Issue 30
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
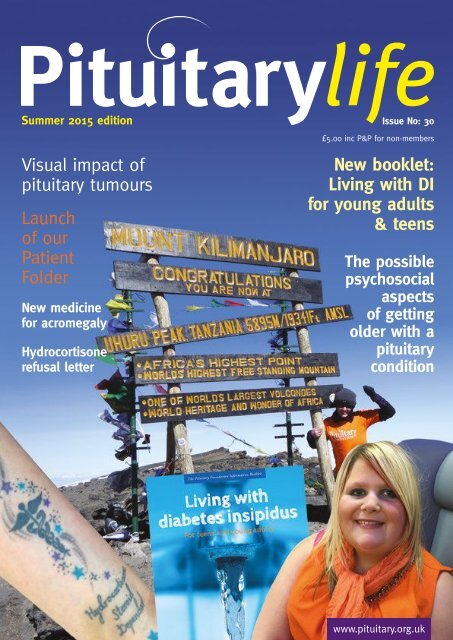
Summer 2015 edition<br />
<strong>Issue</strong> No: <strong>30</strong><br />
£5.00 inc P&P for non-members<br />
Visual impact of<br />
pituitary tumours<br />
Launch<br />
of our<br />
Patient<br />
Folder<br />
New medicine<br />
for acromegaly<br />
Hydrocortisone<br />
refusal letter<br />
New booklet:<br />
Living with DI<br />
for young adults<br />
& teens<br />
The possible<br />
psychosocial<br />
aspects<br />
of getting<br />
older with a<br />
pituitary<br />
condition<br />
Pituitary life | autumn 2012<br />
www.pituitary.org.uk
2<br />
news News<br />
Making progress<br />
contents<br />
Last year was a fantastic year for the<br />
charity in many ways and we have<br />
recently published a new Annual<br />
Review document highlighting our<br />
achievements during 2013/14. We saw<br />
increasing demand for our services,<br />
more patients supported, and a<br />
record breaking record-breaking year<br />
in fundraising, increasing volunteer<br />
numbers and growth across the<br />
organisation generally.<br />
We are proud to say that last year,<br />
of every £1 spent, 85p went towards<br />
supporting patients and our Local Support<br />
Groups’ work in their communities. We’ve<br />
made amazing progress over the past 12<br />
months, but there is so much more to do to<br />
improve awareness and support for patients<br />
and their families. We will now continue to<br />
build on our current achievements and drive<br />
forward our aims of improving awareness,<br />
educating healthcare professionals and<br />
providing support and information to<br />
anyone affected by pituitary conditions.<br />
Please do read a copy of the Annual<br />
Review online, or order a printed copy, so<br />
you can see how the money and support<br />
you contribute to The Foundation is used<br />
effectively. A copy can be downloaded<br />
on our website (www.pituitary.org.<br />
uk/about-us/charity-information) or<br />
News 2-9<br />
Local Support Group news 7<br />
Professional articles 10-11<br />
& 21-26<br />
Raising awareness 13-20<br />
Wall of thanks 16-17<br />
Patients’ stories 27-31<br />
ordered by emailing enquiries@pituitary.<br />
org.uk<br />
Thank you sincerely for continuing<br />
your membership – every member really<br />
does count. We need and appreciate your<br />
help to continue progressing our work to<br />
improve the lives of pituitary patients and<br />
their families ■<br />
Menai Owen-Jones<br />
Chief Executive<br />
Jenny West<br />
Chair of Trustees<br />
New! Pituitary Patient Folder<br />
Have you got our resources you<br />
want to store safely in one place?<br />
Or, have you got appointment<br />
letters, test results and our Emergency<br />
Cards in various envelopes, or wedged<br />
behind the toaster? We have a solution<br />
– our new Pituitary Patient Folder,<br />
with our printed card on the front.<br />
The folder has 20 clear plastic inserts<br />
to easily file all of your pituitary<br />
paperwork. It is a convenient A4 size<br />
to store at home and carry with you to<br />
endocrine appointments; it will help<br />
you find quickly any information you<br />
might need during your appointments.<br />
It will also be invaluable if an<br />
emergency arises – just pick up and take<br />
with you to inform those looking after<br />
you. We are able to offer these folders<br />
(in a choice of purple, orange or green<br />
colours) at a reduced price of £2.00 each<br />
including packing and postage. To order<br />
your folder, please send a cheque for<br />
£2.00 to The Pituitary Foundation, 86<br />
Colston Street, Bristol BS1 5BB, and<br />
marking your envelope ‘Patient Folder’<br />
with a note inside of your preferred<br />
colour. Cheques must be made payable to<br />
“The Pituitary Foundation” Alternatively,<br />
you can order through our website shop ■<br />
Pituitary Life | summer 2015
news News - Awareness Month<br />
3<br />
Awareness Month October 2015<br />
Together, we can make this the best Awareness Month on record! Please have a<br />
look and see which of the below activities you can help with, large or small - it<br />
will make a massive difference!<br />
This October, the main theme of this Awareness Month will be the launch of<br />
the Get Red Flagged Campaign. This campaign is all about encouraging patients<br />
with adrenal insufficiency to register with their local Ambulance Trust. Once<br />
a patient is red flagged on the Trust’s system, if they were to ever call 999, the<br />
call will be flagged for priority attendance to their home address by a vehicle<br />
carrying emergency hydrocortisone. Adrenal crisis is life threatening and<br />
getting red flagged is an important safety precaution.<br />
It would be brilliant news for pituitary awareness if we could increase the<br />
numbers of people getting involved again; 2014 saw a sensational 63% rise from<br />
2013, which will be hard to beat, but we love a challenge! ■<br />
How to get involved<br />
Red flags, with our logo on, will be<br />
printed and sent out as reminders<br />
to support groups and clinics. We<br />
want the pituitary community to be<br />
bombarded by red flags and pictures<br />
of supporters wearing red during<br />
October, we want to make sure everyone<br />
takes notice of this important message.<br />
This is an awareness campaign and the most important way you<br />
can get involved is to get yourself red flagged during October,<br />
through using the information provided by The Foundation. Just<br />
get in touch and we will send you an information factsheet about<br />
what to do. Secondly, you can take a flag and resources to an<br />
endocrine clinic to help with Get Red Flagged awareness. The<br />
Foundation will be sending resources to all pituitary Centres of<br />
Excellence too.<br />
For any queries about getting involved with our Get<br />
Red Flagged awareness campaign please contact Rosa, our<br />
Volunteers, Campaigns & Projects Manager on 0117 370 1316.<br />
The campaign will begin in the autumn, so please remember<br />
if you register to get<br />
involved now, you<br />
will be sent your<br />
resources in early<br />
September, ready<br />
for October ■<br />
To raise awareness and<br />
funds in line with<br />
the Get Red Flagged<br />
campaign supporters are<br />
planning Go Red Days<br />
across the UK.<br />
This can involve anything<br />
from asking your company<br />
to allow a Go Red Day at work, to organising a Red Day<br />
coffee morning. It’s easy - all that’s involved is something red!<br />
This could be wearing a red shirt, T-shirt, tie or socks! For the<br />
more daring, you may even want to dye your hair red or have<br />
your face painted. An easy way to raise money is to charge a<br />
small fee to those wearing red, and you could even bake rediced<br />
cakes to sell. Once you have decided on what you want<br />
to do, please get in touch and we’ll send out your red flags to<br />
help you celebrate going red in style. For help<br />
planning your Go Red event contact Jay<br />
our Fundraising & Marketing Manager<br />
on 0117 370 1314 ■<br />
Do you have time to set up a pituitary<br />
awareness stand for a few hours in<br />
your local community, for example in<br />
a doctor’s surgery or library? If so, we can provide<br />
all the posters, leaflets and balloons you will need. (Remember to<br />
get permission from the venue you are going to use and speak to<br />
us for help in planning your stand.) ■<br />
Pituitary Life | summer 2015
4 News - Awareness Month<br />
If you are unable to get involved with Awareness<br />
Month, but are willing to donate to help fund our<br />
awareness work instead, please fill in the ‘Make a<br />
gift’ section of the Awareness Month insert within<br />
this issue of Pituitary Life. Last year, thanks to your<br />
generosity, we managed to raise an amazing total of<br />
£2568.58 which made our awareness work possible.<br />
Please can you help us again? ■<br />
Give a general pituitary awareness talk in your local<br />
area! This could be anywhere from a local school,<br />
place of work, WI, or Rotary Club. The Foundation<br />
has developed materials to help support people giving<br />
a talk on pituitary conditions. These materials include<br />
PowerPoint slides and notes to read from to make it easier.<br />
Let us know if you’re interested ■<br />
Summer Raffle<br />
Thank you to everyone who has bought raffle tickets so<br />
far. We have raised a fantastic £2800, an increase of<br />
122% on this time last year! Thanks to the collective<br />
efforts of supporters like you, last year’s Summer Raffle<br />
raised £<strong>30</strong>14. We’re hoping that with your help we will<br />
be able to make this year’s Summer Raffle even more<br />
successful than the last. With the closing date on the 26th<br />
June, this is your last chance to request raffle tickets. Please<br />
get in touch with jay@pituitary.org.uk to order your book<br />
of 10 tickets today so you’re in with a chance of winning<br />
one of our fantastic prizes and helping us continue to<br />
support pituitary patients and their families in the process.<br />
As a small charity, all the money we raise plays a vital role in<br />
allowing us to be there for people with pituitary conditions, their<br />
friends and family: 85p of every £1 donated to the charity is spent<br />
on providing support for people affected by pituitary conditions.<br />
This year’s fantastic Summer Raffle prizes are:<br />
1st Prize: A luxury city break in Cardiff in the Mercure<br />
Holland House Hotel and Spa, staying in the Presidential Suite,<br />
including treatments at the hotel and dinner<br />
2nd Prize: Apple iPad<br />
3rd Prize: £50 cash ■<br />
Request your resources<br />
Let us know which activity you are getting involved<br />
in and we will send you the resources you will need.<br />
To do this, just fill in the relevant section of the<br />
Awareness Month insert with this magazine and post<br />
to us. Alternatively, contact our Assistant Administrator,<br />
Emily Graham, at emily@pituitary.org.uk or on 0117<br />
370 1310. Please make sure you let us know about your<br />
awareness activities as this allows us to measure how<br />
much of an impact Awareness Month has around the<br />
UK!<br />
If you would like to take part in an activity that is not<br />
listed above, just let us know as we can still support you<br />
in planning this. The more activity during October the<br />
better!<br />
Please note that all resources will not be posted out<br />
until early September ■<br />
Pituitary Life | summer 2015
News<br />
5<br />
Thank you to all volunteers<br />
We appreciate the amazing work of our volunteers all year round, however,<br />
National Volunteers’ Week is an excellent opportunity to say an EXTRA BIG<br />
thank you! Volunteers’ Week is an annual celebration about the contribution<br />
volunteers make across the UK.<br />
Over the past year, The Pituitary Foundation would never have achieved as much as we have<br />
done without our volunteers’ help. The past year has seen many volunteer highlights including;<br />
reaching a total of 110 volunteers, volunteer Helpline cover rising to over 50%, increased local<br />
support group cover, and the increase in volunteers getting involved in Awareness Month<br />
activities. The staff were delighted to see from feedback this spring that 92.5% of our volunteers<br />
would ‘recommend others to volunteer’.<br />
With our thanks and appreciation for your outstanding commitment, from all the staff at The<br />
Pituitary Foundation ■<br />
To celebrate Volunteers’ Week we<br />
have asked one of our youngest<br />
volunteers, Laura, for her story.<br />
A huge thank you to Laura for her<br />
amazing contributions since joining us.<br />
My name is Laura Duffield and I’m<br />
23 years old. I am a pituitary patient<br />
and the Volunteer Area Coordinator for<br />
the Sheffield Pituitary Support Group. I<br />
currently work full-time as an accounts<br />
assistant for a national coffee shop chain.<br />
I was only three years old when I was<br />
diagnosed with a pituitary condition.<br />
Apparently, I didn’t act like a ‘normal’ child<br />
- I would play for a while then just want to<br />
go to sleep. I used to cover my eyes when<br />
exposed to bright light and, as my condition<br />
deteriorated further, I couldn’t eat anything<br />
without being sick. My concerned parents<br />
persisted with taking me to the doctors<br />
but were made to feel as though they were<br />
being unduly overprotective and paranoid.<br />
They kept being sent away by the doctor<br />
and told that it was nothing more than the<br />
‘terrible twos’.<br />
Back in the 1990s, every child in the<br />
Rotherham area had a routine check-up at<br />
the age of three. Fortunately, this picked<br />
up that something wasn’t quite right with<br />
my eyesight, but despite trying glasses,<br />
there was no improvement. It was only<br />
when an ophthalmologist investigated<br />
further and sent me for an MRI scan<br />
that the tumour was detected and I was<br />
diagnosed with a craniopharyngioma.<br />
Within two weeks of diagnosis (April<br />
1995), I had surgery to remove the tumour<br />
and my pituitary gland. Unfortunately, by<br />
the time I was operated on, the tumour<br />
had become entangled with my optic<br />
nerve, resulting in permanent damage<br />
to my eyesight. I have been left with no<br />
vision in my left eye and only have partial<br />
sight in my right.<br />
Despite having to learn to walk and<br />
talk again after the operation, I managed<br />
well at primary school. I was nominated<br />
and selected for a Child of Achievement<br />
Award, going to London to collect this<br />
and meeting various celebrities. Secondary<br />
school was tough, due to ongoing illness<br />
and regular hospital visits but against all<br />
the odds, I did really well in my GCSEs<br />
and A Levels.<br />
I currently take various medication,<br />
including replacement hormones<br />
(hydrocortisone, thyroxine etc.) and<br />
desmopressin for diabetes insipidus. I<br />
also carry an Efcortesol injection with me<br />
for use in an emergency, should I suffer<br />
an Addisonian crisis. I received regular<br />
growth hormone injections and without<br />
them, I don’t think I would have grown to<br />
be 5 feet 3 inches! I had to stop the growth<br />
hormone injections as a precaution in<br />
2011, when I received the devastating<br />
news that I’d developed a liver tumour.<br />
I had to have an operation to remove<br />
the tumour, losing 75% of my liver, but<br />
fortunately it has since regenerated to<br />
its normal size. As a teenager, I also<br />
used to take Loestrin, but as with the<br />
growth hormone, this medication<br />
was withdrawn as a precaution<br />
following my liver tumour.<br />
I didn’t find out about The Pituitary<br />
Foundation until a few years ago and<br />
only wish I’d found out sooner. The<br />
information and support that’s available<br />
is invaluable. About a year ago, I found<br />
out that the Sheffield Support Group was<br />
close to folding, so I decided to rise to the<br />
challenge and take it over - it’s the best<br />
thing I’ve ever done! I feel as though I’m<br />
helping people with similar conditions<br />
and was surprised to learn just how many<br />
other pituitary patients there are in South<br />
Yorkshire!<br />
Last October, I held a fundraising event<br />
in aid of The Pituitary Foundation, raising<br />
£850 and I’m already planning another<br />
one this year! Out of running the support<br />
group I have met a boyfriend, who is now<br />
a big part of my life! I am very grateful<br />
for all the support my<br />
family and friends<br />
have given me<br />
over the years,<br />
especially my<br />
mum, who<br />
means the<br />
world to<br />
me! ■<br />
Pituitary Life | summer 2015
6 news<br />
Donna’s tattoo<br />
It started three years ago, aged <strong>30</strong>.<br />
I now know I hadn’t felt well for a<br />
long time. It was August and my<br />
husband and I took our three boys,<br />
who were age 11 and twins age seven,<br />
on a two week camping trip where we<br />
had so much fun. But I remember one<br />
night I had a very intense headache -<br />
much worse than normal (I did often<br />
suffer with headaches) but I soldiered<br />
on as us mums do, determined I<br />
