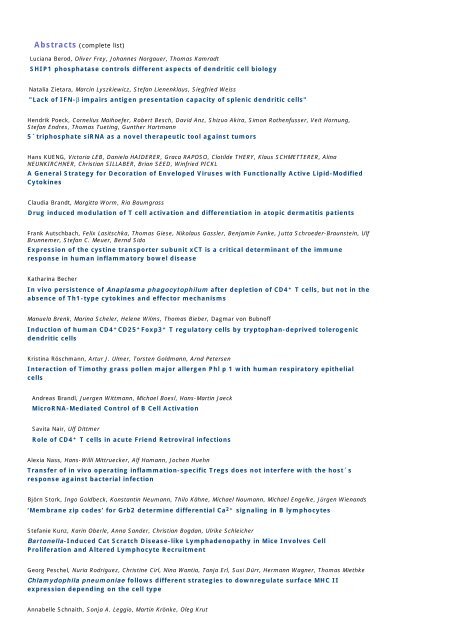
Abstracts (complete list) - Wissenschaft Online
Abstracts (complete list) - Wissenschaft Online
Abstracts (complete list) - Wissenschaft Online
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Abstracts</strong> (<strong>complete</strong> <strong>list</strong>)<br />
Luciana Berod, Oliver Frey, Johannes Norgauer, Thomas Kamradt<br />
SHIP1 phosphatase controls different aspects of dendritic cell biology<br />
Natalia Zietara, Marcin Lyszkiewicz, Stefan Lienenklaus, Siegfried Weiss<br />
"Lack of IFN-β impairs antigen presentation capacity of splenic dendritic cells"<br />
Hendrik Poeck, Cornelius Maihoefer, Robert Besch, David Anz, Shizuo Akira, Simon Rothenfusser, Veit Hornung,<br />
Stefan Endres, Thomas Tueting, Gunther Hartmann<br />
5´triphosphate siRNA as a novel therapeutic tool against tumors<br />
Hans KUENG, Victoria LEB, Daniela HAIDERER, Graca RAPOSO, Clotilde THERY, Klaus SCHMETTERER, Alina<br />
NEUNKIRCHNER, Christian SILLABER, Brian SEED, Winfried PICKL<br />
A General Strategy for Decoration of Enveloped Viruses with Functionally Active Lipid-Modified<br />
Cytokines<br />
Claudia Brandt, Margitta Worm, Ria Baumgrass<br />
Drug induced modulation of T cell activation and differentiation in atopic dermatitis patients<br />
Frank Autschbach, Felix Lasitschka, Thomas Giese, Nikolaus Gassler, Benjamin Funke, Jutta Schroeder-Braunstein, Ulf<br />
Brunnemer, Stefan C. Meuer, Bernd Sido<br />
Expression of the cystine transporter subunit xCT is a critical determinant of the immune<br />
response in human inflammatory bowel disease<br />
Katharina Becher<br />
In vivo persistence of Anaplasma phagocytophilum after depletion of CD4 + T cells, but not in the<br />
absence of Th1-type cytokines and effector mechanisms<br />
Manuela Brenk, Marina Scheler, Helene Wilms, Thomas Bieber, Dagmar von Bubnoff<br />
Induction of human CD4 + CD25 + Foxp3 + T regulatory cells by tryptophan-deprived tolerogenic<br />
dendritic cells<br />
Kristina Röschmann, Artur J. Ulmer, Torsten Goldmann, Arnd Petersen<br />
Interaction of Timothy grass pollen major allergen Phl p 1 with human respiratory epithelial<br />
cells<br />
Andreas Brandl, Juergen Wittmann, Michael Boesl, Hans-Martin Jaeck<br />
MicroRNA-Mediated Control of B Cell Activation<br />
Savita Nair, Ulf Dittmer<br />
Role of CD4 + T cells in acute Friend Retroviral infections<br />
Alexia Nass, Hans-Willi Mittruecker, Alf Hamann, Jochen Huehn<br />
Transfer of in vivo operating inflammation-specific Tregs does not interfere with the host´s<br />
response against bacterial infection<br />
Björn Stork, Ingo Goldbeck, Konstantin Neumann, Thilo Kähne, Michael Naumann, Michael Engelke, Jürgen Wienands<br />
‘Membrane zip codes’ for Grb2 determine differential Ca2+ signaling in B lymphocytes<br />
Stefanie Kunz, Karin Oberle, Anna Sander, Christian Bogdan, Ulrike Schleicher<br />
Bartonella-Induced Cat Scratch Disease-like Lymphadenopathy in Mice Involves Cell<br />
Proliferation and Altered Lymphocyte Recruitment<br />
Georg Peschel, Nuria Rodriguez, Christine Cirl, Nina Wantia, Tanja Erl, Susi Dürr, Hermann Wagner, Thomas Miethke<br />
Chlamydophila pneumoniae follows different strategies to downregulate surface MHC II<br />
expression depending on the cell type<br />
Annabelle Schnaith, Sonja A. Leggio, Martin Krönke, Oleg Krut
Staphylococcus aureus Subverts Autophagy for Induction of Caspase-independent Host Cell<br />
Death<br />
Stella Eugenie Autenrieth, Dirk Middendorf, Ingo Birger Autenrieth<br />
Yersinia enterocolitica induces cell death in splenic dendritic cells: evidence for YopP dependent<br />
and independent mechanisms<br />
Heribert Appelhans, Michael Walther, Andrea Friße, Michael A. Harvey, Stephen A. Judice, Brett A. Stillman, Hans<br />
Peter Seelig<br />
A CE-Certified Autoimmune Disease Diagnostic Protein Microarray<br />
Martina Papadopoulos, Frank Momburg<br />
A complex sequence motif of tapasin stabilizes the TAP2 protein<br />
Andreas Oliver Weinzierl, Dominik Maurer, Florian Altenberend, Nicole Schneiderhan-Marra, Karin Klingel, Oliver<br />
Schoor, Thomas Joos, Hans-Georg Rammensee, Stefan Stevanovic<br />
A cryptic VEGF T-cell epitope: Identification and characterization by mass spectrometry and Tcell<br />
assays<br />
Susanne Tartz, Holger Ruessmann, Jana Kamanova, Peter Sebo, Angelika Sturm, Volker Heussler, Bernhard Fleischer,<br />
Thomas Jacobs<br />
A heterologous prime/boost immunization using recombinant Salmonella and Bordetella<br />
adenylate cyclase induces <strong>complete</strong> protection against P. berghei malaria<br />
Nousheen Zaidi, Timo Herrmann, Daniel Baechle, Sabine Schleicher, Jeannette Gogel, Christoph Driessen, Wolfgang<br />
Voelter, Hubert Kalbacher<br />
A new approach for distinguishing cathepsin E and D activity in antigen processing organelles<br />
Wiebke Hartmann, Markus M. Simon, Bernhard Fleischer, Simone Korten<br />
A new role for granzymes: Suppression of defence against helminths<br />
Elisa Kieback, Jehad Charo, Daniel Sommermeyer, Thomas Blankenstein, Wolfgang Uckert<br />
A new safeguard eliminates TCR gene-modified autoimmune-reactive T cells after adoptive<br />
therapy<br />
Matthias Bros, Frank Jährling, Andrea Renzing, Nadine Wiechmann, Ngoc-Anh Dang, Arne Sutter, Ralf Ross, Jürgen<br />
Knop, Stephan Sudowe, Angelika B. Reske-Kunz<br />
A newly established murine immature dendritic cell line exerts tolerogenic function at its<br />
immature state and upon alternative activation in the presence of glucocorticoid<br />
Iris Watermann, Jeannette Gerspach, Matthias Lehne, Klaus Pfizenmaier, Harald Wajant<br />
A novel CD95L-Prodrug Fusion Protein with tumorselective antitumoral activity<br />
Ines Gütgemann, Jasmin Teresa Ney, Qi Zhou, Christian Kurts, Hubert Schorle, Andreas Limmer, Martina Berg,<br />
Reinhard Büttner<br />
A novel model of antigen recognition in a hepatic tumor microenvironment: c-myc/OVA x<br />
LAPtTA transgenic mice<br />
Peggy Riese, Thomas Ebensen, Claudia Link, Kai Schulze, Michael Morr, Carlos Guzmán<br />
A pegylated derivative of alpha galactosylceramide exhibits improved immune stimulatory<br />
activities<br />
Eva Schlosser, Carolina Otero, Benedikt Kessler, Mariola Edelmann, Rene Brunisholz, Daniel Legler, Marcus Groettrup<br />
A prostate carcinoma antigen reveals a new cytosolic class I processing pathway for<br />
endoplasmic reticulum targeted proteins<br />
Mathias Konstandin, Guido Wabnitz, Hülya Aksoy, Martin Klemke, Thomas Dengler, Yvonne Samstag<br />
A sensitive assay for the quantification of integrin-mediated adhesiveness of human stem cells<br />
and leukocyte subpopulations in whole blood<br />
Heiko Bruns, Frank Stegelmann, Steffen Stenger<br />
Abl-tyrosine kinase modulates immune responses to Mycobacterium tuberculosis
Angelika Stöcklinger<br />
Ablation of Epidermal Langerhans Cells has no Impact on Gene-Gun mediated Immune<br />
Responses<br />
Brigitte Santner-Nanan, Nabila Seddiki, Cindy Zhu, Verena Quent, Anthony Kelleher, Barbara Fazekas de St. Groth,<br />
Ralph Nanan<br />
Accelerated age-dependent transition of human regulatory T cells to effector memory phenotype<br />
Jasmin Herz, Julian Pardo, Hamid Kashkar, Erik Bos, Reinhard Wallich, Peter J. Peters, Elmon Schmelzer, Martin<br />
Krönke, Markus M. Simon, Olaf Utermöhlen<br />
Acid sphingomyelinase is a critical regulator of cytotoxic granule secretion by primary T<br />
lymphocytes<br />
Manuela Rossol, Undine Meusch, Holm Häntzschel, Sunna Hauschildt, Ulf Wagner<br />
Activated CD4 T cells induce TNF production in human monocytes via reverse signalling of<br />
membrane TNF<br />
Milena Josefina Tosiek, Marcus Gereke, Jan Buer, Dunja Bruder<br />
Activation and regulation of autoreactive CD8 T cells in the lung<br />
Xuefang Ren, Marion Schneider, Ying Wang, Lin Xu, Zhenggang Jiang, Fei Ye<br />
Activation induced cell death of CD4+CD25+Foxp3+ T cells by TCR re-stimulation involves a<br />
CD95/CD95L dependent mechanism<br />
Alexei Gratchev, Julia Kzhyshkowska, Sheila Kannookadan, Miriam Ochsenreiter, Anna Popova, Xiaolei Yu, Isabelle<br />
Muller-Molinet, LiMing Gooi, Sergij Goerdt<br />
Activation of a TGF-β-specific multistep gene expression program in mature M2 macrophages<br />
requires glucocorticoid-mediated surface expression of TGF-β receptor II<br />
Umme Amara, Miriam Kalbitz, Andreas Klos, Markus Huber-Lang<br />
Activation of Complement by the Coagulation System<br />
Luisa Cervantes-Barragan, Ulrich Kalinke, Roland Züst, Constantino Lopez-Macias, Volker Thiel, Burkhard Ludewig<br />
Activation of myeloid cells through plasmacytoid dendritic cell-derived type I interferon secures<br />
control of murine coronavirus infection<br />
Alexander Donald McLellan, Patrizia Stoitzner, Jacquie Harper, Sarah Saunderson, Ralph Jack, Anthea Bouwer<br />
Activation of natural killer cells by dendritic cells stimulated with gram positive bacteria<br />
Dimitra Kotsougiani, Birgit Prior, Gertrud Maria Hänsch, Christof Wagner<br />
Activation of T lymphocytes in bacterial infection: production of interferon 4gamma, expression<br />
of the chemokine receptor CXCR6, and up-regulation of Toll-like receptors (TLR) in patients with<br />
implant-associated posttraumatic osteomyelitis<br />
Eva Distler, Catherine Wölfel, Sylvia Köhler, Marion Nonn, Elke Schnürer, Ralf G. Meyer, Christoph Huber, Thomas<br />
Wölfel, Udo F. Hartwig, Wolfgang Herr<br />
Acute myeloid leukemia (AML)-reactive cytotoxic T lymphocyte clones rapidly expanded from<br />
CD8+ CD62L(high)+ T cells of healthy donors prevent AML engraftment in NOD/SCID IL2Rγnull<br />
mice<br />
Sarvari Velaga, Stephan Halle, Sabrina Dähne, Oliver Pabst<br />
Adaptation of Solitary Intestinal Lymphoid Tissue in response to microbial stimulation<br />
Nancy Brewig, Adrien Kissenpfennig, Bernard Malissen, Alexandra Veit, Bernhard Fleischer, Uwe Ritter<br />
Adaptive immune response to Leishmania parasites is induced in the absence of epidermal<br />
Langerhans cells<br />
Gaubert Sophie, Zimmermann Andra, Arbach Olga, Rossa Simone, Thiel Andreas, Voigt Sebastian, Ebell Wolfram<br />
Adenovirus-specific T cell therapy in paediatric stem cell transplants: Isolation and expansion of<br />
donor-derived T lymphocytes
Iris Bellinghausen, Barbara Häringer, Beatrice Lafargue, Tamara Hilmenyuk, Heinz Decker, Joachim Saloga<br />
Allergological implication of the quaternary hexameric structure of the cockroach allergen Per a<br />
3.<br />
Ingrid Schuster, Elfriede Eppinger, Christoph Salat, Bernhard Frankenberger, Joachim Ellwart, Elfriede Nößner, Dirk<br />
Busch, Angela Krackhardt<br />
Allorestricted T cells with high specificity for the FMNL1-derived peptide PP2 show tumor<br />
reactivity but also limited alloreactivity against other MHC alleles – implications for adoptive T<br />
cell therapy using allorestricted T cell receptors<br />
Andrey Bogdanov, Tatyana Rybakova, Nikolai Belyaev<br />
Alpha-fetoprotein impair recovery of cell-mediated immunity normal function after tumor<br />
ablation<br />
Connie Schulze, Petra Heyder, Sandra Franz, Kerstin Sarter, Luis Munoz, Stefan Pöhlmann, Hanns-Martin Lorenz,<br />
Martin Herrmann, Martin Schiller<br />
Alteration of glycocalyx and exposition of mannose residues during apoptosis are essential for<br />
the clearance of apoptotic marterial<br />
Sabine Höpner, Katharina Dickhaut, Jamina Eckhard, Shashank Gupta, Kirsten Falk, Olaf Rötzschke<br />
Amplification of CD4 T cell responses by catalysing antigen-loading through MHC-loading<br />
Enhancer (MLE)<br />
Stefanie Scheu, Philipp Dresing, Richard M. Locksley<br />
An IFNβ Reporter Mouse Model for the Visualization of the Initiation of the Type I Interferon<br />
Response in vivo<br />
Frank Schmitz, Antje Heit, Tobias Haas, Hermann Wagner<br />
An mTOR dependent transport mechanism of cytosolic receptors licenses TLR-independent<br />
recognition of nucleic acids<br />
Linda Sender, Zoe Waibler, Camilla Merten, Roland Hartig, Matthias Gunzer, Peter Reichardt, Ulrich Kalinke, Burkhart<br />
Schraven<br />
An unusual signalling signature suggests a molecular basis for the adverse side effects of antihuman<br />
CD28 superagonistic antibodies<br />
Lorena Martinez Gamboa, Henrik Mei, Karin Reiter, Kristin Kemnitz, Arne Hansen, Florian Emmerich, Abdulgabar<br />
Salama, Thomas Dörner<br />
Analysis of B cell subpopulations in patients with autoimmune thrombocytopenia: effects of<br />
splenectomy and implications for therapy<br />
Timo Lischke, Andreas Hutloff, Richard A. Kroczek<br />
ANALYSIS OF CD4+ T CELL IMMUNITY IN VIVO<br />
Katja Maurer, Ellen Harrer, Andreas Goldwich, Kathrin Eismann, Silke Bergmann, Birgit Schätz, Sandra Müller, Thomas<br />
Harrer<br />
Analysis of CTL mediated immune selection in a dominant HLA B8-restricted CTL Epitope in Nef<br />
Simone Wüst, Denise Tischner, Anna Kleimann, Ralf Gold, Jan P. Tuckermann, Holger M. Reichardt, Fred Lühder<br />
Analysis of Glucocorticoid action in Experimental Autoimmune Encephalomyelitis (EAE)<br />
Anett Schulz, Manuela Rossol, Matthias Pierer, Sybille Arnold, Holm Häntzschel, Christoph Baerwald, Ulf Wagner<br />
Analysis of polymorphisms in the TNFR2 gene in rheumatoid arthritis and possible functional<br />
relevance<br />
Sonja Kothlow, Benjamin Schusser, Nicola Penski, Georg Kochs, Peter Staeheli, Bernd Kaspers<br />
Analysis of potential antiviral Mx activity in the chicken<br />
Andreas Jeron, Susanne Pfoertner, Tanja Toepfer, Jan Buer, Robert Geffers, Andres J Schrader<br />
Analysis of regulatory T cells in renal cell carcinoma<br />
Nicole Warnecke, Burkhart Schraven, Luca Simeoni
Analysis of TCR-mediated MAPK activation in primary T cells.<br />
Eva Billerbeck, Hubert E Blum, Robert Thimme<br />
Analysis of virus specific FoxP3+ regulatory CD8+ T cells<br />
Julia Hoffmann, Ralf-Holger Voss, Ruth Frommolt, Matthias Theobald, Udo Hartwig<br />
Analyzing GVL-immune responses of p53-specific CD8+ cytotoxic T cells to leukemia cell lines<br />
and acute myeloid leukemia in vitro and in vivo in humanized NOD/SCID/IL-2Receptor gammachain<br />
null mice<br />
Heiko Weyd, Lucie Doerner, Andrea Mahr, Nadine Eberhardt, Dagmar Riess, Bjoern Linke, Christine S. Falk, Peter H.<br />
Krammer<br />
Annexin I – an anti-inflammatory signal on the surface of apoptotic cells<br />
Nicole Gerlach, Cassandra James, Ulf Dittmer<br />
Anti-retroviral effects of type I interferon subtypes in vivo<br />
Christina Stöckle, Timo Burster, Thomas Rückrich, Alexander Beck, Christoph Driessen, Arthur Melms, Eva Tolosa<br />
Antigen Processing in the Human Thymus<br />
Patrick C. Rämer, Susanne Haemmerling, Mathias H. Konstandin, Thomas Giese, Thomas J. Dengler, Sivanandam<br />
Vijayshankar<br />
Antigen-presenting capacity and T cell costimulation of endothelial progenitor cells is<br />
comparable to monocytes<br />
Marcela Fajardo-Moser, Christine Hambrecht, Heidrun Moll<br />
Antigen-pulsed dendritic cell-derived exosomes as cell-free vaccines against infection<br />
Christian Schütz, Andreas Mackensen, Jonathan P. Schneck, Jürgen Schölmerich, Mathias Oelke, Martin Fleck<br />
Antigen-specific CD8+ T cell depletion mediated by apoptosis-inducing HLA-A2-Ig based<br />
artificial APCs<br />
Heike Koehler, Andreas Hombach, Hinrich Abken<br />
Antigen-specific T cell activation is repressed by TGF-b which can be overcome by CD28<br />
costimulation<br />
Nonsikelelo Mpofu, Konstantinos Iordanidis, Matthias Hardtke-Wolenski, Micheal. P Manns, Elmar Jaeckel<br />
Antigen-specific, Foxp3 transduced T cells for therapy of type 1 diabetes<br />
Anjana Singh, Miri Blank, Yehuda Shoenfeld, Harald Illges<br />
Antiphospholipid syndrome patients display reduced titers of soluble CD21 in their sera<br />
irrespective of circulating anti-beta-2-glycoprotein-I autoantibodies.<br />
Stefan Lienenklaus, Marcin Lyszkiewicz, Jadwiga Jablonska, Siegfried Weiss<br />
ANTIVIRAL AND ILLUMINATED A NEW MOUSE LINE TO MONITOR β-INTERFERON INDUCTION<br />
Carola Pongratz, Benjamin Yazdanapanah, Hamid Kashkar, Martin Kroenke<br />
Antiviral implications of a convertible HIV-1 directed siRNA library<br />
Cosima Kretz, Bartlomiej Berger, Lucie Dörner, Heiko Weyd, Ingo H. Tarner, Ulf Müller-Ladner, Hanns-Martin Lorenz,<br />
Peter H. Krammer, Annegret Kuhn<br />
Apoptosis in Systemic Lupus Erythematosus: Influence on Immune Response and Peripheral<br />
Tolerance<br />
Katharina Randers, Telja Pursche, Doreen Finke, Kirsten Jacobsen, Robert Hoerster, Christian Brockmann, Holger<br />
Hennig, Tony Marion, Sigfried Goerg<br />
Apoptotic DNA is able to induce in vivo IFN α production within the splenic marginal zone via a<br />
TLR dependent pathway.<br />
Katharina Weibhauser, Bernd Kaspers, Sonja Kothlow
APPLICATION OF THE RCAS RETROVIRAL VECTOR SYSTEM FOR FUNCTIONAL IN VIVO STUDIES<br />
OF THE CYTOKINE BAFF IN THE CHICKEN<br />
Johanna Oberlies, Carsten Watzl, Thomas Giese, Claudia Luckner, Stefan Meuer, Markus Munder<br />
Arginine depletion by human granulocyte arginase impairs NK cell function<br />
Katrin Drögemüller, Martina Deckert, Ulrike Hellmuth, Monika Sakowicz-Burkiewicz, Dirk Reinhold, David Gutmann,<br />
Werner Müller, Dirk Schlüter<br />
Astrocyte gp130-expression is critical for astrocyte survival, downregulation of intracerebral<br />
immune responses and survival of experimental autoimmune encephalomyelitis and Toxoplasma<br />
encephalitis<br />
Mihály Józsi, Stefanie Strobel, Hans-Martin Dahse, Wei-shih Liu, Peter F. Hoyer, Martin Oppermann, Christine Skerka,<br />
Peter F. Zipfel<br />
Autoantibodies block C-terminus of factor H in atypical hemolytic uremic syndrome<br />
Martin Schiller, Isabelle Bekeredjian-Ding, Petra Heyder, Norbert Blank, Klaus Heeg, Hanns-Martin Lorenz<br />
Autoantigens are translocated into apoptotic bodies during apoptosis<br />
Karin Loser, Sandra Balkow, Kerstin Klimmek, Claus Kerkhoff, Wolfgang Nacken, Thomas A. Luger, Stefan Beissert<br />
Autoreactive CD8+ T cell development in CD40L-mediated autoimmunity is controlled by S100A8<br />
and A9 proteins<br />
Bernd Lepenies, Klaus Pfeffer, Michelle Hurchla, Theresa Murphy, Kenneth Murphy, Juliane Oetzel, Bernhard Fleischer,<br />
Thomas Jacobs<br />
B and T lymphocyte attenuator (BTLA) ligation prevents cerebral malaria during P. berghei<br />
ANKA infection<br />
Janine Suffner, Kristin Hochweller, Natalio Garbi, Günter Hämmerling<br />
BAC-transgenic mice for depletion of Foxp3+ regulatory T cells<br />
Matthias Peiser, Juliana Koeck, Burghardt Wittig, Reinhard Wanner<br />
Bacterial lipopeptides activate human Langerhans cells via Toll-like receptor 2<br />
Konrad Bode, Klaus Heeg, Alexander Dalpke<br />
Bacterial origin histone deacetylase inhibitor butyric acid inhibits dendritic cells<br />
Marta Rizzi, Ulrich Salzer, Klaus Warnatz, Stefanie Hamm, Sigune Goldacker, Beate Fischer, Hans Hartmut Peter,<br />
Hermann Eibel<br />
BAFF Receptor expression in CVID patients<br />
Jenny Dieckmann, Susanne Rehfeld, Bernd Kaspers, Sonja Kothlow<br />
BAFF regulates the expression of bcl-2 family members in chicken B cells<br />
Astrid Karbach, Evelyn Rossmann, Veronique Kitiratschky, Heidelore Hofmann, Markus M. Simon, Peter Kraiczy,<br />
Reinhard Wallich<br />
BbCRASP-1 of the Lyme disease spirochetes induces antibodies to nondenatured structural<br />
determinants in humans<br />
Evelyn Rossmann, Peter Kraiczy, Pia Herzberger, Christine Skerka, Michael Kirschfink, Markus M. Simon, Peter F.<br />
Zipfel, Reinhard Wallich<br />
BhCRASP-1 of the relapsing fever spirochete Borrelia hermsii is a factor H and plasminogen<br />
binding protein<br />
Xin Ding, Niklas Beyersdorf, Gregor Blank, Fred Lühder, Kevin Dennehy, Ralf Gold, Thomas Kerkau, Thomas Hünig<br />
Blockade of CD28-B7 interactions by anti-CD28 antibodies protects from immunopathology in<br />
vivo<br />
Tea Gogishvili, Beate Geyer, Susanne Grunewald, Thomas Hünig<br />
Blockade of CD28-mediated co-stimulation ameliorates allergic airway inflammation in mice<br />
Mostafa Jarahian, Carsten Watzl, Yasmin Issa, Peter Altevogt, Frank Momburg
Blockade of natural killer cell-mediated lysis of NCAM140 expressed on tumor cells<br />
Nicole Bethke, Matthias Böthe, Siegfried Kohler, Matthias Niedrig, Andreas Thiel<br />
Bystander activation of recall antigen-specific CD4+ T-cells during primary immunization with<br />
live attenuated yellow fever virus<br />
Olaf Gross, Andreas Gewies, Katrin Finger, Martin Schäfer, Tim Sparwasser, Christian Peschel, Irmgard Förster, Jürgen<br />
Ruland<br />
Card9 controls a non-TLR signaling pathway for innate anti-fungal immunity<br />
Christina Stöckle, Vinod Sommandas, Hubert Kalbacher, Athur Melms, Eleni Adamopoulou, Ekkehard Weber, Christoph<br />
Driessen, Bernhard Boehm, Eva Tolosa, Timo Burster<br />
Cathepsin distribution in primary human antigen presenting cells<br />
Marion Leick, Tanja Hartmann, Susann Ewers, Andrea Diefenbacher, Robert Nibbs, Meike Burger<br />
CCL5 upregulates surface expression of the orphan atypical chemokine receptor CRAM-A/B in a<br />
heparin sulphate dependent manner in pre-B acute lymphoblastoid leukemia cells<br />
Uta Elisabeth Höpken, Susann Winter, Kerstin Krüger, Armin Rehm, Martin Lipp<br />
CCR7 REGULATES LYMPHOCYTE EGRESS AND RECIRCULATION THROUGH BODY CAVITIES<br />
Tim Worbs, TR Mempel, J Bölter, UH von Andrian, R Förster<br />
CCR7-ligands stimulate the intranodal motility of T lymphocytes in vivo<br />
Matthias Krusch, Tina Baessler, Katrin Miriam Baltz, Helmut Rainer Salih<br />
CD137 ligand expression on acute myeloid leukemia cells modulates immune surveillance of<br />
human NK cells identified to express CD137 upon activation<br />
Holger Hoff, Zulema Cabail, Karin Knieke, Marion Rudolph, Heike Hirseland, Barbara Bröker, Monika Brunner-Weinzierl<br />
CD152 (CTLA-4) controls CD28-independently cell cycle progression and resistance against<br />
apoptosis of human T lymphocytes<br />
J. Kolja Hegel, Pushpa Pandiyan, Paula Kolar, Karin Knieke, Steven L. Reiner, Monika Brunner-Weinzierl<br />
CD152 (CTLA-4) utilizes Eomesodermin, but not T-bet, for regulating effector function of<br />
individual CD8 T lymphocytes: Implication for tumor therapy<br />
Karin Knieke, Holger Hoff, Frank Maszyna, Paula Kolar, J. Kolja Hegel, Alf Hamann, Gudrun F. Debes, Monika Brunner-<br />
Weinzierl<br />
CD152 (CTLA-4)- signalling promotes homing to secondary lymphoid organs<br />
Baerbel Keller, Mirzokhid Rakhmanov, Sylvia Gutenberger, Sigune Goldacker, Dirk Holzinger, Elisabeth Nikolopoulus,<br />
Paul Fisch, Hermann Eibel, Hans-Hartmut Peter, Klaus Warnatz<br />
CD21low B Cells Represent a Polyclonally Activated B Cell Population Exposed to Type I<br />
Interferons<br />
Isis Ludwig-Portugall, Emma E. Hamilton-Williams, Christian Kurts<br />
CD25+ regulatory T cells induce peripheral B cell tolerance against non-lymphoid tissue<br />
autoantigens<br />
Christian Becker, Tobias Bopp, Jan Kubach, Franz-Josef Schneider, Edgar Schmitt, Helmut Jonuleit<br />
CD4-mediated, TCR-independent functional activation of human CD4+CD25+ regulatory T cells<br />
Alexander Donald McLellan, Sarah Charlotte Saunderson, Petra Schuberth, Lilija Miller, Amy Charlotte Dunn, Philippa<br />
Anne MacKay, Ralph Wilson Jack<br />
CD40/IL-4-stimulated B cells release exosomes enriched in components of the B cell receptor<br />
complex.<br />
Rachid Marhaba, Margot Zöller<br />
CD44 blocking induces apoptosis by uncoupling Ezrin from the Ras pathway<br />
Annalena Bollinger, Zane Orinska, Silvia Bulfone-Paus
CD8+CD38+ T cells: An newly defined IL-15 dependent regulatory T cell population with effects<br />
in allergic asthma<br />
Katja Lüthje, Svenja Ehrlich, Bernhard Fleischer, Minka Breloer<br />
CD83 expression level affects spleenic B cell maturation<br />
Wiebke Hansen, Simone Reinwald, Astrid M. Westendorf, Carsten Wiethe, Jan Buer<br />
CD83 is involved in the immunosuppressive function of regulatory T cells<br />
Birte Kretschmer, Katja Lüthje, Andreas H. Guse, Svenja Ehrlich, Friedrich Koch-Nolte, Friedrich Haag, Bernhard<br />
Fleischer, Minka Breloer<br />
CD83 modulates B cell function in vivo and in vitro<br />
Thomas Bickert, Andrea Horst, Christoph Wagener, Bernhard Fleischer, Uwe Ritter<br />
CEACAM1 is crucial for lymphvasculogenesis during inflammatory immune responses<br />
Ulf Alexander Wenzel, Sonja Möller, Werner Solbach, Tamas Laskay, Ger van Zandbergen<br />
Cell death regulation controls Leishmania disease development<br />
Norbert Koch, Alexander McLellan, Jürgen Neumann<br />
Chaperone Controlled Assembly and Matched Isotype Pairing of Major histocompatibility<br />
complex Class II Subunits<br />
Johann Poetzl, Catherine Botteron, Daniela Maennel, Anja Lechner<br />
Characterisation of long-lived CCR6 expressing TH cells in the immune response<br />
Bernhard Fleischer, Juliane Ladhoff, Elke Effenberger, Cornelia Doebis, Hans-Dieter Volk, Martina Seifert<br />
Characterisation of NK cell attacks towards MHC class I deficient rat aortic endothelial cells in<br />
vitro<br />
Mirjam Peter, Klaus Heeg, Alexander Dalpke<br />
Characterization of a guanosine-rich suppressive oligodesoxynucleotide which inhibits Toll-like<br />
receptor-9 signaling<br />
Andrea Kiessling, Dagmar Riemann, Susanne Fuessel, Esther Kamphausen, Barbara Seliger<br />
Characterization of expression pattern and regulation of ISGylation system in tumors<br />
Christoph Treese, Franziska Lange, Nadja Hilger, Anja Mittag, Attila Tarnok, Andreas Lösche, Frank Emmerich, Ulrich<br />
Sack<br />
Characterization of fibroblasts eroding cartilage in arthritis<br />
Jan Leipe, Alla Skapenko, Hendrik Schulze-Koops<br />
Characterization of human Interleukin 17 (IL-17)-producing T helper cells (Th17 cells) in<br />
healthy individuals and in patients with rheumatoid arthritis<br />
Michael Mihlan, Mario Hebecker, Markus Huber-Lang, Peter F. Zipfel, Mihály Józsi<br />
Characterization of ligand binding of the human Factor H-related protein 4 (FHR-4) provides<br />
insight into function<br />
Sandra Klein, Cosima Kretz, Nina Oberle, Martin Hartmann, Alexander Enk, Peter H. Krammer, Elisabeth Suri-Payer,<br />
Annegret Kuhn<br />
Characterization of regulatory T cells in human autoimmune diseases with skin manifestations<br />
Björn Kolbe, Ulrike Kolrep, Roland Wagner, Jürgen Schmitz, Ian C.D. Johnston<br />
Characterization of the natural ligand of the plasmacytoid dendritic cell-specific marker CD303<br />
Stefanie Gross, Uwe Trefzer, Wolfram Sterry, Peter Walden<br />
Characterization of tumor-specific versus virus-specific tumor-infiltrating and peripheral blood T<br />
cells from melanoma patients<br />
Marco Frentsch, Regina Starke, Sarah Meier, Gebhardt Friedemann, Dirk Busch, Chiara Romagnani, Andreas Thiel
Characterization of versatile CD8 memory T-cells with potent APC helper function<br />
Shipra Gupta, Sebastian Rieder, Sylvia Escher, Aleksandra Heitland, Wolf-Georg Forssmann, Jörn Elsner, Ulf<br />
Forssmann<br />
Chemokine receptor-mediated intravascular inactivation of leukocytes by a nonglycosaminoglycan(GAG)-binding<br />
variant of NNY-CCL14.<br />
Silvia Capellino, Peter Angele, Werner Falk, Maurizio Cutolo, Rainer H. Straub<br />
Chromaffin-like cells and catecholamine production: role on the inflammatory response in<br />
rheumatoid arthritis (RA) patients<br />
Thomas Bollinger, Monika Bajtus, Annalena Bollinger, Stojan Dimitrov, Werner Solbach<br />
Circadian Rhythm of Regulatory T Cell distribution and function<br />
Nicholas Schwab, Christoph Leder, Chi Wang Ip, Antje Kroner, Klaus-Armin Nave, Klaus Dornmair, Rudolf Martini,<br />
Heinz Wiendl<br />
Clonal expansions of pathogenic CD8+ effector T cells in the CNS of myelin mutant mice<br />
Andreas Grahnert, Steffi Richter, Sunna Hauschildt<br />
Cloning and characterization of an enzymatically active ADP-ribosyltransferase 4 (ART4) from<br />
chicken<br />
Jens Wuerfel, Alina Smorodchenko, Elena Pohl, Johannes Vogt, Eva Tysiak, Robert Glumm, Sven Hendrix, Robert<br />
Nitsch, Frauke Zipp, Carmen Infante-Duarte<br />
CNS-irrelevant T cells enter the brain, cause blood-brain barrier disruption but no cellular<br />
neuropathology<br />
Maria Lawrenz, Alexander Visekruna, Thorsten Joeris, Nicole Schmidt, Anjo Kroesen, Stefan H.E. Kaufmann, Ulrich<br />
Steinhoff<br />
Coherence or Coincidence ? - ERK activation and Immunoproteasomes in Crohn Disease<br />
Marcus Gereke, Jan Buer, Dunja Bruder<br />
Collaboration of the innate and adaptive immune system leads to immunological tolerance in the<br />
lung<br />
Jan Hendrik Niess, Frank Leithauser, Guido Adler, Jörg Reimann<br />
Commensal-driven local TH17 responses trigger inflammatory bowel disease<br />
Maria Diedrichs-Möhring, Georges M.G.M. Verjans, Seerp G. Baarsma, Gerhild Wildner<br />
Comparison of antigen-specific cytokine secretion and proliferation of T lymphocytes in vitro<br />
Vera Jakobi, Swen Wagner, Michael Loos, Franz Petry<br />
Complement activation of Cryptosporidium parvum (Apicomplexa, Protozoa) via the classical<br />
and lectin pathways<br />
Feng Guo, Debra Weih, Elke Meier, Falk Weih<br />
Constitutive alternative NF-?B signaling promotes marginal zone B cell development but disrupts<br />
the marginal sinus and induces HEV-like structures in the spleen<br />
Christian Koble, Jens Derbinski, Bruno Kyewski<br />
CONSTITUTIVE CROSS-PRESENTATION OF ENDOGENOUS SELF- ANTIGENS BY THYMIC<br />
DENDRITIC CELLS<br />
Katja Sabel, Oleg Krut, Martin Krönke, Alexander Klimka<br />
Construction of a recombinant intrabody library to select for inhibitors of intracellular pathogens<br />
Vladimir Kocoski, Norbert Tautz, Eberhard Burkhardt<br />
CONSTRUCTION OF A STABLE TRANSFECTED, PERMANENTLY SECRETING BHK Tet-On CELL LINE<br />
CARRYING THE SINGLE-CHAIN CANINE IL-12 FOR APPLICATION IN THE TUMOR<br />
IMMUNOTHERAPY IN DOG
Alexey Popov, Julia Driesen, Zeinab Abdullah, Claudia Wickenhauser, Tomo Saric, Svenja Debey-Pascher, Trinad<br />
Chakraborty, Martin Krönke, Olaf Utermöhlen, Joachim L. Schultze<br />
Containment of pathogens and induction of the local immune privilege by IDO + denritic cells in<br />
granulomatous infections and its implication for human disease<br />
Kathrin Westphal, Sara Leschner, Holger Loessner, Siegfried Weiss<br />
Containment of tumor colonizing bacteria by host neutrophils<br />
Martin Schlee, Michael Bscheider, Veit Hornung, Andrea Ablasser, Stefan Endres, Gunther Hartmann<br />
Contrasting roles of p38 in TLR signaling<br />
Bishnudeo Roy, Oliver Pabst, Swati Shukla, Sandra Düber, Siegfried Weiss<br />
Contribution of B-1 cells to gut associated humoral immunity<br />
Susanne Kirschnek, Robert Paul, Bianca Obermaier, Georg Häcker, Uwe Koedel<br />
Contribution of cell death in phagocytes and resident cells to the outcome of pneumococcal<br />
meningitis in mice<br />
Gabriele Weintz, Michael Hammer, Ilona Moßbrugger, Leticia Quintanilla-Martinez, Christian Stemberger, Dirk H.<br />
Busch, Roland Lang<br />
Control of inflammation and host resistance during Listeria infection by the MAPK-Phosphatase<br />
DUSP1<br />
Caspar Ohnmacht, Nico van Rooijen, David Voehringer<br />
Cooperation between innate and adaptive immunity during type 2 immune responses in vivo.<br />
Kathrin Schönberg, Gesine Kögler, Johannes Fischer, Markus Uhrberg<br />
Correlation of KIR expression and presence of HLA-C ligands in adult but not neonatal NK cells:<br />
transition from a naïve to an adult NK cell repertoire<br />
Zoe Waibler, Martina Anzaghe, Abdo Konur, Shizuo Akira, Werner Müller, Ulrich Kalinke<br />
CpG 1668 treatment stimulates an anti-inflammatory environment that abrogates CpG 2216<br />
induced type I IFN responses by pDC<br />
Viktor Kölzer, David Anz, Michaela Golic, Cornelia Wurzenberger, Stefan Endres, Carole Bourquin<br />
CpG Oligonucleotide Treatment Alters the Morphological Distribution and Phenotype of<br />
Regulatory T Cells<br />
Wolfgang Kastenmüller, Georg Gasteiger, Ingo Drexler<br />
Cross-competition of CD8+ T cells shapes the immunodominance hierarchy during recall<br />
vaccination<br />
Nanette von Oppen, Linda Diehl, Rene Tolba, Percy Knolle<br />
CROSS-PRESENTING LIVER SINUSOIDAL ENDOTHELIAL CELLS ESTABLISH ANTIGEN-SPECIFIC<br />
ADHESION OF NAÏVE CD8 T CELLS LEADING TO T CELL TOLERANCE IN VIVO<br />
Heinke Conrad, Kerstin Gebhard, Julia Neudorfer, Christian Peschel, Helga Bernhard<br />
Cross-reactivity of HER2p369-377 reactive CTL clones against other HER family members<br />
Mandy Pierau, Engelmann Swen, Thomas Drewes, Thabo Lapp, Dirk Reinhold, Burkhart Schraven, Ursula Bommhardt<br />
Cross-talk between PKB/Akt and TGFβ signalling in T cell activation<br />
Sven Burgdorf, Christian Kurts<br />
Current models and mechanisms of antigen crosspresentation<br />
Jörg Rossbacher, Frank Wilde, Gerd Müller, Martin Lipp<br />
CXCR5 as a therapeutic target in Non Hodgkin lymphomas and autoimmune disease<br />
Sven Hartmann, Antje M. Wengner, Uta E. Hoepken, Peter K. Petrow, Uta Schurigt, Rolf Braeuer, Martin Lipp<br />
CXCR5- and CCR7-dependent lymphoid neo-genesis in a chronic model of antigen-induced<br />
arthritis (AIA)
Tanja Nicole Hartmann, Bretton Summers, Valentin Grabovsky, Eilon Woolf, Ziv Shulman, Eike Buss, Tom Schall,<br />
Marcus Thelen, Ronen Alon<br />
CXCR7 blockage inhibits in human hematopoietic progenitor cells and T cells a CXCR4 subset<br />
specialized in integrin activation by CXCL12 under shear stress conditions<br />
Tobias Bopp, Christian Becker, Matthias Klein, Stefan Klein-Heßling, Alois Palmetshofer, Edgar Serfling, Marc Becker,<br />
Jan Kubach, Schmitt Steffen, Sabine Stoll, Hansjoerg Schild, Martin Staege, Michael Stassen, Helmut Jonuleit, Edgar<br />
Schmitt<br />
Cyclic AMP: The decicive component of naturally occuring regulatory T cell-mediated<br />
suppression<br />
Bianca Paul, Linda Diehl, Alexander Knorre, Percy Knolle, Marc Beyer, Waldemar Kolanus<br />
Cytohesin-3 Links B7H1 mediated Shut-down of the PI3 Kinase Pathway to the Repression of IL-<br />
2 Synthesis in Anergic T cells<br />
Sabrina Hoffmann, Michael Winkler, Marcus Gutscher, Helmut Fickenscher, Carsten Watzl<br />
Cytomegalovirus infected fibroblasts downregulate ligands for the Natural Cytotoxicity receptors<br />
NKp30 and NKp44<br />
Doris Urlaub, Sven Mesecke, Hauke Busch, Roland Eils, Carsten Watzl<br />
Decision making in NK cells<br />
Jochen Maul, Susanne Pförtner, Robert Geffers, Kerstin Kapp, Jan Buer, Martin Zeitz, Rainer Duchmann<br />
Decreased expression of CCR4 on CD4+CD25high regulatory T cells as a possible mechanism for<br />
impaired migration to inflamed mucosa in Crohn´s disease<br />
Mahmoud Sadeghi, Gerhard Opelz, Volker Daniel, Cord Naujokat, Rainer Zimmermann, Angela Huth-Kühne, Caner<br />
Süsal<br />
Decreasing Soluble CD30 and Increasing IFN-γ Plasma Levels are Indicators of Effective Highly<br />
Active Antiretroviral Therapy.<br />
Nadine Voelxen, Sylvia Gutenberger, Hans-Hartmut Peter, Hermann Eibel, Klaus Warnatz<br />
Defective activation of B cells in persistent polyclonal B cell lymphocytosis (PPBL)?<br />
Christine Skerka, Nadine Lauer, Claudia N Keilhauer, Lars Fritsche, Bernhard H.F. Weber, Peter F. Zipfel<br />
Defective Binding of Factor H (Y402H) and FHL-1 to CRP and Collagen in Age Related Macular<br />
Degeneration<br />
Florian Börncke, Beatrix Pollok-Kopp, Mladen V. Tzvetkov, Martin Oppermann<br />
Defective Binding to C-Reactive Protein and Impaired Cofactor Activity of the Allotypic Y402H<br />
Variant of Complement Factor H<br />
Frank Guenther, Gertud Maria Hänsch, Christof Wagner<br />
DEFENCE AGAINST BACTERIAL BIOFILMS: ROLE OF POLYMORPHONUCLEAR NEUTROPHILS<br />
(PMN)<br />
Tobias Schulze, Katrin Räbel, Sven Golfier, Martin Lipp<br />
Deficiency in Sphingosine-1-phosphate receptor 4 (S1P4) results in deviated humoral immune<br />
responses<br />
Anja Erika Hauser, Tobias Junt, Thorsten R. Mempel, Michael W. Sneddon, Steven H. Kleinstein, Sarah E. Henrickson,<br />
Ulrich H. von Andrian, Mark J. Shlomchik, Ann M. Haberman<br />
Definition of Germinal Center B Cell Migration In Vivo Reveals Predominant Intra-zonal<br />
Circulation Patterns<br />
Christine Skerka, Mihály Józsi, Stefanie Strobel, Stefan Heinen, Matthew Edey, Svante L. H. Zipfel, Judith A Goodship,<br />
Timothy H.J. Goodship, Christoph Licht, Peter F. Zipfel<br />
Deletion of CFHR1 and CFHR3 correlates with presence of Factor H autoantibodies in hemolytic<br />
uremic syndrome<br />
Thorsten Feyerabend, Annette Tietz, Herve Luche, Freddy Radtke, Hans Joerg Fehling, Hans Reimer Rodewald
DELETION OF NOTCH-1 IN KIT+ PRO-T CELLS BLOCKS T CELL DEVELOPMENT, BUT DOES NOT<br />
CONVERT T CELL PROGENITORS INTO THYMIC B CELLS<br />
Carsten Wiethe, Alexander Steinkasserer, Manfred Lutz, Andre Gessner<br />
Dendritic cell differentiation state and their interaction with NKT cells determines Th1/Th2<br />
differentiation in the murine model of Leishmania major infection<br />
Stefan A. Kaden, Juergen Schmitz, Gregor Winkels<br />
Dendritic Cell immuno-activating receptor 1 – Characterization of a novel member of the C-type<br />
Lectin family<br />
Marcin •yszkiewicz, Natalia Zi•tara, Manfred Rohde, Kurt Dittmar, Jadwiga Jab•o•ska, Siegfried Weiss<br />
Dendritic cell like function of ER-TR9 + marginal zone macrophages<br />
Kristin Hochweller, Jörg Striegler, Günter J Hämmerling, Natalio Garbi<br />
Dendritic cells control awareness of T lymphocytes for antigen<br />
Mathias Lucas, William Schachterle, Karin Oberle, Peter Aichele, Andreas Diefenbach<br />
Dendritic Cells Prime Natural Killer Cells by trans-Presenting Interleukin 15<br />
Anja Saalbach, Claudia Klein, Ulf Anderegg, Jan C. Simon<br />
Dermal fibroblasts induce maturation of dendritic cells<br />
Elke Pogge von Strandmmann, Boris Böll, Daniel Re, Andreas Engert, Venkateswara Simhadri<br />
Detection of HLA-B associated transcript 3 (BAT3) in sera from Hodgkin Lymphoma patients and<br />
its release from Hodgkin lymphoma cells<br />
Leander Grode, Hans-Heinrich Henneick v. Zepelin, Albrecht Laeufer, Bernd Eisele<br />
Developing a TB vaccine for human use<br />
Stefan Porubsky, Anneliese O. Speak, Bruno Luckow, Vincenzo Cerundolo, Frances M. Platt, Hermann-Josef Gröne<br />
Development and function of invariant natural killer T cells in mice with<br />
isoglobotrihexosylceramide (iGb3) deficiency<br />
Nina Wantia, Tanja Ertl, Christine Cirl, Nuria Rodriguez, Hermann Wagner, Thomas Miethke<br />
Development of a protein and CpG-based vaccination against Chlamydophila pneumoniae<br />
Augustin J Kerkdijk, Gerhard Held, Antje Mueller, Wolfgang L Gross, Michael Pfreundschuh, Jan Voswinkel<br />
Development of a System to Test for Specificity of B-cell Receptors found in Granulomatous<br />
Lesions of Wegeners Granulomatosis patients<br />
Nadja Hilger, Rico Hiemann, Jörg Michel, Ursula Anderer, Martin Weigert, Ulrich Sack<br />
Development of an <strong>complete</strong>ly automatized system for image aquisition and detection of HEp-2<br />
immunofluorescence patterns<br />
Anne Brüstle, Sylvia Heink, Magdalena Huber, Christine Rosenplänter, Christine Stadelmann, Philipp Yu, Enrico Arpaia,<br />
Tak W. Mak, Thomas Kamradt, Michael Lohoff<br />
Development of inflammatory Th17 cells requires interferon regulatory factor 4<br />
Christian Menge, Evelyn A. Nystrom<br />
Dexamethasone depletes γδT cells and alters the activation state and responsiveness of bovine<br />
peripheral blood lymphocyte subpopulations<br />
Christian Menge, William C. Stoffregen, Joachim F.L. Pohlenz, Evelyn A. Nystrom<br />
Dexamethasone differentially down-regulates L-Selectin (CD62L) expression by bovine<br />
lymphocyte subsets in vivo and depletes the intestinal mucosa of intraepithelial γδT cells<br />
Eva Rieser, Monika Braun, Barbara Simm, Barbara Mosetter, Christine S. Falk<br />
Differences between cytotoxicity and cytokine expression are due to different phosphorylation<br />
patterns
Marcel Andre Krüger, Kathrin Kopplin, Nadine Unterwalder, Christian Meisel, Hans-Dieter Volk, Gerald Grütz<br />
Differences in Lipopolysaccharide and Lipid A desensitisation<br />
Jan Diekmann, Olaf Beck, Georg Rauser, Hansjörg Schild, Hermann Einsele, Max S. Topp<br />
Different mechanisms contribute to the immune evasion of Epstein-Barr virus latent membrane<br />
protein 1<br />
Diana Dudziak, Alice O'Kamphorst, Gordon F. Heidkamp, Veit R. Buchholz, Christine Trumpfheller, Chae Gyu Park,<br />
Ralph M. Steinman, Michel C. Nussenzweig<br />
Differential Antigen Processing and Presentation by Dendritic Cell Subsets in vivo<br />
Seray Cetin, Niels Kruse, Andrew Chan, Ralf Gold, Fred Lühder<br />
Differential expression of BDNF mRNA splice variants in mouse brain and immune cells<br />
Ildiko Boross, Christine Lux, Hans-Anton Lehr<br />
Differential expression of IL-17F and IL-17A in the lung of patients affected with<br />
bronchioalveolar cell carcinoma<br />
Markus Kleinewietfeld, Giovanna Borsellino, Adamo Diamantini, Alexander Sternjak, Luca Battistini, Olaf Rötzschke,<br />
Kirsten Falk<br />
Differential expression of VLA-4 by functional Treg and effector CD4+ T cells<br />
Florian Reißfelder, Jutta Schröder-Braunstein, Thomas Giese, Carolin Reiser, Stefan C. Meuer, Bernd Sido<br />
Differential inhibition of human intestinal lamina propria T-lymphocyte activation versus<br />
peripheral blood T cells by the gold-compound auranofin<br />
Svetlana Karakhanova, Karsten Mahnke, Alexander Enk<br />
Differential modulation of B7-H1 expression in pDCs and mDCs upon maturation of dendritic<br />
cells (DCs).<br />
Daniel Engel, Ulrich Dobrindt, Juliane Maurer, Frank Tacke, Christian Kurts<br />
Differential role of CCR2 on Gr1HI and Gr1LO monocyte migration in response to bacterial<br />
infection<br />
Maik Moermann, Mareike Thederan, Christof Wagner, Inaam Nakchbandi, Gertrud Maria Hänsch<br />
Differentiation of the promonocytic cell-line U 937 to osteoclasts by bacterial<br />
lipopolysaccharides: a link between infection and pathological bone resorption.<br />
Kristine Kohl, Sylvia Schnautz, Elisabeth Klein, Thomas Bieber, Susanne Koch<br />
DIFFERENTIATION SIGNALS FOR HUMAN LANGERHANS CELL PRECURSORS IDENTIFIED BY<br />
SEQUENTIAL MIGRATION OF MONOCYTES<br />
Tim Meyer, Susann Beetz, Daniela Wesch, Ina Martens, Dieter Kabelitz<br />
Direct Costimulatory Effect of TLR3 Ligand Poly(I:C) on T cells<br />
Chiara Massa, Christiane Kellert, Esther Kamphausen, Barbara Seliger<br />
Disparate modulation of antigen processing components during maturation of the different<br />
human DC subsets.<br />
Andreas Hombach, Markus Chmielewski, Tobias Riet, Caroline Kopecky, Patrick Schmidt, Nadin Fein, Claudia Ederer,<br />
Anja Hombach, Heike Koehler, Hinrich Abken<br />
Dissecting and modulating a redirected anti-tumor T-cell response for adoptive immunotherapy:<br />
second generation of recombinant immunoreceptors.<br />
Marc A. Blank, Olaf Utermohlen, Holger M. Reichardt, Marco J. Herold<br />
Dissecting the apoptotic pathways induced by Glucocorticoids in T-cells<br />
Annelies Verbrugge, Adelheid Cerwenka<br />
Dissecting the molecular mechanisms involved in the synergy of TREM-1 with TLRs
Sven Burgdorf, Andreas Kautz, Volker Böhnert, Percy Knolle, Christian Kurts<br />
