How does stress increase risk of drug abuse - Addiction Research ...
How does stress increase risk of drug abuse - Addiction Research ...
How does stress increase risk of drug abuse - Addiction Research ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
352<br />
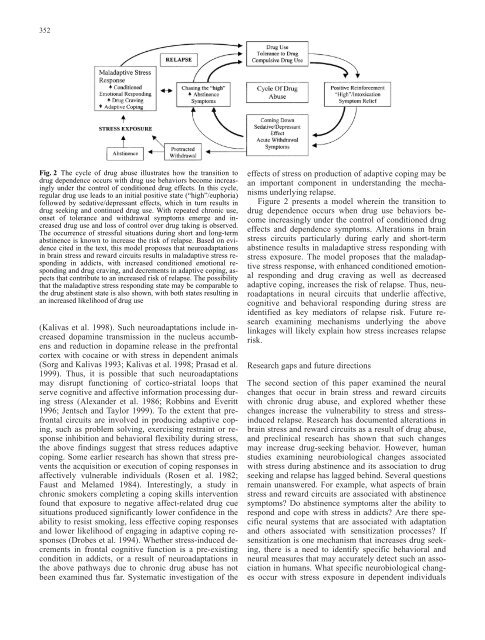
Fig. 2 The cycle <strong>of</strong> <strong>drug</strong> <strong>abuse</strong> illustrates how the transition to<br />
<strong>drug</strong> dependence occurs with <strong>drug</strong> use behaviors become increasingly<br />
under the control <strong>of</strong> conditioned <strong>drug</strong> effects. In this cycle,<br />
regular <strong>drug</strong> use leads to an initial positive state (“high”/euphoria)<br />
followed by sedative/depressant effects, which in turn results in<br />
<strong>drug</strong> seeking and continued <strong>drug</strong> use. With repeated chronic use,<br />
onset <strong>of</strong> tolerance and withdrawal symptoms emerge and <strong>increase</strong>d<br />
<strong>drug</strong> use and loss <strong>of</strong> control over <strong>drug</strong> taking is observed.<br />
The occurrence <strong>of</strong> <strong>stress</strong>ful situations during short and long-term<br />
abstinence is known to <strong>increase</strong> the <strong>risk</strong> <strong>of</strong> relapse. Based on evidence<br />
cited in the text, this model proposes that neuroadaptations<br />
in brain <strong>stress</strong> and reward circuits results in maladaptive <strong>stress</strong> responding<br />
in addicts, with <strong>increase</strong>d conditioned emotional responding<br />
and <strong>drug</strong> craving, and decrements in adaptive coping, aspects<br />
that contribute to an <strong>increase</strong>d <strong>risk</strong> <strong>of</strong> relapse. The possibility<br />
that the maladaptive <strong>stress</strong> responding state may be comparable to<br />
the <strong>drug</strong> abstinent state is also shown, with both states resulting in<br />
an <strong>increase</strong>d likelihood <strong>of</strong> <strong>drug</strong> use<br />
(Kalivas et al. 1998). Such neuroadaptations include <strong>increase</strong>d<br />
dopamine transmission in the nucleus accumbens<br />
and reduction in dopamine release in the prefrontal<br />
cortex with cocaine or with <strong>stress</strong> in dependent animals<br />
(Sorg and Kalivas 1993; Kalivas et al. 1998; Prasad et al.<br />
1999). Thus, it is possible that such neuroadaptations<br />
may disrupt functioning <strong>of</strong> cortico-striatal loops that<br />
serve cognitive and affective information processing during<br />
<strong>stress</strong> (Alexander et al. 1986; Robbins and Everitt<br />
1996; Jentsch and Taylor 1999). To the extent that prefrontal<br />
circuits are involved in producing adaptive coping,<br />
such as problem solving, exercising restraint or response<br />
inhibition and behavioral flexibility during <strong>stress</strong>,<br />
the above findings suggest that <strong>stress</strong> reduces adaptive<br />
coping. Some earlier research has shown that <strong>stress</strong> prevents<br />
the acquisition or execution <strong>of</strong> coping responses in<br />
affectively vulnerable individuals (Rosen et al. 1982;<br />
Faust and Melamed 1984). Interestingly, a study in<br />
chronic smokers completing a coping skills intervention<br />
found that exposure to negative affect-related <strong>drug</strong> cue<br />
situations produced significantly lower confidence in the<br />
ability to resist smoking, less effective coping responses<br />
