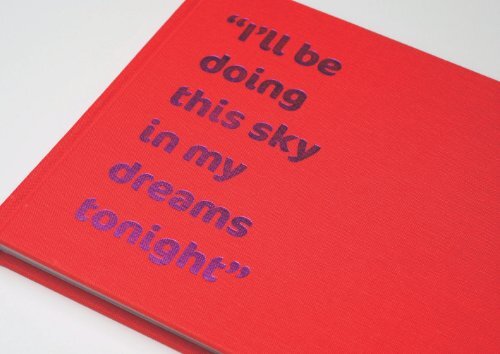
I'LL BE DOING THIS SKY IN MY DREAMS TONIGHT
This document is about validating the importance of creative expression of people who are living within a hospital context. It is based on the assumption that art is about values, beliefs, identity, expression and communication and as such should be a fundamental right of every individual, regardless of whether they are in hospital or not.
This document is about validating the importance of creative expression of people who are living within a hospital context. It is based on the assumption that art is about values, beliefs, identity, expression and communication and as such should be a fundamental right of every individual, regardless of whether they are in hospital or not.
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
“I’ll be doing this sky in my dreams tonight”<br />
Art in Hospital
Published by Art in Hospital, 2006<br />
Printed in an edition of 3000 by Summerhall Press, Edinburgh<br />
ISBN ?<br />
Text © 2006, Penny Rae<br />
Images © 2006, The Artists<br />
All photography © 2006, Carl Cordonnier except where indicated<br />
All rights reserved. No part of this publication may be reproduced in any<br />
form or by any means – graphic, electronic or mechanical, including<br />
photocopying, recording, taping or information storage and retrieval<br />
systems – without the prior written permission from the publishers.<br />
Design: Frozen River
Contents<br />
Positioning Statement Penny Rae 6<br />
Foreword Sir Kenneth Calman 10<br />
Conversations 16
Art in Hospital<br />
A POSITION<strong>IN</strong>G STATEMENT<br />
6<br />
This document is about validating the<br />
importance of creative expression of<br />
people who are living within a hospital<br />
context. It is based on the assumption<br />
that art is about values, beliefs, identity,<br />
expression and communication and<br />
as such should be a fundamental right<br />
of every individual, irregardless of<br />
whether they are in hospital or not.
The first question we asked<br />
ourselves in this study of the<br />
work of Art in Hospital was<br />
how to approach it. What<br />
attitude, state of mind, was<br />
needed in order for the<br />
project’s emotional and artistic<br />
substance to reveal itself? In<br />
the end, the research process<br />
we used was not based on<br />
scientifically proven data, if<br />
such is necessary to make<br />
a convincing case, but on a<br />
process of rational deduction<br />
from individual perspectives,<br />
representing them through<br />
their own words and images.<br />
As we entered into the world<br />
of Art in Hospital, the rules of<br />
interaction between the artists<br />
and participants sometimes<br />
seemed so fluid that they<br />
could only be determined by<br />
the dynamics of each individual<br />
situation. However, what was<br />
clear was that no evaluation<br />
of hospital-based art practice<br />
could be made without some<br />
understanding of context. Art in<br />
healthcare practice is shaped by<br />
a particular place and particular<br />
conditions and a particular<br />
artistic and political moment.<br />
It is designed to respond to<br />
very particular situations.<br />
Unless these situations are<br />
experienced to some degree, is<br />
it very hard for any evaluation<br />
to be responsible or just?<br />
Art in Hospital raises as many<br />
questions as it answers. It is<br />
driven by a belief in people<br />
and a faith in the ability of<br />
art to deal with social crisis.<br />
This document aims simply to<br />
illustrate the extraordinary<br />
journey Art in Hospital is making<br />
for everyone involved in some<br />
way with the organisation;<br />
from health care professionals<br />
to funders, and in particular<br />
for the artists and clients.<br />
We hope it will inspire the<br />
confidence in policy makers<br />
to make a more sustained<br />
and confident commitment<br />
to this kind of partnership.<br />
Penny Rae author<br />
Carl Cordonnier photographer<br />
October 2006<br />
7
8
9
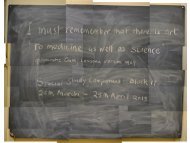
Foreword<br />
by Professor<br />
Sir Kenneth Calman<br />
10<br />
PATRON OF ART <strong>IN</strong> HOSPITAL<br />
CHANCELLOR OF GLASGOW UNIVERSITY
My interest in the arts originated from a love<br />
of literature. During the mid 1980s, I ran an<br />
ethics course for medical students using poems,<br />
plays, texts and the purpose of this was to<br />
help medical students view the world from the<br />
perspective of the artist, and not just the medical<br />
academic. It was an interesting time for me as<br />
we saw these bright medical students begin<br />
to approach their course work with a broader<br />
and more person-orientated approach which<br />
would hopefully make them better doctors.<br />
their being involved in arts and their quality of<br />
life during this time is higher. Medicine is based<br />
on science and the quest for new knowledge. The<br />
arts and humanities however are an important<br />
part of this and may seem to have got lost along<br />
the way. There is now considerable interest in<br />
re-introducing them into the medical curriculum<br />
but not at the expense of medical knowledge. The<br />
medical student needs to know where the heart<br />
is but he also needs to know about emotional<br />
interaction and effective communication.<br />
There were two main questions which were<br />
in my mind. The first was do the arts and the<br />
humanities influence medical professionals, and<br />
secondly do the arts help people with physical<br />
and mental illnesses recover more effectively?<br />
There is scientific evidence for both of these<br />
which is slowly building up. The broader your<br />
outlook on life and the more interesting you<br />
are as a person does allow you to see people<br />
in a different way. In addition, I have seen the<br />
growth and self confidence in patients through<br />
When we founded the Centre for Arts and<br />
Humanities in Health and Medicine we wanted<br />
to try to bring the two worlds together. Simple<br />
things like the environment in the doctors surgery<br />
and looking at the evidence that people felt<br />
better in the waiting room looking out at a garden<br />
rather than brick walls. It seems so obvious yet<br />
