IN THIS ISSUE - Drug Development & Delivery
IN THIS ISSUE - Drug Development & Delivery
IN THIS ISSUE - Drug Development & Delivery
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Drug</strong> <strong>Development</strong> & <strong>Delivery</strong> July/August 2012 Vol 12 No 6<br />
32<br />
month under refrigeration or freezing<br />
conditions.<br />
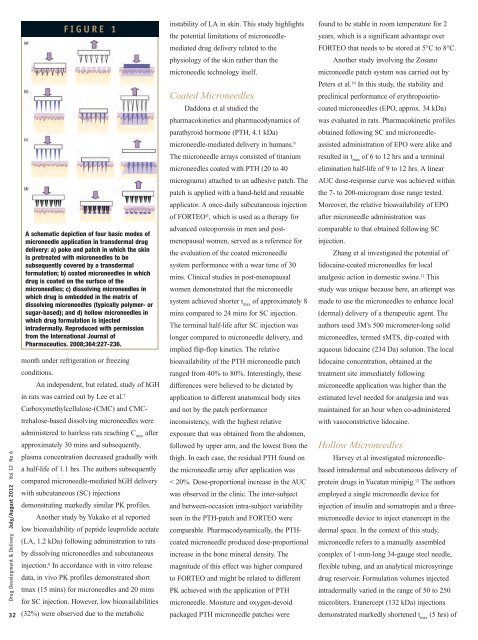
F I G U R E 1<br />
A schematic depiction of four basic modes of<br />
microneedle application in transdermal drug<br />
delivery: a) poke and patch in which the skin<br />
is pretreated with microneedles to be<br />
subsequently covered by a transdermal<br />
formulation; b) coated microneedles in which<br />
drug is coated on the surface of the<br />
microneedles; c) dissolving microneedles in<br />
which drug is embedded in the matrix of<br />
dissolving microneedles (typically polymer- or<br />
sugar-based); and d) hollow microneedles in<br />
which drug formulation is injected<br />
intradermally. Reproduced with permission<br />
from the International Journal of<br />
Pharmaceutics. 2008;364:227-236.<br />
An independent, but related, study of hGH<br />
in rats was carried out by Lee et al. 7<br />
Carboxymethylcellulose-(CMC) and CMC-<br />
trehalose-based dissolving microneedles were<br />
administered to hairless rats reaching C max after<br />
approximately 30 mins and subsequently,<br />
plasma concentration decreased gradually with<br />
a half-life of 1.1 hrs. The authors subsequently<br />
compared microneedle-mediated hGH delivery<br />
with subcutaneous (SC) injections<br />
demonstrating markedly similar PK profiles.<br />
Another study by Yukako et al reported<br />
low bioavailability of peptide leuprolide acetate<br />
(LA, 1.2 kDa) following administration to rats<br />
by dissolving microneedles and subcutaneous<br />
injection. 8 In accordance with in vitro release<br />
data, in vivo PK profiles demonstrated short<br />
tmax (15 mins) for microneedles and 20 mins<br />
for SC injection. However, low bioavailabilities<br />
(32%) were observed due to the metabolic<br />
instability of LA in skin. This study highlights<br />
the potential limitations of microneedle-<br />
mediated drug delivery related to the<br />
physiology of the skin rather than the<br />
microneedle technology itself.<br />
Coated Microneedles<br />
Daddona et al studied the<br />
pharmacokinetics and pharmacodynamics of<br />
parathyroid hormone (PTH, 4.1 kDa)<br />
microneedle-mediated delivery in humans. 9<br />
The microneedle arrays consisted of titanium<br />
microneedles coated with PTH (20 to 40<br />
micrograms) attached to an adhesive patch. The<br />
patch is applied with a hand-held and reusable<br />
applicator. A once-daily subcutaneous injection<br />
of FORTEO ® , which is used as a therapy for<br />
advanced osteoporosis in men and post-<br />
menopausal women, served as a reference for<br />
the evaluation of the coated microneedle<br />
system performance with a wear time of 30<br />
mins. Clinical studies in post-menopausal<br />
women demonstrated that the microneedle<br />
system achieved shorter t max of approximately 8<br />
mins compared to 24 mins for SC injection.<br />
The terminal half-life after SC injection was<br />
longer compared to microneedle delivery, and<br />
implied flip-flop kinetics. The relative<br />
bioavailability of the PTH microneedle patch<br />
ranged from 40% to 80%. Interestingly, these<br />
differences were believed to be dictated by<br />
application to different anatomical body sites<br />
and not by the patch performance<br />
inconsistency, with the highest relative<br />
exposure that was obtained from the abdomen,<br />
followed by upper arm, and the lowest from the<br />
thigh. In each case, the residual PTH found on<br />
the microneedle array after application was<br />
< 20%. Dose-proportional increase in the AUC<br />
was observed in the clinic. The inter-subject<br />
and between-occasion intra-subject variability<br />
seen in the PTH-patch and FORTEO were<br />
comparable. Pharmacodynamically, the PTH-<br />
coated microneedle produced dose-proportional<br />
increase in the bone mineral density. The<br />
magnitude of this effect was higher compared<br />
to FORTEO and might be related to different<br />
PK achieved with the application of PTH<br />
microneedle. Moisture and oxygen-devoid<br />
packaged PTH microneedle patches were<br />
found to be stable in room temperature for 2<br />
years, which is a significant advantage over<br />
FORTEO that needs to be stored at 5°C to 8°C.<br />
Another study involving the Zosano<br />
microneedle patch system was carried out by<br />
Peters et al. 10 In this study, the stability and<br />
preclinical performance of erythropoietin-<br />
coated microneedles (EPO, approx. 34 kDa)<br />
was evaluated in rats. Pharmacokinetic profiles<br />
obtained following SC and microneedle-<br />
assisted administration of EPO were alike and<br />
resulted in tmax of 6 to 12 hrs and a terminal<br />
elimination half-life of 9 to 12 hrs. A linear<br />
AUC dose-response curve was achieved within<br />
the 7- to 200-microgram dose range tested.<br />
Moreover, the relative bioavailability of EPO<br />
after microneedle administration was<br />
comparable to that obtained following SC<br />
injection.<br />
Zhang et al investigated the potential of<br />
lidocaine-coated microneedles for local<br />
analgesic action in domestic swine. 11 This<br />
study was unique because here, an attempt was<br />
made to use the microneedles to enhance local<br />
(dermal) delivery of a therapeutic agent. The<br />
authors used 3M’s 500 micrometer-long solid<br />
microneedles, termed sMTS, dip-coated with<br />
aqueous lidocaine (234 Da) solution. The local<br />
lidocaine concentration, obtained at the<br />
treatment site immediately following<br />
microneedle application was higher than the<br />
estimated level needed for analgesia and was<br />
maintained for an hour when co-administered<br />
with vasoconstrictive lidocaine.<br />
Hollow Microneedles<br />
Harvey et al investigated microneedlebased<br />
intradermal and subcutaneous delivery of<br />
protein drugs in Yucatan minipig. 12 The authors<br />
employed a single microneedle device for<br />
injection of insulin and somatropin and a threemicroneedle<br />
device to inject etanercept in the<br />
dermal space. In the context of this study,<br />
microneedle refers to a manually assembled<br />
complex of 1-mm-long 34-gauge steel needle,<br />
flexible tubing, and an analytical microsyringe<br />
drug reservoir. Formulation volumes injected<br />
intradermally varied in the range of 50 to 250<br />
microliters. Etanercept (132 kDa) injections<br />
demonstrated markedly shortened tmax (5 hrs) of