Issue 28
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
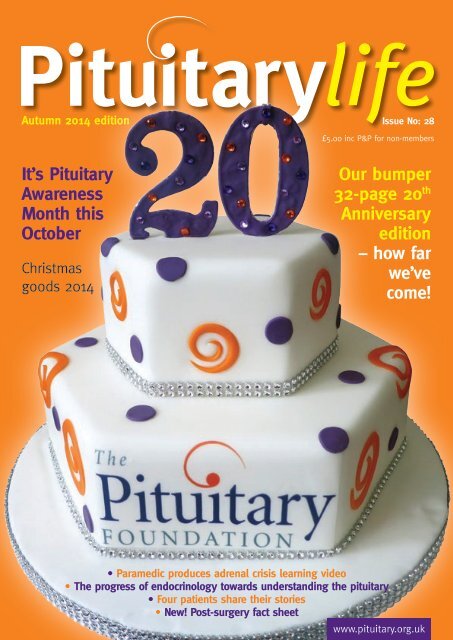
Autumn 2014 edition<br />
<strong>Issue</strong> No: <strong>28</strong><br />
£5.00 inc P&P for non-members<br />
It’s Pituitary<br />
Awareness<br />
Month this<br />
October<br />
Christmas<br />
goods 2014<br />
Our bumper<br />
32-page 20 th<br />
Anniversary<br />
edition<br />
– how far<br />
we’ve<br />
come!<br />
• Paramedic produces adrenal crisis learning video<br />
• The progress of endocrinology towards understanding the pituitary<br />
• Four patients share their stories<br />
• New! Post-surgery fact sheet<br />
Pituitary life | autumn 2012<br />
www.pituitary.org.uk
2<br />
news News<br />
Our 20 th Anniversary –<br />
how far we’ve come<br />
Pat McBride, Editor<br />
I<br />
am delighted, both as a member of<br />
staff and as a patient, to celebrate<br />
20 years of The Foundation. The<br />
original team of trustees Sue Thorn,<br />
Prof Stafford Lightman and Prof John<br />
Wass, set up The Pituitary Foundation in<br />
1994. Sue managed the publication of all<br />
the original leaflets, including writing one<br />
of them, edited the newsletter, dealt with<br />
the patient calls, registered the company<br />
and charity, and helped with the set-up<br />
of the early local groups. As soon as<br />
funds allowed, she worked with the other<br />
trustees to enable The Foundation to<br />
become an independent organisation.<br />
Sue’s contribution to making The<br />
Foundation a success was enormous<br />
and this was recognised at our Training<br />
Weekend in November 2013 when she<br />
and the other founding members were<br />
awarded Honorary Lifetime Membership<br />
of The Foundation.<br />
From our very first national<br />
conference in Bristol in 1997 we have<br />
held ten further national and regional<br />
conferences around the UK; our 20th<br />
anniversary conference in November<br />
will be our 12th. The Foundation’s<br />
first Pituitary News newsletter<br />
was produced in 1996, which<br />
was a mere eight pages, but read<br />
from cover-to-cover by those of<br />
us who, up until then, hadn’t had<br />
any information at all. Over the<br />
years it has undergone many<br />
changes and has evolved<br />
into the glossy, multi-page<br />
Pituitary Life.<br />
Our current booklets are<br />
mainly based on the<br />
original leaflets<br />
we produced<br />
back then, as the<br />
information has<br />
been patientfriendly,<br />
clear<br />
and accurate from the start. Of course,<br />
our resource library has been updated to<br />
reflect newer procedures and treatments<br />
and expanded, to help answer the many<br />
questions you ask. All of our resources<br />
are verified by our Medical Committee.<br />
This committee of 25 members is<br />
made up of consultant endocrinologists,<br />
pituitary surgeons, paediatric<br />
endocrinologists, specialist endocrine<br />
nurses, a psychologist and more recently,<br />
a paramedic. Our wonderful volunteer<br />
base has grown to over 100 – their<br />
commitment and hard work helps so<br />
much to carry on our vital work.<br />
I can clearly remember the day I heard<br />
the Foundation had been launched.<br />
Within minutes, I phoned the number I<br />
was given (by my endocrinologist back<br />
then) and as soon as I spoke to them, I<br />
knew they understood. At last, there was<br />
information to be had and the feeling<br />
of being a ‘rarity’ and alone with this<br />
condition vanished. The eight frustrating<br />
and lonely years from my diagnosis,<br />
without any pituitary knowledge<br />
or support, were over! I have been<br />
privileged to speak with and meet many<br />
courageous and wonderful patients and<br />
their families over<br />
the years. Here’s<br />
to another 20<br />
years (and more)<br />
of support for<br />
all of us with<br />
pituitary<br />
problems ■<br />
contents<br />
News for autumn 2-9<br />
Local Support Group news 7<br />
Professional articles 10-12<br />
(also continued on pages 21-25)<br />
Raising awareness 13-20<br />
(pull out 8 page section)<br />
Wall of thanks 14-15<br />
Patients’ stories 26-31<br />
Newly<br />
extended<br />
Endocrine<br />
Nurse Helpline<br />
hours<br />
It is with thanks to our<br />
generous supporters and<br />
members, that we are in a<br />
position for Alison Milne, our<br />
Endocrine Specialist Nurse to<br />
increase her Helpline hours.<br />
From 8 September 2014, Alison<br />
will hold an extra shift on Mondays<br />
between 10:00am to 1:00pm.<br />
We are delighted to be able to<br />
announce this, as we are aware that<br />
Alison’s Helpline is very popular<br />
and that her support to our<br />
community is greatly needed ■<br />
Pituitary Life | autumn 2014
news News - Awareness Month<br />
3<br />
Awareness Month October 2014<br />
We hope to hugely improve<br />
pituitary awareness across<br />
the UK with our Awareness<br />
Month this year, but we can only do<br />
this with your help!<br />
The Foundation has been preparing<br />
the campaign and awareness activities<br />
for the last few months and we are really<br />
excited about the impact this October<br />
could have, if everyone pulls together.<br />
We’d be delighted if you would help<br />
us to make a big statement this year…<br />
whichever of the below activities you can<br />
help with, large or small, it can make a<br />
massive difference!<br />
This year we are focusing on<br />
improving understanding of adrenal<br />
crisis experienced by steroid dependent<br />
pituitary patients. We are running<br />
an exciting targeted campaign which<br />
involves writing to politicians, and we<br />
have developed a brand new adrenal crisis<br />
leaflet for GPs and A&E staff. There are<br />
also many other fundraising and awareness<br />
activities to get involved with. This year<br />
also happens to be The Foundation’s<br />
20th Anniversary and to help mark this<br />
special occasion and how far we have<br />
come in those twenty years, we are asking<br />
supporters and local groups to hold parties.<br />
If you decide to have a party, please let us<br />
know so that we can promote it on the<br />
website (more information on page 5) ■<br />
Write to your local parliamentary or<br />
assembly member about adrenal crisis.<br />
Email rosa@pituitary.org.uk to be sent the template letter.<br />
We are encouraging everyone to write to their local<br />
politicians, explaining the importance of the lifesaving<br />
steroid hydrocortisone and urging them to<br />
support The Pituitary Foundation’s campaign; this includes<br />
missed, or inadequate, hydrocortisone administration in a<br />
healthcare setting - on the list of NHS Never Events.<br />
What is a ‘Never Event’?<br />
NHS Never Events are serious, largely preventable patient<br />
safety incidents that should not occur in the NHS, if the<br />
available preventative measures have been implemented. The<br />
Never Event list currently includes 25 incidents.<br />
Why should missed or inadequate<br />
administration of hydrocortisone be a<br />
‘Never Event’?<br />
When patients who have adrenal insufficiency (pituitary<br />
patients who have secondary adrenal insufficiency) become<br />
unwell, they can be at risk of going into an adrenal crisis<br />
because their body is unable to naturally increase the output<br />
of steroid from their adrenals to help the body overcome<br />
the illness or stressful situation. Patients taking replacement<br />
steroid (hydrocortisone) need more steroid to prevent them<br />
going into adrenal crisis in the first place, or if the patient<br />
is experiencing an adrenal crisis, to appropriately treat the<br />
adrenal crisis, to prevent a possible life threatening situation.<br />
Unfortunately, too often, healthcare workers do not realise the<br />
urgency of treatment for acute adrenal crisis or fail to heed the<br />
requests of well-informed patients for hydrocortisone. This is<br />
why we believe that missed, or inadequate administration, of<br />
hydrocortisone should become a Never Event.<br />
How can I join this campaign?<br />
Research has been carried out to identify influential MPs,<br />
MSPs, MLAs and AMs with a specific interest in health or<br />
rare disease. (Please see our table of contacts for every area<br />
covered by a Support Group). These researched contacts will<br />
allow a more targeted campaign and hopefully Members of<br />
Parliament, Assembly Members in Wales and Northern Ireland<br />
and Members of the Scottish Parliament will support us in our<br />
campaign. The description of a ‘Never Event’ will be explained<br />
clearly within the template letter.<br />
Pituitary Life | autumn 2014
4 News - Awareness Month<br />
Politicians to contact<br />
Aberdeen South<br />
South Scotland<br />
Birmingham<br />
Brighton / Sussex<br />
Bristol<br />
Cardiff<br />
Central Lancashire<br />
Derby/ Nottingham<br />
Doncaster<br />
Edinburgh<br />
Glasgow<br />
Guildford<br />
Hull West - Hessle<br />
Ipswich and Suffolk<br />
Kent<br />
Leeds<br />
Liverpool<br />
London<br />
Manchester Central<br />
Mid and West Wales<br />
Newcastle<br />
Northern Ireland<br />
Norwich and Norfolk<br />
Oxford<br />
Plymouth and Exeter<br />
Salisbury<br />
Dame Anne Begg (Labour)<br />
Aileen McLeod (Scottish National Party<br />
and sits on the rare diseases Scottish<br />
cross party group)<br />
John Hemming (Lib Dem)<br />
Simon Kirby (Conservative)<br />
Kerry McCarthy (Labour)<br />
Mark Drakeford Minister for Health<br />
and Social Services, (Labour)<br />
Rosie Cooper (Labour)<br />
Anna Soubry (Conservative)<br />
Hugh Bayley (Labour)<br />
Malcolm Chisholm (Labour)<br />
Bob Doris (Scottish National Party)<br />
Anne Milton (Conservative)<br />
Alan Johnson (Labour)<br />
Dan Poulter (Conservative)<br />
Helen Grant (Conservative)<br />
Rachel Reeves (Labour)<br />
Luciana Berger (Labour and<br />
Cooperative)<br />
Norman Lamb Minister of State at the<br />
Department of Health as of 2012 (Lib Dem)<br />
Lucy Powell (Labour)<br />
Rebecca Evans (Labour)<br />
Jenny Chapman (Labour)<br />
Nigel Dodds (Democratic Unionist Party)<br />
Norman Lamb (Lib Dem)<br />
Andrew Smith (Labour)<br />
Ben Bradshaw (Labour)<br />
John Glenn (Conservative)<br />
Sheffield/Crewe and Nantwich Edward Timpson (Conservative)<br />
Shrewsbury<br />
Solent<br />
Swindon<br />
Ian Mearns (Labour)<br />
Caroline Dinenage (Conservative)<br />
Robert Buckland (Conservative)<br />
These are the politicians with the greatest<br />
interest in rare disease issues, regardless<br />
of which parties they are aligned to. We<br />
have researched contact information for<br />
all these politicians which can be found<br />
on The Foundation’s website. Just go to<br />
the ‘Get Involved’ section and then to<br />
‘Campaigns’ tab where you will see the<br />
Awareness Month details. Alternatively,<br />
when you email rosa@pituitary.org.<br />
uk to be sent the template letter, if you<br />
include which politician you are writing<br />
to, we can send you their address.<br />
If you live in an area that is not listed<br />
in the table, we recommend writing to<br />
one of the following, as these politicians<br />
have a particular interest in rare diseases.<br />
The Foundation will also be contacting<br />
these main politicians:<br />
Norman Lamb Lib Dem MP (Minister<br />
of State, the Dept of Heath).<br />
Dame Anne Begg Labour MSP.<br />
Rebecca Evans Labour AM ■<br />
Pituitary Life | autumn 2014
News - Awareness Month<br />
5<br />
Adrenal crisis<br />
leaflet distribution<br />
Help us spread awareness about adrenal crisis to GPs, ambulance<br />
personnel and A&E staff by taking along our brand new leaflet to<br />
your local clinics and hospitals. This is a really worthwhile, but nontime<br />
consuming activity, that everyone can get involved with! We are delighted to<br />
have been able to have a new leaflet designed for Awareness Month. Order yours<br />
today on our website shop or by emailing enquiries@pituitary.org.uk<br />
(These leaflets will be included if you are ordering an awareness pack) ■<br />
It’s The Pituitary<br />
Foundation’s birthday!<br />
An adrenal<br />
crisis is life<br />
threatening!<br />
A pituitary patient<br />
on hydrocortisone,<br />
who is in shock,<br />
been in an accident<br />
or is vomiting,<br />
URGENTLY needs<br />
a higher dose of<br />
hydrocortisone<br />
(usually by 100mg<br />
injection)<br />
l Think - Adrenal<br />
Insufficiency<br />
l Realise<br />
- Adrenal Crisis!<br />
l Act NOW to treat<br />
this patient and<br />
save their life!<br />
www.pituitary.org.uk<br />
Give an<br />
awareness<br />
talk in your<br />
local area<br />
Throw a party during October to celebrate our 20 year anniversary<br />
Parties are a fun way to spread awareness. Pop the kettle on, get baking and<br />
invite some friends round for some sweet treats. A cake sale, raffle and games<br />
are always popular! You may even like to hold a party themed fundraiser in your<br />
office, school, university or college. Order your party pack now to help you plan your<br />
event – email jay@pituitary.org.uk<br />
Making special memories: After you have held your event, make sure you send<br />
us your photos as we intend making a special 20th Anniversary picture collage and we<br />
would love your photo to be included. We want to be able to look back on this photo<br />
in another 20 years with pride, as we celebrate our Ruby Anniversary.<br />
Our ‘Cake me up Selfie Campaign’ will also celebrate our 20th birthday – please<br />
see details of this campaign in your Fundraising Focus pull-out in the middle of this<br />
edition of Pituitary Life ■<br />
This could be anywhere<br />
from a local school,<br />
place of work, WI or<br />
rotary club. The Foundation<br />
has developed materials to help<br />
support people giving a talk<br />
on pituitary conditions. These<br />
materials include PowerPoint<br />
slides and notes to read from, to<br />
make it easier - so let us know if<br />
you’re interested ■<br />
