The treatment of persistent pain - Australian Pain Society
The treatment of persistent pain - Australian Pain Society
The treatment of persistent pain - Australian Pain Society
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Thank you for your many comments regarding the changes we have<br />
initiated in the newsletter. <strong>The</strong> editorial committee appreciates feedback<br />
and has been working hard to commission new articles. I particularly<br />
thank John Quintner, Lorimer Moseley, Sue Inglis and Philip Siddall.<br />
We have over 700 members in our society but only 25% have given<br />
us their correct email address. From time to time our secretariat<br />
sends out a group email message to notify members <strong>of</strong> upcoming<br />
events or updates on the website. If you have changed your email<br />
address please notify the Secretariat<br />
Amal Helou<br />
Editorial 1<br />
President’s Report 1<br />
Attachment style II: <strong>The</strong> <strong>treatment</strong> <strong>of</strong> <strong>persistent</strong> <strong>pain</strong> 2 - 4<br />
Evidence for persisting <strong>pain</strong> as a disease entity 5<br />
Physio Spot 6<br />
IASP News 7<br />
New Members 7<br />
APS Board News 8<br />
Spotlight on members 8<br />
Upcoming Meetings/Announcements/Pigni Report 9<br />
By the time this Newsletter reaches you many <strong>of</strong> us will have returned<br />
from the 10th World Congress on <strong>Pain</strong> held by the IASP in San Diego.<br />
<strong>The</strong>se truly multidisciplinary congresses are at the cutting edge <strong>of</strong> <strong>pain</strong><br />
research and therapy, and ideal places to network with like-minded<br />
colleagues from around the world. <strong>The</strong> 11th World Congress <strong>of</strong> the<br />
IASP will be held in Sydney in 2005, and plans are well advanced<br />
for an exciting meeting. Ge<strong>of</strong>f Gourlay is the Chair <strong>of</strong> the local<br />
arrangements committee, and discusses this further in his IASP report.<br />
If members <strong>of</strong> the <strong>Society</strong> have ideas for an <strong>Australian</strong> <strong>Pain</strong> <strong>Society</strong><br />
Meeting in 2005, perhaps in association with a satellite meeting <strong>of</strong> the<br />
World Congress, please let either Ge<strong>of</strong>f or myself know.<br />
1<br />
AUGUST 2002<br />
Towards the end <strong>of</strong> August a teleconference will be held to further<br />
nursing issues within the <strong>Society</strong>. All nurses are urged to contact their<br />
State PIGNI representative if they want input.<br />
<strong>The</strong> <strong>Society</strong> was represented recently at a National Institute <strong>of</strong> Clinical<br />
Studies (NICS) planning day to examine national initiatives relating to<br />
<strong>pain</strong> management. Issues discussed were; making <strong>pain</strong> more visible in a<br />
hospital setting, reviewing appropriate global <strong>pain</strong> assessment tools,<br />
and mechanisms for implementing clinical guidelines. It is heartening<br />
that the Board <strong>of</strong> NICS has seen <strong>pain</strong> as a focus area.<br />
<strong>The</strong> <strong>Australian</strong> <strong>Pain</strong> <strong>Society</strong>/<strong>Australian</strong> Council and Healthcare Standards<br />
guidelines for Multidisciplinary <strong>Pain</strong> Clinics are due for review, and<br />
Robyn Quinn will Chair a working party to do this. If members have<br />
suggestions or amendments they think should be considered, please<br />
contact Robyn, e-mail robynquinn@msn.com.au.<br />
<strong>The</strong> APS facility directory is also due for a review, and members will be<br />
circulated with an information sheet shortly.<br />
<strong>The</strong> APS/APRA PhD scholarship will be awarded again prior to the start<br />
<strong>of</strong> the 2003 academic year. (See advert in this Newsletter) Those <strong>of</strong> you<br />
who have followed the progress <strong>of</strong> this project must have been<br />
impressed with the presentations <strong>of</strong> the awardees at recent Annual<br />
Scientific Meetings. <strong>The</strong> Chairman <strong>of</strong> the PhD Scholarship Committee,<br />
and the person who developed and launched the project, Ge<strong>of</strong>f<br />
Gourlay, wishes to step down because <strong>of</strong> his IASP work. This is an<br />
important continuing role for the <strong>Society</strong>, and I would welcome<br />
expressions <strong>of</strong> interest for Chairing this committee from members.<br />
This is a rewarding, interesting, and not very demanding role.<br />
At the Strategic Planning Committee meeting the <strong>Society</strong> held last<br />
August, "<strong>pain</strong> in the elderly" was identified as an area for the <strong>Society</strong><br />
to focus on. It has been decided to explore the possibility <strong>of</strong> developing<br />
clinical practice guidelines for <strong>pain</strong> management in nursing homes and<br />
other aged care facilities. Approaches will be made to other interested<br />
bodies, such as the RACGP, <strong>Society</strong> for Geriatric Medicine, Royal<br />
College <strong>of</strong> Nursing, and all the allied health groups. A direct approach<br />
for involvement will also be made to the Federal Government.<br />
Plans are well advanced for the combined <strong>Australian</strong> & New Zealand<br />
<strong>Pain</strong> Societies’ Scientific meeting to be held in March 2003 in Christchurch.<br />
This meeting will see the introduction <strong>of</strong> online abstract submissions.<br />
<strong>The</strong> closing date is 1st November 2002, so hopefully planning is well<br />
ahead for your own submissions - and don't forget whilst you are at<br />
your computer, send us your latest e-mail address. C.Roger Goucke
Suzanne Scott<br />
Multidisciplinary <strong>Pain</strong> Centre, Royal Brisbane Hospital<br />
Robin Murray<br />
<strong>Pain</strong> Management and Research Centre, Royal North Shore Hospital<br />
Health pr<strong>of</strong>essionals who work with<br />
individuals who have <strong>persistent</strong> <strong>pain</strong> have<br />
difficulty at times in accounting for differences<br />
in outcome when those with similar complaints<br />
respond in ways that are unpredictable.<br />
(Pearce, Cramond, Creed, (2001). Bowlby’s attachment theory fits<br />
within the biopsychosocial model <strong>of</strong> <strong>persistent</strong> <strong>pain</strong> and may explain<br />
the sometimes puzzling behaviour <strong>of</strong> these individuals. This article relates<br />
differences in <strong>treatment</strong> outcome to differences in early developmental<br />
histories and examines the influence <strong>of</strong> secure and insecure attachment<br />
