obstetric patients) concluded that H 2 -antagonists<br />
were more efficacious than PPIs for both reducing gastric<br />
volume and increasing gastric pH. 23<br />
European Journal of Anaesthesiology 2011, Vol 28 No 8<br />
Copyright © European Society of Anaesthesiology. Unauthorized reproduction of this article is prohibited.
Perioperative fasting in adults and children 567<br />
As antacids such as 0.3 mol l<br />
1 sodium citrate can<br />
cause nausea and even vomiting, they need not be<br />
administered prior to elective surgery under regional<br />
anaesthesia if the parturient has already received an<br />
H 2 -antagonist or a PPI. However, in the event of emergency<br />
obstetric surgery under general anaesthesia, an<br />
antacid should be administered shortly before induction<br />
of general anaesthesia (e.g. within 20 min) with an H 2 -<br />
antagonist, as time constraints may mean that the efficacy<br />
of H 2 -antagonists cannot be guaranteed at the time<br />
of induction.<br />
Metoclopramide 10 mg can further decrease gastric<br />
volume when used in conjunction with an H 2 -antagonist<br />
prior to elective caesarean section 89 and its use should<br />
be considered prior to both elective and emergency<br />
caesarean section.<br />
Acknowledgements<br />
I.S. has received research funding from Abbott and Anaxsys for<br />
studies unrelated to these guidelines and declares no conflicts of<br />
interest. P.K. has received fees for lectures/consulting and/or study<br />
material from Fresenius Kabi Deutschland GmbH (Bad Homburg,<br />
Germany), ProStrakan Deutschland (Starnberg, Germany),<br />
Merck Sharp & Dohme Corp. (New Jersey, USA), Nutricia<br />
Deutschland (Erlangen, Germany), Essex Pharma (Munich,<br />
Germany) and SonoSite GmbH (Erlangen, Germany). I.M. declares<br />
no conflict of interest.<br />
G.O.S. is part of a £3 million multi-centre trial investigating the<br />
effect of epidural anaesthesia on the second stage of labour and a coauthor<br />
of one of the included studies in the literature review. A.S.<br />
has received gifts of equipment from Schering-Plough but not<br />
related to the content of this guideline.<br />
E.S. has received research funding from the Laerdal Foundation for<br />
Acute Medicine. E.S. is the current President of the Scandinavian<br />
Society of Anaesthesia and Intensive Care and co-author of their<br />
2005 fasting guidelines.<br />
C.S. has received honoraria and speaking fees from Akzo Nobel,<br />
Fresenius, BBraun, Baxter, Abbott, Essex Pharma, GSK and grants<br />
from Abbott, Akzo Nobel, Aspect, Baxter, BBraun, Deltex Medical,<br />
Edwards, Fresenius, GSK, Köhler Chemie, Lilly, MSD, Novalung,<br />
Orion Pharma, Pfizer, Pfrimmer Nutricia and Wyeth. B.V. declares<br />
no competing interests in the last 5 years.<br />
The guidelines group would like to acknowledge the following<br />
individuals who made a valuable contribution to the searching or<br />
reviewing of the literature or who contributed their expertise to the<br />
development of the guidelines: Jan Breuer, Susanna Keilig, Laura<br />
Coleman and Nick Truman.<br />
The guidelines group would also like to acknowledge the following<br />
who reviewed and commented on the draft guidelines, either as<br />
individuals or as representatives of national or international<br />
societies: Muhammad Ajmal, Gabriella Bettelli, Metha Brattwall,<br />
Roland Braun, Jean François Brichant, Valerie Bythell, Akos<br />
Csomos, Gordon Drummond, Gabor Erdoes, Anil Gupta, Jochen<br />
Hinkelbein, Markus Hollmann, Pablo Ingelmo, Ian Jackson, Jean<br />
Joris, Paulo Lemos, Diana Mathioudakis, Claudio Melloni, Victoria<br />
Moral, Oya Ozatamer, Beverly Philip, Felicity Plaat, Paolo Primieri,<br />
Ian Russell, Marc Samama, Daniele Sances, Samantha Shinde,<br />
Daniel Smole, Susanne Sujatta, François Sztark, Claudia Teipelke,<br />
the Dutch Society of Anesthesiology and Bernhard Walder.<br />
Statements of interest of reviewers: Markus Hollmann has received<br />
Lecture fees from Eurocept (The Netherlands), BBraun, Pfizer<br />
Germany, Schering-Plough and Merck, but all are unrelated to<br />
this subject. François Sztark received fees for lectures and<br />
consulting from Fresenius Kabi France and Abbott France and is<br />
co-investigator for Danone Research (study EUDRACT 2009-<br />
A00898–49).<br />
References<br />
1 Brady M, Kinn S, Stuart P. Preoperative fasting for adults to prevent<br />
perioperative complications. Cochrane Database Syst Rev<br />
2003:CD004423.<br />
2 Brady M, Kinn S, Ness V, et al. Preoperative fasting for preventing<br />
perioperative complications in children [review]. Cochrane Database<br />
Systematic Rev 2009:CD005285.<br />
3 Søreide E, Eriksson LI, Hirlekar G, et al. Preoperative fasting guidelines: an<br />
update [review]. Acta Anaesthesiol Scand 2005; 49:1041–1047.<br />
4 Royal College of Nursing. Perioperative fasting in adults and children: an<br />
RCN guideline for the multidisciplinary team. London: Royal College of<br />
Nursing; 2005.<br />
5 Scottish Intercollegiate Guidelines Network, Elliott House, 8-10 Hillside<br />
Crescent, Edinburgh EH7 5EA. 2010. www.sign.ac.uk.<br />
6 Schwartz PJ, Breithardt G, Howard AJ, et al. Task force report: the legal<br />
implications of medical guidelines – a task force of the European Society of<br />
Cardiology. Eur Heart J 1999; 20:1152–1157.<br />
7 American Society of Anesthesiologists Task Force on Preoperative Fasting.<br />
Practice guidelines for preoperative fasting and the use of pharmacologic<br />
agents to reduce the risk of pulmonary aspiration: application to healthy<br />
patients undergoing elective procedures. Anesthesiology 1999; 90: 896–<br />
905.<br />
8 Maltby JR, Sutherland AD, Sale JP, Shaffer EA. Preoperative oral fluids: is a<br />
five-hour fast justified prior to elective surgery? Anesth Analg 1986;<br />
65:1112–1116.<br />
9 Phillips S, Hutchinson S, Davidson T. Preoperative drinking does not affect<br />
gastric contents. Br J Anaesth 1993; 70:6–9.<br />
10 Søreide E, Stromskag KE, Steen PA. Statistical aspects in studies of<br />
preoperative fluid intake and gastric content. Acta Anaesthesiol Scand<br />
1995; 39:738–743.<br />
11 Eriksson LI, Sandin R. Fasting guidelines in different countries. Acta<br />
Anaesthesiol Scand 1996; 40 (8 Pt 2):971–974.<br />
12 Scarr M, Maltby JR, Jani K, Sutherland LR. Volume and acidity of residual<br />
gastric fluid after oral fluid ingestion before elective ambulatory surgery.<br />
CMAJ 1989; 141:1151–1154.<br />
13 Hutchinson A, Maltby JR, Reid CRG. Gastric fluid volume and pH in elective<br />
inpatients. Part I: Coffee or orange juice versus overnight fast. Can J<br />
Anaesth 1988; 35:12–15.<br />
14 Maltby JR, Reid CRG, Hutchinson A. Gastric fluid volume and pH in elective<br />
inpatients. Part II: Coffee or orange juice with ranitidine. Can J Anaesth<br />
1988; 35:16–19.<br />
15 Miller M, Wishart HY, Nimmo WS. Gastric contents at induction of<br />
anaesthesia. Is a 4-h fast necessary? Br J Anaesth 1983; 55:1185–1188.<br />
16 Dubin SA, Jense HG, McCranie JM, Zubar V. Sugarless gum chewing<br />
before surgery does not increase gastric fluid volume or acidity. Can J<br />
Anaesth 1994; 41:603–606.<br />
17 Schoenfelder RC, Ponnamma CM, Freyle D, et al. Residual gastric fluid<br />
volume and chewing gum before surgery. Anesth Analg 2006; 102:415–<br />
417.<br />
18 Søreide E, Holst-Larsen H, Veel T, Steen PA. The effects of chewing gum<br />
on gastric content prior to induction of general anesthesia. Anesth Analg<br />
1995; 80:985–989.<br />
19 Iqbal MS, Ashfaque M, Akram M. Gastric fluid volume and pH: a<br />
comparison of effects of ranitidine alone with combination of ranitidine and<br />
metoclopramide in patients undergoing elective caesarean section. Ann<br />
King Edward Med Coll 2000; 6:189–191.<br />
20 Hong JY. Effects of metoclopramide and ranitidine on preoperative gastric<br />
contents in day-case surgery. Yonsei Med J 2006; 47:315–318.<br />
21 Bala I, Prasad K, Bhukal I, et al. Effect of preoperative oral erythromycin,<br />
erythromycin-ranitidine, and ranitidine-metoclopramide on gastric fluid pH<br />
and volume. J Clin Anesth 2008; 20:30–34.<br />
22 Sustic A, Zelic M, Protic A, et al. Metoclopramide improves gastric but not<br />
gallbladder emptying in cardiac surgery patients with early intragastric enteral<br />
feeding: randomized controlled trial. Croat Med J 2005; 46:239–244.<br />
European Journal of Anaesthesiology 2011, Vol 28 No 8<br />
Copyright © European Society of Anaesthesiology. Unauthorized reproduction of this article is prohibited.
568 Guidelines<br />
23 Clark K, Lam LT, Gibson S, Currow D. The effect of ranitidine versus proton<br />
pump inhibitors on gastric secretions: a meta-analysis of randomised<br />
control trials [review]. Anaesthesia 2009; 64:652–657.<br />
24 Ljungqvist O, Nygren J, Thorell A. Insulin resistance and elective surgery<br />
[review]. Surgery 2000; 128:757–760.<br />
25 Wolfe RR, Allsop JR, Burke JF. Glucose metabolism in man: responses to<br />
intravenous glucose infusion. Metabolism 1979; 28:210–220.<br />
26 Ljungqvist O, Thorell A, Gutniak M, et al. Glucose infusion instead of<br />
preoperative fasting reduces postoperative insulin resistance [review].<br />
J Am Coll Surg 1994; 178:329–336.<br />
27 Van den Berghe GH. Role of intravenous insulin therapy in critically ill<br />
patients [review]. Endocr Pract 2004; 2:17–20.<br />
28 Taniguchi H, Sasaki T, Fujita H, et al. Preoperative fluid and<br />
electrolyte management with oral rehydration therapy. J Anesth 2009;<br />
23:222–229.<br />
29 Kaska M, Grosmanova T, Havel E, et al. The impact and safety of<br />
preoperative oral or intravenous carbohydrate administration versus fasting<br />
in colorectal surgery: a randomized controlled trial. Wien Klin Wochenschr<br />
2010; 122:23–30.<br />
30 Nygren J, Thorell A, Jacobsson H, et al. Preoperative gastric emptying.<br />
Effects of anxiety and oral carbohydrate administration. Ann Surg 1995;<br />
222:728–734.<br />
31 Jarvela K, Maaranen P, Sisto T. Preoperative oral carbohydrate treatment<br />
before coronary artery bypass surgery. Acta Anaesthesiol Scand 2008;<br />
52:793–797.<br />
32 Breuer JP, von Dossow V, von Heymann C, et al. Preoperative oral<br />
carbohydrate administration to ASA III-IV patients undergoing elective<br />
cardiac surgery. Anesth Analg 2006; 103:1099–1108.<br />
33 Gustafsson UO, Nygren J, Thorell A, et al. Preoperative carbohydrate<br />
loading may be used in type 2 diabetes patients. Acta Anaesthesiol Scand<br />
2008; 52:946–951.<br />
34 Henriksen MG, Hessov I, Dela F, et al. Effects of preoperative oral<br />
carbohydrates and peptides on postoperative endocrine response,<br />
mobilization, nutrition and muscle function in abdominal surgery. Acta<br />
Anaesthesiol Scand 2003; 47:191–199.<br />
35 Lobo DN, Hendry PO, Rodrigues G, et al. Gastric emptying of three liquid<br />
oral preoperative metabolic preconditioning regimens measured by<br />
magnetic resonance imaging in healthy adult volunteers: a randomised<br />
double-blind, crossover study. Clin Nutr 2009; 28:636–641.<br />
36 Hausel J, Nygren J, Lagerkranser M, et al. A carbohydrate-rich drink reduces<br />
preoperative discomfort in elective surgery patients. Anesth Analg 2001;<br />
93:1344–1350.<br />
37 Soop M, Nygren J, Myrenfors P, et al. Preoperative oral carbohydrate<br />
treatment attenuates immediate postoperative insulin resistance. Am J<br />
Physiol Endocrinol Metab 2001; 280:E576–E583.<br />
38 Soop M, Nygren J, Thorell A, et al. Preoperative oral carbohydrate treatment<br />
attenuates endogenous glucose release 3 days after surgery. Clin Nutr<br />
2004; 23:733–741.<br />
39 Nygren J, Soop M, Thorell A, et al. Preoperative oral carbohydrate<br />
administration reduces postoperative insulin resistance. Clin Nutr 1998;<br />
17:65–71.<br />
40 Wang ZG, Wang Q, Wang WJ, Qin HL. Randomized clinical trial to<br />
compare the effects of preoperative oral carbohydrate versus placebo on<br />
insulin resistance after colorectal surgery. Br J Surg 2010; 97:317–327.<br />
41 Yuill KA, Richardson RA, Davidson HI, et al. The administration of an oral<br />
carbohydrate-containing fluid prior to major elective upper-gastrointestinal<br />
surgery preserves skeletal muscle mass postoperatively: a randomised<br />
clinical trial. Clin Nutr 2005; 24:32–37.<br />
42 Bisgaard T, Kristiansen VB, Hjortso NC, et al. Randomized clinical trial<br />
comparing an oral carbohydrate beverage with placebo before<br />
laparoscopic cholecystectomy. Br J Surg 2004; 91:151–158.<br />
43 Hausel J, Nygren J, Thorell A, et al. Randomized clinical trial of the effects of<br />
oral preoperative carbohydrates on postoperative nausea and vomiting<br />
after laparoscopic cholecystectomy. Br J Surg 2005; 92:415–421.<br />
44 Faria MS, de Aguilar-Nascimento JE, Pimenta OS, et al. Preoperative<br />
fasting of 2 h minimizes insulin resistance and organic response to trauma<br />
after video-cholecystectomy: a randomized, controlled, clinical trial. World J<br />
Surg 2009; 33:1158–1164.<br />
45 Helminen H, Viitanen H, Sajanti J. Effect of preoperative intravenous<br />
carbohydrate loading on preoperative discomfort in elective surgery<br />
patients. Eur J Anaesthesiol 2009; 26:123–127.<br />
46 Meisner M, Ernhofer U, Schmidt J. Liberalisation of preoperative fasting<br />
guidelines: effects on patient comfort and clinical practicability during<br />
elective laparoscopic surgery of the lower abdomen [German]. Zentralbl<br />
Chir 2008; 133:479–485.<br />
47 Noblett SE, Watson DS, Huong H, et al. Preoperative oral carbohydrate<br />
loading in colorectal surgery: a randomized controlled trial. Colorectal Dis<br />
2006; 8:563–569.<br />
48 Mathur S, Plank LD, McCall JL, et al. Randomized controlled trial of<br />
preoperative oral carbohydrate treatment in major abdominal surgery. Br J<br />
Surg 2010; 97:485–494.<br />
49 Splinter WM, Schreiner MS. Preoperative fasting in children [review].<br />
Anesth Analg 1999; 89:80–89.<br />
50 Cook-Sather SD, Litman RS. Modern fasting guidelines in children [review].<br />
Best Pract Res Clin Anaesthesiol 2006; 20:471–481.<br />
51 Søreide E, Ljungqvist O. Modern preoperative fasting guidelines:<br />
a summary of the present recommendations and remaining<br />
questions [review]. Best Pract Res Clin Anaesthesiol 2006; 20:483–<br />
491.<br />
52 Shime N, Ono A, Chihara E, Tanaka Y. Current practice of preoperative<br />
fasting: a nationwide survey in Japanese anesthesia-teaching hospitals.<br />
J Anesth 2005; 19:187–192.<br />
53 Flick RP, Schears GJ, Warner MA. Aspiration in pediatric anesthesia: is<br />
there a higher incidence compared with adults? Curr Opin Anaesthesiol<br />
2002; 15:323–327.<br />
54 Litman RS, Wu CL, Quinlivan JK. Gastric volume and pH in infants fed<br />
clear liquids and breast milk prior to surgery. Anesth Analg 1994; 79:482–<br />
485.<br />
55 Nicolson SC, Schreiner MS. Feed the babies [editorial]. Anesth Analg<br />
1994; 79:407–409.<br />
56 Cook-Sather SD, Gallagher PR, Kruge LE, et al. Overweight/obesity and<br />
gastric fluid characteristics in pediatric day surgery: implications for fasting<br />
guidelines and pulmonary aspiration risk. Anesth Analg 2009; 109:727–<br />
736.<br />
57 Billeaud C, Guillet J, Sandler B. Gastric emptying in infants with or without<br />
gastro-oesophageal reflux according to the type of milk. Eur J Clin Nutr<br />
1990; 44:577–583.<br />
58 Van der Walt JH, Foate JA, Murrell D, et al. A study of preoperative fasting in<br />
infants aged less than three months. Anaesth Intensive Care 1990;<br />
18:527–531.<br />
59 Bricker SR, McLuckie A, Nightingale DA. Gastric aspirates after trauma in<br />
children. Anaesthesia 1989; 44:721–724.<br />
60 Green SM, Roback MG, Miner JR, et al. Fasting and emergency department<br />
procedural sedation and analgesia: a consensus-based clinical practice<br />
advisory. Ann Emerg Med 2007; 49:454–461.<br />
61 Green SM, Krauss B. Pulmonary aspiration risk during emergency<br />
department procedural sedation: an examination of the role of fasting and<br />
sedation depth [review]. Acad Emerg Med 2002; 9:35–42.<br />
62 Kearney R, Mack C, Entwistle L. Withholding oral fluids from children<br />
undergoing day surgery reduces vomiting. Paediatr Anaesth 1998; 8:331–<br />
336.<br />
63 Schreiner MS, Nicolson SC. Pediatric ambulatory anesthesia: NPO –<br />
before or after surgery? [review]. J Clin Anesth 1995; 7:589–596.<br />
64 Radke OC, Biedler A, Kolodzie K, et al. The effect of postoperative fasting<br />
on vomiting in children and their assessment of pain. Paediatr Anaesth<br />
2009; 19:494–499.<br />
65 Scrutton MJ, Metcalfe GA, Lowy C, et al. Eating in labour. A randomised<br />
controlled trial assessing the risks and benefits. Anaesthesia 1999;<br />
54:329–334.<br />
66 Kubli M, Scrutton MJ, Seed PT, O’Sullivan G. An evaluation of isotonic<br />
‘sport drinks’ during labor. Anesth Analg 2002; 94:404–408.<br />
67 O’Sullivan G, Liu B, Hart D, et al. Effect of food intake during labour on<br />
obstetric outcome: randomised controlled trial. BMJ 2009; 338:b784.<br />
68 Porter JS, Bonello E, Reynolds F. The influence of epidural administration of<br />
fentanyl infusion on gastric emptying in labour. Anaesthesia 1997;<br />
52:1151–1156.<br />
69 Wong CA, Loffredi M, Ganchiff JN, et al. Gastric emptying of water in term<br />
pregnancy. Anesthesiology 2002; 96:1395–1400.<br />
70 Mangesi L, Hofmeyr GJ. Early compared with delayed oral fluids and food<br />
after caesarean section [review]. Cochrane Database Syst Rev<br />
2002:CD003516.<br />
71 Orji EO, Olabode TO, Kuti O, Ogunniyi SO. A randomised controlled trial of<br />
early initiation of oral feeding after cesarean section. J Mater Fetal Neonatal<br />
Med 2009; 22:65–71.<br />
72 Mulayim B, Celik NY, Kaya S, Yanik FF. Early oral hydration after cesarean<br />
delivery performed under regional anesthesia. Int J Gynaecol Obstet 2008;<br />
101:273–276.<br />
73 Teoh WH, Shah MK, Mah CL. A randomised controlled trial on beneficial<br />
effects of early feeding post-Caesarean delivery under regional<br />
anaesthesia. Singapore Med J 2007; 48:152–157.<br />
74 Vanner RG, Goodman NW. Gastro-oesophageal reflux in pregnancy at<br />
term and after delivery. Anaesthesia 1989; 44:808–811.<br />
75 Murray FA, Erskine JP, Fielding J. Gastric secretion in pregnancy. J Obstet<br />
Gynaecol Br Empire 1957; 64:373–381.<br />
76 Davison JS, Davison MC, Hay DM. Gastric emptying time in late pregnancy<br />
and labour. J Obstet Gynaecol Br Commonw 1970; 77:37–41.<br />
European Journal of Anaesthesiology 2011, Vol 28 No 8<br />
Copyright © European Society of Anaesthesiology. Unauthorized reproduction of this article is prohibited.
Perioperative fasting in adults and children 569<br />
77 Nimmo WS, Wilson J, Prescott LF. Further studies of gastric emptying<br />
during labour. Anaesthesia 1977; 32:100–101.<br />
78 Nimmo WS, Wilson J, Prescott LF. Narcotic analgesics and delayed gastric<br />
emptying during labour. Lancet 1975; 1:890–893.<br />
79 Wright PM, Allen RW, Moore J, Donnelly JP. Gastric emptying during<br />
lumbar extradural analgesia in labour: effect of fentanyl supplementation. Br<br />
J Anaesth 1992; 68:248–251.<br />
80 Kelly MC, Carabine UA, Hill DA, Mirakhur RK. A comparison of the effect of<br />
intrathecal and extradural fentanyl on gastric emptying in laboring women.<br />
Anesth Analg 1997; 85:834–838.<br />
81 Wong CA, McCarthy RJ, Fitzgerald PC, et al. Gastric emptying of water in<br />
obese pregnant women at term. Anesth Analg 2007; 105:751–755.<br />
82 Lewis M, Crawford JS. Can one risk fasting the obstetric patient for less<br />
than 4 h? Br J Anaesth 1987; 59:312–314.<br />
83 Rocke DA, Murray WB, Rout CC, Gouws E. Relative risk analysis of factors<br />
associated with difficult intubation in obstetric anesthesia. Anesthesiology<br />
1992; 77:67–73.<br />
84 Dammann HG, Muller P, Simon B. Parenteral ranitidine: onset and duration<br />
of action. Br J Anaesth 1982; 54:1235–1236.<br />
85 Francis RN, Kwik RS. Oral ranitidine for prophylaxis against Mendelson’s<br />
syndrome. Anesth Analg 1982; 61:130–132.<br />
86 Maile CJ, Francis RN. Preoperative ranitidine. Effect of a single intravenous<br />
dose on pH and volume of gastric aspirate. Anaesthesia 1983; 38:324–<br />
326.<br />
87 Levack ID, Bowie RA, Braid DP, et al. Comparison of the effect of two dose<br />
schedules of oral omeprazole with oral ranitidine on gastric aspirate pH and<br />
volume in patients undergoing elective surgery. Br J Anaesth 1996;<br />
76:567–569.<br />
88 Yau G, Kan AF, Gin T, Oh TE. A comparison of omeprazole and ranitidine<br />
for prophylaxis against aspiration pneumonitis in emergency caesarean<br />
section. Anaesthesia 1992; 47:101–104.<br />
89 O’Sullivan G, Sear JW, Bullingham RE, Carrie LE. The effect of magnesium<br />
trisilicate mixture, metoclopramide and ranitidine on gastric pH, volume and<br />
serum gastrin. Anaesthesia 1985; 40:246–253.<br />
European Journal of Anaesthesiology 2011, Vol 28 No 8<br />
Copyright © European Society of Anaesthesiology. Unauthorized reproduction of this article is prohibited.
AAGBI SAFETY GUIDELINE<br />
Pre-operative Assessment and Patient Preparation<br />
The Role of the Anaesthetist<br />
2<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org January 2010
Membership of the working party<br />
(details correct at the start of the working party process)<br />
Dr R Verma<br />
Prof M Y K Wee<br />
Dr A Hartle<br />
Dr V R Alladi<br />
Dr A-M Rollin<br />
Dr G Meakin<br />
Dr R Struthers<br />
Dr J Carlisle<br />
Dr P Johnston<br />
Mrs K Rivett<br />
Mr C Hurley<br />
Chairman<br />
Vice President, AAGBI<br />
Council Member, AAGBI<br />
Council Member, AAGBI<br />
Vice President, Royal College of Anaesthetists<br />
President, Association of Paediatric Anaesthetists<br />
Consultant Anaesthetist, Derriford Hospital<br />
Preoperative Association representative<br />
Vice Chairman, GAT<br />
Patient Liaison Group representative<br />
Royal College of Nursing representative<br />
This guideline has been seen and approved by the Council of the<br />
AAGBI.<br />
The working party is grateful to Dr Helgi Johannsson for his contribution<br />
to this guideline.<br />
1
Contents<br />
1. Recommendations 3<br />
2. Introduction 5<br />
3. Before planned admission 7<br />
4. After planned admission 15<br />
5. After unplanned admission 18<br />
6. Children and young people 19<br />
7. Tests and investigations 22<br />
8. The patient’s perspective 24<br />
References 26<br />
Appendices 29<br />
To be reviewed by 2015.<br />
© Copyright of the Association of Anaesthetists of Great Britain & Ireland. No<br />
part of this book may be reproduced without the written permission of the<br />
AAGBI.<br />
2
1. Recommendations<br />
This guidance has been designed to help anaesthetists provide<br />
high quality pre-operative assessment services and patient<br />
preparation before surgery. In addition it defines the roles and<br />
responsibilities of anaesthetists both after planned and after<br />
unplanned admissions.<br />
Anaesthetists should assume a central role in the organisation<br />
of pre-operative services that encompass much more than<br />
preparing the delivery of anaesthesia.<br />
The anaesthetist has the skills necessary to assess, optimise and<br />
estimate risk and support patients deciding whether to proceed<br />
with surgery and anaesthesia.<br />
Pre-operative anaesthetic assessment should minimise risk for all<br />
patients as well as identify patients at particularly high risk.<br />
The pre-operative anaesthetic clinic should co-operate with<br />
primary care to achieve these aims.<br />
Skilled nurse practitioners are safe and cost-effective in<br />
preparing patients for anaesthesia and should work closely with<br />
anaesthetists with a special interest in pre-operative assessment<br />
and preparation.<br />
After scheduled admissions, anaesthetists must confirm that<br />
patients have been prepared adequately by pre-operative<br />
services so that anaesthesia and surgery can proceed safely.<br />
Tests performed before surgery should be limited to those<br />
recommended by national and local guidelines and protocols.<br />
Most anaesthetic departments should plan for one consultant<br />
whole-time equivalent to run and manage daily high-risk clinics<br />
with appropriate secretarial support.<br />
3
Anaesthetic departments must establish clear pathways of<br />
care for unplanned admissions with surgeons, emergency<br />
departments, critical care and theatre personnel.<br />
Special considerations must be given to children and young<br />
people undergoing anaesthesia and surgery.<br />
Operating sessions and the individual anaesthetist’s job plan<br />
must be arranged to allow time for the anaesthetist responsible<br />
for an individual’s care to visit him/her pre-operatively at an<br />
appropriate time before surgery.<br />
In all but exceptional circumstances this should take place in a<br />
designated reception area, dedicated clinic room or in the ward<br />
ensuring privacy and respecting patients’ dignity, and not in the<br />
anaesthetic room.<br />
Clinical Directors for anaesthesia and theatres should work with<br />
appropriate managers to establish comprehensive and integrated<br />
pre-operative assessment facilities and ensure that there is a lead<br />
anaesthetist for pre-operative assessment.<br />
4
2. Introduction<br />
Preparing a patient for anaesthesia requires an understanding of<br />
the patient’s pre-operative status, the nature of the surgery and<br />
the anaesthetic techniques required for surgery, as well as the<br />
risks that a particular patient may face during this time.<br />
Anaesthetists are in the unique position that they can offer all<br />
of these skills, and the ultimate responsibility for pre-operative<br />
anaesthetic assessment lies with the anaesthetist. Therefore,<br />
anaesthetists should take the lead in organising pre-operative<br />
anaesthetic services.<br />
Patients often have comorbidities that require careful assessment<br />
and co-ordination. Preparation for surgery may take weeks<br />
to achieve, and could therefore potentially cause delay and<br />
cancellation of surgery if not done adequately.<br />
Pre-operative anaesthetic assessment services decrease<br />
cancellations on the day of surgery, improve the patient’s<br />
experience of their hospital admission, and may reduce<br />
complication rates and mortality. The pre-operative visit may<br />
relieve anxiety and answer questions about both the anaesthetic<br />
and surgical processes [1].<br />
Effective communication and a team approach are vital in<br />
the pre-operative period. Complications and malpractice<br />
lawsuits are often attributable to poor preparation and failures<br />
in communication [2]. Essential team members include<br />
anaesthetists, surgeons, physicians and general practitioners.<br />
Specialist anaesthetic pre-operative assessment nurses have<br />
been shown to be safe and effective at pre-operative screening<br />
and should be an integral part of the team [3].<br />
5
The lead anaesthetist for pre-operative assessment and<br />
evaluation should be given the responsibility to:<br />
• Agree and co-ordinate policies and procedures with surgical<br />
and anaesthetic departments.<br />
• Liaise with the lead pre-operative assessment nurse to<br />
establish a comprehensive service with appropriate input<br />
from anaesthetists.<br />
• Ensure with the lead pre-operative assessment nurse that the<br />
pre-operative service nurses receive adequate education<br />
and training to deliver this service safely.<br />
• Ensure that the design of the service delivers a maximum of<br />
18 weeks referral to treatment time (RTT) or less if locally<br />
agreed.<br />
• Ensure that Foundation and Speciality Doctors are able to<br />
acquire the knowledge and competencies required to assess<br />
and prepare a patient for surgery.<br />
Due consideration should be given to vulnerable groups of<br />
patients, (e.g. patients with learning disabilities or severe<br />
physical handicap) who may require a greater degree of support<br />
from family, carers and healthcare personnel.<br />
6
3. Before planned admission<br />
Pre-operative services should:<br />
• Ensure every patient* is fully informed about their proposed<br />
procedure and the interventions that will need to be<br />
undertaken.<br />
• Estimate the level of risk for every patient.<br />
• Ensure every patient* understands their own individual risk<br />
so that they can make an informed decision about whether<br />
to proceed to surgery.<br />
• Identify co-existing medical illnesses and optimally prepare<br />
patients whilst taking into account the urgency of the<br />
operation.<br />
• Identify patients with a high risk of complications in the<br />
peri-operative period and define the appropriate postoperative<br />
level of care (day stay, inpatient, ward, HDU,<br />
critical care).<br />
• Plan discharge.<br />
The visit to the pre-operative clinic also gives the patients an<br />
opportunity to discuss the choices of anaesthetic technique,<br />
methods for pain relief and the risks, in a calmer atmosphere<br />
than immediately before the operation.<br />
Senior anaesthetists with a special interest in pre-operative<br />
assessment are ideally suited to this role.<br />
There are several models available for the pre-operative<br />
anaesthetic assessment clinic, most of which rely both on<br />
anaesthetists and specialist nurses. All hospitals should aim<br />
to provide appropriately staffed clinics. The number of clinics<br />
required will depend on the size and throughput of the<br />
individual trust.<br />
* This assumes that all patients have the capacity to take in the information<br />
provided and make an autonomous decision. For those who do not, attempts<br />
must be made to provide appropriate information and readers are referred to<br />
other guidance on consent issued by the AAGBI and GMC.<br />
7
Pre-operative systems and communication<br />
Recognising that at least 80% of patients could be treated as<br />
day cases (
Pathologies that predictably progress from medical to surgical<br />
treatment, such as aortic aneurysmal disease and osteoarthrosis,<br />
would be particularly suitable for early attempts at optimising<br />
health.<br />
Shortened waits between GP referral and surgery have<br />
decreased the time in which to prepare patients for surgery.<br />
Surgical investigation and pre-operative preparation should<br />
therefore take place in parallel. Early referral by primary care<br />
and surgical teams for pre-operative management will increase<br />
efficiency.<br />
Nurse-led pre-operative assessment<br />
Pre-operative anaesthetic assessment is an extended role for<br />
nurses that has been shown to be safe and cost effective [3-<br />
5]. These nurses usually work as an integral part of the preoperative<br />
team and are a very important link between the<br />
patient and the entire peri-operative team. Physician Assistants<br />
(Anaesthetics) – PA(A) – may also have a role to play.<br />
Nurses should work closely with the anaesthetists involved in<br />
the service and have good communication skills and links with<br />
the rest of the hospital.<br />
Their purpose is to contribute to the pre-operative preparation of<br />
all patients, to identify patients with a high peri-operative risk, to<br />
institute investigations and to refer to the anaesthetist, as well as<br />
to assess patients for suitability for day surgery. In addition, they<br />
will implement the various pre-operative protocols, including<br />
fasting and administration of regular medication, and are able to<br />
answer many of the patient’s questions about their anaesthetic.<br />
Current fasting guidelines are given in Appendix 1.<br />
Protocols should empower the nurses to refer patients to<br />
relevant services such as echocardiography when there is a<br />
9
history of a heart murmur, or pulmonary function tests for chest<br />
disease. These protocols should be written by senior anaesthetic<br />
staff and should be regularly reviewed and updated.<br />
In-clinic spirometry is useful and easy to perform, and may<br />
decrease the number of patients referred for formal pulmonary<br />
function tests.<br />
Pre-operative assessment nurses should co-operate closely<br />
with primary care services, particularly when administration<br />
of specific medication is required, such as subcutaneous<br />
anticoagulation or optimisation of diabetic treatment.<br />
Liaison with secondary care diabetes teams and medical<br />
outreach teams can be particularly helpful and may prevent<br />
unnecessarily long stays in hospitals, both pre- and postoperatively.<br />
It is important that pre-operative assessment nurses have<br />
readily available communication channels with pre-operative<br />
assessment anaesthetists; they should be able to discuss specific<br />
cases and receive feedback from the anaesthetist.<br />
The anaesthetist in the pre-operative<br />
assessment clinic<br />
Senior anaesthetists with a specialist interest in pre-operative<br />
assessment and optimisation should staff pre-operative<br />
assessment clinics with the number of sessions needed being<br />
dependent on the throughput of the hospital and its casemix.<br />
These anaesthetists should see all patients who are potentially at<br />
high risk, make an assessment of the risks and benefits of surgery<br />
and ensure that patients:<br />
• Are confident that they want surgery.<br />
10
• Have balanced the pros and cons of different surgical and<br />
non-surgical alternatives.<br />
• Are receiving optimum treatment if they have significant<br />
medical co-morbities.<br />
• Have had their risks assessed with regard to mortality and<br />
common morbidities.<br />
• Have been informed of these risks and had the opportunity<br />
to discuss them.<br />
• Have been informed how to reduce their risks preoperatively.<br />
• Have been given the opportunity and time to reduce their<br />
risks.<br />
The pre-operative assessment anaesthetist therefore needs<br />
to be skilled at assessing and managing these risks, and in<br />
communicating them both to the patient and to the treating<br />
surgeon [6].<br />
Consultant-to-consultant communication between anaesthetists,<br />
surgeons and critical care physicians is essential, particularly<br />
when the patient is high-risk and the benefits of surgery may<br />
be outweighed by the risks to the patient. Pre-operative<br />
anaesthetists should be able to accept referrals from all<br />
appropriate staff, including GPs, surgeons, pre-operative nurses<br />
and specialist screening clinics.<br />
Multidisciplinary meetings should help anaesthetic consultants<br />
identify and manage high-risk cases, particularly when major<br />
surgery is planned.<br />
Estimating and managing peri-operative risk<br />
Survival and risk in many populations is predictable. Risk<br />
prediction can be used to guide the patient’s pre-operative care<br />
and determine whether the patient needs to see an anaesthetist<br />
in the pre-operative assessment clinic.<br />
11
Anaesthetic, critical care and surgical departments should<br />
discuss risk thresholds for:<br />
• Referral by a pre-operative assessment nurse to an<br />
anaesthetist.<br />
• Pre-operative exercise and drug prescriptions.<br />
• Multidisciplinary team meetings.<br />
• Invasive intra-operative monitoring.<br />
• Post-operative critical care admission and outreach<br />
observation.<br />
These thresholds can be used as markers to help hospitals<br />
determine the level of resources they need to invest to provide<br />
their catchment patient population with adequate pre-operative<br />
services.<br />
A combination of nine variables provide independent prognostic<br />
information:<br />
i. Age<br />
ii. Sex<br />
iii. Socioeconomic status [7]<br />
iv. Aerobic fitness [8-10]<br />
v. Diagnosed ischaemic heart disease (myocardial infarction<br />
and angina)<br />
vi. Diagnosed heart failure<br />
vii. Diagnosed ischaemic brain disease (stroke and transient<br />
ischaemic attacks)<br />
viii. Diagnosed kidney failure [11]<br />
ix. Diagnosed peripheral arterial disease<br />
Pre-operative and post-operative risks of mortality and morbidity<br />
can be estimated with these variables when adjusted for surgical<br />
disease and surgical procedures respectively (see Appendix 2).<br />
Aerobic fitness when measured objectively is an important<br />
12
tool for survival prediction in addition to traditional risk factors<br />
such as hypertension, hypercholesterolaemia, smoking, chronic<br />
obstructive pulmonary disease (COPD) and diabetes [8-10].<br />
In the pre-operative assessment clinic, aerobic fitness can<br />
be estimated with the incremental shuttle walk test or more<br />
precisely quantified with cardiopulmonary exercise testing (CPX/<br />
CPET), which can also diagnose whether aerobic performance is<br />
limited by pulmonary, cardiac or peripheral disease, and may be<br />
a good screening test for ischaemic heart disease [12].<br />
Resources and funding<br />
Setting up pre-operative services where none exist requires<br />
a substantial time commitment in order to put in place the<br />
infrastructure, to recruit staff and to oversee the organisation,<br />
administration and processes at all levels. This may well require<br />
in the region of 5-10 programmed activities per week but this<br />
may vary with the caseload and casemix of the organisation,<br />
and will require the appropriate level of administrative support.<br />
A time commitment is necessary for the lead anaesthetist<br />
adequately to manage the pre-operative service. This role<br />
includes liaison with surgeons, clinicians in other specialties,<br />
doctors in training, primary care, other anaesthetists, theatres<br />
and critical care.<br />
The proportion of patients who would benefit from consultant<br />
pre-operative assessment depends on the type of surgery<br />
undertaken at the hospital, the age and socioeconomic status<br />
of the population and the size of catchment area. Currently,<br />
an average district general hospital might expect to commit<br />
7.5 programmed consultant activities per week to provide one<br />
anaesthetist-led clinic per day (five clinics per week).<br />
The pre-operative assessment clinic provides valuable<br />
opportunities for teaching – of both undergraduate and<br />
13
postgraduate personnel. This may necessitate increased clinic<br />
resources with regard to both the time taken and the space for<br />
trainees and students to see patients.<br />
Cardiopulmonary exercise testing, when undertaken by trained<br />
personnel, takes about 30 minutes to perform and a similar time<br />
to discuss the results with the patient. A specialist anaesthetist<br />
working with a technician should be able to assess between four<br />
and seven patients in a programmed clinical activity.<br />
14
4. After planned admission<br />
Anaesthetists are central to ensuring the safety of patients in the<br />
peri-operative period.<br />
Operating sessions must be planned to allow time for the<br />
anaesthetist responsible for an individual’s care to visit him/<br />
her pre-operatively. This should take place before arrival in the<br />
anaesthetic room in all but exceptional circumstances.<br />
It is the responsibility of the individual anaesthetist giving<br />
the anaesthetic to ensure that the pre-operative assessment is<br />
adequate and that the patient has sufficient information to make<br />
a reasoned decision. It is the responsibility of the Trust to ensure<br />
that sufficient time is made available for this, as a matter of<br />
routine and without undue pressure. Pre-operative anaesthetic<br />
assessment is an integral part of the surgical process, and must<br />
be included in the estimates of time required for the operating<br />
list.<br />
The pre-operative assessment process should have identified<br />
and addressed problems with individual patients, and provided<br />
the patient with appropriate information on the probable perioperative<br />
course. This should allow the pre-operative visit to<br />
focus on the individual patient's needs and concerns.<br />
As a part of the pre-operative visit the anaesthetist should:<br />
• Establish a rapport with the patient and when relevant the<br />
patient’s family.<br />
• Determine the adequacy of pre-operative assessment and<br />
preparation, including arrangements for intra-operative and<br />
postoperative care.<br />
• Confirm the plan and discuss anaesthetic and postoperative<br />
care, including premedication, mode of anaesthesia,<br />
analgesia and anti-emetics.<br />
15
• Ensure the patient is aware of any risks particular to that<br />
patient or associated with specific anaesthetic procedures.<br />
• Ensure the patient understands the nature of the operation<br />
and is happy to proceed (N.B. see footnote on page 7).<br />
• Confirm the availability of HDU or intensive care unit beds<br />
if appropriate, before proceeding.<br />
Anaesthetists in training and non-consultant grades should<br />
discuss high-risk patients with consultant colleagues. The<br />
consultant contacted should ensure that the patient is cared for<br />
by an anaesthetist with the expertise required for that particular<br />
situation. Failure of the pre-operative service to match personnel<br />
to the need of the patient may result in surgery being postponed<br />
until the necessary expertise is available.<br />
Cancellations have a negative impact on patients, families and<br />
clinical services. Where possible, department protocols should<br />
be adhered to and cancellations for idiosyncratic reasons<br />
discouraged.<br />
Occasionally, anaesthetists will cancel surgery in patients who<br />
have been assessed and prepared by another senior anaesthetist.<br />
Anaesthetists should alert their colleagues if there is a failure in<br />
following protocol or when the protocol has been ineffective.<br />
Differences of opinion should be discussed within a department<br />
with the aim of avoiding future cancellations, and protocols<br />
modified accordingly.<br />
If surgery is cancelled the anaesthetist should:<br />
• Explain the reasons for cancellation and ensure that the<br />
patient and his/her family understand what will happen<br />
next.<br />
• Explain the cancellation to the surgical and pre-operative<br />
assessment teams, and primary care where appropriate.<br />
• Clearly document the reason for cancellation and any<br />
16
ecommendations for optimisation in the patient’s medical<br />
notes.<br />
• Take steps to allow surgery to proceed safely at a future<br />
date.<br />
• Address deficiencies in the system to reduce the number of<br />
late cancellations.<br />
17
5. After unplanned admission<br />
Patients requiring anaesthesia after unplanned admission are at<br />
higher risk of medical errors and peri-operative complications<br />
[13]. These patients are often cared for by junior staff.<br />
The standards and principles for the care of elective patients<br />
apply equally to those admitted in an emergency, even though<br />
it is often more difficult to achieve them. Clear pathways of care<br />
for unplanned admissions are vital and should include surgeons,<br />
emergency departments and theatre departments. The purpose<br />
of these pathways should be to enable a high standard of care,<br />
avoid omissions and prevent excessive periods of starvation and<br />
fluid deprivation – particularly in vulnerable groups such as the<br />
elderly.<br />
There must be clear communication between surgeons,<br />
anaesthetists and intensivists with the common goal being the<br />
welfare and best interests of the patient. Often a balance has<br />
to be reached between prevention of deterioration caused<br />
by delaying surgery and the benefit of optimising medical<br />
conditions pre-operatively. Where possible, patients and/or<br />
their next of kin should be included in these discussions. The<br />
risks and benefits of surgery should be explained clearly. These<br />
discussions should be documented clearly in the patient’s<br />
medical notes, particularly when a decision has been made:<br />
• To proceed with anaesthesia when potentially important<br />
investigations have been omitted or when the patient’s<br />
condition has not been optimised.<br />
• Not to proceed with surgery when there is correctable<br />
surgical disease.<br />
High standards of care must be maintained and the patient’s<br />
safety and best interests remain paramount.<br />
18
6. Children and young people<br />
Children and young people have special healthcare needs<br />
because they are physically and emotionally different from<br />
adults, and need the constant care and support of their parents<br />
or guardians [14].<br />
Children should receive care that is integrated and co-ordinated<br />
around their particular needs and the needs of the family. At<br />
least 90% of surgery in children can be performed on a day stay<br />
basis.<br />
They, and their parents, should be treated with respect,<br />
and given the necessary support and information to enable<br />
them to understand and cope with the proposed surgery and<br />
anaesthesia. They should be treated as active partners in<br />
decisions about their health and care, and, where possible, be<br />
able to exercise choice [15].<br />
Before admission<br />
A clear explanation of the proposed surgery and admission<br />
procedures should be given to the parents and the child at the<br />
initial outpatient clinic visit.<br />
Parents and children should be supplied with suitable written<br />
information regarding the proposed surgery and anaesthesia as<br />
well as instructions on what and when the child may eat and<br />
drink before surgery. Such instructions should conform to recent<br />
guidelines [16] (Appendix 1).<br />
Pre-admission care may include attendance at a pre-operative<br />
assessment clinic and/or a pre-admission tour of the hospital.<br />
The pre-operative assessment should include a complete birth<br />
history including the duration of gestation, any difficulties at<br />
19
delivery and the presence of congenital and acquired disease<br />
particularly those affecting the airway or the cardiovascular<br />
system. A history of previous anaesthetics and family history of<br />
anaesthetic problems should be obtained. Sickle-cell screening<br />
should be performed in susceptible populations. The airway<br />
should be assessed and the presence of any loose, usually<br />
deciduous, teeth noted.<br />
Telephone contact on the day before surgery provides an<br />
opportunity to confirm attendance, re-enforce pre-operative<br />
instructions and detect reasons for late cancellation such as<br />
infections or family problems.<br />
After admission<br />
The child should be admitted to a children’s ward or the day<br />
surgery unit staffed by medical and nursing staff trained in<br />
dealing with children and their families. The décor should<br />
be suitable for children, and toys, books, videos and a play<br />
therapist should be available.<br />
Children should not be cared for next to adults and, where<br />
possible, there should also be separate facilities for adolescents<br />
[17].<br />
The law on consent in minors varies across the UK. In England<br />
and Wales, parental consent is usually sought for operations<br />
on a child aged less than 16 years, although the child him/<br />
herself has the right to consent if he/she have achieved sufficient<br />
understanding and intelligence to understand fully what is<br />
proposed, i.e. they are ‘Gillick competent’. However, in cases<br />
in which a child has refused or resisted medical treatment, the<br />
courts have upheld the right of the parents to consent for the<br />
treatment.<br />
In Scotland, parents cannot overturn the decision of a<br />
20
competent minor to refuse treatment. In such cases, much will<br />
depend on the judgement of the doctor as to whether the child<br />
is competent or not, taking into account the importance or<br />
urgency of the proposed operation. In all cases it is important<br />
that staff know who has parental responsibility [18].<br />
The anaesthetist should see the parents and child before<br />
surgery to confirm/perform pre-operative assessment, establish<br />
a rapport, check compliance with guidelines on eating and<br />
drinking, discuss anaesthetic techniques and postoperative pain<br />
relief, and obtain verbal consents, e.g. for nerve blocks and<br />
suppositories.<br />
• All children should be weighed and have their pulse rate<br />
and temperature recorded on admission.<br />
• All communication should be comprehensible to the<br />
parents and the child.<br />
• The possible modes of induction (intravenous/inhalation)<br />
should be discussed and the wishes of the parents and child<br />
complied with where possible.<br />
• If intravenous induction is planned, local analgesic cream<br />
or gel should be applied to possible venepuncture sites in<br />
all but extreme emergencies.<br />
• Selected children may benefit from oral sedative<br />
premedication. This must be carefully timed, and efficient<br />
communication between the theatre team and the ward is<br />
vital.<br />
• Children should be allowed to wear suitable clothing of<br />
their own to theatre.<br />
• Parents should be invited to accompany the child at<br />
induction of anaesthesia and his/her role in the induction<br />
room discussed.<br />
• A ward nurse should be present at induction to escort the<br />
parent back to the ward.<br />
• A parent should be called to the recovery room as soon as<br />
the child is conscious.<br />
21
7. Tests and investigations<br />
Routine pre-operative investigations are expensive, labourintensive<br />
and of questionable value, especially as they may<br />
contribute to morbidity or cause additional delays due to<br />
spurious results.<br />
The National Institute of Healthcare and Clinical Excellence<br />
(NICE) recommends the following pre-operative tests (surgical<br />
severity scores are given in Appendix 3) [19]:<br />
• Electrocardiography: if older than 80; if older than 60 and<br />
surgical severity at ≥ 3; any cardiovascular disease; severe<br />
renal disease.<br />
• Full blood count: if older than 60 and surgical severity<br />
≥ grade 2; all adults if surgical severity ≥ grade 3; severe<br />
renal disease.<br />
• Urea, electrolytes and creatinine: if older than 60 and<br />
surgical severity ≥ grade 3; all adults if surgical severity<br />
grade 4; any renal disease; severe cardiovascular disease.<br />
• Pregnancy test for women who may be pregnant.<br />
• Sickle-cell test on families with homozygous disease or<br />
heterozygous trait; ancestry that is African, Afro-Caribbean,<br />
Asian, Middle-Eastern, east-Mediterranean.<br />
• Chest X-ray: patients scheduled for critical care.<br />
History and examination performed by appropriately trained<br />
and competent personnel remains the most efficient and<br />
accurate way of initially detecting significant morbidity. There<br />
is recent evidence that patients of any age with no major<br />
comorbidities (ASA physical status 1 or 2 – see Appendix<br />
4) presenting for day surgery do not need pre-operative<br />
investigations [20].<br />
Local departmental protocols should determine which<br />
additional tests should be used based upon patient age,<br />
22
comorbidity and complexity of the surgery.<br />
Anaemia ( < 12 g.dl -1 for women and < 13 g.dl -1 for men<br />
should be investigated and treated before planned surgery,<br />
using haematinics such as oral/intravenous iron rather than<br />
transfusion. The urgency and nature of surgery, plus patientspecific<br />
factors, will determine the balance between reversing<br />
anaemia and proceding with surgery. The aim, to avoid perioperative<br />
blood transfusion, is best achieved when hospital<br />
pre-operative services work with other departments and primary<br />
care.<br />
Evaluation of high-risk patients should estimate cardiovascular<br />
risk according to the severity of systemic disease (see Appendix<br />
5), functional capacity and the grade of the planned surgery<br />
[21].<br />
Tests of functional capacity include exercise ECG, CPX testing<br />
and myocardial perfusion scans.<br />
23
8. The patient’s perspective<br />
This document defines the objectives of pre-operative<br />
assessment, emphasising the need to:<br />
• Support all patients as they prepare themselves for surgery.<br />
• Identify important high-risk patients and promote safety.<br />
• Reduce the risk to the patient and optimise the patient’s<br />
condition pre-operatively.<br />
• Identify and mitigate potential anaesthetic difficulties.<br />
• Allay fear, anxiety and lack of understanding through clear<br />
explanation, written information and appropriate discussion.<br />
Many patients, however, will not see an anaesthetist before<br />
admission as they will have been adequately assessed by skilled<br />
practitioners using established protocols. Anaesthetists must<br />
therefore ensure that the information provided not only allows<br />
for efficiency on the day of admission but also addresses any of<br />
the patient’s concerns previously noted. If these concerns are<br />
not adequately dealt with by the practitioner, the patient should<br />
have access to a consultation with an anaesthetist before the<br />
day of operation.<br />
Both assessment before admission and the pre-operative visit<br />
allow patients to:<br />
• Discuss their peri-operative care.<br />
• Ask questions and discuss their fears and anxieties,<br />
particularly about previous anaesthetic experiences.<br />
Communication must be clear, with consistent messages given<br />
to the patient regarding choices for anaesthesia, post-operative<br />
analgesia, prevention and treatment of nausea and vomiting,<br />
pre-operative starvation and any other concerns raised by the<br />
patient.<br />
24
It is extremely important that adequate explanation is given<br />
by anaesthetists and other staff should it become necessary to<br />
postpone surgery. In addition to the impact on the patient’s<br />
medical condition, it is likely to cause considerable disruption<br />
to both their work and their home life.<br />
Information specifically targeted for patients is also available<br />
in the patient information section of the Royal College of<br />
Anaesthetists website (http://www.rcoa.ac.uk)<br />
The prospect of anaesthesia remains daunting for many people.<br />
Given the time constraints of ‘same-day’ admission it may be<br />
difficult for the patients to receive the level of consultation that<br />
would be considered ideal. However, the opportunity to talk to<br />
a doctor who fully understands their needs may ensure a more<br />
confident and co-operative relationship between the patient and<br />
the doctor.<br />
25
References<br />
1. NHS Institute for Innovation and Improvement. Quality and<br />
Service Improvement Tools. http://wwwnodelaysachiever.<br />
nhs.uk/ServiceImprovement/Tools/IT130_PreOpAssessment.<br />
htm (accessed 01/10/09)<br />
2. Greenberg CC, Regenbogen SE, Studdert DM, et al.<br />
Patterns of communication breakdowns resulting in injury<br />
to surgical patients. Journal of the American College of<br />
Surgeons 2007; 204: 533-40.<br />
3. Rushforth H, Burge D, Mullee M, et al. Nurse-led paediatric<br />
pre-operative assessment: an equivalence study. Paediatric<br />
Nursing 2006; 18: 23-9.<br />
4. Rai M, Pandit J. Day of surgery cancellations after nurse-led<br />
pre-assessment in an elective surgical centre: the first 2<br />
years. Anaesthesia 2003; 58: 685-7.<br />
5. Kinley H, Czoski-Murray C, George S, et al. Effectiveness<br />
of appropriately trained nurses in pre-operative assessment:<br />
randomised controlled equivalence/non-inferiority trial.<br />
British Medical Journal 2002; 325: 1323.<br />
6. Geigerenzer G. Reckoning with risk: Learning to live with<br />
uncertainty. London: Penguin, 2003.<br />
7. Alter D, Chong A, Austin P, et al. Socioeconomic status and<br />
mortality after acute myocardial infarction. Annals of<br />
Internal Medicine 2006; 144: 82-93.<br />
8. Win T, Jackson A, Sharples L, et al. Cardiopulmonary<br />
exercise tests and lung cancer surgical outcome. Chest<br />
2005; 127: 1159-65.<br />
26
9. Older P, Hall A, Hader R. Cardiopulmonary exercise testing<br />
as a screening test for perioperative management of major<br />
surgery in the elderly. Chest 1999; 116: 355-62.<br />
10. Carlisle J, Swart M. Mid-term survival after abdominal<br />
aortic aneurysm surgery predicted by cardiopulmonary<br />
exercise testing. British Journal of Surgery 2007; 94: 966-9.<br />
11. Lee TH, Marcantonio ER, Mangione CM, et al. Derivation<br />
and prospective validation of a simple index for prediction<br />
of cardiac risk of major noncardiac surgery. Circulation<br />
1999; 100: 1043-9.<br />
12. Chaudhry S, Arena R, Wasserman K, Hansen JE, Lewis<br />
GD, Myers J, Chronos N, Boden WE. Exercise-induced<br />
myocardial ischemia detected by cardiopulmonary<br />
exercise testing. American Journal of Cardiology 2009; 103:<br />
615-9.<br />
13. Gawande AA, Studdert DM, Orav EJ, Brennan TA, Zinner<br />
MJ. Risk factors for retained instruments and sponges after<br />
surgery. New England Journal of Medicine 2003; 348: 229-<br />
53.<br />
14. The Audit Commission Report. Children first: a study of<br />
hospital services. London: HMSO, 1993.<br />
15. Department of Health. Getting the right start: the national<br />
service framework for children, young people and maternity<br />
services - standard for hospital services. London: HMSO,<br />
2003.<br />
16. Royal College of Nursing. Perioperative fasting in adults<br />
and children. An RCN guideline for the multidisciplinary<br />
team. London: RCN, 2005.<br />
27
17. Hogg C, Cooper C. Meeting the needs of children and<br />
young people undergoing surgery. London: Action for Sick<br />
Children, 2004.<br />
18. British Medical Association. Consent, rights, and choices<br />
in health care for children and young people. London: BMJ<br />
Publishing, 2000.<br />
19. National Institute for Clinical Excellence. Pre-operative<br />
tests, the use of routine pre-operative tests for elective<br />
surgery. London: NICE, 2003.<br />
20. Chung F, Yuan H, Yin L, Vairavanathan S, Wong DT.<br />
Elimination of preoperative testing in ambulatory surgery.<br />
Anesthesia and Analgesia 2009; 108: 467-75.<br />
21. Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007<br />
Guidelines on perioperative cardiovascular evaluation and<br />
care for noncardiac surgery. Journal of the American<br />
College of Cardiology 2007; 50: 1707-32.<br />
28
Appendices<br />
1. Fasting guidelines in adults and children<br />
2. Survival prediction<br />
3. Surgical severity<br />
4. ASA physical status<br />
5. Systemic disease<br />
29
Appendix 1<br />
Fasting guidelines for adults and children<br />
(RCN pre-operative fasting guidelines, 2005)<br />
Adults<br />
Pre-operative fasting in adults undergoing elective surgery – ‘the<br />
2-6 rule’:<br />
• ‘2’ – Intake of water up to 2 h before induction of<br />
anaesthesia.<br />
• ‘6’ – A minimum pre-operative fasting time of 6 h for food<br />
(solids, milk and milk-containing drinks).<br />
• The anaesthetic team should consider further interventions<br />
for patients at higher risk of regurgitation and aspiration.<br />
Post-operative resumption of oral intake in healthy adults:<br />
• Patients should be encouraged to drink when ready,<br />
providing there are no contraindications.<br />
Children<br />
Pre-operative fasting in children undergoing elective surgery –<br />
‘the 2-4-6 rule’:<br />
• ‘2’ – Intake of water and other clear fluid up to 2 h before<br />
induction of anaesthesia.<br />
• ‘4’ – Breast milk up to 4 h before.<br />
• ‘6’ – Formula milk, cow’s milk or solids up to 6 h before.<br />
• The anaesthetic team should consider further interventions<br />
for children at higher risk of regurgitation and aspiration.<br />
30
Post-operative resumption of oral intake in healthly children:<br />
• Oral fluids can be offered to healthly children when they<br />
are fully awake following anaesthesia, providing there are<br />
no contraindications. There is no requirement to drink as<br />
part of the discharge criteria.<br />
Chewing gum<br />
Chewing gum may be allowed up to 2 h before induction of<br />
anaesthesia.*<br />
* This is AAGBI guidance and is not taken from the RCN fasting guidelines.<br />
31
Appendix 2<br />
Survival prediction<br />
Age. The risk of dying doubles every 7 years from the age of<br />
10 so that by 90 years the monthly mortality risk is 5000 times<br />
the risk at the age of 10. Life tables for the United Kingdom,<br />
its constituent countries and individual health authorities are<br />
updated at www.gad.gov.uk<br />
Sex. Men are 1.7 times more likely to die than women the<br />
same age.<br />
Socioeconomic status. The impoverished are twice as likely<br />
to die as the rich.<br />
Aerobic fitness. The predicted peak power in metabolic<br />
equivalents (METs), where 1 MET requires an oxygen<br />
consumption of 3.5 ml.kg -1 .min -1 ;<br />
a) For men 18.4 – (0.16 x age)<br />
b) For women 14.7 – (0.13 x age)<br />
Mortality risk is multiplied by 1.2 for every MET short of<br />
predicted, or by 0.84 for every MET in excess of predicted.<br />
Diagnoses of myocardial infarction, heart failure, stroke,<br />
peripheral arterial disease and renal failure ([creatinine] ><br />
150 µmol.l -1 ) independently multiply long-term mortality risk by<br />
1.5 times. Diagnoses of angina and transient ischaemic cerebral<br />
events multiply risk by 1.2 times (in the absence of MI or stroke<br />
respectively).<br />
Please email john.carlisle@nhs.net for a more detailed and<br />
referenced version including Excel spreadsheets that calculate<br />
individual risk.<br />
32
Appendix 3<br />
Surgical severity (from NICE pre-operative<br />
testing)<br />
Grade 1 examples: diagnostic endoscopy or laparoscopy,<br />
breast biopsy.<br />
Grade 2 examples: inguinal hernia, varicose veins,<br />
adenotonsillectomy, knee arthroscopy.<br />
Grade 3 examples: total abdominal hysterectomy, TURP,<br />
lumbar discectomy, thyroidectomy.<br />
Grade 4 examples: total joint replacement, artery<br />
reconstruction, colonic resection; radical<br />
neck dissection.<br />
33
Appendix 4<br />
ASA physical status<br />
ASA grade 1 A normal healthy patient: i.e. without any<br />
clinically important comorbidity and without a<br />
clinically significant past/present medical history.<br />
ASA grade 2: A patient with mild systemic disease.<br />
ASA grade 3: A patient with severe systemic disease.<br />
ASA grade 4: A patient with severe systemic disease that is a<br />
constant threat to life.<br />
ASA grade 5: A moribund patient who is not expected to<br />
survive without the operation.<br />
ASA grade 6: A declared brain-dead patient whose organs are<br />
being removed for donor purposes.<br />
Adapted from: http://www.asahq.org/clinical/physicalstatus.htm<br />
34
Appendix 5<br />
Systemic disease (from NICE pre-operative<br />
testing)<br />
Cardiovascular disease: ‘mild’<br />
• Mild angina pectoris (no/slight limitation of ordinary<br />
activity, e.g. > 1 flight of stairs).<br />
• Myocardial infarction > 1 month ago (including Q waves on<br />
12 lead ECG).<br />
• Compensated heart failure (no/slight limitation of activity,<br />
comfortable at rest).<br />
Cardiovascular disease: ‘severe’<br />
• Severe or unstable angina pectoris (marked limitation of<br />
ordinary activity).<br />
• Myocardial infarction < 1 month ago.<br />
• Decompensated heart failure (marked limitation of ordinary<br />
activity or symptoms at rest).<br />
• Severe valvular disease (exercise-induced syncope, angina,<br />
dyspnoea, orthopnoea, fatigue, palpitations).<br />
Renal disease: ‘severe’<br />
• Creatinine > 150 µmol.l -1<br />
35
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
Regional Anaesthesia and Patients<br />
with Abnormalities of Coagulation<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
The Obstetric Anaesthetists’ Association<br />
Regional Anaesthesia UK<br />
November 2013
This guideline was originally published in Anaesthesia. If you wish to refer to this<br />
guideline, please use the following reference:<br />
Association of Anaesthetists of Great Britain and Ireland, Obstetric Anaesthetists’<br />
Association and Regional Anaesthesia UK. Regional anaesthesia and patients<br />
with abnormalities of coagulation. Anaesthesia 2013; 68: pages 966-72. This can<br />
be viewed online via the following URL:<br />
http://onlinelibrary.wiley.com/doi/10.1111/anae.12359/abstract
Guidelines<br />
Regional anaesthesia and patients with<br />
abnormalities of coagulation<br />
The Association of Anaesthetists of Great Britain<br />
& Ireland<br />
The Obstetric Anaesthetists Association<br />
Regional Anaesthesia UK<br />
Membership of the Working Party: W. Harrop-Griffiths,<br />
T. Cook, 1 H. Gill, D. Hill, 2 M. Ingram, M. Makris, S. Malhotra,<br />
B. Nicholls, 3 M. Popat, H. Swales 2 and P. Wood<br />
1 Royal College of Anaesthetists<br />
2 Obstetric Anaesthetists’ Association<br />
3 Regional Anaesthesia UK<br />
Summary<br />
Concise guidelines are presented that relate abnormalities of coagulation,<br />
whether the result of the administration of drugs or that of pathological<br />
processes, to the consequent haemorrhagic risks associated<br />
with neuraxial and peripheral nerve blocks. The advice presented is<br />
based on published guidelines and on the known properties of anticoagulant<br />
drugs. Four separate Tables address risks associated with<br />
anticoagulant drugs, neuraxial and peripheral nerve blocks, obstetric<br />
anaesthesia and special circumstances such as trauma, sepsis and massive<br />
transfusion.<br />
© 2013 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of<br />
The Association of Anaesthetists of Great Britain and Ireland.<br />
This is an open access article under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs License,<br />
which permits use and distribution in any medium, provided the original work is properly cited, the use is non-commercial<br />
and no modifications or adaptations are made.<br />
1
Anaesthesia 2013 W. Harrop-Griffiths et al. | Guidelines: patients with abnormalities of coagulation<br />
....................................................................................................<br />
This is a consensus document produced by expert members of a Working<br />
Party established by the Association of Anaesthetists of Great Britain &<br />
Ireland, the Obstetric Anaesthetists’ Association and Regional Anaesthesia<br />
UK. It has been seen and approved by the elected Councils/Committees of<br />
all three organisations.<br />
Accepted: 4 June 2013<br />
• What other statements are available on this topic?<br />
Guidance publications on regional anaesthesia in patients taking anticoagulant<br />
or thromboprophylactic drugs are widely available, two<br />
well-known guidelines having been published by the American Society<br />
of Regional Anesthesia and Pain Medicine (ASRA) [1] or adopted by<br />
the European Society of Regional Anaesthesia and Pain Therapy<br />
(ESRA) [2].<br />
•<br />
Why was this guideline developed?<br />
The available published guidance focuses on neuraxial blockade in<br />
patients receiving drug therapy specifically aimed at modifying<br />
coagulation, but does not address non-neuraxial regional blockade or<br />
patients with abnormalities of coagulation for other reasons. Currently<br />
available guidelines are lengthy and discursive, and do not<br />
lend themselves to use in the acute clinical setting. The remit of the<br />
Working Party that produced these guidelines was to create a concise<br />
document that considered regional anaesthesia of all forms and<br />
abnormalities of coagulation of both therapeutic and pathological<br />
origins.<br />
•<br />
How does this statement differ from existing guidelines?<br />
Although based on the available guidance and on published pharmacokinetic<br />
and pharmacodynamic data pertaining to anticoagulant<br />
drugs, this guidance is considerably more concise.<br />
•<br />
Why does this statement differ from existing guidelines?<br />
These guidelines were developed in order to make useful and concise<br />
guidance available to anaesthetists in the clinical setting.<br />
Anaesthetists are often faced with the question of whether the risks of regional<br />
anaesthetic techniques are increased when performed on patients with<br />
2 © 2013 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of<br />
The Association of Anaesthetists of Great Britain and Ireland.
W. Harrop-Griffiths et al. | Guidelines: patients with abnormalities of coagulation Anaesthesia 2013<br />
abnormalities of coagulation and, if so, whether they are so increased that<br />
the techniques should be modified or avoided. This is not only because the<br />
popularity of regional anaesthesia is on the rise but also because the use of<br />
anticoagulant drugs in the prevention of venous thromboembolism is<br />
expanding, as is the number of different drugs in use. The serious complications<br />
of regional anaesthesia in patients without abnormalities of coagulation<br />
are very rare indeed [3]. For example, in the third National Audit<br />
Project (NAP3), the incidence of vertebral canal haematoma after neuraxial<br />
blockade was 0.85 per 100 000 (95% CI 0–1.8 per 100 000). The extent to<br />
which the risk of haemorrhagic complications is increased in patients with<br />
abnormalities of coagulation is unquantifiable, but likely to be small. The<br />
rarity of the complications means that it is difficult to make accurate estimates<br />
of the incidence of complications related to abnormalities of coagulation,<br />
and therefore offering patients and clinicians advice on the basis of<br />
‘hard data’ is not possible, and is unlikely ever to become possible. We<br />
are therefore reliant on expert opinion, case reports, case series, cohort<br />
studies and extrapolations from drug properties such as the time taken to<br />
achieve peak plasma levels and the known half-lives of drugs.<br />
Published clinical guidance in relation to the risk associated with regional<br />
anaesthesia in patients with abnormalities of coagulation is often binary.<br />
For instance, it is often said that the performance of neuraxial block in<br />
a patient with < 75 9 10 9 .l<br />
1 platelets is not acceptable, whereas its performance<br />
in the presence of > 75 9 10 9 .l<br />
1 platelets is acceptable. However,<br />
there can be no relevant difference in risk or outcome after neuraxial<br />
blockade in two patients, one of whom has a platelet count of 74 9 10 9 1<br />
.l<br />
and the other 76 9 10 9 .l<br />
1 . Risk is a continuum that runs from ‘normal<br />
risk’ to ‘very high risk’, and this guidance seeks to emphasise this point.<br />
This guidance must be interpreted and used after consideration of an<br />
individual patient’s circumstances. None of the advice in this guidance<br />
should be taken as being prohibitive or indicative. An abnormality of<br />
coagulation – however severe – is always a relative contraindication to<br />
the use of a regional anaesthetic technique. However, there may be circumstances<br />
in which, although the use of a regional technique for a<br />
patient with abnormal coagulation may put the patient at significant risk<br />
as a result, the alternative for this patient (often a general anaesthetic)<br />
may expose them to even greater risk. Experienced clinicians should be<br />
involved in decisions about whether or not to perform a regional anaesthetic<br />
technique on a patient with abnormal coagulation, and the patient<br />
with capacity should be given all the information he/she needs to make<br />
an informed choice.<br />
© 2013 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of<br />
The Association of Anaesthetists of Great Britain and Ireland.<br />
3
Anaesthesia 2013 W. Harrop-Griffiths et al. | Guidelines: patients with abnormalities of coagulation<br />
Table 1 Recommendations related to drugs used to modify coagulation. Recommended minimum times are based in most circumstances<br />
on time to peak drug effect + (elimination half-life 9 2), after which time < ¼ of the peak drug level will be present. For those<br />
drugs whose actions are unrelated to plasma levels, this calculation is not relevant. Data used to populate this Table are derived from<br />
ASRA and ESRA guidelines [1, 2] and information provided by drug manufacturers. These recommendations relate primarily to neuraxial<br />
blocks and to patients with normal renal function except where indicated.<br />
Drug<br />
Time to<br />
peak effect<br />
Elimination<br />
half-life<br />
Acceptable time after<br />
drug for block<br />
performance<br />
Acceptable<br />
time after block<br />
Administration<br />
performance<br />
of drug while<br />
or catheter<br />
spinal or epidural<br />
removal for<br />
catheter in place 1 next drug dose<br />
Heparins<br />
UFH sc prophylaxis < 30 min 1–2 h 4 h or normal APTTR Caution 1 h<br />
UFH iv treatment < 5 min 1–2 h 4 h or normal APTTR Caution 2 4h<br />
LMWH sc prophylaxis 3–4 h 3–7 h 12 h Caution 3 4h 3<br />
LMWH sc treatment 3–4 h 3–7 h 24 h Not recommended 4 h 4<br />
Heparin alternatives<br />
Danaparoid prophylaxis 4–5 h 24 h Avoid (consider anti-Xa<br />
levels)<br />
Danaparoid treatment 4–5 h 24 h Avoid (consider anti-Xa<br />
levels)<br />
Not recommended 6 h<br />
Not recommended 6 h<br />
Bivalirudin 5 min 25 min 10 h or normal APTTR Not recommended 6 h<br />
Argatroban < 30 min 30–35 min 4 h or normal APTTR Not recommended 6 h<br />
Fondaparinux prophylaxis 5 1–2 h 17–20 h 36–42 h (consider anti-Xa<br />
levels)<br />
Not recommended 6–12 h<br />
Fondaparinux treatment 5 1–2 h 17–20 h Avoid (consider anti-Xa<br />
levels)<br />
Antiplatelet drugs<br />
NSAIDs 1–12 h 1–12 h No additional precautions No additional<br />
precautions<br />
Aspirin 12–24 h<br />
o<br />
Not relevant;<br />
irreversible effect<br />
No additional precautions No additional<br />
precautions<br />
Not recommended 12 h<br />
No additional<br />
precautions<br />
No additional<br />
precautions<br />
Clopidogrel 12–24 h 7 days Not recommended 6 h<br />
Prasugrel 15–30 min 7 days Not recommended 6 h<br />
Ticagrelor 2 h 8–12 h 5 days Not recommended 6 h<br />
Tirofiban < 5 min 4–8 h 6 8 h Not recommended 6 h<br />
Eptifibatide < 5 min 4–8 h 6 8 h Not recommended 6 h<br />
Abciximab < 5 min 24–48 h 6 48 h Not recommended 6 h<br />
Dipyridamole 75 min 10 h No additional precautions No additional<br />
6h<br />
precautions<br />
Oral anticoagulants<br />
Warfarin 3–5 days 4–5 days INR ≤ 1.4 Not recommended After catheter<br />
removal<br />
4 © 2013 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of<br />
The Association of Anaesthetists of Great Britain and Ireland.
W. Harrop-Griffiths et al. | Guidelines: patients with abnormalities of coagulation Anaesthesia 2013<br />
Table 1. (Continued)<br />
Drug<br />
Time to<br />
peak effect<br />
Elimination<br />
half-life<br />
Acceptable time after<br />
drug for block<br />
performance<br />
Acceptable<br />
time after block<br />
Administration<br />
performance<br />
of drug while<br />
or catheter<br />
spinal or epidural<br />
removal for<br />
catheter in place 1 next drug dose<br />
Rivaroxaban prophylaxis 5<br />
(CrCl > 30 ml.min 1 )<br />
Rivaroxaban treatment 5<br />
(CrCl > 30 ml.min 1 )<br />
3h 7–9 h 18 h Not recommended 6 h<br />
3h 7–11 h 48 h Not recommended 6 h<br />
Dabigatran prophylaxis or treatment 7<br />
(CrCl > 80 ml.min 1 ) 0.5–2.0 h 12–17 h 48 h Not recommended 6 h<br />
(CrCl 50–80 ml.min 1 ) 0.5–2.0 h 15 h 72 h Not recommended 6 h<br />
(CrCl 30–50 ml.min 1 ) 0.5–2.0 h 18 h 96 h Not recommended 6 h<br />
Apixaban prophylaxis 3–4 h 12 h 24–48 h Not recommended 6 h<br />
Thrombolytic drugs<br />
Alteplase, anistreplase,<br />
reteplase, streptokinase<br />
< 5 min 4–24 min 10 days Not recommended 10 days<br />
UFH, unfractionated heparin; sc, subcutaneous; APTTR, activated partial thromboplastin time ratio; iv, intravenous; LMWH, low molecular weight heparin, NSAIDs,<br />
non-steroidal anti-inflammatory drugs; INR, international normalised ratio; CrCl, creatinine clearance.<br />
Notes to accompany Table 1<br />
1 The dangers associated with the administration of any drug that affects coagulation while a spinal or epidural catheter is in place should be considered carefully. There are<br />
limited data on the safety of the use of the newer drugs in this Table, and they are therefore not recommended until further data become available. The administration of<br />
those drugs whose entry in this column is marked as ‘caution’ may be acceptable, but the decision must be based on an evaluation of the risks and benefits of administration.<br />
If these drugs are given, the times identified in the column to the left (‘Acceptable time after drug for block performance’) should be used as a guide to the minimum<br />
time that should be allowed between drug administration and catheter removal.<br />
2 It is common for intravenous unfractionated heparin to be given a short time after spinal blockade or insertion of an epidural catheter during vascular and cardiac<br />
surgery. Local clinical governance guidelines should be followed and a high index of suspicion should be maintained if any signs attributable to vertebral canal<br />
haematoma develop.<br />
3 Low molecular weight heparins are commonly given in prophylactic doses twice daily after surgery, but many clinicians recommend that only one dose be given<br />
in the first 24 h after neuraxial blockade has been performed.<br />
4 Consider increasing to 24 h if block performance is traumatic.<br />
5 Manufacturer recommends caution with use of neuraxial catheters.<br />
6 Time to normal platelet function rather than elimination half-life.<br />
7 Manufacturer recommends that neuraxial catheters are not used.<br />
© 2013 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of<br />
The Association of Anaesthetists of Great Britain and Ireland.<br />
5
Anaesthesia 2013 W. Harrop-Griffiths et al. | Guidelines: patients with abnormalities of coagulation<br />
Table 2 Relative risk related to neuraxial and peripheral nerve blocks in<br />
patients with abnormalities of coagulation.<br />
Higher risk<br />
Normal risk<br />
Block category<br />
Epidural with catheter<br />
Single-shot epidural<br />
Spinal<br />
Paravertebral blocks<br />
Deep blocks<br />
Superficial<br />
perivascular<br />
blocks<br />
Fascial blocks<br />
Superficial blocks<br />
Local infiltration<br />
Examples of blocks in category<br />
Paravertebral block<br />
Lumbar plexus block<br />
Lumbar sympathectomy<br />
Deep cervical plexus block<br />
Coeliac plexus block<br />
Stellate ganglion block<br />
Proximal sciatic block (Labat, Raj, sub-gluteal)<br />
Obturator block<br />
Infraclavicular brachial plexus block<br />
Vertical infraclavicular block<br />
Supraclavicular brachial plexus block<br />
Popliteal sciatic block<br />
Femoral nerve block<br />
Intercostal nerve blocks<br />
Interscalene brachial plexus block<br />
Axillary brachial plexus block<br />
Ilio-inguinal block<br />
Ilio-hypogastric block<br />
Transversus abdominis plane block<br />
Fascia lata block<br />
Forearm nerve blocks<br />
Saphenous nerve block at the knee<br />
Nerve blocks at the ankle<br />
Superficial cervical plexus block<br />
Wrist block<br />
Digital nerve block<br />
Bier’s block<br />
Notes to accompany Table 2<br />
There have only been 26 published reports of significant haemorrhagic complications of peripheral nerve and<br />
plexus blocks [1]. Half of these occurred in patients being given anticoagulant drugs and half in patients with<br />
normal coagulation. Patient harm has derived from:<br />
• Spinal haematoma after accidental entry into the spinal canal during attempted paravertebral blocks as<br />
defined in the Table.<br />
• Exsanguination.<br />
• Compression of other structures, e.g. airway obstruction, occlusion of major blood vessels or tissue ischaemia.<br />
The one death in this series was that of a patient on clopidogrel who underwent a lumbar plexus block and<br />
subsequently exsanguinated. The majority of the 26 cases underwent deep blocks or superficial perivascular<br />
blocks. From these data, and from other data relating to neuraxial blocks, we have placed blocks in the order of<br />
relative risk shown in the Table.<br />
Catheter techniques may carry a higher risk than single-shot blocks. The risk at the time of catheter removal<br />
is unlikely to be negligible.<br />
Ultrasound-guided regional anaesthesia, when employed by clinicians experienced in its use, may decrease<br />
the incidence of vascular puncture, and may therefore make procedures such as supraclavicular blocks safer in<br />
the presence of altered coagulation.<br />
6 © 2013 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of<br />
The Association of Anaesthetists of Great Britain and Ireland.
W. Harrop-Griffiths et al. | Guidelines: patients with abnormalities of coagulation Anaesthesia 2013<br />
Table 3 Relative risks related to neuraxial blocks in obstetric patients with abnormalities of coagulation.<br />
Risk factor Normal risk Increased risk High risk Very high risk<br />
LMWH – prophylactic dose > 12 h<br />
6–12 h<br />
< 6h<br />
< 6h<br />
LMWH – therapeutic dose<br />
> 24 h<br />
UFH – infusion Stopped > 4 h and<br />
APTTR ≤ 1.4<br />
UFH – prophylactic bolus dose<br />
Last given > 4h<br />
12–24 h<br />
Last given < 4h<br />
6–12 h<br />
APTTR above normal range<br />
NSAID + aspirin<br />
Without LMWH<br />
With LMWH dose<br />
12–24 h<br />
With LMWH dose<br />
< 12 h<br />
Warfarin INR ≤ 1.4 INR 1.4–1.7 INR 1.7–2.0 INR > 2.0<br />
General anaesthesia* Starved, not in<br />
labour, antacids<br />
given<br />
Pre-eclampsia Platelets<br />
> 100 9 10 9 1<br />
.l<br />
within 6 h of block<br />
Idiopathic thrombocytopenia Platelets<br />
> 75 9 10 9 .l<br />
1<br />
within 24 h of<br />
block<br />
Intra-uterine fetal death FBC and<br />
coagulation tests<br />
normal within 6 h<br />
of block<br />
Cholestasis INR ≤ 1.4 within<br />
24 h<br />
Platelets 75–<br />
100 9 10 9 .l<br />
and normal<br />
coagulation tests<br />
Platelets<br />
50–75 9 10 9 .l<br />
1 (stable)<br />
No clinical problems<br />
but no investigation<br />
results available<br />
No other clinical<br />
problems but no<br />
investigation results<br />
available<br />
1<br />
Full stomach or in<br />
labour<br />
Platelets<br />
75–100 9 10 9 .l<br />
(decreasing) and<br />
normal coagulation<br />
tests<br />
Platelets<br />
20–50 9 10 9 .l<br />
1<br />
1<br />
Platelets < 75 9 10 9 .l<br />
or abnormal<br />
coagulation tests with<br />
indices ≥ 1.5 or HELLP<br />
syndrome<br />
Platelets < 20 9 10 9 .l<br />
With abruption or<br />
overt sepsis<br />
1<br />
1<br />
© 2013 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of<br />
The Association of Anaesthetists of Great Britain and Ireland.<br />
7
Anaesthesia 2013 W. Harrop-Griffiths et al. | Guidelines: patients with abnormalities of coagulation<br />
LMWH, low molecular weight heparin; UFH, unfractionated heparin; APTTR, activated partial thromboplastin time; NSAID, non-steroidal anti-inflammatory drug; INR,<br />
international normalised ratio.<br />
*Although general anaesthesia is not a risk factor per se for coagulation complications, it is included in this Table to highlight that the alternatives to regional anaesthesia<br />
are not free of risk; thus a risk–benefit comparison is required when choosing one over the other. See notes below.<br />
Notes to accompany Table 3<br />
Risks: The risks are primarily those of vertebral canal haematoma with subsequent cord compression and permanent damage. Realistic alternatives to epidural analgesia<br />
exist in labour, but, for caesarean section, the choice is that of general or neuraxial anaesthesia, and the risks of spinal haematoma in patients with abnormal<br />
coagulation must be weighed against those of general anaesthesia, especially in patients who are in labour and have a full stomach. These risks include hypoxaemia<br />
associated with difficulties maintaining the airway, pulmonary aspiration and thromboembolic complications.<br />
Low platelets: The debate regarding the safety of neuraxial blockade in women with thrombocytopenia is guided by expert consensus opinion in the absence of clinical trials;<br />
it is not therefore possible to give definitive values for a lower limit at which there is an increased risk of haematoma. For normal healthy women, there is no increased<br />
risk of complications with platelet counts > 100 9 10 9 1<br />
.l [4]. A count of > 75 9 10<br />
9 .l<br />
1 has been proposed as an adequate level for regional blocks when there are no<br />
risk factors and the count is not decreasing [5]. In pre-eclampsia, a decreasing platelet count is accompanied by other coagulation abnormalities, and this is assumed to be<br />
the case once the platelet count decreases to below 100 9 10 9 1<br />
.l . If the platelet count is below this value, a coagulation screen should be performed – if this is normal, it<br />
would be reasonable to perform a regional block down to a level of 75 9 10 9 .l<br />
1 , depending on the rate of decrease in platelet count [6]. In idiopathic thrombocytopenic<br />
purpura and gestational thrombocytopenia, there are reduced platelet numbers, but normal function. In these situations, expert opinion is that an experienced anaesthetist<br />
might reasonably perform a neuraxial blockade providing the platelet count is > 50 9 10 9 1<br />
.l and stable, but an individual risk–benefit assessment should be made<br />
[7–11]. It is possible that spinal anaesthesia with platelet counts below this level may be safe if data are extrapolated from that derived from lumbar punctures in nonpregnant<br />
patients performed by haematologists using needles considerably larger than those used by obstetric anaesthetists [9]. A stable level of 40 9 10 9 1<br />
.l may be safe<br />
for lumbar puncture in the absence of other coagulation abnormalities.<br />
The platelet count should be checked before any neuraxial procedure if there is any suspicion of decreasing platelet numbers during routine antenatal testing, signs of the<br />
development of pre-eclampsia, e.g. proteinuria or hypertension, or other clinical features suggesting coagulopathy, placental abruption or if the patient has been given recent<br />
anticoagulant therapy. Platelet numbers can decrease in patients treated with regular heparin for > 4 days. Otherwise, it would not be routine to check platelet numbers<br />
and delay neuraxial block whilst these results are awaited. It would be standard practice to perform a neuraxial procedure within 6 h of the last platelet count and clotting<br />
studies in patients with mild or moderate pre-eclampsia. However, if the patient has severe or fulminating pre-eclampsia or HELLP syndrome, a platelet count and clotting<br />
studies should be checked immediately before performing the procedure, as decreases in platelet count can occur rapidly in these circumstances.<br />
Low molecular weight heparins with aspirin: Treatment with daily LMWH and aspirin 75 mg may be encountered when following NICE guidelines, which recommend<br />
low-dose aspirin for obesity or hypertension. Provided the LMWH is stopped for > 12 h, the platelet count is > 75 9 10 9 1<br />
.l and normal coagulation is confirmed,<br />
neuraxial blocks can be categorised as ‘increased risk’ only.<br />
Intra-uterine fetal death: After intra-uterine death, there is an increased risk of coagulopathy and sepsis, especially in the second week after fetal demise. Coagulation<br />
abnormalities can occur on presentation in about 3% of women with apparently uncomplicated intra-uterine death, and this increases in the presence of abruption<br />
or uterine perforation to around 13% [12]. It is therefore prudent to check coagulation status before any regional procedure. The onset of coagulopathy is variable,<br />
but can be rapid.<br />
Cholestasis: In obstetric cholestasis, coagulopathy may develop as a result of decreased absorption of vitamin K essential for activation of clotting factors. It is important<br />
to check coagulation before regional blockade, but changes do not occur rapidly.<br />
Removal of epidural catheters: The recommendations given in Table 1 for the removal of epidural catheters should be noted.<br />
8 © 2013 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of<br />
The Association of Anaesthetists of Great Britain and Ireland.
W. Harrop-Griffiths et al. | Guidelines: patients with abnormalities of coagulation Anaesthesia 2013<br />
Table 4 Risks of regional anaesthesia in patients with abnormalities of<br />
coagulation – special circumstances.<br />
Trauma<br />
Sepsis<br />
Uraemia<br />
Liver failure<br />
Massive transfusion<br />
Disseminated<br />
intravascular<br />
coagulopathy<br />
The coagulopathy of trauma is precipitated by tissue trauma,<br />
shock, haemodilution, hypothermia, acidaemia and<br />
inflammation. Following major trauma, it is recommended that<br />
an assessment of potential coagulopathy be made before<br />
performing any regional anaesthetic technique.<br />
Severe sepsis is associated with a procoagulant state. Guidelines<br />
support the use of chemoprophylaxis against deep venous<br />
thrombosis. For advice on regional anaesthesia with intercurrent<br />
thromboprophylaxis, refer to Table 1. Septic shock may be<br />
associated with the development of a consumptive coagulopathy.<br />
Clinically significant systemic sepsis remains a relative<br />
contraindication to central neuraxial anaesthesia due to the<br />
presumed increased incidence of epidural abscess and meningitis.<br />
Uraemia may lead to coagulopathy secondary to<br />
thrombocytopenia. It is recommended that all patients with<br />
significant uraemia undergo assessment of platelet number and<br />
function before regional anaesthesia. Platelet function may be<br />
improved by the administration of DDAVP.<br />
Patients with chronic renal impairment may be managed with<br />
regular dialysis. The presence of residual anticoagulation after<br />
heparin administration must be considered in patients after<br />
dialysis, and heparin reversed if indicated. If regional<br />
anaesthesia is performed, the safety of catheter removal must<br />
be considered in patients likely to receive heparin during<br />
further dialysis.<br />
All coagulation factors except factor VIII are synthesised in the<br />
liver. Liver failure is associated with haemostatic abnormality,<br />
the extent of which must be assessed before regional<br />
anaesthetic techniques are performed. There may be<br />
thrombocytopenia and abnormal platelet function due to<br />
associated hypersplenism. Patients in liver failure represent a<br />
high-risk group for general anaesthesia. When regional<br />
anaesthesia is considered as an alternative, coagulopathy must<br />
be assessed and corrected when indicated.<br />
Massive transfusion is associated with altered haemostasis, with<br />
dilution and consumption of coagulation factors being the<br />
primary causes in this pathophysiological change. In assessing<br />
the degree of coagulopathy before regional anaesthetic techniques,<br />
it is recognised that coagulopathy in massive transfusion is a<br />
dynamic situation. Assessment should be made when haemorrhage<br />
is controlled and the patient is cardiovascularly stable. An<br />
assessment of platelet function should ideally occur in patients<br />
who have been given platelet transfusions.<br />
Disseminated intravascular coagulopathy (DIC) is the<br />
pathological activation of coagulation mechanisms in response<br />
to a disease process leading to a consumptive coagulopathy.<br />
A diagnosis of DIC is incompatible with safe neuraxial<br />
blockade. When peripheral blocks are considered, they should<br />
be at compressible sites.<br />
Notes to accompany Table 4<br />
All of the conditions discussed can, in their ‘active’ state, be associated with significant<br />
coagulopathy. When regional anaesthesia is thought to be of potential value, e.g. for postoperative<br />
analgesia, it should be conducted with reference to the guidelines outlined in the<br />
rest of this publication.<br />
© 2013 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of<br />
The Association of Anaesthetists of Great Britain and Ireland.<br />
9
Anaesthesia 2013 W. Harrop-Griffiths et al. | Guidelines: patients with abnormalities of coagulation<br />
Advice is often offered that if regional anaesthesia is to be considered<br />
in a patient with a known abnormality of coagulation, an ‘experienced<br />
anaesthetist’ should perform the procedure. There are, of course,<br />
no hard data to support this suggestion. However, it is advice that the<br />
Working Party supports. It is likely that an experienced regional anaesthetist<br />
will need fewer attempts to gain block success, and it is likely<br />
that the complications related to bleeding are in part related to the<br />
number of attempts at a block. It is reasonable to ask novices to perform<br />
their blocks on patients at ‘normal risk’, reserving attempts in<br />
patients at ‘increased risk’ for experienced clinicians.<br />
Guidance is offered here in the form of four Tables, each with<br />
explanatory notes: Table 1 contains recommendations related to drugs<br />
used to modify coagulation; Table 2 suggests the relative risk related to<br />
the performance of neuraxial and peripheral nerve blocks in patients<br />
with abnormalities of coagulation; Table 3 indicates relative risks related<br />
to obstetric patients; and Table 4 describes risks of regional anaesthesia<br />
in special circumstances.<br />
Some readers may question the absence of a section on haematological<br />
conditions associated with abnormalities of coagulation – why do we<br />
not mention Christmas disease or other forms of haemophilia? Most of<br />
these diseases are the result of the absence or shortage in the body of a<br />
particular clotting factor or group of factors. Most of the patients with<br />
haematological diseases such as these reach surgery in the full knowledge<br />
that they have the disease. The standard treatment of bleeding resulting<br />
from a deficiency of a clotting factor or other contributor to normal coagulation<br />
when faced with surgery is the administration of that factor or<br />
other contributor after guidance from a haematologist. Therefore, for elective<br />
surgery, the solution is almost always the performance of the regional<br />
technique after acceptable normalisation of coagulation on the advice of a<br />
haematologist. In the emergency situation, urgent advice should be sought<br />
from on-call haematologists.<br />
References<br />
1. Horlocker TT, Wedel DJ, Rowlingson JC, et al. Regional anesthesia in the patient receiving<br />
antithrombotic or thrombolytic therapy. Regional Anesthesia and Pain Medicine<br />
2010; 35:64–101.<br />
2. Gogarten W, Van Aken H, Buttner J, Riess H, Wulf H, Burkle H. Regional anaesthesia<br />
and thromboembolism prophylaxis/anticoagulation: revised recommendations of<br />
the German Society of Anaesthesiology and Intensive Care Medicine. Anasthesiologie<br />
und Intensivmedizin 2007; 48: S109–24.<br />
10 © 2013 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of<br />
The Association of Anaesthetists of Great Britain and Ireland.
W. Harrop-Griffiths et al. | Guidelines: patients with abnormalities of coagulation Anaesthesia 2013<br />
3. Cook TM, Counsell D, Wildsmith JAW. on behalf of the Royal College of Anaesthetists<br />
Third National Audit Project. Major complications of central neuraxial block: report<br />
on the Third National Audit Project of the Royal College of Anaesthetists. British<br />
Journal of Anaesthesia 2009; 102: 179–90.<br />
4. Rolbin SH, Abbott D, Musclow E, Papsin F, Lie LM, Freedman J. Epidural anesthesia<br />
in pregnant patients with low platelet counts. Obstetrics and Gynecology 1988; 71:<br />
918–20.<br />
5. Douglas MJ. The use of neuraxial anaesthesia in parturients with thrombocytopenia:<br />
what is an adequate platelet count? In: Halpern SH, Douglas MJ, eds. Evidence Based<br />
Obstetric Anesthesia, 2nd edn. Boston, MA: Blackwell, 2005: 165–77.<br />
6. Sharma SK, Philip J, Whitten CW, Padakandla UB, Landers DF. Assessment of<br />
changes in coagulation in parturients with preeclampsia using thromboelastography.<br />
Anesthesiology 1999; 90: 385–90.<br />
7. Douglas M, Ballem P. Blood disorders. In: Gambling DR, Douglas MJ, McKay RSF,<br />
eds. Obstetric Anaesthesia and Uncommon Disorders, 2nd edn. Cambridge: Cambridge<br />
University Press, 2008: 303–20.<br />
8. Kam PCA, Thompson SA, Liew ACS. Thrombocytopenia in the parturient. Anaesthesia<br />
2004; 59: 255–64.<br />
9. Gill KK, Kelton JG. Management of idiopathic thrombocytopenic purpura in pregnancy.<br />
Seminars in Hematology 2000; 37: 275–89.<br />
10. Van Veen JJ, Nokes T, Makris M. The risk of spinal haematoma following neuraxial<br />
anaesthesia or lumbar puncture in thrombocytopenic individuals. British Journal of<br />
Haematology 2010; 148: 15–25.<br />
11. Frenk V, Camman W, Shankar KB. Regional anesthesia in parturients with low platelet<br />
counts. Canadian Journal of Anesthesia 2005; 52: 114.<br />
12. Maslow AD, Breen TW, Sarna MC, Soni AK, Watkins J, Oriol NE. Prevalence of<br />
coagulation associated with intrauterine fetal death. Canadian Journal of Anesthesia<br />
1996; 43: 1237–43.<br />
© 2013 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of<br />
The Association of Anaesthetists of Great Britain and Ireland.<br />
11
Safe vascular access 2016<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650 Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org May 2016
This guideline was originally published in Anaesthesia. If you wish to refer to this<br />
guideline, please use the following reference:<br />
Association of Anaesthetists of Great Britain and Ireland. Safe vascular access<br />
2016. Anaesthesia 2016; 71: 573-585.<br />
This guideline can be viewed online via the following URL:<br />
http://onlinelibrary.wiley.com/doi/10.1111/anae.13360/full
Anaesthesia 2016<br />
doi:10.1111/anae.13360<br />
Guidelines<br />
Association of Anaesthetists of Great Britain and Ireland*<br />
Safe vascular access 2016<br />
A. Bodenham (Chair), 1 S. Babu, 2 J. Bennett, 3 R. Binks, 4 P. Fee, 5 B. Fox, 6 A. J. Johnston, 7 A. A. Klein, 8<br />
J. A. Langton, 9 H. Mclure 10 and S. Q. M. Tighe 11<br />
1 Consultant, Anaesthesia and Intensive Care, Leeds Teaching Hospitals, Leeds, UK<br />
2 Specialty Doctor, Anaesthesia, North Manchester General Hospital, Manchester, UK<br />
3 Consultant, Anaesthesia, Birmingham Children’s Hospital, Birminham, UK<br />
4 Nurse Consultant, Airedale Hospital, West Yorkshire, UK, and Faculty of Intensive Care Medicine, UK<br />
5 Locum Consultant, Anaesthesia, Belfast Health and Social Care Trust, Belfast, UK<br />
6 Specialist Registrar, Anaesthesia, East Anglia, and Group of Anaesthetists in Training, AAGBI, London, UK<br />
7 Consultant, Anaesthesia and Intensive Care, Addenbrooke’s Hospital, Cambridge, UK<br />
8 Consultant, Anaesthesia, Papworth Hospital, Cambridge, UK<br />
9 Consultant, Anaesthesia, Plymouth Hospitals, Plymouth, and Royal College of Anaesthetists, UK<br />
10 Consultant, Anaesthesia, Leeds Teaching Hospitals, Leeds, UK<br />
11 Consultant, Anaesthesia and Intensive Care, Countess of Chester Hospital, Chester, and AAGBI Council, UK<br />
Summary<br />
Safe vascular access is integral to anaesthetic and critical care practice, but procedures are a frequent source of<br />
patient adverse events. Ensuring safe and effective approaches to vascular catheter insertion should be a priority for<br />
all practitioners. New technology such as ultrasound and other imaging has increased the number of tools available.<br />
This guidance was created using review of current practice and literature, as well as expert opinion. The result is a<br />
consensus document which provides practical advice on the safe insertion and removal of vascular access devices.<br />
.................................................................................................................................................................<br />
*This is a consensus document produced by members of a Working Party established by the Association of Anaesthetists<br />
of Great Britain and Ireland (AAGBI). It has been seen and approved by the AAGBI Board of Directors.<br />
(Date of review: 2020).<br />
These guidelines have been endorsed by the Royal College of Anaesthetists, the Faculty of Intensive Care Medicine, and<br />
the Association of Paediatric Anaesthetists of Great Britain and Ireland.<br />
Accepted: 5 September 2015<br />
Keywords: arterial cannulation; central venous catheterization; complication management; peripheral venous catheters;<br />
vascular access<br />
.................................................................................................................................................................<br />
This is an open access article under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs<br />
License, which permits use and distribution in any medium, provided the original work is properly cited, the use<br />
is non-commercial and no modifications or adaptations are made.<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland 1
Anaesthesia 2016<br />
Bodenham et al. | Safe vascular access guidelines<br />
Recommendations<br />
1 Hospitals should establish systems to ensure patients<br />
receive effective, timely, and safe vascular access.<br />
2 All hospitals should have specific policies for insertion<br />
and removal of vascular access devices including<br />
clear documentation from insertion to removal.<br />
3 Clinicians should be proactive in provision of,<br />
training in and supervision of vascular access.<br />
4 Ultrasound should be used routinely for internal<br />
jugular central venous catheter insertion. The<br />
Working Party recommends its use for all other<br />
central venous access sites, but recognises evidence<br />
is, at present, limited.<br />
5 An understanding of landmark techniques for central<br />
venous cannulation is useful for rare occasions<br />
when ultrasound is not available or cannot be used.<br />
6 The use of ultrasound should be considered early<br />
if arterial or peripheral venous cannulation proves<br />
difficult.<br />
7 Intra-osseous access is useful in emergencies when<br />
intravenous access is difficult. All acute care clinicians<br />
should be familiar with techniques and have<br />
ready access to devices.<br />
8 Clinicians should review processes to improve the<br />
safety and proficiency in vascular access and initiate<br />
regular audit to assess compliance with the<br />
standards identified in this and other guidance.<br />
What other guideline statements are available on this<br />
topic?<br />
There are a small number of existing national and<br />
international guidelines on vascular access [1–5].<br />
Why was this guideline developed?<br />
There is a need for up to date evidence-based guidance<br />
focusing on patient safety. There continues to be cases<br />
of severe morbidity and mortality related to vascular<br />
access [6, 7].<br />
How and why does this publication differ from existing<br />
guidelines?<br />
This is the first UK anaesthetic national guidance in<br />
this field, primarily aimed at safety of insertion and<br />
removal procedures. We also highlight organisational<br />
and training issues.<br />
Introduction<br />
Vascular access is the most common invasive procedure<br />
undergone by patients in secondary care. It is often<br />
poorly undertaken and is the source of considerable<br />
patient discomfort and inconvenience, as well as morbidity<br />
and mortality. Vascular access is essentially a single,<br />
often repetitive, task but providing a quality service<br />
requires more; this includes all aspects of human factors<br />
as well as education, training, audit and technical proficiency.<br />
New technology such as ultrasound and other<br />
imaging has increased the number of tools available.<br />
Peripheral venous cannulation<br />
Peripheral venous cannulation is the commonest, and<br />
probably the most important invasive procedure practised<br />
in hospitals. Principles are summarised in Table 1 [8–11].<br />
An alternative and increasingly used technique is<br />
so called midline catheters [12]. These are approximately<br />
10–20 cm long and inserted into upper arm<br />
veins with ultrasound (as with a peripherally inserted<br />
central catheter, such that the tip lies outside central<br />
veins and are used for short to medium-term access<br />
(e.g. 1–4 weeks antibiotics). They should not be used<br />
for infusions listed as requiring central venous administration.<br />
Table 1 Guide to peripheral cannulation [8–11].<br />
The smallest practical size of cannula should be used.<br />
• Needle guards to reduce needle stick injury are recommended<br />
in all procedures.<br />
• Peripheral insertion is inappropriate for infusion of fluid<br />
with high osmolality (> 500 mOsm.l<br />
1 ) or low (< 5) or<br />
high pH (> 9) or intravenous access for more than<br />
2 weeks.<br />
•<br />
The relative safety of peripheral administration of vasopressors/inotropes<br />
is contentious, but likely to be dependent<br />
on vein size and its blood flow, infusion rate,<br />
individual drug effect and dilution. This is a good area<br />
for future studies.<br />
• Insertion in a limb with lymphoedema should be<br />
avoided, except in acute situations due to increased<br />
risks of local infection.<br />
• Transillumination, ultrasound and infra-red devices may<br />
be useful.<br />
• Routine changes of peripheral cannulae at 72–96 h is<br />
not advocated.<br />
• All cannulae must be flushed after use.<br />
2 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland
Bodenham et al. | Safe vascular access guidelines Anaesthesia 2016<br />
Intra-osseus access<br />
Intra-osseus access (IO) access is useful in emergencies,<br />
when intravenous (IV) access is difficult, and is<br />
faster than central access [13]. It can be used for resuscitation<br />
fluids and drugs. All acute care clinicians<br />
should be familiar with techniques and have ready<br />
access to devices. We suspect that to date this is not<br />
the case in most centres. A number of manual and<br />
automated devices exist.<br />
The tibia and the humerus are preferred sites. For<br />
the tibia, the insertion site is 2 cm distal to the tibial<br />
tuberosity and 1 cm medial to the tibial plateau. Care<br />
is needed to avoid the epiphyseal growth plate in children.<br />
Success is evident by: aspiration of bone marrow<br />
(painful in awake patients); saline flush with no<br />
extravasation; support of the needle by the bone<br />
cortex; and infusion under gravity alone.<br />
Complications include: fracture; extravasation;<br />
osteomyelitis; infection; compartment syndrome;<br />
growth plate injury and pressure necrosis of the skin.<br />
Devices should be removed as soon as suitable IV<br />
access is achieved, ideally within 24 h of placement.<br />
Arterial access<br />
Relative contraindications include severe peripheral vascular<br />
disease, coagulopathy and local synthetic grafts.<br />
There is no evidence to support routine rotation of sites.<br />
Compression of radial and ulnar arteries to assess collateral<br />
perfusion (Allen’s test) is unreliable. Ultrasound can<br />
be used to assess vessel patency and size.<br />
Methods of insertion include: catheter-over-needle;<br />
and catheter-over-wire, i.e. Seldinger or modifications.<br />
A meta-analysis [14] suggested that radial<br />
arterial cannulation with ultrasound is more successful<br />
on first attempt. Major procedural complications<br />
(e.g. permanent ischaemic damage, sepsis, pseudoaneurysm)<br />
are reported to occur in < 1% of cases and<br />
are similar for radial, femoral and brachial sites.<br />
Some studies have found a higher incidence of catheter-related<br />
infection in femoral sites. However, arterial<br />
cannulation is generally considered safest at a suitable<br />
peripheral site if possible.<br />
There have been UK national alerts on severe<br />
hypoglycaemia from misdirected administration of<br />
insulin when glucose solutions are used to flush arterial<br />
lines. The most recent AAGBI guidelines recommend<br />
saline heparin as the only safe solution to<br />
flush catheters [15].<br />
Insertion & removal of central venous<br />
catheters (CVCs)<br />
Device choice<br />
This depends on: patient diagnosis; the intended treatment<br />
(irritant drugs normally require CVC); and<br />
patient choice. Devices should have the appropriate<br />
number of lumens required for the planned usage aiming<br />
to avoid the risks of additional catheter placements<br />
[16]. Smaller diameter devices, if appropriate, reduce<br />
vein trauma on insertion and thereafter. Parenteral<br />
nutrition requires a dedicated lumen. Fixed-length<br />
catheters: 15 cm for right internal jugular vein (IJV),<br />
20 cm for left internal jugular or right axillary/subclavian<br />
vein, and 24 cm for left axillary/subclavian or<br />
femoral vein, are the usual minimum selection length<br />
for adults. See Table 2 for different features [16, 17].<br />
Route of access<br />
Central venous catheters<br />
The internal jugular vein route may have a lower risk<br />
of mechanical complications than the subclavian [1].<br />
Recent work shows catheter-related bloodstream infection<br />
rates are lower in patients in critical care using<br />
the subclavian rather than IJV or femoral routes [18].<br />
Although the groin may have a higher microbial<br />
colonisation rate, tunnelling devices away from the<br />
groin may reduce such risks. Some perceived differences<br />
in complication rates may disappear with optimal<br />
catheter tip positioning between insertion sites.<br />
The right internal jugular/femoral route provides a<br />
straighter course to central veins, making catheter<br />
positioning easier without X-ray guidance. The external<br />
jugular vein is an alternative visible vein, but central<br />
catheter positioning can be difficult.<br />
Peripherally inserted central catheters (PICCs)<br />
These should be used with caution in patients at risk<br />
of ipsilateral lymphoedema and those who may require<br />
an arterio-venous fistula. The basilic and brachial veins<br />
may have a lower thrombosis rate than the cephalic<br />
vein. Ultrasound use may avoid damage to the median<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland 3
Anaesthesia 2016<br />
Bodenham et al. | Safe vascular access guidelines<br />
Table 2 Some features of different central venous catheter devices, all suitable for multiple infusions including veindamaging<br />
substances. Adapted from [16, 17].<br />
Non-tunnelled<br />
Tunnelled<br />
Total implanted<br />
(Ports)<br />
Peripheral insertion<br />
(PICCs)<br />
Features Common use Duration/comments<br />
One to six lumens.<br />
Insertion to subclavian, IJV or<br />
femoral veins.<br />
Some suitable for extra-corporeal<br />
treatments.<br />
One to three lumens. Insertion to<br />
subclavian, IJV or femoral veins (entry).<br />
Tunnelled to exit site.<br />
Dacron cuff anchors device.<br />
One to two lumens.<br />
Insertion to subclavian, IJV, femoral or<br />
upper arm veins (entry).<br />
Tunnelled to port.<br />
One to three lumens.<br />
Insertion to basilic, cephalic and<br />
brachial veins.<br />
Short-term CVC.<br />
Central venous pressure<br />
and ScvO2.<br />
Frequent long-term access.<br />
Haemodialysis/extra-corporeal<br />
treatments.<br />
Frequent long-term access<br />
Complex to insert/remove.<br />
Uses needle access.<br />
Simpler and safer to insert.<br />
Up to 7–10 days.<br />
Routine replacement not<br />
required.<br />
Months/years.<br />
Lower infection than<br />
non-tunnelled catheters.<br />
Months/years.<br />
Lower infection than<br />
tunnelled catheters.<br />
Least lifestyle disruption<br />
1–6 months, or longer.<br />
Suitable for short-term use.<br />
IJV, internal jugular vein; ScvO2, central venous oxygen saturation.<br />
nerve and brachial artery. Use of upper arm veins<br />
avoids the elbow flexure.<br />
Catheter tip position<br />
A poorly positioned catheter tip may increase the risk<br />
of complications, e.g. thrombosis, erosion and pericardial<br />
tamponade [19]. The position of the tip moves<br />
with respiration and patient position. Upper body<br />
CVCs should be positioned with the tip parallel to the<br />
vessel wall, usually in the lower superior vena cava<br />
(SVC) or the upper right atrium (RA). Common sites<br />
for tip misplacement include: high SVC; internal jugular<br />
vein; angled at vein wall; low RA; right ventricle;<br />
innominate vein and subclavian vein.<br />
Assessment of tip position includes: post-insertion<br />
chest X-ray, real-time fluoroscopy, and ECG guidance.<br />
Stenosis or distortion of great veins is common in disease<br />
states particularly with prolonged CVC placement.<br />
Unusual congenital variants (e.g. left SVC) exist [20].<br />
Misplacement can be reduced by the following: use of<br />
the right IJV or femoral veins and pressure over the<br />
IJV may reduce the incidence of IJV malposition when<br />
inserting PICCs or subclavian lines. Catheters and<br />
guidewires may pass centrally more easily on inspiration<br />
as thoracic structures change shape. Ultrasound<br />
can confirm catheter position with supraclavicular,<br />
transthoracic and transoesophageal echocardiographic<br />
views. Electrocardiograpy and electromagnetic guidance<br />
are increasingly used to guide catheter tip positioning<br />
as per recent guidance [21]. Fluoroscopy X-ray contrast<br />
remains the gold standard for imaging.<br />
Most misplaced CVCs are easily identified on chest<br />
X-ray, but signs can be subtle [20]; judicious use of<br />
contrast via the catheter (linogram) is helpful. The limitations<br />
of single plane X-ray imaging must be appreciated.<br />
Clues to misplacement include: pain on injection;<br />
difficulty in aspirating blood from one or more lumens;<br />
or an abnormal pressure waveform, or arterial pattern<br />
blood gas on sampling. Management of misplaced<br />
catheters within central veins includes: using the device<br />
if it is safe to do so; manipulating the position under X-<br />
ray guidance; or replacement, using fluoroscopic guidance<br />
or other imaging as required. Misplacement outside<br />
veins is considered later under complications.<br />
Removal of CVCs<br />
Devices should be removed when they are no longer<br />
required or are causing problems. The patient should<br />
lie flat with the exit site below the heart to reduce risks<br />
of air embolus. Firm digital pressure should be applied<br />
for at least 5 min, followed by an occlusive dressing.<br />
Routine culture of tips is not considered necessary.<br />
Persistent bleeding may require a skin stitch.<br />
Cuffed devices/ports need surgical cut-downs as<br />
they develop complex adherent fibrin sleeves and scar<br />
tissue [22]. Fibrin sleeves are frequently left behind<br />
4 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland
Bodenham et al. | Safe vascular access guidelines Anaesthesia 2016<br />
within the vein (seen as ‘ghosts’ on ultrasound). Very<br />
long-term catheters may become attached to the wall<br />
of SVC/right atrium and cannot be removed by traction<br />
alone; cutting off and leaving in situ or surgical<br />
removal may be required. Devices can become knotted<br />
within veins. Seek advice from vascular surgery or<br />
interventional radiology if difficulties occur.<br />
Procedures in coagulopathic patients<br />
In the presence of a coagulopathy, a more experienced<br />
operator should insert the CVC, ideally at an insertion<br />
site that allows easy compression of vessels. Femoral<br />
access may have a lower risk in this situation. Routine<br />
reversal of coagulopathic abnormality is only necessary<br />
if platelet count < 50 9 10 9 .l<br />
1 , activated partial<br />
thromboplastin time > 1.3 times normal and/or international<br />
normalised ratio > 1.8, as the risk of haemorrhage<br />
is not increased [23]. In selected patients,<br />
different thresholds for correction may be acceptable.<br />
Bleeding risks of insertion and removal vary with<br />
the site, size of device, and operator experience. The<br />
risks of correction (e.g. infection, lung injury, thrombosis)<br />
may exceed that of local bleeding, and it may be<br />
preferable to give blood products if problems occur,<br />
rather than prophylactically.<br />
Difficult central venous catheter insertion<br />
Difficult access occurs frequently [24] and is more<br />
likely with previous multiple attempts, insertion site<br />
scars and long-term access. Distended superficial collateral<br />
veins suggest deeper vein blockage or stenosis.<br />
Doppler ultrasound of great vessels gives limited imaging<br />
of the subclavian vein and SVC; contrast venography/CT/MRI<br />
may be indicated, dependent on urgency.<br />
If difficulty is predicted, insertions should be performed<br />
under X-ray control with appropriate radiation<br />
protection [25]. High-resolution ultrasound should be<br />
used with colour Doppler to study flow. Input from<br />
interventional radiology and surgery may be needed.<br />
A ‘difficult access’ trolley is useful, with additional<br />
instruments, X-ray contrast, sterile drapes and ultrasound<br />
probe covers, standard (18G) and micro-puncture<br />
needles (20-21G), and compatible guidewires<br />
(0.018″ and 0.32″).<br />
Guidewires come in various lengths, with different<br />
coatings and tips (e.g. straight, angled, soft tip or full<br />
‘J’). It is best to be familiar with a small range. Catheters<br />
of 12–24 cm length should be available for adults.<br />
Guidewires should be checked for damage and adherent<br />
clot removed with a wet swab. A selection of<br />
compatible dilators and peel-away sheaths is needed.<br />
Use of a 4–5 Fr introducer sheath allows manipulation<br />
of guidewires while minimising the risk of<br />
damaging the wire or vein; it also acts as a conduit for<br />
contrast injection or advancement of specialist catheters/wires.<br />
X-ray contrast is used to image vascular anatomy,<br />
identify complications and confirm line position/patency.<br />
It may cause anaphylaxis. Contrast nephropathy<br />
is unlikely in doses used for venous access [26].<br />
Paediatric CVC insertion<br />
Provision of CVCs for neonates through to adolescents<br />
is challenging, despite similar techniques to adults.<br />
Children are more likely to be seen with congenital<br />
cardiac anomalies and there is a large range in the size<br />
of vessels, which impacts on procedures and complications<br />
[27]. Most procedures will be conducted under<br />
general anaesthesia, except for peripherally inserted<br />
central catheters.<br />
Catheter choice depends on: vein calibre; indication;<br />
duration of use; severity of illness and operator<br />
experience. Neonatal long lines down to 28G are available.<br />
Umbilical venous catheters remain popular for<br />
short-term use in neonates, despite high complication<br />
rates. Non-tunnelled, 5–6 cm long, 4.5-Fr triple-lumen<br />
CVCs are available for neonates. Tunnelled cuffed<br />
Broviac catheters for long-term use are available down<br />
to 2.7Fr [28].<br />
A full range of sizes of equipment is required.<br />
Operators must be familiar with equipment and procedures.<br />
Typical guidewires are narrower 0.021″ (0.032″<br />
used in adults), and prone to kinking, particularly during<br />
advancement of dilators. The diameter of a ‘J’ tip<br />
may impede advance in a narrow vein. A less curved<br />
tip is preferable. Skin dilators tend to be shorter and<br />
narrower.<br />
X-ray imaging of fine catheters is challenging,<br />
and contrast may be required. There are few data on<br />
the use of electromagnetic or ECG guidance to identify<br />
CVC tip position in children. X-ray guidance<br />
remains standard.<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland 5
Anaesthesia 2016<br />
Bodenham et al. | Safe vascular access guidelines<br />
Chlorhexidine of varying strengths is used for skin<br />
antisepsis before CVC insertion in infants, but efficacy<br />
and safety data comparing solutions is lacking so definitive<br />
guidance cannot be given. Chlorhexidine, in particular<br />
2%, has been associated with skin erythema and<br />
burns in premature infants and caution is advised in<br />
this group; the use of excessive quantities and pooling<br />
on the skin should be avoided [29]. Many centres use<br />
a 0.5% solution as an alternative.<br />
Ultrasound-guided paediatric CVC insertion has<br />
been shown to be superior to landmark techniques<br />
[30]. Superficial vessels and lack of fat allows excellent<br />
imaging. Probes need a small footprint for full skin<br />
contact. Veins are prone to compression by the probe<br />
and access needle, which risks transfixion and damage<br />
to adjacent structures.<br />
Small children are less likely to understand the<br />
importance of their CVC with risks of damage, nor<br />
the risks associated with replacing devices. Implanted<br />
ports may not be tolerated by needle phobic children.<br />
Rapid growth in small children may lead to the tip<br />
migrating.<br />
Peripheral access can be challenging and limit<br />
placement of devices. Loss of peripheral veins is a serious<br />
issue in chronic illness. Prolonged use of CVCs<br />
may lead to central vein thrombosis with difficult or<br />
impossible access. Open surgical cut-down remains a<br />
common technique in paediatric surgery and often<br />
leads to central vein occlusion near the entry site.<br />
Prevention, recognition and<br />
management of central venous<br />
catheter complications<br />
Deaths related to CVCs are often accompanied by<br />
poor documentation [4]. All hospitals should have<br />
clear, specific policies for insertion and documentation<br />
of CVCs (type, insertion site and tip position), and<br />
education on complications and their management.<br />
Publications suggest complication rates of 1–26%<br />
[31]. However, most series are small and lack precise<br />
denominators. Appropriate training and surveillance<br />
should avoid and identify most complications. Discussion<br />
here is limited to more serious, well-recognised<br />
complications (Table 3), which vary in frequency<br />
depending on patient, catheter and operator experience.<br />
There are many other reported rarer complications<br />
listed as case reports in the literature. There is an<br />
increased focus in the UK to reduce the risks of invasive<br />
procedures including universal adoption of WHO<br />
style theatre checklists, definition of so called ‘Never<br />
Events’ (see later), and most recently the introduction<br />
of local and National Safety Standards for Invasive Procedures<br />
(NatSSIPs) [32]. Central venous access and<br />
more central arterial cannulation would be considered<br />
to be within this latter category of invasive procedure.<br />
Infection<br />
Central venous catheter-associated bloodstream infection<br />
can be life-threatening, and is increasingly<br />
regarded as a measure for quality of care. Treatment<br />
should adhere to local guidance and may include CVC<br />
removal [33].<br />
Thrombosis/thrombo-embolism<br />
Thrombosis related to CVCs has a reported incidence<br />
of 3–32% [1], reflecting variations in definition and<br />
imaging, and frequent asymptomatic cases. Prevention<br />
measures include: insertion of the narrowest-bore<br />
catheter possible for treatment needs; placement of the<br />
tip in lower SVC/high right atrium; and early removal.<br />
Evidence suggests that peripherally inserted central<br />
catheters are associated with increased peripheral and<br />
central thrombosis [34]. The femoral route may be<br />
Table 3 Complications of central venous catheter<br />
insertion.<br />
• Infection<br />
s Localised or bloodstream.<br />
• Thrombosis/thromboembolism<br />
s Symptomatic or asymptomatic<br />
• Perforation of vessels and myocardium<br />
s Arterial puncture/tear<br />
s Arterial cannulation<br />
s Venous injury/tear<br />
s Myocardial perforation/cardiac tamponade.<br />
• Pleural collections.<br />
s Pneumothorax<br />
s Haemothorax (haemoperitoneum)<br />
Cardiac arrhythmias<br />
Air embolism<br />
Guidewire/catheter embolism<br />
Catheter occlusion<br />
Catheter breakage/leak/extravasation<br />
Bleeding elsewhere.<br />
Central venous stenosis<br />
• Neurological injury<br />
6 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland
Bodenham et al. | Safe vascular access guidelines Anaesthesia 2016<br />
associated with a higher thrombosis risk [18, 19].<br />
Some retrospective (but not prospective) studies show<br />
an increased thrombosis risk when the subclavian vein<br />
is used long-term [1]. Anticoagulation is not currently<br />
recommended for asymptomatic thrombosis [1], or as<br />
prophylaxis, except for patients at high risk (e.g. previous<br />
DVT or PE) [35].<br />
Thrombosis may present with a poorly functioning<br />
line; a swollen limb; signs of SVC obstruction; pain<br />
over the insertion site; or central embolism. Symptomatic<br />
thrombosis is usually treated with full anticoagulation.<br />
Removal of a functioning CVC depends on<br />
the clinical situation, and ease of re-insertion.<br />
Perforation of great vessels and myocardium<br />
These complications usually occur at insertion and<br />
may cause serious morbidity or mortality. Meticulous<br />
technique, vigilance and early recognition prevent<br />
progression to catastrophe. Bleeding may be evident<br />
externally, but may also be covert, into pleurae, pericardium,<br />
and peritoneum. Once a vessel is perforated<br />
then the guidewire, dilator or catheter may pass into<br />
any adjacent structure or organ, commonly the pleural<br />
space, pericardium, mediastinum or lung in the upper<br />
body.<br />
Arterial puncture<br />
Accidental arterial puncture is reduced with routine<br />
use of ultrasound guidance [1, 36]. It is usually evident<br />
by bright red, pulsatile blood, but confusion may occur<br />
in infants and emergency situations. Manometer tubing<br />
can be attached to a needle or cannula to differentiate<br />
venous from arterial placement. Ultrasound<br />
imaging can confirm the guidewire in the proximal<br />
vein before dilatation. A PO 2 consistent with arterial<br />
blood is strongly suggestive but may reflect atreriovenous<br />
shunting. All tests have flaws; a fuller discussion<br />
is available elsewhere [2].<br />
Needle puncture is managed by removal and digital<br />
pressure. Ultrasound imaging may define the size<br />
of the haematoma, vessel injury and patency. Puncture<br />
of the carotid artery, even with a 21G ‘searching’<br />
needle, may cause stroke, particularly with existing<br />
arterial disease [37]. If the needle also traverses a<br />
vein, there is potential for an aterio-venous fistula.<br />
An expanding neck haematoma in the neck may<br />
fatally compromise the airway [38–40], and require<br />
tracheal intubation and surgical intervention. Haemorrhage<br />
associated with the femoral route may be<br />
concealed in the retroperitoneum. Tense haematomas<br />
elsewhere may require surgical evacuation/repair to<br />
prevent local pressure effects.<br />
Accidental arterial cannulation<br />
The incidence is estimated as 0.1–1% [1]. There may<br />
be excessive bleeding along the guidewire or on passing<br />
dilators and introducers. Activation of high-pressure<br />
alarms on infusion pumps and retrograde flow<br />
within catheter/infusion sets are suggestive. Chest X-<br />
ray may show an abnormal catheter path (to the left<br />
mediastinum), but not if the catheter is in the right<br />
carotid or ascending aorta which are adjacent to the<br />
internal jugular vein and SVC. An arterial waveform<br />
upon pressure transduction (check settings are for<br />
arterial range) confirms arterial positioning. Contrast<br />
injection will demonstrate arterial flow and CT shows<br />
the catheter course. Carotid artery cannulation carries<br />
a higher risk of morbidity and mortality than at other<br />
sites, because of the risk of stroke and local pressure<br />
effects from haemotoma.<br />
Larger catheters/dilators (6Fr or greater) should be<br />
left in place and their safe removal discussed urgently<br />
with interventional radiologists or vascular surgeons.<br />
Management of smaller catheters depends on the<br />
insertion site, presence of arterial disease or thrombus,<br />
and coagulation status; catheters (5Fr or less) are routinely<br />
removed from the femoral artery following radiology<br />
procedures. This is followed by direct pressure<br />
for 10 min, or until haemostasis is achieved, then six<br />
hours bed rest. Such guidance can be followed up for<br />
accidental femoral artery catheterisation. Interventional<br />
radiologists and surgeons should be consulted before<br />
removing larger devices, any arterial catheter from the<br />
neck or chest, or from any site in an anticoagulated<br />
patient [39]. Routine anticoagulation following shortterm<br />
accidental carotid or other artery catheterisation<br />
is not recommended.<br />
Venous tears<br />
This is caused by trauma during insertion or later erosion<br />
of the vein wall. Prevention includes meticulous<br />
insertion technique; avoidance of advancing guidewires<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland 7
Anaesthesia 2016<br />
Bodenham et al. | Safe vascular access guidelines<br />
and dilators against resistance; and firmly holding<br />
guidewires during dilation and catheter advancement.<br />
Poorly positioned catheters need to be repositioned,<br />
e.g. left-sided upper body CVCs that abut the SVC at<br />
an acute angle. Narrow-bore soft catheters and dilators<br />
are less likely to cause perforation.<br />
Venous injury may manifest as a haematoma,<br />
bleeding or extravasation into the mediastinum,<br />
pleura, peritoneum, pericardium or other space. It<br />
may cause haemodynamic compromise, cardiac tamponade,<br />
haemothorax or pleural effusion [38, 40].<br />
The catheter should remain in situ until a vascular<br />
surgical or interventional radiology opinion has been<br />
obtained.<br />
Myocardial perforation/cardiac tamponade<br />
This can be caused by trauma from guidewires or dilators<br />
during insertion, or later erosion by a catheter.<br />
Presentation is usually acute but may be delayed until<br />
infusion of fluids via the catheter. The incidence is<br />
reduced by careful insertion techniques. Infants and<br />
those with dilated cardiomyopathy or previous cardiac<br />
surgery are at higher risk. Guidewires should be<br />
advanced gently and not beyond 20 cm (less in children)<br />
without imaging. Dilators should only be<br />
inserted as far as required to create a tract to the vessel.<br />
Traditionally, it was advocated that catheter tips<br />
should lie above the pericardial reflection but this is<br />
frequently not possible, particularly with left-sided<br />
catheters.<br />
There may be signs of obstructed shock, an<br />
abnormal pressure wave, or cardiac arrest. Chest X-<br />
ray may show an enlarged cardiac outline, which<br />
can be confirmed with echocardiography. Management<br />
involves attempted fluid aspiration through the<br />
catheter, urgent pericardiocentesis or surgical intervention<br />
[40].<br />
Pneumothorax<br />
The incidence of pneumothorax is 0.3–2.3%, highest<br />
with the subclavian route [1, 34]. It is typically caused<br />
by needle penetration of the visceral pleura. Prevention<br />
includes avoiding the subclavian vein, particularly during<br />
early training, and using ultrasound guidance [41].<br />
Recognising a pneumothorax can be difficult. It may<br />
be invisible on initial post-procedure imaging. Staff<br />
and patients should be warned to report late signs and<br />
symptoms.<br />
Treatment options include: observation; administration<br />
of supplemental oxygen; and aspiration; or tube<br />
drainage. Minimal or asymptomatic collections (up to<br />
30% of the pleural cavity) may not require drainage in<br />
spontaneously breathing patients.<br />
Haemothorax<br />
This may occur with central vein or arterial trauma<br />
[42]. The pleurae are low-pressure spaces, where a<br />
large volume of blood can accumulate. Catheters crossing<br />
from a vein or artery into the pleura (or other<br />
space) may be wholly or partially occluding the hole<br />
and bleeding may worsen on removal. Further accumulation<br />
of fluid/blood may occur if the catheter is<br />
used for infusion, resuscitation or dialysis.<br />
There may be clinical signs of respiratory and/or<br />
circulatory failure. Chest X-ray, CT or ultrasound<br />
imaging shows a dense pleural effusion, and aspiration/drainage<br />
of blood confirms the diagnosis. Resuscitation<br />
with drainage and repair of the damaged vessel<br />
may be required.<br />
Cardiac arrhythmias<br />
Arrhythmias may be precipitated by guidewires or<br />
catheters stimulating the heart [43]. They are usually<br />
caused by insertion beyond the predicted length of<br />
catheter for that insertion site, and usually settle on<br />
guidewire/catheter withdrawal. Electrocardiographic<br />
monitoring throughout all upper body CVC insertions<br />
is advisable.<br />
Venous air embolism<br />
Air embolism may be fatal and occur at any time from<br />
insertion to removal. The incidence may be as high as<br />
0.8% [42]. Prevention requires careful insertion/removal<br />
techniques, secure fixation and safe handling<br />
when accessing the catheter. Presentation ranges from<br />
subtle neurological, respiratory or cardiovascular signs<br />
to shock, loss of consciousness and cardiac arrest.<br />
Chronic forms may exist. If suspected, damaged catheters<br />
should be clamped, pressure and wet dressings<br />
applied, and occlusive dressings used. Head-down, left<br />
lateral tilt and attempted aspiration of air via the line<br />
may be useful.<br />
8 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland
Bodenham et al. | Safe vascular access guidelines Anaesthesia 2016<br />
Guidewire and catheter embolus<br />
This risk is increased during difficult or multiple cannulation<br />
attempts of the same vessel, or the presence<br />
of an inferior vena cava filter [44]. Preventative measures<br />
include minimising the length of guidewire<br />
advanced, and maintaining hold of the outside section.<br />
Guidewire counts or mandatory witnessed documentation<br />
of guidewire removal may help identify unaccounted<br />
wires during insertion. Retained guidewires<br />
are usually asymptomatic and recognised incidentally<br />
on X-ray. Guidewire retention is now categorised as an<br />
NHS Never Event [45].<br />
Catheter embolism occurs more often with longterm<br />
devices. Catheter and port hub connections may<br />
fracture/disconnect. Compression of the catheter<br />
between the first rib and clavicle may result in ‘pinchoff’<br />
[46]. Catheters are at risk during removal, especially<br />
cuffed/implanted devices.<br />
Both complications need referral for urgent radiological<br />
or surgical retrieval.<br />
Catheter occlusion<br />
Occlusion may be due to thrombus, fibrin sheath or<br />
precipitation within the catheter. The incidence of<br />
catheter occlusion may be reduced by adhering to<br />
standard procedures for accessing CVCs and managing<br />
failing lines. A Cochrane review of heparin solutions<br />
reported no reduction in intracatheter thrombus [47].<br />
Occlusion is recognised by inability to aspirate or flush<br />
one or more catheter lumens. It is common, and often<br />
managed by a local protocol. A ‘linogram’ may identify<br />
a kinked catheter, aberrant tip position or a fibrin<br />
sheath with reflux of contrast. Thrombolytics can be<br />
used to clear the lumen or surrounding thrombus [48].<br />
In the case of precipitants, strong acid or alkali has<br />
been used to unblock devices.<br />
External catheter breakage<br />
The portion of a CVC outside the body has the potential<br />
to be cut, broken or split. Breakage is more common<br />
in long-term lines. They may be repaired<br />
according to local policy, or replaced.<br />
Extravasation injury<br />
Injury caused by leakage of infusate is usually associated<br />
with catheter damage or withdrawal (placing a<br />
luminal hole outside the vein), or vein perforation.<br />
Rarely, fluid backtracking along a fibrin sheath may be<br />
the cause. High-risk infusates include those with high<br />
or low pH, high osmolality, vasopressors and<br />
chemotherapy agents.<br />
Secure fixation is important to minimise withdrawal,<br />
which may be identified by the loss of a<br />
venous waveform from the proximal lumen of the<br />
catheter. Correct placement of the catheter tip will<br />
help prevent venous erosion and ensure an adequate<br />
length of catheter within the vein.<br />
Leakage of infusate at the insertion site suggests<br />
extravasation; this may be painful and cause tissue<br />
damage. There may be a lack of clinical effect of infusions.<br />
Chest X-ray may reveal a migrated catheter, or a<br />
pleural effusion. Management of extravasation depends<br />
on the nature of the infusate; protocols for extravasation<br />
should be followed. Plastic surgical referral may<br />
be needed if tissue injury occurs.<br />
Nerve injury<br />
This is uncommon [42]. Peripheral or cranial nerves<br />
may be injured. The internal jugular vein is near the<br />
brachial plexus and the vagus. The subclavian vein is<br />
near the brachial plexus. In the upper arm, the<br />
median nerve is adjacent to brachial veins and the<br />
medial cutaneous nerves of forearms next to the<br />
Table 4 Principles of infection prevention for vascular<br />
access.<br />
For peripheral venous access:<br />
Thorough hand washing<br />
Non-sterile gloves<br />
• Skin disinfection with 2% chlorhexidine in 70% alcohol<br />
For peripheral arterial access. As above but this will<br />
generally require sterile gloves to allow procedural palpation<br />
of the artery, and direct handling of needle,<br />
guidewire and catheter.<br />
For central vascular access devices:<br />
Aseptic hand washing<br />
Sterile gown, gloves, hat, facemask<br />
• Surface disinfection with 2% chlorhexidine in 70% alcohol<br />
(or povidone iodine in those sensitive to chlorhexidine),<br />
with air-drying<br />
Large sterile barrier drapes<br />
• preference for upper extremity catheters<br />
Once sited: appropriate anchorage and dressings; aseptic<br />
access techniques; daily site review; and removal at the earliest<br />
opportunity.<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland 9
Anaesthesia 2016<br />
Bodenham et al. | Safe vascular access guidelines<br />
basilic vein. Ultrasound needle guidance should<br />
reduce such risks.<br />
Infection control<br />
The recent Michigan-Keystone project in 103 ICUs in<br />
the US reported major reductions in central venous<br />
catheter (CVC) bloodstream infections from 7.7 to 1.4<br />
per 1000 CVC-patient days [49]. In the UK, the similar<br />
‘Matching Michigan’ project resulted in a reduction<br />
from 3.7 to 1.5 infections per 1000 CVC-patient days<br />
over 20 months [50]. Recent guidelines provide comprehensive<br />
evidence-based recommendations to minimise<br />
such infections. Detailed recommendations on<br />
catheter selection, insertion site, anchorage and dressings,<br />
replacement, removal, management and personal<br />
protection can be found elsewhere [51, 52]. In the<br />
absence of actual or suspected infection, there is no<br />
evidence to support the routine changing of central<br />
venous catheters. Key messages are summarised in<br />
Table 4. Anaesthetists should compare their insertion<br />
techniques and use of devices with these standards.<br />
Training and experience<br />
Descriptions of the competency levels required for<br />
CVC insertion during training and assessment methods<br />
are listed in the current Anaesthesia and ICM<br />
Curricula (annex F, ICM in anaesthesia) (www.rcoa.ac.uk).<br />
Competencies for ultrasound guidance have been<br />
produced [53].<br />
Current training includes: simulation based teaching<br />
(part-task trainers); apprenticeship models; and<br />
courses (local/national, basic/advanced).<br />
The Working Party recommends:<br />
• Phantom or manikin simulation techniques should<br />
be routinely available to improve novice technique.<br />
•<br />
There should be regular training updates for skill<br />
retention, especially for procedures seldom performed<br />
(e.g. IO).<br />
Consent and medicolegal aspects<br />
Consent should follow local and national guidelines<br />
[54]. Written consent is usual for a standalone procedure<br />
or if particular risks are evident. The proposed<br />
side and route of access should be explained, as well as<br />
the potential need to move to other sites. In practice,<br />
much will be verbal as part of a wider discussion of<br />
provision of anaesthesia or critical care. While any<br />
adverse event may lead to a complaint or litigation,<br />
certain serious complications are evident in closed<br />
claim analyses highlighted in the complications section<br />
[38–40]. Early recognition of the problem, referral to<br />
surgery or interventional radiology for help, and correct<br />
management of complications is essential for a<br />
safe outcome.<br />
Use of in situ long-term devices<br />
Many patients already have such devices in situ, e.g.<br />
Hickman tunnelled cuffed type, Groschong valvedtype,<br />
dialysis catheters, peripherally inserted central<br />
catheters, and ports. With appropriate infection control,<br />
such devices can be used for resuscitation, anaesthesia<br />
or critical care. The risks/benefits of inserting<br />
additional CVCs should be assessed. Staff should learn<br />
about such devices and stock port access needles<br />
(Huber type).<br />
Blood should be aspirated and discarded if concentrated<br />
heparin solution locks are in place. Fibrin<br />
sleeves may cause obstruction or an extravasation risk.<br />
Valved catheters preclude CVC pressure monitoring.<br />
Some devices are CT power-injection compatible (e.g.<br />
325 psi rating).<br />
Ultrasound guidance<br />
This has been well covered in the literature. Recent<br />
consensus is that where the technology is affordable<br />
(e.g. in the UK), it should be used routinely for internal<br />
jugular CVCs (unless in emergency or other unusual<br />
situations), and early in other procedures (arterial<br />
and peripheral venous), if difficult [36]. Ultrasound<br />
makes many steps safer including: evaluation of puncture<br />
site; recognition of local pathology; avoidance of<br />
the use of seeker needles, needle guidance; verification<br />
of guidewire/catheters in a vessel; information on central<br />
tip position and recognition of complications.<br />
Two recent Cochrane analyses [55, 56] concluded<br />
a benefit for using ultrasound for CVCs by the internal<br />
jugular vein, but not femoral or axillary/subclavian<br />
routes. The Working Party believe the latter is likely to<br />
relate to a lack of adequate studies, rather than an<br />
inherent failure of ultrasound at other sites, and recommends<br />
that ultrasound guidance should be used for<br />
10 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland
Bodenham et al. | Safe vascular access guidelines Anaesthesia 2016<br />
all routes of access where the vessel cannot be seen<br />
directly or palpated.<br />
Operators need to be adequately trained and<br />
experienced, and use a high-resolution device. It takes<br />
considerable time and practice to become fully competent<br />
in such techniques, and national guidance on<br />
training has not quantified this [53].<br />
Technology is moving quickly developing fast with<br />
smaller, cheaper, simpler to use, higher resolution<br />
machines. The efficacy and cost-effectiveness of echogenic<br />
needles, electromagnetic sensors, needle guides<br />
and other aids is at present unknown and should be a<br />
focus for future studies.<br />
In the UK, given the wide availability of ultrasound,<br />
the Working Party believe it is not practical for<br />
staff to continue to be trained to become fully competent<br />
in all CVC landmark techniques. The only situations<br />
where ultrasound cannot be consistently used are<br />
extensive air emphysema and unavailability of a device<br />
in emergencies. An understanding of landmark techniques<br />
is useful for rare occasions when ultrasound is<br />
not available or not able to be used. Landmark techniques<br />
will still be used in countries where ultrasound<br />
is not available.<br />
Service provision for vascular access<br />
The Working Party suggests that all acute hospitals<br />
should provide the following for all age groups: local<br />
algorithms/guidance for recognition and management<br />
of complications; systems to improve procedures,<br />
training, documentation and equipment.<br />
Anaesthetists may have a prominent role, but<br />
multiple disciplines are involved, depending on the<br />
organisation and treatments provided. Services can be<br />
nominally divided into acute and elective care as<br />
below.<br />
Acute care<br />
Hospitals should organise and provide the following:<br />
1 Timely (24/7) reliable insertion of peripheral<br />
venous cannulae in all acute locations. This should<br />
not necessarily be the sole responsibility of resident<br />
medical staff.<br />
2 Immediate insertion of peripheral IV or<br />
intra-osseous access is required in emergencies.<br />
3 Timely (24/7) insertion of peripheral arterial cannula<br />
in specialised locations (high-dependency<br />
unit, ICU, theatres).<br />
4 Timely (24/7) insertion of short-term CVCs in<br />
specialised locations (high-dependency unit, ICU,<br />
theatres).<br />
Elective care<br />
5 Hospitals must organise and provide the following:<br />
Timely (within 1–3 days) insertion (and<br />
removal) of long-term CVCs in specialised locations<br />
(wards, theatres, radiology) via a dedicated<br />
service. This has been highlighted in the<br />
context of total parenteral nutrition administration<br />
[4].<br />
All acute hospitals will have requirements for<br />
long-term or repeated short-term central venous<br />
access, both in the NHS and independent sector. There<br />
are varied models dependent on local workload,<br />
including: theatre or radiology suite-based, either ad<br />
hoc in an acute setting or on separate standalone lists;<br />
ward-based models, e.g. nurse-led peripherally inserted<br />
central catheter service.<br />
Facilities needed include: procedure room; highresolution<br />
ultrasound; ECG guidance; fluoroscopy;<br />
radiographer; admitting, discharge and recovery areas.<br />
The cost-effectiveness of different models has not been<br />
studied in depth. Savings are possible by rationalising<br />
services, avoiding treatment delays, failed procedures,<br />
and facilitating hospital discharge and outpatient therapy.<br />
Audit<br />
The vascular access organisations, and individual practitioners,<br />
should initiate regular audit processes to<br />
assess compliance with the standards identified in this<br />
guidance. Specialist Societies and Colleges should consider<br />
national audit to set benchmarks (e.g. the NAP<br />
process).<br />
Acknowledgements<br />
AB has received payments from Vygon and Lake medical<br />
for consultancy work. BF has received payments<br />
from BBraun for lecturing. JB has received lecture fees<br />
from Bard Access. AJ has received payments from<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland 11
Anaesthesia 2016<br />
Bodenham et al. | Safe vascular access guidelines<br />
Bard and B Braun for consultancy work/speaker fees.<br />
AK is the Editor-in-Chief of Anaesthesia, and this<br />
manuscript has undergone additional external review<br />
as a result.<br />
References<br />
1. Frykholm P, Pikwer A, Hammarskj€old F, et al. Clinical guidelines<br />
on central venous catheterisation. Acta Anaesthesiologica<br />
Scandinavica 2014; 58: 508–24.<br />
2. Task Force on central venous access. Practice guidelines for<br />
central venous access: a report by the American Society of<br />
Anesthesiologists. Anesthesiology 2012; 116: 539–73.<br />
3. Dariushnia SR, Wallace MJ, Siddiqi NH, et al. Quality improvement<br />
guidelines for central venous access. Journal of Vascular<br />
and Interventional Radiology 2010; 21: 976–81.<br />
4. NCepod. A Mixed Bag. An enquiry into the care of hospital<br />
patients receiving parenteral nutrition. http://www.ncepod.org.uk/2010report1/downloads/PN_report.pdf<br />
(accessed<br />
24/08/2015).<br />
5. Standards for infusion therapy. The Royal College of Nurses,<br />
2010. http://www.bbraun.it/documents/RCN-Guidlines-for-IVtherapy.pdf<br />
(accessed 24/08/2015).<br />
6. http://www.nrls.npsa.nhs.uk/patient-safety-data/organisationpatient-safety-incident-reports/<br />
(accessed 17/10/2015).<br />
7. Hove LD, Steinmetz J, Christoffersen JK, et al. Analysis of<br />
deaths related to anesthesia in the period 1996–2004 from<br />
closed claims registered by the Danish Patient Insurance Association.<br />
Anesthesiology 2007; 106: 675–80.<br />
8. NHS Injectable Medicines Guide. http://medusa.wales.<br />
nhs.uk/ (accessed 19/08/2015).<br />
9. Heinrichs J, Fritze Z, Klassen T, Curtis S. A systematic review<br />
and meta-analysis of new interventions for peripheral intravenous<br />
cannulation of children. Pediatric Emergency Care<br />
2013; 29: 858–66.<br />
10. Webster J, Osborne S, Rickard CM, New K. Clinically-indicated<br />
replacement versus routine replacement of peripheral venous<br />
catheters. Cochrane Database Systematic Reviews 2013; 30:<br />
CD007798.<br />
11. Bowman S, Raghavan K, Walker IA. Residual anaesthesia<br />
drugs in intravenous lines – a silent threat? Anaesthesia<br />
2013; 68: 557–61.<br />
12. http://www.rch.org.au/uploadedFiles/Main/Content/anaes/<br />
a_procedural_guide_to_midline_insertion.pdf. (accessed 17/<br />
10/2015).<br />
13. Anson JA. Vascular access in resuscitation. Is there a role<br />
for the intraosseous route? Anesthesiology 2014; 120: 1015–<br />
31.<br />
14. Shiloh AL, Savel RH, Paulin LM, Eisen LA. Ultrasound guided<br />
catheterization of the radial artery: a systematic review and<br />
meta analysis of randomized control trials. Chest 2011; 139:<br />
524–9.<br />
15. Woodcock TE, Cook TM, Gupta KJ, Hartle A. Arterial line blood<br />
sampling: preventing hypoglycaemic brain injury. Anaesthesia<br />
2014; 69: 380–5.<br />
16. Bishop L, Dougherty L, Bodenham A, et al. Guidelines on the<br />
insertion and management of central venous access devices<br />
in adults. International Journal of Laboratory Hematology<br />
2007; 29: 261–78.<br />
17. O’Grady NP, Alexander M, Burns LA, et al. Guidelines for the<br />
prevention of intravascular catheter-related infections. Clinical<br />
Infectious Diseases 2011; 52: e162–e193.<br />
18. Parienti J-J, Mongardon N, Megarbane, et al. Intravascular<br />
Complications of Central Venous Catheterization by Insertion<br />
Site. New England Journal of Medicine 2015; 373: 1220–9.<br />
19. Ge X, Cavallazzi R, Li C, Pan SM, Wang YW, Wang FL. Central<br />
venous access sites for the prevention of venous thrombosis,<br />
stenosis and infection. Cochrane Database of Systematic<br />
Reviews 2012; 3: CD004084.<br />
20. Gibson F, Bodenham A. Misplaced central venous catheters:<br />
applied anatomy and practical management. British Journal<br />
of Anaesthesia 2013; 110: 333–46.<br />
21. NICE medical technology guidance 2015 [MTG24]. The Sherlock<br />
3CG Tip Confirmation System for placement of peripherally<br />
inserted central catheters. https://www.nice.org.uk/<br />
guidance/mtg24 (accessed 24/08/2015).<br />
22. Hudman L, Bodenham A. Practical aspects of long-term<br />
venous access. Continuing Education in Anaesthesia, Critical<br />
Care and Pain 2013; 13: 6–11.<br />
23. Kander T, Frigyesi A, Kjeldsen-Kragh J, Kalsson H, Rolander F,<br />
Schott U. Bleeding complications after central line insertions:<br />
relevance of pre-procedure coagulation tests and institutional<br />
transfusion policy. Acta Anaesthesiologica Scandinavica 2013;<br />
57: 573–9.<br />
24. Massicotte MP, Dix D, Monagle P, Adams M. Central venous<br />
catheter related thrombosis in children: analysis of the<br />
Canadian Registry of Venous Thromboembolic Complications.<br />
Journal of Paediatrics 1998; 133: 770–6.<br />
25. Miller DL, Va~no E, Bartal G, et al. Occupational radiology protection<br />
in interventional radiology: a Joint Guideline of the<br />
Cardiovascular and Interventional Radiology Society of Europe<br />
and the Society of Interventional Radiology. Cardiovascular<br />
Interventional Radiology 2010; 33: 230–9.<br />
26. Royal College of Radiologists. Standards for Intravascular Contrast<br />
Agent Administration in Adult Patients. Second Edition.<br />
https://www.rcr.ac.uk/sites/default/files/.../BFCR(10)4_Stand_<br />
contrast.pdf (accessed 24/08/2015).<br />
27. Breschan C, Platzer M, Jost R, Stettner H, Likar R. Size of internal<br />
jugular vs subclavian vein in small infants: an observational,<br />
anatomical evaluation with ultrasound. British Journal<br />
of Anaesthesia 2010; 105: 179–84.<br />
28. Arul GS, Livingston H, Bromley P, Bennett J. Ultrasound-guided<br />
percutaneous insertion of 2.7Fr tunnelled Broviac lines in neonates<br />
and small infants. Pediatric Surgery International 2010;<br />
26: 815–8.<br />
29. Medicines and Healthcare products Regulatory Agency, UK.<br />
Chlorhexidine solutions: reminder of the risk of chemical<br />
burns in premature infants. www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON468292<br />
(accessed 17/10/<br />
2015).<br />
30. Gallagher RA, Levy J, Vieiraet RL, et al. Ultrasound assistance<br />
for central venous catheter placement in a pediatric<br />
emergency department improves placement success rates.<br />
Academic Emergency Medicine 2014; 21: 981–6.<br />
31. Nolan JP, Smith RN. Central venous catheters. British Medical<br />
Journal 2013; 347: f6570.<br />
32. Morano SG, Coppola L, Latagliata R, et al. Early and late complications<br />
related to central venous catheters in haematological<br />
malignancies: a retrospective analysis of 1102 patients.<br />
Mediterranean Journal Hematological Infectious Diseases<br />
2014; 6: e2014011.<br />
33. NHS England patient Safety Domain. National Safety Standards<br />
for Invasive Procedures 2015. https://www.england.nhs.uk/patientsafety/never-events/natssips/<br />
(accessed 08/01/<br />
2016).<br />
12 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland
Bodenham et al. | Safe vascular access guidelines Anaesthesia 2016<br />
34. Pikwer A, Akeson J, Lindgren S. Complications associated with<br />
peripheral or central venous routes for central venous cannulation.<br />
Anaesthesia 2012; 67: 65–71.<br />
35. Akl EA, Ramly EP, Kahale LA, et al. Anticoagulation for people<br />
with cancer and central venous catheters. Cochrane Database<br />
of Systematic Reviews 2014; 10: CD006468.<br />
36. Lamperti M, Bodenham AR, Pittiruti M, et al. International<br />
evidence-based recommendations on ultrasound-guided vascular<br />
access. Intensive Care Medicine 2012; 38: 1105–17.<br />
37. Reuber M, Dunkley LA, Turton EP, Bell MD, Bamford JM. Stroke<br />
after internal jugular venous cannulation. Acta Neurologica<br />
Scandinavica 2002; 105: 235–9.<br />
38. Domino KB, Bowdle TA, Posner KL, Spitellie PH, Lee LA, Cheney<br />
FW. Injuries and liability related to central vascular catheters. A<br />
closed claims analysis. Anesthesiology 2004; 100: 1411–8.<br />
39. Pikwer A, Acosta S, Kolbel T, Malina M, Sonesson B, Akeson J.<br />
Management of inadvertent arterial catheterisation associated<br />
with central venous access procedures. European Journal Vascular<br />
and Endovascular Surgery 2009; 38: 707–14.<br />
40. Bodenham A. Reducing major procedural complications from<br />
central venous catheterisation. Anaesthesia 2011; 66: 6–9.<br />
41. Peris A, Zagli G, Bonizzoli M, et al. Implantation of 3951 longterm<br />
central venous catheters: performances, risk analysis,<br />
and patient comfort after ultrasound-guidance introduction.<br />
Anesthesia and Analgesia 2010; 111: 1194–201.<br />
42. Nayeemuddin M, Pherwani AD, Asquith JR. Imaging and management<br />
of complications of central venous catheters. Clinical<br />
Radiology 2013; 68: 529–44.<br />
43. Stuart RK, Baxter JK, Shikora SA, et al. Reducing arrhythmias<br />
associated with central venous catheter insertion or<br />
exchange. Nutrition 1992; 8: 19–21.<br />
44. Abdel-Aal AK, Saddekni S, Hamed MF. Guide wire entrapment<br />
in a vena cava filter: techniques for dislodgement. Vascular<br />
and Endovascular Surgery 2012; 47: 115–23.<br />
45. NHS England, Never Events List 2015/16. www.england.nhs.<br />
uk/wp-content/.../03/never-evnts-list-15-16.pdf. (accessed<br />
24/08/2015).<br />
46. Wu C, Fu J, Feng P, et al. Catheter fracture of intravenous<br />
ports and its management. World Journal of Surgery 2011;<br />
35: 2403–10.<br />
47. Lopez-Briz E, Ruiz Garcia V, Cabello JB, Bort-Marti S, Carbonell<br />
Sanchis R, Buris A. Heparin versus 0.9% sodium chloride<br />
intermittent flushing for prevention of occlusion in central<br />
venous catheters in adults. Cochrane Database of Systematic<br />
Reviews 2014; 10: CD008462.<br />
48. Van Miert C, Hill R, Jones L. Interventions for restoring patency<br />
of occluded central venous catheter lumens. Cochrane Database<br />
of Systematic Reviews 2012; 4: CD007119.<br />
49. Pronovost P1, Needham D, Berenholtz S, et al. An intervention<br />
to decrease catheter-related bloodstream infections in<br />
the ICU. New England Journal of Medicine 2006; 355: 2725–<br />
32.<br />
50. Bion J1, Richardson A, Hibbert P, et al. ‘Matching Michigan’: a<br />
2-year stepped interventional programme to minimise central<br />
venous catheter-blood stream infections in intensive care<br />
units in England. British Medical Journal Quality Safety 2013;<br />
22: 110–23.<br />
51. Loveday HP, Wilson JA, Pratt RJ, et al. EPIC 3: national evidence-based<br />
guidelines for preventing healthcare-associated<br />
infections in NHS hospitals in England. Journal of Hospital<br />
Infection 2014; 86: S1–S70.<br />
52. Association of Anaesthetists of Great Britain and Ireland. Infection<br />
Control in Anaesthesia. Anaesthesia 2008; 63(1027–3): 6.<br />
53. Moureau N, Lamperti M, Kelly LJ, et al. Evidence-based<br />
consensus on the insertion of central venous access devices:<br />
definition of minimal requirements for training. British Journal<br />
of Anaesthesia 2013; 110: 347–56.<br />
54. AAGBI. Consent for Anaesthesia 2006. www.<strong>aagbi</strong>.org/sites/<br />
default/files/consent06.pdf (accessed 24/08/2015).<br />
55. Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound<br />
guidance versus anatomical landmarks for internal<br />
jugular vein catheterization. Cochrane Database of Systematic<br />
Reviews 2015; 1: CD006962.<br />
56. Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound<br />
guidance versus anatomical landmarks for subclavian<br />
or femoral vein catheterization. Cochrane Database of Systematic<br />
Reviews 2015; 1: CD011447.<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland 13
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
Anaesthesia 2016, 71, 1503<br />
Correction<br />
doi:10.1111/anae.13691<br />
Following an item of correspondence, the authors of the guidelines [1] agree that the evidence for pH being an<br />
important determinant for suitability for peripheral intravenous administration of fluids is equivocal and limited.<br />
Therefore, the authors would like to correct the following advice given in the section on peripheral cannulation:<br />
Peripheral insertion is inappropriate for infusion of fluid with high osmolality (> 500 mOsm.l<br />
high pH (> 9) or intravenous access for more than 2 weeks.<br />
1 ) or low (< 5) or<br />
This should read:<br />
Peripheral insertion is inappropriate for some fluids and drugs e.g. high osmolality > 500 mOsm.l<br />
vasopressors or intravenous access for more than 2 weeks. Check local or national guidance.<br />
1 , potent<br />
Reference<br />
1. Bodenham A, Babu S, Bennett J, et al. Association of Anaesthetists of Great Britain and Ireland: Safe vascular access 2016. Anaesthesia<br />
2016; 71: 573–85.<br />
© 2016 The Association of Anaesthetists of Great Britain and Ireland 1503
AAGBI SAFETY GUIDELINE<br />
Safe Management of<br />
Anaesthetic Related Equipment<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org September 2009
Membership of the working party<br />
Dr J A Carter<br />
Dr L W Gemmell<br />
Prof M Y K Wee<br />
Dr C Meadows<br />
Dr T Clutton-Brock<br />
Dr C Waldmann<br />
Dr D Scott<br />
Dr P Bickford-Smith<br />
Dr A Wilkes<br />
Mr C Bray<br />
Mr D McIvor<br />
Mr H Cooke<br />
Ex Officio<br />
Dr R J S Birks<br />
Dr D K Whitaker<br />
Dr A W Harrop-Griffiths<br />
Dr I H Wilson<br />
Dr I G Johnston<br />
Dr E P O’Sullivan<br />
Dr D G Bogod<br />
Chair<br />
AAGBI Honorary Secretary<br />
AAGBI Council Member<br />
Immediate Past GAT Chair<br />
Royal College of Anaesthetists<br />
Intensive Care Society<br />
AAGBI Standards Committee<br />
AAGBI Standards Committee<br />
Medical Device Evaluation Centre<br />
Medicines and Heathcare products<br />
Regulatory Agency<br />
Medicines and Heathcare products<br />
Regulatory Agency<br />
Barema, Trade Association for<br />
Anaesthetic & Respiratory Equipment<br />
President<br />
Immediate Past President<br />
Immediate Past Honorary Secretary<br />
Honorary Treasurer<br />
Honorary Treasurer Elect<br />
Honorary Membership Secretary<br />
Editor-in-Chief, Anaesthesia
Contents<br />
1. Summary 2<br />
2. Introduction 3<br />
3. Responsibility of anaesthetists and Trust or other<br />
healthcare providing organisation 4<br />
4. Standards 8<br />
5. Responsibility of manufacturers and suppliers 10<br />
6. Choosing and trialling equipment 12<br />
7. Public sector procurement regulations and directives<br />
and the process of purchasing 15<br />
8. Commissioning new equipment 19<br />
9. Shared equipment 20<br />
10. Maintenance 21<br />
11. Replacement 24<br />
12. Disposal 25<br />
13. User training 27<br />
14. Incident reporting and investigation 30<br />
15. Audit 33<br />
Glossary of acronyms 33<br />
References 35<br />
Useful numbers and websites 37<br />
To be reviewed by 2015<br />
© Copyright of the Association of Anaesthetists of Great Britain & Ireland. No<br />
part of this book may be reproduced without the written permission of the<br />
AAGBI<br />
1
1. Summary<br />
1.1 Safety, quality and performance considerations must be<br />
included in all equipment acquisition decisions.<br />
1.2 Each directorate should nominate one consultant with<br />
responsibility for equipment management. This Nominated<br />
Consultant should be a member of a Medical Devices<br />
Management Group, which reports directly to the Trust<br />
Board, and he or she should liaise closely with the<br />
Technical Servicing Manager.<br />
1.3 An inventory of all equipment, including donated<br />
equipment, must be held by the technical department for<br />
maintenance and replacement purposes.<br />
1.4 A planned preventative maintenance programme must be<br />
in place.<br />
1.5 There should be a policy to cope with equipment<br />
breakdown.<br />
1.6 A replacement programme which defines equipment life<br />
and correct disposal procedures should be in place.<br />
1.7 Purchase of new equipment should include wide<br />
consultation (especially involving users), and technical<br />
advice to ensure practicality, cost effectiveness and<br />
suitability for purpose.<br />
1.8 There must be a commissioning or acceptance procedure<br />
before any new equipment is put into use.<br />
1.9 All users must be trained in the use of all equipment that<br />
they may use.<br />
1.10 All adverse incidents arising from the use of equipment<br />
must be reported.<br />
2
2. Introduction<br />
The Association of Anaesthetists of Great Britain and Ireland has<br />
long been committed to improving patient safety. The majority<br />
of critical incidents in anaesthesia arise from human error and,<br />
although about 20% of incidents are due to equipment failure,<br />
many incidents that are initially thought to be equipment failure<br />
turn out to be user error or inappropriate use, both of which<br />
indicate a lack of training in the correct use of equipment.<br />
The Association has produced a number of guidelines with<br />
the intention of improving patient safety by reducing human<br />
error and detecting potential equipment failure. These include<br />
Checking Anaesthetic Equipment 3 (2004) and Standards of<br />
Monitoring during Anaesthesia and Recovery Edition 4 (2007)<br />
[1,2]. The Department of Health, through the MHRA, regularly<br />
produces Medical Device Alerts concerning problems with<br />
equipment, and it is essential that all anaesthetists are aware of<br />
relevant publications.<br />
This document gives guidance on choosing, purchasing,<br />
maintaining, replacing and disposing of equipment. It also<br />
emphasises the need to ensure that anaesthetists are trained in<br />
the use of their equipment and that technicians are trained to<br />
maintain the equipment. The MHRA publications, Managing<br />
Medical Devices DB 2006(05) and Devices in Practice – a guide<br />
for health and social care professionals (2008), are written from<br />
a technical point of view and should be used as an adjunct to<br />
the information in this booklet [3,4].<br />
In addition, the MHRA, or their local or national counterpart,<br />
is usually willing and able to give detailed advice on the safe<br />
management of equipment, and their contact details are given<br />
in the appendix.<br />
Throughout this document, the term ‘Trust’ refers to NHS Trusts,<br />
Health Boards, and any other hospital where anaesthetics are<br />
given.<br />
3
3. Responsibility of anaesthetists<br />
and Trust or other healthcare<br />
providing organisation<br />
3.1 The individual anaesthetist<br />
All anaesthetists must be adequately trained in the use of, and<br />
familiar with, all equipment which they use routinely. This<br />
training should be recorded, and individual anaesthetists should<br />
keep their own record of training for appraisal purposes. They<br />
should also be aware of Medical Device Alerts relevant to such<br />
equipment. They should all participate in selection of new<br />
equipment, training in the use of equipment, and reporting<br />
equipment associated incidents.<br />
3.2 The directorate – the nominated consultant or<br />
equipment officer/controller<br />
Anaesthetic directorates should nominate one consultant with<br />
responsibility for equipment (the ‘equipment officer’). The<br />
equipment officer will develop specific expertise with respect to<br />
equipment and be responsible for a co-ordinated approach to its<br />
management (including maintenance and training), replacement<br />
and purchase. He or she may wish to enlist the support of other<br />
colleagues or suitable operating department personnel to assist<br />
with the duties as well as consulting regularly with all members<br />
of the anaesthetic directorate. Identification of the departmental<br />
equipment officer is the responsibility of the clinical director<br />
who should ensure that the individual is identified to the various<br />
heads of the technical department.<br />
Large Trusts will need more than one consultant to fulfil this<br />
role, and an ‘equipment or technical team’, answerable to the<br />
Directorate Management Team, may be required.<br />
4
3.3 Duties of the equipment officer<br />
The equipment officer will represent the directorate on the<br />
Medical Devices Management Group and liaise closely with the<br />
head of the technical department. Their responsibilities include:<br />
• Co-ordinating user input into the choice and procurement<br />
of equipment and ensuring its suitability for the purposes<br />
intended.<br />
• Ensuring that training is available for staff in the use and<br />
care of the equipment and ensuring that appropriate training<br />
records are maintained.<br />
• Acceptance of equipment into service.<br />
• Ensuring that procedures for the use of equipment are<br />
followed.<br />
• Verification of service arrangements and effectiveness.<br />
• Supervision of user servicing tasks.<br />
• Ensuring there are documented contingency arrangements<br />
for patient care in the event of equipment failure.<br />
• Maintaining appropriate records.<br />
• Ensuring that the Trust’s policy applies to all equipment<br />
brought into the Trust irrespective of the source of funding,<br />
e.g. university purchased equipment, loaned and donated<br />
equipment.<br />
• Ensuring that all adverse incidents involving medical<br />
devices are reported in accordance with the instructions<br />
contained in the first Medical Device Alert of each year<br />
(titled ‘All Medical Devices’) issued by the MHRA<br />
and that all MHRA and NPSA safety guidance is distributed<br />
appropriately.<br />
Adequate sessional time to fulfil these duties should be made<br />
available by the Trust.<br />
5
3.4 The Trust - Medical Devices Management Group and<br />
Manager of Technical Servicing<br />
Trusts should establish a Medical Devices Management Group<br />
to develop and implement policies across their organisations.<br />
This group should report directly to the Trust Board, where a<br />
named director should have overall responsibility for medical<br />
equipment.<br />
The responsibility for the technical management of each item of<br />
equipment must be assigned to one department (the ‘technical<br />
department’). Most hospitals have a Manager of Technical<br />
Servicing in post although their title and the department to<br />
which they belong may vary, e.g. department of electronic<br />
and biomedical engineering, department of medical physics or<br />
estates department.<br />
3.5 Inventory of equipment<br />
Technical departments must maintain an ‘inventory of<br />
equipment’ which should include the following information:<br />
• Unique identifier of equipment – item labelled where<br />
possible (if not possible, e.g. endoscope, serial number<br />
recorded).<br />
• Date of purchase and when it was put into service.<br />
• Any specific legal requirements needed and whether they<br />
have been complied with.<br />
• Where it is located, and record of satisfactory<br />
commissioning/installation.<br />
• Recommended service schedule documentation.<br />
• Service arrangements – in-house, supplier, or external<br />
contractor details and service level agreement.<br />
• Service reports.<br />
• Records of incident investigations and product complaints.<br />
• Manual or ‘Instructions For Use’ (IFU) readily available, and<br />
record of where kept.<br />
• End-of-life date.<br />
6
In addition to items for which the technical department has<br />
continuing responsibility, the inventory should also include<br />
items such as laryngoscopes and non-clinical items such as<br />
computers and printers. Although these may not need regular<br />
maintenance they should be included in the replacement<br />
programme.<br />
Every item of equipment, including consumables, must be<br />
identified by a unique number or batch number, and its location<br />
must be recorded. This is particularly important in the case<br />
of equipment recall due to a subsequent fault. All equipment<br />
records should be held on one central record keeping system<br />
where possible, e.g. software database managed by medical<br />
engineering department. If this is not possible, adequate cross<br />
referencing between record systems must be in place. This<br />
is particularly important where equipment may be moved<br />
between sites.<br />
7
4. Standards<br />
4.1 Medical Devices Directive and CE marking<br />
The Medical Devices Directive of the European Union prohibits<br />
the sale of medical devices within the EU that are not CE<br />
(Conformité Européene) marked. A CE mark indicates that<br />
devices meet all essential requirements of the Medical Devices<br />
Directive and are safe and fit for their intended purpose.<br />
However, the CE mark does not indicate clinical efficacy in<br />
all circumstances, therefore user assessment is vital for any<br />
purchase.<br />
4.2 Standards<br />
To ensure suitability for a given task, most devices are<br />
manufactured to one or more verified standards. Standards are<br />
produced by CEN, the Comité Européen de Normalisation,<br />
or European Committee for Standardization, for mechanical<br />
devices, and CENELEC for electrical devices. Many devices<br />
used by anaesthetists use electricity to get mechanical results,<br />
and have to meet standards of both organisations. ISO, the<br />
International Organization for Standardization, and IEC the<br />
International Electrotechnical Commission, produce standards<br />
for the international market. The British Standards Institution<br />
is a national member of the European Organization, and its<br />
standards have gradually been integrated with their European<br />
equivalents.<br />
4.3 CE marking and non-medical equipment<br />
CE marks for medical devices are awarded in four categories<br />
of differing stringency. However, devices intended for nonmedical<br />
use may also bear a CE mark that is indistinguishable<br />
from those on medical devices, but they may not be suitable for<br />
use as medical devices. An example is computer equipment,<br />
including display units and recording devices, which may have<br />
electrical leakage currents which far exceed the safe levels<br />
for use near patients with external pacemakers or central lines<br />
8
that can conduct electricity directly to the heart. A formal risk<br />
assessment by an appropriate expert should be performed,<br />
followed by suitable modification, before such equipment is<br />
used close to patients.<br />
4.4 Non-EU equipment<br />
Equipment purchased outside the European Union may not<br />
carry CE marks. For advice concerning such equipment, see<br />
Medical Devices Regulations 2002 [5]. Use of non-CE marked<br />
medical devices may leave the clinician, and their employer,<br />
open to liability that would otherwise be assumed by the<br />
manufacturer.<br />
4.5 Permissible devices supplied without CE marking<br />
There are three exceptions permissible for a device to be<br />
supplied without a CE mark:<br />
• Custom Made – this is a single device designed and<br />
manufactured specifically for a specific patient as prescribed<br />
by a healthcare professional.<br />
• Device undergoing clinical investigations – the device must<br />
be labelled as such and have the necessary approval<br />
(see CA. ISO 14155).<br />
• Exceptional use on humane grounds.<br />
For both Custom Made and Clinical Trial devices the manufacturer<br />
must adhere to all other requirements for compliance.<br />
9
5. Responsibility of manufacturers<br />
and suppliers<br />
5.1 The Consumer Protection Act, Liability for Defective<br />
Products Act, and the Medical Devices Regulations<br />
The Consumer Protection Act 1988 (CPA) in Britain, the Liability<br />
for Defective Products Act 1991 (LDPA) in Ireland, and the<br />
Medical Devices Regulations in Great Britain and Ireland which<br />
implement the EC Medical Devices Directives into law, embody<br />
the current legislation which describes the manufacturer’s<br />
responsibility with regard to equipment.<br />
5.2 General responsibilities<br />
The CPA, LDPA and Medical Devices Regulations place<br />
absolute responsibility for the safety of products on the manufacturer.<br />
In the event of a defect causing injury, the manufacturer<br />
can be sued by any injured party, i.e. the patient or the<br />
purchaser. This is provided that the device has been used for its<br />
intended purpose, and in accordance with the manufacturer’s<br />
instructions. Negligence need not be proved and it is not<br />
possible for the seller to escape liability by exclusion clauses<br />
in the contract of sale. The manufacturer’s responsibility, as<br />
described in the CPA and LDPA, ends ten years after delivery of<br />
the equipment.<br />
After ten years, the purchaser, but not the patient, could still sue<br />
the manufacturer under the Sale of Goods Act in Britain or the<br />
Sale of Goods and Supply of Services Act in Ireland but it would<br />
probably be difficult to convince the court that the equipment<br />
was still ‘as supplied’.<br />
5.3 Compliance with the regulations and the competent<br />
authority<br />
To place a device on the market a medical device manufacturer<br />
must be in compliance with the applicable European<br />
10
Regulations, including those transposed in each of the member<br />
states, e.g. language requirements. With full compliance a<br />
manufacturer is then able, where applicable, to affix a CE mark<br />
demonstrating compliance with the essential requirements of the<br />
Directive. The Medical Devices Directive and the application of<br />
the CE mark was a legal requirement for all manufacturers with<br />
effect from 14th June 1998, following a 5-year transition period.<br />
Within the United Kingdom and Northern Ireland responsibility<br />
for the enactment and compliance with the Medical Devices<br />
Directives has been assigned to the Medicines and Healthcare<br />
products Regulatory Agency {(MHRA) (Competent Authority<br />
– CA)}, working in conjunction with the respective devolved<br />
administrations of Northern Ireland, Scotland and Wales. The<br />
CA for Ireland is the Irish Medicines Board, Medical Devices<br />
Department.<br />
11
6. Choosing and trialling equipment<br />
6.1 General principles<br />
Choosing anaesthetic equipment should address the<br />
requirements of safety, quality, performance and affordability<br />
(value for money). The selection process should take into<br />
account local and national acquisition policies. The choice of<br />
equipment should incorporate plans for standardisation and<br />
rationalisation to meet existing and future needs. The Medical<br />
Devices Management Group should ensure that acquisition<br />
requirement takes into account the needs and preferences of<br />
all interested parties including the user, the commissioning,<br />
decontamination, maintenance and de-commissioning parties.<br />
6.2 Criteria for choosing<br />
There are many different categories of equipment used in<br />
anaesthesia, ranging from low cost items purchased in large<br />
volumes to high cost items purchased in small numbers.<br />
Purchasers are encouraged to establish a list of available<br />
manufacturers and suppliers. The choice can then be made on<br />
evidence supplied on the following criteria:<br />
• Fitness for intended purpose/application, including ease of<br />
use.<br />
• Safety, quality and performance information from the<br />
manufacturer.<br />
• Rationalising the range of models versus diversity.<br />
• Requirement and availability of training and support<br />
services.<br />
• Single use where appropriate.<br />
• Maintenance, repair support services and availability of<br />
technical support.<br />
• Decontamination and disposal procedures, including<br />
recycling, compatible with local processes.<br />
• Previous performance, reliability and warranty details.<br />
• Lifetime costs.<br />
12
6.3 Assessing equipment and the final choice<br />
Equipment under consideration can be assessed by various<br />
means. A literature review can be carried out to provide the<br />
best evidence. Organisations such as the Centre for Evidencebased<br />
Purchasing (CEP, which was part of the NHS Purchasing<br />
and Supply Agency) and Emergency Care Research Institute (a<br />
US-based organisation) publish reports on various categories<br />
of equipment. For up-to-date information, purchasers should<br />
contact and visit other users, trade exhibitors and sometimes<br />
factories. In particular, previous performance by the<br />
manufacturer in terms of delivery, stock held, training provided<br />
and response to problems are rarely published, but details could<br />
be obtained from users in other Trusts.<br />
The Medical Devices Management Group, including the<br />
anaesthetic equipment officer, should then carefully consider<br />
the options from the information available. Once a choice is<br />
made, a trial should be carried out on the selected equipment<br />
by users. As many users as possible should be encouraged<br />
to participate and to feedback to the equipment officer on an<br />
agreed form. Such forms are often a compulsory part of the<br />
purchasing procedure.<br />
The outcomes from trials of some equipment can be assessed<br />
against the known outcomes from ‘gold standard’ equipment,<br />
for example first time insertion success of laryngeal mask<br />
airways. The manufacturer will usually provide a free loan<br />
of equipment or samples if the products are disposable. It is<br />
important to remember that NHS contract terms impose full<br />
responsibility on the suppliers for equipment on loan. All staff<br />
using loan equipment must be trained by the supplier or an<br />
authorised agent. It is the Trust’s responsibility to ensure that<br />
loan equipment is decontaminated before return to prevent<br />
cross-infection.<br />
To avoid unnecessary duplication of trials, the anaesthetic<br />
13
equipment officer is encouraged to collect all feedback from<br />
the trial and publish the outcome in an appropriate format, for<br />
example at a local or national meeting. The equipment officer<br />
will then recommend the choice of equipment to purchase.<br />
An editorial in Anaesthesia in June 2008 recommended<br />
establishing a Device Evaluation Centre with a panel of experts<br />
to critically appraise available evidence and publish the results<br />
on a website [6]. Individual groups of anaesthetists would be<br />
encouraged to undertake studies with support from the Device<br />
Evaluation Centre in terms of pro formas for ethical approval<br />
and protocols, and statistical help and advice. This would avoid<br />
duplication of trials by individual Trusts and researchers, and<br />
enable rapid removal of inferior products.<br />
6.4 ‘One size suits all’<br />
Having a variety of models for the same purpose can<br />
increase the risk of operator confusion, leading to misuse and<br />
complicating training requirements. In particular, having both<br />
single-use and re-usable equipment intended for the same<br />
purpose could result in re-usable equipment being discarded<br />
and vice versa, resulting in increased costs or potential harm to<br />
the patient and exposing the Trust to risk. Restricting purchase<br />
and stockholding to one type of device reduces these risks and<br />
may reduce maintenance costs. On the other hand, restriction<br />
to one product will increase vulnerability to product faults,<br />
and remove a degree of clinical freedom from individual<br />
practitioners.<br />
6.5 Leasing or purchasing<br />
Consideration should be given whether equipment should be<br />
purchased outright, leased or rented. For example, it may be<br />
more cost effective to rent an expensive item for occasional use<br />
when required.<br />
14
7. Public sector procurement<br />
regulations and directives and the<br />
process of purchasing<br />
7.1 Standing orders and standing financial instructions<br />
(SFIs)<br />
The process of procurement of goods and services in the NHS<br />
is governed by SFIs. There is a financial value for an order or<br />
contract above which a competitive process should be used;<br />
often this is in the region of £15,000 to £30,000.<br />
7.2 Procurement directives<br />
All public sector procurement is subject to the principles of the<br />
Treaty of Rome (transparency and fairness) and the significant<br />
majority (including all medical equipment) is also subject to<br />
the EU Procurement Directives. The Directives were updated<br />
in 2006 to account for the use of eEnablement technologies<br />
in public sector procurement and enable greater flexibility for<br />
complex procurements.<br />
The relevant Directive for medical equipment is the<br />
Procurement Directive 2004/18/EC, 31 March 2004 for Public<br />
Contracts for which the UK Regulation that enforces the<br />
Directive is Public Contracts Regulations SI 2006 No 5 [7,8].<br />
7.3 EU procurement thresholds<br />
The EU Procurement Directives apply to all orders and contracts<br />
for any given organisation (or groups of organisations when<br />
collaborative procurement is undertaken). Splitting lots to avoid<br />
the thresholds contravenes the Directives. A notice of intent<br />
(indicative notice) of known future expenditure should be<br />
placed.<br />
15
EU procurement thresholds<br />
Thresholds applicable from 1 January 2008 are given<br />
below. Thresholds are net of VAT. Public contracts<br />
regulations 2006 - from 1 January 2008<br />
Other public<br />
sector<br />
contracting<br />
authorities<br />
Indicative<br />
notices<br />
SUPPLIES SERVICES WORKS<br />
£139,893<br />
(€206,000)<br />
£509,317<br />
(€750,000)<br />
£139,893<br />
(€206,000)<br />
£509,317<br />
(€750,000)<br />
£3,497,313<br />
(€5,150,000)<br />
£3,497,313<br />
(€5,150,000)<br />
(NB. The Euro values are the reference quantities. The<br />
conversion rate to pounds was based on a exchange rate of 0.68<br />
which may vary).<br />
7.4 Process of purchasing<br />
Most Trusts will use the following process for the purchase<br />
of medical equipment unless it is part of a more complex<br />
procurement. The basic steps involved in this process are:<br />
• Indicative notice (if relevant)<br />
• Advert in the Official Journal of the European Union (OJEU)<br />
• Suppliers express an interest<br />
• Suppliers provide prequalification information (should be<br />
via the NHS supplier information database, SID)<br />
• Short listing and suppliers notified<br />
• Issue of tender<br />
• Presentations by suppliers, visits to suppliers<br />
• Return of completed tender by suppliers<br />
• Evaluation of tenders<br />
• Award notified<br />
• Standstill period (see 7.6)<br />
• Award of contract<br />
16
More guidance on the application can be found on the Office of<br />
Government Commerce and NHS PaSA websites [9,10].<br />
7.5 Purchasing and Supply Agency (PaSA) and ‘Buying<br />
Solutions’<br />
By 2010 the function of PaSA will be taken over by ‘Buying<br />
Solutions’ – the national procurement partner for UK public<br />
services. It is planned that a series of regional support units,<br />
owned by the NHS, will provide a single point of contact for<br />
suppliers in each region.<br />
7.6 Mandatory standstill period<br />
The 2006 UK Regulations also brought into force a<br />
mandatory 10-day standstill period between the notification<br />
of award decision and the date of contract conclusion for all<br />
procurements that are subject to the full scope of the EU public<br />
procurement directives. This is not part of the EU Directives but<br />
follows the Alcatel court case [11].<br />
7.7 Pre-purchase questionnaires<br />
Medical equipment will often be subject to the completion<br />
of a pre-purchase questionnaire (PPQ) by the supplier for the<br />
Trust’s EBME Department. The PPQ is usually completed by the<br />
supplier before or with the order.<br />
7.8 Funding<br />
Major items of equipment (e.g. workstations, monitors) are<br />
funded by the Trust Capital Equipment Committee or similar.<br />
Consumables and items below a threshold figure (usually about<br />
£5000) come out of the directorate or theatre budget.<br />
There should be a planned process of replacement for major<br />
equipment, such as anaesthetic workstations and monitors, so<br />
that each year a proportion of these are replaced in order to<br />
spread the cost. It should be presumed that such equipment<br />
will last about eight years, and the whole life cost taken into<br />
consideration.<br />
17
When negotiating a purchasing agreement for major equipment,<br />
a training package should be included and consideration given<br />
to awarding a servicing agreement. It is often advantageous<br />
to bundle extras into the initial deal rather than pay for<br />
expensive software upgrades at a later date. It is advisable to<br />
compare the complete purchasing agreement from more than<br />
one manufacturer, and in return for notifying the intention to<br />
purchase future equipment from the same company it may<br />
be possible to fix the price for a few years (plus inflation).<br />
This allows the company to plan ahead and the hospital to<br />
standardise equipment.<br />
Advances in technology inevitably give rise to new equipment,<br />
and justification of need through a business case may have to<br />
be submitted to the Trust for approval. In some cases additional<br />
funding has been made available from central sources for<br />
‘essential’ new equipment, such as NICE funding for ultrasound<br />
guided CVC placement. Charitable sources of funding also exist,<br />
e.g. League of Friends, but such organisations prefer not to fund<br />
items which should be bought by the Trust. A personal approach<br />
to such organisations with details of how patient care will be<br />
enhanced is recommended.<br />
18
8. Commissioning new equipment<br />
The MHRA Device Bulletin ‘DB2006(05) Managing Medical<br />
Devices. Guidance for healthcare and social services<br />
organisations’ gives comprehensive advice on commissioning<br />
new equipment [3]. Key major points are summarised below:<br />
• It is important that deliveries of new equipment are<br />
recorded, and go to the right place.<br />
• New anaesthetic equipment, which may not all come at the<br />
same time, has to be unpacked, assembled, recorded on<br />
an inventory, have identifying labels attached, and safety<br />
checks performed. Medical engineering departments will<br />
usually perform these tasks, although sometimes it is the<br />
responsibility of the manufacturer or supplier.<br />
• It should also be noted that Portable Appliance Testing<br />
(PAT) applies to all equipment used in hospitals including,<br />
for example, the coffee machine in the anaesthetic dept.<br />
• Co-ordination between several departments may be<br />
necessary, especially if permanent installation work or<br />
additional services are required.<br />
• Before equipment is used for the first time, full functional<br />
checks must be performed, and staff trained in its use.<br />
• If the equipment uses specialised consumable items,<br />
arrangements to purchase them should be set up well before<br />
the initial stock runs out.<br />
• Loan equipment has to go through a similar process, and<br />
should be subject to a written agreement defining responsibilities<br />
and liabilities.<br />
19
9. Shared equipment<br />
Many types of equipment used by anaesthetists are also used<br />
by other specialties in a variety of locations throughout a<br />
hospital or unit. There are many safety, efficiency and cost<br />
advantages in standardisation. In terms of the patient journey,<br />
for example from admission through accident and emergency,<br />
to radiology, operating theatre, intensive care unit and ward,<br />
the process is considerably simpler and safer if the devices the<br />
patient is attached to all use the same connections to monitoring<br />
devices and infusion systems. It aids staff training and mobility if<br />
similar devices are in use in most areas of a hospital, important<br />
examples being defibrillators and infusion pumps. This may<br />
be facilitated if the equipment officer and the Medical Devices<br />
Management Group liaise closely with the departments using<br />
similar equipment, e.g. intensive care, accident and emergency,<br />
radiology, cardiology and respiratory medicine.<br />
Although departments may wish to compile their own inventory<br />
of equipment for which they have managerial and financial<br />
responsibility, it is a requirement that a database of all such<br />
equipment is maintained by the technical department.<br />
Areas of uncertainty over ownership of equipment should<br />
be clarified. Examples include infusion pumps, patient<br />
controlled analgesia equipment, and blood warmers. It may<br />
be appropriate for some high value items to be shared, and for<br />
commonly used equipment like infusion pumps to be located in<br />
a central store.<br />
The financial implications of asset sharing should be clarified.<br />
Each directorate may have to contribute to the costs of<br />
depreciation, servicing, maintenance and replacement.<br />
Responsibilities for organising and monitoring servicing and<br />
maintenance schedules and for planning replacement must be<br />
defined.<br />
20
10. Maintenance<br />
10.1 Planned preventative maintenance programme<br />
Anaesthetic equipment which is not serviced regularly is liable<br />
to break down with potentially life-threatening consequences.<br />
A planned preventative maintenance programme is essential.<br />
A maintenance log for each device must be kept, linked to the<br />
technical department inventory. A record of all breakdowns<br />
should also be kept. Regular review of each class of item<br />
should reveal the incidence of breakdowns, which could<br />
indicate the need for modification of equipment, frequency<br />
of maintenance or its urgent replacement, or even a need for<br />
further user training.<br />
10.2 Choice of provider<br />
All suppliers must support their equipment, and this includes<br />
maintenance. At the time of purchase, the ‘life time’ cost should<br />
be determined, including the frequency and cost of regular<br />
servicing proposed by the supplier. It is recommended that the<br />
cost of maintenance contracts should be inclusive of emergency<br />
call outs and travel time for engineers, as well as fixed interval<br />
servicing and parts. Cheaper alternatives usually exclude<br />
the cost of emergency call outs and travel time and may be<br />
appropriate for hospitals with sufficient back-up equipment.<br />
Trusts may prefer ‘in-house’ maintenance, as this could have<br />
logistic and cost advantages. The support to be provided by<br />
manufacturers must be defined when equipment is purchased<br />
and should include the provision of service manuals, on-going<br />
technical training and spare parts. If upgrading or modification<br />
of equipment is required at a later date, there are likely to be<br />
additional costs even if the work is to be done in-house. An<br />
annual maintenance budget of at least 10% of the equipment’s<br />
purchase cost is necessary.<br />
Software upgrades must only be undertaken by the supplier.<br />
21
Third party servicing is another option which may be of<br />
particular value for the maintenance of equipment which<br />
requires specialist knowledge and testing, e.g. vaporisers.<br />
Care should be taken to make sure only original equipment<br />
manufacturers (OEM) spare parts are used.<br />
Whichever of these options are chosen, it is essential that they<br />
are fully integrated into the planned maintenance programme.<br />
10.3 Equipment breakdown<br />
The equipment officer should ensure that a complete set of<br />
back-up equipment is available. If it is not, removal of faulty<br />
equipment from service may result in the cancellation of<br />
operating lists with consequent distress to patients and possible<br />
implications for the fulfilment of contracts. The equipment<br />
officer should agree a departmental policy covering the unusual<br />
event that two identical items break down at the same time,<br />
and should support colleagues who invoke this policy. The<br />
policy should be written so that the patient’s best interests are<br />
protected whatever the prevailing circumstances.<br />
In the interests of patient safety, it is essential for all theatres to<br />
keep available manual resuscitation equipment for emergency<br />
use (see Checking Anaesthetic Equipment 3, 2004) [1]. All<br />
theatre staff should be trained in the procedures to be followed<br />
for instances of equipment failure.<br />
10.4 Training in maintenance<br />
Suppliers and their agents are externally audited in all their<br />
procedures, and these include the provision of maintenance.<br />
These standards for quality management systems aid effective<br />
control through the definition and documentation of activities,<br />
the keeping of records to prove that these activities are being<br />
effectively executed and the audit of records by both internal<br />
and external personnel.<br />
22
For ‘in-house’ departments, quality manuals which document<br />
operating policies and procedures need to be verified. These<br />
will cover not only existing activities such as purchasing, repair<br />
and pre-planned maintenance but also other activities such as<br />
document control, corrective action and quality records.<br />
If ‘in-house’ maintenance is chosen, enough time and money<br />
must be allocated for training of technicians to a level<br />
equivalent to that of the supplier so that they are able to provide<br />
a high-quality, safe service. Regular on-going training provided<br />
by the supplier should be the norm.<br />
10.5 Spares<br />
Suppliers have a responsibility to provide spares for seven years<br />
after delivery of the last example of a particular model.<br />
The responsibility for obsolete devices more than seven years<br />
old is that of the Trust, and the need for insurance should be<br />
assessed and acted upon.<br />
10.6 Modifications<br />
If a modification is undertaken on a CE marked device, other<br />
than by the manufacturer, then responsibility for the safety and<br />
liability for the modification changes to the organisation that<br />
has completed the modification. One particular example is if a<br />
device labelled as single-use is reprocessed for further use.<br />
23
11. Replacement<br />
11.1 Planned equipment replacement programme<br />
Equipment must be condemned and replaced before it becomes<br />
unreliable and endangers the patient, and it is recommended a<br />
planned equipment replacement programme, which is phased<br />
over a number of years, is prepared and continuously updated.<br />
This should be planned in conjunction with Trust management<br />
and the finance department. The choice of new equipment<br />
can then be made after appropriate trials, and should take into<br />
account department needs, such as plans for standardisation<br />
and rationalisation (see section 6).<br />
11.2 Timing of equipment replacement<br />
Nationally recognised guidelines on the timing of equipment<br />
replacement do not exist. Therefore it is recommended that<br />
equipment be replaced when it has reached the end of an<br />
agreed time-period, and in consultation with finance officers.<br />
This time period will depend on the type of equipment that<br />
needs replacing.<br />
Replacement of electronic equipment should be considered at<br />
five years and mechanical equipment at eight years. Financial<br />
forecasting should take into account the agreed equipment life<br />
cycle and budgets should be adjusted accordingly to ensure<br />
replacement funding is available, thus avoiding delays and<br />
potential associated patient risks. When delays are inevitable,<br />
clinicians should seek, in writing, an ‘extension of use’ beyond<br />
the agreed time-periods with the relevant medical and financial<br />
officers.<br />
In the past, many items of anaesthetic equipment were<br />
mechanical. Today, most devices contain a high electronic<br />
content, including software. This is placing an increasing burden<br />
on equipment replacement budgets, owing to the increased<br />
pace of obsolescence of electronic equipment.<br />
24
12. Disposal<br />
12.1 General<br />
Unreliable, damaged or worn out equipment should be<br />
removed from service and destroyed. Obsolete but functional<br />
equipment has potential resale value but carries with it liabilities<br />
under the CPA and LDPA. There are companies who can<br />
manage such transactions. The DoH has issued guidelines on<br />
the resale of medical equipment in MHRA DB2006(05) [3].<br />
Alternatively, equipment can be donated to a charity. The donor<br />
has a moral responsibility to ensure that the recipients are given<br />
all relevant information about the equipment.<br />
Full service history, usage, fault log, replacement parts and<br />
decontamination status should be available when equipment is<br />
offered for sale or donation.<br />
Disposed equipment must be removed from the capital asset<br />
register.<br />
12.2 European WEEE Directive<br />
The European WEEE Directive enforces the recovery and<br />
recycling of certain types of electrical and electronic equipment<br />
(EEE) when it is disposed of. The Directive places a requirement<br />
on producers and/or final users to recover and recycle the<br />
equipment in line with specific rules. Producers of electrical and<br />
electronic items are required to register with the Environment<br />
Agency, through organisations referred to as ‘compliance<br />
schemes’, and are required to provide information relating to<br />
material content and recycling [12].<br />
12.3 Re-use of equipment<br />
Equipment that may be used on more than one patient should<br />
be decontaminated or sterilised according to manufacturer’s<br />
instructions and the AAGBI guidelines (see Infection Control<br />
in Anaesthesia 2, 2008) [13]. Some equipment has a limited<br />
25
number of re-uses (e.g. re-usable LMAs) and a record card or<br />
similar device must be used to maintain an accurate record of<br />
the number of re-uses. Any equipment bearing the mark of a<br />
figure 2 with a line crossed through it is for single use only and<br />
must not be re-used.<br />
26
13. User training<br />
13.1 General<br />
Anaesthetists must be trained in the use of all the equipment<br />
that they may use. Training requirements clearly vary widely<br />
between different devices, some requiring little or no additional<br />
training apart from common sense, others being unusable<br />
without complex and specific training. There is little or no<br />
national framework for the standardisation of training in use of<br />
devices in anaesthesia or indeed in any other clinical field, with<br />
the result that currently it is the responsibility of the individual<br />
clinician to ensure that he or she has received the appropriate<br />
training and that it is kept up-to-date. A record of training<br />
received by department members should be kept, and it should<br />
form part of the annual appraisal process.<br />
In more than half of the adverse incidents reported to the<br />
Medicines and Healthcare products Regulatory Agency (MHRA)<br />
there is no readily identifiable equipment fault. Although often<br />
difficult to define precisely, it seems more than reasonable<br />
to assume that many of these have resulted from user related<br />
issues. In some cases it is clear that the user has been the sole<br />
cause of the adverse incident which would not have occurred if<br />
the device had been correctly used.<br />
13.2 Manufacturers’ obligations<br />
Manufacturers of medical devices have a legal obligation to<br />
supply Instructions For Use (IFU) which cover not only how<br />
to use the device but also a description of the intended use of<br />
the device. Using the device outside of the IFU removes much<br />
of the manufacturer’s responsibility and transfers it to the user.<br />
Manufacturers should be encouraged to produce IFUs which<br />
are easy to read and understand; there may be a significant<br />
advantage in producing a summary of the important points or<br />
key instructions. Where practical, these should be available on<br />
the equipment, or held in close proximity.<br />
27
Where new equipment is purchased the amount of training<br />
offered and taken up is very variable. For example, with<br />
complex devices, such as the new generation of anaesthetic<br />
machine workstations, it is usual for manufacturers to supply a<br />
significant amount of user training.<br />
13.3 CCT and CPD<br />
Training in anaesthesia, as described in the CCT documents<br />
published by the Royal College of Anaesthetists, includes<br />
numerous references to anaesthetic related equipment, and both<br />
Primary and Final FRCA examinations cover the basic principles<br />
and more advanced use of a range of medical devices.<br />
Information about new devices and updates on existing ones is<br />
frequently included in Continuing Professional Development<br />
(CPD) programmes, and clinicians should use this as a way of<br />
keeping up-to-date.<br />
13.4 E-learning, simulation and revalidation<br />
E-learning material is now becoming available, in particular<br />
(from the MHRA) on the general principles in using medical<br />
devices safely, e.g. electrosurgery and the anaesthetic machine.<br />
These programmes underline the importance of maintaining<br />
a good understanding of the basic principles behind device<br />
function. For complex devices such as anaesthesia workstations<br />
complementary device-specific educational material is required.<br />
To maintain the necessary independence of bodies with national<br />
regulatory roles means that this type of material will, most<br />
probably, be developed by partnerships between manufacturers,<br />
the Association of Anaesthetists and the Royal College of<br />
Anaesthetists.<br />
There is a coexistent need to develop effective training in the<br />
use of equipment in unanticipated and emergency situations,<br />
particularly in the recognition and management of equipment<br />
failure. These situations fortunately occur infrequently, and<br />
28
anaesthetic simulators already play an important role in<br />
appropriate training.<br />
Users of complex equipment outside of the healthcare setting<br />
(for example in the aviation industry) are subject to much more<br />
clearly defined appropriate training in safety. All responsible<br />
clinicians will use the opportunities provided by CPD to keep<br />
their equipment based skills up-to-date but there are concerns<br />
that the less motivated can still function on a daily basis without<br />
adequate checks on acquisition or retention of skills.<br />
Revalidation of all clinical staff will help to ensure that all<br />
practitioners have up-to-date equipment based skills and have<br />
received appropriate training. Effective training material, with<br />
meaningful assessments, need to be developed. Such material is<br />
already available in some clinical disciplines through e-learning.<br />
29
14. Incident reporting and<br />
investigation<br />
As a profession which emphasises life-long learning, we must<br />
promote an open culture in which all staff will discuss and<br />
report incidents where errors or service failures have occurred.<br />
This encourages the profession to learn from mistakes and<br />
identify any continuing risks.<br />
Each NHS Trust should have risk management systems in place<br />
involving the reporting, analysis, control and prevention of<br />
incidents [14]. It is the responsibility of each anaesthetist to be<br />
aware of the incident reporting procedures of their organisation.<br />
This procedure may include risk managers, medical device<br />
liaison officers and anaesthetic equipment officers.<br />
In addition to the Trust’s local incident reporting system, there<br />
are several organisations, listed below, that may need to be<br />
made aware of adverse incidents associated with anaesthesia.<br />
14.1 Medicines and Healthcare products Regulatory<br />
Agency (MHRA)<br />
The MHRA investigate reports of adverse incidents involving<br />
medical devices or their instructions for use that have led to,<br />
or could lead to, death, life-threatening illness or injury. The<br />
manufacturers of medical devices must report such incidents to<br />
the Competent Authority (the Vigilance System) and investigate<br />
them as part of their post market surveillance responsibilities,<br />
as required by the MDD. Therefore, manufacturers must be<br />
informed of such incidents. However, medical devices (with<br />
any packaging and labelling) which have been involved in an<br />
incident have also to be kept and isolated until MHRA has been<br />
given the opportunity to carry out an investigation.<br />
Where the MHRA investigation concludes there are safety<br />
30
implications for patients or users the Agency will issue a<br />
Medical Device Alert (MDA). MHRA also publish Device<br />
Bulletins and One-Liners to give safety information and<br />
guidance on general safety issues.<br />
There are separate user reporting systems for medical device<br />
incidents which occur within the devolved administrations of<br />
Northern Ireland, Scotland and Wales (see useful numbers and<br />
websites section on page 37).<br />
14.2 National Patient Safety Agency (NPSA)<br />
The NPSA has implemented an anonymised National Reporting<br />
and Learning System across England and Wales. This system<br />
allows reporting of all failures, mistakes, errors and near misses,<br />
with the aim of ensuring that lessons are both learned and<br />
shared throughout the health service. They undertake various<br />
safety initiatives, publish updates on the reports received, and<br />
provide guidance in the form of bulletins and newsletters. The<br />
anonymous reporting allowed under the NPSA system prevents<br />
a full investigation, therefore the NPSA actively encourages<br />
reporting of all medical device incidents directly to the MHRA.<br />
There is an NPSA initiative underway with the Royal College of<br />
Anaesthetists and the AAGBI to institute a specific anaesthetic<br />
reporting system.<br />
14.3 Health and Safety Executive<br />
Incidents involving work-related deaths, major injuries or<br />
injuries resulting in over three days off work, work-related<br />
diseases, and dangerous occurrences (near-miss accidents)<br />
whether involving medical devices or not, should also<br />
be reported under the Reporting of Injuries, Diseases and<br />
Dangerous Occurrences Regulations 1995 (RIDDOR ‘95) to<br />
the relevant enforcing authority for the premises at which the<br />
incident occurred. For healthcare premises, this will usually be<br />
the local office of the Health and Safety Executive (HSE) but<br />
for some it may be the local authority. Further information is<br />
31
available from www.hse.gov.uk<br />
14.4 DoH Estates and Facilities<br />
Incidents involving non-medical equipment, including<br />
engineering plant, parts of the fabric of the building and gas<br />
pipelines should be reported to the Head of Engineering at the<br />
DoH Estates and Facilities in the Department of Health. Further<br />
information is available from www.nhsestates.gov.uk<br />
14.5 Police<br />
The police will investigate where there is the suspicion of<br />
criminal activity, such as malicious tampering with medical<br />
equipment. There is a concordat between the police, HSE and<br />
DoH for the investigation of such incidents; therefore should<br />
the police decide no further action is required the investigation<br />
will pass to the HSE and DoH. Due to the rare and unusual<br />
nature of these investigations there are no established national<br />
guidelines; however advice should be available from your<br />
hospital’s legal department, medical defence organisations,<br />
MHRA and the Association of Anaesthetists.<br />
14.6 Dissemination of safety information to users<br />
Safety information from the MHRA and NPSA is distributed via<br />
the DoH Central Alerting System (CAS) [15]. All internal and<br />
external communications concerning equipment and patient<br />
safety must be cascaded to all the users of equipment through<br />
Trust communication channels.<br />
14.7 Manufacturers<br />
The manufacturer has a legal obligation under the provision<br />
of the European MDD to monitor performance of their devices<br />
in a post production phase, i.e. after placed into clinical<br />
use. Typically this is achieved by a proactive post market<br />
surveillance programme, of which incident reporting may be a<br />
part.<br />
32
15. Audit<br />
15.1 Internal<br />
This is part of the Trust’s clinical governance arrangements and<br />
should consist of regular/annual review of policies and systems<br />
for managing medical equipment.<br />
Healthcare professionals must ensure their own training and<br />
skills remain up-to-date, and this should form part of the annual<br />
staff appraisal.<br />
15.2 External<br />
The Care Quality Commission undertakes audits and inspections<br />
of healthcare organisations regularly to ensure that the MHRA<br />
guidance on safe use of medical devices has been followed.<br />
Strategic Health Authorities audit the performance of Trusts,<br />
including performance against deadlines for action required by<br />
the issue of DoH Safety Alert Broadcast System notices.<br />
Glossary of acronyms<br />
BSI<br />
British Standards Institution<br />
CA<br />
Competent Authority (e.g. in the UK, the MHRA)<br />
CCT Certificate of Completion of Training<br />
CE<br />
Conformité Européene<br />
CEN Comité Européen de Normalisation (For<br />
Mechanical Devices)<br />
CENELEC Comité Européen de Normalisation (For<br />
Electrical Devices)<br />
CEP Centre for Evidence-based Purchasing (part of<br />
PaSA)<br />
CPA Consumer Protection Act 1988<br />
CPD Continuing Professional Development<br />
CVC Central Venous Catheter<br />
33
DB<br />
DoH<br />
EBME<br />
EC<br />
EU<br />
FRCA<br />
HN<br />
HSE<br />
IEC<br />
IFU<br />
ISO<br />
LDPA<br />
LMA<br />
MDA<br />
MDD<br />
MHRA<br />
NICE<br />
OEM<br />
OJEU<br />
PaSA<br />
PAT<br />
PPQ<br />
RIDDOR<br />
SFI<br />
SID<br />
WEEE<br />
Device Bulletin<br />
Department of Health<br />
ElectroBioMedicalEngineering (Hospital<br />
Equipment Technicians)<br />
European Community<br />
European Union<br />
Fellowship of the Royal College of Anaesthetists<br />
Hazard Notice<br />
Health and Safety Executive<br />
International Electrotechnical Commission<br />
Instructions For Use<br />
International Organization for Standardization<br />
Liability for Defective Products Act<br />
Laryngeal Mask Airway<br />
Medical Device Alert<br />
Medical Device Directive<br />
Medicines and Healthcare products Regulatory<br />
Agency<br />
National Institute for Health and Clinical<br />
Excellence<br />
Original Equipment Manufacturer<br />
Official Journal of the European Union<br />
(NHS) Purchasing and Supply Agency<br />
Portable Appliance Testing<br />
Pre-Purchasing Questionnaire<br />
Reporting of Injuries, Diseases and Dangerous<br />
Occurrences Regulations 1995<br />
Standing Orders and Standing Financial<br />
Instructions<br />
Suppliers Information Database<br />
Waste Electrical and Electronic Equipment<br />
34
References<br />
1. Association of Anaesthetists of Great Britain & Ireland.<br />
Checking Anaesthetic Equipment 3, 2004. http://www.<br />
<strong>aagbi</strong>.org/publications/guidelines/docs/checking04.pdf<br />
2. Association of Anaesthetists of Great Britain & Ireland.<br />
Standards of Monitoring during Anaesthesia and Recovery<br />
4, 2007. http://www.<strong>aagbi</strong>.org/publications/guidelines/docs/<br />
standardsofmonitoring07.pdf<br />
3. Medicines and Healthcare products Regulatory Agency.<br />
Device Bulletin, Managing Medical Devices DB2006(05)<br />
http://www.mhra.gov.uk/Publications/Safetyguidance/<br />
DeviceBulletins/CON2025142 [accessed 03.08.09]<br />
4. Medicine and Healthcare products Regulatory Agency.<br />
Devices in Practice - a guide for health and social care<br />
professionals, 2008. http://www.mhra.gov.uk/Publications/<br />
Safetyguidance/Otherdevicesafetyguidance/CON007423<br />
[accessed 03.08.09]<br />
5. Office of Public Sector Information. Statutory Instrument<br />
2002 No. 618, The Medical Devices Regulations. http://<br />
www.opsi.gov.uk/SI/si2002/20020618.htm [accessed<br />
03.08.09]<br />
6. Wilkes AR, Hodzovic I, Latto IP. Introducing new<br />
anaesthetic equipment into clinical practice. Anaesthesia<br />
2008; 63: 571-5.<br />
7. Europa Publications Office. Procurement Directive<br />
2004/18/EC, 31 March 2004 for Public Contracts,Official<br />
Journal of the European Union, http://eur-lex.europa.eu/<br />
LexUriServ/site/en/oj/2004/l_134/<br />
l_13420040430en01140240.pdf [accessed 03.08.09]<br />
35
8. OPSI. Statutory Instrument 2006 No 5 Public Contracts<br />
Regulations http://www.opsi.gov.uk/si/si2006/<br />
uksi_20060005_en.pdf [accessed 03.08.09]<br />
9. Office of Government Commerce. European Procurement<br />
Directives, http://www.ogc.gov.uk/procurement_policy_<br />
and_application_of_eu_rules_european_procurement_<br />
directives.asp [accessed 03.08.09]<br />
10. NHS Purchasing and Supply Agency. EU Tenders, http://<br />
www.pasa.nhs.uk/PASAWeb/Guidance/EUtenders.htm<br />
[accessed 03.08.09]<br />
11. Home Office. Procurement Competitions and the Alcatel<br />
Judgement, http://www.homeoffice.gov.uk/about-us/<br />
freedom-of-information/released-information/foi-archiveabout-us/4115-procurement-alcatel?view=Html<br />
[accessed<br />
03.08.09]<br />
12. Department of Health. Sustainable Development - Waste,<br />
http://www.dh.gov.uk/en/Managingyourorganisation/<br />
Estatesandfacilitiesmanagement/Sustainabledevelopment/<br />
DH_4119635 [accessed 03.08.09]<br />
13. Association of Anaesthetists of Great Britain & Ireland.<br />
Infection Control in Anaesthesia 2, 2008. http://www.<br />
<strong>aagbi</strong>.org/publications/guidelines/docs/infection_control_08.<br />
pdf [accessed 03.08.09]<br />
14. Department of Health. Standards for Better Health, 2004.<br />
http://www.dh.gov.uk/en/publicationsandstatistics/<br />
publications/publicationspolicyandguidance/<br />
dh_4086665 [accessed 03.08.09]<br />
15. Department of Health. Central Alerting System, https://<br />
www.cas.dh.gov.uk/Home.aspx [accessed 03.08.09]<br />
36
Useful numbers and websites<br />
For reporting adverse incidents and further information<br />
MHRA<br />
Tel: 020 7084 3080<br />
Website: www.mhra.gov.uk<br />
Email: aic@mhra.gsi.gov.uk<br />
NPSA<br />
Tel: 020 7927 9500<br />
Website: www.npsa.nhs.uk<br />
Email: enquiries@npsa.nhs.uk<br />
RIDDOR<br />
Tel: 0845 300 9923<br />
Website: www.riddor.gov.uk<br />
Email: riddor@natbrit.com<br />
DoH Estates<br />
Tel: 0113 254 5172<br />
Website: www.nhsestates.gov.uk<br />
Email: nhs.estates@dh.gsi.gov.uk<br />
Northern Ireland<br />
Tel: 028 9052 3704<br />
Website: www.dhsspsni.gov.uk/niaic<br />
Email: niaic@dhsspsni.gov.uk<br />
Scotland<br />
Tel: 0131 275 7575<br />
Website: www.hfs.scot.nhs.uk<br />
Email: enquiries@hfs.scot.nhs.uk<br />
Wales<br />
Tel: 029 2082 3505<br />
Email: health.enquiries@wales.gsi.gov.uk<br />
37
Eire<br />
Tel: 00353 1 676 4971<br />
Website: www.imb.ie<br />
Email: imb@imb.ie<br />
Buying Solutions<br />
Tel: 0345 410 2222<br />
Website: www.buyingsolutions.gov.uk<br />
Email: info@buyingsolutions.gsi.gov.uk<br />
38
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
AAGBI SAFETY GUIDELINE<br />
Skin antisepsis for central<br />
neuraxial blockade<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
September 2014
This guideline was originally published in Anaesthesia. If you wish to refer<br />
to this guideline, please use the following reference:<br />
Association of Anaesthetists of Great Britain & Ireland. Safety guideline:<br />
skin antisepsis for central neuraxial blockade. Anaesthesia (ePub ahead of<br />
print, 3 Sep 2014): doi: 10.1111/anae.12844<br />
This guideline can be viewed online via the following URL:<br />
http://onlinelibrary.wiley.com/enhanced/doi/10.1111/anae.12844/<br />
© The Association of Anaesthetists of Great Britain & Ireland
Guidelines<br />
Safety guideline: skin antisepsis for central<br />
neuraxial blockade<br />
Association of Anaesthetists of Great Britain and<br />
Ireland<br />
Obstetric Anaesthetists’ Association<br />
Regional Anaesthesia UK<br />
Association of Paediatric Anaesthetists of Great<br />
Britain and Ireland<br />
Membership of the Working Party: J. P. Campbell, F. Plaat,<br />
M. R. Checketts, D. Bogod, 1 S. Tighe, 2<br />
A. Moriarty 3 and R. Koerner<br />
1 Obstetric Anaesthetists’ Association, 2 Regional Anaesthesia UK,<br />
3 Association of Paediatric Anaesthetists of Great Britain and Ireland<br />
Summary<br />
Concise guidelines are presented that recommend the method of choice<br />
for skin antisepsis before central neuraxial blockade. The Working Party<br />
specifically considered the concentration of antiseptic agent to use and<br />
its method of application. The advice presented is based on previously<br />
published guidelines, laboratory and clinical studies, case reports, and<br />
on the known properties of antiseptic agents.<br />
....................................................................................................<br />
© 2014 The Association of Anaesthetists of Great Britain and Ireland 1<br />
This is an open access article under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs<br />
License, which permits use and distribution in any medium, provided the original work is properly cited, the use is<br />
non-commercial and no modifications or adaptations are made.
