Mission: Possible - Children's Hospital Boston
Mission: Possible - Children's Hospital Boston
Mission: Possible - Children's Hospital Boston
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
news<br />
August 2007<br />
Children’s<br />
Investing in<br />
asthma education<br />
Asthma is the leading cause of<br />
Inside<br />
hospitalization at Children’s Hos-<br />
pital <strong>Boston</strong> and its rates in New<br />
England are among the highest in the na-<br />
tion. But some of the best ways to improve<br />
asthma outcomes—education and home<br />
interventions—are often not covered by<br />
insurance. To help resolve this problem, Chil-<br />
dren’s partnered with the Asthma Regional<br />
Council (ARC) to make an economic case for<br />
investing in asthma prevention programs.<br />
With the help of researchers at UMass, Lowell<br />
(UML), they conducted a study called Invest-<br />
ing in Best Practices for Asthma. “We found<br />
cost savings across our 20-year review of the<br />
published literature from more than $7 for<br />
every $1 invested in asthma education to as<br />
high as $36 for every $1 invested,” says UML<br />
researcher Polly Hoppin, PhD. The findings<br />
released on July 6, revealing the following:<br />
• Effective asthma education programs can<br />
lead to fewer emergency room visits and<br />
hospitalizations as well as improvements<br />
in quality of life and lung function, which<br />
can, in turn, result in cost savings.<br />
• Home-based interventions are cost-ef-<br />
fective measures that can result in im-<br />
proved health outcomes for patients.<br />
During a home intervention, a trainer<br />
educates families about environ-<br />
mental factors that trigger asthma<br />
(including cockroach or mouse<br />
problems, pet dander, mold, poor<br />
ventilation and/or uncleanliness).<br />
The trainer also educates fami-<br />
continued on page 6<br />
<strong>Mission</strong>: <strong>Possible</strong><br />
Kim Wilson, MD, MPH, a primary care pediatrician<br />
at the Martha Eliot Health Center (MEHC)<br />
and associate director of the Center for International<br />
Pediatrics at Children’s <strong>Hospital</strong> <strong>Boston</strong>, knew she<br />
had to go the extra mile to properly care for the Dominican<br />
patients who make up more than half of her patient<br />
base. But she faced a major stumbling block. Her<br />
patients made regular trips back to the Dominican<br />
Republic (DR) to visit family, sometimes staying for<br />
months or even years at a time, making continual<br />
care difficult. Adding to the problem was the different<br />
ways doctors and patients approach health<br />
care in the two countries.<br />
When a Dominican mother asked if Wilson<br />
could communicate with her child’s doctor<br />
in Baní in the DR back in 2002, Wilson took<br />
it a step further and started the Dominican<br />
Health Alliance to bridge the communication<br />
gap. “There were many things I didn’t<br />
understand about their health care, beliefs<br />
and traditional remedies that I needed to<br />
learn,” she says. For example, in the DR,<br />
preventive care is an unfamiliar concept,<br />
and most families only seek care for<br />
serious illness. So in collaboration with<br />
Sue Torrey, MD, Emergency Department<br />
physician, and other Children’s staff, Wilson<br />
started to travel to<br />
the DR to gain a better<br />
understanding of their<br />
patients’ native health<br />
care system.<br />
The group soon<br />
learned that there was<br />
more to be done than<br />
simply learning about<br />
their culture and health<br />
care system. “The quality<br />
of health care in the DR was<br />
startling,” Wilson says. She<br />
found that many hospitals<br />
lacked basic supplies, relied<br />
on an intermittent water supply<br />
and didn’t have basic infection<br />
control practices in place. She also<br />
learned some sad statistics: Neo-<br />
natal mortality is more than three times higher in the<br />
DR than it is in the United States, and more than 70<br />
percent of all childhood deaths there occur in the first<br />
month of life. Since hospitals’ nurseries have limited<br />
incubators and oxygen, infants must sometimes share,<br />
or go without treatment.<br />
Wilson and her team concentrated their efforts on<br />
improving newborn and maternal care by educating<br />
the public and local medical staff. In addition to<br />
teaching courses on HIV, neonatal resuscitation and<br />
pediatric infection and emergency care, they provided<br />
equipment and medicine to the DR’s main regional<br />
hospital, the Nuestra Señora de Regla <strong>Hospital</strong> Baní,<br />
the only hospital for the province’s 170,000 people.<br />
By last year, the program had blossomed into a nonprofit<br />
organization called Infante Sano (www.infantesano.org),<br />
Spanish for “healthy infant.” Infante Sano<br />
focuses on improving the quality of neonatal and maternal<br />
care by establishing several community outreach<br />
programs in Baní and its surrounding areas designed<br />
