Improving Patient Flow and Reducing Emergency Department ...
Improving Patient Flow and Reducing Emergency Department ...
Improving Patient Flow and Reducing Emergency Department ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
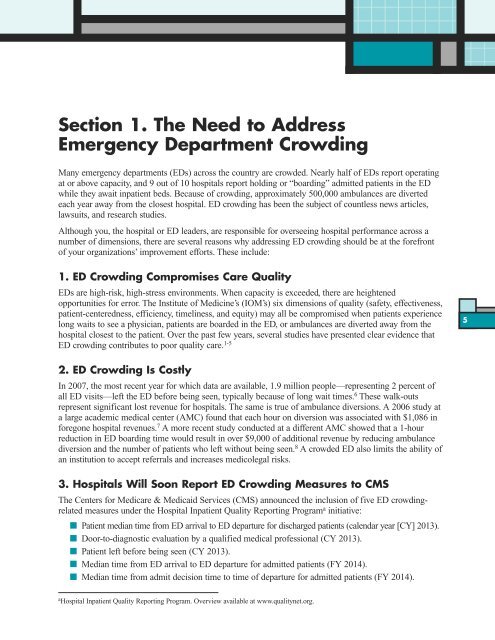
Section 1. The Need to Address<br />
<strong>Emergency</strong> <strong>Department</strong> Crowding<br />
Many emergency departments (EDs) across the country are crowded. Nearly half of EDs report operating<br />
at or above capacity, <strong>and</strong> 9 out of 10 hospitals report holding or “boarding” admitted patients in the ED<br />
while they await inpatient beds. Because of crowding, approximately 500,000 ambulances are diverted<br />
each year away from the closest hospital. ED crowding has been the subject of countless news articles,<br />
lawsuits, <strong>and</strong> research studies.<br />
Although you, the hospital or ED leaders, are responsible for overseeing hospital performance across a<br />
number of dimensions, there are several reasons why addressing ED crowding should be at the forefront<br />
of your organizations’ improvement efforts. These include:<br />
1. ED Crowding Compromises Care Quality<br />
EDs are high-risk, high-stress environments. When capacity is exceeded, there are heightened<br />
opportunities for error. The Institute of Medicine’s (IOM’s) six dimensions of quality (safety, effectiveness,<br />
patient-centeredness, efficiency, timeliness, <strong>and</strong> equity) may all be compromised when patients experience<br />
long waits to see a physician, patients are boarded in the ED, or ambulances are diverted away from the<br />
hospital closest to the patient. Over the past few years, several studies have presented clear evidence that<br />
ED crowding contributes to poor quality care. 1-5<br />
2. ED Crowding Is Costly<br />
In 2007, the most recent year for which data are available, 1.9 million people—representing 2 percent of<br />
all ED visits—left the ED before being seen, typically because of long wait times. 6 These walk-outs<br />
represent significant lost revenue for hospitals. The same is true of ambulance diversions. A 2006 study at<br />
a large academic medical center (AMC) found that each hour on diversion was associated with $1,086 in<br />
foregone hospital revenues. 7 A more recent study conducted at a different AMC showed that a 1-hour<br />
reduction in ED boarding time would result in over $9,000 of additional revenue by reducing ambulance<br />
diversion <strong>and</strong> the number of patients who left without being seen. 8 A crowded ED also limits the ability of<br />
an institution to accept referrals <strong>and</strong> increases medicolegal risks.<br />
3. Hospitals Will Soon Report ED Crowding Measures to CMS<br />
The Centers for Medicare & Medicaid Services (CMS) announced the inclusion of five ED crowdingrelated<br />
measures under the Hospital Inpatient Quality Reporting Programa initiative:<br />
n <strong>Patient</strong> median time from ED arrival to ED departure for discharged patients (calendar year [CY] 2013).<br />
n Door-to-diagnostic evaluation by a qualified medical professional (CY 2013).<br />
n <strong>Patient</strong> left before being seen (CY 2013).<br />
n Median time from ED arrival to ED departure for admitted patients (FY 2014).<br />
n Median time from admit decision time to time of departure for admitted patients (FY 2014).<br />
a Hospital Inpatient Quality Reporting Program. Overview available at www.qualitynet.org.<br />
5