and lower likelihood <strong>of</strong> engaging in adaptive coping responses<br />
(Drobes et al. 1994). Whether <strong>stress</strong>-induced decrements<br />
in frontal cognitive function is a pre-existing<br />
condition in addicts, or a result <strong>of</strong> neuroadaptations in<br />
the above pathways due to chronic <strong>drug</strong> <strong>abuse</strong> has not<br />
been examined thus far. Systematic investigation <strong>of</strong> the<br />
effects <strong>of</strong> <strong>stress</strong> on production <strong>of</strong> adaptive coping may be<br />
an important component in understanding the mechanisms<br />
underlying relapse.<br />
Figure 2 presents a model wherein the transition to<br />
<strong>drug</strong> dependence occurs when <strong>drug</strong> use behaviors become<br />
increasingly under the control <strong>of</strong> conditioned <strong>drug</strong><br />
effects and dependence symptoms. Alterations in brain<br />
<strong>stress</strong> circuits particularly during early and short-term<br />
abstinence results in maladaptive <strong>stress</strong> responding with<br />
<strong>stress</strong> exposure. The model proposes that the maladaptive<br />
<strong>stress</strong> response, with enhanced conditioned emotional<br />
responding and <strong>drug</strong> craving as well as decreased<br />
adaptive coping, <strong>increase</strong>s the <strong>risk</strong> <strong>of</strong> relapse. Thus, neuroadaptations<br />
in neural circuits that underlie affective,<br />
cognitive and behavioral responding during <strong>stress</strong> are<br />
identified as key mediators <strong>of</strong> relapse <strong>risk</strong>. Future research<br />
examining mechanisms underlying the above<br />
linkages will likely explain how <strong>stress</strong> <strong>increase</strong>s relapse<br />
<strong>risk</strong>.<br />
<strong>Research</strong> gaps and future directions<br />
The second section <strong>of</strong> this paper examined the neural<br />
changes that occur in brain <strong>stress</strong> and reward circuits<br />
with chronic <strong>drug</strong> <strong>abuse</strong>, and explored whether these<br />
changes <strong>increase</strong> the vulnerability to <strong>stress</strong> and <strong>stress</strong>induced<br />
relapse. <strong>Research</strong> has documented alterations in<br />
brain <strong>stress</strong> and reward circuits as a result <strong>of</strong> <strong>drug</strong> <strong>abuse</strong>,<br />
and preclinical research has shown that such changes<br />
may <strong>increase</strong> <strong>drug</strong>-seeking behavior. <strong>How</strong>ever, human<br />
studies examining neurobiological changes associated<br />
with <strong>stress</strong> during abstinence and its association to <strong>drug</strong><br />
seeking and relapse has lagged behind. Several questions<br />
remain unanswered. For example, what aspects <strong>of</strong> brain<br />
<strong>stress</strong> and reward circuits are associated with abstinence<br />
symptoms? Do abstinence symptoms alter the ability to<br />
respond and cope with <strong>stress</strong> in addicts? Are there specific<br />
neural systems that are associated with adaptation<br />
and others associated with sensitization processes? If<br />
sensitization is one mechanism that <strong>increase</strong>s <strong>drug</strong> seeking,<br />
there is a need to identify specific behavioral and<br />
neural measures that may accurately detect such an association<br />
in humans. What specific neurobiological changes<br />
occur with <strong>stress</strong> exposure in dependent individuals