to help mothers realize when their pregnancy or infant<br />
are in danger. The organization provides medical supplies<br />
and works with the hospital to develop a plan<br />
for equipment maintenance. Members also produced<br />
videos for local television to train the community<br />
about health issues, and staff make home visits to<br />
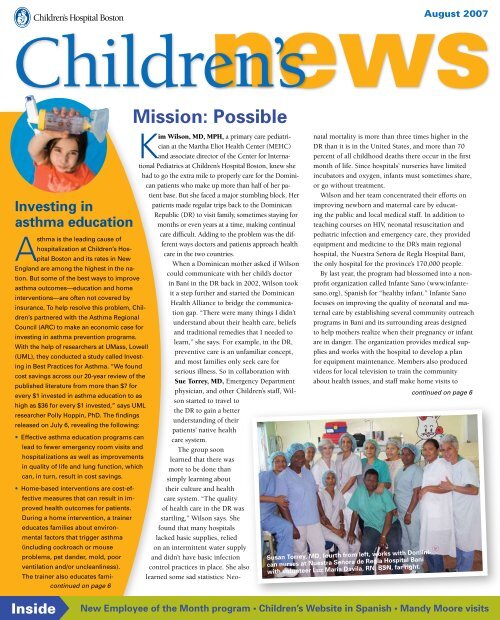
Susan Torrey, MD, fourth from left, works with Dominican<br />
nurses at Nuestra Señora de Regla <strong>Hospital</strong> Baní<br />
with volunteer Luz Maria Davila, RN, BSN, far right.<br />
continued on page 6<br />
Hal turning 17<br />
New Employee of the Month program • Children’s Website in Spanish • Mandy Moore visits
Newborn Medicine A simpler way to check catheter placement<br />
Otolaryngology Neural stem cells may help regrow the cochlea<br />
Hematology/Oncology A faster recovery from marrow transplants<br />
First steps toward a<br />
living cochlear implant<br />
Most cases of deafness are caused by the<br />
dysfunction or death of cells in the cochlea,<br />
the snail-shell-shaped structure in<br />
the inner ear. Douglas Cotanche, PhD, a researcher<br />
in Otolaryngology, now reports that his lab has grown<br />
all the assorted cell types in the cochlea from just one<br />
source: neural stem cells. The study was published<br />
online June 20 by the journal Hearing Research.<br />
Neural stem cells were first isolated from mice<br />
in 1998 by Evan Snyder, MD, PhD, formerly of<br />
Children’s Department of Neurology. Cotanche’s<br />
team implanted the cells deep inside the sound-damaged<br />
cochleas of guinea pigs and mice. Six weeks<br />
later, the cells had migrated throughout the cochlea<br />
and formed satellite cells, spiral ganglion cells and<br />
Schwann cells, which make up the cochlea’s nervous<br />
tissue, as well as the hair cells and supporting cells of<br />
the organ of Corti (the actual hearing organ). “Getting<br />
these cells to integrate into the damaged ear and<br />
make the variety of cochlear cell types is a big step,”<br />
says Cotanche.<br />
The researchers couldn’t show complete rebuilding<br />
of the cochlea, but they believe that with more time<br />
and more stem cells, most of the cochlea could be repopulated.<br />
Cotanche’s next goal is to implant human<br />
neural stem cells in animals and test whether the new<br />
cochlear cells connect with the auditory nerve and<br />
the brain, and whether they respond to sound stimulation—in<br />
other words, whether they restore hearing.<br />
Resident invents a glowing catheter<br />
The placement of central<br />
catheters, which deliver<br />
lifesaving nutrition and<br />
medicine to the most premature<br />
infants, is a “blind” procedure.<br />
The catheter is typically inserted<br />
in the forearm or ankle and advanced<br />
until it reaches a location<br />
near the heart. Only an X-ray can<br />
reveal whether the catheter has<br />
gone astray, veering too close to<br />
the heart, into the neck or even<br />
winding back down the arm.<br />
Adjustments are often required,<br />
leading to delays, more X-rays<br />
and exposure of the infant to<br />
more radiation.<br />
“I thought to myself, there<br />
must be a better way to do this,”<br />
says Farhad Imam, MD, PhD,<br />
a clinical fellow in Newborn<br />
Medicine at Children’s <strong>Hospital</strong><br />
<strong>Boston</strong>, who witnessed several<br />
“misroutings” as a resident in<br />
the Neonatal Intensive Care Unit<br />
(NICU). Imam’s solution was<br />
intuitive: He threaded a central<br />
Farhad Imam, MD, PhD<br />
catheter with an illuminated<br />
fiber-optic wire to make it glow, allowing its progress through the body to be tracked<br />
with the naked eye. After night shifts during his residency and the first year of his NICU<br />
fellowship, Imam spent afternoons testing his design on rabbits. The catheter’s red gleam<br />
was visible through tissue—and even fur.<br />
Initially funded by a Lovejoy Research Award for residents, Imam is now supported<br />
by a Massachusetts Technology Transfer Center grant and he’s con-<br />
tracted with two engineering firms to help build a prototype<br />
Boosting blood stem cells Zebrafish show the way<br />
light-guided catheter over the next year. “The catheter<br />
By systematically screening more than ,500 chemicals in zebrafish, Leonard Zon,<br />
will be most readily usable in newborns,” he<br />
MD, Trista North, PhD, and Wolfram Goessling, MD, PhD, of Children’s Stem<br />
says, “but it should also work in children and<br />
Cell Program, have identified an available drug that ramps up production of blood<br />
possibly in adults.”<br />
stem cells, helping patients recover immune function more quickly after chemotherapy<br />
or bone marrow transplants. The drug, a derivative of prostaglandin E ,<br />
may be tested as early as next year in patients undergoing cord blood transplant for<br />
leukemia. The paper appeared in the June 1 issue of Nature.<br />
Jacqueline Armstrong and Monique<br />
Yoakim-Turk of Children’s Intellectual Property<br />
