National Cancer Prevention Policy - Tobacco Control Supersite
National Cancer Prevention Policy - Tobacco Control Supersite
National Cancer Prevention Policy - Tobacco Control Supersite
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong><br />
2007–09
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong><br />
2007–09
The <strong>Cancer</strong> Council Australia Member Organisations<br />
The <strong>Cancer</strong> Council ACT<br />
159 Maribyrnong Ave<br />
Kaleen Australian Capital Territory 2617<br />
T: (02) 6262 2222<br />
F: (02) 6262 2223<br />
www.actcancer.org<br />
The <strong>Cancer</strong> Council NSW<br />
153 Dowling Street<br />
Woolloomooloo New South Wales 2011<br />
T: (02) 9334 1900<br />
F: (02) 9358 1452<br />
www.cancercouncil.com.au<br />
The <strong>Cancer</strong> Council Northern Territory<br />
Casi House, Unit 1−3/25 Vanderlin Drive<br />
Casuarina Northern Territory 0810<br />
T: (08) 8927 4888<br />
F: (08) 8927 4990<br />
www.cancercouncilnt.com.au<br />
The <strong>Cancer</strong> Council Queensland<br />
553 Gregory Terrace<br />
Fortitude Valley Queensland 4006<br />
T: (07) 3258 2200<br />
F: (07) 3257 1306<br />
www.qldcancer.com.au<br />
The <strong>Cancer</strong> Council Australia is Australia’s peak national non-government cancer organisation. Its members<br />
are the leading state and territory cancer councils, working together to undertake and fund cancer research,<br />
prevent and control cancer, and provide information and support to people affected by cancer.<br />
Citation: The <strong>Cancer</strong> Council Australia 2007. <strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007−09. NSW: The <strong>Cancer</strong><br />
Council Australia.<br />
Copies available from:<br />
The <strong>Cancer</strong> Council Australia, Level 5, Medical<br />
Foundation Building, 92−4 Parramatta Road,<br />
Camperdown NSW 2050<br />
T: (02) 9036 3100<br />
F: (02) 9036 3101<br />
www.cancer.org.au<br />
ISBN 0 947283 88 9<br />
Published May 2007<br />
The <strong>Cancer</strong> Council South Australia<br />
202 Greenhill Road<br />
Eastwood South Australia 5063<br />
T: (08) 8291 4111<br />
F: (08) 8291 4122<br />
www.cancersa.org.au<br />
The <strong>Cancer</strong> Council Tasmania<br />
140 Bathurst Street<br />
Hobart Tasmania 7000<br />
T: (03) 6233 2030<br />
F: (03) 6233 2123<br />
www.cancertas.org.au<br />
The <strong>Cancer</strong> Council Victoria<br />
1 Rathdowne Street<br />
Carlton Victoria 3053<br />
T: (03) 9635 5000<br />
F: (03) 9635 5270<br />
www.cancervic.org.au<br />
The <strong>Cancer</strong> Council Western Australia<br />
46 Ventnor Avenue<br />
West Perth Western Australia 6005<br />
T: (08) 9212 4333<br />
F: (08) 9212 4334<br />
www.cancerwa.asn.au<br />
Prepared by the Publications Unit, The <strong>Cancer</strong> Council Victoria.<br />
This publication may be freely photocopied and distributed, providing the publisher is acknowledged.<br />
Main cover photo and ‘Screening’ photo page 121 by Brian Gilkes; page 175 ‘Immunisation’ photo by Kate<br />
Morris<br />
Thanks to the Australian Institute of Health and Welfare for permission to reproduce Figures 1.1 and 2.1 from<br />
Australian Institute of Health and Welfare & <strong>National</strong> Breast <strong>Cancer</strong> Centre 2006. Breast <strong>Cancer</strong> in Australia:<br />
an overview, 2006. Canberra: AIHW.
C o n t e n t s<br />
Abbreviations 6<br />
The <strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 8<br />
References 10<br />
Section One: Preventable risk factors<br />
<strong>Tobacco</strong> 12<br />
Introduction 12<br />
The link between tobacco and cancer 13<br />
The impact 13<br />
The challenge 15<br />
Effective interventions 20<br />
The policy context 26<br />
Aims 34<br />
References 37<br />
Ultraviolet radiation 41<br />
Introduction 41<br />
The link between ultraviolet radiation and cancer 41<br />
The impact 43<br />
The challenge 44<br />
Effective interventions 46<br />
The policy context 47<br />
Aims 47<br />
References 49<br />
Nutrition 52<br />
Introduction 52<br />
The link between nutrition and cancer 52<br />
The impact 57<br />
The challenge 57<br />
Effective interventions 59<br />
The policy context 63<br />
Aims 64<br />
References 66<br />
Physical activity 71<br />
Introduction 71<br />
How physical activity is measured 72<br />
The link between physical activity and cancer 73<br />
The impact 74<br />
The challenge 75<br />
Effective interventions 76<br />
The policy context 80<br />
Aims 81<br />
References 82<br />
C o n t e n t s
Overweight and obesity 86<br />
Introduction 86<br />
The link between overweight and obesity and cancer 87<br />
The impact 89<br />
The challenge 90<br />
Effective interventions 93<br />
The policy context 98<br />
Aims 99<br />
References 102<br />
Alcohol 107<br />
Introduction 107<br />
The link between alcohol and cancer 107<br />
How the amount of disease caused by alcohol is estimated 110<br />
The impact 111<br />
The challenge 112<br />
Effective interventions 113<br />
The policy context 114<br />
Aims 116<br />
References 117<br />
Section Two: Screening to detect cancer early<br />
Principles of screening 122<br />
Breast cancer 126<br />
Breast cancer in Australia 126<br />
Can breast cancer be prevented? 127<br />
Tests and programs for breast cancer 128<br />
The policy context 130<br />
Potential benefits and adverse effects of breast cancer screening 132<br />
Who should be screened? 132<br />
Aims 133<br />
References 135<br />
Cervical cancer 138<br />
Cervical cancer in Australia 138<br />
Can cervical cancer be prevented? 138<br />
Screening tests and programs for cervical cancer 139<br />
The policy context 140<br />
Potential benefits and adverse effects of cervical cancer screening 141<br />
Who should be screened? 142<br />
Aims 143<br />
References 144<br />
Bowel (colorectal) cancer 145<br />
Bowel cancer in Australia 145<br />
Can bowel cancer be prevented? 145<br />
Tests and programs for bowel cancer 147<br />
The policy context 150<br />
Potential benefits and adverse effects of bowel cancer screening 153<br />
Who should be screened? 154<br />
Aims 154<br />
References 156
Melanoma 161<br />
Melanoma in Australia 161<br />
Can melanoma be prevented? 161<br />
Screening tests for melanoma 161<br />
Rationale for screening for melanoma 162<br />
Would screening be of benefit at this stage? 163<br />
Aims 163<br />
References 163<br />
Prostate cancer 165<br />
Prostate cancer in Australia 165<br />
Can prostate cancer be prevented? 166<br />
Tests for prostate cancer 166<br />
The policy context 168<br />
Potential benefits and adverse effects of prostate cancer screening 170<br />
Aims 171<br />
References 172<br />
Section Three: Immunisation<br />
Human papilloma virus 176<br />
The link between HPV infection and cancer 176<br />
The impact 178<br />
The challenge 179<br />
Effective interventions 180<br />
The policy context 181<br />
Aims 181<br />
References 182<br />
Hepatitis B 186<br />
Introduction 186<br />
The link between hepatitis B infection and cancer 189<br />
The impact 190<br />
The challenge 192<br />
Effective interventions 192<br />
The policy context 195<br />
Aims 197<br />
References 198<br />
List of contributors 202<br />
Index 206<br />
C o n t e n t s
A b b r e v i a t i o n s<br />
AACR Australasian Association of <strong>Cancer</strong> Registries<br />
ABS Australian Bureau of Statistics<br />
ACCC Australian Competition and Consumer Commission<br />
ACN Australian <strong>Cancer</strong> Network<br />
AHRQ Agency for Healthcare Research and Quality<br />
AHTAC Australian Health Technology Advisory Committee<br />
AICR American Institute of <strong>Cancer</strong> Research<br />
AIHW Australian Institute of Health and Welfare<br />
BCC basal cell carcinoma<br />
BMI body mass index<br />
BRCA breast cancer (associated gene)<br />
BSE breast self-examination<br />
CBE clinical breast examination<br />
CDHAC Commonwealth Department of Health and Aged Care<br />
CDHS California Department of Health Services<br />
CDCP Centers for Disease <strong>Control</strong> and <strong>Prevention</strong><br />
CFMDCY Committee on Food Marketing and the Diets of Children and Youth<br />
CGHFBC Collaborative Group on Hormonal Factors in Breast <strong>Cancer</strong><br />
COAG Council of Australian Governments<br />
COSA Clinical Oncological Society of Australia<br />
CTFPHC Canadian Task Force on Preventive Health Care<br />
DHA Department of Health and Ageing (Australian Government)<br />
DHAC Department of Health and Aged Care<br />
DHS Department of Human Services (Victorian Government)<br />
DRE digital rectal examination<br />
FAP familial adenomatous polyposis<br />
FOBT faecal occult blood test<br />
GP general practitioner<br />
HNPCC hereditary non-polyposis colorectal cancer<br />
HPV human papilloma virus<br />
HRT hormone replacement therapy<br />
IARC International Agency for Research on <strong>Cancer</strong><br />
MCDS Ministerial Council on Drug Safety<br />
MSAC Medical Services Advisory Committee<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09
NEACA <strong>National</strong> Expert Advisory Committee on Alcohol<br />
NACCHO <strong>National</strong> Aboriginal Community <strong>Control</strong>led Health Organisation<br />
NATSI Working Party <strong>National</strong> Aboriginal and Torres Strait Islander Working Party<br />
NCCI <strong>National</strong> <strong>Cancer</strong> <strong>Control</strong> Initiative<br />
NCSG <strong>National</strong> <strong>Cancer</strong> Strategies Group<br />
NCSP <strong>National</strong> Cervical Screening Program<br />
NHMRC <strong>National</strong> Health and Medical Research Council<br />
NMSC non-melanoma skin cancer<br />
NOTF <strong>National</strong> Obesity Task Force<br />
NPHP <strong>National</strong> Public Health Partnership<br />
PPV positive predictive value<br />
PSA prostate-specific antigen<br />
RACGP Royal Australian College of General Practitioners<br />
SIGNAL Strategic Inter-Governmental Nutrition Alliance<br />
TCCA The <strong>Cancer</strong> Council Australia<br />
TRUS transrectal ultrasound<br />
UICC International Union Against <strong>Cancer</strong><br />
USDHHS US Department of Health and Human Services<br />
USDHW US Department of Health<br />
UKFSSTI UK Flexible Sigmoidoscopy Screening Trial Investigators<br />
USPSTF US Preventive Services Task Force<br />
UV ultraviolet<br />
VCCR Victorian Cervical Cytology Registry<br />
VCTC VicHealth Centre for <strong>Tobacco</strong> <strong>Control</strong><br />
WCRF World <strong>Cancer</strong> Research Fund<br />
WHO World Health Organization<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
A b b r e v i a t i o n s
T h e N a t i o n a l C a n c e r<br />
P r e v e n t i o n P o l i c y<br />
Australia faces an unprecedented cancer control challenge.<br />
Two years ago, the Australian Institute of Health and Welfare predicted that cancer<br />
incidence would increase by 31% between 2002 and 2011. This means we can expect<br />
more than 115,000 new cancer cases in 2011 (AIHW, AACR, NCSG & McDermid 2005).<br />
More recently, the Australian Burden of Disease Study showed cancer had overtaken<br />
cardiovascular disease as the nation’s biggest disease burden (Begg et al. in press).<br />
Linking cancer incidence to population ageing—an accurate predictor of future trends—<br />
implies an even greater overall increase in cancer incidence in the years after 2011, as the<br />
percentage of Australians aged 65 and over is projected to double by 2051.<br />
The problem will be compounded by a relatively smaller workforce able to support<br />
Australia’s inflated cancer patient base. On current trends, Australia’s obesity epidemic<br />
will also place an unprecedented burden on future cancer services. And people living with<br />
cancer will, quite rightly, have heightened expectations about the nation’s capacity to care<br />
for them, as gradual developments in cancer treatment continue.<br />
The future would be considerably less daunting, however, if we could reach our<br />
potential to reduce cancer incidence through prevention and identify more cancers and<br />
precancerous conditions early, using measures already shown to be effective.<br />
The latest AIHW data shows that around a third of cancer deaths in Australia are attributed<br />
to known avoidable risk factors. Many of the thousands of people who are successfully<br />
treated for cancer could also avoid, reduce or delay the distress of the cancer experience<br />
through appropriate prevention and early detection measures.<br />
Yet as new research reconfirms that cancer is the disease Australians fear more than<br />
any other (Cameron et al. 2006), we continue to fall well short of our capacity to prevent<br />
cancer. Moreover, many of our missed opportunities to prevent cancer also contribute<br />
significantly to the overall community cost of chronic disease in Australia: five of the six<br />
key modifiable cancer risk factors—smoking, poor diet, physical inactivity, overweight/<br />
obesity and alcohol misuse—are all major risk factors for cardiovascular disease, while a<br />
number are also linked to diabetes, depression and asthma (see table below).<br />
Table A.1 Risk factors for chronic disease<br />
Disease Poor<br />
diet<br />
Heart disease<br />
Stroke<br />
<strong>Cancer</strong><br />
Depression<br />
Diabetes<br />
Asthma<br />
Source: Adapted from AIHW 2002<br />
Physical<br />
inactivity<br />
<strong>Tobacco</strong><br />
use<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
Alcohol<br />
misuse<br />
Overweight<br />
and<br />
obesity<br />
High<br />
blood<br />
pressure<br />
High<br />
cholesterol
The <strong>Cancer</strong> Council Australia’s <strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007–09 aims to provide<br />
a blueprint for optimal cancer prevention and early detection in Australia for 2007–09,<br />
drawing on the latest evidence and exploring the impact, risk factors, policy context and<br />
effective interventions. It also provides an opportunity to reflect on the 2004–06 period.<br />
In terms of immediate potential to reduce cancer death, the most significant individual<br />
measure was the Australian Government’s commitment to phase in a population-based<br />
bowel cancer screening program by 2008–09. We publicly welcomed this initiative as an<br />
election commitment in 2004 and the subsequent budget allocation in 2005–06. However,<br />
as 2007 begins, the program’s phase-in remains at an embryonic stage, and public<br />
information is limited on how federal and state/territory governments will work together<br />
to ensure it is built around a rigorous, quality-assured framework. The <strong>Cancer</strong> Council and<br />
its allies will continue to call for the Australian Government to work with all jurisdictions to<br />
deliver a program that is available to all Australians over 50 and adheres to the principles of<br />
best practice summarised in the bowel cancer screening chapter.<br />
In the area of primary prevention, the <strong>Cancer</strong> Council welcomes the tobacco control<br />
progress made in all jurisdictions, particularly the restrictions on smoking in public places,<br />
which will reduce cancer risk among smokers and non-smokers. But, as explored in the<br />
tobacco chapter, a great deal more needs to be done before smoking loses its status as the<br />
cause of the most preventable cancer deaths in Australia.<br />
Another key development was the discovery by a team led by <strong>Cancer</strong> Council Australia<br />
Vice-President Professor Ian Frazer of a vaccine for the human papilloma virus, which<br />
causes cervical cancer. The vaccine’s significance has motivated a new section on<br />
immunisation, which also examines hepatitis vaccination for preventing liver cancer. See<br />
the human papilloma virus and hepatitis B chapters in the immunisation section of the online<br />
edition of the <strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007–09 (published in mid-2007 at www.<br />
cancer.org.au).<br />
HPV immunisation should be particularly effective in developing countries where cervical<br />
cancer is prevalent due to the absence of population-based Pap screening. In Australia,<br />
however, the vaccine’s introduction must not confuse the public about the importance of a<br />
Pap screen program which has delivered the world’s lowest cervical cancer mortality rates<br />
and which remains essential for women in target age groups. The vaccine also exemplifies<br />
the need to develop policy in response to new evidence and emerging issues. So, too,<br />
does the Pap screen program itself, with indications that an increase in screening interval,<br />
from two to three years, warrants consideration in view of the latest evidence.<br />
We welcomed the Government’s commitment to a national skin cancer awareness<br />
campaign, designed to reduce the impact of Australia’s most economically expensive<br />
cancer and the cause of more than 1500 deaths a year. There is a strong case for an<br />
ongoing commitment to such a campaign. Meanwhile, new evidence that excessive sun<br />
avoidance may cause vitamin D deficiency and increase autoimmune disease risk in some<br />
people again shows the importance of incorporating all the latest evidence into effective<br />
policy, as discussed in the skin cancer chapter.<br />
Obesity/overweight, nutrition, physical activity and alcohol are explored with renewed<br />
vigour. While we are gradually winning the battle against preventable disease on some<br />
fronts, the obesity epidemic threatens a reversal of the long-standing trend of future<br />
generations’ life expectancy exceeding that of their parents. Unless steps are taken now<br />
to reduce obesity, particularly among children, bowel and postmenopausal breast cancer<br />
rates may increase significantly beyond what is predicted as part of population ageing.<br />
One positive trend amid this concern is a growing recognition of general practitioners (GPs)<br />
as a pivotal part of chronic disease prevention. General practitioner groups have sought to<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
P r e v e n t i o n p o l i c y
increase their understanding of managing disease risk and, in January 2006, the Council<br />
of Australian Governments announced a number of chronic disease prevention measures<br />
involving GPs. We focus on the role of GPs in cancer prevention on a chapter-by-chapter<br />
basis.<br />
The range of issues covered in the <strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007–09 reflects the<br />
diversity of evidence-based expertise among the external authors and the members of our<br />
Public Health Committee, listed towards the end of this book. My thanks to them all, in<br />
particular the Chair of the Public Health Committee, Ms Dorothy Reading at The <strong>Cancer</strong><br />
Council Victoria, who oversaw the document’s production.<br />
<strong>Cancer</strong> describes a complex range of malignancies. We all hope for a cancer-free future,<br />
for a cure for the disease that claims more Australian lives than any other cause. The<br />
evidence suggests that, rather than a single, miracle cure, reducing the impact of cancer<br />
will be the result of numerous separate developments targeting individual cancers.<br />
Moreover, the evidence shows that the greatest potential gains for reducing cancer<br />
incidence and mortality in Australia are in primary prevention and early detection, using<br />
knowledge we already possess and which is articulated in the <strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong><br />
<strong>Policy</strong> 2007–09.<br />
Mrs Judith Roberts AO<br />
President, The <strong>Cancer</strong> Council Australia<br />
References<br />
Australian Institute of Health and Welfare (AIHW) 2002. Chronic diseases and associated risk factors in<br />
Australia, 2001. Canberra: AIHW.<br />
Australian Institute of Health and Welfare (AIHW), Australasian Association of <strong>Cancer</strong> Registries (AACR),<br />
<strong>National</strong> <strong>Cancer</strong> Strategies Group (NCSG) & McDermid I 2005. <strong>Cancer</strong> incidence projections, Australia 2002 to<br />
2011. Canberra: AIHW, AACR & NCSG.<br />
Begg S, Vos T, Goss J, Barker B, Stevenson C, Stanley L & Lopez AD (in press). The burden of disease and<br />
injury in Australia, 2003. Canberra: AIHW & Brisbane: University of Queensland.<br />
Cameron M, Sambell N, Wakefield M, Hill D 2006. Population change in most feared illnesses and perceived<br />
steps to reduce cancer risk. Presentation at Behavioural Research in <strong>Cancer</strong> <strong>Control</strong> Conference, Brisbane<br />
2006.<br />
10 Section One: Preventable risk factors
Section One:<br />
Preventable risk factors<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
11<br />
P r e v e n t i o n p o l i c y
T o b a c c o<br />
Introduction<br />
12 Section One: Preventable risk factors<br />
Every day, around 43 Australians die from illnesses<br />
caused by smoking, equivalent to over 15,500 deaths<br />
every year. Unless action is taken now, Australians<br />
will continue to die from illnesses caused by smoking<br />
that could have been prevented.<br />
In Australia, cigarette smoking became widespread in the 20th century. At that time,<br />
tobacco was used by many societies, some of which had used it for many centuries;<br />
however, development of the manufactured cigarette in the late 19th century resulted<br />
in increased prevalence and consumption (Winstanley, Woodward & Walker 1995). In<br />
Australia, by the time of the First World War, tobacco smoking had become popular,<br />
particularly the smoking of manufactured cigarettes. By the end of the Second World War,<br />
the earliest date for which Australian data are available, 72% of men and 26% of women<br />
were smokers (Winstanley, Woodward & Walker 1995).<br />
Since the 1970s, various bodies, including the International Union Against <strong>Cancer</strong> and<br />
more recently the World Health Assembly (the governing body of the World Health<br />
Organization), have taken action in recognition of the rising number of deaths caused by<br />
tobacco use. The first ever public health treaty on tobacco that outlines comprehensive<br />
tobacco control strategies, the Framework Convention on <strong>Tobacco</strong> <strong>Control</strong>, was passed<br />
by the World Health Assembly in May 2003. By January 2007, 143 member states of the<br />
World Health Organization were party to the convention, representing over 90% of the<br />
world’s population and making it one of the most extensive and rapidly implemented<br />
pieces of international law in history (WHO 2006).<br />
Australia was one of the first nations to become active in tobacco control, having used a<br />
range of measures, including advertising restrictions, public information, price increases,<br />
and controls on smoking in public places, which have contributed to a significant reduction<br />
in the prevalence of smoking since the mid-1970s. <strong>Tobacco</strong> control remains one of the best<br />
investments governments can make to enhance the health and economic well-being of all<br />
Australians. While progress has been achieved in reducing the prevalence of smoking and<br />
protecting people from the harms of second-hand smoke, smoking continues to contribute<br />
to one of the highest levels of disease burden attributable to a preventable cause. <strong>Tobacco</strong><br />
control must remain a high public policy priority, yet tobacco control initiatives are underfunded<br />
in the context of their demonstrated human and economic effectiveness. At the<br />
same time, efforts to reduce smoking prevalence are undermined by the tobacco industry,<br />
which continues to mislead, deceive and conceal the carnage caused by its deadly and<br />
addictive product, continues to pursue marketing strategies leading to high youth uptake,<br />
and obstructs measures designed to help reduce harm from smoking and exposure to<br />
second-hand smoke.
The link between tobacco and cancer<br />
Pathologists and other medical practitioners first observed a rise in the incidence of lung<br />
cancer in the 1920s and 1930s. Research published in 1950 confirmed that tobacco<br />
smoking was a cause of death and disease, and reports by the Royal College of Physicians<br />
in London in 1962 and the US Surgeon General in 1964 resulted in acknowledgment by<br />
some governments that smoking was a cause of disease (Winstanley, Woodward & Walker<br />
1995). In a 2004 review the US Surgeon General concluded that there was sufficient<br />
evidence to infer a causal relationship between smoking and cancer at the following sites:<br />
bladder, cervix, kidney, larynx, lung, oesophagus, oral cavity and pharynx, pancreas and<br />
stomach; and between smoking and acute myeloid leukaemia.<br />
There is well-documented evidence of the health effects of exposure to second-hand<br />
smoke or ‘passive smoking’. In 1986 a major conclusion of a report by the US Surgeon<br />
General was that involuntary smoking is a cause of disease, including lung cancer, in<br />
healthy non-smokers. This conclusion was supported by reviews published in the same<br />
year by the US <strong>National</strong> Research Council, the International Agency for Research on<br />
<strong>Cancer</strong>, and the Australian <strong>National</strong> Health and Medical Research Council (USDHHS 2006;<br />
Winstanley, Woodward & Walker 1995). In 1992 a US Environmental Protection Agency<br />
report classified cigarette smoke as a class A carcinogen and concluded that exposure<br />
to second-hand smoke causes lung cancer (USDHHS 2006). The 2006 report of the<br />
US Surgeon General on involuntary exposure to tobacco smoke reviews evidence that<br />
reaffirms and strengthens the findings of the 1986 report, concluding that exposure to<br />
second-hand smoke causes lung cancer and also that there is no risk-free level of exposure<br />
to second-hand smoke (see later in this chapter for data on the incidence of cancer and<br />
mortality caused by smoking in Australia).<br />
The impact<br />
In Australia, tobacco smoking kills more than 15,500 Australians each year (Begg et al. in<br />
press). As shown in the Figure 1.1 each year more Australians are killed by tobacco than<br />
by breast cancer, AIDS, traffic and other accidents, murders and suicides combined (AIHW<br />
2006; Begg et al. in press).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
13<br />
T o b a c c o
Figure 1.1 Number of Australians who died in 2004 because of smoking compared with selected other<br />
causes<br />
Causes of death<br />
Falls<br />
Drowning<br />
Transportation accidents<br />
Other accidents<br />
Suicide<br />
Homicide<br />
Breast cancer (females)<br />
AIDS<br />
Smoking*<br />
197<br />
168<br />
116<br />
1,558<br />
1,689<br />
1,335<br />
2,098<br />
2,614<br />
* Note that the estimate for deaths attributable to smoking is based on data for 2003.<br />
Sources: AIHW 2006; Begg et al. in press<br />
14 Section One: Preventable risk factors<br />
15,511<br />
The Australian Burden of Disease Study quantifies the contribution to health status of<br />
mortality, disability, impairment, illness and injury arising from tobacco smoking and other<br />
risk factors. The study found that tobacco is one of the leading risk factors for disease,<br />
being responsible for 7.8% of the total burden of disease in Australia. Only high body mass<br />
creates a greater burden of disease (8.6%) (Begg et al. in press).<br />
Most smokers begin smoking when they are young, and many remain addicted to smoking<br />
for life (Winstanley, Woodward & Walker 1995). As a consequence of their addiction, in<br />
Australia one in two lifetime smokers will die from diseases caused by tobacco, and more<br />
than 22% of these deaths are in people aged under 65 years (AIHW 1998).<br />
<strong>Tobacco</strong> smoking increases the risk of cardiovascular disease, lung disease and cancer,<br />
as well as a number of other conditions (USDHHS 2004). Many of the diseases caused<br />
by smoking are chronic and disabling, and it has been estimated that in the US, for every<br />
premature death caused by smoking in a given year, there were at least 20 smokers living<br />
with a smoking-related disease (USDHHS 2004). Table 1.1 lists the cancers caused by<br />
smoking.<br />
<strong>Tobacco</strong> smoking is a leading cause of cancer, and was estimated to have directly caused<br />
10,592 new cases of cancer (12% of all new cases of cancer) and 7,820 deaths (21.5%<br />
of cancer deaths) in Australia in 2001. Between 1991 and 2001, the incidence rate for<br />
men of cancers attributable to smoking fell by an average of 1.4% per year, while the rate<br />
for women rose by 0.7% per year. These differences are attributable to differences in the<br />
prevalence of smoking among Australian men and women over the past 30 years and the<br />
time lag between exposure to carcinogens and diagnosis of cancer (AIHW & AACR 2004).
Table 1.1 <strong>Cancer</strong> site and percentage of new cancers attributable to smoking in Australia in 2001<br />
Site Males (%) Females (%)<br />
Lung 89 70<br />
Larynx 69 60<br />
Oral cancers 52 42<br />
Renal (kidney) pelvis 51 43<br />
Oesophagus 50 41<br />
Anus 39 29<br />
Bladder 38 28<br />
Vulva – 32<br />
Cervix – 19<br />
Penis 21 –<br />
Pancreas 23 16<br />
Kidney 17 12<br />
Stomach 12 8<br />
Colon/rectum 12 12<br />
Sources AIHW & AACR 2004; Chao et al. 2000; USDHHS 2004<br />
The economic consequences of tobacco use in Australia have been examined, with the<br />
total social costs in 1998−99 having been estimated at $21 billion (Collins & Lapsley<br />
2002). It has also been estimated that the health system costs for lung cancer (85% of<br />
which is attributable to tobacco smoking) amounted to $107 million in 1993−94 (Mathers<br />
et al. 1998). Smoking causes very high levels of ill health and premature death among<br />
Aboriginal and Torres Strait Islander peoples, which adds to the social costs among these<br />
communities (Briggs, Lindorff & Ivers 2003). In Australia in 2001–02, smoking accounted<br />
for more than 291,000 hospital episodes per year, at a cost of $682 million (Hurley 2006).<br />
The challenge<br />
Adults<br />
The prevalence of smoking among Australian adults has been measured by a number<br />
of different surveys: the <strong>National</strong> Drug Strategy Household Survey conducted by the<br />
Australian Institute of Health and Welfare (AIHW 2005); Smoking and Health Surveys<br />
conducted by The <strong>Cancer</strong> Council Victoria (White, Hill et al. 2003); <strong>National</strong> Health Surveys<br />
(ABS 2006); and <strong>National</strong> Aboriginal and Torres Strait Islander Surveys conducted by the<br />
Australian Bureau of Statistics (ABS 1994). Consistent trends have been observed, despite<br />
minor variations in methods between the surveys, so trends over time rather than specific<br />
figures are important foci for policy development (White, Hill et al. 2003).<br />
In 2004 in Australia, 17.4% of people aged 14 years or older were daily smokers, with<br />
a further 3.9% of the population reporting weekly or less than weekly smoking (AIHW<br />
2005). The recent decline in the number of daily smokers among men (18.6%) and women<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
15<br />
T o b a c c o
(16.3%) continues the trends observed over the last 25 years (White, Hill et al. 2003; AIHW<br />
2005).<br />
It has been noted that those smokers who regard themselves as ‘occasional’ or ‘social<br />
smokers’ may make up 29% of all smokers. This segment of smokers holds different<br />
attitudes towards smoking and quitting from other smokers, which has implications for<br />
campaigns and messages for this group of smokers (Morley et al. 2006).<br />
There are specific populations for which smoking rates remain significantly higher than<br />
average, including populations that are socio-economically disadvantaged, Aboriginal and<br />
Torres Strait Islander peoples and male Australians born overseas in particular countries.<br />
Socio-economically disadvantaged populations<br />
The prevalence of smoking in Australia in 2001 among lower blue collar workers (36%)<br />
remained higher than among upper white collar workers (16%), despite the significant<br />
declines in all occupational groups since 1980 observed in surveys of people aged 18 years<br />
or older by The <strong>Cancer</strong> Council Victoria (White, Hill et al. 2003).<br />
Aboriginal and Torres Strait Islander peoples<br />
The prevalence of smoking remains very high among Aboriginal and Torres Strait Islander<br />
peoples. The <strong>National</strong> Aboriginal and Torres Strait Islander health survey of 2004–05<br />
indicated that the prevalence of smoking in people aged 18 years and over has remained<br />
unchanged at 50% since 1995 (ABS 1994); however, the smoking rates among some<br />
remote Aboriginal and Torres Strait Islander communities are much higher (Ivers 2001).<br />
After adjusting for age differences, in 2004 Aboriginal and Torres Strait Islander people<br />
aged 18 years and over were more than twice as likely as non-Indigenous Australians to<br />
be smokers (AIHW 2006). A 2002 survey reported a smoking prevalence of 59% among<br />
Aboriginal health workers in New South Wales (Mark et al. 2005).<br />
Potential contributors to the higher prevalence of smoking among Aboriginal and Torres<br />
Strait Islander peoples include (Briggs, Lindorff & Ivers 2003; AGDHA 2005):<br />
•<br />
•<br />
•<br />
•<br />
•<br />
the effects of historical colonisation and dispossession (disruption and erosion of<br />
language and culture, creation of unhealthy living and social conditions, devaluation of<br />
cultural responses to health problems, general subordination due to racism)<br />
socio-economic disadvantage (the roles of lower levels of education, lower levels of<br />
employment and lower weekly income)<br />
cultural beliefs and strong links to a traditional lifestyle (recognition of homelands,<br />
believing in the important role of elders, and English not being a first language have<br />
been linked to higher prevalence of tobacco use)<br />
enjoyment and addiction (similar to their roles in the maintenance of smoking among<br />
non-Indigenous people)<br />
social contexts and pressures (role of smoking in becoming accepted as part of the<br />
social group, roles of boredom, stress and anxiety).<br />
A lack of knowledge on the health effects of tobacco does not appear to be a major factor<br />
in the higher prevalence of smoking among Aboriginal and Torres Strait Islander peoples<br />
(Briggs, Lindorff & Ivers 2003).<br />
1 Section One: Preventable risk factors
Australians born in particular countries<br />
Smoking rates among Australians born in Australia and in other countries were measured<br />
in the <strong>National</strong> Health Survey 2004–05 for people aged 18 years and over (ABS 2006).<br />
The overall prevalence among men was 24.2%, but smoking was more prevalent among<br />
men born in North Africa and the Middle East (31.9%) and among men born in South East<br />
Asia (28.6%). For women born in Oceania (excluding Australia) the prevalence was 26.3%,<br />
compared with an overall prevalence among women of 18.4% (ABS 2006).<br />
Teenagers<br />
Among secondary students (Table 1.2), rates of smoking decreased in the late 1980s, and<br />
then remained relatively stable in the 1990s (Hill, White & Letcher 1999). Among older<br />
students (those aged 16–17 years), the significant decrease among males and females<br />
between 1999 and 2002 was the first seen in this age group since 1990 (White & Hayman<br />
2004). Among students aged 12–15 years, the prevalence of smoking also declined<br />
between 1996 and 2005.<br />
Table 1.2 Trends in rates of smoking among Australian secondary school children between 1984 and<br />
2005: proportion (%) of students who smoked in the last seven days (age adjusted)<br />
Year Girls<br />
12–15 years<br />
Boys<br />
12–15 years<br />
Girls<br />
16–17 years<br />
Boys<br />
16−17 years<br />
1984 20 19 32 28<br />
1987 14 13 30 26<br />
1990 14 13 28 24<br />
1993 16 15 29 28<br />
1996 16 16 32 28<br />
1999 16 15 29 30<br />
2002 12 10 25 21<br />
2005 7 7 17 16<br />
Sources: Hill, White & Letcher 1999; White & Hayman 2004; White & Hayman 2006<br />
Note that young people who had left school were not included in the national surveys on which this table is based.<br />
There were an estimated 4.3 million ex-smokers among the 16.4 million Australians aged<br />
14 and over in 2004 (AIHW 2005). However, there were still an estimated 2.9 million<br />
Australians who smoked on a daily basis in 2004 (AIHW 2005).<br />
Other challenges<br />
The prevention of more than 17,000 premature deaths in 1998 in Australia can be<br />
attributed to a range of successful tobacco control measures that delivered declines in<br />
smoking from the early 1970s (DHA 2003). However, with almost one in five Australians<br />
continuing to smoke, the nation faces a significant challenge to further reduce smoking<br />
rates and avert major social and economic costs to the community.<br />
Compounding the need to further reduce smoking rates is an expected increase in overall<br />
cancer incidence rates in Australia of around 30% over the next five to 10 years as a result<br />
of population ageing. This trend is likely to continue as the population ages. Reducing<br />
smoking prevalence now would lead to significantly fewer overall cancer diagnoses<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1<br />
T o b a c c o
in the longer-term future, when healthcare services in Australia are likely to be under<br />
unprecedented pressure owing to demographic change.<br />
Despite the progress made in Australia to date, significant challenges to achieving<br />
continued reductions in tobacco-related harm remain. These challenges include the<br />
disproportionate burden of harm among disadvantaged populations, attitudes that<br />
undermine effective tobacco control, the influence of the tobacco industry, and a<br />
reluctance from governments at all levels to take measures to reduce tobacco use<br />
commensurate with the economic and social damage caused by smoking.<br />
Disproportionate tobacco burden<br />
As documented elsewhere in this chapter, socially disadvantaged population groups<br />
bear a disproportionately high tobacco burden in Australia. Evidence increasingly shows<br />
that, as well as causing a growing inequity in health status, smoking among these<br />
groups contributes to a cycle of poverty and disadvantage. Recent research on financial<br />
deprivation and smoking has shown that disadvantaged smokers experience financial<br />
hardship as a result of tobacco use, and are more likely to want to quit smoking, but less<br />
likely to succeed in quitting (Siahpush, Heller & Singh 2005).<br />
Attitudes that undermine effective tobacco control<br />
Resistance to progressive tobacco control can be based on a set of attitudes that are<br />
clearly unsupported by evidence or are based on facile excuses for inaction, yet some of<br />
which are nonetheless cited by social commentators and policy makers to discourage<br />
efforts to reduce the tobacco burden. An important part of ‘de-normalising’ a habit that<br />
causes the extent of preventable death and disease documented in this chapter is to<br />
counter, using evidence, the inaccurate framing of tobacco issues cited as a justification for<br />
tobacco control complacency. Some of the salient catchphrases used to argue against an<br />
increased commitment to tobacco control can be readily debunked in view of the evidence<br />
as follows.<br />
‘We have done everything possible to control tobacco, apart from banning tobacco<br />
altogether.’<br />
This view is contradicted by the evidence, which shows that a comprehensive policy<br />
commitment and sustained campaign funding are highly effective in reducing smoking<br />
rates. In California, which introduced comprehensive tobacco control measures in 1988,<br />
smoking rates have decreased by approximately 38%, from 22.7% to 14% (CDHS 2006).<br />
Jurisdictions such as Canada now have daily smoking rates as low as 13.5% (Canadian<br />
<strong>Tobacco</strong> Use Monitoring Survey 2006). There is every reason to believe that, with<br />
appropriate measures, smoking rates in Australia could be reduced to less than 5%. None<br />
of the required measures would involve banning tobacco products.<br />
‘Australia is doing OK already’ or ‘Australia is doing better than anyone else.’<br />
While Australia should be acknowledged as a world leader in tobacco control policy given<br />
its reforms over the past three decades, more than 17% of Australians still smoke every<br />
day: which corresponds to almost one in five people incurring a 50% risk of dying as a<br />
result of smoking, half of them in middle age. Despite substantial reductions in smoking<br />
rates over the past 30 years, tobacco use remains one of the leading preventable causes<br />
of disease. Over 15,500 Australians die from smoking-caused diseases each year, and lung<br />
cancer rates in women continue to rise.<br />
1 Section One: Preventable risk factors
‘It’s a legal product.’<br />
<strong>Tobacco</strong> is a commercial and regulatory anomaly. Smoking causes a higher disease burden<br />
than the combined use or misuse of all other ‘legal products’ that are rigorously regulated<br />
for safety reasons, including over-the-counter drugs, prescription medicines, pesticides,<br />
alcohol and motor vehicles. On the basis of demonstrated harm, tobacco products are<br />
also under-regulated in comparison with government treatment of other environmental<br />
carcinogens and hazardous consumer products.<br />
‘Smoking provides economic benefits to government and society in general.’<br />
Evidence indicates the opposite: tobacco control is one of the best investments<br />
governments can make. Independent economic analyses clearly demonstrate that smoking<br />
has a high net social and economic cost to the community. Similar analysis has also shown<br />
that a reduction in smoking rates would not harm the economy. There is also objective<br />
evidence for a strong return on investment in tobacco control. The most recent Department<br />
of Health and Ageing analysis on this issue found that every $1 spent on tobacco control<br />
yields $2 in savings, and the consultancy firm Applied Economics concludes that tobacco<br />
control yields better gains than any other public health program expenditure, with a benefit<br />
to cost ratio of 50:1 (Applied Economics 2003).<br />
‘Smoking is an adult choice.’<br />
The vast majority of smokers start smoking while in adolescence, becoming addicted<br />
before they are mature enough to make an adult decision and fully understand the<br />
consequences of nicotine addiction and the harms of smoking (Schofield et al. 1998;<br />
Winstanley, Woodward & Walker 1995). Almost all smokers also say that they regret<br />
starting smoking (Fong et al. 2004). Evidence also shows that most adult smokers are not<br />
fully aware of the dangers of smoking, with a recent survey finding that while two-thirds<br />
identified lung cancer as smoking-related, only one-quarter knew that smoking caused<br />
heart disease and fewer than 10% understood the risk of emphysema, stroke and vascular<br />
problems (Quit Victoria 2006). Around 90% of smokers report regretting ever having<br />
started (Fong et al. 2004).<br />
‘<strong>Tobacco</strong> control is part of a nanny state.’<br />
The argument that government action to reduce smoking rates is restricting personal<br />
freedoms with risk-averse, patronising public policy is debunked by the evidence outlined<br />
against the five arguments discussed above. In addition, most tobacco control measures<br />
are designed to support decisions that people are already making. Every year, 30% to 40%<br />
of smokers attempt to quit, but only one in 10 attempts to quit is successful. <strong>Tobacco</strong><br />
control measures reduce relapse rates and help intending quitters to break their addiction.<br />
Measures are mainly about removing inducements to smoke or providing information,<br />
support and encouragement to quit.<br />
Governments also have a responsibility to protect non-smokers from the increasingly<br />
evident harms of environmental tobacco smoke and to reduce the economic burden, borne<br />
by the wider community, imposed by smoking. The restrictions on smokers imposed over<br />
recent years have attracted overwhelming community support (VCTC 2002).<br />
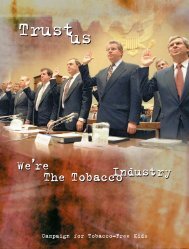
<strong>Tobacco</strong> industry influence<br />
While coordinated efforts to reduce the disease burden of tobacco have made Australia a<br />
challenging market for the tobacco industry compared with nations where there are fewer<br />
controls, almost one in five Australians continues to smoke, with Australian households<br />
spending more than $10 billion on tobacco products per year (ABS 2005).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1<br />
T o b a c c o
<strong>Tobacco</strong> products are among the top 10 best-selling items for a range of retailers, including<br />
supermarket chains, grocery stores, petrol stations and newsagents. The tobacco industry<br />
in Australia was estimated to be worth $6.2 billion in 2002 (VCTC n.d.), with 52 brands of<br />
cigarettes available for sale in June 2003 (Australian Retail <strong>Tobacco</strong>nist 2003). Therefore,<br />
tobacco companies are very well-resourced to counter attempts to reduce smoking rates;<br />
the industry continues to exploit loopholes in tobacco control regulations and to engage<br />
high-powered legal firms when called to account in the courts. The tobacco industry<br />
continues to try to court policy-makers and to adopt a stance of legitimacy and good<br />
corporate citizenship, despite a proven record of deceptive conduct.<br />
Effective interventions<br />
Comprehensive tobacco control strategies, if sufficiently funded, work to reduce tobacco<br />
consumption among both adults and teenage smokers (VCTC 2002). This conclusion is<br />
based on studies from the World Health Organization (WHO 1998) and the US Centers<br />
for Disease <strong>Control</strong> and <strong>Prevention</strong> (CDCP 1999; CDCP 2000; CDCP 2001), and a review<br />
carried out for the World Bank (Jha & Chaloupka 1999).<br />
In Australia over the last 30 years an estimated $8.6 billion has been saved through deaths<br />
avoided and declines in illness and disability due to reduced tobacco use (DHA 2003). It<br />
is estimated that $2 has been saved on health care for each $1 spent on tobacco control<br />
programs to date, with total economic benefits exceeding expenditure by at least 50 to<br />
1. Specific strategies include increasing the prices of tobacco products and changing<br />
social attitudes to smoking through regulation and hard-hitting media campaigns. The<br />
precise impact of any specific strategy has been difficult to assess, as many have been<br />
implemented simultaneously or partially, or in an ad hoc way without comprehensive<br />
evaluation (Chapman 1993). Moreover, all have been opposed and undermined by tobacco<br />
industry activity.<br />
Pivotal to a strategic and coordinated approach to smoking reduction in Australia is the<br />
willingness of governments to commit to, and seek to attain, specific smoking prevalence<br />
targets. Targets can only be achieved if adequate resources are committed to tobacco<br />
control measures in the long term. Evidence shows that it is feasible to achieve a decline of<br />
1% per annum in the prevalence of smoking if tobacco control measures are well-funded<br />
and implemented (CDCP 2001). The speed of the decline depends on government action in<br />
ensuring adequate spending levels as well as appropriate regulation.<br />
The <strong>Cancer</strong> Council encourages the Australian Government to set targets for smoking<br />
prevalence for Australian adults, children and disadvantaged groups, and to allocate<br />
adequate funds for comprehensive tobacco control programs to achieve these targets. In<br />
order to further reduce the unacceptable burden of smoking in Australia, governments and<br />
other institutions involved in public policy will need to build on the demonstrated success<br />
of tobacco control strategies employed in Australia over the past three decades. Priorities<br />
for further action are outlined below.<br />
Continual innovation in tobacco control is required to keep pace with changes in the<br />
smoking-related environment. For example, a growing evidence base showing the<br />
increasing extent of disease linked with smoking demonstrates the need for tobacco<br />
control programs that are commensurate with the burden smoking imposes on the<br />
community. Accumulated evidence showing which approaches to tobacco control are the<br />
most effective should inform government policy. <strong>Policy</strong>-makers must also be able to react<br />
quickly to the tobacco industry’s attempts to exploit loopholes in measures designed to<br />
reduce smoking rates. There are a number of other examples showing the need for flexible,<br />
20 Section One: Preventable risk factors
progressive solutions, as well as evidence that indicates where public policy for tobacco<br />
control in Australia is inadequate.<br />
All jurisdictional governments in Australia have committed, in principle, to the following<br />
general approaches to tobacco control, as each priority is to some extent incorporated into<br />
the <strong>National</strong> <strong>Tobacco</strong> Strategy. However, implementation of the strategy has been gradual,<br />
and the funding commitment is not sufficient to convert policy into effective practice. The<br />
re-establishment of a multi-jurisdictional advisory body drawing on independent expertise<br />
from outside the bureaucracies, such as the former Ministerial <strong>Tobacco</strong> Advisory Group,<br />
would help to guide the implementation of the <strong>National</strong> <strong>Tobacco</strong> Strategy.<br />
The <strong>Cancer</strong> Council Australia outlines the major areas where reform is required below.<br />
Rejection of tobacco industry donations by all political parties, while not explored as<br />
a specific tobacco control measure below, would also be a significant step in ‘denormalising’<br />
smoking and challenging the legitimacy of the tobacco industry.<br />
Recommended funding<br />
Despite the well-documented successes of comprehensive strategies to address tobacco<br />
use and the resultant savings in public finances (DHA 2003), government funding of<br />
tobacco control in Australia is well below optimal. The US Centers for Disease <strong>Control</strong><br />
has developed best practice guidelines for the implementation of comprehensive tobacco<br />
control programs (CDCP 1999). These guidelines draw on evidence-based analyses of<br />
programs implemented in California, Massachusetts and other US states. The guidelines<br />
outline nine program components and estimate a range of annual costs. For a state<br />
with a population under three million people the cost would be US$7–20 per capita, for<br />
populations between three and seven million the cost would be US$6–17 per capita,<br />
and for populations over seven million (e.g. Australia-wide) the cost would be US$5–16<br />
(A$7–21). Recommendations from the VicHealth Centre for <strong>Tobacco</strong> <strong>Control</strong> on how<br />
comprehensive tobacco control programs should be implemented in Australia, based on<br />
the Centers for Disease <strong>Control</strong> best practice guidelines (CDCP 1999), are summarised in<br />
Table 1.3 (VCTC 2003).<br />
Table 1.3 Recommended levels of funding for tobacco control programs (Australian dollars, 2003)<br />
Component A$ million<br />
Community programs 23.25<br />
Chronic disease programs 1.15<br />
School programs 1.65<br />
Enforcement 12.25<br />
Statewide programs 13.07<br />
Counter marketing 64.00<br />
Cessation programs 59.35<br />
Subtotal 174.69<br />
Surveillance and evaluation 8.00<br />
Administration and management 11.80<br />
Total 194.49<br />
Source: VCTC 2003<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
21<br />
T o b a c c o
In 2007, given estimated costs of $200 million and an Australian population of 20.7 million,<br />
the recommended tobacco control measures would cost around A$10 per head. The Better<br />
Health for All Australians Initiative from the Council of Australian Governments (federal,<br />
state and territory governments) provides an opportunity to meet the recommended levels<br />
of investment for tobacco control with its stated intent to: ‘promote healthy lifestyles;<br />
support early detection of lifestyles risks and chronic disease through a new Well Person’s<br />
Health Check (available nationally to people around 45 years old with one or more<br />
identifiable risks that lead to chronic disease); and support lifestyle and risk modification<br />
through referral to services that assist people wanting to make changes to their lifestyle,<br />
for example, give up smoking’ (COAG 2006). Disappointingly, the initial round of funding in<br />
2006 did not include additional funding for tobacco control initiatives, limiting its impact on<br />
cost-effective approaches to health improvement. The <strong>Cancer</strong> Council and its allies working<br />
across all nine jurisdictions in Australia will continue to encourage government to fund<br />
evidence-based tobacco control programs on the basis of their potential to deliver optimal<br />
social and economic gains to the community.<br />
Social marketing campaigns<br />
The <strong>National</strong> <strong>Tobacco</strong> Campaign of the late 1990s (‘Every Cigarette Is Doing You Damage’)<br />
was the first coordinated, multimedia anti-smoking campaign that was run on a national<br />
basis and supported by related activities in jurisdictions (e.g. state Quit programs etc.).<br />
An independent economic evaluation of the campaign, based on a rigorous analysis,<br />
calculated that the $7.1 million invested in the program by the Australian Government in<br />
1997 yielded full cost offsets to the whole economy of $24.2 million, meaning that the<br />
campaign paid for itself three times over. Direct savings to the Australian Government<br />
alone were calculated to be $10.9 million within the year of its implementation (DHA 2000).<br />
Yet the campaign has not been run on a national basis for more than seven years, despite<br />
the clear economic benefits and potential for larger long-term returns. Moreover, evidence<br />
shows that without recurrent commitment to widely accessible information about the risks<br />
of tobacco use, declines in smoking rates can stall or are at risk of reversing.<br />
Based on the success of the <strong>National</strong> <strong>Tobacco</strong> Campaign, and adjusting for inflation,<br />
there is a clear economic case for committing $11 million on a recurrent basis to a new,<br />
evidence-based social marketing campaign. Such a campaign would have a major impact<br />
on bringing smoking rates closer to a feasible 5% of the Australian population and add to<br />
the success of other tobacco control measures.<br />
Elimination of tobacco promotion<br />
When responding to the Government’s review of the <strong>Tobacco</strong> Advertising Prohibition Act,<br />
The <strong>Cancer</strong> Council Australia and allies presented evidence of tobacco industry activity that<br />
contradicted the spirit of the Act and, in some cases, represented potential breaches. On<br />
the basis of that evidence, the <strong>Cancer</strong> Council put forward a number of recommendations<br />
for amending the Act. However, these were not adopted, and the review committee<br />
concluded that no amendments would be made to the Act. An evidence-based case<br />
remains, however, for amending the Act to enact and enforce the following additional<br />
restrictions on tobacco promotion. Recommended measures include:<br />
•<br />
•<br />
amend the definition of ‘tobacco advertisement’ to include the use of imagery that<br />
associates smoking with a desirable lifestyle, and expand the definition of ‘tobacco<br />
product’ to include cigar and cigarette cases (including the slips introduced to conceal<br />
graphic warnings on cigarette packets)<br />
prohibit all advertising and display at the point of sale<br />
22 Section One: Preventable risk factors
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
address smoking in films: for example, classify films with positive depictions of<br />
smoking, and run anti-smoking advertisements before cinema screenings of such films<br />
prohibit the giving of free samples, gifts and other promotional offers aimed at boosting<br />
tobacco sales<br />
prohibit ‘mobile retailing’: sales of tobacco products should be restricted to places that<br />
operate as shops, and shops only, at all times<br />
prohibit vending machines<br />
require all tobacco products to be sold only in prescribed generic packaging that does<br />
not have any colours or branding or information other than that prescribed by regulation<br />
regulate Internet advertising and sales, direct mail/sending of catalogues, and mail order<br />
make it an offence to encourage/employ someone else to run a tobacco advertisement<br />
in breach of the Act<br />
remove exemptions for tobacco advertisements on international flights in and out of<br />
Australia<br />
prohibit marketing outside Australia by Australian companies that would be illegal in<br />
Australia<br />
prohibit false or misleading statements by manufacturers about the addictiveness or<br />
health effects of smoking or exposure to smoke<br />
require tobacco manufacturers to report on all promotional activities and expenditure<br />
and on sales volume<br />
tighten provisions relating to magazines imported from countries with fewer restrictions<br />
on tobacco advertising in periodicals.<br />
There are a number of other recommended amendments, indicating both the extent<br />
to which the Act is limited in achieving its stated aims and the scope for the tobacco<br />
industry to continue to promote its products. The effectiveness of the <strong>Tobacco</strong> Advertising<br />
Prohibition Act is also limited by the relatively small penalties associated with breaches,<br />
particularly in light of the potential revenues associated with recruiting new smokers<br />
through illegal marketing strategies.<br />
While a strengthened <strong>Tobacco</strong> Advertising Prohibition Act would be the appropriate<br />
legislative instrument to further restrict tobacco promotion as described, it is unlikely<br />
that government would call for another general review of the Act in the near future, thus<br />
other approaches to achieve similar results should be considered. For example, direct<br />
approaches to supermarket chains to remove tobacco products from sight have the<br />
potential to further ‘de-normalise’ smoking and assist quitters who are at higher risk of<br />
relapse when cigarettes are in plain view and more readily accessible. In the meantime,<br />
The <strong>Cancer</strong> Council Australia will continue to make the case for incremental amendments<br />
to the Act to phase in the tighter measures described above.<br />
Australia also needs to ensure that the protocols of the World Health Organization<br />
Framework Convention on <strong>Tobacco</strong> <strong>Control</strong>, which was ratified here in 2004, are observed<br />
in the domestic environment, in particular for eliminating loopholes allowing for tobacco<br />
industry sponsorship of sporting events.<br />
Product regulation<br />
As discussed later in this chapter, tobacco products are a regulatory anomaly in view of<br />
the burden that their unregulated availability imposes on the community. All government<br />
jurisdictions in Australia have agreed to the principle of reducing smoking rates through<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
23<br />
T o b a c c o
improved regulation, by collectively endorsing the <strong>National</strong> <strong>Tobacco</strong> Strategy (see later in<br />
this chapter). However, the slow progress of implementation has increased the urgency of<br />
tobacco regulation priorities, which include:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
imposing penalties for misleading statements (see recommended amendments to the<br />
<strong>Tobacco</strong> Advertising Prohibition Act)<br />
banning additives that aid palatability and addictiveness<br />
making reduced ignition propensity cigarettes (shown to significantly reduce fire risk)<br />
mandatory<br />
banning filter venting<br />
making detailed information on the content of all tobacco products publicly available<br />
(possibly on a public domain website)<br />
imposing a ‘polluter pays’ requirement/levy on industry.<br />
Real price increases<br />
As articulated in the <strong>National</strong> <strong>Tobacco</strong> Strategy (see later in this chapter), imposing price<br />
increases on tobacco products through taxation has been shown to directly reduce<br />
smoking rates, and is therefore endorsed as evidence-based tobacco control policy.<br />
Government revenue derived from increased tobacco tax should fund additional smoking<br />
cessation services, to help ensure that people on lower incomes, who already bear a<br />
disproportionate tobacco burden, are better supported to quit smoking.<br />
Accountability<br />
Litigation is an increasingly effective way to help make the tobacco industry accountable<br />
for the death and disease caused by its products and to obtain funds to support tobacco<br />
control measures (Advocacy Institute 2005). The achievements of litigation include<br />
(Daynard 2003):<br />
•<br />
•<br />
•<br />
•<br />
disclosure of documents that demonstrate the intent of the tobacco industry to target<br />
children; deliberately mislead scientists, politicians, and customers about the lethal<br />
and addictive nature of their products; and to conspire with smugglers and money<br />
launderers around the world<br />
verdicts against tobacco companies in tobacco cases in the US, made possible by<br />
the above-mentioned documents, involving punitive damages of millions or billions of<br />
dollars have added to the industry’s confusion and loss of legitimacy and, in the US, the<br />
increasing possibility of bankruptcy further weakens the industry’s position politically<br />
and in the financial community<br />
the first stirrings of responsible behaviour by tobacco companies (Philip Morris now<br />
concedes on its website that cigarette smoking is addictive and causes lung cancer and<br />
other diseases)<br />
media coverage and public discussions about tobacco lawsuits, which educate the<br />
community about addiction and disease caused by smoking.<br />
In Australia the Australian Competition and Consumer Commission has had some success<br />
in enforcing the law against the tobacco industry with respect to its deceptive practices,<br />
with the industry agreeing to court-enforceable undertakings to remove ‘light’ and ‘mild’<br />
brands from sale and pay for corrective advertising. The industry also promptly withdrew<br />
‘split packs’ (see elsewhere in this chapter), which represented a breach of packaging<br />
regulations, following prompt action from the commission. However, the wealthy tobacco<br />
industry is a formidable legal opponent, and the Australian Competition and Consumer<br />
24 Section One: Preventable risk factors
Commission lacks sufficient funds to effectively bring the industry to account. The<br />
Australian Government should adequately fund the Australian Competition and Consumer<br />
Commission to take on the tobacco industry.<br />
Access to smoking cessation aids<br />
The <strong>Cancer</strong> Council Australia recommends improved access to smoking cessation aids<br />
to an extent commensurate with the damage caused by smoking and the percentage of<br />
smokers who would like to quit. Implementation of the other measures articulated in this<br />
section would also require an increase in the availability of smoking aids to help ensure an<br />
optimal return on investment in initiatives such as social marketing campaigns. A range<br />
of products and services needs to be available to support intending quitters, such as<br />
counselling, information and education, and nicotine replacement and pharmacological<br />
products.<br />
Improved tobacco control policy requires:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
promotion of tobacco-dependence treatment as an integral component of cost-effective<br />
health care<br />
increased government funding of the delivery and promotion of non-drug smoking<br />
cessation support services, including Quitlines<br />
increased funding for programs to educate and prompt healthcare providers to identify<br />
and advise patients who smoke to quit, and to refer them to appropriate support<br />
services<br />
implementation of subsidy and access arrangements for pharmacological interventions,<br />
to help ensure that treatment is equitable and cost-effective<br />
tailoring of cessation support services for disadvantaged and high-risk groups, such as<br />
Aboriginal and Torres Strait Islander people<br />
introduction of a Medicare rebate for general practitioners to counsel patients about<br />
smoking cessation or for referral to the Quitline or other effective services.<br />
Smoke-free environments<br />
The restrictions on smoking in public places that gained momentum in the mid-to-late<br />
1980s with bans on smoking in Australian workplaces and domestic flights have extended<br />
to a number of environments, with evidence showing a significant decrease in the health<br />
risks encountered due to second-hand smoke. Smoke-free environments also help to<br />
‘de-normalise’ smoking and encourage smokers to quit. While all Australian jurisdictions<br />
have adopted some bans on smoking in public places, the pace of reform varies, and<br />
opportunities for significant improvement remain. In order for restrictions to reach their<br />
potential to adequately protect all individuals from the dangers of second-hand smoke,<br />
tightening of laws is required in all jurisdictions, with evidence-based recommendations to:<br />
•<br />
•<br />
•<br />
•<br />
eliminate the loopholes/exemptions exploited by pubs and clubs<br />
eliminate ‘high-roller’ room exemptions (e.g. in casinos, where wealthy patrons are<br />
permitted to smoke in enclosed spaces despite the risks to staff)<br />
ban smoking in outdoor dining areas<br />
create smoke-free campuses/higher learning institutions.<br />
There is also a clear case for banning smoking in cars carrying children and pregnant<br />
women.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
25<br />
T o b a c c o
<strong>Tobacco</strong> control strategy for Aboriginal and Torres Strait Islander peoples<br />
The prevalence of smoking among Aborigines and Torres Strait Islanders is around 50%,<br />
more than 2½ times the smoking rate of non-Indigenous Australians. Evidence shows<br />
that smoking among Aborigines and Torres Strait Islander people is a significant cause of<br />
increased cancer mortality and other chronic disease. Indigenous Australians are more<br />
than twice as likely to die within five years of a cancer diagnosis as non-Indigenous cancer<br />
patients, in large part because of the poor prognosis of cancers caused by smoking<br />
(Condon et al. 2005).<br />
The cycle of poverty and disadvantage exacerbated by smoking (discussed elsewhere<br />
in this chapter) is particularly acute among Aborigines and Torres Strait Islander people.<br />
Despite the importance of smoking in the crisis in Indigenous health, efforts to address the<br />
issue have been substantially under-funded. Yet evidence shows that measures to reduce<br />
tobacco use, such as information, education and nicotine replacement therapy, can work<br />
in Indigenous communities if adequately funded and promoted in a culturally appropriate<br />
framework (Briggs, Lindorff & Ivers 2003; Ivers 2004). A tailored approach to tobacco<br />
control for Indigenous people, developed in consultation with Indigenous health groups<br />
such as the <strong>National</strong> Aboriginal Community <strong>Control</strong>led Health Organisation, is essential<br />
to improving the inequity in health outcomes between Indigenous and non-Indigenous<br />
Australians and for breaking the cycle of poverty, poor preventive health and disease.<br />
The policy context<br />
Brief history of tobacco control policy in Australia<br />
Australia’s tobacco control record over the past three decades has been relatively good.<br />
However, governments were initially slow to respond to the evidence demonstrating the<br />
dangers of smoking, and evidence-based tobacco control measures continue to be subject<br />
to delays and insufficient funding across jurisdictions, despite historical evidence showing<br />
the benefits of a strategic approach to reducing smoking rates.<br />
Health authorities in Australia first called for formal government action to reduce tobacco<br />
use in the early 1960s, following international research that demonstrated the serious<br />
health risks associated with smoking. In 1962, health promotion organisations endorsed a<br />
report recommending restrictions on tobacco advertising and the introduction of a public<br />
health education campaign. While it took a decade for government to respond to calls for<br />
tobacco control measures, male smoking rates fell as the news media informed the public<br />
of the dangers of smoking.<br />
The first significant government action, in 1972, was mandatory placement of health<br />
warnings on cigarette packages. From 1973 to 1976, broadcast advertising of cigarettes<br />
was phased out. These two national measures coincided with a major decline in smoking<br />
rates, a trend that has continued, in step with other measures aimed at reducing tobacco<br />
use.<br />
In the 1980s, establishment of preventive health care as a public policy issue, evidence that<br />
smoking was the largest cause of preventable death and disease, and a shift in community<br />
attitudes to smoking, encouraged governments to do more to reduce the tobacco<br />
burden. Passive smoking became a prominent issue in the 1980s because of research<br />
demonstrating the dangers of exposure. The Australian Government legislated to eliminate<br />
smoking from federal workplaces in 1986 and from domestic aircraft in 1987.<br />
2 Section One: Preventable risk factors
State and territory governments, with varying levels of commitment and delay, have<br />
subsequently introduced restrictions on smoking in public places that are subject to<br />
jurisdictional legislation, such as public transport, taxis, and enclosed public places (e.g.<br />
shopping centres, restaurants and theatres and, in some states, pubs and bars). The<br />
Australian Government also banned tobacco advertising in the print media in 1989. In<br />
1992, federal parliament passed the <strong>Tobacco</strong> Advertising Prohibition Act, phasing out most<br />
remaining forms of tobacco advertising by 1995.<br />
Other key tobacco control measures have been excises on tobacco products (deterring<br />
purchase and providing revenue towards the tobacco disease burden) and social marketing<br />
campaigns aimed at raising public awareness of the dangers of smoking.<br />
A milestone social marketing initiative was the Australian Government’s <strong>National</strong> <strong>Tobacco</strong><br />
Campaign run in 1997 and 1998. A government-commissioned independent evaluation of<br />
the campaign found that investment in the first six months of the campaign alone returned<br />
more than double in savings via reduced healthcare costs and life-years saved. Despite this<br />
success, and recommendations from the evaluation team to re-run the campaign, there<br />
has been no coordinated national social marketing campaign aimed at reducing smoking<br />
rates on this scale since then. Because of its success, the campaign has been adapted for<br />
use in other countries.<br />
Figure 1.2 Adult per capita consumption of tobacco products in Australia<br />
Annual amount of toacco dutied per adult over 15 years (kg)<br />
4.0<br />
3.5<br />
3.0<br />
2.5<br />
2.0<br />
1.5<br />
1.0<br />
0.5<br />
Introduction of<br />
manufactured<br />
cigarettes in<br />
Australia<br />
Depression<br />
Uptake by<br />
women<br />
Second<br />
World War<br />
0.0<br />
1903 07 11 15 19 23 27 31 35 39 43 47 51 55 59 63 67 71 75 79 83 87 91 95<br />
YEAR<br />
Source: Compiled by Michelle Scollo, VicHealth Centre for <strong>Tobacco</strong> <strong>Control</strong><br />
Early research on<br />
the health effects<br />
of smoking<br />
Report of the US<br />
Surgeon General<br />
Broadcast tobacco<br />
advertising phased<br />
out<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
Commencement of<br />
Quit campaigns<br />
Introduction of<br />
workplace smoking<br />
bans<br />
New health<br />
warnings<br />
2<br />
T o b a c c o
Australian <strong>National</strong> <strong>Tobacco</strong> Strategy 2004–200<br />
Current national and inter-jurisdictional tobacco control policy is articulated in the<br />
Australian <strong>National</strong> <strong>Tobacco</strong> Strategy 2004–2009. The strategy sets out the intentions<br />
of federal, state and territory governments to work together and collaborate with nongovernment<br />
agencies on a long-term, comprehensive, evidence-based and coordinated<br />
national plan ‘to significantly improve health and to reduce the social costs caused by, and<br />
the inequity exacerbated by, tobacco in all its forms’ (MCDS 2004).<br />
The <strong>Cancer</strong> Council endorses the objectives of the <strong>National</strong> <strong>Tobacco</strong> Strategy, which are,<br />
across all social groups:<br />
•<br />
•<br />
•<br />
•<br />
to prevent uptake of smoking<br />
to encourage and assist as many smokers as possible to quit as soon as possible<br />
to eliminate harmful exposure to tobacco smoke among non-smokers<br />
where feasible, to reduce harm associated with continuing use of and dependence on<br />
tobacco and nicotine.<br />
The <strong>National</strong> <strong>Tobacco</strong> Strategy identifies the following areas for action:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
regulation of tobacco<br />
»<br />
»<br />
»<br />
»<br />
»<br />
»<br />
promotion<br />
place of sale<br />
price (through tobacco tax)<br />
place of use<br />
packaging<br />
products<br />
promotion of Quit and Smokefree messages<br />
cessation services and treatment<br />
community support and education<br />
»<br />
»<br />
informing the community<br />
preventing smoking uptake by children<br />
addressing social and cultural determinants of health<br />
tailoring initiatives for disadvantaged groups<br />
research, evaluation, monitoring and surveillance<br />
workforce development.<br />
Regulation of tobacco promotion<br />
Comprehensive bans on cigarette advertising and promotion were shown to reduce<br />
consumption, but more limited partial bans were found have little or no effect in data from<br />
1970 to 1992 from 22 high-income countries (Jha & Chaloupka 1999). Econometric studies<br />
in high-income countries suggest that comprehensive bans on promotion reduce demand<br />
for tobacco by around 7% (CDCP 1999). When governments ban tobacco advertising in<br />
one medium, the tobacco industry will substitute advertising in other media with little or<br />
no effect on overall marketing expenditure (Jha & Chaloupka 1999). In Australia, tobacco<br />
promotion still occurs at point of sale and on packaging. Research suggests that such<br />
advertising increases positive feelings about cigarette brands (MCDS 2004).<br />
2 Section One: Preventable risk factors
Regulation of place of sale<br />
Regulation of the supply of tobacco products should ensure that they are available to<br />
adults, but are not highly visible and are not sold to children. Laws banning sales to minors<br />
are more effective if the penalties are substantial and the laws are vigorously enforced so<br />
that the probability and cost of being caught outweighs the benefit of continuing illegal<br />
sales (MCDS 2004). Reductions in cigarette consumption by young people, however, have<br />
not always followed increasing sales restrictions. In Australia, the proportion of 12–17-yearolds<br />
who report buying their own cigarettes has declined since 1996, but there has been<br />
a corresponding increase in reports of obtaining cigarettes by having someone else buy<br />
them (White & Hayman 2004).<br />
Regulation of price through tobacco tax<br />
‘Real’ price increases (where increases are not matched by greater earning capacity,<br />
and affordability decreases) can depress demand for cigarettes (Jha & Chaloupka 1999).<br />
Higher prices (usually resulting from taxation increases) induce some smokers to quit,<br />
prevent other people from starting (CDCP 2000), reduce the number of ex-smokers who<br />
relapse, and reduce consumption among continuing smokers. A price rise of 10% on a<br />
pack of cigarettes would be expected to reduce demand by about 4%, but efforts to set an<br />
‘economically optimal’ tax level have produced a wide range of estimates (Jha & Chaloupka<br />
1999). However, effective taxation policy must ensure that increases are real, well<br />
publicised, and occur as often as necessary to maintain effective price rises. It is important<br />
that taxation effects are not insulated or absorbed by economies in manufacturing or<br />
tobacco companies’ pricing policies (Winstanley, Woodward & Walker 1995).<br />
Increasing the price of tobacco products will decrease consumption more in low than in<br />
high-income groups. However, tax increases can cause financial stress for people on low<br />
incomes who continue to smoke. Support for price increases will be more likely if there is<br />
increased investment in supporting people on low incomes to quit (MCDS 2004).<br />
Regulation of place of use<br />
Restrictions on smoking in public places and workplaces will obviously benefit nonsmokers.<br />
Importantly, smokers in workplaces with total bans on smoking are also likely<br />
to reduce the amount they smoke and increase their chances of successfully quitting<br />
(Fichtenberg & Glantz 2002). There is a high level of public support for restricting smoking<br />
in public places in Australia (AIHW 2005).<br />
Regulation of packaging<br />
<strong>Tobacco</strong> product packaging allows information on the product to be communicated to<br />
consumers. Since March 2006 cigarette packages in Australia have been required to carry<br />
colour graphic and text warnings on 30% of the front of the pack and 90% of the back of<br />
the pack. Information on a national Quit website and Quitline number appears on the back<br />
of the pack (DHA 2006). <strong>Tobacco</strong> products in Australia will no longer carry information<br />
about ‘yield’ of components (e.g. nicotine and tar) following concerns that consumers<br />
did not understand this information and acknowledgment that the labelling systems<br />
were based on flawed testing (MCDS 2004). Use of descriptors such as ‘light’ and ‘mild’<br />
has also ceased after the Australian Competition and Consumer Commission found that<br />
the claimed relative health benefits of low yield cigarettes were misleading and likely to<br />
breach the Trade Practices Act (ACCC 2005). However, there is still potential for smokers<br />
to be misled, with continued use of colours and descriptors implying comparative health<br />
benefits, and the mechanism by which deception occurs has not been addressed (King &<br />
Borland 2005).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
2<br />
T o b a c c o
Regulation of products<br />
Possible regulations could be requirements for ‘fire safe’ or reduced ignition propensity<br />
cigarettes (which automatically extinguish when they are not being smoked), and<br />
measures to reduce the addictiveness and palatability of products. A policy is needed ‘to<br />
coordinate regulation of tobacco products and products designed to replace tobacco, in<br />
ways that combine to reduce overall population harm’ (MCDS 2004).<br />
Promotion of Quit and Smokefree messages<br />
Long-term, high-intensity counter-advertising campaigns can reduce consumption<br />
when part of a multi-component program (Jamrozik 2004). Such campaigns also<br />
effectively reduce initiation of tobacco use, in combination with other interventions such<br />
as price increases and school and community programs (CDCP 2000). The <strong>National</strong><br />
<strong>Tobacco</strong> Campaign initiated in 1997 (‘Every Cigarette Is Doing You Damage’) involved<br />
advertisements on television, on radio, in newspapers, and on bus billboards (CDHAC<br />
2004). In a survey conducted to evaluate a 2004 campaign, 48% of smokers reported that<br />
the campaign messages provided encouragement to quit (CDHAC 2004).<br />
Cessation services and treatment<br />
Many people are able to overcome their dependence on tobacco and stop smoking,<br />
although people commonly have multiple attempts before succeeding (MCDS 2004). In<br />
Australia in 2004, 26% of people aged 14 and over described themselves as ex-smokers<br />
(AIHW 2005). The Cochrane Collaboration Methods have found the following interventions<br />
aimed at improving rates of quitting to be effective: brief advice from doctors; nicotine<br />
replacement therapy (via chewing gum, transdermal patch, nasal spray, inhaler, or<br />
tablet); the antidepressant drug bupropion (Zyban); tailored self-help materials; telephone<br />
counselling; and individual or group counselling (Cochrane Library 2006). However,<br />
pharmacotherapies are sometimes not used properly, reducing their efficacy, and clinical<br />
trial results are not always replicated when cessation aids are used in the real world.<br />
Resources to encourage and assist doctors to provide cessation advice include the<br />
Guidelines for prevention activities in general practice (the ‘red book’) and the SNAP guide<br />
on smoking, nutrition, alcohol and physical activity as population health risk factors<br />
(RACGP 2005; RACGP 2004). A study on the application of SNAP in general practice noted<br />
that while verbal advice on smoking cessation advice is reported as being provided ‘very<br />
often’ by 68% of general practitioners, other studies indicate that only 0.6% of patient<br />
encounters involve cessation advice (Amoroso, Hobbs & Harris 2005).<br />
The <strong>National</strong> <strong>Tobacco</strong> Strategy recommends an integrated strategy for cessation services<br />
that would enable coordination of policy and spending by programs covering public health,<br />
medical and pharmaceutical benefits, medical education, development of general practice<br />
and continuing education of virtually all health professionals (MCDS 2004).<br />
Informing the community<br />
Counter-advertising or negative messages about smoking from governments and health<br />
promotion organisations have been found to reduce consumption consistently according<br />
to studies from Australia, North America, Europe and Israel (CDHAC 1999). In general,<br />
the impact is greatest and most sustained when there is low general awareness of the<br />
health risks of smoking (Jha & Chaloupka 1999). In Australia, there is a high level of public<br />
knowledge of illnesses associated with passive smoking, although more could be done to<br />
update the community on new research (VCTC 2002a).<br />
30 Section One: Preventable risk factors
Preventing smoking uptake by children<br />
A recent Australian review of youth tobacco prevention (DHA 2005) notes that prevention<br />
of tobacco uptake is a critical component of any comprehensive tobacco control strategy.<br />
Such efforts have largely focused on young people, given that smoking initiation is most<br />
likely to occur before 18 years of age. Theoretically, prevention or ‘early intervention’<br />
initiatives represent a better long-term solution than cessation initiatives, given the<br />
addictive properties of nicotine. However, effective prevention strategies have remained<br />
largely elusive (DHA 2005).<br />
High-profile campaigns to reset community norms about smoking and help adult rolemodels<br />
to quit can also greatly reduce smoking by children (MCDS 2004). Focusing efforts<br />
on adult smokers is supported by research that demonstrates that mortality can be better<br />
reduced by focusing on current smokers and near-term health problems (Levy, Cummings<br />
& Hyland 2000; Peto et al. 2000). Parental and sibling smoking is a well-established risk<br />
factor for smoking in adolescents (USDHW 1979). When parents who smoke quit before<br />
their children begin smoking, the risk of their children taking up smoking is significantly<br />
reduced (Farkas et al. 1999).<br />
Adolescents (15–17 years) and people aged 18 to 39 years had similar responses to the<br />
Australian <strong>National</strong> <strong>Tobacco</strong> Campaign (White, Tan et al. 2003), suggesting that an adult<br />
approach is more effective with adolescents than a campaign specifically targeting them<br />
(Wakefield, Miller & Roberts 1999). Adolescents showed high campaign awareness<br />
regardless of smoking status, and many felt it was relevant to them, including almost 50%<br />
of non-smokers. In addition, 85% thought that the campaign made smoking seem less<br />
cool and around one-third felt it had discouraged some friends from taking up smoking<br />
(White, Tan et al. 2003).<br />
There is little evidence that school-based programs are effective in the long term in<br />
preventing uptake of smoking. A review by the Cochrane Collaboration identified 23 highquality<br />