wasn’t going to wreck our holiday.<br />
CT scan<br />
On our return I still had a headache and I<br />
felt unwell, weak, even a bit disorientated<br />
but I put it down to having three very<br />
active, lively boys to look after and thought<br />
it would settle when they were back to<br />
school. They went back to school and I<br />
realised I just couldn’t face going to work<br />
(as a teaching assistant at a pre-school).<br />
The following day, I had no strength and<br />
even dropped four pints of milk all over<br />
the floor; my mum then made me phone<br />
the doctors and get an appointment. I went<br />
that day and the locum doctor insisted I<br />
was stressed and depressed, putting me<br />
on antidepressants, but the following day<br />
my mum was unhappy with the diagnosis<br />
and insisted I made an appointment with<br />
my regular doctor. He was very thorough<br />
and agreed it was not depression but felt<br />
because of my weakness, headache and<br />
some vision loss, a CT scan would be a<br />
good place to start and he even bet me a<br />
pound that it would be fine but he needed<br />
to rule a neurological cause out. Within<br />
an hour he phoned me and said to go to<br />
my local hospital straight away as he had<br />
got me an appointment for the same day. I<br />
still didn’t panic, but I could see my mum<br />
was and she called my husband at work<br />
who met us there.<br />
life changing<br />
Wow, then my life changed forever!!! We<br />
sat for two hours after the scan waiting<br />
for someone to give me the all clear (so<br />
I thought), but when we were called back<br />
in, I was told that the scan had shown a<br />
growth and some abnormalities, but they<br />
didn’t treat neuro so they referred my<br />
scans to Derriford hospital which was a<br />
168 miles round-trip away. We were told<br />
we would hear from them within a week.<br />
We went home shocked and with so many<br />
questions!! A growth – where? Cancer?<br />
Abnormalities!!!<br />
pituitary tumour<br />
It was two weeks before we heard<br />
anything - and that was with my husband<br />
chasing, trying to find out who was<br />
looking at the scans and who was going<br />
to look after me. Finally, two months after<br />
my CT, it was made clear to me that I had<br />
a pituitary tumour, which had bled and<br />
five very strange shaped brain aneurisms.<br />
The struggle didn’t stop then because<br />
the local hospital was so far behind with<br />
appointments to see an endocrinologist,<br />
it was a three month waiting list, so I<br />
went private and paid. This appointment<br />
led to me being seen in Derriford within<br />
six weeks and undergoing all the tests.<br />
Meanwhile, I was meeting with various<br />
neurosurgeons to talk through my options,<br />
which at that point, was very bleak due to<br />
the size and shapes of the aneurisms.<br />
endocrine tests<br />
Each endocrine test lead to more<br />
medication - the stress was unbearable. I<br />
was told of the importance of a medical<br />
ID bracelet and how it could potentially<br />
save my life. My parents bought my first<br />
one at the cost of £50 which was so nice,<br />
however, it broke and over the next 12<br />
months I went through five bracelets. It<br />
was also the fact of remembering to put it<br />
on and this caused stress when you were<br />
out and realised you didn’t have it on. It<br />
lead to a conversation one evening with<br />
my mum and husband, who suggested<br />
having it tattooed on; I wasn’t so keen<br />
to start with, but having looked on the<br />
Internet, I changed my mind and decided<br />
it would always be there and it was one<br />
thing I didn’t have to think or stress about<br />
anymore. So I went and had it done and<br />
I’m so pleased I did, it makes me feel safer<br />
and it’s a talking point too. My mum (who<br />
has sadly passed away 18 months ago<br />
from an unknown brain aneurism) and<br />
my husband were right. I’ve undergone<br />
18 operations and a craniotomy in three<br />
years; they have managed to make safe<br />
my aneurisms, for now, but because it has<br />
entailed a lot of operations (with doctors<br />
coming from Milan to treat them), I still<br />
have my tumour!!!<br />
side effects<br />
I take lots of medications and have lots of<br />
side effects!! In fact I’m a totally different<br />
person to who I was, but I’m alive. I<br />
would like to say a massive thanks to The<br />
Pituitary Foundation for their support<br />
and the massive amount of information<br />
online and in the support groups, which<br />
you don’t get told ■<br />
Pituitary life | summer 2015
Local Support Group News<br />
7<br />
This section contains some<br />
brief updates from a few of our<br />
Support Groups around the<br />
UK. For information about our<br />
groups’ meetings and to see if<br />
one of our 32 Support Groups<br />
meet near you, please see our<br />
website, contact Rosa Watkin<br />
on 0117 370 1316, or email<br />
helpline@pituitary.org.uk<br />
Central and North West Lancs<br />
Sadly we have said goodbye to the Area<br />
Co-ordinator Kath McGahran after<br />
many years of running the group. Kath<br />
did a fantastic job and The Foundation<br />
would like to say a huge thank you for<br />
all the time and hard work she put<br />
into the group. The new joint Area<br />
Co-ordinator, Ron Cross, will now<br />
run the group with Phil Buckley who<br />
is continuing as AC. Nick Melling will<br />
be helping to organise events for the<br />
group also. The group will continue<br />
to meet every two months with formal<br />
meetings and meals out. They are always<br />
happy to welcome new members. The<br />
group will next meet on 4 July and 12<br />
September 2015.<br />
Leeds<br />
The Leeds Group meet on the first<br />
Saturday of every month (with the<br />
exception of August when there is<br />
no meeting) in The West Yorkshire<br />
Playhouse restaurant with a 10.<strong>30</strong>am<br />
start. There will be a sign against one<br />
of the bay windows so you can easily<br />
spot them if you are joining them for<br />
the first time. The group is always<br />
happy to welcome new members and<br />
you can find the contact details for<br />
Sally Robertson, Area Co-ordinator, on<br />
our website or by ringing our Helpline.<br />
Recently, the group has enjoyed some<br />
really fascinating meetings with the<br />
recent AGM in April, including a<br />
presentation by Dr Robert Murray,<br />
Consultant Endocrinologist and his<br />
team in Leeds about ‘Advances in the<br />
treatment of pituitary tumours’.<br />
Aberdeen<br />
We are sadly saying goodbye to Jennifer<br />
Gibson who has had to stand down<br />
as Aberdeen’s Area Co-ordinator; we<br />
would like to say a special thank you<br />
for everything she did for the group.<br />
Alison Milne, our Endocrine Nurse,<br />
has kindly offered to run the group in<br />
her spare time as a temporary measure<br />
until another Area Co-ordinator can<br />
take over. Alison can organise two or<br />
three meetings a year. The next date set<br />
is 22 August for a social walk, details<br />
TBC. They are urgently looking for<br />
a new co-ordinator and if anyone is<br />
interested or would like to know more<br />
about the role, please contact Rosa<br />
Watkin on 0117 370 1316, or email<br />
rosa@pituitary.org.uk (Rosa is also<br />
dealing with general group enquiries<br />
until a new co-ordinator is found.)<br />
Ipswich and Suffolk<br />
The Ipswich and Suffolk Group have<br />
regular meetings in Ipswich Hospital<br />
where they share experiences of<br />
pituitary conditions; a member also<br />
attends each pituitary clinic to be there<br />
to offer support to new patients. In<br />
the groups’ recent meetings they<br />
have enjoyed a talk by Jo Pooley,<br />
a paramedic with the Suffolk<br />
Ambulance Service, and held an<br />
informal coffee morning. The group<br />
is next meeting on 27 July, where Dr<br />
Gerry Rayman, head of the Diabetes<br />
& Endocrine Department at Ipswich<br />
Hospital, will be speaking. Dr Rayman<br />
was the instigator of the group along<br />
with Marion Lanyon, the Endocrine<br />
Specialist Nurse. Dr Rayman is giving<br />
up his endocrine clinics to concentrate<br />
on diabetes and his presentations<br />
which he does worldwide; so this talk<br />
is to say ‘Goodbye’. For group details,<br />
email pitips@btinternet.com or ring<br />
our Helpline.<br />
London<br />
London Support Group meetings<br />
are held four times a year and have a<br />
specialist speaker at most meetings. At<br />
the last meeting, the group enjoyed a<br />
talk from Professor Marta Korbonits<br />
on ‘Functioning Tumours’, the type<br />
of tumour that causes the pituitary to<br />
overproduce growth hormone, cortisol<br />
and prolactin. The Professor talked<br />
about all aspects of these conditions<br />
and the treatments available with an<br />
opportunity to ask questions. The<br />
next meetings will be on Saturday<br />
26 September for the annual group<br />
social meeting, then on 11 December<br />
at Hammersmith Hospital. The social,<br />
just for members, will be a Regent’s<br />
Canal trip from Camden Lock to<br />
Little Venice and back again through<br />
Regent’s Park, London Zoo and other<br />
sights (booking is essential).<br />
Contact details for our Support<br />
Groups are on our website or just<br />
call our Helpline ■<br />
Pituitary life | summer 2015
8 news<br />
A patient’s view of their annual review<br />
Your annual appointment<br />
arrives in the post; in fact two<br />
appointment letters are in the<br />
same envelope – the original date was<br />
cancelled (which you never received<br />
anyway) and a new date given for a<br />
week’s time.<br />
You set off from home at 9.00am to<br />
arrive in good time and find parking.<br />
Three car parks are full, so you drive<br />
around for 20 frustrating minutes, hoping<br />
for a space. A quick sprint along corridors,<br />
and flight of stairs to reach the clinic. A<br />
receptionist is checking patients in at the<br />
desk, asking each patient to repeat their<br />
phone number, GP and date of birth –<br />
often asked to be repeated more loudly, in<br />
full hearing of other patients!<br />
The clinic<br />
The walls are bare, except for the odd<br />
poster advertising various diseases and<br />
white boards with illegible doctors’ names<br />
scribbled on…some paintings or local<br />
photos would be nice to look at. The<br />
seating area (probably as in most clinics)<br />
with very hard plastic chairs, faces on<br />
to a general thoroughfare, with patients<br />
parading backwards and forwards,<br />
searching for their various clinics. It’s<br />
a clean and tidy area, but stark. Not a<br />
Pituitary Foundation poster in sight!<br />
One nurse is weighing patients in turn<br />
and three others are ‘busily’ walking in<br />
and out of consulting rooms with files,<br />
their comfortable shoes making that<br />
‘squishing’ noise. The clinic nurses don’t<br />
talk to the waiting group of people, only<br />
as we are checked in and maybe exchange<br />
the odd word at our weigh-in.<br />
After a half hour wait, you are told that<br />
there will be a delay of one hour today<br />
and that we could go and get a cup of tea!<br />
Not many do though, in case they miss<br />
their turn. This delay will be a regular<br />
occurrence found in other medical clinics<br />
and it’s appreciated that sometimes it<br />
simply cannot be helped. However, these<br />
delays can mean patients then also run late<br />
on things they have to do too. The waiting<br />
room fills up; it can appear that patients<br />
who arrive sometime after you, are seen<br />
earlier than you. Staff from other clinics<br />
nearby stop for a chat with your clinic<br />
staff about their social activities. The<br />
waiting patients keep looking to check<br />
if consulting room doors are opening, in<br />
between the distraction of each patient<br />
being called to be weighed. A trip to the<br />
water dispenser is a treat, to stretch your<br />
legs at least! After sitting for one hour<br />
and four minutes, your name is called.<br />
The consultation<br />
An ‘absorbed on several things at once’<br />
consultant greets you; their computer is<br />
also playing up. Consultant asks how you<br />
are. “I’m fine thank you” - your usual<br />
‘annual response’. Your file is open; you<br />
are asked what you are taking (the same<br />
question asked every year) – you reel your<br />
replacement hormones and doses off, as<br />
consultant writes them on the sheet. Have<br />
you ever wondered why patients are asked<br />
this question every visit; is it because the<br />
consultant needs to know that we patients<br />
Pituitary Life | summer 2015
news<br />
9<br />
know what we are taking…?<br />
You are almost done (with<br />
unmistakeable relief from the consultant,<br />
as you are one of those ‘feels-very-wellno-problems-patient’).<br />
You’ll both be<br />
mindful that there are other patients<br />
with very numb backsides in the waiting<br />
room that may well not feel fine. Your<br />
consultant asks when your last scan was.<br />
Apparently, the hospital has transferred<br />
all old paper records to electronic, but<br />
only for the past several years, so a wealth<br />
of your early pituitary history doesn’t<br />
appear to exist. You manage between you<br />
to conclude the outcome of your surgery<br />
and your last scan date.<br />
The mere mention of having an MRI<br />
scan; you shudder inside! You will clearly<br />
recall the scans you have had. No MRI<br />
you’ve had has been up there on your<br />
‘joyous experiences’ list. Do you ever<br />
wonder if your consultant knows just what<br />
an MRI is like to have? Can they imagine<br />
climbing beneath the floorboards at home<br />
to look for a leaking pipe?’ Maybe not, but<br />
bear with me. ‘You are under the floor, in<br />
this tiny space, with the floorboards right<br />
above your face. Now imagine trying to<br />
turn and you get stuck; wedged hard and<br />
cannot move! Are you now claustrophobic<br />
and your panic rising? And then being<br />
pulled out, contrast dye injected into your<br />
vein and pushed back in; within minutes<br />
you’ll have a divine metallic taste in your<br />
mouth and it will feel as though you have<br />
wet yourself? That is what having an MRI<br />
scan can feel like.<br />
The other thing about an MRI that<br />
can cause terror is ‘can the radiologist see<br />
something amiss in your pituitary - or in<br />
your entire brain for that matter’? You get<br />
off the scan table and go off home, none<br />
the wiser but worrying at what might have<br />
shown up – re-growth or other ‘brain<br />
findings’ can be a frightening scenario for<br />
most. If the phone were to ring once you<br />
are home, you almost jump out of your<br />
skin in case it’s about your MRI…!<br />
Editor Note: Not all patients<br />
share this view. One patient says that<br />
she doesn’t find an MRI scary or<br />
unpleasant and meditates whilst lying<br />
there. We understand that headphones<br />
are being offered these days and of<br />
course sedation is available for those<br />
who are claustrophobic. What has your<br />
MRI experience been like? Let me know,<br />
by emailing pat@pituitary.org.uk and<br />
I’ll publish your experiences.<br />
The aftermath<br />
Your consultation takes nine minutes;<br />
you say farewell for another 12 months<br />
and take a ticket to sit in the queue<br />
at phlebotomy for your blood tests.<br />
Phlebotomy is often busy, so another wait,<br />
on another hard seat. Number 60 is called<br />
(you are now a number); unfortunately,<br />
the vein in your left arm won’t behave, so<br />
you come away with both arms plastered,<br />
bruised and sore. You then walk (quite<br />
drained) several hundred yards back to the<br />
car park, pay your extortionate parking<br />
fee and reach home three and a half hours<br />
after you left the house.<br />
You may feel quite emotionally<br />
exhausted after your appointment. There<br />
could be still some uneasiness, visiting<br />
the site of your early treatment and tests.<br />
You will still remember clearly that day of<br />
your diagnosis and being told “You have a<br />
tumour!” and the quite invasive tests you<br />
went through. You might have felt really<br />
quite ill too. The fear of having surgery,<br />
post-op time and slow recovery, plus<br />