Office helped Imam file a patent, recognizing<br />
that a light-guided catheter could save money<br />
and time by replacing the current technique. “Residents<br />
have cool ideas,” says Yoakim-Turk. “They’re new and tend to<br />
question what others don’t anymore.”<br />
Go to Children’s News’ Online Extras at<br />
www.childrenshospital.org/chnews to read more research briefs.<br />
Have research news you would like to share?<br />
Email nancy.fliesler@childrens.harvard.edu or call ext. 5-2426.<br />
Cheonil Kim, MD, attended medical<br />
school in Seoul, Korea, where he was<br />
born, but he knew that once he finished<br />
his degree, he wanted to practice medicine<br />
in the United States. But before he could<br />
leave Korea, he had to serve in the medical<br />
branch of its army. “It was just like that show<br />
M*A*S*H,” he remembers, laughing.<br />
After the army, Kim made the move overseas<br />
and in 1980 began his fellowship at Children’s<br />
<strong>Hospital</strong> <strong>Boston</strong>. From the start, he found<br />
it to be a great fit. “I liked it and they liked<br />
me,” he says. “The families make you feel so<br />
good about working here.” One of the biggest<br />
differences he noticed between American<br />
and Korean hospitals was how patient-doctor<br />
relationships worked. “People are more skeptical<br />
of health professionals in Korea,” he says.<br />
“Families here are positive because they trust<br />
in you—and the institution. That motivates me<br />
to give 100 percent.”<br />
Kim trained in General Surgery for two<br />
years before he decided to make a switch to<br />
Gratitudes<br />
Children’s News | August 2007 www.childrenshospital.org<br />
The secret to his success<br />
DESTINATION:<br />
Children’s<br />
The following letter was sent to Jennifer Finn,<br />
general manager at Fitcorp.<br />
The Nussenbaum family<br />
South Korea<br />
il Kim, MD<br />
Anesthesiologist<br />
Anesthesia. “It takes a certain type of person to<br />
be a surgeon and that wasn’t me,” he says. But<br />
that hasn’t kept Kim out of the operating room<br />
(OR). As an OR director focusing on anesthesia<br />
during otolaryngologic (ears, nose and<br />
throat) surgeries, he ensures that the surgeries<br />
run smoothly, while acting as a liaison between<br />
surgeons, nurses, departments and families.<br />
Despite his success, Kim still considers his<br />
language barrier to be a big challenge. “I give<br />
professional talks, but it’s on a basic level of<br />
communication,” he says. “It helps that I’m<br />
in the medical field, especially at Children’s,<br />
since people really try to understand me in<br />
context, despite my mispronunciations.” He<br />
brushes up on his elocution from time to time<br />
with English lessons and gets a fair amount<br />
of practice talking to his three American-born<br />
sons. Kim considers himself a family man and<br />
attributes this to his heritage. “My cultural<br />
identity is pretty strong,” he says. “I’m very<br />
family-oriented and half of the food I eat is<br />
from my culture—I like the spice.” Although<br />
all of his sons are American, he says, “They<br />
have stronger cultural connections to Korea<br />
than I thought they would—their heritage is<br />
always on their minds, and that’s reflected in<br />
the food they eat.”<br />
Being bilingual has been useful to Kim when<br />
treating Korean-speaking patients over the<br />
years, and many departments have sought his<br />
Dear Jennifer,<br />
translation help. “Even if the family speaks<br />
basic English, they may need clear communication<br />
to feel comfortable. I’m proud to help,”<br />
he says.<br />
Kim knows that the decision he made<br />
decades ago to immigrate to the United States<br />
was the right one. “In Korea, the medical<br />
profession is about fame and prestige,” he says.<br />
“Those weren’t my goals and that’s not my<br />
style,” he says. “Here, it’s about respecting the<br />
individual and quality of care. People appreciate<br />
my work and my presence. I consider that<br />
success.”<br />
Five months ago my teenage son was hospitalized at Children’s<br />
<strong>Hospital</strong> <strong>Boston</strong>. What began as a simple case of mono turned into<br />
a serious illness that ultimately necessitated him having a bone<br />
marrow transplant. My wife and I spent four months at Children’s<br />
with our son, and we continue to return with him on an outpatient<br />
basis during the long recovery period.<br />
During my son’s hospitalization, I managed to set aside time every<br />
day to come to Fitcorp so that I could work out, shower, shave and<br />
try to clear my head. As difficult as this ordeal has been for me<br />
and my family, I cannot even begin to imagine what it would have<br />
been like had I not been able to retreat to Fitcorp. It is hard to put<br />
into words just how important it was to have your club available<br />
to me, even for this short time each day.<br />
I just wanted to thank you so much for making this resource<br />