Distinct antigen uptake and intracellular routing mechanisms for activation of CD4+ and CD8+ T<br />
cells<br />
Astrid Menning, Uta Hoepken, Kerstin Siegmund, Martin Lipp, Alf Hamann, Jochen Huehn<br />
Distinctive role of CCR7 in migration and functional activity of naïve- and effector/memory-like<br />
Treg subsets<br />
Julia Polansky, Jennifer Freyer, Stefan Floess, Karsten Kretschmer, Harald von Boehmer, Alf Hamann, Jochen Huehn<br />
DNA methylation controls foxp3 gene expression<br />
Manije Sabet, Maja Frankuski, Anja Reutzel-Selke, Andreas Pascher, Peter Neuhaus, Johann Pratschke, Katja Kotsch<br />
Donor pretreatment with Simvastatin reduces graft immunogenicity following prolonged cold<br />
ischemia in an experimental model of kidney transplantation<br />
Xiaoqian Wang, Luca Simeoni, Jonathan A. Lindquist, Julio Saez-Rodriguez, Ernst D. Gilles, Stefanie Kliche, Burkhart<br />
Schraven<br />
Dynamics of proximal signaling events after TCR/CD8-mediated induction of proliferation or<br />
apoptosis in mature CD8+ T-cells<br />
Börge Arndt, Burkhart Schraven, Luca Simeoni<br />
Dynamics of TCR signaling events leading to human T-cell proliferation<br />
Stephan Meinke, Philipp Eissmann, Carsten Watzl<br />
Early events in NTB-A signaling<br />
Claudia N. Detje, Hauke Schmidt, Thomas Meyer, Marco Prinz, Ulrich Kalinke<br />
Early type I interferon responses exclude nerotropic viruses from central nervous system<br />
Andrey Bogdanov, Tatyana Rybakova, Anna Nizkorodova, Nikolay Belyaev<br />
Effect of alpha-fetoprotein-activated hematopoietic stem cells on monocytes functional activity<br />
Pablo Ariel Casalis, Martin Griebenow, Maria Laura Zenclussen, Ana Claudia Zenclussen, Hans-Dieter Volk, Christian<br />
Woiciechowsky, Ulrich-Wilhelm Thomale<br />
Effect of injury severity on the local and systemic cytokine expression in a rat model of<br />
traumatic brain injury<br />
Michael Schramm, Ulrike Karow, Albert Haas, Martin Krönke, Olaf Utermöhlen<br />
Effects of Acid SphingoMyelinase on <strong>list</strong>eriocidal activiy of macrophages<br />
Markus Janke, Jens Poth, Thomas Giese, Gunther Hartmann<br />
Effects of immunostimulatory RNA on human granulocyte populations<br />
Özen Sercan, Günter J. Hämmerling, Bernd Arnold, Thomas Schüler<br />
EFFECTS OF INTERFERONγ ON CD8 + T CELL HOMEOSTASIS<br />
Besir Okur, Rainer Glauben, Arvind Batra, Thorsten Stroh, Inka Fedke, Jeannette Pietsch, Martin Zeitz, Britta Siegmund<br />
Effects of Leptin on T helper cell polarisation<br />
Stephan Paxian, Markus P. Kummer, Lars Tatenhorst, Klaus Pfeffer, Frank Kirchhoff, Roland Schmid, Michael T. Heneka<br />
Effects of neuronal and microglial disrupted RelA(p65) in the CNS during neuroinflammatory<br />
disorders<br />
Fanny Edele, Cindy Reinhold, Stefan F. Martin<br />
Efficiency of T cell defence against melanoma depends on the DC immunization route<br />
Prajeeth Chittappen Kandiyil, Thomas Ebensen, Carlos Guzmàn, Reinhold Schmidt, Georg Behrens<br />
Efficient cross-priming induced by the toll-like receptor 2/6 agonist MALP-2<br />
Julius Hafalla, Ana Rodriguez, Fidel Zavala
Efficient development of Plasmodium liver stage-specific memory CD8+ T cells during the course<br />
of blood stage malaria infection<br />
Stefanie Hoyer, Katrin Birkholz, Verena Wellner, Ina Müller, Erwin Schultz, Gerold Schuler, Niels Schaft, Jan Dörrie<br />
Electroporation of TCR-encoding RNA into CD4+ T cells in order to provide T-cell help<br />
Stefanie Helm, Patrick Pankert, Stefanie Eikelmeier, Edward Shang, Hans Ulrich Weltzien, Martina Schnoelzer,<br />
Hermann-Josef Thierse<br />
Elements of the innate immune barrier: Proteomic identification of allergen-protein interactions<br />
in the human epidermis<br />
Benjamin Frey, Luis E. Munoz, Friederike Pausch, Ernst Pöschl, Klaus von der Mark, Martin Herrmann, Udo S. Gaipl<br />
Endogenous AnnexinA5 is Involved in the Immune Reaction Against Allogeneic Cells<br />
Christina Hartwig, Miriam Mazzega, Thomas Tschernig, Detlef Neumann<br />
Endogenous IL-18 in experimentally induced asthma affects cytokine serum levels but is<br />
irrelevant for clinical symptoms<br />
Niklas Engels, Jürgen Wienands<br />
Enhanced signaling of the IgG-BCR is accomplished by tyrosine-phosphorylation of the<br />
cytoplasmic mIgG tail<br />
Fanny Edele, Rosalie Molenaar, Cindy Reinhold, Dominique Gütle, Jan C. Dudda, Reina Mebius, Mathias Hornef, Stefan<br />
F. Martin<br />
Environmental instruction of dendritic cells for T cell homing receptor imprinting<br />
Jana Zeitvogel, Thomas Werfel, Miriam Wittmann<br />
Epidermal stem cells differ in their response to IFN&gamma from other proliferative<br />
keratinocytes<br />
Ellen Andresen, Joern Bullwinkel, Christoph Lange, Holger Heine<br />
Epigenetic regulation of defensin gene expression in lung epithelial cells and COPD<br />
Anke Schütz, Hongqi Lue, Jürgen Bernhagen<br />
ERK1/2-MAPK signaling induced by macrophage migration inhibitory factor (MIF) is influenced<br />
by its CXXC motif<br />
Winfried Barchet, Vera Wimmenauer, Leonid Gitlin, Susan Gilfillan, Marina Cella, Marco Colonna, Gunther Hartmann<br />
Essential Role of MDA-5 in Type I IFN Responses to Poly (I:C) and Encephalomyocarditis<br />
Picornavirus<br />
Roman Karwot, Joachim Maxeiner, Steffen Schmitt, Petra Scholtes, Michael Hausding, Ildiko Boross, Hans Lehr,<br />
Susetta Finotto<br />
Essential role of NFATc2 in CD8+ cells in a murine model of allergic sensitization<br />
Andre Tittel, Daniel Engel, Ulrich Dobrindt, Christian Kurts<br />
Establishing a murine model system to investigate the adaptive immune response against<br />
urinary tract infection<br />
Marion Nonn, Shamsul A. Khan, Eva Distler, Ralf G. Meyer, Leonard D. Shultz, Rupert Handgretinger, Christoph Huber,<br />
Wolfgang Herr, Udo F. Hartwig<br />
Establishment of a NOD/SCID/IL2Rγcnull hematopoietic stem cell transplantation model to study<br />
graft-vs-host and graft-vs-leukemia immune responses of ex vivo modified human T lymphocyte<br />
grafts.<br />
Rainer Wurth, Angelika Bold, Thomas Keller, Ulrike Trahorsch, Peter Voigt, Stefan Schubert, Ulrich Sack<br />
Evaluation and validation of a manual low-cost assay for the monitoring of CD4 counts in HIVinfected<br />
individuals in non-OECD countries<br />
Mathias Fousse, Robert Dinser, Urban Sester, Katinka Albrecht, Mahavir Singh, Hans Köhler, Ulf Müller-Ladner,<br />
Martina Sester
Evaluation of latent tuberculosis infection in patients with inflammatory arthropathies before<br />
treatment with tumour necrosis factor-α blocking drugs using a novel flow-cytometric interferonγ<br />
release assay<br />
Katherina Sewald, Maja Henjakovic, Simone Switalla, Norbert Krug, Armin Braun<br />
Ex vivo Immunomodulatory Testing using Precision Cut Lung Slices: Focus on Dendritic Cells<br />
Ingo Irmler, Mieczyslaw Gajda, Rolf Bräuer<br />
Exacerbation of Antigen induced Arthritis in IFN-γ-deficient Mice as a Result of Unrestricted IL-<br />
17 Response<br />
Gasteiger Georg, Kastenmuller Wolfgang, Sutter Gerd, Drexler Ingo<br />
Exclusive cross-priming of cytotoxic T-cells dictates antigen requisites for MVA vector vaccines<br />
daomin gong<br />
Expression of human GITRL on myeloid dendritic cells enhances their immunostimulatory<br />
function but does not abrogate the suppressive effect of CD4+CD25+ regulatory T cells<br />
Katjana Klages, Anja Stirnweiss, Jörg Reimann, Hansjörg Hauser, Andrea Kröger<br />
EXPRESSION OF INTERFEON REGULATORY FACTOR-1 IN CT26 COLON CARCINOMA CELLS<br />
INDUCES ANTI-TUMOR ACTIVITY<br />
Thorsten Stroh, Arvind Batra, Rainer Glauben, Inka Fedke, Stephen Girardin, Martin Zeitz, Britta Siegmund<br />
Expression of NOD2 but not NOD1 is modulated by pro-inflammatory cytokines in murine<br />
preadipocytes<br />
Cemil Korcan Ayata, Cinthia Farina, Markus Krumbholz, Florian Weisel, Thomas Winkler, Andreas Rosenwald, Reinhard<br />
Hohlfeld, Edgar Meinl<br />
Expression of p75 neurotrophin receptor (p75NTR) and brain derived neurotrophic factor<br />
(BDNF) in germinal centers<br />
Matthias M Gaida, Frank Guenther, Martin Loos, Christof Wagner, Gertrud Maria Hänsch, Helmut Friess, Nathalia<br />
Giese, Wente Moritz<br />
Expression of the chemokine receptor CXCR6 on polymorphonuclear neutrophils (PMN) in<br />
pancreatic tumour specimen and in acute, localised bacterial infections<br />
Eric Keil, Nana Ueffing, Linda Clayton, Ellis Reinherz, Klaus Schulze-Osthoff, Ingo Schmitz<br />
Expression profiling identifies Gadd45β as a novel mediator of negative selection<br />
Silke Meister, Kirsten Neubert, Kai Herrmann, Renate Burger, Martin Gramatzki, Sabine Hahn, Sandra Schreiber,<br />
Ulrich Schubert, Hans-Martin Jäck, Reinhard Voll<br />
Extensive immunoglobulin production sensitizes myeloma cells for proteasome inhibition<br />
Carina Klein, Anja Grahnert, Sunna Hauschildt<br />
Extracellular NAD+ triggers transient [Ca2+]i changes in LPS-activated human monocytes via<br />
P2Y receptors<br />
Anja Grahnert, Erik Schilling, Carina Klein, Sunna Hauschildt<br />
Extracellular NAD + triggers transient [Ca2+ ] i changes in human monocytes via P2X-receptors<br />
Kristin Hochweller, Jörg Striegler, Günter J Hämmerling, Natalio Garbi<br />
Feed-back control of dendritic cell homeostasis<br />
Karsten Kretschmer, Alexander Marson, Garrett M. Frampton, Julia Polansky, Richard A. Young, Harald von Boehmer<br />
Foxp3-dependent gene regulation requires T cell activation<br />
Thomas Quast, Barbara Tappertzhofen, Cora Schild, Waldemar Kolanus<br />
Function of CD81 in dendritic cell migration<br />
Sebastian Dütting, Wolfgang Schuh, Kai Hermann, Christiane Lang, Hans-Martin Jäck, Dirk Mielenz<br />
Function of Swiprosin-2/EFhd1 during B cell development
Cornelia Rosner, Lutz Walter<br />
Functional analysis of MHC class I genes in the rhesus monkey (Macaca mulatta)<br />
Simone Abel, Jan Buer, Wiebke Hansen<br />
Functional analysis of Neuropilin1 in regulatory T cells<br />
Gamze Kabalak, Torsten Matthias, Reinhold E. Schmidt, Torsten Witte<br />
FUNCTIONAL CHARACTERISATION OF ILT6 AS GENETIC RISK FACTOR FOR MULTIPLE<br />
SCLEROSOS AND SJÖGREN’S SYNDROME<br />
Kathrin Gube, Inga Gebuhr, Katrin Vogt, Erik Kwidzinski, Christine Brandt, Hans-Dieter Volk, Birgit Sawitzki<br />
FUNCTIONAL CHARACTERISATION OF THE TOLERANCE ASSOCIATED GENE (TOAG-1)<br />
Susanne Stutte, Sabine Brauer, Irmgard Förster<br />
FUNCTIONAL ROLE OF CCL17 IN ALLERGIC IMMUNE REACTIONS OF THE SKIN<br />
Daniel Reim, Kay Westenfelder, Simone Kaiser-Moore, Sylvia Schlautkötter, Bernhard Holzmann, Heike Weighardt<br />
Functional role of T cells during mixed bacterial peritonitis<br />
Jan Kubach, Petra Lutter, Tobias Bopp, Sabine Stoll, Christian Becker, Jürgen Knop, Stefan Müllner, John Wijdenes,<br />
Edgar Schmitt, Helmut Jonuleit<br />
Galectin-10, a previously unnoted protein essential for the functional activity of human CD4<br />
+CD25+ regulatory T cells<br />
Kerstin Sarter, Connie Schulze, Sandra Franz, Benjamin Frey, Luis Munoz, Udo Gaipl, Martin Herrmann<br />
Galectins contribute to the recognition and clearance of apoptotic cells<br />
Nadja Hilger, Frank Emmrich, Ulrich Sack<br />
Gene expression in microdissected invasive fibroblast isolated from arthritic joints from patients<br />
with RA<br />
Alexander Gerbaulet, Julia Scholten, Thomas Krieg, Karin Hartmann, Axel Roers<br />
Generation of a Mouse Model for Mastocytosis<br />
Dafne Müller, Bettina Meißburger, Katharina Frey, Anette Karle, Ines Höfig, Roland Stork, Roland E. Kontermann<br />
Generation of an improved recombinant bispecific antibody molecule and B7 fusion proteins for<br />
targeted cancer immunotherapy<br />
Kathrin Hofer, Holger Kroenig, Heinke Conrad, Barbara Kast, Christian Peschel, Helga Bernhard<br />
Generation of Th1 lymphocyte clones against an immunodominant epitope of NY-ESO-1<br />
Johannes Stephani, Ronald Naumann, Hermann Wagner, Tim Sparwasser<br />
Generation of TLR- „humanized“ Mice with Bacterial Artificial Chromosome-Technology<br />
Sandra Ehser, Jing-Jing Chuang, Lucian Jiga, Christian Kleist, Flavius Sandra-Petrescu, Gerhard Opelz, Peter Terness<br />
Generation of tolerogenic dendritic cells by treatment with Mitomycin C<br />
Ann-Kristin Mueller, Martina Deckert, Kirsten Heiss, Kristin Goetz, Kai Matuschewski, Dirk Schlüter<br />
Genetically Attenuated Plasmodium berghei Liver Stages Persist and Elicit Sterile Protection<br />
Primarily via CD8 T Cells<br />
Marc Beyer, Sabine Classen, Daniela Eggle, Alexey Popov, Svenja Debey-Pascher, Elmar Endl, Percy A. Knolle, Jim<br />
Riley, Joachim L. Schultze<br />
Genomic screening reveals new proteins specifically expressed by human regulatory CD4+<br />
CD25high FOXP3+ CD127low T cells<br />
Charles Andrew Stewart, Thierry Walzer, Scott Hamilton Robbins, Bernard Malissen, Eric Vivier, Immo Prinz<br />
Germline and rearranged Tcrd transcription distinguish bona fide NK cells and NK-like γδ T cells
Benjamin Wilde, Xin Cai, Sebastian Dolff, Andreas Kribben, Jan Dürig, Christof Specker, Thomas Philipp, Oliver Witzke<br />
GITR and CD134 expression on T-lymphoctyes is associated with disease activity in Wegener's<br />
Granulomatosis<br />
Adjobimey Tomabu, Arndts Kathrin, Satoguina Judith, Hörauf Achim<br />
GITR-GITRL interactions regulate the IgG induction by regulatory T cells<br />
Matthias Krusch, Katrin Miriam Baltz, Tina Baessler, Helmut Rainer Salih<br />
Glucocorticoid-Induced TNF Related Protein (GITR) ligand is spontaneously released by tumor<br />
cells and diminishes anti-tumor reactivity of NK cells<br />
Denise Tischner, Nora Müler, Jens van den Brandt, Andreas Weishaupt, Holger Reichardt<br />
Glucocorticoids exert distinct effects on Experimental Autoimmune Encephalomyelitis<br />
Sabine Stegmaier, Christof Wagner, Gertrud Maria Hänsch<br />
Granzyme B expression in mature polymorphonuclear neutrophils (PMN) and in their precursor<br />
cells<br />
Praxedis Martin, Julian Pardo, Reinhard Wallich, Klaus Ebnet, Sandra Iden, Aynur Ekiciler, Arno Muellbacher, Michael<br />
Huber, Markus M. Simon<br />
Granzyme B is expressed in mouse mast cells in vivo and in vitro and causes delayed cell death<br />
independent of perforin<br />
Gerhard Wingender, Jonathan Braun, James Borneman, Mitchell Kronenberg<br />
Gut derived antigens trigger the final steps of Vα14 iNKT cell differentiation<br />
Dagmar Quandt, Hubert Ludwiczak, Barbara Seliger<br />
Heterogeneous B7-H molecule expression and regulation in RCC and melanoma<br />
Christian Stemberger, Katharina Huster, Martina Koffler, Florian Anderl, Matthias Schiemann, Hermann Wagner, Dirk<br />
Busch<br />
Heterogeneous subset generation from a single naïve CD8+ T cell upon in vivo priming<br />
Wibke Bayer, Simone Schimmer, Dennis Hoffmann, Ulf Dittmer, Oliver Wildner<br />
Heterologous Prime-Boost Vaccination with Ad5 and Fiber Chimeric Adenoviral Vectors Enhances<br />
Immune Protection against Friend Virus<br />
Maren Mönkemeyer, Hans Heiken, Rachel Thomas, Reinhold E. Schmidt, Torsten Witte<br />
Higher risk of CMV reactivation in HIV-1 infected patients homozygous for MICA5.1<br />
Konrad Alexander Bode, Klaus Heeg, Alexander H. Dalpke<br />
Histone deacetylase inhibitor butyric acid of bacterial origin as mediator of tolerance in the<br />
intestinal mucosa<br />
Mareike Schmudde, André Braun, Ulrike Klier, Daniela Pende, Jürgen Sonnemann, Lorenzo Moretta, James F. Beck,<br />
Barbara M. Bröker<br />
Histone deacetylase inhibitors sensitize tumour cells for cytotoxic effects of natural killer cells<br />
Vanessa Witte, Andreas Baur<br />
HIV-1 Nef enhances viral gene expression by linking transcriptional derepression and activation<br />
events<br />
Karsten Gülow, Marcin Kaminski, Peter H. Krammer<br />
HIV-Tat induced generation of Reactive Oxygen Species sensitizes T cells towards Activation-<br />
Induced Cell Death<br />
Claudia Sievers, Kasia Nasilowska, Kerstin Wolk, Robert Sabat, Hans-Dieter Volk, Christian Meisel<br />
HO-1 inhibits constitutive and IFNg-induced HLA-DR expression on myeloid antigen-presenting<br />
cells via inhibition of IFNg receptor signalling and down-regulation of CIITA expression<br />
Nadja Brachwitz, Maria Laura Zenclussen, Andre Sollwedel, Ritschel Stefanie, Hans-Dieter Volk, Ana Claudia<br />
Zenclussen
HO-1 up-regulation increases the number of uNK at the fetal-maternal interface<br />
Jan C. Dudda, Nikole Perdue, Mary Beauchamp, Daniel J. Campbell<br />
Homing receptors CD62L and CD103 mark different subsets of development and function of<br />
Regulatory T cells for suppression of autoimmunity<br />
Otilia Postea, Christian Weber, Andreas Ludwig<br />
Homocysteine-induced adhesive and scavenger activity of endothelial cells involves<br />
upregulation of the transmembrane chemokine CXCL16 by a PPAR-gamma dependent<br />
mechanism<br />
Matthias von Herrath, Christophe Filippi<br />
How viral infections prevent type 1 diabetes by augmenting Treg function<br />
Stefan Welte, Kathrin Pietschmann, Lothar Marischen, Susann Beetz, Ina Martens, Daniela Wesch, Dieter Kabelitz<br />
Human γδ T lymphocytes express pattern recognition receptors<br />
Susann Beetz, Tim Meyer, Ina Martens, Thomas Stempfl, Daniela Wesch, Dieter Kabelitz<br />
Human γδ T lymphocytes can initiate an anti-viral immune response to double-stranded RNA<br />
Thi Thu Hoai Nguyen, Silva Holtfreter, Thi Thu Hong Le, Harald Kusch, Michael Hecker, Susanne Engelmann, Alex van<br />
Belkum, Uwe Völker, Heiman Wertheim, Barbara M. Bröker<br />
Human antibody response to experimental colonization with Staphylococcus aureus<br />
Anja Mayer, Holger Bartz, Fabian Fey, Alexander Dalpke<br />
Human bronchial epithelial cells modify function and phenotype of dendritic cells in<br />
inflammatory settings<br />
Caroline Maas, Shenchu Jin, Oliver Germandi, Gerd Otto, Peter Galle, Dennis Strand, Susanne Strand<br />
Human Chorionic Gonadotropin protects against T cell-mediated liver injury in mice by<br />
downregulating Bim and Puma<br />
Clarissa Mindnich, Sonja Bonness, Kristine Kohl, Sylvia Schnautz, Dagmar von Bubnoff, Dagmar Wilsmann-Theis,<br />
Susanne Koch, Thomas Bieber<br />
HUMAN IN VITRO GENERATED DENDRITIC CELLS EXPRESS THE INDUCIBLE NITRIC OXIDE<br />
SYNTHASE (iNOS)<br />
Annette Paschen, Mostafa Jarahian, Antje Sucker, Sandra Striegel, Iris Moll, Dirk Schadendorf, Frank Momburg<br />
Human Natural Killer (NK) Cells Effectively Kill Autologous Melanoma Cells In Vitro but Limited<br />
NK Cell Infiltration into Tumor Metastasis might Interfere with an Effective Anti-Tumor<br />
Immunity In Vivo<br />
Anja A. Kuehl, Jürgen Westermann, Nina N. Pawlowski, Katja Grollich, Martin Zeitz, Jörg C. Hoffmann<br />
Human peripheral γδ T Cells posses regulatory Potential<br />
Anja Saalbach, Jacqueline Lessig, Jan C Simon, Jürgen Arnhold, Ulf Anderegg<br />
Human Thy-1 induces secretion of matrix metalloproteinase-9 and CXCL8 from neutrophils<br />
Sabrina Laing, Mareike Pilz, Michel Seman, Friedrich Koch-Nolte, Friedrich Haag<br />
Human TNF&alpha is a substrate for modification by ADP-ribosyltransferase-1 (ART1)<br />
Petra Richl, Martin Albers, Henner Morbach, Stephanie Brändlein, H. Peter Vollmers, Hermann Girschick<br />
Humoral immunity against malignant gastric carcinoma cells: molecular characterization and<br />
age-related frequency of SC-1 antibody positive B cells<br />
Gordon Grochowy, Michelle Hermiston, Arthur Weiss, Michael Huber<br />
Hyperactivation of mast cells from CD45 E613R („wedge“) mice<br />
Ursula Ellinghaus, Rudolf Rupec, Oliver Pabst, Ralf Ignatius, Reinhold Förster, Bernd Dörken, Franziska Jundt<br />
IκBα is crucial for marginal zone B cell development
R. Riedl, J. Sommer, K. Prinz, A. Egyed, C. Schellack, A. von Gabain, E. Nagy, K. Lingnau<br />
IC31TM: a novel adjuvant that potently activates Type I immune responses<br />
Alexandra Doerr, Carsten Watzl, Michael Kirschfink<br />
iC3b binding to Raji cells modulates Rituximab- induced antibody-dependent cellular cytotoxicity<br />
(ADCC)<br />
Yvonne Burmeister, Timo Lischke, Anja C. Dahler, Hans-Werner Mages, Kong-Peng Lam, Anthony J. Coyle, Richard A.<br />
Kroczek, Andreas Hutloff<br />
ICOS controls the pool size of effector-memory and regulatory T cells<br />
Eva Nina Huter, Sabine Stoll, Julia Horn, Juergen Knop, Bodo Grimbacher, Helmut Jonuleit<br />
ICOS plays an essential role in the development of anergic and suppressive CD4+ T cells<br />
Johann Röhrl, Thomas Hehlgans<br />
Identification and Biological Characterization of Mouse Beta Defensin 14 – an Ortholog of<br />
Human Beta Defensin 3<br />
Laura Rivino, Federica Sallusto, Antonio Lanzavecchia, Jens Geginat<br />
Identification and characterization of human "context-dependent Tr1/memory" cells.<br />
Andrea Baetz, Christoph Koelsche, Alexander Dalpke<br />
Identification of a nuclear localization signal (NLS) in SOCS1<br />
Theresa Tretter, Ram Kumar Venigalla, Volker Eckstein, Hanns Martin Lorenz<br />
Identification of human B cells with immunoregulatory properties<br />
Tereza Havlova, Anja Tessarz, Vaclav Horejsi, Adelheid Cerwenka<br />
Identification of Key-Players in TREM1/DAP12 Signaling Pathway<br />
Katja Kotsch, Vera Merck, Kristina Kunert, Anja Reutzel-Selke, Andreas Pascher, Hans-Dieter Volk, Peter Neuhaus,<br />
Johann Pratschke<br />
Identification of molecular candidate marker in zero kidney biopsies are indicative for graft<br />
quality<br />
Katja Kotsch, Vera Merck, Kristina Kunert, Anja Reutzel-Selke, Andreas Pascher, Hans-Dieter Volk, Peter Neuhaus,<br />
Johann Pratschke<br />
Identification of molecular candidate marker in zero kidney biopsies are indicative for graft<br />
quality<br />
Wolfram Osen, Mingxia Song, Sabine Soltek, Barbara Leuchs, Julia Steitz, Xuan Duc Ngyuen, Dirk Schadendorf,<br />
Annette Paschen<br />
Identification of novel CD4+ T cell epitopes from human tyrosinase related protein 2 (TRP-2) by<br />
a combinatorial approach based on the immunisation of HLA-transgenic mice with recombinant<br />
Adenovirus and antigen peptide library screening<br />
Josip Zovko, Marco Herold, Christa Kraus, Andrea Peters, Ingolf Berberich<br />
Identification of proteins that influence stability and functionality of the anti-apoptotic Bcl-2<br />
family member A1/Bfl-1<br />
Susanne Berchtold, Edda Fahl, Mathias Hornef, Julia Geisel, Julia-Stefanie Frick, Erwin Bohn<br />
IFIT-2 – a putative novel negative regulator of proinflammatory responses<br />
Uwe Müller, Werner Stenzel, Gabriele Köhler, Gesine Hansen, Nicole Schütze, Reinhard Straubinger, Manfred Blessing,<br />
Andrew McKenzie, Frank Brombacher, Gottfried Alber<br />
IL 13 induces disease promoting type 2 cytokines, alternatively activated macrophages and<br />
allergic inflammation during pulmonary infection of mice with Cryptococcus neoformans<br />
Annette Erhardt, Markus Biburger, Gisa Tiegs<br />
IL-10 AND REGULATORY T CELLS – THE MAIN MEDIATORS OF IMMUNOLOGICAL TOLERANCE<br />
AGAINST CONCANAVALIN A
Anne Schumacher, Paul Ojiambo Wafula, Ana Teles, Hideo Yagita, Hans-Dieter Volk, Ana Zenclussen<br />
IL-10 but not TGF-ß is essential for the suppressor function of Treg cells in murine pregnancy<br />
Hyun-Dong Chang, Jun Dong, Andreas Thiel Thiel, Andreas Radbruch<br />
IL-10 Expression in Th lymphocytes is conditional<br />
Manuel N. D. M. Guerreiro, Anne Marie Asemissen, Gianna Schulz, Il-Kang Na, Jochen Hühn, Sandra Bauer, Eckhard<br />
Thiel, Ulrich Keilholz, Carmen Scheibenbogen<br />
IL-2 induces IL-10 producing regulatory CD3+ T cells in vitro and in vivo<br />
Kerstin Wolk, Ellen Witte, Ute Hoffmann, Wolf-Dietrich Döcke, Stefanie Endesfelder, Khusru Asadullah, Wolfram<br />
Sterry, Hans-Dieter Volk, Bianca Maria Wittig, Robert Sabat<br />
IL-22 Induces Lipopolysaccharide-Binding Protein in Hepatocytes: A Potential Systemic Role of<br />
IL-22 in Crohn's Disease<br />
Daniel Hebenstreit, Elisabeth Maier, Jutta Horejs-Hoeck, Min Li-Weber, Albert Duschl<br />
IL-4 suppresses the Gene Expression of TCF-1 in T cells in a STAT6 dependent way<br />
Manuel Otte<br />
IL-4R – signaling through an alternative signal transduction pathway Manuel Otte, Mario Zaiss,<br />
Susanne Bürgis, Anja Thiel, Georg Schett and André Gessner Institute of Medical Microbiology,<br />
Immunology and Hygiene; University of Erlangen-Nuremberg<br />
Julia-Stefanie Frick, Julia Geisel, Frauke Kahl, Hermann Wagner, Carsten Kirschning, Ingo Autenrieth<br />
IL-6 and maturation govern TLR2 and TLR4 induced TLR agonist tolerance and cross-tolerance in<br />
dendritic cells<br />
Marsilius Mues, Marco Mank, Oliver Griesbeck, Hartmut Wekerle, Florian Kurschus<br />
Imaging Activation: FRET-based Calcium Biosensors in T-Lymphocytes<br />
Thomas G. Berger, Hendrik Schulze-Koops, Michaela Schäfer, Ester Müller, Manfred B. Lutz<br />
Immature and maturation-resistant human dendritic cells generated from bone marrow under<br />
GMP conditions induce allogeneic T cell anergy in vitro<br />
Daniel Nickel, Sven Poppert, Tatjana Zelenski, Nicole Kästner, Heiko Bruns, Axel Schubert, Axel Spahr, Steffen Stenger<br />
Immune modulation mediated by Aggregatibacter actinomycetemcomitans as a possible<br />
mechanism for the development of periodontitis<br />
Jessica Butz, Cordula Fuchs, Barbara Kessler, Heiner Voigt, Daniel Wienhold, Mathias Buettner<br />
Immune reaction of swine after repeated intra-muscular (i. m.) immunization with avian<br />
influenza virus H5<br />
Marcin Wlodarski, Zachary Nearman, Alan Lichtin, Hans-Dieter Volk, Jaroslaw Maciejewski<br />
IMMUNODOMINANT CYTOTOXIC T LYMPHOCYTE EXPANSIONS IN PATIENTS WITH<br />
UNEXPLAINED NEUTROPENIA.<br />
Doreen Haase, Anne Marie Asemissen, Carmen Scheibenbogen<br />
Immunogenic epitopes of the PAX2 transcription factor recognized by colon carcinoma patients<br />
Lukas Frenzel, Zeinab Abdullah, Anja Kriegeskorte, Rebecca Borsutzky, Manoj K. Gupta, Olaf Utermöhlen, Dirk H.<br />
Busch, Martin Krönke, Jürgen Hescheler, Tomo Saric<br />
Immunological properties of murine embryonic stem cell-derived cardiomyocytes<br />
Felix Heymann, Emma E. Hamilton-Williams, Isis Ludwig-Portugall, Susan Quaggin, Jürgen Floege, Hermann-Josef<br />
Gröne, Christian Kurts<br />
Immunopathology of T cell-mediated glomerulonephritis<br />
Nadine Nippe, Katja Gutsche, Mechthild Jung, Gerald Grütz<br />
Immunoregulation of IL-10 induced Autotaxin<br />
Wolfgang G Bessler, Karola Puce, Carsten Kirschning, Maria Huber
Immunostimulating effects of the bacterial extract OM-89<br />
Kerstin Annika Sauer, Joachim Heinrich Maxeiner, Petra Scholtes, Roman Karwot, Hans-Anton Lehr, Mark Birkenbach,<br />
Richard Steven Blumberg, Susetta Finotto<br />
Immunosurveillance of lung melanoma metastasis in EBI-3 (-/-) mice by NK-DCs- induced CD8+<br />
T cells<br />
Henoch Hong, Nupur Bhatnagar, Maren Mönkemeyer, Hans Heiken, Reinhold E. Schmidt, Dirk Meyer-Olson<br />
Impact of HIV-1 Vpr on type I and type II interferon secretion by plasmacytoid dendritic cells<br />
and natural killer cells<br />
Nadine Kämper, Claudia Wegscheid, Jörg Keßler, Norbert Koch<br />
Impact of HLA encoded BAT3 splice variants on MHC class I and class II expression<br />
Diana Fleissner, Jan Buer, Astrid Westendorf<br />
Impact of intestinal dendritic cells for the induction of tolerance or pathology<br />
Johannes Lutz, Werner Müller, Chander Raman, Hans-Martin Jäck<br />
Impaired B Cell Development in the Presence of a Non-Coding IgM mRNA<br />
Verena Moos, Kristina Allers, Thomas Schneider<br />
Impaired innate functions of monocytes and macrophages in Whipple`s disease<br />
Kittan Nicolai A., Bergua Antonio, Haupt Sabrina, Donhauser Norbert, Schuster Philipp, Korn Klaus, Harrer Thomas,<br />
Schmidt Barbara<br />
Impaired plasmacytoid dendritic cell (PDC) innate immune responses in patients with<br />
herpesvirus-associated severe acute retinal necrosis (ARN)<br />
Daniela Wesch, Philine Wrobel, Hamed Shojaei, Hans-Heinrich Oberg, Monika Kunz, Dieter Kabelitz<br />
Implications for the design of γδ T cell-based cancer immunotherapy<br />
Inga Gebuhr, Kathrin Gube, Katrin Vogt, Christian Meisel, Sandra Naundorf, Hans-Dieter Volk, Birgit Sawitzki<br />
Importance of cell surface N-glycosylation for activation of T cell subpopulations<br />
Lydia-Mareen Köper, Andrea Schulz, Hans-Jürgen Ahr, Hans-Werner Vohr<br />
In vitro Differentiation of Skin Sensitizers by Cell Signaling Pathways<br />
Sabine Ring, Karsten Mahnke, Alexander Enk<br />
In vivo activation of injected Tregs precedes the suppression of the elicitation phase of Contact<br />
hypersensitivity reactions independent from spleen and lymph nodes<br />
Sonja Schallenberg, Sabine Ring, Tanja Bedke, Sabrina Schmitt, Kurt Schönfeld, Karsten Mahnke, Elisabeth Suri-<br />
Payer, Alexander H. Enk<br />
In vivo depletion of CD4+CD25+Foxp3+ regulatory T cells does not affect the growth of<br />
established B16 tumors<br />
Alla Skapenko, Joachim R. Kalden, Peter E. Lipsky, Hendrik Schulze-Koops<br />
In vivo function of IL-4-induced Tregs<br />
Marcus Gereke, Karsten Mahnke, Elmar Jäckel, Jan Buer, Dunja Bruder<br />
In vivo induction of tolerance via DEC-205 mediated antigen delivery – therapeutic safety in the<br />
context of infection<br />
Andreas Wieland, Markus Denzel, Jörg Reimann, Reinhold Schirmbeck<br />
In vivo produced complexes of antigen with stress proteins are potent immunogens<br />
Undine Meusch, Manuela Rossol, Holm Häntzschel, Christoph Baerwald, Sunna Hauschildt, Ulf Wagner<br />
Increased Infliximab-induced monocyte apoptosis via reverse signalling of membrane TNF in<br />
patients with rheumatoid arthritis
Joachim Heinrich Maxeiner, Kerstin Annika Sauer, Roman Karwot, Petra Scholtes, Rainer Wiewrodt, Hans-Anton Lehr,<br />
Susetta Finotto<br />
Increased lung tumor in NFATc2 (-/-) mice mediated by defective CD8+ T cells and increased<br />
CD4+CD25+ lung T cells<br />
Matthias Kresse, Ingo Uthe, Heike Weighardt, Irmgard Förster<br />
Inducible ablation of CCL17 positive DC in vivo<br />
Katharina A. Remer, Calin Apetrei, Tobias Schwarz, Heidrun Moll<br />
Induction of a local Th1 response after plasmacytoid dendritic cell-based vaccination protects<br />
mice against infection with Leishmania major<br />
Christine Warmbold, Arthur Ulmer, Thomas Roeder<br />
Induction of inflammatory signal transduction pathways in a Drosophila-derived cell line<br />
Julia Strebovsky, Claus Kaiser, Alexander Dalpke, Klaus Heeg, Holger Bartz<br />
Induction of regulatory T-cells by Toll-like receptor-ligand derived deviant dendritic cells<br />
Ria Baumgrass, Vladimir Pavlovic, Britta Lamottke, Maria Lexberg, Joachim Grün, Uwe Niesner, Andreas Radbruch<br />
Induction of Treg cells by manipulation of TCR signalling<br />
Stephan Fricke, Nadja Hilger, Manuela Ackermann, Peter Ruschpler, Lutz Uharek, Guido Hildebrandt, Jan Matthias<br />
Braun, Frank Emmrich<br />
Induction of xenogenic acute graft versus host disease (aGvHD) in mice<br />
Uta Bussmeyer, Arup Sarkar, Kirsten Broszat, Ger van Zandbergen, Christian Bogdan, Werner Solbach, Friederike von<br />
Loewenich, Tamás Laskay<br />
Infection with Anaplasma phagocytophilum inhibits IFN-&gamma signaling in human<br />
neutrophils<br />
Vilma Urbonaviciute, Barbara G. Fürnrohr, Silke Meister, Petra Heyder, Martin Herrmann, Joachim R. Kalden, Reinhard<br />
E. Voll<br />
Inflammation and immune activation by HMGB1-nucleosome complexes – implications for the<br />
etiopathogenesis of systemic lupus erythematosus<br />
Simone Vallbracht, Birthe Jessen, Sonja Mrusek, Anselm Enders, Peter L. Collins, Christine D. Krempl, Stephan Ehl<br />
Influence of a single viral epitope on T cell response and disease after infection of mice with<br />
respiratory syncytial virus<br />
Torsten Lowin, Rainer H. Straub, Olga Wiesner, Ulf Müller-Ladner, Jörg Schedel<br />
Influence of cortisol on the expression of integrins and intracellular signaling molecules in<br />
synovial fibroblasts in rheumatoid arthritis<br />
Veronika Lukacs-Kornek, Verena Semmling, Christian Kurts<br />
Influence of Cross-Presentation via CCR7<br />
Birgit Weinberger, Ilka Weiskirchner, Beatrix Grubeck-Loebenstein<br />
Influence of latent infection with Cytomegalovirus on Epstein-Barr viral parameters in healthy<br />
elderly individuals: possible interaction of different herpesviruses in immunosenescence<br />
Sandra Martina Dittrich, Elfriede Noessner, Hans Demmelmair, Gernot Desoye, Dolores Schendel, Berthold Koletzko,<br />
Susanne Krauss-Etschmann<br />
Influence of n3/n6 polyunsaturated fatty acids on placental immune responses<br />
Stephan Sudowe, Karina Gisch, Nadine Gehrke, Matthias Bros, Christina Priesmeyer, Angelika B. Reske-Kunz<br />
Inhibition of allergic sensitization and suppression of Th2-mediated airway inflammation by<br />
application of formalin-fixed Staphylococcus aureus-particles<br />
Tobias Frankenberg, Susanne Kirschnek, Hans Häcker, Uwe Koedel, Georg Häcker<br />
Inhibition of apoptosis conserves neutrophil effector function and can contribute to<br />
inflammation in vivo
Martin Raftery, Günther Schönrich<br />
Inhibition of CD1 Antigen Presentation by Human Cytomegalovirus<br />
Dorit Fabricius, Sue O’Dorisio, Sue Blackwell, Bernd Jahrsdörfer, Klaus-Michael Debatin<br />
Inhibition of IFN-α Secretion and Modulation of Immunophenotype and Stimulatory Capacity of<br />
Human Plasmacytoid Dendritic Cell by Vasoactive Intestinal Peptide<br />
Rainer Glauben, Arvind Batra, Thorsten Stroh, Elena Sonnenberg, Inka Fedke, Hans Anton Lehr, Paolo Mascagni,<br />
Martin Zeitz, Britta Siegmund<br />
Inhibition of NF-κB by histone deacetylase inhibitors in models of inflammation-related<br />
tumorigenesis<br />
Dirk Reinhold, Alexander Goihl, Bianca Guth, Uwe Lendeckel, Ute Bank, Michael Täger, Siegfried Ansorge, Jürgen<br />
Faust, Klaus Neubert, Stefan Brocke<br />
Inhibitors of dipeptidyl peptidase IV (DP IV, CD26)-like and of aminopeptidase N (APN, CD13)<br />
enzymatic activity suppress human T cell activation and IL-17 production in vitro and in vivo<br />
Simone Klöter, Max v. Holleben, Bernhard Reis, Klaus Pfeffer, Sandra Beer<br />
Interaction analysis of the adaptor protein SLy2<br />
Pia Herzberger, Corinna Siegel, Christine Skerka, Volker Fingerle, Ulrike Schulte-Spechtel, Bettina Wilske, Volker<br />
Brade, Reinhard Wallich, Peter F. Zipfel, Peter Kraiczy<br />
Interaction of immune regulators factor H and FHL-1 with the Lyme disease spirochete Borrelia<br />
spielmanii sp. nov. is mediated by a plasmid-encoded complement regulator-acquiring surface<br />
protein-1<br />
Nikola Baschuk, Olaf Utermöhlen, Roland Gugel, Gabriele Warnecke, Ulrike Karow, Daniela Paulsen, Frank<br />
Brombacher, Martin Krönke, Wolfgang Deppert<br />
Interleukin-4 impairs granzyme-mediated cytotoxicity of Simian virus 40 large tumor antigenspecific<br />
CTL in Balb/c mice<br />
Michael Meyer-Hermann, Marc Thilo Figge<br />
Interpreting two-photon lymphocyte motility data of the germinal centre: Predictions and<br />
analysis by mathematical models<br />
Astrid M. Westendorf, Wiebke Hansen, Jan Buer<br />
Intestinal antigen display promotes the peripheral induction of antigen specific CD8 + Foxp3 + T<br />
cells<br />
Ilka Knippertz, Andrea Hesse, Eckhart Kaempgen, Gerold Schuler, Alexander Steinkasserer, Dirk. M. Nettelbeck<br />
Intracellular expression of CD40L after adenoviral transduction in combination with IFN-gamma<br />
treatment generates human dendritic cells that both secrete IL-12 and have migratory functions<br />
Silke Overbeck, Peter Uciechowski, M. Leigh Ackland, Dianne Ford, Lothar Rink<br />
Intracellular Zinc Homeostasis in Leukocyte Subsets is Regulated by Different Expression of Zinc<br />
Exporters ZnT-1 to ZnT-9<br />
Benedikt Fritzsching, Jürgen Haas, Fatima König, Eva Pauly, Johannes Pöschl, Peter Krammer, Wolfgang Brück,<br />
Elisabeth Suri-Payer, Brigitte Wildemann<br />
Intracerebral Human Regulatory T Cells: Analysis of CD4+CD25+FOXP3+ T Cells in Brain Lesions<br />
and Cerebrospinal Fluid of Multiple Sclerosis Patients<br />
Sebastian Kreiter, Mustafa Diken, Abderraouf Selmi, Abdo Konur, Michael Koslowski, Christoph Huber, Özlem Türeci,<br />
Ugur Sahin<br />
Intranodal RNA immunisation – a potent method for the induction of immunity by selective<br />
transfection of DC<br />
Stephanie Konrad, Linda Engling, Reinhold E. Schmidt, J. Engelbert Gessner<br />
INVERSE REGULATION OF THE MURINE FcγRIIB AND FcγRIII GENE EXPRESSION BY C5a IS<br />
MEDIATED THROUGH DISTINCT DNA-RESPONSE ELEMENTS<br />
Luise Weigand, Xiaoling Liang, Florian Anderl, Judith van der Griendt, Ingrid Schuster, Andreas Moosmann, Bernhard<br />
Helga, Elfriede Nößner, Dirk Busch, Angela Krackhardt
Investigation of allorestricted peptide-specific T cell responses against Her2/neu – implications<br />
for adoptive T cell therapy in solid cancer<br />
Stefanie Margraf, Carsten Watzl<br />
Investigation of membrane microdomains surrounding Natural Killer cell receptors<br />
Vivienne Engelschalt, J. Engelbert Gessner, Richard A. Kroczek<br />
Involvement of complement and Fc-receptors in the depletion of T cells in vivo<br />
Alexander Fassold, Werner Falk, Rainer H. Straub<br />
Is neuropilin-2 a possible target for the treatment of arthritis?<br />
Selina Christen, Edith Hintermann, Monika Bayer, Urs Christen<br />
JAM-C and its influence on the pathogenesis of type 1 diabetes<br />
Nils Schoof, Frederike von Bonin, Lorenz Trümper, Dieter Kube<br />
Janus kinases are targets of tyrphostin AG17 and HSP90-inhibitor 17-AAG in classical Hodgkin<br />
Lymphoma<br />
Eva Schlecker, Isabel Hartmann, Michael Ackmann, Elisabeth Weiss<br />
KIR2DS2 and interaction with DAP12<br />
Gleb Turchinovich, Jan Kranich, Sonja Schmid, Jürgen Bachl, Jörg Kirberg<br />
Kruppel-like factor 3 (KLF3) affects marginal zone B cell differentiation<br />
Dietmar Zehn, Michael J. Bevan<br />
Lack of peripheral control of low avidity self reactive T cells<br />
Gordon Wilke, Gretel Wittenburg, Claudia Berek<br />
Laser Capture Microdissection and Mircroarray: a Characterisation of Follicular Dendritic Cells<br />
Katja Farhat, Sabine Riekenberg, Jennifer Debarry, Roland Lang, Jörg Mages, Günther Jung, Karl-Heinz Wiesmüller,<br />
Artur J. Ulmer<br />
LIGAND BINDING AND SIGNAL TRANSDUCTION INDUCED BY LIPOPEPTIDES<br />
Christian Draing, Christoph Rockel, Susanne Deininger, Stefanie Sigel, Oliver Dehus, Tamara Rupp, Artur Ulmer,<br />
Thomas Hartung, Corinna Hermann, Sonja von Aulock<br />
Lipoteichoic acid from a lipoprotein diacylglycerol transferase deletion mutant is a potent<br />
immunobiologically active compound<br />
Anna Schurich, Silke Hegenbarth, Jan Böttcher, Sven Burgdorf, Andreas Dolf, Elmar Endl, Christian Kurts, Percy A.<br />
Knolle<br />
Liver sinusoidal endothelial cells are more efficient in cross-presentation than CD8alpha splenic<br />
dendritic cells expressing endocytic receptors devoted to cross-presentation<br />
Matthias Hardtke-Wolenski, Nadja Saal, Konstantinos Iordanidis, Mark S Anderson, Michael P Manns, Elmar Jäckel<br />
Liver specific immune responses related to AIRE mutations<br />
Stephan Borte, Uwe Gerd Liebert, Michael Borte, Ulrich Sack<br />
Long-term cell-mediated immunity following vaccination with live, attenuated measles-mumpsrubella-vaccine<br />
in children with juvenile idiopathic arthritis under treatment with low-dose<br />
Methotrexate and/or tumour necrosis factor α receptor antagonist<br />
Christian Pötschke, Mandy Busse, Annegret Dummer, Tobias Traeger, Wolfram Keßler, Erika Friebe, Marlene Mikulcak,<br />
Claus-Dieter Heidecke, Stefan Maier, Barbara Bröker<br />
Long-term effects of polymicrobial sepsis on the adaptive immune system<br />
Zulema Cabail, Holger Hoff, Heike Hirseland, Steven Nadler, Gerd R. Burmester, Monika C. Brunner-Weinzierl<br />
Longevity of CD28null T Lymphocytes is abrogated by CTLA-4Ig treatment
Anja Siepert, Birgit Sawitzki, H.M. Reichardt, Jochen van den Brandt, Markus Tiedge, Manfred Lehmann, Hans-Dieter<br />
Volk, Petra Reinke<br />
Low dose CNI treatment can control effector function of depletion resistant allo-specific memory<br />
T cells (financial support by Else-Kröner-Fresenius-Stiftung P14/06//A01/06)<br />
Markus Kleinewietfeld, Mireille Starke, Thomas Blankenstein, Kirsten Falk, Olaf Rötzschke<br />
Low dose cyclophosphamide tumor rejection is independent of CD4+ CD25+ regulatory T cells<br />
(Treg)<br />
Juliane Ladhoff, Michael Bader, Sabine Brösel, Elke Effenberger, Isabela Schmitt-Knosalla, Hans-Dieter Volk, Martina<br />
Seifert<br />
Low immunogenicity of rat embryonic stem cell derivatives<br />
Anette Brass, Shiyuan Hong, Nicole Schwarz, George Dubyak, Michel Seman, Friedrich Koch-Nolte, Friedrich Haag<br />
LPS and interferons induce surface expression and activity of ADP-ribosyltransferase ART2.1 on<br />
murine bone marrow-derived macrophages<br />
Christian Schiller, John-Christian Eilert, Maximilian Nitschké, Alexander Seidl, Michael Schleicher, Dolores J. Schendel,<br />
Elisabeth H. Weiss<br />
LST1: a potential transmembrane adaptor protein that modulates cell morphology<br />
Niklas Engels, Gökhan Yigit, Christoph Emmerich, Dirk Czesnik, Detlev Schild, Jürgen Wienands<br />
Lytic replication of Epstein-Barr virus can be induced by LMP2A<br />
Heiko Johnen, Tamara Kuffner, Andrew Cook, Emma Braine, Ben Wu, Roland Stocker, Samuel Norbert Breit<br />
Macrophage Inhibitory Cytokine 1(MIC-1) reduces disease severity in mouse models of arthritis<br />
and atherosclerosis<br />
Katharina Kronenberg, Beate G. Exner, Christine Sattler, James A. Hutchinson, Gudrun E. Koehl, Stefan Farkas, Hans<br />
J. Schlitt, Fred Fändrich, Edward K. Geissler<br />
Macrophages Driven to a Novel State of Activation have Anti-Inflammatory Properties in Mice<br />
Günes Esendagli, Kirsten Bruderek, Torsten Goldmann, Andreas Busche, Detlev Branscheid, Ekkehard Vollmer, Sven<br />
Brandau<br />
Malignant and non-malignant lung tissue areas are differentially populated by natural killer cells<br />
and regulatory T cells in non-small cell lung cancer<br />
Christina Janko, Udo S. Gaipl, Sandra Franz, Nina Ebel, Eberhard Schlücker, Roland Meyer-Pittroff, Martin Herrmann,<br />
Benjamin Frey<br />
Mammalian cells under pressure – Cell death pathways and immunogenicity of dying cells<br />
Christoph Lauer, Michael Basler, Susan D. Demo, Marcus Groettrup<br />
Manipulation of MHC class I antigen presentation by a LMP7-specific inhibitor<br />
Lisa Bruns, Oliver Frey, Christiane Landgraf, Rudolf Volkmer, Thomas Kamradt<br />
Mapping of T cell epitopes in Glucose-6-Phosphate-Isomerase induced arthritis<br />
Peter Kramer, Frank Siebenhaar, Marcus Maurer, Sven Hendrix<br />
Mast cell deficient mice display increased brain inflammation, neurodegeneration and<br />
astrogliosis<br />
Yves Montier, Axel Lorentz, Sigrid Krämer, Stephan C Bischoff<br />
Mast cell mediators stimulate fibroblasts to produce IL-6 that vice versa supports mast cell<br />
survival<br />
Julia Scholten, Alexander Gerbaulet, Giuseppe Testa, Thomas Krieg, Karin Hartmann, Axel Roers<br />
Mast cell-specific Cre/loxP-mediated mutagenesis in vivo<br />
ERIETTA STELEKATI, ZANE ORINSKA, ANNALENA BOLLINGER, SILVIA BULFONE-PAUS<br />
Mast cells modulate CD8+ T cell responses.