starting to take daily hormones, might<br />
have all left their mark.<br />
You feel it’s important to know what<br />
your current blood tests results are, but<br />
these are kept in your file and may only<br />
be sent to your GP after some weeks. You<br />
won’t wish to take your GP’s time up, just<br />
for your results, so you wait until next<br />
year’s appointment to hear about them<br />
then. But, unless you ask, your results<br />
mightn’t be mentioned.<br />
Annual monitoring is of course necessary<br />
and helpful to have your hormone levels<br />
checked, and discuss your condition and<br />
treatments, but the patient’s experience<br />
of coming to clinic can be quite different<br />
to what the consultant, their team and<br />
clinic staff see and believe it to be, as they<br />
routinely carry out their roles with patients<br />
visiting clinic - week in, week out ■<br />
Pituitary life | summer 2015
10 Professional articles<br />
The visual impact of pituitary tumours<br />
By Dr Denize Atan, Consultant in Neuro-ophthalmology, Bristol Eye Hospital<br />
The pituitary gland is an important<br />
gland which sits in the middle of<br />
our brain. It is responsible for<br />
making a number of hormones that<br />
regulate our metabolic rate, responses<br />
to stress, growth, fertility, menstrual<br />
cycle and pregnancy hormones, and<br />
intake/output of fluids.<br />
The most common problem which<br />
affects the pituitary gland is a benign<br />
growth of the gland, also known as an<br />
adenoma. Pituitary adenomas either<br />
produce excessive amounts of pituitary<br />
hormones themselves, or the growth<br />
actually interferes with the production of<br />
pituitary hormones. Our bodies normally<br />
control the levels of these hormones very<br />
precisely, and too high or low levels lead<br />
to ill health. They do not have any direct<br />
influence on our vision. Why then do<br />
problems with the pituitary gland affect<br />
our vision?<br />
The reason is simply this: pituitary<br />
adenomas can affect our vision because of<br />
where they are positioned in the brain, not<br />
because of what they are, or the hormones<br />
they produce.<br />
When a pituitary adenoma reaches<br />
a certain size (>1cm) it is known as a<br />
macroadenoma and it can start to interfere<br />
with the function of the structures around<br />
it. To understand why this is, it is important<br />
to know a little about the anatomy of the<br />
pituitary gland and what lies close to it in<br />
the brain. In other words, growth of the<br />
pituitary gland affects our vision indirectly,<br />
by exerting pressure on the structures that<br />
surround it. A normal pituitary gland, or<br />
a microadenoma (
news Professional articles<br />
11<br />
Figure 2: Patterns of visual impairment caused by a pituitary macroadenoma<br />
Adapted from: http://commons.wikimedia.org/wiki/File:1420_Optical_Fields.jpg<br />
the information it would normally<br />
transmit to the brain via the optic nerve<br />
cannot get through.<br />
What other visual problems<br />
may be caused by a pituitary<br />
macroadenoma?<br />
As mentioned earlier, normal vision<br />
also depends on your eye muscles pulling<br />
both eyes in the right direction to look at<br />
things simultaneously. If your eyes do<br />
not point in exactly in the same direction,<br />
you might see two images instead of<br />
one. This can be very disorientating and<br />
confusing. The reason that a pituitary<br />
macroadenoma can cause double vision<br />
is that the nerves connecting your eye<br />
muscles to your brain are also positioned<br />
very close to the pituitary gland. There are<br />
three nerves that control eye movements,<br />
called the oculomotor, trochlear and<br />
abducent nerves. They are also known as<br />
the third, fourth and sixth cranial nerves.<br />
If any one of these nerves is affected by<br />
a pituitary macroadenoma, it can result in<br />
double vision (Figure 1).<br />
Why is it important to look for<br />
visual problems caused by a<br />
pituitary macroadenoma?<br />
As mentioned earlier, many people may<br />
not be aware of a problem with their<br />
peripheral vision before it becomes quite<br />
advanced and so it is important that you<br />
are screened for any visual problems<br />
resulting from a pituitary macroadenoma.<br />
In addition, some or all of this visual<br />
impairment can be reversed with treatment<br />
of the pituitary macroadenoma – whether<br />
this is medication, surgery or radiotherapy<br />
to shrink the size of the adenoma. As<br />
the adenoma gets smaller, the pressure it<br />
exerts on surrounding structures, including<br />
the visual circuitry, is relieved, leading to<br />
an improvement in vision. Left untreated,<br />
some of this visual impairment may<br />
become permanent. This can sometimes<br />
affect your ability to drive ■<br />
The possible psychosocial aspects of<br />
getting older with a pituitary condition<br />
By Dr Sue Jackson<br />
When we talk about “getting<br />
older”, who are we referring<br />
to? Gerontologists group<br />
older adults into three sub-groups;<br />
the young old (aged 60-75), the old old<br />
(aged 75 to 85), and the oldest old (aged<br />
85 and over). In terms of pituitary<br />
conditions, our knowledge about the<br />
psychosocial aspects of the various<br />
conditions as they relate to adults<br />
is patchy at best. The kind of data<br />
charting the psychosocial issues for<br />
all the conditions across the lifespan<br />
seems to be largely missing. So what<br />
to do? There are very many beliefs and<br />
ideas about ageing, so in this article<br />
I plan to review the commonest ones<br />
and look at what we might therefore<br />
infer about what getting older might<br />
mean for individuals with a pituitary<br />
condition.<br />
It seems to me that there are currently<br />
two almost opposite ways of thinking<br />
about ageing – one view is quite negative<br />
(older age is a miserable time that comes<br />
with poorer health, reduced mobility,<br />
reduced brain power, invisibility, social<br />
Pituitary Life | summer 2015
12 Professional articles<br />
isolation, stigma and discrimination), the<br />
other is more positive (older adulthood is a<br />
time of continuing health and enthusiasm<br />
for living). For the scores of articles about<br />
how age is a state of mind, and how 50<br />
is the new 40, there are a similar number<br />
of articles from people whose experience<br />
of ageing is arguably far less positive. So<br />
what’s going on? Well, the main message<br />
about normal ageing from recent research<br />
seems to suggest that there is a great deal<br />
of individual difference in the experience<br />
of this time of life, meaning the range of<br />
experiences of ageing is potentially vast.<br />
If this hold true for individuals with a<br />
pituitary condition then it seems some<br />
will age well, while some others are likely<br />
to experience difficulties.<br />
Will it be miserable?<br />
Recent research on mood, tends to<br />
suggest that as a nation the trend is for our<br />
later years to be more positive, with fewer<br />
arguments and less worries. But is that<br />
true for people with pituitary conditions?<br />
Data from the Needs Analysis undertaken<br />
for the Pituitary Foundation in 2006<br />
(this report is still available to download<br />
from the Pituitary Foundation website)<br />
suggested that those in the 61+ age group<br />
were significantly less anxious than those<br />
in their middle age (41-60), they also<br />
reported significantly better quality of life<br />
than those in the other age groups and<br />
had significantly less social anxiety than<br />
the other age groups. Of course, you’ll<br />
have already spotted that the data from<br />
the older adults was analysed together,<br />
rather than being explored in relation<br />
to the three sub-groups of older adults<br />
identified at the beginning of this article,<br />
so the real data on the different age<br />
groups is missing.<br />
Will I have poorer health?<br />
A pituitary condition is a chronic<br />
condition, and the Department for Health<br />
(DoH) Chronic Disease Management<br />
Compendium of Information from May<br />
2004 says that 60% of adults in England<br />
report a chronic health problem. They<br />
report data from the United States which<br />
says that 45% of those with a chronic<br />
disease are likely to have more than one<br />
Pituitary life | summer 2015<br />
chronic condition, but for those over the<br />
age of 65 this rises to nearly 70%. These<br />
data would tend to suggest that some<br />
individuals with a pituitary condition may<br />
well develop additional co-morbidities,<br />
but as far as I’m aware, the data on<br />
pituitary patients and their development<br />
of co-morbidities as older adults has yet<br />
to be investigated and reported.<br />
Will I have problems getting<br />
around?<br />
The DoH report identifies a number<br />
of common problems living with comorbidities<br />
can raise for the individuals<br />
concerned:<br />
• Difficulties with activities of daily<br />
living<br />
• Complicated medical regimens that<br />
may require contact with specialist<br />
services and multiple trips to hospital<br />
• Isolation from family and friends<br />
• Development of further comorbidities<br />
(such as depression) that<br />
can be missed<br />
• Development of problems from the<br />
side-effects of treatments.<br />
Their report provides a graph<br />
which illustrates a gradual increase<br />
in the percentage of the population<br />
experiencing limitations on their life, with<br />
a reduced ability to undertake activities<br />
of daily living. So, of the group of<br />
individuals in the nation who only have<br />
one chronic condition, 15% of them<br />
will experience problems in being able<br />
to perform activities of daily living. This<br />
rises to 42% of the population living with<br />
three co-morbidities, and when you get to<br />
those living with five or more, 67% of the<br />
population report problems.<br />
Will I develop cognitive<br />
problems?<br />
Recent research has suggested that the<br />
predictions on the rate of development<br />
of Alzheimer’s disease and vascular<br />
dementias were wrong, and that with an<br />
increase in control of the risk factors<br />
associated with developing dementia (i.e.<br />
weight, blood pressure, and cholesterol)<br />
the percentage of the population likely to<br />
develop such problems have been revised<br />
downward. In terms of memory function,<br />
Denise Boyd & Helen Bee in their 2014<br />
book “Lifespan Development” report<br />
that, generally speaking, the youngest old<br />
(aged 65-75) tend to retain the same kind<br />
of memory function that they’ve always<br />
had, while the old old (aged 75 to 85) and<br />
the oldest old (aged 85 and over) show<br />
some declines in memory function as well<br />
as a slowing in the speed at which they<br />
can remember things, and do unusual, or<br />
unfamiliar, memory tasks.<br />
Will I become invisible and<br />
irrelevant?<br />
In 2011, the results of a survey by the<br />
Nominet Trust reported in the Daily<br />
Mail suggested that more than half of<br />
individuals aged 65+ feel ignored. The<br />
issues raised covered such aspects as the<br />
lack of relevant TV and radio programmes;<br />
older (particularly female) individuals<br />
being less obvious in the media, and a lack<br />
of relevant information for older people<br />
on the Internet (this, despite the large<br />
number of “silver surfers”). People over<br />
50 struggle to find employment, and often<br />
report feeling that the experience they<br />
could bring to the workplace is not sought<br />
or valued by employers. The Patient<br />
Satisfaction Survey undertaken for the<br />
Pituitary Foundation in 2008 (this report<br />
is still available to download from the<br />
Pituitary Foundation website), reported<br />
that two-thirds of respondents who were<br />
in employment felt supported by their<br />
employer, however, this report provided<br />
no breakdown of the information by age<br />
group so is only indicative of a general<br />
trend.<br />
Will I be alone?<br />
Back in the 1960’s a couple of social<br />
scientists (Elaine Cumming & Warren<br />
Earl Henry) suggested that ageing<br />
was associated with what they called<br />
“disengagement”. They reasoned that<br />
as older adults witnessed their friends<br />
passing away, they tended to disengage<br />
from life in preparation for their own<br />
impending death. Their theory has since<br />
been discredited largely due to a lack<br />
of empirical evidence to support it, but<br />
continued on page 21
Raising awareness<br />
special<br />
8 page<br />
13<br />
this section can be pulled out - lift out centre 8 pages from stapled spine<br />
We have continued to be thrilled by the incredible support of all our wonderful<br />
fundraisers and everyone who has donated. We have seen some amazing<br />
fundraising achievements this last few months and you only need to look at<br />
our wall of thanks to see some of the people who have supported us by hosting events,<br />
running, organising quizzes, baking, bag-packing…the list could go on! We’re very happy to<br />
write that this financial year we look on track to raise £500,000! This would be the most raised<br />
in The Pituitary Foundation’s 20 year history! We could not have come close to achieving this goal<br />
without the support of our members and supporters. With your help in the next few weeks, we could achieve this<br />
goal! If you’d be able to donate or fundraise for us, please get in touch as we would love to hear from you. It would<br />
be a massive achievement for a small charity like us to raise half a million pounds and it’s an accomplishment<br />
we’d absolutely love to see happen. With your support, in the next Pituitary Life we hope to<br />
able to say that we’ve achieved this milestone. This would help us lay a firm foundation for a<br />
future where we continue to help pituitary patients and their families ■<br />
Save our Loos campaign<br />
We are looking for members to get involved in the<br />
Save Our Loos campaign, which was launched<br />
at the beginning of June. Councils are currently<br />
shutting down public toilets across the UK and from<br />
speaking with patients who have diabetes insipidus (DI),<br />
we know this is having a real impact on their daily lives.<br />
One in seven public toilets has already been closed by<br />
council cuts. In 11 council areas, including some large<br />
cities, there are no public toilet facilities anywhere. A<br />
Welsh government report recognises the lack of public<br />
facilities can cause isolation, distress, and affects people’s<br />
independence and quality of life. Disability and elderly<br />
care charities have also supported this opinion, but many<br />
closures are still imminent.<br />
Please see the campaigns section on our website today to find<br />
out more about the ways you can get involved with this important<br />
campaign. We need participants to write to<br />
their councillor if there is a public toilet,<br />
local to them, facing closure<br />
(template letters and<br />
information on closures<br />
are available). This<br />
is also an awareness<br />
campaign to support<br />
DI patients, so we will<br />
be publicising useful<br />
resources on the website<br />
throughout the campaign<br />
such as the National Key<br />
Scheme, the Find Toilets app,<br />
The Great British Public Toilet<br />
Map, our free DI toilet cards, and<br />
other useful information ■<br />
pull-out<br />
section<br />
Events record income<br />
Due to all our fundraisers’ support, we have raised a<br />
record amount of money from events! We have raised<br />
over £100,000 from events for the first time ever.<br />
While we celebrate the fundraisers who have raised huge<br />
amounts of money for us, such as our “Team Pituitary”<br />
London Marathon runners who raised a staggering<br />
£45,000 between them, everyone’s contributions – whether<br />
from a cake sale, skydiving or a dress down day - have gone<br />
towards achieving this fantastic amount. We are always<br />
extremely thankful when we receive a donation, but seeing<br />
this total amount representing the cumulative efforts of<br />