available to me and other families of Children’s patients. It is a<br />
wonderful service that you provide to parents who must endure<br />
the nightmare of having a sick child.<br />
Cheonil Kim, MD<br />
Adam Nussenbaum
1<br />
Time Capsule<br />
5 Cottage Wards<br />
10 Carnegie Building<br />
The Time Capsule contains memorabilia pertaining to the history<br />
of the hospital. It will be opened in 2069 to commemorate the<br />
hospital’s bi-centennial.<br />
2<br />
Operating Room/Farley<br />
Building<br />
When Children’s moved to Long-<br />
wood Avenue in 1914, the hospital<br />
constructed a series of small build-<br />
ings behind the Hunnewell Build-<br />
ing. The Operating Room Building,<br />
usually known simply as “Surgical”<br />
or “The OR,” was one of these.<br />
3<br />
Fegan Building<br />
The Fegan Building was built in<br />
1967 for outpatient visits with<br />
patient comfort in mind: More spa-<br />
cious waiting rooms and play areas<br />
replaced the crowded wooden<br />
benches that served as waiting<br />
areas in the old facilities.<br />
4<br />
Time Capsule<br />
Laboratory Study Building<br />
In 1921, a small laboratory build-<br />
ing was constructed behind the<br />
Hunnewell Building, and in 1926,<br />
a second story was added. James<br />
Lawder Gamble, MD, whose work<br />
developed the scientific basis for<br />
oral and intravenous fluid therapy,<br />
worked here and his library has<br />
been reassembled as the Gamble<br />
Reading Room.<br />
The History Trail A walking tour of Children’s <strong>Hospital</strong> <strong>Boston</strong><br />
Since its founding in 1869, Children’s <strong>Hospital</strong> <strong>Boston</strong> has been at the leading edge of patient care, medical research and teaching. Follow the new historic markers<br />
along the Children’s History Trail to learn more about the people, places and achievements of the past—and learn how they inspire us to do great things today.<br />
Operating room, ca. 1900<br />
Outpatient clinic, 19 0s<br />
Dr. Gamble<br />
Wolbach Building<br />
Several wards were constructed in the<br />
area behind the Hunnewell Building to<br />
house medical and surgical patients.<br />
These “cottage wards” (sometimes<br />
called “chicken coops”) were designed<br />
to maximize air and light and to minimize<br />
the spread of infectious diseases.<br />
6<br />
Wolbach Building<br />
Built in 1914 as a hospital for infants and purchased in 1923 by the Harvard School<br />
of Public Health, the Wolbach Building later became a part of Children’s and cur-<br />
rently houses administrative offices. It features many of its original architectural<br />
details, including marble floors and crown molding.<br />
7<br />
Prouty Garden<br />
The Prouty Memorial Gar-<br />
den and Terrace, designed<br />
by the Olmstead Brothers<br />
landscape design firm, was<br />
donated to Children’s in 1956<br />
by Olive Prouty as a memo-<br />
rial to her two deceased<br />
children. The garden, a reg-<br />
istered site with the National<br />
Association for Olmsted<br />
Parks, was honored with a<br />
gold medal by the Massachu-<br />
setts Horticulture Society.<br />
8<br />
Bader Building<br />
The six-story Bader Building<br />
opened in 1930 primarily to treat<br />
children with neuromuscular<br />
diseases. Named in honor of Mr.<br />
and Mrs. L. F. S. Bader, who were<br />
major donors, this building was<br />
one of the most modern hospital<br />
facilities of its time in the United<br />
States.<br />
Silver from the School of<br />
Nursing on display<br />
9<br />
Exhibit Case<br />
This is the main display case of the Children’s Archives<br />
Program. The hospital’s archives were established in 1993<br />
to acquire, preserve and make available the historical<br />
records that document the ongoing history of Children’s,<br />
its staff, volunteers, patients and families.<br />
The Ida C. Smith Building in the<br />
19 0s, one of the “cottage wards.”<br />
Circus Day took place in the 19 0s where<br />
the Prouty Garden is now located<br />
Bader Solarium, 19 0s<br />
The Carnegie Building, built in 1907,<br />
housed medical and surgical research<br />
laboratories and was where doctors<br />
John Enders, Frederick Robbins and<br />
Thomas Weller did work with polio<br />
and other infectious diseases that led<br />
to their receiving the Nobel Prize for<br />
Medicine in 1954.<br />
11 Ambulances<br />
Children’s has long used ambulances to<br />
transport patients, inlcuding the horse-<br />
drawn “barge,” at right.<br />
12<br />
Enders Building<br />
The John F. Enders Pediatric<br />
Research Laboratories, or Enders<br />
Building, opened in 1970 and<br />
was named for John Enders,<br />
PhD, in recognition of his pioneering<br />
work in the study of viruses, includ-<br />
ing polio, mumps and measles.<br />
13<br />
Longwood Row Housing<br />
In the early years after Children’s<br />
relocated from Huntington to<br />
Longwood Avenue, a series of row<br />
houses were built on both sides of<br />
Longwood that served as housing<br />
for medical residents, nurses and<br />
