CLEANASCOPE System Enhances Endoscope Transport & Handling
CLEANASCOPE System Enhances Endoscope Transport & Handling
CLEANASCOPE System Enhances Endoscope Transport & Handling
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Expert Insights<br />
<strong>CLEANASCOPE</strong> <strong>System</strong> <strong>Enhances</strong> <strong>Endoscope</strong><br />
<strong>Transport</strong> & <strong>Handling</strong><br />
<strong>System</strong> Helps Minimize Risk of Cross Contamination,<br />
Improve Efficiency & Reduce Repair Costs<br />
With the number of endoscopy procedures<br />
growing around the world, it is vital that<br />
endoscopes are processed correctly in<br />
order to keep patients and staff safe from the spread<br />
of infection. Along with adhering to rigorous cleaning<br />
and decontamination practices, proper transport and<br />
storage of expensive, delicate endoscopes are crucial<br />
to ensure patient and staff safety and maintain optimal<br />
function. To address the many challenges associated<br />
with the handling of endoscopes, the <strong>CLEANASCOPE</strong><br />
<strong>System</strong> from Advanced Sterilization Products was<br />
designed as a unique storage and transportation<br />
system that reduces the risk of cross contamination<br />
and offers easy visual identification of clean versus<br />
contaminated endoscopes. Benefits of the <strong>CLEANASCOPE</strong><br />
<strong>System</strong> include improved reprocessing safety and<br />
efficiency, and a reduction in equipment repair costs.<br />
Improving <strong>Endoscope</strong> <strong>Handling</strong><br />
According to Libby Thomson, formerly the lead nurse<br />
in the Bowel Cancer Screening Centre and nurse<br />
endoscopist at a leading hospital in the United<br />
Kingdom, hospitals are increasingly focused on<br />
patient and staff safety and providing the highest<br />
level of care. This includes minimizing the risk of<br />
infection associated with endoscopy procedures.<br />
During clinical use, endoscopes are contaminated by<br />
multiple microorganisms, and failure to appropriately<br />
reprocess and handle endoscopes—both contaminated<br />
and clean—can result in nosocomial outbreaks and<br />
serious infections. However, these efforts are<br />
sometimes hampered by insufficient endoscope<br />
handling and transportation practices such as<br />
hospital staff members using open containers to<br />
move dirty endoscopes to the decontamination room.<br />
“<strong>Handling</strong> practices vary widely,” Thomson said. “For<br />
example, in some facilities endoscopes are transported<br />
in open buckets or other containers, which is<br />
inadequate. There is the potential to contaminate<br />
the environment by allowing secretions to fall to the<br />
floor or contaminants to become airborne because the<br />
containers aren’t covered. In addition, because it often<br />
is difficult to hold the container, some staff members<br />
might carry it close to their faces, potentially exposing<br />
them to the risk of infection from contaminated<br />
endoscopes. Similarly, when moving clean endoscopes<br />
back to procedure rooms in open containers, there is<br />
the potential for contamination of the disinfected<br />
instruments.”<br />
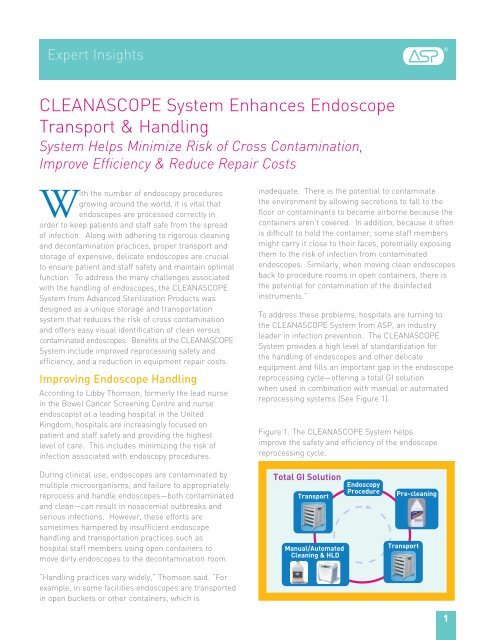
To address these problems, hospitals are turning to<br />
the <strong>CLEANASCOPE</strong> <strong>System</strong> from ASP, an industry<br />
leader in infection prevention. The <strong>CLEANASCOPE</strong><br />
<strong>System</strong> provides a high level of standardization for<br />
the handling of endoscopes and other delicate<br />
equipment and fills an important gap in the endoscope<br />
reprocessing cycle—offering a total GI solution<br />
when used in combination with manual or automated<br />
reprocessing systems (See Figure 1).<br />
Figure 1. The <strong>CLEANASCOPE</strong> <strong>System</strong> helps<br />
improve the safety and efficiency of the endoscope<br />
reprocessing cycle.<br />
Total GI Solution Endoscopy<br />
Procedure<br />
<strong>Transport</strong><br />
Manual/Automated<br />
Cleaning & HLD<br />
Pre-cleaning<br />
<strong>Transport</strong><br />
1
“The liner system is one of the most important reasons why many facilities<br />
are adopting the <strong>CLEANASCOPE</strong> <strong>System</strong>—the color-coded liners take the<br />
guesswork out of endoscope reprocessing.”<br />
According to Thomson, the <strong>CLEANASCOPE</strong> <strong>System</strong><br />
quickly resolves endoscope transport problems. The<br />