Pituitary Life | autumn 2014
6 News - Awareness Month<br />
Organise or take part in an awareness walk<br />
Walk for awareness! We are<br />
asking you to organise a<br />
walk in your area – the<br />
event can be as small or as large as<br />
you want. You can stroll a mile, stride<br />
a midnight marathon, or walk or amble<br />
a 5k in your local park. It is a great way<br />
to keep fit, get your friends, family and<br />
work colleagues involved and collect<br />
sponsorship for your efforts. Every step you take and every<br />
penny raised will be helping to raise awareness – together<br />
we can make a real, positive change to<br />
the pituitary journey. You could even<br />
make your walk light-hearted and eyecatching<br />
by encouraging fancy dress.<br />
Whether all of the participants gather<br />
sponsorship or just a few, the important<br />
thing is the taking part. Last year many<br />
Local Support Groups, members and<br />
supporters all over the country held<br />
walks helping to raise over £4,000 between them. Can you get<br />
your walking boots on this year? ■<br />
Request your<br />
Awareness Pack today<br />
Your kind donations really do make a HUGE difference<br />
to our small charity. If you are unable to get involved with<br />
Awareness Month but are willing to donate to The Pituitary<br />
Foundation instead, please fill in the ‘Make a gift’ section of the<br />
Awareness Month insert within this issue of Pituitary Life. Last<br />
year, thanks to your generosity, we managed to raise a sensational<br />
£1,860 from Awareness Month donations; wouldn’t it be great if<br />
we could exceed the £2,000 mark this year? ■<br />
To request an awareness pack, which contains<br />
all resources and information for you to hold<br />
your awareness event, walk or anniversary party,<br />
please complete the form in the Awareness Month<br />
insert. Or contact Jay, our Fundraising & Marketing<br />
Manager on 0117 370 1314, or Rosa, our Volunteers,<br />
Campaigns & Projects Manager on 0117 370 1316<br />
(alternatively email enquiries@pituitary.org.uk)<br />
Please make sure you let us know about your awareness<br />
activities, as this allows us to measure how much of an<br />
impact Pituitary Awareness Month has around the UK! ■<br />
Pituitary Life | autumn 2014
Local Support Group News<br />
7<br />
This section contains quick<br />
newsflashes from a few of<br />
our Support Groups around<br />
the UK!<br />
To gain extra information and support,<br />
why not take a look on our website to<br />
see if one of our 32 groups meets near<br />
you. Visit www.pituitary.org.uk, or<br />
contact Rosa Watkin on 0117 370 1316,<br />
or email helpline@pituitary.org.uk<br />
LIVERPOOL<br />
A big congratulations to the Liverpool<br />
Support Group who celebrated their<br />
18th Birthday recently! For almost two<br />
decades, the members have tirelessly<br />
supported their fellow patients and<br />
carers, providing information at<br />
friendly, welcoming meetings. 2014<br />
has been another very successful year<br />
for them so far with regular monthly<br />
meetings being held, medical students<br />
visiting and lots of local awareness and<br />
fundraising taking place. The group<br />
have very kindly donated twice to<br />
The Foundation during this summer.<br />
The total of these donations was<br />
an amazing £420 and we are hugely<br />
grateful for their support. We would<br />
like to say an enormous ‘thank you’ to<br />
all the group members.<br />
SOLENT late IT donation -<br />
thank you<br />
We would like to apologise to The<br />
Solent Support Group for leaving<br />
them out of the IT donations thank<br />
you list in the last edition. This was<br />
due to a confusion on our database<br />
about what the donation had been<br />
put towards and we are very sorry for<br />
this error. We are hugely grateful for<br />
the £500 donation from the group,<br />
which was a huge help to us in funding<br />
our new IT equipment! Thank you<br />
to all the group members and the<br />
committee.<br />
The group have all their 2014<br />
meetings planned; for more<br />
information about meeting details<br />
contact Gail on 014<strong>28</strong> 651526.<br />
PLYMOUTH, EXETER, TRURO<br />
and TORBAY<br />
This support group is going from<br />
strength-to-strength under the very<br />
hardworking Area Co-ordinator, Mike<br />
Luxton, who is doing an absolutely<br />
magnificent job! As of this summer,<br />
the group is now covering Torbay as<br />
well as the previous three areas, so<br />
if there are any interested patients<br />
in Torbay do contact Mike at mike.<br />
pituitarylsg@gmail.com or phone<br />
01872 501375. The group now has<br />
well over 50 members and will always<br />
welcome new faces. This group is<br />
known as a roaming group and usually<br />
meets twice a year in each of the<br />
four locations. Meetings are always<br />
in a hospital setting and all meetings<br />
usually have doctors speaking, but<br />
include discussion time for patients<br />
and carers also. Some group members<br />
travel to attend all the meetings but<br />
some just attend their local meeting<br />
which is fine too. The next two<br />
meetings are Torbay on 10 September,<br />
and Truro on 30 September. This<br />
group is providing a much needed<br />
support network in an area that a<br />
couple of years ago had very little<br />
coverage; The Foundation is hugely<br />
grateful to Mike for being such a<br />
dedicated volunteer.<br />
“The support group is like a second<br />
family to me now; we can talk<br />
freely about pituitary and everyone<br />
understands.” (Quote from a support<br />
group member) ■<br />
National Pituitary Conference reminder<br />
Don’t miss the biggest pituitary event of the year - Saturday 8th November 2014! Book your place at our National<br />
Pituitary Conference by calling 0117 370 1316 or via the website shop.<br />
Rates for members are subsidised at just £34. 13s to 25s can attend for just £20. Please book soon to ensure your place,<br />
as this conference is proving very popular. The highly esteemed endocrine team from University College London Hospitals will be<br />
delivering the main sessions, alongside many different workshops covering topics from carers’ rights and benefits, to hydrocortisone<br />
information. The conference venue is easily accessible for central London and there is FREE parking.<br />
Bookings must reach us by October 31st ■<br />
Pituitary Life | autumn 2014
8 News<br />
Hospital management of<br />
hypopituitarism<br />
Ihave had two operations on my<br />
pituitary gland to remove tumours.<br />
I now need to take several pills daily to<br />
replace basic hormones, which were once<br />
controlled by the pituitary gland. One of<br />
these is hydrocortisone, which is needed<br />
to keep me alive.<br />
In the event of a shock to my system,<br />
the pituitary does not trigger the release<br />
of more hydrocortisone and, without<br />
being given extra replacement, I would<br />
die. I’m 67 and I needed a total right hip<br />
replacement. I saw the consultant and<br />
he understood my dilemma regarding<br />
hydrocortisone cover and arranged for<br />
me to see his anaesthetist. Fortunately, he<br />
was aware of the cortisol problems and<br />
“happy” to proceed, so I was sent for<br />
pre-op assessment and a briefing.<br />
On the Wednesday, I went in to<br />
hospital for a total hip replacement.<br />
All hydrocortisone precautions had<br />
been prepared and all staff had been<br />
briefed. After the operation, I was kept<br />
in sterile conditions to minimise the risk<br />
of infection. All medication (including<br />
my hydrocortisone) was administered<br />
as needed – staff changeovers were<br />
seamless, the ward was spotless and the<br />
food was great.<br />
I came out again on the Saturday<br />
afternoon a new man - sore, but pain<br />
free; my life restored.<br />
Well done and thank you to all<br />
concerned.<br />
Diabetes insipidus (DI)<br />
The surgeon and anaesthetist reassuringly<br />
understood about the patient’s<br />
hydrocortisone needs, but the ward staff<br />
had no understanding about hydrocortisone<br />
pre-op and of their DI, post-op.<br />
Pre-op, the patient increased their<br />
hydrocortisone tablets, using their own<br />
supply, whilst waiting for surgery and the<br />
appropriate hydrocortisone cover given<br />
by the surgical team.<br />
Despite explaining about the condition<br />
DI, showing their Patient Care Card<br />
and medication for DI, the ward staff<br />
member hung this up above the patient’s<br />
bed. Confusion still unfortunately exists<br />
that DI means diabetes mellitus ■<br />
New! Translated hydrocortisone<br />
emergency cards<br />
We now have our usual emergency hydrocortisone cards<br />
available in French, Spanish and Turkish for patients who are<br />
travelling to these destinations. The cards are credit-card size to<br />
carry easily in your wallet or purse. One side is in English for your personal<br />
and emergency contact details; the reverse side explains your hydrocortisone<br />
emergency needs in the foreign language. These cards will be available shortly<br />
to order from our website shop, at a cost of £2 each. We will announce on<br />
our website when they are in stock to order ■<br />
Ross Fletcher –<br />
in memorial<br />
We were very saddened to hear<br />
that Ross passed away on 24<br />
July 2014. Ross was a member<br />
of The Foundation from the beginning,<br />
having had successful surgery in 1974 for<br />
a pineal germinoma, but which resulted<br />
in pan-hypopituitarism. In 2004, Ross<br />
suffered a small stroke but continued to<br />
enjoy life, with holidays and his bowling.<br />
In February 2013, Ross suffered a severe<br />
stroke which left him unable to speak<br />
or swallow; he had to be fed through<br />
a tube in his stomach which caused<br />
complications because of his diabetes<br />
insipidus.<br />
During the last three months of his<br />
life, he was stable and his wife, Thea,<br />
managed to bring him home for visits<br />
from his nursing home.<br />
Thea told us that the doctors in the<br />
stroke ward Ross was on, had never<br />
treated a patient with hypopituitarism,<br />
although they did persevere and<br />
eventually manage to stabilise him so<br />
he could be discharged. A contributory<br />
factor of diabetes insipidus appeared on<br />
his death certificate and Thea wanted to<br />
highlight Ross’s experience to prompt<br />
awareness for non-pituitary health care<br />
professionals.<br />
A collection amounting to £200 was<br />
held at Ross’s funeral and we thank<br />
Thea, Ross’s family and friends for their<br />
very kind and generous donations, in his<br />
loving memory. Our sincere condolences<br />
go to Thea and her family ■<br />
Pituitary Life | autumn 2014
News<br />
9<br />
Invitation to participate in a research<br />
study on pituitary conditions<br />
The Pituitary Foundation<br />
is working with Dr Sofia<br />
Llahana, Consultant Nurse in<br />
Endocrinology at UCLH, to conduct a<br />
research study which aims to explore<br />
the health status, quality of life and<br />
educational needs of patients with<br />
pituitary conditions and their families.<br />
The ultimate objective of this study is to<br />
gather baseline information which will<br />
guide future research on developing a<br />
structured self-management programme.<br />
The study will be conducted over 18<br />
months, in two consecutive phases:<br />
1. A questionnaire survey open to all<br />
patients with pituitary conditions<br />
2. Focus group interview with a smaller<br />
number of patients to provide in-depth<br />
exploration of self-management needs<br />
How can you help?<br />
We would be very grateful of your<br />
participation in the study. We anticipate<br />
sending out the questionnaires, along<br />
with detailed information on the study<br />
in October, following ethics approval.<br />
It will take 20-30 minutes to complete it<br />
and you can chose to do this on-line or<br />
on hard copy sent by post. You can also<br />
express your interest to participate in the<br />
focus group interviews which will take<br />
place in London early next year; travel<br />
expenses will be reimbursed.<br />
Participation in the study is voluntary;<br />
only the researcher will have access to<br />
the data which will be anonymised and<br />
presented in a collective matter, with<br />
no means of identifying individual<br />
responses. Although the study may not<br />
have a direct benefit to you at this stage,<br />
it is expected to improve the overall<br />
understanding and raise awareness of<br />
pituitary conditions.<br />
For any queries regarding the study<br />
please contact Sofia Llahana on<br />
sofia.llahana@uclh.nhs.uk<br />
or 0203 447 7584 ■<br />
New! Post–surgery fact sheet<br />
Alison Milne, our endocrine specialist nurse has produced an informative<br />
and patient-friendly fact sheet for patients who are about to have<br />
pituitary surgery. This new Foundation resource will help patients and their<br />
families gain an understanding of the different types of surgery carried out, what to<br />
expect immediately after your operation and the following few weeks and months.<br />
There is also practical advice and tips included, to make you feel as reassured as possible.<br />
This new fact sheet can be requested via email to helpline@pituitary.org.uk or by<br />
ordering from our website shop for a posted hard copy at £2.50, or as a free download.<br />
If you have any questions you want to ask about before or after your surgery,<br />
Alison will always be happy to hear from you. Her number is 0845 450 0377,<br />
Mondays: 10am to 1pm, 6pm to 9pm and Thursdays 9am to 1pm.<br />
Our newly updated Surgery & Radiotherapy booklet is now available too, from<br />
our website shop, to order or download ■<br />
Thank you<br />
The Foundation wishes<br />
to thank Tony Woods<br />
for his hard work and<br />