all our fundraisers is staggering. As the demand for our<br />
services continues to grow, we are enormously thankful to<br />
every one of our fundraisers’ time, energy and commitment<br />
to taking part in events for us ■<br />
Pituitary Life | summer 2015
14 Raising awareness<br />
Ain’t no mountain high enough...<br />
Jemma’s journey<br />
Far beyond my wildest dreams did I ever think I’d be<br />
saying this…..but I’ve just conquered the summit of<br />
Mount Kilimanjaro – “So happy!”<br />
Diagnosed in 2012 following years of frustration and not<br />
knowing what was wrong with me, endless sleepless nights, huge<br />
weight gain, feeling lethargic and depressed to name but a few<br />
of my symptoms. My diagnosis was a relief, to finally find out<br />
that there was something wrong with me and that it wasn’t all in<br />
my head – ironically it turned out it was all in my head! But now<br />
I knew something could be done about it. It took another 18<br />
months of testing to eventually get put forward for surgery and<br />
on 12 August 2013 I had my tumour removed.<br />
Sitting in the hospital the night before my operation I thought,<br />
this is it, this is the start of my new life and I thought about this<br />
quote I had seen – “I want to inspire people, I want someone to<br />
look at me and say because of you I didn’t give up.” That was<br />
when I set myself the challenge of climbing Mount Kilimanjaro<br />
in Tanzania, Africa.<br />
I discovered The Pituitary Foundation whilst in<br />
hospital and straight away joined as<br />
a member. They helped me so much<br />
with the initial stages which can be<br />
so daunting when you first come<br />
out of hospital and have to fend<br />
for yourself with a new, unfamiliar<br />
medical condition. It was<br />
scary, knowing that<br />
Pituitary Life | summer 2015
Raising awareness<br />
15<br />
I had to carry an emergency needle around with me and even<br />
scarier knowing that I might have to use it! They provided me<br />
with lots of reassurance, information packs and visual aids such<br />
as the steroid card to carry around with me. I can remember<br />
endless conversations with Pat, Jay and Alison whether it be via<br />
email or over the phone. I felt they were always there for me.<br />
That’s why I decided to set up a fundraiser for The Pituitary<br />
Foundation. I thought well if I can do this climb I can make<br />
it more worthwhile for others by raising money to help other<br />
people in a similar situation to me. So that was it, my just giving<br />
page – ‘magic happens’ was set up!<br />
In the end I reached a total of £3322.29 I will never forget the<br />
generosity of some people. It didn’t matter how much anyone<br />
donated, it was just the fact that they did and I had people<br />
donating to me whom I hadn’t seen for some 15 years – it truly<br />
was amazing!<br />
hard training<br />
The next six months took to me training hard ready for the climb.<br />
Within weeks I could feel myself getting fitter and I started<br />
seeing results from what I had always strived for but never got.<br />
This is how it feels I thought……to be at the front for once,<br />
as I ran through the finish line, leaving a trail of others behind<br />
me in my cloud of dust! I participated in three tri-athalons that<br />
year and in September 2014 took on the massive challenge of<br />
the off road cycle race from London to Brighton. That was by<br />
far the hardest thing I had ever competed in. 125km, eight and a<br />
half hours of endurance, blood, sweat and tears, but I got there.<br />
Even at my lowest moment as it was getting dark, I was so tired<br />
and cold, I never once thought about giving up. I had to do it.<br />
The sense of achievement as I came hurtling through the ribbon<br />
on Brighton beachfront at 8pm at night was exhilarating!<br />
The strangest thing for me was that in 2014, I did nothing<br />
different to what I had been doing for about 10 years prior. I<br />
ate a normal healthy diet and exercised every day. But this time<br />
it was different. My body had changed and I could now feel the<br />
benefits of having been cured from Cushing’s disease. I lost<br />
around three stone in weight, started getting muscles and felt<br />
generally fit and well. It was a total transformation.<br />
At 9am on 11 October 2014 I did just that. I even unzipped<br />
and stood out of my two big warm coats to reveal my orange<br />
pituitary t-shirt I had been hiding underneath and got that<br />
picture, punching my arm into the air – I did it! The feeling was<br />
quite overwhelming but only lasted for minutes because we were<br />
soon to be rushed back down the mountain to a safer altitude. It’s<br />
quite weird because there was no cheering or hugging between<br />
the group as I envisaged shouting ‘we did it, we did it’ In fact<br />
everyone was quite subdued, not really with it, all the effects of<br />
the altitude<br />
Almost running through the gate at the bottom, passing the<br />
‘congratulations you did it’ sign, saw our porters and guides<br />
greeting us with the notoriously famous song ‘Jambo Bwana’<br />
sung by all on the slopes of the mountain.<br />
Then for the rest of my African adventure. If I have learnt<br />
anything from this illness it’s to seize the day, if there is something<br />
you do not like then change it, if there is something you want to<br />
do, then do it. Life can be short.<br />
quit my job<br />
That’s why I quit my job in the UK and thought once I had<br />
climbed the mountain I would realise my dream of travelling<br />
Africa. So after Zanzibar I spent the next five months touring<br />
Kenya, Uganda and Rwanda, with my highlight being trekking<br />
the mountain gorillas in the Volcans National Park in Rwanda<br />
– always been a childhood dream of mine! Then visiting<br />
Madagsacar, the home to thousands of lemurs. I volunteered<br />
at a game country lodge for six weeks near Johannesburg where<br />
I was amongst all the big wild African animals, taking lion cubs<br />
for walks, feeding the predators, splashing around in a mud pool<br />
with elephants! Oh it was wonderful! I visited Mozambique and<br />
swam with whale sharks, I went to the Kruger National Park<br />
not to mention my final trip over landing from Cape Town all<br />
the way to Nairobi taking in the wonders of Victoria Falls, the<br />
deserts of Namibia, beautiful Botswana, amazing Zambia and<br />
Zimbabwe, stunning Malawi and back up to Tanzania where my<br />
adventure began. It really was the trip of a lifetime.<br />
I just have one more thing to mention, one of my most<br />
treasured times and memories, relevant to me having had<br />
Cushing’s disease: When I was first diagnosed with Cushing’s<br />
disease a lady from South Africa contacted me through a<br />
Facebook ‘Cushing’s patients’ page. Her 12 year old little girl was<br />
going through the same thing as me and was having an operation<br />
to remove her brain tumor only a few days after mine. Even<br />
though we were miles apart, in another country, living different<br />
lives we were going through the same horrible illness. We kept<br />
in contact and exchanged advice, comfort and kind words to<br />
help each other through that time. The little girl’s operation had<br />
some complications but thank fully she came though it well. The<br />
lady had said if I was ever in South Africa to look her up…so<br />
I did. I detoured from Johannesburg on my way to Cape Town<br />
to Durban where they live and I met Prudence and her little girl<br />
Chelyn. What a wonderful meeting and I’m so glad I have two<br />
new friends through something that started as not a very nice<br />
thing but ended magically! ■<br />
Pituitary Life | summer 2015
16 wall of thanks<br />
A date with Mr Grey<br />
– Our thanks to Eleri<br />
Walters who organised a<br />
private screening of “50 shades<br />
of Grey” in her hometown of<br />
Swansea. As well as the year’s<br />
must-see movie guests were<br />
treated to cocktails and a fashion<br />
show, a staggering £<strong>30</strong>00 was<br />
raised in the process!!<br />
Golf for Issy – This proved to be<br />
yet another phenomenal day with 76<br />
golfers turning up for a round of Golf<br />
at Lansdowne Golf Club. Our sincerest<br />
thanks to Issy’s grandfather, Garry Park,<br />
for organising this event. The event<br />
raised a sensational £2713 which takes<br />
the Isabella Andrews Appeal fund to a<br />
monumental £15000.<br />
PhD Project donation<br />
- Mr & Mrs Salt donated £125 for<br />
the PhD project.<br />
Shakespeare Half<br />
Marathon – Congratulations<br />
to Tim Napper who ran the<br />
Shakespeare Half Marathon in<br />
support of brother-in-law, Gez<br />
Thompson. Tim raised a brilliant<br />
£857.88. Gez ran with Tim but<br />
saved his fundraising efforts for<br />
his upcoming Great North Run<br />
challenge!<br />
Thanks to our Birmingham Support<br />
Group who donated £50 to the<br />
Endocrine Nurse Appeal.<br />
Well done to Oscar Barnes who<br />
completed his first Marathon by running<br />
the Brighton Marathon in a very respectable<br />
time of 4 hours 55 minutes. Oscar was<br />
running in memory of brother-in-law, Alex<br />
Hatch, and raised a fabulous amount. This<br />
follows Oscar’s previous fundraising efforts<br />
where he cycled from London to Brighton<br />
and also grew a beard that he subsequently<br />
shaved, raising well over £1000 in the<br />
process. Oscar is pictured here with his wife<br />
Louise, Alex’s sister.<br />
Pituitary Life | summer 2015
17<br />
John Lewis Cribbs Causeway –<br />
Our thanks to shoppers at John Lewis<br />
Cribbs Causeway (Bristol) who voted for<br />
us in the “Community Matters” scheme.<br />
Thanks to your support we received £666!<br />
Alan Andrews, Community Liaison<br />
Co-ordinator , John Lewis said: “The<br />
Partnership’s commitment to working<br />
with the local community, through the<br />
Community Matters scheme makes a real<br />
difference to those in need”.<br />
Liverpool 10K – Congratulations to<br />
pituitary patient, Sarah Elgahmi, who<br />
completed the Liverpool 10K in May.<br />
13 year old fundraiser -<br />
HUGE thank you to 13 year old<br />
Elle Dimbleby !! Over the<br />
festive period Elle had made mince<br />
pies, gingerbread men/trees and<br />
minions, which the train crews of<br />
First Great Western Reading Depot<br />
thoroughly enjoyed!! Elle managed<br />
to raise a fantastic £69.48!!<br />
Swindon Quiz – Thanks to<br />
Catherine Gladwyn who organised<br />
a quiz in her hometown of Swindon and<br />
raised a magnificent £747.50<br />
Golden Wedding Anniversary –<br />
Congratulations to Simon & Val Swancott<br />
who celebrated their Golden Wedding<br />
Anniversary! The generous couple asked<br />
for donations in lieu of gifts to celebrate<br />
this joyous occasion and managed to raise<br />
a fantastic £750 in the process!!<br />
Thank you to the family of the late<br />
Mr William Wernham of Lymm,<br />
Cheshire. They collected £85 in his<br />
memory at his funeral. Such support at<br />
this difficult time is greatly appreciated.<br />
RIP Mr Wernham.<br />
Congratulations to Bill<br />
Graham who cycled<br />
unsupported from England to<br />
the Alps. Bill managed to raise a<br />
staggering £2500 (correct at time<br />
of going to print).<br />
Pituitary Skydive – On June<br />
7th, 25 individuals travelled from<br />
every corner of the country to take<br />
part in the Pituitary Skydive. One<br />
participant, Graham Galley, even cut<br />
short his holiday so that he could take<br />
part. There will be a special feature<br />
in your next issue of Pituitary Life but<br />
so far the daring skydivers look on<br />
course to have raised over £10,000<br />
between them ■<br />
Pituitary Life | summer 2015
18<br />
Professional Raising awareness articles<br />
London Marathon 2015<br />
Sunday 26th April was a fantastic<br />
day for the charity. We saw 10<br />
amazing runners participate in<br />
the Virgin Money London Marathon<br />
and between them the incredible team<br />
managed to raise a whopping £45,000!<br />
We would like to say an absolutely<br />
massive thank you to our amazing team<br />
of runners who ran on behalf of The<br />
Pituitary Foundation.<br />
team pituitary<br />
The team included our very own Trustee,<br />
Tom Sumpster, as well as Manish<br />
Madhvani, Graeme Summers, Nick<br />
Wright, Chris Wright, Matt Osbourne,<br />
Helen Sumner, “Where’s Wally” aka<br />
Hayley White (pictured below), John<br />
Newsham, Sally Arnold and Paul Arnold.<br />
Each runner had their very own<br />
personal reason for running as part of<br />
“Team Pituitary” and our Trustee, Tom<br />
Sumpster, was running to support his son<br />
Zac.<br />
Tom says “Zac was born on 18 January<br />
2013 and at the age of 2 is a cheeky<br />
little monkey, full of fun with the odd<br />
tantrum thrown in here and there. Daily<br />
life includes playgroups, singing and<br />
gymnastics classes and his hero/heroine’s<br />
include Peppa Pig, Batman and Thomas<br />
the Tank Engine ! To look at him when<br />
he is well you would have no idea he has a<br />
rare, potentially life-threatening condition.<br />
Zac has congenital panhypopituitarism<br />
having been born with a very small anterior<br />
pituitary gland and an ectopic posterior<br />
pituitary with no visible stalk. Put simply<br />
he is deficient in several hormones -<br />
growth, sex, cortisol and thyroid. With<br />
the help of modern medicine we are told<br />
Zac will lead a full life - he is injected once<br />
a day with growth hormone and a thyroid<br />
tablet and four times a day with cortisol.<br />
This critical therapy helps to regulate<br />
blood pressure, the immune system,<br />
helping the body respond to stress and<br />
helping the body to balance insulin to<br />
regulate blood/sugar levels.<br />
additional funding<br />
In his two very happy years we have<br />
dealt with four adrenal crises, which<br />
has resulted in hurried calls to the<br />
ambulance service in the middle of<br />
the night, and subsequent hospital<br />
stays in the High Dependancy Unit.<br />
We ran the London Marathon to<br />
raise awareness of pituitary conditions<br />
to provide additional funding for the<br />
Pituitary Foundation so that Zac and<br />
others can benefit from both the support<br />
function the charity provides and I would<br />
like to thank everyone who has generously<br />
supported our efforts”<br />
The Pituitary Foundation would like to<br />
thank all of our “Team Pituitary” runners<br />
for their dedication in preparing for this<br />
event and their amazing support. Thank<br />
you!!<br />
We’d also like to thank everyone<br />
who joined our cheering squad to help<br />
encourage them along at 13.5 and 22<br />
miles. It was a great atmosphere and a<br />
truly memorable day! ■<br />
Manish Madhvani<br />
Pituitary Life | summer 2015
Raising awareness<br />
19<br />
Team Sumpster<br />
Hayley White in Where’s Wally costume<br />
Training for and running marathons and<br />
other endurance events for patients with<br />
adrenal insufficiency<br />
For those patients who are<br />
taking part in marathon events,<br />
we provide general guidance<br />
to help you keep safe and well<br />
whilst running.<br />
Training<br />
During long, slow training it is advised<br />
to keep to your usual daily doses of<br />
hydrocortisone (or prednisolone), but you<br />
can take an extra hydrocortisone 5mg (or<br />
1-2mg prednisolone) after you have been<br />
running for an hour to ninety minutes.<br />
It is important to keep well-hydrated<br />
and have access to fluids during training.<br />
If this is one of your first attempts as<br />
a post-diagnosis return to fitness, you<br />
might feel the need to take a little more<br />
steroid during early training and events.<br />
Therefore, an extra 10mg pre-training and<br />
if felt needed, an extra 5mg, at the end of<br />
your training session should be sufficient.<br />
This should be short term, until your<br />
body becomes accustomed to training<br />
and running distances. Overall, as long<br />
as fitness is built slowly, and training<br />
is completely ‘aerobic’ there should be<br />
little need for extra hydrocortisone or<br />
prednisolone above these amounts. Some<br />
patients find that they need the extra small<br />
doses, even in training, and it is important<br />
to ‘listen to your body’ and also discuss<br />