staff members.<br />
14 Outpatient Visits<br />
In 1938, the Outpatient Department was com-<br />
posed of 25 clinics and handled more than<br />
68,000 visits. Eighty-five doctors took turns<br />
supervising the clinics, which were<br />
available to all patients, regardless of<br />
their parents’ ability to pay. The aver-<br />
age cost to the hospital for each visit<br />
was $1.50 and the average payment<br />
made was 65¢.<br />
Dr. Enders<br />
Carriages outside Hunnewell, 19 0s<br />
15 Hunnewell Building<br />
The oldest continuously occupied build-<br />
ing on campus, Hunnewell is named after<br />
Francis Welles Hunnewell, a major donor to<br />
Children’s and a real estate developer in the<br />
Allston-Brighton neighborhood during the<br />
mid-to-late-19th century.<br />
16 Gardner House<br />
The Gardner House opened<br />
in 1930 and was home to the<br />
School of Nursing through<br />
1978. Nursing students often<br />
gathered in its elegant living<br />
room for high tea. Later, in<br />
the 1980s, families of patients<br />
stayed in the Gardner House’s<br />
family hostel.<br />
Set out on the trail<br />
Take this map, or get a guidebook in the lobby, and walk<br />
around the campus to learn more about each location.<br />
Children’s News | August 2007 www.childrenshospital.org<br />
5<br />
Dr. Weller<br />
Ambulance, 19 0<br />
Longwood Avenue, ca. 19 0<br />
5<br />
4<br />
6<br />
15<br />
7<br />
9<br />
3<br />
16<br />
8<br />
14<br />
2<br />
Hunnewell Building, 19 0s<br />
School of Nursing groundbreaking, 19 9<br />
1<br />
10<br />
13<br />
11<br />
12<br />
© Children’s <strong>Hospital</strong> <strong>Boston</strong> 2007
Dominican Republic continued from page 1<br />
increase awareness. “These interventions are not high-tech or particularly costly,<br />
so it’s very doable,” Wilson says. It’s been going so well, in fact, that she hopes<br />
to expand to more outposts on the Haitian border by January.<br />
When Wilson is back at the MEHC, she draws on her experiences in the DR to<br />
provide more culturally aware care. She knows, for example, that since antibiotics<br />
are available without prescriptions in the DR, her patients are used to taking<br />
them frequently—even to treat minor<br />
viral illnesses. So Wilson makes sure<br />
to explain to patients why this isn’t<br />
always beneficial. After seeing how<br />
entire families, including infants and<br />
young children, travel by moped in the<br />
DR without helmets, she also began<br />
educating her patients about safety<br />
equipment like car seats and bike<br />
helmets. She also learned how to adapt<br />
Kim Wilson, at right, with<br />
Dominican trainees.<br />
medical treatment for patients with<br />
diabetes or asthma, creating a regimen<br />
that they can continue to follow while<br />
they’re visiting family in their home country. This cultural awareness has had a<br />
lasting impact on the many MEHC staff who’ve worked with Wilson.<br />
Infante Sano now has offices in Bani and <strong>Boston</strong>, with 16 Dominican physicians,<br />
nurses, support staff and volunteers. They’ve succeeded in renovating the<br />
special care nursery and the pediatric section of Nuestra Señora de Regla <strong>Hospital</strong><br />
Bani, and opened two clinics in a rural part of the DR late last year. One<br />
specializes in treating malnourished children and the other is a primary care<br />
center. Together, their staff sees more than 300 mothers and children a week.<br />
Still, there’s work to be done. “Our biggest challenge is to have a sustainable<br />
impact,” Wilson says. “It’s very easy to do interventions with a temporary positive<br />
effect, but we want to have a lasting one. We’ve struggled with how to do<br />
that.” That’s why, for now, they’ve transitioned into having a sustained presence<br />
there. But the hard work is gratifying. “What’s really rewarding is that it’s immediately<br />
clear that we’re making a big difference,” Kim says. “I really enjoy seeing<br />
the program grow and the enthusiasm of the people who are so excited to have<br />
the opportunity to improve the care they deliver.”<br />
Exceptional Care<br />
Exceptional Service<br />
Celebrating the first 100 suggestions<br />
On July 9, Children’s <strong>Hospital</strong> <strong>Boston</strong>’s Exceptional Care, Exceptional Service (ECES) program<br />
took a lunch break to honor the first 100 contributors to the ECES suggestions Web site. Since<br />
January, 83 staff members have contributed a total of 110 suggestions on specific ways to improve<br />
the hospital experience and its service. Those who submitted their ideas were invited to a tapas<br />
lunch (replete with a Flamenco guitarist) in the Patient Entertainment Center.<br />
Sandra Fenwick, COO, recognized the ECES team and those who shared their suggestions,<br />
especially the 15 employees whose ideas have already been or are currently being implemented.<br />
Their suggestions include department meet-and-greets for new employees and standardizing<br />