randomised controlled trials of school-based programs to prevent children who<br />
had never smoked becoming smokers (Cochrane Library 2006). The interventions included<br />
information-giving, social influence approaches (representing the majority of studies),<br />
social skills training, and community interventions. There is little evidence that information<br />
alone is effective. Although half of the best quality studies in this group found short-term<br />
effects, the highest quality and longest trial (the Hutchinson Smoking <strong>Prevention</strong> Project)<br />
found no long-term effects from 65 lessons over eight years (Cochrane Library 2006).<br />
Addressing social and cultural determinants of health<br />
Investing in programs that strengthen community and cultural resources (e.g. programs to<br />
reduce the chance of educational failure, family conflict, loss of cultural identity and mental<br />
health problems) may well reduce uptake by young people of smoking (MCDS 2004). Such<br />
investment is crucial in Aboriginal and Torres Strait Islander and other very disadvantaged<br />
communities.<br />
Tailoring initiatives for disadvantaged groups<br />
Several social groups in Australia suffer a particularly high burden of tobacco-related death<br />
and disease (MCDS 2004):<br />
•<br />
•<br />
•<br />
Australian Aboriginal and Torres Strait Islander peoples<br />
people suffering severe and disabling mental illness<br />
people who are institutionalised, including those in custodial settings<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
31<br />
T o b a c c o
•<br />
•<br />
parents/carers and children living in disadvantaged areas<br />
immigrants who left their home countries at a time when the dangers of smoking were<br />
not well understood.<br />
Australian Aboriginal and Torres Strait Islander peoples<br />
In 2004, 50% of Aboriginal and Torres Strait Islander people aged 18 years and over were<br />
current smokers, the same level reported in 1995. During the same period the prevalence<br />
of current smoking (daily, weekly and occasional) among all Australians fell from 27% to<br />
21% (ABS 1994).<br />
An audit by the Centre for Excellence in Indigenous <strong>Tobacco</strong> <strong>Control</strong> produced the<br />
following recommendations to improve and strengthen Indigenous tobacco control<br />
(Adams & Briggs 2005):<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
Improve representation of Indigenous people on boards, advisory groups and in<br />
partnerships for tobacco control.<br />
Each state and territory should establish a process to ensure Indigenous tobacco control<br />
initiatives are sustainable and consistent.<br />
<strong>Tobacco</strong> control training for Aboriginal health workers should be supported through<br />
accredited training delivery.<br />
Professional development training in Indigenous tobacco control should be available.<br />
Organisations that fund tobacco control research should direct a proportion of their<br />
funding to Indigenous tobacco control research.<br />
<strong>Tobacco</strong> control research should include Indigenous people.<br />
Improve accountability of tobacco control organisations to provide services to<br />
Indigenous people.<br />
Develop an Indigenous tobacco control strategy.<br />
Provide a more consistent approach to tobacco control education for young Indigenous<br />
people in schools.<br />
Improve access to nicotine replacement therapies.<br />
Initiatives for other disadvantaged groups<br />
Projects targeting people with mental illness, people in custodial settings, people in<br />
disadvantaged areas, and people with limited English skills operate in some state and<br />
territory jurisdictions (MCDS 2004).<br />
Research, evaluation, monitoring and surveillance<br />
The <strong>National</strong> Drug Strategy Household Survey, which is conducted every three years,<br />
provides comparative data for adult smoking prevalence, but only limited data is currently<br />
available for Aboriginal and Torres Strait Islander peoples and particular cultural groups<br />
(AIHW 2005). Australia’s regular, standardised three-yearly surveys of student smoking are<br />
a valuable resource, providing reliable data about changes in children’s smoking behaviour<br />
since 1984 (White & Hayman 2004). Annual evaluation of the <strong>National</strong> <strong>Tobacco</strong> Campaign<br />
has provided data about smoking knowledge, attitudes and intentions, and Australia is<br />
also contributing to the International <strong>Tobacco</strong> <strong>Control</strong> <strong>Policy</strong> Evaluation Study to provide<br />
information on how tobacco control policies affect smoking cessation (MCDS 2004).<br />
32 Section One: Preventable risk factors
Workforce development<br />
Recruitment and training<br />
Given the focus on policy and regulation, the <strong>National</strong> <strong>Tobacco</strong> Strategy has identified a<br />
need to attract more people from legal, economic, public policy and scientific disciplines<br />
to crucial research and policy jobs. In addition, the importance of the public receiving<br />
accurate information about the health risks of smoking and the effectiveness of various<br />
treatments, policies and programs requires more people skilled in media relations.<br />
Continuing education<br />
As well as the behavioural aspects of smoking, people working in tobacco control need<br />
to better understand the toxicology and epidemiology of tobacco use and the social,<br />
economic and legal aspects of tobacco control. Training for health professionals must<br />
also be addressed as part of a comprehensive policy to treat tobacco dependence. To this<br />
end, the Australian <strong>National</strong> Training Authority has endorsed two units of competency in<br />
smoking cessation as part of the national population health training package.<br />
Access to crucial information<br />
Short term strategies endorsed in the <strong>National</strong> <strong>Tobacco</strong> Strategy are to:<br />
•<br />
•<br />
•<br />
•<br />
better synthesise information about developments internationally<br />
facilitate access to relevant research evidence<br />
facilitate sharing of ideas and resources between states and territories<br />
support biennial Australasian tobacco control conferences.<br />
Framework Convention on <strong>Tobacco</strong> <strong>Control</strong><br />
In 2004 the Australian Government ratified the World Health Organization Framework<br />
Convention on <strong>Tobacco</strong> <strong>Control</strong>. The objective of the convention was to protect present<br />
and future generations from the health, social, environmental and economic consequences<br />
of smoking and exposure to tobacco smoke. Countries that ratify the convention<br />
undertake to implement a range of measures relating to tobacco price and tax increases;<br />
tobacco advertising and sponsorship; regulation of tobacco products; tobacco product<br />
disclosure; packaging and labelling; education, communication, training and public<br />
awareness; cessation measures; illicit trade; sales to minors; support for economically<br />
viable alternatives; liability issues; and scientific and technical cooperation and exchange of<br />
information (WHO 2004).<br />
<strong>Tobacco</strong> Advertising Prohibition Act<br />
The <strong>Tobacco</strong> Advertising Prohibition Act was passed in 1992 to, according to section 3<br />
of the Act, ‘limit the exposure of the public to messages and images that may persuade<br />
them to start smoking, continue smoking, or use, or continue using, tobacco products’;<br />
and ‘to improve public health’. Evidence shows that the Act has worked effectively as a<br />
legislative instrument to limit the exposure of the Australian public to tobacco advertising<br />
through traditional mass media forms of marketing. However, a growing evidence base<br />
also shows that the Act has been ineffective in limiting exposure through other channels of<br />
communication, to which the tobacco industry has increasingly been turning since the Act<br />
was introduced.<br />
In August 2003, the Australian Department of Health and Ageing published an issues paper<br />
as part of the Government’s review of the <strong>Tobacco</strong> Advertising Prohibition Act, inviting<br />
submissions to seek ‘community views on the relevance of the Act’. The <strong>Cancer</strong> Council<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
33<br />
T o b a c c o
Australia in partnership with a number of other health promotion organisations, prepared<br />
a detailed submission documenting why the Act needed amendment to help eliminate the<br />
many ‘guerrilla’ and ‘under the radar’ marketing strategies used by the tobacco industry<br />
to sustain a lucrative market base in Australia. Evidence was presented, in the submission<br />
and at hearings, of strategies that circumvented and contradicted the objectives of the<br />
Act, such as event and venue promotions; point-of-sale marketing; direct marketing and<br />
the use of databases; premiums and value-added promotions; vending machines; internet<br />
marketing; international magazines; ‘buzz’ marketing; sporting and cultural events; and the<br />
promotion of smoking by broadcasters, publishers, film-makers, etc.<br />
Despite the extent of this evidence, supported by separate submissions from health<br />
promotion bodies such as the Royal Australian College of General Practitioners, in April<br />
2005 the Australian Government announced that the <strong>Tobacco</strong> Advertising Prohibition Act<br />
would not be amended, as the review found it to be working well in its current form and<br />
that any gains derived from amendment would be ‘insignificant’. The <strong>Cancer</strong> Council<br />
and its allies will continue to collect evidence on the tobacco industry’s exploitation of<br />
loopholes in the Act. While a general review of the Act is unlikely in the near future,<br />
opportunities may exist for one-off amendments.<br />
Trade Practices Act<br />
The Trade Practices Act (Consumer Product Information Standard) 1974 is the legislative<br />
instrument under which graphic warnings on tobacco packaging were approved by federal<br />
parliament in 2004 and phased in from March 2006. Further amendments to the Act may<br />
facilitate the elimination of tobacco industry innovations such as slips to conceal graphic<br />
smoking warnings on tobacco products and ‘split packs’ enabling people with limited<br />
funds, such as children, to pool their money and break cigarette packets in half. In fact,<br />
prompt court action from the Australian Competition and Consumer Commission forced<br />
the withdrawal of ‘split packs’ less than three weeks after their appearance in October<br />
2006. While this was an encouraging outcome, the introduction of the packs demonstrates<br />
the tobacco industry’s capacity to creatively exploit new markets, a capacity that evidence<br />
shows would be reduced through tighter packaging regulations under the Trade Practices<br />
Act and an updated and more rigorous <strong>Tobacco</strong> Advertising Prohibition Act.<br />
<strong>Tobacco</strong> control: a blue chip investment in public health<br />
Developed by the VicHealth Centre for <strong>Tobacco</strong> <strong>Control</strong> and The <strong>Cancer</strong> Council<br />
Victoria, <strong>Tobacco</strong> control: a blue chip investment in public health details a comprehensive<br />
framework for tobacco control investment based on analysis of the evidence. It makes<br />
recommendations for action by federal, state and territory governments and nongovernment<br />
organisations.<br />
Aims<br />
The <strong>Cancer</strong> Council endorses the objectives of the <strong>National</strong> <strong>Tobacco</strong> Strategy, which are to:<br />
•<br />
•<br />
•<br />
•<br />
prevent the uptake of smoking<br />
encourage and assist as many smokers as possible to quit as soon as possible<br />
eliminate harmful exposure to tobacco smoke among non-smokers<br />
where feasible, reduce the harm associated with continuing use of, and dependence on,<br />
tobacco and nicotine.<br />
34 Section One: Preventable risk factors
What needs to be achieved How The <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
Funding for tobacco control<br />
activities at a level that is<br />
commensurate with the<br />
scale of the harms caused,<br />
and sufficient to achieve<br />
specific declines in the<br />
prevalence of smoking<br />
Informing and reminding<br />
smokers about the harms<br />
of smoking, and motivating<br />
them to quit smoking<br />
Eliminating the promotion<br />
and marketing of tobacco<br />
Regulating tobacco products<br />
to protect the public interest<br />
Encourage the Australian Government to set targets for smoking<br />
prevalence for Australian adults, children and among disadvantaged<br />
groups<br />
Encourage the Australian Government to allocate adequate funds for<br />
comprehensive tobacco control programs to achieve these targets<br />
Continue to develop proposals for funding sources and/or economic<br />
assessments to assist in obtaining the required level of tobacco control<br />
funding<br />
Advocate for the development and implementation of a well-funded and<br />
evaluated social marketing campaign<br />
Participate in national collaboration on the delivery of social marketing<br />
campaigns<br />
Urge the Australian, state and territory governments to eliminate<br />
loopholes in the current legislation and address the remaining avenues of<br />
promotion and marketing of tobacco, with a particular focus on:<br />
• images that portray smoking as desirable, in movies and other popular<br />
culture<br />
• vending machines and mobile retailing of tobacco<br />
• marketing through pack design<br />
• Internet advertising and sales display of tobacco products in retail<br />
settings<br />
• sale of devices designed to conceal health warnings<br />
Continue to identify, document and report any examples of promotion<br />
and marketing of tobacco and its effect on attitudes, knowledge and<br />
behaviour of smokers or those at risk of taking up smoking<br />
Urge the Australian, state and territory governments to regulate tobacco<br />
products to protect the public and smokers, by:<br />
• introducing stronger mechanisms to prevent false or misleading claims<br />
by the tobacco industry about its products<br />
• banning the use of additives in cigarettes that aid palatability and<br />
addictiveness<br />
• requiring that all cigarettes in Australia meet standards for reduced fire<br />
risk<br />
• banning filter venting as part of cigarette design<br />
•<br />
requiring that tobacco companies publish detailed information about<br />
the contents, emissions and design features of all tobacco products<br />
Encourage the Australian, state and territory governments to adopt<br />
licensing schemes to regulate the retailing of tobacco products<br />
Continue to identify, document and report problems that arise from the<br />
absence of regulation of tobacco products, and the harms caused to<br />
smokers as a result<br />
Together with public health groups, examine options and opportunities<br />
for improved regulation of tobacco products<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
35<br />
T o b a c c o
What needs to be achieved How The <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
Further real increases in the<br />
price of tobacco products<br />
Strengthening existing<br />
accountability mechanisms<br />
to hold tobacco companies<br />
to account for the effects of<br />
their unlawful conduct<br />
Improvements in access to<br />
cessation support<br />
Protection of people from<br />
involuntary exposure to<br />
second-hand smoke and<br />
increasing the number of<br />
smoke-free public places<br />
3 Section One: Preventable risk factors<br />
Encourage the Australian Government to increase the excise on tobacco<br />
products at least in line with increases in average weekly earnings<br />
Encourage the Australian Government to ban the sale of duty-free<br />
cigarettes in Australia<br />
Encourage governments to step up measures to prevent evasion of excise<br />
and customs duty on tobacco<br />
Publicly expose examples of the unlawful conduct of tobacco companies,<br />
and demonstrate the ongoing effects of that conduct<br />
Encourage litigation against tobacco companies where this is in the<br />
public interest<br />
Encourage the Australian, state and territory governments to provide<br />
resources and powers to bodies charged with enforcing accountability by<br />
the tobacco industry, including the Australian Competition and Consumer<br />
Commission and state/territory heath authorities<br />
Promote tobacco-dependence treatment as an integral component of<br />
cost-effective health care<br />
Work with governments and other parties to:<br />
• increase funding for Quit services, to meet need<br />
• implement subsidy and access arrangements for pharmacological<br />
assistance for those most in need<br />
• increase the incidence of primary health-care providers referring<br />
patients for cessation advice and assistance<br />
Facilitate the development and use of effective tailored and targeted<br />
support programs for high-risk groups, including Indigenous Australians<br />
Urge state and territory governments to enact strong measures to create<br />
smoke-free environments with a particular focus on:<br />
• ensuring that legislation in relation to smoke-free pubs and clubs<br />
eliminates exposure to second-hand smoke<br />
• ending the exemptions to smoke-free legislation currently provided to<br />
high-roller rooms and other selected gambling venues<br />
• outdoor dining areas<br />
• addressing the need for cars carrying children and pregnant women to<br />
be smoke-free<br />
•<br />
health facilities and campuses<br />
Collaborate with the higher education sector and individual institutions<br />
to encourage smoke-free campuses<br />
Continue to conduct research to demonstrate the importance of smokefree<br />
environments in protecting health, assisting smokers to quit, and<br />
changing public attitudes towards smoking
What needs to be achieved How The <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
Development of targeted<br />
tobacco control strategies<br />
for Indigenous Australians<br />
and others at high risk<br />
Timely implementation of<br />
Australia’s obligations under<br />
the Framework Convention<br />
on <strong>Tobacco</strong> <strong>Control</strong><br />
Effective implementation<br />
and further development<br />
of the Framework<br />
Convention on <strong>Tobacco</strong><br />
<strong>Control</strong> internationally and<br />
regionally<br />
References<br />
<strong>Tobacco</strong><br />
Encourage and support the development of a national tailored tobacco<br />
control strategy for Indigenous Australians, in collaboration with the<br />
<strong>National</strong> Aboriginal Community <strong>Control</strong>led Health Organisation and other<br />
Indigenous health groups<br />
Encourage governments to provide adequate funding and other<br />
resources for the implementation of a tailored tobacco control strategy<br />
for Indigenous Australians<br />
Continue to identify, document and report on tailored tobacco control<br />
interventions for disadvantaged groups<br />
Monitor, and report on, progress of implementation of Framework<br />
Convention on <strong>Tobacco</strong> <strong>Control</strong> measures in Australia<br />
Support Framework Convention on <strong>Tobacco</strong> <strong>Control</strong> implementation in<br />
developing countries in the Western Pacific region<br />
Encourage the Australian Government to play a leading role in the further<br />
development of the Framework Convention on <strong>Tobacco</strong> <strong>Control</strong>, including<br />
developing guidelines, protocols and compliance monitoring<br />
Adams K & Briggs V 2005. Galnya angin (good air): partnerships in Indigenous tobacco control. Melbourne:<br />
Centre for Excellence in Indigenous <strong>Tobacco</strong> <strong>Control</strong>.<br />
Advocacy Institute 2005 Allocation of tobacco control funds. At http://www.advocacy.org/publications/mtc/<br />
allocation.htm. Accessed 31 August 2006.<br />
Amoroso A, Hobbs C & Harris MF 2005. General practice capacity for behavioural risk factor management: a<br />
SNAP-shot of a needs assessment in Australia. Aust J Primary Health 11(2): 120–7.<br />
Applied Economics 2003. Returns on investments in public health: an epidemiological and economic analysis<br />
prepared for the Department of Health and Ageing. Canberra: Commonwealth Department of Health and<br />
Ageing.<br />
Australian Bureau of Statistics (ABS) 2006. <strong>National</strong> Health Survey 2004–05. Sex of person and country of<br />
birth by regular smoker status for persons 18 years and over. Data cells accessed by The <strong>Cancer</strong> Council<br />
Victoria, 1 November 2006.<br />
——— 2005. Australian <strong>National</strong> Accounts: national income, expenditure and product. Table 58. Canberra:<br />
ABS.<br />
——— 1994. <strong>National</strong> Aboriginal and Torres Strait Islander health survey. ABS cat. no. 4190.0. Canberra: ABS.<br />
Australian Competition and Consumer Commission (ACCC) 2005. Low yield cigarettes ‘not a healthier<br />
option’: $9 million campaign. Media release.<br />
Australian Institute of Health and Welfare (AIHW) 2006. Australia’s health 2006. AIHW cat. no. AUS 73.<br />
Canberra: AIHW.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
3<br />
T o b a c c o
——— 2005. 2004 <strong>National</strong> Drug Strategy Household Survey: detailed findings. AIHW cat. no. PHE 66; Drug<br />
Statistics series no. 16. Canberra: AIHW.<br />
——— 1998. The quantification of drug-caused mortality and morbidity in Australia. Canberra: AIHW.<br />
Australian Institute of Health and Welfare (AIHW) & Australasian Association of <strong>Cancer</strong> Registries (AACR)<br />
2004. <strong>Cancer</strong> in Australia 2001. AIHW cat. no. 23; AIHW <strong>Cancer</strong> Series no. 28. Canberra: AIHW.<br />
Australian Retail <strong>Tobacco</strong>nist 2003. April/May vol. 63.<br />
Begg S, Vos T, Goss J, Barker B, Stevenson C, Stanley L & Lopez AD (2007, in press). The burden of disease<br />
and injury in Australia 2003. Canberra: AIHW & Brisbane: University of Queensland.<br />
Briggs VL, Lindorff KJ & Ivers RG 2003. Aboriginal and Torres Strait Islander Australians and tobacco. Tob<br />
<strong>Control</strong> (12 Suppl.): S2:ii5–8.<br />
Business Review Weekly 2002. December 12–18.<br />
California Department of Health Services (CDHS) 2006. Adult smoking prevalence. Sacramento: CDHS.<br />
Canadian <strong>Tobacco</strong> Use Monitoring Survey 2006. Health Canada.<br />
Centers for Disease <strong>Control</strong> and <strong>Prevention</strong> (CDCP) 2001. Investment in tobacco control: state highlights 2001.<br />
Atlanta: Centers for Disease <strong>Control</strong> and <strong>Prevention</strong>.<br />
——— 2000. Strategies for reducing exposure to environmental tobacco smoke, increasing tobacco-use<br />
cessation, and reducing initiation in communities and health-care systems. RR-12. Atlanta: Centers for Disease<br />
<strong>Control</strong> and <strong>Prevention</strong>.<br />
——— 1999. Best practices for comprehensive tobacco control programs. Atlanta: Centers for Disease <strong>Control</strong><br />
and <strong>Prevention</strong>.<br />
Chao A, Thun MJ, Jacobs EJ, Henley SJ, Rodriguez C & Calle EE 2000. Cigarette smoking and colorectal<br />
cancer mortality in the cancer prevention study II. J Natl <strong>Cancer</strong> Inst 92: 1888.<br />
Chapman S 1993. Unravelling gossamer with boxing gloves: problems in explaining the decline in smoking.<br />
BMJ 307(6901): 429–32.<br />
Cochrane Library 2006. Cochrane Collaboration topic: tobacco addiction. http://www.cochrane.org/reviews/<br />
en/topics/94.html. Accessed 31 August 2006.<br />
Collins D & Lapsley H 2002. <strong>National</strong> Drug Strategy monograph series: Counting the cost: estimates of the<br />
social costs of drug abuse in Australia in 1998–9. No. 49. Canberra: Australian Government Department of<br />
Health and Ageing.<br />
Commonwealth Department of Health and Aged Care (CDHAC) 2004. Australia’s <strong>National</strong> <strong>Tobacco</strong> Campaign<br />
evaluation report: volume three. http://www.quitnow.info.au/internet/quitnow/publishing.nsf/content/<br />
evaluation-reports. Accessed 31 August 2006.<br />
——— 1999. Background paper. A companion document to the <strong>National</strong> <strong>Tobacco</strong> Strategy 1999 to 2002–03.<br />
Canberra: CDHAC.<br />
Condon JR, Barnes T, Armstrong BK, Selva-Nayagam S & Elwood JM 2005. Stage at diagnosis and cancer<br />
survival for Indigenous Australians in the Northern Territory. Med J Aust 182(6): 277–80.<br />
Council of Australian Governments (COAG) 2006. Better health for all Australians initiative. http://www.coag.<br />
gov.au/meetings/100206/health. Accessed 31 August 2006.<br />
Daynard RA 2003. Instability in smoking patterns among school leavers in Victoria, Australia. J Public Health<br />
<strong>Policy</strong> 24(3–4): 291–5.<br />
Department of Health and Ageing (Australian Government) (DHA) 2006. <strong>Tobacco</strong> warnings cigarette packs,<br />
Set A. At http://www.health.gov.au/internet/wcms/publishing.nsf/Content/health-pubhlth-strateg-drugstobacco-warning-packs-A.htm.<br />
Accessed 31 August 2006.<br />
——— 2005. Youth tobacco prevention literature review. Canberra: DHA.<br />
3 Section One: Preventable risk factors
——— 2003. Returns on investment in public health: an epidemiological and economic analysis. Canberra:<br />
DHA.<br />
——— 2000. Australia’s <strong>National</strong> <strong>Tobacco</strong> Campaign. Evaluation report volume 2. Canberra: Commonwelath<br />
Department of Health and Aged Care.<br />
Farkas AJ, Distefan JM, Choi WS, Gilpin EA & Pierce JP 1999. Does parental smoking cessation discourage<br />
adolescent smoking? Prev Med 28(3): 213–18.<br />
Fichtenberg CM & Glantz SA 2002. Effect of smoke-free workplaces on smoking behaviour: systematic<br />
review. BMJ 325(7357): 188.<br />
Fong GT, Hammond D, Laux FL, Zanna MP, Cummings KM, Borland R & Ross H 2004. The near-universal<br />
experience of regret among smokers in four countries: Findings from the International <strong>Tobacco</strong> <strong>Control</strong> <strong>Policy</strong><br />
Evaluation Survey. Nicotine and <strong>Tobacco</strong> Research 6:3 S341–51.<br />
Hill D, White V & Letcher T 1999. <strong>Tobacco</strong> use among Australian secondary students in 1996. Aust N Z J<br />
Public Health 23(3): 252–9.<br />
Hurley SF 2006. Hospitalisation and costs attributable to tobacco smoking in Australia: 2001-2002. Med J<br />
Aust 184(1): 45.<br />
Ivers RG 2004. An evidence-based approach to planning tobacco interventions for Aboriginal people. Drug<br />
Alcohol Rev 23(1): 5–9.<br />
Ivers R 2001. Indigenous Australians and tobacco: a literature review. Darwin: Cooperative Research Centre for<br />
Aboriginal and Tropical Health.<br />
Jamrozik K 2004. Population strategies to prevent smoking. BMJ 328(7442): 759–62.<br />
Jha P & Chaloupka F 1999. Curbing the epidemic: governments and the economics of tobacco control.<br />
Washington: The World Bank.<br />
King B & Borland R 2005. What was ‘light’ and ‘mild’ is now ‘smooth’ and ‘fine’: new labelling of Australian<br />
cigarettes. Tob <strong>Control</strong> 14(3): 214–15.<br />
Levy DT, Cummings KM & Hyland A 2000. A simulation of the effects of youth initiation policies on overall<br />
cigarette use. Am J Public Health 90(8): 1311–14.<br />
Mark A, McLeod I, Booker J & Ardler C 2005. Aboriginal health worker smoking: a barrier to lower<br />
community smoking rates? Aborig Isl Health Work J 29(5): 22–6.<br />
Mathers C, Penm R, Sanson-Fisher R, Carter R & Campbell E 1998. Health system costs of cancer in Australia<br />
1993–1994. Australian Institute of Health and Welfare cat. no. HWE 4. Canberra: Australian Institute of Health<br />
and Welfare & <strong>National</strong> <strong>Cancer</strong> <strong>Control</strong> Initiative.<br />
Ministerial Council on Drug Safety (MCDS) 2004. <strong>National</strong> drug strategy: Australia’s integrated framework<br />
2004–2009. At http://www.nationaldrugstrategy.gov.au/internet/drugstrategy/publishing.nsf/Content/<br />
framework0409. Accessed 16 April 2007.<br />
Morley KI et al. 2006 ‘Occasional’ and ‘social’ smokers: potential target groups for smoking cessation<br />
campaigns? Aust N Z J Public Health 30(6): 550–4.<br />
Peto R, Darby S, Deo H, Silcocks P, Whitley E & Doll R 2000. Smoking, smoking cessation, and lung cancer in<br />
the UK since 1950: combination of national statistics with two case–control studies. BMJ 321(7257): 323–9.<br />
Quit Victoria 2006. Research reveals smokers in the dark about health risks. Media release. Melbourne: Quit<br />
Victoria.<br />
Royal Australian College of General Practitioners (RACGP) 2005. Guidelines for preventive activities in general<br />
practice eds M Harris, L Bailey, C Bridges-Webb, J Furler, B Joyner, J Litt, J Smith & Y Zurynski. Sixth edition.<br />
South Melbourne: RACGP.<br />
——— 2004. SNAP: A population health guide to behavioral risk factors in general practice. South Melbourne:<br />
RACGP.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
3<br />
T o b a c c o
Schofield PE, Borland R, Hill DJ, Pattison PE & Hibbert ME 1998. Instability in smoking patterns among<br />
school leavers in Victoria, Australia. Tob <strong>Control</strong> 7(2) 149–55.<br />
Siahpush M, Heller G & Singh G 2005. Lower levels of occupation, income and education are strongly<br />
associated with a longer smoking duration: multivariate results from the 2001 Australian <strong>National</strong> Drug<br />
Survey. Public Health 119(12): 1105–10.<br />
US Department of Health and Human Services (USDHHS) 2006. The health consequences of involuntary<br />
exposure to tobacco smoke: a report of the Surgeon General. Atlanta, GA: US Department of Health and<br />
Human Services, Centers for Disease <strong>Control</strong> and <strong>Prevention</strong>, Coordinating Center for Health Promotion,<br />
<strong>National</strong> Center for Chronic Disease <strong>Prevention</strong> and Health Promotion, Office on Smoking and Health.<br />
——— 2004. The health consequences of smoking: a report of the Surgeon General. Atlanta, GA: U.S.<br />
Department of Health and Human Services, Centers for Disease <strong>Control</strong> and <strong>Prevention</strong>, <strong>National</strong> Center for<br />
Chronic Disease <strong>Prevention</strong> and Health Promotion, Office on Smoking and Health.<br />
US Department of Health and Welfare (USDHW) 1979. Smoking and health: a report of the Surgeon General.<br />
Rockville MD: Public Health Service, Office of Smoking and Health.<br />
VicHealth Centre for <strong>Tobacco</strong> <strong>Control</strong> (VCTC) n.d. The tobacco industry in Australia. Fact sheet. Melbourne:<br />
VCTC.<br />
——— 2003. <strong>Tobacco</strong> control: a blue chip investment in public health: overview document. Melbourne: The<br />
<strong>Cancer</strong> Council Victoria.<br />
——— 2002. Environmental tobacco smoke in Australia. Canberra: Commonwealth Department of Health and<br />
Aged Care.<br />
Wakefield M, Miller C & Roberts L 1999. Comparison of the <strong>National</strong> <strong>Tobacco</strong> Campaign with a targeted<br />
South Australian campaign. In Australia’s <strong>National</strong> <strong>Tobacco</strong> Campaign, evaluation report volume one ed. K<br />
Hassard. Canberra: Commonwealth Department of Health and Aged Care.<br />
White V & Hayman J 2006. Smoking behaviours of Australian secondary students in 2005. Report prepared for:<br />
Drug Strategy Branch, Australian Government Department of Health and Ageing. Monograph series no. 59.<br />
Canberra: Australian Government Department of Health and Ageing, November 2006.<br />
——— 2004. Smoking behaviours of Australian secondary students in 2002. <strong>National</strong> Drug Strategy<br />
Monograph series no. 54. Canberra: Australian Government Department of Health and Ageing.<br />
White V, Hill D, Siahpush M & Bobevski I 2003. How has the prevalence of cigarette smoking changed<br />
among Australian adults? Trends in smoking prevalence between 1980 and 2001. Tob <strong>Control</strong> 12(2 Suppl):<br />
S67–74.<br />
White V, Tan N, Wakefield M & Hill D 2003. Do adult focused anti-smoking campaigns have an impact on<br />
adolescents? The case of the Australian <strong>National</strong> <strong>Tobacco</strong> Campaign. Tob <strong>Control</strong> 12(2 Suppl): S23–9.<br />
Winstanley M, Woodward S & Walker N 1995. <strong>Tobacco</strong> in Australia: facts and issues. Melbourne: Victorian<br />
Smoking and Health Program.<br />
World Health Organization (WHO) 2006. Report of the Open-ended Intergovernmental Working Group on the<br />
WHO Framework Convention on <strong>Tobacco</strong> <strong>Control</strong>. First session. Provisional agenda item 3. Geneva: WHO.<br />
——— 2004. <strong>Tobacco</strong> control legislation. Second edition. An introductory guide. Geneva: WHO.<br />
——— 1998. Guidelines for controlling and monitoring the tobacco epidemic. Geneva: WHO.<br />
40 Section One: Preventable risk factors
U l t r a v i o l e t r a d i a t i o n<br />
Introduction<br />
Melanoma incidence now exceeds lung cancer<br />
incidence. Skin cancer is, in financial terms, the<br />
most costly burden to the health system.<br />
The principal cancer related to excess ultraviolet (UV) radiation is skin cancer. Australia has<br />
the highest rates of skin cancer in the world. Skin cancer includes cutaneous melanoma<br />
and non-melanoma skin cancers (NMSC), namely basal cell carcinoma (BCC) and<br />
squamous cell carcinoma (SCC).<br />
From as early as the 1950s and ‘60s, concern over high skin cancer rates led to limited<br />
community education campaigns programs in Victoria and Queensland. These aimed<br />
to raise public awareness about skin cancer and to increase health professionals’ early<br />
detection of skin cancer.<br />
Since the 1980s, more extensive public health programs aimed at preventing excessive<br />
exposure to UV radiation have been implemented across Australia by cancer organisations<br />
and government health services. The ‘Slip! Slop! Slap!’ and SunSmart slogans, developed<br />
in 1980 and 1987 by The <strong>Cancer</strong> Council Victoria, have been the themes of many<br />
campaigns and are well recognised by Australians in relation to sun protection. The focus<br />
of these skin cancer prevention programs has been on reducing the potential harm of skin<br />
cancer by decreasing exposure to UV radiation and increasing early detection and effective<br />
treatment.<br />
Despite the challenges of evaluating programs aimed at changing sun protection<br />
behaviour, evidence of the effectiveness and cost-efficiency of programs in Australia and<br />
overseas is accumulating. Research is increasingly linking public health programs that<br />
encourage behaviour change to reductions in incidence and mortality.<br />
In addition to this, in Australia, there is evidence that primary prevention programs aimed<br />
at reducing sunlight exposure may be affecting skin cancer rates (Staples et al. 2006) and<br />
that changes in adult behaviour have resulted in some reduction in skin cancer incidence<br />
(Slevin, Clarkson & English 2000).<br />
The link between ultraviolet radiation and cancer<br />
The major causative factor in the development of melanoma and NMSC is UV radiation<br />
exposure (Sun Protection Programs Working Party 1996; Armstrong 2004). Childhood sun<br />
exposure is clearly important. In addition, adult exposure appears to contribute. The exact<br />
exposure needed to develop various skin cancers is not entirely clear. It is likely that both<br />
cumulative and episodic exposures are important, particularly if they cause sunburn.<br />
Based on a review of recalled sun exposure by period of life in studies of melanoma, the<br />
relative risk of melanoma with a history of childhood sunburn is 1.8, while for sunburn in<br />
adulthood it is 1.5 (Whiteman, Whiteman & Green 2001).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
41<br />
U l t r a v i o l e t r a d i a t i o n
In adult life, recreational (intermittent) sun exposure appears to be the strongest<br />
determinant of melanoma risk followed by total lifetime sun exposure and occupational<br />
exposure. Fair skin, which tends to burn easily and tan poorly, is also an important risk<br />
factor for skin cancer (Sun Protection Programs Working Party 1996; English et al. 1997;<br />
Armstrong 2004).<br />
In relation to NMSC, there is evidence that childhood and recreational (that is intermittent<br />
and non-occupational) sun exposure is important in determining the risk of basal cell<br />
carcinoma, while cumulative sun exposure, latitude and occupational exposure are<br />
associated with squamous cell carcinoma (Sun Protection Programs Working Party 1996).<br />
The burden of disease depends on geographical location. Both BCC and SCC rates are<br />
around three times higher in latitudes closer to the equator (Staples, Marks & Giles 1998;<br />
NCCI 2003), where UV radiation is higher.<br />
Impact of ozone depletion<br />
Changes in the stratospheric ozone may also play a role in the incidence of skin cancer.<br />
The ozone layer acts as a barrier to UV radiation. Its depletion over the 20th century has<br />
resulted in higher incident radiation levels reaching the earth’s surface generally. The breakup<br />
of the Antarctic ozone layer has caused profound but localised ozone depletion over<br />
southern land masses (Armstrong 1996).<br />
International measures to protect the ozone layer are showing signs of impact; despite this,<br />
climate change is expected to affect future ozone levels, slowing recovery of the ozone<br />
layer (Severi & English 2004). Due to the large variations in UV radiation levels during the<br />
day, it is difficult to accurately assess what impact ozone depletion has had on overall skin<br />
cancer incidence rates.<br />
Solariums<br />
Artificial UV radiation sources are also hazardous and for this reason solarium use should<br />
be avoided. Recent epidemiological studies have raised the possibility of an association<br />
between solarium use and melanoma (Young 2004; Gallagher, Spinelli & Lee 2005),<br />
however, epidemiological results generally lack consistency. Limited data from long-term<br />
follow-up of patients with severe psoriasis raise the possibility of an increase in SCC and<br />
BCC rates associated with solarium use (Autier 2004). There is no current evidence that<br />
supports the view that exposure to UV radiation through solariums is ‘safe’ or that tanning<br />
in this way protects against skin cancer.<br />
Sunscreens<br />
There has been some debate about the role of sunscreens in skin cancer prevention,<br />
and the potential association of sunscreen use with melanoma risk. A review (Gallagher,<br />
Lee & Bajdik 2004) found mounting evidence that sunscreen can prevent SCC, but no<br />
evidence that it can prevent BCC. It has been suggested that people may use sunscreen<br />
in order to stay longer in the sun and thus may increase their risk of cutaneous melanoma<br />
(IARC 2000). However, Gallagher et al. caution that retrospective case–control studies of<br />
melanoma and sunscreen use should be interpreted with great care, because of subject<br />
recall problems and confounding effects (2004).<br />
Vitamin D<br />
There is good evidence that vitamin D is obtained through sun exposure. There is also<br />
increasing evidence that vitamin D may protect against certain types of cancers (Garland<br />
et al. 1985; Garland et al. 1989; Giovannucci et al. 2006; Boniol, Armstrong & Dore 2006)<br />
42 Section One: Preventable risk factors
and can be beneficial in reducing the risk of osteoporosis. Therefore a balance is required<br />
between avoiding an increase in the risk of skin cancer and achieving enough UV radiation<br />
exposure to maintain adequate vitamin D levels.<br />
For people with fair skin, it has been estimated that adequate vitamin D levels (>50 nmol/l)<br />
can be achieved in summer by exposing the face, arms and hands or an equivalent surface<br />
area for as little as 10 to 15 minutes, either side of the peak UV periods, on most days of<br />
the week (Samanek et al. 2006). In winter, in the southern states of Australia, where UV<br />
radiation levels are less intense, vitamin D levels may be maintained by approximately<br />
two to three hours of sunlight exposure accumulated over a week to the face, arms and<br />
hands or equivalent surface area. In northern states, the amount of sunlight exposure<br />
required to maintain adequate vitamin D levels is significantly less than this. Most people<br />
would achieve sufficient levels of sunlight exposure with normal outdoor activities without<br />
needing to deliberately seek additional sun exposure (TCCA 2006).<br />
However, some people are at risk of vitamin D deficiency, for example, women with dark<br />
skin who wear veils (particularly in pregnancy) and elderly or disabled people in institutional<br />
care or who are housebound. These people may require dietary supplements (Marks et<br />
al. 1995; Nowson & Margerison 2002). In most situations, sun protection to prevent skin<br />
cancer is required during times when the UV Index is moderate or above (>3). At these<br />
levels, it is unlikely to put people at risk of vitamin D deficiency.<br />
The impact<br />
Skin cancer accounts for 81% of all new cases of cancer diagnosed in Australia each year<br />
(AIHW & AACR 2004).<br />
Melanoma and NMSC account for almost 47% of the cancers managed by general<br />
practitioners (AIHW & AACR 2004).<br />
Melanoma<br />
Excluding NMSC, in 2005 melanoma was estimated to be the third most common cancer<br />
diagnosed in Australian women (after breast cancer and colorectal cancer, and the third<br />
most common in Australian men (after prostate and colorectal cancer). Overall melanoma<br />
incidence now exceeds that of lung cancer (AIHW & AACR 2004).<br />
In Australia in 2005, 10,014 people were diagnosed with melanoma (5705 men and 4309<br />
women) (AIHW, AACR, NCSG & McDermid 2005).<br />
In Australia in 2005, there were 1273 deaths from melanoma (862 men and 411 women)<br />
(ABS 2007).<br />
Trends in incidence and mortality<br />
Melanoma is rare in populations of non-European origin (Severi & English 2004).<br />
In Australia the lifetime risk (to age 75 years) of developing melanoma is 1 in 24 for men<br />
and 1 in 33 for women. In 2005 the mean age of first diagnosis for melanoma was 61 years<br />
for men and 57 for women. Between 1991 and 2005 the incidence rate for melanoma<br />
increased on average 1.5% per year among men and 0.9% per year among women (AIHW,<br />
AACR, NCSG & McDermid 2005).<br />
Among younger age groups (< 25), the rate of new cases of melanoma (incidence) is<br />
stable (AIHW & AACR 2004). This is most probably due to a change in sun protection<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
43<br />
U l t r a v i o l e t r a d i a t i o n
ehaviours as a result of public education programs, although it may in part be related to a<br />
change in the racial mix in the Australian population.<br />
Mortality from melanoma rose steadily from 1931 to 1985 with annual rates of increase of<br />
6% in men and 3% in women (Giles & Thursfield 2001).<br />
Since 1990 the rate of death from melanoma in Australia has been relatively stable but<br />
remains twice as high for men compared to women. Mortality rates for men increased<br />
0.7% per year between 1991 and 2005 and mortality rates for women decreased by 0.4%<br />
per year between 1991 and 2005 (AIHW, AACR, NCSG & McDermid 2005; ABS 2007).<br />
Non-melanoma skin cancer (NMSC)<br />
NMSC is the most common cancer in Australia (AIHW & AACR 2004).<br />
Cases of NMSC are not reported routinely to cancer registries but data obtained from<br />
population surveys suggests that 374,000 Australians (equivalent to 1.8% of the<br />
population) are treated for NMSC each year (AIHW & AACR 2004; Staples et al. 2006).<br />
It has been estimated that in 2002 in Australia, 256,000 people were diagnosed with BCC<br />
and 118,000 people were diagnosed with SCC (NCCI 2003).<br />
In Australia in 2002, there were 407 deaths from NMSC (270 men and 137 females) (ABS<br />
2004).<br />
Trends in incidence and mortality<br />
In 2002 the cumulative risks of developing at least one NMSC to age 70 years were 70%<br />
for men and 58% for women. Incidence rates of NMSC have increased from 1985 to 2002.<br />
The increase has been greatest for people 60 years and older while rates for people under<br />
60 have stabilised (Staples et al. 2006).<br />
The rate of treatment (and therefore diagnosis) of new cases of SCC rose by 133%<br />
between 1985 and 2002 and was similar across the sexes. The rate of treatment (and<br />
therefore diagnosis) of new cases of BCC rose by 35% between 1985 and 2002 and was<br />
greater in men (42%) than in women (26%). NMSC rates for both SCC and BCC were<br />
higher in more northerly parts of Australia (NCCI 2003).<br />
Mortality from NMSC decreased overall between 1950 and 1994 but an increase in deaths<br />
among men was noted from the mid-1980s to the mid-1990s, a phenomenon thought to<br />
be related to the HIV/AIDS epidemic (Giles & Thursfield 2001). Mortality rates (2002) are<br />
now 1.6 per 100,000 for men and 0.5 per 100,000 for women (ABS 2004).<br />
NMSC is Australia’s most expensive cancer. More than $264 million (9% of the total costs<br />
of cancer) was spent on diagnosis and treatment in 2000–01 (Staples et al. 2006).<br />
The challenge<br />
Growth in the solarium industry<br />
One of our great challenges is to counter the growing influence of solariums as agencies<br />
that promote the desirability of a tan and potentially expose users to dangerous<br />
UV radiation. The number of solariums and their commercial profile have increased<br />
significantly over the last few years and competition in the industry has led to substantial<br />
publicity and marketing campaigns being waged by solarium operators. Solariums<br />
44 Section One: Preventable risk factors
have been assertively marketed to the young as a health and beauty aid. The number of<br />
establishments in one city alone (Melbourne) increased by more than 650% over five years<br />
to the end of 2001 (Fox 2001). We need to continue to educate the public on the dangers<br />
of solariums and dispel the many solarium myths.<br />
Advocating for solarium regulation<br />
Regulation of the solarium industry also remains a challenge. In the face of a degree<br />
of apparent reluctance by all state and territory governments, and also the Australian<br />
Government, to regulate the solarium industry, there needs to be persistent efforts to<br />
maintain and increase industry standards.<br />
A study of 30 solarium centres in Melbourne during the 2003–04 summer demonstrated<br />
poor compliance by many operators with numerous aspects of the voluntary Australian<br />
Standard: 90% provided access to fair skinned customers and 52% of people aged 16<br />
years were able to buy solarium services without the parental consent the code requires<br />
(Dobbinson, Wakefield & Sambell 2006).<br />
Increases in the desirability of a tan<br />
Despite improving attitudes towards sun protection, there is worrying evidence that<br />
attitudes to tanning and sun protection behaviours are again changing. There are<br />
indications of a recent increase in the desirability of a tan. This is thought to have been<br />
influenced by the growth in the number and profile of commercial solariums and fashions<br />
that have emphasised skimpy clothing with maximum skin exposure. The absence of a<br />
substantial paid mass media campaign around skin cancer may also have played a role.<br />
Given the association between sun protection advertising and people’s attitudes and<br />
behaviours, there needs to be more investment in mass media campaigns to reverse these<br />
trends before they affect skin cancer incidence and mortality.<br />
Explaining the risks and benefits of UV radiation exposure<br />
New debates continue to emerge in relation to the health risks and benefits of UV radiation<br />
exposure in terms of vitamin D. Some of these debates have the potential to confuse<br />
Australians and contaminate the sun protection message. The SunSmart UV Alert is<br />
a useful tool that can help explain when people need to protect themselves from UV<br />
radiation and when protection is not essential. However, this initiative requires monitoring<br />
and further marketing to ensure that the public understands and responds appropriately.<br />
Upskilling GPs in the assessment, diagnosis and treatment of skin cancer<br />
We need to ensure that the knowledge and skills of GPs keeps pace with scientific<br />
developments in the detection and treatment of skin cancer. It is critical that GPs know<br />
how to respond when people ask for a skin cancer check in response to SunSmart<br />
messages that tell them to seek GP advice about any suspicious spot or lesion.<br />
Changing adolescents’ sun exposure patterns<br />
Adolescents generally adopt sun protection behaviours less frequently than adults and it<br />
is more challenging to achieve attitude and behaviour changes among teenagers (Arthey<br />
& Clarke 1995; Mermelstein & Riesenberg 1992; Dobbinson & Hill 2004). Adolescents<br />
spend more time in the sun than any other group. While they have been shown to have a<br />
high level of knowledge on the dangers of sun exposure, they engage in relatively few sun<br />
protection behaviours. We need effective interventions that address adolescents’ growing<br />
perception of sun-tanning as desirable.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
45<br />
U l t r a v i o l e t r a d i a t i o n
Screening for melanoma<br />
There is insufficient Australian research to support a population melanoma screening<br />
program (refer to the chapter on melanoma for more information).<br />
Absence of a long-term coordinated national skin cancer control program<br />
For the first time the Australian Government has committed funds to a national approach,<br />
with $5.5 million being allocated to a social marketing approach delivered over the summer<br />
of 2006–07. However, despite achievements of over 20 years, Australia still lacks a longterm<br />
national skin cancer program. Cooperation continues to grow between the state<br />
cancer councils, but there is also considerable inconsistency in the funding available across<br />
states and territories to implement population-based skin cancer control campaigns.<br />
Effective interventions<br />
After more than 20 years of work, Australia is recognised as having the most extensive,<br />
comprehensive and longest-lasting skin cancer prevention programs in the world. Many<br />
have been based on and modified by extensive research and evaluation (Montague,<br />
Borland & Sinclair 2001).<br />
Skin cancer prevention programs delivered throughout Australia by the state and territory<br />
cancer councils have been formed through needs analysis and formative research that has<br />
guided the development of effective and appropriately targeted strategies.<br />
The <strong>Cancer</strong> Council Australia has a strong commitment to research that facilitates the<br />
development of evidence-based practice. Several state and territory cancer councils fund<br />
epidemiological and behavioural research that provides valuable expertise towards the<br />
development and evaluation of skin cancer prevention and early detection programs.<br />
In 2003, The <strong>Cancer</strong> Council Australia and its members initiated the inaugural national<br />
sun survey to determine attitudes, knowledge and behaviours of the community with a<br />
specific focus on sun protection behaviours and sunburn incidence of Australian children,<br />
adolescents and adults (TCCA, unpublished data). The results of this survey provide<br />
valuable evidence to guide the development of skin cancer prevention strategies.<br />
The health belief model (Egger, Spark & Donovan 2005) guides strategies that might<br />
influence people’s perceived risk, and ability to reduce this risk, within supportive<br />
environments, to motivate behavioural and attitudinal change. Once skin cancer prevention<br />
programs are implemented, evaluation determines the effectiveness of strategies and<br />
possible areas for improvement.<br />
Site-specific interventions targeting settings such as childcare centres, pre-schools,<br />
primary and secondary schools, outdoor recreation settings, workplaces and health care<br />
settings have been shown to help reduce exposure to UV radiation (Glanz, Saraiya &<br />
Briss 2004). Of all settings, school programs have been shown to be most effective for<br />
improving knowledge and attitudes and in some cases improving short-term behaviours.<br />
For skin cancer prevention programs to be most effective, they should adopt a multistrategic<br />
approach that enables a variety of priority groups to be targeted. Glanz,<br />
Saraiya and Briss (2004) recommend that programs use individual-directed strategies,<br />
environmental, policy and structural interventions, media campaigns and community-wide<br />
multi-component interventions.<br />
4 Section One: Preventable risk factors
Buller and Borland (1999) concluded that comprehensive, community-wide programs can<br />
increase sun protection behaviours and reduce UV radiation exposure. These programs are<br />
more effective than smaller-scale interventions since they are delivered through multiple<br />
channels, creating repeated exposure to consistent sun protection messages. Overall,<br />
though more expensive, community-wide interventions may prove to be the most efficient<br />
and cost-effective way to achieve behaviour change.<br />
In addition, skin cancer prevention programs should embrace the recommendations of the<br />
Ottawa Charter (WHO 1986) in relation to public policy development, advocacy strategies,<br />
developing personal skills, reorientating health services and strengthening community<br />
action.<br />
The policy context<br />
Skin cancer prevention can be aided by regulating the solarium industry, effective shade<br />
design by local government, and advocacy and policy for sun protection behaviours in<br />
the workplace. Strategies that increase GPs’ skills in early detection of skin cancer and<br />
encourage people to seek early diagnosis and treatment should also be supported.<br />
Where possible, The <strong>Cancer</strong> Council Australia and its members seek to build strong<br />
partnerships with key stakeholders to support sound skin cancer prevention strategies. This<br />
collaborative approach allows the <strong>Cancer</strong> Council to access valuable advice and feedback<br />
from leading medical, policy and industry representatives, as well as consumers.<br />
Aims<br />
We encourage Australians to protect themselves throughout life against UV radiation,<br />
avoid unnecessary sun exposure and avoid exposure to other sources of UV radiation. Our<br />
aims are to:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
change the attitudes, knowledge and skills of individuals, particularly young people,<br />
about skin cancer and sun protection<br />
develop strategies for the early detection and effective diagnosis of skin cancer<br />
achieve healthy settings, organisations, products, policies and practices that promote<br />
sun protection<br />
strengthen the community’s capacity for coordinated action on skin cancer prevention<br />
inform the design, implementation and evaluation of skin cancer prevention strategies.<br />
What needs to be achieved How The <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
Positive changes in the<br />
attitudes of Australians<br />
towards sun protection with<br />
a particular emphasis on<br />
young people<br />
Encourage the Australian Department of Health and Ageing to develop<br />
and implement a well-evaluated, long-term and comprehensive national<br />
social marketing campaign for children and young people aged 17 to 25<br />
years<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
4<br />
U l t r a v i o l e t r a d i a t i o n
What needs to be achieved How The <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
An increase in knowledge of<br />
the UV Index and application<br />
of the UV Index to sun<br />
protection behaviours<br />
An increased capacity to<br />
monitor behavioural trends<br />
An increased capacity to<br />
monitor epidemiological<br />
trends<br />
An increased capacity to<br />
know what works in relation<br />
to program delivery<br />
Protection of young people<br />
in caring and educational<br />
settings<br />
An increase in the amount of<br />
natural or constructed shade<br />
in public places<br />
Improved sun protection<br />
practices among outdoor<br />
workers<br />
An increase in the early<br />
identification of harmful skin<br />
lesions among older people,<br />
especially men over 50 years<br />
4 Section One: Preventable risk factors<br />
Ensure adequate public information dissemination of the UV Index<br />
through the media and other settings to reach population sub-groups<br />
involved in activities and situations identified at high risk for UV<br />
radiation exposure<br />
Provide training and information to news agencies to support the<br />
widespread use of the UV Index<br />
Every three years implement a national survey of sun protection along<br />
the lines of the Victorian Sun Survey, involving telephone interviews<br />
about sun-related experiences over the previous weekend, and details of<br />
temperature, cloud cover and UV radiation levels<br />
Implement the Primary Schools and Early Childhood Survey nationally<br />
every three years<br />
Conduct a survey of incidence of non-melanoma skin cancer every five<br />
years: the next survey is due in 2007<br />
Undertake specific research and evaluation studies to:<br />
• evaluate skin cancer control strategies<br />
• increase the likelihood of long-term Australian Government investment<br />
in skin cancer prevention<br />
• gather more evidence relating to the economic evaluation of skin<br />
cancer prevention<br />
• lead national and international understanding of what works in<br />
relation to skin cancer prevention<br />
Provide support for the implementation of sun protection policies<br />
and practices by all childcare and pre-school centres across Australia<br />
in conjunction with local, state and territory and Commonwealth<br />
governments<br />
Ensure state and territory governments adopt sun protection policies<br />
and practices in all Australian primary schools: in most states and<br />
territories this will involve continued development and extension of the<br />
<strong>National</strong> SunSmart Schools Program in all primary schools<br />
Determine effective strategies and support their implementation to<br />
improve sun protection practices of students in secondary schools<br />
across Australia<br />
Encourage the adoption of shade provision and construction policies<br />
and building design standards by relevant areas of local, state and<br />
territory and Commonwealth governments<br />
Encourage the inclusion of sun protection policies and practices in all<br />
relevant industrial agreements<br />
Ensure the incorporation of specific provisions for sun protection<br />
practices into existing and future state and territory and Commonwealth<br />
occupational health and safety legislation<br />
Coordinate public relations activity and promotional material to educate<br />
people over 50 years about the importance of early detection
What needs to be achieved How The <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
The safer operation and<br />
promotion of solariums<br />
Increased knowledge of skin<br />
cancer prevention strategies<br />
among key professional<br />
groups<br />
Effective coordinated<br />
policy development and<br />
implementation<br />
Increased knowledge and<br />
skills of medical practitioners<br />
in the early detection and<br />
treatment of melanoma<br />
References<br />
Ultraviolet radiation<br />
Encourage state and territory governments to implement and monitor<br />
legislation to control solarium operation and promotion<br />
Monitor compliance by the solarium industry to the guidelines issued by<br />
the Australian Competition and Consumer Commission (ACCC) and the<br />
AS/NZS 2635:2002 standard for solaria, and draw any non-compliance<br />
with the Trade Practices Act to the ACCC’s attention<br />
Encourage tertiary institutions to include information on sun exposure<br />
and sun protection in relevant education of childcare workers and<br />
teachers, medical practitioners, nurses and health professionals<br />
Develop and maintain evidence-based policy positions about the<br />
relationship between ultraviolet radiation and cancer to complement the<br />
Australian policy context<br />
Ensure effective and coordinated policy development and<br />
implementation to ensure existing policies reflect the best available<br />
evidence<br />
Encourage professional associations to increase GP skills in diagnosis<br />
of early skin cancer in order to avoid missed lesions and reduce<br />
unnecessary lesion removal through accredited training programs<br />
Encourage state and Commonwealth governments to increase access<br />
for all Australians to diagnostic and treatment services, particularly<br />
Australians in rural and remote areas<br />
Armstrong B 1996. An overview: proceedings of the conference on the health consequences of ozone<br />
depletion. <strong>Cancer</strong> Forum (special edition) 20(3): 152–7.<br />
Armstrong BK 2004. How sun exposure causes skin cancer. In <strong>Prevention</strong> of skin cancer, eds DJ Hill, JM<br />
Elwood & DR English. Dordrecht: Kluwer Academic Publishers.<br />
Arthey S & Clarke VA 1995. Suntanning and sun protection: a review of the psychological literature. Soc Sci<br />
Med 40(2): 265–74.<br />
Australian Bureau of Statistics (ABS) 2007. Causes of death, Australia 2005. Cat. no. 3303.0. Canberra: ABS.<br />
——— 2006. Year book Australia, 2006. Cat. no. 1301.0.<br />
——— 2004. Causes of death: Australia summary tables. Cat. no. 33303.0.55.001. Canberra: ABS.<br />
Australian Institute of Health and Welfare (AIHW) & Australasian Association of <strong>Cancer</strong> Registries (AACR)<br />
2004. <strong>Cancer</strong> in Australia 2001. AIHW cat. no. 23; AIHW <strong>Cancer</strong> Series no. 28. Canberra: AIHW.<br />
Australian Institute of Health and Welfare (AIHW), Australasian Association of <strong>Cancer</strong> Registries (AACR),<br />
<strong>National</strong> <strong>Cancer</strong> Strategies Group (NCSG) & McDermid I 2005. <strong>Cancer</strong> incidence projections, Australia 2002 to<br />
2011. Canberra: AIHW, AACR & NCSG.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
4<br />
U l t r a v i o l e t r a d i a t i o n
Autier P 2004. Issues about solaria. In <strong>Prevention</strong> of skin cancer, eds DJ Hill, JM Elwood & DR English.<br />
Dordrecht: Kluwer Academic Publishers.<br />
Boniol M, Armstrong BK & Dore JF 2006. Variation in incidence and fatality of melanoma by season of<br />
diagnosis in new South Wales, Australia. <strong>Cancer</strong> Epidemiol Biomarkers Prev 15(3): 524–6.<br />
Buller DB & Borland R 1999. Skin cancer prevention for children: a critical review. Health Educ Behav 26(3):<br />
317–43.<br />
Dobbinson S & Hill DJ 2004. Patterns and causes of sun exposing and sun protecting behaviour. In<br />
<strong>Prevention</strong> of skin cancer, eds DJ Hill, JM Elwood & DR English. Dordrecht: Kluwer Academic Publishers.<br />
Dobbinson S, Wakefield M & Sambell N 2006. Access to commercial indoor tanning facilities by adults with<br />
highly sensitive skin and by under-age youth: compliance tests at solarium centres in Melbourne, Australia.<br />
Eur J <strong>Cancer</strong> Prev. 15(5): 424–30.<br />
Egger G, Spark R & Donovan R 2005. Health promotion strategies and methods. Second edition. North Ryde:<br />
McGraw-Hill Australia Pty Ltd.<br />
English DR, Armstrong BK, Kricker A & Fleming C 1997. Sunlight and cancer. <strong>Cancer</strong> Causes <strong>Control</strong> 8(3):<br />
271–83.<br />
Fox R 2001. A study into the development of suntanning centres (solariums) in Melbourne 1992–2001.<br />
Melbourne: The <strong>Cancer</strong> Council Victoria.<br />
Gallagher RP, Lee TK & Bajdik CD 2004. Sunscreens: can they prevent skin cancer? In <strong>Prevention</strong> of skin<br />
cancer, eds DJ Hill, JM Elwood & DR English. Dordrecht: Kluwer Academic Publishers.<br />
Gallagher RP, Spinelli JJ & Lee TK 2005. Tanning beds, sunlamps, and risk of cutaneous malignant<br />
melanoma. <strong>Cancer</strong> Epidemiol Biomarkers Prev 14(3): 562–6.<br />
Garland C, Shekelle RB, Barrett-Connor E, Criqui MH, Rossof AH & Paul O 1985. Dietary vitamin D and<br />
calcium and risk of colorectal cancer: a 19-year prospective study in men. Lancet 1(8424): 307–9.<br />
Garland CF, Comstock GW, Garland FC, Helsing KJ, Shaw EK & Gorham ED 1989. Serum 25-hydroxyvitamin<br />
D and colon cancer: eight-year prospective study. Lancet 2(8673): 1176–8.<br />
Giles GG & Thursfield V 2001. Trends in cancer mortality, Australia 1910–1999. Melbourne: The <strong>Cancer</strong> Council<br />
Victoria.<br />
Giovannucci E, Liu Y, Rimm EB, Hollis BW, Fuchs CS, Stampfer MJ & Willett WC 2006. Prospective study of<br />
predictors of vitamin D status and cancer incidence and mortality in men. J Natl <strong>Cancer</strong> Inst 98(7): 451–9.<br />
Glanz K, Saraiya M & Briss P 2004. Impact of intervention strategies to reduce UVR exposure. In <strong>Prevention</strong> of<br />
skin cancer, eds DJ Hill, JM Elwood & DR English. Dordrecht: Kluwer Academic Publishers.<br />
International Agency for Research in <strong>Cancer</strong> (IARC) 2000. Do sunscreens prevent skin cancer? Lyon: World<br />
Health Organization.<br />
Marks R, Foley PA, Jolley D, Knight KR, Harrison J & Thompson SC 1995. The effect of regular sunscreen<br />
use on vitamin D levels in an Australian population. Results of a randomized controlled trial. Arch Dermatol<br />
131(4): 415–21.<br />
Mermelstein RJ & Riesenberg LA 1992. Changing knowledge and attitudes about skin cancer risk factors in<br />
adolescents. Health Psychol 11(6): 371–6.<br />
Montague M, Borland R & Sinclair C 2001. Slip! Slop! Slap! and SunSmart, 1980–2000: Skin cancer control<br />
and 20 years of population-based campaigning. Health Educ Behav 28(3): 290–305.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Control</strong> Initiative (NCCI) 2003. The 2002 national non-melanoma skin cancer survey.<br />
Melbourne: NCCI.<br />
Nowson CA & Margerison C 2002. Vitamin D intake and vitamin D status of Australians. Med J Aust 177(3):<br />
149–52.<br />
50 Section One: Preventable risk factors
Samanek AJ, Croager EJ, Gies P, Milne E, Prince R, McMichael AJ, Lucas RM & Slevin T 2006. Estimates of<br />
beneficial and harmful sun exposure times during the year for major Australian population centres. Med J<br />
Aust 184(7): 338–41.<br />
Severi G & English DR 2004. Descriptive epidemiology of skin cancer. In <strong>Prevention</strong> of skin cancer, eds DJ<br />
Hill, JM Elwood & DR English. Dordrecht: Kluwer Academic Publishers.<br />
Slevin T, Clarkson J & English D 2000. Skin cancer control Western Australia: is it working and what have we<br />
learned? Radiat Prot Dosimetry 91(1–3): 303–6.<br />
Staples M, Marks R & Giles G 1998. Trends in the incidence of non-melanocytic skin cancer (NMSC) treated<br />
in Australia 1985–1995: are primary prevention programs starting to have an effect? Int J <strong>Cancer</strong> 78(2):<br />
144–8.<br />
Staples MP, Elwood M, Burton RC, Williams JL, Marks R & Giles GG 2006. Non-melanoma skin cancer in<br />
Australia: the 2002 national survey and trends since 1985. Med J Aust 184(1): 6–10.<br />
Sun Protection Programs Working Party 1996. Primary prevention of skin cancer in Australia. Canberra:<br />
<strong>National</strong> Health and Medical Research Council.<br />
The <strong>Cancer</strong> Council Australia (TCCA) 2006. Risks and benefits of sun exposure. The <strong>Cancer</strong> Council Australia.<br />
Whiteman DC, Whiteman CA & Green AC 2001. Childhood sun exposure as a risk factor for melanoma: a<br />
systematic review of epidemiologic studies. <strong>Cancer</strong> Causes <strong>Control</strong> 12(1): 69–82.<br />
World Health Organization (WHO) 1986. Ottawa charter for health promotion. Ottawa: WHO.<br />
Young AR 2004. Tanning devices—fast track to skin cancer? Pigment Cell Res 17(1): 2–9.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
51<br />
U l t r a v i o l e t r a d i a t i o n
N u t r i t i o n<br />
Introduction<br />
52 Section One: Preventable risk factors<br />
In Australia, more than 6000 deaths from cancer<br />
each year may be attributed to three major risk<br />
factors: inadequate intake of vegetables and fruit,<br />
inadequate physical activity, and overweight and<br />
obesity.<br />
The importance of food in the prevention of cancer is becoming increasingly recognised.<br />
International variation in cancer rates, combined with the diversity of eating patterns<br />
around the world, is the first line of evidence that food and nutrition play a role in cancer<br />
aetiology. In the past few decades, case–control studies, large prospective cohort studies<br />
and the use of meta-analyses have provided good evidence to support this link. As well,<br />
potential mechanisms of action of specific nutrition components have been identified in<br />
experimental studies.<br />
The study of the influence of nutrition on cancer is a complex area of research.<br />
Contributing to the complexity are obtaining accurate records of what and how much a<br />
person eats, determining the separate and/or combined effects of different foods on cancer<br />
risk, and the long timeframes between dietary exposure and development of disease.<br />
Despite these challenges, there is accumulating evidence to show certain foods and<br />
nutrients can either increase or decrease cancer risk. There is also convincing evidence<br />
that maintaining a healthy body weight can help to reduce cancer risk, and a healthy<br />
diet combined with sufficient physical activity is key to maintaining a healthy body<br />
weight. The recommended eating patterns for reducing cancer risk are consistent with<br />
recommendations for the prevention of cardiovascular disease and type 2 diabetes. Diets<br />
that include vegetables, fruit, grains and cereals (preferably wholegrain), and are low in<br />
fat (particularly saturated fat), salt and energy, support the prevention of all three of these<br />
chronic diseases.<br />
The remainder of this chapter summarises current national recommendations and<br />
population trends concerning food and nutrition. It should be read with the chapters on<br />
physical activity and overweight and obesity. Alcohol, while an aspect of diet, is dealt with<br />
in a separate chapter.<br />
The link between nutrition and cancer<br />
In recent years there have been four major reviews of the epidemiological literature linking<br />
nutrition and cancer:<br />
•<br />
•<br />
World <strong>Cancer</strong> Research Fund and American Institute for <strong>Cancer</strong> Research: Food,<br />
nutrition and the prevention of cancer: a global perspective (WCRF & AICR 1997)<br />
Committee on the Medical Aspects of the Food Supply, UK Department of Health:<br />
Nutritional aspects of the development of cancer (the ‘COMA report’) (UK Department of<br />
Health 1998)
•<br />
•<br />
World Health Organization and Food and Agriculture Organization: Diet, nutrition and the<br />
prevention of chronic diseases (WHO & FAO 2003)<br />
International Agency for Research on <strong>Cancer</strong>: IARC handbooks of cancer prevention<br />
volume 8: fruit and vegetables (IARC 2003).<br />
The updated report from the World <strong>Cancer</strong> Research Fund is due for release at the end of<br />
2007.<br />
An overview of the findings from these reports, plus more recent evidence, is summarised<br />
below.<br />
Fruit and vegetables<br />
Fruit and vegetables are recommended, for their important role as a low-energy-dense<br />
source of nutrients (vitamins, minerals, phytochemicals and fibre) and for their contribution<br />
to weight management, as well as for their probable cancer-protective effect exerted<br />
through a range of bioactive constituents which are plausible anti-cancer agents.<br />
The evidence supporting a protective effect of fruit and vegetables is strongest in relation<br />
to cancers of the digestive tract. Ensuring an adequate intake of fruit and vegetables is<br />
likely to reduce the risk of cancers of the oral cavity, oesophagus, stomach, colorectum and<br />
lung (IARC 2003).<br />
Over the last 10 years there has been a shifting of the evidence relating to the cancer<br />
protectiveness of fruit and vegetables, as outlined in the table below. While earlier reviews,<br />
which mostly relied on the evidence from case–control studies, concluded that fruit and<br />
vegetable consumption convincingly reduces the risk of cancers of the gastrointestinal<br />
tract, more recent prospective studies have not found results to support this (Michels et<br />
al. 2000; Bingham et al. 2003). It is generally believed that fruit and vegetables may help to<br />
indirectly protect against cancer by helping to maintain a healthy body weight.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
53<br />
N u t r i t i o n
Table 1.4 Conclusions of the major nutrition and cancer reports regarding the cancer-protective effect of<br />
vegetables and fruit<br />
Organisation review Highest evidence Moderate evidence Lower evidence<br />
WCRF & AICR 1997 Convincing<br />
Mouth<br />
Pharynx<br />
Oesophagus<br />
Stomach<br />
Colon<br />
Rectum<br />
Lung<br />
UK COMA 1998 Strongly consistent<br />
Oesophagus<br />
54 Section One: Preventable risk factors<br />
Probable<br />
Larynx<br />
Pancreas<br />
Breast<br />
Bladder<br />
Moderate association<br />
Stomach<br />
Colon<br />
Rectum<br />
WHO & FAO 2003 Probable<br />
Oral cavity<br />
Oesophagus<br />
Stomach<br />
Colorectum<br />
IARC 2003 Probable<br />
Oesophagus (fruit &<br />
vegetables)<br />
Stomach (fruit)<br />
Lung (fruit)<br />
Colon-rectum<br />
(vegetables)<br />
Source: Dixon et al. 2004<br />
Possible<br />
Ovaries<br />
Cervix<br />
Endometrium<br />
Thyroid<br />
Liver<br />
Prostate<br />
Kidney<br />
Weak<br />
Breast cancer<br />
Possible<br />
Mouth (fruit &<br />
vegetables)<br />
Pharynx (fruit &<br />
vegetables)<br />
Colon-rectum (fruit)<br />
Larynx (fruit &<br />
vegetables)<br />
Kidney (fruit &<br />
vegetables)<br />
Bladder (fruit)<br />
Stomach (vegetables)<br />
Lung (vegetables)<br />
Ovary (vegetables)
Fruit and vegetables contain an array of protective nutrients and phytochemicals. Despite<br />
many attempts, research has not identified which specific component of fruit or vegetables<br />
provides a cancer-protective effect. A recent review by IARC (2004) suggests cruciferous<br />
vegetables may be important because they contain substantial amounts of glucosinolates,<br />
which are hydrolysed to isothiocyanates and indoles. Experimental studies have shown<br />
that these compounds inhibit carcinogenesis, however these results have only been<br />
partially corroborated by epidemiological studies. It is generally agreed that there is<br />
inadequate evidence to suggest that the consumption of cruciferous vegetables or any<br />
one particular type of fruit or vegetable reduces the risk of cancer—consuming a variety of<br />
fruits and vegetables appears to be the most beneficial (WCRF & AICR 1997; IARC 2004).<br />
Fibre<br />
The current weight of evidence suggests a diet high in fibre could reduce colorectal cancer<br />
risk. The European Prospective Intervention into <strong>Cancer</strong> (EPIC) cohort study confirmed<br />
previous findings that high intakes of dietary fibre reduced the risk of colorectal cancer<br />
(WCRF & AICR 1997; Bingham et al. 2003). Such diets are high in fibre from a range of<br />
sources including wholegrain cereals, fruits and vegetables.<br />
Meat<br />
Research suggests that high red meat consumption, and in particular processed meat<br />
consumption, is associated with an increase in colorectal cancer risk (Norat et al.<br />
2002; Sandhu, White & McPherson 2001). An Australian cohort study has identified an<br />
association between red meat and increased risk of rectal cancer (English et al. 2004).<br />
There has been some inconsistency in the evidence, which may be related to issues<br />
such as the definition of red meat or control of confounding factors such as other related<br />
aspects of diet (fat, low vegetable intake, etc.), but overall results, including findings from<br />
the EPIC cohort study (Norat et al. 2005), support a modest increase in risk.<br />
Some research suggests that eating burnt or charred meat may increase cancer risk;<br />
however, the evidence is not conclusive (Norat & Riboli 2001).<br />
Fish<br />
Experimental studies have shown that omega-3 fatty acids influence cancer development<br />
by lowering inflammation (Rose & Connolly 1999). Fish is a good dietary source of omega-<br />
3 fatty acids. Some epidemiological studies show that higher intakes of fish and/or omega-<br />
3 fatty acids may reduce the risk of developing colorectal cancer and hormone-dependent<br />
cancers such as breast and prostate cancer, but this research can only be described as<br />
suggestive not conclusive (Ralph et al. 2006).<br />
Dietary fat<br />
There has been a great deal of interest in the possible association between fat and cancer.<br />
The World <strong>Cancer</strong> Research Fund report concluded that total fat possibly increased risk of<br />
cancer of the lung, colon, rectum, breast and prostate (WCRF & AICR 1997), although the<br />
UK review did not find sufficient evidence to make any recommendations about fat and<br />
cancer (UK Department of Health 1998).<br />
Current evidence does not indicate a direct link between fat intake and cancer at any site<br />
(Kushi & Giovannucci 2002; Willett 1998). As foods high in fat have a high energy density,<br />
diets high in fat can contribute to obesity (NHMRC 2003a), and obesity is a risk factor for<br />
several cancers (IARC Working Group 2002).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
55<br />
N u t r i t i o n
It may be possible that different types of fat affect cancer differently, as some studies have<br />
suggested that omega-3 fatty acids may reduce the risk of developing colorectal, breast<br />
and prostate cancer (Ralph et al. 2006).<br />
Salt<br />
Diets high in salted foods have been linked to an increased risk of stomach cancer (WCRF<br />
& AICR 1997). The evidence for an increased incidence of stomach cancer in association<br />
with high-salt diets comes from countries where salting of foods (meats) is a common<br />
preserving method. Ecological research has shown that in countries where refrigeration is<br />
commonly used for storage of perishable forms of food, stomach cancer has a relatively<br />
low incidence (Cohen & Roe 1997; Roder 2002).<br />
Dietary supplements<br />
Certain foods that are rich in micronutrients and phytochemicals may play a role in<br />
cancer prevention. Micronutrients include vitamins (e.g. folate, beta-carotene, vitamins<br />
C and E) and minerals (e.g. selenium, calcium). Some biologically active substances or<br />
phytochemicals (e.g. lycopenes, indoles and allicin) have been investigated for cancer<br />
protective properties.<br />
Much of the evidence for dietary supplements is derived from experimental studies and<br />
not properly conducted clinical trials. However the results from the large-scale randomised<br />
controlled trials on the efficacy of dietary supplements to reduce the risk of cancer have<br />
been disappointing. For example, the Alpha-Tocopherol, Beta-Carotene <strong>Cancer</strong> (ATBC)<br />
<strong>Prevention</strong> Trial and Beta-Carotene and Retinol Efficacy Trial (CARET) both showed<br />
increased risk of certain cancers and mortality with supplementation (Bowen et al. 2003;<br />
Leppala et al. 2000; Smigel 1996).<br />
Any diet–cancer association is far more complex than simply supplementing the diet with<br />
micronutrients. Micronutrients ingested in supplement form are often pharmacologically<br />
active, and contain much higher doses than the level of micronutrients someone would<br />
receive in a typical diet. It seems to be the combination and interaction of nutrients and<br />
phytochemicals found together in whole foods that helps reduce the risk of chronic<br />
diseases (WCRF & AICR 1997). The use of supplements in place of a well-balanced diet is<br />
generally not recommended (WCRF & AICR 1997). However some randomised controlled<br />
trials of calcium supplements have shown some potential for lowering the risk of bowel<br />
polyps and cancer (Weingarten, Zalmanovici & Yaphe 2005).<br />
Selenium<br />
Some studies suggest that selenium may be inversely associated with prostate cancer<br />
and colorectal cancer, but most of this evidence comes from trials designed to answer<br />
questions about other types of cancer (Clark et al. 1996; Duffield-Lillico, Dalkin et al. 2003;<br />
Duffield-Lillico, Slate et al. 2003). The evidence of a protective role of selenium in other<br />
types of cancers is weak and inconsistent (Duffield-Lillico et al. 2002; WCRF & AICR 1997;<br />
WHO & FAO 2003). The true effects of selenium require confirmation in independent<br />
trials before new public health recommendations regarding selenium (either from dietary<br />
sources or as supplements) can be made (Combs 2005). The Selenium and Vitamin E<br />
<strong>Cancer</strong> <strong>Prevention</strong> Trial (SELECT) will determine if selenium supplements can protect<br />
against prostate cancer. However the results of this trial will not be available until 2012.<br />
5 Section One: Preventable risk factors
The impact<br />
On a global basis and at current rates, appropriate nutrition and physical activity may<br />
prevent three to four million cases of cancer every year (WCRF & AICR 1997). In Australia,<br />
more than 6000 deaths from cancer each year may be attributed to three major risk factors:<br />
inadequate intake of vegetables and fruit, inadequate physical activity, and overweight and<br />
obesity (Mathers, Vos & Stevenson 1999). These risk factors, through their contribution<br />
to development of cancer alone, are estimated to contribute 3.8% of the total burden of<br />
disease and injury in Australia. Inadequate vegetable and fruit intake has been estimated<br />
to cause 11% of the total cancer burden (Mathers, Vos & Stevenson 1999) and 1.4% of the<br />
total burden of disease in Australia (AIHW 2006).<br />
In Australia, the direct cost of poor diet to the Australian health care system (that is<br />
hospitals, medical expenses, allied health professional services, pharmaceutical expenses<br />
and nursing homes) has been estimated to be in the order of $1.5 billion per year. This<br />
increases to $2.2 billion when indirect costs such as low productivity are included (Lester<br />
1994; Mathers, Vos & Stevenson 1999).<br />
Costs associated with some diet-related cancer have been estimated at $61 million<br />
(1989−90 figures) in direct costs, and $132 million in indirect costs (Crowley et al. 1992).<br />
Increasing average vegetable consumption by one serve/day has been estimated to save<br />
$24.4 million per year from the cost of colorectal, breast, lung and prostate cancers,<br />
and increasing average fruit consumption by one serve/day could save $8.6 million per<br />
year from the costs of breast and lung cancers (Marks et al. 2001). This same report also<br />
estimated that consuming more than one serve of red meat per day accounted for $8.6<br />
million of the total health system cost for colorectal cancer (Marks et al. 2001). Increasing<br />
fruit and vegetable consumption by one serve a day per person would result in direct<br />
health care savings of $180 million a year (Marks et al. 2001). These figures are based on<br />
consumption patterns from the 1995 <strong>National</strong> Nutrition Survey and a meta-analysis of the<br />
diet–cancer relationship conducted in 2001, and therefore may not truly reflect the current<br />
situation.<br />
The challenge<br />
A number of surveys have documented that Australians have below-optimum eating<br />
habits to protect them against overweight, obesity and cancer risk (and other chronic<br />
diseases such as cardiovascular disease and diabetes). The 1983, 1985 and 1995 <strong>National</strong><br />
Nutrition Surveys (ABS & CDHAC 1997) and the Australian Bureau of Statistics’ Apparent<br />
Consumption of Foodstuffs and Nutrients (ABS 2000) data provide an indication of dietary<br />
intakes in Australia. State-based dietary surveys have also been conducted, for example in<br />
Western Australia (Miller & Kose 1996; Hands et al. 2004), Victoria (CSIRO 1993; Catford<br />
2002), and New South Wales (Bauman et al. 2003)<br />
Currently the Australian population does not consume the recommended levels of most<br />
key dietary items, such as vegetables, fruit and wholegrain cereals. Recent trends are<br />
shown in the table below. Over the last 20 years it appears that wholegrain cereal food<br />
intake has increased, but it is still not at recommended levels. Fat intake has reduced, but<br />
is still not low enough, particularly saturated fats. Consumption of vegetables and fruit is<br />
too low, particularly among children.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
5<br />
