The Operating Theatre Journal Digital Edition July 2018
The Operating Theatre Journal Digital Edition July 2018
The Operating Theatre Journal Digital Edition July 2018
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
£2.00<br />
<strong>July</strong> <strong>2018</strong> Issue No. 334 ISSN 1747-728X<br />
<strong>The</strong> Leading Independent <strong>Journal</strong> For ALL <strong>Operating</strong> <strong>The</strong>atre Staff<br />
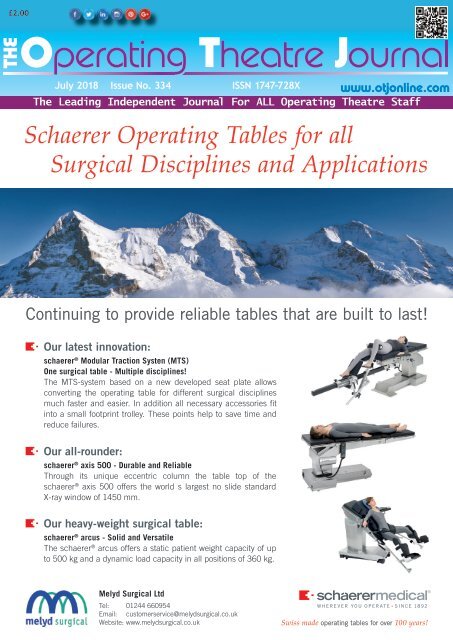
Schaerer <strong>Operating</strong> Tables for all<br />
Surgical Disciplines and Applications<br />
Continuing to provide reliable tables that are built to last!<br />
Our latest innovation:<br />
schaerer ® Modular Traction Systen (MTS)<br />
One surgical table - Multiple disciplines!<br />
<strong>The</strong> MTS-system based on a new developed seat plate allows<br />
converting the operating table for different surgical disciplines<br />
much faster and easier. In addition all necessary accessories fit<br />
into a small footprint trolley. <strong>The</strong>se points help to save time and<br />
reduce failures.<br />
Our all-rounder:<br />
schaerer ® axis 500 - Durable and Reliable<br />
Through its unique eccentric column the table top of the<br />
schaerer ® axis 500 offers the world s largest no slide standard<br />
X-ray window of 1450 mm.<br />
Our heavy-weight surgical table:<br />
schaerer ® arcus - Solid and Versatile<br />
<strong>The</strong> schaerer ® arcus offers a static patient weight capacity of up<br />
to 500 kg and a dynamic load capacity in all positions of 360 kg.<br />
Melyd Surgical Ltd<br />
Tel: 01244 660954<br />
Email: customerservice@melydsurgical.co.uk<br />
Website: www.melydsurgical.co.uk<br />
Swiss made operating tables for over 100 years!
<strong>The</strong> Association for Perioperative Practice<br />
<strong>The</strong> UK’s leading membership association for theatre practitioners<br />
Do you work in<br />
operating theatres?<br />
If so, AfPP can help support you and your career<br />
AfPP Membership Benefits:<br />
Support<br />
Knowledge<br />
Join in,<br />
Join us<br />
• Link member and regional network<br />
• Specialist Interest Groups<br />
• Discussion forums<br />
• Newsletter<br />
• Social networking<br />
• Funding bursaries<br />
• Achievement awards<br />
• Optional Professional Medical<br />
Liability Insurance*<br />
• Job Forum - latest perioperative<br />
job vacancies<br />
Training and Events<br />
• <strong>Journal</strong> of Perioperative Practice<br />
• Online edication<br />
• CPD portfolio and reflective<br />
templates<br />
• Open learning zone<br />
• EBSCO host - scientific journal<br />
archive<br />
• <strong>Journal</strong> archive<br />
• Discounted publications<br />
• Writing for the journal<br />
Advice<br />
Contact us:<br />
membership@afpp.org.uk<br />
01423 881 300<br />
www.afpp.org.uk<br />
• Specialist skills workshops<br />
• Discounted regional and national<br />
educational events<br />
• Speak at events<br />
• Professional clinical advice<br />
• Standards, guidance and best<br />
practice<br />
• Legal advice and representation**<br />
+ Registered membership paid over 12 months by Direct Debit at £8.75 per month, Non-registered membership £7.25 per month,<br />
Student membership £5.00 per month, excludes insurance.<br />
* Full details of the AfPP Professional Indemnity Insurance scheme are available on our website.<br />
Indemnity insurance is an optional membership benefit by application and at additional cost to membership subscription.<br />
** Not valid for Overseas, Retired or Student membership.<br />
<strong>The</strong> Association for Perioperative Practice, Daisy Ayris House, 42 Freemans Way, Harrogate HG3 1DH.<br />
Membership<br />
£8.75 +<br />
per month
<strong>July</strong> <strong>2018</strong> Issue No. 334 ISSN 1747-728X<br />
<strong>The</strong> Leading Independent <strong>Journal</strong> For ALL <strong>Operating</strong> <strong>The</strong>atre Staff<br />
Patient safety<br />
compromised by NHS<br />
understaffing<br />
Royal Colleges join together to reveal results<br />
of annual physician’s survey<br />
Senior doctors have raised new concerns for<br />
patient safety in the NHS across the UK in a new<br />
report released on Tuesday 26 June.<br />
<strong>The</strong> fears are highlighted in “Focus on Physicians<br />
2017 - 18”, the annual census of consultant<br />
physicians and higher speciality trainees (HST)<br />
workforce across the UK. <strong>The</strong> report has<br />
been jointly published by the Royal College of<br />
Physicians and Surgeons of Glasgow, the Royal<br />
College of Physicians of Edinburgh, and the Royal<br />
College of Physicians of London.<br />
<strong>The</strong> survey reveals that more than half of all<br />
consultants and two thirds of trainees reported<br />
frequent gaps in trainees’ rotas, with one in five<br />
respondents saying these are causing significant<br />
problems for patient safety in hospitals , while<br />
three quarters of respondents have highlighted<br />
the workaround solutions they are regularly<br />
having to find.<br />
Other high-level findings include:<br />
• Almost half of advertised consultant posts<br />
remain unfilled because of a lack of suitable<br />
applicants<br />
• Consultants and trainees are working around<br />
10 per cent more than their contracted hours.<br />
This equates to trainees working an extra six<br />
weeks and consultants an extra month unpaid<br />
a year<br />
• Thirty-three per cent of the current consultant<br />
workforce are predicted to reach their<br />
intended retirement age in the next decade.<br />
Medical student places need doubling now to<br />
fill this and the gap left generally by doctors<br />
leaving the profession<br />
• Satisfaction among consultants and trainees<br />
with working in general internal medicine<br />
remains significantly lower than with specialtyworking<br />
Commenting on the findings of the census<br />
Professor David Galloway, President of the Royal<br />
College of Physicians and Surgeons of Glasgow<br />
said: “I’m glad that the three Royal Colleges<br />
have once again joined together to produce this<br />
important piece of work. It’s vital that everyone<br />
involved in the NHS now reflects on these findings<br />
and takes all the action necessary to replicate<br />
best practice and address the challenges that<br />
this document has highlighted.<br />
“What’s of particular concern is the finding<br />
that almost one in five consultants across the<br />
UK reported that rota gaps cause significant<br />
problems for patient safety in their hospital.<br />
This is an unsustainable situation which must be<br />
addressed as a matter of urgency.<br />
“While we welcome short term actions being taken by<br />
governments across the UK to tackle workforce issues,<br />
such as the lifting of the cap on tier 2 visas for NHS staff,<br />
we need consistent and sustained action if we’re to<br />
address this situation in the longer term.<br />
“Government, patients and the medical profession must<br />
work hand in hand if we’re to deliver the best possible<br />
NHS for all.”<br />
Professor Derek Bell OBE, President of the Royal College<br />
of Physicians of Edinburgh, said: “As one of the three<br />
Royal Colleges that commissioned this report, we believe<br />
that Focus on Physicians provides an important snapshot<br />
of the state of play within the medical profession. We<br />
welcome, in particular, that 88% of consultants enjoy<br />
working in their chosen speciality. This indicates a high<br />
level of job satisfaction for consultant specialists.<br />
“Our report also highlights some challenges which must<br />
be tackled head on, and we support any actions which<br />
allow doctors time to care, time to train and time to<br />
research. We believe that these conditions are essential<br />
for job satisfaction, and ultimately for enhancing the<br />
care that our patients receive.”<br />
<strong>The</strong> full census findings can be found at:<br />
https://www.rcpsg.ac.uk/<br />
http://www.rcpe.ac.uk/<br />
https://www.rcplondon.ac.uk/<br />
RCSEd President welcomes<br />
announcement of proposed £20bn<br />
for the NHS but fears it is only the<br />
bare maintenance minimum<br />
Following the Government’s announcement of a<br />
proposed £20bn annual real term increase in NHS<br />
funding in England by 2023-24, Professor Michael<br />
Lavelle Jones, President of the Royal College of<br />
Surgeons of Edinburgh said: “<strong>The</strong> announcement that<br />
the NHS will receive an average 3.4% yearly increase<br />
in NHS funding over the next five years is a significant<br />
step forward and a welcome response to the huge<br />
pressures the service continues to work under.<br />
“However, we do share the concerns expressed<br />
by a range of independent commentators, such as<br />
the Institute of Fiscal Studies, Kings Fund, Health<br />
Foundation and Nuffield Trust, that this represents<br />
the bare minimum that the NHS needs to stabilise<br />
its performance and maintain the current level of<br />
services.<br />
“As the announcement does not appear to cover<br />
important areas such as funding for training, capital<br />
improvements, public health and social care, we are<br />
unsure whether it will be enough to allow the NHS to<br />
expand its workforce and tackle some of the causes of<br />
poor staff morale to make much needed changes such<br />
as integrated care and preventative health.<br />
“That’s why <strong>The</strong> Royal College of Surgeons of Edinburgh,<br />
along with the Federation of Surgical Speciality<br />
Associations and the other surgical Royal Colleges,<br />
are calling for an open and honest debate on the NHS<br />
as it approaches its 70th year. Only through this can<br />
we ensure that the NHS can continue to provide high<br />
quality care and meet the many challenges it faces.”<br />
Inside this issue<br />
State-of-the-art eye<br />
centre opens<br />
Never event at Shropshire<br />
health trust<br />
Patient stayed awake<br />
through 90 minutes<br />
of CPR<br />
RCSEd Faculty of<br />
Pre-Hospital Care<br />
launches new<br />
Diploma<br />
Up to 1,000 patients<br />
suffered harm from<br />
cyber attack<br />
Employers witness<br />
the reserve forces<br />
in action<br />
First UK womb transplant<br />
‘by end of <strong>2018</strong>’<br />
How aspirin may block<br />
bowel tumour<br />
formation<br />
Find out more 02921 680068 • e-mail admin@lawrand.com Issue 334 <strong>July</strong> <strong>2018</strong> 3<br />
P4<br />
P4<br />
P8<br />
P9<br />
P10<br />
P12<br />
P12<br />
P13<br />
Hololens augmented reality<br />
enters the operating<br />
theatre<br />
P14<br />
BRITS ARE PULLING<br />
SICKIES BECAUSE THEY<br />
ARE TOO TIRED<br />
£900 million Future<br />
Leaders investment<br />
Clydebank hospital first to<br />
offer dedicated robotic<br />
surgery<br />
P16<br />
P16<br />
P17<br />
Gene therapy restores paw<br />
function in rats with<br />
spinal cord injury<br />
P17<br />
Pelvic floor problems and<br />
incontinence:<br />
autoprosthesis<br />
Nightingale Health and UK<br />
Biobank announce<br />
major initiative<br />
New Kurt, New Power<br />
UK’s NICE publishes a<br />
Medtech innovation<br />
briefing on PICO<br />
P18<br />
P18<br />
P20<br />
P21<br />
INNOVATION AND REDUCED<br />
COMPLICATIONS IN<br />
THORACIC SURGERY P22<br />
<strong>Digital</strong> system to monitor<br />
recovery room<br />
patients<br />
P22
State-of-the-art eye centre set to transform care for<br />
thousands of patients needing cataract surgery<br />
A brand new state-of-the art £6.7m eye centre<br />
has opened its doors to patients.<br />
<strong>The</strong> new purpose-built centre, which is located<br />
at the Northern General Hospital and follows a<br />
multi-million pound investment from Sheffield<br />
Teaching Hospitals NHS Foundation Trust, is<br />
set to transform care for thousands of patients<br />
needing surgery to treat cataracts, which<br />
commonly affect older people and are the<br />
leading cause of impaired vision throughout<br />
the world.<br />
It is estimated that over half of all people aged<br />
65 and over have some cataract development<br />
in one or both eyes.<br />
Offering some of the best ophthalmic<br />
assessment and surgical facilities in the UK,<br />
the new Northern General Eye Centre is the<br />
first of its kind cataract treatment centre,<br />
providing care for over 5,000 patients across<br />
the Sheffield and South Yorkshire region in<br />
spacious and accessible surroundings.<br />
<strong>The</strong> light, airy facility – which has been<br />
designed with the needs of people with<br />
limited vision in mind – boasts ten consulting<br />
rooms, world-class diagnostic equipment, two<br />
hi-tech operating rooms, a large, welcoming<br />
reception area, dedicated drop off and pick<br />
up points outside the centre, and handy self<br />
check-ins enabling patients to notify staff of<br />
their arrival in a matter of seconds.<br />
As a dedicated centre for cataract surgery,<br />
patients visiting for assessment and treatment<br />
of cataracts will benefit from a unique ‘onestop<br />
approach’. This will mean that they<br />
will now be able to have their outpatient<br />
consultation, all diagnostic tests, preoperative<br />
assessments and consent for surgery<br />
process completed in just one visit, saving<br />
unnecessary repeat trips prior to surgery.<br />
If patients are fit for local anaesthetic<br />
cataract surgery they will be given a date<br />
for their operation before they leave. On the<br />
day of surgery, patients will be seen by the<br />
same consultant they saw at their outpatient<br />
appointment and a named nurse will stay with<br />
them to ‘hold their hand’ during surgery.<br />
Patients often feel nervous prior to having<br />
eye surgery, and research shows that having<br />
a named nurse to accompany them through<br />
the operation decreases anxiety and offers<br />
comfort during the procedure. Refreshments<br />
will also be provided to patients after surgery.<br />
All patients returning for post-operative<br />
check-ups will be able to see their consultant<br />
if necessary and agree a date for surgery in<br />
their other eye if this is needed.<br />
Dalip Malkani, 78, of Bradway, is one of the<br />
first patients in the region to benefit from lifechanging<br />
cataract surgery at the brand new<br />
eye centre. “My vision is much improved in<br />
that eye and the overall quality of my vision<br />
is much better than before,” said the IT<br />
consultant who first started to get a cloudiness<br />
in his vision a year ago and was diagnosed with<br />
a cataract in his right eye.<br />
“<strong>The</strong> staff have been marvellous, they’ve<br />
taken really good care of me and kept me<br />
informed throughout, and I can see things<br />
much more clearly now. My TV looks like it<br />
has much higher resolution than it did before.<br />
I am very fortunate to be in Sheffield and have<br />
world renowned eye specialists.”<br />
Carolyn Wilkie, Operations Director for Head<br />
and Neck services at Sheffield Teaching<br />
Hospital NHS Foundation Trust, said: “We are<br />
delighted to be opening this state-of-the-art<br />
£6.7m facility which will benefit thousands<br />
of patients in the region both now and in<br />
the future. Having cataract surgery can be<br />
a daunting experience, so a huge amount of<br />
planning has gone into the design and set-up of<br />
this building to ensure that every detail, from<br />
patients being able to have a named nurse to<br />
hold their hand throughout surgery to patients<br />
being collected from reception and taken<br />
to the consulting rooms rather than being<br />
called in by the doctor or nurse, improves and<br />