commitment over the years,<br />
during his time on our Trustee<br />
Board. Tony, a patient, has<br />
been able to bring his valuable<br />
experience as a patient and<br />
represent other patients as a<br />
Trustee. We do wish him all the<br />
very best for the future ■<br />
Pituitary Life | autumn 2014
10 Professional articles<br />
Adrenal Insufficiency:<br />
Improving Paramedic Practice<br />
Andy Baines, Advanced Paramedic, North West Ambulance Service<br />
Acute adrenal insufficiency can lead<br />
to severe morbidity and even death if<br />
ineffectively managed. Unfortunately,<br />
in the pre-hospital setting patients<br />
with acute adrenal insufficiency often<br />
receive sub-optimal care. The early<br />
administration of hydrocortisone in<br />
these cases is critical and significantly<br />
improves outcomes to the extent it<br />
can be life-saving. Such therapy is<br />
part of current paramedic practice,<br />
however, there is evidence that<br />
hydrocortisone is rarely used in the<br />
pre-hospital setting. Ultimately,<br />
patients with acute adrenal<br />
insufficiency may currently be suboptimally<br />
managed by paramedics.<br />
Introduction<br />
Adrenal emergencies in the prehospital<br />
field are rare, but when<br />
encountered, the outcome can<br />
be fatal if it is not recognised and treated<br />
rapidly (Shulman 2007). The greatest<br />
challenge for pre-hospital clinicians<br />
is to recognise this elusive condition;<br />
the signs and symptoms may be nonspecific<br />
early in the presentation and<br />
the diagnosis may not be suspected<br />
or immediately clear. Coupled with<br />
the vague nature of the presentation,<br />
a gap in paramedic education means<br />
that the care provided to patients with<br />
acute adrenal insufficiency is not always<br />
optimal (McBride 2012). These factors<br />
combined, suggest that much can be<br />
done to improve the response to this<br />
group of patients. To improve practice,<br />
a project was undertaken to address this<br />
gap in paramedic education.<br />
Defining the problem<br />
Within the 17 years that I have been an<br />
operational paramedic in North West<br />
Ambulance Service (NWAS), I have<br />
encountered several patients who were<br />
adrenal insufficient. The occasions where<br />
I offered the optimal treatment package,<br />
as recommended by the Joint Royal<br />
Colleges Ambulance Liaison Committee<br />
2013 (JRCALC), were after I had received<br />
higher level clinical learning and education.<br />
It would be impractical and negative, to the<br />
current cost improvement programme that<br />
NWAS is facing, to offer this education to<br />
each of its 2200 responding clinicians.<br />
Consequently, this gap in skills and<br />
knowledge has been the driving factor<br />
to develop a package which incorporates<br />
e-learning and a film of a patient’s<br />
journey through an adrenal crisis. An oral<br />
presentation will also be delivered to the<br />
senior paramedics within NWAS. This<br />
blended learning approach is ultimately<br />
more effective as Ruiz (2006) makes<br />
the point that this approach combines<br />
technology and traditional instructor led<br />
training.<br />
The package will be accessible on<br />
NWAS intranet e-learning zone and<br />
be available to all 5000 staff in NWAS.<br />
Once completed, the clinicians will be<br />
able to download a certificate stating<br />
that they have completed the module<br />
and be encouraged to self-reflect on<br />
the new education gained. Reflection in<br />
medicine is seen as vital, as this allows<br />
consideration of the wider context<br />
and the implications of the experience<br />
and the assimilation of the skills or<br />
knowledge into the existing knowledge<br />
base (Branch and Pranjape 2002). The<br />
introduction to the package is illustrated<br />
in figure 1:<br />
Figure 1: Introduction to<br />
NWAS E-Learning Module<br />
Pituitary Life | autumn 2014
Professional articles<br />
11<br />
Quality enhancing solutions<br />
Within the United Kingdom, each<br />
ambulance service clinical quality is<br />
measured through ambulance quality<br />
indicators, these are benchmarked<br />
against other ambulance trusts NHS<br />
England (2013). The system analyses<br />
the clinical care delivered to patients<br />
with common pre-hospital conditions.<br />
Because the conditions reported on are<br />
relatively frequent in the pre-hospital<br />
arena it can be argued that clinicians<br />
largely now offer excellent care. This can<br />
be evidenced by NWAS achieving 97%<br />
stroke care bundle in 2012-2013 (NWAS<br />
stroke care bundle 2013).<br />
As discussed earlier, the prevalence of<br />
adrenal insufficiency is a rare event with<br />
approximately 800 patients in NWAS<br />
area of responsibility. Hahner et al<br />
(2010) report that 42% of these patients<br />
will have at least one adrenal crisis per<br />
year. This would equate to approximately<br />
336 possible pre-hospital presentations.<br />
Taking this into consideration, to arrange<br />
an audit system for adrenal insufficiency,<br />
would be extremely difficult because of<br />
the low expected numbers in comparison<br />
to the 1.4 million patient journeys made<br />
by NWAS annually.<br />
This has led the project to explore<br />
other methods of evaluation, such as<br />
patient involvement and satisfaction,<br />
rather than using traditional ambulance<br />
methods. A patient representative was<br />
heavily involved in the development of<br />
the training package and this package<br />
will be delivered to the patient group<br />
at the monthly meeting in July 2014.<br />
Patient involvement is highlighted by the<br />
Royal College of General Practitioners<br />
statement on safety and quality of care.<br />
One of the key messages is that patients<br />
should be encouraged to be actively<br />
involved in planning their care and the<br />
development of services at practice level<br />
(RCGP curriculum 2013). The Health<br />
Foundation, which is an independent<br />
charity working to improve healthcare<br />
in the United Kingdom, emphasise<br />
the importance of this patient-centred<br />
approach by reporting that if health<br />
staff can engage patients and help them<br />
feel involved, patients are likely to hear<br />
the advice they are given and more<br />
importantly act on it (health.org.2013)<br />
By direct patient involvement with<br />
the patient group and by continuous<br />
interaction with the patient group<br />
representative, a level of achievement<br />
can be claimed. This can be evidenced on<br />
production of the accompanying film of<br />
a patient’s journey through adrenal crisis,<br />
to be displayed on the package which<br />
is displayed in figure two. The patient<br />
states that she “finally feels like someone<br />
is listening and, more importantly, doing<br />
something about it” ■<br />
References<br />
Branch W, Pranjape A (2002)<br />
Feedback and Reflection; Teaching<br />
Methods for Clinical Settings. Academic<br />
Medicine. 2002.77; 1185-1188<br />
Hahner S, Allolio B, (2009)<br />
Therapeutic Management of adrenal<br />
insufficiency. Journal of Clinical<br />
Endocrinology and Metabolism.<br />
April 2009; 94(4); 1059-67.<br />
Health.org Measuring Patient Views<br />
On Health Care Quality<br />
www.health.org.uk<br />
measuringpatientviews.<br />
Assessed on 10/04/2014<br />
Joint Royal Colleges Ambulance<br />
Liaison Committee (2013)<br />
Guidelines. UK Ambulance Services<br />
Clinical Practice Guidelines 2013.<br />
The University of Warwick. Class<br />
Professional Publishing. Bristol.<br />
McBride P (2012) Hydrocortisone<br />
Emergency in Pituitary Patients. Journal<br />
of Paramedic Practice, Vol 4 <strong>Issue</strong> 500<br />
May 2012<br />
National Health Service Statistics<br />
(2013) www. (englandnhs)/<br />
ukstatistics/stat/work-arear/<br />
ambulance-quality-indicators.<br />
Assessed on 07/04/2014<br />
North West Ambulance Service<br />
Quality Accounts (2013)<br />
www.nwas.nhs.uk/media/385086/<br />
quality_account_2013Assessed on<br />
07/04/2014<br />
Royal Colleges of General<br />
Practitioners Curriculum (2010)<br />
Statement of Patient Safety and Quality<br />
of Care. RCGP 30 Euston Square<br />
London NW1 12 FB<br />
Ruiz J, Mintzer M, Issenberg B<br />
(2006) Learning Objects In Medical<br />
Education. Medical Teacher. Vol <strong>28</strong><br />
no 7 pp 599-605<br />
Schulman DP (2007) Adrenal<br />
Insufficiency Still accused Of Morbidity<br />
In childhood Paediatrics. 2007 Feb; 119<br />
(2):e484-94<br />
Figure 2 Voice video: Patient journey through an<br />
adrenal crisis<br />
Pituitary Life | autumn 2014
12<br />
Professional articles<br />
Hydrocortisone Auden tablets:<br />
Following work done by Auden McKenzie to demonstrate uniformity of<br />
distribution for the subdivision of tablets, they can confirm that they have received<br />
approval from the MHRA to include the following statement in the Patient<br />
Information Leaflets (which accompany all packs of Hydrocortisone Auden tablets).<br />
Hydrocortisone Auden Tablets come in two strengths:<br />
• White tablet marked HYD 10 contains 10 mg hydrocortisone. The tablets are<br />
scored so that they can easily be broken into halves or quarters. This can allow<br />
you to take a lower dose of half of a tablet (5mg) or quarter of a tablet (2.5mg).<br />
• White tablet marked HYD 20 contains 20 mg hydrocortisone. The tablets are<br />
scored so that they can easily be broken into halves. This can allow you to take a<br />
lower dose of half of a tablet (10mg).<br />
This information will allow members to break the tablets into halves or quarters<br />
and be confident in the dose that they are taking ■<br />
State of the Nation:<br />
do we need a healthcare revolution?<br />
Dr Sue Jackson, Chartered Psychologist<br />
This is something of an unusual<br />
article, and a little background<br />
might add some clarity. A while<br />
ago I had a discussion with Pat McBride<br />
about possible topics for my new regular<br />
column in Pit Life. Pat told me that the<br />
September issue of Pit Life would be<br />
focused on the 20th anniversary of<br />
The Pituitary Foundation, and then<br />
asked me what I could write that would<br />
be in keeping with that topic. After a<br />
bit of a think, I said I could write an<br />
article that reviewed the state of care<br />
(both medical and psychological) for<br />
individuals with pituitary conditions.<br />
Pat thought this was an excellent topic,<br />
as did other people I talked to. And in<br />
talking about it, I realized just how big<br />
a topic I’d suggested, and how much<br />
work would be required to deliver on my<br />
suggestion. I read a book edited by Linda<br />
Rio (the first mental health professional<br />
to serve on the United States nonprofit<br />
organization, Pituitary Network<br />
Association’s Board of Directors). Rio’s<br />
book is called “The Hormone Factor<br />
Pituitary Life | autumn 2014<br />
in Mental Health: Bridging the Mind-<br />
Body Gap” and comprises a series of<br />
edited chapters, written by a variety of<br />
specialists, which covers pretty much<br />
anything you can think of that might<br />
be relevant to the experience of having<br />
a pituitary condition, from diagnosis<br />
onwards. Basically, Rio and her team of<br />
specialist authors have done my work for<br />
me; so my aim is to review Rio’s book<br />
so that if you want to read it, you know<br />
what to expect, but also to talk about<br />
what Rio’s book suggests to me about<br />
the current state of our healthcare in<br />
relation to pituitary conditions.<br />
Any of you who saw Professor Wass’s<br />
excellent documentary on the history of<br />
hormones will know that we have come a<br />
long way in terms of understanding what<br />
hormones are and what they do. Those<br />
of you who missed his programme, will<br />
find the same information covered in<br />
both the introduction and first chapter<br />
of Rio’s book. While things may have<br />
moved on, there is still more we need to<br />
understand about the endocrine system<br />
and it’s functioning, what happens<br />
when it becomes disordered, and how<br />
to return it to normal functioning. Rio’s<br />
book includes lots of patient stories,<br />
mostly told in their own words, and a<br />
common theme is how difficult it is to<br />
get a diagnosis. Not feeling well, but not<br />
being believed by doctors, incomplete<br />
tests carried out, or tests undertaken but<br />
not followed up. It’s a very sad litany<br />
of distress, and highlights, for me at<br />
least, that while we might understand<br />
more about the endocrine system<br />
and its working, diagnosing problems<br />
associated with the endocrine system<br />
still takes a long time and leaves people<br />
in a difficult situation, affecting their<br />
physical and mental health as well as their<br />
relationships and work life.<br />
Medicine has moved on, and there are<br />
increasingly sophisticated ways to detect<br />
tumours, as well as better techniques to<br />
operate on them. Chapter 13 of Rio’s<br />
book contains an interesting series<br />
of question and answer interviews<br />
between patients and specialist doctors<br />
continued on page 21
Professional news Raising awareness articlesSPECIAL<br />
special<br />
8 page<br />
13<br />
this section can be pulled out - lift out centre 8 pages from stapled spine<br />
The best year EVER!<br />
Thanks to your continued support, our last financial year, year ending June<br />
2014, was the most successful in the history of our charity. Whether you played<br />
our Lottery, donated, walked, ran, swam, cycled, trekked, jumped out of a plane, took<br />
on a zip slide, dressed whackily, held a collection, baked or simply popped on the kettle – we<br />
thank each and every one of you for making it such a successful year. Let’s see if we can build<br />