N u t r i t i o n
Table 1.5 Current trends in consumption and the proportion of the population not consuming<br />
recommended levels of specific foods related to cancer risk<br />
Dietary factor<br />
related to<br />
cancer risk<br />
Vegetable<br />
intake<br />
NHMRC<br />
recommended levels<br />
of consumption<br />
(NHMRC 2003 a & b)<br />
Adults: average of 5<br />
serves per day<br />
Children and<br />
adolescents: minimum<br />
of 2 to 4 serves a day<br />
depending on age<br />
(CDHFS 1998)<br />
Fruit intake Adults: average of 2<br />
serves per day<br />
Children and<br />
adolescents: between<br />
1 and 3 serves a day<br />
depending on age<br />
Cereal, bread,<br />
pasta intake<br />
Adult men: 5−12<br />
serves per day<br />
Adult women: 4−9<br />
serves per day<br />
Children and<br />
adolescents: 3−11<br />
serves per day,<br />
depending on age<br />
Meat intake Moderate serve of<br />
meat: 65−100 g of<br />
cooked red meat, 3−4<br />
times a week (CDHFS<br />
1998)<br />
Children and<br />
adolescents<br />
½–1 serve per day<br />
depending on age<br />
(CDHRS 1998)<br />
5 Section One: Preventable risk factors<br />
Trend in consumption Proportion NOT meeting<br />
minimum levels of<br />
consumption in 1995<br />
Decline in consumption<br />
in both adults and<br />
children 1983−95 (Cook,<br />
Rutishauser & Seelig<br />
2001)<br />
Decline in consumption<br />
in both adults and<br />
children 1983−95 (Cook,<br />
Rutishauser & Seelig<br />
2001)<br />
Slight decline in adults<br />
eating cereal foods on<br />
day of survey 1983−95<br />
(Cook, Rutishauser &<br />
Seelig 2001)<br />
No significant change in<br />
children 1983−95 (Cook,<br />
Rutishauser & Seelig<br />
2001) BUT significant<br />
increase in mean intake<br />
of less healthy cerealbased<br />
products (e.g.<br />
cakes, pies, biscuits)<br />
1985−95<br />
No change in adult<br />
men, declined in<br />
women 1983−95 (Cook,<br />
Rutishauser & Seelig<br />
2001)<br />
Slight rise in children’s<br />
mean intake 1983−95<br />
(Cook, Rutishauser &<br />
Seelig 2001)<br />
Adults: 2 in 3 did not meet the<br />
recommended daily intake for<br />
vegetables (Magarey, McKean &<br />
Daniels 2006)<br />
Children: 2 in 3 did not meet the<br />
recommended daily intake for<br />
vegetables (Magarey, Daniels &<br />
Smith 2001)<br />
Adults: 2 in 3 did not meet<br />
the recommended daily intake<br />
for fruit (Magarey, McKean &<br />
Daniels 2006)<br />
Children: More than half did not<br />
meet the recommended daily<br />
intake for fruit (Magarey, Daniels<br />
& Smith 2001)<br />
Adults: 2 in 3 men and 4<br />
in 5 women did not meet<br />
recommended levels on day of<br />
survey (NHMRC 2003a)<br />
5% of men and 4% of women did<br />
not eat a cereal product on the<br />
day of the survey (McLennan &<br />
Podger 1998)<br />
Children:
Dietary factor<br />
related to<br />
cancer risk<br />
Dietary fat<br />
intake<br />
NHMRC<br />
recommended levels<br />
of consumption<br />
(NHMRC 2003 a & b)<br />
Adults: total fat about<br />
30% of total energy<br />
intake: maximum of<br />
10% of total energy<br />
intake from saturated<br />
fat<br />
Children and<br />
adolescents: total<br />
fat about 30−50% of<br />
total energy intake<br />
(depending on age).<br />
Over 5 years saturated<br />
fat at maximum of<br />
10% of total energy<br />
intake<br />
Salt intake Maximum level of<br />
2300 mg/day: this<br />
includes sodium in<br />
food as well as that<br />
added in cooking or<br />
consumption<br />
Sugar intake < 10% of energy. This<br />
includes all sugars<br />
added to foods by the<br />
manufacturer, cook or<br />
consumer, plus sugars<br />
naturally present in<br />
honey, syrups and fruit<br />
juices (WHO & FAO<br />
2003)<br />
Trend in consumption Proportion NOT meeting<br />
minimum levels of<br />
consumption in 1995<br />
Adults: significant<br />
decline (a positive trend)<br />
in mean intake of total<br />
fats 1983−95 (Cook,<br />
Rutishauser & Seelig<br />
2001)<br />
Children: no significant<br />
change in total fat<br />
intake 1983−95 (Cook,<br />
Rutishauser & Seelig<br />
2001)<br />
No national trend data<br />
available<br />
No national trend data<br />
available<br />
Adults & children: mean total<br />
fat intake and saturated fat<br />
intake on day of survey slightly<br />
exceeded recommended levels<br />
(McLennan & Podger 1998;<br />
Marks et al. 2001)<br />
Adults: 1993 national data<br />
indicate mean sodium intake<br />
higher than recommended levels<br />
(Baghurst et al. 1996)<br />
Children: no data available<br />
(NHMRC 2003b)<br />
Adults: no data available<br />
Children: Mean daily intake<br />
ranged from 7–15% of energy<br />
in girls and 8–14% of energy in<br />
boys (Somerset 2003)<br />
Table adapted from data presented in Body weight, nutrition, alcohol and physical activity: key messages for The <strong>Cancer</strong><br />
Council Australia by Dixon et al. 2004. The interested reader is referred to this document for greater detail.<br />
Specific population groups<br />
Certain population groups have significantly poorer nutrition and are at higher risk of<br />
nutrition-related disease, principally cardiovascular disease and type 2 diabetes (AIHW<br />
2006). The clustering of poor nutrition (both under- and over-nutrition) with smoking,<br />
physical inactivity, lower levels of education and income, and low socio-economic status<br />
signal the need to develop effective interventions targeting these population groups.<br />
Aboriginal and Torres Strait Islander people are particularly at risk, along with residents<br />
in remote areas of Australia and those living on low incomes (SIGNAL 2001; Woods,<br />
Swinburn & Burns 2003). This clustering presents a complex challenge for addressing<br />
nutrition related issues (NATSI Working Party 2001).<br />
Effective interventions<br />
There is mounting evidence about the nature of effective nutrition interventions. Overall the<br />
findings from the literature suggest that diet-related interventions can be effective when<br />
they are multi-focused and sustainable and involve individual and structural change and<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
5<br />
N u t r i t i o n
key stakeholders (Sorensen et al. 1998; Syme 1997; Gill, King & Webb 2005; Thomas et al.<br />
2004; Sahay et al. 2006).<br />
This section focuses on interventions that aim to increase consumption of specific foods<br />
such as vegetables and fruit and that support dietary modification or healthy eating<br />
generally.<br />
Educational interventions focus on changing knowledge, attitudes, skills or the behaviour<br />
of individuals. Environmental interventions create opportunities or remove barriers for<br />
groups of people. With environmental interventions, the emphasis to change health<br />
behaviour moves from the individual to the society that facilitates the unhealthy behaviour.<br />
In the case of nutrition, educational interventions attempt to influence the individual<br />
demand for certain foods such as soft drinks or high fat food. Environmental interventions<br />
attempt to influence the supply of food (e.g. removing soft drinks from vending machines,<br />
increasing fruit and vegetable choices at school canteens or cafeterias).<br />
The US Agency for Healthcare Research and Quality reviewed 92 studies of behavioural<br />
interventions to promote dietary change considered relevant to cancer risk (AHRQ 2000).<br />
In summary, behavioural interventions to increase the intake of fruits and vegetables and<br />
to decrease intake of total fat and saturated fat were assessed as successful, although<br />
child- and adult-focused interventions varied in efficacy. Interventions were more<br />
effective in increasing fruit intake among children and vegetable intake among adults,<br />
and more successful at reducing total fat intake of children rather than adults. In contrast,<br />
interventions with children were less successful than with adults at reducing saturated fat<br />
intake.<br />
Another review, which focused on behavioural interventions to modify fruit and vegetable<br />
intake, found that more than three-quarters of the identified studies reported significant<br />
increases in fruit and vegetable intake, with an average increase of 0.6 servings/day<br />
(Ammerman et al. 2002). Interventions appeared to be more successful at positively<br />
changing dietary behaviour among populations at risk of diseases than among general<br />
healthy populations. Goal setting and the use of small groups seemed to be particularly<br />
promising strategies (Ammerman et al. 2002). Elements of effective interventions include<br />
theoretical basis, family involvement, participatory planning and implementation models,<br />
clear messages, and adequate training and ongoing support for health professionals (Sahay<br />
et al. 2006; Ammerman et al. 2002)<br />
A review of environmental interventions to improve nutrition in children and young people<br />
found that multi-component interventions including an education and environmental<br />
component directed at improving nutrition were most effective, and that children’s<br />
nutritional intake can be modified when their food source is modified (Thomas et al. 2004).<br />
For primary school and high school students, multifaceted interventions (school curricula,<br />
mass media, parent mailings, cafeteria changes) over at least eight to 10 weeks show the<br />
most promise for altering food intake (Thomas et al. 2004). Educational messages targeted<br />
to behaviour change (as opposed to knowledge acquisition) and to specific behaviours<br />
(increase fruit intake, reduce fat intake as opposed to general nutritional changes) are more<br />
successful in changing food behaviours (Thomas et al. 2004).<br />
Reviews of population-based diet interventions have emphasised the need to address<br />
policies that promote structural change and include community involvement in identifying<br />
priorities and interventions (Sorensen et al. 1998; Syme 1997; Gill, King & Webb 2005;<br />
Thomas et al. 2004). Less successful interventions fail to address theories and mediating<br />
variables in behaviour change (AHRQ 2000).<br />
Further work needs to be done on the cost-effectiveness of interventions.<br />
0 Section One: Preventable risk factors
<strong>National</strong> and statewide nutrition promotions<br />
Examples of comprehensive approaches to cancer prevention through modification of diet<br />
and/or physical activity are limited. In 1991, the US <strong>National</strong> <strong>Cancer</strong> Institute launched<br />
the 5-a-Day for Better Health Program, a national, population-based nutrition initiative<br />
to prevent cancer (Heimendinger et al. 1996). The program was a partnership between<br />
the <strong>National</strong> <strong>Cancer</strong> Institute and the vegetable and fruit industry and had multi-strategy,<br />
multi-setting, multi-level and intersectoral components. Evaluation results indicate that<br />
the campaign raised public awareness that vegetables and fruit help reduce cancer risk,<br />
increased vegetable consumption and created an ongoing partnership between health and<br />
agribusiness (Foerster et al. 1995).<br />
In Australia, there have been several statewide campaigns aimed at promoting increased<br />
consumption of vegetables and fruit (e.g. the ‘Go for 2&5’ campaign, Western Australia<br />
2001–2003; Fruit ‘ n’ Veg with Every Meal, Western Australia 1989–93 and South Australia<br />
1990–91; 2 fruit and 5 Vegetables Every Day, Western Australia 1989–93 and Victoria<br />
1992–95; and Eat Well, Tasmania 1997), although these campaigns did not have a specific<br />
cancer prevention focus.<br />
Such campaigns use social marketing strategies to increase public awareness of<br />
dietary recommendations for fruit and vegetable consumption and ultimately increase<br />
consumption. Where available, evaluation shows these campaigns succeeded in promoting<br />
increased awareness, improved public attitudes to fruit and vegetable consumption, and<br />
increased knowledge of the recommended number of serves of fruit and vegetables.<br />
Campaigns sustained for a number of years (e.g. Victoria and Western Australia) increased<br />
reported vegetable and fruit consumption (Dixon et al. 1998; Ejlak, Seal & van Vaetzen<br />
1998; Miller, Pollard & Paterson 1996; Nutrition & Physical Activity Branch 2005). The ‘Go<br />
for 2&5’ campaign in Western Australia resulted in behavioural changes and in the period<br />
2000 to 2003, fruit intake among WA adults increased from 1.6 serves to 2.1 serves while<br />
vegetable intake increased from 2.6 serves to 2.9 serves (Nutrition & Physical Activity<br />
Branch 2005)<br />
Thus, while the evidence is not sufficiently long term, there is general acceptance that a<br />
comprehensive public health program can encourage healthy eating. Such an approach<br />
should encompass education and training, personal health services, mass media,<br />
community action, organisational development, environmental support and economic and<br />
regulatory measures.<br />
Specific cancer prevention interventions<br />
There have been some cancer prevention intervention trials that have examined the<br />
effectiveness of various dietary changes to prevent cancer or cancer precursors (such<br />
as adenomatous polyps). Generally the results from large-scale randomised controlled<br />
trials on the efficacy of dietary supplements to reduce the risk of cancer have been<br />
disappointing. For example, the Alpha-Tocopherol, Beta-Carotene <strong>Cancer</strong> (ATBC) <strong>Prevention</strong><br />
Trial and Beta-Carotene and Retinol Efficacy Trial (CARET) both showed increased risk of<br />
lung cancer and mortality (Bowen et al. 2003; Leppala et al. 2000; Smigel 1996).<br />
The Cochrane Database of Systematic Reviews have concluded that a daily intake of 1 g<br />
of dietary calcium may have a moderate protective effect on the development of colorectal<br />
adenomatous polyps, although this result is only based on two well conducted randomised<br />
controlled trails (Weingarten, Zalmanovici & Yaphe 2005). Dietary interventions to increase<br />
fibre have not shown a statistically significant reduction in the risk of colorectal cancer<br />
(Asano & McLeod 2002).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1<br />
N u t r i t i o n
A large scale randomised controlled trial, the Women’s Health Initiative, randomised<br />
women to a very low fat diet intervention or a usual fat diet (Prentice et al. 2006). Women<br />
on the low fat diet had a 9% lower incidence of breast cancer compared with the control<br />
group, but this result was not statistically significant. However in sub-group analyses,<br />
breast cancer rates were reduced by 22% among women who started with the highest<br />
fat intake (>37% energy from fat) and reduced their fat the most (to 24% after one year)<br />
(Stein 2006). Interestingly, there was suggestive evidence that the low fat diet had a more<br />
protective effect against oestrogen receptor positive breast cancer. Despite the lack of an<br />
apparent effect on colorectal cancer, adenomas were significantly reduced among the low<br />
fat diet group (Stein 2006).<br />
In terms of dietary interventions for cancer survivors, there are only a few successful trials<br />
that suggest that there is hopeful progress in this area. A systematic review of 59 diet<br />
interventions for cancer patients and survivors (mostly with breast cancer) found nonstatistically<br />
significant improvements in overall survival and survival from cancer (Davies<br />
et al. 2006). Most of the included studies in the review were too small and only provided<br />
limited data. A large randomised controlled trial, known as the Women’s Intervention in<br />
Nutrition Study, found that the intervention group who decreased their dietary fat intake<br />
had a lower risk of recurrence of breast cancer (Chlebowski et al. 2005).<br />
General practice<br />
The role of general practice in chronic disease prevention is potentially important, given<br />
that 86% of the population have at least one visit to the general practitioner every year<br />
(RACGP 2005).<br />
A review of primary care interventions found that moderate- or high-intensity counselling<br />
interventions, including the use of interactive health communication tools, can reduce<br />
consumption of saturated fat and increase intake of fruit and vegetables. Brief counselling<br />
of unselected patients by primary care providers appears to produce small changes in<br />
dietary behaviour, but its effect on health outcomes is unclear (Pignone et al. 2003; Steptoe<br />
et al. 2003).<br />
The Royal Australian College of General Practitioners has produced three significant<br />
publications relating to the role of general practice and nutrition. The first, Guidelines for<br />
preventive activities in general practice (the ‘red book’) (RACGP 2005), focuses on the<br />
role of the GP within the consultation, recommending that all adult patients should be<br />
advised to follow the <strong>National</strong> Health and Medical Research Council’s Dietary guidelines for<br />
Australian adults. (Nutrition advice for children should be based on the <strong>National</strong> Health and<br />
Medical Research Council’s Dietary guidelines for children and adolescents in Australia.)<br />
Nutrition advice should be given at two-yearly intervals for adults and on every visit for<br />
children. Their more specific publication: SNAP: A population health guide to behavioural<br />
risk factors in general practice (RACGP 2004) provides more extensive information and<br />
recommendations regarding healthy nutrition (among other common lifestyle risk factors),<br />
focusing on a patient education and behaviour modification approach based upon the<br />
5As (ask, assess, advise, assist, arrange). Lastly, their publication Putting prevention into<br />
practice: guidelines for the implementation of prevention in the general practice setting (the<br />
‘green book’) (RACGP 2006) assists in developing systems in general practice to support<br />
prevention activities at the practice and consultation levels.<br />
In further support of the GP’s role in promoting good nutrition and obesity prevention,<br />
the Commonwealth Department of Health and Ageing, in the 2003/04 budget, funded<br />
the Lifestyle Prescriptions program (commonly known as Lifescripts). Lifescripts is<br />
being implemented through local divisions of general practice, promoting risk factor<br />
management in general practice and primary health care services. Lifestyle prescriptions<br />
2 Section One: Preventable risk factors
are tools for GPs to use when providing lifestyle advice to patients. Advice may be about<br />
quitting smoking, increasing physical activity, eating a healthier diet, maintaining healthy<br />
weight, reducing alcohol consumption, or a combination of these.<br />
The policy context<br />
Commonwealth, state and territory governments are becoming increasingly aware of the<br />
importance of healthy eating in the face of increasing trends to overweight and obesity<br />
among younger and adult Australians. This has resulted in a number of national strategic<br />
agendas including:<br />
•<br />
•<br />
•<br />
•<br />
Healthy weight 2008, Australia’s future. The national action agenda for children and<br />
young people and their families (NOTF 2003).<br />
The Eat Well Australia approach under the SIGNAL <strong>National</strong> Public Health Partnership<br />
(now disbanded), which developed two key action plans: An agenda for action for<br />
public health nutrition 2000–2010 (SIGNAL 2001), which seeks to set the agenda for<br />
and reflect national and state action on nutrition; and the <strong>National</strong> Aboriginal and Torres<br />
Strait Islander nutrition strategy and action plan 2000–2010 (SIGNAL 2001), which sets<br />
a framework for action to respond to the significant diet-related illness experienced by<br />
these Australians.<br />
The Food Standards Code: food standards and regulation fall under the domain of<br />
the statutory authority Food Standards Australia New Zealand. This authority has<br />
responsibility for setting standards for the production and sale of food in Australia,<br />
including food labelling issues such as nutrition and health claims.<br />
Children’s Television Standards: in Australia, food marketing operates under a system<br />
of co-regulation, with the Australian Communications and Media Authority having<br />
responsibility for the Children’s Television Standards, which has some regulations<br />
for limiting television food advertising to children. The Advertising Standards Bureau<br />
administers the industry Codes of Practice developed by Free TV Australia and the<br />
Australian Association of <strong>National</strong> Advertisers, which add very little to the statutory<br />
regulations.<br />
Several state and territory governments have taken steps to mirror or complement the<br />
Eat Well Australia approach, and there is clearly greater recognition of the importance of<br />
having a focus on healthy eating and physical activity as part of obesity and associated<br />
disease prevention (DHS 1997; Northern Territory Government 2001; Queensland Public<br />
Health Forum 2002; NSW Health 2002).<br />
The key challenge now is to move beyond framework development and strategy setting<br />
into comprehensive program implementation.<br />
Two key documents frame the international policy context around nutrition and cancer<br />
prevention:<br />
•<br />
The World Health Organization Global strategy on diet, physical activity and health<br />
was developed through a series of consultations with stakeholders in response to a<br />
request from Member States at the 2002 World Health Assembly. This preventionbased<br />
strategy aims to ‘reduce the risk of chronic non-communicable diseases across<br />
populations by addressing two of the main risk factors, diet and physical activity,<br />
through comprehensive, multi-sectoral interventions’ (WHO 2004).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
3<br />
N u t r i t i o n
•<br />
The International Union Against <strong>Cancer</strong>’s Evidence-based cancer prevention: strategies<br />
for NGOs highlights the need for policy and legislation as part of a multifaceted<br />
approach to improve the nutritional health of populations and individuals (UICC 2004).<br />
Existing recommendations<br />
In general, diet and nutrition recommendations to reduce cancer risk are consistent with<br />
the recommendations of Australian Government health authorities about healthy eating<br />
patterns. The <strong>Cancer</strong> Council Australia endorses the <strong>National</strong> Health and Medical Research<br />
Council Dietary guidelines for Australian adults (NHMRC 2003a), for older Australians<br />
(NHMRC 1999), and for children and adolescents (NHMRC 2003b) and concurs with the<br />
levels of intake of specific food groups recommended by the Australian guide to healthy<br />
eating (CDHFS 1998) and Nutrient reference values (NHMRC 2005).<br />
The <strong>Cancer</strong> Council also acknowledges that its healthy eating recommendations are<br />
consistent with those of other chronic disease prevention groups, such as the <strong>National</strong><br />
Heart Foundation (NHF 2002), with the exception that current research suggests that<br />
limiting alcohol consumption would help prevent cancer.<br />
Aims<br />
Our aims are to encourage the Australian population to:<br />
•<br />
•<br />
•<br />
consume nutritionally adequate and varied diets based primarily on foods of plant origin<br />
such as vegetables, fruit, pulses and wholegrain cereals, as well as lean meats, fish and<br />
low fat dairy products<br />
ensure children have a nutritionally adequate and varied diet along similar lines with<br />
appropriate moderation to suit different age groups<br />
maintain a healthy body weight through a balance of food intake and physical activity.<br />
The <strong>Cancer</strong> Council believes that a national and related state-based comprehensive public<br />
health program is required. Such a program would have an overweight and obesity<br />
focus that would incorporate healthy eating and physical activity with a chronic disease<br />
prevention focus encompassing cancer, diabetes and cardiovascular disease. This would<br />
require collaboration between key organisations in the government, non-government,<br />
medical, education, consumer, media and commercial sectors.<br />
What needs to be achieved How The <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
Increased awareness of the<br />
link between nutrition and<br />
cancer among the general<br />
public and key health<br />
professional groups<br />
Effective coordinated<br />
policy development and<br />
implementation<br />
4 Section One: Preventable risk factors<br />
Monitor and clarify best evidence on the relationship between nutrition<br />
and cancer causation<br />
Ensure key messages are promoted to the public and relevant<br />
health professionals in publications, presentations, programs, media<br />
statements and where opportunities arise<br />
Promote and/or develop complementary primary health resources,<br />
specifically for general practice, to improve evidence-based<br />
interventions by health professionals<br />
Develop and maintain evidence-based policy positions about the<br />
relationship between nutrition and cancer to complement the<br />
Australian policy context<br />
Ensure effective and coordinated policy development and<br />
implementation
What needs to be achieved How The <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
Social marketing campaigns<br />
that promote healthy eating<br />
An increased capacity to<br />
monitor epidemiological trends<br />
An increased capacity to<br />
monitor behavioural trends<br />
More supportive environments<br />
that assist people to make<br />
healthy food choices<br />
An increased capacity to know<br />
what works in relation to<br />
program delivery<br />
Advocate for nationwide social marketing campaigns, that promote<br />
healthy eating across the life course, which are coordinated,<br />
sustainable and far reaching,<br />
Encourage the Australian, state and territory Governments to commit to<br />
long-term investment in promoting healthy eating<br />
Support and deliver effective community interventions at a local and<br />
state level to address healthy eating<br />
Support and conduct high quality epidemiological research further<br />
clarifying the relationship between nutrition and cancer<br />
Support and conduct high-quality behavioural research further<br />
clarifying the barriers and enabling factors for people to adopt healthy<br />
eating<br />
Work towards a better understanding of the determinants of the<br />
obesogenic environment, to inform policy development<br />
Encourage the Australian Government to fund a comprehensive<br />
<strong>National</strong> Nutrition and Physical Activity Survey of both children and<br />
adults, which is conducted, as a minimum on a regular five-year basis<br />
Encourage the Australian Government to address the broader social<br />
and environmental determinants of poor nutrition, in particular:<br />
• call for a ban of television food advertising to children<br />
• develop effective regulatory systems for decreasing the level of food<br />
marketing to children (including television food advertising and other<br />
forms of food marketing)<br />
• improved access to healthy food choices for people who are socially<br />
or geographically disadvantaged<br />
• develop effective regulatory systems for communicating accurate<br />
nutrition and health information on food labels<br />
• improve health literacy for reading food labels<br />
Continue to support and promote the Parents Jury<br />
Participate on the Coalition on Food Advertising to Children<br />
Coordinate public health responses to relevant food regulatory issues,<br />
including changes to food labelling, through participation on the<br />
Coalition on a Healthy Australian Food Supply<br />
Undertake specific research and evaluation studies to:<br />
• evaluate healthy eating interventions<br />
• gather more evidence relating to the economic evaluation of cancer<br />
prevention<br />
• lead national understanding of what works in relation to cancer<br />
prevention<br />
• identify barriers and enabling factors for implementation of these<br />
recommendations in general practice and other health settings<br />
Note: Refer also to the action plans of the physical activity and obesity chapters when considering promotion of nutrition.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
5<br />
N u t r i t i o n
References<br />
Nutrition<br />
Agency for Healthcare Research and Quality (AHRQ) 2000. Efficacy of interventions to modify dietary behavior<br />
related to cancer risk. Evidence report/technology assessment no. 25. Rockville MD: AHRQ.<br />
Ammerman AS, Lindquist CH, Lohr KN & Hersey J 2002. The efficacy of behavioral interventions to modify<br />
dietary fat and fruit and vegetable intake: a review of the evidence. Prev Med 35(1): 25–41.<br />
Asano T & McLeod RS 2002. Dietary fibre for the prevention of colorectal adenomas and carcinomas.<br />
Cochrane Database of Systematic Reviews 1: CD003430<br />
Australian Bureau of Statistics (ABS) 2000. Apparent consumption of foodstuffs and nutrients 1997–98 and<br />
1998–99. ABS cat. no. 4306.0. Canberra: ABS.<br />
Australian Bureau of Statistics (ABS) & Commonwealth Department of Health and Aged Care (CDHAC) 1997.<br />
<strong>National</strong> Nutrition Survey selected highlights Australia 1995. ABS cat. no. 4802.0. Canberra: ABS.<br />
Australian Institute of Health and Welfare (AIHW) 2006. Australia’s health 2006. AIHW cat. no. AUS 73.<br />
Canberra: AIHW.<br />
Baghurst K, Record S & Leppard P 2000. Red meat consumption in Australia: intakes, nutrient contribution<br />
and changes over time. Nutr Dietet 57(4 Suppl): S3–36.<br />
Baghurst K, Record S, Syrette J & Powis G 1996. Food and nutrition in Australia: does five years make a<br />
difference? Adelaide: Commonwealth Scientific and Industrial Research Organisation.<br />
Baranowski T, Lin LS et al. 1997. Theory as mediating variables: why aren’t community interventions working<br />
as desired? Ann Epidemiol S7: S89 –95.<br />
Bauman A, Armstrong T, Davies J, Owen N, Brown W, Bellew B & Vita P 2003. Trends in physical activity<br />
participation and the impact of integrated campaigns among Australian adults, 1997–99. Aust N Z J Public<br />
Health 27(1): 76–9.<br />
Bingham SA, Day NE, Luben R, Ferrari P, Slimani N, Norat T, Clavel-Chapelon F, Kesse E, Nieters A, Boeing H,<br />
Tjonneland A, Overvad K, Martinez C, Dorronsoro M, Gonzalez CA, Key TJ, Trichopoulou A, Naska A, Vineis<br />
P, Tumino R, Krogh V, Bueno-de-Mesquita HB, Peeters PH, Berglund G, Hallmans G, Lund E, Skeie G, Kaaks<br />
R & Riboli E 2003. Dietary fibre in food and protection against colorectal cancer in the European Prospective<br />
Investigation into <strong>Cancer</strong> and Nutrition (EPIC): an observational study. Lancet 361(9368): 1496–1501.<br />
Bowen DJ, Thornquist M, Anderson K, Barnett M, Powell C, Goodman G & Omenn G 2003. Stopping the<br />
active intervention: CARET. <strong>Control</strong> Clin Trials 24(1): 39–50.<br />
Catford J 2002. Why Victorians eat more vegetables and fruit: healthy eating is a public priority. Health of<br />
Victorians: The Chief Officer’s Bulletin 2(1): 1–5.<br />
Chlebowski RT, Blackburn GL, Elashoff C, Thomson MT, Goodman A, Shapiro AE, Giuliano AR, Karanja N,<br />
Hoy MK, Nixon DW & The WINS Investigators 2005. Dietary fat reduction in postmenopausal women with<br />
primary breast cancer: Phase III Women’s Intervention Nutrition Study (WINS). J Clin Oncol 23(16S Part I of II<br />
June supplement): 10.<br />
Clark LC, Combs GF Jr, Turnbull BW, Slate EH, Chalker DK, Chow J, Davis LS, Glover RA, Graham GF, Gross<br />
EG, Krongrad A, Lesher JL Jr, Park HK, Sanders BB Jr, Smith CL & Taylor JR 1996. Effects of selenium<br />
supplementation for cancer prevention in patients with carcinoma of the skin. A randomized controlled trial.<br />
Nutritional <strong>Prevention</strong> of <strong>Cancer</strong> Study Group. JAMA 276(24): 1957–63.<br />
Cohen AJ & Roe FJ 1997. Evaluation of the aetiological role of dietary salt exposure in gastric and other<br />
cancers in humans. Food Chem Toxicol 35(2): 271–93.<br />
Combs GF 2005. Current evidence and research needs to support a health claim for selenium and cancer<br />
prevention. J Nutr 135(2): 343–7.<br />
Commonwealth Department of Health and Family Services (CDHFS) 1998. Australian guide to healthy eating.<br />
Canberra: CDHFS.<br />
Section One: Preventable risk factors
Commonwealth Scientific and Industrial Research Organisation (CSIRO) 1993. What are Australians eating?<br />
Results from the 1985 & 1990 Victorian nutrition surveys. Adelaide: CSIRO (Division of Human Nutrition).<br />
Cook T, Rutishauser I & Seelig M 2001. Comparable data on food and nutrient intake and physical<br />
measurements from the 1983, 1985 and 1995 national nutrition surveys. Canberra: Commonwealth<br />
Department of Health and Aged Care.<br />
Crowley S, Antioch K, Carter R, Waters AM, Conway L & Mathers C 1992. The cost of diet-related disease in<br />
Australia. Canberra: Australian Institute of Health and Welfare.<br />
Davies AA, Davey SG, Harbord R, Bekkering GE, Sterne JA, Beynon R & Thomas S 2006. Nutritional<br />
interventions and outcome in patients with cancer or preinvasive lesions: systematic review. J Natl <strong>Cancer</strong><br />
Inst 98(14): 961–73.<br />
Department of Human Services (DHS) 1997. Healthy eating healthy Victoria: a lasting investment. A strategy<br />
for the implementation of the Victorian Food and Nutrition <strong>Policy</strong>. Melbourne: DHS.<br />
Dixon H, Borland R, Segan C, Stafford H & Sindall C 1998. Public reaction to Victorian ‘2 fruit ‘n’ 5 veg every<br />
day’ campaign and reported consumption of fruit and vegetables. Prev Med 27: 572–82.<br />
Dixon H, Chapman K, Hodge A & Slevin T 2004. Body weight, nutrition, alcohol and physical activity: key<br />
messages for The <strong>Cancer</strong> Council Australia. Unpublished document prepared on behalf of the Nutrition &<br />
Physical Activity Committee of the Public Health Committee, The <strong>Cancer</strong> Council Australia.<br />
Duffield-Lillico AJ, Dalkin BL, Reid ME, Turnbull BW, Slate EH, Jacobs ET, Marshall JR & Clark LC 2003.<br />
Selenium supplementation, baseline plasma selenium status and incidence of prostate cancer: an analysis of<br />
the complete treatment period of the Nutritional <strong>Prevention</strong> of <strong>Cancer</strong> Trial. BJU Int 91(7): 608–12.<br />
Duffield-Lillico AJ, Reid ME, Turnbull BW, Combs GF, Jr., Slate EH, Fischbach LA, Marshall JR & Clark<br />
LC 2002. Baseline characteristics and the effect of selenium supplementation on cancer incidence in a<br />
randomized clinical trial: a summary report of the Nutritional <strong>Prevention</strong> of <strong>Cancer</strong> Trial. <strong>Cancer</strong> Epidemiol<br />
Biomarkers Prev 11(7): 630–9.<br />
Duffield-Lillico AJ, Slate EH, Reid ME, Turnbull BW, Wilkins PA, Combs GF, Jr., Park HK, Gross EG, Graham<br />
GF, Stratton MS, Marshall JR & Clark LC 2003. Selenium supplementation and secondary prevention of<br />
nonmelanoma skin cancer in a randomized trial. J Natl <strong>Cancer</strong> Inst 95(19): 1477–81.<br />
Ejlak J, Seal J & van Vaetzen D 1998. Eat well Tasmania! End of year two survey 1997. Hobart: Tasmanian<br />
Promotion Council & Department of Community and Health Services.<br />
English DR, MacInnis RJ, Hodge AM, Hopper JL, Haydon AM & Giles GG 2004. Red meat, chicken, and fish<br />
consumption and risk of colorectal cancer. <strong>Cancer</strong> Epidemiol Biomarkers Prev 13(9): 1509–14.<br />
Foerster SB, Kizer KW, Disogra LK, Bal DG, Krieg BF & Bunch KL 1995. California’s ‘5 a day––for better<br />
health!’ campaign: an innovative population-based effort to effect large-scale dietary change. Am J Prev Med<br />
11(2): 124–31.<br />
Gill T, King L & Webb K 2005. Best options for promoting healthy weight and preventing weight gain in NSW.<br />
Sydney: NSW Department of Health.<br />
Hands B, Parker H, Glasson C, Brinkman S & Read H 2004. Physical activity and nutrition levels in Western<br />
Australian children and adolescents: report. Perth, WA: Western Australian Government.<br />
Heimendinger J, Van Duyn MA, Chapelsky D, Foerster S & Stables G 1996. The national 5-A-Day for Better<br />
Health Program: a large-scale nutrition intervention. J Public Health Manag Pract 2(2): 27–35.<br />
International Agency for Research on <strong>Cancer</strong> Working Group on the Evaluation of <strong>Cancer</strong>-preventive<br />
Strategies (IARC Working Group) 2002. Handbooks of cancer prevention volume 6: weight control and physical<br />
activity, eds H Vainio & F Bianchini. Lyon, France: IARC Press.<br />
International Agency for Research on <strong>Cancer</strong> (IARC) 2004. IARC handbooks on cancer prevention. Cruciferous<br />
vegetables. Lyon, France: IARC.<br />
——— 2003. IARC handbooks on cancer prevention. Fruit and vegetables. Lyon, France: IARC.<br />
International Union Against <strong>Cancer</strong> (UICC) 2004. Evidence-based cancer prevention: strategies for NGOs—a<br />
handbook for Europe. Geneva: UICC.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
N u t r i t i o n
Kushi L & Giovannucci E 2002. Dietary fat and cancer. Am J Med 113(9B Suppl): S63–70.<br />
Leppala JM, Virtamo J, Fogelholm R, Huttunen JK, Albanes D, Taylor PR & Heinonen OP 2000. <strong>Control</strong>led<br />
trial of alpha-tocopherol and beta-carotene supplements on stroke incidence and mortality in male smokers.<br />
Arterioscler Thromb Vasc Biol 20(1): 230–5.<br />
Lester IH 1994. Recommendations of the workshop to revise nutrition goals and targets, Melbourne, 29<br />
January 1991. In Australia’s food and nutrition (Appendix D). Canberra: Australian Institute of Health and<br />
Welfare.<br />
Magarey A, Daniels LA & Smith A 2001. Fruit and vegetable intakes of Australians aged 2–18 years: an<br />
evaluation of the 1995 <strong>National</strong> Nutrition Survey data. Aust N Z J Public Health 25(2): 155–61.<br />
Magarey A, McKean S & Daniels L 2006. Evaluation of fruit and vegetable intakes of Australian adults: the<br />
<strong>National</strong> Nutrition Survey 1995. Aust N Z J Public Health 30(1): 32–7.<br />
Marks GC, Pang G, Coyne T & Picton P 2001. <strong>Cancer</strong> costs in Australia: the potential impact of dietary change.<br />
Canberra: Australian Food and Nutrition Monitoring Unit.<br />
Mathers C, Vos T & Stevenson C 1999. The burden of disease and injury in Australia. Canberra: Australian<br />
Institute of Health and Welfare.<br />
McLennan W & Podger A 1998. <strong>National</strong> nutrition survey: nutrient intakes and physical measurement. ABS cat.<br />
no. 4805.0. Canberra: Australian Bureau of Statistics.<br />
Michels KB, Edward G, Joshipura KJ, Rosner BA, Stampfer MJ, Fuchs CS, Colditz GA, Speizer FE & Willett<br />
WC 2000. Prospective study of fruit and vegetable consumption and incidence of colon and rectal cancers. J<br />
Natl <strong>Cancer</strong> Inst 92(21): 1740–52.<br />
Miller M, Pollard C & Paterson D 1996. A public health nutrition campaign to promote fruit and vegetables<br />
in Australia. In Multidisciplinary approaches to food choice. Proceedings of Food Choice Conference, ed. A<br />
Worsley. Adelaide: University of Adelaide.<br />
Miller MR & Kose B 1996. What are Western Australians eating? The Perth dietary surveys. In What’s eating<br />
Western Australia? Proceedings of the Nutrition WA Conference. Perth: Health Department of Western<br />
Australia.<br />
<strong>National</strong> Aboriginal and Torres Strait Islander Nutrition Working Party (NATSO Working Party) 2001. <strong>National</strong><br />
Aboriginal and Torres Strait Islander Nutrition Strategy and Action Plan 2000–2010 and first phase activities<br />
2000–2003. Canberra: <strong>National</strong> Public Health Partnerships.<br />
<strong>National</strong> Health and Medical Research Council (NHMRC) 2005. Nutrient reference values for Australia and<br />
New Zealand, including recommended dietary intakes. Canberra: Department of Health and Ageing.<br />
——— 2003a. Dietary guidelines for Australian adults. Canberra: NHMRC.<br />
——— 2003b. Dietary guidelines for children and adolescents in Australia. Canberra: NHMRC.<br />
——— 1999. Dietary guidelines for older Australians. Canberra: NHMRC.<br />
<strong>National</strong> Heart Foundation (NHF) 2002. Healthy eating for the heart. A guide to lowering your blood<br />
cholesterol. Canberra: NHF.<br />
<strong>National</strong> Obesity Task Force (NOTF) 2003. Healthy weight 2008: the <strong>National</strong> Agenda for Children and Young<br />
People and Their Families. Canberra: Australian Government Department of Health and Ageing.<br />
Norat T, Bingham S, Ferrari P, Slimani N, Jenab M, Mazuir M, Overvad K, Olsen A, Tjonneland A, Clavel F,<br />
Boutron-Ruault MC, Kesse E, Boeing H, Bergmann MM, Nieters A, Linseisen J, Trichopoulou A, Trichopoulos<br />
D, Tountas Y, Berrino F, Palli D, Panico S, Tumino R, Vineis P, Bueno-de-Mesquita HB, Peeters PH, Engeset<br />
D, Lund E, Skeie G, Ardanaz E, Gonzalez C, Navarro C, Quiros JR, Sanchez MJ, Berglund G, Mattisson I,<br />
Hallmans G, Palmqvist R, Day NE, Khaw KT, Key TJ, San JM, Hemon B, Saracci R, Kaaks R & Riboli E 2005.<br />
Meat, fish, and colorectal cancer risk: the European Prospective Investigation into <strong>Cancer</strong> and Nutrition. J<br />
Natl <strong>Cancer</strong> Inst 97(12): 906–16.<br />
Norat T, Lukanova A, Ferrari P & Riboli E 2002. Meat consumption and colorectal cancer risk: dose-response<br />
meta-analysis of epidemiological studies. Int J <strong>Cancer</strong> 98(2): 241–56.<br />
Section One: Preventable risk factors
Norat T & Riboli E 2001. Meat consumption and colorectal cancer: a review of epidemiologic evidence. Nutr<br />
Rev 59(2): 37–47.<br />
Northern Territory Government 2001. Food and nutrition policy: action plan 2001–2006. Darwin: Northern<br />
Territory Government.<br />
NSW Health 2002. Strategic direction for public health nutrition 2002–2007. Sydney: NSW Health.<br />
Nutrition & Physical Activity Branch 2005. Go for 2 & 5—campaign summary. Perth: WA Department of<br />
Health.<br />
Pignone MP, Ammerman A, Fernandez L, Orleans CT, Pender N, Woolf S, Lohr KN & Sutton S 2003.<br />
Counseling to promote a healthy diet in adults: a summary of the evidence for the US Preventive Services<br />
Task Force. Am J Prev Med 24(1): 75–92.<br />
Prentice RL, Caan B, Chlebowski RT, Patterson R, Kuller LH, Ockene JK, Margolis KL, Limacher MC, Manson<br />
JE, Parker LM, Paskett E, Phillips L, Robbins J, Rossouw JE, Sarto GE, Shikany JM, Stefanick ML, Thomson<br />
CA, Van HL, Vitolins MZ, Wactawski-Wende J, Wallace RB, Wassertheil-Smoller S, Whitlock E, Yano K,<br />
Adams–Campbell L, Anderson GL, Assaf AR, Beresford SA, Black HR, Brunner RL, Brzyski RG, Ford L, Gass<br />
M, Hays J, Heber D, Heiss G, Hendrix SL, Hsia J, Hubbell FA, Jackson RD, Johnson KC, Kotchen JM, LaCroix<br />
AZ, Lane DS, Langer RD, Lasser NL & Henderson MM 2006. Low-fat dietary pattern and risk of invasive<br />
breast cancer: the Women’s Health Initiative Randomized <strong>Control</strong>led Dietary Modification Trial. JAMA 295(6):<br />
629–42.<br />
Queensland Public Health Forum 2002. Eat well Queensland 2001–2012: smart eating for a healthier state.<br />
Brisbane: Queensland Public Health Forum.<br />
Ralph H, Chapman K, Yu XQ & O’Connell D 2006. The association between omega-3 fatty acid and fish and<br />
the risk of breast, colon, rectum and prostate cancer: a systematic review. Prepared for The <strong>Cancer</strong> Council<br />
NSW.<br />
Roder DM 2002. The epidemiology of gastric cancer. Gastric <strong>Cancer</strong> 5(1 Suppl): 5–11.<br />
Rose DP & Connolly JM 1999. Omega-3 fatty acids as cancer chemopreventive agents. Pharmacol Ther 83(3):<br />
217–44.<br />
Royal Australian College of General Practitioners (RACGP) 2006. Putting prevention into practice: guidelines for<br />
the implementation of prevention in the general practice setting. South Melbourne: RACGP.<br />
——— 2005. Guidelines for preventive activities in general practice, eds M Harris, L Bailey, C Bridges-Webb, J<br />
Furler, B Joyner, J Litt, J Smith & Y Zurynski. South Melbourne: RACGP.<br />
——— 2004. SNAP: A population health guide to behavioral risk factors in general practice. South Melbourne:<br />
RACGP.<br />
Sahay TB, Ashbury FD, Roberts M & Rootman I 2006. Effective components for nutrition interventions: a<br />
review and application of the literature. Health Promot Pract 7(4): 418–27.<br />
Sandhu MS, White IR & McPherson K 2001. Systematic review of the prospective cohort studies on meat<br />
consumption and colorectal cancer risk: a meta-analytical approach. <strong>Cancer</strong> Epidemiol Biomarkers Prev 10:<br />
439–46.<br />
Smigel K 1996. Beta carotene fails to prevent cancer in two major studies; CARET intervention stopped. J<br />
Natl <strong>Cancer</strong> Inst 88(3/4): 145.<br />
Somerset SM 2003. Refined sugar intake in Australian children. Public Health Nutr 6(8): 809–13.<br />
Sorensen G, Emmons K, Hunt MK & Johnston D 1998. Implications of the results of community intervention<br />
trials. Ann Rev Public Health 19:379–416.<br />
Stein K 2006. After the media feeding frenzy: whither the Women’s Health Initiative Dietary Modification<br />
Trial? J Am Diet Assoc 106(6): 794–800.<br />
Steptoe A, Perkins-Porras L, McKay C, Rink E, Hilton S & Cappuccio FP 2003. Behavioural counselling to<br />
increase consumption of fruit and vegetables in low income adults: randomised trial. BMJ 326(7394): 855.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
N u t r i t i o n
Strategic Inter-Governmental Nutrition Alliance (SIGNAL) 2001. Eat well Australia. An agenda for action for<br />
public health nutrition 2000–2010. Canberra: <strong>National</strong> Public Health Partnerships.<br />
Syme SL 1997. Individual vs community interventions in public health practice: some thoughts on a new<br />
approach. Melbourne: Victorian Health Promotion Foundation.<br />
Thomas H, Ciliska D, Micucci S, Wilson-Abra J & Dobbins M 2004. Effectiveness of physical activity<br />
enhancement and obesity prevention programs in children and youth. Hamilton, Canada: City of Hamilton,<br />
Public Health and Community Services.<br />
UK Department of Health 1998. Nutritional aspects of the development of cancer. Report of the Working Group<br />
on Diet and <strong>Cancer</strong> of the Committee on Medical Aspects of Food and Nutrition <strong>Policy</strong>. 48. Norwich, UK: The<br />
Stationery Office.<br />
Weingarten MA, Zalmanovici A & Yaphe J 2005. Dietary calcium supplementation for preventing colorectal<br />
cancer and adnomatous polyps. Cochrane Database of Systematic Reviews 2: CD003548.<br />
Willett WC 1998. Dietary fat intake and cancer risk: a controversial and instructive story. Semin <strong>Cancer</strong> Biol<br />
8(4): 245–53.<br />
Woods B, Swinburn B & Burns C 2003. Eating well in Victoria: food security for all. Melbourne: Deakin School<br />
of Health Sciences.<br />
World <strong>Cancer</strong> Research Fund (WCRF) & American Institute for <strong>Cancer</strong> Research (AICR) 1997. Food, nutrition<br />
and the prevention of cancer: a global perspective. Washington, DC: AICR.<br />
World Health Organization (WHO) 2004. Global Strategy on Diet, Physical Activity and Health. Geneva: WHO.<br />
World Health Organization (WHO) & Food and Agriculture Organization (FAO) 2003. Diet, nutrition and the<br />
prevention of chronic diseases: report of a joint WHO/FAO expert consultation. WHO technical report series<br />
916. Geneva: WHO.<br />
0 Section One: Preventable risk factors
P h y s i c a l a c t i v i t y<br />
Introduction<br />
Less than half of the Australian adult population<br />
achieves the current recommended levels of 150<br />
minutes a week of moderate-intensity physical<br />
activity and less than one-third achieves the higher<br />
level of 60 minutes a day estimated to reduce colon<br />
cancer risk (Cerin et al. 2005).<br />
The study of physical inactivity as a risk factor for chronic disease commenced in the 1950s<br />
and focused on the epidemic of cardiovascular disease in Western countries. A pivotal<br />
review highlighted the public health benefits of regular physical activity (Pate et al. 1995).<br />
This was followed by the US Surgeon General’s report, Physical activity and health, which<br />
summarised the scientific evidence for the health benefits of physical activity (USDHHS<br />
1996). More recently an Australian review has confirmed the dose–response relationship<br />
between physical activity and better health outcomes, specifically all-cause mortality,<br />
cardiovascular disease, stroke, some cancers, type 2 diabetes, depression and obesity<br />
(Bull, Bauman et al. 2004). In addition to the reduction in chronic disease risk, it is clear<br />
that physical activity provides age-specific benefits over a person’s life (Bull, Bauman et al.<br />
2004).<br />
Research on the link between levels of physical activity and specific cancers began during<br />
the 1980s but has increased rapidly over the last decade. Not surprisingly, the most<br />
commonly occurring cancers in men (prostate, lung, colorectal) and in women (breast,<br />
lung, colorectal) have been the subject of most published epidemiological studies. Recent<br />
reviews of physical activity and cancer have identified several hundred relevant studies<br />
(Friedenreich & Orenstein 2002; IARC Working Group 2002; Lee 2003; McTiernan 2003;<br />
Bull, Bauman et al. 2004; Gotay 2005). However, the majority of studies are observational<br />
rather than interventional (McTiernan 2003). More intervention studies are required to<br />
determine the optimal physical activity ‘dose’ for cancer prevention (McTiernan 2003).<br />
The strongest evidence is for two of the most common cancers: breast cancer and colon<br />
cancer. It is also suggested that regular physical activity is associated with a reduction in<br />
all-cancer morbidity and mortality (Bull, Bauman et al. 2004); however this is likely to be<br />
due to the effect of exercise on breast and colon cancer. Whether physical activity reduces<br />
the risk of other cancers, including rectal, endometrial, prostate, testicular, kidney and lung<br />
cancer, remains less certain due to limited and inconclusive data (IARC Working Group<br />
2002; Lee 2003). This remains an active area of research internationally.<br />
Physical activity (along with nutrition) contributes to weight control by contributing to<br />
energy balance. Overweight and obesity have been associated with an increased risk of<br />
several cancers. It is clear that physical activity protects against cancer independently<br />
of its contribution to weight control. Overweight and obesity and physical inactivity are<br />
independent risk factors for cancer (Thune & Furberg 2001; Friedenreich & Orenstein 2002;<br />
IARC Working Group 2002; McTiernan et al. 2003).<br />
More recently, physical activity and physical fitness have been shown to be beneficial to<br />
cancer patients. Despite being a relatively new area of research, physical activity before,<br />
during and after treatment is consistently showing a positive association with cancer<br />
outcomes (Courneya 2003).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1<br />
P h y s i c a l a c t i v i t y
How physical activity is measured<br />
Understanding the ‘dose’ required<br />
The epidemiological research investigating the contribution of physical inactivity to<br />
chronic disease, including cancers, is complicated by the complexities of physical activity<br />
assessment protocols in population-based research (Shephard 2003).<br />
Physical activity is often classified by type. The type, or mode, of physical activity relates<br />
to the specific activity being performed (AIHW 2003). Broadly speaking, the three types of<br />
physical activity are aerobic, resistance and flexibility. Many activities cross more than one<br />
type, for example gymnastics has an aerobic, flexibility and resistance component (Whaley<br />
2006).<br />
Aerobic activities are assessed in terms of energy expenditure, which is a function of<br />
intensity, duration and frequency of activity. Intensity is a measure of how hard an activity<br />
is, duration is the time spent doing the activity and frequency is how many times, usually in<br />
a week, the activity is done (AIHW 2003).<br />
In research, energy expenditure is often calculated in metabolic equivalents (METs). MET<br />
values are multiples of the resting metabolic rate (RMR), that is, 1 MET is the energy used<br />
when sitting quietly. One MET is equivalent to an oxygen uptake of 3.5 mL.kg-1.min-1 or to<br />
a caloric value of 1 kcal.kg-1.hr-1 (4.184 kilojoules per kilogram per hour) (Ainsworth et al.<br />
2000).<br />
Table 1.6 Examples of activities and MET intensities<br />
METs Activity Examples<br />
1.0 Inactivity, quiet Sitting quietly and watching television<br />
3.5 Walking Walking for pleasure<br />
8.0 Bicycling Bicycling, 19–24 km/h, leisure, moderate<br />
8.0 Water activities Swimming, crawl, slow (50 m/min), moderate or light<br />
effort<br />
12.5 Running Running, 12 km/h (5 min/km)<br />
Source: Ainsworth et al. 2000<br />
More commonly the frequency, intensity and duration of physical activity are expressed<br />
separately, or frequency and duration are aggregated to give a total time (in minutes) per<br />
week. Activities are grouped according to intensity, for ease of use.<br />
•<br />
•<br />
Vigorous-intensity activity makes a person short of breath or ‘puff and pant’ (i.e. 7-9<br />
METs).<br />
Moderate-intensity activity is when it is still possible to hold a conversation (i.e. 3-4<br />
METs).<br />
•<br />
Walking includes for recreation, transport or exercise.<br />
(Ainsworth et al. 2000)<br />
Total activity time per week is used to assess whether an individual has completed<br />
sufficient physical activity for a health benefit (see next table). To account for the greater<br />
intensity, time spent in vigorous-intensity activity is weighted by a factor of two (that is,<br />
doubled) when calculating the total activity time per week.<br />
2 Section One: Preventable risk factors
Table 1.7 Definitions of sufficient and insufficient physical activity and sedentary<br />
Term Definition<br />
Sufficient The accumulation of at least 150 minutes of activity over one week in at<br />
least five sessions.<br />
Insufficient The accumulation of some activity but less than 150 minutes of activity<br />
per week.<br />
Sedentary No activity reported over the week.<br />
Source: AIHW 2003<br />
Recall of participation is a known difficulty in the assessment of physical activity. Vigorous<br />
intensity activity is generally reported better than moderate intensity activity (Slattery and<br />
Jacobs 1995). Misclassification of moderate intensity activities would decrease the ability<br />
to detect a real association (IARC Working Group 2002).<br />
The link between physical activity and cancer<br />
The role of physical activity in the prevention of specific cancers continues to be an<br />
active area of research and review (Lee 2003; McTiernan 2003; Roberts & Barnard 2005;<br />
Warburton, Nicol & Bredin 2006).<br />
For the 2002 World Health Report, the World Health Organization systematically reviewed<br />
the evidence on breast and colon cancer (WHO 2002; Bull, Armstrong et al. 2004). In<br />
the same year, the International Agency for Research on <strong>Cancer</strong> (IARC) published its<br />
report, Weight control and physical activity, which included a comprehensive review of the<br />
epidemiological evidence relating to all cancers (IARC Working Group 2002). In 2003, The<br />
<strong>Cancer</strong> Council commissioned a review of the epidemiological literature linking physical<br />
activity and specific cancers (Bauman, Habibullah & Holford 2003), which is summarised<br />
in Getting Australia active II (Bull, Bauman et al. 2004). In the same year, Lee reviewed the<br />
epidemiological evidence for the major cancer sites: breast, colon, rectum, prostate and<br />
lung. Overall the findings are consistent: colon cancer and breast cancer risk decrease with<br />
increasing levels of physical activity (IARC Working Group 2002; Lee 2003; Slattery et al.<br />
1997).<br />
All the reviews have used similar criteria to assess the research design and population<br />
studied: number and characteristics of cancer cases; definition and measurement of<br />
physical activity; estimated time between physical activity exposure and cancer outcome;<br />
and estimated effect size, expressed as an adjusted odds ratio or relative risk (RR).<br />
For colon cancer there is consensus that the risk reduction for physically active men and<br />
women is around 30% to 40% (RR 0.6–0.7), compared with inactive people (IARC Working<br />
Group 2002; Lee 2003; Slattery et al. 1997). By contrast, the evidence for rectal cancer is<br />
inconsistent, with most studies not able to detect a significant difference or reporting a<br />
weak association (Lee 2003; Slattery et al. 1997). There is a dose–response relationship<br />
between physical activity and colon cancer, with optimal protection proffered by 3.5 to 4<br />
hours of vigorous physical activity or 7 to 35 hours of moderate physical activity each week<br />
(Slattery et al. 1997). There remains no clear agreement on the biological mechanism(s) for<br />
the protective effect (Westerlind 2003; Slattery et al. 1997). Current suggestions include<br />
a reduction in gastrointestinal transit time, improvements in immune function, hormone<br />
modulation (insulin, sex hormones and insulin-like growth factor), a reduction in free<br />
radicals and prostaglandin modulation (Westerlind 2003; Slattery et al. 1997).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
3<br />
P h y s i c a l a c t i v i t y
There is consistent epidemiological agreement that physically active women have about a<br />
20% to 30% reduction in breast cancer risk (RR 0.7–0.8) compared with inactive women<br />
(IARC Working Group 2002; Lee 2003). Unlike colon cancer, there is not specific detail on<br />
the optimal dose of physical activity for breast cancer, although it appears that 30 to 60<br />
minutes per day of moderate to vigorous exercise is required to reduce risk. Again there<br />
is evidence of a dose–response relationship: breast cancer risk decreases with increasing<br />
levels of physical activity (Lee 2003). Risk reduction has been reported for both pre- and<br />
post-menopausal women. However it is still unclear which time period(s) in a woman’s<br />
lifespan are most important for physical activity in the development of breast cancer (IARC<br />
Working Group 2002). Like colon cancer, the biological mechanism(s) are not clear. Similar<br />
mechanisms have been postulated, with greater emphasis on oestrogen metabolism (IARC<br />
Working Group 2002; Lee 2003; Westerlind 2003).<br />
There is no consistent evidence of an association between physical activity and other<br />
specific cancers. Endometrial, prostate, testicular, ovarian and lung cancers have been<br />
the subject of the most attention. Although some studies show an association between<br />
physical activity and lung cancer, it is possible that this relationship is confounded by<br />
smoking and/or other lung diseases (IARC Working Group 2002; Lee 2003).<br />
Many questions remain unanswered in this comparatively new area of cancer research.<br />
It appears that more intense and more frequent and longer duration of activity may<br />
generally provide more protection (Bauman, Habibullah & Holford 2003). Further research<br />
is required into the dose–response relationship between physical activity and cancer and<br />
specific cancer sites; the type, frequency, intensity and duration of physical activity; and<br />
the biological mechanisms influencing cancer development (Lee 2003; UICC 2004; Gotay<br />
2005; Roberts & Barnard 2005).<br />
The impact<br />
The population attributable risk (PAR) is often used to assess the relative public health<br />
importance of a risk factor. PAR is a function of the prevalence and strength of the<br />
association between the risk factor and the disease outcome. In the case of physical<br />
inactivity it represents the proportion of cases (for example colon cancer) that could be<br />
prevented if exposure to the risk factor were eliminated, that is, 100% of the population<br />
achieving sufficient physical activity (Bauman 1998; Stephenson et al. 2000). The PAR for<br />
physical inactivity has been estimated for two types of cancer, colon cancer and breast<br />
cancer, as the strongest epidemiological evidence relates to these cancers.<br />
Table 1.8 Estimates of population attributable risk (PAR) for physical activity and cancer<br />
Author Year Breast cancer Colon cancer<br />
Mezzetti et al. 1998 10.6%<br />
Stephenson et al.* 2000 9% 19%<br />
WHO 2002 10% 16%<br />
IARC 2002 11% 13–14%<br />
Slattery 2004 12–14%<br />
* Estimate for the Australian population<br />
Sources: Mezzetti et al. 1998; Stephenson et al. 2000; IARC Working Group 2002; WHO 2002; Smith 2004; Slattery 2004<br />
4 Section One: Preventable risk factors
Broadly speaking, there is agreement between the various estimates. It is likely however<br />
that these underestimate the true PAR. Variation in measurement and definition of physical<br />
activity between studies and the unaccounted-for contribution of physical inactivity to<br />
weight gain are all sources of potential error (IARC Working Group 2002).<br />
In broad terms, therefore, it follows that increasing physical activity could prevent up to<br />
1165 colon cancer and 1297 breast cancer cases annually (AIHW & AACR 2004).<br />
The challenge<br />
Australia has had three national physical activity surveys: in 1997, 1999 and 2000. The<br />
results from the three surveys (see figure below) are of concern, with a discernable<br />
downward trend in the proportion of the population reporting sufficient physical activity.<br />
In 2000, just over half of the adult population (56.8%) achieved the current recommended<br />
levels of 150 minutes per week while the proportion of Australians reporting no physical<br />
activity (sedentary) increased (13.4% in 1997 to 15.3% in 2000) (Bauman, Ford &<br />
Armstrong 2001).<br />
Figure 1.3 Trends in proportion of Australian adults meeting recommended levels of physical activity<br />
Percentage<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Men<br />
63 61<br />
1997<br />
62<br />
Women Total<br />
60<br />
54<br />
57 58<br />
56<br />
1999 2000<br />
YEAR<br />
Source: Bauman, Ford & Armstrong 2001<br />
There has not been a national physical activity survey since 2000 so it is not possible to<br />
make an accurate assessment of the current population physical activity level in Australia.<br />
A number of states have conducted surveys during the intervening period based on the<br />
same instrument, the Active Australia questionnaire. Data from these state-based surveys<br />
show that the downward trend in physical activity has most likely continued.<br />
The data from the 2000 national physical activity survey were re-analysed against three<br />
criteria for achieving sufficient physical activity (Cerin et al. 2005) (refer to figure 1.4<br />
below):<br />
•<br />
<strong>National</strong> physical activity guidelines for adults: accrual of ≥150 minutes of at least<br />
moderate-intensity activity through five or more sessions in the previous week (DHAC<br />
1999).<br />
57<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
5<br />
P h y s i c a l a c t i v i t y
•<br />
•<br />
Moderate-intensity physical activity to reduce colon cancer risk: accrual of ≥420<br />
minutes of at least moderate-intensity activity in the previous week (Slattery et al. 1997).<br />
Vigorous physical activity to reduce colon cancer risk: accrual of ≥210 minutes of<br />
vigorous activity in the previous week (Slattery et al. 1997).<br />
Figure 1.4 Proportion of the population achieving three criteria for sufficient activity<br />
Percentage<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
150 min/wk<br />
Source: Cerin et al. 2005<br />
MEN WOMEN<br />
GENDER<br />
Section One: Preventable risk factors<br />
420 min/wk (moderate) 210 min/wk (vigorous)<br />
The application of different criteria to the data from the 2000 national physical activity<br />
survey highlights that the prevalence of meeting physical activity criteria for colon cancer<br />
prevention is low and much lower than that related to the more generic physical activity<br />
recommendations. Less than half of the population (46%) achieves the recommended<br />
≥150 minutes of at least moderate-intensity activity through five or more sessions in a<br />
week and only 26% meet the colon cancer criteria (Cerin et al. 2005). The same review<br />
also examined the socio-demographic factors associated with achievement of the physical<br />
activity criteria. Across each of the three criteria, physical activity is higher in males than<br />
females, decreases with age and increases with educational attainment (Cerin et al. 2005).<br />
Effective interventions<br />
There is potential to promote higher levels of participation in physical activity in the<br />
Australian population. Several recent reviews and reports have examined the evidence on<br />
effectiveness, key characteristics and best strategies for a population-based approach to<br />
promoting physical activity (Kahn et al. 2002; Bull, Bellew et al. 2004; NPHP 2005).<br />
Be active Australia: a framework for health sector action for physical activity (NPHP 2005)<br />
is the current strategic framework for population-based physical activity promotion in<br />
Australia. The strategic focus of this framework contains three areas: settings, overarching<br />
strategies and population groups. The action areas are summarised below:<br />
1. Settings<br />
• Community environments and organisations<br />
•<br />
Health services
•<br />
•<br />
•<br />
Childcare and out of school hours care<br />
Schools<br />
Workplaces<br />
2. Overarching strategies<br />
•<br />
•<br />
•<br />
•<br />
Communication<br />
Workforce capacity<br />
Evidence, research, monitoring and evaluation<br />
Strategic management and coordination<br />
3. Priority populations<br />
• Aboriginal and Torres Strait Islander peoples<br />
•<br />
Populations with special needs<br />
Be active Australia is underpinned by Getting Australia active II, a major review of physical<br />
activity interventions across different settings and approaches and for different populations<br />
(Bull, Bauman et al. 2004).<br />
Settings<br />
Community environments and organisations<br />
The influence of the environment on physical activity has been the subject of increased<br />
attention for the past decade. It is commonly accepted that the built environment provides<br />
opportunities (and barriers) to physical activity and can facilitate incidental physical activity.<br />
Unfortunately there is a paucity of evidence on the relative contribution of the environment<br />
to physical activity behaviour and there are limited data on the specific environmental<br />
attributes that increase physical activity (McCormack et al. 2004; Giles-Corti 2006).<br />
Environmental improvements require collaboration with and commitment from sectors<br />
outside of health, such as transport and urban planning. The health sector has a role in<br />
education, workforce development and advocacy, as well as contributing to the evidence<br />
base (Giles-Corti 2006).<br />
Health services<br />
Health services, particularly primary health care, are an important setting for individual<br />
physical activity interventions. There is little evidence on the effectiveness of populationbased<br />
physical activity promotion in health services. Health professionals, in particular<br />
general practitioners (GPs) are an accessible, credible source of information for patients<br />
(RACGP 2004). Approximately 85% of Australians visit a GP in any given year (Britt et al.<br />
2005).<br />
Brief interventions for physical activity behaviour change, often based on the transtheoretical<br />
or stages of change model, are recommended for use in general practice<br />
(RACGP 2005). Verbal advice, written materials (such as pamphlets and booklets) and<br />
exercise prescriptions can produce short-term increases in physical activity (Smith<br />
2004). The nature and degree of change is not unexpected given the relatively brief<br />
counselling that patients receive. This could potentially be improved by involving other<br />
health professionals (for example, practice nurses), either in partnership with GPs or<br />
independently, to reinforce health messages and provide more follow-up with patients<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
P h y s i c a l a c t i v i t y
to help them achieve greater and more sustained behavioural changes to their habitual<br />
physical activity behaviours (Smith 2004; Brown 2006).<br />
A number of electronic and paper-based resources are available to assist general practice<br />
to work with patients to improve physical activity, including:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
SNAP: A population health guide to behavioural risk factors in general practice (RACGP<br />
2004)<br />
Lifestyle prescriptions (‘Lifescripts’) (DHA 2005)<br />
Guidelines for preventive activities in general practice (‘the red book’) (RACGP 2005)<br />
Putting prevention into practice: guidelines for the implementation of prevention activities<br />
in the general practice setting (‘the green book’) (RACGP 2006a)<br />
<strong>National</strong> guide to a preventive health assessment in Aboriginal and Torres Strait Islander<br />
peoples (NACCHO 2005).<br />
Childcare and out of school hours care<br />
There is very little published research on the effectiveness of physical activity interventions<br />
in the childcare setting (Timperio, Salmon & Ball 2004); however health promotion<br />
programs targeting childcare centres have proven to be very popular. The demand for<br />
SunSmart Centres and Start Right Eat Right (in Western Australia) suggests that childcare<br />
is a setting very receptive to health promotion interventions.<br />
The majority of out-of-school-hours interventions published were conducted on primaryschool-aged<br />
children in the US, either as after school, summer camp or family-based<br />
interventions. Programs that involved parents were the most effective. Out-of-school-hours<br />
care is a setting that offers considerable promise, but more evidence is needed in an<br />
Australian context and for adolescents (Timperio, Salmon & Ball 2004).<br />
Schools<br />
Schools are frequently identified as an important setting for health promotion. Successful<br />
school-based health promotion can simultaneously improve education and health (WHO<br />
1997). School-based physical activity interventions can be classified into three types:<br />
curriculum-based strategies, environmental change strategies and policy-based strategies<br />
(Timperio, Salmon & Ball 2004). The most successful interventions incorporated a wholeof-school<br />
approach: that is, curriculum-, environmental- and policy-based strategies<br />
(CDCP 1999). Health promotion in schools requires cooperation and collaboration with the<br />
education sector, consistent with the health promoting schools framework (WHO 1997;<br />
NPHP 2005).<br />
Workplaces<br />
Workplace health promotion presents enormous potential to access large numbers of<br />
people at once and improve the health and productivity of the workforce. Up to now,<br />
however, there has been limited evidence supporting the effectiveness of workplace<br />
health promotion programs (Marshall 2004). Workplaces, like other physical and social<br />
environments, provide opportunities and barriers to physical activity. Non-specific<br />
programs and policies that promote incidental physical activity appear to be more<br />
successful and sustainable than individualised or targeted programs in the workplace<br />
(Marshall 2004).<br />
Section One: Preventable risk factors
Strategies<br />
Communication<br />
Communication and community education include mass media (social marketing), printed<br />
material, websites, telephone interventions and community education (Marshall, Owen<br />
& Bauman 2004; NPHP 2005). Overall, mass media successfully raise awareness of<br />
physical activity, measured through recall, but have modest effects on behaviour. Individual<br />
campaigns have reported more success in changing behaviour (Marshall, Owen & Bauman<br />
2004). Interventions using print materials have shown some success in changing physical<br />
activity behaviour in the short term, whereas telephone- and Internet-based interventions<br />
have demonstrated limited success (Marshall, Owen & Bauman 2004).<br />
Workforce capacity<br />
Physical activity promotion is one priority among a range of conflicting and complementary<br />
prevention activities for health professionals (RACGP 2006a; RACGP 2006b). The capacity<br />
of the workforce is limited by the number of health professionals and the time available<br />
to them. All health professionals, not just GPs or those trained in exercise science, should<br />
play a role in increasing physical activity (Brown 2006). Opportunities exist to develop<br />
training packages, both informal and formal, for health (and other) professionals in primary<br />
prevention, specifically physical activity (NPHP 2005). Complementary resources (posters,<br />
pamphlets or brochures) and online support would add value and support for those who<br />
undertake training.<br />
Evidence, research, monitoring and evaluation<br />
There are no national data on the current level of physical activity for Australians. The<br />
most recent data were collected, and reported, in 2000. Since 2000, individual states<br />
and territories have undertaken a range of monitoring and surveillance activities, without<br />
national coordination. Better national coordination of the available data would allow a more<br />
accurate assessment of population physical activity trends over time and evaluation of the<br />
impact of national interventions.<br />
Evidence continues to accumulate to support the protective role of physical activity in<br />
health. Despite this there are specific research areas with conflicting or insufficient data,<br />
including the role of physical activity in cancer prevention beyond breast cancer and colon<br />
cancer and the optimal amount and type of physical activity for weight loss and disease<br />
prevention.<br />
It is clear that there is still a need for more well-designed research to evaluate which<br />
interventions work best, particularly those tailored to specific population groups and/or<br />
settings. The research identifies areas of promise and ‘best bets’, but considerable work<br />
remains to implement and test these approaches on a larger scale in the Australian<br />
context.<br />
Strategic management and coordination<br />
Successful action on physical activity requires strategic leadership and commitment at a<br />
national level as well as a coordinated approach at national, state, territory and local levels,<br />
with good communication between all stakeholders, including the non-government sector<br />
(NPHP 2005). The development of a national framework, Be active Australia, is the first<br />
step to underpinning good public health practice (Bull, Bellew et al. 2004). The absence of<br />
mandated accountability and adequate resourcing at a national level limits the opportunity<br />
for successful implementation of the framework (Bull, Bellew et al. 2004).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
P h y s i c a l a c t i v i t y
Populations<br />
Aboriginal and Torres Strait Islander peoples<br />
The review of interventions with Aboriginal and Torres Strait Islander peoples found very<br />
little published evaluation, despite an increase in the number and diversity of programs in<br />
these communities (Shilton & Brown 2004). There remains a need for much more effort in<br />
this area, in relation to measurement and interventions in urban as well as rural and remote<br />
communities (NACCHO 2005).<br />
Populations with special needs<br />
Populations with special needs are those Australians who face additional barriers to<br />
being physically active. It includes people with a chronic condition, including cancer<br />
(NPHP 2005). The number of cancer survivors (including people living with cancer) in<br />
Australia continues to increase. People who have survived cancer are at increased risk of<br />
many chronic diseases and may have to contend with disability associated with cancer<br />
treatment. Population-based physical activity strategies may not be suitable; rather, small<br />
group or individual interventions would be more appropriate for these groups (NPHP 2005).<br />
The policy context<br />
Policies, reports and strategic plans have been produced by most state and territory<br />
governments, providing direction for improvement in physical activity levels in Australia.<br />
The <strong>Cancer</strong> Council strongly supports the work of other chronic disease prevention<br />
agencies and institutions in the promotion of physical activity.<br />
The <strong>National</strong> physical activity guidelines for Australians (DHAC 1999) includes these<br />
recommendations:<br />
•<br />
•<br />
•<br />
•<br />
Think of movement as an opportunity, not an inconvenience.<br />
Be active every day in as many ways as you can.<br />
Put together at least 30 minutes of moderate-intensity physical activity on most,<br />
preferably all, days.<br />
If you can, also enjoy some regular, vigorous exercise for extra health and fitness.<br />
Australia’s physical activity recommendations for 5–12 year olds and Australia’s physical<br />
activity recommendations for 12–18 year olds (DHA 2004a; DHA 2004b) recommend that:<br />
•<br />
•<br />
Children need at least 60 minutes (and up to several hours) of moderate to vigorous<br />
physical activity every day.<br />
Children should not spend more than two hours a day using electronic media for<br />
entertainment (e.g. computer games, TV, Internet), particularly during daylight hours.<br />
This is a recommended minimum level of activity for children, youth and adults. Higher<br />
levels are likely to give greater benefits.<br />
Colon cancer and breast cancer risk reduces with increasing levels of physical activity. The<br />
optimal risk reduction for colon cancer is achieved at 3.5 to 4 hours of vigorous physical<br />
activity or 7 to 35 hours of moderate physical activity each week (Slattery et al. 1997). The<br />
American <strong>Cancer</strong> Society recommends that 45 to 60 minutes of moderate to vigorous<br />
activity on at least five days of the week is preferable (Kushi et al. 2006).<br />
0 Section One: Preventable risk factors
Aims<br />
The <strong>Cancer</strong> Council Australia recognises the strength of evidence for physical activity in<br />
the prevention of breast and colon cancer and in the reduction of risk for other diseases,<br />
particularly cardiovascular disease and diabetes.<br />
The body of evidence on health benefits of physical activity has led to general public health<br />
recommendations for adults to have 30 minutes of regular, moderate-intensity physical<br />
activity on most days of the week (DHAC 1999). To date, there is insufficient evidence to<br />
support the development of separate public health advice for the prevention of different<br />
illnesses, thus The <strong>Cancer</strong> Council endorses the recommendations that have been put<br />
forward in a consistent fashion by federal, state and territory bodies and other agencies.<br />
The <strong>Cancer</strong> Council’s aims are to encourage the Australian population throughout life to:<br />
•<br />
•<br />
•<br />
maintain at least a minimum level of physical activity: for adults at least 30 minutes of<br />
moderate-intensity activity on most days of the week, for children and adolescents at<br />
least 60 minutes<br />
participate in physical activity of longer duration and higher intensity, to further reduce<br />
colon cancer risk, where possible across the lifespan (consistent with the <strong>National</strong><br />
physical activity guidelines for Australians)<br />
maintain a healthy body weight through a balance of food intake and physical activity.<br />
What needs to be achieved How The <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
Increased awareness of<br />
the link between physical<br />
inactivity and cancer among<br />
the general public and key<br />
health professionals<br />
Effective coordinated<br />
policy development and<br />
implementation<br />
Social marketing campaigns<br />
that promote physical activity<br />
An increased capacity to<br />
monitor epidemiological<br />
trends<br />
Monitor and clarify best evidence on the relationship between physical<br />
inactivity and cancer causation<br />
Ensure key messages are promoted to the public and relevant health<br />
professionals in publications, presentations, programs, media statements<br />
and where opportunities arise<br />
Promote and/or develop complementary primary health resources,<br />
specifically for general practice, to improve evidence-based interventions<br />
by health professionals<br />
Develop and maintain evidence-based policy positions about the<br />
relationship between physical inactivity and cancer to complement the<br />
Australian policy context<br />
Ensure effective and coordinated policy development and<br />
implementation<br />
Advocate for nationwide social marketing campaigns that promote<br />
physical activity across the life course which are coordinated,<br />
sustainable and far-reaching<br />
Encourage the Australian, state and territory governments to commit to<br />
long-term investment to increase the awareness of the health benefits of<br />
physical activity and promote increased participation<br />
Support and deliver effective community interventions at a local, state<br />
and national level to address physical inactivity<br />
Support and conduct high quality epidemiological research further<br />
clarifying the relationship between physical inactivity and cancer<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1<br />
P h y s i c a l a c t i v i t y
An increased capacity to<br />
monitor behavioural trends<br />
More supportive<br />
environments that assist<br />
people to be more physically<br />
active<br />
An increased capacity to<br />
know what works in relation<br />
to program delivery<br />
2 Section One: Preventable risk factors<br />
Support and conduct high quality behavioural research further clarifying<br />
the barriers and enabling factors for participation in physical activity<br />
Work towards a better understanding of the determinants of the<br />
obesogenic environment, to inform policy development<br />
Encourage the Australian Government to fund a comprehensive <strong>National</strong><br />
Nutrition and Physical Activity Survey of children and adults, which is<br />
conducted, as a minimum on a regular five-year basis<br />
Encourage the Australian Government to address the broader social<br />
and environmental determinants of physical inactivity and sedentary<br />
lifestyles<br />
Continue to support and promote the Parents Jury<br />
Undertake specific research and evaluation studies to:<br />
• evaluate physical activity interventions<br />
• gather more evidence relating to the economic evaluation of cancer<br />
prevention<br />
• lead national understanding of what works in relation to cancer<br />
prevention<br />
• identify barriers and enabling factors for implementation of these<br />
recommendations in general practice and other health settings<br />
Note: Refer also to the action plans of the nutrition and obesity chapters when considering promotion of physical activity.<br />
References<br />
Physical activity<br />
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O’Brien WL, Bassett DR Jr, Schmitz<br />
KH, Emplaincourt PO, Jacobs DR Jr & Leon AS 2000. Compendium of physical activities: an update of<br />
activity codes and MET intensities. Med Sci Sports Exerc 32(9 Suppl): S498–504.<br />
Australian Institute of Health and Welfare (AIHW) 2003. The Active Australia Survey: a guide and manual for<br />
implementation, analysis and reporting. Canberra: AIHW.<br />
Australian Institute of Health and Welfare (AIHW) & Australasian Association of <strong>Cancer</strong> Registries (AACR)<br />
2004. <strong>Cancer</strong> in Australia 2001. AIHW cat. no. 23; AIHW <strong>Cancer</strong> Series no. 28. Canberra: AIHW.<br />
Bauman A 1998. Use of population attributable risk (PAR) in understanding the health benefits of physical<br />
activity. Br J Sports Med 32(4): 279–80.<br />
Bauman A, Ford I & Armstrong T 2001. Trends in population levels of reported physical activity in Australia,<br />
1997, 1999 and 2000. Canberra: Australian Sports Commission.<br />
Bauman A, Habibullah M & Holford R 2003. A review of published epidemiological studies 1990–2002, which<br />
examined the relationship between physical activity and cancer. Report for The <strong>Cancer</strong> Council NSW, August<br />
2003 prepared by the NSW Centre for Physical Activity and Health.<br />
Britt H, Miller GC, Knox S, Charles J, Pan Y, Henderson J, Bayram C, Valenti L, Ng A & O’Halloran J 2005.<br />
General practice activity in Australia 2004–05. AIHW cat. no. GEP 18. Canberra: Australian Institute of Health<br />
and Welfare.<br />
Brown WJ 2006. Individual or population approaches to the promotion of physical activity ... is that the<br />
question? J Sci Med Sport 9(1–2): 35–7.