any issues with your endocrinologist.<br />
Marathon day<br />
On race day, most marathoners should<br />
have a fluid and ‘refuelling’ strategy and a<br />
suggested regime is to take an additional<br />
hydrocortisone 5mg at the start of the<br />
race and 5mg when you ‘refuel’. There<br />
should be no need to increase your<br />
hydrocortisone on the day before the race.<br />
Again, fluids will be accessible at points<br />
along the course, ensure your hydration is<br />
optimum before you start and you remain<br />
as hydrated as possible throughout the<br />
run – to hydrate efficiently, don’t gulp<br />
fluids but sip regularly. There will be no<br />
harm on the day by taking a little extra<br />
hydrocortisone.<br />
‘Hitting the wall!’<br />
Runner information from London<br />
Marathon: When you’ve got your<br />
runner number, please fill in the medical<br />
information section on the back. Be<br />
careful not to damage or lose your number<br />
as replacements can’t be issued.<br />
If there’s a risk you may blackout during<br />
the race (for example if you suffer from<br />
fits), please put a red cross on the front<br />
of your number. This can apply to those<br />
with adrenal insufficiency and it needs to<br />
be clearly seen by the race marshals.<br />
Carry hydrocortisone tablets with you<br />
and if you feel you are ‘hitting the wall’,<br />
you can take 5mg or 10mg quickly.<br />
St John Ambulance will again be looking<br />
after first aid at the marathon and will have<br />
the following available on the day:<br />
• 1400 medical, nursing and first aid<br />
volunteers<br />
• 50 specialist crewed ambulances<br />
• <strong>30</strong> cycle response units (first aiders on<br />
bicycles who can weave in and out of<br />
crowds easily)<br />
• 1500 rehydration sachets for<br />
dehydration.<br />
Plan and know where first aid points<br />
are along the route. Keep safe and good<br />
luck! ■<br />
Pituitary Life life | summer 2015
20 Raising awareness<br />
Thanks to you we did it!<br />
We are delighted to say that thanks to everyone who donated to<br />
our Endocrine Nurse Appeal we met our target! We received<br />
part-funding for the post during 2014/2015 and because of<br />
the help of everyone who donated we have now raised the £11,000<br />
that we needed for the remainder of 2015. We were overwhelmed by<br />
everyone’s support and it shows just how fantastic our Endocrine<br />
Nurse, Alison, is. Many people who donated said how Alison had<br />
helped them personally in their time of need and it is wonderful that<br />
so many of you donated to this appeal ■<br />
Feeling<br />
inspired?<br />
If the team have inspired you to take<br />
on a challenge of your own then<br />
why not sign up for an event today?<br />
It doesn’t have to be a marathon.<br />
You could run any distance that is a<br />
challenge to you, whether that’s 5K,<br />
10K, Half Marathon or a Marathon.<br />
Maybe you’d even like to attempt a<br />
different type of challenge<br />
such as a swim, cycle<br />
or triathlon? It doesn’t<br />
matter which challenge<br />
you take on as long<br />
as you know that<br />
whatever you do it will<br />
be greatly appreciated<br />
by us and the pituitary<br />
patients that we<br />
support.<br />
If you would like to<br />
take on a challenge to raise<br />
funds for The Foundation<br />
then please call 0117 370 1314<br />
or e-mail jay@pituitary.org.uk<br />
We will be there to support<br />
you every step of the way, just<br />
as we are there to support<br />
pituitary patients every step of<br />
the way during their pituitary<br />
journey ■<br />
New online resource:<br />
common and rare<br />
endocrine conditions<br />
I<br />
am writing to you regarding Endocrinology, Diabetes & Metabolism<br />
Case Reports, a new online resource that publishes and links together<br />
case reports on common and rare conditions in all areas of clinical<br />
endocrinology, diabetes and metabolism.<br />
This venture is a collaboration between Bioscientifica and several leading<br />
national and international societies around the world; all working together with<br />
the aim to further medical education and clinical practice. This is of particular<br />
importance in our field which encompasses many rare diseases that are often<br />
difficult to conduct clinical studies on. For this reason, case report literature is<br />
immeasurably beneficial, both for treatment and education.<br />
As a patient support group, we know that you are committed to supporting<br />
research in pituitary disease and hope that you can help us by adding a link to<br />
www.edmcasereports.com as a resource on your website.<br />
Your members can benefit by reading about the experiences of others living<br />
with pituitary disease. They may also be able to help other patients living with<br />
this disorder by encouraging their doctors to publish their own case reports.<br />
As this freely accessible database grows, it further enables practitioners to learn<br />
from each other’s experiences ■<br />
Pituitary Life | summer 2015
Professional articles<br />
21<br />
continued from page 12<br />
social isolation and loneliness are a real<br />
concern for some individuals. Boyd &<br />
Bee observe that social networks are<br />
important to older adults, but that there<br />
are gender and ethnic differences in how<br />
such friendships are made, maintained<br />
and used. Remember, The Pituitary<br />
Foundation has a telephone buddy system<br />
that could help some individuals feel less<br />
alone and misunderstood.<br />
What about stigma &<br />
discrimination?<br />
Are other people going to give me a hard<br />
time? A lot of chronic health conditions<br />
(including pituitary conditions) can be<br />
classified as “invisible illnesses”, i.e. they<br />
are not obvious to the casual observer.<br />
Such invisible illnesses are associated with<br />
additional problems, most notably stigma<br />
of varying kinds. Data from The Pituitary<br />
Foundation 2008 Patient Satisfaction<br />
survey provides some support for this, with<br />
22% of respondents agreeing or strongly<br />
agreeing with the statement “I felt I was<br />
discriminated against at work because of<br />
my condition”. While 55% of respondents<br />
agreed or strongly agreed that having a<br />
pituitary condition had reduced their career<br />
prospects; and 42% of respondents agreed<br />
or strongly agreed that having a pituitary<br />
condition had meant that they have had, or<br />
will have to, give up work. Again though,<br />
these data were not disaggregated by age<br />
group so can only be seen as suggestive of<br />
general trends.<br />
People who don’t have a chronic<br />
condition generally do not understand<br />
concepts such as “good day/bad day”.<br />
They genuinely don’t understand why,<br />
if you can do something one day, you<br />
might not be able to do it the next. In<br />
the workplace this can lead to whispering<br />
campaigns, a withdrawal of support<br />
from co-workers and suggestions of<br />
“convenient” attacks of illness in an<br />
attempt to avoid work. Invisible illnesses,<br />
by their very nature, have no external<br />
markers, so others cannot tell the amount<br />
of pain you are dealing with, how tired<br />
you are feeling, whether you are feeling<br />
sick etc. The pressure to constantly have<br />
to educate other people about your<br />
condition can be exhausting. It can be<br />
very frustrating that co-workers can<br />
forget about your condition and start to<br />
make unhelpful demands and comments.<br />
You will find well-meaning folk who will<br />
tell you that it’s all in your mind; that if<br />
you just behave as though you’re fine,<br />
you will be. The Pituitary Foundation<br />
Wellbeing Series leaflet “Relationships &<br />
Communication”, details the commonest<br />
problems in this regard and suggests<br />
some possible coping strategies.<br />
Direct discrimination against older<br />
people can take many forms including<br />
being ignored because of assumed lack<br />
of mental capacity, deafness, and/or<br />
slowness. For example, if an older person<br />
is out with a younger family member,<br />
other people might talk to the younger<br />
person and ignore the older one. This<br />
behaviour seems to be more likely if<br />
the older person is in a wheelchair, or<br />
has some kind of mobility aid. Older<br />
people might find that others talk more<br />
loudly and far more slowly to them, and<br />
quickly get impatient with them (sighing<br />
and tutting). This is an area where there<br />
are striking cultural differences; in some<br />
cultures white hair is taken as a sign of<br />
wisdom, and for a young person to be<br />
allowed to spend time with an older<br />
person is seen as an honour.<br />
Is it all bad?<br />
Research suggests there are some things<br />
that we can do to help us age well, for<br />
example, remaining curious about the<br />
world, learning new skills, having new<br />
experiences, and continuing some kind<br />
of education. The research from lifelong<br />
learning tends to suggest that what you<br />
learn doesn’t matter, and it doesn’t have to<br />
be formal education. All learning seems<br />
to be associated with increased selfconfidence,<br />
which is in turn associated<br />
with an improved ability to deal with<br />
stress. Staying active is also good for us,<br />
not only in terms of physical health, but<br />
also in terms of reducing the risk factors<br />
associated with developing dementia (i.e.<br />
weight, blood pressure, and cholesterol).<br />
However, for some individuals with<br />
a pituitary condition, just doing the<br />
activities of daily living is exhausting, and<br />
the idea of being curious about the world,<br />
engaging in life-long learning, taking up a<br />
creative hobby, or exercising regularly all<br />
feel like too much of an extra burden.<br />
I’ve already said there are large gaps<br />
in our knowledge about the psychosocial<br />
aspects of living with a pituitary condition.<br />
Elsewhere in this magazine you will find<br />
an article about the research that Hayley<br />
Thomas is undertaking at the University<br />
of Plymouth to help us better understand<br />
the issues associated with young people<br />
who have a pituitary condition. It feels to<br />
me that a similar project focused on the<br />
needs of older adults would be very useful<br />
to help us develop a proper understanding<br />
of what it’s like to age with a pituitary<br />
condition ■<br />
Emergency hydrocortisone refusal letter<br />
This letter enclosed free with your magazine has been produced for<br />
patients in the event of an emergency situation, where you are refused<br />
hydrocortisone, by a health care professional (HCP).<br />
If the HCP refuses you hydrocortisone, you or your family can ask the individual<br />
to sign this letter. Once it is signed and dated, this letter could go into your hospital<br />
notes. In any event, if you are in A&E or on a hospital ward, the patient or their family<br />
should insist on the HCP urgently contacting the<br />
endocrinologist on call. Hopefully, this letter<br />
will never need to be signed as the HCP reading<br />
it should understand the necessity of treatment<br />
for the patient’s safety.<br />
Please note: The Foundation cannot become involved in<br />
individual disputes, but our hydrocortisone resources can be<br />
accessed from our website and used by the patient or their<br />
family for information and awareness ■<br />
Emergency Hydrocortisone in Adrenal Insufficiency<br />
Patient’s name: _______________________________________<br />
DOB: ________________________<br />
My Consultant is:<br />
_____________________________________________________<br />
I am a patient with hypopituitarism and adrenal insufficiency. I have<br />
explained to you that, in case of emergency, I need an injection of<br />
hydrocortisone. You have been made aware that refusal to inject<br />
me could be life-threatening.<br />
Please sign below confirming that you have refused to give me<br />
hydrocortisone.<br />
Signed: ____________________________________________<br />
(To be signed by the refusing health professional - Ambulance, A&E or Ward Staff)<br />
Print name: ____________________________________<br />
Date: ______________________________________<br />
Hydrocortisone is a steroid hormone produced by the adrenal gland. It plays a<br />
complex role in regulating body functions and is essential for survival. A good<br />
majority of people with pituitary disease have to take replacement hydrocortisone<br />
daily, as they don’t produce this naturally. Therefore, as they take replacements,<br />
they don’t have the natural surge of cortisol if they become acutely ill, are vomiting<br />
evere shock.<br />
ection is vital! (The patient<br />
his
22 Professional articles<br />
Research Title: Understanding the needs<br />
of children and young individuals with a<br />
pituitary condition Hayley Thomas – PhD at Plymouth University.<br />
It’s fairly well known that there are<br />
big gaps in our understanding about<br />
the psychosocial aspects of living<br />
with a pituitary condition as an adult,<br />
but when it comes to understanding<br />
what it’s like for children and young<br />
people, we know even less. My name is<br />
Hayley Thomas, and I’m undertaking<br />
a PhD at the University of Plymouth<br />
focussed on helping us to understand<br />
what it’s like to have a pituitary<br />
condition as a child or young person.<br />
So far, I’ve identified three areas which<br />
I will explore in my PhD. Firstly, we need<br />
to understand the needs of children<br />
with a pituitary condition, particularly<br />
the psychological and social aspects. We<br />
know that the management of a pituitary<br />
condition can be extremely difficult for<br />
adults, and we are starting to understand<br />
what particular elements require<br />
psychological help and support. We want<br />
to know if it’s the same for children and<br />
young people with the condition.<br />
Secondly, we want to understand the<br />
decision-making that children and young<br />
people engage in with regard to their<br />
treatment. We’re particularly interested to<br />
know how much control children, young<br />
people and their families believe they<br />
have over their care. This is a particularly<br />
difficult topic that involves identifying the<br />
degree to which children and young people<br />
can become involved, in determining their<br />
own treatment plans.<br />
Thirdly, we aim to investigate how<br />
children and young people manage their<br />
conditions. Transition clinics provide a<br />
stepping stone from paediatric care, into<br />
more adult health care services. Transition<br />
clinics hopefully provide the young adult<br />
with the tools needed to manage and<br />
control their condition with confidence,<br />
as well as providing essential support<br />
along the way. The transition clinic model<br />
will be studied, with a view to making<br />
recommendations for future interventions<br />
for young people with pituitary<br />
conditions. It is hoped that this will allow<br />
young individuals to feel empowered to<br />
self-manage their conditions for the rest<br />
of their lives.<br />
So far, I’ve been focusing<br />
on designing a study that is best<br />
suited to making sure that we capture<br />
and properly understand the needs of<br />
children with a pituitary condition at<br />
different ages and stages of treatment.<br />
The plan for the study is coming along<br />
nicely, with the necessary research design<br />
and NHS ethics applications underway.<br />
There are two things that I’m currently<br />
working on where I could really use some<br />
help:<br />
1. I’m looking for Pituitary Foundation<br />
members to form an advisory group<br />
for the research. The main work in<br />
the first instance, is to look at the<br />
research materials that I’m developing,<br />
to make sure that they are suitable for<br />
the different age groups that I will be<br />
working with.<br />
2. I’m also looking for participants who<br />
wish to take part in the study. If you<br />
have a child or young person aged 10<br />
or over, and you would be interested in<br />
talking to me about your experiences<br />
of diagnosis, treatment and life with<br />
the condition, then please get in touch.<br />
Similarly, if you are a young person<br />