telephone greetings and email signatures.<br />
Christine Powers-Perry, executive assistant in Public Affairs, received a special award for<br />
her six outstanding ECES ideas, three of which have already been put into practice. “No idea<br />
is too small if it’s going to change someone’s experience at the hospital,” says Powers-Perry,<br />
who created ECES training badges and designed and created ECES magnets. “The values of<br />
ECES are all things we should be doing to work together and help support the hospital’s mis-<br />
Asthma continued from page 1<br />
lies by teaching them which cleaning products don’t worsen<br />
asthma, how to seal off areas that collect moisture and offering<br />
allergen-free bed and pillow covers or vacuums.<br />
• Non-physician providers (such as nurses, respiratory therapists,<br />
asthma educators and social workers) can provide<br />
effective asthma education and environmental interventions,<br />
often at a lower cost.<br />
“Studies indicate that current approaches to managing asthma<br />
aren’t working for a lot of people,” says Laurie Stillman, director<br />
of the ARC. “This study shows we can improve asthma outcomes<br />
in a cost-effective manner if high-risk patients are given<br />
education and environmental improvements in the home.”<br />
The study also calls on multiple sectors, including payers,<br />
health provider groups, employers and policymakers to play a<br />
role in implementing these programs.<br />
Many of the study’s recommendations are contained in<br />
legislation, filed this year by the <strong>Boston</strong> Urban Asthma Coalition<br />
(BUAC) and Children’s, that would require insurers in Massachusetts<br />
to cover asthma education and in-home environmental<br />
interventions. At a hearing in May, parents of children with<br />
asthma, community health advocates and hospital leaders and<br />
clinicians—including Shari Nethersole, MD, medical director for<br />
community health, and Susan Sommer, RNC, NP, nurse case<br />
manager for the Community Asthma Initiative—testified in support<br />
of the bill before the Joint Committee on Public Health.<br />
With the study’s results to support them, Children’s will<br />
continue working with its partners to bring about the necessary<br />
changes to asthma care. “Too many families, particularly in<br />
low-income communities, are struggling needlessly with the effects<br />
of asthma,” says Lisa Mannix, coordinator of Child Health<br />
Policy and Education at Children’s. “The evidence accumulated<br />
in this business case shows there are interventions that work.<br />
It’s time for decision-makers to take bold action to implement<br />
them on a broader scale.”<br />
Christine Powers-Perry receives her award<br />
from Bess Andrews, director of Public Affairs.<br />
In their own words<br />
Kitty Scott, RN, retired coordinator of Patient Relations<br />
A nurse looks back on 5 years at Children’s<br />
In 1962, I came to Children’s <strong>Hospital</strong> <strong>Boston</strong><br />
as a young nurse with a plan to work at the<br />
hospital for one year and then return home<br />
to Nova Scotia. I’d written a letter to the Nursing<br />
Department explaining my limited experience<br />
and desire for a job. I received a letter<br />
of acceptance with a start date. There was no<br />
interview and I completed my application after I<br />
arrived. My salary was $82 a week.<br />
I was assigned to Division 35, the cardiology/cardiac<br />
surgical unit. My head nurse did not<br />
meet me until I had completed a few days of<br />
orientation and I worked just a few days with a<br />
senior nurse and then was on my own.<br />
There were no intensive care units (ICUs)<br />
at Children’s when I arrived. We cared for<br />
patients who had open heart surgery in the<br />
“Pump Room.” If patients required a ventilator,<br />
they remained in the Recovery Room (now<br />
the Pediatric Advanced Care Unit) but nursing<br />
staff from Division 35 provided the care. In<br />
some cases, patients were so unstable they<br />
remained on the OR table while we cared for<br />
them. Back then, open heart surgery couldn’t<br />
be done until the child reached 45 pounds<br />
because our heart-lung machine wasn’t adapted<br />
for babies, so many children died waiting for<br />
surgery. Some “blue babies” had palliative procedures<br />
done in the hyperbaric chamber, which<br />
was located in the basement of the Harvard<br />
School of Public Health—now the Wolbach<br />
Building. Imagine the challenge of transporting<br />
a baby across the garden to the hospital following<br />
surgery, sometimes in the dark.<br />
In December of 1964, a very exciting thing<br />
occurred. A Cardiac ICU (CICU) was opened<br />
on Division 25, the first pediatric ICU in the<br />
country. I assisted in transferring the first<br />
patient into the unit. A month later, I became<br />
Assistant Head Nurse for the night shift. In<br />
those days, nurses didn’t apply for promotions,<br />
but were chosen by nursing leadership. It<br />
wasn’t unusual to work up to 10 shifts in a row.<br />