on this success for the next year and future years to follow ■<br />
2015 Events<br />
If you would like to take on a challenge to raise funds next<br />
year, then how about the following:<br />
25 May 2015 Bupa London 10K:<br />
We have guaranteed spaces for this event in which you can join<br />
our Celebrity Ambassador, Stephen Campbell Moore, along<br />
with actress, Claire Foy, running the streets of central London,<br />
taking in some of the most amazing sights the City has to offer.<br />
17 July 2015 Pituitary Pen Y Fan climb:<br />
Following the success of this year’s event, where over £2,000<br />
was raised, we will now be making this an annual event. We<br />
would love you to join us.<br />
June 2015 Pituitary Skydive:<br />
Next Spring, due to demand, we are organising a Skydive day in<br />
Swindon. Exact details are yet to be confirmed but it is likely to<br />
be mid-June.<br />
pull-out<br />
section<br />
Christmas goodies:<br />
Included in your Pituitary Life you will find your 2014<br />
Christmas Catalogue. This is full of great gift ideas<br />
for loved ones and sees the return, due to demand, of<br />
The Pituitary Foundation Calendar, this year at a reduced<br />
price of just £5.00, compared to £7.50 in 2012. We expect<br />
these goods to be in high demand, order quickly to avoid<br />
disappointment. *Please note that due to postage costs we have<br />
had to include a minimum order quantity of £5.00* ■<br />
12 April 2015 Brighton Marathon:<br />
We have purchased spaces once again at the Brighton<br />
Marathon. This year our team raised over £3,000; let’s see if we<br />
can get a team together to raise even more during 2015.<br />
If you would like information on any of these events, or if you<br />
would like to take part in an event that is not listed, then please<br />
e-mail jay@pituitary.org.uk or call 0117 370 1314 ■<br />
Christmas Raffle 2014:<br />
Thanks to your incredible support, last year’s Christmas<br />
raffle was the most successful ever, and then this success<br />
continued with the Summer Raffle, which raised almost<br />
twice as much as the previous year. It is a big ask, but we know<br />
that with your continued support we can make this year’s raffle<br />
even more successful. Included in your issue of Pituitary Life is<br />
a book of Raffle tickets. We would be incredibly grateful if you<br />
2015 Calendar<br />
could make every effort to sell these tickets. We have been very<br />
fortunate to have been donated the majority of prizes. We would<br />
like to thank Gail Weingartner (Venture Photography), Rebecca<br />
Coonan (Park House Hotel) and Ed Hughes (£50 cash donation).<br />
Prizes are as follows:<br />
1st Prize = Apple iPad<br />
2nd Prize = Luxury Spa Break for two (worth £400)<br />
3rd Prize = Venture Photography package (worth £245)<br />
4th Prize = £50 Cash ■<br />
Pituitary Life | autumn 2014
14 wall of thanks<br />
We would like to say a huge thank<br />
you to Brian Sutterby,<br />
who nominated us as his chosen<br />
charity during his term as<br />
President of the Rotary Club<br />
of East Hampstead. Thanks<br />
to the generosity and support of<br />
members, a fantastic £1160 was<br />
raised during the year.<br />
If you are a member of a group or<br />
society, could you nominate The<br />
Pituitary Foundation as a chosen<br />
charity or maybe you could hold<br />
a one-off fundraising event? If so,<br />
please e-mail<br />
jay@pituitary.org.uk<br />
Colour Run – Lina Needham, her<br />
sister Coral and husband Andrew<br />
had a great time taking part in the<br />
Colour Run Sunderland judging by the<br />
photos! The three managed to raise a<br />
fantastic £300 in the process.<br />
Springtime Tea: We would like<br />
to thank Mike and Theresa<br />
Beaven for their incredible<br />
efforts at their annual Springtime<br />
Tea, where they managed to raise<br />
a sensational £461<br />
Doctor on the Run! We would<br />
like to thank Dr Sumithra<br />
Giritharan, Registrar at<br />
Salford Royal NHS Foundation<br />
Trust, Endocrine Unit for<br />
completing the Greater<br />
Manchester Run on behalf of The<br />
Foundation!<br />
Thanks to Newcastle Area<br />
Coordinator, Martin Crosby,<br />
who completed two races for us and<br />
managed to raise a staggering £1250!<br />
Three Peaks Challenge:<br />
Friends James Westley and<br />
Callum Smith took on one<br />
of the UK’s toughest endurance<br />
challenges, the UK 3 Peaks –<br />
Snowdon, Scafell Pike and Ben Nevis<br />
managing to complete the incredible<br />
endurance test in under 20 hours.<br />
Congratulations fellas and thanks for<br />
the support.<br />
Poppy Pegler – Congratulations to<br />
Poppy Pegler, 11, who did a 40 foot<br />
sky walk and a zip slide as part of the<br />
AI Awareness fundraising and raised a<br />
sensational £535.35 in the process!<br />
Ian Andrews and friends walked<br />
from Kingswood in Bristol to Weston<br />
Super Mare, in August, to raise funds<br />
towards the “Isabella Andrews<br />
Appeal Fund”. Issy’s dad, Ian, and his<br />
friend walked the arduous 30 plus miles<br />
in a very respectable time and managed<br />
to raise over £800 in the process! This<br />
now takes the total for the Isabella<br />
Andrews Appeal Fund to well over<br />
£10,000 in less than one year.<br />
Pituitary Life | autumn 2014
Professional news articles<br />
15<br />
London to Brighton Cycle:<br />
Thank you to Oscar Barnes, Daniel<br />
McDonald, Catherine Budd,<br />
Brenda McGrandles, Annie O’Brien<br />
and Geoff Macadam, who took on the<br />
London to Brighton cycle for us. The team<br />
look on course to have raised over £2000<br />
between them.<br />
Congratulations to sisters,<br />
Emma McDonald and Ooni Staerk<br />
who did a sky dive in memory of their brother,<br />
Aonghas, who sadly passed away at the tender<br />
age of 14. The daring sisters managed to raise a<br />
sensational £1626.64 between them, in loving<br />
memory of their brother.<br />
Coast to Coast<br />
Challenge: Teenage friends,<br />
John Wilson, Jack<br />
Stephenson, Sam Horn<br />
and Cameron Hunter<br />
began their walk on Monday 14<br />
July 2014 at the town of St Bees;<br />
the walk was 192 miles long,<br />
finishing at Robin Hood Bay<br />
ten days later, on the 24 July!<br />
The boys managed to raise a<br />
spectacular £534 in the process.<br />
Pituitary Pen Y Fan climb: On<br />
30 July walkers joined us in scaling South<br />
Wales’ highest mountain, Pen Y Fan, and<br />
managed to raise a sensational £2300. This<br />
now annual event will take place every July.<br />
Thank you to former Area Coordinator,<br />
Andy Simpson, who walked over 200<br />
miles in June, from Macclesfield to the<br />
Glastonbury festival! Andy raised over<br />
£2000 in the process.<br />
David Black took on the<br />
Brecon Beacons Four<br />
Peaks Challenge and<br />
managed to raise a sensational<br />
£1400 in the process. This trek<br />
encompassed the four peaks of<br />
the Brecon Beacons National<br />
Park and consisted of a 17 mile<br />
trek over rough, challenging<br />
terrain.<br />
Adrenal Insufficiency<br />
Awareness fundraising –<br />
We would like to thank Rachel<br />
Pegler who organised an<br />
Adrenal Insufficiency Awareness<br />
campaign during the Summer and<br />
managed to raise over £1,000! As<br />
part of the fundraising efforts<br />
Tough Mudder Andy! Thank you to<br />
Andy Grant, the son of our Glasgow<br />
Area Co-ordinator, Helen, who completed<br />
“Tough Mudder Scotland” for us in July.<br />
This challenging obstacle course proved no<br />
match for Andy, who managed to raise a<br />
sensational £435.74 in the process!<br />
Photography<br />
fundraising: Our sincere<br />
thanks to Kate Dalton who<br />
has been taking photos and<br />
selling these images online, with<br />
all donations being made to<br />
The Foundation. At the time of<br />
printing Kate had raised £89 ■<br />
Pituitary Life | autumn 2014
16 Raising awareness<br />
Pituitary Life | autumn 2014
news Raising awareness<br />
17<br />
Pituitary Life | autumn 2014
18<br />
Raising awareness<br />
Bradleys Charity of the Year<br />
My name is Richard Greetham,<br />
and I am a Director of<br />
Bradleys Estate Agents, a<br />
33-office organisation covering the<br />
West Country. In May 2013, I was<br />
diagnosed with a pituitary tumour. I<br />
wanted to do something to raise awareness,<br />
but also vitally funds and decided to cycle<br />
around all of my company’s offices - a<br />
total of about 400 miles along some really<br />
difficult climbs and terrain.<br />
I don’t mind admitting, I have<br />
always been somebody that has always<br />
been fairly slow to get my hand my<br />
pocket, when someone wants to be<br />
sponsored for certain things, and one<br />
of the motivators for doing this was<br />
as a punishment to myself, because<br />
people are always doing these things for<br />
a reason, and I now understand those<br />
reasons.<br />
I didn’t know where to start in<br />
terms of fundraising but this is where<br />
working for a large company can make<br />
a difference; you never really know how<br />
popular you are as a person until you take<br />
on a challenge and I can genuinely say, I<br />
work with some amazing, generous and<br />
kind people who together have helped<br />
me raise over £6000 and we are still<br />
collecting money; we have a target of<br />
£10,000 by the end of 2014.<br />
I was genuinely touched by the<br />
amount of colleagues (and now friends)<br />
who took on half marathons, some<br />
of them hurled themselves down 100<br />
mile-an-hour zip wires, which is in Wales,<br />
which quite frankly terrifies the life out<br />
of me, and I would much rather cycle<br />
a long distance than do that. We’ve had<br />
people who put balloons in cars and play<br />
guess the number of balloons to win a<br />
prize. Some staff took pictures of where<br />
they worked and sold them for £5. Other<br />
offices offered photocopying, fax for a<br />
small charge which really worked. Also,<br />
it is amazing how quickly money can be<br />
raised by aiming for small amounts rather<br />
than going for hundreds of pounds in<br />
one hit. I find people are quite happy<br />
to give you a couple of quid rather than<br />
£25 or £30.<br />
I am now near the end of my<br />
challenge, having ridden my 400 miles,<br />
which I thoroughly enjoyed; there wasn’t<br />
a day that I didn’t feel appreciated and<br />
welcomed by the people I work with.<br />
The whole company has got behind the<br />
campaign and made a difference. I am<br />
proud to be a member of The Pituitary<br />
Foundation team and would urge<br />
anybody looking to raise money, to get in<br />
contact with Jay Sheppard who has been<br />
an absolute delight to work with, having<br />
tireless energy and always at the end of<br />
a phone to help. One of the board of<br />
trustees, Mike James, came along and<br />
shared part of the cycle ride with me,<br />
giving up his time coming down from<br />
Bristol to the West Country and facing<br />
some of our hills, which he did and<br />
cherished, and was a delight to ride with.<br />
Our thanks to Richard and<br />
all staff at Bradleys!<br />
If you work for a company no<br />
matter how large or small, could you<br />
nominate The Pituitary Foundation<br />
to benefit as a Charity of the Year<br />
partner? Maybe your company could<br />
support The Foundation by holding<br />
ad hoc fundraising events? Either<br />
way, Jay would love to hear from you.<br />
Please call him on 0117 370 1314<br />
or e-mail jay@pituitary.org.uk ■<br />
Pituitary Life | autumn 2014
Raising awareness<br />
19<br />
Legacy<br />
Awareness Week<br />
8-14 September 2014<br />
Did you know that during 8-14 September it was<br />
Legacy Awareness Week in the UK? Probably<br />
not. This is a topic that many people would rather<br />
not think about, certainly not speak about and a topic, that<br />
many think is not applicable to them.<br />
It’s a common myth that only the rich and famous leave<br />
money to charity when they die. This couldn’t be any<br />
further from the truth. The reality is, that without the gifts<br />
left in Wills by people just like you, we would not be where<br />
we are today.<br />
Charitable legacies have accounted for over 20% of our total<br />
income over the last 5 years and are absolutely vital to The<br />
Foundation as a source of income.<br />
74% of the UK population support<br />
charities and when asked, 35% of people<br />
said they’d happily leave a gift in their Will, once<br />
family and friends had been provided for. The problem is,<br />
only 7% actually do. That’s why, if everyone left money in<br />
a Will for The Foundation, as well as your family, you could<br />
make a huge difference. It could be a little or a lot. So, you<br />
don’t have to be rich and famous to make a contribution<br />
that can make a huge difference. You can all do something<br />
amazing to support pituitary patients just by remembering<br />
us when writing a Will ■<br />
Tax Benefits of leaving a<br />
gift in your Will<br />
You may not know this but there can be<br />
significant Inheritance Tax benefits, if you<br />
leave a gift to a charity. We appreciate that<br />
the most important people to look after are your loved<br />
ones but by leaving a charitable donation you could<br />
actually be leaving your loved ones more.<br />
If you leave a gift to The Foundation then its value will<br />
be deducted from your estate (your money, possessions and<br />
property) before Inheritance Tax is worked out. Gifts made<br />
before your death may also qualify for exemption.<br />
If your estate is liable to Inheritance Tax, you could reduce the amount due by<br />
choosing to give money to charity. You can either leave a fixed sum (known as a<br />
‘Pecuniary Legacy’), or part or all of your estate once other gifts have been distributed<br />
(known as a ‘Residuary Legacy’). You can do this through your Will, or by a<br />
