G G Bodiwala MS F~CS FIC/~ Consultant in Accident & Emer¢~ne ...
G G Bodiwala MS F~CS FIC/~ Consultant in Accident & Emer¢~ne ...
G G Bodiwala MS F~CS FIC/~ Consultant in Accident & Emer¢~ne ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
@<br />
B N Harrop FRCS<br />
Re,.qistrar <strong>in</strong> <strong>Accident</strong> & Emergency<br />
G G <strong>Bodiwala</strong> <strong>MS</strong> <strong>F~CS</strong> <strong>FIC</strong>/~<br />
<strong>Consultant</strong> <strong>in</strong> <strong>Accident</strong> & <strong>Emer¢~ne</strong>¥<br />
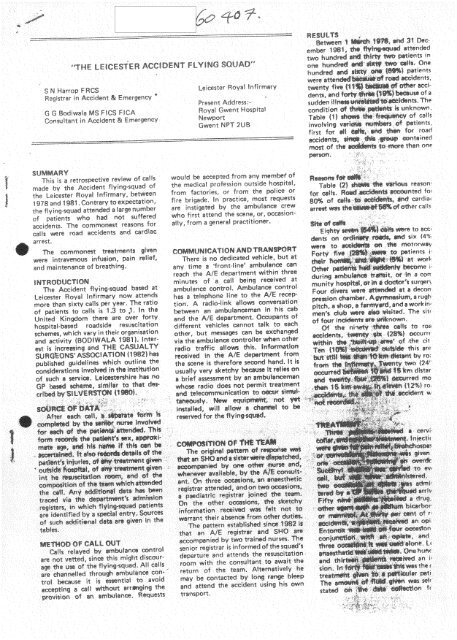
SUMMARY<br />
This is a retrospective review of calls<br />
made bv the <strong>Accident</strong> fiy<strong>in</strong>gosqua d of<br />
the Leicester Rova~ ~nfirmarvo between<br />
! 978 and t981, Contrary to expectation,<br />
the ft/<strong>in</strong>g~5~uad attended a ~ar~ number<br />
of ~atients who had not ~uffered<br />
accidents° The commonest reasons for<br />
calls were ,ned accidents end card~ae<br />
arrest,<br />
The commonest t~eatments ~iven<br />
were <strong>in</strong>travenous <strong>in</strong>fusion, pa<strong>in</strong> relief,<br />
and ma<strong>in</strong>tenance of breath<strong>in</strong>g°<br />
Leicester Rova~ ~nfirmery<br />
Present Address:*<br />
Rova~ Gwent Hospit@<br />
Newport<br />
Gwen~ NPT 2UB<br />
wou~d be accep~d from any mem~¢ of<br />
the medical profe%ion outside hospital<br />
from factories- or from the ~Hce or<br />
fire brigade, ~n practice, most requests<br />
are <strong>in</strong>stigated by the ambulance crew<br />
who first attend the scene, or, occasion °<br />
airy, from a ~nera~ practitioner,<br />
RESULTS<br />
ember !981, @ ~ ~ttended<br />
two hundr~ a~ th{~ ~ #~t~ents <strong>in</strong><br />
sudan iit~ ~nt~o Toe<br />
condition ¢# ~:~1~ ~ ~nknown.<br />
Table {1} ~ ~#’~ of calls<br />
}nVO[V~ v8¢~ @f ~atients,<br />
first fo’t ~1 ~, ~ ~ for road<br />
#~set of th~<br />
- L-<br />
l@-~e than one<br />
Tsb~e {2} ~@ ~ @®S reason"<br />
for c~l}s° R~ m~.~nted ~o,
L<br />
mp~e a~rw~V ~ ~I~ i~t~ ~<br />
m was ~ ~ ~I Q~ven on<br />
mpted t~1 ~ ~ ~v~ ~:~$~ents,<br />
~he {o~o~e~ ~, ~d with<br />
rts furth~ ~ ~ ~ ~t~ent~<br />
red c~ ~ ~rrh~a~ at , TABL~ 3<br />
TABLE 2<br />
RE~ONS FOR-CAL~<br />
No %<br />
Tota~ 43 27<br />
PAT~ ENT$ ~NVOLVED<br />
Of o~e hundred and si×tV one<br />
~;~en# a$~r~, s~×teen (10%) dg~d<br />
at ~:~ ~r~. or ~n the resu~tat~o~ room,<br />
d~oite treatn~nt 9~ven at the ~ne. Fu~<br />
detai~s are ~eck<strong>in</strong>g ~or four patients, one<br />
of whom d~ed ~ the resu~itat~on room°<br />
Of the one hundred and twenty ~even<br />
{79%) patienl~ who surv~ved to ~eave the<br />
re~JseD~t~on room, thirty one {24%)<br />
were sent home with cuts and scratches.<br />
EighW five (67%}, of whom fifty six<br />
(~%} on~v received observation, were<br />
admitted to the wards or treated <strong>in</strong> the<br />
fracture cHnico TwenW four {19%}<br />
patients were critically iHo Eighteen<br />
{75%} of these had received treatment<br />
outside hospital Ten {42%) were ad-<br />
5G RO~ <strong>Accident</strong> ~3 ~1~1 P~t~)<br />
F~H fro~ Height 5 4.5<br />
~4 FaHia~ Ob]e~ 3 ~4 ~S~ 2,5<br />
9 M~h<strong>in</strong>erv ~ 2°5<br />
2 D~v<strong>in</strong># 4 3<br />
~Stab~b~iSh~<strong>in</strong>g)<br />
Cot Thr~t 3 2.5<br />
Spor~ 2 2<br />
Ho~ F~rs I ~¢~ 1<br />
Tota~ 11 ~ 73<br />
w<br />
freq~ueat cau~ ~ ~t~ ~8s ~ ~jurv;<br />
eitlhe~ a~one o~ ~ 8 ~#~ ~h a<br />
an ~ (1%) dged <strong>in</strong> t~ re~$ci~$[o~ h~o ACf {54~ ¢f<br />
} mf~mat~mm<br />
accidenl~, aH pe~r~ ~vive~ u~ ~ve<br />
the re~i~oa ~#mo ~qh~ V ~n#i#~d<br />
four un~n~ous ~tient~ with head<br />
<strong>in</strong>iur~e~, and one ~ wh~h a fractured<br />
femur. N~ne ~%} ~f the ~venteen<br />
pe!~e~ who ~ ~nt~eated ou!~de<br />
hospital, and thirty seven ~87%)of the<br />
fifty five patients who bft the resusc}tation<br />
room, were accompanied b~ at<br />
least one o
I<br />
~#~a of Tteat~#~ Comment<br />
<strong>in</strong>formation !~ven at ~ne<br />
23a ABCE<br />
234 A B D<br />
2 34 NH<br />
234 A8CE<br />
234 B<br />
234<br />
234<br />
34<br />
34<br />
234<br />
"AB<br />
A B<br />
A<br />
*A<br />
NI<br />
3 ~ B<br />
3 a F~#ed<br />
34 BiD<br />
e X<br />
Treatm~nt~ give~ at scene:,<br />
A Intravenous epiate<br />
B Drip<br />
C Fracture ~lntage<br />
D Cewical ~oHar<br />
tono×<br />
CSF ot orrho~8<br />
F ractut~ Zvgoma<br />
Fr~ture Humaru5<br />
Compound fr~ture t~biaifib@a<br />
Abr~io#~<br />
F ~4~U r~ femu~<br />
F r@c~ure f~muf<br />
Fr~ture femur<br />
TFao~ oy ~3. No free1 #r8<br />
Uncomgciou~ from head <strong>in</strong>jury<br />
Now atte~di~ you#% disabJed unit<br />
Scs~p ~aceration<br />
FraeAure femur No other ~n~uW recorded<br />
Tetr~ia F/$ 8~i~ted with e×tractio~ from ~hlc~<br />
Certified dead ~t sc~meo Trsp~:~d beneath lorry<br />
Source of <strong>in</strong>formation:-<br />
! Post mortem report<br />
2 Case notes<br />
3 A & E card<br />
4 Fly<strong>in</strong>g°squad record<br />
GP affeady <strong>in</strong> attendance<br />
Laceration ~iv~r<br />
@@~<br />
Fr~ctsre peta#~<br />
Head i~iu~ w~t~ ~4~<br />
H~ t#jurV with a~ ::+<br />
v " ~A"~ °, ::,<br />
2<br />
.
O<br />
accidents fhs, fh ~-squdq S ~t~endaAca<br />
< ILiFWIvI 3ut Ol~ 1won[r-lois ixi[ie£i[g<br />
=u:e~,qeo SirE’ (t982, :;:onside;s [nat<br />
ttH mos~ COSteffec v~e~ wa~, {J reouc~[tg<br />
giJdt’}~ ~TtOF~a}~[y ?(0[~ Rt;ary d~ssase !s<br />
~o ~rmn tn~ %ene~ai :sub, I( m caro~ac<br />
~esugc! [at<br />
we w~r~ ~}o~ ~IHa COLLINS {I~61<br />
~sqa}red so Perform am:>cna~wnn ,.-q order<br />
T~} re,ease any [rapp~u gatienL ne4her<br />
ma we encou~[e~ an/ sm~at~on wners<br />
like R£DDKH and LNTL£ (1973~. ,we<br />
required to perform a {4enera~ anaesma.<br />
ta: The relative nheq~encV of ~ndustNai<br />
acqden~s ~nd the Possession by ~he [ire<br />
serv;ce o~ qea% v u£r~ng and lack<strong>in</strong>g 9ea~<br />
a~e ~o ~m~rtarw farters wn ch may<br />
eaoi;~n l:~e so.nee ot IU~" dra~r~atic<br />
~ilrJelce. The Oh!~ IXI~K~DII O~<br />
e$~M% at surgery ~r~orisle~ o~ ts~a<br />
hospitai b~ our f~Y~ng-~ua~! was ~he<br />
Performance of ~ ven~s ¢~-do~ On<br />
the sang,~e occas~or where e pa~ent was<br />
~rapped ,.~ a mach<strong>in</strong>e, h~s re~e~ ~e<br />
t~ilitated oy Io~I anaesthe~iao Entoc~×<br />
was u~d on ~ven oc~s~oos= dur<strong>in</strong>g<br />
release or dur<strong>in</strong>g fracture spl<strong>in</strong>ters.<br />
These patients rmght otherwise have<br />
required genera~ anaesthes~m<br />
T~ e PrOPOrtion nf ~nousl’~ dl<br />
Patients attended represents en under<br />
estimate ot the [rue vaaue of rIGs fly<strong>in</strong>@<br />
squad’s funcl on because nsore than one<br />
patient was attended dur<strong>in</strong>q some caJfs<br />
the additJona~ Patients wouad not ati<br />
have reenter attention ~n their own<br />
rignL When seriously iU ~tmnts ~ece~ved<br />
no treatment, this was because of lhe<br />
@ose prox~n-Ht~ of me hosoitat to the<br />
aCCident or ~sndezvous. o~ because the<br />
[t y mg%quad doctors lacked the ne@ssary<br />
skil,. Inevitably some Pa~ents o~ed<br />
before ~he flvMg-souad arrived. HOFF-<br />
MAN [t9821 has shown now much<br />
greater is the potentia~ say nl of Hfa [o<br />
be re;ned by the <strong>in</strong>tsrvennon of bystande~<br />
o~ the crew of an ord<strong>in</strong>ary<br />
ambulance, n ~he <strong>in</strong>terest before ~ns<br />
fty<strong>in</strong>gosquad arNved. The majority of<br />
>t’&’q~ ~1 e~qiraD~T~O~ IrIQ {o qN--~rry ~<br />
%i&~ deDart~ne[~! by radio O! YA£ nurq~<br />
IMO iplIai ~@quIt£Itent,s 0,~ hi£ !fl<strong>in</strong>ts.<br />
Thoegn ne must t! su~tab!v equg31<br />
~1e ~ rarei~ required to ~rtorm che~t<br />
dra{na~ o~ trace~e
,aspon~ib#itv ~e ~ ~e~reQ Fo~ an<br />
,~pa~t~flt ~ ¢8~tt~y covered by<br />
Av~ ~’~ ~ ~etary;<br />
BASKET~, P J F, DIAMOND A W.<br />
and COCHRANE D F<br />
%Jrban mobde resuscr;at~n: Tra<strong>in</strong><br />
{1976~ 4& 377-385.<br />
BOOtWALA. G G<br />
"Fac~s b~h~sd the flyu~g-squads" p,<br />
Wdson D H a~:~ Marsden A K ~Ed};<br />
’~re ot the acutely ~II a.qo <strong>in</strong>lkJre~"<br />
Chiches~e~= #~ile= 1982.<br />
CASUALTY SURGEONS ASSOCIA-<br />
TION: "Gu~dehnes for ~ttmg uo a<br />
nosoitai-based flyml sauad’. Avail.<br />
ab!e ~om Mr G G Bodawala Consu~tan~<br />
m A/E Leicester Rova~ lafirmaryo<br />
COLLINS, J~<br />
~Ofganisa[~o~ an@ ~unC~lOn Ot 8n<br />
accident fly~ng,.squad-, 8r Ned J,<br />
t966, 2 578-580_<br />
HOFFMAN. E;<br />
- ’*-’~ ....... site’° t%ur7 I !, 90-~<br />
6::
F’~ aci:i 7o~c:,,, o :7,’3i~ 766o<br />
5i<br />
Gu i cfe ’!<br />
)<br />
Car e:~ o
- ’ ’<br />
~<br />
707 .... I 0.<br />
R
~ available, height as percentage of expected height for age,<br />
based on the Boston standaxd. This is a measure of<br />
¯ retardation and therefore of past malnutrition.<br />
’ For the qualitative classification of seveze cases the Wellcome<br />
system is proposed. In each group ad~ data should be<br />
= recorded so far as poss~le. It is essenrlal that the criteria for<br />
. <strong>in</strong>clud<strong>in</strong>g children <strong>in</strong> the classification should be clearly laid<br />
,~i~ down.<br />
International comparisons obta<strong>in</strong>ed by these methods would<br />
be extremely valuable.<br />
References<br />
zation T~hm’ca/Rt~oorl Stri~, No. 477. Geneva, WA’LO., 9 .<br />
, Bengoa, I. ~, w/~o C hr~., 1970, 24, ss2. .......<br />
McCance and B. M. Wmaowmn. Lonaoa, t.aurcaub<br />
:i~ 4 ~7HO Chronid~ 1972,26, 160.<br />
,_ s Gomez~ F., a a/.¯~ounud of T~ Ped~i~ l~b 2, 77.<br />
i ::<strong>Accident</strong> Fly<strong>in</strong>g Squad<br />
~ ROGER SHOOK<br />
X t d eea<br />
:’: The c~mc.ept of this research project de~l_oped dur<strong>in</strong>g the early<br />
stages of work<strong>in</strong>g <strong>in</strong> an accident deparmtent <strong>in</strong> 1965, and further<br />
Royal United Hospital, Bath<br />
ROGEK SNOOK, U.D., Senior Casualty O~cer¯ .and Accidmt Medical<br />
O~cer to Bath Ftre Brigade and Ambulance Savice<br />
-<br />
t Stuart, H. C., and Stevenson, S. S., <strong>in</strong> Textbook of P~atr~, ed. W. B.<br />
NeLson, 7th edn., p, 12. Philadelphia, Saugde~L1959.. .....<br />
Seo~ue, N., and Latham, M. C., yourna~ cJ 2 roplcal ~’~amtr~ aria<br />
Enoiromnottal Cldld Health, 1971~ 17¯ 98.<br />
s Waterlow¯ J. C.¯ and Alleyne¯ G. A. O.¯ Admm~ i~ Prou<strong>in</strong> CTunnimT,<br />
1971¯ 25¯ 117 ....<br />
¯ ~~¯ ~.¯ ,. ~ ~ ,.~ _~.,~ ~,..~<br />
~ Mccaace and ~. M~ Wtddow~¯ t~ 91. ~.~¯.~.~,.~u<br />
Ran¯ V. K.¯ and S<strong>in</strong>gh, D.¯ AmericanJom~u O t,a~. ¯ ..... -~<br />
~s Jell~e, 23¯ 83. D. B.¯ and Jell~e¯ B. F. P., ,4mo~anyourna/of C/<strong>in</strong>/m/Nutril~b<br />
a Bmlte~¯ 1971¯ 24¯ H. 1377. J. I..¯ Malemlema, N. T.¯ snd Burge~ A. P., Troffiad and<br />
Geographical Media’s¯ 1969¯ 21, 39- ...........<br />
tt Tmwell, H. C.¯ Tr~ of tl~ ~rya~ ~’oaety o3 ¯ ropwat m~<br />
and Hygiene, 1941¯ 35, 13. ........<br />
ts Watedow¯ J. C.¯ Me.diad Resmrd~ _ .Gouna...l. ~ .p~a~ ~ort .zero., No . _.<br />
t* Brock,.J. F.¯ and Autret, M.¯ World Health Organza,ion. monograph<br />
Ser~¯ No. 8¯ 1952. .............<br />
t~ GalTOW¯ J. S.¯ .4rehi~s Lmbmm~eanos ae Nutr~o~¯ t~o¯ z.o: ~. ..--<br />
~’ McI.~m¯ D. S.¯ Pellet~ P. L.¯ and Read¯ W. W. C.¯ Lazar¯ t~¯ x¯ ~.<br />
t¯ Lan~t¯ 1970¯ 2, 302. ....... ertl NL Younm/~ Nutritio~ 1964,<br />
to Graham¯ G. C.¯ Cor(llmO¯ ~.¯ ana m ¯ h*’ -~<br />
84,71.<br />
Shat~, A., Dema~chi, M., and El-Milli, N., Lo~t, 1972, 2, 143.<br />
~i~ British Me.tfi’¢a/~mrna/¯ 1972¯ 3¯ 569-574<br />
accident services was widened by the fact that hospital equipmen,<br />
was often <strong>in</strong>compatible with that of the ambulance service.<br />
The project developed <strong>in</strong> fotw related stages--lectur<strong>in</strong>g to the<br />
- This paper d~’l~ the organization, evaluation, and<br />
ambulance staff, the organization of an <strong>in</strong>dependently f<strong>in</strong>anced<br />
cost<strong>in</strong>g of an <strong>in</strong>dep~d~tly f<strong>in</strong>anced and operated<br />
and operated accident fly<strong>in</strong>g squad, the <strong>in</strong>troduction of hospital<br />
tra<strong>in</strong><strong>in</strong>g for the ambulancemen, and the <strong>in</strong>vestigation of ambu-<br />
accident fly<strong>in</strong>g squad. 132 acctdenta <strong>in</strong>volv<strong>in</strong>g 302 casuallance design.<br />
ties were attended, six deaths were prevented, medical In 1966 there was Httle literature on the organization of<br />
treatment contributed to the survival of a further four¯ medical attendance at accidents <strong>in</strong> Brita<strong>in</strong>. Hall<br />
and the condition or comfort of many other casualties<br />
was improved. The calls <strong>in</strong> which survival was <strong>in</strong>fluonced<br />
were evenly distributed throughout the three-and-a-halfyear<br />
survey and seven of the I0 so aided were over 16<br />
and under 30 years of age, all I0 be<strong>in</strong>g <strong>in</strong> the work<strong>in</strong>g<br />
~ age group.<br />
The time taken to provide the service was not excessive<br />
and the expense when compared with the overall sav<strong>in</strong>g<br />
was very small The scheme was seen to be equally<br />
suitable for bas<strong>in</strong>g on hospital or general practice or<br />
~ and Coll<strong>in</strong>s*<br />
bad described hospital-based team.’, with medical or nurs<strong>in</strong>g<br />
staff transported respectively by anab~ance and police car, and<br />
Easton’s scheme <strong>in</strong>volv<strong>in</strong>g general p~ctitioners, was npt<br />
started until December 1967. s ¯ * The maj~ pubhcauon ¯ " " IN was.~m<br />
English translauon’ descrFomg ~_of .e~or G681er s o rgm~a" ~n<br />
<strong>in</strong> Heidelberg, West Germany. In this scheme medicaL~eato<br />
ment at accidents was based on the <strong>in</strong>troduction of a large<br />
mobile operat<strong>in</strong>g theatre unit <strong>in</strong> 1957.<br />
These three hospital-based schemes all <strong>in</strong>volved the use of<br />
spechdized transpot~ The alternative, therefore, was m <strong>in</strong>vesti-<br />
both, and work<strong>in</strong>g as an <strong>in</strong>tegrated team with the ambugate the usefulness of one doctor attend<strong>in</strong>g accidents <strong>in</strong> his own<br />
lance service. The use of specialized transport was found car and carry<strong>in</strong>g his own equipment. Thh paper describes the<br />
to be unnecessary. Other benefits of the scheme <strong>in</strong>cluded organization¯ equipment¯ and evaluation of medical attendance<br />
use of the experience of attend<strong>in</strong>g accidonta to ensure by me at the scene of accidents and the <strong>in</strong>tegration of this<br />
relevant and realistic tra<strong>in</strong><strong>in</strong>g for emergency service with<strong>in</strong> the ambulance service dur<strong>in</strong>g the three-and-a-ball-year<br />
~rsonael, and an appreciation of the effect of ambulance period start<strong>in</strong>g <strong>in</strong> November 1967 after a period of feasibility<br />
! ~lgn oa the fremont.<br />
study. On completion of the res~rch Bath City Council then<br />
officially took over the scheme by mak<strong>in</strong>g it a part of the City<br />
Fire and Ambulance Scrvice~ <strong>in</strong>clud<strong>in</strong>g the creation of the<br />
appo<strong>in</strong>tment of accident medical o~iccr.<br />
¯ ~, impetm came from the experience ~ rhanco arrival at theOutl<strong>in</strong>e<br />
of Scheme<br />
’<br />
,<br />
scene of mad 8c~L~.,~t~. m t~e ~ department co~tact<br />
w;th ~_.~ .-~r: oi the emergency services was frequent, and I ORGANIZATION<br />
b~came tncre~n~y aware of the problems that they had to Initially my attendance at road accidents was more <strong>in</strong> the role of<br />
face---<strong>in</strong> particular, cases for which the resuscitative measures an observe:, to study how the emet~cy services organized<br />
required before admission to hospital were beyond both their<br />
tra<strong>in</strong><strong>in</strong>g and equipment. This gap between the ambulance and<br />
themselves, how best to organize medical participation, and.to<br />
build up gradually a relationship ~ the emergen, cY ser)nco<br />
. ~ _<br />
personnel. In fact, this approach set the Fa~ern In~H. ~ r..~<br />
ship that was to cont<strong>in</strong>ue. From the outer m.em<br />
organized<br />
and to comb<strong>in</strong>e<br />
m be<br />
as<br />
available<br />
part of their<br />
m the<br />
team<br />
emergency<br />
at the scene<br />
~nces<br />
of the/<br />
o.n/<br />
/<br />
/
MO. 1--Fire brigade emergency equipment vehicle and accident fly<strong>in</strong>g squad car.<br />
a set-up which encouraged a close and personal work<strong>in</strong>g relationship<br />
<strong>in</strong> which the ambulance staff would actually participate,<br />
to the benefit of all, <strong>in</strong>clud<strong>in</strong>g the patient. At the same time the<br />
ambulanceman could be encouraged to improve his skill <strong>in</strong><br />
assess<strong>in</strong>g priorities.<br />
It was also policy to <strong>in</strong>itiate any treatment and to stabilize<br />
the patient at the scene, and then <strong>in</strong> most cases to allow the<br />
ambulance staff to take over the responsibility for the patient<br />
In the early stages medical equipment was-carried <strong>in</strong> several<br />
cases. This was not satisfactory, howevers and so a resuscitation<br />
box was designed to conta<strong>in</strong> and display all the equipment and<br />
stir be stable <strong>in</strong> a mov<strong>in</strong>g ambulance. Careful choice of equipment<br />
kept the total weight down to 51 lb (23 kg) (37 lb (17 kg)<br />
without the cardiac monitor), and this arrangement, described<br />
<strong>in</strong> more detail elsewhere,’ was most successful <strong>in</strong> practice.<br />
A list of the equipment carried, together with the cost, is given<br />
<strong>in</strong> the Appendix.<br />
COLLECTION OF RF~ULT$<br />
Detailed records were kept of each call, <strong>in</strong>clud<strong>in</strong>g the date,<br />
tim<strong>in</strong>gs, distance travelled, diagram of the scenes vehicles and<br />
casualties <strong>in</strong>volved~ and equipment used. Case histories Were<br />
followed up personally until the eventual outcome of treatment<br />
was know~<br />
The criteria used to categorize the casualties were those used<br />
by the M<strong>in</strong>istry of Transport--that is, slight, seriomh and fatal.<br />
Results<br />
dently and so was available <strong>in</strong> case the patient’s con- DRIVING<br />
dition deteriorated. In practice this policy worked well. Personal<br />
No problems were encountered dur<strong>in</strong>g the research. The<br />
and vehicle identification was an important factor <strong>in</strong> ensur<strong>in</strong>g<br />
acceptance when approach<strong>in</strong>g, work<strong>in</strong>g at, or leav<strong>in</strong>g the scene.<br />
Mediflash green light was found to give adequate vehicle<br />
identification at night and dur<strong>in</strong>g the day to oncom<strong>in</strong>g traffic.<br />
A short over-waistcoat of fluorescent and reflective material A brighter, detachable rotat<strong>in</strong>g beacon would, however, be-<br />
was made and worn at all <strong>in</strong>cidents, and the magnetic flash<strong>in</strong>g<br />
green light (Mediflash) was developed for use on the car when<br />
more effective ff the light<strong>in</strong>g regulations were amended to<br />
travell<strong>in</strong>g to emergencies.<br />
<strong>in</strong>clude doctor’s cars as emergency vehicles. Where <strong>in</strong>dicated<br />
Initially the ambulance control room was <strong>in</strong>formed of my<br />
visual identification was supplemented by the use of a pneu-<br />
whereabouts by the provision of a timetable supplemented by<br />
matic horn. The car was not <strong>in</strong>volved <strong>in</strong> any accidcn~ and <strong>in</strong><br />
comb<strong>in</strong>ation with the use of studded tyres <strong>in</strong> conditiom of ice<br />
periodic telephone calls. This system was far from satisfactory and snow, all <strong>in</strong>cidents were attended without difficulty. Vehicle<br />
and <strong>in</strong>volved only the first 12 calls, while await<strong>in</strong>g delivery of a <strong>in</strong>surance was discussed with the <strong>in</strong>surance agency and no<br />
radiotelephone; the latter completely transformed the scheme. extra premium was required for fully comprehensive cover.<br />
Mobilization of medical aid was therefore through the control<br />
room of the City of Bath’s jo<strong>in</strong>t fire and ambulance service.<br />
The pr<strong>in</strong>cipal advantages of us<strong>in</strong>g one’s own car w¢~ avoidance<br />
As the service also operated a special emergency equipment<br />
of delay <strong>in</strong> mobilization due to wait<strong>in</strong>g for transpo~ to arrive<br />
vehicle (see Fig. 1) for releas<strong>in</strong>g casualtiet trapped <strong>in</strong> any<br />
and load<strong>in</strong>g equipment, freedom of movement when ms call, and<br />
accident situation, it seemed po<strong>in</strong>dess to restrict medical<br />
elim<strong>in</strong>ation of the cost of speciafized transport.<br />
Whenever it was neo:ssary to travel to hospital <strong>in</strong> the ambu-<br />
attendance to road accidents alone. Therefore any <strong>in</strong>cident was lance with the patient a spare ignition key was given to the<br />
attended where medical aid was thought to be required, either nearest policeman so that the car could be moved when desriag<br />
on receipt of the <strong>in</strong>itial 999 call or on the arrival of the first<br />
the road. This proved necessary on 12 calls. On five occasions<br />
vehicle at the <strong>in</strong>cident. Similarly, availability was the police drove the car to the hospital and on the ~ se~n<br />
limited to the Bath ambulance area, and the area covered<br />
was gradually expanded, especially <strong>in</strong>to the Somerset County<br />
the ambulance service returned me to the scene. On all 12<br />
ambulance area. This latter authority then provided a radio-<br />
occasions this help was arranged without del~y and without<br />
any personal <strong>in</strong>tervention.<br />
telephone on the county’s service wavelength.<br />
Special protective cloth<strong>in</strong>g aga<strong>in</strong>*t ~*!~ was found to be<br />
necessary on only one occasion, although a plastic mack<strong>in</strong>tosh<br />
EQUIPMENT<br />
was used <strong>in</strong> heavy ra<strong>in</strong>.<br />
RADIO<br />
The importance of radio contact with the ambulance ~rvice<br />
cannot be overemphasized. Poor communications sooa create<br />
problems <strong>in</strong> any situation, but even more so when tbere is a<br />
degree of urgency, and can then lead to poor relationshlps<br />
between departments. At first a simple radiotelephone was used,<br />
but later a more elaborate <strong>in</strong>stallation <strong>in</strong>cluded a selective<br />
call<strong>in</strong>g device to give automatic warn<strong>in</strong>g of an emergency call,<br />
a portable radio, a "talk-through" switch to enable me to speak<br />
direct to the accident ambulance, and a radio l<strong>in</strong>k to enable any<br />
mobile user or ambulance control to talk direct to the accident o<br />
department. The complete system was quickly accepted by<br />
users and on one occasion (accident 6) contributed to a patient’s<br />
survival, as ~ communication with the ambulance crew<br />
l<br />
i
)<br />
#<br />
4<br />
r ._<br />
!<br />
t<br />
!<br />
0<br />
"’enabled departure of the ambulance to be delayed until I<br />
arrived at the scene. The radio l<strong>in</strong>k with the hospital also<br />
elim<strong>in</strong>ated the delay <strong>in</strong> call<strong>in</strong>g out the accident fly<strong>in</strong>g squad,<br />
which before <strong>in</strong>stallatim <strong>in</strong>velved at least six calls <strong>in</strong> delays<br />
vary<strong>in</strong>g from two to eight m<strong>in</strong>mea.<br />
MEDICAL TREATMENT<br />
Treatment at the scene pr<strong>in</strong>cipally <strong>in</strong>volved hav<strong>in</strong>g the necessary<br />
equipment <strong>in</strong>stantly available very close to the patient,<br />
be<strong>in</strong>g completely familiar with its use, and hav<strong>in</strong>g one person to<br />
act as <strong>in</strong>formed help. The adaptation of resuscitation techniques<br />
to accidents has been described,’ as have the special problems<br />
with the extrication of trapped casualties.’ Dur<strong>in</strong>g the project<br />
it was found that the recognlticat of patterns of <strong>in</strong>jury related to<br />
vehicle damage was of value <strong>in</strong> assess<strong>in</strong>g patients when exam<strong>in</strong>ation<br />
was limited by poor ligh~g, limited access, or fur<br />
cloth<strong>in</strong>g. Entonox (50% oxygen and nitrous oxide) was used for<br />
pa<strong>in</strong> relief at the accident sces~ dur<strong>in</strong>g extrication and <strong>in</strong> the<br />
ambulance. Observatiom <strong>in</strong>clud<strong>in</strong>g pulse and blood pressure<br />
read<strong>in</strong>gs were made <strong>in</strong> 17 cases. Pa<strong>in</strong> relief was effective, rapid<br />
<strong>in</strong> onset, and free from side effects. Muscle spasm was relieved,<br />
bleed<strong>in</strong>g from wounds was not promoted, and the pulse and<br />
blood pressure read<strong>in</strong>gs showed no appreciable change. No<br />
difficulties were encountered when Entonox was given to the<br />
trapped patient held <strong>in</strong> the erect position.<br />
Detailed analysis of the 132 calls showed that 17 were to<br />
various <strong>in</strong>cidents <strong>in</strong>volv<strong>in</strong>g such locations as the river, civil<br />
eng<strong>in</strong>eer<strong>in</strong>g excavations, sewage works, certa<strong>in</strong> home accidents,<br />
and a light aircraft crash. The rema<strong>in</strong>der were to road accidents.<br />
The outcome of calls received and my location on receipt of the<br />
calls are shown <strong>in</strong> Tables I and IL<br />
¯ tam.l z--Outcor~ of the 132CallJ<br />
At <strong>in</strong>cident before del~mre d amb~ ..........<br />
R~ndezv~ with ambulance ............<br />
83<br />
No casualties found on arrival ......<br />
16<br />
ca~lt~ ~hay <strong>in</strong>iu~ ~ ~ "" ¯ ....... ~ ~ 9<br />
Malldous false alarm ................ 4<br />
Unable I0 reach accident <strong>in</strong><br />
1<br />
Distance and time dehy <strong>in</strong> mI .............. 9<br />
Time delay <strong>in</strong> call ............<br />
Distance too great .... 5<br />
~" ""<br />
Po~ ommuni,:adom . "" "" ¯ ..... 2<br />
W~oas ~a~a,atlon f:om ~ ~ ............ 2<br />
oo .... oo .. oo |<br />
~’T.e~...m~ "- .... ....<br />
On~w~..ho, pi~(~.--"-)<br />
",s<br />
LRaa~ ~dt._~ November 1970 .. 5<br />
f~d~,~ .~ .~m .,us~ .... ss<br />
O~du~gaom "ml 108cab)~, ~ .~ ., -re.car ......<br />
34,<br />
( - troru~ ra~o~ ...... I<br />
LTc~-p~me at ~ ~ .... 18<br />
The cars were distributed fairly evenly throughout the project.,<br />
averag<strong>in</strong>g one call every 9-5 days. The <strong>in</strong>cidence of cars<br />
was highest around 12 nmm and between 5 p.m. and 7 p.m. and<br />
11 p.m. and 12 midnigi~ and the <strong>in</strong>cidence of calls was much<br />
higher on Fridays and Saturdays (Figs. 2 and 3). The average<br />
time taken to deal with ese2a call ~ 31 m<strong>in</strong>m~b represent<strong>in</strong>g an<br />
i<br />
- ~o. 2--Dimilmtim of .a~ dmmShout the day.<br />
z<br />
30,<br />
25,<br />
20<br />
~- 15<br />
5<br />
0 H T WT<br />
D~<br />
:7.;<br />
a-(:.<br />
?/.<br />
J F H A H J J A SOND<br />
Month<br />
r~o. 3---Incidence of calls on different days and <strong>in</strong> different months<br />
throughout the year.<br />
571<br />
average work load of 22 mmutes a week. The time taken to<br />
clean equipment after use and make a weekly <strong>in</strong>spection averaged<br />
43 m<strong>in</strong>utes. The average time taken weekly to answer calls and<br />
to clean and ma<strong>in</strong>ta<strong>in</strong> equipment was therefore 65 m<strong>in</strong>utes.<br />
This is to be regarded as a m<strong>in</strong>imum as it does not take <strong>in</strong>to<br />
account keep<strong>in</strong>g records, follow<strong>in</strong>g up case histories, correspondence,<br />
and other duties.<br />
The average time taken for the ambulance to reach the scene<br />
was 8 m<strong>in</strong>utes and for the accident fly<strong>in</strong>g squad 9-5 m<strong>in</strong>utes<br />
(Table III). When these figures are compared with the earfier<br />
f<strong>in</strong>d<strong>in</strong>gs relat<strong>in</strong>g to the outcome of calls they show that where the<br />
TASLe lll---M~an Time spent on Calls and Mean Distance Covtrcd<br />
Time spent on each call ...... 31 (ranm- 4-143~ ra<strong>in</strong>, ~--<br />
Time ambulance took to teach scene "" 8 (range 1 20~" m<strong>in</strong>uT w~<br />
T.ime acci_d~lt fly<strong>in</strong>g squad took to reach scene :: 9"5 (range 1’22) m<strong>in</strong>Ut ~-~<br />
~me spent az,s~e .. -._ ...... 14t (range 2-132) m<strong>in</strong>utes<br />
~tstan. ce traveuea to scene 4.~ (range 0"25o13-5) miles (7.5 (range 0-4-21.7) k<strong>in</strong>)<br />
1oral cttstance travelled 10-3 (range 0-5-29.5) miles (16.5 (range 0-8-47-5~ kn0<br />
call for medical aid was received at an early stage it was possible<br />
to arrive <strong>in</strong> time to offer medical help <strong>in</strong> about 90% of the cases.<br />
The closeness of the ambulance and accident fly<strong>in</strong>g squad<br />
attendance times was due to the ability to mobilize rapidly<br />
after an immediate alert.<br />
Active medical treatment of casualties was undertaken on 22<br />
occasions. In addition two calls <strong>in</strong>volved meet<strong>in</strong>g the ambulance<br />
at hospital for treatment, seven <strong>in</strong>cluded help <strong>in</strong> assessment of<br />
handi<strong>in</strong>g, one concerned advice <strong>in</strong> the management of brom<strong>in</strong>e<br />
burns and <strong>in</strong>halation, and one call <strong>in</strong>volved sort<strong>in</strong>g priorities at a<br />
coach crash." Advice was given at a further five accidents <strong>in</strong><br />
which casualties were trapped and <strong>in</strong>jured but did not require<br />
medical treatment.<br />
Altogether there were 302 casualties, of whom 140 were<br />
slightly <strong>in</strong>jured and 128 seriously <strong>in</strong>jured. Among the latter<br />
there were 34 deaths~25 at the scene and 9 <strong>in</strong> hospital. No<br />
patients died <strong>in</strong> the ambulance. Thirty-three accidents <strong>in</strong>volved<br />
41 casualties be<strong>in</strong>g trapped; of these 18 were seriously <strong>in</strong>jured<br />
and 8 fatally <strong>in</strong>jured. Of the 37 casualties trapped <strong>in</strong> road<br />
accidents 23 were held by the lower limbs, and the mean time<br />
taken to release them was 29 m<strong>in</strong>utes. Although many of the<br />
accidents <strong>in</strong>volved two or more seriously <strong>in</strong>jured casualtiea)<br />
only on one occasion was it particularly difficult to cope with t_~<br />
problems encountered. In this <strong>in</strong>stance three casmdties were<br />
trapped and seriously <strong>in</strong>jured, two <strong>in</strong> one vehicle and one <strong>in</strong> the<br />
other, and this stretched medical resources to the limit. Medical<br />
attendance was therefore of direct value at 38 accidents, or <strong>in</strong><br />
1 <strong>in</strong> 3.5 calls.<br />
Patients who received def<strong>in</strong>itive medical treatment can be<br />
fm~daer aubdi~ded to show where it was probably possible to<br />
prevent a fatal outcome. Six of the casualties would virtuafiy<br />
certa<strong>in</strong>ly have died had they not received this early medical<br />
tremanent, and <strong>in</strong> a further four cases medical treatment made a<br />
major conm~bution to survival. In six <strong>in</strong>stances resuscitation was<br />
unsuccessful, and <strong>in</strong> six medical treatment was of value.<br />
The type of treatment and advice given at the sc~es of the 22<br />
accidents is shown <strong>in</strong> Table IV.
572<br />
¯<br />
:: :: :: :: :: :: :: 2<br />
"" o. 2<br />
Cardiac monitor<strong>in</strong>g ..................<br />
Endotracheai <strong>in</strong>tubation ..........<br />
4<br />
4<br />
nu~vcnous ~ ................<br />
Surgery .. ., ..............<br />
Amputa~on ....<br />
5<br />
6<br />
1<br />
Manipulation of fractug~ ................ 4<br />
Entonox adm<strong>in</strong>istration .............. ..<br />
g<br />
Aspiration of aizway .................. 11<br />
Oxygen admln~tntion ................ 11<br />
First aid before arrival of ambulance ............ 14<br />
General advice .................. 15<br />
Case Reports<br />
MEDICAL TltBAT~ ~SPONSIBLE FOR SURVIVAL<br />
<strong>Accident</strong> I.--A 56-year-old driver collapsed <strong>in</strong> his car. A displaced<br />
denture plate partially obstructed his airway at first, then<br />
completely, with deep cyanosls and muscle spasm hold<strong>in</strong>g the<br />
teeth together. A gag, laryngoscope., and other <strong>in</strong>struments were<br />
used m remove the obstruction, and the aspirator and oxygen<br />
were also used. F<strong>in</strong>al diagnosis: myocardlal <strong>in</strong>farction. He was<br />
eventually discharged.<br />
<strong>Accident</strong> 2.--A 16-year-old motorcyclist was found unconscious<br />
beside his motorcycle and ly<strong>in</strong>g on his back on a steep <strong>in</strong>cl<strong>in</strong>e.<br />
Before the arrival of the ambulance and just after be<strong>in</strong>g turned<br />
on to his side he vomited and the aspirator was required to clear<br />
his airway. Outcome: complete recovery.<br />
<strong>Accident</strong> 3.----A 51-year-old driver was trapped <strong>in</strong> a van after<br />
a collision with a lorry (’Fig. 4). Injuries were: compound fracture<br />
dislocation of talonavicular jo<strong>in</strong>t; compound comm<strong>in</strong>uted fracture<br />
of left u~ia and fibula, with extensive soft-tissue lacerations;<br />
haemarthrosis of left knee; compound commlnuted fracture of left<br />
femur; fractured acetabular rim, acetabulum, and pubic rami;<br />
fractured ribs; lacerations of face, scalp, left hand, and right<br />
knee. Treatment at scene: transfusion of I L of Macrodex, use of<br />
other. Medical aid <strong>in</strong>cluded l~andl<strong>in</strong>g of displaced compound<br />
fractures and the use of the aspirator and oxygen. One Patient<br />
was given 1 litra of <strong>in</strong>travenous Macrodex (and 5 bottles H blood<br />
later) for <strong>in</strong>juries which <strong>in</strong>cluded fractures of the right radius and<br />
ulna, femur, tibia and fibula, ankle, and foot, closed fractu~s ot<br />
the ribs, and lacerations or the left lower leg, right arm, and scalp.<br />
The patients made good recoveries.<br />
<strong>Accident</strong> 6.---A pedestrian aged 22 was <strong>in</strong> mllision with a car.<br />
He was unconscious, and his <strong>in</strong>juries <strong>in</strong>cluded a compound fracture<br />
of the left tibia and fibula, gross disorganization of the soft :i~,<br />
and right tibia and fibula, a compound ¢omn,Jn~ fractu~ of<br />
the right femoral shah and pertrochtmtcric ~ of the neck<br />
of femur, fractuz~ of the sculpula, ribs, and hand, and multiple<br />
face and scalp lacerations. Tff.- ambulance was <strong>in</strong>structed personally<br />
to await my arrival. An <strong>in</strong>fusion was set up and 500 ml<br />
of Macrodex pumped <strong>in</strong>. The severely damaged leg was wrapped<br />
<strong>in</strong> a sterile sheet and placed <strong>in</strong> an <strong>in</strong>flatable, hdl-leg spl<strong>in</strong>t applied<br />
at maximum pressure. Dur<strong>in</strong>g the journey to hospital the ambulance<br />
had to be stopped when the systolic blood pressure dropped<br />
from 70 to 50 mm Hg, and a further 500 ml of Macredex was<br />
transfused rapidly. Further <strong>in</strong>fusion <strong>in</strong> hospital <strong>in</strong>cluded 2 bottles<br />
of plasma and 7 bottles of blood. Amputation of the right leg<br />
b.’Iow the knee was followed by full recovery.<br />
MEDICAL TI~ATMID4T CO~uTnqG TO SURVIVAL<br />
<strong>Accident</strong> 7.---A member of the emergency services collapsed<br />
near a ruptured gas meter when on an emergency fire call and<br />
was unconscious and breath<strong>in</strong>g irregularly when brought out of<br />
the gas-filled build<strong>in</strong>g. He was ventilated with oxygen and connected<br />
to a cardiac monitor, which showed ischaemic changes.<br />
The aspiiator was used m keep the airway clear and oxygen was<br />
given by mask. A period of heavy, central chest pa<strong>in</strong> was followed<br />
by full recovery.<br />
<strong>Accident</strong> 8.--A 19-year-old motorcyclist was <strong>in</strong> collision with<br />
a pedestrian and was seen before the arrival of the ambulance.<br />
He was unconscious and bleed<strong>in</strong>g from the nose, ch<strong>in</strong>, and broken<br />
front tooth sockets. The airway was cleared with the aspirator<br />
(the attend<strong>in</strong>g county ambulance was not equipped with an<br />
aspirator). He eventually made a full recovery.<br />
<strong>Accident</strong> 9.--Two motorcyclists were <strong>in</strong> collision. One aged<br />
24 was unconscious from head <strong>in</strong>juries, and both had compound<br />
fractures of the lower limba. One r~lUired the use of the aspirator<br />
before arrival of the ambulance.<br />
<strong>Accident</strong> IO.--A car driver aged 20 received severe facial <strong>in</strong>juries<br />
<strong>in</strong> a collision with a lorry and was uncon_~-~-~ous. Repeated use<br />
of the aspirator ma<strong>in</strong>ta<strong>in</strong>ed the airway <strong>in</strong> tlg presence of compound<br />
malar and mandibular fractures, displacement of teeth, and<br />
severe facial lacerations. Oxygen was also used. The patient made<br />
a full recovery.<br />
OOMMLner<br />
The op<strong>in</strong>ion that Hves can be saved by early medical treatment<br />
is supported by several necropsy studies. Mackay’ suggested<br />
that 43% of fatally-<strong>in</strong>jured casualties might have had a greater<br />
chance of survival ff medical treatment had been available at the<br />
scene of the accident with<strong>in</strong> l0 m<strong>in</strong>utes. A World Health<br />
Organization report estimated that 15% of early road deaths<br />
lqO. 4--Accide=t 3, show<strong>in</strong>g rescue and resuscitation. (By k<strong>in</strong>d were due to respiratory obstruction. Lauppi," <strong>in</strong> a Series of 300<br />
permission of Bath Evenir~ Chroalde.)<br />
necropsies on road-accident casualties dy<strong>in</strong>g with<strong>in</strong> 48 hours of<br />
mjury, reported that <strong>in</strong> 14"3% respiratory obswaction was the<br />
aspirator and oxygen, manipulation of trapped and fractured legsole<br />
cause of "death. In another series Ruffel-Smith<br />
to permit earlier release, and application of long leg <strong>in</strong>flatable<br />
spl<strong>in</strong>L Outcome: full recovery after treatment, which <strong>in</strong>cluded<br />
transfusion of 2 bottles of plasma and 11 bottles of blood.<br />
<strong>Accident</strong> 4.--A pedestrian aged 20 was struck by a car at night<br />
and thrown through a hedge <strong>in</strong>to a field. He susta<strong>in</strong>ed compound<br />
fractures of the mandible and right tibia and fibula. He was<br />
unconscious and cyanosed and the airway was full of frothy blood.<br />
Immediate use of the aspirator followed by <strong>in</strong>tubadon and tracheal<br />
aspiration cleared the airway without stimulation of reflexes.<br />
Oxygen was also given. He rega<strong>in</strong>ed consciousness on the third<br />
day and recovered fully.<br />
<strong>Accident</strong> 5.--Three casualties aged between 25 and 35 were<br />
trapped and seriously <strong>in</strong>jured, two <strong>in</strong> one vehicle and one <strong>in</strong> the<br />
t" showed<br />
the <strong>in</strong>cidence to be 5%. To the last three series could be added<br />
casualties dy<strong>in</strong>g of blood loss and other reversible causes.<br />
In a series of 34 fatalities it might be reasonably expected that<br />
some deaths would be due to asphyxia or blood loss <strong>in</strong> the<br />
absence of <strong>in</strong>jury <strong>in</strong>compatible with survival. In review<strong>in</strong>g the<br />
necropsy series of this project no such evidence was found,<br />
though if medical treatment had not been available at all the 132<br />
accidents probably examples would then have been seen. Should<br />
the figure of six casualties saved seem a high proportion allowance<br />
must be made that not only is this a selected group of<br />
accidents but also that it conta<strong>in</strong>s accidents <strong>in</strong> situations beside*<br />
those occurr<strong>in</strong>g on the road.