styles on the response <strong>of</strong> <strong>persistent</strong> <strong>pain</strong> sufferers to <strong>treatment</strong>.<br />
Attachment theory is a robust concept that is useful for health<br />
pr<strong>of</strong>essionals when assessing and treating <strong>persistent</strong> <strong>pain</strong>. It may<br />
explain the origins <strong>of</strong> help-seeking and self-caring behaviours <strong>of</strong> these<br />
individuals and help us to understand why certain behaviours are<br />
directed toward pr<strong>of</strong>essionals who are caring for them. At a time <strong>of</strong><br />
need individuals approach a carer in a particular manner and display<br />
certain behaviours that they learned within their family <strong>of</strong> origin.<br />
Children internalise experiences with caretakers and these attachment<br />
experiences become the prototype for their relationships in adult life.<br />
A child who grows up in a caring and nurturing family environment<br />
has the best chance <strong>of</strong> growing to maturity as a self confident adult<br />
with strong self respect, respect for others, and high self efficacy.<br />
In contrast, a child who has to survive in a dysfunctional family<br />
environment, has less chance <strong>of</strong> developing such strong personal<br />
resources. <strong>The</strong> quality and the type <strong>of</strong> the developmental influences<br />
on children determine their manner <strong>of</strong> attachment.<br />
Attachment behaviours become prominent when individuals are<br />
afraid or ill. <strong>The</strong>y approach or avoid their carers according to their<br />
internalised model <strong>of</strong> "self" and "other" at these times.<br />
2<br />
<strong>The</strong> <strong>treatment</strong> <strong>of</strong> <strong>persistent</strong> <strong>pain</strong><br />
<strong>The</strong> key constructs <strong>of</strong> this model are:<br />
1Whether or not the attachment figure is judged to be the<br />
sort <strong>of</strong> person who in general responds to calls for support<br />
and protection, &<br />
2Whether or not the self is judged to be the sort <strong>of</strong> person<br />
anyone, and in particular the person from whom care is<br />
sought, is likely to respond to in a helpful way.<br />
A "carer" is defined here as one with whom the person has a close<br />
emotional bond, or a health pr<strong>of</strong>essional. When individuals have<br />
<strong>persistent</strong> <strong>pain</strong> these carers become the source and the focus <strong>of</strong> help<br />
and support. <strong>The</strong> relationship an individual sets up with any <strong>of</strong> these<br />
carers reflects their model <strong>of</strong> interpersonal relationships. In times <strong>of</strong><br />
need, they are likely to approach a carer with the same behaviours<br />
and intensity that they brought to the relationship with an original<br />
carer such as the mother. It is suggested that this model <strong>of</strong> self and<br />
other is stable throughout life. (Ainsworth, 1982; Bowlby, 1944;<br />
George, Kaplan & Main, 1987).<br />
Attachment theory is relevant to health research and to clinicians because<br />
it has been shown that the particular behaviours that are the outcome<br />
<strong>of</strong> attachment learning determine in part, the ability <strong>of</strong> the individual<br />
to effectively manage and recover from illnesses, traumas or disabilities.<br />
Each <strong>of</strong> the models <strong>of</strong> attachment behaviour favours certain problem<br />
solving strategies. Clinicians generally consider the resources <strong>of</strong> the<br />
patient when considering ways in which information is presented or<br />
in attempting to remedy a problem. Cognitive abilities are usually<br />
taken into account, but it is less likely that the influence <strong>of</strong> emotional<br />
factors related to the individual’s attachment style will be considered.<br />
Our experiences as children influence our subsequent years at least<br />
until we are mature enough to make judgements less coloured by<br />
emotion. Bowlby made his first reports about the detrimental influences<br />
<strong>of</strong> dysfunctional families on children living within these families in<br />
1958. He reported that attachment behaviour is organised, learned<br />
and reinforced or extinguished by social interactions within the family<br />
(Bowlby, 1958). His theories are supported by Ferster and Perrott (1968).<br />
Ainsworth, Blehar, Waters and Wall (1978) classified the attachment<br />
styles <strong>of</strong> children according to their ability to recover from separation<br />
anxiety. Because children are vulnerable when sick or afraid, these<br />
researchers suggested that a strong supportive family environment<br />
not only gives the best possible chance for a child to recover from
illness or injury, it also gives the child a view <strong>of</strong> itself that it is worth<br />
helping. This model <strong>of</strong> the self as worthwhile influences the view <strong>of</strong><br />
other people as being helpful, dependable and trustworthy. <strong>The</strong>ir<br />
sense <strong>of</strong> "felt security" then becomes stable and resilient.<br />
In contrast to secure children, children who are neglected, abused,<br />
or abandoned do not view themselves in the same manner as the<br />
secure group. <strong>The</strong>se insecure children have varying views <strong>of</strong> the self<br />
and diminished confidence in others. <strong>The</strong>ir model <strong>of</strong> attachment<br />
underlies a negative model <strong>of</strong> the world where they must strive to<br />
overcome difficulties in an unstable environment. <strong>The</strong> two<br />
fundamental styles <strong>of</strong> attachment are secure and insecure. <strong>The</strong> factor<br />
which is thought to be common to all insecure individuals is chronic<br />
depression. Children who are unwanted or neglected from birth are<br />
vulnerable to early onset depression, while those who are traumatised<br />
or bereaved, abused or ill are thought to become depressed as a<br />
result <strong>of</strong> the particular problem. (Bowlby, 1944).<br />
Bowlby described two sub-styles <strong>of</strong> insecure adjustment. A child<br />
who had suffered loss such as abandonment or neglect is likely to<br />
become obsessively self-reliant and dismissive <strong>of</strong> others. He labelled<br />
this group "avoidant." Avoidant or dismissive attachment style is<br />
characterised by a strong sense <strong>of</strong> self and a low opinion <strong>of</strong> the ability<br />
<strong>of</strong> others to be dependable or trustworthy. <strong>The</strong>se individuals avoid<br />
being rejected by others by never allowing them to get close enough<br />