Milan Popovic, Ana Teles, Catharina Thuere, Anne Schumacher, Paul Ojiambo Wafula, Hans-Dieter Volk, Ana Claudia<br />
Zenclussen<br />
Mast-cell-associated genes Thp1, Mcpt1 and Mcpt5 are up-regulated after Treg-induced<br />
tolerance at the fetal-maternal interface: new role for mast cells in pregnancy-induced<br />
tolerance?<br />
Kristina Wiege, Syed Raza Ali, Stephanie Konrad, Roland Piekorz, Bernd Nürnberg, Reinhold E Schmidt, J Engelbert<br />
Gessner<br />
MECHANISM OF CELL AND ISOTYPE SPECIFIC Gαi DEPENDENT SIGNALING IN IMMUNE<br />
EFFECTOR CELLS<br />
Marco Wendel, Elisabeth Suri-Payer, Adelheid Cerwenka<br />
Mechanisms of NK cell migration in response to tumors<br />
Barbara C. Rütgen, Wilhelm Gerner, Armin Saalmüller, Sabine E. Hammer<br />
MHC typing in swine: The SLA-haplotype repertoire of Austrian Large White, Landrace, and<br />
Pietrain breeding stocks<br />
J. Albrecht, T. J. Boeld, K. Doser, R. Eder, J. Stahl, R. Andreesen, J. Ermann, M. Edinger, P. Hoffmann<br />
MHC-compatibility between conventional and regulatory T cells is required for suppression of<br />
allospecific T cell responses<br />
Romney Haylett, Lothar Rink<br />
MHC-II Signaling Directs the Activation of NFAT but not NF-κB in B Cells<br />
Karina Stein, Jennifer Debarry, Anna Hanuszkiewicz, Otto Holst, Jörg Mages, Roland Lang, Holger Heine<br />
Microarray analysis of human dendritic cells stimulated with four different bacterial strains with<br />
focus on allergy-protecting mechanisms<br />
Kristina Allers, Désirée Kunkel, Verena Moos, Martin Eisenblätter, Christiane Stahl-Hennig, Annette Schrod, Ralf<br />
Ignatius, Franz-Josef Kaup, Thomas Schneider<br />
Migration patterns of activated versus non-activated non-human primate T lymphocytes:<br />
preferential homing of activated autologous CD8+ T cells in the rectal mucosa<br />
Stefan Wiehr, Thomas Herrmann<br />
Milk-derived immune cells may serve as Trojan Horses in Toxoplasma gondii transmission<br />
Marcin Kaminski, Peter H. Krammer, Karsten Gülow<br />
Mitochondria function as oxidative signalling organelles in activation-induced apoptosis of T<br />
cells.<br />
Martina Anzaghe, Zoe Waibler, Holger Ludwig, Shizuo Akira, Siegfried Weiss, Gerd Sutter, Ulrich Kalinke<br />
Modified vaccinia virus Ankara induces Toll-like receptor independent type I interferon<br />
responses<br />
Christian Jacobi, Jürgen Roemisch, Stefan Meuer, Thomas Giese<br />
Modulation of gene expression by IVIG in healthy donors and multiple sclerosis patients<br />
Anastasia Schneider, Tatiana Binder, Rodica Bernatowicz, Anke Zobywalski, Christine Falk, Anton Hartmann, Dolores<br />
Schendel, Susanne Krauss-Etschmann<br />
MODULATION OF HUMAN DENDRITIC CELLS BY SIX DIFFERENT PROBIOTIC BACTERIAL STRAINS<br />
Irene Wittmman, Diana Aichele, Gerhard Groer, André Gessner, Markus Schnare<br />
Modulation of innate immune responses by recombinant murine bactericidal permeability /<br />
increasing protein through neutralizaton of LPS and Gram-negative bacteria<br />
Stephan Schierer, Andrea Hesse, Ina Mueller, Eckhart Kaempgen, David T. Curiel, Gerold Schuler, Alexander<br />
Steinkasserer, Dirk M. Nettelbeck<br />
Modulation of viability and maturation of human monocyte-derived dentritic cells by oncolytic<br />
adenoviruses<br />
Philip Kruse, Cornelia Rosner, Lutz Walter
Molecular characterisation of the killer cell immunoglobulin-like receptors (KIR) of the rhesus<br />
macaque (Macaca mulatta)<br />
Cary Mac Millan, Alexander Hann, Peter Bannas, Wolfgang Koestner, Friedrich Buck, Friedrich Haag, Friedrich Nolte<br />
Molecular characterization of ADP-ribosylated T cell membrane proteins<br />
Viet Bui, Andreas Diefenbach<br />
Molecular cloning and functional characterization of a novel stimulatory immunoreceptor<br />
expressed by myeloid cells<br />
Susan M Schlenner, Lars A Schneider, Thorsten B Feyerabend, Markus Wunderlin, Hans-Reimer Rodewald<br />
Molecular mechanism of mast cell-mediated innate defense against endothelin and snake venom<br />
sarafotoxin<br />
Jennifer Debarry, Anna Hanuszkiewicz, Otto Holst, Holger Heine<br />
Molecular mechanisms of human dendritic cell stimulation by the Allergy-protective Lactococcus<br />
lactis strain G121<br />
Malte Bachmann, Jens Paulukat, Josef Pfeilschifter, Heiko Mühl<br />
MOLECULAR MECHANISMS OF IFNγ-INDUCED IL-18 BINDING PROTEIN PROMOTER ACTIVATION<br />
AS DETECTED IN HUMAN DLD-1 COLON CARCINOMA CELLS<br />
Maria Papatriantafyllou, Thilo Oelert, Günter Hämmerling, Bernd Arnold<br />
MOLECULAR MECHANISMS OF PERIPHERAL CD8 T CELL TOLERANCE<br />
Tobias Schwerd, Johannes C. Hellmuth, Andreas Schmidt, Hendrik Poeck, Michael Wenzel, Stefan Endres, Simon<br />
Rothenfusser<br />
Molecular mechanisms of virus recognition by Rig-I-like helicases<br />
Petra Riedl, Kurt Reifenberg, Joerg Reimann, Reinhold Schirmbeck<br />
Mono-specific, hepatic CD8 T cell responses primed by cationic peptide/oligonucleotide<br />
complexes suppress viral replication in HBV transgenic mice<br />
Sonja Schmucker, Mario Assenmacher, Anne Richter<br />
Monocytes and myeloid dendritic cells are both able to induce primary activation of naïve MART-<br />
1-specific CD8 + T cells in vitro<br />
Beatrice Jahn-Schmid, Gottfried Fischer, Gabriele Gadermaier, Matthias Egger, Fatima Ferreira, Christof Ebner,<br />
Barbara Bohle<br />
Mugwort pollen allergy as a unique model for the investigation of allergen-specific CD4+T cells<br />
using HLA classII/peptide tetramers<br />
Andreas Junker, Jana Ivanidze, Joachim Malotka, Ingrid Eiglmeier, Hans Lassmann, Hartmut Wekerle, Edgar Meinl,<br />
Reinhard Hohlfeld, Klaus Dornmair<br />
Multiple Sclerosis: T cell receptor transcriptome in distinct brain regions<br />
Felix C. Popp, Elke Eggenhofer, Prezemyslaw Slowik, Philipp Renner, Katharina Kronenberg, Hans J. Schlitt, Pompiliu<br />
Piso, Marc H. Dahlke<br />
MULTIPOTENT MESENCHYMAL STROMAL CELLS INDUCE LONG-TERM ALLOGRAFT ACCEPTANCE<br />
MEDIATED THROUGH IDO<br />
Verena Besche, Christina Glowacki, Nadine Wiechmann, Andrea Renzing, Ngoc-Anh Dang, Stephan Sudowe, Jürgen<br />
Knop, Angelika B. Reske-Kunz, Matthias Bros<br />
Murine dendritic cells exert tolerogenic function at their immature state and upon differentiation<br />
in the presence of dexamethasone<br />
Ulrich Salzer, Chiara Bacchelli, Stephanie Jennings, Allesandro Plebani, Helen Chapel, Hans D Ochs, Simon Urschel,<br />
Bernd H Belohradsky, H Bobby Gaspar, Bodo Grimbacher<br />
Mutations in TACI/TNFRSF13b in patients with CVID – a genetic, immunological and clinical<br />
study in a large patient cohort<br />
Max Bastian, Tobias Braun, Heiko Bruns, Martin Röllinghoff, Steffen Stenger
Mycobacterial Lipopeptides Elicit CD4+ Cytolytic T Lymphocytes in Mycobacterium tuberculosis<br />
Infected Humans<br />
Peter Reichardt, Bastian Dornbach, Song Rong, Stefan Beissert, Faikah Güler, Karin Loser, Matthias Gunzer<br />
Naive B cells generate regulatory T cells in the presence of a mature immunological synapse<br />
Nils Kruse, Arnhild Schrage, Katrin Neumann, Katharina Eulenburg, Friderike Blumenthal-Barby, Simon Fillatreau,<br />
Percy A. Knolle, Martin Zeitz, Alf Hamann, Katja Klugewitz<br />
Naive CD4+ T cells primed by Liver Sinusoidal Endothelial Cells (LSEC) do not differentiate into<br />
cytokine producing effector cells and fail to induce a delayed type hypersensitivity reaction<br />
(DTH)<br />
Benedikt Fritzsching, Eva Pauly, Nina Oberle, Navina Kuss, Katrin Hartmann, Peter Ruf, Johannes Pöschl, Peter<br />
Krammer, Elisabeth Suri-Payer<br />
Naive regulatory T cells: activation and apoptosis sensitization of this novel Treg subpopulation<br />
during the human neonatal period<br />
Manoj Kumar, Norman Putzki, Hans Christoph Diener, Hans Grosse-Wilde, Ernst Kreuzfelder<br />
Natalizumab seems to effect mainly B lymphocytes in patients with Multiple Sclerosis<br />
Stephanie Joachim, Martin Wax, Daniela Kraft, Norbert Pfeiffer, Franz Grus<br />
Neurodegeneration of the optic nerve and changes in antibody profiles after immunization with<br />
heat shock protein 27<br />
Barbara Daller, Michaela Jungbeck, Klaus Pfeffer, Daniela N. Männel, Thomas Hehlgans<br />
Neutralization of LIGHT ameliorates DSS-induced intestinal inflammation<br />
Katrin Birkholz, Niels Schaft, Jan Dörrie, Michael Schwenkert, Christian Kellner, Georg Fey, Gerold Schuler<br />
New strategies for antigen loading of human monocyte-derived DC<br />
Timo Herrmann, Nousheen Zaidi, Hubert Kalbacher<br />
New strategies for the analysis of processed antigens in dendritic cells<br />
Hamid Kashkar, Anke Deggerich, Jens-Michael Seeger, Benjamin Yazdanpanah, Katja Wiegmann, Dirk Haubert, Carola<br />
Pongratz, Martin Krönke<br />
NF-kappaB independent down-regulation of XIAP by bortezomib sensitizes Hodgkin Lymphoma<br />
B-cells against cytotoxic drugs<br />
Michael Kiessling, Peter H. Krammer, Karsten Gülow<br />
NF-kB suppression sensitizes cells towards ROS-induced apoptosis<br />
Maren Claus, Sabine Wingert, Carsten Watzl<br />
NK cell activity is regulated by CD48 - 2B4 (CD244) interaction in cis and in trans<br />
Matthias Krusch, Sorin Armeanu, Ulrich Martin Lauer, Alexander Steinle, Michael Bitzer, Helmut Rainer Salih<br />
NK cell lysis of hepatoma cells following specific induction of NKG2D ligands by the proteasome<br />
inhibitor Bortezomib<br />
Marion Schneider, Xuefang Ren, Ying Wang<br />
NK cell targeting of phagocytic dendritic cells<br />
Cédric VONARBOURG, Andreas DIEFENBACH<br />
NK CELLS EXPRESSING CLASS II MHC MOLECULES: SEPARATE LINEAGE OR JUST NK CELLS ?<br />
Petra Prinz, Ainhoa-Marie Figel, Judith Hosse, Peter J Nelson, Julia S Schleypen, Nicole Baur, Dolores J Schendel,<br />
Christine S Falk, Elfriede Noessner<br />
NK cells with distinct phenotypic and functional profile in the context of myeloid infiltration and<br />
renal cell carcinoma milieu<br />
Rachel Thomas, Maren Mönkemeyer, Gamze Kabalak, Reinhold E. Schmidt, Torsten Witte<br />
NKG2D polymorphism associated with reactivation of CMV in HIV-1 infected patients
Benjamin Stoelcker, Kirsten Krätzel, Günther Eissner, Michael Pfeifer, Christian Schulz<br />
NKG2D-triggered effector function of bronchial epithelial cell activated alloreactive CD8+ T cells<br />
Hansjörg Thude, Kathrin Rebstock, Bärbel Lutz, Jörg Blume, Dagmar Barz<br />
No association of the CD45 C77G gene polymorphism with inflammatory bowel disease in<br />
German patients<br />
Sascha Rutz, Marko Janke, Manuela Krueger, Alexander Scheffold<br />
Notch induces interleukin-10 production by T helper 1 cells<br />
Anne Endmann, Dirk Bumann, Susanne zur Lage, Marcin Lyszkiewicz, Siegfried Weiss, Holger Lößner<br />
Novel Salmonella vaccine strains with in vivo amplifiable antigen expression plasmids<br />
Britta Schneider, Jeannette Gerspach, Sabine Münkel, Harald Wajant, Peter Scheurich, Klaus Pfizenmaier<br />
Novel TRAIL fusion proteins as promising candidates for cancer therapy<br />
Verena Susanne Meyer, Dagmar Sigurdardottir, Wolfgang Kastenmüller, Georg Gasteiger, Ingo Drexler, Stefan<br />
Stevanovic<br />
Novel vaccinia virus T-cell epitopes identified by mass spectrometry of HLA ligands<br />
Kurt Schönfeld, Sabine Ring, Tanja Bedke, Sonja Schallenberg, Karsten Mahnke, Alexander H. Enk<br />
Nucleofection is an effective method to transduce regulatory T cells with different homing<br />
receptors.<br />
Sabrina Schmitt, Karsten Mahnke, Kurt Schönfeld, Svetlana Karakhanova, Alexander H. Enk<br />
Number and function of regulatory T cells in GvHD increase by Extracorporeal Photopheresis<br />
Martin Kolev, Marieta Ruseva, Steffen Thiel, Frederik Hansen, Jens Jensenius<br />
On the role of MBL in a murine model of oral infection with Salmonella typhimurium<br />
Monika Braun, Christine Sers, Ruprecht Kuner, Barbara Simm, Barbara Mosetter, Dolores Schendel, Christine Falk<br />
Oncogenic KRAS-signalling and DNMT activity are involved in immune escape of tumor cells<br />
Varsha Kumar, Jens Stein<br />
Optical ProjectionTomography as a tool for studying the three-dimensional structure of<br />
Seconday Lymphoid Organs*<br />
Mathias Fousse, Ulrich Mack, Tobias Hodapp, Urban Sester, Gerhard W. Sybrecht, Hans Köhler, Martina Sester<br />
OPTIMIZED DIAGNOSIS OF LATENT TUBERCULOSIS INFECTION BY ANALYSIS OF ESAT-6 AND<br />
CFP-10 SPECIFIC T-CELL REACTIVITY USING A RAPID FLOW-CYTOMETRIC ASSAY<br />
Gudrun Szalay, Martina Sauter, Carmen Ruoff, Reinhard Kandolf, Karin Klingel<br />
Osteopontin is not involved in antiviral immunity but in cardiac fibrosis during chronic<br />
enterovirus myocarditis<br />
Stefan Ehlers, Sahar Aly, Klaus Wagner, Sven Malm, Tamas Laskay, Jörg Mages, Roland Lang, Ian Orme, Franz Bange<br />
Oxygen Status of Lung Granulomas in M. tuberculosis-Infected Mice and Guinea Pigs and Causal<br />
Involvement of CXCR3-targeted Chemokines in Granuloma Necrosis<br />
Michal Smida, Anita Posevitz-Fejfar, Burkhart Schraven, Jonathan A. Lindquist<br />
PAG downregulation results in increased proximal signaling but reduced functional outcomes in<br />
primary T cells<br />
Gurumoorthy Krishnamoorthy, Florian C. Kurschus, Klaus Dornmair, Reinhard Mentele, Hans Lassmann, Hartmut<br />
Wekerle<br />
Paradoxical autoimmunity: Molecular self mimicry initiates spontaneous autoimmunity in myelinspecific<br />
T cell receptor transgenic mice deficient of cognate self antigen<br />
Hanna Erdmann, Paul Crocker, Bernhard Fleischer, Thomas Jacobs
Pathogenic Trypanosoma cruzi interacts with the immune modulatory molecule mouse Siglec-E<br />
(sialic acid-binding Ig-like lectin-E)<br />
Jan Dirks, Urban Sester, Daniela Presser, Heinrike Wilkens, Hans Köhler, Martina Sester<br />
PD-1 expression on CMV specific CD4 T cells is associated with viremia and reversible functional<br />
anergy in patients after organ transplantation<br />
Hiroaki Azukizawa, Nobuo Kanazawa, Manfred B. Lutz<br />
Peripheral de novo induction of CD4+ CD25+ Foxp3+ regulatory T cells by steady state<br />
migratory dendritic cells<br />
Fabien Agenes, Jean-Pierre Dangy, Jörg Kirberg<br />
Peripheral inter-clonal competitiveness requires T cell receptor contact to restricting MHC<br />
molecules<br />
Kristina Streyl, Mikhail Nosov, Vijay Kumar Ulaganathan, Hartmut Wekerle, Alexander Flügel<br />
Peripheral milieus license autoaggressive effector T cells to invade their target organ<br />
Sebastian Bunk, Iuliana Suznea, Jan Rupp, Matthias Maass, Michael Przybylski, Albrecht Wendel, Corinna Hermann<br />
Persisting Chlamydia pneumoniae infections are associated with differential immune responses<br />
Nirmal Robinson, Tom Li Stephen, Sonja Meemboor, Wiltrud M. Kalka-Moll, Georg Plum<br />
Phagosomal and endosomal trafficking studies by adenoviral Rab-GFP fusion proteins in primary<br />
cells<br />
Thomas Giese, Claudia Sommerer, Martin Zeier, Stefan Meuer<br />
Pharmacodynamic controlled tapering of Cyclosporine A – a new step towards individualized<br />
immunosuppressive therapy in transplanted patients<br />
Carmen Scheibenbogen, Anne Letsch, Antonia Busse, Sandra Bauer, Alexander Schmittel, Wolf-Karsten Hofmann, Lutz<br />
Uharek, Eckhard Thiel, Ulrich Keilholz<br />
Phase II trial of vaccination with WT1 peptide, GM-CSF, and KLH in patients with acute myeloid<br />
leukemia: immunological, molecular, and clinical results<br />
Kai Schledzewski, Klein Diana, Martin Falkowski, Gerhard Moldenhauer, Jo van Ginderachter, Julia Kzhyshkowska, Lou<br />
de Leij, Gernot Geginat, Bernd Arnold, Sergij Goerdt<br />
Phenotype analysis, cytokine induction and gene expression profiling identify LYVE-1+ tumour<br />
associated macrophages to be a specialized subset of M2 macrophages<br />
Tobias Käser, Wilhelm Gerner, Sabine Hammer, Martina Patzl, Armin Saalmüller<br />
Phenotypic and functional characterisation of porcine CD4 + CD25high regulatory T cells<br />
Stefan Maßen, Dirk Jäger, Inka Seil, Barbara Mosetter, Christine Falk<br />
Phenotypic and functional characterization of KIR-expressing cytotoxic T cells<br />
Esther Wilk, Tibor Horvath, Katy Kalippke, Nadine Wilke, Reinhold E. Schmidt, Roland Jacobs<br />
Phenotypical and functional characteristics of CD20 + T cells<br />
Bernhard Reis, Roland Piekorz, Bernd Nürnberg, Klaus Pfeffer, Sandra Beer<br />
PI3Kγ and δ play combined roles in B cell development<br />
Kerstin Schilling, Bin Hu, Karine Missy, Klaus-Dieter Fischer<br />
Pix proteins in B cell Signalling<br />
Katrin Moser, Oliver Winter, Nicole Haupt, Martin Szyska, Bimba F. Hoyer, Andreas Radbruch, Falk Hiepe, Rudolf A.<br />
Manz<br />
Plasma cell longevity in NZB/W mice<br />
Oliver Winter, Katrin Moser, Nicole Haupt, Martin Szyska, Andreas Radbruch, Rudolf A. Manz<br />
PLASMA CELL SURVIVAL AND DEVELOPMENT IN THE BONE MARROW
Julian Pardo, Christin Urban, Arno Müllbacher, Reinhard Wallich, Christoph Borner, Markus M Simon<br />
Pleiotropism of granzyme B-induced cell death; A means of the host to counter pathogens<br />
evasion strategies of CTL-mediated recovery<br />
Mario Fabri, Alessandra Zingarelli, Eva Flenner, Martina Bessler, Helena Hafke, Wiltrud Maria Kalka-Moll<br />
Polysaccharide modulates CD8+ T cell responses by enhancing TCR cross-linking<br />
Hans-Willi Mittrücker, Steinhoff Ulrich, Stefan H. E. Kaufmann<br />
Poor correlation between BCG vaccination-induced T cell responses and protection against<br />
tuberculosis<br />
Michael Probst-Kepper, Andrea Kroeger, Robert Geffers, Christian Erck, Miguel Godinho, Vitor Martins dos Santos,<br />
Hansjörg Hauser, Jan Buer, Rudi Balling, Siegfried Weiss<br />
POSITIVE FEEDBACK-CONTROL BETWEEN GARP AND FOXP3 IN REGULATORY T CELLS<br />
Nasr Hemdan, Frank Emmrich, Joerg Lehmann, Ulrich Sack<br />
Possible induction or exacerbation of autoimmune diseases by heavy metals through changing<br />
cytokine profiles<br />
Anja Dahten, Dennis Ernst, Dana Hoser, Margitta Worm<br />
PPARγ-ligation improves development of allergen-induced skin inflammation in a murine model<br />
of dermatitis<br />
Luisa Klotz, Indra Dani, Linda Diehl, Ari Waisman, Thomas Klockgether, Percy Knolle<br />
PPARgamma ablation in CD4+ T cells augments T cell responses resulting in enhanced T cell<br />
infiltration of the CNS and increased disease severity during experimental autoimmune<br />
encephalomyelitis<br />
Jürgen Haas, Benedikt Fritzsching, Petra Truebswetter, Peter Krammer, Elisabeth Suri-Payer, Brigitte Wildemann<br />
Prevalence of Newly Generated Naïve Regulatory T-Cells is Critical for Treg Suppressive<br />
Function and Determines Treg Dysfunction in Multiple Sclerosis<br />
Reinhard Maier, Rita De Giuli, Veronika Nindl, Simone Miller, Volker Thiel, Roland Züst, Ari Waisman, Birgit<br />
Ledermann, Burkhard Ludewig<br />
Preventing autoimmune myocarditis through cardiac myosin-specific tolerance<br />
Patrick Vollmar, Stefan Nessler, Bianca Wolff, Sudhakar Reddy Kalluri, Hans-Peter Hartung, Bernhard Hemmer<br />
Preventive and therapeutic effects of the antidepressant venlafaxine on murine experimental<br />
autoimmune encephalomyelitis<br />
Ivan Bogeski, Valentin Mirceski, Markus Hoth<br />
Probing the redox activity of T-lymphocytes deposited at electrode surfaces with voltammetric<br />
methods<br />
Lars-Oliver Tykocinski, Anna Sinemus, Esmail Rezavandy, Bruno Kyewski<br />
Promiscuous gene expression in the thymus - is epigenetic regulation the key?<br />
Thorsten Joeris, Petra Krienke, Ulrike Kuckelkorn, S.H.E. Kaufmann, Ulrich Steinhoff<br />
Proteasome assembly: Competitive integration of constitutive and IFNγ inducible catalytic<br />
subunits<br />
Kirsten Neubert, Silke Meister, Damian Maseda, Kerstin Amann, Reinhard Voll<br />
Proteasome inhibition ameliorates lupus symptomes in NZB/W mice<br />
K. Doser, J. Albrecht, T. J. Boeld, R. Eder, J. Stahl, R. Andreesen, P. Hoffmann, M. Edinger<br />
Protection from graft-versus-host disease by donor CD4+CD25+ regulatory T cells improves B<br />
lymphocyte reconstitution after allogeneic bone marrow transplantation<br />
Aleksandar Backovic, Nikolaus Wick, Georg Wick<br />
PROTEIN SIGNATURES ON SILICONE SURFACE AS BIOMARKERS FOR IMMUNOLOGIC-FIBROTIC<br />
SIDE EFFECTS TO IMPLANTS
Bettina Tosetti, Eva Glowalla, Martin Krönke, Oleg Krut<br />
Proteomics Based Identification of Cell Wall-associated Proteins as Protective Vaccine<br />
Candidates against Staphylococcus aureus<br />
Dirk Haubert, Nina Gharib, Francisco Rivero, Katja Wiegmann, Marianna Hösel, Martin Krönke, Hamid Kashkar<br />
PtdIns(4,5)P-restricted plasma membrane localization of FAN is involved in TNF-induced actin<br />
reorganization<br />
Carina Conrads, Ramona Siemer, Mario Assenmacher, Claudia Niemand<br />
Quality assessment of enriched CD4+CD25+ regulatory T cells<br />
Tatiana Binder, Rodica Bernatowicz, Michael Rothballer, Michael Schmid, Susanne Krauss-Etschmann, Dolores J.<br />
Schendel, Anton Hartmann<br />
QUANTITATION OF LIVE VERSUS DEAD PROBIOTIC BACTERIA<br />
Guido Wabnitz, Urban Sester, Henning Kirchgessner, Yvonne Samstag<br />
Ras/PI3Kinase/cofilin independent activation of human CD45RA+ and CD45RO+ T-cells by<br />
superagonistic CD28 stimulation<br />
Rebekka Wehner, Bärbel Löbel, Martin Bornhäuser, Ernst Peter Rieber, Marc Schmitz<br />
Reciprocal activating interaction between native human blood dendritic cells and NK cells in<br />
antitumor immunity<br />
Andra Schromm, Jörg Howe, Artur Ulmer, Karl-Heinz Wiesmüller, Tobias Seyberth, Günther Jung, Manfred Rössle,<br />
Michel H.J. Koch, Klaus Brandenburg<br />
Recognition of bacterial lipopeptides by human macrophages is critically determined by physicochemical<br />
parameters<br />
Ram Kumar Chowdary Venigalla, Theresa Tretter, Stefan Krienke, Regina Max, Norbert Blank, Volker Eckstein,<br />
Anthony D Ho, Hannes Martin Lorenz<br />
Reduced CD4+CD25- T Cell sensitivity to the suppressive function of CD4+CD25highCD127-/low<br />
Regulatory T Cells in active SLE Patients<br />
Annegret Plege, Katja Borns, Reinhard Schwinzer<br />
Reduction of human anti-pig T cell responses by transgenic expression of human PD-L1 on pig<br />
cells<br />
Niko Föger, Andrew Chan<br />
Redundant versus unique roles of the actin regulatory proteins coronin-1 and coronin-2 in the<br />
immune system<br />
Manuela Ahrendt, Reinhard Pabst, Ulrike Bode<br />
Regeneration of transplanted lymph node fragments in the mesentery to study effects of the gut<br />
lymph on lymph node cytokines and chemokines<br />
Michael Andrzejewski, Nicole Schwarz, Christian Weber, Andreas Ludwig<br />
Regulated shedding of transmembrane chemokines by the metalloproteinase ADAM10 facilitates<br />
detachment of adherent leukocytes<br />
Dirk Brenner, Alexander Golks, Mareike Becker, Christian R. Frey, Rostislav Novak, Friedemann Kiefer, Peter H.<br />
Krammer, Rüdiger Arnold<br />
Regulation of Activation-induced Cell Death by T Cell Receptor-Proximal Signalling<br />
Christina Hartwig, Miriam Mazzega, Hanne Constabel, Georg Behrens, J. Engelbert Gessner, Thomas Tschernig<br />
Regulation of allergic inflammation in a murine asthma model: Antigen uptake via Fcγ-receptors<br />
by DC-subsets, impact on tolerance and immunity<br />
Daniela Sánchez, Sigrid Krämer, Yves Montier, Herbert Schmidt, Stephan C Bischoff<br />
Regulation of human intestinal fibroblasts by Endotoxins and Shiga toxins<br />
Norbert Hüser, Annette Fasan, Monika Semmrich, Bernhard Holzmann, Melanie Laschinger
Regulation of LFA-1 activity: Importance for leukocyte recruitment and alloantigenic T cell<br />
activation in cardiac allograft rejection<br />
Jens Derbinski, Sheena Pinto, Stefanie Rösch, Klaus Hexel, Bruno Kyewski<br />
Regulation of promiscuous gene expression within defined chromosomal regions<br />
Katja Thümmler, Andreas Ramming, Alla Skapenko, Hendrik Schulze-Koops<br />
Regulation of specific immunity by homotypic T cell/T cell interaction<br />
Carl Friedrich Classen<br />
Regulation of the granzyme B inhibitor proteinase inhibitor 9 (PI-9) in monocytes:<br />
Immunomodulating effects of cotrimoxazole<br />
Jennifer Freyer, Stefan Floess, Alf Hamann, Jochen Huehn<br />
REGULATION OF THE MURINE TRANSCRIPTION FACTOR FOXP3<br />
Janine Wehrhahn, Robert Kraft, Sunna Hauschildt<br />
Regulation of TRPM2 channels in human monocytes and macrophages<br />
Christian Erbel, Roland Klingenberg, Sultan Celik, Benjamin Funke, Hardy Schumacher, Nadine Wambsganss, Thomas<br />
Dengler<br />
Regulatorische T Zellen und Signalkaskaden über IL-17 und IL-10 als atheroprotektive<br />
Komponenten in atherosklerotischen Läsionen<br />
Sabine Riekenberg, Katja Farhat, Jennifer Debarry, Holger Heine, Karl-Heinz Wiesmueller, Roland Lang, Artur J. Ulmer<br />
Regulators of G-protein signaling are modulated by bacterial lipopeptides and<br />
lipopolysaccharide<br />
Arthur Liesz, Elisabeth Suri-Payer, Claudia Veltkamp, Henrike Dörr, Clemens Sommer, Thomas Giese, Roland Veltkamp<br />
Regulatory T Cells (Treg) are Important Cerebroprotective Immunomodulators in Acute<br />
Experimental Stroke by an Interleukin-10 Dependent Pathway.<br />
Paula Kolar, Holger Hoff, Karin Knieke, Kolja Hegel, Dagmar Quandt, Monika Brunner-Weinzierl<br />
Regulatory T cells require costimulation by CTLA-4 (CD152)<br />
Ioanna Galani, Marco Wendel, Carola Schellack, Elisabeth Suri-Payer, Adelheid Cerwenka<br />
REGULATORY T CELLS SUPPRESS IFN-γ DEPENDENT LEUKOCYTE ACCUMULATION AND<br />
MACROPHAGE ACTIVATION IN LYMPHOMA<br />
Mario Zaiss, Jochen Zwerina, Karin Polzer, Eva Gückel, Alla Skapenko, Hendrick Schulze-Koops, Nikki Horwood,<br />
Andrew Cope, Georg Schett<br />
Regulatory T cells suppress osteoclast formation- a new link between the immune system and<br />
bone<br />
Florian Eberle, Mehtap Sirin, Klaus Heeg, Alexander Dalpke<br />
Relevance of RNA-mediated immunostimulation for RNA-Interference (RNAi)<br />
Christian Hofmann, Thomas Harrer, Kathrin Eismann, Silke Bergmann, Matthias Schmitt-Haendle, Gerold Schuler, Jan<br />
Dörrie, Niels Schaft<br />
REPROGRAMMING T CELLS WITH A HIV-1-SPECIFICTY BY ELECTROPORATION OF TCR-<br />
ENCODING RNA<br />
Esther Wilk, Katy Kalippke, Sabine Buyny, Reinhold E Schmidt, Roland Jacobs<br />
Response of CD56dim and CD56bright NK cells to Interleukin 21<br />
Elke Scandella, Evelyn Lattmann, Sanjiv Luther, Simone Miller, Tobias Junt, Burkhard Ludewig<br />
Role for lymphoid tissue inducer-like cells in the restoration of immunopathological destruction<br />
of the lymphoid stroma cell network<br />
Adan Chari Jirmo, Claus-Henning Nagel, Beate Sodeik, Reinhold E Schmidt, Georg Behrens
Role of direct versus cross-presentation after acquisition of HSV-1 by murine DC for generating<br />
antiviral immunity<br />
Katharina König, Linda Diehl, Carsten Golletz, Thomas Quast, Waldemar Kolanus, Percy Knolle, Reinhard Büttner,<br />
Lukas C Heukamp<br />
ROLE OF FHL2 IN THE REGULATION OF DENDRITIC CELL MIGRATION<br />
Kerstin Juelke, Andreas Thiel, Chiara Romagnani<br />
Role of inflammatory cytokines in modulating NK cell competence and maturation<br />
Romy Laugks, Patricia Schmidbauer, Bernhard Holzmann, Melanie Laschinger<br />
ROLE OF LFA-1 ACTIVITY REGULATION IN CELL CYCLE CONTROL OF PROLIFERATING T<br />
LYMPHOCYTES<br />
Chiara Cordiglieri, Werner Dammermann, Bo Zhang, Barry Potter, Andreas Guse, Alexander Flügel<br />
Role of NAADP-mediated Ca 2+ signalling in encephalitogenic CD4 + T cells<br />
Annette I. Garbe, Taras Kreslavsky, Harald von Boehmer<br />
Role of Notch in survival, proliferation and differentiation of alpha beta T cell precursors<br />
Varsha Pattu, Bin Qu, Eva.C Schwarz, Tanja Mayer, Carolin Bick, Reiko Trautmann, Markus Hoth, Jens Rettig<br />
Role of SNARE proteins in vesicle fusion at the Immunological Synapse of Cytotoxic T<br />
lymphocytes.<br />
Stefano Majocchi, Natalio Garbi, Günter J Hämmerling<br />
Role of Tapasin-ERp57 heterodimers in the generation of MHC class I/peptide complexes<br />
Carolin Konermann, Daniel Degrandi, Cornelia Beuter-Gunia, Sandra Beer, Klaus Pfeffer<br />
Role of the IFN-γ inducible 65kDa GTPases in pathogen defense<br />
Christiane Habich, Volker Burkart<br />
Role of Toll-like receptor 4 (TLR4) in heat shock protein 60 (hsp60)-mediated beta cell-directed<br />
immune reactivity in non-obese diabetic (NOD) mice<br />
Bernadette Pöllinger, Gurumoorthy Krishnamoorthy, Michael Bösl, Hans Lassmann, Andeas Holz, Hartmut Wekerle,<br />
Florian C. Kurschus*<br />
RR Mouse: Spontaneous relapsing remitting EAE in SJL/J mice expressing a MOG responsive T<br />
cell receptor<br />
Elisa Monzón-Casanova, Christian Söllner, Nico Westphal, Ingolf Berberich, Tohru Miyoshi-Akiyama, Takehiko<br />
Uchiyama, Ingrid Müller, Lutz* Walter, Thomas* Herrmann<br />
RT1Db2: Identification and first functional analysis of a new non-polymorphic MHC class II<br />
molecule<br />
Julia Kzhyshkowska, Alexei Gratchev, Liis Krusell, Srinivas Mamidi, Gail Workman, E. Helene Sage, Sergij Goerdt<br />
Scavenger receptor stabilin-1 links endocytosis and intracellular sorting in alternatively<br />
activated macrophages<br />
Tim Sparwasser, Andrea Hartl, Katharina Lahl, Heinz Fehrenbach, Holger Garn, Harald Renz, Hermann Wagner<br />
Selective depletion of Foxp3+ cells in DEREG mice allows functional analysis of regulatory T cells<br />
during experimental allergic airway inflammation<br />
Ulrike Schleicher, Jan Liese, Claudia Kurzmann, Christian Bogdan<br />
Selective requirement of Toll-like receptor 9 for the activation of natural killer cells in cutaneous<br />
and visceral leishmaniasis<br />
Ulrich Salzer, Jennifer Birmelin, Chiara Bacchelli, Torsten Witte, Ulrike Buchegger-Podbielski, Rita Rzepka, H Bobby<br />
Gaspar, Reinhold E Schmidt, Inga Melchers§, Bodo Grimbacher§<br />
Sequence analysis of TNFRSF13b/TACI in patients with Systemic Lupus Erythematosus<br />
Zeinab Abdullah, Tomo Saric, Hamid Kashkar, Nikola Baschuk, Benjamin Yazdanpanah, Bernd K. Fleischmann, Jürgen<br />
Hescheler, Martin Krönke, Olaf Utermöhlen
Serpin-6 expression protects embryonic stem cells from lysis by antigen-specific CTL<br />
Michael Conzelmann, Michael Rieger, Michael Hess, Ulrich Strohhaecker, Axel Benner, Ute Hegenbart, Anthony D. Ho,<br />
Peter Dreger, Thomas Luft<br />
Serum cytokeratin-18 fragments as sensitive marker of epithelial apoptosis in intestinal and<br />
hepatic graft-versus-host disease<br />
Pia Herzberger, Corinna Siegel, Christine Skerka, Volker Fingerle, Ulrike Schulte-Spechtel, Bettina Wilske, Volker<br />
Brade, Reinhard Wallich, Peter F. Zipfel, Peter Kraiczy<br />
Serum resistance of human pathogenic Borrelia spielmanii sp. nov. correlates with binding of<br />
complement regulators factor H and FHL-1<br />
Anette J. Bauer, Katharina M. Huster, Verena Labi, Roland M. Schmid, Dirk H. Busch, Andreas Villunger, Georg Häcker<br />
Several members of the mitochondrial apoptosis pathway control activated T cell death to<br />
terminate the T cell immune response<br />
Jessica Prüßmeyer, Rory Koenen, Line Fraemohs, Christian Weber, Andreas Ludwig<br />
SHEDDING OF THE JUNCTIONAL ADHESION MOLECULE JAM-A BY THE DISINTEGRIN AND<br />
METALLOPROTEINASE ADAM17 REGULATES NEUTROPHIL TRANSMIGRATION<br />
Oliver Frey, Lisa Bruns, Andreas Reichel, Lars Morawietz, Thomas Kamradt<br />
Short-term depletion of regulatory T cells converts self-limiting arthritis into a chronic disease<br />
Wenhan Li, Stefan Schultz, Nicolas Geis, Michael Kirschfink<br />
shRNA-mediated knockdown of CD59 sensitises tumour cells to complement attack and inhibits<br />
proliferation<br />
David Frommhold, Andreas Ludwig, M. Gabi Bixel, Alexander Zarbock, Annette G. Beck-Sickinger, Alma Zernecke,<br />
Christian Weber, Dietmar Vestweber, Klaus Ley, Markus Sperandio<br />
Sialyltransferase ST3Gal-IV interferes with chemokine-dependent leukocyte adhesion during<br />
inflammation<br />
Andrea Kießling, Juliane Ladhoff, Mir Farzin Mashreghi, Sabine Brösel, Elke Effenberger, Hans-Dieter Volk, Martina<br />
Seifert<br />
Silencing of IFNγ-receptor by siRNA inhibits MHC class II upregulation on endothelial cells<br />
Verena Boschert, Anja Krippner-Heidenreich, Ingo Grunwald, Marie Kühnle, Klaus Pfizenmaier, Peter Scheurich<br />
Single chain TNF, a covalently stabilized TNF derivate<br />
Friedrich Koch-Nolte, Jan Reyelt, Janusz Wesolowski, Kristina Burkert, Nicole Schwarz, Felix Scheuplein, Friedrich<br />
Haag, Vanina Alzogaray, Fernando Goldbaum<br />
Single domain antibodies from llama effectively and specifically block an immunoregulatory T<br />
cell surface enzyme in vivo<br />
Andrej Mantei, Sascha Rutz, Ioanna Andreou, Martin Weber, Alexander Scheffold<br />
siRNA-mediated gene knock-down in primary mouse T cells<br />
Uwe Koelsch, Burkhart Schraven, Luca Simeoni<br />
SIT and TRIM determine T-cell fate in the thymus<br />
Anja Hänsel, Michael Meurer, Ernst Peter Rieber, Knut Schäkel<br />
Slan-dendritic cells (6-Sulfo LacNAc-expressing dendritic cells) in contrast to CD1c+ dendritic<br />
cells express high levels of functional TLR7- and TLR8- receptors<br />
Abudula Abulizi, Annika Grabbe, Markus Brechmann, Christian Polaschegg, Nadine Herrmann, Ingo Goldbeck, Kai<br />
Dittmann, Jürgen Wienands<br />
SLP-65 signal transduction requires SH2-mediated membrane anchoring and a kinaseindependent<br />
adaptor function of Syk<br />
Bernhard Reis, Tanja Scheikl, Norbert Huser, Bernhard Holzmann, Klaus Pfeffer, Sandra Beer<br />
SLy-an Orphan Adaptor Protein Displaying a Nonredundant Role in Lymphocyte Development<br />
and Activation
Max von Holleben, Simone Klöter, Bernhard Reis, Klaus Pfeffer, Sandra Beer<br />
SLy2 represents a new member of a recently identified family of adapter proteins<br />
Bin Qu, Varsha Pattu, Eva C. Schwarz, Tanja Mayer, Jens Rettig, Markus Hoth<br />
SNARE proteins are involed in cytotoxic granule secretion at the immunological synapse.<br />
Simon Frank, Leif Sander, Stephan Bischoff, Axel Lorentz<br />
SNARE proteins in mature primary human mast cells<br />
Manfred Hönig, Ansgar Schulz, Catharina Schütz, Paul Fisch, Tatjana Kersten, Ulrich Pannicke, Markus Rojewski,<br />
Wilhelm Friedrich, Klaus Schwarz<br />
Somatic reversion of lymphocyte subpopulations after HSCT in a patient with JAK3 deficiency -<br />
Evidence for independent αβ- and γδ- T-lineage stem cells<br />
Kevin Thurley, Dorothea Busse, Thomas Höfer<br />
Spatiotemporal Cytokine Dynamics in T-Cell Regulation - A Mathematical Model of IL-2•<br />
•Diffusion and Regulatory T-Cells• (•Treg•)<br />
Ariel H. Achtman, Sven Golfier, Martin Lipp<br />
SPHINGOSINE-1-PHOSPHATE RECEPTOR-4 IS MAINLY EXPRESSED BY LYMPHOID CELLS<br />
Shin-Young Na, Heike Eujen, Catherine Toben, Yi Cao, Anneliese Schimpl, Ralf Gold, Thomas Hünig<br />
Spontaneous development of CD8-mediated EAE in a new transgeneic mouse model<br />
Melinda Czéh, Gerald Willimsky, Thomas Kammertöns, Jehad Charo, Thomas Blankenstein<br />
Sporadic immunogenic cancer induces cytotoxic T lymphocyte unresponsiveness against MHCmismatched<br />
targets<br />
Cornelia Beuter-Gunia, Daniel Degrandi, Sandra Beer, Klaus Pfeffer<br />
SSPII, a new IFN gamma upregulated secretory protein<br />
Maria Lexberg, Hyun-Dong Chang, Andreas Radbruch<br />
Stability and plasticity of IL-17 producing T cells<br />
Anita Correll, Andrea Tuettenberg, Christian Becker, Jürgen Knop, Helmut Jonuleit<br />
Stage-dependent quantification of regulatory T cells and antigen-specific T cell responses in<br />
melanoma patients<br />
Christiane Siewert, Sascha Cording, Markus M. Heimesaat, Oliver Liesenfeld, Stefan Bereswill, Christoph<br />
Loddenkemper, Gunnar Loh, Michael Blaut, Alf Hamann, Jochen Huehn<br />
Stay with friends: commensal microflora drives expansion of Foxp3+ Tregs in gut-associated<br />
lymphoid tissue<br />
Svetlana Karakhanova, Markus Schneider, Johannes Schenkel, Markus Munder<br />
Steroids modulate the T effector cell / TREG / dendritic cell balance during treatment of Graftversus-Host<br />
Disease.<br />
Marcin Wlodarski, Lukasz Gondek, Zachary Nearman, Sandra Zwinger, Hans-Dieter Volk, Jaroslaw Maciejewski<br />
Strategies for quantitation and in-vivo tracking of clonal cytotoxic T-cell responses.<br />
Volker Teichgräber*, Surojit Sarkar*, Vandana Kalia, David Masopust, Laurie Harrington, Antonio Polley, Rafi Ahmed,<br />
E. John Wherry<br />
Strength of stimulus and clonal competition impact the rate of memory CD8 T cell differentiation<br />
Sonja Meemboor, Eva Flenner, Alessandra Zingarelli, Martina Bessler, Wiltrud Kalka-Moll<br />
Streptococcus pneumoniae capsular polysaccharide-mediated CD4+ T cell-dependent immune<br />
response requires IL-6<br />
Daniel Schaefer, Anja Janysek, Jürgen Neumann, Norbert Koch<br />
Strong impact of invariant chain on surface expression of HLA-DQ
Nana Ueffing, Eric Keil, Christian Freund, Ronald Kühne, Klaus Schulze-Osthoff, Ingo Schmitz<br />
Structural and mutational analyses of c-FLIP R reveal requirements for DISC-recruitment<br />
Björn Linke, Heiko Weyd, Lucie Dörner, Andrea Mahr, Peter H. Krammer<br />
Structural Requirements for Annexin 1 Mediated Suppression of Dendritic Cells<br />
Nina Oberle, Nadine Eberhardt, Christine S Falk, Peter H Krammer, Elisabeth Suri-Payer<br />
Suppression Mechanisms of cytokine transcription in human CD4+CD25- T cells upon interaction<br />
with CD4+Foxp3+ regulatory T cells<br />