aged between 18 and 25 and you’d<br />
be willing to talk to me about your<br />
experiences, please get in touch.<br />
If you would like to receive more<br />
information regarding this research, or if<br />
you are interested in being involved in any<br />
aspect of this research, please contact me<br />
via email: hayleylouiset@gmail.com.<br />
Thank you ■<br />
Pituitary Life | summer 2015
Professional articles<br />
23<br />
Trigger words when calling<br />
999 for an ambulance<br />
For adult patients on<br />
hydrocortisone in an emergency<br />
situation<br />
Once you are connected to an<br />
ambulance 999 operator or<br />
call handler, they will ask you<br />
a series of questions to establish<br />
what is wrong. This will allow them<br />
to determine the most appropriate<br />
response as quickly as possible.<br />
Confusion may arise, due to a variety<br />
of trigger words mentioned by patients or<br />
their family, which may not be recognisable<br />
quickly by the call handler, including:<br />
• Pituitary patient<br />
• Has a pituitary condition<br />
• Secondary Addison’s<br />
• Steroid suppression<br />
• Adrenal suppression<br />
• Adrenal insufficiency<br />
• Addison’s crisis<br />
• Hypopituitarism<br />
• Steroid dependant (many conditions<br />
can cause this).<br />
Many ambulance trusts adopted the<br />
trigger words ‘Addisonian crisis’ for their<br />
protocols, following the 2006 JRCALC<br />
guideline, which authorised paramedics<br />
to give injected hydrocortisone for crisis<br />
response, in addition to asthma and<br />
anaphylaxis treatment. It was only in<br />
2013 that JRCALC extended its wording<br />
to make clear that secondary (pituitary)<br />
patients were also covered by this<br />
guideline and suggested that adrenal crisis<br />
should be the preferred term.<br />
Medical alert talisman wording<br />
Our medical committee advises that<br />
patients have ‘Hypopituitarism, on<br />
steroid replacement and at risk of<br />
adrenal crisis’ engraved on their medical<br />
talisman jewellery.<br />
For children who have adrenal<br />
congenital hypoplasia (ACH)<br />
or all other cortisol-deficient<br />
disorders:<br />
The key statement or trigger wording when<br />
calling 999 is Adrenal Insufficiency *<br />
Medical alert talisman wording is Adrenal<br />
Insufficiency.* *(Ref: GOSH) ■<br />
Understanding Cortisol Tests<br />
Alison Milne, Endocrine Specialist Nurse<br />
Cortisol is produced by the adrenal<br />
glands which are controlled by<br />
the pituitary gland. Cortisol levels<br />
are usually high in the morning when<br />
we wake up and then fall gradually<br />
throughout the day - this is called your<br />
diurnal rhythm. Levels of cortisol in<br />
the blood can vary dramatically from<br />
individual to individual. Before we<br />
start discussing blood cortisol levels<br />
it is important to remember that your<br />
results must be interpreted with your<br />
own laboratory reference ranges. They<br />
cannot be compared with other labs or<br />
internet website values.<br />
Common terms used for<br />
cortisol testing<br />
Random cortisol: This means we do not<br />
know exactly where in the individual’s<br />
diurnal rhythm / normal day we are<br />
sampling. We do try where possible to<br />
get a 9am cortisol or, at the very least,<br />
a morning blood sample. In reality, this<br />
is not always possible and therefore, we<br />
should always note the time accurately<br />
on the sample to enable us to assess the<br />
result appropriately. Afternoon cortisol<br />
samples, if borderline low, should really<br />
be reassessed with a morning sample<br />
The ‘normal’ range varies from<br />
180-620nmol/L (Reference: Oxford<br />
Handbook of Endocrinology)<br />
Short Synacthen Test: This is the test that<br />
assesses adrenal cortical function/reserve.<br />
This test is carried out to assess if the<br />
adrenal glands respond appropriately and<br />
produce cortisol when required by the<br />
body. A synthetic dose of the hormone<br />
ACTH (Adrenocorticotrophic Hormone)<br />
which is normally produced by the<br />
pituitary gland is administered.<br />
The patient has a cannula inserted into<br />
a vein to enable us to withdraw blood<br />
more than once and also to administer the<br />
medication.<br />
Cortisol is a stress hormone and<br />
therefore the action of cannulation can<br />
cause an increase in the cortisol level.<br />
Ideally, we should postpone taking our<br />
first sample for at least 15 - 20 minutes.<br />
Blood sample for cortisol level is<br />
obtained at baseline = 0 minutes (after<br />
resting time as explained above).<br />
ACTH level is also obtained at this<br />
sample time.<br />
Synacthen 250mcg is administered<br />
intravenously, followed by a flush to keep<br />
the cannula clear.<br />
Patients may experience a ‘hot flushed’<br />
feeling and/or slight nausea, or a feeling<br />
like ‘butterflies’ in your stomach. These<br />
symptoms usually pass very quickly.<br />
Indeed, some patients do not get any<br />
symptoms at all.<br />
A further blood sample for cortisol is<br />
obtained at <strong>30</strong> minutes. Some centres obtain<br />
a 60 minute cortisol sample. The test is then<br />
complete and the cannula is removed.<br />
There should be no long-lasting effects<br />
from having this test carried out and you<br />
can go about your usual daily activities<br />
following your appointment.<br />
What the results show?<br />
• Initial baseline sample >190nmol/L (><br />
means above)<br />
Pituitary Life | summer 2015
24<br />
Professional articles<br />
• Cortisol levels should peak at around<br />
500nmol/L at <strong>30</strong>minutes<br />
• The increment requires to be at least<br />
200nmol/L from the baseline<br />
NB: these levels are a guide and may well<br />
vary slightly depending on local assays<br />
Cortisol day curves<br />
This is a test that is not frequently used<br />
these days and it seems to vary across the<br />
country whether it is used at all.<br />
Generally, we use this test when you are<br />
on replacement steroid therapy, to assess<br />
the level of steroid within your blood.<br />
This can help to ascertain if you might be<br />
over- or under-replaced. You will be asked<br />
to attend for a certain length of time e.g.<br />
four hours; six hours; eight hours; 12 hours.<br />
Your steroid medication should be withheld<br />
first thing in the morning but bring it with<br />
you to the clinic/hospital. A cannula will<br />
be inserted, resting period should be taken<br />
into consideration as stated above. Initial<br />
baseline cortisol level obtained. You will<br />
then be asked to take your normal dose of<br />
steroid. Hourly blood samples will then be<br />
collected, we do this hourly until your next<br />
steroid dose is due. Following that dose of<br />
steroid, we continue sampling and so on<br />
until the end of the test as requested by<br />
your consultant.<br />
A question I am frequently asked<br />
is: “why is my cortisol level so low/<br />
undetectable at the start of the day<br />
curve?” This is to be expected as we<br />
already know you are steroid dependant.<br />
The results of this test will determine<br />
whether there are any adjustment to<br />
be made to your medication. Patients<br />
are often worried and anxious about<br />
attending for this test, not just because<br />
it can mean a lengthy time in the clinic,<br />
but they are concerned that we will be<br />
enforcing changes to their medication.<br />
Reassuringly, this does not always happen<br />
and indeed, can often just reiterate that<br />
you are on the correct replacement dose.<br />
Insulin Tolerance test<br />
This is the Gold Standard Test for<br />
the assessment of adrenal and growth<br />
hormone reserve.<br />
Cortisol and growth hormone are both<br />
released as part of the stress mechanism<br />
which is triggered by the induced<br />
hypoglycaemia. Blood glucose level must<br />
fall below 2.2mmol/L for an adequate<br />
stimulus.<br />
NB: This test is potentially dangerous<br />
and must be undertaken by experienced<br />
medical personnel. There must be clear<br />
indication that this test is required before<br />
it is performed. A doctor or nurse must<br />
be in attendance at all times.<br />
Contra-indications (reasons for not<br />
performing this test)<br />
• Age over 65 years<br />
• Ischaemic Heart Disease<br />
• Abnormal ECG<br />
• Epilepsy<br />
• Untreated hypothyroidism.<br />
• Severe hypopituitarism 9am Cortisol<br />
< 100nmol/L<br />
Protocol for performing test<br />
Fast overnight (can have tap water only).<br />
Full explanation of procedure and<br />
symptoms to be expected during test must<br />
be explained to patient. Patient’s weight is<br />
obtained to calculate the dose of insulin<br />
required, which will also be determined by<br />
your diagnosis.<br />
ECG (electrocardiograph) tracing<br />
of the heart rhythm to ensure no<br />
abnormalities.<br />
Intravenous cannula inserted (in some<br />
centres you may have two inserted), one<br />
in either arm.<br />
Basal Blood Samples for growth<br />
hormone, cortisol and glucose obtained<br />
(following cannula resting time as described<br />
previously).<br />
Time T=-15 mins & T= 0<br />
Blood Glucose using glucometer<br />
monitored at onset and with further<br />
samples to ensure adequate hypoglycaemia<br />
achieved.<br />
Following the basal sample at T=0,<br />
calculated insulin dose is administered<br />
intravenously.<br />
Samples are obtained as above at <strong>30</strong><br />
minutes, 45 minutes, 60 minutes, 90<br />
minutes and 120 minutes.<br />
Additional samples may be carried out<br />
between T= 0 & T-<strong>30</strong> minutes because<br />
the patient may start to experience<br />
symptoms of hypoglycaemia from around<br />
17 minutes onwards.<br />
The nurse is usually experienced at<br />
picking up the signals that the patient’s<br />
blood sugar is dropping quite rapidly.<br />
Signs of hypoglycaemia<br />
Important to note that some patients can<br />
be asymptomatic or have minimal effects<br />
from the insulin, others may experience<br />
some but not necessarily all of the below<br />
symptoms.<br />
Sweating, clammy, thirsty, hungry, heart<br />
racing, sleepy, lack of concentration and on<br />
occasion, people can be angry and agitated.<br />
If these symptoms are prolonged and<br />
the patient is unable to converse or there is<br />
loss of consciousness the hypoglycaemia<br />
must be reversed. The nurse will already<br />
have the required medication to reverse<br />
hypoglycaemia prepared in advance.<br />
If this is the case sampling should be<br />
continued as adequate stimulus/stress will<br />
have been achieved. Following the test a<br />
carbohydrate containing meal must be<br />
given and taken prior to discharge.<br />
Interpretation<br />
The test cannot be interpreted unless<br />
hypoglycaemia (< 2.2 mmol/L) is<br />
achieved.<br />
An adequate cortisol response is<br />
defined as a rise to greater than 500<br />
nmol/L.<br />
Patients with impaired cortisol<br />
responses i.e. < 500nmol/L but > 400<br />
nmol/L may only need steroid cover for<br />
major illnesses or stresses.<br />
An adequate GH response occurs ><br />
20mU/L.<br />
These values must be interpreted<br />
against your own laboratory reference<br />
range and your consultant/hospital<br />
guidelines.<br />
Glucagon Stimulation test<br />
This may be used to test for cortisol<br />
and growth hormone reserve, when the<br />
Insulin Tolerance Test is contra-indicated.<br />
Fast Overnight (tap water only)<br />
IV cannula inserted (again noting the<br />
resting period as previously explained)<br />
Basal Samples for cortisol, growth<br />
hormone and glucose at T=15 mins and<br />
T=0 mins<br />
Pituitary Life | summer 2015
news Professional articles 25<br />
Administration of Glucagon 1mg (1.5mg<br />
if weight >90kgs)<br />
This is administered by injection<br />
either SC - subcutaneously or IM -<br />
intramuscularly.<br />
Further samples obtained at 90 minutes,<br />
120 minutes, 150 minutes, 180 minutes,<br />
210 minutes and finally, 240 minutes This<br />
test can cause nausea, stomach upset and<br />
headache.<br />
Interpretation<br />
We expect a rise in glucose levels.<br />
Cortisol rises to >500 nmol/L<br />
(nanomoles per litre) and growth<br />
hormone >20mU/L (milliunits per litre)<br />
Some centres may vary slightly on<br />
how and when they perform the above<br />
individual tests but this information is<br />
given as a general guideline to aid your<br />
understanding of what you should expect<br />
from having these tests performed.<br />
As always, I’m happy to take questions<br />
regarding any of the above or other tests<br />
which you would like explained ■<br />
Efcortesol shortage<br />
The latest update (April 2015) from Amdipharm is that Efcortesol should<br />
be back in availability at the end of July. It will be supplied only through<br />
Alliance Healthcare.<br />
Your pharmacist can contact Amdipharm on 0208 588 9100 if they have further<br />
queries. Please be reassured that you can use the powder Solu-Cortef 100mg for the<br />
injection instead. This needs to be mixed with water for injection (2mls), ring your<br />
hospital or our Endocrine Nurse Helpline if you have any queries about this. We are<br />
aware Solu-Cortef is in plentiful supply currently, but if your pharmacist is having<br />
problems, they should contact the manufacturer directly to gain a supply.<br />
When The Foundation contacted AMCo (Amdipharm Mercury Group), about<br />
the availability of Efcortesol which was expected to be in stock during March, they<br />
told us:<br />
“We have had a change in the manufacturer and API source which has caused this<br />
out of stock situation, however we are pleased to let you know that we have resolved<br />
the issues and are expecting the product to be available by July 2015.” They apologise<br />
for any inconvenience caused.<br />
For those patients concerned about not having a HC injection at home,<br />
because of supply issues, we advise in event of emergency, you should always<br />
call an ambulance and state ‘addisonian crisis’ or ‘adrenal crisis’ ■<br />
RESEARCH STUDY<br />
Does Cushing’s disease affect you or someone you<br />
know?<br />
Researchers at selected NHS hospitals are offering paents the opportunity to take<br />
part in a Clinical Research Study of a targeted medical treatment for Cushing’s<br />
disease.<br />
Who can parcipate in the study?<br />
Adult paents with Cushing’s disease who are not suitable for<br />
surgery or who have received prior surgery, and who’s Cushing’s<br />
disease sll requires further treatment; and paents who<br />
have not received radiotherapy in the last 3 years.<br />
Potenal paents will have assessments to determine their<br />
eligibility. If enrolled they will undergo medical examinaons<br />
and assessments, and receive study medicaon.<br />
Paents who parcipate in the study will have their travel costs<br />
reimbursed.<br />
FOR MORE INFORMATION AND TO<br />
FIND THE NEAREST CENTRE<br />
PLEASE CALL THE LEAD RESEARCH<br />
CENTRE ON :<br />
0161 446 8437<br />
CLCI699C2<strong>30</strong>1 Version 1.0, 03‐Sep‐14<br />
Pituitary life | summer 2015
26 Professional articles<br />
New medicine for acromegaly<br />
A<br />
new medicine will soon be<br />
available for certain people<br />
with acromegaly. The brand<br />
name of the medicine is Signifor and<br />
the medical name is pasireotide LAR<br />
(standing for ‘long acting release’).<br />
Acromegaly is caused by a benign<br />
growth on the pituitary gland, which<br />
is found in the front, central part of<br />
the brain.<br />
Doctors are being briefed that Signifor<br />
is suitable for adults where surgery has<br />
not cured their acromegaly (or if surgery<br />
is not an option) and whose disease is not<br />
well controlled with the medicines that<br />
are currently available. 1<br />
Funding for Signifor<br />
In England, the NHS needs to decide<br />
whether it wants to, and can afford, to<br />
make Signifor available to all suitable<br />
patients. This decision may be made next<br />
April, or potentially April 2017 or beyond!<br />
In the meantime, doctors can ask to use<br />
the medicine by making an Individual<br />
Funding Request (an IFR - more<br />
information about IFRs is available on<br />
The Pituitary Foundation website). Before<br />