to provide care or attention.<br />
Those who have been forced to survive traumas such as prolonged<br />
illness, abuse or bereavement were posited by Bowlby to exhibit an<br />
"anxious" attachment style that is characterised by a low sense <strong>of</strong> self<br />
and a distorted view <strong>of</strong> the importance <strong>of</strong> others. However, despite<br />
this distorted sense <strong>of</strong> other’s importance, they may harbour a strong<br />
sense <strong>of</strong> resentment even though they are care-seeking (Bowlby, 1977).<br />
<strong>The</strong>se individuals are typically anxious when they are confronted by<br />
health problems and find it hard to sustain involvement in <strong>treatment</strong>.<br />
Occasionally health workers come into contact with individuals who<br />
are very anxious, very wary <strong>of</strong> contact with others and ambivalent<br />
about their own care. So strongly do these individuals reject others<br />
that a fourth attachment style has been suggested (Bartholemew and<br />
Horowitz, 1991; Hazan and Shaver, 1987). This group <strong>of</strong> avoidant<br />
individuals has been labelled "fearful." <strong>The</strong> fearful group are thought<br />
to consider themselves unworthy and unlovable and expect that<br />
3<br />
<strong>The</strong> <strong>treatment</strong> <strong>of</strong> <strong>persistent</strong> <strong>pain</strong><br />
others will be rejecting, untrustworthy and unavailable. By avoiding<br />
close contact with others they protect themselves from anticipated<br />
rejection (Bartholomew and Horowitz, 1991; Hazan & Shaver, 1987).<br />
It is suggested that these fearful-avoidant individuals are low in<br />
self-respect, while dismissive-avoidant individuals are higher in self<br />
respect but also regard others with suspicion (Bartholomew &<br />
Horowitz, 1991).<br />
<strong>The</strong> fundamental differences between<br />
secure and insecure attachment remain the<br />
most important aspects <strong>of</strong> this research.<br />
A secure individual seeks help when in difficulty and can make<br />
appropriate choices, consistently apply beneficial strategies to<br />
overcoming problems, remain involved in <strong>treatment</strong> and aware <strong>of</strong><br />
their own needs. <strong>The</strong>se health behaviours are very different to those<br />
<strong>of</strong> an insecure individual who may select inappropriate, ineffective or<br />
dangerous strategies to deal with health problems.<br />
Bringing together the constructs <strong>of</strong> attachment style, the role <strong>of</strong> trauma<br />
in childhood, and issues in health care, papers by Sch<strong>of</strong>ferman,<br />
Anderson, Hines Smith and White (1992) and Sch<strong>of</strong>ferman,<br />
Anderson, Hines Smith and Keene (1993) highlighted the issue <strong>of</strong><br />
prejudicial environmental influences on the development <strong>of</strong> somatic<br />
<strong>pain</strong>. In these studies on unsuccessful outcomes <strong>of</strong> back surgery, they<br />
demonstrated a clear and significant correlation between unsuccessful<br />
lumbar spine surgery and a history <strong>of</strong> childhood traumas. This<br />
correlation was seen in single-level, multilevel, primary and repeat<br />
surgeries (Sch<strong>of</strong>ferman et al., 1992; Sch<strong>of</strong>ferman et al., 1993). <strong>The</strong>se<br />
researchers maintain that recognition <strong>of</strong> predictors for<br />
unsuccessful outcome can be useful in avoiding surgery in patients<br />
whose indications for surgery are borderline. <strong>The</strong> greater challenge is<br />
to help the patient who, despite being at high psychological risk for<br />
negative outcome, has severe spinal pathology that will require<br />
surgery. <strong>The</strong>ir conclusions are that preoperative psychological<br />
assessments to assess the influence <strong>of</strong> childhood traumas are critical<br />
in defining patients for whom surgery should be avoided unless<br />
overwhelming spinal pathology is present, or for those patients who<br />
have failed to improve despite previous surgery that has been<br />
technically successful.
Attachment style in health research<br />
Secure attachment style<br />
<strong>The</strong> higher self esteem <strong>of</strong> the secure person with their confidence<br />
that others will support them suggests that secure individuals are<br />
able to seek out and communicate with carers, assess the<br />
appropriateness <strong>of</strong> the services <strong>of</strong>fered and comply with recommended<br />
self-help strategies. <strong>The</strong>ir stability, ability to care for themselves and<br />
strong personal resources enable them to cope and to find support<br />
even when long-term physical problems are present.<br />
Insecure attachment: Anxious style<br />
<strong>The</strong>se individuals who view themselves negatively and others as<br />
positive have a tone <strong>of</strong> communication which idealises health<br />
pr<strong>of</strong>essionals coupled with self-blame and self-depreciating stances<br />
(Mikhail & Henderson, 1994). Initially they are said to be compliant<br />
with self-care strategies but become disillusioned easily and move on<br />
to the next consultant and the next "cure." <strong>The</strong>se individuals are<br />
suggested to be the "doctor shoppers" who accumulate many pills<br />
and procedures and many disappointments about the "failure" <strong>of</strong><br />
the carer and the "failure" <strong>of</strong> the self to be cured.<br />
Insecure attachment : Avoidant style<br />
Those individuals exhibiting an avoidant attachment style respond to<br />
threat by avoiding caretaking figures (Simpson, Rholes & Nelligan,<br />
1992). Approaches to health pr<strong>of</strong>essionals occur only when they<br />
eventually decide they can no longer cope with <strong>pain</strong>. This presentation<br />
as an "emergency" can result in frustration to both carer and cared-for<br />
as the real issues are not obvious and the presentation is highly<br />
emotional. <strong>The</strong> carer may feel pressured to provide immediate relief<br />
that may not be appropriate for the long term. <strong>The</strong> positive view <strong>of</strong><br />
self and negative view <strong>of</strong> others displayed by these individuals helps<br />
them to feel self-sufficient and to view others as unresponsive and<br />
unavailable (Bartholemew, 1990).<br />
4<br />
Avoidance<br />
<strong>The</strong> <strong>treatment</strong> <strong>of</strong> <strong>persistent</strong> <strong>pain</strong><br />
Insecure attachment: Fearful style<br />
<strong>The</strong> negative global view <strong>of</strong> these individuals suggests that they<br />