O<br />
mu-risH MEDXC.~ JOURNAL 2 ~ 1972<br />
¯ Not all accidents <strong>in</strong> the hospital cl<strong>in</strong>ical area were attended,<br />
and so eases not <strong>in</strong>volved <strong>in</strong> this project could be regarded as a<br />
form of "control." A review of all the necropsies <strong>in</strong> this series<br />
was not possible, but from cases seen dur<strong>in</strong>g normal hospital<br />
employment there were three examples of patients who died<br />
from reversible causes, one from asphyxia and two from blood<br />
loss.<br />
Cost<br />
573<br />
free passage through traffic, and good communications. The<br />
policy of organiz<strong>in</strong>g mecLical aid to be available on request,<br />
work<strong>in</strong>g at the scene with the ambulancemen, and tra<strong>in</strong><strong>in</strong>g<br />
them to help rather than tak<strong>in</strong>g a team of assistants was also<br />
important. The area covered was pr<strong>in</strong>cipally that of one ambulance<br />
service, though <strong>in</strong> the <strong>in</strong>stance of accidents <strong>in</strong>volv<strong>in</strong>g<br />
multiple or trapped casualties the area that could be covered<br />
was shown to be greatly extended. The average distance to the<br />
accident scene was under 5 miles (8 k<strong>in</strong>), <strong>in</strong>dicat<strong>in</strong>g that certa<strong>in</strong><br />
patients could still benefit from medical attendance even though<br />
The runn<strong>in</strong>g expenses for the three-and-a-half-years are shown<br />
<strong>in</strong> Table V.<br />
When the capital cost of £927-19i for all the equipment<br />
(see Appendix) is added to the runn<strong>in</strong>g expenses for the threeand-a-half-year<br />
period the total cost is £1,086.71~. Nevertheless,<br />
r~ v--Rum, i~ Bxpema over the Thru-and-a-~-year Pm~d<br />
the ambulance journey time to hospital was relatively short.<br />
such a scheme, if hospital-based, could usefully act as the<br />
nucleus of a scheme <strong>in</strong>volv<strong>in</strong>g and support<strong>in</strong>g peripheral<br />
general-practitioner schemes and would also have appfieation <strong>in</strong><br />
the field of motorway and "major accident" <strong>in</strong>cidents.<br />
The organization of such a scheme is seen as a logical development<br />
of the properly established and <strong>in</strong>dependent accident and<br />
emergency specialty, and shows that the patient’s arrival at the<br />
accident department is not the earliest stage at which medical<br />
P.,dioUc~cc ......<br />
Radio ma<strong>in</strong>temm~ ................<br />
Inturanc* ...................<br />
Batteriea ....................<br />
Petrol ..................<br />
~: -~ :~ :~ "" ::<br />
Total<br />
s-Ts <strong>in</strong>volvement should be directed.<br />
38.75<br />
17"85 This research is based on an M.D. thesis accepted by the<br />
16-80<br />
56"44 University of Bristol <strong>in</strong> 1972 and supported by a grant from<br />
the Peel Medical Research Trust. Acknowledgement is also due<br />
159"52<br />
to the support of the Bath City Council and the medical officer<br />
of health, Dr. R. M. Ross, and the consultants and staff of the<br />
accident departments of St. Mart<strong>in</strong>’s and the Royal United<br />
Hospitals, Bath, and the many firms that donated equipment<br />
to the tcheme.<br />
as all the items of equipment could reasonably be expected to<br />
last for seven years at least, the capital cost could more realisticaily<br />
be spread over that time. If the runn<strong>in</strong>g expenses were to<br />
cont<strong>in</strong>ue at the same level the cost per year would be reduced<br />
from £310-49. (over three-and-a-half-years) to £178-03 (over<br />
seven years). Even the latter could be reduced to £103.60½ by<br />
exclusion of six non-essential items (cardiac monitor, dictaphone,<br />
camera, selective call option on. radiotelephone, tra~cfight<br />
switch, and studded tyres)-<br />
To these figures would have to be added the cost of medical<br />
staff<strong>in</strong>g. This is not easy to assess, however, as only 15% of<br />
calls occurred when I was on duty. A more realistic comparison<br />
could be made with the fees payable to a police surgeon.<br />
With an average of 38 calls a year and an arbitrary fee of £5 a<br />
call this would represent an attendance expense of £190 a year<br />
and an annual reta<strong>in</strong><strong>in</strong>g fee of £100 (at B.M.A. recommended<br />
rates). This would result <strong>in</strong> a total cost per call of £15-86, which<br />
compares very favourably with the average cost per emergency<br />
ambulance call, calculated by the Department of the Environment<br />
to be £15. Us<strong>in</strong>g the Road Research Laboratories cost<strong>in</strong>gs<br />
of road accidents n ts a comparison can be made between the<br />
actual cost of sav<strong>in</strong>g a life by the provision of medical aid and<br />
the overall sav<strong>in</strong>g to the community as a result of reclassify<strong>in</strong>g<br />
that casualty as a serious <strong>in</strong>jury <strong>in</strong>stead of a fatal <strong>in</strong>jury. The<br />
1970 cost<strong>in</strong>g, for fatal <strong>in</strong>jury are £16,809 and for serious <strong>in</strong>jury<br />
£910. These figures represent medical expeusess loss of output,<br />
atxd subj .e~.’ve losses, and the difference of £15,899 represents<br />
the f<strong>in</strong>ancial savmg that results from prevent<strong>in</strong>g a fatal outcome.<br />
Only five of the six casualties saved <strong>in</strong> this series were <strong>in</strong> fact<br />
<strong>in</strong>volved <strong>in</strong> road accidents~ represent<strong>in</strong>g an annual sav<strong>in</strong>g of<br />
1-43 fives. If the figure of £15,899 it multiplied by this factor<br />
and then the total cost of provid<strong>in</strong>g these special medical services,<br />
<strong>in</strong>clud<strong>in</strong>g feet and reta<strong>in</strong>er, is the~ deducted the net annual<br />
sav<strong>in</strong>g to the community <strong>in</strong> provid<strong>in</strong>g th/s sezvice can be<br />
calculated m ~2,135. (T!aa rpl]dity of this cost<strong>in</strong>g <strong>in</strong>terpretation<br />
ha- ~.-m ~a~mled with the ~oad Research Laboratory.)<br />
This scheme was easily organized, <strong>in</strong>expemive, and effective.<br />
Its orgtuimtion would allow it to be based on a hospital or<br />
general practice and did not <strong>in</strong>terfere with other employment.<br />
Moreover, the esther <strong>in</strong>volvement with the patient often made<br />
the diagnosh and treatment less time consum<strong>in</strong>g on return to<br />
the hospk<br />
The success ~ the scheme depended on rapid mobilization,<br />
References<br />
t Hall, H. H., Lancet, 1965, 1, 904.<br />
¯Coll<strong>in</strong>s, J., British Medical Journal, 1966, 2, 578.<br />
¯ J~aston, K., Community. Health, 1970, 2, 81.<br />
: Gogler, E., Ro~.. Aeddents. Manchester, Geigy (U.K.), 1965.<br />
, ",nook, R., M~.cal and Biological Illustration, 1971, 21, 66.<br />
, S~oo.k, ~noot% it., R., lJriu’sh Bri~ Mech’cal ,U~ai~alyo,,.,a, Journal, 1969, 1~, 4, 4, 478.<br />
s Mackay, G. M., British MedicalJournai, 1969, 4, 799.<br />
." Laupptk E.,.S~_wd_z~sc.~ mediz<strong>in</strong>i~ gr~3totsd~’ft, 1954, 335<br />
-- Kune~-.-,mim, ti. p., In/u-y, 1970, 2, 99.<br />
84, .<br />
tt Dawson, R. F. F., Cost of Road Aeddmlu <strong>in</strong> Grmt Brita<strong>in</strong>, Road Research<br />
Laboratory Report LR79. 1967.<br />
Dawson, Kesoarcn .R.F.F., Latmratory Curr_em Report Cost_of LR 396, Road 1971.. Acddosts <strong>in</strong> Great Brita<strong>in</strong>, Road<br />
Appendix<br />
Cost of Equipment (at Time of Purc.hau)<br />
¯ Resuscitation box pa<strong>in</strong>ted white with reflective ~ band and doct~ £<br />
label.<br />
~.....er and two Ysnkath~ msctio~ mmm~ ¯ ¯ 17.9~.<br />
........<br />
P map ~ mat~ mmmt-~ ~ .............. 1241<br />
10.00<br />
ro~ mtravenotm eannulae and mp.-tiem mthetmm ...... ¯ II-15<br />
0.55J<br />
~th <strong>in</strong>trave~m cannulae ( x @ .... ""<br />
p ~ m~us~ (x @ :. :. .... Hs<br />
M.S..A. elbow lmmobiltmr .......... "" "" 5.7o<br />
¯<br />
...........<br />
~.~o<br />
I~ve~ - practifio~nr ~ ........ "" "" 22~0<br />
D ~.~. mnm~ ~ tim ........ um~ ........<br />
-: .. .- .. ~<br />
.... I.$4<br />
.. ,. .. .. ..<br />
Blood cro~mtch mb~ (ho~ml m.om~) .~ ...... 0-25<br />
ecu’oct~ .. ¯ ......... 277.47j<br />
t.om~ (pmmix~. nitrous ostdedogTgta ~ ~ tlk ~llmktt.<br />
-<br />
r2tepma,<br />
vatve,<br />
tic<br />
mmr,,<br />
spl<strong>in</strong>ts<br />
aria<br />
.........<br />
mou~ ....... " - - .... ---- 2"/-5@<br />
. .~oen~.. ton burro drm<strong>in</strong>~ ..... : ......<br />
7.~o<br />
4-25<br />
sp~a bom~U ma mm~ prm mmm~ m,~a mu~ :: :: -- ~v~
Blankets (I wool and. 1 hest-reudai~ foil) ..........<br />
2-90<br />
First-aid kit of dressms~ .btndage, st<strong>in</strong>gs, etc. ........<br />
1.50<br />
..<br />
Rel~eggiv¢ w~.’$t¢oat-type.’l~t~ .... . 2" .... "fL. ..<br />
5"00<br />
4 Wm’n<strong>in</strong>g trumgles (special p y K2.qt| gscnj .... 2-00<br />
Large lured-torch ........ . "" -- "" " " " s~l<br />
2"15<br />
.M<strong>in</strong>or rescue equipment <strong>in</strong>dud<strong>in</strong>s: hacksaw, lemmy tn~ too~ mpem<br />
oo oo oo .. oo oo oo<br />
Mbestos Zloves 2-00<br />
Fire ext<strong>in</strong>guisher .......... .. .. .. 0"92t<br />
12-voh floodlight ............<br />
.. .. 12-00<br />
blediflash ..................<br />
6.30<br />
Medical Aspects of Ambulance Design<br />
ROGER SNOOK<br />
British Medlc.alyoumal, 1972~ 3, 574-578<br />
Summary<br />
Various observations have shown that the <strong>in</strong>terior layout<br />
of many ambulances leaves much to be desired. The<br />
light<strong>in</strong>g levels are <strong>in</strong>adequate, heat loss could be prevehicle<br />
identification and passage through.<br />
could be improved, and measurable differences<br />
exist between the ride characteristics of commercially<br />
available ambulances~ a prototype purpose-built ambulance,<br />
and a private car. Moreover the condition of some<br />
patients may be affected by the motion of the vehicle<br />
either directly or <strong>in</strong>directly. Even though they form a<br />
small percentage of the total number carried, they<br />
represent a very considerable f<strong>in</strong>ancial risk. A personally<br />
conducted survey of ambulance chief officers showed<br />
a deep <strong>in</strong>terest and <strong>in</strong>volvement <strong>in</strong> the upgrad<strong>in</strong>g of the<br />
service with a general dissatisfaction with many of the<br />
vehicles currently available. Hence there is a market for<br />
the purpose-built ambulance, which would benefit the<br />
patient and the ambulanceman alike.<br />
The <strong>in</strong>adequacies of many vehicles currently <strong>in</strong> use as<br />
ambulances have been shown to work aga<strong>in</strong>st the <strong>in</strong>terests<br />
of the patient requir<strong>in</strong>g life support treatment~ and it is<br />
suggested that this warrants urgent attention and action.<br />
A more extensive research project <strong>in</strong>volv<strong>in</strong>g medical<br />
observations on the sup<strong>in</strong>e sick and <strong>in</strong>jured, attendant<br />
task performance, and <strong>in</strong>strumentation analysis of<br />
ear and angular vehicle motions should enable the<br />
~r<br />
mful effects of ride motion to be identified.<br />
None of these <strong>in</strong>vestigations, however, will be of any<br />
value unless they are used <strong>in</strong> develop<strong>in</strong>g future ambulances.<br />
Such development must also parallel an <strong>in</strong>crease<br />
<strong>in</strong> the awareness of the importance bf ambulance design<br />
and its relation to the <strong>in</strong>creased comfort and chance of<br />
survival of the pade~te carried.<br />
There has been relatively tittle research <strong>in</strong>to medical aspects of<br />
ambulance design. With the notable exception of Bothwell’s<br />
patented ambulance specification ~’ most of the published<br />
papers relate to general or outl<strong>in</strong>e specifications of future design<br />
requirements or simply draw attention to the <strong>in</strong>adequacy of<br />
exist<strong>in</strong>g design. London s has said, "although the need for<br />
special ambulances is negligibly small on a commercial scale<br />
this fact does noth<strong>in</strong>g to ease the discomfort of the person<br />
travell<strong>in</strong>g <strong>in</strong> a vehicle designed without the least regard for the<br />
effects of illness and <strong>in</strong>jury." The Committee on Acute Medic<strong>in</strong>e<br />
of the American Society of Anaesthesiologist ss reported that<br />
<strong>Accident</strong> and Ambulance Research, Dunkerton~ Bath<br />
ROGER SNOOK,.M.D., <strong>Accident</strong> Medical Offlcer m Bath Fire Brigade and<br />
Ambulance Servtce<br />
"most vehicles presently /n ~ are uiI~thfa~ory fo~ life<br />
support." ..... " -" .’,<br />
Experience with travell<strong>in</strong>g with patients <strong>in</strong> the ambulance<br />
dur<strong>in</strong>g the research project on provid<strong>in</strong>g medical aid at an<br />
accident s and on <strong>in</strong>terhospital emergency mmsfen <strong>in</strong>dicated<br />
that further <strong>in</strong>vestigations of the ambulance environment were<br />
needed. This paper describes the results of personal observations<br />
and <strong>in</strong>vestigations of such factors as the heat<strong>in</strong>g, light<strong>in</strong>g, sound<br />
<strong>in</strong>sulation, identification, and vehicle motion with reference to<br />
the trearment~ comfort, or condition of the patient. The observations<br />
were made on a variety of commercially available ambulances<br />
<strong>in</strong> service with several local authorities.<br />
The positions <strong>in</strong> the ambulances at which various <strong>in</strong>strament<br />
read<strong>in</strong>gs were taken are <strong>in</strong>dicated <strong>in</strong> Fig. 1.<br />
FIG. 1--Positions <strong>in</strong> ambulancesuwhich various <strong>in</strong>strument read<strong>in</strong>gs were<br />
taken. Measurements taken at pmdtms <strong>in</strong>di.cated .were:.l. T~’~. 2.<br />
Light and sotmd. 3. Vibradon over axle. 4. Vtbrauon wmua wnecma . 5.<br />
Vi[~ration on patiea~s leg. 6. Hot ak curta<strong>in</strong> updraught.<br />
General Destgn<br />
Ambulances transport a variety of patienub <strong>in</strong>clud<strong>in</strong>g sitt<strong>in</strong>g"<br />
cases and rout<strong>in</strong>e and emergency stretcher case~ and so the<br />
<strong>in</strong>terior requirements of the vehiclea vary correspond<strong>in</strong>gly.<br />
The <strong>in</strong>terior layout of most ambulances is <strong>in</strong>flex~ie and makes<br />
treatment of the patient dur<strong>in</strong>g .transit unnecessarily ditficult.<br />
For example, when resuscitation or supportive measures are<br />
required dur<strong>in</strong>g a journey it is an advantage to have the m~cher<br />
centrally mounted. In most presentday ambulances the attendant<br />
either stands or kneels on the floor alongside the stretcher,<br />
which is mounted along the sidewall of the patient ompartment<br />
(Fig, 2).<br />
Ideally the attend<strong>in</strong>g ambulanceman or doctor should be able<br />
to sit at the patient’s head to operate aspiration or ventilation<br />
equipment. To place this attendant’s seat so that it faces<br />
rearward <strong>in</strong>volves mov<strong>in</strong>g the patient nearer to or directly over<br />
the rear axle. By revers<strong>in</strong>g the position of patient and attendant<br />
the former would rema<strong>in</strong> with<strong>in</strong> the wheelbase and the latter<br />
would be able to see where he was go<strong>in</strong>g. This would make it<br />
easier to perform delicate tasks such as <strong>in</strong>sert<strong>in</strong>g an aspirator<br />
mount <strong>in</strong>to the patient’s pharynx, besides reduc<strong>in</strong>g the likeli-<br />
1<br />
t
^<br />
468 THE LANCe"T, FEBRUARY27) 1988
THE LANCET, FEBRUARy 27, 1988<br />
469
578 3 September 1966 Medical Emigration-iSeale<br />
eac~ subsequent year it has fallen at an accelerat<strong>in</strong>g rate. By<br />
1965 there were 750 fewer general practitioners than <strong>in</strong> 1960,<br />
but by 1965 the number from o~¢,seas had ~"2.., t: ~*150 (46%<br />
aearly all of the fall occurr<strong>in</strong>g after 1962. In the early 1950s,<br />
of the total).<br />
Large-scale medical emigration has been a significant aspect<br />
on300theto other400 perhand’year.the~ general practitioners were <strong>in</strong>creas<strong>in</strong>g by of British medic<strong>in</strong>e for over 10 years, and is now a major factor =<br />
¯ contr~ut<strong>in</strong>g to the dw<strong>in</strong>dl<strong>in</strong>g supply of fully tra<strong>in</strong>ed medical ~i¯ I<br />
The number of consultants (exclud<strong>in</strong>g honorary staff and /<br />
locumtenents) <strong>in</strong> England and Wales <strong>in</strong>cttased by 1,034 manpower <strong>in</strong> Brita<strong>in</strong>. In 1964 Professor Abel-Smith wrote<br />
that the loss by emigration of the equivalent of nearly one-<br />
:<br />
between 1962 and 1965, but this was largely offset by a fall of<br />
quarter of the output of the medical schools "’can be regarded ~<br />
933 <strong>in</strong> the number of senior hospital medical officers <strong>in</strong> the<br />
same period,<br />
as a serious matter." In the year 1965 the rate appears to have<br />
risen to one-third of the output of the schools.<br />
In 1960 there were 8,100 junior hospital doctors of registrar ,,<br />
. l<br />
.<br />
grade or below <strong>in</strong> England and Wales. ~y 1965 the number . ~~,<br />
i _~ _ii~ had risen by 2,100, but 1,750 of this <strong>in</strong>crease was due to an<br />
<strong>in</strong>crease <strong>in</strong> doctors born outside the British. Isles. Between Abel~aire~ B’dodi~G~(.lSCvtO. Brias/t Docaz,, a~ Hem, tad =<br />
1962 and 1965 the number of British-born doctors of junior (1964b). B~. mad. Y.,~L<br />
Brit. m,d. y. SutWt.o l~S2o 2, 15.<br />
.<br />
~xspital grades fell by 80. The <strong>in</strong>creas<strong>in</strong>g dependence of the Brit. r~d. y., 1964, 2, 1.<br />
. - !!_<br />
~ospital service upon doctors from overseas is shown by the Overi~diV~ra~on !k~rd (1965). Smiui~ ter 196, ~. ’. ~I42~, ~i."<br />
:act that <strong>in</strong> 1960 2,890 junior hospital doctors <strong>in</strong> England and Scale, I. R. (1962). Brit. mad. y., !, 782. i~<br />
::~ 3~~<br />
~¢ales were born outside the British Isles (36% Of the total), ~ (1964). IbkL, L 1173, .,,<br />
Whitfield, A. G. W. (1963). Lamel, 2. 874.<br />
, " ""~’~4<br />
@<br />
tit. wed. 2F., 1966, 2, 578-.580<br />
/ -.- , ;L |<br />
Organization and Function of an <strong>Accident</strong> Fly<strong>in</strong>g Squad<br />
JOHN COLLINS,* M.B., CH.B., M.ILC.S., L.R.C.P.<br />
X’te first pr<strong>in</strong>ciple for deal<strong>in</strong>g with the seriously <strong>in</strong>~ is to<br />
xnmence treatment as soon as possible. This is most impor-<br />
,nt when urgent resuscitation is required, as with the severely<br />
rocked patient. The accident fly<strong>in</strong>g squad was developed<br />
i this basis, but the team should also be capable of deal<strong>in</strong>g with<br />
~y emergency which requires treatment at the scene of the<br />
cident. The team should be equipped to carry out essential<br />
r~ry, but this should be limited to the m<strong>in</strong>imum necessary,<br />
obviously the place for surgery is under the ideal conditions<br />
the o~.rat<strong>in</strong>g theatre.. The fly<strong>in</strong>g squad should reach ~he<br />
dent ~luickly as poss~le with t~ necessary surgical aid.<br />
The concept of the fly<strong>in</strong>g squad is not a new one. In<br />
many, when the autobahnen were built the seve~ type of<br />
ury which resulted from high-speed accidents demanded a<br />
w organization for their treatment, and mobile operat<strong>in</strong>g<br />
mires were developed. At one time a similar scheme was<br />
roduced by, the Birm<strong>in</strong>gham <strong>Accident</strong> Hospital. Apparently<br />
: ma<strong>in</strong> drawbacks to these schemes were the size and relative<br />
wness of the vehicles.<br />
rhe history of the Derby fly<strong>in</strong>g squad dates from 1955.<br />
a served by the Derbyshire Royal Infirmary is both urban and<br />
¯ al, <strong>in</strong> which there are large <strong>in</strong>dustrial and m<strong>in</strong><strong>in</strong>g concerns<br />
well as agricultural communities. There are also important<br />
works of roads and railways and an airport. Such an area,<br />
h a population of almost half a milliqn, has a considerable<br />
ident potentiaL Seriously <strong>in</strong>jured patients may have long<br />
lances to travel to ~ hospital, and it was considered reason-<br />
: to organize an accident fly<strong>in</strong>g squad based at the hospital,<br />
serve this community. Such "a team would be available to<br />
o<br />
aior Casualty O~icet, Derbyshire Royal Iafirmary.<br />
deal with any patient who might be at risk, because of the time<br />
delay, before reach<strong>in</strong>g surgical aid. The Derby scheme differs<br />
from the experiments <strong>in</strong> Germany and Birm<strong>in</strong>~_gham <strong>in</strong> that it is<br />
designed to treat all types of accident cases ; <strong>in</strong> eleven years the<br />
accent has been ma<strong>in</strong>ly on <strong>in</strong>dustrial <strong>in</strong>juries.<br />
-r mmt<br />
The first problem <strong>in</strong>volved when organiz<strong>in</strong>g the fly<strong>in</strong>g squad<br />
was to equip it adequalr.ly. There were no available standards<br />
for guidance, and a omprelamsive list w’aa pzelxu~ to cover<br />
all possible evennmfities. This list proved to be formidable, as<br />
many articles weire suggested which might be ~ but were<br />
. not essential. Capful prun<strong>in</strong>g t~hmed the r~l~ts con- -<br />
siderably, and eventually a list which appeared to be ~" ~,~.’:-~ i<br />
adequate was agreed. The mggetad immmm drt ames- i<br />
thetic equipment, dress<strong>in</strong>g& spl<strong>in</strong>ts, etc., were assembled to- :~ ....<br />
g~er to assess the amount of spa~_ they would occupy.<br />
This demonstrated that even further reduction was mcessary.<br />
By obta<strong>in</strong><strong>in</strong>g compreased dress<strong>in</strong>gs and m<strong>in</strong>iature equilanent, .i"<br />
where possible, space was saved. Paeumati: plastic spl<strong>in</strong>ts were "<br />
found to be space--sav<strong>in</strong>g and fight. With experience and use -;"<br />
some articles of equipment have been discarded and other) have ~ : ......<br />
been added. By consultation with other departmema, improvemerits<br />
<strong>in</strong> the equipment are onstantly be<strong>in</strong>g considered. On<br />
the whole simple apparatus has been found to be the best because<br />
of the ~ factors of transport and local conditiom. , It was<br />
found convenient to di~da the equipment <strong>in</strong>to two catelga’ies:<br />
the material which must always be taken and the .~’~ial imms ,- !<br />
which should be available when ~ ~eq~sd ~ =":: :’-:<br />
exit equipment ShOuld be <strong>in</strong>speclxal and checked at frecluent "":~<br />
¯ ¯ ° , " .., ":L-" ¯<br />
mtervah, the sur~cal <strong>in</strong>struments aad other such material ~ga-:
¯ 3 September 1966 " <strong>Accident</strong> Fly<strong>in</strong>gSquad--Coll<strong>in</strong>s<br />
579<br />
- trial concerns, m<strong>in</strong>es, and other vulnerable areas, and these are<br />
always available to drivers.<br />
The return journey can be, by comparison with the outward<br />
journey, a much more leisurdy affair. Ambulances are obta<strong>in</strong>ed<br />
¯ from the nearest station, and, although only moderate speeds<br />
are necessary, as the patient is then on treatment, the police<br />
complete their job by escort<strong>in</strong>g the ambulance back to the<br />
hospital.<br />
Certa<strong>in</strong> items of equipment are kept for special types of<br />
<strong>in</strong>cidents. The Siebe Gorman air-breath<strong>in</strong>g apparatus is available<br />
<strong>in</strong> the equipment cupboard for use when the team may be<br />
called to work <strong>in</strong> contam<strong>in</strong>ated or dangerous atmospheres, and<br />
additional masks ax’e available for the use of patients. This is<br />
the type of breath<strong>in</strong>g apparatus used by the fire services.<br />
Fluorescent suits for use on ma<strong>in</strong> roads and the motorway, as<br />
well as helmets and overalls, are available for the protection of<br />
the team when required. The Ambu ventilator and the footoperated<br />
Ambu sucker, which are conta<strong>in</strong>ed <strong>in</strong> a bold-all, are<br />
very convenient and compact. The Brook airway is extremely<br />
useful, and, as a result of its proved value to the Hy<strong>in</strong>g Squad,<br />
Staff<br />
all Derby Borough Police cars and ambulances are now equipped. The staff of the fly<strong>in</strong>g squad is supplied by the casualty<br />
with it. The Beaver ventilator, which is reasonably small anddepartment,<br />
with assistance from other departments. A member<br />
portable, has been adapted for use at the scene of an accident. of the casualty unit, an anaesthetist or another doctor, and a<br />
As it requires ma<strong>in</strong>s voltage, a portable box conta<strong>in</strong><strong>in</strong>g accumu- tra<strong>in</strong>ed nurse comprise the team.<br />
lators and a transistorized <strong>in</strong>vertor, from which a 240-voh i- Each person must be familiar with his ~b and know what<br />
ampere supply is obta<strong>in</strong>ed for several hours, has been developed. equipment is available. The anaesthetist is a useful member<br />
Apart from these special items, there are metres of equip- of the team because the respiratory tract is often <strong>in</strong>voh~l,<br />
merit which can be sent to the scene of a major accident such resuscitation may be required, or a trapped patient may require<br />
as a tra<strong>in</strong> crash so that a casualty-clear<strong>in</strong>g station cure be set up. an anaesthetic before he can be released. Immediate availability<br />
These consist of extra <strong>in</strong>struments, and materials such as is essential, and a member of the casualty staff is always on<br />
blankets, bowls, and other items.<br />
call. .<br />
Portability is a factor to be emphasized. This is particularly<br />
important <strong>in</strong> the Derby area, as the squad has to deal with<br />
m<strong>in</strong><strong>in</strong>g accidents. The equipment has to be carried underground,<br />
over long distances and where walk<strong>in</strong>g may be difficult.<br />
Experience has shown that the conta<strong>in</strong>ers should be robust and<br />
easily carried by one person. Each conta<strong>in</strong>er has a list of its<br />
contents on the outside, and clear <strong>in</strong>structions are pa<strong>in</strong>ted on<br />
each box.<br />
All equipment is constantly available and it is not used for<br />
any other purpose, so that when there is a call for aid there<br />
is no confusion <strong>in</strong> gather<strong>in</strong>g it together. The only substance<br />
that has to be taken from stock is plasma.<br />
Transport<br />
Speed be<strong>in</strong>g the ~ of the service, the idea of us<strong>in</strong>g<br />
mobile operat<strong>in</strong>g theatres, vans, or ambulances was immediately<br />
discarded. A large car was the obvious choice, and arrangements<br />
were made to use a taxi should it be requ~d. The first<br />
call ever received was to a seriously <strong>in</strong>jured man who had been<br />
taken to a distant cottage hospital and was unfit to travel anyfurther<br />
by ambulance. The limitations of us<strong>in</strong>g a taxi were<br />
soon apparent, as it was diff~dt to locate a taxi quickly and<br />
I~ ~dvet ,.~a~ h<strong>in</strong>de~ by ~c ~mlatious.<br />
The Derby Borough Police were consulted and as a result<br />
it was suggested that the fly<strong>in</strong>g squad should be conveyed <strong>in</strong><br />
a police car. This has all the possible advantages, and the<br />
equipment has been des~ned to fit <strong>in</strong>to the boot of the car.<br />
The team proceeds all the way <strong>in</strong> the "police car and where<br />
possible a second police car supplies escort. The Derby Borough<br />
Police have been most cooperative <strong>in</strong> this matter, and usually<br />
a car is at the door oi the casualty deparmaent <strong>in</strong> from three t o<br />
five m<strong>in</strong>utes. Nowadays two cars always attend, and thus moreequipment<br />
can be carded. The police have organized a system<br />
..~ "--l~ww, w" for the squad. As soon as the call is received<br />
police mobile teams are directed to man all oross-roads and<br />
zebra .cross<strong>in</strong>gs and to clear trafl~ In this way, even dur<strong>in</strong>g<br />
times of heavy trkIfic congestion, a police car with sirens, loudhailer,<br />
and lights can usually pass through the town at speed.<br />
If more help or equipment is required extra police ca~ are<br />
readily made a~le, and on one occasion whentwenw-n<strong>in</strong>e<br />
people were/n~,ed, some seriously, <strong>in</strong> a bus crash, fire borough<br />
police cars were used. The Derby Borough Police Force<br />
deserves great credit for their conm~oution to the service, and<br />
<strong>in</strong>deed without it much of the efficiency would be lack<strong>in</strong>g. The"<br />
police have produced detailed maps of mutes to the chief <strong>in</strong>dus-<br />
Method of Call<br />
Any person can request the assistmce of the team. In practice<br />
this usually means that a doctor, nurse, police otFu:er, fire<br />
officer, or ambulance crew has <strong>in</strong>itiated the call. Certa<strong>in</strong> special<br />
arrangements have been made with large <strong>in</strong>dustrial concerns<br />
and the airport for call<strong>in</strong>g the fly<strong>in</strong>g squad. The person<br />
request<strong>in</strong>g assistance is connected by telephone to the casualty<br />
department and is asked to give the location and the approximate<br />
number of casualties. Immediatdy on receipt of a call<br />
the Borough Pofice are <strong>in</strong>formed and the nearest patrol car is<br />
directed to the hospital. A second car is available with<strong>in</strong><br />
m<strong>in</strong>utes, and this car may be used to collect a member of the<br />
team who is on call but not <strong>in</strong> the hospital and take him direct<br />
to the scene of the <strong>in</strong>cident if the first car has loaded the other<br />
members of the team and equipment from the hospital<br />
Major <strong>Accident</strong>s<br />
In preparation for a major accident or disasw.r, a scheme has<br />
been drawn up <strong>in</strong>dicat<strong>in</strong>g the action to be taken to deal with<br />
multiple casualties. In this scheme the fly<strong>in</strong>g squad plays an ¯<br />
important part. Immediately on receipt of a call the fly<strong>in</strong>g<br />
squad would proceed to the scene of the accident and make<br />
a reconnaissance_ The surgeon-<strong>in</strong>-charge would assess the<br />
seriousness of the <strong>in</strong>cident and report hack to the hmpkal by<br />
radio. Further assistance and equipment could be requested<br />
and a clear<strong>in</strong>g station established, ff necessary. In the hospital<br />
a plan for the evacuation of beds has been arranged whereby<br />
the less seriously ill Patients would be transferred to other<br />
hospitals to make room for the admission of casualties, who<br />
would be received by a 1earn stationed <strong>in</strong> the outpatient departme~t.<br />
This scheme for major accidents 1~ been published <strong>in</strong> the<br />
hospital and circulated to all senior staff, wards and departments,<br />
and to all other staff <strong>in</strong>volved, <strong>in</strong>clud<strong>in</strong>g adm<strong>in</strong>istrativ~<br />
and clerical personnd.<br />
In order to have a direct llnk with the hospital a multi-,<br />
channel radio transmitt~/receiver was <strong>in</strong>stalled <strong>in</strong> the casualty<br />
department. By a turn of the switch the different anilmlauce<br />
services which serve the Derbyshire Royal Infirmary can b~.
J 3 September 1966 <strong>Accident</strong> Hy<strong>in</strong>g Squad--Coll<strong>in</strong>s<br />
.-eached. That was the first radio of this type to be <strong>in</strong>stalled<br />
a hospital <strong>in</strong> Great Brita<strong>in</strong>, and the fly<strong>in</strong>g squad requirethe<br />
patient has been made possible by meet<strong>in</strong>g the ambuhnee W]<br />
nears were responsible for its <strong>in</strong>troduction. It is possible, byand<br />
start<strong>in</strong>g the treatment immediately. ~-<br />
~<strong>in</strong>g this apparatus, for the team at the scene of an accident For smooth operation the team must work <strong>in</strong> ~ with -<br />
o talk directly to the staff, <strong>in</strong> the casualty department, and bypolice,<br />
fire, and ambulance<br />
his means any possible errors or mis<strong>in</strong>terpretation of messases<br />
servaam " . It has been emp~ ~:~J ¢all z<br />
to all authorities that, although a call will be answered witbmat some<br />
vhich are rdayed by an ambulance controUer are avoided. It<br />
s also possible for arranrcments for treatment to be made <strong>in</strong><br />
question, particularly when life is at stake, everyone request<strong>in</strong>g ...... 1951<br />
help should bear <strong>in</strong> m<strong>in</strong>d that the departure of the team to aa<br />
~<br />
,dvance of the arrival of a patient at the hospital. The radio<br />
-~:., disct<br />
accident deprives the hospital of medical and nurs<strong>in</strong>g perscmneL ! Law~<br />
,as been used by ambulance crews to summon assistance to an By personal contact with responsible people and an explanation the<br />
ccident, and advice can also be given to crews at the scene<br />
,f an <strong>in</strong>cident. The radio proved so successful that a second<br />
of how the team functions, it has been possible to obta<strong>in</strong> co= ! diflSc<br />
operation <strong>in</strong> the use.of the fly<strong>in</strong>g squad. It has been tmt~- ~: ! patie<br />
eceivcr/trammittcr, on a different frequ~..cy, was <strong>in</strong>stalled so<strong>in</strong><br />
the eleven years of im existence that every od! has K~-.o ; toda:<br />
hat the Derby Borough Ambulance service was brought <strong>in</strong>to<br />
iirect contact with the hospital<br />
reasonable and no " f~" even-with good <strong>in</strong>tent, have -~ | c,u g<br />
been recorded. . .~. :~ ! adwa<br />
.Calls<br />
At first the number of calls on the service were comparatively<br />
.-w, but they have steadily <strong>in</strong>creased over the years. Up to 18<br />
aUs per annum are received at present. In january 1966 there<br />
,ere four calls, whereas <strong>in</strong> February 1966 there were none.<br />
7ith the open<strong>in</strong>g <strong>in</strong> December 1965 of the extension of the M.I<br />
far as Kegworth, which is only eight miles away, an <strong>in</strong>crease<br />
t serious road accidents had been expected, but so far the.re<br />
as o~n one call, to a seriously <strong>in</strong>jured passenger trapped<br />
l a l~lt.<br />
The calls come from a wide variety of <strong>in</strong>dustries ; on~ call was<br />
, release a man trapped <strong>in</strong> a pr<strong>in</strong>t<strong>in</strong>g press, and he required an<br />
~aesthetic before be<strong>in</strong>g released. Another patient was trapped<br />
; the wheel of a crane on an overhead gantry and his partially<br />
vered foot had to be completely amputated to release him.<br />
his was thirty feet above ground: Over the years there have<br />
zn several calls to attend <strong>in</strong>jured m<strong>in</strong>ers. The team goes down<br />
.e pit to the coal-face or to wherever the <strong>in</strong>jured man may be.<br />
ccasionally it has been necessary to treat m<strong>in</strong>ers who have been<br />
jured <strong>in</strong> mach<strong>in</strong>ery underground, and early commeacemeat<br />
<strong>in</strong>travenous therapy, as well as surgical procedures, have been<br />
zdertaken. Supervision of transport of the <strong>in</strong>jured to pit-<br />
~ad, particularly where sp<strong>in</strong>al <strong>in</strong>juries are present, can reduce<br />
e <strong>in</strong>cidence of damage to the sp<strong>in</strong>al cord. On several<br />
casions there have been a number of patients to deal with ; at<br />
:e bus accident 19, and at another 29 patients were <strong>in</strong>volved.<br />
ae team has deah with numerous accidents where people have<br />
en trapped <strong>in</strong> vehicles, and <strong>in</strong> such cases the patient has often<br />
m on phsma while be<strong>in</strong>g released. The team has been<br />
lied to a doctor’s surgery to resuscitate an <strong>in</strong>jured man who<br />
d beena~aken there from work. He had .been <strong>in</strong>jured by a<br />
mper~Thenever a case of severe burn<strong>in</strong>g is notified to the<br />
coop<br />
"i ~ basic eq pment for the fly~g squad comprised surgical " - "7"’ adm!<br />
<strong>in</strong>struments, drums, drugs, and dress<strong>in</strong>gs, and these were avail- --able<br />
from stock. The carry<strong>in</strong>g-cases and portable ma<strong>in</strong>s electric ¯<br />
supply from batteries were made <strong>in</strong> the hospital workshops.<br />
Special items were purchased to improve the service, and ’’"<br />
examples of the more expensive of these are: Pye radio transmitter/receiver,<br />
£200 ; Siebe Gorman breath<strong>in</strong>g apparatus, £70 ;--:~:: !<br />
Ambu resuscitator and sucker, £40 ; Beaver mark II respirator, "~-~ !<br />
£215 ; equipment for test<strong>in</strong>g for radiation hazards, £220. The 7~, i<br />
police have not made any charge for their services.. - ~. ’<br />
(~ha~<br />
bilh3<br />
Beva<br />
to<br />
and<br />
that<br />
<strong>in</strong> n<br />
idea<br />
If y(<br />
: S~t~tnaty ..... .., ~-,~.:. ~.,~,. ! one<br />
2~: me t<br />
The fly<strong>in</strong>g squad <strong>in</strong> Derby has ~ <strong>in</strong> eadstmace for elevea - ~-- : begh<br />
years.<br />
--- the<br />
Essentially the service is ~ion, but surgery has been~,..:~, we s<br />
performed when necessary. -.~,~.:,~ .. Pu<br />
Speed is of vital importance wlma proceed<strong>in</strong>g to an accident..: :’~ " off E<br />
The cooperation of the police is ~sirable and advantageous. ,~.~ ~ jUSt<br />
S<strong>in</strong>ce its <strong>in</strong>ception the squad has been called to deal with a Grat<br />
great variety of accidents. " , _ that<br />
’ Calls for the services of the Derby Fly<strong>in</strong>g Squad have smadily =,: ....<br />
<strong>in</strong>creased <strong>in</strong> numbers and the scopa of its work has gradually ,~<br />
widened.<br />
The success of early treatment of the <strong>in</strong>jured by the fly<strong>in</strong>g L:-,~<br />
squad has amply justified the efforts of the team. ,__<br />
In Derby the fly<strong>in</strong>g squad has been found to be very useful) ~ :<br />
and a plea is made that other areas should seriously consider ~-:~<br />
the advisability of form<strong>in</strong>g timilar teams. " ~’~-"~#-~ ~<br />
:,. -<br />
.<br />
I:<br />
tion<br />
mov,<br />
be<strong>in</strong>~<br />
abRi~<br />
soci~<br />
T!<br />
h~it~<br />
it) f<br />
little<br />
HItiC<br />
the<br />
I5 y<br />
Ithi<br />
they<br />
N.H<br />
The<br />
fiuar<br />
I1<br />
at~$<br />
wog<br />
tion
~ertension, renal disease, and heart failure<br />
stressed the communities without hypertension, let me<br />
aga<strong>in</strong> emphasize that most urban or periurban tropical communities<br />
show blood pressure patterns similar to those seen <strong>in</strong><br />
the United K<strong>in</strong>gdom or <strong>in</strong> North America and have similar or<br />
greater frequencies of <strong>in</strong>dividuals with "high blood pressure."<br />
In most tropical cl<strong>in</strong>ics the majority of subjects seen with raised<br />
blood pressures are classified as essential hypertension, particulariy<br />
those over 40 years of age. A few cases are associated with<br />
underly<strong>in</strong>g renal disease, but it is this group of cases that produces<br />
most of the severe hypertension problems admitted to<br />
hospital. Thus impressions ga<strong>in</strong>ed from hospital admission<br />
studies tend to overemphasize the contribution of renal disease<br />
to the community pattern of blood pressure.<br />
A recent necropsy study from Uganda gives some perspective<br />
on the problem, s* Over a three-year period some 3,000 necropsles<br />
were carried out on patients who had died <strong>in</strong> the hospital;<br />
only 84 cases were f<strong>in</strong>ally diagnosed at necropsy as hypertensive<br />
heart disease, and these fell <strong>in</strong>to four ma<strong>in</strong> groups (see Fig. 2).<br />
Group 1.--Essential hypertension (25 cases). Most of these<br />
¯ were elderly men with cerebrovascular disease as the commonest<br />
s<strong>in</strong>gle cause Of death.<br />
!.<br />
I0.<br />
8<br />
b<br />
4<br />
2<br />
0<br />
8<br />
b<br />
4<br />
2<br />
0<br />
Essential hypertension (25} Dyelonephritis (I
808<br />
e-’tergency which might arise. The service aims to supply an<br />
xperienced accident team which can be mobilized rapid/y, can<br />
travel rapid/y, and is equipped to do the m<strong>in</strong>imum necessary<br />
"<strong>in</strong> the field" before transport<strong>in</strong>g the patient back to hospital.<br />
The system now is well established, works very smoothly, and,<br />
<strong>in</strong> our op<strong>in</strong>ion, reduces both mortality and morbidity and well<br />
justifies the time, money, and effort which it demands.<br />
This paper analyses the calls received, the acti0n taken, and<br />
the patients treated dur<strong>in</strong>g the years 1967-71 <strong>in</strong>clusive.<br />
Analysis of Calls<br />
Mobilization and Duration.--S<strong>in</strong>ce two police vehicles are used<br />
the mobilization time is divided. Dur<strong>in</strong>g 1971 the first vehicle,<br />
carry<strong>in</strong>g the team and immediately needed equipment, averaged<br />
just under four m<strong>in</strong>utes from receipt of the call to mobilization.<br />
The average time for the second car (carry<strong>in</strong>g late or extra<br />
team members and the rema<strong>in</strong>der of the equipment) was six<br />
m<strong>in</strong>utes. The duration of calls is measured from the time of<br />
leav<strong>in</strong>g the department to the time of return. Dur<strong>in</strong>g 1971 this<br />
varied from 10 m<strong>in</strong>utes to 140 m<strong>in</strong>utes, the former be<strong>in</strong>g a call<br />
with subsequent cancellation, and the latter be<strong>in</strong>g a road<br />
traffic accident <strong>in</strong> which after treatment and release of the<br />
tra~g~ed driver he was taken to a casualty department nearer to<br />
.th~ene of the accident. Of.the 79 calls received dur<strong>in</strong>g 1971,<br />
however, 69 (88°.0) lasted less than an hour, the average time<br />
be<strong>in</strong>g 44 m<strong>in</strong>utes. The efficiency of the casualty department is<br />
not greatly affected by the team members’ absence, and the slight<br />
decrease <strong>in</strong> efficiency that does occur is more than balanced by<br />
the speedier transfer of the patient to his f<strong>in</strong>al dest<strong>in</strong>ation, most<br />
of the <strong>in</strong>itial resuscitation hav<strong>in</strong>g been performed before his<br />
admission to the department.<br />
Number of Galls.--The number of calls <strong>in</strong>creased dramatically<br />
dur<strong>in</strong>g 1971 compared with 1970--79 and 46 respectively (Fig. 1).<br />
This was probably due to a comb<strong>in</strong>ation of factors--an <strong>in</strong>crease<br />
70.<br />
60,<br />
50’<br />
40,<br />
I 30,<br />
z<br />
20’<br />
IO,<br />
.Year<br />
FZG. 1--Yearly number of calls recdved by arc/dent<br />
ey<strong>in</strong>g squad.<br />
<strong>in</strong> the number of high velocity road .tam’tic accidents, and an<br />
<strong>in</strong>creas<strong>in</strong>g awareness by the emergency services of the function<br />
of the fly<strong>in</strong>g sq-a d. The team members are constantly advis<strong>in</strong>g<br />
the services of the part they can play, and as a result relationships<br />
with the emergency services are excellent and could not be<br />
improved. No one is ever criticized for a call ~vhich later proves<br />
to have been unnecessary, but they are occasionally rem<strong>in</strong>ded of<br />
the service if <strong>in</strong> one’s op<strong>in</strong>ion the squad should have been<br />
but was not called to a seriously <strong>in</strong>jured patient. This, of course,<br />
leads to a number of unnecessary calls, though at present these<br />
amount to only some 10% of the total. In addition the number<br />
of aborted calls is <strong>in</strong>creas<strong>in</strong>g slowly. These signify early alert of<br />
the fly<strong>in</strong>g squad but subsequent realization that they were<br />
not required, either because the patient was dead or because<br />
he was not as seriously <strong>in</strong>iured as orig<strong>in</strong>ally appeared.<br />
Location of Ca/L--S<strong>in</strong>ce the area served by the fly<strong>in</strong>g squad<br />
mrrxsB ~ic~ jo~a. 30 s~rr~M~<br />
stretches up to 30 miles (48 km) <strong>in</strong> some directions can-out is<br />
not limited to trapped patients. The team often travels to meet<br />
seriously <strong>in</strong>jured patients <strong>in</strong> ambulances, and can thus make<br />
the 40-m<strong>in</strong>ute journey less hazardous. The furthest distance<br />
travelled has been 27 miles (43-5 k<strong>in</strong>) to reach a seriously ill<br />
patient, but a high proportion of calLs (50°o) fall between 5 and<br />
15 miles (8 and 24 k<strong>in</strong>), with about half of the rema<strong>in</strong>der be<strong>in</strong>g<br />
with<strong>in</strong> a 5-mile radius. The outcome of calls received is sho~<br />
<strong>in</strong> Fig. 2.<br />
g<br />
Z<br />
40.<br />
30.<br />
20<br />
I0<br />
P<br />
o ,967 ,47o ,9"7,<br />
Year<br />
FIG. 2---Outcome of calls attended by fly<strong>in</strong>g squad<br />
Squad met -- ’~<br />
ambulance<br />
Type of CalL--The calls have been divided <strong>in</strong>to four ~ ma<strong>in</strong><br />
groups---pit accidents, <strong>in</strong>dustrial (works) accidents, road traffic<br />
accidents, and miscellaneous (<strong>in</strong>clud<strong>in</strong>g domestic, alerts to the<br />
local airport, etc.). Ali the local pits have now closed, but at the<br />
<strong>in</strong>ception of the squad they constituted a large proportion of the<br />
calls (Fig. 3). All the other groups are <strong>in</strong>creas<strong>in</strong>g, but none more<br />
so than the road traffic accidents, which have registered a five.fold<br />
<strong>in</strong>crease <strong>in</strong> the past four years.<br />
SO<br />
4O<br />
,o<br />
o<br />
"Z zo<br />
io<br />
0<br />
Yea r<br />
¯ Road traffic accidents /<br />
x Miscelloneous<br />
o Works<br />
/<br />
¯ Pits /<br />
/ !<br />
/<br />
FIG. 3---Frequent7 of the four ma<strong>in</strong> types of calL<br />
Seasonal DistnT~ution of Calk--S<strong>in</strong>ce road traffic accidents<br />
account for about 65% of all fly<strong>in</strong>g squad calls it seems reasonable<br />
for the total calls to be directly related to high-risk periods<br />
on the roads--altar is, the w<strong>in</strong>ter months (Fig. 4). In fact, whzu<br />
the type of accident is related to the time of year the we=h=<br />
g<br />
Z<br />
20- ¯~/<br />
~./<br />
IS I<br />
0<br />
L<br />
; : - ,.’.:., ¯<br />
I<br />
!<br />
i k<br />
"It<br />
In(<br />
"ck<br />
<strong>in</strong><br />
r~<br />
g~<br />
g~<br />
gn<br />
tlu<br />
T~<br />
04(<br />
O6.(<br />
Z~-(<br />
l&(<br />
2O-(<br />
1<br />
p~1<br />
I-Ic<br />
th=<br />
im fo~<br />
10<br />
mi<br />
col<br />
I~I1<br />
- ¯ .< . im<br />
i.,: II<br />
/"1970<br />
i ~ol<br />
"----.., I/ ..... .<br />
-J;a.- A~I- Jui~- O~:t.- ...........<br />
March Ju~ Sept. Dec. ~ ’"<br />
~o. 4--Se=.mal di~m’bution of all calh ~ce 1967.<br />
I<br />
i<br />
~<br />
TAm<br />
WO<br />
hd
,~ITI~ MEDICAL JOURNAL 30 SEFTEMBER 1972 8O9<br />
3O<br />
O<br />
Road traffic<br />
accidents /<br />
/<br />
/<br />
/<br />
Niscellaneo~us .~x<br />
""---..~....x _..._..~.. x<br />
Works ...~<br />
Pits~ ,~<br />
J..- Ap;,- Jui,- O;,.-<br />
March June Sept. Dec.<br />
tno. 5--Seuonal distribution of the four maln types<br />
of call over a year.<br />
factor is well demonstrated (Fig. 5), the road tra~c accident<br />
total be<strong>in</strong>g the only one with a significant seasonal variation.<br />
This also means that the team members are often work<strong>in</strong>g <strong>in</strong><br />
most adverse weather conditions and therefore have to be<br />
clothed accord<strong>in</strong>gly.<br />
I<br />
~L Time of Day.--When calls are broken down <strong>in</strong>to the period<br />
t which they orig<strong>in</strong>ate the surpris<strong>in</strong>g fact that the total calls<br />
reach a peak <strong>in</strong> the morn<strong>in</strong>g is found. In fact, all groups of<br />
accident reach a peak dur<strong>in</strong>g this time, though road traffic<br />
accidents do present a higher peak around midnight. This latter<br />
group of road traffic accidents are often the most severe, s<strong>in</strong>ce<br />
they usually <strong>in</strong>volve multiple drunken patients.<br />
TABLE I.--Timi~ of Calls throug]lout the Day (Dam for 1967-7I)<br />
Thzw<br />
Road<br />
<strong>Accident</strong>s<br />
Works<br />
laneo~ i<br />
30.01-04.00 hom~<br />
~4~01-0&00 ho~s<br />
~8.01-17.00 hours<br />
12-01-16-00 hours<br />
16-01-20-00 ho~s<br />
20-01-24.00 hours<br />
Total ..<br />
-.<br />
¯ .<br />
.o<br />
¯ .<br />
..<br />
16<br />
8<br />
22<br />
19<br />
29<br />
120<br />
I<br />
II<br />
I0<br />
s2<br />
o<br />
1<br />
12<br />
966<br />
34<br />
Total<br />
17<br />
10<br />
49<br />
41<br />
30<br />
37<br />
I 184<br />
:~ Number of Patients per Coll.--Most calls <strong>in</strong>volved only one<br />
patient, particularly the works, pit, and domestic groups.<br />
However, the road traffic accidents did tend to <strong>in</strong>volve more<br />
~v~<br />
: patient requir<strong>in</strong>g treatment--for example, 90 calls<br />
one patient, 26 calls two patients, 16 carla three or<br />
¯ ~ four patient~ 11 calls 5 to 10 patients, and one call more trmn<br />
10 patients. Although patients <strong>in</strong> these accidents tend to have a<br />
mixture of major and m<strong>in</strong>or <strong>in</strong>juries the team has to be able to<br />
cop~ <strong>in</strong>~ at least, with three or four seriously <strong>in</strong>jm~d<br />
patients. Extra equipment can always be obta<strong>in</strong>ed if necessary.<br />
~ The call <strong>in</strong>volv<strong>in</strong>g more than I0 patients was to an accident<br />
<strong>in</strong>volv<strong>in</strong>g ¯ bus. Ahhough ~ bus conta<strong>in</strong>ed 37 <strong>in</strong>jured people<br />
l ha’.,~ ~__d.~d~l only the two seriously <strong>in</strong>jured patients <strong>in</strong> the<br />
~fiow<strong>in</strong>g patient study.<br />
~ ,~ .<br />
Analysis of Road Traffic <strong>Accident</strong> Patients<br />
Dur<strong>in</strong>g the years 196%71 <strong>in</strong>clusive, 280 patients were treated<br />
by the fly<strong>in</strong>g squad. Of these, five were under the age of 10, the<br />
ages of 14 were not obta<strong>in</strong>ed, and <strong>in</strong> three cases the time of<br />
<strong>in</strong>jury could not be checked. These patients are thus excluded<br />
from further analysis. Seventy-three per cent of the patients<br />
were male. Of the patients with known ages 60% were aged<br />
15-30 years. S<strong>in</strong>ce such a large proportion of the patients were<br />
young and had previously been fit they were potentially more<br />
salvageable than, for example, patients served by a coronary<br />
fly<strong>in</strong>g squad.<br />
AGES OF PATIENTS RELATED TO TIME OF ACCIDENT<br />
The strik<strong>in</strong>g difference <strong>in</strong> ages accord<strong>in</strong>g to the time of day that<br />
the road accidents occurred is shown by plott<strong>in</strong>g the two<br />
extremes graphically (Fig. 6)---namely, the 11-20 and 41-50year<br />
age groups. This difference presumably reflects the social<br />
habits of the tWO groups, carry<strong>in</strong>g the vivid impression that<br />
alcohol is a large contributor to the teenagers’ peak risk period<br />
around midnight. The figures for all ages are given <strong>in</strong> Table II.<br />
20<br />
E = tO<br />
Z<br />
0<br />
Time of day<br />
I)<br />
¯ |l-2yeorO/_/<br />
too. 6--Correlation of time road accidents occur, with two<br />
age groups of patiems.<br />
TABLE II--,~$ of P~olt$ ¢orrel~ed t~it~ Tira~ of Day--Road Tra~¢<br />
<strong>Accident</strong>s Occurred(Data for 1567-71)<br />
¯ Age<br />
(Years)<br />
¯ 11-20 ..<br />
21-30 ..<br />
31-40 ..<br />
41-50 ..<br />
51-60 ..<br />
61-70 ..<br />
Total pttient~<br />
"l’m~ of Day @Ioun)<br />
00-01 04.01 08.01 12.01 16.01 20.01 Total<br />
tO KO KO tO tO to Pc’dents<br />
04.00 08.00 12.00 16.00 20.00 24.00<br />
22 1<br />
19 8<br />
1 2<br />
3 o<br />
1 o<br />
1 0<br />
47 II<br />
m~Parts Injured ar.wrdi~ to Type of <strong>Accident</strong> and (<strong>in</strong> the cme of Road Acddent~) Typt of Vehicle Involved<br />
T~m,! ......<br />
Had<br />
83 4<br />
1585<br />
115<br />
(~est<br />
28 1121<br />
Abdm~<br />
8 23<br />
2<br />
o<br />
15<br />
Pelvis<br />
9<br />
3<br />
1<br />
o<br />
1<br />
14<br />
6 14 11 26 80<br />
11 13 9 14 74<br />
11 5 4 4 27<br />
9 11 7 9 -39<br />
7 5 0 8 21<br />
2 4 3 7 17<br />
46 52 34 68 258<br />
patients’ <strong>in</strong>juries have bee~ subdivided <strong>in</strong>to body areas and<br />
related to type of accident and, <strong>in</strong> the case of road accidents,<br />
to the type of vehicle <strong>in</strong> which the patient was travgfi<strong>in</strong>g.<br />
Head <strong>in</strong>juries dearly constitute a large propo~’on of all <strong>in</strong>juries,<br />
especially <strong>in</strong> car and motor-cycle travellers (Table III). Of all<br />
One<br />
14 2361<br />
26<br />
Arm<br />
Both<br />
3<br />
o I<br />
o<br />
One<br />
34 8672<br />
57<br />
Both<br />
9<br />
8<br />
2 11<br />
21<br />
22 433o<br />
32<br />
Bums<br />
o 1<br />
o
the patients with head <strong>in</strong>jury 60 had solely a head <strong>in</strong>jury and 61<br />
had head plus other serious <strong>in</strong>juries. The type of <strong>in</strong>jury is<br />
dictated by the vehicle (Table II). Motor-car <strong>in</strong>juries are made<br />
up of head, chest~ and limb <strong>in</strong>juries. In lorry accidents the<br />
patient (usually the driver) has lower limb <strong>in</strong>juries, and the<br />
upper body is usually spared. This impression has been so vivid<br />
<strong>in</strong> recent motorway <strong>in</strong>cidents that the team now takes collapsible<br />
Thomas spl<strong>in</strong>ts to any <strong>in</strong>jured lorry drivers. Among motorcyclists<br />
and pedesu’ians head <strong>in</strong>juries predom<strong>in</strong>ate, and occasionally<br />
limb <strong>in</strong>juries occur. Works accidents (apart from m<strong>in</strong>ers<br />
with head <strong>in</strong>juries) usually <strong>in</strong>volve one patient with one limb"<br />
trapped <strong>in</strong> mach<strong>in</strong>ery, and this group is the one which normally<br />
requires true surgical <strong>in</strong>tervention---, for example, amputation.<br />
TREATMENT AT SCENE<br />
The fly<strong>in</strong>g squad aims to provide rapid, essential medical care<br />
at the scene of an accid~mt. Obviously the ideal situation <strong>in</strong> which<br />
to perform surgery or to <strong>in</strong>duce anaesthesia or both is <strong>in</strong><br />
properly equipped hospital surround<strong>in</strong>gs and not <strong>in</strong> a hostile<br />
environment. There are, however, certa<strong>in</strong> therapeutic measures<br />
which must or should be <strong>in</strong>stituted immediatelyNfor example,<br />
efficient analgesia, blood volume replacement, tapp<strong>in</strong>g tension<br />
~ othoraces, <strong>in</strong>tubation and ventilation, and, rarely,<br />
anaesthesia to allow surgery for otherwise impossible<br />
release of a victim (Table IV).<br />
T~ zv~Measura Instituted at Scene of Accidmt<br />
Treatment No. of Occasions ] Treatment No. of Occasion~<br />
Intravenous analgeaht, .. ,. 59 ] General anaesthesia for spf<strong>in</strong>tage .. ,~.<br />
Intramuscular analgesia ..... , Intubafion ........<br />
Drip .. . ...... 104 Sedation ........<br />
.. s~<br />
2<br />
General anaesthesm for release .. 4 ] Ventilation ......<br />
"Anti-shock" measures are obviously the most common treatment<br />
required. Our <strong>in</strong>travenous therapy <strong>in</strong>itially consists of<br />
plasma and dextran 70, with blood be<strong>in</strong>g obta<strong>in</strong>able if required.<br />
MORTALITY<br />
Of the 280 patients treated by the fly<strong>in</strong>g squad 73 die& These<br />
are divided <strong>in</strong> Table V <strong>in</strong>to deaths before arrival of the fly<strong>in</strong>g<br />
squad, dur<strong>in</strong>g attendance of the squad (<strong>in</strong>clud<strong>in</strong>g time spent <strong>in</strong><br />
the casualty department), and <strong>in</strong> hospital after admission.<br />
Only three patients died dur<strong>in</strong>g attendance of the fly<strong>in</strong>g<br />
squad, and these were among 37 patients with severe multiple<br />
<strong>in</strong>juries. (My def<strong>in</strong>ition of severe multiple <strong>in</strong>juries is where<br />
three or more parts of the body are severely <strong>in</strong>jured.) It is<br />
TABIJ vwTime of the 73 Deaths<br />
Type of accident<br />
Pedest- Car<br />
rien<br />
efore arrival of squad 3 26<br />
rar<strong>in</strong>g attendance of<br />
squad .... 0 2<br />
n hospital .. 2 10<br />
Total .... 5 38<br />
lion,/ Motor-! Works Mi~ l- Total<br />
..]<br />
cycle tram ts<br />
4 3 6 (s 4S<br />
0 1 0 ¯ 3<br />
1 2 3 5" 22<br />
5 6 I 8<br />
TABLE VI--S~ ~ Pa6oas admitted to Hospital<br />
tl "/3<br />
Intensive care unit ....<br />
Trauma ward ....<br />
Discharged .... ::<br />
" 43<br />
156<br />
30<br />
,i N’o. of --,-b’~ i<br />
1"~- "~ °ev’la<br />
1O (23%)<br />
7 (4-5%)<br />
0<br />
TABLE vn--lniured PavU of Patients who Died <strong>in</strong> Hospital<br />
No. of i<br />
patients 12<br />
I Head Chest ^halomen<br />
One Both<br />
8 7 4 1 2 2 4 0 I<br />
Arm ~ Mia~ ikma<br />
One Beth<br />
I i<br />
doubtful if anyr2dng can be done for the patients dy<strong>in</strong>g before<br />
arrival of the squad, but the figure of only 22 (11%) deaths out<br />
of 199 viable patients seems a very reasonable one, s<strong>in</strong>ce this<br />
does not <strong>in</strong>clude rout<strong>in</strong>e road traffic cases. (The Heidelberg<br />
Cl<strong>in</strong>ic reports a mortality of about 5% of all road traffic accident<br />
cases admitted’)<br />
The figures for deaths <strong>in</strong> hospital confirm that if the patients’<br />
<strong>in</strong>juries are ~-ious enough to merit admission to any <strong>in</strong>tensive<br />
care unit then the chance of survival is greatly dim<strong>in</strong>ished<br />
(Table VI). Analysis of the <strong>in</strong>juries of patients dy<strong>in</strong>g <strong>in</strong> hospital<br />
(Table VII) shows that the most common <strong>in</strong>juries lead<strong>in</strong>g to<br />
death are head, chest, and abdom<strong>in</strong>al <strong>in</strong>juries (Gogier quoted<br />
head <strong>in</strong>jury as a cause of death <strong>in</strong> 70.2% of his patients) t.<br />
Discussion<br />
Although a selection of powerful analgesics is taken, our normal There have been many attempts to provide an efficient system<br />
rout<strong>in</strong>e <strong>in</strong>itial analgesia is pentazoc~" ¯ (Fortral) 60 rag <strong>in</strong>travenously.<br />
We f<strong>in</strong>d it efficient, rapidly act<strong>in</strong>g, and relatively<br />
free of side effects, its duration of action if given <strong>in</strong>travenously<br />
which would enable doctors to attend at the scene of a serious<br />
accident. Complete mobile "hospitals on wheels" have been<br />
abandoned because they are too slow <strong>in</strong> mobilization. Many<br />
be<strong>in</strong>g about an hour. Thus it does not obscure the cl<strong>in</strong>ical groups of general practitioners have jo<strong>in</strong>ed together and which<br />
picture at subsequent exam<strong>in</strong>ation by neurosurgeon or general ever is nearest to an emergency scene is mobilized to that scene.<br />
surgeon.<br />
This usually has the advantage of rapid gravel but suffers<br />
Induction for general anaesthesia is implemented with a<br />
~Oethrt.act<strong>in</strong>g ohexitone non-barbiturate sodium (Brietal such Sodium). as propanidid If necessary (Epontol) or the<br />
greatly through lack of equipment and f<strong>in</strong>ance and the necessary<br />
cont<strong>in</strong>u<strong>in</strong>g experience <strong>in</strong> the use of such equipment. It is<br />
unreasonable to expect any doctor to <strong>in</strong>tubato someone ly<strong>in</strong>g<br />
anaesthetic can then be cont<strong>in</strong>ued <strong>in</strong> rout<strong>in</strong>e fashion with on a dark, wet road when he has not <strong>in</strong>mbated a patient for<br />
oxygen, nitrous o~de, and halothane delivered by our portable<br />
m<strong>in</strong>iature anaesthetic mach<strong>in</strong>e. There is no place <strong>in</strong> the equip-<br />
perhaps several years. The compromise answer surely lies <strong>in</strong><br />
fly<strong>in</strong>g squads based on the major accident centxeb which can be<br />
ment of the fly<strong>in</strong>g squad for Entonox, s<strong>in</strong>ce they already have a f<strong>in</strong>anced by the hospital and can use tra<strong>in</strong>ed ca~malty staff m<br />
more adaptable form of gas mix<strong>in</strong>g. I am sure, however, that it<br />
is of great value <strong>in</strong> paramedical hands. It is <strong>in</strong>terest<strong>in</strong>g to note<br />
that of the 13 patients given general anaesthesia under most<br />
unsuitable circumstances (Table IV) only one died, the patient<br />
whom emergencies are rout<strong>in</strong>e.<br />
Apart from a weft-equipped team, speed of mebilizati~ and<br />
speed of travel are essential. There is no po<strong>in</strong>t <strong>in</strong> a patie~<br />
rema<strong>in</strong><strong>in</strong>g at the scene if he can be safely tr~pm~ed to hospital<br />
be<strong>in</strong>g an elderly woman with severe multiple <strong>in</strong>juries.<br />
Of the 24 patients <strong>in</strong>mbated 11 died, these <strong>in</strong>clud<strong>in</strong>g five<br />
who were probably already dead but <strong>in</strong> whom resuscitation was<br />
attempted. Of the 15 patients given ventiiation on the .way to<br />
hospital, surpris<strong>in</strong>gly only seven died, these aga<strong>in</strong> <strong>in</strong>clud<strong>in</strong>g a<br />
few hopeless cases.<br />
<strong>in</strong> a shorte: time than k takes for the team to reach him. ¯<br />
The figures show an <strong>in</strong>creas<strong>in</strong>g demand for such a service and<br />
also prove that senior staff must always be ~ available,<br />
although they need not necessarily be with<strong>in</strong> the hospital It is<br />
impossible to justify a fly<strong>in</strong>g squad’s existence statistically <strong>in</strong><br />
terms of mortaEty or morbidity. There are a few cases which<br />
one can state categorically would have had a fatal outcome* but<br />
for the fly<strong>in</strong>g squad’s attendance, but these are rare. However,<br />
the cl<strong>in</strong>ical impression of anyone who travels to the scene or<br />
receives the patients <strong>in</strong> hospital is that these patients benefit<br />
greatly from appropriate early treatment.<br />
References<br />
: Coll<strong>in</strong>s, l, Br<strong>in</strong>’sh Me~’ca!yourna/, 1966, 2, 578.<br />
t C~ler. E ¯ Unfallopfer im Stvassen~erkehv. Basle, Geigy, 1962.<br />
¯Lit~Je, Y~’BnrisS M~i~your~, 19W, 2, VVT.<br />
I t<br />
|<br />
t
622<br />
clear po<strong>in</strong>ter to possible pituitary deficiency and is an important<br />
physical sign <strong>in</strong> newborn boys.<br />
We thank Dr D Stone and Dr A J Frankl<strong>in</strong> for permission to<br />
report their patients. Plasma adrenocorticotrophic hormone was<br />
k<strong>in</strong>dly measured by Professor Lesley H Rees <strong>in</strong> the department of<br />
chemical end?cr<strong>in</strong>ology at St Bartholomew’s Hospital, London.<br />
Other hormone assays were performed <strong>in</strong> the department of chemical<br />
pathology at the H~pital for_Sick Childrem. ~ London.<br />
ReferenCes c ~ ~ ~ ,<br />
I Wil~n ]D, Griff<strong>in</strong> JE, Qeorge _FN, Leshln M. The role _of-gonadal<br />
- steroids <strong>in</strong> sexual differentiae/on. Recent Prog Horm Res 1981 i37:1-39.<br />
Clements JA, Reyes EI, W<strong>in</strong>ter JSD, Fairman--C. Studies on human<br />
- .<br />
.<br />
.<br />
For Debate,. ¯<br />
Paramedics <strong>in</strong> the United K<strong>in</strong>gdom?<br />
A D REDMOND<br />
There is no doubt that until recently the United K<strong>in</strong>gdom<br />
could boast the best ambulance service <strong>in</strong> the wood. This is<br />
no longer’ the case: Standards have not fallen~<strong>in</strong>deed they<br />
have risen. The rest of the world, however, has caught up and<br />
<strong>in</strong> some places has overtaken us. These ambulancemen are no<br />
better tra<strong>in</strong>ed than our own but are better equipped and<br />
allowed to do more. The obvious and best example to quote is<br />
the ambulance system now develop<strong>in</strong>g <strong>in</strong> the United States of<br />
America.<br />
Twenty years ago there was no effective ambulance service<br />
<strong>in</strong>.the United States. In many places any vehicle of suitable<br />
dimension was used to transport a sick or <strong>in</strong>jured patient to<br />
hospital Ironically, the most suitable vehicle to hand was<br />
usually the local hearse. It was no doubt difficult for the<br />
mortician to separate the demands of his patient and the<br />
demands of his profession. To overcome these problems many<br />