declaration to the executors or personal representatives, giving instructions as to how<br />
you would like your legacy to be distributed. If you are leaving money to charity, make<br />
it clear exactly which charity you want to receive your gift. Gifts made to a charity in<br />
the seven years before your death are exempt from Inheritance Tax ■<br />
Thank you<br />
We would like to issue a heartfelt<br />
thank you to the late Rosemary<br />
Evans who left a substantial<br />
gift in her Will to The Pituitary<br />
Foundation. This money will go a<br />
long way towards ensuring that we<br />
can continue to be there for future<br />
generations of pituitary patients.<br />
If you have not pledged a gift<br />
at this moment in time would<br />
you be willing to leave a gift to<br />
The Foundation in your Will?<br />
Remember it doesn’t have to be a<br />
huge donation. We appreciate any<br />
gifts irrespective of size – whether<br />
it’s £10, £100 or £1000, every<br />
penny really does help. Can we<br />
ask that you please notify Jay by<br />
e-mailing jay@pituitary.org.uk ■<br />
Pituitary Life | autumn 2014
20 Raising awareness<br />
Cake me up Selfie<br />
Seeing as it is our 20th Birthday this November, as<br />
well as being Pituitary Awareness Month during<br />
October, we want you to help us celebrate<br />
and raise awareness by taking part in a<br />
“Selfie” campaign. The “Cake me up”<br />
selfie. A ‘selfie’ is a photograph you take of<br />
yourself, usually with your smartphone.<br />
You will all have heard, or quite possibly<br />
taken part in the recent phenomenon that<br />
generated tremendous awareness for breast<br />
cancer charities, the “No Make-up<br />
selfie”? Well, this is our 20th Birthday<br />
twist on this campaign. All you need<br />
to do to take part is take a photo<br />
of yourself, preferably looking as glamourous or wacky as<br />
possible, with a cake in hand to celebrate our birthday!<br />
Please share the details of this campaign to help us raise<br />
as much awareness as possible of this campaign. Keep an eye<br />
out on social media for some well-known faces helping us to<br />
celebrate by taking part in the “Cake me up selfie.” At the<br />
end of November, we will produce a photo montage of all<br />
photographs received, which will be available to purchase<br />
from our website. This would represent a very quirky,<br />
amusing gift for anyone you know who’s taken part.<br />
Don’t forget, the more glamourous, outlandish<br />
and downright wacky that you look - the better!<br />
Help us celebrate our 20th Birthday in style,<br />
whilst helping to raise vital pituitary awareness! ■<br />
Steps:<br />
l Take your selfie and either:<br />
o Text SELF85 £5 to 70070<br />
o Visit www.justgiving.com/Pituitary20thBirthday<br />
l Tweet us your images to @Pituitary_Org using the hashtag #CakeMeUpSelfie<br />
l Tag your images to our Facebook page The Pituitary Foundation (UK)<br />
l Send in hard copies, along with a cheque for £5, made payable to<br />
“The Pituitary Foundation” and post to: Happy Birthday,<br />
The Pituitary Foundation, 86 Colston Street, Bristol, BS1 5BB
Professional articles<br />
21<br />
continued from page 12<br />
highlighting the current state of medicine<br />
in this regard. However, what is also<br />
clear is that some patients continue to<br />
struggle post-operatively despite the<br />
modern techniques and the hormone<br />
replacements available, a point borne<br />
out by the patient stories in Rio’s book<br />
that touch on this topic. I’ve talked<br />
before about the need for a shift away<br />
from the biomedical model that views<br />
the body as something to cure, towards<br />
a bio psychosocial model of healthcare<br />
that takes into account the impact that<br />
the mind and memory have on physical<br />
functioning. This point is made countless<br />
times in Rio’s book by a number of<br />
different specialists, all quoting Harvey<br />
Cushing and his idea that Freud’s<br />
psychoanalytic technique was a backwards<br />
attempt to deal with pituitary disorders<br />
by talking when the root of the problem<br />
was a dysfunctional pituitary gland. It’s<br />
not a case of either/or, I think we need<br />
both medical treatments and psychosocial<br />
support and interventions, and indeed<br />
various of the authors in Rio’s book also<br />
advocate joined up multi-disciplinary<br />
teams to help support patients with<br />
endocrine disorders of all sorts.<br />
But there’s a problem - Robert<br />
Hoffman in Chapter 11 of Rio’s book<br />
makes the point that mental and physical<br />
healthcare have become separated. If<br />
you experience a traumatic event, such<br />
as a car crash, your physical injuries will<br />
be treated in hospital, but any traumatic<br />
stress would have to be discussed with<br />
your GP and then you would have to be<br />
referred to a mental health care service.<br />
But, in thinking about our modern<br />
healthcare system, it occurred to me<br />
there is another problem, i.e. it is set up<br />
to deal with acute (short term) physical,<br />
or mental problems, for example, broken<br />
bones, appendicitis etc. I was chatting to<br />
a recently-retired nurse about this article,<br />
and she told me that I didn’t understand<br />
just how much acute healthcare is now<br />
undertaken in hospitals. She used the<br />
example of appendicitis; when she first<br />
started work, at any given point, half of<br />
the people on the ward would be acute,<br />
but the other half would be staying in for<br />
at least a week post-operatively. She told<br />
me that now a hospital stay following<br />
an appendectomy has reduced to three<br />
days, sometimes less. Virtually all the<br />
patients that are cared for in hospital<br />
now, in her opinion, are acute cases, with<br />
patients and family members of patients,<br />
being expected to take on the burden<br />
of caring for post-operative and chronic<br />
(i.e. long term) conditions including<br />
the administration of complicated drug<br />
regimens and in some cases the use of<br />
complicated medical equipment.<br />
Not only are services fragmented,<br />
but in my experience, healthcare<br />
professionals don’t always seem to<br />
understand what is actually offered or<br />
experienced by patients when they attend<br />
the different services. For example,<br />
there are endless stories of hospitals<br />
discharging patients from hospital<br />
on Friday, with enough drugs for the<br />
weekend, telling them that they can get<br />
more on Monday from their own doctor.<br />
But the primary care service doesn’t work<br />
like that. It’s next to impossible to get a<br />
prescription filled in 24 hours in some<br />
areas, and that’s assuming that you’re well<br />
enough to sort it out. Similarly, there are<br />
endless stories of GPs having a patient<br />
turn up in their surgery, but the hospital<br />
discharge paperwork has not arrived, so<br />
the GP has no idea why they are there, or<br />
what it is they are supposed to be doing.<br />
“But the hospital said…” is a commonly<br />
heard refrain.<br />
And there’s another problem – we<br />
know what recovery looks like for<br />
someone with an acute condition. We<br />
expect them to get over it and resume<br />
their normal activities of living. I doubt<br />
that you need me to tell you that for<br />
individuals with a chronic condition it’s<br />
not like that, and Rio’s book has some<br />
patient stories that bear this out. The<br />
aim of the medical experts in Rio’s book<br />
is to return the body to as near normal<br />
functioning as possible by whatever<br />
combination of medical treatments is<br />
necessary. However, they acknowledge<br />
that the return to normality by this<br />
means doesn’t seem to work for everyone<br />
in that some patients remain significantly<br />
distressed and continue to report<br />
problems in daily functioning, and there<br />
seems to be a great deal of perplexity<br />
as to why this should be the case. It<br />
seems to me that there is a general lack<br />
of understanding that recovery for a<br />
chronic condition looks nothing like<br />
recovery for an acute condition. The<br />
most useful definition of recovery that<br />
I think we could usefully use as an aim<br />
in relation to individuals with a pituitary<br />
condition comes from Anthony (1933)<br />
and is commonly used in mental health<br />
services: “A deeply personal, unique<br />
process of changing one’s attitudes,<br />
values, feelings, goals, skills and/or<br />
roles. It is a way of living a satisfying,<br />
hopeful and contributing life even<br />
with the limitations caused by illness.<br />
Recovery involves the development of<br />
new meaning and purpose in one’s life<br />
as one grows beyond the catastrophic<br />
effects of [mental] illness.” Do we<br />
know enough to be able to do this?<br />
There are some excellent chapters in<br />
Rio’s book that clearly document the<br />
limits of our understanding in relation<br />
to the psychosocial impact of pituitary<br />
conditions, and it is clear that despite<br />
decades of research, there are some<br />
glaring gaps in our knowledge.<br />
Rio’s book has been thoroughly<br />
researched, is well written and has<br />
something for everyone, and that, I<br />
think, is the problem. There is a long list<br />
at the front of the book of all the people<br />
for whom the contents could be relevant,<br />
but I think each would be put off by the<br />
content intended for the others. It’s a<br />
shame, as it deserves to be widely read,<br />
but I’m not convinced that it will be.<br />
I think the final word should go to<br />
the patient advisors at the Future of<br />
Health conference I attended in London<br />
last year, who were very clear that our<br />
current system of GPs as gatekeeper<br />
to fragmented services for physical<br />
and mental health do not serve their<br />
needs. What we need is something<br />
of a healthcare revolution, with more<br />
meaningful engagement with individuals<br />
with chronic conditions, so that<br />
appropriate healthcare services do start<br />
to evolve, preferably with the patients as<br />
experts in living with chronic conditions<br />
guiding the process ■<br />
Pituitary Life | autumn 2014
22 Professional articles<br />
Working towards a single gold standard care<br />
protocol for children and adults with adrenal<br />
insufficiency - brief notes from this meeting<br />
Hosted By UCLH & GOSH CAH Support Group 14 June 2014 meeting<br />
with UK Addison’s Group and The Pituitary Foundation<br />
Note taker: Alice Jackman. My objective<br />
in providing this summary of the<br />
proceedings is to try and convey a few<br />
key points to those parents of pituitary<br />
patients who were unable to make the<br />
meeting. Hopefully these could then<br />
act as a pointer for the start of further<br />
research into what might work better for<br />
their own young person.<br />
Editor note: Due to space limits, this is<br />
an abridged version - the full notes are<br />
freely available for download from<br />
www.cahisus.co.uk<br />
Introduction<br />
Professor Peter Hindmarsh<br />
The impetus for the meeting came<br />
from the story reported in the<br />
Mail about a woman who died<br />
because the attending paramedics told<br />
her ‘you just have a tummy bug’, and they<br />
failed to give her an emergency injection<br />
of hydrocortisone.<br />
What do we mean when we<br />
say adrenal insufficiency?<br />
It is only a shorthand (not a diagnosis)<br />
for what is needed, and is a key phrase<br />
in soliciting appropriate help from the<br />
ambulance services. It is important to<br />
keep the disorders that result in adrenal<br />
insufficiency distinct when providing an<br />
emergency letter, because the different<br />
conditions have different aspects<br />
which need to be considered, once the<br />
emergency injection of hydrocortisone<br />
has been administered.<br />
Problems in adrenal insufficiency<br />
Dr Karavitaki (Adult Endocrinologist Oxford)<br />
gave a brief overview of the functions of<br />
the adrenal glands and listed the incidence<br />
of adrenal insufficiency as follows:<br />
Primary adrenal insufficiency: 93-140 per<br />
million (Arlt & Allolio, 2003)<br />
Secondary adrenal insufficiency: 125-<strong>28</strong>0<br />
per million (Arlt & Allolio, 2003)<br />
The commonest cause for this is too<br />
much steroid therapy, for conditions such<br />
as arthritis<br />
Problems<br />
1) Timing of diagnosis, the following<br />
symptoms noted:<br />
• Anorexia, nausea, vomiting, diarrhoea<br />
• Weight loss<br />
• Dizziness on standing, salt craving<br />
• Increased pigmentation<br />
• Weakness, tiredness<br />
• Abdominal pain<br />
• Joint and muscle pains<br />
2) 50% of patients had symptoms for at<br />
least one year before diagnosis<br />
50% had a crisis which then resulted in<br />
their diagnosis.<br />
3) Cortisol replacement needs to mimic<br />
the natural rhythm of cortisol in<br />
the blood, known as the circadian<br />
rhythm and there are no reliable lab<br />
parameters for correct assessment<br />
and replacement in Addison’s and<br />
hypopituitarism, other than the actual<br />
cortisol concentration. ACTH can<br />
be measured in Addison’s disease, but<br />
this is not so easy to do and requires<br />
special blood samples. However,<br />
ACTH can be measured during a 24-<br />
hour profile.<br />
4) Under-replacement of hydrocortisone:<br />
this results in impairment of wellbeing<br />
and is life-threatening if the<br />
patient experiences an inter-current<br />
illness.<br />
5) Adrenal crisis: Statistics seem to<br />
indicate that, of patients susceptible to<br />
adrenal insufficiency, 8% have a crisis<br />
per year.<br />
Patient education: ensures compliance,<br />
decreases morbidity<br />
- Sick day rules<br />
- Hydrocortisone emergency pack<br />
- Steroid card, medical alert jewellery<br />
- Alert doctors and nurses to the need<br />