All AAGBI guidelines are reviewed to ensure relevance/accuracy and are<br />
updated or archived when necessary. Date of review: 2019.<br />
Accepted: 4 August 2014<br />
• What other guideline statements are available on this topic?<br />
The Royal College of Anaesthetists [1], the American Society of<br />
Anesthesiologists [2] and the American Society of Regional Anesthesia<br />
[3] have all published guidance on prevention of infectious complications<br />
associated with neuraxial techniques.<br />
•<br />
Why was this guideline developed?<br />
Although the current published guidelines comprehensively cover<br />
aseptic technique when performing central neuraxial blockade<br />
(CNB), they are lengthy and discursive documents that are impractical<br />
for use in the acute care setting. The remit of this Working Party<br />
was to produce a concise document that specifically considered<br />
which agent (including the concentration) to use for skin antisepsis<br />
before CNB, and the method of application.<br />
•<br />
How does this statement differ from existing guidelines?<br />
This statement specifically considers which agent to use for skin<br />
antisepsis before CNB, and is more concise than currently available<br />
guidelines. Unlike existing guidance, this statement includes a recommendation<br />
on which concentration of antiseptic agent to use.<br />
•<br />
Why does this statement differ from existing guidelines?<br />
This statement was written to provide useful and concise guidance<br />
for anaesthetists in the clinical setting.<br />
Recommendations<br />
1 Optimum aseptic technique for CNB requires thorough handwashing<br />
with surgical scrub solution and the use of barrier precautions<br />
including the wearing of a cap, mask, sterile gown and gloves, and<br />
the use of a large sterile drape.<br />
2 Chlorhexidine in alcohol should be used for skin antisepsis before<br />
performing CNB.<br />
3 The anaesthetist must be meticulous in taking measures to prevent<br />
chlorhexidine from reaching the cerebrospinal fluid (CSF):<br />
a Chlorhexidine should be kept well away from the drugs and<br />
equipment to be used for CNB and should not be poured into<br />
containers on or near the same surface as the equipment for<br />
2 © 2014 The Association of Anaesthetists of Great Britain and Ireland
CNB. Equipment should be covered or protected while the antiseptic<br />
is applied by swab, applicator or spray.<br />
b The solution must be allowed to dry before the skin is palpated<br />
or punctured.<br />
c The operator should check his/her gloves for contamination with<br />
chlorhexidine. If there is any doubt, they should be changed<br />
before continuing the procedure.<br />
4 Given the lack of convincing evidence of the antimicrobial superiority<br />
of a 2% solution of chlorhexidine in alcohol over a 0.5% solution,<br />
but the presence of clear evidence of the neurotoxicity of<br />
chlorhexidine, the Working Party has concluded that the use of a<br />
0.5% solution should be preferred over a 2% solution for skin antisepsis<br />
before CNB.<br />
5 In children under two months of age, the volume of chlorhexidine<br />
used should be the minimum necessary while still ensuring<br />
antisepsis.<br />
Introduction<br />
The most appropriate and safe antiseptic solution to use on the skin<br />
before CNB remains controversial. A survey of consultant obstetric anaesthetists<br />
in 2009 revealed a wide range of practice across the UK in<br />
terms of both the antiseptic used and its method of application [4].<br />
The ideal antiseptic agent should be effective against a wide range<br />
of micro-organisms, have immediate onset of action, exert a long-term<br />
effect, not be inactivated by organic material (e.g. blood), and have minimal<br />
toxic effects on the skin [3]. Commonly used antiseptic agents for<br />
CNB include chlorhexidine gluconate and povidone iodine. Both of<br />
these antiseptics are available as aqueous and alcoholic solutions.<br />
Chlorhexidine vs povidone iodine<br />
Chlorhexidine gluconate is a potent, broad-spectrum antiseptic that is<br />
effective against nearly all bacteria and yeasts. It has a faster onset and<br />
longer duration of action than povidone iodine, and it retains its efficacy<br />
in the presence of blood. It also has a lower incidence of skin reactions<br />
than povidone iodine [3].<br />
Several investigators have compared the antiseptic efficacy of<br />
chlorhexidine and povidone iodine under a variety of experimental conditions<br />
[5–12]. In all but one investigation [7], chlorhexidine resulted in<br />
a more rapid and superior bactericidal effect that lasted several hours<br />
© 2014 The Association of Anaesthetists of Great Britain and Ireland 3
eyond its initial application. In one of these studies, Kinirons et al. [5]<br />
compared colonisation of epidural catheters following skin preparation<br />
using 0.5% chlorhexidine in alcohol with skin preparation using an<br />
aqueous solution of 10% povidone iodine. Catheters inserted following<br />
the use of chlorhexidine were six times less likely to be colonised than<br />
when povidone iodine had been used.<br />
Chlorhexidine: aqueous vs alcoholic<br />
Sakuragi et al. [10] investigated the effect of chlorhexidine and povidone<br />
iodine on the growth of Staphylococcus aureus (the pathogen most commonly<br />
associated with epidural space infections) in vitro. They found<br />
that both methicillin-resistant and -sensitive strains of the pathogen<br />
grew colonies after exposure for 60 s to aqueous 10% povidone iodine<br />
or aqueous 0.5% chlorhexidine. In contrast, no bacteria grew after 15 s<br />
of exposure to 0.5% chlorhexidine in 80% alcohol.<br />
Chlorhexidine: 0.5% vs 2%<br />
The choice of concentration in the UK and Ireland is between 0.5%<br />
chlorhexidine in 70% alcohol (e.g. Hydrex â solution, Ecolab Ltd, Leeds,<br />
UK) and 2% chlorhexidine in 70% alcohol (e.g. ChloraPrep â ,<br />
CareFusion UK Ltd, Reigate, UK).<br />
Adams et al. [13] compared the efficacy of 2% chlorhexidine in<br />
alcohol with several other antiseptics including 0.5% chlorhexidine in<br />
alcohol against growth of a single strain of Staphylococcus epidermidis<br />
in vitro. In three out of four tests, no difference in efficacy could be<br />
demonstrated. In the fourth test (involving a biofilm with added<br />
human serum), all the antiseptics failed the test of efficacy (log 10<br />
reduction factor in colony-forming units per ml of > 5), although the<br />
failure of 2% chlorhexidine in alcohol was less than for 0.5% chlorhexidine<br />
in alcohol. The authors recommended in-vivo studies to assess<br />
the clinical efficacy of 2% chlorhexidine in alcohol. Crowley et al.<br />
found no difference in bacterial colony counts from skin and epidural<br />
catheter tips after preparation with 0.5% and 2% chlorhexidine in alcohol<br />
[14].<br />
Pratt et al. [15] recommend that before insertion of a central venous<br />
access device, the skin should be decontaminated using 2% chlorhexidine<br />
in 70% alcohol. However, no such guidance exists for CNB, possibly<br />
because of concerns about neurotoxicity associated with<br />
chlorhexidine.<br />
4 © 2014 The Association of Anaesthetists of Great Britain and Ireland
Chlorhexidine, alcohol and neurotoxicity<br />
Recently, the issue of which antiseptic to use before CNB, and in<br />
which concentration, has become contentious. This follows cases of<br />
permanent neurological injury in obstetric patients in which chlorhexidine<br />
was alleged to have been responsible. In one of these cases<br />
[16], a whole syringe of 0.5% chlorhexidine in alcohol was mistakenly<br />
injected into the epidural space; in another case it was suggested that<br />
a syringe of bupivacaine injected spinally had become contaminated<br />
with ‘a measurable quantity’ (defined as 0.1 ml or more) of 0.5%<br />
chlorhexidine in alcohol [17]. All patients developed a chronic adhesive<br />
arachnoiditis with a similar clinical course of progressive neurological<br />
deterioration leading to paraplegia [16–19].<br />
Limited information is available on the risk of neurotoxicity with<br />
chlorhexidine. In 1955, Weston-Hurst reported that the neurotoxic<br />
concentration of aqueous chlorhexidine when injected into the CSF<br />
of monkeys appeared to be in the region of 0.05% [20]. In 1984,<br />
Henschen and Olsen showed that injection of just 5 ll of 0.05%<br />
aqueous chlorhexidine into the anterior chamber of the eye produced<br />
adrenergic nerve degeneration in rats, and the authors postulated that<br />
the thin unmyelinated nerves of the central nervous system might be<br />
equally affected [21]. More recently, Doan et al. found that chlorhexidine<br />
was neurotoxic at a concentration of 0.01% (the lowest concentration<br />
tested) when applied directly to neurons [22]. However, in a<br />
rat model using a radioactive tracer, the same authors estimated<br />
mathematically that provided the antiseptic is allowed to dry fully,<br />
the concentration of antiseptic that could be delivered to the neuaxis<br />
would be extremely low [22].<br />
It has been suggested that alcohol, which constitutes the main component<br />
of chlorhexidine solutions, might be the causative neurotoxic<br />
agent [23]. Alcohol-induced neurolysis is well established and is used<br />
therapeutically in a number of procedures [24]. Accidental injection of a<br />
syringe of alcohol (with or without chlorhexidine) into the epidural<br />
space may therefore be expected to result in neurological injury,<br />
although the effect of the tiny quantities that may contaminate a spinal<br />
needle has been questioned [25].<br />
In a recent editorial on skin antisepsis for CNB [26], the author<br />
concluded that chlorhexidine in alcohol should still be used as the<br />
potential for neurotoxicity was outweighed by the superiority in reducing<br />
surgical site infection. Other bodies have drawn the same conclu-<br />
© 2014 The Association of Anaesthetists of Great Britain and Ireland 5
sion: the Royal College of Anaesthetists (in its Third National Audit<br />
Project (NAP3)) [1], the American Society of Anesthesiologists [2] and<br />
the American Society of Regional Anesthesia [3] all recommend chlorhexidine<br />
in alcohol as the skin disinfectant of choice for CNB. None of<br />
these guidelines specifies the concentration of chlorhexidine to use,<br />
although the authors of the NAP3 report have stated that in their<br />
opinion, based on the limited evidence available, 0.5% chlorhexidine in<br />
alcohol is the optimal skin preparation for CNB [27].<br />
The Working Party is aware that some anaesthetists choose to use<br />
2% chlorhexidine in alcohol because they consider it reduces the risk of<br />
infectious complications compared with the 0.5% solution. As neuraxial<br />
infectious complications are rare, and cases of chronic adhesive arachnoiditis<br />
even rarer, the Working Party acknowledges that there is a lack<br />
of data to support the use of one concentration of chlorhexidine over<br />
another for CNB. However, evidence for the greater efficacy of 2%<br />
chlorhexidine compared with 0.5% is lacking, while the neurotoxicity of<br />
chlorhexidine is well established in vitro and in animal models. It is<br />
consequently the opinion of the Working Party that skin antisepsis for<br />
CNB using 0.5% chlorhexidine in alcohol provides the safest compromise<br />
between the risk of infection and the risk of neurotoxicity. The<br />
Working Party acknowledges that meticulous attention to the method of<br />
application of the antiseptic, and to other infection control precautions,<br />
are likely to be more important factors in reducing the risks of neurotoxicity<br />
and infection than the choice of concentration of chlorhexidine.<br />
Method of application<br />
As it is possible that cases of arachnoiditis have been caused by accidental<br />
contamination with antiseptic of needles, syringes and catheters used<br />
for CNB, a method of skin application that minimises the risk of contamination<br />
of equipment should be used.<br />
Traditionally, antiseptic solutions were poured into a gallipot on the<br />
anaesthetist’s sterile field. However, if there is another open container<br />
for a fluid intended for neuraxial injection (e.g. saline), the potential for<br />
a crossover error is created (the aetiology in one of the reported cases of<br />
arachnoiditis [15]). Moreover, Evans et al. [28] have shown that pouring<br />
chlorhexidine into a gallipot generates splash that spreads at least<br />
40 cm. The authors recommended that antiseptic solutions should not<br />
be poured into containers located on the same tray as equipment for<br />
CNB, and that the equipment should be covered until the back has been<br />
prepared with antiseptic.<br />
6 © 2014 The Association of Anaesthetists of Great Britain and Ireland
Pre-soaked antiseptic sponge applicators (‘swabsticks’) are now<br />
commonly used for skin preparation before central venipuncture and<br />
other procedures. The applicators are manufactured with a reservoir<br />
containing 3 ml or 10.5 ml of antiseptic, and the solution may be dyed<br />
to allow identification of the area of prepared skin. Because the antiseptic<br />
solution is contained within the hollow of the handle, crossover<br />
errors are impossible and fluid spillage should be minimised. However,<br />
it has been observed that leakage of antiseptic solution over the operator’s<br />
gloves may occur via a hole at the end of the handle when the<br />
device is held upside down (the hole below the level of the antiseptic<br />
reservoir) to clean a patient’s back [19]. Currently, the ‘swabstick’ applicators<br />
available in the UK and Ireland contain a 2% solution of chlorhexidine<br />
in alcohol. The manufacturer has advised that a 0.5% version is<br />
unlikely to come onto the market in the near future (CareFusion, personal<br />
communication). The Working Party is aware that some anaesthetists<br />
prefer to use these devices for skin preparation for CNB, and<br />
would encourage the development of applicators containing 0.5%<br />
chlorhexidine in alcohol.<br />
Skin antisepsis before CNB using 0.5% chlorhexidine in 70% alcohol<br />
(Hydrex) from a multi-use spray bottle is widely practised in the UK.<br />
Advocates of this technique argue that contamination is minimised: the<br />
fluid is kept in a closed container and it can be applied at a distance<br />
from the sterile field, before or during preparation of the equipment for<br />
CNB. However, others have suggested that spraying might result in aerosol<br />
contamination of equipment with chlorhexidine and may compromise<br />
sterility by missing an area of skin [29]. Malhotra et al. [30]<br />
showed that a single spray application of 0.5% chlorhexidine in alcohol<br />
sterilised the skin over the lumbar spine in healthy volunteers. The<br />
authors concluded that repeated application was unnecessary, and might<br />
increase the risk of contamination of the CSF if the antiseptic was not<br />
allowed to dry completely. Robins et al. [31] compared application of<br />
chlorhexidine using a spray with application from a sachet in parturients<br />
undergoing combined spinal-epidural anaesthesia. Both techniques<br />
were effective in reducing skin colonisation, but the time to achieve skin<br />
preparation was significantly shorter in the spray group.<br />
Use of chlorhexidine in children<br />
Chlorhexidine has been used for vaginal lavage, whole body cleansing<br />
and umbilical cord care in large, well-designed clinical trials on tens of<br />
thousands of neonates without significant adverse events [32, 33].<br />
© 2014 The Association of Anaesthetists of Great Britain and Ireland 7
Despite chlorhexidine’s proven efficacy, there are concerns about the<br />
risk of skin reactions and percutaneous absorption into the bloodstream,<br />
particularly in preterm and low birth weight infants. Transient<br />
contact dermatitis has been reported in preterm, very low birth weight<br />
infants after long-term placement of chlorhexidine-impregnated dressings<br />
for central venous catheters [34]. However, it has been suggested<br />
that the effect may have been caused by external pressure from the<br />
dressing rather than the chlorhexidine itself [35]. Alcohol-based<br />
chlorhexidine preparations have been reported to cause burns in<br />
infants of 24–26 weeks’ gestational age [36, 37]. There are few data<br />
addressing the potential for chlorhexidine absorption following topical<br />
application. Cowan et al. [38] took blood samples from 24 infants<br />
after whole body bathing with 4% aqueous chlorhexidine and found<br />
that five had detectable chlorhexidine levels. All were < 36 weeks’ gestational<br />
age and the authors suggested that their immature skin was<br />
likely to have increased the permeability of the epidermis. The clinical<br />
significance of traces of chlorhexidine in the blood is unknown. There<br />
are no established values for a safe concentration of chlorhexidine in<br />
the blood, and there are no reports of adverse consequences as a result<br />
of absorption of chlorhexidine in neonates [39]. Because of the limited<br />
safety data in neonates, the Society for Healthcare Epidemiology of<br />
America states that ‘chlorhexidine products are not approved by the<br />
US Food and Drug Administration for children younger than<br />
2 months of age’ [40]. Despite this recommendation, chlorhexidine is<br />
commonly used in neonatal intensive care units in the USA, mostly<br />
for skin preparation and maintenance for central venous access [41].<br />
Allergic reactions to chlorhexidine<br />
Several hypersensitivity reactions due to chlorhexidine have been<br />
described. These include allergic contact dermatitis (commonly after prolonged<br />
and repeated application) [42], contact urticaria [43], photosensitivity<br />
[44], occupational asthma [45] and anaphylaxis [46–48]. Most of<br />
the cases of anaphylaxis to chlorhexidine involved topical application to<br />
mucous membranes [46] and the use of chlorhexidine-impregnated medical<br />
devices (e.g. central venous catheters) [47], although anaphylactic<br />
reactions have also followed application of chlorhexidine to intact skin<br />
[48]. The severity of these cases prompted the Medicines and Healthcare<br />
products Regulatory Agency (MHRA) to issue a Medical Device Alert in<br />
2012 about the potential for anaphylactic reactions due to the use of<br />
medicinal products and medical devices containing chlorhexidine [49].<br />
8 © 2014 The Association of Anaesthetists of Great Britain and Ireland
Other infection control precautions for CNB<br />
Application of antiseptic to the skin is only one component of aseptic<br />
technique before CNB. Both the Association of Anaesthetists of Great<br />
Britain and Ireland and the Obstetric Anaesthetists’ Association have<br />
issued guidance on the other precautions that should be employed [50,<br />
51]. These include thorough handwashing with surgical scrub solution,<br />
the wearing of a cap, mask, sterile gown and gloves, and the use of a<br />
large sterile drape [3]. The Working Party is aware that some anaesthetists<br />
do not employ this level of asepsis for spinals or ‘one-shot’ epidurals,<br />
but believes that full aseptic precautions are required whenever<br />
CNBs are performed. The NAP3 report stated that aseptic technique<br />
had been suboptimal in a number of the reported cases of epidural<br />
abscess [1].<br />
Skin antisepsis for peripheral nerve blocks<br />
These guidelines address only CNBs. However, as the nerves targeted by<br />
some peripheral nerve blocks lie a shorter distance beneath the skin<br />
than the neuraxis, and the evidence of the neurotoxicity of chlorhexidine<br />
is not restricted to the neuraxis, the Working Party considers it<br />
reasonable to recommend that 0.5% chlorhexidine in alcohol be used<br />
for peripheral nerve blocks as well.<br />
Suggestions for further research<br />
The duration of antiseptic action required for different types of CNB<br />
may vary. A single intrathecal injection may only require antisepsis for<br />
a few minutes, whereas insertion of an epidural catheter requires antisepsis<br />
to be maintained throughout the time the catheter remains in<br />
situ. Isopropyl alcohol causes a rapid reduction in the number of skin<br />
micro-organisms, but does not have any residual activity. In comparison,<br />
chlorhexidine exerts an antiseptic effect for up to 24 h [52]. Hibbard<br />
et al. [53] compared the effect of 70% isopropyl alcohol with 2%<br />
chlorhexidine in alcohol on abdominal sites. The authors found that<br />
both maintained antimicrobial activity for at least 6 h, but the chlorhexidine<br />
solution was more effective at 24 h. It may be that isopropyl alcohol<br />
alone could provide adequate antisepsis for a single-injection CNB,<br />
obviating the need for chlorhexidine and therefore avoiding exposure of<br />
the neuraxis to a second neurotoxic substance. A CNB involving an<br />
indwelling catheter, on the other hand, probably requires the more prolonged<br />
action of a chlorhexidine solution. Research is needed comparing<br />
© 2014 The Association of Anaesthetists of Great Britain and Ireland 9
the duration of antimicrobial activity of 0.5–2% chlorhexidine in alcohol<br />
with 70% isopropyl alcohol when used for CNB.<br />
Costerton has shown that S. epidermidis exists at depths of up to<br />
five cell layers in the skin [54]. Dead skin cells are constantly being<br />
shed, along with the colonising bacteria. These, together with sebum,<br />
sweat and environmental material, form an oily layer covering the skin.<br />
It is possible that a single application of antiseptic to the skin removes<br />
bacteria from this oily layer covering the surface, but is ineffective at<br />
removing bacteria at depth. It might be more effective first to apply an<br />
antiseptic that will dissolve this oily surface layer and remove its bacteria.<br />
This could then be wiped away before applying antiseptic again to<br />
remove bacteria living within the epithelium. This ‘apply-wipe-apply’<br />
technique requires both in vitro and in vivo investigation.<br />
Several cases of severe neurological damage have been attributed to<br />
contamination of equipment for CNB with chlorhexidine in alcohol,<br />
caused by splashes, aerosols, or insertion through solution that has not<br />
dried on the skin, or through chlorhexidine crystals that have dried on<br />
the skin [17–19]. Further studies are needed to address the risk of 0.5%<br />
over 2% chlorhexidine in 70% alcohol, and 70% alcohol alone, in causing<br />
neurological damage from such sources of contamination.<br />
Competing interests<br />
FP and DB have provided expert opinions in cases of neurological damage<br />
following neuraxial block, in which the possibility of antiseptic contamination<br />
of injectate was considered. DB has received hospitality from<br />
Care Fusion, manufacturers of Chloraprep, and consequently took no<br />
part in any discussions relating to the use of this product. No external<br />
funding or other competing interests declared.<br />
References<br />
1. Royal College of Anaesthetists. Major Complications of Central Neuraxial Block in<br />
the United Kingdom. Report and Findings of the 3rd National Audit Project of the<br />
Royal College of Anaesthetists, 2009. http://www.rcoa.ac.uk/node/4207<br />
(accessed 08/04/2014).<br />
2. Horlocker TT, Birnbach DJ, Connis RT, et al. Practice advisory for the prevention,<br />
diagnosis, and management of infectious complications associated with neuraxial<br />
techniques. A report by the American Society of Anesthesiologists Task Force on<br />
infectious complications associated with neuraxial techniques. Anesthesiology<br />
2010; 112: 530–45.<br />
3. Hebl JR. The importance and implications of aseptic techniques during regional<br />
anesthesia. Regional Anesthesia and Pain Medicine 2006; 31: 311–23.<br />
10 © 2014 The Association of Anaesthetists of Great Britain and Ireland
4. Bradbury CL, Hale B, Mather I, Suri I. Skin disinfection before spinal anaesthesia for<br />
caesarean section: a survey of UK practice. International Journal of Obstetric Anesthesia<br />
2011; 20: 101–2.<br />
5. Kinirons B, Mimoz O, Lafendi L, Naas T, Meunier J, Nordmann P. Chlorhexidine versus<br />
povidone iodine in preventing colonization of continuous epidural catheters in<br />
children: a randomized, controlled trial. Anesthesiology 2001; 94: 239–44.<br />
6. Sato S, Sakuragi T, Dan K. Human skin flora as a potential source of epidural<br />
abscess. Anesthesiology 1996; 85: 1276–82.<br />
7. Haley CE, Marling-Cason M, Smith JW, Luby JP, Mackowiak PA. Bactericidal activity<br />
of antiseptics against methicillin-resistant Staphylococcus aureus. Journal of Clinical<br />
Microbiology 1985; 21: 991–2.<br />
8. Darouiche RO, Wall MJ, Itani KMF, et al. Chlorhexidine-alcohol versus povidoneiodine<br />
for surgical-site antisepsis. New England Journal of Medicine 2010; 362: 18–<br />
26.<br />
9. Maki DG, Ringer M, Alvarado CJ. Prospective randomised trial of povidone-iodine,<br />
alcohol, and chlorhexidine for prevention of infection associated with central<br />
venous and arterial catheters. Lancet 1991; 338: 339–43.<br />
10. Sakuragi T, Yanagisawa K, Dan K. Bactericidal activity of skin disinfectants on methicillin-resistant<br />
Staphylococcus aureus. Anesthesia and Analgesia 1995; 81: 555–8.<br />
11. Mimoz O, Karim A, Mercat A, et al. Chlorhexidine compared with povidone-iodine<br />
as skin preparation before blood culture. A randomized, controlled trial. Annals of<br />
Internal Medicine 1999; 131: 834–7.<br />
12. Selwyn S, Ellis H. Skin bacteria and skin disinfection reconsidered. British Medical<br />
Journal 1972; 1: 136–40.<br />
13. Adams D, Quayum M, Worthington T, Lambert P, Elliott T. Evaluation of a 2% chlorhexidine<br />
gluconate in 70% isopropyl alcohol skin disinfectant. Journal of Hospital<br />
Infection 2005; 61: 287–90.<br />
14. Crowley L, Preston R, Wong A, et al. What is the best skin disinfectant solution for<br />
labour epidural analgesia? A randomized, prospective trial comparing Chloropreptm,<br />
DuraprepTM and chlorhexidine 0.5% in 70% alcohol Anesthesia and Analgesia<br />
2008; 106: A-A-221.<br />
15. Pratt RJ, Pellowe CM, Wilson JA, et al. Epic 2: National evidence-based guidelines<br />
for preventing healthcare-associated infections in NHS hospitals in England. Journal<br />
of Hospital Infection 2007; 65: S1–64.<br />
16. Sheather M. My epidural hell. Australian Women’s Weekly 30th March, 2011;<br />
http://www.aww.com.au/news-features/in-the-mag/2011/3/my-epidural-hell<br />
(accessed 08/04/2014).<br />
17. Sutcliffe v Aintree Hospitals NHS Trust [2008] EWCA Civ 179.<br />
18. Killeen T, Kamat A, Walsh D, Parker A, Aliashkevich A. Severe adhesive arachnoiditis<br />
resulting in progressive paraplegia following obstetric spinal anaesthesia: a case<br />
report and review. Anaesthesia 2012; 67: 1386–94.<br />
19. Bogod D. The sting in the tail: antiseptics and the neuraxis revisited. Anaesthesia<br />
2012; 67: 1305–20.<br />
20. Weston-Hurst E. Adhesive arachnoiditis and vascular blockage caused by detergents<br />
and other chemical irritants: an experimental study. Journal of Pathology and Bacteriology<br />
1955; 38: 167–78.<br />
© 2014 The Association of Anaesthetists of Great Britain and Ireland 11
21. Henschen A, Olson L. Chlorhexidine-induced degeneration of adrenergic nerves.<br />
Acta Neuropathologica 1984; 63: 18–23.<br />
22. Doan L, Piskoun B, Rosenberg AD, Blanck TJJ, Phillips MS, Xu F. In vitro antiseptic<br />
effects on viability of neuronal and Schwann cells. Regional Anesthesia and Pain<br />
Medicine 2012; 37: 131–8.<br />
23. Patle V. Arachnoiditis: alcohol or chlorhexidine? Anaesthesia 2013; 68: 425.<br />
24. Kocabas H, Salli A, Demir AH, Ozerbil OM. Comparison of phenol and alcohol neurolysis<br />
of tibial nerve motor branches to the gastrocnemius muscle for treatment of<br />
spastic foot after stroke: a randomized controlled pilot study. European Journal of<br />
Physical and Rehabilitation Medicine 2010; 46: 5–10.<br />
25. Miller B. Arachnoiditis: are we accusing the wrong agent(s)? Anaesthesia 2013; 68:<br />
423.<br />
26. Checketts MR. Wash and go – but with what? Skin antiseptic solutions for central<br />
neuraxial block. Anaesthesia 2012; 67: 819–22.<br />
27. Cook TM, Fischer B, Bogod D, et al. Antiseptic solutions for central neuraxial blockade:<br />
which concentration of chlorhexidine in alcohol should we use? British Journal<br />
of Anaesthesia 2009; 103: 456–7.<br />
28. Evans L, Cunningham M, Tilakaratna P. Chlorhexidine droplet splash from a skin<br />
preparation gallipot: effect of height of pouring. Anaesthesia 2013; 68: 1243–6.<br />
29. Girgirah K, MacNab WR. Arachnoiditis: is chlorhexidine spray a safe option? Anaesthesia<br />
2013; 68: 425–6.<br />
30. Malhotra S, Dharmadasa A, Yentis SM. One vs two applications of chlorhexidine/<br />
ethanol for disinfecting the skin: implication for regional anaesthesia. Anaesthesia<br />
2011; 66: 574–8.<br />
31. Robins K, Wilson R, Watkins EJ, Columb MO, Lyons G. Chlorhexidine spray versus<br />
single use sachets for skin preparation before regional nerve blockade for elective<br />
caesarean section: an effectiveness, time and cost study. International Journal of<br />
Obstetric Anesthesia 2005; 14: 189–92.<br />
32. Mullany LC, Darmstadt GL, Khatry SK, et al. Topical applications of chlorhexidine to<br />
the umbilical cord for prevention of omphalitis and neonatal mortality in southern<br />
Nepal: a community-based, cluster-randomised trial. Lancet 2006; 367: 910–8.<br />
33. Tielsch JM, Darmstadt GL, Mullany LC, et al. Impact of newborn skin-cleansing with<br />
chlorhexidine on neonatal mortality in southern Nepal: a community-based, cluster-randomized<br />
trial. Pediatrics 2007; 119: e330–40.<br />
34. Garland JS, Alex CP, Mueller CD, et al. A randomized trial comparing povidoneiodine<br />
to a chlorhexidine gluconate-impregnated dressing for prevention of central<br />
venous catheter infections in neonates. Pediatrics 2001; 107: 1431–6.<br />
35. Visscher M, deCastro MV, Combs L, et al. Effect of chlorhexidine gluconate on the<br />
skin integrity at PICC line sites. Journal of Perinatology 2009; 29: 802–7.<br />
36. Watkins AM, Keogh EJ. Alcohol burns in the neonate. Journal of Paediatrics and<br />
Child Health 1992; 28: 306–8.<br />
37. Reynolds PR, Banerjee S, Meek JH. Alcohol burns in extremely low birthweight<br />
infants: still occurring. Archives of Disease in Childhood Fetal and Neonatal Edition<br />
2005; 90: F10.<br />
38. Cowen J, Ellis SH, McAinsh J. Absorption of chlorhexidine from the intact skin of<br />
newborn infants. Archives of Disease in Childhood 1979; 54: 379–83.<br />
12 © 2014 The Association of Anaesthetists of Great Britain and Ireland
39. Chapman AK, Aucott SW, Milstone AM. Safety of chlorhexidine gluconate used for<br />
skin antisepsis in the preterm infant. Journal of Perinatology 2012; 32: 4–9.<br />
40. Marschall J, Mermel LA, Classen D, et al. SHEA/IDSA practice recommendation:<br />
strategies to prevent central line-associated bloodstream infections in acute care<br />
hospitals. Infection Control and Hospital Epidemiology 2008; 29: S22–30.<br />
41. Tamma PD, Aucott SW, Milstone AM. Chlorhexidine use in the neonatal intensive<br />
care unit: results from a national survey. Infection Control and Hospital Epidemiology<br />
2010; 31: 846–9.<br />
42. Reynolds NJ, Harman RRM. Allergic contact dermatitis from chlorhexidine diacetate<br />
in a skin swab. Contact Dermatitis 1990; 22: 103–28.<br />
43. Wong WK, Goh CL, Chan KW. Contact urticaria from chlorhexidine. Contact Dermatitis<br />
1990; 22: 52.<br />
44. Wahlberg JE, Wennersten G. Hypersensitivity and photosensitivity to chlorhexidine.<br />
Dermatologica 1971; 143: 376–9.<br />
45. Waclawski ER, McAlpine LG, Thomson NC. Occupational asthma in nurses caused by<br />
chlorhexidine and alcohol aerosols. British Medical Journal 1989; 298: 929–30.<br />
46. Wicki J, Deluze C, Cirafici L, Desmeules J. Anaphylactic shock induced by intraurethral<br />
use of chlorhexidine. Allergy 1999; 54: 768–9.<br />
47. Jee R, Nel L, Gnanakumaran G, Williams A, Eren E. Four cases of anaphylaxis to<br />
chlorhexidine impregnated central venous catheters: a case cluster or the tip of the<br />
iceberg? British Journal of Anaesthesia 2009; 103: 614–5.<br />
48. Torricelli R, W€uthrich B. Life-threatening anaphylactic shock due to skin application<br />
of chlorhexidine. Clinical and Experimental Allergy 1996; 26: 112.<br />
49. Medicines and Healthcare Products Regulatory Agency. Medical Device Alert: All Medical<br />
Devices and Medicinal Products Containing Chlorhexidine (MDA/2012/075).<br />
2012. http://www.mhra.gov.uk/Publications/Safetywarnings/MedicalDeviceAlerts/<br />
CON197918?tabName=Problem (accessed 19/04/2014).<br />
50. Association of Anaesthetists of Great Britain and Ireland. Infection control in anaesthesia.<br />
Anaesthesia 2008; 63: 1027–36.<br />
51. Association of Anaesthetists of Great Britain and Ireland and Obstetric Anaesthetists’<br />
Association. Guidelines for Obstetric Anaesthetic Services 3. London: AAGBI,<br />
2013.<br />
52. Carret L, Reverdy ME, Lafforgue C, Falson F, Fleurette J, Freney J. Kinetics of<br />
chlorhexidine on intact skin following a single application. Pathologie Biologie<br />
1997; 45: 737–40.<br />
53. Hibbard JS, Mulberry GK, Brady AR. A clinical study comparing the skin antisepsis<br />
and safety of ChloraPrep, 70% isopropyl alcohol, and 2% aqueous chlorhexidine.<br />
Journal of Infusion Nursing 2002; 25: 244–9.<br />
54. Costerton JW. The Biofilm Primer, 1st edn. Berlin: Springer, 2007.<br />
© 2014 The Association of Anaesthetists of Great Britain and Ireland 13
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
Controlled Drugs in<br />
Perioperative Care<br />
2006<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland,<br />
21 Portland Place, London W1B 1PY<br />
Telephone: 020 7631 1650, Fax: 020 7631 4352<br />
E-mail: info@<strong>aagbi</strong>.org Website: www.<strong>aagbi</strong>.org<br />
January 2006
MEMBERSHIP OF THE WORKING PARTY<br />
Professor Alastair Chambers Chairman. Honorary Secretary, AAGBI<br />
Ms Chrissie Allan<br />
Association for Perioperative Practice<br />
Dr Richard Birks<br />
Honorary Treasuer, AAGBI<br />
Dr Beverly Collett<br />
British Pain Society<br />
Dr John Curran<br />
Royal College of Anaesthetists<br />
Mr Chris Edwards,<br />
Home Office<br />
Dr Ben Fitzwilliams Group of Anaesthetists in Training<br />
Mr Bill Kilvington<br />
Association of Operating Department Practitioners<br />
Dr Peter Nightingale Royal College of Anaesthetists<br />
Dr Anna-Maria Rollin Royal College of Anaesthetists<br />
Dr Cathy Stannard<br />
British Pain Society<br />
Ex Officio<br />
Professor M Harmer<br />
Dr P G M Wallace<br />
Dr D Whitaker<br />
Dr D Dickson<br />
Dr D Bogod<br />
President<br />
Immediate Past President<br />
Immediate Past Honorary Secretary<br />
Honorary Membership Secretary<br />
Editor-in-Chief, Anaesthesia<br />
The working party gratefully acknowledges the assistance of the Royal College<br />
of Nursing and the Royal Pharmaceutical Society of Great Britain who reviewed<br />
and commented on the document<br />
(c) Copyright of the Association of Anaesthetists of Great Britain and<br />
Ireland. No part of this book may be reproduced without the written<br />
permission of the Association of Anaesthetists.
Contents<br />
Section 1. Introduction 3<br />
Section 2. Medicines Act 1968 4<br />
Section 3.<br />
Issue of Controlled Drugs Within the Operating<br />
Department and Key Holding 7<br />
Section 4. Guidelines 8<br />
Section 5. Multiple Dosing 11<br />
Section 6. Solutions for Infusion 12<br />
Section 7. Disposal of Controlled Drugs 14<br />
Appendix 15<br />
References 16<br />
1
SUMMARY OF THE RECOMMENDATIONS<br />
1. Local guidelines should be established to promote good, safe and<br />
legal practice for handling controlled drugs. These must ensure<br />
compliance with the Medicines Act, the Misuse of Drugs Act, the<br />
Misuse of Drugs (Safe Custody) Regulations and the Misuse of<br />
Drugs Regulations.<br />
2. When patient controlled analgesia or other infusion devices are<br />
being used, it is best practice to use pre-filled syringes rather than<br />
make up a solution by diluting ampoules.<br />
3. The Misuse of Drugs Regulations should be amended to take<br />
account changes in the roles and titles of staff in modern clinical<br />
practice. The terms ‘sister or acting sister’ which are widely referred<br />
to are now archaic and should be changed. The Association<br />
recommends that ODPs should be able to be responsible for<br />
possessing and issuing controlled drugs and that senior ODPs could<br />
also have the authority to order controlled drugs.<br />
4. Although controlled drugs must be stored in a secure place this<br />
must allow an appropriate level of access and availability for<br />
immediate clinical use.<br />
5. Unused controlled drugs must be disposed of in an approved<br />
manner and this should be included in local guidelines.<br />
6. The sharing of the contents of any ampoule between patients is poor<br />
practice.<br />
2
SECTION 1. INTRODUCTION<br />
When the Association of Anaesthetists of Great Britain and Ireland<br />
(AAGBI) published a document (1981) on controlled drugs, their use as<br />
far as anaesthetists were concerned was essentially confined to the<br />
anaesthetic rooms and operating theatres. In addition, the quantities of<br />
drugs used were relatively modest.<br />
The situation was different by the time these guidelines were revised in<br />
1994 and developments in clinical practice have continued.<br />
Nowadays patients may receive large doses of opioids as a major part<br />
of their anaesthetic, there is a wide range of controlled drugs available<br />
and the responsibility of anaesthetists in prescribing and administering<br />
controlled drugs has extended not only into the recovery room and<br />
Intensive Therapy Unit, but also to acute and chronic pain services in<br />
all parts of the hospital and home care. An additional factor is the issue<br />
of substance abuse. Because of these extended uses of controlled<br />
drugs, particularly in relationship to acute pain services, a much wider<br />
range of preparations is necessary to meet these requirements, e.g. the<br />
development of Patient Controlled Analgesia (PCA).<br />
This publication recommends what the Association considers best<br />
practice for the safe preparation, distribution and disposal of controlled<br />
drugs to meet current clinical demands in peri-operative care.<br />
3
SECTION 2. MEDICINES ACT 1968<br />
The Medicines Act 1968, together with its secondary legislation,<br />
provides a regulatory scheme of licences, registrations and exemptions<br />
which control all aspects of the production and distribution of all<br />
medicinal products.<br />
A Product Licence is issued when the Medicines and Healthcare<br />
products Regulatory Agency (MHRA) is satisfied regarding a product’s<br />
inherent safety, quality and efficacy for the indicated purpose.<br />
A product licence specifies not only the nature of the drug, but also its<br />
pharmaceutical form, strength and packaging. Thus, for example, an<br />
ampoule of morphine sulphate 30mg may be a licensed product, but,<br />
if used to make and supply a pre-filled syringe or PCA device, the<br />
resulting product will be unlicensed.<br />
As part of the application for a Product Licence, the manufacturer will<br />
have to submit evidence regarding the stability of the product which<br />
will then be assigned a shelf-life.<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
recommends that wherever a pre-filled syringe or PCA device is<br />
marketed as a licensed medicinal product, it should be used in<br />
preference to an equivalent but unlicensed product.<br />
A Manufacturer’s Licence is issued when the Licensing Authority is<br />
satisfied that an applicant can manufacture medicinal products to<br />
acceptable standards, so as to ensure the safety, quality and efficacy of<br />
those products. A manufacturer’s licence enables the holder to produce<br />
either a licensed medicinal product or an unlicensed special. A<br />
manufacturer’s licence may be granted to commercial organisations<br />
and to some NHS hospitals.<br />
Specials are medicinal products in respect of which a Product Licence<br />
is not in existence but which have been made by the holder of a<br />
Manufacturer’s Licence to the order of a medical practitioner.<br />
4
Section 9 of the Medicines Act allows a medical practitioner to prepare<br />
or order a medicinal product for a particular patient. The practitioner<br />
assumes responsibility for all aspects of the safety of such products<br />
including compatibility of ingredients, their stability and sterility. The<br />
patient, or patients, must be named.<br />
A shelf-life of several weeks or months may be appropriate for some<br />
Specials, but it is the responsibility of the manufacturer to ensure that<br />
the shelf-life is supported by suitable stability data. Notice must always<br />
be taken of expiry dates on all products.<br />
Prepared Medicines are medicinal products in respect of which a<br />
Product Licence is not in existence but which have been made under<br />
the supervision of a pharmacist in a retail or hospital pharmacy, neither<br />
of which is the holder of a Manufacturer’s Licence.<br />
This activity is carried out under Section 10 of the Medicines Act which<br />
allows a pharmacist to prepare medicines in accordance with a<br />
prescription given by a medical practitioner or in anticipation of such<br />
a prescription.<br />
Thus, a medicinal product may by classified as:<br />
• a licensed medicine<br />
• a special medicine<br />
• a prepared medicine<br />
Many injectable medicines, although supplied as licensed products,<br />
have to be reconstituted or diluted before administration to the patient<br />
and thus become prepared medicines. When this dilution is carried out<br />
by a registered prescriber, he or she is responsible for seeing that the<br />
procedure is performed properly and accurately.<br />
The working party has given particular consideration to filled syringes<br />
and other devices which are either made up in advance or which<br />
remain with the patient for long periods of time and move with the<br />
patient from one clinical are a to another. A common example are the<br />
medicines used for Patient Controlled Analgesia.<br />
5
In order of preference, the supply of pre-filled syringes and devices<br />
forming part of a PCA or similar system should be as follows:<br />
(i)<br />
A licensed medicinal product wherever such an item is available.<br />
(ii) A ‘special’ produced in a licensed facility which may be a<br />
commercial supplier or hospital pharmacy.<br />
(iii) A prepared medicine made in a retail or hospital pharmacy, under<br />
the direct supervision of a pharmacist.<br />
(iv) Prepared by a trained member of staff near the patient according<br />
to a local protocol.<br />
6
SECTION 3. ISSUE OF CONTROLLED DRUGS<br />
WITHIN THE OPERATING DEPARTMENT AND KEY<br />
HOLDING<br />
The Misuse of Drugs Regulations 2001 place the responsibility for the<br />
possession, safe custody and issue of controlled drugs within hospital<br />
wards and departments with the sister or acting sister in charge of that<br />
ward or department.<br />
Over the last few years, staffing practice in operating departments and<br />
related areas has undergone considerable change; the titles “sister” and<br />
“acting sister” are often no longer used. However, in purely legal terms,<br />
responsibility for the safe custody and issue of controlled drugs rests<br />
with the most senior registered nurse on duty in the department.<br />
Some operating departments have several operating theatres, each of<br />
which will have its own controlled drugs cabinet. The sister or acting<br />
sister in charge of the operating department is responsible for supplies<br />
from all the controlled drugs cabinets. To ensure controlled drugs are<br />
readily available, the sister or acting sister in charge may delegate<br />
control of access (key holding) to another registered nurse or a medical<br />
practitioner (e.g. anaesthetist) or an operating department practitioner<br />
(ODP). This access must be strictly controlled in practice and set out in<br />
locally agreed written guidelines. A registered nurse or an ODP may<br />
remove controlled drugs from a controlled drugs cabinet and return<br />
them to the cabinet on the specific authority of either the sister or a<br />
medical practitioner. However, the responsibility for all controlled<br />
drugs remains with the senior registered nurse on duty, even if the<br />
nurse decides to allow access by others.<br />
As many operating departments are now staffed with ODPs and some<br />
are managed by ODPs, the Association of Anaesthetists of Great Britain<br />
and Ireland believes that the Misuse of Drugs Regulations 2001 should<br />
be amended so that ODPs may also be specifically authorised and be<br />
responsible for possessing and issuing controlled drugs. The<br />
terminology of ‘sister or acting sister’ is now archaic and should<br />
be amended.<br />
7
SECTION 4. GUIDELINES<br />
The development of local guidance is essential. Such guidelines should:-<br />
• recognise and adhere to the relevant legal requirements<br />
• promote good, safe practice<br />
• take account of local staffing arrangements<br />
• not restrict the use of opioids in a manner which would be<br />
detrimental to patient care<br />
• be understood and accepted by all staff<br />
While individual hospitals should have their own local guidelines,<br />
there are a number of points which need to be considered. The<br />
Department of Health Report, Guidelines for the Safe and Secure<br />
Handling of Medicines, (Duthie Report 1988) may be of assistance.<br />
Responsibility<br />
The system established for ordering and security should be that agreed<br />
between the senior pharmacist, the operating department manager and<br />
appropriate senior nursing staff. Current legislation states that<br />
controlled drugs may be requisitioned only by the sister or acting sister<br />
in charge of a department.<br />
Responsibility of individuals within the operating department are those of:<br />
(a) The sister or acting sister in charge for:<br />
(i) ordering, receiving, checking, recording and storing stock;<br />
(ii) recording the amount issued to medical staff;<br />
(iii) returning unused ampoules to stock;<br />
(iv) amending balances accordingly.<br />
8
(b) Medical staff for:<br />
(i) signing for the controlled drugs received in the operating<br />
theatre controlled drugs register;<br />
(ii) properly recording in the patient’s records the amount of<br />
drugs administered;<br />
(iii) returning any unopened ampoules;<br />
(iv) safe disposal of any unused controlled drugs that remain in an<br />
open ampoule or syringe.<br />
(c) The pharmacist for:<br />
(i) supply of controlled drugs to each stock location;<br />
(ii) regular audit of local policies;<br />
(iii) checking controlled drug stocks and registers at least once every<br />
three months.<br />
Issue of drugs from a register to anaesthetists or other prescribers<br />
(a) When controlled drugs are issued, they must be checked by the<br />
prescriber with the nurse (or other designated person) and the<br />
controlled drugs register signed.<br />
(b) The same responsibility and recording procedures apply for the<br />
drawing up of controlled drugs for a PCA or other infusion regimen.<br />
Ordering and Transfer of Drugs<br />
(a) An agreed stock level and usage pattern should be decided between<br />
medical staff and those responsible for ordering.<br />
(b) If computer ordering systems are used, a printout signed by the<br />
sister is required to provide the necessary requisition.<br />
(c) Where ordering is carried out using computer technology, access to<br />
passcodes/terminals should be restricted to designated persons.<br />
9
(d) Controlled drugs coming into the operating department should,<br />
ideally, be received at one central point and distributed from there<br />
to individual operating theatres, or be issued directly to the<br />
controlled drug stock in a specific theatre. There is no legal<br />
requirements for registers to be held at individual theatre level, but<br />
good practice and Department of Health guidance dictates that the<br />
theatre suite register should include a record of all drugs issued for<br />
administration to patients in the individual theatres.<br />
Unused Controlled Drugs<br />
There should be a local protocol describing the procedure for the<br />
disposal of individual doses of controlled drugs which are prepared but<br />
not administered. The Department of Health is expected to issue<br />
guidance on the disposal of controlled drugs shortly.<br />
SECURITY<br />
Controlled drugs must be stored in a secure place. The Misuse of Drugs<br />
(SafeCustody) Regulations 1973 define in great detail the type of<br />
cabinet or safe required and the type of steel, locks and hinges of<br />
which it should be made.<br />
Neither the Misuse of Drugs Act 1971 nor the Safe Custody Regulations<br />
1973 state that controlled drugs must be stored in a double-locked<br />
cabinet, with or without a red light. However, it is worth noting that a<br />
locked refrigerator is a complying receptacle.<br />
Numerous amendments have added substances to, and subtracted<br />
others from, the comprehensive list of those that need or need not be<br />
stored in the controlled drugs cabinet. These relate to Schedule 2<br />
drugs, i.e. the opioids and other potent analgesic agents. They are listed<br />
in the Appendix A. The pharmacist would be able to advise, should<br />
there be any doubts, as to whether a particular drug is subject to the<br />
Safe Custody Regulations.<br />
10
SECTION 5. MULTIPLE DOSING<br />
Containers whose contents are designed to be used for more than one<br />
patient are labelled in such a way as to indicate that they are intended<br />
for multiple use. The contents of any other type of ampoule, whatever<br />
the size, should not be shared between patients.<br />
Financial pressures and a simple wish not to be wasteful of resources<br />
often led anaesthetists to share the contents of one ampoule amongst<br />
multiple syringes. The possibility of mistakes in administration, cross<br />
infection and the admittedly theoretical risk of theft from an open<br />
ampoule are not over-ridden by the small cost benefit of using one<br />
large ampoule rather than several smaller ones. This should not be<br />
construed as including the preparation in pharmacy of individual<br />
prepared syringes.<br />
11
SECTION 6. SOLUTIONS FOR INFUSION<br />
Opioid containing solutions are increasingly being used for parenteral<br />
PCA and epidural analgesia techniques. They commonly contain a<br />
solution of a single controlled drug in diluted format, or a mixture in<br />
combination with a local anaesthetic or other drug.<br />
Preparation<br />
As described in Section II of this document, the Association of<br />
Anaesthetists of Great Britain and Ireland recommends that, wherever<br />
possible, the best practice is that such pharmaceutical preparations<br />
should be purchased from a manufacturer, or prepared under sterile<br />
conditions in a hospital pharmacy. This practice is preferable to<br />
preparing the solution on an individual basis in the operating<br />
department or ward, for the following reasons:-<br />
(a) sterility is guaranteed, which is especially important as the solution<br />
may be administered over several days.<br />
(b) the solution will be clearly labelled, showing the constituent drug(s),<br />
concentration(s), diluent, date of manufacture and expiry date.<br />
Hospitals without a licensed manufacturing facility may prefer to obtain<br />
ready prepared PCA and epidural solutions from a Manufacturers’<br />
Licence holder. This may be another local hospital.<br />
On rare occasions, it may be clinically advisable to administer an unusual<br />
mixture or concentration of drugs. In such cases, it would prudent for the<br />
reasons for this to be documented in the patient’s notes and for senior staff<br />
to be aware of the situation.<br />
Storage<br />
Once prepared, it is recommended that PCA and epidural solutions of<br />
controlled drugs should be supplied in individually sealed bags to<br />
suitable locations such as operating theatres, recovery rooms and labour<br />
wards and post operative wards. Prepared solutions must be accounted<br />
12
for in the ward controlled drug register in the same manner as controlled<br />
drugs.<br />
Solutions must be stored in a complying locked cabinet in each location.<br />
Bags of solution for epidural administration need to be clearly identifiable<br />
and must be stored separately from those for intravenous infusion.<br />
Serious harm to patients can result from the inadvertent parenteral<br />
administration of solutions intended for epidural administration.<br />
13
SECTION 7. DISPOSAL OF CONTROLLED DRUGS<br />
A controlled drug ceases to be classified as such once it is denatured,<br />
dissipated, is not re-usable or has been rendered irretrievable. All drugs,<br />
once disposed of, should be unrecognisable as such. Syringes containing<br />
residual unused controlled drugs should be emptied before being<br />
discarded.<br />
All unused, unopened or out of date products must be returned to the<br />
issuing pharmacy for recording and disposal in accordance with the law.<br />
Sites outside the operating department<br />
It is common practice for infusions of controlled drugs to be set up in<br />
the operating theatre or recovery area. These infusions may then<br />
accompany the patient to the ward. Unused volumes of these infusions<br />
should be disposed of on the ward, thus avoiding unnecessary<br />
transport of controlled drugs (and consequent security implications)<br />
around the hospital.<br />
It is impractical to record the disposal of these volumes in the<br />
controlled drugs register at their site of issue, which may be different<br />
from the site of disposal. In the ward, disposal should be recorded and<br />
a “disposals” page in the controlled drug register should record the site<br />
of drug issue and the volume of drug discarded.<br />
14
APPENDIX<br />
The Misuse of Drugs Act provides the basis of control for certain drugs.<br />
It contains three sets of regulations.<br />
1. The Misuse of Drugs Regulations defines five schedules of drugs.<br />
Schedule 1 contains drugs with no recognised medical use, which are<br />
the most tightly controlled. These include hallucinogens, raw opium<br />
and coca leaf.<br />
Schedule 2 is the most important and covers pharmaceutical opioids<br />
and amphetamines. It is the most relevant to this document and the<br />
routine practice of anaesthesia.<br />
Schedule 3 contains barbiturates and some slimming preparations.<br />
Schedule 4 contains benzodiazepines.<br />
Schedule 5 includes products containing low concentrations of drugs<br />
which would be in Schedule 2 if in a stronger preparation.<br />
There have been various amendments since 1985.<br />
2. The Safe Custody Regulations, followed by several recent<br />
amendments, refers to Schedules 2 and 3, but then actually exempts<br />
many of the Schedule 3 drugs.<br />
A list of the commonly used Schedule 2 drugs include:-<br />
Alfentanil<br />
Cocaine<br />
Diamorphine<br />
Fentanyl<br />
Methadone<br />
Morphine<br />
Pethidine<br />
Remifentanil<br />
3. The Misuse of Drugs (Notifications of a Supply to addicts)<br />
Regulations. Not relevant to this publication.<br />
15
REFERENCES<br />
Report of a Working Party on the use of Controlled Drugs in Operating<br />
Theatres. Association of Anaesthetists of Great Britain and Ireland 1981<br />
(revised 1994)<br />
Medicines Act 1968.<br />
Guidance to NHS Hospitals on the licensing requirements of the<br />
Medicines Act. Published by the Medicines Control Agency now the<br />
Medicines and Healthcare products Regulatory Agency (MHRA).<br />
Misuse of Drugs Act 1971 and its secondary legislation:<br />
The Misuse of Drugs Regulations 2001<br />
The Misuse of Drugs (Safe Custody) Regulations 1973<br />
The Misuse of Drugs (supply to addicts) Regulations 1997<br />
The safe and secure handling of medicines: A team approach. A<br />
revision of the 1988 Duthie report. The Royal Pharmaceutical Society<br />
of Great Britain. 2005 (www.rpsgb.org)<br />
16
21 Portland Place, London W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org<br />
Designed and produced by the r2 Partnership Ltd
Practical advice from the GAT Committee<br />
on surviving the first two years as an anaesthetic trainee<br />
Editor: Dr E H Shewry<br />
GAT Committee<br />
AAGBI<br />
October 2009<br />
1
Welcome<br />
to the first edition of the<br />
Core Survival Guide<br />
I hope this new GAT guide is a useful and<br />
enjoyable read. Starting a new specialty<br />
can be difficult, so I hope this booklet will<br />
answer some of your questions and help<br />
you through those first few weeks and<br />
months. Postgraduate medical training<br />
has changed continuously as this guide<br />
has been developed; please let us know<br />
if there are any top tips we’ve missed and<br />
we’ll aim to add them to the next edition!<br />
Finally, good luck in your new career and<br />
enjoy it!<br />
Liz Shewry<br />
Editor<br />
Vice Chair,<br />
GAT Committee<br />
Acknowledgements<br />
The GAT Committee would like to thank<br />
the Medical Protection Society for its<br />
generous contribution towards the cost<br />
of this publication.<br />
We also wish to thank Dr Nevil Hutchinson<br />
for his contribution in producing the original<br />
SHO Survival Guide.<br />
23
Contents<br />
Foreword 4<br />
1. Introduction 5<br />
2. The Association of Anaesthetists of 6<br />
Great Britain & Ireland and the Group<br />
of Anaesthetists in Training<br />
3. The Royal College of Anaesthetists 8<br />
4. Preparing for the first day as an anaesthetist 8<br />
5. Health and safety 12<br />
6. Portfolio and logbook 12<br />
7. Training in anaesthesia 15<br />
8. Acute Care Common Stem training 24<br />
9. The ARCP (Annual Review of<br />
Competence Progression) 25<br />
10. The Primary FRCA examination 25<br />
11. Getting a ST3 post in anaesthetics 28<br />
12. Anaesthetic training in Scotland 31<br />
13. Anaesthetic training in Northern Ireland 32<br />
14. Professionalism and accountability 33<br />
15. Whom to ask for help? 34<br />
16. Final checklist 36<br />
17. Appendices:<br />
(i) Abbreviations 36<br />
(ii) Useful addresses 37<br />
(iii) Essential reading 38<br />
Disclaimer: The GAT Committee emphasises that this booklet is intended as an introduction to the specialty and<br />
the advice provided must be interpreted as guidance. We acknowledge that the rapid changes in postgraduate<br />
medical training means that although we have ensured that the guidance in this booklet is applicable and up to<br />
date, it may soon need revision. Please use the links for the Royal College of Anaesthetists and the Association of<br />
Anaesthetists of Great Britain & Ireland to augment the information provided in this booklet.<br />
© Copyright of the Association of Anaesthetists of Great Britain & Ireland. No part of this book may be<br />
reproduced without permission of the AAGBI.<br />
23
Foreword<br />
The GAT Committee has produced the<br />
Core Survival Guide as a replacement<br />
to the previous ‘SHO Survival Guide’<br />
– a booklet that most of us found<br />
invaluable during our initial training<br />
years. Its aim is to help you through<br />
those first two years of ‘Core Training’,<br />
as you progress from standing around<br />
feeling like a spare part to being able<br />
to ‘fly solo’ and eventually pass the<br />
Primary FRCA exam and obtain an<br />
ST3 post. It contains many ‘top tips’<br />
to make life just that little bit easier,<br />
and also lists the many benefits of<br />
membership of the AAGBI. This update<br />
has evolved during the many changes<br />
to the structure of medical training over<br />
the last two years, but as always these<br />
things have a tendency to move quickly<br />
and change seems almost continuous.<br />
We recommend that in addition to<br />
utilising this guide you also visit our<br />
web pages at www.<strong>aagbi</strong>.org/gat.htm.<br />
Dr Felicity Howard<br />
GAT Committee Chair<br />
Hard copies of this booklet are being<br />
distributed to anaesthetic departments<br />
and it is available online at<br />
www.<strong>aagbi</strong>.org/gat/publications.htm.<br />
I would like to thank our Vice Chair,<br />
Dr Liz Shewry, for all her hard work in<br />
leading this project, the authors who<br />
have contributed articles to this booklet,<br />
the GAT Committee for their help with<br />
the editing process and the staff at<br />
Portland Place for all their help and<br />
support.<br />
45
Introduction<br />
Anaesthetics has traditionally been a<br />
specialty which junior doctors entered<br />
after two to three years of postgraduate<br />
training. The broad clinical base<br />
developed in those pre-anaesthetic<br />
years has always been a great fallback<br />
to help meet the challenging demands<br />
of the specialty. However, the ongoing<br />
changes in postgraduate medical<br />
training mean that the majority of junior<br />
doctors are now entering anaesthetics<br />
directly following the Foundation<br />
Programme. This means that appropriate<br />
support and guidance are even more<br />
important to ensure the welfare<br />
and success of future anaesthetic<br />
consultants.<br />
The Group of Anaesthetists in Training<br />
(GAT) Committee is formed of elected<br />
representatives from the anaesthetists<br />
in training in the United Kingdom.<br />
We have produced this booklet as an<br />
introduction to the specialty, aimed at<br />
the early training years, and hope you<br />
may gain from some of our personal<br />
experiences. This guide starts from day<br />
one and leads to obtaining a ST3 post.<br />
We hope it will provide some useful<br />
pointers and be an interesting read at<br />
the same time.<br />
45
The Association of Anaesthetists of Great Britain & Ireland<br />
and the Group of Anaesthetists in Training<br />
The Association of Anaesthetists of<br />
Great Britain & Ireland (AAGBI)<br />
was established in 1932 ‘to promote<br />
the development of anaesthesia; to<br />
coordinate the activities of anaesthesia;<br />
to represent anaesthetists and their<br />
interests; and to encourage friendship<br />
among anaesthetists’. It was responsible<br />
for the development of the Faculty of<br />
Anaesthetists of the Royal College of<br />
Surgeons in 1948. This led ultimately to<br />
the formation of the separate College of<br />
Anaesthetists, which received its Royal<br />
Charter in 1992.<br />
Trainee anaesthetists were first<br />
permitted to become associate<br />
members of the AAGBI in 1956, but<br />
they had no representation or voting<br />
rights. The Group of Anaesthetists in<br />
Training (GAT) was established as the<br />
Associates in Training Group in 1967<br />
and was the first single-specialty trainee<br />
representative body in the country. In<br />
1971 it became the Junior Anaesthetists<br />
Group, before changing its name to<br />
GAT in 1991. The membership of<br />
GAT continues to grow year on year<br />
and currently stands at over 3900,<br />
accounting for approximately one-third<br />
of the Association’s membership. GAT<br />
is the only elected body that represents<br />
trainees in anaesthetics at a national<br />
level. All trainee members of the AAGBI<br />
are automatically members of GAT,<br />
and all members of GAT are given the<br />
opportunity to nominate and vote for<br />
members of the GAT Committee.<br />
Besides organising the GAT Annual<br />
Scientific Meeting (ASM), the<br />
Committee represents trainees’ views<br />
on Working Parties, Committees and<br />
Councils of the Association and the<br />
Royal College of Anaesthetists. GAT is<br />
also represented at meetings held by<br />
the Postgraduate Medical Education<br />
and Training Board (PMETB), the British<br />
Medical Association (BMA) and the<br />
Department of Health (DoH). Our role<br />
at these meetings is to represent the<br />
views of anaesthetic trainees and to<br />
pass information back to GAT members.<br />
The GAT Committee runs a number of<br />
seminars aimed primarily at trainees,<br />
such as the Consultant Interview<br />
Seminar. These are continuously<br />
evolving to meet trainees’ needs. We<br />
also hold the flagship ASM at a different<br />
location within the UK each summer.<br />
Other GAT publications include: ‘The<br />
GAT Handbook’ (9 th Edition), the GAT<br />
‘Organising a Year Abroad’ handbook<br />
and ‘Your Career in Anaesthesia’ (for<br />
medical students and FY trainees).<br />
Further information can be found at<br />
www.<strong>aagbi</strong>.org/gat.htm.<br />
67
JOIN THE ASSOCIATION OF ANAESTHETISTS<br />
AND YOU’LL BE IN GOOD COMPANY<br />
10,000 members are already benefiting<br />
from the Association’s unique<br />
membership package:<br />
• Personal injury and life insurance<br />
cover of up to £1 million for patient<br />
transfer<br />
• Free subscription to Anaesthesia -<br />
the renowned international monthly<br />
journal<br />
• Free copies of the Association<br />
guidelines<br />
• Free monthly newsletter Anaesthesia<br />
News keeping you up to date with<br />
new developments<br />
• Special rates for scientific meetings<br />
• Priority booking and special rates for<br />
seminars at Portland Place<br />
• Free advice and information<br />
• Free information handbooks for<br />
trainees & SAS Grade Doctors<br />
• Representation at Westminster and<br />
the DoH<br />
• New AAGBI website with up-todate<br />
news on the Association and<br />
anaesthesia<br />
• Private members’ forum hosted by<br />
Doctors.net<br />
• Opportunities to apply for grants<br />
and awards<br />
• 20% discount on textbooks from<br />
Oxford University Press and<br />
Wiley-Blackwell Publishing<br />
• AAGBI subscription is on the<br />
HMRC approved list of professional<br />
organisations for tax relief<br />
For further details please refer to the application form at the centre of this guide.<br />
Or contact:<br />
Membership Department, Association of Anaesthetists of Great Britain & Ireland<br />
21 Portland Place, London, W1B 1PY<br />
t: 020 7631 8801<br />
e: members@<strong>aagbi</strong>.org<br />
67
The Royal College of Anaesthetists<br />
The Royal College of Anaesthetists<br />
(RCoA) is the professional body<br />
responsible for the specialty of<br />
anaesthetics throughout the United<br />
Kingdom. The Royal Charter gives<br />
the RCoA responsibility for ensuring<br />
excellence in anaesthesia, critical<br />
care and pain management through<br />
setting and maintaining standards<br />
of patient care. In addition to<br />
safeguarding excellence in clinical<br />
care, the responsibilities of the RCoA<br />
include the maintenance of standards<br />
of postgraduate training, governing<br />
examinations and the ongoing<br />
continuing medical education and<br />
professional development of all doctors<br />
working within anaesthesia, pain<br />
management and intensive care. Their<br />
website is: www.rcoa.ac.uk.<br />
The RCoA Tutors (‘College Tutors’)<br />
are trainers who represent the RCoA<br />
and ensure that training is properly<br />
organised, occurs when time-tabled<br />
and is accessible to the trainees. The<br />
College Tutors act as the organisers<br />
and co-ordinators of training. The<br />
delivery of high quality training requires<br />
contributions from all consultants but<br />
the College Tutors are the prime points<br />
of contact for the trainees with the<br />
RCoA.<br />
All UK training hospitals are contained<br />
within schools of anaesthesia. Within<br />
each school an anaesthetist is appointed<br />
as a Programme Director - this is a<br />
deanery appointment - and another as<br />
Regional Advisor, a RCoA appointment.<br />
The Programme Director organises<br />
rotations to ensure exposure to all<br />
appropriate anaesthetic specialities. The<br />
Regional Advisor ensures that standards<br />
of anaesthetic training are maintained,<br />
and represents the policies and views of<br />
the college.<br />
Finally, we recommend that you register<br />
with the RCoA as soon as possible.<br />
Failure to register means you are unable<br />
to apply for the FRCA examination.<br />
Preparing for the first day<br />
as an anaesthetist<br />
Anaesthetics can be an extremely<br />
challenging specialty for any trainee.<br />
With this in mind, there are some<br />
simple things you can do to ease<br />
yourself into this new environment.<br />
Your new hospital should provide you<br />
with an induction pack before you start<br />
and it is perfectly reasonable to ask for<br />
one if you have not received it. This<br />
will give you an idea of the structure<br />
of the department and hospital. The<br />
month before you start is a good time<br />
to contact the College Tutor, the rota<br />
co-ordinator and the ‘novice’ trainees<br />
in the anaesthetic department. The best<br />
person to contact to arrange a time for<br />
this visit is the anaesthetic department<br />
89
co-ordinator or secretary. It always<br />
helps to befriend them and get them<br />
‘on your side’, as they can make your<br />
life easy, or difficult, depending on your<br />
attitude. Although you should be shown<br />
around on your induction day, if you<br />
time a pre-visit correctly, you may be<br />
able to spend time talking to the current<br />
incumbent in your position.<br />
The first day....<br />
Your first one or two days are for<br />
‘induction’ into the Trust and the<br />
Department.<br />
Trust induction<br />
Trusts require all new staff to undergo<br />
a hospital induction. This may be<br />
in the form of lectures or it may be<br />
available online. Some Trusts expect<br />
trainees to complete online modules<br />
before their first day. There are also<br />
other competencies that you are<br />
obliged to complete yearly, such as<br />
manual handling, fire safety and child<br />
protection. You may be expected to<br />
attend a Basic Life Support update. In<br />
addition, you will need to:<br />
• Obtain a security / ID card and<br />
a parking permit when given the<br />
chance as the opening times are<br />
often limited. This may require<br />
having your photo taken.<br />
• Deliver all your personal details<br />
to Human Resources and Payroll<br />
including payslips, GMC Certificate,<br />
P45 / P60. Take the originals along<br />
yourself and ask them to photocopy<br />
them whilst you wait so you can<br />
take the originals away again. If<br />
they get lost you will have to pay for<br />
replacements and the chances are<br />
the Trust will not be forthcoming to<br />
reimburse you for this.<br />
• Attend Occupational Health<br />
bringing a ‘smart card’ if available<br />
and evidence of up-to-date<br />
vaccination status.<br />
• Submit signatures for pharmacy and<br />
pathology.<br />
• Visit the IT department for hospital<br />
login / passwords and to access<br />
email and lab results.<br />
• You may need to attend specific<br />
training sessions to access online<br />
radiology.<br />
• Register with the data controller<br />
before you start an electronic<br />
logbook. (Chapter 6)<br />
Departmental induction:<br />
some suggested aims<br />
Staff - Find out who the following<br />
individuals are: College Tutor, Rota<br />
Co-ordinator, Clinical Lead / Director,<br />
Educational Supervisor.<br />
RCoA Tutor - Every department with<br />
trainees has at least one College Tutor,<br />
who is responsible for overseeing<br />
training according to the guidelines laid<br />
out in the various training documents.<br />
The College Tutor may also act as your<br />
Educational Supervisor or you may<br />
be allocated a separate consultant to<br />
undertake this.<br />
89
Educational Supervisors - An<br />
Educational Supervisor is defined by<br />
PMETB as ‘a trainer who is selected<br />
and appropriately trained to be<br />
responsible for the overall supervision<br />
and management of a specific<br />
trainee’s educational progress …..The<br />
educational supervisor is responsible<br />
for the trainee’s educational agreement.’<br />
You will need a signed educational<br />
agreement to obtain study leave.<br />
Their role is to help plan your training<br />
and reach your personal objectives.<br />
You should arrange to meet them<br />
to formulate an educational plan,<br />
preferably within the first two weeks.<br />
As a novice you will follow a set route,<br />
but if this is a subsequent post then<br />
you should have already considered<br />
how your training should progress.<br />
Most departments have a series of<br />
three to four meetings / appraisals per<br />
post, so at the end of your first meeting<br />
you should make plans for the next. It<br />
is important to keep a signed record<br />
of each meeting. They can assist you<br />
with finding and starting a logbook,<br />
joining the RCoA and understanding<br />
the workplace assessments that you<br />
are required to undertake. Most of<br />
this information can be found on the<br />
RCoA website, but your educational<br />
supervisors may be better able to help<br />
you locate it. It is worth considering the<br />
appropriate time for you to undertake<br />
the Primary FRCA examination early,<br />
as options are now more limited<br />
Study leave - Make sure you are<br />
aware how the annual and study<br />
leave application processes work.<br />
Most departments have rules about<br />
how many trainees of each grade<br />
can be away at one time and keep a<br />
log of current bookings that allows<br />
you to determine availability. It is<br />
important to keep a record of study<br />
leave taken in a Portfolio or Continuing<br />
Professional Development (CPD) diary<br />
as this information may be required at<br />
appraisals and at the Annual Review of<br />
Competence Progression (ARCP).<br />
Annual leave - Planning annual leave<br />
can be very frustrating as a first-comefirst-served<br />
system invariably operates.<br />
Check whether the department requires<br />
prospective cover as if so, you must<br />
swap any on-calls within your leave<br />
period.<br />
Meetings - Obtain lists of departmental<br />
audit, morbidity and mortality meetings,<br />
journal clubs and teaching sessions /<br />
tutorials.<br />
Lockers - As an anaesthetist you will<br />
spend most of your working time in<br />
theatre scrubs. Obtaining a locker is<br />
vital and you should also be issued with<br />
‘theatre shoes’. Be prepared to stand<br />
your ground on this one, and put your<br />
name on the waiting list if required.<br />
Take a padlock/combination lock along<br />
on your first day in case this is required<br />
Access codes - Obtain access codes to<br />
changing rooms and for other doors that<br />
are locked out of hours.<br />
Theatre lists - Discover how to access<br />
theatre lists, whether via email,<br />
electronically or paper, e.g. theatre<br />
reception/secretaries office.<br />
10 11
Equipment competencies - You may be<br />
required to undergo training to ensure<br />
safe use of equipment such as IV, PCA<br />
and epidural pumps, and anaesthetic<br />
machines. These will need to be signed<br />
off and a copy kept in your portfolio.<br />
Computers - Each department will<br />
provide computer access to the internet,<br />
including the GAT website at www.<br />
<strong>aagbi</strong>.org/gat.htm. Find out how to do<br />
this, so you can keep yourself up to<br />
date by visiting the website regularly.<br />
The AAGBI has recently introduced<br />
online accounts for members to allow<br />
them access to specialist facilities such<br />
as Anaesthesia. Signing up with Oxford<br />
Journals will permit free access to the<br />
British Journal of Anaesthesia (BJA) and<br />
its educational supplement (CEACCP).<br />
Medical indemnity - Trainees are often<br />
unsure of the differences between<br />
Crown Indemnity provided by the<br />
NHS Trust and the cover that medical<br />
defence organisations offer. Whereas<br />
Crown Indemnity may cover you for<br />
negligence claims incurred during<br />
your work in the Trust, the defence<br />
organisations will actually support you<br />
by representing your interests at Fatal<br />
Accident Inquiries, Coroners’ Inquests<br />
and GMC hearings. The GAT Committee<br />
consider it essential to maintain<br />
personal medical indemnity cover with<br />
a medical defence organisation. The<br />
AAGBI will insure members against<br />
death and personal injury for up to<br />
£1 million when involved in patient<br />
transfers. This level of cover is not<br />
provided by the majority of medical<br />
defence organisations or by the NHS.<br />
Finally most trainees remember feeling<br />
exhausted during their first few weeks<br />
of anaesthetic training, so you won’t be<br />
alone if you do too!<br />
Induction: orientation<br />
During induction there are certain<br />
places and things that you should be<br />
made aware of. Here is a checklist:<br />
The hospital<br />
• Canteen facilities and opening times<br />
• Library – times and access<br />
• Parking<br />
• Accommodation<br />
• ID page and access<br />
• Hospital facilities, e.g. sports centre<br />
• Occupational health department<br />
• Doctors’ Mess<br />
Anaesthetic department<br />
• On-call room<br />
• Administrative staff<br />
• Rota<br />
• Access codes and telephone<br />
numbers<br />
• Annual and study leave<br />
• College tutor<br />
• Educational Supervisor / Mentor<br />
Theatres<br />
• Department protocols<br />
• Changing room<br />
• Recovery<br />
• Difficult airway trolley<br />
• Paediatric trolley<br />
• Arrest trolley<br />
• Dantrolene – treatment for<br />
malignant hyperthermia<br />
• Intralipid – treatment for LA toxicity<br />
10 11
Other departments<br />
• Day surgery units<br />
• Radiology<br />
• Obstetrics<br />
• Emergency department<br />
• Intensive care unit<br />
• Remote theatres - eye, ECT,<br />
angiography suite<br />
Health and safety<br />
As an anaesthetist patient safety is<br />
paramount. However it is equally<br />
important to ensure your own.<br />
• Whatever your normal practise, it<br />
is vital to become accustomed to<br />
wearing gloves for every patient<br />
contact. Anaesthetics has a high<br />
incidence of exposure to patient<br />
saliva and blood. For certain<br />
procedures a full aseptic technique is<br />
also required, including a mask, hat,<br />
gloves and gown.<br />
• If you suffer a needle stick injury<br />
it is important to follow Trust<br />
protocol. This may require attending<br />
occupational health department<br />
or the emergency department out<br />
of hours.<br />
• Working in theatre involves<br />
transferring patients. Attending a<br />
manual handling course will help<br />
protect you during these manoeuvres.<br />
• It is important to look after your<br />
mental, as well as physical wellbeing.<br />
Training in anaesthetics, as with all<br />
specialties, can be stressful at times.<br />
Please see Chapter 15 on how to<br />
obtain support and advice.<br />
Portfolio and logbook<br />
The RCoA states that ‘at the<br />
commencement of Core Training the<br />
trainee should create a Personal Training<br />
Record or portfolio into which he/she<br />
places all documentation relevant to<br />
training, including details of assessments<br />
completed.’<br />
It is vital to keep detailed<br />
documentation of your training using<br />
a training portfolio. The aim of the<br />
portfolio is to provide factual data<br />
of the training and the professional<br />
development exercises undertaken.<br />
This will ensure that you have all the<br />
required information for your formal<br />
record of assessment and achievement<br />
with your educational supervisor both<br />
at the start of and end of the post.<br />
It should contain the following as a<br />
minimum:<br />
• Up-to-date CV<br />
• Up-to-date logbook summary as per<br />
RCoA recommendations<br />
• All workplace assessments / DOPS /<br />
MiniCEXs / CBDs.<br />
• Appraisals and signed Educational<br />
Agreements<br />
• Training certificates and certificates<br />
of attendance at meetings /<br />
conferences<br />
• Record of audits / surveys / research<br />
or other ongoing projects<br />
• Summaries of MSF (Multi-Source<br />
Feedbacks)<br />
The portfolio will also help you to<br />
12 13
summarise your training, assessment<br />
and achievements before starting formal<br />
training in anaesthetics. The RCoA<br />
provides an example of a portfolio, the<br />
Appraisal Portfolio for Anaesthetists in<br />
Training in the NHS which is available<br />
to download on its website.<br />
You should read the RCoA publications,<br />
‘The CCT in Anaesthesia I: General<br />
Principles’ and, ‘The CCT in<br />
Anaesthesia II: Competency Based<br />
Basic Level Training’ at the start of<br />
your post. Both of these are available<br />
at www.rcoa.ac.uk. Knowing what is<br />
expected of you places you in the best<br />
position to formulate a career plan<br />
with your Educational Supervisor. The<br />
conflict between service provision and<br />
training can be fierce, and as a trainee<br />
you must be prepared to act if your<br />
training requirements are not met. If you<br />
are unaware of the requirements you<br />
may discover the shortcomings of your<br />
training too late. Novice anaesthetists<br />
will tend to follow a specified path,<br />
details of which are given in Chapter 7.<br />
Logbooks<br />
An up-to-date logbook is an essential<br />
requirement for the portfolio as it<br />
provides the evidence of training<br />
exercises undertaken. This should<br />
include all cases in whose anaesthetic<br />
care you were actively involved.<br />
The logbooks will provide a detailed<br />
summary of the cases, level of<br />
supervision, procedures undertaken<br />
(central lines, arterial lines, regional<br />
anaesthesia) and the experience gained.<br />
The link: http://rcoa.ac.uk/index.<br />
asp?PageID=968 lists the electronic<br />
logbooks that are supported by the<br />
college. They include programmes<br />
that are compatible with commonly<br />
available IT platforms, including<br />
Windows, Macintosh, handhelds and<br />
netbooks.<br />
The logbook is a vital part of both the<br />
appraisal and assessment processes.<br />
Keeping up to date with entries is the<br />
only way of maintaining a correct<br />
logbook. Once all the data are entered,<br />
the logbook programme allows you<br />
to produce summaries and reports<br />
(Diagram 1). No identifying information<br />
should be kept within this record,<br />
e.g. hospital number or date of birth.<br />
Trainees should be aware that if taken<br />
off the Trust premises, such electronic<br />
documentation renders them liable<br />
under the Data Protection Act. You are<br />
advised to register as Data Controllers<br />
with the Data Commissioner’s Office<br />
if this applies to you. The cost of this<br />
registration is an annual notification fee,<br />
which will be a lot less than a fine.<br />
Training in anaesthesia<br />
12 13
Royal College of Anaesthetists<br />
Record of Training Period 09/08/07 to 28/08/09<br />
Sample Report<br />
ST Years 1 & 2<br />
Random Hosp NHS Trust<br />
Number of Total % Supervised Solo Teacher 80yrs<br />
Cases<br />
Cardiothoracic 0 0% 0 0 0 0 0 0 0 0<br />
Dental 46 6% 40 6 0 0 0 12 34 0<br />
ENT 42 5% 37 5 0 0 3 8 30 1<br />
General 234 29% 127 107 0 2 1 5 189 37<br />
Gynae 100 12% 23 77 0 0 0 0 98 2<br />
ITU 0 0% 0 0 0 0 0 0 0 0<br />
Maxillo-facial 10 1% 9 1 0 0 2 2 6 0<br />
Misc 29 4% 6 23 0 0 0 0 25 4<br />
Neuro 0 0% 0 0 0 0 0 0 0 0<br />
Obstetrics 112 14% 20 92 0 0 0 0 110 2<br />
Ophthalmics 10 1% 9 1 0 0 0 0 3 7<br />
Orthopaedics 108 13% 17 91 0 1 0 0 98 9<br />
Pain 2 0% 2 0 0 0 0 0 2 0<br />
Plastics 1 0% 1 0 0 0 0 0 1 0<br />
Psych 2 0% 2 0 0 0 0 0 2 0<br />
Radiology 0 0% 0 0 0 0 0 0 0 0<br />
Trauma 37 5% 13 24 0 1 0 2 24 10<br />
Urology 41 5% 15 26 0 0 0 0 36 5<br />
Vascular 31 4% 12 19 0 0 0 0 26 5<br />
Totals 805 333 472 0 4 6 29 684 82<br />
ASA (No of Cases)<br />
Age Criteria (No of Cases)<br />
ASA Total Solo Age Group<br />
1 489 281 80yrs 82<br />
Hours of Work (No of Cases)<br />
Priority (No of Cases)<br />
0800-1800 601 Scheduled 578<br />
1800-0000 164 Urgent 188<br />
0000-0800 40 Emergency 3<br />
Diagram 1: This is an example of an anaesthetic logbook summary, demonstrating the variety of information that can be<br />
stored.<br />
14 15
The current training programme,<br />
overseen by the RCoA, ‘is a<br />
competency-based, supervised,<br />
continuously evaluated and tightly<br />
regulated programme, with the<br />
potential for tailoring to suit individual<br />
requirements and interests’. The<br />
recommended minimum duration of<br />
training is seven years: two years of<br />
Basic Level training (CT1 and 2); two<br />
years of intermediate level training (ST<br />
3 and 4); and three years of advanced<br />
level training (ST 5-7). The actual<br />
duration of training is not fixed to<br />
seven years, but will depend on the<br />
individual needs and the rate at which<br />
the competencies are achieved. The<br />
aim of such a programme is to produce<br />
anaesthetists of high quality.<br />
Core (Basic) Level Training<br />
Overview<br />
Basic level training for anaesthetists<br />
consists of two years training including<br />
a minimum of 21 months in anaesthesia<br />
and three months in intensive care<br />
medicine. Progression depends<br />
on the appropriate competencies<br />
being achieved. The aims during this<br />
important period of an anaesthetist’s<br />
career are: to acquire an overview<br />
of the multi-profession complex<br />
work environment; and to learn the<br />
basic principles of safe and effective<br />
anaesthesia, pain management and<br />
peri-operative resuscitation.<br />
The first six months<br />
Anaesthetists spend the majority of<br />
their time in the theatre suite and it is<br />
important to familiarise yourself with its<br />
workings. The Operating Department<br />
Practitioners (ODPs) will teach as well<br />
as assist, and you will find yourself<br />
relying on their expertise in difficult<br />
situations.<br />
Your patients’ safety is your<br />
responsibility. This not only includes the<br />
obvious, such as ensuring the patient is<br />
asleep, but also safeguarding the patient<br />
by protecting their eyes, pressure points<br />
etc. You will learn the necessary skills<br />
and knowledge during your training,<br />
but when working in an unfamiliar<br />
environment ensure you know the<br />
location of the nearest defibrillator,<br />
emergency drugs and whom to contact<br />
in an emergency.<br />
Many trainees new to anaesthesia<br />
find themselves frustrated during the<br />
first few weeks of work. Having been<br />
competent to work independently<br />
after qualification, you find yourself<br />
back at the beginning, in an unfamiliar<br />
environment, learning the basics under<br />
constant supervision. Knowing what is<br />
expected of you enables you to focus<br />
on what you need to achieve.<br />
The initial assessment of<br />
clinical competency<br />
The first hurdle of training is the<br />
RCoA ‘initial assessment of clinical<br />
competency’. This is at the end of the<br />
14 15
introductory period and is a RCoA<br />
requirement for anaesthetic trainees. It<br />
must be passed before progressing to<br />
indirect clinical supervision and until<br />
this is completed you should have<br />
immediate supervision at all times.<br />
When the assessment takes place<br />
depends on any previous anaesthetic<br />
experience you may have, and the<br />
speed at which you progress. The RCoA<br />
envisages that most trainees would pass<br />
this assessment after three months, and<br />
certainly by six months of training.<br />
The initial assessment of clinical<br />
competency contains six assessments,<br />
each of which must be completed<br />
twice:<br />
1. Pre-operative assessment of patients<br />
2. General anaesthesia (GA) for ASA * 1<br />
or 2 patients without intubation<br />
3. GA for ASA 1 or 2 patients with<br />
tracheal intubation<br />
4. Rapid sequence induction<br />
5. Cardiopulmonary resuscitation<br />
6. Clinical judgement, attitudes and<br />
behaviours<br />
* The ASA (American Society of<br />
Anesthesiologists) grade 1 or 2 patients are<br />
those who are fit and healthy, or have mild<br />
systemic disease.<br />
After completion of this initial<br />
assessment of clinical competency, the<br />
trainee may undertake uncomplicated<br />
general anaesthesia and simple<br />
peripheral nerve blocks under<br />
guidance of a consultant with indirect<br />
supervision. The trainee may commence<br />
solo lists at this time during normal<br />
working hours, but only with the<br />
presence of a trainer working in the<br />
same theatre suite.<br />
Workplace assessments and appraisals<br />
Anaesthetic training is competencybased,<br />
although it currently runs<br />
according to a time-based plan.<br />
Trainees undergo summative<br />
assessments throughout the anaesthetic<br />
training programme. These are designed<br />
to assess whether you have reached<br />
the specified standards in the training<br />
programme, to quantify experience,<br />
and to estimate the individual trainee’s<br />
eligibility to progress to further stages<br />
of training. The RCoA has designed<br />
common tools and documentation that<br />
should be used for workplace based<br />
assessment. For ‘novices’ in anaesthesia<br />
the ‘initial assessment of competency’<br />
takes precedence over the assessments<br />
listed below. The tools used are:<br />
• Multi-Source Feedback (MSF)<br />
• Mini-Clinical Assessment Evaluation<br />
Exercise (MiniCEX)<br />
• Direct Observation of Procedural<br />
Skills (DOPS)<br />
• Case Based Discussion (CBD)<br />
These forms can be downloaded<br />
from the link: http://rcoa.ac.uk/index.<br />
asp?PageID=982<br />
The training programme<br />
16 17
Foundation doctor (two years)<br />
(Or after another specialty e.g. general medicine)<br />
Core training in anaesthetics:<br />
Years 1 and 2<br />
(OR two-year Acute Care Common Stem plus CT2 in anaesthetics)<br />
During which time: Primary Fellowship examination<br />
Competitive application to specialist training in anaesthetics:<br />
Years 3 and 4<br />
During which time: Final Fellowship examination<br />
Specialist training in anaesthetics:<br />
Years 5 to 7<br />
(Potentially including work abroad or a research fellowship)<br />
Certificate of Completion of Training (CCT) awarded<br />
Consultant post<br />
16 17
Supervision of trainees<br />
When working ‘solo’ it is key to know<br />
whom to contact, and exactly how and<br />
how long it will take them to reach you.<br />
More importantly, you should not begin<br />
anything you feel unhappy about. If you<br />
find yourself wondering whether or not<br />
to contact someone senior, you almost<br />
certainly should. It is often during<br />
normal working hours when such lines<br />
of communication become blurred, so<br />
get into the habit of finding out who is<br />
your point of contact before starting a<br />
list on your own.<br />
You are encouraged to seek advice<br />
and/or assistance as early as possible<br />
whenever you are concerned about<br />
patient management. Patient safety<br />
must never be compromised.<br />
Grades of clinical supervision<br />
Clinical supervision of daytime and out<br />
of hours’ duties for anaesthesia falls into<br />
two categories: direct and indirect:<br />
Direct supervision This means working<br />
directly with a senior supervisor who is<br />
actually present or can be within seconds.<br />
This proximity maintains patient safety but<br />
allows a degree of independence in order<br />
to develop confidence.<br />
Indirect supervision Indirect<br />
supervision falls into two categories,<br />
local and distant:<br />
• Local supervision – this means that the<br />
supervisor is on the same geographical<br />
site, is immediately available for<br />
advice and is able to be present within<br />
10 minutes of being called.<br />
• Distant supervision – this means<br />
the supervisor is available rapidly<br />
for advice but is off the hospital site<br />
and/or separated from the trainee by<br />
over 10 minutes.<br />
Named consultant<br />
The RCoA document Guidelines for<br />
the Provision of Anaesthetic Services<br />
(1999) states that ‘all services provided<br />
in the National Health Service are<br />
under the supervision of a consultant.<br />
This applies to all anaesthetic services.<br />
Where trainee or non-consultant career<br />
grade anaesthetists are providing<br />
clinical services this principle must be<br />
applied.’ Anaesthetic departments now<br />
need to ensure that named supervising<br />
consultants are available to all nonconsultant<br />
anaesthetists. When a trainee<br />
is doing a list or a case without a<br />
consultant, he or she should check that<br />
a supervising consultant:<br />
• Has been allocated by the<br />
department<br />
• Is aware that he or she is supervising<br />
a non-consultant<br />
• Is able to assist personally with the<br />
case within an agreed time frame<br />
• Has discussed the anaesthetic<br />
management plan with the nonconsultant<br />
if appropriate<br />
• Has agreed the level and extent of<br />
supervision<br />
Trainees should record the following on<br />
the anaesthetic record:<br />
• The name of the supervising<br />
consultant<br />
• The level of supervision as defined<br />
above<br />
18 19
• Whether the case was discussed<br />
with the supervising consultant and,<br />
if so, the anaesthetic management<br />
plan agreed.<br />
Ultimately, the trainee giving the<br />
anaesthetic is responsible for his or her<br />
own actions. As a qualified medical<br />
practitioner, you are professionally<br />
accountable in your own right.<br />
In summary, it is imperative that you:<br />
• Know when to ask for help<br />
• Know whom to ask for help<br />
• Do not act beyond the level of your<br />
own competence<br />
Many departments operate a starred<br />
consultant scheme. A consultant<br />
working within the same theatre suite<br />
during elective sessions is nominated<br />
to be the focal point for trainees or Staff<br />
and Associate Specialist (SAS) grades<br />
with queries/problems. This consultant<br />
is often paired up with a senior trainee<br />
so that they’re able to leave their theatre<br />
in times of need. In some hospitals the<br />
starred consultant will wish to speak<br />
with a trainee before they start a solo<br />
case or list. In others the consultant may<br />
be floating, for example not attached to<br />
an actual list.<br />
Speak to any trainee and they will<br />
recount a story of being ‘forced’ to take<br />
on something they felt was outside<br />
their comfort zone / above their level<br />
of competence. A common example<br />
is the transfer of a critically ill patient<br />
to another hospital. While we all have<br />
to do things for the first time at some<br />
point during our training, we should<br />
always be able to say no if we feel that<br />
it is in the patient’s best interests. If you<br />
find yourself in such a situation don’t<br />
hesitate to voice your concerns. If you<br />
are working with a senior trainee, tell<br />
them, otherwise inform the consultant<br />
on duty. If you still feel unhappy then<br />
you may have to contact your mentor,<br />
College Tutor, the Head of Department,<br />
or simply another consultant with<br />
whom you get on well. If you feel you<br />
require further help both the BMA and<br />
AAGBI provide such services, as well as<br />
other groups.<br />
Please see Chapter 15 for further details<br />
of how to find help.<br />
Running a list on your own<br />
‘Going solo’ seems sudden and can be<br />
quite daunting but it is actually reached<br />
gradually. Initially you will work with<br />
a senior colleague supervising you<br />
directly in the anaesthetic room and<br />
theatre. This ’one on one’ supervision<br />
will slowly be removed such that you<br />
will provide maintenance of anaesthesia<br />
18 19
unsupervised, then extubation and<br />
then induction. This will progress to<br />
supervision from the coffee room<br />
and you will begin managing single<br />
cases unsupervised until you are<br />
assigned your own theatre list. Here<br />
you will anaesthetise several patients<br />
unsupervised and begin to learn the<br />
art of ‘running a list’. When this day<br />
happens there will be a supervising<br />
consultant available in the theatre<br />
complex and you should make them<br />
aware that this is your first your solo<br />
list. The next step, and perhaps the<br />
biggest one of all, is to progress from<br />
the presence of fellow colleagues in<br />
the theatre suite who are available<br />
for immediate help and support<br />
to anaesthetising with no other<br />
anaesthetists around, i.e. a night on call.<br />
The list that you most often get to<br />
run is the emergency or trauma list.<br />
This can be a challenging experience<br />
as it involves patient assessment,<br />
optimisation of co-morbidities, planning<br />
peri-operative care including postoperative<br />
pain management. With<br />
three months experience in anaesthesia<br />
you will NOT be expected to know<br />
everything or deal with every case, but<br />
to recognise when to ask for advice and<br />
assistance.<br />
The rest of the first six months...<br />
Emphasis is placed on the role of<br />
the anaesthetist in the peri-operative<br />
care of the surgical patient. Thus, a<br />
guided introduction to pre-operative<br />
assessment and post-operative care<br />
is just as important as the practice of<br />
anaesthesia.<br />
The following basic units should be<br />
covered within this six month period:<br />
• Care of the patient<br />
• Anaesthetic equipment<br />
• Basic techniques in general<br />
anaesthesia<br />
• Basic techniques in local<br />
anaesthesia<br />
• Anaesthetic pharmacology<br />
Training for the next 18 months<br />
The following areas of basic training<br />
should be covered in this period:<br />
• Obstetric anaesthesia, analgesia and<br />
resuscitation<br />
• Pain management/ control/ treatment<br />
• The upper airway and its problems<br />
• Peri-operative care of the patient for<br />
major surgery<br />
• Anaesthesia for day case surgery<br />
• Paediatric anaesthesia<br />
• Anaesthesia in the elderly<br />
• Anaesthesia for patients with specific<br />
medical problems<br />
• Intensive care medicine (ICM)<br />
Trainees who have completed a fulltime<br />
basic level training post in ICM<br />
can count up to three months of this<br />
training towards their basic level<br />
training in anaesthesia. Trainees who<br />
enter the Anaesthesia CCT programme<br />
via Acute Care Common Stem (ACCS)<br />
training may also have acquired some<br />
intermediate level ICM competences in<br />
that programme.<br />
During this 18 month period trainees<br />
will widen their experience to<br />
obtain the RCoA Basic Level Training<br />
Certificate and become eligible to<br />
20 21
move to intermediate level training in<br />
anaesthesia, ST3.<br />
By the end of basic level training,<br />
trainees should be able to:<br />
• Undertake the anaesthetic care of<br />
most routine cases<br />
• Assist in the anaesthetic care for<br />
more complex surgery<br />
• Provide anaesthetic care for routine<br />
obstetric practice<br />
• Organise, with the surgical team,<br />
an emergency list; identify potential<br />
problems and seek appropriate help<br />
• Understand the principles<br />
underlying the care of patients<br />
in intensive care and high<br />
dependency units<br />
• Understand the principles of pain<br />
management<br />
• Participate in audit<br />
• Pass an assessment of knowledge<br />
and certain skills by examination<br />
e-Learning<br />
The ‘Integrated Anaesthesia Learning<br />
Portal’ or e-LA is a recently developed<br />
web-based educational resource<br />
produced by the RCoA in partnership<br />
with e-Learning for Healthcare (e-LfH).<br />
It is available, for free, to all UK<br />
anaesthetists practicing in the NHS,<br />
and aims to deliver key knowledge<br />
and concepts from the anaesthetic<br />
curriculum helping trainees to prepare<br />
for the FRCA examination.<br />
e-LA comprises:<br />
• e-Learning Sessions – Knowledge<br />
and scenario-based sessions<br />
covering the first two years of the<br />
anaesthetic curriculum. Each session<br />
takes around 20-30 minutes to<br />
complete.<br />
• e-Library – Access to thousands of<br />
full-text journal articles which have<br />
been cross-referenced and mapped<br />
to the anaesthetic curriculum.<br />
• e-CPD – Articles and associated<br />
MCQs to support general and core<br />
topic based continuing professional<br />
development for trainees and trainers.<br />
• e-Assessment – Formative<br />
assessments with feedback that<br />
will test the user’s understanding of<br />
the knowledge based session and<br />
introduce students to the standard<br />
expected at the FRCA exam.<br />
Simulation medicine<br />
Simulation training is increasingly<br />
being used in medicine and its use<br />
is supported by recent publications<br />
from the Department of Health. ‘The<br />
RCoA encourages the use of simulators<br />
for relevant aspects of postgraduate<br />
training in anaesthesia especially<br />
for events of high importance but<br />
infrequent occurrence (as exampled by<br />
anaphylaxis), for situations where there<br />
might be a high risk to patients, for team<br />
building and working under pressure.<br />
Simulators are also used as assessment<br />
tools in the Primary FRCA Examination.’<br />
Anaesthetic departments are utilising<br />
simulators to varying degrees and<br />
many are currently developing this<br />
service. Now that simulation is a<br />
feature of the primary FRCA it is well<br />
worth familiarising yourself with this<br />
method. If your department does not<br />
20 21
offer simulator training there are many<br />
courses run at the larger simulation<br />
centres across the country.<br />
Basic Level Training Certificate (BLTC)<br />
All trainees progressing to ST3<br />
(Intermediate Level Training), including<br />
those moving from Fixed Term Specialty<br />
Training Appointments, are required to<br />
have the Basic Level Training Certificate<br />
before they can start their intermediate<br />
level training. The BLTC confirms<br />
completion of basic level competencybased<br />
training in anaesthesia and<br />
ICM, of which the second year must<br />
be in the UK. The certificate should be<br />
signed off by at least two designated<br />
consultants, one of whom must be the<br />
College Tutor. There are ten workplace<br />
assessments to get signed up. These are<br />
outlined in ‘The CCT in Anaesthesia<br />
II: Competency Based Basic Level (CT<br />
years 1 and 2) Training and Assessment’<br />
available at www.rcoa.ac.uk. Along<br />
with passing the Primary exam (Chapter<br />
10), these will be the core aims of any<br />
educational planning. Besides these<br />
formal assessments, you should also<br />
have regular appraisals to discuss<br />
matters informally. You must maintain<br />
formal records of both appraisals and<br />
assessments.<br />
Appraisal and assessment<br />
‘The RCoA regards the regular appraisal,<br />
assessment and review of trainees as<br />
an integral part of the postgraduate<br />
educational process. It is also a<br />
non-negotiable requirement for all<br />
doctors employed by the NHS and for<br />
revalidation with the GMC.’ The three<br />
parts of the process are:<br />
1. Appraisal<br />
Appraisal of trainees is intended:<br />
• To provide constructive dialogue<br />
that will identify, anticipate and<br />
lead to action on the strengths<br />
and weaknesses in a trainee’s<br />
performance<br />
• To review educational targets<br />
• To review the results of any<br />
assessments or examinations<br />
• To provide provisional feedback and<br />
support towards progress<br />
• To meet the NHS requirement for the<br />
annual appraisal of all employees<br />
• To facilitate the production of a<br />
personal development plan<br />
• To provide evidence for GMC<br />
revalidation<br />
2. Assessment<br />
The purpose of assessment is to:<br />
Determine fitness for professional<br />
practice. This means more than the<br />
performance of clinical skills, no<br />
matter how complex. Very importantly<br />
it carries an in-built commitment to<br />
standards, and the attitudes which will<br />
maintain those standards throughout<br />
professional life.<br />
Provide evidence of competence in a<br />
trainee. This is to confirm the possession<br />
of the appropriate knowledge, skills<br />
and attitudes required to undertake<br />
safe clinical practice at a level<br />
commensurate with their level of<br />
training.<br />
Provide evidence of confidence and<br />
competence in a consultant. This<br />
22 23
is to confirm the possession of the<br />
confidence, knowledge, skills and<br />
attitudes necessary for independent<br />
professional practice.<br />
3. Annual Review of Competence<br />
Progression (ARCP)<br />
The three key elements supporting<br />
trainees through the training curriculum<br />
are brought together each year in the<br />
ARCP. They are:<br />
Appraisals<br />
Assessments<br />
Planning of trainee’s development<br />
Information taken from the RCoA<br />
publications ‘The CCT in Anaesthetics and<br />
Guidance for Trainers and Trainees’.<br />
Intensive care medicine<br />
Intensive care medicine (ICM) is an<br />
integral part of training in anaesthesia,<br />
with all trainees having to complete<br />
three months during Basic Level<br />
Training and a further six months during<br />
Intermediate Training. However, some<br />
trainees may be interested in dual<br />
accreditation, achieving a CCT in both<br />
anaesthesia and ICM. Anyone interested<br />
in ICM should contact the Intercollegiate<br />
Board for Training in Intensive Care<br />
Medicine (IBTICM) Educational<br />
Supervisor in their hospital, or failing<br />
that the IBTICM Regional Adviser, as<br />
soon as they can. To obtain further<br />
information, go to www.ibticm.org.<br />
Intermediate Training post. On some<br />
rotations, it is possible to end up doing<br />
three months of ICM during a year at<br />
one hospital, and arrive at the next<br />
hospital to find that you are down to<br />
do another three months of ICM. If you<br />
find yourself in this situation, we advise<br />
you to take the matter up with your<br />
College Tutor or Regional Adviser as<br />
soon as possible.<br />
Trainees wishing to obtain dual<br />
accreditation (e.g. advanced level<br />
ICM or intermediate level training)<br />
need six months of acute medicine<br />
experience (of which three months<br />
may be emergency medicine). This<br />
complementary medical experience is<br />
usually acquired at CT1/2 level and the<br />
easiest route to acquire this is via the<br />
ACCS programme.<br />
Intensive care logbook<br />
The Intercollegiate Board for Training in<br />
Intensive Care Medicine has stipulated<br />
that all anaesthetic trainees should<br />
keep a record of cases under their care<br />
in the ICU. This should include cases<br />
that the trainee has admitted, or had<br />
a substantial input into, and also all<br />
procedures.<br />
Attention must be drawn to the fact<br />
that trainees must complete at least<br />
21 months of training in anaesthesia<br />
before they are eligible to move to an<br />
22 23
Workplace based assessment in ICM<br />
IBTICM have made recommendations<br />
for the quantity of workplace based<br />
assessments for the ICM component of<br />
the anaesthesia training programme.<br />
The following is currently suggested as<br />
the minimum number of assessments<br />
required to achieve the basic level of<br />
training (a three month period during<br />
the first two years of training):<br />
Multi Source Feedback x 1<br />
Direct Mini-Clinical Assessment<br />
Evaluation Exercise x 2<br />
Direct Observation of Procedural<br />
Skills x 3<br />
Case based Discussion x 1<br />
For further information see: RCoA ‘The CCT<br />
in Anaesthesia Part II Appendix C, section 7’.<br />
Acute Care Common<br />
Stem training<br />
The Acute Care Common Stem (ACCS)<br />
training programme has emerged as part<br />
of the overhaul of postgraduate medical<br />
training that is ‘Modernising Medical<br />
Careers’.<br />
The ACCS training programme is two<br />
years long and designed to follow<br />
on from the Foundation Training<br />
programme. The rotation consists of<br />
six months of acute General Internal<br />
Medicine, six months of Emergency<br />
Medicine, six months of Intensive<br />
Care Medicine and six months of<br />
Anaesthesia.<br />
The aim of the ACCS programme is to<br />
‘produce trainees able to identify and<br />
manage the acutely unwell patient,<br />
in particular by providing training<br />
in complementary specialties in a<br />
structured programme of training ’ . The<br />
introduction of the programme should<br />
improve the acute clinical skills in<br />
trainees going onto any one of these<br />
specialities.<br />
Since the splitting of training<br />
programmes, trainees are now<br />
considered as Core Trainees (CT)<br />
and must apply again in their chosen<br />
specialty to become a specialty trainee<br />
(ST). Completion of the ACCS rotation<br />
allows entry to CT2 in Anaesthesia<br />
and ST3 in Emergency Medicine and<br />
Acute Medicine. Another benefit of the<br />
programme is that it allows trainees<br />
24 25
to gain the complementary specialty<br />
experience required for a dual ICM<br />
CCT, which is otherwise difficult within<br />
the current training scheme.<br />
As with anaesthetics, ACCS is a<br />
competency-based training programme,<br />
but with different objectives for each<br />
specialty. The RCoA gives further detail<br />
of the training programme in ‘The Acute<br />
Care Common Stem Core Training:<br />
A manual for trainees and trainers’,<br />
available on their website www.rcoa.<br />
ac.uk. And there is a new website for<br />
ACCS trainees: www.accsuk.org.uk.<br />
The ARCP (Annual Review<br />
of Competence Progression)<br />
The ARCP replaces the previous RITA<br />
(Record of In Training Assessment)<br />
process and has been introduced in<br />
line with changes to training via MMC.<br />
It is an annual assessment process for<br />
all trainees which is based on the more<br />
explicit use of evidence to inform the<br />
annual assessment of progress.<br />
In general, appraisal processes are<br />
based around the GMC’s document<br />
‘Good Medical Practice’ (Good Medical<br />
Practice, General Medical Council<br />
2006), which describes the principles<br />
of good medical practice, and the<br />
standards of competence, care and<br />
conduct expected of doctors in all<br />
aspects of their professional work.<br />
These are:<br />
• Good clinical care<br />
• Maintaining good medical practice<br />
• Teaching, training, appraisal<br />
and assessment<br />
• Relationships with patients<br />
• Working with colleagues<br />
• Probity<br />
• Health<br />
The first heading of Good Medical<br />
Practice - good clinical care - is<br />
specialty specific and for the majority<br />
of trainees, the information provided<br />
will be their College logbook and<br />
assessment documents. The other<br />
headings of GMP are common to all<br />
doctors and the information required is<br />
detailed in this document.<br />
The Primary FRCA examination<br />
The Fellowship of the Royal College<br />
of Anaesthetists (FRCA) is a hurdle<br />
to overcome and there are ongoing<br />
changes to the examination structure.<br />
These will be finalised and introduced<br />
progressively over the next few years.<br />
The FRCA is divided into 2 parts,<br />
‘The Primary’ and ‘The Final’. Formal<br />
24 25
assessments of knowledge must be<br />
passed before a trainee can progress<br />
from Basic to Intermediate training<br />
and from Intermediate to Higher<br />
training. These assessments form the<br />
Primary and Final FRCA examinations<br />
or prospectively approved equivalent<br />
qualification.<br />
Passing the primary part of the exam is<br />
a requirement for progression to a ST3<br />
post and intermediate level training.<br />
The Primary exam is designed to assess:<br />
• The candidate’s understanding of the<br />
fundamentals of clinical anaesthetic<br />
practice including equipment and<br />
resuscitation.<br />
• The candidate’s knowledge of the<br />
fundamental principles of anatomy,<br />
physiology, pharmacology, physics,<br />
clinical measurement and statistics<br />
as is appropriate for the discipline of<br />
anaesthesia.<br />
• Whether the candidate’s skills and<br />
attitudes are appropriate to the level<br />
of training.<br />
A full syllabus and exam timetable is<br />
available on the RCoA website (www.<br />
rcoa.ac.uk). People tackle the exam<br />
in different ways but it is important<br />
not to underestimate the amount<br />
of work and commitment required.<br />
Attending one of the many primary<br />
courses helps with preparation. Which<br />
of the many courses to attend comes<br />
down to personal choice and financial<br />
constraints. Do not forget to use the<br />
e-learning package provided by the<br />
RCoA and other websites, e.g. www.<br />
anaesthesiauk.com.<br />
Also use the GAT website for links:<br />
www.<strong>aagbi</strong>.org/gat.htm.<br />
There are 3 parts to the primary<br />
examination:<br />
1. Multiple Choice Questions (MCQ)<br />
2. Objective Structured Clinical<br />
Examination (OSCE)<br />
3. Structured Oral Examination (SOE)<br />
The MCQ<br />
Eligibility to sit the MCQ component<br />
of the Primary FRCA is achieved upon<br />
obtaining a RCoA approved training<br />
post in anaesthesia or ACCS. All<br />
trainees must be registered by the<br />
RCoA.<br />
The MCQ consists of a three hour<br />
multiple choice question paper of<br />
90 questions, each with five stems.<br />
Negative marking has recently been<br />
abandoned and so marks will no longer<br />
be deducted for incorrect answers.<br />
The pass mark is approximately 80%.<br />
The Primary MCQ exam may be<br />
attempted a maximum of five times<br />
and a pass in the MCQ will be valid<br />
for two years; if the Primary has not<br />
been completed by this stage it must be<br />
repeated.<br />
OSCE<br />
The Objective Structured Clinical<br />
Examination (OSCE) consists of up to 18<br />
stations of which 16 count towards the<br />
result. The OSCE lasts approximately<br />
one hour 50 minutes and covers all<br />
aspects of anaesthesia, including<br />
resuscitation, technical skills, anatomy,<br />
26 27
history-taking, physical examination,<br />
communication skills, anaesthetic<br />
equipment, monitoring equipment,<br />
measuring equipment, anaesthetic<br />
hazards and the interpretation of X-rays.<br />
One or more stations may incorporate<br />
the use of an anaesthetic simulator.<br />
The pass mark for each question<br />
depends on its difficulty and the level<br />
of knowledge expected of a ‘borderline’<br />
candidate. The pass mark for the exam<br />
is the sum of all the individual 16 pass<br />
marks and will vary depending on the<br />
combination of questions used.<br />
SOE<br />
From September 2009 there will be<br />
a single Structured Oral Examination<br />
(SOE) or viva examination, which<br />
will be conducted as two separate<br />
sessions. One SOE tests physiology and<br />
pharmacology and the other clinical<br />
anaesthesia, physics and clinical<br />
measurement.<br />
At the first attempt the OSCE and SOE<br />
must be taken at the same sitting. If you<br />
pass one but fail the other component<br />
then you can re-take just the failed<br />
component. As with the MCQ, a pass in<br />
either will be valid for two years.<br />
From September 2009 closed marking<br />
(1, 1+, 2, 2+) has been removed and<br />
now each section of the exam must be<br />
passed in order to gain the<br />
Primary FRCA.<br />
Bibliography for the Primary FRCA<br />
General:<br />
Anaesthesia and Intensive Care A-Z<br />
Yentis SM, Hirsch NP, Smith GB<br />
An excellent first anaesthetic book. A<br />
summary of just about everything you will<br />
come across and much more detailed than<br />
it sounds.<br />
Fundamentals of Anaesthesia<br />
Pinnock C, Lin T, Smith T<br />
This useful basic textbook follows the<br />
primary syllabus.<br />
Oxford Handbook of Anaesthesia<br />
Allman K, Wilson I<br />
Doesn’t teach you the basics, but great for<br />
looking up specific cases prior to a list.<br />
Drugs in Anaesthesia & Intensive Care<br />
Sassada M, Smith S<br />
A pocket guide to all drugs you may come<br />
across, good for tricky MCQ answers,<br />
structuring of drug information for a viva<br />
question and as a reference book<br />
Primary specific:<br />
Basic Physics and Measurement in<br />
Anaesthesia<br />
Kenny G, Davis P<br />
Previously Parbrook, the ‘classic’ physics<br />
textbook.<br />
Respiratory Physiology: The Essentials<br />
West JB<br />
Again, a ‘classic’ primary textbook.<br />
26 27
Pharmacology for Anaesthesia and<br />
Intensive Care<br />
Peck T, Hill S<br />
Excellent pharmacology textbook for FRCA<br />
exam revision.<br />
Essentials of Anaesthetic Equipment<br />
Al-Shaikh B, Stacey S<br />
Excellent for the OSCE.<br />
Guide to the FRCA Examination - The<br />
Primary<br />
The Royal College of Anaesthetists<br />
Contains sample questions, some of which<br />
still appear.<br />
QBase MCQs for the Primary FRCA<br />
series 1, 4, 7<br />
Hammond E, McIndoe A<br />
Anatomy for Anaesthetists<br />
Ellis H<br />
A number of books are also available<br />
based on the Primary FRCA OSCE and<br />
SOE examinations.<br />
Getting an ST3 post in<br />
anaesthetics<br />
Progressing to intermediate level<br />
training:<br />
Before a trainee can progress to<br />
intermediate level training (ST3-4) they<br />
must have:<br />
a) obtained the Basic Level Training<br />
Certificate (BLTC)<br />
b) demonstrated reasonable attitudes<br />
and behaviour<br />
c) passed the Primary FRCA or an<br />
exempting examination<br />
The actual duration of an individual’s<br />
training will be determined by the rate<br />
at which they achieve the necessary<br />
competences. The principles of the UK<br />
CCT training programme are that it:<br />
• is competency based<br />
• is planned<br />
• is evaluated<br />
• has clear objectives<br />
• is supervised<br />
• is delivered by appropriately<br />
appointed trainers<br />
• allows time for study<br />
• accommodates the specific career<br />
needs of individuals<br />
There are certain generic professional<br />
skills, essential to the training of all<br />
specialists that should be covered.<br />
These include:<br />
• Skills, attitude and behaviour<br />
• Communication<br />
• Presentation<br />
• Audit<br />
• Teaching<br />
• Ethics and law<br />
• Management<br />
The Basic Level Training Certificate is<br />
the minimum requirement for an ST3<br />
post and for those who must undergo<br />
further selection before entering<br />
Intermediate Training.<br />
28 29
But, it does not help to answer the<br />
question...<br />
“How do I get onto a Specialty Trainee<br />
rotation?”<br />
So what else might be useful to help<br />
you to stand out during the selection<br />
process?<br />
Word-processing your application<br />
form, checking for spelling mistakes<br />
and having a clearly set out Curriculum<br />
Vitae (CV) is a rather obvious place<br />
to start. Update your CV at least<br />
every six months. Studying the Person<br />
Specifications for upcoming ST3<br />
posts may enable you to tailor your<br />
CV for specific posts. Research and<br />
publications impress selectors and<br />
allow them to differentiate between<br />
candidates with similar qualifications.<br />
A letter in a peer-reviewed journal is<br />
probably the easiest way to start your<br />
publication portfolio. Scan the journals<br />
for topics which are of interest to you or<br />
your department, and ask an interested<br />
consultant to help you submit your first<br />
letter. Once you have joined the AAGBI,<br />
you will receive the Association’s scientific<br />
journal Anaesthesia and the newsletter<br />
Anaesthesia News monthly. These are<br />
obvious publications to target first.<br />
Publishing papers based on research<br />
is more difficult because of the time<br />
required to produce anything substantial.<br />
If you are lucky enough to persuade<br />
someone to allow you to contribute to<br />
a project that is already up and running,<br />
check whether they intend to include<br />
you as one of the authors.<br />
You might consider presenting your<br />
paper orally at one of the many national<br />
or international scientific meetings. The<br />
AAGBI awards the Registrars’ Prize for<br />
an original paper presented at the GAT<br />
Annual Scientific Meeting.<br />
Audit projects, as well as being an<br />
essential part of training, are often a good<br />
way to impress, especially if published.<br />
This is more likely to be the case if you<br />
cover something ‘topical’, or currently<br />
controversial, and include an element<br />
of literature review and discussion.<br />
Completing the audit cycle is vital and<br />
impressive. Furthermore, the AAGBI<br />
awards a trainee poster prize (the Audit<br />
Prize) at the GAT Annual Scientific<br />
Meeting each year, which is audit-based.<br />
Always register your audit with your<br />
hospital audit department to prevent any<br />
unforeseen problems before you start.<br />
There is more to publishing than just<br />
primary clinical research. Case reports<br />
are worth considering whenever you find<br />
yourself involved with a rare or unusual<br />
case. Articles on topics of interest can<br />
also, for example, be sent to Anaesthesia<br />
News or to the RCoA Bulletin. The<br />
AAGBI also awards the Anaesthesia<br />
History Prize jointly with the History<br />
of Anaesthesia Society; each year the<br />
winning essay is presented at the GAT<br />
Annual Scientific Meeting.<br />
Many of those competing for posts<br />
will have completed courses such as<br />
Advanced Life Support (ALS), Advanced<br />
Trauma Life Support (ATLS), European<br />
Paediatric Life Support (EPLS) or<br />
28 29
Advanced Paediatric Life Support (APLS),<br />
and you could consider becoming<br />
an instructor on such a course.<br />
Unfortunately many such courses only<br />
allow you to become instructors if<br />
you are in ST 3 or above. You could<br />
offer your services to your hospital’s<br />
Resuscitation Officers, as they are often<br />
looking for doctors to teach on in-house<br />
resuscitation courses.<br />
Management skills, which can be as<br />
basic as organising a social event for the<br />
department, writing rotas and getting<br />
involved with teaching, also enhance any<br />
application.<br />
Finally, there are other aspects to your<br />
career that may not seem relevant at first<br />
glance but are important in enabling you<br />
to stand out from other candidates. These<br />
include any positions of responsibility<br />
you may have undertaken within the<br />
department or outside of medicine, such<br />
as organising an event or involvement<br />
with charity work. In some regions<br />
having worked abroad in medicine also<br />
gains you points.<br />
30 31
Anaesthetic training in Scotland<br />
Author: Dr Adam M Paul<br />
Since political devolution in 1999, the<br />
Scottish Parliament has had control<br />
over the NHS in Scotland, and with<br />
this employment and training for the<br />
doctors within the NHS. However<br />
Anaesthesia retains a UK wide training<br />
programme, through the Royal College<br />
of Anaesthetists. Therefore a CCT in<br />
Inverness will be exactly the same as<br />
one in Plymouth, but there may be<br />
subtle differences in gaining a training<br />
post and in the working environments.<br />
It is refreshing to see how hard and<br />
how successfully the RCoA and AAGBI<br />
have worked to keep training a UK<br />
wide process despite the increasing<br />
differences between home nation NHS<br />
systems. The AAGBI has a Scottish<br />
Standing Committee, which specifically<br />
looks at Scottish anaesthesia issues<br />
and contains at least one trainee<br />
representative.<br />
Across Scotland there are four schools<br />
of anaesthesia: South-East Scotland<br />
(based in Edinburgh, incorporating<br />
Lothian, Fife and Borders);<br />
East of Scotland (based in<br />
Dundee, incorporating Tayside and<br />
Perthshire); North-East Scotland (based<br />
in Aberdeen and Inverness, also<br />
coordinates the new Highlands and<br />
Islands); and West of Scotland (based<br />
in Glasgow, incorporating Greater<br />
Glasgow and Clyde, Ayrshire and Arran,<br />
Dumfries and Galloway, Forth Valley<br />
and Lanarkshire).<br />
Overall these schools fall under the<br />
governance of NHS Education for<br />
Scotland (NES - http://www.nes.scot.<br />
nhs.uk/) which was set up in 2002 to<br />
allow a coordinated national approach<br />
to medical education - this is what<br />
Medical Education: England (MEE) has<br />
been based on. NES is responsible for<br />
the implementation of MMC Scotland<br />
(http://www.mmc.scot.nhs.uk/). Within<br />
NES there are 7 specialty boards, of<br />
which one is Emergency Medicine and<br />
Anaesthesia.<br />
Overall, the application process is like<br />
elsewhere in the UK, ever evolving, and<br />
candidates must keep up to date using<br />
the above websites. There is no bar to<br />
applying to Scotland as well as other<br />
areas in the UK. Moreover, candidates<br />
can still freely move across borders<br />
between different NHS systems because<br />
the training has been kept UK wide.<br />
30 31
Anaesthetic training in<br />
Northern Ireland<br />
Authors: Dr Paul Johnston, Dr Clive Stanley<br />
Currently in Northern Ireland<br />
postgraduate medical training is<br />
managed by the Northern Ireland<br />
Medical and Dental Training Agency<br />
(NIMDTA).<br />
Local recruitment to anaesthesia for<br />
the 2009 process will take the form<br />
of core training in anaesthesia alone.<br />
This may change for the 2010 process<br />
and beyond. Information pertaining<br />
to a change in this process within<br />
Northern Ireland will be advertised<br />
via the NIMDTA web site. The switch<br />
to core training in 2008 followed<br />
three successful years of run through<br />
training, as a pilot in 2005 / 2006 and<br />
subsequently as part of the national<br />
scheme in 2007.<br />
Core training will consist of a two year<br />
period (CT1, CT2) of initial, basic level<br />
training, which must be successfully<br />
completed (including the Primary FRCA<br />
exam) before a candidate is eligible to<br />
apply competitively for a position at<br />
ST3 level. Following successful entry<br />
to ST3 there will be a five year training<br />
programme, incorporating intermediate<br />
and higher level training, culminating<br />
in the completion of training and the<br />
award of a CCT document. A small<br />
number of anaesthetic posts per year<br />
are allocated to allow ACCS emergency<br />
medicine trainees access to anaesthesia<br />
and intensive care medicine, a<br />
requirement of their training scheme.<br />
ACCS trainees themselves, however, are<br />
no longer recruited into the anaesthesia<br />
training scheme. Currently there are no<br />
FTSTA anaesthesia posts in Northern<br />
Ireland.<br />
Of note, following a recent review of<br />
recruitment to specialty training by the<br />
Health Minister in Northern Ireland,<br />
is that the total number of anaesthetic<br />
training posts is expected to fall slightly<br />
over the coming years. This has been<br />
proposed as an attempt at workforce<br />
planning to match training places to the<br />
expected need for senior and consultant<br />
level medical staff. However, as with<br />
EWTD, preparedness is not yet fully<br />
achieved and reductions in training<br />
numbers seem less likely.<br />
The Northern Ireland Deanery is in<br />
the process of seeking legal advice<br />
concerning its responsibility towards<br />
junior doctors whom it acts to employ.<br />
It is in the process of affirming its<br />
position as a recruitment agency in<br />
order to devolve responsibility for<br />
terms and conditions of employment to<br />
individual Trusts which will hold junior<br />
doctor contracts.<br />
32 33
Professionalism and accountability<br />
Author: Sarah Whitehouse, MPS<br />
Professionalism in the medical world<br />
means constantly adapting to the<br />
changing needs of society. How do you<br />
know what is professional? What are<br />
the standards, who should set them,<br />
and how are these standards judged?<br />
Professionalism as a trainee anaesthetist<br />
is about knowing your limits, being<br />
appropriate and working to reduce risk.<br />
The GMC, as the standard bearer for<br />
professionalism, bases good medical<br />
practice on good clinical care, good<br />
relationships with patients, working<br />
with colleagues, teaching and training,<br />
probity and health.<br />
The GMC’s Good Medical Practice<br />
(2006) states that patients must be able<br />
to trust doctors with their lives and<br />
health, and doctors must show respect<br />
for human life, making the care of<br />
patients their first concern. Anaesthetists<br />
and all other healthcare professionals<br />
should protect and promote the health of<br />
patients and the public, while providing<br />
a good standard of practice and care.<br />
Professional responsibilities go beyond<br />
a mere contract of employment. The<br />
Royal College of Anaesthetists sees<br />
maintaining standards as a core element<br />
of professionalism. Raising the standard<br />
(2006) focuses on audit as part of<br />
clinical governance, looking at ways to<br />
improve patient care.<br />
Professionalism is shown through welldeveloped<br />
communication skills. The<br />
RCoA places emphasis on establishing<br />
the confidence of the patient,<br />
promoting meaningful dialogue, and<br />
communicating any risks in a way that a<br />
patient can understand.<br />
Being professional means treating all<br />
patients equally and with empathy;<br />
even so-called difficult or ‘heart-sink’<br />
patients. Labelling a patient can cause<br />
offence to the patient, blind your<br />
clinical judgment, and cause you to<br />
underestimate the severity of physical<br />
symptoms, perhaps bringing your fitness<br />
to practise into question.<br />
Since 1858, the GMC has promoted<br />
high standards of medical education,<br />
dealing firmly with healthcare<br />
professionals whose fitness to practise<br />
is in doubt. In 2007, the GMC spent<br />
£49.1 million on fitness to practise, and<br />
between April 2006 and February 2007,<br />
there were 389 fitness to practise cases.<br />
Professionalism is not about never<br />
making mistakes, but it is about dealing<br />
with adverse events promptly and<br />
correctly – handling any impact on<br />
patient care, giving a full and frank<br />
account of the facts, apologising where<br />
appropriate, and conducting a critical<br />
incident or significant event review to<br />
reduce recurrence.<br />
32 33
Being professional is about being<br />
prepared if things do go wrong and<br />
having the right indemnity support<br />
when facing challenging medico-legal<br />
situations.<br />
For more information on<br />
professionalism and good medical<br />
practice, or for professional indemnity<br />
advice, visit www.mps.org.uk, or<br />
contact MPS on 0845 605 4000.<br />
Whom to ask for help?<br />
Sometimes things in life don’t go to<br />
plan and are much more difficult than<br />
anticipated. There are always a number<br />
of options and whilst it can seem<br />
that you are the only person having a<br />
particular issue with your training; we<br />
can assure you that you will not be<br />
alone. It is important not to bottle things<br />
up, and it is never seen as a weakness,<br />
but more as a sign of maturity to seek<br />
help when it is required.<br />
Often having a chance to speak to<br />
your fellow colleagues in a social<br />
environment can reassure you that you<br />
are on track and others are having the<br />
same concerns as yourself. If you feel<br />
however that you require more help<br />
there are a number of people you can<br />
turn to.<br />
Many departments now offer a<br />
mentoring programme, where you are<br />
paired up with either a senior trainee or<br />
consultant. Mentors tend to fulfil a more<br />
pastoral role than your educational<br />
supervisor and may be your first point<br />
of contact. If you have not been given a<br />
mentor you can request one.<br />
Others to consider within your place<br />
of work include your Educational<br />
Supervisor, College Tutor, the Head of<br />
Department, Programme Director or<br />
simply another consultant with whom<br />
you get on well. You may prefer to<br />
speak to a non-anaesthetist and there<br />
is normally a nominated consultant as<br />
a point of contact for junior doctors,<br />
or you could consider the Head of<br />
Medical Education.<br />
Sometimes it’s easier to speak to<br />
someone outside the work environment<br />
and many feel more comfortable in this<br />
situation. Your GP is a good starting<br />
point and can refer you on to a third<br />
party if you both agree.<br />
Furthermore, your occupational health<br />
department may also be extremely<br />
helpful and they are worth approaching<br />
for not only physical problems.<br />
If you feel you require further help the<br />
BMA and AAGBI both provide support<br />
services, as do other groups:<br />
34 35
The BMA Counselling Service for<br />
doctors and their families provides<br />
instant access to a telephone<br />
counselling service that operates 24<br />
hours a day, 365 days a year. It is there<br />
to help all doctors and their families<br />
with personal, emotional and workrelated<br />
problems. The BMA’s Doctors<br />
for Doctors Unit deals with a wide<br />
range of problems such as drug and<br />
alcohol problems, bullying at work,<br />
mental health issues, and doctors who<br />
have been referred to the GMC/NCAA.<br />
BMA Counselling Service<br />
Tel: 08459 200 169<br />
BMA Doctors for Doctors Unit:<br />
www.bma.org.uk/doctorsfordoctors<br />
or tel: 020 7383 6739. This service<br />
provides 24 hour support and a number<br />
of these advisors are anaesthetists.<br />
Please note that although the service<br />
is 24 hour, an anaesthetist may not be<br />
available at all times.<br />
practical aspects of their career<br />
management or employment or who<br />
have problems of a less urgent nature<br />
should email wellbeing@<strong>aagbi</strong>.org<br />
or call the AAGBI Secretariat who<br />
will direct your call to members of<br />
Executive or the Welfare Committee as<br />
appropriate.<br />
The AAGBI Welfare Committee has<br />
recently produced a Welfare Resource<br />
Pack. This is available online at http://<br />
www.<strong>aagbi</strong>.org/publications/guidelines/<br />
docs/welfare_resource_pack_2008.pdf.<br />
Further details of help can be<br />
found in the GAT Handbook and<br />
on the Association of Anaesthetists<br />
website: http://www.<strong>aagbi</strong>.org/<br />
memberswellbeing.htm.<br />
Finally, remember you are not alone.<br />
Many anaesthetists will have felt<br />
the same at sometime or have been<br />
through similar experiences - you just<br />
need to ask for support.<br />
The AAGBI recognises the importance<br />
of supporting members’ welfare.<br />
Contact is welcomed from members<br />
with regard to any welfare issue. If for<br />
any reason this does not address your<br />
problem, call the AAGBI during office<br />
hours on 020 7631 1650 or email<br />
wellbeing@<strong>aagbi</strong>.org and you will<br />
be put in contact with an appropriate<br />
advisor.<br />
Members who need to discuss more<br />
34 35
Final checklist<br />
We hope that the information<br />
contained within this guide proves<br />
useful for your future anaesthetic<br />
career.<br />
So, remember to:<br />
• Fill in the form and join the AAGBI<br />
• Register with the Royal College of<br />
Anaesthetists<br />
• Start a logbook today<br />
• Start a portfolio<br />
• Keep a list of all study leave used,<br />
internal and external. This should<br />
include clinical governance<br />
meetings, etc.<br />
• Don’t leave all your workplace<br />
assessments until the last minute!<br />
Appendices<br />
Abbreviations<br />
AAGBI<br />
ACCS<br />
36 37<br />
Association of<br />
Anaesthetists of Great<br />
Britain & Ireland<br />
Acute Care Common Stem<br />
ALS Advanced Life Support /<br />
Advanced Cardiac Life<br />
Support<br />
APLS<br />
Advanced Paediatric Life<br />
Support<br />
ARCP<br />
ASA<br />
ATI<br />
ATLS<br />
BMA<br />
CCT<br />
CT<br />
DoH<br />
EPLS<br />
FRCA<br />
GAT<br />
GMC<br />
IBTICM<br />
ICM<br />
LTFT<br />
Annual Review of<br />
Competence Progression<br />
American Society of<br />
Anesthesiologists<br />
Anaesthetists in Training<br />
in Ireland<br />
Advanced Trauma Life<br />
Support<br />
British Medical<br />
Association<br />
Certificate of Completion<br />
of Training<br />
Core Trainee<br />
Department of Health<br />
European Paediatric Life<br />
Support<br />
Fellow of the Royal<br />
College of Anaesthetists<br />
Group of Anaesthetists in<br />
Training<br />
General Medical Council<br />
Intercollegiate Board for<br />
Training in Intensive Care<br />
Medicine<br />
Intensive Care Medicine<br />
Less-Than-Full-Time<br />
Training
MMC<br />
Modernising Medical<br />
Careers<br />
SAS<br />
Staff and Associate<br />
Specialists<br />
ODP/ODA Operating Department<br />
Practitioner: you will<br />
however notice that they<br />
are often referred to as<br />
Operating Department<br />
Assistant, which was the<br />
title used in previous<br />
years. There may also be<br />
anaesthetic trained nurses<br />
and Physicians’ Assistants<br />
(Anaesthesia) - previously<br />
described as Anaesthetic<br />
Practitioners - within your<br />
department.<br />
OOPT<br />
PALS<br />
PMETB<br />
RCoA<br />
RCSI<br />
Out-of-Programme<br />
Training<br />
Paediatric advanced life<br />
support, now EPLS<br />
Postgraduate Medical<br />
Education and Training<br />
Board<br />
Royal College of<br />
Anaesthetists<br />
Royal College of Surgeons<br />
of Ireland (College of<br />
Anaesthetists)<br />
SpR<br />
ST<br />
Useful Addresses<br />
Specialist Registrar<br />
Specialty Training / Trainee<br />
Group of Anaesthetists in Training<br />
(GAT)<br />
The Association of Anaesthetists of<br />
Great Britain & Ireland<br />
21 Portland Place, London W1B 1PY<br />
tel: 020 7631 1650<br />
fax: 020 7631 4352<br />
email: gat@<strong>aagbi</strong>.org<br />
website: www.<strong>aagbi</strong>.org/gat.htm<br />
The Association of Anaesthetists of<br />
Great Britain & Ireland (AAGBI)<br />
21 Portland Place, London W1B 1PY<br />
tel: 020 7631 1650<br />
fax: 020 7631 4352<br />
email: info@<strong>aagbi</strong>.org<br />
website: www.<strong>aagbi</strong>.org<br />
Royal College of Anaesthetists (RCoA)<br />
35 Red Lion Square, London WC1R<br />
4SG<br />
tel: 020 7092 1500<br />
fax: 020 7092 1730<br />
email: info@rcoa.ac.uk<br />
website: www.rcoa.ac.uk<br />
36 37
RCoA Examinations Department<br />
tel: 020 7908 7312<br />
fax: 020 7636 8280<br />
email: exams@rcoa.ac.uk<br />
The College of Anaesthetists, Royal<br />
College of Surgeons of Ireland (RCSI)<br />
22 Merrion Square North, Dublin 2,<br />
Ireland<br />
tel: 353 1 661 4412<br />
fax: 353 1 661 4374<br />
email: info@coa.ie<br />
website: www.anaesthesia.ie<br />
The Intercollegiate Board for Training<br />
in Intensive Care Medicine (IBTICM)<br />
c/o The Royal College of Anaesthetists<br />
35 Red Lion Square, London WC1R<br />
4SG<br />
tel: 020 7092 1556<br />
fax: 020 7092 1730<br />
Email: ibticm@rcoa.ac.uk<br />
website: www.ibticm.org<br />
The College of Anaesthetists, Royal<br />
College of Surgeons of Ireland (RCSI)<br />
22 Merrion Square North, Dublin 2,<br />
Ireland<br />
tel: 353 1 661 4412<br />
fax: 353 1 661 4374<br />
email: info@coa.ie<br />
website: www.anaesthesia.ie<br />
Anaesthetists in Training in Ireland<br />
(ATI)<br />
PO Box 6526, Dublin 4<br />
email: ati@coa.ie<br />
Website: http://www.anaesthesia.ie/<br />
sections/Default.asp?cms=training_ATI+<br />
Group&cmsid=59_83&id=83&secid=5<br />
The Bernard Johnson advisors<br />
LTFT Training<br />
c/o The Royal College of Anaesthetists<br />
Training Department<br />
35 Red Lion Square, London WC1R<br />
4SG<br />
tel: 020 7092 1553<br />
fax: 020 7092 1730<br />
email: training@rcoa.ac.uk<br />
website: www.rcoa.ac.uk<br />
Essential Reading<br />
• The GAT Handbook – 9th edition.<br />
AAGBI, London, 2009<br />
• The CCT in Anaesthesia I: General<br />
Principles: A manual for trainees and<br />
trainers. Edition 1: January 2007<br />
• The CCT in Anaesthesia II:<br />
Competency Based Basic Level<br />
(ST Years 1 and 2) Training and<br />
Assessment. A manual for trainees<br />
and trainers. Edition 1: January 2007<br />
38 39
38 39
Published by: The Group of Anaesthetists in Training<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
21 Portland Place, London, W1B 1PY<br />
t: 020 7631 1650 f: 020 7631 4352<br />
e: gat@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org/gat.htm<br />
40
Inter-hospital transfer of the critically-ill<br />
patient in the Republic of Ireland<br />
Guidelines for Anaesthetists in referring units<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland,<br />
21 Portland Place, London W1B 1PY<br />
Telephone 020 76311650 Fax 020 7631 4352<br />
www.<strong>aagbi</strong>.org<br />
June 2006
Membership of the working party<br />
CONTENTS<br />
Dr. Rory Page<br />
Dr. Ellen O’Sullivan<br />
Dr. Eamon Tierney<br />
Dr. Brian Pickering<br />
Dr. Anne Bergin<br />
Dr. John Kennedy<br />
Dr. John Loughrey<br />
Dr. Michael Power<br />
Chairman, Working Party / Secretary,<br />
Irish Standing Committee, AAGBI<br />
Convenor, Irish Standing Committee, AAGBI<br />
Deputy Convenor, Irish Standing Committee,<br />
AAGBI<br />
Co-opted, Anaesthetists in Training in Ireland<br />
Member, Irish Standing Committee, AAGBI<br />
Member, Irish Standing Committee, AAGBI<br />
Member, Irish Standing Committee, AAGBI<br />
Co-opted, Irish Intensive Care Society<br />
1. Summary of Recommendations 2<br />
2. Introduction 4<br />
3. Background 5<br />
4. Reasons for transfer in the Republic of Ireland 7<br />
5. Selection of patients requiring anaesthesia care 8<br />
during transfer<br />
6. The transfer 10<br />
7. The base hospital during transfer 12<br />
8. Post-transfer 15<br />
9. The future 16<br />
10. References 17
1. SUMMARY OF RECOMMENDATIONS<br />
1. A 7-day 24-hour inter-hospital retrieval service should be available<br />
for all critically ill patients.<br />
2. Pending the establishment of a full retrieval team for all patients,<br />
extra arrangements for the continuation of the anaesthetic service<br />
need to be put in place in the event of a transfer.<br />
3. Many hospitals caring for critically ill patients on a 24-hour basis<br />
do not have adequate resources to provide the modern standard<br />
of care initially required for these patients prior to transfer. The<br />
funding needs to be put in place to correct these inadequacies.<br />
4. The need for anaesthetic care of a patient during the period of<br />
inter-hospital transfer is determined by the anaesthetic team<br />
attending the patient in the referring hospital.<br />
5. The patient should be resuscitated and his clinical condition<br />
should be as stable as possible before transfer.<br />
6. Any procedures which are reasonably likely to have to be<br />
performed on an emergency basis in the transfer vehicle should be<br />
performed electively in the referring hospital prior to transfer.<br />
7. Interhospital communication between referring teams should be at<br />
an experienced level.<br />
8. Care of the patient during transfer should not be compromised and<br />
should be to a standard as close as possible to that available in an<br />
intensive care unit.<br />
9. Inter-hospital transfer should be undertaken calmly but with<br />
minimum delay. If requested, a police escort should be available<br />
to facilitate travel through traffic black spots or other delays.<br />
Decisions during transfer regarding speed, sirens and degree of<br />
urgency should be determined by the accompanying doctor, in<br />
consultation with the emergency medical technician (EMT) team.<br />
10. Care of the anaesthetist-accompanied patient during transfer is<br />
the responsibility of the referring anaesthetic team. There should<br />
be excellent communication between the referring consultant<br />
anaesthetist and the transfer team en route.<br />
11. The anaesthesia service at the base hospital may need to be<br />
curtailed as a result of losing staff to inter-hospital transfer duties.<br />
12. Each referring and receiving hospital should have a set of guidelines<br />
available to doctors to minimise problems of patient transfer.<br />
<br />
13. Each hospital should have a brief, formal review of each transfer<br />
within a few days of the transfer. This should be led by a<br />
consultant anaesthetist. The purpose of this review would be to<br />
discuss any issues of difficulty that arose during the transfer and to<br />
create policies to help prevent future clinical and organisational<br />
problems.
2. INTRODUCTION<br />
Inter-hospital transfer of the critically ill patient in Ireland necessitates<br />
the accompaniment of a transfer team, usually led by the consultant<br />
anaesthetist at the base hospital. This absence of anaesthesia personnel<br />
from their base hospital has subsequent deleterious effects on the<br />
Department of Anaesthesia’s ability to provide the usual breadth of<br />
service locally.<br />
The purpose of this document is to provide a broad set of guidelines<br />
to consultant anaesthetists and their trainees in referring hospitals as<br />
to how to effect the patient transfer safely and efficiently and how to<br />
maintain the safest possible service at the base hospital in the absence<br />
of the resident non-consultant hospital doctor (NCHD) anaesthetist.<br />
The emphasis of this document is on quality care for all patients.<br />
3. BACKGROUND<br />
From an inter-hospital transport perspective there are three types of<br />
hospitals in Ireland.<br />
1. Many hospitals in urban areas have tertiary speciality units such<br />
as Neurosurgery, Cardiothoracic surgery, Spinal Injuries units,<br />
Paediatric surgery, Haematology and Complex Intensive Care.<br />
These are specialties to which all hospitals may refer. In the main,<br />
the transfer of patients to these hospitals is inward. Occasionally,<br />
however, the transfer is outward to another hospital.<br />
2. Other hospitals, currently described as regional, have varying<br />
degrees of capability to handle complex cases e.g. trauma,<br />
vascular, complex medical cases, complex paediatrics, and<br />
complex maternity on a 24-hour/ 7-day week basis. These<br />
hospitals may transfer patients to the tertiary centres as well as<br />
accepting patients from smaller acute hospitals.<br />
3. The remaining acute units, over twenty in number in General<br />
Hospitals around the country, have large variations in their ability<br />
to deal with acute cases as a result of decentralised policy that<br />
may or may not have reflected local need. Some support acute<br />
adult general surgical, medical, paediatric and maternity services.<br />
Others only have a general adult medical service and a general<br />
surgical service.<br />
Many of these hospitals have a 24-hour accident and emergency<br />
(A&E) service but do not have the staff and facilities to cater for<br />
more complex emergencies. For example, many of these hospitals<br />
do not have an A&E consultant available out-of-hours or even<br />
within the normal 9 to 5 working week, nor do they even all have<br />
experienced A&E doctors at non-consultant level at all times. Not<br />
all A&E departments have a CT scanner available to them on-site<br />
24 hours a day. It is difficult to justify having an A&E department<br />
open for emergencies such as major head injuries or spontaneous<br />
brain haemorrhage without a CT scanner being made immediately
available, and without immediate transfer of the CT images to the<br />
nearest neurosurgical unit. The role for this third layer of hospitals<br />
in the management of critically ill patients is primarily triage,<br />
stabilisation, treatment and / or transfer for further management.<br />
4. REASONS FOR TRANSFER IN THE REPUBLIC<br />
OF IRELAND<br />
Patients are transferred because of their need for specific medical<br />
attention that is not available on-site in the relevant hospital. Examples<br />
of this directed referral include transfer of cardiac patients to one of the<br />
nation’s five cardio-thoracic units (Mater Hospital, Crumlin Hospital,<br />
St. James’ Hospital, Cork University Hospital, University College<br />
Hospital, Galway). Alternatively a patient with multiple injuries may<br />
require referral to a spinal or neurosurgical unit, or a critically ill child<br />
may need transfer to a paediatric ICU.<br />
In addition, patients are also transferred within local HSE areas to<br />
more specialised units for further care, e.g. orthopaedics or intensive<br />
care. An anaesthetist is needed to provide care to those patients whose<br />
requirements include major resuscitation, including management<br />
of the airway and ventilation. This anaesthetic transfer may occur<br />
with further assistance from other disciplines as per national or local<br />
guidelines.<br />
Sometimes the anaesthesia team that is responsible for complex<br />
resuscitative care may make the decision to transfer to another<br />
anaesthetic service rather than to a surgical or medical service<br />
elsewhere. This may be recognition of the existence of limited<br />
resources locally and to obtain more complex treatment elsewhere in<br />
the best interests of the patient.
5. SELECTION OF PATIENTS REQUIRING<br />
ANAESTHESIA CARE DURING TRANSFER<br />
The anaesthetist on call is the person responsible for deciding<br />
whether a patient being transferred requires anaesthetic care during<br />
the transfer. While an intubated patient in hospital does not need a<br />
doctor in attendance at all times, the transfer of an intubated patient<br />
should involve a doctor capable of providing a definitive airway. Other<br />
specialty groups (e.g. A&E medicine) are developing skills in the area<br />
of intubation and ventilation. The Standing Committee is of the view<br />
that it is wholly appropriate for other doctors who possess these skills<br />
to accompany patients, and particularly if they initiate ventilation.<br />
Critically ill children have special needs with regard to transfer.<br />
Special conditions attaching to the transfer of critically ill children are<br />
included in our previous document “Care of the critically ill child in<br />
Irish Hospitals” (Published by the AAGBI and Faculty of Paediatrics,<br />
RCPI, 2005).<br />
Many patients do not need anaesthetic support during inter-hospital<br />
transfer.<br />
These patients include:<br />
• patients who are not likely to need airway or ventilatory support<br />
• patients who are not for resuscitation measures<br />
• patients being transferred for acute definitive management for whom<br />
anaesthesia support will not affect their outcome<br />
• when the request for anaesthetic care during transfer exceeds the<br />
Department of Anaesthesia’s resources to do so safely at that time.<br />
Although the patient would benefit from anaesthesia management<br />
the issue may be one of either delaying transfer until such resources<br />
are available or alternatively sending the patient without an<br />
accompanying anaesthetist but with another doctor.<br />
The Standing Committee is also of the view that, in patients for<br />
whom life-support measures have not been initiated but there exists<br />
a reasonable likelihood that they may become necessary en route to<br />
the receiving hospital, such life-support measures should be initiated<br />
electively prior to transfer. This is in order to avoid the complications<br />
of roadside procedures being performed under sub-optimal conditions.<br />
Such procedures include tracheal intubation, ventilation, peripheral<br />
and central venous cannulation and insertion of chest drains.
6. THE TRANSFER ITSELF<br />
The anaesthesia team transferring a patient must be confident that<br />
the accepting unit understands the patient’s needs and has the<br />
resources to accept them. As a practical point, communication on<br />
as high a level as possible should take place prior to transfer, ideally<br />
Consultant anaesthetist to Consultant anaesthetist but certainly from<br />
one experienced anaesthetist to another. In addition, there should be<br />
senior communication between the referring team in the base hospital<br />
to the admitting team in the receiving hospital.<br />
Telephone communications from the ambulance to the consultant<br />
anaesthetist and the base hospital should always be available.<br />
Key decision-making during transfer is the responsibility of the<br />
transferring anaesthetic team. This team should consult on patient<br />
management issues with the receiving team but the transferring team,<br />
being the team physically attending the patient, should make the key<br />
decisions.<br />
The principle behind safe transfer is that the patient should receive the<br />
same quality of care during transfer as in the base ICU. Care should<br />
be provided by experienced personnel, including a critical care<br />
nurse, an anaesthetist, and, when necessary, other experienced staff.<br />
Although the accompanying anaesthetist is usually in a training grade,<br />
nevertheless he should be sufficiently experienced to complete the<br />
transfer to a high standard of patient care, and with immediate advice<br />
available at all times from the consultant in the base hospital. The<br />
patient should be resuscitated and as stable as possible on departure.<br />
Although inter-hospital transfer is usually urgent, The Standing<br />
Committee feels that there is little to be gained by speeding between<br />
hospitals. Transfer should take place in a calm manner to allow for<br />
the maximum comfort of the patient and team. Sirens and blue lights<br />
should only be used in the case of obstructing traffic. Garda escorts<br />
should be requested in areas of traffic black spots to facilitate calm<br />
and steady progress. The Standing Committee feels that the Emergency<br />
Medical Technician (EMT) ambulance crew should consult the<br />
anaesthetist in this regard.<br />
The transfer team should be covered by insurance cover adequate<br />
to protect it from any claims arising from incidents en route. The<br />
insurance cover should also include cover for members of the transfer<br />
team itself for any injury or loss of employment which might arise<br />
following an accident en route.<br />
10<br />
11
7. THE BASE HOSPITAL DURING TRANSFER<br />
Usually a member of the Department of Anaesthesia is in charge of the<br />
transfer of a critically ill patient both during normal hours and in the<br />
out-of-hours setting. This duty is usually carried out by an anaesthetic<br />
NCHD. In most referring hospitals there is only one anaesthetic NCHD<br />
on call out-of-hours so that the referring hospital is bereft of its only inhouse<br />
anaesthetic doctor for long periods. The consultant on call from<br />
home is the only anaesthetist then available and he must prioritise his<br />
role and resources to balance clinical demands and personnel. This<br />
may leave key areas of the acute hospital service with anaesthetic cover<br />
that is less than optimal. For example, in many hospitals, when the<br />
anaesthetic NCHD on call has left the hospital on inter-hospital duties,<br />
the consultant anaesthetist is left alone to cover the competing needs<br />
of maternity, emergency general surgery, intensive care, resuscitation<br />
and accident/emergency. This is clearly an impossible task, resulting in<br />
the consultant anaesthetist reluctantly having to prioritise certain areas<br />
above others.<br />
The Standing Committee feels than out-of-hours transfers should only<br />
take place when immediate active management of the patient will take<br />
place in the receiving hospital. If surgery, for example, will not take<br />
place until the following day then an early morning transfer should<br />
be arranged rather than conduct an unnecessary middle-of-the-night<br />
transfer with resultant loss of anaesthetic cover locally.<br />
The recommendation of the Standing Committee is that, when an<br />
anaesthetist finds himself alone to cover competing units in the absence<br />
of his colleague on transfer duties, he should hold the obstetric unit,<br />
where present, as his clinical priority. Specifically the anaesthetist<br />
should keep himself free for emergency Caesarean sections. If there<br />
is an epidural service in the obstetric unit it should be temporarily<br />
suspended until the resident anaesthetist returns to base. Secondly, the<br />
single-handed anaesthetist should keep himself free for involvement<br />
in the management of ICU patients to whom he is already clinically<br />
committed.<br />
With regard to provision of anaesthesia for theatre cases other than<br />
Caesarean sections, it is imperative to stress that the provision of<br />
anaesthesia by an anaesthetist to a patient means that he is fully<br />
occupied with that patient to an exclusive level for the duration of the<br />
anaesthetic and cannot become involved in the management of other<br />
patients during that time. The vast majority of non- Caesarean section<br />
cases must therefore be transferred to the nearest appropriate hospital<br />
if surgery is urgent or alternatively must wait until the transferring<br />
anaesthetist returns to base.<br />
The primary recommendation of the Standing Committee is that when<br />
an anaesthetist finds himself single-handedly covering a number<br />
of areas simultaneously, he should contact hospital and nursing<br />
management on duty at that time, and outline the problem of<br />
inadequate anaesthetic cover to them. He should inform management<br />
of his recommendations, as follows:<br />
1. That, until the resident anaesthetist returns, critically ill patients<br />
should not be delivered by ambulance to the A&E department, nor<br />
admitted to the wards. Instead, these cases should be transferred to<br />
the nearest appropriate unit.<br />
2. That he, the anaesthetist on-call, will keep himself free for<br />
emergency Caesarean sections and will not bring any other cases<br />
to theatre. The Standing Committee recognises that, on a very rare<br />
occasion when there is an immediately life-threatening situation,<br />
such as massive haemorrhage or major airway problems, a patient<br />
will have to be brought to theatre immediately as an urgent lifesaving<br />
measure. In this circumstance the anaesthetist should ensure<br />
that the grave state of the patient is carefully documented by the<br />
admitting consultant. The anaesthetist should then inform the<br />
consultant obstetrician and the labour ward that there will be no<br />
anaesthetic cover for Caesarean sections until this urgent patient<br />
has left the operating theatre or alternatively until the transfer team<br />
returns.<br />
3. That the epidural service will be temporarily suspended until the<br />
resident anaesthetist returned.<br />
12<br />
13
4. No other anaesthesia-accompanied transfers can take place until<br />
the return of the first transfer team.<br />
The above situation may pertain less in the normal working hours<br />
when there are more staff members available. In addition the<br />
national mobile Intensive Care Unit (M.I.C.A.S.) is available for<br />
planned inter-hospital transfer 9 to 5 Monday to Friday.<br />
The members of the Department of Anaesthesia should discuss the<br />
problems at the base hospital during inter-hospital transfer:<br />
• within their own department to ensure a consistent response from<br />
all anaesthetists<br />
• at clinical directorate level to ensure hospital-wide plans are put in<br />
place to deal with transfer associated difficulties and<br />
• at the hospital medical board to ensure that consultants in all<br />
specialties are aware of the difficulties.<br />
8. POST-TRANSFER<br />
After a transfer the return to base of the transfer team should be effected<br />
as comfortably and as rapidly as possible.<br />
The Standing Committee wishes to stress that, when a transfer team<br />
returns to base, its members should not be expected to immediately<br />
dive straight into their work schedule without having had a significant<br />
rest break.<br />
There should be a debriefing discussion after each inter-hospital transfer<br />
between the transfer team and the referring hospital consultants.<br />
Problems should be highlighted and policies established to prevent<br />
recurrence of similar problems. Organisational difficulties between<br />
referring and receiving hospitals should be discussed by the relevant<br />
consultants in both hospitals and policies implemented to prevent<br />
recurrence of these difficulties.<br />
Each anaesthetic department should keep formal minutes of these<br />
debriefing sessions. The minutes should be available to inspection on<br />
request by teams from the College of Anaesthetists RCSI and the Irish<br />
Medical Council.<br />
Both referring and receiving hospitals should have a broad set of<br />
guidelines available in their ICU and A&E departments so that doctors<br />
engaged in referring or receiving patient transfers can refer to these<br />
guidelines when confronted by transfer difficulties. These guidelines<br />
should be broad and should cover both clinical and organisational<br />
aspects of patient transfer. The guidelines should be reviewed<br />
annually.<br />
14<br />
15
9. THE FUTURE<br />
The current limited retrieval service run by Dublin hospitals operates<br />
only from 9 to 5, five days a week. In addition the service is available<br />
only to ICU patients and excludes other patients.<br />
A 7-day, 24-hour inter-hospital retrieval service should be available for<br />
all critically ill patients needing transfer. This would include trauma<br />
patients.<br />
Pending this arrangement, all hospitals should have enough levels<br />
of anaesthetic cover to ensure that there is a continuous in-house<br />
anaesthetic presence even when inter-hospital transfers are taking<br />
place.<br />
10. REFERENCES<br />
1. “Transport of the Critically Ill.”<br />
Intensive Care Society of Ireland. 1991.<br />
2. “Care of the Critically Ill Child in Irish Hospitals.”<br />
Association of Anaesthetists of Great Britain and Ireland. 2005<br />
3. “OAA / AAGBI Guidelines for Obstetric Anaesthetic Services 2.”<br />
OAA / AAGBI Revised Edition 2005.<br />
16<br />
17
21 Portland Place, London W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org<br />
Designed and produced by the r2 Partnership Ltd
Day Case and Short Stay Surgery<br />
2<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
The British Association of Day Surgery<br />
May 2011
This guideline was originally published in Anaesthesia. If you wish to refer to<br />
this guideline, please use the following reference:<br />
Verma R, Alladi R, Jackson I, et al. Day case and short stay surgery: 2,<br />
Anaesthesia 2011; 66: pages 417-434<br />
This guideline can be viewed online via the following URL:<br />
http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2044.2011.06651.x/pdf<br />
This guideline has been endorsed by the Association of Surgeons of<br />
Great Britain and Ireland and the Association for Perioperative Practice.<br />
© The Association of Anaesthetists of Great Britain & Ireland and the British Association of Day<br />
Surgery 2011
GUIDELINES<br />
Day case and short stay surgery: 2<br />
Association of Anaesthetists of Great Britain and Ireland<br />
British Association of Day Surgery<br />
Membership of the Working Party: R. Verma (Chairman), R. Alladi,<br />
I. Jackson, I. Johnston, C. Kumar, R. Page, I. Smith, M. Stocker,<br />
C. Tickner, S. Williams and R. Young<br />
This is a consensus document produced by expert members of a Working Party<br />
established by the Association of Anaesthetists of Great Britain and Ireland<br />
(AAGBI) and British Association of Day Surgery (BADS). It has been seen and<br />
approved by the Councils of the AAGBI and BADS.<br />
Summary<br />
1 Day surgery is a continually evolving speciality performed in a range of<br />
ways across different units.<br />
2 In recent years, the complexity of procedures has increased with a wider<br />
range of patients now considered suitable for day surgery.<br />
3 Effective pre-operative preparation and protocol-driven, nurse-led<br />
discharge are fundamental to safe and effective day and short stay surgery.<br />
4 Fitness for a procedure should relate to the patient’s health as<br />
determined at pre-operative preparation and not limited by arbitrary<br />
limits such as ASA status, age or body mass index.<br />
5 Patients presenting with acute conditions requiring urgent surgery can be<br />
efficiently and effectively treated as day cases via a semi-elective pathway.<br />
6 Central neuraxial blockade and a range of regional anaesthetic<br />
techniques, including brachial plexus and paravertebral blocks, can be<br />
used effectively for day surgery.<br />
Re-use of this article is permitted in accordance with the Creative Commons Deed,<br />
Attribution 2.5, which does not permit commercial exploitation.<br />
Ó 2011 The Authors<br />
Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland 1
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
7 Each anaesthetist should develop techniques that permit the patient to<br />
undergo the surgical procedure with minimum stress and maximum<br />
comfort, and optimise his ⁄ her chance of early discharge.<br />
8 Every day surgery unit must have a Clinical Lead with specific interest<br />
in day surgery and whose remit includes the development of local<br />
policies, guidelines and clinical governance.<br />
9 Good quality advice leaflets, assessment forms and protocols are in use<br />
in many centres and are available to other units.<br />
10 Effective audit is an essential component of good care in all aspects of<br />
day and short stay surgery.<br />
11 Enhanced recovery is based on established day surgery principles and<br />
is aimed at improving the quality of recovery after inpatient surgery<br />
such that the patient is well enough to go home earlier and<br />
healthier.<br />
The definition of day surgery in the UK and Ireland is clear: the patient<br />
must be admitted and discharged on the same day, with day surgery as the<br />
intended management. Although still counted as inpatient treatment<br />
(except in the US), 23-h and short stay surgery apply the same principles of<br />
care outlined in this document and can improve the quality of patient care<br />
whilst reducing length of stay.<br />
Since the previous guideline was published in 2005, the complexity of<br />
procedures has increased with a wider range of patients now considered<br />
suitable for day surgery. Despite these advances, the overall rates of day<br />
surgery remain variable across the UK. Whereas the target of 75% of<br />
elective surgery to be performed as day cases from the NHS plan<br />
remains [1], the true picture is difficult to determine, since the only<br />
nationally reported data are limited to 25 procedures [2]. Ten years on,<br />
the advancement of minimally invasive surgery is allowing more<br />
procedures to be performed as day surgery and even higher rates should<br />
be possible.<br />
There was a major drive to promote day surgery around the turn of<br />
this century, but the political focus moved on before all of the lessons<br />
learned were fully implemented [3]. Nevertheless, the recent drive to<br />
reduce length of stay and improve the quality of postoperative recovery<br />
has ensured that day surgery principles are fundamental to modern<br />
patient care. Shortened hospital stays and earlier mobilisation also reduce<br />
the risk of hospital-acquired infections and venous thromboembolism<br />
(VTE).<br />
Ó 2011 The Authors<br />
2 Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
Recent reports<br />
The NHS Modernisation Agency produced an operational guide detailing the<br />
facilities available in, and the management of, day units [4]. This was further<br />
refined in the Ten High Impact Changes document in which the principle of<br />
treating day surgery as the default option for elective surgery was set out [3].<br />
The NHS Institute for Innovation and Improvement has also produced a<br />
document focusing on day case laparoscopic cholecystectomy [5]. Whereas<br />
this document is specific to one procedure, many aspects of the ideal patient<br />
pathway are equally applicable to a wide range of day surgery procedures.<br />
Effective pre-operative assessment and preparation with protocol-driven,<br />
nurse-led discharge are fundamental to safe and effective day and short stay<br />
surgery. Several recent publications provide useful advice on the establishment<br />
and running of both services [6–10].<br />
The British Association of Day Surgery has produced a directory of<br />
procedures that provides targets for day and short stay surgery rates for over<br />
200 different procedures [11]. These procedure-specific targets serve as a<br />
focus for clinicians and managers in the planning and provision of short stay<br />
elective surgery and illustrate the high quality of service achievable in<br />
appropriate circumstances.<br />
In March 2010, the Department of Health published the enhanced<br />
recovery guide that extends day surgery principles to inpatient surgery [12].<br />
Selection of patients<br />
Patients may be referred for day surgery from outpatient clinics, accident<br />
and emergency departments or primary care.<br />
Recent advances in surgical and anaesthetic techniques, as well as the<br />
publication of successful outcomes in patients with multiple comorbidities,<br />
have changed the emphasis in day surgery patient selection. It is now<br />
accepted that the majority of patients are appropriate for day surgery unless<br />
there is a valid reason why an overnight stay would be to their benefit. If<br />
inpatient surgery is being considered it is important to question whether any<br />
strategies could be employed to enable the patient to be treated as a day case.<br />
Full-term infants over 1 month are usually appropriate to undergo day<br />
surgery. A higher age limit is advisable for ex-premature infants (60 weeks<br />
post-conceptional age). The significant risk posed by postoperative apnoea<br />
must be considered and infants with recent apnoea episodes, cardiac or<br />
respiratory disease, family history of sudden infant death syndrome and<br />
Ó 2011 The Authors<br />
Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland 3
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
adverse social circumstances should be considered for overnight admission<br />
and close monitoring. Day surgery units should not perform surgery on<br />
children unless they have suitable staff and facilities.<br />
It is recommended that a multidisciplinary approach, with agreed<br />
protocols for patient assessment including inclusion and exclusion criteria<br />
for day surgery, should be agreed locally with the anaesthetic department.<br />
Patient assessment for day surgery falls into three main categories:<br />
Social factors<br />
(a) The patient must understand the planned procedure and postoperative<br />
care and consent to day surgery.<br />
(b) Following most procedures under general anaesthesia, a responsible<br />
adult should escort the patient home and provide support for the first<br />
24 h.<br />
(c) The patient’s domestic circumstances should be appropriate for<br />
postoperative care.<br />
Medical factors<br />
(a) Fitness for a procedure should relate to the patient’s health as<br />
determined at pre-operative assessment and not limited by arbitrary<br />
limits such as ASA status, age or BMI [13–15].<br />
(b) Patients with stable chronic disease such as diabetes, asthma or epilepsy<br />
are often better managed as day cases because of minimal disruption to<br />
their daily routine.<br />
(c) Obesity per se is not a contraindication to day surgery as even morbidly<br />
obese patients can be safely managed in expert hands, with appropriate<br />
resources. The incidence of complications during the operation or in<br />
the early recovery phase increases with increasing BMI. However,<br />
these problems would still occur with inpatient care and have usually<br />
resolved or been successfully treated by the time a day case patient<br />
would be discharged. In addition, obese patients benefit from the<br />
short-duration anaesthetic techniques and early mobilisation associated<br />
with day surgery [16].<br />
Surgical factors<br />
(a) The procedure should not carry a significant risk of serious complications<br />
requiring immediate medical attention (haemorrhage, cardiovascular<br />
instability).<br />
Ó 2011 The Authors<br />
4 Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
(b) Postoperative symptoms must be controllable by the use of a<br />
combination of oral medication and local anaesthetic techniques.<br />
(c) The procedure should not prohibit the patient from resuming oral<br />
intake within a few hours.<br />
(d) Patients should usually be able to mobilise before discharge although<br />
full mobilisation is not always essential.<br />
Pre-operative preparation<br />
Pre-operative preparation (formerly known as pre-operative assessment) has<br />
three essential components:<br />
1 To educate patients and carers about day surgery pathways.<br />
2 To impart information regarding planned procedures and postoperative<br />
care to help patients make informed decisions – important information<br />
should be provided in writing.<br />
3 To identify medical risk factors, promote health and optimise the<br />
patient’s condition.<br />
All patients must be assessed by a member of the multidisciplinary team<br />
trained in pre-operative assessment for day surgery. Consultant-led and<br />
nurse-run clinics have proved very successful.<br />
Pre-operative preparation is best performed within a self-contained day<br />
surgery facility, where available. This allows patients and their relatives the<br />
opportunity to familiarise themselves with the environment and to meet<br />
staff who will provide their peri-operative care [17]. One-stop clinics,<br />
where pre-operative preparation is performed on the same day as decision<br />
for surgery, offer significant advantages.<br />
Screening questionnaires (Appendix 1), in conjunction with pre-set<br />
protocols, can offer guidance on appropriate investigations, as routine<br />
pre-operative investigations have no relevance in modern anaesthesia.<br />
Although the National Institute of Health and Clinical Excellence<br />
(NICE) guidance on pre-operative investigations [18] is widely<br />
used, one recent study showed no difference in the outcomes of day<br />
surgery patients even when all pre-operative investigations were omitted<br />
[19].<br />
Pre-operative preparation clinics can improve efficiency by enabling<br />
early review of the notes of complex cases, ensuring appropriate<br />
investigations are carried out and that patients are referred for specialist<br />
opinion if deemed necessary.<br />
Ó 2011 The Authors<br />
Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland 5
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
Day surgery for urgent procedures<br />
Patients presenting with acute conditions requiring urgent surgery can be<br />
efficiently and effectively treated as day cases via a semi-elective pathway<br />
[20]. After initial assessment many patients can be discharged home and<br />
return for surgery at an appropriate time, either on a day case list or as a<br />
scheduled patient on an emergency list, whereas others can be immediately<br />
transferred to the day surgery service. This reduces the likelihood of<br />
repeated postponement of surgery due to prioritisation of other cases. A<br />
robust day surgery process is key to the success of this service. Some of the<br />
procedures successfully managed in this manner are shown in Table 1<br />
[21–25]. Essential components of an emergency day surgery pathway are:<br />
1 Identification of appropriate procedures.<br />
2 Identification of a theatre list that can reliably accommodate the<br />
procedure (e.g. a dedicated day surgery list or a flexibly run emergency<br />
theatre list).<br />
3 There should be clear pathways for day surgery in place.<br />
4 The condition must be safe to be left untreated for a day or two and<br />
manageable at home with oral analgesia (standardised analgesic pack for<br />
the patient to take home).<br />
5 There should be provision of clear pre-operative patient information,<br />
ideally in writing.<br />
Documentation<br />
Detailed documentation is important within the day surgery environment<br />
as the patient’s experience is often condensed into a few hours. All aspects<br />
Table 1 Types of urgent surgery suitable for day case procedures.<br />
General surgery Gynaecology Trauma Maxillofacial<br />
Incision and drainage<br />
of abscess<br />
Laparoscopic<br />
cholecystectomy<br />
Laparoscopic<br />
appendicectomy<br />
Temporal artery<br />
biopsy<br />
Evacuation of retained<br />
products of conception<br />
Laparoscopic ectopic<br />
pregnancy<br />
Tendon repair<br />
Manipulation<br />
of fractures<br />
Plating of<br />
fractured<br />
clavicle<br />
Manipulation of<br />
fractured nose<br />
Repair of fractured<br />
mandible ⁄ zygoma<br />
Ó 2011 The Authors<br />
6 Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
of treatment and care must be recorded accurately to ensure that each<br />
patient follows an effective and safe pathway.<br />
Documentation should be a continuum from pre-operative preparation<br />
to discharge and subsequent follow-up. Single care plans reflecting a<br />
multidisciplinary approach are favoured in many units. Variations for<br />
specific groups including children and patients undergoing procedures<br />
under local anaesthesia should be available. Procedure-specific care plans<br />
reflecting integrated care pathways may be used for more complex and<br />
challenging cases [26]. Such care plans are also useful for audit and<br />
evaluating outcome.<br />
Patients should be provided with general as well as procedure-specific<br />
information. This should be given in advance of admission to allow time for<br />
questioning and preparation for same day surgery. Verbal comments should<br />
be reinforced with written material. General information should include<br />
practical details about attending the day surgery unit whereas procedurespecific<br />
information should include clinical information about the patient’s<br />
condition and surgical procedure (Appendix 2). The anaesthetic information<br />
leaflets developed jointly between the AAGBI and the Royal College<br />
of Anaesthetists (RCoA) may also be used [27]. Information for children is<br />
also available [28].<br />
Management and staffing<br />
Every day surgery unit must have a Clinical Lead with specific interest in<br />
day surgery and whose remit includes the development of local policies,<br />
guidelines and clinical governance. A consultant anaesthetist with<br />
management experience is ideally suited to such a role and job plans must<br />
reflect this responsibility [4]. Day surgery must be represented at Board<br />
level [4].<br />
The Clinical Lead should be supported by a day surgery manager who<br />
has responsibility for the day-to-day running of the unit. The manager will<br />
often have a nursing background and should have the knowledge and skills<br />
to make informed decisions and lead on all aspects of day surgery<br />
development.<br />
Nurses, operating department practitioners, physicians’ assistants<br />
(anaesthesia) (PA(A)s), and other ancillary staffing levels will depend<br />
on the design of the facility, casemix, workload and local preferences<br />
and ability to conform to national guidelines. Staff working in these<br />
Ó 2011 The Authors<br />
Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland 7
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
units should be specifically trained in day surgery care. Many units<br />
favour multiskilled staff who have the knowledge and skills to work<br />
within several different areas of the day surgery unit. Efficient use of<br />
resources is best achieved by a well-trained, flexible and multiskilled<br />
workforce [29].<br />
Extended roles facilitate job satisfaction and encourage personal development<br />
and staff retention. Many health care assistants in the day surgery<br />
unit are now able to perform duties traditionally only undertaken by<br />
qualified nurses [30–32]. Individual units should formulate a staffing<br />
structure that takes into consideration local needs.<br />
Each unit should have a multidisciplinary operational group that oversees<br />
the day-to-day running of the unit, agrees policies and timetables, reviews<br />
operational problems and organises audit strategies.<br />
Facilities<br />
Day surgery should ideally be provided in a self-contained unit that is<br />
functionally and structurally separate from inpatient wards and theatres<br />
[33]. It should have its own reception, consulting rooms, ward, theatre<br />
and recovery areas, together with administrative facilities. The operating<br />
theatre and first stage recovery areas should be equipped and staffed to<br />
the same standards as an inpatient facility, with the exception of the<br />
use of trolleys rather than beds. Several patients per day can occupy the<br />
same trolley space, providing far greater efficiency than on wards where<br />
one day case may occupy a bed for a whole day. Car parking or<br />
short stay drop-off and pick-up areas should be provided adjacent to the<br />
unit.<br />
An alternative to a purpose-built unit is the use of a day case ward with<br />
patients transferred to the main operating theatre. This model allows a more<br />
straightforward transition from overnight stay to day case for complex<br />
procedures as there is little impact on theatre equipment or staffing.<br />
However, day case beds dispersed around many wards do not achieve these<br />
efficiencies, nor do they provide the targeted service that is required to<br />
achieve good outcomes.<br />
Typical day unit opening hours would be 07:00–20:00 Monday to<br />
Friday, but with the increasing complexity of surgery many units now open<br />
until about 22:00.<br />
Ó 2011 The Authors<br />
8 Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
Many hospitals provide care for day surgery patients who require<br />
anaesthesia in specialised units, e.g. ophthalmology or dentistry. It may not<br />
be possible or appropriate to centralise these services; however, all such<br />
patients should receive the same high standards of selection, preparation,<br />
peri-operative care, discharge and follow-up as those attending dedicated<br />
day surgery facilities.<br />
Facilities should ensure the maintenance of patients’ privacy and<br />
dignity at all times. Side rooms are particularly useful when caring for<br />
patients requiring an increased level of sensitivity, or for those with<br />
special needs.<br />
Children should be cared for in a facility that reflects their emotional<br />
and physical needs, separate from adult patients and conforming to the<br />
standards required by paediatric units. Nursing staff should be skilled in<br />
paediatric day surgical care. Parents and carers, wherever possible, should<br />
be involved in all aspects of care and appropriate facilities provided for<br />
them.<br />
Anaesthetic management<br />
Day surgery anaesthesia should be a consultant-led service. However, as<br />
day surgery becomes the norm for elective surgery, consideration should<br />
be given to education of trainees as recommended by the RCoA. This<br />
requires appropriate training and provision of senior cover, especially in<br />
stand-alone units. Staff grade and associate specialist anaesthetists who<br />
have an interest in day surgery should be encouraged to develop this as a<br />
specialist interest and take an important role in the management of the<br />
unit.<br />
Appropriate selection and patient preparation is crucial for day surgery.<br />
National guidelines for patient monitoring and assistance for the anaesthetist<br />
should be followed [34, 35].<br />
Anaesthetic techniques should ensure minimum stress and maximum<br />
comfort for the patients and should take into consideration the risks and<br />
benefits of the individual techniques. Analgesia is paramount and must be<br />
long acting but, as morbidity such as nausea and vomiting must be<br />
minimised, the indiscriminate use of opioids is discouraged (particularly<br />
morphine). Prophylactic oral analgesics with long-acting non-steroidal antiinflammatory<br />
drugs (NSAIDs) should be given to all patients if not<br />
contraindicated. For certain procedures (e.g. laparoscopic cholecystectomy)<br />
Ó 2011 The Authors<br />
Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland 9
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
there is evidence that standardised anaesthesia protocols or techniques<br />
improve outcome. Anaesthetists should adhere to such clinical guidelines<br />
where they exist.<br />
Although early mobilisation should be beneficial, extending the range<br />
and complexity of day surgery procedures may increase the risk of VTE.<br />
National guidelines for VTE risk assessment and prophylaxis should be<br />
followed.<br />
Policies should exist for the management of postoperative nausea and<br />
vomiting (PONV) and discharge analgesia. Prophylactic antiemetics are<br />
only recommended in patients with a strong history of PONV, motion<br />
sickness and those undergoing certain procedures such as laparoscopic<br />
sterilisation ⁄ cholecystectomy or tonsillectomy. However, it is important<br />
that PONV is treated seriously once it occurs. Routine use of intravenous<br />
fluids can enhance the patients’ feeling of wellbeing and further reduce<br />
PONV [36].<br />
Regional anaesthesia<br />
Local infiltration and nerve blocks can provide excellent anaesthesia and<br />
pain relief after day surgery. Patients may safely be discharged home with<br />
residual sensory or motor blockade, provided the limb is protected and<br />
appropriate support is available for the patient at home. The expected<br />
duration of the blockade must be explained and the patient must receive<br />
written instructions as to their conduct until normal power and sensation<br />
returns. Infusions of local anaesthesia may also have a place [37]. The use of<br />
ultrasound is increasingly gaining popularity, particularly in upper limb<br />
surgery, and is recognised as a useful tool in several areas of regional<br />
anaesthesia.<br />
Central neuraxial blockade (spinal or caudal) can be useful in day<br />
surgery and is increasing in popularity, although residual blockade may<br />
cause postural hypotension or urinary retention despite the return of<br />
adequate motor and sensory function. These problems can be minimised<br />
by choosing an appropriate local anaesthetic agent or by the use of lowdose<br />
local anaesthetic ⁄ opioid mixtures [38]. Suggested criteria before<br />
attempting ambulation after neuraxial block include the return of<br />
sensation in the perianal area (S4-5), plantar flexion of the foot at preoperative<br />
levels of strength and return of proprioception in the big toe<br />
[39].<br />
Ó 2011 The Authors<br />
10 Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
Sedation is seldom needed but, if used, suggested discharge criteria<br />
should be met and the patient must receive an appropriate<br />
explanation.<br />
Oral analgesics should be started before the local anaesthesia begins to<br />
wear off and also given subsequently on a regular basis.<br />
The patient’s hydration should be checked. Concerns about post-dural<br />
puncture headache (PDPH) have limited the use of spinals in day surgery<br />
patients in the past, but the use of smaller gauge (‡ 25-G) and pencil-point<br />
needles has reduced the incidence to < 1%. Information about PDPH and<br />
what to do if this occurs should be included in the patient’s discharge<br />
instructions as well as the provision of alternative analgesics. Further<br />
information on the use of spinal anaesthesia in day surgery and examples of<br />
patient information leaflets can be found on the BADS website (http://<br />
www.bads.co.uk).<br />
The current nationally agreed curriculum limits the scope of PA (A)s. On<br />
completion of training they are not qualified to undertake regional<br />
anaesthesia or regional blocks [40].<br />
Postoperative recovery and discharge<br />
Recovery from anaesthesia and surgery can be divided into three phases:<br />
1 First stage recovery lasts until the patient is awake, protective reflexes<br />
have returned and pain is controlled. This should be undertaken in a<br />
recovery area with appropriate facilities and staffing [41]. Use of<br />
modern drugs and techniques may allow early recovery to be complete<br />
by the time the patient leaves the operating theatre, allowing some<br />
patients to bypass the first stage recovery area [42]. Most patients who<br />
undergo surgery with a local anaesthetic block can be fast-tracked in<br />
this manner.<br />
2 Second stage recovery ends when the patient is ready for discharge from<br />
hospital. This should ideally be in an area adjacent to the day surgery<br />
theatre. It should be equipped and staffed to deal with common<br />
postoperative problems (PONV, pain) as well as emergencies (haemorrhage,<br />
cardiovascular events). The anaesthetist and surgeon (or a deputy)<br />
must be contactable to help deal with problems. Nurse-led discharge<br />
using agreed protocols is appropriate (Appendix 3). Some of the<br />
traditional discharge criteria such as tolerating fluids and passing urine are<br />
no longer enforced. Mandatory oral intake is not necessary and may<br />
Ó 2011 The Authors<br />
Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland 11
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
provoke nausea and vomiting and delay discharge. Voiding is also not<br />
always required, although it is important to identify and retain patients<br />
who are at particular risk of developing later problems, such as those who<br />
have experienced prolonged instrumentation or manipulation of the<br />
bladder [43]. Protocols may be adapted to allow low-risk patients to be<br />
discharged without fulfilling traditional criteria. Mild postoperative<br />
confusion in the elderly after surgery is common. This is usually<br />
insignificant and should not influence discharge provided social circumstances<br />
permit; in fact, the avoidance of hospitalisation after minor<br />
surgery is preferred [15, 44]. Patients and their carers should be provided<br />
with written information that includes warning signs of possible<br />
complications and where to seek help. Protocols should exist for the<br />
management of patients who require unscheduled admission, especially<br />
in a stand-alone unit.<br />
3 Late recovery ends when the patient has made a full physiological and<br />
psychological recovery from the procedure. This may take several weeks<br />
or months and is beyond the scope of this document.<br />
Postoperative instructions and discharge<br />
All patients should receive verbal and written instructions on discharge and<br />
be warned of any symptoms that might be experienced. Wherever possible,<br />
these instructions should be given in the presence of the responsible person<br />
who is to escort and care for the patient at home.<br />
Advice should be given not to drink alcohol, operate machinery or drive<br />
for 24 h after a general anaesthetic [45]. More importantly, patients should<br />
not drive until the pain or immobility from their operation allows them to<br />
control their car safely and perform an emergency stop. Procedure-specific<br />
recommendations regarding driving should be available.<br />
All patients should be discharged with a supply of appropriate analgesics<br />
and instructions in their use. Analgesia protocols (Appendix 4) relating<br />
to day surgery case mix should be agreed with the pharmacy. Free<br />
pre-packaged take-home medications should be provided as they are<br />
convenient and prevent delays and unnecessary visits to the hospital<br />
pharmacy.<br />
Discharge summary<br />
It is essential to inform the patient’s general practitioner promptly of<br />
the type of anaesthetic given, the surgical procedure performed and<br />
Ó 2011 The Authors<br />
12 Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
postoperative instructions given. Patients should be given a copy of this<br />
discharge summary to have available should they require medical assistance<br />
overnight.<br />
Day surgery units must agree with their local primary care teams how<br />
support is to be provided for patients in the event of postoperative<br />
problems. Best practice is a helpline for the first 24 h after discharge<br />
and to telephone the patient the next day. Telephone follow-up is<br />
highly rated by patients, provides support for any immediate complications,<br />
and is useful for auditing postoperative symptoms and patient<br />
satisfaction.<br />
Audit<br />
Effective audit is an essential component of assessing, monitoring and<br />
maintaining the efficiency and quality of patient care in day surgery units.<br />
Systems should be in place to ensure the routine collection of data regarding<br />
patient throughput and outcomes. There have been a variety of tools<br />
developed to determine patient outcomes. Questionnaires, which rely on<br />
the patients’ completing documentation and returning them to the day<br />
unit, are notoriously inaccurate and response rates are often very low. The<br />
most successful units collect data electronically at all stages of the day<br />
surgery process.<br />
The RCoA’s compendium of audit recipes devotes a section to possible<br />
audits relevant to day surgery [46]. It must be stressed that the most<br />
reliable way of improving service is continuous audit and review of<br />
outcomes rather than one-off snapshots. Information regarding trends in<br />
the patients’ outcomes should be widely distributed amongst the members<br />
of the team.<br />
Audit of day surgery services relate primarily to quality of care and<br />
efficiency. Examples of day surgery processes amenable to audit that have<br />
some measurable outcomes are shown in Table 2.<br />
Audit of patients’ satisfaction should be carried out routinely. A robust<br />
database is helpful; however, the best databases fail to effect change unless<br />
the information is clearly displayed and freely disseminated to the day<br />
surgery users. Monthly graphs and figures detailing all outcomes and trends<br />
should be disseminated to everyone, particularly to key individuals<br />
empowered to influence change.<br />
Ó 2011 The Authors<br />
Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland 13
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
Table 2 Day surgery processes amenable to audit.<br />
Component of process<br />
Outcome measure<br />
Booking process<br />
Patients failing to attend for surgery ⁄ theatre utilisation<br />
Pre-operative preparation Patients cancelled on the day of surgery ⁄ patients failing to<br />
attend<br />
Admission process<br />
Theatre start times<br />
Anaesthesia quality<br />
Unplanned admission rates ⁄ postoperative symptoms<br />
Surgery quality<br />
Unplanned admission rates ⁄ postoperative symptoms<br />
Recovery Discharge times ⁄ unplanned admission rates ⁄<br />
postoperative symptoms<br />
Discharge process<br />
Episodes of unplanned contact with primary care ⁄ out of<br />
hours health services<br />
Postoperative follow-up Episodes of unplanned contact with primary care ⁄ out of<br />
hours health services<br />
Audit<br />
Quality and efficiency improvements<br />
Teaching and training<br />
The RCoA has placed Day Surgery as a core module in all three<br />
components of anaesthetic training: Basic (year 1 ⁄ 2) [47], Intermediate<br />
(year 3 ⁄ 4) [48] and Higher (year 5 ⁄ 6 ⁄ 7) [49]. It also recommends day<br />
surgery as a specialty for advanced level training [50]. However, formal<br />
day surgery training programmes for anaesthetic (and surgical) trainees are<br />
rare.<br />
The competencies required by the RCoA cover the entire day surgery<br />
process, not simply the anaesthetic component. It is essential to design a<br />
well-structured module that provides training in anaesthesia for all<br />
aspects of day surgery and exposure to the organisational challenges of<br />
running a day surgery unit. To facilitate this, it is recommended that<br />
advanced training should take place in a dedicated day surgery unit [50],<br />
yet few such units exist. It is important to remember that high quality<br />
day surgery requires the experience of senior anaesthetists (and surgeons)<br />
and that although the day surgery unit is an ideal environment for<br />
training junior medical staff, relying on them to deliver the service<br />
results in poorer quality patient outcomes and reduced efficiency<br />
[51, 52].<br />
A list of topics that might be included in a day surgery module is shown<br />
in Appendix 5.<br />
Ó 2011 The Authors<br />
14 Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
The training delivery should be audited; some suggestions for this are<br />
given in the RCoA audit compendium [46].<br />
The day surgery unit is an excellent environment for surgical and nursing<br />
training and many of the aspects covered above are equally applicable to<br />
surgical and nursing colleagues.<br />
Day surgery in special environments<br />
A number of complex and highly specialist procedures are beginning to<br />
enter the day surgery arena. Awake craniotomy for tumour resection has<br />
been performed as a day case in the UK [53]. In the interventional X-ray<br />
suite, uterine artery embolisation is a day case procedure, whereas<br />
endovascular aneurysm stents and several other procedures are appropriate<br />
for a short stay approach. Optimal care for these procedures should be<br />
developed by those with expertise in day and short stay surgery, working in<br />
collaboration with specialists in the management of the specific procedure.<br />
Many of these procedures are undertaken in challenging environments,<br />
such as X-ray departments. All the accepted standards for delivery of<br />
anaesthesia, assistance for the anaesthetist, minimal monitoring and the<br />
availability of appropriate recovery (post-anaesthesia care unit (PACU))<br />
facilities should be achieved.<br />
Introducing new procedures to day surgery<br />
The successful introduction of new procedures to day surgery depends on<br />
many factors, including the procedure itself and surgical, nursing and<br />
anaesthetic colleagues. It is important to evaluate the procedure while still<br />
performing it as an overnight stay and identify any steps in the process<br />
that require modification to enable it to be performed as a day case, e.g.<br />
timing of postoperative X-rays, modification of intravenous antibiotic<br />
regimens, physiotherapy input and analgesia protocols [54]. A multidisciplinary<br />
visit to another unit where the procedure is performed<br />
successfully as a day case can be very helpful. Initially limiting the<br />
procedure to a few colleagues (surgeons and anaesthetists) allows an<br />
opportunity to evaluate and optimise techniques and to implement step<br />
changes so that the patient can be discharged safely and with good<br />
analgesia. Support from community nursing can be helpful, especially in<br />
these early stages. Once the procedure has been successfully moved to the<br />
Ó 2011 The Authors<br />
Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland 15
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
day surgery setting it can be expanded to include other surgeons and<br />
anaesthetists as appropriate. Clear clinical protocols help to ensure that all<br />
the lessons learned during the evaluation phase are clearly passed on to<br />
colleagues.<br />
Isolated day surgery units<br />
Many day surgery facilities in the UK and Ireland are isolated and the<br />
number of these is increasing. Currently, there is no set absolute<br />
minimum distance between any stand-alone unit and the nearest acute<br />
or associated hospital, although large distances are uncommon. The<br />
commissioning of any new isolated stand-alone unit requires analysis of<br />
its suitability for the provision of intended services. These facilities may<br />
or may not be purpose-built and the Clinical Lead must be aware of this<br />
in managing any risk. Any association with a nearby acute unit should<br />
be reviewed regularly.<br />
Remoteness is a factor to be considered in the delivery of a safe and<br />
efficient service. A minimum of two anaesthetists on site should be<br />
considered at any one time. Prolonged travel time may be an issue for<br />
visiting staff. On-call commitments must be taken into account so as to<br />
avoid accidents and fatigue either in theatre or when travelling.<br />
The operational policy must agree clear management of certain key<br />
issues. These include:<br />
• Management of patients who cannot be discharged home.<br />
• Management of patients with problems after discharge.<br />
• Appropriate cover for the service and patients until they are<br />
discharged.<br />
• Appropriate patient screening and selection with availability of medical<br />
records.<br />
• Management of medical emergencies, e.g. cardiac arrest and major<br />
haemorrhage, and the availability of materials and skilled personnel to<br />
deal with complications when the anaesthetist is in theatre.<br />
• Transfer agreements with local hospitals and intensive care facilities<br />
• Robust, tested communications between the stand-alone unit, the<br />
nearest acute hospital and the ambulance services.<br />
• Teaching, training and supervision and opportunities for research.<br />
This list is not meant to be exhaustive but gives guidance to some of the<br />
important areas that require consideration.<br />
Ó 2011 The Authors<br />
16 Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
Short stay surgery and enhanced recovery<br />
New approaches to the assessment and management of patients undergoing<br />
more complex surgery are being used to improve the quality of recovery,<br />
reduce the incidence of postoperative complications and reduce lengths of<br />
stay. Many of these techniques are based on the wider application of wellestablished<br />
day surgery principles and are aimed at improving the quality of<br />
recovery so that the patient is well enough to go home sooner. These<br />
strategies are variously called enhanced recovery, fast-track [55], accelerated<br />
or rapid recovery. For any surgical operation there is a large variation in<br />
average lengths of stay in hospitals across the UK and Ireland. Increasing<br />
numbers of hospitals are focusing on the short stay pathway and plan to<br />
manage the majority of their elective patients with stays of fewer than 72 h.<br />
To achieve the maximum benefit from this, hospitals are developing 24-h<br />
stay facilities (some as part of their existing day units) and are embracing<br />
these principles.<br />
Principles of enhanced recovery<br />
Enhanced recovery is the outcome of applying a range of multimodal<br />
strategies that are designed to prepare and optimise patients before, during<br />
and after surgery, ensuring prompt recovery and discharge [12]. Most of<br />
these principles are already well established in day surgery, which can be<br />
considered the ultimate example of enhanced recovery. Anaesthetic<br />
departments should play a major role in this as they can contribute<br />
extensively to all phases of the patients’ management. Many of these<br />
interventions are derived from day surgery.<br />
Pre-operative factors<br />
Pre-operative preparation of the patient plays a crucial role and identifies<br />
additional risk factors and ensures that their medical condition is<br />
optimised. Cardiopulmonary exercise testing provides further information<br />
to enable anaesthetists to discuss these risks with their patients and ensure<br />
that high-risk patients are counselled appropriately. An appropriate level<br />
of intensive or high dependency care can also be put in place if<br />
necessary. Patients and their carers should receive a careful explanation<br />
about the procedure and what will happen to them at every stage of the<br />
peri-operative pathway. This includes resumption of food, drink,<br />
mobilisation and information about discharge and when this is likely<br />
Ó 2011 The Authors<br />
Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland 17
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
to take place. As with day surgery, the provision of written information<br />
is vital.<br />
Patients should usually be admitted on the day of surgery with minimal<br />
starvation times (i.e. 3 h for fluids) and consideration given to the use of<br />
oral carbohydrate loading. Analgesia with paracetamol and NSAIDs<br />
should be started pre-operatively if not contraindicated, and hypothermia<br />
avoided.<br />
Intra-operative factors<br />
Minimally invasive surgery should be combined with use of regional<br />
anaesthesia where possible. Thoracic epidurals or other regional anaesthetic<br />
techniques should normally be used for abdominal surgery in patients likely<br />
to require more than oral analgesia postoperatively. Long acting opioids,<br />
nasogastric tubes and surgical drains should be avoided. Intra-operative fluid<br />
therapy should be goal directed to avoid sodium ⁄ fluid overload and<br />
attention should be paid to maintaining normothermia. Anaesthetic<br />
techniques are otherwise similar to day surgery with the expectation that<br />
patients will mobilise and eat ⁄ drink later in the day.<br />
Postoperative factors<br />
Effective analgesia that minimises the risk of PONV and allows early<br />
mobilisation plays a vital role in enhanced recovery. Systemic opioids<br />
should be avoided where possible and regular oral (or intravenous) analgesia<br />
with simple analgesics (paracetamol and NSAIDs) should be used. For more<br />
invasive procedures, epidural analgesia should be maintained in the<br />
postoperative period. Hydration should be maintained with intravenous<br />
fluids but discontinued as soon as the patient returns to oral fluids, and<br />
PONV should be treated aggressively using a multimodal approach to<br />
therapy.<br />
The patient should be mobilised within 24 h. They should be aware and<br />
encouraged to meet milestones for mobilisation, drinking and eating. This<br />
requires active involvement from both the medical and nursing teams in the<br />
immediate postoperative period. The provision of a specified dining room,<br />
with access to high calorie drinks and where meals can be taken, encourages<br />
the patient to mobilise.<br />
There should be a target discharge date set for which the staff, patients<br />
and relatives should aim, and as in day surgery the discharge should be a<br />
nurse-led process and not dependent on consultant review.<br />
Ó 2011 The Authors<br />
18 Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
The patient’s perspective<br />
A Mayo Clinic study in 2006 showed that patients want their doctors to be<br />
confident, empathetic, humane, personal, forthright, respectful and thorough<br />
[56]. Interestingly, there was no mention of competence, implying<br />
that patients inherently believe their doctors to be competent. A survey<br />
carried out by MORI on behalf of the RCoA in May 2000 found that 35%<br />
of the general public did not believe that anaesthetists were medically<br />
qualified doctors [57]. Hence, there is a credibility gap that anaesthetists<br />
need to address. It is important to ensure that patients are made aware that<br />
anaesthetists are highly qualified professional doctors. The patient information<br />
leaflets produced by the AAGBI and the RCoA can be useful in this<br />
regard.<br />
It is important to realise that to most patients, anaesthesia means general<br />
anaesthesia with loss of consciousness during the procedure, and the patient<br />
sees this as ceding total control to someone else. Nobody is really<br />
completely comfortable with this. The psychology of surrendering control<br />
can result in patient attitudes that may not be explicitly communicated to<br />
the anaesthetist. This can cause a lot of stress and anxiety. Patients are<br />
therefore worried about:<br />
• Never waking up.<br />
• Dying during an operation.<br />
• Waking up during surgery.<br />
• Feeling pain and possibly not being able to make anyone else aware.<br />
In a recent study [58], the top three were identified as being of most<br />
concern to day case patients. The same study highlighted that the factor that<br />
alleviated most anxiety was the presence of a partner or friend, especially<br />
during recovery. Importantly, patients were more receptive to anaesthetists’<br />
visiting and giving information about the procedure than to information<br />
provided by the nursing staff.<br />
Other concerns that are relatively common to patients having a general<br />
anaesthetic are also associated with loss of control:<br />
• Embarrassment about perceived loss of control of bodily functions e.g.<br />
wetting the bed, or saying something inappropriate while still drowsy.<br />
• Nausea and vomiting.<br />
It is important for the anaesthetist to offer reassurances, as this has the<br />
greatest impact compared with delegating this responsibility to the nursing<br />
staff. Apprehensive patients don’t easily absorb big words. Explanations<br />
should be given in simple terms, avoiding jargon and not using emotive<br />
Ó 2011 The Authors<br />
Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland 19
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
language. This is particularly important in helping children understand the<br />
planned procedure and what is to follow. Information provided in writing<br />
before the day of surgery also helps.<br />
A patient about to undergo elective surgery often has contradicting<br />
feelings. On the one hand they are glad that the surgery will cure their<br />
medical problem and provide a life enhancing experience. On the other<br />
hand they are riddled with innumerable anxieties and although it might<br />
seem routine and straightforward to the doctor, the patient will inevitably<br />
view it all very differently. No patient expects surgery to be actually<br />
enjoyable, but what is most appreciated is information delivered by a<br />
respected, highly trained professional, who is empathetic and regards the<br />
patient as a person and not merely as a statistic.<br />
An information leaflet designed to help patients prepare themselves for<br />
day surgery is available on the BADS website [59].<br />
References<br />
1 Department of Health. The NHS Plan. A Plan for Investment. A Plan for Reform.<br />
London: DoH, 2000.<br />
2 NHS Institute for Innovation and Improvement. Better Care, Better Value<br />
Indicators. http://www.productivity.nhs.uk (accessed 03 ⁄ 01 ⁄ 2011).<br />
3 Department of Health NHS Modernisation Agency. 10 High Impact Changes for<br />
Service Improvement and Delivery, 2004. http://www.ogc.gov.uk/documents/<br />
Health_High_Impact_Changes.pdf (accessed 03 ⁄ 01 ⁄ 2011).<br />
4 Department of Health. Day surgery: Operational Guide. Waiting, Booking and<br />
Choice, 2002. http://www.dh.gov.uk/dr_consum_dh/groups/dh_digitalassets/<br />
@dh/@en/documents/digitalasset/dh_4060341.pdf (accessed 03 ⁄ 01 ⁄ 2011).<br />
5 NHS Institute for Innovation and Improvement. Focus On: Cholecystectomy.<br />
Coventry: NHS Institute for Innovation and Improvement, 2006.<br />
6 Association of Anaesthetists of Great Britain and Ireland. Pre-operative Assessment<br />
and Patient Preparation – The Role of the Anaesthetist 2. London: AAGBI, 2010.<br />
7 British Association of Day Surgery. Ten Dilemmas in Preoperative Assessment for<br />
Day Surgery. London: BADS, 2009.<br />
8 British Association of Day Surgery. Organisational Issues in Pre Operative Assessment<br />
for Day Surgery. London: BADS, 2010.<br />
9 British Association of Day Surgery. Ten More Dilemmas in Day Surgery. London:<br />
BADS, 2008.<br />
10 British Association of Day Surgery. Nurse Led Discharge. London: BADS, 2009.<br />
11 British Association of Day Surgery. BADS Directory of Procedures, 3rd edn.<br />
London: BADS, 2009.<br />
Ó 2011 The Authors<br />
20 Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
12 NHS Enhanced Recovery Partnership Programme. Delivering Enhanced recovery.<br />
Helping Patients to Get Better Sooner After Surgery, 2010. http://www.dh.gov.uk/<br />
dr_consum_dh/groups/dh_digitalassets/@dh/@en/@ps/documents/digitalasset/<br />
dh_115156.pdf (accessed 03 ⁄ 01 ⁄ 2011).<br />
13 Ansell GL, Montgomery JE. Outcome of ASA III patients undergoing day case<br />
surgery. British Journal of Anaesthesia 2004; 92: 71–4.<br />
14 Aldwinckle RJ, Montgomery JE. Unplanned admission rates and post discharge<br />
complications in patients over the age of 70 following day case surgery.<br />
Anaesthesia 2004; 59: 57–9.<br />
15 Canet J, Raeder J, Rasmussen LS, et al. Cognitive dysfunction after minor<br />
surgery in the elderly. Acta Anaesthesiologica Scandinavica 2003; 47: 1204–10.<br />
16 Davies KE, Houghton K, Montgomery JE. Obesity and day-case surgery.<br />
Anaesthesia 2001; 56: 1112–5.<br />
17 Lewis S, Stocker M, Houghton K, Montgomery JE. A patient survey to<br />
determine how day surgery patients would like preoperative assessment to be<br />
conducted. Journal of One-day Surgery 2009; 19: 32–6.<br />
18 National Institute for Health and Clinical Excellence. NICE Clinical Guideline<br />
3 — Pre-operative tests. The Use of Routine Preoperative Tests for<br />
Elective Surgery, 2003. http://www.nice.org.uk/CG003 (accessed<br />
03 ⁄ 01 ⁄ 2011).<br />
19 Chung F, Yuan H, Yin L, Vairavanathan S, Wong DT. Elimination of<br />
preoperative testing in ambulatory surgery. Anesthesia and Analgesia 2009; 108:<br />
467–75.<br />
20 Smith I. Emergency day surgery. Journal of One-day Surgery 2009; 19: 2–3.<br />
21 Bhattacharyya M, Gerber B. Minimally-invasive surgical repair of ruptured<br />
Achilles tendon as a day case procedure with early full weight bearing. Journal of<br />
One-day Surgery 2007; 17: 70–5.<br />
22 Howells N, Tompsett E, Moore A, Hughes A, Livingstone J. Day surgery for<br />
trauma patients. Journal of One-day Surgery 2009; 19: 23–6.<br />
23 Mayell AC, Barnes SJ, Stocker ME. Introducing emergency surgery to the day<br />
case setting. Journal of One-day Surgery 2009; 19: 10–3.<br />
24 Miyagi K, Yao C, Lazenby K, Himpson R, Ingham Clark CL. Use of the day<br />
surgery unit for emergency surgical cases. Journal of One-day Surgery 2009; 19:<br />
5–8.<br />
25 Curtis MJ, Samsoon G, Parmar N. Fixation of clavicle fractures: the role of day<br />
surgery? Journal of One-day Surgery 2004; 14: 89–90.<br />
26 British Association of Day Surgery. Examples of Useful Patient Documentation.<br />
http://www.bads.co.uk/bads/joomla/index.php?option=com_content&view=<br />
article&id=60&Itemid=95 (accessed 09 ⁄ 10 ⁄ 2010).<br />
27 Royal College of Anaesthetists and Association of Anaesthetists of Great Britain<br />
and Ireland. You and Your Anaesthetic. Information to Help Patients Prepare<br />
Ó 2011 The Authors<br />
Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland 21
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
for an Anaesthetic, 3rd edn. London: RCoA ⁄ AAGBI, 2008 http://www.rcoa.<br />
ac.uk/docs/PI_yaya.pdf (accessed 03 ⁄ 01 ⁄ 2011).<br />
28 The Royal College of Anaesthetists. Anaesthesia Information for Children and<br />
Young People, 2010. http://www.rcoa.ac.uk/index.asp?PageID=1520 (accessed<br />
03 ⁄ 01 ⁄ 2011).<br />
29 British Association of Day Surgery. Skill Mix and Nursing Establishment for Day<br />
Surgery. London: BADS, 2009.<br />
30 Tickner C. Health care assistant enabled discharge. Journal of One-day Surgery<br />
2009; 17: 106–9.<br />
31 Perioperative Care Collaborative. Delegation: The Support Worker in the Scrub<br />
Role, 2007. http://www.proprius.org.uk/documents/Delegation.pdf (accessed<br />
03 ⁄ 01 ⁄ 2011).<br />
32 Perioperative Care Collaborative. Optimising the Contribution of the Perioperative<br />
Support Worker, 2007. http://www.proprius.org.uk/documents/Perioperative-<br />
Support.pdf (accessed 03 ⁄ 01 ⁄ 2011).<br />
33 Castero C, Bertinato L, Baccaglini U, Drace C, McKee M. Perioperative Care<br />
Collaborative. Copenhagen: WHO European Centre for Health, 2007.<br />
34 Association of Anaesthetists of Great Britain and Ireland. Standards of Monitoring<br />
During Anaesthesia and Recovery 4. London: AAGBI, 2007.<br />
35 Association of Anaesthetists of Great Britain and Ireland. The Anaesthesia Team 3.<br />
London: AAGBI, 2010.<br />
36 Yogendran S, Asokumar B, Cheng DCH, Chung F. A prospective<br />
randomized double-blind study of the effect of intravenous fluid therapy on<br />
adverse outcomes on outpatient surgery. Anesthesia and Analgesia 1995; 80:<br />
682–6.<br />
37 Rawal N, Axelsson K, Hylander J, et al. Postoperative patient-controlled<br />
local anesthetic administration at home. Anesthesia and Analgesia 1998; 86:<br />
86–9.<br />
38 British Association of Day Surgery. Spinal Anaesthesia for Day Surgery Patients.<br />
London: BADS, 2010.<br />
39 Pflug AE, Aasheim GM, Foster C. Sequence of return of neurological function<br />
and criteria for safe ambulation following subarachnoid block. Canadian<br />
Anaesthetists’ Society Journal 1978; 25: 133–9.<br />
40 Joint statement from the Association of Anaesthetists of Great Britain & Ireland<br />
and the Royal College of Anaesthetists. Physicians’ Assistants (Anaesthesia) –<br />
PA(A)s, 2008. http://www.rcoa.ac.uk/docs/PA(A)_JointStatement.pdf<br />
(accessed 03 ⁄ 01 ⁄ 2011).<br />
41 Association of Anaesthetists of Great Britain and Ireland. Immediate Postanaesthetic<br />
Recovery. London: AAGBI, 2002.<br />
42 Lubarsky DA. Fast track in the post-anesthesia care unit: unlimited possibilities?<br />
Journal of Clinical Anesthesia 1996; 8: 70S–2S.<br />
Ó 2011 The Authors<br />
22 Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
43 Pavlin DJ, Pavlin EG, Fitzgibbon DR, Koerschgen ME, Plitt TM. Management<br />
of bladder function after outpatient surgery. Anesthesiology 1999; 91:<br />
42–50.<br />
44 Ward B, Imarengiaye C, Peirovy J, Chung F. Cognitive function is minimally<br />
impaired after ambulatory surgery. Canadian Journal of Anesthesia 2005; 52:<br />
1017–21.<br />
45 Chung F, Kayumov L, Sinclair DR, Edward R, Moller HJ, Shapiro CM. What<br />
is the driving performance of ambulatory surgical patients after general<br />
anesthesia? Anesthesiology 2005; 103: 951–6.<br />
46 Royal College of Anaesthetists. Raising the Standard: A Compendium of Audit<br />
Recipes. London: RCoA, 2006.<br />
47 The Royal College of Anaesthetists. CCT in Anaesthetics. Annex B. Basic Level<br />
Training, 2nd edn. London: RCoA, 2010.<br />
48 The Royal College of Anaesthetists. CCT in Anaesthetics. Annex C. Intermediate<br />
Level Training, 2nd edn. London: RCoA, 2010.<br />
49 The Royal College of Anaesthetists. CCT in Anaesthetics. Annex D. Higher Level<br />
Training, 2nd edn. London: RCoA, 2010.<br />
50 The Royal College of Anaesthetists. CCT in Anaesthetics. Annex E. Advanced<br />
Level Training, 2nd edn. London: RCoA, 2010.<br />
51 Royal College of Surgeons of England. Commission on the Provision of Surgical<br />
Services. Guidelines for Day Case Surgery. London: HMSO, 1992.<br />
52 Hanousek J, Stocker ME, Montgomery JE. The effect of grade of anaesthetist on<br />
outcome after day surgery. Anaesthesia 2009; 64: 150–5.<br />
53 Weidmann C, Grundy P. Day-case awake craniotomy for tumour resection.<br />
Journal of One-day Surgery 2008; 18: 45–7.<br />
54 Hamer C, Holmes K, Stocker M. A generic process for transferring procedures<br />
to the day case setting: the Torbay hospital proposal. Journal of One-day Surgery<br />
2008; 18: 9–12.<br />
55 Wilmore DW, Kehlet H. Recent advances: management of patients in fast track<br />
surgery. British Medical Journal 2001; 322: 473–6.<br />
56 Li JT. The quality of caring. Mayo Clinic Proceedings 2006; 81: 294–6.<br />
57 Corrado M, Carluccio A. Perceptions of anaesthetists – a survey of the general<br />
public research study conducted for the Royal College of Anaesthetists for<br />
National Anaesthesia Day. Royal College of Anaesthetists Newsletter 2000; 51:<br />
319–21 http://www.rcoa.ac.uk/docs/newsletter2000-51.pdf (accessed 03 ⁄ 01 ⁄<br />
2011).<br />
58 Mitchell M. General anaesthesia and day-case patient anxiety. Journal of Advanced<br />
Nursing 2010; 66: 1059–71.<br />
59 Advice for Patients. http://www.bads.co.uk/bads/joomla/images/stories/<br />
downloads/generaladvice.pdf, 2010 (accessed 03 ⁄ 01 ⁄ 2011).<br />
Ó 2011 The Authors<br />
Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland 23
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
Further reading<br />
1 Association for Perioperative Practice. Staffing for Patients in the<br />
Perioperative setting. Harrogate: AfPP, 2008.<br />
2 Department of Health. Getting the right start. National Service Framework<br />
for Children – Standard for Hospital Services. London: DoH, 2003.<br />
3 Department of Health and Children. Children First: National Guidelines<br />
for the Protection and Welfare of Children. London: DoH, 1999.<br />
4 Health Service Executive. HSE National Service Plan 2010. Dublin:<br />
HSE, 2010.<br />
5 Jakobson J. Anaesthesia for Day Case Surgery. New York: Oxford<br />
University Press, 2009.<br />
6 Lemos P, Jarrett P, Philip B eds. Day Surgery Development and Practice.<br />
Porto: International Association for Ambulatory Surgery, 2006.<br />
7 National Association for the Welfare of Children in Hospital. Caring for<br />
children in the Health Services. Just for the Day. London: The Stationery<br />
Office, 1991.<br />
8 National Leadership and Innovation Agency for Healthcare. Day<br />
Surgery in Wales: a guide to good practice. Cardiff: The Welsh Assembly<br />
Government, 2004.<br />
9 NHS Estates. HBN 26 Facilities for Surgical Procedures. Volume 1.<br />
London: The Stationery Office, 2004.<br />
10 NHS Management Executive Value for Money Unit. Day Surgery.<br />
Making it happen. London: HMSO, 1991.<br />
11 NHS Modernisation Agency. National Good Practice Guidelines on<br />
Pre-operative Assessment for Day Surgery. The Stationery Office,<br />
2002.<br />
12 Raeder J. Clinical Ambulatory Anesthesia. New York: Cambridge<br />
University Press, 2010.<br />
13 Scottish Health Planning Note 52: Accommodation for Day Care: Part<br />
1: Day surgery unit. Glasgow: Health Facilities Scotland, 2001.<br />
14 Smith I, ed. Day Care Anaesthesia. Fundamentals of Anaesthesia & Acute<br />
Medicine Series. London: BMJ Books, 2000.<br />
15 The Office of the Comptroller and Auditor General. Accounts of<br />
Public Services 2008. Dublin, Government of Ireland, 2009. http://<br />
www.audgen.gov.ie/documents/annualreports/2008/Appropriation_<br />
Account_2008Rev1.pdf (accessed 11 ⁄ 01 ⁄ 2011).<br />
Ó 2011 The Authors<br />
24 Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
Appendix 1<br />
Sample screening questionnaire for use in day surgery. University Hospital of<br />
North Staffordshire, with permission.<br />
Ó 2011 The Authors<br />
Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland 25
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
Ó 2011 The Authors<br />
26 Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
Appendix 2<br />
Sample patient information sheet for use in day surgery. Royal Surrey County<br />
Hospital NHS Foundation Trust, with permission.<br />
Ó 2011 The Authors<br />
Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland 27
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
Appendix 3<br />
Discharge checklist for day surgery. Reproduced from: British Association<br />
of Day Surgery. Nurse Led Discharge. London: BADS, 2009, with<br />
permission.<br />
Criteria Yes No N ⁄ A Initials Details<br />
Vital signs stable<br />
Orientated to time, place & person<br />
Passed urine (if applicable)<br />
Able to dress & walk (where appropriate)<br />
Oral fluids tolerated (if applicable)<br />
Minimal pain<br />
Minimal bleeding<br />
Minimal nausea ⁄ vomiting<br />
Cannula removed<br />
Responsible escort present<br />
Has carer for 24-h post op<br />
Written & verbal post op instructions<br />
Knows who to contact in an emergency<br />
Follow up appointment<br />
Removal of sutures required?<br />
Referrals made<br />
Dressings supplied<br />
Patient copy of GP letter<br />
Carbon copy of consent<br />
Sick certificate<br />
Has take home medication<br />
Next Dose:<br />
Information leaflet for tablets<br />
Post op phone call required<br />
Discharged by: Nurse’s Signature<br />
___________________________________________________<br />
Date ⁄ Time ____________ Print Name<br />
___________________________________________________<br />
Ó 2011 The Authors<br />
28 Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
Appendix 4a<br />
Acute pain protocol for adult surgery.<br />
Pain intensity<br />
Discharge medication<br />
Doctor’s signature<br />
(sign one box only)<br />
A None None<br />
B Mild Paracetamol 1 g qds<br />
C Moderate Paracetamol 1 g qds<br />
Plus<br />
Ibuprofen 600 mg qds<br />
C* Moderate<br />
(NSAID intolerant)<br />
Paracetamol 500 mg ⁄ codeine<br />
30 mg 1–2 tabs qds<br />
D Severe Paracetamol 500 mg ⁄ codeine<br />
30 mg 1–2 tabs qds<br />
Plus<br />
Ibuprofen 600 mg qds<br />
D* Severe<br />
(NSAID intolerant)<br />
Paracetamol 1 g qds<br />
Plus<br />
Oral morphine 20 mg qds<br />
Appendix 4b<br />
Pain categories for common procedures in the day surgery unit, to be used<br />
in conjunction with the above.<br />
A B C D<br />
EUA ears<br />
Cystoscopy<br />
Restorative<br />
dentistry<br />
Cataract surgery<br />
Grommets ⁄<br />
T-tube removal ⁄<br />
insertion<br />
Prostate biopsy<br />
Sebaceous cyst surgery<br />
Sigmoidoscopy<br />
Skin lesion surgery<br />
Urethral surgery<br />
Anal surgery<br />
Apicectomy<br />
Arthroscopy<br />
Axillary clearance<br />
Breast lumps<br />
Dupuytren’s contracture<br />
Carpal tunnel<br />
decompression<br />
Cervical ⁄ vulval surgery<br />
Hysteroscopy ⁄ D&C<br />
Middle ear surgery<br />
MUA ± steroid injection<br />
Vaginal sling<br />
Varicose vein surgery<br />
Vasectomy<br />
Non-wisdom tooth<br />
extraction<br />
ACL reconstruction<br />
Circumcision<br />
Endometrial ablation<br />
Laparoscopy<br />
Haemorrhoidectomy<br />
Hernia repair<br />
Joint fusions ⁄ osteotomy<br />
Shoulder surgery<br />
Squint surgery<br />
Testicular surgery<br />
Tonsillectomy<br />
Wisdom tooth extraction<br />
Dental clearance<br />
EUA ⁄ MUA, examination ⁄ manipulation under anaesthesia; ACL, anterior cruciate ligament<br />
Ó 2011 The Authors<br />
Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland 29
Guidelines: Day case and short stay surgery<br />
.....................................................................................................................................<br />
Appendix 5<br />
Suitable topics for a training module in day case anaesthesia.<br />
1 Patient selection and preparation:<br />
• The role of patient selection in day surgery<br />
• Medical, social and surgical factors<br />
• Unit protocols for patient selection<br />
• The role of pre-operative preparation in day surgery<br />
• Instructions for ⁄ preparation of patients for day surgery<br />
• Management of patients with complex medical conditions<br />
• Recognition of patients who are unsuitable for day surgery<br />
2 Anaesthetic techniques for day surgery:<br />
• General anaesthetic techniques<br />
• Antiemetic therapy<br />
• Analgesia including the role of nerve blockade<br />
• Fluid therapy<br />
• Airway management<br />
3 Surgical techniques appropriate for day surgery:<br />
• Surgical advances enabling procedures to transfer to day surgery<br />
• Limitations of day surgery<br />
• Risks ⁄ concerns<br />
4 Recovery assessment and discharge criteria:<br />
• Adequacy of analgesia<br />
• Fitness for discharge<br />
• Role of early intervention in prevention of unplanned admissions<br />
• Instructions for patients<br />
• Discharge medication<br />
5 Postoperative follow up and audit:<br />
• Value of postoperative follow-up to patients and the unit<br />
• Use of information technology for audit of outcomes and service development<br />
6 Team working:<br />
• The day unit as a multidisciplinary team<br />
7 Children in the day surgery unit:<br />
• National Service Framework for Children’s requirements for provision of children’s services<br />
• Preparation of children for surgery<br />
8 Management of a day surgery unit:<br />
• Role of day surgery managers<br />
• Role of day surgery within the trust<br />
• Government’s agenda for day surgery<br />
• Booking processes for day surgery<br />
• Knowledge of local and national day surgery performance<br />
• Advances and controversies in day surgery<br />
Ó 2011 The Authors<br />
30 Anaesthesia Ó 2011 The Association of Anaesthetists of Great Britain and Ireland
The Association of Anaesthetists of Great Britain & Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
Website: www.<strong>aagbi</strong>.org<br />
The British Association of Day Surgery<br />
35-43 Lincoln’s Inn Fields, London, WC2A 3PE<br />
Tel: 020 7973 0308<br />
Fax: 020 7973 0314<br />
Email: bads@bads.co.uk<br />
Website: www.bads.co.uk
Peri-operative management of the<br />
surgical patient with diabetes 2015<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
Sept 2015
This guideline was originally published in Anaesthesia. If you wish to refer to this guideline, please use the following<br />
reference:<br />
Association of Anaesthetists of Great Britain and Ireland. Peri-operative management of the surgical patient with diabetes<br />
2015. Anaesthesia 2015; 70: 1427-1440.<br />
This guideline can be viewed online via the following URL:<br />
http://onlinelibrary.wiley.com/doi/10.1111/anae.13233/full
Anaesthesia 2015<br />
Guidelines<br />
doi:10.1111/anae.13233<br />
Peri-operative management of the surgical patient with diabetes<br />
2015<br />
Association of Anaesthetists of Great Britain and Ireland<br />
Membership of the Working Party: P. Barker, P. E. Creasey, K. Dhatariya, 1 N. Levy, A. Lipp, 2<br />
M. H. Nathanson (Chair), N. Penfold, 3 B. Watson and T. Woodcock<br />
1 Joint British Diabetes Societies Inpatient Care Group<br />
2 British Association of Day Surgery<br />
3 Royal College of Anaesthetists<br />
Summary<br />
Diabetes affects 10–15% of the surgical population and patients with diabetes undergoing surgery have greater complication<br />
rates, mortality rates and length of hospital stay. Modern management of the surgical patient with diabetes<br />
focuses on: thorough pre-operative assessment and optimisation of their diabetes (as defined by a HbA1c<br />
< 69 mmol.mol<br />
1 ); deciding if the patient can be managed by simple manipulation of pre-existing treatment during<br />
a short starvation period (maximum of one missed meal) rather than use of a variable-rate intravenous insulin infusion;<br />
and safe use of the latter when it is the only option, for example in emergency patients, patients expected not<br />
to return to a normal diet immediately postoperatively, and patients with poorly controlled diabetes. In addition, it<br />
is imperative that communication amongst healthcare professionals and between them and the patient is accurate<br />
and well informed at all times. Most patients with diabetes have many years of experience of managing their own<br />
care. The purpose of this guideline is to provide detailed guidance on the peri-operative management of the surgical<br />
patient with diabetes that is specific to anaesthetists and to ensure that all current national guidance is concordant.<br />
.................................................................................................................................................................<br />
This is a consensus document produced by members of a Working Party established by the Association of Anaesthetists of<br />
Great Britain and Ireland (AAGBI). It has been seen and approved by the AAGBI Board of Directors. Date of review: 2020.<br />
Accepted: 12 August 2015<br />
• What other guideline statements are available on this<br />
topic?<br />
The NHS Diabetes Guideline for the Peri-operative<br />
Management of the Adult Patient with Diabetes [1] was<br />
published in 2011 by NHS Diabetes (now part of NHS<br />
Improving Quality), and is due to be updated in 2015.<br />
• Why was this guideline developed?<br />
This guideline was developed to improve both the<br />
safety and the outcome of patients with diabetes<br />
undergoing surgical procedures.<br />
.................................................................................................................................................................<br />
This is an open access article under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs<br />
License, which permits use and distribution in any medium, provided the original work is properly cited, the use is<br />
non-commercial and no modifications or adaptations are made.<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland 1
Anaesthesia 2015<br />
Barker et al. | Guidelines on peri-operative management of diabetes<br />
• How and why does this statement differ from existing<br />
guidelines?<br />
The 2011 guideline [1] deals with the whole patient<br />
pathway, from referral for surgery from primary<br />
care to discharge and follow-up. It is too broad in<br />
scope to be a working document for anaesthetists.<br />
This guideline summarises the existing guideline<br />
and focuses specifically on peri-operative care.<br />
Introduction<br />
The demographics describing the dramatic increase in<br />
the number of patients with diabetes are well known.<br />
Patients with diabetes require surgical procedures more<br />
frequently and have longer hospital stays than those<br />
without the condition [2]. The presence of diabetes or<br />
hyperglycaemia in surgical patients has been shown to<br />
lead to increased morbidity and mortality, with perioperative<br />
mortality rates up to 50% greater than the<br />
non-diabetic population [2]. The reasons for these<br />
adverse outcomes are multifactorial, but include: failure<br />
to identify patients with diabetes or hyperglycaemia [3,<br />
4]; multiple co-morbidities including microvascular and<br />
macrovascular complications [5]; complex polypharmacy<br />
and insulin prescribing errors [6]; increased peri-operative<br />
and postoperative infections [2, 7, 8]; associated<br />
hypoglycaemia and hyperglycaemia [2]; a lack of, or<br />
inadequate, institutional guidelines for management of<br />
inpatient diabetes or hyperglycaemia [2, 9]; and inadequate<br />
knowledge of diabetes and hyperglycaemia management<br />
amongst staff delivering care [10].<br />
Anaesthetists and other peri-operative care providers<br />
should be knowledgeable and skilled in the care<br />
of patients with diabetes. Management of diabetes is a<br />
vital element in the management of surgical patients<br />
with diabetes. It is not good enough for the diabetic<br />
care to be a secondary, or sometimes forgotten, element<br />
of the peri-operative care package.<br />
Previous guidelines<br />
In April 2011 NHS Diabetes (now part of NHS<br />
Improving Quality) published a document: NHS Diabetes<br />
Guideline for the Peri-operative Management of<br />
the Adult Patient with Diabetes, in association with the<br />
Joint British Diabetes Societies (JBDS) [1] (an almost<br />
identical version, Management of Adults with Diabetes<br />
Undergoing Surgery and Elective Procedures: Improving<br />
Standards, is available at www.diabetologists-abcd.org.uk/JBDS/JBDS.htm).<br />
This comprehensive guideline<br />
provided both background information and advice to<br />
clinicians caring for patients with diabetes. Some of<br />
the recommendations in that document were due for<br />
review in the light of new evidence and, in addition, it<br />
was felt that anaesthetists and other practitioners caring<br />
for patients with diabetes in the peri-operative period<br />
needed shorter, practical advice. The Association<br />
of Anaesthetists of Great Britain and Ireland (AAGBI)<br />
offered to co-author this shortened guideline, in collaboration<br />
with colleagues involved with the 2011 document.<br />
The previous 2011 NHS Diabetes guidelines<br />
will also be updated in 2015.<br />
The risks of poor diabetic control<br />
Studies have shown that high pre-operative and perioperative<br />
glucose and glycated haemoglobin (HbA1c)<br />
levels are associated with poor surgical outcomes.<br />
These findings have been seen in both elective and<br />
emergency surgery including spinal [11], vascular [12],<br />
colorectal [13], cardiac [14, 15], trauma [16], breast<br />
[17], orthopaedic [18], neurosurgical, and hepatobiliary<br />
surgery [19, 20]. One study showed that the adverse<br />
outcomes include a greater than 50% increase in mortality,<br />
a 2.4-fold increase in the incidence of postoperative<br />
respiratory infections, a doubling of surgical site<br />
infections, a threefold increase in postoperative urinary<br />
tract infections, a doubling in the incidence of myocardial<br />
infarction, and an almost twofold increase in acute<br />
kidney injury [2]. Paradoxically, there are some data to<br />
show that the outcomes of patients with diabetes may<br />
not be different from, or may indeed be better than,<br />
those without diabetes if the diagnosis is known before<br />
surgery [21]. The reasons for this are unknown, but<br />
may be due to increased vigilance surrounding glucose<br />
control for those with a diagnosis of diabetes.<br />
Referral from primary care and<br />
planning surgery<br />
The aim is to ensure that diabetes is as well controlled as<br />
possible before elective surgery and to avoid delays to<br />
surgery due to poor control. The Working Party supports<br />
the consensus advice published in the 2011 NHS<br />
Diabetes guideline that the HbA1c should be<br />
< 69 mmol.mol<br />
1 (8.5%) for elective cases [1], and<br />
2 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland
Barker et al. | Guidelines on peri-operative management of diabetes Anaesthesia 2015<br />
that elective surgery should be delayed if it is<br />
≥ 69 mmol.mol<br />
1 , while control is improved. Changes<br />
to diabetes management can be made concurrently with<br />
referral to ensure the patient’s diabetes is as well controlled<br />
as possible at the time of surgery. Elective surgery<br />
in patients with diabetes should be planned with the aim<br />
of minimising disruption to their self-management.<br />
•<br />
Recommendation: Glycaemic control should be<br />
checked at the time of referral for surgery. Information<br />
about duration, type of diabetes, current<br />
treatment and complications should be made available<br />
to the secondary care team.<br />
Surgical outpatient clinic<br />
The adequacy of diabetes control should be assessed<br />
again at the time of listing for surgery, ideally with a<br />
recorded HbA1c < 69 mmol.mol<br />
1 in the previous three<br />
months. If it is ≥ 69 mmol.mol<br />
1 , elective surgery should<br />
be delayed while control is improved. In a small number<br />
of cases it may not be possible to improve diabetic control<br />
pre-operatively, particularly if the reason for surgery,<br />
such as chronic infection, is contributing to poor control,<br />
or if surgery is semi-urgent. In these circumstances, it<br />
may be acceptable to proceed with surgery after explanation<br />
to the patient of the increased risks. Patients should<br />
be managed as a day case if the procedure is suitable<br />
and the patient fulfils the criteria for day-case surgery<br />
management. Well-controlled diabetes should not be a<br />
contra-indication to day-case surgery.<br />
Patients with poorly controlled diabetes at the time<br />
of surgery will need close monitoring and may need to<br />
start a variable-rate intravenous insulin infusion (VRIII).<br />
• Recommendation: Patients with diabetes should be<br />
identified early in the pre-operative pathway.<br />
Pre-operative assessment<br />
Appropriate and early pre-operative assessment should<br />
be arranged. A pre-operative assessment nurse may<br />
undertake the assessment with support from either an<br />
anaesthetist or a diabetes specialist nurse. It should<br />
occur sufficiently in advance of the planned surgery to<br />
ensure optimisation of glycaemic control before the<br />
date of proposed surgery. The aim is to ensure that all<br />
relevant investigations are available and checked in<br />
advance of the planned surgery, that the patient understands<br />
how to manage his/her diabetes in the peri-operative<br />
period, and that the period of pre-operative<br />
fasting is minimised.<br />
• Recommendation: Tests should be ordered to assess<br />
co-morbidities in line with National Institute for<br />
Health and Care Excellence (NICE) guidance on<br />
pre-operative testing [22]. This should include urea<br />
and electrolytes and ECG for all patients with diabetes;<br />
however, a random blood glucose measurement<br />
is not indicated.<br />
Planning admission (including day surgery)<br />
The aim is to minimise the fasting period, ensure<br />
normoglycaemia (capillary blood glucose (CBG) 6–<br />
10 mmol.l<br />
1 ) and minimise as far as possible disruption<br />
to the patient’s usual routine. Ideally, the patient<br />
should be booked first on the operating list to minimise<br />
the period of fasting. If the fasting period is<br />
expected to be limited to one missed meal, the patient<br />
can be managed by modification of his/her usual diabetes<br />
medication (see below). Patients should be provided<br />
with written instructions from the pre-operative<br />
assessment team about management of their diabetes<br />
medication on the day of surgery, the management of<br />
hypo- or hyperglycaemia in the peri-operative period,<br />
and the likely effects of surgery on their diabetes control.<br />
Patients should be advised to carry a form of glucose<br />
that they can take in case of symptoms of<br />
hypoglycaemia that will not cause surgery to be cancelled,<br />
for example a clear, sugar-containing drink<br />
(glucose tablets may be used instead, but some anaesthetists<br />
may feel they should not be taken within 6 h<br />
of the start of anaesthesia). Patients should be warned<br />
that their blood glucose control may be erratic for a<br />
few days after the procedure.<br />
• Recommendation: When possible, admission should<br />
be planned for the day of surgery, with both the<br />
patient and the ward staff aware of the planned<br />
peri-operative diabetes care, including a plan to<br />
manage hypo- and hyperglycaemia. Surgery should<br />
be scheduled at the start of the theatre list to<br />
minimise disruption to the patient’s glycaemic<br />
control.<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland 3
Anaesthesia 2015<br />
Barker et al. | Guidelines on peri-operative management of diabetes<br />
Management of existing therapy<br />
With appropriate guidance, patients with diabetes<br />
should be allowed to retain control and possession of,<br />
and continue to self-administer, their medication.<br />
Many patients will have several years’ experience and<br />
be expert in self-medication.<br />
The aim is to avoid hypo- or hyperglycaemia<br />
during the period of fasting and the time during and<br />
after the procedure, until the patient is eating and<br />
drinking normally. In people who are likely to miss<br />
one meal only, this can often be achieved by manipulating<br />
the patient’s normal medication using the guidance<br />
provided in Tables 1 and 2.<br />
Glycaemic control in patients with diabetes is a<br />
balance between their carbohydrate intake and utilisation<br />
(for example, exercise). It also depends on what<br />
medication they take and how those medications<br />
work. Some agents (e.g. sulphonylureas, meglitinides,<br />
Table 1 Guideline for peri-operative adjustment of insulin (short starvation period – no more than one missed<br />
meal).<br />
Day of surgery<br />
Insulin<br />
Day before<br />
admission Surgery in the morning<br />
Once daily (e.g. Lantus â , Levemir â , Tresiba â , Insulatard â , Humulin I â , Insuman â )<br />
Evening<br />
Reduce dose Check blood glucose on<br />
by 20% admission<br />
Morning<br />
Reduce dose Reduce dose by 20%; check<br />
by 20% blood glucose on admission<br />
Surgery in the afternoon<br />
Check blood glucose on<br />
admission<br />
Reduce dose by 20%;<br />
check blood glucose on<br />
admission<br />
Whilst a VRIII is<br />
being used*<br />
Continue at 80%<br />
of usual dose<br />
Continue at 80%<br />
of usual dose<br />
Twice daily<br />
Biphasic or ultra-long<br />
acting (e.g. Novomix<br />
30 â , Humulin M3 â ,<br />
Humalog Mix 25 â ,<br />
Humalog Mix 50 â ,<br />
Insuman â Comb 25,<br />
Insuman â Comb 50,<br />
Levemir â , Lantus â )by<br />
single injection, given<br />
twice daily<br />
Short-acting (e.g.<br />
animal neutral,<br />
Novorapid â , Humulin<br />
S â , Apidra â ) and<br />
intermediate-acting<br />
(e.g. animal isophane,<br />
Insulatard â , Humulin I â ,<br />
Insuman â ) by separate<br />
injections, both given<br />
twice daily<br />
No dose<br />
change<br />
No dose<br />
change<br />
Halve the usual morning dose;<br />
check blood glucose on<br />
admission; leave evening meal<br />
dose unchanged<br />
Calculate total dose of morning<br />
insulin(s); give half as<br />
intermediate-acting only in<br />
the morning; check blood<br />
glucose on admission; leave<br />
evening meal dose unchanged<br />
Halve the usual morning<br />
dose; check blood<br />
glucose on admission;<br />
leave the evening meal<br />
dose unchanged<br />
Calculate total dose of<br />
morning insulin(s); give<br />
half as intermediateacting<br />
only in the<br />
morning; check blood<br />
glucose on admission;<br />
leave evening meal<br />
dose unchanged<br />
Stop until eating<br />
and drinking<br />
normally<br />
Stop until eating<br />
and drinking<br />
normally<br />
Three to five injections daily<br />
No dose<br />
change<br />
Basal bolus regimens:<br />
Omit morning and lunchtime<br />
short-acting insulins; keep<br />
basal unchanged*<br />
Premixed morning insulin:<br />
Halve morning dose and omit<br />
lunchtime dose; check blood<br />
glucose on admission<br />
Give usual morning<br />
insulin dose(s); omit<br />
lunchtime dose; check<br />
blood glucose on<br />
admission<br />
Stop until eating<br />
and drinking<br />
normally<br />
* If the patient requires a VRIII then the long-acting background insulin should be continued but at 80% of the dose the patient<br />
usually takes when he/she is well.<br />
VRIII, variable-rate intravenous insulin infusion.<br />
4 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland
Barker et al. | Guidelines on peri-operative management of diabetes Anaesthesia 2015<br />
Table 2 Guideline for peri-operative adjustment of oral hypoglycaemic agents (short starvation period – no more<br />
than one missed meal).<br />
Day of surgery<br />
Surgery in the<br />
Agent<br />
Day before admission morning<br />
Drugs that require omission when fasting owing to risk of hypoglycaemia<br />
Meglitinides<br />
Take as normal Omit morning dose if<br />
(e.g. repaglinide,<br />
nil by mouth<br />
nateglinide)<br />
Sulphonylurea<br />
(e.g. glibenclamide,<br />
gliclazide, glipizide)<br />
Take as normal<br />
Omit morning dose<br />
(whether taking<br />
once or twice daily)<br />
Drugs that require omission when fasting owing to risk of ketoacidosis<br />
SGLT-2 inhibitors*<br />
(e.g. dapagliflozin,<br />
canagliflozin)<br />
No dose change Halve the usual<br />
morning dose; check<br />
blood glucose on<br />
admission; leave<br />
evening meal dose<br />
unchanged<br />
Surgery in the<br />
afternoon<br />
Give morning dose if<br />
eating<br />
Omit (whether taking<br />
once or twice daily)<br />
Halve the usual<br />
morning dose; check<br />
blood glucose on<br />
admission; leave the<br />
evening meal dose<br />
unchanged<br />
Whilst a VRIII is<br />
being used<br />
Stop until eating and<br />
drinking normally<br />
Stop until eating and<br />
drinking normally<br />
Stop until eating and<br />
drinking normally<br />
Drugs that may be continued when fasting<br />
Acarbose Take as normal Omit morning dose if<br />
nil by mouth<br />
DPP-IV inhibitors<br />
(e.g. sitagliptin,<br />
vildagliptin, saxagliptin,<br />
alogliptin, linagliptin)<br />
GLP-1 analogues<br />
(e.g. exenatide,<br />
liraglutide, lixisenatide)<br />
Metformin (procedure<br />
not requiring use of<br />
contrast media†)<br />
Give morning dose if<br />
eating<br />
Stop until eating and<br />
drinking normally<br />
Take as normal Take as normal Take as normal Stop until eating and<br />
drinking normally<br />
Take as normal Take as normal Take as normal Take as normal<br />
Take as normal Take as normal Take as normal Stop until eating and<br />
drinking normally<br />
Pioglitazone Take as normal Take as normal Take as normal Stop until eating and<br />
drinking normally<br />
* Also omit the day after surgery.<br />
† If contrast medium is to be used or the estimated glomerular filtration rate is under 60 ml.min 1 .1.73 m 2 , metformin should be<br />
omitted on the day of the procedure and for the following 48 h.<br />
VRIII, variable-rate intravenous insulin infusion; SGLT-2, sodium-glucose co-transporter-2; DPP-IV, dipeptidyl peptidase-IV;<br />
GLP-1, glucagon-like peptide-1.<br />
insulin and to some extent, thiazolidinediones) act by<br />
lowering glucose concentrations, and doses need to<br />
be modified or the agents stopped during periods of<br />
starvation. Others work by preventing glucose levels<br />
from rising (e.g. metformin, glucagon-like peptide-1<br />
analogues, dipeptidyl peptidase-4 inhibitors); these<br />
drugs may be continued without the risk of hypoglycaemia.<br />
The time of day and the expected duration<br />
of the operation need to be considered, as will<br />
whether a VRIII will be needed. Patients with continuous<br />
subcutaneous insulin infusions only missing one<br />
meal should be advised to maintain their CBG at<br />
6–10 mmol.l<br />
1 . If longer periods of starvation are<br />
predicted, a VRIII should be used and specialist<br />
advice sought.<br />
Tables 1 and 2 have been designed to take all of<br />
these factors into consideration. They are a pragmatic<br />
approach to the pre-operative management of all the<br />
available classes of agent used to manage diabetes.<br />
Use of a variable-rate intravenous insulin<br />
infusion<br />
Variable-rate intravenous insulin infusions are preferred<br />
in: patients who will miss more than one meal;<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland 5
Anaesthesia 2015<br />
Barker et al. | Guidelines on peri-operative management of diabetes<br />
those with type-1 diabetes undergoing surgery who<br />
have not received background insulin; those with<br />
poorly controlled diabetes (defined as a HbA1c<br />
> 69 mmol.mol<br />
1 ); and most patients with diabetes<br />
requiring emergency surgery. Variable-rate intravenous<br />
insulin infusions should be administered and monitored<br />
by appropriately experienced and qualified staff.<br />
An example of a VRIII regimen is provided in<br />
Appendix 1.<br />
Intra-operative care and monitoring<br />
The aim of intra-operative care is to maintain good<br />
glycaemic control and normal electrolyte concentrations,<br />
while optimising cardiovascular function and<br />
renal perfusion. If possible, multimodal analgesia<br />
should be used along with appropriate anti-emetic prophylaxis,<br />
to enable an early return to a normal diet<br />
and the patient’s usual diabetes regimen.<br />
• Recommendation: An intra-operative CBG range of<br />
6–10 mmol.l<br />
1 should be aimed for (an upper limit<br />
of 12 mmol.l<br />
1 may be tolerated at times, e.g. if<br />
the patient has poorly controlled diabetes and is<br />
being managed by a modification of his/her normal<br />
medication without a VRIII). It should be understood<br />
by all staff that a CBG within the range of<br />
6–10 mmol.l<br />
1 is acceptable and that there is no<br />
requirment for a CBG of 6 mmol.l<br />
1 to be the target.<br />
The CBG should be checked before induction<br />
of anaesthesia and monitored regularly during the<br />
procedure (at least hourly, or more frequently if<br />
the results are outside the target range). The CBG,<br />
insulin infusion rate and substrate infusion should<br />
be recorded on the anaesthetic record. Some charts<br />
use colour-coded areas to highlight abnormal<br />
results requiring further intervention or a change<br />
of treatment (see Appendix 2).<br />
Management of intra-operative hyperglycaemia<br />
and hypoglycaemia<br />
If the CBG exceeds 12 mmol.l<br />
1 and insulin has been<br />
omitted, capillary blood ketone levels should be measured<br />
if possible (point-of-care devices are available). If<br />
the capillary blood ketones are > 3 mmol.l<br />
1 or there<br />
is significant ketonuria (> 2+ on urine sticks) the<br />
patient should be treated as having diabetic ketoacidosis<br />
(DKA). Diabetic ketoacidosis is a triad of ketonaemia<br />
> 3.0 mmol.l<br />
1 , blood glucose > 11.0 mmol.l<br />
1 ,<br />
and bicarbonate < 15.0 mmol.l<br />
1 or venous pH < 7.3.<br />
Diabetic ketoacidosis is a medical emergency and specialist<br />
help should be obtained from the diabetes team.<br />
If DKA is not present, the high blood glucose<br />
should be corrected using subcutaneous insulin (see<br />
below) or by altering the rate of the VRIII (if in use).<br />
If two subcutaneous insulin doses do not work, a<br />
VRIII should be started.<br />
Treatment of hyperglycaemia in a patient with type-1<br />
diabetes<br />
Subcutaneous rapid-acting insulin (such as Novorapid<br />
â , Humalog â or Apidra â ) should be given (up to<br />
a maximum of 6 IU), using a specific insulin syringe,<br />
assuming that 1 IU will drop the CBG by 3 mmol.l<br />
1 .<br />
Death or severe harm as a result of maladministration<br />
of insulin, including failure to use the specific insulin<br />
syringe, is a ‘Never Event’. If the patient is awake, it is<br />
important to ensure that the patient is content with<br />
proposed dose (patients may react differently to subcutaneous<br />
rapid-acting insulin). The CBG should be<br />
checked hourly and a second dose considered only<br />
after 2 h.<br />
Treatment of hyperglycaemia in a patient with type-2<br />
diabetes<br />
Subcutaneous rapid-acting insulin 0.1 IU.kg 1 should<br />
be given (up to a maximum of 6 IU), using a specific<br />
insulin syringe. The CBG should be checked hourly<br />
and a second dose considered only after 2 h. A VRIII<br />
should be considered if the patient remains hyperglycaemic.<br />
Treatment of intra-operative hypoglycaemia<br />
For a CBG 4.0–6.0 mmol.l<br />
1 , 50 ml glucose 20%<br />
(10 g) should be given intravenously; for hypoglycaemia<br />
< 4.0 mmol.l<br />
1 a dose of 100 ml (20 g) should<br />
be given.<br />
Fluid management<br />
There is a limited evidence base for the recommendation<br />
of optimal fluid management of the adult diabetic<br />
patient undergoing surgery. It is now recognised that<br />
Hartmann’s solution is safe to administer to patients<br />
6 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland
Barker et al. | Guidelines on peri-operative management of diabetes Anaesthesia 2015<br />
with diabetes and does not contribute to clinically significant<br />
hyperglycaemia [23].<br />
Fluid management for patients requiring a VRIII<br />
The aim is to provide glucose as a substrate to prevent<br />
proteolysis, lipolysis and ketogenesis, as well as<br />
to optimise intravascular volume status and maintain<br />
plasma electrolytes within the normal range. It is<br />
important to avoid iatrogenic hyponatraemia from<br />
the administration of hypotonic solutions. Glucose<br />
5% solution should be avoided. Use of glucose 4%<br />
in 0.18% saline can be associated with hyponatraemia.<br />
The substrate solution to be used should be based<br />
on the patient’s current electrolyte concentrations.<br />
While there is no clear evidence that one type of<br />
balanced crystalloid fluid is better than another, halfstrength<br />
‘normal’ saline combined with glucose is, theoretically,<br />
a reasonable compromise to achieve these<br />
aims. Thus, the initial fluid should be glucose 5% in<br />
saline 0.45% pre-mixed with either potassium chloride<br />
0.15% (20 mmol.l<br />
1 ) or potassium chloride 0.3%<br />
(40 mmol.l<br />
1 ), depending on the presence of hypokalaemia<br />
(< 3.5 mmol.l<br />
1 ).<br />
The Working Party recognises that these fluids<br />
may not be available in all institutions. It is our view<br />
that they should be made available in all areas where<br />
patients with diabetes will be managed. (Hospitals caring<br />
for children will usually have these solutions<br />
already available for general paediatric use).<br />
Fluid should be administered at the rate that is<br />
appropriate for the patient’s usual maintenance<br />
requirements – usually 25–50 ml.kg 1 .day 1 (approximately<br />
83 ml.h 1 for a 70-kg patient) [24].<br />
Very occasionally, the patient may develop hyponatraemia<br />
without signs of fluid overload. In these circumstances,<br />
it is acceptable to prescribe one of the following<br />
solutions as the substrate solution: glucose 5% in saline<br />
0.9% with pre-mixed potassium chloride 0.15%<br />
(20 mmol.l<br />
1 ); or glucose 5% in saline 0.9% with premixed<br />
potassium chloride 0.3% (40 mmol.l<br />
1 ). (Again,<br />
hospitals caring for children will usually have these solutions<br />
available).<br />
Additional Hartmann’s solution or another balanced<br />
isotonic crystalloid solution should be used to<br />
optimise intravascular volume status.<br />
Fluid management for patients not requiring a<br />
VRIII<br />
The aim is to avoid glucose-containing solutions unless<br />
the blood glucose is low. It is important to avoid<br />
hyperchloraemic metabolic acidosis; Hartmann’s solution<br />
should be administered to optimise the intravascular<br />
volume status. If the patient requires prolonged<br />
postoperative fluids (> 24 h), a VRIII should be considered<br />
and glucose 5% in saline 0.45% with pre-mixed<br />
potassium chloride given as above.<br />
Returning to ‘normal’ (pre-operative)<br />
medication and diet<br />
The postoperative blood glucose management plan,<br />
and any alterations to existing medications, should be<br />
clearly communicated to ward staff. Patients with diabetes<br />
should be involved in planning their postoperative<br />
care. If subcutaneous insulin is required in<br />
insulin-na€ıve patients, or the type of insulin or the<br />
time it is to be given is to change, the specialist diabetes<br />
team should be contacted for advice.<br />
Transferring from a VRIII back to oral<br />
treatment or subcutaneous insulin<br />
If the patient has type-1 diabetes and a VRIII has been<br />
used, it must be continued for 30–60 min after the<br />
patient has had their subcutaneous insulin (see below).<br />
Premature discontinuation is associated with iatrogenic<br />
DKA.<br />
Restarting oral hypoglycaemic medication<br />
Oral hypoglycaemic agents should be recommenced at<br />
pre-operative doses once the patient is ready to eat and<br />
drink; withholding or reduction in sulphonylureas may<br />
be required if the food intake is likely to be reduced. Metformin<br />
should only be restarted if the estimated glomerular<br />
filtration rate exceeds 50 ml.min 1 .1.73 m 2 [25].<br />
Restarting subcutaneous insulin for patients already<br />
established on insulin<br />
Conversion to subcutaneous insulin should commence<br />
once the patient is able to eat and drink without nausea<br />
or vomiting. The pre-surgical regimen should be<br />
restarted, but may require adjustment because the insulin<br />
requirement may change as a result of postoperative<br />
stress, infection or altered food intake. The diabetes spe-<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland 7
Anaesthesia 2015<br />
Barker et al. | Guidelines on peri-operative management of diabetes<br />
cialist team should be consulted if the blood glucose<br />
levels are outside the acceptable range (6–12 mmol.l<br />
1 )<br />
or if a change in diabetes management is required.<br />
The transition from intravenous to subcutaneous<br />
insulin should take place when the next meal-related<br />
subcutaneous insulin dose is due, for example with<br />
breakfast or lunch.<br />
For the patient on basal and bolus insulin<br />
There should be an overlap between the end of the<br />
VRIII and the first injection of subcutaneous insulin,<br />
which should be given with a meal and the intravenous<br />
insulin and fluids discontinued 30-60 min later.<br />
If the patient was previously on a long-acting insulin<br />
analogue such as Lantus â , Levemir â or Tresbia â ,<br />
this should have been continued and thus the only<br />
action should be to restart his/her usual rapid-acting<br />
insulin at the next meal as outlined above. If the basal<br />
insulin was stopped, the insulin infusion should be<br />
continued until a background insulin has been given.<br />
For the patient on a twice-daily, fixed-mix regimen<br />
The insulin should be re-introduced before breakfast<br />
or before the evening meal, and not at any other time.<br />
The VRIII should be maintained for 30-60 min after<br />
the subcutaneous insulin has been given.<br />
For the patient on a continuous subcutaneous insulin<br />
infusion<br />
The subcutaneous insulin infusion should be recommenced<br />
at the patient’s normal basal rate; the VRIII<br />
should be continued until the next meal bolus has<br />
been given. The subcutaneous insulin infusions should<br />
not be re-started at bedtime.<br />
Resumption of normal diet<br />
The key to successful management of the surgical<br />
patient with diabetes is resumption of his/her usual<br />
diet. This allows resumption of normal diabetes medication.<br />
Hospital discharge is only feasible once the<br />
patient has resumed eating and drinking.<br />
Other anaesthetic considerations<br />
Use of dexamethasone<br />
Dexamethasone can lead to hyperglycaemia and should<br />
be used with caution in patients with diabetes [26]. If<br />
it is decided that the possible benefits of earlier<br />
resumption of normal diet outweigh the disadvantages<br />
of hyperglycaemia, it should be ensured that the CBG<br />
is measured hourly for at least 4 h after administration.<br />
Use of regional anaesthesia<br />
Local anaesthetic techniques, when used as the sole<br />
anaesthetic, reduce the risk of postoperative nausea<br />
and vomiting. Furthermore, when used as part of the<br />
multimodal technique in general anaesthesia, they have<br />
opioid-sparing actions, with resultant reduction of opioid-related<br />
side-effects. However, evidence suggests<br />
that patients with diabetes are more prone to epidural<br />
abscesses and haemodynamic instability after central<br />
neuraxial blockade (in patients with an autonomic<br />
neuropathy), and, possibly, increased risk of neuropathy<br />
after peripheral nerve blocks [27–29].<br />
Enhanced recovery after surgery<br />
Enhanced recovery of patients undergoing surgery utilises<br />
several strategies to promote earlier resumption of<br />
normal diet, earlier mobilisation, and reduced length<br />
of stay [30]. This has particular relevance for patients<br />
with diabetes as it promotes eating and drinking<br />
(reducing the risk of iatrogenic harm from a VRIII),<br />
and by promoting earlier discharge.<br />
Use of oral carbohydrate loading drinks<br />
Carbohydrate loading may compromise blood glucose<br />
control and should not be used in patients with insulin-treated<br />
diabetes who are likely to have a short period<br />
of fasting. There is some evidence that oral<br />
carbohydrate loading may be safe in patients with<br />
type-2 diabetes [31], and if a VRIII is to be used in<br />
any case there is no reason to withhold oral carbohydrate<br />
loading drinks in any patient with diabetes.<br />
Patients with diabetes requiring<br />
emergency surgery<br />
There are three ways of managing diabetes in the<br />
patient requiring emergency surgery:<br />
1 Modification of normal medication. This is only<br />
possible if the patient is physiologically well and is<br />
being operated on a scheduled list, for example a<br />
8 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland
Barker et al. | Guidelines on peri-operative management of diabetes Anaesthesia 2015<br />
regular trauma list for minor hand surgery, or<br />
evacuation of retained products of conception on<br />
a regular gynaecology list.<br />
2 Use of a VRIII. This should be the default<br />
technique to manage a patient undergoing emergency<br />
surgery because of the unpredictability of<br />
the starvation period caused by the erratic nature<br />
of emergency lists.<br />
3 Use of a fixed-rate intravenous insulin infusion<br />
(see below). This should only be used if the<br />
patient requires immediate surgery and has concurrent<br />
DKA.<br />
The aim is for the patient to be taken to the<br />
1<br />
operating theatre with a CBG of 6–10 mmol.l<br />
1<br />
(6–12 mmol.l may be acceptable), without overt<br />
DKA, and having been adequately resuscitated.<br />
•<br />
Recommendation: In patients undergoing emergency<br />
surgery, the CBG should be checked regularly<br />
(hourly as a minimum whilst acutely unwell),<br />
and a VRIII established using dextrose 5% in saline<br />
0.45% with pre-mixed potassium chloride as the<br />
substrate.<br />
The patient should be checked for ketonaemia<br />
(> 3.0 mmol.l<br />
1 ) or significant ketonuria (> 2+ on<br />
urine sticks) if the CBG exceeds 12 mmol.l<br />
1 . If the<br />
patient has DKA and requires emergency surgery, the<br />
involvement of senior multidisciplinary input from<br />
intensivists, anaesthetists, surgeons and diabetologists<br />
should be considered to agree optimal peri-operative<br />
management. Operating on a patient with DKA carries<br />
significant mortality and should be avoided if at all possible.<br />
The discussion should include: the requirement<br />
for surgery, because DKA can be associated with<br />
abdominal pain (negative laparotomies have been<br />
reported); the area in which the patient should be resuscitated<br />
before theatre; whether saline 0.9% with premixed<br />
potassium chloride or Hartmann’s solution<br />
should be the main resuscitation fluid; whether a VRIII<br />
or a fixed-rate infusion should be used to treat DKA in<br />
theatre; and the area in which the patient will be recovered<br />
after surgery. Recent guidelines and evidence suggest<br />
that a fixed-rate intravenous insulin infusion is<br />
superior to a VRIII in treating DKA in a ward environment<br />
[32]. However, use of a fixed-rate infusion is associated<br />
with hypoglycaemia and requires administration<br />
of glucose 20% if the CBG is under 14 mmol.l<br />
1 .<br />
Early involvement of the diabetes inpatient specialist<br />
team should be sought.<br />
If possible, long-acting insulins (Levemir, Lantus,<br />
Tresiba) should be continued in all patients at 80% of<br />
the usual dose. This is to avoid rebound hyperglycaemia<br />
when intravenous insulin is stopped.<br />
Safety<br />
Errors in insulin prescribing are common and insulin<br />
has been identified as one of the top five high-risk<br />
medications in the inpatient environment [33]. The<br />
wide range of preparations and devices available for<br />
insulin administration (currently > 60) increases the<br />
potential for error. One third of all inpatient medical<br />
errors leading to death within 48 h of the error involve<br />
insulin administration. Common errors include mistakes<br />
when abbreviating the word ‘units’, failure to use<br />
a specific insulin syringe, and errors when preparing<br />
insulin infusions. Use of pre-filled syringes of insulin<br />
for infusion may reduce the risk and should be considered<br />
by Trusts.<br />
Safe use of VRIIIs<br />
Variable-rate intravenous insulin infusions are overused<br />
in the peri-operative setting. Their use is<br />
associated with hypoglycaemia, hyperglycaemia and<br />
ketosis on cessation, and hyponatraemia. There<br />
seems to be a significant risk of hypoglycaemia in<br />
1<br />
patients with a CBG of 4–6 mmol.l and on a<br />
VRIII. Patients often return to surgical wards from<br />
theatre with an intravenous insulin infusion in place<br />
but no directions for its withdrawal. Hospitals<br />
should have written guidelines for both the safe use<br />
of the VRIII and conversion from the VRIII to the<br />
usual diabetes treatment.<br />
To ensure a steady supply of substrate it is recommended<br />
that glucose 5% in saline 0.45% with potassium<br />
chloride 0.15% or 0.3% should be administered<br />
concurrently with the VRIII, at a rate to meet the<br />
patient’s maintenance fluid requirements. It is imperative<br />
that there is hourly monitoring of the CBG (to<br />
keep the CBG at 6–10 mmol.l<br />
1 ), and that in patients<br />
with type-1 diabetes, the VRIII is not discontinued<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland 9
Anaesthesia 2015<br />
Barker et al. | Guidelines on peri-operative management of diabetes<br />
until alternative subcutaneous insulin has been administered.<br />
Metformin<br />
A number of guidelines available for the use of<br />
metformin recommend withdrawing treatment peri-operatively.<br />
However, evidence for this approach is lacking<br />
and there is some evidence that peri-operative continuation<br />
of metformin is safe. Metformin is renally excreted<br />
and renal failure may lead to high plasma levels which<br />
are associated with an increased risk of lactic acidosis<br />
[34]. Metformin should be withheld if there is pre-existing<br />
renal impairment or significant risk of the patient<br />
developing acute kidney injury. Anaesthetists should be<br />
vigilant about the dangers of the use of nephrotoxic<br />
agents, including contract media [35].<br />
Non-steroidal anti-inflammatory drugs (NSAIDs)<br />
There are several additional considerations to the use<br />
of NSAIDs in patients with diabetes, including the<br />
redistribution of renal blood flow in the presence of<br />
hypovolaemia and the risk of oedema, especially if<br />
given concurrently with metformin and glitazones.<br />
Quality control and audit<br />
A number of bodies have published quality standards<br />
pertinent to the peri-operative care of patients with diabetes.<br />
These include NICE, the Royal College of Anaesthetists<br />
(RCoA) and NHS Diabetes (the latter no longer<br />
exists and the Joint British Diabetes Societies Inpatient<br />
Care Group has taken over some of its roles).<br />
National Institute for Health and Care<br />
Excellence<br />
Quality Standard 6, Diabetes in Adults, includes an<br />
auditable standard relating to inpatient care: “People<br />
with diabetes admitted to hospital are cared for by<br />
appropriately trained staff, provided with access to a<br />
specialist diabetes team, and given the choice of selfmonitoring<br />
and managing their own insulin” [36].<br />
Royal College of Anaesthetists<br />
The RCoA’s Guidelines for the Provision of Anaesthetic<br />
Services [37] contains much advice relating to the perioperative<br />
care of patients, including those with diabetes.<br />
In addition, the RCoA publication Raising the<br />
Standard – a Compendium of Audit Recipes contains<br />
details on audit and quality improvement topics pertinent<br />
to patients with diabetes [38]. These focus on<br />
peri-operative care and are suitable for use by anaesthetists<br />
wishing to assess the quality of local provision.<br />
For example, topics include availability of guidelines<br />
for, and management of, chronic medication during<br />
the peri-operative period, and peri-operative fasting.<br />
NHS Diabetes<br />
The NHS Diabetes guideline contains a number of<br />
suggested audit standards covering medication, safety,<br />
training and institutional issues [1].<br />
National Diabetes Inpatient Audit<br />
Whilst the audit standards suggested above may be<br />
used within an organisation, national audit projects<br />
provide a broader picture and allow benchmarking.<br />
The National Diabetes Inpatient Audit (NaDIA) is an<br />
annual snapshot audit of surgical and medical inpatients<br />
with diabetes. The majority of Trusts in<br />
England and Wales are now taking part. The audit is<br />
commissioned by the Healthcare Quality Improvement<br />
Partnership as part of the National Clinical Audit and<br />
Patient Outcomes Programme. The results are available<br />
online in the spring of each year and enable<br />
organisations to assess their performance in caring for<br />
inpatients with diabetes [39].<br />
Included in the audit are questions relating to<br />
whether diabetes management minimises the risk of<br />
avoidable complications, harm resulting from the<br />
inpatient stay, patient experience and the change in<br />
patient feedback on the quality of care since<br />
NaDIA began. Of particular relevance to anaesthetists,<br />
NaDIA includes comparative data on the prevalence of<br />
medication errors, intravenous insulin infusions, glycaemic<br />
control and patient harm. In addition, there<br />
are considerable data from patients’ feedback questionnaires<br />
concerning their experience and involvement in<br />
their own care.<br />
• Recommendation: Anaesthetists interested in perioperative<br />
diabetes management should access the<br />
National Diabetes Inpatient Audit and look up the<br />
results for their own organisation.<br />
10 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland
Barker et al. | Guidelines on peri-operative management of diabetes Anaesthesia 2015<br />
Acknowledgements<br />
This guideline and the text are based in large part on<br />
the guidelines available from the JBDS [1]. The Working<br />
Party and AAGBI are grateful to the JBDS Inpatient<br />
Care Group for permission to use its document<br />
as the basis for this guideline.<br />
Competing interests<br />
No external funding and no competing interests<br />
declared.<br />
References<br />
1. Dhatariya K, Levy N, Kilvert A, et al. NHS Diabetes guideline<br />
for the perioperative management of the adult patient with<br />
diabetes. Diabetic Medicine 2012; 29: 420–33.<br />
2. Frisch A, Chandra P, Smiley D, et al. Prevalence and clinical<br />
outcome of hyperglycemia in the perioperative period in noncardiac<br />
surgery. Diabetes Care 2010; 33: 1783–8.<br />
3. Rayman G. Inpatient audit. Diabetes Update. https://www.diabetes.org.uk/upload/Professionals/publications/Comment_Inpatient%20audit_new.pdf<br />
(accessed 11/08/2015).<br />
4. Hamblin PS, Topliss DJ, Chosich N, Lording DW, Stockigt JR.<br />
Deaths associated with diabetic ketoacidosis and hyperosmolar<br />
coma, 1973-1988. Medical Journal of Australia 1989; 151:<br />
441–2.<br />
5. Stamler J, Vaccaro O, Neaton JD, Wentworth D. Diabetes, other<br />
risk factors, and 12-yr cardiovascular mortality for men<br />
screened in the Multiple Risk Factor Intervention Trial. Diabetes<br />
Care 1993; 16: 434–44.<br />
6. National Patient Safety Agency. Insulin safety. Reducing harm<br />
associated with the unsafe use of insulin products. http://<br />
www.nrls.npsa.nhs.uk/resources/collections/10-for-2010/insulin/?entryid45=74287<br />
(accessed 11/08/2015).<br />
7. Jhanji S, Thomas B, Ely A, Watson D, Hinds CJ, Pearce RM. Mortality<br />
and utilisation of critical care resources amongst highrisk<br />
surgical patients in a large NHS trust. Anaesthesia 2008;<br />
63: 695–700.<br />
8. Pearce RM, Harrison DA, James P, et al. Identification and<br />
characterisation of the high-risk surgical population in the United<br />
Kingdom. Critical Care 2006; 10: R10.<br />
9. Sampson MJ, Brennan C, Dhatariya K, Jones C, Walden E. A<br />
national survey of in-patient diabetes services in the United<br />
Kingdom. Diabetic Medicine 2007; 24: 643–9.<br />
10. George JT, Warriner D, McGrane DJ, et al. Lack of confidence<br />
among trainee doctors in the management of diabetes: the<br />
Trainees Own Perception of Delivery of Care (TOPDOC) Diabetes<br />
Study. Quarterly Journal of Medicine 2011; 104: 761–6.<br />
11. Walid MS, Newman BF, Yelverton JC, et al. Prevalence of previously<br />
unknown elevation of glycosylated hemoglobin in<br />
spine surgery patients and impact on length of stay and total<br />
cost. Journal of Hospital Medicine 2010; 5: E10–4.<br />
12. O’Sullivan CJ, Hynes N, Mahendran B, et al. Haemoglobin A1c<br />
(HbA1C) in non-diabetic and diabetic vascular patients. Is<br />
HbA1C an independent risk factor and predictor of adverse<br />
outcome? European Journal of Vascular and Endovascular Surgery<br />
2006; 32: 188–97.<br />
13. Gustafsson UO, Thorell A, Soop M, Ljungqvist O, Nygren J.<br />
Haemoglobin A1c as a predictor of postoperative hyperglycaemia<br />
and complications after major colorectal surgery. British<br />
Journal of Surgery 2009; 96: 1358–64.<br />
14. Halkos ME, Lattouf OM, Puskas JD, et al. Elevated preoperative<br />
hemoglobin A1c level is associated with reduced long-term<br />
survival after coronary artery bypass surgery. Annals of Thoracic<br />
Surgery 2008; 86: 1431–7.<br />
15. Alserius T, Anderson RE, Hammar N, Nordqvist T, Ivert T. Elevated<br />
glycosylated haemoglobin (HbA1c) is a risk marker in<br />
coronary artery bypass surgery. Scandinavian Cardiovascular<br />
Journal 2008; 42: 392–8.<br />
16. Kreutziger J, Schlaepfer J, Wenzel V, Constantinescu MA. The<br />
role of admission blood glucose in outcome prediction of surviving<br />
patients with multiple injuries. Journal of Trauma –<br />
Injury, Infection and Critical Care 2009; 67: 704–8.<br />
17. Vilar-Compte D, Alvarez de Iturbe I, Martin-Onraet A, et al.<br />
Hyperglycemia as a risk factor for surgical site infections in<br />
patients undergoing mastectomy. American Journal of Infection<br />
Control 2008; 36: 192–8.<br />
18. Shibuya N, Humphers JM, Fluhman BL, Jupiter DC. Factors<br />
associated with nonunion, delayed union, and malunion in<br />
foot and ankle surgery in diabetic patients. Journal of Foot<br />
and Ankle Surgery 2013; 52: 207–11.<br />
19. Chuang SC, Lee KT, Chang WT, et al. Risk factors for wound<br />
infection after cholecystectomy. Journal of the Formosan Medical<br />
Association 2004; 103: 607–12.<br />
20. Ambiru S, Kato A, Kimura F, et al. Poor postoperative blood<br />
glucose control increases surgical site infections after surgery<br />
for hepato-biliary-pancreatic cancer: a prospective study in a<br />
high-volume institute in Japan. Journal of Hospital Infection<br />
2008; 68: 230–3.<br />
21. Kwon S, Thompson R, Dellinger P, Yanez D, Farrohki E, Flum D.<br />
Importance of perioperative glycemic control in general surgery:<br />
a report from the surgical care and outcomes assessment<br />
program. Annals of Surgery 2013; 257: 8–14.<br />
22. National Institute for Health and Care Excellence. Preoperative<br />
Tests: the Use of Routine Preoperative Tests for Elective Surgery.<br />
NICE Guideline CG3, June 2003 www.nice.org.uk/guidance/cg3<br />
(accessed 11/08/2015).<br />
23. Simpson AK, Levy N, Hall GM. Peri-operative i.v. fluids in diabetic<br />
patients – don’t forget the salt. Anaesthesia 2008; 63:<br />
1043–5.<br />
24. National Institute for Health and Care Excellence. Intravenous<br />
fluid therapy in adults in hospital. NICE guideline CG174,<br />
December 2013. www.nice.org.uk/guidance/cg174/evidence<br />
(accessed 11/08/2015).<br />
25. Lipska KJ, Bailey CJ, Inzucchi SE. Use of metformin in the setting<br />
of mild-to-moderate renal insufficiency. Diabetes Care<br />
2011; 34: 1431–7.<br />
26. Geer EB, Islam J, Buettner C. Mechanisms of glucocorticoid-induced<br />
insulin resistance. Endocrinology and Metabolism Clinics<br />
of North America 2014; 43: 75–102.<br />
27. Royal College of Anaesthetists. Major complications of central<br />
neuraxial block in the UK. Third National Audit of The Royal<br />
College of Anaesthetists, January 2009. www.rcoa.ac.uk/nap3<br />
(accessed 11/08/2015).<br />
28. Hebl JR, Kopp SL, Schroeder DR, Horlocker TT. Neurologic complications<br />
after neuraxial anesthesia or analgesia in patients<br />
with pre-existing peripheral sensorimotor neuropathy or diabetic<br />
polyneuropathy. Anesthesia and Analgesia 2006; 103:<br />
1294–9.<br />
29. Reihsaus E, Waldbaur H, Seeling W. Spinal epidural abscess: a<br />
meta-analysis of 915 patients. Neurosurgical Review 2000;<br />
23: 175–204.<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland 11
Anaesthesia 2015<br />
Barker et al. | Guidelines on peri-operative management of diabetes<br />
30. Varadhan KK, Neal KR, Dejong CH, et al. The enhanced recovery<br />
after surgery (ERAS) pathway for patients undergoing<br />
major elective open colorectal surgery: a meta-analysis of<br />
randomized controlled trials. Clinical Nutrition 2010; 29:<br />
434–40.<br />
31. Gustafsson UO, Nygren J, Thorell A, et al. Pre-operative carbohydrate<br />
loading may be used in type 2 diabetes patients.<br />
Acta Anaesthesiologica Scandinavica 2008; 52: 946–51.<br />
32. Joint British Diabetes Societies Inpatient Care Group. The management<br />
of diabetic ketoacidosis in adults, September 2013.<br />
http://www.diabetologists-abcd.org.uk/JBDS/JBDS_IP_DKA_Adu<br />
lts_Revised.pdf) (accessed 11/08/2015).<br />
33. National Patient Safety Agency. The fourth report of the Patient<br />
Safety Observatory. Safety in doses: medication safety incidents<br />
in the NHS, January 2007. www.nrls.npsa.nhs.uk/resources/patient-safety-topics/medication-safety/?entryid45=59822&q=0%<br />
c2%acsafety+in+doses%c2%ac (accessed 11/08/2015).<br />
34. Duncan AI, Koch CG, Xu M, et al. Recent metformin ingestion<br />
does not increase in-hospital morbidity or mortality<br />
after cardiac surgery. Anesthesia and Analgesia 2007; 104:<br />
42–50.<br />
35. Royal College of Radiologists. Standards for Intravascular Contrast<br />
Agent Administration to Adult Patients, 2nd edn. London:<br />
RCR, 2010.<br />
36. National Institute for Health and Care Excellence. Diabetes in<br />
Adults. Quality Standard 6, March 2011. www.nice.org.uk/<br />
guidance/qs6 (accessed 11/08/2015).<br />
37. Royal College of Anaesthetists. Guidelines for the Provision of<br />
Anaesthetic Services 2015. www.rcoa.ac.uk/GPAS2015 (accessed<br />
11/08/2015).<br />
38. Royal College of Anaesthetists. Raising the Standard: A Compendium<br />
of Audit Recipes for Continuous Quality Improvement<br />
in Anaesthesia, 3rd edn, 2012. www.rcoa.ac.uk/<br />
system/files/CSQ-ARB-2012_1.pdf (accessed 11/08/2015).<br />
39. Health and Social Care Information Centre. National Diabetes<br />
Inpatient Audit. www.hscic.gov.uk/diabetesinpatientaudit (accessed<br />
11/08/2015).<br />
12 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland
Barker et al. | Guidelines on peri-operative management of diabetes Anaesthesia 2015<br />
Appendix 1<br />
Example of a variable-rate intravenous insulin infusion prescription. Glucose concentration is usually measured in capillary blood.<br />
Glucose<br />
concentration;<br />
1<br />
mmol.l<br />
Standard rate (use unless otherwise indicated)<br />
No basal insulin<br />
< 4 0.5 IU.h 1 + give<br />
100 ml glucose 20%<br />
intravenously<br />
4.1–6.0 0.5 IU.h 1 + consider<br />
50 ml glucose 20%<br />
intravenously<br />
Basal insulin<br />
continued No basal insulin<br />
STOP + give 100 ml<br />
glucose 20%<br />
intravenously<br />
STOP + consider<br />
50 ml glucose 20%<br />
intravenously<br />
Reduced rate (e.g. insulin-sensitive patients<br />
(i.e. < 24 IU.day 1 ))<br />
0.2 IU.h 1 + give<br />
100 ml glucose 20%<br />
intravenously<br />
0.2 IU.h 1 + give<br />
50 ml glucose 20%<br />
intravenously<br />
Basal insulin<br />
continued No basal insulin<br />
STOP + give 100 ml<br />
glucose 20%<br />
intravenously<br />
STOP + consider<br />
50 ml glucose 20%<br />
intravenously<br />
Increased rate (e.g. insulin-resistant patients<br />
(i.e. > 100 IU.day 1 ))<br />
0.5 IU.h 1 + give<br />
100 ml glucose 20%<br />
intravenously<br />
0.5 IU.h 1 + give<br />
50 ml glucose 20%<br />
intravenously<br />
Basal insulin<br />
continued<br />
STOP + give 100 ml<br />
glucose 20%<br />
intravenously<br />
STOP + consider<br />
6.1–8.0 1 IU.h 1 1 IU.h 1 0.5 IU.h 1 0.5 IU.h 1 2 IU.h 1 2 IU.h 1<br />
8.1–12.0 2 IU.h 1 2 IU.h 1 1 IU.h 1 1 IU.h 1 4 IU.h 1 4 IU.h 1<br />
12.1–16.0 4 IU.h 1 4 IU.h 1 2 IU.h 1 2 IU.h 1 6 IU.h 1 6 IU.h 1<br />
16.1–20.0 5 IU.h 1 5 IU.h 1 3 IU.h 1 3 IU.h 1 7 IU.h 1 7 IU.h 1<br />
20.1–24.0 6 IU.h 1 6 IU.h 1 4 IU.h 1 4 IU.h 1 8 IU.h 1 8 IU.h 1<br />
> 24.1 8 IU.h 1 8 IU.h 1 6 IU.h 1 6 IU.h 1 10 IU.h 1 10 IU.h 1<br />
> 24.1 Ensure insulin is running and that the measured blood glucose concentration is not artefactual<br />
50 ml glucose 20%<br />
intravenously<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland 13
Anaesthesia 2015<br />
Barker et al. | Guidelines on peri-operative management of diabetes<br />
Appendix 2<br />
Example of a variable-rate intravenous insulin infusion regimen observation chart. Reproduced by kind<br />
permission of the Norfolk and Norwich University Hospitals NHS Foundation Trust.<br />
BLOOD GLUCOSE MONITORING CHART (adults, not pregnant)<br />
B<br />
Paent Name:<br />
Hospital Number:<br />
Date of birth:<br />
Consultant:<br />
Date<br />
(dd/mm/yyyy):<br />
Time:<br />
Blood glucose<br />
reading (mmol/L)<br />
OR PATIENT LABEL<br />
A SINGLE reading in a RED area requires acon<br />
TWO consecuve readings in the AMBER areas<br />
require acon<br />
This is the ACCEPTABLE glucose range<br />
This is the IDEAL glucose target range<br />
Ward:<br />
Blood glucose readings (mmol/L)<br />
Ketone levels<br />
Diabetes Inpatient Specialist Nurse bleep - 0407 - available Monday to Friday 9am to 5pm<br />
Urine<br />
Blood<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
++++<br />
+++<br />
++<br />
+<br />
Nil<br />
ALL ACTION TAKEN MUST BE DOCUMENTED IN THE HOSPITAL NOTES<br />
Inials<br />
14 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
Do Not Attempt Resuscitation (DNAR) Decisions<br />
in the Perioperative Period<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org May 2009
Membership of the working party<br />
Dr L Gemmell<br />
Dr M E McBrien<br />
Dr G Heyburn<br />
Ms M Hassell<br />
Dr V Bythell<br />
Mrs K Rivett<br />
Prof J Bion<br />
Dr S Williams<br />
Dr C Stack<br />
Prof A Cunningham<br />
Chairman and AAGBI Honorary<br />
Secretary<br />
Consultant Anaesthetist<br />
Associate Specialist in<br />
Orthogeriatrics<br />
HM Coroner, Cardiff & Vale of<br />
Glamorgan<br />
AAGBI Council Member<br />
Lay Representative, Patient Liaison<br />
Group, RCoA<br />
RCoA<br />
GAT representative<br />
Consultant Anaesthetist<br />
College of Anaesthetists, Ireland<br />
Ex Officio<br />
Dr R J S Birks<br />
Dr D K Whitaker<br />
Dr I H Wilson<br />
Dr I G Johnston<br />
Dr A W Harrop-Griffiths<br />
Dr E O’Sullivan<br />
Dr D G Bogod<br />
President<br />
Immediate Past President<br />
Honorary Treasurer<br />
Honorary Treasurer Elect<br />
Immediate Past Honorary Secretary<br />
Honorary Membership Secretary<br />
Editor-in-Chief, Anaesthesia
Contents<br />
Section 1 Recommendations 2<br />
Section 2 Introduction 4<br />
Section 3 Definitions 6<br />
Section 4 Ethical framework 8<br />
Section 5 Legal framework 9<br />
Section 6<br />
Why is it necessary to review a DNAR<br />
decision before surgery and anaesthesia? 14<br />
Section 7 How to review a DNAR decision 16<br />
Section 8 Conflict resolution 20<br />
Section 9<br />
Duration of the DNAR management<br />
option 22<br />
Section 10<br />
Summary for patients, proxy decision<br />
makers and relatives 23<br />
Section 11 References 25<br />
Appendix 1 28<br />
© Copyright of the Association of Anaesthetists of Great Britain and Ireland.<br />
No part of this book may be reproduced without the written permission of the<br />
AAGBI.<br />
1
1. Recommendations<br />
1. Management of patients with DNAR decisions in the<br />
perioperative period should focus on what resuscitative<br />
measures will be embarked on rather than on what<br />
will not be done.<br />
2. It is essential that patients who may require surgical<br />
procedures with DNAR decisions in place are referred as<br />
early as possible to the anaesthetic and surgical teams.<br />
3. A review of the DNAR decision by the anaesthetist and<br />
surgeon with the patient, proxy decision maker, other doctor<br />
in charge of the patient’s care, and relatives or carers, if<br />
indicated, is essential before proceeding with surgery and<br />
anaesthesia.<br />
4. There are three options for managing the DNAR decision:<br />
Option one: the DNAR decision is to be discontinued.<br />
Surgery and anaesthesia are to proceed with<br />
cardiopulmonary resuscitation (CPR) to be used if<br />
cardiopulmonary arrest occurs.<br />
Option two: the DNAR decision is to be modified to<br />
permit the use of drugs and techniques commensurate with<br />
the provision of anaesthesia.<br />
Option three: no changes are to be made to the DNAR<br />
decision. Under most circumstances this option is not<br />
compatible with the provision of general anaesthesia for any<br />
type of surgical intervention.<br />
5. The agreed DNAR management option should be<br />
documented in the patient’s notes.<br />
6. The DNAR management option should be communicated<br />
to all the healthcare staff managing the patient in the<br />
operating theatre and recovery areas.<br />
2
7. The law provides a clear hierarchy in terms of legal standing<br />
to make DNAR decisions:<br />
a. The competent patient’s direct instructions.<br />
b. The patient’s advance decision or proxy decision maker<br />
if competence is lacking.<br />
c. The senior clinician in charge of the patient’s care, acting<br />
in the patient’s best interests, if there is not a legally valid<br />
advance decision or proxy decision maker for a patient<br />
lacking competence.<br />
8. If, after discussion, there is no agreement on which DNAR<br />
decision option should be adopted, the decision of the<br />
person with the legal right or responsibility for making the<br />
decision should be accepted.<br />
9. If an anaesthetist or other health care provider cannot agree<br />
with the outcome of the review of the DNAR decision, they<br />
must ensure that arrangements are made for another<br />
suitably qualified colleague to take over the role in<br />
accordance with GMC guidelines.<br />
10. If it is unclear who has the right or responsibility to make<br />
the decision, or if there is doubt over the legal validity of an<br />
advance decision or proxy decision maker, or doubt as to<br />
what is in the best interests of the patient, then seek legal<br />
advice immediately.<br />
11. In an emergency, the doctor must make decisions that they<br />
view to be in the best interests of the patient using whatever<br />
information is available.<br />
12. The DNAR management option should, under most<br />
circumstances, apply for the period when the patient is in<br />
the operating theatre and recovery areas. The DNAR<br />
decision should be reinstated when the patient returns to<br />
the ward, unless in exceptional circumstances.<br />
3
2. Introduction<br />
In the past, decisions about treatment and resuscitation status<br />
were often made by doctors with little discussion with the<br />
patient. This paternalistic approach is being replaced with<br />
one based on the concept of autonomy, in which the rights of<br />
an individual to have control over their own body and to be<br />
allowed to make decisions about their medical treatment are<br />
paramount. In this approach, decisions result from a partnership<br />
between the patient and the clinical team and may now involve<br />
proxy decision makers.<br />
DNAR decisions pose a conundrum where patients are<br />
scheduled to undergo anaesthesia because techniques routinely<br />
undertaken in the course of anaesthesia would ordinarily be<br />
classified as resuscitation. Yet it is increasingly common for<br />
patients to be scheduled for anaesthesia and surgery with a preexisting<br />
DNAR decision in place. While this often applies to<br />
older patients, it may also apply to younger patients or children.<br />
These guidelines apply only to adult patients.<br />
Medical conditions that may require anaesthesia for operative<br />
interventions in a patient with a DNAR decision include:<br />
• provision of a support device (e.g. a feeding tube),<br />
• urgent surgery for a condition unrelated to the underlying<br />
chronic problem (e.g. acute appendicitis),<br />
• urgent surgery for a condition related to the underlying<br />
chronic problem but not believed to be a terminal event<br />
(e.g. bowel obstruction),<br />
• procedure to decrease pains (e.g. repair of fractured neck of<br />
femur),<br />
• procedure to provide vascular access.<br />
Guidelines from the American Society of Anesthesiologists (ASA)<br />
have existed to assist in the management of this ethical and<br />
clinical dilemma since 1993 [1] and Canada since 2002 [2], but<br />
4
none have been published in the UK to date.<br />
Revised guidelines providing a framework to support decisions<br />
relating to CPR were published in a joint statement from the<br />
British Medical Association, the Resuscitation Council (UK) and<br />
the Royal College of Nursing in 2007 [3]. This document is<br />
hereafter referred to as the Joint Statement. The Joint Statement<br />
recommends that a DNAR decision is reviewed before surgery<br />
and anaesthesia, but detailed guidance on how the decision<br />
should be managed is not provided.<br />
McBrien and Heyburn have outlined the dilemmas posed by<br />
the need for anaesthesia and surgery in patients with an existing<br />
DNAR decision in place [4]. Although it has been a common<br />
presumption that DNAR decisions should be fully withdrawn<br />
during the perioperative period, this may not be in the<br />
patient’s best interests. A review of the basic legal and ethical<br />
principles involved is needed in order to decide how individual<br />
anaesthetists and anaesthetic departments should manage this<br />
situation.<br />
The AAGBI Council has therefore decided to provide these<br />
guidelines on the management of DNAR decisions in the<br />
perioperative period. This guidance is intended for all clinicians<br />
and healthcare workers involved with adult patients during the<br />
perioperative period, and should be used in conjunction with<br />
the Joint Statement [3].<br />
Decisions regarding DNAR decisions in the perioperative<br />
period form part of the consent process for anaesthesia and<br />
should be viewed as such. The principles outlined in the<br />
AAGBI document ‘Consent for Anaesthesia’ [5], and the GMC<br />
document ‘Consent: patients and doctors making decisions<br />
together’ [6] and Section E ‘Confidentiality and Consent’ in the<br />
Irish Medical Council’s Guide to Ethical Conduct and Behaviour<br />
[7] should also be used in conjunction with these guidelines.<br />
5
3. Definitions<br />
Do not attempt resuscitation (DNAR) decision<br />
DNAR decisions are implemented on the assumption that<br />
cardiopulmonary arrest will be a spontaneous event that is the<br />
culmination of the dying process in a patient who has a terminal<br />
illness or a poor quality of life. These decisions arose out of<br />
the realisation that resuscitation, including cardiopulmonary<br />
resuscitation, is inappropriate in such cases, as it has a poor<br />
outcome and is against the wishes of patients and families.<br />
The Joint Statement provides a framework for the decision<br />
making process in the formation, consequences and<br />
implications of a DNAR decision [3].<br />
In the implementation of a DNAR decision the patient, proxy<br />
decision maker or senior clinician in charge of the patient are<br />
indicating that it is in the patient’s best interests to die naturally<br />
without resuscitative interventions that would be considered<br />
unnecessary and undignified.<br />
Following implementation of the DNAR decision, the patient is<br />
not to be resuscitated with chest compressions, defibrillation of<br />
the heart, artificial respiration or large doses of vasoactive drugs.<br />
However, the highest standards of medical and nursing<br />
care are still to be provided at all times.<br />
Location sensitive DNAR decisions<br />
This is a DNAR decision that is intended to apply in a specific<br />
named location only.<br />
Cardiopulmonary resuscitation (CPR)<br />
CPR is undertaken in an attempt to restore breathing and<br />
spontaneous circulation in a patient in cardiac and/or<br />
respiratory arrest. CPR usually includes chest compressions,<br />
attempted defibrillation, large doses of vasoactive drugs and<br />
ventilation of the lungs.<br />
6
Proxy decision makers<br />
Within these guidelines, this term refers to those who an adult<br />
with capacity has appointed to make decisions about medical<br />
treatment for them once that capacity has been lost. In England<br />
and Wales the legal requirements surrounding the appointment<br />
of a proxy decision maker, known as a Lasting Power of<br />
Attorney (LPA), are covered in the Mental Capacity Act 2005<br />
[8]. In Scotland the proxy decision maker, known as the welfare<br />
attorney, is legislated for in the Adults with Incapacity Act 2000<br />
[9]. In both Northern Ireland and the Republic of Ireland there<br />
are currently no statutory provisions for proxy decision makers<br />
in relation to healthcare decisions.<br />
Competent/incompetent adults<br />
Adults are considered legally unable to make decisions for<br />
themselves if they are unable to:<br />
1. understand the information relevant to the decisions,<br />
2. retain that information,<br />
3. use or weigh that information as part of the process of<br />
making the decisions,<br />
4. communicate the decisions (by talking, sign language, visual<br />
aids or by other means).<br />
Independent Mental Capacity Advocate (IMCA)<br />
The Mental Capacity Act 2005 [8] in England and Wales<br />
includes the provision of a statutory right to advocacy for<br />
people who lack the capacity to make their own decisions<br />
about serious medical treatment or significant changes in their<br />
care arrangements and have no family or friends to support<br />
them. This advocate is called the Independent Mental Capacity<br />
Advocate and is appointed by the local authority or health<br />
board. The role of the IMCA is to indicate to decision makers<br />
the patient’s wishes, feelings, beliefs and values.<br />
7
4. Ethical framework<br />
Advance decisions, such as DNAR decisions, have arisen from<br />
the need for greater respect for patients’ autonomy. Autonomy<br />
forms one of the four principles of biomedical ethics proposed<br />
by Beauchamp and Childress [10], and refers to respect for<br />
the decision making capacities of individuals enabling them<br />
to make informed choices about their healthcare. The other<br />
three principles are beneficence (overall benefit to the patient),<br />
non-maleficence (avoiding the causation of harm) and justice<br />
(fair distribution of benefits to all patients). Unfortunately,<br />
when applied to an ethical dilemma, the four principles often<br />
conflict with each other and so they only provide a framework<br />
for discussion. The paternalistic primary ethical principle of the<br />
past, namely the doctor’s view of the immediate benefit to the<br />
patient, is now in competition with other conflicting principles.<br />
The GMC provides guidance on withholding and withdrawing<br />
life-prolonging treatments [11]. The guiding principle is that<br />
doctors should have respect for human life and make their<br />
patients’ best interests their first concern.<br />
8
5. Legal framework<br />
United Kingdom<br />
The process of devolution within the UK has resulted in<br />
differences in the legal framework between the devolved<br />
nations. However, policies relating to DNAR decisions must<br />
comply with the Human Rights Act 1998 [10] in every legal<br />
setting as this Act applies throughout the UK. A review of the<br />
legal issues surrounding DNAR decisions has been necessary as<br />
a result of changes in society’s expectations which are reflected<br />
in current legislation. The Joint Statement highlights the articles<br />
in the Human Rights Act 1998 that are of particular importance<br />
when considering DNAR decisions [3]. The spirit of the Act,<br />
which aims to promote human dignity and transparent decision<br />
making, is reflected in the recommendations found in the Joint<br />
Statement. A wider review of the implications of the Human<br />
Rights Act in anaesthesia and intensive care was published by<br />
White and Baldwin in 2002 [13], but this did not address the<br />
issue of DNAR decisions in the perioperative period.<br />
The Mental Capacity Act 2005 [8] provides a protective<br />
statutory framework for decision making on behalf of adults who<br />
lack competency in England and Wales. White and Baldwin<br />
have also reviewed the implications of the Mental Capacity<br />
Act in the practice of anaesthesia and intensive care [14]. The<br />
Adults with Incapacity (Scotland) Act 2000 [9] provides a similar<br />
statutory framework for residents in that country. Northern<br />
Ireland currently has no formal legislation covering adults who<br />
lack competency and relies on the common law position that<br />
has developed in this area.<br />
Republic of Ireland<br />
There is currently no specific legislation in relation to advance<br />
decisions in the Republic of Ireland. The Irish Council for<br />
Bioethics has taken the opportunity to examine the ethical and<br />
legal issues surrounding advance directives in the Republic of<br />
Ireland and has published their findings [15].<br />
9
As in the UK, this publication highlights the fact that treatment<br />
carried out without the consent of a competent patient in the<br />
Republic of Ireland is considered both trespass and battery. In<br />
addition, the publication explains that there is currently no<br />
provision for an individual in the Republic of Ireland to make<br />
a legally binding advance decision, or for the appointment<br />
of proxy decision makers to make decisions on matters of<br />
healthcare if and when a patient lacks competence. The Law<br />
Reform Commission in the Republic of Ireland has suggested<br />
that it should be possible for advance decisions to be made<br />
legally binding. They are also considering an amendment to<br />
the existing Powers of Attorney Act 1996 to enable appointed<br />
attorneys to make decisions on minor and routine medical<br />
treatment, in addition to managing the property and affairs<br />
of the person who appointed them, as is the case at present.<br />
Until this becomes law, there is no provision for proxy decision<br />
making for incompetent individuals and the final authority to<br />
make decisions on medical treatment for them rests with the<br />
High Court in Ireland.<br />
Not surprisingly, the lack of clarity in the legal status of advance<br />
decisions such as DNAR decisions in the Republic of Ireland has<br />
led some to express their dissatisfaction with the process there<br />
[16]. The authors of this paper have requested that national<br />
guidance on DNAR decisions is provided in the Republic of<br />
Ireland.<br />
10
Who can implement a DNAR decision?<br />
A DNAR decision may arise:<br />
1. Following the direct instructions of a competent patient.<br />
2. Following a properly executed advance decision by a<br />
patient who now lacks capacity. England and Wales have<br />
different legislation to the rest of the UK concerning advance<br />
decisions:<br />
England and Wales<br />
Advance decisions are covered by the Mental Capacity Act<br />
2005 [8]. To be effective they must:<br />
• Be applicable in the circumstances that have arisen<br />
and include recognition that the patient gives these<br />
instructions ‘even if life is at risk’.<br />
• Be in writing, signed and witnessed.<br />
If an advance decision does not meet these criteria but<br />
appears to set out a clear indication of the patient’s wishes,<br />
it will not be legally binding but should be taken into<br />
consideration in determining the patient’s best interests.<br />
Scotland and Northern Ireland<br />
Advance decisions are not covered by statute but it is likely<br />
that they are binding under common law.<br />
An advance refusal of CPR is likely to be legally binding in<br />
Scotland and Northern Ireland if:<br />
• The patient was an adult at the time the decision was<br />
made (16 years old in Scotland and 18 in Northern<br />
Ireland).<br />
• The circumstances that have arisen are those that were<br />
envisaged by the patient.<br />
11
If an advance decision does not meet these criteria but<br />
appears to set out a clear indication of the patient’s wishes,<br />
it will not be legally binding but should be taken into<br />
consideration in determining the patient’s best interests.<br />
Republic of Ireland<br />
There is no specific legislation in relation to advance<br />
decisions.<br />
3. If a patient lacks capacity and no advance decision exists.<br />
Different legislation regarding proxy decision makers<br />
applies between England and Wales, Scotland, Northern<br />
Ireland and the Republic of Ireland:<br />
England and Wales<br />
If the patient lacks capacity, a decision to implement a<br />
DNAR decision may be made by the person appointed by<br />
the patient’s Lasting Power of Attorney (LPA) as appointed<br />
under the Mental Capacity Act 2005 [8]. Written permission<br />
must have been given to the LPA by the patient, when<br />
competent, to make decisions relating to life-prolonging<br />
treatment.<br />
Under the Mental Capacity Act 2005 [8], a proxy decision<br />
maker must have been instructed in relation to life<br />
sustaining treatment if DNAR is under discussion.<br />
Scotland<br />
If the patient lacks capacity, a decision to implement a<br />
DNAR decision may be made by the patient’s welfare<br />
guardian as appointed under the Adults with Incapacity<br />
(Scotland) Act 2000 [9].<br />
Northern Ireland and the Republic of Ireland<br />
There is no provision for anybody close to the patient,<br />
whether relatives or close friends, to make decisions for the<br />
12
patient if they lack capacity. However, relatives and close<br />
friends should be consulted to determine what the wishes<br />
of the patient would be if they were able to competently<br />
express them.<br />
4. If the patient lacks capacity and there is no advance<br />
decision and no legally empowered proxy decision maker, a<br />
DNAR decision may be implemented by the senior<br />
clinician in charge of the patient’s care. Consultation<br />
with relatives or carers may clearly assist in discovering<br />
any wishes formerly expressed by the patient. In England<br />
and Wales, the Mental Capacity Act 2005 requires an<br />
Independent Mental Capacity Advocate (IMCA) to be<br />
consulted if the patient lacks capacity and has no one<br />
(family, friends or carers) to represent their wishes regarding<br />
‘serious medical treatment’ [8]. The Joint Statement says<br />
that ‘where there is genuine doubt about whether or not<br />
CPR would have a realistic chance of success, or if a DNAR<br />
decision is being considered on the balance of benefits<br />
and burdens, in order to comply with the law an IMCA must<br />
be involved in every case’ [3]. Local guidance should<br />
clearly identify how an IMCA can be contacted. The<br />
role of the IMCA, as with relatives or carers, is to reflect<br />
what the patient’s wishes would have been if they were able<br />
to express them. A relative, carer or IMCA (unless they have<br />
been appointed proxy decision maker) cannot make a<br />
decision about CPR; the decision is that of the treating<br />
clinician.<br />
It must be remembered that patients, relatives, carers and<br />
proxy decision makers cannot demand treatment which<br />
is judged in medical opinion to be against the patient’s<br />
interests.<br />
13
6. Why is it necessary to review a<br />
DNAR decision before surgery and<br />
anaesthesia?<br />
Surgery and anaesthesia constitute a change in the medical<br />
status of a patient with a pre-existing DNAR decision because<br />
of changes in physiology which can add additional risks to<br />
the patient. However, survival rates following cardiac arrest<br />
in the operating theatre are significantly greater than in the<br />
general ward or residential setting where the DNAR decision<br />
was originally intended to apply. Survival rates following<br />
anaesthetic related cardiopulmonary arrest can be as high as<br />
92% [17]. This compares with survival rates of 15-20% after<br />
other in-hospital cardiopulmonary arrests [18]. This therefore<br />
alters the likelihood that CPR in the perioperative period will<br />
be successful and so can impact the original presumptions on<br />
which the DNAR decision was made.<br />
When anaesthesia is considered for a patient with a current<br />
DNAR decision in place the patient and the anaesthetist face<br />
two additional dilemmas. Firstly, anaesthesia itself, whether<br />
regional or general, will promote cardiopulmonary instability<br />
that will require support.<br />
Secondly, many of the routine interventions used in giving an<br />
anaesthetic may be classified as resuscitative measures used<br />
in CPR in another setting. These include the insertion of an<br />
intravenous cannula, administration of intravenous fluids,<br />
insertion of an artificial airway, delivery of oxygen, provision of<br />
respiratory assistance, cardiac monitoring and administration<br />
of vasopressor and other resuscitative drugs. The surgical<br />
procedure itself may also require resuscitative measures to be<br />
implemented.<br />
14
If the anaesthetist was to proceed and strictly obey the<br />
general understanding of a DNAR decision, which excludes<br />
cardiovascular and respiratory support, their actions could be<br />
construed as an act of euthanasia or assisted suicide as they<br />
would be initiating cardiopulmonary compromise and yet be<br />
unable to treat this once it had occurred.<br />
However, if the anaesthetist insists that the DNAR decision is<br />
suspended in order for surgery and anaesthesia to take place,<br />
the patient may be denied their rights to certain Articles of the<br />
Human Rights Act including:<br />
• The right to life (Article 2),<br />
• To be free from inhuman or degrading treatment (Article 3),<br />
• To be free from discriminatory practices, such as ageism, in<br />
respect of these rights (Article 14) [10].<br />
In addition, if an anaesthetist were to treat a patient against their<br />
wishes, for example by implementing CPR when it was clear<br />
that the patient had stated they did not wish this to take place,<br />
this would constitute assault under both the criminal and civil<br />
law. It would also violate the guidance given by the GMC [6].<br />
The Mental Capacity Act 2005 states that an advance decision<br />
must be applicable to the circumstances that subsequently<br />
arise if it is to remain valid [8]. In the case of a DNAR decision<br />
that exists as a result of an advance statement, it is likely that<br />
the circumstance of anaesthesia for an operative procedure<br />
that is considered appropriate will not have been specifically<br />
considered when the advance decision was originally made.<br />
For these reasons, all DNAR decisions must be reviewed before<br />
patients undergo anaesthesia and surgery. The complexity<br />
of these situations makes it essential that decisions regarding<br />
modification of DNAR decisions in the perioperative period<br />
are made by senior staff and, if necessary, with reference to the<br />
hospital’s legal team.<br />
15
7. How to review a DNAR decision<br />
It is important that patients who may require surgical procedures<br />
with DNAR decisions in place are referred as early as possible<br />
to the anaesthetist and surgical team. Time is required to<br />
enable sensitive and effective communication with all the<br />
relevant individuals and to formulate a plan that is acceptable<br />
to all involved with the patients’ care and most importantly<br />
the patients themselves. However, this should be done with<br />
sufficient urgency to avoid delay to surgery in this vulnerable<br />
group of patients.<br />
At the end of the decision making process patients, proxy<br />
decision makers, relatives, carers, friends and IMCAs (if<br />
indicated) should feel that they have received adequate<br />
information in a form they can understand and that the<br />
decisions taken truly reflect the wishes of the patient. If patients<br />
or others feel they have not had the chance to have a proper<br />
discussion with the healthcare team, or are not happy with the<br />
discussions they have had, they should be given the option of<br />
a consultation with other designated individuals within each<br />
hospital.<br />
Emergency situation<br />
In emergency situations it may not be possible to review<br />
a DNAR decision, or any other advance decision, prior to<br />
anaesthesia, surgery or resuscitation as there is insufficient time.<br />
However, attempts must still be made to clarify any advance<br />
decisions that are made known to the doctors involved by<br />
discussion with relatives, proxy decision makers or even the<br />
patient if this is possible.<br />
If an advance decision cannot be discussed with these<br />
individuals, doctors must decide what they view to be in the<br />
best interests of the patient using whatever information is<br />
available.<br />
16
Preoperative phase<br />
Provision must be made for confidential discussion to take<br />
place between the relevant individuals involved in the case:<br />
patient, proxy decision makers, family and carers if appropriate,<br />
anaesthetist, surgeon, physician and nursing staff. The following<br />
points act as guidance to the preliminary assessment of the<br />
patient and enable a treatment plan to be formulated:<br />
a. The patient’s medical condition, including their mental<br />
competence,<br />
b. The surgical intervention required,<br />
c. The history of the DNAR decision including:<br />
• the duration of the decision,<br />
• who was responsible for implementing the decision,<br />
• whether the decision was intended to be ‘location<br />
sensitive’,<br />
• the presumptions on which the decision was based.<br />
The first decision required is whether anaesthesia and surgery<br />
are appropriate, taking into consideration the views of the<br />
patient, relatives, proxy decision makers, surgeons and<br />
anaesthetists. If surgery is deemed appropriate, measures must<br />
be taken to ensure the patient is medically optimised. A decision<br />
must then be taken as to what resuscitative measures are<br />
acceptable in the perioperative period with open, detailed and<br />
frequent communication with the patient, relatives and proxy<br />
decision makers.<br />
Once the plan for the DNAR decision has been agreed, it should<br />
be recorded in the patient’s notes, signed by the relevant parties<br />
and dated. Surgery should proceed as soon as practical after the<br />
decision is made and the medical condition of the patient has<br />
been optimised.<br />
We recommend that one of the following three options is<br />
adopted following review of the DNAR decision, and with<br />
agreement from all the relevant decision makers involved:<br />
17
Option one: The DNAR decision is to be discontinued during<br />
anaesthesia and surgery and fully reinstated once discharged<br />
from the recovery room.<br />
Surgery and anaesthesia are to proceed with CPR to be used if<br />
cardiopulmonary arrest occurs.<br />
Option two: The DNAR decision is to be modified to permit<br />
the use of drugs and techniques commensurate with the<br />
provision of anaesthesia.<br />
In most circumstances, this would include:<br />
1. Monitoring of ECG, blood pressure, oxygenation and any<br />
intraoperative monitors which are considered essential for a<br />
good outcome.<br />
2. Temporary manipulation of the airway and breathing<br />
with intubation and ventilation, when needed; and<br />
with understanding that the patient will be breathing<br />
spontaneously at the end of the procedure.<br />
3. Use of vasopressor or antiarrhythmic drugs to correct<br />
cardiovascular stability related to the provision of anaesthesia<br />
and surgery.<br />
The use of electrical cardioversion or defibrillation to correct<br />
arrhythmias should be considered and discussed with the<br />
patient or proxy decision makers in advance. Attempts of<br />
electrical cardioversion or defibrillation may be considered and<br />
agreed to treat arrhythmias if indicated.<br />
A decision must also be taken about the potential use of chest<br />
compressions. These may be deemed unacceptable in view of<br />
the possible complications involved.<br />
Option three: No changes are to be made to the DNAR<br />
decision.<br />
Under most circumstances this option is not compatible with<br />
the provision of general anaesthesia for any type of surgical<br />
intervention.<br />
18
The patient may wish to undergo a minor surgical procedure<br />
while their DNAR decision remains in place. The anaesthetist<br />
should reach agreement, if possible, with the patient or proxy<br />
decision makers as to exactly what, if any, interventions are<br />
permitted, such as intravenous cannulation, intravenous fluid<br />
administration, sedation, analgesia, monitoring, vasopressor<br />
medication, antiarrhythmic medication, administration of<br />
oxygen or other interventions.<br />
The Joint Statement makes it clear that ‘If a clinician believes<br />
that the procedure or treatment would not be successful with<br />
the DNAR decision still in place, it would be reasonable not to<br />
proceed.’ [3]<br />
Appendix 1 provides an example of a proforma adapted from<br />
the options on page 18. The working party recommends the<br />
adoption of a formal document such as this describing the<br />
procedures the patient has consented to undergo during the<br />
perioperative period. However, it must be remembered that<br />
completing the proforma should not take priority over the<br />
discussion. The purpose of the proforma is to record for clarity<br />
and certainty the decisions that have been made, and the<br />
parties to it. The quality of the medical advice, the exploration<br />
of alternatives and adherence to the patient’s wishes are the<br />
essence of the process.<br />
19
8. Conflict resolution<br />
When dealing with a situation involving the modification of a<br />
pre-existing DNAR decision, the medical team may be faced<br />
with different wishes from the patient, family members and<br />
friends. In attempting to resolve such conflict, the law provides<br />
a clear hierarchy in terms of who can legally make decisions<br />
about the treatment a patient receives:<br />
a) The competent patient’s direct instructions<br />
A competent patient’s direct instructions are always<br />
paramount.<br />
b) The patient’s advance decision or proxy decision<br />
maker<br />
If the patient has made an advance decision and has<br />
appointed a proxy decision maker, and they are both<br />
applicable to exactly the same situation, then which ever<br />
action was taken later (i.e. most recently) takes priority.<br />
It is likely that the situation of anaesthesia and surgery will<br />
not have been considered when making an advance<br />
decision DNAR order which will then invalidate its<br />
application in these circumstances.<br />
The decision will then need to be taken by the proxy<br />
decision maker, if one exists, or the senior clinician in<br />
charge of the patient’s care, as to what management option<br />
should be pursued.<br />
20
c) The senior clinician in charge of the patient’s care<br />
If the patient is not competent to make their own decisions,<br />
and has not appointed a proxy decision maker or made<br />
an advance decision, then the senior clinician in charge<br />
of the patient’s care must make the decision, based on the<br />
patient’s best interests.<br />
Again, consultation with relatives or carers may clearly<br />
assist in discovering any wishes formerly expressed by the<br />
patient. In England and Wales an Independent Mental<br />
Capacity Advocate (IMCA) may be consulted to reflect<br />
the patient’s wishes if there is no relative, friend or carer<br />
to represent the patient. However, the power to make the<br />
decision resides with the treating clinician, not with the<br />
relatives, friend, carers or IMCA.<br />
If, after reasonable effort, agreement or compromise cannot<br />
be reached through dialogue, the decision of the person with<br />
the right or responsibility for making the decision should be<br />
accepted. If there is doubt as to the validity of the appointment<br />
of a proxy decision maker or an advance decision, or what is in<br />
the best interests of the patient, then the Trust legal team should<br />
be contacted immediately for advice. An application may very<br />
quickly be made to court to seek a declaration as to whether a<br />
particular course of action is lawful.<br />
If an anaesthetist or other healthcare provider cannot agree with<br />
the outcome of the review of the DNAR decision, they must<br />
ensure that arrangements are made for another suitably qualified<br />
colleague to take over the role in accordance with GMC<br />
guidelines [19].<br />
21
9. Duration of the DNAR<br />
management option<br />
Intraoperative phase<br />
The DNAR management option should apply for the duration of<br />
the patient’s stay in the theatre environment. If premedication<br />
is prescribed it must be used with extreme caution to avoid<br />
alterations in the patient’s physiological status before transfer to<br />
theatre.<br />
All theatre staff should be made aware of the DNAR<br />
management option of the patient throughout their time in the<br />
theatre suite and recovery area. The anaesthetist and surgeon<br />
involved in preoperative consultation should be present in<br />
theatre throughout the procedure to enable shared responsibility<br />
of resuscitation decisions. In some circumstances this may<br />
not be possible; good communication of decisions from the<br />
preoperative consultation is therefore essential.<br />
Postoperative phase<br />
The DNAR management option should be communicated to the<br />
recovery staff on transfer to the recovery area. This option will<br />
continue until the patient is discharged from the recovery area.<br />
The prior DNAR decision should be reinstated on handover of<br />
the patient to the nursing staff from the ward. In exceptional<br />
circumstances, arrangements may be made to prolong the<br />
DNAR management option following transfer to the ward<br />
postoperatively: for example, if a patient-controlled analgesia<br />
device or epidural infusion is to be used in the postoperative<br />
period. A postoperative review of the patient should be<br />
carried out with communication to the patient, relatives or<br />
proxy decision makers about the perioperative management if<br />
necessary.<br />
There should be regular audits of the management of patients<br />
with DNAR decisions scheduled for surgery.<br />
22
10. Summary for patients, proxy<br />
decision makers and relatives<br />
This section summarises the guidance given in this document<br />
regarding the implications of a DNAR decision, and how the<br />
presumptions on which the DNAR decision was implemented<br />
are altered by the proposed surgery and anaesthesia. This<br />
summary is not intended to be used directly as patient guidance,<br />
but might be useful for lay persons. It is suggested that Trusts<br />
should consider producing appropriate patient guidance on this<br />
matter.<br />
These guidelines apply only to adult patients.<br />
The purpose of reviewing the DNAR decision is to provide an<br />
opportunity for agreement over what treatment will be provided<br />
during surgery and anaesthesia. The three DNAR management<br />
options provide a range of alternatives that should be<br />
considered. The legal hierarchy of the competent patient, their<br />
advance decision or their proxy decision maker, then the senior<br />
clinician in charge of the patient’s care exists to determine who<br />
decides the DNAR management option to be followed.<br />
Although relatives should be involved in decisions about<br />
proposed treatment, they have no legal authority in determining<br />
the DNAR management option. Their inclusion in discussions<br />
for patients who lack capacity is to reflect what the wishes of the<br />
patient would have been if they were able to express them.<br />
It must also be remembered that neither patients nor proxy<br />
decision makers can demand treatment, which is judged in<br />
medical opinion to be against the patient’s interests. Patients<br />
may however refuse treatment, as can proxy decision makers, so<br />
long as they have legal authority to do so. Advance decisions<br />
refusing treatment must be relevant to the situation of the<br />
proposed surgery and anaesthesia.<br />
23
At the end of the decision making process patients, proxy<br />
decision makers, relatives, carers, friends and IMCAs (if<br />
indicated) should feel that they have received adequate<br />
information in a form they can understand and that the<br />
decisions taken truly reflect the wishes of the patient.<br />
Further information on decisions relating to CPR has been<br />
published by the British Medical Association [20], but the<br />
issue of DNAR decisions in the perioperative period is not<br />
considered. If patients feel they have not had the chance to<br />
have a proper discussion with the healthcare team, or are not<br />
happy with the discussions they have had, they should be given<br />
the option of a consultation with other designated individuals<br />
within each hospital.<br />
24
11. References<br />
1. American Society of Anaesthetists Committee on Ethics, 2001.<br />
Ethical guidelines for the anesthesia care of patients with do-notresuscitate<br />
orders or other directives that limit treatment. www.<br />
asahq.org/publicationsAndServices/standards/09.html (accessed<br />
01/08/08).<br />
2. Canadian Anesthesiologists’ Society Committee on Ethics, 2002.<br />
Peri-operative status of ‘do not resuscitate’ (DNR) orders and<br />
other directives regarding treatment. www.cas.ca/members/<br />
sign_in/guidelines/do_not_resuscitate/ (accessed 01/08/08).<br />
3. Resuscitation Council, Decisions Relating to Cardiopulmonary<br />
Resuscitation. A Joint Statement from the British Medical<br />
Association, the Resuscitation Council (UK) and the Royal College<br />
of Nursing, London: 2007. www.resus.org.uk/pages/DNAR.htm<br />
(accessed 18/11/08).<br />
4. McBrien ME and Heyburn G. Anaesthesia 2006; 61: 625–7.<br />
5. Consent for Anaesthesia, 2nd edition 2006. London, The<br />
Association of Anaesthetists of Great Britain and Ireland. www.<br />
<strong>aagbi</strong>.org/publications/guidelines/docs/consent06.pdf (accessed<br />
01/08/08).<br />
6. General Medical Council. Consent: patients and doctors making<br />
decisions together, 2008. www.gmc-uk.org/news/articles/<br />
Consent_guidance.pdf (accessed 01/08/08).<br />
7. Medical Council of Ireland. A Guide to Ethical Conduct and<br />
Behaviour, Sixth Edition, 2004. www.medicalcouncil.ie/<br />
professional/ethics.asp (accessed 18/11/08).<br />
8. Mental Capacity Act 2005. http://www.opsi.gov.uk/ACTS/<br />
acts2005/ukpga_20050009_en_1 (accessed 29.1.09).<br />
9. Adults with Incapacity (Scotland) Act 2000. http://www.opsi.gov.<br />
uk/legislation/scotland/acts2000/asp_20000004_en_1 (accessed<br />
29.1.09).<br />
25
10. Human Rights Act 1998. http://www.opsi.gov.uk/ACTS/acts1998/<br />
ukpga_19980042_en_1 (accessed 29.1.09).<br />
11. Beauchamp TL, Childress JF. Principles of Biomedical Ethics, 5th<br />
edn. Oxford: Oxford University Press, 2001.<br />
12. General Medical Council. Withholding and withdrawing life<br />
prolonging treatments: Good practice in decision-making, 2002.<br />
www.gmc-uk.org/guidance/current/library/witholding_<br />
lifeprolonging_guidance.asp#67 (accessed 18/09/08).<br />
13. White SM, Baldwin TJ. The Human Rights Act, 1998: implications<br />
for anaesthesia and intensive care. Anaesthesia 2002; 57: 882–8.<br />
14. White SM, Baldwin TJ. The Mental Capacity Act 2005 –<br />
implications for anaesthesia and critical care. Anaesthesia 2006;<br />
61: 381-9.<br />
15. Irish Council for Bioethics. Is it time for advance healthcare<br />
directives? Opinion, 2007. www.bioethics.ie/uploads/docs/<br />
AdvanceDirectiveReport.pdf (accessed 18/11/08).<br />
16. Butler MW, Saaidin N, Sheikh AA, Fennell JS. Dissatisfaction with<br />
do not attempt resuscitation orders: A nationwide study of Irish<br />
consultant physician practices. Irish Medical Journal 2006; 99:<br />
208-210.<br />
17. Olsson GL, Hallen B. Cardiac arrest during anaesthesia.<br />
A computer-aided study in 250,543 anaesthetics. Acta<br />
Anaesthesiologica Scandinavica 1988; 32(8): 653–64.<br />
18. Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac<br />
arrest: incidence, prognosis and possible measures to improve<br />
survival. Intensive Care Medicine 2007; 33: 237-45.<br />
19. General Medical Council. Good medical practice, 2006.<br />
www.gmc-uk.org/guidance/good_medical_practice/index.asp<br />
(accessed 01/08/08).<br />
26
20. British Medical Association. Cardiopulmonary resuscitation<br />
model patient information leaflet, 2008. www.bma.org.uk/<br />
health_promotion_ethics/cardiopulmonary_resuscitation/<br />
CPRpatientinformation.jsp (accessed 18/09/08).<br />
27
Appendix 1<br />
DNAR management consent form<br />
This patient has been scheduled for surgery and anaesthesia.<br />
A DNAR decision is already in place. In order for surgery and<br />
anaesthesia to take place, one of the following three options has<br />
been agreed upon.<br />
Option one: The DNAR decision is to be discontinued during<br />
anaesthesia and surgery and fully reinstated once discharged<br />
from the recovery room.<br />
Option two: The DNAR decision is to be modified to permit<br />
the use of drugs and techniques commensurate with the<br />
provision of anaesthesia.<br />
This will include:<br />
1. Monitoring of ECG, blood pressure, oxygenation and any in<br />
traoperative monitors which are considered essential for a<br />
good outcome.<br />
Agreed/ Not agreed<br />
2. Temporary manipulation of the airway and breathing<br />
with intubation and ventilation, when needed; and with<br />
understanding that the patient will be breathing<br />
spontaneously at the end of the procedure.<br />
Agreed/ Not agreed<br />
3. Use of vasopressor or antiarrhythmic drugs to correct<br />
cardiovascular stability related to the provision of anaesthesia<br />
and surgery.<br />
Agreed/ Not agreed<br />
28
4. The use of electrical cardioversion or defibrillation to correct<br />
arrhythmias.<br />
Agreed/ Not agreed<br />
5. The use of chest compressions.<br />
Agreed / Not agreed<br />
Option three: No changes are to be made to the DNAR<br />
decision. Under most circumstances this option is not<br />
compatible with the provision of anaesthesia for any type of<br />
surgical intervention.<br />
The anaesthetist should reach agreement, if possible, with<br />
the patient or proxy decision maker as to exactly what, if any,<br />
interventions are permitted.<br />
Interventions permitted ................................................................<br />
....................................................................................................<br />
....................................................................................................<br />
....................................................................................................<br />
....................................................................................................<br />
....................................................................................................<br />
....................................................................................................<br />
....................................................................................................<br />
29
DNAR management option agreed: Option 1<br />
Option 2<br />
Option 3<br />
The DNAR management option will apply while the patient is<br />
in the operating theatre environment. The DNAR decision is<br />
to be reinstated on discharge from the recovery area unless in<br />
exceptional circumstances.<br />
Signatures<br />
signature of patient with capacity ...............................................<br />
date................................................<br />
OR, if patient does not have capacity<br />
signature of proxy decision maker<br />
instructed in life sustaining treatment...........................................<br />
date..........................................<br />
OR<br />
signature of relative, carer, friend or IMCA<br />
consulted to reflect patient’s wishes.............................................<br />
date............................................<br />
30
AND<br />
signature of clinician in<br />
charge of patient’s care................................................................<br />
date...............................................................<br />
AND/OR<br />
signature of the anaesthetist<br />
who has had the discussion.........................................................<br />
date.........................................................<br />
AND/OR<br />
signature of surgeon, if different to<br />
clinician in charge of patient’s care.............................................<br />
date.............................................<br />
31
32
33
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
Drug and Alcohol Abuse amongst Anaesthetists<br />
Guidance on Identification and Management<br />
2<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org March 2011
Membership of the working party<br />
(Details correct at the start of the working party process)<br />
Dr Diana Dickson<br />
Dr Valerie Bythell<br />
Dr Jane Marshall<br />
Dr Ruth Mayall<br />
Dr Ranjit Verma<br />
Prof Michael Wee<br />
Dr Susan Williams<br />
Chair and AAGBI Welfare Committee Member<br />
AAGBI Council Member<br />
AAGBI Welfare Committee Member<br />
AAGBI Welfare Committee Member<br />
AAGBI Council Member<br />
AAGBI Welfare Committee Chair<br />
GAT Representative<br />
This guideline has been seen and approved by the Council of the<br />
AAGBI.<br />
The working party is grateful to Dr James Clarke, Professor David Hatch,<br />
Mr Blake Dobson, Dr Fiona Moss, Dr Mike Peters, Dr Iain Wilson and Dr<br />
Isabeau Walker for their contributions to this guideline.<br />
The working party would like to acknowledge the helpful advice of Mr Bertie<br />
Leigh of Hempsons Solicitors.<br />
1
Contents<br />
1. Summary 3<br />
2. Introduction 4<br />
3. Factors influencing substance abuse 6<br />
4. The substance abusing anaesthetist 8<br />
5. Initial interventions 12<br />
6. The GMC and substance abusing doctors 14<br />
7. Treatment, support and monitoring 15<br />
8. Return to work 18<br />
References 20<br />
Appendix 1:Definitions 24<br />
Appendix 2:Sources of support 27<br />
Appendix 3:Example of a Trust alcohol and substance 30<br />
abuse policy<br />
Appendix 4:Identifying unsafe drinking habits 35<br />
© The Association of Anaesthetists of Great Britain & Ireland 2011<br />
2
1. Summary<br />
The vast majority of anaesthetists will be unaffected by substance abuse, but<br />
for those few that are affected the consequences can be devastating both for<br />
them and for their patients.<br />
Drug and alcohol abuse is a problem for some anaesthetists, as it is in the<br />
general population. Drug abuse is more common than alcohol abuse in<br />
trainees.<br />
The most immediate risk is of harm to patients.<br />
A report of drug or alcohol abuse in an anaesthetist should be taken seriously<br />
and investigated without delay. Physical or behavioural symptoms at work<br />
indicate advanced addiction.<br />
Anaesthetists are more likely than other doctors to abuse narcotics as a drug<br />
of choice, to abuse drugs intravenously and to be addicted to more than one<br />
drug.<br />
Concerns should be reported to the clinical director in the first instance. A<br />
one-to-one confrontation should be avoided and efforts should be made to<br />
obtain objective evidence.<br />
Clinical managers should be aware of policies and sources of assistance for<br />
managing these doctors.<br />
Many addicted doctors find it difficult to seek help and tend to become<br />
isolated.<br />
There is a danger of self-harm following intervention. Plans must be made<br />
in advance to facilitate treatment and for admission to a specialist unit if<br />
necessary.<br />
The ultimate objective should always be to try and resume a normal pattern<br />
of personal and professional life; this may be difficult particularly for<br />
anaesthetists.<br />
Anaesthetists willing to engage in treatment often experience a significant<br />
improvement in physical, psychological and social wellbeing. Support is<br />
required on a long-term basis.<br />
3
2. Introduction<br />
The vast majority of anaesthetists will be unaffected by substance abuse, but<br />
for those few that are affected the consequences can be devastating both for<br />
them and for their patients.<br />
Illicit drug and alcohol use is relatively common in the general population<br />
and continues to increase in prevalence in many western societies. The<br />
lifetime risk of dependence has been estimated as 7% -15% in doctors [1, 2,<br />
3].<br />
Over 90% of the adult population in the UK drink alcohol, with 31% of men<br />
and 20% of women exceeding the recommended daily intake [4]. Studies<br />
suggest that the incidence in doctors of disorders of alcohol use over a<br />
lifetime is 13-14%, similar to that in the general population [2, 5]. Evidence<br />
suggests that alcohol dependence is more common in older anaesthetists [6,<br />
7], but is less common than in other specialities [8].<br />
Nationally, 10.5% of the population use illicit drugs, particularly in younger<br />
age groups. Drug dependence has been assessed as affecting 2.2% of<br />
the adult population [9]. Doctors are less likely to use illicit drugs than<br />
the general population but more likely to use benzodiazepines and minor<br />
opioids as a result of privileged access [2]. In anaesthetists illicit drug use is<br />
more common under the age of 40 years, and 80% of cases are male [7].<br />
Studies from the US and Australia have reported a 0.4 - 2% prevalence of<br />
drug dependence in anaesthetic trainees [6, 10-12]. Anaesthetists are at a<br />
greatly increased risk of suicide and drug-related death compared to matched<br />
controls in the general population, and the time of highest risk is in the first<br />
five years following graduation [13].<br />
Data from the US indicate that anaesthetists, psychiatrists and emergency<br />
medicine physicians are up to three times more likely to access specialist<br />
treatment facilities for substance abuse disorders than other speciality groups<br />
[6, 8, 14, 15]. Anaesthetists are more likely to abuse opioids as a drug of<br />
choice, to abuse drugs intravenously and to be addicted to more than one<br />
drug [6, 16]. Some of those in treatment actually cited drug availability or<br />
access as a reason for choosing anaesthesia as a career [14]. In 2007, 66%<br />
of the General Medical Council (GMC) annual caseload involved health<br />
problems – 43% involved alcohol abuse, 20% abuse of other substances and<br />
26% involved affective disorders [17].<br />
4
Opioid abuse<br />
The incidence of non-alcohol substance abuse in all grades of anaesthetist<br />
has remained consistent at 1-1.6%, over the last three decades. Rapidly<br />
acting drugs are most commonly used, particularly fentanyl [11, 16, 18].<br />
Rapid tolerance and dependence occur, and tolerance to doses of fentanyl of<br />
over 100 ml.day -1 (5 mg.day -1 ) may develop over a six month period [19].<br />
Propofol abuse<br />
This has been reported since the mid-1990s, with many fatalities. These<br />
were predominantly in anaesthetic trainees, but also in operating department<br />
practitioners and intensive care unit staff. One American survey showed<br />
a 5-fold increase in propofol abuse in anaesthetic trainees over a 10 year<br />
period, with 18% of departments having reported at least one case of<br />
propofol abuse in that decade (incidence 1:1000 anaesthetists per decade).<br />
Of those reported to be abusing propofol the mortality was 28% [20]. Users<br />
may erroneously feel that propofol is safe to use as the quick recovery after<br />
sub-anaesthetic doses prevents overt signs of abuse such as drowsiness.<br />
Death is often the only sign of drug abuse.<br />
Ketamine abuse<br />
Ketamine is known to be a drug of abuse in the general population, with<br />
a prevalence rate of 1.9% [9]. Ketamine abuse has been reported in<br />
anaesthetists [21]. Its short duration of action and predominant use outside<br />
the workplace may account for the paucity of recent literature. Like<br />
propofol, ketamine abuse is best detected by hair sampling.<br />
Cocaine abuse<br />
It is known that cocaine use has escalated recently, with a 6.6% increase in<br />
the general population in the UK in the last year [9]. Anecdotally, cocaine<br />
use has also increased in the medical profession. Cocaine and cannabis are<br />
amongst the five drugs most frequently used by doctors, particularly those in<br />
training [11, 22].<br />
Inhalation agents<br />
In a recent national survey, 22% of anaesthetic departments reported one<br />
or more cases of abuse of inhalational agents, with a mortality rate of 26%.<br />
These agents are often used in conjunction with other substances, often to<br />
ease withdrawal from opioids [23].<br />
Recent review articles that describe the incidence and outcomes of addicted<br />
physicians in general [24-26], and with specific reference to anaesthetists<br />
[27-30] are listed.<br />
5
3. Factors influencing substance abuse<br />
Many factors influencing drug and alcohol abuse are not exclusive to either<br />
doctors or anaesthetists, but some may be particularly relevant to those<br />
undertaking an anaesthetic career.<br />
Environmental factors<br />
The use of alcohol and/or drugs is more acceptable in different social and age<br />
groups. This influences the initial exposure to the substance and ongoing<br />
opportunities for their use. Home or social circumstances are also important<br />
– in one study, 60% of addicted physicians reported physical or emotional<br />
abuse at some stage in their life [31].<br />
Genetic/biochemical factors<br />
There is evidence to suggest that some individuals may have an underlying<br />
susceptibility to addiction; there is a significantly higher risk of dependence<br />
where a parent or other family member is a substance abuser [22, 32]. In<br />
addition, dopamine D2 receptor (DRD2) gene dysfunction and GABA<br />
receptor variants are associated with the risk of addiction [33, 34].<br />
Stress<br />
Anaesthetists often work long hours in an isolated and stressful environment<br />
over which they have little control. Long and unsociable hours of work,<br />
high levels of responsibility, a demanding training and a competitive career<br />
structure may create difficulties for individuals both at work and at home.<br />
There is also the potential in anaesthetic practice for serious medical errors.<br />
Some individuals under stress will use drugs or alcohol as an inappropriate<br />
coping strategy. In an AAGBI study of 1000 anaesthetists in 1997, 92% of<br />
respondents reported consuming alcohol with a median weekly consumption<br />
of 15 units; some anaesthetists reported consumption of up to 70 units per<br />
week [7].<br />
Psychological factors<br />
Approximately one third of all individuals will at some time in their lives<br />
suffer from significant psychological disturbance, usually in the form of<br />
anxiety and/or depression, occasionally progressing to severe mental illness.<br />
In some, this may lead to abuse of several drugs and/or alcohol. Of those<br />
with a mental health disorder, 29% also have an addictive disorder [5].<br />
6
Availability<br />
The fact that anaesthetists have easy access to a wide range of psychoactive<br />
drugs may well influence the likelihood of trying them.<br />
Having become dependent, staying at work helps the addicted doctor to<br />
maintain his/her supply of drugs.<br />
7
4. The substance abusing anaesthetist<br />
Risks<br />
The most immediate risk is of harm to patients.<br />
If the doctor concerned is working while under the influence of drugs or<br />
alcohol there is a risk of harm to patients, and this must be the over-riding<br />
concern. Both decision-making powers and clinical competencies may be<br />
affected with resulting slowed or impaired reactions to urgent situations.<br />
End-stage addicted anaesthetists are so distracted by their addiction that they<br />
are also more likely to take risks.<br />
The second and longer term risk is to the anaesthetist him/herself including<br />
his/her mental and physical health, family and personal relationships and, of<br />
course, career.<br />
Warning signs of alcohol abuse [35]<br />
The first clues that a doctor may have a drug and/or alcohol problem are<br />
often non-specific and not obvious except to the most hawkish of eyes.<br />
Particular attention should be paid to locum doctors, particularly to long-term<br />
locums who have been moving around the country. Doctors with mental<br />
health problems may be at particular risk as some will turn to alcohol or<br />
drugs as a coping strategy. A drink-driving charge should be reported to the<br />
Trust and should be taken seriously<br />
• Subtle change in personality – ‘something not quite right’<br />
• Mood swings and/or anxiety – at times flushed and full of bonhomie, at<br />
other times irascible and irritable<br />
• Gets drunk rather easily at departmental events and behaves bizarrely<br />
and out of character<br />
• Dishevelled appearance, forgetful, disorganised<br />
• Unexplained minor injuries, e.g. facial bruising<br />
• Staff members report the smell of alcohol<br />
• Drug errors, illegible handwriting<br />
• Secretive, socially isolated, regularly turns up late for work, or misses<br />
meetings<br />
• Frequent changes of address<br />
• Marital/relationship problems, call for help from family members,<br />
including children<br />
8
Warning signs of drug abuse [6, 27]<br />
• Behavioural changes<br />
• Needle marks on the arm, long sleeves<br />
• Unexplained regular facial bruising (propofol abuse)<br />
• Physical signs of withdrawal<br />
• Regular absences from theatre<br />
• Volunteering to draw up drugs for others<br />
• Patients in excessive amounts of pain<br />
• Insisting on personally administering opioids in the recovery room<br />
• Excessive or unnecessary prescribing of opioids<br />
• False recording of drug administration<br />
• Improper recording on the anaesthetic record<br />
• Failure to discard wastage<br />
• Over-anxious to give breaks<br />
• Presence in hospital out-of-hours<br />
• Enthusiasm for long, difficult or complicated cases<br />
• Volunteering to work extra shifts or to do extra or late cases on a list<br />
• Offering to stay late, or working overtime especially if likely to be<br />
working alone<br />
Raising concerns<br />
Self-referral<br />
Individuals who self-refer have recognised their need for treatment. They<br />
are likely to seek help from outside agencies and treatment may even have<br />
started without those at work being aware of the problem. Stigmatisation<br />
and the potential loss of livelihood are barriers to self-referral even where an<br />
individual has insight into his/her problem.<br />
Family and friends<br />
While family and friends may not wish to feel that they are betraying the<br />
affected individual they should be made aware that such action is in the best<br />
interests of both patients and the doctor.<br />
Patients<br />
Patients may complain that the doctor smells of alcohol or is acting strangely.<br />
Colleagues and other staff<br />
Altered behaviour is a common sign. Paradoxically, it may be more evident<br />
to those who know them less well, while closer colleagues may rationalise<br />
odd behaviour. An alteration in behaviour on return to theatre after a break<br />
should also raise concern.<br />
9
Locums and trainees<br />
It may be more difficult to obtain evidence about trainees or locums who<br />
rotate to several hospitals for short periods and it is important to work with<br />
regional advisers and schools of anaesthesia.<br />
Doctors in independent practice<br />
They may work at several different hospitals and therefore it may be more<br />
difficult to spot inappropriate patterns of activity. Unless an individual<br />
hospital has a specific protocol, any suspicions should be reported<br />
confidentially to the chairman of the medical staff committee of that hospital.<br />
Taking action is not difficult where the evidence of drug or alcohol abuse is<br />
plain to see. Unfortunately, more often, the changes are subtle and we may<br />
be less alert to them or tend to make excuses for them, and avoid addressing<br />
the possibility of substance abuse. As a result we delay helping for too long.<br />
Where we have such concerns, we have a duty of care, in the interests of<br />
both patients and of the affected doctor, to raise these sooner rather than<br />
later.<br />
Likewise, it is the duty of all anaesthetists, who suspect that they themselves<br />
have, or are developing, substance abuse problems, to refer themselves for<br />
treatment.<br />
Actions that should be taken<br />
What should you do if you suspect an anaesthetic colleague of<br />
substance abuse?<br />
Concerns about an anaesthetist should normally be reported to the clinical<br />
director in the first instance. All those involved including clinical directors<br />
should keep written and confidential records of all relevant interviews and<br />
events, meetings and discussions.<br />
Junior doctors may find it easier to raise the subject with their educational<br />
supervisor or mentor. Non-medical staff may report to their line manager. It<br />
is important that all staff are aware of their duty to relay this information to<br />
the clinical director while maintaining confidentiality.<br />
Hospitals should have a formal policy concerning drug and/or alcohol abuse;<br />
a typical policy is demonstrated in Appendix 3. Clinical directors have a duty<br />
of care to inform the medical director of each case in line with the local Trust<br />
or hospital policy.<br />
10
Where the individual is a trainee, there are specific Trust and deanery<br />
reporting systems. In the case of rotating trainees, information will need to<br />
be passed on when they rotate. This is the responsibility of the college tutor.<br />
Confirming suspicions<br />
Efforts should be made to obtain objective evidence. A single reported<br />
episode of working under the influence of alcohol or drugs may be a marker<br />
of a significant underlying problem and should be considered very seriously<br />
with due investigation.<br />
Evidence must be sought to confirm or refute any report of substance abuse.<br />
Full confidentiality must be maintained during these investigations as there<br />
is always a possibility of malicious reporting. Isolated events reported by<br />
a single witness should be treated with great care, (e.g. drug theft, or drug/<br />
alcohol consumption in the workplace). Prescribing and nursing records<br />
must be examined carefully in order to substantiate the inappropriate use of<br />
drugs.<br />
11
5. Initial interventions<br />
In deciding when or if to intervene, it must be remembered that our first duty<br />
of care is to the patient. A one-to-one confrontation should be avoided.<br />
The term ‘intervention’ is used here to describe the process of enabling the<br />
substance abusing doctor to admit that he/she has a problem that needs<br />
urgent attention. Many abusing doctors are in denial and can only begin<br />
meaningful treatment when they can admit there is a problem.<br />
If there is substantial evidence to suggest that an individual has been abusing<br />
alcohol or drugs and particularly if there is evidence of potential or real<br />
harm to patients, urgent intervention is required. Those with knowledge of<br />
the situation must be prepared to present the evidence regarding the drug<br />
or alcohol abuse. The aim of intervention is to resolve concerns at an early<br />
stage.<br />
Where there are significant allegations, the doctor should be interviewed<br />
by the medical director and the clinical director. Plans must be made in<br />
advance of the interview to facilitate support and treatment, including<br />
identification of specialist treatment centres and other specialised facilities<br />
if available. Many specialist units will provide free assessment. The GMC<br />
will discuss a case and give advice on an anonymous basis ahead of an<br />
intervention. The doctor concerned may find it valuable to be accompanied<br />
by a colleague or other individual representing his/her interests or to be<br />
represented by the British Medical Association (BMA) or similar organisation.<br />
Clinical directors should be familiar with these avenues of help and explore<br />
the possibilities before an intervention (see Appendix 2).<br />
The doctor should be informed of the concerns being raised (without<br />
necessarily divulging the source of information) and any plans for further<br />
investigation or intervention. In this difficult situation the doctor should be<br />
offered the opportunity to undergo an assessment, rather than insisting he/<br />
she has an addiction problem and needs treatment. The process should also<br />
involve occupational health and a psychiatrist with special experience in the<br />
field – this may come via the treatment centre.<br />
It is important to remember that addiction is recognised as a disease [36], and<br />
a substance abusing colleague should be offered treatment as for any other<br />
chronic illness. It is appreciated that a sympathetic attitude may be difficult<br />
if there has been a history of repeated absences, covering for the suspected<br />
doctor and other problems.<br />
12
There is a real possibility of self-harm following intervention. Immediate<br />
referral to a specialist unit may minimise this risk. The doctor concerned<br />
should not be left unsupported following this initial interview. Contact with<br />
a member of the local British Doctors and Dentists Group (BDDG) may be<br />
helpful in this role (see Appendix 2).<br />
Actions to protect patients<br />
Where harm has occurred to a patient as a result of substance abuse<br />
The doctor should be formally excluded from work with a clear statement<br />
as to the reasons for this and what further actions are to be taken. The<br />
GMC should be informed. These actions must be backed up via written<br />
confirmation through the normal disciplinary procedures in the hospital.<br />
The doctor should be offered treatment and support. He/she should be<br />
advised concerning opportunities for support from the BMA and his/her<br />
medical defence organisation, and should also be strongly advised to accept<br />
the plans to initiate treatment.<br />
Where there is clear evidence of abuse but no harm to a patient has<br />
occurred<br />
The doctor should be offered treatment and support, usually through a<br />
mechanism of sick leave. All continuing contact with patients should cease.<br />
The doctor should then be offered an appropriate management plan as<br />
detailed below.<br />
• The doctor accepts that there is a problem. If the situation is largely<br />
confidential then the doctor could be offered psychiatric help outside<br />
his/her own region. If the situation is common knowledge and the<br />
doctor is comfortable with local treatment, this could be provided.<br />
• The doctor refuses to accept that there is a problem. If there is<br />
corroborating evidence to the contrary, the situation is more complex.<br />
The doctor should be asked to consent to random testing of breath,<br />
blood, urine or hair samples as appropriate, under the supervision of<br />
occupational health. No patient contact should be allowed<br />
while further investigation takes place. Referral to an agency in<br />
Appendix 2 is advised for a full independent assessment to take place.<br />
13
6. The GMC and substance abusing doctors<br />
Advice from the GMC must be sought at an early stage where there is any<br />
danger to patients from doctors who are abusing alcohol or drugs. This<br />
will usually be by the medical director who should be in possession of all<br />
available evidence. The GMC has a statutory primary obligation to protect<br />
the public but at the same time aims as far as possible to support doctors in<br />
overcoming their addiction problems through medical supervision.<br />
GMC medical assessment<br />
The GMC will arrange for medical assessment of the doctor to take place,<br />
which will involve two examinations by experts in substance abuse.<br />
Following this a decision will be made as to whether or not the doctor should<br />
have restrictions placed upon his/her registration. The majority of cases are<br />
resolved without the need to appear at Fitness to Practise Panel. In those<br />
cases where restrictions are felt necessary, the GMC will arrange for ongoing<br />
supervision (see Appendix 1). This will be done through an appropriate<br />
supervisor who will report back to the GMC – the supervisor will often have<br />
been one of the experts conducting the original assessments.<br />
The addicted doctor will remain under supervision until the GMC is satisfied<br />
that his/her impairment has been resolved – usually a period of several years<br />
for substance abusing doctors.<br />
Any doctor who appears in court for any reason is automatically referred<br />
to the GMC. This also applies to drink-driving offences. Whether a doctor<br />
is using, abusing, or actually addicted, possession of recreational drugs is<br />
illegal. The GMC does recognise that some kinds of criminal behaviour,<br />
e.g. buying controlled drugs on the street or stealing from employing<br />
organisations, are often driven by addiction, and will arrange for medical<br />
assessment as part of their investigation.<br />
It is in the interests of both the doctor and his/her advisors to ensure that the<br />
best possible medical advice and support is provided in order to optimise the<br />
chances of a return to a satisfactory medical career.<br />
14
7. Treatment, support and monitoring<br />
Treatment<br />
Addiction is a disease that has biological, behavioural, and social<br />
components and any effective treatment must address these issues [19].<br />
Addiction should be managed through professional colleagues and support<br />
agencies listed in Appendix 2.<br />
Treatment may involve admission to hospital or an addiction facility for<br />
detoxification, further physical and psychological assessment, family work,<br />
and introduction to self-help organisations such as Alcoholics Anonymous<br />
or the British Doctors and Dentists Group (BDDG). For doctors, the goal<br />
is typically abstinence, as return to work is not otherwise feasible. Treating<br />
psychiatrists and other professionals usually work with occupational health<br />
physicians in setting up a back-to-work programme, which will involve<br />
a network of professionals including the general practitioner (GP), a<br />
designated workplace supervisor, a mentor (see below), and if the GMC is<br />
involved, a medical supervisor.<br />
Inpatient detoxification and rehabilitation at a specialist unit may be<br />
required. The overall treatment may last for months or years and long periods<br />
of leave may be required.<br />
It must be emphasised that treatment outcomes for doctors have consistently<br />
been shown to be effective and lead to a significant improvement in physical,<br />
psychological and social wellbeing for those doctors willing to engage in a<br />
treatment programme.<br />
The goal of a substance dependent doctor is life-long abstinence from all<br />
mood altering substances.<br />
Signs and symptoms of opioid withdrawal<br />
• Craving<br />
• Restless sleep<br />
• Sneezing, eyes watering, yawning<br />
• Piloerection and recurrent chills<br />
• Pupillary dilatation<br />
• Abdominal and muscle aches and pains<br />
• Nausea, vomiting and diarrhoea<br />
15
Signs and symptoms of stimulant withdrawal<br />
• Increased appetite<br />
• Insomnia or hypersomnia<br />
• Dysphoric mood<br />
• Craving for drugs<br />
• Lethargy and fatigue, depression, suicidal thoughts<br />
Signs and symptoms of alcohol withdrawal<br />
• Tremor: tongue, eyelids, outstretched hands<br />
• Agitation, insomnia<br />
• Transient visual, auditory, tactile hallucinations or illusions<br />
• Nausea, retching, vomiting, sweating<br />
• Delirium tremens – confusion, disorientation, hallucinations, agitation,<br />
pyrexia<br />
• Grand mal convulsions<br />
Support<br />
Addicted doctors feel isolated and need intense and long term support. This<br />
can come from a network of family and close friends. In addition there are<br />
many other agencies that can support the doctor in his/her return to a healthy<br />
life at home and at work (see Appendix 2).<br />
Support is likely to include attendance at self-help groups. This may need to<br />
continue indefinitely as there is a continuing risk of relapse. It is recognised<br />
by Alcoholics Anonymous that those who stop attending regular meetings or<br />
lose contact with peer support group members are more likely to relapse. It<br />
has also been observed that doctors who present for treatment generally do<br />
very well and are less likely to relapse if they regularly attend meetings of the<br />
BDDG in addition to Alcoholics Anonymous or Narcotics Anonymous.<br />
Mentoring<br />
Many doctors find it very valuable to have support and advice from a<br />
colleague outside his/her line management structure.<br />
16
Monitoring<br />
Mandatory biochemical monitoring<br />
This is important especially in the first two years post-treatment when relapse<br />
is most likely to occur. Mandatory testing of breath, hair, urine and blood,<br />
both regularly and at random, should be used to ensure that the individual<br />
remains drug or alcohol abstinent. Hair testing can show the presence of<br />
drugs taken several weeks earlier.<br />
Clinical monitoring by a specialist<br />
Specialist clinical monitoring, such as by a psychiatrist, will enable early<br />
identification of signs or triggers of impending relapse.<br />
Relapse<br />
Relapse may occur with the return to substance abuse in a diagnosed addict<br />
following discharge from a recognised treatment centre or after a period of<br />
abstinence following attendance at Alcoholics or Narcotics Anonymous. The<br />
substance used is not necessarily the initial drug of choice. The belief by<br />
primary opioid abusers that alcohol is an acceptable alternative has led to<br />
many relapses.<br />
Relapse occurs most commonly in the first two years of recovery – the major<br />
risk factors are primary opioid addiction, a co-morbid psychiatric illness and<br />
a family history of substance abuse disorder [32]. Other contributory factors<br />
include previous relapse, failure to focus on abstinence and failure to attend<br />
help groups plus workplace or legal difficulties. If evidence of further abuse<br />
is found the individuals will need to re-enter treatment and their jobs are<br />
likely to be at risk.<br />
17
8. Return to work<br />
The ultimate objective should always be to try and resume a normal pattern<br />
of personal and professional life; this may be difficult, particularly for<br />
anaesthetists (see below).<br />
Where the doctor has been referred to the GMC, the GMC will determine<br />
fitness to practise – whether and when a doctor can return to work.<br />
At a local level the decision to return to work will be a joint decision<br />
involving the doctor, his/her GP, the treating psychiatrist, the medical director<br />
and/or clinical director. Occupational health may also be involved.<br />
There are a number of important considerations that need to be addressed<br />
before a doctor can resume work.<br />
1. Stress in the workplace<br />
If stress in the workplace has been a major contributing factor then it may<br />
be unrealistic for the affected individual to return to the same stresses unless<br />
there has been a fundamental change in the dynamics of the job. The<br />
advantages and disadvantages of return to the same type and place of work<br />
must be discussed in depth with the doctor. If he/she is early in his/her career<br />
then retraining in a different specialty should be considered. This may be<br />
difficult for more senior staff but at the very least, his/her job plan should<br />
be modified realistically. This could include undertaking part time work or<br />
undertaking more administrative or teaching commitments. Return should<br />
be gradual, with allowance made for attending treatment and monitoring<br />
appointments.<br />
2. Drug abuse and anaesthesia<br />
Return to work and continuing in anaesthesia is a subject of much current<br />
debate [26, 30, 37]. Where the operating theatre was the source of drugs<br />
abused, there is some evidence that the risk of relapse in those continuing<br />
employment in the operating theatre is very high [12]. This is usually in<br />
those with the major risk factors for relapse noted above, and those who did<br />
not adhere to recommended treatment and recovery guidelines [15]. The<br />
prospects for those without major risk factors and who were compliant with<br />
treatment and other recommendations are more favourable [32].<br />
Despite earlier reports of poor outcomes in opioid addicted anaesthetists<br />
[12], there are more encouraging recent reports [8, 16]. A significant<br />
proportion of anaesthetists do not relapse and it would therefore be wrong<br />
18
to label all anaesthetists with opioid addiction as being unable to return to<br />
full normal activity. Addiction impairs more doctors than any other disease<br />
[38] but there is evidence that, given the appropriate treatment, follow-up<br />
and support, a large number of addicted anaesthetists do as well as other<br />
specialities in recovery, and remain in anaesthesia [8, 16, 32].<br />
19
References<br />
1. British Medical Association Report on the working group on the misuse<br />
of alcohol and other drugs by doctors. London: BMA, 1998.<br />
2. Hughes PH, Brandenburg N, Baldwin DC, et al. Prevalence of<br />
substance use among US physicians. Journal of the American Medical<br />
Association 1992; 267: 2333-9.<br />
3. Skipper G E. Treating the chemically dependent health professional.<br />
Journal of Addictive Diseases 1997; 16: 67-73.<br />
4. The Health and Social Care Information Centre. NHS Information<br />
Centre Statistics on Alcohol: England 2009; 13-14. http://www.ic.nhs.<br />
uk/webfiles/publications/alcoholeng2009/Final%20Format%20draft%20<br />
2009%20v7.pdf (accessed 25/01/2010).<br />
5. Regier DA, Farmer ME, Rae DS, et al. Co-morbidity of mental disorders<br />
with alcohol and other drug abuse. Journal of the American Medical<br />
Association 1990; 264: 2511-8.<br />
6. Hines R. Substance Abuse in Anesthesia Providers: An Update. Society<br />
of Academic Anesthesiology Associations 2003. http://www.aapd-saac.<br />
org/meetingpapers/2003/hines.pdf (accessed 15/10/2009).<br />
7. Berry CB, Crome IB, Plant M, Plant M. Substance misuse amongst<br />
anaesthetists in the United Kingdom and Ireland. Anaesthesia 2000;<br />
55: 946-52.<br />
8. Skipper GE, Campbell MD, DuPont RL. Anesthesiologists with<br />
substance use disorders; a 5-year outcome study from 16 state physician<br />
health programs. Anesthesia and Analgesia 2009; 109: 891-6.<br />
9. The Health and Social Care Information Centre. NHS Information<br />
Centre Statistics on Drug Misuse: England 2007; http://www.ic.nhs.uk/<br />
webfiles/publications/drugmisuse07/Drugs%20misuse-England%20<br />
2007%20with%20links%20and%20buttons.pdf (accessed 25/1/2010).<br />
10. Weeks AM, Buckland MR, Morgan EB, Myles PS. Chemical<br />
dependence in anaesthetic registrars in Australia and New Zealand.<br />
Anaesthesia and Intensive Care 1993; 21:151-5.<br />
20
11. Booth JV et al. Substance abuse among physicians: a survey of<br />
academic anesthesiology programs. Anesthesia and Analgesia 2002;<br />
95:1024–30.<br />
12. Collins GB, McAllister MS. Jensen M, Gooden TA. Chemical<br />
dependency treatment outcomes of residents in anesthesiology: results<br />
of a survey. Anesthesia and Analgesia 2005; 101:1457–62.<br />
13. Alexander B, Checkoway H, Nagahama SI, Domino KB. Cause-specific<br />
mortality risks of anesthesiologists. Anesthesiology 2000; 93: 922-30.<br />
14. Talbott GD, Gallegos KV, Wilson PO, et al. The Medical Association of<br />
Georgia’s impaired physicians program review of the first 1000<br />
physicians: analysis of specialty. Journal of the American Medical<br />
Association 1987; 257: 2927-30.<br />
15. Gallegos KV, Lubin BH, Bowers C, Blevins JW, Talbott GD, Wilson<br />
PO. Relapse and recovery: Five to ten year follow-up study of<br />
chemically dependent physicians - the Georgia experience. Maryland<br />
Medical Journal 1992; 41: 315-9.<br />
16. Paris RT, Canavan DI. Physician substance abuse impairment:<br />
anesthesiologists vs other specialties. Journal of Addictive Diseases<br />
1999; 18:1-7.<br />
17. Dobson B. GMC Head of Case Review 2010; (personal<br />
communication).<br />
18. Ward CF, Ward GC, Saidman LJ. Drug abuse in anesthesia training<br />
programs. A survey: 1970 through 1980. Journal of the American<br />
Medical Association 1983; 250: 922–5.<br />
19. Berry AJ, Polk SL. Chemical dependence in anesthesiologists: what<br />
you need to know and when you need to know it. American Society<br />
of Anesthesiologists 2002; Committee on Occupational Health of<br />
Operating Room Personnel Taskforce on Chemical Dependence. www.<br />
asahq.org/publicationsAndServices/chemical.pdf. (accessed 24/10/09).<br />
20. Wischmeyer PE, Johnson BR. A survey of propofol abuse in academic<br />
anesthesia programs. Anesthesia and Analgesia 2007; 105:1066-71.<br />
21
21. Moore NN, Bostwick JM. Ketamine dependence in anesthesia<br />
providers. Psychosomatics 1999; 40: 356-9.<br />
22. Lutsky I, Hopwood M, Abram SE, Cerletty JM et al. Use of psychoactive<br />
substances in three medical specialties: anaesthesia, medicine and<br />
surgery. Canadian Journal of Anesthesia 1994; 41:561-7.<br />
23. Wilson JE, Kiselanova N, Stevens Q, et al. A survey of inhalation<br />
anaesthetic abuse in anaesthesia training programmes. Anaesthesia<br />
2008; 63: 616-20.<br />
24. Baldisseri M. Impaired healthcare professional. Critical Care Medicine<br />
2007; 35 (Suppl 2): S106-16.<br />
25. O’Connor P, Spickard Jr A. Physician impairment by substance abuse.<br />
Medical Clinics of North America 1997; 81: 1037-52.<br />
26. Berge K, Seppala MD, Schipper AM. Chemical dependency and the<br />
physician. Mayo Clinic Proceedings 2009; 84: 625-31.<br />
27. American Society of Anesthesiologists Committee on Occupational<br />
Health. Model curriculum on drug abuse for residents in<br />
anesthesiology. www.asahq.org/clinical/curriculum.pdf (accessed<br />
15/10/2009).<br />
28. Bryson EO, Silverstein JH. Addiction and substance abuse in<br />
anesthesiology. Anesthesiology 2008; 109: 905–17.<br />
29. Silverstein JH, Silva DA, Iberti TJ. Opioid addiction in<br />
anesthesiology. Anesthesiology 1993; 79: 354-75.<br />
30. Oreskovich MR, Caldeiro RM. Anesthesiologists recovering from<br />
chemical dependency: can they safely return to the operating room?<br />
Mayo Clinic Proceedings 2009; 84: 576-80.<br />
31. Brewster JM, Kaufmann M. Characteristics and outcomes of doctors in<br />
a substance abuse monitoring programme in Canada: prospective<br />
descriptive study. British Medical Journal 2008; 337:a2098.<br />
32. Domino KB, Horbein TF, Polissar NL, et al. Risk factors for relapse<br />
in health care professionals with substance use disorders. Journal of<br />
the American Medical Association 2005; 293: 1453-60.<br />
22
33. Foll B Le, Gallo A, Strat Y Le, et al. Genetics of dopamine receptors and<br />
drug addiction: a comprehensive review. Behavioural Pharmacology<br />
2009; 20: 1-17.<br />
34. Drgon T, D’Addario C, Uhl GR. Linkage disequilibrium, haplotype<br />
and association studies of a chromosome 4 GABA receptor gene<br />
cluster: Candidate gene variants for addictions. American Journal of<br />
Medical Genetics Part B: Neuropsychiatric Genetics 2006; 141B: 854-<br />
60.<br />
35. Marshall EJ. Doctor’s health and fitness to practise: treating addicted<br />
doctors. Occupational Medicine 2008; 58: 334-40.<br />
36. Morse R, Flavin D. The definition of alcoholism. Journal of the<br />
American Medical Association 1992; 268:1035-9.<br />
37. Earley PH, Berry AJ. Re-entry after addiction treatment: research or<br />
retrain? Anesthesiology 2009; 110:1423-4.<br />
38. Talbott GD, Wright C. Chemical dependency in healthcare<br />
professionals. Occupational Medicine 1987; 2: 581-91.<br />
39. American Psychiatric Association. Diagnostic and Statistical Manual of<br />
Mental Disorders. DSM-IV-TR Criteria for Substance Dependence, 4th<br />
edn (text revision). Washington DC: American Psychiatric Association,<br />
2000.<br />
40. World Health Organization. The ICD-10 classification of mental and<br />
behavioural disorders: clinical descriptions and diagnostic guidelines.<br />
http://www.who.int/substance_abuse/terminology/<br />
ICD10ClinicalDiagnosis.pdf (accessed 19/10/10)<br />
41. Saunders JB, Aasland OG, Babor TF, et al. Development of the alcohol<br />
use disorders identification test (AUDIT): WHO collaborative project on<br />
early detection of persons with harmful alcohol consumption - II.<br />
Addiction 1993; 88: 791-803.<br />
23
Appendix 1: Definitions<br />
The recognition of substance dependence as a disease and its<br />
definitions, some of which are detailed below can be obtained from<br />
the World Health Organization (ICD criteria), the American Psychiatric<br />
Association (Diagnostic and Statistical Manual [DSM] classification)<br />
and American Society of Addiction Medicine websites.<br />
Impairment<br />
An impaired doctor is one who is unable to practice medicine with<br />
reasonable skill and safety to patients because of physical or mental illness,<br />
including deterioration through the ageing process, characterological or<br />
psychiatric difficulties or excessive use of alcohol or other drugs.<br />
Substance abuse (DSM IV-TR criteria) [39]<br />
• Recurrent substance use resulting in a failure to fulfil major role<br />
obligations at work, school or home<br />
• Recurrent substance abuse in situations in which it is physically<br />
hazardous<br />
• Recurrent substance-related legal problems<br />
• Continued substance use despite having persistent or recurrent social<br />
or interpersonal problem caused or exacerbated by the effects of the<br />
substance<br />
The equivalent to substance abuse in the International Classification<br />
of Disease (ICD) is termed ‘harmful use’, and is defined as “A<br />
pattern of psychoactive substance use that is causing damage to<br />
health. The damage may be physical (as in cases of hepatitis from<br />
the self-administration of injected drugs) or mental, (e.g. episodes of<br />
depressive disorder secondary to heavy consumption of alcohol).” [40]<br />
The term ‘substance’ is used to cover alcohol, illicit drugs and prescription<br />
medications taken inappropriately. It is used to describe:<br />
• The use of a substance that leads to impairment in physical and<br />
psychological health and in social dysfunction<br />
• The inappropriate use of prescription drugs<br />
• Use of illegal drug use that will probably lead to harmful health<br />
consequences either by virtue of the quantity of drug or method of use<br />
(e.g. injecting)<br />
There is an important difference between substance abuse and dependence<br />
(addiction).<br />
24
Dependence syndrome (addiction)<br />
The dependence syndrome is “A cluster of physiological, behavioural, and<br />
cognitive phenomena in which the use of a substance or a class of substances<br />
takes on a much higher priority for a given individual than other behaviours<br />
that once had greater value.” [40]<br />
A definite diagnosis should only be made if three or more of the following<br />
criteria have been experienced or exhibited at some time during the previous<br />
year.<br />
a. A strong desire or sense of compulsion to take the substance;<br />
b. Difficulties in controlling substance-taking behaviour in terms of its<br />
onset, termination, or levels of use;<br />
c. A physiological withdrawal state when substance use has ceased or<br />
have been reduced, as evidenced by: the characteristic withdrawal<br />
syndrome for the substance, or use of the same (or closely related)<br />
substance with the intention of relieving or avoiding withdrawal<br />
symptoms;<br />
d. Evidence of tolerance, such that increased doses of the psychoactive<br />
substance are required in order to achieve effects originally produced<br />
by lower doses (clear examples of this are found in alcohol – and opioid<br />
– dependent individuals who may take daily doses sufficient<br />
to incapacitate or kill non-tolerant users);<br />
e. Progressive neglect of alternative pleasures or interests because of<br />
psychoactive substance use, increased amount of time necessary to<br />
obtain or take the substance or to recover from its effects;<br />
f. Persisting with substance use despite clear evidence of overtly harmful<br />
consequences, such as harm to the liver through excessive drinking,<br />
depressive mood states consequent to periods of heavy substance use,<br />
or drug-related impairment of cognitive functioning; efforts should<br />
be made to determine that the user was actually, or could be expected to<br />
be, aware of the nature and extent of the harm. [40]<br />
GMC definitions<br />
1. Your (day-to-day work/surgery etc) must be directly supervised by<br />
a registered medical practitioner of consultant/GP Principal grade. (See<br />
Glossary for full definition)<br />
2. Your (day-to-day work/surgery etc) must be closely supervised by a<br />
registered medical practitioner of consultant/GP Principal grade. (See<br />
Glossary for full definition)<br />
25
3. Your (day-to-day work/surgery etc) must be supervised by a registered<br />
medical practitioner of consultant/GP Principal grade. (See Glossary for<br />
full definition)<br />
Glossary<br />
Directly supervised<br />
The doctor’s work must be directly supervised at all times by a supervising<br />
consultant based in the same place of work. The level of supervision<br />
required is equivalent to that of an FY1 trainee.<br />
Closely supervised<br />
The doctor’s day-to-day work must be supervised by a consultant, who must<br />
be on site and available at all times. The doctor’s work must be reviewed<br />
at least twice per week with the supervising consultant. The level of<br />
supervision required is equivalent to that of a novice anaesthetist.<br />
Supervised<br />
The doctor’s day to day work must be supervised by a consultant, who may<br />
be off site but available on-call. The doctor’s work must be reviewed at least<br />
once a fortnight with the supervising consultant. The level of supervision<br />
required is equivalent to that of a middle grade trainee.<br />
Royal College of Anaesthetists definitions (for comparison):<br />
Direct supervision<br />
Immediately available – in the theatre or available in the theatre suite and<br />
without other responsibilities.<br />
Indirect supervision<br />
Local – on the same geographical site and able to attend within 10 minutes.<br />
Distant supervision<br />
On a different geographical site or unable to attend within 10 minutes.<br />
26
Appendix 2: Sources of support<br />
More details and relevant documents may be found on the AAGBI website,<br />
www.<strong>aagbi</strong>.org/memberswellbeing.htm<br />
Alcoholics Anonymous (AA)<br />
www.alcoholics-anonymous.org.uk 0845 769 7555<br />
Do you think you may have a problem? Check lists: http://www.alcoholicsanonymous.org.uk/newcomers/?pageID=77<br />
The British Doctors and Dentists Group (BDDG)<br />
www.bddg.org 07792 819 966 (national secretary)<br />
This is a countrywide network of doctors and dentists at various stages in<br />
recovery from addiction, who meet on a monthly basis at one of 18 groups<br />
covering the UK. Following initial contact, callers may be put in touch with<br />
a doctor (in some cases another anaesthetist) nearer to their home who may<br />
then introduce a new doctor to the group at the local meetings.<br />
Problems can be discussed at these meetings that may not be appropriate to<br />
discuss at Alcoholics or Narcotics Anonymous meetings; for example, GMC<br />
proceedings and issues surrounding return to work, etc.<br />
There is also an associated families group, where direct relatives of addicted<br />
doctors and dentists can obtain help and support. Each BDDG meeting<br />
usually has a families group. Support for family members of addicted doctors<br />
can be obtained via the Families Group of the BDDG –<br />
www.bddgfamilies.org.uk<br />
Doctors’ Support Line (DSL)<br />
0844 395 3010<br />
A confidential and anonymous peer support helpline for doctors who need<br />
to talk to someone whatever their concerns. Doctors in the group have<br />
themselves been troubled at some stage in their lives, and help is offered to<br />
those who are beginning the process of re-establishing themselves after a<br />
breakdown or other mental crisis.<br />
Doctors’ Support Network (DSN)<br />
www.dsn.org.uk 0871 245 8376<br />
A group with regular meetings throughout the country for help with stress,<br />
burnout, anxiety, depression, psychoses and eating disorders. This may be<br />
helpful for addicted doctors with dual diagnoses.<br />
27
GMC Investigation Team<br />
0161 923 6402 practise@gmc-uk.org<br />
Healthcare Professionals Recovery Group (HPRG)<br />
01327 262 823<br />
These monthly meetings are attended by doctors, dentists, nurses,<br />
pharmacists and other healthcare professionals who have addiction<br />
problems. They too are confidential and offer similar help and support to<br />
that of the BDDG.<br />
Narcotics Anonymous (NA)<br />
www.ukna.org 0300 999 1212<br />
Narcotics Anonymous is for recovering addicts who meet regularly to help<br />
each other stay clean. It is not restricted to those with opioid abuse problems<br />
as the name may suggest, but any drug including tranquillisers, recreational<br />
drugs and alcohol. The website contains some questions and information for<br />
those who think they may have a problem.<br />
Do you think you may have a problem? – checklists may be found at: http://<br />
www.na.org/admin/include/spaw2/uploads/pdf/litfiles/us_english/IP/EN3107.<br />
pdf<br />
The majority of AA or NA meetings are ‘closed’ and are only for recovering<br />
addicts/alcoholics and those who think they may have a drug problem. A<br />
meeting described as ‘open’ may be attended by anyone, e.g. professionals<br />
working with addicts or family members, friends etc. Meetings lists are on<br />
the AA or NA websites with details of open meetings at each venue.<br />
Practitioner Health Programme (PHP)<br />
www.php.nhs.uk 020 3049 4505<br />
This is an NHS funded but entirely confidential service open to doctors and<br />
dentists living or working in the London area. Care is multidisciplinary in<br />
nature and provides appropriate specialist care and support for any doctor<br />
with addiction, mental or physical health concerns. Where inpatient<br />
therapy is thought necessary, this will be organised and funded by the PHP/<br />
NHS. Follow-up, monitoring and help with returning to work are also part of<br />
the services offered. Unfortunately this is currently only available to Londonbased<br />
doctors, but plans for expansion to cover other areas of the country are<br />
in place. Advice can be obtained by phone even if outside the M25 area.<br />
28
Royal Medical Benevolent Fund (RMBF)<br />
www.rmbf.org 0208 540 9194<br />
The RMBF offers financial support and is also developing a helpline. It was<br />
set up by doctors to help colleagues and their dependants in need.<br />
Sick Doctors Trust (SDT)<br />
www.sick-doctors-trust.co.uk 0370 444 5163*<br />
The SDT is an independent charity established over 14 years ago, which<br />
provides a 24-hour helpline manned exclusively by experienced doctors who<br />
are either in recovery from addiction themselves, or trained counsellors. It<br />
provides help and support to doctors who think they may have a problem<br />
with their use of alcohol or other drugs, whether prescribed or not. Calls are<br />
treated with strict confidentiality, and callers may remain anonymous if they<br />
wish.<br />
Help offered includes assessment, advice, referral for treatment when<br />
appropriate and introduction to long term befriending and support services.<br />
The helpline also accepts calls from family members or friends, concerned<br />
colleagues and others.<br />
* please note change of number since publication of the AAGBI<br />
Welfare Resource Pack.<br />
Other resources<br />
Addaction 020 7251 5860<br />
www.addaction.org.uk<br />
Adfam 020 7553 7640<br />
(for families affected by drugs and alcohol) www.adfam.org.uk<br />
Al Anon<br />
(for families/friends of problem drinkers)<br />
020 7403 0888 (24 hours)<br />
www.al-anonuk.org.uk<br />
Alcohol Concern 020 7264 0510<br />
www.alcoholconcern.org.uk<br />
Drinkline 0800 917 8282<br />
National Drugs Helpline 0800 77 66 00<br />
www.talktofrank.com<br />
29
Appendix 3: Example of a Trust alcohol and<br />
substance abuse policy<br />
1. Introduction<br />
The Trust recognises that the prevalence of substance abuse and<br />
alcohol related problems within the general population means that<br />
there will inevitably be members of staff with such problems. Drugs<br />
and alcohol have an impact on cognitive performance and are<br />
associated with cognitive failures at work. This may have implications<br />
for the care of patients and the health and safety of an employee and<br />
his/her colleagues.<br />
1.1 Alcohol and substance abuse related problems at work are defined as:<br />
• any drinking of alcohol<br />
• any use of illicit non-prescribed drugs<br />
• any misuse of prescribed drugs<br />
• any use of any other substance of abuse, e.g. solvents<br />
that has the potential to interfere with an employee’s functioning<br />
and performance in any aspect of his/her job. This definition<br />
covers usage outside the workplace but where the effects have or<br />
may have an impact on an employee’s functioning at work.<br />
Throughout the remainder of this document the term substance will<br />
be used for alcohol, prescribed and non- prescribed drugs and any<br />
other substances used in the circumstances described above.<br />
2. Policy aims<br />
The principal aims of this policy are:<br />
2.1 To ensure that the Trust meets its obligations to safeguard the health,<br />
safety and welfare of its employees and patients using its services.<br />
2.2 To prevent and reduce the incidence of substance related problems in<br />
the workplace.<br />
2.3 To recognise that substance dependency is a health issue and to ensure<br />
that employees experiencing these difficulties have access to<br />
appropriate help.<br />
30
2.4 To foster a climate that will encourage individuals experiencing these<br />
problems to come forward for help in the knowledge that they will<br />
receive support and fair treatment.<br />
2.5 To facilitate the rehabilitation of employees who develop substance<br />
abuse problems.<br />
2.6 To give managers a clear framework within which to deal with<br />
substance abuse problems constructively.<br />
3. General provisions<br />
3.1 No-one will report for duty under the influence of any substance that<br />
affects his/her ability to carry out his/her duties.<br />
3.2 No-one will consume alcohol or use substances of abuse whilst at work,<br />
including breaks.<br />
3.3 Any individual found drunk or under the influence of any substance<br />
on duty will be subject to the Trust’s Disciplinary and Capability<br />
Policy and Procedure. Managers should ensure that the employee<br />
leaves the workplace and arrange to interview him/her after a suitable<br />
interval.<br />
3.4 The supplying of drugs of abuse to other people is a criminal offence.<br />
Any employee found or suspected of undertaking this activity will be<br />
reported to the police.<br />
4. Roles and responsibilities<br />
4.1 The Director of Human Resources is responsible for the implementation<br />
of this policy and ensuring regular review is undertaken.<br />
4.2 Line managers are responsible for ensuring employees are aware of this<br />
policy and for investigating and referring to the Occupational Health<br />
Service (OHS) when an employee is suspected of having a substance<br />
abuse related problem.<br />
4.3 Managers may recognise a problem by a changing attitude to work<br />
by employees which may be evidenced through poor punctuality,<br />
poor attendance, declining performance, the smell of alcohol on the<br />
breath or behaviour suggestive of intoxication, changes in mood<br />
31
and levels of co-operation with colleagues and declining personal<br />
standards of dress and hygiene.<br />
4.4 The OHS is responsible for advising on an affected employee’s fitness<br />
for work and ensuring that the employee who accepts help is referred<br />
on to an appropriate agency. The OHS operates within strict rules of<br />
medical confidentiality and any medical information obtained within<br />
the context of clinical activities will not be released without the consent<br />
of the individual concerned other than in exceptional circumstances as<br />
laid down by the General Medical Council, Nursing and Midwifery<br />
Council etc.<br />
4.5 Employees have a responsibility to ensure that they are fit to undertake<br />
their duties in a safe and appropriate manner at all times.<br />
4.6 Employees are responsible for seeking help if they have a substance<br />
abuse problem that is likely to have an impact on their performance at<br />
work.<br />
4.7 Employees are required to encourage colleagues whom they suspect<br />
have a problem to seek help via the OHS or by discussion with their<br />
line manager. If the colleague refuses to seek help, employees have a<br />
duty to bring their concerns to the attention of their line manager,<br />
otherwise they may be vulnerable in the event of a health and safety<br />
issue.<br />
5. Employees with substance related problems<br />
5.1 It is recognised that substance abuse problems are primarily matters of<br />
health and social concern with which sufferers need help.<br />
5.2 Employees who suspect or are aware that they have a substance abuse<br />
related problem are encouraged to seek medical help through the OHS<br />
(including the staff support and counselling service), their GP, or directly<br />
with an appropriate agency. (See list at Appendix 2).<br />
5.3 Any employee who has been identified as possibly having an<br />
alcohol or substance abuse problem affecting his/her conduct and/<br />
or performance at work will be asked to discuss the matter with his/her<br />
line manager.<br />
5.4 The employee will be offered the opportunity to seek assessment from<br />
32
the OHS who will refer for treatment from an appropriate agency if<br />
necessary. With the employee’s consent the OHS will keep the<br />
employee’s GP informed of progress.<br />
5.5 Whilst the OHS make every effort to arrange an urgent appointment for<br />
employees following a request, in the event of a delay and where<br />
there is concern that an employee may not be fit in the meantime,<br />
the manager, in conjunction with the Divisional Human Resources<br />
Manager, will make a decision as to the appropriate interim action. This<br />
may include special paid leave, suspension on full pay or sick leave.<br />
5.6 In any discussion of an alcohol or drug related problem (whether<br />
at the initiative of the individual or manager) the same rules of<br />
confidentiality would apply with respect to these conditions as to any<br />
other health complaint. However, behaviour associated with misuse<br />
may have to be disclosed where there is evidence of criminal activity,<br />
abuse of a professional position or potential harm to patients or<br />
colleagues.<br />
5.7 Leave to undergo treatment will be dealt with under the normal sick pay<br />
provisions.<br />
5.8 The OHS will advise on fitness to return to work and any job<br />
modification, temporary or permanent redeployment necessary as a<br />
result of the individual’s substance abuse problems.<br />
5.9 An employee identified as having a potential problem who declines<br />
help and whose behaviour or performance at work continues to be a<br />
source of concern will be subject to normal disciplinary procedures.<br />
This may result in termination of employment, which can be on health<br />
grounds in appropriate circumstances.<br />
5.10 It is recognised that relapses do occur. Therefore an employee with an<br />
identified problem who receives help but whose performance<br />
subsequently relapses due to a recurrence of the substance abuse<br />
problem will have the new situation considered on its merits. If<br />
appropriate, a further opportunity to seek/accept help will be offered.<br />
6. Testing for alcohol and substances of abuse in the workplace<br />
6.1 This Trust does not operate a systematic screening programme for the<br />
use of drugs or alcohol.<br />
33
6.2 However, as being under the influence of alcohol or substances of<br />
abuse in the workplace may represent a risk to the safety of the<br />
employee, his/her colleagues or patients, individuals suspected of<br />
abuse may be tested for such substances or markers of misuse as part of<br />
the occupational health assessment.<br />
6.3 Testing will be part of a clinical occupational health assessment and<br />
informed consent will be obtained at the time of testing. The OHS will<br />
monitor employees using blood and/or breath tests for alcohol and<br />
urine testing for drugs and would generally expect to see a return to<br />
normal blood tests and consistently negative urine tests before a return<br />
to work would be considered. On a return to work the employee will<br />
remain under review by the OHS and a system of unannounced testing<br />
will usually be agreed for a period, typically six months. Each<br />
employee is assessed on an individual basis.<br />
6.4 Results of testing are medically confidential and as such are defined as<br />
sensitive personal data under the Data Protection Act. These results<br />
will not be released to the employer or any other third parties without<br />
the consent of the employee. They will assist the occupational health<br />
practitioner in assessing fitness for work and formulating an appropriate<br />
occupational health management plan.<br />
6.5 Refusal to undergo testing or repeated non-attendance will result in the<br />
OHS making recommendations regarding the employee’s fitness to<br />
work on the information available and without the benefit of the test<br />
results.<br />
34
Appendix 4: Identifying unsafe drinking<br />
habits<br />
Over recent years a number of screening questionnaires have been<br />
developed with the objective of identifying hazardous, harmful and<br />
dependent drinking. The 10-item Alcohol Use Disorders Identification Test<br />
(AUDIT) is the gold standard, but shorter versions of this questionnaire<br />
are also available (e.g. AUDIT-C). The AUDIT questionnaires are useful in<br />
detecting problem drinking, but are not diagnostic and should not be used in<br />
isolation. They are freely available on the internet. Readers are referred to the<br />
Department of Health sponsored Alcohol Learning Centre website.<br />
The 10-item AUDIT can be administered as a structured or self-report<br />
interview and takes about 2-3 minutes to complete.<br />
Older screening questionnaires include the CAGE and the Michigan<br />
Alcoholism Screening Test (MAST). These questionnaires tend only to identify<br />
severe or dependent drinking.<br />
AUDIT questionnaire: screen for alcohol misuse [41]<br />
1. How often do you have a drink containing alcohol?<br />
• Never (0)<br />
• Monthly or less (1)<br />
• 2-4 times a month (2)<br />
• 2-3 times a week (3)<br />
• 4 or more times a week (4)<br />
2. How many standard drinks containing alcohol do you have on a typical<br />
day when drinking?<br />
• 1 or 2 (0)<br />
• 3 or 4 (1)<br />
• 5 or 6 (2)<br />
• 7 to 9 (3)<br />
• 10 or more (4)<br />
35
3. How often do you have six or more drinks on one occasion?<br />
• Never (0)<br />
• Less than monthly (1)<br />
• Monthly (2)<br />
• Weekly (3)<br />
• Daily or almost daily (4)<br />
4. During the past year, how often have you found that you were not able<br />
to stop drinking once you had started?<br />
• Never (0)<br />
• Less than monthly (1)<br />
• Monthly (2)<br />
• Weekly (3)<br />
• Daily or almost daily (4)<br />
5. During the past year, how often have you failed to do what was<br />
normally expected of you because of drinking?<br />
• Never (0)<br />
• Less than monthly (1)<br />
• Monthly (2)<br />
• Weekly (3)<br />
• Daily or almost daily (4)<br />
6. During the past year, how often have you needed a drink in the morning<br />
to get yourself going after a heavy drinking session?<br />
• Never (0)<br />
• Less than monthly (1)<br />
• Monthly (2)<br />
• Weekly (3)<br />
• Daily or almost daily (4)<br />
7. During the past year, how often have you had a feeling of guilt or<br />
remorse after drinking?<br />
• Never (0)<br />
• Less than monthly (1)<br />
• Monthly (2)<br />
• Weekly (3)<br />
• Daily or almost daily (4)<br />
36
8. During the past year, have you been unable to remember what<br />
happened the night before because you had been drinking?<br />
• Never (0)<br />
• Less than monthly (1)<br />
• Monthly (2)<br />
• Weekly (3)<br />
• Daily or almost daily (4)<br />
9. Have you or someone else been injured as a result of your drinking?<br />
• No (0)<br />
• Yes, but not in the past year (2)<br />
• Yes, during the past year (4)<br />
10. Has a relative or friend, doctor or other health worker been concerned<br />
about your drinking or suggested you cut down?<br />
• No (0)<br />
• Yes, but not in the past year (2)<br />
• Yes, during the past year (4)<br />
Scoring the audit<br />
Scores for each question range from 0 to 4; thus the maximum score is 40. A<br />
score of 8 or more is associated with harmful or hazardous drinking; a score<br />
of 13 or more in women, and 15 or more in men, is likely to indicate alcohol<br />
dependence.<br />
The AUDIT-C comprises the first three questionnaires of the AUDIT. Anyone<br />
scoring 5 or over on the AUDIT-C is AUDIT-C positive and should go on to<br />
complete the 10-item AUDIT.<br />
37
38
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
Best practice in the<br />
management of epidural<br />
analgesia in the hospital<br />
setting<br />
FACULTY OF PAIN MEDICINE<br />
of The Royal College of Anaesthetists<br />
Royal College of<br />
Anaesthetists<br />
Royal College of<br />
Nursing<br />
Association of<br />
Anaesthetists of Great<br />
Britain and Ireland<br />
British Pain Society<br />
European Society of<br />
Regional Anaesthesia<br />
and Pain Therapy<br />
Association of Paediatric<br />
Anaesthetists of Great<br />
Britain and Ireland<br />
November 2010
Contents<br />
Page<br />
1 Introduction 2<br />
2 Scope of recommendations 2<br />
3 Patient selection and consent 3<br />
4 Personnel, staffing levels and ward environment 3<br />
5 Catheter insertion 4<br />
6 Equipment 5<br />
7 Drugs for epidural analgesia 6<br />
8 Patient monitoring 7<br />
9 Epidural analgesia in children 8<br />
10 Documentation, guidelines and protocols 10<br />
11 Audit and critical incidents 10<br />
12 Education 10<br />
References 11<br />
Guideline development 12<br />
1
1 Introduction<br />
1.1 Epidural analgesia is highly effective for<br />
controlling acute pain after surgery or<br />
trauma to the chest, abdomen, pelvis<br />
or lower limbs. It has the potential to<br />
provide excellent pain relief, minimal<br />
side-effects and high patient satisfaction<br />
when compared with other methods of<br />
analgesia. However, epidural analgesia can<br />
cause serious, potentially life-threatening<br />
complications; safe and effective<br />
management requires a co-ordinated<br />
multidisciplinary approach.<br />
1.2 This document is a revised version of the<br />
guideline published in 2004. 1 In 2009,<br />
the Royal College of Anaesthetists published<br />
the results of a nationwide audit of major<br />
complications associated with central<br />
neuraxial block in the UK. 2 These data have<br />
significantly informed this guideline.<br />
1.3 All practitioners should be aware of the<br />
complications associated with the use of<br />
epidural analgesia. Some complications<br />
can be fatal or result in permanent harm.<br />
Frequent complications include:<br />
hypotension;<br />
respiratory depression (opioid use);<br />
motor block;<br />
urinary retention;<br />
inadequate analgesia;<br />
pruritus (opioid use).<br />
Infrequent but well recognised<br />
complications include:<br />
cardiovascular collapse;<br />
respiratory arrest;<br />
unexpected development of high block,<br />
e.g. catheter migration, intrathecal<br />
injection; local anaesthetic toxicity;<br />
post dural puncture headache syndrome<br />
(including sub-dural haematoma);<br />
drug administration errors (especially<br />
wrong route);<br />
pressure sores;<br />
superficial infection around catheter;<br />
epidural haematoma or abscess;<br />
meningitis;<br />
spinal cord ischaemia;<br />
permanent harm, e.g. paraplegia, nerve<br />
injury.<br />
2 Scope of recommendations<br />
2.1 These guidelines are concerned with the<br />
management of epidural analgesia in<br />
the hospital setting, including continuous<br />
infusions, patient-controlled epidural<br />
analgesia (PCEA) and intermittent top-up<br />
injections. They are not concerned with<br />
the management of epidural analgesia for<br />
obstetrics, palliative care or management of<br />
persistent non-cancer pain.<br />
2.2 The features of an epidural pain<br />
management service are described. These<br />
recommendations should be considered<br />
with other guidelines on the provision of<br />
acute pain services. 3–4<br />
2 Best practice in the management of epidural analgesia in the hospital setting
3 Patient selection and consent<br />
3.1 Patient selection for epidural analgesia should be based<br />
on a careful risk/benefit analysis for each patient. Risk<br />
factors include: impairment of coagulation (pathological or<br />
therapeutic); infection; compromised immunity; duration of<br />
epidural catheterisation; cardiovascular stability; and inadequate<br />
postoperative monitoring capability.<br />
3.2 Continuous epidural analgesia is a significant procedure with<br />
specific and potentially serious complications; therefore,<br />
informed patient consent should be obtained. The process<br />
of obtaining consent should comply with national and local<br />
guidance. There should be a discussion of the risks and<br />
potential benefits of epidural analgesia, including information<br />
on late complications that may occur after discharge from<br />
hospital. A summary of this discussion should be documented<br />
in the patient’s notes. Consent should be facilitated by written<br />
patient information. A suitable leaflet 5 is available on the Royal<br />
College of Anaesthetists’ website; it is not copyrighted and can<br />
be modified to account for local factors.<br />
4 Personnel, staffing levels and ward<br />
environment<br />
4.1 The Department of Anaesthesia should ensure that there are<br />
designated personnel and clear protocols to support the safe<br />
and effective use of epidural analgesia. This should be the<br />
responsibility of a multidisciplinary Acute Pain Service including<br />
a consultant anaesthetist and clinical nurse specialist(s) with<br />
support from pharmacy. 3–4 The service should ensure that<br />
appropriate documentation, administrative routines and audit<br />
are in place.<br />
3
4.2 Ultimate responsibility for the epidural<br />
infusion remains with the practitioner who<br />
instituted it (or supervising consultant if<br />
inserted by a trainee). However, immediate<br />
supervision of the patient may be passed<br />
to the Acute Pain Service and properly<br />
trained ward staff. An agreed form of<br />
communication should be used to facilitate<br />
this transfer of supervision.<br />
4.3 Trainee and Staff and Associate Specialist/<br />
Specialty doctors must possess appropriate<br />
competencies before performing epidural<br />
injections and establishing infusions without<br />
the direct supervision of a consultant or<br />
senior colleague. These are well defined,<br />
regularly reviewed and available from the<br />
Royal College of Anaesthetists and Faculty<br />
of Pain Medicine websites.<br />
4.4 There must be adequate handover of<br />
information between on-call staff about<br />
patients who are receiving epidural<br />
analgesia. Ideally, an up-to-date list of<br />
ongoing epidurals should be maintained<br />
and readily available.<br />
4.5 Nurses with specific training and skills in<br />
the supervision of epidural analgesia and<br />
management of its complications must be<br />
present on the ward and on every shift<br />
(i.e. 24-hour cover). Staffing levels and<br />
expertise should be sufficient to enable<br />
adequate monitoring and care to be given<br />
to all patients receiving epidural analgesia.<br />
These staff must be immediately available<br />
to respond to adverse events. Oxygen<br />
and full resuscitation equipment must be<br />
available.<br />
4.6 Patients receiving epidural analgesia should<br />
be situated close to the nurses’ station, thus<br />
ensuring close supervision. If nursing in a<br />
single room is being considered, a full risk<br />
assessment with respect to the epidural<br />
should be undertaken and staff should be<br />
sure that appropriate monitoring and care<br />
can take place in this environment.<br />
4.7 Before the patient returns to the ward, the<br />
responsible anaesthetist should be assured<br />
that the ward is sufficiently staffed to ensure<br />
safe management of the epidural. A system<br />
of communication should exist to inform<br />
the anaesthetist and theatre staff if this is<br />
inadequate.<br />
4.8 There should be 24-hour access to:<br />
i medical staff, trained and competent<br />
in the management of epidurals,<br />
immediately available to attend patients;<br />
ii senior anaesthetic advice and<br />
availability; and<br />
iii a resuscitation team with a resident<br />
doctor with appropriate competencies.<br />
5 Catheter insertion<br />
5.1 Epidural catheter insertion must be<br />
performed using an aseptic technique. This<br />
should include hand washing, sterile gloves,<br />
sterile gown, hat, mask, appropriate skin<br />
preparation and sterile drapes around the<br />
injection site.<br />
4 Best practice in the management of epidural analgesia in the hospital setting
5.2 The tip of the epidural catheter should be positioned at a spinal<br />
level appropriate for the surgery. A catheter placed in a low<br />
position may be associated with poor analgesia and need for<br />
large volumes of infusion in adults.<br />
5.3 The catheter should be secured in order to minimise<br />
movement in or out of the epidural space. The dressing should<br />
allow easy visibility of the insertion site and catheter.<br />
5.4 Anaesthetists inserting epidural catheters should be aware<br />
of, and adhere to, local infection guidelines (including use of<br />
prophylactic antibiotics in special circumstances).<br />
5.5 Local guidelines should be in place with respect to the insertion<br />
and removal of epidurals in patients on anticoagulants or with<br />
impaired coagulation. All staff should be aware of, and adhere<br />
to, these guidelines.<br />
6 Equipment<br />
6.1 Ideally, equipment for epidural insertion and infusion should<br />
be standardised throughout the institution so that it is familiar<br />
to all staff providing or supervising epidural analgesia. Staff<br />
must be trained in the use of this equipment.<br />
6.2 Infusion pumps should be configured specifically for epidural<br />
analgesia with pre-set limits for maximum infusion rate and<br />
bolus size; lock-out time should be standardised if used for<br />
PCEA. Pumps should be designated for epidural analgesia<br />
only and should be labelled as such. 6 There should be a<br />
documented maintenance programme.<br />
6.3 The epidural infusion system between the pump and patient<br />
must be considered as closed; there should be no injection<br />
ports. An anti-bacterial filter must be inserted at the junction of<br />
epidural catheter and infusion line.<br />
5
6.4 Effective management of epidural analgesia<br />
may require the administration of a bolus<br />
injection of solution into the system. This<br />
may be performed using the syringe within<br />
the pump, thus not breaching the system.<br />
If a separate handheld syringe is used, the<br />
injection must be performed using a strict<br />
aseptic technique. Bolus injections must be<br />
performed by staff with appropriate training<br />
and competencies and more intensive<br />
monitoring of the patient is required<br />
immediately after the injection.<br />
6.5 Epidural infusion lines should be<br />
clearly identified as such. The National<br />
Patient Safety Association (NPSA) has<br />
recommended the use of yellow tubing<br />
to differentiate epidural/spinal lines from<br />
arterial (red), enteral (purple) and regional<br />
(grey) infusions. 7<br />
6.6 In November 2009, the NPSA<br />
recommended that equipment should be<br />
developed that will enable NHS institutions<br />
to perform all epidural, intrathecal and<br />
regional infusions and boluses with devices<br />
that will not connect with intravenous Luer<br />
connectors or intravenous infusion spikes. 8<br />
Practitioners involved in the use of epidural<br />
analgesia should be aware of this project<br />
and respond to further national guidance.<br />
6.7 Resuscitation equipment, oxygen and<br />
appropriate drugs must be readily available<br />
wherever epidural infusions are employed.<br />
7 Drugs for epidural analgesia<br />
7.1 There should be a limited number of<br />
solutions approved and available for<br />
epidural infusions in every hospital. 6<br />
They should be prepared under strict<br />
sterile conditions in specifically designed<br />
units. Many are available commercially.<br />
Any variation from this should occur in<br />
exceptional circumstances only and with the<br />
agreement of the responsible consultant<br />
after a risk/benefit analysis.<br />
7.2 Epidural infusions should be labelled ‘For<br />
Epidural Use Only’. 6<br />
7.3 Epidural infusions should be stored in<br />
separate cupboards or refrigerators from<br />
those holding intravenous and other types<br />
of infusions in order to reduce the risk of<br />
wrong route administration. 6<br />
7.4 The lowest possible effective concentration<br />
of local anaesthetic should be used in order<br />
to preserve motor function as much as<br />
possible. This improves patient satisfaction<br />
and aids detection of neurological<br />
complications. If higher concentrations<br />
are required, the infusion rate should be<br />
reduced periodically to allow assessment of<br />
motor block.<br />
7.5 The use of drugs beyond licence should<br />
be consistent with local hospital guidelines.<br />
and informed by recommendations of the<br />
British Pain Society. 9<br />
6 Best practice in the management of epidural analgesia in the hospital setting
8 Patient monitoring<br />
8.1 Patients must be monitored closely throughout the period of<br />
epidural analgesia. It should be performed by trained staff<br />
aware of its significance and action required in response to<br />
abnormal values. Monitoring should include:<br />
heart rate and blood pressure;<br />
respiratory rate;<br />
sedation score;<br />
temperature;<br />
pain score;<br />
degree of motor and sensory block.<br />
8.2 In addition, requirements for monitoring will be determined by<br />
the nature of the surgery, and condition and age of the patient.<br />
8.3 The frequency of observations should be determined by<br />
normal clinical considerations. With respect to the epidural,<br />
they should be more frequent in the first 12 hours of the<br />
epidural infusion, after top-up injections, changes of infusion<br />
rate and in periods of cardiovascular or respiratory instability.<br />
8.4 Monitoring should follow clear written protocols and<br />
compliance to these should be audited.<br />
8.5 Epidural blockade can cause hypotension. However, when<br />
hypotension occurs after surgery, other common causes<br />
should be considered and excluded, e.g. bleeding, myocardial<br />
insufficiency, sepsis, pulmonary embolus, dehydration.<br />
8.6 Pain scores (at rest and on movement or deep breathing) and<br />
sedation scores will help to identify inadequate or excessive<br />
epidural drug administration. Monitoring protocols should give<br />
clear guidance on actions required if analgesia is inadequate.<br />
8.7 Sedation is often the most sensitive indication of opioidinduced<br />
respiratory depression.<br />
7
8.8 Monitoring of sensory and motor block<br />
is essential for the early detection of<br />
potentially serious complications. The<br />
Bromage Scale is an accepted tool for<br />
the measurement of motor block. 10 An<br />
increasing degree of motor weakness<br />
usually implies excessive epidural drug<br />
administration. However, it can indicate<br />
very serious complications including<br />
dural penetration of the catheter, or the<br />
development of an epidural haematoma<br />
or abscess. Therefore, it is essential<br />
that protocols are in place to manage<br />
the scenario of excessive motor block.<br />
Examples of suitable algorithms and specific<br />
advice on protocols for this situation<br />
are given in the report on the audit of<br />
major complications of central neuraxial<br />
block performed by the Royal College of<br />
Anaesthetists. 2<br />
8.9 An epidural abscess or haematoma can<br />
cause severe, permanent neurological<br />
damage and must be detected and treated<br />
as soon as possible. This diagnosis must<br />
be considered if excessive motor block<br />
does not resolve rapidly after stopping the<br />
epidural infusion. A clear protocol should<br />
be in place describing the actions required<br />
in this situation, including informing senior<br />
anaesthetic staff and immediate availability<br />
of suitable imaging and surgical expertise.<br />
8.10 Records must be kept of the monitoring<br />
described above as well as epidural infusion<br />
rate, total amount used, inspection of<br />
epidural insertion site, patency of intravenous<br />
access and integrity of pressure<br />
areas.<br />
8.11 Staff should be aware that increased or<br />
breakthrough pain may indicate surgical<br />
complications including the development<br />
of compartment syndromes. Special care<br />
should be taken when interpreting physical<br />
signs in patients who may have sustained<br />
neurological damage.<br />
9 Epidural analgesia in children<br />
9.1 All the recommendations in this guideline<br />
apply also to neonates, infants and<br />
children but methods of monitoring and<br />
assessment scores must be appropriate for<br />
developmental age. 11<br />
9.2 Dosing regimens for children must be<br />
adapted for age and weight with maximum<br />
dosage clearly defined to minimise the<br />
risk of cumulative local anaesthetic toxicity,<br />
especially in neonates and infants < three<br />
months of age. 11<br />
9.3 Clear protocols for prescription, monitoring<br />
and troubleshooting of paediatric epidural<br />
infusions should be used. Infusion devices<br />
should be programmed and double<br />
checked with extreme care as there is an<br />
increased risk of error when managing<br />
small infants and neonates. 12<br />
8 Best practice in the management of epidural analgesia in the hospital setting
9.4 Hourly assessments are recommended, especially in the first 12<br />
hours. There should be regular review of the need to continue<br />
the infusion, especially after 48 hours.<br />
9.5 Motor block should be assessed and documented formally<br />
using an age-appropriate assessment. A clear action plan<br />
should be in place if motor block persists or progresses.<br />
9.6 Spread of local anaesthetics in neonates and infants is extensive<br />
and low catheters can be used to provide an effective block for<br />
thoraco-lumbar dermatomes without using unacceptable doses<br />
of local anaesthetic. Whilst caudal catheters are effective, these<br />
can become soiled unless carefully dressed or tunnelled away<br />
from the insertion site.<br />
9.7 Compartment syndrome is a particular concern after very<br />
prolonged procedures, after lower limb surgery and when the<br />
patient has been positioned during surgery in other than the<br />
standard supine position. 12<br />
9.8 An anaesthetist with appropriate competencies and training<br />
should be immediately available to attend a child who is<br />
receiving an epidural infusion.<br />
9.9 The use of drugs beyond licence has been discussed in 7.5.<br />
Specific advice with respect to children has been published by<br />
the Association of Paediatric Anaesthetists of Great Britain and<br />
Ireland. 11<br />
9.10 Written and verbal advice should be provided to patients<br />
and carers alerting them to the signs and symptoms of an<br />
epidural abscess and what to do if they occur. Many children<br />
are discharged before the mean time of onset of these signs<br />
and symptoms. An information leaflet for parents and older<br />
children 13 is available on the Royal College of Anaesthetists’<br />
website.<br />
9
10 Documentation, guidelines<br />
and protocols<br />
10.1 Contemporaneous records must be kept of<br />
events throughout the period of epidural<br />
analgesia. This includes consent, insertion<br />
and removal of the catheter, prescription of<br />
the infusion, monitoring, additional doses<br />
and notes about any complications or<br />
adverse events.<br />
10.2 Safety is enhanced by the use of standard<br />
pre-printed prescription forms rather than<br />
hand written prescriptions that might be<br />
misinterpreted.<br />
10.3 Contact telephone and/or bleep numbers<br />
for expert medical and nursing personnel<br />
must be printed on documents that are<br />
kept on the ward, and near to the patient.<br />
10.4 Protocols and guidelines should include;<br />
overall management of patients with<br />
epidural infusions;<br />
instructions for the use of the pump;<br />
description of the drug concentrations<br />
used in the hospital;<br />
description of infusion rates and how to<br />
adjust them;<br />
instructions for changing epidural solution<br />
bags or syringes;<br />
frequency of observations;<br />
maintenance of intravenous access<br />
throughout the infusion period;<br />
identification and management of early<br />
and late complications;<br />
management of inadequate analgesia;<br />
management of accidental catheter<br />
disconnection;<br />
instructions for removal of the epidural<br />
catheter and monitoring for complications;<br />
insertion and removal of epidural catheters<br />
in patients receiving anticoagulants;<br />
pain management after cessation of the<br />
epidural infusion;<br />
management of opioid and local<br />
anaesthetic toxicity;<br />
mobilisation after epidural removal,<br />
e.g. during enhanced recovery<br />
programmes.<br />
11 Audit and critical incidents<br />
11.1 There should be regular audits concerned<br />
with epidural analgesia. These could<br />
include:<br />
efficacy and patient satisfaction;<br />
incidence of complications;<br />
adherence to management protocols.<br />
11.2 There should be clear procedures for the<br />
reporting of, and response to, critical incidents<br />
associated with the use of epidural analgesia.<br />
12 Education<br />
12.1 There should be formal, documented<br />
training in place for doctors and nurses who<br />
are responsible for supervising patients<br />
receiving epidural analgesia.<br />
12.2 Training programmes should include<br />
induction and regular update sessions and<br />
be commensurate with the responsibilities<br />
of the staff involved.<br />
10 Best practice in the management of epidural analgesia in the hospital setting
References<br />
1 Good practice in the management of continuous epidural analgesia in<br />
the hospital setting. RCoA, London 2004 (www.rcoa.ac.uk/docs/Epid-<br />
Analg.pdf).<br />
2 The 3rd national audit project of the Royal College of Anaesthetists. Major<br />
complications of central neuroaxial block in the United Kingdom. RCoA,<br />
London 2009 (www.rcoa.ac.uk/index.asp?PageID=717).<br />
3 Guidelines for the provision of anaesthetic services. RCoA, London<br />
2009 (www.rcoa.ac.uk/index.asp?PageID=477).<br />
4 Pain management services: good practice. RCoA and BPS, London<br />
2003 (www.rcoa.ac.uk/docs/painservices.pdf).<br />
5 Epidurals for pain relief after surgery. RCoA, London 2008 (www.rcoa.<br />
ac.uk/index.asp?PageID=1499).<br />
6 Patient safety alert: Safer practice with epidurals injections and infusions.<br />
NPSA, London 2007 (www.nrls.npsa.nhs.uk/EasySiteWeb/getresource.<br />
axd?AssetID=60063&type=full&servicetype=Attachment).<br />
7 Design for patient safety: a guide to the design of electronic<br />
infusion devices. NPSA, London 2010 (www.nrls.npsa.nhs.uk/<br />
resources/?EntryId45=68534).<br />
8 Patient safety alert: Safer spinal (intrathecal), epidural and regional<br />
devices – Part B. NPSA, London 2009 (www.nrls.npsa.nhs.uk/<br />
resources/?EntryId45=65259).<br />
9 The use of drugs beyond licence in palliative care and pain management.<br />
A position statement prepared on behalf of the Association for Palliative<br />
Medicine and the British Pain Society. APM and BPS, London 2005<br />
(www.britishpainsociety.org/pub_professional.htm#drugsmain).<br />
10 Description of the Bromage Scale. The 3rd national audit project of the<br />
Royal College of Anaesthetists. Major complications of central neuroaxial<br />
block in the United Kingdom. RCoA, London 2009 (pg 142) (www.rcoa.<br />
ac.uk/index.asp?PageID=717).<br />
11 Good practice in postoperative and procedural pain. APAGBI, London<br />
2008 (www.britishpainsociety.org/pub_professional.htm#apa).<br />
12 Llewellyn N, Moriarty A. The national pediatric epidural audit. Pediatric<br />
Anesthesia 2007;17:520–533 (http://onlinelibrary.wiley.com/<br />
doi/10.1111/j.1460-9592.2007.02230.x/full).<br />
13 An epidural for pain relief after surgery in children. RCoA, London 2009<br />
(www.rcoa.ac.uk/docs/EPRASC.pdf).<br />
11
Guideline development<br />
Members of the working group considered the original version of the guidelines 1 in detail and modified<br />
them in accordance with the current evidence base and recent guidelines published by relevant<br />
professional bodies. Where there was a paucity of evidence to inform changes, these were derived<br />
by obtaining the consensus opinion of the group members. The proposed new guidelines were then<br />
submitted to the governing bodies of the endorsing professional organisations for consideration and<br />
approval. In addition, views of the Regional Advisors of the Faculty of Pain Medicine were obtained.<br />
This process led to further minor changes and the final published version.<br />
The original version 1 did not consider the use of epidurals in obstetric practice. The present working<br />
group decided that this was entirely appropriate as many obstetric factors influence their safe and<br />
effective management.<br />
Members of guideline development group<br />
Professor David Rowbotham (Group Chair, Faculty of Pain Medicine)<br />
Dr Jeremy Cashman (Faculty of Pain Medicine)<br />
Dr David Counsell (British Pain Society)<br />
Ms Felicia Cox (Pain Management Nursing)<br />
Dr Paulah Crawford (Clinical Pharmacist)<br />
Dr John Goddard (Paediatric Anaesthesia and Pain Medicine)<br />
Dr Simon Higgs (Royal College of Nursing)<br />
Dr Roger Laishley (Faculty of Pain Medicine)<br />
Dr Neil Morton (Association of Paediatric Anaesthetists of Great Britain and Ireland)<br />
Dr Barry Nicholls (European Society of Regional Anaesthesia)<br />
Dr Felicity Plaat (Association of Anaesthetists of Great Britain and Ireland)<br />
Professor Ian Power (Faculty of Pain Medicine)<br />
Mrs Kate Rivett (Patient and Public Representative)<br />
Revision date: November 2015<br />
12 Best practice in the management of epidural analgesia in the hospital setting
INSIDE BACK COVER – TO BE LEFT BLANK
faculty of pain medicine<br />
Churchill House 35 Red Lion Square London WC1R 4SG<br />
020 7092 1673/1729 fpm@rcoa.ac.uk<br />
www.rcoa.ac.uk/fpm<br />
© 2010 Design and layout by The Royal College of Anaesthetists<br />
Registered Charity No: 1013887 VAT Registration No: GB 927 2364 18 Registered Charity in Scotland No: SCO37737
Fatigue and Anaesthetists<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650 Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org October 2014
Membership of the working party<br />
(details correct at the start of the working party process)<br />
Dr Kathleen Ferguson<br />
Dr Felicity Howard<br />
Dr Chris Idzikowski<br />
Dr Barry Nicholls<br />
Dr Mike Peters<br />
Dr Felicity Plaat<br />
AAGBI, Chair of working party<br />
GAT<br />
Edinburgh University Sleep Centre<br />
AAGBI<br />
BMA<br />
AAGBI<br />
© The Association of Anaesthetists of Great Britain & Ireland 2014
Contents<br />
1. Preface 2<br />
2. Recommendations 3<br />
3. Introduction 4<br />
4. Why are anaesthetists at risk of fatigue? 6<br />
5. What are the risks? 7<br />
6. How can fatigue be avoided, modified, or managed? 8<br />
7. References 9-11<br />
8. Appendices 1-4 12-16<br />
This is a consensus document produced by expert members of a Working Party<br />
established by the Association of Anaesthetists of Great Britain and Ireland<br />
(AAGBI). It updates and replaces previous guidance published in July 2004. It has<br />
been seen and approved by the AAGBI Board.<br />
• What other guideline statements are available on this topic?<br />
There are several guideline statements published by other healthcare<br />
professional groups within the UK and overseas. Some high fidelity industries<br />
provide evidence-based guidance on fatigue management to their employees<br />
[1-4].<br />
• Why was this guideline developed?<br />
The original guideline (2004) was developed as a reference document for<br />
individuals and departments when considering the effects of hours of work and<br />
type of work undertaken in anaesthesia on clinician’s performance and<br />
wellbeing. The primary goal was to improve patient safety.<br />
• How and why does this statement differ from existing guidelines?<br />
This new guidance is an update on the previous document. Additional research<br />
on the impact of the European Working Time Directive on clinician performance<br />
and fatigue provides new evidence to support the recommendations.<br />
Date of review: 2018<br />
1
1. Preface<br />
The first edition of the Fatigue and Anaesthetists guideline was published in 2004<br />
in paper and extended web versions. The document provided recommendations<br />
on how to anticipate and mitigate the effects of fatigue for anaesthetists in the<br />
workplace. A major driver in producing the document was to reduce risk to patients<br />
by considering the impact of fatigue on anaesthetists’ performance and wellbeing<br />
and thus, in turn, on the incidence of critical incidents in practice.<br />
Since 2004, the effects of the New Deal agreement for junior doctors’ working<br />
hours and the enforcement of the European Working Time Directive (EWTD) have<br />
taxed departments in their ability to deliver service and training. Hours of work<br />
were cut drastically; previously rotas often covered over 80 hours per week. Acute<br />
care specialities have been adversely affected and anaesthesia, in particular, due<br />
to the intensity of out-of-hours work and the number of rotas to be covered by single<br />
departments.<br />
Nine years on, 48 hours are the suggested contractual maximum for job plans.<br />
Out-of-hours rotas have survived the move by variable means: introduction of<br />
hybrid rotas, complex on-call arrangements and full and partial shift patterns. The<br />
resulting squeeze on training time has produced a knock-on effect on consultant<br />
working patterns: many departments have consultants first or second on-call in<br />
theatre, labour ward and intensive care medicine.<br />
Evidence is growing of new working patterns, shift types and their effects in the<br />
healthcare setting. There is also increasing evidence of the detrimental effects of<br />
extended working hours and shift patterns on individual wellbeing [5, 6].<br />
The Fatigue and Anaesthetists publication is being refreshed, adding current<br />
evidence to support the recommendations. Changing service and training demands<br />
plus increased requirement for professional accountability all add to the pressure of<br />
a high-intensity time-pressured job. This AAGBI resource hopes to serve as an aid<br />
to managing fatigue in individuals and departments.<br />
2
2. Recommendations<br />
• In keeping with the General Medical Council (GMC) guidance in Good Medical<br />
Practice [7], every doctor is required to provide safe and effective care and<br />
therefore should be aware of the issues of fatigue. (2004)<br />
• Departments must have a plan to manage staff of all grades who have<br />
undertaken an onerous duty period and consider themselves unfit to continue<br />
work. (2004)<br />
• Job plans should be constructed such that they are not likely to lead to<br />
predictable fatigue. (2004)<br />
• Routine rest breaks should be implemented [8]. (2004)<br />
• Handover protocols should be used before and after every rest break. (2004)<br />
• Rest facilities and on-call rooms should be available for staff to nap during<br />
shifts or sleep post-call. (Updated 2013)<br />
• Resident on-call staff should have suitable accommodation. (2004)<br />
• Refreshments should be available at all times. (2004)<br />
• On-call responsibilities should be reviewed regularly and, particularly in the<br />
older anaesthetist, take into consideration subjective assessment of fatigue<br />
(consider seeking advice from an accredited specialist in occupational<br />
medicine). (Updated 2013)<br />
• Education on fatigue, its causes, mitigating factors, and its impact on healthcare<br />
should be a priority for anaesthesia departments. (New 2013)<br />
3
3. Introduction<br />
What is fatigue?<br />
Fatigue is a subjective feeling of the need to sleep, an increased physiological drive<br />
to fall asleep and a state of decreased alertness [9]. Its consequences include a<br />
decreased capacity to perform mental or physical tasks and are manifest in reduced<br />
physiological performance and cognitive impairment [3]. Inadequate sleep is the<br />
most important single factor impacting on fatigue. Common scenarios leading to<br />
sleep-related fatigue include insufficient sleep, prolonged wakefulness and being<br />
awake when normally one would be asleep [10].<br />
Fatigue may manifest itself in characteristic behaviour patterns that vary between<br />
individuals: yawning and difficulty staying awake, poor concentration and coordination,<br />
head drooping, eye rubbing or heavy eyelids, general feelings of lethargy,<br />
lacking motivation, error events and lapses in attention [4]. As an alternative to<br />
self- or colleague-assessment of observed behaviours, the risk of fatigue may<br />
be quantified subjectively using tools such as the Samn Perelli checklist<br />
(Appendix 1) [11]. Objective assessment is out of the individual’s capability but<br />
subjective assessment along with a sleep diary (Appendix 2) and good practices<br />
can be used to demonstrate appropriate rest during and between periods of work.<br />
What is sleep and how much of it is optimum?<br />
Sleep is a complex physiological process during which the brain remains active<br />
but is less responsive to external stimuli, while undertaking tissue healing and<br />
repair and consolidation of learning and memory. Normal sleep consists of several<br />
phases and is associated with specific EEG patterns and physiological changes.<br />
Sleep follows a diurnal rhythm sleep-wake cycle and is controlled by a circadian<br />
pacemaker in the suprachiasmatic nucleus in the hypothalamus. Research has<br />
demonstrated that the circadian pacemaker would naturally function within a 25-<br />
hour cycle. Light input via the retina and other external stimuli called zeitgebers<br />
act to maintain the sleep-wake cycle within the 24-hour day/night cycle [12, 13].<br />
Sleepiness peaks twice in any 24-hour period: 02.00-04.00 and 13.00-15.00.<br />
The circadian rhythm ensures that the best sleep is achieved when going to bed<br />
between 22.00 and 02.00 and that there is difficulty in sleeping during 08.00-12.00<br />
and 17.00-21.00. The potential adverse impact upon shift workers is obvious.<br />
4
Most adults require eight hours of restorative sleep each night. This varies<br />
between individuals. Restorative sleep may be inadequate due to reduced quality<br />
(awakenings during sleep periods) or insufficient time afforded to sleep. When<br />
sleep is restricted for two or more consecutive nights, a sleep debt accumulates.<br />
Two consecutive nights of restorative sleep is required to recover from significant<br />
sleep loss [14]. Evidence shows that moderate sleep restriction to six hours per<br />
night for two weeks leads to performance reduction equivalent to one night with<br />
total sleep deprivation [15].<br />
When wakefulness is extended beyond what is normal (16-18 hours), cognitive<br />
function is impaired [15, 16]. This may manifest as slow response time, increase in<br />
attention lapse frequency and impaired memory functions, addition and subtraction<br />
ability, and decision-making. Periods of extended wakefulness may be quantified<br />
in terms of the effects of an equivalent blood alcohol level [17]: after 20 hours<br />
of wakefulness (coincident with a circadian low point) performance is impaired<br />
equivalent to that with a blood alcohol of 0.1% (100 mg.100 ml -1 blood). The legal<br />
limit for driving in the UK is 80 mg.100 ml-1 blood. Night workers have been shown<br />
to be at increased risk of vehicle accidents in association with sleep-related fatigue<br />
[18, 19].<br />
Sleep patterns change with age. The requirement for eight hours sleep remains but<br />
the periods of REM sleep are reduced, leading to sleep fragmentation [20]. There<br />
is a reduction in the depth and consolidation of sleep. Older people suffer from<br />
frequent and early awakenings with an exaggerated dip in arousal mid afternoon.<br />
The ability to recover from a sleep debt is decreased and so the older anaesthetist<br />
may be less able to cope with night shift work [21, 22]. Although those over 55<br />
years are considered aged persons in terms of work physiology, intolerance to night<br />
shift and shift work may begin as early as 45-50 years of age. There is considerable<br />
individual variation in susceptibility and physical, psychological and social factors<br />
all play a role [23].<br />
Fatigued individuals may suffer from sleep lapses or ‘microsleeps’ where they<br />
remain unresponsive to external stimuli for very short periods of time (seconds<br />
to minutes). These episodes of sleep are spontaneous, brief and uncontrolled<br />
[24]. Sleep inertia is characterised by a temporary disturbance in performance on<br />
awakening. Its duration depends on the depth of sleep at the time of wakening and<br />
sleep deprivation enhances its appearance [25, 26].<br />
5
4. Why are anaesthetists at risk of fatigue?<br />
Intensity and type of working<br />
Fatigue is a function of time on task; the longer the hours of working, the greater<br />
the risk of fatigue developing [27]. It is also important to recognise that time spent<br />
awake may be substantial given the other demands when balancing daily living and<br />
working. This may be particularly relevant to staff with young families and those<br />
with other responsibilities. There is a near exponential rise in errors associated with<br />
increased time on task. Long shifts (12 hours) lead to a doubling of risk compared<br />
with an eight-hour shift [27]. This must be taken into consideration when planning<br />
for long surgical procedures. The previous working party concluded that ”a 12-hour<br />
working day is not acceptable working practice for an individual anaesthetist of any<br />
grade”. Current evidence would agree with this statement.<br />
The complexity of tasks affects the state of fatigue. Regular activity serves to<br />
reduce fatigue while mundane and lengthy tasks increase the likelihood of fatigue<br />
developing [28].<br />
Sleep disturbance – on-call<br />
On-call patterns of work predispose to poor quality sleep for several possible<br />
reasons: unplanned interruptions move sleep opportunities out of sync with<br />
circadian rhythm and poor timing of zeitgeber stimuli adversely affect the circadian<br />
sleep/wake cycle. In a recent online survey of AAGBI members (Appendix 3), ><br />
60% of respondents reported working out-of-hours as an on-call pattern. This<br />
activity was associated with post-call tiredness and sleep debt.<br />
Sleep deprivation – shift patterns<br />
Individuals who work shift patterns are at risk of developing poor sleep patterns due<br />
to circadian rhythm disruption. The relative risk of adverse incidents increases as<br />
shifts move from morning to afternoon to night. Risk is greatest at the beginning of<br />
a night shift, and increases over successive night shifts from 17% on the first night<br />
to 36% on the fourth [29].<br />
6
5. What are the risks?<br />
Performance and safety<br />
With adverse effects of fatigue on performance and safety accepted, work should<br />
be organised to take place in daytime hours, making use of increased alertness<br />
and peak performance [29, 30]. Regular breaks should be incorporated into the<br />
working day [31] with comprehensive handover protocols used in support [32].<br />
Wellbeing<br />
Evidence is accruing to support claims of an association between impaired health<br />
and sleep disturbance/deprivation. Shift workers may experience poor dietary<br />
habits, peptic ulceration, increased prevalence of obesity and the development<br />
of the diabetic state. Other conditions associated with fatigued shift workers<br />
include hypertension, transient ischaemic attacks and cerebrovascular accidents.<br />
Further research is required to prove causation following a report on an increased<br />
breast cancer risk in Scandinavian nurses working night shifts [33]. Disturbed<br />
circadian homeostasis is implicated in the pathophysiology of these conditions [34].<br />
Individuals should be encouraged to follow good sleep hygiene practices and to<br />
prepare for periods of duty by ensuring adequate restorative sleep before and after<br />
rostered duties.<br />
Service provision<br />
Restricted hours of work, in conjunction with reducing trainee numbers and central<br />
control of career grade expansion, creates a staffing void for service delivery.<br />
Career grade staff cannot fill this gap without appropriate consideration of the<br />
consultant and staff and associate specialist doctor role in job planning and the<br />
effects of fatigue [35].<br />
All grades of anaesthetist perform out-of-hours work either in an on-call capacity<br />
or in shift patterns. The provision of rest breaks within and at the end of periods<br />
of work must be catered for within department rostering [34]. Planning of shifts<br />
must take into account lengths of shift, numbers of nights worked consecutively<br />
and periods of rest before return to work. Rotas should not consist of more than<br />
four nights in a row. Rotas of nine hours provide the minimum effect on cognitive<br />
function but are difficult and costly (staffing) to organise. Rotas in a forward rolling<br />
pattern (day-evening-night) provide the least adverse effects on sleep patterns [18].<br />
The effects of ageing on sleep and fatigue mean that specific consideration must be<br />
made when allocating of out-of-hours duties to the older anaesthetist.<br />
7
6. How can fatigue be avoided, modified, or managed?<br />
Strategies to reduce and mitigate the effects of fatigue include: good sleep<br />
hygiene, techniques to minimise sleep disturbance (Appendix 4), napping, caffeine<br />
ingestion, bright light exposure, regular rest breaks and exercise, avoiding hunger<br />
and dehydration, maintaining alertness and avoiding alcohol ingestion before a<br />
period of duty [2, 3, 36].<br />
Several industries and organisations such as aviation, transport services, the oil<br />
industry and the Queensland Government Health Department [4] have introduced<br />
fatigue management systems into their practices. This proactive approach<br />
to managing fatigue in the workplace is based on education for all levels of the<br />
team. Diary evidence of sleep patterns and hours of work are kept and assessed<br />
to determine the risk to the individual and the service caused by fatigue. The<br />
initiative in Queensland Health is supported by Government legislation [37] and<br />
departments are required to have contingency plans to support staff when fatigue<br />
raises the risk level unacceptably high. Monitoring is routine.<br />
Electronic devices and apps are available, both to facilitate maintaining a diary of<br />
activity and sleep (Appendix 2), and also for self-assessment of mental performance<br />
[38].<br />
Less is known of the effects that non-technical skill development in individuals<br />
and teams may have on the monitoring, reporting and management of fatigue in<br />
medical practice. The recent GMC review of the effects of the EWTD alludes to this<br />
point and highlights this as an area for research in the future [4, 6].<br />
8
7. References<br />
1. Fatigue Risk Management System for Canadian Aviation Industry – An introduction<br />
to Managing Fatigue. Ottawa: Transport Canada, 2007. http://www.tc.gc.ca/eng/<br />
civilaviation/publications/tp14572-6038.htm (accessed 04/06/2013)<br />
2. Managing Shiftwork: Health and Safety Guidance. London: HSE, 2006. http://www.hse.<br />
gov.uk/pubns/priced/hsg256.pdf (accessed 04/06/2013)<br />
3. Managing fatigue in the workplace. London: IPIECA/OGP, 2007 http://www.ogp.org.uk/<br />
pubs/392.pdf (accessed 04/06/2013)<br />
4. Fatigue Risk Management System Resource Pack. Brisbane: Queensland Health, 2009.<br />
http://www.health.qld.gov.au/hrpolicies/other/FRMS_web.pdf (accessed 13/01/2012)<br />
5. The Impact of the Working Time Regulations on Medical Education and Training:<br />
Literature Review. Durham: Durham University, 2012. http://www.gmc-uk.org/The_<br />
Impact_of_the_Working_Time_Regulations_on_Medical_Education_and_Training___<br />
Literature_Review.pdf_51155615.pdf (accessed 04/06/2013).<br />
6. The Impact of the Working Time Regulations on Medical Education and Training:<br />
Final Report on Primary Research. Durham: Durham University, 2012. http://www.<br />
gmc-uk.org/The_Impact_of_the_Working_Time_Regulations_on_Medical_Education_<br />
and_Training___Final_Report_on_Primary_Research.pdf_51157039.pdf (accessed<br />
04/06/2013).<br />
7. Duties of a doctor. London: General Medical Council. http://www.gmc-uk.org/guidance/<br />
good_medical_practice/duties_of_a_doctor.asp (accessed 04/06/2013).<br />
8. The Working Time Regulations 1998 http://www.legislation.gov.uk/uksi/1998/1833/<br />
contents/made (accessed 04/06/2013)<br />
9. Murray D, Dodds C. The effect of sleep disruption on performance of anaesthetists – a<br />
pilot study. Anaesthesia 2003; 58: 520-25.<br />
10. Akerstedt T. Work hours, sleepiness and the underlying mechanisms. Journal of Sleep<br />
Research 1995;4:15-22<br />
11. Estimating aircrew fatigue: a technique with implications to airlift operations. Fort<br />
Belvoir, VA: Defense Technical Information Center Online, 1982. http://www.dtic.mil/cgibin/GetTRDoc?AD=ADA125319<br />
(accessed 04/06/2013).<br />
12. Brain basics: understanding sleep. Bethesda, MD: National Institute of Neurological<br />
Disorders and Stroke. http://www.ninds.nih.gov/disorders/brain_basics/understanding_<br />
sleep.htm (accessed 04/06/2013).<br />
13. Toh KL. Basic science review of circadian rhythm biology and circadian sleep disorders.<br />
Annals of the Academy of Medicine, Singapore 2008; 37: 662-8.<br />
9
14. Bonnet MH. Sleep Deprivation. In: Kryger MH, Roth T, Dement WC, eds. Principles and<br />
Practice of Sleep Medicine. 3rd edn. Philadelphia: Saunders, 2000: 53-71.<br />
15. Von Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional<br />
wakefulness: dose response effects on neurobehavioural functions and sleep physiology<br />
from chronic sleep restriction and total sleep deprivation. Sleep 2003; 26: 117-26.<br />
16. Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, Lilly CM,<br />
Stone PH, Lockley SW, Bates DW, Czeisler CA. Effect of reducing interns’ work hours<br />
on serious medical errors in intensive care units. New England Journal of Medicine<br />
2004; 352: 1838-48.<br />
17. Dawson D, Reid K. Fatigue, alcohol and performance impairment. Nature 1997; 388:<br />
235.<br />
18. Horrocks N, Pounder R. Working the night shift: preparation, survival and recovery- a<br />
guide for junior doctors. Clinical Medicine 2006; 6: 61-7.<br />
19. Horne J, Reyner L. Vehicle accidents related to sleep: a review. Occupational<br />
Environmental Medicine 1999; 56: 289-94.<br />
20. Redline S, Kirchner HL, Quan SF, Gottlieb DJ, Kapur V, Newman A. The effects of age,<br />
sex, ethnicity, and sleep-disordered breathing on sleep architecture. Archives of Internal<br />
Medicine 2004; 164: 406-18.<br />
21. Katz JD. Issues of concern for the aging anesthesiologist. Anesthesia and Analgesia<br />
2001; 92: 1487-92.<br />
22. Folkard S. Shift work, safety, and aging. Chronobiology International 2008; 25: 183-98.<br />
23. Cost G. Di Milia L. Aging and shift work: a complex problem to face. Chronobiology<br />
International 2008; 25: 165-81.<br />
24. Howard SK, Rosekind MR, Katz JD, Berry AJ. Fatigue in anesthesia: implications and<br />
strategies for patient and provider safety. Anesthesiology 2002; 97: 1281-94.<br />
25. Muzet A, Nicolas A, Tassi P, Dewasmes P, Bonneau A. Implementation of napping in<br />
industry and the problem of sleep inertia. Journal Sleep Research 1995; 4(S2): 67-9.<br />
26. Tassi P, Muzet A. Sleep inertia. Sleep Medicine Reviews 2000; 4: 341-53.<br />
27. Folkard S, Tucker P. Shift work, safety and productivity. Occupational Medicine 2003;<br />
53: 95-101.<br />
28. Weinger MB, Englund CE. Ergonomic and human factors affecting anesthetic<br />
vigilance and monitoring performance in the operating room environment.<br />
Anesthesiology 1990; 73: 995-1021.<br />
29. Folkard S, Lombardi DA, Tucker PT. Shiftwork: safety, sleepiness and sleep. Industrial<br />
Health 2005; 43: 20-3.<br />
10
30. Lockley SW, Barger LK, Ayas NT, Rothschild JM, Czeisler CA, Landrigan CP. Effects of<br />
health care provider work hours and sleep deprivation on safety and performance. Joint<br />
Commission Journal on Quality and Patient Safety 2007; 33: 7-18.<br />
31. Tucker P, Folkard S, Macdonald I. Rest breaks and accident risk. Lancet 2003; 361:<br />
680.<br />
32. Safe handover: safe patients. Guidance on clinical handover for clinicians and managers.<br />
London: BMA. http://bma.org.uk/-/media/Files/PDFs/Practical%20advice%20at%20<br />
work/Contracts/safe%20handover%20safe%20patients.pdf (accessed 04/06/2013).<br />
33. Kolstad HA. Nightshift work and risk of breast cancer and other cancers – a critical<br />
review of the epidemiologic evidence. Scandinavian Journal of Work, Environment and<br />
Health 2008; 34: 5-22.<br />
34. Health effects of working unsocial hours and shift work. A briefing paper from the BMA<br />
Board of Science. London: BMA. http://bmaopac.hosted.exlibrisgroup.com/exlibris/<br />
aleph/a21_1/apache_media/77N84N5KQ1LVMF7XR5FUI6MQNG287F.pdf (accessed<br />
04/01/2013).<br />
35. Association of Anaesthetists of Great Britain and Ireland. Working Arrangements<br />
for Consultant Anaesthetists in the United Kingdom. London: AAGBI, 2011. http://<br />
www.<strong>aagbi</strong>.org/sites/default/files/images/working_arrangements_for_consultant_<br />
anaesthetists_web.pdf (accessed 30/12/2013)<br />
36. Garbariono S, Mascialino B, Penco MA, et al. Professional shift-work drivers who adopt<br />
prophylactic naps can reduce the risk of car accidents during night work. Sleep 2004;<br />
27: 1295-302.<br />
37. Work-related fatigue. Summary of recent regulatory developments. Australian<br />
Government, 2006. http://www.safeworkaustralia.gov.au/sites/SWA/about/Publications/<br />
Documents/419/Workrelated_Fatigue_Summay_Recent_Regulatory_Development.pdf<br />
(accessed 04/06/2013).<br />
38. Sleep Well: Your pocket guide to better sleep. Mental Health Foundation; 2011.<br />
http://www.mentalhealth.org.uk/content/assets/PDF/publications/MHF-Sleep-Pocket-<br />
Guide-2011.pdf?view=Standard (accessed 27/03/2014).<br />
11
8. 8. Appendix 1 1<br />
Subjective Subjective assessment assessment of of fatigue fatigue –– Samn Samn Perelli Perelli checklist checklist<br />
(Accessed via via http://www.dtic.mil/cgi-bin/GetTRDoc?AD=ADA125319)<br />
1. Fully alert, wide awake<br />
2. Very lively, responsive, but not at peak<br />
3. Ok, somewhat fresh<br />
4. A little tired, less than fresh<br />
5. Moderately tired, let down<br />
6. Extremely tired, very difficult to concentrate<br />
7. Completely exhausted, unable to function effectively<br />
12
Appendix 2<br />
Sample Sleep Diary<br />
Date and Name Mon Tues Wed Thurs Fri Sat Sun<br />
Time to bed<br />
Time to wake<br />
Hours of sleep<br />
No. of wakenings<br />
Total time awake<br />
How long to fall asleep<br />
How awake did I feel when I got up<br />
1 = wide awake<br />
2 = awake but a little tired<br />
3 = sleepy<br />
Caffeinated drinks and times<br />
Alcoholic drinks and times<br />
Exercise and times<br />
How sleepy did I feel l during the day<br />
1 = so sleepy I struggled to stay awake<br />
2 = somewhat tired<br />
3 = fairly alert<br />
4 = wide awake<br />
1<br />
13
Appendix 3<br />
Membership Questionnaire 1 (Errors and Fatigue countermeasures)<br />
Have you ever napped/fallen asleep/microslept whilst undertaking anaesthesia?<br />
Total number responding 178<br />
Yes<br />
No<br />
89 89<br />
Do you have knowledge of a colleague who has napped/fallen asleep/microslept 120 58<br />
whilst undertaking anaesthesia?<br />
How old are<br />
you in years?<br />
24-29<br />
8<br />
30-34<br />
31<br />
35-39<br />
28<br />
40-44<br />
28<br />
45-49<br />
27<br />
50-54<br />
28<br />
55-59<br />
21<br />
60-64<br />
7<br />
65+<br />
0<br />
Which grade do you work in?<br />
Training<br />
45<br />
SAS<br />
11<br />
Consultant<br />
121<br />
Which pattern of work do you<br />
undertake to provide out-of-hours<br />
service?<br />
Shift<br />
46<br />
Rostered<br />
extended hours<br />
7<br />
On-call<br />
109<br />
Other<br />
13<br />
Have you made mistakes in your work which you relate to tiredness? 127 49<br />
Have you experienced tiredness at your work which you relate to your work pattern? 165 13<br />
Has fatigue affected your personal life outside the workplace? 178 16<br />
How do you counteract fatigue related to your work?<br />
% (n) Always Usually Sometimes Never Rating average<br />
Napping 2.9 (5) 15.6 (27) 59.0 (102) 22.5 (39) 3.01<br />
Caffeine 31.3 (55) 30.1 (53) 28.4 (50) 10.2 (18) 2.18<br />
Leave 5.3 (9) 9.9 (17) 41.6 (71) 43.3 (71) 3.23<br />
Post-call sleep 15.8 (27) 36.3 (62) 32.7 (56) 16.2 (26) 2.47<br />
Sleep debt 12.3 (20) 33.7 (55) 44.2 (72) 9.8 (16) 2.52<br />
Early to bed 9.6 (17) 36.7 (65) 50.8 (90) 2.8 (5) 2.47<br />
↑Activity level 0.6 (1) 19.0 (33) 50.6 (88) 29.9 (52) 3.10<br />
Frequent 1.2 (2) 17.3 (30) 52.6 (91) 28.9 (50) 3.09<br />
breaks<br />
Ask for help 0.6 (1) 4.6 (8) 51.4 (90) 43.4 (76) 3.38<br />
14<br />
14
Membership Questionnaire 2 (Health & Wellbeing)<br />
Have you ever napped/fallen asleep/microslept whilst undertaking anaesthesia?<br />
Total number responding 187<br />
Do you have knowledge of a colleague who has napped/fallen asleep/microslept<br />
whilst undertaking anaesthesia?<br />
How old are 24-29 30-34 35-39 40-44 45-49 50-54 55-59<br />
you in years? 7 34 27 28 28 29 27<br />
Which grade do you work in?<br />
Training<br />
SAS<br />
48<br />
11<br />
Which pattern of work do you Shift<br />
Rostered<br />
undertake to provide out-of-hours<br />
extended hours<br />
service?<br />
48<br />
8<br />
How many hours of sleep do you consider you need 0-5 5.5- 7.5 8-9<br />
each night before work the following day?<br />
4 114 65<br />
How many hours on average do you actually get on 0-5 5.5- 7.5 8-9<br />
nights before clinical work?<br />
15 144 26<br />
Do you think you get sufficient sleep to meet the demands of your job?<br />
Yes No<br />
94 93<br />
Yes No<br />
125 63<br />
60-64 65+<br />
8 0<br />
Consultant<br />
127<br />
On-call Other<br />
113<br />
15<br />
9.5-11 >11<br />
5 0<br />
9.5-11 >11<br />
1 2<br />
Yes No<br />
123 61<br />
Do you regularly have to catch up on sleep following routine clinical duties?<br />
Yes No<br />
55 132<br />
Do you regularly have to catch up on sleep following out-of-hours clinical duties?<br />
Yes<br />
No<br />
146 38<br />
15
Appendix 4<br />
Minimise sleep disturbance:<br />
• Maintain a sleep diary alongside an hours-of-work record<br />
• Regular bedtime and wake-up time<br />
• Sustained adequate sleep<br />
• Two nights of good sleep before work period<br />
• Bedroom quiet, dark and cool<br />
• Avoid heavy eating and drinking before bedtime<br />
• No alcohol, caffeine, nicotine close to bedtime<br />
• No exercise < 3 h before bedtime<br />
16
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
AAGBI SAFETY GUIDELINE<br />
Management of Proximal Femoral Fractures 2011<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org June 2012
This guideline was originally published in Anaesthesia. If you wish to refer to<br />
this guideline, please use the following reference:<br />
Association of Anaesthetists of Great Britain and Ireland. Management of<br />
proximal femoral fractures 2011. Anaesthesia 2012; 67: pages 85-98. This<br />
guideline can be viewed online via the following URL: http://onlinelibrary.<br />
wiley.com/doi/10.1111/j.1365-2044.2011.06957.x/abstract<br />
The following bodies have endorsed this guideline:<br />
Age Anaesthesia Association<br />
The Association for Perioperative Practice<br />
British Orthopaedic Association<br />
The College of Emergency Medicine<br />
© The Association of Anaesthetists of Great Britain 2012
Guidelines<br />
Management of proximal femoral fractures<br />
2011<br />
Association of Anaesthetists of Great Britain<br />
and Ireland<br />
Membership of the Working Party: R Griffiths (Chairman), J Alper,<br />
A Beckingsale, D Goldhill, G Heyburn, J Holloway 1 , E Leaper,<br />
M Parker 2 , S Ridgway, S White, M Wiese 3 and I Wilson<br />
1 Age Anaesthesia Association, 2 British Orthopaedic Association,<br />
3 College of Emergency Medicine<br />
Summary<br />
1. There should be protocol-driven, fast-track admission of patients with<br />
hip fractures through the emergency department.<br />
2. Patients with hip fractures require multidisciplinary care, led by<br />
orthogeriatricians.<br />
3. Surgery is the best analgesic for hip fractures.<br />
4. Surgical repair of hip fractures should occur within 48 hours of<br />
hospital admission.<br />
5. Surgery and anaesthesia must be undertaken by appropriately<br />
experienced surgeons and anaesthetists.<br />
6. There must be high-quality communication between clinicians and<br />
allied health professionals.<br />
Re-use of this article is permitted in accordance with the Creative Commons Deed, Attribution<br />
2.5, which does not permit commercial exploitation.<br />
Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland 1
Anaesthesia 2011<br />
Griffiths et al. | Guidelines: proximal hip fractures<br />
7. Early mobilisation is a key part of the management of patients with<br />
hip fractures.<br />
8. Pre-operative management should include consideration of planning<br />
for discharge from hospital.<br />
9. Measures should be taken to prevent secondary falls.<br />
10. Continuous audit and targeted research is required in order to inform<br />
and improve the management of patients with hip fracture.<br />
..................................................................................................<br />
This is a consensus document produced by expert members of a Working<br />
Party established by the Association of Anaesthetists of Great Britain and<br />
Ireland (AAGBI). It has been seen and approved by the AAGBI Council.<br />
* This article is accompanied by an Editorial. See page 2 of this issue.<br />
Accepted: 11 September 2011<br />
• What other guideline statements are available on this topic?<br />
A number of guidelines concerning best practice management of hip<br />
fracture have recently been published [1–6].<br />
• Why was this guideline developed?<br />
However, existing guidelines are inconclusive about either the involvement<br />
of anaesthetists or the provision of anaesthesia for patients<br />
sustaining hip fracture.<br />
• How and why does this statement differ from existing guidelines?<br />
This guidance is intended specifically to help anaesthetists manage<br />
patients with hip fracture.<br />
In common with other guidelines, this guideline reviews current<br />
evidence regarding best practice anaeathesia. Crucially, however, this<br />
guideline also recommends best practice in the numerous circumstances<br />
where evidence is controversial or incomplete, based on expert consensus<br />
opinion.<br />
Proximal femoral fractures present unique challenges for anaesthetic<br />
departments throughout Great Britain and Ireland, involving the perioperative<br />
care of large numbers of older patients with significant comorbidities.<br />
Despite guidance since the early 1990s concerning best<br />
practice management for these vulnerable patients [1–6], there remains<br />
considerable variation in models of peri-operative care, rehabilitation and<br />
orthogeriatric input.<br />
Approximately 77 000 hip fractures occur in the UK annually,<br />
accounting for 1.5 million bed days, at an inpatient cost of £0.785 billion.<br />
2 Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: proximal hip fractures Anaesthesia 2011<br />
Approximately 65 000 of these occur in England, with a median<br />
postoperative length of stay of 23 days and a 30-day mortality that has<br />
remained consistently around 8–10% for the last two decades – although,<br />
again, there is considerable hospital variation in these figures [6, 7]. The<br />
majority (95%) of hip fractures occur in patients over the age of 60, 75%<br />
occurring in females. Among the elderly, 90% of hip fractures occur after a<br />
simple, mechanical fall from standing height in patients with osteoporotic<br />
bone (Fig. 1) [8]. Other important causes of hip fracture include<br />
neuromuscular pathology, peripheral neuropathy, infection, arrhythmia,<br />
postural hypotension, valvular heart disease and polypharmacy. More than<br />
98% of fractures are repaired surgically, for the purposes of analgesia<br />
and early rehabilitation. Approximately 25% of patients with hip fractures<br />
have at least moderate cognitive impairment (abbreviated mental test<br />
score < 7), 20% are institutionalised, and 50% require walking aids or are<br />
immobile.<br />
As a result of the inadequacies of the evidence base on which most<br />
guidance is founded, there is limited consensus on best-practice anaesthetic<br />
management for hip fracture patients, which this document hopes<br />
to redress.<br />
Neuromuscular status<br />
Cognitive status<br />
Fall Initiation<br />
Fall direction<br />
Energy content and fall height<br />
Fall Descent<br />
Impact location<br />
Soft tissue attenuation<br />
Impact<br />
Bone mineral density<br />
Bone geometry<br />
Structural capacity of the<br />
femur < applied loads<br />
HIP FRACTURE<br />
Figure 1 Mechanical factors leading to a hip fracture.<br />
Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland 3
Anaesthesia 2011<br />
Griffiths et al. | Guidelines: proximal hip fractures<br />
These guidelines will mainly focus on the acute hospital episode,<br />
particularly the pre-operative period, intra-operative management and<br />
immediate postoperative phase. Where evidence is limited, issues controversial<br />
or guidelines uninformative, the Working Party has provided<br />
pragmatic consensus opinions.<br />
In addition, these guidelines will describe the logistics of providing a<br />
high quality service for these patients, together with the important<br />
relationships that must be developed between departments to ensure<br />
quality care.<br />
This has been a multidisciplinary collaboration that has resulted in<br />
advice for anaesthetists and other health-care professionals on how to<br />
create, develop and manage a service for patients with proximal femoral<br />
fracture.<br />
Facilities and services required<br />
Older patients with hip fracture are at risk of significant morbidity and<br />
mortality, both of which can be reduced by prompt surgical fixation of the<br />
fracture and early, effective rehabilitation. This section outlines the<br />
structures and processes required to expedite early surgery and achieve<br />
high quality rehabilitation.<br />
The Department of Health has suggested the following targets for<br />
patients with hip fracture [9]: (i) all patients should be admitted within<br />
4 h of arrival in the emergency department; and (ii) patients should be<br />
operated on by an experienced clinical team within 24 h of a decision<br />
that the patient is fit for surgery. In addition, the British Orthopaedic<br />
Association Standards for Trauma (BOAST) guidelines [10] stipulate that<br />
within 4 h of hospital arrival, hip fracture patients should be admitted to<br />
an appropriate clinical ward area with nursing, orthogeriatric medicine<br />
and surgical expertise appropriate for this often frail patient group;<br />
further, that surgical fixation should not be delayed more than 48 h from<br />
admission unless there are clear reversible medical conditions (see<br />
below).<br />
For many hospitals, achievement of these standards may require<br />
service re-organisation, incorporating the following components.<br />
Multidisciplinary hip fracture management group<br />
This involves a broad collective of stakeholder personnel who meet<br />
regularly in order to discuss and improve the quality and efficiency of hip<br />
fracture care appropriate to a particular hospital. The group may include<br />
trauma co-ordinators, general practitioners, community ⁄ falls assessment<br />
4 Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: proximal hip fractures Anaesthesia 2011<br />
nurses, emergency staff, bed managers, orthopaedic nursing staff and<br />
surgeons, anaesthetists, orthogeriatricians, physio- and occupational<br />
therapists, social workers and rehabilitation services. Trauma coordinators<br />
have a pivotal role, in reducing pre-operative delays, facilitating<br />
interdisciplinary communication and instituting early discharge<br />
planning.<br />
Communication between this group and the hospital’s theatre<br />
management group improves integration of system changes into general<br />
theatre service provision.<br />
Fast-track admission pathway<br />
Most patients with hip fracture are admitted via an emergency department,<br />
where a planned care package should be initiated promptly. The use<br />
of a care pathway proforma focuses patient care and ensures basic quality<br />
standards are met; a number of these exist, which can be tailored to<br />
individual hospitals.<br />
Continuous tracking ⁄ live data systems that regularly update patient<br />
and logistical data may improve management by identifying patients’<br />
location, delays in treatment and relevant clinical information, and may be<br />
used to facilitate clinical audit and business planning.<br />
Trauma lists<br />
Protected trauma lists, separate from general emergency operating lists,<br />
improve the efficiency of trauma service provision. These should be<br />
provided daily, including weekends and bank holidays, and be staffed by<br />
appropriately experienced senior medical and theatre staff. Unless life or<br />
limb-threatening trauma intervenes, the Working Party suggests that hip<br />
fracture surgery is prioritised within operating lists, overriding the<br />
particular subspecialist interest of the senior surgeon assigned to the list.<br />
Multidisciplinary trauma meetings<br />
Daily multidisciplinary trauma meetings, convened before the start of<br />
operating lists, offer excellent opportunities to communicate issues<br />
relating to recent admissions and to plan operative lists and equipment<br />
required for the day ⁄ next day, as well as providing regular teaching and<br />
feedback. Trauma meetings may involve the same staff as above, including<br />
their trainees. Members of the trauma team may change on a daily basis,<br />
so handover of information is a key element. Communication of clinical<br />
information should always involve accurate documentation in patients’<br />
notes in addition to verbal handover.<br />
Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland 5
Anaesthesia 2011<br />
Griffiths et al. | Guidelines: proximal hip fractures<br />
Consultant-delivered service<br />
Older patients with hip fracture experience some of the worst clinical<br />
outcomes among the hospital population. It is not acceptable for these<br />
patients to be anaesthetised by inappropriately experienced trainees.<br />
Ideally, such patients should be anaesthetised by a consultant or<br />
specialist with similar clinical experience. Furthermore, a core group of<br />
consultants with relevant experience of anaesthetising unwell, older<br />
patients should provide the vast majority of the service, rather than<br />
randomly-allocated consultants; one consultant ⁄ specialist should assume<br />
overall clinical leadership for a hip fracture anaesthesia service.<br />
Routine allocation of supernumerary trainee anaesthetists to wholeday<br />
lists allows for greater continuity of care including pre-operative<br />
preparation, postoperative review and interdisciplinary communication, as<br />
well as providing training opportunities relating to orthogeriatric anaesthesia<br />
and regional ⁄ nerve blockade.<br />
Similarly, patients should be operated on by an appropriately<br />
experienced surgeon, in order to minimise operative time and surgical<br />
outcomes (e.g. blood loss, and rate of dislocation ⁄ re-operation).<br />
Operating department<br />
Ideally, all trauma operations should be performed in a specific ‘trauma<br />
theatre’, large enough to allow access for an image intensifier, traction<br />
table, and surgical equipment. Clean air systems, incorporating High<br />
Efficiency Particulate Air Filter (HEPA) and laminar air flow, reduce the<br />
risk of airborne infection. Theatre temperature should be maintained at<br />
20–23 °C and humidity at 50–60%, to reduce the risk of peri-operative<br />
hypothermia.<br />
The minimum theatre team should consist of an operating department<br />
practitioner, two scrub practitioners and a circulator. The theatre<br />
team leader must be experienced in both femoral reconstruction and<br />
replacement procedures, and scrub allocation should take account of the<br />
patient’s health and potential complications previously identified at the<br />
start-of-list team brief. Specialist education is crucial to building a<br />
functional team.<br />
The allocation of a dedicated radiographer per trauma theatre reduces<br />
intra-operative delays.<br />
Stock levels of surgical implants and consumables should anticipate<br />
expected patient numbers, and instrumentation needs should take into<br />
account processing time.<br />
6 Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: proximal hip fractures Anaesthesia 2011<br />
Pre-operative management<br />
Initial management<br />
Hip fractures are painful, particularly on movement. Ambulance transfer<br />
to hospital enables immobilisation and the administration of opioid<br />
analgesia, intravenous fluid therapy and patient warming strategies.<br />
A number of hospitals have successfully introduced ‘fast-track’ triage<br />
systems that allow early clinical recognition of hip fracture (hip pain;<br />
inability to weight-bear; shortened, externally rotated leg on affected<br />
side) with early radiography and diagnosis, enabling rapid ward<br />
admission, from where further medical input and investigations are<br />
carried out.<br />
Close attention should be continued towards analgesia, intravenous<br />
fluid therapy, warming and pressure care during patients’ stay in the<br />
emergency department, particularly if ward admission is delayed beyond<br />
4h.<br />
Early fracture fixation provides the most effective analgesia. In the<br />
interim, a formalised analgesia protocol should be followed. Pain scores, at<br />
rest and on movement, should be recorded before and after the<br />
administration of analgesia. Other scoring systems may be used to assess<br />
pain relief in patients with cognitive dysfunction [11]. Simple analgesics,<br />
such as paracetamol, should routinely be prescribed on a regular basis,<br />
unless contraindicated [12]. Approximately 40% of patients presenting<br />
with hip fracture have at least moderate renal dysfunction (estimated<br />
glomerular filtration rate < 60 ml.min )1 .1.73m )2 ) on admission. Opioids<br />
should be used with caution until urea and electrolyte biochemistry results<br />
have been reviewed, and non-steroidal anti-inflammatory analgesia is<br />
relatively contraindicated [13].<br />
Single-shot ⁄ continuous nerve blocks (femoral ⁄ fascia iliaca [14]) may<br />
be successfully administered by appropriately trained emergency department,<br />
orthopaedic and anaesthetic medical staff [15].<br />
Pre-operative assessment<br />
Traditionally, the pre-operative management of patients with hip fracture<br />
has been by junior orthopaedic staff, with the role of geriatricians limited<br />
to postoperative rehabilitation planning and social placement on discharge<br />
from hospital. More recently, it has become apparent that the increasing<br />
number of elderly, frail patients presenting with hip (and other fragility)<br />
fractures may benefit from earlier, more intensive orthogeriatric input<br />
(Table 1).<br />
Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland 7
Anaesthesia 2011<br />
Griffiths et al. | Guidelines: proximal hip fractures<br />
Table 1 Benefits of early, intensive orthogeriatric input into management<br />
of patients with hip fracture.<br />
• Early identification of patients at increased risk of peri-operative morbidity<br />
and mortality.<br />
• Appropriate additional investigation, indicated by patients’ co-morbidities.<br />
• ‘Pre-optimisation’ of less fit patients before surgery.<br />
• Early rehabilitation and discharge planning.<br />
• Improved interdisciplinary communication between orthogeriatricians, surgeons<br />
and anaesthetists, reducing avoidable admission-to-operation delays.<br />
Pre-operative assessment by the anaesthetist is mandatory, allowing<br />
planning of anaesthetic technique, assessment and communication of perioperative<br />
risk, and pre-optimisation. In order to avoid cancellation on the<br />
day of surgery, a number of hospitals have developed specific information<br />
leaflets for the benefit of orthogeriatricians and orthopaedic surgeons,<br />
identifying particular concerns of relevance to the anaesthetist.<br />
Co-morbidities<br />
The preponderance of elderly patients has been noted above. Approximately<br />
70% of patients will be of ASA physical status 3–4 [6, 7]: 35% have<br />
one co-morbidity; 17% have two; and 7% have three or more [16]. The<br />
most common co-morbidities are cardiovascular disease (35%), respiratory<br />
disease (14%), cerebrovascular disease (13%), diabetes (9%), malignancy<br />
(8%) and treated renal disease (3%).<br />
Recently, a summative scoring system, the Nottingham Hip Fracture<br />
Score (Appendix 1) [17], has been developed to predict postoperative<br />
mortality according to the number of co-morbidities and other factors<br />
(age, male sex, malignancy, pre-operative cognitive function, place of<br />
residence and anaemia), and provides the anaesthetist with information<br />
about outcome that may be discussed with the patient or their relatives.<br />
In addition to assessment of the major systems, the anaesthetist<br />
should also assess the patient with regard to: musculoskeletal abnormalities<br />
(osteoarthritis, kyphoscoliosis, fixed flexion deformities); skin condition<br />
and pressure areas; dentition; and hearing aids.<br />
Polypharmacy<br />
The over-60s consume 60% of the drugs prescribed in the UK; 20% of<br />
people aged over 70 take more than five medications [3]. Polypharmacy<br />
increases the likelihood of adverse drug reactions, which may be<br />
8 Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: proximal hip fractures Anaesthesia 2011<br />
compounded by the limited physiological reserve of this population, and<br />
of which 80% are potentially avoidable [18]. A current medication list<br />
should be reviewed carefully for inappropriate dosing and prescribing, and<br />
potential pharmacokinetic and pharmacodynamic interactions.<br />
Routine pre-operative investigations<br />
Full blood count and urea and electrolyte analyses are required routinely<br />
before surgery. Coagulation studies and chest radiography are required<br />
only if clinically indicated.<br />
Full blood count. Pre-operative anaemia occurs in approximately 40% of<br />
patients, and can result from fracture-related haemorrhage, haemodilution,<br />
poor nutrition and ⁄ or chronic disease. Haemorrhage and<br />
haemodilution may result in a fall in peri-operative haemoglobin<br />
concentration (Hb) equivalent to approximately 2.5 g.dl )1 . Therefore,<br />
patients who are anaemic pre-operatively are likely to be very anaemic<br />
postoperatively, risking myocardial and cerebral ischaemia. It is has been<br />
suggested that older patients require a higher blood transfusion trigger<br />
than is generally used for patients undergoing elective surgery [19], to<br />
the extent that pre-operative transfusion should be considered if Hb is<br />
< 9 g.dl )1 , or Hb is < 10 g.dl )1 with a history of ischaemic heart disease.<br />
If Hb is 10–12 g.dl )1 , two units of blood should be crossmatched. If Hb<br />
is within normal limits, a grouped sample is sufficient. Revision surgery<br />
or periprosthetic fractures incur greater blood loss and require preoperative<br />
crossmatching according to local guidelines. Cell salvage<br />
should be considered for such procedures. After transfusion, repeat Hb<br />
analysis (formal full blood count or point-of-care) is strongly recommended.<br />
Leucocytosis and neutrophilia are common (45% and 60%, respectively)<br />
at presentation, but may be a reactive response to trauma rather<br />
than indicative of infection. Leukocytosis > 17 · 10 9 .l )1 may indicate<br />
infection (commonly of the chest or urine).<br />
A platelet count of 50–80 · 10 9 .l )1 is a relative contraindication to<br />
neuraxial anaesthesia [20]. A platelet count is below 50 · 10 9 .l )1 will<br />
normally require pre-operative platelet transfusion.<br />
Urea and electrolytes. Hypokalaemia is associated with new onset, rapid<br />
ventricular rate atrial fibrillation (AF) peri-operatively. Hyperkalaemia<br />
may indicate rhabdomyolysis if the patient was immobilised and unable to<br />
call for help after falling.<br />
Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland 9
Anaesthesia 2011<br />
Griffiths et al. | Guidelines: proximal hip fractures<br />
Hyponatraemia on admission to hospital is common (17%), and may<br />
indicate infection or result from medication (particularly thiazide<br />
diuretics).<br />
Electrocardiogram (ECG). This is required in all elderly patients with hip<br />
fracture.<br />
Chest radiograph. Routine chest radiographs on admission are not<br />
necessary, but may be useful in patients with newly diagnosed heart failure<br />
or pneumonia.<br />
Special cases<br />
A number of clinical situations merit specific comment since they are<br />
commonly encountered in this group of patients.<br />