local.ommunities developed a volunteer rescue squad. They<br />
fought fires, rescued trapped victims, and transported people<br />
to hospitaL. In an attempt to coord<strong>in</strong>ate the many different<br />
squads, a programme of tra<strong>in</strong><strong>in</strong>g was <strong>in</strong>troduced <strong>in</strong> the early<br />
1970,. This is now widespread and very well organised. The<br />
ambulancemen are referred to as emergency medical technicians,<br />
or EMTs. The basic emergency medical technician has between<br />
80 and 140 hours of tra<strong>in</strong><strong>in</strong>g, which covers basic anatomy and<br />
physiology and simple first aid. This "’simple first aid" does,<br />
however, <strong>in</strong>clude a thorough tra<strong>in</strong><strong>in</strong>g <strong>in</strong> cardiopulmonary<br />
resuscitation. This emphasis on control of the airway and<br />
belief <strong>in</strong> the positive effects.of early cardiopulmonary resuscitation<br />
is a major contribution to the sav<strong>in</strong>g of life. A basic emer-<br />
Stockport Infirmary, Stockport, Cheshlrc<br />
A D REDMOND, MD, FaCSEB, consultant <strong>in</strong> accident and emergency<br />
medic<strong>in</strong>e<br />
Correspondence and requests for repr<strong>in</strong>ts to: Mr A D Redmond.<br />
BRITISH MEDICAL JOURNAL VOLUME 288 25 FEBru~.<br />
sexual development III. Fetal pituitary and serum and<br />
fluid concentrations of LH CG and FSH. J Cl<strong>in</strong> Endocn,<br />
1976 ;~! :9-19.<br />
a Comblatt M, Schwartz R. Hypoglycemia <strong>in</strong> the neonate, <strong>in</strong>.<br />
carbohydrate metabolism <strong>in</strong> <strong>in</strong>fancy. 2rid ed. Philadelphia:<br />
Co Ltd, 1976:178.<br />
Lov<strong>in</strong>ger RD, Kaplan SL, Grumbach MM. Congenital hypo<br />
assooated with neonatal hypoglycemia and microphallus.<br />
secondary to hypothalamic hormone deficiencies..7 Pediatj<br />
1171-81¯<br />
i Moncrief MW, Hill DS, Archer ], Arthur LJH¯ Congenital<br />
pituitary gland and adrenal hypoplasla. Arch Dis Child 1971<br />
’ Leblanc A, Odi~vre M, Hadchouel M, Gendrel D, Cha<br />
Rappaport R; Neonatal eholestasis and hypoglycemia: possi<br />
cortisoi deficiency, y Pediatr 1981 ;99:577-80.<br />
Flatau E, Josefsberg S, Reisner SH, Bialik O, Laron Z: Penile si~<br />
newborn rn-fant.JPediatr 1975;87:663-4.<br />
_ (Accepted II AUgUSt 1983) ~-<br />
gency medical technician can then do further tra<strong>in</strong><strong>in</strong><br />
an <strong>in</strong>termediate emergency medical technician. He has a<br />
60 to 200 hours of tra<strong>in</strong><strong>in</strong>g and will be able to <strong>in</strong>sert<br />
l<strong>in</strong>es, obturator airways, and apply a medical antishock<br />
suit. The obturator airway seals off the oesophagus and<br />
allow air to go down only the trachea. There are many<br />
with this device <strong>in</strong>clud<strong>in</strong>g misplacement <strong>in</strong> the trachea<br />
<strong>in</strong>ducement of vomit<strong>in</strong>g. It is rapidly los<strong>in</strong>g favour <strong>in</strong><br />
United Staies. The medical antishock trouser suit is an<br />
flatable suit put over the legs of the patient <strong>in</strong> an eff0l<br />
<strong>in</strong>crease peripheral resistance and thereby raise the blood<br />
sure. It will also stabilise pelvic fractures. Hav<strong>in</strong>g<br />
this tra<strong>in</strong><strong>in</strong>g the emergency medical technician can then<br />
for even further tra<strong>in</strong><strong>in</strong>g. A cardiac emergency medical map<br />
nician can do all the above, but <strong>in</strong> addition can give drugs<br />
defibrillate patients. A paramedic emergency medical tcc~<br />
does an extra 400 to 800 hours of tra<strong>in</strong><strong>in</strong>g, and is then very<br />
tra<strong>in</strong>ed, and .can give help equivalent to that of a tra<strong>in</strong>ed phy ’~qm<br />
m emergencies. The paramedics can pass endotracheal tulm,<br />
<strong>in</strong>sert central venous l<strong>in</strong>es, and <strong>in</strong>terpret electrocardiograrm<br />
the envy of many a medical registrar.<br />
There are problems, however, with tra<strong>in</strong><strong>in</strong>g techniciam aP<br />
such a high level. As their knowledge and expertise is so m~<br />
and their capabilities are so great the medical profession fed<br />
need to keep a close eye on their activities. Strict and len~<br />
rules are laid down for what they can do at the scene ol D<br />
emergency, and usually any <strong>in</strong>vasive action has to be pro:odd<br />
by permission from the local hospital. In addition, therda~to<br />
the colossal expense of tra<strong>in</strong><strong>in</strong>g these people and equii~<br />
them, radiocommunications there is the added with expense the hos,~ital of provid<strong>in</strong>g Furthermore sophisti ’ ~.1~ .<br />
such a highly tra<strong>in</strong>ed ,,l~.ramedic arrives at the scene, his ~<br />
tra<strong>in</strong><strong>in</strong>g and raison d ~tre is to apply those skills that<br />
been so hard won. Hence the ma<strong>in</strong> drawback with such a sysU~<br />
is delay¯ When the paramedic arrives at the scene he has ~,m<br />
of all to work through a check list. This <strong>in</strong>cludes tak<strong>in</strong>g a hist~<br />
and tak<strong>in</strong>g the patient s blood pressure, pulse, and an ekx-t~
_,*CAL JOURNAL VOLUME 288 25 FEBRUARY 1984<br />
.a~diogram. Trapped or <strong>in</strong>jured patients have to be stabilised<br />
%n a backboard always. If an <strong>in</strong>travenous l<strong>in</strong>e is <strong>in</strong>dicated then<br />
the paramedic has to contact the hospital via radio or telephone,<br />
which all takes time.. There is a grow<strong>in</strong>g concern that <strong>in</strong> the<br />
treatment of trauma this may often be" <strong>in</strong>appropriate and <strong>in</strong><br />
fact life threaten<strong>in</strong>g. The ma<strong>in</strong> cause for concern is <strong>in</strong> the<br />
treatment of penetrat<strong>in</strong>g <strong>in</strong>juries, particularly from gunshot<br />
,ounds and stabb<strong>in</strong>gs. Though we are fortunate not to see<br />
these wounds <strong>in</strong> Brita<strong>in</strong> to the same degree as on the other<br />
side of the Atlantic, they do provide us with an example, albeit<br />
extreme, of what can happen when def<strong>in</strong>itive treatment is delayed.<br />
If a major vessel has been ruptured by a bullet, or some<br />
other penetrat<strong>in</strong>g object, then the patient needs an operation.<br />
Any delay may be fatal. Unless the wounds are so devastat<strong>in</strong>g<br />
that the patient will die immediately or so trivial that there is<br />
no risk of appreciable haemorrhage, then with penetration of a<br />
major vessel the patient has only about 30 m<strong>in</strong>utes <strong>in</strong> wHch to<br />
set def<strong>in</strong>itive surgery. This, however, is usually the time it<br />
t~es for an ambulance to be called, the ambulance to arrive,<br />
~d the paramedics to complete their check list. The patient<br />
therefore arrives <strong>in</strong> the emergencyjj department hav<strong>in</strong>g suffered<br />
s cardiac arrest <strong>in</strong> the ambulance and cannot be resuscitated.<br />
This can best be illustrated with an example. While I was<br />
r/sit<strong>in</strong>g a dist<strong>in</strong>guished medical school <strong>in</strong> the United States. the<br />
follow<strong>in</strong>g case was discussed at a surgical meet<strong>in</strong>g:<br />
At about 11 00 pm a man was shot dur<strong>in</strong>g a garage hold up.<br />
The <strong>in</strong>cident was wimessed and the police were called. The<br />
police arrived at 11 07 pro. The police then called the paramedics,<br />
who.arrived at 11 17 pro. They noted that the patient<br />
,lially conscious and compla<strong>in</strong><strong>in</strong>g of pa<strong>in</strong> around the wound<br />
<strong>in</strong>~ abdomen. The paramedics then began to run through<br />
their check lis% which <strong>in</strong>cluded tak<strong>in</strong>g the patient’s blood pres-<br />
,ure and pulse. Both these were difficult to do and several<br />
attempts were made. An <strong>in</strong>travenous l<strong>in</strong>e was <strong>in</strong>serted and by<br />
the time all this was done the patient was f<strong>in</strong>ally loaded <strong>in</strong>to the<br />
ambulance at 11 32 pro. At 11 42 pro--that is, only 10 m<strong>in</strong>utes<br />
l~ter--the patient arrived <strong>in</strong> the regional trauma centre. The<br />
patient had, however, died <strong>in</strong> the ambulance and could not be<br />
resuscitated. It is obvious from the times stated that ff the<br />
policeman had: simply put the man <strong>in</strong> his car and taken him<br />
straight to the hospita ! , which was only 10 m<strong>in</strong>utes away, or if<br />
the paramedics had taken him straight to the hospital then the<br />
patient would have been talk<strong>in</strong>g and compla<strong>in</strong><strong>in</strong>g of his abdom<strong>in</strong>al<br />
pa<strong>in</strong> when he arrived <strong>in</strong> the trauma centre. The<br />
necropsy showed a perforation of the small bowel and a laceration<br />
to the common iliac ve<strong>in</strong>. These lesions were treatable and<br />
the patient would have lived.<br />
It is becom<strong>in</strong>g clear that <strong>in</strong> the management of trauma efforts<br />
to improve out of hospital care can go only so far. Paramedics<br />
,.re well tra<strong>in</strong>ed, highly skilled, and well motivated. Their role<br />
is that bystanders who <strong>in</strong>itiate cardiopulmonary resuscitation<br />
the moment a cardiac arrest has occurred make a major contribution<br />
to the survival of that patient. An important success<br />
with resuscitation of ventricular fibrillation tak<strong>in</strong>g place out of<br />
hospital can be expected only if cardiopulmonary resuscitation<br />
is started with<strong>in</strong> four m<strong>in</strong>utes of the event and defibrillation<br />
accomplished with<strong>in</strong> eight m<strong>in</strong>ute,. Furthermore, it is not<br />
necessary to have a fully tra<strong>in</strong>ed paramedic arrive on the scene;<br />
a basic emergency medical technician who has received an extra<br />
I0 hours of tra<strong>in</strong><strong>in</strong>g <strong>in</strong> defibrillation can achieve similar results<br />
if he gets there with<strong>in</strong> the eight m<strong>in</strong>utes:<br />
The implications for the United K<strong>in</strong>gdom are obvious. We<br />
already have a well established, well discipl<strong>in</strong>ed, and well<br />
motivated ambulance service. They are experienced <strong>in</strong> the<br />
extrication of patients from vehicles and, along with their fire<br />
and police colleagues, perform an excellent service. The advance,<br />
<strong>in</strong> mmmgement of trauma are to be made not <strong>in</strong> care<br />
received out of hospital but <strong>in</strong> that received <strong>in</strong> hospital. The<br />
American development of trauma centres bears witness to this.*<br />
For patienta who have sutfered seriom trauma the most advantagcous<br />
th<strong>in</strong>g to do is "scoop mad run,’? mad our mnbulance<br />
drivers are good at it. The patient must, however, be scooped<br />
up and run to a trauma centre. Such a place must be.capable of<br />
resuscitat<strong>in</strong>g that patient and provid<strong>in</strong>g mediate surgery by<br />
senior surgeons experienced <strong>in</strong> trauma. If a smaller hospital is<br />
passed en route then so be it. The United State, of America is<br />
accept<strong>in</strong>g this and designat<strong>in</strong>g certa<strong>in</strong> hospitals as trauma<br />
centres. We mtLst do this too.<br />
The advancea <strong>in</strong> coronary cat,, howeverj are to be made<br />
outside the hosp|tal: ~ t<strong>in</strong>t is to tra<strong>in</strong> mo~ of the general<br />
public to <strong>in</strong>itiate cardiopulmonm’y r~tation with<strong>in</strong> the<br />
critical four m<strong>in</strong>ute,. Until our amb~ are equipped<br />
With defibrillator% however, it is unlikely that patients <strong>in</strong><br />
ventrioalar fibrillation will be saved <strong>in</strong> any great numbers. An<br />
ambulance will "probably arrive with<strong>in</strong> eight m<strong>in</strong>utes, but<br />
ambulancer/len can only carry on cardiopulmonary resuscitation<br />
and the ch~mces of that patient surviv<strong>in</strong>g are very poor. If the<br />
ambulancemen had a defibrillator and could reverse ventricular<br />
fibrillation then the day may come when a third of these patients<br />
will be back home with their families, as they are <strong>in</strong> Seattle.<br />
A relatively short time ago we had the best ~mbulance service<br />
<strong>in</strong> the world. The basic structure and the quality of the personnel<br />
still rcana<strong>in</strong>s and <strong>in</strong>deed has improved. All that is lack<strong>in</strong>g is the<br />
provision of defibrillators and once aga<strong>in</strong> our ambulance service<br />
will be the best. ..._---- "<br />
o<br />
References<br />
*-Cobb LA, Hallstrom AP. Community r<strong>in</strong>sed cardiopulmonm’~ resuscimm<br />
the treatment of trauma is, however, limited. The reverse is -_ tion--whnt have we learned ? ~nn N Y ~¢ad Sd 1982;38~:330-42~<br />
-. _- t Trunkey DD. Trauma. Sd ~m 1983 ;2A9 :20-7.<br />
true, or suddeii cardiac arrest. It has been deafly-sl~own-by<br />
- the~rke~ <strong>in</strong> .~ttle that the provision of a highly sHllcd and (~e~xpud 13 October 1883)<br />
fi~t~]~ramedic’team can ~eafly improve the outlook for cardiac<br />
arrests out of hospitaL*<br />
Present figures from S~ttle t~h~v that for episode, o[ventricular<br />
fibrillatioiL outside hospitals, two thirds will be admitted<br />
~,ith a pt~lse and b!ood pressure to hospital. Half of these<br />
W~l go home. Seatde’is fortur~ate <strong>in</strong> that it has’n-enthusiastic<br />
tnd underused fire service. The city burnt down <strong>in</strong> the1890s Does ahitud~ affect th~ read<strong>in</strong>g of bloodpr~sure, dth~ with. a mercury<br />
and has been determ<strong>in</strong>ed never to repeat the episode. It has<br />
or- toith an ana~roid sphygmomanom~t*r ? .....<br />
therefore furnished itself with 32 fire stations for an-18 x6 mile Changes of aldmde may affect the l)Io~i pressure of an <strong>in</strong>dividual,<br />
(~.>" 10 k<strong>in</strong>) city. Furthermore, it has" 14 major hospitals with<strong>in</strong> but they do not have pronounced effects on the record<strong>in</strong>g of that blood<br />
tMs small area. When car_~’ac.arrest occurs it takes 2 m<strong>in</strong>utes- pressure. The convendonai sphygn~, manometer is exposed at both<br />
47 r~conds for a" fire eng<strong>in</strong>e and a-basic ern¢~rgency- medical " ends to prevail<strong>in</strong>g_atmospheric pressure (it is not a barometer).<br />
ttehnician to <strong>in</strong>itiate cardiopulmonary r~uscitat<strong>in</strong>n. Two Similarly, the bellows of the anaeroid sphygmomanometer are ex-<br />
m<strong>in</strong>utes later the <strong>in</strong>termediate .emergency medical t .esOmici~ffiposed to ambient atmospheric pressure, as is the patient <strong>in</strong> whom<br />
arrives, and two m<strong>in</strong>utes after that a paramedic-emerget,cy the blood pressure is measured. Blood pressure is not an absolute<br />
medical technician who passes an (mdotracheal tube, <strong>in</strong>terprets value: it is the pressure difference between the circulatory system<br />
and ambfent atmospheric pressure. Thus if systolic blood pressure is<br />
electrocardiogram, and defibrillates when necessary. The 120 mm Hg and atmospheric pressure is 760 nun Hg absolute systolic<br />
t~ramedic will also stabilise any arrhythmias before transport. pressure will be 880 nun Hg.~R THOMAS, physicist, Glasgow, and<br />
~he other factor that the workers <strong>in</strong> Seattle have established F L~’tm, director, blood pressure unit, Glasgow.<br />
623
5".."<br />
THE LAN~T, AUG1<br />
’q ....: ....’~ -’=:~z~::-:n-ch!cf, Dc:’a...n:que ~ ..... ~ar-.:v °<br />
appreciated :he r,~u- ,.o, e.,.e,t ;, ,,, . for ra~id evacuv_tizn and early<br />
~.a;~-q care when he set up ,’he ..... ’-*--<br />
~te~<br />
,~<br />
"fly<strong>in</strong>g<br />
ambulances’" <strong>in</strong> the first half of:he 19th century but it was<br />
van <strong>in</strong> the latter part of the 1939-45 war that modern<br />
techniques Of resuscitation came to be applied to wounded<br />
peraonneL at ,he,place of <strong>in</strong>iury. Subsequently, dur<strong>in</strong>g the<br />
militar~’confliffts <strong>in</strong> Korea, Vietnam, the Middle East and<br />
more~edentl~ <strong>in</strong> the Falklands, specifically tra<strong>in</strong>ed<br />
’para~c" soldiers provided basic medical care and rapid<br />
eva~anon of the seriously <strong>in</strong>jured. =:7=:.’ ¯ ...<br />
The application of lessons learnt dur<strong>in</strong>g War-time to<br />
ci:51ian experience is often delayed. Nowhere is this more<br />
powerfully exemplified than <strong>in</strong> the establishment of hospital.<br />
based accident fly<strong>in</strong>g squads. In 1955 the first accident fly<strong>in</strong>g<br />
squad was established by Coll<strong>in</strong>s" ’at the accident and<br />
emergency department <strong>in</strong> Derby Royal Infirmary. 1 In the<br />
early 1970s several other centres with<strong>in</strong> the United K<strong>in</strong>gdom<br />
began to appreciate the potential value of such squads, and<br />
the number ofschemes has s<strong>in</strong>ce <strong>in</strong>creased rapidly. In 1982<br />
there were 47 centres throughout the United K<strong>in</strong>gdom with<br />
this facility, but less- than half of these were "active", with<br />
10-100 call-outs per annum. ~<br />
:i~: The two major prev~mbl~ ~ of<br />
trauma are respiratory otmrm=ion and/or<br />
ventilation, and ttypovolaemia. Several<br />
made to quantify ~ components. Lauppi <strong>in</strong>dicate,<br />
14% of patients ~ho died ~6th<strong>in</strong> 2 dal~ ofth~ ~~5<br />
because ofrespi~tory obstructiam. Raffndl-Smi~<br />
the frequency of death from resph’atory ob~,~ ¯<br />
5% ’ In a ma~or sm ........ ,,, ,..z~7~27-~,~ "~<br />
.. . ~ aym i~oc.am~ty otncers fom~’obst~action<br />
<strong>in</strong> 10.7% of patients who died as ~ ¢or,,~ec~<br />
of trauma, but o~y <strong>in</strong> 0-7% of survivors. The~ alto<br />
<strong>in</strong>halavion or’blood ,,~d .............. ~ :-,.-’a~: "<br />
rc;,5~ T:=;’:~,: 4J’i--=:i~’," ...... .... -~ . --~ ,<br />
i-..,:~ .-:a:. v- ~’-~3~-,, ~,~ r_’,~:zents-~.::¯: :’-:.)sequent’- ~k-:~ "<br />
obstructeci airway-at r~ scene of the acddeht.rl~ "%:~,<br />
stud5, of deaths over a 5 y~r period, ofpatieam w~o d:~2 z<br />
hospital as a cons equence oft rauma, " tt~ose wl’~ h~ ~--w~ ’~<br />
obstpaction had less seven= <strong>in</strong>juries a~ meas~ed bya ~:scor<strong>in</strong>g<br />
system than did those without such obsar~-<br />
This f<strong>in</strong>d<strong>in</strong>g strongly implied that airway obstracti~<strong>in</strong>~<br />
a context contributed to morta~. --~ --~’r"=~,; ~ -<br />
The siva,ion<br />
do c.umented. Hoffman showed tl~ for patim~::~<br />
with associated blood Iwas, 59% died imtaml.v amt ~g~.<br />
with<strong>in</strong> 6 h, suggest<strong>in</strong>g that perhaps 25% of d~ll~<br />
hypovolaemia could have been l:a-~,ented; r ~_.~: It<br />
suggested that ~3% of patients who died of trauma fi’ammag:.traffic<br />
accidents did so because of’blood Imps and that lr-l~,Y<br />
of these could have be~n saved by ~dequrae ~,,.~,.<br />
<strong>in</strong>fusion.9 ..........<br />
Although these various studies have be= :~~7<br />
grounds of irreproducibility and subjectivity, it w~-2 a .<br />
nevertheless appear that there is a sizeable propanioa ~<br />
pa:ients whose deaths cou~ have he~a prevr.ated l~tmar~<br />
aid been immediately availabli:.- ...... ~ _ _<br />
ORGANISATION OFFLYING~ADS -_::~ i<br />
THE CASE FOR ACCIDENT FLYING SQUADS<br />
Hav<strong>in</strong>g decide~ Lhat fly<strong>in</strong>g squads have potenti~ wak~<br />
In Gr~{ Brita<strong>in</strong> approximately 6000 people die every year provid<strong>in</strong>g emergency medical care at the scene., mm ~-<br />
as a result of road traffic accidents. Three times this number consider the type ofpersonaeI and equipment best suir~fm<br />
of people are killed <strong>in</strong> accidents <strong>in</strong> other situations and nearly provid<strong>in</strong>g such a service. "::~.~:"<br />
half a million people susta<strong>in</strong> major <strong>in</strong>juries each year from Snook has reported his experimaceofper~onal att~<br />
trauma. It has been suggested tha~ 43°70 of motorcyclists and accident medical officer ~o the Bath Fire and<br />
vehicle occupants who die as a result of road traffic accidents Service;<br />
N’~ ~ ~reat,.r chance o~" ~urvival had medic:.l<br />
..~ :: :. T -~= a,-dabie a~ th: scc.’,.e with<strong>in</strong> ~0 r:aAn of the<br />
.,~;:,~’. it, advocat<strong>in</strong>g a ro!e/br accident/ly<strong>in</strong>g squads it is<br />
~here?ere essential to del<strong>in</strong>eate those groups of patients who<br />
would benefit from the provision of early emergency care.<br />
l° however, a s<strong>in</strong>gl~handed ser~e of this ty:~e La<br />
.1T~.tatlO . ""’" ; "’ : "" r~.;Z7 ":<br />
consist<strong>in</strong>g of senior ,a,?Jt ,~:s from the :tc~-d~::.t arid eme: ~ :department<br />
together with 8ix:t<strong>in</strong>ily tra<strong>in</strong>ed at:rsk-:~: :’2 ,<br />
should attend such calls. In Ed<strong>in</strong>tm~gh, where a fly~ag ~%°- : ,<br />
has been function<strong>in</strong>g for the past $ years, the ~<br />
O. $IMONEN AND O. LAITINEN; REFERENCES--Cont<strong>in</strong>ual ~’~"~’"<br />
17. C.a~ ILM, Croft JD, Petltim~ P, et al..~ ,ew bone formation <strong>in</strong> ost~oporo~is follo..<strong>in</strong>g<br />
treatment with sodium fluo~de. A .oh Intcr~ M~d 1966; 118:11 I- 16.<br />
18. Grove O, Halver B. Trcatracnt of paim’ul mteoporosis with fluo~id~ calcium and<br />
cal¢/ferol. ~lkt~d Get, mot 1978; 8: 167-68.<br />
19. Krokow~ki E. Sodium fluoride <strong>in</strong> tr~tm~nt ofo~mpormh. F~’t$¢f*rafed 1979i 97:<br />
’ 1635-40.<br />
20. Riggs BL, Hodgson SF, Hoffman DL, et al. Treatment of primary esteoporofis with<br />
fluoride and c~lcium. JAM..! 1980; 24~: 446-49.<br />
2 I. R<strong>in</strong>g JD, Kru~ HP. Kuhlen¢ordt F. ~xlium fluoride and calcium (n the treatment of<br />
primary os~eoporosis. M#d Kli, 1982; 7"/ 86--89<br />
22. Riggs BL, Seeman E, Hodpon SF, et al. Effect of the fioorid~/calcium regimen on<br />
ce:t~bral fra~ure o~urr~c~ <strong>in</strong> po~tm~nop~us~l osleoporo~is. N E~I] Msd 1982;<br />
:106: 446-50.<br />
23.8 ikl ~ DD. Fluoride :teat meat ofost ~porosh: a ne’~ look at an old dru<br />
s.<br />
4nn Imtr~ M,’d<br />
’9S3; ~: 1013-15.<br />
-25. Dixo A 5;! ~. N on-hormonal treatment ofos~porosis. Br.W~] 1973; ~’87: 99~- 1000.<br />
26. Dean HT, Arnold FA, Jay Jr P, Knutson JW, Studi~ on mass control of dental cari~<br />
:hroogh fluoridation of the p, ublic water supply. Publ Hcahh R~p 19501 I~:<br />
1403-08.<br />
27..\ta~er FJ. Fluoridation of public water supplies. ] Am Water Works Ass. 1950; 42:<br />
1120-32.
!<br />
~ ’~EL,,.’~CET, at~3t~ST24,1985<br />
_~~m~isea a senior member of medical staff(consultant or<br />
"~"r~.g~’grar grade), one w~aior house officer, and one or more<br />
:~:;¢~trienced nurses. A call-out would therefore deplete the<br />
".~-’omplement of staff <strong>in</strong> the base dqmrtment if arrangements<br />
7 .~rere not made to provide adequate cover. Accord<strong>in</strong>gly most<br />
2~:t,ccidem fly<strong>in</strong>g squads operate from large, usually teach<strong>in</strong>g,<br />
~]~spital accident and ,nmrgeamy departments which have<br />
~N h staff<strong>in</strong>g at senior level<br />
~,Most centres operat<strong>in</strong>g st~ schemes use transport<br />
.~ffovided by the ambulance service and only 6 centres <strong>in</strong> the<br />
~Jjnited K<strong>in</strong>gdom have their own riv<strong>in</strong>g squad vehicle; these<br />
!" vehicles have Usually been funded by public donation or the<br />
~.trea health authority. Despite the crucial nature of<br />
7~mmunication only 60% have their own radio l<strong>in</strong>ks with the<br />
-"emergency services. 2 Considerable experience has been<br />
_.,-,2ned with respec~ to the nature of resuscitative equipment<br />
r.ecessary for the provision of immediate medical care.<br />
Yra~lly the equipment it assigned for use specifically by the<br />
---rag squ~ and added for the vehicle that has been<br />
_._-r2"ed for use Lw the team. Over the past decade such<br />
_7:nee" na- 1-,eco,.v~ F’~’gr(~ssi’,’eiy more ref<strong>in</strong>ed,<br />
~:~mes th~ n:u:*, of ~n;.ova~;o~ made by members o:<br />
:. i.-.g sq~. ~ ~.12 A comiderabie proportion of casualties are<br />
., trap txed and extrication requires SlXCial equipment. This is<br />
~ammally carried by fire service vehicles although several<br />
i~h.-ua~ cari~ a limited range of hydraulicram, saws, shears,<br />
¯ The roadside is not the place for complex medical o r<br />
=~,~lmr#4:al imerventiou. Provided the basic priorities ofairway<br />
~i~ency, ventilation, volume replacement, pa<strong>in</strong> relief, and<br />
(Wlmtage oaa be acIaie~ little more is required <strong>in</strong> the vast<br />
_’~r.:iori~ of eases before tran~er to hospital. The corollary of<br />
-~]s is that it is-not too expensive m ful!y equip a fly<strong>in</strong>g squad;<br />
£~0 000-15 000 would be suff’miem today.<br />
%<br />
EF<strong>FIC</strong>&CY OF FLYING SQUADS<br />
With the wisdom of h<strong>in</strong>dsight, it seems extraord<strong>in</strong>ary that<br />
~0;~o a.~empt was made untit the early 1970s to assess the<br />
:.~:~im~,uence of fly<strong>in</strong>g squads m rndmangmortality or morbidity.<br />
~:~t= Cell!as" orig<strong>in</strong>al paper <strong>in</strong> 1966, his conclusion that "the<br />
- 7 ~c."t~s eft’early treatment of tim <strong>in</strong>jured by the fly<strong>in</strong>g squad<br />
amply justified 1he efforts of the team ’’l was not<br />
supported by objective data. Snook judged that attendance by<br />
_.
¯ 436 ¯ " ":". ÷’:.:~,:~:~ ,::. "-7~.?~’,,.~? :~ "<br />
"rltEL’t.~CE"I<br />
either by a member of one of the~emergency services or a<br />
doctor. Secondly,’ the best results: <strong>in</strong> cardiopulmonary World Health Organisafion<br />
resuscitation out ~ of hospital have occurred ,where lay<br />
bystanders have <strong>in</strong>itiated basic life-support and ~ont<strong>in</strong>ued ; :<br />
~his u.’.=il advanced, cardiac life support is available from APPROPRIATE TE~:I~IOI.OG¥ FOR BIRI’i~:..<br />
speciaEsed services. : - , " -- ..... " ....<br />
" ~ : ..... In April, the European regional office ofthe World R~" "<br />
Organisation, the Pan American Health Organisadoa,<br />
COSCLUSlONS. .............. _k .....<br />
the WHO regional office oftheAmericas held a conf~<br />
The .:didhy of blanket statements <strong>in</strong>dicat<strong>in</strong>g that fl~ ~r’ <strong>in</strong>oo appropriate technology for bixth. The conference, hd~ . i) ~<br />
~q=: ~ ¯’undoubtedly save lives ’m must rema<strong>in</strong> severely Fortaleza, Brazil, was attended hy over 50 participle,<br />
-~:~ ......,~_,e~Lon. Whir can, however, be stated with some re~re~en-.-.,- .~; :~,’:fer,,, o.% :0:r~z
mt Surgery VoL 14/No. 6<br />
S. (1979) Rationaliz<strong>in</strong>g<br />
cn ofacute ankle <strong>in</strong>jur-<br />
;ical exam<strong>in</strong>ation ofthe<br />
wet 2, 1167.<br />
of m<strong>in</strong>or fractures <strong>in</strong><br />
". Injury 5, 213.<br />
~’niveOedical Center,<br />
WI~O sub:<br />
lld be an<br />
chniques<br />
ire of the<br />
.?-<br />
Evaluation of a hospital-based accident fly<strong>in</strong>g<br />
squad us<strong>in</strong>g an <strong>in</strong>jury scor<strong>in</strong>g system<br />
D. F. Gorman and J. Coals<br />
<strong>Accident</strong> Unit, Chester Royal Infirmary<br />
Summary<br />
The records of 250 patients treated by a hospital-based<br />
fly<strong>in</strong>g squad have been analysed retrospectively to<br />
determ<strong>in</strong>e the value of such a unit <strong>in</strong> prevent<strong>in</strong>g death<br />
follow<strong>in</strong>g various types of accident. To facilitate<br />
analysis two analytical methods have been used, one<br />
of which showed that fly<strong>in</strong>g squad action saved two<br />
lives. However, on cl<strong>in</strong>ical grounds we conclude that<br />
measures taken at the scene unequivocally led to the<br />
survival of 6 per cent of those alive at the scene.<br />
S t 3<br />
quantitative assessment made possible by us<strong>in</strong>g<br />
the ISS.<br />
PATIENTS AND METHODS<br />
The Chester Royal Infirmary FS was <strong>in</strong>augurated<br />
<strong>in</strong> 1974. The Chester vehicle is a speciallymodified<br />
estate car, carry<strong>in</strong>g a full range of<br />
resuscitative equipment, experienced nurse(s)<br />
and an experienced doctor, usually ofconsultant<br />
or registrar grade. The vehicle is driven by an<br />
ambulanceman. The squad is summoned by the<br />
emergency services or occasionally a local<br />
INTRODUCTION<br />
General Practitioner when more treatment is<br />
THE value of a hospital-based fly<strong>in</strong>g squad <strong>in</strong> required at the scene of an accident than they<br />
reduc<strong>in</strong>g morbidity and mortality from traffic can provide. S<strong>in</strong>ce the <strong>in</strong>ception of the scheme,<br />
accidents is difficult to assess. Some of the major the FS has also attended non-traumatic emer-<br />
difficulties encountered <strong>in</strong> the epidemiology of gencies.<br />
trauma arise because of the variety of mechan- The first 250 calls, which occurred between<br />
isms caus<strong>in</strong>g <strong>in</strong>jury and the large number of October 1974 and May 1981, have been<br />
<strong>in</strong>dividual <strong>in</strong>juries and comb<strong>in</strong>ation of <strong>in</strong>juries analysed retrospectively by referr<strong>in</strong>g to a log-<br />
which can occur. Such variety prevents assignbook, accident unit notes, <strong>in</strong>patient notes and,<br />
ment of patients <strong>in</strong>to large groups, thereby <strong>in</strong> the case of all those who died as a result of<br />
mak<strong>in</strong>g comparisons and statistically significant trauma, to post-mortem reports. The notes of<br />
conclusions difficult to achieve. Scor<strong>in</strong>g systems patients transferred to other hospitals have been<br />
(AMA Committee, 1971, 1972; Baker et al .... exam<strong>in</strong>ed <strong>in</strong> every case. All data were recorded<br />
1974; Cowley et al., 1974; Baker and O’Neill, on <strong>in</strong>dividual patient record cards which pro-<br />
1976) have therefore been devised <strong>in</strong> a’n~ttempt vided details of day, date and" times of call,<br />
to facilitate such comparisons, despite the scores <strong>in</strong>itiator of~call, geographical location, name and<br />
be<strong>in</strong>g arrived at by summat<strong>in</strong>g different <strong>in</strong>juries. age of patient(s), type of <strong>in</strong>cident, nature of<br />
This paper seeks to utilize one off,systems, . <strong>in</strong>juries, tr~tment given, survival and post-<br />
the Injury Severity Score ~l"(B’fiker, et al., mortem [<strong>in</strong>d<strong>in</strong>gs. and details of nurs<strong>in</strong>g and<br />
1974; Baker and O’Neill, 1976), to produce an medical attendants. In addition, the times of the<br />
objective assessment of the efficacy of~mSpital- 999 calls;and FS call, turnout time, travell<strong>in</strong>g<br />
based Fly<strong>in</strong>g Squad (FS) <strong>in</strong> reduc<strong>in</strong>g mortality time and time spent at the scene of an accident<br />
from traffic and other accidents. Conventional have been recorded <strong>in</strong> most cases.<br />
analysis has been undertaken <strong>in</strong> addition to the An ISS was allocated to each patient attended
e<br />
514 Injury: the British Journal of <strong>Accident</strong> Surgery VOL 14/No. 6<br />
TaMe L Method of cod<strong>in</strong>g <strong>in</strong>juries on the Abbreviated Injury Scale<br />
AIS Code Severity Example<br />
1 M<strong>in</strong>or"<br />
2<br />
Moderate<br />
3<br />
Serious<br />
4 Severe<br />
5 Critical<br />
6 Maximum <strong>in</strong>jury virtually<br />
unsurvivable<br />
9 Unknown<br />
Table II. Method of scor<strong>in</strong>g AIS by type of <strong>in</strong>jury<br />
Superficial laceration<br />
Fractured tibia<br />
Displaced fracture of tibia<br />
Ruptured spleen<br />
Ruptured liver<br />
Massive chest crush<br />
Area Injury AIS AIS 2<br />
Head Unconscious > 1 hour and < 24 hours 4 16<br />
Fracture R transverse process of C7 2<br />
Chest Pulmonary contusion 3 9<br />
Abdomen Ruptured spleen 4 16<br />
Limbs Fracture R superior & <strong>in</strong>ferior public rami 2<br />
Comm<strong>in</strong>uted fracture L femur 3 9<br />
Fracture L humerus, displaced 3<br />
Fracture neck & shaft R humerus with 3<br />
radial nerve palsy<br />
External Laceration of L forehead 1<br />
R cheek 1<br />
R elbow 1<br />
Face R conjunctiva 1<br />
ISS=41 (16+16+9) Patient 203 Call 208<br />
as well as any other patient whose <strong>in</strong>juries would<br />
have merited a call and also received treatment<br />
at the time.<br />
severity scor<strong>in</strong>g<br />
system of scor<strong>in</strong>g was developed by Baker<br />
et al. 0974) and Baker and O’Neill (1976) from<br />
the Abbreviated Injury Seale (AIS) and was<br />
based on analysis of 2128 RTA victims (Baker<br />
¢t al., 1974). For the purposes of scor<strong>in</strong>g, the<br />
body is divided <strong>in</strong>to six regions--head and neck,<br />
face, chest, abdom<strong>in</strong>al and pelvic contents, limbs<br />
and pelvic girdle, and external. Sp<strong>in</strong>al <strong>in</strong>juries<br />
are recorded with<strong>in</strong> one ofthese regions. With<strong>in</strong><br />
each body region an AIS code of 1-6 or 9 is<br />
allocated for each <strong>in</strong>jury as set out <strong>in</strong> the<br />
Abbreviated Injury Scale 1980 Revision (American<br />
Association for Automotive Medic<strong>in</strong>e,<br />
1980). Some examples are given <strong>in</strong> Table I.<br />
Hav<strong>in</strong>g applied the AIS code to each <strong>in</strong>jury,<br />
the maximum s<strong>in</strong>gle score for each of the six<br />
regions is identified and the sum of the squares<br />
ofthe highest AIS code <strong>in</strong> each ofthe three most<br />
severely <strong>in</strong>jured areas is the Injury Severity<br />
Score (ISS). The maximum score for any one<br />
body region is 25 (52) and the maximum ISS is<br />
75 (25+25+25). Any one <strong>in</strong>jury attract<strong>in</strong>g an<br />
AIS score of 6 is automatically awarded an ISS<br />
of 75.<br />
A fatality is not of itselfsufficient to attract an<br />
AIS of 6, the severity of the <strong>in</strong>jury must be<br />
known. An example appears <strong>in</strong> Table II.<br />
Exclud<strong>in</strong>g erythema burns score accord<strong>in</strong>g to<br />
the percentage ofthe body’s surface area affected<br />
as determ<strong>in</strong>ed by the Rule of N<strong>in</strong>es, for example<br />
areas from 6--15 per cent score AIS 2; from<br />
36--90 per cent score AIS 5. In addition, an <strong>in</strong>halation<br />
burn scores AIS 4 or 5 depend<strong>in</strong>g upon<br />
whether artificial ventilation is required (AIS 5)<br />
or not (AIS 4). The ISS takes no account ofoutcome<br />
and is discont<strong>in</strong>uous, with 44 stages<br />
between scores of I and 75; the gaps occur more<br />
frequently as the score of 75 is approached.<br />
i<br />
Gorman and Coals" Evaluation o<br />
Table III. The total number a<br />
fly<strong>in</strong>g squad<br />
Tom/m<br />
Type of cat/ e/~<br />
Trauma 15,<br />
Medical<br />
Surgical<br />
Hoaxes<br />
6;<br />
Aborted I,<br />
Missed rendezvous<br />
Disaster exercise<br />
Total<br />
25q<br />
Table V The number of dear<br />
Cause h<br />
Road traffic accidents<br />
Industrial<br />
Assault<br />
Home<br />
Suicide<br />
Age weight<strong>in</strong>g<br />
It is obvious that older !~<br />
than younger patients to<br />
<strong>in</strong>juries. Baker, (1974) fol<br />
arid 26 were associated wi<br />
tality <strong>in</strong> the respective al<br />
50-69 years and 70+ yt<br />
Analysis to his data from<br />
dent patients admitted<br />
<strong>Accident</strong> Hospital <strong>in</strong> 196<br />
mortality to age and ISS<br />
closely with Baker’s, a<br />
(mean+sd), 29-4+2"5 ;<br />
associated with 50 per ce~<br />
tire age groups 15-44 y~<br />
65 + years. Stoner et al. (<br />
mortality studies ISS mus<br />
Yates (1977) corrected flu<br />
the 45-64 age groups usiz<br />
and <strong>in</strong>cluded a predicted<br />
his modification of Bull’s<br />
age-correction ofall patie~<br />
ate to the 45-64 age gro<br />
study, as is the predicted<br />
In a further publicatic<br />
q
Surgery Vol. 14/No. 6<br />
s 2<br />
6<br />
9<br />
6<br />
9<br />
e<br />
of the squares<br />
0f the l~l~e most<br />
InjurIIleverity<br />
ore for any one<br />
laaximum ISS is<br />
try attract<strong>in</strong>g an<br />
awarded an ISS<br />
ient to attract an<br />
<strong>in</strong>jury must be<br />
Table II.<br />
3re accord<strong>in</strong>g to<br />
ace area affected<br />
aes, for example<br />
re AIS 2; from<br />
ldi~on, an <strong>in</strong>halepend<strong>in</strong>g<br />
upon<br />
¢quired (AIS 5)<br />
account ofout-<br />
~th 44 stages<br />
~ps occur more<br />
pproached.<br />
Gorman and Coals: Evaluation of a hospital-based fly<strong>in</strong>g squad 515<br />
Table II1. The total number and types of calls to the<br />
;fly<strong>in</strong>g squad<br />
/ Type of call<br />
Table IV The <strong>in</strong>itial cause of <strong>in</strong>juries and total<br />
number of patients <strong>in</strong>volved<br />
Total number Total number<br />
of calls of patients No. of<br />
Cause patients<br />
-~;-~ Trauma 156 179 Road traffic accident 131<br />
Medical 68 68 Industrial (<strong>in</strong>clud<strong>in</strong>g farm<strong>in</strong>g) 18<br />
Surgical 3 3 Home 10<br />
Hoaxes 2 0 Assault 5<br />
Aborted 14 0 (20) Suicide attempt 4<br />
Missed rendezvous 6 0 (6) Other 11<br />
Disaster exercise I 0 Total<br />
Total 250 250 179<br />
Table V The number of deaths by cause<br />
Cause No. of patients ISS range<br />
Road traffic accidents 43 17-75<br />
Industrial 8 20-75<br />
Assault 3 16-57<br />
Home 3 25-75<br />
Suicide I 17<br />
Table VI. Time and place of death<br />
lime of death No. of patients ISS range<br />
Dead when Fly<strong>in</strong>g Squad<br />
arrived 14 16-75<br />
Died at the scene 6 25-75<br />
Died <strong>in</strong> transit 4 34-75<br />
Died after arrival at<br />
hospital and with<strong>in</strong> 3<br />
hours 18 26-75<br />
Died 3-24 hours I0 26-75<br />
Died later than 24 hours<br />
after <strong>in</strong>jury 6 17-43<br />
Age weight<strong>in</strong>g<br />
]t is obvious that older patients are more likely<br />
structed a grid ofexpected mortality for different<br />
ISS at different ages above 15 years. Patients<br />
than younger patients to die with less severe were divided <strong>in</strong>to decades and ISS <strong>in</strong>to equal<br />
<strong>in</strong>juries. Baker, (1974) found that ISS of 41, 32 groups 0--4, 5-9, 10-14, etc. An approximate<br />
and 26 were associated with a 50 per.cent mortality<br />
<strong>in</strong> the respective age groups 0-49 years,<br />
probability of mortality was obta<strong>in</strong>ed for each<br />
age group and ISS, for example, age 15-24 years<br />
50-69 years and 70+ years. Apply<strong>in</strong>g Probit with ISS of 35-39 had an approximate prob-<br />
Analysis to his data from 1333 road ti’affic acciability of mortality of 0-4. This grid was based<br />
dent patients admitted to the Birm<strong>in</strong>gham on a further analysis of the 1333 road traffic<br />
<strong>Accident</strong> Hospital <strong>in</strong> 1961, Bull (1975) related accident victims already referred to above (Bull,<br />
mortality to age and ISS. His results compare 1975) and has been used <strong>in</strong> this paper to provide<br />
closely with Baker’s, as-ISS of 39.7+2-9<br />
another method ofdeterm<strong>in</strong><strong>in</strong>g predicted morta-<br />
(mean+sd), 29-4+2-5 and 20-2+1-6 werelity<br />
for patients treated by the FS.<br />
associated with 50 per cent mortality <strong>in</strong> respective<br />
age groups 15.-44 years, 45-64 years and RESULTS<br />
65 + years. Stoner et al. (! 977) affirmed that <strong>in</strong> Table II! illustrates the types ofeall and Table<br />
mortali~ studies ISS must be weighted for age.<br />
Yates (! 977) corrected the ISS of his patients to<br />
IV the precipitat<strong>in</strong>g cause of <strong>in</strong>jury. Table V<br />
the 45-64 age groups us<strong>in</strong>g Bull’s Probit L<strong>in</strong>es<br />
describes the precipitat<strong>in</strong>g cause of death and<br />
and <strong>in</strong>cluded a predicted chance of survival <strong>in</strong><br />
Table VI the place and time of death.<br />
his modification of Bull’s Probit Analysis. This<br />
Two patients were not scored because <strong>in</strong> our<br />
op<strong>in</strong>ion the lesions susta<strong>in</strong>ed could not he scored<br />
age-correction ofall patients to an ISS appropri- adequately us<strong>in</strong>g the ISS system. One patient<br />
ate to the 45-64 age group is utilized <strong>in</strong> this had been struck by lightn<strong>in</strong>g and one was acci-<br />
study, as is the predicted chance of survival. dentally hanged.<br />
In a further publication, Bull (1977) con-<br />
Three patients With relatively low ISS died.<br />
al
O<br />
516 Injury:. the British Journal of <strong>Accident</strong> Surgery Vol. 14/No. 6<br />
The lowest scor<strong>in</strong>g death (ISS= 16) was that of<br />
a man who was already dead when the Fly<strong>in</strong>g<br />
Squad arrived. He had been stabbed with<br />
division of his right common carotid artery and<br />
<strong>in</strong>ternal jugular ve<strong>in</strong> (AIS 4). Two patients had<br />
ISS=IT. One of these died from pulmonary<br />
embolism i0 days aRer self-<strong>in</strong>flicted wounds of<br />
his neck and forearm, the otller was dead before<br />
the arrival of the Fly<strong>in</strong>g Squad and was subsequently<br />
found to have suffered a massive<br />
<strong>in</strong>tra-abdom<strong>in</strong>al haemorrhage due to a ruptured<br />
spleen. He was known to suffer from chronic<br />
lymphatic leukaemia.<br />
Forty-four patients who subsequently died<br />
were alive when the Fly<strong>in</strong>g Squad arrived. These<br />
<strong>in</strong>cluded patients who had fixed dilated pupils,<br />
apnoea and absent major pulses, but on whom<br />
resuscitation was attempted. Scrut<strong>in</strong>y of the<br />
records of these 44 patients revealed that <strong>in</strong><br />
4 cases, earlier <strong>in</strong>sertion of a chest dra<strong>in</strong> Call 4<br />
cases) or earlier <strong>in</strong>travenous <strong>in</strong>fusion (! of the 4<br />
who required a chest dra<strong>in</strong>) might have led to<br />
survival. The ISS scores of these patients were<br />
34, 4 l, 5 l, 54 (chest dra<strong>in</strong>) and 5 ! (IVl).<br />
In regard to delay between the 999 call and the<br />
call for the Fly<strong>in</strong>g Squad (mean 12 m<strong>in</strong>utes and<br />
12.6 m<strong>in</strong>utes respectively), turn-out time (mean<br />
3.9 m<strong>in</strong>utes and 4.4 m<strong>in</strong>utes respectively), or<br />
travell<strong>in</strong>g time (mean 8. ! m<strong>in</strong>utes and 9.3 m<strong>in</strong>utes<br />
respectively), there was no great difference<br />
between the patients who died and those who<br />
survived. Mean time spent at the scene was ! 5.4<br />
m<strong>in</strong>utes for those who died and 27.2 m<strong>in</strong>utes for<br />
those who survived.<br />
One hundred-and-twenty-one patients survived<br />
their <strong>in</strong>juries. Two patients (mentioned<br />
earlier) were not scored, leav<strong>in</strong>g 119 survivors<br />
who were scored. The highest score among the<br />
survivors was 43. Fifty-one patients had scores<br />
between that of the lowest score dy<strong>in</strong>g and the<br />
highest score surviv<strong>in</strong>g. Close scut<strong>in</strong>y of the<br />
records of these 51 patients was undertaken for<br />
evidence that the Fly<strong>in</strong>g Squad improved the<br />
chance of survival. 17 patients had evidence of<br />
hypovolaemic shock and <strong>in</strong> i0 of these <strong>in</strong>fusion<br />
was considered to have improved the chance of<br />
survival, whilst <strong>in</strong> another 4, such treatment was<br />
considered to have saved life.<br />
In addition, 2 patients with scores less than 16<br />
were undoubtedly saved by the rapid adm<strong>in</strong>istration<br />
of large quantities of IV liquids. The first<br />
was a 36-year-old man who had susta<strong>in</strong>ed a<br />
traumatic amputation through the left shoulder<br />
jo<strong>in</strong>t (AIS 3, ISS 9). When the Fly<strong>in</strong>g Squad<br />
arrived he seemed to be moribund with no palpable<br />
pulses. 3 units of Dextran were given<br />
rapidly <strong>in</strong>to a ve<strong>in</strong> <strong>in</strong> his upper right limb as well<br />
as 2 units of plasma and 2 units of O-ve blood<br />
via a phlebotomy at his right ankle. It was<br />
only alter receiv<strong>in</strong>g this quantity by <strong>in</strong>fusion that<br />
the wound began to bleed. Subsequent progress<br />
was uneventful except for an ununited fracture<br />
of his clavicle, which required bone glalt<strong>in</strong>g.<br />
The second patient was a 33-year-old woman<br />
who had fallen through a glass door at home,<br />
susta<strong>in</strong><strong>in</strong>g an extensive wound on her left thigh,<br />
with considerable blQodshed due to complete<br />
division of her femoral artery and ve<strong>in</strong> and long<br />
saphenous ve<strong>in</strong> at about the level of the adductor<br />
open<strong>in</strong>g (AIS 3, ISS 9). Two drips were set up<br />
at the scene and 2 litres were given rapidly; a<br />
further 2.5 litres of blood and plasma were given<br />
with<strong>in</strong> a short time of arriv<strong>in</strong>g at the accident<br />
unit. Another hypovolaemic patient with an ISS<br />
of less than 16 had his prospect of survival<br />
enhanced by early <strong>in</strong>fusion.<br />
Twenty patients were unconscious or had an<br />
impaired level of consciousness at the scene. Of<br />
these, 2 required endotracheal <strong>in</strong>tubation, 5<br />
required <strong>in</strong>sertion of an oral airway, 2 required<br />
suction and/or clear<strong>in</strong>g of debris from their airways,<br />
and the rema<strong>in</strong>der required supervision of<br />
their airways, <strong>in</strong> 3 of these patientsappropriate<br />
management of their airways was considered to<br />
have saved their lives, whilst <strong>in</strong> another 7<br />
patients the prospect of survival was enhanced<br />
by early attention to their airways. Furthermore,<br />
the patient who had been accidentally hanged,<br />
had <strong>in</strong>haled vomitus and was undoubtedly saved<br />
by prompt treatment.<br />
Thus 6 hypovolaemic and 4 unconscious<br />
patients had their lives saved by the Fly<strong>in</strong>g<br />
Squad (10/165, 6.1 per cent) while a further I !<br />
hypovolaemic and 7 unconscious patients had<br />
their chances of survival improved (I 8/! 65, 10-9<br />
per cent). In addition, 4 patients who died might,<br />
with different treatment, hav.e survived (4/165,<br />
2-4 per cent), although 2 of them had an ISS<br />
greater than the highest score of any survivor<br />
and might well have died ultimately.<br />
The distribution of ISS is shown <strong>in</strong> Fig. !<br />
together with all scores corrected to age 45--64<br />
years. N<strong>in</strong>e survivors aged less than 15 years and<br />
2 patients less than ! 5 years who died, have not<br />
had their scores age corrected because the Probit<br />
Analysis described earlier is only applicable to<br />
patients aged ! 5 years or more, thus leav<strong>in</strong>g 166<br />
patients whose ISS have been corrected to that<br />
appropriate to the 45-64 age group.<br />
Clearly it is not realistic to <strong>in</strong>clude patients<br />
already dead <strong>in</strong> the assessment of the treatment<br />
provided by the Fly<strong>in</strong>g Squad. Thus 14 patients<br />
i<br />
I<br />
ooooooooooooooo 7S-<br />
¯ ------- :... 10.<br />
oooo¢ooo<br />
oo<br />
g.’gggl....<br />
ooooooooooo<br />
,$ur~KI {I lg} Died {581.<br />
Uncocrected Scorm<br />
Fig I. The distribution (<br />
dead at the scene befot<br />
Squad have been excl~<br />
survival. Apply<strong>in</strong>g the<br />
vival (Yates, 1977) to t<br />
alive at the scene, ! i0<br />
vive and ! 10 actually<br />
Us<strong>in</strong>g the method de<br />
predicted mortality w~<br />
adult patients alive .<br />
scored. By this me~<br />
expected to die and 42<br />
DISCUSSION<br />
Generally we found tt<br />
apply, except for the 2<br />
not score. Also, sco~<br />
lately our cl<strong>in</strong>ical im]<br />
the exception of some<br />
this series usually stal
"~t Surgery Vol. 14/No. 6<br />
~er right limb as well<br />
units of O-ve blood<br />
ight ankle. It was<br />
Ltity by <strong>in</strong>fusion that<br />
;ubsequent progress<br />
n ununited fracture<br />
bone graft<strong>in</strong>g.<br />
33-year-old woman<br />
;lass door at home,<br />
nd on her left thigh,<br />
d due to complete<br />
y and ve<strong>in</strong> and long<br />
level I e adductor<br />
o drii~were set up<br />
zre given rapidly; a<br />
:i plasma were given<br />
Ang at the accident<br />
¯ patient with an ISS<br />
rospect of survival<br />
:onscious or had an<br />
less at the scene. Of<br />
"heal <strong>in</strong>tubation, 5<br />
I airway, 2 required<br />
ebris from their airuired<br />
supervision of<br />
patients appropriate<br />
,~ was considered to<br />
hilst <strong>in</strong> another 7<br />
~ival was enhanced<br />
rways. Furthermore,<br />
=ccidentally hanged,<br />
s undoubtedly saved<br />
md 4dLnconscious<br />
wed llI~he Fly<strong>in</strong>g<br />
.) while a further ! !<br />
~scious patients had<br />
)roved 08/165, 10.9<br />
:nts who died might,<br />
Lv.e survived (4/165.<br />
)f them had an ISS<br />
ore of any survivor<br />
timately.<br />
is shown <strong>in</strong> Fig. !<br />
rected to age 45-64<br />
than i 5 years and<br />
who died, have po’.<br />
d ~ccau~ ~h¢ P, obit<br />
only applicable to<br />
)re, thus leav<strong>in</strong>g 166<br />
~n corrected to that<br />
group.<br />
to <strong>in</strong>clude patients<br />
~nt of the treatment<br />
=d. Thus 14 patients<br />
Gorman and Coals: Evaluation of a hospital-based fly<strong>in</strong>g squad 517<br />
ISS<br />
was developed from study<strong>in</strong>g <strong>in</strong>juries susta<strong>in</strong>ed<br />
"’’’’’’’’’’’ee" 75’<br />
by road traffic accident victims, this apparent<br />
drawback <strong>in</strong> regard to penetrat<strong>in</strong>g <strong>in</strong>juries is<br />
70’<br />
probably not surpris<strong>in</strong>g and has been remarked<br />
upon by Baker et al. (1974) and Baker and<br />
O’Neill (1976) and by Stoner et al. (1977).<br />
Semmlow and Cone (1976), however, <strong>in</strong> their<br />
e60"<br />
study of 8852 patients from the Ill<strong>in</strong>ois Trauma<br />
Registry (62 per cent of whom were not <strong>in</strong>jured<br />
<strong>in</strong> road accidents) held that the ISS could appropriately<br />
be applied to non-vehicular trauma,<br />
although <strong>in</strong> their series, only 4 per cent of 5502<br />
¯o<br />
patients not <strong>in</strong>jured <strong>in</strong> road traffic accidents had<br />
an ISS greater than 20, compared with 20 per<br />
00¯40<br />
cent of 3350 victims of road traffic accidents¯<br />
ego<br />
The ISS system allowed us to del<strong>in</strong>eate a<br />
ooo<br />
group of 51 surviv<strong>in</strong>g patients <strong>in</strong> whom action<br />
: °°:~ taken by the Fly<strong>in</strong>g Squad could have contri-<br />
e¯<br />
oo buted to survival or even saved life. However,<br />
¯30’ ":e¯<br />
us<strong>in</strong>g the ISS <strong>in</strong> conjunction with the predicted<br />
e¯<br />
eee ¯:.. eeee<br />
o¯ ~::<br />
ego<br />
oooooo<br />
ego chance of survival we were not able to demonstrate<br />
a lower<strong>in</strong>g of actual mortality <strong>in</strong> these 51<br />
oo ~o<br />
ego<br />
!!:<br />
":20.-o0o,<br />
patients. There are several reasons why we were<br />
gig<br />
oo<br />
go<br />
¯go¯<br />
go handicapped <strong>in</strong> this regard. Firstly, the small<br />
sample sizes for any one ISS. Secondly, our <strong>in</strong>-<br />
¯Do¯gooD¯go¯o¯<br />
oooo<br />
gOOD¯<br />
sistence on assign<strong>in</strong>g the lower AIS code whenever<br />
doubt or argument arose <strong>in</strong> regard to<br />
; ........ go¯co¯¯¯¯o¯ 10" ,::|~?|||~:¯=,<br />
oo<br />
oo<br />
go<br />
particular <strong>in</strong>juries. Thirdly, post-mortems were<br />
,,=:~:~o...<br />
oooq,.o<br />
generally.macroscopic and were as a result <strong>in</strong><br />
goD¯O¯¯¯<br />
some respects deficient for our purposes, for<br />
ooooooooooo ¯DO¯De¯O¯<br />
example, shear<strong>in</strong>g <strong>in</strong>jury of the white matter of<br />
Survived 11191 Died (581. Survived (1101 Died 1561 the bra<strong>in</strong> (AIS 5) was reported on only one<br />
Uncorrected Scores Age~orrected Score= occasion from a total of 58 post-mortemg<br />
Fig. I. The distribution of Injury Severity Score.<br />
Fourthly, some of the patients who were found<br />
with some or all ofthe signs such as fixed dilated<br />
pupils, apnoea and absent major pulses, but for<br />
whom resuscitation was nevertheless attempted,<br />
dead at the scene before the arrival of’the Fly<strong>in</strong>gwould<br />
have been classified as dead by other<br />
Squad have been excluded from the analysis ofworkers<br />
and therefore not <strong>in</strong>cluded as potential<br />
survival. Apply<strong>in</strong>g the predicted chance of sursurvivors.<br />
Fifthly, Bull used earlier versions of<br />
vival (Yates, 1977) to the rema<strong>in</strong><strong>in</strong>g ! 52 patientsthe<br />
AIS <strong>in</strong> which some <strong>in</strong>juries were scored<br />
alive at the scene, 110.12 were expected to sur- higher than <strong>in</strong> AIS 80, such as multiple, closed<br />
vive and I i0 actually did survive. fractures of long b2nes which were previously<br />
Us<strong>in</strong>g the method described by Bull (1977) theAIS<br />
code 4 (Baker et al., 1974) now scored AIS<br />
predicted mortality was determ<strong>in</strong>ed for the 152code<br />
3 American Association for Automotive<br />
adult patients alive at the scene who wereMedic<strong>in</strong>e<br />
(1980), and multiple, open fractures of<br />
scored. By this means 44-1 patients were long bones which were previously AIS code 5<br />
expected to die and 42 actually died. (Baker et al., 1974) now scored AIS code 3<br />
American Association for Automotive Medic<strong>in</strong>e<br />
DISCUSSION<br />
(1980). These changes also probably help to<br />
Generally we found the scor<strong>in</strong>g system easy toexpla<strong>in</strong><br />
why <strong>in</strong> both Baker’s and Bull’s series, the<br />
apply, except for the 2 patients whom we couldsurvivor<br />
with the highest scores had ISS=50,<br />
not score. Also, scores seemed to reflect accu- while <strong>in</strong> our series the highest score ofany survirately<br />
our cl<strong>in</strong>ical impression of severity with vor was ISS =43. These factors operate to lower<br />
the exception of some penetrat<strong>in</strong>g <strong>in</strong>juries, <strong>in</strong>the<br />
ISS and therefore <strong>in</strong>appropriately <strong>in</strong>crease<br />
this series usually stabb<strong>in</strong>gs. S<strong>in</strong>ce the systemthe<br />
predicted number of survivors and decrease
518<br />
the difference between actual and predicted<br />
survival.<br />
These 5 po<strong>in</strong>ts apply equally to the alternative<br />
method for determ<strong>in</strong><strong>in</strong>g predicted mortality<br />
(Bull, 1977). Application of this method suggests<br />
that 2 lives were def<strong>in</strong>itely saved by the actions<br />
of the Fly<strong>in</strong>g Squad. Bull has po<strong>in</strong>ted out, however,<br />
that his probability of expected mortality<br />
values are provisional and based on a s<strong>in</strong>gle<br />
limited series.<br />
We consider the ISS to be a valid measure of<br />
<strong>in</strong>jury severity deserv<strong>in</strong>g wider use. It should be<br />
possible to determ<strong>in</strong>e mortality for narrower age<br />
groups than those def<strong>in</strong>ed by Baker and Bull.<br />
The system might well be applicable to audit of<br />
accident and emergency department work and<br />
the assessment of new safety measures such as<br />
the compulsory wear<strong>in</strong>g of seat belts.<br />
Acknowledgements<br />
We wish to acknowledge assistance given by Mr<br />
Michael Holloway, the late Coroner for West<br />
Cheshire and South Clwyd, Drs T. D. S. Holliday<br />
and H. Ingram, <strong>Consultant</strong> Pathologists to<br />
the Chester Royal Infirmary and Mrs K. Gorman<br />
and Mrs M. Ball for their typ<strong>in</strong>g of the<br />
script.<br />
Injury: the British Journal of <strong>Accident</strong> Surge~ Vol. 14/No. 6<br />
REFERENCES<br />
AMA Committee on Medical Aspects of Automotive<br />
Safety (1971) Rat<strong>in</strong>g the severity of tissue damage.<br />
I. The abbreviated scale JAMA 215, 277.<br />
AMA Committee on Medical Aspects of Automotive<br />
Safety (1972) Rat<strong>in</strong>g the severity of tissue damage.<br />
II. The comprehensive scale. JAMA 220, 717.<br />
American Association for Automotive Medic<strong>in</strong>e<br />
(1980) The Abbreviated Injury Scale, 1980 Review.<br />
Baker S. P. and O’Neill B. (1976) The <strong>in</strong>jury severity<br />
score; an update. J. Trauma 16, 882.<br />
Baker S. P., O’Neitt B., Haddon W. Jr. et al. (1974)<br />
The <strong>in</strong>jury severity score; a method for describ<strong>in</strong>g<br />
patients with multiple <strong>in</strong>juries and evaluat<strong>in</strong>g<br />
emergency care. J. Trauma 14, 187.<br />
Bull J. P. (1975) The <strong>in</strong>jury severity score of road<br />
traffic casualties <strong>in</strong> relation to mortality, time of<br />
death, hospital treatment time and disability. <strong>Accident</strong><br />
Analysis and Prevention 7, 249.<br />
Bull J. P. (1978) Measures of severity of <strong>in</strong>jury. Injury<br />
9, 184.<br />
Cowley R. A., Sacco W. J., Gill W. et al. (1974) A<br />
prognostic <strong>in</strong>dex for severe trauma. J. Trauma 14,<br />
1029.<br />
Scmmlow J. L. and Cone R. (1976) Utility of the<br />
<strong>in</strong>jury severity score; a confirmation. Health Serv.<br />
Res. I I, 45.<br />
Stoner H. B., Barton R. N., Little R. A. et al (1977)<br />
Measur<strong>in</strong>g severity of <strong>in</strong>jury. Br. Meal J. 2, 1247.<br />
Yates D. W. (1977) Airway patency <strong>in</strong> fatal accidents.<br />
Br. Med. J. 2, 1249.<br />
Requests for repr<strong>in</strong>ts should be addressed to: Dr D. F. Gorman, Registrar, <strong>Accident</strong> Unit, Chester Royal Infirmary, Chester.<br />
L<br />
Injury. 14.519-522 P~fntet<br />
F ra ctu res ,:<br />
M. E. Blakemore<br />
Birm<strong>in</strong>gham Genera<br />
Surrtrnary<br />
Two cases of fracture, wh<br />
for graft<strong>in</strong>g are presente~<br />
one the ilium. The impl<br />
are discussed.<br />
CASE REPORTS<br />
Case I<br />
A woman aged 63 was a<br />
a height of about 3 fe~<br />
comm<strong>in</strong>uted fi-acture oft<br />
with separation of the ti<br />
the <strong>in</strong>sertion of the anter<br />
it was decided to operat~<br />
cular surface, recogniz<strong>in</strong><br />
preclude stable fixation<br />
the shaft of the tibia. T}<br />
articular fragments and 1<br />
cruciate ligament were<br />
(Fig. 2) and a support<strong>in</strong>g<br />
opposite greater troctm~<br />
then spl<strong>in</strong>ted <strong>in</strong> a plaste:<br />
the patient was allowed<br />
full weight on the teR h<br />
brace h<strong>in</strong>ged at the kn<br />
limb.<br />
Thirteen dad afker Ol<br />
without pa<strong>in</strong> for 6 da<br />
veloped pa<strong>in</strong> <strong>in</strong> the I<br />
Radiography showed<br />
orig<strong>in</strong>at<strong>in</strong>g at the hone<br />
was treated with simpk<br />
patient was then aflow~<br />
from the orig<strong>in</strong>al <strong>in</strong>jur<br />
4) fractures were ¢l<strong>in</strong>ic~<br />
and the patient could t<br />
unaided.<br />
Case 2<br />
A 57-yenr-old man w;<br />
severe cervical spondyl<br />
sion of the nerve root:<br />
decompression and do~
i<br />
I<br />
i<br />
"r"<br />
I .<br />
J i "<br />
i<br />
i<br />
! It<br />
|<br />
! .:<br />
Resuscitation 6, 243-248 { q’4z~.<br />
Role of an accident fly<strong>in</strong>g, squad <strong>in</strong> medical<br />
emergenctes<br />
D, I. ROWLEY* and J. COLLINS<br />
_4co’dent and Emem.]elwy Departmci~t. Dcrh).shirc Ro~’al h-,Jh’,zary, Le,zdua Road.<br />
Derby. U.K.<br />
Summary<br />
A retrospective study of medical cases attended by the Derbyshire Royal Infirmary<br />
<strong>Accident</strong> Fly<strong>in</strong>g Squad demonstrates that of 17 casds only two patients survived to<br />
leave hospital. N<strong>in</strong>e cases of cardiac arrest have been studied <strong>in</strong> further detai!. In a’A of<br />
these cases it was found that diagnosis of arrest had been made~fgre lhe Fly<strong>in</strong>g Squad<br />
was called and that the situation had become extreme before the arrival of the medical<br />
team, In every case the Fly<strong>in</strong>g Squad team took more than 3 ra<strong>in</strong> to arrive, irrespective<br />
of distance. Review of the literature appears to support the conclusion that medical<br />
teams have been of li;tle value when called to cardiac arrest at any distance from the<br />
hospital because of the time lag. It is suggested that more sophisticated primary care<br />
should be available immediately, preferably by highly tra<strong>in</strong>ed ambulance personnel.<br />
Medical teams would give appropriate support to such primary care.<br />
lutrodnetion<br />
An <strong>Accident</strong> Fly<strong>in</strong>g Squad has been develop<strong>in</strong>g <strong>in</strong> Derby, England, s<strong>in</strong>cc !955. The<br />
purpose of this service has beeffsummarised by Coll<strong>in</strong>s (1966) and the practical<br />
problems have been reviewed by Little (1972). The orig<strong>in</strong>al emphasis was upon<br />
<strong>in</strong>dustria! accidents but the service now embraces a whole range of accidents and<br />
"emergenNes, amongst which the road traffic accident predom<strong>in</strong>ates. As illustrated <strong>in</strong><br />
Fig. 1, medical emergencies represent a significant part of the work of the Fly<strong>in</strong>g Squad.<br />
There has been a steady <strong>in</strong>crease <strong>in</strong> demand for the service over the past 4 years. The<br />
aim of the present-study is to ana!yse the progress of medical cases a~tend,*d by the<br />
DcrL.,,i..~:’e - Rexal - ~r.f:rci;r., Accic~er;:<br />
. "r,’_<br />
".c!-ir..z<br />
a!~<br />
Souad-i;,. !c’:7 a veto :r" \~t~.~:’,.<br />
.... ~ .~ -A ~,~3~.CXlII~k,_L:2, cai~.<br />
5<br />
t_’,2LJ-[l.’tl, ,31 I|~;<br />
Patients and methods -<br />
The study is retrospecuve and the diagnoses are those recorded by the senior medica!<br />
officer at the scene. Wherever possible these diagnoses have been confirmed by<br />
Present address: Department of Surgery. Cl:.ase W<strong>in</strong>g, Enfield District Hospital, Enfidd, Middlesex. U.K.<br />
%.<br />
243 " . .... " ....<br />
-: - - . : .:.._ - ~ "~,-~ 2~,2~,r~.~_~
@<br />
I IIIIII 11 I I I II I<br />
244 D. ROWLEY AND J. COLLINS<br />
e,,karl<br />
v’es<br />
7O<br />
60<br />
50<br />
4O<br />
3O<br />
20<br />
10<br />
i~] TOTAL<br />
CALLS<br />
M MEDICAL<br />
CALLS<br />
p<br />
I !<br />
r<br />
1970 1971 1972 1973 1974 1975 1976 1977<br />
YEARS<br />
Fig. J. Distribut,on of calls to the Derbysh!re Royal Infirmary <strong>Accident</strong> Fly<strong>in</strong>g Squad dur<strong>in</strong>g the years<br />
study<strong>in</strong>g the follow-up records or post-mortem reports on the patients. The details of<br />
the Fly<strong>in</strong>g Squad sorties were recorded rout<strong>in</strong>ely by the senior medical officer and an<br />
account of the journey was given by the drivers.<br />
Cardiac arrest was confirmed by us<strong>in</strong>g a Cardio-Aid D<strong>MS</strong> 200 (Simonsen and Weel)<br />
electrocardiograph/defibrillator. This device is a portable and recharge, able electrocardiogram<br />
which will give a crude bipolar readout through the paddles or can be<br />
converted to give a ref<strong>in</strong>ed 12-l<strong>in</strong>e ECG readout. It also possesses the capability to<br />
deliver a graded D.C. shock up to 400 joules (Fig. 2).<br />
~ q<br />
¯.<br />
L;<br />
c~.<br />
<strong>in</strong><br />
A<br />
d<br />
-[
ACCIDENT FLYING SQUADS . 245<br />
l’-~g. 2. Cardio-Aid D<strong>MS</strong>200 (Simonsen and Weel) electrocardiogram/defibrillator. This <strong>in</strong>strument<br />
c.omb<strong>in</strong>~s a crude bipolar electrocardiographic readout with the facility of conversion to a full 12-l<strong>in</strong>e ECG<br />
trace if req~gred.<br />
In all cases, drugs and other equipment were available as follows: sodium<br />
bicarbonate (8.4%) by <strong>in</strong>travenous <strong>in</strong>fusion; adrenal<strong>in</strong>e solution (1:I000). calcium<br />
ct;]oride (iW,..). diazepam, dexamethasone, frusemide, hydrocortisone, isoprenal<strong>in</strong>e.<br />
ligntwane tl’~./.) a~_d practalo!: apparatus for cuffed endotracheal <strong>in</strong>tubation with<br />
-’ :~,,: p:ws,~:’~ vcnfik;tjon and 100’ ,, o~yge:,<br />
Results<br />
All the patients, excep~ for two children hav<strong>in</strong>g their first fit, died ultimately (Table 1).<br />
No patients were successfully resuscitated from a cardiac arrest as diagnosed by<br />
electrocardiographic monitor<strong>in</strong>g. The later n<strong>in</strong>e cases are exam<strong>in</strong>ed further <strong>in</strong> Table 2.<br />
The results reflect the time delay from receiv<strong>in</strong>g the cal! to arriv<strong>in</strong>g at the scene, but<br />
added to lhis is the time taken <strong>in</strong> decid<strong>in</strong>g to call the Squad, which can oniy be guessed.<br />
o- -.