enhances the patients’ experience.<br />
“<strong>The</strong> £6.7m building is a fantastic investment<br />
by Sheffield Teaching Hospitals NHS Foundation<br />
Trust, and not only will patients experience an<br />
extremely high standard of care and have as<br />
much done in one appointment as possible to<br />
avoid unnecessary trips, but by opening up this<br />
facility we will be able to build our services<br />
in the future and ensure that we meet the<br />
increasing demand for cataract eye surgery.”<br />
Cataract surgery is the most commonly<br />
performed operation in the UK, with around<br />
330,000 operations performed each year on<br />
the NHS.<br />
During surgery the lens inside the eye that<br />
has become cloudy is removed and replaced<br />
with an artificial lens to restore clear vision.<br />
If untreated, the clouding can worsen, making<br />
driving and working difficult, and in some<br />
cases, causing complete blindness.<br />
Adult emergency eye care services will<br />
continue to be available from the Royal<br />
Hallamshire Hospital (Monday to Friday,<br />
8.15am to 4.30pm).<br />
For further information about the centre visit<br />
www.sheffieldeyecentre-nhs.uk.<br />
Never event at Shropshire<br />
health trust involved<br />
‘wrong site’ surgery<br />
A serious medical ‘never event’ involving<br />
‘wrong site’ surgery has happened at the<br />
trust running Shropshire’s two main hospitals<br />
<strong>The</strong> never event, named so because they are<br />
incidents that guidelines say should never<br />
happen, was recorded by Shrewsbury and<br />
Telford Hospital NHS Trust (SaTH), which<br />
runs Royal Shrewsbury Hospital and Telford’s<br />
Princess Royal Hospital.<br />
Dr David Lee, chairman of SaTH’s quality<br />
and safety assurance committee, told a<br />
meeting of the trust board yesterday that<br />
an investigation is under way following the<br />
recent incident.<br />
Board members were told it involved ‘wrong<br />
site’ surgery, but the exact details have not<br />
been disclosed.<br />
Dr Lee said the affected patient is currently<br />
recovering.<br />
A report to the board said clinicians have<br />
explained the circumstances to the patient<br />
and family members.<br />
Wrong-site surgery can involve surgery being<br />
performed on the wrong side or site of<br />
the body, the wrong surgical procedure or<br />
surgery on the wrong patient.<br />
In response, the trust’s chief executive<br />
Simon Wright said: “It’s entirely right we<br />
should be taking this extremely seriously.”<br />
<strong>The</strong> trust has recorded two other never<br />
events in the past eight months.<br />
Source: Shropshire Star<br />
<strong>The</strong> next issue copy deadline, Friday 27th <strong>July</strong> <strong>2018</strong><br />
All enquiries: To the editorial team, <strong>The</strong> OTJ Lawrand Ltd, PO Box 51, Pontyclun, CF72 9YY<br />
Tel: 02921 680068 Email: admin@lawrand.com Website: www.lawrand.com<br />
<strong>The</strong> <strong>Operating</strong> <strong>The</strong>atre <strong>Journal</strong> is published twelve times per year. Available in electronic format from the website, www.otjonline.com<br />
and in hard copy to hospitals throughout the United Kingdom. Personal copies are available by nominal subscription.<br />
Neither the Editor or Directors of Lawrand Ltd are in any way responsible for the statements made or views expressed by the contributors.<br />
All communications in respect of advertising quotations, obtaining a rate card and supplying all editorial communications and pictures to the Editor<br />
at the PO Box address above. No part of this journal may be reproduced without prior permission from Lawrand Ltd. © <strong>2018</strong><br />
<strong>Operating</strong> <strong>The</strong>atre <strong>Journal</strong> is printed on paper sourced from Forest Stewardship Council (FSC) approved paper mills and is printed with vegetable based inks. All paper and ink waste is recycled.<br />
<strong>Journal</strong> Printers: <strong>The</strong> Warwick Printing Co Ltd, Caswell Road, Leamington Spa, Warwickshire. CV31 1QD<br />
4 THE OPERATING THEATRE JOURNAL www.otjonline.com
MAT PARTNERS WITH TOLENT CONSTRUCTION FOR RAMSAY<br />
HEALTH CARE’S NEW TEES VALLEY HOSPITAL<br />
Medical Air Technology (MAT) recently completed work at Tees Valley<br />
Hospital, a brand new £23m hospital provided by WW Medical Facilities<br />
and operated by Ramsay Health Care UK, designed to be a bespoke,<br />
patient-centred environment for care and treatment.<br />
<strong>The</strong> hospital is in the grounds of the beautiful 17th century Acklam Hall<br />
and replaces the Tees Valley Treatment Centre. It has 19 beds, consulting<br />
rooms, minor procedure rooms, a diagnostic imaging department, a<br />
physiotherapy department and rehabilitation gym, an inpatient ward<br />
and a day case unit with 12 recovery pods. It also has three ultraclean<br />
operating theatres and an endoscopy suite with recovery room, all<br />
fitted out to the highest standards by MAT, so is able to offer patients<br />
a wide range of surgeries, including orthopaedic procedures. MAT has<br />
a long history of working successfully with Ramsay Health Care and, in<br />
accordance with the client’s wishes, was brought into the Tees Valley<br />
project by the main contractor, Tolent Construction.<br />
MAT provided a turnkey ventilation and equipment package, which<br />
included three ECO-flow ultraclean ventilation (UCV) canopies,<br />
mechanical ventilation systems for the theatres and endoscopy suite<br />
and recovery room, medical gas pendants, surgeons’ panels, operating<br />
lights, pressure stabilisers and firefighter control panels. <strong>The</strong> hospital’s<br />
location close to Acklam Hall, which has a Grade I listing, meant<br />
that the plant room size was restricted to ensure the new building<br />
complemented its historical surroundings. To accommodate this, the<br />
engineers at MAT had to develop a design and ductwork route, unique<br />
to the hospital, that ensured the air handling units fitted into the space<br />
allowed. Dr Andy Jones, Chief Executive of Ramsay Health Care UK,<br />
wanted Tees Valley Hospital to offer “a broader range of services in a<br />
clean, crisp, modern, welcoming environment”, and MAT has helped this<br />
to be realised, providing the hospital with world-class, user-friendly,<br />
energy-efficient operating theatres that will enable and support the<br />
outstanding work of the hospital’s clinical teams.<br />
MAT has worked with Ramsay Health Care UK for many years, installing<br />
operating theatre equipment packages across its hospitals. This year<br />
alone, in addition to Tees Valley Hospital, MAT has installed energyefficient<br />
ECO-flow canopies and other equipment at Rivers Hospital in<br />
Hertfordshire, and Woodland Hospital in Northamptonshire.<br />
MAT FM also holds the service contract for all the hospitals in the group,<br />
ensuring that the critical air system in each facility is compliant and<br />
working correctly, providing a safe environment for patient care and<br />
reducing operating costs.<br />
MAT offers a wide breadth of services so is able to respond flexibly<br />
and quickly to the specific needs of each client. With an in-house<br />
manufacturing facility and dedicated team of highly skilled engineers,<br />
the company makes and supplies bespoke equipment for demanding<br />
clinical arenas. <strong>The</strong>re are several options available, from “equipment<br />
only” packages right up to total turnkey installations, all delivered with<br />
the same commitment to outstanding quality and customer service.<br />
MAT FM can provide a range of competitively priced and highly effective<br />
service and maintenance packages for all core products and turnkey<br />
solutions offered by MAT or other suppliers, ensuring that equipment is<br />
maintained, serviced and validated correctly for optimum performance.<br />
Take a video tour of the new Tees Valley Hospital at:<br />
https://www.gazettelive.co.uk/news/teesside-news/inside-teessidesnew-23m-hospital-14469351<br />
Further information from:<br />
Stephen Taylor, Tel: 0844 871 2100<br />
Email: stephen.taylor@medicalairtechnology.com<br />
www.medicalairtechnology.com<br />
When responding to articles please quote ‘OTJ’<br />
Did YOU know you can read and download<br />
the larger, digital version of <strong>The</strong> <strong>Operating</strong><br />
<strong>The</strong>atre <strong>Journal</strong> for FREE every month?<br />
Simply register at the top right hand corner<br />
of www.otjonline.com and you’ll receive<br />
a notification every time the next issue is<br />
available.<br />
Find out more 02921 680068 • e-mail admin@lawrand.com Issue 334 <strong>July</strong> <strong>2018</strong> 5
An exclusive resource for Practitioners, Nurses, Managers, Clinical Specialists, Anaesthetics, Scrub, PACU, Training & Procurement<br />
ISSN 1747-728X<br />
<strong>The</strong> Leading Independent <strong>Journal</strong> For ALL <strong>Operating</strong> <strong>The</strong>atre Staff<br />
Discover more online!<br />
Join our FREE mailing list at www.otjonline.com and stay in touch with News and Reviews<br />
Queen’s Hospital to help boost health coffers - and here’s how<br />
It comes as Prime Minister <strong>The</strong>resa May has called for action on waste in the NHS<br />
Plastic used in Burton’s Queen’s Hospital’s<br />
operating theatres is now being recycled and<br />
can be sold on to boost health coffers.<br />
<strong>The</strong> Belvedere Road hospital has installed a<br />
recycling machine called a Sterimelt which<br />
turns clinical blue waste, used in operating<br />
theatres, into a product that can make money<br />
for the NHS.<br />
This technology is leading the way as Prime<br />
Minister <strong>The</strong>resa May sent out a call to action<br />
on waste reduction within the NHS.<br />
<strong>The</strong> Prime Minister said that a £20 billion<br />
spending boost to the National Health Service<br />
in the UK would be conditional on them<br />
cutting bureaucracy and waste.<br />
Mrs May, in a speech at the Royal Free Hospital<br />
in London, said: “This must be a plan that<br />
ensures every penny is well spent.<br />
“It must be a plan that tackles waste, reduces<br />
bureaucracy and eliminates unacceptable<br />
variation, with all these efficiency savings<br />
reinvested back into patient care.<br />
“It must be a plan that makes better use of<br />
capital investment to modernise its buildings<br />
and invest in technology to drive productivity<br />
improvements.”<br />
Burton Hospitals NHS Foundation Trust,<br />
which runs Queen’s, started this process with<br />
the installation of a revolutionary recycling<br />
machine called a Sterimelt from multi-awardwinning<br />
Welsh company <strong>The</strong>rmal Compaction<br />
Group.<br />
<strong>The</strong> cutting-edge sustainable recycling<br />
technology has had interest from around<br />
the world and Burton is the first health<br />
service trust in England to have installed this<br />
technology.<br />
Clinical Sterilisation Wrap, the single use<br />
disposable plastic material which is used<br />
in operating theatre’s and for encasing<br />
sterile instruments, is normally mingled with<br />
hazardous material, then incinerated or sent<br />
to special landfill when finished with. This<br />
costs the NHS trust money to dispose of.<br />
However, the Sterimelt machine takes the<br />
blue Sterilisation Wrap and thermally densifies<br />
it into polypropylene blocks that the trust<br />
can then sell on to third party manufacturers<br />
which, in turn, can be made into anything<br />
from a tool box to a plastic hazard warning<br />
sign for water spillages.<br />
Recently, other single use disposable<br />
items have been identified for recycling in<br />
Sterimelt, such as blue polypropylene patient<br />
bed transfer sheets, adding more value to NHS<br />
sustainable recycling.<br />
Other than Burton, <strong>The</strong>rmal Compaction<br />
Group has received interest around England,<br />
particularly in the North East and South West,<br />
for the Sterimelt to be installed in other<br />
trusts, said a spokesman.<br />
Natalie Roddis, the waste and sustainability<br />
officer for Burton Hospitals NHS Foundation<br />
Trust, said: “My colleague James Chadwick<br />
went to a convention where he saw it and<br />
spoke us about it.<br />
“We got in touch with <strong>The</strong>rmal Compaction<br />
Group and they were fantastic and very<br />
responsive. We all jumped into a car and<br />
drove to Wales to see it. We spoke to them<br />
[<strong>The</strong>rmal Compaction Group] and the current<br />
Welsh NHS user about it and it was just as<br />
good as we thought.<br />
“It came at the right time when Blue Planet<br />
was on the TV highlighting plastics (pollution)<br />
in the sea.<br />
“We had it installed in March and we have<br />
not had any problems at all. To get our<br />
uncontaminated clinical waste recycled, it is<br />
fantastic.”<br />
<strong>The</strong> machine has already created interest<br />
from other trusts who have been to Queen’s<br />
Hospital to see it in action.<br />
And Natalie said it is “exciting” to be the<br />
first trust in England to install one of the<br />
revolutionary Sterimelt machines.<br />
She said: “Because it is only the second<br />
commercial Sterimelt to be built by <strong>The</strong>rmal<br />
Compaction Group, there are a couple of<br />
tweaks but the contact we have with the<br />
<strong>The</strong>rmal Compaction Group team means we<br />
just tell them about anything and within a day<br />
or two, they are here from Wales to help us.<br />
“We have had a lot of interest already from<br />
other trusts to come and look at it.”<br />
<strong>The</strong>rmal Compaction Group has won the<br />
Cardiff Business Awards Innovation award<br />
for the Sterimelt, beating three other major<br />
companies to the prestigious trophy.<br />
It also won the Welsh Business Awards<br />
‘Success Thorough Innovation’ category just<br />
three months after final trials on the Sterimelt<br />
and full implementation of the product were<br />
completed at the Aneurin Bevan University<br />
Health Board in South East Wales.<br />
<strong>The</strong>rmal Compaction Group’s sales and<br />
marketing director Thomas Davison-Sebry<br />
said: “It is fantastic to be working with a great<br />
team of people like those at Burton Hospital<br />
NHS Foundation Trust.<br />
“As a private company, at first, we were<br />
unsure how it was going to go with working<br />
with public bodies because this was new to us<br />
but it is incredible.<br />
“We have come up against small issues but we<br />
have worked together as a team, accomplished<br />
and addressed all these and come up with a<br />
fully commercialised machine.<br />
“We have been speaking to people across Asia,<br />
Australia, North America and just recently<br />
signed a distributor in South Africa who are<br />
also enthusiastic about the Sterimelt machine<br />
and can see the potential this possesses<br />
to deliver revenue from waste that would<br />
otherwise be incinerated.”<br />
Source: Derbyshire Live (Jenny Moody)<br />
6 THE OPERATING THEATRE JOURNAL www.otjonline.com
BOA CONGRESS <strong>2018</strong><br />
25th - 28th September, ICC Birmingham<br />
REGISTRATION IS NOW OPEN!<br />
<strong>The</strong> theme for the Congress is<br />
‘Taking stock: Planning the future’<br />
Join us in Birmingham to celebrate our 100th Anniversary!<br />
Register online at:<br />
congress.boa.ac.uk<br />
@BritOrthopaedic #BOAAC British Orthopaedic Association BritOrthopaedic<br />
BOA Congress <strong>2018</strong> (A5) - BESS.indd 1 16/05/<strong>2018</strong> 14:48:09<br />