Beatrix Schumak, Gerhard Wingender, Schwandt Timo, Frank Juengerkes, Thomas Tueting, Percy Knolle, Bernhard<br />
Holzmann, Andreas Limmer<br />
SUPPRESSION OF ADAPTIVE IMMUNE RESPONSES BY TOLL-LIKE RECEPTOR LIGANDS<br />
Christiane A. Opitz, Tobias Lanz, Christian Lutz, Wolfgang Wick, Michael Platten<br />
Suppression of antigen-specific T cell immunity by mesenchymal stem cells: implications for<br />
stem cell therapy of autoimmune diseases.<br />
Andrea Mahr<br />
Suppression of Dendritic Cell Activation by Annexin 1 on the Surface of Apoptotic Cells<br />
Jens Haenig, Manfred B. Lutz<br />
Suppression of mature dendritic cell function by regulatory T cells in vivo is abrogated by CD40<br />
licensing<br />
Yu-Hwa Huang, Eva Tolosa, Heinz Wiendl<br />
Suppressive action of HLA-G-expressing T cells, a novel population of natural regulatory cells, is<br />
independent of antigen-presenting cell, facilitated by TCR-engagement, involves HLA-G-ILT-2<br />
ligation and IL-10<br />
Kathrin Held, Elke Dauber, Michael Loos, Franz Petry<br />
Susceptibility of complement deficient mouse strains to systemic infection with Candida albicans<br />
Liangping Li, Gerald Willimsky, Susanne Seitz, Yaxin Xu, Yongping Li, Lope Estevez Schwarz, Peter Schlag, Thomas<br />
Blankenstein<br />
SV40 LT-immortalized human primary normal and cancerous mammary epithelial cells are<br />
phenotypically similar but can be distinguished in selection medium and 3D culture<br />
Carmen Kroczek, Athanasia Avramidou, Stephan Feller, Christiane Lang, Hans-Martin Jäck, Dirk Mielenz<br />
Swiprosin-1 - molecular switch in B cell receptor signaling?<br />
Anke Osterloh, Ulrich Kalinke, Siegfried Weiß, Bernhard Fleischer, Minka Breloer<br />
SYNERGISTIC AND DIFFERENTIAL MODULATION OF IMMUNE RESPONSES BY HSP60 AND LPS<br />
Nousheen Zaidi, Timo Burster, Vinod Sommandas, Timo Herrmann, Bernhard O. Boehm, Wolfgang Voelter, Hubert<br />
Kalbacher<br />
Synthesis of novel cell penetrating aspartic proteases inhibitors as the targeted inhibitors of<br />
antigen processing<br />
Edith Jasny, Martin Eisenblaetter, Tamara Visekruna, Klara Tenner-Racz, Christiane Stahl-Hennig, Andres Salazar,<br />
Ralph M. Steinman, Klaus Ueberla, Mariagrazia Uguccioni, Ralf Ignatius<br />
Synthetic double-stranded RNA, Poly ICLC, enhances the induction of cellular immune responses<br />
against protein antigens in rhesus macaques<br />
Stefanie Frey, Christine D. Krempl, Stephan Ehl<br />
T cell dependent and T cell independent disease after infection with pneumonia virus of mice<br />
Annette I. Garbe, Jerome P. Jayasekera, Michael C. Carroll, Harald von Boehmer<br />
T cell vaccination with DEC-205-influenza hemagglutinin fusion antibodies
Christof Iking-Konert, Tim Vogl, Matthias Schneider, Konrad Andrassy, Gertrud Maria Hansch<br />
T-lymphocytes in patients with primary vasculitides: Expression of CD11b identifies activated T<br />
cells with the propensity to stimulate polymorphonuclear neutrophils<br />
Sven Meuth, Stefan Bittner, Ole Simon, Heinz Wiendl<br />
Tandem pore domain potassium channels TWIK-related acid-sensitive K+ channel 1 (TASK1)<br />
and TASK3 modulate effector functions of T lymphocytes: a novel therapeutic target for T-cell<br />
mediated autoimmune diseases<br />
Kai Dittmann, Anja Uhmann, Ralf Dressel, Heidi Hahn, Jürgen Wienands<br />
Targeted inactivation of the Hh receptor Ptch abrogates lymphocyte development in mice<br />
Andreas Goldwich, Sabine Hahn, Sandra Schreiber, Ralf Wagner, Manfred Lutz, Eckhardt Kämpgen, Ulrich Schubert<br />
Targeting HIV-1 Gag into the DRiP-Pathway results in enhanced CD8 T cell activation<br />
Stephan Schlickeiser, Katharina Tschimmel, Andreas Meisel, Christian Meisel, Inga Gebuhr, Uwe Pleyer, Hans-Dieter<br />
Volk, Birgit Sawitzki<br />
TARGETING N-GLYCOSYLATION AFFECTS APC FUNCTION IN VITRO AND IN VIVO<br />
Sebastian Temme, Anna Maria Eis-Hübinger, Peter Kuckenberg<br />
Targeting of the major histocompatibility complex class II pathway by herpes simplex virus<br />
type-1 glycoprotein B<br />
Theron Johnson, Karsten Mahnke, Dirk Nettelbeck, Volker Storn, Alexander H. Enk<br />
Targeting of Tumor antigens to dendritic cells (DCs) using a novel single chain fragment variable<br />
Tobias Seibel, Florian Schuetz, Christoph Domschke, Mariana Bucur, Christoph Sohn, Philipp Beckhove<br />
TGFβ and IFN-α regulate Type 1 T-Cell Responses in Primary Breast Carcinomas<br />
Guido Wabnitz, Philipp Lohneis, Yvonne Samstag<br />
The actin bundling protein L-plastin is important for LFA-1 accumulation in the pSMAC of the<br />
immunological synapse<br />
Anne Sappok, Anna S. Wenning, Melodie-Jo Wolfs, Tanja Mayer, Bettina Strauß, Markus Hoth, Eva C. Schwarz<br />
The activation and proliferation of primary human CD4+ T-cells following focal stimulation<br />
Stefanie Kliche, Gael Menasche, Dennis Breitling, Mauro Togni, Xiaoqian Wang, Rico Pusch, Ana Kasirer-Friede,<br />
Theresia E. B. Stradal, Gary A. Koretzky, Burkhart Schraven<br />
THE ADAP/SKAP-55 SIGNALING MODULE REGULATES TCR-MEDIATED INTEGRIN ACTIVATION<br />
THROUGH PLASMA MEMBRANE TARGETING OF RIAM/RAP1<br />
Stephanie Joachim, Joachim Storf, Norbert Pfeiffer, Franz Grus<br />
The Analysis of Antibody Patterns in Glaucoma Patients<br />
Bettina Jux, Markus Frericks, Charlotte Esser<br />
The arylhydrocarbon receptor is a critical regulator of Langerhans cell maturation<br />
Sonja Ortler, Christoph Leder, Michel Mittelbronn, Alla Zozulya, Lieping Chen, Antje Kroner, Heinz Wiendl<br />
The B7-homologue 1 (B7-H1/PD-L1) contributes to confinement of immunopathological CNS<br />
damage: implications for Multiple sclerosis<br />
Thomas Ebensen, Kai Schulze, Peggy Riese, Michael Morr, Carlos A. Guzmán<br />
The bacterial second messenger cdiGMP exhibits promising activity as mucosal adjuvant<br />
Martin Klemke, Elisabeth Kramer, Guido Wabnitz, Mathias Konstandin, Yvonne Samstag<br />
The chemokine SDF-1α induces dephosphorylation of the actin remodelling protein cofilin via a<br />
Gi/Ras/MEK pathway in primary human T cells<br />
Birgit C Viertlboeck, Sonja Schweinsberg, Matthias A Hanczaruk, Ramona Schmitt, Louis du Pasquier, Friedrich W<br />
Herberg, Thomas W Göbel
The chicken leukocyte receptor complex encodes a primordial, activating, high affinity IgY Fc<br />
receptor.<br />
Matthias A. Hanczaruk, Thomas W. Göbel, Birgit C. Viertlboeck<br />
THE CHICKEN TRIGGERING RECEPTOR EXPRESSED ON MYELOID CELLS (TREM)<br />
Barbara Simm, Matthias Witt, Monika Braun, Barbara Mosetter, Rudolf Gruber, Dolores Schendel, Christine Falk<br />
The correlation of CD6 expression with infiltration of NK cells into synovial fluid of Arthritis<br />
patients.<br />
Edgar Serfling, Rene Rost, Wen Chen, Sergei Chuvpilo, Eisaku Kondo<br />
The Crosstalk between NF-kB and NFATc1/aA, the Inducible Short Isoform of NFATc1, Protects<br />
B-Lymphocytes against Apoptosis<br />
Martin Holdener, Edith Hintermann, Eric F. Johnson, Michael P. Manns, Matthias G. von Herrath, Urs Christen<br />
The CYP450 mouse model for autoimmune hepatitis: Breaking of self-tolerance in transgenic<br />
CYP2D6 and wildtype FVB-mice by viral infection<br />
Tarvo Rajasalu, Wolfram Karges, Andreas Spyrantis, Andreas Wieland, Bernhard Böhm, Reinhold Schirmbeck<br />
The diabetogenic, insulin-specific CD8 T cell response primed in the experimental autoimmune<br />
diabetes model in RIP-B7.1 mice<br />
Stephan Thurau, Maria Diedrichs-Möhring, Christiane Hoffmann, Gerhild Wildner<br />
The distribution of uveitogenic GFP+ T cells in a rat model of uveitis<br />
Tobias Haas, Jochen Metzger, Frank Schmitz, Antje Heit, Eicke Latz, Hermann Wagner<br />
The DNA sugar backbone 2-deoxyribose determines Toll-like receptor 9 activation<br />
Dieter Kube, Diana Pinkert, Nils Schoof, Frederike von Bonin, Jennifer Theiss, Fred Schaper, Johannes Bode, Martina<br />
Vockerodt<br />
The EBV oncoprotein Latent Membrane Protein 1 affects the expression of suppressors of<br />
cytokine signaling (SOCS) in transformed B lymphocytes<br />
Dong Wang, Melanie Drenker, Thomas Werfel, Miriam Wittmann<br />
The epidermal inflammatory response in lupus erythematosus shows an autocrine amplification<br />
loop. Major role of TNF&alpha and IL-18.<br />
Andreas Vilcinskas, Boran Altincicek<br />
The greater wax moth Galleria mellonella as a mini-host model for human pathogens and as a<br />
reservoir for novel peptide antibiotics<br />
Leslie Elsner, Vijayakumar Muppala, Mathias Gehrmann, Jingky Lozano, Heike Bickeböller, Thomas Herrmann, Lutz<br />
Walter, Frauke Alves, Gabriele Multhoff, Ralf Dressel<br />
The heat shock protein HSP70 promotes NK cell activity against tumors which express inducible<br />
NKG2D ligands<br />
Aysefa Doganci, Petra Scholtes, Joachim Maxeiner, Roman Karwot, Edgar Schmitt, Hans A. Lehr, I.Cheng Ho, Susetta<br />
Finotto<br />
The IL-2R alpha and IL-2R beta chains differentially regulated allergic airway inflammation in an<br />
experimental in vivo model<br />
Christine S. Falk, Dominik ter Meer, Iris Bigalke, Alexander Buchner, Barbara Mosetter, Barbara Simm, Monika Braun,<br />
Dusan Prevalsek, Dolores Schendel, Hans-Jochem Kolb<br />
The Impact of HLA-C and KIR Genetics on Survival of AML versus ALL Patients following<br />
Haploidentical Bone Marrow / Stem Cell Transplantation.<br />
Kristina Kunert, Constanze Schönemann, Hans-Dieter Volk, Ruth Neuhaus, Andreas Pascher, Claudia Wenzel, Peter<br />
Neuhaus, Johann Pratschke, Katja Kotsch<br />
The impact of KIR/HLA ligand incompatibility on acute rejection episodes after orthotopic liver<br />
transplantation<br />
Mauro Togni, Dirk Reinhold, Burkhart Schraven, Aneegret Reinhold
The importance of adhesion and migration of dendritic cells during the induction of immune<br />
reaction: A role for the adaptor protein SKAP-HOM<br />
Rachid Marhaba, Mario Vitacolonna, Dagmar Hildebrand, Michal Baniyash, Pia Freyschmidt-Paul, Margot Zöller<br />
The importance of myeloid suppressor cells in the regulation of autoimmune effector cells by a<br />
chronic allergic eczema<br />
Michal Smida, Sabine Lindquist, Anita Posevitz-Fejfar, Diana Karitkina, Ramnik Xavier, Brian Seed, Burkhart Schraven,<br />
Jonathan A. Lindquist<br />
The importance of PAG in regulating proximal signaling<br />
Lilli Podola, Hans Jürgen Ahr, Hans-Werner Vohr<br />
THE INDUCTION PHASE OF ALLERGIC ASTHMA INVESTIGATED BY A SHORT-TERM MODEL IN<br />
BROWN NORWAY RATS<br />
Lucie Dörner, Heiko Weyd, Andrea Mahr, Björn Linke, Dagmar Riess, Christine S. Falk, Peter H. Krammer<br />
The influence of apoptotic cells and annexin 1 on peripheral tolerance<br />
Shafaqat Ali, Michael Huber, Christian Kollewe, Werner Falk, Michael U. Martin<br />
The Interleukin-1 Receptor Accessory Protein is essential for Interleukin-33 induced activation<br />
of T cells and mast cells<br />
Manuela Hessmann, Dominik Rueckerl, Toshiyuki Takai, Stefan Ehlers, Christoph Hoelscher<br />
The ITAM-bearing adapter protein DAP12 modulates inflammatory immune responses after<br />
Mycobacterium tuberculosis infection<br />
Veronika Lukacs-Kornek, Sven Burgdorf, Sabine Specht, Miroslaw Kornek, Christian Kurts<br />
The kidney – renal LN system contributes to cross-tolerance against innocuous soluble antigen<br />
Gennadiy Zelinskyy, Sandra Balkow, Simone Schimmer, Tanja Werner, Markus M. Simon, Ulf Dittmer<br />
The level of Friend retrovirus replication determines the cytolytic pathway of CD8+ T cellmediated<br />
pathogen control<br />
Iryna Prots, Alla Skapenko, Jörg Wendler, Stefan Mattyasovszky, Clarisse Yone´, Bernd Spriewald, Harald Burkhard,<br />
Joachim R Kalden, Peter E Lipsky, Hendrik Schulze-Koops<br />
The loss-of-function IL4R single nucleotide polymorphism I50V is associated with early erosive<br />
rheumatoid arthritis<br />
Petra Hoffmann, Tina J. Boeld, Ruediger Eder, Jochen Huehn, Stefan Floess, Udo Baron, Sven Olek, Reinhard<br />
Andreesen, Matthias Edinger<br />
The Naive CD45RA+, But Not The CD127- Subpopulation of Human CD4+CD25high T Cells<br />
Homogeneously Maintains Regulatory T Cell Characteristics Upon In Vitro Expansion<br />
Sandra Düber, Martin Hafner, Elias Hobeika, Michael Reth, Ari Waisman, Karsten Kretschmer, Siegfried Weiss<br />
The origin of B-1a cells: Analysis in mice with inducible B cell development<br />
Ulrich Steinhoff, Alexander Visekruna, Anjo Kroesen<br />
The proteasome controls NF-κB-mediated inflammation in IBD patients<br />
Sandra Kraemer, Regina Krohn, Hongqi Lue, Manfred Dewor, Christian Weber, Jürgen Bernhagen<br />
The pseudo-ELR motif of MIF is required for its functions as CXC arrest chemokine<br />
Nicole Dietrich, Nelson Gekara, Siegfried Weiss<br />
The regulatory mechanisms inviolved in iNOS, TNF-&alpha, and IL-6 induction during host<br />
defence<br />
Uwe Kolsch, Christina Weber, Caroline Ritter, Anna Viehbahn, Thomas Brune<br />
THE REPRODUCTIVITY OF MICE IS INDEPENDENT OF A MHC-I HAPLOTYPE MISMATCH BETWEEN<br />
THE MOTHER AND THE FETUS<br />
Andrey Bogdanov, Tatyana Rybakova, Nikolay Belyaev
The role of alpha-fetoprotein in induction of immunological tolerance to tumor growth: direct<br />
and indirect breaking of tumor immunosurveillance<br />
Filiz Demircik, Ari Waisman<br />
The role of B cells and other antigen presenting cells in infections<br />
Sonja Reißig, Ari Waisman<br />
The Role of CYLD in T cell Development and Regulation<br />
Fabia T.L. Rocha, Rüdiger Arnold, Renate Rutz, Michael Kirschfink<br />
The role of FLIPLong in C5a-modulated spontaneous apoptosis of neutrophils<br />
Denise Bogdanski, Thomas M. Frangen, Christian Schinkel, Gert Muhr, Manfred Köller<br />
The role of IL-17 in the post traumatic phase of polytrauma patients.<br />
Inna Lavrik, Alexander Golks, Dirk Brenner, Julia Hoffmann, Carina Pforr, Peter Krammer<br />
The role of new c-FLIP proteins in life and death of the T cell.<br />
Eva Gueckel, Silke Meister, Mario Zaiss, Sankar Ghosh, Reinhard E. Voll<br />
The role of NF-κB for the development and function of naturally occurring regulatory T cells<br />
Zoran V. Popovic, Roger Sandhoff, Tjeerd P. Sijmonsma, Eva Kiss, Sylvia Kaden, Edgar Tone, Hermann-Josef Gröne<br />
The role of sulfatide SM4s in apoptotic cell uptake and macrophage phenotype alteration<br />
Marko Janke, Michael Peine, Thordis Hohnstein, Lars Morawietz, Alexander Scheffold<br />
THE ROLE OF TH1 AND TH17 T CELLS IN INFLAMMATORY REACTIONS IN VIVO<br />
Jan Liese, Ulrike Schleicher, Christian Bogdan<br />
The role of TLR9 signalling in murine cutaneous leishmaniasis<br />
Paul Gutwein, Anja Schramme, Liliana Schäfer, Hermann-Josef Gröne, Mohamed Sadek, Ingeborg Hauser, Josef<br />
Pfeilschifter<br />
The role of transmembrane and released CXCL16 during inflammatory processes in the kidney<br />
Kai Schulze, Thomas Ebensen, Karina Watzke, Michael Morr, Carlos Guzman<br />
The second messenger 5′GMP is a promising adjuvant for vaccine development<br />
Matthias Eberl, David Vermijlen, Francesco Dieli, Nadia Caccamo, Serena Meraviglia, Giuseppe Cicero, Andrew<br />
Roberts, Bernhard Moser, Hassan Jomaa, Adrian Hayday<br />
The unexpected functional plasticity of human γδ T cells: implications for immunotherapy and<br />
beyond<br />
Rebekka Geiger, Antonio Lanzavecchia, Federica Sallusto<br />
THE “T CELL AMPLIFICATION METHOD” AS A NEW TOOL TO ANALYZE THE REPERTOIRE OF<br />
HUMAN T CELLS<br />
Stefanie Thiele, Andreas Pahl<br />
Therapy of chronic airway diseases with nucleic acids<br />
Arvind Batra, Markus M. Heimesaat, Stefan Bereswill, Jeannette Pietsch, Thorsten Stroh, Rainer Glauben, Inka Fedke,<br />
Martin Zeitz, Britta Siegmund<br />
TLR – expression in cells from adipose tissue – a contribution to chronic inflammation?<br />
Linda Diehl, Anna Schurich, Regina Grochtmann, Silke Hegenbarth, Lieping Chen, Percy Knolle<br />
Tolerogenic maturation of LSEC after cognate T cell interaction promotes B7-H1-dependent CD8<br />
+ T cell tolerance<br />
Elke Gülden, Seiji Imamura, Masaru Ihira, Christiane Habich, Hubert Kolb, Volker Burkart<br />
Toll-like receptor 4: A key regulator of beta-cell directed autoimmunity in a mouse model of type<br />
1 diabetes.
Marina Scheler, Manuela Brenk, Helene Wilms, Thomas Bieber, Dagmar von Bubnoff<br />
Toll-like receptor ligands, and not T cell signals, are strong inducers for Indoleamine-2,3dioxygenase<br />
(IDO),and lead to T cell suppression<br />
Hans-Heinrich Oberg, Jan Lenke, Susann Beetz, Norbert Reiling, Dieter Kabelitz, Daniela Wesch<br />
Toll-like receptor-2 ligands act on Treg to abolish suppression of CD4 + CD25- responder T cell<br />
proliferation and IL-2 production<br />
Elena Babich, Ata-Ur Rasheed, Hans-Peter Rahn, Martin Lipp, Gerd Müller<br />
Tracking follicular B helper T cell differentiation and function by gene expression analysis<br />
Ana Teles, Catharina Thuere, Milan Popovic, Anne Schumacher, Paul Wafula, Hans-Dieter Volk, Ana Zenclussen<br />
Trafficking of regulatory T cells during pregnancy: Expression profile of Treg-related chemokine<br />
and chemokine receptor at the maternal-fetal interface.<br />
Katharina Gropp, Michael Reuter, Gerhard D. Wieland, Christine Skerka, Peter F. Zipfel<br />
Transcription factors EGR-2 and NFkappaB induce chemokine synthesis in macrophages<br />
challenged with the human pathogenic yeast Candida albicans<br />
Yuriy Shebzukhov, Sergei Grivennikov, Andrey Kruglov, Chang-Yi Cui, Ina Wagner, Anna Litvin, Hans-Joachim<br />
Mollenkopf, David Schlessinger, Dmitry Kuprash, Sergei Nedospasov<br />
Transcriptional analysis of lymphoid organs from mice with conditional inactivation of TNF and<br />
LT<br />
Monika Lindemann, Alexandra Schumann, Melanie Fiedler, Camino Valentin-Gamazo, Dietmar Knop, Christoph E.<br />
Broelsch, Michael Roggendorf, Hans Grosse-Wilde<br />
Transfer of adoptive immunity to hepatitis B virus by liver transplantation*<br />
Annette Busch, Thomas Quast, Waldemar Kolanus, Percy Knolle, Andreas Limmer<br />
Transfer of T cell surface molecules to Dendritic cells upon T cell priming involving two distinct<br />
mechanisms differing in quality and time<br />
Jacqueline Moebius, Michael Basler, Marcus Groettrup<br />
TRANSGENIC MICE REVEAL A NOVEL ROLE FOR LMP7 IN TCR TRIGGERED EXPANSION OF T<br />
CELLS<br />
Volker Storn, Karsten Mahnke, Sonja Schallenberg, Theron S. Johnson, Tanja Bedke, Natalio Garbi, Bernd Arnold,<br />
Günter J. Hämmerling, Alexander H. Enk<br />
Treatment of established RMA-Tag tumors via DC directed targeting of tumor antigens is further<br />
improved by depletion of regulatory T cells.<br />
German Salamov, Rupert Holms, Wolfgang G. Bessler, Ravshan Ataullakhanov<br />
Treatment of Hepatitis C Virus Infection with Human Ezrin Peptide One (HEP1) in HIV Infected<br />
Patients<br />
Claudia Stühler, Sarah Lurati, Manik Chatterjee, Ralf C. Bargou, Hermann Einsele, Max S. Topp<br />
Treatment of T lymphocytes with Hsp90 inhibitors selectively kills activated cells while<br />
preserving viability and functionality of resting cells<br />
Kai Zanzinger, Carola Schellack, Gernot Geginat, Adelheid Cerwenka<br />
TREM-1 in infection and cancer<br />
Anna-Maria Herr, Olivia Sövegjarto, Lutz Walter<br />
TRIM proteins: Novel candidates for HIV resistance?<br />
Christiane Desel, Stefan H.E. Kaufmann<br />
Tuberculosis: Efficacy of DNA vaccines encoding dormancy-associated antigens<br />
Jenny Pahne, Subramanya Hegde, Nadine Schröer, Sigrun Smola-Hess
Tumor cell-derived interleukin-6 skews myeloid dendritic cells from an immunostimulatory to a<br />
pro-tumorigenic phenotype<br />
Gerald Willimsky, Melinda Czéh, Christoph Loddenkemper, Johanna Gellermann, Harald Stein, Peter Wust, Thomas<br />
Blankenstein<br />
Tumor immunogenicity, not tumor burden is the primary cause of general cytotoxic T<br />
lymphocyte unresponsiveness<br />
Christoph D. Brenner, Susan King, Imke Wolters, Georg Bornkamm, Martin Röcken, Ralph Mocikat<br />
Tumour control by natural killer cells in a spontaneous mouse lymphoma model<br />
Nicolas Sabarth, Louise Chamberlain, John Tite, Sara Brett, Craigen Jenny<br />
Two-sided effect of T cell help in tolerance breaking and immunodominance<br />
Christian Wahl, Petra Bochtler, Reinhold Schirmbeck, Jörg Reimann<br />
Type I IFN-producing CD4 Valpha14i NKT cells facilitate priming of IL-10-producing CD8 T cells<br />
by hepatocytes<br />
Markus Krumbholz, Hans Faber, Florian Steinmeyer, Lisa-Ann Hoffmann, Hannah Pellkofer, Tania Kümpfel, Tobias<br />
Derfuß, Camelia Ionescu, Michaela Starck, Thomas Giese, Gunther Hartmann, Christian Hafner, Reinhard Hohlfeld,<br />
Edgar Meinl<br />
Type I interferon therapy increases systemic BAFF expression<br />
Susanne Rauchmann, Karin Knieke, Marion Rudolph, Holger Hoff, Monika Brunner-Weinzierl<br />
Ubiquitin-ligases in co-stimulation of T-lymphocytes<br />
Christine Wolff, Peter Härle, Johannes Wildmann, Hugo O. Besedovsky, Rainer H. Straub, Adriana del Rey<br />
Uncoupling of the HPA axis and the sympathetic nervous system in rheumatoid arthritis is linked<br />
to marked changes of norepinephrine levels in the hypothalamus<br />
Sonja Textor, Rosita Accardi, Matthias Dürst, Massimo Tommasino, Lutz Gissmann, Adelheid Cerwenka<br />
Up-regulated expression of activating NK cell receptor ligands in human cervical cancer<br />
Felix Lasitschka, Jutta Schröder-Braunstein, Thomas Giese, Carolin Reiser, Bernd Sido, Stefan C. Meuer<br />
Uptake of Cystine in T-Lymphocytes following CD2 and CD3 stimulation<br />
Meike Winter, Roel Schins, Irmgard Förster<br />
Uptake of nanoparticles in the food by gut-associated dendritic cells<br />
Sascha Barabas, Tanja Bauer, Regina Gary, Petra Lindner, Juha Lindner, Wolfgang Jilg, Hans Wolf, Ludwig Deml<br />
Urea-mediated cross-presentation of soluble Epstein-Barr Virus BZLF1<br />
Emmanuel Prodhomme, Claude Muller<br />
Vaccination against Tobacco Specific N-nitrosamines: Synthesis of a new NNK hapten for the<br />
induction of specific antibodies.<br />
Carsten Alt, Travis Harrison, Akihiro Matsukawa, Charles Litterst, Jon Mirsalis, Annalisa D'Andrea<br />
Vaginal cytokine production as a biomarker for the safety evaluation of microbicide-induced<br />
vaginal irritation<br />
Beatrice Bolinger, Philippe Krebs, Engeler Daniel, Ying Hua Tian, Elke Scandella, Simone Miller, Nicola P. Restifo,<br />
Pierre-Alain Clavien, Burkhard Ludewig<br />
Vascular endothelial cells presenting minor histocompatibility antigen do neither activate nor<br />
tolerize CD8+ T cells<br />
Michaela Kern, Kai Scholz, Ulrich Kalinke, Joachim Schultze, Ulrich Koszinowski, Gunther Hartmann, Percy A. Knolle<br />
Viral infection but not pattern recognition induces functional maturation of tolerogenic liver<br />
endothelial cells leading to induction of effector CD8 T cells<br />
Dennis Lindau, Dagmar Sigurdardottir, Evelyna Derhovanessian, Thomas Leyhe, Graham Pawelec, Stefan Stevanovic,<br />
Lars Stoltze<br />
Visualizing Abeta-specific cytotoxic T cells with HLA tetramers
Patricia Bach, Elisabeth Kamphuis, Bernhard Odermatt, Gerd Sutter, Christian J. Buchholz, Ulrich Kalinke<br />
VSV-G Displaying Retrovirus-Like Particles Induce a Type I IFN Receptor Dependent Switch to<br />
Neutralizing IgG Antibodies<br />
Jessica Nickel, Birgit Löer, Reinhard Bauer, Roland Bornheim, Elisabeth Kremmer, Michael Hoch, Waldemar Kolanus<br />
Wech, a novel intracellular regulator of integrin-dependent cell adhesion<br />
Hamid Kashkar, Jens Michael Seeger, Andreas Hombach, Anke Deggerich, Benjamin Yazdanpanah, Olaf Utermöhlen,<br />
Gerd Heimlich, Hinrich Abken, Martin Krönke<br />
XIAP targeting sensitizes Hodgkin Lymphoma cells for cytolytic T cell attack<br />
Isabel Koch, Reinhard Hoffmann<br />
Yersinia virulence protein YopP inhibits NK cell cytokine production by blocking host cell IL-12<br />
signaling.<br />
Hajo Haase, Lothar Rink<br />
Zinc ions act as a signal in leukocyte activation<br />
Laura Kahmann, Sabine Warmuth, Birgit Plümäkers, Axel M. Gressner, Marco Malavolta, Eugenio Mocchegiani, Lothar<br />
Rink, Peter Uciechowski<br />
Zinc supplementation in the elderly reduces spontaneous inflammatory cytokine release and<br />
restores T cell functions
Luciana Berod, Oliver Frey, Johannes Norgauer, Thomas Kamradt<br />
SHIP1 phosphatase controls different aspects of dendritic cell<br />
biology<br />
Introduction: The signal transduction events underlying Dendritic cell (DC) maturation<br />
involve several molecules working in an orchestrated manner. Between them, the<br />
hematopoietic-restricted protein Src homology 2–containing inositol-5-phosphatase<br />
(SHIP1) may play a significant role by dephosphorylating phosphatidylinositol-3,4,5trisphosphate,<br />
the major PI3K substrate. Here, we show that SHIP1 is involved in DC<br />
differentiation and maturation.<br />
Results: Despite a higher proliferation rate and a faster differentiation, normal<br />
percentages of CD11c BMDC SHIP1 -/- are generated in response to GM-CSF + IL-4<br />
(88.5 vs 85.8 %) compared with WT cells. Moreover, upon LPS or TNF-α-induced<br />
maturation MHC class II and CD86 up regulation is impaired in SHIP1-/- BMDC.<br />
Cytokine production in SHIP1-/- BMDC showed a bias towards lower IL-12 and higher IL-<br />
10 production in response to LPS, as determined by ELISA. Whereas other functional<br />
changes, like antigen uptake downregulation upon LPS treatment were not significantly<br />
affected.<br />
Conclusion: These results indicated that in DC, SHIP1 might act not only as a negative<br />
regulator of PIP3-activated signalling pathways, but also as an activator of certain<br />
events during DC life.
Natalia Zietara, Marcin Lyszkiewicz, Stefan Lienenklaus, Siegfried Weiss<br />
"Lack of IFN-β impairs antigen presentation capacity of<br />
splenic dendritic cells"<br />
Type I interferons (I IFNs) constitute a highly pleiotropic, large cytokine family<br />
composed of a single IFN-β and multiple IFN-α. Thus far, type I IFNs are best known for<br />
their role in protection against viral infections. However in recent years these cytokines<br />
have also been shown to have multiple immunomodulatory functions and therefore play<br />
important role in other diseases including bacterial infections as well as under<br />
autoimmune conditions.<br />
The present study was carried out with the aim to investigate the role of type I IFNs in<br />
antigen presentation. Bone marrow (BM) derived and splenic antigen presenting cells<br />
(APCs) from WT, IFN-β -/- and IFNAR -/- mice were fed with either ovalbumin (OVA)<br />
peptide or whole protein and their capacity to present antigen was tested in proliferation<br />
assay using T cells from OT I or OT II transgenic mice. APCs derived from WT and IFNβ<br />
-/- BM exhibited a comparable capacity for the antigen presentation to CD8 + T cells. In<br />
contrast splenic APCs from IFN-β -/- as well as from IFNAR -/- were found to be highly<br />
impaired in their ability to activate CD4 + T cells and CD8 + T cells. Thus, our results<br />
provide evidence that type I IFNs play a crucial role in antigen presentation via MHC<br />
class I and II molecules
Hendrik Poeck, Cornelius Maihoefer, Robert Besch, David Anz, Shizuo Akira, Simon<br />
Rothenfusser, Veit Hornung, Stefan Endres, Thomas Tueting, Gunther Hartmann<br />
5´triphosphate siRNA as a novel therapeutic tool against<br />
tumors<br />
The cytosolic RNA helicase retinoic acid inducible gene-I (RIG-I) is ubiquitously<br />
expressed suggesting a broad spectrum of target cells and a high therapeutic efficacy in<br />
the immunotherapy of tumors and infections. Latest studies further demonstrate that<br />
uncapped 5'-triphosphate RNA, which can be generated by in–vitro transcription, serves<br />
as a molecular signature for the detection of viral infection by RIG-I. Thus, “infection” of<br />
tumor cells with in–vitro transcribed RNA may represent an important tool to elicit direct<br />
anti-tumor activity. Here we show that the transfection of a 5´-triphosphate siRNA<br />
molecule not only resulted in direct immune activation, apoptosis and relevant RNAimediated<br />
gene-silencing in a murine melanoma cell line, but also elicited strong<br />
immune responses in vitro and in vivo. More importantly, only 5´-triphosphate siRNA,<br />
but not synthetic siRNA, significantly reduced the number of lung metastases in a<br />
murine melanoma model. Interestingly, tumor regression by 5´-triphosphate siRNA was<br />
strongly diminished in NK cell–depleted and IFNAR–deficient mice, but not in TLR7–<br />
deficient mice. Additionally, the administration of 5´-triphosphate siRNA yielded high<br />
numbers of apoptotic tumor cells in vivo and resulted in a down-regulation of murine<br />
Bcl-2 in metastatic lungs of IFNAR-deficient mice indicating that 5´-triphosphate siRNA<br />
displays direct anti-tumor activity in vivo. In conclusion, our results identify 5´triphosphate<br />
siRNA as a novel therapeutic approach combining RNAi and direct antitumor<br />
effects with immunostimulation in one molecule providing the basis for the<br />
development of new therapeutic reagents in the immunotherapy of tumors.
Hans KUENG, Victoria LEB, Daniela HAIDERER, Graca RAPOSO, Clotilde THERY, Klaus<br />
SCHMETTERER, Alina NEUNKIRCHNER, Christian SILLABER, Brian SEED, Winfried PICKL<br />
A General Strategy for Decoration of Enveloped Viruses with<br />
Functionally Active Lipid-Modified Cytokines<br />
Viral particles preferentially incorporate extra- and intracellular constituents of host cell<br />
lipid-rafts, a phenomenon central to pseudotyping. Based on this mechanism we have<br />
developed a system for the predictable decoration of enveloped viruses with functionally<br />
active cytokines that circumvents the need to modify viral proteins themselves. Human<br />
interleukin(hIL)-2, hIL-4, hGM-CSF and murine (m)IL-2 were used as model cytokines<br />
and fused at their C-terminus to the glycosyl phosphatidyl inositol (GPI) acceptor<br />
sequence of the human Fc gamma receptor III (CD16b). We here show that genetically<br />
modified cytokines are all well expressed on 293 producer cells. However, only<br />
molecules equipped with GPI-anchors but not those linked to transmembrane/<br />
intracellular regions of type I membrane proteins are efficiently targeted to lipid-rafts<br />
and consequently to virus-like particles (VLP) induced by MoMLV Gag-Pol. Human IL-4::<br />
GPI and hGM-CSF::GPI co-expressed on VLP were found to differentiate monocytes<br />
towards dendritic cells. Apart from myeloid committed cell types, VLP-bound cytokines<br />
also act efficiently on lymphocytes. Human IL-2::GPI strongly co-stimulated TCR/CD3<br />
dependent T cell activation in vitro and mIL-2::GPI co-activated antigen-specific T cells<br />
in vivo. On a molar basis, the functional activity of VLP bound hIL-2::GPI was found to<br />
be comparable to soluble hIL-2. VLP decorated with hIL-2::GPI and co-expressing a<br />
TCR/CD3 ligand have an IL-2 specific activity of 5 x 10 4 units/mg protein. Virus particles<br />
decorated with lipid-modified cytokines might help to improve viral strains for<br />
vaccination purposes, propagation of factor-dependent cell types, as well as gene<br />
transfer by viral systems in the future.
Claudia Brandt, Margitta Worm, Ria Baumgrass<br />
Drug induced modulation of T cell activation and<br />
differentiation<br />
in atopic dermatitis patients<br />
Atopic dermatitis (AD) is a T cell dependent chronic relapsing inflammatory skin<br />
disorder. Cyclosporine A (CsA) has been shown to be an effective treatment for severe<br />
AD. We studied the effect of low dose CsA therapy on T cell activity and T cell<br />
differentiation in AD patients. Using a whole blood assay we demonstrated that TCR<br />
signalling in peripheral blood T cells of CsA treated AD patients is reduced to 42 % ± 18<br />
but not totally blocked. Such partial inhibition of TCR signalling allowed regulatory T cell<br />
induction under in vitro conditions. Therefore we asked is there an in vivo regulatory T<br />
cell induction, too. Indeed AD patients under low dose CsA therapy have higher<br />
numbers and frequencies of regulatory T cells compared to untreated AD patients. To<br />
evaluate the causal connection between low dose CsA treatment and higher regulatory<br />
T cell numbers we studied individual patients before and during CsA therapy. The data<br />
clearly indicate increased numbers and frequencies of regulatory T cells after onset of<br />
CsA therapy which remained stable during the therapy. The therapeutic effect of low<br />
dose CsA therapy in AD patients could be due to both, inhibition of T cell hyperactivity<br />
and induction of suppressor T cells.
Frank Autschbach, Felix Lasitschka, Thomas Giese, Nikolaus Gassler, Benjamin Funke,<br />
Jutta Schroeder-Braunstein, Ulf Brunnemer, Stefan C. Meuer, Bernd Sido<br />
Expression of the cystine transporter subunit xCT is a critical<br />
determinant of the immune response in human inflammatory<br />
bowel disease<br />
Aims: T-cell receptor reactivity of intestinal lamina propria T cells (LP-T) is critically<br />
dependent on the capacity of local accessory cells, especially mucosal macrophages (LP-<br />
M), to secrete cysteine. For T cells, cysteine is a limiting precursor for glutathione<br />
synthesis, a prerequisite for antigen-dependent proliferation. Production of cysteine by<br />
LP-M requires uptake of the derivative cystine via a membrane transporter. We now<br />
investigated the expression and functional relevance of the cystine transporter system<br />
in tissues and isolated immune cells from normal gut and from patients with<br />
inflammatory bowel disease (IBD).<br />
Methods: Expression of the cystine transporter subunit xCT was analyzed by<br />
quantitative RT-PCR, western-blot (WB) and immunohistology (IH). Glutathione (GSH)<br />
levels were detected by flow cytometry and IH. Cysteine secretion and uptake of [ 35 S]<br />
cystine were measured by in vitro assays.<br />
Results: As compared with peripheral blood monocytes, resident LP-M from normal gut<br />
revealed a defective uptake of cystine which was associated with an absent expression<br />
of the transporter molecule xCT, both in vitro and in situ. In contrast to normal gut<br />
tissues, an enhanced expression of xCT was apparent in IBD samples from patients with<br />
Crohn´s disease and ulcerative colitis (RT-PCR, WB, IH). CD68+ and/or CD14+<br />
mononuclear phagocytes were found to coexpress xCT in inflamed tissues. In vitro, such<br />
macrophages secreted substantial amounts of cysteine, which was associated with an<br />
enhanced GSH content of LP-T in IBD versus normal gut.<br />
Conclusions: Enhanced expression of the cystine transporter subunit xCT by mucosal<br />
macrophages alters the redoxactive microenvironment of LP-T and is a critical<br />
determinant of the immune response in human IBD.
Katharina Becher<br />
In vivo persistence of Anaplasma phagocytophilum after<br />
depletion of CD4 + T cells, but not in the absence of Th1-type<br />
cytokines and effector mechanisms<br />
In vivo persistence of Anaplasma phagocytophilum after depletion of CD4 + T<br />
cells, but not in the absence of Th1-type cytokines and effector mechanisms<br />
Katharina Becher, Yvonne Kern, Birte Steiner, Christian Bogdan and Friederike von<br />
Loewenich<br />
Department of Medical Microbiology and Hygiene, University Clinic of Freiburg, Hermann-<br />
Herder-Straße 11, D-79104 Freiburg, Germany<br />
Anaplasma phagocytophilum is a Gram-negative, obligate intracellular bacterium that is<br />
transmitted by ticks and replicates within neutrophils. In order to further define the<br />
mechanisms of its control in the mammalian host, we studied the course of infection in<br />
transgenic mouse strains with various defects of the immune system. The mice were<br />
systemically infected via i.p. injections of infected SCID mouse blood. At certain time<br />
points of infection, the bacterial load was determined in the blood, spleen and lung by a<br />
quantitative PCR technique. Mice deficient for cytokines and effector molecules involved<br />
in the control of other intracellular pathogens (IL-12p35 -/- , IL-12p35 -/- p40 -/- , IL-4 -/- ,<br />
IFN-gamma -/- , IFN-alphaR -/- , TNF -/- , iNOS -/- , gp91 phox-/- , neutrophil elastase -/- ,<br />
cathepsin G -/- , MCP-1 -/- , perforin -/- , Fas lpr , FasL gld ) were still able to eliminate A.<br />
phagocytophilum. SCID and Rag1 -/- mice developed strikingly increased bacterial loads<br />
in the blood compared to wild-type. SCID mice died after about 21 to 30 days of<br />
infection, but were rescued by the transfer of T cells. Likewise, T cell-deficient nude<br />
mice were not able to control the pathogen, whereas Igα -/- mice (lacking mature Bcells)<br />
cleared the infection. Wild-type mice as well as JHT-mice (no B-cell-receptor)<br />
were resistant against a secondary infection. MHC II -/- mice, CD4-depleted mice or<br />
Tcrb -/- mice showed a low level persistence of Anaplasma. These findings suggest that a<br />
CD4 + T cell-dependent Th1 response plays a role in controlling A. phagocytophilum in<br />
vivo.