246 D. ROWLEY AND J. COLLINS<br />
1¯able 1. Analysis of 17 <strong>in</strong>cidents <strong>in</strong>volv<strong>in</strong>g calls for the fly<strong>in</strong>g squad,<br />
~r,~i,qc 2rT2st<br />
Carcia~ ~,uture<br />
Aortic ane~arysm<br />
Cerebrovascular<br />
accident<br />
No, of patients No, of pattents<br />
~ho died at who died <strong>in</strong> No. of patients<br />
No. of patients the scene hospital who went home<br />
1<br />
9 0<br />
Table 2. Details of calls classified as card iac arrest. Journey times, from receipt of call to arrival at the scene,<br />
and type of subsequent resuscttattve management are shown. D&T. Use of <strong>in</strong>travenous <strong>in</strong>fusion and<br />
endotracheal <strong>in</strong>tubation.<br />
Distance to scene Time for fly<strong>in</strong>g squad Action taken by<br />
of cardiac arrest {miles) to arrive (m<strong>in</strong>) fly<strong>in</strong>g squad<br />
Discussion<br />
3 8 Nil<br />
2 5 Nil<br />
8 -. 10 Nil<br />
12 Not known D&T<br />
10 15 D&T<br />
1.5 3 D&T<br />
l I Not known D&T<br />
3.5 5 D&T<br />
8 10 D&T<br />
Sooriyaarachchi (1976/77) has exam<strong>in</strong>ed t~:e cxi:cr~ences of a resident carmopulmonary<br />
resuscitation team at a general hospital <strong>in</strong> the U.K. In his review of the<br />
literature he notes that similar teams to his claim long-term success <strong>in</strong> 12-23~0 ofcases<br />
attended. His own figures show that of 25 cases attended four survived to leave hospital,<br />
even though a fully tra<strong>in</strong>ed team was available to the personnel monitor<strong>in</strong>g the patients<br />
concerned.<br />
The experiences of a mobile <strong>in</strong>tensive care team outside the hospital are described by<br />
Pantridge & Geddes 11967). They anticipated potential cardiac arrest <strong>in</strong> the case of<br />
myocardial <strong>in</strong>farction by send<strong>in</strong>g a team with at least one doctor and a specially<br />
equipped ambulance with tra<strong>in</strong>ed ambulance personnel to all cases of chest pa<strong>in</strong>. On<br />
i<br />
l<br />
2<br />
0<br />
tl<br />
i<br />
!
i<br />
!<br />
t<br />
l<br />
f.<br />
\<br />
ACCIDENT FLYING SQUADS 247<br />
ten occasions the unit was present at the time of cardiac arrest and subsequently five of<br />
those patients survived to leave hospital. Chamberla<strong>in</strong>, White, B<strong>in</strong>n<strong>in</strong>g. Parker &<br />
Kimber (1973) have a similar organisation; their team attended 57 patients who were<br />
already <strong>in</strong> ventricular fibrillation before the team’s arrival, and only one of these<br />
survived. However, the team was already present at the time of corrlmencement of<br />
ventricular fibrillation <strong>in</strong> a further eight cases, and five of these ultimately survived to<br />
leave hospital.<br />
From Table 2 it can be seen that on no occasion was it possible fo r the Derby team to<br />
reach the scene <strong>in</strong> less than 3 m<strong>in</strong>, irrespective of distance from the hospital to the scene<br />
of the accident. This reflects the problems of hav<strong>in</strong>g to travel most of the journey<br />
tbrm.,~h a built-up area. At all the <strong>in</strong>cidents <strong>in</strong>volv<strong>in</strong>~ cardiac arrest the Fl)<strong>in</strong>g Squad<br />
~mmcdmtc availability. On only two occasmns general practiuonm s ’,, ~ c ~,, ~.~¢m ......<br />
scene, and only one of them had more than the most basic equipment. Ila all the other<br />
cases the ambulance crew was the only primary care service available.<br />
In the cases presented <strong>in</strong> this survey the ambulances were equipped with suction and<br />
M<strong>in</strong>ute Man ventilators. The crews had been tra<strong>in</strong>ed on a standard 6-weeks ambulance<br />
course and rome had had experience with<strong>in</strong> the <strong>Accident</strong> and Emergency Department.<br />
Unless it is <strong>in</strong>tended to extend the services offered by the Fly<strong>in</strong>g Squad to attend al!<br />
emergency calls, the basic primary care must be the central responsibility of the<br />
ambulance organisations, Boughley (1968) has already highlighted the problems of<br />
tra<strong>in</strong><strong>in</strong>g and then ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g a high standard of skill among ambulance personnel,<br />
when the ambulance service workload normally conta<strong>in</strong>s 0.25,°/~ of potentially<br />
dangerous situations. Baskett, Diamond & Cochrane (1976) have made a worthwhile<br />
attempt to overcome the shortcom<strong>in</strong>gs of the present services and the delayed arrival of<br />
a support<strong>in</strong>g medical team. Their use of highly tra<strong>in</strong>ed ambulance men, with sufficient<br />
traimng and skill to pass endotracheal tubes, <strong>in</strong>sert <strong>in</strong>travenous cannulae and perform<br />
cardiac defibrillation, seems to have gone some way to solv<strong>in</strong>g the problem. These<br />
personnel are able to anticipate cardiac arrest and are fully equipped to deal with it at<br />
the moment of recognition. They also have a doctor available if necessary and, s<strong>in</strong>ce<br />
1974 they have had the facility for electrocardiographic telemetry. There are severe<br />
difficulties <strong>in</strong> gett<strong>in</strong>g an objective assessment of this particular scheme.<br />
Suffuzient evidence seems to be accumulat<strong>in</strong>g from the different centres operat<strong>in</strong>g a<br />
resuscitation service outside the hospital to suggest that a high standard of primary<br />
care is required at the scene to compensate for the <strong>in</strong>evitable delays <strong>in</strong> mobilis<strong>in</strong>g a<br />
medical team. A close work<strong>in</strong>g relationship between the paramedical and the Fly<strong>in</strong>g<br />
~quad,~<strong>Accident</strong> and Emergency services is paramount. Furthermore, there seems to be<br />
¯ a place for a group of people <strong>in</strong> the ambulance service possess<strong>in</strong>g a high degree of<br />
tra<strong>in</strong><strong>in</strong>g and everyday experience of emergencies who can support life until <strong>in</strong>tcnsive<br />
c~:,e .:i ~ ,;,.~ ,-.~rvi,’e \Vc conc!ude the,:, a’, t~e presem time, there is little iustification <strong>in</strong><br />
~’7;.’q;~’, . . "g’-Y~:<br />
~el’\;c~: can ~..g ({.\e.,-:.,,e~z.~ ...<br />
Ackno~’ledgraeats<br />
We arc grateful for the critical comments of our colleague, Mr W. A. Fraser-Moodie.<br />
Mr Parsons contributed valuable <strong>in</strong>formation concern<strong>in</strong>g equipment.<br />
" " -. ’,.a ,i,:
248 D, ROWLEY AND J. COLLINS<br />
References<br />
Baskett. P. J. F,, Diamond, A. W. & Cochrane. D. F. ( t976} Urban mobile resuscitation: tra<strong>in</strong><strong>in</strong>g and s~m’vi~,.<br />
Br, ,L Anaes:h. 48, 377-385.<br />
Bol~gh!ey. W. N. F. (1968) <strong>Accident</strong>s, emergencies, and ambulances: a surxey <strong>in</strong> Portsmouth. Brito Meal. J. i,<br />
369-372.<br />
Chamberlai.n, D. A., White. N. M., B<strong>in</strong>n<strong>in</strong>g, R.. Parker, W. S. & Kimber, E, R. (1973) Mobile coronary care<br />
?ro.v;ded ~.~ "’mb.:?w.?=’ ~-r~uazeL ~ri;. ~,,e~.:r: ,.’. 35, 530~P’L<br />
.,z:::, .~k. ,::-L) -’: ~q~¢ .f .taz :.,: ,i.~r,.: r’~"::.,g ~q~’.~d B,~: 5, 241-247.<br />
° ,<br />
I iI<br />
t<br />
i
#<br />
r<br />
<strong>Accident</strong> fly<strong>in</strong>g squads: an objective evaluation of their<br />
role <strong>in</strong> trauma<br />
D J Steedman" and C E Robertson"<br />
An objective evaluation of an Accidcnt Fly<strong>in</strong>g Squad was<br />
performed us<strong>in</strong>g an Injury Severity Scor<strong>in</strong>g system. A<br />
retrospective analysis of 73 trauma patients treated at the<br />
scene failed to confirm the subjective judgement of the<br />
benefits of treatment <strong>in</strong> this group. We recommend that<br />
further studies should be carried out to determ<strong>in</strong>e whether<br />
the failure to document reduction <strong>in</strong> mortality is due to<br />
defects <strong>in</strong> the method of assessment and small patient<br />
numbers or whether it genu<strong>in</strong>ely reflects absence of<br />
benefit of such squads.<br />
There t<strong>in</strong>s been a dramatic <strong>in</strong>crease <strong>in</strong> the number of<br />
hospital based <strong>Accident</strong> Fly<strong>in</strong>g Squads <strong>in</strong> the United<br />
K<strong>in</strong>gdom s<strong>in</strong>ce the tirst scheme was established by Coll<strong>in</strong>s<br />
,’it Derby Royal hlfirmarv <strong>in</strong> 1955 ~ -~. Despite the recem<br />
claims of "’the undoubted value of fly<strong>in</strong>g squads "’~ there ~s<br />
a paucity of objective data to support the role of such<br />
schemes <strong>in</strong> reduc<strong>in</strong>g mortality-and morbidity. Indeed it<br />
has been suggested that it is impossible statistically to<br />
justify a Fly<strong>in</strong>g Squad’s existence. Several workers have<br />
reported on their experience <strong>in</strong> this field of cmergency<br />
medical care. but although considerable detail has been<br />
supplied <strong>in</strong> relation to call outs. evaluation has been based<br />
on subjective assessment: -~,<br />
One of the major difficulties encountered <strong>in</strong> assess<strong>in</strong>g<br />
treatment of traum,~ patients relates to the multiple<br />
<strong>in</strong>juries which are susta<strong>in</strong>ed and to the effect of the<br />
comb<strong>in</strong>ation of these <strong>in</strong>juries, it is essential to def<strong>in</strong>e the<br />
severity of <strong>in</strong>jury <strong>in</strong> a quantitative way before any<br />
statistically significant statement can be made about the<br />
benctits of treatment ". One grad<strong>in</strong>g system for assess<strong>in</strong>g<br />
patacms with multiple <strong>in</strong>juries is the Injury Severity Score<br />
(ISS) ~. has radio communication with the a:nbulance services<br />
and carries a comprehensive range of resuscitative<br />
equipment. The team usually consists of one or two<br />
experienced numbers of nurs<strong>in</strong>g staff, a doctor of<br />
<strong>Consultant</strong> or Registrar grade and one Senior House<br />
Officer, while the van is driven by ambulance personnel.<br />
The first 100 call-outs, which occurred between<br />
January 1980 and February 1983, h:t\e been analysed<br />
retrospectively, h~fi~rmation was obta<strong>in</strong>ed by reference to<br />
the log-book, departmemal records, <strong>in</strong> patient notes and<br />
(<strong>in</strong> all cases who died as a resuh of their <strong>in</strong>juries) to post<br />
mortem reports, l)clails collected <strong>in</strong>cluded: age and scx o1"<br />
patient: type of i~cidem" nature of <strong>in</strong>juries: tre:mnent<br />
given: and survi\’:d,<br />
An <strong>in</strong>jury seventy score was deri\ ed tk~r each patient<br />
tended at the scene b\ the Fly<strong>in</strong>g Squad.<br />
The Abbreviated Injury Scale and the <strong>in</strong>jury severity<br />
score<br />
The Abbreviated In.iury Scale refers to the a’;s:gnmcnt of a<br />
s<strong>in</strong>gle code number on a scale I-6 for specific <strong>in</strong>juries, The 1980<br />
revision of the AIS coma|m; more than 5t~} such <strong>in</strong>jur~<br />
descriptions, Five separate criteria lenergy dissipation, threat to<br />
life. permanent impairment, treatment period and <strong>in</strong>cidence}<br />
were considered <strong>in</strong> the development of the AIS, Thus for each<br />
body region, a rmnor <strong>in</strong>jury would attract an AIS severity code<br />
o1" I: .2 moderate <strong>in</strong>jur~ 2: ,,t:rlous 3: se\erc 4: critical 5: and<br />
Ul,~tXnlitnll <strong>in</strong>jury (uusur\i\;d~lc ~ ilh CI.IFrClII It.’t.’Jllliqucsl f~. [hl<br />
derived from the Abbreviated Injury Scale<br />
tAIS)’. This system has been utilised <strong>in</strong> the present<br />
analysis to evaluate the efficacy of the <strong>Accident</strong> Fly<strong>in</strong>g<br />
Squad based at the Ed<strong>in</strong>burgh Royal Infirmary <strong>in</strong><br />
response to trauma call-outs.<br />
Patients and methods<br />
"[’hc <strong>Accident</strong> and Emergency Department at the<br />
Ed<strong>in</strong>burgh Royal Infirmary is the central <strong>Accident</strong> Unit<br />
rot the Lothian and Border regions with a population of<br />
approximately 750,000, The Fly<strong>in</strong>g Squad was<br />
established <strong>in</strong> 1980 and provides an emergency medical<br />
and nurs<strong>in</strong>g team on a 24-hour basis. The Fly<strong>in</strong>g Squad<br />
vehicle is a specially modified Bedford chassis van which<br />
~,<br />
numerical code I-8 is not a l<strong>in</strong>ear progression and therefore<br />
does not allow for the tak<strong>in</strong>g of an arithmetic me~m ~hen<br />
applied to multiple <strong>in</strong>juries ~,<br />
The Injury Severity Sc~re is derived from the AIS and b;:~.cd<br />
on ~malysis of 2128 road tratlie accident victims <strong>in</strong> Baltimore" ~.<br />
I:or the purl~Scs of In.ltlry Scvcrit~ Scor<strong>in</strong>g Ihe bo-,l\ I~<br />
divided <strong>in</strong>to ~ regiom;: head and neck: face: chest: ,~bdom<strong>in</strong>al<br />
and pelvic contents" limbs and pelvic girdle: and external. An<br />
AIS code of I-h is tl:en assigned to each <strong>in</strong>jury. The ISS is<br />
calculated by add<strong>in</strong>g the squares of the hlghcst AIS code <strong>in</strong> each<br />
o1" the three most severely <strong>in</strong>jured body regions. An example is<br />
sho,wn n -F;ddc I. Fhc ftl:t\ulltun .,,core fi~r an~ one rcgloll i’, 2 ¢<br />
(c\clnd<strong>in</strong>~ tile AIS ¢odc of h). :rod Ilic highc~,t pos,4blc [SS I,;<br />
I1111~, 75. AII~ patict:l alth :ul uliliry se\erc euollgh it~ aliracl all<br />
AIS code ol’~ is aulou~aUc;.dl~ a~ artlcd ;m ISS of 75. The In.lur.~<br />
¯ ~’,erity Set,re pro\~de~, su~t:ddc \\rightist,,’ ft~r the AIS and<br />
all(~vs I~r the proper conlhnlltttt’ql ol" the effects t~l multiple<br />
iujuries<br />
111 mortality studies the ISS \aluc musl be x~cighto.I for age,<br />
fbr older p~tients arc more likely to die from less ,,c\ere mjur~cs<br />
Ih:lll ~ollllgCr i~;lllClltS. Ilulle’ used I)roh! m~;d\sis ~’’ it, l<strong>in</strong>ear~se<br />
.......................................<br />
I)cp;~rtment tff <strong>Accident</strong> and Emeq:ency Medic<strong>in</strong>e, Royal<br />
the mortality da{~ <strong>in</strong> sep~lr;llC age gro~lp,; tn rehll~oa to 13,13<br />
rt~ad traflic accident patics|ts admitted to the Birm<strong>in</strong>gham<br />
hdirm:lry. I_auriston Pl~:ce, Ed<strong>in</strong>burgh. AccidcnL Unil. lie found that an ISS tff 39.7 t 2?9 (mean r SD),<br />
(’,~rrc’,l~t~ldt’nct.’ I~ |) .I Stcedmau. 29.4 ~ 2.5 and 20,2 r I.h ~cre asst~ialed with 5(.)% mort:dity <strong>in</strong><br />
80<br />
Journal ~:¢’tht" Rovt~/ (’ollet, e of Surt~t’rm ~ o[ Ed<strong>in</strong>hur.t,h
TABLE 1<br />
Injury severity scor<strong>in</strong>H<br />
I , I I,’~ I I.%<br />
l{ ~lii~dll!’;ll h;ICm~llOltl;l<br />
!~ ll*llll]’lll ~tll111l!l<br />
l ]*,;q;[ C~lillll’,,lllll<br />
I ~ t~rmc’ I ~ Fib~<br />
llilN~.’I C;]li~" I;It’t’l’~ll roll<br />
%lc~cnlcr-i~’ ~.’Olll u ~,iorl<br />
I’~,. It ol~,-’l it or r,.:;ll li;icnl:H~m~:i<br />
I lilCllll~.’ plrl~l~_’ l:lll]ll ~.<br />
I ~Ic.,’riltio0 l’~ c~’i.’bri~’,\<br />
I%S I- - u . I(~ 41 (’all Tu<br />
UIC Fc,,)¢Ch\c ;IFc llrotl;~*, t. ~ 14 ~¢;.Ir~;, 45-64 )’cars al~tl<br />
f~.~ - \ ca r-, ( there \~ crc" lll’-.tllli,,..’icill ,,.’;l,.,¢s Ill lh,~ 0 - 14 ;.I~.Ii." group<br />
lol lh’,,bll .\rod\ ~4,4. hl our ,,lud.,, age ’,v¢ighi<strong>in</strong>g was produced<br />
b,, i.’orrc~’l<strong>in</strong>g IIi¢ I~S ~;llti¢ oi" pallills IO thai appropriate for<br />
the 4~ -h4 a,2¢ group us<strong>in</strong>g Yalc, s tnodilicaiion ~ el" Bull’s Probil<br />
.mal’.,,i-, (lb-’ I i l:or t’i.;llll]~]C. ,i I’~;llk’[ll ;l~.’cl 71) v. iih illl l,~,~ i>,i"<br />
?l) h,l’, an ~L’--’¢ ,~rr,.f,.’Icd ,;o~rc of 40. "l’;lleS im:ludcd a prcdicled<br />
L’ll,lll~.’L’ ~II ~llr\ I\ ~II III hi’, lllodiliC;l(lOll ali’,.l \~.il~, t, iiliso.l <strong>in</strong> our<br />
,,,’. n ;<strong>in</strong>.if\ ~I~ Io [)r,.’,.ll,..’l lh,: o~,.’r.O] ~.’hilllL’q of ~ur~,’i~,’~ll for those<br />
l~;lllL’lll ’, llull<br />
\~, II0 l~.%’l.q\ l.’d IFI~;IIIIIC[II ;II III,." ~.l.’t.’lil.’,<br />
r-" al~u tlcri\i:tl a grid of CXlk’cicd nlorlalily for dill~:rthll<br />
combitlalkm~, of ISS and age groups above 15 years based on<br />
In,, <strong>in</strong>ilial i.l’ll[l (Tahh: 21. P;llli.’lli’.; ~,\ cr¢ di,, idol <strong>in</strong>lo decade,, ;llld<br />
I~,% mt{~ ,.-qlull group, O-4, 5-9. I0-14 tic, All al’~l’,roxunal
82 .\(I IIll \1 I I "ll\l) ~.)l \11~<br />
TABLE 2<br />
Approximate probability of mortality for different comb<strong>in</strong>ations of ISS and age"<br />
~5<br />
,1()<br />
._<br />
5O<br />
35 4()<br />
3O 35<br />
25 3o<br />
2(). 25<br />
t5, 2u<br />
Ī,t~c O’r)<br />
!.H I.O I.O IA) I.() ! () I )<br />
o.u (Lq I.o I.O I.() I () !,*)<br />
I).7 ( ~ 1),9 l.I) I.D t,11 !31<br />
I1.( (1. ? 1).~ (1. ~)<br />
requir<strong>in</strong>g such specilic air, ray management ,~ur,’ived, 43<br />
patients who survived recdved an <strong>in</strong>tr:|venous <strong>in</strong>fusioll at<br />
the scene, 24 of whom were-noted to have signs ot" hypo-<br />
TABLE 3<br />
Types of call<br />
7"ntal mtmher<br />
Ibtttl ,ttmbcr<br />
l’vpe hi’call ql’c, lls ¢?llt¢tlit,ttt~<br />
trauma 5~ SS<br />
Mctlical 22 22<br />
Aborted Ih (01<br />
Airp~)r~ alert 4 10)<br />
I H 1.11 I()<br />
()¯ I 0.~ 11,(~ O,~ ~) I,I) I,(l<br />
¯ ~ 0.3 0.5 0.6 1~ (19 t 1<br />
(1.2 (), 2 0.2 ll.4 (L ? u s H.q<br />
H, t I).l (1. t 11.2 (. ; (15 D.S<br />
O 0 0 i).l (1. I I1.3 1),5<br />
H (1 O l) 11 (11 t~<br />
(I 11 () 11 (1 () 11.!<br />
l) (1 0 1) 11 i) (1<br />
*lhdl r:<br />
volaenlie shock. This group hlclt~ded 7 p:|tle)]ts ~\ho..,e<br />
transt’cr to the <strong>Accident</strong> alld t!mcrgency l)¢partment<br />
was delayed bet."Ul,,e of ¢)ltr;.ipnlcnt. ")0 paticnt~ received<br />
<strong>in</strong>travenous analgesia, <strong>in</strong>clud<strong>in</strong>g 16 patients reqtttr<strong>in</strong>g<br />
extrication or release fronl imp’dement. 4 patients had a<br />
chest dra<strong>in</strong> <strong>in</strong>~crted. One patient died at the .scene (ISS<br />
2t)), O)lt." patient died on rettlr)llnL, 1.o the <strong>Accident</strong> :1)1,,t<br />
Emcrgcnc.~ l’)clmrtmcnt 11SS33) ’uld 2 paticnt~ died<br />
folio\r<strong>in</strong>g :~dmi,~.,,ion. ouc at 3 da.~s (ISS 2q)and one -)t ,,<br />
tl;l\’n I IS,’q 57).<br />
The distril’)utio)| o(" ISS is gi’,cn m Fig 2 togetl)cr ~=tl)<br />
the corrected scores to the 45-64 age group. The Prt)bil<br />
analysis ~s )1OI al)plit.’;Ihlc to p;lllC)lt’.; trader 13 ~car~.<br />
thercfi~rc 5 children \\ho survived and 2 \vho dled ha~e<br />
not had their score~ corrected. Of the 79 patients who did<br />
............................................ have their scores corrected. 6 wcrc dead when the Fly<strong>in</strong>g<br />
lblal O0 II0 Squad arrived and therefore were excluded fronl the<br />
analysis.<br />
TABLE 4<br />
Precipitat<strong>in</strong>g cause of <strong>in</strong>jury<br />
Nlotlh(’r<br />
of patit, uts<br />
................................................<br />
Road trallic accident 35 62<br />
Industrial works 8 8<br />
Domestic g I 1<br />
Suicide ~ 6<br />
Assault I<br />
TABLE 5<br />
Number of deaths by cause<br />
.\’,), ~# I,~’,¥ rtl/lk~( ’<br />
Road traOic acddent h 2q 75<br />
I)omcsttc a 33 5 [)<br />
Suicide 1 2o 57<br />
Assault I 2()<br />
7btal 5g 88 lbtul 23<br />
Juurnal qf tlw R~o’al Colh’~,e o l’Sur~,e mx y" Ed<strong>in</strong>h trgh
I) J S II II)M \% \%P (" I. ROIH:R I ~()N<br />
If’h" Id’di’illh<br />
TABLE 6<br />
Time and place of death<br />
\’o...f<br />
I )llli’c’lll~i<br />
IYs rlllli~c’<br />
" I)ulld ,, hell ’]~.i,,~ ........................................<br />
~quad arrived 6 51 --75<br />
l)wd :it ,,’cnc ~ 2n 75<br />
I),,cd ~alU. 2-I h,mr,<br />
,I admJ..,m ? 33 75<br />
24 i~,,m, < 2u 57<br />
.\ppl3 m:- Ilk’ p~cdi,’lud chm]cc of ~ur\ ival described h~<br />
’~ah’- h~ lhc IOn’alla!! ’. "7.1 p:divtH,,. ~’q.l ~\cre c\pCClu:l<br />
I~ ",IH~ [\t.’ :illd 5 [) ;l,’lu;llb, MH ~l~.’d.<br />
lhc predicted mortalih li~r lhe 73 p,lticnls alive when<br />
" dw I’b m,.: Squ:Jd anli~{.d u,mg the Ill’.’lliltil.\ grid of Bull"<br />
?3<br />
~ :,~ 14.7 and t 4 patients actualt\ died.<br />
Medical calls<br />
r~enty t~o calls ~crc related to medical conditions. II<br />
pattCllD, rccct\cd ~:ardiopuhnonary resuscitation at the<br />
scene. 3 paucnts ~vcrc successfulh resuscitated, [h)wevcr.<br />
one p;,ucnt ’mh’wquently died on rcu, rn to the <strong>Accident</strong><br />
and I’.mergcnc3 Dcpartmenl and the other 2 patients died<br />
75.<br />
70<br />
60-<br />
SO-<br />
tO<br />
o<br />
]0-<br />
20-<br />
10-<br />
¯ ¯¯ ¯¯¯¯¯<br />
,I<br />
O o ¯<br />
o<br />
ooo<br />
OOOOO<br />
800000000<br />
-~OOOOOOOOOO<br />
8<br />
o<br />
80<br />
o<br />
888888ooooo<br />
~88ooooo<br />
00000000<br />
SURVIV[016LI 01[0 1221 SURVlV[0(S~I 01[01201<br />
UN~ORR[CT[O SCOR[S C~R[U[O S~OR[S<br />
Fig 2 l)iMribution of l~ur~ Sc~¢rily Scores.<br />
4ptH 1986 1 "Ha n’h" 31 \ u,nher 2<br />
"I<br />
83<br />
5 da\’s a11d t4 days follow<strong>in</strong>g admisskm. In 2 further<br />
"’cardiac arrest’" calls the patients had rega<strong>in</strong>ed cardiac<br />
output and \~crc ventilat<strong>in</strong>g spontaneously prior to the<br />
arrival of the Fly<strong>in</strong>g Squad. Both patients survived to<br />
leave hospital.<br />
3 p;nticnts \vh~..i had susta<strong>in</strong>ed a myocardial <strong>in</strong>farction<br />
rccci\cd trc=,tmcnt for arrhythmias and cardiac I~ilurc<br />
before be<strong>in</strong>g transferred to the A & E Departments; 2<br />
’,w\ivcd.<br />
One patient who survived fqtlow<strong>in</strong>g an acute drug<br />
overdose rcquircd ¢ndotrachcal <strong>in</strong>tuhation to ma<strong>in</strong>ta<strong>in</strong> an<br />
adctluatc p:ltcnt airway.<br />
5 other mcdic;d patients who survived rccci\cd<br />
trcatnlK’nt al dK’ st:Cllq Ii)r IIlllSSIVC pulmonary embolism.<br />
;IdUtC hYl~o~:l_\ caemia and Matus ¢l~ilcpticus.<br />
Discussion<br />
rhis suktv i~ i)rc~cntcd as much for it~ method as Ior its<br />
rcsvlts and highhghls the difficulties cncounlcrcd <strong>in</strong><br />
c\ah,atmg the immediate care pro\iCed hv <strong>Accident</strong><br />
Fly<strong>in</strong>g Squads ill relation to trauma. In 1982 a survey<br />
<strong>in</strong>dicated that there \yore 47 ¢cntrcs <strong>in</strong> the United<br />
K<strong>in</strong>gdom which operate such schemes ~. For a method of<br />
emergency care which has been available for 30 years, it<br />
is disturb<strong>in</strong>g that there has been little objective assessment<br />
to confirm the many subJective judgements of benefit.<br />
The ir~troduction of the InJury Severity Score has<br />
facilitated research <strong>in</strong> this field: the first objective<br />
evaluation of :m <strong>Accident</strong> Fly<strong>in</strong>g Squad was performed <strong>in</strong><br />
1983 by Gorman and Coals H from Chester. When the<br />
predicted chance of survival was applied to 152 trauma<br />
patients who received treatment at the scene. I I0.12 were<br />
expected to survive and II0 actually survived, The grid<br />
described by Bull was then used to predict mortality:<br />
accord<strong>in</strong>g to this, 44. I patients were expected to die and<br />
42 actually died.<br />
In our own study there was no obJective evidence<br />
to confirm that treatment carried out at the scene of<br />
the accident saved lives. Failure to demonstrate the<br />
effectiveness of the Fly<strong>in</strong>g Squad may be due to<br />
deficiencies <strong>in</strong> the assessment process rather than to the<br />
use of the Squad per se.<br />
The analytical method we used offers a basis of<br />
comparison of outcome between the populations seen by<br />
the Ed<strong>in</strong>burgh Fly<strong>in</strong>g Squad and that used <strong>in</strong> Bull’s Probit<br />
Analysis. However, there may be many differences<br />
between the populations apart from the use of the Fly<strong>in</strong>g<br />
Squad which =s our particular focus of <strong>in</strong>terest. Certa<strong>in</strong><br />
<strong>in</strong>consistencies also arise <strong>in</strong> the use of the Injury Severity<br />
Score. While the ISS is well validated for blunt trauma ,t<br />
does not appear to reflect accurately the severity of <strong>in</strong>jury<br />
when applied to penetrat<strong>in</strong>g trauma". Injuries associated<br />
with stabb<strong>in</strong>gs and gunshot wounds yield <strong>in</strong>appropriately<br />
low scores us,ng such a scheme. Another situation <strong>in</strong><br />
which difficulty is experienced is <strong>in</strong> ass=gn<strong>in</strong>g scores to<br />
asphyx,atmg-type <strong>in</strong>juries. It is possible that ref<strong>in</strong>ements<br />
of the ISS are required before it can be justifiably<br />
’~, 0"t~-~. ~’:7’-4 "~I~.~-~, ~g~. I ""<br />
_ o<br />
.\
-’~+’9 ~ "<br />
84<br />
:lpplicd t(~ ,\ccidcnt Fly<strong>in</strong>g Squads: <strong>in</strong>deed, it may be that<br />
’cHill2 other scor<strong>in</strong>g system ix ilt2dcss;.lr)’ E~.<br />
Although most Fly<strong>in</strong>g Squads ore designated by the<br />
prelix "’<strong>Accident</strong>", a .signilicant Prot~lortion of their<br />
~t+rkl~+;Id is rt:l;itt:d It+ tllt+’d[t’~.li C+l~,t2g which acct+unled for<br />
one third tel" call,+ respoi+dud tt+ dur<strong>in</strong>g the period of this<br />
study. Objective as’+essment el + their el+licacv <strong>in</strong> this area is<br />
+\ca more diflicult to tlctcrln<strong>in</strong>+, Rowley ~+ reported that<br />
Incdic’al cases attended by the Derby Royal Inlirmary<br />
Fly<strong>in</strong>g Squad represented 20’,% of all the calls, The<br />
outcome for these medical eases was uniforn+ly dismal:<br />
<strong>in</strong>deed, all ultimately died before discharge IYom hospital<br />
except R+r 2 chihJret+ wll~+ h+ld had cpilcptifortn<br />
¢onvtllgi(Ins.<br />
Although the equipment and techniques <strong>in</strong>volved <strong>in</strong> on-<br />
site restl~Cltiltll)ll h;.l\C bcconlc i+rogl’cssi\el) more<br />
sophisticated, it is rckitively mexpel+~ivc to equip a fly<strong>in</strong>g<br />
",tluad---£10.O00 to £20.000 <strong>in</strong>chnd<strong>in</strong>g the vehicle<br />
References<br />
.\~. t’Itll \I I I ",I\ti M)t \lix<br />
t;OvlCCfvlcd ~’’. RUlllliilg c’okts ~lre Ill<strong>in</strong>illl[ll. hut dcpfct~i[lliOiI<br />
of the’ t chicle used ~ill add to the’ t:osts ~ub~tailtialt\.<br />
Nctertholo,s~;. if silt:l+ ~tluads c;.<strong>in</strong> bt2 shOXxll t’o ’qlttr<br />
even o1+¢ life, the) would h~lve amply repaid both their<br />
<strong>in</strong>itial outlay ;rod sul+scqtlcllt runn<strong>in</strong>g co,its, With ncarlx<br />
500,000 persons susta<strong>in</strong><strong>in</strong>g major <strong>in</strong>jury Iron’, trauma <strong>in</strong><br />
the UK each year, the potential u+c of <strong>Accident</strong> Fly<strong>in</strong>g<br />
Squads is great +"<br />
Ilowever, further ,.;ludies are <strong>in</strong>dic:.ltcd to dt~tcr<strong>in</strong><strong>in</strong>c<br />
whether the failure to document objective reductions <strong>in</strong><br />
mortality and morbidit.v is due to dcfcct.s <strong>in</strong> In.jury<br />
Scor<strong>in</strong>g assessment anti small patient numbers, or<br />
whether it genu<strong>in</strong>ely rellccts an absence of benefit <strong>in</strong> the<br />
operatitm of .,+ueh .-,quads In rc.’+ponsc it+ traulna calls.<br />
Acknowlcdgment..+, ()ur th~lllk,~ It+ Dr Kcith l.itt[e for hi,,<br />
hell!lul advice illltl Itl .Sir J I)ou,71ax ,.\licit. ReTionii I i)r,~,ur;ttor<br />
I:i~cal, I’tir i1elllllkSlOll IO t’t;lllllllt’ Ihc iltllOllx.k I’l?ptll’l~<br />
BOI)IWAI.A (J (i. I:al.:tn hl211<strong>in</strong>d lhe Ily<strong>in</strong>,g ktltliltlx, hi: (,+arc ill the aCtltcl\ ill l<strong>in</strong>d iiutlred: Proc’ced<strong>in</strong>t~ ill Vlh hilt’lll,ili~,ii,il<br />
CoI+~IPC~ o1" I’]nicrgcncy Surgery ( 198 1 J. Edit ed hi’ %Vll~on l) I I aBd [tilar~tl’~n #% K. (’llichc’qcr: Jtillll \\"ilc.t
!<br />
ORIGINAL CONTRIBUTION ."<br />
cardiac.~rrest, suwival rates prehospital’<br />
prehoso~tal care, for cardiac arrest<br />
Considerations foX’Improv<strong>in</strong>g Survival From<br />
Out-of-Hospital Cardiac Arrest<br />
S<strong>in</strong>ce the implementation of a paramedic system <strong>in</strong> SPxlttle, yearly survival<br />
rates from out-of-hospital cardiac arrest due to ventricular fibrillation have<br />
a-~raged 25% without any significant <strong>in</strong>crease over the years. Outcorr~ for<br />
arrest associated with other rhythms has been poor: when asystole<br />
first rhythm recorded, .only I% of patients survived; when elec.<br />
tromechanical dissociation was <strong>in</strong>itially present, only 6% survived. For<br />
cases of electrornechanical dissociation, neither the type of rhythm nor the<br />
rbate appear to <strong>in</strong>fluence outcome. ~$urvival from ventricular fibrillation can<br />
e improved by shorten<strong>in</strong>g the delay to <strong>in</strong>itiation of CPR and to defibrilla.<br />
~m. When outcome <strong>in</strong> 244 witnessed arrests was related to the times to<br />
beg<strong>in</strong>n<strong>in</strong>g CPR and to <strong>in</strong>itial defibrillation, mortality <strong>in</strong>creased 3% each<br />
m<strong>in</strong>ute until CPR was begun and 4% a m<strong>in</strong>ute until the first shock was<br />
delivered. New strategies that rn<strong>in</strong>imtze delays appear to have the greatest<br />
promise for improv<strong>in</strong>g survival after cardiac arrest./Weaver WD, Cobb LA,<br />
Hallstrom AP, Copass MK, Ray R, Emery M, Fahrenbruch C: Considerations<br />
for improv<strong>in</strong>g survival from out-of-hospital cardiac arrest. Ann Ernerg Med<br />
October 1986; 1,5:I181.II86.]<br />
INTRODUCTION<br />
A paramedic-staffed prehospital emergency care system has been active <strong>in</strong><br />
Seattle for more than a decade. S<strong>in</strong>ce its beg<strong>in</strong>n<strong>in</strong>g we have monitored the<br />
benefit of provid<strong>in</strong>g such care and have evaluated changes <strong>in</strong> the system<br />
made <strong>in</strong> attempts to improve its efficiency. In this study, we compared survival<br />
rates for cardiac arrest associated with ventricular fibrillation, asystole,<br />
and e|ectromechanical dissociation, and exam<strong>in</strong>ed the cases for factors that<br />
cou~mprove outcome.<br />
MLL~ODS<br />
The Seattle Fire Department provides a tiered out-of-hospital system to<br />
respond to medical emergencies. First responders are firefighters, most of<br />
whom, until recently, were traiited only <strong>in</strong> first aid. S<strong>in</strong>ce 1984 the fire department<br />
has sought to qualify all firefighters at the standard emergency<br />
medical technician (EMT) level. 1 These first-respond<strong>in</strong>g firefighters are located<br />
at 34 fire stations, The ~ response time of the first tier is approximately<br />
three m<strong>in</strong>utes, Paramedics, who are also firefighters, have been<br />
tra<strong>in</strong>ed extensively (more than 2,000 hours of didactic lectures and practical<br />
experience] and are able to manage a wide variety of medical emergencies,<br />
<strong>in</strong>clud<strong>in</strong>g cardiac arrest. Five pm’m’~edic-st~fed units are stationed at four<br />
locations <strong>in</strong> the city and ha~ ~ ~erage :respotise time of six to seven m<strong>in</strong>utes<br />
follow<strong>in</strong>g dispatch."<br />
The fire department responds to approximately 36,000 emergency calls<br />
each year, and two-thirds of the responses are for medical problems. Approxirnately<br />
9,000 of the persons evaluated are transported by fire department<br />
vehicles to a medical facility. Although there was a substantial <strong>in</strong>crease <strong>in</strong><br />
the number of medical emergencies attended dur<strong>in</strong>g the first ten years of<br />
operation, the annual number of cases has been relatively stable s<strong>in</strong>ce 1981<br />
Paramedic stand<strong>in</strong>g orders atrthorize <strong>in</strong>itial treatment <strong>in</strong> cases of cardiac<br />
arrest or hypovolemic shock; all other care beyond first aid is <strong>in</strong>itiated only<br />
after consultation with a physician, who communicates directly w;th pars.<br />
W Douglas Weaver. MD*<br />
Leonard A Cobb. MD*<br />
Alfred P Hallstrom. PhDt<br />
Michael K Copass, MD*<br />
Roberta Ray*<br />
Michael Emery*<br />
Carol Fahrenbruch. <strong>MS</strong>*<br />
Seattle, Wash<strong>in</strong>gton<br />
From the Departments of Medic<strong>in</strong>e* and<br />
Biostatistics.t Harborview Medical Center<br />
and the University of Wash<strong>in</strong>gton, Seattle.<br />
Received for publication May 28, 1985,<br />
Revision received February 11, 1986<br />
Accepted !or publication April 15, 1986.<br />
Presented at the University Association for<br />
Emergency Medic<strong>in</strong>e Annual Meet<strong>in</strong>g <strong>in</strong><br />
Kansas City, Missouri, May 1985.<br />
Supported <strong>in</strong> part by a Grant.<strong>in</strong>.Aid from<br />
the American Heart Association with<br />
contributions <strong>in</strong> part by the American<br />
Heart Association of Wash<strong>in</strong>gton and the<br />
Medic I -- Emergency Medical Services<br />
Foundation.<br />
Address for repr<strong>in</strong>ts: W Douglas Weaver,<br />
MD, Division of Cardiology. Harborview<br />
Medical Center, 325 N<strong>in</strong>th Avenue.<br />
Seattle. Wash<strong>in</strong>gton 98104,<br />
15:10October 1986 Annals of Emergency Medic<strong>in</strong>e 1181/77
1<br />
1<br />
I<br />
- I - 11111 ......................... i ii ................................<br />
SURVIVAL FROM CARDIAC ARREST<br />
Weaver et al<br />
FIGURE 1. Survival rates from out-ofhospital<br />
cardiac arrest due to VF <strong>in</strong><br />
Seattle, March 1970 through March<br />
1985. The early improvement (1970-<br />
1972) was produced by establish<strong>in</strong>g<br />
an <strong>in</strong>itial response tier us<strong>in</strong>g fire<br />
eng<strong>in</strong>e compames to provide CPR, <strong>in</strong>creas<strong>in</strong>g<br />
the number of paramedic<br />
units, and <strong>in</strong>creas<strong>in</strong>g the proportion of<br />
cases receiv<strong>in</strong>g bystqnder-<strong>in</strong>itiated<br />
CPR.<br />
FIGURE 2. Summary of survival from<br />
out.of.hospital cardiac arrest m cases<br />
w~th VF. asystole, and EMD <strong>in</strong>, different<br />
E<strong>MS</strong> systems. Treatment is effective<br />
only for cardiac arrest due to<br />
VE3-Io.13<br />
medics.<br />
For 30 consecutive months, we attempted<br />
to <strong>in</strong>terview all bystanders<br />
present at the time of cardiac collapse<br />
<strong>in</strong> order to esumate the delay from<br />
collapse to telephon<strong>in</strong>g the 911 emergency<br />
number and the delay to <strong>in</strong>itiation<br />
of bystander CPR for those patients<br />
receiv<strong>in</strong>g such care. All emergency<br />
vehicle response times and the<br />
time of treatments delivered [such as<br />
defibrillation) were recorded on magnetic<br />
tape. These record<strong>in</strong>gs permitted<br />
determ<strong>in</strong>ation of the time of imtiauon<br />
of CPR by the fire department and the<br />
time of the <strong>in</strong>itial defibrillator shock.<br />
Survival {hospital.discharge to home)<br />
was tabulated from review of the medical<br />
records. A logistic regression analysis<br />
was used to determ<strong>in</strong>e the effect<br />
of CPR and defibrillation delays on patient<br />
survival rates.<br />
Yearly survival rates for a five-year<br />
period were determ<strong>in</strong>ed for consecutive<br />
patients who presented <strong>in</strong> cardiac<br />
arrest and <strong>in</strong> whom the <strong>in</strong>itial<br />
rhythm was ventncular fibrillation<br />
{VFI, asystole, or electromechanical<br />
dissociation {EMDI. EMD was def<strong>in</strong>ed<br />
as the condition <strong>in</strong> which a QRS<br />
rhythm was present <strong>in</strong>itially and a<br />
state of pulselessness existed or occurred<br />
dur<strong>in</strong>g <strong>in</strong>itial surveillance by<br />
the emergency responders. Patients<br />
who were found alert and who became<br />
pulseless due to VF were excluded,<br />
as were patients with cardiac<br />
arrest associated with trauma. The<br />
cardiac rhythm, as documented by<br />
paramedics, and the <strong>in</strong>itial hemodynamic<br />
status of the patient with<br />
ENID were determ<strong>in</strong>ed from the narrative<br />
report. Patient outcome was<br />
compared for each <strong>in</strong>itial rhythm and<br />
for the <strong>in</strong>itial hemodynamic condition<br />
78/1182<br />
Ventricula~ Fibrillatm~t<br />
Asyst01e<br />
2 ,,~ ~t~ ~,~<br />
of the patient. Discrete variables were<br />
analyzed us<strong>in</strong>g the chi-square test.<br />
RESULTS<br />
Cardiac Rhythm and Outcome<br />
Dur<strong>in</strong>g the 30 consecutive months,<br />
725 patients with VF were discovered<br />
on arrival of paramedics. Tape record<strong>in</strong>gs<br />
of resuscitation efforts were available<br />
<strong>in</strong> two-thirds of these cases (478~<br />
The rema<strong>in</strong>der were not recorded because<br />
of technical malhmction or unavailability<br />
of recorders. There also<br />
was a small portion of cases <strong>in</strong> which<br />
the response time of the emergeqey<br />
vehicle was not known. I~w~ ~of<br />
the patients had a wimessedlb, ardia~ ~’<br />
arrest, and it is only from these cases<br />
that an estimate of collapse could be<br />
2<br />
)6 "4~ 25 ,<br />
343 ~<br />
240 2~24<br />
¯ \ ",,\"<br />
Electromechamcai<br />
Dissocmticm<br />
<strong>in</strong> these 244 cases are representauve<br />
of a!! patients with VF <strong>in</strong>itially discovered<br />
by paramedics.<br />
The most common rhythm associated<br />
with out-of-hospital arrest is<br />
account<strong>in</strong>g ~or about half of all cases.<br />
In the first 15 years of operation, survival<br />
rates from cardiac arrest and VF<br />
averaged 25%, and annual survival<br />
rates have changed little s<strong>in</strong>ce 1973<br />
(Figure I~<br />
a re~e~t<br />
year period, resuscitation was at-<br />
made. In these witnessed cases, 88% tempted m.1,059 patien~ <strong>in</strong> asystolk<br />
cardiac arrest unretatea to trauma<br />
of bystanders were <strong>in</strong>tervaewed and an<br />
estimate of the time of collapse was -: : One hun&ed fifty (14%1 of the vict~,’<br />
made. Thus logistic regression was<br />
were resuscitated and admitted to tl~<br />
hospital, but only 13 ultimately w~,<br />
based on 244 witnessed cases <strong>in</strong> disc2mrged alive -- a survival rate o<br />
which all of these factors were known.<br />
A comparative analysis of <strong>in</strong>terviewed 1%. There were no survivors am~<br />
witnessed cases with tapes versus<br />
those found <strong>in</strong> asystolic arrest relat~<br />
to trauma despite paramedic and ir<br />
non<strong>in</strong>terviewed wimessed cases with- hospital attempts at resuseita<br />
out tapes showed no sagnificant difference<br />
<strong>in</strong> response time of emergency<br />
vehicles. Thus we believe the f<strong>in</strong>d<strong>in</strong>gs<br />
Annals of Emergency Medic<strong>in</strong>e<br />
tion,~:<br />
The outcome for patients di,<br />
covered <strong>in</strong> cardiac arrest and KI~<br />
15:10 Octot~ 1~
e~<br />
100"<br />
80"<br />
60"<br />
40"<br />
s"<br />
,m ~ a, m, 7 mtn<br />
4<br />
| m~n<br />
TI3URATION OF CPR m<strong>in</strong>.[<br />
I<br />
TABLE 1. SurWval follow<strong>in</strong>g treatment <strong>in</strong> 247 patients found <strong>in</strong> ENID<br />
Initial Rhythm ,..<br />
Supraventricular rate ,~ 60 beats/man<br />
Supraventricular rate > 60 beats/man<br />
Idioventricular or not specified.,,<br />
rate ~ 60 beats/man<br />
No. of No. Discharged<br />
Patlent~ Alive (%)<br />
58 0<br />
33 4 (12)<br />
110 4 (4)<br />
2 °, 3 ° atrioventricular block ’:~ 26 1 (4)<br />
i<br />
Ventricular tachycardia ,~ 8 2 (25)<br />
Paced rhythm 3 1 (33)<br />
Unknown .... 9 3 (33)<br />
; 247<br />
TNOo~<br />
15 (6)<br />
the differences between g~oups are significant. The <strong>in</strong>dicated rhythms are<br />
those categorized by paramedics at the scene of the cardiac arrest,<br />
i<br />
dso was pooc In the same five years,<br />
rely 15 of 247 patients (6%}. with<br />
survived, despite vigorous tre~nent<br />
(ventilation; tracheal <strong>in</strong>tubl,ion~<br />
and adm<strong>in</strong>isttation of sodium~bi-<br />
.arbonate, ep<strong>in</strong>ephr<strong>in</strong>e, and someimes<br />
calcium chloride or atrop<strong>in</strong>e~<br />
V’hen patients with EMD were sttat-<br />
Bed accord<strong>in</strong>g to their <strong>in</strong>itial hemo-<br />
:ynamic status on paramedic arriv~<br />
n additional 127 patients were identiied<br />
(94 with both pulse and pre~ure<br />
~itially found, 33 with detectable<br />
ulse only} who subsequently develped<br />
£MD while under paramedic sureillance.<br />
N<strong>in</strong>e of the 94 patients<br />
0%} discovered with both pulse and<br />
[ood pressure and one of the 33 (3%}<br />
’ho had only a palpable pulse sur-<br />
:10 October 1986<br />
2’o<br />
rived. These survival rates are not significantly<br />
different from the rate of<br />
survival <strong>in</strong> the 247 patients who were<br />
found at the outset to be <strong>in</strong> a pulseless<br />
state. The type of <strong>in</strong>itial rhythm, eg,<br />
supraventricular or ventriculm; and <strong>in</strong>itial<br />
rate also appeared not to <strong>in</strong>fluence<br />
survival rates (T~ble 1~<br />
Time to CPR and DeBlnillation<br />
and Survival<br />
In a logistic regression analysis of<br />
survival <strong>in</strong> 244 wimeased arrests with<br />
VI-, both the delay until <strong>in</strong>itiation of<br />
basic life support and the delay until<br />
defibrillation predicted mortality follow<strong>in</strong>g<br />
cardiac arrest. In witnessed<br />
cases, survival rates decreased about<br />
3% with each m<strong>in</strong>ute of delay until<br />
Annals of Emergency Medic<strong>in</strong>e<br />
3<br />
FIGURE 3. Mortality after cardiac at.<br />
rest related to the delay until mitia.<br />
tion of basic life support and to the<br />
duration of CPR until the first defibrillatory<br />
shock was delivered. The<br />
results are from a logistic regression<br />
analysis <strong>in</strong> 244 witnessed cardiac at.<br />
rests <strong>in</strong> which VF was the first docu.<br />
mented rhythm. The relationship of<br />
mortality to four <strong>in</strong>cremental delays<br />
~n ~n~tiat<strong>in</strong>g basic life support is<br />
shown, as is the effect of the delay un.<br />
til delivery of the first defibr~llatory<br />
shock. Mortality rates <strong>in</strong>crease with<br />
the delays until provision of both<br />
basic and advanced life support. Prob.<br />
ability of survival = ! +e -~.9~ -o.o~<br />
Age --0,1787 m<strong>in</strong> to CPR -0.1515 ra<strong>in</strong> of<br />
CPR to first shock).<br />
<strong>in</strong>itiation of CPR, and cont<strong>in</strong>ued to<br />
fall 14% each m<strong>in</strong>utel dur<strong>in</strong>g the period<br />
after <strong>in</strong>itiation of basic life support<br />
to delivery of the first defibrillator,/<br />
shock (Table 2, Figure 3~ When CPR<br />
was begun with<strong>in</strong> three m<strong>in</strong>utes of<br />
collapse and the first shock delivered<br />
shortly thereafter, 23 of 33 such patients<br />
(70%1 survived.<br />
DISCUSSION<br />
Factom shown to be ,u0c~ted with<br />
high survival rates follow<strong>in</strong>g treat.<br />
ment for out-of-hospital cardiac arrest<br />
are a wimessed collapse, bystander<strong>in</strong>itiated<br />
CPR, and a short resuscita.<br />
tion e~lT.2,11,12 In fact, most patients<br />
found <strong>in</strong> VF who ultimately survive<br />
receive little care beyond <strong>in</strong>itial defibrillation<br />
attempts and usually require<br />
three or fewer defibrillatory<br />
shocks for resuscitatiou.2<br />
S<strong>in</strong>ce <strong>in</strong>itiatio~ of the tiered enter.<br />
gency response system <strong>in</strong> 1972, yearly<br />
rat~ for l~tiems<br />
<strong>in</strong> cardiac arrest and VF have rema<strong>in</strong>ed<br />
relatively flat <strong>in</strong> Seattle, about<br />
2~%. Al.though this may be perceived<br />
as a mc~est success, most of the iraprovement<br />
was achieved ten years ago,<br />
and the emergency care system appears<br />
to have had little effect on the<br />
outcome of patients with asysmle or<br />
EMD.<br />
Asystole .and FAVlD ptolmblyl~n~<br />
s~t mote tlum diffemneea <strong>in</strong> the <strong>in</strong>i.<br />
tlal elecui~ ~ of me~ I~<br />
most cases, they are the result of<br />
lengthy delays until beg<strong>in</strong>n<strong>in</strong>g re.<br />
..m tative m._sures. It Rmm ltkel<br />
mat many, such Imtienm may have<br />
collapsed because of VF and tim these.<br />
two conditions are the c~nusequence of<br />
spontaneous defibrillation occmdng<br />
1183/79
SURVIVAL FROM CARDIAC ARREST<br />
"Weaver et al<br />
FIGURE 4. An example of spontaneous<br />
defibriUat~on oc.¢urrmg n<strong>in</strong>e<br />
mmute~ followfng the onset of VF <strong>in</strong> a<br />
patient who had been resuscitated<br />
previously from cardiac arrest and <strong>in</strong><br />
whom irrevocable cerebral <strong>in</strong>jury occurred.<br />
VF followed a short episode of<br />
rapidly conducted atrml flutter. Resuscitative<br />
efforts were not attempted<br />
and spontaneous defibrillation re.<br />
suhed <strong>in</strong> an idiovenmcuJar rhythm.<br />
The rhythm gradually slowed and<br />
asystole was present 31 m<strong>in</strong>utes follow<strong>in</strong>g<br />
arr~t.<br />
many m<strong>in</strong>utes after collapse (Figure<br />
4~ There are several pieces of evidence<br />
to support this. In witnessed cardiac<br />
arrest, VF is the primary rhythm documented<br />
when victims are monitored<br />
soon after collapse34-~z In our series<br />
of patients discovered <strong>in</strong>itially with<br />
&systole, only 237 of 935 cases (25%)<br />
were witnessed to collapse, compared<br />
to two-thirds of patients discovered<br />
with V1-.<br />
A report from suburban K<strong>in</strong>g<br />
County showed a 95% <strong>in</strong>cidence of<br />
VF <strong>in</strong> cases monitored with<strong>in</strong> four<br />
m<strong>in</strong>utes after collapse,, decreas<strong>in</strong>g to<br />
71% for cases first monitored after 12<br />
to 15 m<strong>in</strong>utes.IS Spontaneous defibrillation<br />
appears to occur from<br />
three to 20 m<strong>in</strong>utes or more follow<strong>in</strong>g<br />
the onset of ~ This has been documented<br />
on Hoher tapes <strong>in</strong> victims<br />
who were unattended at the time of<br />
axrest or who received advanced life<br />
support treatments after lengthy delayslS,19<br />
"zl (unpublished data).<br />
The low survival rates associated<br />
with asystole and EMD also may ira..<br />
ply that currently prescribed procedures<br />
and treatments for these<br />
rhythms are <strong>in</strong>effective or possibly<br />
even ~ There ~ a scasc~ty ’o(<br />
mauroll~ s)udies that ~uate drug<br />
ueaumm ~ the ~m~g ,4 card~ ar-<br />
8011184<br />
#<br />
i<br />
17:01 onset of VF<br />
i<br />
17:06 5 m<strong>in</strong>utes later<br />
cases, substantial ga<strong>in</strong>s may be realized<br />
by reduc<strong>in</strong>g both the delay until<br />
<strong>in</strong>itiation of basic life support and defibrillation.<br />
These reductions <strong>in</strong> delay<br />
can most readily be accomplished by<br />
encourag<strong>in</strong>g further community tra<strong>in</strong><strong>in</strong>g<br />
<strong>in</strong> CPR and by provid<strong>in</strong>g first re-<br />
sponders with the equipment and<br />
skills to effect rapid defibrillation. In<br />
several communities, bystander-<strong>in</strong>itiated<br />
CPR has been shown to be associated<br />
with improved survival rates<br />
from cardiac arrest.zA6, ~-aO Th~ effect<br />
is espec~tly true for the subset of<br />
witnessed cases of arrest. Because<br />
most of the effect of bystanders is <strong>in</strong><br />
this subset, the f<strong>in</strong>d<strong>in</strong>g attests to<br />
treatment effectiveness and appears<br />
not to be a result solely due to early<br />
Annals of Emergency Medic<strong>in</strong>e<br />
S<strong>in</strong>ce 1972 more than 370,000<br />
laypersons <strong>in</strong> our community have received<br />
<strong>in</strong>struction <strong>in</strong> CPIL The tram<strong>in</strong>g,<br />
sponsored by the fire department,<br />
requires three hours and emphasizes<br />
how to access the emergency system,<br />
outl<strong>in</strong>es the signs of heart attack and<br />
cardiac arrest, and provides an oppozmmty<br />
manik<strong>in</strong>.<br />
rest, but t,~ available mmlts do not<br />
~ t that q~neohxme, sodium bi-<br />
~mOne, and calcium<br />
r~ ~ Im~ly ~ to the<br />
malor ga<strong>in</strong>s can<br />
usual patient found <strong>in</strong> caxd~ anest<br />
~:ted by sh, m~nj~ the time to<br />
with awm~ or ~tD.2a,z~<br />
fibrillation,<br />
Thus most available data suggest<br />
that &systole and EMD are more often summons of the emergency care sys-<br />
pretezm<strong>in</strong>al conditions, mherendy untem.2~<br />
In communities with exresponsive<br />
to any therapy, primarily tremely rapid emergency response<br />
because of long delays prior to <strong>in</strong>itia- times, the benefit of bystander-<strong>in</strong>itition<br />
of resuscitation. Efforts at <strong>in</strong>ated CPR has not been demonstrate&2<br />
creas<strong>in</strong>g survival rates from cardiac ar- These studies lead us to conclude that<br />
rest can, therdore, most profitably be it is not who <strong>in</strong>itiates such care, but<br />
directed toward improv<strong>in</strong>g the man- <strong>in</strong>stead how quickly resuscitative<br />
agement of patients with VF. In these efforts are begun.<br />
<strong>in</strong> cases<br />
15:10 Octol~r 1<br />
I<br />
""i ¸
i<br />
,rTi<br />
TABLE 2. Survival from out-of-hospital VF related to the delays until CPR and to the ~rst shock<br />
M<strong>in</strong>utes From Collapse<br />
to <strong>in</strong>itiation of CPR<br />
,~3<br />
>3<br />
Total<br />
¯ Survival rates.<br />
tp ~ ,0~ -- row comparison, u~ivarlant analysis.<br />
*P =~ .01 -- column comparison, unlvariant analysis.<br />
t<br />
M<strong>in</strong>utes of CPR to Rrat Shock<br />
,~ 6 7-12 > 12<br />
23 (70%)* 20 (44%) 1 (7%)<br />
42 (39%) 12 (31%) 2 (22%)<br />
651141 (46%)1 33187 (38%)1 3123 (13%)1<br />
| ~ich the response times of pars-<br />
| ~cs are prolonged. For cases of witnessed<br />
arrest <strong>in</strong> which CI’R h/d been<br />
delayed by four m<strong>in</strong>utes and parsmedic<br />
response times.were n<strong>in</strong>e ra<strong>in</strong>utes<br />
or more, eight of 13 victims<br />
162%1 when first responders<br />
mit~d shocks, compared to<br />
seven of 9.6 (27%} when first re-~<br />
slxmders delivered only basic life sup-<br />
~X)ft. 31<br />
rates us<strong>in</strong>g available treatments are<br />
dismal and possibly unalterable.<br />
CONCLUSION<br />
Secondly, tra<strong>in</strong><strong>in</strong>g r~en~ and<br />
cost to extensively implement defibrillation<br />
are prohibitive. In addition,<br />
the relatively small number of uses<br />
per rescuer is <strong>in</strong>adequate to ma<strong>in</strong>ta<strong>in</strong><br />
rhythm recognition skills, Thus a<br />
modified approach us<strong>in</strong>g automatic<br />
external defibrillators is far more prac- REFERENCES<br />
tical, These new automatic devices re- 1. US Department of Transportation<br />
quire substantially less <strong>in</strong>itial and<br />
Emergency Medical technician -- ambuhmce:<br />
Basic tra<strong>in</strong><strong>in</strong>g pmg~am. Instruc-<br />
cont<strong>in</strong>ued tra<strong>in</strong><strong>in</strong>g and may prove tor’s lesson plans. Government Pr<strong>in</strong>t<strong>in</strong>g<br />
useful provided that they are safe for Office, PUbl No. TD 2.208: EM 313, Wash-<br />
~h victim and resene~ are efficient <strong>in</strong>gton DC, 1970.<br />
"~’recogtiz<strong>in</strong>g VI:, and can be imple-<br />
" mented <strong>in</strong> such a way that a substan- 2. Kowalski 11, Thompson BM, Horwitz<br />
L, et al: Bystander CPR <strong>in</strong> prehospital<br />
tial sav<strong>in</strong>gs <strong>in</strong> the time to shock {three coarse ventricular fibrillation. Ann Emerg<br />
m<strong>in</strong>utes or more} can occu~<br />
Med 1984; 13:1016-1020.<br />
An-additional factor affect<strong>in</strong>g ratis<br />
treatment that reduces the<br />
3. Weaver WD, Cobb LA, Copass MK, et<br />
common problem of refibrillation dur-<br />
al: Ventricular defibrillation: A comparative<br />
trial us<strong>in</strong>g 175-I and 320-I shocks.<br />
<strong>in</strong>g resuscitation. The development N F.ngl /Med 1982~307:1101-II06.<br />
and evaluation of pharmacological<br />
~gents to prevent such epi~k)des so 4. Diamond N[ Schofferman T, Elliot W,r:<br />
that peffmmg rhythms =re Factors <strong>in</strong> successful resuscitation by par-<br />
likely to improve subamedics./ACEP 1977~6:42.46.<br />
viva] rates <strong>in</strong> patients with VE There 5. Steuven H, Thompson BM, Apraha-<br />
also appears to be promise <strong>in</strong> new apmian C, et al: Use of calcium <strong>in</strong> prethat<br />
augment pedusion or<br />
attenuate myocardial and cerebral<br />
damage dur<strong>in</strong>g CPR.<br />
Unlike V~, <strong>in</strong> which several new<br />
promis<strong>in</strong>g approaches to treatment ex-<br />
ist, effective strategies aimed at imrov<strong>in</strong>g<br />
outcome for patients dis-<br />
~ered <strong>in</strong> cardiac arrest with asystole<br />
or EMD are not obvious, and survival<br />
d0 October 1986<br />
Annals of Emergency Medic<strong>in</strong>e<br />
TOfM<br />
44/92 (48%)~<br />
57/159 (36%)t<br />
pulmonary resuscitation <strong>in</strong> a paramedic<br />
served metropolitan area. Am [ Public<br />
Heahh 1983~ 73:766-769.<br />
8. Amey BD, Harrison EE, Straub EJ~ Sudden<br />
cardiac death: A retrospective and<br />
prospective study./ACEP 1976;5:429-433.<br />
9. Engman 1~, Campion BC, McBride W~<br />
et al: Mobile coronmry care <strong>in</strong> the man-<br />
~ement of preho~pital cardiac arrest. St<br />
Paul, M<strong>in</strong>nesota, experience. MJnn Med<br />
1976~59:833-835.<br />
I0. BriEp RS, Brown PM, Crabb ME, et<br />
al: The Brighton resuscitation ambulances:<br />
A cont<strong>in</strong>u<strong>in</strong>g experiment <strong>in</strong><br />