Bull FC, Armstrong T, Dixon T, Ham S, Neiman A & Pratt M 2004. Physical inactivity. In Comparative<br />
quantification of health risks: global and regional burden of disease due to selected major risk factors, eds M<br />
Ezzati, A Lopez, A Rodgers & C Murray. Geneva: World Health Organization.<br />
Bull FC, Bauman AE, Bellew B & Brown WJ 2004. Getting Australia active II: an update of evidence on physical<br />
activity. Melbourne: <strong>National</strong> Public Health Partnership.<br />
Bull FC, Bellew B, Schoppe S & Bauman AE 2004. Developments in <strong>National</strong> Physical Activity <strong>Policy</strong>: an<br />
international review and recommendations towards better practice. J Sci Med Sport 7(1 Suppl): 93–104.<br />
Centers for Disease <strong>Control</strong> and <strong>Prevention</strong> (CDCP) 1999. Best practices for comprehensive tobacco control<br />
programs. Atlanta: CDCP.<br />
Cerin E, Leslie E, Bauman A & Owen N 2005. Levels of physical activity for colon cancer prevention<br />
compared with generic public health recommendations: population prevalence and sociodemographic<br />
correlates. <strong>Cancer</strong> Epidemiol Biomarkers Prev 14(4): 1000–2.<br />
Courneya KS 2003. Exercise in cancer survivors: an overview of research. Med Sci Sports Exerc 35(11):<br />
1846–52.<br />
Department of Health and Aged Care (DHAC) 1999. An active way to better health: national physical activity<br />
guidelines for adults. Canberra: DHAC.<br />
Department of Health and Ageing (DHA) 2005. Lifescripts. Canberra: DHA.<br />
——— 2004a. Australia’s physical activity recommendations for 5–12 year olds. Canberra: DHA.<br />
——— 2004b. Australia’s physical activity recommendations for 12–18 year olds. Canberra: DHA.<br />
Friedenreich CM & Orenstein MR 2002. Physical activity and cancer prevention: etiologic evidence and<br />
biological mechanisms. J Nutr 132(11 Suppl): S3456–64.<br />
Giles-Corti B 2006. People or places: what should be the target? J Sci Med Sport 9(5): 357–66.<br />
Gotay CC 2005. Behavior and cancer prevention. J Clin Oncol 23(2): 301–10.<br />
International Agency for Research in <strong>Cancer</strong> Working Group on the Evaluation of <strong>Cancer</strong>-preventive<br />
Strategies (IARC Working Group) 2002. Handbooks of cancer prevention volume 6: weight control and physical<br />
activity, eds H Vainio & F Bianchini. Lyon, France: IARC Press.<br />
International Union Against <strong>Cancer</strong> (UICC) 2004. Evidence-based cancer prevention: strategies for NGOs – a<br />
handbook for Europe. Geneva: UICC.<br />
Kahn EB, Ramsey LT, Brownson RC, Heath GW, Howze EH, Powell KE, Stone EJ, Rajab MW & Corso P 2002.<br />
The effectiveness of interventions to increase physical activity. A systematic review. Am J Prev Med 22(4<br />
Suppl): S73–107.<br />
Kushi LH, Byers T, Doyle C, Bandera EV, McCullough M, McTiernan A, Gansler T, Andrews KS & Thun MJ<br />
2006. American <strong>Cancer</strong> Society guidelines on nutrition and physical activity for cancer prevention: reducing<br />
the risk of cancer with healthy food choices and physical activity. CA <strong>Cancer</strong> J Clin 56(5): 254–81.<br />
Lee IM 2003. Physical activity and cancer prevention—data from epidemiologic studies. Med Sci Sports Exerc<br />
35(11): 1823–7.<br />
Marshall AL 2004. Challenges and opportunities for promoting physical activity in the workplace. J Sci Med<br />
Sport 7(1 Suppl): 60–6.<br />
Marshall AL, Owen N & Bauman AE 2004. Mediated approaches for influencing physical activity: update<br />
of the evidence on mass media, print, telephone and website delivery of interventions. J Sci Med Sport 7(1<br />
Suppl): 74–80.<br />
McCormack G, Giles-Corti B, Lange A, Smith T, Martin K & Pikora TJ 2004. An update of recent evidence of<br />
the relationship between objective and self-report measures of the physical environment and physical activity<br />
behaviours. J Sci Med Sport 7(1 Suppl): 81–92.<br />
McTiernan A 2003. Intervention studies in exercise and cancer prevention. Med Sci Sports Exerc 35(11):<br />
1841–5.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
3<br />
P h y s i c a l a c t i v i t y
McTiernan A, Kooperberg C, White E, Wilcox S, Coates R, Adams-Campbell LL, Woods N & Ockene J 2003.<br />
Recreational physical activity and the risk of breast cancer in postmenopausal women: the Women’s Health<br />
Initiative Cohort Study. JAMA 290(10): 1331–6.<br />
Mezzetti M, Vecchia CL, Decarli A, Boyle P, Talamini R & Franceshi S 1998. Population attributable risk for<br />
breast cancer: diet, nutrition, and physical exercise. J Natl <strong>Cancer</strong> Inst 90(5): 389–94.<br />
<strong>National</strong> Aboriginal Community <strong>Control</strong>led Health Organisation (NACCHO) 2005. <strong>National</strong> guide to a<br />
preventive health assessment in Aboriginal and Torres Strait Islander peoples. Melbourne: Royal Australian<br />
College of General Practitioners.<br />
<strong>National</strong> Public Health Partnership (NPHP) 2005. Be active Australia: a framework for health sector action for<br />
physical activity. Melbourne: NPHP.<br />
Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, Buchner D, Ettinger W, Heath GW & King<br />
AC 1995. Physical activity and public health. A recommendation from the Centers for Disease <strong>Control</strong> and<br />
<strong>Prevention</strong> and the American College of Sports Medicine. JAMA 273(5): 402–7.<br />
Roberts CK & Barnard RJ 2005. Effects of exercise and diet on chronic disease. J Appl Physiol 98(1): 3–30.<br />
Royal Australian College of General Practitioners (RACGP) 2006a. Putting prevention into practice: guidelines<br />
for the implementation of prevention in the general practice setting. Second edition. South Melbourne: RACGP.<br />
——— 2006b. The role of general practice in prevention and health promotion. <strong>Policy</strong> endorsed by the 48th<br />
RACGP Council, 18 May 2006. Melbourne: RACGP.<br />
——— 2005. Guidelines for preventive activities in general practice, eds M Harris, L Bailey, C Bridges-Webb, J<br />
Furler, B Joyner, J Litt, J Smith & Y Zurynski. Sixth edition. South Melbourne: RACGP.<br />
——— 2004. SNAP: A population health guide to behavioural risk factors in general practice. South Melbourne,<br />
Victoria: RACGP.<br />
Shephard RJ 2003. Limits to the measurement of habitual physical activity by questionnaires. Br J Sports<br />
Med 37(3): 197–206.<br />
Shilton TR & Brown WJ 2004. Physical activity among Aboriginal and Torres Strait Islander people and<br />
communities. J Sci Med Sport 7(1 Suppl): 39–42.<br />
Slattery ML 2004. Physical activity and colorectal cancer. Review article. Sports Med 34(4): 239–52.<br />
Slattery ML, Edwards SL, Ma KN, Friedman GD & Potter JD 1997. Physical activity and colon cancer: a public<br />
health perspective. Ann Epidemiol 7(2): 137–45.<br />
Slattery ML & Jacobs DR Jr 1995. Assessment of ability to recall physical activity of several years ago. Ann<br />
Epidemiol 5(4): 292–6.<br />
Smith BJ 2004. Promotion of physical activity in primary health care: update of the evidence on interventions.<br />
J Sci Med Sport 7(1 Suppl): 67–73.<br />
Stephenson J, Bauman A, Armstrong T, Smith B & Bellew B 2000. The costs of illness attributable to physical<br />
inactivity in Australia. Canberra: Commonwealth Department of Health and Aged Care.<br />
Thune I & Furberg A 2001. Physical activity and cancer risk: dose-response and cancer, all sites and sitespecific.<br />
Med Sci Sports Exerc 33(Suppl): S530–50.<br />
Timperio A, Salmon J & Ball K 2004. Evidence-based strategies to promote physical activity among children,<br />
adolescents and young adults: a review and update. J Sci Med Sport 7(1 Suppl): S20–9.<br />
US Department of Health and Human Services (USDHHS) 1996. Physical activity and health: a report of the<br />
Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease <strong>Control</strong><br />
and <strong>Prevention</strong>, <strong>National</strong> Center for Chronic Disease <strong>Prevention</strong> and Health Promotion.<br />
Warburton DE, Nicol CW & Bredin SS 2006. Health benefits of physical activity: the evidence. CMAJ 174(6):<br />
801–9.<br />
4 Section One: Preventable risk factors
Westerlind KC 2003. Physical activity and cancer prevention: mechanisms. Med Sci Sports Exerc 35(11):<br />
1834–40.<br />
Whaley ME 2006. ACSM’s guidelines for exercise testing and prescription. Philadelphia: Lippincott Williams &<br />
Wilkins.<br />
World Health Organization (WHO) 2002. The world health report 2002: reducing the risks, promoting healthy<br />
life. Geneva: WHO<br />
——— 1997. Promoting health through schools: report of a WHO Expert Committee on Comprehensive School<br />
Health Education and Promotion. Geneva: WHO.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
5<br />
P h y s i c a l a c t i v i t y
O v e r w e i g h t a n d<br />
o b e s i t y<br />
Introduction<br />
Obesity is associated with increased risk of cancer of<br />
the colon, breast (post-menopause), endometrium,<br />
kidney, oesophagus and gall bladder. Levels of<br />
overweight and obesity in Australia continue to be a<br />
major health concern. Of particular concern is the<br />
latest estimate that one in four children is overweight<br />
or obese.<br />
Rising rates of overweight and obesity have been described as reaching epidemic<br />
proportions in the developed nations and causing concern in developing nations. Australia<br />
is no exception. Over the last 30 years, rates of overweight and obesity among adults and,<br />
even more worrying, among children, have risen and the rise is accelerating.<br />
Overweight and obesity are a major public health issue: they are an established cause<br />
of morbidity and mortality and are one of the largest risk factors for chronic diseases in<br />
Western countries, particularly increasing the risk of diabetes, cardiovascular disease and<br />
some cancers (WHO & FAO 2003).<br />
There are several ways to measure disease risk associated with overweight and obesity,<br />
including body mass index (BMI) and waist circumference.<br />
BMI is the most commonly used and internationally accepted measure to assess<br />
overweight and obesity (NHMRC 2003a). This is calculated by dividing a person’s<br />
weight (in kilograms) by their height (in metres squared). According to the World Health<br />
Organization’s definitions, adults:<br />
•<br />
•<br />
•<br />
•<br />
with a BMI under 18.5 kg/m2 are classified as underweight<br />
with a BMI of >18.5 to 25 to 30 kg/m2 or higher are classified as obese (WHO & FAO 2003).<br />
As BMI increases from a healthy weight to overweight or obesity, the risk of ill health rises.<br />
Individuals who are obese have a 50% to 100% increased chance of premature death from<br />
all causes compared to individuals with a BMI in the healthy range (WHO 2000).<br />
It should be noted, however, that these classifications are not suitable for children and<br />
adolescents due to age-related growth patterns, and BMI-for-age percentile charts,<br />
developed by the Centers for Disease <strong>Control</strong> and <strong>Prevention</strong>, should be used to assess<br />
overweight and obesity in children. The <strong>National</strong> Health and Medical Research Council<br />
defines the following cut-offs for children and adolescents:<br />
•<br />
•<br />
BMI above the 85th percentile is indicative of overweight<br />
BMI above the 95th percentile is indicative of obesity (NHMRC 2003b).<br />
Section One: Preventable risk factors
The specific cut-off measurements of BMI may not be suitable for all ethnic groups, who<br />
may have equivalent levels of risk at a lower BMI (e.g. Asians) or higher BMI (e.g. Pacific<br />
Islanders or Polynesians).<br />
Measurement of waist circumference may be a simpler valid alternative to BMI for health<br />
promotion (Han et al. 1996).<br />
Waist circumference may also a good predictor of cancer risk. The exact relationship<br />
between increased abdominal fat and increased cancer risk is currently unclear. Significant<br />
increased risk appears to occur when the waist circumference is greater than 102 cm for<br />
men and 88 cm for women (NHMRC 2003c).<br />
Emerging epidemiological data highlight the importance of acting on obesity as a matter<br />
of considerable importance and urgency. The increasing trends to overweight and obesity<br />
among young Australians are particularly worrying. There is mounting evidence of links<br />
between childhood eating behaviour, physical activity trends and obesity, and of their<br />
association with long-term chronic conditions, including some cancers, diabetes and<br />
cardiovascular disease (Dietz 1998; Freedman et al. 1999; WHO 2000; Dunstan et al. 2000;<br />
Ebbeling, Pawlak & Ludwig 2002).<br />
More children and adolescents are displaying the markers of adult chronic diseases, such<br />
as cardiovascular disease, type 2 diabetes and fatty liver disease (Booth et al. 2006).<br />
Obesity essentially results from an imbalance between declining energy expenditure due to<br />
physical inactivity and high energy in the diet. High consumption of energy dense/nutrient<br />
poor foods (excess calories from high sugar or fat foods) is the main determinant of the<br />
obesity epidemic (WHO & FAO 2003).<br />
These trends imply a pattern of rising health costs for governments as well as for<br />
individuals and the community in which they live (Booth et al. 2001).<br />
The link between overweight and obesity and cancer<br />
Obesity (BMI >30 kg/m2) is associated with increased risk of cancer at several sites; the<br />
evidence is clear for cancers of the colon, breast (post-menopause), endometrium, kidney,<br />
oesophagus and gall bladder (IARC Working Group 2002). Overweight (BMI of >25 to<br />
Table 1.9 Proportion of cancer attributable to overweight and obesity and associated factors<br />
Type of cancer Proportion<br />
of incidence<br />
attributable to<br />
overweight or<br />
obesity<br />
Section One: Preventable risk factors<br />
Aspects of the association between overweight or obesity<br />
and cancer<br />
Colon cancer 11% Association seems greater in men than women<br />
Risk not dependent on whether person has been overweight<br />
in early adulthood or later in life<br />
Some evidence that association in women may be increased<br />
by menopausal status and hormone replacement therapy<br />
(HRT) use in the obese (Slattery et al. 2003)<br />
Post-menopausal<br />
breast cancer<br />
Endometrial<br />
cancer<br />
9% Increase in risk of 30% in women with a BMI ≥28 kg/m2<br />
compared to those with a BMI of 25 kg/m2 have a two- to three-fold<br />
increase in risk<br />
Limited evidence suggests risk is similar in pre- and postmenopausal<br />
women<br />
Kidney cancer 25% Individuals with a BMI of ≥30 kg/m2 have a two- to three-fold<br />
increase in risk compared to those below 25 kg/m2<br />
The effect is similar in men and women<br />
Oesophageal<br />
adenocarcinoma<br />
Gall bladder<br />
cancer<br />
Source: Bergstrom et al. 2001, based on figures from Europe<br />
37% Strong association between being overweight and<br />
adenocarcinomas of the lower oesophagus and the gastric<br />
cardia, with a two-fold increase in risk in individuals with a<br />
BMI of >25 kg/m2<br />
24% Limited evidence available but there is a suggestion of almost<br />
a two-fold risk, especially in women<br />
There is also emerging evidence that obesity is associated with increased risk of cancers<br />
of the pancreas and liver, and multiple myeloma and non-Hodgkin lymphoma (Calle et al.<br />
2003).<br />
It is interesting to note that overweight and obesity are risks factors for some of the most<br />
common cancers in Australia, such as colon and breast cancer. With the rising rates of<br />
obesity in Australia, there is concern that this will translate into an increased incidence of<br />
some of the less common cancers associated with obesity.<br />
Up to now we have known that excess body weight increases cancer risk, but there has<br />
been a dearth of evidence to suggest whether losing weight would lower cancer risk.<br />
Recent evidence indicates that weight loss in those who are overweight lowers breast<br />
cancer risk (Eliassen et al. 2006).<br />
Most of the evidence associating body weight with cancer is derived from case–control<br />
and cohort studies. However there has been one large scale randomised controlled<br />
trial, the Women’s Health Initiative, which randomised women to a very low fat diet<br />
intervention or a usual fat diet (Prentice et al. 2006). Unfortunately the Women’s Health<br />
Initiative was not designed to address weight loss, with the intervention group only losing
0.4 kg more weight than the control group. While women on the low fat diet had a 9%<br />
lower incidence of breast cancer compared with the control group, this result was not<br />
statistically significant. However in sub-group analyses, breast cancer rates were reduced<br />
by 22% among women who started with the highest fat intake (>37% energy from fat) and<br />
reduced their fat the most (to 24% after one year) (Stein 2006).<br />
Interestingly, there was suggestive evidence that the low fat diet had a more protective<br />
effect against oestrogen receptor-positive breast cancer. Despite the lack of an apparent<br />
effect on colorectal cancer, adenomas were significantly reduced among the low fat diet<br />
group (Stein 2006).<br />
As well as a healthy body weight being associated with preventing cancer, it is also<br />
associated with preventing cancer recurrence and improving survival for people diagnosed<br />
with cancer (Brown et al. 2003). There is a reasonable level of evidence that weight<br />
management and physical activity positively impacts on quality of life, cancer recurrence<br />
and overall survival for cancer survivors (Brown et al. 2003). Randomised controlled trials,<br />
such as the Women’s Intervention in Nutrition Study, have shown encouraging results of<br />
the effectiveness of nutrition and physical activity interventions in improving outcomes for<br />
cancer survivors (Chlebowski et al. 2005).<br />
The impact<br />
Obesity and its underlying factors of excess energy intake and physical inactivity contribute<br />
substantially to the overall Australian ‘burden of disease’, that is, the overall health<br />
problems based on mortality and disability.<br />
For the first time in Australia, overweight and obesity has overtaken tobacco as the risk<br />
factor responsible for the most significant burden of disease: 8.6% compared with 7.8%<br />
for tobacco (AIHW 2006). Overweight and obesity accounted for 8.8% of the disease<br />
burden for males and 8.3% for females. Even though the burden from tobacco is only<br />
slightly lower than the burden from obesity, it is likely that the obesity burden will continue<br />
to increase, whereas the tobacco impact is declining due to the decreases in smoking<br />
prevalence over the last 40 years.<br />
In Australia, 3% of all cancer deaths have been attributed to a BMI of >25 kg/m2 (Mathers,<br />
Vos & Stevenson 1999). More recent estimates from America suggest that overweight<br />
and obesity may account for 14% of cancer deaths in men and 20% in women (Calle et al.<br />
2003).<br />
US studies have suggested that the effects of obesity on quality of life and on health care<br />
costs are equivalent to 20 years of ageing (Sturm 2002), and that obesity is associated with<br />
at least as much morbidity as poverty, smoking or drinking (Sturm & Wells 2001).<br />
<strong>National</strong>ly, the direct costs of obesity represent a significant proportion of the health care<br />
budget and there is great potential savings from reducing the problem. International<br />
studies on the economic costs of excess body weight, including data from Australia, have<br />
shown that, conservatively, between 2% and 7% of total health care costs may be directly<br />
attributable to overweight and/or obesity (WHO 2002). In Australia in 2003 it was estimated<br />
to equate to about $1.2 billion per year (WHO 2002). Studies of indirect costs of work<br />
workforce participation have shown increased rates of long-term sick leave and premature<br />
disability leading to loss of productivity (WHO 2002).<br />
A recent Australian report estimated that the total financial cost of obesity in 2005 was<br />
$3.7 billion (Access Economics 2006). The total health costs from cancer due to obesity<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
O v e r w e i g h t & o b e s i t y
were $107.3 million in 2005, with 79% of the costs related to bowel and breast cancers.<br />
Given the social and psychological consequences of obesity, intangible costs such as<br />
impaired quality of life are significant, with estimates for obesity-related cancers at $218<br />
million (Access Economics 2006).<br />
Importantly, the escalating cost of health care of an obesity-related disorder, such as<br />
diabetes, has been calculated as almost doubling over time with normal progression of<br />
the disease (Bennett, Magnus & Gibson 2004). This suggests that the economic burden<br />
is not only significant, but is likely to get worse even if there is no further growth in the<br />
prevalence of obesity. Overseas studies have also found that those who are obese attain<br />
lower levels of occupational prestige and lower incomes than non-obese people (Bennett,<br />
Magnus & Gibson 2004). In addition, other studies have found that obese people as a<br />
group receive more sickness and unemployment benefits than people with a healthy body<br />
weight (Bennett, Magnus & Gibson 2004). Indirect costs, which are far greater than direct<br />
costs, include workdays lost, doctor visits, disability pensions and premature mortality, all<br />
of which increase as people go from a healthy weight to overweight or obesity (Wolf &<br />
Colditz 1996).<br />
The challenge<br />
In the 10-year period from 1985 to 1995, the level of combined overweight/obesity in<br />
Australian children more than doubled, while the level of obesity tripled in all age groups<br />
and for both sexes (Cameron et al. 2003).<br />
Adults<br />
There is a lack of recent national data on the levels of overweight and obesity in Australian<br />
adults, as the last <strong>National</strong> Nutrition Survey was conducted in 1995.<br />
The Australian Diabetes, Obesity and Lifestyle Study in 1999−2000 found that the<br />
prevalence of overweight and obesity combined was almost 60% among Australian adults<br />
aged 25 years and over (Cameron et al. 2003). The rate for males was 67% and for females<br />
52%. The prevalence of being overweight was 39%. For adult males it was 48% and for<br />
adult females 30%. The prevalence of obesity was 21% or more than double the rate<br />
observed 15 years earlier: 19% of adult males and 22% of adult females were obese.<br />
According to the five-year follow-up of the Australian Diabetes, Obesity and Lifestyle Study,<br />
more than 600 adults progress from being overweight to being obese every day (i.e. more<br />
than 200,000 annually) (Barr et al. 2006).<br />
The 1995 <strong>National</strong> Nutrition Survey found that the proportion of overweight and/or obesity<br />
increases with age for both males and females (Marks et al. 2001). Adult men seem to<br />
increase their weight rapidly between the ages of 25 and 40 years, while the weight of<br />
women changes most markedly during the menopausal years (45 to 55). Among people<br />
aged 19 to 24 years, one in three males and one in four females are overweight or obese.<br />
Among people aged 45 to 64 years, this rises to three out of four males and almost two out<br />
of three females.<br />
Research has confirmed that weight increases are not just a result of ageing. Younger<br />
people are gaining weight faster than previous generations and weight gain is accelerating<br />
as modern life influences weight patterns. More people are entering adulthood weighing<br />
more. Data shows that those born later in the 20th century (Generation X) will gain weight<br />
as they age at a faster rate than their parents did (Allman-Farinelli et al. 2006a & 2006b).<br />
This is believed to be a result of the increasing obesogenic environment (see description<br />
later in this chapter).<br />
0 Section One: Preventable risk factors
Children<br />
Figure 1.5 Prevalence of overweight and obesity in children aged 7–11 years<br />
Percentage<br />
35<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
BOYS GIRLS<br />
OBESE<br />
OVERWEIGHT<br />
1985 1995 2003 1985 1995 2003<br />
Sources: Magarey, Daniels & Boulton 2001; Sangiorski et al. in press<br />
YEAR<br />
OBESE<br />
OVERWEIGHT<br />
The most recent data on the levels of overweight and obesity in Australian children comes<br />
from the 2004 NSW Schools Physical Activity and Nutrition Survey (SPANS), which<br />
surveyed 5500 children from 5 to 16 years of age (Bauman et al. 2003).<br />
In 2004, almost a quarter of children and young people from kindergarten to Year 10 (aged<br />
five to 16 years) were overweight or obese (25% of boys and 23% of girls) (Bauman et al.<br />
2003). Children aged nine to 12 had some of the highest rates (32% in Year 6 boys and<br />
30% in Year 4 girls). Children from lower socio-economic areas and boys from Middle<br />
Eastern backgrounds were more likely to be overweight or obese (Bauman et al. 2003).<br />
Overweight and obesity is far more common than it used to be. The proportion of school<br />
children who are overweight or obese has increased markedly over the past 20 years. It<br />
appears that in boys, the trend towards being overweight or obese is accelerating (Bauman<br />
et al. 2003). In girls the trend is not accelerating, but is still of concern (Bauman et al.<br />
2003).<br />
A study looking at weight changes among Australian children over three decades found<br />
that between 1985 and 1997, the combined prevalence of overweight and obesity doubled,<br />
and that of obesity trebled among young Australians. The increase over the previous 16<br />
years was far smaller (Booth et al. 2001). In 1985 the prevalence of overweight and obesity<br />
in boys was 11% and 12% in girls, with 1.4% of boys and 1.2% of girls being obese. Only<br />
10 years later, depending upon age, 14% to 26% of boys and 19% to 24% of girls were<br />
overweight or obese. The prevalence of obesity was 2% to 7% in boys and 4% to 6% in<br />
girls (Baur 2001; Magarey, Daniels & Boulton 2001).<br />
Overall there was a statistically significant increase in children’s mean energy intake<br />
between 1983 and 1995. For boys, there was an increase of 1400 kJ per day; for girls,<br />
there was an increase of 900 kJ per day. These increases are much greater than those seen<br />
in adults (Cook, Rutishauser & Seelig 2001). The increase in energy intake was derived<br />
from an increase in foods high in refined sugars, such as soft drinks and confectionery<br />
(Cook, Rutishauser & Seelig 2001).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1<br />
O v e r w e i g h t & o b e s i t y
Obese children have a 25% to 50% chance of progression to adult obesity, and this may<br />
be as high as 78% in older obese adolescents (Must & Strauss 1999). This significant risk<br />
confirms the importance of preventive action.<br />
Specific population groups<br />
The problem of overweight and obesity is so large and widespread throughout the<br />
community that it is difficult to identify any particular group that is not profoundly affected<br />
by the problem. However there are certain groups in the Australian community that bear a<br />
disproportionate burden of this condition.<br />
Data suggest that among Aboriginal Australians and Torres Strait Islanders, overweight<br />
and obesity affect 60% of men and 58% of women (ABS 1995 <strong>National</strong> Health Survey<br />
results, cited in NHMRC 1997; NATSI Working Party 2001). The prevalence of obesity in<br />
males is 25% and in females 28%, compared with an overall population prevalence of<br />
obesity of 18%. Differences in the level of overweight and obesity between Aboriginal and<br />
non-Aboriginal men and women are most pronounced in the younger age groups. High<br />
levels of obesity are found even among the youngest age groups of Aboriginal men and<br />
women and they continue to increase throughout life, up to the sixth decade. However, the<br />
association between overweight and obesity and diseases such as diabetes, cardiovascular<br />
disease and cancers in these communities remains unclear (Guest et al. 1993; Leonard et<br />
al. 2002; Wang & Hoy 2002).<br />
The level of overweight and obesity is higher (up to two to three times) among people<br />
of Southern European and Middle Eastern ethnic origin, when compared to those of<br />
British descent (NSW Health 2003). In contrast, those born in South East Asia had<br />
substantially lower levels of overweight, although care must be taken in interpreting<br />
these figures as the classification system may underestimate overweight in Asian people<br />
(Bennett & Magnus 1994; Bennett 1995; Mathers 1994; NSW Health 2003).<br />
A low social status and low level of education are associated with a higher level of<br />
overweight and obesity, although the effect is more obvious in women and is not as strong<br />
as the relationship between social status and other illnesses (NSW Health 2003). Around<br />
53% of women in the lowest socio-economic group were overweight, compared with 44%<br />
of women in the highest socio-economic group. In addition, 24% of women in the lowest<br />
socio-economic group were obese compared with only 14% of those in the highest group.<br />
There was no significant difference in the number of overweight or obese men in the<br />
highest when compared to the lowest socio-economic groups.<br />
Some data suggest that rural and remote communities have higher levels of overweight<br />
and obesity (NSW Health 2003). The issue of access to appropriate foods and opportunities<br />
to engage in appropriate physical activity are likely to be major contributing factors to these<br />
differentials in rural and remote communities.<br />
The clustering of factors such as low levels of education, low income and food insecurity,<br />
and their association with overweight and obesity levels, requires complex and sensitive<br />
interventions.<br />
2 Section One: Preventable risk factors
Effective interventions<br />
Table 1.10 lists the key physical activity and eating behaviours that need to be increased or<br />
decreased to prevent overweight and obesity.<br />
Most individual studies have been conducted in a very narrow range of settings and relied<br />
heavily on education approaches to small sections of the community. Very few studies<br />
have dealt with environmental, structural or policy change or were conducted on a truly<br />
community-wide basis (Campbell et al. 2005; Reilly et al. 2002; Ebbeling, Pawlak & Ludwig<br />
2002; WHO & FAO 2003; Gill, King & Webb 2005; Summerbell et al. 2003).<br />
Overall the literature states that for an intervention to be effective, initiatives should be<br />
long-lasting, multi-faceted and sustainable, and should target the whole environment<br />
and be behaviourally focused (Campbell et al. 2005; Reilly et al. 2002; Ebbeling, Pawlak &<br />
Ludwig 2002; WHO & FAO 2003; Gill, King & Webb 2005; Summerbell et al. 2003).<br />
Some researchers have proposed a life-course approach to cancer prevention (Uauy &<br />
Solomons 2005). This should start before conception, be followed through childhood and<br />
continue through all stages of the life course, as described in the figure below. Mothers<br />
should start pregnancy with a healthy weight and avoid excessive or low weight gain<br />
during pregnancy. Infant and children’s growth should be regularly assessed to ensure<br />
children to do not gain weight excessively.<br />
Figure 1.6 The life course approach to cancer prevention<br />
DEVELOPMENT OF CANCER<br />
FETAL LIFE INFANCY & CHILDHOOD ADOLESCENCE ADULT LIFE OLDER AGES<br />
Mother’s<br />
nutrition<br />
Fetal growth<br />
Birth weight<br />
Carcinogen<br />
exposure<br />
Source: Uauy & Solomons 2005<br />
Breast feeding<br />
Infections/PEM<br />
Micronutrients<br />
Contaminants<br />
(air, food, water)<br />
Growth rate<br />
Stature<br />
Behaviours<br />
Physical activity<br />
Food choice<br />
Obesity<br />
Carcinogen exposure<br />
Smoking<br />
Contaminants<br />
(air, food, water)<br />
Timing of puberty<br />
Obesity<br />
Physical activity<br />
Inactivity<br />
(exercise & sedentariness)<br />
Carcinogen exposure<br />
AGE<br />
Pregnancy & lactation<br />
Established adult risky behaviours<br />
Diet & physical activity<br />
<strong>Tobacco</strong><br />
Alcohol<br />
Carcinogen exposure<br />
ACCUMULATED RISK<br />
GENETIC SUSCEPTIBILITY TO CANCER<br />
There is general agreement that efforts should be heavily oriented towards prevention<br />
interventions in children because of the greater likelihood of success at a younger age.<br />
More effort needs to be directed at creating environmental and policy changes that will<br />
support the adoption of behaviours conducive to weight control, rather than simply relying<br />
on education approaches.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
3<br />
O v e r w e i g h t & o b e s i t y
Table 1.10 Summary of the strengths of the evidence on factors that might protect or promote against<br />
weight gain and obesity<br />
Evidence Decreases risk Increases risk<br />
Convincing Regular physical activity<br />
High dietary fibre intake<br />
Probable Home and school<br />
environment that supports<br />
healthy food choices for<br />
children<br />
Possible Low glycaemic index foods<br />
Breastfeeding<br />
Insufficient Increased eating frequency Alcohol<br />
* Energy dense foods are high in fat/sugar and energy.<br />
Source: WHO & FAO 2003<br />
4 Section One: Preventable risk factors<br />
High intake of energy dense foods*<br />
Sedentary lifestyles<br />
Heavy marketing of energy-dense foods and fast<br />
food outlets<br />
Sugar-sweetened soft drinks and juices<br />
Adverse social and economic conditions in<br />
developed countries<br />
Large portion sizes<br />
High proportion of food prepared outside of home<br />
Rigid restraint/ periodic disinhibition of eating<br />
patterns<br />
Obesogenic environment<br />
In the past, the usual environment throughout much of Australia enforced a reasonable<br />
degree of physical activity and limited food choice. Today there is access to a wide<br />
variety of cheap, energy dense/nutrient poor foods that are marketed powerfully and the<br />
population is encouraged, directly or indirectly, to avoid expending energy through physical<br />
activity. This has led researchers to describe the environment as ‘obesogenic‘ in that it<br />
inhibits appropriate dietary and physical activity patterns and encourages energy imbalance<br />
(Gebel et al. 2005).<br />
The next table summarises the best options to prevent weight gain based on a framework<br />
for a broad portfolio of actions for tackling weight gain prevention (Gill, King & Webb<br />
2005). This framework considers the level of potential health gain and level of uncertainty<br />
of risk associated with different interventions, and adopts the concept of assessing the<br />
level of ‘promise’ to judge the worth of interventions.
Table 1.11 Best options to prevent weight gain<br />
Target setting Activities<br />
Best options for families Reduce time spent watching TV and other sedentary behaviours<br />
Best options for early<br />
childhood care<br />
Improve parental knowledge and skills through early childhood care facilities<br />
Enhance food service policies in early childhood care facilities<br />
Enhance policies in early childcare facilities to promote physical activity<br />
Best options for schools Establish a network of health promoting schools:<br />
• policy on food and drinks<br />
• school physical environment<br />
• physical activity opportunities<br />
• health education curricula<br />
• programs for out of school hours care<br />
Best options for active<br />
neighbourhoods<br />
Best options for<br />
workplaces<br />
Best options for primary<br />
care<br />
Best options for industry<br />
/ food supply<br />
Best options for media /<br />
marketing<br />
Best options for support<br />
structures<br />
Source: Gill, King & Webb 2005<br />
Active transport<br />
Safe space for exercise facilities<br />
Improve access to food options for families<br />
Increase options for incidental physical activity<br />
Reduce passive work environments<br />
Improve workplace food service options<br />
Improve skills and knowledge of health workers<br />
Work with local suppliers to reduce fat in common foods<br />
Introduce taxation measures and subsidies to make healthy food options<br />
cheaper<br />
Develop a simplified food labelling system indicating energy and fat content<br />
Reduce exposure of children to food advertising<br />
Implement social marketing strategies to support improvement of parents as<br />
healthy role models<br />
Improve monitoring of weight and fitness status<br />
Implement ‘whole of community’ demonstration projects<br />
Individual behaviour change<br />
What research there is has generally focused on individual behaviour change with little<br />
attention to organisational and environmental change. There is a lack of research on the<br />
efficacy of different approaches to high risk, hard-to-reach, low income, and culturally and<br />
linguistically diverse populations that appear to experience higher rates of overweight and<br />
obesity.<br />
Some short-term intense programs are reported as being effective in terms of weight loss,<br />
but there are doubts about sustainability (Huon, Wardle & Szatto 1999; Gortmaker et al.<br />
1999; Sahota et al. 2001). Researchers (Ebbeling, Pawlak & Ludwig 2002) suggest that<br />
these interventions have tended to focus on highly motivated families through specialist<br />
clinics, and that, on the whole, there is little evidence that treatment interventions are<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
5<br />
O v e r w e i g h t & o b e s i t y
more than moderately effective. The relatively small short-term weight losses are generally<br />
reversed in the long term.<br />
Schools and workplaces<br />
Most prevention interventions targeting children and adults have been implemented in<br />
schools and workplaces and have adopted health education and/or behaviour modification<br />
strategies. With a few exceptions, these have largely been shown to be ineffective.<br />
School-based interventions to reduce soft drink intake among children have shown<br />
potential to be effective in preventing excess energy intake and overweight (James<br />
et al. 2004; Ebbeling et al. 2006). Other interventions that show the greatest potential<br />
for reducing obesity in children are those that reduce sedentary behaviours at home<br />
(particularly hours spent viewing TV), and promote physical activity—both in and out of<br />
school hours—as well as improved diet.<br />
Many states in Australia have introduced policy guidelines for school canteens, to address<br />
the need for healthier choices to be available at schools.<br />
Obesity prevention interventions that have tended to fail have been those that addressed<br />
either diet only or physical activity only, that relied primarily on education strategies without<br />
considering environmental influences, or that focused on activities and behaviours that<br />
only occur in limited settings, such as school hours (Ebbeling, Pawlak & Ludwig 2002;<br />
Reilly et al. 2002; Micucci, Thomas & Vohra 2002). One of the challenges in tackling<br />
childhood obesity is the difficulty in engaging and reaching parents. Schools can be a<br />
delivery site for interventions but must consider options to reach the whole family.<br />
<strong>Policy</strong><br />
Although evidence is sparse on the effectiveness of environmental change interventions,<br />
particularly policy and regulatory interventions, they have been proposed as an essential<br />
strategy for combating the obesity epidemic.<br />
There is limited evidence about the effectiveness of economic intervention, such as taxes,<br />
price policies and incentives, in containing or reducing food consumption, particularly<br />
energy dense foods (Goodman & Anise 2006). However, modelling analyses drawing upon<br />
actual market data to track how food purchasing responds to changes in prices suggest<br />
that a combination of increased prices (in the form of taxes) for such nutrients as fat,<br />
saturated fat and sugar and subsidies on high fibre foods could reduce the consumption of<br />
the taxed nutrients as well as total energy intake.<br />
A small body of evidence indicates that reducing the price of fruit, vegetables and other<br />
healthy snacks at the point of purchase (vending machines, cafeterias and supermarkets)<br />
increase their consumption (Anderson et al. 2001; Buscher, Martin & Crocker 2001; French,<br />
Jeffery et al. 1997; French, Story et al. 1997; French et al. 2001; Jeffery et al. 1994; Kristal<br />
et al. 1997).<br />
Although economic measures were an important strategy in tobacco control, there is a<br />
risk that economic policy interventions involving increases in food prices would negatively<br />
impact on low socio-economic groups. Therefore they would need to be carefully<br />
assessed before being implemented. Taxation of soft drinks has been proposed as a<br />
potential strategy, particularly because of the success of taxation of alcoholic drinks in<br />
lowering alcohol consumption. Reduction in intake of soft drinks is associated with obesity<br />
reduction (James et al. 2004; Ebbeling et al. 2006). Soft drinks are a single dietary item that<br />
generally provides little nutrition apart from sugar and energy.<br />
More effective regulation around food marketing has been proposed as an important and<br />
cost-effective strategy for addressing childhood obesity (DHS 2006). Children require<br />
Section One: Preventable risk factors
special consideration with respect to advertising, as they are less able than adults to<br />
understand fully the intent of advertising or its persuasive techniques, and are thus less<br />
able to judge the advertisements critically. The excessive level of food advertising on<br />
Australian televisions contributes to an obesogenic environment (Chapman, Nicholas<br />
& Supramaniam 2006; Neville, Thomas & Bauman 2005). Systematic literature reviews<br />
indicate that food advertising contributes to poor food choices, poor overall diet and thus<br />
increased weight gain and obesity (CFMDCY 2005; Hastings et al. 2003).<br />
All advertising during children’s programs is prohibited in Sweden (since 1991), Norway<br />
(since 1992) and Quebec Canada (since 1980) (Hawkes 2004). In all three cases, the ban is<br />
enforced by a government agency. Children in Quebec who are not exposed to television<br />
food advertising, have significantly less overweight and obesity than the Canadian average<br />
(Shields 2006). A study showed a significantly positive correlation between the number of<br />
television food advertisements and the incidence of children’s overweight across countries<br />
(Lobstein & Dibb 2005). Sweden had the lowest number of food advertisements in this<br />
study and the lowest prevalence of overweight, whereas Australia and the US did not fare<br />
so well (Lobstein & Dibb 2005). The high levels of unhealthy food advertising are also a<br />
concern because of the potential to limit the effectiveness of social marketing campaigns<br />
for healthy foods and lifestyles (Hoek & Gendall 2006).<br />
Broad-based public health interventions<br />
<strong>Prevention</strong> interventions that have adopted a population, community-wide or even<br />
neighbourhood approach, and encompass environmental, legislative and regulatory<br />
change as well as education and behaviour modification strategies, are largely absent and<br />
effectiveness cannot be assessed.<br />
While we lack high-quality evidence on obesity interventions, there is growing knowledge<br />
about the efficacy of broad-based, comprehensive public health interventions in fields<br />
such as tobacco and skin cancer control, HIV/AIDS and road trauma reduction, increased<br />
immunisation rates, decreased coronary heart disease and increased physical activity<br />
(Hawe, Wise & Nutbeam 2001; DHA 2003; Bauman et al. 2002; Bauman et al. 2003; Gill,<br />
King & Webb 2005). The research suggests that effective public health interventions are<br />
sustained, research-based and multi-faceted, and tackle social, cultural, behavioural,<br />
organisational and environmental factors.<br />
Evidence of population-based obesity interventions is weak (because of a modest impact)<br />
or absent (they have not been tried and evaluated). The World Health Organization states:<br />
‘population education strategies will need a solid base of policy and environment-based<br />
changes to be effective in eventually reversing these trends’ (WHO & FAO 2003).<br />
General practice<br />
Although to date there has been insufficient research to provide an evidence base for<br />
the role of the general practitioner (GP) in obesity prevention, their role at the forefront<br />
of providing primary care in Australia is recognised as having ‘enormous potential to<br />
encourage patients to take greater responsibility for their health, which includes changing<br />
lifestyle’ (RACGP 2006).<br />
Several initiatives over recent years have targeted GPs as a crucial point of intervention<br />
in obesity. In 2003 the <strong>National</strong> Health and Medical Research Council published two<br />
guidelines for GPs (Overweight and obesity in adults and Overweight and obesity in children<br />
and adolescents). The guidelines focus on the clinical management of overweight and<br />
obesity to be applied in the general practice consultation.<br />
The Royal Australian College of General Practitioners has produced three significant<br />
publications. The first, Guidelines for preventive activities in general practice (the ‘red book’)<br />
(RACGP 2005) also focuses on the role of the GP within the consultation recommending<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
O v e r w e i g h t & o b e s i t y
a screening approach particularly for children and adolescents. SNAP: A population<br />
health guide to behavioural risk factors in general practice (RACGP 2004) provides more<br />
extensive information and recommendations regarding overweight and obesity (among<br />
other common lifestyle risk factors), focusing on a patient education and behaviour<br />
modification approach based upon the 5As (ask, assess, advise, assist, arrange). Lastly,<br />
Putting prevention into practice: guidelines for the implementation of prevention in the<br />
general practice setting (the ‘green book’) (RACGP 2006) assists in the development of<br />
systems within general practice to support prevention activities at the practice as well as<br />
the consultation level.<br />
In further support of the GP’s role in obesity prevention, the Commonwealth Department<br />
of Health and Ageing, in the 2003/04 budget, funded the Lifestyle Prescriptions program<br />
(commonly known as Lifescripts). Lifescripts is being implemented through local divisions<br />
of general practice, promoting risk factor management in general practice and primary<br />
health care services. Lifestyle prescriptions are tools for GPs to use when providing lifestyle<br />
advice to patients. Advice may be about quitting smoking, increasing physical activity,<br />
eating a healthier diet, maintaining healthy weight, reducing alcohol consumption, or a<br />
combination of these.<br />
The policy context<br />
In 2003, the <strong>National</strong> Obesity Taskforce, with representation from Commonwealth and<br />
state health jurisdictions, developed a four-year national action plan for tackling obesity,<br />
known as Healthy weight 2008: the national action agenda for children and young people<br />
and their families (NOTF 2003). The goals are to:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
achieve healthier weight in children and young people<br />
increase the proportion of children and young people participating in and maintaining<br />
healthy eating and adequate physical activity<br />
strengthen the knowledge, skills, responsibility and resources of all people and<br />
communities to achieve optimal weight<br />
address social and environmental determinants of poor nutrition and physical inactivity<br />
focus action on giving children, young people and families the best possible chance of<br />
maintaining a healthy weight.<br />
A ministerial taskforce to coordinate an anti-obesity campaign was announced in July<br />
2006. It includes government, industry and community representation from the areas of<br />
health, communications, education, and sport.<br />
Healthy weight 2008 was preceded by Acting on Australia’s weight: a strategic plan for<br />
the prevention of overweight and obesity (NHMRC 1997), Eat well Australia: a strategic<br />
framework for public health nutrition, (SIGNAL 2001), and the <strong>National</strong> physical activity for<br />
health action plan (NPHP 2005).<br />
Many of the states and territories have developed frameworks and action plans similar to<br />
the Commonwealth initiative. The New South Wales and Victorian governments held child<br />
obesity summits in 2002 and Queensland held a summit in 2006 to focus attention and<br />
action on rising rates of overweight and obesity in young people.<br />
Internationally, the World Health Organization has adopted a Global Strategy on Diet,<br />
Physical Activity and Health, which was endorsed by the May 2004 World Health<br />
Assembly (WHO 2004). The International Union Against <strong>Cancer</strong> has developed a policy to<br />
Section One: Preventable risk factors
address action on a range of cancer prevention issues including obesity, in Evidence-based<br />
cancer prevention: strategies for NGOs (UICC 2004).<br />
Other relevant food policy contexts include the regulatory systems for food safety and food<br />
marketing. Food standards and regulation fall under the domain of the statutory authority,<br />
Food Standards Australia New Zealand. This has responsibility for setting standards for the<br />
production and sale of food in Australia, including food labelling issues such as nutrition<br />
and health claims.<br />
In Australia, food marketing operates under a system of co-regulation, with the Australian<br />
Communications and Media Authority having responsibility for the Children’s Television<br />
Standards, which include some regulations for limiting food advertising to children. The<br />
Advertising Standards Bureau administers the industry codes of practice developed by Free<br />
TV Australia and the Australian Association of <strong>National</strong> Advertisers, which add very little to<br />
the statutory regulations.<br />
Existing recommendations<br />
The <strong>Cancer</strong> Council Australia supports the <strong>National</strong> Health and Medical Research Council<br />
recommendations in relation to body weight and the maintenance of a balance between<br />
energy intake (healthy eating) and energy output (physical activity). For adults, the<br />
guideline states, ‘Prevent weight gain: be physically active and eat according to your<br />
energy needs’ (NHMRC 2003c). For children, the guideline does not refer specifically to<br />
body weight, but reads, ‘Children and adolescents need sufficient nutritious foods to grow<br />
and develop normally. Growth should be checked regularly for young children. Physical<br />
activity is important for all children and adolescents’ (NHMRC 2003b).<br />
The <strong>Cancer</strong> Council recommends that adults maintain a healthy weight within a BMI<br />
range of 18.5–25 kg/m2. To achieve and maintain a healthy weight, The <strong>Cancer</strong> Council<br />
recommends regular physical activity and eating according to energy needs. Making fruit,<br />
vegetables, cereals and other low fat foods the basis of the diet may assist with achieving<br />
and maintaining healthy body weight.<br />
Aims<br />
Our aims are to encourage the Australian population to:<br />
•<br />
•<br />
•<br />
•<br />
maintain a healthy body weight throughout life by means of a balance of food intake<br />
and physical activity<br />
consume nutritionally adequate and varied diets based primarily on foods of plant origin<br />
such as vegetables, fruit, pulses and wholegrain cereals, as well as lean meats, fish and<br />
low fat dairy products<br />
adopt a physically active lifestyle<br />
ensure children have a nutritionally adequate and varied diet and adopt an active lifestyle<br />
appropriate to different age groups.<br />
We also aim to advocate for more supportive environments to make healthy choices easier<br />
choices.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
O v e r w e i g h t & o b e s i t y
What needs to be achieved How The <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
Increased awareness of the<br />
link between obesity and<br />
cancer among the general<br />
public and key health<br />
professional groups<br />
Effective coordinated<br />
policy development and<br />
implementation<br />
Social marketing campaigns<br />
that promote healthy weight<br />
A reduction in rising rates of<br />
obesity in both children and<br />
adults<br />
An increased capacity to<br />
monitor epidemiological<br />
trends<br />
An increased capacity to<br />
monitor behavioural trends<br />
100 Section One: Preventable risk factors<br />
Monitor and clarify best evidence on the relationship between obesity<br />
and cancer causation<br />
Ensure key messages are promoted to the public and relevant<br />
health professionals in publications, presentations, programs, media<br />
statements and where opportunities arise<br />
Promote and/or develop complementary primary health resources,<br />
specifically for general practice, to improve evidence-based interventions<br />
by health professionals<br />
Develop and maintain evidence-based policy positions about the<br />
relationship between obesity and cancer to complement the Australian<br />
policy context<br />
Ensure effective and coordinated policy development and<br />
implementation<br />
Advocate for nationwide social marketing campaigns that promote<br />
a healthy body weight across the life course, which are coordinated,<br />
sustainable and far reaching<br />
Encourage the Australian Government to commit to long-term<br />
investment in promoting a healthy weight<br />
Support and deliver effective community interventions at a local and<br />
state level to address healthy weight<br />
Contribute to national developments on reducing obesity in Australia<br />
through collaboration and partnerships with major agencies<br />
Recognise the significant public health gains to be made in reducing<br />
rates of obesity in childhood<br />
Support and conduct high-quality epidemiological research further<br />
clarifying the relationship between obesity and cancer<br />
Support and conduct high-quality behavioural research further clarifying<br />
the barriers and enabling factors for people to adopt healthy eating and<br />
physical activity behaviours<br />
Work towards a better understanding of the determinants of the<br />
obesogenic environment, to inform policy development<br />
Encourage the Australian Government to fund a comprehensive <strong>National</strong><br />
Nutrition and Physical Activity Survey of both children and adults, which<br />
is conducted as a minimum on a regular five-year basis
What needs to be achieved How The <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
More supportive<br />
environments that assist<br />
people to make healthy<br />
food choices and provide<br />
opportunities to be physically<br />
active<br />
An increased capacity to<br />
know what works in relation<br />
to program delivery<br />
Encourage the Australian Government to address the broader social and<br />
environmental determinants of poor nutrition and sedentary lifestyles, in<br />
particular:<br />
• call for a ban of television food advertising to children<br />
• develop effective regulatory systems for decreasing the level of food<br />
marketing to children (including television food advertising and other<br />
forms of food marketing)<br />
• improved access to healthy food choices for people who are socially or<br />
geographically disadvantaged<br />
• develop effective regulatory systems for communicating accurate<br />
nutrition and health information on food labels<br />
• improve health literacy for reading food labels<br />
• improve physical environments to increase opportunities for physical<br />
activity<br />
Continue to support and promote the Parents Jury<br />
Participate on the Coalition on Food Advertising to Children<br />
Coordinate public health responses to relevant food regulatory issues,<br />
including changes to food labelling, through participation on the<br />
Coalition on a Healthy Australian Food Supply<br />
Undertake specific research and evaluation studies to:<br />
• evaluate healthy weight interventions<br />
• gather more evidence relating to the economic evaluation of cancer<br />
prevention<br />
• lead national understanding of what works in relation to cancer<br />
prevention<br />
• identify barriers and enabling factors for implementation of these<br />
recommendations in general practice and other health settings<br />
Note: Refer also to the action plans of the physical activity and nutrition chapters when considering promotion of healthy<br />
weight.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
101<br />
O v e r w e i g h t & o b e s i t y
References<br />
Overweight and obesity<br />
Access Economics 2006. The economic cost of obesity. Canberra: Diabetes Australia.<br />
Allman-Farinelli M, King L, Bonfiglioli C & Bauman A 2006a. The weight of time: time influences on overweight<br />
and obesity in women. Sydney: NSW Centre for Overweight and Obesity.<br />
——— 2006b. The weight of time: time influences on overweight and obesity in men. Sydney: NSW Centre for<br />
Overweight and Obesity.<br />
Anderson JV, Bybee DI, Brown RM, McLean DF, Garcia EM, Breer ML & Schillo BA 2001. 5 a day fruit and<br />
vegetable intervention improves consumption in a low income population. J Am Diet Assoc 101(2): 195–202.<br />
Australian Diabetes Obesity and Lifestyle Study 2001. Diabetes and associated disorders in Australia: the<br />
accelerating epidemic. Melbourne: International Diabetes Institute.<br />
Australian Institute of Health and Welfare (AIHW) 2006. Australia’s health 2006. AIHW cat. no. AUS73.<br />
Canberra: AIHW.<br />
Barr ELM, Magliano JD, Zimmet PZ, Polkinghorne KR, Atkins RC, Dunstan DW, Murray SG & Shaw JE<br />
2006. AusDiab 2005: The Australian Diabetes, Obesity and Lifestyle Study. Melbourne: International Diabetes<br />
Institute.<br />
Bauman A, Armstrong T, Davies J, Owen N, Brown W, Bellew B & Vita P 2003. Trends in physical activity<br />
participation and the impact of integrated campaigns among Australian adults, 1997–99. Aust N Z J Public<br />
Health 27(1): 76–9.<br />
Bauman A, Bellew B, Vita P, Brown W & Owen N 2002. Getting Australia active: towards better practice for the<br />
promotion of physical activity. Melbourne, Australia: <strong>National</strong> Public Health Partnership.<br />
Baur LA 2001. Obesity: definitely a growing concern. Med J Aust 174(11): 553–4.<br />
Bennett S 1995. Cardiovascular risk factors in Australia: trends in socioeconomic inequalities. J Epidemiol<br />
Community Health 49(4): 363–72.<br />
Bennett SA & Magnus P 1994. Trends in cardiovascular risk factors in Australia. Results from the <strong>National</strong><br />
Heart Foundation’s Risk Factor Prevalence Study, 1980–1989. Med J Aust 161(9): 519–27.<br />
Bennett SA, Magnus P & Gibson D 2004. Obesity trends in older Australians. AIHW cat. no. AUS42. Canberra:<br />
Australian Institute of Health and Welfare.<br />
Bergstrom A, Pisani P, Tenet V, Wolk A & Adami HO 2001. Overweight as an avoidable cause of cancer in<br />
Europe. Int J <strong>Cancer</strong> 91(3): 421–30.<br />
Booth M, Okely T, Denney-Wilson E, Hardy L, Yang B & Dobbin T 2006. NSW Schools Physical Activity and<br />
Nutrition Survey (SPANS) 2004: summary report. Sydney: NSW Department of Health.<br />
Booth ML, Wake M, Armstrong T, Chey T, Hesketh K & Mathur S 2001. The epidemiology of overweight and<br />
obesity among Australian children and adolescents, 1995–97. Aust N Z J Public Health 25(2): 162–9.<br />
Boyle P, Autier P, Bartelink H, Baselga J, Boffetta P, Burn J, Burns HJ, Christensen L, Denis L, Dicato M, Diehl<br />
V, Doll R, Franceschi S, Gillis CR, Gray N, Griciute L, Hackshaw A, Kasler M, Kogevinas M, Kvinnsland S, La<br />
VC, Levi F, McVie JG, Maisonneuve P, Martin-Moreno JM, Bishop JN, Oleari F, Perrin P, Quinn M, Richards<br />
M, Ringborg U, Scully C, Siracka E, Storm H, Tubiana M, Tursz T, Veronesi U, Wald N, Weber W, Zaridze DG,<br />
Zatonski W & zur Hausen H 2003. European Code Against <strong>Cancer</strong> and scientific justification: third version<br />
(2003). Ann Oncol 14(7): 973–1005.<br />
Brown JK, Byers T, Doyle C, Coumeya KS, Mark-Wahnefried W, Kushi LH, McTieman A, Rock CL, Aziz N,<br />
Bloch AS, Eldridge B, Hamilton K, Katzin C, Koonce A, Main J, Mobley C, Morra ME, Pierce MS & Sawyer KA<br />
2003. Nutrition and physical activity during and after cancer treatment: an American <strong>Cancer</strong> Society guide for<br />
informed choices. CA <strong>Cancer</strong> J Clin 53(5): 268–91.<br />
102 Section One: Preventable risk factors
Buscher LA, Martin KA & Crocker S 2001. Point-of-purchase messages framed in terms of cost, convenience,<br />
taste, and energy improve healthful snack selection in a college foodservice setting. J Am Diet Assoc 101(8):<br />
909–13.<br />
Calle EE, Rodriguez C, Walker-Thurmond K & Thun MJ 2003. Overweight, obesity, and mortality from cancer<br />
in a prospectively studied cohort of US adults. N Engl J Med 348(17): 1625–38.<br />
Cameron AJ, Welborn TA, Zimmet PZ, Dunstan DW, Owen N, Salmon J, Dalton M, Jolley D & Shaw JE<br />
2003. Overweight and obesity in Australia: the 1999–2000 Australian Diabetes, Obesity and Lifestyle Study<br />
(AusDiab). Med J Aust 178(9): 427–32.<br />
Campbell K, Waters E, O’Meara S & Summerbell C 2005. Interventions for preventing obesity in children<br />
(Cochrane review). Cochrane Database of Systematic Reviews 3: CD001871.<br />
Chapman K, Nicholas P & Supramaniam R 2006. How much food advertising is there on Australian<br />
television? Health Promot Int 21(3): 172–80.<br />
Chlebowski RT, Blackburn GL, Elashoff C, Thomson MT, Goodman A, Shapiro AE, Giuliano AR, Karanja N,<br />
Hoy MK, Nixon DW & The WINS Investigators 2005. Dietary fat reduction in postmenopausal women with<br />
primary breast cancer: Phase III Women’s Intervention Nutrition Study (WINS). J Clin Oncol 23(16 Suppl) (Part<br />
I of II): 10.<br />
Committee on Food Marketing and the Diets of Children and Youth (CFMDCY) 2005. Food marketing to<br />
children and youth: threat or opportunity. Washington, DC: Institute of Medicine of the <strong>National</strong> Academies.<br />
Cook T, Rutishauser I & Seelig M 2001. Comparable data on food and nutrient intake and physical<br />
measurements from the 1983, 1985 and 1995 national nutrition surveys. Canberra: Commonwealth<br />
Department of Health and Aged Care.<br />
Department of Health and Ageing (DHA) (Australian Government) 2003. Returns on investment in public<br />
health: an epidemiological and economic analysis. Canberra: DHA.<br />
Department of Human Services (DHS) (Victorian Government) 2006. ACE-Obesity. Assessing costeffectiveness<br />
of obesity interventions in children and adolescents. Summary of results. Melbourne: DHS.<br />
Dietz WH 1998. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics<br />
101(3 Pt 2): 518–25.<br />
Dunstan D, Zimmet P, Welborn P, Sicree T, Armstrong T, Atkins R, Cameron A, Shaw J & Chadban S 2000.<br />
Diabesity and associated disorders in Australia 2000—the accelerating epidemic: the Australian Diabetes,<br />
Obesity and Lifestyle Study (AusDiab): Victorian data report. Melbourne: International Diabetes Institute.<br />
Ebbeling CB, Feldman HA, Osganian SK, Chomitz VR, Ellenbogen SJ & Ludwig DS 2006. Effects of<br />
decreasing sugar-sweetened beverage consumption on body weight in adolescents: a randomized, controlled<br />
pilot study. Pediatrics 117(3): 673–80.<br />
Ebbeling CB, Pawlak DB & Ludwig DS 2002. Childhood obesity: public-health crisis, common sense cure.<br />
Lancet 360(9331): 473–82.<br />
Eliassen AH, Colditz GA, Rosner B, Willett WC & Hankinson SE 2006. Adult weight change and risk of<br />
postmenopausal breast cancer. JAMA 296(2): 193–201.<br />
Freedman DS, Dietz WH, Srinivasan SR & Berenson GS 1999. The relation of overweight to cardiovascular<br />
risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics 103(6 Pt 1): 1175–82.<br />
French SA, Jeffery RW, Story M, Breitlow KK, Baxter JS, Hannan P & Snyder MP 2001. Pricing and promotion<br />
effects on low-fat vending snack purchases: the CHIPS Study. Am J Public Health 91(1): 112–17.<br />
French SA, Jeffery RW, Story M, Hannan P & Snyder MP 1997. A pricing strategy to promote low-fat snack<br />
choices through vending machines. Am J Public Health 87(5): 849–51.<br />
French SA, Story M, Jeffery RW, Snyder P, Eisenberg M, Sidebottom A & Murray D 1997. Pricing strategy to<br />
promote fruit and vegetable purchase in high school cafeterias. J Am Diet Assoc 97(9): 1008–10.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
103<br />
O v e r w e i g h t & o b e s i t y
Gebel K, King L, Bauman A, Vita P, Gill T, Rigby A & Capon A 2005. Creating healthy environments: a review of<br />
links between the physical environment, physical activity and obesity. Sydney: NSW Department of Health and<br />
NSW Centre for Overweight and Obesity.<br />
Gill T, King L & Webb K 2005. Best options for promoting healthy weight and preventing weight gain in NSW.<br />
Sydney: NSW Department of Health.<br />
Goodman C & Anise A 2006. What is known about the effectiveness of economic instruments to reduce<br />
consumption of foods high in saturated fats and other energy-dense foods for preventing and treating obesity?<br />
Copenhagen: WHO Regional Office for Euope.<br />
Gortmaker SL, Peterson K, Wiecha J, Sobol AM, Dixit S, Fox MK & Laird N 1999. Reducing obesity via a<br />
school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med 153(4):<br />
409–18.<br />
Guest CS, O’Dea K, Hopper JL & Larkins RG 1993. Hyperinsulinaemia and obesity in aborigines of southeastern<br />
Australia, with comparisons from rural and urban Europid populations. Diabetes Res Clin Pract 20(2):<br />
155–64.<br />
Han TS, van Leer EM, Seidell JC, Lean ME 1996. Waist circumference as a screening tool for cardiovascular<br />
risk factors: evaluation of receiver operating characteristics (ROC). Obes Res 4(6): 533–47.<br />
Hastings G, Stead M, McDermott L, Forsyth A, MacKintosh A, Raynor M, Godfrey C, Caraher M & Angus<br />
K 2003. Review of the research on the effects of food promotion to children. Glasgow: Centre for Social<br />
Marketing.<br />
Hawe P, Wise M & Nutbeam D 2001. <strong>Policy</strong>- and system-level approaches to health promotion in Australia.<br />
Health Educ Behav 28(3): 267–73.<br />
Hawkes C 2004. Marketing food to children: the global regulatory environment. Geneva: World Health<br />
Organization.<br />
Hoek J & Gendall P 2006. Advertising and obesity: a behavioral perspective. J Health Commun 11(4): 409–23.<br />
Huon GF, Wardle J & Szatto M 1999. Improving children’s eating patterns: intervention programs and<br />
underlying principles. Aust J Nutr Diet 56(3): 156–65.<br />
International Agency for Research in <strong>Cancer</strong> Working Group on the Evaluation of <strong>Cancer</strong>-preventive<br />
Strategies (IARC Working Group) 2002. Handbooks of cancer prevention volume 6: weight control and physical<br />
activity, eds H Vainio & F Bianchini. Lyon, France: IARC Press.<br />
International Union Against <strong>Cancer</strong> (UICC) 2004. Evidence-based cancer prevention: strategies for NGOs—a<br />
handbook for Europe. Geneva: UICC.<br />
James J, Thomas P, Cavan D & Kerr D 2004. Preventing childhood obesity by reducing consumption of<br />
carbonated drinks: cluster randomised controlled trial. BMJ 328(7450): 1237.<br />
Jeffery RW, French SA, Raether C & Baxter JE 1994. An environmental intervention to increase fruit and salad<br />
purchases in a cafeteria. Prev Med 23(6): 788–92.<br />
Kristal AR, Goldenhar L, Muldoon J & Morton RF 1997. Evaluation of a supermarket intervention to increase<br />
consumption of fruits and vegetables. Am J Health Promot 11(6): 422–5.<br />
Leonard D, McDermott R, Odea K, Rowley KG, Pensio P, Sambo E, Twist A, Toolis R, Lowson S & Best JD<br />
2002. Obesity, diabetes and associated cardiovascular risk factors among Torres Strait Islander people. Aust<br />
N Z J Public Health 26(2): 144–9.<br />
Lobstein T & Dibb S 2005. Evidence of a possible link between obesogenic food advertising and child<br />
overweight. Obes Rev 6(3): 203–8.<br />
MacInnis RJ, English DR, Gertig DM, Hopper JL & Giles GG 2004. Body size and composition and risk of<br />
postmenopausal breast cancer. <strong>Cancer</strong> Epidemiol Biomarkers Prev 13(12): 2117–25.<br />
MacInnis RJ, English DR, Hopper JL, Haydon AM, Gertig DM & Giles GG 2004. Body size and composition<br />
and colon cancer risk in men. <strong>Cancer</strong> Epidemiol Biomarkers Prev 13(4): 553–9.<br />
104 Section One: Preventable risk factors
Magarey AM, Daniels LA & Boulton 2001. Prevalence of overweight and obesity in Australian children and<br />
adolescents: reassessment of 1985 and 1995 data against new standard international definitions. Med J Aust<br />
174(11): 561–4.<br />
Marks G, Rutishauer H, Webb K & Picton P 2001. Key food and nutrition data for Australia 1990–1999.<br />
Canberra: Commonwealth Department of Health and Aged Care.<br />
Mathers C 1994. Health differentials among adult Australians 25–64 years. Canberra: Australian Institute of<br />
Health and Welfare.<br />
Mathers C, Vos T & Stevenson C 1999. The burden of disease and injury in Australia. Canberra: Australian<br />
Institute of Health and Welfare.<br />
Micucci S, Thomas H & Vohra J 2002. The effectiveness of school-based strategies for the primary prevention<br />
of obesity and for promoting physical activity and/or nutrition, the major modifiable risk factors for type 2<br />
diabetes: a review of reviews. Hamilton, Canada: Social and Public Health Services Department.<br />
Must A & Strauss RS 1999. Risks and consequences of childhood and adolescent obesity. Int J Obes Relat<br />
Metab Disord 23: S2–11.<br />
<strong>National</strong> Aboriginal and Torres Strait Islander Nutrition Working Party (NATSI Working Party) 2001. <strong>National</strong><br />
Aboriginal and Torres Strait Islander Nutrition Strategy and Action Plan 2000–2010 and first phase activities<br />
2000–2003. Canberra: <strong>National</strong> Public Health Partnerships.<br />
<strong>National</strong> Health and Medical Research Council (NHMRC) 2003a. Dietary guidelines for Australian adults.<br />
Canberra: NHMRC.<br />
——— 2003b. Dietary guidelines for children and adolescents in Australia. Canberra: NHMRC.<br />
——— 2003c. Clinical practice guidelines for the management of overweight and obesity in adults. Canberra:<br />
NHMRC.<br />
——— 1997. Acting on Australia’s weight: a strategic plan for the prevention of overweight and obesity.<br />
Canberra: NHMRC.<br />
<strong>National</strong> Obesity Task Force (NOTF) 2003. Healthy weight 2008: the <strong>National</strong> Agenda for Children and Young<br />
People and Their Families. Canberra: Australian Government Department of Health and Ageing.<br />
<strong>National</strong> Public Health Partnership (NPHP) 2005. Be active Australia: a framework for health sector action for<br />
physical activity. Melbourne: NPHP.<br />
Neville L, Thomas M & Bauman A 2005. Food advertising on Australian television: the extent of children’s<br />
exposure. Health Promot Int 20(2): 105–12.<br />
NSW Health 2003. Report on the weight status of NSW: 2003. Sydney: NSW Health.<br />
Prentice RL, Caan B, Chlebowski RT, Patterson R, Kuller LH, Ockene JK, Margolis KL, Limacher MC, Manson<br />
JE, Parker LM, Paskett E, Phillips L, Robbins J, Rossouw JE, Sarto GE, Shikany JM, Stefanick ML, Thomson<br />
CA, Van HL, Vitolins MZ, Wactawski-Wende J, Wallace RB, Wassertheil-Smoller S, Whitlock E, Yano K,<br />
ms-Campbell L, Anderson GL, Assaf AR, Beresford SA, Black HR, Brunner RL, Brzyski RG, Ford L, Gass M,<br />
Hays J, Heber D, Heiss G, Hendrix SL, Hsia J, Hubbell FA, Jackson RD, Johnson KC, Kotchen JM, LaCroix<br />
AZ, Lane DS, Langer RD, Lasser NL & Henderson MM 2006. Low-fat dietary pattern and risk of invasive<br />
breast cancer: the Women’s Health Initiative Randomized <strong>Control</strong>led Dietary Modification Trial. JAMA 295(6):<br />
629–42.<br />
Reilly JJ, Wilson ML, Summerbell CD & Wilson DC 2002. Obesity: diagnosis, prevention, and treatment;<br />
evidence based answers to common questions. Arch Dis Child 86(6): 392–4.<br />
Royal Australian College of General Practitioners (RACGP) 2006. Putting prevention into practice: guidelines for<br />
the implementation of prevention in the general practice setting. Second edition. South Melbourne: RACGP.<br />
——— 2005. Guidelines for preventive activities in general practice, eds M Harris, L Bailey, C Bridges-Webb, J<br />
Furler, B Joyner, J Litt, J Smith & Y Zurynski. Sixth edition. South Melbourne: RACGP.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
105<br />
O v e r w e i g h t & o b e s i t y
——— 2004. SNAP: A population health guide to behavioural risk factors in general practice. South Melbourne,<br />
Victoria: RACGP.<br />
Sahota P, Rudolf MC, Dixey R, Hill AJ, Barth JH & Cade J 2001. Randomised controlled trial of primary school<br />
based intervention to reduce risk factors for obesity. BMJ 323(7320): 1029–32.<br />
Sangiorski AM, Bell AC, Kremer PK, Swinburn BA in press. High childhood obesity in an Australian<br />
population. Obesity.<br />
Shields M 2006. Measured obesity: overweight Canadian children and adolescents. Nutrition: findings from the<br />
Canadian Community Health Survey. Issue 1. Ottawa: Statistics Canada.<br />
Slattery ML, Ballard-Barbash R, Edwards S, Caan BJ & Potter JD 2003. Body mass index and colon cancer:<br />
an evaluation of the modifying effects of estrogen (United States). <strong>Cancer</strong> Causes <strong>Control</strong> 14(1): 75–84.<br />
Stein K 2006. After the media feeding frenzy: whither the Women’s Health Initiative Dietary Modification<br />
Trial? J Am Diet Assoc 106(6): 794–800.<br />
Strategic Inter-Governmental Nutrition Alliance (SIGNAL) 2001. Eat well Australia. A strategic framework for<br />
public health nutrition. Canberra: <strong>National</strong> Public Health Partnerships.<br />
Sturm R 2002. The effects of obesity, smoking, and drinking on medical problems and costs. Health Aff<br />
(Millwood) 21(2): 245–53.<br />
Sturm R & Wells KB 2001. Does obesity contribute as much to morbidity as poverty or smoking? Public<br />
Health 115(3): 229–35.<br />
Summerbell CD, Ashton V, Campbell KJ, Edmunds L, Kelly S & Waters E 2003. Interventions for treating<br />
obesity in children (Cochrane Review). Cochrane Database of Systematic Reviews 3: CD001872.<br />
Uauy R & Solomons N 2005. Diet, nutrition, and the life-course approach to cancer prevention. J Nutr 135<br />
(12 Suppl): S2934–5.<br />
Wang Z & Hoy WE 2002. Body mass index and mortality in aboriginal Australians in the Northern Territory.<br />
Aust N Z J Public Health 26(4): 305–10.<br />
Wolf AM & Colditz GA 1996. Social and economic effects of body weight in the United States. Am J Clin Nutr<br />
63(3): S466–9.<br />
World Health Organization (WHO) 2004. Global Strategy on Diet, Physical Activity and Health. Geneva: WHO.<br />
——— 2002. Risk to health 2002 world health report. Geneva: WHO.<br />
——— 2000. Obesity, preventing and managing the global epidemic: report of the WHO Consultation on<br />
Obesity. WHO technical report series 894. Geneva: WHO.<br />
World Health Organization (WHO) & Food and Agriculture Organization (FAO) 2003. Diet, nutrition and the<br />
prevention of chronic diseases: report of a joint WHO/FAO expert consultation. WHO technical report series<br />
916. Geneva: WHO.<br />
10 Section One: Preventable risk factors
A l c o h o l<br />
Introduction<br />
Alcohol is a known risk factor for cancer. There is no<br />
evidence to suggest that alcohol may be protective for<br />
any form of cancer.<br />
Alcoholic beverages have both nutritive and psychoactive properties. The history of<br />
alcohol use by humans can be traced back over thousands of years, where it has played<br />
an important role in the culture of a diverse range of communities throughout the world.<br />
Heavy drinking has been associated with Australian culture since the early days of<br />
European settlement (Room 1988).<br />
The <strong>National</strong> Health and Medical Research Council has established Alcohol guidelines for<br />
Australians based on a standard drink (i.e. 10 grams of ethanol). In order to avoid alcoholrelated<br />
harms in the short term, the guidelines recommend no more than six standard<br />
drinks for males and no more than four standard drinks for females during any single<br />
drinking occasion (NHMRC 2001). For individuals drinking more than this, the risk of injury<br />
or death due to short-term harms (e.g. road injury, violent assault, drowning, falls, alcoholic<br />
poisoning) increases significantly. Consumption in excess of these levels is categorised as<br />
either ‘risky’ or ‘high-risk’ depending on the amount drunk.<br />
In relation to long-term harms that can arise from ongoing excessive levels of consumption<br />
(e.g. alcoholic liver cirrhosis, a range of cancers, heart disease and stroke, dependence<br />
and psychosis) the <strong>National</strong> Health and Medical Research Council recommends that males<br />
drink no more than 28 standard drinks over a week and females no more than 14 standard<br />
drinks (NHMRC 2001). Drinkers who consume more than this are at risk of experiencing<br />
‘chronic’ alcohol-related disease and disability. Since chronic alcohol-related illness tends<br />
to develop over a lifetime of drinking, they occur most frequently among people over 45<br />
years of age (NHMRC 2001).<br />
The <strong>National</strong> Health and Medical Research Council alcohol guidelines reflect the fact that<br />
women are more susceptible to adverse effects of alcohol because they typically have a<br />
smaller body size and metabolise alcohol differently (NHMRC 2001).<br />
Information on the health burden attributable to alcohol in Australia largely comes from an<br />
examination of research into its health effects and estimation of the proportion of diseases<br />
(including cancer) attributable to alcohol e.g. (English et al. 1995; Ridolfo & Stevenson<br />
2001; Chikritzhs et al. 2003).<br />
The link between alcohol and cancer<br />
Alcohol is a known risk factor for cancer. In 1988 the International Agency for Research on<br />
<strong>Cancer</strong> classed alcohol as a Group 1 carcinogen (the highest IARC classification in humans)<br />
for cancers of the mouth, pharynx, larynx, oesophagus and liver (IARC 1988).<br />
Nearly 10 years later, the review by the World <strong>Cancer</strong> Research Fund and the American<br />
Institute of <strong>Cancer</strong> Research in 1997 concluded that there was convincing evidence<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
10<br />
A l c o h o l
(the highest level of evidence in this report) that alcohol increases the risk of mouth,<br />
pharyngeal, laryngeal and oesophageal cancers (WCRF & AICR 1997). This review also<br />
found convincing evidence that alcohol increases the risk of primary liver cancer, probably<br />
by way of alcoholic cirrhosis. It found probable evidence that alcohol increases the risk of<br />
colorectal cancer and breast cancer, even at very low levels of consumption. The report<br />
states that risk is a function of the amount of alcohol consumed (WCRF & AICR 1997; IARC<br />
1988).<br />
More recently, the evidence for a significant relationship between alcohol and female<br />
breast cancer has grown, with a number of reviews concluding that the risk of breast<br />
cancer increases with increasing alcohol consumption. An international collaborative metaanalysis<br />
including 53 epidemiological studies concluded that the relative risk of breast<br />
cancer increased by 7.1% (95%CI 5.5−8.7%) for each additional 10 g of alcohol consumed<br />
daily (Hamajima et al. 2002). An Australian meta-analysis concurred with the international<br />
review, finding a significant dose–response relationship for the development of breast<br />
cancer, even at low levels of consumption, and increasing risk with increasing age (Ridolfo<br />
& Stevenson 2001).<br />
The most up to date and compelling review has just been released from IARC in 2007 and<br />
has confirmed that alcohol is a risk factor for the same cancers classified in 1988 and also<br />
for colorectal and breast cancer (IARC 2007).<br />
The table below summarises the current state of evidence showing an association between<br />
alcohol and specific cancer sites. There is convincing evidence that alcohol increases the<br />
risk of cancer of the mouth, pharynx, larynx, oesophagus, colon, rectum, breast and liver<br />
(WCRF & AICR 1997; IARC 1988; English et al. 1995; Single et al. 1999; Bagnardi et al.<br />
2001; Chapman 2003; Ridolfo & Stevenson 2001; IARC 2007).<br />
The overall evidence suggests that alcohol is not a risk factor for cancers of the prostate,<br />
pancreas and bladder (WCRF & AICR 1997; IARC 1988; English et al. 1995; Single et al.<br />
1999; Bagnardi et al. 2001; Chapman 2003; Ridolfo & Stevenson 2001; IARC 2007). For<br />