Manuela Brenk, Marina Scheler, Helene Wilms, Thomas Bieber, Dagmar von Bubnoff<br />
Induction of human CD4 + CD25 + Foxp3 + T regulatory cells by<br />
tryptophan-deprived tolerogenic dendritic cells<br />
Tryptophan catabolism is a tolerogenic effector system to induce anergic T cells and<br />
regulatory T cells (Tregs). Given the crucial importance of DCs in the initiation of a T cell<br />
response, surprisingly little is known about the impact of a high indoleamine 2,3dioxygenase<br />
(IDO)-activity, i.e., a tryptophan-deprived milieu, on DCs themselves. We<br />
show that human monocyte-derived dendritic cells (DCs), when differentiated under<br />
tryptophan-deprived conditions in vitro, acquire potent tolerogenic properties. This<br />
effect is associated with a decreased surface expression of the costimulatory molecules<br />
CD40, CD80, and MHC class II-molecules. In contrast, the inhibitory receptors<br />
Immunoglobulin-like transcript 2 (ILT2), and Immunoglobulin-like transcript 3 (ILT3)<br />
are increased on these DCs. Functionally, tryptophan-deprived DCs show a reduced<br />
capacity to uptake antigens and to stimulate T cells in vitro which can be partly restored<br />
by the addition of an anti-ILT3 Ab. Moreover, we provide evidence that tryptophandeprived<br />
DCs are able to induce CD4 + CD25 + Foxp3 + T regulatory cells with suppressive<br />
functions in an ILT3-dependent fashion. The induction of DCs with tolerogenic properties<br />
by tryptophan deprivation is associated with the induction of an active stress response<br />
pathway mediated by the GCN2 kinase during differentiation of both, immature and<br />
mature DCs. Altogether, these results demonstrate that tryptophan starvation<br />
establishes a regulatory environment for DCs, which, by means of their tolerogenic<br />
properties, favour the enhancement of regulatory T cells.
Kristina Röschmann, Artur J. Ulmer, Torsten Goldmann, Arnd Petersen<br />
Interaction of Timothy grass pollen major allergen Phl p 1<br />
with human respiratory epithelial cells<br />
The bronchial epithelium as a first line of contact of the immune system with the<br />
environment including airborne grass pollen functions as physical barrier and serves as<br />
important immunological regulation system, also involved in allergic reactions like<br />
asthma. Upon activation epithelial cells release inflammatory mediators and cause the<br />
attraction of immuno-competent cells. About 20% of the population of industrialized<br />
countries are suffering from type-I-allergies. Group-I-allergens (e.g. Phl p 1 from<br />
Phleum pratense) cause IgE-reactivity in about 95% of the allergic subjects and exist in<br />
all grass species. We are investigating the interaction of Phl p 1 with human respiratory<br />
epithelium in detail: uptake of the allergen, activation of the cells, route of the allergen<br />
through the epithelial barrier and the potential role of respiratory epithelium as<br />
unprofessional APC. We determined that Phl p 1 activates epithelial cells measured by<br />
release of IL-8 and IL-6. The activity of the allergen cannot be inhibited after preincubation<br />
with mAb blocking the TLR2- and TLR4-signalling pathways, indicating that<br />
contaminating bacterial components are not responsible for the activation of the cells.<br />
However, a <strong>complete</strong> deletion of the biological activity of Phl p 1 after enzymatic<br />
digestion indicates that the allergen itself interacts with the epithelium. After preincubation<br />
with different inhibitors we were able to show the involvement of p38, ERK<br />
and NFκB in the activation of epithelial cells by the allergen. We could also show that Phl<br />
p 1 is taken up by human respiratory epithelium and that these cells can express HLA-<br />
DR. A co-localization of Phl p 1 and HLA-DR and the effective processing of the allergen<br />
by epithelial cells remains to be determined. (Supported by DFG SFB TR22)
Andreas Brandl, Juergen Wittmann, Michael Boesl, Hans-Martin Jaeck<br />
MicroRNA-Mediated Control of B Cell Activation<br />
MicroRNAs (miRNAs) constitute a growing class of small noncoding RNAs that regulate<br />
gene expression mainly at the posttranscriptional level. The regulatory function of<br />
miRNAs has recently been shown to play critical roles in the control of hematopoiesis.<br />
The goal of this project is to determine whether miRNAs function also during the<br />
antigen-induced activation of B lymphocytes. To determine the miRNA profiles in naive<br />
B cells before and after polyclonal activation, we stimulated B cells isolated via magnetic<br />
CD43 beads from spleen with either LPS (simulates T cell-independent activation) or<br />
with a combination of anti-IgM, anti-CD40 and IL4 (simulates T cell-dependent<br />
activation) for various times. The analysis of isolated RNA using miRNA microarray- and<br />
qRT-PCR assays identified about 104 miRNAs in unstimulated B cells. 35 of these were<br />
mostly downregulated after stimulation. In silico analyses with various miRNA target<br />
prediction programs revealed a very interesting and promising set of potential<br />
transcripts whose translation/stability could be controlled by miRNAs during the antigeninduced<br />
activation phase of mature B cells. Among these targets are BCR signalling<br />
molecules and transcription factors that control proliferation, IgH class switch as well as<br />
differentiation in antibody-secreting plasma cells. We will now verify biochemically<br />
potential targets for each the differentially regulated miRNAs and determine the effect<br />
of retrovirally transduced miRNAs on B cell development.
Savita Nair, Ulf Dittmer<br />
Role of CD4 + T cells in acute Friend Retroviral infections<br />
Retroviruses are extremely pathogenic microbes and have accounted for significant<br />
mortality and morbidity worldwide. Cytotoxic T lymphocytes (CTLs) are efficient in<br />
keeping the viral replication under control during acute phase of infections but lose their<br />
protective function during later stages under the suppressive effect of Regulatory T<br />
cells. As a result of this, the virus manages to escape immune surveillance to cause<br />
persistent infections for life. In life-threatening infections such as Human<br />
Immunodeficiency virus (HIV) or Human T-cell leukemia virus (HTLV-1) immune escape<br />
becomes critical. Role of CTLs is well defined in various retroviral infection models but<br />
role of CD4 + T helper cells in retroviral immunity is poorly understood. Hence, we aimed<br />
at characterising the function of CD4 + T cells during the initial phase of infections using<br />
the Friend retrovirus (FV) murine infection model. FV infection causes lethal leukemia in<br />
most strains of mice and the mouse model helps in studying the basic mechanisms of<br />
immunological control and escape in both acute and persistent retroviral infections. In<br />
vivo depletion of CD4 + T cells in acutely infected FV resistant mice strain demonstrated<br />
that CD4 + T cells are important in controlling viral replication in acute FV infections and<br />
onset of erythroleukemia. An ex vivo MHC-II tetramer kinetic analysis of FV-specific CD4<br />
+ T cell responses during acute FV infection showed that maximal activation of CD4 + T<br />
cells are achieved at 10 days post infection correlating with a decrease in viral loads.<br />
Most significantly, FV-specific CD4 + T cells adoptively transferred into mice acutely<br />
infected with FV showed that the transferred cells specifically recognised the FV antigen<br />
in vivo, got activated to express an effector phenotype and produced the anti-viral<br />
cytokine IFN-γ resulting in decreased viral loads. These results indicate that CD4 + T cell<br />
response is vital for the control of virus replication during acute FV infection and for the<br />
resistance of certain mouse strains to virus–induced disease.
Alexia Nass, Hans-Willi Mittruecker, Alf Hamann, Jochen Huehn<br />
Transfer of in vivo operating inflammation-specific Tregs does<br />
not interfere with the host´s response against bacterial<br />
infection<br />
Regulatory T cells (Tregs) play an essential role in regulating inflammatory immune<br />
responses in vivo. In several models it has been shown that Tregs can suppress both<br />
the initiation of immune responses as well as ongoing inflammatory reactions. Little<br />
knowledge exists about the therapeutic use of antigen-specific Tregs to suppress<br />
unwanted immune reactions, while allowing an effective immune response against<br />
invading pathogens at the same time. Here we used a Th1-mediated delayed-type<br />
hypersensitivity (DTH) model for an inflammatory response and analyzed whether a<br />
defined subpopulation of antigen-specific ? +<br />
E Tregs would be able to suppress the DTH<br />
response in the context of a contemporaneous systemic infection with Listeria<br />
monocytogenes. Furthermore, we determined if the presence of high numbers of<br />
inflammation-specific Tregs would influence the immune response against L.<br />
monocytogenes, which mainly takes place within the spleen and liver. ? +<br />
E Tregs turned<br />
out to be potent suppressors of the local inflammation irrespective of the presence or<br />
absence of a systemic bacterial infection. In addition mice adoptively transferred with<br />
antigen-specific Tregs still established an effective immune response against L.<br />
monocytogenes compared to animals not receiving Tregs. Together, our findings<br />
provide evidence that adoptive transfer of antigen-specific Tregs effectively suppresses<br />
inflammatory reactions even in the context of a systemic L. monocytogenes infection<br />
without impairing the host´s pathogen-specific immune response.
Björn Stork, Ingo Goldbeck, Konstantin Neumann, Thilo Kähne, Michael Naumann,<br />
Michael Engelke, Jürgen Wienands<br />
‘Membrane zip codes’ for Grb2 determine differential Ca 2+<br />
signaling in B lymphocytes<br />
The intracellular second messenger Ca 2+ is a key determinant of B cell development,<br />
activation, induction of anergy, or death by apoptosis. The inducible Ca 2+ initiation<br />
complex downstream of the B cell antigen receptor (BCR) is composed of the adaptor<br />
protein SLP-65, Bruton's tyrosine kinase (Btk) and phospholipase C-γ2 (PLC-γ2).<br />
Complex formation allows PLC-γ2 to produce inositol-tris-phosphate (IP3), which<br />
releases Ca 2+ from ER stores into the cytosol followed by entry of extracellular Ca 2+<br />
across the plasma membrane. The relative contribution of intra- and extracellular Ca 2+<br />
fluxes to the total Ca 2+ mobilization profile varies in a developmental stage-specific<br />
manner. This results in differential Ca 2+ signals to ultimately control distinct nuclear<br />
responses and hence cell fate. Our group has shown that fine tuning of the Ca 2+<br />
response involves the intracellular SH2/SH3 domain adaptor protein Grb2, which we<br />
identified as a negative regulator of BCR-induced Ca 2+ signaling. Using a combination of<br />
biochemical, gene targeting and imaging techniques we have now elucidated the mode<br />
of Grb2 action in B cells. We found that following BCR activation, the SH2 domain of<br />
Grb2 binds the tyrosine-phosphorylated adaptor protein Dok-3 (downstream of kinase-<br />
3), which permanently localizes at the inner leaflet of the plasma membrane by virtue<br />
of its PH domain. When recruited to phospho-Dok-3, Grb2 attenuates Btk-dependent<br />
PLC-γ2 activation and IP3 production by interfering with proper formation of the Ca 2+<br />
initiation complex and/or inhibition of Btk activity. However, Grb2 is expressed<br />
throughout the B cell lineage. Maximal Ca 2+ mobilization in mature B cells can be<br />
accomplished by inactivation of Grb2 through translocation of Grb2 to an alternative<br />
transmembrane protein, namely NTAL. Hence, stimulation-dependent relocalization of<br />
Grb2 to distinct submembranous destinations, i.e NTAL or Dok-3, is a critical parameter<br />
to orchestrate the interaction efficiency of Ca 2+ -mobilizing enzymes and to balance BCRinduced<br />
Ca 2+ mobilization.
Stefanie Kunz, Karin Oberle, Anna Sander, Christian Bogdan, Ulrike Schleicher<br />
Bartonella-Induced Cat Scratch Disease-like<br />
Lymphadenopathy in Mice Involves Cell Proliferation and<br />
Altered Lymphocyte Recruitment<br />
In immunocompetent humans the Gram-negative bacterium Bartonella (B.) henselae,<br />
which has a feline reservoir host and is known as facultative intracellular pathogen,<br />
causes cat scratch disease (CSD). The clinical manifestations of CSD are characterized<br />
by a long-lasting, but self-healing enlargement of the draining lymph node which rarely<br />
contains cultivable Bartonella. So far, no data about the immunopathogenic mechanism<br />
leading to this lymphadenopathy exist.<br />
This prompted us to establish a mouse model of CSD. After subcutaneous infection with<br />
a high dose of B. henselae the bacteria were rapidly eliminated, but similar to human<br />
CSD, a striking and long-lasting swelling of the draining lymph node developed. It was<br />
more severe compared to that induced by other Bartonella species. In vivo-proliferation<br />
assays using 5-Bromo-2`-deoxyuridine (BrdU) and the transfer of<br />
carboxyfluoresceinsuccinimidylester (CFSE)-labeled splenocytes revealed that cell<br />
proliferation and a preferential influx of B cells contributed to the observed lymph node<br />
enlargement after Bartonella infection. With respect to possible immunostimulatory<br />
functions of Bartonella, we found that plasmacytoid dendritic cells exposed to Bartonella<br />
in vitro secreted high amounts of interferon (IFN)-α/β. Compared to B. henselae, the<br />
rodent pathogen B. grahamii elicited only a mild lymph node swelling in wildtype mice,<br />
but a severe lymphadenopathy in IFN-α/β receptor-deficient mice. From these data, we<br />
conclude that lymphoproliferation as well as altered immune cell recruitment are<br />
involved in the pathogenesis of B. henselae-induced lymphadenopathy in mice.<br />
Furthermore our data suggest an inhibitory effect of IFN-α/β on the described<br />
lymphadenopathy in mice.
Georg Peschel, Nuria Rodriguez, Christine Cirl, Nina Wantia, Tanja Erl, Susi Dürr,<br />
Hermann Wagner, Thomas Miethke<br />
Chlamydophila pneumoniae follows different strategies to<br />
downregulate surface MHC II expression depending on the<br />
cell type<br />
Chlamydophila pneumoniae (CP), an obligate intracellular bacterium, has developed<br />
several strategies for intracellular survival and to escape from the immune system. One<br />
of the most attractive mechanisms is the downregulation of MHC II in epithelial cells by<br />
degradation of the upstream stimulatory factor-1 (USF-1) by the chlamydial protease<br />
CPAF which is secreted during infection. In WT infected BMDM, where CP does not<br />
replicate as efficient as in epithelial cells, the surface expression of MHC II is<br />
downregulated in comparison with the mock control. Addition of IFNγ one day post<br />
infection did not increase surface MHC II levels compared to IFNγ stimulation alone,<br />
suggesting that infection with CP blocks the stimulatory ability of this cytokine.<br />
However, MyD88 -/- infected BMDM did not show any downregulation of MHC II after<br />
infection, but displayed a substantial upregulation upon infection and subsequent<br />
IFNγ•stimulation. Surprisingly, heat inactivated CP (HI-CP) behaved similar as CP alive.<br />
In addition, RT-PCR to detect CPAF RNA showed no presence of the transcript in WT and<br />
little in MyD88 -/- BMDM, indicating that CPAF may not be involved in MHC II<br />
downregulation in BMDM during infection, but rather a chlamydial PAMP that signals in a<br />
MyD88-dependent manner. By contrary, results obtained from infected WT mouse<br />
embryonic fibroblast (MEFs) showed that HI-CP was not able to impair IFNγ-mediated<br />
MHC II expression. Also, RT-PCR demonstrated the presence of CPAF RNA after<br />
infection and USF-1 was degraded in MEFs after CP infection but not after HI-CP<br />
stimulation. Curiously, USF-1 was upregulated in a MyD88-dependent manner in BMDM<br />
after CP or HI-CP infection, indicating that induction of USF-1 and increased surface<br />
expression of MHC II are not correlated in this cell type. In summary, these data show<br />
that CP prevents IFNγ-induced MHC II upregulation in BMDM via PAMP stimulation<br />
through MyD88-dependent but CPAF-independent mechanism while in MEFs CPAF is<br />
involved and therefore an infection is required.
Annabelle Schnaith, Sonja A. Leggio, Martin Krönke, Oleg Krut<br />
Staphylococcus aureus Subverts Autophagy for Induction of<br />
Caspase-independent Host Cell Death<br />
Staphylococcus aureus is a common bacterial etiology of serious infectious diseases. S.<br />
aureus can invade various types of non-professional phagocytes to produce host cell<br />
death. We show here that shortly after invasion of HeLa cells S. aureus transit to<br />
autophagosomes that was characterized by double membranes and co-localization with<br />
LC3. S. aureus were not able to replicate and produce cell death in autophagy-deficient<br />
atg5 -/- mouse embryonic fibroblasts. S. aureus-containing autophagosomes do not<br />
acidify nor do they acquire lysosome-associated membrane protein-2, indicating that S.<br />
aureus inhibits autophagosome maturation and fusion with lysosomes. Eventually, S.<br />
aureus escape from autophagosomes into the cytoplasm, which results in caspaseindependent<br />
host cell death. S. aureus strains deficient for agr, a global regulator of S.<br />
aureus virulence, were not targeted by autophagy and did not produce host cell death.<br />
Autophagy induction by rapamycin restored both replication and cytotoxicity of agrdeficient<br />
S. aureus strains, indicating that an agr-regulated factor(s) is required for<br />
autophagy-mediated cytotoxicity. The results of this study suggest that rapid induction<br />
of autophagy is essential for S. aureus replication, escape into the cytoplasm, and host<br />
cell killing.
Stella Eugenie Autenrieth, Dirk Middendorf, Ingo Birger Autenrieth<br />
Yersinia enterocolitica induces cell death in splenic dendritic<br />
cells: evidence for YopP dependent and independent<br />
mechanisms<br />
The virulence factor YopP of Yersinia enterocolitica (Ye) induces cell death in mouse<br />
bone marrow-derived dendritic cells (DCs). Here we have investigated whether YopP of<br />
Ye might induce cell death in DCs in vivo. For this purpose, C57BL/6 mice were infected<br />
i.v. with Ye wild type (pYV + ) or with the YopP deficient mutant strain (pYV + ΔyopP).<br />
One, two and three days post infection the number of splenic DCs including<br />
subpopulations as well as the frequency of apoptotic DCs was analyzed by flow<br />
cytometry and immunofluorescence microscopy. Infection of mice with the pYV +<br />
resulted in a higher number of CD11c + cells in the spleen one day post infection<br />
compared to untreated mice. This effect was not observed in the spleen of mice infected<br />
with pYV + ΔyopP, indicating that the rapidly increased number of DCs in the spleen one<br />
day after Yersinia infection is mediated by YopP. Three days post infection the number<br />
of CD11c + cells was three times lower in the spleen of mice infected with pYV +<br />
compared to untreated mice. The decrease in CD11c + cells was associated with<br />
significantly higher numbers of apoptotic and necrotic DCs three days post infection with<br />
the wild type strain pYV + compared to uninfected mice or to mice infected with the YopP<br />
deficient mutant strain pYV + ΔyopP as revealed by immunostaining of active caspase 3,<br />
TUNEL reaction and staining with propidium iodide. However, infection with pYV + ΔyopP<br />
also resulted in a significant, although lower increase of apoptotic DCs suggesting that<br />
part of DC death after Yersinia infection in vivo is caused by mechanisms independent<br />
of YopP. Recent published data suggest, that LPS promotes DC death in bacterial<br />
infections in vivo. Furthermore, analysis of DC subpopulations revealed that Ye induces<br />
cell death predominantly in CD4 + CD8α - DCs. Whether and how this affects priming of T<br />
cells required for the control of Ye infections remains to be shown in future studies.<br />
Taken together, our data demonstrate YopP dependent and YopP independent induction<br />
of DC death in vivo suggesting that YopP, possibly in concert with LPS, induces cell<br />
death in splenic DCs.
Heribert Appelhans, Michael Walther, Andrea Friße, Michael A. Harvey, Stephen A.<br />
Judice, Brett A. Stillman, Hans Peter Seelig<br />
A CE-Certified Autoimmune Disease Diagnostic Protein<br />
Microarray<br />
CombiChip® Autoimmune is an auto-antigen microarray that enables laboratories to<br />
measure the presence of 14 different auto-antibodies associated with collagenosis and<br />
vasculitis-related autoimmune diseases simultaneously from a single serum sample.<br />
Thirteen protein antigens, double stranded DNA, and an internal calibrator (human IgG)<br />
are arrayed on each of 16 pads of nitrocellulose on a coated glass microscope slide<br />
(FAST® Slide). Seventy microliters of diluted patient’s serum is added to each array,<br />
and the presence of reactive antibodies is detected with DY647-conjugated anti-human<br />
IgG. The calibrator, a series of dilutions of human IgG arrayed on each pad, is used to<br />
construct a standard curve to quantify the levels of autoimmune antibodies present<br />
against each antigen. This microspot immunoassay yields reproducible results which are<br />
in good agreement with standard methods such as ELISA and Western Blot. It greatly<br />
reduces assay time and delivers an auto-antibody profile for each patient. This<br />
diagnostic assay has been validated to ensure compliance with the CE guidelines for invitro<br />
diagnostics.
Martina Papadopoulos, Frank Momburg<br />
A complex sequence motif of tapasin stabilizes the TAP2<br />
protein<br />
The type I endoplasmic reticulum (ER) glycoprotein tapasin (Tpn) is essential for loading<br />
of major histocompatibility class I (MHC-I) molecules with an optimal spectrum of<br />
antigenic peptides and for stable expression of the heterodimeric, polytopic TAP peptide<br />
transporter. In a detailed mutational analysis the transmembrane domain (TMD) and ERluminal<br />
connecting peptide (CP) of mouse Tpn were analyzed for their capacity to<br />
stabilize the TAP2 subunit. Replacement of the TMD of Tpn by TMDs from calnexin or<br />
the Tpn-related protein, respectively, <strong>complete</strong>ly abolished TAP2 stabilization after<br />
transfection of Tpn-deficient cells, while TMDs derived from distantly related Tpn<br />
molecules (chicken, fish) were functional. A detailed mutational analysis of the TMD and<br />
adjacent residues in the ER-luminal CP of mouse Tpn was performed to elucidate amino<br />
acids that control the stabilization of TAP2. Single amino acid substitutions, including a<br />
conserved Lys residue in the center of the putative TMD, did not affect TAP2 expression<br />
levels. Mutation of this Lys plus four additional residues, predicted to be neighbors in an<br />
assumed α-helical TMD arrangement, abrogated the TAP2-stabilizing capacity of Tpn. In<br />
the presence of a wild-type TMD, also the substitution of a highly conserved Glu residue<br />
in the CP of Tpn strongly affected TAP2 stabilization. Defective TAP2 stabilization<br />
resulted in impaired cell surface expression of MHC-I molecules. This study thus defines<br />
a novel, spatially arranged motif in the TMD of Tpn essential for stable expression of the<br />
TAP2 protein and a novel protein interaction mode involving an ER-luminal Glu residue<br />
close to the membrane.
Andreas Oliver Weinzierl, Dominik Maurer, Florian Altenberend, Nicole Schneiderhan-<br />
Marra, Karin Klingel, Oliver Schoor, Thomas Joos, Hans-Georg Rammensee, Stefan<br />
Stevanovic<br />
A cryptic VEGF T-cell epitope: Identification and<br />
characterization by mass spectrometry and T-cell assays<br />
The vascular endothelial growth factor A (VEGF) is involved in various physiological<br />
processes such as angiogenesis or wound healing but is also crucial in pathological<br />
events such as tumor growth. Clinical anti-VEGF treatments have been developed which<br />
could already prove to have enormous beneficial effects for cancer patients. In this<br />
article we describe a VEGF-derived CD8 T-cell epitope. The natural HLA ligand<br />
SRFGGAVVR was identified by differential mass spectrometry in two primary renal cell<br />
carcinomas (RCC), significantly over-presented on both tumor tissues. SRFGGAVVR is<br />
derived from a cryptic translated region of VEGF presumably by initiation of translation<br />
at the non-classical start codon CUG499. SRFGGAVVR specific T-cells were generated in<br />
vitro using peptide loaded dendritic cells or artificial antigen presenting cells.<br />
SRFGGAVVR specific CD8+ T-cells were identified by HLA tetramer analysis after in vitro<br />
stimulation. These T-cells were fully functional T-effector cells, which were able to<br />
secrete IFN-gamma upon stimulation and killed tumor cells in vitro. Additionally, we<br />
have quantitatively analyzed VEGF mRNA and protein levels in RCC tumor and normal<br />
tissue samples by gene chip analysis, qRT-PCR, in situ hybridization and bead based<br />
immuno assay. In the future, T-cells directed against VEGF as a tumor associated<br />
antigen may represent a possible way of combining peptide-based anti-VEGF<br />
immunotherapy with already existent anti-VEGF cancer therapies.
Susanne Tartz, Holger Ruessmann, Jana Kamanova, Peter Sebo, Angelika Sturm, Volker<br />
Heussler, Bernhard Fleischer, Thomas Jacobs<br />
A heterologous prime/boost immunization using recombinant<br />
Salmonella and Bordetella adenylate cyclase induces<br />
<strong>complete</strong> protection against P. berghei malaria<br />
Sterile immunity against malaria can be achieved by the induction of cytokine-producing<br />
CD8+ T cells that target infected hepatocytes presenting epitopes of the<br />
circumsporozoite protein (CSP). In the present study we evaluate the protective efficacy<br />
of a heterologous prime/boost immunization protocol based on the delivery of the CD8+<br />
epitope of Plasmodium berghei CSP into the MHC class I presentation pathway, by<br />
either a type III secretion system of live recombinant Salmonella and/or by direct<br />
translocation of a recombinant Bordetella adenylate cyclase toxoid fusion (ACT-CSP)<br />
into the cytosol of CD11b-expressing professional antigen-presenting cells (APC). A<br />
single intraperitoneal application of the recombinant ACT-CSP toxoid, as well as a single<br />
oral immunization with the Salmonella vaccine, induced a specific CD8+ T cell response<br />
and the latter could be further enhanced by repeated application of the live vaccine,<br />
which however conferred only a partial protection on mice against a subsequent<br />
sporozoite challenge. In contrast, a heterologous prime/boost vaccination with the live<br />
Salmonella followed by ACT-CSP led to a significant enhancement of the CSP-specific T<br />
cell response and induced <strong>complete</strong> protection in all vaccinated mice
Nousheen Zaidi, Timo Herrmann, Daniel Baechle, Sabine Schleicher, Jeannette Gogel,<br />
Christoph Driessen, Wolfgang Voelter, Hubert Kalbacher<br />
A new approach for distinguishing cathepsin E and D activity<br />
in antigen processing organelles<br />
Cathepsin E (CatE) and D (CatD) are the major aspartic proteinases in the<br />
endolysosomal pathway. These proteinases exhibit similar specificity and therefore it is<br />
difficult to distinguish between them since known substrates are not exclusively specific<br />
for one proteinase. Here we present a substrate-based assay, which is highly relevant<br />
for immunological investigations since it detects both, CatE and CatD in antigenprocessing<br />
organelles. Therefore it could be used to study the involvement of these<br />
proteinases in protein degradation and the processing of invariant chain. An assay<br />
combining a new monospecific CatE antibody and substrate MOCAc-Gly-Lys-Pro-Ile-Leu-<br />
Phe-Phe-Arg-Leu-Lys(Dnp)-D-Arg-NH2 [where MOCAc is (7-methoxycoumarin-4-yl)<br />
acetyl and Dnp is dinitrophenyl] is presented. This substrate is digested by both<br />
proteinases and therefore can be used to detect the total aspartic proteinase activity<br />
(TAPA) in biological samples. After depletion of CatE by immunoprecipitation, the<br />
remaining activity is due to CatD and the decrease of activity can be assigned to CatE.<br />
The activity of CatE and CatD in cytosolic, endosomal and lysosomal fractions of B cells,<br />
dendritic cells and human keratinocytes was determined. Our data clearly indicate that<br />
CatE activity is mainly located in endosomal and that of CatD in lysosomal<br />
compartments. Hence this assay can also be used for characterization of subcellular<br />
fractions using CatE as an endosomal marker, whereas CatD is a well-known lysosomal<br />
marker. Moreover, the highest TAPA was detected in dendritic cells and the lowest in B<br />
cells. The assay presented exhibits a lower detection limit than common<br />
antibody-based methods without lacking the specificity.
Wiebke Hartmann, Markus M. Simon, Bernhard Fleischer, Simone Korten<br />
A new role for granzymes: Suppression of defence against<br />
helminths<br />
Granzyme (gzm) A and B are major cytotoxic serine proteases of NK cells and cytotoxic<br />
T cells, known to play a key role in the destruction of tumor cells or infected cells.<br />
Recent studies show that gzmB is released by regulatory T (Treg) cells suppressing<br />
effector T cells, antigen-presenting cells, B and NK cells. On the other hand, gzmA and<br />
B can facilitate leukocyte migration by degrading extracellular matrix proteins. Their<br />
role in helminth infection has not been examined so far. As CD4+ T cells, NK cells, B<br />
and Treg cells affect the mixed Th1/Th2 (Th2-biased) immune defence against filariae,<br />
conferred substantially by granulocytes, we investigated the role of gzmA and B during<br />
infection of mice with the rodent filaria Litomosoides sigmodontis. Resistant wildtype<br />
C57BL/6 (wt) mice (infection is finished before worms reach sexual maturity) and<br />
gzmAxB knock out (ko) mice, generated on this background, were naturally infected via<br />
mites. GzmAxB ko mice harboured a lower worm load in the pleural cavity than wt mice<br />
in the early and late phase of infection rendering them hyperresistant. This lower worm<br />
load in ko mice was associated with early reduction of NK and apoptotic cells and a<br />
reduction of Th1 specific IgG2b, but increase of pleural IL-5 compared to wt mice.<br />
Pleural Foxp3+CD4+ Treg cells were detectable early with numbers unaffected by gzmA<br />
or B deficiency and declining with infection. GzmAxB deficiency did not generally<br />
influence leukocyte migration, as size and proportions of leukocyte subpopulations were<br />
unaltered. Therefore, we conclude that a pronounced Th2 response in gzmAxB deficient<br />
mice induced by a still unclear way leads to hyperresistance in this filarial infection and<br />
indicates for the first time a defence-suppressive role of granzymes in an infection.
Elisa Kieback, Jehad Charo, Daniel Sommermeyer, Thomas Blankenstein, Wolfgang<br />
Uckert<br />
A new safeguard eliminates TCR gene-modified autoimmunereactive<br />
T cells after adoptive therapy<br />
The T cell specificity can be redirected by the transfer of TCR genes. The modified T<br />
cells can elicit effector functions against the new target, and adoptive transfer of<br />
redirected T lymphocytes into cancer patients has recently led to clinical success.<br />
However, the adoptive transfer of TCR gene-modified lymphocytes is associated with<br />
potential risks. First, many tumor antigens are also expressed in normal tissue.<br />
Recognition of these antigens on non-tumor cells might lead to autoimmunity. Second,<br />
the introduced TCR chains might form heterodimers with the alpha and beta chains of<br />
the endogenous TCR. The specificity of these mispaired TCRs cannot be predicted and<br />
they might have autoimmune capacity. Third, it has been shown that activation of the<br />
introduced TCR might also trigger signal transduction of the endogenous receptor.<br />
Therefore, it is essential to have the possibility to eliminate autoreactive T cells in vivo<br />
in case of severe side effects.<br />
The strategies developed so far include suicide genes or apoptosis-inducing fusion<br />
constructs. However, they either do not lead to efficient depletion or require purification<br />
of gene-modified cells which might hamper their functionality.<br />
Here, we introduce a novel method to eliminate autoreactive TCR-redirected T cells. By<br />
introducing a myc-tag into the murine OT-I and P14 TCR or the human gp100 TCR it<br />
was possible to deplete T cells in vitro and in vivo with a tag-specific antibody. Tagmodified<br />
TCRs exhibited equal functionality compared to the wild type receptor<br />
concerning MHC-multimer binding and cytokine secretion. In vivo depletion of<br />
adoptively transferred cells entirely prevented disease in an autoimmune mouse model.<br />
Here, OT-I/myc TCR-transduced splenocytes were injected into RIP-mOVA mice which<br />
express the OT-I specific antigen ovalbumin in the beta-islet cells of the pancreas.<br />
Destruction of these cells by the adoptively transferred T lymphocytes led to severe<br />
diabetic disease in untreated control mice. Mice receiving a dose of myc-antibody after<br />
T cell transfer remained healthy and showed no increase in blood glucose levels.
Matthias Bros, Frank Jährling, Andrea Renzing, Nadine Wiechmann, Ngoc-Anh Dang,<br />
Arne Sutter, Ralf Ross, Jürgen Knop, Stephan Sudowe, Angelika B. Reske-Kunz<br />
A newly established murine immature dendritic cell line<br />
exerts tolerogenic function at its immature state and upon<br />
alternative activation in the presence of glucocorticoid<br />
The phenotype and function of murine dendritic cells (DC) is primarily studied using<br />
bone-marrow-derived dendritic cells (BM-DC), but may be hampered by the<br />
heterogenous phenotype of BM-DC due to differential state of maturation. We<br />
characterized a newly established murine DC line (SP37A3) of myeloid origin. During<br />
maintainance in the presence of GM-CSF and M-CSF, SP37A3 cells resemble immature<br />
DC characterized by low expression of MHC II and costimulatory molecules and low T<br />
cell stimulatory capacity. Upon stimulation, SP37A3 cells acquire a mature phenotype<br />
and activate naive T cells as potently as BM-DC. SP37A3 cells at their immature state as<br />
well as upon alternative activation by TNF-a and IL-1ß in the presence of<br />
dexamethasone (DEX) induced regulatory T cells which were anergic upon restimulation<br />
and suppressed proliferation of naive T cells. Alternatively activated SP37A3 cells<br />
displayed lower expression levels of costimulatory molecules and proinflammatory<br />
cytokines as compared with mature cells, as well as upregulated expression of FcgRIIB<br />
and IL-1RA. SP37A3 cells were responsive to DEX even when applied at later time<br />
points during activation suggesting functional plasticity. Taken together, the myeloid DC<br />
line SP37A3 represents a suitable model to study functions of myeloid dendritic cells at<br />
tolerogenic and immunogenic state, circumventing restrictions associated with the use<br />
of primary DC and BM-DC.
Iris Watermann, Jeannette Gerspach, Matthias Lehne, Klaus Pfizenmaier, Harald<br />
Wajant<br />
A novel CD95L-Prodrug Fusion Protein with tumorselective<br />
antitumoral activity<br />
Activation of CD95 induces apoptosis in a variety of tumor cells. The use of soluble<br />
agonists of CD95 in tumor therapy is precluded due to their high systemic toxicity. To<br />
circumvent this problem a CD95L-prodrug was developed that strictly induces CD95<br />
activation in an antigen-dependent manner after processing of tumor-expressed<br />
proteases.<br />
In a tumor model, local application of the prodrug reduced the growth of target antigen<br />
expressing, but not target antigen negative tumor cells, verifying targeted activation<br />
and anti-tumoral action in vivo. Despite this potent apoptosis-inducing activity in tumor<br />
cells in vivo, no side effects have been observed when applied systemically.<br />
Thus, a tumor localized action of the CD95L is ensured by tumor restricted expression of<br />
both, the target antigen and prodrug processing proteases. Here, a novel drug that<br />
fulfills the essential criteria of a target-restricted, anti-tumoral action was developed<br />
that may hold promise for cancer therapies in the future.
Ines Gütgemann, Jasmin Teresa Ney, Qi Zhou, Christian Kurts, Hubert Schorle,<br />
Andreas Limmer, Martina Berg, Reinhard Büttner<br />
A novel model of antigen recognition in a hepatic tumor<br />
microenvironment: c-myc/OVA x LAPtTA transgenic mice<br />
Murine hepatic tumor models to investigate antigen presentation and antigen specific Tcell<br />
recognition are hampered either by the lack of a defined cognate antigen or by the<br />
need to inject tumor cells leading to an artificial change of the local host immune<br />
response. Here, we report the generation of a novel conditional mouse model system of<br />
hepatocellular carcinoma (HCC), in which liver specific antigen presentation and<br />
recognition can be followed. When c-myc/OVA transgenic mice expressing chicken<br />
ovalbumin (OVA) and the proto-oncogene c-myc are crossed with liver specific inducer<br />
mice (LAP tTA), the resulting mice (c-myc/OVA x LAPtTA) develop doxicycline<br />
dependent multinodular tumors, resembling human HCC. Although efficient antigen<br />
presentation by intratumoral dendritic cells occurs, the antigen specific T-cell response<br />
is inefficient: Transferred OVA specific OT1 T-cells are rapidly activated, proliferate and<br />
accumulate in the liver and slightly delayed, in systemic immune organs. However,<br />
these CD8+ T-cells show a partial downregulation of the T-cell receptor and lack<br />
Interferon gamma production indicating T-cell tolerance. This model will be useful in<br />
dissecting antigen-specific and non-specific immune responses during different stages of<br />
hepatocarcinogenesis and testing of immune modulatory strategies within an organ<br />
specific tumor microenvironment.
Peggy Riese, Thomas Ebensen, Claudia Link, Kai Schulze, Michael Morr, Carlos Guzmán<br />
A pegylated derivative of alpha galactosylceramide exhibits<br />
improved immune stimulatory activities<br />
The glycolipid alpha galactosylceramide (alpha GalCer) has immune modulatory<br />
properties, leading to activation of various cell subsets of the innate and adaptive<br />
immune system. However, its poor solubility makes alpha GalCer a suboptimal<br />
compound for in vivo applications. A well-known method to improve the solubility of<br />
chemical compounds in aqueous solutions is the conjugation with polyethylene glycol. A<br />
pegylated derivative of alpha GalCer, called alpha GalCerMPEG, is characterized, which<br />
exhibits improved physiological and biological activities. The new compound is watersoluble<br />
and retains the specificity for the CD1d receptor of alpha GalCer. In vitro studies<br />
showed the same stimulating activities on different subsets of immune cells (dendritic<br />
cells, natural killer cells), even when tested at 33-fold lower concentrations. Natural<br />
killer cells isolated from mice treated with alpha GalCerMPEG have also stronger activity<br />
on Yac-1 cells than those obtained from animals receiving either alpha GalCer or CpG.<br />
Intranasal immunisation studies performed in mice showed, that alpha GalCerMPEG<br />
exerts stronger adjuvant activities than the parental compound alpha GalCer. Coadministration<br />
of beta-galactosidase with alpha GalCerMPEG resulted not only in high<br />
titers of antigen-specific antibodies in serum, but also in the stimulation of stronger Th2<br />
and sIgA responses, both at local and remote mucosal effector sites (i.e., nose, lung,<br />
vagina). The new synthetic derivative alpha GalCerMPEG represents a promising tool for<br />
the development of immune interventions against infectious and non-infectious diseases.
Eva Schlosser, Carolina Otero, Benedikt Kessler, Mariola Edelmann, Rene Brunisholz,<br />
Daniel Legler, Marcus Groettrup<br />
A prostate carcinoma antigen reveals a new cytosolic class I<br />
processing pathway for endoplasmic reticulum targeted<br />
proteins<br />
Proteins that bear an N-terminal endoplasmic reticulum leader peptide are inserted into<br />
the lumen of the endoplasmic reticulum followed by cleavage of the signal peptide and<br />
glycosylation. It has been shown that major histocompatibility complex class I restricted<br />
T cell epitopes can be generated from these glycoproteins by the proteasome after their<br />
retrotranslocation from the endoplasmatic reticulum into the cytosol. In this study we<br />
show that an HLA-A*0201 restricted T cell epitope from prostate stem cell antigen, that<br />
is recognized by prostate carcinoma specific cytotoxic T lymphocytes, encompasses the<br />
cleavage site of the endoplasmic reticulum signal peptidase. This cleavage yields<br />
truncated peptides that fail to bind to HLA-A*0201 and to be recognized by cytotoxic T<br />
lymphocytes. Since processing of prostate stem cell antigen by signal peptidase occurs<br />
immediately after cotranslational insertion, the epitope must be synthesized and<br />
processed from polypeptides that have never reached the endoplasmic reticulum. The<br />
processing of this epitope relies on the activity of the proteasome and the transporter<br />
associated with antigen processing. This is the first example of a new pathway of class I<br />
processing that relies on the failure of endoplasmic reticulum targeted proteins to reach<br />
their compartment of destiny.
Mathias Konstandin, Guido Wabnitz, Hülya Aksoy, Martin Klemke, Thomas Dengler,<br />
Yvonne Samstag<br />
A sensitive assay for the quantification of integrin-mediated<br />
adhesiveness of human stem cells and leukocyte<br />
subpopulations in whole blood<br />
Adhesion of leukocytes is an early step in the formation of adaptive or innate immunity.<br />
Also in chronic inflammatory pathologies like atherosclerosis regulation of adhesiveness<br />
is pivotal for the accumulation of leukocytes within the vessel wall. Therefore, the<br />
quantification of adhesion is crucial for the understanding and monitoring of immune<br />
responses in patients. However, so far functional analysis of leukocyte adhesion was<br />
time consuming and required prior purification of cell populations from peripheral blood.<br />
This reduced the number of samples and cell populations that could be analyzed from<br />
limited patient material. Here we introduce a novel method that enables a rapid<br />
quantification of integrin mediated leukocyte adhesion in human whole blood using flow<br />
cytometry. The quantification relies on soluble multivalent immuncomplexes and is thus<br />
called “ligand-complex-based adhesion assay” (LC-AA). The LC-AA enables evaluation of<br />
both integrin affinity and avidity in T-cells, NK-cells and monocytes from as little as 20•l<br />
whole blood. Furthermore, with the LC-AA for the first time measurement of<br />
adhesiveness of extremely rare cell populations like CD34+ peripheral blood stem cells<br />
can be assessed in the absence of prior purification steps. Finally, small blood volumes<br />
needed for adhesion analysis with the LC-AA allow the evaluation of multiple cell<br />
subpopulations in large sample collectives, e.g. required in clinical studies.
Heiko Bruns, Frank Stegelmann, Steffen Stenger<br />
Abl-tyrosine kinase modulates immune responses to<br />
Mycobacterium tuberculosis<br />
Tyrosine kinases are checkpoints for activation of cellular immune responses. We<br />
hypothesized that Mycobacterium tuberculosis (M.tb.) interferes with tyrosine kinase<br />
function to circumvent killing by the host cell.<br />
We chose to focus on Abl (Abelson) - tyrosine kinase, because it is known to orchestrate<br />
immune response to mycobacterial infection like proliferation, adhesion and apoptosis.<br />
We measured TNF and IFN-gamma release by human PBMC in the presence of the<br />
specific tyrosine kinase inhibitor STI-571. STI-571 treatment inhibited TNF and IFNgamma<br />
release induced by mycobacterial antigens up to 90% (n=7). Furthermore<br />
inhibition of Abl-tyrosine kinase influenced lymphocyte migration. The cell-migration<br />
towards the chemokines CCL21 and CCL5, both required for the containment of<br />
Mycobacterium tuberculosis in granulomas, were affected. Specifically, migration of<br />
PBMC towards CCL21 was enhanced (three-fold), whereas movement towards CCL5 was<br />
reduced.<br />
These findings may be clinically relevant, because STI-571 (Imatinib) is a standard<br />
treatment in chronic myeloid leukaemia. Deviation of cellular immunity as described<br />
here may increase the risk for the occurrence of infectious diseases during Imatinib<br />
therapy.
Angelika Stöcklinger<br />
Ablation of Epidermal Langerhans Cells has no Impact on<br />
Gene-Gun mediated Immune Responses<br />
Gene gun immunization, i.e. bombardment of skin with DNA-coated particles, is an<br />
efficient method for the administration of DNA vaccines. Direct transfection of APC or<br />
cross-presentation of exogenous antigen acquired from transfected non-immune cells<br />
enables MHC-I-restricted activation of CD8+ T cells. Additionally, MHC-II-restricted<br />
presentation of exogenous antigen activates CD4+ T helper cells. Being the principal<br />
APC in the epidermis Langerhans cells (LC) seem ideal candidates to accomplish these<br />
functions. However, the dependence on LC of gene gun-induced immune reactions has<br />
not yet been demonstrated directly. This was primarily hampered by difficulties to<br />
discriminate the contributions of LC from those of other dermal dendritic cells. To<br />
address this problem we have employed Lang-DTR knock-in mice that allow for<br />
selective inducible ablation of LC. LC-deficiency, even over the entire duration of<br />
experiments, did not affect any of the gene gun-induced immune functions examined,<br />
including proliferation of CD4+ and CD8+ T cells, interferon-gamma secretion by spleen<br />
cells, antibody production, cytotoxic T lymphocyte activity, and development of<br />
protective anti-tumor immunity. Together, our data show that gene gun immunization is<br />
capable of inducing humoral and cell-mediated immune reactions independently of LC.
Brigitte Santner-Nanan, Nabila Seddiki, Cindy Zhu, Verena Quent, Anthony Kelleher,<br />
Barbara Fazekas de St. Groth, Ralph Nanan<br />
Accelerated age-dependent transition of human regulatory T<br />
cells to<br />
effector memory phenotype<br />
We and others recently described a method for isolating viable FoxP3+<br />
T regulatory cells (Tregs) by means of the surface phenotype<br />
CD4+CD127loCD25+. In this study, we used the new strategy to measure<br />
Treg numbers, phenotype and function at different ages. Mean<br />
percentages of CD4+CD127loCD25+ Tregs increased only slightly<br />
throughout life, from 6.10% in cord blood to 7.22 % in PBMC from<br />
adults between 20 and 25 years and 7.50% in PBMC from adults over the<br />
age of 60. In all age groups, a higher proportion of Tregs had<br />
acquired a CD45RA- memory phenotype compared with CD4+Foxp3-<br />
conventional T cells. This increase was entirely attributable to<br />
increased Tregs with an effector memory phenotype, whereas central<br />
memory phenotype cells were equally represented within the Treg and<br />
conventional CD4+ T cell populations. Expression of CD95 also differed<br />
between Tregs and conventional CD4+ T cells at all ages. However there<br />
was no difference in the suppressive capacity of the different naïve<br />
and memory Treg subsets. These results suggest that, compared with<br />
their conventional CD4+ T cell counterparts, Tregs undergo<br />
preferential differentiation from a naïve to an effector memory<br />
phenotype, driven by their specificity for self rather than foreign<br />
antigen.
Jasmin Herz, Julian Pardo, Hamid Kashkar, Erik Bos, Reinhard Wallich, Peter J. Peters,<br />
Elmon Schmelzer, Martin Krönke, Markus M. Simon, Olaf Utermöhlen<br />
Acid sphingomyelinase is a critical regulator of cytotoxic<br />
granule secretion by primary T lymphocytes<br />
Granule-mediated cytotoxicity is the major effector mechanism of cytotoxic CD8 + T<br />
cells. The phosholipase acid sphingomyelinase (ASMase) hydrolyzes sphingomyelin into<br />
phospocholine and ceramide and is localized in cytotoxic granules. Therefore, we<br />
hypothesised that ASMase might be involved in the secretion of cytotoxic granules.<br />
We report here that CD8 + T cells from ASMase-deficient (ASMase -/- ) mice are defective<br />
in exocytosis of cytotoxic granules, which results in markedly attenuated cytotoxic<br />
activity and significantly delayed elimination of the Lymphocytic<br />
Choriomeningitis (LCM) virus in vivo. Compared to wild type cytotoxic T cells, ASMase -/-<br />
CD8 + T cells contain equal amounts of granzyme- (gzm) and perforin- specific mRNA<br />
transcripts and functional protein. Strikingly, T cell receptor-mediated release of<br />
cytolytic effector molecules like granzyme A and hexosaminidase is more than ten-fold<br />
reduced in ASMase -/- CD8 + T cells. Cytotoxic granules of ASMase -/- CD8 + T cells are<br />
correctly directed towards the immunological synapse and fusion pores are readily<br />
formed that release low molecular weight dextrans yet retain the macromolecular<br />
complex of serglycin-proteoglycan, granzymes and perforin. Thus ASMase is critically<br />
involved in regulating the secretion of cytotoxic granules of CD8 + T cells.
