You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
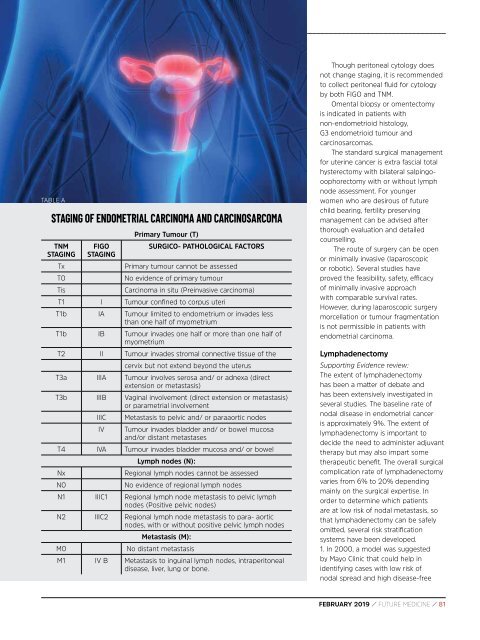
TABLE A<br />
STAGING OF ENDOMETRIAL CARCINOMA AND CARCINOSARCOMA<br />
TNM<br />
STAGING<br />
Tx<br />
T0<br />
Tis<br />
FIGO<br />
STAGING<br />
Primary Tumour (T)<br />
SURGICO- PATHOLOGICAL FACTORS<br />
Primary tumour cannot be assessed<br />
No evidence of primary tumour<br />
Carcinoma in situ (Preinvasive carcinoma)<br />
T1 I Tumour confined to corpus uteri<br />
T1b IA Tumour limited to endometrium or invades less<br />
than one half of myometrium<br />
T1b IB Tumour invades one half or more than one half of<br />
myometrium<br />
T2 II Tumour invades stromal connective tissue of the<br />
cervix but not extend beyond the uterus<br />
T3a IIIA Tumour involves serosa and/ or adnexa (direct<br />
extension or metastasis)<br />
T3b IIIB Vaginal involvement (direct extension or metastasis)<br />
or parametrial involvement<br />
IIIC<br />
IV<br />
Metastasis to pelvic and/ or paraaortic nodes<br />
Tumour invades bladder and/ or bowel mucosa<br />
and/or distant metastases<br />
T4 IVA Tumour invades bladder mucosa and/ or bowel<br />
Nx<br />
N0<br />
Lymph nodes (N):<br />
Regional lymph nodes cannot be assessed<br />
No evidence of regional lymph nodes<br />
N1 IIIC1 Regional lymph node metastasis to pelvic lymph<br />
nodes (Positive pelvic nodes)<br />
N2 IIIC2 Regional lymph node metastasis to para- aortic<br />
nodes, with or without positive pelvic lymph nodes<br />
Metastasis (M):<br />
M0 No distant metastasis<br />
M1 IV B Metastasis to inguinal lymph nodes, intraperitoneal<br />
disease, liver, lung or bone.<br />
Though peritoneal cytology does<br />
not change staging, it is recommended<br />
to collect peritoneal fluid for cytology<br />
by both FIGO and TNM.<br />
Omental biopsy or omentectomy<br />
is indicated in patients with<br />
non-endometrioid histology,<br />
G3 endometrioid tumour and<br />
carcinosarcomas.<br />
The standard surgical management<br />
for uterine cancer is extra fascial total<br />
hysterectomy with bilateral salpingooophorectomy<br />
with or without lymph<br />
node assessment. For younger<br />
women who are desirous of future<br />
child bearing, fertility preserving<br />
management can be advised after<br />
thorough evaluation and detailed<br />
counselling.<br />
The route of surgery can be open<br />
or minimally invasive (laparoscopic<br />
or robotic). Several studies have<br />
proved the feasibility, safety, efficacy<br />
of minimally invasive approach<br />
with comparable survival rates.<br />
However, during laparoscopic surgery<br />
morcellation or tumour fragmentation<br />
is not permissible in patients with<br />
endometrial carcinoma.<br />
Lymphadenectomy<br />
Supporting Evidence review:<br />
The extent of lymphadenectomy<br />
has been a matter of debate and<br />
has been extensively investigated in<br />
several studies. The baseline rate of<br />
nodal disease in endometrial cancer<br />
is approximately 9%. The extent of<br />
lymphadenectomy is important to<br />
decide the need to administer adjuvant<br />
therapy but may also impart some<br />
therapeutic benefit. The overall surgical<br />
complication rate of lymphadenectomy<br />
varies from 6% to 20% depending<br />
mainly on the surgical expertise. In<br />
order to determine which patients<br />
are at low risk of nodal metastasis, so<br />
that lymphadenectomy can be safely<br />
omitted, several risk stratification<br />
systems have been developed.<br />
1. In 2000, a model was suggested<br />
by Mayo Clinic that could help in<br />
identifying cases with low risk of<br />
nodal spread and high disease-free<br />
<strong>FEBRUARY</strong> <strong>2019</strong> / FUTURE MEDICINE / 81