closed, reusable transport trays, carts, and liner<br />
system reduce the risk of cross-contamination from<br />
droplet or airborne contaminants and allow secure<br />
transportation to and from decontamination rooms.<br />
“With the <strong>CLEANASCOPE</strong> trays and mobile cart,<br />
instruments are safely contained, and it is no longer<br />
necessary to carry around soiled equipment in open<br />
containers,” she said.<br />
Eliminating the Guesswork<br />
The <strong>CLEANASCOPE</strong> <strong>System</strong> helps ensure that patients<br />
are not inadvertently exposed to infection risks. The<br />
patented, single-use liner system offers a protective<br />
environment for a disinfected endoscope and provides<br />
clear identification for staff of whether the equipment<br />
is clean or contaminated. After a patient procedure,<br />
the endoscope is wiped down, flushed, and placed in a<br />
<strong>CLEANASCOPE</strong> tray. A red liner cover then is placed<br />
over the tray, ensuring that the endoscope can be<br />
Red & Green Liners Identify Clean<br />
Versus Contaminated <strong>Endoscope</strong>s,<br />
Improving Patient Safety<br />
The <strong>CLEANASCOPE</strong> <strong>System</strong>’s unique colored liners<br />
improve patient safety by signaling to staff whether an<br />
endoscope is clean or dirty. A contaminated endoscope<br />
is placed in a tray and covered with a red liner,<br />
indicating that it is contaminated. Once reprocessed,<br />
the endoscope is covered with a green liner, letting<br />
staff know that is safe to use.<br />
2<br />
Benefits of the<br />
<strong>CLEANASCOPE</strong><br />
Liner <strong>System</strong>:<br />
• Reduces risk<br />
of crosscontamination<br />
• Offers a protective<br />
environment for<br />
endoscopes<br />
• Provides clear<br />
identification<br />
of whether<br />
equipment is clean<br />
or contaminated<br />
• Protects patients<br />
and improves the<br />
efficiency of the<br />
reprocessing cycle<br />
safely and hygienically transported back to the cleaning<br />
room—and alerting staff members that the endoscope<br />
is contaminated. Once the endoscope is reprocessed,<br />
it is placed in a <strong>CLEANASCOPE</strong> tray, with a clean liner,<br />
and covered with a green liner cover, signaling to staff<br />
that it is safe to use for procedures. This unique<br />
liner system helps protect patients and improve the<br />
efficiency of the endoscope reprocessing cycle. (See<br />
Sidebar: Red & Green Liners Identify Clean Versus<br />
Contaminated <strong>Endoscope</strong>s, Improving Patient Safety)<br />
According to Thomson, it can be difficult to differentiate<br />
between clean and dirty endoscopes when a facility<br />
uses open containers. “Equipment can be placed in a<br />
receptacle that isn’t easily identifiable as being dirty,”<br />
she said. “In a busy endoscopy environment, there is<br />
the potential risk of someone picking up that scope<br />
and using it on another patient. Now with the<br />
<strong>CLEANASCOPE</strong> <strong>System</strong>, there is a fail-safe way of<br />
telling whether scopes are clean or dirty, and staff can<br />
make sure instruments are in the appropriate area—<br />
especially important in hectic endoscopy departments.”<br />
The <strong>CLEANASCOPE</strong> <strong>System</strong> also contributes to<br />
increased efficiency. “The ability to quickly, easily, and<br />
safely transport instruments from the procedure room<br />
to the decontamination area and back greatly improves<br />
efficiency,” she said.<br />
“The system works very well. Facilities can place<br />
carts near the endoscopy rooms stocked with clean<br />
endoscopes, and clinical staff members will know<br />
exactly where to go to find what they need. When a<br />
procedure is complete, scopes can be immediately<br />
transported in a covered, color-coded tray to the<br />
decontamination area. Everyone will know what they<br />
are doing, and people in the decontamination room<br />
can quickly see what needs to be cleaned. The liner<br />
system is one of the most important reasons why<br />
many facilities are adopting the <strong>CLEANASCOPE</strong><br />
<strong>System</strong>—the color-coded liners take the guesswork<br />
out of endoscope reprocessing.”<br />
Cutting Repair Costs<br />
Thomson said that another key feature of the<br />
<strong>CLEANASCOPE</strong> <strong>System</strong> is its reusable trays, which<br />
guard against costly equipment repairs by protecting<br />
endoscopes from accidental damage during transport.