for early admission and the need for<br />
extra hydrocortisone before and after<br />
surgery and during stays in hospital,<br />
during severe illness and surgery<br />
5) Osteoporosis: Doses up to 25mg<br />
hydrocortisone do not seem to affect<br />
bone density.<br />
6) Research from Norway and Germany<br />
seems to indicate that patients with<br />
primary or secondary adrenal failure<br />
have a higher level of disability, a<br />
lower quality of life and increased<br />
depression.<br />
7) Metabolic profile: If hydrocortisone<br />
replacement is above 20mg there<br />
appears to be an impact on waist<br />
measurement.<br />
8) Over-replacement: results in impaired<br />
glucose tolerance, and an impaired<br />
lipid profile.<br />
Conclusions:<br />
• There needs to be a greater awareness<br />
of the diagnoses<br />
• It is important to find our optimal<br />
replacement dose to be able to do daily<br />
life. This is what will minimise longterm<br />
morbidity and mortality<br />
• It is vital that patients, support groups<br />
and health professionals all work<br />
together to deal with these challenges ■<br />
Pituitary Life | autumn 2014
news Professional articles<br />
23<br />
Methods of assessing and replacing cortisol<br />
Professor Peter Hindmarsh<br />
The following are options for<br />
assessing cortisol:<br />
One-off blood sample: very<br />
unsatisfactory as cortisol varies hugely<br />
throughout the day and the sample<br />
indicates a snapshot of that moment, but<br />
no idea what is happening during the rest<br />
of the 24-hour period; difficult to relate<br />
to the time the tablet taken, even if the<br />
sample taken 2 hours previously.<br />
Four-hourly day curves: a bit hit and<br />
miss – not nearly enough information,<br />
as cortisol can be cleared at different<br />
rates, you can miss peaks and troughs<br />
and no indicator of what is happening<br />
in the evening and early morning as<br />
hydrocortisone is metabolised differently<br />
in evening.<br />
Urine measurements: need quite a bit<br />
before cortisol is picked up, so it will<br />
identify a high level of cortisol but not so<br />
well for low values. If collected over 24<br />
hours, then it is only looking at cortisol<br />
breakdown products and does not tell<br />
you which dose to alter.<br />
Salivary cortisol: similar problems<br />
to urine as only good when cortisol is<br />
high and also susceptible to different<br />
metabolic patterns in the salivary glands.<br />
What needs to be measured is the<br />
cortisol from the hydrocortisone, which<br />
is being taken to the organs i.e. the<br />
cortisol in the blood!<br />
24-hour blood profiles: the most<br />
revealing solution, usually taken every 20<br />
minutes for study purposes ideally, but<br />
one - two hourly samples are good<br />
Having information from the profile,<br />
it is suggested to start with three to four<br />
doses per day using the distribution<br />
schedule shown in the table.<br />
Beware: oral contraceptive pill leads<br />
to increased cortisol measurements<br />
and a graph was used to illustrate the<br />
remarkable affect the birth control pill<br />
has on the cortisol levels throughout the<br />
24 hour period<br />
There is a limit to how high the levels<br />
of cortisol you can achieve in the blood.<br />
Doubling doses (of<br />
hydrocortisone) does not<br />
double the blood level<br />
10mg=500 nmol/l<br />
30mg=900 nmol/l<br />
50mg=1100 nmol/l<br />
This is because of binding proteins that<br />
get saturated very quickly when high<br />
doses are given, so that more and more<br />
of the dose gets lost in the urine.<br />
Prof Hindmarsh showed graphs<br />
illustrating how double dose and triple<br />
dose do NOT give longer coverage in<br />
time, but peaked higher.<br />
General illness:<br />
Level 1<br />
If you are unwell, temperature of +38C,<br />
Ambulance and Emergency Care<br />
Dr Quen Mok (Ambulance and Emergency Medicine Working Group)<br />
The JRCALC was formed to<br />
improve care in ambulances<br />
on their way to hospital.It is an<br />
advisory group from many backgrounds;<br />
they meet four times a year.<br />
The Panorama programmed illustrated<br />
that there seemed to be a “Post code<br />
lottery of ambulance care in UK”.<br />
JRCALC had a remit to develop, update<br />
and maintain UK ambulance service<br />
clinical and practical guidelines. The<br />
handbook is now 500 pages long and<br />
2013 was the last revision.<br />
In the paediatric section it covers:<br />
General, resuscitation, trauma, medical,<br />
drugs and CBRNE to produce effective,<br />
safe treatment by non-doctors on site.<br />
Paramedics have to work in difficult<br />
environments, with other hazards,<br />
limited drugs, and only 1% of calls<br />
and can take fluids, double your dose<br />
and take an extra DOUBLE dose at 4am<br />
(especially important for children).<br />
There is a natural peak of cortisol at<br />
this time and cortisol levels have been<br />
rising from midnight, and the night time<br />
cortisol dose will have run low, (even if<br />
double, as remember the dose does NOT<br />
last double the time, but peaks higher) so it<br />
is important to adhere to this, especially in<br />
illness to prevent low blood glucose levels.<br />
Level 2<br />
Vomiting: if oral hydrocortisone is not<br />
staying down, give IM hydrocortisone<br />
injection, then go to hospital.<br />
Don’t forget - if you’ve had an<br />
injection, it won’t last longer than tablets,<br />
so give the next dose, no longer than six<br />
hours later.<br />
It is the duty of the endocrinologist<br />
to set up emergency care plans for their<br />
patients, as this must be individualised ■<br />
are for children that need emergency<br />
intervention.<br />
1968 Medicines Act set out that<br />
paramedics are allowed to give medicines.<br />
However, especially with children, getting<br />
the right dose is complicated and to<br />
avoid having to work out on site what the<br />
correct dose would be, the Handbook<br />
has done all the calculations and there<br />
is a ‘Page for Age’ so as to make it<br />
as straightforward as possible for the<br />
paramedics.<br />
Hydrocortisone is most often used for<br />
asthma and adrenal crisis. The biggest<br />
challenge, however, is persuading all the<br />
ambulance trusts to use this national<br />
resource – many trusts still prefer their<br />
local medical boards’ opinions – to the<br />
detriment of their patients. This MUST<br />
become a national conversation ■<br />
Pituitary Life | autumn 2014
24 Professional articles<br />
Care in Accident and Emergency<br />
Dr Rebecca Salter (Imperial Healthcare)<br />
Dr Salter thought that if we could<br />
understand how the emergency<br />
department is set up, we can<br />
interact with it more effectively.<br />
1) Structure of an emergency<br />
department<br />
There are different models: general<br />
department, or a teaching hospital;<br />
there are some paediatric hospitals and<br />
depending on the size of the town,<br />
some hospitals are more hectic than<br />
others.<br />
In an A&E ward, children should have<br />
visual and auditory separation from<br />
adults, and there should be a children’s<br />
nurse.<br />
2) Staffing of an emergency<br />
department<br />
There is a nurse in charge of each<br />
shift, a staff nurse, some Sho/<br />
STI-3 junior doctors - paediatric<br />
or orthopaedic, Registrar ST3-<br />
8 either paediatric or emergency<br />
medicine, Consultant paediatrician or<br />
emergency medicine.<br />
3) Process on arrival<br />
When should you go? Febrile illness,<br />
vomiting/diarrhoea<br />
1. Book in at reception - inform<br />
receptionist of your Emergency Care<br />
Letter (or Patient Care Card -adults)<br />
Pituitary Life | autumn 2014<br />
2. Triage - nurse will assess urgency<br />
of case. Depends on whether<br />
related to condition or not (if you<br />
can phone before arrival and preregister<br />
this can speed things up)<br />
3. You should then be urgently moved<br />
to assessment area and seen quickly<br />
4. You can be taken straight to<br />
paediatrics, registered there and<br />
treatment started, but it is always<br />
dependent on other cases in the<br />
department<br />
4) What you can expect to be<br />
done: this will depend on<br />
which condition you have<br />
• Initial observations<br />
• Bloods - urea and electrolytes,<br />
blood glucose, calcium, cortisol,<br />
17OHP (in CAH), gas, culture,<br />
play specialist - cold spray (local<br />
anaesthetic cream)<br />
• IM/IV Solu-Cortef if not already<br />
given<br />
• IV fluids<br />
• IV hydrocortisone infusion if blood<br />
sugar low, need a bolus of glucose<br />
• Fluid bolus if ‘shocked’<br />
• Contact the endocrine team for<br />
advice<br />
• Contact your GP after attendance<br />
by letter<br />
5) What we (the hospital)<br />
can do to streamline the<br />
process:<br />
• Electronic flagging/special patient<br />
- keep the file updated<br />
• Direct access - some hospitals<br />
do this but it is not always best<br />
practice<br />
• If you have phoned ahead - prearrange<br />
room and appropriate<br />
equipment/drugs<br />
• Endocrine team to liaise with local<br />
specialist with up-to-date clinic letters<br />
• Provide local anaesthetic<br />
• Local emergency departments and<br />
specialist to liaise with endocrine<br />
team regarding acute presentations<br />
• Keep you informed of plans<br />
6) What you can do to help<br />
process:<br />
• Carry your emergency care plan<br />
• Carry recent clinic letter<br />
• If you can, get someone to phone<br />
ahead to your local A&E to warn<br />
them to expect you<br />
• Apply local anaesthetic for injections<br />
• Keep school informed of changes<br />
and check hydrocortisone is in date<br />
• Need to check local A&E has the<br />
clinic letter linked to A&E notes<br />
If A&E are not doing the right<br />
thing:<br />
Politely, but as forcefully as possible,<br />
ask to see the registrar or consultant, “I<br />
want to escalate this”. Point out that your<br />
paperwork shows that “this is an NHS<br />
directive”, or call for the site manager, or<br />
general manager. State: “I can see you are<br />
very busy, but my child is very seriously<br />
ill”. They need to act appropriately,<br />
quickly, and give information quickly.<br />
Extra Information:<br />
Efcortesol is oil based and it can generate<br />
an allergic reaction especially if you have<br />
eczema or asthma - better to use<br />
Solu-Cortef ■
Professional articles<br />
25<br />
Research: Helping young people talk with<br />
doctors and nurses<br />
By Jennifer Downing & Prof. Peter Callery<br />
The COMMEND YOU study<br />
is to trying to find ways to<br />
help healthcare professionals,<br />
young people and parents (if present)<br />
communicate. We are starting to test<br />
the toolkit, developed with the help of<br />
young people with endocrine conditions,<br />
including pituitary conditions, and<br />
parents as well as doctors and nurses.<br />
The toolkit is called ‘Explain’ and is<br />
available on its own website<br />
www.explain.me.uk. Explain is<br />
designed for use at home as well as in<br />
clinics. The site has diagrams to help<br />
explain hypopituitarism and other<br />
endocrine conditions. There is also<br />
information about coming to clinic,<br />
keeping healthy and a glossary of<br />
terms. Much of the text is written as a<br />
response to questions and is followed<br />
by example questions patients may want<br />
to ask healthcare professionals. Health<br />
promotion messages and links to other<br />
information sites are also provided.<br />
A ‘Your <strong>Issue</strong>s/Take Home Messages’<br />
sheet can be downloaded to help young<br />
people tell doctors and nurses what they<br />
want to talk or ask about when they<br />
come to the clinic.<br />
Signing up creates your own private<br />
account to record take home messages<br />
and other notes for future reference.<br />
You can also keep a diary and update a<br />
personal growth chart with your height<br />
and weight.<br />
We are testing the Explain toolkit in<br />
the COMMEND YOU study. Previously<br />
we analysed recordings of consultations<br />
and interviews with young people,<br />
parents, doctors and nurses. We then<br />
developed the Explain toolkit with a<br />
group of young people and their parents.<br />
In this stage participants will test the<br />
Explain toolkit:<br />
• Before a consultation: the ‘Your<br />
<strong>Issue</strong>s’ sheet will be sent to help young<br />
people prepare points and questions<br />
to talk about in clinic. We will also tell<br />
them about the website. After the clinic<br />
appointment patients and parents will<br />
watch back their consultation and talk<br />
to a researcher. They will be asked to<br />
discuss if and how the form and the<br />
website were used in preparation for<br />
the consultation.<br />
• In the consultation: consultations will<br />
be recorded and watched back with<br />
patients and their parents, including<br />
how the website and ‘Your <strong>Issue</strong>s/<br />
Take Home Messages’ sheet was used.<br />
• Post-consultation. Participants will<br />
receive a brief phone call two weeks<br />
after their consultation to ask if<br />
and how they have used any of the<br />
tools since the consultation. Any<br />
benefits, perceived improvements or<br />
outstanding communication needs will<br />
be discussed.<br />
• Patients in the COMMEND YOU<br />
study will also be offered a DVD<br />
recording of their consultation. We<br />
noticed that people could find it<br />
useful to watch the recording of their<br />
consultation during interviews. So<br />
we’re trying this out to see if it can be<br />
helpful as a reminder and to help plan<br />
how to talk with doctors and nurses.<br />
Everyone can see the toolkit and set up a<br />
private account at www.explain.me.uk<br />
Please let us know what you think either<br />