stomach, and lung cancer, the evidence is inconsistent or insufficient to conclude causality.<br />
For lung cancer, the studies generally do not adequately control for confounding from<br />
smoking.<br />
Excessive alcohol consumption carries a strong social stigma in many populations<br />
and most surveys which ask people about the amount of alcohol they consume may<br />
substantially underestimate true levels of consumption (2000). This could result in an<br />
underestimation of the actual carcinogenic effect of the habit and therefore alcohol is<br />
possibly a stronger risk factor than perceived (Stewart & Kleihaus 2003).<br />
Smoking and alcohol together have a synergistic effect on risk of cancers of the larynx,<br />
oropharynx and oesophagus (Jensen et al. 1996; Doll et al. 1999). This means the<br />
combined effects of smoking and alcohol greatly exceed the risk from either one of these<br />
factors alone. Alcohol and tobacco interact in a multiplicative way on the risk of cancers of<br />
the upper aero-digestive tract. For example, compared with the risk for non-smoking nondrinkers,<br />
the approximate relative risks for developing mouth and throat cancer are seven<br />
times greater for those who use tobacco, six times greater for those who use alcohol, and<br />
38 times greater for those who use both tobacco and alcohol (Blot 1992).<br />
This synergistic effect of alcohol and smoking has been estimated to be attributable<br />
for over 75% of cancers of the upper aero-digestive tract in developed countries (Blot<br />
1992). Alcohol has an independent effect on the risk of oral, pharyngeal, laryngeal and<br />
oesophageal cancers, but it is its synergistic effect with smoking that is most significant.<br />
10 Section One: Preventable risk factors
There are also indications that alcohol and hepatitis B virus infection may exert a joint effect<br />
on cancer of the liver (Brechot, Nalpas & Feitelson 1996; Schiff 1997). Also of concern is<br />
the difference noted in liver cancer between Aboriginal Australians and the non-Aboriginal<br />
population; in a West Australian study the incidence and rate of deaths from liver cancer<br />
were 3.5 and 3.6 times higher for Aboriginal males than for non-Aboriginal males<br />
(Thompson & Irvine 2001). This highlights an important area for further investigation and<br />
action.<br />
In conclusion, the association between alcohol consumption and an increased risk of some<br />
cancers has been confirmed. There is a dose–response relationship in most studies after<br />
controlling for potential confounders such as tobacco smoking, and the relations appear to<br />
hold for women as well as men. The relationship is not a straight line, but shows upward<br />
curvature at higher drinking levels (Edwards et al. 1995).<br />
Table 1.12 Evidence of a link between alcohol and cancer<br />
Type of cancer Association between alcohol<br />
and cancer<br />
Level of evidence for causality<br />
Breast Increases risk Convincing<br />
Larynx Increases risk Convincing<br />
Liver Increases risk Convincing<br />
Mouth Increases risk Convincing<br />
Oesophagus Increases risk Convincing<br />
Pharynx Increases risk Convincing<br />
Colon/rectum Increases risk Convincing<br />
Lung Potential risk Insufficient<br />
Stomach Potential risk Insufficient<br />
Bladder Inconsistent and insufficient<br />
evidence of a relationship<br />
Pancreas Inconsistent and insufficient<br />
evidence of a relationship<br />
Prostate Inconsistent and insufficient<br />
evidence of a relationship<br />
Sources: Rehm et al. 2004; IARC 2007<br />
n/a<br />
n/a<br />
n/a<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
10<br />
A l c o h o l
How the amount of disease caused by alcohol is<br />
estimated<br />
The amount of morbidity and mortality which is attributable to drinking alcohol in a<br />
population has typically been estimated using what may be referred to as the ‘populationattributable<br />
fraction method’. Since it is not possible to know about the drinking habits<br />
of all individuals who suffer from disease or injury, it is necessary to apply summary<br />
measures, based (in part) on collections of research studies, of the risk of developing or<br />
dying from a specific condition at various levels of consumption (i.e. relative risk or odds<br />
ratio) (Chikritzhs et al. 2002).<br />
There are two methodological frameworks for quantifying morbidity and mortality<br />
attributable to alcohol:<br />
•<br />
•<br />
The first method is based on the relative risk of death or disease among low-risk, risky<br />
and high-risk drinkers when compared to non-drinkers.<br />
The second method is based on a comparison between risky, high-risk drinkers and lowrisk<br />
drinkers and thus, unlike the first method, is not concerned with abstainers.<br />
In order to estimate the population-attributable fraction due to alcohol for any specific<br />
condition, in addition to condition-specific relative risk estimates, it is also necessary to<br />
have accurate information on the prevalence of alcohol consumption in the community<br />
of interest. Both the framework for estimating relative risks and estimates of drinking<br />
prevalence can dramatically influence the population -attributable fraction. The range of<br />
variability can be demonstrated by comparing population-attributable fraction estimates<br />
made by English and colleagues (English et al. 1995) versus those made by Ridolfo and<br />
Stevenson (2001) in a more recent publication (see Table 1.13 below).<br />
Ridolfo and Stevenson used non-drinkers as the reference group to estimate the<br />
contribution of low-risk, risky and high-risk alcohol consumption and applied drinking<br />
prevalence estimates from a 1998 national survey (Ridolfo & Stevenson 2001). English<br />
and colleagues used low-risk drinkers as the reference group and national consumption<br />
estimates from 1989/90: they were thereby confined to estimating morbidity and mortality<br />
due to risky and high-risk drinking only (English et al. 1995). As a direct result, population<br />
-attributable fractions due to alcohol for cancers—most of which include substantial risk<br />
at low levels of drinking when compared to abstinence—were relatively small compared<br />
to those estimated by Ridolfo and Stevenson. The rationale given for the English et al.<br />
approach was that it was consistent with the public health policy of minimising harm rather<br />
than achieving abstinence. Using low-risk drinkers as the reference group also avoids the<br />
need to incorporate protective effects of low level drinking on cardiovascular disease in<br />
mortality and morbidity estimates (Chikritzhs et al. 2002). It also avoids the difficulty of<br />
using as a reference group current abstainers, who may include both lifelong abstainers<br />
and ‘sick quitters’: those who stopped drinking when they developed health problems.<br />
In order to address the uncertainty and variability in relation to alcohol aetiologic<br />
fractions and subsequent mortality and morbidity estimates for Australia, a consortium<br />
of researchers attempted to establish a consensus position. They recommended that<br />
future estimates use abstainers as the reference group and that results be presented and<br />
disseminated in such a way that both the losses and savings in mortality and morbidity<br />
from each of the drinking levels could be distinguished—as opposed to a single estimate<br />
(Chikritzhs et al. 2002). This approach has subsequently been adopted by national costing<br />
studies and recent estimates of alcohol-attributable morbidity and mortality in Australia<br />
(e.g. Collins & Lapsley 2002; Chikritzhs et al. 2003) and is the most appropriate method for<br />
estimating the effect of alcohol-attributable cancers.<br />
110 Section One: Preventable risk factors
Table 1.13 <strong>Cancer</strong> site and percentage attributable to alcohol<br />
<strong>Cancer</strong> site English et al. (1995) Ridolfo & Stevenson (2001)<br />
Males % Females % Males % Females %<br />
Breast − 3 − 12<br />
Larynx 21 13 51 46<br />
Liver 18 12 39 35<br />
Oesophagus 14 6 46 40<br />
Oropharynx 21 8 40 31<br />
The impact<br />
The harm caused by alcohol, such as the development of cancer and other illnesses and<br />
injuries, has been estimated at 4.9% of the total disease burden in Australia (Mathers, Vos<br />
& Stevenson 1999). At low to moderate intakes, alcohol consumption appears to reduce<br />
the risks of certain conditions, including ischaemic heart disease, stroke and gallstones.<br />
Taking into account these benefits, as well as the harms, alcohol is estimated to be<br />
associated with 2.2% of the total disease burden in Australia (Mathers, Vos & Stevenson<br />
1999). This demonstrates the importance of distinguishing between the effects of drinking<br />
that are low-risk, risky (where the risk of harm increases beyond any possible benefit) and<br />
high-risk (where there is substantial risk of serious harm) (NHMRC 2001).<br />
There is no evidence to suggest that alcohol may be protective for any form of<br />
cancer. Ridolfo and Stevenson estimated that in 1998, 1157 cancer deaths and 3171<br />
hospitalisations were attributable to any level of alcohol consumption (Ridolfo & Stevenson<br />
2001). The number of cancer deaths attributed to alcohol was greater than the combined<br />
total of all deaths attributed to any type of illicit drug (Ridolfo & Stevenson 2001). Over<br />
the years between 1992 and 2001, cancer was the third most common cause of alcoholattributable<br />
death, with only road crash injury and alcoholic liver cirrhosis accounting for<br />
greater numbers of premature deaths (Chikritzhs et al. 2003).<br />
Over half a million hospital episodes (577,269) were estimated to have been caused by<br />
risky or high-risk drinking in the years between 1993 and 2001 (Chikritzhs et al. 2003).<br />
Deaths caused by alcohol contribute substantially to potential years of life lost, which is<br />
a measure of the gap in years between age of death and the age before which death is<br />
considered premature. It has been estimated that about 17 years of life are prematurely lost<br />
for every death caused by risky and high-risk drinking in Australia. This is equivalent to over<br />
52,030 years of life lost every year from premature alcohol-attributable death (Chikritzhs et<br />
al. 2003).<br />
Undoubtedly, alcohol-attributable cancers represent a substantial proportion of the burden<br />
of disease and injury in Australia. The financial cost of disease, injury and crime caused<br />
by alcohol in this country has been estimated to be in excess of $7.6 billion. The exact<br />
proportion attributable to cancer is not clear (Collins & Lapsley 2002).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
111<br />
A l c o h o l
The challenge<br />
Adults<br />
Alcohol is a significant cause of drug-related harm and is one of the highest preventable<br />
causes of death and hospitalisation in Australia (NEACA 2001). According to the 2004<br />
<strong>National</strong> Drug Strategy Household Survey, some 9% of respondents aged 14 years or older<br />
drank alcohol daily, and 41% drank at least weekly (AIHW 2005). Thirty-three per cent of<br />
people drank less often but had drunk in the last 12 months. About 7% were ex-drinkers<br />
and about one in 10 people sampled had never had a full serve of alcohol (AIHW 2005).<br />
In 2004, about 21% of all those surveyed reportedly drank at risky or high-risk levels for<br />
short-term harm, compared to about 10% who were at risk of long-term harm. One in 10<br />
Australians surveyed reported drinking at levels considered risky or high risk for both short-<br />
and long-term harm in the previous 12 months. Males (24%) were more likely to have<br />
consumed alcohol in a risky or high-risk fashion for short-term harm than females (17%)<br />
(AIHW 2005).<br />
Substantial amounts of alcohol are consumed at levels above the <strong>National</strong> Health and<br />
Medical Research Council guidelines for short-term harm. In 2001, some 62% of all alcohol<br />
consumed by Australians aged 14 years and older was drunk during a single drinking<br />
session which exceeded low-risk levels for episodic drinking (e.g. binge drinking). For<br />
younger age groups (both males and females) this proportion was substantially higher and<br />
ranged between 78% and 85%. About 44% of all alcohol reported to have been drunk in<br />
2001 was consumed by people who were at risk or high risk of the long-term effects of<br />
drinking (e.g. various cancers) (Chikritzhs et al. 2003).<br />
Teenagers<br />
Experience with alcohol is common among secondary school students, with use increasing<br />
with age (White & Hayman 2006). By the age of 15 around 90% of students had tried<br />
alcohol, and by age 17, 70% of students had drunk alcohol in the month prior to the<br />
Australian School Students Alcohol and Drug (ASSAD) survey. The proportion of students<br />
drinking in the week prior to the survey increased with age, from around 16% of those<br />
aged 13 to about half of those aged 17 years. At age 13, about 2% of students reported<br />
having drunk beyond low-risk levels for short-term harms; by age 17 the proportion of<br />
students drinking at risky and high-risk levels for short-term harms increased to about<br />
21% (White & Hayman 2006). Analyses of national survey data has also shown that the<br />
proportion of females aged between 14 and 17 years who drank at risky/high-risk levels<br />
for long-term harms increased from 1% in 1998 to 9% in 2001. Among males of the same<br />
age, there was a small decline from 4.3% to 2.7% over the same years (Chikritzhs, Pascal &<br />
Jones 2004).<br />
Aboriginal and Torres Strait Islander peoples<br />
Aboriginal and Torres Strait Islander Australians are more likely to abstain from alcohol<br />
than the general population, nevertheless, alcohol-related problems are of particular<br />
concern for these peoples. The most reliable national survey of Aboriginal and Torres Strait<br />
Islander drinking levels to date (Chikritzhs & Brady 2006) has estimated that about 51% of<br />
Indigenous Australians drink at risky or high-risk levels compared to about 11% among the<br />
non-Indigenous population (AIHW 1995). Deaths from alcohol-attributable conditions are<br />
about two and a half times greater for Aboriginal and Torres Strait Islander peoples when<br />
compared to the general population (Chikritzhs & Brady 2006) and males tend to have<br />
higher levels of consumption than females (AIHW 1995). The consumption of cheap cask<br />
112 Section One: Preventable risk factors
wine is of particular concern for Aboriginal peoples living in rural and remote regions (Gray<br />
et al. 2000).<br />
Trends<br />
In general, from 1998 to 2001, the estimated proportion of the population consuming<br />
alcohol at risky/high-risk levels for chronic harm remained relatively stable among males<br />
and females of all ages, with an increase among girls aged 14 to 17 years and a small<br />
decline among young males being the main exceptions (Chikritzhs et al. 2003).<br />
Adult per capita pure alcohol (i.e. ethanol) consumption in Australia has remained relatively<br />
stable over the past decade and has most recently been estimated at about 9.0 litres,<br />
placing Australians in 22nd place in world rankings (WARC 2004). Beer consumption<br />
contributes to the bulk of all alcohol consumed in Australia, although there has been<br />
a substantial shift from regular to mid/low-strength beers since a tax saving for lower<br />
strength beers was introduced by the Australian Government. The market share of wine<br />
has increased dramatically since the 1960s but has remained relatively stable in recent<br />
years (World Drink Trends 2003).<br />
Effective interventions<br />
Public health policies on reducing alcohol consumption have a strong evidence base,<br />
which derives from research and interventions not necessarily directly related to cancer<br />
control.<br />
Work in various countries has demonstrated public health measures of proven<br />
effectiveness in the following areas:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
retail price influences on alcohol consumption and taxation of alcohol as a prevention<br />
strategy<br />
access to alcohol and the effects of availability on consumption and alcohol-related<br />
problems<br />
restricting advertising and marketing of alcohol<br />
public safety and drinking within particular contexts such as driving or attendance at<br />
sporting venues<br />
community supported intervention programs which focus on enforcing laws in relation<br />
to legal minimum purchase age and drinking to intoxication<br />
giving information about alcohol through mass media campaigns and labelling<br />
individually directed interventions (e.g. brief intervention by general practitioners and<br />
treatment of alcohol dependence by pharmacotherapies or psychosocial interventions).<br />
Successful community-based interventions are typically those which are supported by the<br />
community itself, that are evidence-based and provided with adequate access to relevant<br />
expertise, infrastructure and human resources. A multi-component approach with a focus<br />
on reducing alcohol availability and increasing effective enforcement are fundamental to<br />
the success of community-based interventions (Loxley et al. 2004).<br />
The <strong>National</strong> Alcohol Strategy 2006 to 2009 is a plan for action, designed to reflect<br />
the <strong>National</strong> Drug Strategic Framework and developed through collaboration between<br />
governments, non-government organisations, industry partners and the broader Australian<br />
community. The goal of the <strong>National</strong> Alcohol Strategy is to prevent and minimise alcoholrelated<br />
harm to individuals, families and communities in the context of developing safer<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
113<br />
A l c o h o l
and healthy drinking cultures in Australia. The <strong>National</strong> Alcohol Strategy has focused on<br />
four priority areas: intoxication, public safety and amenity, health impacts, and cultural<br />
place and availability (<strong>National</strong> Alcohol Strategy 2006).<br />
The policy context<br />
It is interesting to note that at the current time, Australia has two sets of alcohol<br />
recommendations produced by the <strong>National</strong> Health and Medical Research Council.<br />
The <strong>National</strong> Health and Medical Research Council considers the effects of alcohol on<br />
cancer in the Australian alcohol guidelines: health risks and benefits developed in 2001<br />
(NHMRC 2001). In these guidelines the <strong>National</strong> Health and Medical Research Council<br />
notes, ‘There is clear evidence to show that alcohol is associated with an increased risk<br />
of cancer overall and that it is a cause of cancer of the mouth, throat and oesophagus.<br />
In addition, the evidence suggests that it may also play a role in other specific cancers.<br />
In particular, further research is needed to clarify the possible role of alcohol in relation<br />
to breast cancer and bowel cancer’ (p. 74). The <strong>National</strong> Health and Medical Research<br />
Council emphasises that, ‘Unlike cardiovascular disease, there is no evidence that alcohol<br />
has any protective effect against cancer, at any level’ (p. 74). Also, in relation to heart<br />
disease, ‘The benefits of alcohol in preventing heart disease can be achieved with as little<br />
as half a standard drink per day … Similar benefits can also be gained from strategies such<br />
as regular exercise, giving up smoking and a healthy diet’ (pp. 68 & 69).<br />
Moreover, recent research suggests that the protective effect of alcohol on cardiovascular<br />
disease may have been exaggerated and many studies which have demonstrated an<br />
apparent increase in cardiovascular disease among non-drinkers have applied faulty<br />
methods and are subject to substantial measurement error (Fillmore et al. 2006).<br />
Thus, <strong>National</strong> Health and Medical Research Council Guideline 12 is also relevant:<br />
•<br />
•<br />
•<br />
•<br />
People who choose not to drink alcohol should not be urged to drink to gain<br />
any potential health benefit and should be supported in their decision not to<br />
drink.<br />
Guideline 1(a) states: To minimise risks and gain benefits in the longer term:<br />
Men should drink an average of no more than four standard drinks a day, and no more<br />
than 28 standard drinks per week<br />
Women should drink an average of no more than two standard drinks a day, and no<br />
more than 14 standard drinks per week.<br />
An Australian standard drink contains 10 g of alcohol (e.g. 425 ml light beer, 285 ml regular<br />
beer, 100 ml wine, 60 ml fortified wine, or 30 ml spirits or liqueurs).<br />
The <strong>National</strong> Health and Medical Research Council Dietary guidelines for Australian adults<br />
released in 2003 have set a lower recommended level of alcohol consumption based on<br />
the energy density of alcohol contributing to weight problems (NHMRC 2003). The dietary<br />
guidelines advise adults:<br />
Limit your alcohol intake if you choose to drink.<br />
Because of alcohol’s effect on both short- and long-term health, and because of<br />
the additional kilojoules it provides in the diets of a society with increasing rates<br />
of obesity, adults—if they drink at all—should limit their average daily intake of<br />
alcohol to no more than two standard drinks a day for men and one standard<br />
drink a day for women.<br />
114 Section One: Preventable risk factors
The <strong>Cancer</strong> Council supports these lower recommendations for alcohol (as specified in the<br />
<strong>National</strong> Health and Medical Research Council Dietary guidelines for Australian adults) as<br />
drinking at these levels is both more appropriate for preventing obesity and decreasing the<br />
risk of all-cause mortality and cancer. The <strong>Cancer</strong> Council recommends that, to reduce the<br />
risk of cancer, alcohol consumption should be limited or avoided. For people who do drink<br />
alcohol, The <strong>Cancer</strong> Council recommends the following:<br />
•<br />
•<br />
For men—an average of no more than two standard drinks a day.<br />
For women—an average of no more than one standard drink a day.<br />
One of the primary aims of the <strong>National</strong> Alcohol Strategy is to improve health outcomes<br />
among all individuals and communities affected by alcohol. To achieve this objective in<br />
relation to cancer, The <strong>Cancer</strong> Council Australia and member cancer councils support<br />
the priority areas and actions outlined in the <strong>National</strong> Alcohol Strategy to reduce alcoholrelated<br />
harms and health consequences.<br />
The role of general practice<br />
The role of general practice in chronic disease prevention is potentially important, given<br />
that 86% of the population have at least one visit to their general practitioner (GP) every<br />
year (RACGP 2005).<br />
However, a review of primary care interventions in relation to alcohol gives mixed results.<br />
While there seemed to be evidence that GP intervention was effective (NHMRC 1996),<br />
this has become less clear in recent years. There still appears to be strong recognition of<br />
the potential for the GP to act as an intervention point (RACGP 2005; Loxley, Toumbourou<br />
& Stockwell 2005) and research is now tending to focusing on how to engage and<br />
train general practice to be more effective in providing alcohol advice (Funk et al. 2005;<br />
McCambridge et al. 2004). Certainly as a single point of intervention, evidence for efficacy<br />
is weakest. However as part of a multi-layered approach that includes policy, community<br />
and family interventions there is more potential for success in reducing at-risk levels of<br />
alcohol consumption (Holmwood 2002; Loxley, Toumbourou & Stockwell 2005).<br />
The Royal Australian College of General Practitioners has produced three significant<br />
publications relating to the role of general practice and alcohol. The first, Guidelines for<br />
preventive activities in general practice (the ‘red book’) (RACGP 2005), focuses on the role<br />
of the GP within the consultation, recommending that all patients should be asked about<br />
the quantity and frequency of alcohol intake and number of alcohol-free days each week<br />
from 14 years of age and those with at-risk patterns of alcohol consumption should be<br />
offered brief advice to reduce their intake. Frequency of assessment varies depending on<br />
level of risk identified. All patients should be asked about frequency and intake every three<br />
years; those with an increased risk (such as people with high blood pressure, liver disease,<br />
pregnancy, etc.) should be asked and given brief advice every 12 months. Patients who<br />
report exceeding the recommended frequency and intake should be followed up monthly<br />
with a brief counselling intervention tailored to reduce alcohol consumption. Drug therapy<br />
is recommended for those patients who are physically or psychologically dependant<br />
or those with psychological, physical or social consequences of excessive alcohol<br />
consumption, and these patients should be followed up at each visit.<br />
Their more specific publication: SNAP: A population health guide to behavioural risk<br />
factors in general practice (RACGP 2004) provides more extensive information and<br />
recommendations regarding alcohol (among other common lifestyle risk factors), focusing<br />
on a patient education and behaviour modification approach based upon the 5As (ask,<br />
assess, advise, assist, arrange). Lastly, their publication Putting prevention into practice:<br />
guidelines for the implementation of prevention in the general practice setting (the ‘green<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
115<br />
A l c o h o l
ook’) (RACGP 2006) assists in developing systems in general practice to support<br />
prevention activities at the practice and consultation levels.<br />
In further support of the GP’s role in promoting a healthy lifestyle and reducing harmful<br />
levels of alcohol, the Commonwealth Department of Health and Ageing, in the 2003/04<br />
budget, funded the Lifestyle Prescriptions program (commonly known as Lifescripts).<br />
Lifescripts is being implemented through local divisions of general practice, promoting<br />
risk factor management in general practice and primary health care services. Lifestyle<br />
prescriptions are tools for GPs to use when providing lifestyle advice to patients. Advice<br />
may be about quitting smoking, increasing physical activity, eating a healthier diet,<br />
maintaining healthy weight, reducing alcohol consumption, or a combination of these.<br />
Existing recommendations<br />
There are a number of initiatives and evidence-based materials that point the way in policy<br />
directions on alcohol control in Australia. Some of the documents and programs that The<br />
<strong>Cancer</strong> Council supports and aims to complement are highlighted below.<br />
•<br />
•<br />
•<br />
The Dietary guidelines for Australian adults, released in 2003 (see discussion above)<br />
(NHMRC 2003).<br />
The <strong>National</strong> Alcohol Strategy 2006–2009: towards safer drinking cultures (<strong>National</strong><br />
Alcohol Strategy 2006)<br />
The Australian alcohol guidelines: health risks and benefits (NHMRC 2001). The <strong>Cancer</strong><br />
Council has developed a lower set of recommendations for safe drinking levels than<br />
what is recommended in these guidelines and supports a revision of these guidelines to<br />
better reflect the growing knowledge of the relationship between alcohol and cancer.<br />
Aims<br />
The <strong>Cancer</strong> Council’s aims are to:<br />
•<br />
•<br />
increase awareness of the link between alcohol consumption and cancer risk among<br />
health authorities, health professionals and the community<br />
encourage efforts to reduce alcohol consumption.<br />
What needs to be achieved How The <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
Increased awareness of the<br />
link between alcohol and<br />
cancer among the general<br />
public and key health<br />
professionals<br />
Effective coordinated<br />
policy development and<br />
implementation<br />
Promote healthy policies<br />
in relation to alcohol<br />
consumption<br />
11 Section One: Preventable risk factors<br />
Monitor and clarify best evidence on the relationship between alcohol<br />
and cancer causation<br />
Ensure alcohol information in key messages is promoted to the public<br />
and relevant health professionals in publications, presentations,<br />
programs, media statements and where opportunities arise<br />
Develop and maintain evidence-based policy positions about the<br />
relationship between alcohol and cancer<br />
Ensure effective and coordinated policy development and<br />
implementation<br />
Identify, analyse and advocate for evidence-based policy initiatives to<br />
reduce alcohol consumption<br />
Act as a role model in the safe consumption of alcohol
An increased capacity to<br />
monitor epidemiological<br />
trends<br />
An increased capacity to<br />
monitor behavioural trends<br />
References<br />
Alcohol<br />
Support and conduct high quality epidemiological research further<br />
clarifying the relationship between alcohol and cancer<br />
Support and conduct high-quality behavioural research to determine if<br />
increased knowledge about the link between alcohol and cancer will<br />
affect behaviour, and what sorts of messages should be communicated<br />
in any social marketing campaigns about responsible use of alcohol<br />
Conduct research to identify barriers and enabling factors for<br />
implementation of these recommendations in general practice and<br />
other health settings<br />
Australian Institute of Health and Welfare (AIHW) 2005. 2004 <strong>National</strong> Drug Strategy Household Survey:<br />
detailed findings. AIHW cat. no. PHE 66; Drug Statistics Series no. 16. Canberra: AIHW.<br />
Australian Institute of Health and Welfare (AIHW) 1995. <strong>National</strong> Drug Strategy Household Survey: urban<br />
Aboriginal and Torres Strait Islander Supplement 1994. Canberra: AIHW.<br />
Bagnardi V, Blangiardo M, La Vecchia VC & Corrao G 2001. A meta-analysis of alcohol drinking and cancer<br />
risk. Br J <strong>Cancer</strong> 85(11): 1700–5.<br />
Blot WJ 1992. Alcohol and cancer. <strong>Cancer</strong> Res 52(7 Suppl): S2119-23.<br />
Brechot C, Nalpas B & Feitelson MA 1996. Interactions between alcohol and hepatitis viruses in the liver. Clin<br />
Lab Med 16: 273–87.<br />
Chapman K 2003. Alcohol and cancer. Unpublished document prepared on behalf of The <strong>Cancer</strong> Council<br />
NSW.<br />
Chikritzhs T & Brady M 2006. Fact or fiction? A critique of the <strong>National</strong> Aboriginal and Torres Strait Islander<br />
Social Survey 2002. Drug Alcohol Rev 25(3): 277–87.<br />
Chikritzhs T, Catalano P, Stockwell T, Donath S, Ngo H, Young D & Matthews S 2003. Australian alcohol<br />
indicators, 1990–2001: patterns of alcohol use and related harms for Australian states and territories. Perth:<br />
<strong>National</strong> Drug Research Institute.<br />
Chikritzhs T, Pascal R & Jones P 2004. Under-age drinking and related harms in Australia. <strong>National</strong> Alcohol<br />
Indicators Bulletin no. 7. Perth, <strong>National</strong> Drug Research Institute, Curtin University of Technology.<br />
Chikritzhs T, Stockwell T, Jonas H, Stevenson C, Cooper-Stanbury M, Donath S, Single E & Catalano P 2002.<br />
Towards a standardised methodology for estimating alcohol-caused death, injury and illness in Australia. Aust<br />
N Z J Public Health 26(5): 443–50.<br />
Collins D & Lapsley H 2002. Counting the cost: estimates of the social costs of drug abuse in Australia in<br />
1998–9. <strong>National</strong> Drug Strategy Monograph Series no. 49. Canberra: Commonwealth Department of Health<br />
and Aged Care.<br />
Doll R, Forman D, La Vecchia C & Wouterson R 1999. Alcoholic beverages and cancers of the digestive tract<br />
and larynx. In Health issues related to alcohol consumption, ed. I Macdonald. London: Blackwell Science.<br />
Edwards G, Anderson P, Babor T, Casswell S, Ferrence R, Giesbrexht N, Godfrey C, Holder H, Lemmens<br />
P, Makela K, Modanik L, Norstrom T, Osterberg E, Romelsko A, Room R, Simpura J & Skog O 1995. The<br />
quantification of drug-caused morbidity and mortality in Australia. New York: Oxford University Press.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
11<br />
A l c o h o l
English DR, Holman CDJ, Milne E, Hulse GK, Codde JP, Bower CI, Corti B, de Klerk N, Knuiman MW,<br />
Kurinczuk JJ, Lewin GF & Ryan GA 1995. The quantification of drug-caused morbidity and mortality in Australia<br />
1995 edition. Canberra: Commonwealth Department of Human Services and Health.<br />
Fillmore K, Stockwell T, Kerr W, Chikritzhs T & Bostrom A 2006. Moderate alcohol use and reduced mortality<br />
risk: systematic error in prospective studies. Addiction Res Theory 14(2): 101–32.<br />
Funk M, Wutzke S, Kaner E, Anderson P, Pas L, McCormack R, Gual A, Barfod S, Saunders J, World Health<br />
Organisation Brief Study Group 2005. A multicountry controlled trial of strategies to promote dissemination<br />
and implementation of brief alcohol intervention in primary health care: findings of a World Health<br />
Organization collaborative study. J Stud Alcohol 66(3): 379–88.<br />
Gray D, Saggers S, Sputore B & Bourbon D 2000. What works? A review of evaluated alcohol misuse<br />
interventions among Aboriginal Australians. Addiction 95(1): 11–22.<br />
Hamajima N, Hirose K, Tajima K, et al. 2002. Alcohol, tobacco and breast cancer—collaborative reanalysis<br />
of individual data from 53 epidemiological studies, including 58,515 women with breast cancer and 95,067<br />
women without the disease. Br J <strong>Cancer</strong> 87(11): 1234–45.<br />
Holmwood C 2002. Alcohol-related problems in Australia: is there a role for general practice? MJA 177:<br />
102–3.<br />
International Agency for Research on <strong>Cancer</strong> (IARC) 2007. Carcinogenicity of alcoholic beverages, vol. 96 of<br />
IARC monographs. Lyon: IARC.<br />
International Agency for Research on <strong>Cancer</strong> (IARC) 1988. Alcohol drinking. Lyon: IARC.<br />
Jensen CM, Paine SL, McMichael AJ & Ewertz M 1996. Alcohol. In <strong>Cancer</strong> epidemiology and prevention.<br />
Second edition, eds D Schotterfeld & T Carroll. New York: Oxford University Press.<br />
Loxley W, Toumbourou J & Stockwell T 2005. A new integrated vision to how to prevent harmful drug use.<br />
MJA 182(2): 54–5.<br />
Loxley W, Toumbourou J, Stockwell T, Haines B, Scott K, Godfrey C, Waters E, Patton G, Fordham RJ, Gray D,<br />
Marshall J, Ryder D, Saggers S, Williams J, Sanci L (eds) 2004. The prevention of substance use, risk and harm<br />
in Australia: a review of the evidence. Canberra: <strong>National</strong> Drug Research Institute and Centre for Adolescent<br />
Health.<br />
Mathers C, Vos T & Stevenson C 1999. The burden of disease and injury in Australia. Australian Institute of<br />
Health and Welfare.<br />
McCambridge J, Platts S, Whooley D & Strang J 2004. Encouraging GP alcohol intervention: Pilot study of<br />
change-orientated reflective listening. Alcohol & Alcoholism 39(2): 146–9.<br />
<strong>National</strong> Alcohol Strategy 2006. The <strong>National</strong> Alcohol Strategy 2006–2009: towards safer drinking cultures.<br />
Canberra: Commonwealth Department of Health and Ageing.<br />
<strong>National</strong> Expert Advisory Committee on Alcohol (NEACA) 2001. <strong>National</strong> alcohol strategy: a plan for action<br />
2001 to 2003–04. Canberra: Commonwealth of Australia.<br />
<strong>National</strong> Health and Medical Research Council (NHMRC) 2003. Dietary guidelines for Australian adults.<br />
Canberra: NHMRC.<br />
——— 2001. Australian alcohol guidelines: health risks and benefits. Canberra: NHMRC.<br />
——— 1996. Guidelines for preventive interventions in primary health care: cardiovascular disease and cancer.<br />
Canberra: NHMRC.<br />
Rehm J, Room R, Monteiro M, Gmel G, Graham K, Rehn N, Sempos C T, Frick U, Jernigan D 2004. Alcohol<br />
use. In Comparative quantification of health risks. Global and regional burden of disease attributable to selected<br />
major risk factors. Volume 1, eds M Ezzati, AD Lopez, A Rodgers, CJL Murray. Geneva: World Health<br />
Organization.<br />
Ridolfo B & Stevenson C 2001. The quantification of drug-caused morbidity and mortality in Australia 1998.<br />
AIHW cat. no. PHE 29. Canberra: Australian Institute of Health and Welfare.<br />
11 Section One: Preventable risk factors
Room R 1988. The dialectic of drinking in Australian life: from the rum corps to the wine column. Aust Drug<br />
Alcohol Rev 7(4): 413–37.<br />
Royal Australian College of General Practitioners (RACGP) 2006. Putting prevention into practice: guidelines for<br />
the implementation of prevention in the general practice setting. Second edition. South Melbourne: RACGP.<br />
——— 2005. Guidelines for preventive activities in general practice M Harris, L Bailey, C Bridges-Webb, J<br />
Furler, B Joyner, J Litt, J Smith & Y Zurynski (eds.). Sixth edition. South Melbourne: RACGP.<br />
——— 2004. SNAP: A population health guide to behavioural risk factors in general practice. South Melbourne,<br />
Victoria: RACGP.<br />
Schiff ER 1997. Hepatitis C and alcohol. Hepatology 26(3) (1 Suppl): S39–42.<br />
Single E, Ashley MJ, Bondy S, Rankin J & Rehm J 1999. Evidence regarding the level of alcohol consumption<br />
considered to be low-risk for men and women. Canberra: Commonwealth Department of Health and Aged<br />
Care.<br />
Stewart B & Kleihaus P (eds) 2003. World cancer report. Lyon: International Agency for Research in <strong>Cancer</strong>.<br />
Stockwell T & Chikritzhs T (eds) 2000. International guide for monitoring alcohol consumption and alcoholrelated<br />
problems. Geneva: WHO.<br />
Thompson N & Irvine JA 2001. Review of cancer among Aboriginal people in Western Australia 2000. Perth:<br />
<strong>Cancer</strong> Foundation of Western Australia.<br />
White V & Hayman J 2006. Australian secondary school students’ use of alcohol in 2005. Report prepared for<br />
Drug Strategy Branch, Australian Government Department of Health and Ageing. Monograph series no. 58.<br />
Canberra: Australian Government Department of Health and Ageing.<br />
White V, Hayman J, Tempany M & Szabo E 2004. Victorian secondary school students use of licit and illicit<br />
substances in 2002: results from the 2002 Australian Secondary School Students’ Alcohol and Drug Survey.<br />
Melbourne: Victorian Government Department of Human Services.<br />
World Advertising Research Centre (WARC) 2004. World drink trends. London: WARC.<br />
World <strong>Cancer</strong> Research Fund (WCRF) & American Institute for <strong>Cancer</strong> Research (AICR) 1997. Summary: Food<br />
nutrition and the prevention of cancer: a global perspective. Washington, DC: AICR.<br />
World Drink Trends 2003. International beverage alcohol consumption and production trends. Henley-on-<br />
Thames: NTC Publications.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
11<br />
A l c o h o l
Section Two:<br />
Screening to detect cancer early
P r i n c i p l e s o f<br />
s c r e e n i n g<br />
Screening refers to the application of a test to a population which has no overt signs or<br />
symptoms of the disease in question, to detect disease at a stage when treatment is more<br />
effective. The screening test is used to identify people who require further investigation to<br />
determine the presence or absence of disease and is not primarily a diagnostic test.<br />
The purpose of screening an asymptomatic individual is to detect early evidence of an<br />
abnormality or abnormalities such as pre-malignant changes (e.g. by Pap test) or early<br />
invasive malignancy (e.g. by mammography) in order to recommend preventive strategies<br />
or treatment that will provide a better health outcome than if the disease were diagnosed<br />
at a later stage.<br />
It is a commonly held belief among health professionals and the community that ‘early<br />
diagnosis’ of cancer is beneficial and therefore screening is bound to be effective.<br />
However, it cannot be assumed that each person who has a screen-detected abnormality<br />
or cancer within a screening program will benefit from that diagnosis. For example, it<br />
is now understood that a substantial proportion of early abnormalities on Pap tests (i.e.<br />
dyplastic changes) will regress without treatment. The potential benefits of organised<br />
population screening program for cancer must thus outweigh any potential harms that<br />
may result in the use of a screening test in people who are otherwise well (Miller 1996)<br />
and there must be strong evidence, preferably from randomised trials, that a screening<br />
program is effective in reducing mortality from cancer.<br />
Principles for the introduction of population screening<br />
The accepted criteria for the assessment of evidence on benefits, risks and costs of cancer<br />
screening are the principles adopted by the World Health Organization (Wilson & Jungner<br />
1968):<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
the condition should be an important health problem<br />
there should be a recognisable latent or early symptomatic stage<br />
the natural history of the condition, including development from latent to declared<br />
disease, should be adequately understood<br />
there should be an accepted treatment for patients with recognised disease<br />
there should be a suitable test or examination that has a high level of accuracy<br />
the test should be acceptable to the population<br />
there should be an agreed policy on whom to treat as patients<br />
facilities for diagnosis and treatment should be available<br />
the cost of screening (including diagnosis and treatment of patients diagnosed) should<br />
be economically balanced in relation to possible expenditure on medical care as a<br />
whole, and<br />
screening should be a continuing process and not a ‘once and for all’ project.<br />
Recommendations for or against population screening interventions are influenced by<br />
the relative strength of the available scientific evidence in relation to these criteria. Most<br />
importantly, there should be sufficient direct evidence from well-conducted studies that<br />
122 Section Two: Screening to detect cancer early
early detection improves health outcomes, and that the benefits of screening outweigh any<br />
potential harms.<br />
Australia currently has three population screening programs for cancer which meet the<br />
World Health Organization criteria. Screening programs for breast, cervical and bowel<br />
cancer are discussed in the following chapters. Two further chapters examine the evidence<br />
for screening for prostate cancer and melanoma and conclude that, at this stage, there is<br />
insufficient evidence to recommend population screening.<br />
The condition<br />
For the disease to be amenable to screening, there must be a latent stage or ‘window’<br />
during which it would be possible to detect the disease before it reaches an advanced<br />
stage. Most cancers are slow growing and many have a pre-invasive or precursor stage<br />
during which early treatment is successful in halting progression to invasive cancer.<br />
For example, pre-malignant lesions of the cervix can be detected by regular Pap tests.<br />
However, the sites of many cancers are not easily visualised and potential screening<br />
tests are insufficiently accurate, so that screening asymptomatic people is ineffective in<br />
detecting early disease.<br />
If detection of cancer at an early stage is possible, it is crucial that appropriate intervention<br />
at that time has the potential to alter the course of the disease. Ideally there should be<br />
strong evidence from well-conducted clinical trials that early treatment or intervention<br />
improves outcome.<br />
Estimation of benefit from early detection on health outcome may be influenced by leadtime<br />
bias and length-time bias.<br />
Lead-time bias refers to the apparent improvement in survival that is seen when screening<br />
advances the time of diagnosis without any change in the actual time of death. In this<br />
case, increased survival merely reflects a greater period of time that the individual is aware<br />
of the presence of cancer.<br />
Length-time bias refers to the tendency of screening to detect a disproportionate number<br />
of cases of slowly progressing cancer compared with more aggressive cases. Rapidly<br />
growing cancers may progress from being undetectable at the time of screening to<br />
symptomatic during the interval between screens and thus are less likely to be detected at<br />
screening or at an early stage.<br />
The screening test (from Miller 1 p. xiii)<br />
The screening test must be sufficiently accurate to detect the condition earlier than in the<br />
absence of screening. Accuracy is measured by considering sensitivity and specificity of<br />
the screening test.<br />
‘Sensitivity’ refers to the ability of a test to correctly identify people who have disease i.e.<br />
the proportion of people with the disease at the time of screening who have a positive<br />
screening test. A test with poor sensitivity will miss cases (persons with disease) and will<br />
produce a large number of false negative results (true cases will be told incorrectly that<br />
they are free of disease).<br />
‘Specificity’ describes the ability of the test to correctly identify people who do not have<br />
the disease. A test with poor specificity will result in a high rate of false positives (healthy<br />
persons will incorrectly test positive and may be subject to more invasive diagnostic<br />
testing).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
123<br />
P r i n c i p l e s o f s c r e e n i n g
Another useful characteristic of a screening test is the positive predictive value (PPV),<br />
which is the likelihood of having disease if the screening test is positive (i.e. true positive).<br />
The PPV depends on the sensitivity and specificity of the test, and whether the condition<br />
is common or rare in the population being screened. In the context of breast cancer<br />
screening, for example, the PPV represents the total number of cancers diagnosed<br />
as a proportion of women who have been recalled for further investigations after<br />
mammography screening.<br />
Finally, the screening test must be acceptable to the population and cause minimal<br />
discomfort, or participation in the screening program will be low. For example, many<br />
women find having a Pap test uncomfortable or embarrassing and are subsequently underscreened.<br />
Substantial resources are consequently required for educational campaigns<br />
to encourage women to undergo Pap tests. Pain on compression is reported by a small<br />
number of women undergoing mammographic screening . Resources are devoted to<br />
radiographer training to address this issue.<br />
Ethical issues in population screening: balance of benefits and harms<br />
‘ The ethical imperative with all medical interventions is to endeavour to ensure<br />
that potential benefits will outweigh harm. This is particularly so of screening. If a<br />
patient asks a doctor for help the doctor is obliged to do his or her best to help but …<br />
(if) ... the doctor initiates a screening program there is a presumption that this must<br />
benefit the patient’ (Fowler & Austoker 1997 p. 1585).<br />
It is very difficult to determine the benefit of screening for an individual. The distinction<br />
between benefits to the community and to individuals needs to be borne in mind when<br />
considering recommendations to participate in organised population screening programs.<br />
Participants in screening programs are ostensibly healthy people, so a program should, at<br />
the very least, be able to demonstrate evidence of an overall benefit to the community and<br />
a minimum of risk that certain individuals may be disadvantaged by the program (Miller<br />
1996). Not only is it important that information on the effectiveness of screening programs<br />
be available, it should also be disseminated widely. Regular monitoring and evaluation of<br />
screening programs is also vital to ensure that effectiveness is maintained and improved<br />
where possible.<br />
Potential harms from screening<br />
It is essential to recognise that an organised population approach to screening, which<br />
ultimately achieves a net health benefit to a community, can result in adverse outcomes for<br />
some individuals.<br />
There is a risk that people who receive false negative results may experience delays in<br />
diagnosis and treatment. Some may develop a false sense of security and ignore warning<br />
symptoms. Increasingly, false negative results can give rise to legal action by people whose<br />
cancers appear to have been missed.<br />
A false positive result can mean that people without the disease undergo follow-up testing<br />
that may be uncomfortable, expensive, and, in some cases, potentially harmful. Rarely, this<br />
can lead to unnecessary treatment. There may be psychological consequences such as<br />
anxiety for both the patient and their family.<br />
For example, a woman with a false positive mammogram undergoing surgical investigation<br />
(e.g. a fine needle biopsy) incurs costs such as anxiety, time lost to the procedure, and<br />
possible adverse effects of the surgery. A person undergoing a colonoscopy as a result of a<br />
124 Section Two: Screening to detect cancer early
false positive faecal occult blood test faces the possibility of a bowel perforation during the<br />
procedure. This risk might be as high as 1 in 1000 (Winawer et al. 1997).<br />
Informed consent<br />
As screening is initiated by ‘the health system’, individuals invited to participate must be<br />
informed, prior to any testing, of potential adverse effects as well as the potential benefits.<br />
There are concerns that false negative results can give rise to legal action by people whose<br />
cancers appear to have been missed. It is important that it is understood that screening<br />
for any disease is never 100% effective and a negative result does not ever constitute a<br />
guarantee that an individual is free of disease. This must be communicated effectively to<br />
the potential participants in a screening program to allow informed consideration of their<br />
involvement before any test is done. Communications must address differences in literacy<br />
and language competency to ensure that individuals are properly informed.<br />
Economic issues in screening<br />
Implementation of possible screening programs will be influenced by consideration of the<br />
equal distribution of limited resources across the whole community for maximum benefit.<br />
Resources allocated to a screening program will lower resources available for other health<br />
needs.<br />
Determining the costs of screening involves the costs of the test and subsequent<br />
diagnostic tests and the costs associated with any hazard of the test as well as the<br />
costs of over-treatment<br />
balanced against<br />
reduced costs of therapy for the primary condition, reduced costs associated with<br />
less expenditure on the treatment of the advanced disease, and the economic<br />
value of the additional years of life gained (Miller 1996 p. 1444).<br />
References<br />
Fowler G & Austoker J 1997. Screening. In Oxford textbook of public health, eds R Detels, WW Holland, J<br />
McEwan & GS Omenn. Third edition. New York: Oxford University Press.<br />
Miller AB 1996. Fundamental issues in screening for cancer. In <strong>Cancer</strong> epidemiology and prevention, eds D<br />
Schottenfeld & J Fraumeni. Second edition. New York: Oxford University Press.<br />
Wilson JMG & Jungner G 1968. Principles and practices of screening for disease. Public health paper. Geneva:<br />
World Health Organization.<br />
Winawer S, Fletcher R, Miller L et al. 1997. Colorectal cancer screening: clinical guidelines and rationale.<br />
Gastroenterol 112: 594–642.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
125<br />
P r i n c i p l e s o f s c r e e n i n g
B r e a s t c a n c e r<br />
Screening mammography is the only tool we have<br />
Breast cancer in Australia<br />
for early detection that has been shown to reduce<br />
population mortality from breast cancer.<br />
In 2005, breast cancer was estimated to be the most common cancer (apart from<br />
non-melanoma skin cancer) diagnosed in women in Australia, with 12,957 new cases<br />
diagnosed. It is estimated that this will increase to 14,818 new cases in 2011 (AIHW,<br />
AACR, NCSG & McDermid 2005). Breast cancer was also the most common cause of<br />
cancer death among Australian women in 2005, with 2,719 deaths recorded (ABS 2007).<br />
Between 1990 and 2005, the rate of deaths from breast cancer decreased by about 2% per<br />
year (ABS 2007; AIHW 2005).<br />
The risk of developing and dying from breast cancer increases with age. In 2005<br />
approximately 23% of women with breast cancer were aged under 50 years, 51% were<br />
aged between 50 and 69 years and 26% were aged 70 years and over. A woman has one<br />
chance in eight of being diagnosed with breast cancer before the age of 85 (AIHW, AACR,<br />
NCSG & McDermid 2005).<br />
Figure 2.1 Time trends in breast cancer age-specific incidence and mortality rates<br />
New cases per 100,000 women<br />
350<br />
300<br />
250<br />
200<br />
150<br />
100<br />
50<br />
0<br />
70+ years<br />
50–69 years<br />
All ages<br />
< 50 years<br />
Approximate commencement of the<br />
BreastScreen Australia Program<br />
1988 1990 1992 1994 1996 1998 2000 2002<br />
12 Section Two: Screening to detect cancer early<br />
Deaths per 100,000 women<br />
140<br />
120<br />
100<br />
INCIDENCE MORTALITY<br />
80<br />
70+ years<br />
60<br />
50–69 years<br />
Approximate commencement of the<br />
40<br />
20<br />
0<br />
BreastScreen Australia Program<br />
All ages<br />
1987, compared to 51.3 deaths per 100,000 women in 2004. A similar pattern of decline in<br />
mortality rates occurred in women aged 70 and over, while rates for women under 50 years<br />
remained consistently below 15 deaths per 100,000 women over the period 1987–2001<br />
(AIHW & NBCC 2006).<br />
Can breast cancer be prevented?<br />
Despite epidemiological evidence of possible risk factors for breast cancer, at this stage<br />
there is limited potential for prevention. Most risk factors are not readily amenable to<br />
change, while lifestyle-related factors that could potentially be modified are associated<br />
with only a small proportion of breast cancer risk. It is important to acknowledge that most<br />
of these risk factors are not established causes of disease, instead serving as surrogate<br />
markers to differentiate individuals at different levels of risk.<br />
Apart from being female, the strongest risk factor for breast cancer is age; in Australia in<br />
2005 the estimated rates of breast cancer varied from 1.5 per 100,000 in women aged<br />
20 to 24 years, to 7.4 per 100,000 in women aged 25 to 29 years, to 305.7 per 100,000 in<br />
women aged 80 to 84 years (AIHW, AACR, NCSG & McDermid 2005).<br />
Having a mother, sister or daughter and/or father, brother or son who has had breast<br />
cancer also increases the risk of breast cancer; the more first-degree relatives affected and<br />
the younger the age of diagnosis, the higher the breast cancer risk. Despite the strength of<br />
family history as a risk factor for breast cancer, inherited genetic susceptibility accounts for<br />
only about 5% of cases; for eight out of nine women who develop breast cancer, there is<br />
no strong family history of the disease (CGHFBC 2001).<br />
Two important genes have been identified that are associated with an inherited<br />
susceptibility to breast and ovarian cancer: BRCA1 and BRCA2). Variations in other genes<br />
have also been associated with breast cancer risk (Singletary 2003).<br />
Other risk factors that are not easily modified include early menarche, late menopause, and<br />
no children or a first child at 30 years or older (Singletary 2003; NBCC 2006).<br />
Breastfeeding is also associated with a reduction in the risk of breast cancer, with women’s<br />
risk decreasing by 4.3% for each year they breastfeed (CGHFBC 2002).<br />
Studies have demonstrated that use of hormone replacement therapy (HRT) is associated<br />
with an increased risk of breast cancer that increases with duration of therapy and age<br />
(Baber, O’Hara & Boyle 2003; Million Women Study Collaborators 2003; Gertig et al.<br />
2003; Rossouw et al. 2002). There is some suggestion that women taking HRT also<br />
have an increased risk of dying from breast cancer (Million Women Study Collaborators<br />
2003). A recent comprehensive Australian review suggests little or no increase in risk for<br />
oestrogen-alone HRT but an increased risk for combination HRT containing oestrogen and<br />
progesterone (NHMRC 2005). Based on the review and Australian incidence figures, it has<br />
been estimated that four additional breast cancers will be seen per 1000 women in their<br />
50s taking combination HRT for five years. The risk decreases with time after cessation of<br />
treatment. A reanalysis of more than 50 studies on oral contraceptives and breast cancer<br />
found a small increase in the risk of developing breast cancer, but this risk returned to<br />
normal within 10 years of discontinuing oral contraceptives (CGHFBC 1996).<br />
Modifiable lifestyle factors have also been shown to have various associations with breast<br />
cancer. There is convincing evidence that alcohol consumption of more than two standard<br />
drinks a day increases the risk of breast cancer (WCRF & AICR 1997; NBCC 2006). It has<br />
been estimated that in Australia, approximately 5% of breast cancers are attributable to<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
12<br />
B r e a s t c a n c e r
alcohol consumption (NBCC 2006). There is evidence of a dose−response relationship with<br />
alcohol consumption, with the relative risk of breast cancer increasing by 7.1% for each<br />
additional 10 g per day of alcohol (CGHFBC 2002). (Refer also to the alcohol chapter.)<br />
Diet, physical activity and the maintenance of a healthy weight may play some role in<br />
protecting against breast cancer. Various reviews have found moderate to weak evidence<br />
of the cancer-protective effect of vegetables and fruit (WCRF & AICR 1997; UK Department<br />
of Health 1998).<br />
The World Health Organization estimates that 10% of breast cancer worldwide can be<br />
attributed to physical inactivity (WHO 2002). An Australian appraisal of the impact of<br />
physical inactivity suggests that the population-attributable risk for breast cancer is 9%<br />
(Stephenson et al. 2000).<br />
A number of reviews have concluded that there is now clear evidence that physical activity<br />
can protect against breast cancer (IARC Working Group 2002; Thune & Furberg 2001). The<br />
risk reduction is around 20% to 40%. The association has been reported for both pre- and<br />
postmenopausal women, but it is as yet unclear which time period(s) in a woman’s lifespan<br />
are most important for physical activity in the development of breast cancer (IARC Working<br />
Group 2002).<br />
Overweight and obesity in postmenopausal women are also associated with increased risk<br />
of breast cancer (Singletary 2003); there is an increase in risk of around 30% in women<br />
with a body mass index at or above 28 kg/m2 compared to those with a body mass index<br />
below 21 kg/m2 (Boyle et al. 2003).<br />
The potential for chemoprevention of breast cancer (in particular oestrogen receptor<br />
positive cancers)—through the use of selective oestrogen receptor modulators such<br />
as tamoxifen and raloxifene and, more recently, aromatase inhibitors—is undergoing<br />
investigation in randomised controlled trials. Evidence suggests that tamoxifen and<br />
raloxifene can reduce the risk of breast cancer by about 50%. However, as tamoxifen is<br />
associated with an increased risk of endometrial cancer, blood clots, uterine bleeding,<br />
hot flushes and other menopausal symptoms, the potential benefits of tamoxifen do<br />
not outweigh the potential risks in otherwise well women (Cuzick et al. 2003). The use<br />
of raloxifene appears to be associated with fewer side effects. None of these drugs is<br />
currently approved for prevention of breast cancer in Australia.<br />
Tests and programs for breast cancer<br />
Mammography<br />
Screening mammography is the best method available for detecting breast cancer early<br />
(IARC 2002). It is the only tool we have for early detection that has been shown to reduce<br />
population mortality from breast cancer.<br />
Research on the effectiveness of mammography screening for breast cancer has occurred<br />
through randomised controlled trials in North America and Europe. These trials have<br />
indicated that the natural history of breast cancer can be interrupted and mortality reduced<br />
through the detection of invasive disease when tumours are small and at an early stage. In<br />
addition, mammography in the context of an organised population screening program is<br />
effective in the detection of a large proportion of early tumours in asymptomatic women.<br />
The International Agency for Research on <strong>Cancer</strong> concluded that routine mammographic<br />
screening reduced risk of dying of breast cancer by 25% in women aged 50 to 69 years<br />
(IARC 2002).<br />
12 Section Two: Screening to detect cancer early
Breast self-examination<br />
Breast self-examination (BSE) as a method of early detection has come under considerable<br />
scrutiny.<br />
Evidence from meta-analyses (Kosters & Gotzsche 2003; Hackshaw & Paul 2003;<br />
Humphrey et al. 2002) and randomised controlled trials (Thomas et al. 2002; Semiglazov<br />
et al. 2003) shows that BSE does not result in a reduction in the size or stage of tumours<br />
at diagnosis or a decrease in mortality from breast cancer. Findings from a UK study that<br />
enrolled a cohort of women comparable to the Australian population demonstrated no<br />
impact of BSE on mortality after 16 years of follow-up (UK Trial of Early Detection of Breast<br />
<strong>Cancer</strong> Group 1999).<br />
Breast awareness<br />
In Australia, even with a fully established mammographic screening program, more than<br />
half of all breast cancers are found by a woman or her doctor after noticing a change in<br />
the breast. Although screen-detected breast cancers are typically smaller, the majority of<br />
non-screen-detected breast cancers are found at an early stage and treated conservatively<br />
(i.e. with surgery that removes as little of the breast as possible). This supports efforts to<br />
promote early detection beyond the mammographic screening program (RACGP 2005,<br />
2006a & 2006b).<br />
In the absence of proof that routine, systematic BSE reduces deaths from breast cancer<br />
across the population, the <strong>National</strong> Breast <strong>Cancer</strong> Centre and The <strong>Cancer</strong> Council Australia<br />
advocate a ‘breast awareness’ approach to encourage women to report new or unusual<br />
breast changes. This involves women being familiar with the normal look and feel of their<br />
breasts, so they may be better able to recognise an unusual change.<br />
Breast awareness encourages familiarity as part of general body awareness and health<br />
care. No specific technique or regularity is promoted, as there is no evidence of the<br />
effectiveness of any one approach.<br />
Because many breast cancers cannot be felt, the breast awareness approach should be<br />
seen as a supplement to—not a substitute for—regular mammograms in women within<br />
the target age range for mammographic screening.<br />
Clinical breast examination<br />
The effectiveness of clinical breast examination (CBE) as a screening method has also<br />
been questioned. The International Agency for Research on <strong>Cancer</strong> concluded that ‘there<br />
is inadequate evidence that screening with clinical breast examination, whether alone or<br />
in addition to screening mammography, can reduce mortality from breast cancer’ (IARC<br />
2002).<br />
The <strong>National</strong> Breast <strong>Cancer</strong> Centre’s position statement on the early detection of breast<br />
cancer (NBCC 2004) summarises the latest evidence. For asymptomatic women at average<br />
risk of breast cancer there is insufficient evidence to encourage CBE as a population<br />
screening tool. However, as there is no evidence to discourage the practice of CBE,<br />
individual women may wish to discuss their specific needs with their doctors. Those at<br />
high risk should discuss ongoing monitoring with their doctors. Options may include CBE.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
12<br />
B r e a s t c a n c e r
The policy context<br />
The national breast cancer screening program, BreastScreen Australia, began in 1991<br />
(BreastScreen Australia 2004a). It is funded by the Australian Government (Giles & Amos<br />
2003) and co-funded and administered by state and territory governments. BreastScreen<br />
services operate under and are measured against the BreastScreen Australia <strong>National</strong><br />
Accreditation Standards (BreastScreen Australia 2004a). The standards are used not only<br />
to drive quality improvement but also to balance the costs and benefits of the program<br />
to women in the target age group. It is a free service that targets asymptomatic women<br />
aged 50 to 69 years and is accessible to all women aged 40 years or above. Women in<br />
the target age range are sent reminders for repeat screens every two years. No doctor’s<br />
referral is required to attend screening, which is performed by two-view mammography.<br />
All mammograms are independently reviewed by two readers, with recall for further<br />
assessment of any abnormalities detected during film reading. The screening services<br />
are delivered through specialised units, either fixed or mobile, that operate as part<br />
of a designated BreastScreen Screening and Assessment Service, which carries out<br />
multidisciplinary assessment of screen-detected abnormalities. All procedures up to the<br />
definitive cytological or histological diagnosis of breast cancer are undertaken within<br />
BreastScreen Australia.<br />
Women in the target group are recruited through direct mail-outs based on the electoral<br />
roll, community education, advertising campaigns, brochures and health care providers<br />
(AIHW 1998). The <strong>Cancer</strong> Council supports recruitment of women through the activities of<br />
its state and territory cancer councils in community education, promotional literature and<br />
the <strong>Cancer</strong> Council Helpline. State and territory cancer councils also support BreastScreen<br />
Australia through professional education and by running cancer registries that monitor and<br />
evaluate the program in relation to cancer rates and mortality.<br />
BreastScreen Australia performance<br />
Participation rate<br />
Monitoring and evaluation are important for BreastScreen Australia. The most recent<br />
national data on breast cancer screening in Australia is in the BreastScreen Australia<br />
monitoring report 2003–04 (AIHW 2007).<br />
The total number of women screened by BreastScreen Australia over the two years<br />
2003–04 was 1,627,115, of whom 70.3% were in the target age group (50 to 69 years). The<br />
proportion of the target group screened (the participation rate) is at 55.6% (2003–04).<br />
There was some variation between participation rates in the states and territories, from a<br />
low of 44.4% in the Northern Territory to a high of 63.1% in South Australia.<br />
Table 2.1 Age-standardised participation by women aged 50–69 years in BreastScreen Australia 2003–04<br />
by states and territories<br />
Australia NSW Vic Qld WA SA Tas ACT NT<br />
Rate % 55.6 50.1 58.8 58.2 56.5 63.1 57.3 51.8 43.4<br />
Source: AIHW 2007<br />
The Australian Bureau of Statistics <strong>National</strong> Health Survey data show that 64% of<br />
Australian women report having a mammogram every two years (ABS 2002). While<br />
not all mammograms will be for cancer screening purposes, this figure suggests that<br />
130 Section Two: Screening to detect cancer early
a significant proportion of women are having mammograms outside the BreastScreen<br />
Australia program. This is of some concern to The <strong>Cancer</strong> Council because it means<br />
data are not recorded and the effects of screening for these women are not evaluated.<br />
If mammography screening is to be successful, it must be provided within an organised<br />
program that adheres to key standards of quality.<br />
Small invasive cancer detection rate<br />
This measures the rate of invasive breast cancers of 15 mm or less diagnosed in women<br />
attending BreastScreen Australia. It is expressed as the number of small cancers detected<br />
for every 10,000 women screened. In 2004, 64% of all invasive breast cancers among<br />
all women aged 40 or over were 15 mm or less. The age-standardised rate for the target<br />
group was 39.1 per 10,000 women for first-round screening and 26.8 per 10,000 women<br />
for subsequent rounds for women aged 40 years and over.<br />
Program sensitivity: interval cancer rate<br />
Program sensitivity is the proportion of invasive breast cancers that are detected by<br />
BreastScreen Australia out of all invasive cancers (interval cancers and screen-detected<br />
cancers) diagnosed in program-screened women during the screening interval. A low<br />
interval cancer rate suggests a successful program. An interval cancer is an invasive breast<br />
cancer that is diagnosed after a screening episode that detected no cancer and before the<br />
next scheduled screening episode.<br />
The age-standardised interval cancer rate for women in the target group 0–12 months after<br />
attending their first screen in 2000–02 was 9.6 per 10,000 following their first screen and<br />
10,1 per 10,000 following subsequent screens.<br />
Detection rate of ductal carcinoma in situ<br />
This indicator measures the rate of ductal carcinoma in situ (DCIS) diagnosed in women<br />
attending BreastScreen Australia. The ability to detect DCIS reflects good quality imaging<br />
and screen film reading. In 2004 the age-standardised DCIS detection rate for women in<br />
the target age group was 19.8 per 10,000 women and in subsequent rounds it was 10.4<br />
per 10,000 women. (For more on DCIS, see below.)<br />
The role of general practice<br />
The role of general practice in breast cancer screening is potentially important, given<br />
that 86% of the population have at least one visit with the general practitioner every year<br />
(RACGP 2005).<br />
General practitioners and general practice team members can contribute to promoting<br />
preventive health behaviours and identifying women at increased or high risk of developing<br />
breast cancer. Promoting breast awareness, mammography screening and individualised<br />
surveillance programs where appropriate are recognised activities of general practice<br />
as outlined in policy and guideline documents produced by Royal Australian College of<br />
General Practitioners (RACGP 2005, 2006a, 2006b). Findings from a national survey of well<br />
women indicated that GP recommendations to their female patients aged 50 to 69 to have<br />
a screening mammogram increased from 35% in 1995 to 62% in 2003. (Barratt et al. 1997;<br />
NBCC 2005)<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
131<br />
B r e a s t c a n c e r
Potential benefits and adverse effects of breast<br />
cancer screening<br />
Screening aims to detect a significant proportion of breast cancers that are small and<br />
of a low grade, enabling better health outcomes from earlier treatment (AIHW, AACR &<br />
NBCC 1999). Research has clearly demonstrated a significant benefit from population<br />
mammography screening for women in the target age group. It has been estimated that<br />
for every 1460 women screened, 13.5 biopsies and 7.4 breast cancers detected, one death<br />
from breast cancer is prevented (AIHW, BreastScreen Australia & NCSP 1999). Screening<br />
10,000 women in this age group is estimated to prevent approximately 10 to 20 deaths<br />
from breast cancer over 10 years (UK Trial of Early Detection of Breast <strong>Cancer</strong> Group 1999).<br />
Mortality benefits from the screening program, if they occur, will not be seen until five to<br />
10 years after a high participation rate is achieved. If 70% of Australian women in the target<br />
group participated in the screening program, death rates from breast cancer for women<br />
over 50 years offered screening would fall by approximately 25% to 30% (AHMAC 1990).<br />
Screening may reduce the trauma associated with treatment. Tumours diagnosed at an<br />
earlier stage and smaller size require less extensive surgery and chemotherapy.<br />
Potential adverse effects of screening<br />
Mammographic screening may have adverse psychological effects for some women.<br />
Of particular concern is increased anxiety experienced as a result of false negative and<br />
false positive results (see introduction to Section 2). The potential negative physical and<br />
psychological effects associated with a false positive test include anxiety induced by fear<br />
of being diagnosed with breast cancer, physical effects of the performance of invasive<br />
diagnostic procedures, diagnosis of non-lethal lesions, and exposure to radiation.<br />
DCIS (where the cancerous cells have not spread beyond the basement membrane of<br />
the breast ducts—described as non-invasive cancer) is often quoted as an example of an<br />
‘over-diagnosed’ breast condition. As recently pointed out by Professor David Roder: ‘The<br />
difficulty is that there is no way currently known to define in-situ lesions with any certainty<br />
as progressive or non-progressive. This definition cannot be made by looking under<br />
the microscope. The potential for over-diagnosis has arisen from statistical inferences,<br />
which are themselves based on assumptions. Differences in estimates are a function of<br />
differences in the assumptions made by researchers, much of which are uncertain and<br />
open to debate’ (GP review 2006).<br />
While the diagnosis and treatment of DCIS is still contested, and general reports suggest<br />
that women found through mammographic screening to have DCIS will be treated by<br />
surgery and/or radiotherapy without evidence of the benefits of treatment having been<br />
established (Rickard 1996), it should be noted that BreastScreen Victoria (2001) reports a<br />
steady decline in the proportion of women diagnosed with DCIS undergoing surgery. The<br />
issues about DCIS should not overwrite the effectiveness of the national breast cancer<br />
screening program in identifying invasive carcinoma of the breast.<br />
Who should be screened?<br />
Evidence of greatest benefit exists for the target age group (women aged 50 to 69 years).<br />
The <strong>Cancer</strong> Council recommends that all women in this age group have a mammogram<br />
every two years through BreastScreen Australia. Debate, however, is increasing around the<br />
benefit of extending screening to women in the decades either side of this age bracket.<br />
132 Section Two: Screening to detect cancer early
An Australian review of the benefits of screening women aged 40 to 49 years concluded<br />
that there is less benefit in screening these women. The benefit is greater for those at the<br />
older end of the age bracket, and for those with a strong family history of breast cancer.<br />
The benefit of screening women aged 40 to 49 years is estimated at approximately onethird<br />
of that of women aged 50 to 69 years (Irwig et al. 1997). BreastScreen Australia policy<br />
states:<br />
BreastScreen Australia selects women for screening on the basis of age alone.<br />
Women aged 40 years and above are eligible. Recruitment strategies will be targeted<br />
at women aged 50–69 years. The age for screening will be monitored and reviewed<br />
as new data becomes available (BreastScreen Australia 2004a).<br />
With increasing life expectancy, the value of screening women over 70 years has also<br />
come under investigation. Barratt et al. (2002) estimate that the benefit of screening<br />
women aged 70 to 79 years to be about 40% to 72% of that achieved in women aged 50<br />
to 69 years; this declines further with increasing age and when quality-of-life adjustment is<br />
made. They estimate that extending screening to women aged 70 to 79 years is relatively<br />
cost-effective and similar to the cost-effectiveness of extending screening to women aged<br />
40 to 49 years. The authors, however, also comment that the estimation of benefits, harms<br />
and costs would be improved with data—now lacking—from randomised trials in the<br />
appropriate age group.<br />
Aims<br />
The <strong>Cancer</strong> Council endorses the major aims of the BreastScreen Australia program (AIHW,<br />
BreastScreen & NCSP 1999):<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
to ensure that the program is implemented in such a way that significant reductions can<br />
be achieved in morbidity and mortality attributable to breast cancer<br />
to maximise the early detection of breast cancer in the target population<br />
to ensure that screening for breast cancer in Australia is provided in dedicated<br />
accredited screening and assessment services as part of the BreastScreen Australia<br />
program<br />
to ensure equitable access for women aged 50–69 years to the program<br />
to ensure that services are acceptable and appropriate to the needs of the eligible<br />
population<br />
to achieve high standards of program management, service delivery, monitoring and<br />
evaluation and accountability (BreastScreen Australia 2004b).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
133<br />
B r e a s t c a n c e r
What we want to achieve How The <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
A 70% two-yearly<br />
participation rate in the<br />
national program by women<br />
in the target group (50–69<br />
years) and access on request<br />
to the program for women<br />
aged 40–49 years and 70<br />
years or more<br />
Referral to appropriate<br />
treatment services and<br />
collection of information<br />
about the outcome of<br />
treatment<br />
Sufficient workforce capacity<br />
to ensure the delivery of<br />
a best practice screening<br />
program to the target<br />
population (women 50–69)<br />
Timely evaluation of new<br />
technologies<br />
<strong>National</strong> evaluation of<br />
BreastScreen performance,<br />
capacity and policy issues<br />
by 2008<br />
134 <strong>National</strong> Section Two: <strong>Cancer</strong> Screening <strong>Prevention</strong> to detect <strong>Policy</strong> cancer 2004 – early 06<br />
Maintain and support education programs to raise awareness in the<br />
community and among health professionals to promote informed<br />
participation of women aged 50–69 years in breast cancer screening<br />
Advocate for government support, including adequate funding, to<br />
ensure targets for participation are met, while maintaining a focus on<br />
equity and access for women Priority should be given to maximising the<br />
participation of Australian Aboriginal and Torres Strait Islander women<br />
and women of culturally and linguistically diverse backgrounds<br />
Recognising that many women have mammograms outside<br />
BreastScreen, advocate for integration of screening of all asymptomatic<br />
women aged 50–69 years into the BreastScreen Australia program<br />
Recognising the importance of providing consistent high-quality care for<br />
women diagnosed with breast cancer in Australia:<br />
• support or advocate for examination of the extent to which women<br />
diagnosed in the screening program are being treated in accordance<br />
with the NHMRC Clinical practice guidelines for the management of<br />
early breast cancer (2001), Management of advanced breast cancer<br />
(2001) and Clinical Practice Guidelines for the Psychosocial Care of<br />
Adults with <strong>Cancer</strong> (2003)<br />
Recognising the importance of informed consumer involvement in<br />
all aspects of breast cancer screening, diagnosis and management,<br />
advocate for active roles for consumers within peak breast cancer<br />
bodies in Australia<br />
Recognising the implications in the short and longer term of radiography<br />
and radiology workforce constraints for BreastScreen Australia,<br />
advocate for increased funding to provide additional places for the<br />
training of radiographers and radiologists<br />
Monitor development of relevant new technologies, (such as digital<br />
mammography and MRI), advocate for rapid evaluation of their<br />
relevance for screening and adoption of those that are positively<br />
evaluated<br />
Support and contribute to national evaluation of the following areas:<br />
• reductions in breast cancer mortality due to screening, risks<br />
associated with screening, program governance and management,<br />
performance trends, accreditation system<br />
• workforce, new technologies and capacity issues<br />
• policy issues such as the appropriate target age range, screening<br />
interval, and screening of women at higher risk or those who present<br />
with symptoms
References<br />
Breast cancer<br />
Australian Bureau of Statistics (ABS) 2007. Causes of death, Australia 2005. Cat. no. 3303.0. Canberra: ABS.<br />