making a funding request, the doctor asks<br />
for permission from their patient and<br />
keeps them informed of whether the<br />
NHS will pay for the medicine.<br />
Doctors in Wales need to apply for<br />
funding for individual patients also, while<br />
the NHS in Scotland will decide in the<br />
spring whether it will make the medicine<br />
available to all patients. Each nation in<br />
the UK makes their own decision about<br />
health, meaning that it is not simple.<br />
Patients who may be suitable<br />
for Signifor<br />
Acromegaly is a rare and serious condition<br />
that can lead to major health problems and<br />
a shorter life. Treatments aim to reduce<br />
these problems and allow a normal length<br />
of life. The aims for effective treatment are:<br />
• Ongoing control of two hormones -<br />
growth hormone (GH) and insulinlike<br />
growth factor 1 (IGF-1)<br />
• To reduce or stabilise the size of the<br />
benign tumour<br />
• Improve signs and symptoms<br />
associated with the disease<br />
• Preserve pituitary function<br />
• Prevent the benign tumour coming<br />
back once reduced or removed 2<br />
These two hormones are not controlled<br />
in many people with acromegaly, despite<br />
them taking maximum doses of current<br />
somatostatin analogues.2 This is where<br />
Signifor comes in.<br />
A clinical trial of nearly 200 people<br />
whose hormones levels were not<br />
controlled on existing medical treatment<br />
compared the effect on patients taking two<br />
doses of Signifor (40mg or 60mg) against<br />
patients taking two other medicines. The<br />
good news is that, comparing Signifor to<br />
the other medicines:<br />
• GH and IGF-1 hormones were<br />
controlled in more people on Signifor<br />
treatment<br />
• the benign tumours were reduced<br />
in size in more people on Signifor<br />
treatment<br />
• Greater improvement in symptoms<br />
were observed in patients on Signifor<br />
than on the other two medicines<br />
As well as the positive benefits, medicines<br />
can cause other unwanted changes, called<br />
side effects. Patients taking Signifor were<br />
more likely to have raised blood sugar,<br />
diabetes and diarrhoea than those taking<br />
the other medicines. While most of these<br />
side effects were mild to moderate, some<br />
patients stopped taking Signifor as a result<br />
of these side effects. Looking overall,<br />
Signifor was well tolerated by patients.<br />
In conclusion, Signifor offers a new<br />
alternative treatment for patients with<br />
acromegaly whose condition is not<br />
controlled by their existing somatostatin<br />
analogues. Research and development of<br />
the medicine was conducted by the Swiss<br />
pharmaceutical company Novartis.<br />
If you have questions about<br />
acromegaly, Signifor or Individual<br />
Funding Requests, please contact us via<br />
the Pituitary Foundation website, helpline<br />
or email support line. You can also request<br />
a booklet about acromegaly ■<br />
References<br />
1. Signifor summary of product characteristics,<br />
Novartis Pharmaceuticals UK<br />
Ltd.<br />
2. Gadelha M et al. Pasireotide versus<br />
continued treatment with octreotide or<br />
lanreotide in patients with inadequately<br />
controlled acromegaly (PAOLA):<br />
a randomised, phase 3 trial. Lancet<br />
Diabetes Endocrinol 2014; 2: 875–84.<br />
New booklet:<br />
Living with<br />
DI for young<br />
adults & teens<br />
This is the first booklet in our<br />
exciting new series for young<br />
adults and teens. Order your<br />
copy though our website shop, or<br />
download for free.<br />
Pituitary Life | summer 2015
news Patients’ stories<br />
27<br />
Marilyn’s story<br />
I<br />
think I was about 28, when I first noticed things were<br />
not right with my health. My tummy was getting larger,<br />
which I put down to getting older as I had always been<br />
about eight stone, even after my children were born.<br />
I muddled along knowing that something was wrong; a few<br />
years later, when my daughter started work (she was in the same<br />
building as myself as we worked at BT) and everyone knew<br />
everyone else - people were asking her if I was pregnant. Before<br />
this, I had had a lot of personal problems, taking on a part-time<br />
job as well as the day one to help with the mortgage etc. I went<br />
to my GP who said I was suffering with stress but I knew it was<br />
more than that as I was going to bed after tea and I didn’t want<br />
to go to work either, but I carried on.<br />
My direct boss, who didn’t know my job, was stamping<br />
her foot at my desk and telling me to get on with it when she<br />
should have been doing some of it herself. I didn’t want to<br />
talk to anyone either. My part-time job lasted for three months<br />
every year and coming to the end of this particular year, things<br />
suddenly started to clear as we had just had a big pay rise at<br />
work. It was only when I was being diagnosed when asked if<br />
I was depressed, I knew what I had gone through and it was<br />
something I never want to happen again.<br />
safari to Kenya<br />
I then started to go on holiday with my friend and my daughter,<br />
on a safari to Kenya and we liked it so much we booked again<br />
for the following year.<br />
In the meantime, I was eating like a horse and coming home<br />
and decorating until the early hours. In fact, my dogs would look<br />
round the door and shrug and say ‘no walk today’ and go to bed.<br />
But in my bad times I would go where no one could see me with<br />
the dogs and cry.<br />
One day, I was in the garden and caught my arm on a dead<br />
twig; the skin immediately shrank back and left an open wound.<br />
I went straight to A&E and the doctor said he wouldn’t be able<br />
to stitch it as the skin would rip, but he managed to do three<br />
stitches; he also asked if I took steroids? I said the only tablets I<br />
took were for headaches - I didn’t even know what steroids were.<br />
By this time, if I banged my shin the same thing happened<br />
and I would end up with an ulcer and bandaged from ankle<br />
to knee. One day at work, I was photocopying and when I<br />
turned round someone had left the bottom drawer of a metal<br />
filing cabinet open and it caught my leg and the same happened<br />
again - the skin shrivelled up, only now it was a bigger wound.<br />
Off again to A&E at a different hospital and two doctors asked<br />
me at different times if I took steroids. Once again, I had two<br />
bandaged legs.<br />
This steroid thing got me thinking, so I went to my GP and<br />
said there must be something in my blood that is causing this<br />
and I said my stomach wasn’t natural either. Her reply was, well<br />
what do you want to know for, do you think there is something<br />
sinister in there? I was about to walk out when she gave me a<br />
note to see a specialist. I duly went and the first thing he said<br />
was “You are carrying too much weight there” and prodded my<br />
stomach; my blood pressure was far too high. He sent me for<br />
an X-ray and when I went back for the results he said my heart<br />
was enlarged and he was thinking hormones, but couldn’t put his<br />
finger on it and would send me to an immunologist.<br />
cyst<br />
Before I got an appointment I was going on holiday again and<br />
I made an appointment with the GP - one who I hadn’t seen<br />
before to get something for my feet as they always felt as though<br />
they were going to burst. He was reading my notes and asked me<br />
Pituitary life | summer 2015
28 Patients’ stories<br />
a few questions and said he thought he knew what was wrong<br />
with me - it could be a cyst.<br />
By now, going to and from work, I couldn’t get up the stars<br />
at the stations without hauling myself up by the spindles under<br />
the banister and was convinced I would soon be in a wheel chair.<br />
When I arrived back from holiday there was an appointment<br />
for me to attend Withington Hospital where I was asked<br />
questions and told to crouch down - of course, I couldn’t get<br />
up again. The doctor called the consultant and said “I think we<br />
have a ‘Cushing’s” and to me “Could you come to Christies on<br />
Monday?” This was 20 years after I knew there was something<br />
wrong, as you know when your body is not up to scratch. Whilst<br />
in Christies for the week, I had to collect all my urine and had my<br />
blood taken early morning and midnight. At the end of the week<br />
the ward doctor came to me and said they had found ACTH in<br />
my blood but not in my urine, we will have to go back to the lab.<br />
I also had a scan but nothing showed up.<br />
back for results<br />
I went back about a month later for the results the doctor said<br />
we had a discussion about you last week and there is nothing we<br />
can do. I asked him what did he mean - if it was in my blood<br />
it should have been in my urine as well. “OK” he said, do me<br />
another 48-hour collection and I’ll take some more blood, and<br />
when it was all analysed it was there in both, but they had to find<br />
out where the growth was.<br />
Back in Christies for a week again and then to have sinus<br />
sampling at Manchester Royal. I would go as a sitting patient and<br />
come back on a stretcher. They also gave me a vial of drug to<br />
take with me. I was sitting in the waiting room and a sister came<br />
out and said it’s not as bad as you think. In I went and there were<br />
about a dozen people in there. What would happen was hollow<br />
wires would be threaded through my veins from my groins until<br />
they reached the pituitary, I also had a cannula in my arm, they<br />
injected the drug and after 15 minutes blood was taken from the<br />
three points at exactly the same second (or near enough); then<br />
again, after another eight minutes and again, near the end of the<br />
half hour, then the blood was taken straight to another hospital<br />
for analysis; I went back to Christies and bed for a couple of<br />
days. I went back a couple of weeks later and was told good<br />
news the tumour was on the right side and I would have to go<br />
down to the Radcliffe Infirmary in Oxford for the operation.<br />
This was now November 1991. I was lucky as my brother lives<br />
in Hertfordshire, so accommodation was no problem.<br />
lumbar puncture<br />
Two days after my op, the doctor came to take the plugs out of<br />
my nose and said he could heat the hospital with me I was so<br />
hot. The next day, my nurse asked why I wouldn’t open my eyes,<br />
I didn’t answer him and they were just going to do a lumbar<br />
puncture when they noticed my back was covered in a rash. They<br />
had given me penicillin three days before my op to stop infection<br />
- I was allergic to penicillin. Fortunately, I didn’t have to have a<br />
plug from my thigh. As soon as they changed the antibiotic I was<br />
a different person and going about the hospital and into Oxford<br />
town to the shops. The hospital is in the old buildings and very<br />
quaint. I just had three stitches under my top lip.<br />
blood tests<br />
When I got home, it was straight into Christies for blood tests<br />
and lo and behold there was ACTH again. I was given bags of<br />
tablets, to no avail, so the consultant said there was only one<br />
way: a bilateral adrenalectomy, which I had in April 1993. I had<br />
the op at Christies on the Wednesday and on Friday when my<br />
partner (husband now) came to visit, the doctor was shouting<br />
down the phone for any ambulance to get me to Withington into<br />
ICU (Christies don’t have an ICU for obvious reasons). I knew<br />
nothing since before my op, only this little anaesthetist bustling<br />
into the ward saying I didn’t know you were on my list - drink<br />
this and I had gone in seconds. I had been back on the ward<br />
for some days when I felt tightness in my leg and woke up next<br />
morning to a pulmonary embolism which was seen to PDQ.<br />
When I got home after about three weeks, I was ok and<br />
eventually decided to take medical retirement and redundancy<br />
and got a job in a charity shop three days a week.<br />
In 1997 I asked for another scan as Christies had then got an<br />
MRI only to find that my growth had regrown. To save another<br />
op, I had 15 doses of radiotherapy and a few weeks later got<br />
married and went on a wildlife expedition in Borneo.<br />
I had an adrenalectomy and radiotherapy and for some reason,<br />
I now have Nelsons Syndrome instead of Cushing’s.<br />
treatment for asthma<br />
Two years ago, after being ill for some months and the GP<br />
treating me for asthma - I kept telling him about my stomach<br />
which was now bigger than a football and absolutely solid and<br />
I could only walk a few paces before I had to stop as I couldn’t<br />
breathe, so I spent the time sitting in a chair. Eventually he<br />
decided to send me into Glan Clwyd Hospital (we now live in<br />
North Wales) to see what was wrong with me. I then found out<br />
that I had heart failure. One of the tests I had this year was a 24-<br />
hour monitor and the cardiac doctor thought my heart problem<br />
was probably due to everything, especially my enlarged heart.<br />
Whenever I have any blood tests though, they are always perfect.<br />
I was 70 last May with the normal aches and pains of an oldie,<br />
my walking isn’t too good but I manage, and my condition hasn’t<br />
stopped me from going on holiday. I think now I have been going<br />
to Africa every year since 1989 and is now in my blood as they say,<br />
but with all the troubles there we have decided Sri Lanka may be<br />
better.<br />
And to finish on a funny note, the surgeons who performed<br />
my adrenalectomy were coming to see me every day on the ward,<br />
in ICU and on the ward later, (they work at both hospitals); one<br />
day they asked me if I had any pains in my tummy, I said “No,<br />
but no doubt you hoofed everything out and hoofed it back<br />
again” and he said “You’re not far wrong and actually we were<br />
calling you Lazarus”, so that’s how bad I was ■<br />
Pituitary Life | summer 2015
Patients’ stories<br />
29<br />
Mike’s story - twenty five years on<br />
I<br />
sat up in bed one morning in January<br />
and suddenly realised it is 25 years<br />
since I was diagnosed with a pituitary<br />
tumour and having it removed later in<br />
that year. Perhaps now is the time to<br />
reflect on the events of the last quarter<br />
of a century on my life.<br />
In the late 1980s I began to feel extremely<br />
tired and unwell and despite several visits to<br />
my GP we failed to get to the bottom of<br />
it. I was sent to see a liver consultant who<br />
did some extensive tests and I ended up<br />
being sent home with some tablets and the<br />
thought it could be the dreaded ME (very<br />
much in fashion at that time).<br />
We move on a year and major company<br />
restructuring following a takeover,<br />
resulted in our move to Oxford and while<br />
making Bristol staff redundant I suffered<br />
a heavy nose bleed and was taken to<br />
Frenchay hospital by my MD. By the time<br />
I got there the bleeding had stopped and<br />
after a cursory look was sent home.<br />
In mid-1990 I was working in Oxford<br />
late one evening when I began to experience<br />
severe pains in my left arm so decide to<br />
drive to the John Radcliffe Hospital where<br />
I was admitted for a couple of days hooked<br />
up to a monitor and parted with a fair<br />
amount of blood plus a twenty four hour<br />
urine collection.<br />
The registrar came to see me and said no<br />
heart attack but hormones detected in my<br />
urine. I was sent home and referred to Dr<br />
Burke, an Endocrinologist, who saw me in<br />
August and by then I was experiencing very<br />
severe hot flushes every few hours.<br />
While I was meeting Dr Burke I had a<br />
real supersonic flush and he immediately<br />
sent me off for an x-ray of my head and a<br />
pituitary tumour was discovered.<br />
After more tests and scans, I was<br />
operated on by Mr Richard Kerr at the<br />
Oxford Radcliffe Infirmary (no longer<br />
exists - now a college). He is now President<br />
of the Society of British Neurological<br />
Surgeons and at the time gave me one<br />
piece of advice. Be prepared not to be<br />
taken seriously when you return to work<br />
as you have no scar. How true!<br />
Well, here I am 48 years old, with a<br />