Alcohol dependence. Alcohol dependence is common, under-diagnosed<br />
and a risk factor for falls [21]. Patients are at risk of significant perioperative<br />
morbidity.<br />
Atrial fibrillation. All patients in AF should have a ventricular rate<br />
< 100.min )1 . Factors that may lead to new or fast AF include<br />
hypokalaemia and hypomagnesaemia, hypovolaemia, sepsis, pain and<br />
hypoxaemia. If treatment of these is ineffective, acute ventricular rate<br />
control may be achieved using beta-blockers (metoprolol) or verapamil<br />
[22].<br />
Anticoagulation. A third of patients presenting with hip fracture take<br />
aspirin regularly. There is a risk of significant bleeding if aspirin is taken in<br />
combination with other thromboprophylactic medication. Aspirin may be<br />
withheld during inpatient stay, unless indicated for unstable angina or<br />
recent ⁄ frequent transient ischaemic attacks. About 4% of patients take<br />
clopidogrel, which inhibits platelet function, and this should alert the<br />
anaesthetist to myocardial ischaemia or cardiac stents. Clopidogrel is<br />
generally not stopped on admission, especially in patients with drugeluting<br />
coronary stents. Surgery should not be delayed, nor platelets<br />
administered prophylactically, but marginally greater blood loss should be<br />
expected. Novel antiplatelet therapies include prasugrel, eptifibatide,<br />
abciximab and tirofiban.<br />
Warfarin is taken by approximately 5% of patients presenting with hip<br />
fracture. Hospital guidelines concerning the peri-operative management of<br />
10 Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: proximal hip fractures Anaesthesia 2011<br />
patients taking warfarin should be followed; in general, the International<br />
Normalised Ratio (INR) should be < 2 for surgery and < 1.5 for neuraxial<br />
anaesthesia. Small amounts of vitamin K may be used to ‘reverse’ the<br />
effects of warfarin; supplemental peri-operative anticoagulation with<br />
heparins is usually indicated. Prothrombin complex concentrates rapidly<br />
reverse the effects of warfarin but are expensive and rarely indicated.<br />
Warfarin should be recommenced 24 h after surgery, although some<br />
departments recommence it later on the day of surgery.<br />
The advice of haematologists should be sought if in doubt about the<br />
peri-operative management of patients on chronic anticoagulant therapy.<br />
Regular anticoagulant medication requires that the anaesthetist balance<br />
the attendant risks of neuraxial and lumbosacral plexus blockade (ie<br />
haemorrhage and neuropraxia) against the benefits of these procedures for<br />
the elderly.<br />
Chest infection. Pre-operative chest infection requires prompt antibiotic<br />
therapy, along with supplemental oxygen, intravenous fluids and<br />
physiotherapy. Expedited surgery under regional anaesthesia is preferred,<br />
enabling early mobilisation, analgesia and improved co-operation with<br />
postoperative physiotherapy.<br />
Diabetes. Approximately 9% of patients with hip fracture are diabetic.<br />
Hospital guidelines concerning the peri-operative management of diabetic<br />
patients should be followed. Hyperglycaemia is not a reason to delay<br />
surgery unless the patient is ketotic and ⁄ or dehydrated.<br />
Dialysis. Dialysed patients may develop renal bone disease and anaemia.<br />
Although surgery is normally tailored around the patient’s dialysis, urgent<br />
surgery may necessitate heparin-free dialysis.<br />
Heart murmur. Unrecognised calcific aortic stenosis is an important<br />
cause of anaesthesia-related mortality. There is considerable debate<br />
concerning the postponement of surgery pending echocardiography, but<br />
a majority of clinicians favour proceeding to surgery with modification of<br />
their technique towards general anaesthesia and invasive blood pressure<br />
monitoring, with the proviso that patients should undergo echocardiography<br />
in the early postoperative period.<br />
Echocardiography may be indicated: (i) to establish left ventricular<br />
function if the patient is breathless at rest or on low level exertion; or (ii) to<br />
investigate the severity of an ejection systolic murmur heard in the aortic<br />
Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland 11
Anaesthesia 2011<br />
Griffiths et al. | Guidelines: proximal hip fractures<br />
area, particularly if significant aortic stenosis is suggested by two or more<br />
of: a history of angina on exertion; unexplained syncope or near syncope; a<br />
slow rising pulse; an absent second heart sound; or left ventricular<br />
hypertrophy on the ECG without hypertension (although clinical signs of<br />
aortic stenosis can be difficult to elicit [23]).<br />
Implantable cardioverter defribrillators (ICD) and pacemakers. Increasingly,<br />
ICDs are implanted to try and prevent sudden cardiac death from<br />
dangerous cardiac arrhythmias; they may also have a pacemaker function.<br />
As with pacemakers, there is a risk both of unipolar diathermy’s delivering<br />
an arrhythmogenic shock to the myocardium, and of peri-operative failure<br />
of the device. Early pre-operative consultation with a cardiologist is<br />
required, both to establish the type of device and to develop a plan for<br />
intra-operative management of patients.<br />
Pre-operative optimisation<br />
All acute hospitals should develop a specific protocol for the resuscitation<br />
of patients with hip fracture, with particular regard to: monitoring<br />
(pulse oximetry, respiratory rate, ECG, non-invasive blood pressure<br />
measurement, core temperature and static ⁄ dynamic pain scores);<br />
cannulation and intravenous fluid therapy; analgesia; thermoregulation;<br />
and pressure care. These protocols may be commenced during ambulance<br />
transfer, but are mandatory once the patient has been admitted to<br />
the hospital.<br />
Subsequently, important co-morbidities should be recognised and<br />
treated without unnecessarily delaying surgery, in order to minimise<br />
that patient’s specific risks of surgery and anaesthesia. This is a<br />
multidisciplinary task, involving input from and communication between<br />
orthogeriatricians, anaesthetists, surgeons, nursing staff and physiotherapists.<br />
Timing of surgery<br />
Ideally, surgery should be performed within 48 h of hospital admission<br />
after hip fracture [2, 9], with a new target of 36 h having been introduced<br />
in England and Wales in April, 2010. Currently, 80% of hospitals achieve a<br />
mean admission to operation time of less than 48 h [6].<br />
Meta-analyses [24, 25] indicate that delaying surgery beyond 48 h<br />
from admission is associated with prolonged inpatient stay, increased<br />
morbidity (pressure sores, pneumonia, thromboembolic complications)<br />
and increased mortality (if delay is prolonged).<br />
12 Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: proximal hip fractures Anaesthesia 2011<br />
There is no evidence to suggest that outcome is improved by delaying<br />
surgery to allow pre-operative physiological stabilisation. However, the<br />
benefits of expedited surgery must be balanced against the risks of certain<br />
untreated conditions (Table 2).<br />
Ethical considerations<br />
A number of ethical considerations arise in the treatment of elderly<br />
patients with hip fracture.<br />
Consent and mental capacity<br />
Approximately 25% of patients with hip fracture have moderate or<br />
severe cognitive impairment, and a further 15–25% have mild cognitive<br />
impairment. In order for patients to consent to, or refuse, surgical<br />
repair of hip fracture, they must be able to do so voluntarily, based on<br />
a decision made on information about the procedure presented to<br />
them. The patient must have capacity to make a decision; that is,<br />
he ⁄ she must be able to understand the information, remember it and<br />
use it to reach a decision. In this age group, the ability to assimilate<br />
information and communicate decisions may be impaired by poor<br />
vision, hearing or speech, and steps should be taken to overcome these<br />
problems.<br />
If the patient lacks capacity, then treatment may be provided<br />
according to the Mental Capacity Act 2005 [26] (MCA) (in Scotland,<br />
the Adults with Incapacity (Scotland) Act 2000). Essentially, it remains the<br />
Table 2 Reasons for delaying surgery for hip fracture that the Working<br />
Party considers acceptable and unacceptable.<br />
Acceptable<br />
• Haemoglobin concentration < 8 g.dl )1 .<br />
• Plasma sodium concentration < 120 or<br />
> 150 mmol.l )1 and potassium<br />
concentration < 2.8 or > 6.0 mmol.l )1 .<br />
• Uncontrolled diabetes.<br />
• Uncontrolled or acute onset<br />
left ventricular failure.<br />
• Correctable cardiac arrhythmia with a<br />
ventricular rate > 120 .min )1 .<br />
• Chest infection with sepsis.<br />
• Reversible coagulopathy.<br />
Unacceptable<br />
• Lack of facilities or theatre space.<br />
• Awaiting echocardiography.<br />
• Unavailable surgical expertise.<br />
• Minor electrolyte abnormalities.<br />
Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland 13
Anaesthesia 2011<br />
Griffiths et al. | Guidelines: proximal hip fractures<br />
doctors’ decision to administer treatment that is deemed to be both<br />
necessary and in the patient’s best interests; doctors should be prepared to<br />
justify their decisions to treat ⁄ deny ⁄ withdraw treatment to the courts if<br />
necessary. Decisions must not be biased by reference to the patient’s age.<br />
Doctors must consult relatives about treatment decisions, and should seek<br />
to ascertain whether the patient had previously written an advanced<br />
directive, or appointed a Lasting Power of Attorney. The Courts may be<br />
consulted if there is uncertainty about a patient’s management or if there<br />
is dispute between clinical staff and relatives.<br />
Rationing of healthcare<br />
Implicit in the anti-discriminatory tenor of both the MCA and the Human<br />
Rights Act 1998 is the requirement to provide equal access to, and<br />
administration of, medical treatment (for example, high dependency unit<br />
(HDU) care) to all patients, regardless of age and infirmity. This is at odds<br />
with common law, which appears to support the rationing of services<br />
within the NHS, and the issue remains unresolved in law. Doctors are not<br />
obliged to deliver treatment that they consider to be futile or not in the<br />
patient’s best interests.<br />
Do not attempt resuscitation (DNAR) decisions<br />
A joint statement from the British Medical Association, the Resuscitation<br />
Council (UK) and the Royal College of Nursing provides the framework<br />
under which DNAR decisions are made and ratified [27].<br />
Do not attempt resuscitation decisions are increasingly prevalent<br />
among the patient population with hip fracture, and may proscribe<br />
cardiopulmonary resuscitation in the event of arrest. Although DNAR<br />
decisions are presumed not to apply during surgery and anaesthesia,<br />
resuscitation may not be in the patient’s best interests, or even desired by<br />
the patient. The AAGBI has recognised these potential difficulties, and<br />
issued guidance [28].<br />
Discussions about DNAR should precede surgery, and anaesthetists<br />
must take steps to make themselves aware of the outcome of these<br />
discussions.<br />
Intra-operative management<br />
Surgical considerations<br />
A number of hip fracture classification systems exist. Generally, 50% of<br />
fractures are intracapsular, the remainder extracapsular (Fig. 2).<br />
14 Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: proximal hip fractures Anaesthesia 2011<br />
Intracapsular fractures<br />
Intracapsular fractures include subcapital, transcervical and basicervical<br />
fractures, and may be displaced or undisplaced. Blood loss from an<br />
intracapsular fracture at the time of injury is minimal because of the poor<br />
vascular supply at the fracture site and tamponade effected by the capsule.<br />
Occasionally, undisplaced fractures may be treated conservatively, but<br />
there is a 30–50% risk of subsequent displacement. Current preference is<br />
for all undisplaced intracapsular fracture to be treated by internal fixation<br />
with multiple screws or a sliding hip screw.<br />
Untreated, disruption to the capsular blood supply of the head of the<br />
femur by a displaced intracapsular fracture can lead to avascular necrosis<br />
of the bone, resulting in a painful hip of limited function. Therefore,<br />
surgical treatment involves hemiarthroplasty; even then, intracapsular<br />
fracture is associated with longer-term arthritis, and increasingly, total hip<br />
arthroplasty is preferred for younger patients.<br />
Compared to uncemented arthroplasty, cemented arthroplasty<br />
improves hip function and is associated with lower residual pain<br />
postoperatively.<br />
Figure 2 Common sites of proximal femoral fractures. Arrows show the<br />
insertion of the joint capsule.<br />
Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland 15
Anaesthesia 2011<br />
Griffiths et al. | Guidelines: proximal hip fractures<br />
Extracapsular fractures<br />
These include inter- and subtrochanteric fractures, and can be further<br />
divided into groups related to the degree of comminution.<br />
Blood loss from cancelleous bone is greater, such that the total blood<br />
loss from an extracapsular fracture may exceed one litre; the greater the<br />
degree of comminution and the larger the bone fragments, the greater the<br />
blood loss. In addition, greater periosteal disruption causes extracapsular<br />
fractures to be considerably more painful than an intracapsular fracture.<br />
Extracapsular fractures can be treated conservatively, healing after 6–<br />
8 weeks of traction and bed rest, but such management is associated with<br />
increased morbidity and mortality, and a considerably reduced chance of<br />
the patient returning home.<br />
Invariably, extracapsular fractures are fixed surgically, using either a<br />
sliding hip screw (intertrochanteric fractures) or less commonly, a<br />
proximal femoral intramedullary nail (subtrochanteric fractures).<br />
Anaesthetic considerations<br />
Regional anaesthesia for hip fracture surgery requires blockade of the<br />
lateral cutaneous nerve of the thigh and femoral, obturator, sciatic and<br />
lower subcostal nerves, and can only be reliably achieved in the conscious<br />
patient with neuraxial blockade. General anaesthesia requires additional<br />
administration of postoperative analgesia, most commonly in the form of<br />
peripheral nerve blockade. Poor analgesia in the immediate postoperative<br />
period increases morbidity.<br />
There is a minimal evidence base for determining the optimal<br />
anaesthetic technique for patients undergoing hip fracture surgery.<br />
Consequently, anaesthetists tend to adhere to a technique with which they<br />
are familiar, roughly half administering neuraxial anaesthesia and the<br />
remainder general anaesthesia. Furthermore, the wide range of drugs and<br />
dosages used obscures determination of the best technique using audit data.<br />
Based on a 2004 Cochrane systematic review of anaesthesia for hip<br />
fracture surgery [29], that suggested that regional anaesthesia may<br />
reduce the incidence of postoperative confusion, the Scottish Intercollegiate<br />
Guidelines Network has produced the only recommendation<br />
concerning choice of anaesthetic technique, namely that ‘Spinal ⁄<br />
epidural anaesthesia should be considered for all patients undergoing<br />
hip fracture repair, unless contraindicated.’ [1]. Until such time as<br />
evidence is published that confirms regional anaesthesia is superior<br />
to general anaesthesia or vice versa, the Working Party endorses<br />
this recommendation. This endorsement is supported by a recent<br />
16 Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: proximal hip fractures Anaesthesia 2011<br />
meta-analysis suggesting that regional anaesthesia ‘is the technique of<br />
choice (although) the limited evidence available do(es) not permit a<br />
definitive conclusion to be drawn with regard to mortality or other<br />
outcomes’ [30].<br />
Of greater importance, whichever technique is used, is that anaesthesia<br />
is sympathetic to the limited physiological reserve and co-morbidities<br />
of older patients [31].<br />
The Working Party does not support the administration of opioid<br />
analgesics as the sole adjunct to anaesthesia for this patient group, due to<br />
the relatively greater risk of respiratory depression and postoperative<br />
confusion. Peripheral nerve blockade should always be considered,<br />
therefore, as an adjunct to spinal or general anaesthesia, to extend the<br />
period of postoperative non-opioid analgesia.<br />
Neuraxial anaesthesia<br />
The Working Party recommends that either spinal anaesthesia or<br />
general anaesthesia is administered, as simultaneous administration<br />
is associated with precipitous falls in intra-operative blood pressure<br />
[32].<br />
Postoperative epidural analgesia (including combined spinal-epidural<br />
anaesthesia) provides good postoperative analgesia, but may limit early<br />
mobilisation after surgery, and for this reason is less commonly used in the<br />
UK.<br />
Spinal (subarachnoid) anaesthesia is commonly used, with or without<br />
sedation. Conceptually, spinal anaesthesia for hip fracture fixation in<br />
elderly patients should be viewed distinctly from spinal anaesthesia for<br />
caesarean section in younger patients. Lower doses of intrathecal<br />
bupivacaine (< 10 mg) appear to reduce associated hypotension [32,<br />
33]. Attempted lateralisation of subarachnoid anaesthesia using hyperbaric<br />
bupivacaine with the patient positioned laterally (with the fractured hip<br />
inferior) may ameliorate hypotension. Co-administration of intrathecal<br />
opioids prolongs postoperative analgesia; fentanyl is preferred to<br />
morphine or diamorphine, which are associated with greater respiratory<br />
and cognitive depression [34].<br />
Sedation may be provided, but should be used cautiously in the very<br />
elderly. Midazolam and propofol are commonly used. Ketamine may be<br />
used, theoretically to counteract hypotension, but may be associated with<br />
postoperative confusion.<br />
Supplemental oxygen should always be provided during spinal<br />
anaesthesia.<br />
Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland 17
Anaesthesia 2011<br />
Griffiths et al. | Guidelines: proximal hip fractures<br />
General anaesthesia<br />
Reduced doses of intravenous induction agents should be administered.<br />
Inhalational induction is well tolerated by the elderly and allows for<br />
maintenance of spontaneous ventilation. There remains debate about<br />
whether mechanical ventilation is preferred to spontaneous ventilation.<br />
Paralysis and tracheal intubation are associated with greater physiological<br />
derangement than spontaneous ventilation, but proponents argue that<br />
mechanicalventilationreducestheriskofperi-operativeaspirationandallows<br />
greater control of arterial carbon dioxide levels. Intra-operative hypoxaemia<br />
is common, and higher inspired oxygen concentrations may be required.<br />
Peripheral nerve blockade<br />
Blockade of the femoral, obturator and lateral cutaneous nerve of the thigh<br />
may be sufficient for peri-operative analgesia. The most reliable method of<br />
blocking all three is the psoas compartment block, although this risks a<br />
degree of neuraxial blockade and formation of a deep haematoma in<br />
recently anticoagulated patients.<br />
Anterior approaches (femoral nerve ⁄ fascia iliaca block) do not<br />
reliably block all three nerves, but reduce postoperative analgesia<br />
requirements, and are more amenable to ultrasound-guided placement<br />
and continuous catheter infusions postoperatively [15].<br />
Wound infiltration with local anaesthetic is insufficiently analgesic.<br />
High volume, low concentration pericapsular ⁄ periosteal injection of local<br />
anaesthetic agents has not been assessed.<br />
Pre- or postoperative peripheral nerve blockade may be used to<br />
supplement either general or spinal anaesthesia.<br />
Monitoring<br />
Minimum standards for monitoring include the continual presence of the<br />
anaesthetist, pulse oximetry, capnography, ECG and non-invasive blood<br />
pressure monitoring [35]. Core temperature monitoring should be used<br />
routinely. Point-of-care Hb analysers (e.g. Hemocue, or similar) should be<br />
used routinely at the end of surgery to assess the degree of anaemia and<br />
guide blood transfusion.<br />
Given the high incidence of significant co-morbidities in this<br />
population, there should be a low threshold for considering further<br />
monitoring equipment, which may include:<br />
• Invasive blood pressure monitoring [36], particularly for patients with<br />
limited left ventricular function or valvular heart disease.<br />
18 Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: proximal hip fractures Anaesthesia 2011<br />
• Central venous pressure (CVP) monitoring, for patients with limited left<br />
ventricular function or undergoing revision ⁄ periprosthetic fracture<br />
surgery.<br />
• Cardiac output monitoring. Transoesophageal Doppler guided fluid<br />
therapy may reduce hospital stay in patients undergoing general<br />
anaesthesia for hip fracture surgery. Transthoracic Doppler probes are<br />
becoming available for use in sedated or awake patients. Dilution<br />
techniques (e.g. LiDCO) are increasingly accurate, and may be used in<br />
conjunction with invasive blood pressure monitoring.<br />
• Bispectral index (BIS) monitors may be used to optimise the depth of<br />
anaesthesia and avoid potential cardiovascular depression. Initial BIS<br />
levels may be abnormally low in alcoholic patients and patients with<br />
dementia.<br />
• Cerebral oxygen saturation [37]. The homeostatic regulation of cerebral<br />
blood flow is poor in older patients, and depressed further by<br />
anaesthesia. Detection of reduced cerebral oxygen saturation may be<br />
associated with reduced postoperative cognitive dysfunction.<br />
Supplemental pain relief<br />
Regular paracetamol administration should continue throughout the perioperative<br />
period. Non-steroidal anti-inflammatory drugs should be used<br />
with extreme caution in hip fracture patients, and are contraindicated<br />
in those with renal dysfunction. Similarly, opioids (and tramadol) should<br />
be used with caution in patients with renal dysfunction: oral opioids<br />
should be avoided, and both dose and frequency of intravenous opioids<br />
should be reduced (e.g. halved). Codeine should not be administered, as it<br />
is constipating, emetic and associated with peri-operative cognitive<br />
dysfunction.<br />
Thromboprophylaxis<br />
Venogram and ventilation ⁄ perfusion studies have shown a prevalence of<br />
37% for deep vein thrombosis (DVT) and 6% for PE (pulmonary<br />
embolism) [38], although clinical symptoms are only seen in 1–3% of<br />
DVTs and 0.5–3% of PEs in patients with hip fracture. Fondaparinux or<br />
low molecular weight heparins are commonly prescribed and may<br />
impact on the anaesthetic technique: low molecular weight heparin<br />
should be administered between 18:00 and 20:00 to minimise the risk of<br />
bleeding related to neuraxial anaesthesia during hip surgery on daytime<br />
trauma lists. Thromboembolism stockings or intermittent compression<br />
devices should be employed intra-operatively, in addition to ensuring the<br />
Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland 19
Anaesthesia 2011<br />
Griffiths et al. | Guidelines: proximal hip fractures<br />
patient remains warm and well-hydrated. Expedited surgery and<br />
mobilisation, and regional anaesthesia, may reduce the risk of DVT<br />
further.<br />
Antibiotics<br />
Antibiotics should be administered within one hour of skin incision.<br />
Hospital antibiotic protocols should be followed.<br />
Pressure care<br />
Older patients are particularly susceptible to pressure damage. Patients<br />
should be positioned sympathetically during surgery, to avoid the<br />
development of pressure sores and ⁄ or neuropraxia. Excessive flexion<br />
and internal rotation of the non-operative hip should be resisted during<br />
dynamic hip screw insertion.<br />
The skin of older patients is thin and liable to be damaged by minimal<br />
trauma. Care should be taken when removing dressings or diathermy<br />
plates, and when moving the patient.<br />
Thermoregulation<br />
Older patients are susceptible to intra-operative hypothermia, particularly<br />
during longer procedures [39]. Active warming strategies should always be<br />
employed and continued postoperatively.<br />
Intravenous fluids<br />
Optimised peri-operative fluid management reduces morbidity and<br />
hospital stay [40]. Many patients become hypovolaemic before surgery,<br />
and pre-operative fluid therapy should be prescribed routinely. Cardiac<br />
output-guided fluid administration appears to reduce hospital stay and<br />
improve outcome [41].<br />
Bone cement implantation syndrome (BCIS)<br />
This is characterised by hypoxia, hypotension, or both, and ⁄ or unexpected<br />
loss of consciousness, around the time of cementation, prosthesis<br />
insertion, reduction of the joint or, occasionally, limb tourniquet deflation<br />
in a patient undergoing cemented bone surgery [42]. The incidence in hip<br />
fracture surgery is uncertain. Several mechanisms may contribute to a<br />
multimodal aetiology, including fat ⁄ platelet ⁄ fibrin ⁄ marrow emboli and<br />
stimulated release of vasoactive mediators. The risk of BCIS may be<br />
reduced by good surgical technique (including medullary lavage, good<br />
20 Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: proximal hip fractures Anaesthesia 2011<br />
haemostasis before cement insertion, use of a cement gun to enable<br />
retrograde cement insertion, venting of the femur, minimising the length<br />
of the prosthesis and minimising the force applied to it during insertion)<br />
and good anaesthetic technique (including increasing the inspired oxygen<br />
concentration at the time of cementation, avoiding intravascular volume<br />
depletion, and using additional haemodynamic monitoring in high-risk<br />
patients).<br />
The treatment of BCIS includes delivery of 100% oxygen, fluid<br />
resuscitation (guided by CVP measurement) and vasoactive ⁄ inotropic<br />
support.<br />
Postoperative management<br />
Patients with hip fracture remain at relatively high risk of complications in<br />
the early postoperative phase, and may require a prolonged period of<br />
monitoring in the anaesthetic recovery unit or, less commonly, the<br />
HDU ⁄ ICU. There is recognition that some patients may not be nursed in<br />
the most appropriate place following hip fracture surgery. The Working<br />
Party recommends that hip fracture patients should receive ward care with<br />
a nurse:patient ratio of 1:4, with regular input from physicians specialised<br />
in medicine for the elderly [4].<br />
Analgesia<br />
Peripheral nerve blockade is rarely effective beyond the first postoperative<br />
night. Analgesia requirements vary considerably after fracture fixation,<br />
particularly during remobilisation. Regular paracetamol administration<br />
should continue [11], augmented by carefully prescribed opioid analgesia,<br />
as indicated. Pain evaluation should be included as part of routine<br />
postoperative nursing observations.<br />
Oxygen<br />
Older patients are at risk of postoperative hypoxia, and supplemental<br />
oxygen should be administered postoperatively for at least 24 h. Oxygenation<br />
and respiratory function improve with mobilisation.<br />
Fluid balance<br />
Hypovolaemia is common. Early oral fluid intake should be encouraged,<br />
rather than routine prescription of intravenous fluids. Urinary catheters<br />
should be removed as soon as possible, to reduce the attendant risk of<br />
urinary tract infection.<br />
Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland 21
Anaesthesia 2011<br />
Griffiths et al. | Guidelines: proximal hip fractures<br />
Postoperative cognitive dysfunction ⁄ acute confusional state<br />
This is common (25%) in patients with hip fracture, interrupting routine<br />
management and rehabilitation. Treatment involves multimodal optimisation<br />
of postoperative care requiring adequate analgesia, nutrition,<br />
hydration, electrolyte balance, appropriate medication, bowel habit and<br />
mobilisation, in conjunction with identifying and treating complications<br />
such as chest infection, silent myocardial ischaemia and urinary tract<br />
infection [43]. Drugs such as haloperidol or lorazepam should only be<br />
used to control symptoms in the short term. Cyclizine should be used with<br />
caution in older persons, due to its antimuscarinic side effects.<br />
Nutrition<br />
Up to 60% of patients with hip fracture are clinically malnourished on<br />
admission to hospital. The calorie and protein density of hospital food is<br />
often poor, and mortality (and possibly length of stay) may be reduced<br />
through the administration of nutritional supplementation and employment<br />
of dietetic assistants [44, 45].<br />
Rehabilitation<br />
The rehabilitation process constitutes the majority of a patient’s<br />
inpatient stay after hip fracture, and continues for some time after<br />
discharge.<br />
Rehabilitation is ideally co-ordinated by orthogeriatricians, and is<br />
aimed at providing a patient-centred package of care that attempts to<br />
return the patient to levels of activity and residence similar to their prefracture<br />
status. To this end, patients usually require input from<br />
physiotherapists, occupational therapists, social workers, nursing staff<br />
and their own relatives. Secondary prevention of falls and osteoporosis<br />
should be actively considered in the early postoperative period, as<br />
subsequent fragility fracture or periprosthetic fracture is associated with a<br />
particularly poor prognosis.<br />
Anaesthetists may become involved in secondary surgical management<br />
(e.g. wound debridement, prosthesis revision) or in the provision of<br />
longer-term analgesia or HDU facilities.<br />
Printed information describing the typical care pathways for hip<br />
fracture patients should be available for patients, carers and relatives.<br />
Outcomes<br />
Outcomes vary considerably in the UK.<br />
22 Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: proximal hip fractures Anaesthesia 2011<br />
Mortality<br />
Mortality after hip fracture has remained relatively unchanged for the last<br />
two decades. Currently, 8.4% of patients die within 30 days of surgery [6].<br />
However, it has been suggested that up to half of postoperative deaths are<br />
potentially preventable [46]. Thirty-day mortality is increased for older,<br />
sicker, male patients. Up to 15–30% of patients die within a year of<br />
surgery.<br />
Length of acute inpatient stay<br />
This is between eight and 30 days, with a mean of 16 days [6].<br />
Discharge destination<br />
Only 44% of patients admitted from home are discharged back to their<br />
own homes within 30 days of surgery. A further 22% are discharged to a<br />
residential or nursing home, and discharge may become prolonged in<br />
waiting for admission to these facilities.<br />
Audit and research<br />
Cochrane reviews have consistently recognised the relative dearth of<br />
evidence on which to base best practice guidance with regards to the<br />
clinical management of patients presenting with hip fracture. Consequently,<br />
practice varies widely across the country, as several audits have<br />
shown [6, 7], resulting in wide variations in patient outcome.<br />
Clinical audit is fundamental to the process of improving the quality<br />
of patient care. Local audit enables physicians both to identify specific<br />
areas of care that could be improved, and to assess performance<br />
longitudinally. National audit enables hospitals to compare performance<br />
against other hospitals, and identify specific paragons of practice that may<br />
they might adopt. A number of audit tools are available for anaesthetists:<br />
Hip Fracture Perioperative Network (HFPN)<br />
This is an NHS-sponsored network developed under the auspices of the<br />
Age Anaesthesia Association, with the aim of improving evidence-based<br />
(anaesthetic) care for patients with hip fracture in the UK. The HFPN<br />
website [47] includes freely available database and annual report templates<br />
that anaesthetists may use to audit hip fracture care in their own hospitals,<br />
as well as ideas for research, specimen patient information leaflets, preoperative<br />
care information for junior surgeons, and hip fracture care<br />
pathway proformas.<br />
Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland 23
Anaesthesia 2011<br />
Griffiths et al. | Guidelines: proximal hip fractures<br />
National Hip Fracture Database (NHFD)<br />
The NHFD is a collaboration between the British Orthopaedic Association<br />
and the British Geriatrics Society, with the main aim ‘to focus attention on<br />
hip fracture both locally and nationally, benchmark its care across the<br />
country, and use continuous comparative data to create a drive for sustained<br />
improvements in clinical standards and cost effectiveness’ [48]. All eligible<br />
hospitals in the UK (except Scotland) are registered, with regular<br />
contributions of data from over 75% of eligible hospitals, concerning in<br />
excess of 130 000 patients (2011). The NHFD has recently begun to collect<br />
data about anaesthetic methods used for hip fracture surgery.<br />
Patient information<br />
The provision of good quality information for patients is a key component<br />
of the consent process, and is fundamental to good practice as detailed by<br />
the General Medical Council [49] and AAGBI [50].<br />
The Working Party recommends that each department produce a<br />
written information leaflet or booklet. It is essential that patients and<br />
relatives are involved in the process. Typically, such information would<br />
include basic surgical information about the injury with more detailed<br />
information the anaesthetic considerations. Anaesthetic options, including<br />
intended benefits and risks, should be explained clearly. An alternative to<br />
an anaesthetic information leaflet might be a more comprehensive<br />
document developed with multidisciplinary input from nurses, surgeons,<br />
physiotherapist, occupational therapists, etc. The Working Party recommends<br />
that, where possible, information should be evidence-based.<br />
A specimen patient information sheet is freely available from the<br />
HFPN website [47], and may be edited to apply to the hip fracture care<br />
pathway of specific hospitals.<br />
Appendix 2 lists areas where information for patients can be found.<br />
Training<br />
The elderly patient with a proximal femoral fracture offers multiple<br />
opportunities to learn and demonstrate specific core outcomes, knowledge<br />
and skills within ‘units of training’ set out in the Royal College of<br />
Anaesthetists’ 2010 curriculum [51].<br />
The Working Party recommends that basic level trainees (CT1-2)<br />
participate in the multidisciplinary peri-operative care of patients with hip<br />
fracture (e.g. through participation in orthogeriatric and acute pain ward<br />
rounds, and pre-operative assessment), as well as receiving training in the<br />
24 Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: proximal hip fractures Anaesthesia 2011<br />
theory of intra-operative care of the elderly and practical experience of<br />
relevant nerve block and regional anaesthetic techniques.<br />
Intermediate level trainees (ST3-4) should be encouraged to become<br />
more independent in patient assessment, and should aim to manage the<br />
moderate- to high-risk patient with indirect local support only.<br />
Higher level trainees (ST5-7) should be encouraged to undertake<br />
independent trauma list planning, prioritisation and management, with<br />
senior advice. This will, undoubtabley, reveal numerous potential<br />
management, teamwork and leadership opportunities; all essential<br />
domains of Common Competencies of Medical Practice. The trainee<br />
may also develop roles in teaching medical students and more junior<br />
trainees.<br />
Advanced training ⁄ fellowship posts (ST6-7) undertaken in hospitals,<br />
for example specialising in regional anaesthesia or anaesthesia for the<br />
elderly, may provide the potential for a trainee for develop a specific<br />
interest in the peri-operative care of older trauma patients. Higher level<br />
trainees should be encouraged to participate in audit and research<br />
involving patients with hip fracture.<br />
Acknowledgement<br />
The Working Party acknowledges the assistance of Prof. Opinder Sahota<br />
and Dr Iain Moppett, Queen’s Medical Centre, Nottingham.<br />
Competing interests<br />
RG and SW have advised both the National Institute for Health and<br />
Clinical Excellence (during development of Clinical Guideline 124 (The<br />
management of hip fracture in adults)) and the NHFD, and are<br />
respectively, Lead Clinician and Research Co-ordinator for the HFPN.<br />
MJP has received honoraria from a number of commercial companies for<br />
giving lectures on different aspects of hip fracture treatment and advising<br />
on hip fracture treatments, and he has received royalties from BBraun Ltd<br />
related to the design and development of an implant used for the internal<br />
fixation of intracapsular hip fractures.<br />
References<br />
1. Scottish Intercollegiate Guidelines Network. Management of hip fracture in older<br />
people. National clinical guideline 111. 2009. http://www.sign.ac.uk/pdf/<br />
sign111.pdf (accessed 30 ⁄ 08 ⁄ 2011).<br />
2. British Orthopaedic Association and British Geriatrics Society. The care of patients with<br />
fragility fracture. 2007. http://www.nhfd.co.uk/ (accessed 30 ⁄ 08 ⁄ 2011).<br />
Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland 25
Anaesthesia 2011<br />
Griffiths et al. | Guidelines: proximal hip fractures<br />
3. Royal College of Physicians. National clinical audit of falls and bone health in older<br />
people. November, 2007. http://old.rcplondon.ac.uk/clinical-standards/ceeu/<br />
Documents/fbhop-execsummary.pdf (accessed 30 ⁄ 08 ⁄ 2011).<br />
4. National Confidential Enquiry into Patient Outcome and Death. An age old problem. A<br />
review of the care received by elderly patients undergoing surgery. http://<br />
www.ncepod.org.uk/2010eese.htm (accessed 30 ⁄ 08 ⁄ 2011).<br />
5. The National Institute for Health and Clinical Excellence. Clinical Guideline 124. The<br />
management of hip fracture in adults. 2011. http://www.nice.org.uk/nicemedia/<br />
live/13489/54918/54918.pdf (accessed 30 ⁄ 08 ⁄ 2011).<br />
6. The National Hip Fracture Database. National Report, 2011. http://www.nhfd.co.<br />
uk/003/hipfractureR.nsf/NHFDNationalReport2011_Final.pdf (accessed 30 ⁄ 08 ⁄<br />
2011).<br />
7. White SM, Griffiths R, Holloway J, Shannon A. Anaesthesia for proximal femoral<br />
fracture in the UK: first report from the NHS Hip Fracture Anaesthesia Network<br />
(HIPFAN). Anaesthesia 2010; 65: 243–8.<br />
8. Hayes WC, Myers ER, Robinovitch SN, Van Den Kroonenberg A, Courtney AC,<br />
McMahon TA. Etiology and prevention of age-related hip fractures. Bone 1996; 18:<br />
S77–86.<br />
9. NHS Institute for Innovation and Improvement. Delivering Quality and Value.<br />
November, 2005. http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4122355.pdf<br />
(accessed 30 ⁄ 08 ⁄ 2011).<br />
10. British Orthopaedic Association Standards for Trauma (BOAST) 1. Hip fracture in the<br />
older person. September, 2007. http://www.boa.ac.uk/en/publications/boast/<br />
(accessed 30 ⁄ 08 ⁄ 2011).<br />
11. Royal College of Physicians, British Geriatrics Society and The British Pain Society. The<br />
assessment of pain in older people. October, 2007. http://www.bgs.org.uk/<br />
Publications/Clinical%20Guidelines/pain%20concise%20guidelines%20WEB.pdf<br />
(accessed 30 ⁄ 08 ⁄ 2011).<br />
12. Cuvillon P, Ripart J, Debureaux S, et al. Analgesia after hip fracture repair in<br />
elderly patients: the effect of a continuous femoral nerve block: a prospective<br />
and randomised study. Annales Francaises d’Anesthesie et de Reanimation 2007; 26:<br />
2–9.<br />
13. White SM, Rashid N, Chakladar A. An analysis of renal dysfunction in 1511 patients<br />
with fractured neck of femur: the implications for perioperative analgesia. Anaesthesia<br />
2009; 64: 1061–5.<br />
14. Foss NB, Kristensen BB, Bundgaard M, et al. Fascia iliaca compartment blockade for<br />
acute pain control in hip fracture patients: a randomized, placebo-controlled trial.<br />
Anesthesiology 2007; 106: 773–8.<br />
15. Parker MJ, Griffiths R, Appadu BN. Nerve blocks (subcostal, lateral cutaneous, femoral,<br />
triple, psoas) for hip fractures. Cochrane Database of Systematic Reviews 2002; 1:<br />
CD001159.<br />
16. Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative<br />
complications on mortality after hip fracture in elderly people: prospective observational<br />
cohort study. British Medical Journal 2005; 331: 1374–9.<br />
17. Maxwell MJ, Moran CG, Moppett IK. Development and validation of a preoperative<br />
scoring system to predict 30 day mortality in patients undergoing hip fracture surgery.<br />
British Journal of Anaesthesia 2008; 101: 511–7.<br />
18. White SM. Including the very elderly in clinical trials. Anaesthesia 2010; 65: 778–80.<br />
26 Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: proximal hip fractures Anaesthesia 2011<br />
19. Foss NB, Kristensen MT, Jensen PS, Palm H, Krasheninnikoff M, Kehlet H. The effects of<br />
liberal versus restrictive transfusion thresholds on ambulation after hip fracture<br />
surgery. Transfusion 2009; 49: 227–34.<br />
20. Horlocker TT, Wedel DJ, Benzon H, et al. Regional anesthesia in the anticoagulated<br />
patient: defining the risks (the second ASRA Consensus Conference on Neuraxial<br />
Anesthesia and Anticoagulation). Regional Anesthesia and Pain Medicine 2003; 28:<br />
172–97.<br />
21. Hallgren MA, Hogberg P, Andreasson S. Alcohol consumption and harm among elderly<br />
Europeans: falling between the cracks. European Journal of Public Health 2010; 20:<br />
616–7.<br />
22. The Task Force for the Management of Atrial Fibrillation of the European Society of<br />
Cardiology (ESC). Guidelines for the management of atrial fibrillation. European Heart<br />
Journal 2010; 31: 2369–429.<br />
23. Chambers J. Aortic stenosis: is common but often unrecognised. British Medical<br />
Journal 2005; 330: 801–2.<br />
24. Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip<br />
fracture patients? Systematic review, meta-analysis and meta-regression. Canadian<br />
Journal of Anesthesia 2008; 55: 146–54.<br />
25. Khan SK, Kalra S, Khanna A, Thiruvengada MM, Parker MJ. Timing of surgery for hip<br />
fractures: a systematic review of 52 published studies involving 291,413 patients.<br />
Injury 2009; 40: 692–7.<br />
26. White SM, Baldwin TJ. The Mental Capacity Act, 2005. Implications for anaesthesia and<br />
intensive care. Anaesthesia 2006; 61: 381–9.<br />
27. British Medical Association, Resuscitation Council (UK) and the Royal College of<br />
Nursing. Decisions relating to cardiopulmonary resuscitation. October, 2007. http://<br />
www.resus.org.uk/pages/dnar.pdf (accessed 30 ⁄ 08 ⁄ 2011).<br />
28. Association of Anaesthetists of Great Britain and Ireland. DNAR decisions in the<br />
perioperative period. May, 2009. http://www.<strong>aagbi</strong>.org/publications/guidelines/<br />
docs/dnar_09.pdf (accessed 30 ⁄ 08 ⁄ 2011).<br />
29. Parker MJ, Handoll HHG, Griffiths R. Anaesthesia for hip fracture surgery in adults.<br />
Cochrane Database of Systematic Reviews 2004; 18: CD000521.<br />
30. Luger TJ, Kammerlander C, Gosch M, et al. Neuroaxial versus general anaesthesia in<br />
geriatric patients for hip fracture surgery: does it matter. Osteoporosis International<br />
2010; 21: S555–72.<br />
31. Association of Anaesthetists of Great Britain and Ireland. Anaesthesia and perioperative<br />
care of the elderly. December 2001. http://www.<strong>aagbi</strong>.org/publications/<br />
guidelines/docs/careelderly01.pdf (accessed 30 ⁄ 08 ⁄ 2011).<br />
32. Wood R, White SM. Anaesthesia for 1131 patients undergoing proximal femoral<br />
fracture repair: effects on blood pressure, fluid administration and perioperative<br />
anaemia. Anaesthesia 2011; 66: 1017–22.<br />
33. Ben-David B, Frankel R, Arzumonov T, Marchevsky Y, Volpin G. Minidose bupivacainefentanyl<br />
spinal anesthesia for surgical repair of hip fracture in the aged. Anesthesiology<br />
2000; 92: 6–10.<br />
34. Hindle A. Intrathecal opioids in the management of acute postoperative pain.<br />
Continuing Education in Anaesthesia, Critical Care and Pain 2008; 8: 81–5.<br />
35. Association of Anaesthetists of Great Britain and Ireland. Recommendations for<br />
standards of monitoring during anaesthesia and recovery. 4th ed. March 2007.<br />
Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland 27
Anaesthesia 2011<br />
Griffiths et al. | Guidelines: proximal hip fractures<br />
http://www.<strong>aagbi</strong>.org/publications/guidelines/docs/standardsofmonitoring07.pdf<br />
(accessed 30 ⁄ 08 ⁄ 2011).<br />
36. National Confidential Enquiry into Perioperative Deaths. Extremes of age. November,<br />
1999. http://www.ncepod.org.uk/pdf/1999/99full.pdf (accessed 30 ⁄ 08 ⁄ 2011).<br />
37. Minville V, Asehnoune K, Salau S, et al. The effects of spinal anesthesia on cerebral<br />
blood flow in the very elderly. Anesthesia and Analgesia 2009; 108: 1291–4.<br />
38. National Institute for Health and Clinical Excellence. Clinical guideline 92. Venous<br />
thromboembolism: reducing the risk of venous thromboembolism (deep vein<br />
thrombosis and pulmonary embolism) in patients admitted to hospital. March,<br />
2010. http://www.nice.org.uk/nicemedia/live/12695/47920/47920.pdf (accessed<br />
30 ⁄ 08 ⁄ 2011).<br />
39. National Institute for Health and Clinical Excellence. Clinical guideline 65. Inadvertent<br />
perioperative hypothermia: the management of inadvertent perioperative hypothermia<br />
in adults. April, 2008. http://www.nice.org.uk/nicemedia/live/11962/40432/<br />
40432.pdf (accessed 30 ⁄ 08 ⁄ 2011).<br />
40. Price JD, Sear JJW, Venn RRM. Perioperative fluid volume optimization following<br />
proximal femoral fracture. Cochrane Database of Systematic Reviews 2004, Issue 1.<br />
CD003004.<br />
41. Sinclair S, James S, Singer M. Intraoperative intravascular volume optimisation and<br />
length of hospital stay after repair of proximal femoral fracture: randomised<br />
controlled trial. British Medical Journal 1997; 315: 909–12.<br />
42. Donaldson AJ, Thomson HE, Harper NJ, Kenny NW. Bone cement implantation<br />
syndrome. British Journal of Anaesthesia 2009; 102: 12–22.<br />
43. Björkelund KB, Hommel A, Thorngren KG, Gustafson L, Larsson S, Lundberg D.<br />
Reducing delirium in elderly patients with hip fracture: a multi-factorial intervention<br />
study. Acta Anaesthesiologica Scandinavica 2010; 54: 678–88.<br />
44. Duncan DG, Beck SJ, Hood K, Johansen A. Using dietetic assistants to improve the<br />
outcome of hip fracture: a randomised controlled trial of nutritional support in an<br />
acute trauma ward. Age and Aging 2006; 35: 148–53.<br />
45. Foss NB, Jensen PS, Kehlet H. Risk factors for insufficient perioperative oral nutrition<br />
after hip fracture surgery within a multi-modal rehabilitation programme. Age and<br />
Aging 2007; 36: 538–43.<br />
46. Foss N, Kehlet H. Mortality analysis in hip fracture patients: implications for design of<br />
future outcome trials. British Journal of Anaesthesia 2005; 94: 24–9.<br />
47. The Hip Fracture Perioperative Network. http://www.networks.nhs.uk/hipfractureanaesthesia<br />
(accessed 30 ⁄ 08 ⁄ 2011).<br />
48. The National Hip Fracture database. http://www.nhfd.co.uk/ (accessed<br />
30 ⁄ 08 ⁄ 2011).<br />
49. General Medical Council. Consent: patients and doctors making decisions together.<br />
June, 2008. http://www.gmc-uk.org/static/documents/content/Consent_0510.pdf<br />
(accessed 30 ⁄ 08 ⁄ 2011).<br />
50. Association of Anaesthetists of Great Britain and Ireland. Consent for anaesthesia.<br />
2nd ed. January 2006. http://www.<strong>aagbi</strong>.org/publications/guidelines/docs/<br />
consent06.pdf (accessed 30 ⁄ 08 ⁄ 2011).<br />
51. Royal College of Anaesthetists. Curriculum for a CCT in Anaesthetics. 2 ed.<br />
August, 2010. http://www.rcoa.ac.uk/index.asp?PageID=1479 (accessed 30 ⁄ 08 ⁄<br />
2011).<br />
28 Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland
Griffiths et al. | Guidelines: proximal hip fractures Anaesthesia 2011<br />
52. Wiles MD, Moran CG, Sahota O, Moppett IK. Nottingham Hip Fracture Score as a<br />
predictor of one year mortality in patients undergoing surgical repair of fractured neck<br />
of femur. British Journal of Anaesthesia 2011; 106: 501–4.<br />
Appendix 1<br />
Nottingham Hip Fracture Score<br />
A score out of ten is derived by adding weighted scores for eight criteria<br />
(a). The total score may then be used to predict the risk of a patient dying<br />
within 30 days of hip fracture surgery (b), a figure that may be used to<br />
stratify patient-specific surgical risk during the process of consent, and in<br />
order to identify patients who may benefit from more intensive levels of<br />
peri-operative care. The score may also be used to predict 1-year<br />
postoperative mortality [52].<br />
(a) Derivation of score.<br />
Variable<br />
Points<br />
Age 66–85 years 3<br />
Age 86 ‡ older 4<br />
Male 1<br />
Haemoglobin concentration £ 10 g.dl )1 on admission to hospital 1<br />
Abbreviated mental test score £ 6 ⁄ 10 on admission to hospital 1<br />
Living in an institution 1<br />
More than one co-morbidity 1<br />
Active malignancy within last 20 years 1<br />
(b) Predicted 30-day mortality.<br />
Score<br />
Predicted 30-day postoperative mortality<br />
0 0<br />
1 1%<br />
2 2%<br />
3 4%<br />
4 6%<br />
5 10%<br />
6 15%<br />
7 23%<br />
8 22%<br />
9 45%<br />
10 57%<br />
Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland 29
Anaesthesia 2011<br />
Griffiths et al. | Guidelines: proximal hip fractures<br />
Appendix 2<br />
Resources for patients and relatives<br />
There is excellent guidance, with examples, available on how to develop<br />
and produce information leaflets from the following:<br />
• Royal College of Anaesthetists (http://www.rcoa.ac.uk/index.asp?PageID=69):<br />
You and your anaesthetic; Anaesthesia explained.<br />
• British Orthopaedic Association (http://www.boa.ac.uk/en/patientinformation/olderhip):<br />
Guidance for older patients with hip fractures.<br />
• NHS Brand Guidelines (http://www.nhsidentity.nhs.uk/tools-and-resources/patient-information):<br />
Patient information: a general resource<br />
for producing written information for patients.<br />
30 Anaesthesia ª 2011 The Association of Anaesthetists of Great Britain and Ireland
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
The Royal College of<br />
Anaesthetists<br />
The Association of<br />
Anaesthetists of Great<br />
Britain and Ireland<br />
The Good Anaesthetist<br />
Standards of Practice for Career Grade Anaesthetists<br />
February 2010
The Royal College<br />
of Anaesthetists<br />
The Association of<br />
Anaesthetists of<br />
Great Britain and<br />
Ireland<br />
The Good Anaesthetist<br />
Standards of Practice for Career Grade Anaesthetists<br />
Prepared by the Joint Committee on Good Practice<br />
ISBN: 978-1-900936-00-2<br />
Published February 2010 by the Royal College of Anaesthetists.<br />
Design and layout by the Royal College of Anaesthetists.<br />
This publication will be reviewed in 2011.<br />
© The Royal College of Anaesthetists 2010<br />
All rights reserved. No part of this framework may be reproduced or transmitted in any<br />
form or by any means, electronic or mechanical, including photocopying, recording or any<br />
information storage or retrieval system without prior permission of the Royal College of<br />
Anaesthetists.<br />
Whilst the Royal College of Anaesthetists has endeavoured to ensure that the document is<br />
as current as possible at the time it was published, it can take no responsibility for matters<br />
arising from circumstances which may have changed, or information which may become<br />
available subsequently.<br />
All enquiries in regard to this document should be addressed to:<br />
Professional Standards Directorate<br />
The Royal College of Anaesthetists<br />
Churchill House<br />
35 Red Lion Square<br />
London WC1R 4SG<br />
email: standards@rcoa.ac.uk<br />
Page 1
Contents ❚<br />
Foreword 4<br />
Introduction 5<br />
Notes on terminology 6<br />
Related guidelines and sources of information 7<br />
Domain A: knowledge, skills and performance<br />
Attribute 1: maintain your professional performance 8<br />
Attribute 2: apply knowledge and experience to practice 10<br />
Attribute 3: keep clear, accurate and legible records 12<br />
Domain B: safety and quality<br />
Attribute 4: put into effect systems to protect patients and improve care 14<br />
Attribute 5: respond to risks to safety 16<br />
Attribute 6: protect patients and colleagues from any risk posed by your health 18<br />
Domain C: communication, partnership and teamwork<br />
Attribute 7: communicate effectively 20<br />
Attribute 8: work constructively with colleagues and delegate effectively 22<br />
Attribute 9: establish and maintain partnerships with patients 24<br />
Domain D: maintaining trust<br />
Attribute 10: show respect for patients 26<br />
Attribute 11: treat patients and colleagues fairly and without discrimination 28<br />
Attribute 12: act with honesty and integrity 30<br />
Prepared by the Joint Committee on Good Practice | Page 3
Foreword ❚<br />
This document represents the distillation of many previous publications related to the standards<br />
of practice expected of clinicians delivering anaesthesia. These standards have been mapped<br />
to the generic standards in the Framework for Appraisal and Assessment published by the<br />
General Medical Council (GMC) in 2008. In this document they defined four domains and three<br />
attributes in each domain. There are then standards within each attribute, 75 in all, which every<br />
doctor with a licence to practise must meet.<br />
Our specialty standards must, and indeed do, map to all of these 75 generic standards but<br />
also include those that effectively define the current practice of anaesthesia. They have been<br />
ratified by the Joint Committee on Good Practice (JCGP) of the Royal College of Anaesthetists<br />
(RCoA) and Association of Anaesthetists of Great Britain and Ireland (AAGBI) and will be regularly<br />
reviewed and updated as necessary.<br />
It is these specialty specific standards that we have submitted to the GMC and which will<br />
underpin all aspects of revalidation for anaesthetists. At first glance they appear daunting, but<br />
in practice they simply describe activities we all do, and which are usually reviewed in annual<br />
appraisal. It is worth taking some time to compare what information we each have to support<br />
our claim to meet these standards (usually in our appraisal documents) and therefore identify<br />
where we might be sensible to gather more supporting information (or ‘evidence’) before our<br />
next appraisal.<br />
Acknowledgements<br />
We are extremely grateful to the many individuals who have contributed their time in preparing<br />
the original document and those who assisted in the revisions for this new document. In<br />
particular, we wish to thank Professor David Hatch and Dr Maria Rollin in their role as primary<br />
authors; Mr Charlie McLaughlan (Director of Professional Standards), Mr Don Liu (Revalidation<br />
Project Manager), Dr Judith Hulf CBE (Revalidation Lead, Academy of Medical Royal Colleges),<br />
Dr Kirstyn Shaw (Revalidation Manager, Academy of Medical Royal Colleges) for their input; and,<br />
finally, Councils for both the RCoA and AAGBI, the JCGP and the RCoA Patient Liaison Group for<br />
their help in assisting with the revisions.<br />
Professor C Dodds<br />
RCoA Revalidation Lead<br />
February 2010<br />
Page 4 | The Good Anaesthetist | Standards of Practice for Career Grade Anaesthetists
Introduction ❚<br />
The Good Anaesthetist has been compiled to set standards for career grade anaesthetists working<br />
in hospital settings within and/or outside of the NHS. It provides a structured framework detailing<br />
the minimum standards that anaesthetists are expected to meet. In particular, the framework can<br />
be used to reflect on practice and identify knowledge areas, skills and attitudes for professional<br />
development. The Good Anaesthetist also underpins the revalidation process for the specialty. It<br />
maps a number of generic and specialty standards to the 12 attributes, as set out in the GMC<br />
Framework for Appraisal and Assessment (2008), which anaesthetists are required to demonstrate<br />
they are continuing to meet through supporting information and during annual appraisal.<br />
The Good Anaesthetist is also intended for use by patients, to provide an informed understanding<br />
of the standards that can be reasonably expected from a competent career grade anaesthetist.<br />
The list of standards is not intended to be exhaustive, but to indicate the range of knowledge,<br />
skills and attitudes in the pattern of practice expected of a career grade anaesthetist. The<br />
standards that are generic to all doctors are drawn principally from Good Medical Practice (2006)<br />
and can be found in the GMC Framework for Appraisal and Assessment. These generic standards<br />
have been incorporated into The Good Anaesthetist and have been supplemented by standards<br />
agreed by the JCGP of the Royal College of Anaesthetists (RCoA) and Association of Anaesthetists<br />
of Great Britain and Ireland (AAGBI). The vast majority listed have been defined as the essential<br />
minimum standards. Anaesthetists who repeatedly fail to conform to the minimum standards<br />
without good and sufficient reason may place their licence to practise at risk during the<br />
revalidation process.<br />
Within each attribute we have grouped the standards according to a shared identifiable<br />
characteristic, i.e. a knowledge, skill, attitude or function area. No one individual standard<br />
should be given a greater degree of importance, including the standard at the beginning of<br />
each group. The groups are a practical way to help anaesthetists approach revalidation in an<br />
organised and focused manner. Anaesthetists will be required to collect supporting information<br />
in each attribute and consideration of standards, when grouped together according to a shared<br />
characteristic, will provide focus for this activity.<br />
Good practice in anaesthesia is dependent not only on the knowledge levels, skills and attitudes<br />
of the individual but also on co-operation from organisations – in particular, in the provision of<br />
adequate resources and time. All anaesthetists should bring to the attention of their employing<br />
organisations any deficiency in resources which impacts on meeting the standards listed in The<br />
Good Anaesthetist and which subsequently influence the quality of medical care and patient safety.<br />
Prepared by the Joint Committee on Good Practice | Page 5
Notes on terminology ❚<br />
The standards listed in The Good Anaesthetist are derived from Good Medical Practice (2006) and<br />
from the work carried out by the JCGP. In Good Medical Practice the terms ‘you must’ and ‘you<br />
should’ are used and the same convention is applied throughout The Good Anaesthetist.<br />
■ ■<br />
■ ■<br />
■ ■<br />
‘An anaesthetist must’ – is used for an overriding duty or principle.<br />
‘An anaesthetist should’ – is used when providing an explanation of how that overriding duty<br />
is to be met.<br />
‘An anaesthetist should’ – is also used where a duty or principle will not apply in all situations<br />
or circumstances, or where there are factors outside your control that affect whether you can<br />
comply with the guidance.<br />
‘Ensure’ is used where anaesthetists must do all that is within their control to make sure that the<br />
event takes place.<br />
Page 6 | The Good Anaesthetist | Standards of Practice for Career Grade Anaesthetists
Related guidelines and sources of information ❚<br />
We have provided references to other guidance to illustrate how the standards in The Good<br />
Anaesthetist can be interpreted and applied in practice. References are placed within the<br />
appropriate attribute, although many of the guidelines cited cover a number of issues and are<br />
applicable to several attributes.<br />
For the sake of brevity we have not cited the following high level good practice guidelines<br />
because they are applicable to all 12 attributes. It is therefore worth referring to the following:<br />
The General Medical Council<br />
››<br />
Good medical practice, 2006.<br />
The Royal College of Anaesthetists and The Association of Anaesthetists of<br />
Great Britain and Ireland<br />
››<br />
Good practice: a guide for departments of anaesthesia, critical care and pain<br />
management (3rd edition), 2006.<br />
The Royal College of Anaesthetists<br />
››<br />
Guidelines for the provision of anaesthetic services (3rd edition), 2009.<br />
The Royal College of Anaesthetists and The Pain Society<br />
››<br />
Pain management services: good practice, 2003.<br />
The guidelines referenced in The Good Anaesthetist have been developed by the GMC, RCoA<br />
or AAGBI. We have only listed those which are currently active. There are a number of other<br />
guidance documents produced by professional bodies including the specialist societies, which<br />
may be relevant to your job plan and professional practice. These guidelines should be referred<br />
to as they may also illustrate how the standards in The Good Anaesthetist can be applied. The Good<br />
Anaesthetist will be made available online as a web based resource. As we develop this area of<br />
work we will include links to the full text of all relevant guidance documents as they are published.<br />
Prepared by the Joint Committee on Good Practice | Page 7
Domain A: knowledge, skills and performance<br />
Attribute 1: maintain your professional performance<br />
Standards<br />
➣➣<br />
An anaesthetist must maintain knowledge of the law and other regulation relevant to<br />
their practice.<br />
❏❏<br />
An anaesthetist must adhere to the laws and codes of practice relevant to their work.<br />
➣➣<br />
An anaesthetist must keep knowledge and skills up to date.<br />
❏❏<br />
An anaesthetist should regularly update relevant knowledge and skills in relation<br />
to clinical practice to comply with core, higher and advanced level requirements of<br />
continuing professional development (CPD).<br />
❏❏<br />
An anaesthetist should regularly update relevant knowledge and skills in relation to<br />
wider clinical practice.<br />
❏❏<br />
An anaesthetist should learn and practise new improved techniques for patient<br />
wellbeing and safety.<br />
➣➣<br />
An anaesthetist must participate in professional development and educational<br />
activities.<br />
❏❏<br />
An anaesthetist should formulate a personal development plan.<br />
❏❏<br />
An anaesthetist should attend hospital and departmental educational meetings.<br />
❏❏<br />
An anaesthetist should seek opportunities to learn from colleagues locally and<br />
elsewhere.<br />
❏❏<br />
An anaesthetist should retain records of CPD activities to support the revalidation<br />
process.<br />
❏❏<br />
An anaesthetist must be truthful in recording CPD activities.<br />
➣➣<br />
An anaesthetist must take part in regular and systematic audit.<br />
❏❏<br />
An anaesthetist should participate actively in departmental or hospital audit meetings<br />
on a regular basis.<br />
❏❏<br />
An anaesthetist should reflect upon and evaluate personal practice at regular intervals.<br />
Page 8 | The Good Anaesthetist | Standards of Practice for Career Grade Anaesthetists
Domain A: knowledge, skills and performance<br />
Attribute 1: maintain your professional performance<br />
Explanatory notes<br />
Maintaining professional performance is both a necessary and continuous process due to medical,<br />
scientific and technological advances and changes in patient expectations. Realisation of these<br />
advances and meeting of those expectations by the profession as a whole, in the day to day practice of<br />
anaesthesia, pain medicine and intensive care, are dependent on individual doctors keeping up to date<br />
with new knowledge and skills and applying them locally and nationally. Individual commitment to<br />
this process requires planned and regular participation in the core, higher and advanced level areas of<br />
continuing professional development (CPD), and also regular review of clinical practice against current<br />
best practice and defined evaluation criteria.<br />
An important aspect of keeping up to date is knowledge of current legal, regulatory and professional<br />
codes which influence clinical and professional practice, e.g. controlled drug provision.<br />
Related guidelines and sources of information<br />
The General Medical Council<br />
››<br />
Guidance on CPD online (accessed 23 November 2009) www.gmc-uk.org/education.<br />
The Royal College of Anaesthetists<br />
››<br />
Continuing professional development guidelines (2nd edition), 2010 (in press).<br />
››<br />
Raising the standard: a compendium of audit recipes (2nd edition), 2006.<br />
Prepared by the Joint Committee on Good Practice | Page 9
Domain A: knowledge, skills and performance<br />
Attribute 2: apply knowledge and experience to practice<br />
Standards<br />
➣➣<br />
In providing care an anaesthetist must recognise and work within the limits of their<br />
competence.<br />
❏❏<br />
When a problem arises outside their area of competence an anaesthetist must seek help<br />
from a suitable colleague.<br />
❏❏<br />
An anaesthetist must act promptly and appropriately when anaesthetic complications<br />
arise and be familiar with the operation of resuscitation equipment and current<br />
resuscitation guidelines.<br />
❏❏<br />
An anaesthetist must take urgent appropriate action if a patient has suffered harm<br />
through misadventure or for any other reason.<br />
❏❏<br />
An anaesthetist must use safe, regularly maintained equipment which has been checked<br />
before use, and use equipment and techniques with which he or she is familiar.<br />
➣➣<br />
An anaesthetist must adequately assess the patient’s condition.<br />
❏❏<br />
An anaesthetist must assess the patient before anaesthesia and devise an appropriate<br />
plan of anaesthetic management.<br />
➣➣<br />
An anaesthetist must provide or arrange advice, investigations or treatment where<br />
necessary.<br />
❏❏<br />
An anaesthetist must prescribe drugs or treatment, including repeat prescriptions, safely<br />
and appropriately.<br />
❏❏<br />
An anaesthetist must take steps to alleviate pain and distress whether or not a cure may<br />
be possible.<br />
❏❏<br />
An anaesthetist must provide effective treatments based on the best available evidence.<br />
❏❏<br />
An anaesthetist should consider appropriate local or nationally agreed guidelines when<br />
planning an anaesthetic.<br />
❏❏<br />
An anaesthetist must consult colleagues, or refer patients to colleagues, when this is in<br />
the patient’s best interest.<br />
➣➣<br />
If they are involved in teaching, an anaesthetist must apply the skills, attitudes and<br />
practice of a competent teacher/trainer.<br />
❏❏<br />
An anaesthetist should support the College Tutor in the teaching and clinical supervision<br />
of anaesthetic trainees.<br />
❏❏<br />
An anaesthetist should participate actively in the professional development of trainees.<br />
❏❏<br />
An anaesthetist should participate in the assessment of trainees, having undertaken the<br />
necessary training.<br />
❏❏<br />
An anaesthetist should contribute to the teaching of medical and other students.<br />
❏❏<br />
An anaesthetist should adopt a multidisciplinary approach to learning and teaching.<br />
❏❏<br />
An anaesthetist should help to foster a culture of lifelong learning.<br />
Page 10 | The Good Anaesthetist | Standards of Practice for Career Grade Anaesthetists
Domain A: knowledge, skills and performance<br />
Attribute 2: apply knowledge and experience to practice<br />
Explanatory notes<br />
Patients rely on anaesthetists to utilise and apply their expert knowledge and experience when making<br />
professional judgements, dealing with complex situations and solving clinical problems. However, on<br />
the other hand, given the rate of scientific and technological advances in medicine the majority of<br />
patients do not expect anaesthetists to be the fountain of all knowledge. In return for this recognition,<br />
anaesthetists must work within the limits of their competence; and where appropriate consult or seek<br />
advice from other sources or refer patients to colleagues, including those from other specialties, who<br />
do have the necessary experience and expertise.<br />
An environment where patient care prospers is one where all members of the healthcare team can<br />
learn from one another. Anaesthetists must therefore share their knowledge, skills and expertise by<br />
engaging in the education, training and professional development of colleagues. This educational role<br />
also includes undertaking reliable and honest formative assessment of students and trainees; providing<br />
constructive feedback to them as appropriate.<br />
Related guidelines and sources of information<br />
The General Medical Council<br />
››<br />
Good practice in prescribing medicines: supplementary guidance, 2008.<br />
››<br />
Withholding and withdrawing life-prolonging treatments: good practice in decision making, 2006.<br />
The Royal College of Anaesthetists<br />
››<br />
Cardiopulmonary resuscitation: standards for clinical practice and training, 2004.<br />
››<br />
Good practice in the management of continuous epidural analgesia in the hospital setting, 2004.<br />
››<br />
Local anaesthesia for intraocular surgery, 2001.<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
››<br />
Checking anaesthetic equipment (3rd edition), 2004.<br />
››<br />
Day surgery (2nd edition), 2005.<br />
››<br />
Do not attempt resuscitation (DNAR) decisions in the peri-operative period, 2009.<br />
››<br />
Guidelines for the management of a malignant hyperthermia crisis, 2007.<br />
››<br />
Peri-operative management of the morbidly obese patient, 2007.<br />
››<br />
Pre-hospital anaesthesia. AAGBI safety guideline, 2009.<br />
››<br />
Pre-operative assessment: the role of the anaesthetist, 2001.<br />
››<br />
Safe management of anaesthetic related equipment, 2009.<br />
››<br />
Suspected anaphylactic reactions associated with anaesthesia (4th edition). AAGBI safety guideline, 2009.<br />
Prepared by the Joint Committee on Good Practice | Page 11
Domain A: knowledge, skills and performance<br />
Attribute 3: keep clear, accurate and legible records<br />
Standards<br />
➣➣<br />
In providing care an anaesthetist must keep clear, accurate and legible records.<br />
❏❏<br />
An anaesthetist should enter their name and GMC number on the anaesthetic record<br />
sheet, in addition to the name of the patient and their details; non-consultants should<br />
record the name of their consultant supervisor.<br />
❏❏<br />
An anaesthetist should only use recognised abbreviations in keeping clear and legible<br />
records.<br />
➣➣<br />
In providing care an anaesthetist must make records at the same time as the events<br />
they are recording or as soon as possible afterwards.<br />
❏❏<br />
An anaesthetist should ensure that the anaesthetic record sheet or hospital notes are up<br />
to date as soon as practicable after the management of complications which have arisen<br />
unexpectedly.<br />
❏❏<br />
An anaesthetist should make an accurate, legible, contemporaneous record of the timing<br />
and doses of drugs and fluids administered such that a colleague could take over the<br />
administration of the anaesthetic if necessary.<br />
❏❏<br />
An anaesthetist should ensure that the results of physiological monitoring of the patient<br />
are recorded at appropriate intervals.<br />
➣➣<br />
An anaesthetist must record clinical findings, decisions, information given to patients,<br />
drugs prescribed and other information or treatment.<br />
❏❏<br />
An anaesthetist should make a written record of the pre-operative assessment and<br />
discussion, including any specific consent for regional anaesthesia or other procedures<br />
when necessary.<br />
❏❏<br />
An anaesthetist should complete an entry in the hospital incident reporting system<br />
following a critical incident.<br />
Page 12 | The Good Anaesthetist | Standards of Practice for Career Grade Anaesthetists
Domain A: knowledge, skills and performance<br />
Attribute 3: keep clear, accurate and legible records<br />
Explanatory notes<br />
The basic premise for keeping good quality medical records in anaesthesia, pain medicine and intensive<br />
care is to facilitate communication amongst colleagues, and ensure the effective and safe continuation<br />
of care of patients at different times and by different team members. It is therefore particularly<br />
important that critical incidents, complications and unexpected events are accurately documented.<br />
A secondary, but important, premise is that records (provided patients have been informed and they<br />
do not object) are an important resource when it comes to auditing areas of anaesthesia care and<br />
reviewing cases for educational purposes.<br />
Related guidelines and sources of information<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
››<br />
Information management: guidance for anaesthetists, 2008.<br />
Prepared by the Joint Committee on Good Practice | Page 13
Domain B: safety and quality<br />
Attribute 4: put into effect systems to protect patients and improve care<br />
Standards<br />
➣➣<br />
An anaesthetist must respond constructively to the outcome of audit, appraisals and<br />
performance reviews or assessments.<br />
❏❏<br />
An anaesthetist must participate in the annual appraisal process.<br />
➣➣<br />
An anaesthetist must take part in systems of quality assurance and quality<br />
improvement.<br />
❏❏<br />
An anaesthetist should co-operate with internal and external reviews.<br />
➣➣<br />
An anaesthetist must comply with risk management and clinical governance<br />
procedures.<br />
❏❏<br />
An anaesthetist should participate in relevant national reporting schemes.<br />
❏❏<br />
An anaesthetist must cooperate with legitimate requests for information from<br />
organisations monitoring public health.<br />
➣➣<br />
An anaesthetist must provide information for confidential enquiries and significant<br />
event reporting.<br />
❏❏<br />
An anaesthetist must report suspected adverse drug reactions.<br />
➣➣<br />
An anaesthetist must ensure arrangements are made for the continuing care of the<br />
patient where necessary.<br />
❏❏<br />
An anaesthetist should ensure that on-call teams have a range of skills sufficient to<br />
manage any reasonable predictable clinical eventuality.<br />
❏❏<br />
An anaesthetist must write clear instructions for post-operative care including pain relief,<br />
oxygen therapy and fluid management as necessary.<br />
❏❏<br />
An anaesthetist must ensure that there is continuous supervision of a patient receiving<br />
anaesthesia. If in exceptional circumstances you are required to leave the theatre, you<br />
must ensure that the patient is supervised by another anaesthetist or appropriately<br />
trained assistant following a handover in accordance with AAGBI guidelines.*<br />
❏❏<br />
An anaesthetist must ensure that recovering patients are observed on a one-to-one<br />
basis by an anaesthetist, recovery nurse or other properly trained member of staff<br />
in accordance with AAGBI guidelines** until they have regained airway control and<br />
cardiovascular stability and are able to communicate.<br />
Page 14 | The Good Anaesthetist | Standards of Practice for Career Grade Anaesthetists
Domain B: safety and quality<br />
Attribute 4: put into effect systems to protect patients and improve care<br />
Explanatory notes<br />
Anaesthetists have a duty of care in ensuring patient safety at all times. This duty applies at both<br />
systems and individual patient care levels. Taking part in data collection exercises and reporting<br />
significant events and complications are vital in developing an organisational culture whereby issues<br />
that could potentially affect patient safety can be systematically identified. The duty of care extends,<br />
whether you are on or off duty, to making sure that competent members of staff are involved in the<br />
provision of safe and continuous care of patients. Patient safety, including measures to foresee and<br />
prevent any adverse incidents that may arise, should be given due consideration in any service or<br />
performance review, including the annual appraisal.<br />
Related guidelines and sources of information<br />
The General Medical Council<br />
››<br />
Raising concerns about patient safety, 2008.<br />
The Royal College of Anaesthetists<br />
››<br />
Syringe labelling in critical care areas, 2004.<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
››<br />
Controlled drugs in perioperative care, 2006.<br />
››<br />
Immediate postanaesthetic recovery, 2002.**<br />
››<br />
Interhospital transfer. AAGBI safety guideline, 2009.<br />
››<br />
Provision of anaesthetic services in magnetic resonance units, 2002.<br />
››<br />
Recommendations for standards of monitoring during anaesthesia and recovery (4th edition), 2007.*<br />
››<br />
Recommendations for the safe transfer of patients with brain injury, 2006.<br />
››<br />
Theatre efficiency: safety, quality of care and optimal use of resources, 2003.<br />
Prepared by the Joint Committee on Good Practice | Page 15
Domain B: safety and quality<br />
Attribute 5: respond to risks to safety<br />
Standards<br />
➣➣<br />
An anaesthetist must report risks in the healthcare environment to their employing or<br />
contracting bodies.<br />
❏❏<br />
An anaesthetist should respond promptly to risks posed by patients.<br />
❏❏<br />
An anaesthetist must follow infection control procedures and regulations.<br />
❏❏<br />
An anaesthetist must safeguard and protect the health and well being of vulnerable<br />
people, including children and the elderly and those with learning disabilities.<br />
➣➣<br />
An anaesthetist must take action where there is evidence that a colleague’s conduct,<br />
performance or health may be putting patients at risk.<br />
❏❏<br />
An anaesthetist should be able to recognise when a colleague may be putting patients<br />
at risk because of poor performance, misconduct or health reasons.<br />
❏❏<br />
An anaesthetist should listen impartially to medical, nursing and other colleagues when<br />
they express concerns about a fellow anaesthetist, and discuss such concerns only in an<br />
appropriate forum.<br />
❏❏<br />
An anaesthetist must take action and inform the clinical director or other responsible<br />
person if necessary when a colleague may be putting patients at risk, and keep a written<br />
record of the action taken.<br />
Page 16 | The Good Anaesthetist | Standards of Practice for Career Grade Anaesthetists
Domain B: safety and quality<br />
Attribute 5: respond to risks to safety<br />
Explanatory notes<br />
Risks to patient safety can come from several, sometimes unexpected, sources. Responsibilities in<br />
regard to occupational health and safety laws apply to all employees in an organisation. However, there<br />
are some risks that only a doctor, with their expertise and experience, will be able to recognise. Risk to<br />
patient safety may stem from a poorly performing doctor in your team. If this risk could potentially or<br />
does already affect patient safety, depending on seriousness, appropriate action must be taken in line<br />
with local Trust and national procedures. The poorly performing doctor may be a close colleague or a<br />
senior member of the clinical team, but your overriding duty is to take appropriate steps if there is a risk<br />
to patient safety. Poor performance may be due to ill health; another reason to take appropriate action,<br />
in helping a fellow colleague.<br />
Related guidelines and sources of information<br />
The General Medical Council<br />
››<br />
0–18 years: guidance for all doctors, 2007.<br />
››<br />
Raising concerns about patient safety, 2008.<br />
The Royal College of Anaesthetists<br />
››<br />
Child protection and the anaesthetist: safeguarding children in the operating theatre –<br />
intercollegiate document, 2007.<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
››<br />
Anaesthesia and peri-operative care of the elderly, 2001.<br />
››<br />
Infection control in anaesthesia (2nd edition). AAGBI safety guideline, 2008.<br />
Prepared by the Joint Committee on Good Practice | Page 17
Domain B: safety and quality<br />
Attribute 6: protect patients and colleagues from any risk posed by your health<br />
Standards<br />
➣➣<br />
An anaesthetist should make arrangements for accessing independent medical advice<br />
when necessary.<br />
❏❏<br />
An anaesthetist must seek advice and help from a suitably qualified professional in<br />
accordance with GMC guidance if you know that you may have a serious condition<br />
which either could affect your performance or is transmissible to patients.<br />
❏❏<br />
An anaesthetist should access professional counselling, advice, support and help services<br />
if they are suffering from any mental health problem, including addiction, which could<br />
potentially affect their professional judgement or performance.<br />
➣➣<br />
An anaesthetist must make arrangements to protect patients and colleagues from their<br />
own health or other problem.<br />
❏❏<br />
An anaesthetist should be immunised against common serious communicable diseases<br />
where vaccines are available.<br />
❏❏<br />
An anaesthetist should hand over duties to a colleague if judgement or ability is<br />
temporarily impaired due to stress, tiredness or illness.<br />
❏❏<br />
An anaesthetist must not work under the influence of alcohol or drugs.<br />
❏❏<br />
An anaesthetist should take reasonable steps to stay healthy.<br />
Page 18 | The Good Anaesthetist | Standards of Practice for Career Grade Anaesthetists
Domain B: safety and quality<br />
Attribute 6: protect patients and colleagues from any risk posed by your health<br />
Explanatory notes<br />
Looking after patients should not distract an anaesthetist from looking after their own physical and<br />
mental health. A healthy anaesthetist is one who can contribute fully to a team and, in turn, the<br />
effective provision of medical care. Patients have a right to expect safe treatment. This expectation<br />
extends to doctors whose health poses no risk in their professional relationships with patients. You<br />
must seek formal advice if you think your own health is putting patients at risk or you feel it is limiting<br />
your ability as a doctor to function effectively. Dependence on alcohol or drugs falls into this category,<br />
as do stress and fatigue.<br />
Related guidelines and sources of information<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
››<br />
Fatigue and anaesthetists, 2004.<br />
››<br />
Welfare resource pack, 2008.<br />
Prepared by the Joint Committee on Good Practice | Page 19
Domain C: communication, partnership and teamwork<br />
Attribute 7: communicate effectively<br />
Standards<br />
➣➣<br />
An anaesthetist must communicate clearly and effectively with colleagues within and<br />
outside the team.<br />
❏❏<br />
An anaesthetist must pass on information to colleagues involved in, or taking over, the<br />
care of your patient.<br />
❏❏<br />
An anaesthetist should communicate directly with senior and specialist medical<br />
colleagues when appropriate.<br />
❏❏<br />
An anaesthetist should communicate effectively with all members of the team to ensure<br />
resources are used to best effect for the delivery of patient care.<br />
❏❏<br />
An anaesthetist should explain to assistants and other staff what your requirements are<br />
likely to be in advance of inducing anaesthesia.<br />
➣➣<br />
An anaesthetist must visit and explain to patients and/or involved parties after surgery<br />
when something has gone wrong.<br />
❏❏<br />
An anaesthetist should meet with close relatives by appointment when asked to do so to<br />
discuss when things have gone wrong.<br />
❏❏<br />
An anaesthetist must be considerate to those close to the patient.<br />
❏❏<br />
An anaesthetist should ensure that a witness is present when explaining what went<br />
wrong with a patient and/or involved parties, and that the incident and patient visit are<br />
both adequately documented in the clinical records.<br />
➣➣<br />
An anaesthetist must keep patients informed about the progress of their care.<br />
❏❏<br />
An anaesthetist must listen to patients and respect their views about their health.<br />
❏❏<br />
An anaesthetist must give patients the information they need in order to make decisions<br />
about their care in a way they can understand.<br />
❏❏<br />
An anaesthetist should encourage questions when possible and allow time to listen<br />
to the concerns of patients, guardians or parents before and, where possible, after an<br />
anaesthetic or therapeutic procedure.<br />
❏❏<br />
An anaesthetist must respond to patients’ questions.<br />
❏❏<br />
An anaesthetist must answer questions openly and honestly.<br />
Page 20 | The Good Anaesthetist | Standards of Practice for Career Grade Anaesthetists
Domain C: communication, partnership and teamwork<br />
Attribute 7: communicate effectively<br />
Explanatory notes<br />
Effective provision of care in anaesthesia, pain medicine and intensive care requires anaesthetists<br />
to utilise a number of communication skills. Listening, questioning and providing instructions to<br />
colleagues are just some of the skills that are necessary within a functioning multidisciplinary setting.<br />
Non-verbal forms of communication are just as important as verbal ones.<br />
Patients are very much seen as partners and contributors in the provision of their own healthcare.<br />
Whether they can effectively contribute to this partnership is dependent on information provided by<br />
their doctor in ways that can be easily understood. Again, this is very much dependent on a doctor’s<br />
communication skills. Mistakes, as in any other area of life, can occur in medical practice. When a<br />
mistake has been made, whether a complaint has followed or not, an informed and appropriate<br />
explanation must be given to the patient or a close family member.<br />
Related guidelines and sources of information<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
››<br />
Catastrophes in anaesthetic practice: dealing with the aftermath, 2005.<br />
Prepared by the Joint Committee on Good Practice | Page 21
Domain C: communication, partnership and teamwork<br />
Attribute 8: work constructively with colleagues and delegate effectively<br />
Standards<br />
➣➣<br />
An anaesthetist must treat colleagues fairly and with respect.<br />
❏❏<br />
An anaesthetist should respect the skills and contributions of other members of the<br />
anaesthetic, medical and nursing team.<br />
❏❏<br />
An anaesthetist should encourage multidisciplinary team working.<br />
❏❏<br />
An anaesthetist should ensure that the work content of job plans and on-call rotas is<br />
fairly distributed among colleagues.<br />
➣➣<br />
An anaesthetist must support colleagues who have problems with their performance,<br />
conduct or health.<br />
❏❏<br />
An anaesthetist should always be willing to advise and help colleagues.<br />
❏❏<br />
An anaesthetist should support colleagues undergoing rehabilitation after their illness or<br />
returning to work after a period of absence for any reason.<br />
➣➣<br />
An anaesthetist should act as a positive role model for colleagues.<br />
❏❏<br />
An anaesthetist should provide appropriate professional support and encouragement for<br />
trainees, staff and associate specialist grade (SAS) doctors and other anaesthetists under<br />
their supervision.<br />
❏❏<br />
An anaesthetist should attend hospital promptly when requested and only leave when<br />
appropriate to do so.<br />
❏❏<br />
An anaesthetist should be prepared to work flexibly within the department.<br />
❏❏<br />
An anaesthetist should ensure that they are aware of being placed on a roster to cover<br />
emergency operating lists and on-call duties.<br />
❏❏<br />
An anaesthetist must make sure that when on-call they can easily be contacted.<br />
❏❏<br />
An anaesthetist should arrange annual, professional and study leave in advance in<br />
accordance with local departmental policy.<br />
➣➣<br />
An anaesthetist must ensure that colleagues to whom they delegate have appropriate<br />
qualifications and experience.<br />
❏ ❏ An anaesthetist with a management role should confirm that the on-call staff work<br />
within their competencies.<br />
Page 22 | The Good Anaesthetist | Standards of Practice for Career Grade Anaesthetists
Domain C: communication, partnership and teamwork<br />
Attribute 8: work constructively with colleagues and delegate effectively<br />
Explanatory notes<br />
Anaesthetists usually function as members of departments and multidisciplinary teams in order to<br />
provide safe and effective care to patients. Developing good relationships with colleagues is important,<br />
as well as understanding and respecting their professionalism, roles and views. Anaesthetists are<br />
commonly leaders of clinical teams and should therefore ensure that ineffective team working does not<br />
compromise patient care. Displaying the behaviours and attitudes of a positive role model is often the<br />
first step in achieving this.<br />
Related guidelines and sources of information<br />
The General Medical Council<br />
››<br />
Management for doctors, 2006.<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
››<br />
The anaesthesia team (2nd edition), 2005.<br />
››<br />
Consultant trainee relationships – a guide for consultants, 2001.<br />
››<br />
Guidance on the 2003 (new) contract and job planning for consultant anaesthetists, 2005.<br />
››<br />
Guidance on the supervision of non-consultant anaesthetists, 2008.<br />
Prepared by the Joint Committee on Good Practice | Page 23
Domain C: communication, partnership and teamwork<br />
Attribute 9: establish and maintain partnerships with patients<br />
Standards<br />
➣➣<br />
An anaesthetist should encourage patients to take an interest in their health and take<br />
action to improve and maintain it.<br />
❏❏<br />
An anaesthetist must support patients in caring for themselves.<br />
❏❏<br />
An anaesthetist should engage in the education of patients and the wider public.<br />
❏❏<br />
An anaesthetist should promote the specialty of anaesthesia in the wider public interest.<br />
➣➣<br />
An anaesthetist must be satisfied that they have consent or other valid authority before<br />
they undertake any examination or investigation, provide treatment or involve patients<br />
in teaching or research.<br />
❏❏<br />
An anaesthetist should ensure that patients have understood the nature and purpose of<br />
any proposed treatment or investigation and any significant risk or side effects associated<br />
with it, enabling them to make an informed choice of anaesthetic technique by giving<br />
clear explanation of the advantages and disadvantages of the options available, using<br />
terms that a patient can understand and relate to when giving consent.<br />
❏❏<br />
An anaesthetist must abide with local research ethics committee and multicentre<br />
research ethics committee guidelines when carrying out research.<br />
Page 24 | The Good Anaesthetist | Standards of Practice for Career Grade Anaesthetists
Domain C: communication, partnership and teamwork<br />
Attribute 9: establish and maintain partnerships with patients<br />
Explanatory notes<br />
It has been recognised that good professional relationships with patients is fundamental to the practice<br />
of medicine. Establishing a partnership, which is built on trust, will allow an anaesthetist to influence<br />
the patient’s approach and attitude to their treatment and care over time. Trust is gained through an<br />
anaesthetist’s professionalism, which covers not only their knowledge and clinical skills but also their<br />
ability to empathise with, understand and respect the views and feelings of patients. This is a process<br />
and the same consideration must also be given when obtaining patient consent. It is not just a signing<br />
of an appropriate consent form but involves listening to a patient’s concerns and anxieties, answering<br />
their questions and providing information in a way they can understand. Having an anaesthetic, an<br />
admission to critical care or the requirement for pain medicine are often parts of medical care about<br />
which patients are most anxious.<br />
Related guidelines and sources of information<br />
The General Medical Council<br />
››<br />
Consent: patients and doctors making decisions together, 2008.<br />
››<br />
Maintaining boundaries: supplementary guidance, 2006.<br />
››<br />
Making and using visual and audio recordings of patients: guidance for doctors, 2002.<br />
››<br />
Research: the role and responsibility of doctors, 2002.<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
››<br />
Consent for anaesthesia (2nd edition), 2004.<br />
Prepared by the Joint Committee on Good Practice | Page 25
Domain D: maintaining trust<br />
Attribute 10: show respect for patients<br />
Standards<br />
➣➣<br />
An anaesthetist must implement and comply with systems to protect patient<br />
confidentiality.<br />
❏❏<br />
An anaesthetist must maintain patient confidentiality at all times.<br />
➣➣<br />
An anaesthetist must be polite, considerate and honest and respect patients’ dignity<br />
and privacy.<br />
❏❏<br />
An anaesthetist should promote trust with patients through courteous behaviour,<br />
honest discussions and respect for their right to privacy and dignity, whether conscious<br />
or unconscious.<br />
❏❏<br />
An anaesthetist must treat each patient fairly and as an individual.<br />
Page 26 | The Good Anaesthetist | Standards of Practice for Career Grade Anaesthetists
Domain D: maintaining trust<br />
Attribute 10: show respect for patients<br />
Explanatory notes<br />
Politeness, consideration, honesty and respect are recognised social norms in any professional working<br />
environment. Showing respect to patients includes respecting their privacy. Without assurances about<br />
privacy, patients may be reluctant to seek help from doctors or part with the necessary information so that<br />
doctors can provide safe and effective care. Patient confidentiality is therefore a duty for all doctors but it<br />
is not an absolute. Information can or should be disclosed in certain circumstances, e.g. to satisfy a legal<br />
requirement, and under certain conditions, as stipulated by the latest GMC guidance on confidentiality.<br />
Related guidelines and sources of information<br />
The General Medical Council<br />
››<br />
Confidentiality, 2009.<br />
››<br />
Maintaining boundaries: supplementary guidance, 2006.<br />
››<br />
Personal beliefs and medical practice: supplementary guidance, 2008.<br />
Prepared by the Joint Committee on Good Practice | Page 27
Domain D: maintaining trust<br />
Attribute 11: treat patients and colleagues fairly and without discrimination<br />
Standards<br />
➣➣<br />
An anaesthetist must be honest and objective when appraising or assessing colleagues<br />
and when writing references.<br />
❏❏<br />
An anaesthetist must not exaggerate competence or fail to mention significant<br />
weaknesses in a reference.<br />
❏❏<br />
An anaesthetist should be honest and open in relations with colleagues.<br />
❏❏<br />
An anaesthetist should provide references, reports or signed documents within a<br />
reasonable time.<br />
❏❏<br />
An anaesthetist should ensure that an applicant is aware that a reservation would be<br />
expressed when writing a reference for him or her.<br />
➣➣<br />
An anaesthetist must respond promptly and fully to complaints.<br />
❏❏<br />
An anaesthetist should, if appropriate, give an apology to the patient and their relatives<br />
and explain in understandable terms what occurred when an untoward incident took<br />
place.<br />
❏❏<br />
An anaesthetist should respond constructively to any complaints received and cooperate<br />
with any relevant complaints procedures or formal inquiry into the treatment of<br />
a patient.<br />
➣➣<br />
An anaesthetist must provide care on the basis of the patient’s needs and the likely<br />
effect of treatment.<br />
❏❏<br />
An anaesthetist must act in the patient’s interest at all times.<br />
❏❏<br />
An anaesthetist must not allow their personal prejudice to affect the treatment or<br />
management of a patient under their care.<br />
❏❏<br />
An anaesthetist should consider the clinical needs of the patient and the professional<br />
needs of colleagues when planning a clinical session.<br />
Page 28 | The Good Anaesthetist | Standards of Practice for Career Grade Anaesthetists
Domain D: maintaining trust<br />
Attribute 11: treat patients and colleagues fairly and without discrimination<br />
Explanatory notes<br />
Engaging with your colleagues fairly and without discrimination, irrespective of their gender, age, race,<br />
sexuality, economic status, lifestyle, culture and religious or political belief, is essential when working<br />
as part of a team. The reverse of this is your right to work without being subject to discrimination.<br />
Consideration of a colleague’s competence and performance must be based on honest and objective<br />
decisions and judgements. Honesty and objectivity must also be applied in your professional<br />
relationships with patients. Best practice involves the recognition and acknowledgement of different<br />
needs in helping patients access medical care on an equal basis.<br />
Complaints must also be managed fairly and without discrimination. Not all complaints by patients<br />
are a result of a mistake; but complaints have risen in recent years due in part to general expectations<br />
increasing and tolerances decreasing. If justified, an anaesthetist should respond promptly and<br />
appropriately to any complaint.<br />
Related guidelines and sources of information<br />
The General Medical Council<br />
››<br />
Personal beliefs and medical practice: supplementary guidance, 2008.<br />
››<br />
Withholding and withdrawing life-prolonging treatments: good practice in decision making, 2006.<br />
››<br />
Writing references: supplementary guidance, 2007.<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
››<br />
Consultant trainee relationships – a guide for consultants, 2001.<br />
››<br />
Management of anaesthesia for Jehovah’s Witnesses (2nd edition), 2005.<br />
Prepared by the Joint Committee on Good Practice | Page 29
Domain D: maintaining trust<br />
Attribute 12: act with honesty and integrity<br />
Standards<br />
➣➣<br />
An anaesthetist must ensure that they have adequate indemnity or insurance cover for<br />
their practice.<br />
➣➣<br />
An anaesthetist must be honest in financial and commercial dealings.<br />
❏❏<br />
An anaesthetist must inform patients about any fees and charges before starting<br />
treatment.<br />
❏❏<br />
An anaesthetist must ensure any published information about their services is factual<br />
and verifiable.<br />
❏❏<br />
An anaesthetist should not undertake private practice or any other commitment which<br />
would prevent them from fulfilling rostered clinical NHS duties.<br />
➣➣<br />
An anaesthetist must be honest in any formal statement or report, whether written or<br />
oral, making clear the limits of your knowledge or competence.<br />
Page 30 | The Good Anaesthetist | Standards of Practice for Career Grade Anaesthetists
Domain D: maintaining trust<br />
Attribute 12: act with honesty and integrity<br />
Explanatory notes<br />
Honesty and integrity form the cornerstone of medical professionalism. Divergence away from these<br />
virtues, regardless of where an anaesthetist may be working (e.g. the NHS or private healthcare sector),<br />
risks diminishing the trust placed in anaesthetists and the profession by patients, colleagues and the<br />
public. In providing information about yourself, your services and others, honesty is reflected by the<br />
accuracy and verifiability of that information. Fulfilling contractual and professional obligations to their<br />
employer and patients will demonstrate the integrity of an anaesthetist.<br />
Related guidelines and sources of information<br />
The General Medical Council<br />
››<br />
Acting as an expert witness: supplementary guidance, 2008.<br />
››<br />
Conflicts of interest: supplementary guidance, 2008.<br />
››<br />
Reporting criminal and regulatory proceedings within and outside the UK:<br />
supplementary guidance, 2008.<br />
››<br />
Taking up and ending appointments: supplementary guidance for doctors, 2008.<br />
››<br />
Writing references: supplementary guidance, 2007.<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
››<br />
Guidance on the 2003 (new) contract and job planning for consultant anaesthetists, 2005.<br />
››<br />
Independent practice, 2008.<br />
››<br />
Voluntary code of practice for billing private patients, 2008.<br />
Prepared by the Joint Committee on Good Practice | Page 31
The Royal College of Anaesthetists<br />
Churchill House | 35 Red Lion Square | London WC1R 4SG<br />
020 7092 1500 www.rcoa.ac.uk info@rcoa.ac.uk<br />
Design and layout by The Royal College of Anaesthetists<br />
The Association of Anaesthetists of Great<br />
Britain and Ireland<br />
21 Portland Place | London W1B 1PY<br />
020 7631 1650 www.<strong>aagbi</strong>.org info@<strong>aagbi</strong>.org
The Royal College of<br />
Anaesthetists<br />
The Association of<br />
Anaesthetists of Great<br />
Britain and Ireland<br />
Good Practice<br />
A guide for departments of anaesthesia,<br />
critical care and pain management<br />
Third edition<br />
2006
The Royal College of<br />
Anaesthetists<br />
The Association of Anaesthetists<br />
of Great Britain and Ireland<br />
Prepared by the Joint Committee on Good Practice<br />
Association of Anaesthetists of Great Britain and Ireland<br />
Professor M Harmer (Chairman)<br />
Dr J Chestnut<br />
Dr I Wilson<br />
Dr D Saunders (Sick Doctors Scheme)<br />
Royal College of Anaesthetists<br />
Sir Peter Simpson<br />
Dr A-M Rollin<br />
Dr J Curran<br />
Dr A Lim<br />
Professor D J Hatch (Professional Standards Advisor)<br />
Mrs A Murray (Patient Liaison Group)<br />
Mr C McLaughlan (Professional Standards Director)<br />
Regional Adviser<br />
Dr J Clarke<br />
Lead Postgraduate Dean<br />
Professor S Field<br />
National Clinical Assessment Service<br />
Professor A Scotland<br />
British Pain Society<br />
Dr B Collett<br />
Intensive Care Society<br />
Professor M Mythen
The Royal College of Anaesthetists<br />
Churchill House 35 Red Lion Square London WC1R 4SG<br />
tel: 020 7092 1500 fax: 020 7092 1730<br />
email: info@roca.ac.uk web: www.rcoa.ac.uk<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
21 Portland Place London W1B 1PY<br />
tel: 020 7631 1650 fax: 020 7631 4352<br />
email: info@<strong>aagbi</strong>.org web: www.<strong>aagbi</strong>.org<br />
Design and layout by The Royal College of Anaesthetists<br />
© Royal College of Anaesthetists and Association of<br />
Anaesthetists of Great Britain and Ireland.<br />
This Guidance may, however, be freely reproduced for<br />
teaching purposes.<br />
October 2006.<br />
The document will be reviewed in 2009.
Contents<br />
Foreword 5<br />
Summary 6<br />
Chapters<br />
1 Introduction and background 7<br />
2 The ethical framework 15<br />
3 Duty of care for anaesthetists 18<br />
4 Professional and clinical guidelines 21<br />
5 Audit: setting, monitoring and reviewing standards 22<br />
6 Continuing professional development 27<br />
7 Record keeping 30<br />
8 Leadership, management and administration 33<br />
9 The poorly performing anaesthetist 37<br />
References 44<br />
Bibliography of current guidance from 46<br />
central organisations<br />
Appendix 1: core topics 49
Good Practice Guide 2006<br />
<br />
Foreword<br />
All doctors practising anaesthesia, critical care and pain management have a primary duty to<br />
provide the best care of patients that they can, whether they practise as consultants, nonconsultant<br />
career grade doctors or trainees, and whether in the National Health Service or<br />
in the independent sector.<br />
The stimulus for the first edition (1998) of this document Good Practice – A Guide for<br />
Departments of Anaesthesia came from a meeting convened in April 1997 by the Chief<br />
Medical Officer (England), Sir Kenneth Calman, at which all acute clinical services were urged<br />
to produce benchmarks of good practice for their specialty.<br />
The Royal College of Anaesthetists (the College) and the Association of Anaesthetists of<br />
Great Britain and Ireland (the Association) set up a joint working party to address this issue.<br />
The working party’s remit was:<br />
❚<br />
❚<br />
❚<br />
to collate current agreed guidelines and standards which specify good practice<br />
to consider how these guidelines and standards could be applied at individual<br />
departmental and national level to ensure patient safety<br />
to offer guidance on the identification and management of poorly performing anaesthetists.<br />
The first edition of the Good Practice document brought together advice, recommendations<br />
and information which reviewed the basis of good practice in anaesthesia, critical care and pain<br />
management. It also summarised the methods by which the medical profession was regulated<br />
and gave guidance to anaesthetists and anaesthetic departments about how departments<br />
could set, maintain and monitor standards of good practice within a changing environment.<br />
The importance of corporate ownership of standards within a department and local regulation<br />
of good practice was emphasised. The document set down as requested the benchmarks<br />
for anaesthetic practice in the context of the many changes which marked the end of the last<br />
Millennium. It was welcomed in both anaesthetic and wider medical circles.<br />
Subsequently, the Association and the College set up a Joint Committee on Good Practice to<br />
develop and advise on some of the themes in the Good Practice document. Many of the<br />
initiatives of the late 1990s have evolved to such an extent that it became clear that the Good<br />
Practice document would require regular review and updating. Such occurred in 2002 with<br />
updating of regulatory issues and reflection of best current practice.<br />
This, the third edition of the Good Practice Guide, is the result of further review and updating<br />
of the previous documents to provide appropriate and current advice on the various aspects<br />
that constitute good practice. Further guidance pertaining to pain management is under<br />
development by the British Pain Society.<br />
We, the Presidents of the Royal College of Anaesthetists and the Association of Anaesthetists<br />
of Great Britain and Ireland, commend this guidance to all involved in anaesthesia, critical<br />
care and pain management.<br />
Dr David Whitaker,<br />
President, Association of Anaesthetists<br />
of Great Britain and Ireland<br />
Dr Judith Hulf,<br />
President,<br />
Royal College of Anaesthetists
Good Practice Guide 2006<br />
Summary<br />
The way in which medicine is practised and the social and political environment in which doctors’<br />
work have changed dramatically in recent years. Recent developments in the provision of NHS<br />
care within the independent sector have again raised concerns over standards of practice.<br />
From early in 2007 anaesthetists and patients will increasingly encounter the new nonmedically<br />
qualified member of the anaesthesia team – the anaesthesia practitioner (AP).<br />
Three phases of recruitment and training are under way for APs in partnership with hospitals<br />
and universities in England, Scotland and Northern Ireland. The Phase 1 students will<br />
qualify to practise on successful completion of 27 months of training and shortly after the<br />
publication of this document. Working under the direct supervision of an anaesthetist, the<br />
AP will be initially indemnified under local arrangements; however, following a period on a<br />
voluntary register held by the College, all aspects of registration for the AP will be taken on<br />
by a national regulator, most likely to be the Health Professions Council. The AP programme,<br />
initiated by the Department of Health (DH) and endorsed by the College and the Association,<br />
is the only one in the United Kingdom (UK) which has been formally accepted by patients and<br />
anaesthetists as safe and appropriate.<br />
Anaesthetists in the UK have an excellent record of adapting to these changes while<br />
maintaining very high standards of patient care. However, concerns have been expressed<br />
by Government, public bodies and the media about the continuing ability of doctors to<br />
regulate themselves. These concerns will only be allayed as doctors demonstrate clearly<br />
their ability to maintain high standards throughout the NHS. Indeed, quality of care has<br />
become the centrepiece of the Government’s approach, though at the same time there is<br />
now acknowledgement that chronic underfunding has contributed to many of the problems<br />
in the NHS. There is a major challenge to ensure that, as funding improves, standards are<br />
maintained and best use is made of such funding.<br />
This third edition of Good Practice – A guide for departments of anaesthesia, critical<br />
care and pain management, updates information and sets out the standards which the<br />
Association of Anaesthetists and the Royal College of Anaesthetists believe should characterise<br />
the delivery of anaesthetic services. It is vital that departments of anaesthesia and individual<br />
anaesthetists continue to provide a high quality service and care for patients. It is the wish<br />
of the Councils of the College and the Association that departments audit their practice and<br />
delivery of anaesthetic services against the benchmarks in this Good Practice document.<br />
Where departments do so, standards of practice will be maintained, anaesthetists will<br />
continue to develop their knowledge and skills and the likelihood of poor practice will be<br />
greatly reduced.
Good Practice Guide 2006<br />
<br />
Chapter 1: Introduction and background<br />
The organisational changes in medicine and in the way it is practised continue at an<br />
alarming rate. Against a background of raised public expectations of both the National<br />
Health Service and of individual doctors, and in a climate of blame and litigation, the<br />
problems within medical practice seem to have increased rather than receded. At<br />
the very least, the changes and recommendations initiated in 1998 have reinforced a<br />
greater awareness among all doctors of the wide responsibilities they carry for their<br />
patients, and the demands on them to demonstrate that their knowledge, skills and<br />
attitudes are being continually updated and critically assessed.<br />
1.1 Contemporary issues 1–5<br />
Recent years have not only seen major changes in medicine due to scientific advances<br />
and technological developments but also changes in the social context within which<br />
doctors work. In the latter half of the 20th Century, the culture of paternalism on the<br />
one hand and deference on the other, rightly, largely disappeared. The population<br />
in general and patients in particular have become better informed about health<br />
matters and decisions about their healthcare. Doctors have accepted that they and<br />
their patients are partners and they now practise in this climate of better patient<br />
knowledge and of co-operation. Simultaneously, time medical practice takes place<br />
within a political and economic framework over which the medical profession has little<br />
control, but in which it is expected by both politicians and patients to make the system<br />
work efficiently and effectively.<br />
Increasingly in the last few years, doubts have been expressed about the ability of<br />
the medical profession to set and maintain standards of practice and to deal with<br />
those whose knowledge, skills and attitudes are deficient. Every case of alleged poor<br />
performance, whether in clinical practice, professional conduct or personal ethics,<br />
serves to reinforce that perceived view. Despite the many changes in management<br />
and the systems in which doctors work, professionally led regulation of the medical<br />
profession is still accepted as the ultimate method for dealing with matters of poor<br />
performance, though deficiencies in the robustness of this have been challenged by<br />
Dame Janet Smith in her report of the Shipman Enquiry. The basis for this system is that<br />
medicine involves knowledge, skills and attitudes which those without a medical training<br />
or specific training cannot adequately evaluate and regulate. On the other hand, the<br />
importance of the perspective provided by a strong non-medical input is now widely<br />
recognised. The maintenance of professionally led regulation can only be expected<br />
to remain extant if the overall performance of doctors is seen and agreed to be of a<br />
consistently acceptable standard and if the profession deals promptly and effectively<br />
with those of its membership who fall below such a standard. It is right, therefore, that<br />
Government, the DH, the profession, the media and the public should continue to take<br />
steps to ensure the reinforcement of the regulatory process.
Good Practice Guide 2006<br />
The key questions are:<br />
How do doctors set standards?<br />
How do doctors maintain standards?<br />
How are these standards revised when necessary?<br />
How does the profession ensure compliance with these standards?<br />
How does the profession publicly demonstrate this is taking place?<br />
This Guide for anaesthetists and departments of anaesthesia, critical care and<br />
pain management addresses these questions within the framework of the General<br />
Medical Council’s document Good Medical Practice. 6 The relevant paragraphs<br />
from the document are indicated in italics.<br />
Throughout this document, the terms ‘anaesthetist’ and ‘anaesthetic practice’<br />
are used to refer to all anaesthetists involved in clinical anaesthesia and<br />
perioperative care, in critical care, in acute and chronic pain management, and<br />
in obstetric care.<br />
1.2 The traditional system of regulation<br />
Since the Medical Act of 1858 which set up the General Medical Council (GMC), a<br />
complex set of arrangements has developed for professional regulation. These<br />
consist of:<br />
The General Medical Council (GMC)<br />
The Postgraduate Medical Education Board (PMETB)<br />
The Medical Royal Colleges and their Faculties<br />
National professional organisations<br />
Contracts of employment<br />
The GMC sets the framework within which UK medical schools undertake basic medical<br />
training. It is required to include on the Medical Register all whom the universities<br />
deem qualified. From the outset the GMC has had powers to remove from the Register<br />
those whom it finds guilty of serious professional misconduct and subsequently to<br />
restrict, supervise or suspend the practice of doctors whose health or performance<br />
may place patients at risk.<br />
PMETB sets the generic principles, standards and outcomes, onto which individual<br />
specialties map their training and assessment programmes. Standards of practice<br />
within the medical specialties are regulated by the Royal Colleges in so far as they set<br />
up training programmes and examinations under PMETB, establish the requirements<br />
for the recognition of training departments and lay down criteria for appointment to<br />
consultant posts. Hitherto, their regulatory powers have been confined to training and<br />
have not included the activities of consultants. This is gradually changing, especially<br />
in the areas of continuing education and professional development and increasingly<br />
in the development of criteria for revalidation.
Good Practice Guide 2006<br />
<br />
A further part of setting and maintaining standards is the ‘guidance’ which the<br />
Colleges and professional associations issue about clinical care and the safe provision<br />
of services. The Association has been particularly active in this field over the past<br />
two decades and has issued guidance on a wide range of subjects. While these<br />
documents are without statutory authority they have, together with guidance from<br />
the College and other groups, and with the support of the body of the specialty,<br />
become the benchmarks by which doctors involved in anaesthesia are expected to<br />
practise. They also set out the requirements which purchasers and providers need<br />
to meet to enable anaesthetists to deliver high quality services. These activities<br />
of the College, the Association and other specialist bodies are supported by their<br />
educational programmes.<br />
In addition to all these initiatives, doctors are subject to a range of legislation and<br />
to their contracts of employment with the accompanying disciplinary procedures.<br />
Individual Trusts are required to work under NHS employment guidelines, which<br />
include all aspects of their clinical duties, including local performance assessment.<br />
They are also influenced by the activities of the civil courts and by the demands of<br />
their own defence societies.<br />
During the early 1990s, in response to increasing concerns about the profession’s ability<br />
to set and monitor standards and demonstrate that they were adhered to, the profession<br />
initiated further regulatory developments. In 1995, there was a national conference on<br />
the core values of medicine 7 and the Royal Colleges also introduced continuing medical<br />
education for consultants. If individuals failed to meet the prescribed targets, they<br />
might no longer be able to teach and supervise trainees. If a department failed to meet<br />
them, recognition for training would be at risk. Requirements for continuing medical<br />
education for non-consultant career grades were also introduced. In April 2000, the<br />
Royal College of Anaesthetists issued a revised scheme for Continuing Professional<br />
Development (CPD). The College believes it is a professional necessity for all career<br />
grade anaesthetists to take part in CPD. This includes those who are full-time or parttime,<br />
those who are locum anaesthetists, those engaged wholly in independent practice<br />
and those affiliated to non-UK Colleges or Faculties.<br />
The organisation of programmes of CPD is expected to make a major contribution<br />
to the standards of practice. In addition, the College incorporated into CPD the list<br />
of core topics; these are topics in which an individual specialist working in a typical<br />
hospital and participating in the emergency on-call rota should have up-to-date<br />
knowledge and proficiency.<br />
The GMC and PMETB together have a statutory responsibility to co-ordinate all phases<br />
of medical education, a responsibility which in the past it has discharged in relation<br />
to undergraduate and postgraduate education up until entry into the career grades.<br />
In future it will also, through its CPD board working in close collaboration with the<br />
Medical Royal Colleges and others, co-ordinate CPD for all career grade doctors. It<br />
is clearly essential that CPD schemes meet the criteria required for revalidation. This<br />
attests to the importance with which these activities are regarded.
10 Good Practice Guide 2006<br />
1.3 Recent developments in regulation<br />
1.3.1 The General Medical Council<br />
1.3.1.1 Medical Act 1995<br />
In July 1997, the GMC’s new procedures for assessing the performance of doctors<br />
under the 1995 Medical (Professional Performance) Act, 8 came into force. These<br />
procedures enable the GMC to assess formally a doctor’s clinical and professional<br />
performance, including tests of knowledge and skills where there is reason to believe<br />
that these may be seriously deficient.<br />
The GMC has powers to require doctors to undergo further training, to restrict their<br />
practice or to suspend them from practice, initially for a limited period but indefinitely<br />
if deficiencies are not remedied. The boundaries between these procedures and the<br />
NHS complaints and disciplinary procedures and the criteria for referral to the GMC<br />
are set out in the GMC document, Maintaining Good Medical Practice. 9<br />
1.3.1.2 Revalidation<br />
The GMC has also initiated changes which will result in all doctors having to undergo a<br />
process of revalidation, in order to maintain their licence to practise. Although this was<br />
planned to commence in 2004, its start has been delayed pending a review by the CMO,<br />
following publication of the Shipman report. The appraisal system will form the basis of<br />
the process for most doctors and there will also be a major lay input into the assessment of<br />
doctors for revalidation. Individual specialties will have a major involvement in setting the<br />
standards by which doctors are judged. It seems likely that several different elements will<br />
contribute to the process including regular satisfactory appraisals which must incorporate<br />
the development and fulfilment of a personal development plan and verified evidence of<br />
personal performance, which will vary between specialties. This could include personal<br />
audit, multi-professional feedback (360 o ) or evidence from hospital performance figures.<br />
The final element will be a positive sign-off by the employer that there are no causes for<br />
concern. The Academy of Medical Royal Colleges has been working to try to develop<br />
systems which will be equable across specialties and throughout the whole country.<br />
1.3.2 Government 10<br />
The governmental initiatives outlined below refer to England. Equivalent bodies<br />
are present or are being set up in Scotland, Wales and Northern Ireland.<br />
1.3.2.1 White Paper<br />
The White Paper, The New NHS, 10 published in December 1997, made it clear that<br />
practitioners must accept responsibility for developing and maintaining standards within<br />
their local NHS organisations. Self-regulation was strengthened and extended into the<br />
local clinical community. Chief executives are now held accountable for the quality of<br />
the services provided by their Trust. Through clinical governance and the appraisal<br />
system, chief executives have been provided with the tools whereby they should be able<br />
to encourage medical practitioners to keep their skills up to date and should have an<br />
early warning of impending problems and the means to rectify them. The quality of local<br />
clinical services is now overseen by the Healthcare Commission with statutory powers to<br />
ensure that local systems are in place to monitor and improve quality.
Good Practice Guide 2006 11<br />
1.3.2.2 The National Clinical Assessment Service (NCAS) (formerly Authority) 11<br />
In April 2001, the National Clinical Assessment Authority (NCAA) was established and<br />
represents part of the Government’s commitment to quality assurance in the health<br />
service. In April 2005, following the Arm’s Length Bodies Review, the NCAA became<br />
part of the National Patient Safety Agency (NPSA), changing its name to the National<br />
Clinical Assessment Service (NCAS).<br />
NCAS provides a service to NHS organisations and organisations that provide healthcare<br />
services to the NHS, as well as to doctors and dentists themselves, aimed at helping<br />
them tackle performance problems at an early stage, earlier than is current practice.<br />
One of its key aims is to help avoid the inappropriate use of suspension or exclusion,<br />
which was so often the case in the past, causing great damage to services and to doctors<br />
themselves. Concerns about a doctor’s performance should be tackled locally and<br />
problems hopefully resolved. If not, doctors can be referred to NCAS which can provide<br />
a range of advice, support and assessment services which are aimed at recommending<br />
how to proceed. It may suggest a range of possible options, for example, that the doctor<br />
should return to work, should have a period of retraining organised and implemented<br />
through the postgraduate dean, or perhaps should be referred to the GMC. It will be<br />
the responsibility of the Health Authority or Trust to implement any recommendations.<br />
NCAS now has more than five years of experience in this work, and evaluation of its work<br />
has shown evidence of earlier resolution of even complex and challenging cases and<br />
of substantial reductions in inappropriate use of suspension and exclusion. Evaluation<br />
reports are available from the NCAS website at: www.ncas.npsa.nhs.uk or directly from<br />
them by email: ncas@ncas.npsa.nhs.uk.<br />
The College has been working closely with the Association of Anaesthetists and NCAS<br />
to develop a portfolio of documents to advise over issues of poor performance. This<br />
has been achieved under the umbrella of the Joint Committee on Good Practice. It is<br />
hoped that, wherever possible, NCAS and the Joint Committee can work together so<br />
that, effectively, there is a single point of contact for all concerns. It is often difficult<br />
to discover initially whether the perceived problems are with the system, an individual<br />
or a group of clinicians. The documents available include advice to Trusts, advice<br />
to College/NCAS visitors and advice on retraining, and, for individual referral, the<br />
confidential ‘sick doctor’ scheme still operates.<br />
The Government expects the profession to deliver a uniformly high standard of practice<br />
throughout the NHS and will continue to look to individual healthcare professionals to<br />
be responsible for the quality of their clinical practice.<br />
1.3.2.3 The National Patient Safety Agency (NPSA) 12<br />
The NPSA was established in September 2001 with the remit to identify errors in the process<br />
of patient care and enable such errors to be reduced in a blame free environment. In this<br />
regard the College Critical Incident Reporting System has been adopted in full with minor<br />
modifications for use by the agency. The results obtained from this anonymous reporting<br />
will be collected from all NHS hospitals and will be used to reduce risks to patients.
12 Good Practice Guide 2006<br />
1.3.3 The Academy of Medical Royal Colleges (AoMRC)<br />
The Academy of Medical Royal Colleges is a common forum for College representatives<br />
to meet to discuss items of mutual interest and from which a common voice can be<br />
formulated to negotiate with Government, the GMC and other bodies. It does not<br />
devalue the status of the individual Colleges but allows a stronger position to be<br />
adopted in areas of common interest.<br />
1.3.4 The Postgraduate Medical Education and Training Board (PMETB)<br />
PMETB is a regulatory authority which has replaced both the Specialist Training Authority<br />
(STA) and the Joint Committee for Postgraduate Training in General Practice (JCPTGP). It<br />
is independent of the Department of Health and answers to the Secretary of State. It<br />
launched in September 2005 and is charged with quality assuring all aspects of medical<br />
education, training and assessment, ensuring that programmes and curricula are fit for<br />
purpose, and appropriately validated. It will be responsible for delivering all aspects<br />
of Modernising Medical Careers, though responsibility for Foundation training, and<br />
particularly the first pre-registration year, will be shared with the GMC.<br />
1.3.5 The British Medical Association (BMA)<br />
The BMA represents the whole medical profession, is the interface between doctors,<br />
their employers and the public and can exercise an overview of the different specialties.<br />
It takes on board the terms and conditions of service and speaks for the profession<br />
in discussions of remuneration and in disputes, and in how the NHS can best provide<br />
a comprehensive service for all patients.<br />
1.4 Local standard setting and regulation 13<br />
The culture in which doctors work is still often not conducive to the admission of deficiencies,<br />
which tend to be regarded as a sign of weakness, and ignored or covered up. There are<br />
gaps between central guidance, regulation and the individual doctor. The introduction of<br />
annual appraisal from April 2001, as a contractual obligation, has emphasised the need for<br />
the regular and constructive review of the way in which the employee is keeping up to date<br />
with the developments in theoretical knowledge, with the preservation of practical skills and<br />
with the retention of appropriate attitudes. It is expected that the appraisal process will be<br />
informed from a number of sources, representative of all the areas in which the individual<br />
doctor works, including the private sector. Appraisal is designed to be a constructive nonconfrontational<br />
developmental process. As well as the responsibility of individual doctors<br />
for their own professional development, it is also necessary for the sense of corporate<br />
responsibility to be further developed within departments. This need is highlighted by the<br />
changes which have taken place in the way in which medicine has been practised during<br />
the past decade, the main features of which are as follows.<br />
1.4.1 Team working<br />
It has become unusual for doctors to work as isolated individuals; in hospital practice,<br />
they are usually members of departments which provide a service. This has long been<br />
the model in anaesthesia. On a different level, doctors also function as members of<br />
multidisciplinary healthcare teams. While they are commonly the leaders of clinical<br />
teams, their ability to care for patients depends vitally on the skills of other doctors
Good Practice Guide 2006 13<br />
and healthcare professionals. In such cases, the details of an individual anaesthetist’s<br />
practice may be little known to colleagues in the same department.<br />
1.4.2 Continuity of care<br />
Doctors have increasing concerns about the quality of their lives apart from their<br />
work. This has been particularly reflected in the reduction in working hours of<br />
trainees. Consultants, while theoretically having continuous responsibility for patients<br />
under their care, frequently hand this over to an on-call colleague at night and at<br />
weekends. This issue is dealt with in more detail in Chapter 3.<br />
1.4.3 Management<br />
The NHS has a complex management system which often defines the limits of what<br />
doctors can do. Many clinicians are involved in healthcare management as clinical<br />
leads, clinical directors and medical directors. It is important that those undertaking<br />
these roles are properly trained and resourced in terms of time free from other<br />
clinical responsibilities.<br />
1.4.4 Complaints<br />
When a patient complains it is because of dissatisfaction with some aspect of their<br />
care which may range from an administrative error to dissatisfaction with their clinical<br />
management. At the same time, expectations have increased and patients’ tolerances<br />
have decreased. Not all mistakes result in a complaint and not all complaints are<br />
because of a mistake. The management of complaints must focus firstly on complaints<br />
avoidance by ensuring that systems are in place so that problems are minimised.<br />
The Clinical Negligence Scheme for Trusts (CNST) 14 allows Trusts to target areas of<br />
repeated adverse events. Complaints are often multifaceted but good communication<br />
with patients will often defuse potentially difficult situations and minimise the causes<br />
for complaint. For this to develop in a constructive manner there is need for a culture<br />
of openness. Where local action fails to resolve a complaint then an independent<br />
review panel can be convened. Complaints are now a fact of working life and the best<br />
way to minimise their impact is to deal with them quickly, fairly and openly.<br />
These changes have major implications for the organisation of medical work and the<br />
provision of patient care. They also emphasise the need for local, corporate regulation.<br />
The former President of the GMC, Sir Donald Irvine, has summarised professional<br />
regulation and standard setting in the following way:<br />
Figure 1 Routes of accountability<br />
Individual doctors Clinical team National bodies<br />
➠<br />
Personal standards<br />
➠<br />
➠<br />
Local collective standards<br />
➠<br />
➠<br />
National professional<br />
standards<br />
➠<br />
Self-assessment Local audit External review
14 Good Practice Guide 2006<br />
The key to the effective working of these arrangements is to be found at a local level.<br />
Anaesthetists are used to working as members of a department, and teamworking<br />
is usually accepted from an early stage of an anaesthetist’s career. The<br />
corporate standards and ethos of departments of anaesthesia, critical care and pain<br />
management provide the most effective way of ensuring high standards of patient<br />
care, preventing any decline in an individual’s performance and recognising when a<br />
deterioration occurs.<br />
Several requirements are essential for departments to work in this way. These include:<br />
❚<br />
❚<br />
❚<br />
an effective and constructive system of appraisal<br />
an agreed system of continuing medical education and professional development<br />
methods of dealing sensitively and effectively with those anaesthetists whose<br />
clinical and professional standards fall below an acceptable level.<br />
At a national level, there are a series of initiatives to allow for the development of<br />
national standards and monitoring of such standards. Figure 2 gives a diagrammatic<br />
summary of some of the mechanisms involved in the setting, delivery and monitoring<br />
of these standards. The National Institute for Health and Clinical Excellence and<br />
the different National Service Frameworks are designed to give national standards<br />
of service. Professional Self-Regulation and Clinical Governance allied to Life Long<br />
Learning are designed to give dependable local delivery. In England the process<br />
is monitored by the Healthcare Commission, the National Performance Framework<br />
and National Patient and Users Surveys. Equivalent bodies and procedures are<br />
operational or planned in Scotland, Wales and Northern Ireland.<br />
Figure 2 Standards – setting, delivering, monitoring<br />
➠<br />
National Institute for Health and<br />
Clinical Excellence<br />
National Service Frameworks<br />
➠<br />
Clear standards of service<br />
➠<br />
Professional Self-Regulation<br />
Clinical Governance<br />
Life Long Learning<br />
➠<br />
Dependable local delivery<br />
➠<br />
Healthcare Commission<br />
National Performance Framework<br />
National Patient and Users Surveys<br />
➠<br />
Monitored standards<br />
The Association and the College believe that where anaesthetists corporately take the<br />
responsibility in the light of agreed advice for setting local standards and complying<br />
with them there will be:<br />
❚<br />
❚<br />
❚<br />
a high level of professional satisfaction within departments<br />
continuously rising standards of perioperative care for patients<br />
considerable influence exerted throughout the hospital.
Good Practice Guide 2006 15<br />
6, 15–18<br />
Chapter 2: The ethical framework<br />
The apparently straightforward relationship of mutual Trust and respect between<br />
doctors and patients has been complicated by changes, summarised in the<br />
introduction, which have taken place in both medicine and society in recent years.<br />
Various groups and individuals have developed an ethical framework which sets out<br />
what is required of doctors if they are to merit and retain the Trust of patients and<br />
the public. The ethical framework within which anaesthetists should practise may be<br />
summarised under four main headings:<br />
❚<br />
❚<br />
❚<br />
❚<br />
Professional competence.<br />
Professional relationships with patients and colleagues.<br />
Public duties.<br />
Probity.<br />
2.1 Professional competence<br />
In providing care you must recognise and work within the limits of your<br />
competence.<br />
A doctor’s first duty is to work for the benefit of patients. This requires a detailed,<br />
up-to-date knowledge of the particular area in which the doctor works together with<br />
proficiency in the skills which practice in that area requires. The time has passed<br />
when the basic medical undergraduate training and subsequent specialist training<br />
equipped those in anaesthesia, critical care and pain management with the knowledge<br />
and skills for a career-long practice of high standard. The rate at which advances are<br />
made in all aspects of the care of patients is so great that every anaesthetist needs to<br />
be involved in a programme of continuing education and training at local and national<br />
level. With such a rapid rate of change, anaesthetists will develop particular areas of<br />
expertise which should be available to colleagues within a department.<br />
However, while the benefits of modern peri-operative care are obvious, most<br />
anaesthetic procedures carry some risk of harm to patients. Audit of both individual<br />
practice and the service provided by a department is essential if these risks are to be<br />
minimised and benefits maximised.<br />
2.2 Professional relationships<br />
2.2.1 With patients 19–20<br />
Patients must be able to trust doctors with their lives and health.<br />
Having an anaesthetic, an admission to critical care or the requirement for pain<br />
management are often parts of the peri-operative care about which patients are the<br />
most anxious. The degree of trust and confidence patients have in their anaesthetist<br />
is crucially dependent on the relationship the anaesthetist establishes with them.<br />
Courtesy is the essential prerequisite. It is also important to give a clear explanation<br />
of what the anaesthetic and peri-operative care involve in language which the patients
16 Good Practice Guide 2006<br />
can understand. Patients’ concerns and anxieties should be listened to, their questions<br />
answered and information should be given to enable them to face the operative and<br />
peri-operative care with confidence. The anaesthetist should also ensure that the<br />
patient understands and has signed the appropriate consent form for the procedure<br />
to be undertaken. Often written information can be helpful, particularly for same day<br />
admissions and day case surgery where the pre-operative visit by the anaesthetist<br />
may of necessity be brief. 21 A collection of leaflets on anaesthesia and anaesthetic<br />
risk are available from the College for this purpose. Care by the anaesthetist should<br />
never be prejudiced by a patient’s gender, age, culture, background, education, race<br />
or life style. Interpreters should be available and consideration should be given to the<br />
production of appropriate translated written material. It is not best practice to rely on<br />
the patient’s family for interpreting facilities.<br />
Patients in pain management clinics may also display a variety of concerns and emotions.<br />
Empathetic handling of these patients is essential for a mutually successful outcome.<br />
Chaperones should be routinely available for outpatient consultations and examinations.<br />
If a mistake is made or a complication occurs during the course of a patient’s perioperative<br />
care which affects outcome or may have implications for a future anaesthetic, it must<br />
be discussed openly and honestly with the patient and where appropriate with relatives.<br />
This discussion should be recorded in the patient’s notes.<br />
2.2.2 With colleagues<br />
Para 41: Most doctors work in teams with colleagues from other professions.<br />
You must:<br />
❚<br />
❚<br />
respect the skills and contributions of your colleagues<br />
communicate effectively with colleagues within and outside the team.<br />
Anaesthetists working in the NHS necessarily work as members of departments of<br />
anaesthesia, critical care and pain management. In the provision of peri-operative care,<br />
obstetrics, critical care and pain management they work with other doctors and health<br />
professionals. The ability to work harmoniously in departments and teams is essential if<br />
patients are to be cared for properly. Anaesthetists will often take the lead in decision making,<br />
and robust debate within departments and with other groups is an essential component<br />
in providing a high quality anaesthetic service. However, there is no place in modern<br />
departments of anaesthesia for individuals who pursue their clinical practice and style of<br />
personal conduct irrespective of the views and wishes of their colleagues. Professional<br />
independence is important and variety is healthy, both in clinical practice and personal<br />
style, but the limits of acceptable behaviour must be recognised by all concerned.<br />
2.3 Public duties<br />
Like other doctors, anaesthetists practise in a service with limited resources. While<br />
these resources could be significantly increased if there was the political will to do so,<br />
there is still debate whether it is possible to fund from public sources all that medicine<br />
can do. As members of society, therefore, anaesthetists have a duty to see that public
Good Practice Guide 2006 17<br />
2.4 Probity<br />
funds are used responsibly. If this is to be reconciled with the duty to bring benefit to<br />
individual patients, anaesthetists must base their clinical practice on the best available<br />
evidence and run their departments efficiently.<br />
If factors in the working environment are threatening the safety of patients,<br />
anaesthetists have an ethical duty to take appropriate action. This may mean declining<br />
to provide certain types of anaesthetic care, critical care and pain management until<br />
the deficiencies have been rectified.<br />
As responsible members of society, doctors should be honest in their financial<br />
dealings, in their approach to patients and in all matters involved with their work, their<br />
teaching responsibilities and in research. An anaesthetist’s contract of employment<br />
and job plan set out the contractual obligation to the employer. Failure to meet these<br />
obligations is a disciplinary offence.<br />
While, in employment terms, NHS and independent practice are separate, in professional<br />
terms they are often closely related. Anaesthetists are largely dependent on surgeons<br />
for their access to independent practice and the possibility exists for this relationship<br />
to compromise an anaesthetist’s independence. One way of preventing this is by NHS<br />
anaesthetists organising themselves in clinical groupings to optimise patient care and<br />
auditing their independent sector work in the same way that they audit their NHS work.<br />
2.5 Research<br />
2.6 Health<br />
Research is vital in improving care for present and future patients. Doctors involved in<br />
research have an ethical duty to show respect for human life and people’s autonomy.<br />
It is essential that there is a partnership between the participants and the healthcare<br />
team, based on trust. There must be respect for the patients’ and volunteers’ rights<br />
to make decisions about their involvement, their privacy and dignity, and at all times<br />
they must be treated with politeness and consideration. 22<br />
The GMC 6 has issued guidance to doctors on what measures to take to protect<br />
themselves and others, including patients, from infection by serious communicable<br />
diseases such as hepatitis B. 23<br />
It includes guidance on what to do if a healthcare worker suffers a needlestick injury,<br />
and how to implement appropriate infection control measures. Those involved<br />
in ‘exposure prone procedures’ may have to modify their professional practice.<br />
Anaesthetists, however, are seldom involved in these procedures, described by the DH<br />
as ‘those where the risk that injury to the healthcare worker could result in exposure<br />
of the patient’s open tissues to the blood of the healthcare worker’.<br />
It is equally important for departments and Trusts to have in place mechanisms to<br />
support colleagues during periods of illness or following a clinical catastrophe. 24
18 Good Practice Guide 2006<br />
Chapter 3: Duty of care for anaesthetists<br />
The nature of anaesthetic practice means that most anaesthetists have a varying work<br />
pattern with duties performed in several sites within both the public and independent<br />
sectors. This diversity of activity means that an anaesthetist may be involved in<br />
the care of patients in a variety of sites for a variety of durations. Concerns have<br />
been raised as to the responsibility of the anaesthetist in the on going care that has<br />
followed the anaesthetic intervention.<br />
It is important to remember that, just like any other doctor, an anaesthetist has a<br />
recognised ‘duty of care’ to patients. The term ‘duty of care’ is a legal phrase defining<br />
whether a doctor (or other healthcare worker) can be held to be responsible for the care<br />
of an individual patient. However, it may be more helpful to try to look at the issue more<br />
from the GMC’s approach to doctors’ responsibilities than from a legal one.<br />
Levels of responsibility vary. At times an anaesthetist will:<br />
a<br />
b<br />
have a responsibility to be physically present with the patient, such as whilst<br />
administering a general anaesthetic. If in exceptional circumstances the<br />
anaesthetist has to leave the patient they must delegate responsibility to another<br />
appropriate person in line with GMC guidance on delegation: 6<br />
Para 54: ‘When you delegate care or treatment you must be satisfied<br />
that the person to whom you delegate has the qualifications, experience,<br />
knowledge and skills to provide the care or treatment involved. You<br />
must always pass on enough information about the patient and<br />
the treatment they need. You will still be responsible for the overall<br />
management of the patient.’’<br />
share responsibility with other healthcare professionals, being available for advice and<br />
help such as during the postoperative recovery period. The nature and intensity of such<br />
help will vary from the immediate postoperative recovery period until the end of the<br />
‘episode of care’, whenever that happens to be. The GMC also gives guidance on this:<br />
Para 41: ‘Healthcare is increasingly provided by multi-disciplinary<br />
teams. Working in teams does not change your personal accountability<br />
for your professional conduct and the care you provide’.<br />
Para 50: ‘Sharing information with other healthcare professionals is<br />
important for safe and effective patient care.’<br />
c be asked to provide care when not on duty. Anaesthetists also have a responsibility<br />
to ensure that satisfactory arrangements for the delivery of care are in place to<br />
cover periods when they are not available. In the NHS, this is usually assured by<br />
the ‘on-call’ system and other local departmental arrangements, but this is not<br />
always the case in the independent sector. In the past surgeons have fallen foul of<br />
the GMC for not making proper arrangements to deal with emergency postoperative<br />
complications arising when they are not available; there is no theoretical reason why<br />
anaesthetists should be treated differently.
Good Practice Guide 2006 19<br />
Para 48: ‘You must be satisfied that, when you are off duty, suitable<br />
arrangements have been made for your patients’ medical care. These<br />
arrangements should include effective hand-over procedures involving<br />
clear communication with healthcare colleagues.’<br />
The GMC guidelines cited above are of necessity written in generic terms and include<br />
the concept of ‘an episode of care’ without defining the precise meaning of the term.<br />
For a surgeon or a physician, that ‘episode of care’ might reasonably relate to a<br />
period of time in hospital or a specific consultation. The situation for anaesthetists<br />
is less clear as the ‘episode of care’ could be interpreted as ranging from just the<br />
period of anaesthesia, through to the complete duration of hospital confinement. For<br />
anaesthetists practising invasive pain management, the ‘period of care’ could even<br />
extend to include the complete period of treatment (possibly lasting years).<br />
Notwithstanding the fundamental principles of a ‘duty of care’ but to provide some<br />
clarification of the situation, the following are suggestions to quantify the term ‘episode of<br />
care’ within the variability of activities undertaken by anaesthetists. They are constructed<br />
on the basis of the extent of any intervention or the duration of action of medications<br />
administered in the course of anaesthesia and postoperative management.<br />
1<br />
2<br />
Outpatient consultation (including pre-assessment)<br />
The episode of care ends when the patient leaves the consulting room. In<br />
the case of repeated consultations such as for chronic pain management, the<br />
cessation of a particular episode of care does not mean that there is not an on<br />
going general duty of care to the patient particularly if a course of treatment has<br />
followed that consultation.<br />
Day case surgery<br />
For the majority of day case surgical patients, the episode of care lasts from<br />
the initial pre-operative visit on the day of surgery through to discharge from<br />
hospital. Should the patient require admission as a result of an anaesthetic<br />
incident, the episode of care shall extend until the patient has fully recovered<br />
from the effects of that incident or the care of the patient has been transferred<br />
to another person. Should admission be as a consequence of the surgical<br />
procedure, the episode of care for the anaesthetist will cease as for a standard<br />
in-patient (see below).<br />
3 Inpatient anaesthesia<br />
There is a wide range of anaesthetic involvement in patients admitted for a<br />
variety of surgical procedures. For all cases, the principle should be that the<br />
episode of care extends from the initial pre-operative visit through to the<br />
cessation of the effect of drugs administered during and immediately following<br />
the anaesthetic. In the case of opioid analgesic drugs administered as part of<br />
the anaesthetic, the episode of care related to that drug shall cease with the<br />
administration of subsequent analgesic medication (i.e. it has worn off). In the<br />
case of local or regional anaesthesia, the episode of care shall end with the<br />
recovery of normal sensation and muscle power.
20 Good Practice Guide 2006<br />
4<br />
The postoperative prescription of drugs does not in itself imply a continuing<br />
‘episode of care’ as long as there is a clear line of responsibility for the care of<br />
the patient relevant to drugs prescribed (e.g. for patient-controlled analgesia,<br />
there is a protocol involving follow up by an acute pain service, or equivalent).<br />
Use of neuraxial blockade for postoperative analgesia<br />
The principle should be that the duty of care shall continue until such time as<br />
the effect of the intervention ceases. In the case of intrathecally-administered<br />
opioids, that would be the need for additional analgesic medication. For epidural<br />
analgesia, the episode of care would cease with the removal of the epidural and<br />
the recovery of normal sensation and motor power.<br />
5 Implanted drug-delivery systems<br />
These may be used for chronic pain management. In this instance, the<br />
‘implanting’ physician retains responsibility until the device is removed. This<br />
implies a long-term responsibility but the care can be shared with others (on-call<br />
availability for any problems) or transferred to others (transfer of care back to<br />
the original referring physician).<br />
In the case of any complication of anaesthesia or analgesia, the anaesthetist shall<br />
retain responsibility for the patient until such time as that care is transferred to<br />
someone else.<br />
In the event of circumstances preventing the anaesthetist from being available throughout<br />
an episode of care (e.g. booked annual leave on the day following major surgery and<br />
use of epidural analgesia), it is the duty of the anaesthetist to ensure that appropriate<br />
support and monitoring are available for the patient. This may be in the form of transfer<br />
of care to a colleague or through a mechanism such as an acute pain service.<br />
The anaesthetist does not have a requirement to provide care beyond the end of the<br />
‘episode of care’ but it would be seen as good practice to retain an interest in the on<br />
going progress of any patient with whom there has been professional involvement.
Good Practice Guide 2006 21<br />
Chapter 4: Professional and clinical<br />
guidelines<br />
Over the last 20 years, guidelines published by the College, the Association and other<br />
specialist organisations have played a key part in developing and maintaining high<br />
standards of anaesthetic care in the UK. Modern peri-operative care is complex; it is<br />
provided by many different anaesthetists working with other doctors and healthcare<br />
professionals. Wards are increasingly busy and are often short of staff, and staff of all<br />
disciplines looking after patients change frequently during each 24-hour period. There<br />
is, therefore, very considerable potential for mistakes to be made.<br />
It is widely accepted that the practice of individual anaesthetists may vary where<br />
evidence supports a range of different techniques. However, under certain<br />
circumstances and in those areas where the patient is not being immediately and<br />
personally supervised by the anaesthetist, such as in the recovery room, high<br />
standards of care are more likely to be maintained if there are agreed guidelines<br />
within a department and hospital. Where such guidelines have been agreed by<br />
members of a department, they should normally be adhered to.<br />
Guidelines are particularly appropriate where:<br />
A problem is life threatening:<br />
For example – management of the difficult airway<br />
– cardiopulmonary resuscitation<br />
– management of massive bleeding<br />
– acute hypersensitivity (anaphylaxis)<br />
A problem is unusual:<br />
For example – abnormal haemoglobins<br />
– malignant hyperthermia<br />
A problem is routine but is managed by different people in different<br />
wards and departments:<br />
For example – blood ordering schedule<br />
– postoperative pain relief<br />
– day case anaesthesia<br />
– peri-operative management of diabetes<br />
– endocarditis prophylaxis<br />
– pre-operative investigation<br />
– pre-operative starvation<br />
In many areas national guidelines are available which may need to be amended<br />
according to local circumstances. In other areas, notably in the way particular<br />
services are provided, local guidelines are often necessary. These should be based<br />
on available evidence and audited, reviewed and revised regularly.
22 Good Practice Guide 2006<br />
Chapter 5: Audit: setting, monitoring and<br />
reviewing standards<br />
Para 14: ‘You must work with colleagues and patients to maintain and<br />
improve the quality of your work and promote patient safety. In particular<br />
you must:<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
maintain a folder of information and evidence, drawn from your<br />
medical practice<br />
reflect regularly on your standards of medical practice in accordance<br />
with GMC guidance on licensing and revalidation<br />
take part in regular and systematic audit<br />
take part in systems of quality assurance and quality improvement<br />
respond constructively to the outcome of audit, appraisals and<br />
performance reviews, undertaking further training where necessary<br />
help to resolve uncertainties about the effects of treatment<br />
contribute to confidential enquiries and adverse event recognition and<br />
reporting, to help reduce risk to patients<br />
report suspected adverse drug reactions in accordance with the relevant<br />
reporting scheme.’<br />
Clinical audit is a quality improvement process which seeks to improve patient care and<br />
outcomes through systematic review against explicit criteria leading to implementation<br />
of change if required. 25 It is a key component of clinical governance. Regular<br />
review by departments of anaesthesia of what anaesthetists do and how they do it<br />
is essential for maintaining high standards of practice. Audit became a contractual<br />
obligation for doctors in the early 1990s. The GMC considers it to be part of good<br />
practice. 6 The Government White Paper, The New NHS, 26 places great emphasis<br />
on clinical governance and ‘measuring progress’ in six areas: health improvement;<br />
fair access to services; effective delivery of appropriate healthcare; efficiency; the<br />
experience of patients and their carers; and health outcomes of NHS care. The White<br />
Paper also puts in place clear alternative regulatory mechanisms which will be used if<br />
the profession fails to regulate itself effectively. At the time of publication, the review<br />
Good Doctors, Safer Patients was still in consultation.<br />
In order to assist departments in developing appropriate audit programmes, the<br />
College has produced an anaesthetic audit recipe book, Raising the Standard. 27<br />
This document, which is regularly updated, should act as a catalyst to promote local<br />
departmental audit. It describes a list of audits which should be undertaken in all<br />
branches of anaesthetic, critical care and pain management practice. Clearly, all audits<br />
cannot be undertaken simultaneously nor is the list intended to be prescriptive.
Good Practice Guide 2006 23<br />
5.1 Local audit<br />
Audit which is properly conducted plays an important part in:<br />
❚<br />
❚<br />
❚<br />
improving patient care<br />
improving the provision of anaesthetic services<br />
continuing medical education.<br />
Traditionally, audit is considered under three headings – the structure, process and<br />
outcome of care. The key to effective audit is the audit cycle (Figure 3) whereby<br />
information and data are collected, analysed and reviewed; changes are agreed and<br />
standards set; the changes are implemented and after a period of time the cycle is<br />
repeated. As the process continues, each cycle aspires to a higher level of care.<br />
Figure 3 The audit cycle<br />
Collect information and data<br />
Implement change<br />
Analyse and review<br />
Different routes into the cycle include:<br />
Agree change and set standards<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
individual case reports of mortality and morbidity<br />
reviews of critical incidents<br />
perceptions of patients and other healthcare workers about the anaesthetic service<br />
complaints about the anaesthetic service<br />
formal reviews of areas of clinical practice and service provision.<br />
All the above should feed into a departmental audit programme.<br />
5.2 The audit programme<br />
The audit programme of an anaesthetic department should follow a regular pattern<br />
and the following is recommended:<br />
Monthly<br />
Two to three times a year<br />
Annually<br />
Review of deaths, complications,<br />
unexpected outcomes (e.g. unplanned<br />
admission to ICU or HDU), critical incidents<br />
Joint audits with other departments, e.g.<br />
surgeons, obstetricians, paediatricians<br />
Review of anaesthetic record keeping<br />
Every two to three years<br />
Review of local guidelines<br />
In addition, departments should review practice against national guidelines as they<br />
are published and thereafter every two to three years. It is also good practice for
24 Good Practice Guide 2006<br />
individual anaesthetists to undertake on going personal audits of particular aspects<br />
of their own work.<br />
Departments should keep written summaries of audit meetings as reference<br />
documents for subsequent reviews.<br />
The College has developed national audit projects within anaesthesia. These will<br />
provide valuable data (first results published in the BJA in September 2005) and also<br />
provide benchmarks against which a department can compare itself.<br />
Nationally, the specialty of anaesthesia has a long record of effective audit in the<br />
Confidential Enquiries into Maternal Deaths (now the Confidential Enquiry<br />
into Maternal and Child Health), National Confidential Enquiry into Patient<br />
Outcome and Death and Scottish Audit of Surgical Mortality. Both the College<br />
and the Association encourage anaesthetic departments to contribute to national<br />
reporting systems and also implement recommendations which follow review of<br />
critical incidents.<br />
5.3 Critical incidents 28–31<br />
The College definition of a critical incident is ‘an event which led to harm or could have<br />
led to harm if it had been allowed to progress’. It should be preventable by a change<br />
of practice. The College has defined two ways of grading critical incidents based on<br />
outcome and the degree of preventability.<br />
5.3.1 Outcome<br />
❚ No effect.<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
Transient abnormality unnoticed by the patient, e.g. laryngospasm.<br />
Transient abnormality with full recovery, e.g. headache.<br />
Potentially permanent but not disabling damage, e.g. chipped tooth.<br />
Potentially permanent disabling damage, e.g. stroke.<br />
Death.<br />
5.3.2 Preventability<br />
❚ Probably preventable within current resources, e.g. failure to perform a preoperative<br />
machine check.<br />
❚<br />
❚<br />
❚<br />
❚<br />
Probably preventable with reasonable extra resources, e.g. failure to detect<br />
oesophageal intubation (which could be obviated by capnography).<br />
Possibly preventable within current resources, e.g. pneumothorax during<br />
insertion of a central venous line, which might be prevented by better teaching/<br />
supervision.<br />
Possibly preventable with reasonable extra resources, e.g. inability to replace<br />
unwell anaesthetist because of inadequate staffing which might be prevented by<br />
more cover.<br />
Not obviously preventable by any change in practice, e.g. idiosyncratic drug reaction.
Good Practice Guide 2006 25<br />
Each department should have a critical incident co-ordinator whose job it is to<br />
receive reports, discuss them confidentially with the reporter and ensure accuracy of<br />
reporting. Incidents should be well documented in the patient’s notes and reviewed<br />
at a department’s audit meeting.<br />
While errors are an integral part of everyday life, an error during the giving of an<br />
anaesthetic may have serious implications for both the patient and the anaesthetist.<br />
Understanding the causes of error is an important way of preventing it from occurring<br />
again. Critical analysis of errors has been successfully applied in the aviation industry<br />
and has resulted in changes in equipment, recruitment and training policies. This<br />
approach has been successfully adapted to anaesthesia.<br />
Anaesthetists are part of a complex system of patient care, and deficiencies in that<br />
system may contribute to untoward events during anaesthesia. 32 Under Health and<br />
Safety Legislation 33 there is a requirement to report certain events to the Health<br />
and Safety Executive for review. The Act places upon all staff an obligation to report<br />
clinical and non-clinical incidents which are likely to have a bearing on the quality,<br />
safety or efficiency of care provided.<br />
Two principal reporting systems should be used. Firstly, the Royal College of<br />
Anaesthetists in collaboration with the NPSA have distributed a reporting database<br />
to all departments which should be used for all events. From this, reports can be<br />
printed for use at department morbidity and mortality meetings. The NPSA was<br />
created to implement a mandatory reporting system to detect and learn from data on<br />
adverse incidents. The emphasis is on learning and development and not on blame. 34<br />
Secondly, many Trusts use a Trust reporting system which should be used additionally<br />
for events which have caused harm to the patient, staff or to the reputation of the<br />
Trust. Trusts should be encouraged to endorse the use of both systems, as they<br />
should complement each other. It is sensible practice for a Trust to have a common<br />
reporting system with reports being collated by a risk manager.<br />
Many anaesthetists have taken on the role of clinical governance lead within their<br />
Trust or department. It is suggested that this role be clearly defined in their job plan<br />
and that adequate time and resource be allocated. 35<br />
5.4 Confidentiality 19<br />
The maintenance of confidentiality about complications and critical incidents within<br />
the specialty is essential if both national reporting and local audit are to be honest<br />
and comprehensive and anonymity assured. Nevertheless, all anaesthetists have<br />
a responsibility to monitor the structure, process and outcome of the care which<br />
their department provides. Where patterns of poor care emerge or where specific<br />
events have implications for the Trust, they have a duty to share that information with<br />
other clinicians, healthcare workers and managers. Where actual harm has occurred,<br />
patients must always be informed as soon as possible.
26 Good Practice Guide 2006<br />
5.5 Audit of critical care services<br />
Comprehensive Critical Care 36 published by the Department of Health in 2000<br />
recommended that ‘a data collecting culture promoting an evidence base must be<br />
recognised as an integral part of the delivery of critical care and an essential part of<br />
the Trust’s clinical governance and risk management programme’. Clinicians should,<br />
therefore, insist that sufficient clerical and administrative support is provided for<br />
data collection in critical care and high dependency units. They should also ensure<br />
that their Trust provides details of activity employing the Augmented Care Period<br />
(ACP) dataset to the DH for incorporation in hospital episode statistics. Auditing and<br />
assessing activity are essential in service planning at Trust level to meet clinical needs<br />
as well as nationally to inform future development.<br />
Clinical outcome between critical care units is particularly difficult to compare in<br />
view of the varying case mix and severity of illness of the patients involved. It is<br />
recommended, therefore, that all units are involved in a system of national comparative<br />
audit such as the Intensive Care National Audit and Research Centre (ICNARC) or<br />
its Scottish equivalent. This not only requires an efficient system of data collection<br />
and enthusiasm from the doctors and nurses involved to ensure data accuracy and<br />
completeness, but also a willingness to examine variations in performance from the<br />
nationally predicted norms and initiate any change in practice that may be required<br />
for improvement.<br />
Regular clinical reviews and morbidity and mortality meetings should be undertaken<br />
involving all staff in the unit including medical, nursing, paramedical and other<br />
support staff in addition to multidisciplinary involvement of referring clinicians. The<br />
number and process of transfers of critically ill patients outwith the critical care unit<br />
either within hospital or between hospitals should be audited and any critical incidents<br />
recorded and acted upon. This requires not only co-operation between Trusts within<br />
the established critical care networks, but also review at a national level.<br />
5.6 Audit of pain management services<br />
Both acute and chronic pain management services should conduct regular audit and<br />
critical incident discussion involving all staff members. Patient involvement with service<br />
audit is important. Internal audit is essential to monitor service effectiveness, efficiency<br />
and deficits and allows services to discuss treatment options fully with patients. Interhospital<br />
audit allows ‘benchmarking’ against other pain management services and<br />
can be a valuable learning tool. Recommended topics for pain management audit are<br />
included in Raising the Standard. 27
Good Practice Guide 2006 27<br />
Chapter 6: Continuing professional<br />
development (CPD) 37<br />
Para 12: ‘You must keep your knowledge and skills up-to-date throughout<br />
your working life.’<br />
Para 16: ‘If you are involved in teaching, you must develop the skills, attitudes<br />
and practices of a competent teacher.’<br />
CPD is a requirement of good medical practice and an integral part of the<br />
maintenance of professional standards. It embraces both theoretical knowledge<br />
and the acquisition and development of skills needed in the fields of communication,<br />
teaching, management and clinical duties.<br />
CPD is an essential part of the life of all doctors, and is required for appraisal,<br />
clinical governance and revalidation. The exact amount and type of CPD activity are<br />
a matter for the individual but must be sufficient to satisfy personal and regulatory<br />
requirements. A review of CPD activity should be an integral part of the anaesthetist’s<br />
annual appraisal within the Trust; that review requires not only an accurate record but<br />
some indication of the benefit of specific activities. A complete record of CPD activity<br />
is an integral part of the process of revalidation by the GMC.<br />
Maintenance of CPD is also required by the College for recognition as a teacher of<br />
trainee anaesthetists: it follows that a department cannot be approved for training<br />
unless a majority of consultant anaesthetists in that department are up to date with<br />
their CPD requirements. The College no longer seeks details of specific CPD but<br />
assumes successful annual appraisal to be evidence of appropriate activity.<br />
CPD must be cost effective and undertaken by all grades of medical staff including<br />
non-consultant career grades.<br />
6.1 Funding for CPD<br />
Because CPD is a mandatory requirement for appraisal and in the long run revalidation,<br />
it follows that employers, Trusts or otherwise, should ensure that adequate funding is<br />
available for this purpose. If for some reason it is not available, then pressure must<br />
be applied through the management structure, by the professional bodies both within<br />
and without the Trust to correct shortfalls in educational and study leave budgets.<br />
6.2 Finding time for CPD<br />
CPD should largely take place during normal working hours. For anaesthetists<br />
this may cause considerable problems. Internal CPD, such as departmental audit<br />
meetings, may require the cancellation of operating lists but the inevitable requests<br />
for exceptions to attendance must be resisted and genuine emergency work provides<br />
the only valid reason for absence. Joint meetings with surgical groups can help solve<br />
this dilemma. External CPD may also lead to cancellation of clinical activities and,<br />
while this is regrettable, unfortunately it may sometimes be necessary.
28 Good Practice Guide 2006<br />
6.3 Monitoring of CPD<br />
Personal records must be kept of all CPD activity. It is necessary to obtain a certificate<br />
of attendance when attending any external courses or meetings, and organisers of<br />
meetings which are approved for CPD purposes are required to provide a certificate<br />
of attendance for each attendee. Proof of attendance at meetings such as internal<br />
audit meetings and journal clubs should also be maintained in the form of CPD diary<br />
records/photocopies of departmental diaries or attendance registers.<br />
Deficiencies of individuals, or within a department, should be acknowledged so that<br />
attempts can be made to fill or correct them. A list of skills available to train others<br />
should also be recorded.<br />
6.4 Directed CPD<br />
Usually, anaesthetists decide for themselves what type of CPD to undertake. However, at<br />
each annual appraisal, the appraiser may suggest other forms of CPD in order to train<br />
the anaesthetist for new clinical or management activities required for the organisation.<br />
This should be welcomed. At the same time, at each annual appraisal, the anaesthetist<br />
should raise with the appraiser any area of CPD that they believe is required in order to<br />
fill deficiencies in areas within the individual’s current scheduled duties.<br />
6.5 Range of activities<br />
CPD embraces a large range of useful activities including:<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
visiting other hospitals or centres of excellence<br />
learning or improving management skills<br />
improving teaching ability<br />
use of anaesthetic simulators<br />
interactive learning.<br />
In the revised 2005 College CPD document (see: www.rcoa.ac.uk/docs/CPD_<br />
guidelines.pdf), attention was drawn to the great benefit of spending sessions with<br />
consultant colleagues. The anaesthetists undertaking this should be rostered as<br />
supernumeraries for such sessions.<br />
6.6 Limitations to CPD<br />
It is unreasonable to expect all consultants to be able to anaesthetise all patients<br />
presented to them throughout their career, be they on a routine operating list or as an<br />
emergency. It is essential that individuals know their own professional limitations, and<br />
act within them. Within an anaesthetic department, it is essential that all necessary<br />
skills are present, and that a system is in place so that they can be deployed at the<br />
time and place required. The clinical director must ensure that the corporate CPD of<br />
the department achieves these targets. An individual, however senior, must never be<br />
reluctant to ask for help nor should a colleague refuse to provide it.
Good Practice Guide 2006 29<br />
However, when anaesthetists are rostered to cover emergency duties, it is essential<br />
that they undertake CPD appropriate to cover every type of emergency likely to be<br />
encountered on that particular roster. In order to assist this, the College CPD revised<br />
system incorporates a list of core topics.<br />
6.7 Core topics<br />
The expanded list of ‘core topics’ in anaesthesia (Appendix 1) is based upon the<br />
original list agreed by the Union of European Medical Specialists (UEMS) in 1998.<br />
Each topic is divided into clinical challenges, knowledge and skills.<br />
These are topics that an individual specialist working in a typical hospital and<br />
participating in the emergency on-call rota should have up-to-date knowledge of and<br />
proficiency in, but may be modified in the light of their individual responsibilities.
30 Good Practice Guide 2006<br />
Chapter 7: Record keeping<br />
Para 3 (f): ‘In providing care you must keep clear, accurate and legible<br />
records, reporting the relevant clinical findings, the decisions made, the<br />
information given to patients, and any drugs prescribed or other investigation<br />
or treatment.’ 6<br />
The King’s Fund Organisation Audit Hospital Accreditation Programme has set a<br />
standard for health records in its Organisational Standards criteria, 38 which states:<br />
‘There is an accurate health record which enables the patient to receive<br />
effective continuing care, enables the healthcare team to communicate<br />
effectively, allows another doctor or professional members of staff to assume<br />
care of the patient at any time, enables the patient to be identified without<br />
risk or error, facilitates the collection of data for research, education and<br />
audit and can be used in legal proceedings.’<br />
If this standard of record keeping is not maintained and professional requirements are<br />
not being met, patients, and possibly staff, are put at risk. It cannot be emphasised too<br />
strongly that in medico-legal cases the outcome is often dependent on the anaesthetic<br />
record. An untidy, illegible, scantily completed chart may be taken as indirect evidence<br />
of shoddy or inattentive care. 39 Furthermore, the examination of medical records<br />
forms part of the GMC’s fitness to practise procedures (see Chapter 9). The record<br />
must be such that if another doctor were required to take over the case, this record<br />
would allow systematic and ready access to all the information required.<br />
7.1 The content of the anaesthetic record<br />
There is no standard anaesthetic record in the UK. However, in recent years both the<br />
Association and the College have set out what they regard as the minimum data set<br />
for an anaesthetic record. 40 The GMC uses this information for assessment purposes<br />
in what it considers to be essential recorded information. While the format of the<br />
anaesthetic record is a matter for local preference, the record should contain:<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
basic data entry: names of surgeon(s) and anaesthetist(s), date, operation.<br />
Where the anaesthetist is a trainee or SAS grade doctor, the name of the<br />
supervising consultant should be recorded (see 8.2.4 for level of supervision)<br />
patient identification: name, date of birth, gender, hospital number<br />
pre-operative assessment: relevant history, physical examination, drugs,<br />
allergies, ASA grade<br />
anaesthetic technique: induction and maintenance technique, including<br />
anaesthetic agents used, recorded in detail<br />
intravenous drugs administered: clear record of pre-operative and intraoperative<br />
drugs given, doses and time of administration
Good Practice Guide 2006 31<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
equipment monitoring: record of anaesthetic machine and circuit check, relevant<br />
equipment monitoring such as FiO 2<br />
(always) and pressure alarms<br />
patient monitoring used: this should be in accordance with the recommendations<br />
of the Association of Anaesthetists 41<br />
physiological variables recorded: time based chart recordings of relevant<br />
parameters including pre-induction values<br />
frequency of record of physiological variables: frequent recording from induction<br />
depending on patient stability, but not less frequently than every ten minutes for<br />
pulse, blood pressure, oxygen saturation and end-tidal carbon dioxide<br />
fluid balance: evidence of venous cannulation; record of fluids administered;<br />
blood loss where relevant<br />
postoperative pain relief: clear and appropriate postoperative analgesic orders<br />
other postoperative instructions: oxygen therapy, immediate postoperative fluids<br />
and monitoring to Association standards. 42<br />
Any discussions the anaesthetist has with the patient or a responsible adult acting<br />
for the patient about anaesthetic techniques, risks, special procedures etc should be<br />
documented either on the anaesthetic records or in the body of the clinical notes.<br />
A printed record of each anaesthetic should be included in the patient’s case notes,<br />
wherever practicable.<br />
In addition:<br />
❚<br />
❚<br />
❚<br />
it is particularly important that critical incidents and complications are accurately<br />
documented<br />
where it is necessary for a case to be handed over from one anaesthetist to<br />
another, this should be noted, as should decisions shared with other clinicians<br />
and staff<br />
if a patient is unexpectedly admitted to ICU or HDU the reasons for doing so<br />
should be recorded.<br />
7.2 Other uses for anaesthetic records<br />
Computerised records provide detailed information about both individual and<br />
departmental practice. However, they are most valuable for auditing specific areas of<br />
anaesthetic care. Records are also a useful tool of personal audit particularly when<br />
used with three or four colleagues for case-based discussions.<br />
Patients’ notes, including the anaesthetic record, are confidential documents and the<br />
GMC, therefore, requires that patients’ consent to disclosure of information for research,<br />
teaching and audit must be obtained unless the data have been effectively anonymised. 19
32 Good Practice Guide 2006<br />
7.3 Critical care<br />
Critical care practice requires a full assessment of each patient at least once per<br />
24- hours. This should be documented in full, including abnormal results, changes<br />
in treatment and reasons for them, and forward plans. Results should be charted in<br />
such a way that trends can be easily identified.<br />
Current trainee work patterns often result in patient care changing hands several<br />
times a day. Accordingly, it is vital that medical notes record each change in care<br />
and the reasons for it. They should include procedures performed, discussions with<br />
relatives, outcomes of investigations and decisions to reduce or withdraw support.<br />
The aim is for transparent documentation which allows any other doctor to take over<br />
the patient’s care at any point.<br />
7.4 Pain management<br />
7.4.1 Outpatient<br />
As in all other out patient clinics, comprehensive records must be kept, detailing history,<br />
examination, investigations, treatment and outcomes. Copies of correspondence to<br />
general practitioners, consultants and other health professionals should be retained<br />
within the hospital notes.<br />
Discussions about treatment options and potential side effects should be documented,<br />
along with a record of consent, if required.<br />
7.4.2 Inpatient<br />
7.4.2.1 Acute pain management<br />
There should be a record of the management of acute pain, including pain assessments<br />
and treatment, in the hospital notes. These are necessary to foster continuity of care.<br />
7.4.2.2 Chronic and cancer pain<br />
Detailed clinical notes should be made in the patient’s clinical record when the pain<br />
management service is involved in managing in-patients with chronic pain or cancer<br />
pain. The pain service should ensure that colleagues are kept informed when patient<br />
care is being shared.<br />
Further to this document, an additional publication is being produced in conjunction<br />
with The British Pain Society regarding chronic pain management.
Good Practice Guide 2006 33<br />
Chapter 8: Leadership, management and<br />
administration<br />
Para 42: ‘If you are responsible for leading a team, you must follow the<br />
guidance in Management for Doctors.’ 43<br />
A department of anaesthesia, critical care and pain management should provide<br />
a clinical service of high quality within a defined budget and, where appropriate,<br />
training facilities to the standard required by the College. While good administrative<br />
arrangements are necessary within a department, the key to achieving these is<br />
effective and efficient leadership. This should be provided by a designated head of<br />
service who is responsible for all the activities of the department.<br />
8.1 Head of department<br />
In many Trusts this is the clinical director. However, in some Trusts, the department<br />
of anaesthesia is part of another directorate and the clinical director is not an<br />
anaesthetist. Under these circumstances it is necessary to have an anaesthetist who<br />
takes responsibility for all aspects of the anaesthetic service. He/she may be the lead<br />
clinician in anaesthesia, the head of service or the chairman of the department. In<br />
this guidance, the term ‘clinical director’ refers to the designated anaesthetist with<br />
management responsibility for all the activities in which the department of anaesthesia<br />
is engaged. To encourage efficient rostering and use of resources it is recommended<br />
that the department of anaesthesia, critical care and pain management should have<br />
management responsibility for operating departments, 39 intensive care and pain relief<br />
services, though it is recognised that there are other models which work satisfactorily.<br />
The clinical director is appointed by, and is accountable to, the chief executive for the<br />
management of the anaesthetic service. However, the director cannot function without<br />
the support of consultant and other colleagues and must therefore be acceptable<br />
to them. Some years of consultant experience are usually necessary before being<br />
appointed to such a post. In some hospitals there has been a tendency to appoint<br />
clinical directors primarily because of their management capability, but it is the qualities<br />
of good leadership which are essential. These are fundamentally the ability to provide<br />
direction and generate trust. Giving support, guidance, inspiration and confidence to<br />
colleagues is the foundation upon which the success of a department is built.<br />
8.2 Role within the department of anaesthesia<br />
8.2.1 Staff management<br />
The clinical director must ensure that there is an equitable distribution of work within<br />
the department with efficient rostering to meet all the activities which it undertakes.<br />
This includes the proper management of annual, study and professional leave.<br />
All consultants are required to have a job plan specifying their contractual obligations,<br />
which should be reviewed and agreed annually. This is a good opportunity, along
34 Good Practice Guide 2006<br />
with preparation for appraisal, for consultants to assess their own programmes and<br />
workloads, professional development and needs, the overall work of the department,<br />
their role within it and the resources available to them and their department, 44 Nonconsultant<br />
career grade anaesthetists should also have clearly defined programmes<br />
of work. 45 As for consultant staff, adequate arrangements must be in place for their<br />
continuing medical education and professional development.<br />
While the day-to-day responsibility for trainees rests with the College tutor, the<br />
quality of the clinical work which they undertake is the responsibility of the clinical<br />
director. The clinical director also has responsibility for all other staff within the<br />
directorate, although they will normally be managed by the appropriate business or<br />
nurse manager.<br />
Close liaison between the College tutor and the clinical director is needed to ensure<br />
that the training requirements of the College are met. A mentoring system between<br />
consultants and trainees is strongly recommended. 46 This promotes support for and<br />
communication with trainees.<br />
Poor performance among anaesthetists is fortunately rare. Nevertheless, the<br />
clinical director has a duty to promote high standards, identify poor performance in<br />
colleagues and take whatever action is necessary to protect patients from harm. This<br />
is discussed in detail in Chapter 9 of this Guidance.<br />
8.2.2 Budgets<br />
The operational control of the directorate’s finances normally will be within the<br />
remit of the business manager. However, the clinical director has a responsibility to<br />
ensure that the anaesthetic service is adequately resourced for the commitments it<br />
undertakes but keeps within the agreed budget allocated to it.<br />
8.2.3 Communication<br />
Good communications within the directorate are essential if it is to run efficiently and if<br />
all staff are to feel involved in the department and content in their work. Without good<br />
communications misunderstandings easily arise and inaccurate perceptions quickly<br />
take root. Informal discussions, regular, minuted meetings, letters, memoranda,<br />
notice boards and emails form an essential communications network. It should be<br />
recognised that emails are disclosable documents and that if emails are sent outside<br />
of the NHS system, then this method of communication is not secure and should not<br />
be used for patient information. Time given to communication pays considerable<br />
dividends in getting things done with the support of colleagues, particularly if it is<br />
backed up by a personal concern for people’s welfare.<br />
In a directorate which manages the operating theatres, clear lines of communication<br />
with surgeons and theatre staff are necessary. A theatre users’ group/committee is<br />
a useful forum by which this can be achieved.
Good Practice Guide 2006 35<br />
Anaesthetists who hold out-patient clinics should communicate effectively with the<br />
patient’s general practitioner and the referring doctor (if this is not the GP). It is now<br />
recommended that letters should normally also be copied to the patient.<br />
8.2.4 Guidelines<br />
The College and the Association consider it necessary that, for some areas of the<br />
anaesthetic service and clinical practice, departments should have clear guidelines.<br />
These should be issued during the induction of every newly appointed anaesthetist to<br />
the anaesthetic department. Guidelines should state explicitly how the supervision of<br />
trainees and SASGs is implemented.* The clinical director should ensure that agreed<br />
guidelines are complied with and regularly reviewed. This is part of the audit cycle<br />
which is a key feature of a successful department. 21<br />
8.2.5 Delegation<br />
The work of a modern anaesthetic department is complex. Effectiveness and<br />
efficiency are enhanced when named anaesthetists, with appropriate experience and<br />
skills, have responsibility for particular areas for which they are accountable to the<br />
clinical director.<br />
Examples are:<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
rostering and management of leave<br />
equipment<br />
audit<br />
continuing medical education and professional development<br />
training<br />
specialist services including critical care, obstetrics, paediatrics, acute pain and<br />
chronic pain<br />
clinical governance.<br />
8.2.6 Contract discussions<br />
The clinical director or Lead Clinician should undertake contract negotiations with health<br />
service commissioners for anaesthetic, critical care and pain management services.<br />
8.3 Role outside the department of anaesthesia<br />
The clinical director of anaesthesia has a key part to play in the overall running of a<br />
Trust, in determining and implementing policy, and should be a member of the Trust’s<br />
operational board. Anaesthetists work in many different departments of a hospital<br />
and are therefore well placed to have an overview of the opportunities and problems<br />
within it. Good working relationships with other clinical directors are needed if the<br />
anaesthetic department is to work well throughout a hospital.<br />
*The principles of supervision are defined in: The CCT in Anaesthesia I: General Principles. A manual for<br />
trainees and trainers (www.rcoa.ac.uk/docs/CCTpti.pdf).
36 Good Practice Guide 2006<br />
It is self-evident that while the work undertaken by anaesthetists – both in nature<br />
and volume – is mostly generated by other clinicians, anaesthetists do have a major<br />
contribution to make to the successful accomplishment of that work. 47 Purchasers,<br />
therefore, need to understand the full nature and range of functions that a modern<br />
anaesthetic service can offer to patients, how it operates and the constraints within<br />
which it operates.<br />
8.4 Support 48–49<br />
Clinical directors need both time and support to do the job. They should have a<br />
separate contract for this part of their work with an agreed job description. Adequate<br />
sessional time must be made available. Individual Trusts may make specific financial<br />
arrangements with clinical directors but it is not recommended that a clinical director<br />
should have a full programme of clinical work.<br />
Clinical directors should be supported by and work closely with business and nurse<br />
managers as well as have ready access to specialist managers in such areas as<br />
finance and personnel. They must also be provided with adequate personal and<br />
secretarial assistance and information technology facilities.
Good Practice Guide 2006 37<br />
Chapter 9: The poorly performing<br />
anaesthetist<br />
Para 43: ‘You must protect patients from risk of harm posed by another<br />
colleague’s conduct, performance or health.’<br />
In its guidance to doctors on Good Medical Practice the GMC sets out the standards<br />
of performance it expects from medical practitioners. These include the provision<br />
of good clinical care for patients, maintaining a proper professional relationship<br />
with patients and working constructively within medical and multidisciplinary teams.<br />
Evidence of departure from the standards described under these general headings<br />
may be used to support a complaint to the GMC of impaired fitness to practise. Every<br />
doctor when aware of bad practice by another doctor, especially where this may lead<br />
to harm to patients, has a duty to take appropriate action.<br />
The management of the poorly performing anaesthetist is governed by a complex set<br />
of arrangements. It is also a very sensitive issue and there is considerable scope for<br />
the problem to be mishandled. This Chapter therefore summarises:<br />
❚<br />
❚<br />
❚<br />
methods within departments of anaesthesia for preventing the performance of its<br />
members from falling below an acceptable standard<br />
objectives in managing the poorly performing anaesthetist<br />
the terms used in Department of Health and GMC documents.<br />
It also provides guidance on how clinical directors should proceed in the event of<br />
concerns arising about an anaesthetist’s performance.<br />
Concerns about a doctor’s conduct or capability can come to light in a wide variety of<br />
ways, for example:<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
concerns expressed by other clinical or non-clinical staff<br />
review of performance against job plans<br />
concerns raised at appraisal<br />
clinical governance or clinical audit<br />
complaints by patients or relatives<br />
information from regulatory bodies<br />
litigation following allegations of negligence<br />
information from the police or coroner.<br />
If inadequate performance has been suspected or detected it can be dealt with at<br />
three different levels:
38 Good Practice Guide 2006<br />
❚<br />
❚<br />
❚<br />
Locally where it is apparent that some improvement in skills, knowledge or<br />
behaviour is required, the clinical director may recommend that further training<br />
or other action is required and this may be arranged by the local department.<br />
Where more serious concerns are evident regarding a doctor’s performance,<br />
the Trust (in England, Wales and Northern Ireland) should contact the National<br />
Clinical Assessment Service (NCAS) at the earliest opportunity. The number<br />
of doctors who have been suspended from work for long periods is a cause<br />
for concern, and the issue was investigated in detail by the National Audit<br />
Office. 50 (The phrase ‘exclusion from work’ is now used to avoid confusion with<br />
‘suspension’ of the right to practise which may be imposed by the GMC). Trusts<br />
are now required to discuss the case fully with the chief executive, medical<br />
director, Director/Head of Human Resources, NCAS and other interested parties<br />
(such as the police where there are serious criminal allegations) whenever<br />
exclusion is being considered. 51<br />
Where a very serious problem has occurred, a doctor may be immediately<br />
excluded and referred directly to the GMC. In these cases the above parties must<br />
discuss the case at the earliest opportunity following the exclusion.<br />
9.1 Prevention of poor performance<br />
The aim of clinical governance, which is now widely implemented in the NHS, is to<br />
secure better quality care, and observance of its key principles should help in the<br />
maintenance of professional standards. 52<br />
Although designed to support improvements in practice, the introduction of a<br />
mandatory system of annual appraisal within the NHS should help to identify poorly<br />
performing individuals at an early stage. Appraisal, a formative process in which both<br />
appraiser and appraised agree a professional development plan based on identified<br />
and agreed areas of need, should be seen as quite different from assessment, in<br />
which identified strengths and weaknesses may have implications for an individual’s<br />
career. Although assessments are important elements of the RITA process for trainees,<br />
they will not be used for non-training grades until the time comes for the five-yearly<br />
revalidation of their medical registration. However, if potentially serious performance<br />
issues arise in the appraisal process, the appraisal should be suspended whilst the<br />
appraising doctor ensures that they are addressed urgently, especially if they pose a<br />
threat to patient safety.<br />
The culture within an anaesthetic department is central in maintaining high standards<br />
of anaesthetic practice. Where little attention is paid to efficient running of the<br />
department, record keeping, agreement on clinical guidelines, audit and local and<br />
central programmes of continuing education, standards are likely to fall. The local<br />
implementation of the recommendations already made in this Good Practice Guide will<br />
go a long way to maintain the standards of performance of individual anaesthetists.<br />
The recommendations provide the framework set by the Association and the College<br />
within which anaesthetists are expected to practise and hence the benchmarks by<br />
which they may be assessed. Anaesthetists should concentrate on maintaining
Good Practice Guide 2006 39<br />
overall standards within their department and take appropriate steps to prevent any<br />
individual’s performance from becoming seriously deficient. However, anaesthetists in<br />
general and clinical directors in particular also need to understand the procedures to<br />
be followed if seriously deficient performance in a colleague is suspected.<br />
9.2 Objectives in managing the poorly performing anaesthetist<br />
Identifying and managing the poorly performing anaesthetist is always difficult. The<br />
person concerned will be a colleague, and often a friend, sometimes of long standing.<br />
It is not easy to view the situation objectively and it helps, therefore, to have clear<br />
objectives. Fundamentally there are always three:<br />
❚<br />
❚<br />
❚<br />
9.3 Terminology<br />
To protect patients from harm. This is the primary objective which must always<br />
be uppermost.<br />
To ensure that the anaesthetist is treated justly. Procedures should be fair and open.<br />
To provide opportunities for the anaesthetist to improve their performance. 53<br />
A poorly performing anaesthetist is one whose performance is outside the accepted<br />
limits of practice. Within these limits an anaesthetist may adopt practices which<br />
are different from those of other departmental colleagues provided that there is a<br />
reasonable body of anaesthetists who would practise in a similar way.<br />
9.3.1 Department of Health terminology<br />
In its publications Supporting doctors, protecting patients 54 and Assuring the<br />
Quality of Medical Practice, 55 the Government indicated its intention to introduce<br />
a new approach to the way in which poor clinical performance is dealt with in the<br />
NHS, complementing the reforms proposed by the GMC, Medical Royal Colleges and<br />
other professional bodies. It proposed a change from the traditional approach using<br />
disciplinary solutions applied late in the day to one that attempts to identify problems<br />
early so that doctors can be helped by educational measures.<br />
In December 2003 the Department of Health issued the document High Professional<br />
Standards in the Modern NHS; a framework for the initial handling of<br />
concerns about doctors and dentists in the NHS, under cover of HSC 2003/012.<br />
This framework has now been completed. 51 All NHS bodies were required by 1 June<br />
2005 to implement the framework, and it has been agreed with Monitor that it should<br />
be issued to NHS Foundation Trusts as advice. The framework replaces the previous<br />
disciplinary procedures for doctors as set out in circular HC(90)9 as well as the<br />
‘three wise men’ panels provided for in HC(82)13. It abolishes the right of appeal<br />
to the Secretary of State held by certain doctors under Para 190 of the Terms and<br />
Conditions of Service.<br />
The framework, which has been drafted in close association with NHS Employers<br />
and the NCAS and agreed with the British Medical Association and the British Dental<br />
Association, consists of five parts:
40 Good Practice Guide 2006<br />
Part I: Action when a concern arises<br />
Part II: Restriction of practice and exclusion<br />
Part III: Conduct hearings and disciplinary matters<br />
Part IV: Procedures for dealing with issues of capability<br />
Part V: Handling concerns about a practitioner’s health<br />
The key changes are that:<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
❚<br />
the distinction between personal and professional misconduct is abolished.<br />
Doctors and dentists employed in the NHS will be disciplined for misconduct<br />
under the same locally based procedures as any other staff member<br />
there is a single process for handling capability issues about the practitioner’s<br />
professional competence closely tied in with the work of the NCAS<br />
health issues are routinely dealt with through the occupational health service<br />
the employing Trust is squarely responsible for the disciplining of its medical and<br />
dental staff – not outsiders<br />
there is scope to bring in expert advice for panels considering capability issues<br />
the capability panel will be handled by an independent chair<br />
the same disciplinary procedures will apply to all doctors and dentists employed<br />
in the NHS.<br />
Where there are concerns about a doctor’s clinical performance that cannot be<br />
resolved locally, the employer will refer the doctor to NCAS. This may initiate an<br />
assessment of the doctor’s clinical performance and give advice on any action to be<br />
taken. It is, however, an advisory body, and the employer will remain responsible for<br />
dealing with the problem, either by local resolution in accordance with the framework<br />
or by referral to the GMC.<br />
9.3.2 GMC terminology 56<br />
The law governing the way in which the GMC handles complaints about doctors<br />
changed on 1 November 2004.<br />
Under the new procedures, complaints about doctors no longer follow separate<br />
streams for health, performance and conduct. Instead, the GMC looks at the doctor’s<br />
fitness to practise in the round, assesses whether it is impaired, and determines if any<br />
impairment requires action on the doctor’s registration.<br />
For anaesthetists this encompasses the whole spectrum of peri-operative care, critical<br />
care and pain management which they are trained to provide. Failure in one area may<br />
be regarded as evidence of poor performance, as would failure to seek help from a<br />
colleague if an anaesthetist’s knowledge and skill were inadequate for the level of<br />
care required for a given patient. In practice, repeated patterns of poor performance<br />
rather than a single episode are more likely to lead to concern.
Good Practice Guide 2006 41<br />
Fitness to practise may be impaired by reason of misconduct, criminal conviction or caution,<br />
determination by another regulatory body, deficient performance or ill health. When<br />
dealing with performance or health issues, the GMC tries to identify areas where remedial<br />
action such as retraining or medical treatment is possible, whilst protecting patients from<br />
harm. It is also well known, for example, that the practice of anaesthesia is very stressful<br />
and there is continuing concern about the suicide rate among anaesthetists.<br />
The GMC has power to impose conditions on a doctor’s registration, to suspend it<br />
or to erase the doctor from the register. In future, only doctors with a licence will<br />
be allowed to practise clinically, and apart from erasure the above sanctions will be<br />
applied to the licence rather than to registration. Under the new regulations the<br />
GMC also has the power to issue a warning where a doctor’s fitness to practise is<br />
not impaired but there has been a significant departure from the principles set out in<br />
Good Medical Practice. Warnings will be disclosed to the doctor’s employer and<br />
any enquirer for a period of five years.<br />
9.4 Which procedure should be followed?<br />
Most performance, health and conduct problems in doctors are best handled locally,<br />
using the Trust’s agreed procedures. This is the responsibility of a Trust’s medical<br />
director. Clinical directors must ensure that appropriate informal and formal procedures<br />
are in place within a directorate to monitor the quality of clinical practice and discuss<br />
any performance issues with the medical director at the earliest possible stage. In cases<br />
involving trainees, responsibility will be shared with the postgraduate dean.<br />
The procedure to be followed depends on the nature of the concerns about the<br />
poorly performing anaesthetist.<br />
9.4.1 Local procedures to be followed within a Trust<br />
9.4.1.1 Concerns which are initially non-specific and where patients<br />
may or may not be immediately at risk<br />
Gather discreetly as much information as possible. Ignore hearsay evidence and<br />
try to establish the facts. Anyone making an allegation against a colleague must<br />
be prepared to support it in writing. It is almost always helpful to consult trusted,<br />
senior colleagues before deciding how to proceed. If concerns appear to be wellfounded<br />
but not serious, it may be sufficient for one or two colleagues to bring them<br />
informally to the doctor’s attention, together with appropriate advice. If the concerns<br />
are serious, or if the anaesthetist has no insight into the problem, he/she should be<br />
informed that the clinical director must be involved at an early stage. This enables<br />
the clinical director to see the issues in perspective and for a range of options to be<br />
considered about how best to proceed. It may also be helpful later should the clinical<br />
director be criticised by the anaesthetist concerned or by other colleagues.<br />
Advice can also be obtained from the College and the Association. clinical directors<br />
may find the Association’s document on Stress in Anaesthetists particularly helpful. 57<br />
The details of the Association’s Sick Doctor Scheme are also set out in this publication.<br />
The GMC has an advisory service for medical directors.
42 Good Practice Guide 2006<br />
9.4.1.2 Concerns where patients are clearly at risk or informal discussions<br />
have failed to resolve issues under the previous section (9.4.1.1)<br />
The clinical director and medical director should be contacted urgently. NCAS should<br />
also be contacted, especially when exclusion is being considered.<br />
The medical director, who is responsible for deciding which particular procedure should<br />
be followed, may wish to seek help from the Association and the College in providing<br />
impartial advice. The clinical director, however, may be asked to be the investigating<br />
officer. This is appropriate as the clinical director is thoroughly familiar with accepted<br />
standards of practice and the day-to-day running of the department of anaesthesia and<br />
understands how anaesthesia is practised locally. The clinical director’s responsibility<br />
is to provide the medical director with the facts and such information and advice as are<br />
required for the medical director to decide how to proceed.<br />
9.4.2 Procedures outside a Trust<br />
9.4.2.1 National Clinical Assessment Service (formerly Authority) (NCAS)<br />
NCAS (formerly Authority) was established to improve arrangements for dealing with<br />
the poor clinical performance of doctors, and its advisory and assessment services<br />
are aimed at enabling NHS Trusts in England, Wales and Northern Ireland to handle<br />
cases quickly and fairly, reducing the need to use disciplinary procedures to resolve<br />
problems. A similar scheme is being developed in Scotland. It has helped to avoid<br />
formal or informal suspension, including the so-called ‘gardening leave’ in 85% of<br />
cases referred to it where this was being considered by the Trust.<br />
A Trust in England can seek advice from NCAS about a doctor whom it thinks is poorly<br />
performing at any stage in the handling of the case. NCAS has developed a staged<br />
approach to the services it provides NHS Trusts and practitioners. This involves:<br />
❚<br />
❚<br />
❚<br />
❚<br />
immediate telephoned advice, available 24 hours<br />
advice, then detailed supported local case management<br />
advice, then detailed NCAS clinical performance assessment<br />
support with planning and implementing recommendations arising from assessment.<br />
9.4.2.2 Ombudsman<br />
Where the issues are not clear or where there is doubt as to the case to be answered,<br />
referral can be made to the NHS Ombudsman for assistance in resolving the problem.<br />
9.4.2.3 Referral to the GMC<br />
The criteria for referral to the GMC’s Fitness to Practise procedures include:<br />
❚<br />
❚<br />
❚<br />
where local action by the Trust, with or without advice from NCAS, would be<br />
impractical or has been tried but has failed to resolve the problem<br />
where local action has resolved the immediate local issue but the matter has<br />
wider implications<br />
where the problems are so serious that immediate referral to the GMC is clearly<br />
required regardless of whether or not local action may also be appropriate.
Good Practice Guide 2006 43<br />
Referral should be considered if the anaesthetist fails to display appropriate insight into<br />
the problems, has left the district but may have taken those problems to another area of<br />
the country or has moved exclusively into private practice. In particular the GMC may be<br />
the only body able to take effective action where serious problems arise in relation to a<br />
doctor working as a transient locum or working solely in non-NHS practice.<br />
Performance and health issues are unlikely to require immediate referral to the GMC<br />
if the anaesthetist has insight into the problem and is willing to co-operate with local<br />
initiatives to help resolve the concerns.<br />
Finally, remember in any investigation into a colleague’s performance:<br />
❚<br />
❚<br />
keep records of everything: conversations, telephone calls, meetings and<br />
interviews. These may be needed at a later stage<br />
do not jump to conclusions about the outcome of the investigation. Patient and<br />
persistent investigation to establish the facts and openness with the colleague<br />
concerned are the only ways to protect patients, maintain standards and act justly.<br />
It is very difficult to maintain confidentiality during an investigation of a colleague’s<br />
performance. Inevitably, rumours spread and colleagues worry about what is<br />
happening. It is important, therefore, to keep colleagues informed in general terms<br />
only but at the same time keeping confidential the details of the enquiry until it has<br />
been completed.
44 Good Practice Guide 2006<br />
References<br />
1 Klein R. The state of the profession: the politics of the double bed. BMJ 1990;301:700–702.<br />
2 Stacey M. The GMC and professional accountability. Pub Pol and Admin 1989;4:12–27.<br />
3 Rosenthal MM. The incompetent doctor: behind closed doors. Open University Press, Buckingham 1995.<br />
4 Smith R. Profile of the GMC: the day of judgement comes closer. BMJ 1989;298:1241–1244.<br />
5 Lock S. Regulating doctors. BMJ 1989;299:137–138.<br />
6 Good Medical Practice. GMC, London 2006.<br />
7 Core Values Conference. Core values for the medical profession in the 21st century. BMA, London 1995.<br />
8 Performance Procedures. GMC, London 1997.<br />
9 Maintaining Good Medical Practice. GMC, London 1998.<br />
10 The new NHS. DH, Stationery Office, London 1997.<br />
11 The National Clinical Assessment Authority, London 2001 (www.ncaa.nhs.uk).<br />
12 The National Patient Safety Agency (Establishment and Constitution) Order. Statutory Instrument No:1743, London 2001.<br />
13 Irvine D. The performance of doctors II: Maintaining good practice, protecting patients from poor performance.<br />
BMJ 1997;314:1613–1615.<br />
14 National Health Service (Clinical Negligence Scheme) Regulations. CNST 1996.<br />
15 Beauchamp TL, Childress JF. Principles of Biomedical Ethics. Third edition. OUP, Oxford 1989.<br />
16 Berwick DM. Medical associations: guilds or leaders? BMJ 1997;314:1564.<br />
17 Calman K. The profession of medicine. BMJ 1994;309:1140–1143.<br />
18 Smith R. Medicine’s core values. BMJ 1994;309:1247–1248.<br />
19 Seeking patients’ consent: the ethical considerations. GMC, London 1998.<br />
20 Confidentiality: Protecting and Providing Information. GMC, London 2000.<br />
21 Anaesthesia under examination. The Audit Commission. Audit Commission Publications, Abingdon 1997:92.<br />
22 Research: The role and responsibilities of doctors. GMC, London 2002.<br />
23 Hepatitis B infected Healthcare Workers. Health Service Circular HSC 2000/020.<br />
24 Catastrophies in Anaesthetic Practice. AAGBI, London 2005.<br />
25 Principles for Best Practice in Clinical Audit. NPSA, Radcliffe Medical Press 2002 (also available via www.nelh.nhs.uk).<br />
26 The New NHS. DH, Stationery Office 1997:63–67.<br />
27 Raising the Standard: A compendium of audit recipes for continuous quality improvement in anaesthesia. Second<br />
edition. RCoA, London 2006.<br />
28 Craig J, Wilson ME. A survey of anaesthetic misadventures. Anaesthesia 1981;36:933–936.<br />
29 Kumar V. An analysis of critical incidents in a teaching department for quality assurance: a survey of mishaps during<br />
anaesthesia. Anaesthesia 1988;33:879–883.<br />
30 Williamson JA, Webb RK, Pryor GL. Anaesthesia safety and the critical incident technique. Australia Clinical<br />
Review 1985;6:57–61.<br />
31 Cooper JB, Newbower RS, Kitz RJ. An analysis of major errors and equipment failures in anaesthesia management:<br />
considerations for prevention and detection. Anesthesiology 1984;60:34–42.<br />
32 Runciman WB et al. The Australian Incident Monitoring Study. System failure: an analysis of 2000 incident reports.<br />
Anaesth Intensive Care 1993:21:684–695.<br />
33 Health and Safety at Work Act. Risks and Diseases of Dangerous Occurrences Regulations (RIDDOR). HSE 1974.<br />
34 The National Patient Safety Agency (www.npsa.nhs.uk).<br />
35 A Practical Handbook for Improving Clinical Audit – NHS Clinical Governance Support Team, March 2005.<br />
36 Comprehensive Critical Care planning and managing critical care capacities. DH, London 2000 (www.doh.gov.<br />
uk/compcritcare/planning.htm).<br />
37 The Doctor as a Teacher. GMC, London 1999.<br />
38 Standard of Records. The King’s Fund Organisation Audit.<br />
39 Utting JE. Pitfalls in anaesthetic practice. BJA 1987;59:888–890.<br />
40 New guidelines for anaesthetic records. RCoA Newsletter 1996;27:8–9.<br />
41 Recommendations for Standards of Monitoring during Anaesthesia and Recovery. AAGBI, London 2000.
Good Practice Guide 2006 45<br />
42 Efficiency of Theatre Services. AAGBI, London 1989.<br />
43 Management for doctors: guidance from the General Medical Council. GMC, London 2006.<br />
44 Guidance on Contracts and Workloads for Consultant Anaesthetists. AAGBI, London 1997.<br />
45 Non-Consultant Career Grade Anaesthetists. AAGBI, London 1998.<br />
46 Consultant trainee relationships. A guide for consultants. AAGBI, London 2001.<br />
47 Anaesthesia under examination. The Audit Commission. Audit Commission Publications, Abingdon 1997:4–7.<br />
48 Anaesthesia under examination. The Audit Commission. Audit Commission Publications, Abingdon 1997:91–104.<br />
49 Departments of Anaesthesia: secretariat and accommodation. AAGBI, London 1992.<br />
50 The Management of Suspensions of Clinical Staff in NHS Hospital and Ambulance Trusts in England. The National<br />
Audit Office. The Stationery Office, London 2003.<br />
51 Maintaining High Professional Standards in the Modern NHS. DH, 2005.<br />
52 Achieving Improvements through Clinical Governance: a progress report on implementation by NHS Trusts. The<br />
National Audit Office. The Stationery Office, London 2003.<br />
53 When things go wrong. Practical steps for dealing with the problem doctor, version 1. Association of Trust<br />
medical directors. Cheadle 1997.<br />
54 Supporting Doctors, Protecting Patients. Consultation Paper on recognising and dealing with poor clinical<br />
performance of doctors in the NHS in England. DH, London 2000 (www.gov.uk/pub/docs/doh/cmodev.pdf).<br />
55 Assuring the Quality of Medical Practice: Implementing Supporting Doctors, Protecting Patients. DH, London 2001.<br />
56 Referring a doctor to the GMC: a guide for individual doctors, medical directors and clinical governance managers.<br />
GMC, London 2004.<br />
57 Stress in Anaesthetists. AAGBI, London 1997.
46 Good Practice Guide 2006<br />
Bibliography of current guidance from<br />
central organisations<br />
General documents<br />
Department of Health<br />
A First Class Service: Quality in the New NHS. Wetherby, 1998.<br />
An Organisation with a Memory. Report of an Expert Group on Learning from adverse events<br />
in the NHS chaired by the Chief Medical Officer, 2000.<br />
Building a safer NHS for patients. Implementing an organisation with a memory, 2001.<br />
Maintaining high professional standards in the modern NHS: Doctors’ and dentists’ disciplinary<br />
framework, 2005.<br />
Modernising Medical Careers, 2004.<br />
Quality in the new NHS (HSC1999/154), 1999.<br />
Supporting Doctors, Protecting Patients. The Stationary Office, London 1999.<br />
The New NHS. Modern, Dependable, 1997.<br />
The NHS Plan: a Plan for Investment, a Platform for Reform, 2000.<br />
General Medical Council<br />
Good Medical Practice, 2006.<br />
Management in Healthcare – the Role of Doctors, 1999.<br />
Research: The Role and Responsibilities of Doctors, 2002.<br />
Serious Communicable Diseases, 1997.<br />
The Doctor as a Teacher, 1999.<br />
The anaesthetist’s working environment<br />
Association of Anaesthetists of Great Britain and Ireland<br />
Anaesthetic Related Equipment. Purchase, maintenance and replacement, 1994.<br />
Controlled Drugs in Perioperative Care, 2006.<br />
Department of Anaesthesia: Secretariat and Accommodation, 1992 (currently under revision).<br />
Drug and Alcohol Abuse Amongst Anaesthetists: Guidance on Identification and Management, 2000.<br />
Guidance on Contracts and Workload for Consultant Anaesthetists, 2005.<br />
Infection Control in Anaesthesia, 2002.<br />
Theatre Efficiency, 2003.<br />
Joint Committee on Good Practice (RCoA & AAGBI)<br />
Departmental Portfolio, 2002.<br />
Good Practice – a guide for departments of anaesthesia, critical care and pain<br />
management (third edition).<br />
Guide for Appraisal, 2000.<br />
Personal Folder Supplement to Form 3 of the NHS Appraisal Folder, 2002.<br />
Royal College of Anaesthetists<br />
Information for patients – Risks associated with having an Anaesthetic, 2005.<br />
Raising the Standard: A compendium of audit recipes for continuous quality improvement in<br />
anaesthesia. Second edition, 2006.<br />
Raising the Standard: Information for Patients, 2003.
Good Practice Guide 2006 47<br />
Provision of services<br />
Association of Anaesthetists of Great Britain and Ireland<br />
Anaesthesia in Great Britain and Ireland: a physician only service, 1996.<br />
Anaesthetists and Non-acute Pain Management (jointly with the RCoA and British Pain Society), 1993.<br />
Day Case Surgery, 2005.<br />
Immediate Post Anaesthetic Recovery, 2002.<br />
Non-Consultant Career Grade Anaesthetists, 1998 (under revision).<br />
OAA/AAGBI Guidelines for Obstetric Anaesthesia Services, 2005.<br />
Provision of Anaesthetic Services in Magnetic Resonance Units, 2002.<br />
Provision of Pain Services, 1997.<br />
Risk Management, 1998.<br />
Surgery and General Anaesthesia in General Practice Premises, 1995.<br />
The Role of the Anaesthetist in the Emergency Service, 1991.<br />
Intensive Care Society<br />
Allied Health Professional and Healthcare Scientists Critical Care Staffing Guidance, 2003.<br />
Standards for Intensive Care Units, 1997.<br />
Royal College of Anaesthetists<br />
Guidance on the Provision of Anaesthetic Services, 1999–2006.<br />
Guidance on the Provision of Paediatric Anaesthetic Services, 2004.<br />
Pain after Surgery (jointly with RCS England), 1990.<br />
Pain Management Services – Good Practice, 2003.<br />
Royal College of Surgeons of England<br />
Day Case Surgery, 1992.<br />
Clinical practice<br />
Association of Anaesthetists of Great Britain and Ireland<br />
Anaesthesia and Anaesthetists: Information for Patients and their Relatives, 1997.<br />
Anaesthesia and Peri-operative Care of the Elderly, 2001.<br />
Blood Transfusion and the Anaesthetist – Blood Component Therapy, 2005.<br />
Catastrophies in Anaesthetic Practice, 2005.<br />
Checking Anaesthetic Equipment (3), 2004.<br />
Consent for Anaesthesia (2), 2006.<br />
Day Case Surgery, 2005.<br />
Good Practice in the Management of Continuous Epidural Analgesia in the Hospital Setting<br />
(with RCoA and others), 2004.<br />
HIV and other Blood Borne Viruses, 1992 & 1996.<br />
Immediate Post Anaesthetic Recovery, 2002.<br />
Recommendations for Standards of Monitoring during Anaesthesia and Recovery (3), 2000.<br />
Recommendations for the Transfer of Patients with Acute Head Injuries to Neurosurgical Units, 1996.<br />
Suspected Anaphylactic Reactions Associated with Anaesthesia (3), 2003.<br />
General Medical Council<br />
Confidentiality: Protecting and Providing Information, 2004.<br />
Seeking Patients’ Consent: The Ethical Considerations, 1998.<br />
Withdrawing and Withholding Life-prolonging Treatments – Good Practice in Decision Making, 2002.
48 Good Practice Guide 2006<br />
Intensive Care Society<br />
Guidelines for Adult Organ Donation, 2004.<br />
Guidelines for the Transport of the Critically Ill Adult, 2002.<br />
Point of Care Testing in Critical Care, 2004.<br />
The Process of Consent within the Intensive Care Unit.<br />
Royal College of Anaesthetists<br />
Cardiopulmonary Resuscitation: Standards for Clinical Practice and Training (joint<br />
statement with Royal College of Physicians of London, Intensive Care Society<br />
and Resuscitation Council), 2004.<br />
General Anaesthesia, Sedation and Resuscitation in Dentistry (jointly with<br />
Faculty of Dental Surgery), 1991.<br />
Good Practice in the Management of Continuous Epidural Analgesia in the Hospital Setting<br />
(with AAGBI and others), 2004.<br />
Implementing and Ensuring Safe Sedation Practice for Healthcare Procedures in<br />
Adults (Report of an Intercollegiate Working Party of the Academy of Medical<br />
Royal Colleges), 2001.<br />
Local Anaesthesia for Intraocular Surgery, 2001.<br />
Recommendations on Anaesthetic Records. RCoA Newsletter 1996;27:8–9.<br />
Standards and Guidelines for General Anaesthesia for Dentistry, 1999.<br />
Royal College of Surgeons of England<br />
Sedation by non-anaesthetists, 1993.<br />
Working relationships<br />
Association of Anaesthetists of Great Britain and Ireland<br />
Consultant trainee relationships – a guide for consultants, 2001.<br />
Fatigue and Anaesthetists, 2004.<br />
Management of Anaesthesia for Jehovah’s Witnesses, 2005.<br />
Preoperative Assessment – The role of the Anaesthetist, 2001.<br />
Stress in Anaesthesia, 1997.<br />
The Anaesthesia Team, 2005.<br />
General Medical Council<br />
Management in Healthcare: the Role of Doctors, 1999.<br />
Continuing education and professional development<br />
Association of Anaesthetists of Great Britain and Ireland<br />
Guidance on the 2003 (New) Contract and Job Planning for Consultant Anaesthetists, 2005.<br />
Department of Health<br />
Learning for Delivery: Making connections between post qualification learning/continuing<br />
professional development and service planning, 2004.<br />
Royal College of Anaesthetists<br />
CPD Guidelines, 2005.<br />
Guidance on Appraisal for Anaesthetists, 2000.<br />
Personal Development Planning for the NCCG Anaesthetist, 2003.<br />
Role of Non-Medical Staff in the Delivery of Anaesthesia Services, 2002.
Good Practice Guide 2006 49<br />
Appendix 1: core topics<br />
Airways<br />
Clinical challenges<br />
1 Anticipated or predicted difficult airway (cervical spondylosis, micrognathia, dental abscess patient).<br />
2<br />
3<br />
4<br />
5<br />
6<br />
7<br />
8<br />
9<br />
Unexpected difficult airway (normal airway assessment, difficulty first revealed at attempt at<br />
intubation).<br />
Failed intubation – this will include the use of airway adjuncts to through cricothyroid puncture<br />
techniques.<br />
Foreign body in the airway.<br />
Management of a patient for elective tracheostomy (e.g. major head and neck surgery, patients in ITU).<br />
Management of a patient for emergency tracheostomy (trauma, acute upper airway obstruction).<br />
Surgery for emergency conditions affecting the upper airway – bleeding, infection, tumour etc.<br />
Shared airway management – types of devices available, how to use them.<br />
Safe extubation and management of unanticipated airway obstruction in the recovery period.<br />
Knowledge<br />
1 Knowledge of anatomy of upper and lower airways.<br />
2<br />
3<br />
4<br />
5<br />
6<br />
7<br />
Advances in understanding of physiology of airway obstruction.<br />
Methods of assessment of likely difficulty in airway management.<br />
Airway adjunct devices available (and their relative strengths and weaknesses).<br />
Difficult airway strategies and protocols.<br />
Failed intubation algorithms.<br />
Causes and management of postoperative airway obstruction.<br />
Skills<br />
1 Use of airway adjuncts.<br />
2<br />
3<br />
Advanced techniques, especially fibreoptic intubation.<br />
Practice in the use of failed intubation algorithms including surgical airway access.<br />
Emergency and major surgery<br />
Clinical challenges<br />
1 Major trauma – multiple systems (principles of ATLS for non-ATLS card carrying members).<br />
2<br />
3<br />
4<br />
5<br />
Chest trauma for the non-cardiothoracic anaesthetist. Blunt chest trauma (as part of major trauma<br />
and as an isolated event).<br />
Leaking and ruptured abdominal aortic aneurysm.<br />
Critically ill patient from ITU going to theatre.<br />
Perforated viscus in the medically compromised patient (e.g. elderly patient with ischaemic heart<br />
disease and perforated caecum or sigmoid).<br />
6 Maintenance of body homeostasis during prolonged surgical procedures.
50 Good Practice Guide 2006<br />
Knowledge<br />
1 Developments and advances in the overall management of these patients – better understanding of the<br />
role of temperature control, fluid management, intra-operative renal support, permissive hypotension.<br />
2<br />
3<br />
4<br />
5<br />
6<br />
7<br />
8<br />
Principles of management of the physiological insults from the disease processes.<br />
Principles of massive blood transfusion.<br />
Advances in surgical management and the implications for the anaesthetist.<br />
Chest drain management principles – insertion, transport etc.<br />
Advances in management of techniques such as one-lung ventilation.<br />
The role of the relevant non-technical skills, e.g. limitations on human performance and the<br />
techniques to help compensate for this.<br />
Principles surrounding choice of monitoring techniques.<br />
Skills<br />
1 Application of ATLS principles (rather than obtaining ATLS certification).<br />
2<br />
3<br />
4<br />
5<br />
Chest Drain Management skills where relevant.<br />
Management of one lung ventilation.<br />
Non-technical skills – opportunity to apply the knowledge.<br />
Insertion and use of invasive and non-invasive monitoring.<br />
Fluid management<br />
Clinical challenges<br />
1 Major haemorrhage.<br />
2<br />
3<br />
4<br />
5<br />
Major fluid loss (burns, sequestration).<br />
Blood transfusion policies.<br />
Diagnosis and management of coagulopathies.<br />
Advances in oxygen carrying substances/blood substitutes.<br />
Knowledge<br />
1 Advances in understanding of physiology of fluid therapy – types of fluids, aggressive vs<br />
non-aggressive therapy etc.<br />
2<br />
3<br />
4<br />
5<br />
6<br />
7<br />
Principles of massive blood replacement.<br />
Principles of fluid therapy for major burns.<br />
Practice from recognised expert centres, e.g. organisation of major haemorrhage packs.<br />
Coagulopathy – monitoring of coagulopathy, role of different type of factor replacements, relevant<br />
risks of infection etc.<br />
Advances in new fluid therapies.<br />
Awareness of relevant guidelines, e.g. SIGN.<br />
Skills<br />
1 Use of associated equipment, e.g. rapid infusing and warning devices, bedside measurement devices.
Good Practice Guide 2006 51<br />
Intensive care medicine<br />
Clinical challenges<br />
1 Current uses of inotropes and other vaso-active drugs.<br />
2<br />
3<br />
4<br />
5<br />
Methods of ventilation for different types of pulmonary disorder.<br />
Management of the septic patient.<br />
Multi-organ failure.<br />
Discontinuation of treatment and organ donation.<br />
Knowledge<br />
1 Update on pathophysiology of relevant condition, e.g. sepsis, multi-organ failure etc.<br />
2<br />
3<br />
4<br />
5<br />
6<br />
7<br />
Update on cardiovascular pharmacology – specific drugs including relative indications and<br />
contra-indications.<br />
Update on renal support and implications for peri-operative management.<br />
Update on antimicrobial therapy.<br />
Update on respiratory support – types of ventilation, weaning etc.<br />
Severity scoring and assessment of brain function.<br />
Procedures for organ donation.<br />
Skills<br />
1 Familiarisation with ventilators and infusion devices.<br />
Invasive monitoring<br />
Clinical challenges<br />
1 Inserting the devices (what devices are currently available).<br />
2<br />
3<br />
Using the information from the devices.<br />
Trouble-shooting problems.<br />
Knowledge<br />
1 The current position on the relevant indications and contra-indications.<br />
2<br />
3<br />
4<br />
What devices are available along with their relative advantages and disadvantages.<br />
How to deal with common problems.<br />
Knowledge of current guidelines (NICE).<br />
Skills<br />
1 The use of ultrasonic location devices.<br />
2<br />
3<br />
Setting up the devices (anaesthetists who do not routinely use such devices in elective work may be<br />
using them in very ill emergency patients and not be familiar with how to configure monitors etc).<br />
Techniques for challenging cases, e.g. approaches other than internal jugular and subclavian.<br />
Major trauma<br />
Clinical challenges<br />
1 The role of the anaesthetist in major incidents (general principles of triage, immediate care etc).<br />
2<br />
3<br />
Current practices in individual major trauma cases. Available techniques, indications for use<br />
etc. (pelvic fracture fixation, diagnosis and management of blunt abdominal trauma in cases of<br />
suspected bleeding, e.g. ruptured spleen).<br />
The patient with a head injury and/or other potential life-threatening injuries.<br />
4 Anaesthesia for investigation of the major trauma patient (CT scanning).
52 Good Practice Guide 2006<br />
Knowledge<br />
1 Advanced Life Support & Advanced Trauma Life Support principles.<br />
2<br />
3<br />
4<br />
5<br />
Updates on advances in surgical management, e.g. pelvic fractures, gun shot wounds.<br />
Updates in the management of the head injured patient.<br />
Updates in the management of the patient with spinal column and spinal cord injury.<br />
Major incident management, including triage and the role of the anaesthetist.<br />
Skills<br />
1 The key skills for ALS and ATLS.<br />
Obstetrics<br />
Clinical challenges<br />
1 Non-obstetric surgery for the parturient.<br />
2<br />
3<br />
4<br />
5<br />
6<br />
7<br />
8<br />
9<br />
Resuscitation of the parturient. For those covering obstetric rotas but not practising regularly.<br />
General anaesthesia for emergency Caesarean section.<br />
Regional anaesthesia for emergency Caesarean section.<br />
Management of major haemorrhage (ante-partum, intra-partum or post partum) and<br />
coagulopathies.<br />
Neonatal resuscitation.<br />
Analgesia and anaesthesia for labour and delivery.<br />
Difficult or failed intubation.<br />
Post dural puncture headache.<br />
Knowledge<br />
1 Update on current management of the parturient.<br />
2<br />
3<br />
4<br />
5<br />
6<br />
7<br />
Update on eclampsia and pre-eclampsia.<br />
Update on pharmacology in relation to the parturient and foetus.<br />
Principles of management of mothers with cardiac disease.<br />
Management of major haemorrhage and coagulopathy.<br />
Failed intubation protocols for obstetric practice.<br />
Management of post dural puncture headache.<br />
Skills<br />
1 Basic Neonatal Life Support for those with an emergency obstetric commitment – the needs will vary<br />
depending on local resources.<br />
2<br />
Those providing emergency rota cover should also be familiar with the equipment available and<br />
relevant for emergencies – infusion systems, invasive monitoring equipment etc.<br />
Occasional emergencies<br />
Clinical challenges<br />
1 Serious medical conditions (endocrine, neurological, cardiorespiratory).<br />
2<br />
3<br />
4<br />
Accidental injuries (drowning, burns).<br />
Anaphylaxis.<br />
Advanced Life Support (adults).<br />
5 Paediatric Life Support.
Good Practice Guide 2006 53<br />
Knowledge<br />
1 Updates in treatment and management of the various medical conditions.<br />
2<br />
3<br />
Update on treatment of drowning and burns.<br />
Familiarisation with current protocols for emergency conditions.<br />
Skills<br />
1 Ability to apply the relevant protocols.<br />
2<br />
Those skills necessary for the relevant protocols.<br />
Paediatrics<br />
Clinical challenges<br />
1 Resuscitation of the neonate.<br />
2<br />
3<br />
4<br />
Management of paediatric emergencies that may present at A&E (upper airway problems, trauma,<br />
acute infections with major cardiorespiratory components).<br />
Transfer of sick children.<br />
Provision of analgesia.<br />
Knowledge<br />
1 Updates in current management principles.<br />
2<br />
3<br />
4<br />
5<br />
Current equipment and its indications and contra-indications.<br />
Principles of fluid balance in children.<br />
Management options for pain.<br />
Principles of stabilisation and transfer.<br />
Skills<br />
1 Relevant airway skills and use of airway adjuncts.<br />
2<br />
Current approaches to cardiovascular access and stability.<br />
Pain management<br />
Clinical challenges<br />
1 Management of the adult postoperative patient.<br />
2<br />
3<br />
4<br />
5<br />
Management of the patient with acute pain pre-operatively.<br />
Management of acute pain from non-surgical causes (fractured ribs, pancreatitis, acute myocardial<br />
infarction, sickle cell etc).<br />
Trouble shooting of problems with regional block (unilateral block, missed segment etc).<br />
Management of patients with chronic pain conditions.<br />
Knowledge<br />
1 Update in physiology of pain and pharmacology of relevant drugs.<br />
2<br />
3<br />
4<br />
5<br />
Update in non-pharmacological methods.<br />
Update in management strategies for specific conditions.<br />
Challenges and how to deal with them.<br />
Current protocols and guidelines for managing infusion devices, PCA, epidural infusions etc.<br />
Skills<br />
1 The ability to use the relevant equipment.<br />
2<br />
(The ability to site regional blocks is dealt with in regional techniques below).<br />
3 Ability to apply relevant protocols.
54 Good Practice Guide 2006<br />
Postoperative complications<br />
Clinical challenges<br />
1 The patient who cannot breathe adequately postoperatively.<br />
2<br />
3<br />
4<br />
The patient who is bleeding and requires to go back to theatre.<br />
Recognition and management of complications in the early postoperative period (airway obstruction,<br />
shivering, nausea and vomiting, pain).<br />
Sudden collapse from cardiovascular event.<br />
Knowledge<br />
1 Factors causing reduced respiratory capacity.<br />
2<br />
3<br />
4<br />
5<br />
6<br />
Investigation of patient who cannot breathe adequately.<br />
Principles of fluid and blood therapy (see fluid management).<br />
Options for management of shivering, PONV and pain.<br />
Management of airway problems (see airways section above, knowledge 7).<br />
Update of theoretical knowledge of causes of sudden collapse and resuscitation.<br />
Skills<br />
1 Maintenance of appropriate level of resuscitation skills.<br />
Regional techniques<br />
Clinical challenges<br />
1 Identification and management of problems (intra-operative unilateral block, missed segment etc),<br />
hypotension, total spinal block, extensive block.<br />
2<br />
3<br />
4<br />
Identification and management of local anaesthetic toxicity.<br />
Management of non-obstetric patient with dural puncture headache (post spinal or post epidural).<br />
Neurological damage.<br />
Knowledge<br />
1 Relevant anatomy of blocks.<br />
2<br />
3<br />
4<br />
5<br />
Update on pharmacology of local anaesthetic drugs.<br />
Indications and contra-indications.<br />
Management of complications of local anaesthetic blocks.<br />
Investigation of neurological damage.<br />
Skills<br />
1 Ability to perform blocks.<br />
2<br />
Ability to use relevant equipment (nerve location devices, infusion pumps etc).<br />
Transfer of the critically ill patient<br />
Clinical challenges<br />
1 Critically ill patients to ITU in other centres.<br />
2<br />
3<br />
4<br />
Transfer of head injured patients.<br />
Transfer of burned patients.<br />
Stabilisation of child prior to transfer.<br />
5 Air transfer.
Good Practice Guide 2006 55<br />
Knowledge<br />
1 Update of impact on pathophysiology of transfer.<br />
2<br />
3<br />
4<br />
5<br />
The logistical and practical aspects – what equipment to have available, what drugs to take etc.<br />
The challenges presented by different groups – the burned patient, the head injured patient, the<br />
patient in single or multiple organ failure being taken to ITU.<br />
Familiarisation with existing protocols.<br />
Additional problems of air transfer.<br />
Skills<br />
1 Most of the challenges are organisational, which includes familiarity with the relevant equipment in<br />
addition to the key non-technical skills.