how many waiting rooms are dreary and dismal<br />
places. So it’s not just those who are health<br />
professionals who need to think differently, it’s<br />
architects, planners and many others. There<br />
is a chance with new hospital buildings to look<br />
11
12<br />
holistically at the treatment of patients and to<br />
use architecture and design to endorse a holistic<br />
approach to treatment. Design has also to be<br />
about creating a vibrant community whether that<br />
is for a hospital or any other kind of institution.<br />
The arts seem to engender a sense of community.<br />
For me the Angel of the North is a particularly<br />
strong symbol of the nurturing positive<br />
community spirit. It has transformed peoples’<br />
sense of pride in Gateshead, which is now<br />
associated with the home of the angel. When<br />
we think about quality of life the qualities are<br />
those which make people happy and from all my<br />
anecdotal and personal experience, engagement<br />
as a participant or as a spectator in the arts,<br />
these activities help to improve quality of life and<br />
perhaps even more appropriately when people<br />
are unwell. To influence the acceptance of arts<br />
in healthcare has to come from people who are<br />
really in a position to change attitudes and policy.<br />
When I was the Government’s Chief Medical<br />
Officer and people knew that I was interest in<br />
the arts I like to think that it did allow people to<br />
think differently. People in influential positions<br />
must always recognise the importance of their<br />
voice. By endorsing the movement you give<br />
people permission to move ahead. I have always<br />
advocated the use of arts in the teaching of ethics<br />
to doctors. While I believe that science remains<br />
absolutely critical to medical teaching I also<br />
believe that the arts are fundamentally necessary<br />
to improve quality of life and the development<br />
of a fully rounded person. Relationships between<br />
those who fund the arts and those who fund<br />
hospitals are essential. I suspect that more<br />
partnerships need to take place and people<br />
must be encouraged to think outside their own<br />
professional box and learn from people with<br />
different professional backgrounds. A louder<br />
voice should be coming from those working<br />
within the arts and healthcare. Organisations<br />
like Art in Hospital have huge amounts of<br />
‘evidence’ that their work is valuable. Dedicated<br />
arts spaces in hospital are desirable. There is<br />
a strong enough body of evidence now to endorse<br />
the fact that an artist’s role can be critical in<br />
the overall care of patients. Arts specialists
are often still excluded from decisions about<br />
patient care. I hope it will not be long before they<br />
are seen to be part of the patient care team.<br />
Exposure to the arts and a measure of peoples’<br />
reaction to involvement in the arts is thus very<br />
important. Humour as a component of this also<br />
makes people feel better. Story telling, and<br />
art in itself, may never relieve the symptoms<br />
but feeling valued, and being part of the<br />
story can go a long way towards recovery.<br />
leads to creativity both for patients and for the<br />
artist’s own work. I think many artists would<br />
say their own work has developed positively<br />
through their work with people in hospitals.<br />
We should not try to limit the development of<br />
arts and healthcare but see it as an opportunity<br />
for improving the quality of life for all concerned.<br />
Professor Sir Kenneth Calman, April 2006<br />
I sometimes use the analogy of the bucket. A<br />
bucket filled with love, care, compassion or<br />
whatever you wish to call it. The general idea is<br />
that patients take out of the bucket and doctors<br />
and other health professionals fill it. This is a<br />
false model. There is always some love, care and<br />
compassion and even humour in the bucket that<br />
patients put in and doctors take out. It is I think<br />
the same with artists who work in hospital, they<br />
put their skills and vision and training into the<br />
bucket but they receive a remarkable amount<br />
back in return and it is that partnership which<br />
13
14
15
16<br />
Barbara<br />
McEwan<br />
Gulliver<br />
DIRECTOR AND FOUNDER, ART <strong>IN</strong> HOSPITAL<br />
I started working as an Artist in a hospital in<br />
1989. At that time, artists working in hospitals<br />
were completely isolated and there was<br />
little or no recognition from either the arts<br />
funding bodies or the health boards of the<br />
value of this kind of work, whether it was in<br />
visual arts, theatre, dance or music. I found<br />
an inspired hospital manager who worked<br />
with me on putting together a proposal for<br />
a pilot programme of visual art work and we<br />
established our first art room at Belvidere<br />
hospital in Glasgow. With The Glasgow School<br />
of Art we established a student placement<br />
scheme and Art in Hospital was born.<br />
Our first exhibition was in an empty ward in<br />
December 1991. It was the result of the work of<br />
the previous year. Disused hospital wards make<br />
brilliant gallery spaces. We received funding for<br />
a second year of activity and in 1993 we were<br />
able to employ two part time artists, who were<br />
recent graduates of The Glasgow School of Art.<br />
We had our first public exhibition in 1994 ‘From<br />
a staircase to a banister to the colours in the sky.’<br />
After we were successful in receiving funding<br />
from the health board, the project was expanded<br />
to two more hospitals. I wanted to develop an<br />
artistic practice that reflected my own values<br />
and priorities which are about a belief in the<br />
empowerment of the individual in an institutional<br />
context. It is about an emotional response to art,<br />
the feel of a brush on a piece of paper, the joy<br />
of colour, the texture of paint. We have begun<br />
to touch the surface with new media projects,<br />
digital animation, video but we have much more<br />
to do. I want to offer the artists flexibility in<br />
their approaches to working with patients but<br />
I also have to constantly demonstrate that this<br />
particular model of practice is cost effective.