prehospital care by ambulance staff. Br<br />
Med / 1976~2:1161-1165.<br />
11. Thompson I~, Hallstrom AP, Cobb<br />
LA: Bystander-<strong>in</strong>itiated c~rdiopulmonary<br />
resuscitation <strong>in</strong> the matmgemont of ventricular<br />
fibrillation. Ann Inters Med<br />
1979;90:737-740.<br />
12. Eisenberg <strong>MS</strong>, Bergner L, Hallstrom<br />
AP: Who shall ltve~ Who shall dieL <strong>in</strong><br />
Sudden Cardiac De~th tn the CommtmJ.<br />
ty. New York, Praeger Publishers, 1984, pp<br />
48-49.<br />
13. Harrison EE, Amey BD: The use of<br />
calcium chloride <strong>in</strong> cardiac resuscitation<br />
(abstract~ Circnlatio~ 1982~66:!1-348.<br />
14. MeJd W~, ~ ~ Trombold IC, et<br />
al: Successhtl resuscitation of two near Mmultaneous<br />
cues of cardiac ar~st with a<br />
review of fifteen cases occurr<strong>in</strong>g dur<strong>in</strong>g<br />
supervised e~ends~ Citcu/atioa 1976~53:<br />
187-189.<br />
15. Enns T, Tweed WA, Donen N: Prehospital<br />
cardiac rhythm dotetiomtion <strong>in</strong> a<br />
hospital cardiac arrest. Ann Emerg Med system provid<strong>in</strong>g only basic life support.<br />
1983~ 12:136-139.<br />
Ann Emerg Med 1983~12:478-481.<br />
6. Myerberg R[, Conde CA, Sung R[0 et al: 16. Roth R, Stewart RD, Rogers K, et al:<br />
Cl<strong>in</strong>ical, electrophysiolngic and hemo- Out-of-huspital cardiac arrest: Factors asdynamic<br />
profile of patients resuscitated sociated with survival. Ann Emerg Med<br />
from prehospital cardiac arrest. Am ~ Med 1984~ 13:237-243.<br />
1980~68:568-576.<br />
17. Liberthson KR, N~gel EL, Hirschman<br />
7. Guzy PM, Pearce ML, Greenfield S: WC, et al: Pathophysiologic observations<br />
The survival benefit of bystander cardio- <strong>in</strong> prehospital ventricular fibrillation =nd<br />
118$/81
O<br />
P<br />
SURVIVAL FROM CARDIAC ARREST<br />
" Weaver et al<br />
sudden death. Circulation 1974)49:<br />
790-798.<br />
18. Hallstrom AP, Eisenberg <strong>MS</strong>, Bergner<br />
L: The persistence of ventricular fibrillation<br />
and its implication for evaluat<strong>in</strong>g<br />
E<strong>MS</strong>. Emerg Health Serv Qtr 1983j1:<br />
41-49.<br />
19. Nikolic G, Bishop RL, S<strong>in</strong>gh JB: Suddenculauon<br />
death 1982i66:218-225.<br />
dur<strong>in</strong>g holter monitor<strong>in</strong>g. Cir-<br />
20. W<strong>in</strong>ke RA: Ambulatory electrocardiography<br />
and the diagnosis, evaluation,<br />
and treatment of chronic ventricular arrhythmias.<br />
Prog Cardiovas Dis 1980i<br />
23:99-128.<br />
21. H<strong>in</strong>kle LE, Argyros DC, Hayes JC, et<br />
al: Pathogenesis of an unexpected sudden<br />
death: Role of early cycle ventricular premature<br />
contractions. Am ] Cgrch’ol 1977)<br />
39:873-879.<br />
22. Steuven HA, Thompson B, Apraha-<br />
mian C, et al: Lack of effectiveness of calcium<br />
chloride <strong>in</strong> refractory asystole. Ann<br />
Emerg Med 1985~14:630-632.<br />
23. Steuven HA, Thompson B, Aprahamian<br />
C, et al: The effectiveness of calcium<br />
chloride <strong>in</strong> refractory electrome.<br />
chanical dissociation. Ann £merg Med<br />
1985; 14:626-629.<br />
24. Cobb LA, Hallstrom AP: Communi.<br />
ty-based cardiopulmonary resuscitation:<br />
What have we learned? Arm NY Acad Sci<br />
1982)382:330-341,<br />
25. Lund 1, Skulberg A: Cardiopulmonary<br />
resuscitation by lay people. Lancet 1976;<br />
2:207-214.<br />
26. Copley DP, Mantle |A, Rogers W]: Improved<br />
outcome for prehospital cardiopul.<br />
monary collapse with resuscitation by bystanders.<br />
Circulation 1977)56:901-905.<br />
27. Eisenberg M, Bergner L, Hallstrom A:<br />
Paramedic programs and out-of-hospital<br />
82/1186 Annals of Emergency Medic<strong>in</strong>e<br />
cardiac arrest. I. Factors associated with<br />
successful resuscitation. Am I Public<br />
Health 1979;69:30.38.<br />
28. Twee~ WA, Bristow G, Donen N: Resuscitation<br />
from cardiac arrest: Assessment<br />
of a system provid<strong>in</strong>g only basic lit¢<br />
support outside of hospit~. Can Meal Asso¢<br />
] 1980)122:297-300.<br />
29. Ver teai L, Wilson L, Glick N: Cardiac<br />
arrest: Comparison of paramedic and conventional<br />
ambulance services. Can Med<br />
Asso¢ ] 1983)128:809-813.<br />
30. Cumm<strong>in</strong>s RO, Eisenberg <strong>MS</strong>: Prehospital<br />
cardiopulmonary resuscitation.<br />
Is it eff.ec~ive? ]AMA 1985~253:2408-<br />
2412.<br />
31. Weaver WD, Copass MK, Buff D, et ah<br />
Improved neurologic recovery and survival<br />
after,early defibrillation. Circ~at.fon<br />
1984;69:943-948.<br />
: ..,,, "<br />
,÷’ T<br />
’" L,<br />
.,<br />
i:
CHARLES M. BURNS, MD, FRCSC*<br />
4. <strong>Accident</strong>-Injury Organization: Canadian Overview<br />
Trauma from motor vehicle accidents is<br />
a major health-care problem, result<strong>in</strong>g <strong>in</strong><br />
enormous economic losses to the coun-<br />
~srYaand reason<br />
is second<br />
for hospitalization<br />
only to heart<br />
<strong>in</strong><br />
disease<br />
Canada.<br />
Fund<strong>in</strong>g for research and accident-<strong>in</strong>jury<br />
programs is critically low,<br />
National and prov<strong>in</strong>cial trauma registries<br />
must be developed to provide data<br />
that can be used appropriately to plan<br />
and monitor the strategy of accident<br />
health-care and prevention programs,<br />
Manitoba, which has <strong>in</strong> place a trauma<br />
registry, has a prov<strong>in</strong>ce-wide trauma systern<br />
compris<strong>in</strong>g two comprehensive<br />
trauma units and seven regional centras<br />
located strategically In the catchment<br />
areas of the major centres, A comparison<br />
of the performance of this system with<br />
that of hospitals <strong>in</strong> Baltimore has shown<br />
that the Manitoba system provides an<br />
equal level of care. The author recommends<br />
that a trauma system be astal)fished<br />
<strong>in</strong> regions of one to two million<br />
population, Each region should have one<br />
to three comprehensive trauma services<br />
a number of regional trauma eerv-<br />
~j~es<br />
¯ each strategicaBy located.<br />
W’rth appropriate fund<strong>in</strong>g for trauma<br />
care. the propose d system would pay for<br />
itself. "--<br />
From the Department of Surgery, Health<br />
Sciences Centre, University of Manitoba,<br />
W<strong>in</strong>nipeg, Man.<br />
Presented as part of a symposium on the<br />
organization of trauma care at the 53rd<br />
annual meet<strong>in</strong>g of the Royal College of<br />
Physicians and Surgeons of Canada by the<br />
Royal College <strong>in</strong> cooperation with the<br />
Trauma Association of Canada, the Canadian<br />
Association of General Surgeons, the<br />
Canadian Orthopaedic Association and the<br />
Canadian Association of Plastic Surgeons,<br />
Montreal, PQ, Sept. 11, 1984<br />
*Associate Professor of Surgery, University<br />
of Manitoba. Director of Trauma Services,<br />
Health Sciences Centre, W<strong>in</strong>nipeg, Man.<br />
Accepted for pubfication June 6, 1985<br />
Repr<strong>in</strong>t requests to: Dr. C.M. Burns, Rm.<br />
160. Old Basic Sciences Build<strong>in</strong>g, 753<br />
McDermot Ave., W<strong>in</strong>nipeg, Man. R3E 07"6<br />
Lee treumatismas subis lore d’accidents<br />
de le route repr6sentent un probl6me<br />
majaur de lo<strong>in</strong>s de osnt6; lie r6sultent en<br />
des pertas 6conomiques importantas<br />
pour le pays st lie vlennent au second<br />
rang derri6re les maladies cardlaquas<br />
comme cause d’hospitalisotion au<br />
Canada, N6anmo<strong>in</strong>s lea subventions b le<br />
recherche et aux progremmes de so<strong>in</strong>s<br />
aux victimea d’accidents sont critiquement<br />
bas,<br />
On dolt 6tablir des listes natlonale et<br />
prov<strong>in</strong>clalas des traumstismas subis lore<br />
d’accidents af<strong>in</strong> d’accumuler las donn6es<br />
qui permettront de pianifier et de surveillerle<br />
stret6gie des so<strong>in</strong>s aux victimes<br />
d’accidents et calle des progremmas de<br />
pr6vantion. Le Manitoba qui a une talle<br />
lista, poes~le un syst6me de so<strong>in</strong>s posttreumatiques<br />
comprenant deux unit6s de<br />
so<strong>in</strong>J complsts pour traumatis6s et sept<br />
centras r6gionaux situ6s strat6piquement<br />
darts le circonacription des grands cantres.<br />
Comparetivemant au syst6me qui<br />
pr6vaut dens les h6pitaux de Baltimore,<br />
on peut dire que le systkrne manitobaln<br />
offre un nlveau de so<strong>in</strong>s satisfaisant.<br />
L’auteur recommande qu’un service de<br />
so<strong>in</strong>s pour traumatis6s solt 6tabli darts<br />
chaque grand h6pital et qu’une unit6<br />
r(q~omale soit raise sur pied dana chaque<br />
r6glon comptant de un i deux millions de<br />
population.<br />
Avac les fonds approprkSs, le syst6me<br />
propo~5 sereit rentable.<br />
<strong>in</strong> a large <strong>in</strong>crease <strong>in</strong> the total number of<br />
fatalities and <strong>in</strong>jured and disabled persons<br />
over the past 30 years. Also the escalat<strong>in</strong>g<br />
hospital costs, welfare and property<br />
loss have seriously dra<strong>in</strong>ed the Canadian<br />
economy. To ease this burden, government<br />
and foundation fund<strong>in</strong>g should support<br />
the development of a national<br />
trauma program.<br />
The Canadian Picture<br />
The total ~ars of life lost annually<br />
through motor vehicle accidents is greater<br />
than the total of all cardiac and respiratory<br />
deaths,<br />
Rush<strong>in</strong>g the accident victim to the nearest<br />
hospital and then f<strong>in</strong>d<strong>in</strong>g a doctor is no<br />
longer an acceptable way to manage a<br />
traumatized patient. Modern data<br />
process<strong>in</strong>g, communications, transport,<br />
and sophisticated pre- and <strong>in</strong>hospital<br />
medical care should be coord<strong>in</strong>ated to<br />
provide a high standard of health care for<br />
such victims. An accident-<strong>in</strong>jury program<br />
should be directed prov<strong>in</strong>cially and coord<strong>in</strong>ated<br />
nationally.<br />
The rate of accident <strong>in</strong>juries has been<br />
kept under reasonable control through the<br />
efforts of government agencies, but the<br />
greater numbers of motor vehicles and the<br />
expansion of heavy <strong>in</strong>dustry have resulted<br />
n Lawson <strong>in</strong> 1977 estimated<br />
Canada’s yearly economic loss from accidents<br />
to be $2.5 to $4 billion. 2 In 19~,4<br />
these losses may well double that figure.<br />
Motor vehicle accidents account for 30%<br />
to 40% of the total accident deaths <strong>in</strong><br />
Canada annually. The risk of accident to<br />
the Canadian driver is 20~0 greater than<br />
that to the US driver and 50% greater by<br />
miles driven. Less than 1% of the<br />
research dollar goes to trauma research<br />
and organization of a health-care program<br />
for accident <strong>in</strong>jury (Gordon J.<br />
Gutelius JR: Unpublished data, I9"/5).<br />
Between 1960 and 1975, the numben<br />
of motor vehicle drivers and passengen<br />
~jm~! k=zea~l~O~ ~=1 Zel/o fewe~ tivcly (Fig. 1), while the <strong>in</strong>cidence of<br />
motorcycle accident <strong>in</strong>jury; <strong>in</strong>ctea.u~l<br />
almost 1000%) The relatively sm.,;l<br />
<strong>in</strong>crease <strong>in</strong> pedestrians <strong>in</strong>jured attesu to<br />
effective countermeasures. However.<br />
these 20 000 victims are among the mo~t<br />
severcly <strong>in</strong>jured and suga<strong>in</strong> the mo~t<br />
severe ongo<strong>in</strong>g disability as a group.<br />
The Traffic Injury Research Found~<br />
don of Canada studied blood alcohol<br />
levels of victims <strong>in</strong> 1647 fatal traffic accidents<br />
<strong>in</strong> 1976 (Table 1). 3 impairment<br />
levels (more than 17 retool/L) of blood<br />
alcohol were found <strong>in</strong> 25~ to $2~ of ~"<br />
tiros <strong>in</strong> the categories exam<strong>in</strong>ed. The~e<br />
figures are particularly important bec2"~<br />
frequently <strong>in</strong>nocent people <strong>in</strong> anodgg<br />
vehicle<br />
The <strong>in</strong>cidence<br />
are <strong>in</strong>volved<br />
of traffic<br />
<strong>in</strong> the<br />
accident<br />
accident.<br />
deatht<br />
and <strong>in</strong>juries for 1977 is compared, by<br />
prov<strong>in</strong>ce <strong>in</strong> Fig. 2. 3 It is notable that the<br />
~= gVIRGERY
I i<br />
J<br />
!<br />
number <strong>in</strong>jured (i.e., anyone show<strong>in</strong>g any<br />
evidence of <strong>in</strong>jury or compla<strong>in</strong><strong>in</strong>g of pa<strong>in</strong>)<br />
is about 40 times the number of deaths.<br />
While Ontario and Manitoba had among<br />
’gO0<br />
110<br />
the lowest fatality rates, their <strong>in</strong>jury rates<br />
were among the highest. The development<br />
of accident-<strong>in</strong>jury programs <strong>in</strong> Ontario<br />
and Manitoba may have contributed to<br />
these favourable statistics.<br />
Develop<strong>in</strong>g Organization for Trauma<br />
Care and Prevention <strong>in</strong> Canada<br />
Trauma Registries<br />
The registry system is be<strong>in</strong>g studied at<br />
seven hospitals across Canada. Trauma<br />
registries that <strong>in</strong>clude <strong>in</strong>jury severity<br />
scor<strong>in</strong>g 4.~ <strong>in</strong> addition to detailed records<br />
of all fatalities and <strong>in</strong>juries for patients<br />
admitted to hospital <strong>in</strong>dicate clear priorities-for<br />
research and strategy when<br />
develop<strong>in</strong>g prehospital and <strong>in</strong>hospital<br />
accident health-care programs. The<br />
present <strong>in</strong>complete estimates of the<br />
impact of trauma on the Canadian economy<br />
could be more accurately estimated.<br />
Improved health-care programs for the<br />
<strong>in</strong>jured and appropriate preventive measures<br />
would result <strong>in</strong> substantial sav<strong>in</strong>gs<br />
not to mention reduced suffer<strong>in</strong>g.<br />
Table I-Blood Alcohol Content Among Fatally Injured Drivers<br />
bV Vehicle Type. Seven Prov<strong>in</strong>ce* Aggregates. Canada, 1976<br />
Blood alcohol level<br />
Im<strong>in</strong>imum % of victims)<br />
No. of fatal<br />
i Drivers of accidents Positivet Impairedt<br />
i Automobiles 1 119 47 38<br />
Truclrs;v~ns 291 49 42<br />
iMeto~cyc,~s 153 40 29<br />
Tractor trai~ 32 25 25<br />
. Snowmobiles 52 60 !<br />
52<br />
, "Pr<strong>in</strong>ce Ed’ccerd Island, New Bnmswick, Ontario. Manitoba, Saskatchewan. Alberta and British Columbia.<br />
, t> 2 mmolL<br />
i*> 17 mr,~L<br />
t Source: Traffic Injmy Remarch Foundation of Canada, Analysis of Fatal Traffic Crashes 1976.<br />
o<br />
Persons<br />
,.,.,;.TT;O.rT<br />
Killed.<br />
Rate per 100 OO0 Population,<br />
1977<br />
Canada<br />
:i~.~::.:i~:~::-~:-.:.!-:’::ii!ii~i%i:~::~:i::l~l Newfoundland<br />
I J! ! , , ’~i Ii<br />
Pr<strong>in</strong>ce Edward !~ ~<br />
’ Island<br />
";L:Lb’:’:: +. :’::-:+v,.<br />
I<br />
Nova Scotia<br />
New Brunswick<br />
:<br />
Quebec<br />
Ontario<br />
Manitoba<br />
Persons Injured,<br />
Rate per 100 OOO Population,<br />
000 I:K)O<br />
:i:~:::~::~:~:?l<br />
Saskotchewan<br />
L I I I I I<br />
!<br />
L ¯ ’: " : : .: . i<br />
Alberta<br />
I : I I<br />
P’::: :. : ¯ "1 ]<br />
i Br~sh Columbia<br />
I I I I~ i I Yukon<br />
Nm’thweot I Tecritodes<br />
0 5 10 15 20 25 30 35 40 45 50 0 200 400 600 8001000 1200<br />
FIG. 2--Incidence of traffic deaths and <strong>in</strong>juries by prov<strong>in</strong>ce for 197"/.<br />
The data obta<strong>in</strong>ed from trauma registries<br />
could be used to strengthen epidemiologic,<br />
research and treatment programs,<br />
to assess priorities <strong>in</strong> different geographic<br />
regions, to develop appropriate prehospitat<br />
health care, to def<strong>in</strong>e the strategy,<br />
location and type of ambulance services<br />
re~luired <strong>in</strong> each region and to decide on<br />
the type of ambulance service to be used<br />
regionally,<br />
The Manitoba trauma registry.--Our<br />
registry, the only one <strong>in</strong> Canada at<br />
present, was developed us<strong>in</strong>g the<br />
ICD.9.CM 6 Manitoba Health Services<br />
Commission discharge data, which lists<br />
all <strong>in</strong>juries, complications, procedures<br />
and associated diseases for each victim<br />
admitted to hospital.<br />
The <strong>in</strong>itial data is scored, assign<strong>in</strong>g a<br />
specific abbreviated <strong>in</strong>jury score (AIS) to<br />
each <strong>in</strong>jury. ~ A computer algorithm was<br />
developed to assign this AIS scale as a<br />
score to s<strong>in</strong>gle <strong>in</strong>juries, 1 and 2 be<strong>in</strong>g<br />
m<strong>in</strong>or <strong>in</strong>juries and scores of 3, 4 and 5<br />
<strong>in</strong>dicat<strong>in</strong>g life-threaten<strong>in</strong>g <strong>in</strong>juries. In the<br />
patient with multiple <strong>in</strong>juries the <strong>in</strong>jury.<br />
severity score (ISS) ~ is automatically<br />
scored by a computer program. Scores below<br />
15 are considered m<strong>in</strong>or <strong>in</strong>juries and<br />
those above as life-threaten<strong>in</strong>g <strong>in</strong>juries.<br />
The AIS/80 scor<strong>in</strong>g of <strong>in</strong>juries: was<br />
modified to reflect more accurately the<br />
threat to life. The scor<strong>in</strong>g table and the<br />
computer algorithm were forwarded to<br />
Professor E. MacKenzie, Johns Hopk<strong>in</strong>s<br />
University and seven trauma centres<br />
across Canada for further de\elopment<br />
and study: Every effort should be made<br />
to ma<strong>in</strong>ta<strong>in</strong> a uniform national scor<strong>in</strong>g<br />
system.<br />
Prehospital Services <strong>in</strong> Canada<br />
A Manitoba study (’Fig. 3) of 364 prehospital<br />
deaths for 1980, 1981 and 1982<br />
<strong>in</strong>dicates thai 15~ of the victims had<br />
m<strong>in</strong>or-<strong>in</strong>jur~ severity sco[es. Detailed<br />
study is needed to establish why victims<br />
with such low scores died dur<strong>in</strong>g the prehospital<br />
period and to determ<strong>in</strong>e methods<br />
of prevention.<br />
CA~Ea<br />
0t r J]<br />
im<br />
FIG. 3--Prehospital deaths <strong>in</strong> Manitoba for<br />
1980, 1981, 1982. White bars = those with<br />
m<strong>in</strong>or-<strong>in</strong>jury severity score (ISS less than 15).<br />
dolled bars : those with life-threaten<strong>in</strong>g <strong>in</strong>jury<br />
severity score (ISS more than I5).<br />
VOLUME 28. NO. 6. NOVEMBER 1985 I THE CANADIAN JOURNAL OF SURGERY 483
O<br />
O<br />
Prehospital services <strong>in</strong>’ Canada are at<br />
’ vary<strong>in</strong>gstages of development. Ontario,<br />
Manitoba, Saskatchewan and British<br />
Columbia provide prov<strong>in</strong>cial fund<strong>in</strong>g for<br />
ambulance services and programs for<br />
tra<strong>in</strong><strong>in</strong>g ambulance attendants to the<br />
levels of emergency medical attendant<br />
(EMA) I and II. Paramedic programs<br />
(EMA III level) have been developed <strong>in</strong><br />
Vancouver and 12 centres <strong>in</strong> Alberta.<br />
Saskatchewan, Manitoba and Ontario are<br />
<strong>in</strong>itiat<strong>in</strong>g tra<strong>in</strong><strong>in</strong>g at this level. These programs<br />
are of great value <strong>in</strong> treat<strong>in</strong>g acute<br />
medical emergencies, <strong>in</strong> cases where<br />
extraction of the victim from a motor<br />
vehicle is prolonged and when delivery<br />
time to the hospital is extended. Rural<br />
areas would benefit most from such services.<br />
Unfortunately, there are no largeregion<br />
dispatch<strong>in</strong>g centres anywhere <strong>in</strong><br />
Canada at present. The German system<br />
of regional dispatch should be studied for<br />
adoption <strong>in</strong> Canada.<br />
Ontario has <strong>in</strong> place, through its community<br />
college system, an educational<br />
program for the tra<strong>in</strong><strong>in</strong>g of emergency<br />
medical attendants <strong>in</strong> its ambulance services.<br />
This is the first prov<strong>in</strong>ce-wide program<br />
<strong>in</strong> Canada. Except for Montreal,<br />
Quebec and the eastern prov<strong>in</strong>ces have<br />
accomplished little <strong>in</strong> the development of<br />
a coord<strong>in</strong>ated prehospital-care system.<br />
There, a physician is assigned to certa<strong>in</strong><br />
high-risk ambulance runs. This system<br />
may provide <strong>in</strong>terest<strong>in</strong>g data for comparison<br />
with the EMA programs; it may<br />
prove to be more effective and cost efficient.<br />
A trauma registry, us<strong>in</strong>g a Standard<br />
national scor<strong>in</strong>g system, would allow for<br />
valuable comparative studies between<br />
centres us<strong>in</strong>g differ<strong>in</strong>g prehospital<br />
systems.<br />
The development of the emergency<br />
physician specialty and the advanced<br />
trauma life support (ATLS) course has<br />
upgraded the lx)tential standard of <strong>in</strong>jury<br />
care <strong>in</strong> the fh’st hour after <strong>in</strong>jury. Unfortunately,<br />
the services result<strong>in</strong>g from these<br />
developments are usually found only <strong>in</strong><br />
large urban centres. Regional trauma<br />
units, strategically located, us<strong>in</strong>g data<br />
from registry studies, would provide<br />
appropriate resources for rural regions.<br />
Air-ambulance systems exist <strong>in</strong> almost<br />
every prov<strong>in</strong>ce and have provided a valuable<br />
resource for the transport of trauma<br />
victims long distances to sophisticated<br />
trauma centres. These, however, are not<br />
well coord<strong>in</strong>ated and seldom carry<br />
appropriately tra<strong>in</strong>ed medical attendants.<br />
Air-ambulance services are provided<br />
almost entirely by fixed-w<strong>in</strong>g aircraft,<br />
which, <strong>in</strong> Canada, are probably the most<br />
appropriate. Capital cost, ma<strong>in</strong>tenance,<br />
available crew and distances <strong>in</strong> Canada<br />
are factors that strongly support development<br />
of fixed-w<strong>in</strong>g ambulance services<br />
first. Specific regions, isolated from fixedw<strong>in</strong>g<br />
evacuation where a high risk of acci-<br />
dent <strong>in</strong>jury has been demonstrated, might<br />
be considered for helicopter services.<br />
In northern Canada are now almost<br />
250 000 people who are exposed to an<br />
<strong>in</strong>creas<strong>in</strong>g <strong>in</strong>cidence of accident <strong>in</strong>jury<br />
associated with heavy <strong>in</strong>dustry (oil exploration,<br />
lumber<strong>in</strong>g, m<strong>in</strong><strong>in</strong>g). Army resct, e<br />
units, which are available at four levels<br />
of expertise and response <strong>in</strong> a number of<br />
regions, could be strategically located to<br />
provide rapid triage and evacuation of the<br />
<strong>in</strong>jured to appropriate centres <strong>in</strong> the<br />
south. Regional trauma centres <strong>in</strong> Whitehorse,<br />
Yellowknife and northern Quebec<br />
might provide such services us<strong>in</strong>g army<br />
paramedical attendants. The armed services<br />
personnel would derive practical<br />
experience and the population a valuable<br />
service at no extra expense.<br />
Trauma Cenlres<br />
In 1977, the trauma committee of the<br />
Canadian Association of General Surgeons<br />
and now the Trauma Association<br />
of Canada designated 21 comprehensivecare<br />
centres. In addition, it is proposed<br />
CASES<br />
120<br />
100<br />
8O<br />
6O<br />
4O<br />
1<br />
4<br />
?<br />
that regional trauma centres, havm~<br />
staff at least one surgeon experienced <strong>in</strong><br />
trauma care, be developed <strong>in</strong> each of the<br />
catchment areas of the major centres. At<br />
present, Manitoba is the only prov<strong>in</strong>ce<br />
that has this system <strong>in</strong> place.<br />
The trauma system was developed by<br />
the medical profession not by legislation<br />
It has had po deleteriou~ ,mp;.:~ on the<br />
heath-care system as it was developed<br />
dur<strong>in</strong>g a phase when regionalization was<br />
tak<strong>in</strong>g place.<br />
The Manitoba system.--In Manitoba<br />
the trauma hospital system <strong>in</strong>cludes two<br />
comprehensive trauma units, both <strong>in</strong><br />
W<strong>in</strong>nipeg, and seven regional traunm<br />
units across the prov<strong>in</strong>ce. Of patients ~,h<br />
life-threaten<strong>in</strong>g <strong>in</strong>juries, 55% are admitted<br />
<strong>in</strong>itially to a trauma-unit hospital,<br />
suggest<strong>in</strong>g the appropriate strategic location<br />
of these hospitals across the<br />
prov<strong>in</strong>ce. Of the patients with lifethreaten<strong>in</strong>g<br />
<strong>in</strong>juries who are not <strong>in</strong>iti~,dly<br />
admitted to the trauma-unit hospitals,<br />
75% are referred <strong>in</strong>to the system with<strong>in</strong><br />
the first 48 hours after <strong>in</strong>jury. Obviously<br />
not all life-threaten<strong>in</strong>g <strong>in</strong>juries need be<br />
¯CASE80EATH8<br />
¢TU ~ 2S8 46<br />
2 CTU (B) 87 14<br />
$ RTU 61 1<br />
4 01"HER WP~ IO0 ¯<br />
8 011tER MAN (A) 44 t<br />
6 OTHER MAN (B) 88<br />
? NURSING 8TN. 7<br />
¯<br />
11-20 21~30 31-40 41-50 81&up<br />
INJJRY SEVERffY SCORE<br />
FIG. 4--Initisd admission of patients with multiple or life-threaten<strong>in</strong>g <strong>in</strong>juries (1SS more<br />
than 15). Comprehensive trauma unit A, which <strong>in</strong>cludes trauma service, treats majority o| such.<br />
patients. CTU = comprehensive trauma unit, RTU = t~llional trsums unit, WPG - wwmpeg,<br />
MAN = Manitoba.<br />
Injury<br />
severity<br />
score<br />
11-20<br />
21-30<br />
31-40<br />
41-50<br />
>50<br />
Table ,-Comparison of Comprehensive Trauma Units A and B by SundvaJ<br />
Probability to Discharge and Accord<strong>in</strong>g to Injury Sevedty Score<br />
Unit A Unit B _<br />
No. patients Survival No. patients Sur~vd<br />
(deaths) probability (deaths)<br />
117 (1) 0.992 48 10) 1.000<br />
89 118) 0.798 28 (7) 0.750<br />
20 18) 0.600 915) 0.455<br />
20113) 0.350 212) 0.000<br />
916} 0.334 0 0.000 ..~<br />
[
I<br />
treated <strong>in</strong> a trauma-unit hospital; some<br />
can be successfully and well treated outside<br />
the system. However, those victims<br />
suffer<strong>in</strong>g multiple <strong>in</strong>juries and almost<br />
100% of those suffer<strong>in</strong>g head <strong>in</strong>jury of<br />
life-threaten<strong>in</strong>g severity (ISS more than<br />
15) are immediately transferred to the<br />
trauma-unit system (Fig. 4).<br />
Of the two comprehensive trauma units<br />
<strong>in</strong> W<strong>in</strong>nipeg, unit A has a special trauma<br />
service, while unit B does not. Comparison<br />
of survival probability at the two<br />
units shows that <strong>in</strong> each <strong>in</strong>jury severity<br />
category except ISS 11 to 20, the probability<br />
of survival was higher <strong>in</strong> unit A<br />
(Table !I). This observation suggests that<br />
it is important to have <strong>in</strong>itial triage and<br />
total trauma health care coord<strong>in</strong>ated by<br />
a team of trauma surgeons from the time<br />
of admission throughout the critical<br />
phase. Such a resource probably should<br />
be available for every ! to 2 million population<br />
group across the country.<br />
While the statistical significance of<br />
these figures may be questionable, the<br />
actual numbers speak for themselves.<br />
Numerous variables not <strong>in</strong>cluded <strong>in</strong><br />
statistical analyses are controlled <strong>in</strong> a<br />
large registry experience.<br />
A comparison of the performance of<br />
the Manitoba trauma health-care system<br />
with that reported from six sophisticated<br />
hospitals <strong>in</strong> Baltimore (Fig. 5) shows that<br />
<strong>in</strong> both 0 to 49- and 50 to 69-year age<br />
tUURY ~Vl~RtTy SCORE - MAtleTQtA<br />
/ toe-. ~ ~ /<br />
,,a’°’~loe)<br />
a,.F!G. S--Comparison of performance (prob-<br />
¯ -n,v m sursival) of trauma patients <strong>in</strong><br />
Manitoba ssstem and that of similar patients<br />
<strong>in</strong> six Baltimore hospitals, l,DS0 (50% mortality<br />
po<strong>in</strong>t) was used as measure of performance.<br />
Patients dead on arrival at hospital<br />
acre excluded. Dotted l<strong>in</strong>es connect po<strong>in</strong>ts<br />
based on fewer than 10 cases. Circles = 0 to<br />
49 )ears, triangles = 50 to 69 .~ears, squares<br />
"~ "/0 )ears and older.<br />
FOLUME 28, NO.<br />
,<br />
groups, the survival probability" <strong>in</strong><br />
Manitoba .was equal to or greater than<br />
tor produc<strong>in</strong>g this result could be the<br />
that <strong>in</strong> Baltimore as measured by the<br />
prov<strong>in</strong>cial trauma program.<br />
LDS0 (50% mortality po<strong>in</strong>t). Only <strong>in</strong> the Fund<strong>in</strong>g<br />
over ?0-year age group did Baltimore rate<br />
better than Manitoba. It is possible that<br />
Trunkey<br />
the smaller number of cases <strong>in</strong> this<br />
category <strong>in</strong> Baltimore skewed the results.<br />
Given the limitations of this gross measuremem<br />
of standard of care, one might<br />
conclude that the trauma-system program<br />
<strong>in</strong> Manitoba is provid<strong>in</strong>g a satisfactory<br />
level of care. If trauma registries, us<strong>in</strong>g<br />
identical scor<strong>in</strong>g systems, were available<br />
<strong>in</strong> other prov<strong>in</strong>ces, comparisons could be<br />
made. S<strong>in</strong>ce the Manitoba fatality rate by<br />
miles driven and by number of vehicles<br />
registered is the lowest <strong>in</strong> the country and<br />
the <strong>in</strong>jury rate is among the highest, a fac-<br />
7 demonstrated the mismatch<br />
of years of life lost and’the level of fund<strong>in</strong>g<br />
<strong>in</strong> the United States for three<br />
categories of disease (Fig. 6).<br />
Trauma is concentrated <strong>in</strong> the under<br />
39-year age group (our greatest natural<br />
resource with the longest life expectancy).<br />
Because of this, the costs of disability and<br />
the loss of productivity are ongo<strong>in</strong>g and<br />
cumulative. This results <strong>in</strong> a great economic<br />
dra<strong>in</strong> on the country. In fact, the<br />
discrepancy clearly demonstrates the<br />
<strong>in</strong>appropriate level of support given by<br />
"governments and research foundations to<br />
develop health care for what is the major<br />
pandemic affect<strong>in</strong>g North American<br />
society.<br />
In Canada, the level of fund<strong>in</strong>g for<br />
trauma care is likely to be much lower<br />
than that <strong>in</strong> the US even though the risk<br />
to the Canadian population as drivers of<br />
motor vehicles is much higher than that<br />
<strong>in</strong> the US. If we corrected this discrepancy<br />
and did noth<strong>in</strong>g more, the proposed<br />
trauma health-care system would pay for<br />
itself.<br />
Conclusions<br />
Prov<strong>in</strong>cial trauma registries and a<br />
national trauma registry should be developed<br />
to provide the uniforn: dam on<br />
which to build a health-care system based<br />
on logical strategy and health-care priorities.<br />
Epidemiologic, basic and cl<strong>in</strong>ical<br />
research programs should be developed<br />
to monitor the performance of the accident<br />
program and <strong>in</strong>dicate where<br />
improvement <strong>in</strong> strategy and health care<br />
is needed.<br />
Trauma services <strong>in</strong> comprehensive<br />
trauma units and a regional trauma unit<br />
should be developed <strong>in</strong> each area of ! to<br />
2 million population density.<br />
Federal, prov<strong>in</strong>cial and research foundation<br />
fund<strong>in</strong>g priorities should be reexam<strong>in</strong>ed<br />
and allocated where the grow<strong>in</strong>g<br />
need is great. We cannot ignore the<br />
projection made by Campbell and La~son<br />
s that <strong>in</strong> the next 10 years there will be<br />
64 000 lives lost and 3 000 000 <strong>in</strong>juries<br />
suffered <strong>in</strong> Canada.<br />
The Manitoba Accidem Injury Health Care<br />
Project was supported by donations from the<br />
follow<strong>in</strong>g sources: Manitoba Health Services<br />
Commission, Murphy Foundation <strong>in</strong>c.. W.<br />
Garfield Weston Foundation, James Richardson<br />
& Sons Ltd., McKeag Realty Ltd., General<br />
Distributors of Canada, Dionian Industries<br />
Ltd., Monarch Life Assurance Company,<br />
Manitoba Medical Services Foundation. Inc.,<br />
Great-West Life Assurance Company. W<strong>in</strong>nipeg<br />
Cl<strong>in</strong>ic Research Institute& The Paul H.T<br />
FIG. 6--Mismatch of )ears of life lost and Thorlakson Research Foundation. Inc...\loffat<br />
fund<strong>in</strong>g for trauma <strong>in</strong> United States (after Communications Led., Monarch Industries<br />
Trunkey DDT).<br />
Ltd., Cargill Gra<strong>in</strong> Company Ltd., P.L. &<br />
A.M. Ashdown, Mrs. M.E. Mcimosh.<br />
6, NOVEMBER 1985 / THE CANADIAN JOURNAL OF SURGERY 48~
[{e ferenees<br />
I. Canada. Department of National Health and Welfare: A<br />
"~’ew Perspective on the tleolth of Canadians. A K~ork<strong>in</strong>g<br />
Docu,~, "nt. (,:at 82-538E). Department of Supply and Serv.<br />
ices, Otta~a. 1974<br />
2 L ,,~s ~O’~ J J: The costs of rt~d acciOems and [heir application<br />
<strong>in</strong> ecc[ omic evaluation of safety programs. Present.<br />
ed al [he Annual Conference of the Roads ,~,~<br />
cidents. Poison<strong>in</strong>g. and Violence m Canada an Overview,<br />
Department of Supply and Services. Ottawa. 1980<br />
4. BAKER SP. O’NEILL Ii HADDON V." JR. LONG W11: The<br />
<strong>in</strong>juPy se~rity ~’ore: a method for describ<strong>in</strong>g patients with<br />
multiple <strong>in</strong>juries and evaluat<strong>in</strong>g emergency care. J Trauma<br />
1974; 14:187-96<br />
5. American Association for Automotive Med;.¢i~, Commhtee<br />
on Injury Scal<strong>in</strong>g: The Abbreviate~/ Injury Scale, 1980<br />
Revision, American Association for Automotive Medic<strong>in</strong>e,<br />
Morton Grove, IlL. 1980<br />
Trampprta[ion Assocultion of Canada. O~[awa. Sept. :978 6. International Classification of Diseases. 9th Rev.. Cl<strong>in</strong>i.<br />
3. Canada, Department of National Heahh and Welfare: AS: .~.~ ca/Modification, Commission on Professional and Hosp-<br />
HANS-J(~RG OESTERN, MD<br />
Health Statistics. Ann Arbor, Mich., 1978<br />
7. TRU,’,;KEV DD: Trauma. <strong>Accident</strong>al and <strong>in</strong>tentional <strong>in</strong> iuties<br />
account for more years of life lost <strong>in</strong> the i ¯ " . .~tn<br />
cancer and heart disease. Among the ~r2,~rt~pd t’~rrtc~[~<br />
are improved preventive efforts. ~ t:a~’y and further<br />
research. Sci A, ’ .~; Z49(2): 28-35<br />
8. CAMPBELL (’:[~. ~ ~,,’SON J J: Prospects for road safety<br />
<strong>in</strong> the *P’~. P,’~sented at the Annual Conference of [he<br />
p ~er’ ~-I Transportation Association of Canada, W<strong>in</strong>-<br />
-.,~g. Sept. 1981<br />
5. The German Model for Rescue of Traumatized Patients<br />
<strong>Accident</strong>s and their sequelae are the<br />
e ma<strong>in</strong> cause of death In Germany among<br />
people under 40 years of age. The cost<br />
<strong>in</strong> disability payments and lost work<br />
averages $40 000 per <strong>in</strong>jury. The author<br />
describes the German system for trauma<br />
rescue.<br />
The aims of rescue care <strong>in</strong> Germany<br />
are to reduce the <strong>in</strong>terval between <strong>in</strong>jury<br />
and hospital admission and to br<strong>in</strong>g the<br />
patient to the right hospital, bypass<strong>in</strong>g<br />
smaller hospitals if necessary.<br />
Ambulance rescue systems are of two<br />
types: the stationary, <strong>in</strong> which the physician<br />
travels with the ambulance, and the<br />
rendezvous, <strong>in</strong> which the physician and<br />
ambulance, travell<strong>in</strong>g separately, meet at<br />
the accident site. At the beg<strong>in</strong>n<strong>in</strong>g of the<br />
1970s the air-rescue system was started<br />
and now comprises 32 stations and 25<br />
BO-105 helicopters.<br />
The Hannovar experience shows that<br />
of the <strong>in</strong>itial diagnoses made at the accie<br />
dent site by helicopter rescue service,<br />
51..9% of victims had head <strong>in</strong>juries,<br />
35.5% fractures of extremities, 17.0%<br />
From the Trauma Department, Hannover<br />
,Medical School, Hannover, West Germany<br />
Presented as part of a symposium on the<br />
organization of trauma care at the 33rd<br />
annual meet<strong>in</strong>g of the Royal College of<br />
Physicians and Surgeons of Canada by the<br />
Royal College <strong>in</strong> cooperation with the<br />
Trauma Association of Canada, the Canadian<br />
Association of General Surgeons, the<br />
Canadian Orthopaedic Association and the<br />
Canadian Association of Plastic Surgeons,<br />
Montreal, PQ, Sept. 11, 1984<br />
Accepted for publication June 6, 1985<br />
Repr<strong>in</strong>t requests to: Dr. Hans-J6rg<br />
Oestern, Professor of Surgery, Trauma<br />
Department, Hannover Medical School,<br />
Konstanty-Gutschow.Str. 8, 3000 Hannover<br />
61. West Germany<br />
thoracic trauma, 10.2% abdom<strong>in</strong>al<br />
trauma and 7.6% sp<strong>in</strong>al fractures.<br />
Because of respiratory <strong>in</strong>sufficiency or<br />
unconsciousness with danger of aspiration,<br />
12.0% of the patients had to be<br />
<strong>in</strong>tubatad endotracheally. One hundred<br />
and twenty-two patients with a cl<strong>in</strong>icid<br />
diagnosis of death were successfully<br />
resuscitated at the accident scene. A<br />
study compar<strong>in</strong>g the efficiency of the<br />
helicopter and ambulance systems<br />
showed that as the severity of the <strong>in</strong>judes<br />
Increases, the death rate is greater<br />
<strong>in</strong> the group rescued by ambulance. Of<br />
22 accidents <strong>in</strong>volv<strong>in</strong>g rescue he,coptars,<br />
7 (32%) resulted <strong>in</strong> at least one<br />
death. Between 1973 and 1983. 16<br />
doctors, pilots or attendants were killed.<br />
En Aliemagne, los accidents at leurs<br />
s~luelles sont les pdncipales causes de<br />
chez les mo<strong>in</strong>s de 40 ans. Les<br />
coots en paiements pour Incapacit~ et en<br />
perta de travail atteignent an moyenne<br />
40 0005 par bleesure. L’auteur dimdt le<br />
syst&me allemand de sauvetage des traumatis6s.<br />
Les buts des operations de seuvetege<br />
an Aliemagne sent de r~Kluire I’<strong>in</strong>tarvalle<br />
6coul6 entre la bleesum et I’ardv6e il<br />
I’h6pitai, at de dirigar le patient vars<br />
I’h6pitei le plus appropri6 m6me a’li faut,<br />
chem<strong>in</strong> feisant, ignoror de plus petite<br />
h6pitaux quand cela s’av6m n6ceesaire.<br />
Lea syst&mes de aauvetago arnbulancler<br />
sent de deux types: atationnaire, alors<br />
qua le m~dec<strong>in</strong> voyage avec I’ambulance;<br />
de rendez-vous, quand le ndtdec<strong>in</strong><br />
at I’ambulance, voyageant s6par~mant,<br />
convergent vars le lieu de I’accident. Au<br />
d~but des ann~ec 70, un syst~me de<br />
sauvetage par air a ~t~ mis~ur pied; li<br />
comprend ma<strong>in</strong>tenant 32 stations at 25<br />
h6licopt&res BO-105.<br />
L’exp~rlence de Hannovre d&montre<br />
qua Iors du diagnostic <strong>in</strong>itial felt sur los<br />
lieux de I’accident par les services de<br />
sauvetage par h~licopt~)re, 51.9% des<br />
victimes souffraient de traumatismes cdtnlens,<br />
35.5% de fractures des extr~mit~s,<br />
17.0% de traumedsmes thoreciques,<br />
10.2% de traumetismes<br />
abdom<strong>in</strong>aux at 7.6% de fractures sp<strong>in</strong>ales.<br />
~, cause d’<strong>in</strong>suffisance respiratoire<br />
ou de perte de conscience avec danger<br />
d’espiration, 12.0% des patients ont dO<br />
8tre <strong>in</strong>tub6 par vole andotrach~mle. Cent<br />
v<strong>in</strong>gt-doux patients consicl0r~m cl<strong>in</strong>icluement<br />
comma morte ont pu ~tre r6anim~s<br />
am rmu de I’acctdent. Une ~tude comparant<br />
I’efficacit~ des systlm~es pe~ ambulance<br />
at par h~licoptkre a montr~<br />
qu’avec I’augmantation de la gravit~ des<br />
blessures, la mortalit~ ~teit plus grande<br />
¯ dens le groupe secouru par ambulance.<br />
Dens 22 accidents impikluant des h~lF<br />
coptAms de sauvatage, 7 (32%) ont<br />
entra<strong>in</strong>~ ou mo<strong>in</strong>s une mortalitY. Entre<br />
1973 at 1983, 16 ndtdectrm,.pilotes ou<br />
<strong>in</strong>flrmlers ont 6t6 tu6s.<br />
In Germany, motor vehicle accidents and<br />
their sequelae are the ma<strong>in</strong> cause of death<br />
amoag people under 40 years of age. The<br />
death toll from trauma <strong>in</strong> 1983 <strong>in</strong> the<br />
country was 50000, of which 11 747 were<br />
from traffic accidents. Injuries <strong>in</strong> that<br />
year totalled 500 691. The cost of these<br />
<strong>in</strong>juries <strong>in</strong> lost work and disability is<br />
alarm<strong>in</strong>g, amount<strong>in</strong>g to an average of<br />
$40 000 per <strong>in</strong>jury.<br />
There is statistical evidence of a correlation<br />
betweer~ the time of the accident,<br />
the start of treatment and the outcome;<br />
that is, the shorter the rescue time, the<br />
better are the results (Figs. I and 2). What<br />
can we do to optimize the management<br />
of acute <strong>in</strong>juries?<br />
486 VOLUME 28, NO. 6, NOVEMBER 1985 / THE CANADIAN JOURNAL OF SURGERY
Aims of Rescue Care<br />
In Germany our aims <strong>in</strong> the care of the<br />
severely <strong>in</strong>jured patient are as follows:<br />
¯ Reduce the rescue <strong>in</strong>terval; that is,<br />
start treatment early at the scene of the<br />
accident.<br />
¯ Br<strong>in</strong>g the patient to the right hospital,<br />
bypass<strong>in</strong>g smaller hospitals not<br />
properly equipped to handle severe<br />
trauma.<br />
¯ Shorten the transportation time.<br />
Rescue Systems <strong>in</strong> Germany<br />
Our emergency ambulance service was<br />
begun about 20 years ago. It br<strong>in</strong>gs the<br />
doctor to the scene of the accident so that<br />
he can start resuscitation immediately.<br />
The service comprises two systems -- the<br />
stationary and the rendezvous.<br />
In the stationary system, an ambulance<br />
is situated near the hospital and is dispatched<br />
by the rescue control centre to<br />
accidents with<strong>in</strong> a radius of 8 km. The<br />
obvious disadvantage of this system is<br />
that it takes too long to arrive at the scene<br />
of an accident any distance from the<br />
hospital.<br />
The rendezvous system is used mostly<br />
<strong>in</strong> rural districts or <strong>in</strong> towns that have<br />
only one emergency vehicle. A doctor on<br />
call is delivered to the scene by a specially<br />
equipped car manned by the local fire<br />
department. He may, when necessary, use<br />
his own car. Simultaneously, an ambu-<br />
i i 1 I -<br />
~ 10 18 20 25~<br />
FIG. 1--Relation between survival and start<br />
of treatment.<br />
I<br />
lance is sent to the scene of the accident.<br />
This is an excellent system and a good<br />
way to providt early medical help.<br />
Rescue Helicopter Service<br />
In the last year, 25 267 missions were<br />
performed by rescue helicopters. The<br />
Federal Republic of Germany started the<br />
present air-rescue system dur<strong>in</strong>g the<br />
1970s. It now comprises 32 stations and<br />
25 Be-105 helicopters. With an optimal<br />
effective radius of 50 km, medical emergency<br />
help is available to 90°70 of the<br />
country’s population with<strong>in</strong> 15 m<strong>in</strong>utes.<br />
Under the disaster control organiza-<br />
tion, the pilots are provided by the Federal<br />
M<strong>in</strong>istry of the Interior and medical<br />
attendants by various private local rescue<br />
organizations and fire brigades. Doctors<br />
are assigned by the base hospitals. The<br />
German automobile club is responsible<br />
for adm<strong>in</strong>istration and cost account<strong>in</strong>g of<br />
the rescue flights. It also negotiates contracts<br />
with the <strong>in</strong>surance organizations.<br />
Operat<strong>in</strong>g costs are reimbursed by accident<br />
and health <strong>in</strong>surance organizations<br />
with<strong>in</strong> the communities and cities to the<br />
respective doctor.<br />
i I<br />
I<br />
!I<br />
I<br />
FIG. 3--L<strong>in</strong>es of communication to rescue<br />
control centre. ADAC = German automobile<br />
club. Dotted l<strong>in</strong>es represent radio ommunt.<br />
cation, solid l<strong>in</strong>es telephone communication..<br />
75% /<br />
-" .,-!--- #7--. _,4z___<br />
/ /7 .7<br />
"1 Y ,y /<br />
°%i/I , /, , /I , J I l<br />
30sec 1ra<strong>in</strong> 2 3 5 10 15 30 1hour 2 5 10 15<br />
FIG. 2--Relation between different types of emergency, <strong>in</strong>terval without treatment and<br />
OUtcome.<br />
f<br />
All emergency calls are channelled to<br />
the rescue control centre <strong>in</strong> the area,<br />
which is <strong>in</strong> four-channel contact with the<br />
police. The control centre coord<strong>in</strong>ates and<br />
activates all ground-rescue vehicles and<br />
the rescue helicopter with<strong>in</strong> its area of<br />
responsibility (Fig. 3). A paramedic and<br />
an emergency care physician are assigned<br />
to each helicopter, which is equipped for<br />
safeguard<strong>in</strong>g the vital functions of the<br />
<strong>in</strong>jured victim, treat<strong>in</strong>g shock and provid<strong>in</strong>g<br />
<strong>in</strong>itial treatment of <strong>in</strong>juries, and also<br />
provid<strong>in</strong>g safe transport to the hospital.<br />
The important factor of air rescue by<br />
helicopters compared with conventional<br />
land-bound ambulance rescue, is that<br />
through the early application of medical<br />
measures by a physician the <strong>in</strong>terval<br />
without therapy is greatly shortened.<br />
An <strong>in</strong>vestigation carried out <strong>in</strong> 1971<br />
showed that even <strong>in</strong> a large city like Hannever,<br />
it took more than 20 m<strong>in</strong>utes to<br />
get 64070 of accident victims to the hospital<br />
by ambulance. In 26%, more than 30<br />
m<strong>in</strong>utes elapsed before they were treated<br />
by a doctor <strong>in</strong> a hospital and <strong>in</strong> none of<br />
these cases was effective treatment<br />
<strong>in</strong>itiated before admission. The rescue<br />
helicopter reached the accident site <strong>in</strong> less<br />
than 10 m<strong>in</strong>utes after be<strong>in</strong>g notified <strong>in</strong> at<br />
least 60% of cases.<br />
Treatment at the <strong>Accident</strong> Scene<br />
The <strong>in</strong>itial diagnoses made at the accident<br />
scene for the years 1972 to 1983 are<br />
shown <strong>in</strong> Table I. Head <strong>in</strong>juries were the<br />
most common. Almost 65070 of the<br />
patients were <strong>in</strong> shock. In cases of extensive<br />
hypovolemia, two or three large-bore<br />
catheters are used and the patient is<br />
<strong>in</strong>fused, preferably with crystalloid solution.<br />
If necessary, 2000 mL or more of<br />
fluid may be <strong>in</strong>fused before the victim<br />
reaches hospital.<br />
The procedures carried out at the accident<br />
scene by either the ambulance or<br />
helicopter-rescue system are listed <strong>in</strong><br />
Table II. Because of respiratory <strong>in</strong>sufficiency<br />
or unconsciousness with danger of<br />
aspiration, 12.007o of the patients had to<br />
be <strong>in</strong>tubated endotracheally. So as not to<br />
restrict the availability of the rescue<br />
helicopter, only 31070 of the victims were<br />
thus transported dur<strong>in</strong>g the period 1972<br />
to 1983. They were patients who required<br />
cont<strong>in</strong>uous medical observation or had<br />
<strong>in</strong>juries, such as vertebral fractures,<br />
requir<strong>in</strong>g smooth transport.<br />
Table I-Injmles Diagnosed at<br />
<strong>Accident</strong> Scene, 1972 to 1983<br />
Injury %<br />
Head <strong>in</strong>jury 51.9<br />
Fractures of extremities 35.5<br />
Thoracic trauma 17.0<br />
Abdom<strong>in</strong>al trauma 10.2<br />
Sp<strong>in</strong>al fractures 7.6 i<br />
VOLUME 28, NO. 6, NOVEMBER 1985 / THE CANADIAN JOURNAL OF SURGERY 487
Helicopter versus Ambulance<br />
cue <strong>in</strong> Hannover and more than 13 000<br />
missions, the effectiveness of this system<br />
To compare the effectiveness of for all <strong>in</strong>volved is without question.<br />
helicopter versus ambulance rescue, we However, there is <strong>in</strong>creas<strong>in</strong>g criticism<br />
carried out a prospective study of 48 trau- from laymen and doctors and a resistance<br />
matized patients. The study was restricted to the establishment of new centres on the<br />
to patients with one or more <strong>in</strong>juries caus- grounds of pollution and cost control. So<br />
<strong>in</strong>g shock and an estimated blood loss of the question is frequently asked, how<br />
1000 mL <strong>in</strong> the first hour. Children under many lives have really been saved by the<br />
15 years old and patients with cranio- helicopter? This question cannot be<br />
cerebral trauma were excluded. answered accurately.<br />
In group 1, aggressive treatment was One hundred and twenty-two patients<br />
started at the site of the accident by the with a cl<strong>in</strong>ical diagnosis of death were<br />
doctor from the rescue helicopter. In successfully resuscitated at the accident<br />
group 2, patients were transported by site. There are certa<strong>in</strong>ly more positive<br />
ambulance, without a physician, to the effects from prompt on-the-scene treat-<br />
nearest hospital, but because of the severe ment, us<strong>in</strong>g helicopter rescue, than from<br />
<strong>in</strong>jury were transferred to our hospital. spectacular resuscitations of moribund<br />
open fracture. Naturally, the time factor<br />
has a significant bear<strong>in</strong>g on the end result<br />
regardless of the quality of primary care.<br />
Risks of Helicopter Rescue<br />
How safe is the rescue helicopter sYstem?<br />
Between 1973 and 1983, 146 300 rescue<br />
missions were carried out <strong>in</strong> the Federal<br />
Republic of Germany and there were<br />
22 accidents <strong>in</strong>volv<strong>in</strong>g rescue helicopters<br />
-- a rate of i accident per 6648 missions.<br />
Of the 22 helicopter accide"-t~, t (32°70)<br />
resulted <strong>in</strong> at least f, ne death each. Durhag<br />
this period, :6 doctors, pUots or attendant~<br />
were killed.<br />
Causes of Helicopter <strong>Accident</strong>s<br />
It was noted that group 1 patients patients. Life-threaten<strong>in</strong>g complications<br />
reached hospital <strong>in</strong> less than half the time at the site of the accident and dur<strong>in</strong>g Nearly 60% of these accidents were due<br />
despite the fourfold greater distance from transport are prevented, especially to human failure and the rema<strong>in</strong>der were<br />
the hospita! to the site of the accident obstructions of the airway, and through secondary to technical failure. The higher<br />
(Table III). In these patients, an average adequate early and aggressive treatment, risk associated with rescue helicopter<br />
of 711 mL of fluid was <strong>in</strong>fused before complications result<strong>in</strong>g from shock are flights was due to lack of extensive<br />
arrival at hospital, while patients <strong>in</strong> group decreased.<br />
navigatory preparation, land<strong>in</strong>gs <strong>in</strong><br />
2 received an average of 230 mL and<br />
unfamiliar or narrow areas, busy streets,<br />
many of them received no <strong>in</strong>fusion at all. Management of Open Fractures and and hous<strong>in</strong>g developments, flights made<br />
Accord<strong>in</strong>gly, the systolic blood pressure Infection<br />
<strong>in</strong> poor weather conditions, undue haste,<br />
of group 2 patients on admission to our<br />
and extensive <strong>in</strong>volvement of the crew<br />
cl<strong>in</strong>ic was only 92.3 mm Hg. On average, A card<strong>in</strong>al rule at the accident scene is associated with <strong>in</strong>creased risk.<br />
the shock <strong>in</strong>dex (heart rate divided by to avoid further soft-tissue <strong>in</strong>jury. We Critics of air rescue note the restricted<br />
systolic pressure) <strong>in</strong> this group was 1.18. strongly recommend that fracture/ be conditions <strong>in</strong> an aircraft and the limited<br />
The levels of the helicopter group clearly realigned or reduced where possible at the possibilities for therapy dur<strong>in</strong>g flight.<br />
show the results of better primary treat- scene to relieve pressure on the <strong>in</strong>jured This is only partially true, and external<br />
ment -- an average systolic pressure of soft tissues. Swell<strong>in</strong>g and the spread of heart massage can be performed dur<strong>in</strong>g<br />
119.4 mm Hg and shock <strong>in</strong>dex of 0.88. hematoma are reduced by plac<strong>in</strong>g a sterile flight <strong>in</strong> extreme cases. On the other<br />
To f<strong>in</strong>d out the effects of this circula- dress<strong>in</strong>g over the wound and immobiliz- hand, the speed of the rescue helicopter<br />
tory replacement, the subsequent course <strong>in</strong>g the extremity <strong>in</strong> a pneumatic spl<strong>in</strong>t. allows a patient early treatment accord-<br />
of the patients was immstigated. Twa In our cl<strong>in</strong>ic, 59°7o of the open fractures hag to <strong>in</strong>dividual requirement <strong>in</strong> a special-<br />
patients of group 2 died <strong>in</strong> the emergency have already received field treatment ized hospital even when it is not the<br />
department. Almost half of the patients with<strong>in</strong> about 20 m<strong>in</strong>utes of <strong>in</strong>jury from nearest one. True contra<strong>in</strong>dications to<br />
<strong>in</strong> this group had to be treated <strong>in</strong> an <strong>in</strong>ten- a resident who accompanied the rescue<br />