NOTES
Design and layout by The Royal College of Anaesthetists
Reducing the risk from cemented<br />
hemiarthroplasty for hip fracture 2015<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
British Orthopaedic Association<br />
British Geriatric Society<br />
February 2015
This guideline was originally published in Anaesthesia. If you wish to refer<br />
to this guideline, please use the following reference:<br />
Association of Anaesthetists of Great Britain and Ireland. Safety guideline:<br />
reducing the risk from cemented hemiarthroplasty for hip fracture 2015.<br />
Anaesthesia 2015, 70, pages 623–626.<br />
This guideline can be viewed online via the following URL:<br />
http://onlinelibrary.wiley.com/doi/10.1111/anae.13036/full<br />
© The Association of Anaesthetists of Great Britain & Ireland
Guidelines<br />
Safety guideline: reducing the risk from<br />
cemented hemiarthroplasty for hip fracture<br />
2015<br />
Association of Anaesthetists of Great Britain and<br />
Ireland<br />
British Orthopaedic Association<br />
British Geriatric Society<br />
Membership of the Working Party: R. Griffiths, S. M. White,<br />
I. K. Moppett, M. J. Parker, 1<br />
T. J. S. Chesser, 1 M. L. Costa, 1 A. Johansen, 2 H. Wilson 2 and<br />
A. J. Timperley<br />
1 British Orthopaedic Association<br />
2 British Geriatric Society<br />
Summary<br />
Concise guidelines are presented for the preparation and conduct of<br />
anaesthesia and surgery in patients undergoing cemented hemiarthroplasty<br />
for hip fracture. The Working Party specifically considered recent<br />
This is an open access article under the terms of the Creative Commons<br />
Attribution-NonCommercial-NoDerivs License, which permits use and<br />
distribution in any medium, provided the original work is properly<br />
cited, the use is non-commercial and no modifications or adaptations<br />
are made.<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
1
publications highlighting complications occurring during the peri-operative<br />
period [1, 2]. The advice presented is based on previously published<br />
advice and clinical studies.<br />
....................................................................................................<br />
This is a consensus document produced by expert members of a Working<br />
Party established by the Association of Anaesthetists of Great Britain and<br />
Ireland, with representatives from the British Orthopaedic Association<br />
and British Geriatric Society. It has been seen and approved by the<br />
elected Boards/Councils/Committees of all three organisations.<br />
All AAGBI guidelines are reviewed to ensure relevance/accuracy and are<br />
updated or archived when necessary. Date of review: 2020.<br />
Accepted: 13 February 2015<br />
• What other guideline statements are available on this topic?<br />
The National Patient Safety Agency (NPSA) issued an alert in 2009,<br />
about the use of bone cement during hip arthroplasty [3]. Specialtyfocused<br />
advice has been published by both anaesthetists [4] and<br />
surgeons [5].<br />
•<br />
Why was this guideline developed?<br />
The Anaesthesia Sprint Audit of Practice (ASAP) [1] collected prospective<br />
information on bone cement implantation syndrome (BCIS)<br />
[6]. The audit revealed evidence of cardiovascular compromise in<br />
some patients undergoing cemented hemiarthroplasty for hip fracture.<br />
•<br />
How does this statement differ from existing guidelines?<br />
This document has been a collaborative effort by anaesthetists, surgeons<br />
and orthogeriatricians. It highlights the need for joint decision<br />
making, teamworking and attention to detail during the peri-operative<br />
period.<br />
•<br />
Why does this statement differ from existing guidelines?<br />
This is the first multidisciplinary clinical guidance on peri-operative<br />
management of this clinical problem.<br />
Recommendations<br />
There should be a three-stage process to reduce the incidence of problems<br />
in patients undergoing cemented hemiarthroplasty for hip fracture:<br />
1. Identification of patients at high risk of cardiorespiratory compromise:<br />
2 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
a) Increasing age;<br />
b) Significant cardiopulmonary disease;<br />
c) Diuretics;<br />
d) Male sex.<br />
2. Preparation of team(s) and identification of roles in case of severe<br />
reaction:<br />
a) Pre-operative multidisciplinary discussion when appropriate;<br />
b) Pre-list briefing and World Health Organization Safe Surgery<br />
checklist ‘time-out’.<br />
3. Specific intra-operative roles:<br />
a) Surgeon:<br />
Inform the anaesthetist that you are about to insert cement;<br />
Thoroughly wash and dry the femoral canal;<br />
•<br />
Apply cement in retrograde fashion using the cement gun<br />
with a suction catheter and intramedullary plug in the femoral<br />
shaft;<br />
•<br />
Avoid vigorous pressurisation of cement in patients judged<br />
to be at risk of cardiovascular compromise (see below).<br />
b) Anaesthetist:<br />
Ensure adequate resuscitation pre- and intra-operatively;<br />
• Confirm to surgeon that you are aware that he/she is about<br />
to prepare/apply cement;<br />
•<br />
Maintain vigilance for signs of cardiorespiratory compromise.<br />
Use either an arterial line or non-invasive automated<br />
blood pressure monitoring set on the ‘stat’ mode during/<br />
shortly after application of cement. Early warning of cardiovascular<br />
collapse may be heralded by a drop in systolic<br />
pressure. During general anaesthetic, a sudden drop in endtidal<br />
pCO 2 may indicate right heart failure and/or catastrophic<br />
reduction in cardiac output;<br />
• Aim for a systolic blood pressure within 20% of pre-induction<br />
value;<br />
• Prepare vasopressors in case of cardiovascular collapse.<br />
Introduction<br />
This guidance is aimed at clinicians involved in the intra-operative management<br />
of patients undergoing cemented arthroplasty. The guidance<br />
does not include the consenting process, or the choice of surgical intervention,<br />
which is covered in existing national guidelines [7], although<br />
the Working Party acknowledges that these are vital parts of the process<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
3
y which patients undergo such surgery, and that the usual requirements<br />
for individualised treatment and supplying patients with appropriate<br />
information must apply.<br />
Bone cement implantation syndrome<br />
Surgical instrumentation of the femoral canal has been associated with significant<br />
cardiovascular compromise [1, 5]. This phenomenon can occur<br />
with any such surgery, especially procedures that breach the femoral canal,<br />
such as intramedullary nailing and cemented and uncemented hip<br />
implants, but the risk has been particularly highlighted in frail patients<br />
undergoing cemented hemiarthroplasty following hip fracture.<br />
During surgery, significant cardiovascular compromise can occur<br />
during preparation of the femoral canal, during insertion of the cement<br />
(if used for fixation) and/or prosthesis, and when the hip is reduced [6].<br />
Compared with uncemented prostheses, the use of cemented prostheses<br />
for hip fracture surgery increases the likelihood of pain-free mobility<br />
after surgery [8], reduces the risk of re-operation and is associated with<br />
a lower mortality rate at 30 days [8–11]. However, an adverse cardiovascular<br />
event has been associated with cemented hemiarthroplasty and this<br />
is sometimes referred to as ‘bone cement implantation syndrome’<br />
(BCIS) [6].<br />
Adverse cardiovascular events occur in approximately 20% of hip<br />
fracture operations in which a cemented prosthesis is used [1, 2]. The<br />
severity of the reaction is indicated in Table 1.<br />
Certain patient factors are associated with an increased risk of<br />
severe cardiovascular events during cemented hemiarthroplasty, in particular<br />
increasing age, male sex, significant cardiopulmonary disease and<br />
use of diuretic medication [2, 11]. These factors are also associated with<br />
increased 30-day mortality, though the magnitude of the association is<br />
far greater for BCIS itself [2].<br />
Table 1 Incidence of adverse effects during arthroplasty using a cemented<br />
prosthesis [1, 2].<br />
Grade 1<br />
Arterial saturation < 94% or > 20% fall in<br />
~20%<br />
systolic blood pressure<br />
Grade 2<br />
Arterial saturation < 88% or hypotension<br />
~3%<br />
> 40% fall in systolic blood<br />
pressure or loss of consciousness<br />
Grade 3 Cardiopulmonary resuscitation required ~1%<br />
4 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Administrative and human factor aspects<br />
In patients with the above risk factors, discussion between surgeons, anaesthetists<br />
and orthogeriatricians should consider how best to minimise<br />
the early peri-operative risks of mortality and morbidity, given the<br />
known benefits of surgical intervention [10]. Surgeons and anaesthetists<br />
can also modify peri-operative practice both to reduce the risk of cardiovascular<br />
events and to improve outcome in the event of such an<br />
Table 2 Specific intra-operative surgical and anaesthetic roles for reducing<br />
the incidence and management of BCIS.<br />
Conduct of surgery<br />
Conduct of<br />
anaesthesia<br />
Ask the anaesthetist to confirm that he/she has<br />
heard your instruction to the theatre team that<br />
you are about to prepare the femoral canal for<br />
cement and prosthesis insertion<br />
Carefully prepare, wash and dry the femoral canal.<br />
Use of a pressurised lavage system is<br />
recommended to clean the endosteal bone of<br />
fat and marrow contents<br />
Use a distal suction catheter on top of an<br />
intramedullary plug. Insert the cement from a<br />
gun in retrograde fashion on top of the plug<br />
and pull the catheter out as soon as it is<br />
blocked with cement.<br />
Do not use excessive manual pressurisation or<br />
pressurisation devices in patients at higher risk<br />
of cardiovascular events (see above for risk factors)<br />
Ensure that the patient is adequately hydrated before<br />
induction of and during anaesthesia<br />
Maintain vigilance for possible cardiovascular events<br />
once the femoral head is removed and the surgeon<br />
has verbally indicated his/her intent to instrument<br />
the femoral canal<br />
Confirm to the surgeon that you are aware of<br />
preparation of the femoral canal for cement and<br />
prosthesis insertion<br />
Aim to maintain the systolic blood pressure within<br />
20% of pre-induction values throughout surgery,<br />
using vasopressors and/or fluids. Invasive blood<br />
pressure monitoring is indicated for patients at<br />
higher risk<br />
Be ready to give vasopressors, e.g. metaraminol/<br />
adrenaline in case of cardiovascular collapse<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
5
event (Table 2) [11]. All hip fracture surgery should be undertaken or<br />
directly supervised by appropriately experienced anaesthetists and surgeons<br />
and on planned trauma lists [7].<br />
All members of the theatre team should be aware of the problems<br />
associated with femoral instrumentation and the use of cemented prostheses.<br />
The potential for adverse events should be identified for each patient<br />
as part of both the pre-list briefing before starting a theatre list and at the<br />
World Health Organization Safe Surgery checklist ‘time-out’ immediately<br />
before surgery. In the event of a severe reaction or cardiopulmonary arrest,<br />
theatre staff should be aware of their defined roles in resuscitating the<br />
patient, as described in the Coventry ‘cement curfew’ and modified<br />
according to individual hospital operating procedures [12].<br />
References<br />
1. National Hip Fracture Database. Anaesthesia Sprint Audit of Practice, 2014.<br />
https://www.rcplondon.ac.uk/sites/default/files/national_hip_fracture_database_<br />
anaesthesia_sprint_audit_of_practice_asap.pdf (accessed 19/12/2014).<br />
2. Olsen F, Kotyra M, Houltz E, Ricksten SE. Bone cement implantation syndrome in<br />
cemented hemiarthroplasty for femoral neck fracture: incidence, risk factors, and<br />
effect on outcome. British Journal of Anaesthesia 2014; 113: 800–6.<br />
3. National Patient Safety Agency. Mitigating surgical risk in patients undergoing hip<br />
arthroplasty for fractures of the proximal femur, 2009. http://www.nrls.npsa.nhs.uk/<br />
alerts/?entryid45=59867 (accessed 19/12/2014).<br />
4. Safe Anaesthesia Liaison Group. Patient Safety Update, 1 October 2011 to 31<br />
December 2011. http://www.rcoa.ac.uk/system/files/CSQ-PS-PSU-DEC2011.pdf<br />
(accessed 19/12/2014).<br />
5. Timperley AJ, Whitehouse SL. Mitigating surgical risk in patients undergoing hip<br />
arthroplasty for fractures of the proximal femur. Journal of Bone and Joint Surgery<br />
[British] 2009; 91-B: 851–4.<br />
6. Donaldson AJ, Thomson HE, Harper NJ, Kenny NW. Bone cement implantation syndrome.<br />
British Journal of Anaesthesia 2009; 103: 12–22.<br />
7. National Institute for Health and Care Excellence. Hip fracture: the management of<br />
hip fracture in adults, 2011. www.nice.org.uk/guidance/cg124 (accessed 19/12/<br />
2014).<br />
8. Parker MJ, Gurusamy KS, Azegami S. Arthroplasties (with and without bone<br />
cement) for proximal femoral fractures in adults. Cochrane Database of Systematic<br />
Reviews 2010; 6: CD001706.<br />
9. Yli-Kyyny T, Sund R, Hein€anen M, Venesmaa P, Kr€oger H. Cemented or uncemented<br />
hemiarthroplasty for the treatment of femoral neck fractures? Acta Orthopaedica<br />
2014; 85: 49–53.<br />
10. Costain DJ, Whitehouse SL, Pratt NL, Graves SE, Ryan P, Crawford RW. Perioperative<br />
mortality after hemiarthroplasty fixation method. A study based on the Australian<br />
Orthopaedic Association National Joint Replacement Registry. Acta Orthopaedica<br />
2011; 82: 275–81.<br />
6 © 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
11. Griffiths R, Parker M. Bone cement implantation syndrome and proximal femoral<br />
fracture. British Journal of Anaesthesia 2015; 114: 6–7.<br />
12. Scrase A, Horwood G, Sandys S. Coventry, ‘‘Cement Curfew’’: team training for<br />
crisis. Anaesthesia News 2014; 327: 8–9.<br />
© 2015 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland<br />
7
The Association of Anaesthetists of Great Britain & Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
Website: www.<strong>aagbi</strong>.org<br />
British Orthopaedic Association<br />
35-43 Lincoln’s Inn Fields, London, WC2A 3PE<br />
Tel: 020 7405 6507<br />
Website: www.boa.ac.uk<br />
British Geriatric Society<br />
Marjory Warren House, 31 St John’s Square<br />
London, EC1M 4DN<br />
Tel: 020 7608 1369<br />
Website: www.bgs.org.uk
UK National Core Competencies for Post-anaesthesia Care 2013<br />
Immediate Post-anaesthesia Recovery 2013 supplement
CONTENTS<br />
Glossary of terms 3<br />
Introduction 5<br />
Competency 1 Communication 7<br />
Competency 2 Professional development 9<br />
Competency 3 Clinical leadership 10<br />
Competency 4 Clinical governance 11<br />
Competency 5 Assessment and management of the airway 13<br />
Competency 6 Assessment and management of breathing 16<br />
Competency 7 Assessment and management of the circulation 17<br />
Competency 8 Assessment of level of consciousness 18<br />
Competency 9 Monitoring during recovery 19<br />
Competency 10 Intravenous access and fluid balance 21<br />
Competency 11 Applied knowledge of pharmacology in peri-operative care 22<br />
Competency 12 Management of postoperative pain, nausea and vomiting 24<br />
Competency 13 Recovery emergencies 26<br />
Competency 14 Post surgical care 29<br />
Appendix 1 31<br />
2
GLOSSARY OF TERMS<br />
AAGBI<br />
AIMS<br />
AVPU<br />
BARNA<br />
BVM<br />
CODP<br />
CPAP<br />
CPD<br />
DVT<br />
ECG<br />
GCS<br />
HDU<br />
HPC<br />
ICU<br />
LMA<br />
MH<br />
NCEPOD<br />
NES<br />
NIBP<br />
NMC<br />
NPSA<br />
ODP<br />
PACU<br />
Association of Anaesthetists of Great Britain and Ireland<br />
Anaesthetic Incident Monitoring Study<br />
Alert, Verbal, Pain Unresponsive scoring system for conscious level<br />
British Anaesthetic and Recovery Nurses Association<br />
Bag, valve, mask ventilation<br />
College of Operating Department Practitioners<br />
Continuous positive airway pressure<br />
Continuing professional development<br />
Deep vein thrombosis<br />
Electrocardiogram<br />
Glasgow Coma Scale<br />
High dependency unit<br />
Health Professionals Council<br />
Intensive care unit<br />
Laryngeal mask airway<br />
Malignant hyperpyrexia<br />
National Confidential Enquiry into Patient Outcome and Death<br />
NHS Education Scotland<br />
Non-invasive blood pressure<br />
Nursing and Midwifery Council<br />
National Patient Safety Agency<br />
Operating department practitioner<br />
Post-anaesthesia care unit<br />
3
PCA<br />
pCO2<br />
PDP<br />
PONV<br />
PPE<br />
QIS<br />
RAE<br />
RCN<br />
RCS<br />
SaO2<br />
SPSP<br />
ETT<br />
Patient controlled analgesia<br />
Partial pressure of carbon dioxide<br />
Personal development plan<br />
Postoperative nausea and vomiting<br />
Personal protective equipment<br />
NHS Quality Improvement Scotland<br />
Ring/Adair/Elwyn endotracheal tubes<br />
Royal College of Nursing<br />
Royal College of Surgeons<br />
Oxygen saturation<br />
Scottish Patient Safety Programme<br />
Tracheal tube<br />
4
INTRODUCTION<br />
The provision of safe care during recovery from anaesthesia and surgery relies heavily on investment in the education and training of post-anaesthesia care<br />
unit (PACU) staff. Maintenance of standards requires continual update such as resuscitation skills, application of new techniques and advances in pain<br />
management. PACU staff are specialists and often play a key role in the education of others, including other theatre staff, ward-based nurses, midwives and<br />
trainee doctors. All PACU staff should receive training, tailored to meet the needs of the individual and the local service but meet the national standards<br />
defined in this document.<br />
The concept of recovery rooms was first discussed and documented in the late 19 th century as anaesthesia was evolving. The importance of specialist<br />
nursing care for postoperative patients was recognised [1]. A study during the 1940s in the United States recommended the continuing development of the<br />
recovery room as being an essential part of the post-anaesthesia care pathway. This study highlighted, amongst other factors, airway obstruction as a key<br />
factor contributing to potentially preventable postoperative deaths [2].<br />
Dramatic advances in anaesthesia and surgery over the last 150 years have contributed significantly to the fall in morbidity and mortality. Nonetheless deaths<br />
still occur during the recovery phase of postoperative care. The National Confidential Enquiry into Peri-operative Outcome and Death (NCEPOD) addressed<br />
this issue in its 2001 report Changing the way we operate [3] and stated “Immediately after surgery all patients not returning to a special care area (e.g. ICU or<br />
HDU) need to be nursed by those trained and practised in the postoperative recovery area. If there are separate arrangements for staffing the operating<br />
theatre out of hours, these must include the provision of specialised recovery staff.”<br />
A review of recovery room critical incidents was published by the Anaesthetic Incident Monitoring Study in 2002 [4] that detailed the proportion and type of<br />
incidents encountered in recovery rooms in Australia and the United States and called for ongoing education and quality assurance programmes to be<br />
developed to reduce these events.<br />
A report released by NHS Quality Improvement Scotland (2003) demonstrated that not all staff who recover patients postoperatively are fully trained to the<br />
required standard and that much of the recovery training was on an ad hoc and informal basis raising particular concerns in remote locations such as<br />
remotely located operating theatres and the radiology departments [5].<br />
Basic training for PACU starts with achievement of entry-level competence during nursing or operating department practitioner (ODP) training programmes of<br />
learning. This individual requires supervision and mentoring until he/she has acquired the competencies to care safely and successfully for a patient in the<br />
PACU. Thereafter they are expected to maintain, develop and enhance their practice through practical experience, further learning and continuing<br />
professional development. They will be expected to populate and maintain a lifelong portfolio of experience during their training and working life. Registered<br />
practitioners with current experience of working in the PACU are able to have prior qualifications and experience recognised.<br />
The competencies required by PACU staff are both professional and clinical. The professional components are:<br />
• Communication<br />
• Professional development<br />
• Clinical leadership<br />
• Clinical governance<br />
5
The clinical components are:<br />
• Assessment and management of the airway<br />
• Assessment and management of breathing<br />
• Assessment and management of the circulation<br />
• Assessment of consciousness<br />
• Monitoring during the immediate postoperative phase<br />
• Intravenous access and fluid balance<br />
• Applied knowledge of pharmacology in peri-operative care<br />
• Management of postoperative pain,<br />
• Management of postoperative nausea and vomiting (PONV)<br />
• Management of surgical and anaesthetic emergencies<br />
In specialised areas of surgery, such as paediatrics and obstetrics, additional specific competencies are required.<br />
This document uses work previously published by Quality Assuring Continuing Professional Development and by NHS Education Scotland. The three<br />
relevant documents are A Route to Enhanced Competence in Perioperative Practice for Operating Department Practitioners and Nurses. (NHS<br />
Education for Scotland. A Route to Enhanced Competence in Perioperative Practice for Operating Department Practitioners and Nurses. Edinburgh:<br />
NES, 2002.)<br />
Core Competencies for Anaesthetic Assistants 2011 http://www.nes.scot.nhs.uk/media/4239/anaesthetic_core_competencies_2011.pdf and<br />
Portfolio of Core Competencies for Anaesthetic Assistants 2012 http://www.nes.scot.nhs.uk/media/1410332/nesd0050_smaad_portfolio_2012.pdf<br />
This document has been modified following consultation with other stakeholders across Great Britain and Ireland (see appendix 1). All standards and<br />
recommendations described in this document should be applied to all recovery areas where anaesthesia is administered including obstetric, cardiology,<br />
radiology, dental and mental health units as well as community hospitals.<br />
References<br />
1. Radford M. Recovery nursing services: An evolution. British Journal of Perioperative Nursing 2003; 13:155-8,160-1.<br />
2. Hatfield A, Tronson M. The Complete Recovery Room Book, 4 th edition. New York: Oxford University Press, 2009.<br />
3. NCEPOD. Changing the Way we Operate. www.ncepod.org.uk/pdf/2001/01full.pdf (accessed 18/10/12).<br />
4. Kluger MT, Bullock MFM. Recovery room incidents: a review of 419 reports from the Anaesthetic Incident Monitoring Study (AIMS). Anaesthesia 2002;<br />
57: 1060-66.<br />
5. Healthcare Improvement Scotland. National Overview September 2005, Anaesthesia – Care Before, During and After Anaesthesia.<br />
http://www.healthcareimprovementscotland.org/idoc.ashx?docid=b19010c9-13fc-4f4a-be49-916919990246&version=-1 (accessed 18/10/12).<br />
6. Association of Great Britain and Ireland. Immediate Post-anaesthesia Recovery 2013. Anaesthesia 2013; 68: 288-97.<br />
6
COMPETENCY 1: COMMUNICATION<br />
Competency 1 Knowledge and skills Suggested indicators<br />
1.1 Apply effective communication skills in<br />
order to promote clinically effective patient<br />
care.<br />
Understands and applies principles of good<br />
communication with patients, carers and<br />
peri-operative team members.<br />
Assess, plan, implement and evaluate<br />
individualised care using a recognised nursing<br />
framework in collaboration with all members of<br />
the multidisciplinary team.<br />
1.2 Establish and maintain effective,<br />
professional relationships with patients, carers<br />
and staff in all disciplines.<br />
Provides accurate, concise and relevant verbal<br />
and written information related to peri-operative<br />
patient care.<br />
Alerts appropriate members of the<br />
multidisciplinary team to changes in patientʼs<br />
condition.<br />
Acquires knowledge of Guidelines for records<br />
and record keeping (Nursing and Midwifery<br />
Council (NMC), 2004) and Standards of<br />
conduct, performance and ethics (Health<br />
Professionals Council (HPC), 2003).<br />
Demonstrates use of information technology<br />
including computers and data management<br />
skills.<br />
Uses appropriate listening and responding<br />
skills to develop relationships with patients,<br />
carers and staff.<br />
Interpret an anaesthetic chart that includes<br />
pre-operative assessment and intraoperative<br />
observations of vital signs and documentation<br />
of fluids and drugs administered.<br />
Communicate changes in patientʼs<br />
observations appropriately.<br />
Treat patients in a non-judgmental manner,<br />
maintaining their dignity at all times.<br />
Demonstrate concern and respect for patients<br />
and carers.<br />
7
Articulates role within peri-operative<br />
team Demonstrates knowledge of<br />
teamwork strategies related to the perioperative<br />
environment.<br />
Use effective communication strategies with<br />
patients, anaesthetists and surgeons.<br />
1.3 Apply the principles of good communication<br />
to promote trust and confidence.<br />
Educates and informs patients and carers<br />
attending the PACU.<br />
Complies with local and national policies and<br />
protocols regarding record keeping.<br />
Keeps accurate and comprehensive records.<br />
Recognise patientʼs feelings of vulnerability.<br />
Provide reassurance, comfort and appropriate<br />
physical and psychological support.<br />
Maintain patient records completely and<br />
accurately.<br />
1.4 Admission of patient to PACU. Understands admission protocol for PACU.<br />
Describes preparation of PACU for receiving a<br />
patient into the unit.<br />
Identifies patients not suitable for admission to<br />
PACU.<br />
Safely admit patient to PACU including<br />
mandatory documentation.<br />
Start discharge planning of patient to<br />
appropriate area.<br />
1.5 Discharge of patient from PACU. Understands discharge criteria for the unit.<br />
Explains significance of each criterion for<br />
patients well being.<br />
Understands the process for discharge from<br />
PACU to trained staff accepting the patient into<br />
their care.<br />
Identify patient fit for discharge and meeting<br />
agreed discharge criteria.<br />
Ensure completion of relevant documentation.<br />
Handover care to appropriately trained staff<br />
maintaining patient dignity including full<br />
documentation of the process.<br />
8
COMPETENCY 2: PROFESSIONAL DEVELOPMENT<br />
Competency 2 Knowledge and skills Suggested indicators<br />
2.1 Demonstrate personal continuing<br />
professional development (CPD) in recovery<br />
skills.<br />
2.2 Contribute to the continuing professional<br />
development needs of the multidisciplinary<br />
team.<br />
2.3 Contribute and promote an environment<br />
that encourages CPD.<br />
Keeps a professional portfolio of learning and<br />
experience gained.<br />
Recognises own limitations, identifies<br />
professional development needs and develops<br />
a personal development plan (PDP).<br />
Uses appropriate resources and reflective<br />
practice to enhance knowledge and skills.<br />
Demonstrates personal accountability for<br />
ensuring own clinical competence.<br />
Contributes to peri-operative teaching<br />
programmes by promoting clinically effective<br />
practice.<br />
Supports and assesses learners.<br />
Offers clinical supervision to others as<br />
appropriate.<br />
Participates in performance appraisal<br />
programmes.<br />
Develops and delivers teaching appropriate to<br />
the PACU environment.<br />
Demonstrates ability to develop and access<br />
learning resources.<br />
Maintain a personal portfolio.<br />
Undertake appraisal and document evidence of<br />
achievements.<br />
9
COMPETENCY 3: CLINICAL LEADERSHIP<br />
Competency 3 Knowledge and skills Suggested indicators<br />
3.1 Demonstrate leadership skills in order to<br />
enhance patient care.<br />
3.2 Support and promote clinical effectiveness<br />
by developing an evidence-based approach to<br />
postoperative care.<br />
Develops autonomy in own role within the<br />
recovery room.<br />
Makes effective clinical decisions and manages<br />
resources.<br />
Shows evidence of research awareness.<br />
Adapts clinical practice in light of current<br />
research.<br />
Motivates and supports others in developing<br />
evidence-based practice.<br />
10
COMPETENCY 4: CLINICAL GOVERNANCE<br />
Competency 4 Knowledge and skills Suggested indicators<br />
4.1 Identify and manage risks and<br />
hazards.<br />
4.2 Understand how to recognise a<br />
critical incident or near miss and follow<br />
local and national reporting<br />
mechanisms.<br />
4.3 Participate and contribute to a<br />
quality assurance strategy.<br />
Understands the principles, issues<br />
and factors relating to risk<br />
management.<br />
Uses knowledge appropriately to<br />
eliminate or reduce these risks.<br />
Understands critical incidents, their<br />
definition, actions required including a<br />
worked example.<br />
Aware of local and national critical<br />
incident reporting policies.<br />
Uses knowledge of national and local<br />
measures of quality assurance to<br />
develop and participate in high<br />
quality peer review audit.<br />
Apply manual handling techniques appropriately using available<br />
aids. Attend regular updates.<br />
Demonstrate safe management of clinical waste, sharps, drugs<br />
and chemicals.<br />
Use personal protective equipment (PPE) and be aware of<br />
infection control principles.<br />
Comply with national and local guidance on single-use items and<br />
medical device decontamination.<br />
Report and feedback on critical incidents.<br />
Complete local critical incident forms satisfactorily.<br />
Critical incidents that may occur include:<br />
Acute or sub-acute airway obstruction<br />
Cardiopulmonary arrest<br />
Need for cardiovascular support (inotropes, vasoconstrictors,<br />
anti-arrhythmics)<br />
Inadequate reversal of neuromuscular blocking drugs<br />
Need for urgent review of patient by anaesthetist.<br />
Need for ventilatory support (CPAP, tracheal intubation,<br />
lung ventilation)<br />
Severe pain that is difficult to control Unduly prolonged stay<br />
in PACU (>2 h) Significant hypothermia (
4.4 Demonstrate and promote the<br />
delivery of recovery care within a<br />
professional, ethical and legal<br />
framework.<br />
4.5 Demonstrate personal and<br />
professional accountability in relation<br />
to the role of recovery of the<br />
postoperative patient.<br />
Discusses and applies the principles<br />
of ethical, legal and professional<br />
issues affecting patient care,<br />
ensuring appropriate documentation<br />
that follows national and local<br />
directives. Understands the<br />
importance of confidentiality.<br />
Applies the principles of<br />
accountability to the care of the<br />
patient following surgery. Practises<br />
within the limitations of personal<br />
scope of practice and, where<br />
appropriate seeks guidance and<br />
support from colleagues when<br />
exposed to new or unfamiliar<br />
procedures or situations.<br />
Awareness of concept of:<br />
informed consent in adults and children<br />
legal issues relating to patients with learning disabilities or mental<br />
health difficulties<br />
patient groups including Jehovahʼs Witnesses and advance patient<br />
directives.<br />
Adhere to the NMC and HPC codes of conduct.<br />
http://www.<strong>aagbi</strong>.org/sites/default/files/Jehovah%27s%20Witnesse<br />
s_0.pdf<br />
Take on appropriate responsibility.<br />
Show recognition of own limitations with reflection on<br />
performance.<br />
12
COMPETENCY 5: ASSESSMENT AND MANAGEMENT OF THE AIRWAY<br />
Competency 5 Knowledge and skills Suggested indicators<br />
5.1 Apply knowledge of the anatomy and<br />
physiology of the upper airway<br />
tomanagement of the airway in the PACU.<br />
5.2 Can maintain an airway during emergence<br />
from anaesthesia.<br />
Understands those aspects of the anatomy of<br />
the upper airway which are relevant to airway<br />
management including physiological changes<br />
to the airway postoperatively as a<br />
consequence of anaesthesia and surgery.<br />
Can recognise signs of upper airway<br />
obstruction or compromised airway using the<br />
ʻlook, listen and feelʼ approach.<br />
Can perform simple manoeuvres to establish<br />
a clear airway:<br />
effective head tilt chin lift<br />
jaw-thrust<br />
oropharyngeal suction<br />
insertion of an appropriate oropharyngeal<br />
or nasopharyngeal airway.<br />
Describe the anatomy and physiology of the<br />
upper airway.<br />
Discuss the physiological changes caused by<br />
anaesthesia and surgery.<br />
Discuss oxygen requirements in the immediate<br />
postoperative period.<br />
Describe signs of partial and complete airway<br />
obstruction.<br />
Demonstrate manoeuvres to clear the airway<br />
on a patient or manikin as described in<br />
immediate life support (ILS) course<br />
curriculum.<br />
5.2a Assist in maintaining an airway during<br />
bag and mask ventilation.<br />
Can hold a face mask in position, ensuring a<br />
gas-tight seal, or perform manual intermittent<br />
positive pressure ventilation (IPPV).<br />
Can identify suitable breathing systems.<br />
Can describe features of self-inflating bag and<br />
demonstrate its use.<br />
Demonstrate ability to perform either role in<br />
two-person bag and mask ventilation as<br />
described in the immediate life support (ILS)<br />
course curriculum.<br />
Demonstrate bag-valve-mask (BVM)<br />
technique for ventilatory support using an<br />
Ambu self- inflating bag or similar.<br />
Explain need of proficiency in this skill in the<br />
theatre suite, PACU and during intra-hospital<br />
patient transfer.<br />
13
5.3 Understands features of oxygen delivery<br />
equipment.<br />
Demonstrates familiarity with and use of<br />
face masks: (types, design features, including<br />
fixed and variable performance designs).<br />
nasal cannulae<br />
nebulisers<br />
breathing circuits including T-pieces<br />
piped gases and oxygen flowmeters<br />
oxygen cylinders.<br />
Choose an oxygen delivery system appropriate<br />
for a particular patient.<br />
Explain rationale behind choice.<br />
5.4 Can set up and assist the anaesthetist with<br />
emergency intubation of the trachea.<br />
Sets up intubation equipment tray / trolley. Able<br />
to test the equipment.<br />
Can select appropriate tracheal tube (TT).<br />
Positions the patient appropriately and assists<br />
the anaesthetist with routine intubation of the<br />
trachea.<br />
Assist in elective intubation of patient or<br />
manikin.<br />
Calculate TT size (diameters and lengths)<br />
using standard formulae.<br />
Explain morbidity associated with use of<br />
incorrect tube size.<br />
5.5 Ability to select appropriate airway<br />
equipment for use in an emergency.<br />
Demonstrates detailed knowledge of<br />
emergency airway equipment, including salient<br />
features of each and their use.<br />
Demonstrates detailed knowledge of laryngeal<br />
mask airway (LMA), TT and other methods of<br />
securing the airway.<br />
Describe indications for use of straight and<br />
curved bladed laryngoscopes, specialised<br />
laryngoscopes, forceps, bougies and<br />
introducers.<br />
Describe indications for the use of<br />
LMA<br />
intubating LMA<br />
TT (including double lumen, RAE and<br />
microlaryngeal tubes)<br />
cricothyroidotomy and tracheostomy.<br />
14
5.6 Demonstrate ability to place a LMA<br />
in an adult patient.<br />
5.7 Awareness of risks and complications of<br />
removing an airway.<br />
Ability to assess when it is safe to do so.<br />
5.8 Ability to prepare and check appropriate<br />
suction equipment.<br />
Demonstrates LMA placement in an adult<br />
patient equating to ILS course standard. (PACU<br />
staff need to be proficient in using an LMA in an<br />
emergency).<br />
Objectively assesses patientʼs neuromuscular<br />
function.<br />
Prepares and positions patient for removal of<br />
airway devices.<br />
Appropriate airway management following<br />
removal.<br />
Demonstrates knowledge of types of suction<br />
catheters and their appropriate use.<br />
Site an LMA in a manikin.<br />
Demonstrate appropriate management for<br />
removal of airway devices.<br />
Describe the range of suction equipment<br />
available. Demonstrate the assembly and use<br />
of appropriate equipment.<br />
5.9 Ability to prepare and check appropriate<br />
airway equipment.<br />
Demonstrates knowledge of oxygen<br />
administration devices and masks.<br />
Describe the range of airway equipment<br />
available. Demonstrate the assembly and<br />
correct use of appropriate devices.<br />
15
COMPETENCY 6: ASSESSMENT AND MANAGEMENT OF BREATHING<br />
Competency 6 Knowledge and skills Suggested indicators<br />
6.1 Can apply knowledge of the anatomy and<br />
physiology of the respiratory system to<br />
assessing the adequacy of breathing in<br />
patients in the PACU.<br />
6.2 Can apply knowledge of effects of<br />
pharmacology of anaesthetic agents and of<br />
surgery upon the respiratory system.<br />
Understands those aspects of the anatomy and<br />
physiology of the respiratory system in<br />
controlling breathing.<br />
Understands effects of anaesthesia and<br />
surgery on respiration.<br />
Understands the effects of anaesthesia and<br />
surgery on respiratory function.<br />
6.3 Can assess respiration. Describes postoperative patterns of respiration.<br />
Describe the signs of obstructed breathing.<br />
Can describe, identify and use equipment used<br />
for assessing the respiratory system.<br />
Describe the anatomy and physiology of the<br />
respiratory system.<br />
Discuss the physiological changes caused by<br />
anaesthesia and surgery and the changes in<br />
oxygen requirements in the immediate<br />
postoperative period.<br />
Describe the signs and symptoms of<br />
inadequate reversal of neuromuscular blockade<br />
and central respiratory depression. See<br />
competency 11.<br />
Describe the mechanism of inspiration and<br />
expiration and factors controlling respiration.<br />
Assess the airway, chest movement,<br />
respiratory rate, rhythm and colour.<br />
Accurately measure respiratory rate.<br />
Can identify use of accessory muscles and<br />
presence of tracheal tug.<br />
Demonstrate safe use of pulse oximeters and<br />
stethoscopes.<br />
6.4 Can identify patients with pre-existing<br />
respiratory disease.<br />
Recognises patients with pre-existing<br />
respiratory disease and the effects of surgery<br />
and anaesthesia.<br />
Identify and demonstrate appropriate<br />
management of patients with respiratory<br />
insufficiency.<br />
6.5 Can identify patients at risk of postoperative<br />
hypoxia and manage appropriately.<br />
Can identify signs and symptoms of hypoxia,<br />
respiratory depression and impending<br />
respiratory failure.<br />
Understands the use of appropriate monitoring<br />
equipment.<br />
Describe hypoxia and cyanosis. Uses<br />
Use pulse oximetry and capnography<br />
appropriately.<br />
16
COMPETENCY 7: ASSESSMENT AND MANAGEMENT OF THE CIRCULATION<br />
Competency 7 Knowledge and skills Suggested indicators<br />
7.1 Can apply knowledge of the anatomy and<br />
physiology of the cardiovascular system to<br />
manage cardiopulmonary circulation in the<br />
PACU.<br />
7.2 Can measure arterial pressure in<br />
postoperative patients and recognise<br />
deviations from the norm.<br />
7.3 Understand use of intravenous fluids to<br />
support the circulation.<br />
7.4 Understands the use of vasoactive drugs<br />
to treat heart rate and arterial pressure in the<br />
PACU.<br />
Understands those aspects of the anatomical<br />
and physiological changes to the<br />
cardiovascular system postoperatively as a<br />
consequence of anaesthesia and surgery.<br />
Measures arterial pressure and assess<br />
peripheral perfusion.<br />
Understands the importance of autoregulation<br />
and factors that affect it.<br />
Describes signs of circulatory abnormalities.<br />
Can perform manoeuvres to support circulation<br />
appropriately.<br />
Demonstrates knowledge about:<br />
intravenous infusion sets<br />
fluid bags<br />
pressure bags and infusors<br />
fluid warmers.<br />
Knows where the drugs are located.<br />
Understands methods of administration of:<br />
atropine<br />
glycopyrronium<br />
metaraminol<br />
ephedrine<br />
adrenaline<br />
GTN.<br />
Describe the anatomy and physiology of the<br />
cardiovascular system.<br />
Discuss the physiological changes caused by<br />
anaesthesia and surgery.<br />
Describe common circulatory problems<br />
encountered in the immediate postoperative<br />
period.<br />
Demonstrate ability to measure and interpret<br />
arterial pressure in the postoperative period<br />
and communicate with relevant staff.<br />
Demonstrate appropriate management to<br />
optimise circulation.<br />
Demonstrate manoeuvres to correct circulation<br />
such as elevation of legs, Trendelenberg and<br />
reverse Trendelenberg.<br />
Explain use of appropriate fluids for different<br />
patient groups.<br />
Explain rationale of choice of fluids.<br />
Demonstrate appropriate management of<br />
patients requiring fluid resuscitation.<br />
See competency 10.<br />
Identify and describes preparation and<br />
indication for each drug according to local drug<br />
protocols.<br />
17
COMPETENCY 8: ASSESSMENT OF LEVEL OF CONSCIOUSNESS<br />
Competency 8 Knowledge and skills Suggested indicators<br />
8.1 Can assess conscious level in the<br />
postoperative patient and take appropriate<br />
action.<br />
Can use appropriate assessment tools.<br />
Understands the effects of anaesthesia and<br />
surgery on the level of consciousness.<br />
Understands locally and nationally used<br />
assessment tools for conscious level e.g. the<br />
Glasgow Coma Scale (GCS) and Alert, Verbal,<br />
Pain, Unresponsive (AVPU) scores.<br />
Describe the relevant physiology of the central<br />
nervous system.<br />
Discuss the changes caused to the levels of<br />
consciousness by anaesthesia and surgery and<br />
describe common problems encountered in the<br />
immediate postoperative period.<br />
Uses appropriate assessment tools to<br />
measure, record and interpret return to<br />
consciousness of the postoperative patient.<br />
18
COMPETENCY 9: MONITORING DURING RECOVERY<br />
Competency 9 Knowledge and skills Suggested indicators<br />
9.1 Can undertake full patient assessment on<br />
admission to the PACU and in the immediate<br />
postoperative period.<br />
9.2 Demonstrate knowledge of monitoring<br />
equipment used in PACU including normal<br />
parameters and need for interventions when<br />
outside these parameters.<br />
9.2a Can establish routine monitoring.<br />
Understands physiological consequences of<br />
surgery and anaesthesia.<br />
Able to use and identify abnormalities using:<br />
Pulse oximeters including indications for<br />
arterial blood gas sampling.<br />
Capnographs including significance of<br />
end-tidal CO2 values.<br />
Invasive arterial pressure lines including<br />
recognition and management of hyperand<br />
hypotension.<br />
ECG including basic interpretation of rate,<br />
rhythm and ischaemia. Understands<br />
indications for performing a 12 lead EGC.<br />
Temperature probes and warming<br />
devices.<br />
Recognises signs and symptoms of<br />
adequate neuromuscular function.<br />
Urine output as an indicator of renal<br />
function.<br />
Able to assess wound drainage and<br />
surgical procedure.<br />
Demonstrate ability to assess airway,<br />
breathing, circulation, conscious level, drug<br />
therapy, dressings, drains and fluid balance.<br />
Set up routine monitoring of SpO2, NIBP,<br />
ECG and temperature.<br />
Demonstrate ability to establish<br />
capnography measurement, use nerve<br />
stimulator and urimeter appropriately.<br />
Perform 12-lead ECG and document<br />
accurately.<br />
Measure temperature using appropriate<br />
equipment and take appropriate action to<br />
maintain normothermia.<br />
Use a urimeter.<br />
Record wound drainage accurately. Change<br />
drain bottles. Troubleshoot and manage<br />
wound drainage systems.<br />
19
9.3 Perform charting of physiological data and<br />
describes patientʼs clinical status appropriately<br />
to the anaesthetist and other staff members.<br />
Understand the significance of trends.<br />
9.4 Uses available near-patient testing as a<br />
monitoring tool.<br />
Can measure haemoglobin (Hb) and blood<br />
glucose concentrations and describe risks<br />
associated with abnormal values.<br />
9.5 Can assist during establishment of central<br />
venous and invasive arterial pressure<br />
monitoring.<br />
9.6 Able to record and interpret data from<br />
invasive central venous and arterial monitors,<br />
identifying values outside normal parameters.<br />
Can set up a pressure transducer and take<br />
blood samples from central venous and arterial<br />
lines.<br />
Able to chart monitor values using standard<br />
symbols.<br />
Recognises adverse trends which indicate risk.<br />
Identifies common artefacts.<br />
Describes patientʼs clinical status to the<br />
anaesthetist. Able to alert staff to adverse<br />
monitoring trends pre-empting development of<br />
life-threatening emergencies.<br />
Able to use near-patient testing for Hb and<br />
blood glucose and describe risks associated<br />
with abnormal values.<br />
Shows knowledge of normal parameters and<br />
actions to be taken when values are abnormal.<br />
Understands relevance in paediatric patients.<br />
Can calibrate near-patient testing machines<br />
(using manufacturersʼ guidelines).<br />
Able to prepare the necessary equipment.<br />
Assists in positioning and supporting the<br />
patient, skin preparation and helping to prevent<br />
accidental movement during the procedure.<br />
Shows knowledge of complications and risk<br />
factors.<br />
Able to recognise complications and act<br />
appropriately.<br />
Understands indications for invasive<br />
monitoring.<br />
Able to set up, attach and calibrate<br />
pressure transducers and maintain<br />
patency of lines. Able to take blood<br />
samples from these lines.<br />
Accurately monitor and record physiological<br />
parameters.<br />
Describe the appropriate course of action for<br />
abnormal trends and adverse events.<br />
Able to use Situation, Background,<br />
Assessment, Recommendation (SBAR)<br />
methodology to communicate with appropriate<br />
professional colleagues.<br />
Attain certification of competency for all nearpatient<br />
testing equipment in use.<br />
Describe the process and discuss the principle<br />
risks.<br />
Monitor and record physiological data<br />
accurately.<br />
Describe appropriate course of action<br />
for adverse readings or abnormal<br />
trends.<br />
20
COMPETENCY 10: INTRAVENOUS ACCESS AND FLUID BALANCE<br />
Competency 10 Knowledge and skills Suggested indicators<br />
10.1. Can set up intravenous infusion equipment. Able to set up intravenous infusions, including<br />
fluid-warming devices, pressure bags,<br />
volumetric infusers and volumetric pumps.<br />
Undertake training on equipment used<br />
locally.<br />
10.2 Understand basic principles and participates<br />
in postoperative fluid management.<br />
10.3 Knowledge of equipment associated with<br />
transfusion of blood and blood products.<br />
10.4 Understands the principles involved in safe<br />
administration of crystalloids, colloids, blood and<br />
blood products.<br />
Understands postoperative fluid maintenance<br />
Demonstrates ability to accurately record fluid<br />
balance including fluid intake and losses.<br />
Understands use of equipment for<br />
administration and warming of blood and<br />
blood products.<br />
Understands clinical aspects of blood and blood<br />
products administration including safety checks<br />
and documentation.<br />
Able to recognise and manage an adverse<br />
reaction to transfusions.<br />
Accurately monitor and record fluid balance.<br />
Recommend appropriate measures in the<br />
event of adverse readings and trends.<br />
Ensure acquisition of current Better Blood<br />
Transfusion competency.<br />
Familiar with indications for transfusion of<br />
Crystalloids<br />
Colloids<br />
concentrated red cells<br />
platelets<br />
fresh<br />
frozen<br />
plasma<br />
cryoprecipitae salvaged red cells.<br />
See competency 7.3.<br />
10.5 Knowledge of safe placement and use of<br />
nasogastric tubes.<br />
Aware of local protocols regarding safe<br />
administration of blood products.<br />
Understands the rationale of use of salvaged<br />
blood and the workings of cell-savers.<br />
Understands the indications for the use of<br />
nasogastric tubes and checks for accurate<br />
placement.<br />
http://www.<strong>aagbi</strong>.org/sites/default/files/red_cell_<br />
08.pdf<br />
http://www.<strong>aagbi</strong>.org/sites/default/files/cell%20_s<br />
alvage_2009_amended.pdf<br />
Demonstrates appropriate management of<br />
nasogastric tubes and confirmation of<br />
accurate placement.<br />
21
COMPETENCY 11: APPLIED KNOWLEDGE OF PHARMACOLOGY IN PERIOPERATIVE CARE<br />
Competency 11 Knowledge and skills Suggested indicators<br />
11.1 Can calculate appropriate doses and<br />
concentrations in clinical use.<br />
11.2 Understands the clinical indications,<br />
location, preparation, and labelling of drugs<br />
relevant to the PACU.<br />
Able to calculate doses and concentrations in<br />
clinical use (as per local policy).<br />
Prepares drugs for administration during<br />
emergencies.<br />
Familiar with safe practice and local policies.<br />
Aware of clinical indications, complications,<br />
side effects and clinical preparation of<br />
following drugs as well as their labelling and<br />
storage location within the PACU including<br />
local Standard Operating Procedures for<br />
Controlled Drugs:<br />
antacids<br />
inotropes<br />
pressor agents<br />
vasodilators<br />
antiarrhythmics anticoagulants<br />
bronchodilators<br />
steroids<br />
antibiotics<br />
antiemetics<br />
intravenous induction agents<br />
anticholinergics<br />
sedatives and their antagonists<br />
non-steroidal analgesics<br />
opioids and their antagonists<br />
suxamethonium<br />
non-depolarising neuromuscular<br />
blocking agents and reversal agents<br />
respiratory stimulants<br />
local anaesthetic agents<br />
Attain local course certification.<br />
Describe local intravenous drug administration<br />
policies.<br />
22
11.3 Can set up patient-controlled analgesia<br />
(PCA) equipment and other infusion devices.<br />
11.4 Can set up equipment to deliver nebulised<br />
drugs.<br />
Understands the principles of PCA including<br />
knowledge of PCA pumps and safety features.<br />
Demonstrates knowledge of opioid<br />
pharmacology.<br />
Understands local protocols, standard<br />
operating procedures and monitoring.<br />
Understands the principles of epidural<br />
administration of local anaesthetics and<br />
opioids.<br />
Demonstrates knowledge of pharmacology of<br />
local anaesthetics and opioids (see<br />
competency 11.2).<br />
Demonstrates knowledge of pumps used for<br />
continuous epidural analgesia infusions in line<br />
with local protocols and monitoring.<br />
Understands the principles of nebulised drug<br />
administration.<br />
Demonstrates knowledge of pharmacology of<br />
nebulised drugs.<br />
Understands local protocols and monitoring of<br />
patients on nebulised drugs.<br />
Set up a PCA pump according to local<br />
protocols.<br />
Monitor patient appropriately.<br />
Attain certificate of competency in use of locally<br />
provided PCA pumps.<br />
Set up an epidural infusion according to local<br />
protocols.<br />
Monitor patients appropriately.<br />
Attain certification of competency in use of<br />
epidural pumps in local use.<br />
Set up a nebuliser to deliver drugs.<br />
23
COMPETENCY 12: MANAGEMENT OF POSTOPERATIVE PAIN, NAUSEA AND VOMITING<br />
Competency 12 Knowledge and skills Suggested indicators<br />
12.1 Assess and manage postoperative pain. Can describe pain pathways including<br />
physiology of pain transmission.<br />
Use pain scoring tool and knowledge of pain<br />
physiology to select appropriate techniques for<br />
pain management.<br />
12.2 Can match prescribed analgesia to<br />
patientʼs pain score.<br />
Understands how the following analgesic<br />
techniques can modify transmission of pain<br />
sensation:<br />
opioids<br />
paracetamol<br />
nonsteroidal analgesics<br />
local anaesthetics.<br />
Select and deliver appropriate prescription to<br />
achieve adequate analgesia before discharge<br />
from the PACU.<br />
12.3 Management of side effects of analgesics. Understands side effects and complications of<br />
the following analgesic techniques:<br />
opioids<br />
paracetamol<br />
nonsteroidal analgesics<br />
local anaesthetics.<br />
Recognise side effects and complications<br />
associated with administration of analgesics.<br />
Act promptly and appropriately to minimise<br />
morbidity.<br />
Administer naloxone according to local<br />
protocols.<br />
Explain dermatome chart and the significance<br />
of levels of neuraxial block.<br />
Explain local protocols for management of local<br />
anaesthetic toxicity (see competency 13.9).<br />
24
12.4 Can manage patients with central<br />
neuraxial and peripheral nerve block.<br />
Understands indications, side effects,<br />
complications and rationale for:<br />
spinal anaesthesia<br />
epidural analgesia<br />
regional nerve blockade.<br />
Is aware of specialist nursing care needed for<br />
patients in these groups.<br />
Explain structure and function of the spinal<br />
column.<br />
Explain signs and symptoms of:<br />
dural puncture headache<br />
high spinal block<br />
migration of epidural catheter.<br />
Measure sensory and motor blockade and<br />
record extent of block using a dermatome chart.<br />
Administers epidural top-ups in accordance<br />
with local protocols.<br />
12.5 Can assess PONV. Demonstrates knowledge of the physiology and<br />
pathophysiology of PONV Including knowledge<br />
of risk factors.<br />
Assess and manage PONV using local<br />
protocols and multi-modal therapy.<br />
25
COMPETENCY 13: RECOVERY EMERGENCIES<br />
Competency 13 Knowledge and skills Suggested indicators<br />
13.1 Knows how to contact<br />
anaesthetic, surgical and other<br />
appropriate staff for assistance.<br />
Is aware of the importance of calling<br />
for urgent help when needed.<br />
Well versed with local<br />
communication protocols for<br />
contacting appropriate clinicians.<br />
Explain mechanisms in place to contact appropriate members of staff for<br />
assistance.<br />
13.2 Can perform ILS. Demonstrates knowledge of ILS.<br />
Understands local protocols for<br />
access and use of defibrillators<br />
and support.<br />
Attain current certification of attendance of locally approved ILS course –<br />
Ref: ILS Resuscitation Council (UK).<br />
13.3 Recognises significant<br />
cardiac dysrhythmias.<br />
13.4 Understands principles of<br />
managing the shocked patient.<br />
13.4a Recognises and<br />
understands principles of<br />
managing anaphylaxis.<br />
Understands the aetiology,<br />
relevance, and management of<br />
significant cardiac dysrhythmias.<br />
Understands types and grades of<br />
shock, their significance, and<br />
principles of management.<br />
Demonstrate knowledge of<br />
anaphylactic shock management<br />
guidelines published by the<br />
AAGBI.<br />
http://www.<strong>aagbi</strong>.org/sites/default/files/anaphylaxis_2009_0.pdf<br />
http://www.<strong>aagbi</strong>.org/sites/default/files/ana_web_laminate_final.pdf<br />
26
13.5 Recognises pathophysiology<br />
of malignant hyperthermia (MH)<br />
including management of patient<br />
with proven MH susceptibility.<br />
13.6 Recognises and<br />
understands principles of<br />
managing suxamethonium<br />
apnoea.<br />
13.7 Can implement local<br />
protocol for management of<br />
sudden life-threatening<br />
haemorrhage.<br />
13.8 Can describe detailed<br />
management of patient with latex<br />
allergy.<br />
Demonstrate knowledge of MH<br />
management guidelines published<br />
by the AAGBI.<br />
Can prepare dantrolene in an<br />
emergency situation.<br />
Understands causes of<br />
suxamethonium apnoea, its<br />
significance and principles of<br />
management.<br />
Understands local protocol for<br />
management of sudden lifethreatening<br />
haemorrhage including<br />
use of rapid infusors / warmers<br />
where available.<br />
Understands pathophysiology and<br />
clinical management of latex allergy<br />
including use of local protocols.<br />
http://www.<strong>aagbi</strong>.org/sites/default/files/MH%20guideline%20for%20web%2<br />
0v2.pdf<br />
http://www.<strong>aagbi</strong>.org/sites/default/files/MH%20task%20allocations%20for%<br />
20web.pdf<br />
http://www.<strong>aagbi</strong>.org/sites/default/files/MH%20recommended%20contents<br />
%20for%20web.pdf<br />
Participate in local simulation using date-expired dantrolene.<br />
Set up pressure infusors for rapid infusion of fluids.<br />
Explain major blood transfusion protocols.<br />
Explain rationale and use of tourniquets and pressure dressings to reduce<br />
blood loss.<br />
Identify latex allergy patient and explain risk factors.<br />
Source and prepare equipment and environment safe for use in patients<br />
with latex allergy.<br />
13.9 Can describe detailed<br />
management of patient with local<br />
anaesthetic toxicity.<br />
Demonstrates knowledge of<br />
severe local anaesthetic toxicity<br />
management published by the<br />
AAGBI.<br />
Be aware of location of Intralipid.<br />
http://www.<strong>aagbi</strong>.org/sites/default/files/la_toxicity_2010_0.pdf<br />
http://www.<strong>aagbi</strong>.org/sites/default/files/la_toxicity_notes_2010_0.pdf <br />
27
13.10 Short term management of<br />
a patient requiring unexpected<br />
ventilation in the PACU.<br />
13.11 Understand appropriate<br />
specialty specific complications,<br />
side effects and principles of<br />
management.<br />
Understands the indications for<br />
short-term postoperative<br />
ventilation.<br />
Demonstrates knowledge of local<br />
protocols including documentation<br />
and relevant nursing interventions<br />
in these patients.<br />
Fat embolism<br />
Pulmonary embolism<br />
Amniotic fluid embolism<br />
Glycine induced<br />
hyponatraemia<br />
Orthopaedic cement<br />
Unstable cervical spine.<br />
Prepare a recovery bay, ventilator and essential equipment for<br />
postoperative ventilation.<br />
Describe local protocols for the care of a ventilated patient in the PACU.<br />
Seek appropriate support from other clinical staff as appropriate.<br />
Explain local protocols for these complications.<br />
28
COMPETENCY 14: POST SURGICAL CARE<br />
Competency 14 Knowledge and skills Suggested indicators<br />
14.1 Thromboembolic<br />
prophylaxis.<br />
14.2 Management of<br />
normothermia.<br />
14.3 Management of the<br />
diabetic patient.<br />
Demonstrate knowledge of risk<br />
factors and current local<br />
prophylaxis regimens and<br />
understand clinical reasons for<br />
variance.<br />
Understands importance of<br />
normothermia and indications for<br />
intra-operative hypothermia and<br />
postoperative management.<br />
Understands importance of<br />
normoglycaemia and use of<br />
insulin infusion pumps. Able to<br />
determine blood glucose levels<br />
using near-testing equipment.<br />
Adherence to current thromboembolic prophylaxis regimens.<br />
Use of available equipment to promote normothermia and hypothermia<br />
where clinically appropriate.<br />
Maintenance of normoglycaemia in diabetic patients with appropriate<br />
intervention of clinicians to maintain normoglycaemia. Institute therapy to<br />
maintain normoglycaemia in diabetic patients using appropriate, protocols,<br />
equipment and clinical guidance.<br />
14.4 Surgical site inspection. Ability to assess the operative site<br />
including dressings for<br />
complications.<br />
Communicate effectively between theatre teams and PACU staff with<br />
regard to surgical site and dressing complications. Establish parameters<br />
for surgical interventions.<br />
14.5 Orthopaedic and other<br />
stabilising casts.<br />
Recognises poor circulation<br />
secondary to oedema or failing<br />
circulation.<br />
Explain clinical signs and symptoms of complications associated with the<br />
use of plasters, casts and splints.<br />
14.6 Circulatory observations. Observes peripheral circulation and<br />
pulses.<br />
Explain use of ultrasound Doppler and appropriate charting to<br />
demonstrate adequate peripheral circulation and demonstrate an<br />
understanding of the limitations of Doppler assessment.<br />
29
14.7 Urinary catheters and<br />
bladder irrigation systems.<br />
Accurately documents urinary<br />
output and demonstrate<br />
understanding of bladder irrigation<br />
systems with knowledge of<br />
including issues associated with<br />
poor output.<br />
14.8 Wound drainage. Accurately records wound drainage<br />
and understands the principles of<br />
reinfusion systems.<br />
Demonstrates understanding of<br />
individual patient parameters where<br />
surgical intervention may be<br />
appropriate.<br />
Accurately document urine output.<br />
Use bladder irrigation systems and indicate clearly need for surgical<br />
intervention.<br />
Explain factors requiring intervention while monitoring wound drains.<br />
14.9 Specialist dressings. Demonstrate knowledge of<br />
surgical specific dressings.<br />
14.10 Surgery specific care. Demonstrate knowledge of<br />
surgical specific care required<br />
by individual patient.<br />
30
APPENDIX 1<br />
Stakeholder groups consulted were:<br />
Association for Perioperative Practice<br />
British Anaesthetic and Recovery Nurses Association<br />
College of Operating Department Practitioners<br />
Royal College of Nursing<br />
Royal College of Surgeons<br />
31
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
INDEPENDENT PRACTICE<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland,<br />
21 Portland Place, London W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
www.<strong>aagbi</strong>.org<br />
April 2008
Members of the Working Party<br />
Dr W Harrop-Griffiths (Chairman) Honorary Secretary, AAGBI<br />
Dr D K Whitaker<br />
Dr D Bogod<br />
Dr M Wee<br />
Dr D Dickson<br />
Dr S McDevitt<br />
Dr N Denny<br />
Dr M Ward<br />
Dr J Carter<br />
President, AAGBI<br />
Editor-in-Chief, Anaesthesia<br />
Vice President, AAGBI<br />
Council Member, AAGBI<br />
Council Member, AAGBI<br />
Council Member, AAGBI<br />
Former Vice President, AAGBI<br />
Former Vice President, AAGBI<br />
Ex Officio<br />
Dr I Wilson<br />
Dr I Johnston<br />
Dr R Birks<br />
Dr L Gemmell<br />
Honorary Treasurer, AAGBI<br />
Honorary Membership Secretary, AAGBI<br />
President Elect, AAGBI<br />
Honorary Secretary Elect, AAGBI
Contents<br />
Key Points 2<br />
Introduction 3<br />
Good Practice 5<br />
Getting started in Independent Practice 9<br />
Billing issues in Private Practice 13<br />
Indemnity for Independent Practice 14<br />
Independent Medicolegal Practice 16<br />
Independent Practice in Pain Medicine 20<br />
Independent Practice in Intensive Care 22<br />
Chambers and Group Practice 26<br />
Resources and Useful Contacts 29<br />
1
Key Points<br />
• Independent practice should only be conducted by fully trained and<br />
suitably experienced doctors. The minimum requirements include<br />
a registerable medical degree, FRCA or equivalent, a certificate of<br />
completion of training or equivalent, and entry in the appropriate<br />
specialist register of the General Medical Council.<br />
• Maintenance of the highest possible standards of ethics, medical<br />
care and clinical governance is mandatory in the performance of<br />
independent practice, as it is for NHS practice.<br />
• Consultants with NHS contracts must take every possible step to ensure<br />
that their private practice does not adversely impact on their NHS<br />
duties.<br />
• Consultants should only practise in hospitals in which they have been<br />
given practising privileges or admitting rights.<br />
• Consultants conducting private practice should have appropriate<br />
medical indemnity.<br />
• Consultants should keep clear and accurate records of their private<br />
practice activities.<br />
• Groups or partnerships of consultants should be established under<br />
legally acceptable agreements.<br />
2
Introduction<br />
Information about independent practice is not commonly available and yet<br />
it is often the subject of questions asked by members. The purpose of this<br />
booklet is to provide a background to independent practice in Great Britain<br />
& Ireland and to provide advice and guidance for those consultants involved<br />
in private practice.<br />
Before the start of the National Health Service in 1948, independent practice<br />
was the main source of income for anaesthetists in this country. With the<br />
advent of the NHS, a number of provident societies merged to form the<br />
British United Provident Association (BUPA) to preserve freedom of choice in<br />
healthcare and to help patients afford choice in terms of where, when and by<br />
whom they were treated. BUPA had some 80% of the insurance market in the<br />
1950s, and private practice represented about 6% of acute medical activity,<br />
largely concentrated in the major metropolitan centres. At this time, insurers<br />
provided patients with a single combined benefit towards both anaesthetist’s<br />
and surgeon’s fees, and it was not until 1975 that, following successful<br />
representations by the AAGBI, this was divided into separate surgical and<br />
anaesthetic benefits.<br />
In 1975, the health minister Barbara Castle closed all pay beds in NHS<br />
hospitals, and this resulted in a major expansion of independent hospital<br />
facilities, rapidly doubling the number of private beds. BUPA purchased its<br />
first group of hospitals, and US businesses invested heavily to establish what<br />
is now the largest hospital provider (BMI/Netcare) and other hospital groups.<br />
This considerably improved the quantity and quality of private facilities<br />
available. The current size of the UK private healthcare market is around £4<br />
billion, with 7.5 million insured patients (12.7% of the population). About 2.8<br />
million patients are insured by BUPA, who now have 41% of the insurance<br />
market. About 19% of the market is self-pay.<br />
As with any activity, there are pros and cons to independent practice.<br />
The advantages include additional income, more clinical freedom and an<br />
opportunity to develop closer relationships with colleagues and patients. The<br />
disadvantages include the additional time spent in practice, out-of-hours and<br />
antisocial working, and a need for flexibility. Consultants may also need to<br />
be on call for their private patients and will work more often on their own.<br />
Anyone doing private practice will be required to pay a higher medical<br />
3
indemnity subscription, have more complicated accounts and must make sure<br />
that their private work does not conflict with their NHS contract.<br />
The main purpose of private practice is the income that it generates. No<br />
consideration of private practice is complete without a clear description of<br />
the difference between benefits and fees.<br />
Benefits are what insurance companies pay out on behalf of patients according<br />
to the terms of their policy contract with them.<br />
Fees are what consultants charge patients for their professional services.<br />
These two terms should never be confused, and they should not be used<br />
interchangeably. Most private medical insurers (PMIs) make their benefit<br />
schedules available to consultants. Some, such as the Western Provident<br />
Association (WPA), make their schedule publicly available (http://www.wpa.<br />
org.uk). A small number of PMIs do not publish their benefit schedules. The<br />
AAGBI is of the view that all PMIs should make their benefit tables public.<br />
No organisation can set consultants’ private practice fees. If any membership<br />
organisation such as the AAGBI were to attempt to set fees, it would attract<br />
unwelcome interest from the Office of Fair Trading (OFT). It is for the<br />
individual consultants to determine their own fees themselves.<br />
Anyone considering conducting private practice should consider the matter<br />
fully before embarking on it. Although it provides financial and other rewards,<br />
it demands the very highest ethical, clinical and financial standards. Private<br />
practice income is difficult to estimate accurately over time, and the private<br />
practitioner must always put clinical governance and cooperation with<br />
colleagues ahead of financial gain.<br />
4
Good Practice<br />
Doctors should treat their private patients to the same clinical standards<br />
that they treat their NHS patients and vice versa. Therefore, all the guidance<br />
documents and recommendations that set standards of care for NHS patients<br />
should be presumed to be valid for private patients. Guidance documents<br />
for anaesthesia are issued by the Royal College of Anaesthetists (RCoA), the<br />
AAGBI, the British Medical Association (BMA) and the General Medical<br />
Council (GMC). The Healthcare Commission (HCC) has responsibility<br />
for setting and assessing standards in the private sector as well as in the<br />
NHS. The National Institute for Health and Clinical Excellence (NICE) also<br />
produces recommendations, most of which are directly relevant to the private<br />
sector. The websites of all these bodies are given in the Resources Section.<br />
The anaesthetist in private practice should be well versed in all relevant<br />
publication and national guidelines. Active membership of subspecialty<br />
societies is strongly recommended in order to maintain current knowledge in<br />
the areas of practice conducted in both public and private sectors.<br />
Practising anaesthesia in private hospitals commonly involves working in<br />
isolation, often being the only anaesthetist in an operating theatre suite or in the<br />
whole hospital. The qualifications necessary for appointment to a substantive<br />
NHS Consultant Anaesthetist should be considered those necessary to provide<br />
private anaesthetic care: a registerable medical degree; FRCA or equivalent<br />
qualification as judged by the RCoA; a Certificate of Completion of Training<br />
(CCT) or equivalent; entry as an anaesthetist in the Specialist Register of the<br />
GMC. Some private hospitals only award practising privileges to doctors<br />
who hold or who have held a substantive consultant appointment in an NHS<br />
hospital; others consider this not to be necessary.<br />
Anaesthetists who do private work should be appraised to standards similar<br />
to those pertaining in the NHS. If the anaesthetist holds an NHS contract,<br />
appraisal should prove easy to arrange. If the anaesthetist practises only in<br />
the private sector, he or she should make arrangements to be appraised by<br />
a suitably trained and certified colleague. The anaesthetist should maintain<br />
appropriate Continuing Professional Development training in subspecialties<br />
practised in the private sector and should be prepared to prove this to the<br />
appropriate authorities.<br />
5
Anaesthetists practising in the private sector should adhere and conform to<br />
appropriate Clinical Governance requirements as determined by the private<br />
hospitals and agreed by the Medical Advisory Committees of these hospitals.<br />
Anaesthetists should only practise in private hospitals in which they have been<br />
awarded Admitting Rights or Practising Privileges. They should conform to the<br />
regulations and guidelines adopted by the private hospital. The private hospital<br />
has the responsibility for ensuring that the Medical Advisory Committee has<br />
approved these regulations and guidelines, and that all anaesthetists are<br />
informed of the regulations and guidelines relevant to them. The hospital<br />
should make the anaesthetist aware of its disciplinary procedures. There have<br />
been instances of private hospitals demanding that consultants make all the<br />
details of their annual appraisal available. The AAGBI believes that the details<br />
of an anaesthetist’s appraisal documentation are confidential, but that it is<br />
reasonable for a hospital to be given written confirmation that an anaesthetist<br />
has successfully undergone an appraisal process.<br />
An anaesthetist should not undertake cases in the private sector for which he<br />
or she is not appropriately trained, experienced and in ongoing practice. This<br />
usually means that an anaesthetist who has an NHS appointment will have a<br />
similar clinical portfolio in both sectors. Anaesthetists should keep a logbook<br />
of cases done in the private sector and should be prepared to provide the<br />
information contained therein to appropriate supervising bodies.<br />
The anaesthetist has an ongoing clinical responsibility to a private patient<br />
that continues into the postoperative period. However, this responsibility<br />
has limits, and we suggest that the anaesthetist makes the limits clear to the<br />
surgeon and other healthcare professionals involved in the patient’s care.<br />
Such limits may be:<br />
• Until postoperative high dependency or intensive care is no longer<br />
needed or is handed over to an intensivist or another anaesthetist.<br />
• For patients not requiring intensive or high dependency care, the limits<br />
of the anaesthetist’s care may be when the patient is:<br />
- Awake and discharged from the recovery room<br />
- Physiologically stable and satisfactory<br />
- Free from significant postoperative pain, nausea and vomiting<br />
- Not receiving intravenous opioid treatment, e.g. patient-controlled<br />
analgesia<br />
6
- Not receiving neuraxial or peripheral local anaesthetic infusions<br />
- Free from the short-term effects of peripheral or neuraxial<br />
nerve blocks<br />
Any care provided by an anaesthetist beyond these limits may be separately<br />
chargeable if the patient has been warned of this before treatment. It is<br />
reasonable to expect an anaesthetist to be available for a private patient for<br />
the period during which the early and predictable complications of surgery<br />
may occur. However, we suggest that this period should not normally exceed<br />
24 – 48 h and should certainly cease at the discharge of the patient from<br />
hospital.<br />
For anaesthetists who work in both the NHS and the private sector, there will<br />
be times at which the demands of these two practices will seem to clash. The<br />
New Consultant Contract is specific about the conduct expected of an NHS<br />
consultant with regard to private practice. A copy of the contract and specific<br />
guidance can be found on the BMA website. The following general points are<br />
worthy of consideration:<br />
• Private practice should not normally be conducted in contracted NHS<br />
hours but may on occasion be acceptable provided it causes minimal<br />
disruption and has the support of both colleagues and managers.<br />
• Scheduled private practice should not normally be undertaken when<br />
on call for NHS patients. However, if the private practice is performed<br />
in the consultant’s base NHS hospital, this may be acceptable to<br />
colleagues and managers.<br />
• The BMA Code of Conduct for Private Practice states that “There<br />
will be circumstances in which consultants may reasonably provide<br />
emergency treatment for private patients during time when they are<br />
scheduled to be working or are on call for the NHS. Consultants should<br />
make alternative arrangements to provide cover where emergency<br />
work of this kind regularly impacts on NHS commitments”. If one of<br />
your existing private patients unexpectedly develops a complication<br />
that requires the urgent presence of an anaesthetist, it is therefore<br />
acceptable to leave NHS duties or to delay them provided adequate<br />
cover is given for those NHS patients under your care. Under these<br />
uncommon circumstances it might be acceptable to delay the start of<br />
7
an elective list; it would not be acceptable to abandon an NHS patient<br />
in an operating theatre or recovery room unless a suitable colleague is<br />
willing and able to take over care.<br />
Good practice in the private sector involves treating all patients to the highest<br />
standards while maintaining appropriate skills and knowledge. Patients<br />
in both the NHS and private sector are entitled to high standards of care<br />
provided by competent professionals.<br />
8
Getting started in Independent Practice<br />
Before embarking on independent practice, it is important to get advice from<br />
a chartered accountant about your tax situation and to get advice from one of<br />
your colleagues who is an experienced independent practitioner. If you have<br />
joined a group practice, then the best person to ask may be the person who<br />
runs the group.<br />
Admitting rights<br />
Before you can work in a private hospital, you will need to obtain what<br />
are variously known as admitting rights or practising privileges. All private<br />
hospitals should have a Medical Advisory Committee (MAC) that comprises<br />
consultants of all subspecialties, one of whom will be the chairman. The<br />
senior manager of the hospital should grant practising privileges to consultants<br />
who meet the standards set by the MAC. Practising privileges are not awarded<br />
by right; some hospitals may refuse to award them even to consultants who<br />
meet the criteria set by the MAC. The private hospital will provide you with<br />
the necessary application forms on request. It may be a good idea to make an<br />
appointment to meet with the senior manager of the hospital before seeking<br />
practising privileges. Take advice on this from a colleague who already<br />
works in the hospital. The hospital’s requirements for the award of practising<br />
privileges are likely to include:<br />
• A curriculum vitae<br />
• Documentary evidence of relevant qualifications and completion of<br />
subspecialty training<br />
• A current and valid GMC certificate<br />
• Proof of membership of a medical defence organisation (MDO)<br />
• Evidence of hepatitis B immunit<br />
• Proof of recent successful appraisal<br />
• A Criminal Records Bureau (CRB) Enhancement Disclosure or the<br />
following documents that will allow the hospital to acquire one:<br />
o A completed CRB application form<br />
o A passport, driving licence and recent utility bill confirming<br />
home address<br />
9
Some of these documents will need to be updated annually, and you<br />
should expect the hospital to ask for ongoing evidence that you fulfil their<br />
requirements for the maintenance of practising privileges.<br />
Registration with PMIs<br />
Before a PMI will pay you directly for treating their customers, you will need<br />
to register with them. This may involve providing copies of documents that<br />
will satisfy the PMI that you are suitably qualified to provide medical care to<br />
their customers. A list of the larger PMIs along with their contact details is<br />
provided in the Resources Section.<br />
Accountants<br />
All consultants conducting private practice should seek and heed advice from<br />
an accountant with experience in private medical practice. Accountants will<br />
provide invaluable advice on billing, banking, taxation and expenses. They<br />
will also be very helpful when planning pensions and eventual retirement from<br />
both NHS and private practice. The fee that an accountant charges for work<br />
done that relates to private medical practice is a tax-deductible expense.<br />
Billing<br />
The keeping of accurate records is the key to efficient billing. You should keep<br />
a record of the following for every patient you treat:<br />
• Name<br />
• Address<br />
• Telephone numbers<br />
• Date of birth<br />
• Insurance details (PMI, registration number, authorisation number)<br />
• Date of procedure<br />
• The hospital at which the procedure was performed<br />
• Surgeon (if any)<br />
• Procedures performed (both narrative and OPCS codes)<br />
• Any unusual occurrences or circumstances<br />
10
A logbook or database that contains this information will obviously contain<br />
confidential information. Electronic records come under the terms of the<br />
Data Protection Act, and appropriate registration and data protection are<br />
required. A secure backup of all data should be kept. Many consultants<br />
starting in private practice choose to do their own billing and to keep their<br />
own accounts. The consultant should keep precise and careful records of<br />
the date and amount billed, and the date and amount received. Commercial<br />
software packages are available that will facilitate this process. However,<br />
as practice volumes in increase, many opt to pay others to do their billing<br />
and financial record-keeping. An increasing number of commercial billing<br />
services are available. Consultants working in a partnership or group practice<br />
often directly employ someone to do the billing or have an established<br />
arrangement with a commercial billing service. Consultants whose wives,<br />
husbands or partners have no income or whose earnings are less than the<br />
threshold for higher-rate income tax may benefit financially from paying their<br />
partners to do the billing.<br />
Setting fees<br />
Each consultant should determine his or her own fees. Agreeing with a group<br />
of local consultants to charge the same fee as other group members can<br />
be considered anti-competitive and should be avoided unless the group is<br />
trading as a partnership with an established legal identity. If there is doubt<br />
about the trading status of a group of anaesthetists, expert legal advice should<br />
be sought.<br />
Banking<br />
Take advice from your accountant on how to manage your bank accounts.<br />
Most consultants who conduct private practice maintain a separate bank<br />
account that is wholly dedicated to their private practice. You should keep a<br />
full and accurate record of all payments into this account and all payments<br />
made from it.<br />
Tax<br />
Never forget that you will have to pay tax on the money that you have earned,<br />
so take advice from your accountant. Many wise anaesthetists ring-fence 40%<br />
of their private practice income in a separate account so that they always have<br />
the money available to pay the tax when a demand arrives on the doorstep.<br />
11
Investigations by the Inland Revenue<br />
Every year, a number of doctors is investigated by the Inland Revenue. Most<br />
are chosen at random, some are chosen because they have drawn attention to<br />
themselves in some way. A tax investigation is time-consuming and costly for<br />
the individual concerned. It is possible to take out an annual insurance policy<br />
to cover the costs of an investigation; consultants should consider taking out<br />
this sort of insurance.<br />
12
Billing issues in Private Practice<br />
The publication of this guideline document coincides with that of the “AAGBI<br />
Voluntary Code of Practice for Billing Private Patients”, to which the reader<br />
should refer for advice on billing in independent practice.<br />
It is illegal for the AAGBI or any other professional body to set medical fees.<br />
However, the individual anaesthetist is free to set his or her fees according to a<br />
variety of factors that he or she may feel are pertinent. These might include:<br />
• The time taken to provide the service, including pre-operative, intraoperative<br />
and postoperative care<br />
• The training, qualifications and experience necessary to provide<br />
medical care safely<br />
• The complexity of the medical care provided<br />
• The rarity of the anaesthetic skills necessary to provide safe and<br />
effective care.<br />
• The risk to the patient of the procedures being performed<br />
• The time of day and day of the week that the service is provided and<br />
the degree of surgical urgency<br />
• The risk to the anaesthetist of providing the service<br />
Anaesthetists should review their fees on an annual basis.<br />
There are occasionally problems when privately insured patients are admitted<br />
to NHS hospitals with medical conditions requiring emergency surgery.<br />
Most of these patients are entitled to be treated by the NHS without charges<br />
being made. Some patients in these circumstances choose to be treated on<br />
a private basis. In general, PMIs will not pay benefits to anaesthetists under<br />
these circumstances unless the patient signs a declaration that they wish to<br />
be treated privately. If the patient is incapable of expressing such a wish or<br />
signing such a form but his or her next of kin requests private treatment, the<br />
next of kin should sign a declaration waiving NHS treatment and requesting<br />
private treatment. Such declarations should be acquired before treatment is<br />
given.<br />
13
Indemnity for Independent Practice<br />
Under NHS indemnity, NHS bodies take direct responsibility for costs and<br />
damages arising from clinical negligence in which employers are vicariously<br />
liable for the acts and omissions of their healthcare professional staff, including<br />
locums whether “internal” or provided by an external agency. An anaesthetist<br />
employed by one Trust working in another Trust as part of a formal agreement<br />
between the Trusts is also covered by NHS indemnity. A consultant<br />
undertaking contracted NHS work in a private hospital would also normally<br />
be covered by the NHS Litigation Authority (NHSLA). NHS indemnity does not<br />
cover the defence of staff involved in disciplinary proceedings conducted by<br />
statutory bodies like the GMC, police investigations arising from professional<br />
practice or Good Samaritan acts. Clinical negligence means actual or alleged<br />
negligence or breach of duty in connection with the provision of clinical<br />
services. A Good Samaritan act is the provision of clinical services related to<br />
a clinical emergency, accident or disaster when the anaesthetist is not present<br />
in his or her professional capacity but as a bystander. NHS indemnity does not<br />
normally extend to private practice, whether conducted in the independent<br />
sector or in NHS hospitals.<br />
It is therefore essential for all anaesthetists, especially those undertaking private<br />
practice, to be a member of a medical defence organisation (MDO) or have<br />
some other form of appropriate insurance cover. This indemnity will cover<br />
clinical negligence claims, complaints procedures, Good Samaritan acts,<br />
advice on legal and ethical dilemmas arising from professional practice, GMC<br />
enquiries, disciplinary procedures, inquests and fatal accident enquiries, and<br />
police investigations arising from professional practice. Absence of protection<br />
will leave the anaesthetist exposed in the event of a claim, and this may lead<br />
to professional and financial ruin.<br />
In the UK, there are three main MDOs – the Medical Defence Union (MDU),<br />
the Medical Protection Society (MPS) and the Medical and Dental Defence<br />
Union of Scotland (MDDUS). All three organisations are mutual companies<br />
and they do not have legally binding contracts with their subscribers. Their<br />
benefits are discretionary on the decision of their boards. In choosing suitable<br />
cover, one should carefully consider not just the actual costs but also the<br />
detail of the benefits and services offered by the company. The subscriptions<br />
for the above three medical organisations are based on a scale according to<br />
specialty and private income, excluding income from medicolegal work and<br />
14
taking into account legitimate private practice expenses. It is also important<br />
to note that, in the event of a claim, the MDO will require documentary proof<br />
that the full subscription had been paid for indemnity cover. Subscriptions to<br />
MDOs are allowable expenses against private practice earnings.<br />
Policies with commercial companies are on a ‘claims made’ basis. This means<br />
that the insured doctor is only covered for claims arising from incidents<br />
which both occur and are reported whilst the policy is in force. When the<br />
policy expires, so does the cover unless a run-off payment is made. The<br />
mutual organisations offer ‘occurrence or incident-based’ schemes that<br />
give protection for claims arising from incidents that occurred during the<br />
subscription period no matter when they are reported, even if it is many<br />
years after that subscription had ceased. These provide ongoing protection at<br />
retirement or death – the latter prevents one’s estate being liable for claims.<br />
The MDU introduced a version of ‘claims made’ membership in 1992, known<br />
as contemporary, which offered lower subscriptions, particularly in the first<br />
five years. The cover for this policy ceases unless a run-off payment is made<br />
and this is equivalent to approximately one year’s normal premium. When a<br />
doctor switches to another organisation or company, his or her previous risk<br />
is usually covered by the new organisation or company. It is wise to get this<br />
confirmed in writing from the new organisation or company.<br />
It is not possible to cover all aspects of indemnity in the NHS or private<br />
practice in the limited confines of this guidance and some aspects are<br />
complex. Readers are advised to consult the relevant defence organisations<br />
for further information pertaining to their personal circumstances from the<br />
web addresses given in the Resources Section.<br />
15
Independent Medicolegal Practice<br />
Medicolegal work can be divided into personal injury and negligence. The<br />
former entails examining clients who are making claims for injuries that they<br />
have sustained outside the medical arena, often occupational in nature, e.g.<br />
repetitive strain injury or back pain, or following an accident, e.g. whiplash<br />
or nerve damage leading to a chronic regional pain syndrome. While much<br />
of this work is performed by orthopaedic colleagues, it can provide a useful<br />
source of income for the chronic pain specialist, who will often encounter<br />
patients in need of a report in the course of their daily duties.<br />
However, this section of the guidance is about clinical negligence work and<br />
the role of the medicolegal expert. There are some misconceptions about<br />
medicolegal experts, so let’s deal with these first.<br />
You have to be old to be an expert. No, in fact any consultant anaesthetist<br />
is, almost by definition, an expert in anaesthesia, although not necessarily an<br />
expert in all branches of anaesthesia – it is unwise to stray outside those areas<br />
of practice that you encounter on a regular basis. An expert has to be able<br />
to: derive a likely sequence of events from a bundle of documents, largely<br />
clinical records; explain those events in terms that an intelligent layman<br />
can understand; decide (often by reference to the literature) whether the<br />
standard of care contained in those events would be regarded as acceptable<br />
practice by a reasonable body of his or her peers; write all of this down in a<br />
logical, accessible manner; and – very rarely – hold his or her own in what<br />
many regard as the ultimate viva voce, the conference with Counsel or an<br />
appearance in the witness box. Yes, your qualifications and expertise will be<br />
compared to those of the expert retained by the other side, but this is a very<br />
minor issue; the calm, honest, modest and well-prepared expert will always<br />
come over well.<br />
Experts sell their souls to the lawyers. This is completely untrue. Expert<br />
witnesses have always been meant to be impartial and, whichever side has<br />
instructed them, their report should be neutral. This has, in the past, been more<br />
honoured in the breach than in the observance, but recent guidance from the<br />
Department of Constitutional Affairs, in the form of the Civil Procedure Rules<br />
means that the expert’s duty to the Court has been formalised, and the days<br />
of the so-called ‘hired gun’ are well and truly over. Modern experts should<br />
16
eschew being labelled as ‘claimant’ or ‘defence’ practitioners. Indeed, recent<br />
reforms mean that they might even be instructed jointly by both sides.<br />
Do I want to do it?<br />
Expert witness work has some distinct advantages. You are not beholden to<br />
surgeons for independent income, and the bulk of the work can be done from<br />
the comfort of your own home. The research needed to produce a report<br />
can be enlightening and educational in its own right. The rewards can be<br />
substantial, although you will be fortunate indeed to achieve an hourly rate<br />
that matches that of independent clinical practice.<br />
However, it is not an easy option. Deadlines are rarely flexible and recent<br />
reforms have made them tighter than ever. There can be no short-cuts in<br />
writing a report; flaws are very quickly and publicly shown up if the case<br />
gets to Court. Reports are very rarely unchallenged, even by the team that has<br />
instructed you, so if you find it difficult to accept criticism, this is not a job<br />
for you. Good organisational skills are essential, especially as your practice<br />
expands, and you will need a well-ordered and persistent billing service. And,<br />
of course, medicolegal practitioners can get into very hot water indeed if they<br />
are perceived as having stepped outside their field of expertise.<br />
So how do I get started?<br />
Word of mouth remains the best way to get your first instructions. Somewhere<br />
near you is an expert in anaesthesia with more work than he or she can<br />
handle. Ask them if you can help out, or offer to write a draft report on<br />
a simple case so that they can get an idea of your abilities. Solicitors are<br />
looking for someone who can deliver a sensible, logical, readable report that<br />
addresses the key issues, who can do it on time, and who will not overstate<br />
the strengths of the case only to retract later when under pressure.<br />
In the past, most experts have learned on the job, but this is far from ideal,<br />
and there are now courses that the aspiring practitioner can attend. Action<br />
Against Medical Accidents (AvMA) have transformed over the years from an<br />
aggressive pressure group into a powerful and respectable training and policysetting<br />
organisation. Details of courses, including ‘Getting Started as a Clinical<br />
Negligence Expert’, can be found on their website. Other commercial bodies<br />
offer similar courses and even the chance to stand up and be cross-examined<br />
in a court hired for the day, although the costs can be rather prohibitive.<br />
17
Moving on<br />
There are also organisations out there that act as forums for medicolegal<br />
practitioners and represent their interests, such as the Academy of Experts<br />
and the Expert Witness Institute. These bodies provide useful advice to<br />
their members, and membership – which requires references from solicitors<br />
and/or barristers – is an indication to instructing solicitors that you know<br />
what you are doing. They represent a useful next step to advancing your<br />
medicolegal career, although very few solicitors will instruct you on the basis<br />
of membership of one of these organisations alone. AvMA holds a register of<br />
practitioners that does appear to be widely used by claimant solicitors looking<br />
for an expert. Inclusion is out of the expert’s control but seems to be based<br />
on a good history of producing high quality reports. The Resources Section<br />
contains website addresses for the organisations mentioned above.<br />
As timeframes for conducting cases and costs are being forced down by the<br />
courts, solicitors are looking more avidly for fast turn-around times and low<br />
costs when selecting experts. A fixed-price preliminary report is now often<br />
the first recourse for the solicitor who wants a quick opinion as to whether<br />
a case has merit, and this approach has been sanctioned by the courts and<br />
professional bodies. The ability to provide a two = to three-page report<br />
within two weeks of receipt of records often leads to further instruction in the<br />
same and other cases, although this does need careful organisation and time<br />
management.<br />
A final word of caution<br />
As with every other area of medical practice, there are great pressures to<br />
reduce the amount of money that doctors can earn as experts. The Legal<br />
Services Commission (formerly the Legal Aid Board) has stated that expert<br />
fees should be capped at levels that are far below the sort of rates currently<br />
charged, and are actively in consultation to achieve this end. At the same<br />
time, there is a drive towards improving quality by introducing accreditation,<br />
through a process that is still far from clear.<br />
You will, of course, have taken out professional liability insurance with<br />
one of the MDOs for your clinical practice, but be aware that this does not<br />
necessarily provide cover for medicolegal work. You can fall foul of doctors<br />
whom you have unfairly castigated in a report, of patients who feel that you<br />
have not been sufficiently supportive of their claim, or of lawyers who are<br />
18
dissatisfied with the service you provided. Medicolegal insurance is available<br />
from all the major MDOs and costs very little – make sure you are covered!<br />
It is tempting to take on every case that comes through your door – after all,<br />
it is flattering to have your opinion sought. However, always ask yourself the<br />
following questions before agreeing to help:<br />
• Can I deliver within the requested time-frame?<br />
• Is this within my area of expertise?<br />
• Do I have any conflict of interests, e.g. close friendship or professional<br />
relationship with any of the doctors involved?<br />
• Can I take on the extra work that will inevitably arise through requests<br />
for clarification, further comments, responses to challenges from the<br />
other side, conferences with Counsel, and Court appearances?<br />
19
Independent Practice in Pain Medicine<br />
Independent practice in Pain Medicine should only be undertaken by those<br />
with the appropriate training and experience. In most cases this will mean<br />
that the consultant holds or has held a substantive NHS consultant post that<br />
includes regular work in this subspecialty.<br />
Standards of practice<br />
There should be no difference in the standard of care provided to NHS or<br />
private patients. Similarly, clinical pain medicine decision-making and casemix<br />
should be similar for an individual consultant in both public and private<br />
sectors. The only exception to this would be differences in care relating to the<br />
time available to consult with the patient, the limitations of waiting lists and<br />
the form of therapies funded by the NHS and PMIs.<br />
Clinic facilities<br />
Clinics should be held in an environment in which access to adequate and<br />
appropriate support facilities is available. This should include adequate<br />
facilities for consultation and examination of patients, chaperone facilities,<br />
resuscitation equipment and access to appropriate clinical investigations.<br />
Facilities for more complex investigations and scans should be available but<br />
not necessarily present on site.<br />
Interventions<br />
If any form of intervention is undertaken, suitable sterile conditions, equipment<br />
and nursing support should be available, along with recovery facilities if<br />
sedation or anaesthesia is given. Major interventions may demand operating<br />
theatre facilities, trained nurses and radiological facilities. Patients should<br />
follow a defined and documented pathway of pre-operative assessment,<br />
informed consent, procedure, recovery, ward care and discharge.<br />
Mode of practice<br />
When practising in pain medicine, the anaesthetist’s mode of practice more<br />
resembles that of a surgeon than an anaesthetist. A pain specialist will need to<br />
arrange for outpatient consultation facilities to be made available by a private<br />
hospital or he or she may rent private consulting rooms. Referrals will come<br />
from General Practitioners (GPs), consultant colleagues, physiotherapists,<br />
osteopaths or chiropractors. When the referral does not come from a GP, it<br />
is good practice to notify the patient’s GP and to ensure that the GP is fully<br />
20
informed about the progress of the treatment. A pain specialist may well have<br />
to invest in secretarial and administrative support.<br />
On-call cover<br />
A consultant will need to be on call and available for their own patients<br />
throughout any hospital admission. They will also need to provide some form<br />
of availability at other times for their patients who are undergoing treatment.<br />
It is advisable to arrange cross-cover with one or more colleagues in the same<br />
specialty. This allows adequate cover for patients during holidays and other<br />
absences.<br />
Multidisciplinary work<br />
Although it is less usual for pain consultants in private practice to run<br />
multidisciplinary clinics, referral pathways to the relevant allied health<br />
professionals such as physiotherapists, occupational therapists, psychologists<br />
and pharmacists should be available in order to provide appropriate standards<br />
of care.<br />
Fees<br />
Fees should be set in accordance with the advice set out in the section on<br />
“Billing issues” above. Most PMIs provide schedules of benefit maxima for<br />
pain therapy procedures.<br />
Indemnity<br />
Consultants undertaking independent practice in pain medicine will require<br />
full indemnity from their MDO, which should be informed of the exact nature<br />
of the consultant’s practice, i.e. the relative proportions of the consultant’s<br />
income that are sourced from pain management and from purely anaesthetic<br />
practice.<br />
21
Independent Practice in Intensive Care<br />
Responsibility for patients admitted to an Intensive Care Unit (ICU)<br />
When a private patient requires admission to an ICU, their medical management<br />
should become the responsibility of one clinician who should be a recognised<br />
intensivist. A recognised intensivist is a clinician with appropriate training<br />
and experience who holds or has held a substantive consultant’s post that<br />
includes clinical responsibilities for patients in intensive care. This clinician<br />
should be the only consultant to charge the patient for their services. Only if<br />
the intensivist requests another consultant, e.g. a cardiologist, to attend the<br />
patient should any other consultant charge be made.<br />
Postoperative intensive care as a ‘routine’ part of anaesthesia<br />
Many major surgical procedures are followed by a short and predictable<br />
stay in an ICU, e.g. cardiac bypass or aortic aneurysm surgery. In these<br />
circumstances, and if the patient’s postoperative treatment and course are<br />
uncomplicated, it is common practice for the anaesthetist who has managed<br />
the patient before and during surgery to be responsible for the patient while<br />
in the ICU. The fee charged by the consultant anaesthetist should include<br />
this routine ICU care. However, if intensive care extends beyond this routine<br />
postoperative period, usually taken to be a period of no more than 24 h,<br />
responsibility for the patient’s ongoing care should become the responsibility<br />
of an intensivist, who should be able to make separate charges for the patient’s<br />
care. If the anaesthetist providing the anaesthetic care is also an intensivist, he<br />
or she can make additional charges after the first 24 h in the ICU provided the<br />
patient has been given appropriate warning that this may happen.<br />
Unexpected postoperative ICU admission<br />
In the event of a private patient unexpectedly requiring postoperative ICU<br />
management, the patient’s medical management should be handed over to<br />
an intensivist, who will make appropriate charges.<br />
Standard of care<br />
The same standard of care should be provided to patients in the ICUs of<br />
both independent and NHS hospitals. Equipment and beds should comply<br />
with existing national standards. Adequate numbers of intensive care trained<br />
nursing staff must be available to manage the required patient dependency.<br />
Junior medical staff with intensive care training, including airway management<br />
22
skills and resuscitation, must be immediately available. An on-call consultant<br />
intensivist without other responsibilities should be available at all times.<br />
Transfer of patients from independent hospitals to NHS ICUs<br />
Many independent hospitals do not have adequate Level 3 ICU facilities, and<br />
patients may therefore need to be transferred to an appropriate NHS hospital.<br />
The independent hospital should have in place a contractual agreement with<br />
a neighbouring NHS ICU to provide transfer of a sick private patient to the<br />
NHS ICU or, if full, provide transfer to an ICU where a bed is available.<br />
Patients may elect either to continue to be fee-paying or to become an NHS<br />
patient if they are entitled to receive free NHS care. If the patient is too sick<br />
to make a decision, then they remain a private patient in an NHS hospital<br />
until such time as they are competent to express their preference. Under these<br />
circumstances, some PMIs will try to claim that, if the patient is entitled to<br />
NHS care, they will no longer provide cover after such a transfer. Patients,<br />
or their next of kin, should be told that this is not usually the case and they<br />
should be advised to contact their relative’s PMI to seek confirmation of<br />
continued private patient status.<br />
If no retrieval contract has been agreed, it remains the responsibility of the<br />
independent hospital to undertake the transfer of the patient. Such transfers<br />
must be prearranged in accordance with Intensive Care Society guidelines,<br />
with the availability of appropriate monitoring and equipment. Accompanying<br />
medical and nursing staff should have suitable training and experience in<br />
transporting critically ill patients.<br />
Charging for ICU services<br />
Some elements of ICU management may be charged as individual procedures.<br />
For example, the procedure of percutaneous tracheostomy requires both an<br />
operator (intensivist) and an anaesthetist, and both may submit accounts for<br />
the procedure. Most ICU management is a combination of procedures, ward<br />
rounds, therapy adjustments and waiting for these adjustments to work, and<br />
availability. This work may be charged as an hourly rate for actual attendance<br />
or as a daily rate taking on-call availability into account. A fixed daily charge<br />
for each patient covering all procedures may be more practical for billing<br />
purposes, and more acceptable to PMIs. As for anaesthetic fees, the actual<br />
rate charged is up to the individual, but in calculating the rate it may be<br />
helpful to consider the degree of expertise required and the length of training<br />
undertaken to become an intensivist.<br />
23
Accurate records of procedures undertaken and time spent treating patients<br />
should be kept, in case submitted accounts are questioned either by the<br />
patients or their healthcare insurance companies.<br />
Charging for ward consultations<br />
Requests for consultation for possible ICU admission should be charged at the<br />
rate of a complex outpatient referral, and may be repeated over consecutive<br />
days if indicated. Intensivists may also oversee a patient’s management in the<br />
first few days after discharge from ICU, and may charge for this at a suitable<br />
daily attendance rate.<br />
Charging for patient transfers<br />
If a patient is transferred from an independent hospital to a hospital with<br />
ICU facilities, the accompanying consultant anaesthetist or intensivist may<br />
charge for their services. This may most appropriately be at an hourly rate to<br />
include stabilising the patient for transfer, and the time taken to perform the<br />
handover.<br />
“Fixed cost” cases and intensive care<br />
Many independent hospitals offer “Fixed cost” packages for uninsured<br />
patients. Hospitals offering such packages should have made arrangements in<br />
advance to cover unexpected complications, including unanticipated critical<br />
care requirements and transfer to NHS facilities. Such arrangements may<br />
include a contingency fund to cover additional medical and hospital fees, or<br />
an increased payment for each case to cover such complications.<br />
The 2003 Consultant Contract<br />
Under the terms of the new consultant contract, independent practice should<br />
not be undertaken during NHS time except with the explicit permission of<br />
the employing NHS hospital management. It is not considered permissible to<br />
be paid twice for the same event. This is a problem for intensivists who may<br />
be asked to take over the management of private patients during their normal<br />
NHS duties.<br />
The agreement between the BMA and the Department of Health relating<br />
to the new consultant contract allows for some independent practice to be<br />
undertaken alongside a consultant’s scheduled NHS duties at the discretion of<br />
their NHS employers. This may be taken to cover the situation where an NHS<br />
Intensive Care Unit contains the occasional private patient.<br />
24
Otherwise, the options are:<br />
• Invoice the patient for the intensive care services provided and then<br />
pay the fee directly to the hospital. This may cause problems with tax<br />
records.<br />
• Invoice the patient, keep the fee, then reimburse the hospital in time<br />
spent looking after patients.<br />
• If the work is undertaken outside of contracted NHS time as defined<br />
in the individual’s job plan, it is acceptable to invoice the patient and<br />
keep the fee.<br />
• Arrange either for a colleague to undertake the management of<br />
the patient, or for this colleague to cover the intensivist’s NHS<br />
responsibilities in order to avoid such a conflict of interest.<br />
• Formalise an agreement with Trust management that allows intensivists<br />
to charge for the management of private patients on the basis they are<br />
a source of additional income to NHS hospitals and as such a suitable<br />
mutually agreeable solution should be possible between clinicians and<br />
management.<br />
25
Chambers and Group Practice<br />
For anaesthetists, the prospect of practice in the independent sector may be<br />
a lonely one, as for many their introduction to private practice soon after<br />
appointment to consultant status is as a single-handed practitioner. Many<br />
will find that an established group practice already exists and if their job plan<br />
makes them attractive to the established group or they express an interest in<br />
becoming part of the group, an invitation to join might be forthcoming soon<br />
after appointment. Within the specialties such as anaesthesia, radiology and<br />
pathology, group practice is particularly attractive as a result of the usually<br />
discrete episodes of direct patient responsibility.<br />
The advantages of group practice<br />
Sharing:<br />
Maximising:<br />
Practice costs and expenses<br />
Practice accommodation and secretarial assistance<br />
Administrative responsibilities<br />
Practice cover and on-call<br />
Specialty expertise, i.e. not everyone in the group<br />
needs to be able to cover all specialties<br />
Income<br />
Free and off-call time<br />
Strength in negotiating with private hospitals,<br />
Treatment Centres and PMIs<br />
The disadvantages of group practice<br />
Loss of:<br />
Practice and professional autonomy<br />
Income, if your personal practice becomes very busy<br />
or only involves high-value procedures<br />
Tax advantage of paying a low-earning partner for<br />
secretarial services.<br />
For an increasing number of anaesthetists, the concept of group practice<br />
has of late been particularly attractive, and it is important to understand<br />
the terminolgy in use. Group practices generally fall into one of two types:<br />
chambers or partnerships.<br />
26
Chambers<br />
This title has been borrowed from the legal profession in the UK. Here,<br />
following completion of his or her training, a new barrister must find a seat or<br />
“tenancy” in a set of chambers. Chambers are groups of barristers, and tend<br />
to comprise between 20 and 60 barristers. The term can equally be used to<br />
describe any group of professionals who choose to work together and who<br />
share rent and facilities such as the service of secretaries and other support<br />
staff. Most chambers offer a system whereby the members contribute to these<br />
common expenses by paying a percentage of their gross income. However,<br />
there is no profit-sharing as in a partnership (see below), and individual<br />
members of the group keep the fees they themselves earn beyond what they<br />
have to pay towards the chambers expenses.<br />
Partnerships<br />
This title has a much more significant legal meaning under UK law whereby<br />
a partnership is a type of business entity in which partners share the profits<br />
or losses of the business undertaking in which they have all invested. The<br />
shares may be equal (equity partnership) or may be fractional, based upon the<br />
seniority or some other factor that varies only by the consent of all partners. A<br />
true partnership must have a legally drafted partnership agreement signed by<br />
all partners and there should be regular partnership meetings.<br />
Generally, partners have an obligation of strict liability to third parties injured<br />
by the partnership. Partners may have joint liability or joint and several<br />
liability depending upon circumstances. The liability of limited partners is<br />
limited to their investment in the partnership, hence the term Limited Liability<br />
Partnership. Without a legally drafted partnership agreement, the group acting<br />
as a partnership will be regarded in law as a “sham” partnership and will not<br />
benefit from the legal advantages of a real partnership, such as the ability for<br />
all partners to charge the same fee without an accusation of price fixing.<br />
The key to the success of a partneship rests in a sense of mutual trust between<br />
partners so that there is a feeling that the work is genuinely being shared<br />
equally. One important element in achieving this feeling is the important<br />
part played by the partnership manager who allocates work according<br />
to the agreed partnership rules laid down in the agreement. Partnership<br />
administration can be largely left to the salaried partnership manager who<br />
acts under the immediate direction of the elected partnership chairperson.<br />
Larger partnerships may also choose to appoint a partnership secretary and a<br />
27
treasurer, but the arrangements of the partnership executive are matters to be<br />
decided by the members of the partnership with professional advice from their<br />
nominated legal and financial advisors.<br />
Since partners are jointly responsible for third party damage, one important<br />
item that must be agreed at the onset is the individuals’ responsibility for<br />
medical indemnity insurance, which should ideally be made an absolute<br />
obligation for continued membership of the partnership. Some partnerships<br />
take on the responsibility of payment on behalf of the individuals to avoid<br />
any inadvertent lapses.<br />
28
Resources and useful contacts<br />
Medical Defence Union<br />
Medical and Dental Defence Union of Scotland<br />
Medical Protection Society<br />
www.the-mdu.com<br />
www.mddus.org.uk<br />
www.mps.org.uk<br />
Academy of Experts<br />
Action Against Medical Accidents<br />
Association of Anaesthetists of Great Britain & Ireland<br />
Criminal Records Bureau<br />
Department of Constitutional Affairs<br />
Expert Witness Institute<br />
General Medical Council<br />
Healthcare Commission<br />
Intensive Care Society<br />
Legal Services Commission<br />
National Institute for Health and Clinical Excellence<br />
National Patient Safety Agency<br />
NHS Litigation Authority<br />
Office of Fair Trading<br />
Royal College of Anaesthetists<br />
Small Claims Court<br />
The British Pain Society<br />
UK Department of Health<br />
www.academy-experts.org<br />
www.avma.org.uk<br />
www.<strong>aagbi</strong>.org<br />
www.crb.gov.uk<br />
www.dca.gov.uk<br />
www.ewi.org.uk<br />
www.gmc-uk.org<br />
www.healthcarecommission.org.uk<br />
www.ics.ac.uk<br />
http://www.legalservices.gov.uk<br />
www.nice.org.uk<br />
www.npsa.nhs.uk<br />
www.nhsla.com<br />
www.oft.gov.uk<br />
www.rcoa.ac.uk<br />
www.hmcourts-service.gov.uk<br />
www.britishpainsociety.org<br />
www.dh.gov.uk<br />
AXA PPP<br />
BCWA<br />
BUPA<br />
CIGNA<br />
Norwich Union<br />
Standard Life<br />
WPA<br />
www.axappphealthcare.co.uk<br />
www.bcwa.co.uk<br />
www.bupa.co.uk<br />
www.cigna.co.uk<br />
www.norwichunion.com/health<br />
www.standardlifehealthcare.co.uk<br />
www.wpa.org.uk<br />
29
30
31
21 Portland Place, London W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
AAGBI SAFETY GUIDELINE<br />
Infection Control in Anaesthesia<br />
2<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland,<br />
21 Portland Place, London W1B 1PY<br />
Telephone: 020 7631 1650<br />
E-mail: info@<strong>aagbi</strong>.org Website: www.<strong>aagbi</strong>.org<br />
October 2008
Membership of the Working Party<br />
Dr Leslie Gemmell<br />
Dr Richard Birks<br />
Dr Patrick Radford<br />
Professor Don Jeffries CBE<br />
Dr Geoffrey Ridgway<br />
Mr Douglas McIvor<br />
Chairman, Honorary Secretary Elect<br />
President Elect<br />
Royal College of Anaesthetists<br />
Emeritus Professor of Virology, University of London<br />
Consultant Microbiologist<br />
Medicines and Healthcare Products Regulatory Authority<br />
Ex officio<br />
Dr David Whitaker<br />
Dr William Harrop-Griffiths<br />
Dr Iain Wilson<br />
Dr Ian Johnston<br />
Dr David Bogod<br />
President<br />
Honorary Secretary<br />
Honorary Treasurer<br />
Honorary Membership Secretary<br />
Editor-in-Chief, Anaesthesia<br />
This guideline was originally published in Anaesthesia. If you wish to refer to this guideline, please<br />
use the following reference:<br />
Anaesthesia 2008, 63; 1027-36
Anaesthesia, 2008, 63, pages 1027–1036<br />
doi:10.1111/j.1365-2044.2008.05657.x<br />
.....................................................................................................................................................................................................................<br />
GUIDELINES<br />
Infection Control in Anaesthesia<br />
Association of Anaesthetists of Great Britain and Ireland<br />
Membership of the Working Party: Gemmell L, Chair; Birks R, President Elect; Radford P, Royal<br />
College of Anaesthetists representative; Jeffries D, National Institute for Health and Clinical<br />
Excellence; Ridgway G, consultant microbiologist; McIvor D, Medicines and Healthcare Products<br />
Regulatory Authority; Executive Officers of AAGBI, ex officio<br />
This is a consensus document produced by expert members of a Working Party established by the Association of<br />
Anaesthetists of Great Britain and Ireland (AAGBI). It updates and replaces previous guidance published in<br />
2002.<br />
1.0. Summary<br />
(1) A named consultant in each department of anaesthesia<br />
should liaise with Trust Infection Control<br />
Teams and Occupational Health Departments to<br />
ensure that relevant specialist standards are established<br />
and monitored in all areas of anaesthetic<br />
practice.<br />
(2) Precautions against the transmission of infection<br />
between patient and anaesthetist or between patients<br />
should be a routine part of anaesthetic practice.<br />
In particular, anaesthetists must ensure that hand<br />
hygiene becomes an indispensable part of their<br />
clinical culture.<br />
(3) Anaesthetists must comply with local theatre infection<br />
control policies including the safe use and disposal of<br />
sharps.<br />
(4) Anaesthetic equipment is a potential vector for<br />
transmission of disease. Policies should be documented<br />
to ensure that nationally recommended<br />
decontamination practices are followed and audited<br />
for all reusable anaesthetic equipment.<br />
(5) Single use equipment should be utilised where<br />
appropriate but a sterile supplies department (SSD)<br />
should process reusable items.<br />
(6) An effective, new bacterial ⁄ viral breathing circuit<br />
filter should be used for every patient and a local<br />
policy developed for the re-use of breathing circuits<br />
in line with manufacturer’s instructions. The AAGBI<br />
recommends that anaesthetic departments should<br />
consider changing anaesthetic circuits on a daily basis<br />
in line with daily cleaning protocols.<br />
(7) Appropriate infection control precautions should be<br />
established for each anaesthetic procedure, to include<br />
maximal barrier precautions for the insertion of central<br />
venous catheters, spinal and epidural procedures and<br />
any invasive procedures in high risk patients.<br />
2.0. Introduction<br />
The Association of Anaesthetists of Great Britain and<br />
Ireland (AAGBI) published guidelines in 2002 on problems<br />
relating to infection control in anaesthetic practice.<br />
In addition to AAGBI Officers and Council members,<br />
representation included the Royal College of Anaesthetists<br />
and the Medicines and Healthcare Products Regulatory<br />
Authority (MHRA). This is an updated version of<br />
that guidance document.<br />
Healthcare organisations now have a legal responsibility<br />
to implement changes to reduce healthcare associated<br />
infections (HCAIs). The Health Act 2006 provided the<br />
Healthcare Commission with statutory powers to enforce<br />
compliance with the Code of Practice for the Prevention<br />
and Control of Healthcare Associated Infection (The<br />
Code). The Code provides a framework for NHS Bodies<br />
to plan and implement structures and systems aimed at<br />
prevention of HCAIs. The Code sets out criteria that<br />
mandate NHS bodies, including Acute Trusts, and which<br />
ensure that patients are cared for in a clean environment.<br />
Anaesthetists should be in the forefront of ensuring<br />
that their patients are cared for in the safest possible<br />
environment. Further advice can be obtained from the<br />
Department of Health (DOH) website http://www.<br />
clean-safe-care.nhs.uk.<br />
Ó 2008 The Authors<br />
Journal compilation Ó 2008 The Association of Anaesthetists of Great Britain and Ireland 1027
Infection control in anaesthesia Anaesthesia, 2008, 63, pages 1027–1036<br />
.....................................................................................................................................................................................................................<br />
3.0. General principles<br />
Healthcare providers have responsibilities under the<br />
Health and Safety at Work Act 1974; offences against<br />
the Act are covered by Criminal Law. The Control of<br />
Substances Hazardous to Health (COSHH) Regulations 1999<br />
have been considered part of the Health and Safety at Work<br />
Act; the Act ensures that Trusts are responsible for the<br />
health and safety of their employees and others (including<br />
visitors and patients), and the control and management of<br />
the risk of infection. As part of the Health Act 2006, the<br />
Department of Health (DOH) released the Code of Practice<br />
for the Prevention and Control of Healthcare Associated<br />
Infections [1].<br />
Trust Chief Executives are accountable for ensuring<br />
that care delivered within each Trust meets relevant<br />
standards. Trusts should have Infection Control Committees<br />
and Infection Control Teams responsible for<br />
preparing policies and monitoring compliance with<br />
appropriate standards. A microbiologist should be designated<br />
to provide advice on microbiological aspects of<br />
decontamination and sterilisation. The AAGBI Working<br />
Party recommends that a named consultant in each<br />
Department of Anaesthesia should liaise with the Infection<br />
Control Team and the Occupational Health Department<br />
to ensure that relevant standards are established and<br />
monitored in all areas of anaesthetic practice.<br />
The environment<br />
Hospital environmental hygiene encompasses a wide<br />
range of routine activities that are important in the<br />
prevention of HCAI. The hospital must be visibly clean<br />
and acceptable to patients, visitors and staff. Statutory<br />
requirements must be met in relation to safe disposal of<br />
clinical waste, laundry and linen. Bed occupancy should<br />
ensure enough time between patient admissions to ensure<br />
adequate cleaning and decontamination of the patient<br />
area.<br />
The Code of Practice enshrines in law the duty of<br />
Trusts to maintain a clean and appropriate environment<br />
for patients including the fabric of the building and related<br />
structures. Operating theatres and associated areas should<br />
be designed and maintained to the standards defined<br />
in Health Building Note 26, Facilities for Surgical Procedures<br />
published in 2004. Microbiological commissioning and<br />
monitoring of operating theatre suites should adhere to<br />
national recommendations.<br />
Standard precautions<br />
Anaesthetists will be involved in the care of patients who<br />
may harbour potentially pathogenic organisms, which<br />
may not be obvious or readily identifiable. Precautions<br />
aimed at preventing the transmission of organisms<br />
between patient and anaesthetist or between patients<br />
must be a routine part of anaesthetic practice.<br />
The AAGBI recommends the use of Standard Precautions,<br />
which incorporate additional safeguards for specific<br />
procedures and patients, including single-use gloves, fluid<br />
resistant masks with a transparent face shield and gowns<br />
[2]. Precautions are recommended for all patients regardless<br />
of their diagnosis or presumed infectious status and<br />
must be implemented when there is a possibility of<br />
contact with:<br />
1 Blood.<br />
2 All other body fluids.<br />
3 Non-intact skin.<br />
4 Mucous membranes.<br />
Preventative measures should be based on the likelihood<br />
of an infectious agent being present, the nature of<br />
the agent and the possibility of dispersion, e.g. splashing.<br />
A standard set of precautions should be established for<br />
every invasive procedure (see below) with additional risk<br />
assessment of each patient to determine extra and specific<br />
precautions that may be appropriate.<br />
Hand hygiene<br />
Anaesthetists must ensure that good hand hygiene becomes<br />
an indispensable part of their clinical culture<br />
Hand-mediated transmission is the major contributing<br />
factor to infection associated with healthcare [3]. Effective<br />
hand decontamination immediately before every episode<br />
of direct patient contact will result in a significant<br />
reduction in the transfer of potential pathogens and a<br />
decrease in the incidence of preventable HCAI [4].<br />
Despite consistent advice, staff often neglect hand hygiene<br />
when caring for patients.<br />
At the start of every session, and when visibly soiled or<br />
potentially contaminated, hands must be washed with<br />
liquid soap and water. When there is no soiling, the<br />
Hand Hygiene Liaison Group advocates that staff should<br />
use an antimicrobial hand rub between patients or<br />
activities [5] as this is effective and quicker. It is vital to<br />
ensure that the whole hand and fingers (particularly the<br />
tips), are exposed to the hand rub. Antimicrobial hand<br />
rub is not effective in preventing cross infection with<br />
Clostridium difficile.<br />
Trusts must ensure that sinks, soap and antimicrobial<br />
hand rubs are conveniently placed to encourage regular<br />
use. Watches and jewellery (including dress rings<br />
and wrist adornments) must be removed at the beginning<br />
of each clinical session, before regular hand decontamination<br />
begins. Cuts and abrasions must be covered with<br />
waterproof dressings, which must be changed as appropriate.<br />
Staff with dermatitis, psoriasis or other skin<br />
conditions should consult with the Occupational Health<br />
Department for further advice.<br />
Ó 2008 The Authors<br />
1028 Journal compilation Ó 2008 The Association of Anaesthetists of Great Britain and Ireland
Anaesthesia, 2008, 63, pages 1027–1036<br />
Infection control in anaesthesia<br />
.....................................................................................................................................................................................................................<br />
The Code of Practice states that policies should be<br />
directly tied to the clinical governance framework and<br />
regularly reviewed under a system of audit, revision and<br />
update.<br />
Gloves<br />
It is important to undertake a risk assessment regarding<br />
the safe use of gloves. Although they may offer some<br />
protection against inoculation with blood-borne viruses,<br />
incorrect use of gloves could actually spread infection<br />
between patients.<br />
Sterile gloves must be worn for invasive procedures and<br />
contact with sterile sites. Non-sterile examination gloves<br />
must be worn for contact with mucous membranes, nonintact<br />
skin and all activities that carry a risk of exposure to<br />
blood, body fluids, secretions and excretions. All blood<br />
and body fluids, substances, secretions and excretions may<br />
be considered to be potentially infective regardless of the<br />
perceived risk of the source.<br />
Gloves must be worn as single-use items. They should<br />
be put on immediately before an episode of patient<br />
contact and removed as soon as the activity is completed,<br />
and before contact with fomites, including curtains, pens,<br />
clinical notes, keyboards and telephones. Gloves should<br />
be changed between patients and between different<br />
procedures on the same patient. Gloves must be disposed<br />
of as clinical waste and hands should be washed or<br />
decontaminated following the removal of gloves. It has<br />
been demonstrated that 98% of anaesthetists’ contact with<br />
patients’ blood could be prevented by routine use of<br />
gloves [6].<br />
Gloves of an acceptable quality must be available in all<br />
clinical areas. Latex-free gloves must be available for use<br />
for staff or patients who have an allergy or sensitivity to<br />
rubber gloves.<br />
Facemasks<br />
The use of facemasks to decrease the incidence of<br />
postoperative wound infection has been questioned<br />
[7, 8]. However, masks with a face shield should be<br />
worn when there is a risk of blood, body fluids, secretions<br />
and excretions splashing into the face and eyes. Masks<br />
must also be worn by anaesthetists when carrying out a<br />
sterile procedure under full aseptic conditions (see later).<br />
If worn, masks should not be taken down to speak and<br />
should be changed if they become damp or contaminated.<br />
Masks must only be handled by the ties. Correctly fitting<br />
facemasks may also give some protection to the anaesthetist<br />
against inhaling infected droplets from the respiratory<br />
tracts of patients with infectious respiratory<br />
diseases.<br />
The Working Party is aware that the wearing of masks<br />
remains an area of contention in many Trusts and<br />
conflicting evidence may be cited [9, 10]. In view of<br />
the continuing controversy about the wearing of masks,<br />
the Working Party suggests that local protocols should be<br />
agreed about their use in hospitals.<br />
Theatre caps<br />
Theatre personnel in most UK operating theatres wear<br />
disposable headgear although there is little evidence for<br />
the effectiveness of this practice except for scrub staff in<br />
close proximity to the operating field [11]. However,<br />
theatre caps should be worn in laminar flow theatres<br />
during prosthetic implant operations, and it is the<br />
Working Party’s view that their general use should<br />
continue.<br />
Theatre suits and gowns<br />
The skin of staff working in the operating theatre is a<br />
major source of bacteria that have the potential for being<br />
dispersed into the air. Clean theatre suits should be<br />
available for all staff in theatre. Full body, fluid-repellent<br />
gowns should be worn where there is a risk of extensive<br />
splashing of blood, body fluids, secretions and excretions.<br />
Sterile gowns should be worn when invasive procedures<br />
are undertaken. Disposable plastic aprons are often worn<br />
on wards in situations where there is a risk of physical<br />
soiling of clothing in order to prevent transmission of<br />
infection between patients.<br />
Contaminated clothing should be changed and safely<br />
discarded into an appropriate receptacle at the earliest<br />
opportunity.<br />
There is little evidence to show that wearing surgical<br />
attire outside the theatre and returning to the theatre<br />
without changing increases surgical wound infection<br />
rates. With the widespread move to admission on the<br />
day of surgery, the times when anaesthetists will have to<br />
leave theatre have increased and repeated changing will<br />
impact on theatre efficiency. Local policies must be<br />
developed and reflect the necessity for ‘theatre discipline’<br />
and allay perceived concerns of patients and visitors. Local<br />
policies should be agreed between all theatre users and<br />
Trusts must ensure adequate provision of appropriate<br />
clothing. The DoH guidance on Uniforms and Workwear<br />
[12] also recognises that there is little evidence that<br />
work clothes pose a significant hazard in terms of<br />
increased infection rates.<br />
Shoes and overshoes<br />
Special footwear should be worn in the operating<br />
department and cleaned if contaminated or after every<br />
use. Trusts should ensure that a system for cleaning<br />
theatre footwear is in place in each theatre suite. Plastic<br />
overshoes may increase bacterial contamination of floors<br />
[13] and, in addition, hands become contaminated when<br />
Ó 2008 The Authors<br />
Journal compilation Ó 2008 The Association of Anaesthetists of Great Britain and Ireland 1029
Infection control in anaesthesia Anaesthesia, 2008, 63, pages 1027–1036<br />
.....................................................................................................................................................................................................................<br />
overshoes are put on or removed. Their use is not<br />
recommended.<br />
Movement within the theatre complex<br />
To reduce airborne contamination, general traffic in and<br />
out of the operating theatre itself should be kept to a<br />
minimum. Doors should be kept closed to ensure the<br />
efficiency of the ventilation system.<br />
Moving patients on their beds into the operating<br />
theatre may increase the bacterial count on floors, but it is<br />
claimed that this is of little significance if bed linen is<br />
changed before transfer [14]. All used linen must be<br />
handled safely to minimise the risk of contamination of<br />
the environment and staff. Used bed linen must be<br />
handled with care to reduce the release of small fomite<br />
particles into the air – bed linen should be ‘bagged’ by the<br />
bed or patient trolley. The use of separate trolleys from<br />
ward to transfer area and transfer area to table has not<br />
been shown to have benefit [15] although this practice<br />
continues in many operating areas.<br />
If entering the operating theatre itself, visitors should<br />
change into theatre suits and wear designated footwear.<br />
Order of patients<br />
There should be a written hospital policy requiring<br />
accurate printed theatre lists to be available prior to the<br />
scheduled date. ‘Dirty cases’, i.e. patients likely to disperse<br />
microbes of particular risk to other patients, should be<br />
identified before surgery and theatre staff should be<br />
notified. These patients should be scheduled last on an<br />
operating list to minimise risk. Where this is not possible,<br />
the Hospital Infection Society (HIS) advises that a<br />
plenum-ventilated operating theatre should require a<br />
minimum of 15 min before proceeding to the next case<br />
after a ‘dirty’ operation [16].<br />
The most probable routes for transmission of infection<br />
between successive patients are airborne or on items and<br />
surfaces that have been in contact with the patient.<br />
Appropriate cleaning of the operating theatres between<br />
all patients should be undertaken. Whenever there is<br />
visible contamination with blood or other body materials,<br />
the area must be disinfected with sodium hypochlorite<br />
(according to local protocols) and then cleaned with<br />
detergent and water. Floors of the operating room should<br />
be disinfected at the end of each session.<br />
Safe use and disposal of sharps<br />
Accidental injury has long been recognised as an occupational<br />
hazard in the healthcare setting. Accidental<br />
inoculation with infected blood, however small in<br />
amount, presents a significant risk to anaesthetists.<br />
In the UK, 16% of occupational injuries occurring<br />
in hospitals are attributed to sharps injuries. These are<br />
predominantly caused by needles and are associated<br />
mainly with venepuncture, administration of intravenous<br />
drugs and recapping of needles. These should be<br />
preventable by adhering to national guidelines and agreed<br />
standards [17]:<br />
• Sharps must not be transferred between personnel and<br />
handling should be kept to a minimum.<br />
• Needles must not be bent or broken prior to use or<br />
disposal.<br />
• Needles and syringes must not be disassembled by hand<br />
prior to disposal.<br />
• Needles should not be recapped or resheathed.<br />
• Used sharps must be discarded into an approved sharps<br />
container at the point of use.<br />
• The sharps container should be sealed and disposed of<br />
safely by incineration when about two-thirds full or in<br />
use for more than four weeks, whichever is sooner.<br />
Sharps containers must comply with BS 7320:1990 –<br />
‘Specification for sharps’.<br />
• Blunt aspirating needles should be used for drawing up<br />
drugs.<br />
• Needle protection devices may reduce needlestick<br />
injuries but require further evaluation before widespread<br />
use can be advised.<br />
Preventing contamination of drugs<br />
Drugs and fluids require safe handling by anaesthetists,<br />
who should follow local protocols for preparation and<br />
administration to prevent contamination.<br />
Syringes and needles are sterile, single-use items and,<br />
after entry or connection to a patient’s vascular system<br />
or attachment to infusions, a syringe and needle should<br />
be considered contaminated and used only for that<br />
patient. A syringe must not be used for multiple<br />
patients even if the needle is changed. Before use,<br />
prepared syringes and needles should be stored in a<br />
clean container and syringes capped to avoid contamination.<br />
After use or at the end of the anaesthetic, all<br />
used syringes with needles should be discarded into an<br />
approved sharps container.<br />
Care must be taken when drawing up drugs. Single use<br />
ampoules should be discarded after the required amount<br />
of drug is drawn up and not re-used for subsequent<br />
patients. Ampoules can be kept for identification purposes<br />
and discarded at the end of the list. Multiple-use ampoules<br />
are not recommended.<br />
All infusions, administration sets or items in contact<br />
with the vascular system or other sterile body compartments<br />
are for single-patient use. An aseptic technique<br />
should be used when preparing infusions and breaks ⁄ taps<br />
in lines should be kept to a minimum. Injection ports<br />
should be maintained with a sterile technique, kept free<br />
of blood and covered with a cap when not in use.<br />
Ó 2008 The Authors<br />
1030 Journal compilation Ó 2008 The Association of Anaesthetists of Great Britain and Ireland
Anaesthesia, 2008, 63, pages 1027–1036<br />
Infection control in anaesthesia<br />
.....................................................................................................................................................................................................................<br />
Connections and injection ports in intravenous lines<br />
should be kept to a minimum. Three-way taps should be<br />
avoided if practicable. Needle-free Luer injection devices<br />
should be used to cover exposed female Luer injection<br />
ports. These are easily cleaned before and after drug<br />
administration, do not harbour blood in crevices and also<br />
reduce the need for needles, resulting in a reduction of<br />
needlestick injuries.<br />
infection. ‘Guidance on Decontamination’ prepared by<br />
the MHRA and DoH provides guidelines for the safe<br />
reprocessing of medical devices [19, 20]. It is recommended<br />
that each department identifies a designated<br />
consultant who, in conjunction with the appropriate<br />
bodies in their Trust, will develop specific guidelines for<br />
anaesthetic practice which satisfy national recommendations<br />
and that these practices are audited on a regular basis.<br />
4.0. Anaesthetic equipment and infection<br />
control<br />
Items of anaesthetic equipment may become contaminated<br />
either by direct contact with patients, indirectly via<br />
splashing, by secretions or from handling by staff.<br />
Contamination is not always visible and all used pieces<br />
of equipment must be assumed to be contaminated and<br />
disposed of or, if reusable, undergo a process of decontamination.<br />
The Code of Practice has specific requirements<br />
for the decontamination of surgical equipment<br />
and other equipment used in patient care. There is a need<br />
to designate a person who is responsible for ensuring<br />
equipment cleanliness.<br />
Single-use equipment<br />
Where appropriate, single-use disposable equipment will<br />
remove the difficulties of re-use and decontamination<br />
procedures. The use of such equipment is to be encouraged.<br />
However, there are problems of cost, storage and<br />
disposal of single-patient use devices, and for some<br />
equipment there is no feasible disposable alternative.<br />
The balance between single-use items and re-usable<br />
equipment will require local determination based on an<br />
assessment of patient safety, the available facilities and cost.<br />
Packaging should not be removed until the point of use for<br />
infection control, identification, traceability in the case of<br />
a manufacturer’s recall, and safety.<br />
A multidisciplinary research team at the University of<br />
Nottingham has carried out a study investigating the use<br />
and re-use of single-use devices in English NHS operating<br />
theatres. The published paper clarified some of the issues<br />
around single-use devices such as single-use equipment<br />
that must be immediately discarded after use, e.g. suction<br />
catheters, and some that may be re-used in the same<br />
patient in the same episode, e.g. disposable laryngoscope<br />
blades [18].<br />
Decontamination<br />
Decontamination is a combination of processes including<br />
cleaning, disinfection and ⁄ or sterilisation used to make a<br />
re-usable item safe to be handled by staff and safe for<br />
further use on patients. Effective decontamination of<br />
re-usable devices is essential in reducing the risk of<br />
Decontamination processes<br />
Cleaning – removal of foreign material from an item.<br />
This usually involves washing with a detergent to remove<br />
contamination followed by rinsing and drying. All<br />
organic debris, e.g. blood, tissue or body fluids, must be<br />
removed before disinfection or sterilisation, as its presence<br />
will inhibit disinfectant or sterilant from contacting<br />
microbial cells. Cleaning before sterilisation is of the<br />
utmost importance in the effectiveness of decontamination<br />
procedures in reducing the risk of transmission of<br />
prions.<br />
Low Level Disinfection – kills most vegetative bacteria<br />
(except TB and endospores), some fungi and some viruses<br />
using disinfectants such as sodium hypochlorite, 70%<br />
alcohol and chlorhexidine.<br />
High Level Disinfection – kills vegetative bacteria (not<br />
all endospores), fungi and viruses. With sufficient contact<br />
time (often several hours), these high level disinfectants<br />
may produce sterilisation, e.g. the use of aldehydes,<br />
peracetic acid and chlorine dioxide.<br />
Sterilisation – A process used to render an object free<br />
from viable micro-organisms, including all bacteria,<br />
spores, fungi and viruses, with techniques such as<br />
autoclaving (but see prions later).<br />
Risk assessment<br />
The choice of equipment and ⁄ or the level of cleanliness<br />
⁄ disinfection ⁄ sterility required of re-usable items may<br />
be assessed against the risk posed to patients of transmission<br />
of infection during any procedure in which the<br />
equipment is employed. It has been proposed by the<br />
MHRA Microbiology Advisory Committee that three<br />
levels should be considered:<br />
1 High Risk – the device will penetrate skin or<br />
mucous membranes, enter the vascular system or a<br />
sterile space – these devices require sterilisation.<br />
2 Intermediate Risk – the device will be in contact<br />
with intact mucous membranes or may become<br />
contaminated with readily transmissible organisms –<br />
these devices require high level disinfection or<br />
sterilisation.<br />
Ó 2008 The Authors<br />
Journal compilation Ó 2008 The Association of Anaesthetists of Great Britain and Ireland 1031
Infection control in anaesthesia Anaesthesia, 2008, 63, pages 1027–1036<br />
.....................................................................................................................................................................................................................<br />
3 Low Risk – the device contacts intact skin or does not<br />
contact patient directly – these devices require low<br />
level disinfection or cleaning.<br />
Infection control policy<br />
Anaesthetic face masks<br />
Although normally in contact with intact skin, these<br />
items are frequently contaminated by secretions from<br />
patients and have been implicated in causing crossinfection<br />
[21]; local disinfection is not normally effective<br />
. These items should be single-use items or should<br />
be sterilised between patients by an audited Sterile<br />
Supplies Department in accordance with the manufacturer’s<br />
instructions.<br />
Airways and tubes<br />
Oral airways, nasal airways and tracheal tubes should be<br />
of single-use type since they readily become contaminated<br />
with transmissible organisms [22] and blood [23].<br />
Ideally, supraglottic airways should be of the singlepatient<br />
use type but the re-usable design is in common<br />
use and many anaesthetists perceive it as being less<br />
traumatic. Therefore, a supraglottic airway designed for<br />
repeated use should be sterilised (in an audited SSD) no<br />
more often than the manufacturer recommends. A<br />
supraglottic airway used for tonsillectomy or adenoidectomy<br />
should not be used again (see section on Prion<br />
Diseases). The AAGBI recommends single-use supraglottic<br />
airways.<br />
Catheter mounts – angle pieces<br />
It is recommended that these items are single-patient use<br />
type.<br />
Anaesthetic breathing systems<br />
The AAGBI has previously recommended that ‘an<br />
appropriate filter should be placed between the patient<br />
and the breathing circuit (a new filter for each patient)’.<br />
Although it appears that pleated hydrophobic filters<br />
have a better filtration performance than most electrostatic<br />
filters, the clinical relevance of this has yet to be<br />
established [24, 25]. The MHRA have also warned of the<br />
difficulty in assessing the performance of breathing filters<br />
in MDA ⁄ 2004 ⁄ 013.<br />
Until 2001 manufacturers of disposable anaesthetic<br />
breathing circuits supplied these as non-reusable items. In<br />
practice, most UK departments of anaesthesia used these<br />
circuits for more than one patient or for more than one<br />
operating session in conjunction with the use of a new<br />
filter for each patient. In 2006, the MHRA re-emphasised<br />
in Devices Bulletin DB 2006(04) the clinical and legal<br />
implications of re-use of devices labelled for single use and<br />
the AAGBI firmly supports their recommendations.<br />
Therefore, departments may follow the manufacturer’s<br />
recommendations for use for up to 7 days. However, to<br />
ensure consistency in the infection control process, the<br />
Working Party recommends that circuits are disposed of<br />
when the anaesthetic machine and monitors are cleaned<br />
(see below). The AAGBI recommends that anaesthetic<br />
circuits are routinely changed on a daily basis. If<br />
visibly contaminated or used for highly infectious cases,<br />
e.g. tuberculosis, the circuits should be changed between<br />
patients and safely discarded. No attempt should be made<br />
to reprocess these items.<br />
Anaesthetic machines<br />
Routine daily sterilisation or disinfection of internal<br />
components of the anaesthetic machine is not necessary if<br />
a bacterial ⁄ viral filter is used between patient and circuit.<br />
However, manufacturers’ cleaning and maintenance policies<br />
should be followed, and bellows, unidirectional<br />
valves and carbon dioxide absorbers should be cleaned<br />
and disinfected periodically. All the surfaces of anaesthetic<br />
machines and monitors should be cleaned on a daily basis<br />
with an appropriate disinfectant or immediately if visibly<br />
contaminated.<br />
Laryngoscopes<br />
As with anaesthetic facemasks, laryngoscopes are known<br />
to become contaminated during use. Current practices<br />
for decontamination and disinfection between<br />
patients are frequently ineffective, leaving residual<br />
contamination that has been implicated as a source of<br />
cross-infection [26, 27]. Blades are also regularly<br />
contaminated with blood [28], indicating penetration<br />
of mucous membranes, which places these items into a<br />
high-risk category. Proper cleaning of laryngoscope<br />
blades is of great importance before decontamination<br />
⁄ sterilisation, particularly of residue around light<br />
sources or articulated sections. New purchases should<br />
be of a design that is easy to clean. Although repeated<br />
autoclaving may affect the function of laryngoscopes<br />
[29], the Working Party recommends that re-usable<br />
laryngoscope blades should be sterilised by an audited<br />
SSD between patients, following the manufacturers’<br />
instructions. Plastic sheaths may be used to cover blades<br />
and handles to reduce contamination but it has been<br />
noted, especially with blade covers, that these have<br />
created difficulties during tracheal intubation.<br />
There are an increasing number of inexpensive, singleuse<br />
laryngoscope blades and handles of improving design<br />
available, and their use is to be encouraged. The choice of<br />
blade must be dictated by Departments of Anaesthesia.<br />
Ó 2008 The Authors<br />
1032 Journal compilation Ó 2008 The Association of Anaesthetists of Great Britain and Ireland
Anaesthesia, 2008, 63, pages 1027–1036<br />
Infection control in anaesthesia<br />
.....................................................................................................................................................................................................................<br />
Traditional blades should be available at all times in case<br />
difficulty is encountered.<br />
Laryngoscope handles also become contaminated with<br />
micro-organisms and blood during use, and they should<br />
be washed ⁄ disinfected and, if suitable, sterilised by SSDs<br />
after every use. The knurled handles of laryngoscopes<br />
cannot be cleaned reliably manually if covered in blood or<br />
body fluids.<br />
Anaesthetists should show great care when handling<br />
laryngoscopes: wear gloves during intubation and place<br />
used instruments in a designated receptacle to prevent<br />
contamination of surfaces, pillows and drapes.<br />
Fibreoptic bronchoscopes<br />
These are expensive items which cannot be autoclaved.<br />
Decontamination is dependent on sufficient contact time<br />
with high level disinfectants and it is particularly important<br />
that the washing and cleaning process removes all<br />
tissue residues from the lumens. Decontamination is best<br />
achieved with an automated system. National guidelines<br />
for care of these instruments have been provided by the<br />
MDA, now the MHRA, DoH and NHS Estates [18, 30,<br />
31, and 32].<br />
With the uncertainty of the future implications of<br />
variant Creutzfeld Jakob Disease (CJD), these items<br />
should have a unique identifier which should be recorded<br />
at every use to permit future tracing.<br />
Bougies<br />
Re-use of these items has been associated with crossinfection<br />
[33]. Manufacturers recommend that a gum<br />
elastic bougie may be disinfected up to five times between<br />
patients and stored in a sealed packet. It is preferable that<br />
alternative single-use intubation aids are employed when<br />
possible.<br />
Surfaces<br />
The surfaces of anaesthetic machines and monitoring<br />
equipment, especially those areas which are likely to<br />
have been touched by the gloved hand that has been in<br />
contact with blood or secretions, should be regarded as<br />
contaminated and should be cleaned at the earliest<br />
opportunity, probably between patients. Local policies<br />
should be in place to ensure that all equipment that<br />
touches intact skin, or does not ordinarily touch the<br />
patient at all, is cleaned with a detergent at the end<br />
of the day or whenever visibly contaminated. This<br />
includes non-invasive blood pressure cuffs and tubing,<br />
pulse oximeter probes and cables, stethoscopes,<br />
electrocardiographic cables, blood warmers etc., and<br />
the exterior of anaesthetic machines and monitors.<br />
Items such as temperature probes should be for single<br />
patient use.<br />
Oxygen masks and tubing<br />
Single-patient use products should be used.<br />
Resuscitation equipment<br />
Single-patient use equipment should be kept in a sealed<br />
package or should be resterilised between patients<br />
according to the manufacturer’s instructions. All training<br />
equipment should be handled similarly.<br />
5.0. Prion diseases<br />
Transmissible Spongiform Encephalopathies (TSEs) are a<br />
group of illnesses in which there is progressive neurological<br />
degeneration associated with characteristic pathological<br />
changes. TSEs are caused by abnormal prions,<br />
which are infectious proteins. Microscopic traces of<br />
tissue often remain on surgical instruments after washing<br />
and autoclaving or disinfecting and any prion protein in<br />
these traces could still transmit the disease if inoculated<br />
into another patient. However, successive washing after<br />
use reduces the concentration so that, after about 10<br />
decontamination cycles, infectivity becomes negligible<br />
[34].<br />
Variant Creutzfeldt-Jakob disease (vCJD) is a TSE<br />
caused by the same prion protein that causes Bovine<br />
Spongiform Encephalopathy (BSE) in cattle. After an<br />
incubation period of several years, the disease shows itself<br />
as a progressive degeneration of the brain leading to<br />
death. It is similar to sporadic CJD, which has been spread<br />
by neurosurgical instruments, dura mater grafts and<br />
pituitary extracts. However, while sporadic CJD prion<br />
protein is to be found only in brain, spinal cord and<br />
posterior eye, the prion protein of vCJD can also be<br />
found in lymph nodes, appendix and tonsils. Prion<br />
protein becomes detectable in tissues in the later period<br />
of incubation and is present in higher concentrations once<br />
the disease becomes manifest [34]. Advice on the<br />
detection and prevention of prion diseases is available<br />
from the Advisory Committee on Dangerous Pathogens<br />
(ACDP), the Spongiform Encephalopathy Advisory<br />
Committee (SEAC) and the National Institute for Health<br />
and Clinical Excellence [35]. The CJD Incidents Panel<br />
Advice advises on the prevention of transmission of CJD<br />
in specific cases [36, 37].<br />
Tonsillectomy and adenoidectomy<br />
Lymphoid tissue, including that of the adenoid and tonsil,<br />
is of ‘medium infectivity’ for vCJD and it is possible that a<br />
patient undergoing surgery could be incubating this<br />
disease. Surgeons routinely operate with traceable reusable<br />
instruments in accord with latest national advice,<br />
since single-use instruments were associated with excessive<br />
bleeding and risks of CJD transfer are low [38].<br />
Ó 2008 The Authors<br />
Journal compilation Ó 2008 The Association of Anaesthetists of Great Britain and Ireland 1033
Infection control in anaesthesia Anaesthesia, 2008, 63, pages 1027–1036<br />
.....................................................................................................................................................................................................................<br />
Tracheal tubes, supraglottic airways and oral airways<br />
should be destroyed after use for these operations as they<br />
can be contaminated by infectious tissue and batch<br />
cleaning may cause transfer of protein from one device<br />
to another [39].<br />
Theoretically, a laryngoscope blade used at the end of<br />
surgery or for emergency re-intubation could become<br />
contaminated. However, the Working Party’s estimate is<br />
that the risk is extremely small and probably less than<br />
those posed by the use of a disposable laryngoscope for<br />
what could be a difficult laryngoscopy. Therefore, the<br />
recommendation is that single-use laryngoscopes are<br />
not mandatory in anaesthesia for tonsil and adenoid<br />
surgery. Those purchasing laryngoscopes with single-use<br />
blades (and other single-use devices) have a responsibility<br />
to ensure that the performance of the instruments is at<br />
least as good as that of the standard reusable alternatives.<br />
Anaesthetic management of cases of CJD<br />
This advice covers known cases, suspected cases and those<br />
who are at risk of developing CJD. Isolation is not<br />
needed. Standard (‘universal’) precautions are essential.<br />
Blood and other samples should be labelled ‘Biohazard’.<br />
Invasive procedures such as central venous cannulation<br />
and spinal anaesthesia mandate the use of full aseptic<br />
procedures, including mask and eye protection. The area<br />
around where invasive procedures are performed should<br />
be clear enough to allow easy mopping of spillages. High<br />
infectivity tissues are those in the brain, spinal cord and<br />
posterior eye; medium risk tissues for CJD are those in the<br />
anterior eye and olfactory epithelium – any needles or<br />
probes used by anaesthetists near these tissues will be<br />
disposable. In vCJD, lymphoid tissue is also classed as<br />
having medium infectivity. In these circumstances, it is<br />
advisable that any laryngoscope used after the tonsil has<br />
been operated on or any bronchoscope used for biopsy on<br />
patients in this group should be treated as potentially<br />
contaminated. These instruments should either be<br />
destroyed (easily done with single-use laryngoscopes) or<br />
should be quarantined pending advice. Such advice can<br />
be obtained from the CJD Incidents Panel.<br />
Transmission of vCJD by transfusion of blood<br />
and blood products<br />
Although only three cases have been discovered, this is<br />
the only route of transfer of vCJD as yet shown to be<br />
from medical interventions. The National Blood Transfusion<br />
Service repeatedly updates its procedures so as to<br />
reduce the tiny risk of transfer of prions, viruses and<br />
bacteria [40]. Procedures include leucodepletion and<br />
sourcing most plasma products from outside the UK.<br />
Anaesthetists can further decrease the risk by minimising<br />
the use of blood and blood products.<br />
Summary: how to reduce the risk of transmission<br />
of prion disease<br />
1 Adherence to the same universal precautions as for<br />
other potential infections.<br />
2 Minimising the use of transfusion of blood and blood<br />
products.<br />
3 Use of SSD decontamination and sterilisation with<br />
tracing for all reusable equipment.<br />
4 Ensuring that any instrument that contacts the brain,<br />
spinal cord or dura is destroyed afterwards.<br />
5 The employment of single-use equipment when this is<br />
as reliable and safe as the re-usable alternatives.<br />
6 Destroying or quarantining instruments used on cases<br />
who may have CJD and for those known to be at risk.<br />
7 Ensuring that all airway devices used during tonsillectomy<br />
and adenoidectomy are discarded after use.<br />
6.0. Infection control precautions for<br />
anaesthetic procedures<br />
Carrying out procedures in an operating theatre does not<br />
pose a lower risk of infection than other hospital locations<br />
and the risk of infection depends on the procedure and on<br />
the level of barrier protection rather than the surrounding<br />
environment [41].<br />
Maximal barrier precautions<br />
Maximal barrier precautions involve full hand washing,<br />
the wearing of sterile gloves and gown, a cap, mask and<br />
the use of a large sterile drape [42]. The skin entry site<br />
should be cleaned with an alcoholic chlorhexidine<br />
gluconate solution or alcoholic povidone-iodine solution<br />
[43]. The antiseptic should be allowed to dry before<br />
proceeding.<br />
Certain invasive anaesthetic procedures require this<br />
optimum aseptic technique:<br />
• Insertion of central venous catheters.<br />
• Spinal, epidural and caudal procedures.<br />
The Working Party is aware that many anaesthetists do<br />
not employ this level of asepsis for ‘one-shot’ spinals or<br />
epidurals but believes that, when central neural spaces are<br />
penetrated, full aseptic precautions are required.<br />
Comprehensive guidelines have been prepared for<br />
insertion and maintenance of central venous catheters<br />
[44] and are commended to all anaesthetists. The use of<br />
care bundles has been advocated by IHI (Institute of<br />
Health Improvement) to reduce catheter related bacteraemias.<br />
Originally developed in the USA, Care Bundles<br />
is an approach that systematically appraises clinical<br />
processes. It is based on measuring the actual provision<br />
of therapeutic interventions according to standards,<br />
informed by evidence, which local clinicians set themselves<br />
[45].<br />
Ó 2008 The Authors<br />
1034 Journal compilation Ó 2008 The Association of Anaesthetists of Great Britain and Ireland
Anaesthesia, 2008, 63, pages 1027–1036<br />
Infection control in anaesthesia<br />
.....................................................................................................................................................................................................................<br />
Other barrier precautions<br />
Certain invasive procedures do not require full barrier<br />
precautions as above but nevertheless demand appropriate<br />
aseptic techniques. Such precautions involve the wearing<br />
of sterile gloves and use of small drapes, although similar<br />
attention is required to hand washing and skin preparation.<br />
These procedures include:<br />
• Peripheral regional blocks.<br />
• Arterial line insertion.<br />
Peripheral venepuncture or intramuscular injection in<br />
low-risk patients will involve handwashing, non-sterile<br />
gloves and skin preparation with propyl alcohol. Peripheral<br />
intravenous catheters are a significant source of<br />
nosocomial bacteraemias and care is required.<br />
High-risk patients<br />
Certain patients may be especially vulnerable to infection,<br />
e.g. the immunocompromised, or offer particularly high<br />
risk of transmitting infection, e.g. tuberculosis and HIV.<br />
For the immunocompromised, maximal barrier precautions<br />
are required for all invasive procedures and similarly,<br />
where there is a high infection risk, staff should concentrate<br />
not only on preventing cross-infection between<br />
patients but in protecting themselves by ensuring compliance<br />
with all precautions.<br />
7.0. References<br />
1 DoH The Health Act 2006. Code of Practice for the Prevention<br />
and Control of Health Care Associated Infections.<br />
2 National Association of Theatre Nurses. Universal Precautions<br />
and Infection Control in the Peri-Operative Setting. Harrogate:<br />
NATN, 1997.<br />
3 Stone SP, Teare L, Cookson BD. The evidence for hand<br />
hygiene. Lancet 2001; 357: 479–80.<br />
4 Pittet D, Hugonnet S, Harbarth S, et al. Effectiveness of a<br />
hospital wide programme to improve compliance with hand<br />
hygiene. Lancet 2000; 356: 1307–12.<br />
5 Teare L, Cookson B, Stone S. Hand hygiene. British Medical<br />
Journal 2001; 323: 411–12.<br />
6 Kristensen M, Sloth E, Jensen TK. Relationship<br />
between anaesthetiprocedure and contact of anesthesia<br />
personnel with patient body fluids. Anesthesiology 1990; 73:<br />
619–24.<br />
7 Orr NW. Is a mask necessary in the operating theatre? Annals<br />
of the Royal College of Surgeons of England 1981; 63: 390–2.<br />
8 Mitchell NJ, Hunt S. Surgical face masks in modern<br />
operating rooms – a costly and unnecessary ritual? Journal of<br />
Hospital Infection 1991; 18: 239–42.<br />
9 McLure HA, Tallboys CA, Yentis SM, Azadian BS. Surgical<br />
face masks and downward disposal of bacteria. Anaesthesia<br />
1998; 53: 624–6.<br />
10 Philips BJ, Ferguson S, Armstrong P, Anderson P, Anderson<br />
FM, Wildsmith JAW. Surgical face masks are effective in<br />
reducing bacterial contamination caused by dispersal from<br />
the upper airway. British Journal of Anaesthesia 1992; 69:<br />
407–8.<br />
11 Humphreys H, Russell AJ, Marshall RJ, Ricketts VE, Reeves<br />
DS. The effect of surgical theatre headgear on bacterial counts.<br />
Journal of Hospital Infection 1991; 19: 175–80.<br />
12 DoH Uniforms and Workwear. An Evidence Base for<br />
Developing Local Policy, Department of Health, 2007.<br />
13 Humphreys H, Marshall RJ, Ricketts UE, Russell AJ,<br />
Reeves DG. Theatre overshoes do not reduce operating<br />
theatre floor bacterial counts. Journal of Hospital Infection 1991;<br />
17: 117–23.<br />
14 Litsky BY, Litksy W. Bacterial shedding during bedstripping<br />
of reusable and disposable linens as detected by the<br />
high volume air sampler. Health Laboratory Science 1971; 8:<br />
29–34.<br />
15 Lewis DA, Weymond G, Nokes CM, et al. A bacteriological<br />
study of the effect on the environment of using a one or two<br />
trolley system in theatre. Journal of Hospital Infection 1990; 15:<br />
35–53.<br />
16 Hospital Infection Society: Behaviours and Rituals in the<br />
Operating Theatre – A Report from the Hospital Infection Society<br />
Working Group on Infection Control in Operating Theatres.<br />
Hospital Infection Society, 2002.<br />
17 Health Service Advisory Committee. Safe disposal of clinical<br />
waste. Sheffield HSE, 1999; 68.<br />
18 Rowley E, Dingwall R. The use of single-use devices in<br />
anaesthesia: balancing the risks to patient safety. Anaesthesia<br />
2007; 62: 569–74.<br />
19 Sterilisation, disinfection and cleaning of medical equipment.<br />
Guidance on decontamination from the Microbiology<br />
Advisory Committee to Department of Health Medical<br />
Devices Agency MDA. London 2002, 2005, 2006.<br />
20 NHS Decontamination Programme. Department of Health<br />
(UK). http://www.dh.gov.uk/en/Managingyourorganisation/<br />
Leadershipandmanagement/Healthcareenvironment/<br />
NHSDecontaminationProgramme/index.htm (accessed 15<br />
July 2008).<br />
21 MacCallum FO, Noble WC. Disinfection of anaesthetic face<br />
masks. Anaesthesia 1960; 15: 307.<br />
22 Miller DH, Youkhana I, Karunaratne WU, Pearce A. Presence<br />
of protein deposits on cleaned re-usable anaesthetic equipment.<br />
Anaesthesia 2001; 56: 1069–72.<br />
23 Chrisco JA, Devane G. A descriptive study of blood in the<br />
mouth following routine oral endotracheal intubation.<br />
Journal of American Association of Nurse Anesthetists 1992; 60:<br />
379–83.<br />
24 Wilkes AR. Breathing system filters. British Journal of<br />
Anaesthesia. CEPD Review. 2002; 2: 151–4.<br />
25 Wilkes AR, Benbough JE, Speight SE, Harmer M.<br />
The bacterial and viral filtration performance of breathing<br />
system filters. Anaesthesia 2002; 55: 458–65.<br />
26 Ballin MS, McCluskey A, Maxwell S, Spilsbury S.<br />
Contamination of laryngoscopes. Anaesthesia 1999; 54:<br />
1115–6.<br />
27 Esler MD, Baines LC, Wilkinson DJ, Langford RM.<br />
Decontamination of laryngoscopes: a survey of national<br />
practice. Anaesthesia 1999; 54: 587–92.<br />
Ó 2008 The Authors<br />
Journal compilation Ó 2008 The Association of Anaesthetists of Great Britain and Ireland 1035
Infection control in anaesthesia Anaesthesia, 2008, 63, pages 1027–1036<br />
.....................................................................................................................................................................................................................<br />
28 Phillips RA, Monaghan WP. Incidence of visible and<br />
occult blood on laryngoscope blades and handles. Journal<br />
of American Association of Nurse Anesthetists 1997; 65: 241–6.<br />
29 Bucx MJ, Veldman DJ, Beenhakker MM, Koster R. The<br />
effect of steam sterilisation at 134°C on light intensity<br />
provided by fibrelight Macintosh laryngoscopes. Anaesthesia<br />
1999; 54: 875–8.<br />
30 Device Bulletin DB2002 (05) Decontamination of<br />
Endoscopes. London: MDA, 2002.<br />
31 Transmissible spongiform encephalopathy agents: safe<br />
working and the prevention of infection, annex F<br />
(Decontamination of endoscopes, amended 2005). Advisory<br />
Committee of Dangerous Pathogens and Spongiform<br />
Encephalopathy Advisory Committee. http://www.<br />
advisorybodies.doh.gov.uk/acdp/tseguidance/index.htm<br />
(accessed 15 July 2008).<br />
32 HTM 2030, Washer Disinfectors. London: NHS Estates, 1997.<br />
The Stationary Office.<br />
33 Jerwood DC, Mortiboy D. Disinfection of gum elastic<br />
bougies. Anaesthesia 1995; 50: 376.<br />
34 Transmissible spongiform encephalopathy agents. safe<br />
working and the prevention of infection. Guidance from the<br />
(updated website): http://www.advisorybodies.doh.gov.uk/<br />
acdp/tseguidance/index.htm (accessed 15 July 2008).<br />
35 Patient safety and the reduction of risk of transmission of<br />
Creutzfeldt-Jakob disease (CJD) via interventional procedures.<br />
National Institute for Health and Clinical Excellence<br />
interventional procedure guidance 196, available via the<br />
NICE website: http://www.nice.org.uk (accessed 15 July<br />
2008).<br />
36 Health Protection Agency CJD Panel: information and<br />
advice. http://www.hpa.org.uk/infections/topics_az/cjd/<br />
incidents_panel.htm (accessed 15 July 2008).<br />
37 CJD Incidents Panel Fifth Annual Report to the<br />
Advisory Committee on Dangerous Pathogens on Transmissible<br />
Spongiform Encephalopathies (2006): website as<br />
above.<br />
38 Re-introduction of Re-usable instruments for tonsil surgery.<br />
Press release from the UK Department of Health, 14<br />
December 2001.<br />
39 Richards E, Brimacombe J, Laupau W, Keller C. Protein<br />
cross-contamination during batch cleaning and autoclaving<br />
of the ProSeal TM laryngeal mask airway. Anaesthesia 2006;<br />
61: 431–3.<br />
40 Current information from the UK and Scottish blood<br />
transfusion services. http://www.blood.co.uk/hospitals/<br />
library and http://www.scotblood.co.uk (accessed 15 July<br />
2008).<br />
41 Pearson ML Hospital Infection Control Practices Advisory<br />
Committee. Guidelines for prevention of intravascular<br />
device related infections. Infection Control and Hospital<br />
Epidemiology 1994; 15, 227–30.<br />
42 Fletcher SJ, Bodenham AR. Catheter-related sepsis:<br />
an overview. British Journal of Intensive Care 1999; 9: 74–80.<br />
43 Maki DG, Ringer M, Alvacado CJ. Prospective<br />
randomised trial of providone-iodine, alcohol, and<br />
chlorhexidine for prevention of infection associated with<br />
central venous and arterial catheters. Lancet 1991; 338:<br />
339–43.<br />
44 Pratt RJ, Pellowe C, Loveday HP, et al. The Epic Project –<br />
Guidelines for preventing infections associated with the<br />
insertion and maintenance of central venous catheters. Journal<br />
of Hospital Infection 2001; 47: (Suppl) S47–67.<br />
45 Implement the central line bundle. http://www.ihi.org/<br />
IHI/Topics/CriticalCare/IntensiveCare/Changes/<br />
ImplementtheCentralLineBundle (accessed 15 July 2008).<br />
Ó 2008 The Authors<br />
1036 Journal compilation Ó 2008 The Association of Anaesthetists of Great Britain and Ireland
21 Portland Place, London W1B 1PY<br />
Telephone: 020 7631 1650<br />
Fax: 020 76314352<br />
E-mail: info@<strong>aagbi</strong>.org<br />
Website: www.<strong>aagbi</strong>.org
AAGBI SAFETY GUIDELINE<br />
Interhospital Transfer<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland,<br />
21 Portland Place, London W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org<br />
February 2009
MEMBERSHIP OF THE WORKING PARTY<br />
Dr D Goldhill<br />
Dr L Gemmell<br />
Dr D Lutman<br />
Dr S McDevitt<br />
Dr M Parris<br />
Dr C Waldmann<br />
Dr C Dodds<br />
Chairman, Consultant Anaesthetist,<br />
Royal National Orthopaedic Hospital<br />
Honorary Secretary Elect, AAGBI<br />
Consultant Anaesthetist, Great<br />
Ormond St Hospital<br />
Council Member, AAGBI<br />
Group of Anaesthetists in Training<br />
Consultant Anaesthetist, Royal<br />
Berkshire Hospital<br />
Royal College of Anaesthetists<br />
Ex-Officio<br />
Dr D K Whitaker<br />
Dr R J S Birks<br />
Dr I H Wilson<br />
Dr A W Harrop-Griffiths<br />
Dr I G Johnston<br />
Dr D G Bogod<br />
President<br />
President Elect<br />
Honorary Treasurer<br />
Honorary Secretary<br />
Honorary Membership Secretary<br />
Editor-in-Chief, Anaesthesia<br />
© Copyright of the Association of Anaesthetists of Great Britain and Ireland.<br />
No part of this book may be reproduced without the written permission of the AAGBI.
CONTENTS<br />
Section 1 Recommendations ..............................................................2<br />
Section 2<br />
Section 3<br />
Section 4<br />
Section 5<br />
Section 6<br />
Section 7<br />
Section 8<br />
Section 9<br />
Background..........................................................................3<br />
Introduction.........................................................................4<br />
The decision to transfer........................................................5<br />
Stabilisation before transfer..................................................7<br />
Accompanying the patient...................................................8<br />
Monitoring, drugs and equipment......................................10<br />
The ambulance..................................................................11<br />
Documentation and handover............................................13<br />
Appendix ..........................................................................................14<br />
References ..........................................................................................15<br />
1
Section 1<br />
Recommendations<br />
1. Transfer can be safely accomplished even in extremely ill patients.<br />
Those involved in transfers have the responsibility for ensuring that<br />
everything necessary is done to achieve this.<br />
2. The need for transfers between hospitals is likely to increase. Transfers<br />
for non-clinical reasons should only take place in exceptional<br />
circumstances and ideally only during daylight hours.<br />
3. The decision to transfer must involve a senior and experienced<br />
clinician.<br />
4. Hospitals should form transfer networks to coordinate and manage<br />
clinically indicated transfers.<br />
5. Networks should take responsibility for ensuring that arrangements can<br />
be made for accepting transfers to an agreed protocol with minimal<br />
administrative delays.<br />
6. Protocols, documentation and equipment for transfers should be<br />
standardised within networks.<br />
7. All doctors and other personnel undertaking transfers should have the<br />
appropriate competencies, qualifications and experience. It is highly<br />
desirable that this should include attendance at a suitable transfer<br />
course.<br />
8. A professional, dedicated transfer service has many advantages and is<br />
the preferred method of transferring suitable patients.<br />
9. Hospitals must ensure that suitable transfer equipment is provided.<br />
10. Hospitals must ensure that they have robust arrangements to ensure that<br />
sending personnel on a transfer does not jeopardise other work within<br />
the hospital.<br />
11. Hospitals must ensure that employees sent on transfers have adequate<br />
insurance cover and are made aware of the terms and limitations of this<br />
cover.<br />
12. Arrangements must be in place to ensure that personnel and equipment<br />
can safely and promptly return to base after the transfer.<br />
13. Details of every transfer must be recorded and subject to regular audit<br />
and review.<br />
2
Section 2<br />
Background<br />
The AAGBI Council decided to commission a Working Party to produce<br />
guidelines in the usual format of the Association to provide instruction and<br />
help to those arranging transfers and those involved with the actual transfer of<br />
the patients between hospitals.<br />
A large number of interhospital transfers already take place and the number<br />
is likely to increase. Anaesthetists are commonly involved in transferring<br />
the sickest of these patients. This has the potential to affect an Anaesthetic<br />
Department’s budget and ability to maintain a service and on-call rotas.<br />
This document addresses transfers between hospitals, not within a hospital.<br />
However, the principles for the safe movement of patients are also applicable<br />
to transport within a hospital.<br />
3
Section 3<br />
Introduction<br />
In 1997 it was estimated that over 11,000 critically ill patients were transferred<br />
between intensive care units in the UK [1]. The majority of transfers are for<br />
appropriate clinical reasons for patients requiring care not available in the<br />
referring hospital. Such specialist care includes neuroscience, paediatrics,<br />
burns, spinal injury, etc. There is a limited number of paediatric and neonatal<br />
centres with high-level critical care support. Transfer of critically ill children<br />
must be a consideration in any hospital with an emergency department. Many<br />
transfers are undertaken for non-clinical reasons commonly related to the<br />
relative lack of critical care beds. It is government policy that these transfers<br />
should be as few as possible and contained within critical care transfer<br />
groups [2]. A relatively small percentage of patients transferred between<br />
hospitals involve repatriations of patients previously transferred. Patients may<br />
be transferred from the emergency department, critical care units, operating<br />
theatres, wards or other areas of the hospital. Transfers often occur outside of<br />
normal working hours and take place at short notice [3]. During the transfer<br />
the patient is in a noisy, difficult and potentially dangerous environment and<br />
the transferring medical team is operating independently. All hospitals that<br />
may be involved in transfers must ensure that the appropriate personnel,<br />
equipment, training and support are available. In the past, inexperienced<br />
doctors with inadequate training, supervision and equipment carried out<br />
many of the transfers [1,3-5]. Although the situation has improved, in many<br />
regions of the country there are still significant limitations in the process of<br />
arranging and carrying out a transfer.<br />
This booklet should be read in conjunction with ‘Recommendations for the<br />
Safe Transfer of Patients with Brain Injury’ published by the Association of<br />
Anaesthetists in 2006 (http://www.<strong>aagbi</strong>.org/publications/guidelines/docs/<br />
braininjury.pdf). Other guidelines have been published including those from<br />
the Intensive Care Society ([6] available from www.ics.ac.uk). This booklet<br />
is not intended to be an in-depth document on transfer but should be read in<br />
conjunction with these and other guidelines.<br />
4
Section 4<br />
The decision to transfer<br />
It is essential that a systematic approach is taken to the process of patient<br />
transfer; starting with the decision to transfer, through the pre-transfer<br />
stabilisation, and then the management of the transfer itself. This will<br />
encompass all the stages including skilled evaluation, communication,<br />
documentation, monitoring and treatment, handover and return to base.<br />
Education and preparation are central to any safe transfer.<br />
The decision to transfer must not be taken lightly. It has the potential to expose<br />
the patient and transferring staff to additional risk, requires trained personnel,<br />
specialised equipment and a vehicle, and may result in additional expense<br />
and worry for carers and relatives. A senior doctor, normally a consultant,<br />
should therefore be involved in making this decision. Documentation of the<br />
decision should include the name of the doctor making the decision with their<br />
grade and contact details, and the date and time at which the decision was<br />
made. Reasons for the decision should be given including whether it is for<br />
clinical or non-clinical reasons.<br />
Once the decision is made a hospital and medical team must agree to take<br />
the patient. In much of the United Kingdom critical care transfer groups have<br />
been established with a role of co-ordinating and facilitating transfers within<br />
a network. If a critical care bed is required, direct consultant-to-consultant<br />
contact is often the best way to make arrangements. In the appropriate<br />
circumstances and for the right patient many intensive care units are able<br />
to accommodate patients at short notice. However, the further away the<br />
referring hospital and the more tenuous the links, the less responsibility the<br />
accepting hospital is likely to feel. We would therefore strongly advise groups<br />
of hospitals to form networks to facilitate and organise transfers.<br />
Most of the country is covered by bed bureaux such as the Emergency<br />
Bed Service (EBS). They contact critical care units on a regular basis and<br />
are able to provide some indication of the availability of beds. They do<br />
not take responsibility for arranging the transfer and it is still necessary to<br />
negotiate directly with individual units. Once a critical care unit has agreed<br />
to accept a patient it is necessary for the patient’s medical team to arrange<br />
for the appropriate medical speciality in the receiving hospital to take overall<br />
responsibility for the patient during their admission to that hospital.<br />
5
This process may require many telephone calls and take several hours [7].<br />
Streamlining this process should be a responsibility for a transfer network.<br />
The process of arranging the transfer must be documented including the<br />
name, grade and contact details of those making the arrangements both at the<br />
referring and receiving centres, the date and time of calls made and details of<br />
any advice received.<br />
A limited number of retrieval services able to perform transfers exist in the UK,<br />
mainly covering paediatric patients. A professional, dedicated transfer service<br />
has many advantages and is the preferred method of transferring suitable<br />
patients. Networks should aim to fund and develop such teams. Members of<br />
these teams have the training and competencies to undertake transfers; such<br />
teams have appropriate equipment and can work with the ambulance service,<br />
hospitals and other interested parties on protocols and guidelines. They also<br />
ensure that transfers can be safely achieved without compromising the work<br />
of the transferring hospital.<br />
Although these services are extremely welcome they cannot be relied upon<br />
to provide a service at short notice and at all times [8-10]. Every hospital that<br />
may transfer patients must have suitable arrangements in place for providing<br />
transfers. Most transfers are in an ambulance by road. There is an increasing<br />
number of transfers in rotary and fixed wing aircraft. Air transfers confer<br />
additional hazards and expense and require further training [11,12].<br />
6
Section 5<br />
Stabilisation before transfer<br />
Although transfers are potentially associated with additional risk to patients<br />
[13-15], they can be safely accomplished even in extremely ill patients [16-<br />
18]. Generally, a transfer should not be undertaken until the patient has<br />
been resuscitated and stabilised. All hospitals involved in transfers must<br />
ensure that they have appropriate arrangements in place for this. It may be<br />
several hours after the decision to transfer before the transfer can take place.<br />
It may be necessary to secure the airway, and many patients will require<br />
a tracheal tube or tracheostomy with appropriate end-tidal carbon dioxide<br />
monitoring. Appropriate venous access must be in place and monitoring<br />
instituted. Continuous invasive blood pressure measurement is the best<br />
technique for monitoring blood pressure during the transfer of ill patients.<br />
Treatment should not be delayed while waiting for the transfer. The accepting<br />
hospital may be able to provide advice on the immediate management in<br />
specialised situations. A ‘scoop and run’ philosophy is only appropriate on<br />
rare occasions when the urgency of the situation and the need for definitive<br />
treatment will limit the time available for stabilisation before transfer. For<br />
example, transfer of a patient with a leaking aortic aneurysm to a vascular<br />
centre may be time-critical. Even in these situations the transfer should not<br />
begin until essential management and monitoring has been undertaken. It<br />
is good practice to establish the patient on the transport ventilator and other<br />
equipment for a period of time before they are moved.<br />
7
Section 6<br />
Accompanying the patient<br />
A critically ill patient should be accompanied by a minimum of two<br />
attendants. The precise requirement for accompanying personnel will depend<br />
upon the clinical circumstances in each case. The level of a patient’s critical<br />
care dependency provides a guide to the personnel who should accompany<br />
them [19]. A senior doctor, normally a consultant, should take the decision<br />
on who should accompany the patient. Before departure the senior individual<br />
undertaking the transfer should be satisfied with the state of the patient and<br />
all other aspects associated with the transfer. Many patients do not need<br />
anaesthetic support during interhospital transfer.<br />
These patients include:<br />
• patients who are not likely to need airway or ventilatory support<br />
• patients for whom attempting cardiopulmonary resuscitation would<br />
be inappropriate<br />
• patients being transferred for acute definitive management for whom<br />
anaesthesia support will not affect their outcome<br />
Levels of patients’ critical care needs as a guide to transfer requirements.<br />
The decision should be made by a senior doctor [19]<br />
Level 0:<br />
Patients whose needs can be met through normal ward care in an acute<br />
hospital should not usually need to be accompanied by a doctor, nurse or<br />
paramedic.<br />
Level 1:<br />
At risk of their condition deteriorating, or those recently relocated from higher<br />
levels of care and whose needs can be met on an acute ward with additional<br />
advice and support from the critical care team will require a paramedic<br />
ambulance crew and may require a nurse, paramedic and/or medical escort.<br />
Level 2:<br />
Requiring more detailed observation or intervention including support for a<br />
single failing organ system or post-operative care and those stepping down<br />
from higher levels of care must be escorted by competent, trained and<br />
experienced personnel, usually a doctor and a nurse or paramedic.<br />
8
Level 3:<br />
Patients requiring advanced respiratory support alone or basic respiratory<br />
support together with support of at least two organ systems. This level<br />
includes all complex patients requiring support for multi-organ failure. These<br />
patients must be escorted by competent, trained and experienced personnel,<br />
usually a doctor and a nurse or paramedic.<br />
When the request for anaesthetic care during transfer exceeds the Department<br />
of Anaesthesia’s ability to do this safely, decisions about priority and relative<br />
risk may have to be taken. Although the patient would benefit from anaesthesia<br />
management, the issue may be one of either delaying transfer until resources<br />
are available or sending the patient without an accompanying anaesthetist<br />
but with another doctor. Anaesthetic Departments should use interhospital<br />
transfers to provide doctors with training and experience under the direct<br />
supervision of an experienced transfer team.<br />
All individuals involved in the transport of critically ill patients should be<br />
suitably competent, trained and experienced. A competency-based training<br />
curriculum is being developed by the Royal College of Anaesthetists. There<br />
are generic training courses available but consideration should be given to the<br />
development of local Trust and Network training and simulation programmes.<br />
Good communication skills are essential. Each Trust should have a designated<br />
consultant who is responsible for secondary transfers, guideline production<br />
and training and audit.<br />
While safety is of paramount importance during transfer, there is always a<br />
remote possibility of an ambulance being involved in an accident resulting in<br />
death or serious injury to staff. The insurance situation in these circumstances<br />
is complex. It is essential that all members of staff who might be involved<br />
in transporting patients and their employers ensure that adequate financial<br />
arrangements are in place for themselves and their dependents in the event of<br />
an accident and that they are made aware of the terms and limitations of this<br />
cover. In addition, the AAGBI has negotiated insurance for all their members<br />
involved in the transport of critically ill patients. Details of the appropriate<br />
insurance schemes and the cover benefit of membership are available from<br />
the AAGBI (www.<strong>aagbi</strong>.org). The AAGBI also recommends that doctors<br />
involved with the transfer of patients are members of a medical defence<br />
organisation.<br />
9
Section 7<br />
Monitoring, drugs and equipment<br />
Patients with level 1, 2 or 3 critical care needs will require monitoring during<br />
the transfer. Monitoring needs to be established and secure before the transfer<br />
is started. This may require the insertion of central venous lines, arterial lines<br />
and equipment for measuring cardiac output, as well as end-tidal carbon<br />
dioxide monitoring.<br />
The personnel involved in the transfer should ensure that they have adequate<br />
supplies of the necessary drugs. These may include sedatives, analgesics,<br />
muscle relaxants, and inotropes. Many of these drugs are best prepared<br />
beforehand in pre-filled syringes. The patient should be established on the<br />
medication to be used during the transfer before the transfer commences.<br />
As much of the equipment as possible should be mounted at or below the<br />
level of the patient. In particular, large arrays of vertical drip stands should be<br />
avoided. This allows unhindered access to the patient and improves stability of<br />
the patient trolley. All equipment should be robust, durable and lightweight.<br />
Electrical equipment must be designed to function on battery when not<br />
plugged into the mains. Additional batteries should be carried in case of<br />
power failure. Portable monitors should have a clear illuminated display and<br />
be capable of displaying ECG, arterial oxygen saturation, non-invasive blood<br />
pressure, two invasive pressures, capnography and temperature. Non-invasive<br />
blood pressure may rapidly deplete battery power and is unreliable when<br />
there is external movement and vibration. Alarms should be visible as well<br />
as audible in view of the loud background noise levels.<br />
Portable mechanical ventilators should have, as a minimum, disconnection<br />
and high pressure alarms, the ability to supply positive end expiratory pressure<br />
and variable inspired oxygen concentration, inspiratory : expiratory ratio,<br />
respiratory rate and tidal volume. In addition, the ability to provide pressurecontrolled<br />
ventilation, pressure support and continuous positive airway<br />
pressure is desirable. Additional equipment for maintaining and securing the<br />
airway, intravenous access, etc should also be available.<br />
Ideally, all equipment within a Critical Care Network should be standardised<br />
to enable the seamless transfer of patients without, for example, interruption of<br />
drug therapy or monitoring due to incompatibility of leads and transducers.<br />
10
Section 8<br />
The ambulance<br />
The European Committee for Standardisation has published specifications for<br />
ambulances. Private transport services may use Type C mobile ICU vehicles.<br />
These will have 240V AC power, a secure critical care trolley and carry a<br />
ventilator and syringe drivers. It is more usual to request an ambulance from<br />
the local ambulance service to perform the transfer. This is a likely to be a<br />
Type B or equivalent vehicle that has 12V electric sockets, oxygen supply and<br />
limited monitoring and other equipment.<br />
Before transfer it is essential to ascertain what needs to be taken with the<br />
patient to support the transfer. The oxygen supply and battery operated<br />
equipment must be more than sufficient for the anticipated duration of the<br />
transfer. Unless a transfer service is used, everything except the oxygen<br />
supply usually has to be supplied by the transferring hospital. Hospitals<br />
involved in transfers must ensure that the appropriate equipment is available<br />
for likely transfers at all times.<br />
The standard ambulance trolley is ill-suited to patient transfers. Ideally, it<br />
should be able to carry all the equipment including oxygen supply, a ventilator,<br />
syringe drivers, suction and backup batteries. These items should be placed<br />
below the patient, and the trolley should be secured within the ambulance to<br />
allow free access to all sides with a fixation capable of withstanding up to 10<br />
G in all directions. It is not acceptable to place items on the patient’s trolley<br />
or on shelves within the vehicle. Gravity feed drips are unreliable in moving<br />
vehicles. Sufficient syringe or infusion pumps are required to enable essential<br />
fluids and drugs to be delivered. Pumps should preferably be mounted below<br />
the level of the patient and infusion sets fitted with anti-siphon devices.<br />
Portable warm-air devices for maintaining the patient’s temperature can be<br />
useful and can also be mounted on the patient’s trolley.<br />
A major issue relating to safety during transport is the speed of travel. For<br />
the majority of cases high-speed travel is not necessary and the safety of all<br />
passengers and other road users is paramount. Medical personnel present<br />
may offer advice as to the patient’s clinical condition and the speed of travel<br />
but they should be aware of the requirements of the Road Traffic Act in such<br />
cases. The decision to use blue lights and sirens rests with the ambulance<br />
driver. The goal is to facilitate a smooth and rapid transfer with the minimum<br />
acceleration and deceleration. A police escort may be required through<br />
11
heavily congested areas, but not all police authorities provide this service.<br />
Staff should remain seated at all times and wear the seat belts provided. If,<br />
despite meticulous preparation, unforeseen clinical emergencies arise and<br />
the patient requires intervention, this should not be attempted in a moving<br />
ambulance. The vehicle should be stopped appropriately in a safe place and<br />
the patient attended to. Where staff may be required to move outside the<br />
vehicle, high visibility clothing must be worn. On safety issues all staff in the<br />
vehicle must obey the instructions of the crew.<br />
Air transport should be considered for longer journeys where road access is<br />
difficult or when, for other reasons, it may be quicker. Perceived speed of<br />
air transport must be balanced against organisational delays and inter-vehicle<br />
transfers at either end of the journey. Helicopters vary in size, capacity and<br />
range. They generally provide a less comfortable, more cramped environment<br />
than a road ambulance or pressurised fixed wing aircraft. In addition, they are<br />
expensive and have a poorer safety record.<br />
The transport of patients by air presents medical escorts with many problems<br />
unique to this mode of travel. Staff involved in aeromedical transport must<br />
have both a high level of expertise, specialist knowledge and practical training.<br />
Staff without appropriate training should not undertake aeromedical transfers.<br />
Minimum requirements include safety training, evacuation procedures for the<br />
aircraft and basic on-board communication skills (particularly for helicopters).<br />
However, more advanced training in aeromedical transport medicine is<br />
desirable. Training should also address the special physical, physiological<br />
and psychological stresses that are important when flying as well as provide<br />
a detailed knowledge of how medical conditions can be affected by this<br />
environment and the necessary precautions needed to facilitate safe transfer.<br />
12
Section 9<br />
Documentation and handover<br />
Clear records should be maintained at all stages. This is a legal requirement<br />
and should include details of the patient’s condition, reason for transfer,<br />
names of referring and accepting consultants, clinical status prior to transfer<br />
and details of vital signs, clinical events and therapy given during transport.<br />
Standard documentation should be developed across networks and be<br />
used for both intra-hospital and interhospital transport. The clinical record<br />
should briefly summarise the patient’s clinical status before, during and after<br />
transport, including relevant medical conditions, environmental factors and<br />
therapy given. This should include a core data set for audit purposes and the<br />
transport team should be able to retain a duplicate. There should be a process<br />
to investigate specific problems, including delays in transportation.<br />
Clear information should be given to the transport team before departure about<br />
the location of the receiving area for the formal handover of the patient. On<br />
arrival at the receiving hospital, there should be a formal handover between<br />
the transport team and the receiving medical and nursing staff who will<br />
assume responsibility for the patient’s care. Handover should include a verbal<br />
and written account of the patient’s history, vital signs, therapy and significant<br />
clinical events during transport. X-rays, scans and other investigation results<br />
should be described and handed over to receiving staff.<br />
After handover, the transport team is relieved of the duty of care to the patient,<br />
who is now in the medical care of the receiving hospital. This is an important<br />
part of the transfer of care and the status of the patient should be formally<br />
noted by the receiving team. It should be noted that the ambulance crew<br />
or air crew may not always be able to return the transfer team whence they<br />
came. The transfer team should be prepared to return home by taxi or other<br />
appropriate means and therefore thought should be given to clothing, the<br />
amount of equipment to be carried and the means of payment for the return<br />
journey.<br />
13
APPENDIX<br />
1 Departure checklist<br />
Do attendants have adequate competencies, experience, knowledge<br />
of case, clothing, insurance?<br />
Appropriate equipment and drugs?<br />
Batteries checked?<br />
Sufficient oxygen?<br />
Trolley available?<br />
Ambulance service aware or ready?<br />
Bed confirmed? Exact location?<br />
Case notes, X ray films, results, blood collected?<br />
Transfer chart prepared?<br />
Portable phone charged?<br />
Contact numbers known?<br />
Money or cards for emergencies?<br />
Estimated time of arrival notified?<br />
Return arrangements checked?<br />
Relatives informed?<br />
Patient stable, fully investigated?<br />
Monitoring attached and working?<br />
Drugs, pumps, lines rationalised and secured?<br />
Adequate sedation?<br />
Still stable after transfer to mobile equipment?<br />
Anything missed?<br />
14
References<br />
1. Mackenzie PA, Smith EA, Wallace PG. Transfer of adults between<br />
intensive care units in the United Kingdom: postal survey. British<br />
Medical Journal 1997; 314: 1455-6.<br />
2. Department of Health. Comprehensive Critical Care. a review of adult<br />
critical care services. 2000. London, Department of Health.<br />
3. Gray A, Gill S, Airey M, Williams R. Descriptive epidemiology of adult<br />
critical care transfers from the emergency department. Emergency<br />
Medicine Journal 2003; 20: 242-6.<br />
4. Jameson PP, Lawler PG. Transfer of critically ill patients in the Northern<br />
region. Anaesthesia 2000; 55: 489.<br />
5. Spencer C, Watkinson P, McCluskey A. Training and assessment<br />
of competency of trainees in the transfer of critically ill patients.<br />
Anaesthesia 2004; 59: 1248-9.<br />
6. Guidelines for the transport of the critically ill adult. 2002. London,<br />
The Intensive Care Society.<br />
7. Duke GJ, Green JV. Outcome of critically ill patients undergoing<br />
interhospital transfer. The Medical Journal of Australia 2001; 174: 122-<br />
5.<br />
8. Vos GD, Nissen AC, Nieman FH et al. Comparison of interhospital<br />
pediatric intensive care transport accompanied by a referring<br />
specialist or a specialist retrieval team. Intensive Care Medicine 2004;<br />
30: 302-8.<br />
9. Bellingan G, Olivier T, Batson S, Webb A. Comparison of a specialist<br />
retrieval team with current United Kingdom practice for the transport<br />
of critically ill patients. Intensive Care Medicine 2000; 26: 740-4.<br />
10. Belway D, Henderson W, Keenan SP, Levy AR, Dodek PM. Do<br />
specialist transport personnel improve hospital outcome in critically ill<br />
patients transferred to higher centers? A systematic review. Journal of<br />
Critical Care 2006; 21: 8-17.<br />
11. Diaz MA, Hendey GW, Bivins HG. When is the helicopter faster? A<br />
comparison of helicopter and ground ambulance transport times. The<br />
Journal of Trauma 2005; 58: 148-53.<br />
12. Dewhurst AT, Farrar D, Walker C, Mason P, Beven P, Goldstone JC.<br />
Medical repatriation via fixed-wing air ambulance: a review of patient<br />
characteristics and adverse events. Anaesthesia 2001; 56: 882-7.<br />
15
13. Bercault N, Wolf M, Runge I, Fleury JC, Boulain T. Intrahospital<br />
transport of critically ill ventilated patients: a risk factor for ventilatorassociated<br />
pneumonia--a matched cohort study. Critical Care Medicine<br />
2005; 33: 2471-8.<br />
14. Fan E, Macdonald RD, Adhikari NK et al. Outcomes of interfacility<br />
critical care adult patient transport: a systematic review. Critical Care<br />
2005; 10: R6.<br />
15. Waydhas C. Intrahospital transport of critically ill patients. Critical Care<br />
1999; 3: R83-R89.<br />
16. Gebremichael M, Borg U, Habashi NM et al. Interhospital transport of<br />
the extremely ill patient: the mobile intensive care unit. Critical Care<br />
Medicine 2000; 28: 79-85.<br />
17. Penner GE, Brabson TA, Bunk C. Are interfacility ground transports<br />
of patients utilizing intra-aortic balloon pumps safe? Prehospital<br />
Emergency Care 2001; 5: 395-8.<br />
18. Uusaro A, Parviainen I, Takala J, Ruokonen E. Safe long-distance<br />
interhospital ground transfer of critically ill patients with acute severe<br />
unstable respiratory and circulatory failure. Intensive Care Medicine<br />
2002; 28: 1122-5.<br />
19. The Intensive Care Society. Levels of critical care for adult patients.<br />
2002. London, The Intensive Care Society.<br />
16
17
21 Portland Place, London W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
Management of<br />
Anaesthesia for<br />
Jehovah’s Witnesses<br />
2nd edition<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland,<br />
21 Portland Place, London W1B 1PY<br />
Telephone: 020 7631 1650, Fax: 020 7631 4352<br />
E-mail: info@<strong>aagbi</strong>.org Website: www.<strong>aagbi</strong>.org<br />
November 2005
Members of the Working Party<br />
Dr Mike E Ward<br />
Dr John Dick<br />
Dr Stephanie Greenwell<br />
Dr Ellen O’Sullivan<br />
Dr Ranjit Verma<br />
Dr David K Whitaker<br />
Chairman of the working party<br />
Group of Anaesthetists in Training<br />
Vice-President<br />
Council Member<br />
Council Member<br />
Immediate Past Honorary Secretary<br />
Ex Officio<br />
Prof Mike Harmer<br />
Dr Peter G M Wallace<br />
Dr Richard Birks<br />
Prof W Alastair Chambers<br />
Dr Diana Dickson<br />
Dr David Bogod<br />
President<br />
Immediate Past President<br />
Honorary Treasurer<br />
Honorary Secretary<br />
Honorary Membership Secretary<br />
Editor-in-Chief, Anaesthesia<br />
The Working Party would like to acknowledge the helpful advice of<br />
Mr Bertie Leigh of Hempsons Solicitors and Geraldine Hickey of<br />
McCann Fitzgerald Solicitors (Ireland)<br />
1
2
Recommendations<br />
1. Wherever possible, consultant staff (anaesthetists and surgeons)<br />
should be directly involved throughout the care of Jehovah’s Witness<br />
patients.<br />
2. Departments of Anaesthesia should review their procedure for being<br />
alerted at an early stage of the scheduling of Jehovah’s Witness patients<br />
for elective surgery.<br />
3. Departments should keep a regularly updated list of those senior<br />
members prepared to care for followers of the Jehovah’s Witness<br />
faith.<br />
4. In an emergency, an anaesthetist is obliged to care for a patient in<br />
accordance with the patient’s wishes.<br />
5. Properly executed Advance Directives must be respected and special<br />
Jehovah’s Witness consent forms should be widely available for use as<br />
required.<br />
6. All Jehovah’s Witnesses must be consulted individually, whenever<br />
possible, to ascertain what treatments they will accept.<br />
7. Discussions with individual Jehovah’s Witness patients should be fully<br />
documented and their acceptance or rejection of treatments recorded<br />
and witnessed.<br />
8. In the case of children, local procedures for application to the High<br />
Court for a ‘Specific Issue Order’ should be reviewed and available for<br />
reference.<br />
9. In Scotland. In the case of children, local procedures for application to<br />
the Court of Session or appropriate Sheriff Court should be reviewed<br />
and available for reference.<br />
10. In Ireland. In the case of children, application to District Court for<br />
child to be placed under Emergency Care Order should be reviewed<br />
and available for reference.<br />
11. A ‘Specific Issue Order’ or equivalent should only be applied for when<br />
it is felt to be entirely necessary to save the child in an elective or semielective<br />
situation.<br />
12. In a life-threatening emergency in a child unable to give competent<br />
consent, all life-saving treatment should be given, irrespective of the<br />
parents’ wishes.<br />
3
SECTION 1<br />
1. Introduction<br />
1.1 The first edition of this guidance [1] was published in March 1999 and<br />
was received by the members of both the Association of Anaesthetists<br />
of Great Britain and Ireland (the Association) and the Watch Tower Bible<br />
and Tract Society of Britain (the official organisation for British Jehovah’s<br />
Witnesses) with some acclaim.<br />
1.2 Since then there has been a continuing debate surrounding the ethical and<br />
practical consequences of consent for medicine as well as developments<br />
in the areas of ‘Oxygen Therapeutics’, blood transfusion medicine and<br />
alternative blood sparing technologies.<br />
1.3 In his Report for 2003 entitled On the State of Public Health, the UK<br />
Department of Health’s Chief Medical Officer, Professor Liam Donaldson,<br />
stated that he believed too many unnecessary blood transfusions were<br />
being given in England [2]. He added, “The gift of blood is too often<br />
squandered by unnecessary and inappropriate use”, and expressed<br />
concern at the fall in the donor pool (down by one fifth in 4 years). He<br />
further suggested that transfusion is unnecessary unless the haemoglobin<br />
falls below 7 g/dl, and proposed that only consultants, and not junior<br />
staff, should be allowed to order blood and blood products.<br />
1.4 The management of Jehovah’s Witness patients was briefly reviewed in<br />
the Royal College of Anaesthetists’ publication Continuing Education in<br />
Anaesthesia, Critical Care & Pain[3].<br />
1.5 This present report has been prepared by the Association and advises<br />
on the anaesthetic management of patients belonging to the Jehovah’s<br />
Witness faith.<br />
4
SECTION 2<br />
2. Beliefs and their Implications for the Anaesthetist<br />
2.1 Every competent adult patient is entitled to refuse to consent to medical<br />
treatment for good reason, bad reason or no reason. No opinion should<br />
be attributed to a patient simply because they are a member of a religious<br />
or political group. In this guide we seek to describe the views held by<br />
most mainstream Elders of the community of Jehovah’s Witnesses in the<br />
hope that this will assist anaesthetists in advising and treating individual<br />
Jehovah’s Witness patients. However, there is no substitute for seeking the<br />
views of the individual patient who happens to be a Jehovah’s Witness at<br />
the time when decisions have to be made. Doctors must be aware at all<br />
times that all patients are entitled to change their minds and that the only<br />
thing that matters is what treatment the patient wishes to have at the time<br />
when the decision has to be taken.<br />
2.2 It is estimated that there are nearly 6.5 million Jehovah’s Witnesses in 235<br />
countries worldwide and about 150, 000 in Great Britain and Ireland.<br />
2.3 Recent knowledge of the risk of transmission of disease and other<br />
complications of blood transfusion have in many cases been cited as<br />
further support for the Jehovah’s Witnesses’ refusal to accept blood<br />
transfusion. Increasing awareness of this risk generally by the medical<br />
profession has altered views on the need for transfusion and altered our<br />
perception of the problems occurring as a result of acute unexpected<br />
blood loss.<br />
2.4 The Jehovah’s Witness movement is some 120 years old, having been<br />
founded in North Eastern United States of America. It is an actively<br />
proselytising Christian organisation that originally had objections to other<br />
medical treatments such as vaccinations and inoculations, although these<br />
are now largely accepted. In 1945, the Watch Tower Bible and Tract<br />
Society (the name of the group’s legal publishing entity) promulgated<br />
the views that adherents to the faith should not receive allogenic blood.<br />
Some adherents of the faith choose to extend this prohibition to include<br />
blood products. The explanation for these beliefs is their interpretation<br />
of Genesis 9:3, 4, Leviticus 17:11, 12 and Acts 15:28, 29 (Appendix<br />
1), all of which describe the prohibition of the consumption of blood.<br />
The established Jehovah’s Witnesses’ interpretation of this is that an<br />
individual’s life is represented by their blood. The prohibition of blood<br />
transfusion is a deeply held core value and is a sign of respect for the<br />
sanctity of life.<br />
5
2.5 It may be helpful to regard these rules under the following two<br />
headings:<br />
2.5.1 Treatment generally regarded as unacceptable by Jehovah’s<br />
Witnesses:<br />
• Transfusion of whole blood, packed red cells, white cells, plasma<br />
(FFP), and platelets<br />
• Preoperative autologous blood collection and storage for later<br />
reinfusion (pre-deposit)<br />
2.5.2 Matters that Jehovah’s Witnesses recognise as being of personal<br />
choice:<br />
Each Witness decides whether he/she wishes to accept the<br />
following as a matter of individual choice. It is therefore important<br />
to discuss with each patient whether or not these are acceptable.<br />
• Blood salvage (intra and post-operative), haemodilution,<br />
haemodialysis, and cardiac bypass<br />
• Blood ‘fractions’ of plasma or cellular components (eg albumin,<br />
immunoglobulins, clotting factors)<br />
• Whilst haemoglobin based oxygen carrying solutions are not<br />
yet licensed in the UK, they may soon be available and may be<br />
acceptable to some Jehovah’s Witness patients.<br />
• Transplantation, including solid organ, bone, tissue etc<br />
• Epidural blood patch (see below)<br />
2.6 It should be remembered that no absolute rules regarding blood<br />
products exist. Some Witnesses are willing to accept the use of plasma<br />
protein fraction (PPF) or components such as albumin, immunoglobulins<br />
and haemophilic preparations, when asked individually. Other clinical<br />
interventions may also need to be dealt with on a personal basis. Organ<br />
transplantation, for example, is not specifically forbidden for Jehovah’s<br />
Witnesses, and each individual is expected to reach his or her own<br />
decision.<br />
2.7 Cardiac bypass may be accepted provided the pump is primed with nonblood<br />
fluids and blood is not stored in the process. Auto transfusion is<br />
acceptable to many Jehovah’s Witnesses. Jehovah’s Witnesses will not<br />
accept pre-operative collection, storage and later re-infusion of blood.<br />
2.8 The use of an epidural blood patch may be acceptable to some Jehovah’s<br />
Witnesses [4].<br />
6
2.9 Administration of blood to a competent patient, against their will and<br />
in conflict with their genuinely held beliefs, has been likened by the<br />
Witnesses to rape. It will not result in expulsion from the community if it<br />
was carried out against the expressed wishes of the patient but may have<br />
as deep a psychological effect as forceful sexual interference.<br />
2.10 Because of the variability between individual beliefs, it is common for a<br />
Witness patient to wish to consult with the Elders of the community for<br />
help in reaching a decision regarding accepting blood-product related<br />
medical treatment. Most active communities (in 42 key locations in<br />
Great Britain and Ireland, generally based in the major cities) maintain<br />
a committee of Elders, known as the ‘Hospital Liaison Committee for<br />
Jehovah Witnesses’, which can be contacted and whose telephone<br />
numbers are generally lodged with the local hospital switchboards served<br />
by the committee. Appendix 2 gives the main contact numbers for the<br />
national central committees.<br />
2.11 The local Hospital Liaison Committee can also act as a local resource for<br />
information regarding the beliefs and practices of Jehovah’s Witnesses.<br />
They are generally aware of up to date research and clinical practice in<br />
the area of bloodless surgery and have access to a great deal of reference<br />
material and information.<br />
2.12 Hospital Liaison Committees also hold a schedule of clinicians experienced<br />
in treating patients in accordance with the wishes of Jehovah’s Witnesses.<br />
These clinicians may be prepared to give advice if consulted or even<br />
accept transfer of the patient’s care.<br />
2.13 The Working Party suggests that departments of anaesthesia have<br />
available a list of anaesthetists willing to manage such patients.<br />
7
SECTION 3<br />
3. The legal position in respect of anaesthesia and consent<br />
3.1 Jehovah’s Witnesses are generally well informed, both about their legal<br />
position and the options for treatment. Any competent adult is entitled<br />
to accept surgery but also specifically to exclude certain aspects of<br />
management, such as the administration of a blood transfusion. The<br />
recent recommendations from the Department of Health in respect<br />
of consent forms provide for the inclusion of a box for the patient to<br />
complete, and this may contain specific exclusions from the consent.<br />
Most practising Jehovah’s Witnesses will carry with them an Advance<br />
Directive document. Appendix 3 gives the full wording of a typical<br />
directive which specifically states that “in the event of emergency<br />
treatment including general anaesthesia and surgery….” it forbids the<br />
administration of blood or blood components. The advance directive<br />
goes on to state “my express refusal of blood is absolute and is not to be<br />
overridden in any circumstances”. It is important to realise that individual<br />
Jehovah’s Witnesses may have different views, and the doctor’s obligation<br />
is to respect the wishes of the individual patient.<br />
3.2 It is the view of this Working Party that such an advance medical<br />
directive by a competent adult, if properly signed and witnessed, must<br />
be respected unless there is evidence that the patient has changed their<br />
view since the directive was executed.<br />
3.3 The Working Party strongly recommends that the views held by each<br />
Jehovah’s Witness patient should be ascertained to find out which aspects<br />
of treatment are acceptable and which are not.<br />
3.4 To administer blood to a patient who has steadfastly refused to accept it<br />
by either the provision of an advance directive or by its exclusion in a<br />
consent form is unlawful and ethically unacceptable. It may also lead to<br />
referral to the General Medical Council, criminal and/or civil proceedings<br />
[5].<br />
3.5 In the management of an unconscious patient whose status as a Jehovah’s<br />
Witness may be unknown, the doctor caring for the patient will be<br />
expected to perform to the best of his ability, and this may include the<br />
administration of blood transfusion. However, there may be opinions put<br />
forward by relatives or associates of the patient suggesting that the patient<br />
would not accept a blood transfusion even if that resulted in death. Such<br />
relatives should be invited to produce evidence of the patient’s status as<br />
8
a Jehovah’s Witness. It is not uncommon for Jehovah’s Witnesses to lodge<br />
a copy of their advance directives with their General Practitioner, who<br />
should be contacted.<br />
3.6 Children of Jehovah’s Witnesses below the age of 16 years may cause<br />
particular difficulty. The wellbeing of the child is overriding and, if the<br />
parents refuse to give permission for blood transfusion, it may be necessary<br />
to apply for a ‘Specific Issue Order’ via the High Court in order legally<br />
to administer the blood transfusion (see below and Appendix 4 for the<br />
procedure to follow). It is important, however, before this serious step is<br />
taken, that two doctors of consultant status should make an unambiguous<br />
clear and signed entry in the clinical record that blood transfusion is<br />
essential, or likely to become so, to save life or prevent serious permanent<br />
harm. In the event that a court order is sought, it is essential [5] that the<br />
parents be given the opportunity to be properly represented and are kept<br />
fully informed of the practitioners’ intention to apply for the order.<br />
In Scotland such an application for a ‘Specific Issue Order’ is made to<br />
the Court under Section 11 of the Children (Scotland) Act 1995<br />
In Ireland an application is made for an Emergency Care Order to the<br />
District Court under Section 12 or 13 of the Child care Act 1991<br />
In the case of young people over 12 years who are capable of understanding<br />
the issues, the anaesthetist may be able to rely upon their consent (see<br />
Section 5).<br />
The management of a child of a Jehovah’s Witness in an emergency<br />
situation who is likely to succumb without the immediate administration<br />
of blood is viewed in law in a different light. In this situation, application<br />
to the courts will be too time-consuming and the blood should be<br />
transfused without consulting the court. The courts are likely to uphold<br />
the decision of the doctors who give blood.<br />
Most hospitals provide a special Jehovah’s Witness consent form but, if<br />
that is not forthcoming, the Hospital Liaison Committee of the Jehovah’s<br />
Witnesses has a suitable form available (See Appendix 3). It may also be<br />
advisable to make a separate clear entry in the patient’s clinical notes<br />
to the effect that the patient has refused the administration of blood or<br />
blood products under any circumstances. However the extent of the<br />
prohibition should be clearly set out, because of the range of opinions<br />
identified in paragraph 2.5 above.<br />
9
SECTION 4<br />
4. Clinical Management<br />
4.1 Preoperative<br />
4.1.1 It is essential that surgeons who are aware that an elective patient<br />
is a Jehovah’s Witness should alert the anaesthetic department as<br />
soon as possible in order to ensure that a consultant anaesthetist<br />
is prepared to manage the patient’s care. Early warning of any<br />
potential intervention that could lead to the need for blood or<br />
blood products is also advisable.<br />
4.1.2 Anaesthetists have the right to refuse to anaesthetise an individual<br />
in an elective situation but should attempt to refer the case to a<br />
suitably qualified colleague prepared to undertake it. The surgeon<br />
should be informed as soon as possible if any difficulty ensues. In<br />
an emergency, the anaesthetist is obliged to provide care and must<br />
respect the patient’s competently expressed views.<br />
4.1.3 Major procedures can be carried out in stages in order to limit<br />
acute blood loss, and the choice of operative technique may also<br />
influence outcome; for example bilateral procedures could be<br />
performed in two unilateral stages.<br />
4.1.4 Increasingly, obstetric or major lower limb procedures may be<br />
performed under local or regional anaesthesia alone and, in this<br />
situation, some patients may change their mind when confronted<br />
with the need for a blood transfusion as a life saving measure. Any<br />
change in the patient’s views at this point should be regarded as a<br />
modification in the scope of consent and should be witnessed. A<br />
contemporaneous entry should be made in the patient’s anaesthesia<br />
and clinical record. Whether or not a patient who has received<br />
sedation will be competent to vary the consent which they have<br />
previously given will depend upon the facts of the case. Broadly<br />
speaking the law holds that a patient has capacity to consent to<br />
treatment if they are capable of receiving advice from a doctor, of<br />
understanding that advice, of balancing the issues in their mind and<br />
uttering their wishes. They do not need to be able to give a full and<br />
detailed discourse on the finer points of religion or pharmacology<br />
that may be involved in their decision, simply to decide whether<br />
or not they want to have the blood or blood products in question.<br />
Where a patient has consented to receive blood which the doctor<br />
10
elieved was immediately necessary in order to save their life, if<br />
the Court accepts that that belief is reasonably held it should not<br />
criticise the doctor for acting upon the consent of the patient.<br />
4.1.5 The introduction of an antenatal alert of the anticipated delivery<br />
of a child to a Jehovah’s Witness mother can also be beneficial so<br />
that appropriate senior staff will be available. This arrangement<br />
should apply to booking of delivery dates by both obstetricians<br />
and midwives.<br />
4.1.6 Full pre-operative investigations and consultations with the patient<br />
should take place as early as possible in order to ascertain the<br />
degree of limitation on intra-operative management.<br />
4.1.7 At the pre-operative visit it is very important to take the<br />
opportunity to see the patient without relatives or members of the<br />
local community who may influence and impede full and frank<br />
discussion of the acceptability of certain forms of treatment. At<br />
this stage, treatments that are regarded as acceptable should be<br />
established and the patient and staff made fully aware of the risks<br />
of refusal of blood or blood products. Agreed procedures and<br />
unacceptable treatments should be entered into the clinical notes<br />
and signed as a record and witnessed by the patient. Such entries<br />
should be both dated and timed.<br />
At the patient’s request, family members or members of the Hospital<br />
Liaison Committee for Jehovah’s Witnesses may be part of these<br />
discussions. Their prime role should be to avoid confrontation and<br />
assist understanding on both sides.<br />
These family or Hospital Liaison Committee members may<br />
however hold stronger views than those of the patient and, with<br />
the patient’s agreement, they should be excluded if their presence<br />
is detrimental to the patient’s peace of mind and mental comfort.<br />
4.1.8 Pre-operative anaemia should be investigated and treated. The<br />
use of recombinant erythropoetin to improve haemoglobin levels<br />
has been documented but is a slow treatment that might not be<br />
clinically justified or cost effective. It may be beneficial, however, to<br />
improve the iron stores by pre-administration of iron supplements.<br />
Discussion of an individual case with a haematologist could be<br />
beneficial.<br />
11
4.2 Intra-operative Management<br />
4.2.1 Consideration should be given, before surgery, to one or more of<br />
a number of techniques to reduce intra-operative blood loss, such<br />
as: careful positioning to avoid venous congestion, hypotensive<br />
anaesthesia, use of tourniquets where appropriate, meticulous<br />
haemostasis, use of vasoconstrictors and haemodilution.<br />
4.2.2 A ‘cell saver’ system may be acceptable to the Jehovah’s Witness<br />
and can be used in certain operations where blood loss is unlikely<br />
to result in blood contamination. Nevertheless, discussions of the<br />
use of a cell saver should be carried out with the patient to assess<br />
acceptability.<br />
4.2.3 A number of drugs have been used in an effort to reduce fibrinolysis,<br />
increase coagulability and reduce blood loss; eg tranexamic acid<br />
and aprotinin [6].<br />
4.3 Postoperative Care<br />
4.3.1 Postoperative blood loss should be carefully monitored and<br />
accurately recorded. Simple manoeuvres (e.g. direct compression)<br />
or early surgical intervention (e.g. re-exploration) may reduce<br />
overall blood loss.<br />
4.3.2 In some peripheral orthopaedic surgery, such as total knee<br />
replacement, postoperative wound drainage of blood can be<br />
reinfused, using special filter-drainage systems.<br />
4.3.3 In the event of massive blood loss it may be necessary to consider<br />
elective ventilation to enhance oxygen delivery [7].<br />
4.3.4 Active cooling in the postoperative period has also been described<br />
to reduce oxygen consumption and increase dissolved oxygen<br />
carriage, but this technique is not widely accepted [8].<br />
4.3.5 Hyperbaric oxygen therapy has been described in the management<br />
of anaemia following severe blood loss. Swift reversal of hypoxia is<br />
possible but the technique has limited application. Nevertheless,<br />
referral for hyperbaric therapy may be considered if an appropriate<br />
facility is available [9].<br />
12
5. Paediatric Considerations<br />
5.1 Young adults of sound mind aged 16–18 years have a statutory right<br />
in England and Wales to consent to procedures on their own account<br />
and there is no legal requirement to obtain additional consent from a<br />
parent or guardian. The patient’s consent takes precedence over parental<br />
objections. Parents may give lawful consent to a young adult unable to<br />
consent in their own right, because of decreased consciousness.<br />
In Scotland, young persons aged 16 or over have an exclusive right to<br />
determine their own medical treatment. The parent has no right to consent<br />
or interfere; similarly, recourse to the Courts would not be available.<br />
In Ireland a person is considered adult for the purposes of consent to<br />
medical treatment at the age of 16 and there is no legal requirement to<br />
obtain additional consent from parent or guardian (Section 23 of the<br />
Non-Fatal Offences against the Person Act 1997).<br />
5.2 In England and Wales children younger than 16 years may be<br />
competent to give their own consent if they demonstrate a clear grasp<br />
of the proposed treatment and the risks, benefits or consequences of<br />
acceptance or rejection of a proposed treatment. This is referred to as<br />
‘Gillick-competence’. However, this is likely only to apply to children<br />
above the age of 12 years, but could for more minor procedures apply<br />
much younger.<br />
A situation could be envisaged where a child under the age of 16 years,<br />
of Jehovah’s Witness parents, were to consent to an elective blood<br />
transfusion in the face of parental opposition. Consent in this situation<br />
would be sound provided that the child could show evidence of ‘Gillick<br />
competence’.<br />
5.3 Although children aged 16–18 years are capable of consenting to any<br />
medical procedure, so that consent of another person is not necessary,<br />
the law expressly states that this does not invalidate the right of others to<br />
consent on their behalf. If the patient is in an acute emergency situation it<br />
will be lawful for an anaesthetist to proceed on the basis of the consent of<br />
either parent. Where time permits, the court should be asked to resolve<br />
the position.<br />
In Scotland, a young person aged 16 or over can only be treated against<br />
their wishes in cases where the young person has some mental incapacity,<br />
in which case a parent or agency could aquire rights by being appointed<br />
as guardian.<br />
13
In Ireland the issue of the “mature minor” has not been judicially<br />
considered and it is unclear whether young people under the age of 16<br />
are permitted to give consent and whether the Irish Courts would adopt a<br />
principle of competence similar ‘Gillick’. Similarly it is not clear whether<br />
the Irish Courts would accept that minors are capable of refusing medical<br />
treatment. The Irish judiciary are reluctant to intervene to overrule parental<br />
decisions and will do so only in exceptional cases. However each case<br />
must be judged on its merits and where there are life threatening issues<br />
the Courts may favour the personal rights of the child over family and<br />
parental considerations.<br />
In an unreported case in March 2003 the Gardai were called to to a<br />
hospital after the parents of a two-year-old boy refused to allow him a<br />
blood transfusion on religious grounds. The Gardai made an application<br />
under the Child Care Act and the transfusion proceeded. In another case<br />
the High Court ordered that a child be made a Ward of Court to enable<br />
her to be treated with blood products. In this case the five-month-old<br />
baby girl required life saving open heart surgery. [10]<br />
5.4 Consent to give blood products in the face of opposition by both child<br />
and parents is illustrated by a case involving a 14-year-old burns victim<br />
[11]. Both the child and the parents, with strongly held beliefs, refused<br />
a transfusion required to manage severe burn injuries. It was found by<br />
the Family Court, following the opinion of an expert in child psychiatry,<br />
that these beliefs were founded upon the context of her own family<br />
experience alone and that there was a distinction between a view of that<br />
kind and the constructive formulation of an opinion which occurred with<br />
adult experience.<br />
While it was accepted that the patient’s opinions were firmly held, they<br />
were necessarily based upon a limited understanding of matters and that<br />
she was not in possession of all the details which it would be right and<br />
appropriate to have in mind when making such a decision. The Official<br />
Solicitor was appointed to act as ‘guardian ad litem’ and consent to give<br />
blood products was granted.<br />
5.5 This point was further discussed in the High Court in England in 2003<br />
[12] where it was found to be in the best interests of a Jehovah’s Witness<br />
patient (nearly 17 years old) to receive blood products where the risk<br />
to life was immediately threatening and there was no other form of<br />
treatment available. A useful Case Study is available to further explore<br />
this point [13].<br />
14
5.6 On 1st April 2001 under the provisions of the Criminal Justice and Court<br />
Services Act, the Children and Family Court Advisory and Support<br />
Service – (CAFCASS) was set up. This is a national Non-Departmental<br />
Public Body for England and Wales that safeguards and promotes the<br />
welfare of children involved in family court proceedings. It is accountable<br />
to Parliament through the Department for Education and Skills. CAFCASS<br />
is independent of the courts, social services, education and health<br />
authorities and all similar agencies. It brings together the services<br />
previously provided by:<br />
• The Family Court Welfare Service<br />
• The Guardian ad Litem Services<br />
• The Children’s Division of the Official Solicitor.<br />
15
6. Consequences of Bloodless Anaesthesia and Surgery<br />
6.1 Financial Consequences<br />
6.1.1 Cost of care<br />
Special equipment for, and additional theatre time spent in the<br />
conservation of blood carries an increased cost to the hospital.<br />
Depending on the specialty and complexity of the surgery, theatre<br />
time costs between £7 and £15 a minute [14].<br />
Maintaining a patient with a low haemoglobin level following<br />
surgery without transfusion may also carry an additional cost in<br />
days spent in HDU or ITU. National figures indicate that each<br />
additional day spent in an HDU bed costs £543 and in an ITU bed<br />
£1266 [15]. Occupation of these beds also further denies access<br />
of an already scarce resource to other patients in need of higher<br />
dependency and intensive care.<br />
Access to hyperbaric oxygen facilities is limited to only 30 sites<br />
in the UK and session costs vary. There is an additional cost of<br />
transfer of the patient to these centres.<br />
6.1.2 Costs of Cell Saver<br />
The cost of blood salvage machinery varies. Prices range from<br />
£5,000 to £14,000, with the price of disposables ranging between<br />
£70 and £100.<br />
6.1.3 Savings in Costs of Blood<br />
The price of a unit of blood has risen dramatically in the last<br />
decade, especially since leucodepletion has been added to the<br />
preparation process. The current national price of a unit of packed<br />
cells is around £132, a unit of FFP around £35 and a unit of platelets<br />
around £217 [16].<br />
6.2 Consequences of avoidance of blood transfusion errors and<br />
disease<br />
Incorrect blood components transfused (or “wrong blood”) account for<br />
75% of all reports to the Serious Hazards of Transfusion working group<br />
(SHOT) in 2003. The risk of death from an acute haemolytic reaction<br />
is quoted as 0.67 per million units (British Committee for Standards in<br />
Haematology guidelines, http://www.bcshguidelines.com). The rates of<br />
transfusion-transmitted infections are estimated to be 1 in several million<br />
16
transfusions for HIV, 1 in 30 million for Hep C, and 1 in 1 million for Hep<br />
B. (Data from the SHOT annual report for 2003, published July 2004).<br />
The transmission rate for vCJD is unknown. There have been two reports<br />
to date of possible vCJD transmission secondary to blood transfusions<br />
from donors who subsequently developed vCJD [17].<br />
6.3 Use of Erythropoetin And Recombinant Factor VIIa<br />
6.3.1 Erythropoetin<br />
The acceptance of either of the two erythropoetin products<br />
currently available in Britain does not raise any religious issues for<br />
patients who are Jehovah’s Witnesses.<br />
6.3.1.1 Autologous blood pre-donation<br />
Erythropoetin is licensed for autologous blood predonation<br />
in the UK and Ireland and should be commenced four<br />
weeks before to surgery. However, Jehovah’s Witnesses<br />
do not accept autologous predonation.<br />
6.3.1.2 Increasing haemoglobin levels preoperatively<br />
The use of erythropoetin to boost haemoglobin levels<br />
before surgery may be considered. However this is<br />
an unlicensed use of erythropoetin in Ireland and the<br />
UK. The exact dose required has not been established<br />
and the patient would require careful monitoring.<br />
Erythropoetins will not be indicated in patients with<br />
history of cardiovascular or ischaemic heart disease,<br />
unstable angina or at risk of venothromboembolism.<br />
6.3.1.3 Post-operative use of erythropoetin in Jehovah’s Witness<br />
patients<br />
Erythropoetin is not licenced for post-operative use in<br />
any patient group, although it has been successfully used<br />
to treat acute anaemia [18].<br />
6.3.2 Recombinant Factor VIIa (rFVIIa)<br />
rFVIIa is indicated for the treatment of bleeding episodes in patients with<br />
haemophilia A or B, with inhibitors to Factors VIII or IX. It has also been<br />
used in cases of refractory thrombocytopenia, and there have been a<br />
number of case reports of its successful use in Jehovah’s Witness patients<br />
particularly after cardiac surgery [19]. rFVIIa has also been used to<br />
correct the coagulation and platelet defects in Jehovah’s Witness patients<br />
with cirrhosis to allow invasive procedures to be performed [20].<br />
17
6.4 Other considerations<br />
6.4.1 Stress and Anxiety for Anaesthetists and Surgeons<br />
It is well recognised that both surgeons and anaesthetists regard<br />
any limitation on their clinical freedom to be stressful, and this<br />
added stress is likely to be even greater when the consequences<br />
of the limitation may result in an otherwise avoidable death.<br />
This should be clearly and calmly explained to the patient, their<br />
relatives or representatives so that all parties are clear as to the<br />
consequence of their expressed wishes.<br />
A clinician may refuse to participate in an elective procedure if he<br />
feels that the patient’s request is unreasonable or inappropriate in<br />
his hands (para 4.1.2). This freedom of action is not present in an<br />
emergency when a practitioner may find himself participating in a<br />
procedure against his will and with compromised clinical freedom.<br />
Departments of both anaesthesia and surgery should have a<br />
procedure to deal with this situation, such as the maintainance<br />
of a register of clinicians who are prepared to be involved in<br />
procedures within the limitations imposed by Jehovah’s Witness<br />
patients.<br />
6.4.2 Ethical Dilemmas<br />
Working within restrictions imposed by Jehovah’s Witness<br />
patients can result in diversion of hospital resources from other<br />
patients who have a medically indicated need for them. Examples<br />
are significant periods in ITU or HDU, the use of a hyperbaric<br />
chamber or temporary dialysis.<br />
6.4.3 Effects on Other Patients<br />
Excessive resources, including the extra time necessary to complete<br />
bloodless surgery safely, used by these special patients in order to<br />
satisfy their religious beliefs may result in a lack of resources being<br />
available to other patients.<br />
6.4.4 Effects on Members of Hospital Staff<br />
The ripple effect on other members of the theatre teams and ward<br />
staff may also be profound. Full briefing of ALL members of the<br />
expanded team can avoid feelings of frustration and anger which<br />
may be directed at the patient, their relatives or representatives.<br />
Ideally this should be done before surgery so that all support can<br />
be provided to the patient and staff as required.<br />
18
Counselling may be required for the anaesthetic and surgical<br />
team who may feel that, whilst adhering to the patient’s expressed<br />
wishes, they have been unable to provide an optimal level of care<br />
that has resulted in a significant morbidity or even death during<br />
their care.<br />
19
7. Conclusion<br />
7.1 The Association of Anaesthetist of Great Britain and Ireland remains<br />
firmly of the view that all patients are entitled to take individual decisions<br />
about matters respecting their treatment which are important to them. It<br />
is the doctor’s duty to advise the patient clearly about their professional<br />
assessment of the patient’s needs and it is the patient’s right to decide<br />
what should be done to his or her body. Once the patient’s views have<br />
been clearly articulated they should be recorded and respected. This<br />
is based squarely on a respect for the patient’s right of autonomy and<br />
to decide what is done with and to their body. Any wilful flouting of a<br />
patient’s clearly recorded wishes in this fashion will be a serious matter<br />
which may expose the transgressor to punishment in the GMC and is<br />
liable as an offence against the criminal law.<br />
The Association has some sympathy with the anxieties and frustration<br />
experienced by anaesthetists asked to practice what they may feel to<br />
be suboptimal care. Nevertheless it is our view that a full explanation<br />
by both sides to the other of their needs, concerns and the potential<br />
consequences of their actions should help to mitigate these stressors.<br />
Discussion between the parties is a tenet of the Consent process.<br />
7.2 As the recent paper [3] in the Royal College of Anaesthetist’s Continuing<br />
Medical Education Journal states “Many of the techniques developed<br />
for use in Jehovah’s Witness patients will become standard practice in<br />
years to come in an effort to conserve blood stocks and reduce the need<br />
for transfusion”. Our experience in this area of anaesthetic practice may<br />
have positive developments which can be extended to other areas.<br />
20
References<br />
1. Management of Anaesthesia for Jehovah’s Witnesses, AAGBI March<br />
1999<br />
2. Annual Report of the Chief Medical Officer – 2003 On the State of the<br />
Public Health.<br />
www.publications.doh.gov.uk/cmo/annualreport2003/index.htm<br />
3. Milligan LJ and Ballamy MC, Anaesthesia and critical care of Jehovah’s<br />
Witnesses. Continuing Education in Anaesthesia, Critical Care & Pain<br />
2004; 4: 35-39<br />
4. Bearb ME and Pennant 1987. Epidural Blood Patch in a Jehovah’s Witness<br />
Anesthesia and Analgesia 1987; 66: 1052<br />
5. ReT All England Law Reports 1992; 4:647-70.<br />
6. Royston D. Blood-sparing Drugs: Aprotinin, Tranexamic Acid, and<br />
Epsilon-Aminocaproic Acid. In International Anesthesiology Clinics 1995;<br />
Vol 33:155-79.<br />
7. Ashley E. Anaesthesia for Jehovah’s Witnesses. British Journal of Hospital<br />
Medicine 1997; Vol 58:375-380.<br />
8. Baker CE, Kelly GD and Perkins GD. BJA 1998; Vol 81: 256-259.<br />
9. P. L. McLoughlin, T. M. Cope and J. C. Harrison Hyperbaric oxygen<br />
therapy in the management of severe acute anaemia in a Jehovah’s<br />
Witness Anaesthesia 1999; 54, 891-895<br />
10. Personal Communication Geraldine Hickey of McCann FitzGerald<br />
Solicitors Ireland<br />
11. Blood Transfusion Refusal – Best interests of minor Jehovah Witness.<br />
Medical Litigation 1998; 8-9 [Re L (A Minor) (FamD: The President, June<br />
10, 1998 10 Pages].<br />
12. Re P (Minor) [2003] EWHC 2327<br />
13. http://www.ethics-network.org.uk/Cases/previous/process.htm<br />
14. Personal Communicational Northumbria Health Care NHS Trust<br />
21
15. NHS Reference Costs 2003 and National Tariff 2004, Department of<br />
Health, 2004<br />
16. Personal Communication from the National Blood Service, and<br />
https://www.blood.co.uk/<br />
17. Llewelyn CA et al. Possible transmission of variant Creutzfeldt-Jakob<br />
disease by blood transfusion. The Lancet 2004; 363: 417-421.<br />
18. Atabek U, Alvarez R, Pello MJ, Alexander JB, Camishion RC, Curry<br />
C, Spence RK. Erythropoetin accelerates hematocrit recovery in postsurgical<br />
anemia. Am Surg. 1995; 61(1):74-7.<br />
19. Tanaka, Kenichi A. M.D.; Waly, Amr A. M.D. +; Cooper, William A.<br />
M.D.; Levy, Jerrold H. M.D. Treatment of Excessive Bleeding in Jehovah’s<br />
Witness Patients after Cardiac Surgery with Recombinant Factor VIIa<br />
(NovoSeven(R)). Anesthesiology 2003; 98 :(6), 1513-5.<br />
20. Papatheodoridis G.V.; Chung S.; Keshav S.; Pasi J.; Burroughs A.K.<br />
Correction of both prothrombin time and primary haemostasis<br />
by recombinant factor VII during therapeutic alcohol injection of<br />
hepatocellular cancer in liver cirrhosis. Journal of Hepatology, 1999; 31:<br />
(4),747-750.<br />
22
Appendix 1<br />
The Holy Bible – Authorised King James Version<br />
Genesis Chapter 9, Verses 3–4<br />
3. Every moving thing that liveth shall be meat for you; even as the green<br />
herb have I given you all things.<br />
4. But flesh with the life thereof, which is the blood thereof, shall ye not<br />
eat.<br />
Leviticus Chapter 17, Verses 11–12<br />
11. For the life of the flesh is in the blood: and I have given it to you upon the<br />
altar to make an atonement for your souls: for it is the blood that maketh<br />
an atonement for the soul.<br />
12. Therefore I said unto the children of Israel, No soul of you shall eat blood,<br />
neither shall any stranger that sojourneth among you eat blood.<br />
Acts Chapter 15, Verse 28–29<br />
28. For it seemed good to the Holy Ghost, and to us, to lay upon you no<br />
greater burden than these necessary things;<br />
29. That ye abstain from meats offered to idols, and from blood, and from<br />
things strangled, and from fornication: from which if ye keep yourselves,<br />
ye shall do well. Fare ye well.<br />
23
Appendix 2<br />
Hospital Liaison Committees – Contact Numbers<br />
Hospital Information Services<br />
IBSA House, The Ridgeway, London, NW7 1RN<br />
020 8906 2211<br />
his@uk.jw.org<br />
Belfast Ken McGuire 07801 632151 ken.mcguire@belfasthlc.co.uk<br />
Birmingham Roy Jackson 07889 648508 roy@jw-hlc.org<br />
Cardiff David Newman 07860 794807 d.newman@swwales-hlc.org.uk<br />
Dublin Mark Scully 00 353 87 1209019 mark.scully@hlc.ie<br />
Glasgow Harry Crawford 07711 367409 harry@hlcglasgow.co.uk<br />
London North Brian Brooks 07931 714369 brian.brooks@hlcln.org.uk<br />
London South Peter Foster 07947 046330 pf1@london.com<br />
24
Appendix 3<br />
Full Wording of suggested “Jehovah’s Witness Consent/Release”<br />
GENERAL CONSENT FORM EXCLUDING<br />
BLOOD TRANSFUSION<br />
Your Trust or Authority:<br />
Patient Information...........................................................................................<br />
Patient’s Surname ............................................................................................<br />
Other Name (s)............... Hospital Unit Number....... Date of Birth....................<br />
DOCTOR – (this part to be completed by Registered Medical Practitioner)<br />
NATURE OF OPERATION, INVESTIGATION OR TREATMENT:<br />
I confirm that I have explained the operation investigation or treatment, and such<br />
appropriate options as are available and the type of anaesthetic, if any (general/<br />
regional/sedation) proposed, to the patient in terms which in my judgment are<br />
suited to the understanding of the person named below. I further confirm that I<br />
have emphasised my clinical judgment of the potential risks to the patient and/<br />
or person who nonetheless understood and imposed the limitation expressed<br />
below.<br />
I acknowledge that this limited consent will not be over-ridden unless revoked<br />
or modified.<br />
Signature.......................................... Date.................................<br />
Name of Registered Medical Practitioner...........................................................<br />
PATIENT (this part to be completed by the patient)<br />
I...............................................................................................................................(name)<br />
Confirm that I have read the words above and have consented to undergo<br />
the above named procedure. I confirm that the doctor named on this form<br />
has explained to me the nature and purpose of the procedure and the type of<br />
25
anaesthetic that he proposes to use, that I have consented to undergo both. I have<br />
also agreed to his using non- blood volume expanders and pharmaceuticals that<br />
control haemorrhage and/or stimulate the production of red blood cells. I also<br />
consent to his using other drugs routinely used in the course of an anaesthetic.<br />
However, I have told the doctor that I am one of Jehovah‘s Witnesses with firm<br />
religious convictions. With full realization of the implications of this position and<br />
knowledge that it may pose additional risks to my health or life, I have decided<br />
to impose the following further restrictions on what the doctors may do in the<br />
course of the operation. I do so exercising my own choice. I expressly withhold<br />
my consent to the following:<br />
1. Allogenic blood;<br />
2. Primary blood components including<br />
a. red cells<br />
b. white cells<br />
c. plasma<br />
d. platelets<br />
3. Any sample of my blood being used for cross-matching.<br />
4. I also object to the following: (please insert any other restrictions that you<br />
wish to impose):<br />
I understand that I am free to delete any of the words which appear above in<br />
order to modify these restrictions.<br />
I understand that this limitation of consent will remain in force and bind all those<br />
treating me unless and until I expressly revoke it.<br />
I understand that the procedure may not be done by the doctor who is treating me<br />
so far and that the express limitation of my consent to this procedure described<br />
above will be regarded as absolute by all the doctors who treat me, and will not<br />
be overridden in any circumstances by a purported consent of a relative or other<br />
person or body unless I have identified them to the hospital and appointed them<br />
in writing with authority to act as my proxy.<br />
I understand that such refusal will be regarded as remaining in force and binding<br />
upon those who care for me even though I may be unconscious or affected<br />
by medication or medical condition rendering me incapable of expressing my<br />
wishes and that doctors treating me will continue to be bound by my refusal<br />
even though they may believe that the treatment is immediately necessary in<br />
order to save my life.<br />
26
I further consent to any other procedure that may be immediately necessary to<br />
save my life or health, but I attach the same restrictions I have described above<br />
to the performance of that procedure.<br />
I further understand that details of my treatment and any consequences resulting<br />
will not be disclosed to any other person without my express consent or that of<br />
my authorised proxy unless required by law.<br />
Signature............................... Dated ..............................................<br />
Witnessed by.........................<br />
Of..........................................<br />
Dated..............................................<br />
27
Appendix 4<br />
Simplified Procedure for Application to Courts for a ‘Specific Issue Order’<br />
1. Child and parents refuse consent to treatment. Doctors believe treatment<br />
must be given, in the best interests of the child. This would not be an<br />
emergency situation – if it is, the doctor should act in the best interests of<br />
the child, having taken a second opinion, and record his actions carefully<br />
in the medical records.<br />
2. Doctors seek advice from their Trust Legal Department or Chief Executive<br />
who in turn seeks solicitors’ advice. Parents should be kept informed and<br />
invited to case conferences.<br />
3. If solicitors advise proceeding, they will involve CAFCASS whose function<br />
is to represent the interests of minors or others who are ‘incompetent’.<br />
A member of the CAFCASS staff, or a solicitor appointed by them, will<br />
probably wish to see the parents and the child, to discuss the situation.<br />
CAFCASS may then instruct solicitors and counsel to act on the child’s<br />
behalf.<br />
4. The Trust applies to the High Court (in Scotland the Court of Session or<br />
Sheriff Court) for an order giving consent to the proposed treatment. The<br />
terms of the proposed order should be discussed in advance with the<br />
CAFCASS representative.<br />
5. A hearing might be held in public, but with the names of the family,<br />
the hospital and the doctors directly involved kept confidential, when<br />
the doctor(s) recommending treatment would give evidence, based on<br />
a previously prepared affidavit. The Court will wish the doctor to state<br />
the reasons for the recommended treatment, together with other options<br />
considered and the reasons for discarding those options. Independent<br />
expert advice may also be required. CAFCASS may call their own<br />
experts to give evidence. The parents may wish to have separate legal<br />
representation.<br />
6. The Court may grant the order and may impose further conditions. The<br />
Court’s paramount consideration will be the welfare of the child.<br />
7. The Trust and the doctors then consider how best to proceed in<br />
accordance with the Court’s ruling.<br />
8. The Trust may be required to pay a proportion of the legal costs of<br />
CAFCASS, as well as its own.<br />
28
Procedure for cases<br />
involving children<br />
under 18<br />
See sections 3.6, 3.7<br />
& Appendix 4<br />
Parents refuse consent for<br />
essential transfusion for immediate<br />
or anticipated need even after<br />
careful and complete counselling<br />
If child capable of giving<br />
consent and does so,<br />
respect his wishes<br />
If life threatening,<br />
take second opinion,<br />
administer life-saving<br />
transfusion, document<br />
fully and inform Legal<br />
Dept/Manager<br />
If non-emergency, approach Trust Legal<br />
Dept/Duty Manager to seek advice<br />
from Trusts Solicitors. Keep parents<br />
informed of intentions<br />
Trust’s solicitors contact CAFCASS<br />
who will probably interview<br />
parents, child & medical staff<br />
CAFCASS will act on the<br />
child’s behalf<br />
Trust applies to High Court (in Scotland<br />
the Court or Sheriff Court) for Order giving<br />
consent for proposed treatment<br />
Public Hearing (Court will be asked to rule that names of family,<br />
hospital and doctors remain confidential). Doctors give evidence<br />
of need & lack of alternatives. CAFCASS will represent the child.<br />
The Parents may be heard and have legal representation.<br />
Court may grant order and may impose other conditions.<br />
Court’s paramount consideration will be child’s best interest<br />
Trust’s doctors proceed according to<br />
Court ruling.<br />
NB Trust may be required to pay part of<br />
costs of CAFCASS<br />
29
21 Portland Place, London W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org<br />
Designed and produced by Cox Design Ltd
AAGBI Safety Guideline<br />
Management of Severe Local Anaesthetic Toxicity<br />
1<br />
Recognition<br />
2<br />
Immediate<br />
management<br />
3<br />
Treatment<br />
Signs of severe toxicity:<br />
• Sudden alteration in mental status, severe agitation or loss of consciousness,<br />
with or without tonic-clonic convulsions<br />
• Cardiovascular collapse: sinus bradycardia, conduction blocks, asystole and<br />
ventricular tachyarrhythmias may all occur<br />
• Local anaesthetic (LA) toxicity may occur some time after an initial injection<br />
• Stop injecting the LA<br />
• Call for help<br />
• Maintain the airway and, if necessary, secure it with a tracheal tube<br />
• Give 100% oxygen and ensure adequate lung ventilation (hyperventilation may<br />
help by increasing plasma pH in the presence of metabolic acidosis)<br />
• Confirm or establish intravenous access<br />
• Control seizures: give a benzodiazepine, thiopental or propofol in small<br />
incremental doses<br />
• Assess cardiovascular status throughout<br />
• Consider drawing blood for analysis, but do not delay definitive treatment to do<br />
this<br />
In circulatory arrest<br />
• Start cardiopulmonary resuscitation<br />
(CPR) using standard protocols<br />
• Manage arrhythmias using the<br />
same protocols, recognising that<br />
arrhythmias may be very refractory to<br />
treatment<br />
• Consider the use of cardiopulmonary<br />
bypass if available<br />
Without circulatory arrest<br />
Use conventional therapies to treat:<br />
• hypotension,<br />
• bradycardia,<br />
• tachyarrhythmia<br />
Give intravenous<br />
lipid emulsion<br />
(following the regimen overleaf)<br />
• Continue CPR throughout treatment<br />
with lipid emulsion<br />
• Recovery from LA-induced cardiac<br />
arrest may take >1 h<br />
• Propofol is not a suitable substitute<br />
for lipid emulsion<br />
• Lidocaine should not be used as an<br />
anti-arrhythmic therapy<br />
Consider intravenous<br />
lipid emulsion<br />
(following the regimen overleaf)<br />
• Propofol is not a suitable substitute<br />
for lipid emulsion<br />
• Lidocaine should not be used as an<br />
anti-arrhythmic therapy<br />
4<br />
Follow-up<br />
• Arrange safe transfer to a clinical area with appropriate equipment and suitable<br />
staff until sustained recovery is achieved<br />
• Exclude pancreatitis by regular clinical review, including daily amylase or lipase<br />
assays for two days<br />
• Report cases as follows:<br />
in the United Kingdom to the National Patient Safety Agency<br />
(via www.npsa.nhs.uk)<br />
in the Republic of Ireland to the Irish Medicines Board (via www.imb.ie)<br />
If Lipid has been given, please also report its use to the international registry at<br />
www.lipidregistry.org. Details may also be posted at www.lipidrescue.org<br />
Your nearest bag of Lipid Emulsion is kept<br />
This guideline is not a standard of medical care. The ultimate judgement with regard to a particular clinical procedure or treatment plan<br />
must be made by the clinician in the light of the clinical data presented and the diagnostic and treatment options available.<br />
© The Association of Anaesthetists of Great Britain & Ireland 2010
Immediately<br />
Give an initial intravenous bolus<br />
injection of 20% lipid emulsion<br />
1.5 ml.kg –1 over 1 min<br />
and<br />
Start an intravenous infusion of 20%<br />
lipid emulsion at 15 ml.kg –1 .h –1<br />
after 5 min<br />
Give a maximum of two repeat<br />
boluses (same dose) if:<br />
• cardiovascular stability has not<br />
been restored or<br />
• an adequate circulation<br />
deteriorates<br />
Leave 5 min between boluses<br />
A maximum of three boluses can be<br />
given (including the initial bolus)<br />
and<br />
Continue infusion at same rate, but:<br />
Double the rate to 30 ml.kg –1 .h –1 at<br />
any time after 5 min, if:<br />
• cardiovascular stability has not been<br />
restored or<br />
• an adequate circulation deteriorates<br />
Continue infusion until stable and<br />
adequate circulation restored or<br />
maximum dose of lipid emulsion given<br />
Do not exceed a maximum cumulative dose of 12 ml.kg –1<br />
An approximate dose regimen for a 70-kg patient would be as follows:<br />
Immediately<br />
Give an initial intravenous bolus<br />
injection of 20% lipid emulsion<br />
100 ml over 1 min<br />
and<br />
Start an intravenous infusion of 20%<br />
lipid emulsion at 1000 ml.h –1<br />
after 5 min<br />
Give a maximum of two repeat<br />
boluses of 100 ml<br />
and<br />
Continue infusion at same rate<br />
but double rate to 2000 ml.h –1 if<br />
indicated at any time<br />
Do not exceed a maximum cumulative dose of 840 ml<br />
This AAGBI Safety Guideline was produced by a Working Party that comprised:<br />
Grant Cave, Will Harrop-Griffiths (Chair), Martyn Harvey, Tim Meek, John Picard, Tim Short and Guy Weinberg.<br />
This Safety Guideline is endorsed by the Australian and New Zealand College of Anaesthetists (ANZCA).<br />
© The Association of Anaesthetists of Great Britain & Ireland 2010
Anaesthesia 2016, 71, 352<br />
Corrections<br />
In [1], the Figure 2 legend should be amended from:<br />
Figure 2 Ultrasound screen captures of block administration, with needle advanced cranio-caudally. 1 ribs, 2 serratus anterior<br />
muscle, 3 intercostal muscle, 4 local anaesthetic.<br />
to:<br />
Figure 2 Ultrasound screen captures of block administration, with needle advanced cranio-caudally. 1 paraspinal muscles,<br />
2 local anaesthetic, 3 intercostal muscles, 4 ribs.<br />
Reference<br />
1. Roue C, Wallaert M, Kacha M, Havet E. Intercostal/paraspinal nerve block for thoracic surgery. Anaesthesia 2015; 71: 112–3.<br />
doi:10.1111/anae.13383<br />
In the Guidelines [1] by Harrop-Griffiths et al., the notes to accompany Table 2 stated that there was one death in a<br />
patient who underwent lumbar plexus block. This was incorrect, and should read:<br />
“The one death in this series was that of a patient on clopidogrel who underwent a lumbar sympathetic<br />
block...”<br />
Reference<br />
1. Harrop-Griffiths W, Cook T, Gill H, Hill D, Ingram M, Makris M, Malhotra S, Nicholls B, Popat M, Swales H, Wood P (Working Party). The<br />
Association of Anaesthetists of Great Britain & Ireland & The Obstetric Anaesthetists’ Association Regional Anaesthesia UK. Regional anaesthesia<br />
and patients with abnormalities of coagulation. Anaesthesia 2013; 68: 966–72.<br />
doi:10.1111/anae.13380<br />
352 © 2016 The Association of Anaesthetists of Great Britain and Ireland
AAGBI: Consent for anaesthesia 2017<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650 Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org January 2017
This guideline was originally published in Anaesthesia. If you wish to refer to this guideline, please use the following reference:<br />
Association of Anaesthetists of Great Britain and Ireland. AAGBI: Consent for anaesthesia 2017. Anaesthesia 2017; 72: 93-105.<br />
This guideline can be viewed online via the following URL:<br />
http://onlinelibrary.wiley.com/doi/10.1111/anae.13762/full
Anaesthesia 2017<br />
Guidelines<br />
doi:10.1111/anae.13762<br />
AAGBI: Consent for anaesthesia 2017<br />
Association of Anaesthetists of Great Britain and Ireland<br />
S. M. Yentis, 1 A. J. Hartle, 2 I. R. Barker, 3 P. Barker, 4 D. G. Bogod, 5 T. H. Clutton-Brock, 6 A. Ruck<br />
Keene, 7 S. Leifer, 8 A. Naughton 9 and E. Plunkett 10<br />
1 Consultant Anaesthetist, Chelsea and Westminster Hospital, London and Honorary Reader, Imperial College<br />
London, UK; Vice-President, AAGBI (Working Party Chair from July 2015)<br />
2 Consultant Anaesthetist, Imperial College Healthcare NHS Trust, London, UK; President, AAGBI (to Sept 2016;<br />
Working Party Chair to July 2015)<br />
3 Specialist Registrar in Anaesthesia, Imperial rotation, London, UK (present position: Consultant Anaesthetist,<br />
Imperial College Healthcare NHS Trust, London, UK)<br />
4 Consultant Anaesthetist, Norfolk and Norwich University Hospitals, Norwich, UK; member, AAGBI Board of Directors<br />
5 Consultant Anaesthetist, Nottingham University Hospitals NHS Trust, Nottingham, UK<br />
6 Reader, University of Birmingham, Birmingham, UK; Council member, Royal College of Anaesthetists (to Feb. 2016)<br />
7 Barrister, 39 Essex Chambers, London; Honorary Research Lecturer University of Manchester, UK; Visiting Research<br />
Fellow, King’s College London, UK<br />
8 Specialist Registrar in Anaesthesia, Manchester rotation, Manchester, UK; member, AAGBI Group of Anaesthetists in<br />
Training (GAT) Committee<br />
9 Lay member, AAGBI Board of Directors<br />
10 Specialist Registrar in Anaesthesia, Birmingham School of Anaesthesia, Birmingham, UK; member, AAGBI GAT<br />
Committee<br />
Summary<br />
Previous guidelines on consent for anaesthesia were issued by the Association of Anaesthetists of Great Britain and<br />
Ireland in 1999 and revised in 2006. The following guidelines have been produced in response to the changing ethical<br />
and legal background against which anaesthetists, and also intensivists and pain specialists, currently work, while<br />
retaining the key principles of respect for patients’ autonomy and the need to provide adequate information.<br />
The main points of difference between the relevant legal frameworks in England and Wales and Scotland, Northern<br />
Ireland and the Republic of Ireland are also highlighted.<br />
.................................................................................................................................................................<br />
Correspondence to: S. M. Yentis.<br />
E-mail: s.yentis@imperial.ac.uk<br />
Accepted: 22 October 2016<br />
Keywords: anaesthesia; assessment; consent; medicolegal; pre-operative<br />
This is a consensus document produced by expert members of a Working Party established by the Association of<br />
Anaesthetists of Great Britain and Ireland. It has been seen and approved by the AAGBI Board of Directors. Date of<br />
review: 2022.<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland. 1<br />
This is an open access article under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs License, which permits use and<br />
distribution in any medium, provided the original work is properly cited, the use is non-commercial and no modifications or adaptations are made.