This benefit is especially important as hospitals<br />
face growing financial pressures and must safeguard<br />
expensive instrumentation, including flexible<br />
endoscopes, which are prone to handling damage<br />
and costly to repair. According to the literature:<br />
• At least half of endoscopes in hospital settings may<br />
be unavailable for use because of repair needs. 1<br />
• Damaged endoscopes can be expensive to repair,<br />
disrupt a facility’s capacity to provide endoscopy<br />
services, and potentially compromise patient safety. 2<br />
• Approximately 70-90% of endoscope damage may be<br />
attributed to improper handling. 3–5<br />
• Proper endoscope care and handling can dramatically<br />
improve the lifespan of an endoscope. 3<br />
According to Thomson, the <strong>CLEANASCOPE</strong> <strong>System</strong><br />
trays help reduce endoscope damage. “The trays<br />
are well-sized, so you don’t need to tightly coil the<br />
endoscope for transport, reducing damage,” she said.<br />
“Also, having endoscopes safely in individual covered<br />
trays prevents accidental damage during transport to and<br />
from the decontamination area. That’s very important in<br />
busy endoscopy departments. Facilities have experienced<br />
less repair time and cost for endoscopes since they<br />
started using the <strong>CLEANASCOPE</strong> <strong>System</strong>.”<br />
This is critical, Thomson said, as the instruments are<br />
expensive, with endoscopes costing from $20,000 to<br />
more than $80,000 each. 3,6 The financial impact is<br />
exacerbated because damaged endoscopes can lead to<br />
canceled procedures and delays in patient treatment.<br />
Focus on Standards<br />
According to Thomson, the positive experience of<br />
hospitals with the <strong>CLEANASCOPE</strong> <strong>System</strong> is<br />
indicative of a growing focus on instrument processing<br />
standards and infection prevention in the United<br />
States, Europe, and around the world.<br />
Many professional organizations, hospitals, and endoscopy<br />
centers have developed guidelines to govern the transport<br />
and handling of these fragile, high-priced instruments.<br />
Professional organizations in the U.S., including the<br />
Association of Perioperative Registered Nurses (AORN)<br />
and the Society of Gastroenterology Nurses and<br />
Associates (SGNA), have issued guidelines or recommended<br />
practices calling for the transport of endoscopes<br />
in a covered receptacle at all times. 7,8 In the United<br />
Kingdom, the Joint Advisory Group (JAG) on GI Endoscopy<br />
also has issued similar standards regarding the<br />
transport of endoscopes. 9 (See Sidebar: Guidelines for<br />
<strong>Transport</strong>ing and <strong>Handling</strong> Flexible <strong>Endoscope</strong>s)<br />
In the United Kingdom, Thomson served as a JAG lead<br />
nurse advisor and said that in recent accreditation visits<br />
to facilities, there has been an increased concentration<br />
on reviewing and improving decontamination practices,<br />
including endoscope transport and storage. “When we<br />
started decontamination assessments, things were not<br />
in good shape,” she said. “Now, most units have made<br />
significant investments to improve their practices, and<br />
standards are rapidly rising. Endoscopy departments<br />
worldwide are spending the money to improve services,<br />
and there is more emphasis on using equipment such<br />
as the <strong>CLEANASCOPE</strong> <strong>System</strong>.<br />
“With endoscopy, we must be vigilant to prevent<br />
putting patients and staff at risk,” Thomson continued.<br />
“As a result, we want to always minimize exposure to<br />
infections, and the <strong>CLEANASCOPE</strong> <strong>System</strong> provides a<br />
key solution. Every time there’s an infection outbreak<br />
in a hospital, there is an investigation. When you<br />