by submitting feedback through the site<br />
or directly to us at<br />
Jennifer.downing@manchester.ac.uk ■<br />
Pituitary Life | autumn 2014
26 Patients’ stories<br />
A rugby player’s pituitary journey<br />
My life was pretty simple. I was<br />
27, had a girlfriend of eight<br />
years, with a child called Lewis,<br />
(who I call my son after bringing him<br />
up since he was 18 months old), a son<br />
called Jordan aged four, a house and of<br />
course a job! I was working for Lloyds<br />
TSB Private Banking. My whole life was<br />
normal; get up, get the kids up, get off<br />
to work, get home, feed the kids, get the<br />
kids to bed (eventually) and spend an<br />
hour or so with Paula catching up on the<br />
day’s events. The other joy in my life was<br />
rugby! I am a HUGE Rugby Union fan<br />
and was playing for my local team.<br />
At the start of 2006 I started to<br />
feel tired; it was put down to the drag<br />
of everyday life and a busy work-life<br />
balance. With the tiredness, I had also<br />
developed these excruciating headaches;<br />
you would find me clutching my head in<br />
Pituitary Life | autumn 2014<br />
my arms and squeezing. The headaches<br />
were almost unbearable. But as we do, we<br />
struggle on, which I did. So my life at<br />
this point felt like hell, I was always tired,<br />
had no energy to enjoy my family, wanted<br />
to go to bed constantly, my headaches<br />
were now so painful, my eyesight had got<br />
worse. I had stopped playing rugby, and<br />
had lost my way.<br />
In 2008 I was rushed in to Frenchay<br />
Hospital, Bristol with a brain tumour<br />
the size of a lemon. After two lifesaving<br />
operations and six weeks of<br />
radiotherapy, I am lucky to say I am alive.<br />
Since June 2008, I have undergone many<br />
other tests following the discovery of<br />
a dysfunctioning pituitary gland. The<br />
results of these tests have confirmed<br />
that I have hypopituitarism, I am growth<br />
hormone deficient, I have diabetes<br />
insipidus, I need to take hydrocortisone<br />
(steroid which replaces the body’s natural<br />
production of cortisol) twice-a-day,<br />
and also I have a deficiency in the male<br />
hormone testosterone, which I replace<br />
daily. Hormones make us the people we<br />
are, and it is hard to come to terms with<br />
not being who you were.<br />
When dealing with all the changes<br />
to my mind and body, I found myself<br />
feeling alone and with lots of questions<br />
unanswered. I didn’t feel like I could<br />
continually ask my GP things, because<br />
the surgery didn’t seem like they<br />
understood things either. Then, one<br />
evening while searching the Internet for<br />
answers, I came across The Pituitary<br />
Foundation. It gave me an insight into all<br />
my conditions. I learnt more in that one<br />
evening than I had for the two months<br />
of consultant and GP meetings! I could<br />
take my time and read things through,<br />
print off information and give to my<br />
family to read, so they understood what<br />
was going on.<br />
Over the past two years The<br />
Foundation has helped me in my<br />
everyday living. For instance, helping me<br />
to secure a radar key, which has saved<br />
many an embarrassing moment when<br />
desperate for the toilet! The Foundation’s<br />
Emergency Hydrocortisone booklet<br />
has saved my life recently when I was<br />
involved in an accident. Because of this<br />
booklet, the ambulance crew were able<br />
to identify my need for an emergency<br />
hydrocortisone injection and prevented<br />
any further complications. I have phoned<br />
and spoken to Helpline operators, who<br />
have put my mind at rest and given me<br />
sound advice on matters I was unsure of.<br />
For me The Foundation has made<br />
me feel a part of something. A sense<br />
of belonging. I used to feel alone and<br />
confused about what was happening to<br />
me. But now I feel I know exactly what’s<br />
happening and how it’s affecting me<br />
and I can plan and organise my life so<br />
much better. To know there are other
Patients’ stories<br />
27<br />
people out there experiencing what<br />
I’m going through helps towards the<br />
self-healing. I can’t speak highly enough<br />
of The Foundation, and the support it<br />
offers because it has helped me get to<br />
where I am today and enjoy life again<br />
after a horrendous ordeal. Without The<br />
Foundation and the support I have<br />
received I believe I would not be back<br />
to work full time as a Bank Manager, be<br />
back playing my beloved rugby every<br />
Saturday and be the father I am to my<br />
three children.<br />
2014 update<br />
This update couldn’t come at a timelier<br />
manner to allow me to highlight the<br />
importance of our support network<br />
because, without all of them, I would not<br />
be here today.<br />
This update couldn’t have come at<br />
a better time for me personally either,<br />
to allow me to reflect on the past few<br />
years. Since my story was written,<br />
the positives are: we’ve moved to our<br />
perfect home in Martock, Somerset.<br />
Our three boys are now Lewis 15,<br />
Jordan eleven and Blake six; all three<br />
are growing up into amazing boys, who<br />
make me proud each and every day even<br />
when they are fighting! I am still here<br />
battling on every day now; I put that<br />
down as a positive to highlight that it is<br />
so very easy to become complacent.<br />
My struggles:<br />
Weight gain: I am the heaviest I have<br />
ever been; two flights of stairs leave me<br />
huffing and puffing. Now, I’m a relative<br />
fit 33 year old rugby player but with the<br />
recent increase of my hydrocortisone<br />
my weight has increased. Body shape:<br />
my body shape changes throughout the<br />
testosterone cycle<br />
My biggest struggle is my mind<br />
Every day reminded of what I’ve been<br />
through. Mood swings, depression<br />
and tiredness have all pulled me to the<br />
lowest points over the last six months,<br />
so much so, in my last endocrinologist<br />
appointment in July, I broke down and<br />
admitted I couldn’t cope any longer.<br />
The hamster wheel of life was moving<br />
too quickly for me to keep up. With my<br />
condition, I couldn’t determine if it was<br />
just normal to not feel like you could<br />
cope, because of our busy lives, or, if it<br />
was down to my hormones not being at<br />
the correct levels to be able to cope. Dr<br />
Bickerton was extremely supportive and<br />
as a result of blood tests has increased<br />
my Levothyroxine and hydrocortisone. A<br />
month on, I am happy to say I can now<br />
cope with the hamster wheel of life and<br />
the dark clouds that were inside my head<br />
have totally gone. I am now no longer<br />
the miserable husband or dad, but the<br />
happy full-of-life one again. The increase<br />
in my medication has improved our lives<br />
so much, it’s amazing.<br />
Keep talking<br />
If you take one thing away from reading<br />
my update, take this. What we go<br />
through never stops. We battle on, not<br />
knowing what we are battling, until we<br />
get the results of tests. Our bodies and<br />
minds control themselves and it’s out of<br />
our control sometimes.<br />
Keep talking; write a diary so you can<br />
see what worked well and what didn’t.<br />
Sometimes, by looking back you can<br />
see how far you’ve come. Use whatever<br />
support The Pituitary Foundation offers,<br />
that suits your needs. If it’s a buddy, a<br />
telephone call to the endocrinologist<br />
nurse, or printing off an information<br />
leaflet. Keep in contact with your<br />
endocrinologist and be honest. I broke<br />
down in my last review, instead of being<br />
the brave stubborn man I usually am,<br />
and by doing that, my hormones are to<br />
the level they should be and WHAT a<br />
surprise, I can cope again!<br />
I would like to thank The Pituitary<br />
Foundation and my wife Paula, who is<br />
my ROCK (she knows me better then<br />
I know myself), for all the fantastic<br />
support you have provided me and the<br />
people around me ■<br />
Pituitary Life | autumn 2014
<strong>28</strong> Patients’ stories<br />
Hilary’s story<br />
I<br />
have idiopathic diabetes insipidus or DI. That is, I don’t<br />
have it as a result of something like a pituitary tumour or<br />
head injury, but it just happened out of the blue and the<br />
consultant can’t say what caused it. It is quite rare anyway<br />
but I think having it for no reason is rarer still. The word<br />
idiopathic comes from the Greek words ‘idios’ and ‘pathos’<br />
meaning literally one’s own suffering, but I have my own way<br />
of remembering it. The doctor’s an idiot and the diagnosis<br />
is pathetic. Actually I don’t believe that at all, as getting a<br />
diagnosis was one of the best things that happened to me.<br />
Diabetes insipidus simply means ‘dilute urine’ and, when<br />
undiagnosed, you pass an awful lot of that and you drink vast<br />
amounts of whatever liquid is to hand, to try to assuage a<br />
terrible thirst. It is caused by a part of the posterior pituitary<br />
gland, which should normally secrete vasopressin (the<br />
antidiuretic hormone), stopping working. This should normally<br />
control the retention of water in the body. So much for the<br />
theory - in practice, undiagnosed DI is a bit of a nightmare.<br />
addicted to water<br />
It all started when I noticed I was needing to drink water at<br />
meal times. It got bad enough to go to the doctor who, quite<br />
naturally, sent me for tests for diabetes mellitus. Diabetes<br />
insipidus, despite the name, has nothing to do with diabetes<br />
mellitus. When the tests for what is commonly called just<br />
‘diabetes’ turned out normal, I was sent to see an endocrine<br />
consultant. He told me that ninety percent of the people he<br />
saw with my problem were addicted to water. He told me to try<br />
chewing gum. It took a whole year to get bad enough to have<br />
a water deprivation test to see if I had DI, by which time I was<br />
completely filling two large five gallon plastic containers with<br />
urine in less than twenty four hours and needing to drink and<br />
pee all the time.<br />
nightly ritual<br />
I have a story to illustrate what a problem drinking and peeing<br />
all the time is. My husband and I were running a small business<br />
and to save money we were living in a touring caravan. There<br />
was a double bed in the van with two bunk beds. It was my<br />
ritual every night to put a row of bottles of water by the double<br />
bed, so I could drink after I had been to the loo. The symptoms<br />
were non-stop, day and night. Because he was being woken<br />
every time I got up to go to the loo in the caravan’s portable<br />
toilet, my husband decided to sleep in one of the bunk beds.<br />
One night while turning in his bed, he pulled a muscle. He went<br />
to the doctor and was given anti-inflammatory drugs in spite of<br />
saying he had a problem with his stomach. Unfortunately, they<br />
gave him a stomach ulcer. He was drinking milk all the time to<br />
help the ulcer. We went to the seaside for a break and stayed in<br />
a B&B. In the middle of the night, my husband had run out of<br />
milk and I had run out of drinks. We got up, threw our clothes<br />
on, dashed downstairs and drove at speed to an all night garage.<br />
We nearly held up the bemused attendant as my husband<br />
demanded a large bottle of milk and I ordered the largest bottle<br />
of drink they had in the place. It is funny to recall it now, but<br />
were both in deadly earnest at the time!<br />
water deprivation test<br />
By the end I was feeling quite unwell. It is not life-threatening<br />
as long as you keep drinking, but it is very unpleasant. The<br />
water deprivation test for the diagnosis is horrible, as you<br />
cannot drink for several hours. I remember having ice cubes,<br />
but an endocrine nurse who I was at a recent test with has no<br />
recollection of that. They have to stop the test when you start<br />
getting dehydrated, which happens quite soon as you pee out<br />
all the liquid in your body.<br />
There is no way of curing a switched off hormone, but<br />
controlling it is easy. I just use a nasal spray of synthetic<br />
vasopressin twice a day and the symptoms go away. I have to<br />
make sure I am fully stocked with nasal spray, but diabetes<br />
insipidus is one of the conditions for which you do not have<br />
to pay prescription fees ■<br />
Pituitary Life | autumn 2013
Patients’ stories<br />
29<br />
Lawrence’s story<br />
It all started in the year 2000. I had a<br />
good job, was very fit and enjoyed a lot<br />
of water sport.<br />
I lived in my own flat, worked hard<br />
and played hard without giving a thought<br />
to the welfare of my body. Looking<br />
back, I guess I was one of the lucky<br />
ones, as no matter what I ate or drank I<br />
always remained slim and healthy, or so it<br />
appeared.<br />
In October 2000 I noticed my vision<br />
was not as good as it was; it just looked<br />
misty and for a few days I put it down<br />
to fatigue and presumed it would get<br />
better. As it was certainly not getting<br />
any better, I went to the opticians. They<br />
had a good look and though my vision<br />
was by now quite poor they could not<br />
see a problem with my eyes and told<br />
me to “See how it goes.” I was not at all<br />
satisfied with that advice and asked for<br />
another appointment the following week,<br />
but unfortunately got the same response.<br />
I was really quite worried, so I went to<br />
see my doctor. He just said I was working<br />
too hard and should go to the gym! I<br />
then asked to see a specialist and was<br />
referred to the local hospital.<br />
MRI scan<br />
When I saw the consultant, after a full<br />
eye examination and despite my poor<br />
vision, he also told me that he could<br />