Doctor: Patient stayed awake through 90 minutes of CPR<br />
A case report said that a man was showing unusual signs of conscious awareness while a medical team performed CPR on<br />
him after he suffered cardiac arrest<br />
COPENHAGEN, Denmark — A new case report said a man who underwent cardiac arrest showed unusual signs of conscious awareness while a<br />
medical crew performed CPR on him.<br />
CNN reported that the medical team performed CPR on the 69-year-old man for 90 minutes when he suffered cardiac arrest shortly after being<br />
admitted to a hospital for indigestion and nausea.<br />
“At this time, paramedics were still in the room, and CPR was initiated immediately,” Dr. Rune Sarauw Lundsgaard said. “Due to a recent event<br />
with another patient, the cardiac arrest team was in the next room, and advanced CPR was initiated shortly after. This means that two paramedics<br />
and four hospital porters were shifting in pairs of two at performing the CPR. <strong>The</strong> patient had no electrical activity in the heart at any time. <strong>The</strong><br />
heart only functioned because of the manual compressions.”<br />
Lundsgaard said the patient occasionally showed signs of conscious awareness while CPR was performed on him.<br />
“As soon as CPR was initiated, the patient opened his eyes,” he said. “When CPR was performed, the patient was able to respond to verbal<br />
communication by moving eyes, lifting hands and legs and nodding his head. <strong>The</strong> patient’s wife was present and able to hold his hand.”<br />
Dr. Sam Parnia, who led a study on the topic in 2014, said it is extremely unusual for patients to show such a level of consciousness during CPR.<br />
“It is exceedingly rare for people to have actual awareness with external signs of being conscious as is being discussed in this case report,” Parnia<br />
said. “All the studies of CPR have demonstrated that there is insufficient blood flow to the brain (approximately 15 percent of baseline blood flow)<br />
to allow for the return of brain stem reflexes and consciousness with external signs of being awake.”<br />
Parnia added that “it is much more likely to have people waking up during compressions when the additive effect on an already beating heart<br />
raises the blood pressure to a sufficient level to provide enough blood flow to the brain.”<br />
Lundsgaard said CPR is usually stopped when a patient begins to appear conscious.<br />
“Normally, chest compressions are stopped once the patient shows signs of life or spontaneous breathing,” he said. [When] the patient moved, we<br />
stopped CPR, and immediately the patient went unconscious due to his nonfunctioning heart. This was done several times with the same result.”<br />
Dr. Parnia said the team performed CPR for much longer than is customary.<br />
“Most hospitals will stop at around 20 minutes. However, based on results of studies, it is recommended to continue for at least 45 minutes. This<br />
is unusual,” he said.<br />
Despite the lifesaving efforts, the team was unable to save the patient.<br />
“<strong>The</strong> cardiac arrest team in our case was very affected by the situation,” Lundsgaard said. “For me, having to tell the patient that we were unable<br />
to save his life ... and that in a minute we will stop chest compressions and you will not survive was a challenging situation.”<br />
Lundsgaard said the incident brought up the issue of sedating patients during CPR.<br />
“<strong>The</strong> question of sedation during CPR is not new, but sedation is not routinely performed during CPR,” he said. “We know from anesthesia that<br />
accidental awareness during operations often leads to post-traumatic distress and decreased quality of life. One might suspect that awareness<br />
during CPR may be just as stressful.”<br />
Source www.ems1.com<br />
8 THE OPERATING THEATRE JOURNAL www.otjonline.com
JRI Orthopaedics celebrates gold standard ratings<br />
for hip replacement systems<br />
“<strong>The</strong> 13A* rating demonstrates<br />
the abundance of evidence about<br />
the Furlong as one of the best<br />
performing stems on the market –<br />
cemented or uncemented.”<br />
JRI Orthopaedics’s, state-of-the-art manufacturing facility in Sheffield<br />
JRI Orthopaedics’ pioneering<br />
uncemented hip implant system<br />
has been awarded the highest<br />
rating by ODEP – the Orthopaedic<br />
Data Evaluation Panel - in<br />
recognition of its clinical<br />
performance.<br />
<strong>The</strong> multi-award-winning company<br />
has received a 13A* rating – the<br />
highest possible award – from<br />
ODEP for both its long-established<br />
Furlong® Uncemented H.A-C<br />
coated hip stem and CSF® cup.<br />
JRI Orthopaedics was the first<br />
company in the world to produce a<br />
hip implant with a Hydroxyapatite<br />
(HAC) coating enabling a biological<br />
bond with the patient’s bone and<br />
so the prospect of a hip for life.<br />
<strong>The</strong> Furlong HAC stem was<br />
launched in 1985 and is now one<br />
of the leading uncemented hips<br />
on the UK market. It is one of only<br />
six such products to be given the<br />
gold standard 13A* rating by ODEP.<br />
ODEP independently assess<br />
whether orthopaedic products<br />
have reached quality performance<br />
benchmarks in accordance with<br />
the National Institute for Health<br />
and Care Excellence (NICE)<br />
guidelines for survivorship of total<br />
hip replacements.<br />
John Suggitt, Senior Product<br />
Manager at Sheffield-based JRI<br />
Orthopaedics, said: “ODEP ratings<br />
provide a simple, independently<br />
verified assessment of the<br />
strength of evidence of an<br />
implant, assessed against national<br />
clinical best practice guidelines by<br />
an independent panel of experts.<br />
“We are absolutely delighted to<br />
have received the highest 13A*<br />
rating for the Furlong® HAC hip<br />
stem and CSF® Acetabular Cup.<br />
“Only six uncemented stems and<br />
cups have 13 A* ratings and so we<br />
feel very proud to be part of such<br />
an exclusive club of excellence.<br />
ODEP award ratings for clinical<br />
evidence at three, five, ten<br />
and now 13 years of total hip,<br />
knee and shoulder replacement<br />
products.<br />
JRI Orthopaedics’s next<br />
generation uncemented hip<br />
replacement system, the Furlong<br />
Evolution®, was launched in 2012<br />
and has just received an ODEP 5A*<br />
rating – the highest award after<br />
five years of impressive clinical<br />
evidence.<br />
John added: “We manufacture<br />
and supply products that<br />
provide the best solutions for<br />
joint replacement, repair and<br />
reconstruction allowing patients<br />
to have a better quality of life for<br />
longer.<br />
“<strong>The</strong> 5A* ODEP rating for the<br />
Evolution® shows just how<br />
good this technology is and that<br />
the next generation is just as<br />
good which is why these hip<br />
replacements come with our 20-<br />
year warranty.”<br />
JRI Orthopaedics has worldclass<br />
expertise in the design,<br />
development and manufacture<br />
of a portfolio of orthopaedic<br />
implants and systems which<br />
deliver the best solutions in<br />
joint reconstruction, repair and<br />
regeneration.<br />
JRI Orthopaedics’s<br />
Furlong® Uncemented<br />
H.A-C coated hip stem<br />
which is made at the<br />
company’s state-ofthe-art<br />
manufacturing<br />
facility in Sheffield.<br />
<strong>The</strong> company, which<br />
employs over 100 people at<br />
its showcase manufacturing<br />
facility in Chapeltown, has<br />
internationally recognized<br />
research and development<br />
capabilities.<br />
Earlier this year JRI<br />
Orthopaedics was acquired<br />
by China’s leading<br />
orthopaedic implant<br />
company AK Medical in a<br />
£16.7M deal. <strong>The</strong> company,<br />
which was wholly owned<br />
by the charity Orthopaedic<br />
Research UK (ORUK), is now part<br />
of one of the world’s largest<br />
3D-printed orthopaedic implant<br />
manufacturers.<br />
<strong>The</strong> synergy created by combining<br />
the two businesses will create a<br />
larger and stronger group within<br />
the international orthopaedic<br />
sector.<br />
Latest ODEP ratings can be found<br />
at www.odep.org.uk<br />
When responding to articles please quote ‘OTJ’<br />
RCSEd Faculty of Pre-Hospital Care launches new Diploma in Urgent Medical Care<br />
<strong>The</strong> Royal College of Surgeons of Edinburgh (RCSEd), Faculty of Pre-Hospital<br />
Care, is the first medical Royal College to develop a Diploma in Urgent<br />
Medical Care (DipUMC RCSEd), targeted at the many thousands of nurses,<br />
doctors and paramedics that provide essential healthcare across the UK<br />
when GP surgeries are closed.<br />
Colville Laird, Convener for Examinations in Urgent Medical Care RCSEd,<br />
explained: “<strong>The</strong> diploma is to start the thinking about professional<br />
development in this important area of healthcare. For example, the<br />
Government has said it wants 15,000 more paramedics. Career progression<br />
and professional development in this vital area of healthcare needs support<br />
because much of the healthcare patients experience will be delivered by this<br />
group of multi-professional practitioners, which includes nurses, paramedics<br />
and doctors providing out-of-hours (OOH)/Urgent Care services.”<br />
Pre-hospital Emergency Medicine is an established sub-speciality of medicine<br />
provided by a broad range of practitioners: first aiders; paramedics; doctors;<br />
nurses; first responders; and emergency service professionals that include<br />
the police, fire and armed forces. <strong>The</strong> role of the RCSEd’s Faculty is to set<br />
and maintain clinical standards for practitioners in this evolving specialty.<br />
<strong>The</strong> new Diploma in Urgent Medical Care exam will focus on the timely<br />
recognition, diagnosis and management of conditions and situations in urgent<br />
care settings, which can present a variety of challenges to practitioners.<br />
Practitioners will already have skills equivalent to level 7 of the<br />
Skills for Health Career Framework for Health, and be able to<br />
demonstrate knowledge and skills to manage complex and atypical<br />
cases. <strong>The</strong> syllabus includes the care of patients from all age<br />
groups from neonates to the very elderly.<br />
Students will self-study for the two-day exam supported by an<br />
extensive syllabus and study guidance available on the RCSEd<br />
website. Day one of the exam is a written paper, and day two oral<br />
is a structured oral exam. Applications for the diploma close on 2<br />
November <strong>2018</strong>, and the two-day exam takes place at the RCSEd<br />
in Edinburgh on 12 and 13 March 2019.<br />
Colville Laird concludes: “We hope that by setting up a postgraduate<br />
diploma open to a multi-professional group of healthcare<br />
practitioners we will raise the awareness of continuing professional<br />
development (CDP) in an essential area of healthcare provision.”<br />
For more information about the work of the Faculty go to<br />
https://fphc.rcsed.ac.uk/my-fphc/about-us<br />
For more information about the Diploma in Urgent Medical Care go<br />
to https://www.rcsed.ac.uk/exams/exam-entry?calId=5a512efa-<br />
1345-44e8-a209-ef6d47d0b12d&locName=Edinburgh<br />
Find out more 02921 680068 • e-mail admin@lawrand.com Issue 334 <strong>July</strong> <strong>2018</strong> 9
Up to 1,000 patients suffered<br />
harm from medical devices<br />
hit by a cyber attack<br />
As many as 1,000 patients suffered harm from medical devices hit by a<br />
cyber attack, according to a new survey conducted by researchers at<br />
the University of California San Diego. <strong>The</strong> results were announced at<br />
the HIMSS Healthcare Security Forum recently.<br />
Commenting on this, Garrett Sipple, managing consultant at Synopsys’<br />
Software Integrity Group, said “This is another example of recognising<br />
the importance of security as it plays a role in maintaining the safety<br />
and effectiveness of medical devices. Medical devices often move<br />
through long product development cycles that can make them slow to<br />
react to new cybersecurity threats, especially if cybersecurity wasn’t<br />
even a key consideration in the development process.<br />
Cyber-attacks aren’t the only side effect to consider when it comes to<br />
medical device security. In a survey Synopsys ran with Ponemon last<br />
spring, it was found that in 38% of cases where a medical device had<br />
been breached, inappropriate health care had been delivered to the<br />
patient – and that could be lethal.<br />
One of the prevalent themes in this document is the critical role that<br />
systems must play in the healthcare sector, because there is shared<br />
responsibility among regulators, manufacturers, healthcare providers,<br />
and patients. While software security has been discussed for many<br />
years, fewer people are talking about systems security and integrating<br />
security into systems engineering. <strong>The</strong> healthcare industry must solve<br />
this problem at the system-of-systems level, as well as for individual<br />
products like MRI machines and patient monitors.<br />
Well known technical activities such as static code analysis are<br />
important, but so are non-technical elements like risk management<br />
processes and program-level prioritisation of resources based on<br />
identified risk.<br />
Many of the recommendations are already understood and documented.<br />
One specific example is the recommendation that stronger mechanisms<br />
are<br />
“<strong>The</strong><br />
needed,<br />
measures<br />
but there<br />
Sir Bruce<br />
is no<br />
Keogh<br />
silver bullet.<br />
outlined<br />
That<br />
during<br />
concept<br />
his speech<br />
is fully embodied<br />
last night<br />
in<br />
will<br />
the<br />
be<br />
BSIMM<br />
instrumental<br />
framework.<br />
in supporting<br />
BSIMM identifies<br />
healthcare<br />
a superset<br />
professionals<br />
of 113<br />
to<br />
security<br />
identify<br />
the early signs and enable them to act, Health Education England’s new<br />
activities that have been used to build security into systems. Leveraging<br />
education and training materials will be particularly relevant as will a<br />
this superset to identify new activities is one step organisations can<br />
clinical network approach to care where professionals and organisations<br />
take. <strong>The</strong> key message from this is that evaluating security at every<br />
work together across a dened geographical area – this helps to bring<br />
layer in a product or system lifecycle – systems, software, firmware,<br />
a safe, standardised and equitable approach to care.<br />
hardware – is the only way to fundamentally build security into a<br />
product.”<br />
Further “As a college, reading: we https://www.fiercehealthcare.com/tech/ucsdmedical-device-cybersecurity-patient-harm-advamed-legacy-devices<br />
Child Health Record to include information for parents on how to tell<br />
have updated the national template for the Personal<br />
if your child is ill, and for health professionals, have recently launched<br />
Paediatric Care Online (PCO-UK) – an online decision support tool,<br />
providing specialist diagnostic advice to help ensure children get the<br />
right treatment at the earliest opportunity.<br />
“To support this, I now urge paediatricians and all healthcare<br />
professionals to utilise the resources Sir Bruce has outlined. Collectively<br />
we www.facebook.com/<strong>The</strong>OTJ<br />
can slow down the grip of this deadly disease and reduce the number<br />
of children who come face to face with it.”<br />