Manuela Rossol, Undine Meusch, Holm Häntzschel, Sunna Hauschildt, Ulf Wagner<br />
Activated CD4 T cells induce TNF production in human<br />
monocytes via reverse signalling of membrane TNF<br />
Activated CD4 T cells are able to activate human monocytes by direct cell-cell contact,<br />
which leads to the production of pro-inflammatory cytokines. This process is believed to<br />
be important in chronic inflammatory diseases like rheumatoid arthritis (RA). Previously,<br />
we described membrane TNF expressed on activated T cells and TNF receptor (TNFR) 1<br />
and 2 expressed on monocytes as ligand/receptor pair responsible for monocyte<br />
activation. Now we propose a second mechanism participating in T cell-monocyte cell<br />
contact, namely reverse signalling of membrane TNF in which TNF acts as a signal<br />
transducing receptor.<br />
Several lines of evidence indicate the involvement of TNF reverse signalling in T cellmediated<br />
monocyte activation. (i) Membrane TNF is expressed on monocytes and<br />
TNFR2 is expressed on activated T cells. (ii) Blockade of TNFR2 on activated CD4 T cells<br />
by antibodies led to a diminished TNF production and Erk phosphorylation in monocytes.<br />
(iii) Resting CD4 T cells transfected with a TNFR2 plasmid induced TNF production in<br />
monocytes. (iv) Knockdown of TNFR2 on CD4 T cells by specific siRNA led to a<br />
decreased TNF production in monocytes. (v) Crosslinking of membrane TNF on<br />
monocytes by a plate-bound TNFR2:Ig construct induced a strong production of TNF.<br />
This TNF production depends on activation of MAP kinase Erk and casein kinase 1, the<br />
enzyme responsible for TNF phosphorylation.<br />
In conclusion, we identified reverse signalling of membrane TNF as a second pathway<br />
leading to TNF production in T cell-mediated monocyte activation. Accordingly,<br />
monocytes of RA patients treated with an anti-TNF antibody did not respond to<br />
activated T cells of healthy donors, pointing to a possible blockade of membrane TNF<br />
reverse signalling due to the anti-TNF antibody.
Milena Josefina Tosiek, Marcus Gereke, Jan Buer, Dunja Bruder<br />
Activation and regulation of autoreactive CD8 T cells in the<br />
lung<br />
The lung mucosa as it is positioned between the body and environment has to keep the<br />
balance between immunity and tolerance. To better understand mechanisms of<br />
induction and regulation of CD8 T cell-mediated immune responses in the lung we<br />
investigate an SPC-HAxCL4 transgenic mouse. This mouse expresses a model antigen<br />
(viral hemagglutinin, HA) in alveolar epithelial cells type II of the lung simultaneously<br />
with transgenic CD8 T cells of HA-specificity providing an autoimmune environment in<br />
the lung. Autoreactive CD8 lymphocytes escape from clonal deletion in the thymus and<br />
migrate to the lung. Histopathological analysis of SPC-HAxCL4 mice reveals progressing<br />
with age formation of lymphocytic infiltrations in the lung, resembling inducible<br />
secondary lymphoid tissue; nevertheless the disease is not lethal suggesting presence<br />
of some regulatory mechanisms.<br />
HA-specific lymphocytes of SPC-HAxCL4 mice, regardless of their autoreactive potential<br />
and infiltration of the lung, show naïve phenotype. In contrast while reisolated, HA-<br />
specific CD8 T cells respond in vitro to their specific antigen by massive proliferation<br />
which excludes their anergic phenotype.<br />
To investigate the acute form of CD8 T cell-mediated autoimmune response, we<br />
perform adoptive transfers of HA - specific CD8 lymphocytes into SPC-HA mice<br />
expressing HA in the lung epithelium.<br />
Surprisingly, CD8 T cells when transferred naïve, fail to proliferate and do not cause<br />
airway inflammation. In contrast, when cotransferred together with in vitro preactivated<br />
CD4 T cells of the same antigen specificity, naïve CD8 cells migrate to the<br />
draining BLN and the lung where they proliferate and trigger inflammation. These data<br />
suggest the importance of T helper cells in facilitating processes of priming and homing<br />
of autoreactive CD8 lymphocytes in the lung.<br />
The next matter of interest is the role of CD4 cells of HA-specificity in maintaining self-<br />
tolerance in SPC-HAxCL4 mice as well as the conditions under which the tolerance could<br />
be broken.
Xuefang Ren, Marion Schneider, Ying Wang, Lin Xu, Zhenggang Jiang, Fei Ye<br />
Activation induced cell death of CD4+CD25+Foxp3+ T cells by<br />
TCR re-stimulation involves a CD95/CD95L dependent<br />
mechanism<br />
In order to better understand how regulatory T cells (Treg) would be modulated, we<br />
isolated murine CD4+CD25+T cells from naive BALB/c or DO11.10 mice by MACS<br />
(magnetic cell sorting). Treg were functionally verified by suppressing an 3H cell<br />
proliferation assay. RT-PCR and intracellular staining were applied to detect the<br />
expression of Foxp3 in these cells. To induce actvation induced cell death (AICD), Treg<br />
from BALB/c mice were stimulated with anti-CD3/CD28 antibodies, and those from<br />
DO11.10 mice were incubated with OVA323-339 peptide plus antigen presenting cells<br />
(APCs), respectively. SuperArray and Real-time PCR were established to detect the<br />
apoptosis gene expression pattern in Treg. Flow cytometry was performed to determine<br />
the apoptosis of Treg. The influence of anti-FasL, anti-TRAIL neutralizing antibody and<br />
zVAD-fmk on AICD of Treg was evaluated.<br />
Results: CD4+CD25+Foxp3+ Treg act to suppress activation of the immune system and<br />
thereby maintain immune system homeostasis and tolerance to self. Management of<br />
Treg during an immune response is very significant. To augment Treg is advantageous<br />
in autoimmune disease, allergy and organ transplantation. On the contrary, depletion of<br />
Treg is beneficial to cancer patients. Activation induced cell death (AICD) is one of the<br />
main mechanisms for T cell contraction in vivo. We show here CD4+CD25+T cells from<br />
murine splenocytes could be successfully classified by MACS with 98% purity and<br />
specifically express Foxp3 which is the ‘master control gene’ for Treg cells and<br />
demonstrated suppression of proliferation of CD4+CD25-T cells. Treg can be induced to<br />
AICD by TCR re-stimulation, which may reach up to 39-45• following in vitro<br />
activationfor 7 days. The results of SuperArray and real-time PCR showed different gene<br />
expression patterns of TNF family members in freshly isolated Treg and activated Treg.<br />
TCR re-stimulation of Treg in vitro revealed a CD95/CD95L dependent pathway toward<br />
AICD. These findings open up to more detailed investigation of Treg modulatory events<br />
in vivo.
Alexei Gratchev, Julia Kzhyshkowska, Sheila Kannookadan, Miriam Ochsenreiter, Anna<br />
Popova, Xiaolei Yu, Isabelle Muller-Molinet, LiMing Gooi, Sergij Goerdt<br />
Activation of a TGF-β-specific multistep gene expression<br />
program in mature M2 macrophages requires glucocorticoidmediated<br />
surface expression of TGF-β receptor II<br />
Alternatively activated (M2) macrophages regulate steady state-, cancer- and<br />
inflammation-related tissue remodeling. They are induced by Th2-cytokines and<br />
glucocorticoids (GC). The responsiveness of mature macrophages to transforming<br />
growth factor (TGF)-β a cytokine involved in inflammation, cancer and atherosclerosis is<br />
currently controversial. Recently, we demonstrated that interleukin-17 receptor B<br />
(IL17RB) is up-regulated in human monocyte derived macrophages differentiated in the<br />
presence of Th2 cytokine IL-4 and TGF-β1. Here we show that mature human<br />
macrophages differentiated in the presence of IL-4 and dexamethasone (M2IL-4/GC )<br />
respond to TGF-β by 5-fold induction of IL17RB mRNA. Further TGF-β induced a gene<br />
expression program comprising 111 genes in mature human M2IL-4/GC , but not M2IL-4 which includes transcriptional/signalling regulators (ID3, RGS1) as early response<br />
genes, and immune modulators (ALOX5AP, IL17RB) as well as atherosclerosis-related<br />
genes (ALOX5AP, ORL1, APOC1, APOC2, APOE) as late response genes. Analysis of<br />
molecular mechanism underlying GC/TGF-β cooperation revealed that surface<br />
expression of TGF-βRII was high in M2GC and M2IL-4/GC , but absent from M2IL-4 , while<br />
the expression of TGF-βRI/II mRNA, TGF-βRII total protein and surface expression of<br />
TGF-βRIII were unchanged. TGF-βRII surface expression was dependent on GC dose in<br />
a range of physiological to therapeutic GC concentrations and determined the strength<br />
and duration of Smad2-phosphorylation-mediated signaling. In summary, mature<br />
human M2 macrophages made permissive to TGF-β by GC-induced surface expression<br />
of TGF-βRII activate in response to TGF-β1 a multistep gene expression program<br />
featuring traits of macrophages found within an atherosclerotic lesion.
Umme Amara, Miriam Kalbitz, Andreas Klos, Markus Huber-Lang<br />
Activation of Complement by the Coagulation System<br />
Introduction: Both, the complement and the coagulation system belong to the "first line<br />
of defence" and undergo massive activation early after severe injury. A dialogue<br />
between the two cascades has often been proposed but the precise molecular pathways<br />
of this interaction are still unclear. To elucidate the mechanisms involved, the effects of<br />
various coagulation factors on generation of the complement activation products C3a<br />
and C5a was investigated.<br />
Methods: In vitro cleavage of C5 or C3 in presence or absence of various coagulation<br />
factors (F) was determined in a time- and dose-dependent manner by ELISA and<br />
Immunoblotting. Biological activity of the cleavage products was also assessed by C3adependent<br />
mast cell (HMC-1)- and C5a-dependent neutrophil-chemotactic activity. Oneway<br />
ANOVA and Tukey multiple comparison test, p
Luisa Cervantes-Barragan, Ulrich Kalinke, Roland Züst, Constantino Lopez-Macias,<br />
Volker Thiel, Burkhard Ludewig<br />
Activation of myeloid cells through plasmacytoid dendritic<br />
cell-derived type I interferon secures control of murine<br />
coronavirus infection<br />
The secretion of type I interferons (IFN) is one of the fundamental aspects of the innate<br />
immune response against viruses. However, the role of type I IFNs in the pathogenesis<br />
of coronavirus infections has not yet been fully clarified, neither its importance for<br />
particular coronavirus infected cell populations. We have shown recently that<br />
plasmacytoid dendritic cell derived type I interferons (IFNs) are of prime importance for<br />
the initial control of mouse hepatitis virus (MHV) infection (Cervantes-Barragan Blood.<br />
2007 109:1131-7). In the present study, we have determined the major target cell<br />
populations of type I IFNs. To this end, we have first generated a series of chimeric<br />
mice expressing the type I interferon receptor (IFNAR) either on hematopoietic or nonbone<br />
marrow-derived cells. Early control of MHV depended mainly on IFNAR expression<br />
on hematopoietic cells. To establish which leukocyte subset responds most efficiently to<br />
type I IFN, mice conditionally deficient for the type I interferon receptor (IFNAR) on<br />
different leukocyte subsets were infected with MHV. This genetic analysis revealed that<br />
IFNAR expression on macrophages/neutrophils and dendritic cells is of prime<br />
importance for the early containment of MHV within secondary lymphoid organs, while<br />
IFN activity on B cells or T cells is not required for the clearance of MHV infection. Taken<br />
together, our results indicate that the protection of macrophages/neutrophils and<br />
CD11c-positive dendritic cells through type I IFN is essential for the control of murine<br />
coronavirus infection.
Alexander Donald McLellan, Patrizia Stoitzner, Jacquie Harper, Sarah Saunderson,<br />
Ralph Jack, Anthea Bouwer<br />
Activation of natural killer cells by dendritic cells stimulated<br />
with gram positive bacteria<br />
Interferon-gamma (IFNγ) release by natural killer (NK) cells plays a key role in the<br />
resolution of cancer or viral infection. We have previously shown that the cell wall<br />
components of Gram-positive bacteria stimulate a rapid release of IFNγ from human and<br />
murine leukocytes. The effect has also been found to be mimicked by the cell wall<br />
component lipoteichoic acid (LTA) but not by other Toll-like receptor-agonists. NK cell<br />
activation requires membrane-contact with bacteria-stimulated dendritic cells (DC), but<br />
is independent of the adhesion molecule LFA-1 and the NK cell activation molecule<br />
NKG2D. IL-12 and IL-18 expression was found to be essential for NK cell activation.<br />
Activation of DC/NK with whole bacteria was maintained in TLR2-/- and TLR4-/-<br />
backgrounds, however the stimulation of DC/NK with the cell wall component LTA was<br />
lost in the TLR4-/- background, further fuelling the controversy surrounding the role of<br />
this TLR in the recognition of Gram-positive bacteria. Despite inducing potent cytokine<br />
secretion in DC/NK cells, Gram-positive cell wall stimulation did not lead to increased<br />
natural or antibody-dependent (ADCC) cytotoxicity of NK cells against the NK-sensitive<br />
target YAC-1 or antibody sensitised A20 cells. We are currently investigating the in vivo<br />
potential of these adjuvants to drive NK cell activation and Th1 polarisation for the<br />
treatment of tumours or infectious diseases.
Dimitra Kotsougiani, Birgit Prior, Gertrud Maria Hänsch, Christof Wagner<br />
Activation of T lymphocytes in bacterial infection: production<br />
of interferon 4gamma, expression of the chemokine receptor<br />
CXCR6, and up-regulation of Toll-like receptors (TLR) in<br />
patients with implant-associated posttraumatic osteomyelitis<br />
Implant-associated posttraumatic osteomyelitis is caused by bacterial biofilms, mostly<br />
consisting of staphylococci species that colonize devices used for osteosynthesis, such<br />
plates, nails, or screws, or prosthesis for joint replacement. In most cases, removal of<br />
the infected implant is required. During surgery, cells having infiltrated the infected site<br />
can be collected for phenotypical and functional characterization. Predominantly highly<br />
activated polymorphonuclear neutrophils (PMN) were found as well as T lymphocytes,<br />
the latter amounting to approximately 20 % of infiltrated cells. The majority of the<br />
infiltrated T cells expressed CXCR6, a homing receptor for non-lymphoid tissue, while<br />
CXCR6 expression on peripheral T cells was well below 20 %.<br />
The infiltrated T cells, particularly the CD8+CD28-, produced 4gamma IFN, while the<br />
peripheral blood T cells obtained from the same patient did not. Moreover, again<br />
predominantly on the infiltrated T-cells Toll-like receptors were expressed. TLR1, TLR2<br />
or TLR4 were found on small, but conspicuous T-cell populations that also expressed<br />
CD11b+. The data lead to the following conclusion: persistent, localised bacterial<br />
infections lead to the activation of T cells, and their infiltration into the infected site. It<br />
is feasible that by producing 4gamma IFN the T cells enhance the efficiency of the local<br />
effector cells, particularly of the PMN, and thereby support the local host defence.
Eva Distler, Catherine Wölfel, Sylvia Köhler, Marion Nonn, Elke Schnürer, Ralf G.<br />
Meyer, Christoph Huber, Thomas Wölfel, Udo F. Hartwig, Wolfgang Herr<br />
Acute myeloid leukemia (AML)-reactive cytotoxic T<br />
lymphocyte clones rapidly expanded from CD8+ CD62L(high)<br />
+ T cells of healthy donors prevent AML engraftment in NOD/<br />
SCID IL2Rγnull mice<br />
Current in vitro techniques for isolating acute myeloid leukemia (AML)-reactive cytotoxic<br />
T lymphocytes (CTLs) from healthy donors are of relatively low efficiency and yield<br />
responder populations with unknown biological significance. We established an<br />
allogeneic mini-mixed lymphocyte-leukemia culture (mini-MLLC) approach by<br />
stimulating donor CD8+ T cells with HLA class I-matched primary AML blasts in<br />
microtiter plates. Before culture, CD8+ T cells were separated into CD62L(high)+ and<br />
CD62L(low)+/neg subsets enriched for naive/central memory and effector memory<br />
cells, respectively. In 8 different related and unrelated donor/AML pairs, numerous CTL<br />
populations were isolated that specifically lysed myeloid leukemias in association with<br />
various HLA-A, -B, or -C alleles. These CTLs expressed T-cell receptors of single Vβ<br />
chain families, indicating their clonal origin. The majority of CTL clones were obtained<br />
from mini-MLLCs initiated with CD62L(high)+ cells. Using antigen-specific stimulation,<br />
multiple CTL populations were amplified to 10e8-10e10 cells within 6-8 weeks. Two<br />
representative CTL clones were capable of <strong>complete</strong>ly preventing the engraftment of<br />
human primary AML blasts in NOD/SCID IL2Rγnull mice. We concluded that the mini-<br />
MLLC approach allows the efficient in vitro expansion of AML-reactive CTL clones from<br />
CD8+CD62L(high)+ precursors of healthy donors. These CTLs can inhibit AML<br />
engraftment in immunodeficient mice, suggesting their potential biological relevance.
Sarvari Velaga, Stephan Halle, Sabrina Dähne, Oliver Pabst<br />
Adaptation of Solitary Intestinal Lymphoid Tissue in response<br />
to microbial stimulation<br />
Besides Peyer´s patches, solitary intestinal lymphoid tissue (SILT) provides a structural<br />
platform to efficiently initiate immune responses in the murine small intestine. SILT<br />
consists of dynamic lymphoid aggregates that are heterogeneous in size and<br />
composition, ranging from small clusters of mostly lineage-negative cells known as<br />
cryptopatches to larger isolated lymphoid follicles rich in B cells. Here we report a novel<br />
technique that allows monitoring the dynamic behaviour of individual SILT over time.<br />
We demonstrate that colonization of germ free mice with commensal bacteria provokes<br />
an adjustment of the spectrum of SILT to that observed under specific pathogen free<br />
conditions by the conversion of pre-existing lymphoid structures into larger-sized SILT.<br />
Further enhanced microbial stimulation by means of oral infection with the<br />
enteropathogen Salmonella yields SILT that exceed the size spectrum of structures<br />
observed under pathogen free conditions. Salmonella directly infects SILT triggering a<br />
vigorous inflammatory response and immunopathology that leads to enlargement and<br />
morphological destruction of SILT. However, neither colonisation of germ free mice nor<br />
infections trigger the de novo formation of lymphoid tissue. The functional analysis of<br />
chemokinereceptor and integrin-deficient mouse strains indicates that the adaptation of<br />
SILT in response to microbial stimulation is mediated by a unique population of lineage<br />
negative SILT cells expressing the stem cell factor receptor cKit, chemokinereceptor<br />
CXCR5 and lymphotoxinα. In conclusion, our findings establish SILT, a lymphoid<br />
compartment frequently neglected in earlier studies, as a bona fide lymphoid tissue in<br />
the intestine that acts as a major site for Salmonella invasion and ensuing mucosal<br />
pathology.
Nancy Brewig, Adrien Kissenpfennig, Bernard Malissen, Alexandra Veit, Bernhard<br />
Fleischer, Uwe Ritter<br />
Adaptive immune response to Leishmania parasites is induced<br />
in the absence of epidermal Langerhans cells<br />
Epidermal Langerhans cells (LCs) represent a subset of dendritic cells (DCs), which<br />
appear in the outer compartment of the skin. The biological role of this DC<br />
subpopulation still remains controversial. In the experimental model of leishmaniasis<br />
LCs were discussed to be critical for regulation of cutaneous immune reactions.<br />
However, recently it was documented that dermal-derived DCs rather than epidermal<br />
LCs might represent the key players in experimental leishmaniasis. These contradictory<br />
findings might be explained by the overlapping phenotype of epidermal-derived LCs and<br />
dermal-derived DCs. To answer the question whether LCs are indeed involved in T cell<br />
mediated immune response against Leishmania (L.) major, knock-in mice expressing a<br />
diphteria toxin receptor under the control of the langerin (CD207) gene were used to<br />
conditionally ablate LCs. Following depletion, mice were infected subcutaneously into<br />
the footpad with L. major parasites and the immune response in the footpad draining<br />
lymph node (LN) and at the site of infection was analyzed over the time.<br />
Investigation of i) the course of infection, ii) the production of L. major-specific<br />
immunoglobulines and iii) the development of a memory T cell response revealed no<br />
differences between LC-ablated and control mice, indicating a minor role for LCs in the<br />
immune response against experimental leishmaniasis. To examine the cellular immune<br />
response in skin draining LNs cells were isolated and restimulated with soluble<br />
Leishmania antigen. We detected comparable proliferation of antigen specific CD4+ T<br />
cells in LC-ablated and control mice. In contrast, the proliferation of CD8+ T cells<br />
occured just up to day 10 after infection and was significantly diminished in LC-ablated<br />
mice. Therefore, we assume that LCs interact transiently with CD8+ T cells, known to<br />
play a minor role in the high dose infection model of experimental leishmaniasis, but not<br />
with CD4+ T cells.<br />
In conclusion, this is the first study demonstrating that epidermal LCs are dispensable<br />
for the induction of a protective immune response against Leishmania parasites.
Gaubert Sophie, Zimmermann Andra, Arbach Olga, Rossa Simone, Thiel Andreas,<br />
Voigt Sebastian, Ebell Wolfram<br />
Adenovirus-specific T cell therapy in paediatric stem cell<br />
transplants: Isolation and expansion of donor-derived T<br />
lymphocytes<br />
Human adenoviruses rarely cause severe clinical symptoms in healthy children and<br />
adults. However, they become a critical issue for immunocompromised patients and<br />
result in significant morbidity and mortality in allogeneic haematopoietic stem cell<br />
transplant children. Antiviral medication has not been unequivocally effective,<br />
encouraging new strategies. Virus-specific T cells are described as a key component in<br />
immunity against adenoviruses.<br />
In our lab a protocol was developed to generate adenovirus-specific T cell lines for<br />
paediatric haematopoietic stem cell-transplant patients under Good Manufacturing<br />
Practices, in order to infuse these cells in the early post transplant period. Starting with<br />
100 ml whole blood from the designated allogeneic healthy donor we stimulate<br />
peripheral mononuclear cells with a defined mix of overlapping peptides covering the<br />
hexon protein primary sequence (PepMix). Reactive cells are selected for interferongamma<br />
secretion using the CliniMacs device in a class A environment. Positively sortedcells<br />
are expanded for at least two weeks with autologous feeder cells and a cytokine<br />
cocktail. When ready, the T cell line is phenotyped for its specificity and cytotoxicity<br />
using autologous B-LCL, tested for the microbiological and viral status, and<br />
cryopreserved in three aliquots for prophylactic infusions on day +20, +60 and +100<br />
post-transplant with a cell dose of 1 x 107/m² body surface of the recipient. Our<br />
validation runs demonstrate that the final product contains variable mixtures of NKcells,<br />
CD4+ and CD8+ T-cells with specificity higher than 60 %. Further details of the<br />
protocol and clinical trials will be discussed.
Iris Bellinghausen, Barbara Häringer, Beatrice Lafargue, Tamara Hilmenyuk, Heinz<br />
Decker, Joachim Saloga<br />
Allergological implication of the quaternary hexameric<br />
structure of the cockroach allergen Per a 3.<br />
Cockroach allergens play a very important role in allergic diseases, especially asthma.<br />
The major allergen of the American cockroach (Periplaneta americana), Per a 3,<br />
naturally occurs as isoforms of hexamers. The aim of this study was to investigate<br />
whether the hexameric structure of Per a 3 influences its allergenicity and<br />
immunogenicity. Therefore, we compared the different effects of native hexamers and<br />
dissociated monomers of cockroach hemolymph extracts, containing almost only Per a 3<br />
proteins, on proliferation and Th1/Th2 cytokine production of CD4+ T cells in coculture<br />
with allergen-pulsed monocyte-derived dendritic cells as well as the leukotriene release<br />
of basophils. In Periplaneta americana-sensitized and non-sensitized donors the<br />
monomer was internalized faster by immature DC and induced higher proliferation and<br />
IFN-gamma production than the native hemolymph extracts (hexamers). While in nonsensitized<br />
donors IL-4 and IL-5 as well as IL-10 production were also increased after<br />
stimulation with monomeric Per a 3-pulsed DC, Th2 cytokine and IL-10 production were<br />
only enhanced in Periplaneta americana-sensitized donors using hexameric Per a 3pulsed<br />
DC. Furthermore, in the leukotriene release assay the monomer was less<br />
effective than the hexamer. Our data indicate that the quaternary structure can<br />
influence both allergenicity and immunogenicity, also depending on the sensitization<br />
status. In addition, the monomeric variant of Per a 3 allergens could be a possible<br />
candidate for a specific immunotherapy because the IgE-mediated allergic reaction and<br />
the Th2-inducing capacity are diminished while the Th1-inducing capacity is retained.
Ingrid Schuster, Elfriede Eppinger, Christoph Salat, Bernhard Frankenberger, Joachim<br />
Ellwart, Elfriede Nößner, Dirk Busch, Angela Krackhardt<br />
Allorestricted T cells with high specificity for the FMNL1derived<br />
peptide PP2 show tumor reactivity but also limited<br />
alloreactivity against other MHC alleles – implications for<br />
adoptive T cell therapy using allorestricted T cell receptors<br />
Cell-based immunotherapy in settings of allogeneic stem cell transplantation or donor<br />
leukocyte infusions has curative potential, especially in hematological malignancies.<br />
However, this approach is severely restricted due to graft-versus-host-disease (GvHD).<br />
Therefore, we aimed to generate HLA-A2-allorestricted T cells with defined specificity<br />
using the CLL-associated antigen Formin-related protein in leukocytes 1 (FMNL1) as<br />
target.<br />
After stimulation with peptide-pulsed T2 cells, we were able to isolate an HLA-A2allorestricted<br />
effector T cell clone specifically recognizing the peptide FMNL1-PP2<br />
(RLPERMTTL) derived from FMNL1. Potent lytic effector functions were observed against<br />
different tumor cell lines and EBV-transformed B cells. The T cells showed also reactivity<br />
against CLL cells.<br />
Investigating the specificity of this T cell clone, we observed high peptide specificity<br />
against T2 cells pulsed with the specific peptide, but not T2 cells pulsed with seven<br />
different control peptides. Moreover, T2 cells presenting the highly homologous HDAC6derived<br />
peptide RLAERMTTR in an HLA-A2-restricted manner were not recognized.<br />
However, the T cell clone was reactive against different HLA-A2 subtypes as well as two<br />
out of 16 HLA-A2- samples. Peptide pulsing of HLA-A2 subtypes increased target<br />
recognition in several cases indicating that the selected peptide might be presented by<br />
these HLA-A2 subtypes. Concerning the two HLA-A2- samples which have been<br />
recognized, MHC-restriction could be specified in one case to HLA-A*3303 by testing<br />
A*3303-transfected C1R cells. In this case peptide pulsing did not increase specific<br />
recognition of target cells suggesting that another peptide may be recognized in the<br />
context of HLA-A*3303.<br />
These data indicate that highly peptide-specific allorestricted T cells may harbour<br />
polyspecificity against different peptides and MHC molecules which can result in<br />
unpredicted cytotoxicity. This is certainly of special interest for the use of allorestricted<br />
peptide-specific T cell receptors for adoptive transfer.
Andrey Bogdanov, Tatyana Rybakova, Nikolai Belyaev<br />
Alpha-fetoprotein impair recovery of cell-mediated immunity<br />
normal function after tumor ablation<br />
It was shown tumor successfully grown when it were thought of as having escaped from<br />
immunosurveillance. Tumor-induced immunosuppression based on changing of immune<br />
cells functional activity, structure and viability. At that, tumor produces many factors<br />
that may involve in suppression of anti-tumor immunity. One of prospective factor is<br />
alpha-fetoprotein (AFP), which induced disorders of certain immunity effector reactions<br />
in vitro and provides immunosuppression in overproducing transgenic mice. We<br />
investigated the role of exogenous AFP in immunosuppression maintaining after noncancerous<br />
tumor ablation. In result, AFP exposures lead to derangement of normal<br />
function recovery of cell-mediated immunity after tumor nodule ablation. Thus, cytolytic<br />
activities of NK-, NKT- and •D8+ T cells as well as PHA-induced proliferations of NKT-<br />
and •D8+ T cells were much more low that in placebo-injected animals. Moreover,<br />
induced production of IFN-γ and TNF-α from NK cells and •D8+ T cells as well secretions<br />
of IFN-γ from NKT cells and TNF-β from •D8+ T cells were inhibited compare with<br />
placebo-injected animals. Dendritic cells from AFP-injected animals showed weak<br />
antigen-presenting ability and suppressed secretion of IL-12, IL-18 and IL-23. In<br />
addition, they secreted IL-10, PGE2 and TGF-β1, which not detected in placebo-injected<br />
animals. Investigation of effector •D4+ T cells demonstrated still higher Th2 cells<br />
prevalence on Th1 cells in AFP-injected animals whereas Th1 cells quantity was higher<br />
that Th2 cells in placebo-injected animals. Besides, TGF-β1- and IL-10-produced<br />
hematopoietic stem cells as well as functionally active of Th3- and Treg1 cells presented<br />
in spleen of AFP-injected animals. At that, values of all investigated parameters of AFPinjected<br />
animals were higher or similar with same parameters of tumor-bearing animals’<br />
prior tumor rejection. Consequently, AFP maintains and in some cases elevates tumorinduced<br />
immunosuppression through direct and/or indirect (via activation regulatory T<br />
cells and hematopoietic stem cells) ways even after tumor ablation.
Connie Schulze, Petra Heyder, Sandra Franz, Kerstin Sarter, Luis Munoz, Stefan<br />
Pöhlmann, Hanns-Martin Lorenz, Martin Herrmann, Martin Schiller<br />
Alteration of glycocalyx and exposition of mannose residues<br />
during apoptosis are essential for the clearance of apoptotic<br />
marterial<br />
Apoptosis and removal of apoptotic cells are essential for the maintenance of<br />
homeostasis in multicellular organisms. Defects in these processes lead to the<br />
development of autoimmune diseases. To date, a variety of receptors regulating uptake<br />
of apoptotic cells are known. Recently, alterations of sugar residues on the surface of<br />
apoptozing cells were observed. Thus, we wanted to characterize changes in the<br />
glycocalyx of dying lymphocytes. Further, we wanted to analyze whether these changes<br />
are important for the clearance of apoptotic cells. We analyzed the binding of lectins to<br />
apoptotic lymphocytes and subcellular fragments shed from these cells. A receptor for<br />
poly-mannose residues expressed on dendritic cells is DC-SIGN (DCS). To substantiate<br />
the role of DCS for the engulfment of apoptotic material we used Raji cells stably<br />
transfected with DCS (Raji-DCS). Engulfment by Raji-DCS and untransfected Raji cells<br />
of apoptotic material was compared.<br />
Apoptozing lymphocytes showed an early binding of Maakia amurensis lectin I (MAL I)<br />
and Sambuccus nigra agglutinine (SNA) (2h after apoptosis induction). These lectins<br />
recognize sialic acid residues. Further, on we detected a time dependent increase in the<br />
binding of Narcissus pseudonarcissus lectin (NPn), Griffonia simplificolia lectin II (GSL<br />
II) and Ulex europaeus agglutinine I (UEA I). NPn recognizes poly-mannose, GSL II is<br />
specific for N-acetyl-glucosamine, and UEA I for fucose residues. These lectins also<br />
bound to subcellular fragments shed from apoptozing cells. Co-incubation of subcellular<br />
fragments with Raji-DCS as well as untransfected Raji cells revealed that the uptake of<br />
subcellular fragments depends on the presence of DCS. Untransfected Raji cells showed<br />
a significantly attenuated and delayed engulfment of apoptotic material.<br />
Taken together we found an alteration of the glycocalyx on the surface of apoptotic cells<br />
as well as subcellular fragments shed from these cells during apoptosis. The recognition<br />
of altered glycocalyx especially of mannose residues by DCS is crucial for the<br />
engulfment of apoptotic material.
Sabine Höpner, Katharina Dickhaut, Jamina Eckhard, Shashank Gupta, Kirsten Falk,<br />
Olaf Rötzschke<br />
Amplification of CD4 T cell responses by catalysing antigenloading<br />
through MHC-loading Enhancer (MLE)<br />
In previous studies we identified a set of small molecular compounds which have the<br />
capacity to enhance loading of peptides/proteins onto MHCII molecules. We showed the<br />
enhancement of antigen-loading on soluble as well as membrane bound MHCII-<br />
Molecule. In particular adamantanethanole (AdEtOH) strongly accelerates the antigenloading<br />
rate. This effect is obvious for HLA-DR molecules expressing Glycine at position<br />
beta 86 of the pocket P1, which is located in the binding site. The dimorphic position<br />
(Glycine/Valine) determines the depth of the conserved pocket P1 in the MHC-molecule.<br />
MLEs transiently occupies the P1 and stabilizing the receptive conformation, which leads<br />
to rapid ligand exchange.<br />
We are able to show the correlation between the depth of the pocket P1 and allelespecificity.<br />
Additionally there is evidence for using allele-specific compounds, like<br />
AdEtOH as molecular tools for amplifying immune reactions in vivo.<br />
In mouse models we could obtain strongly enhanced specific CD4+- T-cell response<br />
against tumour associated antigens (TAA) by using MLE as vaccine additive<br />
(“adjuvant”). However the observation of rapid ligand exchange from outside by MLEs<br />
could be a risk factor for allergy or autoimmune diseases and gives rise to investigate<br />
environmental factors, which acts by the mechanism of MLEs. Preliminary data show<br />
modulation of autoimmune reaction in EAE-models using AdEtOH. So far, it is important<br />
to investigate the role of MLE in tumour vaccination as well as autoimmunity functions<br />
of small molecular compounds.
Stefanie Scheu, Philipp Dresing, Richard M. Locksley<br />
An IFNβ Reporter Mouse Model for the Visualization of the<br />
Initiation of the Type I Interferon Response in vivo<br />
Type I interferons (IFNs) were initially identified on the basis of their antiviral activities.<br />
However, recent studies place these cytokines at the interface between the innate and<br />
adaptive immune system, with additional important roles in bacterial and parasitic<br />
infections and antitumoral and immunomodulatory features. Structurally, type I IFNs<br />
can be grouped into a protein family of multiple IFNα subtypes, encoded by at least 13<br />
different genes in the mouse, and a single IFNβ subtype. The canonical pathway for<br />
IFNα/β production is initiated by the IRF-3 mediated expression of IFNβ leading to a<br />
positive feedback loop via the IFN type I receptor and IRF-7. Although the interferon<br />
produced first in most situations is IFNβ the celltypes responsible for this initial<br />
production remain unclear. To reveal the identity of these IFNβ producers in vitro and in<br />
vivo we created an IFNβ reporter knock in mouse which expresses the enhanced yellow<br />
fluorescent protein (eYFP) from a bicistronic mRNA linked by an IRES to the endogenous<br />
IFNβ message. In vitro experiments with bone marrow derived macrophages (BMDM)<br />
and dendritic cells (BMDDCs) show IFNβ production from distinct cell subpopulations in<br />
response to defined pathogen compounds. The highest frequencies of IFNβ/YFP + cells<br />
were observed in BMDMs after poly(I:C) treatment. This response was already<br />
detectable 4 hours after poly(I:C) stimulation with a peak at 24 hours. A small<br />
population of GMCSF-grown BMDDCs produced IFNβ after poly(I:C), CpG or LPS<br />
treatment whereas FLT3-L cultured B220 + pDCs responded mainly to CpG. Initial in vivo<br />
data show that after poly(I:C) injection IFNβ producing CD11c + cells localized to the<br />
marginal zone and T cell areas of the spleen whereas in lymph nodes accumulations of<br />
IFNβ producing cells could be observed in the subcapsular sinus. Additional data will be<br />
presented validating these IFNβ/YFP reporter mice as a valuable tool for the<br />
visualization and characterization of IFNβ producing cells in vitro and in vivo after<br />
challenge with defined pathogen compounds or in infection models.
Frank Schmitz, Antje Heit, Tobias Haas, Hermann Wagner<br />
An mTOR dependent transport mechanism of cytosolic<br />
receptors licenses TLR-independent recognition of nucleic<br />
acids<br />
Nucleic acid recognition by innate receptors constitutes an integral part of the<br />
mammalian anti-viral immune responses. The endosomally expressed Toll-like receptors<br />
(TLR)-3 and -9 recognize natural and synthetic double stranded (ds)RNA and single<br />
stranded (ss)DNA, respectively. The synthetic mimics of dsRNA, Poly I:C, and ssDNA<br />
(CpG-ODN) have been reported to display synergistic activation of innate immune cells<br />
and subsequent enhanced production of type I interferons, ultimative leading to<br />
increased cytotoxic T cell responses.<br />
When stimulating myeloid dendritic cells (mDC) with those ligands, we made the<br />
unexpected observation, that the production of interferon alpha (IFNa), so far<br />
considered a key feature of plasmacytoid DCs, is independent of TLR-3 and -9. The<br />
restricted translocation of both ligands to endosomal/lysosomal compartments leads us<br />
to hypothesize that the non-TLR nucleic acid receptors RIG-I and Mda5 are involved. To<br />
date, these receptors are described to operate exclusively in the cytosol. To elucidate<br />
the mechanism allowing cytosolic receptors to respond to endosomally located ligands,<br />
we investigated the role of autophagy, a process for transport of cytosolic material to<br />
lysosomes. Indeed, chemical inhibitors of autophagy did significantly reduce the<br />
observed IFNa production. Further, rapamycin, and inductor of autophagy operating at<br />
the cellular kinase mTOR was capable to increase the cellular response both to CpG-<br />
ODN plus Poly I:C and to Poly I:C alone.<br />
These findings suggest a novel transport mechanism of cytosolic receptors to<br />
endosomes/lysosomes for the recognition of extracellular nucleic acids. Ultimatively,<br />
this process may mechanistically explain the immunogeneicity of apoptotic host-cells to<br />
induce tumor-protective T cell responses.
Linda Sender, Zoe Waibler, Camilla Merten, Roland Hartig, Matthias Gunzer, Peter<br />
Reichardt, Ulrich Kalinke, Burkhart Schraven<br />
An unusual signalling signature suggests a molecular basis<br />
for the adverse side effects of anti-human CD28<br />
superagonistic antibodies<br />
Superagonistic CD28 antibodies (CD28SA) activate T-lymphocytes without concomitant<br />
perturbation of the TCR/CD3-complex. In rats and mice they induce the preferential<br />
expansion of regulatory T-cells and can be used for the treatment of autoimmune<br />
diseases. Therefore, it was proposed that CD28SAs might also be applicable for<br />
humans. However, a phase I clinical trial using the CD28 superagonist TGN1412 showed<br />
that the reactivity of human T-cells towards CD28SA-mediated stimulation dramatically<br />
differs from the response of mouse, rat and even monkey T-cells. The molecular basis<br />
for the severe side effects of CD28SAs in humans is as yet unclear. Here we show that<br />
two distinct CD28SAs (commercially available ANCD28.1 and original TGN1412) induce<br />
a delayed and weak but extremely sustained calcium response in human, but not in<br />
rhesus or cynomolgus monkey T-cells. The sustained Ca++-signal is accompanied by a<br />
global and extended activation of the major intracellular signalling pathways. Together<br />
these signals culminate in the synthesis of high amounts of pro-inflammatory cytokines,<br />
most notably IFNgamma and TNFalpha but also IL-2, -4, -5 and -10. Our findings<br />
suggest a molecular basis for the dramatic side effects that CD28 superagonists produce<br />
when administered to humans.
Lorena Martinez Gamboa, Henrik Mei, Karin Reiter, Kristin Kemnitz, Arne Hansen,<br />
Florian Emmerich, Abdulgabar Salama, Thomas Dörner<br />
Analysis of B cell subpopulations in patients with autoimmune<br />
thrombocytopenia: effects of splenectomy and implications<br />
for therapy<br />
Background: Evidences of B cell depletion (i.e. by anti-CD20, Rituximab) strongly<br />
supports an immunopathogenic role of B cells in autoimmune diseases, including RA,<br />
SLE and autoimmune thrombocytopenia (ITP). Disturbances of B cell homeostasis have<br />
been identified in patients with SLE and Sjögren’s syndrome. Because Rituximab as well<br />
as splenectomy are effective treatment options in severe ITP, and autoantibodies<br />
against platelets surface antigens represent an immunopathogenic key element in this<br />
entity, B cell abnormalities are expected to be of great importance for the disease.<br />
Therefore, we analysed distribution and activation of B cell subsets in peripheral blood<br />
samples from ITP patients and healthy donors (HD).<br />
Methods: B cell subsets were defined by FACS analysis of surface CD19 and CD27 in<br />
peripheral blood samples from non-splenectomized ITP patients (ITP) and patients in<br />
remission after splenectomy (“ITP-spl”), either splenectomized more than two years ago<br />
(“long-term-spl”) or less than 6 months ago (“recent-spl”), and HD. Activation of cell<br />
subsets was assessed by measurement of surface expression of CD95, CD38, ICOS-L,<br />
HLA-DR and the chemokine receptors CXCR3, CXCR4 and CXCR5. Migration capacity of<br />
B cells was assessed by chemotaxis assays towards CXCR3, CXCR4 and CXCR5 ligands.<br />
Results: Frequency of memory B cells was significantly decreased in ITP-spl patients<br />
compared to ITP patients without splenectomy or HD. Remarkably, this effect was more<br />
pronounced in long-term-spl patients. Differences were confirmed comparing absolute<br />
numbers of memory B cells between long-term-spl patients and HD, while no significant<br />
differences were observed for naïve or total B cells. Assessment of activation showed<br />
elevated number of CD95 expressing cells in ITP patients (either splenectomized or not)<br />
when compared to HD in all B cell subsets, indicating a steady activation state even<br />
after splenectomy. Cells expressing CXCR3 were reduced in all B cell subsets, specially<br />
in long-term-spl patients, while no differences were observed in cells expressing CXCR4<br />
nor CXCR5. Analysis of migration capacity towards CXCR4 or CXCR5 ligands showed<br />
also no differences between subsets when compared to HD, while CXCR3+ cells from<br />
ITP patients showed an increased migration towards CXCR3 ligands.<br />
Conclusion: Splenectomy apparently favours clinical remission in ITP patients through<br />
removal of the site of platelets destruction, and also leads to significant reduction of<br />
memory B cells. Our observations indicate different dynamics and regulation of diverse<br />
B cell subsets. Identification of splenic survival factors for memory B cells may have the<br />
potential for new therapeutic approaches targeting specific B cell subsets.
Timo Lischke, Andreas Hutloff, Richard A. Kroczek<br />
ANALYSIS OF CD4+ T CELL IMMUNITY IN VIVO<br />
We intend to study the development of CD4+ T cell memory in vivo. In a first step,<br />
many of the in vitro data on the expression of cell surface communication molecules<br />
have to be re-derived from in vivo experiments. To establish a baseline for future<br />
experiments aimed at defining the influence of inflammatory agents on the development<br />
of CD4+ T cell memory, we have adoptively transferred transgenic, ovalbumin (OVA)specific<br />
CD4+ T cells into syngeneic murine recipients, which were subcutaneously<br />
immunized with OVA + lipopolysaccharide. The draining lymph nodes were removed at<br />
defined time points and the OVA-specific CD4+ T cells were analysed for the expression<br />
of activation markers such as CD69 and CD25, and for the expression of the<br />
costimulatory molecules 4-1BB, OX40, ICOS, PD-1, and BTLA. CD69 and CD25 became<br />
detectable already 6 h after immunization on most OVA-specific CD4+ T cells; 4-1BB<br />
was hardly expressed at all. Expression of OX40 and ICOS could be seen at 12 h, with<br />
maxima at 24 h and 48 h, respectively. The kinetics for PD-1 and BTLA, the negative<br />
regulators of T cell activation, were more extended. Further, we determined the exact<br />
expansion and contraction kinetics of CD4+ T cells using CSFE labelling. In the late<br />
phase of the immune response (days 5 – 21), we recorded the development of OVA<br />
specific CD4+ CD44+ CD62L− effector-memory and CD44+ CD62L+ central-memory T<br />
cells, but did not observe the appearance of FoxP3+ regulatory T cells. The degree of T-<br />
B interaction was assessed by measuring the serum levels of OVA-specific IgG1, IgG2a,<br />
and IgG2b. This comprehensive analysis of the CD4+ T cell response will be<br />
instrumental for the future dissection of the decision points for memory formation in<br />
vivo.
Katja Maurer, Ellen Harrer, Andreas Goldwich, Kathrin Eismann, Silke Bergmann, Birgit<br />
Schätz, Sandra Müller, Thomas Harrer<br />
Analysis of CTL mediated immune selection in a dominant HLA<br />
B8-restricted CTL Epitope in Nef<br />
Objectives: To study the role of CTL escape for disease progression in HIV-1-infection<br />
we analyzed the CTL response to the dominant HLA B8-restricted CTL epitope<br />
FLKEKGGL (FL8) in HIV-1 Nef.<br />
Design: Fifty seven HLA-I-typed patients at different stages of HIV-1 infection were<br />
included in this study. One subject was used for longitudinal analyses.<br />
Methods: HIV-1 nef genes derived from plasma or PBMC were analyzed by PCR based<br />
sequencing. Nef FL8 - specific immune responses were detected by gamma-IFN<br />
ELISPOT using freshly isolated PBMCs and synthetic peptides. CTL lines were generated<br />
by peptide stimulation.<br />
Results: We could detect a significant correlation between mutations in the Nef epitope<br />
FL8 and the presence of the HLA-B8 allele. Mutations within the FL8 epitope decreased<br />
CTL recognition depending on the individual CTL line. The longitudinal analysis of a HIV-<br />
1-infected patient with good control of HIV-1 viremia for several years demonstrated<br />
the emergence of a K to Q – mutation at position P5 with rising viremia and disease<br />
progression.<br />
Conclusion: Our data demonstrate a strong selection pressure on the Nef FL8 epitope by<br />
CTL. The longitudinal analysis in a patient indicate an important role of CTL escape<br />
mutations for disease progression.
Simone Wüst, Denise Tischner, Anna Kleimann, Ralf Gold, Jan P. Tuckermann, Holger<br />
M. Reichardt, Fred Lühder<br />
Analysis of Glucocorticoid action in<br />
Experimental Autoimmune Encephalomyelitis (EAE)<br />
Currently application of high-dose glucocorticoids (GCs) is the standard therapy of acute<br />
relapses in multiple sclerosis. Despite their widespread use, the mechanisms of GC<br />
action in the treatment of neuroinflammatory disorders are not yet fully understood.<br />
This refers to the cell-types that are targets of GCs, the question whether genomic or<br />
rather non-genomic mechanisms are involved and the processes that are modulated. In<br />
order to address these questions, we made use of the well-established MOG35-55<br />
induced EAE model in the C57Bl/6 mouse.<br />
Therapeutic and preventive administration of dexamethasone ameliorates the disease<br />
course in a dose-dependent manner. To elucidate the role of the GR in mediating this<br />
effect we used heterozygous GR knock-out mice and hematopoietic stem cell chimeras.<br />
These experiments revealed that the cytosolic GR is a prerequisite for most GC actions<br />
since the therapeutic efficacy of high doses of dexamethasone was very low and<br />
transient in these models as demonstrated by the clinical scores and histological<br />
analysis of CNS inflammation. Induction of EAE in different conditional GR knock-out<br />
mice showed that, at the cellular level, expression of the GR in T cells is essential for<br />
the beneficial effects of GCs in neuroinflammatory diseases. At present experiments are<br />
under way that should help to identify the processes and genes that are specifically<br />
targeted by GCs in T cells. With the new knowledge in hands we anticipate that<br />
therapeutic approaches for multiple sclerosis may be improved.
