AAHAM Q4 '21
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
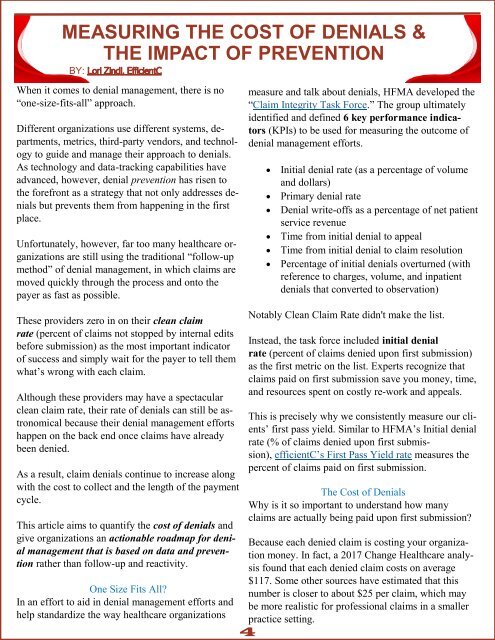
MEASURING THE COST OF DENIALS &<br />
THE IMPACT OF PREVENTION<br />
BY:<br />
When it comes to denial management, there is no<br />
“one-size-fits-all” approach.<br />
Different organizations use different systems, departments,<br />
metrics, third-party vendors, and technology<br />
to guide and manage their approach to denials.<br />
As technology and data-tracking capabilities have<br />
advanced, however, denial prevention has risen to<br />
the forefront as a strategy that not only addresses denials<br />
but prevents them from happening in the first<br />
place.<br />
Unfortunately, however, far too many healthcare organizations<br />
are still using the traditional “follow-up<br />
method” of denial management, in which claims are<br />
moved quickly through the process and onto the<br />
payer as fast as possible.<br />
measure and talk about denials, HFMA developed the<br />
“Claim Integrity Task Force.” The group ultimately<br />
identified and defined 6 key performance indicators<br />
(KPIs) to be used for measuring the outcome of<br />
denial management efforts.<br />
• Initial denial rate (as a percentage of volume<br />
and dollars)<br />
• Primary denial rate<br />
• Denial write-offs as a percentage of net patient<br />
service revenue<br />
• Time from initial denial to appeal<br />
• Time from initial denial to claim resolution<br />
• Percentage of initial denials overturned (with<br />
reference to charges, volume, and inpatient<br />
denials that converted to observation)<br />
These providers zero in on their clean claim<br />
rate (percent of claims not stopped by internal edits<br />
before submission) as the most important indicator<br />
of success and simply wait for the payer to tell them<br />
what’s wrong with each claim.<br />
Although these providers may have a spectacular<br />
clean claim rate, their rate of denials can still be astronomical<br />
because their denial management efforts<br />
happen on the back end once claims have already<br />
been denied.<br />
As a result, claim denials continue to increase along<br />
with the cost to collect and the length of the payment<br />
cycle.<br />
This article aims to quantify the cost of denials and<br />
give organizations an actionable roadmap for denial<br />
management that is based on data and prevention<br />
rather than follow-up and reactivity.<br />
One Size Fits All?<br />
In an effort to aid in denial management efforts and<br />
help standardize the way healthcare organizations<br />
4<br />
Notably Clean Claim Rate didn't make the list.<br />
Instead, the task force included initial denial<br />
rate (percent of claims denied upon first submission)<br />
as the first metric on the list. Experts recognize that<br />
claims paid on first submission save you money, time,<br />
and resources spent on costly re-work and appeals.<br />
This is precisely why we consistently measure our clients’<br />
first pass yield. Similar to HFMA’s Initial denial<br />
rate (% of claims denied upon first submission),<br />
efficientC’s First Pass Yield rate measures the<br />
percent of claims paid on first submission.<br />
The Cost of Denials<br />
Why is it so important to understand how many<br />
claims are actually being paid upon first submission?<br />
Because each denied claim is costing your organization<br />
money. In fact, a 2017 Change Healthcare analysis<br />
found that each denied claim costs on average<br />
$117. Some other sources have estimated that this<br />
number is closer to about $25 per claim, which may<br />
be more realistic for professional claims in a smaller<br />
practice setting.