Louise Silverton, Director for Midwifery at the Royal College of<br />
Midwives, said: “Severe sepsis can and does kill. Though it is rare, it<br />
can be catastrophic for pregnant and postnatal women.<br />
Nurse Led Clinics - Preoperative assessment<br />
(2-Day Programme)<br />
“Sepsis remains a leading cause of maternal death. That is why it is so<br />
important that we do all we can to identify it as soon as possible so that<br />
it can be treated. It is also important not to forget newborn babies who<br />
can succumb to infection very quickly.<br />
Thursday 5th and Friday 6th <strong>July</strong> <strong>2018</strong><br />
“Midwives <strong>The</strong> Royal Marsden should certainly Education “think and sepsis” Conference where Centre there is deterioration<br />
in Stewart’s the health Grove, of either Chelsea, mother SW3 or 6JJbaby. This means we need the right<br />
number of midwives so that they can deliver the best possible care,<br />
<strong>The</strong> study days are aimed at nurses and other health care professionals<br />
including in the postnatal period.<br />
with an interest in preoperative assessment; they will cover a wide<br />
range of clinical and organisational topics facilitated by specialist<br />
“Having nurses and the consultant right numbers anaesthetists. of staff will also help to ensure continuity<br />
of care and carer for women. Midwives who know the woman will be<br />
better For further equipped information to spot and changes to book in the your woman’s place please condition visitand identify<br />
problems www.royalmarsden.nhs.uk/studydays<br />
such as sepsis developing.”<br />
TCI & BIS Practicum<br />
Friday 21st September <strong>2018</strong><br />
<strong>The</strong> Royal Marsden Education and Conference Centre<br />
Stewart’s Grove, London, SW3 6JJ<br />
A highly practical one day course delivering:<br />
- Consultant led teaching and advice, by clinicians using TCI and BIS<br />
everyday<br />
- Small group ‘hands on’ clinical workshops, using simulation with<br />
BIS<br />
- Problem solving and trouble shooting<br />
- TCI in a wide range of settings<br />
For further information and to book your place please visit<br />
www.royalmarsden.nhs.uk/studydays<br />
Exenterative Surgery for Pelvic Cancers:<br />
Current Practices and Future Directions<br />
Thursday 27th - Friday 28th September <strong>2018</strong><br />
<strong>The</strong> Royal Marsden Education and Conference Centre<br />
Stewart’s Grove, London, SW3 6JJ<br />
Professor This conference Helen Stokes-Lampard, presents new Chair information of the Royal concerning College GPs, opioids said:<br />
“Sepsis examining is a scientific huge worry and for clinical GPs as subjects initial germane symptoms to can patients be similar and<br />
to practitioners.<br />
other common illnesses, and the College is putting a lot of effort<br />
into Novel helping opioid-related family doctors topics recognise and updates potential on existing sepsis issues and ensure will seek that<br />
patients to educate rapidly those receive who appropriate deal with opioids assessment in whatever and treatment. professional<br />
“We capacity. have produced a toolkit, in partnership with NHS England, which<br />
brings For further together information existing and guidance, to book your training place materials please visit and patient<br />
information www.royalmarsden.nhs.uk/studydays<br />
to encourage us all to ‘think sepsis, talk sepsis and treat<br />
sepsis’.<br />
“We are pleased to be working with NHS England to raise awareness<br />
and improve outcomes for patients. It really could save lives.”<br />
Anna Crossley, Professional Lead for Acute, Emergency & Critical<br />
Care at the RCN, said: “Sepsis is a life-threatening condition and early<br />
identication is the key to survival, but it can be difcult to diagnose<br />
and often symptoms can be mistaken for a u-like illness. This is why<br />
raising<br />
<strong>The</strong><br />
awareness<br />
11th Royal<br />
among carers,<br />
Marsden<br />
health<br />
Pain<br />
care professionals<br />
and Opioid<br />
and the<br />
public is so vital. Even though Conference<br />
there has been good progress to improve<br />
diagnosis, a cohesive national plan is needed to ensure that healthcare<br />
professionals Thursday are 16th supported – Friday and equipped 17th to November identify and treat <strong>2018</strong> sepsis<br />
early.<br />
<strong>The</strong> Royal Marsden Education and Conference Centre<br />
“If Stewart’s sepsis is Grove, not recognised London, SW3 quickly, 6JJ it can lead to shock, multiple organ<br />
failure and death, which is why early detection is critical to start<br />
treatment This conference within the presents hour. Nurses new and information health care concerning support workers, opioids<br />
who examining see their scientific patients and on clinical a regular subjects basis, germane and are to often patients the and rst<br />
healthcare practitioners. worker to see them, are well placed to recognise the signs<br />
of sepsis early and raise the alarm. If a person has signs or symptoms<br />
Novel opioid-related topics and updates on existing issues will seek<br />
that indicate possible infection, think ‘could this be sepsis?’ and act<br />
to educate those who deal with opioids in whatever professional<br />
fast to raise the alarm, wherever you are.<br />
capacity.<br />
https://www.england.nhs.uk/wp-content/uploads/2015/08/Sepsis-<br />
For further information and to book your place please visit<br />
Action-Plan-23.12.15-v1.pdf<br />
www.royalmarsden.nhs.uk/conferences<br />
twitter.com/OTJOnline<br />
10 Find out more 02921 680068 • e-mail admin@lawrand.com THE OPERATING THEATRE JOURNAL Issue 316 January www.otjonline.com<br />
2017 7
<strong>The</strong>atres and Anaesthesia<br />
Conference <strong>2018</strong><br />
“Patient Centred Care”<br />
n<br />
<strong>The</strong> Leeds<br />
Teaching Hospitals<br />
NHS Trust<br />
Saturday 13th October <strong>2018</strong>, 09:00 - 16:00<br />
Bridge Community Church, Rider Street, Leeds, LS9 7BQ<br />
Think<br />
Drink<br />
Patient<br />
Engagement<br />
Leeds<br />
Improvement<br />
Method<br />
Day case<br />
Challenge<br />
Tickets<br />
£40<br />
To book a place please visit:<br />
https://theatres-and-anaesthesia.eventbrite.co.uk/<br />
As all Getinge Flow models, the Flow-c hav<br />
For more information please contact Vicky Tye via:<br />
Email: v.tye@nhs.net Tel: 0113 206 5580<br />
feature.This safety mechanism overrules th<br />
and oxygen if the O2 level should drop belo<br />
Getinge to launch the Flow-c Anesthesia Machine at the<br />
Euroanaesthesia Congress<br />
Getinge, a leading global provider of innovative medical technology, announced its<br />
attendance at <strong>The</strong> Euroanaesthesia Congress (ESA) in Copenhagen which ran from June<br />
2 – 4, <strong>2018</strong> and the official launch of the Flow-c Anesthesia Machine. Euroanaesthesia<br />
is Europe’s largest annual event showcasing the latest developments in the field of<br />
anesthesia, perioperative medicine, intensive care, emergency medicine and pain<br />
treatment and this event was expected to attract over 5000 participants.<br />
‘We are excited to announce that Getinge will launch the Flow-c Anesthesia Machine<br />
at this major international event. Flow-c is a compact anesthesia machine where<br />
every detail has been designed to ease the daily work, enabling cost-efficient and<br />
safe treatment for patients, says Markus Stirner-Schilling, Senior Director, Acute Care<br />
<strong>The</strong>rapies, Global Commercial Operations.<br />
sia Machine<br />
About Flow-c:<br />
Based on the world-class Servo ventilator platform and with the same innovative<br />
technology as Flow-i, the Flow-c ensures superior ventilation performance with the<br />
power and precision needed to ventilate all patient categories.<br />
“<strong>The</strong> Flow-c is designed to simplify everyday anesthesia workflow in the fast-paced<br />
gy, announces OR.<strong>The</strong> today intuitive its attendance and easy to use touch screen gives one point of control for all<br />
functions, and the system’s operational simplicity saves time and contributes to<br />
June 2 – improved 4, <strong>2018</strong> mobility and the official in the ORs,” says Lena Evander, Director Product Management<br />
is Europe’s Anesthesia largest at annual Getinge. event<br />
, perioperative<br />
Despite<br />
medicine,<br />
its compact<br />
intensive<br />
design, Flow-c packs in a great rail length using every millimeter<br />
t is expected of space. to attract <strong>The</strong> stepless over 5000 rails allow monitors, tables and other accessories to be added<br />
where it best suits the user. And with the neatly routed back, covered by specially<br />
designed panels, Flow-c minimizes the clutter of hoses and cables, and contributes to<br />
an improved hygiene and safety in the OR.<br />
c Anesthesia Machine at this major<br />
As all Getinge Flow models, the Flow-c have the unique O2Guard to prevent hypoxia<br />
ere every as detail a standard has been feature.This designed safety mechanism overrules the clinician´s settings and<br />
nt for patients, increases says Markus the flow Stirner-<br />
of fresh gas and oxygen if the O2 level should drop below 21%.<br />
rcial Operations. Read more and watch the film about the new Getinge Flow-c:<br />
https://www.getinge.com/int/product-catalog/flow-c-anesthesia-machine<br />
When responding to articles please quote ‘OTJ’<br />
Please visit the booth to ‘experience the flo<br />
Find out more 02921 680068 • e-mail admin@lawrand.com Issue 334 <strong>July</strong> <strong>2018</strong> 11<br />
ame innovative technology as Flow-
Employers witness the<br />
reserve forces in action<br />
Employers within the NHS were recently invited to observe reservist<br />
training taking place at the North Atlantic Treaty Organisation (NATO)<br />
Saber Strike exercise in Poland.<br />
During the visit, employers were able to witness first-hand how<br />
beneficial the training exercises were for the reservists and how these<br />
skills can be transferred into the NHS workforce.<br />
Clinicians from the UK worked side by side with medics from the<br />
US army’s 212 combat support hospital during the exercise, which<br />
consisted of two weeks training, involving 19 countries and 18,000<br />
troops. Throughout the exercise, NHS reservists tackled complex<br />
training scenarios including major incidents and chemical, biological,<br />
radiological and nuclear attacks.<br />
David Cox, senior operating department practitioner at University<br />
Hospitals Coventry & Warwickshire NHS Trust said:<br />
“Prior to the visit to Poland, I was not fully aware of the range of<br />
medical specialities supplied by reservists. I now have much more<br />
awareness and a fuller understanding of what reservists can do.<br />
“<strong>The</strong>y have a broader range of experience in challenging situations,<br />
where team work and flexibility are essential. By being a reservist, it<br />
demonstrates the motivation and commitment of the individual.<br />
“I would say to any employer with reservists as part of their workforce:<br />
your staff will be committed, motivated and have a broader range of<br />
clinical experiences in emergency care. This ultimately enables better<br />
standards of patient care within the NHS.”<br />
Heena Asher, general manager of Stroke and Neurosciences at Imperial<br />
College healthcare NHS Trust added:<br />
“I was overwhelmed at the size of the training exercise and the<br />
partnership with the US Army. I was amazed by the levels of respect,<br />
focus and coordination between the reservists to deliver clinical care.<br />
“<strong>The</strong> exercise made it very clear that reservists shine as leaders, inspire<br />
their colleagues and are focused on getting things right the first time.<br />
“As a trust, we need to ensure that we’re doing everything we can to<br />
support reservists so that we attract these people with such expert<br />
qualities to work in our organisation.”<br />
To find out more about recruiting and supporting reservists in your NHS<br />
workforce, visit our dedicated web pages - http://www.nhsemployers.<br />
org/your-workforce/retain-and-improve/managing-your-workforce/<br />
supporting-the-armed-forces-in-the-nhs.<br />
Are You Linkedin ?<br />
Join our Group<br />
<strong>The</strong> <strong>Operating</strong> <strong>The</strong>atre <strong>Journal</strong><br />
When responding to articles please quote ‘OTJ’<br />
in TM<br />
First UK womb transplant ‘by end of <strong>2018</strong>’<br />
<strong>The</strong> surgeon planning to do the first womb transplant in the UK says<br />
he hopes to carry out the first operations “before the end of <strong>2018</strong>”.<br />
Mr Richard Smith, clinical lead at the charity Womb Transplant UK, also<br />
said that they plan to use living donors.<br />
In 2015, approval was given for 10 womb transplants in the UK, but<br />
these were from deceased donors, whose hearts are still beating.<br />
Now the team plans to use both live and cadaveric donors.<br />
Mr Smith, a consultant gynaecologist at Queen Charlotte’s and Chelsea<br />
Hospital in London, said this was because the procedure to retrieve a<br />
womb from a living donor was now simpler and safer, with the surgery<br />
time cut from 12 to four hours.<br />
Around 750 women in the UK have approached the team to enquire<br />
about transplantation.<br />
Womb Transplant UK says it has enough funds to pay for three transplants<br />
but will need hundreds of thousands of pounds more to complete a<br />
total of 15 transplants - five of these with living, related donors.<br />
Around 6,000 women in the UK were born without a womb, while others<br />
lose their uterus to cancer.<br />
At present, their only chance of having a genetically-related child is<br />
through surrogacy.<br />
A global review of womb transplants has found that the procedure is a<br />
“major advance” but requires strictly controlled clinical trials.<br />
Writing in BJOG: An International <strong>Journal</strong> of Obstetrics and<br />
Gynaecology, a team of doctors in Japan said while womb transplants<br />
offer “great hope” for women born without a uterus, the practice is<br />
still experimental.<br />
Womb transplants to date:<br />
Womb transplants have been carried out in 10 countries: Saudi Arabia,<br />
Turkey, Sweden, US, China, Czech Republic, Brazil, Germany, Serbia<br />
and India.<br />
• 2014 - woman in Gothenburg, Sweden gives birth to a baby boy using<br />
a transplanted womb in world first. <strong>The</strong> 36-year-old mother received<br />
the donated womb from a friend in her 60s<br />
• 2017 - woman in Dallas, Texas gives birth to a baby, in the first<br />
successful procedure in the US<br />
• 42 women worldwide have received transplanted wombs<br />
• 11 babies have been born, eight of them in Sweden<br />
Surgical risk<br />
<strong>The</strong> paper is the first global review of womb transplantation.<br />
It says surgical risk is the major concern due to the difficulty of obtaining<br />
the uterine veins which run along the pelvic floor.<br />
In a trial in Sweden involving nine patients, the average time to remove<br />
the uterus from a living donor was 11.5 hours, with 4.5 hours for the<br />
recipient surgery.<br />
A team in China reduced the time of living donor organ retrieval to<br />
six hours using robot-assisted surgery, and the ovarian vein as an<br />
alternative to the uterine veins.<br />
How would the procedure work in the UK?<br />
• Women being considered for a womb transplant will undergo clinical<br />
and psychological investigations as would any potential living donors<br />
• Living donors are likely to be the mother or sister of the recipient<br />