Anett Schulz, Manuela Rossol, Matthias Pierer, Sybille Arnold, Holm Häntzschel,<br />
Christoph Baerwald, Ulf Wagner<br />
Analysis of polymorphisms in the TNFR2 gene in rheumatoid<br />
arthritis and possible functional relevance<br />
The gene for TNF receptor 2 (TNFR2) is located on chromosome 1p36.2, a region, which<br />
has already been described to be associated with susceptibility to autoimmune diseases.<br />
To determine a possible association of TNFR2 polymorphisms with rheumatoid arthritis<br />
(RA), PCRs with sequence specific primers were carried out to identify known<br />
polymorphisms in RA patients and controls. The frequency of the rare allele of the 1668<br />
T/G polymorphism, which is located in the 3´UTR of the TNFR2 gene, was higher in RApatients<br />
than in healthy controls (4.6% vs. 2.7%, OR 1.77, p=0.029). The<br />
polymorphism which leads to an amino acid change (position 676, Met/Arg) and the<br />
other two polymorphisms (1663 G/A, 1690 T/C) in the 3´UTR were equally distributed<br />
in RA patients and controls.<br />
Next we analyzed the expression of TNFR2 on immune cells in donors with the RA<br />
associated 3´UTR polymorphism or the 676 T/G polymorphism with a resulting amino<br />
acid change. The 3´UTR polymorphism resulted in a decreased expression of TNFR2 on<br />
CD4 T cells and monocytes in patients with RA, while the 676 T/G polymorphism had no<br />
influence on the expression of the protein on the surface of these cells. As the 676 T/G<br />
polymorphism results in an amino acid change, functional studies were carried out for<br />
this polymorphism. We previously described a TNFR2 dependent cell contact assay,<br />
which might resemble the pro-inflammatory milieu in RA. Monocytes of donors with and<br />
without the polymorphism were co-cultured with activated, fixed T cells and cytokine<br />
production was measured. We observed a decreased production of TNF, IL-8 and<br />
soluble TNFR2 in monocytes of healthy donors and RA patients with the 676 T/G<br />
polymorphism. The effects are specific for T cell induced monocyte activation, because<br />
neither LPS induced nor spontaneous production of TNF, IL-8 and soluble TNFR2 are<br />
dependent on the polymorphism.<br />
In summary, a 3´UTR polymorphism in the TNFR2 gene is associated with RA and leads<br />
to a diminished cell surface expression of the protein. The functional 676 T/G<br />
polymorphism results in a decreased cytokine production in an inflammatory setting.
Sonja Kothlow, Benjamin Schusser, Nicola Penski, Georg Kochs, Peter Staeheli, Bernd<br />
Kaspers<br />
Analysis of potential antiviral Mx activity in the chicken<br />
The chicken is a natural host of influenza A virus and the relevance of avian FLUAV<br />
infections for human health and the poultry industry is highlighted by the ongoing<br />
pandemic H5N1 outbreak. One of the key players in antiviral defence against FLUAV is<br />
the type I IFN system and studies in mice identified PKR and Mx proteins as main<br />
effectors of the IFN-induced antiviral state. Mx proteins are present in all vertebrates<br />
and belong to the dynamin superfamily of large GTPases. In the chicken, Mx was<br />
initially described as a cytoplasmic protein that lacks antiviral activity. But recent<br />
studies revealed that the chicken Mx gene is highly polymorphic and suggested that an<br />
Asn/Ser polymorphism at amino acid position 631 might determine antiviral activity.<br />
To examine whether the 631Asn isoform of Mx does mediate resistance against FLUAV<br />
infection embryo fibroblasts (CEF) from individual chicken embryos with defined<br />
homozygous Mx 631 genotype were generated. To induce Mx expression these cells<br />
were preincubated with different concentrations of chIFN&alpha and subsequently<br />
infected with different avian influenza viruses ChIFN treatment of CEF induced a dose<br />
dependent antiviral state and was effective for all viruses tested. Mx protein was<br />
detected in cells of both Mx isoforms but no differences in antiviral activity could be<br />
observed. To exclude additional polymorphisms in the Mx genes of these cells, identical<br />
chMx constructs differing only in AS631 were generated and are analysed for their<br />
antiviral properties.<br />
Hence further detailed studies will be necessary to finally identify factors which<br />
influence antiviral Mx activity in the chicken and IFN mediated resistance to FLUAV<br />
infection.
Andreas Jeron, Susanne Pfoertner, Tanja Toepfer, Jan Buer, Robert Geffers, Andres J<br />
Schrader<br />
Analysis of regulatory T cells in renal cell carcinoma<br />
In many cancer diseases an increased frequency of peripheral CD4+CD25+ regulatory T<br />
cells (Treg) could be observed correlated with poor prognosis of cancer patients.<br />
Therefore we characterized human Treg cells from patients with renal cell carcinoma<br />
(RCC), which is known to be an immunogenic tumor.<br />
Using magnetic cell separation we isolated highly pure CD4+CD25+ Treg and naïve CD4<br />
+CD25- T cells from the peripheral blood of 12 RCC patients and 11 healthy donors. In<br />
FACS analyses we confirmed elevated levels of peripheral CD4+CD25+ Treg cells in RCC<br />
patients. These cells were further analysed for expression profiles on the Human Treg<br />
Chip, a self-developed customized oligonucleotide microarray representing 350 Treg<br />
associated genes.<br />
Significant differentially expressed genes between CD4+CD25+ and naïve CD4+CD25-<br />
T cells were conducted to gene ontology resulting in a functional clusterization of the<br />
corresponding genes. We observed association to apoptosis, cell cycle, proliferation,<br />
signal transduction and regulation of transcription as well as to categories like<br />
cytokines, chemokines and surface receptors. Combining gene regulation and the<br />
functional background of the affected molecules we concluded that Treg cells derived<br />
from RCC patients might be less responsive to apoptotic stimuli, which might promote<br />
their accumulation in the periphery and hereby also tumor immune escape.<br />
Further experiments will compare peripheral Treg cells to tumor surrounding Treg cells<br />
to identify new targets explaining a potential crosstalk between tumor and Treg cell.
Nicole Warnecke, Burkhart Schraven, Luca Simeoni<br />
Analysis of TCR-mediated MAPK activation in primary T cells.<br />
The mitogen-activated protein kinase (MAPK) family includes three major wellcharacterized<br />
groups of kinases: the extracellular signal-regulated protein kinases<br />
(ERK), the p38 MAP kinases and the c-Jun NH2-terminal kinases (JNK). In immune<br />
cells, MAPKs preside to the regulation of lymphocyte development as well as to both the<br />
innate and the adaptive immune responses. T cells possess multiple possible ways to<br />
activate MAPKs. Previous data had suggested that RasGRP is required for ERK activation<br />
and positive selection while Grb2 regulates another branch of the TCR-mediated<br />
signaling cascade leading to JNK and p38 activation and negative selection in the<br />
thymus. To assess how MAPKs are activated in peripheral T lymphocytes, we performed<br />
RNA interference by using short interfering RNA (siRNA). Efficient downregulation of<br />
RasGRP1, but not of Grb2 or Sos1, resulted in a severe reduction of TCR-mediated Erk<br />
phosphorylation in human primary T cells. Thus, similar to thymocytes, also peripheral T<br />
cells activate ERK via a pathway involving RasGRP. Surprisingly, when we suppress<br />
Grb2 or Sos1 expression we found that ERK phosphorylation was enhanced. Finally, we<br />
demonstrated that Grb2 and Sos1 are dispensable during TCR-mediated JNK and p38<br />
phosphorylation in primary human T cells, thus indicating that JNK and p38 activation<br />
occurs through different mechanisms in mature in comparison to immature T cells. In<br />
summary, our data suggest that in primary T lymphocytes Grb2/Sos1 are not positive<br />
regulators of MAPK activation but rather appear to be component of a negative<br />
regulatory complex required to inhibit T-cell activation.
Eva Billerbeck, Hubert E Blum, Robert Thimme<br />
Analysis of virus specific FoxP3+ regulatory CD8+ T cells<br />
Regulatory T cells have been shown to be involved into the suppression of virus specific<br />
T cell responses. Recent studies focused on the regulatory CD4+CD25+ T cell subset,<br />
however, very little information is currently available about the role of regulatory CD8+<br />
T cells in virus infections. To address this important issue, we analyzed the expression<br />
of the regulatory T cell specific transcription factor FoxP3 in HCV-, Flu-, EBV- and CMVspecific<br />
CD8+ T cells from the blood of chronically HCV infected patients and healthy<br />
controls ex vivo and after peptide-specific stimulation. Of note, we did not see a<br />
significant FoxP3 expression in virus-specific CD8+ T cells ex vivo. However, in vitro<br />
stimulation of human PBMC with HCV- or Flu -specific peptides gives rise to two distinct<br />
antigen-specific T cell populations: FoxP3- and FoxP3+ CD8+ T cells. Of note, the<br />
expansion of HCV- and Flu specific FoxP3+ CD8+ T cells was blocked by IL-2- and IL-10neutralizing<br />
antibodies. The HCV- and Flu-specific FoxP3+ CD8+ T cells displayed typical<br />
surface markers of CD4+ regulatory T cells, such as GITR and CTLA-4 and had a cellcell<br />
contact dependent suppressive activity. Interestingly, the stimulation of PBMC with<br />
CMV specific peptides did not induce the generation of virus specific FoxP3+ regulatory<br />
CD8+ T cells. In sum, our results indicate that stimulation with a defined viral antigen<br />
leads to the expansion of two different cell populations: FoxP3- memory/ effector as<br />
well as FoxP3+ regulatory virus-specific CD8+ T cells that may contribute to the<br />
suppression of virus-specific T cells in a strict antigen-specific manner.
Julia Hoffmann, Ralf-Holger Voss, Ruth Frommolt, Matthias Theobald, Udo Hartwig<br />
Analyzing GVL-immune responses of p53-specific CD8+<br />
cytotoxic T cells to leukemia cell lines and acute myeloid<br />
leukemia in vitro and in vivo in humanized NOD/SCID/IL-<br />
2Receptor gamma-chain null mice<br />
Graft-vs-leukemia (GVL) immune responses are of key interest in allogeneic<br />
hematopoietic stem cell transplantation and are mediated by donor T-cells recognizing<br />
hematopoietic minor-histocompatibility-antigens as well as common leukemiaassociated<br />
antigens (e.g. WT1, p53). Adoptive transfer of leukemia-specific T cells<br />
would potentially increase GVL-immunity in the absence of graft-versus-host disease<br />
(GVHD). Using a C57BL/6 HLA-CyA2-Kb transgenic mouse model, we generated HLA-A2<br />
restricted, human p53- and PRAME-peptide specific CD8+ cytotoxic T lymphocytes<br />
(CTLs), which are able to recognize p53 peptide epitopes presented by p53-transfected<br />
tumor cells (e.g., EL4-A2Kb-p53, Saos2/143) as well as various leukemia cell lines<br />
naturally expressing p53 or PRAME (e.g., HL60, KG-1 and PCI13) as shown by 51Crrelease<br />
and CFSE-labelling based cytotoxicity assays. In ongoing experiments, p53specific<br />
CTL are also being tested for cytolytic activity to acute myeloid leukemia (AML)<br />
blasts, and results demonstrate AML-reactivity to selected samples.<br />
The potential of p53-specific CTL to mount GVL-immunity in vivo without GVHD is<br />
currently evaluated in a tumor protection model using NOD/SCID IL2R common gamma<br />
chain deficient (gamma c null) mice. After co-culture of CTL and p53 expressing tumor<br />
cells for 24h in vitro followed by adoptive transfer into NOD/SCID/IL2Rgamma c null<br />
recipients previously engrafted with purified HLA-A2+ CD34+ stem cells, persistence of<br />
tumor and human B cells as well as GVL-reactivity are examined by genomic PCR and<br />
flow cytometry, and the results will be presented.<br />
In summary, our results suggest that HLA-A2 restricted p53 specific CD8+ T cells are a<br />
promising tool to confer GVL immunity in the absence of GVHD.
Heiko Weyd, Lucie Doerner, Andrea Mahr, Nadine Eberhardt, Dagmar Riess, Bjoern<br />
Linke, Christine S. Falk, Peter H. Krammer<br />
Annexin I – an anti-inflammatory signal on the surface of<br />
apoptotic cells<br />
In multicellular organisms, apoptotic cell death takes place continuously to remove<br />
excess cells, maintaining tissue homeostasis. To preclude the release of noxious cellular<br />
contents and the development of autoimmunity, dying cells are rapidly cleared by<br />
neighbouring phagocytes, such as macrophages or dendritic cells (DC), which reside in<br />
peripheral tissues as sentinels of the immune system. Under steady state conditions,<br />
the uptake of apoptotic cells does not lead to an autoimmune response, even though<br />
many self-antigens are presented by professional antigen presenting cells. We reasoned<br />
that apoptotic cells might play an active part in preventing autoimmunity by modulating<br />
DC activity, possibly leading to the development of “tolerogenic” DC or to the induction<br />
of regulatory/anergic T cells. In an attempt to define signals on the surface of apoptotic<br />
cells involved in this process, we raised monoclonal antibodies against apoptotic cells<br />
and screened for their ability to differentiate between live and apoptotic cells. Using this<br />
approach, the lipid binding protein annexin I was identified on the surface of early<br />
apoptotic cells by an antibody which we named DAC5. Blocking experiments with DAC5<br />
as well as addition of recombinant annexin I confirmed a role of this protein in<br />
suppression of pro-inflammatory cytokine secretion by DC. Our results indicate that<br />
annexin I acts as an anti-inflammatory signal suppressing immune responses against<br />
self antigens, possibly contributing to the induction of peripheral tolerance.
Nicole Gerlach, Cassandra James, Ulf Dittmer<br />
Anti-retroviral effects of type I interferon subtypes in vivo<br />
Type I interferons (IFN) play a very important role in the innate immunity against viral<br />
infections. In mice type I IFN belongs to a multigene family including 14 IFNα subtypes<br />
and a single IFNβ subtype. IFNα/β is produced very early after infection and induces an<br />
antiviral state in the cells. Interestingly, individual IFNα subtypes differ in their<br />
biological activity. However, nothing is known yet about the exact biological function of<br />
IFNα subtypes in a retroviral infection. In the current study we have used the Friend<br />
retrovirus model to determine the differences in the antiviral effects of the IFNα<br />
subtypes (1, 4, 6, and 9) as well as to analyse the mode of action of these subtypes in<br />
vivo.<br />
After FV infection of mice only IFNα4 and IFNα9 mRNA transcripts could be detected in<br />
splenocytes. However, IFNα subtypes 1, 4, 6 and 9 were all biologically active against<br />
FV in vitro, but differed in their relative biological efficacies. Treatment of FV-infected<br />
mice with the IFNα subtypes IFNα1, IFNα4 and IFNα9, but not IFNα6 led to a reduction<br />
to various degrees of the viral load. IFNα subtype therapy regulated the cytokine<br />
production in the plasma of FV-infected mice and thus may modulate the subsequent<br />
innate and adaptive immune responses. Along these lines decreased viral load after<br />
IFNα1 treatment correlated with augmented FV-specific CD8+ T-cell and NK-cell<br />
responses, whereas the lower viral load in the IFNα4 and IFNα9 treated mice exclusively<br />
correlated with the activation of NK-cells in the spleen. The current results show that<br />
treatment of virus infections with selected IFNα subtypes can be an effective antiviral<br />
therapy. The knowledge about the different antiviral properties of the IFNα subtypes<br />
against retroviruses may facilitate their clinical use in retroviral infections in the future.
Christina Stöckle, Timo Burster, Thomas Rückrich, Alexander Beck, Christoph<br />
Driessen, Arthur Melms, Eva Tolosa<br />
Antigen Processing in the Human Thymus<br />
The interaction of the TCR of developing thymocytes with peptide-MHC complexes on<br />
thymic antigen presenting cells (APC) is crucial for T cell development, both for the<br />
positive selection of “useful” thymocytes as well as the negative selection of<br />
autoreactive and potentially harmful thymocytes. Therefore, the self-peptide-<br />
MHC complexes displayed by thymic APC such as dendritic and epithelial cells shape the<br />
T cell repertoire of each individual. These peptides are generated by intracellular<br />
proteases such as the cathepsins and AEP (MHC-II). Proteolytic destruction of potential<br />
T cell epitopes from self-antigens will lead to a lack of presentation and<br />
consequently, escape of autoreactive T cells recognising these epitopes. To draw a<br />
picture of the processes that govern generation or destruction of self-epitopes in<br />
thymic APC we studied the antigen processing machinery and self-antigen processing in<br />
the human thymus using a combination of approaches including RT-PCR, active site<br />
labeling and in vitro digests with lysosomes from separated APC subsets. While in<br />
peripheral dendritic cells the main immunogenic epitope of myelin basic protein is<br />
destroyed by cathepsin G, thymic DC <strong>complete</strong>ly lack CatG activity. Epitope destruction<br />
in these cells is dominated by cathepsin S and AEP. Thymic DC therefore<br />
differ remarkably in their antigen processing machinery from their peripheral<br />
counterparts.
Patrick C. Rämer, Susanne Haemmerling, Mathias H. Konstandin, Thomas Giese,<br />
Thomas J. Dengler, Sivanandam Vijayshankar<br />
Antigen-presenting capacity and T cell costimulation of<br />
endothelial progenitor cells is comparable to monocytes<br />
Endothelial progenitor cells (EPC) home to sites of vascular repair and therefore have<br />
potential implications in vascular diseases and in allogenic transplant settings. This<br />
study aimed to investigate the antigen presenting capacity of EPC and their T cell<br />
costimulatory capacity compared to HUVEC and monocytes.<br />
EPCs were isolated from PBMCs by adhesion to fibronectin. Coculture assays of EPC,<br />
HUVEC and monocytes were performed with allogenic CD4 T cells and were quantified<br />
by thymidine incorporation. Cytokine production was assessed by qRT-PCR (Light<br />
Cycler).<br />
Flow-cytometric analyses revealed an expression of endothelial antigens (e.g. KDR) as<br />
well as monocytic antigens (e.g. CD14). In PHA-based CD4 costimulation assays, EPC<br />
induced similar stimulation indices (35) compared to monocytes (30), while HUVECinduced<br />
proliferation was clearly less (~20). This T cell activation was strongly<br />
dependent on B7-CD28 interaction, as blocking with CTLA-4 fusionprotein resulted in<br />
70% decrease of proliferation. In addition, costimulation with EPC resulted in 6-fold<br />
upregulation of IL-2 mRNA after 8h, comparable to monocytes (7x), but significantly<br />
stronger than HUVEC (1.5x).<br />
In contrast to HUVEC, EPC activate naïve CD4/CD45RA T cells. Stimulation of PHAactivated<br />
naïve T cells with EPC resulted in a stimulation index of 380, similar to<br />
monocytes (340), while HUVEC failed to induce such strong proliferation (30).<br />
EPC were moreover able to present antigen in a HLA-DR restricted way. The peptide 85<br />
B MTB was effectively presented to DR3A3 hybridoma, a cell line specifically recognizing<br />
this peptide presented via HLA-DR. After preincubation of EPC with 85 B MTB, IL-2<br />
production of the hybridoma was 20fold increased.<br />
In conclusion, although EPC exhibit endothelial-like surface markers, functional<br />
characteristics place these cells more in a monocytic lineage. This is further supported<br />
by tests of antigen-presentation in which EPC resemble APCs more than actual<br />
endothelial cells. These findings will pertain to the use of endothelial precursors<br />
especially in a transplant setting.
Marcela Fajardo-Moser, Christine Hambrecht, Heidrun Moll<br />
Antigen-pulsed dendritic cell-derived exosomes as cell-free<br />
vaccines against infection<br />
Dendritic cells (DC) are the most potent antigen-presenting cells of the immune system<br />
with the unique capacity to initiate and regulate adaptive immune responses. We<br />
previously demonstrated that susceptible mice immunized with bone marrow-derived<br />
DC (BMDC) that had been pulsed ex vivo with Leishmania major antigens and activated<br />
with CpG were protected against infection. DC secrete a 60-100 nm diameter<br />
membrane vesicle population of endocytic origin, called exosomes. Besides MHC and<br />
costimulatory molecules, DC-derived exosomes bear several adhesion proteins, which<br />
are probably involved in their specific targeting and immunological properties. We<br />
investigated the capacity of exosomes secreted by antigen-pulsed and CPG-activated<br />
BMDC to induce protective immunity against leishmaniasis. Our data indicate that<br />
treatment with exosomes derived from antigen-pulsed and CpG-activated BMDC elicit a<br />
Th1-biasted Leishmania-specific immune response in vivo and confer long-lasting<br />
protection against infection. These data encourage us to further investigate the<br />
mechanisms responsible for the immunostimulatory capacity of DC-derived exosomes in<br />
vivo and in vitro in order to exploit their full potential as vaccination tools.
Christian Schütz, Andreas Mackensen, Jonathan P. Schneck, Jürgen Schölmerich,<br />
Mathias Oelke, Martin Fleck<br />
Antigen-specific CD8+ T cell depletion mediated by apoptosisinducing<br />
HLA-A2-Ig based artificial APCs<br />
Different cell based immunotherapy strategies have been developed to specifically<br />
modulate T cell mediated immune responses. To expand CD8+ T cells in antigenspecific<br />
fashion, we previously generated an “artificial-Antigen-Presenting-Cell” (aAPC)<br />
by immobilizing soluble HLA-A2-Ig dimer molecules and anti-CD28-mAb onto microbeads.<br />
Here we present phenotypical and functional data of aAPC-based “Killer-artificial-<br />
Antigen-Presenting-Cells” (•aAPC), generated to overcome problems related to current<br />
cell-based approaches for the treatment of autoimmunity. •aAPC were generated by<br />
coupling different amounts of an apoptosis-inducing α-Fas(CD95)-mAb onto the<br />
previously established aAPC. FACS-analysis revealed multiple HLA-A2-Ig based-•aAPC<br />
phenotypes, which induced Fas-mediated apoptosis in Jurkat T cells at different levels.<br />
To test, whether •aAPC could also be used to eliminate unwanted cytotoxic T<br />
lymphocytes (CTL) in an antigen-specific fashion, additional co-culture experiments<br />
were established with CMVpp65- and Melan-A26-35 specific CTL. High levels of<br />
apoptosis were only observed in CMVpp65 or Melan-A26-35 specific CTL co-cultured<br />
with •aAPC loaded with the corresponding peptide. Control •aAPC pulsed with a nonspecific<br />
peptide did not induce apoptosis in CTL. Elimination of specific CTL by cognate<br />
peptide-pulsed •aAPC was time and ratio dependent, not due to activation-induced-celldeath<br />
(AICD), and almost <strong>complete</strong>ly abrogated in the presence of a blocking α-FasmAb.<br />
This study demonstrates for the first time, that HLA-A2-Ig based-•aAPC can be used to<br />
eliminate unwanted CTL in an antigen-specific fashion through induction of Fasmediated<br />
apoptosis. Future studies will exploit this novel •aAPC technology to<br />
determine its potential for the treatment of autoimmune diseases and prevention of<br />
allograft rejections.
Heike Koehler, Andreas Hombach, Hinrich Abken<br />
Antigen-specific T cell activation is repressed by TGF-b which<br />
can be overcome by CD28 costimulation<br />
Solid tumors are frequently protected from a cellular anti-tumor attack by an<br />
immunological barrier, the predominant mediators of which are thought to be IL-10 and<br />
TGF-b. We explored the impact of these cytokines on the individual, tumor-specific T<br />
cell effector functions upon antigen engagement. Isolated, naïve CD4+ and CD8+ T<br />
cells were antigen-specifically redirected towards CEA+ tumor cells by expression of a<br />
recombinant T cell receptor (immunoreceptor) which binds CEA and triggers T cell<br />
activation via CD3z. Immunoreceptor activated T cells secrete IFN-g, proliferate, and<br />
lyse CEA+, but not CEA- tumor cells. Whereas IL-10 has no direct effect on<br />
immunoreceptor triggered effector functions of both CD4+ and CD8+ T cells, TGF-b<br />
represses proliferation, but neither IFN-g secretion nor specific cytolytic activities. TGFb<br />
mediated repression of proliferation is reverted by B7-CD28 costimulation.<br />
Consequently, combined CD28-CD3z signaling via recombinant immunoreceptor<br />
converts antigen-triggered T cell proliferation largely resistant to TGF-b mediated<br />
repression. This demonstrates that TGF-b induced suppression of a specific anti-tumor T<br />
cell attack is not primarily due to repression of cytolytic activities but indirectly to<br />
repression of T cell proliferation which, however, can be overcome by costimulatory<br />
CD28-CD3z signaling providing a strategy to overcome TGF-b mediated immunological<br />
tumor protection.
Nonsikelelo Mpofu, Konstantinos Iordanidis, Matthias Hardtke-Wolenski, Micheal. P<br />
Manns, Elmar Jaeckel<br />
Antigen-specific, Foxp3 transduced T cells for therapy of type<br />
1 diabetes<br />
In vitro expanded antigen specific CD4+CD25+ regulatory T cells (Tregs), have been<br />
shown to suppress autoimmune diabetes, suggesting a novel approach to cellular<br />
immunotherapy for autoimmunity. However to interfere with ongoing disease requires<br />
at least 10 6 in vitro expanded antigen specific Tregs which are difficult to obtain from a<br />
polyclonal repertoire. Hence an alternative approach would be to instruct naïve or<br />
antigen specific CD4+ T cells to obtain regulatory function. Indeed retroviral<br />
transduction of antigen specific T cells with Foxp3, a Treg lineage specific transcription<br />
factor, results in the generation of Tregs that can interfere with established<br />
autoimmunity in a non-lymphopenic nonobese diabetic (NOD) mouse model. However,<br />
conditions for transduction into NOD T cells have not yet been optimized. Furthermore<br />
very little is known about the in vivo effect of these Foxp3 transduced antigen specific T<br />
cells. Here we show that ecotropic pseudotyped viruses are more efficient at<br />
transducing NOD CD4+ T cells than VSVG pseudotyped viruses. In addition retroviral<br />
transduction of Foxp3 into NOD CD4+ primary T cells carrying the transgenic TCR from<br />
an islet Ag-specific T cell clone, BDC2.5, confers a Treg phenotype on these cells as<br />
they exhibit Treg signature characteristics such as in vitro anergy, suppressive capacity<br />
and upregulation of CD62L, CD25 and GITR. Adoptive transfer of Foxp3 transduced BDC<br />
T cells into NOD recipients shows that the cells home and proliferate in an antigen<br />
specific manner.
Anjana Singh, Miri Blank, Yehuda Shoenfeld, Harald Illges<br />
Antiphospholipid syndrome patients display reduced titers of<br />
soluble CD21 in their sera irrespective of circulating anti-beta-<br />
2-glycoprotein-I autoantibodies.<br />
B cells have a central role in the development of many autoimmune diseases, relating to<br />
their mechanism of activation, genetics and the successful application of anti-B-cell<br />
therapy. The membrane protein complex CD19/CD21 couples innate immune<br />
recognition by the complement system to the activation of B cells. A soluble form of the<br />
complement receptor CD21 (sCD21) is shed from the lymphocyte surface. sCD21 is able<br />
to bind all known ligands such as CD23, sCD23, Epstein-Barr-Virus and C3d in immune<br />
complexes. The levels of sCD21 in the serum may modulate the immunity. Here, we<br />
show the serum levels of sCD21 in sera of Antiphospholipid syndrome (APS) patients.<br />
APS is an autoimmune disorder in which autoantibodies cause heart attack, stroke and<br />
miscarriage. APS might may appear as primary or in association with Systemic Lupus<br />
erythromatosus (SLE) and other autoimmune diseases. Here we ask whether APS<br />
patients have different sCD21 titers compared to healthy persons and whether sCD21<br />
levels correlate with the presence of anti-ß2-GPI autoantibodies. We show that<br />
autoimmune APS patients have significantly reduced amounts of sCD21 in their sera,<br />
irrespective of the presence of anti-ß2-GPI autoantibodies. In our APS patients cohort<br />
additional SLE, vasculities, DVT (Deep vein thrombosis), fetal loss or thrombosis did not<br />
correlate to the reduced level of sCD21.
Stefan Lienenklaus, Marcin Lyszkiewicz, Jadwiga Jablonska, Siegfried Weiss<br />
ANTIVIRAL AND ILLUMINATED<br />
A NEW MOUSE LINE TO MONITOR β-INTERFERON INDUCTION<br />
Type I Interferons have been reported to be involved in a wide variety of diseases like<br />
viral and bacterial infections as well as inflammatory, allergic and autoimmune<br />
reactions. Within the group of Type I IFNs which consists of more than 10 α-IFNs and a<br />
single β-IFN, β-IFN has been shown to play a central role. In fibroblasts the <strong>complete</strong><br />
Type I IFN response depends on the presence of this “immediate early” interferon.<br />
Although this regulatory function has been carefully described, up to now the impact on<br />
Type I IFN dependent disease is poorly understood. Since spleen cells in contrast to<br />
fibroblasts can produce α-IFNs independent of β-IFN a key question is which cells are<br />
the Type I IFN producers in various situations. To adress this questions we generated a<br />
new mouse line in which the β-IFN gene can be inactivated tissue specifically. The cre<br />
mediated deletion places a luciferase gene under the β-IFN promoter and thus allows<br />
the sensitive detection of the β-IFN producing cells. Here we demonstrate the β-IFN<br />
monitoring capacity after deletion of the floxed β-IFN allele in the whole mouse. The<br />
heterozygote mice have an intact Type I IFN response and at the same time express<br />
luciferase if β-IFN is induced. Detecting the light emission we follow the β-IFN producers<br />
in uninduced as well as in virus infected mice. This new mouse line provides a powerful<br />
tool to pinpoint the β-IFN producing cells in different diseases and to characterise their<br />
function in the induction of the Type I IFN response.
Carola Pongratz, Benjamin Yazdanapanah, Hamid Kashkar, Martin Kroenke<br />
Antiviral implications of a convertible HIV-1 directed siRNA<br />
library<br />
RNA interference (RNAi) has been recognized as a powerful gene therapy strategy<br />
against RNA viruses like human immunodeficiency virus (HIV). However, the efficacy of<br />
transiently transfected or stably expressed RNAi is limited by the rapid development of<br />
escape mutant viruses. Here we describe the construction of a genome-wide<br />
randomized lentiviral RNAi library directed against HIV type-1. Employing appropriate<br />
selection procedures we have selected approximately 484 short interfering RNA<br />
sequences. Potent siRNA sequences were subcloned into a lentiviral expression cassette.<br />
The possible regulatory effects of the shRNA vectors on HIV expression were assessed<br />
by co-transfection with an HIV-derived pNL4.3-luc expression vector followed by a<br />
luciferase assay. More than 50% of the lentiviral expression cassettes proved to inhibit<br />
HIV-driven luciferase expression by greater than 70%. These siRNAs will be scrutinized<br />
for their binding to conserved or variable regions of HIV, respectively, and tested for<br />
their suitability of long-term inhibition of wild type HIV isolates.
Cosima Kretz, Bartlomiej Berger, Lucie Dörner, Heiko Weyd, Ingo H. Tarner, Ulf Müller-<br />
Ladner, Hanns-Martin Lorenz, Peter H. Krammer, Annegret Kuhn<br />
Apoptosis in Systemic Lupus Erythematosus:<br />
Influence on Immune Response and Peripheral Tolerance<br />
Systemic lupus erythematosus (SLE), a human autoimmune disease, is associated with<br />
abnormal immune responses; however, the pathogenesis of SLE is still not well<br />
understood. It has been suggested that accumulation of apoptotic cells in the tissue and<br />
circulation is associated with this disease. Several reports proposed that a <strong>complete</strong> and<br />
safe disposal of apoptotic remnants might be crucial for the maintenance of peripheral<br />
tolerance. Furthermore, it has been demonstrated that dendritic cells (DCs) cocultivated<br />
with apoptotic cells are suppressed in their production of inflammatory<br />
signals. The aim of this study was to investigate whether an impaired clearance of<br />
apoptotic cells or a defect in the apoptotic pathway itself is responsible for the<br />
manifestation of SLE. DCs derived from peripheral blood mononuclear cell samples were<br />
analyzed regarding their functionality in clearance of apoptotic cells. Preliminary data<br />
suggest that DCs of patients with SLE are highly sensitive to inflammatory stimuli. In<br />
addition, we observed that the activation of patients’ DCs could still be suppressed by<br />
apoptotic tumor cells. To determine if tolerance can be induced by apoptotic cells of SLE<br />
patients, we co-cultivated apoptotic neutrophils with U-937, a tumor cell line displaying<br />
DC qualities. Interestingly, we observed an increase of inflammatory parameters in<br />
some of the patients in contrast to normal healthy donors when apoptotic neutrophils<br />
were used. These data support our hypothesis that there is a molecular defect in<br />
peripheral tolerance in SLE patients, which might be due to impaired apoptosis. Further<br />
analysis is necessary to understand the mechanism and impact of these findings and to<br />
allow therapeutic approaches in the future.
Katharina Randers, Telja Pursche, Doreen Finke, Kirsten Jacobsen, Robert Hoerster,<br />
Christian Brockmann, Holger Hennig, Tony Marion, Sigfried Goerg<br />
Apoptotic DNA is able to induce in vivo IFN α production<br />
within the splenic marginal zone via a TLR dependent<br />
pathway.<br />
Introduction: Systemic lupus erythematosus is a multigenic autoimmune disease related<br />
to impaired waste disposal and elevated levels of Interferon alpha. Here we provide<br />
evidence that targeting of apoptotic DNA towards the splenic marginal zone explains<br />
TLR-9 pathway dependent elevated levels of Interferon alpha in lupus susceptible<br />
complement C4 deficient mice.<br />
Methods: Levels of intravascular DNA of wt mice or C4null mice were determined by<br />
ELISA and TUNEL dotblot assay. C57/Bl6 wildtype mice were injected with 4 µg<br />
apoptotic or native DNA with or without prior treatment with chloroquin. Splenic CD11b<br />
cells were isolated 6h later by magnetic cell sorting, mRNA was purified and IFN α and<br />
TLR9 were measured by RT-PCR.<br />
Results: We found that the levels of DNA were significantly higher in serum of C4null<br />
mice than in wt mice, but TUNEL dotblot assay detected apoptotic DNA in both mice.<br />
Application of apoptotic DNA showed a significant increase of Interferon alpha mRNA<br />
and TLR-9 in CD11b+ cells whereas native DNA resulted just in a minimal increase.<br />
Prior treatment with chloroquine reduced the expression of Interferon alpha and TLR-9<br />
mRNA in CD11b+ cells.<br />
Conclusion: Here we demonstrate that untreated C4null mice have elevated levels of<br />
intravascular DNA, which may be of apoptotic origin and that targeting of apoptotic DNA<br />
towards the marginal zone increases levels of Interferon mRNA in C4null mice as well as<br />
in wt mice. Blockade of in vivo TLR signal transduction with chloroquine prevented the<br />
apoptotic DNA dependent interferon alpha activation, demonstrating that endogenous<br />
apoptotic DNA plays an important role for the induction of interferon alpha SLE.
Katharina Weibhauser, Bernd Kaspers, Sonja Kothlow<br />
APPLICATION OF THE RCAS RETROVIRAL VECTOR SYSTEM<br />
FOR FUNCTIONAL IN VIVO STUDIES OF THE CYTOKINE BAFF<br />
IN THE CHICKEN<br />
We recently showed that ChBAFF, the chicken homolog of the mammalian B cell<br />
activating factor of the TNF family (BAFF), is an essential survival factor for peripheral<br />
mature chicken B cells. To further analyze the influence of ChBAFF especially on<br />
immature prebursal and bursal B cells, in vivo studies must be performed. We examined<br />
whether for this purpose the delivery of selected genes into developing embryos by<br />
RCAS based retroviral gene transfer provides an alternative to standard methods like<br />
protein injection.<br />
We generated RCAS-BP(A) vectors for the overexpression of chBAFF and the in vivo<br />
neutralization of the cytokine expressing the cross-reacting soluble human decoy<br />
receptor BCMA. Following the injection of day 3 embryos with infected fibroblasts stable<br />
expression of the retrovirally induced transgenes was detected both in chicken embryos<br />
and in birds up to more than two months of age. Immunhistochemical staining for viral<br />
protein revealed virus replication in all examined tissues giving strong positive signals in<br />
endothelial cells and the medulla of bursal follicles. To determine the biological activity<br />
of RCAS expressed proteins, B cell numbers in peripheral blood and spleen were<br />
analysed by means of flow cytometry and immunohistochemistry. 2 week old BAFF<br />
transgenic birds showed a more than 2-fold increase in B cell numbers in peripheral B<br />
cell compartments In contrast, neutralization of BAFF activity by BCMA-Fc expression<br />
lead to the nearly <strong>complete</strong> absence of B cells in secondary lymphoid tissues. BAFF<br />
overexpression also significantly increased amounts of serum immunoglobulins. Effects<br />
of transgen proteins were detectable for the <strong>complete</strong> examination period, though at<br />
two month of age differences decreased, probably due to homeostatic control<br />
mechanisms.<br />
These results demonstrate that the RCAS retroviral vector system can be effectively<br />
applied for the expression of soluble molecules and is a valuable tool to overcome the<br />
limitations of functional in vivo studies in the chicken.<br />
This work was supported by the “Elite-Förderung Bayern” and the DFG (GRK 1029).
Johanna Oberlies, Carsten Watzl, Thomas Giese, Claudia Luckner, Stefan Meuer,<br />
Markus Munder<br />
Arginine depletion by human granulocyte arginase impairs NK<br />
cell function<br />
The arginine-hydrolysing enzyme arginase is constitutively expressed by human<br />
granulocytes (PMN). Upon PMN cell death arginase is liberated and depletes arginine in<br />
the microenvironment. This amino acid depletion suppresses T cell proliferation and<br />
cytokine secretion and emerges as a key mechanism of immunosuppression during<br />
chronic inflammation.<br />
Here we show that PMN arginase also severely impairs several functions of primary<br />
human NK cells as well as lymphokine-activated killer cells (LAK). In arginine-free<br />
medium or medium depleted of arginine by liberated PMN arginase, NK cell proliferation<br />
and IL12/IL-18-induced IFN-&gamma secretion are severely diminished. We also see<br />
impairment of NK cell degranulation in the context of arginine depletion. NK cell viability<br />
is unaffected by the absence of arginine. The mechanism of NK cell suppression by<br />
arginine depletion is likely posttranscriptional since mRNA transcript frequency is<br />
unaffected upon NK cell activation in the absence of arginine. Finally, the arginase<br />
inhibitor N-&omega-hydroxy-nor-L-arginine is able to restore NK cell functions<br />
<strong>complete</strong>ly in our experimental system. Arginase inhibitors therefore seem to be<br />
promising pharmacological agents to treat unwanted suppression of the adaptive (T<br />
cell) as well as innate (NK cell) immune system.
Katrin Drögemüller, Martina Deckert, Ulrike Hellmuth, Monika Sakowicz-Burkiewicz,<br />
Dirk Reinhold, David Gutmann, Werner Müller, Dirk Schlüter<br />
Astrocyte gp130-expression is critical for astrocyte survival,<br />
downregulation of intracerebral immune responses and<br />
survival of experimental autoimmune encephalomyelitis and<br />
Toxoplasma encephalitis<br />
In cerebral inflammatory diseases, there is robust astrocyte activation; however their in<br />
vivo function is largely unknown. To study their role in experimental autoimmune<br />
encephalomyelitis (EAE), we generated mice deficient in astrocytic expression of gp130<br />
(GFAP-Cre gp130fl/fl), the signal transducing receptor for cytokines of the IL-6 family.<br />
numbers of GFAP+ astrocytes were strongly reduced in experimental autoimmune<br />
encephalomyelitis (EAE) of GFAP-Cre gp130fl/fl mice. Clinically, GFAP-Cre gp130fl/fl<br />
mice were characterized by a significantly more severe EAE and finally succumbed to<br />
chronic EAE, whereas control mice recovered. Histopathologically, inflammation and<br />
demyelination were more intense, widespread and persisted in GFAP-Cre gp130fl/fl<br />
mice. In addition, GFAP-Cre gp130fl/fl mice were significantly impaired in control of<br />
Toxoplasma gondii ultimately dying of a necrotizing Toxoplasma encephalitis (EAE).<br />
While GFAP+ astrocytes of infected gp130fl/fl control mice were activated and increased<br />
in number, which was associated with effective parasite control and survival of TE,<br />
GFAP-Cre gp130fl/fl mice lossed GFAP+ astrocytes during TE. In vitro, survival of T.<br />
gondii-infected, LPS- and TNF-stimulated astrocytes was also gp130-dependent. Thus,<br />
astrocytes are of crucial importance in EAE and TE, and gp130 is a critical survival<br />
factor of astrocytes in inflammatory CNS disorders.
Mihály Józsi, Stefanie Strobel, Hans-Martin Dahse, Wei-shih Liu, Peter F. Hoyer, Martin<br />
Oppermann, Christine Skerka, Peter F. Zipfel<br />
Autoantibodies block C-terminus of factor H in atypical<br />
hemolytic uremic syndrome<br />
Atypical hemolytic uremic syndrome (aHUS) is a severe renal disease and is associated<br />
with defective complement regulation. Mutations in several complement regulating<br />
genes and also factor H (FH)-specific autoantibodies have been described in aHUS<br />
patients. Our aim was to investigate the role of FH-autoantibodies in aHUS.<br />
Plasma samples of 51 aHUS patients were screened and FH-autoantibodies were<br />
identified in five cases, which corresponds to ~10% of the patients. Specificity was<br />
confirmed by removal of IgG from the plasma, which eliminated FH binding. Isolated<br />
IgG bound to FH and to its C-terminal fragment SCR19-20 in ELISA, and reacted with<br />
FH in Western blot assay. Furthermore, FH binding activity was contained in the F(ab’)2<br />
fragments of isolated patient IgG. For mapping of binding epitopes, recombinant FH<br />
deletion mutants were used in ELISA. This approach localized for all five autoantibodies<br />
the binding site to SCR19-20 of FH. C-terminal binding of the five FH-autoantibodies<br />
was verified in competition assays using recombinant FH fragments and domain mapped<br />
monoclonal antibodies.<br />
C3b-binding of FH was reduced by addition of patient IgG in ELISA. In hemolysis<br />
assays, patients’ plasma caused increased lysis of sheep erythrocytes. In one patient<br />
the autoantibody titer was followed during treatment. Plasma exchanges were effective<br />
in reducing the FH-autoantibody titer, which was accompanied by improvement in<br />
clinical parameters.<br />
Our data indicate that FH-autoantibodies associated with aHUS block the C-terminus of<br />
FH, which is essential for binding to C3b and to cellular surfaces. Autoantibody binding<br />
may also reduce the stability or alter the conformation of FH. These effects may result<br />
in a reduced FH activity and contribute to the development of aHUS.
Martin Schiller, Isabelle Bekeredjian-Ding, Petra Heyder, Norbert Blank, Klaus Heeg,<br />
Hanns-Martin Lorenz<br />
Autoantigens are translocated into apoptotic bodies during<br />
apoptosis<br />
Dysregulation of apoptosis and clearance of apoptotic debris contributes to the<br />
development of autoimmune disease like systemic lupus erythematodes (SLE). A<br />
hallmark of apoptosis is the formation of membrane vesicles (apoptotic bodies) which<br />
separate from the dying cell. In the present study we analyzed whether nuclear<br />
antigens are translocated into apoptotic bodies and whether apoptotic bodies are<br />
effectively engulfed by monocyte derived phagocytes. We found an accumulation of<br />
nuclear antigens within apoptotic bodies. In detail, we detected an accumulation of<br />
DNA, histones and ribonuclear proteins. Interestingly, other cytoplasmic molecules like<br />
p53, Hsp 70, cytochrome C, prohibitin, Lamin B and NUMA were excluded from<br />
apoptotic bodies. Purified apoptotic bodies were rapidly engulfed, when coincubated<br />
with monocyte derived phagocytes. In this context it is important to note that those<br />
molecules which accumulated in apoptotic bodies are preferred targets of the<br />
autoimmune response in SLE. Our data suggest that during apoptosis “immunogenic<br />
molecules” are actively translocated into apoptotic bodies. This is followed by an<br />
effective engulfement of apoptotic bodies by environmental phagocytes. In autoimmune<br />
diseases a defective clearance of apoptotic bodies or a dysregulation of apoptotic body<br />
formation may contribute to the development of autoimmunity and the formation of<br />
autoantibodies against structures present in apoptotic bodies.
Karin Loser, Sandra Balkow, Kerstin Klimmek, Claus Kerkhoff, Wolfgang Nacken,<br />
Thomas A. Luger, Stefan Beissert<br />
Autoreactive CD8+ T cell development in CD40L-mediated<br />
autoimmunity is controlled by S100A8 and A9 proteins<br />
CD40-CD40L signaling is involved in the development of autoimmunity and transgenic<br />
(tg) overexpression of CD40L in basal keratinocytes spontaneously leads to systemic<br />
autoimmunity as evidenced by autoantibodies, nephritis, proteinuria, and autoimmune<br />
dermatitis, which can be adoptively transferred by injecting CD8+ T cells into naive<br />
recipient mice. To identify genes involved in the development of MHC class I-restricted<br />
autoreactivity gene expression profiling of sorted CD8+ T cells from CD40L tg mice<br />
before and after onset of disease was performed and surprisingly, an increased<br />
expression of S100A8 and A9 genes both members of the S100 family of Ca-binding<br />
proteins was detected. To determine the functional relevance of S100A8/A9 expression<br />
for the development of autoimmunity in vivo, CD40L tg mice were crossed to S100A8/<br />
A9-/- mutants. Interestingly, CD40LxS100A8/A9-/- mice showed significantly reduced<br />
autoimmune dermatitis and markedly decreased numbers of skin lesion infiltrating<br />
lymphocytes. Since CD40L tg mice show renal IgG/IgM depositions and<br />
glomerulonephritis, renal function was analyzed in CD40LxS100A8/A9-/- mice.<br />
Importantly, CD40LxS100A8/A9-/- mice showed a <strong>complete</strong> loss of nephritis, renal<br />
immunoglobulin depositions, and proteinuria indicating normal kidney function.<br />
Additionally, the activation status of lymph node CD8+ T cells was determined in<br />
CD40LxS100A8/A9-/- mice demonstrating a decreased expression of cytotoxic/<br />
autoreactive markers like CD43 and granzyme B. CD8+ T cells isolated from<br />
CD40LxS100A8/A9-/- mice produced significantly reduced amounts of IL-17 a cytokine<br />
which has been suggested to mediate the inflammation associated with several<br />
autoimmune diseases. Moreover, adoptively transferred CD8+ T cells from<br />
CD40LXS100A8/A9-/- mice failed to elicit autoimmune dermatitis in recipient mice<br />
indicating that the expression of S100A8/A9 proteins may be critically involved in the<br />
pathogenesis of autoreactive MHC class I-restricted T cells in CD40L-induced systemic<br />
autoimmunity.
Bernd Lepenies, Klaus Pfeffer, Michelle Hurchla, Theresa Murphy, Kenneth Murphy,<br />
Juliane Oetzel, Bernhard Fleischer, Thomas Jacobs<br />
B and T lymphocyte attenuator (BTLA) ligation prevents<br />
cerebral malaria during P. berghei ANKA infection<br />
BTLA (CD272) is a coinhibitory receptor that is expressed on T and B cells and dampens<br />
T cell activation. In this study, we analyzed the function of BTLA during infection with P.<br />
berghei ANKA. This strain provokes a strong activation of T cells that is in C57BL/6 mice<br />
associated with a pathology that resembles cerebral malaria in humans. During the<br />
course of infection we found an induction of BTLA in several organs, which was either<br />
due to up-regulation of BTLA expression on activated T cells in the spleen or due to<br />
infiltration of BTLA-expressing T cells into several organs. In the brain we observed a<br />
marked induction of BTLA and its ligand HVEM during cerebral malaria, which was<br />
accompanied by an accumulation of predominantly CD8+ T cells, but also of CD4+ T<br />
cells. Application of an anti-BTLA mAb caused a significantly reduced incidence of<br />
cerebral malaria compared to control Ig. Treatment with this antibody also led to a<br />
decreased number of T cells that sequestered into the brain of P. berghei ANKA-infected<br />
mice. Our findings indicate that BTLA/HVEM interactions are functionally involved in<br />
sequestration of T cells in brain capillaries and that BTLA engagement is of importance<br />
to prevent immunopathology during infection with P. berghei ANKA. This study suggests<br />
that BTLA is a potential target for therapeutic interventions in severe malaria and might<br />
also have implications for the treatment of other inflammatory processes.