In addition to a modest raise, this new position<br />
gave me every other weekend off—regular<br />
staff nurses worked eight-hour shifts and<br />
worked two out of three weekends. Providing<br />
adequate coverage was the priority, and the<br />
nurses’ personal lives came second. As nurses,<br />
we wore totally white uniforms, white shoes<br />
and stockings, and, of course, the cap that<br />
represented the school of nursing from which<br />
we graduated.<br />
Parents did not stay at<br />
the hospital at night unless<br />
the child was critically ill,<br />
and at 8 p.m., all visitors<br />
left. Parents were not<br />
encouraged to participate<br />
in their child’s care, so the<br />
staff nurses provided all<br />
care, except perhaps an<br />
occasional diaper change<br />
or bottle feeding. Except at<br />
the highest level of nursing<br />
administration, nurses were<br />
not involved in decisionmaking<br />
of the hospital. Staff<br />
nurses did not serve on any<br />
hospital-wide committees<br />
and annual reviews were<br />
done by the supervisors<br />
with no peer input. Promotions<br />
meant getting farther<br />
and farther away from the<br />
bedside.<br />
Fourteen years ago, when I was the Nurse<br />
Recruiter, I was asked to hire for a part-time<br />
position in Patient Relations. A decision had been<br />
made that a nurse should fill this opening. However,<br />
it seemed that no nurses were interested<br />
because no one applied. After a number of weeks,<br />
my director came by to ask me if I would consider<br />
the position. With much trepidation, I decided<br />
to move into this new role while I continued to<br />
do nurse recruitment.<br />
After accepting the fact that an angry call<br />
was not directed at me personally, and that<br />
there are people one simply cannot please, I<br />
learned as much as I could about billing and<br />
insurance practices. I settled in and found<br />
my last job at Children’s as challenging and<br />
satisfying as caring for critically ill patients. I<br />
have enjoyed the more complicated cases and<br />
the challenges of situations involving Risk<br />
Management and the Office of Legal Counsel.<br />
Patient Relations allowed me to use my people<br />
skills, clinical knowledge and familiarity with<br />
the hospital and its players to address the ma-<br />
jority of challenges that came my way. It was a<br />
great job for an old nurse!<br />
Since my early days, I have seen so many<br />
changes—more than can be mentioned! In addition<br />
to the fantastic advances in medical care,<br />
we have gone from one small CICU and several<br />
small “care rooms” to two large, state-of-theart<br />
ICUs. Parents can visit 24 hours a day and<br />
are encouraged to participate in their child’s<br />
care. RN evaluations are done with peer input.<br />
There is a Clinical Ladder that allows nurses to<br />
advance but remain involved in direct patient<br />
care. Most staff work 12-hour shifts and have<br />
two out of three weekends off—not on. Now,<br />
nurses wear brightly colored scrubs and there<br />
is less formality than in the “old days.”<br />
Children’s is an amazing place and I am<br />
very proud to have worked here for so many<br />
years. I have had eight different positions and<br />
enjoyed the challenges and satisfaction of them<br />
all, whether it’s been providing direct care to<br />
the patients as a staff nurse or contributing to<br />
the care in other ways. I’m leaving feeling very<br />
good that I chose to be a nurse.<br />
Do you know how many units (pints) of blood Children’s<br />
collected in 006? Including donations from the Blood<br />
Mobile and donations of whole blood, platelets and double<br />
red blood cells from the Blood Donor Center, the total was<br />
10,858 units!<br />
sion,” she says. To make a suggestion, go to http://web2.tch.harvard.edu/eces/formESS.cfm.<br />
6 Children’s News | August 2007 www.childrenshospital.org<br />
7<br />
Kitty Scott, RN
This month’s<br />
En Español…Children’s <strong>Hospital</strong> <strong>Boston</strong> has just launched<br />
a Spanish version of the hospital Web site for our Spanish<br />
speaking patients and providers. The site features information<br />
such as directions, how to prepare your child for a hospital<br />
stay, health tips, descriptions of our main clinical services and<br />
more. Check it out at www.childrenshospital.org/espanol.<br />
Family Advocacy Day<br />
It all happened at Children’s <strong>Hospital</strong> <strong>Boston</strong>!<br />
Talking politics…Four patients from Children’s headed to Washington,<br />
DC, for Family Advocacy Day, sponsored by the National Association of<br />
Children’s <strong>Hospital</strong>s, in late June. The patients shared their health histories<br />
with senators and congressmen from their home states of Maine, New Hamp-<br />
shire, Massachusetts and Rhode Island to promote the reauthorization of the State<br />
Children’s Health Insurance Programs, the passage of the Children’s Health Care<br />