experience considerable anxiety and hostility in interpersonal matters,<br />
stemming from a history <strong>of</strong> abuse, neglect and / or trauma<br />
(Bartholemew & Horowitz, 1991). When anxiety increases they<br />
retreat and avoid seeking help (Simpson et al., 1992). When help is<br />
finally sought they present as hopeless and helpless and their distress<br />
may encourage health pr<strong>of</strong>essionals to recommend psychiatric care<br />
for their perceived suicidal intentions. Mikhail (1994) suggested that<br />
this situation serves to intensify the feelings <strong>of</strong> rejection experienced<br />
by these people and increases their punitive view <strong>of</strong> self.<br />
Summary<br />
Health pr<strong>of</strong>essionals generally seek to understand differences in <strong>pain</strong><br />
presentation through a multidisciplinary assessment <strong>of</strong> the individual.<br />
<strong>The</strong>y also educate individuals in positive coping strategies in order<br />
to help them develop the self-efficacy needed to manage chronic<br />
<strong>pain</strong>. Psychological assessment includes an assessment <strong>of</strong> the<br />
individual’s developmental history as well as an appraisal <strong>of</strong> their<br />
cognitive skills, and psychological <strong>treatment</strong>s may be essential when<br />
<strong>pain</strong>-related behaviours associated with insecure attachment styles<br />
are present. This may prevent such individuals needing long-term<br />
involvement with <strong>pain</strong> clinicians.<br />
Attachment theory provides a sound evidence based approach that<br />
gives an insight into the patient’s world and philosophy <strong>of</strong> life.<br />
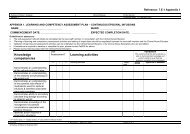
1. secure<br />
Value <strong>of</strong> the self = high<br />
Value <strong>of</strong> others = high<br />
• stable / autonomous<br />
• organised • active copers<br />
• problem solvers<br />
3. insecure-avoidant/dismissive<br />
Value <strong>of</strong> the self = low<br />
Value <strong>of</strong> others = low<br />
• dismissing <strong>of</strong> intimacy<br />
• obsessively self-reliant<br />
• relationship stressed<br />
• distrusting & aggressive<br />
• chronic depression - early onset<br />
Anxiety<br />
Attachment style: An explanatory model<br />
2. insecure-preoccupied<br />
Value <strong>of</strong> the self = low<br />
Value <strong>of</strong> others = high<br />
• dysfunctional • disorganised<br />
• compulsive caregivers<br />
• ambivalent & anxious<br />
• chronic depression<br />
2. insecure-preoccupied<br />
Value <strong>of</strong> the self = low<br />
Value <strong>of</strong> others = low<br />
• anxious & avoidant<br />
• helpless & distressed<br />
• disoriented • passive aggressive<br />
• chronic depression
� References<br />
1 AINSWORTH, M.D. (1982).<br />
Attachment: Retrospect and prospect, in C.M. Parkes and J.<br />
Stevenson- Hinde (eds.) <strong>The</strong> Place <strong>of</strong> attachment in Human<br />
Behaviour (pp.3-30), London: Tavistock.<br />
2. AINSWORTH, MD, BLEHAR, MC, WATERS, E, & WALL, S (1978).<br />
Patterns <strong>of</strong> attachment: A psychological study <strong>of</strong> the strange<br />
situation. Sydney: John Wiley & Sons.<br />
3. BARTHOLOMEW, K. (1990).<br />
Avoidance <strong>of</strong> intimacy: An attachment perspective.<br />
Journal <strong>of</strong> Social and Personal Relationships, 7, 147-178.<br />
4. BARTHOLOMEW, K., & HOROWITZ, L.M. (1991).<br />
Attachment styles among young adults: A test <strong>of</strong> a four-category<br />
model. Journal <strong>of</strong> Personality and social psychology, 61(2), 226-244.<br />
5. BOWLBY, J. (1944). Forty-four juvenile thieves (ii).<br />
International Journal <strong>of</strong> Psychoanalysis, 25, 107-128.<br />
6. BOWLBY, J. (1958). <strong>The</strong> nature <strong>of</strong> the child’s tie to his mother.<br />
International Journal <strong>of</strong> Psychoanalysis, 42, 317-340.<br />
7. FERSTER, C.B., & PERROTT, M.C. (1968).<br />
Behaviour Principles. New York: New Century. Pp 104-116.<br />
8. GEORGE, C., KAPLAN, M., & MAIN, M. (1987).<br />
<strong>The</strong> adult attachment interview, in M.Main (ed.) Behaviour and<br />
the Development <strong>of</strong> Representational Models <strong>of</strong> Attachment:<br />
Five Methods <strong>of</strong> Assessment.<br />
9. HAZAN, C., & SHAVER, P. (1987).<br />
Romantic love conceptualised as an attachment process.<br />
Journal <strong>of</strong> Personality and Social Psychology, 52, 511-524.<br />
10. MIKHAIL, S., HENDERSON, P., & TASCA, G. (1994).<br />
An interpersonally based model <strong>of</strong> chronic <strong>pain</strong>: An application<br />
<strong>of</strong> attachment theory. Clinical Psychology Review, 14(1), 1-16.<br />
11. PEARCE, S., CRAMOND, T., & CREED, P. (2001).<br />
Attachment style and chronic <strong>pain</strong> syndrome.<br />
<strong>Australian</strong> <strong>Pain</strong> <strong>Society</strong> Newsletter, May, 2-4.<br />
12. SCHOFFERMAN, J., ANDERSON, D., HINES, R., SMITH, G., &<br />
WHITE, A. (1992). Childhood psychological trauma correlates with<br />
unsuccessful lumbar spine surgery. Spine, 17(Suppl.), S138-144.<br />
13. SCHOFFERMAN, J, ANDERSON, D, HINES, R, SMITH, G, KEANE, G.1993<br />
Childhood psychological trauma & chronic refractory low-back <strong>pain</strong>.<br />
Clinical Journal <strong>of</strong> <strong>Pain</strong>, 9, 260-265.<br />
14. SIMPSON, J.A., RHOLES, W.S., & NELLIGAN, J.S. (1992).<br />
Support seeking and support giving within couples in an anxietyprovoking<br />
situation: <strong>The</strong> role <strong>of</strong> attachment styles.<br />
Journal <strong>of</strong> Personality and Social Psychology, 62(3), 434-446.<br />
5<br />
Michael Cousins<br />
Chair <strong>of</strong> Anaesthesia and <strong>Pain</strong> Management<br />
Royal North Shore Hospital and <strong>The</strong> University <strong>of</strong> Sydney<br />
I have deliberately used the term "<strong>persistent</strong> <strong>pain</strong>" as it is a<br />
convenient way <strong>of</strong> describing how some patients who begin with<br />
acute <strong>pain</strong>, pass into a transitional phase where the <strong>pain</strong> does indeed<br />
"persist". This is a very important phase for us to study as it is clearly<br />
not a normal situation, and poses the very significant risk that the<br />
patient will develop "long term persisting <strong>pain</strong>". As a side issue, I<br />
would like to propose that we consider adopting <strong>persistent</strong> <strong>pain</strong> rather<br />
than chronic <strong>pain</strong> for the following two reasons:<br />
1Chronic <strong>pain</strong> has developed some extremely unfortunate<br />
connotations which will be difficult to change; and<br />