sive care unit longer than 10 days. In com- vehicle to the scene. The benefits of this<br />
Table V-Cause of Death<br />
parison, almost two thirds of group 1 early care are substantial: a 3.507o <strong>in</strong>fec- Cause Group 1 Group 2<br />
patients could be moved out of the <strong>in</strong>tention rate when primary care was<br />
sive care unit after 1 to 3 days. The aver- adm<strong>in</strong>istered by air ambulance personnel<br />
Adult respiratory<br />
age duration <strong>in</strong> the <strong>in</strong>tensive care unit was as opposed to a 22.2070 rate <strong>in</strong> patients<br />
distress syndrome - 3<br />
Sepsis 2 3<br />
only half as long <strong>in</strong> group 1 as <strong>in</strong> group who reached the trauma centre by way of E~tion 1 2<br />
2 (Table IV).<br />
another hospital with<strong>in</strong> 10 hours of<br />
With respect to cause of death, a high<br />
<strong>in</strong>jury. In the latter case, <strong>in</strong>fection<br />
Totals 3 8<br />
Overall death rate, % 11.8, 38.0<br />
rate of respiratory <strong>in</strong>sufficiency was noted occurred <strong>in</strong> every fifth patient with an<br />
<strong>in</strong> group 2. This complication is generally<br />
recognized as a result of <strong>in</strong>adequately<br />
treated hypovolemic shock. The overall<br />
Table Ill-Comparison of the Effactivemss of Helicopter<br />
and Ground Rescue Methods <strong>in</strong> Trauma <strong>in</strong>juries <strong>in</strong> Germany<br />
death rate <strong>in</strong> group 2 was more than 3.5<br />
times that <strong>in</strong> group I (Table V).<br />
After almost 12 years’ use of air res-<br />
Factor<br />
Distance from accident site to hospital, km<br />
Interval between <strong>in</strong>jury and <strong>in</strong>itial treatment, m<strong>in</strong><br />
Volume replacement dur<strong>in</strong>g transport, mL<br />
Group 1<br />
28.1<br />
22.2<br />
711<br />
Group 2<br />
7,2<br />
47.0<br />
230<br />
Table II-Procedures Performed at <strong>Accident</strong><br />
Scene, 1972 to 1983. by ~ or Rescue.<br />
HeScoptor personnel<br />
% of<br />
Procedure patients<br />
Volume replacement 31.3<br />
Control of bleed<strong>in</strong>g 29.1<br />
Spl<strong>in</strong>t<strong>in</strong>g of fractures 18.7<br />
Intubation and ventilation 12.0<br />
Resuscitation 4.9<br />
Duration of<br />
treatment, d<br />
Table W-Duration of Treatment <strong>in</strong> ~ Care Unit*<br />
Group 1. % Group 2. %<br />
1- 3<br />
4-10<br />
11-20<br />
> 20 I<br />
62.9 14.3<br />
14.8 33.3<br />
7.4 28.5<br />
14.8 14.4<br />
*9.5% of patients <strong>in</strong> group 2 died with<strong>in</strong> 1 h of arrival M hospital.<br />
488 VOLUME 28, NO. 6, NOVEMBER 1983 / THE CANADIAN JOURNAL OF SURGERY
f<br />
helicopter transport, such as an unresolved<br />
pneumothorax, are rare.<br />
Condudons<br />
Our rescue system works and without<br />
a doubt <strong>in</strong> the densely populated areas of<br />
Europe such a system of air rescue could<br />
be used <strong>in</strong> the same way as <strong>in</strong> Germany<br />
and Switzerland. For less-densely populated<br />
areas, an extended " numbers of missions can be flown. quickly? Perhaps it requires only the<br />
The questiom of political and econom- <strong>in</strong>itiative of <strong>in</strong>dependent or private<br />
ical value is not easy to answer, because organizations. The Federal Republic of<br />
it is difficult to estimate the f<strong>in</strong>ancial Germany’s helicopter air rescue system<br />
value of a rescued life. Even with thiswas<br />
<strong>in</strong>itiated by the German automobile<br />
reservation, the political economist Baum club which, together with the Federal<br />
(personal communication) calculates the M<strong>in</strong>istry of the Interior, started the first<br />
favourable value of the air-rescuesystem rescue helicopter service <strong>in</strong> Munich.<br />
to be at least comparable to that of us<strong>in</strong>g Today, this club still acts as an impetus<br />
seat belts.<br />
for further development of air rescue and<br />
missions radius Why are air-rescue systems <strong>in</strong> wealthy supplies valuable help with adm<strong>in</strong>istration<br />
should be considered, so that sufficient <strong>in</strong>dustrial countries not <strong>in</strong>stituted more and accounts.<br />
ATLAS OF STOMAL PATHOLOGY. A.<br />
Fnmch<strong>in</strong>i, B. Cola and PJ.d’E. Stevens.<br />
112 pp. lUnst. Raven Press, New York,<br />
1~3. $70. ISBN 88-85937-37-2.<br />
The surgical literature conta<strong>in</strong>s much <strong>in</strong>formation<br />
on the technical aspects of creat<strong>in</strong>g stomas.<br />
In spite of this, stomas are often carelessly or<br />
improperly fashioned, with resultant morbidity,<br />
embarrassment and distress to patients.<br />
This book, written from a pathologic rather<br />
than a surgical perspective, provides a valuable<br />
addition to the literature. It properly and<br />
comln~he~.siveiy descrihes the consequences of<br />
poorly constructed stomas and illustrates <strong>in</strong><br />
detail the gamut of other processes that affect<br />
stomas.<br />
The book is well organized <strong>in</strong>to 10 chapters,<br />
2 of which deal comprehensively with primary<br />
and secondary stomal conditions. The chapter<br />
on primary stomal conditions deals with<br />
such problems as poor site, edema, ischemia,<br />
¯ .’t~ction, prolapse, hernia and sk<strong>in</strong> lesions.<br />
Each one is well illustrated with co[our photographs.<br />
This is perhaps the strongest attribute<br />
and raison d’etre of the book, for, as<br />
Professor Brian Brooke emphasizes <strong>in</strong> his<br />
preface, "Stomas have to be seen to be<br />
believed...for stoma problems all too often<br />
beggar description".<br />
Other chapters cover such topics as stomal<br />
problems <strong>in</strong> radiotherapy, gynecology and<br />
obstetrics, and pediatrics. There are also chapters<br />
on problems of obta<strong>in</strong><strong>in</strong>g a cont<strong>in</strong>ent<br />
stoma and special problems of ostomates,<br />
<strong>in</strong>clud<strong>in</strong>g psychic and metabolic disturbances.<br />
This book is not a comprehensive treatise<br />
covet<strong>in</strong>g all aspects of stomai management -nor<br />
does it claim to be. However, as a beautifully<br />
illustrated atlas of morbid conditions<br />
affect<strong>in</strong>g stomas, it fills a void <strong>in</strong> the literature.<br />
it would make a worthy addition to the library<br />
of surgeons or residents <strong>in</strong>volved <strong>in</strong> the care<br />
of ostomates and would he a valuable reference<br />
for enternstomai therapists.<br />
WILLIAM G. POLLETT, MD, FRCSC<br />
Assistant Professor of Surgery,<br />
Memorial University of Newfoundland,<br />
St, John’s, Nfld.<br />
AIB 3V6<br />
Canada Limited, Toronto, 1984. $46.20.<br />
ISBN 0-’/216-9081-S.<br />
For surgeons practis<strong>in</strong>g solo at a distance from<br />
a University centre, where residents help the<br />
staff to keep abreast of the current literature,<br />
it is a pleasure to f<strong>in</strong>d a book of this calibre<br />
that presents the current th<strong>in</strong>k<strong>in</strong>g of many<br />
authorities on a problem that plastic surgeons<br />
must deal with on a regular basis.<br />
The first few chapters cover care of the burn<br />
wound <strong>in</strong> general and serve as an excellent<br />
review for all members of the burn team. The<br />
chapter on <strong>in</strong>halation <strong>in</strong>jury is superb, while<br />
chapters that deal with specific treatment of<br />
the various elements of the face provide a reference<br />
and put the latest state-of-the-art ideas <strong>in</strong><br />
perspective. These chapters are also an excel.<br />
lent source of detailed <strong>in</strong>formation for members<br />
of the profession who do not deal with<br />
fa~ burns on a regular basis. The three chapters<br />
deal<strong>in</strong>g with nurs<strong>in</strong>g, and physical and<br />
occupational therapy re<strong>in</strong>force the concept of<br />
a team approach, which is essential <strong>in</strong> the care<br />
of any burn victim. The bibliography is an outstand<strong>in</strong>g<br />
source of material for further detailed<br />
read<strong>in</strong>g and represents an excellent literature<br />
review.<br />
The only criticism of the volume lies <strong>in</strong> its<br />
illustrations, some of which are out of place.<br />
In some areas, more detailed follow-up photngraphs<br />
would have added considerably to the<br />
flow of the book.<br />
This text should he on the bookshelves of<br />
all plastic surgeons and, more importantly, <strong>in</strong><br />
the library of every emergency room regardless<br />
of the size of the hospital.<br />
DUNCAN R. BROWN, MD, FRCSC<br />
No. 7, Endeca Place,<br />
402-5th Avenue S,<br />
Lethbridge, Alta.<br />
TIJ 0T5<br />
CURRENT SURGICAL THERAPY<br />
1984-1985. John L. Cameron. 613 pp.<br />
illust, C.V. Mnsby Company Ltd.,<br />
Toronto, 1984. Price not stated. ISBN<br />
0-941158-20-9.<br />
This text was designed to update surgical<br />
BURNS OF THE HEAD AND NECK. management for the practis<strong>in</strong>g general surgeon.<br />
Thomas L. Wachtel and David H. Frank. It is well organized and is easy and <strong>in</strong>terest<strong>in</strong>g<br />
216 pp. Illust. W.B. Sanaders Company to read. Most of the contributors are recog-<br />
VOLUME 28, NO. 6, NOVEMBER 1985 / THE CANADIAN JOURNAL SURGERY OF<br />
Ill I II I I II<br />
nized authorities <strong>in</strong> their fields. Some sections<br />
are better written than others, which is not<br />
unusual for multiauthored texts, but the overall<br />
quality of the presentations is good. Illustrations<br />
have been kept to a m<strong>in</strong>imum and there<br />
are many <strong>in</strong>stances where an <strong>in</strong>formative illus-<br />
. tration or table would have streaml<strong>in</strong>ed the<br />
text. For example, a table list<strong>in</strong>g antibiotics,<br />
with <strong>in</strong>dications, doses, toxicity and drug <strong>in</strong>teractions<br />
as an appendix would have saved a<br />
search of the text for the <strong>in</strong>formation. Some<br />
authors discussed only their own approach to<br />
a problem but others <strong>in</strong>cluded other options<br />
for evaluation and comparison. It would have<br />
helped the reader if some references to suggested<br />
approaches were cited so that the source<br />
material could be reviewed. Some authors,<br />
however, did <strong>in</strong>clude selective references that<br />
were helpful. A few sections, such as those on<br />
small-bowel tumours and bowel diverticula,<br />
were too detailed <strong>in</strong> relation to their importance.<br />
There should have been a section on surgical<br />
jaundice with new methods for diagnosis<br />
and treatment.<br />
In general, this text provides a practical<br />
approach to new techniques <strong>in</strong> surgery and<br />
should be of <strong>in</strong>terest to the cl<strong>in</strong>ical surgeon as<br />
¯ well as the surgeon <strong>in</strong> tra<strong>in</strong><strong>in</strong>g. It is not meant<br />
to replace standard texts, which <strong>in</strong>clude anatomy<br />
and pathophysiology as well as a comprehensive<br />
coverage of a subject.<br />
HARVEY H. SIGMAN, MD, FRCSC, FACS<br />
Department of Surgery,<br />
The Sir Mortimer B. Davis-Jewish<br />
General Hospital,<br />
3755 C&e Ste-Cather<strong>in</strong>e,<br />
Montreal, PQ<br />
H3T IE2<br />
KAPLAN’S FUNCTIONAL AND SURGI-<br />
CAL ANATOMY OF THE HAND. 3rd<br />
ed. Morton Sp<strong>in</strong>ner. 446 pp. Illust. J.B.<br />
Lipp<strong>in</strong>cott Company, Philadelphia, 1994.<br />
$87.50 (US). ISBN 0-397-$9593-3.<br />
The first two editions of Kaplan’s text were<br />
published <strong>in</strong> 1953 and 1965 respectively. Dr.<br />
Kaplan had asked Dr. Morton Sp<strong>in</strong>ner to help<br />
with this third edition, but when he died before<br />
its completion, Sp<strong>in</strong>ner became the editor. Ten<br />
contributors participated.<br />
cont<strong>in</strong>ued on page 544<br />
489
The Problem of Cardiac Arrest <strong>in</strong><br />
the Community<br />
RICHARD CRAMPTON, DM<br />
Out-of-hospital cardiac arrests constitute 350,000 cases yearly<br />
<strong>in</strong> the United States and 60,000 <strong>in</strong> the United K<strong>in</strong>gdom. Prompt<br />
resuscitation (CPR) by lay persons and fast defibrillation by paramedics<br />
have had epidemiologic consequences on both sides of<br />
the Atlantic. In Seattle there are 20.6 and <strong>in</strong> Brighton 10.0 longterm<br />
life-saves yearly per 100,000 persons. In Piedmont Virg<strong>in</strong>ia,<br />
coronary deaths fell 16% for persons 30-69 years old and 25%<br />
for those of all ages; prehospital life-saves accounted for 23%<br />
and 8% of each respective reduction. S<strong>in</strong>ce CPR by lay persons<br />
~<br />
ow triples the long-term survival rate when coupled with preospital<br />
defibrillation, favorable benefit-to-cost ratios can be effected<br />
by add<strong>in</strong>g advanced life support and citizen CPR to an<br />
extant ambulance system. Meticulous direct and <strong>in</strong>direct medical<br />
control by the physician assures the highest quality of CPR and<br />
early cardiac care (ECC). Diagnostic procedures like electroprovocation<br />
identify high-risk patients. Changes of behavior and<br />
diet, new drugs, new operations, and external and implantable<br />
automated devices reduce sudden deaths. In the future, automated<br />
defibrillation by first responders and tra<strong>in</strong>ed lay persons<br />
(<strong>in</strong>clud<strong>in</strong>g members of families of hlgh-dsk patients) should <strong>in</strong>crease<br />
the number of early survivors who become candidates for<br />
long-term therapy with drugs, operations, and devices. (Am J<br />
Emerg Med 1984;2:204-209)<br />
In the 18 years s<strong>in</strong>ce the <strong>in</strong>troduction of mobile <strong>in</strong>tensive<br />
care <strong>in</strong> Belfast, Northern Ireland, ~’2 thousands<br />
of lives have been saved and morbidity decreased by<br />
this type of emergency service. 3’4 Application of Pantridge’s<br />
conceptt-3 upgraded American emergency<br />
~ ervices and thereby affected the national toll of<br />
50,000 deaths yearly from cardiac arrest. Improvements<br />
<strong>in</strong> ambulance services <strong>in</strong> Brighton ~ and<br />
Ed<strong>in</strong>burgh6 reviews quantifiable effects of the implementation of<br />
mobile coronary care upon sudden cardiac death <strong>in</strong><br />
the community, <strong>in</strong> the United States and Europe.<br />
EMERGENCY CORONARY CARE IN THE<br />
VIRGINIA PIEDMONT<br />
In 1970, a retrospective survey of the frequency,<br />
time, duration of symptoms, and site of deaths <strong>in</strong> the<br />
city of Charlottesville and Albemarle County, Virg<strong>in</strong>ia,<br />
for I%3-1%9, <strong>in</strong>dicated that two hospital coronary<br />
care units <strong>in</strong>troduced <strong>in</strong> 1966 did not reduce community<br />
mortality from coronary disease<br />
likewise reduced the yearly total of 60,000<br />
out-of-hospital cardiac arrests <strong>in</strong> Brita<strong>in</strong>. This paper<br />
From the Division of Cardiology, and Emergency Medical Service,<br />
University of Virg<strong>in</strong>ia, Charlottesville, Virg<strong>in</strong>ia.<br />
Supported <strong>in</strong> part by the Charles A. Frueauff Foundation, New<br />
York City; by the Robert Wood Johnson Foundation Emergency<br />
Medical Communications Network, project 1420; and by the<br />
Thomas Jefferson Emergency Medical Services System, DHEW<br />
project 03-H-000, 366-02.<br />
Presented at the First International Conference on Cardiac Arrest<br />
and Resuscitation, Brighton, England, October 19-21,<br />
1982.<br />
Address repr<strong>in</strong>t requests to Dr. Crampton: 158 Medical Center,<br />
University of Virg<strong>in</strong>ia, Charlottesville, VA 22908.<br />
7 (Fig. I); the<br />
survey confirmed an earlier report. 8 From 1967 to 1969<br />
there were 677 coronary deaths, 382 <strong>in</strong> the hospital<br />
and 295 out of the hospital. Us<strong>in</strong>g Pantridge’s utopian<br />
predictions from observations <strong>in</strong> Belfast, 9 and estimat<strong>in</strong>g<br />
from a retrospective survey the theoretically<br />
preventable coronary deaths dur<strong>in</strong>g the first two hours<br />
of symptoms, it was hypothesized that riaobile coronary<br />
care might reduce mortality <strong>in</strong> the community by<br />
27%} 0 From 1971, volunteer ambulance workers provided<br />
emergency transport and cardiopulmonary resuscitation<br />
(CPR), and physicians and nurses provided<br />
emergency cardiac care (ECC). Initially, the system<br />
added to the extant ambulance systemtt-t6 was modeled<br />
on Pantridge’s system begun <strong>in</strong> I%6 at the Royal<br />
Victoria Hospital, Belfast, t’2 and later modified <strong>in</strong> the<br />
light of experiences reported from medical, paramedic,<br />
and basic emergency systems <strong>in</strong> Miami, Seattle,<br />
Columbus, New York, Los Angeles, and Virg<strong>in</strong>ia<br />
Beach. t7-26<br />
In 1971-1973, the predicted reduction of 27% <strong>in</strong><br />
community mortality from coronary disease nearly<br />
matched the observed 25% reduction. No significant<br />
fall occurred <strong>in</strong> 1974 despite the apparent ma<strong>in</strong>tenance<br />
of reduced numbers of coronary deaths. Only 8% of<br />
the life-saves <strong>in</strong> persons aged 30 to 99 years were attributable<br />
to prehospital resuscitation with long-term<br />
survival. 4 However, <strong>in</strong> persons aged 30-69 years, survival<br />
after prehospital resuscitation constituted 23%<br />
of the 16% fall <strong>in</strong> coronary deaths. If prehospital lifesaves<br />
were discounted, no significant change would<br />
have taken place <strong>in</strong> prehospital coronary deaths for<br />
the cohort described. 4 As a consequence of earlier outof-hospital<br />
emergency care, preventable deaths when<br />
the patient is received by the ambulance and taken to<br />
the emergency department should contribute, theoret-<br />
Key Words: Cardiac arrest, community, defibrillation, medical<br />
control, resuscitation, sudden death.<br />
204
i.<br />
ically, to the reduction of mortality from coronary disease.3.9,<br />
t t- 16<br />
The reason for the decl<strong>in</strong>e <strong>in</strong> coronary deaths <strong>in</strong> the<br />
Charlottesville-Albermarle community rema<strong>in</strong>s unclear.<br />
A concomitant spontaneous decl<strong>in</strong>e associated<br />
with a national American trend appeared unlikely, because<br />
coronary deaths <strong>in</strong> Virg<strong>in</strong>ia simultaneously rose<br />
by 6%. 4 Very early ECC may have had an effect by<br />
avert<strong>in</strong>g cardiopulmonary arrest due to ventricular fibrillation<br />
or asystole, as was first predicted by<br />
Pantridge 9 and as has been subsequently demonstrated.<br />
3<br />
uJ 400<br />
_J<br />
13.<br />
0<br />
LU<br />
bl-t/.~,Mt-"l LJN ¯ ,CARDIAC ARRES1 IN IHE COMMUNITY<br />
" 350 ...............................<br />
g<br />
EMERGENCY CORONARY CARE IN THE COMMUNITY<br />
Data from the United Statestr,zT-35 and Europe36-48 suggest that prehospital ECC <strong>in</strong> the community has a<br />
favorable effect (Figs. 2 and 3). Likewise, study of agespecific<br />
prehospital life-saves (Fig. 4) suggests that<br />
cost/benefit analyses might prove useful. Physicians<br />
and nurses no longer provide prehospital ECC <strong>in</strong> most<br />
American communities, despite the fact that these<br />
professionals participated <strong>in</strong> many feasibility trials.<br />
The performances of paramedics, <strong>in</strong>termediate emergency<br />
medical technicians (EMTs), and basic EMTs<br />
have been evaluated, and the latter personnel appear<br />
less effective than the former two groups. 3t.33 Brief<br />
tra<strong>in</strong><strong>in</strong>g of EMTs <strong>in</strong> recognition of ventricular fibrillation<br />
and <strong>in</strong> the delivery of transthoracic direct current<br />
countershocks has <strong>in</strong>creased the number of longterm<br />
survivors. 3t,33 Nevertheless, cl<strong>in</strong>ical therapeutic<br />
pr<strong>in</strong>ciples such as correct<strong>in</strong>g acute dysautonomia, reliev<strong>in</strong>g<br />
the pa<strong>in</strong> of ischemia, and stabiliz<strong>in</strong>g rhythm<br />
should not be abandoned, s<strong>in</strong>ce prevention of cardiac<br />
arrest due to ventricular fibrillation or asystole also<br />
reduces morbidity and mortality. 3’9’t3-tr,49<br />
Long-term survival after out-of-hospital cardiac arrest<br />
has considerably <strong>in</strong>creased because of prehospital<br />
CPR by members of the public (Fig. 5, Table I). Two<br />
to six life-saves per I00,000 were achieved by CPR<br />
alone with transport to the emergency department for<br />
defibrillation, <strong>in</strong> Wash<strong>in</strong>gton’s K<strong>in</strong>g County, 31’33 W<strong>in</strong>nipeg,<br />
4° and Reykjavik and suburbs. ~ Basic life support<br />
(CPR) provided 4 m<strong>in</strong>utes or less after collapse<br />
from ventricular fibrillation, comb<strong>in</strong>ed with direct current<br />
countershoek adm<strong>in</strong>istered 8 m<strong>in</strong>utes or less from<br />
the time of collapse, 5° yielded 50% long-term survival.<br />
Clearly, CPR did not replace advanced life support.<br />
Maximum impact was atta<strong>in</strong>ed only when the two procedures<br />
were comb<strong>in</strong>ed. For ventricular fibrillation,<br />
immediate defibrillation would be the ideal therapy.<br />
However, despite the system delays of ambulance response<br />
plus return, it rema<strong>in</strong>s a remarkable achievement<br />
of aggressive prehospital CPR that delayed defibrillation<br />
<strong>in</strong> the emergency department had significant<br />
impact. 31"33"4°’~<br />
200<br />
6061 62636465666768 697071 72 73 74<br />
YEAR<br />
FIGURE i. In Charlottesville and Aibemarle County, Virg<strong>in</strong>ia,<br />
observed community coronary deaths (black bars), paired with<br />
yearly expected deaths (white bars), rose significantly <strong>in</strong> 1964 (P <<br />
0.01) and fell significantly <strong>in</strong> 1971-1973 (P < 0.005, < 0.005, <<br />
0.0001). Hospital coronary care units, opened <strong>in</strong> 1966, had no impact.<br />
Prehospital basic and advanced life support begun <strong>in</strong> 1971 thus<br />
reduced deaths significantly.<br />
Nagel suggested that prehospital ECC contributed<br />
5% to reduction of coronary mortality <strong>in</strong> the USA, st<br />
but this figure seems low. In Seattle, 90 to I00 resuscitated<br />
victims of ventricular fibrillation survive each<br />
year, constitut<strong>in</strong>g a reduction of about 10% <strong>in</strong> coronary<br />
mortality for that community. 52 The paramedic<br />
service <strong>in</strong> K<strong>in</strong>g County, Wash<strong>in</strong>gton, reduced coronary<br />
mortality <strong>in</strong> the community by 8.4%. 32 In piedmont<br />
Virg<strong>in</strong>ia, a 16% to 25% reduction took place (Fig.<br />
I). 4 The end po<strong>in</strong>t of resuscitation and defibrillation<br />
with long-term survival is easy to measure. Indubitably,<br />
when prevention of death occurs, although it is<br />
exceed<strong>in</strong>gly difficult to estimate, it certa<strong>in</strong>ly contributes<br />
significantly to the efficiency of prehospital coronary<br />
care. 3,9,t6<br />
Estimates of costs and benefits <strong>in</strong> prehospital ECC<br />
are difficult if not impossible. In piedmont Virg<strong>in</strong>ia,<br />
prehospital CPR and ECC doubled admissions to the<br />
community’s hospital coronary care units, t3"52 Both<br />
theoretic53 and pragmatic ~ models for assess<strong>in</strong>g the<br />
impact of prehospital ECC yielded measurably favorable<br />
economic impact. The cost of add<strong>in</strong>g prehospital<br />
ECC to an extant ambulance system provided a complementary<br />
cost/benefit ratio of 40:1. =6 However, no<br />
costs and benefits of CPR by citizens were budgeted.<br />
In the Seattle assessment, the expense of CPR begun<br />
by lay persons was <strong>in</strong>corporated. 54 If Acton’s<br />
assessment53 is applied, CPR by lay persons <strong>in</strong> Seattle<br />
favorably <strong>in</strong>fluenced a large number of life-saves and<br />
yielded a cost/benefit ratio of 1:7. 3"55 Future <strong>in</strong>vestigation<br />
of community age-specific life-saves (Fig. 4)<br />
might yield even higher ratios with greater economic<br />
leverage. Such studies are urgently needed if emer-<br />
250<br />
205
AMERICAN JOURNAL OF EMERGENCY MEDICINE ¯ Volume 2, Number 3 ¯ May 1984<br />
ILl<br />
J<br />
ILl 13.<br />
O<br />
O<br />
16<br />
12<br />
ILl<br />
> 4<br />
STL COLKCW SA C-A MIA LA CIN MIN<br />
l-,z<br />
LIJ<br />
0<br />
LIJ<br />
0 BR RO RE GO ED CO BE HE Wi DU NO<br />
ILl<br />
Lk<br />
.J<br />
O O<br />
CH-ALB EDNBRG RYKJVK HLSNKI OSLO L ANG SETL SETL WlNN REYK<br />
FIGURE 2 (above, left). American prehospital life-saves per 100,000 people per year from basic and advanced life support <strong>in</strong> Seattle (STL),<br />
Columbus (COL), K<strong>in</strong>g County, Wash<strong>in</strong>gton, (KCW), San Antonio (SA), Charlottesville and Albemarle County (C-A), Miami (M[A), Los<br />
Angeles (LA), C<strong>in</strong>nic<strong>in</strong>ati (C[N), and M<strong>in</strong>neapolis (M[N). (Data derived from references 16 and 27-35.)<br />
FIGURE 3 (above, right). European and Canadian prehospital life-saves (black bars) and averted cardiac arrests (hatched bar) per 100,000<br />
people per year from basic and advanced life support <strong>in</strong> Brighton (BR), Rotterdam (RO), Reykjavik (RE), Gotenberg (GO), Ed<strong>in</strong>burgh (ED),<br />
Copenhagen (CO), Belfast (BE), Hels<strong>in</strong>ki (HE), W<strong>in</strong>nipeg (WD, Dundee (DU), and Nott<strong>in</strong>gham (NO). (Data derived from references 36-48.)<br />
OF[GURE 4. Age-spcc~c life-saves per 100,000 people per year for Charlottesville and Albcmarle County (CH-ALB), ages 30 to 69 years<br />
(black bar), F_,d<strong>in</strong>~r~ (EDNBRG), ages 20 to 69 years (hatched bar), Reykjavik (RYKJVK), ages < 91 years (white bar), and Hels<strong>in</strong>ki<br />
(HLSNKD, ages < 65 years (cross-hatched bar). (Data derived from references 15, 38, 39, and 46.)<br />
FIGURE 5. Survival rates with (black bars) and without (white bars ) cardiopulmonary resuscitation by lay persons <strong>in</strong> Oslo, Los Angeles<br />
(L ANG), Seattle suburbs (SE]’L*), Seattle city (SETL**), W<strong>in</strong>nipeg (W[NN) and Reykjavik (REYK). (Data derived from references 27.40,<br />
46, 50, 70, and 71.)<br />
gency services and lay CPR programs are to receive<br />
their fair share of community resources.<br />
MEDICAL CONTROL OF EMERGENCY CORONARY CARE<br />
The medical profession is obligated to susta<strong>in</strong> a high<br />
quality of prehospital ECC. Medical control comprises<br />
direction by the physician of all emergency care rendered<br />
by basic and <strong>in</strong>termediate EMTs, paramedics,<br />
and nurses and physicians <strong>in</strong> the field, and direction<br />
of personnel, such as ambulance dispatchers, <strong>in</strong>volved<br />
<strong>in</strong> emergency communications. Indirect functions of<br />
the physician consist of development and use of protocols<br />
for treatment, review of cases, and assessment<br />
206<br />
45<br />
30<br />
15<br />
of results; development of programs for tra<strong>in</strong><strong>in</strong>g<br />
EMTs, paramedics, dispatchers, nurses, and physicians;<br />
and development of programs for citizens <strong>in</strong><br />
CPR. The physician becomes the direct medical controller<br />
when supervis<strong>in</strong>g, by radio or telephone, the<br />
on-the-spot provider of ECC before and dur<strong>in</strong>g ambulance<br />
transport. 56 By exercis<strong>in</strong>g both direct and <strong>in</strong>direct<br />
control, the physician can guarantee a high<br />
quality of prehospital ECC with maximum favorable<br />
results: 7<br />
Supervision by the physician <strong>in</strong>cludes develop<strong>in</strong>g a<br />
citizenry tra<strong>in</strong>ed to perform CPR. Given the frequency<br />
of sudden cardiac death and the favorable cost/benefit<br />
ratio, sufficient numbers of persons <strong>in</strong> neighborhoods
TABLE 1.<br />
CRAMPTON ¯CARDIAC ARREST IN THE COMMUNITY<br />
Influence of Prehospital Cardiopulmonary Resuscitation by Lay Persons on Discharge from the Hospital<br />
Community No. of Cases<br />
Osl°rl<br />
Suburban Seattle<br />
631<br />
so<br />
487<br />
SeattleZr<br />
Los Angeles<br />
316<br />
72<br />
120<br />
W<strong>in</strong>nipeg<br />
170<br />
.4°<br />
226<br />
Reykjavik’46 222<br />
Total 217-’---2<br />
* Defibrillation limited to hospital emergency department.<br />
should learn CPR. 58 Families of persons at high risk<br />
of sudden cardiac death should have members tra<strong>in</strong>ed<br />
to render CPR. First responders such as police, fire,<br />
rescue squads, and custodians also should become<br />
providers of CPR, as should selected persons work<strong>in</strong>g<br />
<strong>in</strong> offices, stadiums, factories, theaters, concert halls,<br />
and major transportation carriers and term<strong>in</strong>als. S<strong>in</strong>ce<br />
external automated defibrillation may soon become<br />
feasible for use by lay persons, they should be tra<strong>in</strong>ed<br />
m this technique as well. This is particularly true for<br />
families of persons at high risk of sudden cardiac<br />
death. 59<br />
The future appears promis<strong>in</strong>g and excit<strong>in</strong>g. Recognition<br />
and understand<strong>in</strong>g of sudden death are improv<strong>in</strong>g<br />
60-62 After out-of-hospital cardiac arrest, prediction<br />
of recovery, z7,63 determ<strong>in</strong>ants of survival, 64 and<br />
selection of antiarrhythmic therapy 65,66 can be approached<br />
rationally. Change of behavior and diet, and<br />
new drugs, operations, and automated implantable 67<br />
and external6S, 69 devices, have already reduced sudden<br />
cardiac deaths. Improvement <strong>in</strong> prehospital resuscitation<br />
and emergency services should augment this<br />
trend. 7° The diagnostic procedure of electroprovocation<br />
of cardiac arrhythmias has del<strong>in</strong>eated management<br />
of the population at risk of a second sudden car-<br />
o diac death.65,66 Automated defibrillation by EMTs,<br />
first responders, and tra<strong>in</strong>ed lay persons, <strong>in</strong>clud<strong>in</strong>g<br />
members of families of high-risk patients, should <strong>in</strong>crease<br />
survivors who become candidates for long-term<br />
therapy with drugs, operations, and devices. =.69<br />
Out-of-hospital ECC has reduced death and morbidity<br />
from coronary heart disease <strong>in</strong> selected communities<br />
<strong>in</strong> the western world. It appears to be cost<br />
effective as an emergency measure. Its efficacy trebles<br />
when comb<strong>in</strong>ed with CPR by lay persons. Meticulous<br />
medical control by the physician will provide and susta<strong>in</strong><br />
a high quality of ECC. Thus, the physician responsible<br />
for medical control holds the key to effective<br />
ECC for the community <strong>in</strong> the future.<br />
Long-term Survival<br />
Cardiac Episode Lay CPR No Lay CPR<br />
Not documented 27/75 43/556<br />
All cardiac arrests 25/108 451379<br />
Ventricular fibrillation 471109 43/207<br />
Ventricular fibrillation 12/49 4/71<br />
Not documented 9/55 3/115<br />
Ventricular tachycardia 16/65 8/161<br />
and fibrillation<br />
All cardiac arrests 16/38 5/184<br />
152/499 151/1673<br />
(30.5%) (9.0%)<br />
The author thanks T. W. B. Crampton for the illustrative computer<br />
graphics and Drs. W. M. O’Brien, J. Alexander, and D. L.<br />
Kaiser for statistical help.<br />
REFERENCES<br />
1. Pantridge JF, Geddes JS. Cardiac arrest after myocardial<br />
<strong>in</strong>farction. Lancet 1966;1:807-808.<br />
2. Pantridge JF, Geddes JS. A mobile <strong>in</strong>tensive care unit <strong>in</strong> the<br />
management of myocardial <strong>in</strong>farction. Lancet 1967;<br />
2:271-273.<br />
3. Pantridge JF, Adgey AAJ, Geddes JS, et al. The Acute Coronary<br />
Attack. New York: Grune & Stratton, 1975.<br />
4. Crampton RS. Prehospital coronary care <strong>in</strong> the Virg<strong>in</strong>ia<br />
piedmont and United States, <strong>in</strong> Adgey AAJ (ed). Acute<br />
Phase of Ischemic Heart Disease and Myocardial Infarction.<br />
The Hague, Boston, London: Mart<strong>in</strong>us Nijhoff,<br />
1982:119.<br />
5. Mac<strong>in</strong>tosh AF, Crabb ME, Gra<strong>in</strong>ger R, et al. The Brighton<br />
resuscitation ambulances: Review of 40 consecutive survivors<br />
of out-of-hospital cardiac arrest. Br Med J<br />
1978;1:1115-1118.<br />
6. Vetter N J, Pocock S, Julian DG. Measur<strong>in</strong>g the effect of a<br />
mobile coronary care unit upon the community. Br Heart<br />
J 1979;41:418-425.<br />
7. Stillerman R, Aldrich RF, McCormack RC, et al. Coronary<br />
artery disease (CAD): Death <strong>in</strong> a community before and<br />
after the advent of hospital coronary care units. Circulation<br />
1970;42(Supp1111):202.<br />
8. Oliver MF, Julian DG, Donald KW. Problems <strong>in</strong> evaluat<strong>in</strong>g<br />
coronary care units: Their responsibilities and their relation<br />
to the community. Am J Cardiol 1967;20:465-474.<br />
9. Pantridge JF. Mobile coronary care. Chest 1970;58:229-<br />
234.<br />
10. Aldrich RF, Stillerman R, McCormack RC, etal. Sudden coronary<br />
artery disease (CAD): Death <strong>in</strong> a community and<br />
the prospective role of mobile coronary care (MCCU). Circulation<br />
1970;42(Supp11111:83.<br />
11. Crampton RS, Stillerman R, Gascho JA, et al. Prehospital<br />
coronary care <strong>in</strong> Charlottesville and Albemarle County. Va<br />
Med Month 1972;99:1191 - 1196.<br />
12. Crampton RS, Aldrich RF, Stillerman R, et al. Prehospital<br />
cardiopulmonary resuscitation <strong>in</strong> acute myocardial <strong>in</strong>farction.<br />
N Engl J Med 1972;286:1320-1321.<br />
13. Crampton RS, Aldrich RF, Gascho JA, et al. Reduction of<br />
prehospital, ambulance and community coronary death<br />
207
AMERICAN JOURNAL OF EMERGENCY MEDICINE ¯ Volume 2, Number 3 ¯ May 1984<br />
rates by the community-wide emergency cardiac care<br />
system. Am J Med 1975;58:151-165.<br />
14. Crampton RS, Gascho J, Mart<strong>in</strong> E. Tak<strong>in</strong>g coronary care to<br />
,the patient. Lancet 1978;1:1145-1146.<br />
15. Crampton RS. Mobile coronary care: Evaluation of efficiency,<br />
<strong>in</strong> Donoso E, Lipski J (eds). Acute Myocardial Infarction.<br />
New York: Stratton Intercont<strong>in</strong>ental, 1978:27-<br />
36.<br />
16. Crampton RS. Prehospital advanced cardiac life support:<br />
Evaluation of a decade of experience. Top Emerg Med<br />
1980;1:27-36.<br />
17. Nagel EL, Hirschman JC, Mayer PW, et al. Telemetry of<br />
physiologic data: An aid to fire-rescue personnel <strong>in</strong> a metropolitan<br />
area. South Med J 1968;61:598-601.<br />
18. Nagel EL, Hirschman JC, Nussenfeld, SR et al. Telemetrymedical<br />
command <strong>in</strong> coronary and other mobile emergency<br />
care system. JAMA 1970;214:332-338.<br />
19. Cobb LA, Conn RD, Samson WE, et al. Early experiences <strong>in</strong><br />
the management of sudden death with a mobile <strong>in</strong>tensive/<br />
coronary care unit. Circulation 1970;41-42(Supp1111):144.<br />
Baum RS, Alvarez H, Cobb LA. Survival after resuscitation<br />
from out-of-hospital ventricular fibrillation. Circulation<br />
1974;50:1231-1235.<br />
Lewis RP, Fulkerson PK, Stang JM, et al. The Columbus<br />
emergency medical service system. Ohio State Med J<br />
1979;75:391-394.<br />
22. Grace W J, Chadbourn JA. The mobile coronary care unit.<br />
Dis Chest 1969;55:452-455.<br />
23. Lambrew CT. Experience <strong>in</strong> telemetry of the electrocardiogram<br />
to a base hospital. Heart Lung 1974;3:756-764.<br />
24. Lewis A J, Criley JM. An <strong>in</strong>tegrated approach to acute coronary<br />
care. Circulation 1974;50:203-205.<br />
25. Criley JM, Lewis A J, Ailshie GE. Mobile emergency care<br />
units: Implementation and justification. Adv Cardiol<br />
1975;15:9-24.<br />
26. Edwards BW. Medical control and the volunteer rescue<br />
squad. J Emerg Med Serv 1981 ;6:38-42.<br />
27. Thompson RG, Hallstrom AP, Cobb LA. Bystander-<strong>in</strong>itiated<br />
cardiopulmonary resuscitation <strong>in</strong> the management of<br />
ventricular fibrillation. Ann Intern Med 1979;90:737-740.<br />
28. Lewis RP, Lanese RR, Stang JM, et al. Reduction of mortality<br />
from prehospital myocardial <strong>in</strong>farction by prudent<br />
patient activation of mobile coronary care system. Am<br />
Heart J 1982;103:123-130.<br />
29. Keller MD. ,a, study of the impact of mobile coronary care<br />
units, <strong>in</strong> Emergency Medical Services Systems Research<br />
Projects. Wash<strong>in</strong>gton, DC: DHEW Publication No (PHS)<br />
79-3220, 1979:74.<br />
30. Hoffer EP. Emergency medical serv=ces. N Engl J Med<br />
1979;301:1118-1121.<br />
31. Eisenberg <strong>MS</strong>, Bergner L, Hallstrom A. Out-of-hospital cardiac<br />
arrest: Improved survival with paramedic serv=ces.<br />
Lancet 1980;1:812-815.<br />
32. Eisenberg M, Bergner L, Hallstrom A. Paramedic programs<br />
and out-of-hospital cardiac arrest: I1. Impact on community<br />
mortality. Am J Public Health 1979;69:39-42.<br />
33. Eisenberg <strong>MS</strong>, Copass MK, Hallstrom AP, et al. Treatment<br />
of out-of-hospital cardiac arrests with rapid defibrillation<br />
by emergency medical technicians. N Engl J Med<br />
1980;302:1379-1 383.<br />
34. Myerburg RJ, Conde CA, Sung R J, et al. Cl<strong>in</strong>ical electrophysiologic<br />
and hemodynamic profile of patients resuscitated<br />
from prehospital cardiac arrest. Am J Med<br />
1980;68:568- 576.<br />
35. Rockswold G, Sharma B, Ruiz E, et al. Follow-up of 514<br />
consecutive patients with cardiopulmonarv arrest outside<br />
the hospital. JACEP 1979;8:216- 220.<br />
208<br />
36. Webb SW. Mobile coronary care. Lancet 1974;1:559-560.<br />
37. Mac<strong>in</strong>tosh AF, Crabb ME, Gra<strong>in</strong>ger R, et al. The Brighton<br />
resuscitation ambulances: Review of 40 consecutive survivors<br />
of out-of-hospital cardiac arrest. Br Med J<br />
1978;1:1115-1118.<br />
38. Vetter N J, Pocock S, Julian DG. Measur<strong>in</strong>g the effect of a<br />
mobile coronary care unit upon the community. Br Heart<br />
J 1979;41:418-425.<br />
39. Siltanen P, Sundberg S, Hytonen I. Impact of a mobile coronary<br />
care unit on the sudden coronary mortality <strong>in</strong> a<br />
community. Acta Med Scand 1979;205:195-200.<br />
40. Tweed WA, Bristow G, Donen N. Resuscitation from cardiac<br />
arrest: Assessment of a system provid<strong>in</strong>g only basic life<br />
support outside of hospital. Can Med Assoc J 1980;<br />
122:297-300.<br />
41. McNeill GP, Bouchier lAD, Watson H. Mobile coronary care<br />
available to the general public. Lancet 1979;1:975.<br />
42. Hill JD, Hampton JR, Mitchell JRA. A randomized trial of<br />
home-versus-hospital management for patients with suspected<br />
myocardial <strong>in</strong>farction. Lancet 1978;1:837-841.<br />
43. Hampton JR, Dowl<strong>in</strong>g M, Nicholas C. Comparison of results<br />
from a cardiac ambulance manned by medical or nonmedical<br />
personnel. Lancet 1977;1:526-529.<br />
44. Studd C. The Brighton experience with resuscitation ambulances.<br />
Am J Emerg Med 1984;2:275-276.<br />
45. Hart HN. Integrated approach to prehospital coronary care<br />
=n Rotterdam. Am J Emerg Med 1984;2:225-229.<br />
46. Gudjonsson H, Baldv<strong>in</strong>sson E, Oddsson G, et al. Results of<br />
attempted cardiopulmonary resuscitation of patients<br />
dy<strong>in</strong>g suddenly outside the hospital <strong>in</strong> Reyjavik and the<br />
surround<strong>in</strong>g area, 1976-1979. Acta Med Scand<br />
1982 ;212:247- 251. ""<br />
47. Holmberg S, Wennerblom B. Out-of-hospital cardiac arrest:<br />
Effect of special ambulances <strong>in</strong> G6teborg on mortality.<br />
Am J Emerg Med 1984;2:222-224.<br />
48. Pedersen A. In Copenhagen. Brighton Conference Abstracts.<br />
London:British Heart Foundation, 1982:38.<br />
49. Crampton RS, Michaelson SP, Aldrich RF, et al. Prehospital<br />
care for myocardial <strong>in</strong>farction. N Engl J Med 1974;<br />
291:418.<br />
50. Eisenberg <strong>MS</strong>, Bergner B, Hallstrom A. Paramedic programs<br />
and out-of-hospital cardiac arrest: I. Factors associated<br />
with successful resuscitation. Am J Public<br />
Health 1979;69:30-38.<br />
51. Nagel EL. Prehospital care as a cause for coronary heart<br />
disease mortality decl<strong>in</strong>e, <strong>in</strong> Havlik RJ, Fe<strong>in</strong>leib M (eds).<br />
Proceed<strong>in</strong>gs of a Conference on the Decl<strong>in</strong>e <strong>in</strong> Coronary<br />
Heart Disease Mortality. Wash<strong>in</strong>gton, DC: DHEW Publ No<br />
(NIH) 79-1610, 1979.<br />
52. Adgey AAJ, Crampton RS. Hospital or home for acute myocardial<br />
<strong>in</strong>farction: Another look at whether or not we<br />
should bother to care. Am Heart J 1981 ;102:473-477.<br />
53. Sidel VW, Acton J, Lown B. Models for the evaluation of<br />
prehospital coronary care. Am J Cardiol 1969;24:674-<br />
688.<br />
54. Hallstrom A, Eisenberg <strong>MS</strong>, Bergner L. Model<strong>in</strong>g the effectiveness<br />
and cost-effectiveness of an emergency service<br />
system. Soc Sci Med 1 981 ;15C:13-17.<br />
55. Crampton RS. The role of organized medic<strong>in</strong>e <strong>in</strong> provid<strong>in</strong>g<br />
education about cardiopulmonary resuscitation, <strong>in</strong><br />
Greenberg HM, Dwyer EM Jr (eds). New York, Ann NY<br />
Acad Sci 1982;382:324-329.<br />
56. Committee on Emergency Medical Services. Medical Control<br />
<strong>in</strong> Emergency Medical Services Systems. Wash<strong>in</strong>gton,<br />
DC: National Academy Press 1981.<br />
57. Pozen MW, D’Agost<strong>in</strong>o RB, Sytkowski PA, et al. Effectiveness<br />
of a prehospital medical control system: An analysis
i<br />
i<br />
i<br />
I<br />
!<br />
!<br />
I<br />
i<br />
i<br />
!<br />
I<br />
O<br />
p<br />
of the <strong>in</strong>teraction between emergency room physician<br />
and paramedic. Circulation 1981 ;63:442-447.<br />
58. McEIroy CR. Citizen CPR: The role of the lay person <strong>in</strong> prehospital<br />
care. Top Emerg Med 1980;1:37-46.<br />
59. Friedberg CK. Introduction: Symposium, myocardial <strong>in</strong>farction<br />
(Part 1). Circulation 1972;45:179.<br />
60. Sonneblick EH, Lesch M (eds). Sudden Cardiac Death. New<br />
York: Grune & Stratton, 1981.<br />
61. Greenberg HM, Dwyer EM Jr (eds). Sudden Coronary Death.<br />
Ann NY Acad Sci 1982;382:1-484.<br />
62. Adgey AAJ (ed). Acute Phase of Ischemic Heart Disease and<br />
Myocardial Infarction. Boston: Mart<strong>in</strong>us Nijhoff, 1982.<br />
63. Longstreth WT, Diehr P, Inui TS. Prediction of awaken<strong>in</strong>g<br />
after out-of-hospital cardiac arrest. N Engl J Med 1983;<br />
308:1378-1382.<br />
64. Swerdlow CD, W<strong>in</strong>kle RA, Mason JW. Determ<strong>in</strong>ants of survival<br />
<strong>in</strong> patients with ventricular tachyarrhythmias. N Engl<br />
J Med 1983;308:1436-1442.<br />
65. Rusk<strong>in</strong> JN0 DiMarco JP, Garan H. Out-of-hospital cardiac<br />
arrest: Electrophysiologic observations and selection of<br />
long-term anti-arrhythmic therapy. N Engl J Med<br />
1980 ;303:607-13.<br />
CRAMPTON II CARDIAC ARREST IN THE COMMUNITY<br />
66. Garan H, Rusk<strong>in</strong> JN, DiMarco JP et al. Electrophysiologic<br />
studies before and after myocardial revascularization <strong>in</strong><br />
patients with life-threaten<strong>in</strong>g ventricular arrhythmias. Am<br />
J Cardiol 1983;51:519-24.<br />
67. Mirowski M, Reid PR. Mower MM, et al. Term<strong>in</strong>ation of malignant<br />
ventricular arrhythmias with an implanted automatic<br />
defibrillator <strong>in</strong> human be<strong>in</strong>gs. N Engl J Med<br />
1980;303:322-324.<br />
68. Jaggarao NSV, Heber M, Gra<strong>in</strong>ger R, et al. Use of an automated<br />
external defibrillator-pacemaker by ambulance<br />
staff. Lancet 1982;2:73-75.<br />
69. Diack AW, Welborn WS, Rullman RG et al. An automatic<br />
cardiac resuscitator for emergency treatment of cardiac<br />
arrest. Med Instrum 1979;13:78-81.<br />
70. Jacobsen S (ed). Resuscitation. Cl<strong>in</strong>ics <strong>in</strong> Emergency Medic<strong>in</strong>e.<br />
New York: Churchill Liv<strong>in</strong>gston, 1983.<br />
71. Lund I, Skulberg A. Cardiopulmonary resuscitation by lay<br />
people. Lancet 1976;2:702-704.<br />
72. Guzy PM, Pearce ML, Greenfield, S, et al. Effectiveness of<br />
citizen cardiopulmonary resuscitation dur<strong>in</strong>g out-of-hospital<br />
emergencies <strong>in</strong> metropolitan Los Angeles. Circulation<br />
(Suppl II) 1979;60:46.<br />
2O9
908<br />
Occasional Surve!<br />
Management of cardiac arrest<br />
of resuscitation services<br />
ROGER- H JONES<br />
Abstract .... ~ - - -<br />
A survey of the English health regions identified n<strong>in</strong>e<br />
ambulance based resuscitation schemes. Their structure<br />
and function are heterogeneous and their impact on<br />
patient survival is often speculatlve.~There is considerable<br />
medical, paramedical, and lay enthusiasm for<br />
resuscitation schemes but this cannot be harnessed until<br />
medlcolegal uncerta<strong>in</strong>ties are removed and guidel<strong>in</strong>es<br />
for development are set out. Better documentation of<br />
the benefits of exist<strong>in</strong>g schemes should be undertaken<br />
so that. advanced tra<strong>in</strong><strong>in</strong>g of ambulance personnel can<br />
proceed rationally.<br />
Introduction<br />
I<br />
Every year <strong>in</strong> England and Wales over 100 000 people die from<br />
ischaemic heart diseaseF Many of these deaths are sudden or<br />
unheralded, and over half of the victims die before they reach<br />
hospital. Figures from the United States/are similar, with<br />
650 000 deaths each year, and, "s<strong>in</strong>ce 60-70% of sudden deaths<br />
caused by cardiac arrest occur before hospitalisation it is clear<br />
that the community. ,,s deserves to be. regarded as the ulumate"<br />
coronary care umt. The community, and the primary health<br />
care team <strong>in</strong> particular, has clear educational, preventive, and<br />
therapeutic responsibilities <strong>in</strong> relation to ischaemic heart disease<br />
but when these measures fail, how are we to respond ?<br />
elSelc9e76~sD;mP era~ed~h~ft ~:l~us~r~:;eSmaut;dq~tp;n d ~a m<br />
bulances manned by ambulancemen who have received tra<strong>in</strong><strong>in</strong>g<br />
<strong>in</strong> advanced techniques significantly affects the overall mortality<br />
rate of patients suffer<strong>in</strong>g from acute myocardial <strong>in</strong>farction" and<br />
recommended that "authorities are advised to defer the <strong>in</strong>troduction<br />
of new and the extension of exist<strong>in</strong>g advanced tra<strong>in</strong><strong>in</strong>g<br />
schemes for ambulance.men." No further directives have been<br />
issued s<strong>in</strong>ce then; none the less several schemes are <strong>in</strong> operation.<br />
While attempt<strong>in</strong>g to set up a local resuscitation scheme, we<br />
found that basic <strong>in</strong>formation about the exf, ent of resuscitation<br />
schemes <strong>in</strong> England was not available, and there is certa<strong>in</strong>ly no<br />
consensus view about the most effective way <strong>in</strong> which schemes<br />
should be organised. A survey was undertaken to try to answer<br />
these questions. (R H Jones, Upjohn Travell<strong>in</strong>g Fellowship<br />
Report, 1982.*)<br />
*Copies may be obta<strong>in</strong>ed from the librarian, Royal College of General<br />
Practitioners, 14 Pr<strong>in</strong>ces Gate, Hyde Park, London $W7 1PU.<br />
Andover) I-lant$ SPI0 3LD<br />
ROGER H JONES, MRCr, bmcor, general practitioner<br />
Correspondence and requests for repr<strong>in</strong>ts to: 56 Junction Rd, Andover,<br />
Hants SP10 3QU.<br />
I IIIIIII I<br />
BRITISH MEDICAL JOURNAL VOLUM~ 287 I OCTOBE<br />
<strong>in</strong> the community: a survey<br />
Methods - -<br />
Because it seemed likely that most resuscitation schemes woui<br />
based on the ambulance service, <strong>in</strong>itial approaches were mad<br />
letter to the regional ambulance officers Of the 11 English reg<br />
ambulance set-ices (the four 71~ames regions <strong>in</strong> Greater L~<br />
are served by one ambuFance service). Contact was also made ~:<br />
headquarters and branch representatives of the Associati~<br />
Emergency Medical Technicians (AEMT) and the British Associi<br />
of Immediate Care Scheme (BASICS).<br />
When the replies from the regional ambulance officers<br />
available ambulance based schemes <strong>in</strong> their regions were visited<br />
documented, us<strong>in</strong>g a structured <strong>in</strong>terview. Dur<strong>in</strong>g this <strong>in</strong>qui~<br />
discovered several other schemes <strong>in</strong> the early stages of developr{<br />
but, with the exception of the new Nott<strong>in</strong>gham coronary ambul, ~<br />
scheme, these are not <strong>in</strong>cluded <strong>in</strong> the analysis. Throughout<br />
survey all my <strong>in</strong>quiries were answered and I received-the fti<br />
cooperation from everyone concerned.<br />
W~sltcrn ) ~.<br />
\<br />
nO<br />
c...,_. :
J<br />
.CAL JOURNAL vOLUME 287 1 OCTOBER 1983<br />
//ever, it is <strong>in</strong>structive to comment briefly on the regions <strong>in</strong><br />
,~ere are no resuscitation ambulance schemes.<br />
:EGIONS WITH NO RESUSCITATION SCHEMES<br />
Northern region--The question of resuscitation schemes never<br />
ceres to have arisen here.<br />
North western region--Except for a coronary ambulance service<br />
~ascd on Wythenshawe Hospital, Manchester, which closed down<br />
,ccause of lack of funds, there have been no schemes <strong>in</strong> this region.<br />
rhere is certa<strong>in</strong>ly an awareness of the potential medicolegal problems<br />
ris<strong>in</strong>g because of lack of national direction.<br />
Mersey reglon--Aithough advanced tra<strong>in</strong><strong>in</strong>g for ambulancemen has<br />
,een started <strong>in</strong> Liverpool, there have been no resuscitation ambulance<br />
chemeS.<br />
West Midlands region--There was a "limited tra<strong>in</strong><strong>in</strong>g exercise" <strong>in</strong><br />
esuscitation <strong>in</strong> the Hereford and Worcester area, which has now<br />
:nded, and an advanced tra<strong>in</strong><strong>in</strong>g scheme operates <strong>in</strong> Warwickshire.<br />
East A nglla region--The possibility of develop<strong>in</strong>g advanced tra<strong>in</strong><strong>in</strong>g<br />
.chemes <strong>in</strong> Cambridge was mooted some years ago but the idea<br />
"oundered on the question of medicolegal responsibility.<br />
London region--Some years hgo the London Ambulance service<br />
vas mov<strong>in</strong>g towards the tra<strong>in</strong><strong>in</strong>g of ambulance personnel <strong>in</strong> the use<br />
ff monitor<strong>in</strong>g and defibrillation equipment, but these proposals<br />
vere abandoned because of the DHSS circular mentioned above, s<br />
S, dvanced tra<strong>in</strong><strong>in</strong>g <strong>in</strong> <strong>in</strong>tubation and <strong>in</strong>travenous <strong>in</strong>fusion techniques<br />
aas, however, cont<strong>in</strong>ued. A rather unusual coronary ambulance<br />
;ervice~h~ed on the cardiology department at St Bartholomew’s<br />
,qospit~rves the City of London between 9 am and 5 pm from<br />
~ondays "rom the cardiology to Fridays. or The .accident coronary d epartme..nt, ambulance a is nurse statT tr.om ed by me a accalae=t regi.~rar"<br />
tepartment, a technicum from the medical elcctrontca aepartm...,<br />
md sometimes a medical student. Each year the ambulance ss called<br />
mt between 300 and 400 times and about 20 casualties are defibrillated.<br />
Leeds--This scheme was started iust before the 1976 DHSS<br />
:ircular ’~ was issued; it was an experimental scheme based on electro-<br />
:ardiogram radiotelemetry and speech l<strong>in</strong>ks between specially staffed<br />
and equipped vehicles and the coronary care unit at Leeds General<br />
Infirmary. The trial was limited and failed to Show any benefit for<br />
pauents. It was possibie to provide cover only between 9 am and<br />
5 pro, and dur<strong>in</strong>g the 15 month trial period six patients were defibrillated,<br />
none of .whom survived. The DHSS circular discouraged<br />
extension of this experiment.<br />
REGIONS WITH RESUSCITATION SCHEMES<br />
Eight centres were exam<strong>in</strong>ed <strong>in</strong> detail to document the activities<br />
of ambulance based resuscitation schemes: Alton, Andover, Avon,<br />
Bcighton, Gloucester, Nott<strong>in</strong>gham, Oxford, and York.<br />
A It o n<br />
This new scheme is <strong>in</strong> Alton, a country town of 15 000 <strong>in</strong>habitants<br />
that is 15 miles from the nearest general h.ospital. The scheme was<br />
set up by a general practiti-oner and.tra<strong>in</strong><strong>in</strong>g is open to all ambulance<br />
personnel. In 18 months three patients have been-successfully<br />
resuscitated with n<strong>in</strong>e further unsuccesgful attempts. The r~dicolegal<br />
position of ambulance personnel rema<strong>in</strong>s ambiguous, however, but<br />
*he scheme is at present proceed<strong>in</strong>g as a pilot project.-.<br />
Andover ._<br />
The Andover scheme developed because of the successful activities<br />
m nearby Alton. It is based on a country town of 35 000 <strong>in</strong>habitants<br />
which is also about 15 miles from the nearest district hospital. The<br />
scheme, once aga<strong>in</strong>, was developed by a general practitioner and is<br />
supported by charitable funds. The adm<strong>in</strong>istrative and medicolegal<br />
problems here, however, are even more complex, and at present,<br />
although monitor<strong>in</strong>g and defibrillation equipment is carried <strong>in</strong> the<br />
ambulances, ambulance personnel may use only the monitors;<br />
defibrillators are used only by general practitioners.<br />
A yon<br />
Avon has a longstand<strong>in</strong>g, advanced tra<strong>in</strong><strong>in</strong>g scheme developed by<br />