——— 2002. <strong>National</strong> Health Survey. Summary of results 2001. ABS cat. no. 4364.0. Canberra: ABS.<br />
Australian Health Ministers Advisory Council (AHMAC) 1990. Breast cancer screening in Australia: future<br />
directions. Australian Institute of Health <strong>Prevention</strong> Program Evaluation Series no. 1. Canberra: AHMAC.<br />
Australian Institute of Health and Welfare (AIHW) 2007. BreastScreen Australia monitoring report 2003–04.<br />
Canberra: AIHW.<br />
——— 2005. State and territories GRIM (General Record of Incidence of Mortality) books. Canberra: AIHW.<br />
——— 1998. Breast and cervical cancer screening in Australia 1996–97. AIHW cat. no. CAN 3; <strong>Cancer</strong> Series<br />
no. 8. Canberra: AIHW.<br />
Australian Institute of Health and Welfare (AIHW), Australasian Association of <strong>Cancer</strong> Registries (AACR) &<br />
NHMRC <strong>National</strong> Breast <strong>Cancer</strong> Centre (NBCC) 1999. Breast cancer in Australian women 1982–1996. AIHW<br />
cat. no. CAN 6. Canberra: AIHW.<br />
Australian Institute of Health and Welfare (AIHW), Australasian Association of <strong>Cancer</strong> Registries (AACR),<br />
<strong>National</strong> <strong>Cancer</strong> Strategies Group (NCSG) & McDermid I 2005. <strong>Cancer</strong> incidence projections, Australia 2002 to<br />
2011. Canberra: AIHW, AACR & NCSG.<br />
Australian Institute of Health and Welfare (AIHW), BreastScreen Australia & <strong>National</strong> Cervical Screening<br />
Program (NCSP) 1999. Breast and cervical cancer screening in Australia 1996–1997. Canberra: Australian<br />
Institute of Health and Welfare.<br />
Australian Institute of Health and Welfare (AIHW) & <strong>National</strong> Breast <strong>Cancer</strong> Centre (NBCC) 2006. Breast<br />
cancer in Australia: an overview, 2006. AIHW cancer series no. 34. cat no. CAN 29. Canberra: AIHW.<br />
Baber RJ, O’Hara JL & Boyle FM 2003. Hormone replacement therapy: to use or not to use? Med J Aust<br />
178(12): 630–3.<br />
Barratt A, Cockburn J, Lowe J, Paul C, Perkins J & Redman S 1997. Report on the 1996 Breast Health Survey.<br />
Kings Cross, NSW: NHMRC <strong>National</strong> Breast <strong>Cancer</strong> Centre.<br />
Barratt A, Mannes P, Irwig L, Trevena L, Craig J & Rychetnik L 2002. <strong>Cancer</strong> screening. J Epidemiol<br />
Community Health 56(12): 800–902.<br />
Boyle P, Autier P, Bartelink H, Baselga J, Boffetta P, Burn J, Burns HJ, Christensen L, Denis L, Dicato M, Diehl<br />
V, Doll R, Franceschi S, Gillis CR, Gray N, Griciute L, Hackshaw A, Kasler M, Kogevinas M, Kvinnsland S, La<br />
VC, Levi F, McVie JG, Maisonneuve P, Martin-Moreno JM, Bishop JN, Oleari F, Perrin P, Quinn M, Richards<br />
M, Ringborg U, Scully C, Siracka E, Storm H, Tubiana M, Tursz T, Veronesi U, Wald N, Weber W, Zaridze DG,<br />
Zatonski W & Zur Hausen H 2003. European Code Against <strong>Cancer</strong> and scientific justification: third version<br />
(2003). Ann Oncol 14(7): 973–1005.<br />
BreastScreen Australia 2004a. BreastScreen Australia quality improvement program. Canberra: BreastScreen<br />
Australia.<br />
——— 2004b. <strong>National</strong> accreditation standards: BreastScreen Australia Quality Improvement Program. Revised<br />
edition. Canberra: BreastScreen Australia.<br />
Collaborative Group on Hormonal Factors in Breast <strong>Cancer</strong> (CGHFBC) 2002. Breast cancer and breastfeeding:<br />
collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50,302<br />
women with breast cancer and 96,973 women without the disease. Lancet 360(9328): 187–95.<br />
——— 2001. Familial breast cancer: collaborative reanalysis of individual data from 52 epidemiological<br />
studies including 58,209 women with breast cancer and 101,986 women without the disease. Lancet<br />
358(9291): 1389.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
135<br />
B r e a s t c a n c e r
——— 1996. Breast cancer and hormonal contraceptives: collaborative reanalysis of individual data on<br />
53,297 women with breast cancer and 100,239 women without breast cancer from 54 epidemiological<br />
studies. Lancet 347(9017): 1713–27.<br />
Cuzick J, Powles T, Veronesi U, Forbes J, Edwards R, Ashley S & Boyle P 2003. Overview of the main<br />
outcomes in breast cancer prevention trials. Lancet 361(9354): 296–300.<br />
Gertig DM, Erbas B, Fletcher A, Amos A & Kavanagh AM 2003. Duration of hormone replacement therapy,<br />
breast tumour size and grade in a screening programme. Breast <strong>Cancer</strong> Res Treat 80(3): 267–73.<br />
Giles GG & Amos A 2003. Evaluation of the organised mammographic screening programme in Australia.<br />
Ann Oncol 14(8): 1209–11.<br />
GP review 2006. Informed decisions. GP review May: 32.<br />
Hackshaw AK & Paul EA 2003. Breast self-examination and death from breast cancer: a meta-analysis. Br J<br />
<strong>Cancer</strong> 88(7): 1047–53.<br />
Humphrey LL, Helfand M, Chan BK & Woolf SH 2002. Breast cancer screening: a summary of the evidence<br />
for the U.S. Preventive Services Task Force. Ann Intern Med 137(5 Part 1): 347–60.<br />
International Agency for Research in <strong>Cancer</strong> Working Group on the Evaluation of <strong>Cancer</strong>-preventive<br />
Strategies (IARC Working Group) 2002. Handbooks of cancer prevention volume 6: weight control and physical<br />
activity eds H Vainio & F Bianchini. Lyon, France: IARC Press.<br />
International Agency for Research on <strong>Cancer</strong> (IARC) 2002. Handbooks of cancer prevention volume 7: breast<br />
cancer screening, eds H Vainio & F Bianchini. Lyon, France: IARC Press.<br />
Irwig L, Glasziou P, Barratt A & Salkeld G 1997. Review of the evidence about the value of mammographic<br />
screening in 40–49 year old women. Kings Cross, NSW: <strong>National</strong> Breast <strong>Cancer</strong> Centre.<br />
Kosters JP & Gotzsche PC 2003. Regular self-examination or clinical examination for early detection of breast<br />
cancer (Cochrane review). Cochrane Database of Systematic Reviews 2: CD003373.<br />
Million Women Study Collaborators 2003. Breast cancer and hormone replacement therapy in the Million<br />
Women Study. Lancet 362(9382): 419–27.<br />
<strong>National</strong> Breast <strong>Cancer</strong> Centre (NBCC) 2006. Report on the status of breast cancer risk factors. Unpublished<br />
report.<br />
——— 2005. <strong>National</strong> Breast <strong>Cancer</strong> Centre breast health technical report. Camperdown NSW: NBCC.<br />
——— 2004. Early detection of breast cancer: position statement. Camperdown NSW: NBCC.<br />
<strong>National</strong> Health and Medical Research Council (NHMRC) 2005. Hormone replacement therapy: a summary of<br />
the evidence. Canberra: NHMRC.<br />
Productivity Commission 2006. Report on government services 2006. Canberra: Australian Government<br />
Productivity Commission.<br />
Rickard M 1996. The increasing detection of DCIS: lessons for Australia. Kings Cross: <strong>National</strong> Breast <strong>Cancer</strong><br />
Centre.<br />
Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford<br />
SA, Howard BV, Johnson KC, Kotchen JM & Ockene J 2002. Risks and benefits of estrogen plus progestin in<br />
healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled<br />
trial. JAMA 288(3): 321–33.<br />
Royal Australian College of General Practitioners (RACGP) 2006a. Putting prevention into practice: guidelines<br />
for the implementation of prevention in the general practice setting. Second edition. South Melbourne: RACGP.<br />
——— 2006b. The role of general practice in prevention and health promotion. <strong>Policy</strong> endorsed by the 48th<br />
RACGP Council, 18 May 2006. Melbourne: RACGP.<br />
——— 2005. Guidelines for preventive activities in general practice, eds M Harris, L Bailey, C Bridges-Webb, J<br />
Furler, B Joyner, J Litt, J Smith & Y Zurynski. Sixth edition. South Melbourne: RACGP.<br />
13 <strong>National</strong> Section Two: <strong>Cancer</strong> Screening <strong>Prevention</strong> to detect <strong>Policy</strong> cancer 2004 – early 06
Semiglazov VF, Manikhas AG, Moiseenko VM, Protsenko SA, Kharikova RS, Seleznev IK, Popova RT,<br />
Migmanova NS, Orlov AA, Barash NI, Ivanova OA & Ivanov VG 2003. Results of a prospective randomized<br />
investigation [Russia (St Petersburg)/WHO] to evaluate the significance of self-examination for the early<br />
detection of breast cancer]. Vopr Onkol 49(4): 434–41.<br />
Singletary SE 2003. Rating the risk factors for breast cancer. Ann Surg 237(4): 474–82.<br />
Stephenson J, Bauman A, Armstrong T, Smith B & Bellew B 2000. The costs of illness attributable to physical<br />
inactivity in Australia. Canberra: Commonwealth Department of Health and Aged Care.<br />
Thomas DB, Gao DL, Ray RM, Wang WW, Allison CJ, Chen FL, Porter P, Hu YW, Zhao GL, Pan LD, Li W, Wu<br />
C, Coriaty Z, Evans I, Lin MG, Stalsberg H & Self SG 2002. Randomized trial of breast self-examination in<br />
Shanghai: final results. J Natl <strong>Cancer</strong> Inst 94(19): 1445–57.<br />
Thune I & Furberg A 2001. Physical activity and cancer risk: dose-response and cancer, all sites and sitespecific.<br />
Med Sci Sports Exerc 33(Suppl): S530–50.<br />
UK Department of Health 1998. Nutritional aspects of the development of cancer. Report of the Working<br />
Group on Diet and <strong>Cancer</strong> of the Committee on Medical Aspects of Food and Nutrition <strong>Policy</strong>. Norwich, UK:<br />
The Stationery Office.<br />
UK Trial of Early Detection of Breast <strong>Cancer</strong> Group 1999. 16-year mortality from breast cancer in the UK Trial<br />
of Early Detection of Breast <strong>Cancer</strong>. Lancet 353: 1909–14.<br />
World <strong>Cancer</strong> Research Fund (WCRF) & American Institute for <strong>Cancer</strong> Research (AICR) 1997. Food, nutrition<br />
and the prevention of cancer: a global perspective. Washington, DC: AICR.<br />
World Health Organization (WHO) 2002. Risk to health 2002 world health report. Geneva: WHO.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
13<br />
B r e a s t c a n c e r
C e r v i c a l c a n c e r<br />
In Australia, a vaccine that prevents the majority<br />
of cervical cancer is now available. The vaccine<br />
will have a profound impact on Australia’s cervical<br />
screening program, and in the future will influence<br />
changes to national policy. However, Pap tests will<br />
remain important in preventing cancer of the cervix.<br />
Cervical cancer in Australia<br />
In 2005 estimates, cancer of the cervix accounted for 610 new cancers in Australian<br />
women (AIHW, AACR, NCSG & McDermid 2005). The lifetime risk of a woman developing<br />
cervical cancer before the age of 75 years is 1 in 233 (AIHW, AACR, NCSG & McDermid<br />
2005). In Australia in 2004, cervical cancer accounted for 212 deaths (AIHW 2006).<br />
Between 1991 (when Australia’s <strong>National</strong> Cervical Screening Program commenced) and<br />
2005, the incidence of cervical cancer among women aged 20 to 69 halved from 17.2 per<br />
100,000 women to 7.3 in 2005 (AIHW, AACR, NCSG & McDermid 2005). The mortality<br />
rate has also declined from 4.0 in 1991 to 1.8 in 2004 (AIHW 2006), and is now among the<br />
lowest in the world (IARC 2002).<br />
Mortality data from 2001 to 2004 in Queensland, South Australia, Western Australia and<br />
the Northern Territory indicate that Indigenous women have a mortality rate attributable to<br />
cervical cancer of 9.9 per 100,000 women. This is more than four times the corresponding<br />
death rate of non-Indigenous women (2.1 per 100,000 women) (AIHW 2006).<br />
Can cervical cancer be prevented?<br />
The human papilloma virus (HPV) has been identified in 99.7% of cervical cancer<br />
specimens (Walboomers et al. 1999). While HPV is clearly necessary for the development<br />
of cervical cancer, it is certainly not sufficient (Walboomers et al. 1999). Worldwide, there<br />
are estimated to be 326 million adult women who are infected with HPV. This compares<br />
with approximately 450,000 new cases of cervical cancer worldwide each year (Bosch<br />
2000). Clearly cervical cancer is a very rare outcome of HPV infection.<br />
HPV is a sexually transmitted infection and almost all individuals become infected with<br />
HPV within two to five years of initiating sexual activity (Wright et al. 2006). HPV can<br />
be classified into high and low-risk types based on the strength of their association with<br />
cervical cancer. Co-factors that increase the risk of cervical cancer progressing in women<br />
who have a persistent high-risk HPV infection include exposure to tobacco smoke, more<br />
than five full-term pregnancies, the use of oral contraceptives for five years or more,<br />
immunosuppression, and presence of antibodies to Chlamydia trachomatis or to herpes<br />
simplex virus type 2 (IARC 2005).<br />
13 Section Two: Screening to detect cancer early
A vaccine to prevent HPV infection<br />
A vaccine designed to prevent two of the most common types of high-risk HPV (HPV<br />
16 and 18) is available in Australia, and from April 2007 was included on the <strong>National</strong><br />
Immunisation Schedule.<br />
HPV types 16 and 18 are responsible for up to 70% of cervical cancers (Munoz et al.<br />
2003), and clinical trials have found the vaccine to be 100% effective (Wright et al. 2006).<br />
The vaccine is highly effective when given to females who are not already infected with<br />
the HPV types included in the vaccine. Therefore, it is recommended that the vaccine be<br />
administered prior to commencement of sexual activity (Wright et al. 2006). As the vaccine<br />
does not protect against all types of HPV that cause cervical cancer, vaccinated women<br />
should have regular Pap tests.<br />
In sexually active women, the most important measure to prevent cervical cancer is regular<br />
Pap tests.<br />
See the human papilloma virus chapter in the immunisation section of the online edition of<br />
the <strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007–09 (published in June 2007 at www.cancer.org.<br />
au).<br />
Screening tests and programs for cervical cancer<br />
The Pap test<br />
Cervical cancer is one of the few cancers where screening can detect precancerous cell<br />
growth. These abnormalities can be treated, preventing the development of cancer. The<br />
Pap test (named after its developer, Dr George Papanicolaou) is the most widely used<br />
cancer screening test in the world (Eurogin 2003). Typically, cervical cancer takes 10 years<br />
or more to develop. Abnormalities detected by a Pap test can be monitored, or, if required,<br />
further investigated and early treatment initiated.<br />
Cervical screening with the Pap test began in British Columbia (Canada) in 1949. Although<br />
no randomised controlled trials evaluating screening have been conducted, a large number<br />
of observational studies have shown a strongly protective effect of screening (USPSTF<br />
1996). In particular, substantial declines in mortality and incidence of cervical cancer have<br />
been demonstrated after the introduction of screening programs.<br />
Other screening technologies<br />
In the past decade, a desire to improve the sensitivity of the Pap test and an increased<br />
understanding about the role of HPV has led to the development of new screening<br />
technologies.<br />
Liquid-based cytology<br />
Liquid-based cytology is a technique where the cervical cells collected on the sampling<br />
instruments are suspended in liquid. At the laboratory the liquid sample is filtered to<br />
remove unnecessary material such as blood, bacteria and other matter. The cells are then<br />
deposited as a single layer onto a slide, stained and examined under a microscope.<br />
As new technologies are evaluated for adoption, appropriate consideration must be given<br />
to how they will improve the cervical screening program in terms of sensitivity, specificity,<br />
cost-effectiveness and quality of life. An Australian Government review in Australia by<br />
the Medical Services Advisory Committee in 2002 concluded that there is insufficient<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
13<br />
C e r v i c a l c a n c e r
evidence to suggest that liquid-based cytology is superior to the conventional Pap test, and<br />
recommended that public funding not be supported for this screening test in Australia at<br />
this time (MSAC 2002). Further research is ongoing into the use of this technology.<br />
HPV DNA testing<br />
Due to the relationship between persistent infection with high-risk types of HPV and<br />
the development of cervical cancer, testing for the presence of HPV DNA in cervical cell<br />
specimens has the potential to identify women at increased risk of developing cervical<br />
cancer. Commercially available HPV DNA testing kits can detect 13 high-risk types of HPV.<br />
Several countries have developed guidelines recognising the role of HPV testing as a<br />
primary screening test and in the management of abnormal cervical cell abnormalities (Cox<br />
& Cuzick 2006). The International Agency for Research on <strong>Cancer</strong> states that it is likely<br />
longer screening intervals could be achieved using HPV DNA testing as a screening test<br />
(IARC 2005). Currently in Australia, HPV DNA testing is recommended for use in women<br />
following treatment of a high-grade abnormality. The test is used to determine whether the<br />
virus has been cleared from the body (NCSP 2005).<br />
International studies continue to investigate the role of HPV DNA testing for triaging lowgrade<br />
cervical abnormalities and as a primary screening tool.<br />
The policy context<br />
In Australia, screening for cervical cancer was introduced on an ad hoc basis in the 1960s.<br />
Guidelines on cervical screening programs published in 1986 by the World Health<br />
Organization and the International Agency for Research on <strong>Cancer</strong> were used as a basis<br />
for a review of cervical screening in Australia. The review was conducted on behalf of<br />
Australian Health Ministers Advisory Council (AIHW, BreastScreen Australia & NCSP 1999).<br />
Following this review, cervical screening was organised into a structured program known<br />
today as the <strong>National</strong> Cervical Screening Program; this was implemented in 1991 as a joint<br />
initiative of the Australian, state and territory governments.<br />
State and territory cancer organisations have been involved in a coordinating role in the<br />
establishment of state Pap test registries and recruitment of women to the screening<br />
program. In some states and territories, cancer councils maintain an important role in<br />
cervical screening programs.<br />
Existing recommendations<br />
The <strong>National</strong> Cervical Screening Program policy developed in 1991 provides guidelines for<br />
which women need screening and how often screening should occur. It states:<br />
1.<br />
2.<br />
Routine screening with Pap tests should be carried out every two years for women who<br />
have no symptoms.<br />
All women who have ever been sexually active should start having Pap tests between<br />
the ages of 18 and 20 years, or one or two years after beginning sex, whichever is later.<br />
In some cases, it may be appropriate to start screening before 18 years of age.<br />
3.<br />
Pap tests may cease at the age of 70 years for women who have had two normal Pap<br />
tests within the last five years. Women over 70 years who have never had a Pap test,<br />
or who request a Pap test, should be screened (Cervical <strong>Cancer</strong> <strong>Prevention</strong> Taskforce<br />
1991).<br />
140 Section Two: Screening to detect cancer early
It is anticipated that the introduction of the HPV vaccine will, in the future, influence<br />
changes to this national policy.<br />
Recent changes to guidelines<br />
Women with abnormal Pap test results should be managed in accordance with the<br />
<strong>National</strong> Health and Medical Research Council guidelines Screening to prevent cervical<br />
cancer: guidelines for the management of asymptomatic women with screen detected<br />
abnormalities (NCSP 2005). After extensive review, these guidelines were endorsed by the<br />
<strong>National</strong> Health and Medical Research Council in 2005 and came into effect in July 2006.<br />
Pap test quality<br />
One indicator of Pap test quality is the proportion of tests where an endocervical<br />
component is present. Presence of an endocervical component in 80% of Pap tests is<br />
generally considered acceptable. It is sometimes difficult to obtain the endocervical<br />
component when taking a Pap test in older women. There is some indication that the<br />
proportion of Pap tests lacking an endocervical component has increased over time. In<br />
Victoria, this has increased from 17.3% in 2000 to 22.1% in 2005 (VCCR 2006).<br />
The role of general practice<br />
In Australia, approximately 80% of Pap tests are taken by GPs (AIHW & AACR 2004) and<br />
therefore GPs play an important role in cervical screening in this country. GPs also play<br />
an important role in recruiting women who have never had a Pap test or are significantly<br />
under-screened.<br />
In November 2001, the Australian Government introduced a cervical screening Practice<br />
Incentive Payment to support general practices to enhance cervical cancer screening.<br />
The program has a number of components. Accredited practices receive a payment on<br />
registering for the scheme. GPs also receive a Special Incentive Payment when they<br />
perform a Pap test from unscreened and under-screened women aged between 20 and<br />
69 years. Finally, in order to encourage general practices to adopt a systematic approach<br />
to cervical screening, practices receive an outcomes payment when they reach a target<br />
screening rate (NCSP 2006). In May 2006, 91.7% of practices in Australia were signed on<br />
to participate in these activities (Medicare Australia 2006).<br />
Potential benefits and adverse effects of cervical<br />
cancer screening<br />
Rationale<br />
It has been estimated that screening using the Pap test has the potential to reduce<br />
squamous cell carcinoma of the cervix by up to 90% (AIHW, BreastScreen Australia &<br />
NCSP 1999).<br />
In Australia, the age-standardised incidence rate for cervical cancer declined by an average<br />
of 6.2% each year between 1991 and 2001. Mortality rates have also fallen by an average<br />
of 5.2% per year since 1991 (AIHW & AACR 2004). These gains can be attributed, in part,<br />
to the success of the <strong>National</strong> Cervical Screening Program.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
141<br />
C e r v i c a l c a n c e r
Potential adverse effects<br />
No screening test is 100% accurate. A Pap test every two years is about 90% accurate and<br />
is currently the best available protection against cervical cancer for women who have ever<br />
had sex. Like all screening tests, the Pap test is performed on asymptomatic women. False<br />
positive results as well as false negative results may occur.<br />
Even minor abnormalities can cause anxiety for some women. Women who receive false<br />
negative results may experience delays in diagnosis or treatment. False negative results<br />
may also create a false sense of security that may cause warning symptoms to be ignored.<br />
Who should be screened?<br />
All women who have ever been sexually active should commence having Pap tests<br />
between the ages of 18 and 20 years, or within two years after beginning sex, whichever is<br />
later (Cervical <strong>Cancer</strong> <strong>Prevention</strong> Taskforce 1991).<br />
Who has been screened?<br />
Cervical cytology registers in Australia provide information on the majority of women who<br />
undergo screening, although an estimated 1% to 3% of women choose not to be included<br />
on the register (AIHW, BreastScreen Australia & NCSP 1999). In the two years between<br />
January 2003 and December 2004, the participation rate for cervical cancer screening in<br />
Australia was 60.7% for the target population of women aged 20 to 69 years (AIHW 2006).<br />
Table 2.2: Participation rates in the <strong>National</strong> Cervical Screening Program by age group, Australia<br />
2003−04<br />
Age group 20–24 25–29 30–34 35–39 40–44 45–49 50–54 55–59 60–64 65–69<br />
Percentage 47.8 58.1 62.8 63.8 64.3 65.9 64.0 66.6 57.2 49.6<br />
Source: AIHW 2006<br />
Participation in screening is highest in the age groups 30–34 to 55–59 but declines sharply<br />
after the age group of 55–59. The participation rate across the age groups 40–69 increased<br />
slightly in 2003–04 compared to 2001–02 (AIHW 2006).<br />
Australia’s two-yearly screening interval is conservative, with many countries<br />
recommending three years or more between tests. The International Agency for Research<br />
on <strong>Cancer</strong> recommend three-yearly screening for women aged 25 to 49 and five-yearly<br />
screening for women aged 50 to 64 (IARC 2005)—a recommendation that the NHS<br />
Cervical Screening Programme in the United Kingdom has recently adopted. Data from<br />
Victoria show that if participation in cervical screening is measured over a three-year time<br />
interval, then the participation rate in women aged 20 to 69 years is close to 80% (VCCR<br />
2006).<br />
Adherence to the recommended two-yearly screening interval is not optimal. Among<br />
women who received a negative Pap test report in February 2000, 26.2% were re-screened<br />
before two years had elapsed (AIHW 2006). Early re-screening increases the cost of the<br />
program and reduces cost-effectiveness.<br />
142 Section Two: Screening to detect cancer early
Recruitment<br />
Women in the target age group are recruited by a variety of initiatives determined mainly at<br />
the state/territory level.<br />
Recruitment strategies are implemented for particular population sub-groups, such as older<br />
women, Australian Aboriginal and Torres Strait Islander women and women from culturally<br />
diverse backgrounds (AIHW, BreastScreen Australia & NCSP 1999).<br />
Aims<br />
The <strong>Cancer</strong> Council aims to maximise participation in the cervical screening program of<br />
eligible women and contribute to improvements in the program.<br />
What we want to achieve How The <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
Maximum screening<br />
participation of eligible<br />
women<br />
Maximum vaccine uptake<br />
among eligible girls and<br />
young women and ensure<br />
screening messages remain<br />
visible<br />
Ongoing evaluation of the<br />
effectiveness and efficiency of<br />
the screening program, so as<br />
to inform policy and program<br />
development<br />
Promote and foster participation in cervical cancer screening,<br />
particularly among women in under-screened populations<br />
Collaborate with Indigenous communities to improve rates of cervical<br />
screening among Australian Aboriginal and Torres Strait Islander<br />
women<br />
Develop systems to ensure that data are collected on Indigenous status<br />
to enable evaluation of program effectiveness<br />
Work with all relevant health professionals to reduce early re-screening<br />
Work with all relevant health professionals and consumers to increase<br />
adherence to the updated guidelines: Screening to prevent cervical<br />
cancer: guidelines for the management of asymptomatic women with<br />
screen detected abnormalities (NCSP 2005)<br />
Promote participation in HPV immunisation programs to eligible girls<br />
and young women, with particular emphasis on population groups most<br />
at risk, such as Indigenous communities<br />
Work with all relevant health professionals and consumers to ensure<br />
women are aware that, vaccinated or not, Pap tests remain important in<br />
preventing cancer of the cervix<br />
Advocate for, and contribute expert advice to, the review of evidence in<br />
relation to:<br />
• a change in national policy following the introduction of the HPV<br />
vaccine<br />
• a change to the screening interval and age at first screen<br />
• investigation of new technologies<br />
•<br />
timely implementation of review findings<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
143<br />
C e r v i c a l c a n c e r
References<br />
Cervical cancer<br />
Australian Institute of Health and Welfare (AIHW) 2006. Cervical screening in Australia 2003–2004. AIHW cat.<br />
no. 28; <strong>Cancer</strong> Series no. 33. Canberra: AIHW.<br />
Australian Institute of Health and Welfare (AIHW) & Australasian Association of <strong>Cancer</strong> Registries (AACR)<br />
2004. <strong>Cancer</strong> in Australia 2001. AIHW cat. no. 23; AIHW <strong>Cancer</strong> Series no. 28. Canberra: AIHW.<br />
Australian Institute of Health and Welfare (AIHW), Australasian Association of <strong>Cancer</strong> Registries (AACR),<br />
<strong>National</strong> <strong>Cancer</strong> Strategies Group (NCSG) & McDermid I 2005. <strong>Cancer</strong> incidence projections, Australia 2002 to<br />
2011. Canberra: AIHW, AACR & NCSG.<br />
Australian Institute of Health and Welfare (AIHW), BreastScreen Australia & <strong>National</strong> Cervical Screening<br />
Program (NCSP) 1999. Breast and cervical cancer screening in Australia 1996–1997. Canberra: AIHW.<br />
Bosch F 2000. Clinical cancer and HPV: a worldwide perspective. In Proceedings of the Fourth International<br />
Multidisciplinary Congress: Eurogin 2000. Bologna: Italy.<br />
Cervical <strong>Cancer</strong> <strong>Prevention</strong> Taskforce 1991. Screening for the prevention of cervical cancer. Canberra:<br />
Department of Health, Housing and Community Services.<br />
Cox T & Cuzick J 2006. HPV DNA testing in cervical cancer screening: from evidence to policies. Gynecol<br />
Oncol 103(1): 8–11.<br />
Eurogin 2003. Conclusions: cervical cancer control, priorities and new directions. International charter. 1–22.<br />
International Agency for Research on <strong>Cancer</strong> (IARC) 2005. IARC handbooks on cancer prevention. Cervix<br />
cancer screening. Lyon, France: IARC.<br />
——— 2002. Globocan 2002. At http://www-dep.iarc.fr. Accessed 16 April 2007.<br />
Medical Services Advisory Committee (MSAC) 2002. Liquid based cytology for cervical screening. MSAC<br />
reference 12a. Canberra: Australian Government Department of Health and Ageing.<br />
Medicare Australia 2006. Medicare Australia statistical reporting: approved practices in the quarterly<br />
calculations by activity. Participation in the PIP. Through Medicare Australia / Health statistics / Statistical<br />
reporting / Divisions of general practice. Accessed 26 November 2006.<br />
Munoz N, Bosch FX, de Sanjose S, Herrero R, Castellsague X, Shah KV, Snijders PJ & Meijer CJ 2003.<br />
Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med<br />
348(6): 518–27.<br />
<strong>National</strong> Cervical Screening Program (NCSP) 2006. Information for health professionals. At http://www.<br />
cervicalscreen.health.gov.au/internet/screening/publishing.nsf/Content/professionals. Accessed 16 April 2007.<br />
——— 2005. Screening to prevent cervical cancer: guidelines for the management of asymptomatic women<br />
with screen detected abnormalities. Canberra, Commonwealth of Australia.<br />
<strong>National</strong> Health and Medical Research Council (NHMRC) 2005. Screening to prevent cervical cancer:<br />
guidelines for the management of asymptomatic women with screen detected abnormalities. Canberra:<br />
NHMRC.<br />
US Preventive Services Task Force (USPSTF) 1996. The guide to clinical preventive services, 2nd edition.<br />
Washington: US Department of Health and Human Services, Office of Disease <strong>Prevention</strong> and Health<br />
Promotion.<br />
Victorian Cervical Cytology Registry (VCCR) 2006. Statistical report 2005. Melbourne: VCCR.<br />
Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJ, Peto J, Meijer CJ &<br />
Munoz N 1999. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol<br />
189(1): 12–19.<br />
Wright TC, Bosch FX, Franco EL, Cuzick J, Schiller JT, Garnett GP & Meheus A 2006. HPV vaccines and<br />
screening in the prevention of cervical cancer; conclusions from a 2006 workshop of international experts.<br />
Vaccine 24 (3 Suppl): S251–61.<br />
144 Section Two: Screening to detect cancer early
B o w e l ( c o l o r e c t a l )<br />
c a n c e r<br />
Bowel cancer is the most common potentially fatal<br />
cancer in Australians and is expected to increase<br />
in incidence by more than 30% over the next five<br />
to 10 years as our population ages. Populationbased<br />
screening for bowel cancer, currently being<br />
introduced in Australia, can reduce mortality by<br />
30% to 40% in people screened.<br />
Bowel cancer in Australia<br />
Bowel cancer, also known as colorectal or large bowel cancer, is a major health problem<br />
in Australia. One in 18 men and one in 25 women is likely to develop the disease. In 2005,<br />
there were estimated to be 14,237 new cases of bowel cancer—7,765 in men and 6,472<br />
in women—representing 14.5% of all new cases of cancer (excluding non-melanoma skin<br />
cancer). The incidence rate rises steadily with advancing age and most cases occur after<br />
the age of 50. Between 1991 and 2005, age-adjusted rates of bowel cancer incidence<br />
remained steady in men and slowly increased in women. In the 10-year period 2001–11,<br />
the number of new cases of bowel cancer is projected to increase by about one-third<br />
(AIHW, AACR, NCSG & McDermid 2005).<br />
In 2005, there were 4171 deaths in Australia from bowel cancer: 2330 in men and 1641<br />
in women. Bowel cancer was the second most common cause of death from cancer over<br />
all, as well as being the third most common cause of death from cancer in men (after<br />
lung and prostate cancers) and the third most common in women (after breast and lung<br />
cancers) (ABS 2007). Between 1991 and 2005, the death rate for bowel cancer fell by 2.5%<br />
per annum for men and by 2.6% for women (ABS 2007; AIHW 2005). Despite the trend<br />
towards better survival, bowel cancer remains an important cause of premature death in<br />
Australia.<br />
In Indigenous communities, where incidence rates are believed to be under-recorded,<br />
bowel cancer is the third most common cancer affecting men and the fourth most<br />
common affecting women (ABS & AIHW 2005). The survival rate from bowel cancer<br />
is lower for Indigenous than non-Indigenous Australians (Condon et al. 2004). It is also<br />
recognised that Aboriginal people and Torres Strait Islanders often have co-morbidities that<br />
may hinder the effectiveness of cancer treatments (Valery et al. 2006).<br />
Can bowel cancer be prevented?<br />
Evidence shows that bowel cancer is associated with a number of modifiable and<br />
unmodifiable risk factors.<br />
Important risk factors that cannot be addressed through lifestyle or behavioural change<br />
include a personal history of bowel cancer, advanced adenoma, chronic inflammatory<br />
bowel disease or a strong family history of bowel cancer (ACN Revision Committee<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
145<br />
B o w e l c a n c e r
2005). Two specific syndromes, which have a defined inherited genetic basis, are familial<br />
adenomatous polyposis (FAP) and hereditary non-polyposis colorectal cancer (HNPCC).<br />
HNPCC (also known as Lynch Syndrome) is also associated with an excess of cancers at<br />
other sites, including the endometrium and ovary. Clinical surveillance of individuals with<br />
these risk factors, as set out in The <strong>Cancer</strong> Council Australia’s Australian <strong>Cancer</strong> Network<br />
Clinical practice guidelines for the prevention, early detection and management of colorectal<br />
cancer, is recommended.<br />
Bowel cancer is also being increasingly linked to lifestyle and in recent decades, there has<br />
been considerable interest in identifying modifiable risk factors.<br />
The main focus of research into preventable risk factors associated with bowel cancer<br />
has been in relation to diet (including nutritional supplements), body weight and lifestyle<br />
factors such as physical activity, intake of aspirin and other non-steroidal anti-inflammatory<br />
drugs, and smoking (ACN Revision Committee 2005). A comprehensive overview of diet<br />
and cancer, published in 1997, estimated that changes in diet and physical activity could<br />
reduce the incidence of bowel cancer by 66% to 75% (WCRF & AICR 1997). (See the<br />
chapters on alcohol, nutrition, obesity and physical activity for more information.)<br />
Obesity, particularly central (around the waist) obesity, is an independent risk factor for<br />
bowel cancer and adenomas (IARC Working Group 2002; MacInnis et al. 2004).<br />
A number of studies have shown that smoking is a risk factor for bowel cancer and<br />
precancerous adenomas (Kune et al. 1992; Chao et al. 2000; Giovannucci 2001; Limburg et<br />
al. 2003; Anderson et al. 2003). The report from the <strong>Cancer</strong> <strong>Prevention</strong> Study II estimated<br />
that, in the US, approximately 12% of deaths from bowel cancer among both men and<br />
women were attributable to smoking (Chao et al. 2000).<br />
The review released from IARC in 2007 has confirmed that alcohol is a risk factor for the<br />
same cancers classified in 1988 and also for colorectal and breast cancer (IARC 2007).<br />
Aspirin has been shown to have potential in preventing bowel cancer (Sandler et al. 2003;<br />
Benamouzig et al. 2003; Chan et al. 2005). Findings from the Nurses’ Health Study and<br />
the Women’s Health Study indicate that the benefit is not evident until after more than a<br />
decade of regular aspirin consumption (Chan et al. 2005; Cook et al. 2005). Adverse effects<br />
of aspirin include acute upper gastrointestinal bleeding (Weil et al. 1995). After reviewing<br />
research into the effects of aspirin and non-steroidal anti-inflammatory drugs, the<br />
Australian <strong>Cancer</strong> Network stated that ‘it is reasonable to consider aspirin as prophylaxis<br />
in adenoma bearers’ but that ‘aspirin has not had broad scientific approval for use as a<br />
colorectal tumour chemo-preventive in individuals at average risk, because of uncertainties<br />
about the optimal dosage and duration of use, and adverse effects’ (ACN Revision<br />
Committee 2005).<br />
General practitioners and their teams have an important role in bowel cancer prevention.<br />
As they see 86% of the Australian population every year, they ‘have enormous potential to<br />
encourage patients to take greater responsibility for their health’ (RACGP 2006). Australian<br />
Doctor surveyed 1246 Australians in 2006, with 56% reporting they would act on advice<br />
from their GP in relation to lifestyle changes such as losing weight, quitting smoking and<br />
doing more exercise: all shown to reduce the risk of bowel cancer (Howe 2006).<br />
The Royal College of General Practitioners has published two key documents to support<br />
preventive work in general practice. The Guidelines for preventive activities in general<br />
practice (the ‘red book’) (RACGP 2005) is a guide listing who is most at risk, and<br />
evidence-based recommendations for screening or preventive care for a number of<br />
conditions including cancers. The other is Putting prevention into practice: guidelines for<br />
the implementation of prevention in the general practice setting (the ‘green book’) (RACGP<br />
2006). While there is evidence to show the benefits of GP preventive activities, there are<br />
many barriers, including the lack of time in typical general practice consultations. Solutions<br />
14 Section Two: Screening to detect cancer early
could focus on: how to use this time most effectively; the role of e-health measures such<br />
as follow-up, recall, and desktop prompts; non-GP measures such as practice nurse<br />
involvement; and non-clinical staff measures such as utilising waiting room opportunities.<br />
Tests and programs for bowel cancer<br />
Rationale<br />
Population-based screening provides an important opportunity to reduce bowel cancer<br />
mortality and morbidity. The combination of prevention measures, such as those outlined<br />
above, and population-based screening, has even greater potential to reduce the impact of<br />
bowel cancer in Australia.<br />
Research indicates that most bowel cancers develop from adenomatous polyps<br />
(adenomas); a small adenoma may grow into advanced cancer over an estimated 10 years.<br />
It should be recognised that it is common for middle-aged or elderly people to have one<br />
or more adenomas, most of which (estimated at around 19 out of 20) never progress to<br />
cancer.<br />
Adenomas are described as ‘advanced’ when certain features, such as larger size (10<br />
mm or more in diameter) are present. These features act as markers of greater likelihood<br />
of progression to cancer and greater risk for cancer elsewhere in the large bowel. Once<br />
cancer has developed, growth may occur gradually over 12 to 24 months or even longer.<br />
While the cancer remains confined to the bowel wall (stage A), surgical resection gives<br />
cure rates around 90% (ACN Revision Committee 2005).<br />
Most people with advanced adenomas and many with early stage cancer experience none<br />
of the symptoms that would alert them or their doctor to the presence of bowel cancer. For<br />
people diagnosed with bowel cancer, the pathological stage of development of the tumour<br />
at the time of diagnosis, as well as the treatments that follow, will affect their prognosis.<br />
Survival rates for bowel cancer are strongly related to stage, with five-year case survival<br />
rates found in South Australia (where statewide data is available) to be:<br />
•<br />
•<br />
•<br />
•<br />
88% for Stage A, when the cancer is contained within the bowel wall<br />
70% for Stage B, when the cancer has extended through the bowel wall, but with no<br />
lymph nodes affected<br />
43% for Stage C, when the cancer is present in the lymph nodes<br />
7% for Stage D, when the cancer cannot be removed by surgery or has spread to other<br />
areas of the body.<br />
There is an upward trend in these survival figures, due to a number of factors, including<br />
improvements in surgical technique and more widespread use of adjuvant chemotherapy<br />
and radiotherapy (ACN Revision Committee 2005).<br />
The two objectives of bowel cancer screening are 1) to prevent cancer by identifying and<br />
removing precancerous, advanced adenomas and 2) to diagnose and treat early stage,<br />
curable cancer.<br />
The evidence on screening for bowel cancer was reviewed in a report for the Australian<br />
Health Technology Advisory Committee (AHTAC 1997). The report concluded that the<br />
efficacy of screening based on the faecal occult blood test had been demonstrated, and<br />
that the best approach to mass screening of the Australian population required definition:<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
14<br />
B o w e l c a n c e r
such as pilot studies to assess acceptance by the target population, feasibility and costeffectiveness.<br />
Guidelines for the prevention, early detection and management of bowel cancer,<br />
incorporating the Australian Health Technology Advisory Committee recommendations on<br />
screening, were developed by the Australian <strong>Cancer</strong> Network and endorsed by the <strong>National</strong><br />
Health and Medical Research Council in 1999 (NHMRC, COSA & ACN 1999) and again in<br />
2005 (ACN Revision Committee 2005).<br />
Three screening tools for the early detection of bowel cancer are commonly available:<br />
the FOBT, sigmoidoscopy, and colonoscopy (ACN Revision Committee 2005). Two other<br />
tools—computerised tomographic (CT) colonography (also known as virtual colonoscopy)<br />
and faecal DNA testing—may have a future role in screening but are still undergoing<br />
evaluation (Van Dam et al. 2004; Cotton et al. 2004; Davies, Miller & Coleman 2005;<br />
Osborn & Ahlquist 2005).<br />
Faecal occult blood tests (FOBTs)<br />
<strong>Cancer</strong>s in the large bowel have a tendency to produce low-grade bleeding (Macrae &<br />
St John 1982; St John et al. 1992). The detection of blood in small (often not visible)<br />
concentrations in the faeces provides the basis for use of FOBTs in screening for bowel<br />
cancer.<br />
With FOBTs, blood can be detected through the chemical or immunochemical properties<br />
of haem and haemoglobin. The chemical tests, most of which use guaiac-impregnated<br />
slides as the test system, depend on detection of the chemical activity of haem. Certain<br />
foods and medications have the potential to interfere with test results so dietary<br />
modification may be required—usually avoiding red meat and vitamin C supplements for<br />
several days. The immunochemical tests utilise antibodies to human globin and are not<br />
affected by diet or medications. (For further discussion of the properties of the tests refer<br />
to Young, Macrae & St John 1996; Young et al. 2002.)<br />
FOBTs are simple tests that can be done at home. Depending on the particular test,<br />
samples are collected from either two or three bowel actions. The samples are then<br />
sent to a laboratory for analysis to check for the presence of blood. As bleeding may<br />
be intermittent, the presence of blood in even one sample should be investigated by<br />
colonoscopy (see below).<br />
Bowel cancer will be identified in 5% to 10% of those with a positive FOBT, an adenoma<br />
will be identified in another 20% to 35%, and bleeding will be due to a non-neoplastic<br />
cause such as haemorrhoids in the remainder. However, as shown by FOBT-based<br />
randomised controlled trials and other large studies, the likelihood of finding bowel cancer<br />
is between 12 and 40 times greater in a person with a positive FOBT than in someone<br />
whose test shows no evidence of bleeding (Mandel et al. 1993; Mandel et al. 1999;<br />
Alexander & Weller 2003).<br />
A false negative result from the FOBT (i.e. no bleeding detected in a person who actually<br />
has bowel cancer or an advanced adenoma) may occur because of intermittent blood loss,<br />
uneven distribution of blood in the faeces or, in the case of chemical tests, because of<br />
intake of vitamin C supplements (Young, Macrae & St John 1996). The choice of FOBT also<br />
affects false negative rates, as different tests may have different thresholds for detection<br />
of blood, and therefore for cancer. The chemical test used in the European randomised<br />
controlled trials has a sensitivity for cancer of only 50% (Hardcastle et al. 1996; Kronborg et<br />
al. 1996) whereas many newer chemical and immunochemical tests have a sensitivity for<br />
cancer in the range 70% to 90% (Allison et al. 1996).<br />
14 Section Two: Screening to detect cancer early
Periodic testing is recommended, as a negative (i.e. normal) result does not rule out<br />
the possibility of future development of bowel cancer. Evidence from the European<br />
randomised controlled trials, which used a low-sensitivity test repeated two-yearly for 10<br />
years, suggests that this approach would lead to a reduction of 15% to 18% in mortality<br />
from bowel cancer among those offered screening (Hardcastle et al. 1996; Kronborg et<br />
al. 1996). The reduction in mortality was estimated to be 30% to 40% among those who<br />
actually performed the test (Jorgensen, Kronborg & Fenger 2002; Scholefield et al. 2002).<br />
Sigmoidoscopy<br />
Sigmoidoscopy involves tube examination of the rectum and the lower part of the colon<br />
(i.e. the section of large bowel closest to the anus). The sigmoidoscope may be rigid (best<br />
suited for examining the rectum) or flexible (reaching into the lower part but unable to<br />
examine the upper part of the colon).<br />
Flexible sigmoidoscopy allows examination of the area where 55% to 60% of bowel<br />
cancers and advanced adenomas occur (AHTAC 1997). When abnormalities are detected,<br />
a tissue sample (biopsy) can be collected for pathological examination. The sensitivity<br />
for detection of neoplastic lesions depends on the proficiency of the sigmoidoscopist.<br />
Adenoma detection rates were shown to vary considerably between examiners in<br />
several large studies (Atkin et al. 2004; Pinsky et al. 2005), highlighting the need for<br />
comprehensive training and the auditing of outcomes. In 2005, an international task force<br />
issued detailed recommendations to assist with quality improvement (Levin et al. 2005).<br />
Evidence from several case−control studies indicates that screening by flexible<br />
sigmoidoscopy should lead to a substantial reduction in the death rate from bowel cancer<br />
(Selby et al. 1992; Newcomb et al. 1992). Major randomised controlled trials using flexible<br />
sigmoidoscopy for screening are currently underway in the US, UK and Italy (Gohagan et<br />
al. 2000; UKSSTI 2002; Segnan et al. 2002). Progress results from the three trials show the<br />
screening procedure to be feasible, safe and well accepted (Weissfeld et al. 2005; Wardle,<br />
Miles & Atkin 2005; Segnan et al. 2002).<br />
The Australian Health Technology Advisory Committee report stated that the evidence<br />
is sufficient to warrant consideration of sigmoidoscopic screening as an alternative (or<br />
a complement) to FOBT screening, but noted that mortality data from the randomised<br />
controlled trials will not be available for several more years (AHTAC 1997).<br />
Colonoscopy<br />
A colonoscope is similar to a flexible sigmoidoscope but is much longer. Interest in using<br />
colonoscopy as a screening tool relates to its ability to detect a very high proportion<br />
of bowel cancers and advanced adenomas by examination of the entire length of the<br />
large bowel. It allows biopsies to be taken from any suspected abnormalities as well as<br />
enabling most adenomas and some polypoid cancers to be completely removed during the<br />
examination.<br />
Many studies have shown that colonoscopy has around 95% sensitivity for detection of<br />
cancer (Leaper et al. 2004; Robertson et al. 2005; Singh et al. 2006). The sensitivity for<br />
detection of adenomas varies according to their size and site within the large bowel (Rex<br />
et al. 1997). As with sigmoidoscopy, sensitivity for detection of lesions depends on the<br />
proficiency of the examiner, again highlighting the need for comprehensive training and<br />
the auditing of outcomes. In 2002, the US Multi-Society Task Force on Colorectal <strong>Cancer</strong><br />
produced a detailed report on key performance indicators for colonoscopy (Rex et al.<br />
2002).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
14<br />
B o w e l c a n c e r
Colonoscopy is the recommended follow-up test for those with positive findings at FOBT<br />
or screening sigmoidoscopy. It is also recommended as the primary tool for cancer<br />
surveillance in people with an increased risk of bowel cancer. When it is not possible to<br />
examine the total length of the bowel by colonoscopy, a CT colonography or barium enema<br />
should be performed.<br />
The overall appropriateness of colonoscopy as the primary tool in population screening is<br />
much less certain. Acceptability of the procedure is limited by its invasive nature and the<br />
need for vigorous bowel preparation and sedation. The feasibility of providing colonoscopy<br />
for the five million Australians at average risk is also doubtful, given the high cost of the<br />
procedure, workforce and other logistic issues, and the required diversion of resources<br />
away from other health services.<br />
Of even greater importance, there is no high level evidence to support use of colonoscopy<br />
in population screening (ACN Revision Committee 2005). In 2001, the Canadian Task Force<br />
on Preventive Health Care stated that there was insufficient evidence to include or exclude<br />
colonoscopy as an initial screening test in people at average risk (CTFPHC 2001). Similarly,<br />
in 2002, the US Preventive Services Task Force was unable to find direct evidence that<br />
screening colonoscopy was effective in reducing the bowel cancer mortality rate (USPSTF<br />
2002).<br />
The policy context<br />
In 1999, in line with the Australian Health Technology Advisory Committee and the<br />
<strong>National</strong> Health and Medical Research Council recommendations, the <strong>National</strong> <strong>Cancer</strong><br />
<strong>Control</strong> Initiative developed a proposal for a feasibility study for bowel cancer screening in<br />
the general population (NCCI 1999). The recommendations were formulated by an expert<br />
group that included representatives of the cancer councils. In response to this proposal,<br />
funds were set aside in the May 2000 federal budget to mount a four-year national<br />
feasibility study based on biennial screening using immunochemical FOBTs.<br />
The Population Screening Section of the Department of Health and Ageing then assumed<br />
responsibility for planning the <strong>National</strong> Bowel <strong>Cancer</strong> Screening Pilot Study. The Health<br />
Insurance Commission (known as Medicare Australia), cancer councils, and many other<br />
interested groups participated in the planning process. Three pilot sites—Mackay in<br />
Queensland, and defined suburbs in Adelaide and Melbourne—were chosen for the<br />
feasibility study, which was conducted between November 2002 and June 2004. The Pilot<br />
Evaluation Report concluded that a nationally coordinated bowel cancer screening program<br />
in Australia would be feasible, acceptable and cost effective (Healthcare Management<br />
Advisors 2005).<br />
In the 2005/06 federal budget, the Australian Government announced that it would provide<br />
$43.4 million over three years (including $7.8 million for the precursor pilot programs) to<br />
phase in a nationally coordinated, population-based bowel cancer screening program.<br />
The Department of Health and Ageing formed a new Bowel <strong>Cancer</strong> Screening Section to<br />
develop and coordinate the program.<br />
In August 2006 the Government confirmed that the <strong>National</strong> Bowel <strong>Cancer</strong> Screening<br />
Program would begin by inviting people who turn 55 or 65 years of age between 1 May<br />
2006 and 30 June 2008, and those who were invited to participate in the pilot, to complete<br />
an FOBT in their own home and return it by post to a laboratory for analysis. (Australia<br />
Post gave its approval.) Following consultation with state and territory governments,<br />
invitations to eligible participants would be issued on either a postcode or birth date basis<br />
and delivered through the mail. Nearly one million people were expected to be invited to<br />
150 Section Two: Screening to detect cancer early
participate in the initial phase; the first invitations were issued in Queensland on 7 August<br />
2006.<br />
A national bowel cancer screening register is set up within Medicare Australia. The<br />
register is responsible for issuing invitations and FOBTs, monitoring all data and arranging<br />
follow-up notifications for participants who receive positive FOBT results but do not have<br />
colonoscopies. It also runs the national Information Line.<br />
According to the Government, program implementation will be incremental and influenced<br />
by funding availability and healthcare system capacity, including colonoscopy and surgical<br />
services in each state and territory. The results of the first phase of <strong>National</strong> Bowel <strong>Cancer</strong><br />
Screening Program are expected to be reviewed prior to the 2008/09 federal and state/<br />
territory budgets. This review is expected to guide decisions about further implementation<br />
of the program.<br />
The <strong>Cancer</strong> Council fully supports and applauds the Australian Government’s introduction<br />
of a national bowel cancer screening program using faecal occult blood testing. As the<br />
program takes shape across Australia, the <strong>Cancer</strong> Council encourages all governments to<br />
ensure issues of access, quality and equity remain paramount. The availability of timely,<br />
high-quality colonoscopy following a positive FOBT will be an important issue affecting<br />
the success of the program, particularly in rural and remote areas where access may be<br />
limited.<br />
Appreciating the need for gradual implementation in the first instance, the <strong>Cancer</strong> Council<br />
encourages the Australian Government to make the necessary commitments, to ensure<br />
that the program becomes available to as many at-risk Australians as possible, in the<br />
shortest possible time.<br />
No upper age limit has been set for screening. Decisions about continued participation by<br />
the elderly are likely to be based on their personal preference and general state of health,<br />
and the perceived balance between benefits of screening and harms related to the followup<br />
investigations required in those with positive screening tests.<br />
Screening for people at increased risk of bowel cancer<br />
The Australian Health Technology Advisory Committee report on colorectal cancer<br />
screening noted that a national approach to population screening for people without<br />
symptoms would need to be complemented by a national policy for groups potentially<br />
at increased risk for bowel cancer: individuals with a family history of bowel cancer, or a<br />
personal history of bowel adenoma, bowel cancer or inflammatory bowel disease (AHTAC<br />
1997). GPs are well positioned to determine bowel cancer risk on the basis of family history<br />
and to instigate appropriate management, again consistent with guidelines (RACGP 2005;<br />
ACN Revision Committee 2005; McMurrick, Dorien & Shapiro 2006).<br />
The Australian <strong>Cancer</strong> Network Clinical practice guidelines for the prevention, early detection<br />
and management of colorectal cancer defines three categories of people in relation to risk<br />
for bowel cancer based on their family history of the disease.<br />
•<br />
•<br />
In the first category, people who have just one first-degree relative with bowel cancer<br />
are advised to have the same screening as those at average risk, provided their relative<br />
was diagnosed with cancer at or over the age of 55.<br />
The second category includes people with two or more first-degree relatives with bowel<br />
cancer (on the same side of the family) or one first-degree relative diagnosed under the<br />
age of 55 years. Because of their greater risk for cancer, screening is generally based on<br />
periodic (usually every five years) colonoscopy.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
151<br />
B o w e l c a n c e r
•<br />
The third category covers members of families with definite or suspected FAP or<br />
HNPCC. People with FAP usually have hundreds of small polyps throughout their<br />
bowel, some of which become malignant if not removed. HNPCC is not associated with<br />
polyposis but, like FAP, is caused by an inherited change in a gene. The place of genetic<br />
testing and recommendations about surveillance and prophylactic surgery are described<br />
in chapter 7 of the guidelines (ACN Revision Committee 2005).<br />
Detailed recommendations for surveillance by colonoscopy in those with past bowel<br />
cancer or adenoma are also set out in the Australian <strong>Cancer</strong> Network guidelines.<br />
Culturally appropriate communication<br />
Announcements made with the 2005/06 federal budget stated that Aboriginal and Torres<br />
Strait Islander communities will be invited to participate in the screening program from age<br />
45. The pilot evaluation showed that culturally and linguistically diverse communities and<br />
Aboriginal people and Torres Strait Islanders lacked awareness of bowel cancer screening<br />
issues. This was a major barrier against participation (Woolcott Research 2004). Culturally<br />
appropriate education and resources, as well as engagement with local health workers, will<br />
be needed to address the particular needs of these communities (Woolcott Research 2004)<br />
and to ensure that their participation, or non-participation, is based on informed choice.<br />
The role of general practice<br />
General practitioners (GPs) have an important role at critical points in the <strong>National</strong> Bowel<br />
<strong>Cancer</strong> Screening Program (DHA 2006). These include:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
determining the appropriateness of screening for individual patients (e.g. those with<br />
significant co-morbidities, or those who’ve recently undergone screening outside the<br />
national program)<br />
assessing high-risk individuals and managing them according to <strong>National</strong> Health and<br />
Medical Research Council guidelines<br />
receiving FOBT results where the participant has nominated a GP<br />
managing participants with a positive FOBT<br />
notifying the central registry of outcomes.<br />
GPs also have an important role in recognising and assessing individuals with symptoms<br />
that could be related to cancer, and in whom diagnostic investigations (rather than<br />
screening) are required (ACN Revision Committee 2005; McMurrick, Dorien & Shapiro<br />
2006). Symptoms include:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
bleeding from the back passage or any sign of blood in a bowel motion<br />
an unexplained and persistent change in bowel actions<br />
unexplained tiredness<br />
lower abdominal pain<br />
a persistent feeling of fullness.<br />
A recommendation from a GP has been shown to enhance participation rates in bowel<br />
cancer screening using FOBTs (Cole et al. 2002). It has been shown to be the most highly<br />
rated attribute that would encourage participation in bowel cancer screening (Salkeld et<br />
al. 2003). Over 90% of a population group surveyed responded that they would be likely or<br />
very likely to have an FOBT every two years if a doctor recommended this (Epidemiology<br />
Services Unit 2004). Pilot program invitees who did not participate indicated they were<br />
152 Section Two: Screening to detect cancer early
likely to do so if reinvited, especially if recommended by a GP (DHA 2005). Given this, it<br />
is not unreasonable to expect that a proactive approach by GPs in identifying their eligible<br />
patients and recommending their involvement in the screening program, may enhance<br />
participation rates. Whilst there is evidence that GPs support bowel cancer screening, GPs<br />
have also articulated a need for further education about this activity (Turner et al. 2006;<br />
Tong et al. 2004).<br />
It is anticipated that the national screening program will increase awareness of bowel<br />
cancer and bowel cancer screening in the broader population, including those not currently<br />
eligible for the screening program. GPs will be in a position to respond to this demand by<br />
managing patients according to current guidelines (RACGP 2005; ACN Revision Committee<br />
2005).<br />
Potential benefits and adverse effects of bowel<br />
cancer screening<br />
Potential benefits<br />
As discussed earlier, bowel cancer screening using FOBTs has the potential to significantly<br />
reduce mortality from bowel cancer. Monitoring systems in South Australia found that only<br />
15% of bowel cancers are detected at the earliest point, Stage A (AHTAC 1997). Thus an<br />
important potential benefit of screening is to detect early stage, curable cancers in those<br />
without any clinical evidence of disease (ACN Revision Committee 2005). A screening<br />
program also has the potential to detect advanced adenomas, allowing them to be<br />
removed before progressing to bowel cancer.<br />
Thus, the benefits of bowel cancer screening are two-fold: providing opportunities for both<br />
prevention and early detection. It is predicted that a fully implemented screening program<br />
could save close to 2000 lives per year (Macrae 2005).<br />
Potential adverse effects<br />
Bowel cancer screening may result in adverse psychological and physical effects due to<br />
false positive tests. The potential adverse effects include anxiety induced by fear of having<br />
bowel cancer, anxiety related to diagnosis of lesions of doubtful clinical significance and<br />
complications of invasive diagnostic procedures (specifically colonoscopy). In several<br />
studies, anxiety due to positive test results was shown to decrease after investigation<br />
of the cause, with no evidence of long-term harm after screening (Lindholm et al. 1997;<br />
Wardle et al. 1999; Parker et al. 2002). The need to provide timely follow-up investigations<br />
following a positive result from an FOBT has important implications for the national<br />
program, as delays in the provision of colonoscopy may lead to high levels of anxiety.<br />
The most significant adverse effect is the potential for physical harm linked to exposure<br />
to colonoscopy. Colonoscopy is performed as a day case procedure and usually requires<br />
sedation. It can produce severe complications such as perforation, haemorrhage or death<br />
and carries a remote risk of transmitting infections. In a review of six prospective studies<br />
of colonoscopy, about one in 1000 patients suffered perforation, three in 1000 suffered<br />
major haemorrhage, and between one and three in 10,000 died as a result of the procedure<br />
(Winawer et al. 1997). In two more recent studies, the findings were similar, overall<br />
morbidity being 0.4% (Dafnis et al. 2001; Gatto et al. 2003). A review of a large Australian<br />
hospital experience supported the conclusions of these other studies and reported a<br />
mortality rate of 0.004% in outpatients having the procedure (Viiala et al. 2003).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
153<br />
B o w e l c a n c e r
Despite the possibility of adverse consequences of screening, distress generated by<br />
diagnosis of an advanced cancer when there has been no opportunity for early detection<br />
by screening also needs to be taken into consideration (ACN Revision Committee 2005).<br />
Who should be screened?<br />
Randomised controlled trials at the population level indicate that screening tests for faecal<br />
occult blood reduce overall mortality from colorectal cancer in populations selected on the<br />
basis of age. These have shown benefit for people aged 45–50 years and upward. Costeffectiveness<br />
studies also demonstrate that age influences cost-effectiveness. Together<br />
with the observation that risk increases four-fold between ages of 40 and 50 years, these<br />
lead to the recommendation that screening of average risk people should commence at<br />
age 50 years (NHMRC 2005).<br />
Although the <strong>National</strong> Health and Medical Research Council guidelines do not suggest<br />
an upper age for screening, it is common for population-based screening programs to do<br />
so. There is no clear evidence on the best age to cease screening for bowel cancer. In the<br />
randomised controlled trials using FOBT, the upper age at the time of entry ranged from<br />
75 (Kronborg et al. 1996) to 80 years (Mandel et al. 1993). With increasing age, bowel<br />
cancer becomes more prevalent, but the potential for years of life saved through screening<br />
decreases. In addition, follow up colonoscopies may be less well tolerated among the<br />
elderly and participation is likely to drop off after the age of 70 (Hardcastle et al. 1996).<br />
Further cost-effectiveness research is needed to establish an appropriate upper age for the<br />
<strong>National</strong> Bowel <strong>Cancer</strong> Screening Program.<br />
Aims<br />
The <strong>Cancer</strong> Council aims to maximise participation of eligible people in the bowel cancer<br />
screening program and contribute to developments in knowledge to improve that program.<br />
What we want to achieve How The <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
Increased awareness among<br />
the general public and key<br />
health professional groups<br />
of the links between bowel<br />
cancer and nutrition, physical<br />
activity, obesity, alcohol<br />
consumption and smoking<br />
cessation<br />
A high-quality, well resourced<br />
national bowel cancer<br />
screening program capable<br />
of reaching 70% two-yearly<br />
participation of people over<br />
50 years of age by 2012<br />
154 Section Two: Screening to detect cancer early<br />
Advocate for a whole-of-government approach incorporating social<br />
marketing, policy reform and research, administered through a<br />
partnership involving all jurisdictions and peak health bodies (the<br />
success of the integrated <strong>National</strong> <strong>Tobacco</strong> Campaign of the late 1990s<br />
provides an excellent example on which to draw)<br />
Ensure key messages are promoted to the public and relevant<br />
health professionals in publications, presentations, programs, media<br />
statements and where opportunities arise<br />
Promote and/or develop primary health resources, specifically for<br />
general practice, to improve evidence-based interventions by health<br />
professionals<br />
Advocate for a whole-of-government agreement to a comprehensive,<br />
evidence-based screening program with adequate funding to reach the<br />
target population
What we want to achieve How The <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
A process of quality<br />
assurance and continuous<br />
improvement in the national<br />
bowel cancer screening<br />
program<br />
Sufficient workforce capacity<br />
to ensure colonoscopy wait<br />
times for a positive FOBT<br />
are under 30 days (for<br />
both screening program<br />
participants and those who<br />
have screened outside the<br />
program)<br />
Maximum participation of<br />
eligible people in bowel<br />
cancer screening<br />
Referral to appropriate<br />
treatment services and<br />
collection of information<br />
about the outcome of<br />
treatment<br />
Advocate for the development of mandatory national training and<br />
accreditation standards for colonoscopy provision<br />
Advocate for government to build a formal, ongoing evaluation<br />
mechanism into the program to ensure regular monitoring and periodic<br />
evaluation. Evaluation should address:<br />
• overall outcomes relating to the impact of the program on bowel<br />
cancer mortality and morbidity<br />
• economic outcomes relating to the cost-effectiveness of the program<br />
and barriers to optimising participation among the target population<br />
• process outcomes relating to the performance of the program against<br />
its stated objectives<br />
• potential barriers to evaluation, notably fast-tracking cancer<br />
registrations to facilitate timely evaluation of program outcomes<br />
• sufficient resources to enable stated objectives to be achieved<br />
• periodic review of the target screening age group<br />
Support professionals such as general practitioners to contribute to the<br />
program’s efficiency and effectiveness<br />
Advocate for increase government funding and service redevelopment<br />
initiatives to increase colonoscopy capacity and ensure wait times are<br />
minimised<br />
Advocate for government support, including adequate funding, to<br />
ensure targets for participation are met, while maintaining a focus<br />
on equity and access. Priority should be given to maximising the<br />
participation of Australian Aboriginal and Torres Strait Islander<br />
communities and people of culturally and linguistically diverse (CALD)<br />
backgrounds, as they are likely to be under-screened<br />
Assist in developing tailored communications strategies, to promote and<br />
foster participation among specific population groups (e.g. Aboriginal<br />
and Torres Strait Islander and CALD communities)<br />
Recognising the importance of providing consistent high quality care for<br />
people diagnosed with bowel cancer in Australia:<br />
• support or advocate for examination of the extent to which people<br />
diagnosed in the screening program are being treated in accordance<br />
with the NHMRC Clinical practice guidelines for the prevention, early<br />
detection and management of colorectal cancer (2005)<br />
•<br />
encourage data collection that includes stage and outcome measures<br />
as well as qualitative information on patient experience<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
155<br />
B o w e l c a n c e r
References<br />
Bowel (colorectal) cancer<br />
Alexander F & Weller D 2003. Evaluation of the UK colorectal cancer screening pilot. Edinburgh: Department of<br />
Community Health Services.<br />
Allison JE, Tekawa IS, Ransom LJ & Adrain AL 1996. A comparison of fecal occult blood tests for colorectal<br />
cancer screening. N Engl J Med 334: 155–9.<br />
Anderson JC, Attam R, Alpern Z, Messina CR, Hubbard P, Grimson R, Ells PF & Brand DL 2003. Prevalence of<br />
colorectal neoplasia in smokers. Am J Gastroenterol 98(12): 2777–83.<br />
Atkin W, Rogers P, Cardwell C, Cook C, Cuzick J, Wardle J & Edwards R 2004. Wide variation in adenoma<br />
detection rates at screening flexible sigmoidoscopy. Gastroenterology 126(5): 1247–56.<br />
Australian Bureau of Statistics (ABS) 2007. Causes of death, Australia 2005. Cat. no. 3303.0. Canberra: ABS.<br />
Australian Bureau of Statistics (ABS) & Australian Institute of Health and Welfare (AIHW) 2005. The health<br />
and welfare of Australia’s Aboriginal & Torres Strait Islander peoples. Canberra: ABS.<br />
Australian <strong>Cancer</strong> Network Colorectal <strong>Cancer</strong> Guidelines Revision Committee (ACN Revision Committee)<br />
2005. Guidelines for the prevention, early detection and management of colorectal cancer. Sydney: The <strong>Cancer</strong><br />
Council Australia and ACN.<br />
Australian Health Technology Advisory Committee (AHTAC) 1997. Colorectal cancer screening. Canberra:<br />
Commonwealth Department of Health and Family Services.<br />
Australian Institute of Health and Welfare (AIHW) 2005. State and territories GRIM (General Record of<br />
Incidence of Mortality) books. AIHW: Canberra.<br />
Australian Institute of Health and Welfare (AIHW), Australasian Association of <strong>Cancer</strong> Registries (AACR),<br />
<strong>National</strong> <strong>Cancer</strong> Strategies Group (NCSG) & McDermid I 2005. <strong>Cancer</strong> incidence projections, Australia 2002 to<br />
2011. Canberra: AIHW, AACR & NCSG.<br />
Benamouzig R, Deyra J, Martin A, Girard B, Jullian E, Piednoir B, Couturier D, Coste T, Little J & Chaussade S<br />
2003. Daily soluble aspirin and prevention of colorectal adenoma recurrence: one-year results of the APACC<br />
trial. Gastroenterology 125(2): 328–36.<br />
Calle EE, Rodriguez C, Walker-Thurmond K & Thun MJ 2003. Overweight, obesity, and mortality from cancer<br />
in a prospectively studied cohort of US adults. N Engl J Med 348(17): 1625–38.<br />
Canadian Task Force on Preventive Health Care (CTFPHC) 2001. Colorectal cancer screening.<br />
Recommendation statement from the Canadian Task Force on Preventive Health Care. Can Med Assoc J<br />
165(2): 206–8.<br />
Chan AT, Giovannucci EL, Meyerhardt JA, Schernhammer ES, Curhan GC & Fuchs CS 2005. Long-term use<br />
of aspirin and nonsteroidal anti-inflammatory drugs and risk of colorectal cancer. JAMA 294(8): 914–23.<br />
Chao A, Thun MJ, Jacobs EJ, Henley SJ, Rodriguez C & Calle EE 2000. Cigarette smoking and colorectal<br />
cancer mortality in the cancer prevention study II. J Natl <strong>Cancer</strong> Inst 92: 1888.<br />
Cole SR, Young GP, Byrne D, Guy JR & Morcom J 2002. Participation in screening for colorectal cancer based<br />
on a faecal occult blood test is improved by endorsement by the primary care practitioner. J Med Screen 9(4):<br />
147–52.<br />
Condon JR, Barnes T, Cunningham J & Armstrong BK 2004. Long-term trends in cancer mortality for<br />
Indigenous Australians in the Northern Territory. Med J Aust 180(10): 504–7.<br />
Cook NR, Lee IM, Gaziano JM, Gordon D, Ridker PM, Manson JE, Hennekens CH & Buring JE 2005. Lowdose<br />
aspirin in the primary prevention of cancer: the Women’s Health Study: a randomized controlled trial.<br />
JAMA 294(1): 47–55.<br />
Cotton PB, Durkalski VL, Pineau BC, Palesch YY, Mauldin PD, Hoffman B, Vining DJ, Small WC, Affronti J,<br />
Rex D, Kopecky KK, Ackerman S, Burdick JS, Brewington C, Turner MA, Zfass A, Wright AR, Iyer RB, Lynch<br />
15 Section Two: Screening to detect cancer early
P, Sivak MV & Butler H 2004. Computed tomographic colonography (virtual colonoscopy): a multicenter<br />
comparison with standard colonoscopy for detection of colorectal neoplasia. JAMA 291(14): 1713–19.<br />
Dafnis G, Ekbom A, Pahlman L & Blomqvist P 2001. Complications of diagnostic and therapeutic<br />
colonoscopy within a defined population in Sweden. Gastrointest Endosc 54(3): 302–9.<br />
Davies RJ, Miller R & Coleman N 2005. Colorectal cancer screening: prospects for molecular stool analysis.<br />
Nat Rev <strong>Cancer</strong> 5(3): 199–209.<br />
Department of Health and Ageing (DHA) (Australian Government) 2006. <strong>National</strong> Bowel <strong>Cancer</strong> Screening<br />
Program. Information for general practitioners. Canberra: DHA.<br />
——— 2005. Bowel cancer knowledge, perceptions and screening behaviours: knowledge, attitudes and<br />
practice pre- and post-intervention surveys (2002 and 2004.) Final report. Canberra: Commonwealth of<br />
Australia.<br />
Epidemiology Services Unit 2004. Bowel <strong>Cancer</strong> Screening Pilot Program: knowledge, attitudes & practices<br />
pre- and post-intervention surveys (2002 & 2004). Final report. Canberra: Department of Health and Ageing<br />
(Australian Government).<br />
Gatto NM, Frucht H, Sundararajan V, Jacobson JS, Grann VR & Neugut AI 2003. Risk of perforation after<br />
colonoscopy and sigmoidoscopy: a population-based study. J Natl <strong>Cancer</strong> Inst 95(3): 230–6.<br />
Giovannucci E 2001. An updated review of the epidemiological evidence that cigarette smoking increases risk<br />
of colorectal cancer. <strong>Cancer</strong> Epidemiol Biomarkers Prev 10(7): 725–31.<br />
Gohagan JK, Prorok PC, Hayes RB & Kramer BS 2000. The Prostate, Lung, Colorectal and Ovarian (PLCO)<br />
<strong>Cancer</strong> Screening Trial of the <strong>National</strong> <strong>Cancer</strong> Institute: history, organization, and status. <strong>Control</strong> Clin Trials<br />
21(6 Suppl): S251–2.<br />
Hardcastle JD, Chamberlain JO, Robinson MHE, Moss SM, Amar SS, Balfour TW, James PD & Mangham CM<br />
1996. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet 348: 1472–7.<br />
Healthcare Management Advisors 2005. Australia’s Bowel <strong>Cancer</strong> Screening Pilot and beyond. Final evaluation<br />
report. Canberra: Australian Government Department of Health and Ageing.<br />
Howe M 2006. Open to change. Australian Doctor 27 April.<br />
International Agency for Research on <strong>Cancer</strong> (IARC) 2007. Carcinogenicity of alcoholic beverages, vol. 96 of<br />
IARC monographs. Lyon: IARC.<br />
International Agency for Research on <strong>Cancer</strong> Working Group on the Evaluation of <strong>Cancer</strong>-preventive<br />
Strategies (IARC Working Group) 2002. Handbooks of cancer prevention volume 6: weight control and physical<br />
activity, eds H Vainio & F Bianchini. Lyon, France: IARC Press.<br />
Jorgensen OD, Kronborg O & Fenger C 2002. A randomised study of screening for colorectal cancer using<br />
faecal occult blood test. Results after 13 years and seven biennial screening rounds. Gut 50: 29–32.<br />
Kronborg O, Fenger C, Olsen J, Jorgensen OD & Sondergaard O 1996. Randomised study of screening for<br />
colorectal cancer with faecal-occult-blood test. Lancet 348: 1467–71.<br />
Kune GA, Kune S, Vitetta L & Watson LF 1992. Smoking and colorectal cancer risk: data from the Melbourne<br />
Colorectal <strong>Cancer</strong> Study and brief review of literature. Int J <strong>Cancer</strong> 50: 369–72.<br />
Leaper M, Johnston MJ, Barclay M, Dobbs BR & Frizelle FA 2004. Reasons for failure to diagnose colorectal<br />
carcinoma at colonoscopy. Endoscopy 36(6): 499–503.<br />
Levin TR, Farraye FA, Schoen RE, Hoff G, Atkin W, Bond JH, Winawer S, Burt RW, Johnson DA, Kirk<br />
LM, Litin SC & Rex DK 2005. Quality in the technical performance of screening flexible sigmoidoscopy:<br />
recommendations of an international multi-society task group. Gut 54(6): 807–13.<br />
Limburg PJ, Vierkant RA, Cerhan JR, Yang P, Lazovich D, Potter JD & Sellers TA 2003. Cigarette smoking<br />
and colorectal cancer: long-term, subsite-specific risks in a cohort study of postmenopausal women. Clin<br />
Gastroenterol Hepatol (1): 202–10.<br />
Lindholm E, Berglund B, Kewenter J & Haglind E 1997. Worry associated with screening for colorectal<br />
carcinomas. Scand J Gastroenterol 32(3): 238–45.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
15<br />
B o w e l c a n c e r
MacInnis RJ, English DR, Hopper JL, Haydon AM, Gertig DM & Giles GG 2004. Body size and composition<br />
and colon cancer risk in men. <strong>Cancer</strong> Epidemiol Biomarkers Prev 13(4): 553–9.<br />
Macrae FA 2005. Screening for colorectal cancer: virtually there. Med J Aust 182:52.<br />
Macrae FA & St John DJ 1982. Relationship between patterns of bleeding and Hemoccult sensitivity in<br />
patients with colorectal cancers or adenomas. Gastroenterology 82(5 Pt 1): 891–8.<br />
Mandel JS, Bond JH, Church TR, Snover DC, Bradley GM, Schuman LM & Ederer F 1993. Reducing mortality<br />
from colorectal cancer by screening for fecal occult blood. N Engl J Med 328: 1365–71.<br />
Mandel JS, Church TR, Ederer F & Bond JH 1999. Colorectal cancer mortality: effectiveness of biennial<br />
screening for fecal occult blood. J Natl <strong>Cancer</strong> Inst 91(5): 434–7.<br />
McMurrick P, Dorien S & Shapiro J 2006. Bowel cancer: guide for the GP. Aust Fam Physician 35(4): 192–7.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Control</strong> Initiative (NCCI) 1999. Screening for early detection of colorectal cancer: a national<br />