If we focus our attention on the transitional phase, as<br />
2<br />
described above, the patient and public perception will<br />
shift towards an appreciation that we are trying to prevent<br />
patients from suffering <strong>pain</strong> on a permanent basis.<br />
<strong>The</strong> evidence for persisting <strong>pain</strong> as a disease entity, falls under the<br />
categories <strong>of</strong>: � basic science � clinical manifestations<br />
� psychological changes � unhelpful environmental adaptations<br />
With respect to the basic science <strong>of</strong> persisting <strong>pain</strong>, there is now<br />
overwhelming evidence that there is a neurobiological process<br />
associated with tissue and nerve injury which poses at least the<br />
potential for a continuum from the acute to <strong>persistent</strong> phase.<br />
Unfortunately, most animal models must be regarded as very much<br />
representing only the acute phase, since they have neglected to<br />
investigate the occurrence and persistence <strong>of</strong> behavioural changes<br />
that have been well identified in humans. However, recent experiments<br />
by Kevin Keay, Richard Bandler and Associates from our group, have<br />
identified an exciting new avenue <strong>of</strong> studying the transitional phase in<br />
animals. This may provide the opportunity for some clinically relevant<br />
investigation <strong>of</strong> some <strong>of</strong> the changes that have been identified in<br />
largely acute models such as:<br />
� pathophysiology in the form <strong>of</strong> spontaneous firing <strong>of</strong><br />
damaged peripheral and nervous system neurons, including<br />
"burst firing" in thalamus and associated brain areas;<br />
� neuroanatomical reorganisation <strong>of</strong> dorsal horn apparently<br />
under control <strong>of</strong> growth factors such as NT3 and BDNF;
� potential death <strong>of</strong> inhibitory neurons due to excessive release<br />
<strong>of</strong> nitrous oxide, with associated interference with inhibitory<br />
neuro-transmitters such as GABA;<br />
� genetic changes associated with long term increase response<br />
<strong>of</strong> neurons; neuroanatomical reorganisation at a brain level,<br />
resulting in increased central representation <strong>of</strong>"<strong>pain</strong>ful areas".<br />
Clinically detectable abnormalities associated with persisting <strong>pain</strong> can<br />
sometimes be difficult to document. On the other hand, patients with<br />
syndromes such as complex regional <strong>pain</strong> syndrome (CRPS) can<br />
manifest striking changes including secondary hyperalgesia, allodynia,<br />
hyperpathia, vasomotor changes, abnormalities in motor function<br />
and trophic changes. It is possible that such clinical abnormalities<br />
may be directly linked to the pathophysiology, which has been<br />
identified in animal models, however, such a linkage has yet to be<br />
made. An exciting opportunity to link abnormalities identified at a<br />
basic level with clinical abnormalities may lie in the use <strong>of</strong> magnetic<br />
resonance spectroscopy (MRS). Philip Siddall and Annie Woodhouse,<br />
in collaboration with Pr<strong>of</strong>essor Carolyn Mountford, have developed<br />
capabilities to detect regional abnormalities in brain function which<br />
seem to show specific patterns for different <strong>pain</strong> states.<br />
Perhaps the strongest evidence currently available is from the clinical<br />
psychology literature where a substantial number <strong>of</strong> abnormalities<br />
have been documented in patients with persisting <strong>pain</strong> including;<br />
high levels <strong>of</strong> anxiety, depression, feelings <strong>of</strong> hopelessness and<br />
helplessness, fear avoidance behaviour, etc. Currently the only factors<br />
that have been identified as being important in the progression from<br />
an acute to a <strong>persistent</strong> phase are in the psychological domain, and<br />
the only available studies relate to patients with low back <strong>pain</strong>. It<br />
would thus seem important to study patients following surgery and<br />
trauma to examine whether psychological factors may also be<br />
important in these areas.<br />
Despite the shortcomings in some <strong>of</strong> the currently available evidence,<br />
there is increasing evidence from the basic and clinical sciences that<br />
persisting <strong>pain</strong> does become a disease entity regardless <strong>of</strong> the<br />
underlying causes <strong>of</strong> the <strong>pain</strong>. Clearly, the primary objective is to<br />
treat any underlying causes. However, there is also a concern now<br />
that such <strong>treatment</strong> <strong>of</strong> underlying causes should be carried out<br />
expeditiously. Otherwise the processes associated with persisting <strong>pain</strong><br />
may move into a <strong>persistent</strong> phase, such that <strong>treatment</strong> <strong>of</strong> the<br />
underlying condition may no longer result in a reversal <strong>of</strong> the <strong>pain</strong><br />
process.<br />
6<br />
This month, the physio spot is introducing<br />
(not that they need introduction!)<br />
Tina Souvlis and Bill Vincenzino<br />
Tina and Bill are doing research at the Department <strong>of</strong> Physiotherapy,<br />
University <strong>of</strong> Queensland, in the area <strong>of</strong> central analgesic and motor<br />
effects associated with manual therapy. Obviously, this is an important<br />
area for anyone doing manual therapy – the more we understand<br />
about why and how these techniques work, the more we promote<br />
targeted and effective intervention.<br />
Comments invited: l.moseley@mailbox.uq.edu.au<br />
Manual therapy and <strong>pain</strong> relief<br />
What reasons spring to mind about the effectiveness <strong>of</strong> manual<br />
therapy? To most people the thought <strong>of</strong> "putting something back<br />
into place" or "getting things moving" ie the biomechanical effects<br />
are paramount. However, musculoskeletal <strong>pain</strong> is one <strong>of</strong> the main<br />
reasons for attendance at physiotherapy clinics. Physiotherapists<br />
along with other medical and health practitioners have long used<br />
manual therapy techniques in the relief <strong>of</strong> <strong>pain</strong>. <strong>The</strong>se techniques<br />
include both manipulation such as a high velocity thrust techniques,<br />
passive oscillatory mobilisation and more recently mobilisation<br />
techniques incorporating active movement.<br />
Manual therapy has long been known anecdotally to be effective<br />
in the management <strong>of</strong> <strong>pain</strong> and the <strong>treatment</strong> <strong>of</strong> musculoskeletal<br />