17
18<br />
From the outset, there are certain criteria which<br />
are essential for me to. We employ only practicing<br />
and professional artists. When I interview artists,<br />
I look at their practice, whether in painting,<br />
drawing, printmaking, film, video or sculpture<br />
but I equally consider their communication skills.<br />
We establish dedicated art spaces in each of<br />
the hospitals we work in. I feel it is essential to<br />
work in a non clinical space in an environment<br />
which is notably different to the wards.<br />
I think of Art in Hospital as giving back choices<br />
to people who have temporarily had choices<br />
removed from them and developing stronger<br />
links between medicine, treatment, care and<br />
artistic practice, which have traditionally been<br />
seen as having no relationship. Health care is<br />
seen as structured and functional; art is seen<br />
as slightly anarchic and needing freedom not<br />
context. The reality is less divided. Artists are<br />
open and responsive to changing situations and<br />
health care professionals are also concerned<br />
about individuality and quality of life for patients.<br />
In 2006 we have over eighteen artists employed<br />
across nine hospitals. Since we began, we have<br />
had sixty five exhibitions, we have undertaken<br />
projects in France, Switzerland and Belgium.<br />
We have exhibited at ten Glasgow Art Fairs.<br />
I want Art in Hospital to be a model for other<br />
health boards and to suggest a new way of<br />
working between health boards and arts<br />
funding bodies. I want to look at our work<br />
in partnership with hospitals in Europe and<br />
internationally and I want eventually to<br />
see artists, patients, hospital Clinical Staff,<br />
Administrative Staff all endorsing the important<br />
place of art in a hospital environment.<br />
The potential and the demand for<br />
expansion of our work is endless.
19
20
21
22
Liz Cameron<br />
THE RIGHT HON.THE LORD PROVOST<br />
COUNCILLOR LIZ CAMERON<br />
I have watched the work of Art in Hospital<br />
develop for the last 13 years and I emphatically<br />
endorse its success. Care for the elderly is of<br />
particular interest for me and I have always<br />
seen the results of their work in physical<br />
rehabilitation. I believe wholeheartedly in their<br />
approach of sharing skills and facilitating a<br />
creative environment for the people they are<br />
working with. Not only is it transforming for them<br />
mentally and emotionally; nursing staff have<br />
talked to me about the improvements they see<br />
in patients’ confidence, level of mental alertness<br />
and even in their physical conditions. I think<br />
their work is pioneering and I am delighted to be<br />
associated with it and support it. It is important<br />
to remember that health doesn’t just mean an<br />
absence of sickness but a state of well being.<br />
I remember walking into the hospital at<br />
Blawarthill Hospital and seeing artists working,<br />
intent and absorbed. Then I realised that most<br />
of the patients were in their 80’s and it was an<br />
uplifting moment that I will remember for ever.<br />
I’m also delighted that Art in Hospital have<br />
such a prominent place at the Glasgow Art<br />
Fair. The organisation is an integral part<br />
of the arts in Glasgow. The work is of such<br />
high quality that it comes as no surprise to<br />
me that it sells so well. The quality control<br />
comes from the patients being supported by<br />
talented and dedicated professional artists.<br />
Alzheimers doesn’t so much as run in my<br />
family, it gallops and I want to know that if I<br />
am hospitalised and need constant care when<br />
I get older that there will be talented and<br />
dedicated artists sharing their skills with me, so<br />
I have very selfish reasons too for supporting<br />
so completely the work of Art in Hospital.<br />
23
24
25
Bridget McConnell<br />
EXECUTIVE DIRECTOR OF CULTURE & SPORT<br />
GLASGOW CITY COUNCIL<br />
26<br />
What is sometimes perceived as social<br />
engineering through art is often criticised but I<br />
believe wholeheartedly in the transformational<br />
power of art and its worth and value to<br />
individual lives. My involvement with Art in<br />
Hospital is at policy level, ensuring that work<br />
like this is not marginalised but an integral part<br />
of Glasgow’s arts policy. In the field of health<br />
care for the elderly, the emphasis seems to be<br />
shifting from the importance of prolonging life<br />
for its own sake to an acceptance that quality<br />
of life must be provided at every stage of life.<br />
In the same way, evaluation of arts policies<br />
in this area cannot simply be about numbers<br />
but must also take into account anecdotal<br />
evidence about the value to patients and<br />
health care workers of art and arts practice.<br />
We need to have more advocates at opinion<br />
forming level to ensure revenue funding<br />
for organisations that work in this area.
Arts projects in health care work when the artists<br />
do not compromise on the quality of work and the<br />
sharing of all their skills. No one wants access to<br />
mediocrity, everyone wants access to excellence.<br />
This is why Art in Hospital is so successful. Skilled<br />
and talented professional artists are employed<br />
in a way that firstly allows them to share their<br />
experience and secondly allows them the time<br />
and space to continue their own professional<br />
development. All the artists I have seen working<br />
within the Art in Hospital projects are committed<br />
to what they are doing. Their communication skills<br />
and levels of involvement with patients and health<br />
care staff is the cornerstone of their success.<br />
27<br />
As a possible model for funding and access to the<br />
arts in hospital, I am particularly interested in the<br />
GP referral scheme that currently applies to sport<br />
and would like to see it extended to arts practice.