• <strong>The</strong> recipient will need to take immunosuppressant drugs following<br />
the transplant and throughout pregnancy to prevent their body<br />
rejecting the donor organ<br />
• After six months, if there are no complications, the woman will have<br />
frozen embryos implanted, created from her eggs and her partner’s<br />
sperm<br />
• If all goes well, the baby will be delivered by caesarean section<br />
between 35-37 weeks gestation<br />
• Couples will be given the option of trying for two pregnancies<br />
• Once it is no longer needed, the womb will be removed to allow the<br />
recipient to stop taking immunosuppressant drugs<br />
Mr Smith told the BBC that after a preliminary selection process,<br />
the team was in contact with around 50 women who were potential<br />
recipients.<br />
Some of these women had close relatives who were willing to donate<br />
their wombs.<br />
He said: “<strong>The</strong> new method of live donor retrieval changes the equation<br />
to make it much safer.<br />
“It is still major surgery but the risk of clot formation, DVT and damage<br />
to pelvic organs is greatly reduced, making it an acceptable approach.”<br />
<strong>The</strong> surgery will take place in NHS transplant centres, but the costs will<br />
be paid for by the charity, and team members will give their services<br />
free.<br />
Source: BBC News Fergus Walsh<br />
12 THE OPERATING THEATRE JOURNAL www.otjonline.com
Registered Anaesthetic Technician<br />
North Shore & Waitakere Hospital & Elective Surgical Centre<br />
Waitemata District Health Board<br />
New Zealand<br />
• Diverse<br />
• Team Culture<br />
• Variation of specialties<br />
If you are an Anaesthetic Technician who is interested in joining our<br />
dynamic, proactive hardworking team on a permanent basis, long with<br />
extending your practice; then we want to hear from you<br />
You will be joining a team of 40 Registered Anaesthetic Technicians who<br />
collectively cover three sites working 24/7. You will need to have a broad<br />
range of experience in many surgical and anaesthetic specialities including:<br />
ENT, Obstetrics, Gynaecology, and Emergency Department, Intensive care,<br />
also being part of the Cardiac Arrest team and out of hospital transfer.<br />
You will need to have the following:<br />
• Excellent communication skills and will fit seamlessly into our multidisciplinary<br />
team.<br />
• Registered Anaesthetic Technician or eligible to be registered with the<br />
Medical Sciences Council of New Zealand.<br />
To be considered for this position or to view the position description,<br />
please apply online at: www.wdhbcareers.com<br />
For further information please email Julie Bromley<br />
julie.bromley@waitematadhb.govt.nz<br />
View the Benefits for working for Waitemata District Health Board<br />
www.wdhbcareers.com/Benefits<br />
Job code: NOR03459<br />
Closing date: 31st <strong>July</strong> <strong>2018</strong><br />
www.wdhbcareers.com<br />
www.operatingtheatrejobs.com<br />
Wish You Were Here<br />
<strong>Operating</strong> Department Practitioners/RGNs:<br />
We are currently recruiting <strong>The</strong>atre Practitioners<br />
with either Scrub and First Assistant or Recovery<br />
and Advanced Life Support qualifications, to work<br />
in Torquay.<br />
This is a great opportunity to join a dedicated<br />
theatre team and receive a variety of benefits, in<br />
addition to a competitive salary.<br />
So if you are keen to flourish and grow beside the<br />
sea, we would love to hear from you. Interested?<br />
<strong>The</strong>n please visit our website to apply or telephone:<br />
01803 321640 for further information<br />
https://www.atscloud.co.uk/ramsayhealthcare/<br />
vacancies.aspx?lstLocation=15<br />
How aspirin may block bowel<br />
tumour formation<br />
Researchers have shed light on how taking aspirin can help to prevent<br />
bowel cancer. <strong>The</strong>y found that the painkiller blocks a key process linked<br />
to tumour formation.<br />
Regular use of aspirin is known to reduce a person’s risk of developing<br />
colon cancer but the drug’s tumour-fighting properties have not been<br />
well understood.<br />
Researchers at the University of Edinburgh, funded by the MRC and<br />
BBSRC, focused on a structure found inside cells called the nucleolus.<br />
Activation of the nucleolus is known to drive tumour formation and its<br />
dysfunction has also been linked to Alzheimer’s and Parkinson’s.<br />
<strong>The</strong> team tested the effects of aspirin on cells grown in the lab and on<br />
tumour biopsies from colon cancer patients.<br />
<strong>The</strong>y found that aspirin blocks a key molecule called TIF-IA, which is<br />
essential for the nucleolus to function.<br />
Not all colon cancer patients respond to aspirin but the researchers say<br />
their findings could help pinpoint those most likely to benefit.<br />
Aspirin has side effects that include internal bleeding and it can cause<br />
certain types of stroke. Long term use is not recommended. <strong>The</strong><br />
researchers say the study paves the way for the development of new,<br />
safer therapies that mimic aspirin’s effects.<br />
Dr Lesley Stark of the Cancer Research UK Edinburgh Centre, MRC<br />
Institute of Genetics & Molecular Medicine at the University of<br />
Edinburgh, said: “We are really excited by these findings as they suggest<br />
a mechanism by which aspirin may act to prevent multiple diseases. A<br />
better understanding of how aspirin blocks TIF-IA and nucleolar activity<br />
provides great promise for the development of new treatments and<br />
targeted therapy.”<br />
<strong>The</strong> research, published in Nucleic Acid Research, was also supported<br />
by Worldwide Cancer Research, Bowel and Cancer Research and <strong>The</strong><br />
Rosetrees Trust.<br />
This article is adapted from materials supplied by the University of<br />
Edinburgh.<br />
Find out more 02921 680068 • e-mail admin@lawrand.com Issue 334 <strong>July</strong> <strong>2018</strong> 13
Hololens augmented reality enters the operating<br />
theatre at Imperial College<br />
Hololens augmented reality technology is being used during surgery at<br />
Imperial College. We spoke to Dr Philip Pratt about introducing the AR<br />
headsets into the operating theatre.<br />
Imperial College London is trialling Microsoft’s mixed reality Hololens<br />
headsets for skin graft surgeons at St Mary’s Hospital, London.<br />
While at first glance, the Microsoft Hololens headset appears identical<br />
to a VR headset, this technology in fact creates a ‘mixed’, rather than<br />
virtual, reality.<br />
This is where a layer of augmented reality is overlayed on top of the<br />
physical world, and can be used to enhance our perception of physical<br />
objects. <strong>The</strong> tech has currently found applications in manufacturing and<br />
construction, but is now being used, perhaps to most groundbreaking<br />
effect, in medicine.<br />
“We have these incredible machines in the basement of the hospital<br />
- the CT and MRI scanners - that can essentially give us pictures of<br />
what’s inside the patient...We can see all of that on the screen, but the<br />
way that information is currently used in the operating theatre is so<br />
antiquated,” says Dr Philip Pratt, research fellow at the Department of<br />
Surgery and Cancer at Imperial College London.<br />
Now, using the Hololens headsets, Pratt wants to give surgeons access<br />
to these images while they are actually performing surgery, starting<br />
with skin grafts at St Mary’s Hospital, London.<br />
Skin grafts are suitable for the types of injury which result in trauma<br />
to the flesh - for example, those resulting from car accidents or severe<br />
burns.<br />
To heal the area, a piece of healthy skin is taken from a different part of<br />
the body and attached to the damaged area. However, importantly, it<br />
must be attached in a location where it can be connected with a blood<br />
supply, to ensure the skin does not die.<br />
<strong>The</strong>refore, locating the position of major blood vessels under the skin<br />
surface is of the utmost importance in this type of surgery. In most<br />
hospitals around the world, this form of surgery involves a painstaking<br />
process where a sterile ruler is used to map out measurements taken<br />
from a scan, making multiple, small incisions on the skin’s surface.<br />
Another option is to use an instrument which amplifies blood flow,<br />
the Doppler Ultrasound Probe, to try to detect the location of blood<br />
vessels.<br />
“That’s a very approximate method and there’s no guarantee that<br />
where x marks the spot, you’ve actually got the right place. It’s very<br />
important that when you make your incisions, you’re exactly on top<br />
of the vessels of interest - it can take a long time to locate,” says Dr<br />
Pratt. “Time in operating theatres is very precious, you’ve got a lot of<br />
surgeons in the room and time is money,” he says, pointing out that it’s<br />
also preferable to reduce the amount of time patients need to be kept<br />
under general anaesthetic.<br />
----S ubscribe<br />
to the OTJ<br />
Information on the location of blood vessels is available from a CT<br />
scan - something that has been around since the ‘70s. However, it has<br />
been hard to mirror this two dimensional information onto the patient’s<br />
body. Until Hololens, that is.<br />
“Hololens came along and I immediately thought, yes, this is a classic<br />
clinical problem that we can use the technology to help solve,” says Dr<br />
Pratt. “Because what surgeons want to do is visualise the interior of the<br />
patient and overlay that information intraoperatively.”<br />
<strong>The</strong> technology is currently being used in the hospital for any cases that<br />
require lower limb reconstructive surgeries.<br />
<strong>The</strong> Hololens ability to tether the overlayed images onto physical<br />
landmarks means that the accuracy of the image mapping is crucially<br />
preserved even when the body part moves. However, as this is the<br />
first time the technology has been used in this setting, lower limb<br />
surgeries were selected because the large, rigid bone structures in the<br />
legs means that there is less movement of the blood vessels when the<br />
patient changes position.<br />
With a background in robotic surgery, Dr Pratt himself wrote the code<br />
for the software used in the hospital. He points out that to work, he had<br />
to make the technology as simple to use as possible.<br />
“[<strong>The</strong> surgeons] did adapt to it very quickly. It has to be very intuitive<br />
in terms of how you manipulate the images, how you align images to<br />
the patient. If it takes someone more than you know 30 seconds or a<br />
minute to get the hang of it, then you’ve not done the job properly.”<br />
So far, the feedback from surgeons has been overwhelmingly positive.<br />
“<strong>The</strong>y’re delighted with it,” he says.<br />
So, what could be next for the tech? Some of the immediate future<br />
applications also involve surgery where locating particular blood<br />
vessels is imperative.<br />
An obvious area where this is true is breast reconstructive surgery,<br />
following breast cancer for example. Another potential area is colon<br />
or rectum cancers, where an MRI scan identifying the tumour could<br />
be projected onto the area during surgery to ensure that all of the<br />
malignant tissue is excised. However, as this involves more fluid,<br />
flexible structures, it will be more challenging to map imagery onto this<br />
area of the body.<br />
However - despite being a pioneer of innovation in the medical sphere<br />
- Dr Pratt cautions against over-zealous attitudes towards technology.<br />
“We have to go first to the problem and not the solution,” he says. “It’s<br />
not about taking a piece of technology and finding something to use it<br />
for. Instead, we have to start with a problem and then find the most<br />
appropriate technology to help it.”<br />
Right now, the technology can only be used by hospitals associated with<br />
Imperial College, including St Mary’s, Charing Cross and Hammersmith<br />
Hospitals. However, Dr Pratt is focused on increasing the number of case<br />
studies conducted using the technology, with the goal of eventually<br />
having the technology rolled out to every hospital in the UK.<br />
This will involve a laborious, regulatory process before it can become<br />
a standardised tool across the NHS. But this aim remains firmly within<br />
the sights of the tech.<br />
“My driving motivation behind this is to see it used as often and as<br />
geographically widespread as possible,” says Dr Pratt. “I want it to be<br />
not just in one hospital or 10 hospitals, but 100 or 1,000 hospitals.<br />
That’s definitely part of the grand scheme.”<br />
Delivered to your door every month<br />
It’s easy to subscribe, just visit our website at www.otjonline.com and pay via Card or Paypal.<br />
Have your own personal copy of the <strong>Operating</strong> <strong>The</strong>atre <strong>Journal</strong><br />
Subscribing to the OTJ costs just £14.00 per year to cover delivery in the UK,<br />
For corporate and overseas customers just £24.00<br />
Visit: www.otjonline.com/subscription.php<br />
or Email: admin@lawrand.com<br />
Source: Computerworld UK (Laurie Clarke)<br />
14 THE OPERATING THEATRE JOURNAL www.otjonline.com<br />
----<br />
--------------------------------
www.<strong>Operating</strong><strong>The</strong>atreJobs.com<br />
A one-stop resource for ALL your theatre related Career opportunities<br />
View the latest vacancies online !<br />
<strong>The</strong>atre Practitioners Recovery Nurses Anaesthetic Nurses ODPs<br />
Scrub Practitioners Nurse Practitioners Medical Representatives<br />
and Clinical Advisers<br />
Find out more 02921 680068 • e-mail admin@lawrand.com Issue 334 <strong>July</strong> <strong>2018</strong> 15
An exclusive resource for Practitioners, Nurses, Managers, Clinical Specialists, Anaesthetics, Scrub, PACU, Training & Procurement<br />
ISSN 1747-728X<br />
<strong>The</strong> Leading Independent <strong>Journal</strong> For ALL <strong>Operating</strong> <strong>The</strong>atre Staff<br />
Congratulations you are reading the extended <strong>Journal</strong> online!<br />
BRITS ARE PULLING SICKIES<br />
BECAUSE THEY ARE TOO<br />
TIRED TO WORK<br />
A staggering quarter of Brits are routinely “too tired” to go to work and<br />
one in twenty workers have called in sick up to four times in the last<br />
year due to feeling sleep deprived after either a poor quality or not<br />
enough sleep the night before according to new research from Bensons<br />
for Beds.<br />
Bensons for Beds has conducted a sleep wellness survey which looked<br />
into the nation’s sleep patterns and found that the average adult gets<br />
just six hours of sleep per night, despite claiming they need at least<br />
eight hours in order to feel rested!<br />
Of those that do drag themselves into the office, one fifth have nodded<br />
off on public transport commuting to work, and people admitted to also<br />
falling asleep in meetings and at their desks.<br />
70 percent say a poor night’s sleep and tiredness affects their ability to<br />
do their job effectively, with 60 percent of the 2,500 full-time workers<br />
surveyed claiming that work and family stresses were the biggest<br />
causes of anxiety. However, almost a quarter of Brits blame their sleep<br />
problems on their partner’s snoring!<br />
Harveys Chief Customer Officer, Henry Swift said: “At Bensons for Beds,<br />
we take sleep and wellness seriously which is why our in-store experts<br />
are on hand every day to help you get the best night’s sleep you can.<br />
We have everything you need to get the most out of your bedroom<br />