very stressful job asking ‘where do I go<br />
from here?’ (No Pituitary Foundation at<br />
this time - you lucky people today in the<br />
same situation, have wonderful support at<br />
no cost).<br />
As I recovered (back at work early at<br />
the insistence of my FD) tests continued<br />
to establish replacement hormone needs<br />
and I threw myself back into my job and<br />
returned to my active lifestyle (mainly<br />
walking).<br />
I am a very positive person but I<br />
suddenly realised, after about three<br />
months, this approach was not working so<br />
I talked to my wife Anne and my daughters<br />
about what to do next. I decided the best<br />
way forward was not to try and beat or<br />
ignore the condition but to work with it<br />
and this I have done successfully to the<br />
present day, although old age is having an<br />
effect as well!!<br />
What do I mean by that? Well, I<br />
discovered mornings are good, afternoons<br />
bad; so I started work as early as I could<br />
i.e. this is being written in the early<br />
morning, as after 2pm I am usually pretty<br />
useless. This has worked for me and since<br />
then life has been a bit easier.<br />
Close family and friends have been very<br />
supportive, apart from one close family<br />
member who told me I needed anger<br />
management. I can tell you that showed<br />
a complete lack of understanding and it<br />
hurt very much.<br />
In the next ten years I walked up<br />
several mountains in Wales, including<br />
Snowdon and also completed several<br />
National Trails, the West Highland Way,<br />
Great Glen Way and St Cuthbert’s Way<br />
among others.<br />
In about 1994, Dr Burke retired and was<br />
replaced by Prof John Wass (co-founder<br />
of The Pituitary Foundation) and I realised<br />
what good hands my wellbeing had been<br />
placed in. In 1997, following a five year<br />
scan, it was discovered my tumour was<br />
growing again and the decision was made to<br />
have 28 sessions of radiotherapy over four<br />
weeks at the Churchill Hospital and despite<br />
being knocked for six, I continued to work<br />
all through the treatment (every weekday at<br />
8am). I recovered from this setback and was<br />
made redundant in another reorganisation<br />
in June 2000. We decide to move back west<br />
to be near our children but I continued to<br />
see Prof Wass at the OCDEM centre at<br />
the Churchill Hospital. John Wass retired<br />
from the NHS and I discovered that one<br />
of his young registrars at Oxford, Dr Karin<br />
Bradley, was now a consultant operating at<br />
the Bristol Royal Infirmary. I asked her if she<br />
would take my case on and to date I have an<br />
annual appointment to see her. A successful<br />
transfer for lucky me; from that comment<br />
you can gather I am looked after very well.<br />
I joined The Pituitary Foundation in<br />
2000 through the Bristol Support Group.<br />
They are a tremendous crowd of people<br />
and our ethos of helping watch each other<br />
has worked wonders. I am still an active<br />
member of the Group and also volunteer<br />
at the National Support Office - think I<br />
must hold some sort of record for folding<br />
raffle tickets!<br />
In my 70th year I walked Hadrian’s Wall<br />
with Anne’s cousin, Ian. No other word<br />
than ‘wow’ would describe the scenery<br />
and I was sponsored to raise funds for<br />
The Foundation,<br />
I would still love to walk another trail<br />
but think age is catching up on me and<br />
I have picked up other health problems<br />
on the way i.e. Type 2 Diabetes, hardened<br />
arteries and kidney stones to name a few.<br />
I am still walking around three miles a day<br />
mostly along the sea front here in Weston<br />
Super Mare. I am now 73 and hope to<br />
go on for a good few more years with<br />
the support of my family, The Pituitary<br />
Foundation and my consultant, Dr Karin<br />
Bradley, and her team.<br />
Bearing in mind the danger of repeating<br />
myself, my great belief is this condition<br />
cannot be beaten but if you work with it,<br />
the quality of life you should achieve is<br />
good ■<br />
Pituitary Life | summer 2015
<strong>30</strong><br />
Patients’ stories<br />
Pat’s Story – a carer’s review, 11 years on<br />
Looking back over the last 12 years,<br />
since Tony had his diagnosis,<br />
(pituitary apoplexy from a macro<br />
prolactinoma) we have at times had<br />
quite a roller coaster of a ride!<br />
The Endocrine Team at the Queen<br />
Elizabeth Hospital carefully monitored<br />
his condition in order to stabilise his<br />
medication, and he is now checked on<br />
an annual basis. It took two years for<br />
him to recover the confidence to drive<br />
again. This seemed to me to be a bleak<br />
time whilst I came to terms with Tony’s<br />
limitations and frustrations.<br />
a life saver!<br />
I was finally able to persuade him to attend<br />
The Pituitary Foundation Birmingham<br />
and West Midlands Local Support Group.<br />
For me it was a life saver! Wayne, the Coordinator,<br />
ran the group with his mother as<br />
carer support. She helped me, by allowing<br />
me to voice my feelings of concern and<br />
inadequacy. I looked forward to talking<br />
to her and others at the meetings, and was<br />
glad to see how it helped Tony to talk to<br />
others too.<br />
Our GP practice found the diagnosis<br />
very interesting, and a medical student<br />
who happened to be spending time with<br />
one of the doctors was told that she<br />
should feel very honoured to have met a<br />
pituitary patient, as most doctors never<br />
see one in the whole of their career!<br />
We have a very supportive family who<br />
encouraged me to go back to doing some<br />
of my hobbies. I was able to rejoin my<br />
dressmaking class and a fitness class,<br />
whilst Tony was kept an eye on. We<br />
even ventured on holiday in our touring<br />
caravan, with our sons helping by towing<br />
us there and back. The site managers<br />
were brilliant in placing us conveniently,<br />
so that Tony had as little distance as<br />
possible to walk. I found this holiday<br />
terrifying at first, as I felt isolated from the<br />
help we had got used to. Being a retired<br />
Occupational Therapist didn’t help, as I<br />
felt inadequate.<br />
I decided to become a volunteer at the<br />
QE, when Tony was fit enough to be<br />
left, as a way of giving something back<br />
to the hospital that had saved his life.<br />
I still do this and enjoy the work I do<br />
very much.<br />
In 2008, our LSG Co-ordinator<br />
resigned as he was moving away, and<br />
so, that July we held our first meeting<br />
as Joint Area Co-ordinators to avoid<br />
its closure. As a result of this, we have<br />
met some lovely, interesting people<br />
and attended The Foundation Training<br />
Days and Conferences.<br />
Our constant problem has been the<br />
fact that Tony was already an insulin<br />
dependent Diabetic type 2, as this<br />
can confuse symptoms at times. For<br />
instance, he had an Adrenal Crisis in<br />
January 2012, which I mistook for a<br />
Hypo at first. When the glucose failed<br />
to improve his condition, I realised<br />
that his condition had become serious<br />
and called an ambulance. During his<br />
admission, Sherwin, one of the Specialist<br />
Endocrine Nurses, came to demonstrate<br />
to Tony and me how to inject emergency<br />
hydrocortisone. We told him that we ran<br />
the Local Support Group, and he agreed<br />
to come to a meeting to show all the<br />
members. Everyone was given an orange<br />
to practice on!<br />
sleep clinic<br />
Tony has been a volunteer gardener at a<br />
nearby local hospital now for over two<br />
years. This has been a relief for me and an<br />
outlet for him. He has been able to start a<br />
new interest in a work environment, giving<br />
us both our own space. He loves working<br />
again and the team have developed quite<br />
a status at the hospital for what they do.<br />
At his annual review in the pituitary<br />
clinic in 2013, I mentioned that Tony still<br />
seemed very sleepy, as he kept dozing off<br />
when he sat down. Arrangements were<br />
made for him to have testosterone levels<br />
checked, and referral to the Sleep Clinic as<br />
he may have sleep apnoea. As it happened,<br />
both needed attention. He was told that<br />
although the increase in testosterone may<br />
help, Tony was overweight and this causes<br />
fat to sit around the neck and press on<br />
the airway during sleep. He was given<br />
a mask and machine to help, which had<br />
to be used every night. Fortunately, his<br />
condition was considered to be mild,<br />
and, although he had to declare it to the<br />
DVLA, he was still able to drive. He was<br />
furious with me for telling the consultant<br />
that he fell asleep, and blamed me for him<br />
being expected to wear the mask!<br />
For Tony this was the final spur to lose<br />
weight. He spoke to his GP, who was<br />
pleased to refer him through the NHS<br />
scheme to Weight Watchers. I am very<br />
proud of Tony’s commitment! He has<br />
lost 27lbs, achieved his goal, resulting<br />
in normal readings for his sleep and a<br />
reduced need for insulin. The mask and<br />
machine went back and now he very rarely<br />
needs to take insulin four times a day, as<br />
he did before. For the first time both he<br />
and I feel that at last he is in control of<br />
his wellbeing.<br />
We have just celebrated our 50th<br />
Wedding Anniversary, and have several<br />
events planned over the year. We have a<br />
wonderful, caring family, who still keep<br />
an eye on the ‘Old Chap’! We both want<br />
people to know that, yes, for patients and<br />
their carers, there is a future!! ■<br />
Pituitary Life | summer 2015
news Patients’ stories<br />
31<br />
John’s story - continued from last issue<br />
Editor note: We apologise, due<br />
to a design oversight, that some<br />
of John’s story from the spring<br />
2015 edition (no. 29) was missed;<br />
this excerpt below is from the<br />
last column on page 21 to first of<br />
upper columns on page 22.<br />
Before we flew back to Bermuda<br />
we had to attend a week long<br />
business conference which was<br />
a nightmare. Trying to outwardly<br />
maintain the appearance that all was<br />
well yet not being able to see properly<br />
was very difficult.<br />
On our return, I had a visual field test<br />
which verified the absence of peripheral<br />
vision and sent for an MRI, which<br />
revealed a pituitary tumour pressing on<br />
the optic nerve. Bermuda didn’t have the<br />
resources or expertise to deal with this<br />
type of condition so I was referred to the<br />
Lahey Clinic in Boston for a full diagnosis.<br />
We left a warm and sunny Bermuda and<br />
arrived in Boston on a bitter cold mid-<br />
October day. As I recall, we headed<br />
straight to the shops to buy enough warm<br />
clothes and boots to last for the long<br />
weekend we thought we would be there.<br />
US neurosurgeon<br />
We met with Dr Freidburg, Chairman<br />
of the Lahey Hospital Trust and one of<br />
the preeminent neurosurgeons in the US.<br />
After a day of further tests the diagnosis<br />
was confirmed. Dr Freidburg had a space<br />
in his calendar to operate the following<br />
Friday – Halloween - and outlined the<br />
procedure. The transsphenoidal removal<br />
of the tumour would take about 2 ½ hours<br />
and entail a two day stay in hospital with a<br />
further two weeks of recuperation before<br />
being allowed to fly back to Bermuda.<br />
Our long weekend was expanding...<br />
In the event the op took almost six<br />
hours as the tumour was old and fibrous<br />
and proved difficult to remove. It tore<br />
the arachnoid and spinal fluid started<br />
leaking which had to be packed with<br />
tissue from my thigh. A full craniotomy<br />
was scheduled for the following week.<br />
Afterwards I spent two weeks in intensive<br />
care and a further three on the ward.<br />
From there I was discharged to a local<br />
hotel and attended the hospital daily for<br />
further postoperative checks. Boston had<br />
experienced a very heavy snowfall, which<br />
delayed us even further and we eventually<br />
got back to Bermuda seven weeks after<br />
we had left.<br />
return to work<br />
I had lost a huge amount of weight and<br />
strength but slowly started recovering and<br />
did a phased return to work over the next<br />
couple of months. Within two years I was<br />
able to take part in a 15 mile charity walk<br />
coming in the top five.<br />
However, I came to realise that I<br />
was less sharp-minded than previously<br />
and in an industry answerable<br />
to shareholders and variable<br />
market conditions the pressure<br />
was intense. I struggled with<br />
things I had formerly taken in<br />
my stride and suffered bouts<br />
of depression. Boardroom<br />
decisions were being made<br />
that I did not agree with<br />
but didn’t have the energy<br />
to fight, so I resigned. It<br />
offers little consolation that the<br />
company failed soon after.<br />
We left Bermuda and<br />
returned to our house in Kent and I<br />
attempted to form a new company but it<br />
was evident that my drive and energy had<br />
gone and I shelved the project.<br />
After a year of doing no work I felt<br />
I needed to do something and took a<br />
junior position with a broker in London,<br />
which was mostly enjoyable - although<br />
the 90 minute commute less so! The<br />
company was taken over two years later<br />
and I happily accepted redundancy. By<br />
now I had to take stock of our finances<br />
and knew that if we ‘tightened our belts’<br />
I could afford to give up work in my mid-<br />
50s and appreciate that I was incredibly<br />
lucky to be able to do so. I could also play<br />
a bigger part in looking after my then 2<br />
year old grandson and found this to be<br />
great fun and immensely therapeutic ■<br />
If you would like to share your patient<br />
or family member’s story in Pituitary<br />
Life, please contact pat@pituitary.<br />
org.uk or write your story and send<br />
to The Pituitary Foundation, 86<br />
Colston Street, Bristol, BS1 5BB.<br />
Pituitary life | summer 2015
FREE Will offer<br />
Following the success of our FREE Will trial we<br />
are delighted to be able to announce that we have<br />
extended this offer. Gifts in Wills are a vital source of<br />
income for The Pituitary Foundation and enable us to be<br />
there to support future generations of pituitary patients<br />
in their hour of need.<br />
What we are offering<br />
We are offering you, our valued members, a FREE Will writing<br />
service (worth £100). You would make your Will over the<br />
telephone, in the comfort and privacy of your own home.<br />
(As we have committed Members living all over the country<br />
it would be impossible for a small organisation like us to offer<br />
a face-to-face service). Compass Wills and Estate Planning are<br />
specialist estate planners and have over 20 years’ experience<br />
in the field, so you can be assured of a quality, professional<br />
service (www.compass-advisors.co.uk). They will talk you<br />
through each step to make the process as easy and simple as<br />
possible.<br />
Next steps<br />
If you would like a free Will, please either call or e-mail Compass<br />
Wills and Estate Planning quoting the reference “Pituitary” as<br />
soon as possible:<br />
• Telephone – 01792 893200 Office opening hours: (Mon-<br />
Fri 9am-5pm)<br />
• E-mail – alyson.dyer@compass-wills.co.uk ■<br />
Find us on<br />
Facebook<br />
This edition is funded by Novartis<br />
The views expressed by the contributors are not necessarily those of The Pituitary<br />
Foundation. All information given is general - individual patients can vary and<br />
specific advice from your medical advisors should always be sought.<br />
We do not endorse any companies nor their products featured in this edition.<br />
© 2015 The Pituitary Foundation<br />
• Registered company number 3253584<br />
• Registered charity number 1058968<br />
The Pituitary Foundation<br />
86-88 Colston Street, Bristol, BS1 5BB<br />
helpline@pituitary.org.uk www.pituitary.org.uk<br />
Editor of Pituitary Life: Pat McBride<br />
Working to support pituitary patients<br />
Printed by Moulton printers www.moultonprinting.com.<br />
Designed by www.forestgraphics.net