28
29
David McQuatt<br />
DEVELOPMENT MANAGER<br />
30<br />
Art in Hospital is constantly evolving as an<br />
organisation and as a body of artists. We are<br />
trying to consolidate our work but at the same<br />
time we want to move forward with new ways<br />
of involvement and new practice. I see part<br />
of our role as being to validate the concept of<br />
peoples’ privacy within an institution. That<br />
means offering them the choice to come into<br />
an environment that suggests new ways of<br />
expressing themselves personally. It means<br />
helping to find a form of visual expression for<br />
people that is non-judgemental and in which<br />
no one makes assumptions about what people<br />
can or cannot do simply because they are in a<br />
hospital situation. That’s the basic philosophy of<br />
the organisation for me. The process follows of<br />
creating work and the finished work is at the end<br />
of the line and all are important, but no moment<br />
is more important for me than when someone<br />
picks up that pencil, brush or charcoal for the<br />
very first time and makes that initial mark. The<br />
strength of our work is shown by the demand<br />
for us to open our practice to more units, more<br />
nursing homes, more hospitals, more artists.<br />
Our resources are constantly stretched and<br />
difficult decisions are constantly having to<br />
be made. We would like to offer more artists,<br />
more time for development, for discussion,<br />
for evaluation and widen access to all.<br />
Current levels of funding make it impossible.
31
32
John Lieser<br />
PATIENT AND ARTIST<br />
I wasn’t allowed to do art at school because I had<br />
a German surname. I had to do the sweeping up<br />
instead. I think my early paintings were terrible<br />
but the artists encouraged me to persevere. I’ve<br />
only missed 2 art sessions in the last 3 years. It’s<br />
the most important thing I do. It’s the only time<br />
I lose myself and forget about the cancer. I’m in<br />
a wee world of my own. I feel warm and secure. I<br />
started out by just looking at the paintings in the<br />
books and sometimes I just sat there and looked<br />
at the flowers. It’s difficult to explain the feeling<br />
when they told me someone had bought one of<br />
my paintings at the Art Fair. It was unbelievable.<br />
I was choked up. I think it was one of the most<br />
important moments in my life. Can you imagine?<br />
Someone paid for one of my paintings, then took<br />
it home and hung it on their wall. Unbelievable.<br />
33
Irene Florence<br />
SENIOR PROJECT MANAGER<br />
34<br />
I don’t believe in altruism. I do a job that<br />
brings immense satisfaction and it is a job that<br />
includes frail and vulnerable people. I think<br />
the demand for our work will always be there.<br />
Initially, other health care workers can be wary<br />
of us and of what we do, but then become very<br />
receptive. I think that we’re in quite a privileged<br />
position compared to the care staff. They are<br />
having to cope with primary care needs whilst<br />
we are there to help to release creativity in<br />
people and give them back some choices. As<br />
artists we all have lots of ideas as to how to<br />
develop projects; ideas are never a problem<br />
but resourcing them is problem. I would<br />
describe our work as person centred but within<br />
the parameters of prescribed hospital life.<br />
My own practice has been clearly influenced<br />
by the people I work with here. I am working in<br />
hospitals with people who are very hesitant and<br />
unsure of the materials they are working with,<br />
whether its charcoal, acrylics, pastels or oils.<br />
When I’m in my own studio I try much harder<br />
now to let go with my materials and to enjoy<br />
them. I know I have become more confident<br />
in the use of texture, colour and surface.
we are<br />
there to<br />
help to<br />
release<br />
creativity<br />
in people.<br />
35
36
37
Winnie<br />
PATIENT AND ARTIST<br />
38<br />
I’ll be doing this sky in my dreams<br />
tonight. I know I won’t be able to<br />
sleep unless I get that sky right. You<br />
see I’m a learner with a capital ‘L’.<br />
The simple fact is that I was unhappy<br />
before I started painting and I’ve<br />
been happy since. Once a week’s<br />
just not enough. I should be painting<br />
every day. I should always have<br />
been painting. It would have kept<br />
me out of trouble. I’ve always been<br />
in trouble. My parents despaired of<br />
me. There were all sorts of troubles<br />
in my life. I was married three times<br />
and all my husbands died. I sit in<br />
this room with my paints and I feel<br />
joy, hope and happiness. I’m at one<br />
with the world for the first time.
I’m at one with<br />
the world for<br />
39<br />
the first time.