have solid procedures in place so staff can look at<br />
an endoscope and know it is clean with a visual sign,<br />
you can reduce the chance that a contaminated<br />
endoscope is the cause. If the scopes are clean,<br />
you’re not transporting infections. Guidelines have<br />
been a big driver for change, and it’s a small price<br />
to pay to get something like this into place” ■<br />
Guidelines for <strong>Transport</strong>ing &<br />
<strong>Handling</strong> Flexible <strong>Endoscope</strong>s:<br />
• AORN recommends that endoscopes be transported<br />
“…in a manner that preserves the sterilization/<br />
disinfection status of the endoscope.” 7<br />
• SGNA recommends transporting endoscopes<br />
in closed containers to avoid chances for cross<br />
contamination. Its guidelines state that, when<br />
transporting an endoscope to the reprocessing<br />
area, an enclosed container will prevent escape<br />
of airborne and droplet contaminants. 8 Experts<br />
emphasize that it is important to consider both the<br />
protection of the apparatus and the environment<br />
during transport. 10<br />
• CDC guidelines state that, “A protocol should be<br />
developed that ensures the user knows whether<br />
an endoscope has been appropriately cleaned and<br />
disinfected,” and endoscopes should be stored<br />
“in a manner that will protect them from damage<br />
or contamination.” 11<br />
• The UK National Health Service’s National<br />
Endoscopy Programme guidelines require that<br />
“endoscopes are transported to the decontamination<br />
area in a covered receptacle that is of an appropriate<br />
size as to avoid contaminating the environment,”<br />
and when transporting an instrument to and from<br />
the endoscopy unit, “endoscopes are transferred<br />
in a receptacle with a hard lid that completely<br />
encloses the endoscope.” 9<br />
3
References<br />
1. Leiner D. Implementing cost-effective ways to reduce endoscope repair expenses. Biomed Instrum Technol.<br />
2003;37:201–204.<br />
2. Dix K. Scope cleaning and repair: top 10 ways to keep scopes happy. Infection Control Today. 2008.<br />
http://www.infectioncontroltoday.com/articles/scope-cleaning-and-repair.html. Accessed June 26, 2008.<br />
3. Dilulio R. Service solutions: protecting your endoscope investment. 24X7. October 2006.<br />
http://www.24x7mag.com/issues/articles/2006-10_05.asp. Accessed June 26, 2008.<br />
4. Ellis K. <strong>Endoscope</strong> cleaning and repair: keeping valuable scopes fit for duty. EndoNurse. 2006.<br />
http://www.endonurse.com/articles/2006/11/endoscope-cleaning-and-repair.aspx. Accessed April 30, 2009.<br />
5. Ellis K. <strong>Endoscope</strong> repair: perspectives and advice from industry experts. EndoNurse. 2005.<br />
http:/www.endonurse.com/articles/521feat1.html. Accessed June 26, 3008.<br />
6. Dix K. Scope leak testing. EndoNurse. 2007. http://www.endonurse.com/articles/07aprfeat2.html. Accessed<br />
Sept. 24, 2009.<br />
7. Conner R, Reno D. AORN Standards, Recommended Practices and Guidelines. Denver, CO: AORN; 2006.<br />
8. Society of Gastroenterology Nurses and Associates Inc (SGNA). Standards of Infection Control in Reprocessing of<br />
Flexible Gastrointestinal <strong>Endoscope</strong>s. 2007.<br />
9. National Endoscopy Programme: Decontamination Standards for Flexible <strong>Endoscope</strong>s. Leicester, England: Joint<br />
Advisory Group on GI Endoscopy; 2009.<br />
10. Thomas L. <strong>Transport</strong>ing the endoscope. Gastroenterol Nurs. 2005;28:145–146.<br />
11. Rutala W, Weber D. HICPAC Guideline for disinfection and sterilization in healthcare facilities, 2008: Centers for<br />
Disease Control and Prevention;16, 87.<br />
33 Technology Drive • Irvine CA 92618 • (888) 783-7723<br />
www.aspjj.com<br />
<strong>CLEANASCOPE</strong> is a registered trademark of Medicart International Limited.<br />
© Ethicon, Inc. 2010 AD-100319-01-US_A