environment, which is crucial to set you on your way to a good night’s<br />
sleep. Our Comfort Station Adaptive, for example, uses our unique<br />
body-track technology to help you find the perfect mattress firmness<br />
and our exclusive iGel range with temperature regulating technology,<br />
warms you up when you get too cold, and cools you down when you<br />
get too hot.”<br />
Stephanie Romiszweski, Sleep Physiologist at the Sleepy Head Clinic<br />
added: “Making sure your bedroom environment is suitable for you<br />
is the first step to achieving the most out of sleep. Once you have<br />
done this, if you are still struggling to sleep it’s time to look at your<br />
behaviour. Try and keep a regular wake time, and whilst having the<br />
same sleep ‘opportunity’ is important, it doesn’t mean going to bed<br />
when you are anxious or not sleepy just because the clock on the wall<br />
says so.<br />
“Only go to bed once you are really sleepy and spend the rest of your<br />
sleep opportunity enjoying yourself and finding things that make you<br />
feel good. That way work and the days events are less likely to impact<br />
on the quality of your sleep. Remember it’s all about quality and not<br />
quantity<br />
£900 million Future Leaders<br />
investment will sustain the UK as<br />
global home of research talent<br />
Business Secretary Greg Clark recentl unveiled a major new £900<br />
million investment in the UK Research and Innovation Future Leaders<br />
Fellowship Scheme.<br />
<strong>The</strong> inaugural UKRI Future Leaders Fellowship Scheme will receive £900<br />
million over the next 11 years, with six funding competitions and at<br />
least 550 fellows awarded over the next three years.<br />
<strong>The</strong> investment will provide up to seven years of funding for earlycareer<br />
researchers and innovators, including support for part-time<br />
awards and career-breaks, providing flexibility to researchers to tackle<br />
ambitious and challenging research questions.<br />
Business Secretary Greg Clark said: “We are a nation of innovators, with<br />
some of the world’s greatest inventions created on British soil – from<br />
penicillin to the first computer program. We want to retain our global<br />
reputation as a destination for world-class scientists and researchers,<br />
by providing opportunities to find and nurture the next Ada Lovelace<br />
and Isaac Newtons.<br />
“I want the UK to remain the go-to destination for the best researchers<br />
and innovators and that is why we are investing in the rising stars of<br />
research and innovation to develop the new products and technologies<br />
of tomorrow.”<br />
Previous investment in new talent has funded research into new cancer<br />
drugs and developed critical technology which will bring us driverless<br />
cars. Today’s announcement will build on this success and boost the<br />
pipeline of talent needed to build a Britain fit for the future. <strong>The</strong><br />
money, which is part of the single biggest investment in science in 40<br />
years, will help ensure the UK invests 2.4% of GDP in R&D by 2027 and<br />
becomes the most innovative economy by 2030.<br />
Chief Executive of UK Research and Innovation, Professor Sir Mark<br />
Walport said: “Talented people are the energy and engine of new<br />
knowledge, new ideas and new opportunities. <strong>The</strong> long-term investment<br />
announced today means the UK will continue to attract and grow<br />
the very best, supporting those who want to solve the most difficult<br />
questions whether they are in frontier science, our evolving society or<br />
our changing economy.”<br />
www.ukri.org<br />
www.<strong>Operating</strong><strong>The</strong>atreJobs.com<br />
A one-stop resource for ALL your theatre related Career opportunities<br />
View the latest vacancies online !<br />
16 THE OPERATING THEATRE JOURNAL www.otjonline.com
Clydebank hospital first to<br />
offer dedicated robotic surgery<br />
system to chest patients<br />
A Scottish hospital has become the first in the UK to dedicate a stateof-the-art<br />
robotic surgery system for the use of lung patients, a move<br />
which could have a transformational impact on recovery times. <strong>The</strong><br />
£1.3million Da Vinci system enables surgeons to perform operations<br />
through a few small incisions, instead of more invasive procedures<br />
which take longer to heal.<br />
While the machine has been installed at several NHS facilities across<br />
the country, the one installed at the Golden Jubilee National Hospital<br />
in Clydebank is the first to be used solely by a thoracic services unit.<br />
Clinicians believe the system will pay for itself in the long term by<br />
allowing patients to return home quicker and require less care as their<br />
outcomes are improved.<br />
Cardiothoracic consultant Alan Kirk, who has used the Da Vinci on<br />
lung patients, said: “It is probably standard of care for most urology<br />
or prostate cancer work and recently over the past five years in the<br />
UK people have diversified and started using it for chest surgery. “We<br />
are the first unit in the whole of the UK to buy one specifically for lung<br />
surgery. “Although it looks very complicated, it’s really an extension of<br />
what we already do on a keyhole and minimally invasive platform, but<br />
this takes things one stage further forward. “Over the past five years,<br />
we’ve gone from big open operations for lung cancer to 80 per cent of<br />
our lung cancer procedures now being done by conventional keyhole<br />
surgery and now there is a natural extension of that, which we hope<br />
and anticipate will result in improved patient outcomes.”<br />
Mr Kirk added his colleagues at other hospitals had to compete with<br />
various departments for access to their respective Da Vinci system. He<br />
continued: “Our plan over the next 18 months is to develop this to the<br />
stage that those who need or want robotics will be able to get it. One of<br />
the reasons we are at this stage is that we are one of the biggest units<br />
in the UK. “But we now have the ability to operate on more people<br />
with lung cancer – of which there are 4,600 cases in Scotland each year.<br />
Twenty years ago, only 10 per cent got an operation. Now it’s in excess<br />
of 25 per cent.” <strong>The</strong> robotics system also benefits the surgeons who use<br />
it as well as the patients.<br />
“<strong>The</strong> vision you get is high-definition and in 3D and is fantastic,”<br />
added Mr Kirk. “You’re looking at 360 articulation, which you cannot<br />
have working under your own hand. <strong>The</strong> precision of the surgery, the<br />
dexterity, and the vision makes it better for all.” <strong>The</strong>re are currently<br />
38 units delivering lung cancer and chest surgery across the UK, eight<br />
of which have access to robotics. Case study: Climbing the stairs a<br />
week after surgery is no problem for one patient Living on the top floor<br />
of a tenement block with no lift could seem a daunting prospect for<br />
many patients recovering at home from major surgery. But Geraldine<br />
MacAulay, 55, is already able to routinely scale the more than 80<br />
steps to her flat in Glasgow’s leafy west end district, despite having<br />
undergone treatment in April at the Golden Jubilee National Hospital<br />
in Clydebank.<br />
<strong>The</strong> optometrist was diagnosed that same month with adenocarcinoma,<br />
a malignant tumour formed from glandular structures in epithelial tissue.<br />
This meant she had to undergo a lower left lobectomy, which entailed<br />
the removal of part of the lower left lobe of her lung due to cancer.<br />
Such surgery would previously have entailed a long and often painful<br />
period of convalescence due to its invasive nature. Instead, Geraldine is<br />
managing her recovery by simply taking four paracetamol tablets each<br />
day. It follows surgery using a state-of-the-art Da Vinci system, which<br />
is controlled by a surgeon from a console in the operating theatre. <strong>The</strong><br />
hospital is the first unit in the UK to dedicate such a robotics system to<br />
lung patients within its thoracic services team. “<strong>The</strong> diagnosis was a<br />
bolt out of the blue,” she told <strong>The</strong> Scotsman. “It was mooted around two<br />
weeks before that my operation would be something more unusual. “I<br />
was quite happy. I was of course pleased with anything that would give<br />
me a better outcome, and to support something progressive. Geraldine<br />
was in hospital for five nights, and was back “out and about” just a<br />
week later. “It’s a daunting prospect having any kind of surgery as well<br />
as being diagnosed with cancer,” she continued. “But my situation was<br />
definitely helped, despite the traumatic experience of being diagnosed,<br />
by having an easier experience (post-surgery)<br />
Gene therapy restores paw function<br />
in rats with spinal cord injury<br />
Medical Research Council (MRC)-funded researchers at King’s College<br />
London have shown that rats with spinal cord injuries can re-learn<br />
skilled hand movements after being treated with a gene therapy.<br />
People with spinal cord injury often lose the ability to perform<br />
everyday actions that require coordinated hand movements, such as<br />
writing, holding a toothbrush or picking up a drink. Regaining hand<br />
function is the top priority for patients and would dramatically improve<br />
independence and quality of life. No regenerative treatments are<br />
currently available.<br />
<strong>The</strong> researchers, whose work is published in the journal Brain, tested<br />
a new gene therapy for regenerating damaged tissue in the spinal cord<br />
that could be switched on and off using a common antibiotic.<br />
Professor Elizabeth Bradbury from the Institute of Psychiatry,<br />
Psychology & Neuroscience (IoPPN) said: “What is exciting about our<br />
approach is that we can precisely control how long the therapy is<br />
delivered by using a gene switch. This means we can hone in on the<br />
optimal amount of time needed for recovery. Gene therapy provides a<br />
way of treating large areas of the spinal cord with only one injection,<br />
and with the switch we can now turn the gene off when it is no longer<br />
needed.”<br />
After a traumatic spinal injury, dense scar tissue forms which prevents<br />
new connections being made between nerve cells. <strong>The</strong> gene therapy<br />
causes cells to produce an enzyme called chondroitinase which can<br />
break down the scar tissue and allow networks of nerve cells to<br />
regenerate.<br />
Most human spinal cord injuries occur at the neck level and affect all<br />
four limbs. <strong>The</strong> researchers gave the gene therapy to rats with spinal<br />
injuries that closely mimicked the kind of human spinal injuries that<br />
occur after traumatic impacts such as car crashes or falls.<br />
Dr Emily Burnside from the IoPPN explains: “Rats and humans use a<br />
similar sequence of coordinated movements when reaching and grasping<br />
for objects. We found that when the gene therapy was switched on for<br />
two months the rats were able to accurately reach and grasp sugar<br />
pellets. We also found a dramatic increase in the spinal cord of the<br />
rats, suggesting that new connections had been made in the networks<br />
of nerve cells.”<br />
<strong>The</strong> researchers had to overcome a problem with the immune system<br />
recognising and removing the gene switch mechanism. To get around<br />
this, the researchers worked with colleagues in the Netherlands to add<br />
a ‘stealth gene’ which hides the gene switch from the immune system.<br />
Professor Joost Verhaagen at the Netherlands Institute for Neuroscience<br />
says: “<strong>The</strong> use of a stealth gene switch provides an important safeguard<br />
and is an encouraging step toward an effective gene therapy for spinal<br />
cord injury. This is the first time a gene therapy with a stealth on/off<br />
switch has been shown to work in animals.”<br />
<strong>The</strong> gene therapy is not yet ready for human trials. While the ability<br />
to switch a therapeutic gene off provides a safeguard, the researchers<br />
found a small amount of the gene remained active even when switched<br />
off. <strong>The</strong>y are now working on shutting the gene down completely and<br />
moving towards trials in larger species.<br />
<strong>The</strong> research is funded by the International Spinal Research Trust and<br />
Wings for Life, as well as the MRC.<br />
We are pleased to accept<br />
clinical articles for publication<br />
within the pages of<br />
<strong>The</strong> <strong>Operating</strong> <strong>The</strong>atre <strong>Journal</strong><br />
Please send for the attention of the<br />
Editor at:<br />
admin@lawrand.com<br />
Source: <strong>The</strong> Scotsman Chris McCall<br />
Find out more 02921 680068 • e-mail admin@lawrand.com Issue 334 <strong>July</strong> <strong>2018</strong> 17
Pelvic floor problems and incontinence:<br />
autoprosthesis significantly improves<br />
quality-of-life<br />
Meeting of the International Urogynecological Association in Vienna under the leadership of MedUni Vienna/Vienna General Hospital<br />
Due to their anatomical difference and also the particular stresses<br />
associated with pregnancy and childbirth, incontinence and pelvic<br />
floor problems are particularly prevalent in women. Apart from<br />
incontinence, women can also develop pelvic floor muscle weakness,<br />
overstretching of the pelvic connective tissue and displacement of<br />
the pelvic organs. <strong>The</strong>ir quality-of-life can be significantly improved<br />
by surgical transplantation of endogenous tissue to strengthen the<br />
affected area of the pelvic floor.<br />
“This is therefore a form of autoprosthesis,” summarises Heinz Kölbl,<br />
Head of the Division of General Gynecology and Gynecologic Oncology at<br />
the Department of Obstetrics and Gynecology, MedUni Vienna/Vienna<br />
General Hospital. Kölbl is also head of the local organising committee<br />
for the 43rd Annual Meeting of IUGA (International Urogynecological<br />
Association), the largest conference in the world in this field, which will<br />
took place in the Austria Center Vienna on 27 – 30 June <strong>2018</strong>.<br />
In this surgical procedure – which is performed when conservative<br />
techniques or medications have failed to achieve the desired result<br />
– endogenous tissue is taken from an area adjacent to the affected<br />
area, tautened and allowed to scar over, thereby producing the desired<br />
strength. Says Kölbl: “On average that improves quality-of-life for<br />
affected patients by at least 30%.” Research is also being conducted<br />
into the use of external stem cell tissue. Says Kölbl: “It is our vision<br />
that, in future, we will be able to insert external tissue that is even<br />
stronger and more functional, using minimally invasive techniques.”<br />
Currently many patients still suffer a relapse, requiring a second or<br />
even third operation to strengthen their pelvic floor.<br />
Viennese pelvic floor unit is a world leader<br />
<strong>The</strong> pelvic floor unit within MedUni Vienna/Vienna General Hospital’s<br />
Department of Obstetrics and Gynecology is a world leader – a fact that<br />
is underscored by the large number of urogynecological conferences<br />
held in Vienna. <strong>The</strong> ESGE 27th International Congress of the European<br />
Society of Gastrointestinal Endoscopy will also be held in Vienna in<br />
October – with the focus on women’s health. Researchers in Vienna are<br />
currently conducting studies using GenePatterns to develop risk profiles<br />