40
Dr Paul Knight<br />
CONSULTANT PHYSICIAN<br />
MEDIC<strong>IN</strong>E FOR THE ELDERLY<br />
In 1991 I was given the management of the care<br />
for the elderly unit and part of my understanding<br />
of that brief was to enhance the quality of life<br />
for people in the unit. Provision of artists and<br />
dedicated art spaces within hospitals are not part<br />
of the strategic thinking within primary care but<br />
I believe there should be strategic partnerships<br />
between health boards and those organisations<br />
which fund the arts. In the same way that funding<br />
partnerships are necessary, a holistic approach<br />
to care is also essential; not just in the hospital<br />
but when possible in the hospital outreach<br />
programmes. Joint working should become<br />
an ethos. Everyone has such severe budgetary<br />
restraints that it’s the only way forward for this<br />
kind of work. It’s easy to say that for a relatively<br />
modest investment, there are very high returns. I<br />
can see that the work is far more than diversional.<br />
There are the workshops, the exhibitions, the<br />
Art Fair and lots of other public moments. I can<br />
understand now how important this work is.<br />
Projects like Art in Hospital develop from a kernel<br />
and are nurtured by one enthusiastic protagonist.<br />
In this case it was Barbara Gulliver.<br />
41
42
43
44
Lucy Bates<br />
PROJECT MANAGER<br />
ART <strong>IN</strong> HOSPITAL<br />
I enjoy applying the skills that<br />
I have learnt to support other<br />
peoples’ work. Our work is<br />
not about analysis; the results<br />
may be therapeutic but I am<br />
not a therapist. I am an Artist<br />
sharing what I know. Working<br />
in a group is an important part<br />
of the process. A third focus is<br />
created between ourselves and<br />
the patients. We are relating<br />
to each other through art and<br />
achievement and process. It’s a<br />
very different conversation to<br />
illness, treatments and doctors.<br />
We are<br />
relating to<br />
each other<br />
through art.<br />
45
46
47
52
53
Claire Simpson<br />
SENIOR ARTS DEVELOPMENT OFFICER<br />
GLASGOW CITY COUNCIL<br />
54<br />
I look at Art in Hospital in the same way I look at<br />
any professional visual arts organisation working<br />
in the city. I don’t pigeon hole them within a<br />
social context because they’re all professional<br />
artists who are developing their own practice at<br />
the same time as sharing their skills and training<br />
with a particularly venerable section of the<br />
community. I don’t see how you can make a rigid<br />
distinction between this kind of work and any<br />
other professional practice. I imagine the work<br />
the artists do in the Glasgow hospitals feeds<br />
into their practice in the same way as any other<br />
important life experience feeds their practice.
55
Charlotte Donovan<br />
ARTIST, ART <strong>IN</strong> HOSPITAL<br />
56<br />
The ultimate<br />
wish would be<br />
dedicated art<br />
space on every<br />
hospital site.<br />
The ultimate wish would be dedicated art<br />
space on every hospital site. Each one would<br />
have open access for visitors, staff, patients<br />
and visitors. There would be exhibitions,<br />
performances, residencies, public art<br />
programmes, artists’ studios. They would be<br />
living, vibrant non-institutional spaces within<br />
the necessary confines of the hospitals.<br />
I hope that health care professionals are gradually<br />
understanding and endorsing the place of the<br />
artist’s work in hospitals. There is still a sense that<br />
all the other professionals working in a health care<br />
context have their place but that the Artist remains<br />
on the periphery. As artists we are often working<br />
up to five hours a day with individual patients,<br />
more hours than any other member of staff.
57
Marielle Macleman<br />
58<br />
ARTIST COORD<strong>IN</strong>ATOR, ARTS <strong>IN</strong><br />
PALLIATIVE CARE, ART <strong>IN</strong> HOSPITAL
It’s hard to dispel the myth that we’re<br />
therapists. We are artists who have<br />
made a choice to spend time working<br />
here at the hospice. We are not here to<br />
analyse. For us this is not a therapeutic<br />
practice but an artistic practice. Our<br />
discussions with patients are about<br />
colour and light and materials. Each<br />
time I look at the walls of this room, I<br />
see extraordinary stories. Over there<br />
I can see the sun setting over the loch<br />
painted by someone who has a brain<br />
tumour. The landscape next to it was<br />
painted by a man who has just relearnt<br />
to use his left hand. That series of small<br />
paintings have been done by someone<br />
who has lost all verbal skills and needed<br />
a way to say thank you to her carers. Not<br />
long ago, we were visited by a man who<br />
wanted to collect his mother’s paintings.<br />
She had died some weeks previous<br />
to his visit and he said it was the only<br />
legacy he had of her. There is a lot of<br />
colour and a lot of laughter in this room.<br />
59
Loretto Fernie<br />
PATIENT AND ARTIST<br />
60<br />
I’d love to have<br />
gone to Art School.<br />
I would never have<br />
missed a class.<br />
I’d have been the<br />
first one in and the<br />
last one out.<br />
I’m an insomniac. I only sleep<br />
for an hour or so at a time. I<br />
used to lie there awake, just<br />
worrying and thinking. Now I<br />
keep my paints and my easel<br />
by my bed and when I wake<br />
up I paint. Sometimes I get<br />
my best ideas in the night.<br />
Since I started painting I’ve<br />
cut down on my smoking. I<br />
used to smoke about 60 a day<br />
and now I smoke about 15.<br />
I would paint all day and all night<br />
if I could. I’d love to have gone<br />
to Art School. I would never have<br />
missed a class. I’d have been the<br />
first one in and the last one out.