initiative for the new millennium. Melbourne: NCCI.<br />
<strong>National</strong> Health and Medical Research Council (NHMRC) 2005. Clinical practice guidelines for the prevention,<br />
early detection and management of colorectal cancer. Canberra: NHMRC.<br />
<strong>National</strong> Health and Medical Research Council (NHMRC), Clinical Oncological Society of Australia (COSA)<br />
& Australian <strong>Cancer</strong> Network (ACN) 1999. Guidelines for the prevention, early detection and management of<br />
colorectal cancer (CRC). Canberra: NHMRC.<br />
Newcomb PA, Norfleet RG, Storer BE, Surawicz TS & Marcus PM 1992. Screening sigmoidoscopy and<br />
colorectal cancer mortality. J Natl <strong>Cancer</strong> Inst 84: 1572–5.<br />
Osborn NK & Ahlquist DA 2005. Stool screening for colorectal cancer: molecular approaches.<br />
Gastroenterology 128(1): 192–206.<br />
Parker MA, Robinson MH, Scholefield JH & Hardcastle JD 2002. Psychiatric morbidity and screening for<br />
colorectal cancer. J Med Screen 9(1): 7–10.<br />
Pignone M, Saha S, Hoerger T, Mandelbatt J 2002. Cost-effectiveness analyses of colorectal cancer<br />
screening: A systematic review for the US Preventive Services Task Force. Ann Intern Med 137: 94–104.<br />
Pinsky PF, Schoen RE, Weissfeld JL, Kramer B, Hayes RB & Yokochi L 2005. Variability in flexible<br />
sigmoidoscopy performance among examiners in a screening trial. Clin Gastroenterol Hepatol 3(8): 792–7.<br />
Rex DK, Bond JH, Winawer S, Levin TR, Burt RW, Johnson DA, Kirk LM, Litlin S, Lieberman DA, Waye JD,<br />
Church J, Marshall JB & Riddell RH 2002. Quality in the technical performance of colonoscopy and the<br />
continuous quality improvement process for colonoscopy: recommendations of the US Multi-Society Task<br />
Force on Colorectal <strong>Cancer</strong>. Am J Gastroenterol 97(6): 1296–308.<br />
Rex DK, Cutler CS, Lemmel GT, Rahmani EY, Clark DW, Helper DJ, Lehman GA & Mark DG 1997.<br />
Colonoscopic miss rates of adenomas determined by back-to-back colonoscopies. Gastroenterology 112(1):<br />
24–8.<br />
Robertson DJ, Greenberg ER, Beach M, Sandler RS, Ahnen D, Haile RW, Burke CA, Snover DC, Bresalier<br />
RS, Keown-Eyssen G, Mandel JS, Bond JH, Van Stolk RU, Summers RW, Rothstein R, Church TR, Cole<br />
BF, Byers T, Mott L & Baron JA 2005. Colorectal cancer in patients under close colonoscopic surveillance.<br />
Gastroenterology 129(1): 34–41.<br />
Royal Australian College of General Practitioners 2006. Putting prevention into practice: guidelines for the<br />
implementation of prevention in the general practice setting. South Melbourne: RACGP.<br />
——— 2005. Guidelines for preventive activities in general practice, eds M Harris, L Bailey, C Bridges-Webb, J<br />
Furler, B Joyner, J Litt, J Smith & Y Zurynski. South Melbourne: RACGP.<br />
Salkeld GP, Solomon MJ, Short L & Ward J 2003. Measuring the importance of attributes that influence<br />
consumer attitudes to colorectal cancer screening. ANZ J Surg 73(3): 128–32.<br />
Sandler RS, Halabi S, Baron JA, Budinger S, Paskett E, Keresztes R, Petrelli N, Pipas JM, Karp DD, Loprinzi<br />
CL, Steinbach G & Schilsky R 2003. A randomized trial of aspirin to prevent colorectal adenomas in patients<br />
with previous colorectal cancer. N Engl J Med 348(10): 883–90.<br />
15 Section Two: Screening to detect cancer early
Scholefield JH, Moss S, Sufi F, Mangham CM & Hardcastle JD 2002. Effect of faecal occult blood screening<br />
on mortality from colorectal cancer: results from a randomised controlled trial. Gut 50(6): 840–4.<br />
Segnan N, Senore C, Andreoni B, Aste H, Bonelli L, Crosta C, Ferraris R, Gasperoni S, Penna A, Risio M,<br />
Rossini FP, Sciallero S, Zappa M & Atkin WS 2002. Baseline findings of the Italian multicenter randomized<br />
controlled trial of ‘once-only sigmoidoscopy’––SCORE. J Natl <strong>Cancer</strong> Inst 94(23): 1763–72.<br />
Selby JV, Friedman GD, Quesenberry CP Jr & Weiss NS 1992. A case–control study of screening<br />
sigmoidoscopy and mortality from colorectal cancer. N Engl J Med 326: 653–7.<br />
Singh H, Turner D, Xue L, Targownik LE & Bernstein CN 2006. Risk of developing colorectal cancer following<br />
a negative colonoscopy examination: evidence for a 10-year interval between colonoscopies. JAMA 295(20):<br />
2366–73.<br />
St John DJ, Young GP, McHutchison JG, Deacon MC & Alexeyeff MA 1992. Comparison of the specificity and<br />
sensitivity of Hemoccult and HemoQuant in screening for colorectal neoplasia. Ann Intern Med 117: 376–82.<br />
Tong S, Hughes K, Oldenburg B & Del Mar C 2004. Would general practitioners support a population-based<br />
colorectal cancer screening programme of faecal-occult blood testing? Intern Med J 34(9–10): 532–8.<br />
Towler B, Irwig L, Glasziou P, Weller D & Silagy C 1998. A systematic review of the effects of screening for<br />
colorectal cancer using the faecal occult blood test, Hemoccult. BMJ 317: 559–65.<br />
Turner GB, Chin MW, Foster NM, Emery J & Forbes GM 2006. Attitudes of Western Australian general<br />
practitioners to colorectal cancer screening. Med J Aust 185(4): 237.<br />
UK Flexible Sigmoidoscopy Screening Trial Investigators (UKSSTI) 2002. Single flexible sigmoidoscopy<br />
screening to prevent colorectal cancer: baseline findings of a UK multicentre randomised trial. Lancet<br />
359(9314): 1291–300.<br />
US Preventive Services Task Force (USPSTF) 2002. Screening for colorectal cancer: recommendation and<br />
rationale. Ann Intern Med 137(2): 129–31.<br />
Valery PC, Coory M, Stirling J & Green AC 2006. <strong>Cancer</strong> diagnosis, treatment, and survival in Indigenous and<br />
non-Indigenous Australians: a matched cohort study. Lancet 367(9525): 1842–8.<br />
Van Dam J, Cotton P, Johnson CD, McFarland BG, Pineau BC, Provenzale D, Ransohoff D, Rex D, Rockey D &<br />
Wootton FT III 2004. AGA future trends report: CT colonography. Gastroenterology 127(3): 970–84.<br />
Viiala CH, Zimmerman M, Cullen DJ & Hoffman NE 2003. Complication rates of colonoscopy in an Australian<br />
teaching hospital environment. Intern Med J 33(8): 355–9.<br />
Wardle J, Miles A & Atkin W 2005. Gender differences in utilization of colorectal cancer screening. J Med<br />
Screen 12(1): 20–7.<br />
Wardle J, Taylor T, Sutton S & Atkin A 1999. Does publicity about cancer screening raise fear of cancer?<br />
Randomised trial of the psychological effect of information about cancer screening. BMJ 319(7216): 1037–8.<br />
Weil J, Colin-Jones D, Langman M, Lawson D, Logan R, Murphy M, Rawlins M, Vessey M & Wainwright P<br />
1995. Prophylactic aspirin and risk of peptic ulcer bleeding. BMJ 310(6983): 827–30.<br />
Weissfeld JL, Schoen RE, Pinsky PF, Bresalier RS, Church T, Yurgalevitch S, Austin JH, Prorok PC & Gohagan<br />
JK 2005. Flexible sigmoidoscopy in the PLCO cancer screening trial: results from the baseline screening<br />
examination of a randomized trial. J Natl <strong>Cancer</strong> Inst 97(13): 989–97.<br />
Winawer SJ, Fletcher RH, Miller L, Godlee F, Stolar MH, Mulrow CD, Woolf SH, Glick SN, Ganiats TG, Bond<br />
JH, Rosen L, Zapka JG, Olsen SJ, Giardiello FM, Sisk JE, Van Antwerp R, Brown-Davis C, Marciniak DA &<br />
Mayer RJ 1997. Colorectal cancer screening: clinical guidelines and rationale. Gastroenterology 112: 594–642.<br />
Woolcott Research 2004. A qualitative evaluation of opinions, attitudes and behaviours influencing the Bowel<br />
<strong>Cancer</strong> Screening Pilot Program. Final report. Canberra: Australian Government Department of Health and<br />
Ageing.<br />
World <strong>Cancer</strong> Research Fund (WCRF) & American Institute for <strong>Cancer</strong> Research (AICR) 1997. Summary: food<br />
nutrition and the prevention of cancer: a global perspective. Washington, DC: AICR.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
15<br />
B o w e l c a n c e r
Young GP, Macrae FA & St John DJB 1996. Clinical methods for early detection: basis, use, and evaluation. In<br />
<strong>Prevention</strong> and early detection of colorectal cancer, eds GP Young, P Rozen & B Levin. London: WB Saunders<br />
Company.<br />
Young GP, St John DJ, Winawer SJ & Rozen P 2002. Choice of fecal occult blood tests for colorectal cancer<br />
screening: recommendations based on performance characteristics in population studies: a WHO (World<br />
Health Organization) and OMED (World Organization for Digestive Endoscopy) report. Am J Gastroenterol<br />
97(10): 2499–507.<br />
1 0 Section Two: Screening to detect cancer early
M e l a n o m a<br />
Melanoma in Australia<br />
Currently there is no conclusive scientific evidence<br />
that population screening for melanoma reduces<br />
mortality from this disease.<br />
Australia has the highest incidence of melanoma in the world. In 2005, an estimated<br />
10,014 Australians (5705 men and 4309 women) were diagnosed with melanoma.<br />
Excluding non-melanoma skin cancer, melanoma was the third most common cancer<br />
diagnosed in Australian women (after breast and colorectal cancer), and the third most<br />
common in Australian men (after prostate and colorectal cancer) in 2005. In 2005 there<br />
were 862 deaths from melanoma in men and 411 in women (ABS 2007).<br />
Can melanoma be prevented?<br />
Melanoma is potentially almost totally preventable. Exposure to excess ultraviolet (UV)<br />
radiation is the major environmental factor in its development and one which is amenable<br />
to behavioural intervention. More information on prevention of melanoma is included in the<br />
chapter on ultraviolet radiation.<br />
Screening tests for melanoma<br />
The screening tests proposed for early detection of melanoma include total body skin<br />
examination by a health care professional or skin self-examination. Detection of a<br />
suspicious lesion constitutes a positive screening test for which further investigation is<br />
required. Melanoma is confirmed by skin biopsy (ACN & NHMRC 1999).<br />
Skin examination by a GP or specialist<br />
Although differences have been reported between the effectiveness of specialists and<br />
GPs in detecting malignant melanoma (Morrison, O’Loughlin & Powell 2001), a systematic<br />
review concluded that there was insufficient evidence to prove an overall difference (Chen<br />
et al. 2001). Nevertheless, a number of studies have indicated that the benign-to-malignant<br />
ratio of pigmented skin lesions is very high (around 30:1) in the general practice setting in<br />
Australia (Del Mar et al. 1994; Marks et al. 1997).<br />
The ability of GPs to conduct screening for melanoma is an important pre-condition for the<br />
introduction of a screening program, but little information is available on this. In a large trial<br />
of population screening in Queensland using whole-body skin examinations, 2.5% of all<br />
suspicious skin lesions detected by GPs were confirmed as melanoma giving an estimated<br />
specificity of 86.1% (Aitken et al. 2006). The melanomas detected during that screening<br />
program tended to be less advanced, similar to results found in other screening programs<br />
(Geller et al. 2003).<br />
Another factor to be considered in screening for melanoma is the proportion of the<br />
body examined. Melanoma is more likely than non-melanoma skin cancers to appear on<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1 1<br />
M e l a n o m a
sites of the body not normally exposed to the sun. One study estimated that detection<br />
of melanomas was six times more likely with a total body skin examination (Rigel et al.<br />
1986), but a smaller subsequent study found little advantage in total body examination<br />
(De Rooij et al. 1996). While screening of visible areas of the body has been demonstrated<br />
to be well accepted (Girgis et al. 1996), a total body skin examination raises the issue of<br />
embarrassment as a barrier to repeated screening. However, a recent study found that only<br />
8% of participants said that they agreed or strongly agreed that having a skin examination<br />
would be embarrassing (Janda et al. 2004).<br />
A critical issue in regards to screening by GPs or specialists is to determine the<br />
significance of including relatively new diagnostic techniques in the screening process.<br />
Dermoscopy (surface microscopy) is a well-researched technique that uses inexpensive<br />
hand-held surface microscopes allowing a significant increased melanoma diagnostic<br />
ability in a specialist setting (Kittler et al. 2002). It has also been shown to improve the<br />
sensitivity for melanoma diagnosis by 38% in a study using Australian GPs (Westerhoff,<br />
McCarthy & Menzies 2000). There have been a number of computer programs developed<br />
to analyse digitalised dermoscopy images. These have been widely promoted by the<br />
manufacturers for use in the general community. However, they are still in the research<br />
and development phase and there are no data as yet to show they are superior to a welltrained<br />
and experienced clinician using dermoscopy. Trials using dermoscopy and handheld<br />
digital monitoring devices within general practice are currently underway in Western<br />
Australia. Further research is required to determine their value in community screening for<br />
melanoma.<br />
Self-examination<br />
Studies have shown a tendency by subjects to under-report or demonstrate poor selfassessment<br />
of pigmented skin lesions (Borland, Marks & Noy 1992; Hanrahan et al. 1995),<br />
which may have significant ramifications for self-referral to screening (Eiser et al. 2000;<br />
Melia et al. 2000). Most studies examining detection of melanoma have found that the<br />
majority of melanomas are first detected by the patient (Koh et al. 1992; McPherson et<br />
al. 2006). However, in one of these studies only about 4% of patients who detected the<br />
melanoma themselves did so during a deliberate skin self-examination (McPherson et al.<br />
2006).<br />
Rationale for screening for melanoma<br />
Interest in screening for melanoma is based on the potential for detection and treatment of<br />
significantly thinner melanomas, since people in whom thinner melanomas are detected<br />
and excised experience a better outcome than those detected with more advanced<br />
disease.<br />
For non-melanoma skin cancer, early detection of squamous cell carcinoma can also<br />
reduce the rate of deaths if treated early, while for basal cell carcinomas for which the rates<br />
of death are much lower, the benefits of screening would relate to reductions in illness,<br />
costs and inconvenience (NHMRC 1997).<br />
This discussion will focus on screening in relation to melanoma.<br />
1 2 Section Two: Screening to detect cancer early
Would screening be of benefit at this stage?<br />
Despite no formalised screening program in Australia, mortality from melanoma in younger<br />
cohorts is improving. This may reflect either earlier presentation of tumours or increased<br />
detection of clinically irrelevant indolent melanomas (AIHW & AACR 2004).<br />
Existing community awareness is leading to successful screening and early detection<br />
both at the request of individuals and opportunistically from their health care providers.<br />
To reduce mortality further, an organised screening program would need to significantly<br />
enhance early diagnosis beyond what is currently being achieved.<br />
An additional concern relates to rapidly growing melanoma. A recent study suggests that<br />
one-third of melanomas grow rapidly (at 0.5 mm or more of tumour thickness per month)<br />
(Liu et al 2006). These are unlikely to be detected early at an annual screening program.<br />
Evidence is insufficient at present to recommend for or against routine screening for<br />
melanoma of the general asymptomatic population. This is consistent with the current<br />
position of the US Preventive Services Task Force (AHRQ 2005).<br />
Aims<br />
The <strong>Cancer</strong> Council’s aims are to:<br />
•<br />
•<br />
encourage research to determine the impact of new diagnostic technologies<br />
(dermoscopy and digital monitoring) in general practice<br />
encourage further research to determine whether screening for melanoma in Australia<br />
would reduce illness and death and whether implementation would be practical and<br />
acceptable to the community.<br />
References<br />
Melanoma<br />
Agency for Healthcare Research and Quality (AHRQ) 2005. Guide to clinical preventive services. AHRQ<br />
Publication no. 05-0570, June 2005. Rockville MD: AHRQ.<br />
Aitken JF, Janda M, Elwood M, Youl PH, Ring IT & Lowe JB 2006. Clinical outcomes from skin screening<br />
clinics within a community-based melanoma screening program. J Am Acad Dermatol 54(1): 105–14.<br />
Australian Bureau of Statistics (ABS) 2007. Causes of death, Australia 2005. Cat. no. 3303.0. Canberra: ABS.<br />
Australian <strong>Cancer</strong> Network (ACN) & <strong>National</strong> Health and Medical Research Council (NHMRC) 1999. Clinical<br />
practice guidelines for the management of cutaneous melanoma. Canberra: ACN.<br />
Australian Institute of Health and Welfare (AIHW) & Australasian Association of <strong>Cancer</strong> Registries (AACR)<br />
2004. <strong>Cancer</strong> in Australia 2001. AIHW cat. no. 23; AIHW <strong>Cancer</strong> Series no. 28. Canberra: AIHW.<br />
Borland R, Marks R & Noy S 1992. Public knowledge about characteristics of moles and melanomas. Aust J<br />
Public Health 16(4): 370–5.<br />
Chen SC, Bravata DM, Weil E & Olkin I 2001. A comparison of dermatologists’ and primary care physicians’<br />
accuracy in diagnosing melanoma: a systematic review. Arch Dermatol 137(12): 1627–34.<br />
De Rooij MJ, Rampen FH, Schouten LJ & Neumann HA 1996. Total skin examination during screening for<br />
malignant melanoma does not increase the detection rate. Br J Dermatol 135(1): 42–5.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1 3<br />
M e l a n o m a
Del Mar C, Green A, Cooney T, Cutbush K, Lawrie S & Adkins G 1994. Melanocytic lesions excised from the<br />
skin: what percentage are malignant? Aust J Public Health 18(2): 221–3.<br />
Eiser JR, Pendry L, Greaves CJ, Melia J, Harland C & Moss S 2000. Is targeted early detection for melanoma<br />
feasible? Self-assessment of risk and attitudes to screening. J Med Screen 7(4): 199–202.<br />
Geller AC, Zhang Z, Sober AJ, Halpern AC, Weinstock MA, Daniels S, Miller DR, Demierre MF, Brooks DR<br />
& Gilchrest BA 2003. The first 15 years of the American Academy of Dermatology skin cancer screening<br />
programs: 1985–1999. J Am Acad Dermatol 48(1): 34–41.<br />
Girgis A, Clarke P, Burton RC & Sanson-Fisher RW 1996. Screening for melanoma by primary health care<br />
physicians: a cost-effectiveness analysis. J Med Screen 3(1): 47–53.<br />
Hanrahan PF, Hersey P, Watson AB & Callaghan TM 1995. The effect of an educational brochure on<br />
knowledge and early detection of melanoma. Aust J Public Health 19: 270–4.<br />
Janda M, Elwood M, Ring IT, Firman DW, Lowe JB, Youl PH & Aitken JF 2004. Prevalence of skin screening<br />
by general practitioners in regional Queensland. Med J Aust 180(1): 10–15.<br />
Kittler H, Pehamberger H, Wolff K & Binder M 2002. Diagnostic accuracy of dermoscopy. Lancet Oncol 3(3):<br />
159–65.<br />
Koh HK, Miller DR, Geller AC, Clapp RW, Mercer MB & Lew RA 1992. Who discovers melanoma? J Am Acad<br />
Dermatol 26: 914–19.<br />
Liu W, Dowling JP, Murray WK, McArthur GA, Thompson JF, Wolfe R & Kelly JW 2006. Rate of growth in<br />
melanomas: characteristics and associations of rapidly growing melanomas. Arch Dermatol. 142: 1551–8.<br />
Marks R, Jolley D, McCormack C & Dorevitch AP 1997. Who removes pigmented skin lesions? J Am Acad<br />
Dermatol 36(5 Pt 1): 721–6.<br />
McPherson M, Elwood M, English DR, Baade PD, Youl PH & Aitken JF 2006. Presentation and detection of<br />
invasive melanoma in a high-risk population. J Am Acad Dermatol 54: 783–92.<br />
Melia J, Harland C, Moss S, Eiser JR & Pendry L 2000. Feasibility of targeted early detection for melanoma: a<br />
population-based screening study. Br J <strong>Cancer</strong> 82(9): 1605–9.<br />
Morrison A, O’Loughlin S & Powell FC 2001. Suspected skin malignancy: a comparison of diagnoses of<br />
family practitioners and dermatologists in 493 patients. Int J Dermatol 40(2): 104–7.<br />
<strong>National</strong> Health and Medical Research Council (NHMRC) 1997. Preventive interventions in primary health care:<br />
cardiovascular disease and cancer. Canberra: NHMRC.<br />
Rigel DS, Friedman RJ, Kopf AW, Weltman R, Prioleau PG, Safai B, Lebwohl MG, Eliezri Y, Torre DP & Binford<br />
RT, Jr. 1986. Importance of complete cutaneous examination for the detection of malignant melanoma. J Am<br />
Acad Dermatol 14(5 Pt 1): 857–60.<br />
Westerhoff K, McCarthy W & Menzies S 2000. Increase in the sensitivity for melanoma diagnosis by primary<br />
care physicians using skin surface microscopy. Br J Dermatol 143(5): 1016–20.<br />
1 4 Section Two: Screening to detect cancer early
P r o s t a t e c a n c e r<br />
<strong>Cancer</strong> of the prostate is a common and important<br />
health problem. Its early diagnosis and subsequent<br />
treatment present a dilemma for medical practitioners<br />
and consumers. Since advantages of testing and<br />
treatment are not clear-cut, individual men who<br />
decide to be tested for prostate cancer should be able<br />
to do so on the basis of informed consent, having<br />
access to full information about the potential benefits<br />
and risks associated with testing. Preliminary findings<br />
suggest that introduction of a national education<br />
program for general practitioners to improve decision-<br />
making relating to the use of prostate-specific antigen<br />
Prostate cancer in Australia<br />
testing would be cost-effective.<br />
In 2005, prostate cancer is projected to be the most common cancer (apart from nonmelanoma<br />
skin cancer) diagnosed in Australian men, with an estimated 12,529 new cases<br />
(AIHW, AACR, NCSG & McDermid 2005).<br />
Prostate cancer mainly affects men in older age groups. Over 85% of new cases and over<br />
96% of deaths occur in men over 60 years of age. It is rare in men under 45 years.<br />
Although the incidence of prostate cancer increases with age, the threat to life from<br />
prostate cancer decreases with age because the disease generally develops and<br />
progresses slowly. This means that men diagnosed with prostate cancer who are older<br />
than 75 years or have fewer than 10 years life expectancy are considered to be least at risk<br />
of dying of prostate cancer.<br />
Men who are diagnosed at an earlier age (e.g. in their 50s) are most at risk of dying from<br />
prostate cancer (Baade, Steginga et al. 2005). This is because it is probable that they will<br />
live long enough for their prostate cancer to progress to a life-threatening stage and are<br />
less likely to die from competing causes. It is also important to note that, irrespective of the<br />
risk it poses, a diagnosis of prostate cancer at any age can have a major impact on a man’s<br />
quality of life.<br />
The incidence of prostate cancer was relatively stable until 1989 but, between 1990 and<br />
1994, there was a dramatic rise in the number of new cases reported (AIHW & AACR<br />
2004). This has been attributed to increased detection of the disease due to many more<br />
investigations, particularly case-finding using PSA testing, which was introduced around<br />
1990 (see below). However, between 1994 and 1997 the age-standardised prostate cancer<br />
incidence rate fell by 30%. Since then, there has been little change between the 1998 and<br />
2005 rate, indicating that the surge-effect from the previously undetected cases has been<br />
accommodated and the practice of early detection has stabilised.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1 5<br />
P r o s t a t e c a n c e r
The mortality rate from prostate cancer, which is significantly lower than the incidence rate,<br />
decreased by 1.9% per annum between 1991 and 2005, when 2,946 deaths were reported<br />
(ABS 2007).<br />
The burden of prostate cancer is likely to increase with the ageing of the Australian<br />
population, and this has major public health and economic implications (Weller et al. 1998).<br />
Can prostate cancer be prevented?<br />
The causes of prostate cancer are poorly understood. Geographical and racial differences<br />
in rates of prostate cancer provide compelling evidence that environmental and lifestyle<br />
factors are involved (Weller et al. 1998). Age and family history are the strongest risk<br />
factors in Australia. Researchers continue to examine other possible risk factors, including<br />
diet, weight and physical activity. An effective approach to primary prevention of prostate<br />
cancer has not yet been identified (Harris & Lohr 2002).<br />
Chemoprevention is being investigated but is not in routine use. A trial examining selenium<br />
and vitamin E (The SELECT trial) is in progress, with results not anticipated until 2013<br />
(Klein 2004). An analysis of the screening arm of the prostate, lung, colorectal and ovarian<br />
(PLCO) cancer trial does not show a benefit for supplementation with the micronutrient<br />
antioxidants vitamin E, beta-carotene and vitamin C (Kirsh et al. 2006).<br />
An Australian review noted that there is little evidence that could define risk groups<br />
sufficiently for targeted screening activities (Weller et al. 1998). One possible exception<br />
is men with a strong family history of prostate cancer. Men with a first-degree relative<br />
diagnosed with prostate cancer have a two-and-a-half times greater risk of being<br />
diagnosed, with some evidence that the risk is higher if the relative was diagnosed before<br />
the age of 60 years (Johns & Houlston 2003). The genetic basis has not been identified,<br />
though men carrying mutations of the breast cancer susceptibility genes BRCA1 or BRCA2<br />
gene have an increased risk of several types of cancer, including prostate cancer (Liede et<br />
al. 2000). The questions of whether, when and how often such people should be monitored<br />
have yet to be addressed.<br />
Tests for prostate cancer<br />
Prostate-specific antigen test<br />
The prostate-specific antigen (PSA) test is commonly used to try to detect prostate cancer.<br />
It measures the amount of PSA in blood.<br />
PSA levels can be raised due to a range of conditions. In studies of men aged 45 to 80<br />
years, 7% to 13% had a PSA level greater than 4 ng/ml; of these, 10% to 30% were<br />
identified as having prostate cancer on biopsy (USPSTF 2005). The level of PSA used to<br />
justify biopsy is commonly set at 4 ng/ml. Some have advocated a cut-off of 2.5 ng/ml<br />
(Punglia et al. 2003), since it is estimated that 25% to 30% of prostate cancers are detected<br />
with a PSA between 2.5 and 4 ng/ml (Pepe et al. 2006). However, increased sensitivity<br />
by use of a lower level will decrease specificity, leading to a higher rate of unnecessary<br />
biopsies and an increase in over-diagnosis (see below).<br />
Accuracy may be improved by taking into account a man’s age, since PSA levels increase<br />
with age due to benign enlargement of the prostate. It may also be improved by measuring<br />
the proportion of free to total or complexed PSA, since men with prostate cancer tend to<br />
1 Section Two: Screening to detect cancer early
have lower levels of free PSA than men who don’ t have prostate cancer. However, there is<br />
no consensus yet on either of these measurements (Harris & Lohr 2002; Stenman 1997).<br />
Digital rectal examination<br />
Another form of testing is digital rectal examination. This test involves manual examination<br />
of the prostate gland through the rectum. Some abnormalities may be felt but it is not<br />
possible to feel all of the prostate. A cancer that is in a part of the prostate gland out of the<br />
doctor’ s reach—estimated to be 25% to 35% of the prostate—may be missed (USPSTF<br />
2005). In addition, small (stage A or T1) cancers cannot be felt. Wide variations in reporting<br />
occur between doctors (AHTAC 1996).<br />
Transrectal ultrasound and biopsy<br />
Neither the PSA test nor DRE, alone or together, is a truly accurate test for prostate cancer.<br />
If abnormalities are detected by a PSA test or DRE, tissue specimens will be needed for<br />
diagnosis, usually via transrectal ultrasound (TRUS) imaging to permit spatial positioning of<br />
biopsy needles. The needle biopsy procedure involves eight to 10 or more cores of tissue<br />
being removed for examination under a microscope. Even though tissue is taken from a<br />
number of locations, and most malignant cancers will be detected, it is not possible to say<br />
with complete certainty that a negative result excludes the presence of cancer. The test<br />
carries risks of infection and bleeding (AHTAC 1996).<br />
Test limitations and implications<br />
The sensitivity and specificity of the screening tests available for prostate cancer cannot be<br />
determined with certainty (i.e. confirmed by pathology tests on tissue samples) because<br />
biopsies are generally not done on people with negative screening tests (USPSTF 2005).<br />
Only the positive predictive value—the probability of cancer when the test is positive—can<br />
be calculated with any confidence, but this also is subject to methodological difficulties<br />
from the needle biopsy (USPSTF 2005).<br />
A recent study where 2950 men with ‘normal’ PSA values (
Participants in the ERSPC trial completed a questionnaire on health before screening and<br />
then twice subsequently if they were diagnosed with prostate cancer. Mental and self-rated<br />
overall health worsened significantly immediately after diagnosis (P
•<br />
•<br />
a monitoring mechanism be put in place to ensure that the Australian Health Technology<br />
Advisory Committee position on screening is reviewed when significant developments<br />
occur<br />
a comprehensive education program on the risks and benefits of prostate cancer testing<br />
be introduced for GPs, their patients and the community.<br />
The <strong>Cancer</strong> Council Australia and state and territory cancer councils were active in the<br />
establishment in 1998 of the <strong>National</strong> Prostate <strong>Cancer</strong> Collaboration to foster clinical,<br />
laboratory and epidemiological research, as well as research and programs in education. In<br />
1999 the group became the Australian Prostate <strong>Cancer</strong> Collaboration. Its aim is to develop<br />
strategies for the control of prostate cancer to decrease mortality and increase quality of<br />
life.<br />
The role of general practice<br />
Recent reports suggest that GPs are poorly resourced to assist their patients making an<br />
informed choice on prostate cancer testing. Only half or less of the GPs who responded<br />
to a survey were aware of guidelines published by the Royal Australasian College of<br />
General Practitioners and The <strong>Cancer</strong> Council Australia—both of which recommend against<br />
population screening (Ward, Young & Sladden 1998).<br />
A meeting about informed choice for prostate cancer testing in general practice (Pinnock<br />
2004) reported that:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
studies on how patients make medical decisions indicate that non-systematic factors<br />
such as old beliefs, anecdotes and salient experiences are more common than a<br />
systematic weighing up of pros and cons (see also Farrell, Murphy & Schneider 2002;<br />
Steginga et al. 2002)<br />
testing is often requested for medico-legal reasons. The process and content of an<br />
informed choice discussion needs to reflect medico-legal obligations<br />
criteria have been developed to assess which decision aids are likely to be most<br />
effective in helping patients become informed and make decisions<br />
the barriers GPs face in fully informing patients with diverse backgrounds and<br />
knowledge need to be better understood<br />
particular skills are needed in order to communicate complex issues such as uncertainty<br />
and risk to patients<br />
complicating factors are men’s lack of access to primary care services, particularly<br />
in rural areas, poor general knowledge of male health in the community and high<br />
prevalence of anxiety about urinary symptoms.<br />
Preliminary findings suggest that the introduction of a national education program for<br />
GPs to improve decision-making relating to the use of PSA testing would be cost effective<br />
(Stone et al. 2005). Evaluations of the GP education workshops have shown that as<br />
participants’ knowledge about PSA testing and level of understanding increased, they were<br />
more likely to initiate discussions with patients about the risks and benefits of testing, and<br />
they were more confident in doing so (Metcalfe et al. 2006; Steginga et al. 2005).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1<br />
P r o s t a t e c a n c e r
Potential benefits and adverse effects of prostate<br />
cancer screening<br />
Refer to the introduction to Section Two for the World Health Organization criteria that<br />
need to be satisfied before population screening for a disease may be introduced. Central<br />
to this is the need for evidence that screening for the disease, with subsequent early<br />
treatment, is effective in improving health outcomes. In relation to prostate cancer, the<br />
question is whether detection of tumours using currently available tests will result in<br />
benefits for most patients.<br />
The difficulty regarding early detection of prostate cancer is that first, depending on the<br />
age of the patient, many cancers found through screening will not be life threatening.<br />
Second, it is currently not possible to distinguish with certainty those cancers that will be<br />
life threatening. It has been estimated that prostate cancer is present in 30% to 40% of<br />
men aged more than 50 years, but only one in four of these cancers will result in clinical<br />
symptoms and one in 14 will cause death (Weller et al. 1998).<br />
Would population screening be of benefit at this stage?<br />
The current state of knowledge does not satisfy the World Health Organization criterion<br />
that there should be an accepted treatment for patients with recognised disease. It is<br />
possible that intervention through early detection will cause more harm than good, for<br />
example in the risks posed by treatment (see below).<br />
The problem of over-diagnosis<br />
A major concern with screening is that it will diagnose cancers which, if left undetected,<br />
would never have caused morbidity or mortality. This is known as over-diagnosis. One<br />
estimate using mathematical modelling puts the over-diagnosis rate as high as 50%<br />
(Draisma et al. 2003). It has been estimated that most prostate cancer detected by<br />
commonly promoted testing strategies would not have caused morbidity or mortality<br />
(McGregor et al. 1998; Draisma et al. 2003). Over-diagnosis results in unnecessary<br />
treatment with high risks of urinary incontinence, bowel problems (especially following<br />
radiation) and erectile dysfunction (Begg et al. 2002).<br />
Prostate cancer treatment issues<br />
The major treatment options following detection of prostate cancer are active treatment<br />
(surgical removal of the prostate or radiation therapy) or observational treatment (watchful<br />
waiting) (AHTAC 1996).<br />
Our knowledge of which prostate cancers are life threatening and which are not is limited.<br />
In the European Randomised study of screening for prostate cancer, the patients in the<br />
Rotterdam section were screened by PSA, DRE and transrectal ultrasound. A subset of<br />
patients who would have qualified for a surveillance program were identified: those with<br />
a Gleason score less than or equal to 3+3, PSA density less than 0.2 and a maximum PSA<br />
level of 15 ng/ml. Those who met the above arbitrary criteria who chose watchful waiting<br />
did not do worse than those who had active treatment at a mean follow-up to 80.8 months<br />
(Roemeling et al. 2006).<br />
Limitations of studies comparing the effectiveness of treatments occur because most<br />
information on treatment by surgical removal of the prostate comes from uncontrolled<br />
case series and cohort studies that indicate survival following surgery is high. However,<br />
1 0 Section Two: Screening to detect cancer early
ecause surgical patients are usually younger and have less advanced disease, it is difficult<br />
to separate out the effects of treatment efficacy and selection bias.<br />
In practice there is a wide variation in treatment decisions. Treatments for early prostate<br />
cancer differ in the proportion of patients who are likely to experience side effects such as<br />
erectile problems, incontinence and bowel symptoms.<br />
Current clinical practice supports active intervention, particularly among men whose life<br />
expectancy exceeds 10 years with aggressive and early onset of disease.<br />
Randomised controlled trials comparing options are difficult to conduct, but a recent study<br />
compared watchful waiting with immediate radical prostatectomy in 695 men with newly<br />
diagnosed early stage prostate cancer. Prostatectomy led to a significant reduction in<br />
both metastatic disease and disease-specific mortality, and, after eight to 10 years, overall<br />
mortality (Holmberg et al. 2002; Bill-Axelson et al. 2005).<br />
Radiation therapy is widely practised in Australia, particularly among older patients and<br />
those with more aggressive or later stage (high-risk) cancers. Newer techniques, delivering<br />
radiation therapy aimed at increasing the radiation dose while minimising effects on<br />
adjacent tissues, are becoming increasingly available. An analysis of 60,290 men with low<br />
and moderate grade organ-confined prostate cancer, on the <strong>National</strong> <strong>Cancer</strong> Institute’s<br />
Surveillance, Epidemiology and End Results (SEER) Program showed better survival for<br />
men under and over 60 years if they received surgery or brachytherapy rather no definitive<br />
treatment (Tward et al 2006).<br />
Because it has not been possible to prove definitively that treatments differ in effectiveness<br />
(NHMRC 2003), the incorporation of patient preference into treatment decisions is widely<br />
endorsed (Weller et al. 1998; NHMRC & ACN 2003).<br />
Aims<br />
The <strong>Cancer</strong> Council Australia supports:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
advocating for and contributing expert advice to the development of decision-making<br />
tools for informed choice about prostate cancer testing, for medical practitioners and<br />
consumers, based on the best available evidence<br />
contributing to the development and implementation of community education relating<br />
to the prostate and prostate cancer<br />
monitoring and supporting research on population screening and testing for prostate<br />
cancer to inform the development of policy and communication strategies<br />
seeking opportunities to work with health related agencies, health professionals and<br />
consumers to increase understanding of the prostate and prostate cancer<br />
addressing the issues which cause inequities in access and outcomes in prostate<br />
cancer, such as living in rural and remote Australia, by developing models where<br />
information and multidisciplinary care can be accessed by those groups.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1 1<br />
P r o s t a t e c a n c e r
References<br />
Prostate cancer<br />
Australian Bureau of Statistics (ABS) 2007. Causes of death, Australia 2005. Cat. no. 3303.0. Canberra: ABS.<br />
Australian Health Technology Advisory Committee (AHTAC) 1996. Prostate cancer screening: summary of<br />
the review prepared by the Australian Health Technology Advisory Committee. Canberra: Commonwealth<br />
Department of Health and Family Services.<br />
Australian Institute of Health and Welfare (AIHW) 2006. Australia’s health 2006. AIHW cat. no. AUS 73.<br />
Canberra: AIHW.<br />
Australian Institute of Health and Welfare (AIHW) & Australasian Association of <strong>Cancer</strong> Registries (AACR)<br />
2004. <strong>Cancer</strong> in Australia 2001. AIHW cat. no. 23; AIHW <strong>Cancer</strong> Series no. 28. Canberra: AIHW.<br />
Australian Institute of Health and Welfare (AIHW), Australasian Association of <strong>Cancer</strong> Registries (AACR),<br />
<strong>National</strong> <strong>Cancer</strong> Strategies Group (NCSG) & McDermid I 2005. <strong>Cancer</strong> incidence projections Australia, 2002 to<br />
2011. Canberra: AIHW.<br />
Baade PD, Steginga SK, et al. 2005. Communicating prostate cancer risk: what should we be telling our<br />
patients. Med J Aust 182: 472–5.<br />
Bangma CH, Kranse R, Blijenberg BG & Schroder FH 1995. The value of screening tests in the detection<br />
of prostate cancer. Part II: Retrospective analysis of free/total prostate-specific analysis ratio, age-specific<br />
reference ranges, and PSA density. Urology 46(6): 779–84.<br />
Begg CB, Riedel ER, Bach PB, Kattan MW, Schrag D, Warren JL & Scardino PT 2002. Variations in morbidity<br />
after radical prostatectomy. N Engl J Med 346(15): 1138–44.<br />
Bill–Axelson A, Holmberg L, Ruutu M, Haggman M, Andersson S-O, Bratell S, Spangberg A, Busch C,<br />
Nording S, Garmo H, Palmgren J, Adami H-O, Norlen BJ & Johansson J-E 2005. Radical prostatectomy<br />
versus watchful waiting in early prostate cancer. N Engl J Med 352(19): 1977–84.<br />
Ciatto S, Bonardi R, Lombardi C, Cappelli G, Castagnoli A, D’Agata A, Zappa M & Gervasi G 2001. Predicting<br />
prostate biopsy outcome by findings at digital rectal examination, transrectal ultrasonography, PSA, PSA<br />
density and free-to-total PSA ratio in a population-based screening setting. Int J Biol Markers 16(3): 179–82.<br />
Coory MD & Baade PD 2005. Urban–rural differences in prostate cancer mortality, radical prostatectomy and<br />
prostate-specific antigen testing in Australia. Med J Aust 182(3): 112–15.<br />
Draisma G, Boer R, Otto SJ, Cruijsen van der I, Damhuis RA, Schroder FH & de Koning HJ 2003. Lead times<br />
and overdetection due to prostate-specific antigen screening: estimates from the European Randomized<br />
Study of Screening for Prostate <strong>Cancer</strong>. J Natl <strong>Cancer</strong> Inst 95(12): 868–78.<br />
Farrell MH, Murphy MA & Schneider CE 2002. How underlying patient beliefs can affect physician–patient<br />
communication about prostate-specific antigen testing. Eff Clin Pract 5(3): 120–9.<br />
Gattellari M & Ward JE 2005. Men’s reactions to disclosed and undisclosed opportunistic PSA screening for<br />
prostate cancer. Med J Aust 182(8): 386–9.<br />
Harris R & Lohr KN 2002. Screening for prostate cancer: an update of the evidence for the US Preventive<br />
Services Task Force. Ann Intern Med 137(11): 917–29.<br />
Holmberg L, Bill-Axelson A, Helgesen F, Salo JO, Folmerz P, Haggman M, Andersson SO, Spangberg A,<br />
Busch C, Nordling S, Palmgren J, Adami HO, Johansson JE, Norlen BJ & The Scandinavian Prostatic <strong>Cancer</strong><br />
Group Study Number 4 2002. A randomized trial comparing radical prostatectomy with watchful waiting in<br />
early prostate cancer. N Engl J Med 347(11): 781–9.<br />
Johns LE & Houlston RS 2003. A systematic review and meta-analysis of familial prostate cancer risk. BJU Int<br />
91(9): 789–94.<br />
Kirsh VA, Hayes RB, Mayne ST, Chatterjee N, Subar AF, Dixon LB, Albanes D, Andriole GL, Urban DA & Peters<br />
U 2006. Supplemental and dietary vitamin E, beta-carotene, and vitamin C intakes and prostate cancer risk. J<br />
Natl <strong>Cancer</strong> Inst 98(4): 245–54.<br />
1 2 Section Two: Screening to detect cancer early
Klein EA 2004. Selenium and vitamin E cancer prevention trial. Ann N Y Acad Sci 1031: 234–41.<br />
Korfage IJ, de Koning HJ, Roobol M, Schroder FH & Essink-Bot ML 2006. Prostate cancer diagnosis: the<br />
impact on patients’ mental health. Eur J <strong>Cancer</strong> 42(2): 165–170.<br />
Kupelian P, Kuban D, Thames H, Levy L, Horwitz E, Martinez A, Michalski J, Pisansky T, Sandler H, Shipley W,<br />
Zelefsky M & Zietman A 2005. Improved biochemical relapse-free survival with increased external radiation<br />
doses in patients with localized prostate cancer: the combined experience of nine institutions in patients<br />
treated in 1994 and 1995. Int J Radiat Oncol Biol Phys 61(2): 415–19.<br />
Liede A, Metcalfe K, Hanna D, Hoodfar E, Snyder C, Durham C, Lynch HT & Narod SA 2000. Evaluation of<br />
the needs of male carriers of mutations in BRCA1 or BRCA2 who have undergone genetic counseling. Am J<br />
Hum Genet 67(6): 1494–504.<br />
Luo LY, Shan SJ, Elliott MB, Soosaipillai A & Diamandis EP 2006. Purification and characterization of human<br />
kallikrein 11, a candidate prostate and ovarian cancer biomarker, from seminal plasma. Clin <strong>Cancer</strong> Res 12(3<br />
Pt 1): 742–50.<br />
McGregor M, Hanley JA, Boivin JF & McLean RG 1998. Screening for prostate cancer: estimating the<br />
magnitude of overdetection. Can Med Assoc J 159(11): 1368–72.<br />
Metcalfe R, Russell R, McAvoy B, Tse J, Sutherland G & Hoey L 2006. Promoting shared decision making and<br />
informed choice for the early detection of prostate cancer: Development and evaluation of a GP education<br />
program. <strong>Cancer</strong> Forum 30(1): 38–42.<br />
<strong>National</strong> Health and Medical Research Council (NHMRC) & Australian <strong>Cancer</strong> Network (ACN) 2003. Clinical<br />
practice guidelines: evidence–based information and recommendations for the management of localised<br />
prostate cancer. Canberra: NHMRC.<br />
Pepe P, Panella P, D’Arrigo L, Savoca F, Pennisi M & Aragona F 2006. Should men with serum prostatespecific<br />
antigen < or =4 ng/ml and normal digital rectal examination undergo a prostate biopsy? A literature<br />
review. Oncology 70(2): 81–9.<br />
Pinnock CB 2004. PSA testing in general practice: can we do more now? Med J Aust 180(8): 379–81.<br />
Pinnock CB, Weller DP & Marshall VR 1998. Self-reported prevalence of prostate-specific antigen testing in<br />
South Australia: a community study. Med J Aust 169(1): 25–8.<br />
Potosky AL, Davis WW, Hoffman RM, Stanford JL, Stephenson RA, Penson DF & Harlan LC 2004. Five-year<br />
outcomes after prostatectomy or radiotherapy for prostate cancer: the prostate cancer outcomes study. J<br />
Natl <strong>Cancer</strong> Inst 96(18): 1358–67.<br />
Punglia RS, D’Amico AV, Catalona WJ, Roehl KA & Kuntz KM 2003. Effect of verification bias on screening<br />
for prostate cancer by measurement of prostate-specific antigen. N Engl J Med 349(4): 335–42.<br />
Roemeling S, Roobol MJ, Postma R, Gosselaar C, van der Kwast TH, Bangma CH & Schroder FH 2006.<br />
Management and survival of screen-detected prostate cancer patients who might have been suitable for<br />
active surveillance. Eur Urol 50(3): 475–82.<br />
Schroder FH, Kranse R, Rietbergen J, Hoedemaeke R & Kirkels W 1999. The European Randomized Study<br />
of Screening for Prostate <strong>Cancer</strong> (ERSPC): an update. Members of the ERSPC, Section Rotterdam. Eur Urol<br />
35(5–6): 539–43.<br />
Selley S, Donovan J, Faulkner A, Coast J & Gillatt D 1997. Diagnosis, management and screening of early<br />
localised prostate cancer. Health Technol Assess 1(2): 1–96.<br />
Smith DP & Armstrong BK 1998. Prostate-specific antigen testing in Australia and association with prostate<br />
cancer incidence in New South Wales. Med J Aust 169(1): 17–20.<br />
Steginga SK, Occhipinti S, Gardiner RA, Yaxley J & Heathcote P 2002. Making decisions about treatment for<br />
localized prostate cancer. BJU Int 89(3): 255–60.<br />
Steginga SK, Pinnock C, Baade PD, Jackson C, Green A, Preston J, Heathcote P & McAvoy B 2005. An<br />
educational workshop on the early detection of prostate cancer. Aust Fam Physician 34(10): 889–91.<br />
Stenman UH 1997. Prostate-specific antigen, clinical use and staging: an overview. Br J Urol 79 (1 Suppl):<br />
S53–60.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1 3<br />
P r o s t a t e c a n c e r
Stone CA, May FW, Pinnock CB, Elwood M & Rowett DS 2005. Prostate cancer, the PSA test and academic<br />
detailing in Australian general practice: an economic evaluation. Aust N Z J Public Health 29: 349–57.<br />
Thompson IM, Pauler DK, Goodman PJ, Tangen CM, Lucia MS, Parnes HL, Minasian LM, Ford LG, Lippman<br />
SM, Crawford ED, Crowley JJ & Coltman CA Jr 2004. Prevalence of prostate cancer among men with a<br />
prostate-specific antigen level < or =4.0 ng per milliliter. N Engl J Med 350(22): 2239–46.<br />
Tward JD, Lee CM, Pappas LM, Szabo A, Gaffney DK & Shrieve DC 2006. Survival of men with clinically<br />
localized prostate cancer treated with prostatectomy, brachytherapy, or no definitive treatment: impact of age<br />
at diagnosis. <strong>Cancer</strong> 107(10): 2392–400.<br />
US Preventive Services Task Force (USPSTF) 2005. The guide to clinical preventive services 2005. Washington:<br />
Agency for Healthcare Research and Quality.<br />
Ward J, Young J & Sladden M 1998. Australian general practitioners’ views and use of tests to detect early<br />
prostate cancer. Aust N Z J Public Health 22: 374–80.<br />
Ward JE, Hughes AM, Hirst GH & Winchester L 1997. Men’s estimates of prostate cancer risk and selfreported<br />
rates of screening. Med J Aust 167(5): 250–3.<br />
Weller D, Pinnock C, Aldeman C, Moss J & Doust J 1998. Screening for prostate cancer: update of the 1996<br />
AHTAC report. Unpublished document on behalf of the Australian <strong>Cancer</strong> Network. Adelaide: Department of<br />
Evidence-based Care and General Practice, Flinders University of South Australia.<br />
1 4 Section Two: Screening to detect cancer early
Section Three:<br />
Immunisation<br />
www.cancer.org.au
H u m a n p a p i l l o m a v i r u s<br />
HPV<br />
1 Section Three: Immunisation<br />
Prophylactic vaccination against human papilloma<br />
virus (HPV) 16/18 has the potential to prevent up<br />
to 70% of cervical cancers. The <strong>National</strong> Cervical<br />
Screening Program has been effective at reducing<br />
cervical cancer incidence and mortality, and the<br />
vaccine offers the potential to further decrease the<br />
incidence of and mortality from this disease.<br />
Species specific papilloma viruses infect a range of animals including humans. Over 100<br />
different types of HPV have been identified. The majority of HPV types infect only epithelial<br />
cells of the skin and mucosa. Most produce no evident disease. Some HPV types have<br />
been associated with anogenital and aerodigestive diseases (Baseman & Koutsky 2005).<br />
Some produce proliferative lesions (warts) of skin and genital skin, and these tend to be<br />
grouped as low and high risk based on their potential to cause malignancy.<br />
There are in excess of 40 anogenital HPV types, about 15 of which are oncogenic (high<br />
risk) (Schiffman & Kjaer 2003). Anogenital HPVs are the most common sexually transmitted<br />
infections.<br />
Transmission<br />
Genital HPVs are primarily transmitted through sexual contact (genital-genital or genital<br />
anal), though this need not include penetrative sexual intercourse. Other modes of<br />
transmission, including perinatal, digital, oral and autoinoculation, are less common<br />
(IARC 1995). HPV infections are thought to be established in the basal epithelium through<br />
abrasion or microtrauma of the superficial epithelium (Lowy & Schiller 2006). In sexually<br />
active adults acquisition of HPV is common. Prevalence among sexually active young<br />
women is high at around 20% to 25% (Ho et al 1998). Repeated testing of teenagers over a<br />
three-year period has documented a cumulative prevalence rate of 44% (95% CI, 40 to 48)<br />
(Woodman et al 2001). Infection may be with one or more HPV subtypes and these may<br />
change over time (NHMRC 2005).<br />
The link between HPV infection and cancer<br />
HPV infections can induce the development of either benign or malignant lesions. Benign<br />
lesions include non-genital and anogenital skin warts, oral and laryngeal papillomas<br />
and anogenital mucosal condylomata (Lowy & Schiller 2006). Persistent infection with<br />
high-risk HPVs are generally subclinical, but can result in the development of a range of<br />
anogenital tumours including cancers of the cervix, anus, penis, vulva and vagina (Lowy<br />
& Schiller 2006). It has been estimated that HPV infections are present in over 80% of<br />
anal cancers (Frisch et al. 1999, Daling et al. 2004), 40% of penile cancers, 40% of vulval<br />
and vaginal cancers, and nearly 100% of cervical cancers (Parkin 2006). An association of<br />
HPV infection with squamous cell carcinomas of the head and neck has been established<br />
and HPV infection is thought to contribute to 3% and 12% of cancers of the mouth and<br />
oro-pharynx respectively (Parkin 2006). The role of HPV infection in the development of
epithelial carcinomas of the bladder, oesophagus and lung is being studied (Persing &<br />
Prendergast 1999).<br />
The role of HPV infection in the aetiology of a range of anogenital and other cancers has<br />
been demonstrated. However, the HPV vaccines currently available have principally been<br />
tested for and aimed at reducing cervical cancer incidence. The following summary will<br />
focus on HPV infection and cervical cancer.<br />
HPV and cervical cancer<br />
The association between HPV and cervical cancer was not determined until the 1970s,<br />
and it wasn’t until the mid-1990s that the primary role of HPV in the development of<br />
cervical cancer was definitely confirmed (Eurogin 2003). Research has now distinguished<br />
between high-risk (oncogenic) and low-risk (non-oncogenic) types of HPV, and persistent<br />
infection with high-risk types of HPV is now recognised to be a necessary precursor to the<br />
development of cervical cancer (Nobbenhuis et al. 1999).<br />
Oncogenic and non-oncogenic HPVs cause low-grade squamous intraepithelial lesions<br />
(LSIL) of the cervix (Baseman & Koutsky 2005). It was believed that the development of<br />
cervical cancer involved progression from low to moderate to high-grade intraepithelial<br />
lesions (HSIL). However, natural history studies suggest that low and high-grade cervical<br />
lesions are distinct HPV processes (Baseman & Koutsky 2005). LSIL represent the transient<br />
appearance of viral infection where the HPV-infected epithelium undergoes differentiation<br />
and maturation and displays minor cellular abnormalities (Baseman & Koutsky 2005).<br />
Longitudinal studies were conducted in Brazil (Schlecht et al, 2003) and the Netherlands<br />
(Nobbenhuis et al. 2001) to examine the natural history of low grade cervical neoplasia.<br />
Schlecht et al. (2003) reported that, in the absence of intervention, only a minority of LSIL<br />
progressed to HSIL (mean progression time 86.4 months, 95% CI, 81.9 to 90.9), with the<br />
majority (78%) of LSIL regressing in less than one year (mean regression time 10.5 months,<br />
95% CI, 8.1 to 12.9). The regression rates reported by the Dutch (Nobbenhuis et al, 2001)<br />
were slightly lower, 37.2% (95% CI, 24.8 to 49.6) at 12 months, and 54.9% (95% CI, 41.9<br />
to 67.9) at 24 months, which probably reflects their stricter definition of regression (two<br />
negative follow-up Pap tests).<br />
HSIL occurs when HPV infects immature cells and prevents maturation and differentiation,<br />
resulting in the replication of immature cells and the accrual of genetic changes that can<br />
lead to cervical cancer (Baseman & Koutsky 2005). Cervical screening data shows the<br />
incidence of HSIL is 0.7% (VCCR 2005) and is most commonly found amongst women in<br />
their twenties, declining rapidly with age (NHMRC 2005). In an unscreened population, it<br />
is estimated that between one third and two thirds of women will develop cervical cancer<br />
after HSIL, although the time to development of cancer is variable. (Schiffman & Kjaer<br />
2003) The world age standardised incidence rate of cervical cancer is 26.9 per 100,000,<br />
peaking at age 54 years (Gustafsson et al. 1997).<br />
It is estimated that it takes an average of 10 years from HPV infection to malignant<br />
progression (Schiffman & Kjaer 2003). The steps involved in HPV-induced cervical<br />
carcinogenesis include HPV infection, HPV persistence, progression to precancer and<br />
invasion (Schiffman & Kjaer 2003). Most HPV infections are transient and clearance of<br />
HPV infection and regression of precancerous changes can occur (Schiffman & Kjaer<br />
2003). The majority of type-specific HPV infection clears within two years (Richardson et al.<br />
2003). The mean time for regression of precancerous changes is longer in women infected<br />
with high-risk HPV types (mean duration of regression 13.8 – 17.1 months) compared to<br />
low-risk HPV types (mean duration of regression 7.7 – 8.9 months) (Schlecht et al. 2003).<br />
Precancerous changes also persist longer and progress faster in women infected with<br />
high-risk HPVs (Schlecht et al. 2003), and those with HIV infection (Ferenczy et al. 2003).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1<br />
H u m a n p a p i l l o m a v i r u s
The impact<br />
About 70% of invasive cervical cancers are caused by HPV 16 and 18 (Munoz et al. 2003)<br />
and about 90% of genital warts are caused by HPV 6 or 11 (Von Krogh 2001).<br />
Cervical cancer is the second most common cancer, and the third most common cause of<br />
cancer deaths in women worldwide (Figure 3.1). Eighty per cent of cervical cancer cases<br />
occur in the developing world (Jones 1999).<br />
Figure 3.1 Female cancer incidence and mortality worldwide: leading sites of new cancer and cancer<br />
death 2002<br />
Breast<br />
Cervix uteri<br />
Colon and rectum<br />
Lung<br />
Stomach<br />
Ovary etc.<br />
Corpus uteri<br />
Liver<br />
Oesophagus<br />
Leukaemia<br />
Non-Hodgkin lymphoma<br />
Pancreas<br />
Thyroid<br />
Oral cavity<br />
Melanoma of skin<br />
Brain, nervous system<br />
Kidney etc.<br />
Bladder<br />
Multiple myeloma<br />
Nasopharynx<br />
Other pharynx<br />
Hodgkin lymphoma<br />
Larynx<br />
Mortality<br />
Incidence<br />
0 5 10 15 20 25 30 35 40<br />
Age-standardised rate per 100,000 women<br />
Source: Ferlay et al. 2004<br />
In 2005 in Australia, there were 610 estimated cases of cervical cancer (AIHW 2006)<br />
and there were 212 deaths in 2004 (AIHW 2005), making cervical cancer the 12th most<br />
common cause of cancer in women and 16th most common cause of cancer death (AIHW<br />
& AACR 2004). Approximately 80% of cervical cancers occur in less developed countries<br />
and this is largely attributable to the absence of organised population-based cervical cancer<br />
screening programs (Monsonego et al. 2004). HPV has been identified in 99.7% of cervical<br />
cancer specimens (Walboomers et al. 1999). The estimated lifetime risk for women of one<br />
or more genital HPV infection is 75%.<br />
Worldwide there are estimated to be 326 million adult women who are infected with HPV.<br />
In comparison, there are approximately 450,000 new cases of cervical cancer worldwide<br />
each year (Bosch 2000); thus, HPV is considered necessary but not sufficient for the<br />
development of cervical cancers.<br />
1 Section Three: Immunisation
The challenge<br />
Stigmatisation of cervical cancer as a sexually transmitted disease<br />
HPV is a sexually transmitted infection and most individuals become infected with HPV<br />
within two to five years of initiating sexual activity (Wright et al. 2006). Risk factors for HPV<br />
transmission include age at first sexual intercourse, age of the woman and her partner,<br />
the number of sexual partners and other surrogate indicators for the likelihood that a<br />
sexual partner is infected with HPV (Schlecht et al. 2003). Prophylactic vaccines must be<br />
administered to individuals prior to virus exposure. This ideally prevents the establishment<br />
of the HPV infection by eliminating the virus at the time of, or shortly after, exposure to<br />
HPV. This is achieved by stimulating the immune system to produce neutralising antibodies<br />
that bind to certain areas of the virus, preventing it from attaching to the host cell (Devaraj,<br />
Gillison & Wu 2003).<br />
Parents may be reluctant to involve their young daughters in a vaccination program<br />
that is linked to sexual activity. However, cervical cancer should be considered as a rare<br />
complication of oncogenic HPV infection rather than as a sexually transmitted disease.<br />
Overall, the impact of the HPV vaccines on cervical cancer will be influenced by uptake<br />
of the vaccine by the population. In turn, the uptake of the vaccines will be influenced by<br />
perceived benefits and risks. Therefore communication strategies with health professionals,<br />
parents, women and adolescents which are sensitive to culture, religion and age are<br />
required to support uptake of the HPV vaccine.<br />
Encouraging high levels of uptake in the indigenous community<br />
Immunisation should positively impact on under-screened groups and populations with<br />
a higher incidence of cervical cancer. In Australia, Aboriginal women are more than four<br />
times more likely to die of cervical cancer than other Australian women (AIHW 2006).<br />
This difference is in part due to lower participation of this group in the <strong>National</strong> Cervical<br />
Screening Program. Vaccinating Aboriginal girls and women should reduce the incidence<br />
and mortality from cervical cancer but this will require better understanding of their barriers<br />
to participation. Targeted efforts are required for this at-risk population.<br />
Confusion about the importance of continuing to screen<br />
Confusion about HPV vaccination and cervical screening may lessen compliance with<br />
cervical screening in the vaccinated population. The currently available vaccines target<br />
only two or four of the 40 HPV types infecting the anogenital tract, therefore effective<br />
communication strategies will be required to ensure women still participate in the <strong>National</strong><br />
Cervical Screening Program.<br />
The duration and scope of protection provided by the vaccine is unknown<br />
Current level 1 evidence supports the delivery of the vaccine to young women who have<br />
not yet commenced sexual activity and have therefore not yet been infected with the virus.<br />
The level of protection provided to older, sexually active women or boys is under evaluation<br />
in clinical trials (Kahn & Burk 2007). As this information becomes available, changes may<br />
need to be made to the delivery of the vaccine and the communication strategy.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1<br />
H u m a n p a p i l l o m a v i r u s
Effective interventions<br />
<strong>National</strong> Cervical Screening Program<br />
Between 1991 and 2002 the incidence of cervical cancer almost halved among women<br />
aged 20 to 69 (AIHW 2006) and the mortality from cervical cancer in Australia is among<br />
the lowest in the world. The decline in incidence and mortality, in part, is attributable to the<br />
success of the <strong>National</strong> Cervical Screening Program (see pages 138 to 144).<br />
Prophylactic vaccine<br />
Prophylactic vaccination against HPV 16/18 has the potential to prevent up to 70% of<br />
cervical cancers. While the <strong>National</strong> Cervical Screening Program has been effective at<br />
reducing cervical cancer incidence and mortality, the vaccine offers the potential to further<br />
decrease the incidence of and mortality from this disease. Internationally the greatest<br />
impact of the vaccine will be in countries without an organised screening program, in<br />
conditions of nutrient deficiency and where HIV is endemic (Gravitt & Shah 2005).<br />
Two HPV L1 VLP vaccines have been developed commercially. Cervarix is a bivalent HPV<br />
16/18 vaccine developed by GlaxoSmithKline. The vaccine is given as an intra-muscular<br />
injection in a three-step protocol at zero, one and six month intervals (Stanley, Lowy &<br />
Frazer 2006). Gardasil, developed by Merck and Co. Inc., is a quadrivalent HPV 16/18/6/11<br />
L1 VLP vaccine delivered by an intra-muscular injection at zero, two and six month<br />
intervals (Stanley, Lowy & Frazer 2006).<br />
Early studies have shown the HPV vaccines to be safe and well tolerated (Giles & Garland<br />
2006). Results demonstrate that both vaccines are effective at protecting against persistent<br />
cervical HPV 16/18 infection and associated disease (Stanley, Lowy & Frazer 2006). Trials<br />
have shown almost universal seroconversion in vaccinated subjects (Giles & Garland<br />
2006) and 100% efficacy for preventing persistent infection. The quadrivalent vaccine<br />
was shown to confer additional protection in women against HPV 6/11-induced mucosal<br />
and cutaneous genital disease (Stanley, Lowy & Frazer 2006). The vaccines have been<br />
shown to be safe and effective in preventing infection with HPV 16 and 18. The duration of<br />
protection conferred by the vaccine beyond five years is under evaluation in clinical trials<br />
(Kahn & Burk 2007).<br />
In the short term the impact of the HPV vaccines will be a reduction in cervical dysplasia.<br />
The long-term impact is a reduction in the incidence and mortality from cervical cancer.<br />
Taken together this translates to a reduction in treatment costs as well as psychological<br />
and medical morbidity (Lowy & Schiller 2006).<br />
The impact of the vaccine on other anogenital cancers and aero-digestive cancers is not<br />
presently known.<br />
The prophylactic vaccine and the development of therapeutic vaccines together with<br />
emerging new technologies in screening present the opportunity to progressively reduce<br />
HPV-associated malignancy and in doing so significantly decrease the burden of cervical<br />
cancer on the community (Roden & Wu 2003).<br />
Therapeutic vaccine<br />
Worldwide it is estimated that there are 100 million women infected with high-risk HPV<br />
types, and five million women have persistent infections which may result in anogenital<br />
cancers (Giles & Garland 2006).<br />
1 0 Section Three: Immunisation
The goals of a therapeutic vaccine could include: clearing an existing HPV infection,<br />
preventing the development and progression of lesions, and eliminating existing lesions<br />
and possibly cancers (Devaraj, Gillison & Wu 2003).<br />
When available, the impact of the therapeutic vaccine will include less invasive and<br />
disfiguring treatment options for women with pre-existing HPV lesions (Brinkman et al.<br />
2005), potentially lessening the treatment costs and psychosocial impact on women.<br />
However such vaccines are at least 10 years from market.<br />
The policy context<br />
In 2006 the Therapeutics Goods Administration approved the quadrivalent HPV vaccine<br />
Gardasil for use in women aged nine to 26 and males aged nine to 15 .<br />
Since April 2007, free HPV vaccination in Australia has been provided through schoolbased<br />
programs to girls aged between 12 and 18. From July 2007 until 30 June 2009, the<br />
HPV vaccine will be made available through general practitioners and other immunisation<br />
providers for females aged 12 to 18 who did not receive the vaccine through the schoolbased<br />
program. Females aged 18 to 26 are eligible to receive the free vaccine, however,<br />
the full course of three doses must be completed before the end of June 2009. Under the<br />
<strong>National</strong> HPV Vaccination Program the HPV vaccine is not funded for males and is not<br />
available as a PBS product.<br />
In 2007 the TGA approved the bivalent vaccine Cervarix for use in women aged 12 to 45<br />
– this vaccine is not available as part of the free vaccination program and is not available as<br />
a PBS product.<br />
Aims<br />
As the prophylactic HPV vaccine is made available in Australia there are a number of public<br />
health challenges which need to be addressed.<br />
What needs to be achieved How The <strong>Cancer</strong> Council Australia and its members (the state<br />
and territory cancer councils) will do this<br />
Maximised uptake of the<br />
prophylactic vaccine and effective<br />
communication<br />
Immunisation of populations with<br />
higher incidences and poorer<br />
outcomes<br />
Promote uptake of the vaccine and compliance with the<br />
vaccination schedule among adolescent girls and young women<br />
Devise a clear and culturally and age-sensitive communication<br />
strategy<br />
Communicate information about HPV in a way which meets the<br />
information needs of the public and health professionals<br />
Provide information in a culturally sensitive manner<br />
Focus on strategies to facilitate vaccination among Aboriginal<br />
women, who have a higher incidence of and mortality from cervical<br />
cancer than the rest of the Australian population, and recent<br />
immigrants from high prevalence countries.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1 1<br />
H u m a n p a p i l l o m a v i r u s
What needs to be achieved How The <strong>Cancer</strong> Council Australia and its members (the state<br />
and territory cancer councils) will do this<br />
Ensure that the <strong>National</strong> Cervical<br />
Screening Program continues to<br />
have high participation by relevant<br />
women<br />
1 2 Section Three: Immunisation<br />
Communicate clearly about the role of cervical screening in<br />
vaccinated women, to limit confusion and prevent reduced<br />
compliance with screening<br />
Devise approaches to managing different screening schedules, if<br />
changes in the frequency of screening are indicated for vaccinated<br />
women<br />
Monitor and evaluate the program Set up data processes to capture and monitor vaccination data<br />
Match vaccination data with screening program data and state<br />
cancer registries<br />
Research on therapeutic vaccine Advocate for continued research on the application and effect of<br />
therapeutic vaccines on regression of lesions and cancers. Studies<br />
on the acceptability of a vaccine as treatment also need to be<br />
undertaken<br />
Further research Advocate for further research in:<br />
• vaccine efficacy and booster requirements<br />
• two versus three doses<br />
• epidemiology and vaccination of boys – issue of herd immunity<br />
• infant vaccination efficacy<br />
• adult vaccination efficacy<br />
• uptake and acceptability of the vaccine in non-English speaking<br />
communities<br />
• barriers to screening<br />
• most effective way of screening for cervical cancer in a<br />
vaccinated population<br />
• genotype replacement over time<br />
References<br />
Australian Institute of Health and Welfare (AIHW) 2006. Cervical screening in Australia<br />
2003–2004. AIHW cat. no. 28; <strong>Cancer</strong> Series no. 33. Canberra: AIHW.<br />
——— 2005. <strong>Cancer</strong>: cervical screening. At www.aihw.gov.au/cancer/screening/cervical/<br />
cervical.cfm viewed 5 September 2007.<br />
Australian Institute of Health and Welfare (AIHW) & Australasian Association of <strong>Cancer</strong><br />
Registries (AACR) 2004. <strong>Cancer</strong> in Australia 2001. AIHW cat. no. 23; AIHW <strong>Cancer</strong> Series<br />
no. 28. Canberra: AIHW.<br />
Baseman JG & Koutsky LA 2005. The epidemiology of human papillomavirus infections. J<br />
Clin Virol 32 (1 Suppl): S16–24.<br />
Bosch F 2000. Clinical cancer and HPV: a worldwide perspective. In Proceedings of the<br />
Fourth International Multidisciplinary Congress: Eurogin 2000. Bologna, Italy.
Brinkman JA, Caffrey AS, Muderspach LI, Roman LD & Kast WM 2005. The impact of<br />
anti HPV vaccination on cervical cancer incidence and HPV induced cervical lesions:<br />
consequences for clinical management. Eur J Gynaecol Oncol 26(2): 129–42.<br />
Daling JR, Madeleine MM, Johnson LG, Schwartz SM, Shera KA, Wurscher MA, Carter JJ,<br />
Porter PL, Galloway DA & McDougall JK 2004. Human papillomavirus, smoking, and sexual<br />
practices in the etiology of anal cancer. <strong>Cancer</strong> 101(2): 270-280.<br />
Devaraj K, Gillison ML & Wu TC 2003. Development of HPV vaccines for HPV-associated<br />
head and neck squamous cell carcinoma. Crit Rev Oral Biol Med 14(5): 345–62.<br />
Eurogin 2003. Conclusions: cervical cancer control, priorities and new directions.<br />
International charter. 1–22.<br />
Ferenczy A, Coutlee F, Franco E & Hankins C 2003. Human papillomavirus and HIV<br />
coinfection and the risk of neoplasias of the lower genital tract: a review of recent<br />
developments. CMAJ 169(5): 431-434.<br />
Ferlay J, Bray F, Pisani P & Parkin P 2004. Globocan 2002. <strong>Cancer</strong> incidence, mortality and<br />
prevalence worldwide. [IARC <strong>Cancer</strong>Base No. 5, version 2.0]. Lyon, IARCPress.<br />
Frazer IH 2004. <strong>Prevention</strong> of cervical cancer through papillomavirus vaccination. Nat Rev<br />
Immunol 4(1): 46–54.<br />
Frisch M, Fenger C, van den Brule AJ, Sorensen P, Meijer CJ, Walboomers JM, Adami HO,<br />
Melbye M & Glimelius B 1999. Variants of squamous cell carcinoma of the anal canal and<br />
perianal skin and their relation to human papillomaviruses. <strong>Cancer</strong> Res 59(3): 753-757.<br />
Garcia-Hernandez E, Gonzalez-Sanchez JL, Andrade-Manzano A, Contreras ML, Padilla S,<br />
Guzman CC, Jimenez R, Reyes L, Morosoli G, Verde ML & Rosales R 2006. Regression of<br />
papilloma high-grade lesions (CIN 2 and CIN 3) is stimulated by therapeutic vaccination<br />
with MVA E2 recombinant vaccine. <strong>Cancer</strong> Gene Ther 13(6): 592–7.<br />
Giles M & Garland S 2006. Human papillomavirus infection: an old disease, a new vaccine.<br />
Aust N Z J Obstet Gynaecol 46(3): 180–5.<br />
Gravitt PE & Shah KV 2005. A virus-based vaccine may prevent cervical cancer. Curr Infect<br />
Dis Rep 7(2): 125–31.<br />
Gustafsson L, Ponten J, Bergstrom R & Adami HO 1997. International incidence rates of<br />
invasive cervical cancer before cytological screening. Int J <strong>Cancer</strong> 71(2): 159-165.<br />
Ho GY, Bierman R, Beardsley L, Chang CJ and Burk RD 1998. Natural history of<br />
cervicovaginal papillomavirus infection in young women. N Engl J Med 338(7):423–428.<br />
International Agency for Research on <strong>Cancer</strong> (IARC) 1995. IARC monographs on the<br />
evaluation of carcinogenic risks to humans. Volume 64. Human papillomaviruses: summary<br />
of data reported and evaluation. Lyon, France: IARC.<br />
Jones SB 1999. <strong>Cancer</strong> in the developing world: a call to action. BMJ 319: 505–8.<br />
Kahn JA & Burk RD 30-6-2007. Papillomavirus vaccines in perspective. Lancet 369(9580):<br />
2135-2137.<br />
Lowy DR & Schiller JT 2006. Prophylactic human papillomavirus vaccines. J Clin Invest<br />
116(5): 1167–73.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1 3<br />
H u m a n p a p i l l o m a v i r u s
Mahdavi A & Monk BJ 2005. Vaccines against human papillomavirus and cervical cancer:<br />
promises and challenges. Oncologist 10(7): 528–38.<br />
Monsonego J, Bosch FX, Coursaget P, Cox JT, Franco E, Frazer I, Sankaranarayanan R,<br />
Schiller J, Singer A, Wright TC Jr, Kinney W, Meijer CJ, Linder J, McGoogan E, Meijer C<br />
2004. Cervical cancer control, priorities and new directions. Int J <strong>Cancer</strong> 108(3): 329-333.<br />
Munoz N, Bosch FX, de Sanjose S, Herrero R, Castellsague X, Shah KV, Snijders PJ &<br />
Meijer CJ 2003. Epidemiologic classification of human papillomavirus types associated<br />
with cervical cancer. N Engl J Med 348(6): 518-527.<br />
<strong>National</strong> Health and Medical Research Council 2005. Screening to prevent cervical cancer:<br />
guidelines for management of asymptomatic women with screen detected abnormalities.<br />
Canberra: NHMRC.<br />
Nobbenhuis MA, Helmerhorst TJ, van den Brule AJ, Rozendaal L, Voorhorst FJ, Bezemer<br />
PD, Verheijen RH & Meijer CJ 2001. Cytological regression and clearance of high-risk<br />
human papillomavirus in women with an abnormal cervical smear. Lancet 358(9295): 1782-<br />
1783.<br />
Nobbenhuis MA, Walboomers JM, Helmerhorst TJ, Rozendaal L, Remmink AJ, Risse<br />
EK, van der Linden HC, Voorhorst FJ, Kenemans P & Meijer 1999. Relation of human<br />
papillomavirus status to cervical lesions and consequences for cervical-cancer screening: a<br />
prospective study. Lancet 354(9172): 20–5.<br />
Parkin DM 2006. The global health burden of infection-associated cancers in the year 2002.<br />
Int J <strong>Cancer</strong> 118(12): 3030–44.<br />
Persing DH & Prendergast FG 1999. Infection, immunity, and cancer. Arch Pathol Lab Med<br />
123(11): 1015–22.<br />
Richardson H, Kelsall G, Tellier P, Voyer H, Abrahamowicz M, Ferenczy A, Coutlee F &<br />
Franco EL 2003. The natural history of type-specific human papillomavirus infections in<br />
female university students. <strong>Cancer</strong> Epidemiol Biomarkers Prev 12(6): 485–90.<br />
Roden R & Wu TC 2003. Preventative and therapeutic vaccines for cervical cancer. Expert<br />
Rev Vaccines 2(4): 495–516.<br />
Rous P & Kidd JG 1938. The carcinogenic effect of a papilloma virus on the tarred skin of<br />
rabbits: description of the phenomenon. J Exp Med 67: 399–428.<br />
Schiffman M & Kjaer SK 2003. Chapter 2: Natural history of anogenital human<br />
papillomavirus infection and neoplasia. J Natl <strong>Cancer</strong> Inst Monogr (31): 14–19.<br />
Schlecht NF, Platt RW, Duarte-Franco E, Costa MC, Sobrinho JP, Prado JC, Ferenczy<br />
A, Rohan TE, Villa LL & Franco EL 2003. Human papillomavirus infection and time to<br />
progression and regression of cervical intraepithelial neoplasia. J Natl <strong>Cancer</strong> Inst 95(17):<br />
1336–43.<br />
Shope R & Weston Husrt E 1933. Infectious papillomatosis of rabbits. J Exp Med 58:<br />
607–24.<br />
Stanley M, Lowy DR & Frazer I 2006. Chapter 12: Prophylactic HPV vaccines: underlying<br />
mechanisms. Vaccine 24 (3 Suppl): S106–13.<br />
Von Krogh G 2001. Management of anogenital warts (condylomata acuminata). Eur J<br />
Dermatol 11(6): 598-604<br />
1 4 Section Three: Immunisation
Victorian Cervical Cytology Registry 2006. Statistical report 2005. Melbourne: Victorian<br />
Cervical Cytology Registry.<br />
Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJF,<br />
Peto J, Meijer CJLM & Munoz N 1999. Human papillomavirus is a necessary cause of<br />
invasive cervical cancer worldwide. J Pathol 189: 12–19.<br />
Woodman CB, Collins S, Winter H, Bailey A, Ellis J, Prior P, Yates M, Rollason TP & Young<br />
LS 2001. Natural history of cervical human papillomavirus infection in young women: a<br />
longitudinal cohort study. Lancet 357(9271):1831–1836.<br />
Wright TC, Bosch FX, Franco EL, Cuzick J, Schiller JT, Garnett GP & Meheus A 2006. HPV<br />
vaccines and screening in the prevention of cervical cancer; conclusions from a 2006<br />
workshop of international experts. Vaccine 24 (3 Suppl): S51–61.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1 5<br />
H u m a n p a p i l l o m a v i r u s
H e p a t i t i s B<br />
Introduction<br />
At least 25% of those with chronic hepatitis B<br />
infection will develop hepatocellular cancer<br />
The hepatitis B virus (also known as HBV) was discovered in the 1960s; however, chronic<br />
hepatitis B infection (also known as CHB) was suspected as a cause of liver cancer from<br />
the early 1940s (Heymann 2004).<br />
Hepatitis B is a hepadnavirus that contains partially double-stranded DNA (Heymann 2004).<br />
The outer surface of the virus contains the hepatitis B surface antigen (HBsAg). Other<br />
important antigenic components are the hepatitis B core antigen (HBcAg), and hepatitis<br />
B e antigen (HBeAg). These antigenic components form the foundation of serological<br />
diagnosis of hepatitis B infection and immunity (Heymann 2004).<br />
Hepatitis B replicates almost exclusively in the liver but very high concentrations of<br />
virus are released into the blood, so that most tissues and body fluids are infectious.<br />
Transmission occurs through percutaneous or mucous membrane contact with infected<br />
blood or body fluids. This can occur by needle/syringe sharing, sexual intercourse and<br />
even in household settings, possibly through the use of shared objects, such as razor<br />
blades, where infectious virus has been shown to persist for up to a week (Lavanchy<br />
2004; Previsani, Lavanchy & Zuckerman 2004; Tawk et al. 2006a). The major mode<br />
of transmission on a global level is from mother to child, around the time of birth. If a<br />
pregnant woman has active or chronic hepatitis B infection and presence of HBeAg<br />
(indicating higher levels of hepatitis B viral load), the risk of infection in her newborn infant<br />
is 90% (Previsani, Lavanchy & Zuckerman 2004). During much of the last century, blood<br />
transfusions were a potential source of hepatitis B but the Australian Red Cross Blood<br />
Service has routinely screened all donated blood products and organ donors for a number<br />
of viruses, including hepatitis B, which has been screened for since 1975.<br />
Hepatitis B infection causes symptomatic acute hepatitis in approximately 30% to 50% of<br />
adults, but in young children, particularly those aged less than one year, infection is usually<br />
asymptomatic (Heymann 2004). The incubation period is 45 to 180 days and the period of<br />
communicability extends from several weeks before the onset of acute illness usually to<br />
the end of the period of acute illness.<br />
Acute illness is indistinguishable from other forms of hepatitis and symptoms include<br />
fever, jaundice, malaise, anorexia, nausea and vomiting, abdominal pain, myalgia and the<br />
passage of dark-coloured urine and light-coloured stools. During recovery, malaise and<br />
fatigue may persist for many weeks. Fulminant hepatitis, which occurs in approximately<br />
1% of cases, is a clinical syndrome of sudden onset occurring in people without preexisting<br />
liver disease, and results in severe impairment of liver function, sometimes with<br />
cerebral oedema and encephalopathy.