for subsequent major pelvic floor damage. “So that we can potentially<br />
establish in advance that women from the high-risk group should not<br />
be allowed to give birth naturally, for example, in order to prevent<br />
subsequent incontinence or other pelvic floor damage,” explains Kölbl,<br />
who is also a member of MedUni Vienna/Vienna General Hospital’s<br />
Comprehensive Cancer Center. A similar risk profile already exists for<br />
women who are less than 160 cm tall: they should no longer be allowed<br />
to give birth naturally, if the embryo weighs more than 4,000 g. Says<br />
Kölbl: “That would give them a 100% risk of developing pelvic floor<br />
problems.”<br />
One in three women has bladder problems over the course of her life<br />
and one in 25 women experiences pelvic floor problems after childbirth.<br />
And around 3% of all women are affected by symptomatic forms of<br />
pelvic floor prolapse.<br />
For more information: www.iugameeting.org<br />
Nightingale Health and UK Biobank announce major initiative to analyse<br />
half a million blood samples to facilitate global medical research<br />
Comprehensive metabolic biomarker profiles of the world’s largest health database to be analysed in 30 months.<br />
Nightingale Health, the Finnish innovator of an internationally<br />
recognized blood biomarker technology for studying chronic diseases,<br />
will analyse the biomarker profiles of 500,000 blood samples from UK<br />
Biobank. <strong>The</strong> ground-breaking research initiative was announced today<br />
at the UK Biobank Scientific Conference <strong>2018</strong> in London.<br />
Nightingale’s biomarker profiling technology will be used to analyse UK<br />
Biobank blood samples by measuring metabolic biomarkers that recent<br />
studies have found are predictive of future risk for heart disease, type<br />
2 diabetes and many other common chronic diseases. Until recently,<br />
technological constraints and prohibitive costs have prevented the<br />
analysis of comprehensive metabolic data from large-scale biobank<br />
collections, but this process has been made viable by Nightingale’s<br />
technology, which measures over 200 metabolic biomarkers in a single<br />
blood test.<br />
This initiative will further enrich the world’s most detailed public<br />
health database provided by the UK Biobank.<br />
Professor Sir Rory Collins, UK Biobank’s Principal Investigator, said<br />
the commitment by Nightingale to perform these assays would allow<br />
researchers around the world to advance health research more quickly.<br />
He expects the combination of these biomarker data with the detailed<br />
health information that participants have already provided to generate<br />
many new insights. “We are delighted to see these novel blood sample<br />
analyses being done in UK Biobank,” said Professor Collins. “We already<br />
have an enormous amount of information about the lifestyles and<br />
genetic make-up of the participants in UK Biobank, as well as about<br />
their health, and are currently conducting imaging studies of their<br />
brains, hearts and bodies. Providing the medical research community<br />
with these additional high quality metabolic biomarker data on such<br />
a large scale will enhance discovery science and population science,<br />
providing opportunities to benefit patient care and public health.”<br />
“Analysing 500,000 blood samples from a single study with Nightingale’s<br />
comprehensive biomarker profiling technology allows us to uncover<br />
metabolic signatures that reflect a risk for future disease onset, as<br />
well as their underlying risk factors. We anticipate this detailed<br />
molecular readout of the health state, combining both lifestyle and<br />
genetic makeup, will result in a wealth of scientific applications from<br />
the research community. This will be relevant not only to the British<br />
population but also yield ground-breaking science and enhanced drug<br />
development opportunities with a global public health impact,” said<br />
Dr. Peter Würtz, Scientific Director and Founder, Nightingale Health.<br />
Nightingale Health’s technology has been previously used to analyse<br />
more than 500,000 blood samples from over 200 cohort studies and<br />
clinical trials around the globe, with more than 150 peer-reviewed<br />
publications showcasing how the detailed metabolic biomarker data<br />
provide novel insights into health and disease.<br />
“Nightingale’s mission is strongly linked to scientific evidence<br />
generation. This means working with world-leading institutions and<br />
biosample collections to continuously improve the understanding of<br />
health and disease. Our aim is to translate this understanding into<br />
improved early prediction of diabetes and cardiovascular diseases,<br />
achieving better healthcare for everyone. Our initiative with the UK<br />
Biobank demonstrates Nightingale’s unwavering commitment towards<br />
supporting innovative medical science carried out by researchers from<br />
across the world,” said Teemu Suna, CEO and Founder, Nightingale<br />
Health.<br />
<strong>The</strong> initiative corresponds to over 10 million EUR investment in UK<br />
Biobank and will be funded by Nightingale Health, with analyses of<br />
UK Biobank samples being performed at Nightingale’s laboratory in<br />
Finland. In line with the founding principles of the UK Biobank, this<br />
metabolomic data will be incorporated back into the UK Biobank’s<br />
resource following a 9 months exclusivity period for Nightingale Health<br />
and made openly available to the scientific community.<br />
For more information, please visit https://www.nightingalehealth.com<br />
18 THE OPERATING THEATRE JOURNAL www.otjonline.com
NNATIONAL CONFERENCE *<br />
INNOVATION AND EFFICIENCY IN THE<br />
<strong>Operating</strong> <strong>The</strong>atre<br />
Department<br />
6 th<br />
ATIONAL CONFERENCE *<br />
Tuesday, 13th November <strong>2018</strong> Crowne Plaza, City Centre, LIVERPOOL £279pp<br />
<strong>The</strong> 6th national <strong>Operating</strong> <strong>The</strong>atre Department conference<br />
focus is on efficiency, innovation and effectiveness which is<br />
reflected prominently in the programme.<br />
<strong>The</strong>re is an excellent mix of evidence and cases from clinical practice from all over the UK and<br />
Ireland. <strong>The</strong> event is an opportune resource to network with nationwide colleagues providing<br />
evidence, anecdote and information to take back to your own operating theatres.<br />
Attended by <strong>The</strong>atre Managers, Senior <strong>Operating</strong> Department and Perioperative Practitioners,<br />
Educationalists, Nurses, ODPs, Clinical Managers and Government leads.<br />
INCLUDES:<br />
• Re-defining metrics for change and improvement<br />
in theatres<br />
• Efficiency under pressure - A Quality Champion Project<br />
• Financial effectiveness in the <strong>Operating</strong> <strong>The</strong>atres<br />
• <strong>The</strong> Empty Recovery Room<br />
• ISO 9001:2015 industrial standard for a clinical area?<br />
• Debriefing as an education tool in the <strong>Operating</strong> <strong>The</strong>atre<br />
• How Intra Operative Cell Salvage transformed our<br />
department and Trust<br />
• Development of an innovative collaborative approach<br />
to Peri-operative training programmes<br />
HOW TO<br />
BOOK<br />
Online: www.mkupdate.co.uk E: bookings@mkupdate.co.uk<br />
T: 01768 773030 and SMS: 07375 032963 (Mon - Fri)<br />
CONFERENCES<br />
professionals<br />
training professionals<br />
since 1992<br />
M&K Update Ltd, Keswick, Cumbria CA12 5AS<br />
Tel: 01768 773030<br />
www.mkupdate.co.uk
New Kurt, New Power | PatientSafe Network<br />
New Kurt, New Power<br />
<strong>The</strong>re would always be the laggards who would do everything they<br />
could to maintain the status quo.<br />
<strong>The</strong> closer the messengers got to delivering the change the greater the<br />
bullying and intimidation would become. All the messengers had to do<br />
was put up with all the shit that was flung their way.<br />
Please note – the Please Kurts note – the depicted Kurts depicted in these in images and this and story this are not story real are not real<br />
Someone told Old Kurt that clearly displaying his name and role was<br />
Someone told Old Kurt that clearly displaying his name and role was better for communication, team<br />
better for communication, team work and ultimately patient safety and<br />
work and ultimately patient safety and care.<br />
care.<br />
Old Kurt was offended having never done this before. He felt he was being told he hadn’t been doing his<br />
Old Kurt was offended having never done this before. He felt he was<br />
job to the best of his ability. He was understandably a bit annoyed.<br />
being told he hadn’t been doing his job to the best of his ability. He was<br />
understandably a bit annoyed.<br />
New Kurt, New Power | PatientSafe Network<br />
And so he looked for ways to rebuff what had been said:<br />
<strong>The</strong>y knew they’d be able to, having been exposed to far worse and<br />
realising what was at stake.<br />
Eventually Old Kurt relented (in this story he does anyway).<br />
It took Old Kurt a while and required a lot of searching within himself<br />
and yes, courage.<br />
He had to accept that displaying his name and role, for others to clearly<br />
see, was better. He was actually a better doctor providing better care<br />
than he had before just because he took this simple step – after all<br />
caring for patients was his job.<br />
And so he looked for ways to rebuff what had been said:<br />
world ‘Show – connected me the evidence’ as they – was were an old favourite. through It wouldn’t social work media here platforms though. It was and obvious the that internet. <strong>The</strong>re was no denying it any more – it was obvious – and his head hurt<br />
‘Show displaying me ones name the and evidence’ role made it – easier was for an people old to favourite. remember (Old It Kurt, wouldn’t like most of work his here less from thinking about it.<br />
though. colleagues, had It kept was it to obvious himself that that he’d struggled displaying to remember ones others name names). and role made it<br />
‘Cost’ – he could try this angle, yet he’d seen some staff using a pen to write And their names so another and roles step onin the right<br />
easier for people to remember (Old Kurt, like most of his colleagues,<br />
Further, collaborative teams were now openly gathering supportive data on the initiative from all over the<br />
direction was taken – towards a<br />
their had heads kept – pretty it to himself much for that free. he’d struggled to remember others names). culture which welcomes change and<br />
https://www.psnetwork.org/new-kurt-new-power/[02/07/<strong>2018</strong>, 12:37:23]<br />
Further, collaborative teams were now openly gathering supportive improvement.<br />
‘Infection data on control’ the initiative – Old Kurt from loved all over his cotton the world hats – so connected couldn’t as use they infection were control as an angle to<br />
Something else amazing happened<br />
maintain through the status social quo. media He platforms considered and going the internet. back to using disposable hats but – his New College Kurt had found just putthat through<br />
out a ‘Cost’ statement – he supporting could try this reusable angle, hats yet over he’d disposable seen some ones staff (no using evidence a pen of differences<br />
wearing his<br />
in<br />
name<br />
infection<br />
& role hat meant<br />
to write their names and roles on their heads – pretty much for free. others felt more confident in doing<br />
rates and reusable hats being better for the environment).<br />
so. <strong>The</strong>y were less likely to feel<br />
‘Infection control’ – Old Kurt loved his cotton hats so couldn’t use threatened by the intimidation.<br />
infection control as an angle to maintain the status quo. He considered<br />
<strong>The</strong> only remaining line of attack was the most primitive of all – bullying, threats and Staff intimidation. within theatre He<br />
going back to using disposable hats but his College had just put out a<br />
now communicated more easily on numerous<br />
could statement attack the supporting way the message reusable was hats being over delivered. disposable He ones asked (no for evidence it to be softened different and things. presented Resultantly as the camaraderie in his theatre complex<br />
was much greater than it had ever been.<br />
a nice of way differences to support in infection team introductions. rates and reusable But it was hats more being than better that, wasn’t for the it – he knew that – it had<br />
environment).<br />
clinical outcome implications.<br />
<strong>The</strong> only remaining line of attack was the most primitive of all – bullying,<br />
threats and intimidation. He could attack the way the message was<br />
So then<br />
being<br />
he<br />
delivered.<br />
chose to attack<br />
He asked<br />
the messengers<br />
for it to be softened<br />
and galvanised<br />
and presented<br />
others to<br />
as<br />
do<br />
a<br />
the<br />
nice<br />
same.<br />
way to support team introductions. But it was more than that, wasn’t<br />
Yet despite – he knew this the that messengers – it had clinical persisted outcome because implications. they knew the message was right.<br />
So then he chose to attack the messengers and galvanised others to do<br />
<strong>The</strong> messengers, the same. being human themselves, appreciated what humans were like – perhaps one of the<br />
reasons Yet the despite message this was the conceived messengers in the persisted first place because – it’s visual they nature knew the would display to everyone how<br />
much<br />
message<br />
we resist<br />
was<br />
change.<br />
right.<br />
<strong>The</strong> messengers, being human themselves, appreciated what humans<br />
<strong>The</strong>re were would like always – perhaps be the one laggards of the who reasons would the do message everything was they conceived could to in maintain<br />
Staff<br />
the<br />
also<br />
status<br />
started<br />
quo.<br />
to think – ‘if there’d been so much resistance to adopt<br />
the first place – it’s visual nature would display to everyone how much this simple change what else had been resisted‘.<br />
we resist change.<br />
Staff also felt more empowered to change their work environments in<br />
the interest of patient welfare. Further because of the internet and<br />
social networks they were able to collaborate rapidly and effectively<br />
on thousands of other projects seeing them to fruition. <strong>The</strong>y delivered<br />
brilliant solutions to problems they’d been blinded to in the past.<br />
New Kurt was much happier in the New Power workplace which he’d<br />
helped create.<br />
So we’re his colleagues.<br />
And everyone lived happily ever after.<br />
(Well almost. At least things started heading in the right direction.<br />
<strong>The</strong>re is still a tonne of work to do).<br />
New Power by Jeremy Heimans & Henry Timms.<br />
20 THE OPERATING THEATRE JOURNAL www.otjonline.com<br />
<strong>The</strong> closer the messengers got to delivering the change the greater the bullying and intimidation would
UK’s NICE publishes a Medtech innovation briefing on PICO<br />
for the prophylactic use in surgically closed incisions to<br />
reduce surgical site complications<br />
Smith & Nephew, the global medical technology business, announces that the UK’s National Institute for Health and Care Excellence (NICE) has<br />
issued a Medtech innovation briefing (MIB) on the use of PICO Single Use Negative Pressure Wound <strong>The</strong>rapy (sNPWT).<br />