61
Sharon Goodlet<br />
SENIOR PROJECT MANAGER, ART <strong>IN</strong> HOSPITAL<br />
Working for Art in Hospital is ideal for artists<br />
as they have time to work alone in the studio<br />
as well as time working with the patients.<br />
The isolation and self-absorption that is often<br />
a problem for some artists is reduced by<br />
the very intensive time with the patients.<br />
62<br />
There is always an element of surprise working<br />
with elderly residents. I worked with an 86 year<br />
old woman who had left school at 13 to look after<br />
her brothers and discovered painting through<br />
Art in Hospital. She had amazing energy and<br />
experimented with a wide range of materials. She<br />
was very talented. Her enthusiasm for painting<br />
changed her life at 86. Her story inspired me<br />
and in turn renewed an enthusiasm for my own<br />
work. Those stories aren’t unusual and many<br />
of us working as artists within the project are<br />
constantly refreshed by the enthusiasm and<br />
dedication of the patients. I’ve found that<br />
artists who no longer work with traditional<br />
materials become drawn to them again through<br />
their time spent working with patients.<br />
I’ve worked with a number of the different<br />
client groups. With the elderly in the<br />
Mansionhouse Unit, with clients through<br />
the Epilepsy Connection, with the physically<br />
disabled rehab unit. I’ve also worked on<br />
preparing work for the Art Fair, which is<br />
often an important boost to the patients<br />
whose work is selected and sold.<br />
We could do a lot more if we were adequately<br />
resourced to develop. We could create more<br />
dedicated workshop spaces and have more<br />
exhibitions. We could spend more time in<br />
staff training and develop our skills. I see<br />
healthcare staff attitudes changing when<br />
they see the results of what we do. Open<br />
days are important where people can see
the work and understand the process and give<br />
the artists a higher profile in the hospitals.<br />
We’re all pushed for time. We have lots of<br />
contact time with patients, there aren’t the<br />
resources to allow us to develop ideas and<br />
talk amongst other artists about what works<br />
and why as much as we like. It would be great<br />
to employ a fundraiser, someone to market<br />
and promote the work, and a curator to keep<br />
the exhibitions fresh across the hospitals.<br />
63
64
Sandra Anderson<br />
PATIENT AND ARTIST<br />
I’m working on a painting<br />
now that was inspired by<br />
my holiday in Yorkshire.<br />
It’s a painting of the<br />
North York Moors. I’m<br />
trying to bring back the<br />
light from my holiday.<br />
I remember looking out at<br />
the cliffs, the lighthouse,<br />
the tractors in the fields.<br />
It’s all there. I’ve just got<br />
to try to bring it back<br />
and put it here. I had<br />
my first brain tumour<br />
around my 38 th birthday.<br />
65
Kirsty Stansfield<br />
ARTIST, ART <strong>IN</strong> HOSPITAL<br />
66<br />
I work with digital media and the person centred<br />
approach that is the ethos of Art in Hospital very<br />
much reflects my own approach to making and<br />
researching work. Process is very important to<br />
me, in both my own art practice and my work<br />
with Art in Hospital. It is not about setting goals.<br />
It’s ongoing and has to be seen as long term in<br />
the way we build relationships and trust. I think<br />
the art room is often perceived as an oasis in the<br />
hospital. It can be seen as good and bad that we’re<br />
not part of multi-disciplinary care teams within the<br />
hospital. On one hand it gives us autonomy and<br />
independence but it does mean we are always on<br />
the edge. I think what we do is to make space to<br />
allow people to find something within themselves.
I begin new sessions by<br />
introducing myself on the<br />
wards. I describe the art space.<br />
I ask people to come and visit<br />
the space and when they do<br />
come, I encourage them to<br />
respond to the materials in<br />
their own way. I think when<br />
people are given the opportunity<br />
they can communicate an<br />
idea or a thought visually<br />
which they wouldn’t<br />
normally say using words.<br />
At the moment I’m creating a<br />
project about reduced personal<br />
space and I’m looking at how<br />
people relate to personal objects<br />
in such a reduced environment.<br />
For example, there can be four<br />
people living in a ward and<br />
their personal possessions are<br />
reduced to clothing and one<br />
or two framed photographs.<br />
Working with people with<br />
dementia, for example, can<br />
be rewarding and can also be<br />
very frustrating. There can be<br />
sessions when no two words<br />
relate to each other and other<br />
days when everything flows<br />
for that same individual.<br />
Sometimes people have to walk<br />
past the art room many times<br />
before they actually come in,<br />
and even then it takes another<br />
few weeks before they have the<br />
confidence to do anything. We<br />
have to be patient and ready to<br />
help them build on this over time.<br />
Bill created a video postcard<br />
to send to his daughter in<br />
Canada. He had never held<br />
a video camera before and<br />
he immediately created a<br />
very personal relationship<br />
with it, both in front of and<br />
behind the camera. He filmed<br />
other residents too and they<br />
responded to the camera<br />
very positively. There would<br />
have been a very different<br />
response if I had been holding<br />
the camera. As artists working<br />
in this way, we sometimes<br />
have to make ourselves<br />
invisible. Our role becomes<br />
to help people translate a<br />
thought or an idea by sharing<br />
the creative skills we have.<br />
67
68
Daisy Richardson<br />
ARTIST, ART <strong>IN</strong> HOSPITAL<br />
As an artist it is rewarding<br />
to share what you know<br />
with someone else and to<br />
see amazing results simply<br />
from that information being<br />
passed on. Perhaps we can<br />
be credited with providing<br />
some of the pieces in the<br />
jigsaw but the overall concept<br />
and result belongs to the<br />
individuals we are working<br />
with. The art rooms are an<br />
essential part of our work. They<br />
counteract the impersonal<br />
and often sterile atmosphere<br />
of the hospital and provide<br />
a neutral space for us all.<br />
There are very few rewarding<br />
ways of supporting yourself as<br />
an Artist. This is one of them.<br />
When an individual piece of work<br />
is completed for the first time<br />
by one of the patients, you can<br />
see an amazing pride in that<br />
achievement and it’s always<br />
backed up by support from<br />
other patients in the room.<br />
The training programmes offered<br />
to us are really important and<br />
I’ve picked up lots of new skills<br />
through attending them.<br />
Overall I’ve become more<br />
patient by my involvement in<br />
this kind of work, which has to<br />
be good for my own practice.<br />
69
Alice Shambrook<br />
PATIENT AND ARTIST<br />
70<br />
The paintings don’t feel as though they come<br />
from me. The paint and the brushes take over. I<br />
think I’ve got an Artist’s name. ‘Alice Shambrook’.<br />
I used to work for years and years in a shop in<br />
Sauchiehall Street opposite Glasgow School<br />
of Art. I used to stand in the doorway of the<br />
shop and look up at the School of Art and all<br />
the magic that spilled out of there. Now I’m<br />
an Artist and I’m a part of that same magic.<br />
When I had my stroke I felt like a nobody and a<br />
nothing. Now I feel like someone special when<br />
people say ‘Alice, is that your painting over<br />
there?’ and I say ‘Yes, that’s my painting.’<br />
You see art should be part of the world of<br />
all the ordinary people like me who never<br />
had a chance to be part of the magic.