a consultant anaesthetist at Frenchay Hospital. Almost a quarter of<br />
the region’s ambulance personnel have been tra<strong>in</strong>ed, and electrocardiogram<br />
monitor<strong>in</strong>g and defibrillation equipment is now available<br />
at 10 of the county’s 11 ambulance stations. In addition, three mobile<br />
resuscitation units with fixed electrocardiographic and defibrillation<br />
equipment carry a range of fluids and <strong>in</strong>travenous drugs. In 1981<br />
cardiac arrest was treated 49 times, and 37 patients were defibrillated.<br />
Brighton<br />
The well known Brighton coronary ambulance programme 4j<br />
orig<strong>in</strong>ally set out to provide a specially equipped ambulance and a<br />
doctor to travel rapidly to suspected coronary victims. It was quickly<br />
appreciated that it was more appropriate to tra<strong>in</strong> the ambulance<br />
personnel, and there are now over 30 well tra<strong>in</strong>ed ambulancemen<br />
who are expert <strong>in</strong> <strong>in</strong>terpret<strong>in</strong>g electrocardiograms, skilled at <strong>in</strong>tubation,<br />
defibrillation, and <strong>in</strong>travenous therapy, and able to adm<strong>in</strong>ister a<br />
variety of <strong>in</strong>travenous drugs. In 1981 31 out of 128 defibrillations<br />
were successful. In addition to this advanced tra<strong>in</strong><strong>in</strong>g programme, a<br />
successful exercise <strong>in</strong> community education <strong>in</strong> cardiopulmonary<br />
resuscitation is under way--the Brighton Save a Life Campaign~<br />
which has already <strong>in</strong>structed about 18 000 members of the public.<br />
Gloucester<br />
969<br />
Gloucester has an advanced tra<strong>in</strong><strong>in</strong>g scheme with many similarities<br />
to the Avon scheme, although some details of the tra<strong>in</strong><strong>in</strong>g programme<br />
differ. About a quarter of the ambulance staff <strong>in</strong> the county have<br />
received advanced tra<strong>in</strong><strong>in</strong>g, and there are 15 mobile resuscitation<br />
units at 10 of the 12 stations. This scheme <strong>in</strong>teracts with an immediate<br />
care scheme based on 20 general practitioners <strong>in</strong> west<br />
Gloucestershire.<br />
/<br />
Nott<strong>in</strong>gham<br />
The Nott<strong>in</strong>gham experimental coronary ambulance schemes were<br />
started <strong>in</strong> 1973 when a s<strong>in</strong>gle ambulance with cardiac monitor<strong>in</strong>g<br />
equipment and a defibrillator came <strong>in</strong>to service; over the next’few<br />
years the efficacy of this scheme was tested experimentally, firstly,<br />
with comparisons of the responses of ord<strong>in</strong>ary ambulances and<br />
coronary ambulances to emergencies, then with th~’ixaclusion of a<br />
hospital doctor <strong>in</strong> the ambulance crew on alternate days, and, f<strong>in</strong>ally,<br />
with the exclusion of general practitioner <strong>in</strong>itiated calls and assessment<br />
of the effect of the service <strong>in</strong> response to 999 calls only.’ This<br />
study showed no difference <strong>in</strong> prchospital mortality between patients<br />
carried by coronary ambulances and those carried by_ rout<strong>in</strong>e ambulances.<br />
At the end of~tliis study the .coro~tary ambulance service<br />
was discont<strong>in</strong>ued.<br />
The scheme is now be<strong>in</strong>g redeveloped. The lessons learnt from the<br />
experiments <strong>in</strong> the past eight years <strong>in</strong>clude the sugges-tiOn tb_at<br />
detailed tra<strong>in</strong><strong>in</strong>g <strong>in</strong> drug adm<strong>in</strong>istration and endotracheal <strong>in</strong>tubation<br />
are probably less important than early "monitor<strong>in</strong>g and-defibrillation<br />
for Victims of myocardial <strong>in</strong>farction. The new scheme will.cover a<br />
population of about 500 000 with !0 emergency vehicles. A coro_nary<br />
register is be<strong>in</strong>g established <strong>in</strong> N’oit<strong>in</strong>gha-m so-that-d_caths from<br />
ischaemic heart disease can be recorded before the scheme becomes<br />
operational and reviewed after the scheme has started. There-are<br />
further plans to develop a pi-ogramme of community education <strong>in</strong><br />
cardiopulmonary resuscitation. - -<br />
Oxford<br />
The Oxford scheme, a more recent countywideadvanced tra<strong>in</strong><strong>in</strong>g<br />
scheme, started <strong>in</strong> 1978. The thorough tra<strong>in</strong><strong>in</strong>g programme has<br />
produced 48 tra<strong>in</strong>ed personnel out of an establishment of 142 <strong>in</strong><br />
Oxfordsbire. There are 16 monitor-defibrillator units <strong>in</strong> use throughout<br />
the county and 39 accident and emergency vehicles. In 1981<br />
23 patients were defibrillated. A community cardiopulmonary
O ,<br />
O<br />
970<br />
resuscitation scheme <strong>in</strong> Oxfordshire began <strong>in</strong> 1981, and 52 <strong>in</strong>structors<br />
and almost 1000 members of the public have now been tra<strong>in</strong>ed. In<br />
1981 36 patients required <strong>in</strong>tubation and 23 were defibrillated.<br />
York<br />
All 42 ambulance personnel <strong>in</strong> York have been tra<strong>in</strong>ed to use their<br />
monitor-defibrillators, of which six are available<strong>in</strong> the city ambulances.<br />
The emphasis, as <strong>in</strong> the proposed Nott<strong>in</strong>gham scheme, is on early<br />
defibrillation rather than detailed tra<strong>in</strong><strong>in</strong>g <strong>in</strong> <strong>in</strong>tubation and <strong>in</strong>fusion<br />
techniques, Between 1970 and 1981 13 of the 181 defibrillations<br />
resulted <strong>in</strong> ultimate recovery.<br />
The table summarises the features of these corofiary ambulance<br />
schemes. General practitioner <strong>in</strong>volvement refers to th e cooperation<br />
of general practitiof:ers <strong>in</strong> tra<strong>in</strong><strong>in</strong>gand <strong>in</strong> the dayto day-runn<strong>in</strong>g of<br />
the-scheme. The~ two Hampshire schemes were started by general<br />
practitioners and the Gloucester scheme <strong>in</strong>teracts with a group of<br />
immediate care doctors, but the rema<strong>in</strong>der have little contact with<br />
local primary care doctors, although there are BASICS groups <strong>in</strong><br />
Oxfordshire, Somerset, and Bristol.<br />
OTHER SCHEMF.$<br />
Association of Emergency Medical Technicians (AEMT)<br />
The Association of Emergency Medical Technicians is an association<br />
for paramedical personnel <strong>in</strong>terested or active <strong>in</strong> emergency care.<br />
About 700 ambfi]ancemen are members of AEMT, which has 43<br />
branches throughout the country. The tra<strong>in</strong><strong>in</strong>g programme is quite<br />
separate from the ambulance service advanced tra<strong>in</strong><strong>in</strong>g programme<br />
and is organised on guidel<strong>in</strong>es which have been agreed with BASICS.<br />
In addition the AEMT provides an <strong>in</strong>surance <strong>in</strong>demnity for £500 000<br />
aga<strong>in</strong>st malpractice claims.<br />
British Association for Immediate Care (BA SIC.S)<br />
/<br />
The British Association for Immediate Care is an organisation of<br />
medical practitioners who have an <strong>in</strong>terest <strong>in</strong> immediate care. At<br />
present about 1350 belong to the 44 schemes <strong>in</strong> England. Each scheme<br />
is organised <strong>in</strong> response to local needs, but <strong>in</strong> general BASICS sets<br />
out to deal with accidents rather than medical emergencies. A survey<br />
of the 14 largest BASICS groups, account<strong>in</strong>g for over 60% of the<br />
total membership, suggests that ready access to electrocardiogram<br />
monitor<strong>in</strong>g and defibrillation equipment is the exception rather than<br />
the rule.<br />
Discussion<br />
Provision of mobile resuscitation facilities for deal<strong>in</strong>g with<br />
cardiac arrest occurr<strong>in</strong>g outside hospital is patchy, and if not<br />
chance then serendipity seems to have guided their development.<br />
Clearly non-cl<strong>in</strong>ical determ<strong>in</strong>ants operate <strong>in</strong> the development<br />
of coronary ambulance and mobile resuscitation programmes;<br />
taken together with evidently widely differ<strong>in</strong>g<br />
perceptions of the role of the ambulance service an unevenness<br />
of approach is <strong>in</strong>evitable.<br />
What is perhaps most unsatisfactory about the development of<br />
resuscitation strategies is their uncerta<strong>in</strong> value, both <strong>in</strong> the<br />
Some features of resuscitation ambulance schemes<br />
BRITISH MEDICAL JOURNAL VOLUME 287 I¯:OCTOBER 1983<br />
absolute sense of sav<strong>in</strong>g life and <strong>in</strong> the relative sense of the<br />
appropriateness of divert<strong>in</strong>g funds and energies which might be<br />
better used elsewhere. Few attempts have been made to tackle<br />
this difficult and important question. There seem to be three :<br />
different approaches to manag<strong>in</strong>g out of hospital cardiac arrest,<br />
exemplified <strong>in</strong> the various schemes which have been surveyed: -<br />
firstly, a perception of chest pa<strong>in</strong> and myocardial <strong>in</strong>farction as a -<br />
medical emergency requir<strong>in</strong>g urgent medical attention and<br />
hospital admission; secondly, an attempt to provide a much~<br />
wider range of skills to deal with ffauma and medical and<br />
surgical emergencies as well as cardiac arrest; xhirdly, the _ ~<br />
provision O f less advanced but equally mob!le expertise With the<br />
emphasis on early defibrillation and basic life support.<br />
The emphasis <strong>in</strong> the Brighton Scheme is0n the first of these, ~-~<br />
although the resuscitation ambulances respond to a variety of- =other<br />
life threaten<strong>in</strong>g emergencies; the second is the basis for -<br />
the Oxford, Avon, and Gloucester schemes; and the-third ~-.<br />
underlies plann<strong>in</strong>g for the new Nott<strong>in</strong>gham scheme and is the ~<br />
basis for the York city ambulance scheme and also of the<br />
general practitioner related schemes <strong>in</strong> Alton and Andover. The<br />
third must also be taken as the rationale for those general<br />
practitioner based- immediate care groups hav<strong>in</strong>g access to<br />
defibrillators. - -<br />
The Brighton resuscitation ambulance programme is probably<br />
the best known and most widely reported, although the<br />
home versus hospital question of the management of myocardial<br />
<strong>in</strong>farction rema<strong>in</strong>s unresolved and there are commonsense<br />
reasons for regard<strong>in</strong>g flash<strong>in</strong>g blue lights and high<br />
technology as arrythmogenic. There is a sense, too, <strong>in</strong> which<br />
primary care is bypassed when chest pa<strong>in</strong> means a 999 call and<br />
hospital admission. The Brighton ambulance personnel are<br />
probably the best tra<strong>in</strong>ed <strong>in</strong> cardiac care and their expertise<br />
and ability to adm<strong>in</strong>ister drugs may contribute greatly to the ~<br />
management of cardiac arrest, although Hampton and his<br />
colleagues have cast some doubt on the impact on survival of<br />
these abilities. 7 The resuscitation ambulances also respond to<br />
other, non-cardiac emergencies, such as drown<strong>in</strong>g, trauma,<br />
drug overdose, and hypoglycaemia.<br />
The second approach to manag<strong>in</strong>g cardiac arrest outside<br />
hospital forms one element of a much more comprehensive<br />
view of the value of paramedical tra<strong>in</strong><strong>in</strong>g for ambulance personnel.<br />
Although good documentation would massively enhance<br />
their credibility, the mobile resuscitation units and the staff<br />
with advanced tra<strong>in</strong><strong>in</strong>g <strong>in</strong> Avon, Oxford, and Gloucester are a<br />
most impressive development. Correction of hypovolaemic<br />
shock before admission to hospital, for example, must be judged<br />
a potentially life sav<strong>in</strong>g contribution, and the versatility of these<br />
ambulance crews, evident when review<strong>in</strong>g the reports of<br />
patients whom they have helped, is beyond doubt. In dist<strong>in</strong>ction<br />
to a "pure" coronary care approach these schemes appear to<br />
require no justification, although their revenue consequences<br />
are not <strong>in</strong>considerable. Unfortunately th1976 DHSS circular<br />
acted as a damper on advanced tra<strong>in</strong><strong>in</strong>g of this type."<br />
Thirdly, limited resuscitation by early defibrillation (assumed<br />
to be performed <strong>in</strong> a sett<strong>in</strong>g of basic cardiopulmonary resuscitation<br />
capabilities) avoids some of the tra<strong>in</strong><strong>in</strong>g, organisational, and<br />
f<strong>in</strong>ancial consequences of more elaborate schemes. This seems<br />
a second best buy for the ambulance service but is probably<br />
ideal when cooperation between the ambulance service and<br />
Brighton and<br />
Alton Andover Avon Hast<strong>in</strong>gs Gloucester Nott<strong>in</strong>gham Oxford York<br />
No of years runn<strong>in</strong>g 2 1 10 8 10 4 12<br />
No of tra<strong>in</strong>ed personnel 12 11 50 43 55 ~ 48 42<br />
Intubatlon-<strong>in</strong>fusion tra<strong>in</strong>ed<br />
+<br />
+ +<br />
} + 0<br />
Able to adm<strong>in</strong>ister drugs 0 ~ ~ + ~)<br />
0<br />
0<br />
Specially fitted vehicles 0 0 + + + 0 +0 +<br />
Significant charitable fund<strong>in</strong>g + ÷ + + + 0 + ÷<br />
Community cardiopulmonary resuscitation<br />
programme<br />
0 0 0 0<br />
General practitioner <strong>in</strong>volvement<br />
÷ 0 +0 o 0 0
oDICAL JOURNAL VOLUME 287<br />
I OCTOBER 1983<br />
¯ practice is good. It does seem more sensible, however,<br />
clatively expensive and bulky electrocardiogram monitor<strong>in</strong>g<br />
.d defibrillation equipment to be carried by the ambulances<br />
rather than be<strong>in</strong>g handed from general practitioner to general<br />
practitioner <strong>in</strong> an immediate care scheme. On the other hand, a<br />
recent report on the management of myocardial <strong>in</strong>farction by<br />
,,immediate care doctors ’’8 stated that an appreciable number<br />
to3 out of 511) of patients died <strong>in</strong> the presence of their general<br />
practitioner. This, it was suggested, argued for the wider use of<br />
defibrillators by general practitioners.<br />
This may be one way <strong>in</strong> which primary care doctors can<br />
contribute to "the ultimate coronary care unit" but there are<br />
others. At present general practitioner and ambulance based<br />
resuscitation schemes make only a small impression on the<br />
number of sudden deaths <strong>in</strong> the community. The reason for<br />
the delay <strong>in</strong> develop<strong>in</strong>g more widespread advanced tra<strong>in</strong><strong>in</strong>g for<br />
ambulance personnel has already been mentioned but there<br />
seems little doubt that when political, f<strong>in</strong>ancial, legal, and<br />
attitud<strong>in</strong>al difficulties have been overcome, greater opportunities<br />
for deal<strong>in</strong>g with out of hospital cardiac arrest will arise. This<br />
survey showed that <strong>in</strong> many areas, particularly country districts,<br />
there is great potential for fruitful cooperation between general<br />
practitioners and the ambulance service. This might be expressed<br />
as <strong>in</strong>volvement <strong>in</strong> immediate care arrangements,<br />
contribution to tra<strong>in</strong><strong>in</strong>g, and support of proposals for extend<strong>in</strong>g<br />
the role of ambulance personnel.<br />
On a wider front, tl~.e potential of any resuscitation scheme<br />
cannq~ realised without widespread tra<strong>in</strong><strong>in</strong>g of the public <strong>in</strong><br />
the p~ffciples of cardiopulmonary resuscitation. In Seattle<br />
about one third of the population have received such <strong>in</strong>struction<br />
and this probably accounts for the high success rate of the<br />
resuscitation there which undoubtedly saves about 100 lives<br />
each year.* Despite this, only <strong>in</strong> Brighton and Oxford have<br />
resuscitation ambulance programmes acted as a stimulus for<br />
public education <strong>in</strong> cardiopulmonary resuscitation, and this is a<br />
further area <strong>in</strong> which general practitioners may contribute to<br />
the out of hospital management of cardiac arrest.<br />
Are antiprostagland<strong>in</strong>s of any value <strong>in</strong> treat<strong>in</strong>g the irritable bwwel<br />
~yndrome ?<br />
Possibly, but it is too early to be sure. Diarrhoea is the predom<strong>in</strong>ant<br />
feature <strong>in</strong> a few patients with the irritable bowel syndrome. These<br />
patients often have raised concentrations of prostagland<strong>in</strong> E, <strong>in</strong> their<br />
: jcjunaL,[luid,, and <strong>in</strong> six such patients an uncontrolled trial 9 f ~dometh~25<br />
mg four times-daily cut the stool volume and frequency<br />
by ha1~q’hese prelim<strong>in</strong>ary results need to be confirmed <strong>in</strong> a placebo<br />
controlled trial s<strong>in</strong>ce many patients with the irritable bowel syndrome<br />
respond well to placebos. Meanwhile, it may be relevant that <strong>in</strong><br />
’ patients with this syndrome who develop diarrhoea <strong>in</strong> response to<br />
specific foods.the co. ncetitration of prostagland<strong>in</strong> E~ <strong>in</strong> rectal fluid<br />
rises when they are challenged with the food <strong>in</strong>-question.* Aga<strong>in</strong>,<br />
these are early f<strong>in</strong>d<strong>in</strong>gs, and the precise role of prostagland<strong>in</strong>s <strong>in</strong><br />
the i-rritable bowel syndrome with diarrhoea is far from clear.~<br />
g llEgXOi% reader <strong>in</strong> medic<strong>in</strong>ei Bristol.<br />
- : Bukhave H Rask-Mad~n J=Prostagland<strong>in</strong> E, <strong>in</strong> jejunal fluids and its potential<br />
-. "" diagnostic value for select<strong>in</strong>g patient¯ with <strong>in</strong>domethacm-sen¯mve dmrrhoea.<br />
.i. EurJClln lwuest1981;U:191-3. . " - ...... - "~ ~ood<br />
Juries VA, McLaut~hlan l r, Shormouse .M,’worgman e,, taunter j~. r<br />
<strong>in</strong>tolerance- a major factor <strong>in</strong> the pathogene¯i¯ of irrttable bowel ¯ynurome.<br />
Lancet 1982]ii:U15-7. ~ "<br />
What is the risk of a person ~vho has had one coronary thrombosis hav<strong>in</strong>g<br />
another attack ?<br />
For the purposes of this reply I will assume that the subject has<br />
survived their first myocardial <strong>in</strong>farction by at least one month. The<br />
Fram<strong>in</strong>gham study <strong>in</strong>dicates that for men, the average annual<br />
mortality will be 5% a year for the next 10 years, between three and<br />
971<br />
There is obviously a great deal of enthusiasm among doctors<br />
and ambulance staff who want to contribute to the prehospital<br />
care of the critically ill. Whereas on one hand it will be a waste<br />
if this enthusiasm rema<strong>in</strong>s untapped and unchannelled for want<br />
of national direction, on the other, the DHSS is unlikely to<br />
support extension of resuscitation services unless they can be<br />
shown to represent money well spent.<br />
I am grateful for the support of a Royal College of General Practitioners<br />
Upjohn Travell<strong>in</strong>g Fellowship which enabled me to undertake<br />
this study, and for the help and hospitality extended by all<br />
whom I contacted, <strong>in</strong> particular Dr Hugh Bethell (Alton), Mr Cliff<br />
Beaver (Avon), Mr R Gra<strong>in</strong>ger and Mr L Relf (Brighton), Mr<br />
George James (Gloucester), Professor John Hampton (Nott<strong>in</strong>gham),<br />
Mr Geoff Plumb and Mr Peter Scott (Oxford), and Mr Eddie Semon<br />
(York).<br />
References<br />
t Office of Population Censuses and Surveys. Mortallty statistics 1979:<br />
England and Wales. London: H<strong>MS</strong>O, 1981.<br />
¯ American<br />
monary resuscitation<br />
Heart Association.<br />
and emergency<br />
Standards<br />
care.<br />
and guidel<strong>in</strong>es<br />
JAMA 1980;244:453-509.<br />
for cardiopul-<br />
s Department of Health and Social Security. Health Servic~ Development.<br />
Ambulance Serolce: advanced tra<strong>in</strong><strong>in</strong>g for ambulancema~. London:<br />
DHSS, 1976. (HN(76)204.)<br />
4 Briggs RS, Brown PM, Crabb ME, et al. The Brighton resuscitation<br />
ambulances: a cont<strong>in</strong>u<strong>in</strong>g experiment <strong>in</strong> prehnspital care by ambulance<br />
staff. Br Med J 1976;ii:1161-5.<br />
i Mack<strong>in</strong>tosh AF, Crabb ME, Gra<strong>in</strong>ger R, et al. The Brighton resuscitation<br />
ambulances: review of 40 consecutive survivors of out-of-hospital<br />
cardiac arrest. Br MedJ 1978;i:1115-8.<br />
¯ Hampton JR1 Nicholas C. Randomised trial of a mobile coronary care unit<br />
for emergency calls. Br MedJ 1978;i:1118-21.<br />
7 Hampton JR, Dowl<strong>in</strong>g M, Nicholas C. Comparison of results from a<br />
cardiac ambulance manned by medical or non-medical personnel<br />
Lancet 19771i:526-9.<br />
8 Rawl<strong>in</strong>s DC. Study of the management of suspected cardiac <strong>in</strong>farction<br />
by British immediate care doctors. Br MedJ 1981;282:16T7-9.<br />
* Thompson.RG, Hallstrom AP, Cobb LA. BysumderTim~tiat.e! :1 ..c~.diopulmonary<br />
resuscitanon m the management ot venmcmar nonttatton.<br />
Annals Intern Med 1979;90:737-40.<br />
four times that of the general population, t Women have a higher<br />
mortality <strong>in</strong> the first year but fare similarly thereafter. Most of the<br />
deaths will be cardiac. Thirteen per cent of Fram<strong>in</strong>gham men and<br />
40% of women had a further non-fatal myocardial <strong>in</strong>farction with<strong>in</strong><br />
five years of the first attack. The Fram<strong>in</strong>gham data are important<br />
because they <strong>in</strong>clude all eases of myocardial <strong>in</strong>farction occurr<strong>in</strong>g <strong>in</strong> a<br />
def<strong>in</strong>ed community irrespective of whether they were admitted to<br />
hospital. Considerably more <strong>in</strong>formatiofi is available from studies of<br />
subjects discharged from hospital after myocardial <strong>in</strong>farction. Lurla<br />
assembled 10 069 subjects who had recovered from acute myocardial<br />
<strong>in</strong>farction from various studies and noted that five year mortality<br />
dusters at 30% to 35%.* Many of these studies, however, <strong>in</strong>cluded<br />
subjects with previous episodes of_myocardia! <strong>in</strong>faret<strong>in</strong>n. A recent<br />
study from this side of the Atlantic reported -on the mortality of men -<br />
under 60 surviv<strong>in</strong>g tbeir first myocardial <strong>in</strong>farction or episode of<br />
unstable ang<strong>in</strong>a b~- at least 28 days. ~ For m3ioeardial <strong>in</strong>faretlon2<br />
five, 10, and 15 year mortality percentages were 2,2, 40, and 59, rather<br />
more than three times that of the general population. This paper<br />
conta<strong>in</strong>s a review of 22 other studies of post<strong>in</strong>farction mortality.<br />
Subjects more likely to die after myocardial <strong>in</strong>farction are older;<br />
those with larger <strong>in</strong>farcts as evidenced by complications such as<br />
heart failure; hypertensive subjects; and those who cont<strong>in</strong>ue to<br />
smoke. Beta-blockade may improve survival <strong>in</strong> suitable subjects but<br />
this effect is modest and probably less than the effect of stopp<strong>in</strong>g<br />
smok<strong>in</strong>g.~t M GRAHAM, consultant cardiologist, Dubl<strong>in</strong>.<br />
t Kannel WB Sorlic P McNamara PM. Prognosis after <strong>in</strong>itial myocardial <strong>in</strong>farction:<br />
the Fram~ngham study. AmJ Cardlol 1979;44:53-9.<br />
t Lurla MH, Knoke JD, Wach¯ JS, Luria MA. Survival after recovery from acute<br />
myocardial <strong>in</strong>farction. Two and five year prognostic <strong>in</strong>dices. Am ~ JVled 1979;<br />
Graham 67:7-14. I, Mulcahy R, Hickey N, O’Neill W, Daly L. Natural hi¯tory of coronary<br />
heart disease: a study of 586 men surviv<strong>in</strong>g an <strong>in</strong>itial acute attack. Am HeartJ<br />
1983; 105:249-57.
Who scores<br />
<strong>in</strong> trauma?<br />
David Steedman and Col<strong>in</strong> R0berts0n<br />
Trauma is the commonest cause of death<br />
between the ages of I and 34 years <strong>in</strong> the<br />
United K<strong>in</strong>gdom¯ I Improvements <strong>in</strong><br />
prehospital care and trauma management<br />
with<strong>in</strong> hospital are necessary if reductions<br />
are to be achieved." Quantitative measures<br />
of the severity of <strong>in</strong>jury, of proven<br />
reliability and validity, are essential to<br />
permit appropriate resource allocation, the<br />
prediction of outcome and the evaluation<br />
of emergency medical care, 3’4<br />
Estimatesof<strong>in</strong>jury severity appear <strong>in</strong> the<br />
earliest known surgical text, the Smith<br />
I’apyrus. s <strong>in</strong> World War !! a system was<br />
,~ i~tcwhich sments of depended blood loss, on cl<strong>in</strong>ical but it was crude,<br />
ult to apply and lacked a numerical<br />
scale/’The first widely recognised <strong>in</strong>jury<br />
~calc was developed for <strong>in</strong>vestigation of<br />
light aircraft accidents7 and later applied to<br />
road traffic accidents by the Cornell<br />
Injuries Research Group.S Over the next 20<br />
years a variety of systems emerged from<br />
multidiscipl<strong>in</strong>ary crash <strong>in</strong>vestigation<br />
teams, but they were often not comparable<br />
and each had limitations. ~ An attempt to<br />
establish a uniform rat<strong>in</strong>g system and<br />
standardise the language used <strong>in</strong> describ<strong>in</strong>g<br />
<strong>in</strong>juries led to the development of the first<br />
Abbreviated lnjurv Scale (AIS) <strong>in</strong> 1971. ~(~<br />
The latest revision’AIS 85 ~l conta<strong>in</strong>s more<br />
than 1201) separate <strong>in</strong>jury descriptions.<br />
¯ Abbreviated’ refers to the assignment of<br />
a s<strong>in</strong>gle code number on a scale of I (m<strong>in</strong>or<br />
<strong>in</strong>jury) to 6 (major <strong>in</strong>jury--unsurvivable<br />
with current techniques) for specific<br />
<strong>in</strong>juries. The AIS is non-l<strong>in</strong>ear and has<br />
when applied to patients with<br />
~ ationS<br />
pie <strong>in</strong>juries as it is not possiblc to<br />
derive an anthmchc mean value. "<br />
However it is utilised <strong>in</strong> the derivation of<br />
the lnjurv Severity Score (ISS) to assess<br />
multiply <strong>in</strong>jured patientsfl ~<br />
The ISS is the most widely used system<br />
for measur<strong>in</strong>g the cumulative effects of<br />
¯ 14<br />
<strong>in</strong>juries. For scormg purposes, the bodyis<br />
divided <strong>in</strong>to six regions: head and neck:<br />
face; chest; abdom<strong>in</strong>al and pelvic contents;<br />
limbs and pelvic girdle; and external.<br />
With<strong>in</strong> each body region an AIS code is<br />
assigned to each <strong>in</strong>jury¯ The ISS is<br />
calculated by summ<strong>in</strong>g the squares of the<br />
highest A IS code <strong>in</strong> each of the three most<br />
Dr Steedman is a ,Senior Registrar and Dr<br />
Robertson a Cort~ultant <strong>in</strong> the Departments<br />
of <strong>Accident</strong> and Emergency Medic<strong>in</strong>e of the<br />
Royal <strong>in</strong>firmary and Western (;eneral<br />
l lospital, Ed<strong>in</strong>burgh.<br />
severely <strong>in</strong>jured body regions. The ISS has<br />
been shown to correlate closely with<br />
morbidity and mortality from road traffic<br />
is<br />
accidents " and other types of blunt<br />
trauma. 1~,,17 The importance of age<br />
weight<strong>in</strong>g <strong>in</strong> mortality studies has been<br />
confirmed by Bull; Ls and by us<strong>in</strong>g Probit<br />
analysis ’LD 50" values can be derived for<br />
different age groups, based on the ISS.<br />
Effective systems for prehospital triage<br />
are fundamental to the provision of<br />
emergency care for trauma patients,<br />
Indices of severity based on physiological<br />
parameters,~S 2°obta<strong>in</strong>able at accident<br />
scenes, assist <strong>in</strong> identify<strong>in</strong>g high risk<br />
patients and permit appropriate allocation<br />
of available resources. One such system,<br />
the Trauma Score (TS) devised by<br />
Champion and co-workers, 2~ comb<strong>in</strong>es<br />
cardiorespiratory parameters and the<br />
Glasgow Coma Scale 22 and has been<br />
correlated with patient outcome <strong>in</strong> nearly<br />
40110 trauma patients. 23 An important<br />
application of the Trauma Score is <strong>in</strong><br />
comlf<strong>in</strong>ation with the Injury Severity<br />
Score, when comparisons can be made<br />
between predicted and actual patient<br />
outcome, thus provid<strong>in</strong>g a useful <strong>in</strong>dex of<br />
patient care--the TRISS metbodok~gy<br />
(Traun~a Score, ISS, age comb<strong>in</strong>ation<br />
<strong>in</strong>dex).-’4<br />
Trauma constitutes a major health<br />
problem <strong>in</strong> the United K<strong>in</strong>gdom: however<br />
research <strong>in</strong> this field has]acked the<br />
necessary f<strong>in</strong> anci al support de spite cl aims<br />
that the quality of patient care is less than<br />
2~ 26<br />
optimal. -’ While’thecurrently available<br />
,scor<strong>in</strong>g systems are not perfect (for<br />
example difficulty arises <strong>in</strong> scor<strong>in</strong>g<br />
penetrat<strong>in</strong>g <strong>in</strong>jury us<strong>in</strong>g the ISS) future<br />
ref<strong>in</strong>ements <strong>in</strong> their methodology and<br />
application will improve their accuracy.<br />
Even so: thcy provide powerful cl<strong>in</strong>ical and<br />
research tools. Their adoption by research<br />
z7 i<br />
¯<br />
teams, ntensl "v" ists zs and <strong>Accident</strong> and<br />
Emergency cl<strong>in</strong>icians29 will facilitate audit<br />
and direct improvements <strong>in</strong> the<br />
management traum a victims.<br />
References<br />
I. Office of Population Census and Surveys.<br />
Deaths by cause. 198.5. I.,ondon:<br />
Government Statistical Service, 1986.<br />
2. Tnmkey 1). Trauma. Scientific American<br />
1983; 249: 2(I--7.<br />
3. Gibson G. Indicesofseverity for emer’gency<br />
medical evaluative studies. Int J Health Serv<br />
1981 : I I: 597-5,,22.<br />
4. Caytcn (’(;, Fvans W, Severity <strong>in</strong>dices and<br />
their implications for Ihc cmcrgency medical<br />
services research and evaluation. J Trauma<br />
1979; lq: 98-102.<br />
5. Breasted JH. 1"he Edw<strong>in</strong> Smith Papyrus.<br />
Chicago: The University of Chicago Press,<br />
19~).<br />
6. Grant RT. Ment’orandum on the<br />
ob~rvat ions required <strong>in</strong> cases of wound<br />
shock. BMJ 1941; 2: 332-6.<br />
7. DeHaven H. The site. frequency and<br />
dangerousness of <strong>in</strong>jury susta<strong>in</strong>ed by g00<br />
survivors of light plane accidents. Crash<br />
<strong>in</strong>jury research. New York: Cornell<br />
University. 1952.<br />
8. Ryan G A. Garret JW. A quantitative scale of<br />
impact <strong>in</strong>jury. Publication CA I. No.<br />
VT- 1823- R34. Buffalo: Cornell I Iniversity,<br />
1968.<br />
9. Petrucelli E. States JD, Ha<strong>in</strong>es LH. The<br />
Abbreviated Injury Scale: evolution, usage<br />
and future adaptability. Accid Anal Prey<br />
1981 ; 13: 29-35,<br />
10. Committee on medical aspects of automotive<br />
safety. Rat<strong>in</strong>g the severity of ti~ue damage<br />
I : The Abbreviated Scale, JA MA 1971 ; 215:<br />
277-80,<br />
11. Committee on <strong>in</strong>jury scal<strong>in</strong>g. The<br />
Abbreviated Iniury Scale: 1985 Revision.<br />
American Association for Automotive<br />
Medic<strong>in</strong>e, 1985.<br />
12. BulIJP. Measuresoftheseverityof<strong>in</strong>jury,<br />
Injury 1978; 8:184-7.<br />
13. Baker SP, @’Neill B, Hadden W, Jr Long<br />
WB. The Injury ,Severity ,Score: a method for<br />
de~rib<strong>in</strong>gpatients with multiple <strong>in</strong>juries and<br />
evaluat<strong>in</strong>g emergency care. J Trauma 1974;<br />
14: 187-96.<br />
14. Baker SP, O’Neill B. The Injury Severity<br />
Score: an update. J Trauma 1076; 16: ~82-5.<br />
15. Bull JP. The Injury Severity Score of road<br />
traffic casualties <strong>in</strong> relation to mortality,<br />
time of death, hospital treat meat time and<br />
disability. AccidAnal Prev 1975; 7: 24q-55.<br />
16. SemmlowJ.L,Cone R. Utilityofthe Injury<br />
Severity Score: a confirmation, lteahh Serv<br />
Res 1976; I I: 4.5-52.<br />
17, Stoner liB, Barton RN, Little RA. Yates<br />
DW. Measur<strong>in</strong>g the ~verity of <strong>in</strong>jury¯ BMJ<br />
1977; 2: 1247-9.<br />
18. Kirkpatrick JR. YoiJmans RL. Trauma<br />
Index¯ An aide <strong>in</strong> the evaluation of <strong>in</strong>jury<br />
victims. J Trauma 1971 ; I I : 71 I- 14.<br />
19. Champion HR, Sacco WJ. tlannan DS,<br />
Leppcr RI,, el al, A~scssment of <strong>in</strong>jury<br />
severity: The Triage Index. (’tit (’are Med<br />
1980;8:201-8.<br />
20. Gormican SP. CRA <strong>MS</strong> Scale: field triage of<br />
trauma victims. Ann Emerg Med 1982; I 1:<br />
132-5.<br />
21. Champion H R, Sacco WJ. Camazzo A J,<br />
Copes W, Fouty WJ. Trauma Score. Crit<br />
CareMed 1981 ;9: 672-6.<br />
22, TeasdaleG.Jennet B. As~smentofcoma<br />
and impaired qonsciousne~s: a practical<br />
scale. Lancet 1974; 2: 81-4.<br />
23. Champion HR. Field triage 0ftrauma<br />
patients. Ann Emerg Med 1982; I 1 : 160-1.<br />
24. Champion HR, Sacco WJ. Hunt TK,<br />
Trauma severity scor<strong>in</strong>g to predict mortality.<br />
WorldJ Surg 1983" 7:4--11.<br />
25, The responsibility of emergency medic<strong>in</strong>e<br />
towards the prevention of road accidents.<br />
Arch Emerg Med 1986, 3: 157-76.<br />
26. Trunkey D. Towards optimal trauma care.<br />
Arch Emerg Med 1986: 2: 181-95.<br />
27. Little RA, Frayn KN, Randall PE. Stoner<br />
HB. Maycock PF. Plasma catecholam<strong>in</strong>e<br />
concentrations <strong>in</strong> acute states of stress and<br />
trauma. Arch Emerg Med 1985; 2: 46-7.<br />
28, MorganCJ, Branthwaite MA. Severity<br />
scor<strong>in</strong>g <strong>in</strong> <strong>in</strong>tensive care. BMJ 1986; 292:<br />
1546.<br />
29. Steedman D J, Robertson CE. AOUADS:<br />
an objective evaluation of<br />
their role <strong>in</strong> trauma. J Roy ColI Surg Ed<br />
1986; 31 : 80--4.<br />
-- (’ARI OI:TIII:CRrFR’AI I YII I MAY/JI.INE 11:/87 VOI.3NO3
e<br />
e<br />
ORIGINAL CONTRIBUTION<br />
emergency medical services, cardiac arrest, <strong>in</strong>-hospital resuscitation;<br />
resuscitation, cardiac arrest<br />
In-Hospital Resuscitation Follow<strong>in</strong>g<br />
Unsuccessful Prehospital Advanced<br />
Cardiac Life Support: ’Heroic Efforts’<br />
Or an Exercise <strong>in</strong> Futility?.<br />
From our emergency department logbook we identified 281 consecutive patients<br />
transported to the Regional Medical Center at Memphis follow<strong>in</strong>g<br />
failed prehospital advanced cardiac life support (ACLS). Medical records<br />
were obta<strong>in</strong>ed for 240 cases (85.4%). Initial cardiac rhythms <strong>in</strong> the EL) <strong>in</strong>cluded<br />
ventricular fibrillation or pulseless ventricular tachycardia (29%),<br />
electromechanical dissociation (18%), and asystole (51%). Thirty-two patients<br />
(13.3%) were successfully resuscitated <strong>in</strong> the EL), but only four (1.7%)<br />
survived to hospital discharge. Two patients had good neurologic outcomes;<br />
both degenerated to cardiac arrest shortly prior to arrival <strong>in</strong> the EL). The<br />
rema<strong>in</strong><strong>in</strong>g two survivors were discharged to nurs<strong>in</strong>g homes with severe neurologic<br />
deficits. Of the 41 cases for whom no medical records could be<br />
found, 39 were noted <strong>in</strong> our logbook to have died <strong>in</strong> the EL). No record of<br />
subsequent hospital admission could be found for the other two. Both are<br />
presumed to have died. Failure to respond to prehospital ACLS predicts nonsurvival<br />
and may warrant cessation of efforts <strong>in</strong> the field. Future programs<br />
and research efforts <strong>in</strong> the management of out-of-hospital cardiac arrest<br />
should be focused on optimal provision of prehospital care prior to the onset<br />
of irreversible deterioration. [Kellermann AL, Staves DR, Hackman BB: Inhospital<br />
resuscitation follow<strong>in</strong>g unsuccessful prehospital advanced cardiac<br />
life support: ’Heroic efforts’ or an exercise, <strong>in</strong> futility? Ann Emerg IVied lane<br />
1988;17:589-594.]<br />
INTRODUCTION<br />
Despite two decades of dramatic advances <strong>in</strong> emergency cardiac care, a<br />
majority of victims of out-of-hospital cardiac arrest fail to respond to prehospital<br />
efforts at resuscitation.Va In many metropolitan areas, paramedics<br />
emergently transport patients who fail to respond to prehospital advanced<br />
cardiac life support IACLS) to the nearest hospital for cont<strong>in</strong>ued efforts at<br />
resuscitation.<br />
A decision to transport a patient <strong>in</strong> refractory cardiac arrest commits a<br />
paramedic crew to hazardous high-speed driv<strong>in</strong>g. The emergency department<br />
must rapidly mobilize available personnel to cont<strong>in</strong>ue the attempt of resuscitation.<br />
Any patient successfully resuscitated then is admitted to an <strong>in</strong>tensive<br />
care unit, often for a stormy hospital course.<br />
Reports have failed to focus on this important subgroup of patients. Information<br />
regard<strong>in</strong>g the cl<strong>in</strong>ical outcomes of these patients has been scant. No<br />
studies have directly exam<strong>in</strong>ed the personnel and monetary costs associated<br />
with decisions to cont<strong>in</strong>ue resuscitation efforts despite unsuccessful prehospital<br />
ACLS. Our study was conducted to exam<strong>in</strong>e these issues.<br />
METHODS<br />
The Regional Medical Center at Memphis is a 435-bed, adult, acute care<br />
hospital supported, <strong>in</strong> part, by the government of Shelby County, Tennessee.<br />
The hospital and its ED are staffed by residents and faculty of the University<br />
of Tennessee, Memphis. The ED at the Regional Medical Center averages<br />
65,000 visits annually and is the po<strong>in</strong>t of entry for three-quarters of all nonobstetric<br />
admissions.<br />
Emergency medical services {E<strong>MS</strong>) for the City of Memphis are provided<br />
by the Memphis Fire Department {MFD) E<strong>MS</strong> Bureau. The Bureau operates<br />
14 ambulances staffed by two paramedics each, who are authorized to pro-<br />
17:6 June 1988 Annals of Emergency Medic<strong>in</strong>e<br />
Arthur L Kellermann, MD, MPH<br />
Diane R Staves, MD<br />
Bela B Hackman, MD<br />
Memphis, Tennessee<br />
From the Departments of Medic<strong>in</strong>e<br />
and Community Medic<strong>in</strong>e, University<br />
of Tennessee, Memphis, Tennessee.<br />
Received for publication August 20, 1987.<br />
Revision received January 18, 1988.<br />
Accepted for publication February 10.<br />
1988.<br />
Presented at the Society for General<br />
nternal Medic<strong>in</strong>e National Meet<strong>in</strong>g <strong>in</strong><br />
San Diego, California. April 1987.<br />
Address for repr<strong>in</strong>ts: Arthur Kellermann,<br />
MD. MPH, Division of Emergency<br />
Medic<strong>in</strong>e, Department of Medic<strong>in</strong>e. 877<br />
Jefferson. Room G071. Memphis.<br />
Tennessee 38103.<br />
589/63<br />
I
OA<br />
~p<br />
UNSUCCESSFUL PREHOSPITAL RESUSCITATION<br />
Kellermann, Staves & Hackman<br />
FIGURE 1. Outcome of refractory prehospital<br />
carch’ac arrest.<br />
vide ACLS under the medical control<br />
of on-l<strong>in</strong>e physicians. All units carry<br />
defibrillators. S<strong>in</strong>ce 1979, all units also<br />
have been equipped with-automatic,<br />
oxygen-powered cardiopulmonary resuscitators.<br />
Paramedics are authorized<br />
to perform endotracheal <strong>in</strong>tubation<br />
and adm<strong>in</strong>ister a wide range of cardiac<br />
drugs. MFD paramedic response times<br />
for emergency runs average five m<strong>in</strong>utes<br />
from call to arrival on scene.<br />
Dur<strong>in</strong>g the study <strong>in</strong>terval, all MFD<br />
paramedic units followed the 1980 to<br />
1986 guidel<strong>in</strong>es for cardiac resuscitaion<br />
developed by the American Heart<br />
ssociation.4 In cases <strong>in</strong>volv<strong>in</strong>g ven-<br />
tricular fibrillation or pulseless ventricular<br />
tachycardia, paramedics were<br />
authorized to deliver up to three defibrillatory<br />
shocks prior to establish<strong>in</strong>g<br />
contact with an on-l<strong>in</strong>e physician.<br />
Additional resuscitative measures meluded<br />
immediate endotracheal <strong>in</strong>tubation,<br />
hyperventilation with oxygen,<br />
establishment of peripheral venous<br />
access, and adm<strong>in</strong>istration of IV ep<strong>in</strong>ephr<strong>in</strong>e,<br />
lidoca<strong>in</strong>e, and/or atrop<strong>in</strong>e as<br />
<strong>in</strong>dicated.<br />
Accord<strong>in</strong>g to MFD statistics, onscene<br />
time <strong>in</strong> cases <strong>in</strong>volv<strong>in</strong>g unsuccessful<br />
prehospital resuscitation averages<br />
approximately 22 m<strong>in</strong>utes. S Unfortunately,<br />
comprehensive records of<br />
each prehospital cardiac resuscitation<br />
were not kept dur<strong>in</strong>g the study <strong>in</strong>terval.<br />
Therefore, case-specific data regard<strong>in</strong>g<br />
<strong>in</strong>dividual cardiac arrest cirumstances<br />
and details regard<strong>in</strong>g each<br />
rehospital resuscitation attempt were<br />
unavailable. Dur<strong>in</strong>g the study <strong>in</strong>terval,<br />
all MFD cardiac arrest patients who<br />
failed to respond to prehospital ACLS<br />
received cont<strong>in</strong>uous mechanical CPR<br />
dur<strong>in</strong>g emergency transportation to<br />
the nearest hospital.<br />
We retrospectively identified,<br />
through our ED logbook, all adult<br />
patients transported to the Regional<br />
Medical Center at Memphis by ambulance<br />
follow<strong>in</strong>g nontraumatic, outof-hospital<br />
cardiac arrest who arrived<br />
without a palpable pulse or blood<br />
pressure between November 11, 1983,<br />
and January 6, 1986. A total of 219<br />
cases were identified. In addition, we<br />
prospectively identified 62 cases between<br />
January 7 and December 15,<br />
1986. Patients who arrived by automobile<br />
and patients who susta<strong>in</strong>ed a<br />
cardiac arrest only after arrival <strong>in</strong> the<br />
64/590<br />
1<br />
¯ Died <strong>in</strong> ED<br />
28 (11.7%)<br />
ED were excluded. Pa<strong>in</strong>stak<strong>in</strong>g file<br />
searches through medical records<br />
yielded 240 of 281 charts (85.4%).<br />
All available records were reviewed<br />
by one of the authors to identify the<br />
present<strong>in</strong>g cardiac rhythm <strong>in</strong> the ED,<br />
total time of the ED resuscitation<br />
effort, major ED management, and ED<br />
outcome. We def<strong>in</strong>ed a "successful" resuscitation<br />
as reestablishment of a<br />
pulse and blood pressure sufficient to<br />
susta<strong>in</strong> life and permit admission of<br />
the patient to an ICU. For patients resuscitated<br />
<strong>in</strong> the ED and admitted to<br />
the hospital, we noted length of hospital<br />
stay, hospital outcome, and disposition.<br />
Functional status at discharge<br />
was determ<strong>in</strong>ed us<strong>in</strong>g implicit criteria<br />
(ie, good recove~ able to return home<br />
without significant deficits; moderate<br />
disability’ able to return home but requir<strong>in</strong>g<br />
assistance with some aspects<br />
of daily life; severe disability" dependent<br />
on others for daily support).<br />
Estimates of ED personnel use were<br />
calculated us<strong>in</strong>g documented durations<br />
of ED resuscitation and conservative<br />
estimates of the total number<br />
of personnel <strong>in</strong>volved. ED charges for<br />
cardiac resuscitation are the same regardless<br />
of the duration of the resuscitation<br />
attempt or the total number of<br />
personnel <strong>in</strong>volved. ICU and ward bed<br />
charges were calculated based on documented<br />
lengths of stay and standard<br />
hospital room charges. Medications,<br />
Annals of Emergency Medic<strong>in</strong>e<br />
(n = 240)<br />
4 (1.6%)<br />
208 (86.7%)<br />
[] Died <strong>in</strong> hospital [] Survived to discharge<br />
supplies, and professional fees were<br />
not <strong>in</strong>cluded. All charges are expressed<br />
<strong>in</strong> 1986 dollars.<br />
RESULTS<br />
Absence of a pulse was confirmed<br />
on arrival to the ED <strong>in</strong> all 240 cases <strong>in</strong><br />
which documentation was available.<br />
Two hundred eight of 240 patients<br />
(87%) were <strong>in</strong>tubated successfully prior<br />
to arrival; the rema<strong>in</strong>der were be<strong>in</strong>g<br />
ventilated by esophageal obturator mrway<br />
or bag-valve-mask. Endotracheal<br />
<strong>in</strong>tubation was completed m all cases<br />
with<strong>in</strong> two m<strong>in</strong>utes follow<strong>in</strong>g arrival<br />
<strong>in</strong> the ED.<br />
Present<strong>in</strong>g cardiac rhythms <strong>in</strong> the<br />
ED <strong>in</strong>cluded ventricular fibrillation or<br />
pulseless ventricular tachycardia <strong>in</strong> 69<br />
cases (29%), electromechanical dissociation<br />
(EMD) <strong>in</strong> 43 (18%), asystole<br />
<strong>in</strong> 122 (51%), and other rhythms <strong>in</strong> six<br />
(2.5%). Follow<strong>in</strong>g arrival, resuscitation<br />
efforts followed 1980 to 1986 ACLS<br />
guidel<strong>in</strong>es. 4 Transthoracic or transvenous<br />
pac<strong>in</strong>g was attempted <strong>in</strong> 30<br />
cases (13%); successful capture was<br />
noted <strong>in</strong> 19 (8%), but pulses were established<br />
<strong>in</strong> only three (1%). Pericardiocentesis<br />
was attempted <strong>in</strong> 19 (8%)<br />
cases, but transient cl<strong>in</strong>ical benefit<br />
was noted <strong>in</strong> only one.<br />
In the ED, physicians were able to<br />
successfully reestablish a pulse and<br />
blood pressure <strong>in</strong> 32 of 240 cases<br />
(13.3%). Patients found to be <strong>in</strong> ven-<br />
17:6 June 1988<br />
i
e<br />
e<br />
Cases<br />
12<br />
10<br />
8<br />
6<br />
4<br />
2<br />
0 1<br />
(N = 32)<br />
[] Survived to discharge ¯ Died dur<strong>in</strong>g hospitalization<br />
7 9 11 13 15 17 19 21 23 25 27 29 31 33 35 37 39 41<br />
Number of days 2<br />
TABLE 1. ED and hospital room charges follow<strong>in</strong>g refractory prehospital<br />
carch’ac arrest<br />
(N = 281)<br />
ED $284/case x 281 cases - $ 79,804<br />
ICU $554/day x 119 days - $ 65,926<br />
Ward $212/day x 70 days -$ 14,840<br />
Total $160,570<br />
Charges expressed ~n 1986 dollars; excludes charges for drugs, laboratory, supplies.<br />
and professional fees.<br />
tricular fibrillation or pulseless ventricular<br />
tachycardia on arrival to the<br />
ED were resuscitated more often than<br />
patients found <strong>in</strong> other rhythms (22%<br />
vs 9.9%; chi-square P < .02). All patients<br />
successfully resuscitated were<br />
admitted to an ICU.<br />
Only four patients (1.6%) survived<br />
to hospital discharge (Figure 1). Despite<br />
more frequent <strong>in</strong>itial resuscitation,<br />
patients who presented to the<br />
ED with ventricular fibrillation or<br />
pulseless ventricular tachycardia were<br />
no more likely to survive to hospital<br />
discharge (two of 69 [2.9%] vs two of<br />
171 [1.2%]; chi-square P = .22). One<br />
of these four survivors actually responded<br />
to prehospital ACLS with reestablishment<br />
of a pulse and blood<br />
pressure at the scene but had a second<br />
cardiac arrest less than two m<strong>in</strong>utes<br />
prior to arrival at the Regional Medical<br />
Center. A second patient deteriorated<br />
en route from ventricular tachycardia<br />
with a pulse and blood pressure<br />
to ventricular fibrillation shortly before<br />
arrival. Both were resuscitated<br />
and subsequently discharged home<br />
with good neurologic outcomes.<br />
The rema<strong>in</strong><strong>in</strong>g two patients failed<br />
to respond at any po<strong>in</strong>t to prehospital<br />
ACLS but were resuscitated successfully<br />
<strong>in</strong> the ED. Both were eventually<br />
17,6 June 1988<br />
discharged to nurs<strong>in</strong>g homes with severe<br />
neurologic deficits follow<strong>in</strong>g<br />
prolonged hospital stays (Figure 2).<br />
Of the 41 patients for whom no record<br />
could be found, 39 were noted <strong>in</strong><br />
our logbook to have died <strong>in</strong> the ED. In<br />
the rema<strong>in</strong><strong>in</strong>g two cases, no specific<br />
ED outcome was recorded. A search of<br />
<strong>in</strong>patient files and ICU admission logbooks<br />
failed to reveal the name of<br />
either patient with<strong>in</strong> 24 hours of arrival<br />
<strong>in</strong> the ED. Both are presumed to<br />
have died.<br />
Resuscitation attempts were cont<strong>in</strong>ued<br />
<strong>in</strong> the ED a mean of 33.2 +<br />
16.6 m<strong>in</strong>utes (range, six to 163 m<strong>in</strong>utes).<br />
The respond<strong>in</strong>g team usually<br />
consisted of a staff physician, a resident,<br />
one to two <strong>in</strong>terns, two ED<br />
nurses, a ward clerk, and an anesthesiologist<br />
or certified nurse anesthetist.<br />
Total personnel time spent <strong>in</strong> resuscitation<br />
attempts exceeded 1,100 personhours.<br />
Dur<strong>in</strong>g our study <strong>in</strong>terval the standard<br />
hospital charge associated with<br />
an ED resuscitation at the Regional<br />
Medical Center was $284, regardless<br />
of the duration of the resuscitation or<br />
consumption of supplies. The 32 patients<br />
successfully resuscitated <strong>in</strong> the<br />
ED spent a total of 119 days <strong>in</strong> an ICU;<br />
70 days were spent on general medical<br />
Annals of Emergency Medic<strong>in</strong>e<br />
;FI;<br />
FIGURE 2. Outcome of refractory prehospital<br />
cardiac arrest -- length of<br />
hospital stay.<br />
wards. The 1986 room rate for a day <strong>in</strong><br />
the ICU was $554; the room charge<br />
for a ward bed was $212. Based on<br />
these figures, total ED and hospital<br />
room charges for the study group exceeded<br />
$160,000 (Table 11.<br />
DISCUSSION<br />
S<strong>in</strong>ce the pioneer<strong>in</strong>g work of Pantridge<br />
and Geddes,6, 7 prehospital<br />
emergency cardiac care has become<br />
established <strong>in</strong> many major metropolitan<br />
centers. Cobb, 8 Nagel,9 Eisenberg,<br />
lo and others n have shown that<br />
well-tra<strong>in</strong>ed paramedics can reliably<br />
deliver defibrillatory shocks, start IV<br />
l<strong>in</strong>es, perform endotracheal <strong>in</strong>tubation,<br />
and successfully resuscitate<br />
many victims of out-of-hospital cardiac<br />
arrest. In 1980, Eisenberg, Copass,<br />
Hallstrom, et all2 demonstrated the<br />
superiority of prehospital ACLS <strong>in</strong><br />
comparison to basic EMT services.<br />
Of the variables that have been<br />
shown to be associated with suecessful<br />
resuscitation follow<strong>in</strong>g cardiac<br />
arrest, the most important one amenable<br />
to system <strong>in</strong>tervention is the<br />
total duration of time to defibrillation.2,<br />
a In cases <strong>in</strong>volv<strong>in</strong>g delays to defibrillation<br />
of more than three to four<br />
m<strong>in</strong>utes, early prowsion of CPR improves<br />
the chances for s:lbsequent resuscltation,3,4,1a,<br />
14 Most patients who<br />
respond to prehospital emergency cardiac<br />
care do so early <strong>in</strong> a resuscitation<br />
effortA5 Few survive resuscitation attempts<br />
last<strong>in</strong>g longer than 30 m<strong>in</strong>utes.<br />
16<br />
Given these clearly developed pr<strong>in</strong>ciples,<br />
it is no surprise that patients<br />
who fail to respond to prehospital<br />
ACLS rarely survive emergency trans-<br />
591/65<br />
I<br />
|
~ tudy<br />
UNSUCCESSFUL PREHOSPITAL RESUSCITATION<br />
Kellermann, Staves & Hackman<br />
portation to the hospital for subsequent<br />
efforts at <strong>in</strong>-hospital resuscitation.<br />
Fewer still survive to hospital<br />
discharge. While patients <strong>in</strong> our study<br />
arriv<strong>in</strong>g <strong>in</strong> ventricular fibrillation or<br />
ventricular tachycardia were more frequently<br />
resuscitated <strong>in</strong> the ED, it appears<br />
that the prolonged period of<br />
CPR associated with these cases precluded<br />
long-term survival with good<br />
neurologic function. If the two patients<br />
<strong>in</strong> our series who ma<strong>in</strong>ta<strong>in</strong>ed a<br />
spontaneous pulse and blood pressure<br />
until two m<strong>in</strong>utes prior to arrival at<br />
our hospital are excluded, no patient<br />
<strong>in</strong> our series could be considered to<br />
have had a satisfactory outcome.<br />
Several potential limitations to our<br />
deserve comment. All of our<br />
atients were adult victims of nontraumatic<br />
cardiac arrest. Conclusions<br />
based on a series of adult patients may<br />
not apply to prolonged resuscitation<br />
attempts <strong>in</strong>volv<strong>in</strong>g pediatric patients..<br />
Likewise, persons susta<strong>in</strong><strong>in</strong>g cardiac<br />
arrest follow<strong>in</strong>g penetrat<strong>in</strong>g trauma<br />
have been shown to benefit from a<br />
comb<strong>in</strong>ation of aggressive prehospital<br />
care, rapid transport, and immediate<br />
<strong>in</strong>-hospital surgical managementAz Conventional wisdom and several<br />
case reports dictate that hypothermic<br />
patients warrant determ<strong>in</strong>ed efforts at<br />