Quality Act and funding for the Children’s <strong>Hospital</strong>s Graduate Medical Education<br />
Program.<br />
Workouts for community<br />
children…A new high-tech<br />
fitness center for children,<br />
GoKids <strong>Boston</strong>, recently opened at UMass <strong>Boston</strong>,<br />
with Children’s support. The center will investigate the<br />
science and practice of improving fitness in children<br />
and provide exercise programs for children with health<br />
challenges. At the grand opening, Sandra Fenwick,<br />
chief operating officer, gave a speech and local chil-<br />
dren got to test out the excergaming—kid-friendly<br />
exercise equipment that has interactive, built-in games.<br />
Latino youth<br />
recognition…In<br />
an effort to recognize high-achieving Latino middle schoolers, Children’s is<br />
sponsoring a series of Latino youth recognition days at Fenway Park. The<br />
first one was June 15 and the second was July 16; the last one will be held<br />
Sept. 3. At the events, the students are recognized during pre-game, on-<br />
field ceremonies and given certificates of recognition by Red Sox players<br />
David “Big Papi” Ortiz, Wily Mo Peña, Julio Lugo and Alex Cora. El Mundo<br />
newspaper and the Red Sox developed the project to encourage academic excellence and are giving out more<br />
than 500 Sox tickets to inner-city youth.<br />
More Mandy…On July 16, actress/singer Mandy<br />
Moore wowed patients throughout the hospital,<br />
including this young patient-reporter Ashley during<br />
the Midweek Morning Show taping in the 10NW<br />
playroom. Moore stopped by to visit patients before<br />
giving a Mix 98.5 concert at the Prudential Center.<br />
Online Extras at<br />
www.childrenshospital.org/chnews…<br />
Our new anti-violence art and poetry contest • Martha<br />
Eliot Health Center’s Car Seat Checkpoint event • HIV<br />
testing turnout at the Martha Eliot Health Center •<br />
Research briefs • NASCAR’s visit • Transforming Care<br />
at the Bedside project • National Kidney Foundation<br />
donates Sox tickets<br />
Editor: Erin Graham<br />
Designers: Javier Amador-Peña,<br />
Patrick Bibbins<br />
Contributors: Louise Cobb, Nancy<br />
Fliesler, Lisa Mannix, Sheila Spalding<br />
Department of Public Affairs<br />
and Marketing<br />
Children’s <strong>Hospital</strong> <strong>Boston</strong><br />
21 Autumn St., 2nd Floor<br />
<strong>Boston</strong>, MA 02115<br />
(617) 355-6420<br />
VP of Public Affairs and Marketing:<br />
Michelle Davis<br />
Director of Public Affairs:<br />
Bess Andrews<br />
Manager of Public Affairs:<br />
Matthew Cyr<br />
GoKids <strong>Boston</strong> gym<br />
Ashley interviewed Mandy<br />
Moore for the Midweek<br />
Morning Show<br />
More News online at www.childrenshospital.org/chnews<br />
© 2007, Children’s <strong>Hospital</strong> <strong>Boston</strong>. All rights reserved.<br />
Upcoming events<br />
Employee<br />
summer bash<br />
Children’s <strong>Hospital</strong> <strong>Boston</strong>’s annual<br />
summer party, Cowboys Around the<br />
World, will take place August 1, 11 a.m.<br />
to 5 p.m. in the hospital cafe. Stop by<br />
for BBQ, music and entertainment. On<br />
August 2, 10:30 p.m. to 12 a.m., there<br />
will be an event for night shift employees.<br />
Invitations were distributed with<br />
your paycheck on July 27th.<br />
MEHC health fair<br />
You’re invited to attend the annual<br />
Martha Eliot Health Center (MEHC)<br />
health fair August 25, 11 a.m. to 3 p.m.<br />
in the MEHC parking lot. This year’s<br />
health fair will promote physical activity,<br />
sports, healthy eating, education<br />
and youth empowerment. There will be<br />
free preventive and chronic disease<br />
screenings for attendees and staff will<br />
offer assistance in obtaining health<br />
coverage, including Medicaid, Medicare<br />
and Commonwealth Care.<br />
Latino Heritage<br />
Month celebrations<br />
The first of many Children’s events<br />
celebrating Latino Heritage Month will<br />
be the <strong>Boston</strong> Harbor Salsa and Latin<br />
Dance Cruise on Sept. 16, 7 to 10 p.m.<br />
Enjoy the charge of Latin music and<br />
dance, get some exercise, explore the<br />
skyline from the harbor and mingle<br />
with your coworkers at Children’s<br />
private area on the top deck. The<br />
cruise and post-cruise party, including<br />
a salsa lesson, is $20; with a dinner<br />
buffet it’s $30. Sign up for tickets for<br />
you and guests at Human Resources<br />
by Aug. 31.<br />
Exceptional Service<br />
Employee of the<br />
Month<br />
Human Resources (HR) is happy to<br />
announce Employee of the Month, a<br />
new recognition program as a part of<br />
the Exceptional Care, Exceptional Service<br />
(ECES) initiative. Nominating a coworker<br />
or staff member is a wonderful<br />
way to recognize the outstanding<br />
performance, service and teamwork of<br />
a fellow employee/staff who exemplifies<br />
ECES standards. Visit the HR Web<br />
page for more information.<br />
Do you have news?<br />
Email: news@childrens.harvard.edu<br />
or call (617) 355-6420.