I think<br />
I’ve got<br />
an artist’s<br />
name.<br />
71
Dr Keith Beard FRCP Edin<br />
CONSULTANT PHYSICIAN,<br />
MEDIC<strong>IN</strong>E FOR THE ELDERLY,<br />
VICTORIA <strong>IN</strong>FIRMARY, GLASGOW<br />
72<br />
Flashes of realization come to me through<br />
personal experiences. I remember one long<br />
stay patient. She used to crochet dishcloths<br />
for the hospital fairs. They were grey and<br />
I remember always associating the grey<br />
dishcloths she was crocheting with her as a<br />
person. Then one day I saw that she had gone<br />
to the art room with one of the artists. She<br />
was completing an acrylic painting of flowers<br />
in very vivid primary colours and I suddenly<br />
realized that I’d completely missed the point.<br />
For a very long time after that incident, I related<br />
to my patients in a different kind of way and<br />
I hope that incident will remain with me as<br />
long as I am working with elderly people.
The other important moment for me in relation<br />
to Art in Hospital was when I finally understood<br />
that the artists weren’t trying to prove<br />
anything through the work they were doing<br />
with patients. They were open, non-prejudiced,<br />
non-judgemental and weren’t setting any goals.<br />
Barbara had always explained to me that the<br />
work wasn’t therapy but I needed to understand<br />
that by seeing it. There was simply an open<br />
acceptance of everyone’s ability and the artists<br />
were sharing these values with my patients.<br />
There was absolutely no sense of imposition.<br />
I don’t know how to measure success in this area<br />
of work. I don’t know if it reduces dependency<br />
on medication. I don’t know if a growth in self<br />
confidence and happiness means a lesser sense<br />
of dependence. There is speculation amongst<br />
my colleagues that the art workshops keep<br />
some of our patients going. I personally had<br />
a patient who I firmly believe found an added<br />
strength to get through her surgery because of<br />
wanting to get back to an unfinished painting.<br />
But to actually measure the cost and benefit<br />
in this area is extraordinarily difficult. What I<br />
do know is that Art in Hospital has been going<br />
for over 13 years and innumerable people have<br />
benefited from this project. Let’s face it, within<br />
the current financial constraints and pressures<br />
of the National Health Service a lot of people<br />
must be lobbying to keep them going. I think<br />
of myself as a Lobbyist for Art in Hospital and<br />
strongly defend their funding wherever I go.<br />
I remember Art in Hospital producing a patient,<br />
Crawford Mitchell’s solo painting show. It was<br />
an extraordinary event but the real moment for<br />
me came later, when I was watching him create<br />
new work in the hospital. He knew exactly what<br />
he was doing and he was clear and focused. As<br />
he became ill and started to disappear, so too<br />
did his work. I think it was at that time that<br />
I understood the work of Art in Hospital.<br />
73
74
Chris Aiton<br />
PATIENT AND ARTIST<br />
I feel relaxed and peaceful<br />
when I’m here. I’ve never been<br />
forced or even asked to come.<br />
It was just a suggestion that<br />
I might enjoy myself. But it’s<br />
more than enjoyment working<br />
with the artists. It’s something<br />
that makes me feel very proud.<br />
I used to knit and I was always<br />
knitting for the family. Now I<br />
paint and that’s what the family<br />
get from me now, my painting.<br />
It’s completely brilliant doing<br />
painting. My family think it<br />
is too. They all came down<br />
to the Art Fair. Everyone got<br />
dressed up and they all came<br />
down to see my painting.<br />
I used to knit…<br />
now I paint.<br />
75
76
77
Maria Vannini<br />
OCCUPATIONAL THERAPY ASSISTANT<br />
78<br />
…the nursing staff<br />
think of Sam in<br />
relation to his art,<br />
Sam, the Artist…<br />
The artists bring a sense of wonder that is so<br />
often lost in an institution. You can call it what<br />
you like but I call it wonder. It would be disastrous<br />
to lose that from this hospital for patients and<br />
staff. The artists have a very special way of seeing<br />
the patients. When people spend large periods<br />
of time in hospitals they become very dependent<br />
and somehow through the art patients are given<br />
back some of that lost independence. What a gift?<br />
Sam never painted before. It’s hard to believe<br />
that now because the nursing staff think of<br />
Sam in relation to his art, Sam, the artist who<br />
is always painting. With his growth in selfconfidence<br />
and self-esteem I have seen a<br />
new physical and mental strength in him.<br />
Sarah had always refused to join any group.<br />
Now I see her confidant, happy and smiling.<br />
She still won’t go to any other group but<br />
she doesn’t miss going to the art room.
79
Alex McKenzie<br />
DIRECTOR OF NORTH GLASGOW<br />
COMMUNITY HEALTH CARE PARTNERSHIP<br />
80<br />
The role of the NHS in Continuing Care is changing<br />
dramatically. Care for the Elderly is becoming less<br />
about clinical intervention and more and more<br />
about ensuring continuing quality of life.<br />
A care package should in theory comprehensively<br />
include priority services and non mainstream<br />
services. Once patients have been discharged<br />
from hospital, we have to consider rehabilitation<br />
and a range of activities to enhance quality of life<br />
and most importantly to avoid readmittance.