<strong>The</strong> MIB reports the prophylactic use of PICO as a potentially more effective alternative to standard surgical dressings in the prevention of surgical<br />
site complications (SSCs). This is the first and only MIB published by NICE on an NPWT device for preventing SSCs.<br />
Complications from surgical incisions are a significant economic and human burden, costing an approximate £1 billion 1 to the NHS each year and<br />
contributing to significant morbidity and mortality in the UK and globally. A recent World Union of Wound Healing Societies consensus guidelines<br />
reports that up to 60% of surgical site infections (SSIs) are preventable 2 .<br />
<strong>The</strong> prophylactic use of the PICO system is proven to be effective in reducing SSCs, including SSIs and dehiscence (wound rupturing) of the surgical<br />
incision, in patients at elevated risk of SSCs 7 .<br />
<strong>The</strong> PICO dressing has a proprietary AIRLOCK Technology that uniformly and consistently delivers NPWT across a surgical incision and the<br />
surrounding zone of injury generated naturally by the incision itself 3,4 . This proprietary feature is designed to help reduce the risk of wound<br />
complications by reducing post-operative fluid, swelling and associated tension around a closed surgical incision compared with standard<br />
dressings 5,6 . <strong>The</strong> combination of these actions helps reduce the risk of surgical wound dehiscence 7 and SSIs 7 , the 2 most common SSCs.<br />
Evidence shows how the prophylactic use of PICO resulted in fewer complications, and in earlier discharge from hospitals, reducing length of stay,<br />
on average by more than 8 days, in closed laparotomy wounds after abdominal surgery 8 *, which has the potential to release bed days for the NHS.<br />
In patients undergoing primary hip and knee arthroplasties, it was estimated that care with PICO enabled cost savings of more than £7,000 per<br />
high-risk patient (BMI ≥35 or ASA ≥3) compared with care with standard dressings 9 **.<br />
Read more about NICE’s finding here: http://www.smith-nephew.com/PICOMIB<br />
Ms Pauline Whitehouse, Consultant General and Colorectal Surgeon, Worthing Hospital, said, “Following the introduction of PICO into our Trust<br />
for moderate- to high-risk incisions, we quickly noticed a significant reduction in superficial surgical site infections. We have now introduced PICO<br />
across the Trust and are seeing similar reductions in infective complications for other specialities”.<br />
MIBs are objective information on device and diagnostic technologies to aid local decision-making by clinicians, managers and procurement<br />
professionals. <strong>The</strong>y are NICE advice, designed to support NHS and social care commissioners and staff who are considering using new medical<br />
devices, and other medical or diagnostic technologies. <strong>The</strong> briefing will help avoid the need for organisations to produce similar information<br />
locally, saving staff time and resources. MIBs are commissioned by NHS England and produced in support of the NHS 5-Year Forward View,<br />
specifically as one of a number of steps that will accelerate innovation in new treatments and diagnostics.<br />
As part of the MIB, NICE conducted a thorough review of the published and peer-reviewed data from a variety of meta-analyses and randomised<br />
controlled trials (RCTs). <strong>The</strong> effectiveness of PICO in reducing SSCs has been examined in 10 RCTs and multiple observational studies. A recently<br />
published 1,839 patient meta-analysis demonstrated the efficacy of PICO, used prophylactically, significantly reducing SSIs by 58% in closed surgical<br />
incisions compared with standard care 5 ***.<br />
PICO is suitable for use in both hospital and community settings, and is approved for a number of indications, including surgically closed incision<br />
sites.<br />
“NICE MIBs are a great resource for NHS organisations, and are often a reference used by healthcare systems beyond the UK. Today we are<br />
delighted to see the NICE MIB support for the prophylactic use of PICO as an effective alternative for clinicians who look to reduce their rates of<br />
surgical site complications. This will provide them with the confidence to use PICO for their at-risk patients and procedures, in support of their<br />
efforts to achieve better economic and clinical outcomes,” said Paolo Di Vincenzo, Smith & Nephew’s SVP of Advanced Wound Management. “With<br />
PICO, we are keeping Smith & Nephew at the forefront of delivering pioneering solutions that continue to improve current standards of care, by<br />
reducing the burden and delivering better clinical and economic outcomes. PICO has shown significant clinical results in reducing life-threatening<br />
infections on closed surgical incisions, which has contributed significantly to improved patient outcomes, in a cost-effective portable solution”.<br />
For more information about Smith & Nephew, please visit our website www.smith-nephew.com,<br />
follow @SmithNephewplc on Twitter or<br />
visit SmithNephewplc on Facebook.com.<br />
References:<br />
1. Guest J et al, Health economic burden that different wound types impose on the UK’s National Health Service. Int Wound J 2016; doi: 10.1111/<br />
iwj.12603<br />
2. World Union of Wound Healing Societies (WUWHS) Consensus Document. Closed surgical incision management: understanding the role of NPWT.<br />
Wounds International, 2016<br />
3. Data on File. DS/17/253/R. Project Opal PICO 7 System Stability Testing - Initial Time Point. October 2017<br />
4. Malmsjö M et al. Biological effects of a disposable, canisterless Negative Pressure Wound <strong>The</strong>rapy system (in-vitro). Eplasty 2014; 14:e15<br />
5. Selvaggi F et al., New Advances in Negative Pressure Wound <strong>The</strong>rapy (NPWT) for Surgical Wounds of Patients Affected with Crohn’s Disease.<br />
Surgical Technology International XXIV; 83- 89<br />
6. Loveluck et al (2016) Biomechanical modeling of forces applied to closed incision during NPWT eplasty16e20<br />
7. Strugala, V. and Martin, R. Meta-analysis of comparative trials evaluating a prophylactic single-use negative pressure wound therapy system<br />
for the prevention of surgical site complications. Surgical Infections (2017). DOI 10.1089/sur.2017.156<br />
8. O’Leary, Donal Peter et al. 2017. “Prophylactic Negative Pressure Dressing Use in Closed Laparotomy Wounds Following Abdominal Operations.”<br />
Annals of Surgery. Jun 265(6): 1082-1086<br />
9. Nherera LM, Trueman P, Karlakki SL. Cost-effectiveness analysis of single-use negative pressure wound therapy dressings (sNPWT) to reduce<br />
surgical site complications (SSC) in routine primary hip and knee replacements. Wound Repair Regen. April 2017. doi:10.1111/wrr.12530<br />
Find out more 02921 680068 • e-mail admin@lawrand.com Issue 334 <strong>July</strong> <strong>2018</strong> 21
NEW EVIDENCE SHOWS ASSOCIATION BETWEEN INNOVATION<br />
AND REDUCED COMPLICATIONS IN THORACIC SURGERY<br />
Studies presented at the European Society of Thoracic Surgeons meeting examine the impact of innovation on<br />
both patient outcomes and hospital costs<br />
Exciting data from the 26th European Society of Thoracic Surgeons meeting shows an association between innovation, and improved patient<br />
outcomes and lowered hospital costs. Two studies presented at an Ethicon* sponsored symposium show that significantly lower rates of bleeding<br />
complications occurred when ECHELON FLEX Powered Staplers where used, [1] and how a first of its kind lung model can identify the cause of<br />
air leaks post-surgery. [2] With such complications proving costly and dangerous for patients, finding ways to minimize risk is vitally important. 1,2<br />
Findings from the first real-world study exploring the impact of powered staplers compared to manual devices in video-assisted thoracoscopic<br />
surgery (VATS) for lung cancer, found that bleeding complications dropped by nearly half when surgeons used a powered stapler. <strong>The</strong> study which<br />
has been published in Advances in <strong>The</strong>rapy, also found a nearly 10% reduction in total hospital costs, and one day sooner discharge from the<br />
hospital associated with the powered-stapling procedures.1<br />
“This real-world study shows stapler choice really does matter in significantly reducing bleeding complications and lowering overall costs in VATS<br />
lobectomy procedures. <strong>The</strong> results in favor of powered stapling devices in thoracic surgery are compelling,” said lead study author Daniel L. Miller,<br />
MD, Chief, General Thoracic Surgery at WellStar Health System, Mayo Clinic Care Network in Marietta, GA.<br />
A lobectomy is a surgical procedure where an entire lobe of the lung is removed due to lung cancer, infection, chronic obstructive pulmonary<br />
disease (COPD) or benign tumors. [3] Between 2-10% of lobectomies result in bleeding complications. [4],[5]<br />
Findings from a lung model study, published in IEEE Transactions on Biomedical Engineering, found that unlike any system before, the novel ex-vivo<br />
model was able to successfully replicate a person’s breathing both under ventilated and natural conditions. Developed by Ethicon, in partnership<br />
with leading experts in thoracic surgery, the new model simulates the various physiologic environments experienced by an isolated lung during<br />
the perioperative period, allowing researchers to monitor how and why air leaks happen. 2 Researchers will now be able to explore under clinically<br />
relevant conditions, the possible ways to reduce the risk of air leaks, 2 a post-operative complication that occurs in 24% of lobectomies and<br />
associated with an almost doubled increase in hospital mortality. [6]<br />
“We continue to take aim at critical clinical issues such as hemostasis complications through the development of innovative devices like ECHELON<br />
FLEX Powered Staplers and the generation of meaningful clinical and real-world evidence that fills knowledge gaps, validates outcomes and<br />
better informs everyday decision making,” said Edmund Kassis, MD, Ethicon Sr. Medical Director for Thoracic Surgery.<br />
This year, more than 310,000 adults all over Europe will be diagnosed with lung cancer, and it is approximated that only 18% will survive for longer<br />
than five years. Lung cancer is the biggest cancer killer worldwide, causing more deaths than breast and prostate cancer combined. [7]<br />
*Ethicon represents the products and services of Ethicon, Inc., Ethicon Endo-Surgery, LLC and certain of their affiliates. Ethicon Endo-Surgery, Inc.<br />
is the legal manufacturer of ECHELON FLEX Powered Staplers. All other trademarks are the property of their respective owners.<br />
References<br />
[1] Miller DL, Roy S, Kassis ES. et al. Impact of powered and tissuespecific<br />
endoscopic stapling technology on clinical and economic<br />
outcomes of video-assisted thoracic surgery lobectomy procedures:<br />
a retrospective, observational study. Advances in <strong>The</strong>rapy (<strong>2018</strong>).<br />
https://doi.org/10.1007/s12325-018-0679-z.<br />
[2] Klassen C, Eckert CE, Wong J. et al. Ex Vivo Modeling of<br />
Perioperative Air Leaks in Porcine Lungs. IEEE Transactions on<br />
Biomedical Engineering (<strong>2018</strong>). https://ieeexplore.ieee.org/<br />
document/8325303/<br />
[3] American Lung Association. Lobectomy. Available at: www.<br />
lung.org/lung-health-and-diseases/lung-procedures-and-tests/<br />
lobectomy.html. Accessed May <strong>2018</strong>.<br />
[4] Kent M, et al. Open, video-assisted thoracic surgery, and robotic<br />
lobectomy: review of a national database. Ann Thorac Surg.<br />
2014;97:236-444.<br />
[5] Based on Ethicon (2016) internal analysis of data from 26,955<br />
lobectomy procedures captured in Premier Perspective database<br />
for the period of 2008- 2014.<br />
[6] Yoo A, Ghosh SK, Danker W. et al. Burden of air leak complications<br />
in thoracic surgery estimated using a national hospital billing<br />
database. ClinicoEconomics and Outcomes Research. 2017;9:378-<br />
383.<br />
[7] Lung Cancer Europe. Our Diagnosis. Available at:<br />
www.lungcancereurope.eu/lung-cancer/. Accessed May <strong>2018</strong>.<br />
www.facebook.com/<strong>The</strong>OTJ<br />
<strong>Digital</strong> system to monitor<br />
recovery room patients<br />
Adelaide - SA Health is to implement a digital health solution in the<br />
form of a post-surgery cloud-based patient monitoring system. <strong>The</strong><br />
system will be fitted into the Royal Adelaide Hospital.<br />
<strong>The</strong> new platform has been developed by Allscripts, working<br />
in collaboration with iProcedures. <strong>The</strong> platform is called the<br />
iPro Post-Anaesthesia Care Unit module (PACU), and it enables<br />
recovery room nurses to record patients’ post-operative data, with<br />
metrics collected in real time. For nurses this requires the use of<br />
resuscitation skills, knowledge and application of new techniques<br />
and the application of pain management.<br />
iProcedures delivers software solutions to streamline the<br />
perioperative workflow in hospitals; this includes technologies<br />
like iPro Anesthesia, which is a mobile application that aims to<br />
improve documentation and patient safety. Allscripts is a Health IT<br />
technology solutions company.<br />
<strong>The</strong> platform was developed by anaesthesiologists with a focus on<br />
improving patient safety, documentation, hospital efficiency and<br />
medication management, according to the Healthcare Information<br />
and Management Systems Society. <strong>The</strong> comprehensive end-to-end<br />
solution is used to generate a complete, compliant and legible<br />
anaesthesia record.<br />
To date over one thousand patients have been administered in<br />
the system across 33 operating theaters, where all; vital signs are<br />
automatically tracked. Discussing this, Royal Adelaide Hospital’s<br />
AIMS project manager Paul Dawkins stated: “When you get<br />
anaesthetists going out of their way to visit you to thank you for<br />
AIMS, you know it is doing a good job.”<br />
Source: <strong>Digital</strong> <strong>Journal</strong> TIM SANDLE<br />
22 THE OPERATING THEATRE JOURNAL www.otjonline.com
Advanced Surgical Practice (MSc)<br />
Part-time distance learning programme<br />
Postgraduate Certificate and Postgraduate Diploma exit points available<br />
For those who wish to increase their knowledge of surgical practice in order to help improve patient<br />
care. Graduates have reported that this programme has led directly to promotion, and many were<br />
stimulated to pursue academic careers.<br />
<strong>The</strong> modular approach allows you to evaluate care from an evidence-based perspective, starting<br />
with admission and preoperative preparation through to postoperative care and discharge.<br />
A range of other programmes are also available including Pain Management, Critical Care, and<br />
standalone CPD modules.<br />
Contact us to find out more<br />
pgtmedadmissions@cardiff.ac.uk<br />
+44 (0)29 20687214<br />
www.cardiff.ac.uk/medicine
VISIT US<br />
Stand 21<br />
AfPP Residential<br />
Conference<br />
University of York<br />
9th – 12th August<br />
Your first<br />
choice in<br />
respiratory<br />
care<br />
Intersurgical provide flexible<br />
patient solutions for use within<br />
emergency care and the hospital<br />
environment for:<br />
<strong>The</strong> complete solution from<br />
the respiratory care specialists<br />
• Airway Management<br />
• Anaesthesia<br />
• Critical Care<br />
• Oxygen and Aerosol <strong>The</strong>rapy<br />
View our full product range:<br />
www.intersurgical.co.uk/products<br />
lnteract with us<br />
Quality, innovation and choice<br />
www.intersurgical.co.uk