Anaesthesia 2017 Yentis et al. | AAGBI: Consent for anaesthesia 2017<br />
• What other guidelines are available on this topic?<br />
Previous guidance was published by the Association<br />
of Anaesthetists of Great Britain and Ireland<br />
(AAGBI) in 1999 [1] and this was revised in 2006<br />
[2]. Guidance on consent to examination and treatment<br />
was published by the General Medical Council<br />
(GMC) in 2008 [3] and the Department of<br />
Health (DoH) in 2009 [4]. The British Medical<br />
Association and Law Society have published<br />
guidance on the assessment of mental capacity in<br />
2015 [5].<br />
• Why was this guideline developed?<br />
There have been a number of changes in the ethical<br />
and legal context around delivery of healthcare<br />
since the last AAGBI guidance, in particular new<br />
case law and increasing emphasis on consumerism<br />
and patient-centred care.<br />
• How and why does this statement differ from existing<br />
guidelines?<br />
The previous AAGBI guidance has been updated<br />
and input received from intensivists and pain<br />
specialists as well as anaesthetists. In addition,<br />
some guidance is offered for the increasingly different<br />
systems in the devolved nations and in Ireland.<br />
Recommendations<br />
(The legal frameworks for decision-making in relation<br />
to those lacking capacity in Scotland, Northern Ireland<br />
and the Republic of Ireland are not the same as that<br />
in England and Wales, although the guiding principles<br />
are largely the same. The body of this guidance is<br />
based on the law as it applies in England and Wales; a<br />
comparative table is provided at the end to highlight<br />
the main differences (Appendix 1, Supporting Information)).<br />
1 Information about anaesthesia and its associated<br />
risks should be provided to patients as early as<br />
possible, preferably in the form of an evidencebased<br />
online resource or leaflet that the patient<br />
can keep for future reference. Those undergoing<br />
elective surgery should be provided with information<br />
before admission, preferably at pre-assessment<br />
or at the time of booking, but the duty remains<br />
on the anaesthetist to ensure that the information<br />
is understood.<br />
2 Immediately before induction of anaesthesia, for<br />
example in the anaesthetic room, is not an acceptable<br />
time to provide elective patients with new<br />
information other than in exceptional circumstances.<br />
3 The amount and the nature of information that<br />
should be provided to the patient should be determined<br />
by the question: ‘What would this particular<br />
patient regard as relevant when coming to a<br />
decision about which of the available options to<br />
accept?’<br />
4 At the end of an explanation about a procedure,<br />
patients should be asked whether they have any<br />
questions; any such questions should be addressed<br />
fully and details recorded.<br />
5 Anaesthetists should record details of the elements<br />
of a discussion in the patient record, noting the<br />
risks, benefits and alternatives (including no treatment)<br />
that were explained.<br />
6 A separate consent form, signed by the patient, is<br />
not required for anaesthetic procedures that are<br />
done to facilitate another treatment.<br />
7 Consent is an ongoing process, not a single event,<br />
and may require repeated discussion and/or confirmation,<br />
with documentation at every stage.<br />
8 For a course of treatment (e.g. for chronic pain),<br />
consent to continue should be confirmed and documented<br />
before each individual component, and<br />
any changes to risks, benefits or alternatives discussed<br />
fully.<br />
9 If patients insist they do not want to know about<br />
the risks of a procedure (including anaesthesia),<br />
the consequences of this should be explained; this<br />
discussion should be recorded in writing and the<br />
patient given the opportunity to change his/her<br />
mind. Patients should understand that there may<br />
be risks but should not have a detailed explanation<br />
forced upon them if unwilling.<br />
10 The Mental Capacity Act 2005 (MCA) [6] confirms<br />
that adults should be presumed to have<br />
capacity to consent to medical treatment. If there<br />
are reasonable grounds for concluding otherwise,<br />
these must be documented. The MCA places a<br />
duty upon all those concerned with care to make<br />
efforts to reverse or minimise temporary incapacity<br />
to enable patients to make their own decisions<br />
2 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland.
Yentis et al. | AAGBI: Consent for anaesthesia 2017 Anaesthesia 2017<br />
and, where it is not possible to do so, to treat<br />
patients lacking capacity in their best interests.<br />
Adults may make an advance decision to refuse<br />
treatment or appoint a proxy to decide upon their<br />
behalf using a lasting power of attorney (LPA). A<br />
valid and applicable advance decision or a decision<br />
of a validly appointed health and welfare LPA is legally<br />
binding, as is the decision of a court-appointed<br />
deputy with the appropriate powers.<br />
11 Anaesthetists should be aware of the different<br />
frameworks that apply in relation to consent (and<br />
who can consent on behalf of the patient) with<br />
respect to patients aged 16 and 17 and those<br />
under 16.<br />
12 When planning to allow trainees or others to use<br />
an opportunity presented by a clinical encounter<br />
for training in practical procedures, the anaesthetist<br />
should make every effort to minimise risk<br />
and maximise benefits, and should consider alternative<br />
ways of achieving the same end. Specific<br />
consent for such procedures may or may not be<br />
required depending on the circumstances.<br />
A set of ‘frequently asked questions’ (FAQs) (relating<br />
to England and Wales and Northern Ireland, with<br />
a version adapted for Scotland and a note relating to<br />
the Republic of Ireland) is also provided in Appendix 2,<br />
Supporting Information.<br />
Introduction<br />
The need for consent before treatment is firmly<br />
embedded in modern healthcare. These guidelines –<br />
the third produced by the Association of Anaesthetists<br />
of Great Britain and Ireland (AAGBI) – draw upon<br />
previous versions [1, 2] and other guidance [3–5] in<br />
the context of the particular roles of anaesthetists,<br />
intensivists and pain specialists in providing clinical<br />
care, against a backdrop of evolving legal and ethical<br />
frameworks in which they work. In light of the different<br />
legal frameworks that now apply in the devolved<br />
nations and in the Republic of Ireland, the body of<br />
this guidance limits itself to the legal framework that<br />
applies in England and Wales (although the guiding<br />
principles are largely the same). A table highlights the<br />
key differences in the legal frameworks in Scotland,<br />
Northern Ireland and the Republic of Ireland<br />
(Appendix 1, Supporting Information). (n.b. the word<br />
‘treatment’ is used in this document to indicate both<br />
treatment in the usual sense, that is, something used<br />
to ‘treat’ (alleviate) something, and also an anaesthetic<br />
intervention such as general/regional anaesthesia, etc).<br />
The importance of consent<br />
Ethical aspects<br />
Clinicians have an ethical obligation to respect<br />
patients’ autonomy – that is, their right to be involved<br />
in decisions that affect them. In medicine, this is<br />
reflected in the requirement to obtain consent for<br />
treatment, which can only be valid if adequate information<br />
is supplied and the patient has the capacity to<br />
understand it and make a balanced decision, free from<br />
coercion [7]. Patients may change their minds and<br />
withdraw consent at any time, so long as these conditions<br />
still apply.<br />
The need to respect autonomy sometimes conflicts<br />
with other obligations, such as the principle of beneficence<br />
(doing good). For example, patients may decline<br />
life-saving treatment, and this decision must be<br />
respected if they have capacity.<br />
Professional aspects<br />
Respect for autonomy and the need for consent is<br />
emphasised in professional guidance as being central<br />
to the doctor–patient relationship. The GMC’s guidance<br />
in 2008 confirmed that doctors should tell their<br />
patients what the latter wanted to know, not what the<br />
doctors thought they should know [3].<br />
Patients also have an interest in knowing what is<br />
going to happen to them and what they should expect<br />
during a course of treatment or other medical encounter.<br />
It is a professional obligation to explain such<br />
things to patients, to give them the opportunity to ask<br />
questions and to provide honest answers.<br />
Legal aspects<br />
The legal requirements for valid consent reflect the ethical<br />
ones: it must be given voluntarily by an appropriately<br />
informed patient, who has the capacity to exercise a<br />
choice – even if this choice appears irrational. Pain, illness<br />
and premedication do not necessarily make a<br />
patient incapable of consenting to treatment [7].<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland. 3
Anaesthesia 2017 Yentis et al. | AAGBI: Consent for anaesthesia 2017<br />
Touching a patient without consent or approaching<br />
him/her with a needle, irrespective of outcome,<br />
may lead to a claim of assault or battery. Far more<br />
common, although, is a claim of negligence after a<br />
complication has occurred, on the basis that had a<br />
warning been given, the patient would not have agreed<br />
to the treatment and the complication would not have<br />
occurred [8]. Case law suggests that a doctor might<br />
still be found negligent even if the patient would have<br />
undergone the treatment had he/she been warned [9,<br />
10], reflecting the importance that the law accords to<br />
the duty to respect patients’ autonomy. In addition,<br />
Articles 3, 8 and/or 9 of the European Convention on<br />
Human Rights might feasibly be invoked if consent is<br />
not sought from patients before treatment [10, 11].<br />
The treating doctor is responsible for ensuring that<br />
the patient has consented to the treatment. For<br />
patients referred for investigations requiring anaesthesia,<br />
for example MRI, consent for the investigation<br />
should be sought by the referring doctor or local radiologist,<br />
while consent for anaesthesia should be sought<br />
by the anaesthetist providing anaesthesia.<br />
For many decades, legal decisions concerning consent<br />
have been based on the Bolam principle [12], that<br />
is, whether the doctor seeking consent did so (i.e.<br />
provided enough information) in accordance with a<br />
responsible body of clinical opinion. The courts subsequently<br />
stressed that such a clinical opinion must be<br />
rational and stand up to logical analysis [13]. Recent case<br />
law (Montgomery v Lanarkshire Health Board) has confirmed<br />
that the Bolam principle no longer applies in<br />
matters of consent, and that a doctor needs to provide all<br />
‘material risks’ to a patient, with materiality defined as:<br />
“... whether a reasonable person in the patient’s position<br />
would be likely to attach significance to the risk, or the<br />
doctor should reasonably be aware that the particular<br />
patient would be likely to attach significance to it” [10] –<br />
thus bringing the law in line with previous professional<br />
guidance from the GMC in 2008 [3, 14]. There are only<br />
three exceptions to this rule: i) the patient has expressed<br />
a fixed desire not to know the risks; ii) discussion of the<br />
risks would pose a serious threat (beyond merely causing<br />
distress) to the patient (e.g. suicide); and iii) in ‘circumstances<br />
of necessity’ where urgent treatment is needed<br />
but the patient lacks capacity, and where the treatment<br />
that is being delivered is in his/her best interests.<br />
Patients must be informed of alternative treatments,<br />
the risks associated with them and the option<br />
of not receiving treatment; not doing so may invalidate<br />
consent and result in a negligence claim [10, 15].<br />
Capacity, best interests and<br />
voluntariness<br />
Capacity<br />
The MCA provides the legal framework in England<br />
and Wales for protecting and supporting people whose<br />
capacity may be impaired [6]. It reinforces that capacity<br />
should be assumed unless proven otherwise (Section<br />
1(2)), sets out how to make decisions where a<br />
person does not (despite being supported) have the<br />
capacity to make his/her own decisions (Sections 1(5)<br />
and (4)) and introduced several new roles, bodies and<br />
powers (see Table 1).<br />
Those over 16 years have the legal capacity to<br />
consent to a medical procedure if they are able to<br />
understand, retain, use and weigh the relevant information,<br />
and communicate their decision [3, 6, 16]. In<br />
most instances, it is for the person treating the patient<br />
to decide whether the patient has the capacity or not.<br />
Assumptions relating to capacity based on age,<br />
Table 1 Summary of the Mental Capacity Act (2005)’s<br />
main features and provisions [6].<br />
Statutory<br />
principles<br />
Roles/institutions<br />
created<br />
Other<br />
A person must be assumed to have<br />
capacity unless proved otherwise<br />
A person must be given all practicable<br />
help to make his/her own decision<br />
before being treated as lacking capacity<br />
A person must not be treated as lacking<br />
capacity merely because he/she makes<br />
an unwise decision<br />
An intervention or decision made on<br />
behalf of a person lacking capacity<br />
must be in his/her best interests.<br />
The intervention or decision made on<br />
behalf of a person lacking capacity<br />
must cause the least restriction of<br />
his/her rights and freedom of action to<br />
achieve the stated purpose<br />
Court of Protection<br />
Lasting power of attorney<br />
Independent Mental Capacity Advocates<br />
Deputies<br />
Advance decisions to refuse treatment<br />
confirmed in law<br />
Applies to anyone over 16 years old<br />
4 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland.
Yentis et al. | AAGBI: Consent for anaesthesia 2017 Anaesthesia 2017<br />
appearance or behaviour must not be made [3, 17],<br />
and nor should they be made about a patient’s capacity<br />
to make decisions on the basis of a particular condition,<br />
for instance a learning disability. Furthermore,<br />
patients cannot be treated as lacking capacity to consent<br />
to or refuse medical procedures unless all practicable<br />
steps to support them to do so have been taken<br />
without success [6].<br />
The decision made by the patient does not have to<br />
be sensible, rational or well considered. Furthermore, a<br />
patient should not be treated as being unable to make a<br />
decision merely because the decision that he/she makes<br />
is one that appears unwise to the treating professionals<br />
[6]. However, a highly irrational decision that is based<br />
on a persistent misinterpretation of the information<br />
presented may indicate that the patient does not, in<br />
fact, have the capacity to make the decision within the<br />
meaning of the MCA (in practice, determining incapacity<br />
on the grounds of irrationality is fraught with difficulty;<br />
in such a situation, legal advice should be<br />
sought). Under the MCA, the patient’s inability to<br />
make the decision must be because of an impairment of<br />
or disturbance in the functioning of their mind or<br />
brain, in the absence of which he/she has the capacity<br />
no matter how impaired his/her reasoning process is.<br />
(See also Voluntariness, below, in relation to concerns<br />
that a patient’s decisions may be made under duress).<br />
Refusal of treatment by an adult with capacity is<br />
legally binding, even if refusal is likely to result in the<br />
patient’s death [18]. The position in relation to 16-<br />
and 17-year-olds is addressed below.<br />
Capacity is issue-specific: patients may have capacity<br />
to consent to simple procedures but not complex<br />
ones [19, 20].<br />
A lack of decision-making capacity may be the<br />
predictable result of a condition (e.g. Alzheimer’s disease,<br />
Huntingdon’s dementia), the temporary result of<br />
an event (e.g. unconsciousness following intoxication,<br />
head injury or during general anaesthesia), or the permanent<br />
result of an event (e.g. perinatal brain damage<br />
or persistent vegetative state).<br />
Mental illness may impair a patient’s capacity to<br />
provide valid consent for treatment. However, a person<br />
receiving treatment for mental illness (even if he/she is<br />
detained under the Mental Health Act 1983 (MHA))<br />
should not be assumed to be incapable of providing<br />
valid consent for medical, surgical or dental treatment.<br />
The consent of a patient detained under the MHA is<br />
not required for any medical treatment of the patient’s<br />
mental disorder if that treatment is being given under<br />
the provisions of Part 4 of the MHA. However, the<br />
patient’s consent, or a second opinion, is required<br />
before the administration of electroconvulsive therapy<br />
(ECT), which also cannot be given where the patient<br />
has made an advance decision refusing ECT, or a<br />
health and welfare attorney or court-appointed deputy<br />
refuses the treatment. When the patient is not capable<br />
of consenting, or refuses treatment, ECT can be given<br />
in an emergency if the authorised practitioner certifies<br />
the patient’s lack of capacity or refusal, and that the<br />
treatment is likely to alleviate or prevent deterioration<br />
in the patient’s condition. Licence to treat in this way<br />
in an emergency would also extend to the use of general<br />
anaesthesia for administering ECT [21].<br />
Best interests<br />
If a patient lacks capacity, practitioners must make a<br />
clear record of the grounds on which they have<br />
reached this decision, the treatment that will be undertaken,<br />
and how this treatment will be in the patient’s<br />
best interests. The courts have made clear that ‘best<br />
interests’ for these purposes involve consideration of<br />
the patient’s ‘welfare in the widest sense, not just medical<br />
but social and psychological; they must consider the<br />
nature of the medical treatment in question, what it<br />
involves and its prospects of success; they must consider<br />
what the outcome of that treatment for the patient is<br />
likely to be; they must try and put themselves in the<br />
place of the individual patient and ask what his attitude<br />
to the treatment is or would be likely to be; and<br />
they must consult others who are looking after him or<br />
interested in his welfare, in particular for their view of<br />
what his attitude would be’ [22]. The process of best<br />
interests decision-making is designed to ensure that<br />
the decision that is made is right for the patient ‘as an<br />
individual human being’, which may or may not<br />
accord with the decision that appears wise to the treating<br />
professionals [22, 23]. The MCA stresses that family<br />
members (and where appropriate, other persons<br />
close to the patient) must be consulted when considering<br />
patients’ best interests [6], but failure to do so<br />
should not compromise care in an emergency. If a<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland. 5
Anaesthesia 2017 Yentis et al. | AAGBI: Consent for anaesthesia 2017<br />
patient lacking capacity is to undergo serious medical<br />
treatment (defined in the context of a fine balance<br />
between risks and benefits, or of the ‘serious consequences’<br />
that may arise) but no family members or<br />
close friends are available, consultation with an Independent<br />
Mental Capacity Advocate should be sought,<br />
under Sections 35-37 of the MCA [6].<br />
Patients who are aware that they are likely to lose<br />
capacity to make decisions, either temporarily or permanently,<br />
may choose to prepare an ‘advance decision’<br />
(often known as ‘advance directive’ or ‘living will’),<br />
stating which treatments they would refuse in the<br />
event that their treating team consider them indicated<br />
(see below).<br />
A patient may also have made an LPA. This is a<br />
legal document that allows patients to appoint another<br />
person(s) to make decisions on his/her behalf in the case<br />
of incapacity. Two types of LPA exist (health/welfare<br />
and property/financial affairs), and they must be registered<br />
with the Office of the Public Guardian for them to<br />
have effect (this process may take up to several weeks; if<br />
needed more urgently an application may have to made<br />
to the Court of Protection). Only an attorney under a<br />
health and welfare LPA can have any power to make<br />
decisions in relation to medical treatment, and an attorney<br />
has no power to refuse life-sustaining treatment<br />
unless the document contains specific provision to that<br />
effect (a health and welfare deputy can never have the<br />
power to refuse life-sustaining treatment). Enduring<br />
powers of attorney (EPA), which can no longer be made<br />
but many of which are still used, could only give the<br />
attorney power to make decisions in relation to property<br />
and financial affairs; an attorney under an EPA can<br />
therefore never make healthcare decisions on behalf of a<br />
patient. In some circumstances, a patient lacking capacity<br />
to make decisions may have a court-appointed deputy,<br />
who may (depending on the terms of their<br />
appointment) have powers to make some healthcare<br />
decisions, but will never have the power to refuse lifesustaining<br />
treatment.<br />
Voluntariness<br />
For a decision by an individual to be valid, it must<br />
have been taken voluntarily, that is, without coercion<br />
[3, 7]. In general, it is good practice for the clinician<br />
who is seeking consent to indicate whether he/she<br />
favours one therapeutic option over another, but the<br />
imbalance of power and influence in the doctor–patient<br />
relationship means that the vulnerable patient<br />
may feel coerced by the doctor’s enthusiasm. Anaesthetists<br />
seeking consent should be aware of this and<br />
not allow their preferences to override the patient’s<br />
autonomy [4].<br />
Coercion can occur when patients are influenced<br />
by the beliefs or preferences of friends or relatives.<br />
This is more likely to arise where a child with capacity<br />
is accompanied by a parent, in areas where both parties<br />
have a major stake in the outcome, such as obstetrics,<br />
or in certain cultures. Where such a situation is<br />
suspected, anaesthetists should seek to speak to the<br />
patient away from a potentially coercive influence.<br />
Legal advice should be sought where anaesthetists are<br />
not clear whether a patient’s inability to make decisions<br />
about his/her medical treatment is down to an<br />
impairment or disturbance in the functioning of his/<br />
her mind or brain, or the duress to which he/she may<br />
be being subjected by family members or friends [7].<br />
Such situations must be handled very carefully, particularly<br />
if English is not the first language of any participant.<br />
A ‘whole team’ approach is always best, but is<br />
essential in obstetric and/or paediatric cases, with early<br />
consultant involvement.<br />
Information and the consent process<br />
Information about anaesthesia and related procedures<br />
is not exclusively provided by anaesthetists, but the<br />
anaesthetist caring for the patient is responsible for the<br />
discussion with the patient regarding that procedure.<br />
This can be delegated to someone else, providing that<br />
the person is suitably trained and qualified with adequate<br />
knowledge of what is planned, including an<br />
understanding of the risks. He/she must also act in<br />
accordance with the GMC’s guidance [3].<br />
Timing<br />
Information about anaesthesia and its associated risks<br />
should be provided to patients as early as possible, preferably<br />
in the form of an evidence-based online resource or<br />
leaflet that the patient can keep for future reference (see<br />
e.g. http://www.labourpains.com/UI/Content/Content.as<br />
px?ID=5; http://www.<strong>aagbi</strong>.org/news/information-public/<br />
information-about-anaesthesia-adults). Those undergoing<br />
6 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland.
Yentis et al. | AAGBI: Consent for anaesthesia 2017 Anaesthesia 2017<br />
elective surgery should be provided with information<br />
before admission, preferably at pre-assessment or the time<br />
of booking, but the duty remains on the anaesthetist to<br />
ensure that the information is understood. This is particularly<br />
important for patients admitted on the day of surgery<br />
– increasingly the norm in modern surgical practice –<br />
where the opportunity for prolonged discussion is limited.<br />
Patients should be informed that they will meet the anaesthetist<br />
before their operation, so that further queries and<br />
discussions can take place before finally consenting to<br />
anaesthesia. Consent can only be valid if the patient is sufficiently<br />
informed and understands the broad nature of<br />
the procedure [4, 24, 25].<br />
The anaesthetist must be satisfied that patients<br />
have been given sufficient time to come to a considered<br />
view after they have been provided with relevant<br />
information about their treatment, and have had the<br />
opportunity for adequate discussion, even if admitted<br />
on the same day as surgery. The time required for this<br />
will depend on the patient and the nature of the procedure.<br />
Immediately before induction of anaesthesia,<br />
for example in the anaesthetic room, is not an acceptable<br />
time to provide elective patients with new information<br />
other than in exceptional circumstances. The<br />
importance of allowing sufficient time for the consenting<br />
process is illustrated by a recent case in which it<br />
was held to be unacceptable to inform a patient who<br />
had specifically arranged to have surgery performed by<br />
a particular surgeon, as she was about to enter the<br />
operating theatre, that her surgery would be performed<br />
by a different surgeon, since there was insufficient<br />
time for her to make an informed and free<br />
decision [26].<br />
Standards for provision of information<br />
Sufficient time must be allowed for the process of consent<br />
to take place during the pre-operative visit.<br />
The amount and the nature of information that<br />
should be disclosed to the patient should as far as possible<br />
be determined by the question: ‘What would this<br />
particular patient regard as relevant when coming to a<br />
decision about which – if any – of the available<br />
options to accept?’ [4].<br />
Individual anaesthetists and departments may wish<br />
to use nationally available written information or to<br />
produce their own (e.g. see http://www.rcoa.ac.uk/docu<br />
ment-store/you-and-your-anaesthetic; https://www.rcoa.<br />
ac.uk/node/428; http://www.labourpains.com/UI/Con<br />
tent/Content.aspx?ID=5). Written information should<br />
be available in languages commonly read by local<br />
patients. Braille and large-print versions should be<br />
available for situations where impaired vision is likely<br />
(e.g. information about local anaesthesia for cataract<br />
surgery). Translators or readers must be available for<br />
those patients unable to read the written information<br />
provided. If the patient does not speak English then<br />
consent must take place with the use of an interpreter,<br />
and must not rely on family members or friends to<br />
translate, ensuring the accuracy of the information<br />
provided and reducing any coercive influence.<br />
Information may only be withheld if providing it<br />
would pose a serious threat to a patient’s health, not<br />
just because the anaesthetist feels it may make a<br />
patient anxious or deter him/her from undergoing a<br />
beneficial procedure. Conversely, any information that<br />
might lead a patient to cancel or defer a procedure<br />
should be considered significant. If patients insist they<br />
do not want to know about anaesthesia or a procedure,<br />
the consequences of not understanding the procedure/<br />
anaesthesia should be explained, particularly as it may<br />
mean their consent is not valid. This discussion should<br />
be recorded and the patient provided with the opportunity<br />
to change his/her mind. Basic information about<br />
the nature of the procedure should always be provided;<br />
however, detailed information should not be forced<br />
upon patients who have repeatedly indicated that they<br />
do not want to hear it [27].<br />
In broad terms, patients must understand to what<br />
they are consenting. Therefore, anaesthetists should tell<br />
the patient: i) what procedures are intended, and why;<br />
ii) what the significant, foreseeable risks of these procedures<br />
are, and their consequences; and iii) what the<br />
alternatives are, including having no treatment. When<br />
deciding how much information to provide, anaesthetists<br />
must consider the relevance of information<br />
from their judgement of the patient’s perspective, and<br />
mention significant hazards. A broad summary of what<br />
should be included in most cases is provided in<br />
Table 2, although the information given should always<br />
be according to what a particular patient wants to<br />
know and the likelihood of outcomes in that specific<br />
case, given the patient’s medical history, the nature of<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland. 7
Anaesthesia 2017 Yentis et al. | AAGBI: Consent for anaesthesia 2017<br />
Table 2 Broad summary of information appropriate for patients during the consenting process (n.b. the anaesthetist<br />
should be guided by what each particular patient wants to know, rather than a proforma list, and with consideration<br />
of what the incidence of risks might be in that patient).<br />
Common components<br />
of anaesthetic technique<br />
Specific aspects related to<br />
procedure or condition<br />
Common/significant<br />
side-effects<br />
Serious side-effects<br />
Fasting; administration and effects of premedication; transfer from ward to anaesthetic room;<br />
cannula insertion; non-invasive monitoring; induction of general and/or local anaesthetic;<br />
monitoring throughout surgery by the anaesthetist; intra-operative drugs/fluids; intra-operative<br />
discomfort/awareness of the procedure/surroundings, etc, if awake/sedated; transfer to recovery<br />
area; return to ward; postoperative analgesia/anti-emetics/fluids; techniques of a sensitive nature,<br />
e.g. insertion of an analgesic suppository<br />
Alternative techniques where appropriate, including if one technique fails (e.g. general anaesthesia<br />
for caesarean section as an alternative to regional anaesthesia, or if the latter is inadequate)<br />
Invasive monitoring and associated risks; recovery in a critical care environment; sedation;<br />
intubation/tracheotomy<br />
Nausea and vomiting; sore throat; damage to teeth/lips; cognitive dysfunction; numbness/<br />
weakness/return of pain after local anaesthetic techniques; suxamethonium pains; post-dural<br />
puncture headache<br />
Nerve/eye damage; awareness during anaesthesia; death<br />
the surgery and its urgency. It is the anaesthetist’s<br />
responsibility to make reasonable efforts to judge what<br />
would be particularly significant risks or complications<br />
to his/her patient, for example the risk of vocal cord<br />
damage from general anaesthesia if the patient is a<br />
professional singer. Where possible, estimates of the<br />
incidence of risks should be given and the discussion<br />
recorded (see below).<br />
All patients should be given the opportunity to ask<br />
questions and honest answers should be provided. The<br />
courts have emphasised the importance of medical professionals’<br />
recognising that they are engaged in a dialogue<br />
with the patients they are treating, and tailoring<br />
that dialogue to the needs of the individual patient [10].<br />
Many questions relate to the operation itself. The<br />
anaesthetist should not provide information about the<br />
surgical procedure beyond his/her capability.<br />
Documentation<br />
As in previous versions of this guidance, the Working<br />
Party’s view continues to be that a signed consent<br />
form is not necessary for anaesthetic procedures that<br />
are done to facilitate another treatment, since it is the<br />
process of consent itself that is important; a signed<br />
form is evidence that a consent process has been<br />
undertaken but does nothing to validate or invalidate<br />
the consent. Furthermore, the anaesthetic can be considered<br />
a component of another treatment (e.g. anaesthesia<br />
for surgery) or as part of a larger and interrelated<br />
process (e.g. epidural pain relief for childbirth),<br />
rather than a treatment in itself (see FAQs, Appendix 2,<br />
Supporting Information).<br />
Whether consent is oral or written, it is essential<br />
for anaesthetists to document clearly both a patient’s<br />
agreement to the intervention and the discussions that<br />
led up to that agreement, including the patient’s questions<br />
and the responses given. This can be done on a<br />
standard consent form, on the anaesthetic record or<br />
separately in the patient’s notes. Anaesthetic departments<br />
may wish to design anaesthetic records to document<br />
the discussions and agreement to specific modes<br />
of anaesthesia and interventions. A proforma may be<br />
useful – but as a guide to the conversation, not as a<br />
checklist to be ticked off without recording further<br />
detail. Documentation is particularly important where<br />
a patient wishes to reverse a previously documented<br />
decision, or circumstances when the patient’s decision<br />
goes against the anaesthetist’s advice, for example if a<br />
patient wishes to convert to general anaesthesia during<br />
apparently effective regional anaesthesia, or alternatively<br />
to continue with regional anaesthesia despite<br />
suboptimal anaesthesia in the view of the anaesthetist.<br />
Sometimes, the anaesthetic procedure is the primary<br />
therapeutic intervention. Examples include invasive procedures<br />
for the treatment of chronic pain, epidural<br />
blood patch for the treatment of post-dural puncture<br />
headache or placement of a central line for chemotherapy<br />
or parenteral nutrition. In these circumstances, and<br />
8 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland.
Yentis et al. | AAGBI: Consent for anaesthesia 2017 Anaesthesia 2017<br />
especially when the procedure is carried out in the operating<br />
theatre complex, many Trusts insist that a DoH<br />
consent form be completed and signed by the patient as<br />
evidence that consent has been given, and the Working<br />
Party’s advice is that local procedures should be followed.<br />
For a course of treatment (e.g. repeated nerve<br />
blocks), consent to continue should be confirmed before<br />
each individual component, with any changes to the<br />
risks, benefits or alternatives discussed fully [28].<br />
Qualified consent<br />
Some patients, for religious or other personal reasons,<br />
may qualify their general consent to treatment by<br />
refusing specific aspects of that treatment. Doctors<br />
must respect these wishes as far as possible.<br />
Jehovah’s Witnesses, for example, may differ in<br />
their interpretations of the acceptability of blood transfusions.<br />
Most Jehovah’s Witnesses will refuse homologous<br />
blood transfusion; however, some will accept<br />
autologous or cell-salvaged blood. Cardiopulmonary<br />
bypass with non-haematogenous primes and organ<br />
transplantation are usually regarded as acceptable [29].<br />
If a patient gives qualified consent, a record should<br />
be made in the hospital notes indicating that the patient<br />
has been informed of the likely consequences of this<br />
decision, together with the reasons why such a treatment<br />
was proposed in the first instance. If the patient remains<br />
adamant, attention should be drawn to the clause on the<br />
consent form that specifies the patient’s right to list procedures<br />
for which consent is not agreed. The doctor<br />
should also make a note of the precise nature of the<br />
restriction that has been imposed by the patient and the<br />
explanation of risks that took place.<br />
Qualified consent does not remove a patient’s right<br />
to reasonable and proper care, including provision of all<br />
other forms of treatment that are appropriate in the circumstances.<br />
If an individual anaesthetist does not feel<br />
capable of providing proper care consistent with the<br />
patient’s wishes, then he/she can refuse to treat the<br />
patient, provided that no additional harm is likely to<br />
result from that refusal, and make reasonable attempts<br />
to find a different anaesthetist who is willing to treat the<br />
patient. However, in an emergency when treatment is<br />
immediately necessary, the anaesthetist should attempt<br />
to comply with the wishes of a patient who has capacity.<br />
Advance decisions (‘advance<br />
directives’, ‘living wills’) and ‘Do not<br />
attempt resuscitation’ decisions<br />
Adult patients with capacity who anticipate future<br />
incapacity through illness may indicate their preferences<br />
for future treatment by completing an advance<br />
decision, to take effect if they do not have the capacity<br />
to consent to or refuse specific medical treatments. For<br />
example, patients may indicate that they do not wish<br />
to undergo life-saving surgery if they suffer from<br />
dementia when they are older. Many Jehovah’s Witnesses<br />
carry with them an advance decision forbidding<br />
the administration of blood or blood components.<br />
Although an advance decision to refuse routine<br />
treatment does not have to be in writing, one to refuse<br />
life-sustaining treatment must be in writing, must be<br />
witnessed, and must make clear that it is to apply to<br />
the treatment even if life is at risk [6]. An advance<br />
decision that is valid and applicable to the treatment<br />
in question is legally binding [6]. Wherever possible,<br />
anaesthetists should check whether a patient has made<br />
a relevant advance decision to refuse treatment.<br />
When a situation falls fully within the terms of the<br />
advance decision, clinicians should respect the terms<br />
unless there is good evidence that the patient did not<br />
have capacity to make the advance decision, or that<br />
the patient has changed his/her mind since signing it<br />
[31].<br />
Advance decisions cannot authorise doctors to do<br />
anything outside the law, or compel them to carry out<br />
a specific form of treatment, for example continue lifesustaining<br />
treatment that is not in a patient’s best<br />
interests, or provide a treatment the primary intention<br />
of which is to hasten death [22].<br />
‘Do not attempt resuscitation’ (DNAR) decisions<br />
are not advance decisions. Consideration as to the<br />
likely appropriateness of resuscitation must, however,<br />
be based wherever possible on discussion with the<br />
patient (or, where the patient is unable to take part in<br />
the discussion, those close to the patient). Further<br />
guidance on DNAR decisions is available elsewhere<br />
[27]. The Working Party is aware of current work<br />
being done to produce similar guidance encompassing<br />
wider emergency treatment, beyond DNAR alone<br />
(Recommended Summary Plan for Emergency Care<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland. 9
Anaesthesia 2017 Yentis et al. | AAGBI: Consent for anaesthesia 2017<br />
and Treatment (previously Emergency Care and Treatment<br />
Plan); see https://www.resus.org.uk/consultations/<br />
respect/).<br />
Special circumstances<br />
Obstetrics<br />
Drugs, fatigue, pain or anxiety may compromise the<br />
capacity of an adult parturient, but do not necessarily<br />
lead to incapacity unless the degree of compromise is<br />
severe.<br />
Labour is the wrong time to burden women with<br />
excessive information. Every obstetric unit must provide,<br />
in early pregnancy, advice about pain relief and<br />
anaesthesia during labour and delivery [32]. An anaesthetist<br />
must be involved in preparing this information<br />
and approve the final version. Any patient who wishes<br />
to discuss techniques with an anaesthetist must be able<br />
to do so. Nevertheless, the patient must still be provided<br />
with appropriate information at the time of the<br />
procedure, the details of which must be documented.<br />
Birth plans often include references to analgesia<br />
and anaesthesia. If a woman loses capacity during<br />
labour, the birth plan should be treated as representing<br />
an advance decision, and any documented refusal of<br />
therapy must be respected. However, a presumption of<br />
capacity remains in these circumstances. Therefore,<br />
women who have capacity and who request epidural<br />
analgesia during labour, despite recording a refusal in<br />
their birth plan, must have their request respected, and<br />
the decision documented as above.<br />
In law, a pregnant woman with capacity can refuse<br />
any treatment for any reason, even if this puts the<br />
unborn child at risk of harm or death. An emergency<br />
court order to authorise treatment may be requested<br />
in such circumstances, but will only be granted if the<br />
court concludes that the woman lacks the relevant<br />
decision-making capacity and that the treatment is in<br />
her best interests.<br />
In general, 16- and 17-year-old parturients are to<br />
be regarded as adults from the point of view of making<br />
decisions about interventions, and children younger<br />
than this may be considered as having capacity depending<br />
upon the circumstances (see below). Units should<br />
therefore have guidelines in place to ensure that these<br />
patients receive age-appropriate information and advice<br />
and access to an anaesthetist if needed.<br />
Critical care<br />
The principles of consent for patients receiving critical<br />
care are the same as in the general population; however,<br />
many will lack capacity because of their underlying<br />
condition or essential therapy (e.g. sedation).<br />
Chronic pain<br />
Anaesthetic interventions for patients with chronic<br />
pain are often primary in nature – that is, the intervention<br />
is intended to be therapeutic, rather than facilitating<br />
a more definitive procedure to take place.<br />
When this is the case, written, signed consent on conclusion<br />
of the consent process is recommended, and is<br />
often a Trust requirement. Guidance is available from<br />
the Faculty of Pain Medicine at the Royal College of<br />
Anaesthetists for specialists performing specific interventional<br />
procedures (see http://www.rcoa.ac.uk/faculty-of-pain-medicine/guidelines).<br />
16- and 17-year-olds<br />
In England and Wales, 16- and 17-year-olds (often<br />
referred to as ‘young people’) are covered by the MCA<br />
and are presumed to have the capacity to consent to<br />
treatment, including the administration of an anaesthetic,<br />
as if they were adults. Where a capable young<br />
person has given consent, it is not then necessary to<br />
obtain consent from his/her parent or guardian. Consent<br />
can also be given by those with parental responsibility<br />
(see https://www.gov.uk/parental-rights-responsi<br />
bilities/who-has-parental-responsibility; https://e-justice.<br />
europa.eu/content_parental_responsibility-302-IE-en.do?<br />
clang=en) for the young person, whether or not he/she<br />
lacks capacity. The closer the young person is to the<br />
age of maturity and the more that he/she objects to<br />
the proposed treatment (especially if it is invasive or<br />
serious), the more cautious healthcare professionals<br />
should be about relying upon the consent of a person<br />
with parental responsibility; rather, consideration<br />
should be given to applying to court. The court can<br />
override the refusal of treatment of a capable young<br />
person if he/she is likely to suffer irreversible harm as<br />
a result of his/her refusal.<br />
Children<br />
Children (for these purposes, those under the age of<br />
16) are not presumed to have capacity to consent to<br />
10 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland.
Yentis et al. | AAGBI: Consent for anaesthesia 2017 Anaesthesia 2017<br />
treatment, unless the doctor decides that the child ‘has<br />
sufficient intelligence and understanding to appreciate<br />
fully what is proposed’ (i.e. ‘Gillick competence’ [20]).<br />
The degree of understanding they will need to show<br />
will vary depending upon the nature of the procedure<br />
and the severity of the condition being treated. A capable<br />
child should understand the treatment and its<br />
effects, and the consequence of non-treatment. If<br />
capacity fluctuates, the child should be considered as<br />
lacking capacity. Capable children should be encouraged<br />
to inform their parents about treatment, but the<br />
doctor must still respect their right to confidentiality<br />
and a refusal to permit disclosure to the parents.<br />
Consent may be provided for children lacking<br />
capacity by a person with parental responsibility, provided<br />
the treatment for which the consent is given is in<br />
the child’s best interests. Usually, parents (or those with<br />
parental responsibility) will make the decision, although<br />
they themselves must be capable of making the decision<br />
and it must be made in the child’s best interests. Either<br />
parent may give consent; but other family members cannot<br />
give consent on behalf of the parents. If there is disagreement<br />
between the parents, the courts may limit the<br />
power of one parent to refuse treatment that is in the<br />
best interests of the child. If both parents refuse, an<br />
application may be made to the court to overrule the<br />
parents. Where a Gillick competent child refuses treatment,<br />
healthcare professionals can, in principle, rely<br />
upon the consent of a person with parental responsibility,<br />
but they should always consider whether it is necessary<br />
to obtain the authority of the court.<br />
In life-threatening situations, parental authorisation<br />
should be obtained if possible and, in default, application<br />
should be made to the court if necessary. Whatever<br />
happens, the best interests of the child must be put first<br />
and treatment that is immediately essential to safeguard<br />
the child’s life or health should not be denied in the<br />
absence of parental authorisation, even if there is no<br />
time to get court authority (although it should be noted<br />
that it is usually possible to find a judge within an hour).<br />
Individual judgment must be exercised in determining<br />
the degree of restraint that is acceptable to achieve induction<br />
of anaesthesia in an uncooperative child, even<br />
when the parents appear to consent to have the child<br />
restrained. When faced with a child who is uncontrollable<br />
for whatever reason, the anaesthetist should<br />
consider ceasing treatment, giving an appropriate explanation<br />
to the parent or representative, and arranging necessary<br />
future treatment for the child.<br />
Research and audit<br />
The need for participants’ consent and for review by an<br />
independent Research Ethics Committee is no different<br />
in anaesthetic and related research to that in any other<br />
area of medical research, and anaesthetists are referred<br />
to the copious guidelines and regulations that already<br />
exist (e.g. at http://www.hra.nhs.uk/research-community/).<br />
Particular considerations apply in relation to<br />
patients who do not have the capacity to consent to participation<br />
in research studies; in such cases, a relative or<br />
other person may be appointed as a ‘consultee’ to advise<br />
researchers as to the patient’s preferences, and patients<br />
may be recruited into emergency research without prior<br />
consent if specific criteria are met [33].<br />
Learning/maintaining practical skills<br />
Although practical procedures can be rehearsed and<br />
practised on manikins – and, to a lesser extent, volunteers<br />
– most learning and maintaining of practical<br />
skills occurs during patients’ care (unlike research, in<br />
which the process is usually extra to care).<br />
It may be difficult to define what constitutes a single<br />
‘procedure’ since most can be separated into several<br />
components. In addition, practitioners learn from every<br />
procedure they do. It is therefore impossible to seek<br />
patients’ consent for every aspect of every ‘procedure’<br />
in which there may be a learning component. The<br />
Working Party endorses the following approach [34]:<br />
• The risks and benefits of each procedure and its<br />
components, both to the patient concerned and to<br />
society in general, must be considered.<br />
• The harms should be minimised as much as possible,<br />
for example by close supervision, prior practice<br />
on manikins, etc.<br />
• The benefits should be maximised as much as possible,<br />
for example by close supervision, and targeting<br />
skills to practitioners most likely to use them in<br />
the future.<br />
• Alternatives should be considered, for example<br />
other ways of learning/maintaining skills, other<br />
techniques.<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland. 11
Anaesthesia 2017 Yentis et al. | AAGBI: Consent for anaesthesia 2017<br />
In some cases, for example an anaesthetist inexperienced<br />
in fibreoptic orotracheal intubation wishing to<br />
learn the technique unsupervised during general anaesthesia,<br />
patients’ specific consent should be sought since<br />
there may be additional risks from inexperienced use<br />
and there are limited benefits to the patient. In other<br />
cases, for example an experienced endoscopist using<br />
the fibrescope as part of his/her routine technique,<br />
specific consent would not be required since the risks<br />
have been minimised and the benefits maximised, and<br />
the technique constitutes part of the general procedure<br />
of ‘orotracheal intubation’ (so long as the associated<br />
risks remain equivalent to or less than the alternatives).<br />
However, if a particular patient wishes to discuss<br />
intubation, for example if he/she is especially<br />
concerned about damage to teeth or sore throat, the<br />
anaesthetist should provide more details, as for any<br />
other aspect of anaesthesia – upholding the principle<br />
that disclosure of information should be flexible<br />
according to what the individual patient wants to<br />
know. It should also be remembered that patients have<br />
the right to know who is doing what to them, and<br />
how qualified they are [3, 34]. This right is not diminished<br />
by the fact that they may be under the influence<br />
of anaesthesia at the time of the intervention.<br />
The same principles apply to supervision of others:<br />
the supervising anaesthetists should include trainees’<br />
and their own experience as part of their assessment<br />
of overall risks and benefits, including the need to<br />
minimise the former and maximise the latter, as<br />
described above.<br />
Sometimes anaesthetists are approached by medical<br />
students and paramedical staff wishing to learn/<br />
maintain skills, for example in airway management.<br />
Such individuals are not only less skilled than anaesthetists<br />
but also not medically qualified, making the<br />
risk/benefit assessment even more important. The<br />
Department of Health’s guidance states that patients’<br />
specific consent is not required for procedures done<br />
by students if such procedures are part of patients’<br />
normal care. However, the Working Party considers<br />
that this depends on the student’s competence and<br />
the risks involved. For example, while it would be<br />
acceptable for a novice to hold a facemask under<br />
supervision without specific consent, since the risks<br />
are minimal, tracheal intubation is more invasive and<br />
requires a greater level of competence before the<br />
patient’s specific consent is no longer required. In<br />
particular, the Working Party strongly opposes the<br />
practice whereby students or paramedics move<br />
between anaesthetic rooms to ‘do’ intubations, with<br />
no consideration of these issues.<br />
The above approach is equally applicable to<br />
patients who lack capacity to give consent, so long as<br />
it is concluded that specific consent would not be<br />
required. If the patient may lack capacity to give specific<br />
consent to a procedure, the same considerations set<br />
out above under Capacity, best interests and voluntariness<br />
should be applied. There is no necessary bar to a<br />
student carrying out such a procedure but particular<br />
care will need to be taken by those supervising them.<br />
Acknowledgements<br />
The Working Party is grateful to Dr Chris Danbury,<br />
Legal and Ethical Policy Unit, Faculty of Intensive<br />
Care Medicine/Intensive Care Society (FICM/ICS), and<br />
Dr R. Searle, Faculty of Pain Medicine, Royal College<br />
of Anaesthetists, for comments. We are also grateful<br />
to: Mr Colin McKay, Chief Executive, Mental Welfare<br />
Commission for Scotland, Mr Michael Graham, Cleaver<br />
Fulton Rankin Solicitors, Belfast, and Dr Ciaran<br />
Craven, Merchants Quay Chambers, Dublin, for drafting<br />
Appendix 1; to Dr D. Ray, Consultant in Anaesthesia<br />
and Critical Care, Royal Infirmary of Edinburgh<br />
and Honorary Clinical Senior Lecturer, University of<br />
Edinburgh, Mr C. McKay, Chief Executive, Mental<br />
Welfare Commission for Scotland, and Mrs N. Shippin,<br />
Legal Adviser and Director, Central Legal Office,<br />
NHS National Services Scotland, for adapting the Scottish<br />
version of Appendix 2; and to Drs Peter Maguire,<br />
Tim Bennett and Aidan Cullen, Consultant Anaesthetists,<br />
Daisy Hill Hospital, Newry, Northern Ireland,<br />
for comments and suggestions relating to Northern<br />
Ireland.<br />
Competing interests<br />
SMY, AH, DGB and THCB have provided expert witness<br />
reports for the court on the instructions of both<br />
claimants and defendants, and/or HM Coroner. SMY<br />
was a member of the working group that wrote the<br />
GMC’s guidance on consent [6]. AH is his Trust’s<br />
Lead Clinician for the MCA, and has written and<br />
12 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland.
Yentis et al. | AAGBI: Consent for anaesthesia 2017 Anaesthesia 2017<br />
broadcast on issues related to capacity and consent.<br />
ARK regularly acts in proceedings before the Court of<br />
Protection involving the MCA, and has acted in proceedings<br />
on the instructions of the FICM/ICS. He is<br />
on the FICM/ICS Legal and Ethical Policy Unit, and<br />
has provided assistance to the Resuscitation Council<br />
(UK)/British Medical Association/ Royal College of<br />
Nursing on their Guidance on Decisions relating to<br />
Cardiopulmonary Resuscitation [27].<br />
References<br />
1. Association of Anaesthetists of Great Britain and Ireland. Information<br />
and consent for anaesthesia. London: AAGBI, 1999.<br />
http://www.<strong>aagbi</strong>.org/sites/default/files/consent99.pdf (accessed<br />
20/10/2016).<br />
2. Association of Anaesthetists of Great Britain and Ireland. Consent<br />
for anaesthesia 2. London: AAGBI, 2006. http://www.aag<br />
bi.org/sites/default/files/consent06.pdf (accessed 20/10/<br />
2016).<br />
3. General Medical Council. Consent: patients and doctors making<br />
decisions together. London: GMC, 2008. http://www.gmc-uk.<br />
org/guidance/ethical_guidance/consent_guidance_contents.asp<br />
(accessed 20/10/2016).<br />
4. Department of Health. Reference guide to consent for examination<br />
or treatment. London: DoH, 2009. https://www.<br />
gov.uk/government/uploads/system/uploads/attachment_da<br />
ta/file/138296/dh_103653__1_.pdf (accessed 20/10/2016).<br />
5. British Medical Association and Law Society. Assessment of<br />
mental capacity: a practical guide for doctors and lawyers,<br />
4th edn. Nottingham: Law Society Publishing, 2015.<br />
6. The Mental Capacity Act 2005. http://www.legislation.<br />
gov.uk/ukpga/2005/9/contents (accessed 20/10/2016).<br />
7. Re T (Adult: Refusal of Treatment) [1993] Fam 95.<br />
8. White SM, Baldwin TJ. Consent for anaesthesia. Anaesthesia<br />
2003; 58: 760–74.<br />
9. Chester v Afshar [2004] UKHL 41.<br />
10. Montgomery v Lanarkshire Health Board [2015] UKSC 11.<br />
11. The Human Rights Act 1998. http://www.legislation.gov.uk/<br />
ukpga/1998/42/contents (accessed 20/10/2016).<br />
12. Bolam v Friern Hospital Management Committee [1957] 2 All<br />
ER 118.<br />
13. Bolitho v City and Hackney Health Authority [1997] 4 All ER.<br />
14. Bogod D, McCombe K. Paternalism and consent: has the law<br />
finally caught up with the profession? Anaesthesia 2015; 70:<br />
1016–9.<br />
15. Janet Birch v University College London Hospital NHS Foundation<br />
Trust [2008]. EWHC 2237.<br />
16. Kings College Hospital NHS Foundation Trust v C & Another<br />
[2015] EWCOP 80.<br />
17. General Medical Council. Treatment and care towards the end<br />
of life: good practice in decision making. London: GMC, 2010.<br />
http://www.gmc-uk.org/Treatment_and_care_towards_the_end<br />
_of_life___English_1015.pdf_48902105.pdf (accessed 20/10/<br />
2016).<br />
18. B v An NHS Trust [2002] EWHC 429 (Fam).<br />
19. Re W [2002] EWHC 901.<br />
20. Gillick v West Norfolk and Wisbech AHA [1986] AC 112.<br />
21. The Mental Health Act 1983 s58(3)(b). http://www.legislati<br />
on.gov.uk/ukpga/1983/20/contents (accessed 20/10/2016).<br />
22. Aintree v James [2013] UKSC 67.<br />
23. Wye Valley NHS Trust v B [2015] EWCOP 60.<br />
24. Al Hamwi v Johnston [2005] EWHC 206.<br />
25. Smith v Tunbridge Wells HA [1994] 5 Med LR 334.<br />
26. Kathleen Jones v Royal Devon and Exeter NHS Foundation<br />
Trust (unreported; see http://www.pibriefupdate.com/cont<br />
ent/law-journal-summaries/news-category-2/3447-late-switchof-surgeon-can-this-invalidate-consent-jones-v-royal-devon-andexeter-nhs-foundation-trust-james-counsell-outer-temple-chambers<br />
(accessed 20/10/2016)).<br />
27. British Medical Association, Resuscitation Council (UK) & Royal<br />
College of Nursing. Decisions relating to cardiopulmonary<br />
resuscitation. London: BMA/RCUK/RCN, 2014. https://www.resus.org.uk/dnacpr/decisions-relating-to-cpr/<br />
(plus new statement<br />
2015 https://www.resus.org.uk/dnacpr/decisionsrelating-to-cpr-new-statement/)<br />
(accessed 20/10/2016).<br />
28. Bartley v Studd [1995] Medical Law Monitor 2(8) 1.<br />
29. Association of Anaesthetists of Great Britain and Ireland. Management<br />
of anaesthesia for Jehovah’s Witnesses, 2nd edn. London:<br />
AAGBI, 1999. https://www.<strong>aagbi</strong>.org/sites/default/files/<br />
Jehovah’s%20Witnesses_0.pdf (accessed 20/10/2016). OR new<br />
AAGBI guidelines on blood transfusion if ready (due 2016) &<br />
appropriate.<br />
30. HE v A Hospital NHS Trust [2003] EWHC 1017 (Fam).<br />
31. Obstetric Anaesthetists’ Association & Association of Anaesthetists<br />
of Great Britain and Ireland. OAA/AAGBI Guidelines<br />
for obstetric anaesthetic services 2013. London: AAGBI, 2013.<br />
https://www.<strong>aagbi</strong>.org/sites/default/files/obstetric_anaesth<br />
etic_services_2013.pdf (accessed 20/10/2016).<br />
32. Health Research Authority. Adults unable to consent for themselves.<br />
http://www.hra.nhs.uk/resources/before-you-apply/<br />
consent-and-participation/adults-unable-to-consent-for-themsel<br />
ves/ (accessed 20/10/2016).<br />
33. Yentis SM. The use of patients for learning and maintaining<br />
practical skills. Journal of the Royal Society of Medicine 2005;<br />
98: 299–302.<br />
34. General Medical Council. Good Medical Practice. London: GMC,<br />
2013. http://www.gmc-uk.org/guidance/good_medical_practice.asp<br />
(accessed 20/10/2016).<br />
Supporting Information<br />
Additional Supporting Information may be found in<br />
the online version of this article:<br />
Appendix S1. Summary of the main differences in<br />
the legal framework for decision-making in relation to<br />
those lacking capacity in England and Wales and those<br />
in Scotland, Northern Ireland and the Republic of Ireland.<br />
Appendix S2a. Frequently asked questions regarding<br />
consent (England and Wales and Northern Ireland).<br />
Appendix S2b. Frequently asked questions regarding<br />
consent (Scotland).<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd on behalf of Association of Anaesthetists of Great Britain and Ireland. 13
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
Management of a Patient with Suspected<br />
Anaphylaxis During Anaesthesia<br />
SAFETY DRILL<br />
(Revised 2009)<br />
Immediate management<br />
∙∙<br />
∙∙<br />
∙∙<br />
∙∙<br />
∙∙<br />
∙∙<br />
∙∙<br />
Use the ABC approach (Airway, Breathing, and Circulation). Team-working enables several tasks to be<br />
accomplished simultaneously.<br />
Remove all potential causative agents and maintain anaesthesia, if necessary, with an inhalational agent.<br />
CALL FOR HELP and note the time.<br />
Maintain the airway and administer oxygen 100%. Intubate the trachea if necessary and ventilate the lungs<br />
with oxygen.<br />
Elevate the patient’s legs if there is hypotension.<br />
If appropriate, start cardiopulmonary resuscitation immediately according to Advanced Life Support<br />
Guidelines.<br />
Give adrenaline i.v.<br />
◦◦<br />
Adult dose: 50 µg (0.5 ml of 1:10 000 solution).<br />
◦◦<br />
Child dose: 1.0 µg.kg -1 (0.1 ml.kg -1 1:100 000 solution).<br />
∙∙<br />
∙∙<br />
Several doses may be required if there is severe hypotension or bronchospasm. If several doses of<br />
adrenaline are required, consider starting an intravenous infusion of adrenaline.<br />
Give saline 0.9% or lactated Ringer’s solution at a high rate via an intravenous cannula of an appropriate<br />
gauge (large volumes may be required).<br />
◦◦<br />
Adult: 500 - 1 000 ml<br />
◦◦<br />
Child: 20 ml.kg -1<br />
∙∙<br />
Plan transfer of the patient to an appropriate Critical Care area.<br />
CONTINUED OVERLEAF<br />
© The Association of Anaesthetists of Great Britain & Ireland 2009
Secondary management<br />
∙∙<br />
Give chlorphenamine i.v. Adult: 10 mg<br />
Child 6 - 12 years: 5 mg<br />
Child 6 months - 6 years: 2.5 mg<br />
Child
The use of blood components<br />
and their alternatives 2016<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
July 2016
This guideline was originally published in Anaesthesia. If you wish to refer<br />
to this guideline, please use the following reference:<br />
Association of Anaesthetists of Great Britain and Ireland. AAGBI<br />
guidelines: the use of blood components and their alternatives 2016<br />
Anaesthesia 2016; 71: 829-842.<br />
This guideline can be viewed online via the following URL:<br />
http://onlinelibrary.wiley.com/doi/10.1111/anae.13489/full
Guidelines<br />
AAGBI guidelines: the use of blood<br />
components and their alternatives 2016<br />
A. A. Klein, 1 P. Arnold, 2 R. M. Bingham, 3 K. Brohi, 4 R. Clark, 5<br />
R. Collis, 6 R. Gill, 7 W. McSporran, 8 P. Moor, 9 R. Rao Baikady, 10<br />
T. Richards, 11 S. Shinde, 12 S. Stanworth 13 and T. S. Walsh 14<br />
1 Consultant, Department of Anaesthesia and Intensive Care, Papworth<br />
Hospital, Cambridge, UK and Chair, AAGBI Working Party<br />
2 Consultant, Department of Paediatric Anaesthesia, Alder Hey<br />
Children’s Hospital, Honorary Lecturer, University of Liverpool,<br />
Liverpool, UK<br />
3 Consultant, Department of Paediatric Anaesthesia, Great Ormond<br />
Street Hospital for Children, London, UK<br />
4 Professor, Centre for Trauma Sciences, Barts Health NHS Trust and<br />
Queen Mary University of London, London, UK<br />
5 Specialist Trainee, Department of Anaesthesia, Glasgow Royal<br />
Infirmary, Glasgow, UK and Group of Anaesthetists in Training<br />
6 Consultant, Department of Anaesthesia, University Hospital of Wales,<br />
Cardiff, UK and Obstetric Anaesthetists’ Association<br />
7 Consultant, Department of Anaesthesia, University Hospital Southampton,<br />
UK, Royal College of Anaesthetists and Association of Cardiothoracic<br />
Anaesthetists<br />
8 Transfusion Practitioner, The Royal Marsden Hospital, London, UK<br />
9 Consultant, Department of Anaesthesia, Derriford Hospital, Plymouth,<br />
UK and Defence Anaesthesia representative<br />
10 Consultant, Department of Anaesthesia, The Royal Marsden Hospital,<br />
London, UK<br />
11 Professor, Division of Surgery and Interventional Science, University College<br />
Hospital, London, UK and Royal College of Surgeons<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 1<br />
This is an open access article under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs<br />
License, which permits use and distribution in any medium, provided the original work is properly cited, the use is<br />
non-commercial and no modifications or adaptations are made.
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
12 Consultant, Department of Anaesthesia, Southmead Hospital, Bristol,<br />
UK and Honorary Secretary, AAGBI<br />
13 Consultant, Department of Haematology, Oxford Radcliffe Hospitals,<br />
Oxford, UK, and NHS Blood and Transplant<br />
14 Professor, Department of Anaesthetics, Critical Care and Pain<br />
Medicine, Edinburgh University, Edinburgh, UK<br />
Summary<br />
Blood transfusion can be life-saving. Anaesthetists regularly request and<br />
administer blood components to their patients. All anaesthetists must be<br />
familiar with indications and appropriate use of blood and blood components<br />
and their alternatives, but close liaison with haematology specialists<br />
and their local blood sciences laboratory is encouraged.<br />
Considerable changes in approaches to optimal use of blood components,<br />
together with the use of alternative products, have become apparent<br />
over the past decade, leading to a need to update previous<br />
guidelines and adapt them for the use of anaesthetists working throughout<br />
the hospital system.<br />
....................................................................................................<br />
Endorsed by the Royal College of Anaesthetists and the Network for<br />
Advancement of Transfusion Alternatives (NATA).<br />
Keywords: anaemia and coagulation, blood crossmatch, FFP indications,<br />
major haemorrhage, transfusion<br />
Accepted: 11 March 2016<br />
Recommendations<br />
1 All patients should have their haemoglobin concentration (Hb)<br />
measured before listing for major elective surgery.<br />
2 Patients who are anaemic by the World Health Organization definition<br />
(Hb men < 130 g.l<br />
1 , women < 120 g.l<br />
1 ) should be investigated<br />
before elective surgery and treated appropriately, and elective<br />
non-urgent surgery other than caesarean section should be delayed.<br />
3 Where blood transfusion is anticipated, this and alternatives to<br />
transfusion should be discussed with the patient before surgery, and<br />
this should be documented.<br />
2 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
4 Red blood cells should be transfused one unit at a time, and the<br />
patient’s Hb should be checked before each unit transfused, unless<br />
there is ongoing bleeding or a large deficit that needs correcting.<br />
5 The use of intra-operative cell salvage and tranexamic acid administration<br />
should be considered in all non-obstetric patients where blood<br />
loss > 500 ml is possible and in traumatic and obstetric major haemorrhage.<br />
6 Blood components should be prescribed for small children by volume<br />
rather than number of units.<br />
7 Every institution should have a massive transfusion protocol which is<br />
regularly audited and reviewed.<br />
8 Group O red cells for transfusion should be readily available in the<br />
clinical area, in case haemorrhage is life-threatening. Group-specific<br />
red cells should be available within a very short time<br />
(15–20 min) of the laboratory receiving correctly-labelled samples<br />
and being informed of the emergency requirement for blood.<br />
9 During major haemorrhage due to trauma and obstetrics, consideration<br />
should be given to transfusing red cells and FFP in preference<br />
to other intravenous fluid.<br />
10 Patients who continue to actively bleed should be monitored by pointof-care<br />
and/or regular laboratory tests for coagulation, fibrinogen and<br />
platelet counts or function, and a guide for transfusion should be FFP if<br />
INR > 1.5, cryoprecipitate if fibrinogen < 1.5 g.l<br />
1 and platelets if platelet<br />
count < 75 9 10 9 .l<br />
1 .<br />
What other guidelines are available on this topic?<br />
A number of other guidelines are available, some of which are quite recent,<br />
but none cover the breadth of UK anaesthetic practice (Appendix 1).<br />
Why was this guideline developed?<br />
There is a need for a relevant up-to-date clinical guidance for practising<br />
UK anaesthetists, critical care staff and those from other specialities and<br />
backgrounds, based on evidence where possible and with a focus on<br />
safety.<br />
How and why does this publication differ from<br />
existing guidelines?<br />
This is an updated guideline that also brings three previous AAGBI<br />
guidelines together (blood component therapy, 2005; massive haemorrhage,<br />
2010; and red cell transfusion, 2008).<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 3
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
Introduction<br />
Transfusion medicine is changing rapidly in response to new developments.<br />
Considerable changes in approaches to transfusion, together with<br />
the use of alternative agents, have become apparent over the past decade.<br />
Blood transfusion can be life-saving, but this is a scarce and costly<br />
resource. There is increased focus on appropriate transfusion practice to<br />
ensure quality of service provision, and transfusion has been proposed<br />
as a quality indicator in surgical care. Blood transfusion usage remains<br />
high, particularly in trauma, obstetrics, critical care and cardiovascular<br />
surgery.<br />
Anaesthetists are frequently involved in transfusion decisions, the<br />
administration of blood and blood components and as part of the team<br />
managing any major haemorrhage. However, the use of allogeneic blood<br />
components has serious implications and warrants careful consideration<br />
[1]. As a consequence, there has recently been an expansion of interest<br />
in safeguarding and checklists, blood conservation, preservation techniques,<br />
coagulation profiling and the use of haemostatic agents. Appropriate<br />
use of blood components in patient care is of utmost importance.<br />
Several recent major research publications that have looked at transfusion<br />
practice were aimed at patient safety, outcomes and individualised<br />
care, including: use of restrictive transfusion protocols; adjuvant<br />
therapies; substitution of blood components with pooled factor concentrates;<br />
and use of point-of-care (POC) testing to target specific component<br />
use (see http://onlinelibrary.wiley.com/doi/10.1111/anae.2014.70.<br />
issue-s1/issuetoc).<br />
It is essential that our practice of blood transfusion is safe and<br />
based on current, scientific, evidence-based knowledge. A multidisciplinary<br />
approach that aims to benefit patients by the reduction in inappropriate<br />
transfusions is paramount. This working party aims to<br />
formalise guidance on the clinical indications and risks of transfusion,<br />
blood conservation and the transfusion process.<br />
Patient blood management<br />
Patient blood management is a patient-based approach aimed at reducing<br />
the utilisation of blood transfusion and improving the patient’s clinical<br />
outcome and safety, and focuses on the optimisation of three factors<br />
peri-operatively: patient, surgical and anaesthetic. It has been recommended<br />
as a standard of care in the UK National Health Service [2]. It<br />
focuses on three ‘pillars’ of care in surgical patients: detection and<br />
4 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
Table 1 Patient blood management – measures that should be taken in<br />
patients who are expected to bleed during surgery.<br />
Pre-operative<br />
-Pre-operative Hb should be measured, recorded and optimised as<br />
required<br />
-Elective surgery should be postponed in patients with untreated anaemia<br />
-Review and consider stopping antiplatelet and anticoagulant medication<br />
seven days before surgery<br />
-Consider minimally invasive or laparoscopic surgical technique<br />
-Point-of-care testing should be available with appropriate training.<br />
Intra-operative<br />
-Position patient carefully to maintain venous drainage<br />
-Use patient warming to maintain temperature > 36°<br />
-Consider cell salvage if blood loss > 500 ml anticipated<br />
-Consider giving tranexamic acid 1 g if blood loss > 500 ml anticipated<br />
-Apply restrictive transfusion threshold (Hb 70–80 g.l<br />
1 depending on<br />
patient characteristics and haemodynamics)<br />
-Consider use of topical haemostatic agents.<br />
Postoperative<br />
-Maintain oxygen delivery, targeting oxygen saturation levels > 95%<br />
-Single unit blood transfusion policy – re-assess Hb concentration and<br />
clinical need between units<br />
-Postoperative drains or cell salvage.<br />
treatment of peri-operative anaemia; reduction of peri-operative blood<br />
loss; and harnessing and optimising the patient-specific physiological<br />
reserve of anaemia [3] (Table 1).<br />
Anaemia<br />
Pre-operative anaemia is common, occurring in up to a third of patients<br />
before surgery, and associated with worse outcomes. All patients should<br />
have their Hb checked before listing for surgery. Patients who are anaemic<br />
(Hb in men < 130 g.l<br />
1 , women < 120 g.l<br />
1 ) should be investigated<br />
and the cause treated appropriately [4]. Patient pathways and pre-assessment<br />
clinics should be established to allow timely and appropriate management,<br />
and elective surgery should be delayed if required [5].<br />
Cell salvage<br />
The use of cell salvage should be considered for high- or medium-risk<br />
surgery in non-obstetric adult patients where blood loss > 500 ml is<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 5
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
likely, and in obstetric major haemorrhage. In patients with malignancy<br />
or obstetric haemorrhage, a leucocyte filter must be used. Bacterial contamination<br />
of the surgical field remains a contra-indication. Cell salvage<br />
may also be continued in the postoperative period [6].<br />
Other aspects of patient blood management are discussed throughout<br />
these guidelines.<br />
Process for transfusion<br />
Administering the wrong blood type in error (with the risk of ABO<br />
incompatibility) is the most serious outcome of blood transfusion. Most<br />
of these incidents are due to the failure of the final identity checks carried<br />
out between the patient (at the patient’s side) and the blood to be<br />
transfused. All members of staff involved in the administration of a<br />
blood component must be trained and competency-assessed as per local<br />
policy. Local policy will also stipulate if this is a one- or two-person<br />
bedside check, with each person performing the check independently<br />
[7]. Red cell transfusions must be completed within 4 h of removal from<br />
the blood fridge. All prescriptions for transfusion must be documented<br />
in the patient record, either on the anaesthetic chart or on the drug/<br />
fluid prescription chart. Local policy for confirmation of the transfusion<br />
must be followed – it is a legal requirement that 100% of blood components<br />
must be traceable [8]. Where blood transfusion is anticipated, this<br />
should be discussed with the patient before surgery and valid consent to<br />
receive transfusion should be documented [9]. Patients should be<br />
informed that they have received blood or blood components before discharge<br />
from hospital as they will otherwise be unaware; they should also<br />
be informed that this removes them from the donor pool. It is also<br />
important that the patient’s general practitioner is informed.<br />
The following guidance is for a manual checking process at the bedside;<br />
the preferred system is an electronic transfusion management system.<br />
-The patient must be positively identified. All patients receiving blood<br />
components should be wearing an identification wristband containing<br />
four core identifiers – first name, last name, date of birth and patient<br />
identification number.<br />
-Immediately before the transfusion, check the component next to the<br />
patient, against the prescription.<br />
-Check the four core identifiers on the compatibility label attached to<br />
the blood component with the identification attached to the patient. If<br />
6 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
there are any discrepancies, do not proceed and call the transfusion<br />
laboratory.<br />
-Check that the compatibility label attached to the blood component<br />
has the same blood group and 14-digit component donation number<br />
(or batch number for coagulation factors) as the sticker on the blood<br />
component.<br />
-Visually check the blood component for any leakage, discolouration or<br />
presence of any clots or clumps.<br />
-Check the expiry date and time.<br />
Transfusing an unidentified patient<br />
All hospitals should have a clear local policy for transfusion of patients<br />
whose identity is unknown. In emergency situations or where the<br />
patient cannot immediately be identified, the patient should still have<br />
identification attached stating unknown male or female and a unique<br />
identification number. The blood sample sent to the transfusion laboratory<br />
should contain these exact details.<br />
In the event that the patient’s identity becomes known, new identification<br />
must be attached to the patient and a new transfusion sample<br />
collected and fully labelled with the known patient’s details.<br />
Monitoring for adverse events or reactions during transfusions<br />
Clinical observations should include heart rate, blood pressure, temperature<br />
and respiratory rate, as per local guidelines (national guidelines<br />
define a minimum of pre-transfusion, at the end of transfusion and 15<br />
min after transfusion). If there are any signs of a transfusion reaction,<br />
such as tachycardia, rash, breathlessness, hypotension or fever, stop the<br />
transfusion and contact the laboratory immediately [10]. Management<br />
may include the administration of antihistamine or steroid drugs, or<br />
intramuscular/intravenous adrenaline if life-threatening [11]. Diagnosis<br />
of a transfusion reaction during ongoing haemorrhage may be difficult,<br />
but if concern arises, the documentation should be double-checked for<br />
administration errors and further analyses performed as per local protocols.<br />
Transferring blood with a patient<br />
Blood components should be transferred with patients at high risk of<br />
requiring transfusion en route or immediately on arrival. There should<br />
be effective communication between the blood transfusion laboratories<br />
involved, according to regional policy. Blood components must be<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 7
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
transported in a storage box suitable to maintain their integrity, along<br />
with accompanying paperwork, and careful handover is required. When<br />
the patient arrives at their destination, the receiving transfusion laboratory<br />
should be immediately informed that blood was transported. The<br />
patient should be issued with a new identity wristband, a new sample<br />
taken for cross-match and more blood issued; until this is available,<br />
blood transferred with the patient may be administered if required.<br />
Red blood cell transfusion<br />
Red blood cell (RBC) transfusion is potentially life-saving for the treatment<br />
of blood loss (Major haemorrhage – see next section). In patients<br />
who do not have active bleeding and in normovolaemic patients, the Hb<br />
should be measured before and after every unit of RBC transfused. Nearpatient<br />
measurement of Hb may be particularly useful, but laboratory<br />
measurement remains the gold standard. Haemoglobin concentration is<br />
dependent on both red cell mass and plasma volume; it may fall due to<br />
haemodilution due to intravenous fluid administration. In the bleeding<br />
patient, haemoglobin concentration may remain falsely elevated despite<br />
significant blood loss due to inadequate fluid resuscitation.<br />
Other potential indications for RBC transfusion are clinical signs<br />
and biochemical markers of inadequate oxygen delivery, such as elevated<br />
blood lactate concentration, a low Ph and low central or mixed venous<br />
oxygen saturation.<br />
Optimum haemoglobin transfusion trigger<br />
Recent publications comparing more liberal transfusion strategies (typical<br />
transfusion trigger Hb 90–100 g.l<br />
1 ) with more restrictive strategies<br />
(typical transfusion trigger Hb 70–80 g.l<br />
1 ) did not show any difference<br />
in patient outcomes [12, 13]. Therefore, a general Hb threshold of<br />
70 g.l<br />
1 should apply as a guide for red cell transfusion. Uncertainty<br />
remains for patients with ischaemic heart disease, including acute coronary<br />
syndrome and after cardiac surgery [14], and higher thresholds<br />
(80 g.l<br />
1 ) may be more appropriate in such circumstances.<br />
Major haemorrhage<br />
Major haemorrhage is variously defined as loss of more than one blood<br />
volume within 24 h (around 70 ml.kg 1 , > 5 l in a 70 kg adult); 50%<br />
of total blood volume lost in < 3 h; or bleeding in excess of<br />
150 ml.min 1 . A pragmatic clinically-based definition is bleeding which<br />
leads to a systolic blood pressure of less than 90 mm Hg or a heart<br />
8 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
rate of more than 110 beats.min 1 . Major haemorrhage is a significant<br />
cause of mortality and morbidity in the peri-operative setting. Appropriate<br />
and effective management integrates multiple factors, including:<br />
recognition; communication; timely delivery of blood products; and<br />
application of definitive modalities of treatment (surgery and interventional<br />
radiology) [15].<br />
Major haemorrhage protocol<br />
Policies should be defined in an institutional major haemorrhage protocol.<br />
Activation of a protocol should result in the immediate release and<br />
administration of blood components for initial resuscitation, without<br />
prior approval from a haematologist. Such protocols perform best when<br />
specific to clinical areas such as the emergency department or the labour<br />
ward, and are designed to include robust and clearly understood activation<br />
and communication from bedside to laboratory. Their activation<br />
should also mobilise other resources, such as additional (senior) staff<br />
including portering, blood warmers, pressure infusers and cell salvage<br />
devices [16].<br />
A clear mechanism for the escalation of a team response and for<br />
identifying individuals with sufficient seniority and experience to undertake<br />
the key roles of team leader (senior anaesthetist) and co-ordinator<br />
is essential to the process, as is enabling a single point of contact with<br />
the laboratory and other support services.<br />
Initial resuscitation<br />
Most major haemorrhage packs will contain four units of RBCs and<br />
four units of FFP (equivalent to 15–20 ml.kg 1 in a standard adult);<br />
platelet concentrate may also be provided. Administration should be via<br />
wide-bore intravenous access, or intra-osseous access until the former<br />
can be obtained.<br />
Group O red cells should be readily available and transfused if<br />
haemorrhage is life-threatening. It is essential to give group O Rh-negative<br />
red cells to children and women of childbearing potential, but<br />
group O Rh-positive red cells may be used in adult men.<br />
Group-specific red cells should be rapidly made available (within<br />
15–20 min) by the laboratory after receiving a correctly labelled blood<br />
group sample and being informed of the emergency requirement for<br />
blood. Emergency Group O red cells should continue to be provided<br />
where timely and safe issue of group-specific red cells is not possible.<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 9
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
Haemostatic resuscitation<br />
This describes the process of restoring and sustaining normal tissue perfusion<br />
with the emphasis on preservation of effective clotting. Coagulopathy<br />
is associated with haemorrhage (consumption) and transfusion<br />
of blood products (dilution), as well as mechanism of injury in trauma;<br />
this may exacerbate the haemorrhage and resultant morbidity. Point-ofcare<br />
or laboratory testing should be used to guide management.<br />
During resuscitation, the following should be prevented/treated:<br />
hypothermia; acidosis; hypocalcaemia (aim for ionised calcium<br />
> 1.0 mmol.l<br />
1 ); and hyperkalaemia.<br />
Special situations<br />
Critical care<br />
Anaemia is prevalent during critical illness. In addition to blood loss and<br />
sampling, haemodilution and impaired erythropoiesis may be important<br />
contributors [17]. Patients with anaemia demonstrate biochemical abnormalities<br />
similar to those with chronic inflammatory diseases.<br />
Although biochemical markers of tissue hypoxia, notably blood<br />
lactate concentration, are frequently elevated, evidence does not support<br />
increasing oxygen delivery with RBC transfusion when the Hb is<br />
> 70 g.l<br />
1 , unless the patient has cardiac disease [18].<br />
One important group of patients admitted to ICU are patients with<br />
haematological malignancies. Overall, patients with cancer form one of<br />
the larger groups of recipients of blood components. However, unlike<br />
other patient groups, the anaemia in patients with haematological malignancies<br />
reflects an underlying bone marrow failure, and therefore, it is<br />
unclear to what extent findings from the majority of randomised trials<br />
conducted in surgery or general critical care can be extrapolated to cancer,<br />
although the same broad principles of restrictive use of red cells commonly<br />
apply (70–80 g.l<br />
1 for red cell transfusion).<br />
Obstetrics<br />
Estimating blood loss at delivery is notoriously difficult, and every effort<br />
should be made to directly measure abnormal bleeding across all settings<br />
in the delivery suite [19]. Early recognition of bleeding by changing<br />
bed linen and pads immediately after delivery and systematically<br />
weighing new blood-soaked pads correlates with the fall in Hb concentration<br />
and improves outcome.<br />
As soon as abnormal bleeding is recognised, > 500 ml after a vaginal<br />
delivery and > 1000 ml after a caesarean delivery, the obstetrician,<br />
10 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
anaesthetist and senior midwife should attend the mother. Blood should<br />
be taken for full blood count (Hb), clotting studies, group and screen,<br />
and a venous blood gas for rapid Hb measurement and lactate<br />
(> 2 mmol.l<br />
1 is an indicator of shock). Cell salvage is recommended if<br />
abnormal bleeding occurs during caesarean section, and a leucocyte filter<br />
should be used for autotransfusion of processed blood.<br />
Severe early consumptive coagulopathy is associated with abruption,<br />
amniotic fluid embolus and severe bleeding with pre-eclampsia. Early<br />
use of FFP before RBC may be required.<br />
Postpartum haemorrhage associated with atony or trauma is unlikely<br />
to be associated with haemostatic impairment unless the diagnosis is<br />
delayed. Protocol-led use of blood products will lead to overtransfusion of<br />
FFP in the majority of cases [20]. If coagulation tests are not known, then<br />
FFP should be withheld until four units of RBC have been given. If no<br />
coagulation results are available and bleeding is ongoing, then, after four<br />
units of RBC, four units of FFP should be infused and 1:1 ratio of RBC–<br />
FFP transfusion maintained until the results of haemostatic tests are<br />
known. Point-of-care (POC) testing is recommended in this setting [21].<br />
Hypofibrinogenaemia, below normal levels for pregnancy, predicts<br />
the risks of ongoing postpartum haemorrhage. The normal plasma fibrinogen<br />
concentration in pregnancy is 4–6 g.l<br />
1 , and a laboratory Clauss<br />
fibrinogen of < 3 and especially < 2 g.l<br />
1 , with ongoing bleeding, is associated<br />
with progression to major obstetric bleeding [22]. Fibrinogen<br />
replacement with cryoprecipitate or fibrinogen concentrate should be considered<br />
in these circumstances, if there is bleeding.<br />
Monitoring of haemostatic function in obstetric haemorrhage is particularly<br />
important; laboratory testing is often too slow during obstetric<br />
haemorrhage, and therefore, POC testing is preferred. Tests should include<br />
plasma fibrinogen concentration or POC equivalent [21]. With ongoing<br />
bleeding, any abnormalities should be treated, as this indicates significant<br />
haemostatic impairment in the obstetric patient. Platelet transfusions are<br />
rarely required and should only be given once the platelet count is known.<br />
Tranexamic acid reduces total blood loss and should be given if<br />
postpartum haemorrhage is severe (> 500 ml after a vaginal delivery<br />
and > 1000 ml after a caesarean delivery), at an initial dose of 1 g.<br />
Paediatrics<br />
There is little direct evidence to guide the use of blood products in children,<br />
and generally the guidance intended for adults can be safely<br />
applied to children with some modifications (specifically in transfusion<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 11
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
volumes). ‘Restrictive’ approaches to transfusion are appropriate for<br />
almost all children older than 3 months of age. Higher transfusion<br />
thresholds are often applied to neonates and children with congenital<br />
heart disease. Although thresholds are not clearly defined, there is evidence<br />
that quantities of transfusion can be reduced in these patients by<br />
applying moderately restrictive thresholds for transfusion without<br />
adverse effect on outcome [23, 24]. Neonates should receive components<br />
specified for neonatal use, including cytomegalovirus-negative blood<br />
products.<br />
The volume of blood to be administered requires modification<br />
depending on the size of the patient. It is recommended that blood in<br />
children should be prescribed in volume rather than number of units.<br />
In practice, sensible rounding to the nearest unit will be more efficient.<br />
• A transfusion of 10 ml.kg 1 of RBC should increase Hb by approximately<br />
20 g.l<br />
1 .<br />
• Cryoprecipitate should be given in a dose of 5–10 ml.kg 1 .<br />
• Platelets should be given in a dose of 10–20 ml.kg 1 .<br />
• Fresh frozen plasma may be given in doses of 10–15 ml.kg 1 .<br />
Tranexamic acid can be used in children: a loading dose of 15 mg.kg 1<br />
followed by infusion 2 mg.kg 1 .h 1 should be used in trauma [25].<br />
With technical refinements, cell salvage can be useful in children,<br />
even if the absolute volume of blood loss is less than 500 ml [26].<br />
Major haemorrhage is rare in children outside of highly specialist<br />
areas of practice. The guidance suggested for adults can be generally<br />
applied, though requires an awareness of the size of the child and the<br />
clinical context of the bleeding. Blood volume of a child is estimated at<br />
70 ml.kg 1 but may be as high as 100 ml.kg 1 in newborns. Devices for<br />
vascular access and rapid administration of blood should be appropriate<br />
for the size of the child and rate of blood loss. Children are at particular<br />
risk of electrolyte imbalance and hypothermia during rapid administration<br />
of blood products.<br />
Trauma<br />
During active bleeding, follow the principles of damage control resuscitation:<br />
Early haemorrhage control<br />
Ensure clinical treatment is constantly directed towards haemorrhage<br />
control. Use temporary haemostatic devices (pressure, tourniquets, etc.)<br />
12 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
followed as soon as practically possible by surgery or interventional<br />
radiological control of haemorrhage.<br />
Permissive hypotension<br />
Do not try to normalise blood pressure during active haemorrhage.<br />
Maintain a minimum acceptable preload and blood pressure with volume<br />
resuscitation alone; this may need to be modified in the presence<br />
of trauma in head and spinal injuries. The use of vasopressors should<br />
be avoided during active haemorrhage.<br />
Avoid crystalloid and colloid administration<br />
During uncontrolled haemorrhage, avoid clear fluids for volume resuscitation<br />
unless there is profound hypotension and no imminent availability<br />
of blood products.<br />
Target trauma-induced coagulopathy<br />
Deliver blood products empirically at first, and use laboratory or pointof-care<br />
tests of coagulation to guide therapy as soon as available [27].<br />
Give tranexamic acid 1 g immediately, but avoid if more than 3 h<br />
after injury, unless there is ongoing evidence of hyperfibrinolysis (as<br />
suggested by POC testing).<br />
Whilst haemorrhage is being controlled, administration of RBC and<br />
FFP in a ratio of 1:1 should be used to replace fluid volume [28]. Consider<br />
the administration of cryoprecipitate (two pools) and platelets (one<br />
adult therapeutic dose) until test results are available and bleeding is<br />
controlled. Once control is achieved, blood components should be<br />
administered as guided by testing at the earliest opportunity (see Monitoring<br />
section, blood components).<br />
Cardiac surgery<br />
Anaemic patients have an increased risk of mortality and complications<br />
following cardiac surgery [29]. Elective cardiac surgery should not be<br />
undertaken in an anaemic patient without prior investigation and treatment<br />
as considered necessary.<br />
Viscoelastic testing is recommended to guide transfusion [30]. The<br />
use of local transfusion protocols guided by point-of-care testing may<br />
lead to appropriate transfusion with reduced costs. The evidence base<br />
for the efficacy of fresh frozen plasma is minimal and of poor quality<br />
[31].<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 13
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
The effect of cardiopulmonary bypass on platelet function may<br />
make the use of a higher platelet count (> 75 9 10 -9 .l<br />
1 ) necessary after<br />
bypass.<br />
There is no clear evidence of the benefit of platelet function analysis<br />
except in those patients who have taken PY12 receptor inhibitors such<br />
as clopidogrel within 5 days of surgery [32].<br />
Monitoring<br />
Laboratory testing<br />
Traditional tests such as APTT and PT/INR have been standardised for<br />
the monitoring of anticoagulants and are designed to diagnose and<br />
manage factor deficiencies such as haemophilia. Standardisation within<br />
laboratories has made the results very reliable.<br />
The PT and APTT were not designed to monitor coagulation deficiencies<br />
during haemorrhage and suggested INR and APTT ratios or<br />
triggers, which are widely quoted to guide coagulation product replacement,<br />
are based on small historic studies that have little relevance today.<br />
Slow turnaround time also means that the results do not reflect the<br />
dynamic clinical situation during ongoing haemorrhage [33].<br />
Point-of-care testing<br />
Point-of-care testing has a shorter turnaround time and represents a<br />
more global and therefore more relevant reflection of coagulation status<br />
[34]. Point-of-care testing is increasingly popular for general and<br />
cardiac surgery, trauma units, intensive care and obstetrics. Point-ofcare<br />
testing for Hb concentration is commonly used, such as blood<br />
gas analysis or the HemoCue â (€Angelholm, Sweden), which both correlate<br />
well with laboratory measurements [35]. The activated clotting<br />
time (ACT) is also well validated and should be used routinely whenever<br />
heparin is administered, particularly in cardiac and vascular<br />
surgery.<br />
Targeted blood component therapy based on POC testing has been<br />
shown to be safe and effective, and to decrease blood product usage.<br />
However, there are currently no studies that show improved patient outcome<br />
compared with standard treatment [32].<br />
At the current time, there are two commercially available semi-automated<br />
viscoelastic machines that use similar technology: thromboelastometry<br />
(ROTEM, TEM International, Munich, Germany) and<br />
thromboelastography (TEG, Haemonetics Corp, Braintree, MA, USA).<br />
One manufacturer cannot be recommended above the other.<br />
14 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
There are no universal algorithms across the specialities, and local<br />
protocols are required based on institutional procedures. There is limited<br />
interchangeability between TEG and ROTEM, and development<br />
and validation of separate treatment algorithms for the two devices are<br />
required [36].<br />
There are concerns about standardisation of both assays with poor<br />
quality control and assurance and a wide variation in results between<br />
centres [37]. It is good practice to pair coagulation samples and send a<br />
second sample for laboratory-based analysis.<br />
Drugs<br />
An increasing number of patients take either anticoagulants or antiplatelet<br />
agents. All patients require careful pre-operative medication optimisation<br />
before surgery. The management of drugs related to antithrombotic therapy<br />
in the peri-operative setting is a common problem, balancing bleeding<br />
risk with thrombosis.<br />
Patients at high risk (> 10% risk of thrombotic events per year)<br />
of thrombosis should be considered for bridging anticoagulation, or<br />
in the following circumstances:<br />
-venous thromboembolic event within the last 3 months, or<br />
-prosthetic (mechanical) heart valve<br />
Bridging anticoagulation usually consists of low molecular weight heparin.<br />
The dose and type of the low molecular weight heparin depends on the<br />
patient’s weight, timing of surgery, type of procedure and thrombotic risks.<br />
Warfarin (Vitamin K antagonist)<br />
The international normalised ratio (INR) is used to monitor the effectiveness<br />
of warfarin. In most situations, INR is maintained between 2.0<br />
and 2.5.<br />
The peri-operative management of warfarin is summarised in<br />
Table 2. In patients with atrial fibrillation on warfarin, routine use of<br />
bridging anticoagulation with low molecular weight heparin before surgery<br />
is not recommended.<br />
For emergency reversal of warfarin, prothrombin complex concentrate<br />
(PCC) 50 IU.kg 1 is recommended. Intravenous vitamin K<br />
(10 mg) may also be given, but this may preclude re-warfarinisation<br />
for a number of days. Fresh frozen plasma is an alternative if PCC<br />
is not available [37], but should not be used as elective prophylaxis<br />
in patients taking warfarin.<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 15
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
Table 2 Peri-operative optimisation of warfarin anticoagulation for<br />
major surgery. Bridging with LMWH required for high-risk patients,<br />
patients who suffered recent thromboembolic events or patients with<br />
mechanical prosthetic heart valves.<br />
Day 5 Days 4, 3, 2 Day 1 Surgery Postoperative<br />
Last dose of<br />
warfarin.<br />
Treatment dose LMWH<br />
(consider Vitamin K if<br />
INR > 2.5<br />
Half treatment<br />
dose LMWH<br />
Omit<br />
LMWH.<br />
Check<br />
INR<br />
Prophylactic<br />
LMWH until<br />
warfarin is<br />
commenced.<br />
INR, international normalised ratio; LMWH, low molecular weight heparin.<br />
Novel oral anticoagulants<br />
Novel oral anticoagulants have more predictable pharmacodynamics and<br />
a faster onset of action with a shorter half-life than warfarin. There are<br />
currently three drugs on the market; these are increasingly used for<br />
management of patients with atrial fibrillation; after stroke and transient<br />
ischaemic attacks; and prophylaxis/management of venous thromboembolism<br />
[38].<br />
Their half-life varies, especially in the presence of renal impairment.<br />
Currently, there are no specific routine coagulation tests to determine<br />
their effectiveness. Regarding antidotes, the United States Food and<br />
Drug Administration and the European Commission have recently<br />
approved the first of these, idarucizumab (Praxbind, Boehringer Ingelheim<br />
International, Ingelheim am Rhein, Germany), for the emergency<br />
reversal of dabigatran; other antidotes are currently undergoing clinical<br />
trials.<br />
Dabigatran is a direct thrombin inhibitor. Half-life depends on<br />
extent of renal impairment (normally 48–72 h). For major elective surgery,<br />
neuraxial blockade and in patients with renal dysfunction, the drug<br />
should be stopped 5 days before surgery. For others, it can be stopped<br />
3 days before surgery.<br />
Rivaroxaban and apixaban are direct factor Xa inhibitors. Half-life<br />
is 5–13 h and is less dependent on renal function. For major elective<br />
surgery, neuraxial blockade and in patients with renal dysfunction, the<br />
drug should be stopped 3 days before surgery, otherwise stop 24–48 h<br />
before surgery.<br />
If surgery is urgent, consider PCC 50 IU.kg 1 , correct other abnormal<br />
coagulation tests and check platelets. Bridging anticoagulation is not<br />
16 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
required except in patients with recent (< 3 months) history of pulmonary<br />
embolism or deep venous thrombosis.<br />
Antiplatelet drugs<br />
These drugs cause irreversible inhibition of platelets; replenishment of<br />
platelets occurs at a rate of 10–15% per day. The restoration of normal<br />
platelet function depends on the individual drug and dosage.<br />
Aspirin inhibits the production of thromboxane. It should be continued<br />
for most procedures until the day before surgery. In patients at<br />
low risk of cardiovascular events having major surgery and those undergoing<br />
high-risk procedures such as intracranial surgery, aspirin should<br />
be discontinued 5 days before the procedure.<br />
Clopidogrel is an oral, thienopyridine-class antiplatelet agent, and<br />
the active metabolites circulate for up to 18 h after the last dose. Clopidogrel<br />
should be stopped 7 days before surgery unless point-of-care testing<br />
is used to check platelet function.<br />
The drugs prasugrel and ticlopidine are also thienopyridine-class<br />
antiplatelet drugs similar to clopidogrel. The same recommendations as<br />
for clopidogrel apply to the above drugs.<br />
Antiplatelet drugs and non-cardiac surgery in patients with<br />
coronary stents<br />
The management of these drugs in patients with coronary stents in situ<br />
depends on the type of stent, time after the coronary event and surgery<br />
type (major vs minor). Communication with the cardiology team is key.<br />
Elective surgery should be postponed for at least 4–6 weeks after<br />
bare metal stent implantation and 6 months after drug-eluting stent<br />
implantation. Aspirin may be continued during the peri-operative<br />
period except in closed space surgery such as intracranial and spinal<br />
surgery.<br />
For emergency surgery, management depends on the antiplatelet<br />
agent and when the last dose was taken. Platelet transfusion should be<br />
reserved as an additional measure for critical bleeding.<br />
Drugs that decrease blood loss<br />
Tranexamic acid is a synthetic derivative of the amino acid lysine that<br />
inhibits plasminogen activation, thus preventing impairment of fibrinolysis.<br />
In the last few years, there is increased evidence that its use may reduce<br />
bleeding in trauma, cardiac surgery and other major surgery. Seizures have<br />
been reported when high doses are given, but there is little evidence of<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 17
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
other side effects [39]. Dose is variable, but 1 g bolus is recommended,<br />
and an additional infusion of 500 mg.h 1 may also be considered [40].<br />
Aprotinin is a serine protease inhibitor antifibrinolytic which acts<br />
by inactivating free plasmin. The drug was withdrawn from the market<br />
in 2007 due to safety issues with increased incidence of renal impairment<br />
and anaphylactic reactions. Recently, regulators have licensed the<br />
drug only for myocardial revascularisation (coronary artery bypass surgery)<br />
[41].<br />
Blood components<br />
Before administration of any blood component, the patient’s details<br />
should be checked against those on the bag (see red blood cell transfusion<br />
section). Blood components have specific storage and expiry times.<br />
Every effort must be made to avoid wastage.<br />
In haematological malignancy, the clinical team must be consulted<br />
before administering blood components because of the need for specific<br />
requirements. The transfusion threshold may be different to non-haematological<br />
patients. A small number of patients require transfusion with<br />
irradiated blood components to prevent them developing transfusionassociated<br />
graftversus-host<br />
disease (TA-GVHD), which is rare, but usually fatal. Patients<br />
with the following conditions require irradiated blood: congenital immunodeficiency<br />
states, for example Di-George’s syndrome; allogeneic bone marrow<br />
transplant recipients and donors; autologous bone marrow-transplanted<br />
patients; Hodgkin’s lymphoma; purine analogue therapy including new<br />
agents clofarabine and bendamustine; and patients who receive antithymocyte<br />
globulin (anti-CD52) therapy (alemtuzumab) [42].<br />
Fresh frozen plasma<br />
Fresh frozen plasma is leucodepleted plasma rapidly frozen to below<br />
25 °C to maintain the integrity of labile coagulation factors. The use<br />
of FFP has increased significantly in the past few years [38]. Given that<br />
anti-HNA and anti-HLA antibodies occur at higher frequency in multiparous<br />
women, implementation of male-only plasma in component therapy<br />
began in the UK in 2003, and this has reduced the incidence of<br />
transfusion-related acute lung injury (TRALI) [43].<br />
Fresh frozen plasma can be thawed using a dry oven (10 min),<br />
microwave (2–3 min) or in a water bath (20 min). Thawed FFP can be<br />
used for up to 24 h as long as it is stored at 4 °C. This time has<br />
recently been extended to 5 days when stored at 4 °C for use in major<br />
18 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
haemorrhage associated with trauma. Once out of the fridge, it must be<br />
used within 30 min, and once thawed, it should never be refrozen.<br />
Approximate volume per bag is 300 ml.<br />
Fresh frozen plasma contains all the factors of the soluble<br />
coagulation system, including the labile factors V and VIII to a varying<br />
degree. The fibrinogen content of four units of FFP is approximately<br />
2 g, compared with approximately 4 g fibrinogen in two pools of<br />
cryoprecipitate.<br />
Fresh frozen plasma should be the same group as the patient. If the<br />
blood group is unknown, group AB FFP is preferred, as it does not contain<br />
any anti-A or anti-B. If group O FFP is given to non-group O children,<br />
it should be high-titre (HT) negative. The recommended<br />
therapeutic dose is 15 ml.kg 1 .<br />
To reduce the risk of variant Creutzfeldt–Jakob disease, FFP for use<br />
in all those born in 1996 or later is sourced outside of the UK and has<br />
undergone viral inactivation (either with methylene blue or solvent<br />
detergent treatment).<br />
Indications for FFP use include the following:<br />
• replacement of coagulation factors during major haemorrhage, particularly<br />
trauma and obstetrics;<br />
acute disseminated intravascular coagulation (DIC) with bleeding;<br />
• in patients who are actively bleeding and whose INR is > 1.5 (or<br />
POC equivalent);<br />
• immediate reversal of warfarin-induced haemorrhage when PCC is not<br />
available (PCC is the first choice);<br />
• thrombocytopenic purpura usually with plasmapheresis preferably<br />
using pathogen-inactivated FFP; and<br />
• replacement of coagulation factors when specific factors are not<br />
available (uncommon).<br />
There is a very limited role for FFP in the management of (mild–<br />
moderate) coagulation abnormalities frequently seen in many nonbleeding<br />
critically ill patients before invasive procedures. Fresh frozen<br />
plasma is not recommended for routine use in patients with cirrhosis/<br />
liver disease unless significant coagulopathy is identified, as again current<br />
understanding indicates that isolated abnormalities of the PT or<br />
APPT do not reflect a ‘balanced haemostasis’. Fresh frozen plasma<br />
should not be used simply as routine circulatory volume replacement.<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 19
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
Cryoprecipitate<br />
Cryoprecipitate is also a leucodepleted plasma product containing concentrated<br />
factor VIII, von Willebrand factor, fibrinogen, factor XIII and<br />
fibronectin, produced by further processing of FFP. It is stored<br />
at 25 °C; once thawed for administration, it can be kept at ambient<br />
temperature for 4 h, and should not be kept in the fridge again [42].<br />
In the UK, it is mainly available as pooled bags of five units, 100–<br />
200 ml per bag. It is also available as one unit of 20–40 ml. Each single unit<br />
has 400–450 mg of fibrinogen, and pools of five units contain at least 2 g.<br />
The adult dose is two pools; transfuse using a standard blood giving<br />
set with a 170- to 200-lm filter.<br />
Indications for cryoprecipitate include the following:<br />
• hypofibrinogenaemia due to major haemorrhage and massive transfusion.<br />
There is increased use of cryoprecipitate in major trauma,<br />
obstetric haemorrhage<br />
and cardiac surgical bleeding. During major haemorrhage,<br />
fibrinogen should be maintained > 1.5 g.l<br />
1 , except in active obstetric<br />
haemorrhage where fibrinogen should be maintained > 2 g.l<br />
1 ;<br />
combined liver and renal failure with bleeding;<br />
bleeding associated with thrombolytic therapy;<br />
• disseminated intravascular coagulation with fibrinogen < 1.0 g.l 1 ;<br />
and<br />
• advanced liver disease, to maintain fibrinogen level > 1.0 g.l 1 .<br />
Cryoprecipitate for use in all those born in 1996 or later is made<br />
from FFP sourced outside of the UK and has undergone viral inactivation<br />
with methylene blue. These components are available as single units<br />
for smaller children and pooled units for older children and young<br />
adults.<br />
Platelets<br />
Platelets are either made from pooled buffy coat-derived platelets from<br />
four whole blood donations, suspended in platelet additive solution and<br />
the plasma of one of the four donors (who is male), or as an adult therapeutic<br />
dose obtained from a single donor by apheresis donation. Both<br />
can be used interchangeably; NHSBT recommends that recipients born<br />
on or after 1st January 1996 should receive apheresis donation platelets<br />
where possible.<br />
20 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
There is increased use of platelets in the last few years. The greatest<br />
demand is for haemato-oncology patients; platelets should not be<br />
administered to patients with chemotherapy-induced thrombocytopenia<br />
in the absence of bleeding, unless their platelet count is < 10 9 10 9 .l<br />
1 .<br />
The risk of transmission of bacterial infection (1 in 12,000) is higher<br />
than other blood components because platelets are stored at 22 °C. This<br />
risk is reduced by bacterial screening before release.<br />
Platelets do not have to be the same group as the patient, but where<br />
group O platelets are given to a non-group O child they should be selected<br />
to be high-titre negative. D-negative children and women of childbearing<br />
potential should receive D-negative platelets because of the small risk of<br />
developing immune anti-D.<br />
Platelet concentrate should be stored at 22 °C with constant gentle<br />
agitation in an approved incubator. Platelets must not be placed in a<br />
refrigerator. Transfusion should ideally be commenced within 30 min of<br />
removal from the platelet storage incubator. Each pack contains 250–<br />
350 ml; platelet count in the pack is > 2.4 9 10 10 .l<br />
1 per adult dose,<br />
and transfusion should lead to an increase in the patient’s platelet count<br />
by approximately 30 9 10 9 .l<br />
1 . The patient’s platelet count should be<br />
repeated after transfusion.<br />
A standard adult therapeutic dose should be infused over a period of<br />
30 min through a standard blood administration set or platelet administration<br />
set incorporating a 170- to 200-lm filter. Do not give through a set<br />
that has already been used for red cells. No drugs should be added directly<br />
to the unit of platelets.<br />
Indications for platelets include the following:<br />
• prevention and treatment of bleeding due to thrombocytopenia or<br />
platelet function defects.<br />
• If patient is actively bleeding, transfuse to a platelet count<br />
> 75 9 10 9 1<br />
.l<br />
If not bleeding, the following triggers should be applied:<br />
routine prophylactic use: 10 9 109 .l<br />
1 ;<br />
• prophylactic use with additional risk factors (e.g. Sepsis):<br />
10 – 20 9 10 9 .l<br />
1 ;<br />
other major surgery or invasive procedures: 50 9 109 .l<br />
1 ;<br />
• neuraxial blockade: 50 9 109 .l<br />
1 ; and<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 21
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
• prophylactic use in closed compartment surgery (eye, brain):<br />
100 9 10 9 .l<br />
1 .<br />
In the UK, the availability of platelets is centralised and will depend<br />
on the demand and distance from nearest blood centre. Clinicians need<br />
to be aware of local laboratory arrangements and normal time interval<br />
for obtaining platelets from central storage.<br />
Special blood components<br />
Prothrombin complex concentrate<br />
Prothrombin complex concentrate (in the UK) comes as four-factor<br />
concentrate containing factors II, VII, IX and X, with protein S, C and<br />
heparin. It can be rapidly reconstituted providing a high concentration<br />
of these four clotting factors in a small volume. It is indicated in<br />
acquired factor deficiency and for urgent reversal of warfarin. There is<br />
limited evidence for use in any other setting.<br />
Fibrinogen concentrate<br />
There has been considerable interest in fibrinogen concentrate. It is<br />
widely used in mainland Europe in the management of bleeding following<br />
surgery or trauma. Recent trials in cardiac surgery have not shown<br />
any benefit from its use. It is only licensed for use in congenital<br />
hypofibrinogenaemia in the UK.<br />
Recombinant factor viia<br />
Licensed for use in haemophiliacs with inhibitors. It is the most potent<br />
thrombin generator available at present. Late use in the exsanguinating<br />
patient is almost always associated with no benefit, a high risk of mortality<br />
and thrombotic complications. Following cardiac surgery, it has<br />
been shown to reduce re-operation rates and transfusion in the bleeding<br />
patient. However, its use may increase the risk of thrombotic complications<br />
and its use except under haematological direction cannot be recommended<br />
[44].<br />
Acknowledgements<br />
AK is the Editor-in-Chief of Anaesthesia, and has received research<br />
funding and honoraria from Pharmacosmos and CSL Behring. RB has<br />
received educational support from Pharmacosmos. RG has received honoraria<br />
from CSL Behring and Octapharma. TR has received research<br />
funding and honoraria from Vifor Pharma and Pharmacosmos. RC has<br />
22 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
received research funding from CSL Behring and TEM International.<br />
No other conflicts of interest declared.<br />
References<br />
1. Bolton-Maggs PHB, Cohen H. Serious Hazards of Transfusion (SHOT) haemovigilance<br />
and progress is improving transfusion safety. British Journal of Haematology 2013;<br />
163: 303–14.<br />
2. NHS Blood and Transplant. Patient Blood Management: Optimising the Care of<br />
Patients who may need Transfusion. http://hospital.blood.co.uk/media/27420/<br />
140804-1-25447-bookmark-patient-blood-management.pdf (accessed 08/11/<br />
2015).<br />
3. Clevenger B, Mallett SV, Klein AA, Richards T. Patient blood management to reduce<br />
surgical risk. British Journal of Surgery 2015; 102: 1325–37.<br />
4. Kotze A, Harris A, Baker C, et al. British Committee for Standards in Haematology<br />
Guidelines on the identification and management of pre-operative anaemia. British<br />
Journal of Haematology 2015; 171: 322–31.<br />
5. Clevenger B, Richards T. Pre-operative anaemia. Anaesthesia 2015; 70: 20–e8.<br />
6. Ashworth A, Klein AA. Cell salvage as part of a blood conservation strategy in<br />
anaesthesia. British Journal of Anaesthesia 2010; 105: 401–16.<br />
7. National Patient Safety Agency. Safer Practice Notice 14: Right patient, right blood.<br />
October 2006. NPSA/2006/14. http://www.nrls.npsa.nhs.uk/resources/clinicalspecialty/emergency-medicine/?Entryid45=59805<br />
(accessed 08/11/2015).<br />
8. Medicines and Healthcare Products Regulatory Authority. Blood Safety and Quality<br />
Regulations, 2005. http://www.shotuk.org/wp-content/uploads/2010/03/12-David-<br />
Churchward.pdf (accessed 08/11/2015).<br />
9. Advisory Committee on the Safety of Blood, Tissues and Organs (sabto). Patient Consent<br />
for Blood Transfusion, 2011. https://www.gov.uk/government/publications/<br />
patient-consent-for-blood-transfusion (accessed 01/12/2015).<br />
10. British Committee for Standards in Haematology Guidelines on the Administration<br />
of Blood Components, 2009. http://www.bcshguidelines.com/documents/<br />
Admin_blood_components_bcsh_05012010.pdf (accessed 08/11/2015).<br />
11. Tinegate H, Birchall J, Gray A, et al. British Committee for Standards in Haematology.<br />
Blood Transfusion Task Force Guideline on the investigation and management<br />
of acute transfusion reactions. British Journal of Haematology 2012; 159:<br />
143–53.<br />
12. Salpeter SR, Buckley JS, Chatterjee S. Impact of more restrictive blood transfusion<br />
strategies on clinical outcomes: a meta-analysis and systematic review. American<br />
Journal of Medicine 2014; 127: 124–31.<br />
13. Holst LB, Petersen MW, Haase N, Perner A, Wetterslev J. Restrictive versus liberal<br />
transfusion strategy for red blood cell transfusion: systematic review of randomised<br />
trials with meta-analysis and trial sequential analysis. British Medical Journal 2015;<br />
350: h1354.<br />
14. Murphy GJ, Pike K, Rogers CA, et al. Liberal or restrictive transfusion after cardiac<br />
surgery. New England Journal of Medicine 2015; 372: 997–1008.<br />
15. British Committee for Standards in Haematology. A practical guideline for the<br />
haematological management of major haemorrhage, 2015. Http://www.<br />
bcshguidelines.com/documents/Major_Haemorrhage.pdf (accessed 08/11/2015).<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 23
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
16. Gill R. Practical management of major blood loss. Anaesthesia 2015; 70: 54–e20.<br />
17. Retter A, Barrett NA. The management of abnormal haemostasis in the ICU. Anaesthesia<br />
2015; 70: 121–e41.<br />
18. Retter A, Wyncoll D, Pearse R, et al. Guidelines on the management of anaemia<br />
and red cell transfusion in adult critically ill patients. British Journal of Haematology<br />
2013; 160: 445–64.<br />
19. Lilley G, Burkett-St-Laurent D, Precious E, et al. Measurement of blood loss during<br />
postpartum haemorrhage. International Journal of Obstetetric Anesthesia 2015; 24:<br />
8–14.<br />
20. Collis RE, Collins PW. Haemostatic management of obstetric haemorrhage. Anaesthesia<br />
2015; 70: 78–e28.<br />
21. Mallaiah S, Barclay P, Harrod I, Chevannes C, Bhalla A. Introduction of an algorithm<br />
for ROTEM-guided fibrinogen concentrate administration in major obstetric haemorrhage.<br />
Anaesthesia 2015; 70: 166–75.<br />
22. Collins PW, Lilley G, Bruynseels D, et al. Fibrin-based clot formation as an early and rapid<br />
biomarker for progression of postpartum hemorrhage: a prospective study. Blood 2014;<br />
124: 1727–36.<br />
23. Kirpalani H, Whyte RK, Anderson C, et al. The premature infants in need of transfusion<br />
(PINT) study: a randomized, controlled trial of a restrictive (low) versus liberal<br />
(high) transfusion threshold for extremely low birth weight infants. Journal of Pediatrics<br />
2006; 149: 301–7.<br />
24. New HV, Grant-Casey J, Lowe D, Kelleher A, Hennem S, Stanworth SJ. Red blood cell<br />
transfusion practice in children: current status and areas for improvement? A study<br />
of the use of red blood cell transfusions in children and infants. Transfusion 2014;<br />
54: 119–27.<br />
25. Royal College of Paediatrics and Chuild Health. Major trauma and the use of<br />
tranexamic acid in children, 2012. Http://www.rcpch.ac.uk/system/files/<br />
protected/page/Major Trauma and the Use of Tranexamic Acid in Children -<br />
Evidence Statement 2012-11.pdf (accessed 08/11/2015).<br />
26. Cholette JM, Powers KS, Alfieris GM, et al. Transfusion of cell saver salvaged blood<br />
in neonates and infants undergoing open heart surgery significantly reduces RBC<br />
and coagulant product transfusions and donor exposures: results of a prospective,<br />
randomized, clinical trial. Pediatric Critical Care Medicine 2013; 14: 137–47.<br />
27. Cap A, Hunt BJ. The pathogenesis of traumatic coagulopathy. Anaesthesia 2015;<br />
70: 96–e34.<br />
28. Hall S, Murphy MF. Limitations of component therapy for massive haemorrhage: is<br />
whole blood the whole solution? Anaesthesia 2015; 70: 511–4.<br />
29. Klein AA, Collier TJ, Brar MS, et al. The incidence and importance of anaemia in<br />
patients undergoing cardiac surgery in the UK - the first Association of Cardiothoracic<br />
Anaesthetists national audit. Anaesthesia 2016; 71: 627–35.<br />
30. National Institute for Health and Care Excellence (NICE). Viscoelastic point-of-care<br />
testing to assist with the diagnosis, management and monitoring of haemostasis:<br />
a systematic review and cost-effectiveness analysis. https://www.nice.org.uk/<br />
guidance/dg13/documents/detecting-managing-and-monitoring-haemostasisviscoelastometric-pointofcare-testing-rotem-teg-and-sonoclot-systems-diagnosticsassessment-report2<br />
(accessed 08/11/2015).<br />
24 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
31. Besser MW, Ortmann E, Klein AA. Haemostatic management of cardiac surgical<br />
haemorrhage. Anaesthesia 2015; 70: 87–e31.<br />
32. Corredor C, Wasowicz M, Karkouti K, Sharma V. The role of point-of-care platelet<br />
function testing in predicting postoperative bleeding following cardiac surgery: a<br />
systematic review and meta-analysis. Anaesthesia 2015; 70: 715–31.<br />
33. Fowler A, Perry DJ. Laboratory monitoring of haemostasis. Anaesthesia 2015; 70:<br />
68–e24.<br />
34. Mallett SV, Armstrong M. Point-of-care monitoring of haemostasis. Anaesthesia<br />
2015; 70: 73–e26.<br />
35. Skelton VA, Wijayasinghe N, Sharafudeen S, Sange A, Parry NS, Junghans C. Evaluation<br />
of point-of-care haemoglobin measuring devices: a comparison of Radical-7 TM<br />
pulse co-oximetry, hemocue â and laboratory haemoglobin measurements in<br />
obstetric patients. Anaesthesia 2013; 68: 40–5.<br />
36. Hildyard C, Curry N. Point-of-care testing: a standard of care? Anaesthesia 2015;<br />
70: 1113–8.<br />
37. Quarterman C, Shaw M, Johnson I, Agarwal S. Intra- and inter-centre standardisation<br />
of thromboelastography (TEG). Anaesthesia 2014; 69: 883–90.<br />
38. Van Veen JJ, Makris M. Management of peri-operative anti-thrombotic therapy.<br />
Anaesthesia 2015; 70: 58–e23.<br />
39. Sharma V, Katznelson R, Jerath A, et al. The association between tranexamic acid<br />
and convulsive seizures after cardiac surgery: a multivariate analysis in 11 529<br />
patients. Anaesthesia 2014; 69: 124–30.<br />
40. Hunt BJ. The current place of tranexamic acid in the management of bleeding.<br />
Anaesthesia 2015; 70: 50–e18.<br />
41. Ortmann E, Besser MW, Klein AA. Antifibrinolytic agents in current anaesthetic practice.<br />
British Journal of Anaesthesia 2013; 111: 549–63.<br />
42. Challis M, Marrin C, Vaughan RS, Goringe A. Who requires irradiated blood products?<br />
Anaesthesia 2011; 66: 620–1.<br />
43. Hart S, Cserti-Gazdewich CM, McCluskey SA. Red cell transfusion and the immune<br />
system. Anaesthesia 2015; 70: 38–e16.<br />
44. Gill R, Herbertson M, Vuylsteke A, et al. Safety and efficacy of recombinant activated<br />
factor VII: a randomized placebo-controlled trial in the setting of bleeding<br />
after cardiac surgery. Circulation 2009; 120: 21–7.<br />
Appendix 1<br />
Other available guidelines.<br />
National Institute for Health and Care Excellence (NICE) 2015<br />
(http://www.nice.org.uk/guidance/indevelopment/gid-CGWAVE0663?)<br />
British Committee for Standards in Haematology, 2012-15<br />
(http://www.bcshguidelines.com/4_haematology_guidelines.html?Dtype=<br />
Transfusion&dpage=0&sspage=0&ipage=0#gl)<br />
Practice Guidelines for Peri-operative Blood Management – American<br />
Society of Anesthesiologists (http://anesthesiology.pubs.asahq.org/<br />
article.aspx?Articleid=2088825)<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 25
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
Management of severe perioperative bleeding – Guidelines from<br />
the European Society of Anaesthesiology (2013) (http://anest-rean.lt/wpcontent/uploads/2013/05/Management_of_severe_perioperative_bleeding_.<br />
2.pdf)<br />
Network for the Advancement of Patient Blood Management,<br />
Haemostasis and Thrombosis<br />
(NATA) (http://www.nataonline.com)<br />
National Blood Authority Australia PBM Guidelines (http://<br />
www.blood.gov.au/pbm-guidelines)<br />
26 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
The use of blood components<br />
and their alternatives 2016<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
July 2016
This guideline was originally published in Anaesthesia. If you wish to refer<br />
to this guideline, please use the following reference:<br />
Association of Anaesthetists of Great Britain and Ireland. AAGBI<br />
guidelines: the use of blood components and their alternatives 2016<br />
Anaesthesia 2016; 71: 829-842.<br />
This guideline can be viewed online via the following URL:<br />
http://onlinelibrary.wiley.com/doi/10.1111/anae.13489/full
Guidelines<br />
AAGBI guidelines: the use of blood<br />
components and their alternatives 2016<br />
A. A. Klein, 1 P. Arnold, 2 R. M. Bingham, 3 K. Brohi, 4 R. Clark, 5<br />
R. Collis, 6 R. Gill, 7 W. McSporran, 8 P. Moor, 9 R. Rao Baikady, 10<br />
T. Richards, 11 S. Shinde, 12 S. Stanworth 13 and T. S. Walsh 14<br />
1 Consultant, Department of Anaesthesia and Intensive Care, Papworth<br />
Hospital, Cambridge, UK and Chair, AAGBI Working Party<br />
2 Consultant, Department of Paediatric Anaesthesia, Alder Hey<br />
Children’s Hospital, Honorary Lecturer, University of Liverpool,<br />
Liverpool, UK<br />
3 Consultant, Department of Paediatric Anaesthesia, Great Ormond<br />
Street Hospital for Children, London, UK<br />
4 Professor, Centre for Trauma Sciences, Barts Health NHS Trust and<br />
Queen Mary University of London, London, UK<br />
5 Specialist Trainee, Department of Anaesthesia, Glasgow Royal<br />
Infirmary, Glasgow, UK and Group of Anaesthetists in Training<br />
6 Consultant, Department of Anaesthesia, University Hospital of Wales,<br />
Cardiff, UK and Obstetric Anaesthetists’ Association<br />
7 Consultant, Department of Anaesthesia, University Hospital Southampton,<br />
UK, Royal College of Anaesthetists and Association of Cardiothoracic<br />
Anaesthetists<br />
8 Transfusion Practitioner, The Royal Marsden Hospital, London, UK<br />
9 Consultant, Department of Anaesthesia, Derriford Hospital, Plymouth,<br />
UK and Defence Anaesthesia representative<br />
10 Consultant, Department of Anaesthesia, The Royal Marsden Hospital,<br />
London, UK<br />
11 Professor, Division of Surgery and Interventional Science, University College<br />
Hospital, London, UK and Royal College of Surgeons<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 1<br />
This is an open access article under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs<br />
License, which permits use and distribution in any medium, provided the original work is properly cited, the use is<br />
non-commercial and no modifications or adaptations are made.
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
12 Consultant, Department of Anaesthesia, Southmead Hospital, Bristol,<br />
UK and Honorary Secretary, AAGBI<br />
13 Consultant, Department of Haematology, Oxford Radcliffe Hospitals,<br />
Oxford, UK, and NHS Blood and Transplant<br />
14 Professor, Department of Anaesthetics, Critical Care and Pain<br />
Medicine, Edinburgh University, Edinburgh, UK<br />
Summary<br />
Blood transfusion can be life-saving. Anaesthetists regularly request and<br />
administer blood components to their patients. All anaesthetists must be<br />
familiar with indications and appropriate use of blood and blood components<br />
and their alternatives, but close liaison with haematology specialists<br />
and their local blood sciences laboratory is encouraged.<br />
Considerable changes in approaches to optimal use of blood components,<br />
together with the use of alternative products, have become apparent<br />
over the past decade, leading to a need to update previous<br />
guidelines and adapt them for the use of anaesthetists working throughout<br />
the hospital system.<br />
....................................................................................................<br />
Endorsed by the Royal College of Anaesthetists and the Network for<br />
Advancement of Transfusion Alternatives (NATA).<br />
Keywords: anaemia and coagulation, blood crossmatch, FFP indications,<br />
major haemorrhage, transfusion<br />
Accepted: 11 March 2016<br />
Recommendations<br />
1 All patients should have their haemoglobin concentration (Hb)<br />
measured before listing for major elective surgery.<br />
2 Patients who are anaemic by the World Health Organization definition<br />
(Hb men < 130 g.l<br />
1 , women < 120 g.l<br />
1 ) should be investigated<br />
before elective surgery and treated appropriately, and elective<br />
non-urgent surgery other than caesarean section should be delayed.<br />
3 Where blood transfusion is anticipated, this and alternatives to<br />
transfusion should be discussed with the patient before surgery, and<br />
this should be documented.<br />
2 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
4 Red blood cells should be transfused one unit at a time, and the<br />
patient’s Hb should be checked before each unit transfused, unless<br />
there is ongoing bleeding or a large deficit that needs correcting.<br />
5 The use of intra-operative cell salvage and tranexamic acid administration<br />
should be considered in all non-obstetric patients where blood<br />
loss > 500 ml is possible and in traumatic and obstetric major haemorrhage.<br />
6 Blood components should be prescribed for small children by volume<br />
rather than number of units.<br />
7 Every institution should have a massive transfusion protocol which is<br />
regularly audited and reviewed.<br />
8 Group O red cells for transfusion should be readily available in the<br />
clinical area, in case haemorrhage is life-threatening. Group-specific<br />
red cells should be available within a very short time<br />
(15–20 min) of the laboratory receiving correctly-labelled samples<br />
and being informed of the emergency requirement for blood.<br />
9 During major haemorrhage due to trauma and obstetrics, consideration<br />
should be given to transfusing red cells and FFP in preference<br />
to other intravenous fluid.<br />
10 Patients who continue to actively bleed should be monitored by pointof-care<br />
and/or regular laboratory tests for coagulation, fibrinogen and<br />
platelet counts or function, and a guide for transfusion should be FFP if<br />
INR > 1.5, cryoprecipitate if fibrinogen < 1.5 g.l<br />
1 and platelets if platelet<br />
count < 75 9 10 9 .l<br />
1 .<br />
What other guidelines are available on this topic?<br />
A number of other guidelines are available, some of which are quite recent,<br />
but none cover the breadth of UK anaesthetic practice (Appendix 1).<br />
Why was this guideline developed?<br />
There is a need for a relevant up-to-date clinical guidance for practising<br />
UK anaesthetists, critical care staff and those from other specialities and<br />
backgrounds, based on evidence where possible and with a focus on<br />
safety.<br />
How and why does this publication differ from<br />
existing guidelines?<br />
This is an updated guideline that also brings three previous AAGBI<br />
guidelines together (blood component therapy, 2005; massive haemorrhage,<br />
2010; and red cell transfusion, 2008).<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 3
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
Introduction<br />
Transfusion medicine is changing rapidly in response to new developments.<br />
Considerable changes in approaches to transfusion, together with<br />
the use of alternative agents, have become apparent over the past decade.<br />
Blood transfusion can be life-saving, but this is a scarce and costly<br />
resource. There is increased focus on appropriate transfusion practice to<br />
ensure quality of service provision, and transfusion has been proposed<br />
as a quality indicator in surgical care. Blood transfusion usage remains<br />
high, particularly in trauma, obstetrics, critical care and cardiovascular<br />
surgery.<br />
Anaesthetists are frequently involved in transfusion decisions, the<br />
administration of blood and blood components and as part of the team<br />
managing any major haemorrhage. However, the use of allogeneic blood<br />
components has serious implications and warrants careful consideration<br />
[1]. As a consequence, there has recently been an expansion of interest<br />
in safeguarding and checklists, blood conservation, preservation techniques,<br />
coagulation profiling and the use of haemostatic agents. Appropriate<br />
use of blood components in patient care is of utmost importance.<br />
Several recent major research publications that have looked at transfusion<br />
practice were aimed at patient safety, outcomes and individualised<br />
care, including: use of restrictive transfusion protocols; adjuvant<br />
therapies; substitution of blood components with pooled factor concentrates;<br />
and use of point-of-care (POC) testing to target specific component<br />
use (see http://onlinelibrary.wiley.com/doi/10.1111/anae.2014.70.<br />
issue-s1/issuetoc).<br />
It is essential that our practice of blood transfusion is safe and<br />
based on current, scientific, evidence-based knowledge. A multidisciplinary<br />
approach that aims to benefit patients by the reduction in inappropriate<br />
transfusions is paramount. This working party aims to<br />
formalise guidance on the clinical indications and risks of transfusion,<br />
blood conservation and the transfusion process.<br />
Patient blood management<br />
Patient blood management is a patient-based approach aimed at reducing<br />
the utilisation of blood transfusion and improving the patient’s clinical<br />
outcome and safety, and focuses on the optimisation of three factors<br />
peri-operatively: patient, surgical and anaesthetic. It has been recommended<br />
as a standard of care in the UK National Health Service [2]. It<br />
focuses on three ‘pillars’ of care in surgical patients: detection and<br />
4 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
Table 1 Patient blood management – measures that should be taken in<br />
patients who are expected to bleed during surgery.<br />
Pre-operative<br />
-Pre-operative Hb should be measured, recorded and optimised as<br />
required<br />
-Elective surgery should be postponed in patients with untreated anaemia<br />
-Review and consider stopping antiplatelet and anticoagulant medication<br />
seven days before surgery<br />
-Consider minimally invasive or laparoscopic surgical technique<br />
-Point-of-care testing should be available with appropriate training.<br />
Intra-operative<br />
-Position patient carefully to maintain venous drainage<br />
-Use patient warming to maintain temperature > 36°<br />
-Consider cell salvage if blood loss > 500 ml anticipated<br />
-Consider giving tranexamic acid 1 g if blood loss > 500 ml anticipated<br />
-Apply restrictive transfusion threshold (Hb 70–80 g.l<br />
1 depending on<br />
patient characteristics and haemodynamics)<br />
-Consider use of topical haemostatic agents.<br />
Postoperative<br />
-Maintain oxygen delivery, targeting oxygen saturation levels > 95%<br />
-Single unit blood transfusion policy – re-assess Hb concentration and<br />
clinical need between units<br />
-Postoperative drains or cell salvage.<br />
treatment of peri-operative anaemia; reduction of peri-operative blood<br />
loss; and harnessing and optimising the patient-specific physiological<br />
reserve of anaemia [3] (Table 1).<br />
Anaemia<br />
Pre-operative anaemia is common, occurring in up to a third of patients<br />
before surgery, and associated with worse outcomes. All patients should<br />
have their Hb checked before listing for surgery. Patients who are anaemic<br />
(Hb in men < 130 g.l<br />
1 , women < 120 g.l<br />
1 ) should be investigated<br />
and the cause treated appropriately [4]. Patient pathways and pre-assessment<br />
clinics should be established to allow timely and appropriate management,<br />
and elective surgery should be delayed if required [5].<br />
Cell salvage<br />
The use of cell salvage should be considered for high- or medium-risk<br />
surgery in non-obstetric adult patients where blood loss > 500 ml is<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 5
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
likely, and in obstetric major haemorrhage. In patients with malignancy<br />
or obstetric haemorrhage, a leucocyte filter must be used. Bacterial contamination<br />
of the surgical field remains a contra-indication. Cell salvage<br />
may also be continued in the postoperative period [6].<br />
Other aspects of patient blood management are discussed throughout<br />
these guidelines.<br />
Process for transfusion<br />
Administering the wrong blood type in error (with the risk of ABO<br />
incompatibility) is the most serious outcome of blood transfusion. Most<br />
of these incidents are due to the failure of the final identity checks carried<br />
out between the patient (at the patient’s side) and the blood to be<br />
transfused. All members of staff involved in the administration of a<br />
blood component must be trained and competency-assessed as per local<br />
policy. Local policy will also stipulate if this is a one- or two-person<br />
bedside check, with each person performing the check independently<br />
[7]. Red cell transfusions must be completed within 4 h of removal from<br />
the blood fridge. All prescriptions for transfusion must be documented<br />
in the patient record, either on the anaesthetic chart or on the drug/<br />
fluid prescription chart. Local policy for confirmation of the transfusion<br />
must be followed – it is a legal requirement that 100% of blood components<br />
must be traceable [8]. Where blood transfusion is anticipated, this<br />
should be discussed with the patient before surgery and valid consent to<br />
receive transfusion should be documented [9]. Patients should be<br />
informed that they have received blood or blood components before discharge<br />
from hospital as they will otherwise be unaware; they should also<br />
be informed that this removes them from the donor pool. It is also<br />
important that the patient’s general practitioner is informed.<br />
The following guidance is for a manual checking process at the bedside;<br />
the preferred system is an electronic transfusion management system.<br />
-The patient must be positively identified. All patients receiving blood<br />
components should be wearing an identification wristband containing<br />
four core identifiers – first name, last name, date of birth and patient<br />
identification number.<br />
-Immediately before the transfusion, check the component next to the<br />
patient, against the prescription.<br />
-Check the four core identifiers on the compatibility label attached to<br />
the blood component with the identification attached to the patient. If<br />
6 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
there are any discrepancies, do not proceed and call the transfusion<br />
laboratory.<br />
-Check that the compatibility label attached to the blood component<br />
has the same blood group and 14-digit component donation number<br />
(or batch number for coagulation factors) as the sticker on the blood<br />
component.<br />
-Visually check the blood component for any leakage, discolouration or<br />
presence of any clots or clumps.<br />
-Check the expiry date and time.<br />
Transfusing an unidentified patient<br />
All hospitals should have a clear local policy for transfusion of patients<br />
whose identity is unknown. In emergency situations or where the<br />
patient cannot immediately be identified, the patient should still have<br />
identification attached stating unknown male or female and a unique<br />
identification number. The blood sample sent to the transfusion laboratory<br />
should contain these exact details.<br />
In the event that the patient’s identity becomes known, new identification<br />
must be attached to the patient and a new transfusion sample<br />
collected and fully labelled with the known patient’s details.<br />
Monitoring for adverse events or reactions during transfusions<br />
Clinical observations should include heart rate, blood pressure, temperature<br />
and respiratory rate, as per local guidelines (national guidelines<br />
define a minimum of pre-transfusion, at the end of transfusion and 15<br />
min after transfusion). If there are any signs of a transfusion reaction,<br />
such as tachycardia, rash, breathlessness, hypotension or fever, stop the<br />
transfusion and contact the laboratory immediately [10]. Management<br />
may include the administration of antihistamine or steroid drugs, or<br />
intramuscular/intravenous adrenaline if life-threatening [11]. Diagnosis<br />
of a transfusion reaction during ongoing haemorrhage may be difficult,<br />
but if concern arises, the documentation should be double-checked for<br />
administration errors and further analyses performed as per local protocols.<br />
Transferring blood with a patient<br />
Blood components should be transferred with patients at high risk of<br />
requiring transfusion en route or immediately on arrival. There should<br />
be effective communication between the blood transfusion laboratories<br />
involved, according to regional policy. Blood components must be<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 7
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
transported in a storage box suitable to maintain their integrity, along<br />
with accompanying paperwork, and careful handover is required. When<br />
the patient arrives at their destination, the receiving transfusion laboratory<br />
should be immediately informed that blood was transported. The<br />
patient should be issued with a new identity wristband, a new sample<br />
taken for cross-match and more blood issued; until this is available,<br />
blood transferred with the patient may be administered if required.<br />
Red blood cell transfusion<br />
Red blood cell (RBC) transfusion is potentially life-saving for the treatment<br />
of blood loss (Major haemorrhage – see next section). In patients<br />
who do not have active bleeding and in normovolaemic patients, the Hb<br />
should be measured before and after every unit of RBC transfused. Nearpatient<br />
measurement of Hb may be particularly useful, but laboratory<br />
measurement remains the gold standard. Haemoglobin concentration is<br />
dependent on both red cell mass and plasma volume; it may fall due to<br />
haemodilution due to intravenous fluid administration. In the bleeding<br />
patient, haemoglobin concentration may remain falsely elevated despite<br />
significant blood loss due to inadequate fluid resuscitation.<br />
Other potential indications for RBC transfusion are clinical signs<br />
and biochemical markers of inadequate oxygen delivery, such as elevated<br />
blood lactate concentration, a low Ph and low central or mixed venous<br />
oxygen saturation.<br />
Optimum haemoglobin transfusion trigger<br />
Recent publications comparing more liberal transfusion strategies (typical<br />
transfusion trigger Hb 90–100 g.l<br />
1 ) with more restrictive strategies<br />
(typical transfusion trigger Hb 70–80 g.l<br />
1 ) did not show any difference<br />
in patient outcomes [12, 13]. Therefore, a general Hb threshold of<br />
70 g.l<br />
1 should apply as a guide for red cell transfusion. Uncertainty<br />
remains for patients with ischaemic heart disease, including acute coronary<br />
syndrome and after cardiac surgery [14], and higher thresholds<br />
(80 g.l<br />
1 ) may be more appropriate in such circumstances.<br />
Major haemorrhage<br />
Major haemorrhage is variously defined as loss of more than one blood<br />
volume within 24 h (around 70 ml.kg 1 , > 5 l in a 70 kg adult); 50%<br />
of total blood volume lost in < 3 h; or bleeding in excess of<br />
150 ml.min 1 . A pragmatic clinically-based definition is bleeding which<br />
leads to a systolic blood pressure of less than 90 mm Hg or a heart<br />
8 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
rate of more than 110 beats.min 1 . Major haemorrhage is a significant<br />
cause of mortality and morbidity in the peri-operative setting. Appropriate<br />
and effective management integrates multiple factors, including:<br />
recognition; communication; timely delivery of blood products; and<br />
application of definitive modalities of treatment (surgery and interventional<br />
radiology) [15].<br />
Major haemorrhage protocol<br />
Policies should be defined in an institutional major haemorrhage protocol.<br />
Activation of a protocol should result in the immediate release and<br />
administration of blood components for initial resuscitation, without<br />
prior approval from a haematologist. Such protocols perform best when<br />
specific to clinical areas such as the emergency department or the labour<br />
ward, and are designed to include robust and clearly understood activation<br />
and communication from bedside to laboratory. Their activation<br />
should also mobilise other resources, such as additional (senior) staff<br />
including portering, blood warmers, pressure infusers and cell salvage<br />
devices [16].<br />
A clear mechanism for the escalation of a team response and for<br />
identifying individuals with sufficient seniority and experience to undertake<br />
the key roles of team leader (senior anaesthetist) and co-ordinator<br />
is essential to the process, as is enabling a single point of contact with<br />
the laboratory and other support services.<br />
Initial resuscitation<br />
Most major haemorrhage packs will contain four units of RBCs and<br />
four units of FFP (equivalent to 15–20 ml.kg 1 in a standard adult);<br />
platelet concentrate may also be provided. Administration should be via<br />
wide-bore intravenous access, or intra-osseous access until the former<br />
can be obtained.<br />
Group O red cells should be readily available and transfused if<br />
haemorrhage is life-threatening. It is essential to give group O Rh-negative<br />
red cells to children and women of childbearing potential, but<br />
group O Rh-positive red cells may be used in adult men.<br />
Group-specific red cells should be rapidly made available (within<br />
15–20 min) by the laboratory after receiving a correctly labelled blood<br />
group sample and being informed of the emergency requirement for<br />
blood. Emergency Group O red cells should continue to be provided<br />
where timely and safe issue of group-specific red cells is not possible.<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 9
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
Haemostatic resuscitation<br />
This describes the process of restoring and sustaining normal tissue perfusion<br />
with the emphasis on preservation of effective clotting. Coagulopathy<br />
is associated with haemorrhage (consumption) and transfusion<br />
of blood products (dilution), as well as mechanism of injury in trauma;<br />
this may exacerbate the haemorrhage and resultant morbidity. Point-ofcare<br />
or laboratory testing should be used to guide management.<br />
During resuscitation, the following should be prevented/treated:<br />
hypothermia; acidosis; hypocalcaemia (aim for ionised calcium<br />
> 1.0 mmol.l<br />
1 ); and hyperkalaemia.<br />
Special situations<br />
Critical care<br />
Anaemia is prevalent during critical illness. In addition to blood loss and<br />
sampling, haemodilution and impaired erythropoiesis may be important<br />
contributors [17]. Patients with anaemia demonstrate biochemical abnormalities<br />
similar to those with chronic inflammatory diseases.<br />
Although biochemical markers of tissue hypoxia, notably blood<br />
lactate concentration, are frequently elevated, evidence does not support<br />
increasing oxygen delivery with RBC transfusion when the Hb is<br />
> 70 g.l<br />
1 , unless the patient has cardiac disease [18].<br />
One important group of patients admitted to ICU are patients with<br />
haematological malignancies. Overall, patients with cancer form one of<br />
the larger groups of recipients of blood components. However, unlike<br />
other patient groups, the anaemia in patients with haematological malignancies<br />
reflects an underlying bone marrow failure, and therefore, it is<br />
unclear to what extent findings from the majority of randomised trials<br />
conducted in surgery or general critical care can be extrapolated to cancer,<br />
although the same broad principles of restrictive use of red cells commonly<br />
apply (70–80 g.l<br />
1 for red cell transfusion).<br />
Obstetrics<br />
Estimating blood loss at delivery is notoriously difficult, and every effort<br />
should be made to directly measure abnormal bleeding across all settings<br />
in the delivery suite [19]. Early recognition of bleeding by changing<br />
bed linen and pads immediately after delivery and systematically<br />
weighing new blood-soaked pads correlates with the fall in Hb concentration<br />
and improves outcome.<br />
As soon as abnormal bleeding is recognised, > 500 ml after a vaginal<br />
delivery and > 1000 ml after a caesarean delivery, the obstetrician,<br />
10 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
anaesthetist and senior midwife should attend the mother. Blood should<br />
be taken for full blood count (Hb), clotting studies, group and screen,<br />
and a venous blood gas for rapid Hb measurement and lactate<br />
(> 2 mmol.l<br />
1 is an indicator of shock). Cell salvage is recommended if<br />
abnormal bleeding occurs during caesarean section, and a leucocyte filter<br />
should be used for autotransfusion of processed blood.<br />
Severe early consumptive coagulopathy is associated with abruption,<br />
amniotic fluid embolus and severe bleeding with pre-eclampsia. Early<br />
use of FFP before RBC may be required.<br />
Postpartum haemorrhage associated with atony or trauma is unlikely<br />
to be associated with haemostatic impairment unless the diagnosis is<br />
delayed. Protocol-led use of blood products will lead to overtransfusion of<br />
FFP in the majority of cases [20]. If coagulation tests are not known, then<br />
FFP should be withheld until four units of RBC have been given. If no<br />
coagulation results are available and bleeding is ongoing, then, after four<br />
units of RBC, four units of FFP should be infused and 1:1 ratio of RBC–<br />
FFP transfusion maintained until the results of haemostatic tests are<br />
known. Point-of-care (POC) testing is recommended in this setting [21].<br />
Hypofibrinogenaemia, below normal levels for pregnancy, predicts<br />
the risks of ongoing postpartum haemorrhage. The normal plasma fibrinogen<br />
concentration in pregnancy is 4–6 g.l<br />
1 , and a laboratory Clauss<br />
fibrinogen of < 3 and especially < 2 g.l<br />
1 , with ongoing bleeding, is associated<br />
with progression to major obstetric bleeding [22]. Fibrinogen<br />
replacement with cryoprecipitate or fibrinogen concentrate should be considered<br />
in these circumstances, if there is bleeding.<br />
Monitoring of haemostatic function in obstetric haemorrhage is particularly<br />
important; laboratory testing is often too slow during obstetric<br />
haemorrhage, and therefore, POC testing is preferred. Tests should include<br />
plasma fibrinogen concentration or POC equivalent [21]. With ongoing<br />
bleeding, any abnormalities should be treated, as this indicates significant<br />
haemostatic impairment in the obstetric patient. Platelet transfusions are<br />
rarely required and should only be given once the platelet count is known.<br />
Tranexamic acid reduces total blood loss and should be given if<br />
postpartum haemorrhage is severe (> 500 ml after a vaginal delivery<br />
and > 1000 ml after a caesarean delivery), at an initial dose of 1 g.<br />
Paediatrics<br />
There is little direct evidence to guide the use of blood products in children,<br />
and generally the guidance intended for adults can be safely<br />
applied to children with some modifications (specifically in transfusion<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 11
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
volumes). ‘Restrictive’ approaches to transfusion are appropriate for<br />
almost all children older than 3 months of age. Higher transfusion<br />
thresholds are often applied to neonates and children with congenital<br />
heart disease. Although thresholds are not clearly defined, there is evidence<br />
that quantities of transfusion can be reduced in these patients by<br />
applying moderately restrictive thresholds for transfusion without<br />
adverse effect on outcome [23, 24]. Neonates should receive components<br />
specified for neonatal use, including cytomegalovirus-negative blood<br />
products.<br />
The volume of blood to be administered requires modification<br />
depending on the size of the patient. It is recommended that blood in<br />
children should be prescribed in volume rather than number of units.<br />
In practice, sensible rounding to the nearest unit will be more efficient.<br />
• A transfusion of 10 ml.kg 1 of RBC should increase Hb by approximately<br />
20 g.l<br />
1 .<br />
• Cryoprecipitate should be given in a dose of 5–10 ml.kg 1 .<br />
• Platelets should be given in a dose of 10–20 ml.kg 1 .<br />
• Fresh frozen plasma may be given in doses of 10–15 ml.kg 1 .<br />
Tranexamic acid can be used in children: a loading dose of 15 mg.kg 1<br />
followed by infusion 2 mg.kg 1 .h 1 should be used in trauma [25].<br />
With technical refinements, cell salvage can be useful in children,<br />
even if the absolute volume of blood loss is less than 500 ml [26].<br />
Major haemorrhage is rare in children outside of highly specialist<br />
areas of practice. The guidance suggested for adults can be generally<br />
applied, though requires an awareness of the size of the child and the<br />
clinical context of the bleeding. Blood volume of a child is estimated at<br />
70 ml.kg 1 but may be as high as 100 ml.kg 1 in newborns. Devices for<br />
vascular access and rapid administration of blood should be appropriate<br />
for the size of the child and rate of blood loss. Children are at particular<br />
risk of electrolyte imbalance and hypothermia during rapid administration<br />
of blood products.<br />
Trauma<br />
During active bleeding, follow the principles of damage control resuscitation:<br />
Early haemorrhage control<br />
Ensure clinical treatment is constantly directed towards haemorrhage<br />
control. Use temporary haemostatic devices (pressure, tourniquets, etc.)<br />
12 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
followed as soon as practically possible by surgery or interventional<br />
radiological control of haemorrhage.<br />
Permissive hypotension<br />
Do not try to normalise blood pressure during active haemorrhage.<br />
Maintain a minimum acceptable preload and blood pressure with volume<br />
resuscitation alone; this may need to be modified in the presence<br />
of trauma in head and spinal injuries. The use of vasopressors should<br />
be avoided during active haemorrhage.<br />
Avoid crystalloid and colloid administration<br />
During uncontrolled haemorrhage, avoid clear fluids for volume resuscitation<br />
unless there is profound hypotension and no imminent availability<br />
of blood products.<br />
Target trauma-induced coagulopathy<br />
Deliver blood products empirically at first, and use laboratory or pointof-care<br />
tests of coagulation to guide therapy as soon as available [27].<br />
Give tranexamic acid 1 g immediately, but avoid if more than 3 h<br />
after injury, unless there is ongoing evidence of hyperfibrinolysis (as<br />
suggested by POC testing).<br />
Whilst haemorrhage is being controlled, administration of RBC and<br />
FFP in a ratio of 1:1 should be used to replace fluid volume [28]. Consider<br />
the administration of cryoprecipitate (two pools) and platelets (one<br />
adult therapeutic dose) until test results are available and bleeding is<br />
controlled. Once control is achieved, blood components should be<br />
administered as guided by testing at the earliest opportunity (see Monitoring<br />
section, blood components).<br />
Cardiac surgery<br />
Anaemic patients have an increased risk of mortality and complications<br />
following cardiac surgery [29]. Elective cardiac surgery should not be<br />
undertaken in an anaemic patient without prior investigation and treatment<br />
as considered necessary.<br />
Viscoelastic testing is recommended to guide transfusion [30]. The<br />
use of local transfusion protocols guided by point-of-care testing may<br />
lead to appropriate transfusion with reduced costs. The evidence base<br />
for the efficacy of fresh frozen plasma is minimal and of poor quality<br />
[31].<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 13
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
The effect of cardiopulmonary bypass on platelet function may<br />
make the use of a higher platelet count (> 75 9 10 -9 .l<br />
1 ) necessary after<br />
bypass.<br />
There is no clear evidence of the benefit of platelet function analysis<br />
except in those patients who have taken PY12 receptor inhibitors such<br />
as clopidogrel within 5 days of surgery [32].<br />
Monitoring<br />
Laboratory testing<br />
Traditional tests such as APTT and PT/INR have been standardised for<br />
the monitoring of anticoagulants and are designed to diagnose and<br />
manage factor deficiencies such as haemophilia. Standardisation within<br />
laboratories has made the results very reliable.<br />
The PT and APTT were not designed to monitor coagulation deficiencies<br />
during haemorrhage and suggested INR and APTT ratios or<br />
triggers, which are widely quoted to guide coagulation product replacement,<br />
are based on small historic studies that have little relevance today.<br />
Slow turnaround time also means that the results do not reflect the<br />
dynamic clinical situation during ongoing haemorrhage [33].<br />
Point-of-care testing<br />
Point-of-care testing has a shorter turnaround time and represents a<br />
more global and therefore more relevant reflection of coagulation status<br />
[34]. Point-of-care testing is increasingly popular for general and<br />
cardiac surgery, trauma units, intensive care and obstetrics. Point-ofcare<br />
testing for Hb concentration is commonly used, such as blood<br />
gas analysis or the HemoCue â (€Angelholm, Sweden), which both correlate<br />
well with laboratory measurements [35]. The activated clotting<br />
time (ACT) is also well validated and should be used routinely whenever<br />
heparin is administered, particularly in cardiac and vascular<br />
surgery.<br />
Targeted blood component therapy based on POC testing has been<br />
shown to be safe and effective, and to decrease blood product usage.<br />
However, there are currently no studies that show improved patient outcome<br />
compared with standard treatment [32].<br />
At the current time, there are two commercially available semi-automated<br />
viscoelastic machines that use similar technology: thromboelastometry<br />
(ROTEM, TEM International, Munich, Germany) and<br />
thromboelastography (TEG, Haemonetics Corp, Braintree, MA, USA).<br />
One manufacturer cannot be recommended above the other.<br />
14 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
There are no universal algorithms across the specialities, and local<br />
protocols are required based on institutional procedures. There is limited<br />
interchangeability between TEG and ROTEM, and development<br />
and validation of separate treatment algorithms for the two devices are<br />
required [36].<br />
There are concerns about standardisation of both assays with poor<br />
quality control and assurance and a wide variation in results between<br />
centres [37]. It is good practice to pair coagulation samples and send a<br />
second sample for laboratory-based analysis.<br />
Drugs<br />
An increasing number of patients take either anticoagulants or antiplatelet<br />
agents. All patients require careful pre-operative medication optimisation<br />
before surgery. The management of drugs related to antithrombotic therapy<br />
in the peri-operative setting is a common problem, balancing bleeding<br />
risk with thrombosis.<br />
Patients at high risk (> 10% risk of thrombotic events per year)<br />
of thrombosis should be considered for bridging anticoagulation, or<br />
in the following circumstances:<br />
-venous thromboembolic event within the last 3 months, or<br />
-prosthetic (mechanical) heart valve<br />
Bridging anticoagulation usually consists of low molecular weight heparin.<br />
The dose and type of the low molecular weight heparin depends on the<br />
patient’s weight, timing of surgery, type of procedure and thrombotic risks.<br />
Warfarin (Vitamin K antagonist)<br />
The international normalised ratio (INR) is used to monitor the effectiveness<br />
of warfarin. In most situations, INR is maintained between 2.0<br />
and 2.5.<br />
The peri-operative management of warfarin is summarised in<br />
Table 2. In patients with atrial fibrillation on warfarin, routine use of<br />
bridging anticoagulation with low molecular weight heparin before surgery<br />
is not recommended.<br />
For emergency reversal of warfarin, prothrombin complex concentrate<br />
(PCC) 50 IU.kg 1 is recommended. Intravenous vitamin K<br />
(10 mg) may also be given, but this may preclude re-warfarinisation<br />
for a number of days. Fresh frozen plasma is an alternative if PCC<br />
is not available [37], but should not be used as elective prophylaxis<br />
in patients taking warfarin.<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 15
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
Table 2 Peri-operative optimisation of warfarin anticoagulation for<br />
major surgery. Bridging with LMWH required for high-risk patients,<br />
patients who suffered recent thromboembolic events or patients with<br />
mechanical prosthetic heart valves.<br />
Day 5 Days 4, 3, 2 Day 1 Surgery Postoperative<br />
Last dose of<br />
warfarin.<br />
Treatment dose LMWH<br />
(consider Vitamin K if<br />
INR > 2.5<br />
Half treatment<br />
dose LMWH<br />
Omit<br />
LMWH.<br />
Check<br />
INR<br />
Prophylactic<br />
LMWH until<br />
warfarin is<br />
commenced.<br />
INR, international normalised ratio; LMWH, low molecular weight heparin.<br />
Novel oral anticoagulants<br />
Novel oral anticoagulants have more predictable pharmacodynamics and<br />
a faster onset of action with a shorter half-life than warfarin. There are<br />
currently three drugs on the market; these are increasingly used for<br />
management of patients with atrial fibrillation; after stroke and transient<br />
ischaemic attacks; and prophylaxis/management of venous thromboembolism<br />
[38].<br />
Their half-life varies, especially in the presence of renal impairment.<br />
Currently, there are no specific routine coagulation tests to determine<br />
their effectiveness. Regarding antidotes, the United States Food and<br />
Drug Administration and the European Commission have recently<br />
approved the first of these, idarucizumab (Praxbind, Boehringer Ingelheim<br />
International, Ingelheim am Rhein, Germany), for the emergency<br />
reversal of dabigatran; other antidotes are currently undergoing clinical<br />
trials.<br />
Dabigatran is a direct thrombin inhibitor. Half-life depends on<br />
extent of renal impairment (normally 48–72 h). For major elective surgery,<br />
neuraxial blockade and in patients with renal dysfunction, the drug<br />
should be stopped 5 days before surgery. For others, it can be stopped<br />
3 days before surgery.<br />
Rivaroxaban and apixaban are direct factor Xa inhibitors. Half-life<br />
is 5–13 h and is less dependent on renal function. For major elective<br />
surgery, neuraxial blockade and in patients with renal dysfunction, the<br />
drug should be stopped 3 days before surgery, otherwise stop 24–48 h<br />
before surgery.<br />
If surgery is urgent, consider PCC 50 IU.kg 1 , correct other abnormal<br />
coagulation tests and check platelets. Bridging anticoagulation is not<br />
16 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
required except in patients with recent (< 3 months) history of pulmonary<br />
embolism or deep venous thrombosis.<br />
Antiplatelet drugs<br />
These drugs cause irreversible inhibition of platelets; replenishment of<br />
platelets occurs at a rate of 10–15% per day. The restoration of normal<br />
platelet function depends on the individual drug and dosage.<br />
Aspirin inhibits the production of thromboxane. It should be continued<br />
for most procedures until the day before surgery. In patients at<br />
low risk of cardiovascular events having major surgery and those undergoing<br />
high-risk procedures such as intracranial surgery, aspirin should<br />
be discontinued 5 days before the procedure.<br />
Clopidogrel is an oral, thienopyridine-class antiplatelet agent, and<br />
the active metabolites circulate for up to 18 h after the last dose. Clopidogrel<br />
should be stopped 7 days before surgery unless point-of-care testing<br />
is used to check platelet function.<br />
The drugs prasugrel and ticlopidine are also thienopyridine-class<br />
antiplatelet drugs similar to clopidogrel. The same recommendations as<br />
for clopidogrel apply to the above drugs.<br />
Antiplatelet drugs and non-cardiac surgery in patients with<br />
coronary stents<br />
The management of these drugs in patients with coronary stents in situ<br />
depends on the type of stent, time after the coronary event and surgery<br />
type (major vs minor). Communication with the cardiology team is key.<br />
Elective surgery should be postponed for at least 4–6 weeks after<br />
bare metal stent implantation and 6 months after drug-eluting stent<br />
implantation. Aspirin may be continued during the peri-operative<br />
period except in closed space surgery such as intracranial and spinal<br />
surgery.<br />
For emergency surgery, management depends on the antiplatelet<br />
agent and when the last dose was taken. Platelet transfusion should be<br />
reserved as an additional measure for critical bleeding.<br />
Drugs that decrease blood loss<br />
Tranexamic acid is a synthetic derivative of the amino acid lysine that<br />
inhibits plasminogen activation, thus preventing impairment of fibrinolysis.<br />
In the last few years, there is increased evidence that its use may reduce<br />
bleeding in trauma, cardiac surgery and other major surgery. Seizures have<br />
been reported when high doses are given, but there is little evidence of<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 17
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
other side effects [39]. Dose is variable, but 1 g bolus is recommended,<br />
and an additional infusion of 500 mg.h 1 may also be considered [40].<br />
Aprotinin is a serine protease inhibitor antifibrinolytic which acts<br />
by inactivating free plasmin. The drug was withdrawn from the market<br />
in 2007 due to safety issues with increased incidence of renal impairment<br />
and anaphylactic reactions. Recently, regulators have licensed the<br />
drug only for myocardial revascularisation (coronary artery bypass surgery)<br />
[41].<br />
Blood components<br />
Before administration of any blood component, the patient’s details<br />
should be checked against those on the bag (see red blood cell transfusion<br />
section). Blood components have specific storage and expiry times.<br />
Every effort must be made to avoid wastage.<br />
In haematological malignancy, the clinical team must be consulted<br />
before administering blood components because of the need for specific<br />
requirements. The transfusion threshold may be different to non-haematological<br />
patients. A small number of patients require transfusion with<br />
irradiated blood components to prevent them developing transfusionassociated<br />
graftversus-host<br />
disease (TA-GVHD), which is rare, but usually fatal. Patients<br />
with the following conditions require irradiated blood: congenital immunodeficiency<br />
states, for example Di-George’s syndrome; allogeneic bone marrow<br />
transplant recipients and donors; autologous bone marrow-transplanted<br />
patients; Hodgkin’s lymphoma; purine analogue therapy including new<br />
agents clofarabine and bendamustine; and patients who receive antithymocyte<br />
globulin (anti-CD52) therapy (alemtuzumab) [42].<br />
Fresh frozen plasma<br />
Fresh frozen plasma is leucodepleted plasma rapidly frozen to below<br />
25 °C to maintain the integrity of labile coagulation factors. The use<br />
of FFP has increased significantly in the past few years [38]. Given that<br />
anti-HNA and anti-HLA antibodies occur at higher frequency in multiparous<br />
women, implementation of male-only plasma in component therapy<br />
began in the UK in 2003, and this has reduced the incidence of<br />
transfusion-related acute lung injury (TRALI) [43].<br />
Fresh frozen plasma can be thawed using a dry oven (10 min),<br />
microwave (2–3 min) or in a water bath (20 min). Thawed FFP can be<br />
used for up to 24 h as long as it is stored at 4 °C. This time has<br />
recently been extended to 5 days when stored at 4 °C for use in major<br />
18 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
haemorrhage associated with trauma. Once out of the fridge, it must be<br />
used within 30 min, and once thawed, it should never be refrozen.<br />
Approximate volume per bag is 300 ml.<br />
Fresh frozen plasma contains all the factors of the soluble<br />
coagulation system, including the labile factors V and VIII to a varying<br />
degree. The fibrinogen content of four units of FFP is approximately<br />
2 g, compared with approximately 4 g fibrinogen in two pools of<br />
cryoprecipitate.<br />
Fresh frozen plasma should be the same group as the patient. If the<br />
blood group is unknown, group AB FFP is preferred, as it does not contain<br />
any anti-A or anti-B. If group O FFP is given to non-group O children,<br />
it should be high-titre (HT) negative. The recommended<br />
therapeutic dose is 15 ml.kg 1 .<br />
To reduce the risk of variant Creutzfeldt–Jakob disease, FFP for use<br />
in all those born in 1996 or later is sourced outside of the UK and has<br />
undergone viral inactivation (either with methylene blue or solvent<br />
detergent treatment).<br />
Indications for FFP use include the following:<br />
• replacement of coagulation factors during major haemorrhage, particularly<br />
trauma and obstetrics;<br />
acute disseminated intravascular coagulation (DIC) with bleeding;<br />
• in patients who are actively bleeding and whose INR is > 1.5 (or<br />
POC equivalent);<br />
• immediate reversal of warfarin-induced haemorrhage when PCC is not<br />
available (PCC is the first choice);<br />
• thrombocytopenic purpura usually with plasmapheresis preferably<br />
using pathogen-inactivated FFP; and<br />
• replacement of coagulation factors when specific factors are not<br />
available (uncommon).<br />
There is a very limited role for FFP in the management of (mild–<br />
moderate) coagulation abnormalities frequently seen in many nonbleeding<br />
critically ill patients before invasive procedures. Fresh frozen<br />
plasma is not recommended for routine use in patients with cirrhosis/<br />
liver disease unless significant coagulopathy is identified, as again current<br />
understanding indicates that isolated abnormalities of the PT or<br />
APPT do not reflect a ‘balanced haemostasis’. Fresh frozen plasma<br />
should not be used simply as routine circulatory volume replacement.<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 19
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
Cryoprecipitate<br />
Cryoprecipitate is also a leucodepleted plasma product containing concentrated<br />
factor VIII, von Willebrand factor, fibrinogen, factor XIII and<br />
fibronectin, produced by further processing of FFP. It is stored<br />
at 25 °C; once thawed for administration, it can be kept at ambient<br />
temperature for 4 h, and should not be kept in the fridge again [42].<br />
In the UK, it is mainly available as pooled bags of five units, 100–<br />
200 ml per bag. It is also available as one unit of 20–40 ml. Each single unit<br />
has 400–450 mg of fibrinogen, and pools of five units contain at least 2 g.<br />
The adult dose is two pools; transfuse using a standard blood giving<br />
set with a 170- to 200-lm filter.<br />
Indications for cryoprecipitate include the following:<br />
• hypofibrinogenaemia due to major haemorrhage and massive transfusion.<br />
There is increased use of cryoprecipitate in major trauma,<br />
obstetric haemorrhage<br />
and cardiac surgical bleeding. During major haemorrhage,<br />
fibrinogen should be maintained > 1.5 g.l<br />
1 , except in active obstetric<br />
haemorrhage where fibrinogen should be maintained > 2 g.l<br />
1 ;<br />
combined liver and renal failure with bleeding;<br />
bleeding associated with thrombolytic therapy;<br />
• disseminated intravascular coagulation with fibrinogen < 1.0 g.l 1 ;<br />
and<br />
• advanced liver disease, to maintain fibrinogen level > 1.0 g.l 1 .<br />
Cryoprecipitate for use in all those born in 1996 or later is made<br />
from FFP sourced outside of the UK and has undergone viral inactivation<br />
with methylene blue. These components are available as single units<br />
for smaller children and pooled units for older children and young<br />
adults.<br />
Platelets<br />
Platelets are either made from pooled buffy coat-derived platelets from<br />
four whole blood donations, suspended in platelet additive solution and<br />
the plasma of one of the four donors (who is male), or as an adult therapeutic<br />
dose obtained from a single donor by apheresis donation. Both<br />
can be used interchangeably; NHSBT recommends that recipients born<br />
on or after 1st January 1996 should receive apheresis donation platelets<br />
where possible.<br />
20 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
There is increased use of platelets in the last few years. The greatest<br />
demand is for haemato-oncology patients; platelets should not be<br />
administered to patients with chemotherapy-induced thrombocytopenia<br />
in the absence of bleeding, unless their platelet count is < 10 9 10 9 .l<br />
1 .<br />
The risk of transmission of bacterial infection (1 in 12,000) is higher<br />
than other blood components because platelets are stored at 22 °C. This<br />
risk is reduced by bacterial screening before release.<br />
Platelets do not have to be the same group as the patient, but where<br />
group O platelets are given to a non-group O child they should be selected<br />
to be high-titre negative. D-negative children and women of childbearing<br />
potential should receive D-negative platelets because of the small risk of<br />
developing immune anti-D.<br />
Platelet concentrate should be stored at 22 °C with constant gentle<br />
agitation in an approved incubator. Platelets must not be placed in a<br />
refrigerator. Transfusion should ideally be commenced within 30 min of<br />
removal from the platelet storage incubator. Each pack contains 250–<br />
350 ml; platelet count in the pack is > 2.4 9 10 10 .l<br />
1 per adult dose,<br />
and transfusion should lead to an increase in the patient’s platelet count<br />
by approximately 30 9 10 9 .l<br />
1 . The patient’s platelet count should be<br />
repeated after transfusion.<br />
A standard adult therapeutic dose should be infused over a period of<br />
30 min through a standard blood administration set or platelet administration<br />
set incorporating a 170- to 200-lm filter. Do not give through a set<br />
that has already been used for red cells. No drugs should be added directly<br />
to the unit of platelets.<br />
Indications for platelets include the following:<br />
• prevention and treatment of bleeding due to thrombocytopenia or<br />
platelet function defects.<br />
• If patient is actively bleeding, transfuse to a platelet count<br />
> 75 9 10 9 1<br />
.l<br />
If not bleeding, the following triggers should be applied:<br />
routine prophylactic use: 10 9 109 .l<br />
1 ;<br />
• prophylactic use with additional risk factors (e.g. Sepsis):<br />
10 – 20 9 10 9 .l<br />
1 ;<br />
other major surgery or invasive procedures: 50 9 109 .l<br />
1 ;<br />
• neuraxial blockade: 50 9 109 .l<br />
1 ; and<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 21
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
• prophylactic use in closed compartment surgery (eye, brain):<br />
100 9 10 9 .l<br />
1 .<br />
In the UK, the availability of platelets is centralised and will depend<br />
on the demand and distance from nearest blood centre. Clinicians need<br />
to be aware of local laboratory arrangements and normal time interval<br />
for obtaining platelets from central storage.<br />
Special blood components<br />
Prothrombin complex concentrate<br />
Prothrombin complex concentrate (in the UK) comes as four-factor<br />
concentrate containing factors II, VII, IX and X, with protein S, C and<br />
heparin. It can be rapidly reconstituted providing a high concentration<br />
of these four clotting factors in a small volume. It is indicated in<br />
acquired factor deficiency and for urgent reversal of warfarin. There is<br />
limited evidence for use in any other setting.<br />
Fibrinogen concentrate<br />
There has been considerable interest in fibrinogen concentrate. It is<br />
widely used in mainland Europe in the management of bleeding following<br />
surgery or trauma. Recent trials in cardiac surgery have not shown<br />
any benefit from its use. It is only licensed for use in congenital<br />
hypofibrinogenaemia in the UK.<br />
Recombinant factor viia<br />
Licensed for use in haemophiliacs with inhibitors. It is the most potent<br />
thrombin generator available at present. Late use in the exsanguinating<br />
patient is almost always associated with no benefit, a high risk of mortality<br />
and thrombotic complications. Following cardiac surgery, it has<br />
been shown to reduce re-operation rates and transfusion in the bleeding<br />
patient. However, its use may increase the risk of thrombotic complications<br />
and its use except under haematological direction cannot be recommended<br />
[44].<br />
Acknowledgements<br />
AK is the Editor-in-Chief of Anaesthesia, and has received research<br />
funding and honoraria from Pharmacosmos and CSL Behring. RB has<br />
received educational support from Pharmacosmos. RG has received honoraria<br />
from CSL Behring and Octapharma. TR has received research<br />
funding and honoraria from Vifor Pharma and Pharmacosmos. RC has<br />
22 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
received research funding from CSL Behring and TEM International.<br />
No other conflicts of interest declared.<br />
References<br />
1. Bolton-Maggs PHB, Cohen H. Serious Hazards of Transfusion (SHOT) haemovigilance<br />
and progress is improving transfusion safety. British Journal of Haematology 2013;<br />
163: 303–14.<br />
2. NHS Blood and Transplant. Patient Blood Management: Optimising the Care of<br />
Patients who may need Transfusion. http://hospital.blood.co.uk/media/27420/<br />
140804-1-25447-bookmark-patient-blood-management.pdf (accessed 08/11/<br />
2015).<br />
3. Clevenger B, Mallett SV, Klein AA, Richards T. Patient blood management to reduce<br />
surgical risk. British Journal of Surgery 2015; 102: 1325–37.<br />
4. Kotze A, Harris A, Baker C, et al. British Committee for Standards in Haematology<br />
Guidelines on the identification and management of pre-operative anaemia. British<br />
Journal of Haematology 2015; 171: 322–31.<br />
5. Clevenger B, Richards T. Pre-operative anaemia. Anaesthesia 2015; 70: 20–e8.<br />
6. Ashworth A, Klein AA. Cell salvage as part of a blood conservation strategy in<br />
anaesthesia. British Journal of Anaesthesia 2010; 105: 401–16.<br />
7. National Patient Safety Agency. Safer Practice Notice 14: Right patient, right blood.<br />
October 2006. NPSA/2006/14. http://www.nrls.npsa.nhs.uk/resources/clinicalspecialty/emergency-medicine/?Entryid45=59805<br />
(accessed 08/11/2015).<br />
8. Medicines and Healthcare Products Regulatory Authority. Blood Safety and Quality<br />
Regulations, 2005. http://www.shotuk.org/wp-content/uploads/2010/03/12-David-<br />
Churchward.pdf (accessed 08/11/2015).<br />
9. Advisory Committee on the Safety of Blood, Tissues and Organs (sabto). Patient Consent<br />
for Blood Transfusion, 2011. https://www.gov.uk/government/publications/<br />
patient-consent-for-blood-transfusion (accessed 01/12/2015).<br />
10. British Committee for Standards in Haematology Guidelines on the Administration<br />
of Blood Components, 2009. http://www.bcshguidelines.com/documents/<br />
Admin_blood_components_bcsh_05012010.pdf (accessed 08/11/2015).<br />
11. Tinegate H, Birchall J, Gray A, et al. British Committee for Standards in Haematology.<br />
Blood Transfusion Task Force Guideline on the investigation and management<br />
of acute transfusion reactions. British Journal of Haematology 2012; 159:<br />
143–53.<br />
12. Salpeter SR, Buckley JS, Chatterjee S. Impact of more restrictive blood transfusion<br />
strategies on clinical outcomes: a meta-analysis and systematic review. American<br />
Journal of Medicine 2014; 127: 124–31.<br />
13. Holst LB, Petersen MW, Haase N, Perner A, Wetterslev J. Restrictive versus liberal<br />
transfusion strategy for red blood cell transfusion: systematic review of randomised<br />
trials with meta-analysis and trial sequential analysis. British Medical Journal 2015;<br />
350: h1354.<br />
14. Murphy GJ, Pike K, Rogers CA, et al. Liberal or restrictive transfusion after cardiac<br />
surgery. New England Journal of Medicine 2015; 372: 997–1008.<br />
15. British Committee for Standards in Haematology. A practical guideline for the<br />
haematological management of major haemorrhage, 2015. Http://www.<br />
bcshguidelines.com/documents/Major_Haemorrhage.pdf (accessed 08/11/2015).<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 23
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
16. Gill R. Practical management of major blood loss. Anaesthesia 2015; 70: 54–e20.<br />
17. Retter A, Barrett NA. The management of abnormal haemostasis in the ICU. Anaesthesia<br />
2015; 70: 121–e41.<br />
18. Retter A, Wyncoll D, Pearse R, et al. Guidelines on the management of anaemia<br />
and red cell transfusion in adult critically ill patients. British Journal of Haematology<br />
2013; 160: 445–64.<br />
19. Lilley G, Burkett-St-Laurent D, Precious E, et al. Measurement of blood loss during<br />
postpartum haemorrhage. International Journal of Obstetetric Anesthesia 2015; 24:<br />
8–14.<br />
20. Collis RE, Collins PW. Haemostatic management of obstetric haemorrhage. Anaesthesia<br />
2015; 70: 78–e28.<br />
21. Mallaiah S, Barclay P, Harrod I, Chevannes C, Bhalla A. Introduction of an algorithm<br />
for ROTEM-guided fibrinogen concentrate administration in major obstetric haemorrhage.<br />
Anaesthesia 2015; 70: 166–75.<br />
22. Collins PW, Lilley G, Bruynseels D, et al. Fibrin-based clot formation as an early and rapid<br />
biomarker for progression of postpartum hemorrhage: a prospective study. Blood 2014;<br />
124: 1727–36.<br />
23. Kirpalani H, Whyte RK, Anderson C, et al. The premature infants in need of transfusion<br />
(PINT) study: a randomized, controlled trial of a restrictive (low) versus liberal<br />
(high) transfusion threshold for extremely low birth weight infants. Journal of Pediatrics<br />
2006; 149: 301–7.<br />
24. New HV, Grant-Casey J, Lowe D, Kelleher A, Hennem S, Stanworth SJ. Red blood cell<br />
transfusion practice in children: current status and areas for improvement? A study<br />
of the use of red blood cell transfusions in children and infants. Transfusion 2014;<br />
54: 119–27.<br />
25. Royal College of Paediatrics and Chuild Health. Major trauma and the use of<br />
tranexamic acid in children, 2012. Http://www.rcpch.ac.uk/system/files/<br />
protected/page/Major Trauma and the Use of Tranexamic Acid in Children -<br />
Evidence Statement 2012-11.pdf (accessed 08/11/2015).<br />
26. Cholette JM, Powers KS, Alfieris GM, et al. Transfusion of cell saver salvaged blood<br />
in neonates and infants undergoing open heart surgery significantly reduces RBC<br />
and coagulant product transfusions and donor exposures: results of a prospective,<br />
randomized, clinical trial. Pediatric Critical Care Medicine 2013; 14: 137–47.<br />
27. Cap A, Hunt BJ. The pathogenesis of traumatic coagulopathy. Anaesthesia 2015;<br />
70: 96–e34.<br />
28. Hall S, Murphy MF. Limitations of component therapy for massive haemorrhage: is<br />
whole blood the whole solution? Anaesthesia 2015; 70: 511–4.<br />
29. Klein AA, Collier TJ, Brar MS, et al. The incidence and importance of anaemia in<br />
patients undergoing cardiac surgery in the UK - the first Association of Cardiothoracic<br />
Anaesthetists national audit. Anaesthesia 2016; 71: 627–35.<br />
30. National Institute for Health and Care Excellence (NICE). Viscoelastic point-of-care<br />
testing to assist with the diagnosis, management and monitoring of haemostasis:<br />
a systematic review and cost-effectiveness analysis. https://www.nice.org.uk/<br />
guidance/dg13/documents/detecting-managing-and-monitoring-haemostasisviscoelastometric-pointofcare-testing-rotem-teg-and-sonoclot-systems-diagnosticsassessment-report2<br />
(accessed 08/11/2015).<br />
24 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
Klein et al. | AAGBI blood transfusion guidelines 2016 Anaesthesia 2016<br />
31. Besser MW, Ortmann E, Klein AA. Haemostatic management of cardiac surgical<br />
haemorrhage. Anaesthesia 2015; 70: 87–e31.<br />
32. Corredor C, Wasowicz M, Karkouti K, Sharma V. The role of point-of-care platelet<br />
function testing in predicting postoperative bleeding following cardiac surgery: a<br />
systematic review and meta-analysis. Anaesthesia 2015; 70: 715–31.<br />
33. Fowler A, Perry DJ. Laboratory monitoring of haemostasis. Anaesthesia 2015; 70:<br />
68–e24.<br />
34. Mallett SV, Armstrong M. Point-of-care monitoring of haemostasis. Anaesthesia<br />
2015; 70: 73–e26.<br />
35. Skelton VA, Wijayasinghe N, Sharafudeen S, Sange A, Parry NS, Junghans C. Evaluation<br />
of point-of-care haemoglobin measuring devices: a comparison of Radical-7 TM<br />
pulse co-oximetry, hemocue â and laboratory haemoglobin measurements in<br />
obstetric patients. Anaesthesia 2013; 68: 40–5.<br />
36. Hildyard C, Curry N. Point-of-care testing: a standard of care? Anaesthesia 2015;<br />
70: 1113–8.<br />
37. Quarterman C, Shaw M, Johnson I, Agarwal S. Intra- and inter-centre standardisation<br />
of thromboelastography (TEG). Anaesthesia 2014; 69: 883–90.<br />
38. Van Veen JJ, Makris M. Management of peri-operative anti-thrombotic therapy.<br />
Anaesthesia 2015; 70: 58–e23.<br />
39. Sharma V, Katznelson R, Jerath A, et al. The association between tranexamic acid<br />
and convulsive seizures after cardiac surgery: a multivariate analysis in 11 529<br />
patients. Anaesthesia 2014; 69: 124–30.<br />
40. Hunt BJ. The current place of tranexamic acid in the management of bleeding.<br />
Anaesthesia 2015; 70: 50–e18.<br />
41. Ortmann E, Besser MW, Klein AA. Antifibrinolytic agents in current anaesthetic practice.<br />
British Journal of Anaesthesia 2013; 111: 549–63.<br />
42. Challis M, Marrin C, Vaughan RS, Goringe A. Who requires irradiated blood products?<br />
Anaesthesia 2011; 66: 620–1.<br />
43. Hart S, Cserti-Gazdewich CM, McCluskey SA. Red cell transfusion and the immune<br />
system. Anaesthesia 2015; 70: 38–e16.<br />
44. Gill R, Herbertson M, Vuylsteke A, et al. Safety and efficacy of recombinant activated<br />
factor VII: a randomized placebo-controlled trial in the setting of bleeding<br />
after cardiac surgery. Circulation 2009; 120: 21–7.<br />
Appendix 1<br />
Other available guidelines.<br />
National Institute for Health and Care Excellence (NICE) 2015<br />
(http://www.nice.org.uk/guidance/indevelopment/gid-CGWAVE0663?)<br />
British Committee for Standards in Haematology, 2012-15<br />
(http://www.bcshguidelines.com/4_haematology_guidelines.html?Dtype=<br />
Transfusion&dpage=0&sspage=0&ipage=0#gl)<br />
Practice Guidelines for Peri-operative Blood Management – American<br />
Society of Anesthesiologists (http://anesthesiology.pubs.asahq.org/<br />
article.aspx?Articleid=2088825)<br />
© 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland 25
Anaesthesia 2016 Klein et al. | AAGBI blood transfusion guidelines 2016<br />
Management of severe perioperative bleeding – Guidelines from<br />
the European Society of Anaesthesiology (2013) (http://anest-rean.lt/wpcontent/uploads/2013/05/Management_of_severe_perioperative_bleeding_.<br />
2.pdf)<br />
Network for the Advancement of Patient Blood Management,<br />
Haemostasis and Thrombosis<br />
(NATA) (http://www.nataonline.com)<br />
National Blood Authority Australia PBM Guidelines (http://<br />
www.blood.gov.au/pbm-guidelines)<br />
26 © 2016 The Authors. Anaesthesia published by John Wiley & Sons Ltd<br />
on behalf of Association of Anaesthetists of Great Britain and Ireland
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
The Anaesthesia Team<br />
3<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org May 2010
Membership of the working party<br />
(details correct at the start of the working party process)<br />
Dr R J S Birks<br />
Dr V R Alladi<br />
Ms J Angell<br />
Dr R Broomhead<br />
Prof W A Chambers*<br />
Dr R Griffiths<br />
Prof C M Kumar<br />
Dr I H Wilson<br />
Chairman and AAGBI President<br />
Council Member, AAGBI<br />
PA(A) Representative, RCoA<br />
GAT representative<br />
Vice President, AAGBI<br />
Council Member, AAGBI<br />
Council Member, RCoA<br />
Honorary Treasurer, AAGBI<br />
This guideline has been seen and approved by the Council of the<br />
AAGBI.<br />
The working party acknowledges the assistance of Ms Diane Gilmour (AfPP),<br />
Mr Bill Kilvington (CODP) and Dr David Whitaker (AAGBI Immediate Past<br />
President).<br />
*Prof Chambers is chair of the PA(A) project steering group run by NHS<br />
Education for Scotland.<br />
1
Contents<br />
1. Recommendations 3<br />
2. Introduction 4<br />
3. Organisation and management 5<br />
4. Pre-operative assessment 7<br />
5. The operating department 8<br />
6. Recovery post-anaesthetic care unit (PACU) 14<br />
7. Postoperative pain management 16<br />
References 18<br />
To be reviewed by 2015.<br />
© Copyright of the Association of Great Britain & Ireland. No part of this<br />
book may be reproduced without the written permission of the AAGBI.<br />
2
1. Recommendations<br />
Comprehensive peri-operative care can only be provided by an anaesthesia<br />
team led by consultant anaesthetists. All members of the team must be<br />
trained to nationally agreed standards.<br />
Effective pre-operative assessment of patients for anaesthesia and surgery is<br />
vital in the modern setting. It reduces cancellations, promotes efficient bed<br />
usage and can allay patients’ anxieties. It does not replace the need for the<br />
anaesthetist’s pre-operative visit.<br />
Anaesthetists must have dedicated qualified assistance wherever anaesthesia<br />
is administered, whether in the operating department, the obstetric unit or<br />
any other area.<br />
Recovery (post-anaesthetic care unit) areas must have sufficient numbers of<br />
trained staff available throughout all operating hours. If operating occurs<br />
over the whole of a 24-hour period, the PACU area must be open for the<br />
whole 24 hours.<br />
All acute hospitals providing inpatient surgical services must have an acute<br />
pain team led by a consultant anaesthetist.<br />
The AAGBI supports the concept of common training schemes for operating<br />
department staff that share objectives and lead to the development of<br />
common working practices, pay, conditions and career opportunities.<br />
Close monitoring of the development of the physicians’ assistant (anaesthesia)<br />
role, with particular reference to maintenance of standards, will continue.<br />
Only those who have trained and qualified within a recognised UK<br />
programme should practice in the role.<br />
The AAGBI believes the recommendations in this document should apply to<br />
all nations of the UK.<br />
3
2. Introduction<br />
It is now over 20 years since the Association of Anaesthetists of Great Britain<br />
& Ireland (AAGBI) made recommendations on assistance for anaesthetists.<br />
This was the first development of the anaesthesia team concept. The<br />
team approach has continued to develop even in the five years since this<br />
document was last published.<br />
Anaesthetists increasingly work with non-medical personnel in all aspects<br />
of patient care. These relationships within the team are described in this<br />
document. In the context of this document, the term ‘anaesthetist’ includes<br />
all grades: consultants, SAS grades, specialist doctors and trainees unless<br />
specified.<br />
Pre-operative assessment clinics are now a feature of most hospitals and<br />
trusts. These must be effective and efficient if they are to improve the safety<br />
and quality of patient care.<br />
As this publication goes to press, most trusts/hospitals have put into place the<br />
surgical checking procedures pioneered by the World Health Organization<br />
and endorsed by the National Patient Safety Agency (NPSA), the AAGBI<br />
and others. This should be a routine team discipline afforded to all<br />
patients undergoing surgery and emphasises the importance of teamwork.<br />
Anaesthetic aspects are described in this publication.<br />
Devolution of nations within the UK has led to different emphasis in different<br />
areas of practice and has sometimes hindered the development of uniform<br />
national standards, particularly in the field of assistance for anaesthetists. We<br />
believe uniform standards should be the goal.<br />
The role of physicians’ assistants (anaesthesia) (PA(A)s) is commented upon in<br />
this publication. It is not clear to what extent and how the role of the PA(A)<br />
will develop.<br />
4
3. Organisation and management<br />
Organisation of comprehensive anaesthetic services requires considerable<br />
knowledge, effort and expertise.<br />
Each acute hospital facility should have a designated head of anaesthesia<br />
services responsible for all activities in which anaesthetists are engaged. This<br />
individual will usually be the clinical director and should have managerial<br />
and budgetary control of the service. In some hospitals, the clinical director<br />
of anaesthesia may be responsible for the whole of the operating services.<br />
In some, the department of anaesthesia is part of another directorate. If<br />
this is the case, it is necessary to have an identified lead anaesthetist to<br />
take responsibility for all aspects of the anaesthesia service. For the sake of<br />
simplicity this publication refers to this individual as the clinical director.<br />
Whatever the wider directorate structure, the budget for anaesthesia services<br />
should be controlled by anaesthetists.<br />
The clinical director’s role<br />
The clinical director is responsible to the chief executive for the safety of the<br />
local service. He/she must ensure that the recommended national standards<br />
of staffing and facilities are in place to provide a high quality anaesthesia<br />
service throughout the peri-operative period and in all areas where<br />
anaesthesia is performed.<br />
Sufficient resources must be committed to recruiting and training staff and<br />
to encourage continued professional development to ensure successful<br />
revalidation. The clinical director must be provided with management<br />
support, usually in the form of a business manager and clinical service<br />
manager, as well as having sufficient contracted time to undertake his/<br />
her duties. In addition to management responsibilities, the clinical director<br />
must offer support, guidance and encouragement to all members of the<br />
department. Recognition of the importance of the training responsibility of<br />
the NHS is essential.<br />
The role of other consultants<br />
The clinical director will usually delegate some operational aspects of the<br />
anaesthesia team. It is often helpful to have a lead consultant to provide<br />
medical supervision in specialist areas such as day surgery, obstetric<br />
anaesthesia, training (the College tutor), safety and postoperative pain<br />
control. A rota co-ordinator, who has a good knowledge of the local service<br />
and skill-mix of anaesthetists should be appointed and supported in the role.<br />
5
The role of the clinical service manager<br />
Non-medical staff involved in the anaesthesia team are normally managed<br />
by a senior operating department practitioner (ODP) or a senior nurse,<br />
responsible to a clinical service manager.<br />
Modern anaesthesia services are complex and the clinical service<br />
manager will usually work closely with other departments or managers.<br />
Responsibilities of the senior manager will include:<br />
• Careful co-ordination of pre-operative assessment that requires<br />
communication with surgeons, the medical records department,<br />
outpatient clinics and all related departments; the individual leading this<br />
service should work closely with a lead anaesthetist,<br />
• Maintaining adequate staffing with trained anaesthesia assistants in the<br />
operating department,<br />
• An appropriately staffed PACU,<br />
• Ensuring an adequate skill-mix of staff is available 24 hours a day, 7 days<br />
a week. There may be advantages in rotating trained staff with common<br />
skills between theatres, PACU and high dependency and intensive<br />
care units depending on local circumstances,<br />
• An acute pain service that should be a routine part of the anaesthesia<br />
team and adequately staffed by trained nurses working with an<br />
anaesthesia lead,<br />
• Regular audit of all components of the anaesthesia service, not<br />
only for the efficient use of resources, but also for clinical quality and<br />
safety.<br />
There is therefore a need for close communication with all users of the<br />
service. A multidisciplinary theatre users’ committee is often useful for<br />
ensuring common goals, co-operation and motivation across specialties.<br />
A theatre governance group should review all clinical incidents and safety<br />
guidance and ensure patient safety is seen as a priority by the hospital.<br />
6
4. Pre-operative assessment<br />
Assessment before anaesthesia is the responsibility of the anaesthetist.<br />
However, pre-operative assessment before the date of surgery achieves<br />
several desirable objectives. It ensures that patients are prima facie fit for<br />
anaesthesia and surgery, and that all likely investigations will be completed<br />
and available at the time of admission. It thus minimises the disruption<br />
caused by late cancellation or postponement and their adverse effects<br />
on theatre utilisation and bed occupancy, not to mention the distress and<br />
inconvenience to patients and their relatives or carers. It enhances efficiency<br />
and ensures a higher level of overall patient care. It also gives an opportunity<br />
for patients to express concerns they may have about anaesthesia and<br />
surgery.<br />
Good practice dictates that all patients should be seen by an anaesthetist<br />
before undergoing an operation that requires the services of an anaesthetist.<br />
Ideally, this should be the doctor who is to give the anaesthetic. Although it<br />
is the anaesthetist who is responsible for deciding whether a patient is fit for<br />
anaesthesia, other professional groups may be involved in the pre-operative<br />
assessment process.<br />
Pre-operative assessment is now commonly carried out by a specially trained<br />
multidisciplinary team led by, and with access to, a consultant anaesthetist,<br />
in the pre-operative assessment clinic. In the clinic, nursing, ODP and other<br />
trained staff play an essential role when, by working to agreed protocols, they<br />
screen and assess patients for fitness for anaesthesia and surgery [1].<br />
It is important to be clear about the boundaries between the remit of the<br />
pre-anaesthesia assessment team and the responsibilities of the anaesthetist.<br />
The AAGBI feels that it is inappropriate for a non-anaesthetist to promise a<br />
particular type of premedication, anaesthetic technique or postoperative pain<br />
management and that the decision to proceed (with anaesthesia) cannot be<br />
delegated. It is essential, in all but a dire emergency, that the anaesthetising<br />
anaesthetist should see patients pre-operatively in a quiet ward, theatre<br />
reception area or theatre admissions unit rather than in a busy operating<br />
theatre.<br />
It is not within the remit of this document to go into the details of the<br />
running of pre-operative assessment clinics. This is addressed in the AAGBI<br />
publication on pre-operative assessment (2010) [1].<br />
7
5. The operating department<br />
Management<br />
The operating department must have a manager who is responsible for<br />
ensuring an efficient and effective service. This individual will be responsible<br />
for ensuring the provision of adequately trained staff and ongoing audit of<br />
activity, whatever the local directorate structure. Proper use of resources<br />
and optimum throughput of patients depends on maintaining good<br />
communication between anaesthetists, surgeons and operating department<br />
staff.<br />
World Health Organization (WHO) Surgical Safety Checklist [2]<br />
In 2008 the WHO produced a core set of standards for the peri-operative<br />
period within the operating department. The NPSA has endorsed these<br />
standards and issued guidance on how they should be implemented. An<br />
executive and clinical lead is appointed to implement the surgical safety<br />
checklist within each organisation where surgery is performed.<br />
The checklist is completed for each patient who undergoes any surgical<br />
procedure; this includes those done under local anaesthesia.<br />
An accurate record, either paper or electronic, confirming that the checklist<br />
is complete must be entered into the clinical notes by a registered member of<br />
the team; this could be a surgeon, anaesthetist, nurse or ODP.<br />
The whole process is designed to reduce the mistakes or omissions that occur<br />
during surgical procedures by improving team communication. A briefing<br />
and debriefing with all theatre staff should occur at the beginning and end<br />
of the list. For individual patients we describe the rest of the process with<br />
particular reference to anaesthesia.<br />
Sign in<br />
This is performed before induction of anaesthesia. The anaesthetic<br />
equipment must be formally checked in accord with AAGBI machine check<br />
guidelines (currently under review) [3]. There must be written verification<br />
of this process. Patient monitoring should be attached in compliance with<br />
the AAGBI guideline [4].The anaesthesia team should confirm the ‘sign<br />
in’ checks before induction of anaesthesia. They include patient identity,<br />
surgical site marking, medication, allergies, airway and risk of blood loss.<br />
When the patient is unable to confirm the necessary information, this can be<br />
provided by carers or significant others.<br />
8
Time out<br />
This procedure should be completed before the start of the surgical<br />
intervention. All members of the operating department team must introduce<br />
themselves to each other, unless already known. The surgeon, anaesthetist<br />
and registered practitioners verbally confirm the identity of the patient, the<br />
site of surgery and the procedure. At this stage any anticipated adverse events<br />
should be discussed. In particular, the anaesthesia team may wish to highlight<br />
any patient co-morbidities. The anaesthetist should pay particular attention<br />
to monitoring the patient throughout surgery, maintaining normothermia and<br />
ensuring that there are no issues with any of the equipment used by the team.<br />
The anaesthesia team must pay particular attention to the site of surgery<br />
when regional blocks are being performed.<br />
Sign out<br />
This takes place before any member of the team leaves the operating<br />
theatre at the end of each case. Of particular concern to the whole theatre<br />
team is the checking of swabs and accurate measurement of fluid loss, key<br />
concerns for the patient in the recovery period. The postoperative recovery<br />
and management plan should be discussed and information relayed to the<br />
recovery practitioner.<br />
The WHO checklist is new (as of May 2010) to most units and may be<br />
subject to local/minor modification as time progresses.<br />
NB. In Scotland the process is slightly different. Briefing and de-briefing are as<br />
above. Then in three parts:<br />
i. Sending for the patient: name, procedure and ward check,<br />
ii. Surgical pause: before the commencement of anaesthesia the<br />
anaesthetist and assistant, surgeon operating, and theatre team member<br />
check name, date of birth, armband, consent, allergies,<br />
thromboprophylaxis, antibiotics and staff competencies,<br />
iii. End of procedure: swab and instrument count.<br />
9
Assistance for the anaesthetist<br />
Trained assistance for the anaesthetist must be provided wherever anaesthesia<br />
is provided.<br />
The safe administration of anaesthesia cannot be carried out single handedly;<br />
competent and exclusive assistance is necessary at all times.<br />
The clinical director must insist on adequate resources to employ, train and<br />
develop sufficient numbers of assistants to ensure a safe anaesthesia service<br />
in accordance with good practice.<br />
If appropriate basic resources are not available, the clinical director should<br />
limit clinical practice so that safe, quality-based patient care is ensured.<br />
Anaesthetic room<br />
The anaesthetist and trained assistant are joined in some units by a third<br />
member of staff to help with any untoward emergency, obese patients, carers<br />
in the anaesthetic room, and so on. In any event, a third person should<br />
be available in close proximity to the anaesthetic room to help with any<br />
unforeseen problem.<br />
The AAGBI recommends that a trained anaesthesia assistant should always<br />
be immediately available and present during anaesthesia. Only in extreme<br />
emergencies, as judged by the anaesthetist, should anaesthetic intervention<br />
proceed without a trained assistant, e.g. acute unforeseen airway/bleeding<br />
problems.<br />
The role of the anaesthesia assistant<br />
The current trend is towards multi-skilling where most professionals in the<br />
operating department are able to perform many tasks including assisting<br />
the anaesthetist, assisting the surgeon, working in the recovery area and<br />
undertaking administrative duties. However, patterns of work must ensure<br />
that skills are maintained. Staff assigned to the role of anaesthetic assistant<br />
should not have any other duties that would prevent them from providing<br />
dedicated assistance to the anaesthetist during anaesthesia.<br />
Training<br />
Assistance for the anaesthetist may be provided by ODPs or adequately<br />
trained, registered nurses. Whatever the background, the training for all<br />
anaesthesia assistants must comply fully with national standards. Employment<br />
of staff without a qualification that complies with national standards is<br />
not acceptable. Learners are accepted for formal training as anaesthesia<br />
10
assistants, but they must be supervised at all times by a registered practitioner.<br />
There should be a programme of continuing professional development and<br />
training for all anaesthesia assistants.<br />
Operating Department Practitioners (ODPs)<br />
There are now 27 universities and colleges providing qualifications for ODPs;<br />
these are based in England, Wales and Scotland. ODPs must have completed<br />
an approved programme that confers eligibility to apply for registration with<br />
the Health Professions Council (HPC). Currently for an ODP to enter the<br />
HPC register they must complete a two-year Diploma HE, although a degree<br />
programme is under development.<br />
ODPs became a statutorily regulated profession (within the HPC) in October<br />
2004. There are almost 10,000 ODPs registered with the HPC.<br />
Nurses<br />
Qualified nurses are already registered professionals but require additional<br />
training before taking on the duties of an anaesthesia assistant. In England<br />
until 2002, the recognised national qualification of competency for nurses<br />
as anaesthesia assistants was the English National Board qualification (ENB<br />
182).<br />
Universities now provide postgraduate nurse training and have developed<br />
theatre courses to replace the ENB 182. At most universities these comprise<br />
three core modules and three optional modules, including anaesthesia.<br />
There are no standard competencies and the courses may differ in length<br />
and content. The AAGBI would like to see the development of nationally<br />
recognised competencies for nurses assisting the anaesthetist. However,<br />
the courses led by local universities are in the main of a high standard and<br />
have some national guidance. A nurse should not assist an anaesthetist until<br />
successful completion of such a course.<br />
Qualified nurses can still train as ODPs, either through the NVQ route (until<br />
2008) or by APL (accreditation of prior learning) with a university ODP<br />
provider. They cannot complete an award that entitles them to the title of<br />
ODP unless they complete the full Dip HE in ODP award.<br />
In Scotland, nurses assisting anaesthetists now have to achieve a series of<br />
competencies devised by NHS Education Scotland. The courses to achieve<br />
these competencies are administered by individual hospitals.<br />
11
Professional associations<br />
Continuing education and support is offered by three organisations: the<br />
College of Operating Department Practitioners (CODP), the Association for<br />
Perioperative Practice (AfPP) and the British Association of Anaesthetic &<br />
Recovery Nurses (BARNA).<br />
Physicians’ Assistants (Anaesthesia) – PA(A)s [5]<br />
The AAGBI has previously stated that the highest standards of anaesthesia<br />
can only be achieved by a physician-only service. However, in response<br />
to a potential workforce crisis in 2002 the Royal College of Anaesthetists<br />
(RCoA) and Department of Health reported on the potential for development<br />
of a non-medical role as part of a consultant-led anaesthesia team to<br />
enhance flexibility and service provision whilst maintaining the highest<br />
standards of safety. [6] The AAGBI engaged with the pilot project run by<br />
the Modernisation Agency to ensure that the model developed would work<br />
effectively in NHS practice.<br />
The AAGBI believes that the workforce concerns envisaged in 2002 have<br />
not yet materialised but recognises that the full impact of the EWTD and<br />
increasingly consultant-based service provision has yet to be determined.<br />
Numbers of trained PA(A)s are low and numbers employed in the future will<br />
be determined by local departments and their staffing needs. The AAGBI<br />
would like to reiterate that all PA(A)s are required to practice within the<br />
guidelines of the RCoA/AAGBI (available on both websites), and consultants<br />
working with them should ensure that they are supported to the required<br />
standard.<br />
In 2009 there were around 70 trained PA(A)s nationally (
the establishment of a Managed Voluntary Register. Formal registration is<br />
currently being sought with the Health Professions Council.<br />
Whether in the NHS or private sector, two PA(A)s to one consultant<br />
anaesthetist should remain the maximum, and PA(A)s working in this<br />
way should each have their own qualified assistance. There is as yet no<br />
equivalence for those wishing to enter the PA(A) profession from abroad. The<br />
AAGBI does not recommend employing PA(A)s who have not trained in the<br />
UK programme.<br />
It should again be emphasised that at the end of their initial training<br />
PA(A)s are not qualified to undertake regional, obstetric or paediatric<br />
anaesthesia, or be involved in initial airway management of the acutely ill or<br />
injured, as described in the AAGBI/RCoA standards document. [9]<br />
As before, the situation will be monitored continuously by the AAGBI.<br />
13
6. Recovery post-anaesthetic care unit<br />
(PACU)<br />
The AAGBI published guidance on the required facilities for the safe recovery<br />
from anaesthesia in 2002 [10]. (This guidance is being reviewed and the<br />
revised edition will be published in 2010). There is, however, a need to<br />
re-emphasise the principles outlined in that report and to emphasise the<br />
recommendations on staffing and training.<br />
The responsibility of anaesthetists for the care of their patients extends into<br />
the postoperative period and includes the management of postoperative pain<br />