We all see the benefits of the work<br />
of Art in Hospital although the<br />
measurable benefits are less easy<br />
to document. I have to measure<br />
numbers, capacities, facilities.<br />
The arts funders have to support<br />
us with the non measurable<br />
benefits of the arts, because their<br />
evaluation systems must take<br />
into account the artists and the<br />
work, which we, within the health<br />
sector cannot do. The aspirations<br />
that we have for holistic provision<br />
for elderly people are much<br />
greater than what we can provide<br />
financially. I can only see those<br />
tensions getting worse. We are<br />
currently looking at social models<br />
of care for the elderly and how to<br />
deliver social care models more<br />
effectively. The pilot projects we<br />
set up with Art in Hospital are in<br />
recognition of those changes<br />
in thinking.<br />
81
82
83
Maureen Henderson O<strong>BE</strong><br />
DIRECTOR OF NURS<strong>IN</strong>G<br />
GREATER GLASGOW NHS<br />
84<br />
I first found out about Art in Hospital in 1993 at<br />
Cowglen as part of the Continuing Care facility.<br />
I began by seeing the work as diversional therapy<br />
and welcomed it in that context but over the last<br />
10 years my views have changed as I understand<br />
the work more. It’s essential for Art in Hospital<br />
to continue and I honestly believe that the<br />
majority of nursing staff are of the same opinion.
There are so many negative stories<br />
about the health service; it’s good to<br />
have a success story. Art in Hospital<br />
has a real credibility because of the<br />
sensitivity the artists have to working<br />
within the confines of a hospital and<br />
because of the quality of work the<br />
patients produce with the support<br />
of the artists. I remember talking to<br />
someone who had been in the art<br />
sessions who told me it was the first<br />
time he had something different to<br />
talk to his relatives about. There’s<br />
an important knock on effect too.<br />
Families can gain a new respect for their<br />
relatives who they may have begun to<br />
see primarily as a patient. That can be<br />
very important for example in a family<br />
discussion about the future of a patient.<br />
85<br />
Life is very dull for people in long term<br />
care. I was delighted to see that Art in<br />
Hospital had extended their services<br />
to the spinal and rehabilitation units.
86
Sam O’Boyle<br />
PATIENT AND ARTIST<br />
I was brought up in the East End<br />
of Glasgow and you didn’t do<br />
art in the East End of Glasgow<br />
when I was a boy. I come to<br />
paint here now twice a week.<br />
I’d come every day if the artists<br />
were here. I like to work with<br />
acrylic. I like charcoal too, but<br />
it’s difficult to control my hands<br />
so the charcoal smudges easily<br />
if you can’t keep a steady hand.<br />
I’ve tried water colours too but<br />
somehow I always go back to<br />
acrylics for the effect I want.<br />
87
88
Maggie Maxwell<br />
VISUAL ARTS OFFICER, SCOTTISH ARTS COUNCIL<br />
Hospitals are microcosms of communities<br />
and within every community, there is always<br />
an Artist. It is a fundamental given with<br />
Art in Hospital that the artists are always<br />
professionally trained and interested in their<br />
own practice. I never question that assurance.<br />
Because of this principle, there is a consistently<br />
high quality of engagement and of work.<br />
I have always fought for the arts funding bodies to<br />
recognize this area of work and to mainstream it<br />
as core provision. Sustainable funding is essential<br />
for the development of the work. It has to be<br />
about partnerships between the arts funders and<br />
the health boards. Between us all, there has to be<br />
an endorsement of artists working in institutions<br />
like hospitals, hospices, day care centres.<br />
In the end it comes down to basic humanity<br />
doesn’t it? Doctors, administrators, patients,<br />
artists, managers. We all know the value of this<br />
kind of provision, we all want to offer it to<br />
patients, we all want to support artists who<br />
choose to work in this field. We see the results.<br />
All of this goes without saying. The problem is<br />
putting the jigsaw together so that we maximize<br />
funding opportunities and take these projects<br />
forward. The evidence base is growing and now<br />
there are mapping exercises to monitor what<br />
is happening in the area of art and health.<br />
89
90
91
Gill Keith<br />
OUTPATIENT AND ARTIST<br />
92<br />
I remember this incredible feeling of relief when I<br />
first found the art space at the hospital. I nearly cried<br />
when someone offered me a choice of teas and a<br />
choice of biscuits. Actually, I think I did cry, with relief.<br />
The circumstances of my life had changed traumatically<br />
overnight and the contact with the artists was the first<br />
time that I was offered the opportunity to acknowledge<br />
that change and to express what was happening inside<br />
my head. It was a totally safe space for that expression<br />
and there were no expectations or assumptions<br />
about what I could or couldn’t do. The artists gave me<br />
information. They responded to what I was trying to say<br />
visually and allowed me to process those thoughts.<br />
Art in Hospital provided me with a level of sanity and self<br />
recognition that I thought I had almost lost. I didn’t know<br />
how to do ‘life’ any more in this new situation. I remember<br />
the feeling of self-affirmation when I was painting and I<br />
realised that the way I felt when I was painting was the<br />
way I had to make myself feel in my day to day life.
93
94
95
ART <strong>IN</strong> HOSPITAL ACKNOWLEDGES SUPPORT FROM<br />
96<br />
This document was made possible through additional funds outwith the core programme.