conditions. In addition, meta-analyses carried out looking at spinal<br />
manual therapy in the management <strong>of</strong> both cervical and lumbar spine<br />
<strong>pain</strong> conditions have demonstrated positive short-term effects.<br />
Although, there is a growing body <strong>of</strong> literature into the biomechanical<br />
effects <strong>of</strong> manual therapy until relatively recently there has been little<br />
research carried out into other potential neurophysiological mechanisms<br />
by which these types <strong>of</strong> <strong>treatment</strong>s may exert some <strong>of</strong> their effects.<br />
<strong>The</strong> potential for spinal manual therapy to activate endogenous <strong>pain</strong><br />
reliving mechanisms was hypothesized by Wright (1995). Since then,<br />
a number <strong>of</strong> studies have demonstrated that spinal and peripheral<br />
manual therapy can produce analgesia which is significantly greater<br />
than that produced by placebo or control techniques in a range <strong>of</strong><br />
conditions. <strong>The</strong> hypoalgesia produced by these <strong>treatment</strong>s have<br />
consistently been shown to be specific to mechanical <strong>pain</strong> thresholds.<br />
Manual therapy <strong>treatment</strong>s do not change thresholds to thermal<br />
<strong>pain</strong>. This change in mechanical threshold is immediate in onset, it is<br />
not reversible by naloxone and does not demonstrate tolerance to
epeated dosing. In short, the characteristics <strong>of</strong> this response seem to<br />
suggest non-opioid mechanisms.<br />
In addition to the hypoalgesic effects, many studies have postulated<br />
a motor effect following spinal manual therapy. Depending on the<br />
techniques used and muscles tested, studies have shown that there<br />
may be facilitation <strong>of</strong> motor effects or perhaps inhibition <strong>of</strong> muscle spasm<br />
associated with <strong>pain</strong>. An increase in both peripheral and central measures<br />
<strong>of</strong> sympathetic nervous system activity have also been demonstrated<br />
to occur in conjunction with these motor and <strong>pain</strong> relieving effects.<br />
<strong>The</strong>se effects have also been demonstrated over a number <strong>of</strong> studies.<br />
This tripartite effect <strong>of</strong> hypoalgesia, activation <strong>of</strong> the sympathetic<br />
system and motor facilitation may be regulated by a center such as<br />
the periaqueductal gray area <strong>of</strong> the midbrain which has connections<br />
to multiple systems through nuclei in the rostroventral medulla.<br />
It is tempting to assume that the techniques described as manual<br />
therapy are limited to producing biomechanical or perhaps even<br />
psychological effects. <strong>The</strong> implications <strong>of</strong> such a widespread<br />
response over a number <strong>of</strong> systems is that the afferent input via<br />
manual therapy is a sufficient stimulus to also activate a coordinated<br />
response including the descending <strong>pain</strong> inhibitory systems.<br />
This research is progressing and more evidence as to the mechanisms<br />
and effectiveness <strong>of</strong> manual therapy as well as other physiotherapeutic<br />
tools will hopefully emerge. Please contact us if you would like to<br />
enquire about these studies or to comment.<br />
Tina Souvlis t.souvlis@shrs.uq.edu.au<br />
Bill Vicenzino b.Vicenzino@shrs.uq.edu.au<br />
Department <strong>of</strong> Physiotherapy, University <strong>of</strong> Queensland. Brisbane.<br />
Reference WRIGHT, A., Hypoanalgesia post manipulative therapy,<br />
Manual <strong>The</strong>rapy, 1 (1995) 11-16.<br />
<strong>The</strong> <strong>Society</strong> would like to welcome new members to the APS<br />
Steve Brimstone Psychology<br />
Anne Burke Psychology<br />
Louise Chapple Nursing<br />
Janet Mosquera Psychology<br />
Kerrie Noonan Psychology<br />
Maryanne Sparrow <strong>Pain</strong> Management<br />
Anne Ward Nursing<br />
7<br />
<strong>The</strong>re is feverish<br />
activity at the IASP<br />
Secretariat in Seattle<br />
preparing for the San Diego World <strong>Pain</strong><br />
Congress in a couple <strong>of</strong> weeks time.<br />
At the time <strong>of</strong> writing this piece (late July), registration numbers<br />
march steadily towards the 4000 mark which is very close to the<br />
number predicted by the Secretariat about 6 months ago. Over the<br />
last decade or so, an interesting trend in Congress registration<br />
numbers has arisen in that Congresses sited in Europe have a larger<br />
number <strong>of</strong> delegates compared to those in North America. Congress<br />
sites have oscillated between UK / Europe and North America save<br />
the 1990 World Congress in Adelaide. Delegate numbers in San Diego<br />
has great implications for the 2005 Congress in Sydney which, as I<br />
have said previously, is only the second time a World <strong>Pain</strong> Congress<br />
has been sited in the Southern Hemisphere. <strong>The</strong> IASP Council, Local<br />
Arrangements Committee for the 2005 Congress and the <strong>Australian</strong><br />
<strong>Pain</strong> <strong>Society</strong> Board <strong>of</strong> Directors wish all APS members to become<br />
ambassadors for the 2005 Sydney meeting both here and abroad.<br />
After 2005, it will be a considerable time period before the vast<br />
number and diversity <strong>of</strong> <strong>pain</strong> experts, clinicians and researchers in all<br />
<strong>pain</strong> disciplines will grace our shores at the one time. Thus, Sydney<br />
2005 does represent a unique opportunity for all trainees and<br />
practitioners to learn the latest developments and we must all make<br />
every effort to promote the meeting to all, ie members and non-APS<br />
members alike.<br />
<strong>The</strong>re is already great interest in arranging a number <strong>of</strong> Satellite<br />
meetings to the main Sydney meeting. Various groups are already<br />
assessing potential sites that will be in desirable geographical locations.<br />
At the present time, I have been approached informally by at least 4<br />
groups already with a view to arranging satellite meetings around<br />
the Sydney World Congress.<br />
<strong>The</strong> other important issue I wish to bring to your attention is possible<br />
participation <strong>of</strong> APS members in the various IASP Taskforces and<br />
Committees. <strong>The</strong>se Taskforces and Committees serve a vital function<br />
that essentially maps the current and future direction <strong>of</strong> the<br />
International Association. Consequently, I believe it is most important<br />
to have as wide as possible participation <strong>of</strong> APS members in the various<br />