not see a problem, and that I should<br />
therefore have a second appointment<br />
to see him in a month. By this point I<br />
could not drive, as I could not see well<br />
enough and to again be told that there<br />
was no answer to my difficulties was<br />
very alarming. My mother then made an<br />
appointment for me at a private hospital<br />
in Colchester. When I saw this consultant<br />
(although I could not see him!) he felt<br />
I should have immediate tests and an<br />
MRI scan. I was by now feeling very<br />
unwell and as a result of my MRI scan,<br />
was admitted promptly to Oldchurch<br />
Hospital in Romford.<br />
When in hospital I was given<br />
medication that helped me get some<br />
of my vision back. It was such a relief<br />
but I had no idea what lay ahead. I had<br />
been in hospital for some time having<br />
tests, but still with no idea what could be<br />
wrong – until the day came, when I met<br />
a man who pulled my bed curtain round<br />
and said he wanted to talk to me. He<br />
asked if I knew what was wrong with<br />
me. I said I had no idea. I was a very laidback<br />
27 year old, until I found out what<br />
was wrong. “You have a brain tumour”<br />
he said. He explained this was what was<br />
causing the problems with my vision and<br />
what they were going to do (he was, in<br />
fact, my surgeon). I asked “What are my<br />
chances of coming through this?” As his<br />
description was quite unpleasant, all I<br />
could remember from that point on were<br />
the words “50/50”. He did say other<br />
things but they all seemed insignificant<br />
after that.<br />
being grateful<br />
It seemed to me that my life had come<br />
as close to ending as flipping a coin.<br />
‘50/50’ resonated in my head a lot, but it<br />
was made so much easier by the constant<br />
stream of visitors I had, and cards, even<br />
from my customers (I was a very happy<br />
Lawrence after<br />
Lawrence before<br />
Chrysler Jeep salesman). I was thankful<br />
that I had had a great life. Being grateful<br />
for that kept me going and I started to<br />
think that if my time had come, then I<br />
had had a great time being here.<br />
After surgery I did not feel able to<br />
speak or move but could communicate<br />
by wiggling my feet. Anyway, I have just<br />
realised this is going on a bit so will get<br />
on to the bits you are probably more<br />
wanting to read. I just wanted to tell you<br />
how I got to this next part!<br />
In my mother’s words, “You just<br />
ballooned in front of us”, and I did. I<br />
went in to hospital a size <strong>28</strong>” waist and<br />
after surgery I was getting bigger and<br />
bigger. Two weeks later, I came home<br />
Pituitary Life | autumn 2013
30 Patients’ stories<br />
to stay at my mother’s. I had been in<br />
hospital for a month. I could hardly walk<br />
and used two sticks. My pituitary gland<br />
had been removed during surgery and<br />
I now had a number of medications<br />
to take, including steroids. I felt, and<br />
looked, unrecognisable to myself. I had<br />
to buy a complete new wardrobe of XL<br />
clothes and 42” waist jeans AND new<br />
shoes, as even my feet had grown! I felt<br />
enormous but just thought I would lose<br />
weight and get back to my old self.<br />
slow but gradual progress<br />
After three months I returned to my<br />
own home having made slow but gradual<br />
progress. Over the next ten years, I tried<br />
many ways to lose weight but nothing<br />
worked for me. I clearly remember going<br />
to the doctor at 17 stone pleading for<br />
help. I knew there MUST be a way. He<br />
said, and I remember it so vividly, “IT’S<br />
UNLIKELY YOU WILL BE ABLE TO<br />
LOSE WEIGHT, BUT IF YOU ARE<br />
CAREFUL YOU CAN PROBABLY<br />
MAINTAIN IT.” ‘Maintain it,’ I thought,<br />
‘I don’t want to maintain 17 stone.’ I used<br />
to love to run but now it hurt to walk.<br />
I felt I ate healthily but generally I was<br />
extremely unhappy. I was single (I’d had a<br />
long-term girlfriend) and found it hard to<br />
hold down a job. I would have been very<br />
happy, then, if in fact I had not made it<br />
through surgery. I could no longer do<br />
any of the hobbies I had enjoyed before<br />
and thought “What’s the point?”<br />
constanty tired<br />
I plodded on. A few highs, a lot of lows.<br />
I had four TIAs over a short period<br />
and then, after collapsing and a week in<br />
hospital, I was told I had Type 2 diabetes.<br />
My sleep was awful, I was constantly<br />
tired, and that’s how it went on.<br />
My mother then discovered the Raw<br />
Food Coach, Karen Knowler and we<br />
went to one of her raw food workshops.<br />
I really enjoyed the food she made,<br />
but the turning point was that she lent<br />
me a DVD about some people in the<br />
USA who went raw and reversed their<br />
diabetes; it was called ‘Raw for Thirty<br />
Days’. Since my illness, I had thought<br />
that if I had enough money I would go<br />
to a health retreat and stay there until I<br />
felt well again or at least more alive. I was<br />
up one night researching such retreats,<br />
in case I won the lottery, and found<br />
one that had recently opened, offering<br />
really good deals. It later came up in<br />
conversations with my family and it was<br />
agreed that I should go.<br />
I was there for three weeks, mainly<br />
juicing and eating plant based food. It<br />
was a very simple place but it changed,<br />
if not SAVED, my life. We walked,<br />
rebounded and drank lots of juice, with<br />
the addition of plant-based foods. Also, I<br />
had been suffering from a skin condition,<br />
which I had been on antibiotics for<br />
months for. While I was there my<br />
skin totally cleared up and I stopped<br />
my antibiotic medication. I checked<br />
my blood sugars frequently and they<br />
became, and remain, very stable, which<br />
has allowed me to change my diabetic<br />
medication.<br />
running again<br />
One evening, I went for a walk. I was<br />
reminiscing to myself about how much<br />
I used to like to run and wondered if<br />
I could do it again, as I felt so well. I<br />
broke into a jog and was smiling from<br />
ear-to-ear. Then I broke into a full-blown<br />
run, almost a sprint. Being big, I felt<br />
like a jumbo jet taking off but was also<br />
ecstatic that I had run again. I went into<br />
the house and managed to puff out the<br />
words that I had just been running. I<br />
sat for a moment with the other guests<br />
and then got up and did it again. Just to<br />
be able to run again was amazing, even<br />
though it felt somewhat unnatural!<br />
After three weeks, at my last weigh<br />
in, I had lost exactly a stone. I was now<br />
16 stone and absolutely overjoyed. I<br />
had found a way. As soon as I got<br />
home, I put my microwave on EBay<br />
and replaced it with a juicer. I juiced<br />
and made what I called ‘Super Salads’ all<br />
the time. I bought my own rebounder<br />
(mini-trampoline). My skin looked<br />
amazing and my blood sugars were still<br />
very stable. I did not deny myself any<br />
particular foods, but mostly drank juice<br />
and ate salads. I carried on...and two<br />
years later I had gone from a 38” to a<br />
34” (now 32”) waist and was able to finish<br />
a 10K run in Greenwich Park dressed as<br />
Father Christmas in aid of The Pituitary<br />
Foundation. It was a massive landmark for<br />
me. In the same year, I also went wakeboarding<br />
which, writing about it now, I<br />
still can’t quite believe it. I never thought<br />
I would be able to do any type of water<br />
sports again. I also went snow-boarding<br />
(on a dry ski-slope) and it felt amazing to<br />
do some of the things I used to enjoy.<br />
two years on<br />
Another two years on and I still felt<br />
great. I was unfortunately in and out of<br />
work, partly down to redundancies and<br />
partly down to just totally the wrong jobs<br />
for me, but I would take almost anything<br />
as I so wanted to work. Whether in paid<br />
or voluntary work – I usually took a<br />
green juice for lunch!<br />
talk on juices<br />
For over a year I have been working<br />
part-time whilst seeking full-time work.<br />
People have noticed the ongoing positive<br />
changes in me and asked me to make<br />
them juices also. This has happened<br />
more and more and led to me giving a<br />
talk on juices at my local hospital and<br />
also at a complimentary healthcare<br />
centre. As well as these, I was even asked<br />
by a local businessman to give three juice<br />
demonstrations at his companies.<br />
the juice guy<br />
I still have occasional check-ups with<br />
my endocrinologist but juicing has<br />
had a profoundly beneficial effect on<br />
my condition and thereby positively<br />
influenced the amount of medications<br />
I need to take. People have referred to<br />
me as ‘The Juice Guy’ and I cannot think<br />
of a better title, especially as my friends<br />
and family have seen the transformation<br />
happen in front of them since I became<br />
a Juicerholic!<br />
Looking back, if I had not gone<br />
through all that I would probably still be<br />
selling prestige cars which at the time I<br />
thought was great, but I would far rather<br />
be doing something positive and healthy<br />
with a thought for the wellbeing of<br />
myself and others ■<br />
Pituitary Life | autumn 2013
Patients’ stories<br />
31<br />
Michael’s story<br />
A photo of me enjoying a driving day at the Severn Valley Railway back in the summer. My instructor is on my left.<br />
In late 2012, I became aware that I<br />
had developed blurred vision in my<br />
left eye. I attended my opticians in<br />
January and was alarmed to discover that I<br />
could not read the top letter on the vision<br />
chart with my left eye, even with the aid of<br />
the various corrective lenses provided by<br />
my optician. He referred me immediately<br />
to Queen Mary’s Hospital Sidcup, who<br />
carried out various tests and ranged a<br />
further appointment for me in March.<br />
Towards the end of February, I<br />
became concerned that my condition<br />
was worsening and attended A&E at<br />
the Western Eye Hospital in London<br />
on 27 February. Again, a number of<br />
tests were carried out and a provisional<br />
diagnosis of non-arteritic ischaemic optic<br />
neuropathy was reached. I attended a<br />
follow-up appointment on 19 April when<br />
this diagnosis was confirmed. A further<br />
appointment to test visual fields was<br />
arranged for 21 June.<br />
Early in June, vision in my right eye<br />
began to deteriorate rapidly; I therefore<br />
attended Moorefield’s A&E on 5 June.<br />
Moorefield’s conducted a further series<br />
of tests and offered me an appointment<br />
with a neuro-ophthalmologist on 12<br />
June, with the option of re-presenting at<br />
A&E if I noticed a further decline in my<br />
right eye vision (by this time my left eye<br />
vision was non-existent). My right eye<br />
vision was declining on a day-to-day basis<br />
by now and so I duly presented again at<br />
Moorefield’s A&E on 8 June. Again, a<br />
variety of tests were carried out and the<br />
thinking was that (rather unluckily!) I had<br />
suffered another non-arteritic ischaemic<br />
optic neuropathy, this time in my right<br />
eye. I was about to be discharged, but<br />
after speaking to the consultant, the duty<br />
doctor decided to send me for a brain<br />
scan.<br />
This revealed the presence of a large<br />
(egg-sized) tumour on my pituitary gland,<br />
which was impinging on my optic nerve<br />
and causing the reduction in sight. It was<br />
successfully removed by Mr Barazi and<br />
team at Kings College Hospital shortly<br />
afterwards and I am pleased to say that<br />
my vision in both eyes has returned to<br />
around the level it was this time last<br />
year, i.e. before I became aware that<br />
there was a problem. The consultant<br />
ophthalmologist at Kings has described<br />
this recovery as ‘remarkable’.<br />
No criticism of any individuals or<br />
institutions is intended here, but the key<br />
point is the timing of the brain scan. It<br />
would clearly have helped if this had<br />
been provided at an earlier stage, and<br />
there may be a lesson here for others<br />
(both patients and physicians) who find<br />
themselves faced with a similar situation.<br />
I’m delighted to report that I’ve had no<br />
further problems, and have responded<br />
well to ongoing endocrine treatment.<br />
Post script: At my most recent<br />
ophthalmology appointment at King’s<br />
they told me that there is irreversible<br />
damage to the retina in my left eye. It<br />
is probable that this would not have<br />
occurred had the tumour been diagnosed<br />
earlier. The practical effect of this is that<br />
should I decide to have lens replacement<br />
surgery at a later date, any improvement<br />
in my left eye would only be marginal.<br />
But I would stress that, given all the<br />
circumstances, I am extremely happy<br />
with the outcome ■<br />
Pituitary Life | autumn 2013
Find us on<br />
Facebook<br />
The views expressed by the contributors are not necessarily those of The Pituitary<br />
Foundation. All information given is general - individual patients can vary and<br />
specific advice from your medical advisors should always be sought.<br />
We do not endorse any companies nor their products featured in this edition.<br />
© 2014 The Pituitary Foundation<br />
• Registered company number 3253584<br />
• Registered charity number 1058968<br />
• Registered address: 86 Colston Street, Bristol, BS1 5BB<br />
The Pituitary Foundation<br />
86-88 Colston Street, Bristol, BS1 5BB<br />
helpline@pituitary.org.uk www.pituitary.org.uk<br />
Editor of Pituitary Life: Pat McBride<br />
Working to support pituitary patients<br />
Printed by Moulton printers www.moultonprinting.com.<br />
Magazine production supported by Pfizer Limited.<br />
Design: www.forestgraphics.net