and postoperative nausea and vomiting (PONV). Emergence from anaesthesia<br />
is potentially hazardous and patients require close observation until recovery<br />
is complete. Care must be transferred to staff who have been specially trained<br />
in recovery procedures and reached prescribed competencies. Currently<br />
these are often locally devised but the AAGBI is working to promote the<br />
development of national competencies. All recovery staff should have<br />
achieved their recognised local competencies.<br />
While patients remain in the PACU there must always be a suitably trained<br />
anaesthetist (and surgeon) immediately available within the hospital.<br />
Close collaboration between the anaesthetist and the surgeon is particularly<br />
important at this time so that clear instructions are given to recovery staff.<br />
Transfer to recovery area<br />
The anaesthetist should be satisfied that the recovery staff are competent to<br />
take responsibility for the patient before care is transferred. No fewer than<br />
two staff should be present when there is a patient in the PACU who does not<br />
fulfil the criteria for discharge to the ward [10]. If this level of staffing cannot<br />
be assured, the anaesthetist should stay with the patient until satisfied that the<br />
patient is fit to return to the ward.<br />
Recommendations on the transfer of the patient from the operating theatre to<br />
the PACU are outlined in the AAGBI’s publication referred to above [10].<br />
Immediate recovery<br />
Continuous individual observation of each patient is required on a oneto-one<br />
basis until the patient is able to maintain their own airway. The<br />
recovery staff, therefore, must not have any other duties at this time. Failure<br />
to provide adequate care for patients during this period of vulnerability,<br />
14
in which the possibility of serious complications is well recognised, may<br />
prove catastrophic for the patient and could result in serious medico-legal<br />
consequences for the hospital. In hospitals with an emergency surgical<br />
service, appropriately staffed recovery facilities must be available throughout<br />
the 24 hours.<br />
A post-anaesthesia care plan should be implemented for each patient which<br />
includes monitoring to ensure satisfactory cardiorespiratory function, fluid,<br />
pain and PONV management, and the administration of other drugs to<br />
agreed protocols. These have been the subject of previous advice [4]. Careful<br />
records must be maintained (increasingly in electronic form) and recovery<br />
staff must be able to interpret the information and initiate appropriate action<br />
where necessary. Staff must also be able to assess the suitability of transfer of<br />
patients to the next level of care.<br />
Dedicated recovery staff must be trained in immediate and advanced<br />
resuscitation techniques.<br />
Discharge<br />
The patient should remain in a suitably equipped PACU until all the criteria<br />
for discharge have been met. Discharge must be based on a carefully<br />
worded protocol or on the personal instructions of the anaesthetist.<br />
Recommendations on the criteria for discharge from the recovery area have<br />
been published previously and are currently being reviewed [10].<br />
Management<br />
The optimal management structure for the PACU should be influenced by the<br />
directorate of anaesthesia. There must be clear lines of communication with<br />
other relevant directorates and departments.<br />
Training and qualifications<br />
All staff who work in the recovery area should have received appropriate<br />
training and have achieved recognised competencies. The core skills<br />
required are summarised in our published work [10].<br />
Personnel who are in training may work in PACUs but must be supervised<br />
by trained staff. Staffing levels should not be depleted to fill deficits in other<br />
areas of the hospital, although rotation between staff within the operating<br />
department should be encouraged to maintain skills. All staff must have<br />
access to further professional development and there should be appropriate<br />
study leave.<br />
15
7. Postoperative pain management<br />
Background<br />
All hospitals performing major surgery should have a multidisciplinary<br />
acute pain team with an anaesthetist in overall charge (the majority having<br />
a sessional commitment by a consultant to acute pain) and a senior nurse<br />
running the service on a day-to-day basis, following predefined protocols.<br />
In 1997, an Audit Commission report [11] recommended more effective<br />
collaboration between the anaesthetist, surgeon and nurses.<br />
A high quality acute pain management service should include identifying the<br />
patient’s individual requirements on admission and then ‘tracking’ the patient<br />
from the surgical ward, through recovery, critical care if appropriate and back<br />
to the ward.<br />
The acute pain team<br />
Potential members of an acute pain team include:<br />
• A consultant anaesthetist(s) with sessional commitments to the team,<br />
• Trainee anaesthetists, as part of the on-call team and as part of their<br />
modular training in pain management,<br />
• SAS and specialist doctors in anaesthesia,<br />
• A nurse team to manage the day to day follow-up of patients made up<br />
of specialist nurse/nurse practitioners who have had specific training in<br />
the management of acute pain,<br />
• Nurses in training,<br />
• ODPs,<br />
• A pharmacist,<br />
• A physiotherapist,<br />
• Secretarial and audit department support.<br />
Consultant responsibility<br />
It is important that postoperative pain be controlled immediately on recovery<br />
from anaesthesia. The pain team must therefore be involved from an early<br />
stage with PACU staff and the consultant responsible for the pain service has<br />
an obvious role in PACU and other critical care areas. This role will involve<br />
the design and implementation of pain management protocols and the<br />
education and training of staff.<br />
Roles of non-medical personnel<br />
A lead nurse should be responsible for running the service on a day-to-day<br />
16
asis within the limits defined by protocols. The lead nurse is responsible<br />
for liaison between PACU, critical care areas and the wards, troubleshooting<br />
problems and referring problem patients to medical staff. They also have<br />
an important role in education. Potential additional roles for the acute pain<br />
team are the placing of intravenous cannulae, administering appropriate<br />
drugs intravenously and topping up epidurals. The appropriateness of the<br />
delegation of any of these tasks is obviously influenced by the location in<br />
which they were used, with different roles being appropriate in the HDU,<br />
recovery and general ward.<br />
The pharmacy has a role in the provision of drugs for the acute pain team. It<br />
should also be involved in maintaining the range of drugs required for the<br />
service, the evaluation of new drugs and education. This important role is<br />
enhanced by nominating a specific pharmacist to the team.<br />
An important aim of postoperative analgesia is restoration of function and this<br />
can be assessed by the ward physiotherapist who should be involved with<br />
the acute pain team and may be a source of secondary referrals.<br />
Standards of practice<br />
The majority of pain services are delivered on the basis of protocols that have<br />
been drawn up by consultation between anaesthetists, surgeons and staff<br />
from PACU and general wards. Because there are local differences in both<br />
the role of nurses and the extent of their remit, there will be variations in the<br />
protocols between hospitals. The pain team should be responsible for the<br />
implementation of a system to introduce, disseminate and review protocols<br />
for all grades of staff caring for postoperative patients and for continuing audit<br />
of the service.<br />
Educational implications<br />
The educational implications are two-fold: education of the team members<br />
and education by the team members.<br />
Anaesthetists must play a major role in educating the members of the acute<br />
pain team, in collaboration with the lead nurse. Appropriate aspects of<br />
training should also be addressed by other members of the team.<br />
17
References<br />
1. The Association of Anaesthetists of Great Britain and Ireland. Pre-<br />
Operative Assessment and Patient Preparation - The role of the<br />
Anaesthetist 2. London: AAGBI, 2010.<br />
2. World Health Organization. Surgical Safety Checklist. Switzerland:<br />
WHO, 2009.<br />
3. The Association of Anaesthetists of Great Britain and Ireland. Checking<br />
Anaesthetic Related Equipment 3. London: AAGBI, 2004 (currently<br />
being reviewed).<br />
4. The Association of Anaesthetists of Great Britain and Ireland.<br />
Recommendations for Standards of Monitoring During Anaesthesia and<br />
Recovery 3. London: AAGBI, 2000 (revised in 2007).<br />
5. The Royal College of Anaesthetists. Physicians Assistants (Anaesthesia)<br />
[PA(A)]. http://www.rcoa.ac.uk/index.asp?PageID=761(accessed<br />
23/02/2010.)<br />
6. The Royal College of Anaesthetists. The Role of Non-Medical Staff in<br />
the Delivery of Anaesthesia Services. London: RCoA, 2002.<br />
7. The Royal College of Anaesthetists. Bulletin of the Royal College of<br />
Anaesthetists; 50. London: RCoA, 2008.<br />
8. The Royal College of Anaesthetists and The Royal College of<br />
Ophthalmologists. Local Anaesthesia for Intraocular Surgery. London:<br />
RCoA, 2001.<br />
9. The Association of Anaesthetists and The Royal College of Anaesthetists.<br />
Physicians’ Assistants (Anaesthesia) - PA(A)s - supervision and limitation<br />
of scope of practice. http://www.rcoa.ac.uk/docs/PA(A)_JointStatement.<br />
pdf (accessed 26.02.10).<br />
10. The Association of Anaesthetists of Great Britain and Ireland.<br />
Immediate Postanaesthetic Recovery. London: AAGBI, 2002 (currently<br />
being reviewed).<br />
11. Department of Health. Briefing Anaesthesia under Examination Audit<br />
Commission Report. Oxford: DoH, 1997.<br />
18
19
20
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
AAGBI SAFETY GUIDELINE<br />
Suspected Anaphylactic Reactions<br />
Associated with Anaesthesia<br />
4<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org July 2009
This guideline was originally published in Anaesthesia. If<br />
you wish to refer to this guideline, please use the following<br />
reference:<br />
Association of Anaesthetists of Great Britain and Ireland.<br />
Suspected anaphylactic reactions associated with anaesthesia.<br />
Anaesthesia 2009; 64: pages 199-211<br />
This guideline can be viewed online via the following URL:<br />
http://www3.interscience.wiley.com/cgi-bin/fulltext/121583621/<br />
PDFSTART
GUIDELINES<br />
Suspected Anaphylactic Reactions<br />
Associated with Anaesthesia<br />
Association of Anaesthetists of Great Britain and Ireland<br />
Membership of the Working Party: N J N Harper, Chairman;<br />
T Dixon; P Dugué; D M Edgar; A Fay; H C Gooi; R Herriot;<br />
P Hopkins; J M Hunter; R Mirakian; R S H Pumphrey;<br />
S L Seneviratne; A F Walls; P Williams; J A Wildsmith; P Wood.<br />
Ex Officio: A S Nasser 1 , R K Powell 1 , R Mirakhur 2 , J Soar 3 ,<br />
Executive Officers, AAGBI<br />
1 British Society for Allergy and Clinical Immunology<br />
2 Royal College of Anaesthetists<br />
3 Resuscitation Council UK<br />
This is a consensus document produced by expert members of a Working Party<br />
established by the Association of Anaesthetists of Great Britain and Ireland<br />
(AAGBI). It updates and replaces previous guidance published in 2003.<br />
Summary<br />
(1) The AAGBI has published guidance on management of anaphylaxis<br />
during anaesthesia in 1990, 1995 and 2003. This 2008 update was<br />
necessary to disseminate new information.<br />
(2) Death or permanent disability from anaphylaxis in anaesthesia may be<br />
avoidable if the reaction is recognised early and managed optimally.<br />
(3) Recognition of anaphylaxis during anaesthesia is usually delayed<br />
because key features such as hypotension and bronchospasm more<br />
commonly have a different cause.<br />
Re-use of this article is permitted in accordance with the Creative Commons Deed,<br />
Attribution 2.5, which does not permit commercial exploitation.<br />
Ó 2009 The Authors<br />
Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland 1
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
(4) Initial management of anaphylaxis should follow the ABC approach.<br />
Adrenaline (epinephrine) is the most effective drug in anaphylaxis and<br />
should be given as early as possible.<br />
(5) If anaphylaxis is suspected during anaesthesia, it is the anaesthetist’s<br />
responsibility to ensure the patient is referred for investigation.<br />
(6) Serum mast cell tryptase levels may help the retrospective diagnosis of<br />
anaphylaxis: appropriate blood samples should be sent for analysis.<br />
(7) Specialist (allergist) knowledge is needed to interpret investigations for<br />
anaesthetic anaphylaxis, including sensitivity and specificity of each<br />
test used. Specialist (anaesthetist) knowledge is needed to recognise<br />
possible non-allergic causes for the ‘reaction’. Optimal investigation<br />
of suspected reactions is therefore more likely with the collaboration<br />
of both specialties.<br />
(8) Details of specialist centres for the investigation of suspected<br />
anaphylaxis during anaesthesia may be found on the AAGBI website<br />
http://www.<strong>aagbi</strong>.org.<br />
(9) Cases of anaphylaxis occurring during anaesthesia should be reported<br />
to the Medicines Control Agency and the AAGBI National<br />
Anaesthetic Anaphylaxis Database. Reports are more valuable if the<br />
diagnosis is recorded following specialist investigation of the reaction.<br />
(10) This guidance recommends that all Departments of Anaesthesia<br />
should identify a Consultant Anaesthetist who is Clinical Lead for<br />
anaesthetic anaphylaxis.<br />
Introduction<br />
The AAGBI published its first guidelines on suspected anaphylactic reactions<br />
in 1990. Subsequent revisions were published in 1995 and 2003. The current<br />
guidelines incorporate advice from a large number of clinical immunologists,<br />
allergists and anaesthetists throughout the UK. In common with the 1995 and<br />
the 2003 editions, this report is published jointly with the British Society for<br />
Allergy and Clinical Immunology (BSACI).<br />
This document is intended to be concordant with, and complementary<br />
to, the 2007 Scandinavian Clinical Practice Guidelines, the 2008 Resuscitation<br />
Council UK guidelines and the BSACI guidelines: Investigation of<br />
suspected anaphylaxis during anaesthesia.<br />
These guidelines apply only to suspected anaphylactic reactions associated<br />
with anaesthesia and it is presupposed that the patient is in the care of a<br />
trained anaesthetist.<br />
Ó 2009 The Authors<br />
2 Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
Objectives<br />
(1) To clarify the definitions used in allergy and anaphylaxis.<br />
(2) To review the epidemiology of anaesthesia-related anaphylaxis.<br />
(3) To provide advice on the recognition of anaesthetic anaphylaxis.<br />
(4) To make recommendations on the immediate management and initial<br />
investigation of suspected anaesthetic anaphylaxis.<br />
(5) To make recommendations concerning the further investigation of<br />
suspected anaesthetic anaphylaxis.<br />
(6) To assist anaesthetists in obtaining access to a specialist centre for<br />
comprehensive investigation of suspected anaesthetic anaphylaxis.<br />
(7) To assist anaesthetists to provide appropriate information to the<br />
specialist centre.<br />
(8) To make recommendations about the reporting and collection of data<br />
on anaesthetic anaphylaxis in Great Britain and Ireland.<br />
Definitions<br />
The term ‘anaphylaxis’ has been used for all types of acute life-threatening<br />
illness triggered by abnormal sensitivity (hypersensitivity) to a trigger agent,<br />
and for apparently spontaneous attacks with similar features (idiopathic<br />
anaphylaxis). This has made it difficult to define. The EAACI Nomenclature<br />
Committee proposed the following broad definition [1]:<br />
Anaphylaxis is a severe, life-threatening, generalized or systemic hypersensitivity<br />
reaction.<br />
Minor, localised or non-systemic reactions are outside the definition of<br />
anaphylaxis. Anaphylaxis may be divided into ‘allergic anaphylaxis’ and<br />
‘non-allergic anaphylaxis’. The clinical features of allergic anaphylaxis<br />
and non-allergic anaphylaxis may be identical. The EAACI committee<br />
proposed the term ‘allergic anaphylaxis’ should be used only when the<br />
reaction is mediated by an immunological mechanism (such as IgE, IgG, or<br />
complement activation by immune complexes). An anaphylactic reaction<br />
mediated by IgE antibodies, such as to amoxicillin, is referred to as ‘IgEmediated<br />
allergic anaphylaxis’.<br />
The term ‘anaphylactoid’ reaction had been introduced for non-<br />
IgE-mediated anaphylactic reactions but the EAACI committee has<br />
recommended this term should no longer be used. This proposal has not<br />
been universally accepted. An authoritative recent American practice<br />
parameter [2] states: ‘Anaphylaxis is defined … as a condition caused by an<br />
Ó 2009 The Authors<br />
Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland 3
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
IgE-mediated reaction [2]. Anaphylactoid reactions are defined as those<br />
reactions that produce the same clinical picture as anaphylaxis but are not IgE<br />
mediated.’ In these guidelines we will follow the European (EAACI)<br />
nomenclature.<br />
Anaphylaxis is not a homogeneous process: the pathways, mediators,<br />
time course and response to treatment depend on the trigger agent, its route<br />
and rate of administration, the nature of the patient’s hypersensitivity and<br />
the state of health of the patient, including incidental pathology such as<br />
respiratory or cardiovascular disease and the effects of concomitant<br />
medication such as b-blockers and ACE inhibitors. Although anaphylaxis<br />
commonly involves respiratory, cutaneous and circulatory changes, variations<br />
such as shock with gastrointestinal disturbance or shock alone are<br />
possible. Alternatively, reactions may be fatal without significant shock<br />
except as the terminal event following respiratory arrest [3]. Angioedema<br />
and urticaria may be features of anaphylaxis but commonly result from<br />
mechanisms other than anaphylaxis.<br />
Intravascular volume redistribution is an important component of<br />
anaphylactic shock. Cardiac output may be decreased as a result of reduced<br />
coronary artery perfusion pressure as well as impaired venous return. Local<br />
release of mediators may cause coronary artery spasm and there may be<br />
features of acute left or right ventricular failure. Myocardial ischaemia with<br />
ECG changes is expected within minutes of anaphylactic shock becoming<br />
severe.<br />
Asphyxia may be due to upper airway occlusion caused by angioedema,<br />
or bronchospasm with mucus plugging of the lower airways; the latter most<br />
commonly occurs in patients taking daily treatment for asthma. Both these<br />
processes may occur simultaneously in patients reacting to foods, latex,<br />
b-lactam antibiotics or aspirin.<br />
Anaphylaxis usually resolves in 2–8 h but secondary pathology arising<br />
from the reaction or its treatment may prolong this. Resolution is complete<br />
except when cerebral hypoxia at the peak of the reaction has caused<br />
significant brain damage, or when disordered clotting leads to bleeding.<br />
Acknowledgements<br />
The involvement of the British Society for Allergy and Clinical Immunology<br />
and the Clinical Immunology and Allergy section of the British<br />
Society for Immunology is gratefully acknowledged. In addition, the<br />
working party wishes to acknowledge the assistance of the following:<br />
Ó 2009 The Authors<br />
4 Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
Sr Alex Farragher Specialist Immunology Nurse<br />
Mr Chris Hirst AAGBI Anaphylaxis website designer<br />
Dr David Noble<br />
Dr Martin Shields<br />
References<br />
1 Johansson SGO, Bieber T, Dahl R, et al. Revised nomenclature for allergy for<br />
global use: Report of the Nomenclature Review Committee of the World<br />
Allergy Organization, October 2003. Journal of Allergy and Clinical Immunology<br />
2004; 113: 832–6.<br />
2 Joint Task Force on Practice Parameters. The diagnosis and management<br />
of anaphylaxis: an updated practice parameter. Journal of Allergy and Clinical<br />
Immunology 2005; 115: S483–523.<br />
3 Pumphrey RSH. Lessons for management of anaphylaxis from a study of fatal<br />
reactions. Clinical and Experimental Allergy 2000; 30: 1144–50.<br />
Epidemiology<br />
Geographical variation<br />
Most reports on anaesthesia-related anaphylaxis originate from France,<br />
Australia, New Zealand and the United Kingdom. Other case series have<br />
been described from Scandinavia and the USA. The true incidence and<br />
their associated morbidity and mortality remain poorly defined. Both the<br />
accuracy and completeness of reporting is not optimal.<br />
10% of anaesthesia-related reactions reported to the UK Medicines<br />
Control Agency (MCA) were fatal. These data should be interpreted with<br />
caution because it is likely that many less-severe reactions are not reported<br />
[1]. Reactions that are accepted as side-effects of certain drugs, for instance,<br />
histaminergic reactions due to atracurium and mivacurium, may be underreported.<br />
During a time period of over 6 years only 361 reactions were<br />
reported to the MCA. In a 2-year period 789 reactions were reported in<br />
France in a comparable population where there is a well-established culture<br />
of reporting anaesthesia-related reactions [2].<br />
Based on studies in Australia and France, the incidence of anaphylaxis<br />
during anaesthesia has been estimated at between 1 in 10 000 and 20 000<br />
[3, 4]. The true incidence of anaphylaxis during anaesthesia in the UK is<br />
not known. By extrapolating the French and Australian data to the UK, it is<br />
estimated that there are approximately 500 severe reactions in the UK each<br />
year. Anaphylactic reactions are more common when drugs are given<br />
intravenously.<br />
Ó 2009 The Authors<br />
Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland 5
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
In one large study an immune basis was demonstrated in two-thirds of<br />
patients investigated for anaphylaxis [2]: the remainder comprised nonallergic<br />
anaphylaxis and mechanisms other than anaphylaxis. The tests<br />
currently available for the diagnosis of anaesthetic anaphylaxis are imperfect.<br />
Skin tests and blood tests have limited sensitivity and specificity and their<br />
positive and negative predictive value varies between drugs.<br />
Patient characteristics (age, sex, ethnicity, smoking etc)<br />
Neuromuscular blocking drugs and latex appear to cause anaphylaxis more<br />
commonly in female patients. There appears to be a connection between<br />
smoking and antibiotic anaphylaxis, possibly because smokers may become<br />
sensitised by exposure to repeated courses of antibiotics for respiratory tract<br />
infections. Individuals with a history of atopy, asthma or allergy to some<br />
foods appear to be at increased risk of latex allergy but not anaphylaxis to<br />
neuromuscular blocking drugs or antibiotics [2, 5]. Anaphylaxis associated<br />
with radiographic contrast media appears to be associated with atopy [6].<br />
Patients with asthma or taking b-blocking drugs may suffer a more severe<br />
reaction. Some of these reactions may be refractory to conventional<br />
therapy.<br />
Possible environmental sensitising agents<br />
The prevalence of anaphylactic reactions to neuromuscular blocking agents<br />
(NMBAs) is reported to be at least six times more frequent in some<br />
countries [7, 8]: it is considerably more common in Norway than in<br />
Sweden. Quaternary ammonium ions (QAI) are proposed to be the<br />
allergenic epitopes in NMBAs. Common environmental chemicals such as<br />
toothpastes, washing detergents, shampoos, and cough medicines share<br />
these allergenic epitopes with the NMBAs [8]. Numerous possibilities exist<br />
for a predisposed individual to become sensitised to QAIs and thus be at risk<br />
of developing anaphylaxis to NMBAs during anaesthesia. In a recent<br />
Scandinavian survey, use of certain cough medicines was found to be the<br />
only significant difference in environmental chemical exposure [8]. In<br />
Norway, but not Sweden, cough syrups containing pholcodine are available<br />
without prescription. IgE-antibodies to pholcodine were seen in 6% of a<br />
general population (blood donors) in Norway but not in Sweden (0%).<br />
Muscle relaxants<br />
Approximately 60% of cases of anaesthesia-related anaphylaxis are thought<br />
on the basis of skin tests to be due to neuromuscular blocking agents.<br />
Ó 2009 The Authors<br />
6 Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
Mivacurium and atracurium are associated with non-allergic anaphylaxis in<br />
which release of mediators (notably histamine) from mast cells exactly<br />
imitates allergic anaphylaxis. Cisatracurium, although sharing a benzylisoquinolinium<br />
structure, is not associated with non-allergic anaphylaxis,<br />
although several cases of allergic anaphylaxis have been reported. It is<br />
generally accepted that succinylcholine is the NMBA most likely to<br />
be associated with allergic anaphylaxis, although rocuronium has been<br />
implicated in a similar number of cases in France.<br />
The prevalence of sensitisation to NMBAs in the community is higher<br />
than the incidence of reactions would suggest. In one study, approaching<br />
10% of the general population exhibited skin reactivity to NMBAs, an<br />
incidence that far exceeds the incidence of anaphylaxis on administration of<br />
these drugs during anaesthesia [9]. A previous history of specific drug<br />
exposure is not necessary, particularly for neuromuscular blocking drugs. A<br />
history of previous exposure is found in fewer than 50% of patients who are<br />
allergic to neuromuscular blocking drugs. Conversely, an uneventful<br />
exposure may sensitise an individual to subsequent administration of the<br />
drug.<br />
Cross-sensitivity between different NMBAs is relatively common,<br />
probably because they share a quaternary ammonium epitope. If anaphylaxis<br />
to an NMBA is suspected, the patient should undergo skin prick<br />
testing with all the NMBAs in current use. If a patient demonstrates a<br />
positive skin prick test (SPT) to an NMBA, the patient should be warned<br />
against future exposure to all NMBAs if possible. If it is mandatory to use an<br />
NMBA during anaesthesia in the future, it would seem appropriate to<br />
permit the use of an NMBA which has a negative skin test, accepting that a<br />
negative skin test does not guarantee that anaphylaxis will not occur.<br />
The apparent excess of cases of anaphylaxis to rocuronium in some<br />
countries should be interpreted with caution until much more data have<br />
been collected. Large sample sizes are needed to estimate the true incidence:<br />
if the true incidence is 1 in 5000, a sample size of 7 million would be<br />
needed to have a 95% chance of being within 5% of the true value [10].<br />
There is a need for further epidemiological studies.<br />
Latex<br />
Latex hypersensitivity is the second most common cause of anaesthesiarelated<br />
anaphylaxis in many studies (up to 20% of cases). However, the<br />
incidence of anaphylaxis to latex is considerably less than would be<br />
suggested by the prevalence of positive skin tests or positive IgE tests. It<br />
Ó 2009 The Authors<br />
Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland 7
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
appears that the incidence may be waning, at least in some countries;<br />
possibly as a result of a change or decline in the use of latex gloves. Certain<br />
patient groups are more susceptible to latex anaphylaxis (see Appendix II).<br />
Antibiotics<br />
Approximately 15% of anaesthesia-related anaphylactic episodes are due to<br />
antibiotics. This proportion has increased in recent years and may merely<br />
mirror increased exposure to antibiotics in the community [2, 11]. The<br />
pre-operative history is important. Although only a minority of patients<br />
who report allergy to antibiotics have a true allergy, the consequence<br />
of anaphylaxis to intravenous antibiotics may be catastrophic, and selfreporting<br />
should be taken seriously. Skin testing is only approximately 60%<br />
predictive of clinical hypersensitivity. Penicillins and cephalosporins which<br />
share the b-lactam ring are responsible for approximately 70% of antibioticinduced<br />
anaphylaxis. Many antibiotics possess a b-lactam ring:<br />
• Benzylpenicillin, phenoxymethylpenicillin<br />
• Flucloxacillin, temocillin<br />
• Amoxicillin, ampicillin, co-amoxiclav<br />
• Co-fluampicil<br />
• Piperacillin, ticarcillin,<br />
• Pivmecillinam HCl<br />
• Cephalosporins<br />
• Aztreonam<br />
• Ertapenem, imipenem with cilastatin, meropenem<br />
The structure of the side chains attached to the b-lactam ring is also<br />
important in determining the response of the immune system. First<br />
generation cephalosporins and cefamandole share a similar side chain with<br />
penicillin and amoxicillin. A recent meta-analysis suggested that patients<br />
who are allergic to penicillin or amoxicillin have a higher incidence of<br />
allergic reactions to first generation cephalosporins and cefamandole, but<br />
not other cephalosporins [12]. The issue is complicated because the<br />
classification of cephalosporins relates to their antimicrobial activity rather<br />
than their chemical structure.<br />
First generation cephalosporins<br />
• Cefalexin (cephalexin)*<br />
• Cephaloridine<br />
Ó 2009 The Authors<br />
8 Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
• Cephalothin<br />
• Cefazolin<br />
• Cefradine (cephradine)*<br />
• Cefadroxil*<br />
Second generation cephalosporins<br />
• Cefaclor*<br />
• Cefamandole<br />
• Cefuroxime*<br />
Third generation cephalosporins<br />
• Cefixime*<br />
• Cefotaxime*<br />
• Cefpodoxime*<br />
• Ceftazidime*<br />
• Ceftriaxone*<br />
Fourth generation cephalosporins<br />
• Cefepime<br />
• Cefpirome<br />
*Listed in the British National Formulary.<br />
Local anaesthetics<br />
Anaphylactic reactions to local anaesthetic drugs are very uncommon. Local<br />
anaesthetic esters are more likely than amides to provoke a Type lV allergic<br />
reaction. Preservatives such as methyl-paraben or metabisulphites may be<br />
responsible in some cases. It has been suggested that inadvertent intravascular<br />
injection of a local anaesthetic or the systemic absorption of adrenaline<br />
may be responsible for many of the reported reactions. Reactions occurring<br />
in the dental chair may also be associated with idiopathic angioedema or<br />
latex allergy.<br />
Opioids<br />
Opioids are an uncommon cause of anaesthesia-related anaphylaxis.<br />
Diagnosis is difficult and the true incidence is unknown. Morphine,<br />
pethidine and codeine are well-known to cause non-specific histamine<br />
release which precludes diagnostic skin testing. The diagnosis of opioid<br />
Ó 2009 The Authors<br />
Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland 9
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
anaphylaxis often rests on a careful history and the exclusion of other<br />
possibilities. Challenge testing may be appropriate in some cases but may be<br />
performed only in specialist centres.<br />
Anaesthetic induction agents<br />
Anaphylaxis to propofol is very uncommon. The antigenic determinant<br />
may be the isopropyl groups. It has been stated that patients with egg allergy<br />
or soy allergy should avoid propofol but there is no strongly-supportive<br />
evidence. It has been suggested that propofol anaphylaxis is more likely if<br />
lignocaine is added to reduce pain on injection: there is no evidence to<br />
support this suggestion. Anaphylaxis to thiopental has become extremely<br />
uncommon, probably reflecting the decline in its use. A small number of<br />
cases of midazolam anaphylaxis have been reported.<br />
Non-steroidal anti-inflammatory drugs (NSAIDs)<br />
Several mechanisms may be responsible for reactions to NSAIDs.<br />
Inhibition of the PGE 2 pathway leads to excessive leukotriene synthesis<br />
and subsequent mediator release, causing urticaria or bronchospasm. IgEmediated<br />
reactions may also occur in relation to some NSAIDs. Fatal<br />
anaphylaxis has been described after oral administration of NSAIDs.<br />
Halogenated volatile anaesthetics<br />
There are no published reports of anaphylaxis to halogenated volatile<br />
anaesthetics. The rare fulminant form of hepatitis associated with halothane<br />
has an immune basis which is unrelated to anaphylaxis.<br />
Colloids<br />
Intravenous colloids are responsible for approximately 4% of all perioperative<br />
anaphylactic reactions. In one study, gelatin solutions were<br />
responsible for 95% of the intravenous colloid reactions. It has been stated<br />
that the incidence may be greater with the urea-linked gelatins compared with<br />
the modified fluid gelatins. Intravenous gelatin solutions should be avoided in<br />
patients with a history of allergy to gelatin-containing vaccines. Anaphylaxis<br />
to intravenous dextrans has been reported, with an incidence similar to the<br />
modified fluid gelatins. Anaphylaxis to hydroxyethyl-starch is rare.<br />
Antiseptics and disinfectants<br />
Reactions to chlorhexidine have come into greater prominence in recent<br />
years. There appears to be a significant difference in incidence between<br />
Ó 2009 The Authors<br />
10 Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
countries [13]. Reactions range from contact dermatitis to life-threatening<br />
anaphylaxis. Anaphylaxis has occurred when chlorhexidine was used as an<br />
antiseptic for urological and gynaecological procedures as well as insertion<br />
of central venous and epidural catheters. The chlorhexidine coating of<br />
certain central venous catheters has been implicated in such reactions. It is<br />
prudent to allow skin disinfectant to completely dry before beginning an<br />
invasive procedure. Anaphylaxis to polyvinylpyrrholidine as povidoneiodine<br />
or as an excipient for oral medicines occurs but is rare.<br />
Miscellaneous agents<br />
Many agents to which patients may be exposed during anaesthesia may be<br />
associated with anaphylaxis, including aprotinin, protamine, heparins,<br />
radiological contrast material, dyes and oxytocin. Anaphylaxis to glycopyrronium<br />
and neostigmine may occur very rarely.<br />
References<br />
1 Axon AD, Hunter JM. Editorial III: Anaphylaxis and anaesthesia – all clear now?<br />
British Journal of Anaesthesia 2004; 93: 501–4.<br />
2 Mertes PM, Laxenaire MC, Alla F. Anaphylactic anaphylactoid reactions<br />
occurring during anaesthesia in France in 1999–2000. Anesthesiology 2003; 99:<br />
536–45.<br />
3 Fisher MM, Baldo BA. The incidence and clinical features of anaphylactic<br />
reactions during anesthesia in Australia. Annales Francaises d’Anesthesie et de<br />
Reanimation 1993; 12: 97–104.<br />
4 Laxenaire MC. Epidemiology of anesthetic anaphylactoid reactions. Fourth<br />
multicenter survey (July 1994-December 1996). Annales Francaises d’Anesthesie et<br />
de Reanimation 1999; 18: 796–809.<br />
5 Laxenaire MC, Mertes PM. Anaphylaxis during anaesthesia. Results of a<br />
two-year survey in France. British Journal of Anaesthesia 2001; 87: 549–58.<br />
6 Lang DM, Alpern MB, Visintainer PF, Smith ST. Increased risk for anaphylactoid<br />
reaction from contrast media in patients on beta-adrenergic blockers or<br />
with asthma. Annals of Internal Medicine 1991; 115: 270–6.<br />
7 Laake JH, Rottingen JA. Rocuronium and anaphylaxis – a statistical challenge.<br />
Acta Anaesthesiologica Scandinavica 2001; 45: 1196–203.<br />
8 Florvaag E, Johansson SG, Oman H, et al. Prevalence of IgE antibodies to morphine.<br />
Relation to the high and low incidences of NMBA anaphylaxis in Norway<br />
and Sweden, respectively. Acta Anaesthesiologica Scandinavica 2005; 49: 437–44.<br />
9 Porri F, Lemiere C, Birnbaum J, et al. Prevalence of muscle relaxant sensitivity<br />
in a general population: implications for a preoperative screening. Clinical and<br />
Experimental Allergy 1999; 29: 72–5.<br />
Ó 2009 The Authors<br />
Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland 11
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
10 Fisher M, Baldo BA. Anaphylaxis during anaesthesia: current aspects of diagnosis<br />
and prevention. European Journal of Anaesthesiology 1994; 11: 263–84.<br />
11 Moss J. Allergy to anesthetics. Anesthesiology 2003; 99: 521–3.<br />
12 Pichichero ME, Casey JR. Safe use of selected cephalosporins in penicillinallergic<br />
patients: a meta-analysis. Otolaryngology-Head and Neck Surgery 2007; 136:<br />
340–7.<br />
13 Garvey LH, Roed-Petersen J, Menne T, Husum B. Danish Anaesthesia<br />
Allergy Centre – preliminary results. Acta Anaesthesiologica Scandinavica 2001; 45:<br />
1204–9.<br />
Recognition and clinical diagnosis of anaphylaxis<br />
In a closely monitored patient such as during anaesthesia, when a fall in<br />
blood pressure, change in heart rate or difficulty with ventilation are<br />
noticed, anaphylaxis is so rarely the cause that inevitably treatment is given<br />
for another diagnosis before anaphylaxis is recognised; the response to this<br />
treatment has commonly delayed or even prevented recognition of the true<br />
cause. It is therefore probable that many grade I and II acute allergic<br />
reactions to anaesthetic drugs are missed. Conversely, a cause other than<br />
allergic anaphylaxis seems more likely in around one-third of the patients<br />
referred to specialist centres for investigation of suspected anaphylaxis<br />
during anaesthesia.<br />
Previous history<br />
Any clue that appropriately raises anticipation of anaphylaxis will be helpful.<br />
A previous history of reaction to anaesthetic drugs, antibiotics, other drugs,<br />
chlorhexidine or latex should obviously lead to appropriate avoidance.<br />
Because it is always possible the wrong trigger factor was identified, the<br />
exact details of exposure leading to any previous reaction should be sought<br />
during the pre-operative assessment. Cross-reactivity between non-anaesthetic<br />
drugs such as pholcodine or environmental chemicals containing<br />
quaternary ammonium groups such as cosmetics and detergents has been<br />
proposed as the source of sensitivity to opioids and muscle relaxants: a<br />
history of cutaneous sensitivity to cosmetics or rashes from cough medicines<br />
should raise caution.<br />
Anaphylaxis to amoxicillin and cephalosporins is commonest in asthmatic<br />
smokers who have had multiple courses of these antibiotics without<br />
reacting: the symptoms of anaphylaxis in such a patient are likely to be<br />
initially misinterpreted (quite reasonably) as those expected from anaesthesia<br />
in an asthmatic smoker.<br />
Ó 2009 The Authors<br />
12 Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
Clinical features<br />
Although anaesthesia-related anaphylaxis usually results from intravenous<br />
drug administration, administration by other routes, for example cutaneous,<br />
mucosal ⁄ vesical peritoneal, intra-articular or intramuscular may be responsible.<br />
Clinical features include hypotension, tachycardia or bradycardia;<br />
cutaneous flushing, rash or urticaria; bronchospasm; hypoxia; angioedema<br />
and cardiac arrest. If an adverse event such as hypotension or bronchospasm<br />
occurs during anaesthesia it is appropriate to suspect anaphylaxis unless<br />
there exists a significantly more likely cause.<br />
Tachycardia is not invariable: bradycardia is seen in approximately 10%<br />
of patients with allergic anaphylaxis during anaesthesia. Hypotension is the<br />
sole clinical feature in approximately 10% of patients and is likely to be<br />
exaggerated in patients undergoing anaesthesia with neuraxial blockade.<br />
Widespread flushing or urticaria is seen in the majority of patients but the<br />
absence of cutaneous signs does not exclude anaphylaxis. Bronchospasm<br />
may be more common in patients with pre-existing asthma.<br />
Clinical features<br />
Allergic<br />
anaphylaxis<br />
(n = 518), n (%)<br />
Non-allergic<br />
anaphylaxis<br />
(n = 271), n (%)<br />
Cardiovascular 387 (74.7) 92 (33.9)<br />
Arterial hypotension 90 (17.3) 50 (18.4)<br />
Cardiovascular collapse 264 (50.8) 30 (11.1)<br />
Bradycardia 7 (1.3) 2 (0.7)<br />
Cardiac arrest 31 (5.9) –<br />
Bronchospasm 207 (39.8) 52 (19.2)<br />
Cutaneous signs 374 (71.9) 254 (93.7)<br />
Angioedema 64 (12.3) 21 (7.7)<br />
Clinical features of allergic anaphylaxis and non-allergic anaphylaxis occurring during<br />
anaesthesia in France between 1st Jan 1999 and 31st Dec 2000. Mertes PM et al. Anesthesiology<br />
2003; 99: 536–45.<br />
The clinical features usually occur within a few minutes but may be<br />
delayed by up to an hour. Substances to which the clinical reaction may be<br />
delayed include latex, antibiotics, intravenous colloids and Cidex OPA<br />
(used to disinfect surgical instruments). However, an immediate response<br />
does not exonerate these substances. The clinical features of anaphylaxis<br />
to neuromuscular blocking agents usually develop rapidly. Deflation of a<br />
surgical tourniquet may induce anaphylaxis if the allergen has been<br />
sequestered in the limb.<br />
Ó 2009 The Authors<br />
Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland 13
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
Immediate management<br />
These management guidelines presuppose that the patient is in the care of an<br />
appropriately-trained anaesthetist and full resuscitation facilities and appropriate vital<br />
signs monitors are available.<br />
There is a wide spectrum of severity and combinations of clinical<br />
features. Although management should be tailored to the individual patient,<br />
there is consensus that adrenaline should be given as early as possible. In<br />
addition to having alpha-agonist activity, adrenaline is a valuable betaagonist<br />
which is inotropic and a bronchodilator, and reduces further<br />
mediator release.<br />
Other causes of hypotension or difficulty in ventilation should be<br />
excluded, for example a misplaced tracheal tube or equipment failure.<br />
Immediate management<br />
1 Use the ABC approach (Airway, Breathing, Circulation). Teamworking<br />
enables several tasks to be accomplished simultaneously.<br />
2 Remove all potential causative agents (including IV colloids, latex and<br />
chlorhexidine) and maintain anaesthesia, if necessary, with an inhalational<br />
agent.<br />
3 Call for help and note the time.<br />
4 Maintain the airway and administer oxygen 100%. Intubate the trachea if<br />
necessary and ventilate the lungs with oxygen.<br />
5 Elevate the patient’s legs if there is hypotension.<br />
6 If appropriate, start cardiopulmonary resuscitation immediately according<br />
to Advanced Life Support Guidelines.<br />
7 Administer adrenaline intravenously. An initial dose of 50 lg (0.5 ml of<br />
1 : 10 000 solution) is appropriate (adult dose). Several doses may be<br />
required if there is severe hypotension or bronchospasm.<br />
8 If several doses of adrenaline are required, consider starting an intravenous<br />
infusion of adrenaline (adrenaline has a short half-life).<br />
9 Administer saline 0.9% or lactated Ringer’s solution at a high rate via an<br />
intravenous cannula of an appropriate gauge (large volumes may be<br />
required).<br />
Secondary management<br />
1 Administer chlorphenamine 10 mg IV (adult dose).<br />
2 Administer hydrocortisone 200 mg IV (adult dose).<br />
Ó 2009 The Authors<br />
14 Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
3 If the blood pressure does not recover despite an adrenaline infusion,<br />
consider the administration of an alternative intravenous vasopressor<br />
according to the training and experience of the anaesthetist, for example<br />
metaraminol.<br />
4 Treat persistent bronchospasm with an intravenous infusion of salbutamol.<br />
If a suitable breathing-system connector is available, a metered-dose<br />
inhaler may be appropriate. Consider giving intravenous aminophylline<br />
or magnesium sulphate.<br />
5 Arrange transfer of the patient to an appropriate Critical Care area.<br />
6 Take blood samples (5–10 ml clotted blood) for Mast Cell Tryptase as<br />
follows:<br />
a Initial sample as soon as feasible after resuscitation has started – do not<br />
delay resuscitation to take the sample.<br />
b Second sample at 1–2 h after the start of symptoms.<br />
c Third sample either at 24 h or in convalescence (for example in a<br />
follow-up allergy clinic). This is a measure of baseline tryptase levels as<br />
some individuals have a higher baseline level.<br />
d Ensure that the samples are labelled with the time and date.<br />
7 Liaise with the hospital laboratory (see Appendix lll: Mast cell Tryptase).<br />
Drug doses in children<br />
Adrenaline<br />
Intramuscular<br />
> 12 years: 500 lg IM (0.5 ml of a 1 : 1000 solution)<br />
300 lg IM (0.3 ml of a 1 : 1000 solution) if the child is small<br />
6–12 years: 300 lg IM (0.3 ml of a 1 : 1000 solution)<br />
Up to 6 years: 150 lg IM (0.15 ml of a 1 : 1000 solution)<br />
Intravenous<br />
Intravenous adrenaline may be used in children in acute areas such as<br />
operating theatres or intensive care units by those familiar with its use and if<br />
IV access is already available. Great care should be taken to avoid dose<br />
errors when preparing drug dilutions. Prepare a syringe containing 1 ml<br />
of 1 : 10 000 adrenaline for each 10 kg body weight (0.1 ml.kg )1 of<br />
1 : 10 000 adrenaline solution = 10 lg.kg )1 . Titrate to response, starting<br />
with a dose of one-tenth of the contents of the syringe, i.e. 1 lg.kg )1 .<br />
Often a child will respond to as little as 1 lg.kg )1 . In smaller children,<br />
further dilution may be needed to allow dose titration (check carefully<br />
Ó 2009 The Authors<br />
Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland 15
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
for decimal point and concentration errors). The intramuscular route is<br />
preferred where there is no venous access or where establishing venous<br />
access would cause a delay in drug administration.<br />
Hydrocortisone<br />
> 12 years: 200 mg IM or IV slowly<br />
6 to 12 years: 100 mg IM or IV slowly<br />
6 months to 6 years: 50 mg IM or IV slowly<br />
< 6 months: 25 mg IM or IV slowly<br />
Chlorphenamine<br />
> 12 years: 10 mg IM or IV slowly<br />
6 to 12 years: 5 mg IM or IV slowly<br />
6 months to 6 years: 2.5 mg IM or IV slowly<br />
< 6 months: 250 lg.kg )1 IM or IV slowly<br />
Later investigations to identify the causative agent<br />
Any patient who has a suspected anaphylactic reaction associated with<br />
anaesthesia should be investigated fully, but investigations should not<br />
interfere with the immediate treatment of the patient. The anaesthetist who<br />
administered the anaesthetic or the consultant anaesthetist in charge of the<br />
patient is responsible for ensuring that the reaction is investigated.<br />
The patient should be referred to a specialist Allergy or Immunology<br />
centre that has appropriate experience of investigating this type of problem.<br />
Anaesthetic departments should identify a lead anaesthetist for anaesthetic<br />
anaphylaxis. Referral pathways should be agreed prospectively with the appropriate<br />
specialist centre.<br />
Criteria for referral to a specialist centre for investigation<br />
Patients in whom allergic or non-allergic anaphylaxis is suspected should be<br />
referred to a specialist clinic for investigation. A patient should be referred if<br />
there is any of the following:<br />
1 Unexplained cardiac arrest during anaesthesia.<br />
2 Unexplained, unexpected hypotension (for example a decrease of<br />
mean arterial pressure of more than 30 mmHg) which requires active<br />
treatment.<br />
Ó 2009 The Authors<br />
16 Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
3 Unexplained, unexpected bronchospasm, particularly if the bronchospasm<br />
is severe, causes a significant decrease in oxygen saturation and is<br />
relatively resistant to treatment.<br />
4 Widespread rash, flushing or urticaria.<br />
5 Angioedema.<br />
A detailed analysis of events surrounding the suspected anaphylactic<br />
reaction must be undertaken. The time of onset of the reaction in relation to<br />
induction and other events is the most important information. All drugs and<br />
other agents to which the patient was exposed before and during the<br />
anaesthetic as well as their timing in relation to the reaction must be recorded.<br />
Details sent to the specialist centre along with a letter of referral must<br />
include:<br />
• A legible photocopy of the anaesthetic record<br />
• A legible photocopy of the recovery room chart<br />
• Legible photocopies of drug charts<br />
• A description of the reaction and time of onset in relation to induction<br />
• Details of blood tests sent and their timing in relation to the reaction<br />
• Contact details of the surgeon and the general practitioner<br />
A standard referral proforma is useful (see Appendix S1 in Supporting<br />
Information).<br />
Tests performed at the specialist centre<br />
Skin tests<br />
Patients should be referred for skin testing as soon as possible after the<br />
clinical event. Skin testing can be performed as soon as the patient has made<br />
a full clinical recovery and the effects of any antihistamine given to treat<br />
the reaction have fully worn off. Skin tests can provide confirmation of<br />
sensitisation to a specific drug but must be interpreted within the clinical<br />
context. There are a variety of techniques and several different criteria are<br />
used for positivity [1–4] so skin testing must be performed by suitably<br />
trained and experienced personnel.<br />
A histamine solution and physiological saline are used as positive and<br />
negative controls respectively. Drugs with anti-histamine activity must be<br />
discontinued a few days before testing. There is no need to discontinue oral<br />
or inhaled steroids.<br />
Skin prick tests are usually done on the volar surface of the forearm. A<br />
drop of the drug is placed on the skin and the skin pricked through the drop<br />
with a lancet. The results are read after 15–20 min.<br />
Ó 2009 The Authors<br />
Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland 17
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
Intradermal tests may be performed where skin prick tests are negative.<br />
Although they are more sensitive, they are less specific, more difficult to<br />
interpret and more likely to precipitate a systemic reaction. Intradermal tests<br />
are usually performed on the forearm or back. 0.02 to 0.05 ml of a dilute<br />
solution is injected intradermally and the results read after 20–30 min.<br />
Both skin prick tests and intradermal tests are widely used in the diagnosis<br />
of IgE mediated allergic reactions though the diagnostic value of a positive<br />
test for most drugs is limited due to lack of subsequent challenge data. If the<br />
mechanism is unknown a negative test is unreliable.<br />
All drugs used during anaesthesia may be tested and lists of non-irritant<br />
dilutions have been compiled for both skin prick tests and intradermal tests<br />
[5]. Skin tests are most useful for latex, beta lactam antibiotics and NMBAs.<br />
They are also useful for induction agents, protamine [6] and chlorhexidine.<br />
Intradermal testing may be more reliable for propofol [2]. Skin tests are not<br />
usually performed for opioids because false positive results are common.<br />
However, skin prick testing appears to be informative for the synthetic<br />
opioids fentanyl and remifentanil. Skin tests are not useful for NSAIDs,<br />
dextrans or iodinated radiological contrast media [6] because anaphylaxis to<br />
these agents is not usually IgE-mediated.<br />
Patch tests are the mainstay of diagnosis for contact allergic reactions and<br />
may be useful for diagnosing exanthematous drug rashes but are not helpful<br />
in eliciting the cause of suspected anaphylactic reactions occurring during<br />
anaesthesia.<br />
References<br />
1 Pepys J, Pepys EO, Baldo BA, Whitwam JG. Anaphylactic ⁄ anaphylactoid<br />
reactions to anaesthetic and associated agents. Anaesthesia 1994; 49: 470–5.<br />
2 Fisher MMcD, Bowey CJ. Intradermal compared with prick testing in the<br />
diagnosis of anaesthetic allergy. British Journal of Anaesthesia 1997; 79: 59–63.<br />
3 Berg CM, Heier T, Wilhelmsen V, Florvaag E. Rocuronium and cisatracuriumpositive<br />
skin tests in non allergic volunteers: determination of drug concentration<br />
thresholds using a dilution titration technique. Acta Anaesthesiologica Scandinavica<br />
2003; 47: 576–82.<br />
4 Leynadier F, Sansarricq M, Didier JM, Dry J. Prick tests in the diagnosis<br />
of anaphylaxis to general anaesthetics. British Journal of Anaesthesia 1987; 59:<br />
683–9.<br />
5 Prevention of allergic risk in Anaethesia. Societe Francaise d’Anesthesie et de<br />
Reanimation, 2001. http://www.sfar.org/allergiefr.html [accessed 8 October<br />
2008].<br />
Ó 2009 The Authors<br />
18 Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
6 Fisher M, Baldo BA. Anaphylaxis during anaesthesia: current aspects of diagnosis<br />
and prevention. European Journal of Anaesthesiology 1994; 11: 263–84.<br />
Blood tests<br />
Appropriate further blood investigations depend on the drug in question,<br />
and the experience of the specialised laboratory service. Blood samples<br />
for specific IgE tests may be taken at the time of the reaction, or soon<br />
afterwards during that hospital admission. If the results are negative these<br />
tests should be repeated when the patient is seen at the specialist centre in<br />
case the initial results might be falsely negative due to possible consumption<br />
of relevant IgE antibodies during the reaction. The most commonly used<br />
test for allergen-specific IgE uses target allergen or drug bound onto a<br />
three-dimensional sponge-like solid matrix or ‘CAP’ and a fluorescent<br />
detection system. The Radio-AllergoSorbent Test (RAST) uses a radioactive<br />
detection system: it is now rarely used but the name has persisted in<br />
common use.<br />
Specific IgE antibodies against succinylcholine (thiocholine ester) can be<br />
assayed in serum but the sensitivity is relatively poor (30–60%). Tests for<br />
serum IgE antibodies against other neuromuscular blocking drugs are not<br />
available in the UK. Specific IgE antibodies against several antibiotics can<br />
be assayed. These include amoxicilloyl, ampicilloyl, penicilloyl G, penicilloyl<br />
V and cefaclor, however the diagnostic value of these tests is less well<br />
defined. Tests for specific antibodies against latex, chlorhexidine and bovine<br />
gelatin are available.<br />
The presence of drug-specific IgE in serum is evidence of allergic<br />
sensitisation in that individual and provides a possible explanation of the<br />
mechanism and specific drug responsible for the reaction. It is not in itself<br />
proof that the drug is responsible for the reaction. It is important to<br />
emphasise that attribution of cause and effect is a judgement made after<br />
considering all the clinical and laboratory information relevant to the<br />
reaction.<br />
Experimental tests<br />
There is much research into ways of improving the in vitro elucidation of<br />
anaphylaxis. In addition to tissue-bound mast cells, circulating basophils are<br />
also involved in anaphylaxis. During anaphylaxis, proteins such as CD63<br />
and CD203c become newly or increasingly expressed on the surface of<br />
Ó 2009 The Authors<br />
Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland 19
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
basophils. These can be detected by flow cytometry which forms the basis<br />
of experimental drug-induced basophil stimulation tests.<br />
Appendix I<br />
Frequently asked questions<br />
Should I give a test dose of IV antibiotic?<br />
No. Predictive testing would require serial challenges with increasing doses,<br />
starting with a minuscule dose and allowing at least 30 min between each<br />
dose. This approach is impossible within the constraints of an operating list.<br />
Should I avoid cephalosporins in a patient who gives a history suggestive of penicillin<br />
allergy?<br />
Most patients who give a history of a penicillin-related rash are not allergic<br />
to cephalosporins. However, there are now many suitable alternatives to<br />
cephalosporins and, unless there are compelling bacteriological indications,<br />
it would be appropriate to consider avoiding first and second generation<br />
cephalosporins. If there is a convincing history of penicillin-related<br />
anaphylaxis, the case for avoiding first and second generation cephalosporins<br />
is stronger.<br />
Should I use crystalloid or colloid in the immediate management of anaphylaxis?<br />
There is no evidence that one is better than the other. If an IV colloid has<br />
already been given to the patient before the appearance of clinical signs of<br />
anaphylaxis, it should be discontinued and either replaced by crystalloid or<br />
replaced by a colloid of a different class; e.g. replace a gelatin-based colloid<br />
with a starch-based colloid.<br />
Should I give an H2-blocking drug as part of the immediate management of<br />
anaphylaxis?<br />
There is no evidence to support the use of H2-blocking drugs in this<br />
situation.<br />
What should I do if a patient with a convincing history of cardio-respiratory collapse<br />
during a previous anaesthetic presents for emergency surgery without having been<br />
investigated for anaphylaxis?<br />
1 Covert cardiac or respiratory disease should be sought in accordance with<br />
normal pre-operative practice.<br />
Ó 2009 The Authors<br />
20 Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
2 It may be possible to exclude latex allergy by taking a detailed history<br />
from the patient. If this is impossible, a latex-free environment should be<br />
provided.<br />
3 Inhalational agents are likely to be safe unless the previous collapse was<br />
due to malignant hyperthermia.<br />
4 If previous records are available:<br />
a It would be appropriate to avoid all drugs given during the previous<br />
anaesthetic before the onset of cardio-respiratory collapse, with the<br />
exception of inhalational agents.<br />
b If the patient received a neuromuscular blocking drug before the<br />
collapse, then all neuromuscular blocking drugs should be avoided if<br />
possible because cross-sensitivity is common.<br />
5 If previous records are not available:<br />
a It would be appropriate to avoid all neuromuscular blocking drugs if<br />
possible (the anaesthetist will need to assess the balance of risks).<br />
b Drugs used in local and regional anaesthesia are likely to be safe;<br />
allergy to amide local anaesthetic drugs is extremely rare.<br />
c It would be appropriate to avoid chlorhexidine preparations if possible;<br />
allergy to povidone iodine is less common than allergy to chlorhexidine.<br />
d The previous reaction may have been the result of non-allergic<br />
anaphylaxis; it would be appropriate to avoid drugs that are known to<br />
release histamine, for example morphine.<br />
6 There is no evidence that pre-treatment with hydrocortisone or<br />
histamine-blocking drugs will reduce the severity of anaphylaxis.<br />
What should I say to a patient who wishes to be screened for anaesthetic allergy<br />
pre-operatively?<br />
Unless there is a history suggestive of previous anaesthetic anaphylaxis, preoperative<br />
screening is of no value. The sensitivity and specificity of skin<br />
tests and blood tests is relatively low. If the pretest probability is very low,<br />
i.e. there is no positive history, neither a negative test nor a positive test is<br />
likely to be predictive of outcome.<br />
Should I avoid propofol in patients who are allergic to eggs, soya or nuts?<br />
There is no published evidence indicating that propofol should be avoided<br />
in patients who are allergic to eggs, soya or nuts. Propofol contains purified<br />
egg phosphatide and soya-bean oil. It is likely that the manufacturing<br />
process removes or denatures the proteins responsible for egg allergy and<br />
Ó 2009 The Authors<br />
Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland 21
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
soya allergy. However, a cautious approach would seem to be appropriate<br />
in patients with egg allergy or soya allergy.<br />
I don’t have a specialist allergy centre nearby. Should I do my own skin-testing?<br />
The results of skin tests are very technique-dependent and their interpretation<br />
requires specialist training and experience.<br />
Appendix II<br />
Latex allergy<br />
Latex is a natural rubber derived from the sap of a tree (Hevea brasiliensis)<br />
found in Asia which contains several water-soluble proteins, designated<br />
Hev b 1- Hev b 13. Patient contact with natural rubber latex (NRL) during<br />
anaesthesia may occur via several routes including the airway, mucous<br />
membranes, surgical wounds and parenteral injection. An anaphylactic<br />
reaction to NRL during anaesthesia may be immediate, or may be delayed<br />
for up to an hour. The clinical manifestations of NRL anaphylaxis during<br />
anaesthesia tend to be less severe than anaphylaxis due to neuromuscular<br />
blocking drugs.<br />
Classification of latex reactions<br />
1 Systemic reaction: a Type 1 hypersensitivity reaction involving<br />
specific IgE to Hev proteins, mostly to Hev b 5&6. This is the most<br />
severe but least frequent reaction and occurs in genetically predisposed<br />
individuals. The symptoms consist of itching, swelling, rhinitis,<br />
asthma and anaphylaxis. This allergy is life long. A proportion of<br />
sensitized individuals also react to certain fruits cross reacting with<br />
latex proteins.<br />
2 Contact dermatitis: a delayed Type IV hypersensitivity reaction<br />
consisting of an eczematous reaction starting 24–48 h after repeated<br />
skin or mucosal contact with additives used during rubber production.<br />
This is a T cell-mediated, non-life-threatening reaction. It may,<br />
however, predispose the individual to a more severe systemic<br />
reaction.<br />
3 Clinical non-immune-mediated reaction: irritant dermatitis resulting<br />
from a mild irritant effect of the powder in the gloves and that of<br />
disinfectants, sweating etc. This is the most frequent reaction, is limited<br />
to the contact area and is characterised by itching, irritation and blistering<br />
at the side of contact.<br />
Ó 2009 The Authors<br />
22 Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
High risk individuals<br />
Approximately 8% of the population is sensitized to latex but only 1.4% of<br />
the population exhibits latex allergy. The following groups are at increased<br />
risk:<br />
• Patients with atopy<br />
• Children undergoing multiple surgical procedures, such as spina bifida,<br />
or children undergoing surgery at a very young age<br />
• Patients with severe dermatitis of their hands<br />
• Healthcare professionals<br />
• Patients with allergy to fruits; most frequently banana, chestnut and<br />
avocado<br />
• Industrial workers using protective gear<br />
• Occupational exposure to latex<br />
Pre-operative assessment<br />
A history of pre-operative symptoms suggestive of latex allergy is present in<br />
approximately a quarter of patients who develop intra-operative NRL<br />
anaphylaxis. A thorough history, including an occupational history, should<br />
be part of the pre-operative assessment. It is useful to ask specifically<br />
whether contact with balloons, condoms or latex gloves provokes itching,<br />
rash or angioedema.<br />
Pre-operative testing<br />
If the clinical history is positive or equivocal, the patient should be referred<br />
for testing before the surgical procedure and surgery should proceed only in<br />
an emergency. In the preoperative situation, it is particularly important to<br />
exclude IgE-mediated sensitivity. The choice of test: either a blood test for<br />
latex-specific IgE, or skin testing may depend on local availability. Current<br />
tests have a sensitivity of approximately 75–90%; skin prick testing may be<br />
more sensitive than blood tests for specific IgE. It is important that skin<br />
prick tests are performed by trained staff. It may be appropriate to proceed<br />
to challenge testing in some patients.<br />
Peri-operative precautions<br />
• If NRL allergy is diagnosed pre-operatively, avoidance is mandatory.<br />
• Care should be taken to avoid introducing additional, unrelated hazards<br />
when latex precautions are implemented in the operating theatre.<br />
• Latex allergy should be recorded in the case-notes and on the patient’s<br />
wrist bracelet.<br />
Ó 2009 The Authors<br />
Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland 23
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
• The surgical team and the nursing and anaesthetic support teams should<br />
be alerted.<br />
• There is no evidence that premedication with an anti-histamine or<br />
steroid is useful.<br />
• The operating theatre should be prepared the night before to avoid<br />
the release of latex particles and the patient should be scheduled first<br />
on the list. Evidence is limited regarding the need for this degree of<br />
caution in operating theatres where all latex gloves are of the nonpowdered<br />
type.<br />
• A ‘Latex allergy’ notice should be placed on the doors to the anaesthetic<br />
room and operating theatre.<br />
• Staff traffic should be limited.<br />
• Absolute use of synthetic gloves when preparing equipment and during<br />
anaesthesia, surgery and postoperative care.<br />
• Non-essential equipment should be removed from the vicinity of the<br />
patient.<br />
• The anaesthetic and surgical areas must contain only latex free products.<br />
• Only latex-free dressings and tapes should be applied.<br />
• Equipment in resuscitation boxes and trolleys must contain only latex<br />
free material.<br />
Postoperative investigation of possible latex anaphylaxis<br />
If skin testing and specific IgE testing is negative or equivocal in the<br />
presence of a suggestive history, it may be appropriate for the patient<br />
to proceed to a provocation test with the finger of a latex glove. This<br />
procedure must be performed by trained staff and resuscitation facilities<br />
must be available. Patch testing by an expert is useful in the diagnosis of<br />
delayed (Type lV) hypersensitivity to rubber.<br />
Hospital Latex-Allergy Policy<br />
It is recommended that all hospitals have a latex-allergy policy which<br />
should address the following:<br />
• A named clinical lead for latex allergy<br />
• Instructions for accessing latex-allergy testing<br />
• Latex allergy precautions in the ward and clinic settings<br />
• Latex allergy precautions in the operating theatre environment<br />
• Avoidance of latex sensitization in employees<br />
• Liaison with pharmacy and equipment-procurement departments<br />
Ó 2009 The Authors<br />
24 Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
Further reading<br />
Demaegd J, Soetens F, Herregods L. Latex allergy: a challenge for anesthetists. Acta<br />
Anaesthesiologica Belgica 2006; 57: 127–135.<br />
Mari A, Scala E, D’Ambrosio C, Breitenerder H, Wagner S. Latex allergy with a<br />
cohort of non at risk subjects with respiratory symptoms: prevalence of latex<br />
sensitization and assessment of diagnostic tools. International Archives of Allergy and<br />
Immunology 2007; 143: 135–143.<br />
Bousquet J, Flahault A, Vandemplas O, Ameille J, et al. Natural rubber latex allergy<br />
among health care workers: a systematic review of the evidence. The Journal of<br />
Allergy and Clinical Immunology 2006; 118: 447–54.<br />
Mertes PM, Laxenaire MC, Alla F. Anaphylactic and anaphylactoid reactions<br />
occurring during anesthesia in France in 1999-2000. Anesthesiology 2003; 99:<br />
536–545.<br />
Suli C, Lorini M, Mistrello G, Tedeschi A. Diagnosis of latex hypersensitivity:<br />
comparison of different methods. European Annals of Allergy and Clinical<br />
Immunology 2006; 38: 24–30.<br />
Appendix III<br />
Mast cell tryptase<br />
1 Mast cells are found within many tissues including lung, intestine and<br />
skin. Tryptase is a protease enzyme which acts via widespread protease<br />
activated receptors (PARs). There are two types of tryptase; a and b,<br />
each of which has several subtypes. Mature b-tryptase is stored in<br />
granules in mast cells and is released during anaphylaxis by a calciumdependent<br />
mechanism. a-tryptase is secreted constitutively by mast cells<br />
and is the form normally found in the blood in health. a-tryptase is<br />
elevated in systemic mastocytosis. Pro-b-tryptase is also secreted<br />
constitutively by mast cells.<br />
2 The normal functions of tryptase include modulation of intracellular<br />
calcium ion and intestinal chloride ion transport in addition to<br />
mediating relaxation of smooth muscle in vascular endothelium and<br />
bronchial smooth muscle. In inflammation, tryptase stimulates the<br />
release of pro-inflammatory interleukins and stimulates further tryptase<br />
secretion by neighbouring mast cells.<br />
3 A variety of pathways may combine to produce anaphylaxis, depending<br />
on the trigger and the susceptibility of the patient. Typically anaphylaxis<br />
results from mast cell activation, and typically this will cause release of<br />
mast cell b-tryptase into the circulation.<br />
4 Anaphylaxis may be caused by basophil or complement activation, both of<br />
which are not associated with a rise in mast cell tryptase. A raised tryptase<br />
Ó 2009 The Authors<br />
Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland 25
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
concentration is therefore a marker of anaphylaxis, but anaphylaxis does<br />
not always cause a raised concentration. The greater the rise in concentration,<br />
the greater the probability this was caused by an anaphylactic<br />
reaction but a normal concentration does not disprove anaphylaxis.<br />
5 A rise in serum tryptase simply indicates mast cell degranulation and<br />
does not discriminate between allergic and non-allergic anaphylaxis. It<br />
has been stated that the rise in serum tryptase concentration may be less<br />
marked in non-allergic anaphylaxis.<br />
6 During anaphylaxis, tryptase peaks by approximately 1 h and its half-life<br />
in the circulation is about 2 h: the concentration therefore falls rapidly<br />
following an anaphylactic reaction.<br />
7 The most widely used assay for tryptase is the ImmunoCAP Ò<br />
fluorescence enzyme immunoassay (FEIA) which measures the sum<br />
of a and b-tryptase concentrations. A raised resting concentration is<br />
usually due to a-tryptase, secreted constitutively by the increased<br />
numbers of mast cells in systemic mastocytosis.<br />
8 Although the current tryptase assay has a high specificity, its sensitivity is<br />
relatively low and some cases of anaphylaxis may be missed.<br />
9 The sensitivity and specificity of the tryptase assay depends on the cutoff<br />
point that is chosen to indicate anaphylaxis. Because there is a wide<br />
variation in the base-line plasma concentration of tryptase, the change<br />
in tryptase concentration is more helpful than the absolute concentration<br />
in reaching a diagnosis.<br />
10 Intravenous fluid replacement is usually required during treatment of a<br />
reaction. This fluid will dilute the blood and causes a fall in the<br />
concentration of tryptase measured. This must be taken into account<br />
when evaluating the measured concentration.<br />
11 Following death, the circulation stops and tryptase is no longer removed<br />
from the circulation; samples taken postmortem are helpful in evaluating<br />
whether the terminal events were related to anaphylaxis. A raised<br />
tryptase concentration found at autopsy has lower predictive value than<br />
a sample taken during life. b-tryptase may be raised in trauma or<br />
myocardial infarction.<br />
Further reading<br />
Fisher MM, Baldo BA. Mast cell tryptase in anaesthetic anaphylactoid reactions.<br />
British Journal of Anaesthesia 1998; 80: 26–29.<br />
Enrique E, Garcia-Ortega P, Sotorra O, Gaig P, Richart C. Usefulness of UniCAP<br />
Tryptase fluoroimmunoassay in the diagnosis of anaphylaxis. Allergy 1999; 54:<br />
602–606.<br />
Ó 2009 The Authors<br />
26 Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland
Suspected anaphylactic reactions associated with anaesthesia<br />
.....................................................................................................................................<br />
Payne V, Kam PCA. Mast cell tryptase: a review of its physiology and clinical<br />
significance. Anaesthesia 2004; 59: 695–703.<br />
Brown SGA, Blackman KE, Heddle RJ. Can serum mast cell tryptase help diagnose<br />
anaphylaxis? Emergency Medicine Australasia 2004; 16: 120–124.<br />
Appendix IV<br />
Useful websites<br />
http://www.<strong>aagbi</strong>.org<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
http://www.bsaci.org<br />
The British Society for Allergy and Clinical Immunology<br />
http://www.immunology.org<br />
The British Society for Immunology<br />
http://www.resus.org.uk<br />
Resuscitation Council UK<br />
http://www.eaaci.net<br />
The European Academy of Allergology and Clinical Immunology<br />
http://www.mhra.gov.uk<br />
The Medicines and Healthcare products Regulatory Agency<br />
Supporting Information<br />
Additional Supporting information may be found in the online version of<br />
this article:<br />
Appendix S1 Anaesthetic Anaphylaxis Referral Form.<br />
Please note: Wiley-Blackwell are not responsible for the content or<br />
functionality of any Supporting materials supplied by the authors. Any<br />
queries (other than missing material) should be directed to the<br />
corresponding author for the article.<br />
Ó 2009 The Authors<br />
Journal compilation Ó 2009 The Association of Anaesthetists of Great Britain and Ireland 27
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
Appendix 2a<br />
Frequently asked questions regarding consent (n.b. relating to England and Wales). Please note:<br />
i) When the new Mental Capacity (Northern Ireland) Act 2016 comes into force in Northern Ireland, the<br />
relevant legal provisions in England and Wales and in Northern Ireland will be very similar; for more<br />
information see http://www.legislation.gov.uk/nia/2016/18/contents.<br />
ii)<br />
iii)<br />
For information about the implications of the new Assisted Decision-Making (Capacity) Act 2015 in the<br />
Republic of Ireland, see<br />
http://www.hse.ie/eng/about/Who/qualityandpatientsafety/nau/AssistedDecisionMaking/).<br />
A separate document [Appendix 2b] relates to Scotland.<br />
1. Can obtaining consent for anaesthesia be delegated to another healthcare professional?<br />
It is recommended that the person who gains consent for anaesthesia from a patient is the anaesthetist who will<br />
perform the case. However, for logistical reasons this is not always possible. The person taking consent should<br />
always be an anaesthetist or a physician’s assistant in anaesthesia (PA(A)) who understands the risks and benefits<br />
of the anaesthetic technique and also the alternatives. Surgeons and pre-operative assessment nurses should not<br />
be expected to take consent from patients for general or regional anaesthesia, although this may form part of<br />
their discussion about the procedure. Surgeons may take consent for procedures under local anaesthetic that<br />
they are going to administer.<br />
2. How soon before the procedure should consent be taken?<br />
Consent is a process and not a fixed point in time. The consent process for anaesthesia begins when the<br />
procedure necessitating anaesthesia is first discussed with the patient. At that point the mode of anaesthesia<br />
should be mentioned and written information about anaesthesia should be provided. (For urgent or emergency<br />
cases, provision of written information is not always practical or possible.) For elective cases, further information<br />
can be given at the pre-operative assessment visit. If the patient is seen by an anaesthetist at this point, consent<br />
may be taken for anaesthesia and any associated procedures. However, consent must still be confirmed on the<br />
day of the procedure by the anaesthetist. Verification that consent has been given should be done again in the<br />
anaesthetic room, although this should not be the place where risks, alternatives and additional procedures are<br />
discussed.<br />
3. For how long does consent remain valid?<br />
Consent is event-specific and there is no defined length of time for which it remains valid. It should be taken in<br />
advance of the procedure in question and confirmed immediately before the procedure. It may be withdrawn at<br />
any time.<br />
4. Do patients need to receive written information about anaesthesia and its risks?
Elective patients should be offered written information about anaesthesia and the associated risks. Patients<br />
undergoing urgent or emergency surgery may also benefit from receiving written information although this is not<br />
always possible in practice.<br />
5. What steps should I take to ensure that information is understood?<br />
Potential barriers to comprehension include: language differences; communication difficulties; poor numerical<br />
literacy (quantifying risk); medical illiteracy (understanding medical conditions or terminology); preference for<br />
types of learning (visual or auditory); presence of pain and/or psychological and emotional distress; and lack of<br />
time. The consent process should involve presentation of information in a way that the patient can understand.<br />
This may involve the use of an interpreter, patient information leaflets (translated as required), infographics,<br />
diagrams, credible patient information websites and involvement of a family member, friend or other healthcare<br />
professional. Sufficient time must be allowed for the process and a phased approach may be necessary, allowing<br />
the patient time to absorb information before making a decision.<br />
6. Which risks of anaesthesia do I need to document that I have discussed with the patient?<br />
Ideally, all of the risks that have been discussed should be documented. Anaesthetic charts should have space for<br />
documentation of the discussion leading to consent. Some charts employ a tick-box system as an aide memoire;<br />
such systems can be useful but care must be taken to ensure that they are accurately completed.<br />
7. Should I discuss a technique as a possible option even if I don’t feel I have the skills to use it, e.g. shoulder block<br />
for shoulder surgery?<br />
Discussion of the treatment options should in general include alternative techniques, but it would be<br />
unreasonable to require inclusion of an exhaustive list of treatments that are not available to that patient (thus<br />
the Montgomery ruling states that patients are entitled to decide: “which, if any, of the available forms of<br />
treatment to undergo” and that they should be made aware of: “any material risks involved in any recommended<br />
treatment, and of any reasonable alternative or variant treatments” [10]. The range of ‘reasonable’ anaesthetic<br />
techniques that should be discussed will depend on the individual anaesthetist's ability to provide them and their<br />
availability in that institution/setting, as well as the degree to which they are used in general to provide<br />
anaesthesia for the procedure in question. Thus, for example, it would be standard modern practice to discuss<br />
regional anaesthesia for caesarean section as the preferred option, but to include also discussion of general<br />
anaesthesia both as a technique in its own right and as a back-up technique should regional anaesthesia fail. It is<br />
also accepted practice to offer regional anaesthesia for other procedures, e.g. shoulder surgery, but it is not<br />
universal practice to offer this as the preferred option in all centres, although there are anaesthetists (and units)<br />
that might argue it should be. The Working Party accepts that opinions as to the preference for and availability of<br />
such techniques vary, and would suggest that anaesthetists present and explain the technique that is their/their<br />
unit's standard practice, whilst explaining that there are other techniques that are used elsewhere/by others, and<br />
that the patient may have heard of. If the patient has strong views/preferences around the use of e.g. a regional
or another technique, to the point where he/she would even consider seeking treatment elsewhere, then this<br />
should be discussed with patient and surgeon, along with the implications of such a course of action.<br />
8. What level of detail of anaesthetic technique do I need to discuss with the patient?<br />
Discussion of a treatment (or anaesthetic) should include those components that are of importance to that<br />
patient. However, it would be unreasonable to list every drug and technique that together constitute<br />
‘anaesthesia’, so that the patient may ‘approve’ each one; thus the Montgomery ruling states: “The doctor's duty<br />
is not therefore fulfilled by bombarding the patient with technical information which she cannot reasonably be<br />
expected to grasp” [10]. The broad range of information considered appropriate for discussion with patients<br />
during the consenting process in most cases is provided in Table 2 of the consent guidance [link]; further<br />
discussion should be guided by the patient’s wishes.<br />
9.What level of risk requires me to inform the patient about a particular complication?<br />
It is occasionally stated that complications with a risk < 1% do not need to be discussed with a patient. However,<br />
what might constitute a ‘material risk’ to a particular patient does not depend on its size. The Montgomery ruling<br />
states that: “...the assessment of whether a risk is material cannot be reduced to percentages. The significance of<br />
a given risk is likely to reflect a variety of factors besides its magnitude: for example, the nature of the risk, the<br />
effect which its occurrence would have upon the life of the patient, the importance to the patient of the benefits<br />
sought to be achieved by the treatment, the alternatives available, and the risks involved in those alternatives. The<br />
assessment is therefore fact-sensitive, and sensitive also to the characteristics of the patient” [10].<br />
10. What should I do if a patient indicates that he/she does not wish to know about the risks of anaesthesia?<br />
A patient who refuses to hear about the risks of anaesthesia should be given the opportunity to change his/her<br />
mind and this may require a repeat appointment. Information should not be forced upon a patient and so if a<br />
patient repeatedly indicates that he/she does not wish to hear about the risks of anaesthesia then the<br />
implications of this should be explained and the details of this conversation must be documented in the notes.<br />
11. Is a signed consent form for anaesthesia recommended?<br />
No, a signed consent form for anaesthesia is not recommended if the anaesthesia or anaesthetic procedure is<br />
done to facilitate another treatment (e.g. anaesthesia for surgery) or as part of a larger and inter-related process<br />
(e.g epidural pain relief for childbirth). The statement in the Montgomery ruling, above (see FAQ 8) goes on to<br />
state: “The doctor's duty is not therefore fulfilled by bombarding the patient…, let alone by routinely demanding<br />
her signature on a consent form” [10].<br />
For procedures done as primary therapeutic interventions, e.g. interventional pain procedures, local<br />
practices/policies should be followed and this may include a written consent form.
12. If a patient signs a surgical consent form mentioning general or regional anaesthesia, do I need to discuss the<br />
risks associated with anaesthesia with him/her?<br />
Yes. Unless the patient has received accurate information about the anaesthetic and the risks and alternatives, it<br />
cannot be said that he/she has given his/her consent. A signature on a form does not remove the requirement for<br />
a discussion to take place.<br />
13. My patient is refusing a treatment that is clearly in his/her best interests; does this mean he/she lacks<br />
capacity?<br />
A patient’s capacity to decide is not defined according to whether or not the patient’s decision is in what his/her<br />
doctor believes to be his/her best interests, so if a treatment decision appears not to be sensible, rational or well<br />
considered, it does not necessarily mean that the patient lacks capacity to make it. However, if a decision is highly<br />
irrational and based on persistent misinterpretation it may be that the patient is suffering a mental illness, in<br />
which case a specialist clinical opinion should be sought, since deeming incapacity on the grounds of irrationality<br />
is unlawful.<br />
14. Who can determine whether a patient has capacity?<br />
In most cases, this will be the responsibility of the person providing the treatment and therefore taking consent. If<br />
you doubt your patient’s capacity, the GMC’s Good Medial Practice guidance states that you need to seek advice<br />
from others involved in his/her care and those close to the patient, who may have knowledge of his/her usual<br />
abilities and methods of communication. Gaining opinions of colleagues with specialist experience, for example<br />
neurologists, psychiatrists and speech and language therapists, is also advised. If you are still unsure about a<br />
patient’s capacity, the GMC states that legal advice should be sought, since application to a court may be<br />
appropriate.<br />
15. Under what circumstances can someone else consent on a patient’s behalf?<br />
A person can consent on behalf of another person: (i) if a healthcare proxy has been appointed through a lasting<br />
power of attorney, and the attorney has the power to make the decision in question; (ii) if a court has appointed a<br />
deputy with the appropriate powers; or (iii) if the patient is a child or young person, in which case his/her parents<br />
or those with parental responsibility, local authorities or the courts may consent (although children and young<br />
people should be involved as much as possible in decisions about their care, even when they are not able to make<br />
decisions on their own).<br />
16. When does an Independent Medical Capacity Advocate (IMCA) need to be consulted?<br />
An IMCA should be consulted to assist with decision-making when a patient over 16 lacks capacity, and a<br />
treatment is proposed that is felt by medical professionals to be in his/her best interests but there are no family<br />
or friends to consult. The IMCA acts to represent the patient and will decide if the best interests’ framework has<br />
been appropriately followed, but the IMCA does not make the decision him/herself. If the IMCA feels that due
process has not been followed, he/she will issue a formal challenge. More information about IMCAs can be found<br />
at http://www.scie.org.uk/publications/imca/information/doctors.asp.<br />
17. What if the medical teams disagree as to what is in the patient’s best interests if he/she doesn’t have<br />
capacity?<br />
Assessing the best interests of somebody lacking capacity requires consideration of that person’s point of view,<br />
and what his/her decision would be under the circumstances were he/she to have capacity. Assessment of<br />
somebody's best interests is a process rather than an event, and must take into account any evolving factors<br />
including the urgency and seriousness of the situation. The Mental Capacity Act 2005 includes a checklist for<br />
assessing best interests that includes: ensuring a non-judgemental, non-discriminatory approach; taking acount of<br />
all relevant circumstances including the possibility that the person might regain capacity later; enabling the<br />
person to participate as much as possible; considering his/her wishes, feelings, beliefs and values; and seeking the<br />
views of others (e.g. relatives) where appropriate. No one person or group of people has the ultimate say in<br />
determining best interests over any other, and it is feasible that different people/groups might apply the above<br />
process and conclude that different treatment options represent the patient's best interests. If consensus cannot<br />
be reached, then a Clinical Ethics Committee could be consulted if one exists, but the ultimate decision would rest<br />
with the Court of Protection. An exception to this would be in the case of a valid lasting power of attorney or<br />
court-appointed deputy, when the decision between treatment options would rest with the attorney/deputy (but<br />
even their decisions may be referred to the Court of Protection if they are disputed). See<br />
http://www.39essex.com/content/wp-content/uploads/2016/08/Capacity-Assessments-Guide-August-2016.pdf.<br />
18. Is there a specified lower age limit for ‘age of consent’?<br />
No. Under 16, the treating doctor may decide that the child has 'sufficient intelligence and understanding to<br />
appreciate fully what is proposed'. Young persons (16- and 17-year-olds) are presumed to have the capacity to<br />
consent.<br />
19. Who has parental responsibility?<br />
Mothers automatically have parental responsibility from birth. There are different conditions for whether fathers<br />
and same-sex partners have parental responsibility in the devolved nations and Ireland (see<br />
https://www.gov.uk/parental-rights-responsibilities/who-has-parental-responsibility and https://ejustice.europa.eu/content_parental_responsibility-302-IE-en.do?clang=en).<br />
Other people who may have parental<br />
responsibility are: someone who has successfully applied for it; a legally appointed guardian; a person with a<br />
residence order for that child; the local authority designated to care for that child; or a person with an emergency<br />
protection order for that child.<br />
20. What resources are available to help children, young people and their parents understand about the risks of<br />
anaesthesia?
The AAGBI in association with the Royal College of Anaesthetists and the Association of Paediatric Anaesthetists<br />
of Great Britain and Ireland have produced a selection of leaflets and activities for this purpose as part of the<br />
‘Anaesthesia information for children and young people’ project (see http://www.<strong>aagbi</strong>.org/news/informationpublic/information-about-anaesthesia-children-and-young-people).<br />
21. What other resources can I use to help me with the consent process?<br />
The AAGBI and the Royal college of Anaesthetists have also produced a series of information leaflets for adults<br />
(see http://www.<strong>aagbi</strong>.org/news/information-public/information-about-anaesthesia-adults). Some of the other<br />
specialist societies also have information available. In the UK, guidance is available from the GMC (see<br />
http://www.gmc-uk.org/guidance/ethical_guidance/consent_guidance_index.asp).<br />
If your patient lacks capacity to consent and has nobody whom he/she is willing for you to consult, the<br />
Independent Mental Capacity Advocate (IMCA) service should be used (see<br />
https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/365629/making-decisionsopg606-1207.pdf).<br />
22. What should I do if a patient has given consent for a particular anaesthetic technique and the situation<br />
changes and I think an alternative is indicated? (e.g. a laparoscopic procedure is changed to an open procedure<br />
and regional analgesia is now indicated.)<br />
If the patient has not consented to a particular technique before induction of anaesthesia, then any alternatives<br />
must be in the patient’s best interests. The risks and benefits to that patient must be carefully considered, along<br />
with any preferences expressed during the pre-operative discussion. Ideally, possible changes in circumstance,<br />
e.g. the risk of conversion of laparoscopic cholecystectomy to open, should be anticipated and discussed preoperatively.<br />
23. If the anaesthetist responsible for the case changes, does the consent process need to be repeated?<br />
The anaesthetist caring for the patient is the one responsible for the discussions with that patient regarding that<br />
procedure. If you are satisfied that consent was appropriately taken by someone suitably qualified and trained,<br />
then it is acceptable to continue without repeating the consent process – though it would be good practice to<br />
introduce yourself and confirm consent.<br />
24. Do I need to seek specific consent for an arterial line or central venous catheter?<br />
If this is an intended or likely procedure as part of a patient’s care then it should be discussed with the patient,<br />
along with a discussion of any significant risks and consequences. If the need arises unexpectedly once the patient<br />
is anaesthetised, any additional procedures must be in the patient’s best interests. The decision to perform such<br />
procedures must be recorded in the patients’ notes.<br />
n.b. all websites accessed on 20/10/2016. References refer to those in the main article document.
Appendix 2b<br />
Frequently asked questions regarding consent (n.b. relating to Scotland). (A separate document [Appendix 2a]<br />
relates to England and Wales, and Northern Ireland. For information about the implications of the new Assisted<br />
Decision-Making (Capacity) Act 2015 in the Republic of Ireland, see<br />
http://www.hse.ie/eng/about/Who/qualityandpatientsafety/nau/AssistedDecisionMaking/).<br />
1. Can obtaining consent for anaesthesia be delegated to another healthcare professional?<br />
It is recommended that the person who gains consent for anaesthesia from a patient is the anaesthetist who will<br />
perform the case. However, for logistical reasons this is not always possible. The person taking consent should<br />
always be an anaesthetist or a physician’s assistant in anaesthesia (PA(A)) who understands the risks and benefits<br />
of the anaesthetic technique and also the alternatives. Surgeons and pre-operative assessment nurses should not<br />
be expected to take consent from patients for general or regional anaesthesia, although this may form part of<br />
their discussion about the procedure. Surgeons may take consent for procedures under local anaesthetic that<br />
they are going to administer.<br />
2. How soon before the procedure should consent be taken?<br />
Consent is a process and not a fixed point in time. The consent process for anaesthesia begins when the<br />
procedure necessitating anaesthesia is first discussed with the patient. At that point the mode of anaesthesia<br />
should be mentioned and written information about anaesthesia should be provided. (For urgent or emergency<br />
cases, provision of written information is not always practical or possible.) For elective cases, further information<br />
can be given at the pre-operative assessment visit. If the patient is seen by an anaesthetist at this point, consent<br />
may be taken for anaesthesia and any associated procedures. However, consent must still be confirmed on the<br />
day of the procedure by the anaesthetist. Verification that consent has been given should be done again in the<br />
anaesthetic room, although this should not be the place where risks, alternatives and additional procedures are<br />
discussed.<br />
3. For how long does consent remain valid?<br />
Consent is event-specific and there is no defined length of time for which it remains valid. It should be taken in<br />
advance of the procedure in question and confirmed immediately before the procedure. It may be withdrawn at<br />
any time.<br />
4. Do patients need to receive written information about anaesthesia and its risks?<br />
Elective patients should be offered written information about anaesthesia and the associated risks. Patients<br />
undergoing urgent or emergency surgery may also benefit from receiving written information although this is not<br />
always possible in practice.
5. What steps should I take to ensure that information is understood?<br />
Potential barriers to comprehension include: language differences; communication difficulties; poor numerical<br />
literacy (quantifying risk); medical illiteracy (understanding medical conditions or terminology); preference for<br />
types of learning (visual or auditory); presence of pain and/or psychological and emotional distress; and lack of<br />
time. The consent process should involve presentation of information in a way that the patient can understand.<br />
This may involve the use of an interpreter, patient information leaflets (translated as required), infographics,<br />
diagrams, credible patient information websites and involvement of a family member, friend or other healthcare<br />
professional. Sufficient time must be allowed for the process and a phased approach may be necessary, allowing<br />
the patient time to absorb information before making a decision.<br />
6. Which risks of anaesthesia do I need to document that I have discussed with the patient?<br />
Ideally, all of the risks that have been discussed should be documented. Anaesthetic charts should have space for<br />
documentation of the discussion leading to consent. Some charts employ a tick-box system as an aide memoire;<br />
such systems can be useful but care must be taken to ensure that they are accurately completed.<br />
7. Should I discuss a technique as a possible option even if I don’t feel I have the skills to use it, e.g. shoulder block<br />
for shoulder surgery?<br />
Discussion of the treatment options should in general include alternative techniques, but it would be<br />
unreasonable to require inclusion of an exhaustive list of treatments that are not available to that patient (thus<br />
the Montgomery ruling states that patients are entitled to decide: “which, if any, of the available forms of<br />
treatment to undergo” and that they should be made aware of: “any material risks involved in any recommended<br />
treatment, and of any reasonable alternative or variant treatments” [10]. The range of ‘reasonable’ anaesthetic<br />
techniques that should be discussed will depend on the individual anaesthetist's ability to provide them and their<br />
availability in that institution/setting, as well as the degree to which they are used in general to provide<br />
anaesthesia for the procedure in question. Thus, for example, it would be standard modern practice to discuss<br />
regional anaesthesia for caesarean section as the preferred option, but to include also discussion of general<br />
anaesthesia both as a technique in its own right and as a back-up technique should regional anaesthesia fail. It is<br />
also accepted practice to offer regional anaesthesia for other procedures, e.g. shoulder surgery, but it is not<br />
universal practice to offer this as the preferred option in all centres, although there are anaesthetists (and units)<br />
that might argue it should be. The Working Party accepts that opinions as to the preference for and availability of<br />
such techniques vary, and would suggest that anaesthetists present and explain the technique that is their/their<br />
unit's standard practice, whilst explaining that there are other techniques that are used elsewhere/by others, and<br />
that the patient may have heard of. If the patient has strong views/preferences around the use of e.g. a regional<br />
or another technique, to the point where he/she would even consider seeking treatment elsewhere, then this<br />
should be discussed with patient and surgeon, along with the implications of such a course of action.
8. What level of detail of anaesthetic technique do I need to discuss with the patient?<br />
Discussion of a treatment (or anaesthetic) should include those components that are of importance to that<br />
patient. However, it would be unreasonable to list every drug and technique that together constitute<br />
‘anaesthesia’, so that the patient may ‘approve’ each one; thus the Montgomery ruling states: “The doctor's duty<br />
is not therefore fulfilled by bombarding the patient with technical information which she cannot reasonably be<br />
expected to grasp” [10]. The broad range of information considered appropriate for discussion with patients<br />
during the consenting process in most cases is provided in Table 2 of the consent guidance [link];further<br />
discussion should be guided by the patient’s wishes.<br />
9. What level of risk requires me to inform the patient about a particular complication?<br />
It is occasionally stated that complications with a risk < 1% do not need to be discussed with a patient. However,<br />
what might constitute a ‘material risk’ to a particular patient does not depend on its size. The Montgomery ruling<br />
states that: “...the assessment of whether a risk is material cannot be reduced to percentages. The significance of<br />
a given risk is likely to reflect a variety of factors besides its magnitude: for example, the nature of the risk, the<br />
effect which its occurrence would have upon the life of the patient, the importance to the patient of the benefits<br />
sought to be achieved by the treatment, the alternatives available, and the risks involved in those alternatives. The<br />
assessment is therefore fact-sensitive, and sensitive also to the characteristics of the patient” [10].<br />
10. What should I do if a patient indicates that he/she does not wish to know about the risks of anaesthesia?<br />
A patient who refuses to hear about the risks of anaesthesia should be given the opportunity to change his/her<br />
mind and this may require a repeat appointment. Information should not be forced upon a patient and so if a<br />
patient repeatedly indicates that he/she does not wish to hear about the risks of anaesthesia then the<br />
implications of this should be explained and the details of this conversation must be documented in the notes.<br />
11. Is a signed consent form for anaesthesia recommended?<br />
No, a signed consent form for anaesthesia is not recommended if the anaesthesia or anaesthetic procedure is<br />
done to facilitate another treatment (e.g. anaesthesia for surgery) or as part of a larger and inter-related process<br />
(e.g epidural pain relief for childbirth). The statement in the Montgomery ruling, above (see FAQ 8) goes on to<br />
state: “The doctor's duty is not therefore fulfilled by bombarding the patient…, let alone by routinely demanding<br />
her signature on a consent form” [10].<br />
For procedures done as primary therapeutic interventions, e.g. interventional pain procedures, local<br />
practices/policies should be followed and this may include a written consent form.<br />
12. If a patient signs a surgical consent form mentioning general or regional anaesthesia, do I need to discuss the<br />
risks associated with anaesthesia with him/her?
Yes. Unless the patient has received accurate information about the anaesthetic and the risks and alternatives, it<br />
cannot be said that he/she has given his/her consent. A signature on a form does not remove the requirement for<br />
a discussion to take place.<br />
13. My patient is refusing a treatment that he/she clearly needs; does this mean he/she lacks capacity?<br />
A patient’s capacity to decide is not defined according to whether or not the patient’s decision is what his/her<br />
doctor believes that he/she needs, so if a treatment decision appears not to be sensible, rational or well<br />
considered, it does not necessarily mean that the patient lacks capacity to make it. However, if a decision is highly<br />
irrational and based on persistent misinterpretation it may be that the patient is suffering a mental illness, in<br />
which case a specialist clinical opinion should be sought, since deeming incapacity on the grounds of irrationality<br />
is unlawful.<br />
14. Who can determine whether a patient has capacity?<br />
In most cases, this will be the responsibility of the person providing the treatment and therefore taking consent. If<br />
you doubt your patient’s capacity, the GMC’s Good Medial Practice guidance states that you need to seek advice<br />
from others involved in his/her care and those close to the patient, who may have knowledge of his/her usual<br />
abilities and methods of communication. Gaining opinions of colleagues with specialist experience, for example<br />
neurologists, psychiatrists and speech and language therapists, is also advised. If you are still unsure about a<br />
patient’s capacity, the GMC states that legal advice should be sought, since application to a court may be<br />
appropriate.<br />
15. How do I proceed if the patient does not have capacity to consent to the treatment?<br />
Part 5 of the Adults with Incapacity (Scotland) Act 2000 (‘the AWI Act’) sets out the procedures to be followed. In<br />
most cases, the treating doctor grants a certificate (a ‘section 47 certificate’) confirming his/her opinion that the<br />
patient is incapable of making a decision in relation to the treatment in question, and setting out the treatment<br />
being authorised under the certificate. Assessing the appropriate treatment for somebody lacking capacity<br />
requires consideration of that person’s point of view, and what his/her decision would be under the<br />
circumstances, were he/she to have capacity. Assessment of the treatment that somebody needs is a process<br />
rather than an event, and must take into account any evolving factors including the urgency and seriousness of<br />
the situation. The AWI Act aims to protect people who lack capacity to make particular decisions, but also<br />
supports their involvement in making decisions about their own lives as far as they are able to do so. The<br />
principles to be followed include: considering the benefit of the procedure or treatment to the person; using the<br />
option that restricts the person’s freedom as little as possible; taking the person’s past and present wishes into<br />
account; consulting with relevant others including primary carers, nearest relative, named person, attorney or<br />
guardian (if there is one); and encouraging the person to use existing skills and develop new skills.<br />
16. What if the medical teams disagree as to what treatment the patient needs if he/she does not have capacity?
It is feasible that different people/groups might apply the above process and conclude that different treatment<br />
options are needed. Ultimately, the responsibility rests with the doctor granting the section 47 certificate,<br />
although attempts should be made to reach a consensus among the clinical team, and to consult others (e.g. a<br />
Clinical Ethics Committee if one exists). If there is serious concern about the decision, formal authorisation from<br />
the sheriff court could be obtained by applying for an intervention order under the AWI Act.<br />
17. Under what circumstances can someone else consent on a patient’s behalf?<br />
A person can consent on behalf of another adult: (i) if the patient has appointed a welfare attorney, it has been<br />
confirmed the patient lacks capacity, and the welfare attorney has the power to make the decision in question; (ii)<br />
if the sheriff court has appointed a welfare guardian with the appropriate powers; or (iii) if the patient is a child or<br />
young person, in which case his/her parents or those with parental responsibility, local authorities or the courts<br />
may consent (although children and young people should be involved as much as possible in decisions about their<br />
care, even when they are not able to make decisions on their own).<br />
18. What if the welfare attorney or welfare guardian disagrees with the treating doctor?<br />
Guardians or attorneys cannot demand a treatment that the treating doctor does not believe is clinically justified.<br />
But if they have the appropriate power, they can withhold consent to medical treatment. In such cases, if<br />
agreement cannot be reached, the medical practitioner can seek an independent opinion under s50 of the AWI<br />
Act from a medical practitioner nominated by the Mental Welfare Commission. The nominated medical<br />
practitioner can override the refusal of the attorney or guardian. Ultimately, any interested party can appeal to<br />
the Court of Session for a final decision.<br />
19. Is there a specified lower age limit for ‘age of consent’?<br />
No. A child under 16 may give consent where the treating doctor believes that he/she is capable of understanding<br />
the nature and the possible consequences of the procedure or treatment proposed. Young persons aged 16 or<br />
more are presumed to have the capacity to consent.<br />
20. Who has parental responsibility?<br />
Mothers automatically have parental responsibilities and rights – only a court order can take any of these away. A<br />
father also has these responsibilities and rights but only if:<br />
• he was married to the child’s mother at the time of (or since) the child’s conception, or<br />
• he has been given the responsibilities and rights by a court order, or<br />
• he has made and registered together with the mother, a Parental Responsibilities and Rights Agreement.<br />
The Family Law (Scotland) Act 2006 states that when the birth is registered by both parents and the father’s name<br />
is on the child’s birth certificate, full and equal parental responsibilities and rights are given. This applies only<br />
from May 2006 and is not retrospective.
The position in same-sex relationships is more complicated. When a woman is a parent by virtue of<br />
section 42 of the Human Fertilisation and Embryology Act (HFEA) 2008, i.e. when she is in a civil partnership with<br />
the child’s mother, she will automatically have parental responsibilities and rights. If a woman is the child’s<br />
second female parent by virtue of section 43 of HFEA 2008, i.e. when the mother has agreed that she should be<br />
the child’s second parent and she is registered as such, she will automatically have parental responsibilities and<br />
rights. Where none of these principles applies, there are two ways that a father or the child’s second female<br />
parent can obtain these responsibilities and rights:<br />
• by agreement with the mother (if the mother has not been deprived of some or all of her parental<br />
responsibilities and rights). This agreement must stipulate the date upon which the father or second<br />
female parent is to acquire the responsibilities and rights, and the agreement must be in a prescribed<br />
form and registered in the Books of Council and Session.<br />
• by applying to the Sheriff Court or Court of Session under the Children (Scotland) Act 1995.<br />
The provisions apply only where the child has been conceived as a result of assisted reproduction. If the child is<br />
conceived as a result of sexual intercourse, the civil partner or female cohabitant will not be the child’s parent<br />
though she may accept that child as a child of the family.<br />
Other people who may have parental responsibility are: someone who has successfully applied for it; a<br />
legally appointed guardian; a person with a residence order for that child; the local authority designated to care<br />
for that child; or a person with an emergency protection order for that child.<br />
21. What resources are available to help children, young people and their parents understand about the risks of<br />
anaesthesia?<br />
The AAGBI in association with the Royal College of Anaesthetists and the Association of Paediatric Anaesthetists<br />
of Great Britain and Ireland have produced a selection of leaflets and activities for this purpose as part of the<br />
‘Anaesthesia information for children and young people’ project (see http://www.<strong>aagbi</strong>.org/news/informationpublic/information-about-anaesthesia-children-and-young-people).<br />
22. What other resources can I use to help me with the consent process?<br />
The AAGBI and the Royal college of Anaesthetists have also produced a series of information leaflets for adults<br />
(see http://www.<strong>aagbi</strong>.org/news/information-public/information-about-anaesthesia-adults). Some of the other<br />
specialist societies also have information available. In the UK, guidance is available from the GMC (see<br />
http://www.gmc-uk.org/guidance/ethical_guidance/consent_guidance_index.asp). Sources of further advice,<br />
include the AWI Code of Practice on part 5 (see http://www.gov.scot/Publications/2010/10/20153801/0), the<br />
Mental Welfare Commission guidance on Consent to Treatment (see<br />
http://www.mwcscot.org.uk/media/51774/Consent%20to%20Treatment.pdf), and on the use of the AWI in<br />
General Hospitals (see http://www.mwcscot.org.uk/media/340709/awi_in_general_hospitals_final_2.pdf).
23. What should I do if a patient has given consent for a particular anaesthetic technique and the situation<br />
changes and I think an alternative is indicated? (e.g. a laparoscopic procedure is changed to an open procedure<br />
and regional analgesia is now indicated.)<br />
If the patient has not consented to a particular technique before induction of anaesthesia, then the risks and<br />
benefits to that patient of any alternatives must be carefully considered, along with any preferences expressed<br />
during the pre-operative discussion. Ideally, possible changes in circumstance, e.g. the risk of conversion of<br />
laparoscopic cholecystectomy to open, should be anticipated and discussed pre-operatively.<br />
24. If the anaesthetist responsible for the case changes, does the consent process need to be repeated?<br />
The anaesthetist caring for the patient is the one responsible for the discussions with that patient regarding that<br />
procedure. If you are satisfied that consent was appropriately taken by someone suitably qualified and trained,<br />
then it is acceptable to continue without repeating the consent process – though it would be good practice to<br />
introduce yourself and confirm consent.<br />
25. Do I need to seek specific consent for an arterial line or central venous catheter?<br />
If this is an intended or likely procedure as part of a patient’s care then it should be discussed with the patient,<br />
along with a discussion of any significant risks and consequences. If the need arises unexpectedly once the patient<br />
is anaesthetised, the decision to perform any additional procedures must be recorded in the patients’ notes.<br />
n.b. all websites accessed on 20/10/2016. References refer to those in the main article document. See main<br />
article document for acknowledgements.
AAGBI SAFETY GUIDELINE<br />
Arterial line blood sampling: preventing<br />
hypoglycaemic brain injury<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
September 2014
This guideline was originally published in Anaesthesia. If you wish to refer<br />
to this guideline, please use the following reference:<br />
Association of Anaesthetists of Great Britain and Ireland. Arterial line blood<br />
sampling: preventing hypoglycaemic brain injury 2014. Anaesthesia 2014,<br />
69: pages 380–385<br />
This guideline can be viewed online via the following URL:<br />
http://onlinelibrary.wiley.com/doi/10.1111/anae.12536/abstract<br />
© The Association of Anaesthetists of Great Britain & Ireland
Guidelines<br />
Arterial line blood sampling: preventing<br />
hypoglycaemic brain injury 2014<br />
The Association of Anaesthetists of Great Britain<br />
and Ireland<br />
Membership of the Working Party: T. E. Woodcock, T. M. Cook,<br />
K. J. Gupta and A. Hartle<br />
Summary<br />
Drawing samples from an indwelling arterial line is the method of<br />
choice for frequent blood analysis in adult critical care areas. Sodium<br />
chloride 0.9% is the recommended flush solution for maintaining the<br />
patency of arterial catheters, but it is easy to confuse with glucose-containing<br />
bags on rapid visual examination. The unintentional use of a<br />
glucose-containing solution has resulted in artefactually high glucose<br />
concentrations in blood samples drawn from the arterial line, leading to<br />
insulin administration causing hypoglycaemia and fatal neuroglycopenic<br />
brain injury. Recent data show that it remains a common error for<br />
incorrect fluids to be administered as arterial line flush infusions.<br />
Adherence to the National Patient Safety Agency’s 2008 Rapid Response<br />
Report on this topic may not be enough to prevent such errors. This<br />
guideline makes detailed recommendations on the prescription, checking<br />
and administration of arterial line infusions in adult practice. We also<br />
make recommendations about storage, arterial pressure monitoring and<br />
sampling systems and techniques. Finally, we make recommendations<br />
about glucose monitoring and insulin administration. It is intended that<br />
adherence to these guidelines will reduce the frequency of sample<br />
© 2014 The Association of Anaesthetists of Great Britain and Ireland 1<br />
This is an open access article under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs<br />
License, which permits use and distribution in any medium, provided the original work is properly cited, the use is<br />
non-commercial and no modifications or adaptations are made.
contamination errors in arterial line use and capture events, when they<br />
do occur, before they cause patient harm.<br />
....................................................................................................<br />
This is a consensus document produced by expert members of a Sprint<br />
Working Party established by the Association of Anaesthetists of Great<br />
Britain and Ireland (AAGBI). It has been seen and approved by the<br />
AAGBI Board.<br />
Accepted: 5 November 2013<br />
• What other guideline statements are available on this topic?<br />
In July 2008, a National Patient Safety Agency (NPSA) Rapid Response<br />
Report was released [1], highlighting examples of patient harm resulting<br />
from glucose-containing flush infusions contaminating blood samples<br />
drawn from arterial lines [2, 3]. Subsequently, it was reported to<br />
the Safe Anaesthesia Liaison Group in 2011 that the NPSA had<br />
received 169 further incident reports, featuring 31 glucose monitoring<br />
errors (personal communication, Prof. D. Cousins, NHS England).<br />
The Medicines and Healthcare products Regulatory Authority<br />
(MHRA) issued a Drug Safety Update on the issue in 2012 [4].<br />
•<br />
Why was this guideline developed?<br />
Experiment and experience show that compliance with the procedures<br />
required in the NPSA’s 2008 Rapid Response Report, even with good<br />
sampling technique using a simple open arterial line system, is not sufficient<br />
to prevent injury or death arising from sample contamination<br />
error. In a series of 102 cases where a glucose-containing solution was<br />
incorrectly infused, sample contamination error occurred in 30 (personal<br />
communication, Prof. D. Cousins, NHS England). Recent data<br />
show that using incorrect arterial line fluid infusions is a common<br />
error, with an average of one such event reported to the National<br />
Reporting and Learning System every week [5]. More than 30% of<br />
intensive care units have reported recent arterial line errors, with a further<br />
30% reporting errors from operating theatres or the emergency<br />
department [5]. In one case, neuroglycopenia contributed to the<br />
patient’s death [6].<br />
•<br />
How and why does this statement differ from existing guidelines?<br />
The Working Party identified three error-prone processes that can<br />
lead to iatrogenic hypoglycaemia. Our recommendations are<br />
2 © 2014 The Association of Anaesthetists of Great Britain and Ireland
designed to address each of these processes and reduce the likelihood<br />
of active errors and latent risks leading to patient harm [7]. The<br />
error-prone processes are:<br />
• use of arterial flush solution (prescription, dispensing, checking<br />
and administration)<br />
• blood sampling technique for glucose concentration measurement<br />
• administration of insulin to treat apparent hyperglycaemia.<br />
•<br />
For each error-prone procedure, the Working Party systematically<br />
considered whether it was possible or practicable to: eliminate the<br />
procedure; apply safeguard technology; use warning or alarm systems;<br />
specify training requirements for practitioners; and protect the<br />
patient from the consequences of occasional error.<br />
The evidence that informs these guidelines mostly concerns arterial<br />
blood sampling in adult patients. Our recommendations can also be<br />
applied to venous cannulae that are flushed and used for blood sampling.<br />
There may be additional considerations for paediatric practice<br />
that are outside our remit.<br />
Basic knowledge for all practitioners<br />
‘Dextrose’ and ‘glucose’ are interchangeable biological terms for dextrorotatory<br />
glucose (C 6 H 12 O 6 ). Figure 1 illustrates the arrangement of<br />
‘open’ and ‘closed’ systems for maintaining patency and drawing blood<br />
samples from flushed vascular access systems. The open system has a<br />
single three-way tap, close to the vascular catheter, that is used for both<br />
removing residual flush solution and obtaining the blood sample. The<br />
volume of residual fluid between the sampling point and the bloodstream<br />
is referred to as the dead space. To prevent contamination of a<br />
blood sample with flush solution, it has been recommended that 39<br />
dead space volume be withdrawn and discarded (or saved for return to<br />
the circulation) before a sample is taken [8]. However, bench-top experiments<br />
have shown that significant glucose contamination of the blood<br />
sample occurs even with 59 dead space removal when using an open<br />
arterial line sampling system with a glucose 5% flush solution [9]. A<br />
solution of glucose 5% contains approximately 280 mmol.l<br />
1 , hence<br />
contamination of a 1-ml blood sample with just 0.03 ml flush solution<br />
would conceal true hypoglycaemia or make a normal sample hyperglycaemic,<br />
potentially leading to inappropriate insulin therapy. Erroneous<br />
administration of glucose 10% or 20% would result in even greater<br />
© 2014 The Association of Anaesthetists of Great Britain and Ireland 3
Figure 1 Open and closed systems for sampling from arterial lines. The syringe indicated is for removal of dead<br />
space volume and the red arrow indicates the sample drawing point.<br />
4 © 2014 The Association of Anaesthetists of Great Britain and Ireland
contamination. With sodium chloride 0.9% flush, only gross sample<br />
contamination (e.g. due to incorrect sampling technique) will cause dangerous<br />
sampling errors. Contamination of a sample with heparinised<br />
saline also leads to artefactually increased phosphate concentrations.<br />
Erratic or highly varying sequential test results should heighten the suspicion<br />
of blood sample contamination error.<br />
The closed system has a port for removal of dead space beyond a<br />
separate sampling point and, if used as intended by its designers, effectively<br />
eliminates the risk of significant contamination of the sample [9].<br />
Moreover, it reduces the risk of bacteraemia and minimises wastage of<br />
blood because the withdrawn flush and blood can be returned to the<br />
circulation without opening the system.<br />
Nervous tissue is not able to sustain functional or basal metabolic<br />
activity during hypoglycaemia, and prolonged neural glucose deprivation<br />
(neuroglycopenia) leads to permanent or fatal neural injury. Hypoglycaemia<br />
reduces conscious level and causes sympathetically mediated symptoms<br />
of anxiety, tachycardia, tachypnoea, pupillary dilation and<br />
sweating. Beta-blocker therapy blunts some of these symptoms. Hypoglycaemia<br />
is difficult to diagnose clinically in patients with an altered<br />
level of consciousness and in those treated with exogenous catecholamines.<br />
In these patients, practitioners should therefore check for hypoglycaemia<br />
in the presence of a new increase in heart rate or respiratory<br />
rate, sweating, convulsions, pupillary changes, or a fall in conscious<br />
level. Continuous electroencephalography has the potential to detect<br />
neuroglycopenia in monitored patients [10]. Fatal neuroglycopenic brain<br />
injury can occur within two hours of the onset of hypoglycaemia [2].<br />
Neuroglycopenia is therefore not reliably prevented by routine checking<br />
of glucose levels (e.g. once per nursing shift) with blood from an alternative<br />
site.<br />
Sodium chloride 0.9% with glucose 5% has been recommended as<br />
an intravenous fluid for use in paediatric practice [11]. Figure 2 illustrates<br />
how this fluid is particularly easy to confuse with sodium chloride<br />
0.9%. Currently, at least twelve other fluids containing combinations of<br />
sodium chloride, glucose and potassium exist for use in a variety of clinical<br />
circumstances. They all carry increased risk of misidentification,<br />
accidental use as arterial line flush solution and glucose contamination<br />
of blood samples.<br />
Peripheral glucose testing by pricking a finger or ear lobe may be inaccurate<br />
in patients with poor peripheral perfusion, on vasopressor therapy,<br />
or with severe peripheral oedema [12]. Continuous intravascular glucose<br />
© 2014 The Association of Anaesthetists of Great Britain and Ireland 5
(a)<br />
(b)<br />
Figure 2 Appearance of sodium chloride 0.9% and glucose 5% fluid bag<br />
(a) when placed inside a pressure bag and (b) when removed, showing<br />
the ease of confusion with plain sodium chloride. Reproduced from [6],<br />
with permission.<br />
monitoring is under development for introduction into clinical practice<br />
[13, 14], but until that technique is established, it is necessary to draw<br />
frequent blood samples for glucose analysis to guide insulin therapy in<br />
critically ill patients.<br />
Recommendations<br />
The Working Party’s recommendations apply to any clinical areas where<br />
blood is sampled from arterial access devices and includes critical care<br />
areas, operating theatres and emergency departments.<br />
Policy and training<br />
Hospitals must raise awareness among relevant staff of the serious<br />
patient harm that can result from arterial line sample contamination<br />
errors and must have a policy that defines local procedures for arterial<br />
line use, including prescribing, administering and monitoring flush<br />
solutions and blood sampling technique.<br />
Policies about the prescribing, administering and monitoring of<br />
intravenous infusions and policies about intravenous insulin therapy<br />
6 © 2014 The Association of Anaesthetists of Great Britain and Ireland
should be cross-referenced to the arterial line and blood sampling<br />
policy.<br />
All staff involved in the insertion of, management of, or sampling<br />
from, arterial lines must be appropriately trained and competent to deliver<br />
the standards set out in the policy, and performance against these<br />
standards should be regularly audited.<br />
Fluids for flush infusions<br />
Sodium chloride 0.9%, with or without heparin, should be the only solution<br />
to be used for arterial line infusion and flushing. Blood sampling<br />
from a cannula lumen that carries other solutions is not recommended.<br />
Identifying arterial lines<br />
Arterial infusion lines must be clearly identifiable. Labels and colour differentiation<br />
are appropriate measures to achieve this.<br />
Fluid stock and storage<br />
In clinical areas that use arterial lines, bags of sodium chloride 0.9% for<br />
use as arterial line flush should be stored away from fluids for intravenous<br />
use. Bags should be stored in a suitable receptacle and not scattered<br />
across a shelf.<br />
Only those fluid solutions in regular use should be stored in a<br />
clinical area. For example, sodium chloride 0.9% with glucose 5%,<br />
which is recommended for use in paediatric practice, should not be<br />
stored in clinical areas where paediatric practice is unusual. If practicality<br />
dictates that such solutions must be stored, an additional risk<br />
assessment and management plan must be made to prevent their<br />
erroneous use.<br />
Prescription and setting up<br />
An arterial line flush solution must be documented by prescription or<br />
record of administration (e.g. anaesthetic chart) or standard operating<br />
procedure as defined in the hospital’s arterial line policy.<br />
The flush solution must be independently double-checked by a second<br />
practitioner before setting up and attaching to an arterial line. Also<br />
known as independent validation, an independent double-check of a<br />
high-alert medication is a procedure in which two clinicians separately<br />
check, alone and apart from each other, then compare results of each<br />
component of prescribing, dispensing and verifying the high-alert medication<br />
before administering it to the patient [15].<br />
© 2014 The Association of Anaesthetists of Great Britain and Ireland 7
Pressurising devices<br />
All pressurising devices must be designed to permit unimpaired inspection<br />
of the contained flush infusion bag while in use. A fully transparent<br />
front panel is strongly recommended.<br />
Checking during use<br />
The flush infusion bag must be independently double-checked at least<br />
once during each nursing shift and whenever nursing care of the patient<br />
is handed over. This double-check must include removal of the flush<br />
bag from its pressurising device (Fig. 2).<br />
Sampling techniques<br />
To avoid sample contamination with flush infusions, the use of ‘closed’<br />
arterial line sampling systems is recommended.<br />
Where an ‘open’ system is to be used for blood sampling, inevitable<br />
contamination must be kept to a minimum by making the dead space<br />
volume between the sampling port and the arterial lumen as small as<br />
practicable in the clinical situation. The syringe used for removal of<br />
dead space volume must be readily distinguishable from the sampling<br />
syringe. Throughout the sampling process and until the sample syringe<br />
is removed, the sampling technique must avoid flush solution’s entering<br />
the dead space, the sample or any three-way tap at the sampling site.<br />
Glucose concentration thresholds<br />
When an arterial line is used to take blood samples for measurement of<br />
blood glucose concentrations, a value that is unexpectedly high must<br />
trigger a medical review and a check of the blood sampling system for<br />
possible sample contamination error. The source of the blood sample<br />
should be checked to ensure no possibility of sample contamination. If<br />
this is not possible, a confirmatory sample must be drawn from the<br />
most appropriate alternative site.<br />
Initiating and increasing insulin infusions<br />
Before commencing an insulin infusion in a patient not previously<br />
known to be an insulin-dependent diabetic and before increasing an<br />
insulin infusion rate above a policy-defined threshold (e.g. 6 IU.h 1 )on<br />
the basis of samples drawn from a flushed line, there must be a medical<br />
review. The source of the blood sample should be checked to ensure no<br />
possibility of sample contamination. If this is not possible, a confirmatory<br />
sample must be drawn from the most appropriate alternative site.<br />
8 © 2014 The Association of Anaesthetists of Great Britain and Ireland
Abnormal blood tests<br />
A blood test that shows an unexpected abnormality or unusual variation<br />
from previous results should prompt a check of the source of the blood<br />
sample to ensure no possibility of sample contamination. If this is not<br />
possible, a confirmatory sample must be drawn from the most appropriate<br />
alternative site.<br />
Recording trends in measured glucose levels and physiological<br />
variables<br />
Variations in blood chemistry and vital signs are easier to appreciate<br />
from a graphic trend display, which may facilitate earlier detection of<br />
hypoglycaemia. Graphic trend displays, particularly of glucose readings<br />
and of vital signs including heart rate and respiratory rate, are recommended.<br />
Monitoring for signs of hypoglycaemia<br />
Hypoglycaemia should be considered and specifically checked for in any<br />
sedated or unconscious patient receiving insulin therapy who exhibits a<br />
new increase in heart rate or respiratory rate, or sweating, pupillary<br />
changes or a fall in conscious level.<br />
Incident reporting<br />
Any incident causing potential or actual patient harm related to contamination<br />
of blood samples obtained from an arterial line should be<br />
reported to both local and national incident reporting systems. Any<br />
incident causing patient harm must be disclosed to the patient or his/<br />
her next of kin in accordance with local policy.<br />
National monitoring of incidents<br />
National patient safety organisations should monitor the occurrence of<br />
incidents relating to arterial line and flush infusion errors to determine<br />
whether further actions are needed to reduce their incidence.<br />
Engineered solutions<br />
Equipment manufacturers, pharmaceutical suppliers and clinicians should<br />
engage in a collaboration to develop safer systems for the prevention of<br />
arterial cannula clotting. Potential solutions to be considered will include:<br />
• highly visible and easily distinguishable fluid bags for exclusive use<br />
with arterial pressure monitoring and sampling systems.<br />
© 2014 The Association of Anaesthetists of Great Britain and Ireland 9
• special connections between the fluid bag and the arterial pressure<br />
monitoring and sampling system.<br />
• integrated systems, possibly incorporating both the above solutions.<br />
Supporting healthcare providers when errors occur<br />
When errors occur, staff and organisations must “promise to learn and<br />
commit to act” [16]. It is often the systems, procedures, conditions, environment<br />
and constraints faced by healthcare providers that lead to patient<br />
safety problems. Rather than blame individuals, trust should be placed in<br />
the goodwill and good intentions of the staff and attention focused on<br />
learning from (and remembering) errors [16, 17].<br />
Acknowledgements<br />
We are grateful to all individuals and organisations who provided comments<br />
on the first draft of this guideline, and to the following people who<br />
attended a Consensus Conference for Stakeholders at 21 Portland Place<br />
on 10 October 2013: Chris Quinn (Beckton Dickson); Iswori Thakuri and<br />
Markku Ahtiainen (British Anaesthetic and Recovery Nurses Association);<br />
Catherine Plowright (British Association of Critical Care Nurses); Tim<br />
Lewis (College of Operating Department Practitioners); Jane Harper<br />
(Intensive Care Society); Caroline Wilson (Group of Anaesthetists in<br />
Training); Archie Naughton (AAGBI Lay Representative); Desmond Watson<br />
(Medical and Dental Defence Union of Scotland); Gary Duncum and<br />
Hayley Bird (Smiths Medical); Sharon Maris (Teleflex); Clare Crowley<br />
and Mark Tomlin (UK Clinical Pharmacy Association); Graham Milward<br />
(Vygon).<br />
Competing interests<br />
No external funding and no competing interests declared.<br />
References<br />
1. National Patient Safety Agency. Infusions and sampling from arterial lines. Rapid<br />
Response Report. NPSA/2008/RRR006. http://www.nrls.npsa.nhs.uk/resources/?<br />
EntryId45=59891 (accessed 01/08/2013).<br />
2. Sinha S, Jayaram R, Hargreaves CG. Fatal neuroglycopaenia after accidental use of a<br />
glucose 5% solution in a peripheral arterial cannula flush system. Anaesthesia<br />
2007; 62: 615–20.<br />
3. Panchagnula U, Thomas AN. The wrong arterial line flush solution. Anaesthesia<br />
2007; 62: 1077–8.<br />
4. Medicines and Healthcare products Regulatory Authority. Glucose solutions: false<br />
blood glucose readings when used to flush arterial lines, leading to incorrect insulin<br />
10 © 2014 The Association of Anaesthetists of Great Britain and Ireland
administration and potentially fatal hypoglycaemia. Drug Safety Update 2012; 5:<br />
A2. http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON175433<br />
(accessed 01/08/2013).<br />
5. Leslie R, Gouldson S, Habib N, et al. Management of arterial lines and blood sampling<br />
in intensive care: a threat to patient safety. Anaesthesia 2013; 68: 1114–19.<br />
6. Gupta KJ, Cook TM. Accidental hypoglycaemia caused by an arterial flush drug error:<br />
a case report and contributory causes analysis. Anaesthesia 2013; 68: 1178–87.<br />
7. Reason J. Human error: models and management. British Medical Journal 2000;<br />
320: 768–70.<br />
8. Burnett RW, Covington AK, Fogh-Andersen N. Recommendations on whole blood<br />
sampling, transport, and storage for simultaneous determination of pH, blood<br />
gases, and electrolytes. International Federation of Clinical Chemistry Scientific Division.<br />
Journal of the International Federation of Clinical Chemistry 1994; 6: 115–20.<br />
9. Brennan KA, Eapen G, Turnbull D. Reducing the risk of fatal and disabling hypoglycaemia:<br />
a comparison of arterial blood sampling systems. British Journal of Anaesthesia<br />
2010; 104: 446–51.<br />
10. Remvig LS, Elsborg R, Sejling AS, et al. Hypoglycemia-related electroencephalogram<br />
changes are independent of gender, age, duration of diabetes, and awareness status<br />
in type 1 diabetes. Journal of Diabetes Science and Technology 2012; 6: 1337–44.<br />
11. National Patient Safety Agency. Reducing the risk of hyponatraemia when administering<br />
intravenous infusions to children. Patient Safety Alert. NPSA/2007/22.<br />
http://www.nrls.npsa.nhs.uk/resources/?EntryId45=59809 (accessed 01/08/<br />
2013).<br />
12. Jacobi J, Bircher N, Krinsley J, et al. Guidelines for the use of an insulin infusion for the<br />
management of hyperglycemia in critically ill patients. Critical Care Medicine 2012;<br />
40: 3251–76.<br />
13. Beier B, Musick K, Matsumoto A, Panitch A, Nauman E, Irazoqui P. Toward a continuous<br />
intravascular glucose monitoring system. Sensors (Basel) 2011; 11: 409–24.<br />
14. Romey M, Jovanovic L, Bevier W, Markova K, Strasma P, Zisser H. Use of an intravascular<br />
fluorescent continuous glucose sensor in subjects with type 1 diabetes<br />
mellitus. Journal of Diabetes Science and Technology 2012; 6: 1260–6.<br />
15. ISMP Medication Safety Alert! Nurse Advize-ERR Volume 6 Edition 12 December 2008.<br />
http://www.ismp.org/Newsletters/nursing/Issues/NurseAdviseERR200812.pdf<br />
(accessed 13/10/2013).<br />
16. National Advisory Group on the Safety of Patients in England. A promise to learn, a<br />
commitment to act – improving the safety of patients in England. https://www.<br />
gov.uk/government/uploads/system/uploads/attachment_data/file/226703/Ber<br />
wick_Report.pdf (accessed 13/10/2013).<br />
17. Smith A. Lest we forget: learning and remembering in clinical practice. Anaesthesia<br />
2013; 68: 1099–103.<br />
© 2014 The Association of Anaesthetists of Great Britain and Ireland 11
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
Assistance for the Anaesthetist<br />
A Report by the Irish Standing Committee of the<br />
Association of Anaesthetists of Great Britain & Ireland<br />
2007<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland,<br />
21 Portland Place, London W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
www.<strong>aagbi</strong>.org<br />
October 2007
Membership of the working party<br />
Dr Brian Pickering<br />
Dr Ellen O’Sullivan<br />
Dr Rory Page<br />
Dr Anne Bergin<br />
Dr David Honan<br />
Dr John Kennedy<br />
Dr J Loughrey<br />
Dr Carlos McDowell<br />
Dr John McAdoo<br />
Chairman, Working Party<br />
Convenor, Irish Standing Committee,<br />
AAGBI<br />
Secretary, Irish Standing Committee,<br />
AAGBI<br />
Member, Irish Standing Committee,<br />
AAGBI<br />
Member, Irish Standing Committee,<br />
AAGBI<br />
Member, Irish Standing Committee,<br />
AAGBI<br />
Member, Irish Standing Committee,<br />
AAGBI<br />
Co-opted, Irish Standing Committee,<br />
AAGBI<br />
Co-opted, President Irish College of<br />
Anaesthetists
Table of Contents<br />
1. Summary..............................................................................................2<br />
2. Introduction..........................................................................................3<br />
3. Survey of Availability of Assistance for the Anaesthetist.........................3<br />
Setting for Anaesthetic Delivery............................................................3<br />
Anaesthetic Assistance Availability........................................................4<br />
Anaesthetic Assistance Rostering...........................................................4<br />
Anaesthetic Assistance Training.............................................................5<br />
The Future............................................................................................5<br />
4. Detailed Recommendations..................................................................6<br />
Setting for Anaesthetic Delivery............................................................6<br />
Anaesthetic Assistance Availability........................................................6<br />
Anaesthetic Assistance Rostering...........................................................7<br />
Anaesthetic Assistance Training.............................................................7<br />
The Future............................................................................................8<br />
5. Appendix .............................................................................................9<br />
6. References..........................................................................................12
Section 1-Summary<br />
1. The availability of assistance to the anaesthetist is considered to be<br />
of fundamental importance to the safe conduct of anaesthesia, as<br />
recommended by the AAGBI.<br />
2. The Irish Standing Committee considers the availability of trained<br />
assistance to the Irish anaesthetist to be inadequate in relation to the<br />
standards set by the AAGBI.<br />
3. Anaesthetic assistance is most often provided by nursing staff without<br />
a dedicated anaesthetic role.<br />
4. Anaesthetic departments currently have little role in the rostering of<br />
anaesthetic assistants. Communications between anaesthetic assistant<br />
managers and anaesthetic departments are informal and may benefit<br />
from a more structured approach<br />
5. The absence of a nationally identifiable core competency programme<br />
for anaesthetic assistants has led to variable practices within Irish<br />
hospitals.<br />
6. Off-site locations are particularly vulnerable to practice variances<br />
and should be paid special attention when considering anaesthetic<br />
assistance.<br />
7. Early discussion about perceived inadequacies or potentially unsafe<br />
practices should be encouraged.<br />
8. Managers and fund holders should understand the role of the<br />
anaesthetic department in identifying failures in the provision of<br />
adequate anaesthetic assistance. Once notified of inadequacies,<br />
anaesthetic department recommendations should be acted upon in<br />
a timely fashion. Failure to act upon these recommendations should<br />
be cause for the withdrawal of anaesthetic services from the affected<br />
area.<br />
9. The Committee recommends the development of a national core<br />
competencies programme that will contribute to a quality improvement<br />
in anaesthesia delivery.
Section 2-Introduction<br />
The availability of assistance to the anaesthetist is considered to be of<br />
fundamental importance to the safe conduct of anaesthesia 1 . The presence of<br />
such assistance has been shown to reduce the incidence of adverse anaesthetic<br />
events and to improve patient outcome 2 . The purpose of this review by the<br />
Irish Standing Committee of the Association of Anaesthetists of Great Britain<br />
and Ireland (AAGBI) is to place in context the current status of anaesthetic<br />
assistance in Irish hospitals and to make recommendations for the future<br />
development of this service. Our core findings are informed by the results<br />
of our national “Survey of Availability of Assistance for the Anaesthetist”,<br />
conducted during 2006-2007, and the resultant Committee discussions. In<br />
addition, recent changes to Irish legislation 3 mean that there is now a statutory<br />
requirement for the availability of trained anaesthetic assistance during<br />
the conduct of certain procedures, e.g. electroconvulsive therapy (ECT) in<br />
psychiatric hospitals. This is the first time that this requirement has been in<br />
place and we are unaware of any other jurisdiction in which this is the case.<br />
The issues raised for Irish anaesthetists are unclear at present but we believe<br />
that this report addresses a significant information gap and may serve as a<br />
template for future developments.<br />
Section 3-Survey of Availability of Assistance for the<br />
Anaesthetist<br />
This survey was conducted during 2006-2007. The questionnaire was sent to<br />
all accredited training departments registered with the College of Anaesthetists<br />
RCSI. Twelve training departments responded. The key results are summarised<br />
below. (A more detailed view of the questionnaire and of the response is<br />
included in the Appendix).<br />
Setting for Anaesthetic Delivery<br />
The respondents were from a range of hospitals that, in the opinion of the<br />
Committee, represent a cross section of settings in which anaesthesia is<br />
conducted in Ireland. A majority of departments indicated that they regularly
provide cover for off-site locations. These included interventional radiology,<br />
magnetic resonance imaging, computerised tomography scanning, cardiac<br />
catheterisation, cardioversion, endoscopy and ECT.<br />
Responses were received from a number of sub-specialty hospitals including<br />
those that provide paediatric and obstetric services. These settings have<br />
unique assistance requirements.<br />
Anaesthetic Assistance Availability<br />
The availability of trained assistance was generally poor. Only a minority<br />
of hospitals replied that they always have a trained assistant present during<br />
anaesthesia (25%), and most departments did not have trained assistance<br />
available in all of the areas in which they provided anaesthetic cover (62.5%).<br />
About half of the departments replied that they could identify recurrent<br />
circumstances, e.g. time or location, within their hospital that resulted in lack<br />
of adequate assistance being available. One quarter of departments could<br />
recall an instance of error or near miss that could be directly attributed to the<br />
non-availability of assistance for the anaesthetist.<br />
Anaesthetic Assistance Rostering<br />
In Ireland almost all anaesthetic assistants are nurses. As such, anaesthetic<br />
assistants are rostered by a nurse manager in the theatre complex. The<br />
individual manager may be a designated senior anaesthetic nurse or may be<br />
the co-ordinating senior theatre nurse. No department surveyed has input into<br />
the rostering of anaesthetic assistance. Anaesthetic departments are generally<br />
unaware of the criteria employed by nurse managers when deciding who<br />
should be rostered to provide anaesthetic assistance. Only 25% of nurses<br />
rostered were from a dedicated pool of anaesthetic or recovery nurses. The<br />
remainder were from the theatre pool of nurses. This situation continued outof-hours<br />
but 25% of hospitals responded that assistance was more likely to be<br />
drawn from a non-dedicated pool of nurses during this time.
Anaesthetic Assistance Training<br />
There is enormous variability in the type of training that anaesthetic assistants<br />
receive throughout Ireland. The majority of respondents were unclear as to<br />
the exact training that their assistants had received. One hospital has its own<br />
in-house training programme. Some assistants had been on an anaesthetic<br />
assistant training course. Of those departments that knew what training<br />
was provided, the majority response was that the assistants had some local<br />
“on the job” training or exposure to anaesthesia during a theatre course.<br />
Some departments indicated that they were involved in the development of<br />
local training programmes but five departments responded that they had no<br />
involvement in the training of anaesthetic assistants in their hospital.<br />
The Future<br />
Nearly all departments responded that the current level of anaesthetic assistance<br />
available to Irish anaesthetists was inadequate (88%). Non-nursing assistance<br />
for the anaesthetist would be acceptable to the majority of departments (75%)<br />
and most felt that the College of Anaesthetists in conjunction with individual<br />
hospitals should be at the forefront of developing future training programmes.<br />
Many departments felt that lack of communication and interaction between<br />
anaesthetists and those responsible for rostering of assistants was a significant<br />
barrier to their provision. Training deficiencies were identified as another key<br />
barrier.
Section 4-Detailed Recommendations<br />
The following recommendations are the consensus opinion of the Irish<br />
Standing Committee of the AAGBI.<br />
Setting for Anaesthetic Delivery<br />
The Committee notes that most departments provide anaesthetic cover in a<br />
wide variety of off-site locations. It is well recognised that these environments<br />
pose particular challenges for the anaesthetist and can be associated with<br />
higher rates of critical or near-miss incidents. As such, the Committee<br />
recommends that the provision of adequate assistance in these settings<br />
should be a priority for all stakeholders. Settings that fail to provide adequate<br />
assistance should be considered unsafe environments and departments of<br />
anaesthesia should be supported by hospital management to ensure that any<br />
recommendations regarding the provision of assistance in these settings are<br />
complied with.<br />
Anaesthetic Assistance Availability<br />
There is an unacceptably high level of lack of assistance for the anaesthetist<br />
and this could result in critical incidents or near misses within Irish hospitals.<br />
The Committee is of the opinion that adequate assistance should be<br />
immediately available at any site where an anaesthetist is expected to provide<br />
anaesthetic cover.<br />
Departments of anaesthesia should be supported in establishing reporting<br />
mechanisms that identify recurrent circumstances which result in the nonprovision<br />
of adequate assistance for the anaesthetist. Inadequacies thus<br />
identified should be discussed at a departmental level and reported to hospital<br />
managers as appropriate.<br />
Hospital managers should understand the critical importance of anaesthetic<br />
assistance and the dangers that the lack of trained and competent assistance<br />
poses to patient safety. It is the department of anaesthesia’s responsibility to<br />
make hospital management aware of any significant deficiencies. Service<br />
provision should not be undertaken in circumstances in which there is a<br />
resulting identified risk to patient safety. The department of anaesthesia
should be the recognised identifier of such risks and their recommendations<br />
on these matters should be acted upon.<br />
Anaesthetic Assistance Rostering<br />
As the majority of anaesthetic assistants are currently recruited from the nursing<br />
profession, the principle responsibility for rostering should remain with nurse<br />
managers. Communication between relevant departments of anaesthesia<br />
and nurse managers appears to be poor in many of the centres that replied<br />
to our survey. There appears to be significant potential for improvement in<br />
the communication between these key stakeholders. Early discussion about<br />
perceived inadequacies or potentially unsafe rostering practices should be<br />
encouraged.<br />
The skill mix of those individuals rostered for anaesthetic assistance duties<br />
should be discussed and agreed between nurse managers and the department<br />
of anaesthesia. Rostering from a dedicated pool of anaesthetic assistants<br />
is preferable to alternative arrangements. This will encourage a culture of<br />
anaesthetic safety awareness and service development. It is recommended<br />
that agency staff are not rostered to provide anaesthetic assistance.<br />
Rostering arrangements should be transparent. An agreed mechanism should<br />
be put in place to identify those areas in which anaesthetic assistance will<br />
be required on a daily basis. The anaesthetic assistant co-ordinator should<br />
meet with the anaesthetic co-ordinator on a daily basis to discuss service<br />
requirements. This meeting should identify those areas that have particular<br />
assistant requirements and it should identify those areas where no immediate<br />
assistance is rostered. Service planning can then take place in consultation<br />
with the duty anaesthetist rostered to provide anaesthesia.<br />
Anaesthetic Assistance Training<br />
The Committee notes the efforts that have been made at a local level to<br />
introduce training programmes and the success of certain individual training<br />
courses. However, the training of anaesthetic assistants varies widely<br />
throughout Ireland. There are no national, identifiable core competencies<br />
that an individual should attain before being considered a trained anaesthetic
assistant. As such there is little guidance available on who should be<br />
considered competent to act as an anaesthetic assistant. It is the opinion of<br />
the Committee that the lack of a national standard could contribute to errors<br />
or near misses during the peri-operative period. This is most critical in off-site<br />
or isolated areas.<br />
The Future<br />
The Committee recommends the development of a national core competencies<br />
programme consistent with the Scottish Medical and Scientific Committee<br />
published report “Core Competencies for the Anaesthetic Assistant” 4 as<br />
endorsed by the AAGBI. Such a development should identify a multidisciplinary<br />
group involving key stakeholders and should be funded as a Health Service<br />
Executive initiative guided by the Irish Standing Committee of the AAGBI<br />
and the College of Anaesthetists. A national training programme should be<br />
established to train a new generation of anaesthetic assistants. Consideration<br />
should be given to the entry into such a training program of individuals from<br />
non-nursing backgrounds. In the Committee’s opinion, a national training<br />
programme would result in a significant improvement in the quality of<br />
anaesthesia delivery in the Republic of Ireland. This is consistent with the<br />
views expressed in the Hanly Report 5 , “Teamwork in Anaesthesia” 1 and<br />
“Response to Hanly Report” 6 previously published by the AAGBI.
Appendix<br />
Anaesthetic Department Questionnaire<br />
Setting for Anaesthesia Cover<br />
Median [range]<br />
How many beds are in your hospital? 255 [69-680]<br />
How many ICU beds are in your hospital? 4.5 [0-26]<br />
How many theatres do you provide cover for? 2.5 [1-10]<br />
How many off-site locations do you provide cover for? 1 [0-4]<br />
Availability<br />
Is trained assistance for the anaesthetist available YES (37.5%)<br />
in every area that anaesthesia is provided? NO (62.5%)<br />
Is a trained assistant always present during anaesthesia? YES (25%)<br />
NO (75%)<br />
In what circumstances may an assistant not be available? (text entry)<br />
Are there any recurrent circumstances (location or time of YES ( 50%)<br />
anaesthesia) that cause your department particular difficulty? NO (50%)<br />
In the past year, have there been any instances of error or YES (25%)<br />
near miss that could be attributed to the non-availability NO (75%)<br />
of assistance in your department?
Rostering<br />
Who is responsible for the rostering of anaesthetic assistants? (text entry)<br />
Is assistance from dedicated pool of anaesthetic/ Dedicated 25%<br />
recovery nurses or from general pool of theatre nurses? General 75%<br />
Is this the same at night? YES 75%<br />
NO 25%<br />
Do you roster agency staff to provide assistance for the YES (0%)<br />
anaesthetist? NO (100%)<br />
What criteria do you employ when deciding who should<br />
be rostered to provide assistance for the anaesthetist? (text entry)<br />
In the past year, have there been any instances of error or YES (12.5%)<br />
near miss that could be attributed to the rostering of NO (87.5%)<br />
assistance in your department?<br />
Training<br />
Specify the anaesthesia assistance training that those personnel<br />
rostered for assistant duty have received.<br />
10
What training does your department provide for anaesthesia<br />
assistants? (text entry)<br />
In the past year, have there been any instances of error or YES 12.5%<br />
near miss that could be attributed to gaps in anaesthetic NO 87.5%<br />
assistance training in your department?<br />
The Future<br />
In your opinion:<br />
1. Is the current level of anaesthetic assistance adequate? YES 12.5%<br />
NO 87.5%<br />
2. Is non-nursing assistance for the anaesthetist acceptable? YES 75%<br />
NO 25%<br />
3. Where is the most appropriate place to base future<br />
anaesthetic assistance training programmes?<br />
University 12.5% College of Anaesthetists 62.5%<br />
School of Nursing 12.5% Individual hospitals 62.5%<br />
4. What, if any, are the barriers to providing adequate assistance for the<br />
anaesthetist? (text entry)<br />
11
References<br />
1. The Anaesthesia Team, Section 5 “Assistance for the Anaesthetist”<br />
(2005) – AAGBI guideline. http://www.<strong>aagbi</strong>.org<br />
2. Impact of Anaesthesia Management Characteristics on Severe<br />
Morbidity and Mortality Arbous, M Sesmu et al. Anesthesiology<br />
2005; 102: 257-68.<br />
3. Mental Health Act 2001, Section 59(2) “Rules Governing the Use of<br />
ECT”- (2006) Mental Health Commission R-S59 (2)/01/2006.<br />
4. Core Competencies for the Anaesthetic Assistant- (2006) Scottish<br />
Medical and Scientific Committee.<br />
5. The Hanly Report – June 2003.<br />
6. Response to Hanly Report – (2005) Irish Standing Committee<br />
AAGBI. http://www.<strong>aagbi</strong>.org<br />
12
13
21 Portland Place, London W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
The Newsletter<br />
of the<br />
Association<br />
of Anaesthetists<br />
of Great Britain<br />
and Ireland<br />
ISSN 0959-2962 No. 349<br />
AUGUST 2016<br />
SPECIAL ISSUE:<br />
Age and the<br />
Anaesthetist<br />
A report of a working party of the AAGBI, endorsed by the<br />
Royal College of Anaesthetists, with a joint editorial by Andrew Hartle,<br />
President, AAGBI and Liam Brennan, President, RCoA
The life changing<br />
POWER OF<br />
ULTRASOUND<br />
We believe in the power of visualisation: the life changing<br />
improvements to patient outcomes through ultrasound.<br />
We share that belief and vision with the clinicians who<br />
drive the capabilities and value of our products.<br />
Collaborative, connected, cost effective<br />
Our shared objectives are made real through an unremitting<br />
focus on quality, patient safety and value.<br />
The SonoSite family is built on four essential pillars: durability,<br />
reliability, ease of use and education. Connect with our<br />
community and bring the benefits of SonoSite excellence to<br />
your patients.<br />
For more information about these systems and SonoSite<br />
excellence visit www.sonosite.com/uk or contact your local<br />
customer service representative on 01462-341151.<br />
SonoSite iViz<br />
SonoSite X-Porte<br />
SonoSite SII<br />
SonoSite Edge II<br />
Editorial<br />
This issue of Anaesthesia News is devoted to print publication of ‘Age and<br />
the Anaesthetist’. Why has the AAGBI taken this unusual step? It is simply<br />
this: the single biggest challenge facing the NHS is to respond to the vastly<br />
increased demands of an ageing population, not just for our patients but<br />
also for the staff on whom they depend. Quick fixes balance the books; but<br />
recent 'bailouts' mixed cash with efficiencies so this is not sustainable long<br />
term. As more patients live even longer, real term funding per person must<br />
increase to maintain current service provision. Lifestyle changes and new<br />
drugs may both extend life further; one costs little, one (inevitably) costs lots.<br />
Commissioned and approved by the Board of the AAGBI, endorsed by<br />
Council of the RCoA, ‘Age and the Anaesthetist’ has a distinguished<br />
authorship led by former RCoA President Peter Hutton, whose original<br />
idea it was. What began as a lecture has evolved through being an AAGBI<br />
'glossy' to the comprehensive analysis of the impact of age on the individual<br />
anaesthetist, their clinical practice, patients, retirement and the wider NHS.<br />
What has emerged is unlike anything produced previously by either the<br />
AAGBI or the RCoA; devoted to a single topic like a guideline, closer in size<br />
to one of the GAT or SAS Handbooks.<br />
This publication could not be better timed. English trainees will soon have<br />
a new contract, although we now know it isn't one they have agreed.<br />
Negotiations on a new English consultant contract are advanced, but a final<br />
offer has yet to be made. Pension changes have already been introduced,<br />
with the ageing population as one of the major drivers. More people living<br />
longer with more comorbidities will undoubtedly put more strain on the<br />
affordability of healthcare and healthcare workers are not immune to these<br />
pressures.<br />
The implications for anaesthetists of these demographic changes are not<br />
just theoretical. We will all face clinical, personal, financial, ethical and many<br />
other challenges. Contract and pension changes mean all consultants<br />
starting in post today will have to work until they are at least 68 to receive<br />
their pension in full. That extra eight years of service compared to the status<br />
quo may be crucial in determining how those affected cope with longer<br />
working hours, on-call, or shift work. We both (aged 51 and 56) take much<br />
longer to recover from disturbed nights on-call, and would not relish more of<br />
the same in ten years time (and neither may our patients!)<br />
Anaesthetists are not age-immune. Increasing pensionable ages mean all<br />
stakeholders must acknowledge that consultants (or SAS doctors) at 35 and<br />
65 have different and varying mental and physical strengths (particularly<br />
around 24/7 service) which must be intrinsic to job and career plans.<br />
The NHS* evolves in response to the electoral cycle as much as service<br />
needs. It now needs a long-term, sustainable strategy agreed openly by<br />
all major political parties, or to be removed from party politics. Other areas<br />
affecting generations (climate change, pollution, energy and water supply,<br />
pensions) suggest it sometimes requires a disaster to effect change.<br />
Our specialty doesn’t need to wait for a disaster; we hope ‘Age and the<br />
Anaesthetist’ may play a major part in guiding decision-making by our<br />
members, employers and politicians as they prepare themselves and the<br />
NHS for whatever the future holds.<br />
Contents<br />
1.0: Executive Summary 04<br />
2.0: Introduction – what is the problem? 05<br />
3.0: Societal changes and financial issues 06<br />
3.1: Life expectancy 06<br />
3.2: Financial provision for retirement 07<br />
3.3: The current conflicted situation 09<br />
4.0: Age, physiological changes and comorbidities 10<br />
4.1: The ageing process and its impact on<br />
organ function 10<br />
4.2: The role of comorbidity 12<br />
4.3: Healthy life expectancy and survivorship<br />
in good health 13<br />
4.4: Summary of key factors 13<br />
5.0: Workforce patterns and workforce issues 14<br />
5.1: Time in employment and retirement patterns<br />
of the general population 14<br />
5.2: Employment patterns and the retirement<br />
intentions of medical staff 15<br />
5.3: Wellbeing at work: making work possible 16<br />
5.4: The public’s expectations of older professionals 17<br />
5.5: Other professional groups and human factors 19<br />
6.0: Implications for the future: practical aspects<br />
to be addressed 21<br />
6.1: Considerations for the anaesthetist 21<br />
6.2: Considerations for the employer 23<br />
6.3: The role of the Government 25<br />
6.4: The role of the public 26<br />
Appendix 1: Working party members 26<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
21 Portland Place, London W1B 1PY<br />
Telephone: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: anaenews@<strong>aagbi</strong>.org<br />
Website: www.<strong>aagbi</strong>.org<br />
Anaesthesia News<br />
Managing Editor: Upma Misra<br />
Editors: Phil Bewley (GAT), Nancy Redfern, Richard Griffiths, Sean Tighe,<br />
Mike Nathanson, Rachel Collis, Felicity Platt, Gerry Keenan and Elizabeth McGrady<br />
Address for all correspondence, advertising or submissions:<br />
Email: anaenews@<strong>aagbi</strong>.org<br />
Website: www.<strong>aagbi</strong>.org/publications/anaesthesia-news<br />
Andrew Hartle<br />
President, AAGBI<br />
Liam Brennan<br />
President, RCoA<br />
Editorial Assistant: Rona Gloag<br />
Email: anaenews@<strong>aagbi</strong>.org<br />
Design: Chris Steer<br />
AAGBI Website & Publications Officer<br />
Telephone: 020 7631 8803<br />
Email: chris@<strong>aagbi</strong>.org<br />
Printing: Portland Print<br />
SONOSITE and the SONOSITE logo are trademarks and registered trademarks of FUJIFILM SonoSite, Inc. in various jurisdictions.<br />
FUJIFILM is a trademark and registered trademark of FUJIFILM Corporation in various jurisdictions. All other trademarks are the property of their respective owners.<br />
Copyright © 2016 FUJIFILM SonoSite, Inc. All rights reserved. Subject to change. 2422 04/16<br />
*it is likely that the future will see<br />
divergence of the taxation, funding and<br />
political models of the NHS in England<br />
Copyright 2016 The Association of Anaesthetists of Great Britain and Ireland<br />
The Association cannot be responsible for the statements or views of the contributors.<br />
No part of this newsletter may be reproduced without prior permission.<br />
Advertisements are accepted in good faith. Readers are reminded that<br />
Scotland, Wales and Northern Ireland.<br />
Anaesthesia News cannot be held responsible in any way for the quality<br />
Anaesthesia News August 2016 • Issue 349<br />
or correctness of products or services offered in advertisements. 3
Age and the<br />
Anaesthetist<br />
1.0: Executive Summary<br />
• The effects of ageing are inevitable, but the rates of physical<br />
and psychological change are highly variable from person<br />
to person. A one-size retirement strategy cannot fit all and<br />
necessarily be compatible with patient safety. Although the<br />
volume of data is small, there is evidence emerging that the<br />
anaesthetist’s age per se, could be a risk factor for anaesthetic<br />
safety.<br />
The report of a working party of the AAGBI*<br />
Working Party Members<br />
Peter Hutton (Chair)<br />
Mary Baker MBE<br />
Carol Black DBE<br />
Tony Giddings<br />
Richard Griffiths (AAGBI)<br />
William Harrop-Griffiths (RCoA)<br />
Guy Hirst<br />
Nancy Redfern (AAGBI)<br />
David Shipway<br />
*This report has been endorsed by the Royal College of Anaesthetists<br />
For citation purposes:<br />
Hutton P, Baker M, Black C, et al. Age and the Anaesthetist. AAGBI<br />
Working Party Report. March 2016. Anaesthesia News 2016; 349: 3-27.<br />
‘Every generation<br />
Blames the one before<br />
And all of their frustrations<br />
Come beating on your door’<br />
• There are considerable benefits to be obtained from reviewing<br />
how other safety-critical industries, such as airline, nuclear<br />
power, transport, fire-fighting, and oil extraction, have managed<br />
the problems of the ageing employee. These have involved<br />
considerations of hours of work, optimisation of the workplace<br />
and competence testing.<br />
• The NHS, as the major employer of anaesthetists, has an onus<br />
upon it to anticipate the demographic workforce changes<br />
that will parallel the planned increases in retirement age and<br />
to make appropriate adjustments to the working environment,<br />
working practices and the job plans of older workers.<br />
• As the public ages, the proportion of patients with significant<br />
comorbidities who require anaesthesia will increase. Older<br />
anaesthetists will need to remain capable of managing this<br />
population. Given the current nature of annual appraisal and<br />
revalidation, the possibility of introducing processes to confirm<br />
workplace competency needs to be considered.<br />
• The public has a reasonable expectation that professional<br />
groups will manage their practitioners to ensure they are<br />
capable of undertaking the duties for which they are employed.<br />
It is important that anaesthesia acts now to anticipate the<br />
problems of the future. Leaving things to natural evolution and<br />
chance is a too high-risk strategy to be compatible with both<br />
patient safety and the best interests of individual anaesthetists.<br />
• The implications of increased life expectancy and economic<br />
projections have resulted in unprecedented pressures on the<br />
long-term payment of state and salary-related pensions.<br />
• There are demonstrable positive returns in wellbeing and<br />
income from remaining in employment, but the effects of<br />
removing a mandatory retirement age on safety-critical jobs,<br />
such as that of an anaesthetist, have not been evaluated.<br />
• Current retirement patterns in medicine may well reflect ‘selfselection’<br />
in terms of an individual being able to carry out the<br />
demands of a consultant post safely. From the best available<br />
data, > 40% of consultants expressed an intention to retire<br />
between 56 and 60, with a similar percentage intending to<br />
go before 65 years. Only 3% intended to continue beyond<br />
65 and at present the over-65s on the UK’s General Medical<br />
Council (GMC) register represent £115 billion and is increasingly difficult to contain.<br />
The combination of these factors and their projected costs is a huge<br />
burden for current and future governments. The single most effective<br />
strategy to manage the increasing costs is simply to decrease the<br />
period for which government-funded pensions (work-related and<br />
basic state) are paid to individuals. Since it is not possible to affect<br />
the date of death, this has resulted in the UK Government increasing<br />
the retirement age for both the basic state pension [4] and public<br />
sector salary schemes, and increasing a person’s monthly financial<br />
contributions to the latter.<br />
These changes will impact on medical staff in two ways:<br />
• In order to make adequate pension provision for their own future,<br />
they may have to stay in work longer than they had intended.<br />
• The patient population will age and present with more<br />
comorbidities, adding greater complexity to routine surgical<br />
procedures.<br />
Increasing the retirement ages of medical staff in the presence<br />
of greater patient complexity is an open-ended experiment with<br />
considerable potential for adverse outcomes for all concerned.<br />
It is important for those in work to understand the implications for<br />
themselves in providing finance for their retirement while retaining a<br />
high quality of delivery of care, and for employers to make changes<br />
that enable older workers to remain at work.<br />
This report on Age and the Anaesthetist looks at the various facets of<br />
this new social and professional construct with a view to assessing<br />
and anticipating its impact on our specialty and its practitioners. In<br />
doing so, it not only evaluates the consequences for anaesthetists<br />
themselves, but also touches on the implications for the wider<br />
workplace environment and for other staff with whom we work.<br />
Note: All references in this document can be found<br />
with the online version of this issue<br />
Mike and the Mechanics, 1988<br />
www.<strong>aagbi</strong>.org/AgeandtheAnaesthetist<br />
4 Anaesthesia News August 2016 • Issue 349 Anaesthesia<br />
Anaesthesia<br />
News<br />
News<br />
August<br />
August<br />
2016<br />
2016 • Issue<br />
Issue<br />
349<br />
349 5
3.0: Societal changes<br />
and financial issues<br />
3.1: Life expectancy<br />
Life expectancy is defined as the average number of years of life<br />
remaining at a particular age. It is a blunt metric that when applied to<br />
the newborn is used to describe the average duration of life of a defined<br />
population set. It includes many factors including infant mortality,<br />
country, profession, gender, the supply of food, the effects of wars and<br />
epidemics, and the diseases associated with age. Importantly, what<br />
total life expectancy at birth does not do is to predict with any accuracy<br />
the age at which those who have reached adulthood actually die.<br />
It is frequently stated that over millennia, life expectancy has continued<br />
to increase. While statistically true, this unrefined statement conceals<br />
the causes of this trend. There are many cases in ancient history of<br />
people living to an age which would meet current expectations.<br />
Sophocles died aged 90 in 406 BC, and Socrates died aged 70 in<br />
399 BC. This anomaly of the typical age at death differing from life<br />
expectancy is clearly explained in the figure below 1 which plots the<br />
probability of dying against age in ancient Rome.<br />
1000 live births – the lowest rate on record. This compares with 11.1<br />
deaths in 1981, a 62% decrease. In the last 15–20 years, there has<br />
however, been a marked change in society’s demographics that has<br />
been due to the increasing numbers of adults surviving into old age,<br />
i.e. a genuine increase in life expectancy based on longevity rather than<br />
improvements in child and maternal health. Data from the UK’s 2011<br />
Census [5] showed that in England and Wales, 1 in 6 of the population<br />
was aged > 65 years, whereas only 1 in 16 of the population was<br />
aged < 5 years. The current life expectancy in the UK as people age is<br />
shown in the table below.<br />
Life expectancy by sex and age. National Life Tables, Office for<br />
National Statistics, UK, 2011–2013<br />
Current age; years<br />
Male life<br />
expectancy;<br />
years<br />
40 40.3 43.6<br />
45 35.6 38.8<br />
Female life<br />
expectancy;<br />
years<br />
50 31.0 34.1<br />
Probability of death<br />
The probability of dying at a given age in the Roman Empire<br />
It can be seen that, at birth, the infant mortality rate was over 1 in 3,<br />
yet for those who survived birth, this rate of mortality did not return<br />
until > 60 years of age. The death rate from 15–35 years of approximately<br />
10% was the effect of warfare on men and maternal death in women.<br />
Since antiquity, infant mortality has steadily decreased, and with it both<br />
the average life expectancy at birth and the size of the population have<br />
increased. In the UK, the infant mortality rate in England and Wales<br />
continues to decrease; in 2011, there were just 4.2 infant deaths 2 per<br />
55 26.6 29.5<br />
60 22.3 25.1<br />
65 18.3 20.8<br />
70 14.5 16.7<br />
75 11.2 13.0<br />
80 8.2 9.6<br />
85 5.8 6.8<br />
This trend, first noted over two decades or so ago, continues. For both<br />
mortality and disability, overall health has improved substantially in<br />
absolute terms in the UK between 1990 and 2010. During this period,<br />
life expectancy increased by 4.2 years [6]. Illustrative projections are<br />
as follows:<br />
• About one-third of babies born in 2012 in the UK are expected to<br />
survive to celebrate their 100th birthday.<br />
• More than 95,000 people aged 65 in 2012 are expected to<br />
celebrate their 100th birthday in 2047.<br />
• The total number of centenarians is projected to rise from 14,500<br />
in 2012 to 110,000 in 2035.<br />
• 10% of current 65-year-old males and 15% of current 65-year-old<br />
females will become centenarians.<br />
As the population ages and more people become economically inactive<br />
(discussed more fully in Section 3.3), more of the burden of providing<br />
public finance from taxation falls on the young, who are decreasing in<br />
number. This is a major funding problem for the Government.<br />
This trend towards an older population with a higher median age<br />
and requiring more taxable income from the young for its support is<br />
also true worldwide, as shown in the diagram below from the World<br />
Health Organization [7]. In 2010, an estimated 524 million people<br />
were aged 65 or older (8% of the world’s population). By 2050, this<br />
number is expected to nearly triple to about 1.5 billion, representing<br />
16% of the world’s population. Although developed countries have the<br />
oldest population profiles, the vast majority of older people – and the<br />
most rapidly ageing populations – are in less developed countries.<br />
Between 2010 and 2050, the number of older people in less developed<br />
countries is projected to increase more than 250%, compared with a<br />
71% increase in developed countries. This raises major issues for<br />
overseas aid policies.<br />
3.2: Financial provision for retirement<br />
Private pensions<br />
The plight of those having insufficient funds to live out their life in relative<br />
comfort was first addressed in the 18th century by the Presbyterian<br />
Church in Scotland. Under the Law of Ann (1672), the widow and<br />
children of a deceased minister of the Church of Scotland received<br />
only half a year’s stipend in the year of the minister’s death. After that<br />
they faced penury. Two ministers, Robert Wallace and Andrew Webster,<br />
along with the Professor of Mathematics at Edinburgh, Colin Maclaurin,<br />
decided to tackle this injustice.<br />
In gathering data they found that there were approximately ‘930<br />
ministers in life at all times’, of whom ‘27 died yearly’, leaving ‘280<br />
widows living at any one time’ [8]. From annual premiums paid by<br />
ministers, the Fund for a Provision for the Widows and Children of the<br />
Ministers of the Church of Scotland 3 was established. The contributions<br />
were set at a level so that, when invested, there was sufficient income<br />
to meet the payments to the beneficiaries. This was the first actuarial<br />
forecast to determine what contributions had to be made during one’s<br />
working life to provide for benefits during retirement or after death.<br />
As such, it formed the model for innumerable other ‘fully-funded’<br />
independent schemes. The Universities Superannuation Scheme, and<br />
most industrial company and private pensions, are structured in this<br />
way. Many clinical academics are in the Universities Superannuation<br />
Scheme.<br />
As a result of the increasing longevity of new entrants, most of these<br />
actuarially-determined private pensions are moving away from final<br />
salary benefits (where the pension is a proportion of the final salary<br />
determined by the number of years of contributions), to defined benefit<br />
schemes where the returns relate to the individual’s total contributions<br />
made and estimated years of life rather than the final salary.<br />
1<br />
Figure taken from the work of Parkin and presented by Harlow M, Laurence R. Growing Up and Growing Old in Ancient Rome. London: Routledge, 2002. Fig 1.1, p 9.<br />
2<br />
An infant death is defined as the death of a child aged less than 1 year old.<br />
3<br />
This grew steadily from its inception to become the general insurance and pension fund now known as Scottish Widows.<br />
6 Anaesthesia News August 2016 • Issue 349 Anaesthesia News August 2016 • Issue 349 7
The pace of private pension reform has accelerated over the past<br />
decade. The Pensions Act 2008 instructed that all employees over 22<br />
years of age and below the state pension age 4 should be automatically<br />
enrolled into a qualifying workplace pension scheme between 2012<br />
and 2016. From October 2017, all private sector employers have<br />
to contribute a minimum of 3% to an employee’s pension with the<br />
employee contributing at least 4%.<br />
‘Old-age’ or basic state pensions<br />
In the UK an ‘old-age’ or basic state pension is paid from current<br />
taxation to everybody reaching the state pension age who has made<br />
compulsory or voluntary National Insurance contributions during the<br />
whole or part of their working lifetime.<br />
Publically funded pensions of this type, which aimed to provide<br />
support during the life remaining when work was no longer possible,<br />
were introduced (probably as a political manoeuvre to wrong-foot his<br />
socialist opponents) by Bismarck, the Chancellor of Germany, in the<br />
Old Age and Disability Insurance Bill of 1889. This provided a state<br />
pension funded jointly by those in work and the state for all those<br />
retired from work and > 70-years-old. Less than 10% of the population<br />
lived to benefit.<br />
In Britain at the beginning of the 20th century, the only general<br />
support for old age was the Poor Law. None but a small number of<br />
people received a proper pension or had made private insurance<br />
provision. The consequent extent of poverty in the elderly resulted in<br />
Lloyd George’s Old Age Pensions Act (1908) [9], which paid a noncontributory,<br />
means-tested pension to each person aged over 70 from<br />
1 January 1909. Through a series of subsequent legislative initiatives<br />
over ensuing years, the pensionable age was set at 60 for women and<br />
65 for men. The National Insurance Act (1946) created a universal<br />
social insurance system based around flat-rate benefits (at the same<br />
level for all contingencies) in return for flat-rate contributions. This still<br />
forms the basis for the current basic state pension. On average, the<br />
benefits from the basic state pension represent over half the incomes<br />
of those currently retired [10].<br />
Of great importance in state-funded pensions is the ‘support ratio’,<br />
which is an important indicator of the pressures that demographics<br />
pose for a state pension system. It measures how many people there<br />
are of working age (20–64 years) relative to the number of retirement<br />
age (over 65 years): this is effectively the ratio of the number of<br />
economically active people in relation to those drawing benefits. Data<br />
from the Organisation for Economic Co-operation and Development<br />
[11] shows the following for the UK from 1950 to 2050.<br />
Year<br />
Support ratio<br />
1950 7.2 to 1<br />
1980 5.1 to 1<br />
2010 3.5 to 1<br />
2050 1.8 to 1<br />
It is clear that the situation pertaining to when the welfare state started<br />
is very different from that today, and things will get steadily worse.<br />
Sometime before 2050, on average, two working people will be paying<br />
the full basic state pension for one retired person.<br />
To manage these unprecedented trends, the Pensions Act (2007)<br />
introduced a number of changes to state pensions. The most important<br />
was to provide for gradual increases in the state pension age for men<br />
and women, from 65 to 68 between 2024 and 2046. The Pensions Bill<br />
(2011) speeded up the pace of the increases of the 2007 Act: women’s<br />
state pension age would rise to 65 by November 2018 and for both<br />
4<br />
This is the age determined by government at which the basic state pension will be paid.<br />
men and women would reach 66 by 2020. The 2013/14 Pensions Bill<br />
and the Chancellor's 2013 Autumn Statement set out a framework<br />
within which the state pension age would be regularly reviewed in the<br />
future. They anticipated that an increase to 68 years and, later, to 69<br />
years would occur sooner than in previous estimates.<br />
Public sector employment pensions<br />
It has been the norm for many years for employees in the public sector<br />
to be enrolled automatically in a final salary pension scheme. However,<br />
there are no individual ‘pension pots’ with people’s names on them; the<br />
pension contributions made over a professional lifetime are not saved<br />
as hypothecated taxes for future use. Furthermore, even if there were<br />
proper ‘pension pots’, the total contributions throughout life would not<br />
meet the lifetime benefits.<br />
The NHS (and the public sector in general) thus has an ‘unfunded’,<br />
or ‘pay-as-you go’, scheme paid out of general taxation as part of the<br />
cost of providing public services. In its elemental form this is essentially<br />
a Ponzi scheme whereby younger workers pay taxes to support<br />
those who have retired. Long-term, such a scheme only works when<br />
the population is growing and when most retirees do not live for too<br />
long. When there is a national financial crisis or low economic growth<br />
combined with a simultaneous increase in beneficiaries, maintaining<br />
these payments is a major problem for the Government.<br />
The four largest pay-as-you-go public sector schemes [12] are:<br />
• The Armed Forces Pension Scheme (covering the UK).<br />
• The Principal Civil Service Pension Scheme (for England, Scotland,<br />
Wales and some employees in Northern Ireland).<br />
• The NHS Pension Scheme (for England and Wales).<br />
• The Teachers’ Pension Scheme (for England and Wales).<br />
These four schemes have accounted for over 75% of total payments<br />
from UK public service pay-as-you-go pension schemes in recent<br />
years. They are all of the defined benefit type, in which the pension<br />
that a retired employee receives depends on the final salary earned<br />
and the number of years of service. In accordance with their terms and<br />
conditions, the schemes usually pay a lump sum when an employee<br />
retires, followed by a regular pension until the death of the pensioner<br />
and any eligible dependents. Combined, the schemes had 6.5 million<br />
members at 31 March 2009, comprising 2.75 million current staff, 1.59<br />
million previous employees who had earned pensions but were not yet<br />
eligible to draw them, and 2.13 million pensioners, i.e. there were fewer<br />
people contributing than there were those eligible to draw benefits.<br />
These schemes have a major current and future funding problem. Total<br />
payments to pensioners in the four schemes increased by 38% (a 26%<br />
real-terms increase), in the decade from 2000 to 2010, the dominant<br />
factor being the 23% increase in the number of pensions paid.<br />
3.3: The current conflicted situation<br />
Through legislation, the Government sets:<br />
• An annual allowance for the maximum amount of pensionable<br />
contributions that qualify for tax relief in any one year.<br />
• A cap (the lifetime allowance) on the maximum total pension assets<br />
an individual can hold without incurring extra tax on its benefits.<br />
The Finance Act (2011) contained a number of changes to the tax<br />
regime for both private and public sector funded pensions of which the<br />
most important were:<br />
• A decrease in the annual contributions allowance from £255,000 in<br />
2010/11 to £50,000 from 2011/12 onwards.<br />
• A decrease in the lifetime allowance from £1.8 million to £1.5 million<br />
from April 2012. Any amounts in excess of the lifetime allowance<br />
are subject to a tax charge of 25% (in addition to income tax) if the<br />
benefits are paid as a pension, or a 55% tax charge if they are paid<br />
as a lump sum.<br />
For many NHS doctors (and especially those who have made additional<br />
private pension provision), the lifetime allowance is being reached in<br />
their late 50s or early 60s. It is calculated as 5 :<br />
Private pension assets + NHS lump sum + (20 x the annual NHS<br />
pension)<br />
For a doctor with no additional private pension, retiring from an annual<br />
salary of £100,000 per annum with 40 years’ contributions results in a<br />
lifetime allowance of:<br />
£150,000 (lump sum) + (20 x £50,000) = £1,150,000<br />
The lifetime allowance was introduced in 2006 at a level of £1.5 million.<br />
It then increased each year to 2010, when it reached a level of £1.8<br />
million. Since 2010, there have been a number of pension reforms that<br />
have led to the lifetime allowance being further reduced. The current<br />
level of the lifetime allowance in the 2015–16 tax year is £1.25 million and<br />
this will reduce further to £1 million from April 2016 6 as the Government<br />
tries to decrease its expenditure on pension tax relief.<br />
The financial paradox of this for doctors and other professionals (who<br />
in relation to the general population have earnings and pension benefits<br />
well into the upper quartile), is that whereas the Government would<br />
like them to continue to work and contribute to the economy through<br />
productivity and taxation (to optimise pension returns and minimise<br />
tax contributions), they are retiring on financial grounds while still fit for<br />
work. Some, but not all, return to work after retirement. In this situation,<br />
once having officially retired and returned, the new contract will have no<br />
continuation of time-accumulated benefits such as sick leave.<br />
As a result of the progressive cost of meeting retirement benefits, public<br />
sector schemes have recently undergone significant modifications.<br />
Following changes for new joiners and existing members who opted to<br />
convert in 2008, on 1 April 2015 the NHS pension scheme was modified<br />
again [13]. The 2015 NHS Scheme is a Career Average Revalued<br />
Earnings scheme. This is a form of defined benefit pension scheme,<br />
which means you get a guaranteed level of benefit at retirement payable<br />
according to a fixed formula related to totalled annual contributions.<br />
In a Career Average Revalued Earnings scheme, your pension reflects<br />
your pensionable pay throughout your career. The pension you earn<br />
each year is based on actual pensionable pay in that ‘scheme year’<br />
and is increased by a set rate linked to inflation (known as ‘revaluation’)<br />
each year up to retirement or leaving. A ‘scheme year’ runs from 1 April<br />
of one year to 31 March of the following year. The final pension payable<br />
is calculated by adding together the revalued pensions earned in each<br />
year of membership. Under these new arrangements:<br />
• The normal pensionable age at which benefits can be taken<br />
without reduction is the same as the state pension age at that time,<br />
i.e. the normal NHS ‘contributory’ pensionable age will increase as<br />
set by the future legislation that defines the state pensionable age.<br />
At present, this means it will be 66 years for both men and women<br />
by 2020.<br />
• Employees can contribute until they are 75.<br />
• Members’ contributions vary from 5% to 14.5% (increasing with<br />
salary), and the employer pays 14%. The Government has reserved<br />
the right to alter these figures.<br />
• The Pensions Policy Institute estimates that reforms to the NHS<br />
pension schemes will decrease the average value of the benefit<br />
offered across all scheme members by more than a third [14].<br />
• An important feature of the new scheme is that because pension<br />
benefits are accumulated annually, it more easily allows for career<br />
breaks and for reduced hours closer to retirement age.<br />
In summary, the current situation is confusing. On the one hand, the<br />
imposition of the lifetime allowance on existing final salary schemes is<br />
encouraging earlier retirements for high earners such as consultants.<br />
On the other hand, the future will see higher contributions, lower benefits<br />
and an increasing age at which contributory and state pensions will be<br />
paid. Furthermore, the application of the lifetime allowance will decrease<br />
the appetite for making further conventional private pension provision.<br />
It is clear that future arrangements will not match the traditional NHS<br />
pension benefits. The age of retirement will increase and individuals<br />
will be increasingly responsible for their own financial provision in<br />
retirement.<br />
Very importantly, the effect of the proposed changes on the health of<br />
older consultants, their ability to maintain complex sophisticated skills<br />
and their ability to care for an increasingly complex patient population<br />
appears not to have been considered.<br />
5<br />
The annual pension is multiplied by 20 to calculate the ‘virtual pot’ that would be required to generate the value of the annual pension from an annuity at 5%. Since the global<br />
financial crisis there have been very low or zero interest rates, but the multiplier has not been adjusted. If it ever were to be adjusted, the effect on tax payable on pension income<br />
could be considerable.<br />
6<br />
Data from the Pensions Advisory Service. http://www.pensionsadvisoryservice.org.uk<br />
8 Anaesthesia News August 2016 • Issue 349 Anaesthesia News August 2016 • Issue 349 9
4.0: Age, physiological<br />
changes and comorbidities<br />
4.1: The ageing process and its impact<br />
on organ function<br />
The ageing process<br />
Ageing is a complex biological process that remains inadequately<br />
understood. It is characterised by a progressive decrease in organ<br />
reserve that increases the vulnerability of an individual to organ<br />
dysfunction and failure. However, ageing is very unpredictable and<br />
its effects are heterogeneous. Genetic factors interact with those of<br />
the environment to influence both rate and extent of ageing. Twin<br />
concordance studies suggest that 25% of ageing variation can be<br />
accounted for by genetics, while 50% is due to environmental factors<br />
[15–18]. While a range of environmental agents is known to play a role,<br />
how these will affect the ageing of each exposed individual is extremely<br />
difficult to predict. The average progress of ageing in a cohort is<br />
predictable, but the individuals within it show large and unpredictable<br />
variability.<br />
Impact of ageing on organ function<br />
Ageing may affect physical performance in three broad categories:<br />
1. Disruption of physiological rhythms. Physiological circadian<br />
rhythms such as sleep and endocrine axes are altered with ageing.<br />
2. Loss of physiological complexity. Results in functional decline<br />
of the organism by diminishing the range of available, adaptive<br />
responses to the innumerable stressors of everyday life [19].<br />
3. Homeostenosis. This represents the progressive loss<br />
of physiological reserves and inability to compensate for<br />
physiological stressors. Its most extreme manifestation is frailty.<br />
In the frail individual, most physiological reserves are employed to<br />
maintain basal organ function. A subsequent external challenge<br />
may result in loss of organ function. In the frail, this typically<br />
presents with failure of complex neurophysiological processes<br />
such as ambulation, balance, continence and cognition. This is<br />
shown as a conceptual graphic below [20].<br />
The processes of ageing are diverse and, even before a state of frailty<br />
is reached, ageing can affect physical performance. Circadian rhythm<br />
disruption and an inability to adapt to changes in the sleep-wake cycle<br />
may have implications for 24-hour working in advanced age [21].<br />
Cardiovascular changes include those of anatomical and decreased<br />
physiological variation in heart rate [22]. Both these lead to an overall<br />
reduction in cardiovascular peak performance [23]. Similar changes<br />
are seen across other key organ systems, e.g. ageing also affects<br />
parameters of pulmonary function with decreases seen in the forced<br />
expired volume in one second (FEV1) and the forced vital capacity [24].<br />
Neurological ageing is characterised by neuronal loss and decrease in<br />
white matter volume [25]. Changes also occur at a cellular level, with<br />
reduction in receptor expression and neurotransmitter function [26].<br />
These factors translate into measurable neurocognitive parameters,<br />
including decreases in cognitive processing speed [27].<br />
Decreased neurocognitive testing performance is seen with advancing<br />
age in a range of cognitive domains [28], but particularly within<br />
executive planning and function. Presbyacusis [29] and presbyopia<br />
[30] may also affect sensory input into the ageing neurological system<br />
[31]; this may synergistically combine with neurocognitive ageing to<br />
affect physical performance.<br />
The effects on the major organ systems are summarised in the table<br />
below [32].<br />
While physical changes are unlikely to affect the ability of an<br />
anaesthetist to function on a day-to-day basis in the workplace, the<br />
equivalent subtle changes in neurological, sensory and cognitive<br />
function may be of greater significance. Also, individuals ageing even<br />
at normal rates [33] may only rarely be exposed to stressor events of<br />
sufficient magnitude to unmask the loss in neurophysiological reserve.<br />
It would be bad for patient safety if such a situation arose unexpectedly<br />
during anaesthesia.<br />
Homeostenosis and frailty<br />
Age related physiological changes<br />
(adapted from Chester & Rudolph [32])<br />
Mechanism of<br />
change<br />
Molecular,<br />
structural and<br />
organ level<br />
changes and<br />
systemic<br />
effects<br />
Blood pressure Pulse and cardiac output Respiratory Hormonal/immunological<br />
• oxidative and<br />
mechanical<br />
damage to vascular<br />
endothelium<br />
• heightened<br />
inflammatory<br />
response from<br />
cytokines, growth<br />
factors, collagen,<br />
elastases and<br />
proteinases<br />
• decreased arterial wall<br />
pliability<br />
• increased left<br />
ventricular wall<br />
thickness<br />
• diastolic dysfunction<br />
• increased pulse<br />
pressure<br />
• desensitisation of<br />
sympathetic receptors<br />
disrupts intracellular<br />
signalling<br />
• decreased baroreflexes<br />
• delayed responses<br />
• decreased cardiac<br />
output and increased<br />
resting heart rate<br />
• maximum heart rate is<br />
more limited with age<br />
• increased elastases<br />
degrade elastic tissue<br />
and reduce compliance<br />
with dilation of<br />
airspaces<br />
• altered chest wall shape<br />
• increased work of<br />
breathing<br />
• altered diaphragm<br />
shape<br />
• decreased compliance<br />
• air trapping with<br />
increased residual<br />
volumes and decreased<br />
tidal volumes<br />
• increased respiratory<br />
rate compensates for<br />
less tidal volume<br />
• decreased T-cell function<br />
with reduced immunity<br />
• changes in hypothalamic<br />
activity<br />
• Increase in dysfunctional/<br />
deficient hypothalamic<br />
mineralocorticoid receptors<br />
• increased night-time<br />
cortisol levels<br />
• reduced ability to maintain<br />
body heat with less<br />
subcutaneous fat, reduced<br />
peripheral vasoconstriction<br />
• dysregulated circadian<br />
rhythm<br />
• loss of muscle mass<br />
10 Anaesthesia News August 2016 • Issue 349 Anaesthesia News August 2016 • Issue 349 11<br />
Compensation<br />
to stress<br />
• reduction in<br />
• less sympathetic • weakened respiratory • loss of heat maintenance<br />
endogenous cellular responsiveness<br />
muscles, less<br />
and thermogenesis<br />
repair capability<br />
hinders ability of<br />
compliant chest wall,<br />
mechanisms with<br />
due to damaged<br />
cardiovascular system and increased work<br />
heightened vulnerability to<br />
cardiomyocytes and to adjust when<br />
of breathing diminish<br />
hot and cold stressors<br />
vascular endothelium stimulated<br />
ability to adapt to stress • lower core body<br />
• altered intracellular • less adaptability in • less sensitivity of<br />
temperature hinders<br />
protein expression<br />
heart rate is associated chemoreceptors and<br />
ability to regulate body<br />
• mitochondrial ageing with falls, frailty<br />
mechanoreceptors<br />
temperature<br />
and changes in signal<br />
causes decreased<br />
transduction cascades<br />
response to hypoxia<br />
• loss of responsiveness<br />
and hypercapnia<br />
to sympathetic stimuli<br />
Age related physiological changes (adapted from Chester & Rudolph [32])
4.2: The role of comorbidity<br />
The relationship between comorbidity and age<br />
Though the processes of ageing result in loss of physiological reserve,<br />
primary organ failure and disease are not considered parts of the normal<br />
ageing process. However, the accumulation of chronic comorbidity,<br />
and importantly multimorbidity, is closely associated with advancing<br />
age. Not only is the presence of comorbidity associated with increased<br />
mortality, but so is poor health and physical function. Data reporting<br />
the prevalence of multimorbidity have historically been scarce. A recent<br />
landmark UK population study [34] reported that by the age of 50, half<br />
the population had acquired at least one comorbidity, with 65% having<br />
multimorbidity by the age of 65.<br />
Impact of ill health and comorbidity on the ability to work<br />
The presence or absence of comorbidity is of limited use in determining<br />
its effect on an individual’s ability to function in the workplace. Although<br />
reported limitation is more useful, this depends on the role fulfilled by<br />
that individual. The application of population-wide data to a highly<br />
selected population of anaesthetists with a very specific defined skillset<br />
therefore has its weaknesses. However, the data sources quoted above<br />
and immediately below describe high rates of impaired dexterity (8%),<br />
stamina (11%) and mobility (13%) within the working population, which,<br />
importantly, increase significantly after the age of 65. These may have<br />
implications for anaesthetists towards the end of their working life.<br />
Effects of physical or mental health conditions lasting > 12<br />
months. Office for National Statistics, UK, 2013<br />
4.3: Healthy life expectancy<br />
and survivorship in good health<br />
Despite the presence of significant longstanding disability and limitation<br />
of function, life expectancy in the UK continues to increase. At the age<br />
of 65, life expectancy ranges from 18 years for men to 20.7 years for<br />
women. Approximately 60% of this further life expectancy will be spent<br />
in good health, indicating that the current conventional retirement age<br />
does not reflect impending disability and poor health status. Data from<br />
the Office for National Statistics are shown below [36].<br />
Projected survival, health status and disability at birth and<br />
65 years. Derived from self-reported prevalence of limiting<br />
longstanding illness and disability data (2009–11) and life<br />
expectancy tables (2011–13). Office for National Statistics, UK.<br />
Multimorbidity and age<br />
Longstanding limiting illness and disability<br />
Percentage of physical parameters affected by physical or mental<br />
health, by age<br />
Affected<br />
parameter<br />
Age<br />
25–44; %<br />
Age<br />
45–64; %<br />
Age<br />
65–74; %<br />
Age ><br />
75; %<br />
Sex<br />
Healthy life expectancy at birth<br />
Life<br />
expectancy;<br />
years<br />
Healthy life<br />
expectancy;<br />
years<br />
Actual<br />
years of<br />
‘not good’<br />
health<br />
Proportion<br />
of life<br />
spent<br />
in good<br />
health; %<br />
In addition to physical health problems, mental health disorders<br />
increase in prevalence with age. They are closely associated with<br />
combined physical and mental comorbidity, which is present in 18%<br />
of patients ≥ 65. Although these patients are at or above current<br />
retirement age, this study also found that nearly two thirds of people<br />
with combined physical and mental health comorbidity were aged <<br />
65 years. Although multimorbidity is more prevalent in older people,<br />
approximately half of the multimorbid population in the UK is aged<br />
below 65. This indicates that physical and mental health problems<br />
affect large numbers of the working-age population. These data are<br />
similar to rates of self-reported longstanding illness and disability for<br />
the UK population derived by the Office for National Statistics in 2013<br />
[35].<br />
Self-reported prevalence of longstanding illness and disability.<br />
Office for National Statistics, UK, 2013<br />
Age; years Male % Female % All %<br />
24–44 19 22 21<br />
45–64 42 42 42<br />
Arguably, more important than knowing the prevalence of comorbidity<br />
or multimorbidity is understanding how these conditions affect the<br />
physical function and lifestyle of an individual. UK data from the Office<br />
for National Statistics provides information on self-reported limiting<br />
conditions, i.e. illnesses which require a change to life activities [35].<br />
Self-reported prevalence of longstanding illness and disability<br />
that limit life activities. Office for National Statistics, UK, 2013<br />
Age; years Male % Female % All %<br />
24–44 9 11 10<br />
45–64 21 23 22<br />
65–74 33 31 32<br />
> 75 45 49 47<br />
These data illustrate that although self-reported longstanding illness<br />
and disability is common within the working population, increasing<br />
from 21% (between ages 24–44) to 42% (between ages 45–64),<br />
the limitation of life activities associated with this is significantly less<br />
common. Only 10% of those aged 24–44 years and 22% of those aged<br />
45–64 are limited by their condition. This increases a further 10% to<br />
32% of those aged 65–74.<br />
Vision 2 4 7 16<br />
Hearing 1 4 9 21<br />
Mobility 5 13 22 42<br />
Dexterity 3 8 11 21<br />
Learning,<br />
comprehension<br />
and<br />
concentration<br />
2 3 2 4<br />
Memory 2 4 5 12<br />
Mental health 5 6 2 2<br />
Male 78.4 64.2 14.2 81.9<br />
Female 82.4 66.1 16.3 80.2<br />
Healthy life expectancy at age 65<br />
These data pertain to the entire UK population, and therefore<br />
Social skills and<br />
are unlikely to be perfectly reflective of the working population of<br />
behaviour<br />
65–74 59 55 57<br />
anaesthetists. They do not account for illness or disability starting in<br />
1 1 0 0<br />
youth in people who never reach the workplace, nor does it account for<br />
socioeconomic status. Multimorbidity correlates closely with increasing<br />
Other 5 6 9 7<br />
> 75 68 70 69<br />
social deprivation, and these data may therefore over-predict poor<br />
health and disability in the selected population that is the subject of<br />
this report.<br />
12 Anaesthesia News August 2016 • Issue 349 Anaesthesia News August 2016 • Issue 349 13<br />
Stamina,<br />
breathing and<br />
fatigue<br />
4 11 16 25<br />
Sex<br />
Life<br />
expectancy;<br />
years<br />
Healthy life<br />
expectancy;<br />
years<br />
Actual<br />
years of<br />
‘not good’<br />
health<br />
Male 18 10.7 7.3 59.3<br />
Female 20.7 12.1 8.6 58.6<br />
4.4: Summary of key factors<br />
Proportion<br />
of life<br />
>65 years<br />
spent<br />
in good<br />
health; %<br />
1. Ageing is a complex and heterogeneous process. Biological and<br />
chronological ageing are not synonymous, and the course of<br />
ageing in an individual is difficult to predict.<br />
2. Ageing results in progressive loss of physiological reserve, which<br />
is characterised by homeostenosis, loss of physiological variability<br />
and disruption of native physiological rhythms.<br />
3. Comorbidity is increasingly prevalent with advancing age. Variation<br />
in patterns of comorbidity is seen within populations between<br />
diverse socioeconomic groups.<br />
4. Longstanding disability increases with age, but is significantly<br />
prevalent in the working age population. A large proportion of<br />
these people have limitations in their function.<br />
5. Life expectancy in the UK is increasing, with approximately 60% of<br />
remaining life expectancy at age 65 expected to be characterised<br />
by self-reported good health.
5.0: Workforce patterns<br />
and workforce issues<br />
5.1: Time in employment and retirement<br />
patterns of the general population<br />
It is important to review employment trends in the general population.<br />
As well as medical staff being part of this population and hence subject<br />
to its characteristics, the trends also describe the population whose<br />
health the Government will be responsible for managing with a view to<br />
keeping them economically active.<br />
rather than the condition itself – is by far the main predictor of leaving<br />
work. In addition, the presence of three or more doctor-diagnosed<br />
conditions is strongly related to cessation of work. Another key factor<br />
that will influence the ability of the Government to modify the public<br />
sector pension bill is the current retirement pattern. To change this<br />
requires a massive culture shift. The current data on employment rates<br />
are shown below.<br />
The European Commission, in preparing for the future needs of its<br />
ageing population, commissioned a study into the impact of chronic<br />
disease on the retirement age in the EU. This was undertaken by the<br />
Dutch National Institute for Public Health and the Environment and<br />
published in 2012 [37]. At the time of their survey, the normal retirement<br />
age across Europe varied from 57 years in Greece to 67 in Norway,<br />
with the UK then having 60 for women and 65 for men. They concluded<br />
the following:<br />
• The burden of chronic diseases on Europeans of retirement age<br />
is substantial and will increase due to population ageing and<br />
prevailing lifestyle risks.<br />
• Poor health has an impact on the labour participation of older<br />
workers.<br />
• Chronic diseases among older European workers contribute to<br />
economic costs.<br />
• Musculoskeletal and cardiovascular complaints were the main<br />
causes of early retirement in the health services 7 .<br />
One metric was emphasised as being an important vector of whether<br />
or not people remained in employment. This was the percentage of<br />
each age group reporting a longstanding illness or health problem;<br />
this is shown in the figure below.<br />
People in the EU reporting chronic health issues by age<br />
categories in 2010 (Eurostat 8 2012)<br />
It can be seen that between the ages of 60 and 65, the 50% rate is<br />
passed. This does not indicate that all these people will be unfit for<br />
work, but may mean that earlier employment may have to be modified<br />
to accommodate a change in health status. It is a very important to<br />
note that the review indicated that self-perception of poor health –<br />
The EU average employment rate (%) by age category in 2011<br />
(source: Eurostat 2012)<br />
It is very important to note that for whatever the various causes, labour<br />
participation decreases progressively after the age of 50.<br />
Putting the above findings together results in these conclusions:<br />
• When the state pensionable age is increased, as is planned in the<br />
UK, if people continue to work, the number of older workers with<br />
a chronic disease and activity limitations due to health problems<br />
will also increase.<br />
• Effective interventions will be needed to improve the work<br />
participation of people with a chronic disease.<br />
• The reasons for retirement will not be entirely determined by<br />
health or the self-perception of health. Some of those retiring will<br />
be doing so because they are economically able to, or because<br />
they need to care for a loved one, or simply because they dislike<br />
their work.<br />
The crucial point is that in order to meet the Government’s planned<br />
intentions for the normal pensionable age in the NHS pension scheme<br />
to become equal to the state pensionable age (so as to allow retirement<br />
without an actuarial penalty), a huge change to current retirement<br />
patterns is required. It means that approximately three times as many<br />
people at present in the 60–64 age group and nearly ten times as<br />
many as are at present in the 65–69 age group would have to remain<br />
in employment. It is highly unlikely that this will be the case and many<br />
individuals will end up taking reduced benefits when compared with<br />
the present retirees. Perversely, it may also encourage an increase in<br />
attempts to retire on grounds of ill health so that the pension entitlement<br />
is ‘made-up’ to what it would be at the state pensionable age.<br />
7<br />
This includes all health workers, not just medical staff.<br />
8<br />
Eurostat is a directorate of the European Commission responsible for the collection of data. This was the data source used to inform the 2012 RIVM report referenced in<br />
reference 37. It can be accessed at http://www.ec.europa.eu/eurostat<br />
5.2: Employment patterns and the<br />
retirement intentions of medical staff<br />
Getting data on the retirement intentions of consultant medical staff is<br />
difficult. The most basic approach is to look at the age distribution of<br />
doctors registered with the GMC. The current situation is shown in the<br />
table below [38].<br />
14 Anaesthesia News August 2016 • Issue 349 Anaesthesia News August 2016 • Issue 349 15<br />
Age group<br />
Number of doctors<br />
≤ 25 10,715 3.9%<br />
26–35 76,139 27.8%<br />
36–45 80,350 29.3%<br />
46–55 57,796 21.1%<br />
56–65 31,672 11.6%<br />
> 65 13,344 4.9%<br />
No birth date 3,837 1.4%<br />
Total 273,853 100.0%<br />
Proportion of the<br />
workforce<br />
Doctors (all grades) registered with the GMC in 2016<br />
Clearly these data must be interpreted with caution since, over time,<br />
there has been an increasing number of doctors registered per year.<br />
At present there are nearly 86,000 doctors on the specialist register, of<br />
whom 11.5% are anaesthetists. The number of specialist registrants<br />
has increased by over 50% from 2005. These will however be occupying<br />
the earlier years in the table below. The important figure to note is that<br />
between the decade 46–55 years to the decade 56–65 years there<br />
is a reduction of nearly 50% in continued employment, and between<br />
the decade 56–65 years to over 65 years there is a further nearly<br />
60% reduction. These reductions will have a number of confounding<br />
variables buried within them, but the decrements are so great that for<br />
medical staff to continue in employment as the Government intends<br />
requires a massive change in end-of-career decisions.<br />
Accepting that there will be some specialty differences, probably the<br />
best information to date on retirement intentions is that from a survey<br />
undertaken by the Federation of the Royal Colleges of Physicians of<br />
the UK in 2011 [39]. The intended ages of retirement are shown below.