IASP activities and earnestly urge APS members to think about this
issue. It is a requirement that all members <strong>of</strong> IASP Committees and<br />
Taskforces must be IASP members (<strong>Australian</strong> <strong>Pain</strong> <strong>Society</strong> membership<br />
is insufficient) and this is not unreasonable if you think about it.<br />
<strong>The</strong> current Directory <strong>of</strong> Members is the appropriate source to see<br />
the options for your consideration. If you are interested, please<br />
contact one <strong>of</strong> the APS Board members and they will arrange to<br />
have your name considered. Clearly, we are not in a position to<br />
guarantee that you will actually be <strong>of</strong>fered a position <strong>of</strong> your choice.<br />
What I can say is that historically, there has been regular and<br />
frequent representation; past members have contributed significantly<br />
and this has been appreciated by the IASP. So go to it!<br />
Ge<strong>of</strong>f Gourlay<br />
Directors' Meeting 30th September 2002<br />
� Planning commenced for the 2004 ASM in Canberra<br />
Provisional dates 7-11 March 2004<br />
Convenor Ge<strong>of</strong>f Speldewinde<br />
� Teleconference PIGNI – August 28<br />
� Approval for refundable deposit for block booking <strong>of</strong> Qantas<br />
flights to Christchurch for the 2003 ASM<br />
� Abstracts online. Website engineering $1,000 approved<br />
� Review <strong>of</strong> the ACHS/APS <strong>pain</strong> facility guidelines<br />
Shared costs with ACHS $2,000 approved<br />
� 2005 local organising committee financial support $6,000<br />
approved<br />
� Possibility <strong>of</strong> a Queensland satellite meeting for 2005 in<br />
association with the World Congress.<br />
� Elections due 2003: call for nominations to be sent by<br />
November 2002<br />
� APS / APRA PhD Scholarship applications to close Nov 2002<br />
� NICS awaiting minutes <strong>of</strong> exploratory meeting held 29 July 2002<br />
� Possibility <strong>of</strong> developing clinical practice guidelines on <strong>pain</strong> in<br />
the elderly with other interested organisations<br />
� Facility directory template to send to members to be developed<br />
C. Roger Goucke<br />
8<br />
Julien P. de Jager FRACP<br />
President, <strong>Australian</strong> Rheumatology Association<br />
Interviewed by Dr Sue Inglis<br />
Who was/is your most influential mentor? I ‘ve had many, but the<br />
late Dr Brian Billington, gastroenterologist at Prince <strong>of</strong> Wales Hospital,<br />
and Dr Milton Cohen at St Vincent's Hospital in Sydney (still very<br />
much alive) would top the list.<br />
Most challenging patient? A young lawyer with severe destructive<br />
rheumatoid arthritis who was very poorly compliant with <strong>treatment</strong>,<br />
requiring narcotics for <strong>pain</strong> relief, bilateral hip replacements, requiring<br />
knee, metacarpal replacements and triple fusions <strong>of</strong> her feet. We<br />
finally had a showdown where I requested she find another<br />
rheumatologist and since then we have got along famously!<br />
Most rewarding experience in medicine? Seeing a young lady with<br />
severe juvenile arthritis and SLE go into remission on therapy, then<br />
graduate from Uni, and marry a great young man. <strong>The</strong>se rewards come<br />
every week mixed with all the <strong>treatment</strong> failures and adverse reactions!<br />
What would you advise those starting out in the field?<br />
Never give up, whether it is passing exams or puzzling out a problem,<br />
and do it all for the people we are committed to serve. <strong>The</strong>re is good<br />
in everyone, but make the most <strong>of</strong> those inspirational patients who<br />
carry you through difficult times with the others.<br />
How has medicine changed since you started out? We have<br />
come full circle, I think. I am from a family <strong>of</strong> lawyers and was inspired<br />
to do medicine by our family doctor, and family friends who were<br />
doctors, with their incredible dedication. <strong>The</strong>n during training (70s and<br />
early 80s) the world was all about satisfying the individual, and<br />
technological advances. This isolated many doctors from the very thing<br />
that makes medicine so worthwhile. It is pleasing to see the curricula<br />
<strong>of</strong> medical schools, and the emphasis in general practice in the last<br />
10 or more years redressing that. We are back to the situation where<br />
our responsibility is first to the patients and their needs.<br />
If you weren’t a doctor what would you like to be?<br />
I have never wanted to do anything else.<br />
What book are you reading at the moment?<br />
Peter Carey's ‘True History <strong>of</strong> the Kelly Gang’.<br />
Your favourite saying? "Send not to know for whom the bell tolls,<br />
it tolls for thee", by John Donne who was vicar <strong>of</strong> St Paul's. <strong>The</strong><br />
preceding lines are usually omitted, but are even more inspirational<br />
"Any man's death diminishes me, because I am involved in mankind".<br />
Julien P de Jager, FRACP, President, <strong>Australian</strong> Rheumatology Association<br />
dejager@ozemail.com.au
<strong>Pain</strong> Conference Canberra<br />
7 -11 March 2004<br />
<strong>The</strong> planning for this meeting is underway in a preliminary<br />
sense with a local organising committee being grouped<br />
(not yet finalised and will probably be a little fluid for a while).<br />
DC Conferences, with usual efficiency, has arranged the dates<br />
during our annual Canberra Week in sunny & warm March 2004.<br />
We are actively considering the following 3 themes:<br />
1. 'Musculoskeletal' issues, possibly in a conjoint effort with<br />
Australasian Faculty <strong>of</strong> Musculoskeletal Medicine<br />
2. Placebo in <strong>pain</strong> management.<br />
3. Exploring psychological constructs 'beyond' CBT<br />
ie what else is relevant?<br />
However planning is still at the embryonic stage and we<br />
welcome ideas from the membership. Please send these to<br />
Ge<strong>of</strong>frey Speldewinde: email gspeld@capitalrehab.com.au<br />
Please reply as soon as possible as the themes will be firmed up<br />
over the next 2 months.<br />
Ge<strong>of</strong>frey Speldewinde<br />
for the Conference Organising Committee<br />
AUSTRALIAN PAIN SOCIETY APS and<br />
AUSTRALIAN PAIN RELIEF ASSOCIATION APRA<br />
PhD Scholarship<br />
<strong>The</strong> APS is a Multidisciplinary <strong>Society</strong> whose charter is to improve the education,<br />
research and development, diagnosis and <strong>treatment</strong> <strong>of</strong> all forms <strong>of</strong> <strong>pain</strong>.<br />
APRA is a registered charity with the <strong>Australian</strong> Taxation Office and<br />