Chronic hepatitis B infection occurs when the immune response fails to clear acute<br />
infection. Markers of chronic hepatitis B infection are the persistence of HBsAg, with or<br />
without HBeAg, for more than six months after initial infection. This is further determined<br />
by the presence of hepatitis B DNA. Chronic infection occurs in 1% to 5% of adults, but<br />
is more common in immunocompromised persons and considerably more common in<br />
infants infected around the time of birth (up to 90%) (Heymann 2004; Lavanchy 2004;<br />
Ocama, Opio & Lee 2005; Previsani, Lavanchy & Zuckerman 2004). People with chronic<br />
hepatitis B infection, particularly those who are HBeAg positive, can transmit hepatitis B to<br />
others via the routes discussed above.<br />
The complications of chronic hepatitis B infection include progression to cirrhosis in up to<br />
30% of cases (Fattovich et al. 2004; Villeneuve 2005). Cirrhosis is a serious liver disease<br />
associated with chronic and often widespread destruction of liver substance occurring<br />
over a period of several years. Because liver inflammation can be totally symptomless,<br />
progression of inflammation to cirrhosis can occur without the knowledge of the patient.<br />
Chronic hepatitis B infection is the major cause of hepatocellular carcinoma (HCC)<br />
worldwide (Lavanchy 2005; WHO 2004).<br />
Australia<br />
Hepatitis B infection is a notifiable condition in Australia. There are two case definitions<br />
applied to notifications of hepatitis B: incident and unspecified.<br />
•<br />
•<br />
Incident hepatitis B is recorded when there is no evidence of hepatitis B infection in<br />
the past 24 months and serological markers such as HBsAg and IgM core antigen are<br />
present or hepatitis B DNA and IgM core antibodies are present. In 2005, 245 cases<br />
of incident hepatitis B were reported to the <strong>National</strong> Notifiable Diseases Surveillance<br />
System (NNDSS 2007). Of the people with incident hepatitis B notified in 2005, 46%<br />
reported injecting drug use exposure and 34% reported sexual exposure (NNDSS 2007).<br />
Unspecified hepatitis B, defined where a person does not meet the criteria for a<br />
newly acquired hepatitis B infection but has laboratory evidence of hepatitis B infection,<br />
accounted for 6396 notifications in 2005 (NNDSS 2007).<br />
The Northern Territory has the highest reported rates of incident and unspecified<br />
notifications of hepatitis B; chronic hepatitis B infection is considered endemic in<br />
Aboriginal and Torres Strait Islander communities. Studies undertaken in the mid-1990s<br />
indicated that up to 25% of rural Aboriginal populations were HBsAg positive (Fisher &<br />
Huffam 2003; O’Sullivan et al. 2004; Wood et al. 2005). A large proportion of chronic<br />
hepatitis B infection cases occur among people born in Asia and the Pacific Islands and<br />
also among people born in other hepatitis B-endemic areas such as the Middle East,<br />
Mediterranean and central or northern Africa (O’Sullivan et al. 2004; Tawk et al. 2006a),<br />
with the vast majority of these cases presumed to have been acquired overseas. In<br />
addition, Australian and overseas-born children of parents from these hepatitis B endemic<br />
regions, who were born prior to the introduction of the universal infant hepatitis B<br />
vaccination program in Australia, are at an increased risk of acquiring hepatitis B, either<br />
perinatally or through horizontal transmission.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1<br />
H e p a t i t i s B
Figure 3.1 shows the number of incident hepatitis B notifications from 1993 to 2006 (mean<br />
notifications per year = 315) and Figure 3.2 shows the number of unspecified notifications<br />
from 1991 to 2006, total over 90,000 notifications during those 15 years (NNDSS 2007).<br />
Figure 3.1 Incident hepatitis B notifications 1993–2006<br />
Number<br />
450<br />
400<br />
350<br />
300<br />
250<br />
200<br />
150<br />
100<br />
50<br />
0<br />
1993 1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006<br />
Year<br />
Source: NNDSS 2007<br />
Figure 3.2 Unspecified hepatitis B notifications, 1991–2006<br />
Number<br />
10000<br />
9000<br />
8000<br />
7000<br />
6000<br />
5000<br />
4000<br />
3000<br />
2000<br />
1000<br />
0<br />
Source: NNDSS 2007<br />
1 Section Three: Immunisation<br />
1991 1992 1993 1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006<br />
Year
Global<br />
Globally, an estimated two to three billion people have been infected with hepatitis B and<br />
of these, more than 400 million suffer from chronic hepatitis B infection (Goldstein et al.<br />
2005; Lavanchy 2004; Lavanchy 2005; WHO 2004). At least 25% of those with chronic<br />
hepatitis B infection will develop hepatocellular cancer (HCC), making HCC the tenth<br />
leading cause of death worldwide (Ghany & Doo 2004; Lavanchy 2004; Lavanchy 2005;<br />
Previsani, Lavanchy & Zuckerman 2004).<br />
Over 75% of people with chronic hepatitis B infection reside in the Asia-Pacific region<br />
(Lesmana et al. 2006). Within this region is the Western Pacific Region, which consists<br />
of 37 countries, including Australia (WHO 2004). Australia, New Zealand and Japan are<br />
all considered low prevalence countries (Clements et al. 2006; Lesmana et al. 2006). In<br />
the Western Pacific Region, hepatitis B seroprevalence estimates range from less than<br />
1% to 20%. China has the highest prevalence and accounts for more than a third of the<br />
global burden of chronic hepatitis B infection. Vietnam, Taiwan and the Philippines also<br />
report hepatitis B seroprevalence rates of up to 20% (Clements et al. 2006; Lesmana et al.<br />
2006). There are approximately 280,000 deaths in the Western Pacific Region each year<br />
attributable to complications arising from hepatitis B infection. Over 90% of these deaths<br />
are due to hepatitis B acquired decades earlier at birth or during childhood (Clements et<br />
al. 2006). Hepatitis B vaccination has been introduced into the Western Pacific Region to<br />
improve hepatitis B control in this region.<br />
The link between hepatitis B infection and cancer<br />
An association between chronic liver damage from any cause and hepatocellular<br />
carcinoma (HCC) was well known before the discovery of hepatitis B (Kew 2002). It was<br />
obvious that countries with very high chronic infectious hepatitis rates were also among<br />
those with the highest prevalence of HCC (Bosch & Ribes 2002). The introduction of<br />
serologic tests for hepatitis B in the late 1960s further supported the connection between<br />
chronic hepatitis B infection and HCC. In 1994 hepatitis B was classified as a carcinogen<br />
by the International Agency for Research on <strong>Cancer</strong> (IARC 1997). Case–control studies<br />
from various regions of the world have consistently demonstrated that chronic hepatitis<br />
B infection is more common among HCC cases than controls (IARC 1997). A number of<br />
studies have demonstrated the geographic coincidence between hepatitis B endemicity<br />
and HCC prevalence (Beasley et al. 1981; Chan et al. 2004; Craxi & Camma 2005;<br />
Heymann 2004; Lee, Hsieh & Ko 2003; Lok 2004).<br />
Multiple factors appear to play a role in the progression of chronic hepatitis B infection<br />
to HCC, with chronic inflammation and cytokine effect playing a major role in the<br />
development of fibrosis and ongoing hepatocyte generation. Hepatitis B DNA has also<br />
been demonstrated to be integrated into cellular DNA in samples of HCC (Brechot 2004;<br />
Chang et al. 2005; Hayashi & Di Bisceglie 2005). Various other viral factors associated<br />
with HCC development include the hepatitis B genotype, viral mutations and high viral<br />
load (Brechot 2004; Chan et al. 2004; Chen et al. 2006; McGlynn & London 2005; Tang et<br />
al. 2004; Yu et al. 2005). The direct involvement of the hepatitis B virus in carcinogenesis<br />
has now been shown to be related to expression of several hepatitis B proteins (Bonilla &<br />
Roberts 2005; Brechot 2004). The product of the HB X gene, the X protein, has multiple<br />
oncogenic effects. The hepatitis B X gene transactivates other genes, including those<br />
involved in cell turnover, and is found in an integrated form in almost all hepatitis B-related<br />
cancers. More rapid progression may occur in the presence of environmental carcinogens<br />
such as aflatoxins in the diet. However, people with chronic hepatitis B infection from<br />
endemic regions retain their high risk of HCC even if they migrate to countries with low<br />
levels of environmental carcinogens. Women are less likely to maintain persistent hepatitis<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1<br />
H e p a t i t i s B
B infection than men, or to develop HCC if they remain carriers through middle age.<br />
The incidence of HCC is two to four times greater in men than in women. This may be<br />
explained, in part, by the fact that males are generally more likely to be co-infected with<br />
hepatitis C, consume alcohol and smoke cigarettes (McGlynn & London 2005).<br />
The greatly increased risk of developing HCC associated with chronic hepatitis B infection<br />
was unequivocally demonstrated by surveys of middle-aged male civil servants in Taiwan<br />
(Beasley et al. 1981). In this study, 22,707 men were prospectively followed for HBsAg<br />
status and mortality. Forty-one subjects died from HCC and all but one were HBsAg<br />
negative. A similar increase in risk for people with chronic hepatitis B infection has been<br />
reported from many different countries, with both high and low overall adult hepatitis B<br />
prevalence rates. The risk of HCC from chronic hepatitis B infection is far higher than that<br />
observed among individuals with liver cirrhosis from other causes (Cantarini et al. 2006).<br />
The impact<br />
Worldwide, there were more than 600,000 deaths due to primary liver cancer in 2002<br />
(Perz et al. 2006). Among primary liver cancers worldwide, hepatocellular carcinoma (HCC)<br />
represents the major histologic type and is likely to account for 70% to 85% of cases<br />
(Perz et al. 2006). HCC is the tenth leading cause of death from any condition and is the<br />
fifth most common malignancy in males and the eighth in females (Lavanchy 2004; WHO<br />
2004). Hepatitis B and C infections account for an estimated 78% of HCC globally (53%<br />
and 25%, respectively); however, the relative percentage of HCC cases linked to hepatitis B<br />
(and/or hepatitis C) varies by geographic setting. In addition to HCC, an estimated 446,000<br />
cirrhosis deaths related to hepatitis B and C occurred in 2002 (Perz et al. 2006). The lifetime<br />
risk of death from hepatitis B-related HCC or cirrhosis is estimated to be 25% for a person<br />
who becomes chronically infected during childhood (Bonilla & Roberts 2005; Roberts &<br />
Kemp 2007).<br />
Data on the incidence and mortality from primary liver cancers in Australia are shown<br />
in Tables 3.1 and 3.2 below. The majority of liver cancers are HCC (as determined by<br />
ICD-10 code C22.0), but these data include other tumours such as cholangiocarcinoma,<br />
hepatoblastoma and tumours without histological confirmation. These data demonstrate<br />
the increase in primary liver cancers between 2001 and 2005, similar to that reported<br />
elsewhere (Amin et al. 2007) and to what has been seen in the past two decades, when the<br />
incidence of HCC almost doubled in both men (from 2.06 to 3.97 per 100,000) and women<br />
(from 0.57 to 0.99 per 100,000) from 1978 to 1997 (Law et al. 2000).<br />
Precise information regarding the number of cases of HCC due to hepatitis B infection<br />
Australia-wide is not available. However, a recent longitudinal study in NSW using data<br />
linkage found that of 2072 cases of HCC identified from 1990 to 2002, 323 (15.6%), 267<br />
(12.9%) and 18 (0.8%) were linked to hepatitis B, hepatitis C and hepatitis B/hepatitis C coinfection<br />
notifications respectively (Amin et al. 2007). A younger age at diagnosis of HCC<br />
and birth outside of Australia (particularly Asia) were associated with hepatitis B-linked<br />
cases. However, the rates of hepatitis B and C infection among people with HCC in this<br />
study may have been underestimated due to limitations of the data used in the analysis<br />
and factors such as underreporting and testing of hepatitis B and C infection, particularly<br />
in earlier years. A smaller Victorian study of 96 people with cirrhosis who had developed<br />
HCC reported that approximately 15% were HBsAg positive (and 30% hepatitis C antibody<br />
positive) (Kemp et al. 2005).<br />
1 0 Section Three: Immunisation
The rise in HCC is thought to be associated with a number of factors, many of which are<br />
related to hepatitis B (and hepatitis C) infection. An analysis of HCC epidemiology in an<br />
Australian tertiary hospital from 1975–2002 reported that between 1995 and 2002, people<br />
with HCC were more likely to be male, aged less than 64 years, non-Caucasian and born<br />
overseas, in comparison to patients with HCC between 1975 and 1983 (Roberts & Kemp<br />
2007). This is consistent with an increase in the average age of immigrants from highrisk<br />
hepatitis B endemic countries, bringing more individuals into the age groups at risk.<br />
Secondly, the prevalence of chronic hepatitis C has risen in Australia and is associated<br />
with HCC cases. Co-infection with hepatitis C and hepatitis B is known to increase the<br />
risk of developing HCC (Amin et al. 2006a; Amin et al. 2006b; Amin et al. 2007). A recent<br />
Australian study describing cancer incidence in people with hepatitis B, hepatitis C or a<br />
co-infection with both viruses found that the risk of HCC was 20 to 30 times greater than in<br />
the uninfected population (Amin et al. 2006a).<br />
Although in developed countries the mean duration from onset of chronic hepatitis B<br />
infection to the diagnosis of HCC is 35 years (Craxi & Camma 2005), in countries where<br />
hepatitis B is highly endemic, HCC can develop in children and across all age groups but is<br />
uncommon before the age of 30 (Lavanchy 2005; McGlynn & London 2005; Raza, Clifford<br />
& Franceschi 2007; Villeneuve 2005). Given that since 1991 there have already been over<br />
90,000 chronic hepatitis B infection cases notified in Australia, the future burden of HCC<br />
will continue for many years to come, before the impact of the universal hepatitis B vaccine<br />
on HCC will become apparent.<br />
Table 3.1 Incidence data for primary liver cancers from 2005 compared with 2001 #<br />
New cases ASR* % change ASR<br />
(last 10 years)<br />
% of all<br />
cancer<br />
% increase in cases<br />
2001–2005<br />
Male 718 7.4 +2.9% 1.3% 62%<br />
Female 261 2.2 +4.8% 0.6% 53%<br />
*ASR = age standardised rate per 100,000 (Australian 2001 population standard)<br />
# Includes intrahepatic bile duct cancer<br />
Source: AIHW et al. 2005<br />
Table 3.2 Mortality data for primary liver cancers #<br />
Deaths ASR* % change p.a. ASR (last 10 years)<br />
Male 596 6.1 +1.9%<br />
Female 346 2.9 +4.6%<br />
*ASR = age standardised rate per 100,000 (Australian 2001 population standard)<br />
# Includes intrahepatic bile duct cancer<br />
Source: AIHW 2005<br />
In 2001, the direct costs of managing people with chronic hepatitis B infection in Australia<br />
were estimated to range from $1233 for a person with non-cirrhotic chronic hepatitis B<br />
infection to $144,392 for a person requiring a liver transplant. Direct costs for HCC were<br />
$11,753 and the average cost for palliative care for a person with chronic hepatitis B<br />
infection and HCC was $6307 (Butler et al. 2004).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1 1<br />
H e p a t i t i s B
The challenge<br />
Hepatitis B is transmitted through percutaneous or mucous membrane contact with<br />
infected blood or body fluids: in healthcare and other settings, by needle/syringe sharing,<br />
in sexual intercourse and possibly through the sharing of household items, such as razor<br />
blades. Worldwide, transmission is most common from mother to child, around the time<br />
of birth. The challenge is to protect against transmission wherever possible. <strong>Prevention</strong><br />
measures are described below.<br />
Effective interventions<br />
Vaccination<br />
The hepatitis B vaccine has been available for over 20 years and was the world’s first<br />
cancer prevention vaccine (Beasley et al. 1983; van der Sande et al. 2006). In the early<br />
1980s, a plasma-derived hepatitis B vaccine prepared from the inactivated plasma of<br />
people with chronic hepatitis B infection was used in Australia and internationally. In the<br />
late 1980s, a hepatitis B vaccine manufactured by recombinant DNA technology became<br />
available and replaced the plasma-derived vaccine in most countries, including Australia<br />
(Yu, Cheung & Keeffe 2004). The gene for the major ‘surface’ antigen (HBsAg) of the<br />
hepatitis B virus is expressed in yeast cells. The hepatitis B vaccines currently available<br />
in Australia are monovalent, meaning the vaccine only contains hepatitis B antigen,<br />
or combination vaccines that contain hepatitis B antigen and other antigens such as<br />
diphtheria, tetanus, pertussis, Haemophilus influenzae type B, poliomyelitis and hepatitis A<br />
antigens (NHMRC 2008).<br />
In Australia during the early 1980s, hepatitis B vaccination was initially administered to<br />
at-risk groups such as healthcare workers. In 1987, hepatitis B vaccination of infants born<br />
to mothers who were hepatitis B surface-antigen-positive commenced. In 1997, routine<br />
adolescent hepatitis B vaccination was introduced, followed by universal infant vaccination<br />
in May 2000. The adolescent program will continue until all children born since 2000 reach<br />
adolescence (NHMRC 2008; Williams 2002).<br />
The Australian <strong>National</strong> Immunisation Program currently includes a single dose of hepatitis<br />
B vaccine at birth or up to eight days of age followed by three doses of hepatitis B vaccine<br />
at two, four and either six or 12 months of age. Adolescents aged between 12 and 15<br />
years receive either a two-dose schedule (adult dose vaccine) administered at a 0 and four-<br />
(or six-) month interval; or a three-dose schedule (paediatric dose vaccine) at 0, one- and<br />
six-monthly intervals, predominantly through school-based programs. Adults receive a<br />
three-dose schedule of hepatitis B vaccine administered at 0, one and six-monthly intervals<br />
(AHC 2006; Yuen et al. 2004).<br />
Hepatitis B vaccines are recommended in adults (or those not previously immunised) in the<br />
following at-risk groups (NHMRC 2008; Williams 2002):<br />
•<br />
•<br />
•<br />
•<br />
•<br />
household contacts of people with acute and chronic hepatitis B<br />
sexual contacts of people with acute and chronic hepatitis B<br />
people on haemodialysis, people who are HIV-positive and other adults with impaired<br />
immunity<br />
injecting drug users<br />
recipients of concentrated blood products<br />
1 2 Section Three: Immunisation
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
people with chronic liver disease and/or hepatitis C (who are seronegative for<br />
hepatitis B)<br />
residents and staff of facilities for people with intellectual disabilities<br />
people adopting children from overseas<br />
liver transplant recipients (who are seronegative for hepatitis B)<br />
inmates and staff of long-term correctional facilities<br />
healthcare workers, ambulance personnel, dentists, embalmers, tattooists and bodypiercers<br />
police, members of the armed forces and emergency services staff if at risk of exposure<br />
to body fluids<br />
funeral workers and other workers who have regular contact with human tissue, blood<br />
or body fluids and/or used needles or syringes<br />
people travelling to regions of intermediate or high endemicity, either long term or for<br />
frequent short terms<br />
sex industry workers.<br />
Although vaccine-induced antibody levels decline with time and may become<br />
undetectable, booster doses are not recommended in immuno-competent individuals after<br />
a primary course, as there is good evidence that a completed primary course of hepatitis<br />
B vaccination provides long-lasting protection (NHMRC 2008; Williams 2002). This applies<br />
to children and adults, including those at risk of occupational exposure, such as healthcare<br />
workers and dentists (Fitzsimons et al. 2005; Petersen et al. 2004).<br />
During the late 1980s, perinatal transmission of hepatitis B was recognised as the major<br />
factor leading to virus persistence and chronic liver disease and HCC. Vaccination of<br />
newborn infants of mothers with chronic hepatitis B infection was shown to be effective in<br />
reducing viral transmission, especially if combined with administration of ‘hyperimmune’<br />
hepatitis B immunoglobulin (HBIG) at birth. Hepatitis B vaccine given in combination with<br />
one dose of HBIG to babies within 12–24 hours after birth is around 85% to 95% effective<br />
in preventing hepatitis B infection (Beasley et al. 1983; Chang & Chen 2002; Kripke 2007;<br />
Lee et al. 2006; Petersen et al. 2004; WHO 2004; Yu, Cheung & Keeffe 2004). In Australia,<br />
all antenatal women are tested for hepatitis B or the hepatitis B status of mother is<br />
determined upon presentation in labour if unknown. Infants born to hepatitis B surfaceantigen-positive<br />
mothers or those of unknown status should receive HBIG at birth as well<br />
as the hepatitis B vaccine.<br />
The effect of vaccination on carriage rates in vaccinated age cohorts has been reported<br />
in many countries (Chang 2003; Chang et al. 2005; Chang & Chen 2002; Clements et al.<br />
2006; Chen 2005; Yu, Cheung & Keeffe 2004). More time must elapse before these cohorts<br />
reach the age of greatest HCC prevalence, but already some countries with previously<br />
very high HCC rates, such as Taiwan, have observed statistically significant reductions in<br />
young, vaccinated age groups (Chang & Chen 2002; Yuen et al. 2004). Taiwan introduced<br />
a universal hepatitis B vaccination program for infants in 1984; while HCC is uncommon in<br />
children, the reported incidence of HCC fell by 75% in children aged six to nine years who<br />
were born after the program started (Chang 2003; Lee, Hsieh & Ko 2003).<br />
The use of the hepatitis B vaccine and HBIG has been shown to be cost effective even<br />
in countries such as Australia with a low prevalence of hepatitis B. In the late 1990s, the<br />
World Health Organization advised the introduction of universal vaccination for all infants<br />
born in countries where the prevalence of chronic hepatitis B infection exceeded 2%.<br />
However, universal hepatitis B vaccination has been undertaken only sporadically in many<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1 3<br />
H e p a t i t i s B
countries, primarily due to limited resources. Data from the World Health Organization<br />
in 2005 indicate that although 158 out of 192 (82%) of member states had introduced a<br />
routine infant immunisation program, only 119 countries could report coverage of three<br />
doses at levels greater than 80% (ACT-HBV APSCM 2006; WHO 2004). As such, hepatitis<br />
B and its complications remain a global concern (WHO 2004).<br />
Other interventions<br />
Transmission of hepatitis B in healthcare settings has been greatly reduced by screening<br />
of blood donations prior to transfusion or manufacture of blood products, and screening<br />
of organ donors prior to transplant (Hilleman 2003). In addition, the use of standard<br />
precautions in the clinical setting to minimise transmission of blood-borne viruses and<br />
other infection control measures—such as the use of disposable equipment, sterilisation of<br />
multi-use equipment and the correct disposal of sharps, body fluids and other body parts—<br />
has further minimised the risk of hepatitis B transmission in the healthcare setting.<br />
Treatment of chronic hepatitis B infection, cirrhosis and HCC<br />
The medical treatment of people with established chronic hepatitis B infection is targeted<br />
at reducing the hepatitis B replication, which in turn can potentially prevent or slow<br />
progression to cirrhosis and HCC.<br />
In a very small percentage of people with chronic hepatitis B infection, there may be<br />
resolution of the infection. The choice of therapy varies, depending on the viral load<br />
and extent of hepatic damage; however, the ultimate aim of treatment is sustained viral<br />
suppression that results in normal ALT levels, a decrease in hepatitis B DNA and prevention<br />
of the sequelae of infection (ACT-HBV APSCM 2006; Okanoue & Minami 2006). Nucleoside<br />
analogue drugs such as lamivudine and entecavir suppress hepatitis B virus replication<br />
very effectively, although emergence of resistance is a serious problem, particularly in the<br />
case of lamivudine (ACT-HBV APSCM 2006; Fung & Lok 2004; Locarnini & Omata 2006).<br />
PEG-interferon suppresses hepatitis B replication in a majority of individuals and achieves<br />
sustained virological control (ongoing low or undetectable levels of hepatitis B viraemia) in<br />
about a third (ACT-HBV APSCM 2006; Farrell & Teoh 2006; Ghany & Doo 2004; Hoofnagle<br />
et al. 2007). Virological control, whether spontaneous or after treatment, greatly reduces<br />
the subsequent risk of HCC; however, it has no effect on the course of established liver<br />
cancer. As most people with chronic hepatitis B infection are completely asymptomatic,<br />
a policy of monitoring and treating those with the highest risk of HCC (e.g. those with<br />
hepatitis B viral load above 2000 IU/mL and age above 40 years) may be the most effective<br />
strategy. This would require effective screening and detection programs to identify people<br />
with chronic hepatitis B infection.<br />
Treatment of HCC itself is difficult because of the multifocal nature of the tumour and<br />
its inaccessibility. Techniques for destruction of tumour nodules depend on accurate<br />
localisation, and, although they do prolong life, they are seldom curative. Unfortunately<br />
blood tests for tumour markers have not proved reliable as screening tests, and effective<br />
chemotherapy is still lacking (Hilleman 2003; Kemp et al. 2005; O’Brien, Kirk & Zhang<br />
2004). Imaging techniques have been employed to monitor known carriers, especially<br />
those who have developed cirrhosis and/or are entering middle age. Liver transplantation<br />
and removal of the entire liver is regarded as the most likely treatment to achieve cure, but<br />
prior spread beyond the liver may already have occurred and this has proved difficult to<br />
assess (Kemp et al. 2005).<br />
1 4 Section Three: Immunisation
The policy context<br />
The bleak outcome of HCC makes prevention an especially desirable public and personal<br />
health policy. <strong>Prevention</strong> of persistent hepatitis B infection by universal infant vaccination<br />
is clearly the most significant measure, and since 2000 it has achieved global acceptance<br />
and support (Hipgrave, Maynard & Biggs 2006; WHO 2004). It will be many years before<br />
this is manifested in a falling prevalence of HCC. In the meantime, treatment of established<br />
hepatitis B infection and reduction of exposure to other factors that increase the risk of<br />
developing chronic liver disease, such as alcohol and aflatoxins, can reduce the proportion<br />
of infected people who develop chronic liver disease and HCC. The appropriate schedules<br />
for early tumour detection in people with established cirrhosis have yet to be established in<br />
Australia and there are also ongoing evaluations of different methods of surgical treatment<br />
(Roberts & Kemp 2007).<br />
Primary prevention of hepatitis B by vaccination is now provided for all Australian infants<br />
as part of the <strong>National</strong> Immunisation Program described above. This provides optimum<br />
protection against infection in early life, when the likelihood of developing persistent<br />
infection is very high, and also provides ongoing immunity into adolescence and adult life.<br />
Uptake of hepatitis B vaccine in Australian children is very good, with three-dose coverage<br />
reported in 94.7% of infants aged 12 months and 95.9% of children aged two years (ACIR<br />
2006).<br />
However, despite good vaccine coverage in infants, children and school-based delivery to<br />
unimmunised adolescent groups in Australia, hepatitis B vaccination has been consistently<br />
underused by adults in high-risk groups who would not have been targeted by universal<br />
infant and childhood immunisation because of their age (Tawk et al. 2006b; Yuen et al.<br />
2004). Low vaccine uptake rates among high-risk adults have generally been due to a<br />
lack of awareness, failure to identify and offer vaccination to at-risk persons, the cost<br />
of accessing the hepatitis B vaccine and failure to complete a course of the hepatitis<br />
B vaccine. At-risk groups, in particular people from culturally and language diverse<br />
communities, Indigenous Australians, injecting drug users, inmates of correctional facilities<br />
and men who have sex with men, need to have ready access to hepatitis B vaccines,<br />
potentially via targeted campaigns.<br />
There is evidence that universal immunisation of infants and children in Australia is having<br />
an impact, with the number of cases of acute hepatitis B declining between 2001 and<br />
2006 from 415 to 295 (from 2.1 to 1.6 per 100,000 population) (NHMRC 2008). It is likely<br />
that these declining rates also reflect changing practices among other risk groups, such<br />
as sex workers and intravenous drug users. However, while incident hepatitis B may<br />
have declined as a result of vaccination, the impact from the pool of people with chronic<br />
hepatitis B infection—many of whom may not be recognised as such—is still to be felt.<br />
It will be several more decades before they reach middle age, when HCC is most likely<br />
to develop. In most high prevalence countries, vaccination was introduced even more<br />
recently so that adult immigrants from these countries still have high hepatitis B carriage<br />
rates (Farrell & Teoh 2006; Tawk et al. 2006a; Tawk et al. 2006b). This means that for many<br />
years to come the pool of adult hepatitis B carriers in Australia will be relatively static or<br />
may even grow, as will the prevalence of hepatitis B-related HCC.<br />
There are two options for reducing the disease burden from those with established chronic<br />
hepatitis B infection. The first is to treat people with chronic hepatitis B infection before<br />
they develop cirrhosis. There is good evidence that the risk of HCC is greatly reduced if<br />
viral replication is controlled either spontaneously or with treatment. Although between<br />
0.5% and 1% of the adult population have chronic hepatitis B infection with detectable<br />
virus in their blood, a minority are aware of their infected status or assessed for treatment<br />
(Gidding et al. 2007; O’Sullivan et al. 2004; Wood et al. 2005). Apart from antenatal<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1 5<br />
H e p a t i t i s B
screening, case finding has not been promoted as a public health priority, and there is<br />
generally no systematic arrangement for referral and assessment of individuals who are<br />
found to be HBsAg positive in the course of ordinary medical care, although many of these<br />
are notified under the current laboratory-based reporting system. Cost–benefit analyses of<br />
hepatitis B treatment strategies do not yet include the expense of case finding, and there<br />
is debate in the literature about the benefit of treatment of non-cirrhotic patients, whose<br />
infection may clear spontaneously over time.<br />
The second option for reducing the disease burden of HCC is to institute screening for<br />
cancer nodules in the livers of people with established cirrhosis. If small and single, the<br />
nodules can be treated by resection of the affected lobe of the liver. If large or multiple,<br />
injection of the lesions with cytotoxic drugs may prolong life (Craxi & Camma 2005;<br />
Hilleman 2003; Kemp et al. 2005). In summary, the current approaches to secondary<br />
prevention of HCC in those with established hepatitis B infection have not yet attained a<br />
sufficiently firm scientific basis to justify their introduction on a nationwide scale.<br />
In 2006, the Australian Hepatitis Council issued a position paper outlining a number of<br />
actions that members believe are necessary to address hepatitis B in Australia. These<br />
include (ACT-HBV ANZLC 2007; AHC 2006):<br />
•<br />
•<br />
•<br />
•<br />
•<br />
the development and implementation of a national hepatitis B strategy<br />
the development of health maintenance and support resources for people with chronic<br />
hepatitis B infection<br />
broad research that encompasses both the social and health impacts of hepatitis B<br />
infection<br />
representation of people living with chronic hepatitis B infection on any national<br />
strategic council and an ongoing campaign to raise awareness of hepatitis B<br />
vaccinations and treatment among high-risk groups.<br />
Despite the gains that will be made through universal vaccination of infants, many further<br />
measures require consideration in an overall strategy to reduce the future burden of<br />
disease from HCC<br />
.<br />
1 Section Three: Immunisation
Aims<br />
What needs to be achieved How <strong>Cancer</strong> Council Australia and its members (the state and<br />
territory cancer councils) will do this<br />
Increased awareness of the<br />
link between hepatitis B<br />
Infection and liver cancer<br />
among those at high risk<br />
and key health professional<br />
groups<br />
Immunisation of populations<br />
with higher incidences and<br />
poorer outcomes<br />
Monitor and evaluate the<br />
vaccination program<br />
Effective coordinated policy<br />
to support development<br />
and implementation of<br />
a <strong>National</strong> Hepatitis B<br />
Strategy<br />
Timely evaluation of new<br />
technologies<br />
Monitor and clarify best evidence on the relationship between hepatitis B<br />
and liver cancer causation<br />
Ensure key messages are promoted to those at high risk and relevant<br />
health professionals via publications, presentations, programs, media<br />
statements and wherever opportunities arise<br />
Promote and/or develop primary health resources, specifically for general<br />
practice, to improve evidence-based interventions by health professionals<br />
in the field of hepatitis B prevention and treatment.<br />
Advocate for and support screening and vaccination among recent<br />
immigrants from high prevalence countries and for Indigenous<br />
Australians.<br />
Advocate to government for funding and establishment of data processes<br />
to capture and monitor vaccination data at a <strong>National</strong> level<br />
Match vaccination data with screening program data and state cancer<br />
registries<br />
Develop and maintain evidence-based policy positions about the<br />
relationship between HBV infection and cancer in the Australian context<br />
Identify, analyse and advocate for evidence-based policy initiatives to<br />
reduce alcohol consumption in populations at risk for hepatitis B related<br />
disease<br />
Monitor development of relevant new technologies, (such as ultrasound<br />
and MRI), advocate for rapid evaluation of their relevance and adoption<br />
of those that are positively evaluated<br />
Further research Support and conduct high quality epidemiological research further<br />
clarifying the relationship between chronic hepatitis B infection and<br />
cancer in the Australian population.<br />
Support and conduct high-quality behavioural research to determine:<br />
• the barriers and enabling factors for people from target at-risk<br />
populations to participation in a HBV monitoring and HCC prevention<br />
program<br />
• whether increased knowledge about the link between hepatitis B virus<br />
infection and liver cancer can affect behaviour<br />
•<br />
identify key messages for social marketing campaigns about hepatitis<br />
B vaccination, early liver disease diagnosis and management (including<br />
responsible use of alcohol).<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1<br />
H e p a t i t i s B
References<br />
ACT-HBV Asia-Pacific Steering Committee Members (ACT-HBV APSCM) 2006. Chronic hepatitis B: treatment<br />
alert. Liver Int 26: 47–58.<br />
ACT-HBV Australia and New Zealand Local Chapter (ACT-HBV ANZLC), ed. GJ Dore 2007. Hepatitis B in<br />
Australia: responding to a diverse epidemic. ACT-HBV Asia-Pacific.<br />
Amin J, Dore GJ, O’Connell DL, Bartlett M, Tracey E, Kaldor JM & Law MG 2006a. <strong>Cancer</strong> incidence in<br />
people with hepatitis B or C infection: a large community-based linkage study. J Hepatol 45(2): 197–203.<br />
Amin J, Law MG, Bartlett M, Kaldor JM & Dore GJ 2006b. Causes of death after diagnosis of hepatitis B or<br />
hepatitis C infection: a large community-based linkage study. Lancet 368(9539): 938–45.<br />
Amin J, O’Connell D, Bartlett M, Tracey E, Kaldor J, Law M & Dore G 2007. Liver cancer and hepatitis B and<br />
C in New South Wales, 1990–2002: a linkage study. Aust N Z J Public Health 31(5): 475–82.<br />
Australian Childhood Immunisation Register (ACIR) 2006. Medicare Australia, December.<br />
Australian Hepatitis Council (AHC) 2006. Position Paper: Addressing Hepatitis B. AHC.<br />
Australian Institute of Health and Welfare (AIHW) 2005. State and territories GRIM (General Record of<br />
Incidence of Mortality) books. Canberra: AIHW.<br />
Australian Institute of Health and Welfare (AIHW), Australasian Association of <strong>Cancer</strong> Registries (AACR),<br />
<strong>National</strong> <strong>Cancer</strong> Strategies Group (NCSG) & McDermid I 2005. <strong>Cancer</strong> incidence projections, Australia 2002 to<br />
2011. Canberra: AIHW, AACR & NCSG.<br />
Beasley RP, Hwang LY, Lee GC, Lan CC, Roan CH, Huang FY & Chen CL 1983. <strong>Prevention</strong> of perinatally<br />
transmitted hepatitis B virus infections with hepatitis B immune globulin and hepatitis B vaccine. Lancet<br />
2(8359): 1099–1102.<br />
Beasley RP, Hwang LY, Lin CC & Chien CS 1981. Hepatocellular carcinoma and hepatitis B virus. A<br />
prospective study of 22,707 men in Taiwan. Lancet 2(8256): 1129–33.<br />
Bonilla GR & Roberts LR 2005. The role of hepatitis B virus integrations in the pathogenesis of human<br />
hepatocellular carcinoma. J Hepatol 42(5): 760–77.<br />
Bosch FX & Ribes J 2002. The epidemiology of primary liver cancer: global epidemiology. In Viruses and liver<br />
cancer, ed. E Tabor. Amsterdam: Elsevier Science.<br />
Brechot C 2004. Pathogenesis of hepatitis B virus-related hepatocellular carcinoma: old and new paradigms.<br />
Gastroenterology 127(5 Suppl 1): S56–61.<br />
Butler JR, Pianko S, Korda RJ, Nguyen S, Gow PJ, Roberts SK, Strasser SI & Sievert W 2004. The direct<br />
cost of managing patients with chronic hepatitis B infection in Australia. J Clinical Gastroenterol 38(3 Suppl):<br />
S187–92.<br />
Cantarini MC, Trevisani F, Morselli-Labate AM, Rapaccini G, Farinati F, Del Poggio P, Di Nolfo MA, Benvegnu<br />
L, Zoli M, Borzio F, Bernardi M & Italian Liver <strong>Cancer</strong> (ITA.LI.CA) group 2006. Effect of the etiology of viral<br />
cirrhosis on the survival of patients with hepatocellular carcinoma. Am J Gastroenterol 101(1): 91–8.<br />
Chan HL, Hui AY, Wong ML, Tse AM, Hung LC, Wong VW & Sung JJ 2004. Genotype C hepatitis B virus<br />
infection is associated with an increased risk of hepatocellular carcinoma. Gut 53(10): 1494–8.<br />
Chang MH 2003. Decreasing incidence of hepatocellular carcinoma among children following universal<br />
hepatitis B immunization. Liver Int 23(5): 309–14.<br />
Chang MH, Chen TH, Hsu HM, Wu TC, Kong MS, Liang DC, Ni YH, Chen CJ, Chen DS & Taiwan Childhood<br />
HCC Study Group. 2005. <strong>Prevention</strong> of hepatocellular carcinoma by universal vaccination against hepatitis B<br />
virus: the effect and problems. Clin <strong>Cancer</strong> Res 11(21): 7953–7.<br />
Chang MW & Chen DS 2002. <strong>Prevention</strong> of hepatocellular carcinoma by hepatitis B immunization. In Viruses<br />
and liver cancer, ed. E Tabor. Amsterdam: Elsevier Science.<br />
Chen CJ, Yang HI, Su J, Jen CL, You SL, Lu SN, Huang GT, Iloeje UH & REVEAL-HBV Study Group 2006. Risk<br />
of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. JAMA 295(1):<br />
65–73.<br />
1 Section Three: Immunisation
Chen DS 2005. Long-term protection of hepatitis B vaccine: lessons from Alaskan experience after 15 years.<br />
Ann Intern Med 142(5): 384–5.<br />
Clements CJ, Baoping Y, Crouch A, Hipgrave D, Mansoor O, Nelson CB, Treleaven S, van Konkelenberg R<br />
& Wiersma S 2006. Progress in the control of hepatitis B infection in the Western Pacific Region. Vaccine<br />
24(12): 1975–82.<br />
Craxi A & Camma C 2005. <strong>Prevention</strong> of hepatocellular carcinoma. Clin Liver Dis 9(2): 329–46.<br />
Farrell GC & Teoh NC 2006. Management of chronic hepatitis B virus infection: a new era of disease control.<br />
Intern Med J 36(2): 100–13.<br />
Fattovich G, Stroffolini T, Zagni I & Donato F 2004. Hepatocellular carcinoma in cirrhosis: incidence and risk<br />
factors. Gastroenterology 127(5 Suppl 1): S35–50.<br />
Fisher DA & Huffam SE 2003. Management of chronic hepatitis B virus infection in remote-dwelling<br />
Aboriginals and Torres Strait Islanders: an update for primary healthcare providers. Med J Aust 178(2): 82–5.<br />
Fitzsimons D, François G, Hall A, McMahon B, Meheus A, Zanetti A, Duval B, Jilg W, Böcher WO, Lu SN,<br />
Akarca U, Lavanchy D, Goldstein S, Banatvala J & Van Damme P 2005. Long-term efficacy of hepatitis B<br />
vaccine, booster policy, and impact of hepatitis B virus mutants. Vaccine 23(32): 4158–66.<br />
Fung SK & Lok AS 2004. Treatment of chronic hepatitis B: who to treat, what to use, and for how long? Clin<br />
Gastroenterol Hepatol 2(10): 839–48.<br />
Ghany MG & Doo EC 2004. Management of chronic hepatitis B. Gastroenterol Clin North Am 33(3): 563–79.<br />
Gidding HF, Warlow M, MacIntyre CR, Backhouse J, Gilbert GL, Quinn HE & McIntyre PB 2007. The impact<br />
of a new universal infant and school-based adolescent hepatitis B vaccination program in Australia. Vaccine<br />
online 13 August: 1–5.<br />
Goldstein ST, Zhou F, Hadler SC, Bell BP, Mast EE & Margolis HS 2005. A mathematical model to estimate<br />
global hepatitis B disease burden and vaccination impact. Int J Epidemiol 34(6): 1329–39.<br />
Hayashi PH & Di Bisceglie AM 2005. The progression of hepatitis B- and C-infections to chronic liver disease<br />
and hepatocellular carcinoma: epidemiology and pathogenesis. Med Clin North Am 89(2): 371–89.<br />
Heymann DL 2004. Hepatitis, viral. In <strong>Control</strong> of communicable diseases manual, ed. DL Heymann, 18th<br />
edition. Washington, DC: American Public Health Association.<br />
Hilleman MR 2003. Critical overview and outlook: pathogenesis, prevention, and treatment of hepatitis and<br />
hepatocarcinoma caused by hepatitis B virus. Vaccine 21(32): 4626–49.<br />
Hipgrave DB, Maynard JE & Biggs BA 2006. Improving birth dose coverage of hepatitis B vaccine. Bull World<br />
Health Organ 84(1): 65–71.<br />
Hoofnagle JH, Doo E, Liang TJ, Fleischer R & Lok AS 2007. Management of hepatitis B: summary of a clinical<br />
research workshop. Hepatology 45(4): 1056–75.<br />
International Agency for Research on <strong>Cancer</strong> (IARC) 1997. Hepatitis viruses. IARC Monographs volume 59.<br />
Lyon, France: IARC Press.<br />
Kemp W, Pianko S, Nguyen S, Bailey MJ & Roberts SK 2005. Survival in hepatocellular carcinoma: impact of<br />
screening and etiology of liver disease. J Gastroenterol Hepatol 20(6): 873–81.<br />
Kew MC 2002. Hepatitis B virus in the etiology of hepatocellular carcinoma. In Viruses and liver cancer, ed. E<br />
Tabor. Amsterdam: Elsevier Science.<br />
Kripke C 2007. Hepatitis B vaccine for infants of HBsAg-positive mothers. Am Fam Physician 75(1): 49–50.<br />
Lavanchy D 2004. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging<br />
prevention and control measures. J Viral Hepat 11(2): 97–107.<br />
Lavanchy D 2005. Worldwide epidemiology of HBV infection, disease burden, and vaccine prevention. J Clin<br />
Virol 34 (1 Suppl): S1–3.<br />
Law MG, Roberts SK, Dore GJ & Kaldor JM 2000. Primary hepatocellular carcinoma in Australia, 1978–1997:<br />
increasing incidence and mortality. Med J Aust 173(8): 403–5.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
1<br />
H e p a t i t i s B
Lee C, Gong Y, Brok J, Boxall EH & Gluud C 2006. Hepatitis B immunisation for newborn infants of hepatitis<br />
B surface antigen-positive mothers. Cochrane Database of Systematic Reviews (2): CD004790.<br />
Lee CL, Hsieh KS & Ko YC 2003. Trends in the incidence of hepatocellular carcinoma in boys and girls in<br />
Taiwan after large-scale hepatitis B vaccination. <strong>Cancer</strong> Epidemiol Biomarkers Prev 12(1): 57–9.<br />
Lesmana LA, Leung NW, Mahachai V, Phiet PH, Suh DJS, Yao G & Zhuang H 2006. Hepatitis B: overview of<br />
the burden of disease in the Asia-Pacific region. Liver Int 26: 3–10.<br />
Locarnini S & Omata M 2006. Molecular virology of hepatitis B virus and the development of antiviral drug<br />
resistance. Liver Int 26: 11–22.<br />
Lok AS 2004. <strong>Prevention</strong> of hepatitis B virus-related hepatocellular carcinoma. Gastroenterology 127(5 Suppl<br />
1): S303–9.<br />
McGlynn KA & London WT 2005. Epidemiology and natural history of hepatocellular carcinoma. Best Pract<br />
Res Clin Gastroenterol 19(1): 3–23.<br />
<strong>National</strong> Health and Medical Research Council (NHMRC) 2008. The Australian Immunisation Handbook, 9th<br />
edn. Canberra: Australian Government Department of Health and Ageing.<br />
NNDSS 2007. Annual Report <strong>National</strong> Notifiable Diseases Surveillance System 2005. Commun Dis Intell<br />
31(1): 14–21.<br />
O’Brien TR, Kirk G & Zhang M 2004. Hepatocellular carcinoma: paradigm of preventive oncology. <strong>Cancer</strong><br />
Journal 10(2): 67–73.<br />
O’Sullivan BG, Gidding HF, Law M, Kaldor JM, Gilbert GL & Dore GJ 2004. Estimates of chronic hepatitis B<br />
virus infection in Australia, 2000. Aust N Z J Public Health 28(3): 212–16.<br />
Ocama P, Opio CK & Lee WM 2005. Hepatitis B virus infection: current status. Am J Med 118(12): 1413.<br />
Okanoue T & Minami M 2006. Update of research and management of hepatitis B. J Gastroenterol 41(2):<br />
107–18.<br />
Perz JF, Armstrong GL, Farrington LA, Hutin YJ & Bell BP 2006. The contributions of hepatitis B virus and<br />
hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol 45(4): 529–38.<br />
Petersen KM, Bulkow LR, McMahon BJ, Zanis C, Getty M, Peters H & Parkinson AJ 2004. Duration of<br />
hepatitis B immunity in low risk children receiving hepatitis B vaccinations from birth. Pediatr Infect Dis J<br />
23(7): 650–5.<br />
Previsani N, Lavanchy D & Zuckerman AJ 2004. Hepatitis B. In Viral hepatitis, ed. IK Mushahwar. Geneva:<br />
World Health Organization.<br />
Raza SA, Clifford GM & Franceschi S 2007. Worldwide variation in the relative importance of hepatitis B and<br />
hepatitis C viruses in hepatocellular carcinoma: a systematic review. Br J <strong>Cancer</strong> 96(7): 1127–34.<br />
Roberts SK & Kemp W 2007. Hepatocellular carcinoma in an Australian tertiary referral hospital 1975–2002:<br />
change in epidemiology and clinical presentation. J Gastroenterol Hepatol 22(2): 191–6.<br />
Tang B, Kruger WD, Chen G, Shen F, Lin WY, Mboup S, London WT & Evans AA 2004. Hepatitis B viremia is<br />
associated with increased risk of hepatocellular carcinoma in chronic carriers. J Med Virol 72(1): 35–40.<br />
Tawk HM, Vickery K, Bisset L, Lo SK, Selby W, Cossart YE & Infection in Endoscopy Study Group 2006a. The<br />
current pattern of hepatitis B virus infection in Australia. J Viral Hepat 13(3): 206–15.<br />
Tawk HM, Vickery K, Bisset L, Selby W, Cossart YE & Infection in Endoscopy Study Group 2006b. The impact<br />
of hepatitis B vaccination in a Western country: recall of vaccination and serological status in Australian<br />
adults. Vaccine 24(8): 1095–1106.<br />
van der Sande MA, Waight P, Mendy M, Rayco-Solon P, Hutt P, Fulford T, Doherty C, McConkey SJ,<br />
Jeffries D, Hall AJ & Whittle HC 2006. Long-term protection against carriage of hepatitis B virus after infant<br />
vaccination. J Infect Dis 193(11): 1528–35.<br />
Villeneuve JP 2005. The natural history of chronic hepatitis B virus infection. J Clin Virol 34 (1 Suppl): S139–42.<br />
200 Section Three: Immunisation
Williams A 2002. Reduction in the hepatitis B related burden of disease – measuring the success of universal<br />
immunisation programs. Commun Dis Intell 26(3): 458–60.<br />
Wood N, Backhouse J, Gidding HF, Gilbert GL, Lum G & McIntyre PB 2005. Estimates of chronic hepatitis B<br />
virus infection in the Northern Territory. Commun Dis Intell 29(3): 289–90.<br />
World Health Organization (WHO) 2004. Hepatitis B vaccines. Wkly Epidemiol Rec 79(28): 255–63.<br />
Yu AS, Cheung RC & Keeffe EB 2004. Hepatitis B vaccines. Clin Liver Dis 8(2): 283–300.<br />
Yu MW, Yeh SH, Chen PJ, Liaw YF, Lin CL, Liu CJ, Shih WL, Kao JH, Chen DS & Chen CJ 2005. Hepatitis B<br />
virus genotype and DNA level and hepatocellular carcinoma: a prospective study in men. J Natl <strong>Cancer</strong> Inst<br />
97(4): 265–72.<br />
Yuen MF, Lim WL, Chan AO, Wong DK, Sum SS & Lai CL 2004. 18-year follow-up study of a prospective<br />
randomized trial of hepatitis B vaccinations without booster doses in children. Clin Gastroenterol Hepatol<br />
2(10): 941–5.<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
201<br />
H e p a t i t i s B
List of contributors
Authors<br />
Dr Cleola Anderiesz BSc (Hons), PhD, Grad<br />
Cert H.Ec (HPV chapter)<br />
Kate Broun BAppSci (Health Promotion)<br />
(Hons) (Cervical cancer chapter)<br />
Manager<br />
PapScreen Victoria<br />
Kathy Chapman BSc, MNutrDiet* (Nutrition<br />
and Obesity chapters)<br />
Nutrition Program Manager<br />
The <strong>Cancer</strong> Council NSW<br />
Dr Tanya Chikritzhs PhD, Post GradDip (Epi<br />
& Biostats), BA (Hons) (Alcohol chapter)<br />
Senior Research Fellow<br />
<strong>National</strong> Drug Research Institute<br />
Curtin University<br />
Professor Yvonne Cossart (Hepatitis B<br />
chapter)<br />
Bosch Professor<br />
Department of Infectious Diseases and<br />
Immunology<br />
The University of Sydney<br />
Alison Evans PhD (Breast cancer chapter)<br />
Acting Deputy Director<br />
<strong>National</strong> Breast <strong>Cancer</strong> Centre<br />
Associate Professor Dorota Gertig MBBS,<br />
MHSC, ScD, FAFPHM (Principles of<br />
Screening chapter)<br />
Medical Director<br />
Victorian Cervical Cytology Registry<br />
Paul Grogan* (<strong>Tobacco</strong> chapter)<br />
Advocacy Manager<br />
The <strong>Cancer</strong> Council Australia<br />
Dr Jane Jeffs BAppSc (Med Lab Sc), PhD,<br />
MASM (Hepatitis B chapter)<br />
Immunisation Handbook and <strong>Policy</strong><br />
Coordinator<br />
The Children’s Hospital at Westmead<br />
Tracey Johnston BA (Hons) (Breast cancer<br />
chapter)<br />
Communications Officer<br />
BreastScreen Victoria Coordination Unit<br />
Ellen Kerrins BN (UNSW), RN, Post Grad<br />
OncNsg* (Prostate cancer chapter)<br />
Group Executive<br />
<strong>Cancer</strong> <strong>Control</strong> Programs<br />
The <strong>Cancer</strong> Council South Australia<br />
Dr Simone Lee BSc, MND, PhD (Nutrition<br />
chapter)<br />
Coordinator Public Health Nutrition<br />
<strong>Cancer</strong> <strong>Prevention</strong> Unit<br />
The <strong>Cancer</strong> Council South Australia<br />
Dr Kristine Macartney BMedSci, MBBS<br />
(Hons), MD, FABP (USA) (Hepatitis B<br />
chapter)<br />
Deputy Director, <strong>Policy</strong> Support<br />
The <strong>National</strong> Centre for Immunisation<br />
Research and Surveillance (NCIRS)<br />
Postgraduate Clinical Fellow, Department of<br />
Infectious Diseases and Microbiology<br />
The Children’s Hospital at Westmead<br />
Professor Ian Olver MD, PhD, CMin, FRACP,<br />
FAChPM, MRACMA* (Prostate cancer<br />
chapter)<br />
Chief Executive Officer<br />
The <strong>Cancer</strong> Council Australia<br />
Alison Peipers BEd, GradDipTEFL* (Bowel<br />
cancer chapter)<br />
Deputy Director<br />
<strong>Cancer</strong> Education Unit<br />
The <strong>Cancer</strong> Council Victoria<br />
Steve Pratt APD, MAAESS, BSc (Human<br />
Movement), BSc (Nutrition and Food<br />
Science), GradDip (Dietetics), GradCert<br />
(Food Technology) (Physical activity<br />
chapter)<br />
Nutrition and Physical Activity Coordinator<br />
The <strong>Cancer</strong> Council Western Australia<br />
Craig Sinclair BEd (Sec), PostGrad Rec,<br />
PostGrad OrgBehav, MPPM* (Ultraviolet<br />
radiation and Melanoma chapters)<br />
Director<br />
<strong>Cancer</strong> Education Unit<br />
The <strong>Cancer</strong> Council Victoria<br />
Professor James St John MD, FRCP, FRACP<br />
(Bowel cancer chapter)<br />
Honorary Senior Associate<br />
The <strong>Cancer</strong> Council Victoria<br />
Anita Tang BA, MALP* (<strong>Tobacco</strong> chapter)<br />
Director, Health Strategies<br />
The <strong>Cancer</strong> Council NSW<br />
Susan Upham (Physical activity chapter)<br />
GP Education Project Coordinator<br />
The <strong>Cancer</strong> Council Western Australia<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
203<br />
L i s t o f c o n t r i b u t o r s
Noni Walker MPH, BSc, Postgraduate<br />
Diploma in Nutrition and Dietetics (<strong>Tobacco</strong><br />
chapter)<br />
Walker Shanley Consultancy<br />
*Members of The <strong>Cancer</strong> Council Australia’s<br />
Public Health Committee 2006–07<br />
Contributors/reviewers<br />
Professor Annie S Anderson BSc, PhD, SRD<br />
Centre for Public Health Nutrition Research<br />
Department of Medicine<br />
University of Dundee<br />
Sandy Angus BSSc*<br />
Senior Project Officer (Indigenous),<br />
Queensland Cervical Screening Program<br />
<strong>Cancer</strong> Screening Services Unit<br />
Population Health/Public Health Services<br />
Unit<br />
Queensland Health<br />
Gaël Castillo Bachelor of Business Systems<br />
Office of the Director<br />
The <strong>Cancer</strong> Council Victoria<br />
Professor Simon Chapman PhD<br />
Director of Research<br />
School of Public Health A27<br />
University of Sydney<br />
Professor Kate Conigrave FAChAM,<br />
FAFPHM, PhD<br />
Staff Specialist<br />
Drug Health Services<br />
Royal Prince Alfred Hospital<br />
Conjoint Associate Professor<br />
School of Public Health and Departments of<br />
Psychological Medicine and Medicine<br />
University of Sydney<br />
Kay Coppa RN, GradDipHealthScience<br />
(Primary Health Care), MPH<br />
Skin <strong>Cancer</strong> <strong>Prevention</strong> Manager<br />
The <strong>Cancer</strong> Council NSW<br />
Levinia Crooks BA (Hons), DipEd<br />
Chief Executive Officer<br />
Australasian Society for HIV Medicine<br />
(ASHM)<br />
Levinia Crooks BA (Hons), DipEd<br />
Chief Executive Officer<br />
Australasian Society for HIV Medicine<br />
(ASHM)<br />
204 <strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
Professor Chris Del Mar MA, MB BChir,<br />
MD, FRACGP, FAFPHM<br />
Dean, Faculty of Health Sciences and<br />
Medicine<br />
Bond University<br />
Associate Professor Greg Dore BSc, MBBS,<br />
PhD, FRACP, MPH<br />
Head, Viral Hepatitis Clinical Research<br />
Program<br />
<strong>National</strong> Centre In HIV Epidemiology and<br />
Clinical Research<br />
University of New South Wales<br />
Associate Professor Peter Foley BMedSc,<br />
MBBS (Monash), MD (Melbourne), FACD<br />
Department of Medicine (Dermatology)<br />
The University of Melbourne<br />
St Vincent’s Hospital Melbourne<br />
Dr Linda Foreman MBBS, MPH, FRACGP*<br />
General Practitioner, Chandlers Hill Surgery<br />
GP Advisor<br />
The <strong>Cancer</strong> Council South Australia<br />
Professor Ian Frazer FAA, MB, ChB, MD<br />
Director, Diamantina Institute for <strong>Cancer</strong>,<br />
Immunology and Metabolic Medicine<br />
The University of Queensland<br />
Susan Greenbank BAppSci (Health<br />
Promotion)*<br />
Manager, <strong>Prevention</strong> and Early Detection<br />
Unit<br />
The <strong>Cancer</strong> Council Queensland<br />
Professor Mark Harris MBBS, DRACOG,<br />
FRACGP, MD<br />
Professor of General Practice<br />
Executive Director, Centre for Primary<br />
Health Care and Equity<br />
School of Public Health and Community<br />
Medicine<br />
University of NSW<br />
Darlene Henning BA (Psychology)<br />
Coordinator, General Practice Program<br />
<strong>Cancer</strong> Education Unit<br />
The <strong>Cancer</strong> Council Victoria<br />
Dr Chris Karapetis MBBS, FRACP, MMedSc<br />
Senior Consultant Medical Oncologist<br />
Department of Medical Oncology, Flinders<br />
Medical Centre<br />
And Senior Lecturer, Flinders University
Associate Professor John Kelly MDBS,<br />
FACD<br />
Head, Victorian Melanoma Service<br />
The Alfred<br />
Rachel Laws BSc (Nutrition), MSc (Nutrition<br />
& Dietetics)<br />
Research Fellow<br />
UNSW Research Centre for Primary Health<br />
Care & Equity<br />
School of Public Health & Community<br />
Medicine<br />
UNSW<br />
Professor Evie Leslie BAppSci (Phys Ed),<br />
MHN, PhD<br />
Associate Professor of Public Health<br />
Deakin University<br />
Dr Rosemary Lester MBBS, MPH, MS<br />
(Epid), FAFPHM<br />
Assistant Director, Public Health Branch<br />
Communicable Disease <strong>Control</strong> Unit<br />
Department of Human Services<br />
Belinda Lowcay BBehavSc*<br />
Primary Health Care Coordinator<br />
<strong>Cancer</strong> <strong>Prevention</strong> Unit<br />
The <strong>Cancer</strong> Council South Australia<br />
Jane Martin BA (Hons), MPH<br />
Senior <strong>Policy</strong> Adviser<br />
Obesity <strong>Policy</strong> Coalition (The <strong>Cancer</strong> Council<br />
Victoria, Diabetes Victoria and Deakin<br />
University)<br />
Rosemary Moore<br />
Editor, Publications Unit<br />
The <strong>Cancer</strong> Council Victoria<br />
Jennifer Muller<br />
Senior Director<br />
<strong>Cancer</strong> Screening Services Unit<br />
Queensland Health<br />
Meg Murchland BA (Lib & Inf Mgmt),<br />
GDPH<br />
<strong>Cancer</strong> <strong>Control</strong> Programs Information<br />
Officer<br />
The <strong>Cancer</strong> Council South Australia<br />
Carole Pinnock PhD<br />
Chair, Education Committee<br />
Australian Prostate <strong>Cancer</strong> Collaboration<br />
Principal Research Scientist, Urology Unit<br />
Repatriation General Hospital, Daws Park,<br />
South Australia<br />
Dorothy Reading BA, DipEd*<br />
Senior Strategic Consultant<br />
The <strong>Cancer</strong> Council Victoria<br />
And Chair, Public Health Committee<br />
The <strong>Cancer</strong> Council Australia<br />
Lesley Rowlands MPH<br />
Research Assistant<br />
Victorian Cytology Service<br />
Dr Marion Saville MBChB, Am Bd (Anat<br />
Path & Cytopath), FIAC, Grad Dip Med<br />
(Clin Epi)<br />
Director, Victorian Cytology Service<br />
Terry Slevin BA (Hons), MPH<br />
Director, Education and Research<br />
The <strong>Cancer</strong> Council Western Australia<br />
Associate Professor Suzanne Steginga PhD<br />
Director of Community Services and<br />
Research Programs<br />
The <strong>Cancer</strong> Council Queensland<br />
Philippa Thomson BA, BEd<br />
Research Administrative Assistant,<br />
Research Management Unit<br />
The <strong>Cancer</strong> Council Victoria<br />
Vicky Thursfield<br />
Information Manager, <strong>Cancer</strong> Epidemiology<br />
Centre<br />
The <strong>Cancer</strong> Council Victoria<br />
Dr Justin Tse MBBS, MMed, FRACGP<br />
Sub-dean, Royal Melbourne Hospital<br />
Clinical School<br />
Royal Melbourne Hospital<br />
The University of Melbourne<br />
Elmer V Villanueva MD, ScM, FRIPH<br />
Epidemiologist<br />
<strong>National</strong> Breast <strong>Cancer</strong> Centre<br />
Dr Vicky White<br />
Deputy Director, Centre for Behavioural<br />
Research in <strong>Cancer</strong><br />
The <strong>Cancer</strong> Council Victoria<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
205<br />
L i s t o f c o n t r i b u t o r s
Index
A<br />
alcohol 107 – 119<br />
aims of The <strong>Cancer</strong> Council<br />
Australia 116<br />
alcohol-related health impacts<br />
deaths 111<br />
disease burden<br />
how disease burden is calculated<br />
110<br />
economic costs 111<br />
social costs 111<br />
alcohol control measures 107,<br />
113<br />
access 113<br />
community interventions 113<br />
media / advertising 113<br />
<strong>National</strong> Alcohol Strategy 113,<br />
116<br />
NHMRC guidelines 107<br />
pricing 113<br />
primary care / GPs 113<br />
public safety 113<br />
reports and guidelines<br />
Alcohol guidelines for Australians<br />
107, 116<br />
GP guidelines 115<br />
Lifescripts 116<br />
NHMRC dietary guidelines<br />
115, 116<br />
surveys and reports<br />
ASSAD 112<br />
link between alcohol and<br />
cancer<br />
and smoking 108<br />
cancer types 108<br />
bowel/colorectal cancer 108,<br />
146<br />
breast cancer 108<br />
evidence for other cancers 109<br />
larynx 107<br />
liver 107<br />
mouth 107<br />
oesophagus 107<br />
other diseases 107<br />
pharynx 107<br />
women and risk 107<br />
prevalence of risky, high-risk<br />
and binge drinking 112<br />
Aboriginal and Torres Strait<br />
Islander peoples 112<br />
adults 112<br />
drinking trends 113<br />
teenagers 112<br />
B<br />
bowel cancer 145 – 160<br />
aims of The <strong>Cancer</strong> Council<br />
Australia 154, 155<br />
benefits and risk from bowel<br />
screening 153<br />
colonoscopy complications<br />
124, 153<br />
detecting advanced adenoma<br />
153<br />
false positive results 153<br />
psychological effects 153, 154<br />
reduce mortality 153<br />
deaths 145<br />
detection and screening 147<br />
colonoscopy 149, 150, 153<br />
faecal occult blood tests 148,<br />
151<br />
role of general practice 146,<br />
152, 153<br />
screening rationale 147<br />
sigmoidoscopy 149<br />
incidence 145<br />
Aboriginal and Torres Strait<br />
Islander peoples 145<br />
men 145<br />
women 145<br />
national bowel cancer<br />
screening program 123,<br />
150, 151<br />
Aboriginal and Torres Strait<br />
Islander peoples 152<br />
pilot program 150<br />
role of general practice 152,<br />
153<br />
screening for people at<br />
increased risk 151, 152<br />
who should be screened? 150,<br />
154<br />
prevention 145<br />
aspirin 146<br />
Clinical practice guidelines<br />
146<br />
preventable risk factors 146<br />
risk factors 145<br />
advanced adenoma 145<br />
alcohol 146<br />
chronic inflammatory bowel<br />
disease 145<br />
Clinical practice guidelines<br />
146<br />
family history 145<br />
FAP 146<br />
HNPCC 146<br />
nutrition 146<br />
obesity and overweight 74<br />
personal history of bowel<br />
cancer 145<br />
reducing risk through physical<br />
activity 74<br />
breast cancer 126 – 137<br />
aims of The <strong>Cancer</strong> Council<br />
Australia 133, 134<br />
benefits and risks from breast<br />
screening 124, 132<br />
DCIS ‘over-diagnosis’ 132<br />
false negative and false positive<br />
results 124<br />
psychological effects 132<br />
reducing deaths 132<br />
deaths 126<br />
detection and screening<br />
breast awareness 129<br />
effectiveness 129<br />
breast self-examination 129<br />
effectiveness 129<br />
clinical breast examination<br />
129<br />
effectiveness 128<br />
mammography 128<br />
effectiveness 128<br />
role of general practice 131<br />
incidence 126<br />
national breast cancer<br />
screening program 123<br />
BreastScreen Australia performance<br />
130<br />
who should be screened? 132,<br />
133<br />
prevention 128<br />
risk factors 127<br />
alcohol 127<br />
being female 127<br />
family history 127<br />
gene variations 127<br />
HRT 127<br />
increasing age 127<br />
obesity and overweight (postmenopause)<br />
74<br />
other risk factors 127<br />
reducing risk with physical<br />
activity 74<br />
C<br />
cervical cancer 138 – 144<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
20<br />
I n d e x
aims of The <strong>Cancer</strong> Council<br />
Australia 143<br />
benefits and risks from cervical<br />
screening 141<br />
false negative and false positive<br />
results 142<br />
reducing deaths 141<br />
causes / risk factors 138<br />
antibodies for Chlamydia or<br />
herpes 138<br />
HPV 138, 139<br />
immunosuppression 138<br />
oral contraceptives 138<br />
pregnancies 138<br />
smoking 138<br />
detection and screening<br />
other screening technologies<br />
139, 140<br />
Pap test 139<br />
national cervical cancer<br />
screening program 123,<br />
140<br />
changes to guidelines 141<br />
role of general practice 141<br />
who should be screened? 140,<br />
142<br />
vaccine 9, 139<br />
H<br />
hepatitis B 9, 109, 186<br />
human papilloma virus 9, 138,<br />
139, 140, 141, 143<br />
M<br />
melanoma 161 – 164<br />
aims of The <strong>Cancer</strong> Council<br />
Australia 163<br />
deaths 161<br />
detection and screening 161<br />
dermoscopy 162<br />
rationale for screening for<br />
melanoma 162<br />
role of general practice 161,<br />
162<br />
self-examination 162<br />
skin examination by doctor 161<br />
incidence 161<br />
insufficient evidence for<br />
population screening<br />
123, 163<br />
prevention 161<br />
N<br />
nutrition 52 – 70<br />
aims of The <strong>Cancer</strong> Council<br />
Australia 64, 65<br />
improving nutrition: approaches<br />
and programs 59<br />
behavioural interventions 60<br />
economic benefits 57<br />
environmental interventions 60<br />
general practice 62<br />
programs<br />
Eat Well Australia 63<br />
Healthy Weight 2008 63<br />
specific cancer prevention<br />
interventions 61<br />
statewide programs 61<br />
reports and regulation<br />
Australian Guide to Healthy<br />
Eating 64<br />
Children’s Television Standards<br />
63<br />
Food Standards Code 63<br />
<strong>National</strong> Nutrition Survey<br />
57<br />
NHMRC dietary guidelines<br />
64<br />
UICC cancer prevention<br />
strategies 64<br />
WHO Global Strategy on<br />
diet 63<br />
improving nutrition: barriers to<br />
effective interventions<br />
Aboriginal and Torres Strait<br />
Islander peoples 59<br />
current consumption trends 58<br />
disadvantaged groups 59<br />
link between poor nutrition and<br />
cancer 52<br />
bowel cancer 146<br />
deaths 57<br />
dietary fat 55<br />
dietary supplements 56<br />
disadvantaged groups 59<br />
economic costs 57<br />
fibre 55<br />
fish 55<br />
fruit and vegetables 53, 54, 55<br />
meat 55<br />
salt 56<br />
20 <strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
O<br />
selenium 56<br />
overweight and obesity 86 – 106<br />
aims of The <strong>Cancer</strong> Council<br />
Australia 99<br />
approaches and programs to<br />
help prevent overweight<br />
and obesity 93, 94<br />
body mass index (BMI) 86<br />
children and adolescents 86<br />
childcare 95<br />
children 86, 93<br />
addressing the obesogenic<br />
environment 94<br />
families 95<br />
food industry 95, 96<br />
individual behaviour change<br />
95<br />
life course approach 93<br />
media / advertising 95<br />
neighbourhoods 95<br />
policy 96<br />
primary care / GPs 95<br />
public health interventions 97<br />
reports<br />
Acting on Australia’s weight<br />
98<br />
Eat well Australia 98<br />
GP guidelines 97<br />
Healthy weight 2008 98<br />
Lifescripts 97<br />
<strong>National</strong> physical activity for<br />
health action plan 98<br />
Overweight and obesity in<br />
adults 97<br />
Overweight and obesity in<br />
children and adolescents<br />
97<br />
WHO Global Strategy 98<br />
schools 95<br />
tax on soft drinks 96<br />
waist circumference measurement<br />
86, 87<br />
workplaces 95<br />
burden of disease 14, 89<br />
deaths 89<br />
economic costs 87, 89, 90<br />
social costs 90<br />
quality of life 90<br />
link between overweight and<br />
obesity and cancer<br />
bowel / colon cancer 146
east cancer (post-menopause)<br />
87, 88<br />
cancer types 86, 88<br />
colon cancer 86, 87, 88<br />
endometrial cancer 86, 87, 88<br />
gall bladder cancer 86, 87, 88<br />
kidney cancer 86, 87, 88<br />
oesophageal cancer 86, 87, 88<br />
weight loss and reduction in<br />
cancer risk 88<br />
prevalence of overweight and<br />
obesity<br />
‘epidemic’ in Australia 8, 86<br />
Aboriginal and Torres Strait<br />
Islander peoples 92<br />
adults 86, 90<br />
children 86, 87, 91<br />
disadvantaged groups 92<br />
Middle Eastern origin 86, 92<br />
rural communities 92<br />
southern European origin 86,<br />
92<br />
P<br />
physical activity 71 – 85<br />
aims of The <strong>Cancer</strong> Council<br />
Australia 81, 82<br />
approaches and programs<br />
to encourage physical<br />
activity<br />
Aboriginal and Torres Strait<br />
Islander peoples 80<br />
Australia’s physical activity<br />
recommendations for 12-<br />
18 year olds 80<br />
Australia’s physical activity<br />
recommendations for 5-12<br />
year olds 80<br />
Be Active Australia 76<br />
childcare 78<br />
community environments and<br />
organisations 76<br />
disadvantaged people 80<br />
GPs 77, 78<br />
health services 77<br />
<strong>National</strong> physical activity<br />
guidelines for Australians<br />
80, 81<br />
national programs 75<br />
population trends in physical<br />
activity 75, 76<br />
schools 78<br />
strategies<br />
communications and media<br />
79<br />
GPs 79<br />
research 79<br />
workplaces 78, 79<br />
links between physical activity<br />
and cancer prevention<br />
75<br />
breast cancer 73, 74, 75, 80<br />
colon cancer 73, 80<br />
other cancers 74<br />
links between physical<br />
inactivity and cancer<br />
71, 73<br />
bowel / colon cancer 146<br />
breast cancer 71<br />
colon cancer 71<br />
how physical activity is measured<br />
72<br />
overweight and obesity 71<br />
types of cancer 71<br />
prostate cancer 165 – 174<br />
aims of The <strong>Cancer</strong> Council<br />
Australia 171<br />
benefits and risk from prostate<br />
screening (potential) 170<br />
difficulty of distinguishing lifethreatening<br />
cancers 170<br />
over-diagnosis 170<br />
treatment issues 170, 171<br />
causes / risk factors 166<br />
age 166<br />
family history 166<br />
deaths 165, 166<br />
detection 166<br />
digital rectal examination 167<br />
future screening prospects<br />
168<br />
PSA 166, 167<br />
test limitations 167, 168<br />
who has been tested? 168<br />
role of general practice 169<br />
transrectal ultrasound and<br />
biopsy 167<br />
incidence 165<br />
insufficient evidence for<br />
population screening<br />
123, 168, 170<br />
prevention 166<br />
chemoprevention 166<br />
S<br />
screening<br />
economic issues 125<br />
informed consent 124<br />
potential harms 124<br />
principles 122<br />
WHO criteria 122<br />
T<br />
tobacco 12 – 40<br />
aims of The <strong>Cancer</strong> Council<br />
Australia 34, 35, 36, 37<br />
link between tobacco and<br />
cancer 13<br />
anal cancer 15<br />
bladder cancer 15<br />
bowel / colorectal cancer 15<br />
cervical cancer 15<br />
kidney cancer 15<br />
laryngeal cancer 15<br />
lung cancer 15<br />
oesophageal cancer 15<br />
oral cancers 15<br />
other diseases 14, 19<br />
pancreatic cancer 15<br />
passive smoking and cancer<br />
13<br />
penis cancer 15<br />
stomach cancer 15<br />
types of cancer associated<br />
with tobacco 13, 15<br />
bowel cancer 146<br />
vulval cancer 15<br />
smoking prevalence 15, 17<br />
Aboriginal and Torres Strait<br />
Islander peoples 16<br />
adults 27<br />
country of birth 17<br />
socially disadvantaged 16, 18<br />
teenagers 17<br />
tobacco control: barriers to<br />
effective interventions<br />
attitudes that undermine effective<br />
intervention 18, 19<br />
tobacco industry 12, 19<br />
tobacco control measures 9, 12<br />
Aboriginal and Torres Strait<br />
Islander peoples 26, 32<br />
disadvantaged people 31, 32<br />
economic benefits 19, 20<br />
funding 21<br />
health warnings 26<br />
history of policy in Australia<br />
26<br />
litigation 24<br />
<strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09<br />
20<br />
I n d e x
preventing smoking uptake 31<br />
price increases 24<br />
product regulation 22, 23, 24,<br />
28, 29<br />
programs<br />
<strong>National</strong> <strong>Tobacco</strong> Campaign<br />
22, 27, 32<br />
<strong>National</strong> <strong>Tobacco</strong> Strategy<br />
24, 28, 30, 33<br />
Quit 30<br />
Smoke-free 30<br />
reports and legislation<br />
health surveys 15<br />
International <strong>Tobacco</strong><br />
<strong>Control</strong> <strong>Policy</strong> Evaluation<br />
Study 32<br />
<strong>National</strong> Drug Strategy<br />
Household Survey 32<br />
<strong>National</strong> <strong>Tobacco</strong> Strategy<br />
21<br />
<strong>Tobacco</strong> Advertising Prohibition<br />
Act 22, 23, 27, 33<br />
<strong>Tobacco</strong> control: a blue<br />
chip investment in public<br />
health 34<br />
Trade Practices Act 34<br />
WHO Framework Convention<br />
on <strong>Tobacco</strong> <strong>Control</strong><br />
23, 33<br />
smoke-free environments 25,<br />
28<br />
smoking cessation aids 25<br />
workplace development 33<br />
workplaces 26<br />
tobacco related health impacts<br />
chronic disease 14<br />
deaths 13, 14, 17, 18<br />
economic costs 14<br />
social costs 15<br />
U<br />
ultraviolet radiation 41 – 50<br />
aims of The <strong>Cancer</strong> Council<br />
Australia 47, 48, 49<br />
link between UV radiation and<br />
skin cancer 41<br />
adult exposure 42<br />
basal cell carcinoma 41<br />
incidence 44<br />
childhood exposure 41<br />
impact of ozone depletion 42<br />
melanoma 41<br />
incidence 43<br />
screening 46<br />
solariums 42<br />
squamous cell carcinoma 41<br />
incidence 44<br />
skin cancer: barriers to<br />
effective interventions<br />
absence of a national program<br />
46<br />
concerns about vitamin D<br />
deficiency 42, 45<br />
desirability of a tan 45<br />
growth in solarium industry 44<br />
skin cancer prevention<br />
approaches and<br />
programs 41, 46, 47<br />
changing adolescents’ attitudes<br />
45<br />
Slip! Slop! Slap! 41<br />
sunscreen 42<br />
upskilling GPs 45, 47<br />
UV Alert 45<br />
210 <strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007 – 09
The <strong>National</strong> <strong>Cancer</strong> <strong>Prevention</strong> <strong>Policy</strong> 2007–09 advocates for a concerted and<br />
comprehensive national approach to the prevention of cancer in Australia.<br />
Preventing cancer means that the pain, inconvenience and distress of cancer are<br />
avoided—not only for people with disease, but also for their families and friends. Our<br />
health system also benefits; resources and time can be allocated elsewhere as the<br />
burden of treating this disease reduces.<br />
This policy has been carefully researched and reviewed. International knowledge about<br />
risk is presented, along with evidence of effective interventions and strategies relevant to<br />
the Australian context. We outline program structures that could be suitable for helping a<br />
wide range of people.<br />
We recommend actions for a national impact. For these actions to be effective, the<br />
cancer councils and government need to bring together our strengths—our capacities to<br />
lead, implement and resource.<br />
www.cancer.org.au