resuscitation and adequate rewarm<strong>in</strong>g~<br />
because an unknown number of victims<br />
of severe hypothermia may respond<br />
to prolonged resuscitation and<br />
survive with good neurologic function.<br />
1 S- 20<br />
Prior to June 1986, comprehensive<br />
data regard<strong>in</strong>g the prehospital manement<br />
of cardiac arrest were not col-<br />
~g<br />
lected or ma<strong>in</strong>ta<strong>in</strong>ed by the MFD. We<br />
are, therefore, unable to comment on<br />
the specific circumstances surround<strong>in</strong>g<br />
each cardiac arrest episode or the<br />
precise quality of prehospital cardiac<br />
care. We believe, however, that any mtercommunity<br />
differences m the quality<br />
of prehospital cardiac care are likely<br />
to be reflected <strong>in</strong> vary<strong>in</strong>g rates of<br />
prehospital resuscitation, rather than<br />
<strong>in</strong> different rates of subsequent <strong>in</strong>-hospital<br />
resuscitation.<br />
Some may consider our poor rate of<br />
survival follow<strong>in</strong>g unsuccessful prehospital<br />
ACLS to be specific to the<br />
MFD E<strong>MS</strong> bureau or our study <strong>in</strong>stitution.<br />
In a subsequent review of<br />
the literature, we have identified<br />
seven additional studies from six cities<br />
or metropolitan counties <strong>in</strong> which<br />
patients fail<strong>in</strong>g to respond to prehospital<br />
ACLS were transported to the<br />
66/59")<br />
nearest hospital. 9,21-26 Of 1,164 patients,<br />
six (0.5%) were noted to survive<br />
to hospital discharge (Table 2).<br />
Four of these six <strong>in</strong>itially responded to<br />
prehospital ACLS but susta<strong>in</strong>ed a second<br />
cardiac arrest shortly before arrival<br />
<strong>in</strong> the ED. The functional status of<br />
these survivors at discharge was not<br />
specified.<br />
Based on our data and the results of<br />
others, we conclude that failure to respond<br />
to prehospital ACLS on the<br />
scene with reestablishment of a blood<br />
pressure and pulse is highly predictive<br />
of death prior to hospital discharge.<br />
Comb<strong>in</strong><strong>in</strong>g our results with those<br />
noted, only ten of more than 1,440 patients<br />
(0.69%) have been reported to<br />
have survived to hospital discharge<br />
after arriv<strong>in</strong>g <strong>in</strong> cardiac arrest follow<strong>in</strong>g<br />
prehospital ACLS. 9,21-26 Six of<br />
these ten survivors actually had a<br />
pulse and blood pressure at the time<br />
the decision to transport was made. In<br />
<strong>in</strong>dividual cases, failure to respond to<br />
emergency cardiac care may reflect<br />
long down times without CPR, delays<br />
to defibrillation, long E<strong>MS</strong> response<br />
times, refractory <strong>in</strong>itial arrythmias<br />
(eg, asystole), or perhaps other unspecflied<br />
factors. Regardless of the factor(s)<br />
associated with failure to respond <strong>in</strong><br />
any given case, patients unsuccessfully<br />
resuscitated at the scene rarely survive<br />
to hospital discharge.<br />
A decision to transport a patient to<br />
the hospital follow<strong>in</strong>g unsuccessful<br />
prehospital ACLS is associated with<br />
high costs and considerable risks.<br />
More than 1,100 hours of skilled ED<br />
personnel time were <strong>in</strong>volved <strong>in</strong> our<br />
series, a number approximately equal<br />
to one person work<strong>in</strong>g 40 hours a<br />
week for more than six months. The<br />
32 patients resuscitated <strong>in</strong> our ED accounted<br />
for an additional 189 bed-days<br />
of ICU and ward hospitalization. ED<br />
and hospital room charges alone exceeded<br />
$160,000.<br />
In contrast to the ten survivors of<br />
refractory out-of-hospital cardiac arrest<br />
identified by our study and literature<br />
review, 159 motor vehicle deaths<br />
<strong>in</strong>volv<strong>in</strong>g ambulances <strong>in</strong> emergency<br />
use were reported to the National<br />
Highway Traffic Safety Adm<strong>in</strong>istration<br />
between 1977 and 1985.27 Many of<br />
these deaths <strong>in</strong>volved pedestrians,<br />
drivers, or passengers of non-E<strong>MS</strong> vehicles.<br />
The National Association of<br />
State E<strong>MS</strong> directors recently has<br />
noted that 25 EMTs and paramedics<br />
nationwide died as a result of highspeed<br />
ambulance driv<strong>in</strong>g between Jan-<br />
Annals of Emergency Medic<strong>in</strong>e<br />
uary 1, 1983, and May 31, 1986. 28 C<br />
of these deaths <strong>in</strong>volved a MFD par,<br />
medic who died <strong>in</strong> an ambulance accident<br />
<strong>in</strong> 1984.29 While the annual toll<br />
of serious but nonfatal <strong>in</strong>juries as a result<br />
of ambulance-related motor vehicle<br />
accidents is undoubtedly higher,<br />
the magnitude of this figure is unknown.<br />
A few E<strong>MS</strong> systems have adopted<br />
policies that permit paramedic units<br />
to cease efforts <strong>in</strong> the field <strong>in</strong> selected<br />
cases of refractory out-of-hospital cardiac<br />
arrest after consultation with an<br />
on-l<strong>in</strong>e physician, za,2s Based on our<br />
data, we believe these policies justified.<br />
They should be more widely implemented<br />
by well-supervised E<strong>MS</strong><br />
systems offer<strong>in</strong>g comprehensive prehospital<br />
ACLS.<br />
Both of the patients <strong>in</strong> our study<br />
who survived with good neurologic<br />
outcomes and four of the six survivors<br />
identified by our literature review had<br />
a pulse and blood pressure at the time<br />
the decision to transport was made.<br />
Initial response to prehospital ACLS<br />
appears to select those patients who<br />
are likely to benefit from cont<strong>in</strong>ued<br />
emergency cardiac care, because virtuaUy<br />
all ultimately successful resuscitations<br />
follow<strong>in</strong>g out-of-hospital cardiac<br />
arrest are accomplished at the<br />
scene.lS,3o CPR alone rarely susta<strong>in</strong>s<br />
cardiac and cerebral function long<br />
enough to permit successful transport<br />
to an <strong>in</strong>-hospital resuscitation teamA2<br />
Despite consistent CPR by automatic<br />
resuscitation devices, more<br />
than 70% of our patients were <strong>in</strong><br />
asystole or electromechanical dissociation<br />
by the time they arrived <strong>in</strong><br />
our ED. Given the <strong>in</strong>evitable deterioration<br />
that occurs dur<strong>in</strong>g prolonged<br />
CPR, it appears that little is ga<strong>in</strong>ed<br />
from transport<strong>in</strong>g patients <strong>in</strong> refractory<br />
cardiac arrest to expensive hospitalbased<br />
technology.<br />
E<strong>MS</strong> policies that mandate transport<br />
to the nearest hospital <strong>in</strong> cases of<br />
refractory out-of-hospital cardiac arrest<br />
may actually compromise a patient’s<br />
chances for survival by encourag<strong>in</strong>g<br />
a "load and go" approach rather<br />
than determ<strong>in</strong>ed efforts at prehospital<br />
ACLS. Many of the 32 patients resuscitated<br />
<strong>in</strong> the ED dur<strong>in</strong>g our study<br />
might have responded sooner and had<br />
better outcomes if efforts had been<br />
cont<strong>in</strong>ued <strong>in</strong> the field beyond the<br />
po<strong>in</strong>t that a decision to transport was<br />
made. In other than exceptional cases,<br />
high-speed transport to the hospital<br />
should never be considered an accept-<br />
17:6 June 1988
e<br />
e<br />
Miami8<br />
1970-73<br />
TABLE 2. Outcome of patients present<strong>in</strong>g to the ED <strong>in</strong> cardiac arrest despite prehospital ACLS<br />
Brighton, England .18<br />
1974-76<br />
Miami19 235<br />
1975-78<br />
Suburban Kansas City 2o 225<br />
1979<br />
Sacramento County 21 4601-<br />
1979-81<br />
San Francisco 22 49<br />
1986<br />
Milwaukee 23 93<br />
1986<br />
Memphis 281<br />
1984-87<br />
No. Patients<br />
Survived to<br />
Discharge Comments<br />
102 0 Explicit policy to transport nonresponders. Total <strong>in</strong>cludes<br />
only patients <strong>in</strong> refractory ventricular fibrillation follow<strong>in</strong>g<br />
unsuccessful prehospital emergency cardiac care. An<br />
unknown percentage of 199 additional patients shocked<br />
<strong>in</strong>to asystole or EMD. These are not <strong>in</strong>cluded <strong>in</strong> group<br />
total.<br />
@<br />
UNSUCCESSFUL PREHOSPITAL RESUSCITATION<br />
Kellermann, Staves & Hackman<br />
pears to be litde justification for policies<br />
that encourage rapid transport to<br />
the hospital follow<strong>in</strong>g unsuccessful<br />
prehospital ACLS. In the vast majority<br />
of cases, failure to reestablish spontaneous<br />
cardiac activity at the scene<br />
sufficient to generate a pulse after determ<strong>in</strong>ed<br />
prehospital efforts at resuscitation<br />
warrants cessation of efforts <strong>in</strong><br />
the field and pronouncement of death.<br />
On the other hand, <strong>in</strong>itial response to<br />
treatment followed by recurrent cardiac<br />
arrest warrants cont<strong>in</strong>ued efforts,<br />
<strong>in</strong>clud<strong>in</strong>g transport to the nearest hospital<br />
ED.<br />
Given our present understand<strong>in</strong>g of<br />
the physiologic limits of prolonged<br />
cellular ischemia, we question the<br />
wisdom of cont<strong>in</strong>ued research <strong>in</strong>to<br />
costly hospital-based technology for<br />
the management of refractory out-ofhospital<br />
cardiac arrest. We believe further<br />
<strong>in</strong>vestments <strong>in</strong> tra<strong>in</strong>mg~ program<br />
development, and cl<strong>in</strong>ical research<br />
should be focused on the optimal<br />
provision of prehospital emergency<br />
cardiac care, prior to the onset of irreversible<br />
deterioration.<br />
We are <strong>in</strong>debted to the <strong>in</strong>ternal medic<strong>in</strong>e<br />
housestaff of the University of Tennessee<br />
and the nurses and unit assistants <strong>in</strong> the<br />
emergency department of the Regional<br />
Medical Center at Memphis, without<br />
whom this study would not have been<br />
possible. We are also <strong>in</strong>debted to Carol<br />
Conway for preparation of this manuscript.<br />
REFERENCES<br />
I. Lown B: Sudden cardiac death: The major<br />
problem confront<strong>in</strong>g contemporary cardiology.<br />
Am ] Cardiol 1979;43:313-328.<br />
2 Eiscnberg <strong>MS</strong>, Bergner L, Hallstrom A~, et al:<br />
cardiac death. Sci Am 1986~245:37-43.<br />
Standards and guidel<strong>in</strong>es for cardiopulmo.<br />
mary resuscitation ICPRJ and emergency cardiac<br />
care IECCJ. lAMA 1986;255:2905-2914.<br />
4. Standards and guidel<strong>in</strong>es for cardiopulmomary<br />
resuscitation (CPR) and emergency cardiac<br />
care (ECCJ. lAMA 1980i244:453-509.<br />
S. Unpublished data, Memphis Fire Depart.<br />
merit, E<strong>MS</strong> Bureau, 1987.<br />
6. Pantridge JE Geddes IS: Cardiac arrest after<br />
myocardial <strong>in</strong>farction. Lancet 1966;1:807-808.<br />
7. Pantridge JF, Geddes IS: A mobile <strong>in</strong>tensive<br />
care unit <strong>in</strong> the management of myocardial <strong>in</strong>farction.<br />
Lancet 1967;2:271-273.<br />
8. Cobb LS, Baum RS, Alvarez H, et al: Resuscitation<br />
from out-of-hospital ventticular fibrillation:<br />
Four-year follow-up. Circulatl’on 1975;52<br />
68/504<br />
(suppl III~:223-228.<br />
9. Liberthson PR, Nagel SL Hirschman JC, et<br />
al: Prehospital ventricular defibrillation: Prognosis<br />
and follow-up course. 1V Engl I Med<br />
1974;291:317-321.<br />
I0. Eisenberg <strong>MS</strong>, Bergner L, Hallstrom AP:<br />
Out-of-hospital cardiac arrest: Improved survival<br />
with paramedic services. Lancet 1980;1:<br />
812-816.<br />
II. Hearn T: The development of emergency<br />
medical services, <strong>in</strong> Eisenberg <strong>MS</strong>, Bergner L,<br />
Hallstrom AP (edsl: Sudden Cardiac Death <strong>in</strong><br />
the Community. New York, Praeger Publish<strong>in</strong>g,<br />
1984, p 29-43.<br />
12. Eisenberg <strong>MS</strong>, Copass MK, Hallstrom AP, et<br />
al: Management of out-of-hospital cardiac arrest:<br />
Failure of basic emergency medical techni.<br />
clan services, lAMA 1980;243:1049.1051.<br />
13. Eisenberg <strong>MS</strong>, Bergner L, Hallstrom AP:<br />
Cardiac resuscitation <strong>in</strong> the community: Importance<br />
of rapid provision and implications for<br />
program plann<strong>in</strong>g, lAMA 1979;241:1905.1907.<br />
14. Cumm<strong>in</strong>s RO, Eisenberg ME, Hallstrom AP,<br />
et al: Survival of out-oLhospital cardiac arrest<br />
with early <strong>in</strong>itiation of cardiopulmomary resuscitation.<br />
Am I Emerg Med 1985;3:114.118.<br />
15. Weaver WD, Cobb LA, Hallstrom A~, et al:<br />
Considerations for improv<strong>in</strong>g survival from outof-hospital<br />
cardiac arrest. Ann Emerg Med<br />
1986;15:1181-1186.<br />
16. Smith pl- Bodai BI: Guidel<strong>in</strong>es for discont<strong>in</strong>u<strong>in</strong>g<br />
prehospital CPR <strong>in</strong> the emergency department<br />
-- A review. Ann Emerg Med<br />
1985; 14:1093 - 1098.<br />
17. Copass MK, Oreskovich MR, Bladengroen<br />
MR, et al: Prehospital cardiopulmomary resuscitation<br />
of the critically <strong>in</strong>jured patient. Am l<br />
Surg 1984;148:20-26.<br />
18. Southwick FS, Dalgfish PH: Recovery after<br />
prolonged asystolic cardiac arrest <strong>in</strong> profound<br />
hypothermia. A case report and literature review.<br />
lAMA 1980;243:1250-1253.<br />
19. Bristow G, Smith R, Lee J, et al: Resuscitation<br />
from cardiopulmonary arrest dur<strong>in</strong>g accidental<br />
hypothermia due to exhaustion and exposure.<br />
Can Med Assoc I 1977;117:227-279.<br />
20. Siebke H, Rod T, Breivik H, et al: Survival<br />
after forty ni<strong>in</strong>utes submersion without cerebral<br />
sequelae. Lancet 1975;1:1275-1277.<br />
21. Mack<strong>in</strong>tosh AI., Crabb ME, Gra<strong>in</strong>ger R, et<br />
al: The Brighton resuscitation ambulances: Review<br />
of 40 consecutive survivors of out-of-hospital<br />
cardiac arrest. Br Med I 1978;1:115-118.<br />
22. Myerburg RI, Conde CA, Sung RJ, et al:<br />
Cl<strong>in</strong>ical, electrophysiologic and hemodynamic<br />
profi!e of patients resuscitated from prehospital<br />
cardiac arrest. Am I Meal 1980;68:568-576.<br />
23. Szczygiel M, Wright R, Wagner E, et al:<br />
Prognostic <strong>in</strong>dicators of ultimate long-term survival<br />
follow<strong>in</strong>g advanced life support. Ann<br />
Eraerg Med 1981jI0:566-570.<br />
24. Smith pl, Bodai BI: Guidel<strong>in</strong>es for discont<strong>in</strong>u<strong>in</strong>g<br />
cardiopulmonary resuscitation <strong>in</strong> the<br />
emergency department after prehospital, nonparamedic<br />
directed cardiac arrest. West l Med<br />
1985;143:402-405.<br />
Annals of Emergency Medic<strong>in</strong>e<br />
L<br />
25. Geehi EC, Lewis FR, Auerbach PS: Fa~ure<br />
of open-heart massage to improve survival after<br />
prehospital non-traumatic cardiac arrest {letterL<br />
N Engl ] Med 1986;314:1189.1190.<br />
26. Aprahamian C, Thompson BM, Gruchow<br />
H~, et al: Decision mak<strong>in</strong>g <strong>in</strong> prehospital sudden<br />
cardiac arrest. Ann Emerg Med 1986;15:<br />
445-449.<br />
27. Luchtar S, personal cOmmunication, National<br />
Highway Traffic Safety Adm<strong>in</strong>istration,<br />
1987.<br />
28. Hume El~ personal communication, Center<br />
for Health and Regulation, Council of State<br />
Governments, 1987.<br />
29. Phillips JB: A matter of equity. IE<strong>MS</strong><br />
1986~ 11:6-7.<br />
30. Eisenberg <strong>MS</strong>, Cumm<strong>in</strong>s RO: Term<strong>in</strong>ation<br />
of CPR <strong>in</strong> the prehospital arena {editotialL Ann<br />
Eraerg Med 1985; 14:1106-1107.<br />
31. White DJ: Transthoracic pac<strong>in</strong>g <strong>in</strong> cardiac<br />
asystole. Am I Emerg Med 1983;3:264-266.<br />
32. Hedges JR, Syverud S, Delsey WC: Develop-<br />
.ments <strong>in</strong> transcutaneous and transthoraclc pac<strong>in</strong>g<br />
dur<strong>in</strong>g bradysystolic arrest. Ann Emerg Med<br />
1984; 13:822-827.<br />
33. Cobb LA, Werner IA, Tronghbangh BG: Sudden<br />
cardiac death I: A decade’s experience with<br />
out-of-hospital resuscitation. Modern COncepts<br />
Cardiovasc Disease 1980;49:31.36.<br />
34. Eisenberg <strong>MS</strong>, Copass MK, Hallstrom A~, et<br />
al: Treatment of out-of-hospital cardiac arrest<br />
with rapid defibrillation by emergency medical<br />
technicians. N Engl ] Med 1980;302:1379.1383<br />
35. Stultz K, Brown D, Shug V, et al: Prehospital<br />
defibrillation performed by emergency medical<br />
technicians <strong>in</strong> rural communities. N Engl IMed<br />
1984;310:219-223.<br />
36. Phillips SI, Ballent<strong>in</strong>e B, Slon<strong>in</strong>e D, et al:<br />
Percutaneous <strong>in</strong>itiation of cardiopulmomary bypass.<br />
Ann Thorac Surg 1983;36:223-225.<br />
37. Lev<strong>in</strong>e R, Gorayeb M, Safar P, et al: Emergency<br />
cardiopulmomary bypass after prolonged<br />
cardiopulmonary resuscitation basic life support<br />
<strong>in</strong> dogs improves survival labstract L Ann<br />
Emerg Med 1986;15:627.<br />
38. Mart<strong>in</strong> GB, Nowak RM, Carden DL, et al:<br />
Femoro-femoro cardiopulmomary bypass <strong>in</strong> the<br />
atrreraest~t ent of prolonged can<strong>in</strong>e cardiopulmonarv<br />
6~. nt lanstraetL Ann Emerg Med 1986j15":<br />
39. Weaver WD, Copass MK, Hill DL, et al:<br />
Cardiac arrest treated with a new automatic external<br />
defibrillator by out-of-hospital first responders.<br />
Am ] Carddiol 1986;57:1017-1021.<br />
40. Cumm<strong>in</strong>s RO, Eisenberg <strong>MS</strong>, Litw<strong>in</strong> PE, et<br />
al: Automatic external defibrillators used by<br />
emergency medical technicians: A controlled<br />
cl<strong>in</strong>ical trial, lAMA 1987;257:1605-1610.<br />
41. Stults KR, Brown DD, gerber RE: Efficacy<br />
of an automated external defibrillator <strong>in</strong> the<br />
management of out-of-hospital cardiac arrest:<br />
Validation of the diagnostic algorithm and <strong>in</strong>itial<br />
cl<strong>in</strong>ical experience <strong>in</strong> a rural environment.<br />
Circulation 1986;73:701-709.<br />
42. Eisenberg <strong>MS</strong>, Hallstrom AP, Carter WB, et<br />
al: Emergency CPR <strong>in</strong>struction via telephone.<br />
Am I Public Health 1985;75:47.50.<br />
17:6 June 1988
I<br />
I<br />
i<br />
t<br />
J<br />
i<br />
] I<br />
i<br />
!<br />
J I<br />
II 1<br />
International Notes<br />
The Brighton Resuscitation Ambulance Service has<br />
been <strong>in</strong> operation s<strong>in</strong>ce 1971. The service covers a<br />
population of 300,000, which rises to half a million<br />
dur<strong>in</strong>g the summer months, and serves an area with<strong>in</strong><br />
a five-mile radius of Brighton and Hove. This coastal<br />
resort is a popular retirement area and has a high percentage<br />
of elderly residents.<br />
OPERATIONAL DETAILS<br />
Tra<strong>in</strong>ed Personnel<br />
The service currently has 30 advanced life support<br />
tra<strong>in</strong>ed personnel, two thirds of whom are based at the<br />
Hove Ambulance Station and the rema<strong>in</strong>der at the<br />
Brighton Ambulance Station. The operational target is<br />
to ma<strong>in</strong>ta<strong>in</strong> four ambulances, each manned with a m<strong>in</strong>imum<br />
oi ~ one paramedic and one ambulanceman; <strong>in</strong><br />
reality, there are often two paramedics per vehicle.<br />
These highly tra<strong>in</strong>ed paramedic ambulancemen are<br />
under the control of the East Sussex Ambulance<br />
Headquarters <strong>in</strong> Eastbourne.<br />
Operational Coord<strong>in</strong>ation<br />
Emergency calls from medical practitioners and<br />
calls to the 999 phone number are routed by British<br />
Telecommunications directly to these headquarters.<br />
From the headquarters control room, an appropriate<br />
duty paramedic is beeped. Upon return<strong>in</strong>g to his vehicle,<br />
which may be <strong>in</strong> or return<strong>in</strong>g to a station or at<br />
a standby location, he receiVes a direct radio message<br />
gwmg the location of the emergency.<br />
From the Department of Cardiology, Royal Sussex County Hospital;<br />
Brighton, England.<br />
Presented at the First International Conference on Cardiac Arrest<br />
and Resuscitation, Brighton, England, October 19-21,<br />
1982.<br />
Address repr<strong>in</strong>t requests to Dr. Studd: Department Of Cardiology,<br />
Royal Sussex County Hospital, Brighton, England BN2<br />
5BE.<br />
Key Words: Ambulance, emergency medical service, paramedic,<br />
resuscitation.<br />
Equipment<br />
The Brighton Ex pperience with<br />
Resuscitation Ambulances<br />
CLIVE STUDD, MD<br />
Standard equipped ambulances are used (these ambulances<br />
normally carry a comprehensive range of<br />
equipment) plus ECG/defibrillator and the personal resuscitation<br />
kit of the <strong>in</strong>dividual paramedic. Recently,<br />
Heart Aid ® and Pace Aid® devices have been carried<br />
and are undergo<strong>in</strong>g evaluation.<br />
Selection and Tra<strong>in</strong><strong>in</strong>g of Personnel<br />
Ambulancemen with at least two years of service<br />
may be scheduled for advanced tra<strong>in</strong><strong>in</strong>g if they achieve<br />
a satisfactory result <strong>in</strong> a basic anatomy and physiology<br />
exam<strong>in</strong>ation organized by the ambulance headquarters.<br />
Advanced tra<strong>in</strong><strong>in</strong>g starts with a six-month period,<br />
dur<strong>in</strong>g which lectures <strong>in</strong> resuscitation are given once<br />
a week. This is followed by a one-month full-time attachment<br />
to the coronary care unit and the <strong>in</strong>tensive<br />
therapy unit of the Royal Sussex County Hospital.<br />
Success <strong>in</strong> the exam<strong>in</strong>ation at the end of this tra<strong>in</strong><strong>in</strong>g<br />
permits the personnel to undertake defibrillation. Follow<strong>in</strong>g<br />
a six-month period of further field work, personnel<br />
undertake five days’ tra<strong>in</strong><strong>in</strong>g <strong>in</strong> <strong>in</strong>tubation and<br />
<strong>in</strong>travenous cannulation. Satisfactory performance<br />
dur<strong>in</strong>g this tra<strong>in</strong><strong>in</strong>g permits the ambulancemen to function<br />
as fully tra<strong>in</strong>ed personnel. Annual refresher periods<br />
of five days are tailored to <strong>in</strong>dividual requirements,<br />
and cont<strong>in</strong>ual review of <strong>in</strong>dividual performance<br />
is undertaken through regular meet<strong>in</strong>gs and discussion<br />
of specific cases.<br />
Pr<strong>in</strong>ciples of Tra<strong>in</strong><strong>in</strong>g<br />
The follow<strong>in</strong>g pr<strong>in</strong>ciples of tra<strong>in</strong><strong>in</strong>g have been applied:<br />
1. Ambulancemen should be able to deal effectively<br />
with all common life-threaten<strong>in</strong>g emergencies.<br />
2. Invasive procedures capable of caus<strong>in</strong>g great<br />
harm should be avoided.<br />
3. Drug therapy should have a wide marg<strong>in</strong> of<br />
safety.<br />
4. The course of <strong>in</strong>struction should be sufficiently<br />
275
AMERICAN JOURNAL OF EMERGENCY MEDICINE ¯ Volume 2, Number 3 ¯ May 1984<br />
comprehensive to generate confidence with<strong>in</strong> the ambulancemen<br />
of their ability to cope with all but the<br />
most unusual cases.<br />
5. Their competence should enable them to perform<br />
without recourse to telemetry or central radio control.<br />
RESULTS<br />
The average number of calls per day handled is 33,<br />
with a response time (from receipt of call by headquarters<br />
to arrival at the scene) of 21% by 4 m<strong>in</strong>utes,<br />
40% by 5 m<strong>in</strong>utes, 61% by 6 m<strong>in</strong>utes, 75% by 7 m<strong>in</strong>utes,<br />
and 82% by 8 m<strong>in</strong>utes, with a mean response<br />
time of 5.4 m<strong>in</strong>utes. These figures are well with<strong>in</strong> the<br />
Department of Health and Social Security recommended<br />
times, but of course are somewhat slower<br />
than one would ideally like to see.<br />
Of approximately 12,000 emergency calls <strong>in</strong> 1981,<br />
O<br />
O<br />
29 attempted resuscitations were made for out-of-<br />
hospital cardiac arrest. Ten of these cardiac arrests<br />
occurred <strong>in</strong> the presence of ambulance staff, and all<br />
those patients were subsequently discharged from<br />
hospital <strong>in</strong> satisfactory condition. Retrospective analysis<br />
has shown that 21 of the 129 patients were considered<br />
unresuscitable. This leaves 98 patients who<br />
were thought to be resuscitable. Of these 98, 21 survived<br />
and the rema<strong>in</strong>der died, Of these 21 survivors,<br />
52% received basic cardiac life support (BCLS) before<br />
the arrival of the ambulance. Of the 77 patients who<br />
died, only 28.6% received BCLS. The total of 31 survivors<br />
from our population represents approximately<br />
10 per 100,000.<br />
As a measure of the efficiency of our resuscitative<br />
measures, we have established that of the 31 patients<br />
276<br />
receiv<strong>in</strong>g BCLS, 26 received BCLS with<strong>in</strong> 4 m<strong>in</strong>utes<br />
and advanced cardiac life support (ACLS) with<strong>in</strong> 8<br />
m<strong>in</strong>utes, and I l survived. This survival figure for this<br />
subgroup is 43%, which is comparable to the figure<br />
quoted by Eisenberg et aL l<br />
Of those 33 receiv<strong>in</strong>g bystander CPR, there was no<br />
significant difference <strong>in</strong> the adequacy of CPR between<br />
survivors and nonsurvivors.<br />
We are, of course, <strong>in</strong>terested <strong>in</strong> long-term survival.<br />
From our 1974- 1976 records, we know that of 18 patients<br />
under the age of 65 who were work<strong>in</strong>g before<br />
out-of-hospital arrest, 14 returned to work. From the<br />
31 survivors <strong>in</strong> 1981, 26 were alive at five months, and<br />
long-term follow-up of previous years’ survivors has<br />
shown a 77% survival at two years.<br />
CONCLUSIONS<br />
I. The implementation of comprehensive advanced<br />
tra<strong>in</strong><strong>in</strong>g of ambulancemen is feasible.<br />
2. The use of advanced tra<strong>in</strong>ed ambulancemen<br />
work<strong>in</strong>g <strong>in</strong>dependently <strong>in</strong> emergency vehicles is effective<br />
and not costly.<br />
3. The pattern of survival when related to the use<br />
of BCLS and ACLS supports the extension of CPR<br />
tra<strong>in</strong><strong>in</strong>g <strong>in</strong>to the community.<br />
4. Improved ambulance response times would be<br />
beneficial to those patients denied BCLS.<br />
REFERENCES<br />
1. Eisenberg <strong>MS</strong>, Bergner L, Hallstrom A. Survivors of out-ofhospital<br />
cardiac arrest: Morbidity and long-term survival.<br />
Am J Emerg Med 1984;2:189-192.
~t<br />
L,~9-03-09 16;.,30 01 383 6418 B M J EDITORIAL 014<br />
@<br />
*It<br />
A full list of authors is given<br />
at the end ofthis paper<br />
Correspondence to: Mr M J<br />
Allen, L¢i¢~teJ Royal<br />
! nfirmary, Leicester<br />
LEI 5WW<br />
Br Mt~+? 19~t9.2~I 65 |.4<br />
MIDDLES<br />
FOR THE URGENT AI7ENTION<br />
..... e ..J<br />
FROM ....... ....<br />
NUMBER OF SHEETS...-~-. ......<br />
BMJ FAX 01 383 6418<br />
BMJ PI1ONE<br />
01 383 6355<br />
Cop<strong>in</strong>g with the early stages of the MI disaster: at the scene and<br />
on arrival at hospital<br />
Staff of the accident and emergency departments of Derbyshire Royal Infirmary, Leicester Royal<br />
Infirmary, and Queen’s Medical Centre, Nott<strong>in</strong>gham<br />
Last month Kirsh et al reported how the 88 <strong>in</strong>itial to prevent leak<strong>in</strong>g fuel from ignit<strong>in</strong>g. This made the<br />
survivors of the Boe<strong>in</strong>g 737 aircrash were treated <strong>in</strong>embankment<br />
extren~ly slippery. Ropes, ladders, and<br />
hospital and on the outcome three weeks after the steps dug by mounta<strong>in</strong> rescue teams proved extremely<br />
crash.’ Here we describe how the three ma<strong>in</strong> hospitals’ useful for the qgik., lllum<strong>in</strong>ation was poor at first. As<br />
accident and emergency services coped with the the rescue operation progressed, with removal of<br />
disaster <strong>in</strong> its <strong>in</strong>itial stages: at the scene of the accident victims and wreckage cavities of 3-5 m appeared <strong>in</strong> the<br />
and on arrival at hospital.<br />
tail and rear fuxlage, necessitat<strong>in</strong>g the use of ropes to<br />
At 8 26 pm on Sunday 8 January 1989 a Boe<strong>in</strong>g 737 lower doctors to patients.<br />
with 126 passengers and crew on board crashed <strong>in</strong>to<br />
the western embankment of the Ml motorway just<br />
south of junction 24 after an attempt to make an<br />
emergency land<strong>in</strong>g at East Midlands airport. The crash<br />
occurred on the borders of three counties: Derbyshire,<br />
Leicestershire, and Nott<strong>in</strong>ghamshire (fig 1). Thus<br />
plans for deal<strong>in</strong>g with a major accident were activated,<br />
entail<strong>in</strong>g police, fire, ambulance, and medical services<br />
Nott<strong>in</strong>glutm<br />
from each of the counties. This had the adva.ttage that<br />
more thai, ~deq~mt¢. hcadth care ~rvloee were avadabte @<br />
but th~ disadvantage of complex organisafional and<br />
communication problems. Coord<strong>in</strong>ation was essential<br />
to the rescue operation.<br />
Initial response<br />
At about 830 pm the accident and emergency<br />
departments of the three ma<strong>in</strong> hospitals (Derbyshire<br />
Royal Infirmary, Leicester Royal Infirmary, and<br />
Queen’s Medical Centre, Nott<strong>in</strong>gham) were alerted<br />
about an aircraft attempt<strong>in</strong>g an emergency land<strong>in</strong>g at<br />
Past Midlands airport (a common call for any hospital<br />
<strong>in</strong> the vic<strong>in</strong>ity of an airport).<br />
There was tome confusion and <strong>in</strong>itial confirmation<br />
of a major disaster was not received at any centre. As<br />
the crash happened dur<strong>in</strong>g a peak time for people to<br />
v~atch television the early news flashes prompted the<br />
response of most of the staff who came <strong>in</strong>to the<br />
"departments thus byparadng the telephone call <strong>in</strong><br />
system for major ditaster=.<br />
Fly<strong>in</strong>g squads were sent from the three hospitals,<br />
and subsequently two back up =quads with extra<br />
equipment wer= dispatched from Leicetter Royal<br />
Infirmary and Derbyshire Royal Infirmary.<br />
The accne<br />
On impact the aircraft broke <strong>in</strong>to three sections: the<br />
tail, ma<strong>in</strong> fuselage, and cockpit (fig 2). Victims were<br />
trapped by twisted wreckage <strong>in</strong> the flipped tail and the<br />
front and rear sections of the fuselage. In the ma<strong>in</strong><br />
fuselage the floor had collapsed <strong>in</strong>to the cargo hold and<br />
<strong>in</strong>jured people were trapped by collapsed seat frames,<br />
which had concert<strong>in</strong>aed.<br />
Access to the aircraft and victims was difficult for<br />
several reasons. The embankment sloped about 30 ° to<br />
the horizontal and was thickly wooded. The airport fire<br />
services had sprayed foam on to the aircraft and hillside<br />
B.Vi] vo~ t’~t: 298 11 MARCH 1989 651<br />
rm I-,tl~,~’omJ.<br />
Memben of the ~<strong>in</strong>g uluads divided <strong>in</strong>to teams ofa.<br />
doctor and a nurse. The team from Derby operated <strong>in</strong><br />
the tail section, that from Nott<strong>in</strong>sham <strong>in</strong> the adjacent<br />
~1 and rear fuselage u~:tion, and that from Lek:euer<br />
<strong>in</strong> the ma<strong>in</strong> fuselage and cockpit. Equipment was<br />
limited to what could be carried <strong>in</strong> e pocket and<br />
treatment restricted by access until patients wee=<br />
partially or completely extricated from the wreckage.<br />
Coord<strong>in</strong>ation among the teams became established<br />
once all the squads were on site, although there was<br />
some delay because of the difficulty <strong>in</strong> identify<strong>in</strong>g<br />
medical staff. In addition, the nature and location of<br />
the wreckage made communication among the teams<br />
extremely diffk’~|t.
@<br />
Triage po<strong>in</strong>t<br />
¢,~a.z tt - lwfiCt, a.,xfi~ a’orn <strong>in</strong> #J ~d~u<br />
Th. tiros ~wmvuatton of aLa~ut 40 patients was tO a<br />
triage po<strong>in</strong>t on the motorway, but rapid transport<br />
to Queen’s Medical Centre by ambulance crews on<br />
<strong>in</strong>struction f~rn their control centre and the demand<br />
for medical ’teams on the aircraft caused this triage<br />
po<strong>in</strong>t to disappear. Once the triage po<strong>in</strong>t was reestablished,<br />
equipped, and staffed it became the focal<br />
po<strong>in</strong>t for the medical services. Patients were reassessed<br />
at this po<strong>in</strong>t before be<strong>in</strong>g transferred to hospital,<br />
although conditions were less than ideal.<br />
Types of <strong>in</strong>|uries<br />
Most of the survivors had multiple pelvic and leg<br />
<strong>in</strong>juries attd to a lesser extent trauma to the skull,<br />
spree, alsd chest. Abdonf<strong>in</strong>al <strong>in</strong>juries were rare.<br />
A subsequent analysis of all <strong>in</strong>juries showed that 83<br />
.i~tie!:ts susta<strong>in</strong>ed 324 separate <strong>in</strong>juries (table I). These<br />
mjurtes were coded accord<strong>in</strong>g to the 1985 revision of<br />
the abbreviated miury scale.’ The grades of <strong>in</strong>jury<br />
were tabulated aga<strong>in</strong>st the six body regions that were<br />
used for the calculation of <strong>in</strong>iury severity scores.’<br />
Although the scor<strong>in</strong>g system orig<strong>in</strong>ated from statistics<br />
from road traffic acddents, it has become the univerully<br />
prefcrrod system for assess<strong>in</strong>g the severity of<br />
impact <strong>in</strong>juries. Table II shows the mean score and the<br />
?Aatz t--Abbrepimod iajury teals (AIS) ~ode for 324 <strong>in</strong>juria <strong>in</strong> B3<br />
patWnt~ 1 ’slues ar~ nambers of <strong>in</strong>j~rrics ’<br />
AI$ code<br />
Bed.~ ~eJ,,~ ! 2 3 4 ~ Thud<br />
Hced o, neck<br />
F~c¢<br />
2 4 5 2 2<br />
4<br />
I S<br />
Cheer 2<br />
4 ?<br />
6<br />
? 4 22<br />
L ~. I¢ pclCiC ¢t’~t ents " trcmitica ~r Ixdvi¢ Iprdh: |0 S ! I 17<br />
.!<br />
Iczlcrnal<br />
84 68 ] }}-<br />
104 4 I 109<br />
Total 117 111 86 7 ~ ~.4<br />
<strong>in</strong>jury .~verity Score<br />
Unit<br />
Umv~ndt). Hmpilal, Noct<strong>in</strong>gl~m<br />
Derbyshire Royal Infirmary<br />
[.t’kesler Royal lnRrmery<br />
No tsrp~tiet~ls<br />
38<br />
2~1<br />
20<br />
Ransc<br />
l.,T~<br />
1-34<br />
| .43<br />
M¢lm<br />
9.6<br />
12" I<br />
14.5<br />
Nn ~f patk’nts<br />
with scott. ~ :6<br />
9<br />
7<br />
6<br />
Total<br />
S3 1-4~ ! t "5 22<br />
range and the numbers of put..’ngs with scores o’<br />
greater than ]6 for each centre.<br />
Treatment<br />
Treatment was focused on the patients who were<br />
trapped <strong>in</strong> the aircraft as those who were not trapped<br />
were rapidly transferred to hospital bythe <strong>in</strong>itial<br />
wave of ambul.m~.., crews. PYiorities were ~---’l~,o<br />
.~rways, estabhsh<strong>in</strong>g access to the circulation "1~<br />
<strong>in</strong>travenous fluids and analgesia, and apply<strong>in</strong>g spl<strong>in</strong>ts<br />
when possible. The victims were reassessed at the<br />
triage po<strong>in</strong>t, once it was re-established, with regard to<br />
life threaten<strong>in</strong>g <strong>in</strong>juries and the above priorities.<br />
Transfer to hospital was then organised.<br />
With the pattern of <strong>in</strong>juries from this <strong>in</strong>cident large<br />
supplies of <strong>in</strong>travenous fluids, adm<strong>in</strong>istration sets,<br />
analgesia, and spl<strong>in</strong>ts were required. Further requirements<br />
for these items were relayed to the base hospitals,<br />
but they took some time to arrive. Some supplies were<br />
never received.<br />
’rrll~apofl ~" *<br />
The <strong>in</strong>itial coord<strong>in</strong>ation el" the three ambulance<br />
Evacuation by ambulance ~o Queen’s Medical C.¢ntr~<br />
and Derbyshire Royal Inf<strong>in</strong>mu? was comparatively<br />
easy as they were the aearest cemres on the least<br />
congested routes.<br />
As the rescue became oqlmised it was controlled by<br />
the chief ambulance of’ricer oa tit:. ,As tufa-marion w~s<br />
relayed at, the dlstributiot; of patients among the three<br />
hospitalg, fln.th4~1.1 ~il~s were.redirected accord<strong>in</strong>gly.<br />
The roads had become ongested by this time and<br />
helJcopter~, two Sea K<strong>in</strong>~p and two Wes~xes, were<br />
used to transport <strong>in</strong>jured peup]e to Leicester Royal<br />
Infirmary (fly<strong>in</strong>g time n<strong>in</strong>e m<strong>in</strong>utes). This was despite<br />
the patients’ obvious concern about further air travel.<br />
Communication<br />
<strong>in</strong> one centre excellent direr communication was<br />
achieved between staff at the scene and thr.~e at the<br />
base hospital by the use of a cellular telephong.<br />
This, however, did not Wevent confus<strong>in</strong>g rumours<br />
spread<strong>in</strong>g ft’m~ mher ~ Communication between<br />
the site and the other two hospitals was thought<br />
to be <strong>in</strong>adequate, althotlgh the cellular telephone was<br />
used to a~erta<strong>in</strong> where the i~ured people had been<br />
taken and to redire~ them accordFu~iy. As far as we arc<br />
aware there was no <strong>in</strong>tercommunication between the<br />
three hospitals.<br />
As with all disasters, cmmmmlcadou was criticis~l.<br />
It should be ~ed, however, tim com0entional, day<br />
to day methods of taxnmmimk~a mano~ be used<br />
when a di~aer has o¢cmr~. ~g’t’¢a hmutrt.d people<br />
were on site throtigll~t varle~ ~ of the regu¢<br />
operation and had a lot of~ to relate.<br />
Communicatio~ betwem tl~ aizgraft and the triap<br />
po<strong>in</strong>t was ~mm~y dil~ah, IP.aq~,st~ for equipment<br />
had to be relayed verlxdly md could berune quite<br />
distorted. Comidem~ time mid be l<strong>in</strong>t by nurses<br />
climb<strong>in</strong>g dowh from the upper nadtes of the emMnkment,<br />
where ti~: ¢ociq~t real freat fuselage section<br />
were located, to the triage ~ to ~ for equipment.<br />
The only method of mahmtk~ an update on the<br />
rescue operation was toclimbmd scramble around the<br />
aircraft. This took about 20 w.i~utea.<br />
Initial respom~ of hospttaib<br />
USE OF .~AFF<br />
All three ho~. "utls found that they had more than<br />
enough med:cal staffand <strong>in</strong> some <strong>in</strong>stances an excess.<br />
BMJ VOLUg~ 298 I I M^ReH 1989
~ .-..<br />
@<br />
@<br />
,~ . ,.~nt,~:,:~t~ m~" grade and sl.~:alty<br />
of both doctors and nurses.<br />
[n each hospital one consultant <strong>in</strong> accident and<br />
emergency medic<strong>in</strong>e took charge of the triage po<strong>in</strong>t<br />
and another the resuscitation room. The doctors <strong>in</strong> the<br />
accident snd emergency departments formed teams<br />
and <strong>in</strong> one centre were clearly identified with tabards<br />
and sashes. Each team worked <strong>in</strong> a designated area.<br />
The specialty coord<strong>in</strong>ator reta<strong>in</strong>ed a supervisory role<br />
and did not participate <strong>in</strong> treat<strong>in</strong>g <strong>in</strong>dividual patients.<br />
Once the <strong>in</strong>itial resuscitation procedures had been<br />
carried out patients were then transferred to the<br />
admitt<strong>in</strong>g teams. The flow of patients through the<br />
departments was too rapid <strong>in</strong> some <strong>in</strong>stances ow<strong>in</strong>g to a<br />
lack of <strong>in</strong>formation on numbers of patients and the<br />
severity of their <strong>in</strong>juries. The automatic response was<br />
to treat patients rapidly+ keep<strong>in</strong>g the accident and<br />
emergency departments clear. The <strong>in</strong>itial transfer of<br />
patients from the scene was extremely fast, thus<br />
apply<strong>in</strong>g pressure on thc deparunents to treat the<br />
patients as quickly as possible.<br />
More than one entrance po<strong>in</strong>t to the department also<br />
caused confusion at one centre.<br />
t30~:U~X’rlON<br />
Difficulty was encountered <strong>in</strong> the documentation of<br />
the patients and the decipher<strong>in</strong>g of rapidly made notes<br />
<strong>in</strong> the accident and emergency departments. Each<br />
hospital used its own system of documentation at the<br />
scene of the crash, which proved confus<strong>in</strong>g. Often<br />
triage labels were absent on admission, and the<br />
<strong>in</strong>formation conta<strong>in</strong>ed <strong>in</strong> those present was of little<br />
value,<br />
Hav<strong>in</strong>g only one copy of notes with each patient<br />
caused problems at the base hospitals.<br />
Lessons to be learnt<br />
In general the three centres dealt with the survivors<br />
extremely well. The follow<strong>in</strong>g po<strong>in</strong>ts were thought to<br />
be important.<br />
AT "riie SCENE<br />
(1) The identification of key staff should be<br />
improved, which would make coord<strong>in</strong>ation and communication<br />
much easier.<br />
(2) On arrival of the first fly<strong>in</strong>g squad teams an<br />
assessment should be made of the pattern and type of<br />
<strong>in</strong>juries requir<strong>in</strong>g treatment. Appropriate equipment<br />
accompanied by a nurse should be requested and transferred<br />
to the scene. Specific specialist staff requirements<br />
could sis0 b¢ mobilised at this po<strong>in</strong>t.<br />
(3) The triage po<strong>in</strong>t should be clearly identified and<br />
illum<strong>in</strong>ated, with one nurse <strong>in</strong> charge of all of the<br />
equipment.<br />
(4) A tmified system of categoris<strong>in</strong>g patients would<br />
be advantageous. At this <strong>in</strong>cident each hospital had its<br />
own particular methods of labell<strong>in</strong>g, which ~aus~<br />
problen~. Such a unified system should be extended<br />
throughout the oumry because of the constant movemeat<br />
ofjunlor staff from place to place.<br />
(S)Evl~-uetlon by helicopter proved to be extremely<br />
useful. The helicopters used could handle up to 10"<br />
patient~l on stretchers, medical staff be<strong>in</strong>g able to<br />
eccot~pany them and give treatment with comparative<br />
ease. m addition, relief staff and additional equipment<br />
could be easily transferred to the. scene.<br />
(6) Provision should be made for the changeover of<br />
medical staff if the time required at the scene of the<br />
disaster is prolonged.<br />
(7) The cellular telephone was <strong>in</strong>valuable, allow<strong>in</strong>g<br />
direct communication between the scene of the disaster<br />
and the base hospital. When more than one centre<br />
is concerned, however, methods should exist for<br />
communication between hospitals.<br />
~8; ltand held radios with transmitt<strong>in</strong>g and ret’eiv<strong>in</strong>g<br />
capabilities would have been btneficial fo~ ask<strong>in</strong>g for<br />
equipment and staffand pass<strong>in</strong>g on <strong>in</strong>formation on the<br />
numbers of patients and the stages of extrication. To<br />
have had more than four sets (three for the aircraft and<br />
one for the triage po<strong>in</strong>t)+ however, would have created<br />
havoc on the airwaves.<br />
(9) When more than one centre is concerned with<br />
receiv<strong>in</strong>g the survivors of a dis<strong>in</strong>ter the patienus<br />
should be appropriately distributed hat--ares.<br />
This would require regular communication betweea~<br />
hospitals aswell as between the hospitals and the scene:<br />
(10) In any major disaster hazardo0s conditions may<br />
exist; <strong>in</strong> this <strong>in</strong>stance the hazards were 77 000 iitres of<br />
aviation fuel and the slippery terra<strong>in</strong>. Provision should<br />
therefore be made for treat<strong>in</strong>g possible <strong>in</strong>juries tO<br />
rescuc teams, and care should be taken not to clo~ the<br />
<strong>in</strong>cident too soon.<br />
AT THE HOSPITAL<br />
(11 The call out I~r~tCln should be looked at closely.<br />
Perhaps each specialty concerned should be responsible<br />
for its own call out of staff.<br />
(2) In this-pprticular disaster there were over 80<br />
<strong>in</strong>jm, ed people and one hospital alone would probably<br />
not have been able to cope with trem<strong>in</strong> 8 the,t all.<br />
Provision should therefore be made <strong>in</strong> disaster<br />
plann<strong>in</strong>g for lxmlble ooperation with neighbour<strong>in</strong>g<br />
hospitals and plans formulated on how communications<br />
would take place.<br />
(3) A good method for the Identification ~ medical<br />
and nurs<strong>in</strong>g staff would be useful and allow a more<br />
effectiV~ ~ 6f’tl~lP~kllis,., ~: -+<br />
(4) A simple’diagram to illustrate the <strong>in</strong> juri~ ~misht<br />
have been helpful. $imi~Hyil,l,lcordnnhm+t,h,boxes<br />
to tick for tetanus and antibiotic prophylaxis along<br />
with the analgesia given might have been beneficial.<br />
(5) Communications with<strong>in</strong> the hospital proved<br />
difficult. The u~e of "walkie talkies" by key sufffwould<br />
improve the flow of patients.<br />
(6) A systemised approach to the ~tatton of<br />
patients is required, and a copy of the notes should be<br />
left for the records of the accident and emergency<br />
departments.<br />
(7) A consultant radiologist should be <strong>in</strong>cluded <strong>in</strong><br />
each major disaster team and <strong>in</strong> the call out system.<br />
Discussion<br />
¯ Each disaster presents its own problems. Disaster<br />
practice exercises tend to con~ntrate on airports or<br />
major <strong>in</strong>dustrial complexes, where the potential exists<br />
for many people to be hurt. There should, however, be<br />
an element of flexibility to cater for the unexpected. In<br />
this <strong>in</strong>cident the aviation fuel fortunately did not ignite<br />
and alter the pattern of<strong>in</strong>juri~.<br />
A major disaster stretches tl~ remurg~ of the<br />
emergency servk’~t tu an exLren~. The extremity was<br />
not reached at this <strong>in</strong>cident bqa:ause of the capabilltigs<br />
of three major disaster plans.<br />
The six’~"ficity of the phms ~ frota day to day<br />
rout<strong>in</strong>e. Thu~d~hl 0¢t~’"tiid~ what should<br />
h, ve h*ppen~l ~ wha did +~. ThJ. led to<br />
crittclsm at debrief<strong>in</strong>g sessions; m<strong>in</strong>e crilktsms may be<br />
justified, song impossibl© to relolve. <hotqgh dug<br />
theo beh<strong>in</strong>d em <strong>in</strong><br />
this can be di~R. to ~:~0 Im~mse of the<br />
unfamiliarity and devlatlon fi-0m ~lim:.<br />
At the scene chaos and confusion were commlled<br />
more by regularity than by the disaster plan. The first<br />
40 patients transferred to Queen’s Medical C~tre,<br />
Nott<strong>in</strong>gham, had little triage or tr~tng’m at the scene<br />
becau~ of the sheer numbers of ambulances available<br />
to "scoop and run." This they did ss is their normal<br />
practice. They cannot be expected to wait for the<br />
~tO qwISO±IO~ " ~ ~ Rtbo gqg 10 Zg:gt 60-g0-6~6t<br />
6.~
O<br />
L<br />
arrival of medical teams with organised triage po<strong>in</strong>ts.<br />
To the receiv<strong>in</strong>g hospital this was a considerable izhqux<br />
of patients who had not received prehospital care, and<br />
staff <strong>in</strong> the hospital did not know how many more were<br />
to come or the extent of their <strong>in</strong>juries as they had no<br />
communications with those at the scene. This applied<br />
pressure on the accident and emergency departments<br />
to process the patients as fast as possible. The conditlon<br />
of several patients deteriorated <strong>in</strong> the x ray<br />
department and may not have done so had this<br />
pressure on rapid assessment and management not<br />
been present.<br />
To have many doctors available on site was an"<br />
advantage. To have volunteers present who were not<br />
from the fly<strong>in</strong>g squad system, although admirable, did,<br />
however, cause some concern to the site medical<br />
officer, who was not aware of their capabiJiti~ or<br />
lidlhatione <strong>in</strong> an unsupervised environment <strong>in</strong> which<br />
communication was bad. Had the triage po<strong>in</strong>t been<br />
~mtabllsh.d e~Lier, or the :sh~: mcd.[~al o[fi~cr I:~u<br />
more ldenfifiablc, better control could have existed.<br />
The triage po<strong>in</strong>t could be recognised from boxes of<br />
colloid, adm<strong>in</strong>istration sets, and familiar faces <strong>in</strong> the<br />
crowd of lum<strong>in</strong>ous jackets.<br />
The fly<strong>in</strong>g squad functioned well <strong>in</strong> a situation uot<br />
far removed from their usual practice by splitt<strong>in</strong>g <strong>in</strong>to<br />
teams of two to treat the trapped’patients <strong>in</strong> various<br />
sections of the wreckage <strong>in</strong> cramped, awkward, and<br />
dangerous conditions. The extent of their role can be<br />
gauged from the supplies used~ The familiarity and<br />
ease with which they operated <strong>in</strong> this <strong>in</strong>cident empha.<br />
s/seal one of the arguments for their existence.<br />
Despite the arguments and criticisms this <strong>in</strong>cident<br />
has produced with<strong>in</strong> the medical profession the casualties<br />
received treatment that would be extremely<br />
NHS Review<br />
Radical change of policy on NHS pay<br />
Roger Dyson<br />
.<br />
This is tl’~ fourth <strong>in</strong> I<br />
series ofanides which ,~<br />
comment on the whit~<br />
~=y~k’~. ~r .<br />
~m~mum~ll~<br />
i~m~<br />
~_.._~’r~.<br />
~<br />
TI~. s~_ie~<br />
The government’s review of the NHS confirms a trend<br />
towarda . pay devolution alread Y underway<br />
<strong>in</strong> Whitley<br />
~il agreements and offers self govern<strong>in</strong>g hospitals iraqi .~St ~n~ted li~ onaitiOnS scope to~t Of emnlovment <strong>in</strong>dependently | Tk..~. <strong>in</strong> sett<strong>in</strong>g<br />
devglopments constitute a rem~ka’ble ch~uge <strong>in</strong>" "~’";<br />
~ philosophy that will do more to chan~ the<br />
(s~u4~ ¯ r ,. ~ on Is ~e~<br />
"" ¯<br />
~ of the NHS than other more immedia !<br />
~si~ smtherev’ ’ ~ y<br />
~. ..... ~ ~<br />
~ew. In parucular the rapid<br />
~xums~on-o~ pay devolution raises a longer term<br />
..... ether health professionals.<br />
"r +<br />
’’~ J At mational level the review makes clear that "the<br />
Iovernment’s objective throughout the service is progrestively<br />
to <strong>in</strong>troduce greater flexibility <strong>in</strong> order to<br />
allow managers to relate pay rates to local labour<br />
markets and to reward <strong>in</strong>dividual performance." This<br />
process has already started and <strong>in</strong>c/udes both grad<strong>in</strong>g<br />
and pay flexibility.<br />
~. Department of Aduh sad<br />
~".umst<strong>in</strong>uial Education,<br />
UM~y of Keela, Kse~,<br />
Su,5ord~hh~ $T5 5~G<br />
Rog~ Dymn, I’HD, director<br />
Two major grad<strong>in</strong>g flexibility agreements were<br />
<strong>in</strong>troduced <strong>in</strong> 1988 for nurses and for medical laboratory<br />
scientific officers. Despite many faults, the cl<strong>in</strong>ical<br />
grad<strong>in</strong>g review <strong>in</strong> nurs<strong>in</strong>g has <strong>in</strong>troduced a structure<br />
with several opportunities for grad<strong>in</strong>g flexibifity and<br />
h~gher pay <strong>in</strong> the future. The <strong>in</strong>troduction of more<br />
&M~] ~*-~m:+s¢.s primary nurs<strong>in</strong>g and cl<strong>in</strong>ical nurs<strong>in</strong>g specialist posts is<br />
654<br />
difficult to improve upon, given the disastrous nature<br />
of this <strong>in</strong>cident. Lessons have been learnt. We empha.<br />
sise that such good medical care would not have been<br />
possible without the excellent ooperation, deification,<br />
and help from our olleagues from the f~e, polk~, and<br />
am~ servk~s as well as ~ helicopter crews and<br />
mounta<strong>in</strong> rmc~ teams.<br />
Wc dmak the deporuments of medical ~u~on<br />
l~’rb)~hite and L,ekater Royal hb~mnri,.s for ~ help~<br />
and ~ BmT~ for his editorial help.<br />
S ~--,, -. m ~eene [at me scene); Dr D Baker, Dr N ,<br />
Boucher, Dr S Dave, Dr A Dove, Dr S Dexter, Dr N French,<br />
Dr J Mason, Dr D Miller, Dr ] Vanuim, Dr D Virdee, Dr T:<br />
. parua~.~; ,.,~:mre ~a/l~.: Dr A Morris, Dr S i~<br />
rema<strong>in</strong>, Mr P Prltty, Ms Jme Warn (phmoBrapher) Oft the .....<br />
scene); D~ M Dco~, Dr l Gordon, Dr W Malone, Dr L<br />
OIi-,~r, Dr A Watt, Dr D qC~Ul~, Dr J’ W~st~a, ~ A leja~4.-<br />
Moodie (<strong>in</strong> the depsrunent); L¢iccuo Royal l~rmary: Dr L<br />
Beaumont, Dr C Harper, Dr I Hume, Dr S Mard©., Dr M<br />
Mowbnty, Dr M Underwood, Mr M Allem, Mr D Barton, Mr<br />
J Harper (at the scene); Dr V Cheppel, Dr J Dive, r, Dr A<br />
McCaskie, Dr G Siqlh, Dr M Thompson, Mr G Bodiwals,<br />
Mr D D~Cruz, Mr i Pimir, Mr D Qumu~ (<strong>in</strong> the depsn.<br />
meat).<br />
s~n’ad~<br />
,,,- ,,mmuou:. ~ pay flexibifiw has already been<br />
proposed to the nurses’ pay review body <strong>in</strong> the<br />
mantgcmcnt side’s evidence, and <strong>in</strong> the current negotiations<br />
with the adm<strong>in</strong>istrative and clerical Whidey<br />
ouncil the management’s representatives are press<strong>in</strong>g<br />
for some local pay devolution on the back of a<br />
completely new and more flexible grad<strong>in</strong>g structure, In<br />
these negotiations the Department of Health gives<br />
the impression of be<strong>in</strong>g determ<strong>in</strong>ed to press ahead<br />
irresp~tive of the opposition of the staff sial. F to the<br />
pr<strong>in</strong>cipk of local pay devolution.<br />
Much has yet to be decided about the range of pay<br />
~J VOLUME 298 l I ~4A~CH 1989<br />
t<br />
t<br />
T<br />
B<br />
£1