works closely with the APS to support educationl and research in <strong>pain</strong>.<br />
<strong>The</strong> <strong>Australian</strong> <strong>Pain</strong> <strong>Society</strong> and the <strong>Australian</strong> <strong>Pain</strong> Relief Association have<br />
funded three PhD Scholarships over the last 4 years (one in conjunction with CSL).<br />
<strong>The</strong> stipend for this Scholarship is AUD20,000 per annum and the APS will<br />
provide some financial support to allow the candidate to attend the<br />
Annual Scientific Meeting <strong>of</strong> the <strong>Society</strong>.<br />
<strong>The</strong> award is to enable full time research leading to a Doctor <strong>of</strong> Philosophy<br />
or equivalent, at any recognised <strong>Australian</strong> University. <strong>The</strong> applicant must be<br />
an <strong>Australian</strong> citizen and the applicant and his/her supervisor must be members<br />
<strong>of</strong> the APS. <strong>The</strong> funded project can be related to any aspect <strong>of</strong> the mechanisms,<br />
diagnosis or <strong>treatment</strong> <strong>of</strong> acute or chronic <strong>pain</strong>. Further information about the PhD<br />
Scholarship, including the Conditions <strong>of</strong> Award, can be obtained from the Secretariat:<br />
DEADLINE 15 NOVEMBER 2002<br />
APS Secretariat: DC Conferences • PO Box 571 Crows Nest NSW 1585<br />
Phone 02 9954 4400 • Fax 02 9954 0666<br />
Email APS@dcconferences.com.au<br />
9<br />
Australasian Academy <strong>of</strong> Cerebral Palsy and<br />
Developmental Medicine Inaugural Conference<br />
20 - 21 September 2002 • <strong>Australian</strong> National Maritime Museum<br />
Darling Harbour, Sydney, Australia<br />
PIAA International Section Conference 2002<br />
Physician Insurers Association <strong>of</strong> America International Section<br />
in association with MDA, MDAV & UMP<br />
‘Minimising Medical Error and Limiting Liability ... a work in progress’<br />
10 - 12 October 2002 • <strong>The</strong> Regent Hotel • Sydney, Australia<br />
A Combined Meeting: <strong>Australian</strong> <strong>Pain</strong> <strong>Society</strong> 24th ASM &<br />
New Zealand <strong>Pain</strong> <strong>Society</strong> 10th ASM<br />
9 - 13 March 2003 • Christchurch Convention Centre Christchurch,<br />
New Zealand<br />
ISPP 2003 • 6th International Symposium on Paediatric <strong>Pain</strong>.<br />
<strong>Pain</strong> in Childhood: <strong>The</strong> Big Questions<br />
15 - 19 June 2003 • Sydney Convention Centre<br />
Darling Harbour, Sydney, Australia<br />
Contact the APS Secretariat for further details:<br />
Phone 02 9954 4400 • email aps@dcconferences.com.au<br />
APS Secretariat Website www.dcconferences.com.au<br />
APS Website www.apsoc.org.au<br />
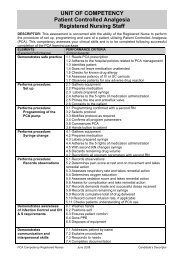
Report from <strong>Pain</strong> Interest Group – Nursing Issues<br />
From Julieanne James on behalf <strong>of</strong> the PIG-NI organising committee<br />
<strong>The</strong> half day seminar "Nurse Initiated <strong>Pain</strong> Management" was held on Sunday 24<br />
March preceding the APS Annual Scientific Meeting. <strong>The</strong> speakers were well<br />
received with enthusiastic positive feedback. <strong>The</strong>re were just over 200 registrants<br />
and information from the Responder Questions are outlined below. We would like<br />
to thank the following companies for their generous and ongoing support <strong>of</strong> this<br />
meeting. Abbott Australasia, AstraZeneca, Ansell International, Baxter Healthcare,<br />
CSL Limited, Jansen Cilag, Medtronic, Mundipharma & the Royal College <strong>of</strong> Nursing.<br />
Represented regions <strong>of</strong> registrants:<br />
67% from NSW; 8% QLD; 6% VIC; WA, SA, ACT & TAS were all 4% and under.<br />
Areas <strong>of</strong> practice<br />
Acute 30%; Chronic16%; Palliative14%; Critical Care 13%;<br />
Surgical Nursing 7%; Several other areas 20%
Website: www.apsoc.org.au • Password for members site: Placebo<br />
President: Dr C. Roger Goucke<br />
WA <strong>Pain</strong> Management Centre • Sir Charles Gairdner Hospital<br />
QE2 Medical Centre, Hospital Ave Nedlands WA 6009<br />
Tel 08 9346 3263 • Fax 08 9346 3481<br />
Vice President: Dr Carolyn Arnold<br />
Caulfield <strong>Pain</strong> Management Research Centre<br />
260 Kooyong Rd, Caulfield VIC 3162<br />
Tel 03 9276 6834 • Fax 03 9276 6675<br />
Treasurer: Dr Paul J Graziotti<br />
Sir Charles Gairdner Hospital 199 Cambridge St, Wembley WA 6014<br />
Tel 08 9388 8289 • Fax 08 9386 5927<br />
Secretary: Dr Bruce Rounsefell<br />
Royal Adelaide Hospital <strong>Pain</strong> Clinic, North Terrace, SA 5000<br />
Tel 08 8222 5403 • Fax 08 8222 5904<br />
ACT State Councillor: Dr Ge<strong>of</strong>frey Speldewinde<br />
15 Napier Close Deakin ACT 2600<br />
Tel 02 6282 6240 • Fax 02 6282 5510<br />
NSW State Councillor: Dr Raj Sundaraj<br />
60 Derby Street, Kingswood NSW 2747<br />
Tel 02 4722 8100 • Fax 02 4722 8388<br />
Newsletter Editor: Ms Amal Helou<br />
<strong>Pain</strong> Management Centre QE2, Royal Prince Alfred Hospital<br />
59 Missenden Rd, Camperdown NSW 2050<br />
Tel 02 9515 9739 • Fax 02 9515 9751<br />
Email amalh@diab.rpa.cs.nsw.gov.au<br />
Website Coordinator: Dr John Corry<br />
Suite B6, 161 Strickland Crescent, Deakin ACT 2600<br />
Tel 02 6285 1833 • Fax 02 6285 2280<br />
Website www.apsoc.org.au • Email apsoc@org.au<br />
10<br />
QLD State Councillor: Dr James P O’Callaghan<br />
Arnold Janssen Centre 259 Wickham Tce Brisbane QLD 4000<br />
Tel 07 3831 0383 • Fax 07 3834 6481<br />
SA State Councillor: Dr Timothy J Semple<br />
<strong>Pain</strong> Clinic Royal Adelaide Hospital Adelaide SA<br />
Tel 08 8222 5403 • Fax 08 8222 5163<br />
TAS State Councillor: Ms Kerry Merse<br />
Hobart <strong>Pain</strong> Clinic Calvary Hospital<br />
49 Augusta Rd, Lenah Valley TAS 7008<br />
Tel 03 6228 2700 • Fax 03 6278 9005<br />
VIC State Councillor: Ms Lyn Boag<br />
Multidisciplinary <strong>Pain</strong> Centre, Parkville<br />
MECRS PO Box 7000, Carlton South 3053<br />
Tel 03 8387 2258 • Fax 03 8387 2141<br />
WA State Councillor: Ms Sally Greenway<br />
St John <strong>of</strong> God Hospital<br />
65 Rupert St, Subiaco, WA 6008<br />
Tel 08 9382 6111 • Fax 08 9382 6115<br />
Secretariat: DC Conferences P/L PO Box 571, Crows Nest NSW 1585<br />
Tel 02 9954 4400 • Fax 02 9954 0666<br />
Email aps@dcconferences.com.au<br />
IASP 909 NE 43rd St, Suite 306, Seattle WA 98105-6020 USA<br />
Tel 1.206-547-6409 • Fax 1. 206-547-1703<br />
Email iaspdesk@ juno.com<br />
New website www.iasp-<strong>pain</strong>.org<br />
IASP LIAISON: Dr Ge<strong>of</strong>f Gourlay<br />
<strong>Pain</strong> Management Unit, Flinders Medical Centre, Bedford Park SA 5042<br />
Tel 08 8204 5346 • Fax 08 8374 1758<br />
Email Ge<strong>of</strong>f.Gourlay@Flinders.edu.au