Nederlands tijdschrift voor anesthesiologie - Nederlandse ...
Nederlands tijdschrift voor anesthesiologie - Nederlandse ...
Nederlands tijdschrift voor anesthesiologie - Nederlandse ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
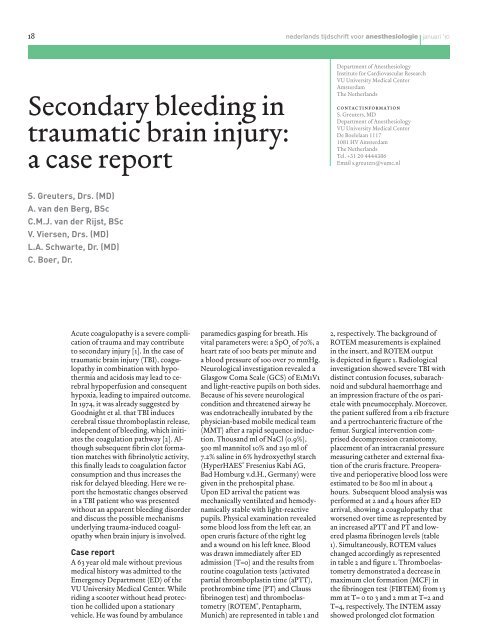
18 nederlands <strong>tijdschrift</strong> <strong>voor</strong> <strong>anesthesiologie</strong> | januari '10<br />
Secondary bleeding in<br />
traumatic brain injury:<br />
a case report<br />
S. Greuters, Drs. (MD)<br />
A. van den Berg, BSc<br />
C.M.J. van der Rijst, BSc<br />
V. Viersen, Drs. (MD)<br />
L.A. Schwarte, Dr. (MD)<br />
C. Boer, Dr.<br />
Acute coagulopathy is a severe complication<br />
of trauma and may contribute<br />
to secondary injury [1]. In the case of<br />
traumatic brain injury (TBI), coagulopathy<br />
in combination with hypothermia<br />
and acidosis may lead to cerebral<br />
hypoperfusion and consequent<br />
hypoxia, leading to impaired outcome.<br />
In 1974, it was already suggested by<br />
Goodnight et al. that TBI induces<br />
cerebral tissue thromboplastin release,<br />
independent of bleeding, which initiates<br />
the coagulation pathway [2]. Although<br />
subsequent fibrin clot formation<br />
matches with fibrinolytic activity,<br />
this finally leads to coagulation factor<br />
consumption and thus increases the<br />
risk for delayed bleeding. Here we report<br />
the hemostatic changes observed<br />
in a TBI patient who was presented<br />
without an apparent bleeding disorder<br />
and discuss the possible mechanisms<br />
underlying trauma-induced coagulopathy<br />
when brain injury is involved.<br />
Case report<br />
A 63 year old male without previous<br />
medical history was admitted to the<br />
Emergency Department (ED) of the<br />
VU University Medical Center. While<br />
riding a scooter without head protection<br />
he collided upon a stationary<br />
vehicle. He was found by ambulance<br />
paramedics gasping for breath. His<br />
vital parameters were: a SpO 2 of 70%, a<br />
heart rate of 100 beats per minute and<br />
a blood pressure of 100 over 70 mmHg.<br />
Neurological investigation revealed a<br />
Glasgow Coma Scale (GCS) of E1M1V1<br />
and light-reactive pupils on both sides.<br />
Because of his severe neurological<br />
condition and threatened airway he<br />
was endotracheally intubated by the<br />
physician-based mobile medical team<br />
(MMT) after a rapid sequence induction.<br />
Thousand ml of NaCl (0.9%),<br />
500 ml mannitol 10% and 250 ml of<br />
7.2% saline in 6% hydroxyethyl starch<br />
(HyperHAES ® Fresenius Kabi AG,<br />
Bad Homburg v.d.H., Germany) were<br />
given in the prehospital phase.<br />
Upon ED arrival the patient was<br />
mechanically ventilated and hemodynamically<br />
stable with light-reactive<br />
pupils. Physical examination revealed<br />
some blood loss from the left ear, an<br />
open cruris facture of the right leg<br />
and a wound on his left knee. Blood<br />
was drawn immediately after ED<br />
admission (T=0) and the results from<br />
routine coagulation tests (activated<br />
partial thromboplastin time (aPTT),<br />
prothrombine time (PT) and Clauss<br />
fibrinogen test) and thromboelastometry<br />
(ROTEM ® , Pentapharm,<br />
Munich) are represented in table 1 and<br />
Department of Anesthesiology<br />
Institute for Cardiovascular Research<br />
VU University Medical Center<br />
Amsterdam<br />
The Netherlands<br />
contactinformation<br />
S. Greuters, MD<br />
Department of Anesthesiology<br />
VU University Medical Center<br />
De Boelelaan 1117<br />
1081 HV Amsterdam<br />
The Netherlands<br />
Tel. +31 20 4444386<br />
Email s.greuters@vumc.nl<br />
2, respectively. The background of<br />
ROTEM measurements is explained<br />
in the insert, and ROTEM output<br />
is depicted in figure 1. Radiological<br />
investigation showed severe TBI with<br />
distinct contusion focuses, subarachnoid<br />
and subdural haemorrhage and<br />
an impression fracture of the os parietale<br />
with pneumocephaly. Moreover,<br />
the patient suffered from a rib fracture<br />
and a pertrochanteric fracture of the<br />
femur. Surgical intervention comprised<br />
decompression craniotomy,<br />
placement of an intracranial pressure<br />
measuring catheter and external fixation<br />
of the cruris fracture. Preoperative<br />
and perioperative blood loss were<br />
estimated to be 800 ml in about 4<br />
hours. Subsequent blood analysis was<br />
performed at 2 and 4 hours after ED<br />
arrival, showing a coagulopathy that<br />
worsened over time as represented by<br />
an increased aPTT and PT and lowered<br />
plasma fibrinogen levels (table<br />
1). Simultaneously, ROTEM values<br />
changed accordingly as represented<br />
in table 2 and figure 1. Thromboelastometry<br />
demonstrated a decrease in<br />
maximum clot formation (MCF) in<br />
the fibrinogen test (FIBTEM) from 13<br />
mm at T= 0 to 3 and 2 mm at T=2 and<br />
T=4, respectively. The INTEM assay<br />
showed prolonged clot formation