These data clearly confirm the discrepancy between the retirement<br />
intentions of the consultant workforce and the objectives of public<br />
sector retirement policy. A total of 47% expressed an intention to retire<br />
between 56 and 60, and a further 43% intended to retire before 65. Only<br />
3% intended to work beyond that age. The two most common reasons<br />
cited for wanting to retire were pressure of work and domestic reasons,<br />
with dissatisfaction with the NHS following close behind.<br />
Voluntary early retirements were also studied in a 2011 survey published<br />
by the British Medical Association [40], which found that retirements<br />
before the age of 60 had increased by 72% in the previous year. The<br />
proportion of retiring consultants each year who took retirement early<br />
had almost doubled from 7.3% in 2006 to 14% in 2011. If these figures<br />
remain unchanged as retirement intentions, possibly also stimulated by<br />
the financial problems associated with exceeding the lifetime allowance,<br />
there is a very significant professional problem ahead that affects both<br />
the service capability of the NHS and doctors’ personal lives.<br />
5.3: Wellbeing at work: making<br />
work possible<br />
The changes to pensions regulations not only affect medical staff – they<br />
affect all workers in the NHS. Others in doctors’ workplaces will also be<br />
increasing in age and, in interacting with them, mutual allowances may<br />
have to be made. As a result of this and other considerations, wellbeing<br />
at work relates to more than just the individual: it includes their health,<br />
colleagues, and the matrix of hours and facilities within which they carry<br />
out their job. There is considerable financial and social loss to those<br />
absent from work, and going to work needs to be recognised as the<br />
healthier option. The importance of work and health in people’s lives was<br />
explored by Dame Carol Black’s report Working for a healthier tomorrow<br />
[41]. This review was not instigated primarily to meet the future changes<br />
planned in pensions reform, but its findings and conclusions have<br />
considerable impact on them. In essence, it sought to establish the<br />
foundations for a broad consensus around a new vision for health and<br />
work in the UK. At the heart of this vision were three principal objectives:<br />
• Prevention of illness and promotion of health and wellbeing.<br />
• Early intervention for those who develop a health condition.<br />
• An improvement in the health of those out of work so that everyone<br />
with the potential to work has the support they need to do so.<br />
A shift in attitudes is necessary to ensure that employers and employees<br />
recognise not only the importance of preventing ill health, but also the<br />
key role the workplace can play in promoting health and wellbeing.<br />
Over the past decades, the focus has been on health and safety in the<br />
workplace – and great strides have been made in this regard - but little<br />
was done to address positive health and wellbeing. Research specially<br />
commissioned for the Black Report found considerable evidence that<br />
health and wellbeing programmes produced economic benefits across<br />
all sectors and all sizes of business; in other words, good health is good<br />
business.<br />
The review identified that health and wellbeing are not just medical<br />
issues. The nature and characteristics of the jobs people do are critically<br />
important in terms of satisfaction, reward and control. Good management<br />
also leads to good health, wellbeing and improved performance. Line<br />
managers have a role in identifying and supporting people with health<br />
conditions to help them to carry on with their responsibilities or to adjust<br />
responsibilities when necessary. In the future this could become a<br />
critical path towards keeping all grades of older workers in the NHS in<br />
employment. Medical staff will need to play their part in this process.<br />
For those who develop health conditions, their roles will need to be<br />
underpinned by changes in ideas of fitness for work. It is inappropriate<br />
to be at work unless you have the appropriate fitness; being at work<br />
when unwell normally impedes recovery. Employers have significant<br />
scope to facilitate an employee’s early return from sickness absence.<br />
Early, regular and sensitive contact with employees during sickness<br />
absences can be a key factor in enabling an early return. Tackling<br />
stigma around ill health and disability is key to enabling more people<br />
with health conditions to stay in work. This is particularly true for those<br />
with mental ill health, as many organisations fail to recognise the full<br />
value of the contribution they can make.<br />
Changing perceptions will also require greater public engagement<br />
with the benefits of work to health, increasing expectations of what<br />
makes a job good and of the support people with health conditions<br />
should expect to enable them to remain in or return to work. A lack<br />
of understanding about the relationship between work and a person’s<br />
health, and the omission of this evidence from professional training,<br />
has meant that despite best intentions, the work-related advice that<br />
healthcare professionals give to their patients can be overly cautious<br />
and may not be in the best interests of the patient in the long term.<br />
Emerging evidence suggests that, for many people, early interventions<br />
help to prevent short-term sickness absence from progressing to<br />
long-term sickness absence and ultimately the inability to work. In a<br />
subsequent report [42] that tackled the issue of absence from work<br />
because of sickness, it was noted that much sickness absence and<br />
inactivity follows common health conditions that, given the right support,<br />
are compatible with work, although sometimes work patterns need to<br />
change. Sickness absence in the NHS varies significantly. Sickness<br />
absence data in the NHS are presented in terms of percentage of<br />
working time lost, and different NHS workforces have markedly different<br />
absence rates. Ambulance staff have the highest aggregated sickness<br />
absence rate (6.3%) followed by healthcare assistants and other<br />
support staff (6.21%). By contrast, nursing, midwifery and health visiting<br />
learners had the lowest rate (1.05%) followed by medical and dental<br />
staff (1.21%). Generally, NHS absence rates have decreased in recent<br />
years, particularly in those job areas exhibiting above average absence.<br />
One of the great social conundrums of our time has been revealed by<br />
the Marmot Report [43], which was commissioned on behalf of the<br />
Department of Health. This studied the effects of inequalities on health.<br />
These are reflected in the NHS workplace through the wide spectrum of<br />
people working there. There is a social gradient in health: the lower a<br />
person’s social position, the worse his or her health. Health inequalities<br />
result from social inequalities, so action on health inequalities requires<br />
action across all the social determinants of health. While within England<br />
there are nowhere near the extremes of inequalities in mortality and<br />
morbidity seen globally, inequality is still substantial, and the Marmot<br />
Report calls for urgent action. In England, people living in the poorest<br />
neighbourhoods will, on average, die seven years earlier than people<br />
living in the richest neighbourhoods. Even more disturbing, the average<br />
difference in disability-free life expectancy is 17 years. Thus, people in<br />
poorer areas not only die sooner, but they will also spend more of their<br />
shorter lives with disability. The combined effect of social class and the<br />
importance of employment (as described above in the Black Report)<br />
can be seen in the figure below 9 .<br />
Social class, employment and mortality rates<br />
There is an important link between the findings of the Marmot Report<br />
and the planned changes to state and public sector pensions in the<br />
UK. Assuming that the late 60s is the pensionable age towards which<br />
England is moving, > 30% will have a limiting disability when aged ><br />
65 years. The Marmot Report concludes that if society wishes to have<br />
a healthy population working for longer, it is essential to take action to<br />
increase the general level of health and to flatten the social gradient.<br />
It can therefore be inferred that alone, the planned pensions legislation<br />
changes will probably fail to meet their intended targets. What is<br />
required alongside these changes is a wholesale change in the way<br />
society views health and work. For people to work longer, the workplace<br />
needs to promote health and wellbeing and make sure that everybody<br />
with the potential to work has the support they need to do so. The<br />
NHS employs persons from all social classes; to enable them all to<br />
play their part as economically active members of society, there also<br />
needs to be attention focused on the reduction of inequalities in order<br />
to transform illness, disability and dependency into continued good<br />
health and social engagement through work.<br />
5.4: The public’s expectations of older<br />
professionals<br />
Trust and professional regulation<br />
The relationship between medical staff and patients is in constant<br />
evolution and, if the media are to be believed, appears to be<br />
moving away from ‘blind faith’ towards accountability, challenge and<br />
measurement of competence. This is encouraged by individual doctor<br />
performance league tables and the sort of user, infection and mortality<br />
ratings shown on the NHS Choices website. Despite this, patient<br />
satisfaction on an individual basis remains high and, in May 2015, ><br />
95% of inpatients treated by NHS Trusts and Foundation Trusts would<br />
have recommended their provider to friends or family [44]. The question<br />
for this publication is: ‘How does the age of the medical practitioner<br />
affect the public’s reasonable right to expect that the medical staff it<br />
sees are competent?’<br />
In a series of Reith Lectures entitled A Question of Trust, Onora<br />
O’Neill examined the relationship between those receiving and those<br />
providing professional services [45]. She argued that although at times<br />
the relationship would break down and disappointment would result,<br />
the essential factor in any lay-professional relationship was trust. If<br />
there was no trust and an innate responsibility to provide good care on<br />
trust, all the possibly recordable numerically accountable data could<br />
not substitute for it. In her view, the need for, and acceptance of, trust<br />
is both crucial and self-evident, and any erosion of it is to everybody’s<br />
detriment. While trust is still possible on a person-to-person basis, the<br />
public, Government and media nevertheless (and with good reason)<br />
require certain groups, of whom the medical profession is one, to be<br />
regulated within the law and to adhere to specified standards and<br />
behaviours. The need for this is well accepted by society as a means<br />
of containing at least the worst of professional lapses through control<br />
of the Medical Register. More recently, with the introduction of annual<br />
appraisal and revalidation, the GMC is now seen as not only regulating<br />
serious offences but also managing ongoing quality control throughout<br />
a professional lifetime. Unfortunately, although the public may see<br />
revalidation as providing a guarantee of minimum satisfactory quality<br />
standards, there is evidence that the process at times has considerable<br />
gaps. People still present to the GMC who have had a series of<br />
satisfactory annual appraisals and a few even end up subsequently<br />
in jail. The question is: How should the public be reassured about an<br />
older doctor’s competence?<br />
Evidence relating age to competence<br />
A good starting point is to review available evidence of when things<br />
have gone wrong. Perhaps the first point to make is that whatever<br />
correlation is being looked at with respect to underperformance or<br />
reporting, males always outnumber females, both in absolute numbers<br />
and proportionately. The National Clinical Assessment Service 10<br />
has been collecting data since its inception in 2001. Referrals made<br />
in 2009/10 (the latest data available), show patterns similar to those<br />
observed in earlier years [46], and the incidence of referral related to<br />
age is shown below [47]. In this diagram, H & C are specialist medical<br />
staff working in hospitals and the community.<br />
It can be seen that for hospital consultants, unlike general practitioners,<br />
there is no strong correlation with age. On the other hand, in terms of<br />
GMC referrals [48], between 2010 and 2013 for those on the specialist<br />
register in the 30–50 year old group, the referral rate was 7.6%, as<br />
compared with 13% for those aged > 50. These rather unrefined GMC<br />
metrics do not give any information about the subset close to or above<br />
the usual retirement age. In the UK, there is currently little information<br />
on the relationship between doctors’ age and their competence,<br />
particularly around and above the ‘normal’ retirement age.<br />
In the USA, the situation is different because there are no equivalent<br />
pensions similar to those of the UK public sector. Consequently,<br />
there are greater financial drivers to keep people at work, but these<br />
are not necessarily in the public’s best interest, and this has been a<br />
regular topic of discussion in newspapers such as the Washington<br />
Post [49], in which continued employment of elderly medical staff has<br />
been questioned. It reports that 42% of physicians are > 55-years-old<br />
and 21% are > 65-years-old – a considerable contrast with the UK.<br />
Probably the oldest clinically practising living physician was Ephraim<br />
Engleman, who worked until his death at the age of 104 [50] as Director<br />
of the Rosalind Russell Medical Research Centre for Arthritis at the<br />
University of California. At a different medical centre, the dangers of<br />
being too respectful to age and reputation were demonstrated when a<br />
patient bled to death during a routine cholecystectomy [51]. When the<br />
hospital investigated this event, which was caused by a revered mentor<br />
of several generations of surgeons, they found that for six years, junior<br />
staff had always ordered extra blood for his laparoscopic procedures,<br />
and the anaesthesia department always put an experienced consultant<br />
with him because it was common knowledge that the surgical risks<br />
were greater. The surgeon’s colleagues and the hospital were<br />
essentially accommodating his deficiencies rather than tackling the<br />
root of the problem.<br />
The problem of the ageing surgeon was reviewed in some detail by<br />
Blasier, an American orthopaedic surgeon [52], during a symposium<br />
on clinical risk and judicial reasoning. He concluded that both<br />
anecdotal evidence and objective testing suggest that age causes a<br />
deterioration in physical and cognitive performance, and that surgeons<br />
were reluctant to plan for retirement. In addition, he indicated that<br />
conventional outcome measures are unable to detect a progression of<br />
substandard outcomes that are unacceptable clinically but insufficient<br />
to trigger an institutional response.<br />
9<br />
This is reproduced in the Marmot report and is taken from: Bethune A. Unemployment and Mortality. In Drever F and Whitehead<br />
M (Eds.) Health inequalities: Decennial supplement. ONS Series DS no. 15. London: The Stationery Office, 1997.p 156–67.<br />
10<br />
Since 2013, NCAS has been an operating division of the NHS Litigation Authority.<br />
16 Anaesthesia News August 2016 • Issue 349 Anaesthesia News August 2016 • Issue 349 17
The removal of an age-related retirement date in the UK<br />
The problems in the UK are further complicated by the combination of<br />
the pressure to work longer to meet the criteria for a full pension in the<br />
presence of anti-age discrimination legislation. The Equality Act 2010,<br />
and the Employment Equality (Repeal of Retirement Age Provisions)<br />
Regulations 2011, came into force on 6 April 2011 in England, Scotland<br />
and Wales [53]. These regularised several aspects of public and<br />
personal life with respect to the prevention of discrimination, and from<br />
October 2012 it was not possible for employers to require employees<br />
to retire on the grounds of age alone. At a stroke this removed the<br />
safety valve of being able to remove employees known or thought<br />
to be underperforming when they reached the accepted retirement<br />
age for their employment. If they do not want to stop work, an older<br />
employee now has to be shown to be unable to satisfactorily undertake<br />
the content of their job description. The situation is further complicated<br />
because there is an onus on the employer to respond to a request to<br />
make a change in a job description ‘in a reasonable manner’ [54], and<br />
guidance has been issued by the Advisory Conciliation and Arbitration<br />
Service [55]. Changes to a job description can be requested by the<br />
employer or the employee. Case law is developing on disputes in<br />
which these requests have not resulted in mutual agreement. It is now<br />
established that an employee cannot demand changes to their job that<br />
are convenient to them if they do not meet the corporate objectives of<br />
the employer. Similarly, the employer has to make ‘reasonable’ efforts to<br />
accommodate a request if the corporate objectives can still be achieved<br />
if the request were granted.<br />
The impact of the removal of the fixed retirement age has been reviewed<br />
by the Health and Safety Executive (HSE) in relation to ‘safety critical<br />
work’ [56]. This included occupations in the airline, nuclear power,<br />
transport, fire-fighting and oil extraction industries. Anaesthesia is<br />
clearly ‘safety critical work’ but no medical specialties were specifically<br />
reviewed by the HSE. Their methodology and analysis is nevertheless<br />
highly relevant. In summary, their key messages relevant to an older<br />
consultant were:<br />
• While there is evidence that cognitive and physical abilities decline<br />
with increasing age, these do not necessarily have a negative<br />
impact on performance at work. Studies of age have found huge<br />
inter-individual variations in performance.<br />
• The relationship between chronological age and performance is<br />
neither simple nor straightforward. A number of factors including<br />
functional capacity for work, work demands, work environment,<br />
stress, shift work, expertise, and attitudes towards work and<br />
retirement are relevant. There was a critical age for increasing<br />
intolerance to night work as age progressed, but this was again<br />
individually variable.<br />
• It is the specific combination of demands and complexity required<br />
by a job that makes it potentially highly demanding, as opposed to<br />
the job title itself. Individuals are able to use different strategies to<br />
compensate for age-related declines in performance, such as their<br />
expertise, job knowledge, education and high motivation. However,<br />
when job demands exceed the overall capacity of a worker, they<br />
may no longer be able to compensate for any decline.<br />
• There is evidence of ‘healthy worker’ effects, whereby individuals<br />
self-select to move into less demanding jobs, or retire as their<br />
ability to carry out a job decreases. There is also evidence of ‘safe<br />
worker’ effects where rigorous screening standards mean that<br />
workers lose their licence to work, e.g. pilots and offshore workers.<br />
• There is a paucity of information about the performance of older<br />
workers in very demanding jobs. For example, the extent of ‘healthy<br />
worker’ effects or ‘safe worker’ effects within demanding jobs is<br />
unknown. The extent to which these effects act as a safeguard<br />
against safety critical outcomes is also unknown.<br />
• More longitudinal research is required in order to investigate<br />
decrements in performance over a working life.<br />
The present position with regard to anaesthetists<br />
• The relationships between patients and doctors remain very good,<br />
with a high degree of trust. Part of this places a responsibility on<br />
doctors both individually and collectively to ensure a high standard<br />
of clinical practice is delivered.<br />
• The changes in the public sector pension arrangements, coupled<br />
with the removal of age-related compulsory retirement from<br />
clinical practice, create a situation in which doctors who are<br />
underperforming because of age may go undetected. Current<br />
audits lack the sensitivity to identify subtle but significant changes<br />
in performance, and there have been many situations in which<br />
clinicians have been inappropriately ‘carried’ by colleagues and<br />
institutions when they should have ceased clinical practice.<br />
• There is no simple relationship between age and performance, and<br />
there are huge individual variations. While there is evidence that<br />
cognitive and physical abilities decline with increasing age, these<br />
do not necessarily have a negative impact on performance at work.<br />
However, there will come a point when the job demands exceed the<br />
overall capacity of an individual worker to compensate.<br />
• In employment outside medicine, there is evidence that individuals<br />
self-select to move into less demanding jobs, or retire as their ability<br />
to carry out a job decreases. The safety implications for the public<br />
of the ability to modify the job content of an anaesthetist with age<br />
are obvious. So also is the need to detect those without the insight<br />
to ‘self-select’ when their workplace performance is declining.<br />
• Although the volume of literature is small, there is however<br />
increasing evidence that within anaesthesia, older age per se<br />
could be an independent risk factor for safe practice. Should this<br />
risk become established as true by continuing audit and evidence<br />
collection, and what can be done about it, is considered in<br />
Section 6.<br />
5.5: Other professional groups<br />
and human factors<br />
Other professional groups<br />
As acknowledged above, several ‘high-stakes’ industries (airline,<br />
nuclear power, transport, fire-fighting and oil extraction), have taken<br />
steps to try to ensure that their professionals are performing to proper<br />
standards throughout their working lives and have had to modify<br />
their processes as regulations and legislation have changed. There<br />
are lessons to be learned from this and it is useful to take the airline<br />
industry, which has long had age, fitness and competency barriers to<br />
continued employment, as an example.<br />
Historically, national aviation authorities grew up in response to the<br />
increasing aviation activity after the Second World War, and in 1947<br />
the International Civil Aviation Organisation was established. In 2003, a<br />
European Aviation Safety Agency was created, but individual member<br />
states have their own national authorities. In the UK, this body is the<br />
Civil Aviation Authority, which works closely with the European Aviation<br />
Safety Agency to promote the highest common standards of safety<br />
and environmental protection.<br />
A pilot’s competence on a specific aircraft is confirmed by the granting<br />
of a licence by the Civil Aviation Authority. The pilot is subsequently<br />
checked on a six-monthly basis for technical, handling and crew<br />
resource management (equivalent to team management) competence<br />
over a two-day period. This time is also used to refresh skills in dealing<br />
with abnormal and emergency situations on a rotational basis, so all<br />
possible scenarios are covered every three years. Every training pilot<br />
is checked either by a Civil Aviation Authority inspector or a senior<br />
examiner every three years, as well as by ad hoc standardisation<br />
checks. In addition, all pilots have a two-yearly line check in which an<br />
authorised training captain observes a crew operate a commercial flight.<br />
Medical checks covering past medical events, eyesight, hearing, ECG,<br />
lung function, haematology, biochemistry and urine are mandatory.<br />
These have to be repeated at yearly or six-monthly intervals, depending<br />
on the class of aircraft.<br />
It is worthy of note that pilots generally get apprehensive about their<br />
six-monthly competency checks in the simulators. This raised level of<br />
anxiety can, and sometimes does, cause degraded performance levels.<br />
Debriefing after the event usually precipitates an admission from the<br />
pilot that the cause of the reduction in performance was as a result of<br />
‘life stresses’ rather than cognitive degradation. In all airlines there have<br />
been cases of performance degradation stimulated by more sinister<br />
medical issues. It is therefore important to try to differentiate between<br />
the causes so that retraining and remedial actions are appropriately<br />
instigated.<br />
Until 1 October 2006, British Airways had a maximum age for pilots<br />
of 55 even though their Civil Aviation Authority licence allowed for a<br />
maximum age of 60, and most other British and international airlines<br />
had a policy of a maximum age of 60. Issues of restraint of trade and<br />
ageism subsequently forced British Airways to fall in line with the Civil<br />
Aviation Authority’s maximum age limit. Now, in the UK, pilots, like all<br />
other workers, have been freed from an upper age limit by legislation,<br />
although they still have to pass regular competency tests. The ‘effects of<br />
age’ problem has been tackled internationally by the International Civil<br />
Aviation Organisation. It developed the concept of an ‘incapacitation<br />
risk’ occurring to a pilot during the cockpit on any given flight, and<br />
made the important point that:<br />
• Not all causes of death or fatal conditions posed an incapacitation<br />
risk because the disease develops slowly, e.g. most malignant<br />
disease.<br />
• Not all incapacitations necessarily pose a risk of death, e.g. a faint<br />
or a transient ischaemic attack.<br />
Accidents due to simultaneous double incapacitation from physical<br />
disease, i.e. both pilots incapacitated at the same time, are extremely<br />
rare; none having occurred for > 40 years. European Aviation Safety<br />
Agency aircraft design standards state that the average probability<br />
per flight per hour of a ‘catastrophic failure’ must be ‘extremely<br />
improbable’, with a probability per flight hour of the order of < 1 x 10 -9 .<br />
Its presentation of this concept is shown in the figure below.<br />
Deaths per million in UK males which impacts on the<br />
incapacitation risk with age<br />
It can be seen from the figure that up to age 65, the mortality rate is still<br />
< 1% per year, which approximately equates to 1 death per 1,000,000<br />
hours. With two pilots, the probability of both dying is (1 x 10 -6 ) x (1<br />
x 10 -6 ), which equals (1 x 10 -12 ). This probability is 1,000 times less<br />
than that set by the European Aviation Safety Agency 11 . Surveys on<br />
pilot performance [57] concluded similarly to the HSE that: ‘Overall,<br />
the scientific record has not resulted in a clear specification of the<br />
relationship between age, cognitive function, and pilot performance’.<br />
Further data demonstrated that although there was a measurable<br />
reduction in performance in those aged > 60 years, it still stood<br />
significantly above the licence requirements. It was recognised that<br />
there was considerable individual variation but that performance up to<br />
the age of 65 years is not now seen as an issue by the industry. As a<br />
result of these reviews, the Civil Aviation Authority now specifies that<br />
in two-pilot civilian passenger aircraft, pilots can be licensed up to the<br />
age of 65 years, but either the pilot in charge or the co-pilot must be <<br />
60 years [58].<br />
It is clear from the measured experiences of the airline industry that<br />
there are many similar findings to those observed anecdotally in<br />
medicine and to the conclusions of the Health and Safety Executive<br />
review (see ref 56 earlier). With ageing, there remains very wide<br />
individual variation. Health has a measurable impact, there are regular<br />
competency checks, and risk is mitigated by combining professionals<br />
of different ages.<br />
Human factors<br />
Human error is known to occur during the practice of medicine, but<br />
for > 20 years, its genesis has been known more as a problem of<br />
psychology or engineering rather than medicine [59]. The words of<br />
George Santayana, the Spanish philosopher – ‘Those who do not<br />
remember the past are condemned to repeat it’ – are particularly<br />
apposite because doctors make the same mistakes again and<br />
again, sometimes over decades [60,61]. Command, control and<br />
more regulation appear not to have significantly decreased failure at<br />
the doctor-patient interface. It is surely naïve to think that if we go on<br />
11<br />
These calculations are based on population death rates, which are not the same as ‘incapacitation incidents’ while flying, but the methodology establishes the principle.<br />
18 Anaesthesia News August 2016 • Issue 349 Transfer Anaesthesia of principle News to August anaesthesia 2016 • has Issue important 349 messages for being the only anaesthetist on site out of hours.<br />
19
prescribing the same remedies, we will get a different result. As Cicero<br />
observed around 140 BC, ‘Any man can make mistakes, but only an<br />
idiot persists in his error’. His view was supported over two thousand<br />
years later by Einstein in his observations on experimental science<br />
when he said ‘Insanity is doing the same thing over and over again,<br />
and expecting a different result’. We need the help of better systems<br />
and a change in organisational culture.<br />
In other high-risk industries, research into human factors and safety<br />
science has substantially changed the culture of organisations and<br />
the management of risk because their leaders have realised that their<br />
future, their jobs and their profits depend on it. The same impact of<br />
human factors research has not yet been felt in hospitals. Perhaps<br />
this is because consultants usually go unchallenged and, as they age,<br />
they persist with established mental pathways. After all, accepted<br />
practice is where the majority of errors and harm arise.<br />
Medical experts are quick and productive, and most of the time<br />
they get it right, but when they don’t, perhaps due to an incorrect<br />
perception, assumption or communication, or because they are the<br />
victims of confirmation bias, the risks are much greater than in those<br />
of the novice who is full of self-doubt. In his book Thinking Fast and<br />
Slow [62], Daniel Kahneman has helped us to grasp how we make<br />
decisions and the benefits and risks of each process. Being mindful<br />
of this science is an important safeguard in understanding what we<br />
and others do, especially when, as experts, we make rapid, intuitive<br />
choices that feel effortless and right. In these conditions, our normally<br />
competent but possibly ageing brain does not invite us to pause and<br />
consider. That step requires another team member, a ‘second brain’,<br />
to challenge us. This is a crucial benefit of team working and of open<br />
relationships in medicine and in management, and as we age these<br />
become of much greater potential importance. Established consultants<br />
are particularly vulnerable to delusions of adequacy and resistant to<br />
change, particularly if it means unlearning a cherished habit. They may<br />
need to be rewired.<br />
Unlearning and relearning are complex and time-consuming<br />
processes. Furthermore, new behaviours commonly revert to older<br />
habits when there is distraction, stress or urgency, so there may<br />
be a particular vulnerability for retrained doctors faced with these<br />
conditions. It is difficult but at times necessary to change one’s habits<br />
and what one believes; only by recognising the importance of human<br />
factors in the workplace can this be achieved.<br />
Human factors optimisation is about designing systems that are<br />
resilient to unanticipated events and addressing problems by<br />
modifying the design of the system to support people better [63]. In a<br />
nutshell, the aim of human factors optimisation is 'modifying systems<br />
to make it easy for people to do the right thing'. Such interventions<br />
develop environments that are intrinsically safer than before, and<br />
have great potential to mitigate the errors and changes associated<br />
with ageing. For them to be introduced first requires an acceptance<br />
that error is normal and is only a moral issue when it is known to be<br />
avoidable or undeclared. When it occurs, it is never just one person’s<br />
fault, it is a system failure and the primary determinant of safety is<br />
one of organisational culture. To quote Don Berwick [64], ‘In the end,<br />
culture will trump rules, standards and control strategies every single<br />
time and achieving a vastly safer NHS will depend far more on major<br />
cultural change than on a new regulatory regime’. Some in leadership<br />
positions in healthcare have yet to understand and adopt these<br />
principles; they think that identifying culprits is corrective. They blame<br />
individuals alone for errors and ignore the cultural and systems factors<br />
that are so contributive. Such leaders need help because although<br />
they are probably doing their best they ‘don’t know what they don’t<br />
know’. It is a risk for all of us, and especially those older members in<br />
the workplace.<br />
Conclusions<br />
Medicine is not unique in having to address the continued employment<br />
of an ageing worker who has to perform to a highly sophisticated<br />
professional standard. Other industries have, through systematic<br />
research and audit, found and solved problems that medicine has,<br />
to date, really only recorded at an anecdotal level. There is much that<br />
can be learned from them both in their approach and in their solutions.<br />
Two things come through as constant themes. The first is that while<br />
there is evidence that cognitive and physical abilities decline with age,<br />
these are highly individually variable and do not necessarily prevent<br />
continued employment at a safe level. The second is that human<br />
factors are increasingly being recognised as vectors for error, and that<br />
working in properly functioning teams and modifying the environment<br />
can have very considerable safety advantages. This is particularly<br />
relevant to ageing professionals who may warrant some special<br />
consideration in this regard: perhaps at the end of one’s career there<br />
should be an appreciation that a safe working environment is one with<br />
which one is familiar.<br />
6.0: Implications for the<br />
future: practical aspects<br />
to be addressed<br />
Anaesthesia is a safety-critical occupation that in the UK has very high<br />
standards of practice and very low levels of morbidity and mortality. It<br />
is clear from this review that the plan to maintain more people in work<br />
to an older age than at present, in the presence of an increasingly<br />
complex patient population, has significant, potential safety<br />
implications. The actual effect on patient safety cannot be calculated<br />
in advance with any accuracy. There are four key stakeholder groups<br />
involved, each of which has responsibility and a contribution to make<br />
in trying to maintain the current levels of safe practice. These are:<br />
• The anaesthetists themselves.<br />
• The organisations that employ anaesthetists and maintain their<br />
workplaces.<br />
• The Government, through national and health policies.<br />
• The public who use the health services.<br />
The sections below try to identify the factors relevant to each of these<br />
groups. It should be emphasised that these are rapidly developing<br />
areas of consideration and what is written is in no way definitive in its<br />
scope: recommendations are highly likely to change over time.<br />
6.1: Considerations for the anaesthetist<br />
The first and greatest commandment for anaesthetists, both<br />
individually and as a professional group, is to accept that extending<br />
their clinical working lives will bring problems, and that planning for<br />
the consequences of change is essential. Although the evidence for<br />
age-related problems is still emerging, there are clear trends.<br />
Evidence that there is a problem<br />
In 2012, Tessler et al. [65] reviewed a ten year period of anaesthesia<br />
activity in British Columbia, Quebec and Ontario with respect to<br />
the age of anaesthetist and litigation events. In general, older<br />
anaesthesiologists tended to care for fewer patients and were involved<br />
in less complex procedures. They found that when compared to<br />
anaesthesiologists < 50 years of age, those > 65 had an incidence of<br />
being involved in litigation that was 50% higher and, of those medicolegal<br />
cases, almost twice as many had a disabled patient outcome.<br />
In 2013, a survey of Canadian anaesthesiologists [66] reviewed the<br />
age of those practising. It found that:<br />
• 68% were < 54 years old.<br />
• 22% were 55–64 years old.<br />
• 7% were 65–74 years old.<br />
• 3% were >75 years old.<br />
Canada, like the UK, has anti-age discrimination legislation, and the<br />
review discussed the personal and institutional problems that the<br />
removal of a statutory retirement age is bringing. The problem of<br />
ageing in the workplace has also been highlighted by the Anaesthesia<br />
Continuing Education Committee (ACECC). Their Welfare of<br />
Anaesthetists Special Interest Group has studied the Retirement and<br />
Late Career Options for the older professional [67].<br />
20 Anaesthesia News August 2016 • Issue 349 Anaesthesia News August 2016 • Issue 349 21
These three publications incorporate and discuss several common<br />
themes:<br />
• There is good neurophysiological evidence that after the age<br />
of approximately 60, processing speed (dealing with incoming<br />
information quickly and efficiently), short-term memory, the ability<br />
to retain new information and vigilance all decline. However, there<br />
is great inter-individual variability and the impact of ageing on<br />
each individual’s performance at work is different: many older<br />
anaesthetists in good health will be able to continue to perform<br />
well.<br />
• Age-related physical health problems can impact on performance.<br />
The incidence of many chronic conditions (e.g. musculoskeletal<br />
problems and cataracts), and of acute illness (e.g. ischaemic<br />
heart disease) increases with age, as does a decrement in visual<br />
acuity, hearing loss and some aspects of cognitive function.<br />
Some health problems (e.g. hypothyroidism), are not always easy<br />
to spot and may go unrecognised by both the individual and their<br />
colleagues until well advanced.<br />
• Quality of sleep worsens with age and sleep becomes shorter.<br />
Tiredness has an effect on older doctors’ performance and mood.<br />
Being on-call can be highly disruptive to sleep, even when not<br />
called out. There is a decrease in the capacity to adapt to shift<br />
work with increasing age: older workers’ cognitive performance<br />
may be more impaired during night work but they may be less<br />
aware of their degree of impairment.<br />
• Decreased job satisfaction, irritability, burnout, anxiety, depression<br />
and fatigue are more common in older practitioners, and these,<br />
combined with fear of failure and challenges to self-esteem, can<br />
impact on the decision to retire.<br />
• Older anaesthetists may be slower at recognising and managing<br />
new situations, but can be quick to respond when they are not tired<br />
and are able to draw on previous experience. Older practitioners<br />
may rely heavily on previous experience, intuitively recognising<br />
patterns and making ‘routinised’ automatic rapid responses to<br />
developing situations without employing conscious analysis and<br />
reasoning [68]. As physicians age, they are perhaps more likely<br />
to make errors from placing undue weight on first impressions, i.e.<br />
premature closure.<br />
• There was complete agreement that the path towards eventual<br />
retirement (whenever that was) needed active management.<br />
Waiting passively for an adverse event to signal professional<br />
failure was definitively not the way forward.<br />
Detecting and managing underperformance<br />
While the conclusion is that ageing anaesthetists can present problems<br />
to themselves and their patients, and that problems with ageing<br />
anaesthetists will become more frequent, it is far from clear what should<br />
be done to address the situation and to protect patients. Tessler and<br />
Shrier [65] demonstrated that older anaesthetists are more likely to<br />
make errors in even simple cases. A frequently stated assumption then<br />
follows that older anaesthetists should not undertake complex cases,<br />
but where is the hard evidence for specific individuals? While it is true<br />
that, on an individual basis, a number of practitioners choose to try<br />
to scale down the complexity and intensity of their workload, and are<br />
probably showing laudable insight in doing so, does this have to be<br />
applied as a rule at a particular age?<br />
Baxter et al.[66] suggested ways in which anaesthetists could tailor<br />
their practice to address their individual situations, and how hospital<br />
management could get the best from the older clinician. They concluded<br />
that ‘a more structured approach to tapering clinical activities and<br />
planning retirement may benefit both individuals and departments of<br />
anaesthesia and may ultimately improve patient safety’. This proactive<br />
methodology was echoed by the ACECC and also discussed by<br />
Redfern and Gallagher [68]. Examples of suggested actions are:<br />
• Progressively scaling-down activities, with a gradual move to a<br />
shorter working week, elimination of on-call night shifts, more time<br />
for assessment of patients with complex medical problems, help<br />
with more complex cases, or, when appropriate, a modification in<br />
the scope of practice to avoid predictable difficulties.<br />
• Older individuals typically receive less feedback on their<br />
performance, but may find it more difficult to recognise when their<br />
skills deteriorate because they rely more on pattern recognition<br />
than analytic cognitive processes. Doing a list with a consultant<br />
colleague, observing and discussing each others’ practice, is<br />
useful and can assist in overcoming potential errors.<br />
• Always working in a theatre complex where there are other<br />
anaesthetists readily available to advise or assist in crises,<br />
whether with clinical issues or with personal health, is helpful. This<br />
also overcomes the ‘incapacitation incident’ discussed in Section<br />
5.5. Careful consideration should be given to the advisability of<br />
working in remote sites, including those in the independent sector.<br />
• The design of CPD and remedial training should take into account<br />
the needs of the older workforce. Traditional, lecture-based CPD<br />
may be less useful to the older practitioner than group activities<br />
in which participants discuss clinical management and receive<br />
feedback from peers [69]. Maintaining a commitment to teaching<br />
and learning from trainees can only be good.<br />
The big issue to be addressed is that given the impact the ageing<br />
anaesthetist can have on patient safety, how are they to be confirmed<br />
as being fit for purpose within their clinical job plan? Although there<br />
are several tools used for the cognitive assessment of physicians,<br />
these do not evaluate crisis management and may not pick up subtle<br />
changes in performance. Workplace assessments are an obvious<br />
possibility, but these can be fraught with numerous problems, not least<br />
of which is the lack of accepted methodology and frequency of review.<br />
Does the ‘assessment situation’ (either in real time or by retrospective<br />
review of cases) replicate the ‘real thing’? What if the assessor was<br />
once the trainee of the ageing ‘examinee’? Would inappropriate power<br />
dynamics and oversensitivity to a person’s feelings influence the<br />
findings and conclusions? How would one manage an unsatisfactory<br />
outcome? Would patients deserve to be informed about any limitations<br />
on the scope of an individual’s practice? It is however, in principle,<br />
surely important for both the older anaesthetist and their colleagues<br />
to regard peer observation and confirmation of competence (or<br />
otherwise) as helpful and in patients’ interests, and not as a challenge<br />
to their personal professionalism. This may in the future become a<br />
professional commitment, with confirmations of competence from<br />
observation etc. starting at five-year intervals earlier in a career but<br />
progressing to perhaps bi-annually at greater ages. Another factor in<br />
reducing anxiety in older workers is the minimisation of changes to<br />
their working environment, both in terms of location, equipment and<br />
personnel.<br />
To overcome some of the disadvantages of workplace assessment,<br />
simulation training has been suggested for older anaesthetists in the<br />
pre-retirement phase of their careers. Evidence exists that knowledge<br />
and skill sets are transferred from the simulated environment to the<br />
clinical setting, both for procedural skills, and non-technical skills<br />
for crisis management. However, using simulation as a summative<br />
assessment tool might be problematic, as validity has not been tested<br />
in this age group. Boulet and Murray [70] conclude that ‘it is not clear<br />
how judgments of minimal competence should or could be made’.<br />
Return to work after illness<br />
Another problem that already exists is that of anaesthetists returning<br />
to work from non-trivial illness (e.g. myocardial infarction, transient<br />
ischaemic attacks and depression). Such an event is more common<br />
in the older age group, and diseases recur. Measures that could be<br />
put in place that would enhance patient safety with respect to older<br />
anaesthetists in this situation could include:<br />
• A gradual and planned return to work, at an appropriate pace to<br />
allow stamina and confidence to re-build.<br />
• Never working in an isolated site or alone without anaesthetists<br />
in adjoining theatres.<br />
• Identification of a younger buddy.<br />
• Having known support readily available to assist in crises (clinical<br />
events or personal health).<br />
• Specifying appropriate clinical duties more closely.<br />
• Considering changes (perhaps temporary) to job plans.<br />
• Considering changes to the annual appraisal process and<br />
combining them with a medical report of fitness for employment.<br />
Summary<br />
A reasonable summary of the present position is to say that:<br />
• There will be an increase in the number of older anaesthetists in<br />
the workplace in future, and there need to be plans in place to<br />
manage this demographic shift.<br />
• There is evidence emerging that some older anaesthetists may<br />
have a reduced clinical performance that can be adverse to<br />
patient safety.<br />
• There is a widespread belief that older anaesthetists need<br />
enhanced monitoring of their workplace performance.<br />
• It would be valuable to introduce some sort of process to confirm<br />
competence within the individual’s job plan before problems<br />
arise.<br />
• Annual appraisal needs to be tailored specifically to the older<br />
practitioner so as to allow a genuine two-way interchange of<br />
information both to optimise the anaesthetist’s job plan and to<br />
maximise patient safety.<br />
• Older anaesthetists need to recognise that performance<br />
deteriorates with age, and they need to be both self-aware and<br />
proactive in addressing concerns they have about themselves.<br />
Individual anaesthetists have a responsibility to demonstrate<br />
insight into the potential impacts of ageing, and to ensure that<br />
their health remains compatible with their job requirements.<br />
• Older anaesthetists should comply with reasonable requests<br />
from their department with respect to their planned duties. If<br />
changes are needed, it is vital that the clinical director ensures<br />
the older anaesthetist understands the reasons for change, and<br />
that their perspective is taken into account in decision-making.<br />
• Although ageing processes are known to be individually variable,<br />
it may be necessary for the purposes of practicality to introduce<br />
some arbitrary age ranges or limits within or at which age-related<br />
factors are reviewed.<br />
For a successful outcome, there will be complementary features of<br />
departmental policy that need to be introduced that will mirror the<br />
responsibilities of the individual practitioner, and these are considered<br />
in the next section. To plan a good future for patients, individual<br />
anaesthetists and departments, older workers must be supported<br />
and not left to form yet another ‘lost tribe’.<br />
6.2: Considerations for the employer<br />
In increasing the age at which NHS pensions can be withdrawn<br />
without actuarial decrement, the Government has created an openended,<br />
uncontrolled experiment for departments and hospitals that<br />
have to accommodate the demographic shift in retirement age while<br />
maintaining patient safety. In addition, if the NHS is to have enough<br />
staff to meet ever-increasing demands, it will need to retain older<br />
workers. As with anaesthetists themselves, the first thing departments<br />
and hospitals have to do is to recognise the problems ahead, plan for<br />
them and be prepared to commit resources in terms of time and cost<br />
to maintaining safety.<br />
General principles<br />
A passive ‘wait and see’ and ‘hope for the best’ approach cannot be<br />
justified on the available safety data related to ageing. Organisations<br />
must therefore ensure that job plans, CPD and the work environment<br />
are designed and adapted to meet the needs of older workers.<br />
Clinical directors and departments that take a strategic approach,<br />
with effective job planning and appropriate involvement of human<br />
resources and occupational physicians, are likely to get the most from<br />
their older workforce.<br />
All employers ought to be able to trust anaesthetists to adhere to<br />
professional standards. With more people in the future working<br />
22 Anaesthesia News August 2016 • Issue 349 Anaesthesia News August 2016 • Issue 349 23
eyond the age at which they would choose to retire, there is a potential<br />
for this trust to be broken more frequently than it is at present, since<br />
older physicians are less likely to follow guidelines [66]. Current GMC<br />
guidelines (Good Medical Practice Domain 2 [71]) make it clear that<br />
there is an inherent responsibility to comply with workplace policies.<br />
Adherence to these by medical staff is a reasonable expectation of the<br />
employer.<br />
Departments and Clinical Directors have a responsibility to ensure<br />
that the working environment addresses the needs of older workers.<br />
Equipment should be easy to see and hear. Hearing becomes<br />
progressively less sensitive, and cataracts, glaucoma and macular<br />
degeneration are all more common with advancing age. Beeps and<br />
alarms need to be sufficiently flexible to cater for normal age-related<br />
hearing loss [68], and drug labels and monitor displays should be highcontrast<br />
and in large print [72].<br />
When an anaesthetist has a chronic or relapsing condition, it is useful for<br />
the Clinical Director to involve the Consultant Occupational Physician<br />
in ensuring the individual is well enough to meet the demands of their<br />
job, to help in redesigning job plans when needed, and to optimise<br />
the working environment. A formal assessment of the workplace to<br />
identify an individual’s specific needs may be helpful, e.g. provision<br />
of appropriate seating in theatre for someone with musculoskeletal<br />
problems.<br />
Job plans<br />
Individual job plans must take appropriate account of the impacts<br />
of ageing. Over time, older anaesthetists’ work patterns will need<br />
adjustment. Changes made should play to the individual’s strengths,<br />
and ensure continued involvement in the department. Job satisfaction<br />
and a sense of being valued by colleagues are important in retaining<br />
older colleagues in the workforce. Appropriate job planning might<br />
include daytime weekend work instead of overnight on-call, flexible<br />
working, shorter hours, less isolated working and less demanding or<br />
less stressful lists. A change of role might be appropriate for some,<br />
perhaps involving pre-operative assessment clinic work, undergraduate<br />
or postgraduate education, clinical governance or other non-clinical<br />
roles.<br />
Because the impact of ageing is very variable, the timing and nature<br />
of changes to job plans will be different for different individuals. It is<br />
therefore difficult to provide indicative age ranges at which such changes<br />
should be considered. It is also possible that some individuals may<br />
demand changes that suit them, but that are difficult or unreasonable<br />
for the department to accommodate. This can produce strains that will<br />
need to be overcome.<br />
Irrespective of the increase in statutory retirement age (as described in<br />
Section 5.4), the Repeal of Retirement Age Provisions Regulations 2011<br />
came into force on 6 April 2011 in England, Scotland and Wales. One<br />
of the consequences of this was that, from October 2012, it was not<br />
possible for employers to require employees to retire on the grounds<br />
of age alone. This means that an enforced retirement would have to be<br />
a proportionate means of achieving a legitimate aim of the employer.<br />
In practice, justifying such a retirement is likely to be difficult unless<br />
the employer can provide evidence that there is a decline in either<br />
intellectual or physical performance, which is linked to an increase in<br />
age that prevents the job being done properly.<br />
The current situation is that if a person is performing satisfactorily and<br />
wishes to continue to work in the same post without change, they<br />
cannot be prevented from doing so on the grounds of age alone. If<br />
changes are desired to the job description, these can be requested<br />
by the employer or the employee. Case law is developing on disputes<br />
in which these requests do not result in agreement. However, it has<br />
been established that an employee cannot demand changes to their<br />
job which convenience them but do not meet the corporate objectives<br />
of the employer. Similarly, the employer has to make ‘reasonable’<br />
efforts to accommodate a request if the corporate objectives can still<br />
be attained if the request were granted. The Department of Work and<br />
Pensions [73], in its description of good employment practice, says:<br />
‘Part-time or flexible working can be an important way of enabling<br />
employees of all ages to stay in work, or return to work, while meeting<br />
their wider personal needs. For many older employees flexible working<br />
is a popular option as it allows them to make a gradual transition<br />
between full-time work and retirement. 60 per cent of over 50s would<br />
like to continue working past State Pension age, but on a part-time<br />
basis… Flexible working options can help employers to retain skilled<br />
and experienced staff. It can also help employers to manage the flow<br />
of work, whether on a day to day basis or over the longer-term. Benefits<br />
can include less downtime...or covering peak business periods’.<br />
In summary, a person at or over retirement age has identical rights<br />
and limitations to a younger person who requests a change to their<br />
job description, and it is good practice for both parties to approach the<br />
situation appreciating the objectives and views of the other.<br />
The approach of other industries<br />
The HSE, in its review of the management of safety critical occupations<br />
[56], recommends surveillance for, and the development of, intervention<br />
strategies for employers of older workers to be complemented by an<br />
assessment tool.<br />
The Work Ability Index [74], developed by the Swedish Institute of<br />
Occupational Health, is an example of a validated instrument used<br />
by occupational physicians to assess work ability during health<br />
examinations. This questionnaire asks the employee about:<br />
• Current work ability compared with lifetime best.<br />
• Work ability in relation to the demands of the job.<br />
• Number of current diseases diagnosed by a physician.<br />
• Estimated work impairment due to diseases.<br />
• Sick leave during the past year.<br />
• An employee’s own prognosis of work ability two years from now.<br />
• Mental resources.<br />
This generates a useful matrix of information from which to discuss<br />
future plans with a trained appraiser who understands the needs of<br />
the older worker and the factors that influence continued enjoyment<br />
of work. The decision to continue working or to retire is influenced by<br />
workplace performance, personal health, job satisfaction, working<br />
hours, financial status, pension arrangements, family commitments,<br />
peer-retirement norms, employer attitudes and availability of work.<br />
While not recommending this tool above others, it has had wide<br />
usage and is validated: it is an example of how other safety critical<br />
occupations have approached assessment. Assessment is common<br />
in other industries and, although well-recognised for airline pilots,<br />
analogous processes are already in place for such occupations as<br />
miners, professional road drivers, engine drivers, oil rig workers,<br />
sailors, air traffic controllers and nuclear power workers. ‘Why are<br />
anaesthetists not subject to something similar?’ is a legitimate question<br />
to ask. This will need a change of culture to one of acceptance by both<br />
anaesthetists and employers that peer monitoring and assessment is<br />
not a challenge to personal professionalism. Instead it is, or should<br />
be, an essential part of professionalism, and it needs to be recognised<br />
that this is a considerable time commitment for all concerned. To<br />
achieve the right outcome, it needs to be done properly, not squeezed<br />
in or fitted between existing commitments. At present, once consultant<br />
grade is achieved, there appears to be little or no appetite from either<br />
employee or employer to make consultant staff subject to regular<br />
workplace scrutiny of their clinical performance.<br />
6.3: The role of the Government<br />
It is clear from this review that the Government has the unenviable<br />
task of managing the increasingly complex health needs of an ageing<br />
population whose expectations of what is possible are rising in the<br />
presence of:<br />
• Probable future low economic growth.<br />
• A shortage of natural resources and energy.<br />
• An increasing ratio of economically unproductive to productive<br />
members of the population.<br />
The Government is in a difficult position. It has made an understandable<br />
start by moving towards a situation in which people provide more<br />
for their own retirement. In making savings in public expenditure<br />
by reducing pension costs, it has gone directly to the biggest<br />
lever it can pull. In addition the Government is already subject to<br />
recommendations of its own making. In 2004, the English Department<br />
of Health [75] said that ‘the reduction of inequality in health outcomes<br />
is a key objective, which is to be achieved through local action as well<br />
as national planning’. In 2007, the Office of Science and Technology<br />
[76] made it clear that ‘Health inequalities result from many interlinking<br />
factors, of which relative poverty and socioeconomic grouping are the<br />
main drivers. The greatest variations are seen in the elderly’.<br />
As previously described (Section 5.3), in 2010 the Marmot Report<br />
echoed these views. However, it is important to question whether a<br />
reduction in inequality is politically achievable, and whether there is<br />
an acceptable cost in achieving it. Approximately 2,700 years ago, it<br />
was written that ‘There will always be poor people in the land’ 12 and<br />
Aristotle 13 , who saw social differences as inevitable, said ‘The worst<br />
form of inequality is to try to make unequal things equal’. In 2014, a<br />
rather concerning health economics analysis by Bognar and Hirose<br />
[77] concluded that, in a developed democracy operating within a<br />
limited financial envelope, the pursuit of health equality may be<br />
counterproductive to many. They asked: ‘How much overall health<br />
should society sacrifice (i.e. in the better-off) for reducing the social<br />
inequality in health?’ These are political rather than health questions<br />
and the answers are not obvious. The Government’s stated policy on<br />
health equality, although laudable, may have a major impact on the<br />
service but not deliver the goals it intends. It is clear that the balance<br />
between health need and health expenditure requires constant<br />
review. It is certain that modifications to policy and solutions that limit<br />
demand will inevitably arise. How the Government will develop those<br />
policies that limit demand, or even if this is politically possible, is by<br />
no means clear. Some of the most contentious measures, which are<br />
currently not officially being considered, are:<br />
• Allowing co-funding of care within the NHS when a patient can<br />
afford it and wants it.<br />
• Facilitating and encouraging ‘self-help’ by local groups on a<br />
voluntary basis within the context of community care.<br />
• Setting a maximum cost for any specific pathway of care, and<br />
in particular for terminal illness. A fixed NHS Personal Maternity<br />
Care budget has recently been suggested [78].<br />
• Establishing a hypothecated health tax to augment health<br />
expenditure raised from general taxation. This possibility is<br />
receiving increasing consideration within parliament [79].<br />
• Admitting publically that everything cannot always be delivered<br />
to everybody on all occasions, i.e. there needs to be an ethical<br />
policy on healthcare rationing.<br />
Whatever approach the Government and politicians take, underlying<br />
the whole issue of quality is the fact that clinical honesty will not be<br />
achieved in practice without political honesty of purpose for the NHS.<br />
Watch this space.<br />
12<br />
Deuteronomy 15:11 – 7th century BCE.<br />
13<br />
Paraphrase from Aristotle, Book VII 3.5, 1325.b.<br />
24 Anaesthesia News August 2016 • Issue 349 Anaesthesia News August 2016 • Issue 349 25
6.4: The role of the public<br />
Appendix 1: Working party members<br />
The responsibilities of the public are more difficult to describe than<br />
their interests. Lifelong, free at the point of service ‘cradle to grave’<br />
healthcare has existed for over 60 years in the UK, and is now<br />
embedded as a part of British expectation. The NHS Constitution<br />
[80] was launched in an attempt to try to clarify what patients’ and<br />
employees’ rights and responsibilities were. Section 3b describes<br />
the patients’ and public’s responsibilities. These are:<br />
• Recognise that you can make a significant contribution to your<br />
own, and your family’s, good health and wellbeing, and take<br />
personal responsibility for them.<br />
• Register with a GP practice – the main point of access to NHS<br />
care as commissioned by NHS bodies.<br />
• Provide accurate information about your health, condition and<br />
status.<br />
• Keep appointments or cancel within reasonable time.<br />
• Follow the course of treatment that you have agreed, and talk to<br />
your clinician if you find this difficult.<br />
• Participate in important public health programmes such as<br />
vaccination.<br />
• Ensure that those closest to you are aware of your wishes about<br />
organ donation.<br />
• Give feedback – both positive and negative – about your<br />
experiences and the treatment and care you have received.<br />
• Treat NHS staff and other patients with respect.<br />
Peter Hutton (Chair)<br />
Peter is a consultant anaesthetist with a focus on<br />
neuroanaesthesia and trauma at the University<br />
Hospital Birmingham, and Honorary Professor of<br />
Anaesthesia at the University of Birmingham. He<br />
also undertakes Medical Examiner duties. During<br />
his career he has served on a number of national<br />
bodies such as the GMC and from 2007–2009 was joint clinical lead<br />
for unscheduled care for NHS London. He is a past Council Member<br />
of the AAGBI and was formerly President of the Royal College of<br />
Anaesthetists (2002–2003) and Chair of the Academy of Medical<br />
Royal Colleges (2002–2004). He established and chaired a Home<br />
Office Ethics Group to manage the ethical aspects of forensic DNA<br />
Analysis (2008–2010), and in the recent past was the Independent<br />
Hospital Consultant Advisor to the two Mid-Staffs inquiries. In 2014<br />
he was appointed by the Home Office to lead a review of Forensic<br />
Pathology services in England and Wales.<br />
Mary Baker MBE<br />
Tony Giddings<br />
Tony is a retired a consultant general and vascular<br />
surgeon who also holds a pilot’s licence. He has had<br />
a long-term practical and research interest in surgical<br />
organisation, performance and safe systems. A<br />
former Council Member of the Royal College of<br />
Surgeons, he was also President of the Association<br />
of Surgeons of Great Britain and Ireland. He was a reviewer for the<br />
original Mid-Staffs inquiry and a special adviser to the Parliamentary<br />
Health Committee.<br />
He continues to research and teach on patient safety and in promoting<br />
a better understanding of the opportunities for improvement in health<br />
services and the wellbeing of practitioners. Through films he has<br />
helped to show healthcare staff their familiar world with new eyes, and<br />
with new insights into human factors. He believes that we have much<br />
more to do to apply what we already know to make better use of our<br />
skills and to reduce inappropriate blame and avoidable harm.<br />
Richard Griffiths (AAGBI)<br />
Guy Hirst<br />
Guy was a British Airways pilot from 1972 until<br />
2006, during which time he flew over 18,000 hours<br />
and was a Training Captain on DC 10 and Boeing<br />
747-400 aircraft. In 1999 he was promoted to be a<br />
Training Standards Captain, responsible for training,<br />
developing and revalidating British Airways training<br />
pilots on behalf of the Civil Aviation Authority. Guy was one of the<br />
pioneers of the introduction of Human Factors (HF) Training into Airline<br />
culture.<br />
Since 2001 Guy has been running training and coaching programmes<br />
in association with many healthcare organisations in the UK. He<br />
has also been involved with several research projects, particularly<br />
in the operating theatre environment. Guy is the co-founder of Risky<br />
Business (http://www.risky-business.com) He is the Aviation Expert for<br />
ITV news and recently appeared in a BBC Horizon programme entitled<br />
How to Avoid Mistakes in Surgery.<br />
Nancy Redfern (AAGBI)<br />
These are all laudable responsibilities, but what is lacking is an open<br />
public discussion about the quantity and content of healthcare that<br />
can be provided across the NHS with the current funding. Many visits<br />
to primary care and A&E departments are known to be unnecessary<br />
and waste resources. For the NHS to be able to pursue better<br />
methods of managing serious illness, the public will have to use<br />
the services more sparingly, and have a better understanding of the<br />
costs of what is provided.<br />
Mary is a sociologist whose professional life has<br />
been spent representing the interests of patients<br />
and relatives, culminating as the former CEO of the<br />
Parkinson’s Disease Society. She is the Immediate<br />
Past President of the European Brain Council, Past<br />
President of the European Federation of Neurological Associations, a<br />
Consultant to the World Health Organization and Chair of the Working<br />
Group on Parkinson’s Disease. Academic appointments include<br />
Associate Membership of the Health Services Research Unit, University<br />
of Oxford and Visiting Fellow within the London School of Economics<br />
Health Centre. For her work, Mary has received Honorary Doctorates<br />
from the Universities of Surrey and Aston. She had Honorary Fellowship<br />
conferred by the Faculty of Pharmaceutical Medicine. In 2009 she<br />
received the prestigious British Neuroscience Association Award<br />
for Outstanding Contribution to British Neuroscience and for Public<br />
Service, followed in 2014 by the Dana/EDAB Lifetime Achievement<br />
Award for Outreach on Behalf of Brain Research.<br />
Following postgraduate clinical training in the East<br />
Midlands and California and undertaking a BJA<br />
Research Fellowship and completing an MD (1995)<br />
in Leicester, Richard was appointed to his present<br />
post of consultant anaesthetist at Peterborough &<br />
Stamford Hospitals in 1996. He was an examiner for<br />
the FRCA (2003–2012) and was elected to the Council of the AAGBI<br />
in 2008. Here he served as Honorary Secretary and is currently a Vice<br />
President. He chaired AAGBI working parties into Proximal Femoral<br />
Fractures and Surgery in the Elderly.<br />
Richard has pursued a major interest in peri-operative medicine in<br />
older adults, specifically around hip fractures. He founded the NHS Hip<br />
Fracture Perioperative Network in 2007 and co-led the observational<br />
study, Anaesthesia Sprint Audit of Practice (ASAP). He was awarded<br />
the Dudley Buxton medal by the Royal College of Anaesthetists for<br />
promoting the understanding of the science of anaesthesia in 2014.<br />
Nancy is Honorary Membership Secretary of the<br />
AAGBI and a Consultant Anaesthetist. Throughout<br />
her 29 years of consultant practice, her interests have<br />
been in education and professional development.<br />
Following a stint as College Tutor and Programme<br />
Director, she worked part-time as Associate Dean<br />
managing flexible training and developing a system to support and<br />
manage doctors who became ill. This led to work on the ‘expert<br />
group’ of the National Clinical Assessment Service. For her Diploma<br />
in Education she reviewed ways of managing and supporting doctors<br />
in difficulty. As Specialty Dean Director, she managed 56 different<br />
disciplines, contributed regularly to the Conference of Postgraduate<br />
Medical Deans and was Lead Dean for two specialties. She established<br />
mentoring both in the Northern Deanery and at the AAGBI, and now<br />
reaps the benefit, using mentors to ensure she contributes in ways she<br />
enjoys in her senior years.<br />
Carol Black DBE<br />
William Harrop-Griffiths (RCoA)<br />
David Shipway<br />
Introducing this as a social concept through public education will be<br />
difficult but necessary. If the public does not respond to calls for better<br />
usage, funds will inevitably dry up, and rationing without rationale will<br />
become the norm unless there are personal funds to bridge the gap.<br />
There is evidence that rationing is already happening internationally<br />
[81]. With the increased use of pre-assessment clinics because of<br />
the increased age and complexity of patients, these locations could<br />
gradually become the places where ‘worthwhile use of resource’<br />
decisions are taken [82]. To be able to retain the trust of the public,<br />
discussions with patients and relatives need to be open and honest.<br />
This again requires proper public information and education to allow<br />
conversations to be undertaken against the background of an ethical<br />
framework acceptable to society and supported by the Government.<br />
Dame Carol Black is Principal of Newnham College<br />
Cambridge, Expert Adviser on Health and Work to<br />
the Department of Health England and to Public<br />
Health England, and Chairman of the Nuffield Trust<br />
for Health Policy. She is also a member of the Welsh<br />
Government’s Bevan Commission on Health in<br />
Wales, and Chair of the RSSB’s Health and Wellbeing Policy Group.<br />
In November 2011 when National Director for Health and Work she<br />
completed as Co-Chair an independent review for the UK Government<br />
of sickness absence in Britain. The recommendations of this report<br />
are now being put in place, with for example a national Fit for Work<br />
Service. Professor Black is a Past President of the Royal College<br />
of Physicians, and a past-Chair of the Academy of Medical Royal<br />
Colleges. The Centre she established at the Royal Free Hospital in<br />
London continues to be internationally renowned for the research and<br />
treatment of connective tissue diseases such as scleroderma.<br />
William is a Consultant Anaesthetist and Honorary<br />
Clinical Senior Lecturer at Imperial College Healthcare<br />
NHS Trust, London, UK. He graduated in 1981 from<br />
Oxford University and St Thomas’s Hospital, London<br />
and trained in London and Seattle. He was President<br />
of the AAGBI from 2012–2014, and is a Council<br />
Member of the Royal College of Anaesthetists. He is the Chair of<br />
NHS England’s National Safety Standards for Invasive Procedures<br />
Group, and has great enthusiasm for regional anaesthesia with<br />
clinical interests in orthopaedic, obstetric and vascular anaesthesia.<br />
William is an Associate Editor of the journal Regional Anesthesia &<br />
Pain Medicine. He is fond of speaking in public, and his lectures have<br />
often been described as ‘a victory of style over content’. He takes this<br />
as a compliment.<br />
David is a Consultant Physician and Gerontologist<br />
at St Mary’s Hospital, Imperial College Healthcare<br />
NHS Trust, London. He is an atypical geriatrician,<br />
and subspecialises in the peri-operative care of old<br />
and multimorbid patients undergoing surgery. David<br />
trained at Oxford University, and completed his<br />
postgraduate medical training in London. He undertook specialist<br />
fellowship training in peri-operative medicine at Guy’s and St Thomas’<br />
NHS Foundation Trust. Since his appointment at St Mary’s Hospital,<br />
he has established a new service delivering embedded peri-operative<br />
geriatric medical care within the department of surgery. He has<br />
published in the field of peri-operative medicine and the implications of<br />
the ageing population for surgical services and training. His specialist<br />
interests are frailty and cognitive impairment in the peri-operative<br />
setting.<br />
26 Anaesthesia News August 2016 • Issue 349 Anaesthesia News August 2016 • Issue 349 27
15 th Anaesthesia, Pain and Critical Care Update<br />
Friday 30 th September & Saturday 1 st October 2016<br />
Royal Armouries, Armouries Drive, Leeds LS10 1LT<br />
REGISTRATION<br />
08:00 - 08:45: Registration, Coffee, Trade Stands<br />
08:45 - 09:00: Welcome address - Dr Velu Guruswamy, Leeds, Organising Secretary<br />
SESSION 1 (Chairs – Prof Ravi Mahajan & Dr Mahesh Shah)<br />
09:00 - 09:25: Management of Critically unwell parturients<br />
Dr Audrey Quinn , Middlesborough 2B06, 3B00<br />
09:25 - 09:50: Day to day challenges in Paediatric Anaesthesia<br />
Dr Stephanie Bew, Leeds 2D02, 3D00<br />
09:50 - 10:15: Trauma Anaesthesia - lessons learnt & is there a fixed recipe<br />
Dr Martin Drezner, Leeds 2A02, 3A10<br />
10 :15 -10:30: Discussion<br />
10:30 - 11:00: Coffee break, Trade Stands, Posters<br />
SESSION 2 (Chairs – Prof Rajinder Mirakhur & Dr Ravi Marthi)<br />
11:00 - 11:25: Paediatric Anaesthesia in India - remembering ‘Taare Zameen Par’<br />
Prof (Retd) Rebecca Jacob, India 3J00<br />
11:25 - 11:50: Patient safety first<br />
Dr Liam Brennan, President RCoA 3I00<br />
11:50 - 12:15: Is Medical profession under threat in UK<br />
Dr Anthea Mowat, Deputy Chair BMA, London 3J00<br />
12:15 - 12:30: Discussion<br />
12:30 - 13:30: Lunch , Posters, Trade Stands<br />
SESSION 3 A (Chairs – Dr Roop Kishen & Dr Shivkumar Singh)<br />
13:30 - 14:45: Free paper presentation<br />
SESSION 3B (Chairs – Dr Ranjit Verma & Dr Nalini Malarkkan)<br />
13:30 - 13:55: Acute Brain Injury - Optimum management from DGH to Tertiary Center<br />
Dr Tonny Veenith, QEH, Birmingham 2F01, 3F00<br />
13:55 - 14:20: Acute pain in Chronic pain patients<br />
Dr Barani Ganesan, Leeds 3E00<br />
14:20 - 14:45: Why people fail in Revalidation<br />
Ms Tista Chakravarthy- Gannon, Lead Regional Advisor, GMC, London 3J00<br />
14:45 - 15:00: Discussion<br />
15:00 - 15:30: Coffee, Trade Stands and Posters<br />
SESSION 4 (Chairs – Dr Abhiram Mallick & Dr Jayavanth Kini)<br />
15:30 - 15:55: Peri-operative Medicine<br />
Dr Ramani Moonesinghe, London 2A06, 2A07<br />
15:55 - 16:20: Oxygen Insufflation in Difficult Airway<br />
Dr Anil Patel, President, DAS 1C02, 3A01<br />
16:20 - 16:30: Discussion<br />
SESSION 5 (Chairs – Prof Monsukh Popat & Dr Pawan Gupta)<br />
16:30 - 17:15: Debate – This house believes consultants being resident on call<br />
is the way forward for the NHS 3J00<br />
Supporting the notion - Dr Simon Tomlinson, Manchester,<br />
Against the notion - Dr Hamish McLure, Leeds<br />
(RCOA Approved 6 CPD points)<br />
Organsied by BAOIA. Charity Dinner with Mr Sunil Gavaskar.<br />
Further details and registration, visit www.baoia.co.uk<br />
Workshops on 1 st October 2016<br />
WS 1 - Airway workshop (AW)<br />
Dr Sonal Sonwalkar / Dr Heather Gorton<br />
Regional Anaesthesia (RA)<br />
Dr Sameer Bhandari / Dr Vinay Shanthi<br />
WS 2 UL (UPPER LIMB / TRUNK)<br />
WS 3 LL (LOWER LIMB / CNB)<br />
WS 4 - Simulation workshop (SW)<br />
Organiser TBC<br />
09.00-<br />
12.30<br />
13.30-<br />
16.30<br />
WS1 WS2 WS3 WS4<br />
AW UL - SW<br />
AW - LL SW<br />
Each delegate can attend 2 of 4 workshops<br />
(RCOA Approved 6 CPD points)<br />
EARLY BIRD<br />
BOOKING CLOSES<br />
26 SEPTEMBER<br />
2016<br />
ANNUAL<br />
SCIENTIFIC<br />
MEETING<br />
2016<br />
BOOKING NOW OPEN<br />
Torquay 16-18 November 2016<br />
Riviera Centre<br />
Torquay<br />
ABSTRACTS<br />
SUBMISSION DEADLINE<br />
05 SEPTEMBER<br />
2016<br />
• WORKSHOPS<br />
• PRO/CON DEBATES<br />
• EXPERT CASE DISCUSSION<br />
• ODP SIMULATION SESSION<br />
• ORAL PRESENTATIONS<br />
• INDUSTRY EXHIBITION<br />
www.das2016.co.uk<br />
DAS_Bulletin_Ad_2016.indd 1 24/06/2016 14:18<br />
TRAVEL GRANTS/IRC FUNDING<br />
The International Relations Committee (IRC)<br />
offers travel grants to anaesthetists who<br />
are seeking funding to work, or to deliver<br />
educational training courses or conferences,<br />
in low and middle-income countries.<br />
Please note that grants will not normally be considered for<br />
attendance at congresses or meetings of learned societies.<br />
Exceptionally, they may be granted for extension of travel<br />
in association with such a post or meeting. Applicants<br />
should indicate their level of experience and expected<br />
benefits to be gained from their visits, over and above<br />
the educational value to the applicants themselves.<br />
For further information and an application form<br />
please visit our website:<br />
http://www.<strong>aagbi</strong>.org/international/irc-fundingtravel-grants<br />
or email secretariat@<strong>aagbi</strong>.org<br />
or telephone 020 7631 1650 (option 3)<br />
Closing date: 19 September 2016<br />
C<br />
M<br />
Y<br />
CM<br />
MY<br />
CY<br />
CMY<br />
K<br />
11 th West of England<br />
Anaesthesia Update<br />
11 th West of England Anaesthesia Update Conference<br />
Based in Chalet Hotel St Christoph Austria<br />
Talks cover a wide range of topics in anaesthesia, pain and ICM<br />
15 CPD points RCOA<br />
Flights from Bristol, Gatwick, Southampton and other airports nationwide<br />
All grades of Anaesthetist from everywhere welcome.<br />
ROYAL COLLEGE OF PHYSICIANS<br />
16 th – 20 rd January 2017<br />
St Christoph am Arlberg (nr St Anton), Austria<br />
Visit: www.weauconf.com<br />
7TH NOVEMBER 2016<br />
LONDON<br />
The<br />
Preoperative<br />
Association<br />
NATIONAL CONFERENCE<br />
ACCREDITED WITH 5 CEPD POINTS<br />
TOPICS TO INCLUDE: Preoperative Optimisation in Primary Care / “Getting it right first<br />
time” Model Hospital / Perioperative Medicines Guide / Obstructive Sleep Apnoea /<br />
Hypertension Guidelines Update / Perioperative Medicine Curriculum / Revalidation<br />
for Nurses / ECG Workshop / Perioperative Quality Improvement Programme<br />
ABSTRACT FOR PRESENTATIONS OR POSTERS TO BE SUBMITTED BY 9TH SEPTEMBER 2016<br />
Open to all healthcare professionals involved in the preoperative assessment of<br />
the surgical patient. For full details and to book your place, please contact us:<br />
W: WWW.PRE-OP.ORG / T: 020 7631 8896
THE ROYAL COLLEGE OF ANAESTHETISTS<br />
CPD STUDY DAY<br />
BELFAST<br />
Wednesday, 28 September 2016<br />
The Waterfront Hall, Belfast<br />
£200 (£150 for RCoA registered trainees)<br />
Event organiser: Dr B Darling<br />
Lectures on the day may include:<br />
■ Anaesthesia for bariatric surgery<br />
■ Interventional radiology in the management of strokes<br />
■ Pre-hospital health emergency management system<br />
■ Fast track total knee arthroplasty<br />
■ Analgesia for acute surgical pain<br />
■ The GMC: working for patients<br />
■ The GMC: working with doctors<br />
■ How doctors cure crime<br />
5<br />
CPD<br />
CREDITS<br />
st<br />
21Annual Scientic Meeting 2016<br />
Friday, 4 th November 2016<br />
Oxford Town Hall, Oxford<br />
Improving patients’ outcomes<br />
Sessions:<br />
• Pain in orthopaedic patients: whose pain is it?<br />
• Pushing the boundaries of regional anaesthesia<br />
for orthopaedic surgery<br />
• Working together to improve patients’ outcomes<br />
Follow @RCoA_Events<br />
Find us on Facebook<br />
events@rcoa.ac.uk | 020 7092 1673 | www.rcoa.ac.uk/events<br />
Abstract submission deadline: 23 rd September<br />
Register at www.bsoa.org.uk<br />
Registration fees from £ 50.<br />
Approved by the RCoA for 5.0 CPD credits<br />
Essentials of Anaesthesia in the<br />
Developing World<br />
Focused Intensive Care<br />
Echocardiography (FICE) Course<br />
Training the Trainers<br />
Resuscitation Update for<br />
Consultants<br />
Cardiff Ultrasound Guided<br />
Regional Anaesthesia with<br />
Cadaveric Anatomy<br />
Cardiff Perioperative Hands-on<br />
Transoesophageal<br />
Echocardiography (TOE)<br />
Symposium<br />
Date<br />
15th September 2016<br />
13th & 14th October 2016<br />
22 November 2016<br />
Course Full<br />
NEW date coming in Autumn!<br />
Dates Available are:<br />
20-22 September 2016<br />
15-17 November 2016<br />
12th &13th September 2016<br />
Course Details<br />
A 1 day fun, interactive and informative course offering an<br />
introduction to working in the developing world. There will be<br />
simulation demonstrations and participants can experience<br />
equipment used applicable to the developing world.<br />
FICE accreditation course for the Intensive Care Society<br />
(ICS) and British Society of Echocardiography (BSE).<br />
A 2 day multi professional simulation course offering 10 CPD<br />
points for those interested in Simulation Education.<br />
A half day refresher course on managing cardiac arrest in<br />
adults.<br />
A 2 day practical hands-on course that course enables you to<br />
optimize and interpret the ultrasound machine’s information<br />
and to apply it to real-world clinical procedures.<br />
A 3 day practical course for all specialists who wish to<br />
perform perioperative transoesophageal echocardiography.<br />
Symposium Course Details<br />
A 2 day lecture based course for all specialists who wish<br />
to gain expert knowledge of transoesophageal<br />
echocardiography.<br />
Courses for Clinicians<br />
Course Fee<br />
£100<br />
Earlybird price by 26th Aug or £120<br />
thereafter. (including<br />
lunch/refreshments)<br />
£150<br />
(including lunch/refreshments)<br />
£240<br />
Earlybird price by 20th Sept or £280<br />
thereafter.(including lunch/refreshments)<br />
£60<br />
(including lunch/refreshments)<br />
£260<br />
(including lunch/ refreshments)<br />
£400<br />
(including lunch/refreshments)<br />
£450<br />
(including lunch/refreshments)<br />
Research & Statistics Courses Statistics Course Details<br />
£80 Earlybird price by 1st Oct or £100<br />
Simple Statistics Excel & SPSS 21st October 2016<br />
A 1 day course open to all health care workers who wish<br />
to gain statistical experience.<br />
thereafter. (including<br />
Lunch/Refreshments)<br />
Introduction to Research 15th & 16 December 2016<br />
Research Course Details - 10 CME Points from the<br />
Royal College of Anaesthetists. A 2 day course covering<br />
all research competencies of the 2010 high syllabus in<br />
research<br />
£150 Earlybird price by 20th Nov or<br />
£180 thereafter. (including<br />
lunch/refreshments)<br />
To Register:<br />
11th October 2016<br />
click on this Link: https://form.jotformeu.com/cmhabc/Courses<br />
Website: For more information www.bmc.wales<br />
Trainees and<br />
medical students<br />
Download the latest edition<br />
of the GAT Handbook<br />
an-august16.indd 2 06/06/2016 13:01<br />
OA2016_inz88x124.indd 1 17.6.16 13:4<br />
Covering all aspects of anaesthesia training<br />
experience in the UK:<br />
• Guidance on applying for training jobs<br />
• Tips and advice on developing your CV in<br />
sub-speciality areas<br />
• Including maternity leave, working less-than-full-time<br />
and keeping out of trouble in your career<br />
An invaluable resource for trainees and trainers alike.<br />
Download your free copy of the new GAT Handbook TODAY<br />
www.<strong>aagbi</strong>.org/GAThandbook<br />
THE GAT<br />
HANDBOOK<br />
TWELTH EDITION<br />
With<br />
interactive<br />
links – find<br />
what you<br />
need easily
Over<br />
£71,000<br />
raised<br />
so far<br />
£25,000 still to raise. Help us achieve our target<br />
Only 2 months to go!<br />
In this Olympic Year, help us save thousands of lives around the world by donating to Lifeboxes for Rio.<br />
Help us to reach our target of £96,000 to buy 600 Lifebox Pulse Oximeters - that’s the same as the number<br />
of Team GB athletes attending the Olympic and Paralypmic Games in Rio.<br />
Become a Lifeboxes for Rio fundraiser today<br />
www.<strong>aagbi</strong>.org/LifeboxesForRio<br />
Together we can save thousands of lives around the world<br />
where patients are at risk of death from hypoxia.<br />
AAGBI Foundation: Registered as a charity in England & Wales no. 293575 and in Scotland no. SC040697<br />
Lifebox: Registered as a charity in England & Wales (1143018)<br />
Second City Cycle: bike ride to<br />
Annual Congress Birmingham 2016<br />
The final lap of Lifeboxes for Rio draws<br />
closer, we still have £25,000 left to raise<br />
For the last four years, our fearless team of cyclists have peddled up and<br />
down the UK, to the AAGBI Annual Congress. This year is no different!<br />
The Annual Congress 2016, is being held in the second city: Birmingham.<br />
In aid of the AAGBI’s fundraising campaign, Lifeboxes for Rio, the bike<br />
ride will navigate its way along the towpaths of the longest canal in<br />
England: The Great Union Canal.<br />
The proposed starting day will be Saturday 10 September, leaving from<br />
AAGBI HQ in London and arriving in Birmingham<br />
12 September. The stopovers will be in:<br />
Day 1: Tring Day 2: Harpole Day 3: Birmingham<br />
Each year the AAGBI celebrates, recognises and awards the work of individuals and teams<br />
within the anaesthesia profession.<br />
Abstract Submission<br />
You’re invited to submit an abstract for poster presentation<br />
at WSM London 2017. The deadline to submit an abstract<br />
is Wednesday 31 August 2016. A preliminary review of<br />
abstracts received will determine which abstracts will be<br />
accepted for poster presentation. If accepted, your abstract will<br />
be published in a fully referenceable online supplement to the<br />
Anaesthesia journal. Authors of the best poster(s) will be awarded<br />
‘Editors’ Prizes.<br />
NELA Prize<br />
NELA will also be sponsoring a Trainee poster prize at the WSM<br />
London 2017. This prize will be for the best poster that uses your<br />
hospital's NELA data to bring about an improvement in care.<br />
AAGBI<br />
Innovation Award<br />
The annual AAGBI Prize for Innovation in Anaesthesia,<br />
Critical Care and Pain.<br />
The AAGBI Prize for Innovation 2017 promotes innovation<br />
in anaesthesia and intensive care. The award is open to all<br />
anaesthetists, intensivists and pain specialists in Great Britain and<br />
Ireland and will be presented at WSM London 2017. The emphasis is<br />
on new ideas contributing to patient safety, high quality clinical care<br />
and improvements in the working environment.<br />
The deadline to apply for the AAGBI Innovation Award is Friday 30<br />
September 2016. Find out more about the AAGBI Innovation Award<br />
visit www.<strong>aagbi</strong>.org/innovation<br />
To find out more and start planning your abstract submission,<br />
visit www.wsmlondon.org/content/abstract-submissions<br />
For further information and a route map please visit<br />
www.<strong>aagbi</strong>.org/cycle<br />
Find out more – visit www.wsmlondon.org
ANNUAL CONGRESS<br />
BIRMINGHAM<br />
14 -16 September 2016<br />
Sessions include:<br />
• ICS for non-intensivists • Blood pressure • Ethics<br />
• Workforce • Tools of the trade • Hot topics in training<br />
Keynotes:<br />
Andy McCann, Performance Coach, DNA Definitive – Walking the tightrope:<br />
dynamic resilience in action<br />
Professor Alistair Burns, Manchester – Dementia: a challenge for everyone<br />
Professor Paul Myles, Melbourne – Quality of recovery and disability-free survival<br />
Practical workshops, poster presentation,<br />
social events and more!<br />
JUST OVER A<br />
MONTH TO GO -<br />
HAVE YOU BOOKED<br />
YOUR PLACE YET?<br />
European<br />
Accreditation Council<br />
for Continuing<br />
Medical Education<br />
(EACCME)<br />
applied for<br />
BOOK NOW<br />
www.annualcongress.org<br />
AAGBI1<br />
@AAGBI
Recommendations for the Safe Transfer of<br />
Patients with Brain Injury<br />
2006<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland,<br />
21 Portland Place, London W1B 1PY<br />
Telephone 020 76311650 Fax 020 7631 4352<br />
www.<strong>aagbi</strong>.org<br />
May 2006
MEMBERSHIP OF THE WORKING PARTY<br />
Dr PA Farling<br />
Dr PJD Andrews<br />
Dr S Cruickshank<br />
Dr I Johnston<br />
Dr B Matta<br />
Prof DK Menon<br />
Dr E Moss<br />
Dr MP Parris<br />
Dr M Power<br />
Dr M Smith<br />
Dr DK Whitaker<br />
Ex Officio<br />
Professor M Harmer<br />
Professor WA Chambers<br />
Dr A W Harrop-Griffiths<br />
Dr RJS Birks<br />
Dr IH Wilson<br />
Dr DE Dickson<br />
Dr D Bogod<br />
Chairman of Working Party and Immediate<br />
Past President Neuroanaesthesia Society of<br />
Great Britain & Ireland<br />
Chairman Neuro-intensive Care & Emergency<br />
Medicine Section, European Society of Intensive<br />
Care Medicine<br />
Immediate Past Honorary Treasurer Neuroanaesthesia<br />
Society of Great Britain & Ireland<br />
Council Association of Anaesthetists of Great Britain<br />
& Ireland<br />
Honorary Secretary Neuroanaesthesia Society of<br />
Great Britain & Ireland<br />
Intensive Care Society<br />
Royal College of Anaesthetists<br />
Group of Anaesthetists in Training<br />
Honorary Secretary Intensive Care Society of Ireland<br />
President Neuroanaesthesia Society of Great Britain<br />
& Ireland<br />
President Elect Association of Anaesthetists of<br />
Great Britain and Ireland<br />
President<br />
Honorary Secretary<br />
Honorary Secretary Elect<br />
Honorary Treasurer<br />
Honorary Treasurer Elect<br />
Honorary Membership Secretary<br />
Editor-in-Chief Anaesthesia<br />
The Joint Royal Colleges Ambulance Liaison Committee has endorsed this document.<br />
Significant contributions were received from The Society of British Neurological<br />
Surgeons and from Dr Stephen Hancock, Consultant Paediatric Intensivist.<br />
The Association of Anaesthetists of Great Britain and Ireland wishes to record its<br />
sincere thanks for the support and advice given by the Neuroanaesthesia Society of<br />
Great Britain and Ireland in publication of this document.<br />
© This document was first published in December 1996 by the Association of<br />
Anaesthetists of Great Britain and Ireland, 9 Bedford Square London WC1B 3RA<br />
© Copyright of the Association of Anaesthetists of Great Britain and Ireland. No part of<br />
this book may be reproduced without the written permission of the Association of<br />
Anaesthetists.
CONTENTS<br />
Section I Summary and Recommendations 02<br />
Section II Background 03<br />
Section III Introduction 04<br />
Section IV Organisation and Communication 05<br />
Section V Staffing Requirements and Standards 07<br />
Section VI Preparation for the Transfer 08<br />
Section VII The Transfer 11<br />
Section VIII Equipment and Drugs 13<br />
Section IX Education and Training 15<br />
Section X Resource Implications for Transfer of Patients 17<br />
with Brain Injuries<br />
References 18<br />
Appendices 19<br />
1
SECTION I - SUMMARY AND RECOMMENDATIONS<br />
1. High quality transfer of patients with brain injury improves outcome.<br />
2. There should be designated consultants in the referring hospitals and<br />
the neuroscience units* with overall responsibility for the transfer of<br />
patients with brain injuries.<br />
3. Local guidelines on the transfer of patients with brain injuries<br />
should be drawn up between the referring hospital trusts, the<br />
neurosciences unit and the local ambulance service. These should<br />
be consistent with established national guidelines. Details of the<br />
transfer of responsibility for patient care should also be agreed.<br />
4. While it is understood that transfer is often urgent thorough<br />
resuscitation and stabilisation of the patient must be completed<br />
before transfer to avoid complications during the journey.<br />
5. All patients with a Glasgow Coma Scale (GCS) less than or equal to<br />
8 requiring transfer to a neurosciences unit should be intubated and<br />
ventilated, as should any patients with the indications detailed in<br />
Appendix 1.<br />
6. Patients with brain injuries should be accompanied by a doctor with<br />
appropriate training and experience in the transfer of patients with<br />
acute brain injury. They must have a dedicated and adequately<br />
trained assistant. Arrangements for medical indemnity and personal<br />
accident insurance should be in place.<br />
7. The standard of monitoring during transport should adhere to<br />
previously published standards.[1]<br />
8. The transfer team must be provided with a means of communication<br />
- a mobile telephone is suitable.<br />
9. Education, training and audit are crucial to improving standards of<br />
transfer.<br />
* Throughout this document the term acute neuroscience unit is taken<br />
to include neurology, neurosurgery, neuroanaesthesia, neurocritical<br />
care and neuroradiology.<br />
2
SECTION II - BACKGROUND<br />
In 1996 the Association of Anaesthetists (AAGBI) and the<br />
Neuroanaesthesia Society (NASGBI) published Recommendations for<br />
the Transfer of Patients with Acute Head Injuries to Neurosurgical<br />
U n i t s. Since 1996 a number of organisations have published<br />
guidelines relating to transfer.[2-8] However, it was felt that it would<br />
be beneficial to provide an up-to-date resource to be distributed to<br />
members of the AAGBI. The National Service Framework for long term<br />
conditions has implications for neurological patients.[9] Changes in<br />
clinical practice, for example the development of intrava s c u l a r<br />
treatment of subarachnoid haemorrhage,[10] will increase the number<br />
of transfers of patients with non-traumatic brain injury. It wa s ,<br />
therefore, considered appropriate to extend the scope of the guideline<br />
to include all patients with acute brain injury. Ideally the transfer of<br />
paediatric patients will be undertaken by staff experienced in the<br />
transfer of critically ill children.<br />
Supplementary electronic material can be obtained from many of the<br />
sources that are detailed in the References section of this document.<br />
3
SECTION III - INTRODUCTION<br />
Patients with neurotrauma or other acute brain injury often receive<br />
their initial treatment at a local hospital, which may not have a<br />
neurosciences unit. As a result, many patients with serious brain<br />
injuries have to be transferred urgently between hospitals by road<br />
ambulance, or occasionally by air. In some areas Critical Care<br />
Networks and transfer groups have been established according to<br />
national directives.[11] While no precise time targets have been set<br />
between injury and surgery, a maximum of 4 hours is aimed at because<br />
it is clear that the sooner an expanding haematoma is evacuated, the<br />
better for the patient.<br />
Transfer of patients with brain injury is potentially hazardous if poorly<br />
executed.[12] Patients can come to harm as a result and ultimate<br />
neurological outcome may be adversely affected. This can be avoided<br />
if sound principles are applied. The main causes of secondary brain<br />
damage are raised intracranial pressure (ICP), hypotension, hypoxia,<br />
hy p e rcarbia, cardiovascular instability and hy p e r pyrexia. Most<br />
principles of safe transfer are common to all seriously ill patients but<br />
there are some specific features that apply in particular to those with<br />
acute brain injury. These principles apply equally to transfer of patients<br />
both within and between hospitals.<br />
These recommendations are provided for those responsible for<br />
planning, managing and undertaking transfer of brain injured patients.<br />
They aim to supply not only practical guidelines for ensuring safe<br />
transfer of individual patients, but also principles of organisation to<br />
assist in local negotiation when establishing new or improving existing<br />
transfer arrangements.<br />
4
SECTION IV - ORGANISATION AND<br />
COMMUNICATION<br />
Safe transfer of patients with brain injuries requires an effective<br />
partnership between the referring hospitals, the neurosciences unit and<br />
the ambulance service.<br />
Local guidelines should be agreed between the referring hospitals and<br />
the neurosciences unit in advance. They should be subject to regular<br />
review and audit. The guidelines will include:<br />
• which patients should be referred,<br />
• when a transfer should be made,<br />
• who is responsible for accepting the patient,<br />
• the preparations and arrangements for the journey itself so that there<br />
is no unnecessary delay,<br />
• when the responsibility for the patient is transferred from the<br />
referring to the receiving team.<br />
Anaesthetists should be involved in agreeing local guidelines that are<br />
consistent with established national and international guidelines.<br />
Guidelines do not replace clinical judgement but they provide a safe<br />
framework within which judgement can be exercised.<br />
Every hospital to which the ambulance services take patients with<br />
serious brain injuries must have facilities for resuscitation and<br />
diagnosis, including 24-hour access to computerised tomography.<br />
Appropriate staff and equipment should be available to ensure a safe<br />
transfer to the neurosciences unit when necessary. There should be a<br />
designated consultant within that hospital who has ove ra l l<br />
responsibility for secondary transfers and a consultant at the<br />
neurosciences unit who has ove rall responsibility for receiv i n g<br />
transfers. These duties should be recognised in job plans.<br />
Education and training are crucial to improving standards of transfer.<br />
Appropriate resources must be provided by those who plan and<br />
5
purchase these services. They must be available to all professionals<br />
who share responsibility for the safety of the patient. There are obvious<br />
advantages in having a common philosophy of care and standardised<br />
terminology, such as those provided by the Advanced Trauma Life<br />
Support (ATLS) system and the GCS. A modified GCS should be used<br />
for paediatric patients.[3]<br />
Good verbal and written communications are vital. This is especially<br />
so at the time of referral and when a patient is handed over at the end<br />
of the transfer. They will include precise details of where, within the<br />
neurosciences centre, the patient is to be taken. The ambulance<br />
service appreciate an early warning to facilitate their arrangements.<br />
6
SECTION V - STAFFING REQUIREMENTS AND<br />
STANDARDS<br />
Expediency should not dictate the level of expertise available for the<br />
transfer of patients. Critically ill patients with acute brain injuries must<br />
be accompanied by a doctor with suitable training, skills,<br />
competencies and experience of brain injury transfer.<br />
It must be recognised that a trainee alone in an ambulance is working<br />
in an unsupervised capacity. Changes in working patterns may reduce<br />
the availability of trainees for transfers and consultant time for transfers<br />
must be built into manpower projections. Account should be taken of<br />
shift arrangements when deciding who should accompany the patient.<br />
A dedicated trained assistant must be provided for the escorting doctor.<br />
This might be an appropriately trained operating department<br />
practitioner, nurse or paramedic.<br />
Employers must ensure that there is appropriate medical indemnity<br />
i n s u rance for such transfers. In addition, the Association of<br />
Anaesthetists (AAGBI) recommends that doctors are members of<br />
medical defence organisations. Adequate death and personal injury<br />
insurance must also be provided for the members of the transfer team<br />
by the employer; existing employer insurance may be inadequate and<br />
local arrangements should be clarified. Details of appropriate<br />
insurance schemes are available from the AAGBI (www.<strong>aagbi</strong>.org) and<br />
such cover is a benefit of membership.<br />
7
SECTION VI - PREPARATION FOR THE TRANSFER<br />
Many critical care networks have reached consensus with local<br />
ambulance providers to ensure that all Trusts have common standards<br />
of transfer equipment. These developments are highly desirable, and<br />
likely to result in better organisation and delivery of patient care<br />
The decision to transfer a patient with a brain injury must be made by<br />
senior medical staff at the referring hospital in consultation with senior<br />
staff at the neurosciences unit, who should provide written advice on<br />
neurosurgical management. Thorough resuscitation and stabilisation<br />
of the patient before transfer is the key to avoiding complications<br />
during the journey. The fundamental requirement before transfer is to<br />
ensure satisfactory oxygen delivery. A mean blood pressure greater<br />
than 80 mmHg (paediatric values - appendix III), PaO2 greater than 13<br />
kPa and PaCO2 between 4.5 – 5.0 kPa should be achieved.<br />
Monitoring should include:<br />
pupillary size and reaction to light<br />
ECG<br />
pulse oximetry<br />
invasive blood pressure<br />
urine output by urinary catheter<br />
capnography<br />
central venous pressure monitoring where indicated<br />
temperature (preferably core and peripheral)<br />
Investigations undertaken prior to transfer should include:<br />
arterial blood gas estimation<br />
chest, lateral cervical spine pelvis, and other appropriate X-rays [13]<br />
haematology FBC and coagulation screen<br />
biochemistry blood sugar<br />
other investigations as appropriate<br />
blood should be cross matched if appropriate, and sent in the<br />
transferring ambulance (not in a separate taxi)<br />
8
A p p ropriate re s p i ra t o ry support must be established. Tra ch e a l<br />
intubation during transfer is difficult and dangerous. All patients with<br />
a GCS of 8 or less require intubation prior to transfer. In addition,<br />
whatever the baseline GCS, intubation should be considered if the<br />
GCS has fallen by 2 or more points. Intubation is essential if there is a<br />
fall of 2 or more points in the motor score. Intubation requires<br />
adequate sedation and muscle relaxation to avoid an increase in (ICP),<br />
and measures to prevent aspiration of gastric contents. This will<br />
normally involve rapid sequence induction with in-line stabilisation of<br />
the cervical spine. After intubation, appropriate drugs should be<br />
employed to maintain sedation, analgesia and muscle relaxation,<br />
(preferably administered by syringe driver), while avoiding hypotension<br />
and reduced cerebral perfusion pressure (CPP). Patients should be<br />
ventilated with the aim of achieving a PaO2 greater than 13 kPa and a<br />
PaCO2 of 4.5 – 5.0 kPa unless there is clinical or radiological evidence<br />
of raised intracranial pressure when more aggressive hyperventilation<br />
is justified (but not below 4 kPa). If hyperventilation is used the FIO2<br />
should be increased.<br />
Inspired oxygen should be guided by blood gas estimations before<br />
departure. Expired carbon dioxide should be monitored continuously.<br />
A chest drain should be inserted if a pneumothorax is present or<br />
considered a potential problem, eg due to fractured ribs. Underwater<br />
seals should normally be replaced by leaflet valve (Heimlich type)<br />
drainage systems. Chest drains should not be clamped.[2] A large bore<br />
orogastric tube should be passed and left on free drainage (not<br />
nasogastric in case the patient has a base of skull fracture).<br />
Intravenous volume loading should be undertaken with crystalloid or<br />
colloid initially to maintain or restore satisfactory peripheral perfusion,<br />
blood pressure and urine output. 5% Dextrose should be avoided and<br />
blood products should be given as required. Hypovolaemic patients<br />
tolerate transfer poorly and the circulating volume should be normal or<br />
supra-normal before transfer, preferably with a haematocrit over 30%.<br />
A central venous catheter may be useful to optimise filling pressures<br />
and for the administration of drugs and fluids during the transfer.<br />
9
A patient who remains hypotensive despite resuscitation must not be<br />
transported until all possible causes of the hypotension have been<br />
identified and the patient stabilised.<br />
Correction of major haemorrhage takes precedence over transfer. It is<br />
important that these measures are not omitted in an attempt to speed<br />
transfer of the patient, as resultant complications may be impossible to<br />
deal with once the journey has begun.<br />
Persistent hypotension will adversely affect neurological outcome.<br />
When other causes of hypotension have been excluded, consider the<br />
judicious use of inotropes/vasopressors to offset the hypotensive effects<br />
of sedative agents.<br />
If the patient has had a seizure, loading with anticonvulsant agents<br />
(usually phenytoin) should be considered prior to transfer. Unstable or<br />
compound long bone fractures should have preliminary toilet and be<br />
splinted to provide neurovascular protection and analgesia.<br />
If the transfer team has not been involved in the initial stages they<br />
should familiarise themselves with treatment already given and<br />
independently assess the general status of the patient before departure.<br />
All lines and tubes must be fixed securely and ready access to them<br />
ensured.<br />
The transfer team should confirm the availability of an appropriate<br />
transfer vehicle and check the function of all equipment, including<br />
battery charge status.[14] Oxygen requirements for the journey<br />
including possible delays should be estimated and should include<br />
driving gas requirements of the ventilator. A minimum reserve of<br />
oxygen and drugs should be one hour or twice the estimated journey<br />
time. If transfer times are unduly long, it may be necessary to arrange<br />
for back up oxygen supplies to be made available en route if possible.<br />
Before departure, case notes, X-rays, a referral letter and investigation<br />
reports should be collated and any required blood or blood products<br />
collected. The neurosciences unit should be contacted and informed of<br />
the estimated journey time.<br />
10
SECTION VII - THE TRANSFER<br />
The transfer team should be relieved of all other duties, be<br />
appropriately dressed, equipped and insured. Ideally, the transfer team<br />
should be involved in the initial resuscitation and management of the<br />
patient. If this is not possible, they should receive a formal hand-over<br />
from the resuscitation team. All notes (or photocopies), X-rays, CT<br />
scans, blood results and cross-matched blood should accompany the<br />
patient. The duty consultant anaesthetist in the referring hospital<br />
should be made aware of the planned transfer. All monitoring<br />
equipment should be checked, connected to the patient and securely<br />
mounted so that it cannot fall on to the patient during transfer or cause<br />
injury to ambulance occupants in the event of an accident.<br />
The patient should be transferred onto the transport trolley/stretcher,<br />
properly secured and padded with due regard to any possible spinal<br />
injury.[2, 15] The patient should be positioned with a 20° head up tilt.<br />
The development of ambulance trolleys that allow this degree of tilt,<br />
while maintaining spinal immobilisation, should be encouraged. Most<br />
transfers will be by land ambulance but for transfers over longer<br />
distances local protocols may include transfer by air.[16]<br />
During transfer, patient management will be centred upon maintaining<br />
oxygenation and adequate blood pressure and minimising rises in ICP.<br />
Monitoring ECG, invasive blood pressure, SpO2, PECO2, temperature,<br />
pupillary size and reaction to light, and the administration of drugs<br />
and other infusions should be continued.<br />
A paper record must be maintained during the transfer. This may be<br />
aided by a dictaphone or by the electronic memory in monitors. The<br />
development of standardised documentation is encouraged and many<br />
critical care networks have developed local transfer documentation.<br />
Transfers should be undertaken smoothly and not at high speed.<br />
The transfer team should be equipped with a mobile telephone to<br />
contact the neurosciences unit and their base hospital en route.<br />
11
A patient who has been made physiologically stable before departure<br />
is more likely to remain so for the duration of the transfer, although<br />
there is still the need for constant vigilance and prompt action to deal<br />
with complications. If, despite thorough preparation, there is a need to<br />
perform any procedure during the transfer this should be done with the<br />
ambulance brought to a halt.<br />
Staff at the neurosciences unit should be available to receive a<br />
comprehensive hand-over following which they assume responsibility<br />
for the patient’s care. Notes, X-rays, scans and a copy of the transfer<br />
record should be left with the receiving staff. The neurosciences unit<br />
should be prepared to provide the transfer team with refreshments.<br />
A protocol should be established to ensure the immediate return of the<br />
referring team with their equipment to their hospital. Often a contract<br />
exists with a local taxi firm for this purpose. Personal injury insurance<br />
should also cover the return journey.<br />
The referring team should keep a copy of the summary and transfer<br />
record for audit purposes.<br />
The relatives should be notified about the transfer by the referring<br />
hospital, but they should not normally accompany the patient in the<br />
ambulance.<br />
12
SECTION VIII - EQUIPMENT AND DRUGS<br />
All equipment must be serviced regularly, ch e cked daily and<br />
rechecked immediately before any transfer. If the ambulance ventilator<br />
is to be used then it must be checked before departure, as should the<br />
ambulance oxygen supply and suction. It is advisable before<br />
purchasing any new equipment to consult the ambulance service, to<br />
ensure that it is compatible with the oxygen and power supply in their<br />
vehicles.<br />
The patient should receive the same standard of phy s i o l o g i c a l<br />
monitoring during transfer as they would receive in an intensive care<br />
unit. The transfer team must be familiar with all of the equipment and<br />
drugs in the transfer kit and the transfer vehicle.<br />
Essential equipment to go with the patient in the ambulance<br />
The following equipment should be readily available, purpose<br />
designed, dedicated for transfers and be stored in a suitable container<br />
which should have some form of seal, which when broken, would<br />
indicate that the equipment has been used and requires restocking and<br />
checking:<br />
1. Portable mechanical ventilator with airway pressure and minute<br />
volume monitor, and disconnect alarm<br />
2. Adequate supply of oxygen for the journey, including unforeseen<br />
delays (see Section VI)<br />
3. Portable battery powered multifunction monitor to include:<br />
• ECG<br />
• invasive blood pressure monitoring<br />
• non invasive blood pressure monitoring as a backup<br />
• central venous pressure monitoring<br />
• pulse oximetry<br />
• capnography<br />
• temperature<br />
13
4. Other equipment<br />
• suction<br />
• battery powered syringe pumps<br />
• battery powered IV volumetric pumps (infusion by gravity is<br />
unreliable during transfer)<br />
• intubation equipment<br />
• self-inflating bag, valve and mask<br />
• venous access equipment<br />
• chest drain equipment<br />
• DC defibrillator<br />
• spare batteries<br />
• warming blanket<br />
5. An adequate supply of essential drugs to go with the patient<br />
• Hypnotics, eg propofol or midazolam<br />
• muscle relaxants, eg atracurium, vecuronium,- suxamethonium<br />
may be required for re-intubation<br />
• analgesics, eg alfentanil, fentanyl,<br />
• anticonvulsants, eg diazepam, thiopentone<br />
• mannitol 20%, furosemide<br />
• vasoactive drugs, eg ephedrine, dopamine, noradrenaline<br />
• resuscitation drugs as in hospital resuscitation boxes<br />
• intravenous fluids<br />
6. Communication equipment<br />
It is essential that the transfer team should be able to communicate<br />
easily with the designated consultant or his deputy in the referring<br />
hospital and the neurosurgical team during the transfer. The benefits of<br />
a mobile telephone which can be pre-programmed with useful<br />
numbers outweigh the minimal risk of it interfering with electronic<br />
equipment.[17]<br />
7. Paediatric equipment<br />
The transfer of paediatric patients will require size specific equipment<br />
and staff experienced in the transfer of critically ill children.[6,7,18]<br />
14
SECTION IX - EDUCATION AND TRAINING<br />
Good practice depends upon sound education, adequate resources of<br />
expertise, time for training and a commitment to quality throughout all<br />
levels of the organisation. Ensuring and facilitating good educational<br />
standards and arrangements will be a function of the consultant<br />
responsible for inter-hospital transfers.<br />
The fundamental requirement is that every doctor, nurse and<br />
paramedic likely to be involved in the transfer of seriously brain<br />
injured patients has had formal training in the theoretical and practical<br />
aspects of the subject. This will include:<br />
• the principles of managing a patient with an acute brain injury;<br />
• the principles and practice of ATLS;<br />
• the adverse physiological changes associated with moving the<br />
patient;<br />
• manual handling of the patient;<br />
• practical aspects of working in an ambulance or aircraft;<br />
• knowledge of the equipment and drugs used in transfer;<br />
• the legal and safety aspects of transfer;<br />
• communications.<br />
The setting in which this education is provided will vary locally.<br />
Learning opportunities will range from mandatory induction courses<br />
for new hospital staff to formal multidisciplinary training courses on<br />
transfer medicine. The latter are now run in a number of centres, and<br />
m ay be particularly appropriate for consultants responsible for<br />
developing and maintaining the standards of transfer.[19] All doctors,<br />
nurses and other allied health professionals who are new to a hospital<br />
should attend teaching sessions to learn local arrangements and<br />
policies and meet the staff involved.<br />
Much of the educational value of any training post comes from gaining<br />
clinical experience under supervision. The designated tra n s f e r<br />
consultant should be aware of the educational opportunities offered by<br />
transfers of patients with brain injuries to the neurosciences unit. It is<br />
15
important to involve those who take part in regular interdepartmental<br />
audit. This will include A&E personnel, anaesthetists, paramedics, etc.<br />
Participation of the neurosciences unit in such audit is particularly<br />
valuable.<br />
The quality of transfer should be audited, and critical incidents<br />
recorded. Such information is invaluable in refining and improving<br />
local transfer protocols. Appropriate audit tools for transfer are<br />
available from the Royal College of Anaesthetists.[20]<br />
16
SECTION X - RESOURCE IMPLICATIONS FOR T R A N S F E R<br />
OF PATIENTS WITH BRAIN INJURIES<br />
Without adequate resources it is not possible to have a good quality<br />
transfer service. Each organisation that provides acute healthcare<br />
should recognise that this requires specific funding which should be<br />
considered in discussions with purchasers. Resources include staff and<br />
equipment that may be similar to, and shared with, those used for other<br />
secondary transfers including the movement of ICU patients within the<br />
hospital. It should be recognised that there are significant resource<br />
implications to the transferring hospital on-call anaesthetic team.<br />
Hospitals involved in transfer of patients with brain injuries should set<br />
aside a budget for this work. The budget will include the capital<br />
equipment, the cost of which will depend upon its complexity and the<br />
demand placed upon it, as well as the cost of servicing, maintenance,<br />
insurance and renewal/upgrading at appropriate intervals. Portable<br />
equipment will need regular battery replacement and will have a<br />
shorter life than static equipment. There must be adequate provision for<br />
clothing and personal insurance.<br />
The responsibilities of the designated consultant for transfers include<br />
logistics, training, audit and liaison between the parties involved and<br />
may require dedicated programmed activities in job plans. Rotas of<br />
doctors and nurses must take account of this work and allow staff of<br />
adequate seniority to be released from other duties.<br />
Retrieval teams have been set up in some regions eg Northern Ireland<br />
[21] and are of particular importance in paediatric practice.[22]<br />
However, the speed of transfer required for head injuries may not<br />
permit a team to travel from the neuroscience centre. In addition, on<br />
a rare occasion two transfers may be required simultaneously, hence<br />
the referring hospitals will have to maintain the capability to transfer<br />
transfer patients with a time-critical lesion. This means that any unit<br />
potentially admitting children with head trauma should have a<br />
contingency to undertake such a transfer and have an appropriate kit<br />
with paediatric equipment ready for use. In an ideal world the funding<br />
of suitably situated retrieval teams would not be an issue.<br />
17
REFERENCES<br />
1. Association of Anaesthetists of Great Britain and Ireland. Recommendations for standards of<br />
monitoring (3rd ed). London: Association of Anaesthetists of Great Britain and Ireland, 2000.<br />
2. Intensive Care Society. Guidelines for the transport of the critically ill adult. Intensive Care<br />
Society 2002 h t t p : / / w w w. i c s . a c . u k / d ow n l o a d s / icstransport2002mem.pdf<br />
3. NICE Guidelines. Head injury: triage, assessment, investigation & early management of head<br />
injury in infants, children & adults. HMSO 2003 http://www.nice.org.uk<br />
4. Early management of patients with head injury. SIGN publication No.46 Aug 2000 ISBN<br />
1899893 27 X 2000 www.sign.ac.uk<br />
5. Brain Trauma Foundation: American Association of Neurological Surgeons’ joint section on<br />
neurotrauma & critical care: Guidelines for the management of severe head injury. J<br />
Neurotrauma 1996; 13: 641-734<br />
6. Paediatric Intensive Care Society. Standards for paediatric intensive care, including standards<br />
of practice for the transport of the critically ill child. Bishop’s Stortford: Saldatore Ltd, 1996.<br />
7. Paediatric Intensive Care Society. Standards document 2001<br />
8. Warren J, Fromm RE, Orr RA et al. Guidelines for the inter-and intrahospital transport of<br />
critically ill patients. Critical Care Medicine 2004; 32: 256-262<br />
9. National Service Fra m e work for long term conditions.<br />
h t t p : / / w w w. d h . g ov. u k / P u b l i c a t i o n s A n d S t a t i s t i c s / P u b l i c a t i o n s / P u b l i c a t i o n s Po l i cy A n d G u i d a n c e /<br />
PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4105361&chk=jl7dri<br />
10. Molyneux A. International Subarachnoid Aneurysm Trial (ISAT) Lancet 2002; 360: 1267-74<br />
11. Neuroscience Critical Care Report progress in developing services Aug 2004<br />
http://www.modern.nhs.uk/criticalcare/5021/7117/20040%20DoH-Neurosciences.pdf<br />
12. Andrews PJD, Piper IR, Dearden NM. Secondary insults during intrahospital transport of<br />
head-injured patients. Lancet 1990; 335: 327-330.<br />
13. Morris CG Mullan B. Clearing the cervical spine after polytrauma. Anaesthesia 2004; 59:<br />
755-61<br />
14. Medical vehicles and their equipment - Road ambulances EN 1789:1999<br />
http://www.cenorm.be<br />
15. http://www.vca.gov.uk/vehicle/ambul.shtm<br />
16. Air, water and difficult terrain ambulances – Part 2: Operational and technical requirements<br />
for the continuity of patient care EN 13718-2:2002 http://www.cenorm.be<br />
17. New advice issued on the use of mobile phones in hospitals. Ref 2004/0287<br />
http://www.dh.gov.uk<br />
18. Guidance on the Provision of Paediatric Anaesthetic Services Chapter 7, Guidelines on the<br />
Provision of Anaesthetic Services, Published by the Royal College of Anaesthetists, January<br />
2005 http://www.rcoa.ac.uk/docs/Paeds.pdf<br />
19. Mark J. Transfer of the critically ill patient. Anaesthesia News July 2004 ISSN0959-2962<br />
20. Raising the Standard: A compendium of audit recipes (February 2000) Section 9: Anaesthesia<br />
outside theatres http://www.rcoa.ac.uk/docs/section9.pdf<br />
21.The Northern Ireland Critical Care Transfer Service. www.nisca.org/niccats<br />
22. Children’s Acute Transport Service www.cats.nhs.uk<br />
18
APPENDIX I<br />
INDICATIONS FOR INTUBATION AND<br />
VENTILATION FOR TRANSFER AFTER BRAIN INJURY<br />
• GCS 8 or less<br />
• Significantly deteriorating conscious level (i.e. fall in motor score of<br />
two points or more)<br />
• Loss of protective laryngeal reflexes<br />
• Hypoxaemia (PaO2 < 13 kPa on oxygen)<br />
• Hypercarbia (PaCO2 > 6 kPa)<br />
• Spontaneous hyperventilation causing PaCO2 < 4.0 kPa<br />
• Bilateral fractured mandible<br />
• Copious bleeding into the mouth (e.g. from skull base fracture)<br />
• Seizures<br />
An intubated patient should be ventilated with muscle relaxation, and<br />
appropriate sedation and analgesia. Aim for a PaO2 > 13 kPa, PaCO2<br />
4.5 – 5.0 kPa unless there is clinical or radiological evidence of raised<br />
intracranial pressure when more aggressive hyperventilation is justified<br />
to a PaCO2 of not less than 4 kPa. If hyperventilation is used the FIO2<br />
should be increased.<br />
19
APPENDIX II<br />
TRANSFER CHECKLIST FOR NEUROSURGICAL PATIENTS<br />
SYSTEM<br />
CHECKLIST<br />
Respiration PaO2 > 13 kPa?<br />
PaCO2 < 5 kPa?<br />
Airway clear?<br />
Airway protected adequately?<br />
Intubation and ventilation required?<br />
Circulation BP mean > 80 mmHg? (adults)<br />
Pulse < 100/min? (adults)<br />
Peripheral perfusion?<br />
Two reliable large iv cannulae in situ?<br />
Estimated blood loss already replaced?<br />
Arterial line?<br />
Central venous access if appropriate?<br />
Head injury GCS?<br />
GCS trend (improving/deteriorating)?<br />
Focal signs?<br />
Skull fracture?<br />
Seizures controlled?<br />
Raised ICP appropriately managed?<br />
Other injuries Cervical spine injury (cervical spine protection), chest<br />
injury, fractured ribs, pneumothorax excluded?<br />
Intrathoracic, intra-abdominal bleed?<br />
Pelvic, long bone fracture?<br />
Extracranial injuries splinted?<br />
Escort<br />
Doctor & escort adequately experienced?<br />
Instructed about this case?<br />
Adequate equipment and drugs?<br />
Can use equipment and drugs?<br />
Sufficient oxygen supplies?<br />
Case notes and X-rays?<br />
Transfer documentation prepared?<br />
Where to go in the neurosurgical unit?<br />
Telephone numbers programmed into mobile phone?<br />
Mobile phone battery fully charged?<br />
Name and bleep number of receiving doctor?<br />
Money in case of emergencies?<br />
20
APPENDIX III<br />
ADDITIONAL INFORMATION FOR PAEDIATRICS<br />
Most paediatric critical care networks operate an emergency retrieval<br />
service [22]. The most appropriate method of transfer to the<br />
neurosurgical centre or PICU should be identified according to the<br />
clinical situation. The choice is between an emergency retrieval and<br />
one way transfer by the referring hospital team.<br />
The local referring hospital team should always transfer time critical<br />
cases to avoid delay:<br />
• rapidly expanding space occupying lesion e.g. extradural<br />
• penetrating injury<br />
• uncontrollable bleeding from skull base<br />
If CT scanning is unavailable in the referring unit for any reason then<br />
a time critical one way transfer should also occur.<br />
Age specific mean arterial blood pressure targets to maintain CPP [22]<br />
Age<br />
Mean arterial blood pressure (mmHg)<br />
< 3months 40 - 60<br />
3 months – 1 year 45 -75<br />
1 – 5 years 50 - 90<br />
6 – 11 years 60 - 90<br />
12 – 14 years 65 - 95<br />
21
21 Portland Place, London W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org<br />
Designed and produced by the r2 Partnership Ltd
AAGBI SAFETY GUIDELINE<br />
Care of the Critically Ill Child<br />
in Irish Hospitals 2015<br />
Published by<br />
The Association of Anaesthetists of Great Britain & Ireland<br />
June 2015
Membership of the working party<br />
Dr G Maloney<br />
Dr M J White<br />
Dr K Bailey<br />
Dr A Bergin<br />
Dr D Corcoran<br />
Dr I Lambert<br />
Dr D Doherty<br />
Joint Chair, Convenor of Irish Standing Committee<br />
Joint Chair<br />
Honorary Secretary/Honorary Treasurer of Irish Standing Committee<br />
Consultant Anaesthetist<br />
Consultant Paediatrician<br />
Consultant Paediatrician<br />
Paediatric Intensive Care Consultant Anaesthetist<br />
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0<br />
International License
Contents<br />
1. Neonatal resuscitation in hospitals that have no paediatric service 3<br />
2. Neonatal resuscitation in hospitals that have a paediatric service 6<br />
3. Care of the critically ill child in hospitals without a paediatric service 7<br />
4. Care of the critically ill child in general hospitals with a paediatric service 9<br />
5. Inter-hospital transfer – current practice 10<br />
6. National neonatal and paediatric retrieval services 11<br />
7. Summary 12<br />
Date of review: 2019<br />
1
Introduction<br />
Recent health controversies regarding the delivery of infants outside maternity units,<br />
combined with areas of difficulty in caring for critically ill older children in general hospitals,<br />
have prompted the Irish Standing Committee of the Association of Anaesthetists of Great<br />
Britain and Ireland and the Faculty of Paediatrics, RCPI, to review some aspects of<br />
paediatric care in general hospitals, both with and without paediatric and/or maternity units.<br />
Many general anaesthetists are worried that expectations of the service they can provide to<br />
critically ill children might be too great but, on the other hand, general paediatricians do not<br />
have the skills and ongoing experience to deal with critically ill ventilated children requiring<br />
intensive care. All anaesthetists nowadays have a paediatric module in their training but,<br />
because of a lack of ongoing experience, many anaesthetists worry about losing their<br />
paediatric intensivist skills. This problem in relation to the management of the critically ill<br />
child outside a specialist paediatric hospital is not exclusive to the Republic of Ireland, and<br />
we are aware that this debate is also occurring elsewhere.<br />
2
1. Neonatal resuscitation in hospitals that have no paediatric service<br />
Several hospital sites outside Dublin provide acute medical services but do not have paediatric<br />
cover. It is not an uncommon occurrence for these units to be required to manage a newborn<br />
infant, either as a result of the mother presenting in precipitate labour and delivering on-site<br />
or when the infant is born outside the hospital and is brought in by a parent or the ambulance<br />
services. In most cases such infants may only require basic support such as feeding and<br />
temperature control. On occasion, however, these infants, as a result of prematurity or other<br />
problems, may require more significant interventions such as airway management and<br />
intravenous fluids. The absence of paediatric staff at these sites means that all initial support<br />
will be provided by general adult clinicians and nurses. All possible steps should be taken to<br />
minimise obstetric and neonatal attendances at these units; however it is important that each<br />
of the non-paediatric units have agreed protocols to guide staff when such attendances do<br />
occur and that they are equipped to provide a basic level of neonatal resuscitation and care.<br />
It is suboptimal for doctors or nurses to be required to manage clinical problems in which<br />
they are not trained or in which they do not have recent and continuing experience. In that<br />
context it is acknowledged that all assistance provided by medical and nursing staff is in<br />
accordance with the principle of providing limited emergency medical care. Practitioners are<br />
simply required to do their best given the circumstances. It should also be acknowledged<br />
that the generally thin layers of staffing in the non-obstetric/non-paediatric units around the<br />
country mean that it is possible that, in a given situation, no anaesthetist may be available to<br />
attend an obstetric/neonatal case because they are occupied with another emergency. The<br />
following is recommended on this issue:<br />
1.1 Minimising risk<br />
• Health Service Executive (HSE) hospital groups with responsibility for any acute<br />
medical hospital unit without an obstetric/paediatric department should make every<br />
effort to ensure maximum public awareness as to which hospital sites do, and<br />
which do not, provide these services. This is particularly important when those who<br />
may have language difficulties are housed by the HSE near such a unit. A special<br />
effort needs to be made to ensure that these vulnerable individuals understand<br />
that if they have a pregnancy-related problem, they should proceed to the nearest<br />
designated maternity unit.<br />
• Each hospital site without obstetric/paediatric services should have clear signage at<br />
the entrance detailing the hospital sites within the region where these services are<br />
provided.<br />
• All ambulance and general practitioner on-call services should be given clear<br />
instructions that all acute obstetric and paediatric referrals should be directed to the<br />
appropriate hospital.<br />
3
1.2 Communication needs<br />
In the opinion of the working party, communication failure is probably the most common<br />
contribution to negative outcomes in these situations. It is incumbent on hospital management<br />
and clinicians to ensure that clear, prescriptive communication pathways have been thought<br />
through in each unit so that the non-expert has rapid access to advice from an obstetrician<br />
and/or paediatrician when an incident arises. Dedicated communication infrastructure may<br />
be needed, such as dedicated bleep systems, but each unit should address its own individual<br />
needs in this area.<br />
1.3 Equipment and facility needs<br />
• All non-paediatric sites should have the basic equipment required for neonatal<br />
resuscitation and stabilisation readily available for use.<br />
• Facility to provide less than 100% oxygen and to blend oxygen is required.<br />
• All non-paediatric sites should have a designated facility where neonatal<br />
equipment is located and where short-term emergency neonatal care can be<br />
delivered.<br />
• Hospital management should ensure that there is adequate training of staff in<br />
neonatal resuscitation and maintenance of the necessary equipment in all nonpaediatric<br />
sites especially in the emergency department where most clinical<br />
events will occur.<br />
1.4 Guidelines for management of newborn infants and imminent deliveries<br />
presenting to a non-paediatric unit<br />
• If the infant is active and well, transport of the mother and infant to the appropriate<br />
obstetric/paediatric unit should be arranged. Management of the infant can be<br />
discussed with the on-call consultant paediatrician prior to transfer.<br />
• If the infant is significantly premature or is unwell, the on-call consultant anaesthetist,<br />
if available, should attend to assist with the management of the baby.<br />
• Ongoing management of a sick infant and transport arrangements should be<br />
organised in consultation with the on-call consultant paediatrician in the designated<br />
unit.<br />
• Ideally, transport of a sick neonate should be conducted by paediatric staff. In the<br />
absence of the National Neonatal Transport Service, which at the time may be<br />
directed to other high risk neonatal transfers and is based in Dublin, there should<br />
be capacity to provide dependable neonatal support at short notice from within<br />
each region to give a timely response. At present staffing levels, it may not always<br />
4
e possible for paediatric personnel to attend such a delivery outside their own<br />
hospital. Responsibility for resourcing such a service remains with the HSE.<br />
• If a woman presents in an advanced stage of labour, and delivery is judged to<br />
be imminent, she should be moved immediately to the designated area within the<br />
hospital where she can deliver her baby and neonatal care can be provided.<br />
• If neonatal resuscitation is required over and above normal supportive care, the<br />
on-call consultant anaesthetist, if not otherwise involved in emergency care, should<br />
attend to assist in the resuscitation.<br />
• The on-call consultant obstetrician and paediatrician in the regional unit should be<br />
informed as soon as possible and they will guide further management of the mother<br />
and baby and advise on transfer.<br />
5
2. Neonatal resuscitation in hospitals that have a paediatric service<br />
• Neonatal resuscitation is the responsibility of the paediatric service, which will ensure<br />
adequate availability of trained personnel at all times. All paediatric units should be<br />
in a position to ensure the on-site presence, throughout a 24 hour period, of at least<br />
one staff member capable of performing full neonatal resuscitation, in accordance<br />
with the American Academy of Pediatrics neonatal resuscitation programme.<br />
• All paediatric personnel attending any delivery in the labour ward or theatre must<br />
have completed the American Academy of Pediatrics neonatal resuscitation<br />
programme. This should be updated at the end of every two-year period.<br />
• The anaesthetist's responsibility during a caesarean section is towards the care of<br />
the mother.<br />
• There will be occasions, however, when paediatric staff may require the support<br />
of anaesthetic colleagues to assist with resuscitation of an infant. If a consultant<br />
anaesthetist and a non-consultant hospital anaesthetist are present, and if the<br />
mother is stable, the consultant anaesthetist may assist in the neonatal resuscitation<br />
if so requested, provided that the consultant paediatrician has been called to attend.<br />
• In a situation where a non-consultant doctor has not yet completed the American<br />
Academy of Paediatrics Neonatal Resuscitation course (e.g. at the beginning of<br />
January and July when staff change jobs), he/she should only attend the labour<br />
ward or theatre while accompanied by another member of staff with up-to-date<br />
neonatal resuscitation qualifications.<br />
• Acutely ill neonatal patients from the community should be directed to the appropriate<br />
paediatric centre rather than the maternity hospitals.<br />
6
3. Care of the critically ill child in hospitals without a paediatric service<br />
There are currently ten acute general hospital sites outside Dublin providing acute medical<br />
services that do not have paediatric cover. It is not uncommon for these sites to be required<br />
to manage a critically ill child, either as a result of a traumatic injury or an acute medical<br />
condition. Every effort should be made to minimise the frequency of these attendances but<br />
when they do occur, it is important that there are clear, concise and workable guidelines for<br />
clinical management.<br />
3.1 Minimising risk – the National Clinical Paediatric Programme<br />
recommends<br />
• There should be consensus among all units in a region regarding the age criteria<br />
for a paediatric patient.<br />
• HSE with responsibility for any acute medical hospital unit without a paediatric<br />
service should take robust steps to ensure maximum public awareness of which<br />
hospital sites do, and which do not, provide these services.<br />
• Where vulnerable populations who may have language difficulties are housed by<br />
the HSE near units without paediatrics, specific, targeted communication intiatives<br />
may be needed to ensure their understanding that, if their child is acutely unwell,<br />
they should proceed to the nearest designated paediatric unit.<br />
• Each hospital site without a paediatric service should have clear signage at the<br />
entrance detailing the hospital sites within the region where these services are<br />
provided.<br />
• Paediatric Advanced Life Support/Advanced Paediatric Life Support (PALS/APLS)<br />
training should be available to front-line staff in non-paediatric hospitals. It is<br />
recommended that an APLS certified or suitably trained staff member should be on<br />
duty at all times.<br />
• The ambulance service should be given clear instructions that all ill children<br />
should be taken to the nearest hospital with a paediatric service. The ambulance<br />
service should only take an ill child to a non-paediatric hospital site in extreme<br />
circumstances such as a child requiring active cardiopulmonary resuscitation or<br />
with an upper airway obstruction.<br />
• General practitioner/GP on-call services should be given clear instructions that all<br />
acute paediatric referrals should be directed to the appropriate site.<br />
7
3.2 Who is in charge?<br />
Children with injuries/surgical problems and children with acute medical emergencies (e.g.<br />
status epilepticus, acute severe asthma, meningococcal sepsis or diabetic ketoacidosis)<br />
should continue to be placed under the care of adult clinicians prior to transfer. In units with<br />
an emergency department consultant on-site, it may be agreed locally that he/she should<br />
take primary responsibility for critically ill children. Where there is anaesthetic involvement,<br />
care should be jointly anaesthetic with the admitting clinician. The admitting clinician and/or<br />
anaesthetist should consult directly with the paediatric consultant in the receiving hospital<br />
prior to transfer.<br />
With the expected introduction of paediatric retrieval, clinical responsibility will transfer to<br />
the Retrieval Team on departure from the referring hospital. The consultant paediatrician<br />
assumes clinical responsibility when the child arrives in the receiving hospital.<br />
3.3 Paediatric clinical guidelines<br />
It is the responsibility of each non-paediatric hospital unit to have a set of paediatric<br />
guidelines available which cover the management of the common paediatric emergencies.<br />
These guidelines should be facilitated by the paediatricians and other relevant consultant<br />
specialists in the region.<br />
3.4 Paediatric resuscitation trolleys<br />
Each non-paediatric hospital unit should have a formal paediatric resuscitation trolley set up<br />
in the A&E department. The use of the Broselow tape system is strongly recommended for<br />
the management of the child in the A&E setting.<br />
3.5 Paediatric drug formulary<br />
The British National Formulary for Children is now widely accepted as the standard paediatric<br />
formulary in Ireland. An up-to-date copy of this publication should be available in all nonpaediatric<br />
A&E departments, with new editions replacing old as they are published. APLS/<br />
PALS manuals should also be available.<br />
The Our Lady’s Children’s Hospital, Crumlin, formulary and prescribing guide app is available<br />
for download from the iTunes Store for a small fee.<br />
8
4. Care of the critically ill child in general hospitals with a paediatric service<br />
Children are admitted to the hospital under the care of a paediatrician or surgeon. If they are<br />
deemed to be critically ill, the admitting consultant (paediatrician or surgeon) should consult<br />
with the anaesthetic consultant about admission to ICU or ventilated transfer to another<br />
centre as they deem appropriate. Management in ICU should be jointly anaesthetic and<br />
paediatric (or surgical). Some hospitals have high dependency areas on the paediatric unit<br />
and it may be appropriate to maintain children requiring respiratory support in this setting<br />
with appropriately trained nurses.<br />
The AAGBI recognises the dilemma faced by general anaesthetists who feel they are<br />
working outside their usual area of practice when dealing with critically ill children. The best<br />
local expertise should be used in the management of these children. The anaesthetist is<br />
generally the most skilled person available to deal with intubation and ventilation of children<br />
outside the neonatal period.<br />
A decision whether to transfer the child to a paediatric intensive care unit is made jointly by<br />
the local hospital clinicians and the paediatric intensivist. Referring hospitals should seek<br />
telephone advice from the tertiary paediatric intensive care unit (PICU) using the centralised<br />
telephone referral (1890-213-213) and online via http://www.hse.ie/go/picu. This is the<br />
only avenue of referral to PICU in the Republic of Ireland, regardless of the nature of the<br />
presenting complaint. Initial communication should be a consultant-to-consultant referral<br />
between the referring physician and receiving paediatric intensivist.<br />
In general, critically ill children presenting outside of the tertiary paediatric centres should be<br />
resuscitated, stabilised and prepared for transfer to a PICU. Should a decision be made to<br />
admit a child to an adult ICU, the child’s care should be shared by the admitting consultant<br />
and the consultant anaesthetist. Ongoing telephone advice from the paediatric intensivist<br />
should be readily available.<br />
Care of a critically ill child in an adult ICU should only occur in exceptional circumstances.<br />
There should be local protocols and guidelines readily available for the management<br />
of mechanical ventilation, physiological monitoring, intravenous fluid and medication<br />
administration, which reflects current practice in PICU. The centralised referral line and<br />
website should be considered as a resource to guide the management of paediatric patients<br />
under these circumstances.<br />
There are some situations when, after consultation with the tertiary unit, a critically ill child<br />
may not be transferred out, such as:<br />
• When there is no paediatric intensive care bed available in the tertiary centre.<br />
• When the child is too ill to transfer.<br />
• When the outcome is deemed to be very poor, or when brainstem death has<br />
occurred. Care of a child with a neurological determination of death for the purposes<br />
of organ donation is a niche area in medicine, best done by PICUs with practice and<br />
protocols for this.<br />
9
Nursing care of the critically ill child requires ICU and paediatric nursing expertise. Ideally<br />
the nurse managing the child should have PICU training. However in situations where this<br />
is not available, nursing may be provided by the joint management of an ICU nurse and a<br />
paediatric nurse. It is the responsibility of hospital management to ensure the availability<br />
of appropriately trained nursing staff to meet the needs of critically ill children. Suitable<br />
equipment should be available both in the emergency department and in the ICU.<br />
Training: In spite of the fact that all anaesthetists undergo a paediatric module during training,<br />
the Group recognises that loss of paediatric skills is an issue.<br />
APLS training with regular updates for all staff who may be involved with critically ill children<br />
is desirable, alongside available supranumary clinical sessions in anaesthesia and PICU<br />
available in the paediatric hospitals.<br />
5. Inter-hospital transfer – current practice<br />
Children undergoing treatment in general hospitals with paediatric departments may need<br />
to be referred to a specialist paediatric unit for investigation and/or treatment. The manner<br />
in which such transfer is carried out will depend on the severity of the child’s condition, and<br />
the urgency of transfer.<br />
Where the condition is serious and has already warranted admission to the ICU, common<br />
current practice is for the ICU anaesthetic staff to accompany the patient. This arrangement<br />
has the obvious benefit that specialised interventions such as mechanical ventilation are<br />
supervised by the trained staff, but at the same time takes specialist staff away from the<br />
primary admitting unit.<br />
It is recommended that a member of the paediatric team also accompanies such critically<br />
ill patients. While the specialist interventions are quite properly the remit of the ICU doctor<br />
(almost always anaesthesia staff), the underlying condition may well be more familiar to<br />
paediatricians.<br />
It is apparent that this joint approach, while carrying obvious benefits for the paediatric<br />
patient, is not the universally adopted practice. The AAGBI recommends a joint paediatric/<br />
anaesthetic approach.<br />
The AAGBI recognises that transfers will inevitably be required without direct input from the<br />
National Retrieval Service. It is recommended that the most senior personnel are available<br />
to accompany the child, both from paediatrics, anaesthetics and an experienced paediatric<br />
nurse.<br />
10
6. National neonatal and paediatric retrieval services<br />
Among consultants working in paediatrics and anaesthetics there is consensus that, for<br />
critically ill children who need to be transferred to tertiary units, a ‘paediatric retrieval system’<br />
is required. This has been demonstrated to provide optimal, specialised PICU facilities<br />
during an especially hazardous phase of the child’s management. This service already<br />
exists for newborns up to the age of 6 weeks (National Neonatal Transport Service) and for<br />
adults (Mobile Intensive Care Ambulance Service). Children outside these age groups are<br />
currently denied this service. The National Neonatal Transport Service is awaiting funding<br />
to extend its service to 24 hours, 7 days a week.<br />
The need for a nationwide paediatric retrieval service has been well accepted internationally<br />
and this document should be viewed as a strong recommendation for the implementation of<br />
such a service, available 24 hours a day and 7 days a week.<br />
The transport team should consist of members as determined by the paediatric hospital.<br />
The team requires access to road ambulance and occasionally air transport. The provision,<br />
staffing and day-to-day management of the paediatric service should be under the control of<br />
the paediatric receiving hospitals.<br />
11
7. Summary<br />
The purpose of this document is to provide guidelines to improve the quality of care of<br />
critically ill children.<br />
The AAGBI recognises that care of critically ill infants and children outside a paediatric<br />
hospital is a problematic area for hospital management, nurses, clinicians, paediatricians<br />
and general anaesthetists.<br />
Mothers in labour should be encouraged to attend hospitals with an on-site obstetric and<br />
paediatric service, and to bypass hospitals which do not have these services. HSE should<br />
put in place signage and communication lines to ensure that this occurs.<br />
When, in spite of the above, a newborn baby or woman in advanced labour presents<br />
to a hospital without paediatric or obstetric departments, and if there is a need for more<br />
resuscitation of the infant than standard supportive care, the consultant anaesthetist or their<br />
delegate, and any other consultants deemed necessary, should assist in the resuscitation<br />
of the infant. Paediatricians and anaesthetists in general hospitals, when presented with a<br />
critically ill child, should arrange for jointly conducted safe and rapid transfer of the child to<br />
a PICU.<br />
There is a need for national 7-day/24-hour neonatal and paediatric retrieval services. These<br />
services should be managed centrally by the neonatal intensive care services of tertiary<br />
maternity hospitals for critically ill neonates and the paediatric intensive care services of<br />
tertiary paediatric hospitals, to ensure prompt and safe transfer of critically ill children and<br />
newborns. Until these retrieval services become available, a joint anaesthetic/paediatric<br />
team should transfer critically ill children with advice from the receiving unit. All staff that may<br />
be involved with critically ill children should be trained in paediatric advanced life support.<br />
12
13
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
Catastrophes in Anaesthetic Practice –<br />
dealing with the aftermath<br />
2005<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland,<br />
21 Portland Place, London W1B 1PY<br />
Telephone: 020 7631 1650, Fax: 020 7631 4352<br />
E-mail: info@<strong>aagbi</strong>.org Website: www.<strong>aagbi</strong>.org<br />
September 2005
MEMBERSHIP OF THE WORKING PARTY<br />
Dr Michael Wee<br />
Dr David Bogod<br />
Prof Alastair Chambers<br />
Prof Michael Harmer<br />
Dr Iain Wilson<br />
Dr David Saunders<br />
Dr Barbara Bahlmann<br />
Mrs Sandy Gaskins<br />
Dr Sara Hunt<br />
Dr Janet Prentice<br />
Chair, Association of Anaesthetists of<br />
Great Britain and Ireland (AAGBI)<br />
Editor-in-Chief, Anaesthesia<br />
Honorary Secretary, AAGBI<br />
President, AAGBI<br />
Council member, AAGBI<br />
Council member, Royal College of Anaesthetists<br />
Group of Anaesthetists in Training<br />
Chartered Psychologist<br />
Chair, Group of Anaesthetists in Training<br />
Doctors Support Network<br />
Acknowledgements: Mr Bertie Leigh of Hempsons Solicitors and Dr Stuart<br />
White, Consultant Anaesthetist for their helpful comments on the document.<br />
Review Date June 2010
CONTENTS<br />
Section 1. Summary 2<br />
Section 2. Introduction 3<br />
Section 3. Actions to take after the event 5<br />
Section 4. The role of the anaesthetic department 9<br />
Section 5. The Trust response 10<br />
Section 6. How a catastrophe may affect you personally 13<br />
Section 7. Critical incident stress debriefing (CISD) 17<br />
Section 8. Medico-legal issues and the GMC 19<br />
Section 9. Sources of help 24<br />
Section 10. References and further reading 27<br />
1
SECTION 1. SUMMARY<br />
• The majority of anaesthetists are likely to be involved with an<br />
anaesthetic catastrophe at some point in their careers.<br />
• The psychological impact on staff following death or serious injury<br />
to a patient should not be underestimated.<br />
• It is vital that members of the anaesthetic department support the<br />
anaesthetist and a senior colleague or mentor should be assigned to<br />
this role.<br />
• Contemporaneous records of the event must be kept.<br />
• The clinical commitment of the anaesthetist concerned should be<br />
reviewed immediately by the clinical director.<br />
• A team approach should be adopted to breaking bad news with<br />
relatives. This should not be done over the telephone.<br />
• The task of breaking bad news should not be carried out by a trainee<br />
or staff grade or associate specialist (SAS) doctor without a<br />
consultant present.<br />
• Each hospital must have a procedure for dealing with and<br />
investigating catastrophic events.<br />
• Critical incident stress debriefing by trained facilitators with further<br />
psychological support may assist individuals to recover from the<br />
traumatic event.<br />
• Anaesthetists are strongly advised to be a member of a medical<br />
defence organisation.<br />
2
SECTION 2. INTRODUCTION<br />
Although deaths due to anaesthesia are extremely uncommon with an<br />
estimated incidence of 0.5-0.8 per 100,000 anaesthetics 1,2, we are all<br />
likely to experience a death on the operating table at some point in our<br />
careers. In the majority of cases, death is expected and the cause<br />
understood. However, when death or serious injury is unexpected, the<br />
experience can be extremely traumatic for all concerned including the<br />
theatre team, ward and ancillary staff. The 2000-2002 Confidential<br />
Enquiry into Maternal and Child Health report recommended that<br />
anaesthetists and staff who were involved in a maternal death should<br />
receive supportive counselling 3 .<br />
A survey of two hundred and fifty one anaesthetists from twelve NHS<br />
hospitals in England showed that 92% had experienced an intraoperative<br />
death; 60% of deaths were expected occurring mainly in<br />
emergency surgery (80%). 4<br />
Whether a death is 'expected' or 'unexpected' may be irrelevant, as the<br />
anaesthetist involved may be emotionally affected by any intraoperative<br />
death or serious injury to the patient. The training and ethos<br />
of anaesthesia to avoid harm and maintain patient safety at all times<br />
puts additional stress on the anaesthetist. 5-9 The psychological effects<br />
of an intra-operative death or serious injury on a background of<br />
continuing stress, may tip the balance towards acute personal,<br />
psychological or physical disaster. 10<br />
When a death or serious injury occurs in a private hospital, the<br />
anaesthetist may feel particularly vulnerable. Private hospitals may not<br />
have the support systems which are available in the NHS. However, it<br />
is the responsibility of the chief executive officer or the general<br />
manager of the private hospital to put in motion their governance and<br />
risk management systems to deal with a catastrophe.<br />
It is incumbent on colleagues, hospital, Trust, family and society in<br />
general to provide practical help and support to the anaesthetist<br />
3
involved according to individual needs. This is part of good clinical<br />
and corporate governance, and risk management.<br />
Unfortunately, research into the effects and management of intraoperative<br />
deaths is minimal. The aim of this document is to suggest<br />
pragmatic ways of dealing with the aftermath of a death or serious<br />
injury during anaesthesia.<br />
4
SECTION 3. ACTIONS TO TAKE AFTER THE EVENT<br />
Consult departmental guidelines if available. 11<br />
a) Immediate Actions<br />
Records<br />
Keep an accurate and contemporaneous record of the anaesthetic and<br />
event. These should be legible, timed, dated and signed. Electronically<br />
stored monitoring records should be printed and filed in the notes. If<br />
stored monitoring records are unavailable, recordings should be made<br />
on the basis of recollection as accurately as possible and preferably<br />
corroborated by staff who were present at the time. Where practical,<br />
it is advisable during attempted resuscitation to allocate one member<br />
of the team to record times, the personnel involved, interventions<br />
including details of all drugs, fluids used and outcomes. Original notes<br />
and charts must not be altered in any way at a later date. Amendments<br />
and additions must be recorded separately, timed, dated and signed.<br />
If the anaesthetist is unable to write notes immediately, a full<br />
retrospective account must be made as soon as possible. It is essential<br />
that this account concurs with the records in the notes and the<br />
recordings from the monitors or explains the discrepancy. The date<br />
and time of this retrospective record should be noted and signed (in<br />
black ink to allow photocopying). Any subsequent entries to the<br />
contemporaneous notes should be made in the same way. If it has not<br />
already been recorded, the anaesthetist should document details of the<br />
discussions with the patient pre-operatively regarding the risks of<br />
anaesthesia and surgery. It is important to keep copies of the records<br />
and make personal notes as these may be required later (see Section<br />
8).<br />
Dealing with the anaesthetist<br />
For trainees or SAS grades, the responsible consultant should attend in<br />
person and deal with the situation. A consultant anaesthetist should<br />
inform a colleague who should attend the hospital and assist with the<br />
5
aftermath. A decision will need to be made whether the anaesthetist<br />
should continue with his/her list or on-call. There is no standard<br />
advice in this situation although individual Trusts may have their own<br />
policies which should be followed (see Section 5). The decision is best<br />
made after assessing the situation between the anaesthetist involved, a<br />
senior colleague and the clinical director.<br />
Dealing with the patient<br />
In the event of a death, inform the Coroner (England and Wales) or<br />
Procurator Fiscal (Scotland) and the patient's general practitioner as<br />
soon as possible by telephone or other immediate means. The Coroner<br />
or Procurator Fiscal may decide to conduct their own investigation.<br />
The anaesthetist involved should contact his/her defence organisation.<br />
It is important to complete a Trust critical or adverse incident form.<br />
In the event of death, all lines, tubes and other equipment connected<br />
to the patient must be left in place. If there is any cause for concern<br />
regarding the placement of the endotracheal tube, its position should<br />
be confirmed and recorded by an independent anaesthetist. The body<br />
should be transferred to an appropriate area for further investigation if<br />
necessary. In some circumstances, the Coroner may instruct a<br />
pathologist to investigate. At a later stage after the body has been<br />
prepared for viewing, the relatives may attend to pay their last respects.<br />
Although it may be difficult to do, in the event of a medical catastrophe<br />
where the patient survived, it is important for the anaesthetist<br />
concerned to take an interest in the progress of the patient. This will<br />
involve regular visits to the ITU or rehabilitation unit. Failure to do so<br />
may paint a negative perception that the anaesthetist did not care.<br />
Regular communication with the family is also helpful.<br />
Dealing with relatives<br />
Breaking bad news should not be done over the telephone. It will be<br />
necessary to invite the relatives to come to hospital informing them that<br />
some complication had occurred but no details should be given. There<br />
may be pressure from the relatives to get information over the phone<br />
6
ut this should be politely and firmly resisted without antagonism. If<br />
there is no immediate family to accompany the relative, ask the relative<br />
to bring a friend. Some hospitals have established a bereavement<br />
service which can be helpful for grieving relatives.<br />
The interview with the family<br />
This will consist of an initial interview, possibly followed by more<br />
depending on the situation. Find a suitable quiet and comfortable<br />
room free from interruption for the interview. Do not speak to the<br />
family on your own or allow the surgical team to do this. A team<br />
approach is essential.<br />
Before the interview, decide who should be the spokesperson. Speak<br />
to the family with your surgical colleague who may already have<br />
encountered members of the family prior to the operation. Other team<br />
members should include theatre or ward staff, chaplaincy staff and<br />
other support staff including an interpreter if appropriate. A senior<br />
colleague should accompany trainees and SAS doctors for support.<br />
Explain the 'bad news' first in a straightforward and honest way,<br />
followed by answering any questions which may arise. If the cause of<br />
the disaster is known, then this should be explained in lay language.<br />
Giving an apology does not imply fault. However, if no cause has<br />
been identified, do not speculate or offer an opinion. Take time, listen<br />
and empathise. Use an interpreter in cases where understanding of<br />
English is limited. Give the family the time to take in the bad news and<br />
do not give them too much information initially.<br />
Other members of the team interviewing the family can contribute<br />
during questioning led by the spokesperson. If appropriate, inform the<br />
relatives that a full investigation will take place and that this may take<br />
some time. If appropriate, reassure the relatives that all that could be<br />
done was done to keep their relative alive and that their relative was<br />
not in pain or aware during the resuscitation attempts. This knowledge<br />
may be comforting to them.<br />
7
It may be necessary to conduct a second interview after a relatively<br />
short period of time to give further information, answer questions or to<br />
clarify certain issues. Further interviews may be necessary in the<br />
future.<br />
b) 'Later' Actions<br />
Equipment and drugs<br />
The clinical director or a consultant not involved with the incident<br />
should take responsibility for checking the patient and equipment. If<br />
there is suspicion of equipment failure or a hazard affecting the theatre,<br />
a decision may be made to take the theatre or anaesthetic machine out<br />
of commission until further notice.<br />
All anaesthetic equipment, drug syringes and ampoules should be<br />
kept, and moved to a secure store room for investigation. An accurate<br />
record should be made of all the checks undertaken including time<br />
and date of inspection. All disposable equipment including syringes<br />
and ampoules, airway devices etc. should be kept in a secure box.<br />
Further investigation may be required by medical equipment<br />
maintenance personnel, manufacturers or toxicologists.<br />
Dealing with the theatre team<br />
The team should be initially debriefed at a time to suit all staff and<br />
preferably within a few hours of the catastrophe. The aim is to provide<br />
and record information, and to gain feedback while details are still<br />
fresh. It is also useful to allay anxieties or misconceptions experienced<br />
by members of the theatre team. The presence of a trained counsellor<br />
may be useful to assist staff traumatised by the event (see Section 6).<br />
Dealing with the media<br />
The media may try to approach staff at the hospital or at home. A Trust<br />
manager trained with dealing with the media should be the only<br />
person communicating with them. All media enquiries should be<br />
directed to this manager.<br />
8
SECTION 4. THE ROLE OF THE DEPARTMENT OF<br />
ANAESTHESIA<br />
It is vital that members of the anaesthetic department support the<br />
anaesthetist who may be stressed and traumatised. 12 A stressed<br />
anaesthetist will be more prone to making errors. (see Sections 6 and 7)<br />
It is important to listen to the individual and encourage him/her to talk<br />
and refrain from being judgemental. Informal, sympathetic peer<br />
review with a few colleagues is often useful. Keep all conversations<br />
confidential. At a later date, when the cause of the catastrophe is<br />
known, a departmental mortality and morbidity meeting may be useful<br />
to inform and learn lessons from the incident.<br />
An experienced and sympathetic senior anaesthetic colleague should<br />
be assigned to act as mentor and provide support for as long as<br />
necessary. The mentor should be known and accepted by the<br />
anaesthetist concerned. Members of the department may have to take<br />
over the involved anaesthetist's duties including on call commitments,<br />
for a period of time.<br />
The anaesthetist will feel particularly vulnerable when a catastrophe<br />
occurs in a private facility. It is the responsibility of the concerned<br />
anaesthetist to inform his/her colleagues of the catastrophe in order to<br />
obtain as much assistance as possible. The assistance from the<br />
department and colleagues should not be any less than if the<br />
catastrophe had occurred in an NHS facility.<br />
9
SECTION 5. THE TRUST RESPONSE<br />
Each Trust should have a policy detailing the response to serious<br />
incidents. Medical managers are responsible to the Chief Executive for<br />
managing the process.<br />
Following a serious incident, the Trust should immediately review the<br />
safety of patients and staff, the clinical systems, drugs and equipment<br />
employed, and any implications for the NHS at large. Every Trust is<br />
different and specific roles will differ. Communication between all<br />
involved must be a high priority to ensure that timely, effective action<br />
is taken.<br />
Out of hours, depending on the nature of the incident, the on-call<br />
consultant and duty manager must be informed.<br />
The role of the Clinical Director (CD)<br />
Working with their manager, the CD is responsible for Trust patient<br />
safety in anaesthesia. The CD should make an assessment of the nature<br />
of the incident to determine whether the catastrophe could recur or put<br />
other patients or staff at risk.<br />
Urgent actions:<br />
• Secure the area or equipment until investigated.<br />
• Identify and support all staff involved. The anaesthetist should be<br />
interviewed as soon as possible and, after discussion, a decision<br />
made regarding continuation of work.<br />
• Keep a record of all actions.<br />
• Check that the relatives have been contacted, and cared for.<br />
Contact the patient's GP.<br />
• Ascertain if there is any evidence of an equipment or drug problem.<br />
• Ascertain if there is any evidence of poor staff performance or<br />
system failure.<br />
• If there is suspicion of a criminal act, the police need to be<br />
contacted.<br />
• Contact the GP.<br />
10
• Check that the Coroner (England and Wales) or Procurator Fiscal<br />
(Scotland) has been informed.<br />
• Ensure that an incident form has been completed and the Trust<br />
governance team is involved. They will liaise with Health & Safety<br />
Executive (HSE), Medicines and Healthcare Products Regulatory<br />
Agency (MHRA), National Patient Safety Agency (NPSA) and other<br />
NHS organisations as necessary.<br />
Follow up actions:<br />
• Report findings to the Medical Director as soon as possible (within<br />
24 hours). Discuss the incident, and decide plans for an initial<br />
investigation.<br />
• Initiate support for the anaesthetist involved. Meet the anaesthetist<br />
along with another colleague who will be asked to mentor the<br />
individual to provide support. Regular meetings should be<br />
scheduled with the mentor. Depending on the nature of the<br />
incident, explain the next steps which will usually involve contact<br />
with the Medical Director and possibly the legal department. Keep<br />
notes of this meeting.<br />
• After discussion, consider taking the anaesthetist off call or duty and<br />
arrange for a few days leave while the incident is investigated. The<br />
anaesthetist may need support on return by working with a<br />
colleague for a short time. Involve Occupational Health if illness is<br />
a possibility.<br />
• Together with the appropriate manager ensure that the relevant<br />
theatre staff are supported, and have been debriefed.<br />
• Arrange for statements to be made by all who were present during<br />
the incident using the Trust proforma. Statements should be<br />
descriptions of what happened rather than interpretations of events.<br />
Statements may be legally disclosable in the future, so accuracy and<br />
care is essential.<br />
The role of the Medical Director (MD)<br />
The MD will work with the CD to ensure that all appropriate steps have<br />
been taken following the incident. In consultation with the Chief<br />
Executive Officer, the MD will decide the nature of the inquiry<br />
11
equired for the incident. This is a rapid decision based on the<br />
available evidence, and may be an internal or external inquiry. The<br />
NPSA Incident Decision Tree is useful at this stage. Serious incidents<br />
will require a root cause analysis. The inquiry should be started within<br />
two weeks and report its findings within six weeks.<br />
Most deaths or serious injury have a clinical explanation, and the likely<br />
underlying cause can be determined. The Coroner or Procurator Fiscal<br />
will determine whether an Inquest/Inquiry will be required.<br />
The MD will take responsibility for organising contact with the media.<br />
Outcome from the inquiry may result in a number of possible actions:<br />
• Personnel issues may require Occupational Health review, possible<br />
disciplinary action including the GMC or retraining issues. The<br />
National Clinical Assessment Authority (NCAA) may need to be<br />
involved.<br />
• Deaneries and the Royal College of Anaesthetists may become<br />
involved for trainees.<br />
• Equipment report to the MHRA and HSE.<br />
• Prevention of future incidents utilising a systems approach for risk<br />
management.<br />
12
SECTION 6. HOW A CATASTROPHE MAY AFFECT<br />
YOU PERSONALLY<br />
The following symptoms are 'common' feelings to have after a<br />
traumatic incident. It is also important for colleagues and family to<br />
recognise these symptoms and offer help.<br />
Reliving the event<br />
The impressions left by the event may be so strong that it is re-lived<br />
long after it actually happened. Flashbacks and daydreams are<br />
common, as is re-experiencing of the feelings that surfaced during or<br />
after the event. Sometimes you may suddenly start to feel as if the<br />
original event is about to happen again. This can be alarming, but be<br />
assured that it is not unusual.<br />
Shock<br />
It could be that you don't feel anything for a while; instead you feel<br />
numb, exhausted and cold and it can become difficult to do everyday<br />
things.<br />
Restless and Wound-up<br />
You may find it difficult to rest and concentrate. You may also have<br />
problems sleeping. You may become irritable and tearful.<br />
Doom and Gloom<br />
You may feel the world is no longer a safe place and that the future is<br />
no longer bright. You may feel vulnerable and disappointed with life.<br />
Anger<br />
Strong feelings of rage or anger about what has happened can occur.<br />
You may feel strongly towards those you feel had some responsibility<br />
for what happened, or just that nothing is fair.<br />
13
Fear<br />
You may become afraid of new things, or of being left alone; leaving<br />
your loved ones; or of just going out. Other fears centre on breaking<br />
down, losing control, having unbearably intense feelings or worry that<br />
the original event might happen again.<br />
Guilt<br />
Often people feel guilty and wonder whether more could have been<br />
done.<br />
Relationships<br />
Stresses and strains previously taken as being part of life can appear<br />
unbearable to someone who had been through a traumatic incident. A<br />
tendency to withdraw from close contact with relatives, friends and<br />
colleagues is often observed. This can lead to additional problems.<br />
Longer term relationship problems can get worse and you can feel that<br />
'absolutely nobody understands what I am going through'.<br />
Physical Effects<br />
Your body also reacts to the trauma, sometimes straight away and<br />
sometimes much later on. You may feel the following:-<br />
• Tiredness. All traumatic incidents are demanding on the body and<br />
use up a lot of energy. This may continue after the incident is over.<br />
You may stay hyper-aroused for a long time and eventually become<br />
exhausted.<br />
• Muscle Tension. Being wound-up for too long can be unpleasant.<br />
Stiffness and tension can lead to localised pains, headaches,<br />
dizziness, breathing and swallowing problems.<br />
• Other effects. As the body works overtime, you can become aware<br />
of palpitations, hands shaking, or that you are sweating excessively.<br />
You may also get nausea, diarrhoea or menstrual problems.<br />
You may experience some or all of these reactions only occasionally,<br />
or all the time. It is important to remember they are all recognised and<br />
a natural consequence of the event, and are a sign that you are coping<br />
with something that is very difficult for a person to deal with.<br />
14
Typically reactions start to lessen within a week or so before fading<br />
away altogether over a longer period of time. If they do not, then it is<br />
important that you should take the initiative and talk to someone about<br />
your reactions to extreme stress.<br />
Longer Term Reactions<br />
Some feelings may not occur until later and you may not notice them<br />
until someone else points them out. Try not to become defensive. You<br />
may lose confidence in pursuing everyday activities and things that you<br />
once did without a second thought can become difficult for a time.<br />
You may become emotionally detached, feeling cut off from people to<br />
whom you are usually close, or become irritable and annoyed with<br />
them.<br />
What you can do to help yourself<br />
The most important thing is to avoid bottling up feelings you have<br />
about what happened, however shocked or surprised you may be. Be<br />
careful - accidents happen more frequently after severe stress,<br />
especially in the home or on the road.<br />
• Cooperate with all investigations.<br />
• Get support from a senior colleague or mentor and arrange regular<br />
meetings.<br />
• Talk about the event with your colleagues and your relatives.<br />
Talk to others who are not directly involved with the situation (see<br />
Section 9).<br />
• Try not to isolate yourself.<br />
• Get colleagues to help with difficult cases and take up some of your<br />
duties.<br />
• Don't smoke or drink too much or self-medicate. Consult your<br />
general practitioner.<br />
• Give yourself time to recover.<br />
15
When to ask for help<br />
Sometimes events are too severe (or too personal) for reactions to<br />
improve with time. If this happens to you, you might want more help,<br />
particularly if:<br />
• Memories, dreams and images of the traumatic event continue to<br />
intrude on your consciousness, making you feel frightened and<br />
deprived of rest.<br />
• Your bodily sensations remain overwhelming.<br />
• Your feelings are not giving you any peace.<br />
• You remain exhausted, wound-up and feel 'burnt out'.<br />
• Your work performance is affected.<br />
• You have to keep active to avoid feeling upset.<br />
• You have nightmares or sleep problems.<br />
• You have nobody to openly share your feelings.<br />
• You find yourself getting uncontrollably angry.<br />
• You feel lonely and isolated.<br />
• You feel or become accident prone and cannot concentrate.<br />
• Your relationships suffer, or other people comment that you've<br />
changed.<br />
• You find yourself relying on medication or alcohol.<br />
If you experience any of the above, talk to a close colleague or mentor<br />
and get some help.<br />
16
SECTION 7. CRITICAL INCIDENT STRESS<br />
DEBRIEFING (CISD)<br />
Psychological debriefing is a set of procedures which includes Critical<br />
Incident Stress Debriefing (CISD) and on-going psychological<br />
counselling. These activities involve the giving of information aimed at<br />
preventing psychological morbidity and aiding recovery after a<br />
traumatic event. CISD was developed to reduce immediate distress<br />
and identify individuals likely to develop longer term psychological<br />
problems.<br />
There has been some controversy on the efficacy of CISD. 13 It was<br />
originally developed to be carried out by trained facilitators in order to<br />
mitigate stress responses amongst emergency responders. Some<br />
research has questioned its efficacy 14,15 but these may have been based<br />
on groups that have not been managed by appropriately trained<br />
counsellors or on participants who have not been followed up with<br />
further psychological support.<br />
Appropriately trained and experienced counsellors can advise on the<br />
structure and process of debriefing sessions. 16 Although CISD was<br />
originally designed to be carried out in large groups made up of all<br />
those affected by the trauma, there is growing evidence that it may be<br />
more effective initially to group participants by professional role or<br />
make trained counsellors available both on-site and off-site to suit<br />
individual preferences. 17 If large group sessions are thought to be<br />
advisable, these can be arranged at a later date.<br />
Whatever CISD process is decided upon, Trusts must ensure that any<br />
affected member of staff has the opportunity to see a trained counsellor<br />
within the first 72 hours after the event.<br />
Doctors are notoriously reluctant to seek professional help and some<br />
anaesthetists will continue to feel traumatised long after the event.<br />
Although Trusts have a duty of care towards staff, each individual also<br />
17
has a responsibility to ensure they are fit to work. It is important for<br />
colleagues and mentors to recognise signs of stress and remind<br />
individuals of the psychological resources available to them.<br />
18
SECTION 8. MEDICO-LEGAL ISSUES AND THE GMC<br />
Any professional involved in a medical catastrophe in their practice<br />
should want to encourage and assist in an investigation into what, if<br />
anything, went wrong and why. While the prospect of medico-legal<br />
consequences will weigh heavily on the mind of any anaesthetist<br />
involved in a catastrophic outcome, it should be remembered that very<br />
few such cases actually result in a formal disciplinary hearing or action<br />
for compensation. Adherence to the guidelines in this document<br />
should mean that the concerns of all parties will be adequately<br />
addressed, which will minimise the bad feeling that sometimes drives<br />
relatives to seek legal redress.<br />
The wheels of medico-legal processes turn slowly and memory can<br />
become very inaccurate as time passes. The best explanation for one's<br />
actions is a comprehensive, contemporaneous and accurate record of<br />
events (see Section 3); these should be stored in an appropriate<br />
location and may need to be kept for many years. Your defence<br />
organisation, mentor and department will be able to help you prepare<br />
for any medico-legal or disciplinary investigations.<br />
Legal Representation<br />
If the incident happened in your employing NHS Trust, then you are<br />
covered by your employer for civil litigation, i.e. negligence claims<br />
through the NHSLA (National Health Service Litigation Authority). 18<br />
However, it is always advisable to also have legal cover via one of the<br />
medical defence organisations, who should be informed of any<br />
unexpected death of a patient in your care. Personal representation of<br />
this sort is particularly important if there is any possibility of<br />
disagreement or dispute between you and your Trust, if the incident<br />
involves a private patient (in which case you are not covered by your<br />
NHS employer) or if there is any possibility of criminal charges being<br />
brought against you.<br />
19
Suspension<br />
It is not unusual for a clinician involved in a major untoward incident<br />
to be asked to stop clinical work pending the investigation of an<br />
incident. Sometimes this is by agreement to alter or change duties, and<br />
on occasion it takes the form of suspension by the employer.<br />
Suspension is, at least officially, a neutral measure aimed at protecting<br />
the individual, the Trust and its patients while inquiries are conducted.<br />
The suspended clinician will be kept on full pay, although admitting<br />
privileges to local private hospitals are nowadays usually curtailed for<br />
the duration. The anaesthetist may well be barred from visiting the<br />
Trust, and will be strongly advised not to discuss the matter in question<br />
with the media. Suspension should nowadays be a short-term<br />
measure, only employed to allow the facts to be clarified and<br />
appropriate disciplinary procedures to be considered.<br />
Possible sequence of events<br />
• Internal inquiry<br />
• Coroner's inquest (England and Wales) or Procurator Fiscal's<br />
(Scotland) Investigation<br />
• Criminal prosecution<br />
• GMC investigation<br />
• Civil litigation<br />
Internal Inquiry<br />
It is very likely that an unexpected peri-operative death or serious<br />
injury will lead to an internal inquiry. This is a fact-finding exercise,<br />
usually conducted by a senior clinician (often the medical or clinical<br />
director) who will interview and take statements from everyone<br />
involved. If asked to attend for interview, it is advisable to inform your<br />
medical defence organisation who may offer to send one of their<br />
representatives to accompany you; in any event, it is a good idea to<br />
take a trusted colleague or mentor along.<br />
20
Inquests<br />
In England and Wales, suspicious or unexpected deaths have to be<br />
reported to the Coroner, who will then decide whether to hold an<br />
Inquest. Coroners have wide powers of discretion as to which cases<br />
they wish to investigate. If in any doubt, clinicians are strongly<br />
recommended to inform the Coroner's Officer. The system is different<br />
in Scotland where sudden or unexpected deaths are investigated by the<br />
Procurator Fiscal who has the authority to ask for the assistance of the<br />
police in his/her investigation and may call a Fatal Accident Enquiry.<br />
Inquests often happen many months after the death, so good recordkeeping<br />
is essential. The Inquest is an enquiry into the identity of the<br />
deceased and, more importantly, the cause of death: it is not supposed<br />
to be about allocation of blame or determining negligence. However,<br />
there is an increasing tendency for interested parties - particularly the<br />
family of the deceased - to instruct legal representatives who are able,<br />
at the Coroner's discretion, to indulge in a degree of cross-examination<br />
of the witnesses. If the Coroner is persuaded that there is a genuine<br />
wider public interest in the outcome, then he/she may even choose to<br />
empanel a jury, at which point the Inquest starts to become more like<br />
a traditional adversarial Law Court. The Trust will provide legal cover<br />
for these situations but, again, the concerned anaesthetist is strongly<br />
advised to consult his/her own defence organisation in plenty of time<br />
before the Inquest.<br />
Criminal Prosecution<br />
Any clinician would be very concerned at the thought of a police<br />
investigation following a catastrophic outcome. Previously very<br />
unusual, police involvement has become more common following<br />
recent high-profile events such as the Shipman Inquiry and disasters<br />
involving blocked anaesthetic tubing and intrathecal administration of<br />
vincristine. 20-22 If they feel that there are suspicious circumstances or,<br />
perhaps more likely, that one or more of the clinicians have been<br />
grossly negligent, the police may recommend to the Crown<br />
Prosecution Service that criminal proceedings should be pursued;<br />
occasionally, the Coroner's verdict may encourage such action.<br />
21
The potential implications of a criminal prosecution cannot be<br />
overstated. Gross negligence, i.e. "reckless disregard for the welfare of<br />
the patient" attracts a charge of manslaughter which, if proven, will<br />
inevitably lead to erasure from the medical register and, often,<br />
imprisonment. Even if cleared of such a charge, the accompanying<br />
media publicity and stigma will often profoundly impact upon the<br />
clinician's professional and private life.<br />
General Medical Council (GMC)<br />
The GMC requires doctors in practice to take appropriate action if they<br />
are aware of concerns about another individual's ability to practice<br />
safely. This requirement extends to medical directors who may feel it<br />
appropriate or necessary to report an incident which might indicate a<br />
problem with a doctor's competence or performance. The GMC will<br />
let the individual know that they have received a complaint or<br />
comment about them and invite a response; once again it is vital to<br />
inform one's medical defence organisation as early as possible.<br />
Following initial investigation, the GMC case examiners may decide<br />
that no further action is warranted, issue a formal warning or refer the<br />
case to the Fitness to Practice Panel for final adjudication. 23 The case<br />
examiners can also ask the Interim Orders Committee to consider<br />
temporary suspension from, or restrictions to, the doctor's practice<br />
while investigation is underway. Once again, if this does eventually<br />
proceed to a formal hearing, the time delay can be very significant and<br />
the importance of good contemporaneous notes is vital.<br />
The NHS does not provide doctors with legal representation for GMC<br />
hearings. Membership of a medical defence organisation is strongly<br />
recommended.<br />
22
Civil Litigation<br />
A possible outcome of an unexpected peri-operative death or serious<br />
injury is a civil case for negligence being brought against the Trust (if<br />
NHS) or the individual practitioner (if private). This is a slow process,<br />
with prolonged preliminary stages designed to minimise the number of<br />
cases coming to Court, and the anaesthetist will often have little idea<br />
of what is happening after his/her initial involvement in supplying a<br />
witness statement. It is not unusual for civil cases to drag on for five<br />
years or more after the precipitating event. If it is a child who has<br />
suffered injury, the claim may not be made for many years.<br />
There are a number of reasons why the NHSLA may decide that a civil<br />
suit should be settled out of court. It is often a frustrating experience<br />
for anaesthetists who are confident that they could defend their own<br />
actions in a public arena, but there may be other aspects of the case<br />
which cannot be defended. It may be worth making vigorous<br />
representations to the NHSLA if it seems that such an action will be<br />
contemplated, although decisions are often made on pragmatic<br />
grounds and rarely reversed. At the time of writing, the Central Legal<br />
Office, the Scottish equivalent of the NHSLA, appears to be taking a<br />
more aggressive stance in defending doctors who they feel have not<br />
been negligent.<br />
Should you be called to give evidence, it is essential to have good<br />
quality records and to spend as much time as necessary rehearsing the<br />
facts of the case; it is very difficult to jog one's memory from a large<br />
bundle of case notes in the stressful environment of the witness box. It<br />
is advisable to go over the events of the case with a colleague and, if<br />
unfamiliar with the workings of the law, visit the court beforehand to<br />
get an idea of layout, behaviour and protocol. Try not to get flustered<br />
by cross-examination, answer politely, slowly and truthfully,<br />
addressing the Judge at all times, and do not be tempted into giving an<br />
expert opinion.<br />
23
SECTION 9. SOURCES OF HELP<br />
Consult your medical defence organisation in the first instance.<br />
Support services within the NHS<br />
Occupational Health Department<br />
Every NHS Trust has an Occupational Health Department that provides<br />
advice on the effects of work on health and the effects of health on<br />
work. Each NHS Trust provides a confidential counselling service for<br />
staff. Arrangements vary between Trusts but it is often linked with the<br />
Occupational Health Department.<br />
General Practitioner<br />
All doctors should be registered with a local GP. If you feel that the<br />
stress of your job, or of any particular incident at work, is affecting your<br />
health, you should make an appointment to see your GP. GP practices<br />
often have access to counselling services.<br />
Phone based resources<br />
Doctors' SupportLine<br />
0870 765 0001 www.doctorssupport.org<br />
Confidential, anonymous telephone helpline for doctors with any<br />
concerns whether work related or not. Staffed by trained volunteer<br />
doctors. Open 36 hours / week<br />
BMA Counselling Line<br />
08459 200 169<br />
Confidential counselling service for discussing personal, emotional<br />
and work-related problems. Available 24 hours / day; 365 days / year.<br />
For BMA members and their families only.<br />
Samaritans<br />
08457 909090 www.samaritans.org<br />
Confidential emotional support for people who are experiencing<br />
feelings of despair, including those contemplating suicide. Available<br />
24 hours / day; 365 days / year.<br />
24
AAGBI Sick Doctor's Scheme<br />
020 7631 1650<br />
This service is currently under review. Please contact the AAGBI for<br />
information.<br />
Web based resources<br />
Support4Doctors<br />
www.support4doctors.org<br />
A website run by the Royal Medical Benevolent Fund that aims to put<br />
doctors and their families in touch with a range of organisations who<br />
can help. Covers areas such as: Work & Career; Money & Finance;<br />
Health & Well-Being; Family & Home.<br />
BMA Doctors for Doctors<br />
www.bma.org.uk then click on doctors health and wellbeing.<br />
A web-based resource pack intended as a self-help tool to aid doctors<br />
in accessing appropriate help for any difficulties in which they may<br />
find themselves. For BMA members.<br />
BMJ Careers Discrimination Matching Scheme<br />
www.bmjcareers.com/discrimination/<br />
It provides the opportunity for doctors who feel that they have been<br />
discriminated against in some way, to receive informal support from<br />
another doctor. Communication is purely electronic.<br />
Support Groups and similar resources<br />
Doctors' Support Network<br />
0870 321 0 642 www.dsn.org.uk<br />
Confidential self-help support group for doctors with mental health<br />
problems.<br />
Meetings around the UK; Newsletter; email support groups.<br />
25
Sick Doctors Trust<br />
0870 444 5163 www.sick-doctors-trust.co.uk<br />
Undertake to provide early intervention and treatment for doctors<br />
suffering from addiction to alcohol or other drugs, thus protecting<br />
patients while offering hope, recovery and rehabilitation to affected<br />
colleagues and their families.<br />
Suspended Doctors Group of the Society of Clinical Psychiatrists<br />
01725 513367 (Dr Peter Tomalin)<br />
Confidential support for any hospital doctor who has been suspended,<br />
including advice based on the experience of others. Also has a<br />
network of psychiatrists around the country to whom doctors can be<br />
referred if they are becoming unwell.<br />
Financial Support<br />
Royal Medical Benevolent Fund<br />
020 8540 9194 www.rmbf.org<br />
Provides support ranging from specialist information and advice to<br />
financial assistance.<br />
Royal Medical Foundation<br />
01372 821011<br />
www.royalmedicalfoundation.org<br />
Provides support to medical practitioners and/or their dependants who<br />
find themselves in financial hardship.<br />
BMA Charities<br />
020 7383 6334<br />
Established to help all doctors (not just BMA members) and their<br />
dependants in times of need.<br />
26
SECTION 10. REFERENCES AND FURTHER READING<br />
1. Lunn JN, Hunter AR, Scott DB. Anaesthesia-related surgical<br />
mortality. Anaesthesia 1983;38:1090-94.<br />
2. Australian and New Zealand College of Anaesthetists. Safety of<br />
anaesthesia-related mortality, 1997-1999. http://www.anzca.edu.au/<br />
publications/reports/mortality/mort_97_1.htm.<br />
3. Why Mothers Die 2000-2002. Confidential Enquiries into<br />
Maternal and Child Health. RCOG Press, London.<br />
4. White SM, Akerele O. Anaesthetists' attitudes to intraoperative<br />
death. Personal communication from Dr. Stuart White.<br />
5. Bacon AK. Death on the table. Anaesthesia 1989; 44:245-8.<br />
6. Bacon AK. Major anaesthetic mishaps- handling the aftermath.<br />
Current Anaesthesia and Critical Care 1990, 1:253-7.<br />
7. Aitkenhead AR. Anaesthetic disasters: handling the aftermath.<br />
Anaesthesia 1997; 52: 477-82.<br />
8. White SM. Death on the table. Editorial. Anaesthesia 2003;<br />
58:515-9.<br />
9. Smith IC and Jones MW. Surgeon's attitudes to intraoperative<br />
death: a questionnaire survey. British Medical Journal 2001,<br />
322:896-7.<br />
10. Hawton K, Clements A, Sakarovitch C, Simkin S and Deeks DJ.<br />
Suicide in doctors: a study of risk according to gender, seniority<br />
and specialty in medical practitioners in England and Wales 1979-<br />
1995. Journal of Epidemiology and Community Health 2001;<br />
55:296-300.<br />
11. Cooper JB, Cullen DJ, Eichhorn JH, Philip JH and Holzman S.<br />
Administrative guidelines for response to an adverse anaesthesia<br />
event. Journal of Clinical Anaesthesia 1993; 5:79-84.<br />
12. Stress in Anaesthetists. 1997. Association of Anaesthetists of Great<br />
Britain and Ireland. http:/www.<strong>aagbi</strong>.org/pdf/28doc.pdf.<br />
13. Kenardy JA. The current status of psychological debriefing. British<br />
Medical Journal 2000; 321:1032-3.<br />
14. Everly, G. & Boyle, S. 2001. Critical Incident Stress Debriefing<br />
CISD: A Meta-analysis. Ellicott City, MD: International Critical<br />
Incident Stress Foundation.<br />
27
15. Emmerik AAP, Kamphuis JH, Hulsbosch AM and Emmelkamp<br />
PMG. Single session debriefing after psychological trauma: a<br />
meta analysis. The Lancet 2002; 360:766-71.<br />
16. Mitchell J T. 2003. Not always as it appears. CISM Perspectives.<br />
www.cismperspectives.com<br />
17. Carr K R. 2003. Critical Incident Stress Debriefings for Cross-<br />
Cultural Workers: Harmful or helpful? MMCT. PO Box OS-3063<br />
Osu-Accra, Ghana, West Africa. http://www.mmct.org/ article9/ htm<br />
18. http://www.nhsla.com/NR/rdonlyres/B0148219-A94C-469D-<br />
A5FC-127A418926E8/0/AVeryBriefGuideforClinicians.pdf<br />
19. http://www.dh.gov.uk/PolicyAndGuidance/HumanResources<br />
AndTraining/ModerninsingProfessionalRegulation/DoctorsAnd<br />
DentistsDisciplinaryFrameworkArticle/fs/en?CONTENT_ID=40727<br />
71&chk=x9pnf/<br />
20. http://www.the-shipman-inquiry.org.uk/<br />
21. Carter JA. Checking anaesthetic equipment and the Expert Group<br />
on Blocked Anaesthetic Tubing (EGBAT). Anaesthesia 2004; 59:<br />
105-7.<br />
22. http://news.bbc.co.uk/1/hi/health/3133076.stm<br />
23. http://www.gmc-uk.org/probdocs/fitness to practice guidance/<br />
factsheets/fitness to practice procedures explained.pdf.<br />
28
29
21 Portland Place, London W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org<br />
Designed and produced by the r2 Partnership Ltd
AAGBI SAFETY GUIDELINE<br />
Blood Transfusion and the Anaesthetist<br />
Intra-operative Cell Salvage<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org September 2009
Membership of the working party<br />
Prof M Y K Wee<br />
Dr D Thomas<br />
Dr R Verma<br />
Ms J Jones<br />
Dr S Catling<br />
Dr J Isaac<br />
Dr F Howard<br />
Mrs S Milton<br />
Ex Officio<br />
Dr R J S Birks<br />
Dr D K Whitaker<br />
Dr L W Gemmell<br />
Dr A W Harrop-Griffiths<br />
Dr I H Wilson<br />
Dr I G Johnston<br />
Dr E P O’Sullivan<br />
Dr D G Bogod<br />
Chair and AAGBI Vice President<br />
Joint Chair, UK Cell Salvage Action<br />
Group<br />
AAGBI Council Member<br />
UK Cell Salvage Action Group<br />
UK Cell Salvage Action Group<br />
Royal College of Anaesthetists<br />
GAT Chair<br />
Association for Perioperative Practice<br />
President<br />
Immediate Past President<br />
Honorary Secretary<br />
Immediate Past Honorary Secretary<br />
Honorary Treasurer<br />
Honorary Treasurer Elect<br />
Honorary Membership Secretary<br />
Editor-in-Chief, Anaesthesia<br />
Acknowledgements<br />
The working party is grateful to Danny McGee, representing<br />
the College of Operating Department Practioners and Catherine<br />
Howell representing the UK Cell Salvage Action Group.
Contents<br />
1 Recommendations 2<br />
2 Introduction 3<br />
3 Getting organised and competencies 4<br />
4 Operative indications 7<br />
5 Technical aspects 8<br />
6 Special circumstances 10<br />
7 Financial considerations 14<br />
References 15<br />
Appendices 18<br />
Endorsements and/or Support<br />
This guideline has the endorsement and/or support of the<br />
following bodies:<br />
• British Orthopaedic Association<br />
• College of Anaesthetists of Ireland<br />
• Royal College of Obstretricians & Gynaecologists<br />
• Royal College of Surgeons in Ireland<br />
• Royal College of Surgeons of Edinburgh<br />
• Royal College of Surgeons of England<br />
• Vascular Anaesthesia Society of Great Britain & Ireland<br />
• Vascular Society of Great Britain & Ireland<br />
To be reviewed by 2014<br />
© Copyright of the Association of Anaesthetists of Great Britain & Ireland. No<br />
part of this book may be reproduced without the written permission of the<br />
AAGBI<br />
1
1. Recommendations<br />
• The use of Intra-operative Cell Salvage (ICS) reduces the<br />
demand on allogeneic (donor) red cells and is a cost effective<br />
measure.<br />
• Trusts should provide the resources required to set up and<br />
maintain an ICS service in a safe, appropriate and cost<br />
effective manner.<br />
• Each Trust needs to ensure there is a clinical lead for ICS.<br />
• A member of the theatre management team is responsible for<br />
ensuring overall management and facilitation of the ICS<br />
service.<br />
• All personnel using ICS must be adequately trained and<br />
competent in its use.<br />
• Pre-operative assessment clinics should provide information<br />
on ICS to patients.<br />
• All ICS cases undertaken require documentation and audit of<br />
use to enable future service planning and quality assurance.<br />
2
2. Introduction<br />
The challenge to ensure a safe and adequate supply of blood<br />
components for transfusion continues. It has been recognised<br />
that there are morbidities associated with the immunological<br />
complications of allogeneic blood transfusion. The cost of<br />
allogeneic blood components is increasing as testing and<br />
processing to avoid transfusion transmitted infection becomes<br />
more sophisticated. An additional concern is that the donor pool<br />
is decreasing.<br />
The use of ICS reduces the demand on allogeneic (donor)<br />
red cells and is a cost effective measure. The Chief Medical<br />
Officer’s National Blood Transfusion Committee in England<br />
document ‘Strategies for Blood Conservation’ recommends<br />
three main strategies to reduce demand: ICS, better education of<br />
practitioners, and better pre-operative patient preparation.<br />
Analysis of a recent survey showed that 53% of UK hospitals<br />
now use ICS [1]. The principal aim of this document is to<br />
facilitate and promote the safe and competent use of ICS to<br />
enhance patient care.<br />
3
3. Getting organised and<br />
competencies<br />
Greater awareness of the need for blood conservation should<br />
help influence clinicians to make wider use of autologous blood<br />
recovery techniques.<br />
Lead ICS clinician<br />
The lead clinician should ideally be someone working in the<br />
theatre setting, i.e. a consultant anaesthetist or surgeon and a<br />
member of the Hospital Transfusion Committee. Their role is to<br />
provide information, support and direction. This includes:<br />
• Responsibility for the overall ICS programme within an<br />
organisation.<br />
• Ensuring that agreed procedures and protocols are adhered<br />
to.<br />
• Informing clinical staff about the benefits of the autologous<br />
programme.<br />
• Identifying clinical situations where cell salvage can be used.<br />
• Advising on the use of ICS in special circumstances, e.g.<br />
malignancy, sepsis, and obstetrics.<br />
• Developing a safe out of hours ICS service where<br />
appropriate.<br />
4
Operational management<br />
Operational manager<br />
A senior member of the theatre management team should<br />
be responsible for the organisation and facilitation of the ICS<br />
service by:<br />
• Identifying a member of staff who will take on the role of coordinating<br />
the cell salvage service.<br />
• Being involved in the purchase of equipment and service<br />
contracts.<br />
• Liaising with the lead ICS clinician to produce and<br />
implement local protocols and guidelines.<br />
ICS co-ordinator<br />
In larger Trusts, there may be a need for a cell salvage coordinator.<br />
The co-ordinator should be fully trained and<br />
competent in the operation of all types of cell salvage machines<br />
used in an organisation. The cell salvage co-ordinator is a<br />
member of the theatre staff who is responsible for:<br />
• Delivering and recording of training and competency<br />
assessment.<br />
• Arranging for cell salvage to be available at the clinician’s<br />
request. If the service is not available, this should be<br />
reported to the lead ICS manager and clinician.<br />
• Maintaining records of all procedures undertaken to ensure<br />
accurate auditing and quality assurance.<br />
• Providing information for the Hospital Transfusion Committee<br />
(HTC) and national audits as appropriate.<br />
5
Competencies<br />
Documents supporting competency assessment are available on<br />
the Better Blood Transfusion website:<br />
www.transfusionguidelines.org.uk.<br />
Click on Better Blood Transfusion Toolkit on the left hand menu,<br />
then Appropriate Use and then UK Cell Salvage Action Group.<br />
Alternatively most search engines will take you straight to the<br />
relevant section if you insert ‘UK Cell Salvage Action Group’.<br />
6
4. Operative indications<br />
ICS is indicated in surgery with:<br />
• Anticipated blood loss of >1000mls or >20% Estimated<br />
Blood Volume.<br />
• Patients with a low Hb or increased risk factors for bleeding.<br />
• Patients with multiple antibodies or rare blood types.<br />
• Patients with objections to receiving allogeneic (donor)<br />
blood.<br />
In cases with Jehovah’s Witnesses where a decision to use ICS is<br />
made, this should be discussed with the patient pre-operatively<br />
and informed consent obtained. All blood salvaged will need to<br />
be labelled clearly. Use of the standard UK label issued for cell<br />
salvage is recommended. It is essential that any adverse events<br />
whether clinical or technical are reported to Serious Hazards of<br />
Transfusion (SHOT).<br />
Procedures which may be suitable for ICS<br />
(See Appendix 1 on page 18).<br />
7
5. Technical aspects<br />
The surgical team should be aware of the technical issues<br />
relating to the quality of cell salvage.<br />
During surgery, blood loss can be removed from the operative<br />
site by a combination of suction and swabs. Depending on the<br />
type of surgery, blood loss to swabs during surgery has been<br />
estimated at between 30% and 50% of the total surgical blood<br />
loss. By washing swabs, the blood that is normally discarded<br />
can be collected and the overall efficiency of red cell recovery<br />
improved.<br />
ICS should be temporarily discontinued when substances not<br />
licensed for intravenous (IV) use are present within the surgical<br />
field and could potentially be aspirated into the collection<br />
reservoir. The standard theatre suction should be used to<br />
aspirate the surgical field and the wound should be irrigated<br />
with copious 0.9% sodium chloride before resuming ICS.<br />
Examples of substances that should not be aspirated into the ICS<br />
system include:<br />
• Antibiotics not licensed for IV use<br />
• Iodine<br />
• Topical clotting agents<br />
• Orthopaedic cement<br />
To optimise the yield and quality of salvaged blood a large bore<br />
suction tip (minimum 4mm, e.g. Yankauer sucker) should be<br />
used and surface skimming minimised. Try to avoid aspirating<br />
blood mixed with large quantities of air from the surgical field.<br />
8
To reduce haemolysis the vacuum pressure should always be set<br />
as low as practicable.<br />
A standard blood administration set is usually adequate.<br />
There are special circumstances where additional filters are<br />
recommended (see overleaf).<br />
9
6. Special circumstances<br />
The decision to use blood that is potentially contaminated<br />
with bacteria, amniotic fluid or malignant cells should be<br />
made by the clinicians caring for the patient, taking into<br />
account the latest evidence and consideration of the risks<br />
and benefits for the individual patient.<br />
Malignancy<br />
The manufacturers of ICS devices do not recommend its use<br />
in patients undergoing surgery for malignant disease. This is<br />
due to concerns about the possibility of malignant cells being<br />
reinfused and giving rise to metastases. However, in addition<br />
to the many reports in the literature of the use of ICS in cancer<br />
surgery without obviously leading to early metastasis, two recent<br />
studies have shown no difference in biochemical recurrence or<br />
long term survival after radical prostatectomy and cystectomy<br />
between patients receiving ICS and those that received no blood<br />
[2,3].<br />
A recent prospective study of hepatocarcinoma surgery also<br />
showed no difference in recurrence rates between those who<br />
did and did not receive cell salvaged blood [4].<br />
In contrast, there is evidence that allogeneic transfusion is<br />
independently associated with an increased rate of both<br />
postoperative infection and disease recurrence [5-8].<br />
Consequently, in April 2008 the use of ICS in urological<br />
malignancies was approved by NICE [9]. ICS can now be<br />
used routinely during surgery for urological malignant disease.<br />
Aspiration of blood from around the tumour site should be<br />
avoided to minimise contamination of salvaged blood with<br />
malignant cells. There is in vitro evidence that blood filtration<br />
through leucodepletion filters significally reduce malignant<br />
10
cell numbers. Some clinicians use a leucodepletion filter (Pall<br />
Leukoguard RS) to reduce the reinfusion of malignant cells<br />
which may be contaminating the cell salvaged red cells, whilst<br />
others reinfuse unfiltered without apparent problems. It is<br />
important to remember the manufacturers’ guidance on the use<br />
of these filters by not pressurising the reinfusion bag.<br />
Obstetrics<br />
The main concern surrounding the use of ICS during obstetric<br />
haemorrhage is the risk of reinfusing fetal contaminants with<br />
the theoretical risk of causing amniotic fluid embolus (AFE).<br />
However, to date there are no proven cases in the literature<br />
of AFE caused by reinfusion of salvaged blood, and the use<br />
of cell salvage in obstetrics is approved by NICE. The use<br />
of leucodepletion filters in this situation has also shown a<br />
significant reduction in contamination from amniotic fluid [10-<br />
13].<br />
ICS is being increasingly used in the UK in obstetrics for women<br />
at risk from massive obstetric haemorrhage during caesarean<br />
section [14]. In the year 2005-2006, 38% of UK maternity units<br />
used ICS, and 28% included the use of ICS in their Massive<br />
Obstetric Haemorrhage (MOH) protocol [15]. Early theoretical<br />
concerns over amniotic fluid embolism have not been borne out<br />
in clinical practice, and 80% of maternity units identified lack<br />
of training, rather than safety concerns, as the barrier to more<br />
frequent use of ICS.<br />
Obstetric use also raises the concern of reinfusion of fetal red<br />
cells from the operative field, as the cell saver cannot distinguish<br />
fetal from maternal red cells [16]. If the mother is rhesus<br />
negative (and the fetus RhD positive) the extent of maternal<br />
exposure should be determined by Kleihauer testing as soon<br />
as possible and a suitable dose of Anti D given. (N.B. the RhD<br />
negative mother would be routinely receiving Anti D after<br />
obstetric haemorrhage).<br />
11
Bowel contamination<br />
The use of ICS in the presence of bowel contents is contraindicated<br />
by the manufacturers unless there is catastrophic<br />
haemorrhage. However, the evidence indicates that wound<br />
infection rates after laparotomy for abdominal injuries is no<br />
different for patients receiving allogeneic or cell salvaged<br />
blood, with no correlation between organisms grown from the<br />
cell saved blood and those causing postoperative pneumonias,<br />
bacteraemias or urinary tract infections [17,18].<br />
A recent prospective RCT of laparotomy for abdominal trauma<br />
showed that ICS significantly reduced allogeneic blood usage<br />
with no effect on postoperative infection or mortality [18].<br />
While salvage from grossly contaminated fields should be<br />
avoided, procedures involving bowel resection may use ICS for<br />
at least part of the procedure.<br />
If deemed clinically necessary the following practical tips may<br />
help:<br />
• Initial evacuation of the soiled abdominal contents.<br />
• Additional washing (increasing the volume of IV normal<br />
saline [0.9% NaCl] which the machine uses to wash the<br />
salvaged blood).<br />
• Ensure use of broad spectrum antibiotics.<br />
It is unlikely that bowel contamination in such traumatised<br />
individuals will lead to problems in decision making about<br />
the use of ICS, but hopefully the points raised can enable all<br />
concerned to make an informed management choice.<br />
12
N.B. SHOT has received a few recent reports of hypotension<br />
that appear to be temporally related to reinfusion of cell<br />
salvaged blood. The clinical/equipment details of each case are<br />
currently being investigated to establish whether there are any<br />
common features. The web version of this document will be<br />
updated accordingly.<br />
13
7. Financial considerations<br />
To keep the cost argument simple, it becomes self evident that<br />
if there is a machine available and a competent operator, then<br />
the direct and recurring costs can be quite easily calculated.<br />
Each 250 ml of salvaged and washed red cells is equivalent to<br />
a unit of concentrated red cells, e.g. SAGM. Both have a similar<br />
volume and haematocrit and therefore could be regarded as<br />
therapeutically equal, if time is allowed for the stored red cells<br />
to become biochemically active.<br />
The current red cell unit cost in the UK is approximately £140<br />
(although the price has been intentionally held steady for some<br />
years). The disposable costs vary depending on which cell<br />
salvage machine is being used, but range from approximately<br />
£100 to £170. One can see that at this level saving an average<br />
of 1 to 1.5 units of red cell equivalent per case salvaged will<br />
cover the disposable costs. As prices will inevitably change it is<br />
recommended that readers bear in mind the date of publication<br />
of this booklet.<br />
If the hardware for cell salvage is not available within the<br />
Trust where you work you may find a generic business<br />
case helpful. Readers requiring a generic business case,<br />
which can be adapted to their own circumstances can<br />
obtain this by going straight to the UK Cell Action Salvage<br />
Group area of the Better Blood Transfusion Website as<br />
explained on page 6 or by placing ‘UK Cell Salvage Action<br />
Group’ in a search engine.<br />
14
References<br />
1. UK CSAG National Questionnaire April 2007.<br />
http://transfusionguidelines.org.uk/docs/pdfs/bbt-03_icsagnewsletter-01_20080420.pdf<br />
(accessed 17.01.09).<br />
2. Neider AM, Carmack AJK, Sved PD, Kim SS, Manoharan<br />
M, Soloway MS. Intra-operative cell salvage during radical<br />
prostatectomy is not associated with greater biochemical<br />
recurrence rate. Adult Urology 2005; 65: 30-4.<br />
3. Neider AM, Manoharan M, Yang Y, Soloway MS. Intraoperative<br />
cell salvage during radical cystectomy does not<br />
affect long term survival. Adult Urology 2007; 69; 881-4.<br />
4. Muscari F, Suc B, Vigouroux D, et al. Blood salvage<br />
autotransfusion during transplantation for<br />
hepatocarcinoma: does it increase the risk of neoplastic<br />
recurrence? Transplant International 2005; 18 (11): 1236-<br />
9.<br />
5. Kinoshita Y, Udagawa H, Tsutsumi K, et al. Usefulness of<br />
autologous blood transfusion for avoiding allogeneic<br />
transfusion and infectious complications after esophageal<br />
cancer resection. Surgery 2000; 127: 185-92.<br />
6. Jones KR, Weissler MC. Blood transfusion and other risk<br />
factors for recurrence of cancer of the head and neck.<br />
Archives of Otolaryngology - Head and Neck Surgery<br />
1990; 16: 304-9.<br />
7. Woolley AL, Hogikyan ND, Gates GA, Haughey BH,<br />
Schechtman KB, Goldenberg JL. Effect of blood transfusion<br />
on recurrence of head and neck carcinoma. Retrospective<br />
review and meta-analysis. Annals of OtoRhinoLaryngology<br />
1992; 101: 724-30.<br />
15
8. Takemura M, Osugi H, Higashino M, Takada N, Lee S,<br />
Kinoshita H. Effect of substituting allogeneic blood<br />
transfusion with autologous blood transfusion on outcomes<br />
after radical oesophagectomy for cancer. Annals of<br />
Thoracic and Cardiovascular Surgery 2005; 11: 293-330.<br />
9. National Institute for Heath and Clinical Excellence. No<br />
258. April 2008. http://www.nice.org.uk/Guidance/IPG258/<br />
Guidance/pdf/English (accessed 17.01.09).<br />
10. National Institute for Heath and Clinical Excellence. No<br />
144 November 2005. http://guidance.nice.org.uk/IPG144<br />
(accessed 17/01/09).<br />
11. The Confidential Enquiry into Maternal and Child Health<br />
(CEMACH). Saving Mothers’ Lives: reviewing maternal<br />
deaths to make motherhood safer - 2003-2005. The<br />
Seventh Report on Confidential Enquiries into Maternal<br />
Deaths in The United Kingdom. London: CEMACH:<br />
http://www.cmace.org.uk/Publications/CEMACH-<br />
Publications/Maternal-and-Perinatal-Health.aspx<br />
(accessed 21/07/08).<br />
12. Waters JH, Biscotti MD, Potter PS, Phillipson E. Amniotic<br />
fluid removal during cell salvage in the caesarean section<br />
patient. Anesthesiology 2000; 92: 1531-6.<br />
13. Sullivan I, Faulds J, Ralph C. Contamination of salvaged<br />
maternal blood by amniotic fluid and fetal red cells during<br />
elective caesarean section. British Journal of Anaesthesia<br />
2008; 101(2): 225-9.<br />
14. Allam J, Cox M, Yentis SM. Cell salvage in obstetrics.<br />
International Journal of Obstetric Anesthesia 2008; 17:37-<br />
45.<br />
16
15. Teig M, Harkness M, Catling S, Clarke V. Survey of cell<br />
salvage use in obstetrics in the UK. International Journal of<br />
Obstetric Anesthesia 2007; 16: S30.<br />
16. Catling SJ, Williams S, Fielding AM. Cell salvage in<br />
obstetrics: an evaluation of the ability of cell salvage<br />
combined with leucocyte depletion filtration to remove<br />
amniotic fluid from operative blood loss at caesarean<br />
section. International Journal of Obstetric Anesthesia 1999;<br />
8: 79-84.<br />
17. Ozmen V, McSwain NE, Nichols RL, Smith J, Flint<br />
LM. Autotransfusion of potentially culture-positive blood<br />
in abdominal trauma: preliminary data from a prospective<br />
study. Journal of Trauma 1992; 32: 36-9.<br />
18. Bowley DM, Barker P, Boffard ND. Intra-operative blood<br />
salvage in penetrating abdominal trauma: a randomised,<br />
controlled trial. World Journal of Surgery 2006; 30: 1074-<br />
80.<br />
Websites<br />
www.transfusionguidelines.org.uk<br />
www.<strong>aagbi</strong>.org<br />
www.nataonline.com<br />
www.bbts.org.uk<br />
17
Appendix 1<br />
Procedures and situations which may be suitable for ICS<br />
Vascular Surgery, Trauma<br />
& Orthopaedics<br />
Open aortic aneurysm repair -<br />
(elective and emergency)<br />
Splenic/liver trauma<br />
Spinal surgery<br />
Revision hip replacement<br />
Pelvic and femoral fractures<br />
(In primary hip and knee<br />
replacement it may be better<br />
to consider post operative<br />
drainage systems)<br />
Urology<br />
Radical cystectomy<br />
Radical prostatectomy<br />
Nephrectomy<br />
Pelvic clearance<br />
General Surgery<br />
Hepatectomy<br />
Abdominal/thoracic trauma<br />
Emergency laparotomy<br />
Cardiac<br />
All major procedures (post-op<br />
drainage may be of use if<br />
mediastinal drainage is of high<br />
volume)<br />
18
Obstetric<br />
Emergency use: major<br />
obstetric haemorrhage at<br />
caesarean section, laparotomy<br />
for postpartum haemorrhage<br />
genital tract trauma, etc.<br />
Elective use: anticipated<br />
haemorrhage at caesarean<br />
section, e.g. placenta praevia/<br />
accreta, large fibroid uterus,<br />
etc.<br />
Gynaecology<br />
All major procedures, e.g.<br />
pelvic clearance<br />
Head and Neck<br />
Major procedures<br />
Jehovah’s Witnesses or<br />
any patient refusing<br />
a blood transfusion<br />
Consideration should also be<br />
given to post-op drainage and<br />
reinfusion where indicated<br />
All surgical procedures where<br />
blood loss is expected to have<br />
an impact<br />
Maximum benefit of cell salvage can be gained by<br />
capture of emergency cases which often require large<br />
volume blood component support.<br />
19
Appendix 2<br />
Diagram of ICS set-up<br />
Drawn for the UK ICS Action Group by Medical Illustration<br />
Department - University Hospital of South Manchester NHS<br />
Foundation Trust.<br />
20
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
AAGBI SAFETY GUIDELINE<br />
Checking Anaesthetic Equipment 2012<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland<br />
21 Portland Place, London, W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org June 2012
This guideline was originally published in Anaesthesia. If you wish to refer to<br />
this guideline, please use the following reference:<br />
Association of Anaesthetists of Great Britain and Ireland. Checking<br />
Anaesthetic Equipment 2012. Anaesthesia 2012; 67: pages 660-68. This<br />
guideline can be viewed online via the following URL: http://onlinelibrary.<br />
wiley.com/doi/10.1111/j.1365-2044.2012.07163.x/abstract<br />
© The Association of Anaesthetists of Great Britain 2012
Guidelines<br />
Checking Anaesthetic Equipment 2012<br />
Association of Anaesthetists of Great Britain and<br />
Ireland<br />
Membership of the Working Party: A. Hartle (Chair), E. Anderson,<br />
V. Bythell, L. Gemmell, H. Jones 1 , D. McIvor 2 , A. Pattinson 3 ,<br />
P. Sim 3 and I. Walker<br />
1 Royal College of Anaesthetists<br />
2 Medicines and Healthcare products Regulatory Agency<br />
3 British Association of Anaesthetic and Respiratory Equipment<br />
Manufacturers Association<br />
Summary<br />
A pre-use check to ensure the correct functioning of anaesthetic<br />
equipment is essential to patient safety. The anaesthetist has a primary<br />
responsibility to understand the function of the anaesthetic equipment and<br />
to check it before use. Anaesthetists must not use equipment unless they<br />
have been trained to use it and are competent to do so. A self-inflating bag<br />
must be immediately available in any location where anaesthesia may be<br />
given. A two-bag test should be performed after the breathing system,<br />
vaporisers and ventilator have been checked individually. A record should<br />
be kept with the anaesthetic machine that these checks have been done.<br />
The ‘first user’ check after servicing is especially important and must be<br />
recorded.<br />
Reuse of this article is permitted in accordance with the Creative Commons Deed, Attribution<br />
2.5, which does not permit commercial exploitation.<br />
Anaesthesia ª 2012 The Association of Anaesthetists of Great Britain and Ireland 1
Anaesthesia 2012<br />
Hartle et al. | Checking anaesthetic equipment<br />
..................................................................................................<br />
This is a consensus document produced by expert members of a Working<br />
Party established by the Association of Anaesthetists of Great Britain and<br />
Ireland (AAGBI). It has been seen and approved by the AAGBI Council.<br />
This article is accompanied by an Editorial. See page 571 of this issue.<br />
You can respond to this article at http://www.anaesthesiacorrespondence.com<br />
Accepted: 18 March 2012<br />
• What other guideline statements are available on this topic?<br />
Guidelines on checking anaesthetic equipment have been published by<br />
the Association of Anaesthetists of Great Britain and Ireland (AAGBI),<br />
and amongst others, the American Society of Anesthesiologists, the<br />
Australian and New Zealand College of Anaesthetists and the World<br />
Federation of Societies of Anesthesiologists.<br />
• Why was this guideline developed?<br />
The increasing sophistication and diversity of anaesthesia workstations<br />
made the AAGBI’s existing guideline less universally applicable.<br />
Incidents reported to the Medicines and Healthcare products<br />
Regulatory Agency (MHRA), National Patient Safety Agency (NPSA)<br />
and AAGBI also highlighted priority checks that would avoid harm.<br />
• How does this statement differ from existing guidelines?<br />
The checklist specifies outcomes rather than processes and covers all the<br />
equipment necessary to conduct safe anaesthesia, not just the<br />
anaesthesia workstation. It has been written by Officers and Council<br />
members of the AAGBI in conjunction with representatives of the Royal<br />
College of Anaesthetists (RCoA), MHRA, NPSA and manufacturers. It<br />
was modified after a consultation with the membership of the AAGBI<br />
and industry. It has been trialled and modified in simulator settings on<br />
different machines. It has been endorsed by the Chief Medical Officers<br />
of England, Scotland, Wales and Northern Ireland.<br />
• Why does this statement differ from existing guidelines?<br />
The guideline reflects anaesthetic practice and staffing in the UK and<br />
Ireland and is applicable to any anaesthetic machine, including those yet<br />
to be developed.<br />
The pre-use check to ensure the correct functioning of anaesthetic<br />
equipment is essential to patient safety. The importance of this pre-use<br />
check is recognised worldwide and the check has been included in the<br />
2 Anaesthesia ª 2012 The Association of Anaesthetists of Great Britain and Ireland
Hartle et al. | Checking anaesthetic equipment Anaesthesia 2012<br />
World Health Organization’s Surgical Safety Checklist [1]. The AAGBI<br />
published the third edition of Checking Anaesthetic Equipment in 2004,<br />
and this has gained widespread acceptance in the profession. Changes in<br />
anaesthetic equipment and introduction of microprocessor-controlled<br />
technology necessitate continued revision of this document.<br />
This new edition of the safety guideline updates the procedures<br />
recommended in 2004 and places greater emphasis on checking all of the<br />
equipment required. A Working Party was established in 2009 comprising<br />
Officers and Council Members of the AAGBI and representatives of the<br />
Group of Anaesthetists in Training (GAT), RCoA, MHRA and the British<br />
Association of Anaesthetic and Respiratory Equipment Manufacturers<br />
Association (BAREMA). The Working Party reviewed the 2004 guideline,<br />
together with guidelines published by other organisations, and in addition<br />
reviewed incidents reported to the MHRA and the National Reporting and<br />
Learning Service (NRLS) of the NPSA [2]. The accompanying Checklist for<br />
Anaesthetic Equipment 2012 has been completely reformatted (Fig. 1).<br />
There are two new checklists – the first to be completed at the start of<br />
every operating session, the second a short set of checks before each case.<br />
The detail of how to perform these checks is given in this safety guideline.<br />
The first draft was circulated to the membership of the AAGBI and to<br />
manufacturers for comments, and the guideline amended in the light of<br />
these. Several versions of the checklist were trialled in simulators using<br />
different machines. The final version of the checklist was then submitted<br />
for further usability tests in simulators. The guideline and checklists have<br />
been endorsed by the Chief Medical Officers of England, Scotland, Wales<br />
and Northern Ireland.<br />
The principles set out in previous guidelines have governed<br />
amendments in this new edition. It must be emphasised that failure to<br />
check the anaesthetic machine and ⁄ or the breathing system features as a<br />
major contributory factor in many anaesthetic misadventures, including<br />
some that have resulted in hypoxic brain damage or death. The RCoA<br />
recognises the importance of these safety checks, and knowledge of them<br />
may be tested as part of the FRCA examination [3].<br />
The anaesthetist has a primary responsibility to understand the<br />
function of the anaesthetic equipment and to check it before use<br />
Anaesthetists must not use equipment unless they have been trained to use<br />
it and are competent to do so [4]. The NHS Clinical Negligence Scheme<br />
for Trusts and NHS Quality Improvement Scotland require that hospitals<br />
ensure all personnel are trained to use and to check relevant equipment<br />
Anaesthesia ª 2012 The Association of Anaesthetists of Great Britain and Ireland 3
Anaesthesia 2012<br />
Hartle et al. | Checking anaesthetic equipment<br />
Figure 1 Checklist for Anaesthetic Equipment 2012.<br />
[5, 6]. This may take place at induction for new staff or at the introduction<br />
of new equipment. This responsibility may be devolved to the department<br />
of anaesthesia, but where such a department does not exist other<br />
4 Anaesthesia ª 2012 The Association of Anaesthetists of Great Britain and Ireland
Hartle et al. | Checking anaesthetic equipment Anaesthesia 2012<br />
This checklist is an abbreviated version of the publication by the Association of Anaesthetists of Great Britain and<br />
Ireland 'Checking Anaesthesia Equipment 2012'.<br />
Figure 1 (Continued).<br />
arrangements must be made. A record of training must be kept. The use of<br />
routine checks and associated checklists is an important part of training in<br />
anaesthesia, and is part of the RCoA’s Competency Based Training.<br />
Anaesthesia ª 2012 The Association of Anaesthetists of Great Britain and Ireland 5
Anaesthesia 2012<br />
Hartle et al. | Checking anaesthetic equipment<br />
Modern anaesthetic workstations<br />
The AAGBI checklist for anaesthetic equipment is applicable to all<br />
anaesthetic workstations and should take only a few minutes to perform. It<br />
represents an important part of safe patient care. It is not intended to<br />
replace the manufacturer’s pre-anaesthetic checks, and should be used in<br />
conjunction with them. For example, some modern anaesthetic workstations<br />
will enter a self-testing cycle when the machine is switched on, in<br />
which case those functions tested by the machine need not be retested by<br />
the user. The intention is to strike the right balance so that the AAGBI<br />
checklist for anaesthetic equipment is not so superficial that its value is<br />
doubtful or so detailed that it is impractical to use. Manufacturers may<br />
also produce checklists specific to their device; these should be used in<br />
conjunction with the AAGBI checklist for anaesthetic equipment.<br />
The checking procedure described covers all aspects of the anaesthetic<br />
delivery system from the gas supply pipelines, the machine and breathing<br />
systems, including filters, connectors and airway devices. It includes an<br />
outline check for ventilators, suction, monitoring and ancillary equipment.<br />
The anaesthetic equipment must be checked by trained staff on a<br />
routine basis using the checklist and according to the manufacturer’s<br />
instructions, in every environment where an anaesthetic is given. A record<br />
should be kept with the anaesthetic machine that these checks have<br />
been done.<br />
Each hospital must ensure that all machines are fully serviced at the<br />
regular intervals designated by the manufacturer and that a service record<br />
is maintained. As it is possible for errors to occur when reassembling an<br />
anaesthetic machine, it is essential to confirm that the machine is correctly<br />
configured for use after each service. The ‘first user’ check after servicing<br />
is especially important and must be recorded.<br />
Equipment faults may develop during anaesthesia that were either not<br />
present or not apparent on the pre-operative check. This may be caused by<br />
pipeline failure, electrical failure, circuit disconnection or incorrect<br />
configuration, etc. An immediate and brief check of equipment should<br />
be made if there is a critical incident involving a patient, even if the<br />
equipment was checked before the start of the case, as the incident may be<br />
caused by a primary problem with the equipment.<br />
The checking procedure described in this publication is reproduced in<br />
an abbreviated form, as a sheet entitled Checklist for Anaesthetic<br />
Equipment 2012 (Fig. 1). This laminated sheet should be attached to each<br />
anaesthetic machine and used to assist in the routine checking of<br />
anaesthetic equipment.<br />
6 Anaesthesia ª 2012 The Association of Anaesthetists of Great Britain and Ireland
Hartle et al. | Checking anaesthetic equipment Anaesthesia 2012<br />
Procedures for checking anaesthetic equipment<br />
The following checks should be carried out at the beginning of each<br />
operating theatre session. In addition, specific checks should be carried out<br />
before each new patient during a session or when there is any alteration or<br />
addition to the breathing system, monitoring or ancillary equipment.<br />
It is the responsibility of the anaesthetist to make sure that these checks<br />
have been performed, and the anaesthetist must be satisfied that they have<br />
been carried out correctly. In the event of a change of anaesthetist during an<br />
operating session, the status of the anaesthetic equipment must be<br />
confirmed, including that a formal check has been performed.<br />
Before using any anaesthetic equipment, ventilator, breathing system<br />
or monitor, it is essential to be fully familiar with it. Modern anaesthetic<br />
workstations are complex devices. It is essential that anaesthetists have full<br />
training and formal induction for any machines they may use. A quick<br />
‘run-through’ before the start of an operating session is not acceptable.<br />
Careful note should be taken of any information or labelling on the<br />
anaesthetic machine that might refer to its current status.<br />
Alternative means of ventilation<br />
The early use of an alternative means of ventilation (a self-inflating bag<br />
that does not rely on a source of oxygen to function) may be life-saving. A<br />
self-inflating bag must be immediately available in any location where<br />
anaesthesia may be given [7, 8]. An alternative source of oxygen should be<br />
readily available.<br />
Perform manufacturer’s machine check<br />
Modern anaesthesia workstations may perform many of the following<br />
checks automatically during start-up. Users must know which are included<br />
and ensure that the automated check has been performed.<br />
Power supply<br />
Check that the anaesthetic workstation and relevant ancillary equipment<br />
are connected to the mains electrical supply (where appropriate) and<br />
switched on. The anaesthetic workstation should be connected directly to<br />
the mains electrical supply, and only correctly rated equipment connected<br />
to its electrical outlets. Multisocket extension leads must not be plugged<br />
into the anaesthetic machine outlets or used to connect the anaesthetic<br />
machine to the mains supply.<br />
Hospitals should have back-up generators, and many operating<br />
theatres will have their own back-up system. Anaesthetists should know<br />
Anaesthesia ª 2012 The Association of Anaesthetists of Great Britain and Ireland 7
Anaesthesia 2012<br />
Hartle et al. | Checking anaesthetic equipment<br />
what is available where they are working. Back-up batteries for anaesthetic<br />
machines and other equipment should be charged.<br />
Switch on the gas supply master switch (if one is fitted).<br />
Check that the system clock (if fitted) is set correctly.<br />
Gas supplies and suction<br />
To check the correct function of the oxygen failure alarm involves<br />
disconnecting the oxygen pipeline on some machines, whilst on machines<br />
with a gas supply master switch, the alarm may be operated by turning the<br />
master switch off. As repeated disconnection of gas hoses may lead to<br />
premature failure of the Schrader socket and probe, these guidelines<br />
recommend that the regular pre-session check of equipment includes a ‘tug<br />
test’ to confirm correct insertion of each pipeline into the appropriate socket.<br />
It is therefore recommended that, in addition to these checks, the<br />
oxygen failure alarm must be checked on a weekly basis by disconnecting<br />
the oxygen hose whilst the oxygen flowmeter is turned on, and a written<br />
record kept. In addition to sounding an alarm, which must sound for at<br />
least 7 s, oxygen failure warning devices are also linked to a gas shut-off<br />
device. Anaesthetists must be aware of both the tone of the alarm and also<br />
which gases will continue to flow on the particular model of anaesthetic<br />
machine in use.<br />
Medical gas supplies<br />
Identify and take note of the gases that are being supplied by pipeline,<br />
confirming with a ‘tug test’ that each pipeline is correctly inserted into the<br />
appropriate gas supply terminal. Note that excessive force during a ‘tug<br />
test’ may damage the pipeline and ⁄ or gas supply terminal.<br />
1 Check that the anaesthetic apparatus is connected to a supply of oxygen<br />
and that an adequate reserve supply of oxygen is available from a spare<br />
cylinder.<br />
2 Check that adequate supplies of any other gases intended for use are<br />
available and connected as appropriate. All cylinders should be securely<br />
seated and turned off after checking their contents.<br />
3 Carbon dioxide cylinders should not be present on the anaesthetic<br />
machine. Where a blanking plug is supplied this should be fitted to any<br />
empty cylinder yoke.<br />
4 Check that all pressure gauges for pipelines connected to the anaesthetic<br />
machine indicate 400–500 kPa.<br />
8 Anaesthesia ª 2012 The Association of Anaesthetists of Great Britain and Ireland
Hartle et al. | Checking anaesthetic equipment Anaesthesia 2012<br />
5 Check the operation of flowmeters, where these are present, ensuring that<br />
each control valve operates smoothly and that the bobbin moves freely<br />
throughout its range without sticking. If nitrous oxide is to be used, the<br />
anti-hypoxia device should be tested by first turning on the nitrous oxide<br />
flow and ensuring that at least 25% oxygen also flows. Then turn the<br />
oxygen flow off and check that the nitrous oxide flow also stops. Turn on<br />
the oxygen flow and check that the oxygen analyser display approaches<br />
100%. Turn off all flow control valves. (Machines fitted with a gas supply<br />
master switch will continue to deliver a basal flow of oxygen).<br />
6 Operate the emergency oxygen bypass control and ensure that flow<br />
occurs from the gas outlet without significant decrease in the pipeline<br />
supply pressure. Ensure that the emergency oxygen bypass control<br />
ceases to operate when released.<br />
Suction<br />
Check that the suction apparatus is functioning and all connections are<br />
secure; test for the rapid development of an adequate negative pressure.<br />
Breathing system and vaporisers<br />
Whole breathing system<br />
Check all breathing systems that are to be used and perform a ‘two-bag<br />
test’ before use, as described below [9]. Breathing systems should be<br />
inspected visually and inspected for correct configuration and assembly.<br />
Check that all connections within the system and to the anaesthetic<br />
machine are secured by ‘push and twist’. Ensure that there are no leaks or<br />
obstructions in the reservoir bags or breathing system and that they are<br />
not obstructed by foreign material. Perform a pressure leak test (between<br />
20 and 60 cmH 2 O on the breathing system by occluding the patient-end<br />
and compressing the reservoir bag.<br />
Vaporisers<br />
Manual leak testing of vaporisers was previously recommended routinely.<br />
It should only be performed on basic ‘Boyle’s’ machines and it may be<br />
harmful to many modern anaesthetic workstations. Refer to the<br />
manufacturer’s recommendation before performing a manual test.<br />
Check that the vaporiser(s) for the required volatile agent(s) are fitted<br />
correctly to the anaesthetic machine, that any locking mechanism is fully<br />
engaged and that the control knobs rotate fully through the full range(s).<br />
Ensure that the vaporiser is not tilted. Turn off the vaporisers.<br />
Anaesthesia ª 2012 The Association of Anaesthetists of Great Britain and Ireland 9
Anaesthesia 2012<br />
Hartle et al. | Checking anaesthetic equipment<br />
Check that the vaporiser(s) are adequately filled but not overfilled, and<br />
that the filling port is tightly closed.<br />
Manual leak test of vaporiser<br />
1 Set a flow of oxygen of 5 l.min )1 and with the vaporiser turned off,<br />
temporarily occlude the common gas outlet. There should be no leak<br />
from any part of the vaporiser and the flowmeter bobbin (if present)<br />
should dip.<br />
2 Where more than one vaporiser is present, turn each vaporiser on in<br />
turn and repeat this test. After this test, ensure that the vaporisers and<br />
flowmeters are turned off.<br />
Changing and filling vaporisers during use. It may be necessary to<br />
change a vaporiser during use. Where possible, repeat the leak test; failure<br />
to do so is a common cause of critical incidents [10]. Some anaesthetic<br />
workstations will automatically test vaporiser integrity.<br />
It is only necessary to remove a vaporiser from a machine to refill it if<br />
the manufacturer recommends this. Vaporisers must always be kept<br />
upright. Tilting a vaporiser can result in delivery of dangerously high<br />
concentrations of vapour [11].<br />
Carbon dioxide absorber<br />
Inspect the contents and connections and ensure there is adequate supply<br />
of carbon dioxide absorbent. Check the colour of the absorbent.<br />
Alternative breathing systems<br />
For Bain-type and circle co-axial systems, perform an occlusion test on the<br />
inner tube and check that the adjustable pressure limiting (APL) valve,<br />
where fitted, can be fully opened and closed.<br />
Correct gas outlet<br />
Particular care must be exercised in machines with an auxiliary common<br />
gas outlet (ACGO). Incidents of patient harm have resulted from<br />
misconnection of a breathing system to an ACGO or misselection of the<br />
ACGO [12].<br />
Whenever a breathing system is changed, either during a case or a list,<br />
its integrity and correct configuration must be confirmed. This is<br />
particularly important for paediatric lists when breathing systems may<br />
be changed frequently during a list.<br />
10 Anaesthesia ª 2012 The Association of Anaesthetists of Great Britain and Ireland
Hartle et al. | Checking anaesthetic equipment Anaesthesia 2012<br />
Ventilator<br />
Check that the ventilator is configured correctly for its intended use. Ensure<br />
that the ventilator tubing is securely attached. Set the controls for use and<br />
ensure that adequate pressure is generated during the inspiratory phase.<br />
Check that alarms are working and correctly configured.<br />
Check that the pressure relief valve functions correctly at the set pressure.<br />
Two-bag test<br />
A two-bag test should be performed after the breathing system, vaporisers<br />
and ventilator have been checked individually [9].<br />
1 Attach the patient-end of the breathing system (including angle piece<br />
and filter) to a test lung or bag.<br />
2 Set the fresh gas flow to 5 l.min )1 and ventilate manually. Check the<br />
whole breathing system is patent and the unidirectional valves are<br />
moving (if present).<br />
3 Check the function of the APL valve by squeezing both bags.<br />
4 Turn on the ventilator to ventilate the test lung. Turn off the fresh gas<br />
flow or reduce to a minimum. Open and close each vaporiser in turn.<br />
There should be no loss of volume in the system.<br />
Breathing systems should be protected with a test lung or bag when<br />
not in use to prevent intrusion of foreign bodies.<br />
Scavenging<br />
Check that the anaesthetic gas scavenging system is switched on and<br />
functioning. Ensure that the tubing is attached to the appropriate exhaust<br />
port of the breathing system, ventilator or anaesthetic workstation [13].<br />
Monitoring equipment<br />
Check that all monitoring devices, especially those referred to in the<br />
AAGBI’s Standards of Monitoring during Anaesthesia and Recovery<br />
guidelines [14], are functioning and that appropriate parameters and<br />
alarms have been set before using the anaesthetic machine. This includes<br />
the cycling times, or frequency of recordings, of automatic non-invasive<br />
blood pressure monitors. Check that gas sampling lines are properly<br />
attached and free from obstruction or kinks. In particular, check that the<br />
oxygen analyser, pulse oximeter and capnograph are functioning correctly<br />
and that appropriate alarm limits for all monitors are set. Be aware of the<br />
‘default’ alarm settings if using these.<br />
Anaesthesia ª 2012 The Association of Anaesthetists of Great Britain and Ireland 11
Anaesthesia 2012<br />
Hartle et al. | Checking anaesthetic equipment<br />
Gas monitoring lines are often the cause of a significant leak; check that<br />
they are properly attached and any sampling ports not in use have been<br />
blanked off. To eliminate the need to change the sampling line repeatedly,<br />
the gas monitoring line should be assembled as an integral part of the<br />
breathing circuit by attaching it proximal to the patient breathing filter.<br />
Airway equipment<br />
These include bacterial filters, catheter mounts, connectors and tracheal<br />
tubes, laryngeal mask airways, etc.; check that these are all available in the<br />
appropriate sizes, at the point of use, and that they have been checked for<br />
patency.<br />
A new, single-use bacterial filter and angle piece ⁄ catheter mount must<br />
be used for each patient. It is important that these are checked for patency<br />
and flow, both visually and by ensuring gas flow through the whole<br />
assembly when connected to the breathing system, as described below.<br />
Check that the appropriate laryngoscopes are available and function<br />
reliably. Equipment for the management of the anticipated or unexpected<br />
difficult airway must be available and checked regularly in accordance with<br />
departmental policies [15]. A named consultant anaesthetist must be<br />
responsible for difficult airway equipment and the location of this<br />
equipment should be known.<br />
Total intravenous anaesthesia (TIVA)<br />
When TIVA is used there must be a continuous intravenous infusion of<br />
anaesthetic agent or agents; interruption from whatever cause may result<br />
in awareness. A thorough equipment check is therefore the most<br />
important step in reducing the incidence of awareness. Anaesthetists<br />
using TIVA must be familiar with the drugs, the technique and all<br />
equipment and disposables being used.<br />
The Safe Anaesthesia Liaison Group (SALG) has produced safety<br />
guidance on guaranteeing drug delivery during TIVA [16]; SALG made<br />
the following recommendations:<br />
1 An anti-reflux ⁄ non-return valve should always be used on the<br />
intravenous fluid infusion line when administering TIVA.<br />
2 Sites of intravenous infusions should be visible so that they may be<br />
monitored for disconnection, leaks or infusions into subcutaneous<br />
tissues.<br />
3 Clinical staff should know how to use, and to check, the equipment<br />
before use.<br />
12 Anaesthesia ª 2012 The Association of Anaesthetists of Great Britain and Ireland
Hartle et al. | Checking anaesthetic equipment Anaesthesia 2012<br />
4 Organisations should give preference to purchasing intravenous<br />
connectors and valves that are clearly labelled.<br />
Ancillary and resuscitation equipment<br />
Check that the patient’s trolley, bed or operating table can be tilted headdown<br />
rapidly. A resuscitation trolley and defibrillator must be available in<br />
all locations where anaesthesia is given and checked regularly in<br />
accordance with local policies.<br />
Equipment and drugs for rarely encountered emergencies, such as<br />
malignant hyperthermia and local anaesthetic toxicity must be available<br />
and checked regularly in accordance with local policies. The location of<br />
these must be clearly signed [17, 18].<br />
Single-use devices<br />
Any part of the breathing system, ancillary equipment or other apparatus<br />
that is designated ‘single-use’ must be used for one patient only, and not<br />
reused. Packaging should not be removed until the point of use, for<br />
infection control, identification and safety. (For details of decontamination<br />
of reusable equipment, see the AAGBI safety guideline Infection Control in<br />
Anaesthesia [19].)<br />
Machine failure<br />
In the event of failure, some modern anaesthetic workstations may default<br />
to little or no flow, or oxygen only with no vapour. Users must know the<br />
default setting for the machine in use. Alternative means of oxygenation,<br />
ventilation and anaesthesia must be available.<br />
‘Shared responsibility’ equipment<br />
As a member of the theatre team, the anaesthetist will share responsibility<br />
for the use of other equipment, e.g. diathermy, intermittent compression<br />
stockings, warming devices, cell salvage and tourniquets, but should have<br />
received appropriate training. Involvement with this equipment, especially<br />
‘trouble shooting’ problems that arise intra-operatively, must not be<br />
allowed to distract anaesthetists from their primary role.<br />
Recording and audit<br />
A clear note must be made in the patient’s anaesthetic record that the<br />
anaesthetic machine check has been performed, that appropriate<br />
monitoring is in place and functional, and that the integrity, patency<br />
and safety of the whole breathing system has been assured. A logbook<br />
Anaesthesia ª 2012 The Association of Anaesthetists of Great Britain and Ireland 13
Anaesthesia 2012<br />
Hartle et al. | Checking anaesthetic equipment<br />
should also be kept with each anaesthetic machine to record the daily presession<br />
check and weekly check of the oxygen failure alarm. Modern<br />
anaesthesia workstations may record electronic self tests internally. Such<br />
records should be retained for an appropriate time. Documentation of the<br />
routine checking and regular servicing of anaesthetic machines and patient<br />
breathing systems should be sufficient to permit audit on a regular basis.<br />
Recovery<br />
There must be clear departmental procedures for the daily and other<br />
checks of equipment that is used in recovery. This may also include preuse<br />
checks of patient-controlled analgesia and epidural pumps, etc. [20].<br />
Disclaimer<br />
The AAGBI cannot be held responsible for failure of any anaesthetic<br />
equipment as a result of a defect not revealed by these procedures.<br />
References<br />
1. National Patient Safety Agency. WHO Surgical Safety Checklist NPSA ⁄ 2009 ⁄<br />
PSA002 ⁄ U1, January 2009, NPSA. http://www.nrls.npsa.nhs.uk/resources/<br />
?entryid45=59860 (accessed 09 ⁄ 04 ⁄ 12).<br />
2. Cassidy CJ, Smith A, Arnot-Smith J. Critical incident reports concerning anaesthetic<br />
equipment: analysis of the UK National Reporting and Learning System (NRLS) data<br />
from 2006–2008. Anaesthesia 2011; 66: 879–88.<br />
3. Royal College of Anaesthetists. CCT in Anaesthetics Annex B Basic Level Training<br />
Edition 2 Version 1.2, August 2010. http://www.rcoa.ac.uk/index.asp?PageID=1479<br />
(accessed 29 ⁄ 01 ⁄ 2012).<br />
4. Association of Anaesthetists of Great Britain & Ireland. Safe Management of<br />
Anaesthetic Related Equipment, 2009. http://www.<strong>aagbi</strong>.org/publications/guidelines/docs/safe_management_2009.pdf<br />
(accessed 29 ⁄ 01 ⁄ 2012).<br />
5. NHS Litigation Authority. NHSLA Risk Management Standards for Acute Trusts Primary<br />
Care Trusts and Independent Sector Providers of NHS Care, January 2010. London:<br />
NHSLA, 2010.<br />
6. NHS Quality Improvement Scotland. Clinical Standards for Anaesthesia July 2003.<br />
http://www.nhshealthquality.org/nhsqis/files/ANAES_STND_JUL03.pdf (accessed<br />
29 ⁄ 01 ⁄ 2012).<br />
7. Medicines and Healthcare products Regulatory Agency. MDA ⁄ 2005 ⁄ 062 07<br />
November 2004 http://www.mhra.gov.uk/Publications/Safetywarnings/MedicalDeviceAlerts/CON2022493<br />
(accessed 29 ⁄ 01 ⁄ 2012).<br />
8. Medicines and Healthcare products Regulatory Agency. MDA ⁄ 2010 ⁄ 036 06 May 2010<br />
http://www.mhra.gov.uk/Publications/Safetywarnings/MedicalDeviceAlerts/<br />
CON081785 (accessed 29 ⁄ 01 ⁄ 2012).<br />
9. Australian and New Zealand College of Anaesthetists. Recommendations on Checking<br />
Anaesthesia Delivery Systems, 4.2.3.4.2, 2003. http://www.anzca.edu.au/<br />
resources/professional-documents/ps31.html (accessed 29 ⁄ 01 ⁄ 2012).<br />
14 Anaesthesia ª 2012 The Association of Anaesthetists of Great Britain and Ireland
Hartle et al. | Checking anaesthetic equipment Anaesthesia 2012<br />
10. Medicines and Healthcare products Healthcare Regulatory Agency. MDA ⁄ 2010 ⁄ 052<br />
02 June 2010 http://www.mhra.gov.uk/Publications/Safetywarnings/MedicalDeviceAlerts/CON085024<br />
(accessed 29 ⁄ 01 ⁄ 2012).<br />
11. Medicines and Healthcare products Regulatory Agency. MDA ⁄ 2003 ⁄ 039 06<br />
November 2003 http://www.mhra.gov.uk/Publications/Safetywarnings/Medical<br />
DeviceAlerts/CON008613 (accessed 29 ⁄ 01 ⁄ 2012).<br />
12. Medicines and Healthcare products Regulatory Agency. MDA ⁄ 2011 ⁄ 108 01 December<br />
2011 http://www.mhra.gov.uk/Publications/Safetywarnings/MedicalDeviceAlerts/<br />
CON137664 (accessed 29 ⁄ 01 ⁄ 2012).<br />
13. Medicines and Healthcare products Regulatory Agency. MDA ⁄ 2010 ⁄ 21, 10 March<br />
2010. http://www.mhra.gov.uk/Publications/Safetywarnings/MedicalDeviceAlerts/<br />
CON076104 (accessed 29 ⁄ 01 ⁄ 2012).<br />
14. Association of Anaesthetists of Great Britain & Ireland. Standards of Monitoring during<br />
Anaesthesia and Recovery 4, 2007. http://www.<strong>aagbi</strong>.org/publications/guidelines/<br />
docs/standardsofmonitoring07.pdf (accessed 29 ⁄ 01 ⁄ 2012).<br />
15. Difficult Airway Society. Recommended Equipment for Management of Unanticipated<br />
Difficult Intubation, July 2005. http://www.das.uk.com/equipmentlistjuly2005.htm<br />
(accessed 29 ⁄ 01 ⁄ 2012).<br />
16. Safe Anaesthesia Liaison Group. Guaranteeing Drug Delivery in Total Intravenous<br />
Anaesthesia, September 2009. http://www.<strong>aagbi</strong>.org/news/docs/tiva_infonov09.pdf<br />
(accessed 29 ⁄ 01 ⁄ 2012).<br />
17. Association of Anaesthetists of Great Britain & Ireland. Management of a Malignant<br />
Hyperthermia Crisis, 2007. http://www.<strong>aagbi</strong>.org/publications/guidelines/docs/<br />
malignanthyp07amended.pdf (accessed 29 ⁄ 01 ⁄ 2012).<br />
18. Association of Anaesthetist of Great Britain & Ireland. Management of Severe Local<br />
Anaesthetic Toxicity 2, 2010. http://www.<strong>aagbi</strong>.org/publications/guidelines/docs/<br />
standardsofmonitoring07.pdf (accessed 29 ⁄ 01 ⁄ 2012).<br />
19. Association of Anaesthetists of Great Britain & Ireland. Infection Control in<br />
Anaesthesia 2, 2008. http://www.<strong>aagbi</strong>.org/publications/guidelines/docs/infection_control_08.pdf<br />
(accessed 29 ⁄ 01 ⁄ 2012).<br />
20. Association of Anaesthetists of Great Britain & Ireland. Immediate Post anaesthetic<br />
Recovery, 2002. http://www.<strong>aagbi</strong>.org/publications/guidelines/docs/postanaes02.pdf<br />
(accessed 29 ⁄ 01 ⁄ 2012).<br />
Anaesthesia ª 2012 The Association of Anaesthetists of Great Britain and Ireland 15
21 Portland Place, London, W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org
This checklist is an abbreviated version of the publication by the Association of Anaesthetists of Great Britain and<br />
Ireland 'Checking Anaesthesia Equipment 2012'. It was originally published in Anaesthesia.<br />
If you wish to refer to this guideline, please use the following reference: Checklist for anaesthetic equipment 2012.<br />
Anaesthesia 2012; 66: pages 662–63. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2044.2012.07163.x/abstract
VOLUNTARY CODE OF PRACTICE<br />
FOR BILLING PRIVATE PATIENTS<br />
Published by<br />
The Association of Anaesthetists of Great Britain and Ireland,<br />
21 Portland Place, London W1B 1PY<br />
Telephone 020 7631 1650 Fax 020 7631 4352<br />
www.<strong>aagbi</strong>.org<br />
April 2008
Contents<br />
Introduction 1<br />
Summary of recommendations 2<br />
General comments 3<br />
Before treatment 4<br />
During treatment 7<br />
After treatment 8<br />
Emergencies 10<br />
Appendices 11
Introduction<br />
The Association of Anaesthetists of Great Britain & Ireland (AAGBI) has<br />
produced this Voluntary Code of Practice for Billing Private Patients in<br />
response to requests from members and in order to guide members in<br />
matters relating to invoicing patients for private medical services. The private<br />
health market is experiencing change, and there is pressure for anaesthetists’<br />
fees to be paid directly by third parties as part of a treatment “package” or<br />
network. The AAGBI believes it important that the direct professional and<br />
contractual relationship between consultant anaesthetist and private patient<br />
be maintained. The guidance provided in this document underlines this<br />
relationship and gives advice on how to invoice patients. The idea behind<br />
this document is not to provide a mandatory method for managing financial<br />
issues in private practice but to offer a voluntary code of practice to which<br />
members can subscribe if they wish. Those who do may choose to indicate<br />
their compliance with this code in their invoices.<br />
The AAGBI would welcome comments on this document from members,<br />
patients and PMIs.<br />
Will Harrop-Griffiths<br />
Honorary Secretary, for the Independent Practice Committee of the AAGBI<br />
1
1.0 Summary of recommendations<br />
1.1 Consultants set the fees that they charge their patients. Private<br />
Medical Insurers (PMIs) set benefit levels for their customers. There<br />
is no necessary correlation between fees and benefits.<br />
1.2 Once a patient has agreed to the fee to be charged by the consultant<br />
for a procedure, there exists a contract under which the patient<br />
becomes liable for the payment of the fee, regardless of whether or<br />
not the patient holds private medical insurance.<br />
1.3 Consultants should charge transparent and reasonable fees, and<br />
should make every effort to inform their patients of the fees before<br />
surgery.<br />
1.4 Insured patients should be encouraged to check the benefit levels<br />
provided by their particular policy with their PMIs before undergoing<br />
surgery.<br />
1.5 The fee charged should ideally include the totality of the care<br />
involved in the planned procedure. Any additional fees should be<br />
disclosed to the patient before surgery.<br />
1.6 Consultants may send invoices to the patients, their PMIs or both.<br />
The AAGBI recommends that consultants always send the invoice<br />
to the patient. A copy of the invoice may also be sent to insured<br />
patients’ PMIs.<br />
2
2.0 General comments<br />
2.1 When a consultant anaesthetist (henceforth “consultant”) offers<br />
medical care to a private patient in return for a disclosed fee and<br />
the patient agrees to this arrangement, a contract is created in which<br />
the patient is wholly responsible for the payment of the consultant’s<br />
fee.<br />
2.2 This contract is not affected by the fact that the patient is a subscriber<br />
to a PMI; the patient remains ultimately responsible for payment of<br />
the fee but the PMI may pay some or all of the fee to the consultant<br />
on behalf of the patient.<br />
2.3 Consultants set the level of the fees that they charge; PMIs set the<br />
benefit limits for their customers. The benefits provided by PMIs<br />
to their customers allow the payment of consultants’ fees wholly<br />
or in part. There is thus no necessary correlation between the fees<br />
charged by consultants and the benefits paid by PMIs.<br />
2.4 There exists no legally enforceable contract between a consultant<br />
and a PMI except where both parties enter willingly into such a<br />
contract.<br />
2.5 Private patients will remain responsible for payment of a consultant’s<br />
fee under the contract between them unless the consultant agrees to<br />
accept that the responsibility for payment should be confined to the<br />
PMI or other third party.<br />
3
3.0 Before treatment<br />
3.1 Whenever possible, the consultant should inform the patient before<br />
treatment of the likely fee 1 or explain how it will be determined<br />
unless he is prepared to limit his fee to whatever that patient’s<br />
benefit maxima may happen to be 2 . Where, as often happens,<br />
patients take the decision to undergo an operation before they have<br />
spoken to their anaesthetist, they should be advised to contact the<br />
consultant anaesthetist if they wish to be told more about the fee<br />
that will be charged.<br />
3.2 The scope of the fee quoted by the consultant should be explained.<br />
It may for example be a totalled fee for all the planned elements of<br />
the expected treatment process, such as:<br />
3.2.1 Routine pre-operative evaluation whether performed shortly<br />
before surgery or some time in advance;<br />
3.2.2 Intra-operative care, including payments to assistants or<br />
consultant colleagues for services provided during the<br />
treatment;<br />
3.2.3 All drugs and equipment used in connection with the<br />
procedure;<br />
3.2.4 Invasive monitoring lines used before, during or after<br />
surgery;<br />
3.2.5 The performance of peripheral or neuraxial regional<br />
anaesthetic or analgesic techniques supplementary to or in<br />
place of general anaesthesia; and<br />
1 A sample letter is provided in Appendix 1<br />
2 If the consultant is prepared to accept whatever benefit the PMI offers for the procedure,<br />
he need not warn the patient of his fee. If he does not warn the patient of the<br />
fee, he should not demand that the patient pay any shortfall if the PMI benefit is less<br />
than the fee charged.<br />
4
3.2.6 Postoperative care, to include HDU and ICU care, and the<br />
management of continuous neuraxial of peripheral analgesic<br />
techniques.<br />
3.3 If the fee quoted does not cover the totality of planned care, the<br />
consultant should tell the patient and clearly describe the additional<br />
fees that may be charged.<br />
3.4 The patient should be warned that if the procedure and care differs<br />
from that planned, the fee may also vary, but that this variation will<br />
be fixed by the same means 3 . If any specific variations are envisaged<br />
these should be described at least in outline and the fee scales<br />
explained.<br />
3.5 The consultant may choose to provide a separate estimate of HDU<br />
or ICU fees. This is advisable where it is less likely that these costs<br />
may be incurred.<br />
3.6 The consultant should recommend that all patients check the<br />
benefit levels that are available for the treatment under the policy<br />
held with the PMI.<br />
3.7 The patient should be told that he is ultimately responsible for the<br />
payment of the fee or the payment of any shortfall.<br />
3.8 The consultant may wish to ask the patient to sign a financial<br />
agreement before the treatment in which the patient guarantees that<br />
the consultant’s fee will be paid.<br />
3.9 If the consultant chooses not to be paid directly by the PMI, the<br />
patient should be told as long before the planned treatment as<br />
possible.<br />
3 If the fee for the planned procedure is, for instance, 125% of the benefit maximum<br />
provided by the patient’s PMI, then the fee for the procedure actually performed<br />
would be expected to be approximately 125% of the benefit maximum offered by<br />
the PMI for the actual procedure performed.<br />
5
3.10 The consultant should tell the patient if he knows that he is not<br />
recognised for benefits by the patient’s PMI.<br />
3.11 The consultant should keep a record of the fee quoted to the<br />
patient.<br />
3.12 It is acceptable for a consultant to request payment of fees in<br />
advance of treatment under certain circumstances.<br />
3.13 Sometimes fees are in fact negotiated by a third party on behalf<br />
of the doctor. The fee set by the consultant anaesthetist may be<br />
agreed with the patient by the surgeon or by the surgeon’s secretary<br />
or other agent. Sometimes it will be by a hospital administrator.<br />
Consultant anaesthetists must ensure that their agents have a clear,<br />
complete and up-to-date list of their charges and that they make a<br />
record of precisely what has been agreed.<br />
3.14 Sometimes, particularly in emergencies or where there are<br />
linguistic problems, the patient’s agreement will be given by an<br />
accompanying relative or other agent acting on their behalf. In all<br />
these circumstances it is vital to ensure that the representative has<br />
the authority of the principal they represent. Parents and spouses<br />
have ostensible authority to negotiate on behalf of their children<br />
and partners; in all other cases the doctor will be wise to ensure that<br />
there is a binding agreement with someone identifiable.<br />
3.15 If separate charges are to be made by the consultant in respect of<br />
anaesthetic agents, other drugs or equipment, he should ensure that<br />
the patient appreciates this.<br />
6
4.0 During treatment<br />
4.1 If the consultant surgeon and anaesthetist plan to use a coding<br />
system, e.g. CCSD codes, when billing the patient, they should<br />
agree the code or codes relating to the procedure or procedures<br />
performed, and should ensure that members of the operating theatre<br />
staff are informed of these codes.<br />
4.2 In choosing codes, the consultants should agree upon the code or<br />
codes that best describe the procedure or procedures performed,<br />
bearing in mind that some codes are specifically constructed so as<br />
to include the performance of more than one procedure. Consultants<br />
should not break up the elements of a single surgical or anaesthetic<br />
procedure into its constituent parts in order to maximise the benefit<br />
provided to the patient by his PMI.<br />
7
5.0 After treatment<br />
5.1 Accounts 4 should be sent to the patient, the patient’s PMI or to<br />
both 5 .<br />
5.1.1 If the consultant agrees to set his fee within the PMI’s benefit<br />
maxima, he can send an account only to the PMI if he so<br />
wishes. Alternatively, he can send an account to the patient<br />
and a copy to the PMI (or vice versa), making clear that he<br />
has done so.<br />
5.1.2 If the consultant’s fee is likely to be in excess of the PMI’s<br />
benefit, he would be wise to send an account to the patient<br />
and, if he so wishes, a copy to the PMI (or vice versa). He<br />
should make clear to the patient whether he wishes the<br />
patient to forward the account to the PMI or whether he has<br />
sent a copy to the PMI.<br />
5.1.3 If the patient does not hold private medical insurance or<br />
if the consultant does not wish to be paid directly by the<br />
PMI, the consultant should send an account to the patient<br />
and should ask to be paid directly by the patient. Under<br />
these circumstances, the consultant should offer to provide<br />
the patient with a receipt so that the patient can then claim<br />
benefits from his PMI if he has one.<br />
5.1.4 If a consultant uses a billing service, he should consider<br />
himself responsible for the fees charged in the bills sent on<br />
his behalf and for the way in which the fees are collected.<br />
5.2 Only one invoice (and copy if appropriate) should be sent for each<br />
discrete treatment episode.<br />
4 A sample invoice is provided in Appendix 2.<br />
5 The AAGBI recommends that consultants always send the invoice to the patient. A<br />
copy of the invoice may also be sent to insured patients’ PMIs.<br />
8
5.6 Consultants are not obliged to put a CCSD code on their accounts,<br />
unless they have entered into an agreement with the patient or his<br />
PMI to do so, but may assist the patient if codes are included in the<br />
account.<br />
5.7 The consultant may include a descriptive narrative of the procedures<br />
performed in the account in order to assist correct coding by the<br />
PMI but should not do so in order to maximise benefit payment.<br />
5.8 The consultant should not normally allocate portions of his fee to<br />
particular codes or narratives. The fee should represent the whole<br />
amount payable for the entire treatment episode.<br />
5.9 The consultant may, if it has been specified as a term of the contract,<br />
set a time limit for payment and should detail any penalties or<br />
additional payments that will be incurred by late payment.<br />
9
6.0 Emergencies<br />
6.1 Emergency treatment is more complex and carries more risk than<br />
elective treatment. It also frequently takes longer than elective<br />
treatment and is often more disruptive of the doctor’s life, being<br />
conducted outside routine working hours. Thus the doctor will<br />
frequently feel it is appropriate to charge a higher fee.<br />
6.2 Some procedures specified by CCSD codes are always performed<br />
as emergencies and the PMIs’ benefit maxima associated with those<br />
procedures may take this into account.<br />
6.3 Other procedures specified by CCSD codes are commonly<br />
performed electively so that benefit maxima are less likely to cover<br />
the fees consultants charge for acting in an emergency. Where the<br />
consultant charges a higher fee because of some factor particular<br />
to the case, such as the fact that it has been performed as an<br />
emergency, then this should be made clear to assist the patient in<br />
explaining the situation to the PMI.<br />
6.4 The consultant should make every effort to warn the patient of<br />
his fee in advance of surgery but this may not be possible in an<br />
emergency, in which case the patient, or whoever has contracted<br />
on their behalf, will have incurred a liability to meet a fee that is<br />
reasonable in the circumstances.<br />
6.5 The fee that will be reasonable in the circumstances will take into<br />
account the issues mentioned in 6.1 above. If the patient cannot<br />
be warned of the fee in advance of surgery, the fee that will be<br />
reasonable in the circumstances will be based on the appropriate fee<br />
for the equivalent elective procedure, with an additional proportion<br />
added to the extent that the factors described in paragraph 6.1<br />
arise.<br />
10
Appendix 1<br />
PRO FORMA LETTER FROM SURGEON TO PATIENT IN ADVANCE OF SURGERY<br />
<br />
<br />
<br />
Dear ,<br />
I am writing to confirm that your admission has been arranged to the on at for surgery that afternoon. It is essential<br />
you have nothing to eat after on the morning of admission. You may<br />
drink clear fluids until and the ward staff will then advise on fluid<br />
intake.<br />
Mr ’s fee for <br />
will be approximately £. In addition, the approximate fee for<br />
the anaesthetist, Dr , will be £.<br />
If you wish to make a claim from your medical insurance company, please<br />
obtain a claim form, complete the subscriber’s section and give it to the<br />
admissions officer on admission.<br />
You are advised to check with your insurance company the level of your<br />
cover and the exact allowances to which you are entitled under the terms and<br />
conditions of your particular policy. Many insurance companies do settle the<br />
surgeon’s and anaesthetist’s fees in full but in some cases a shortfall occurs.<br />
Payment of any shortfall is your responsibility. If in doubt, I suggest that you<br />
send a copy of this letter to your insurance company, asking them to send you<br />
an agreement in writing as to of the above fees they will cover.<br />
Yours sincerely,<br />
<br />
Secretary to <br />
11
Appendix 2<br />
EXAMPLE OF AN INVOICE<br />
To Mr A Patient<br />
Address<br />
Dr H Featherstone FRCA<br />
Consultant Anaesthetist<br />
For Professional Services<br />
At the John Snow Hospital on 29/2/2008<br />
21 Portland Place<br />
London W1B 1PY<br />
Tel: 020 7631 1650<br />
PMI Ref: HF 04786<br />
Provider Ref: 152320<br />
Procedure:<br />
Ectomy and refashioning<br />
CCSD Code: X2365<br />
£325.00<br />
Terms: payment within 30 days<br />
Either: If you have insurance please forward this to your insurers<br />
Or:<br />
A copy of this invoice has been forwarded to your insurers<br />
With compliments<br />
12
13
21 Portland Place, London W1B 1PY<br />
Tel: 020 7631 1650<br />
Fax: 020 7631 4352<br />
Email: info@<strong>aagbi</strong>.org<br />
www.<strong>aagbi</strong>.org