Janine Suffner, Kristin Hochweller, Natalio Garbi, Günter Hämmerling<br />
BAC-transgenic mice for depletion of Foxp3+ regulatory T cells<br />
It is well-documented that Foxp3+CD4+ CD25+ T cells, so called regulatory T cells<br />
(Tregs), play a fundamental role for the maintenance of self-tolerance. In order to<br />
analyse Treg function in vivo, we generated a novel BAC-transgenic mouse line,<br />
expressing eGFP, the diphtheria toxin receptor, and luciferase under the control of the<br />
Foxp3 locus. These Foxp3 GDL mice offer unique opportunities to study biology and<br />
function of Treg cells. Live Foxp3+ (GFP+) cells can be positively selected by flow<br />
cytometry. After treatment with 30ng DT/g bw for three times, we observed efficient<br />
depletion of luciferin expressing cells, visible in bioluminescence imaging (IVIS), as well<br />
as <strong>complete</strong> depletion of GFP+.<br />
The transfer of in vivo depleted CD4+ cells from Foxp3-GDL mice into Rag2-/- recipient<br />
mice resulted in severe colitis, weight loss and death of the recipient mice. This shows<br />
that DT treatment effectively depleted regulatory T cells necessary for prevention of<br />
colitis in immunodeficient recipients.<br />
Although we efficiently deplete all eGFP+ cells, the efficiency of depletion of CD4+ Foxp3<br />
+ cells varied between different mouse lines. Hence, the BAC does not appear to be<br />
expressed in all Foxp3+ cells. We observed that continuous depletion of GFP+Foxp3+<br />
Tregs leads to homeostatic expansion of the remaining GFP-Foxp3+ Tregs. Foxp3+ cells<br />
expanded most rapidly in the blood, followed by the spleen. GFP-Foxp3+ cells in<br />
mesenteric LN and thymus did not expand within 7 days.<br />
Further investigation includes the thymic involvement in homeostatic expansion of<br />
Tregs, the expansion of Tregs in different peripheral organs, and assessment of<br />
proliferative capacity and factors required for homeostatic expansion in the periphery.
Matthias Peiser, Juliana Koeck, Burghardt Wittig, Reinhard Wanner<br />
Bacterial lipopeptides activate human Langerhans cells via<br />
Toll-like receptor 2<br />
Dendritic cells (DCs) are central in linking the innate with the adaptive immune system.<br />
They are known to be equipped with a plethora of pathogen-detecting Toll-like receptors<br />
(TLRs). However, the pattern of TLRs on epidermal DCs, the Langerhans cells (LCs)<br />
remained as yet poorly characterized. As detected by monoclonal antibodies, we show<br />
that LCs from human skin express TLR1, 2, 5, 6, and 9, the cognate receptors for<br />
detection of bacterial-derived molecules. Langerin+LCs generated from monocytes and<br />
sorted by the CD1c molecule (CD1c+MoLCs) acquired a matured phenotype when<br />
activated by lipopolysaccharide (LPS), peptidoglycan (PGN), macrophage-activating<br />
lipopeptide 2 (MALP2) and lipopeptide Pam3CSK4. In human epidermal LCs, the TLR2<br />
ligand PGN, the TLR2/1 ligand Pam3CSK4, and the TLR2/6 ligand Pam2CSK4 enhanced<br />
the expression of the costimulatory molecules CD86 and CD40. TLR2-triggering<br />
lipopeptides activated CD1c+MoLCs by inducing IL-1 receptor-associated kinase (IRAK)<br />
1 phosphorylation, secretion of the proinflammatory cytokines interleukin (IL)-6 and<br />
tumor necrosis factor (TNF)α and migration in response to chemokines CCL19 and<br />
CCL21. Upregulation of TNFα and IL-6, nuclear factor-κB (NFκB) activation and<br />
proliferation of allogeneic CD4+T cells could be blocked by TLR2-specific antibodies in<br />
TLR2-stimulated CD1c+MoLCs. Coblocking of the TLR2 heterodimeric receptors by anti-<br />
TLR1/anti-TLR2 and anti-TLR2/anti-TLR6 indicated an exclusive role of TLR2 in IL-6<br />
induction in human LCs. Collectively, these findings demonstrate that TLR2 expressed<br />
by LCs mediates inflammatory responses to lipopeptides and plays a central role in<br />
sensing bacterial pathogens in human skin.
Konrad Bode, Klaus Heeg, Alexander Dalpke<br />
Bacterial origin histone deacetylase inhibitor butyric acid<br />
inhibits dendritic cells<br />
Posttranslational modifications of histones by acetylation are a major mechanism to<br />
modify chromatin structure and gene expression in eukaryotic DNA. In a recent work we<br />
could show that histone deacetylase (HDAC) inhibitors like trichostatin A or<br />
suberoylanilide hydroxamic acid (SAHA) in non-apoptotic concentrations strongly inhibit<br />
Toll-like receptor (TLR)-induced cytokine induction of dendritic cells. In the present<br />
work we investigated whether the HDAC inhibitor butyric acid, a product of the<br />
metabolism of some anaerobic bacteria, also inhibits dendritic cell activation by TLRs.<br />
We can show in bone marrow derived dendritic cells that butyric acid strongly inhibits<br />
the expression of several TLR induced cytokines like IL-12p40, IFNβ and TNFα on<br />
protein (ELISA and FACS-analysis) and mRNA (real-time RT-PCR) level. Whereas TLR<br />
stimulation resulted in transient histone H4 acetylation at selected regions of the IL-<br />
12p40 promoter as shown by chromatin immunoprecipitation, butyric acid induced a<br />
hyperacetylation of the whole IL-12p40 locus for a prolonged period. HDAC inhibitors<br />
had no effects on upstream NFκB activation and nuclear translocation as well as on MAP<br />
kinase signaling (immuno-blot and gel-shift) but recruitment of selected transcription<br />
factors to the IL-12p40 promoter region was impaired in the presence of butyric acid.<br />
The results give evidence that butyric acid affects immune cells by inhibiting HDACs.<br />
This might indicate that butyric acid is involved in the induction of tolerance towards the<br />
physiological bacterial flora in the mucosa of the intestine.
Marta Rizzi, Ulrich Salzer, Klaus Warnatz, Stefanie Hamm, Sigune Goldacker, Beate<br />
Fischer, Hans Hartmut Peter, Hermann Eibel<br />
BAFF Receptor expression in CVID patients<br />
BAFF Receptor (BAFF-R) is a member of the TNF-R superfamily and is expressed mainly<br />
on mature B cells. Common variable immune deficiency (CVID) is a primary immune<br />
deficiency characterized by hypogammaglobulinemia. Several genetic defects<br />
contributing to this phenotype have been identified (mutations in ICOS gene, TACI<br />
gene, CD19 gene). Our group recently identified a deletion mutation within the BAFF-R<br />
gene, removing the transmembrane domain of the protein. The homozygous mutation<br />
precludes the syntheses of functional BAFF-R. Therefore, B cell development in the<br />
BAFF-R deficient patient is arrested at the transitional B cell stage. As a result, the<br />
patient lacks IgG-producing plasmacells and is severely B lymphopenic.<br />
Searching for additional BAFF-R mutations we screened a subgroup of our cohort of<br />
CVID patients with very low number of B cells in peripheral blood (
Jenny Dieckmann, Susanne Rehfeld, Bernd Kaspers, Sonja Kothlow<br />
BAFF regulates the expression of bcl-2 family members in<br />
chicken B cells<br />
BAFF (B-cell activating factor of the TNF-family) is a central regulator of B cell<br />
homeostasis in mammals and birds. In vitro and in vivo studies with recombinant<br />
ChBAFF protein have shown that in contrast to man and mice in the chicken BAFF is not<br />
only involved in the regulation of mature B cells but also in the development of very<br />
early B cells stages in the bursa of Fabricius, the chickens unique primary B cell organ.<br />
ChBAFF does not induce cell proliferation but rather acts as an anti-apoptotic factor. To<br />
analyze whether this anti-apoptotic activity is mediated by the regulated expression of<br />
bcl-2 family members, detailed expression studies for chicken homologues of pro- and<br />
anti-apoptotic members of this key protein family in apoptosis were performed by<br />
means of RT-PCR and quantitative RT-PCR.<br />
ChBAFF is mainly expressed in an autocrine way by B cells in the bursa, where all bcl-2<br />
family members showed varying but continuous expression during embryogenesis and<br />
post hatch with significantly increased bok expression around hatch.<br />
For the characterization of BAFF effects in vivo the retroviral gene transfer system RCAS<br />
was used to either overexpress the cytokine or generate a functional BAFF knockdown<br />
by expressing the soluble decoy receptor huBCMA. Though cytokine overexpression did<br />
significantly increase the peripheral B cell number it did not affect the size of the<br />
embryonic and post hatch bursal B cell compartment or change the expression levels of<br />
bcl-2 family members in the bursa. In contrast, BAFF neutralisation significantly<br />
decreased both peripheral and bursal B cell pools. Strikingly, the few remaining B cells<br />
in the bursa of BCMA transgenic birds showed enhanced BAFF expression and massively<br />
increased amounts of anti-apoptotic bcl-2 and Nr13 mRNA. This suggests that in the<br />
bursa effects of the highly expressed endogenous BAFF are maximal and cannot be<br />
further enhanced by cytokine overexpression, but if endogenous BAFF signalling is<br />
blocked only those B cells survive which succeed to produce high amounts of BAFF and<br />
anti-apoptotic proteins.<br />
This work was supported by the DFG (GRK 1029).
Astrid Karbach, Evelyn Rossmann, Veronique Kitiratschky, Heidelore Hofmann, Markus<br />
M. Simon, Peter Kraiczy, Reinhard Wallich<br />
BbCRASP-1 of the Lyme disease spirochetes induces<br />
antibodies to nondenatured structural determinants in<br />
humans<br />
Pathogenic species of the Borrelia (B.) burgdorferi sensu lato complex express<br />
complement regulator-acquiring surface proteins (CRASP) that bind serum factor H and<br />
factor H-like protein 1 (FHL-1). The binding of factor H and FHL-1 to the bacterial<br />
surface is thought to locally increase the efficiency of C3b cleavage and simultaneously<br />
downregulate the alternative complement cascade. BbCRASP-1 is the dominant factor H<br />
and FHL-1 binding protein. Inactivation of BbCRASP-1 increases sensitivity to<br />
complement in vitro, and the introduction of BbCRASP-1 into serum-sensitive B. garinii<br />
strains imparts partial serum resistance suggesting that BbCRASP-1 plays an important<br />
role in immune evasion. Von Lackum et al. demonstrated that spirochetes express<br />
BbCRASP-1 in the mouse skin at tick bite site for 72 h post infection. However, it is still<br />
debated whether spirochetes express BbCRASP-1 during infection in humans. The goal<br />
of this study was to investigate BbCRASP-1 specific antibody responses in Lyme disease<br />
patients. We have compared the reactivity of serum antibodies derived from patients for<br />
various B. burgdorferi antigens, including BbCRASP-1, VlsE and OspC. The quality of<br />
antibodies generated during natural infection was analyzed by using nondenatured and<br />
denatured forms of the three recombinant outer surface proteins. In summary, the data<br />
obtained suggest that spirochetes express BbCRASP-1 during infection in humans.<br />
However, antibodies generated are exclusively directed towards nondenatured<br />
structural determinants of the protein. These findings may have important implications<br />
for the analysis of humoral immune responses to proteins in general.
Evelyn Rossmann, Peter Kraiczy, Pia Herzberger, Christine Skerka, Michael Kirschfink,<br />
Markus M. Simon, Peter F. Zipfel, Reinhard Wallich<br />
BhCRASP-1 of the relapsing fever spirochete Borrelia hermsii<br />
is a factor H and plasminogen binding protein<br />
Borrelia (B.) hermsii is the most frequent tick-borne relapsing fever agent in North<br />
America and is transmitted to humans through the bites of infected Ornithodoros ticks.<br />
B. hermsii employs several mechanisms to persist in the blood and evade immune<br />
response. Antigenic variation is clearly important to escape humoral immunity.<br />
Complement may be more important in opsonization and phagocytosis. Here we<br />
identified a novel member of the complement regulator acquiring surface protein<br />
(CRASP) family expressed by B. hermsii and designated BhCRASP-1. The ability to bind<br />
the complement regulators, factor H (FH) and factor H related protein 1 (FHR-1) but not<br />
FH-like protein 1 (FHL-1) has important implications for the host-pathogen interaction.<br />
In this study, we demonstrate that pathogens that bind FH exploit the regulatory<br />
activity of this protein, which serves to control C3b deposition and C3 convertase<br />
activity. BhCRASP-1 specifically interacts with the short consensus repeat 20 of FH.<br />
Heterologous expression of BhCRASP-1 in the serum-sensitive B. burgdorferi B313<br />
strain protects transformed B313 cells to some extent from complement-mediated<br />
killing. Furthermore, we show that FH and plasminogen can bind concurrently to<br />
BhCRASP-1, however via distinct, non-overlapping domains. Binding of plasminogen to<br />
BhCRASP-1 in the presence of host-derived urokinase-type plasminogen activator (uPA)<br />
leads to the formation of active plasmin that degrades high molecular weight<br />
glycoproteins, such as fibrinogen. Our findings will be helpful to further elucidate the<br />
molecular basis of B. hermsii interactions with host factors in the pathogenesis of<br />
relapsing fever.
Xin Ding, Niklas Beyersdorf, Gregor Blank, Fred Lühder, Kevin Dennehy, Ralf Gold,<br />
Thomas Kerkau, Thomas Hünig<br />
Blockade of CD28-B7 interactions by anti-CD28 antibodies<br />
protects from<br />
immunopathology in vivo<br />
Co-stimulation through CD28 achieved either by interactions of CD28 with B7 molecules<br />
or by agonistic anti-CD28 antibodies is critically involved in the initiation of T cell<br />
responses.<br />
Here we have studied the in vitro and in vivo properties of a novel mouse anti-mouse<br />
CD28 antibody, E18, which recognizes an epitope close to the B7 binding site. In vitro,<br />
both, the intact antibody and its Fab fragment, <strong>complete</strong>ly blocked the binding of B7<br />
molecules to CD28 expressed on mouse thymocytes. E18 Fab also inhibited T cell<br />
proliferation after stimulation with anti-CD3 or the superantigen staphylococcal<br />
enterotoxin B (SEB) in vitro, while the intact antibody triggered suboptimal costimulation.<br />
Application of E18 mAb to normal BALB/c mice in vivo or to newborn<br />
thymus organ cultures in vitro selectively reduced the generation of CD25+ FoxP3+<br />
regulatory T cells (Treg cells). In the periphery, a single injection of 250 •g E18 to adult<br />
BALB/c mice led to a gradual loss of CD4+ T cells from secondary lymphoid organs,<br />
while not reducing Treg cell frequencies among CD4 cells. Even after weekly treatment<br />
with 100 •g E18/ mouse for a period of 26 weeks only a two-fold reduction in Treg cell<br />
frequencies among CD4+ cells was observed, which thoroughly rebounded after<br />
cessation of treatment. Preventive application of E18 mAb prior to in vivo stimulation<br />
with SEB strongly reduced the proliferation of responding Vβ8+ CD4+ T cells. The<br />
capacity of mAb E18 to inhibit effector T cell responses in vivo translated into protection<br />
from acute graft versus host disease-associated lethality and provided efficient<br />
treatment for experimental autoimmune encephalomyelitis. This work was supported by<br />
grants from the DFG (Hu295/8), the GHS (1.01.1/06/001) and the Wilhelm Sander-<br />
Stiftung (2005.133.1).
Tea Gogishvili, Beate Geyer, Susanne Grunewald, Thomas Hünig<br />
Blockade of CD28-mediated co-stimulation ameliorates<br />
allergic airway inflammation in mice<br />
Allergic airway inflammation is characterized by a Th2-mediated immune response and<br />
cytokines, such as IL-4, IL-5 and IL-13 are predominantly responsible for eliciting the<br />
pathogenic changes. Activation of naïve T-cells involves not only engagement of the<br />
TCR by antigen, but also requires signals delivered through co-stimulation. Recent<br />
studies have demonstrated the central role of CD28 in the induction of allergic airway<br />
inflammation and immunotherapeutic options selectively targeting CD28 have been<br />
suggested to be desirable. To investigate the requirement for CD28 for functional<br />
activity of T-cells we examined the effects of an aCD28 mAb, which interferes with<br />
CD28-B7 interaction, in a murine model of allergic airway inflammation. Treatment with<br />
mAb was started before or after the allergic state had been established. Blockade of costimulation<br />
by aCD28 mAb moderately reduced the number of CD4+ T cells. This effect<br />
was associated with the reduced production of Th2 cytokines to the side of<br />
inflammation. Interestingly, treatment with aCD28 did not influence IL-10 and IFNgamma<br />
secretion. Examination of the airways demonstrated that OVA/Alum<br />
sensitization led to infiltration of eosinophils, which was significantly reduced after<br />
administration of aCD28. Moreover, total IgE was only slightly reduced, whereas<br />
synthesis of OVA-specific IgE was significantly inhibited in treated groups. Thus, our<br />
data demonstrate that blockade of co-stimulation with aCD28 mAb reduces Ag-driven<br />
immune response in a murine model of allergic airway inflammation.
Mostafa Jarahian, Carsten Watzl, Yasmin Issa, Peter Altevogt, Frank Momburg<br />
Blockade of natural killer cell-mediated lysis of NCAM140<br />
expressed on tumor cells<br />
Expression of the neural cell adhesion molecule (NCAM) on malignant cells of<br />
neuroendocrine, epithelial and hematopoeitic origin has been reported but its role for<br />
tumor cell recognition by the immune system remained uncertain so far. We have<br />
studied the cytotoxicity of the natural killer (NK) cell line NK92 and polyclonal NK cells<br />
from different donors against NCAM-deficient and NCAM-transfected tumors. While the<br />
pancreatic carcinoma PANC-1 and the glioblastoma T98G showed no enhanced<br />
susceptibility to NK lysis after NCAM transfection, de novo NCAM expression in HeLa<br />
cervical carcinoma, SHEP neuroblastoma and the multiple myeloma lines RPMI-8226<br />
and LP-1 was associated with significantly decreased lysis by NK cells. Binding of an<br />
NCAM-specific monoclonal antibody to NCAM-positive target cells was able to reverse<br />
the reduced lysis susceptibility. Conjugate formation of NCAM-expressing tumor cells<br />
with NK cells was blocked and could be restored by anti-NCAM. NK cell-expressed NCAM<br />
molecules which might engage in homotypic cis- or trans-interactions had no apparent<br />
inhibitory function. The known cis-ligands of NCAM, heparan sulfate proteoglycan and<br />
L1-CAM, were also not directly involved in NK inhibition. ICAM-1 cell surface expression<br />
was down-modulated in NCAM-transfected HeLa cells. ICAM-1 is involved in killer cell<br />
immune synapse formation. Its downmodulation may therefore contribute to the<br />
reduced lysis of NCAM-expressing target cells. We conclude that aberrant expression of<br />
NCAM on tumor cells of different histogenetic origin can lead to inhibition of target cell<br />
recognition and lysis by NK cells.
Nicole Bethke, Matthias Böthe, Siegfried Kohler, Matthias Niedrig, Andreas Thiel<br />
Bystander activation of recall antigen-specific CD4+ T-cells<br />
during primary immunization with live attenuated yellow<br />
fever virus<br />
Immunization with the attenuated yellow fever virus 17D-204 confers protection in the<br />
majority of vaccinees. However, the underlying mechanisms for the generation of<br />
specific cellular immunity have remained unclear so far. To gain insight into vaccinationinduced<br />
immunological processes we have analyzed absolute and relative frequencies of<br />
various immunocyte subsets and assessed yellow fever vaccine-specific and bystander<br />
activated CD4+ T-cells.<br />
Human blood was obtained from 8 healthy volunteer donors before and at 8 time points<br />
after vaccination with yellow fever virus 17D-204. Absolute and relative frequencies of<br />
CD4, CD8, DC, NK and B-cell subsets were analyzed by multicolour flow cytometry.<br />
Antigen-specific CD154+ CD4+ T-cell were analyzed for expression of IL-2, IFNγ, TNFα,<br />
IL-4 and IL-10 after stimulation with yellow fever vaccine 17D-204, recall antigens<br />
(CMVpp65, TT) and SEB.<br />
Hitherto all vaccinees responded with significant generation of yellow fever vaccinespecific<br />
CD154+ CD4+ T-cells with maximum responses for IL-2, IFNγ, TNFα and IL-4<br />
between day 10-14. In 6 out of 8 donors increased frequencies of CMV and/or TTspecific<br />
CD154+ CD4+ T-cells peaked shortly before or in parallel to the appearance of<br />
yellow fever vaccine-specific T-cells.<br />
Our data demonstrate that primary yellow fever immunization induces vaccine-specific<br />
CD4+ T-cells but also mobilizes recall antigen-specific CD4+ T-cells with polyfunctional<br />
features.
Olaf Gross, Andreas Gewies, Katrin Finger, Martin Schäfer, Tim Sparwasser, Christian<br />
Peschel, Irmgard Förster, Jürgen Ruland<br />
Card9 controls a non-TLR signaling pathway for innate antifungal<br />
immunity<br />
Fungal infections are increasing worldwide with the dramatic rise in immunodeficiencies<br />
including AIDS. However, immune responses to fungi are poorly understood. Dectin-1 is<br />
the major mammalian pattern recognition receptor for the fungal component zymosan.<br />
It represents the prototype of innate non-Toll like receptors (TLRs) containing<br />
immunoreceptor tyrosine-based activation motifs (ITAMs) related to those of adaptive<br />
antigen receptors. Here we identify Card9 as a key transducer of Dectin-1 signaling.<br />
While being dispensable for TLR/MyD88 induced responses, Card9 controls Dectin-1/Syk<br />
mediated myeloid cell activation, cytokine production and innate anti-fungal immunity.<br />
Card9 couples to Bcl10 and regulates with Bcl10/Malt1 zymosan induced NF-κB<br />
activation. Yet, Card9 is dispensable for antigen receptor signaling that utilizes Carma1<br />
to link to Bcl10/Malt1. Thus, our results define a novel innate immune pathway and<br />
indicate that evolutionary distinct ITAM receptors of the innate and adaptive system<br />
employ diverse adaptor proteins to selectively engage the conserved Bcl10/Malt1<br />
module.
Christina Stöckle, Vinod Sommandas, Hubert Kalbacher, Athur Melms, Eleni<br />
Adamopoulou, Ekkehard Weber, Christoph Driessen, Bernhard Boehm, Eva Tolosa,<br />
Timo Burster<br />
Cathepsin distribution in primary human antigen presenting<br />
cells<br />
Distinct proteases are required for the processing of antigens in order to make them<br />
suitable for loading onto major histocompatibility complex (MHC) class II molecules for<br />
presentation to CD4+ T cells. Several classes of cathepsins, including cysteine and<br />
aspartate, are involved in this processing. In addition, we recently described a serine<br />
protease cathepsin G (CatG) as a new member of this antigen processing machinery.<br />
CatG was detected in primary human B cells, in contrast to B cell lines and active CatG<br />
was evident in primary human dendritic cells (DC), but not in monocyte-derived DC. In<br />
vitro experimentation demonstrated that CatG degraded the immunodomminant T cell<br />
epitope of the multiple sclerosis-associated autoantigen myelin basic protein (MBP).<br />
Here we directly compared the cathepsin distribution of primary B cells with both DC<br />
subsets: myeloid DC (mDC) and plasmacytoid DC (pDC). Higher levels of CatG and<br />
CatD were found in pDC compared to mDC or B cells. During maturation of mDC CatG<br />
expression was decreased, resulting in suppressed T cell activation when pulsed with<br />
tetanus toxoid C-fragment (TTC). The expression of other cathepsins was to a large<br />
extent unchanged. We therefore propose that CatG is crucial in processing of TTC in<br />
primary human mDC.
Marion Leick, Tanja Hartmann, Susann Ewers, Andrea Diefenbacher, Robert Nibbs,<br />
Meike Burger<br />
CCL5 upregulates surface expression of the orphan atypical<br />
chemokine receptor CRAM-A/B in a heparin sulphate<br />
dependent manner in pre-B acute lymphoblastoid leukemia<br />
cells<br />
Chemokines work as cellular recruitment molecules. Specific combinations of<br />
chemokines, chemokine receptors, and adhesion molecules determine which subgroups<br />
of leukocytes migrate and what their destinations are. These migratory processes are<br />
also regulated by the availability and binding of chemokines on endothelial layers by<br />
interactions with glycosaminoglycans and atypical chemokine receptors that are<br />
described as silent or decoy receptors. Here, we report that pre-B acute lymphoblastoid<br />
leukemia cells Nalm6 and G2 express transcripts of a rare distributed splice variant of<br />
the atypical orphan receptor CRAM-A. These pre-B cells show high surface expression of<br />
CRAM in connection with CCL5-mediated functional responses. We investigated these<br />
responses in detail in Nalm6 cells that do not express any of the known CCL5 receptors<br />
but still specifically phosphorylate ERK1/2 in response to CCL5 stimulation. CCL5 did not<br />
induce calcium responses or migration in Nalm6 cells. CRAM-A/B transfected cell lines<br />
also did not show any migratory responses but a change in actin polymerization<br />
together with ERK1/2 phosphorylation. In addition, CCL5-induced p44/42<br />
phosphorylation was not inhibited by pertussis toxin suggesting that CRAM-A/B does not<br />
signal via Gi proteins. Intriguingly, CRAM surface expression on Nalm6 cells is<br />
specifically upregulated in response to CCL5 but not to other chemokines. The<br />
upregulation of surface expression follows distinct time and concentration kinetics and is<br />
mediated by heparin sulfate binding of CCL5 together with CCL5 binding to CRAM.<br />
Radioactive ligand binding assays also indicate low affinity CCL5 binding directly to<br />
CRAM. Our results characterize CRAM-A/B as belonging to the group of atypical<br />
chemokine receptors that rather play a role in modulating chemokine induced immune<br />
responses than in triggering direct motility.
Uta Elisabeth Höpken, Susann Winter, Kerstin Krüger, Armin Rehm, Martin Lipp<br />
CCR7 REGULATES LYMPHOCYTE EGRESS AND RECIRCULATION<br />
THROUGH BODY CAVITIES<br />
Continous lymphocyte circulation from the blood into non-lymphoid tissues and from<br />
there back to local lymphoid organs via afferent lymphatics maintains immune<br />
surveillance under homeostatic as well as inflammatory conditions. We recently showed<br />
that the CC chemokine receptor CCR7 controls not only homeostatic B and T cell<br />
trafficking to and within secondary lymphoid organs, but also homeostatic recirculation<br />
of lymphocytes through non-lymphoid epithelial tissues. Lack of CCR7 results in a<br />
massive accumulation of lymphocytes with the development of ectopic lymphoid follicles<br />
in the gastric mucosa, and age-dependent histomorphological changes with profound<br />
cystic hyperplasia and an increased rate of mucosal proliferation.<br />
Here, we demonstrate that CCR7 deficiency also results in disturbed lymphocyte<br />
reciculation through body cavities. Lack of CCR7 leads to a significant increase of T- and<br />
B lymphocyte numbers within the peritoneal and pleural cavity. To address the<br />
molecular basis of lymphocyte accumulation in body cavities, we adoptively transferred<br />
biotinylated splenocytes derived from either wt or CCR7-/- mice into the peritoneal<br />
cavities of wt recipients. Twenty four hours after adoptive transfer of biotinylated<br />
splenocytes derived from either wt or CCR7-/- mice into the peritoneal cavities of wt<br />
recipients, the amount of recirculated donor lymphocytes was determined in the<br />
draining parathymic lymph nodes by flow cytometric analysis and immunohistology.<br />
Thus, peritoneal accumulation of lymphocytes is caused by impaired egress of CCR7<br />
deficient lymphocytes from the peritoneum via the afferent lymphatics to the draining<br />
lymph nodes and this process is highly dependent on CCR7 expression. We conclude<br />
that the homeostatic chemokine receptor CCR7 serves as a central regulator in<br />
peripheral lymphocyte recirculation and cellular homeostasis at peripheral sites.
Tim Worbs, TR Mempel, J Bölter, UH von Andrian, R Förster<br />
CCR7-ligands stimulate the intranodal motility of T<br />
lymphocytes in vivo<br />
In contrast to lymphocyte homing, little is known about molecular cues controlling the<br />
motility of these cells within lymphoid organs. Applying two-photon intravital<br />
microscopy in mice, we demonstrate that signals provided by the chemokine receptor<br />
CCR7 enhance the intranodal motility of CD4+ T cells. Analyzing motility properties of<br />
adoptively transferred T cells in the T cell area of wild type recipients we observed a<br />
33% reduction of the average cell velocity and a 55% reduction of the mean motility<br />
coefficient of CCR7-deficient CD4+ T cells compared to wild type cells. Both parameters<br />
were similarly reduced once adoptively transferred wild type T cells were analyzed in<br />
the T cell area of lymph nodes of plt/plt mice, which lack CCR7-ligands. Importantly,<br />
systemic application of the CCR7-ligand CCL21 was sufficient to rescue the motility of<br />
wild type T cells inside the T cell area of plt/plt recipients. Comparing the movement<br />
behavior of T cells in subcapsular areas, which are devoid of detectable amounts of<br />
CCR7-ligands even in wild type mice, we failed to reveal any differences in wild type<br />
and plt/plt recipients. Furthermore, in both wild type and plt/plt recipients subcutaneous<br />
injection of the CCR7-ligand CCL19 induced the rapid recruitment of highly motile T cells<br />
into the subcapsular region. Together, these data identify CCR7 and its ligands as<br />
important chemokinetic factors stimulating the basal motility of CD4+ T cells inside<br />
lymph nodes in vivo.
Matthias Krusch, Tina Baessler, Katrin Miriam Baltz, Helmut Rainer Salih<br />
CD137 ligand expression on acute myeloid leukemia cells<br />
modulates immune surveillance of human NK cells identified<br />
to express CD137 upon activation<br />
Studies of haploidentical bone marrow transplantation (BMT) suggest that NK cells play<br />
an important role in immunosurveillance of leukemia, and acute lymphoblastic<br />
leukemias (ALL) were shown to be less susceptible to NK-mediated lysis than acute<br />
myeloid leukemia (AML). NK cell reactivity is governed by a balance of activating and<br />
inhibitory receptors including various members of the TNF receptor (TNFR) family. The<br />
TNFR family member CD137/4-1BB has been shown to stimulate proliferation and IFN-γ<br />
production, but not cytotoxicity of NK cells in mice. Surprisingly, yet nothing is known<br />
regarding the consequences of CD137-CD137 ligand (CD137L) interaction for NK cell<br />
reactivity in humans. Here we report that NK cells express CD137 upon stimulation with<br />
activating cytokines like IL-2 or IL-15. In addition, we demonstrate that primary acute<br />
myeloid leukemia (AML) cells of patients express CD137L in 14 of 34 (41%) cases.<br />
CD137L expression in AML was not associated with expression of HLA-class I, CD80/86<br />
or ligands for the activating immunoreceptor NKG2D. Reverse signaling via CD137L into<br />
AML cells induced the release of the immunoregulatory cytokines IL-10 and TNF.<br />
Furthermore, AML-expressed CD137L stimulated both cellular cytotoxicity and IFN-γ<br />
production of CD137-expressing NK cells, since NK cell reactivity was significantly<br />
reduced by addition of blocking CD137 antibodies in coculture assays. Taken together,<br />
our data indicate that CD137 is inducibly expressed and mediates different effects in<br />
human compared to murine NK cells. Furthermore, CD137L expression substantially<br />
influences tumor immunoediting by AML cells and modulates NK cell-mediated<br />
immunosurveillance of leukemia.
Holger Hoff, Zulema Cabail, Karin Knieke, Marion Rudolph, Heike Hirseland, Barbara<br />
Bröker, Monika Brunner-Weinzierl<br />
CD152 (CTLA-4) controls CD28-independently cell cycle<br />
progression and resistance against apoptosis of human T<br />
lymphocytes<br />
The activation of T-lymphocytes is tightly controlled by positive and negative costimulatory<br />
receptors. Primary costimulatory molecules are CD28 and CD152 (CTLA-4)<br />
of the Ig-superfamily. Both are stimulated by the same ligands B7-1 (CD80) and B7-2<br />
(CD86) on antigen-presenting cells. While CD28 is mediating positive co-stimulatory<br />
signals the crosslinking of CD152 leads to cell-cycle arrest and reduced production of<br />
cytokines, but CD28 as well as CD152-mediated signals induce resistance against<br />
activation-induced cell death (AICD). A subpopulation of human T-helper cells (CD4+)<br />
and cytotoxic T cells (CD8+) that has lost the expression of CD28 (CD28null T cells)<br />
show reduced proliferation and longevity. In this study we could show that despite the<br />
loss of CD28 expression these cells are able to express CD152 at their cell surface<br />
shortly after beginning of their stimulation. Their surface CD152 is functional as the<br />
serological blockade of CD152 leads to enhanced proliferation of CD4 and CD8 CD28null<br />
T lymphocytes. In addition we were able to show that blockade of CD152 signal<br />
transduction using CD152 Fab-fragments during stimulation leads to enhanced induction<br />
of apoptosis. The anti-apoptotic effect of CD152 was confirmed by cross-linking of<br />
CD152 which leads to reduced activation of caspases. The CD152-mediated resistance<br />
against apoptosis is mediated by enhanced activation of the anti-apoptotic kinase Akt.<br />
Thus, surface CD152 expression and CD152-mediated signalling is independent of CD28signalling.<br />
These data also demonstrate that CD152 initiates CD28-independent<br />
induction of anti-apoptotic signalling pathways.
J. Kolja Hegel, Pushpa Pandiyan, Paula Kolar, Karin Knieke, Steven L. Reiner, Monika<br />
Brunner-Weinzierl<br />
CD152 (CTLA-4) utilizes Eomesodermin, but not T-bet, for<br />
regulating effector function of individual CD8 T lymphocytes:<br />
Implication for tumor therapy<br />
Immune responses of CD8 T lymphocytes are primarily regulated by positive and<br />
negative costimulatory molecules such as CD28 and CD152 (CTLA-4), respectively. We<br />
were able to show that surface expression of CD152 is highly up regulated on activated<br />
CD8 T lymphocytes already during primary immune responses, suggesting a prominent<br />
regulatory role. Traditionally, CD152 blockade or deficiency was thought to only<br />
increase CD4 T cell help or enhance the overall frequency of cytotoxic CD8 T cells<br />
responding an antigenic stimulus. We could now reveal that CD152 enhances effector<br />
functions (cytotoxicity and cytokine response) of individual CD8 T cells. Mechanistically,<br />
we could demonstrate that signals induced by CD152 reduce the frequency of IFNgamma<br />
and GranzymeB expressing CD8 T cells independently of T-bet by selectively<br />
inhibiting Eomesodermin downstream of the ERK/MAPK pathway. Enhanced cytotoxicity<br />
of individual CD8 cells primed in the absence of CD152 signaling could be demonstrated<br />
in vivo. These novel insights could explain the efficacy of anti CD152 treatment for<br />
tumor rejection.
Karin Knieke, Holger Hoff, Frank Maszyna, Paula Kolar, J. Kolja Hegel, Alf Hamann,<br />
Gudrun F. Debes, Monika Brunner-Weinzierl<br />
CD152 (CTLA-4)- signalling promotes homing to secondary<br />
lymphoid organs<br />
Migration of antigen-experienced T cells to secondary lymphoid organs is important for<br />
immune responses. Here, we show that CD152 (CTLA-4), known as a major down<br />
regulator of T-cell responses, enhanced CD4 T cell migration towards CCL19, a<br />
chemokine involved in directing lymphocytes to lymph nodes and leaving tissues.<br />
Paralleling the enhanced chemotaxis, CD152 signalling increased T cell expression of<br />
CCL19 binding receptor CCR7. Importantly, the CD152-mediated signals amplified the<br />
migration of Th1 cells to lymph nodes in vivo indicating an unexpected role for CD152 in<br />
the orchestration of effector T cell recirculation through secondary lymphoid organs.
Baerbel Keller, Mirzokhid Rakhmanov, Sylvia Gutenberger, Sigune Goldacker, Dirk<br />
Holzinger, Elisabeth Nikolopoulus, Paul Fisch, Hermann Eibel, Hans-Hartmut Peter,<br />
Klaus Warnatz<br />
CD21low B Cells Represent a Polyclonally Activated B Cell<br />
Population Exposed to Type I Interferons<br />
Most patients with common variable immunodeficiency (CVID) exhibit a severely<br />
disturbed homeostasis of the circulating B cell pool. About 10% of these patients are<br />
characterized by the expansion of B cells with an unusually low expression of CD21.<br />
These CD21lowCD38low B cells exhibit an activated phenotype with increased cell size<br />
and elevated levels of CD86. Spectrotyping of sorted cells identified a polyclonal origin<br />
of CD21low B cells. A similar expansion of CD21low B cells in SLE as well as HIV<br />
infected patients suggested a potential role of type I interferon stimulation. Gene<br />
expression analysis for MxA, OAS1 and IFIT1 of FACS sorted CD21low B cells versus<br />
naive B cells of HD and CVID patients confirmed the interferon signature in CD21low B<br />
cells. Since HHV8 was suggested as a possible pathogen in a subgroup of CVID patients<br />
we tested our patients with expanded CD21low B cells and granulomatous disease, but<br />
could not confirm a role of HHV8 in our cohort. Currently we are investigating polyclonal<br />
activation of B cells via different Toll like receptors as a possible source of CD21low B<br />
cell differentiation.
Isis Ludwig-Portugall, Emma E. Hamilton-Williams, Christian Kurts<br />
CD25+ regulatory T cells induce peripheral B cell tolerance<br />
against non-lymphoid tissue autoantigens<br />
To study mechanisms of peripheral B cell tolerance against non-lymphoid tissue<br />
autoantigens we generated transgenic RIP-OVA/HEL (ROH) mice expressing the model<br />
antigens, OVA and HEL in pancreatic islets. T cells in these mice were not centrally<br />
tolerant to OVA, because double transgenic ROHxOT-I mice produced OVA specific CD8<br />
+ T cells (OT-I cells) and became diabetic. When ROH mice were immunized with OVA,<br />
we observed OVA specific IgG titers at day 21, suggesting that CD4+ cells able to<br />
switch Ig subclass were present. Nevertheless, titers in ROH mice were much lower than<br />
in nontransgenic controls, indicating specific tolerance. When we depleted CD25+ cells<br />
with the PC61 mAb, autoantibody production was <strong>complete</strong>ly restored, whereas titers<br />
against the foreign model antigen ßGal were unaffected. These findings suggested that<br />
regulatory tolerance suppressed autoantibody production, rather then deletion of<br />
autoreactive B or T cells.<br />
To investigate whether this tolerance was induced in the periphery, we injected naïve<br />
HEL-specific B cells form the transgenic IgHEL donor mice into ROH mice and analysed<br />
their phenotypical changes. After 3 days we detected neither proliferation, nor changes<br />
in IgHEL cell numbers, nor B cell receptor (BCR) downregulation. After 22 days numbers<br />
of IgHEL cells in transgenic recipients were reduced, and surviving cells showed reduced<br />
expression of the BCR. IgMa produced by IgHEL cells rapidly vanished in transgenic<br />
mice, even when specific help was provided. Thus, IgHEL cells were peripherally<br />
tolerized to a non-lymphoid tissue autoantigen. We conclude that peripheral B cell<br />
tolerance against autoantigens in nonlymphoid tissues can be maintained by CD25+<br />
Treg
Christian Becker, Tobias Bopp, Jan Kubach, Franz-Josef Schneider, Edgar Schmitt,<br />
Helmut Jonuleit<br />
CD4-mediated, TCR-independent functional activation of<br />
human CD4+CD25+ regulatory T cells<br />
CD4 coreceptors exert complex regulatory effects on T cell activation and function. We<br />
recently showed that engagement of CD4 by specific anti-CD4 antibodies induce<br />
suppressive activity in human CD25+Foxp3+ regulatory T cells (Tregs). CD4 mediated<br />
activation of Tregs acts independently of TCR stimulation but elicits comparable<br />
suppressive activity resulting in efficient suppression of effector T cell proliferation and<br />
cytokine production. Examination of the proximal CD4 signaling events in Tregs after<br />
CD4 ligation shows phosphorylation of the zeta-associated protein-70 which relays<br />
signals to downstream signaling components. Selective inhibition of lck activity during<br />
anti-CD4 stimulation prevents induction of suppressive function in CD25+ Tregs. In<br />
contrast to Tregs, CD4 ligation of CD4+CD25- T cells by anti-CD4 cross-linking does not<br />
induce suppressive activity.<br />
Here we show that the HIV-derived CD4 binding envelope glycoprotein gp120 is a<br />
potent functional activator of human Tregs. Upon stimulation with gp120, Tregs<br />
substantially increase production of cAMP, a second messenger previously shown to be<br />
essentially involved in Treg-mediated suppression. These results demonstrate that<br />
suppressive activity in human Tregs can be directly triggered by gp120, suggesting that<br />
immune dysfunctions associated with HIV infection might in part result from CD4mediated<br />
Treg activation by the virus.
Alexander Donald McLellan, Sarah Charlotte Saunderson, Petra Schuberth, Lilija<br />
Miller, Amy Charlotte Dunn, Philippa Anne MacKay, Ralph Wilson Jack<br />
CD40/IL-4-stimulated B cells release exosomes enriched in<br />
components of the B cell receptor complex.<br />
Exosomes are lipid-bound nanovesicles released by a variety of cell types and have<br />
been proposed to play a role in antigen presentation, immunoregulation and viral<br />
transmission. Recent work in our lab has shown that exosomes are not present in the<br />
blood of normal humans or mice. Moreover, primary leukocytes do not release<br />
exosomes unless subjected to potent activation signals. High level exosome release was<br />
stimulated when splenic B cells were cultured with activated-T cell membranes and this<br />
was found to be dependent on IL-4 and CD40L signalling. B cell exosomes expressed<br />
high levels of MHC-I, MHC-II and B220, as well as components of the B cell receptor<br />
complex (BCR), namely surface-IgM, CD19 and the tetraspanins CD81 and CD9 (a<br />
marker of marginal zone B cells). Although CD40/IL-4-stimulated B cells secreted a<br />
range of other immunoglobulin isotypes (IgA, IgG1, IgG2a/2b & IgG3), IgM was the<br />
predominant isotype enriched on the surface of exosomes. This suggests that the<br />
exosome pathway may intersect with antigen uptake and processing mediated by the<br />
BCR complex. We propose that blood-borne antigen entering the marginal sinus of the<br />
spleen is processed by antigen-specific marginal zone B cells which then release<br />
exosomes containing Ig-bound antigen for transfer to other cell types, such as dendritic<br />
cells.
Rachid Marhaba, Margot Zöller<br />
CD44 blocking induces apoptosis by uncoupling Ezrin from the<br />
Ras pathway<br />
The adhesion molecule CD44 is involved in a large array of functions including<br />
hematopoeisis, lymphocytes homing, migration, activation and apoptosis. The CD44<br />
gene comprises 20 exons divided into two groups; standard and variable exons. The<br />
standard exons are common to all CD44 glycoproteins and lead to the expression of the<br />
CD44 standard isoform (CD44s). The variable exons are expressed by alternative<br />
splicing in a cell type- and activation state- dependent manner, and lead to the<br />
generation of several CD44 variant isoforms (CD44v). We have previously shown that<br />
CD44 crosslinking provides a co-stimulatory signal for the TCR signaling whereas<br />
CD44v6 and CD44v7 deliver signals independently of the TCR engagement. In this<br />
work, we studied the effect of CD44 blocking on T cell proliferation and induction of<br />
apoptosis and the underlying mechanism. We found that CD44 blocking induces<br />
apoptosis of T cells. This effect is associated with a strong inhibition of ERK and JNK<br />
phosphorylation. CD44 blocking correlates with the loss of CD44-associated Ezrin and<br />
inhibits complex formation between Ezrin and Ras leading to the MAPK activation. These<br />
results suggest that CD44, via an interaction with an unknown cellular ligand, delivers<br />
signals leading to cell proliferation and inhibition of apoptosis.
Annalena Bollinger, Zane Orinska, Silvia Bulfone-Paus<br />
CD8+CD38+ T cells: An newly defined IL-15 dependent<br />
regulatory T cell population with effects in allergic asthma<br />
Regulatory T-cells (Tregs) are of essential importance to achieve peripheral tolerance<br />
toward self and harmless alloantigens. The family of Tregs is composed of so called<br />
naturally occurring and induced Tregs, wherein the characterisation of CD8+ Tregs just<br />
has begun. However, CD8+ T-cells are essential players for establishment of an<br />
adequate immune responses. Impaired Treg function is associated with a breakdown of<br />
tolerance causing autoimmune diseases or allergy. In this context, IL-15, as an<br />
interleukin with various activating actions on T-cells, has been shown to exert strong<br />
effects on the course of allergy via influencing both effector T-cells and Tregs. Based on<br />
this background we postulated that IL-15 regulated CD8+ Tregs may play an important<br />
role in prevention of allergy.<br />
In this study, we characterized a very first IL-15 modulated CD8+ Treg population<br />
phenotypically and functionally for the C57 BL/6 murin system. We elucidated CD38, a<br />
transmembrane NAD-glycohydrolase with pleiotropic functions, as an IL-15 sensitive<br />
molecule. Its surface expression clearly correlates with well defined Treg markers, such<br />
as CD25, glucocorticoid-induced tumour necrosis factor receptor (GITR), the forkhead/<br />
winged helix transcription factor foxp3 and others. Concerning functional aspects, we<br />
found a suppressive capacity of CD8+CD38+ T-cells toward antigen-specific CD8 and<br />
CD4 T-cell proliferation, which was additionally associated with a decreased level of IL-2<br />
and an increase of IL-10. Furthermore, we have established the Ovalbumin/asthma in<br />
vivo model for the use of C57 BL/6 mice in context with regulatory T-cells and allergy.<br />
Investigations of the effect mediated by CD8+CD38+ T cells elucidated a clear function<br />
in down-regulating TH2 associated IL-6 release in the bronchioalveolarlavage (BAL).<br />
Taken together, we determined an IL-15 sensitive CD8+CD38+ Treg population acting<br />
as a regulator of allergic asthma.<br />
Funded by SFB/Transregio 22, A14
Katja Lüthje, Svenja Ehrlich, Bernhard Fleischer, Minka Breloer<br />
CD83 expression level affects spleenic B cell maturation<br />
The murine transmembrane glycoprotein CD83 is an important regulator for both:<br />
thymic T cell maturation and peripheral T cell response. CD83 deficiency leads to a<br />
block in the thymic maturation of CD4 + T cells and addition of soluble CD83 was shown<br />
to suppress peripheral T cell responses in vivo and in vitro. Recently we showed that<br />
CD83 that is expressed by activated B cells, is also involved in the regulation of B cell<br />
function. CD83 overexpression in CD83 transgenic (tg) mice led to a dramatically<br />
reduced Ig response to TD and TI model antigens in vivo that was due to CD83<br />
expression on the B cells themselves.<br />
Here, we investigate the B cell development in CD83 overexpressing transgenic (tg)<br />
mice and in CD83 mutant (mut) mice that display dramatically reduced amounts of<br />
CD83. Analysis of B220 + cells in the bone marrow revealed no difference in the<br />
percentage of IgM - CD43 - pre B cells. Analysis of the spleenic B cell pool highlighted an<br />
increase in transitional B cells and a reciprocal decrease in follicular B cells. Employing<br />
two independent CD83tg mouse strains, we further showed that the intensity of CD83<br />
expression was positively correlated to accumulation of transitional B cells in the spleen.<br />
Since CD83tg bone marrow displayed the same impaired maturation upon<br />
transplantation into irradiated wild-type hosts the accumulation of immature B cells in<br />
the spleen was not induced by CD83 expression on stromal cells but rather due to CD83<br />
expression on hematopoetic stem cells.<br />
While the number of transitional and follicular B cells in CD83 mutant mice was normal<br />
a decreased maturation of marginal zone B cells was observed. This altered maturation<br />
of marginal zone B cells was only partially reverted to normal upon transplantation of<br />
CD83 deficient bone marrow into wild-type hosts and therefore may be due to both:<br />
CD83 deficiency on somatic and on bone marrow derived cells.<br />
Taken together we provide evidence that CD83, in addition to its well described role in<br />
thymic T cell maturation, is also involved in B cell development. In contrast to T cell<br />
maturation where CD83 is necessary to be present on non hematopoetic thymic<br />
epithelial cells we show that CD83 expression on hematopoetic cells, presumably the<br />
transitional B cells themselves, plays a role in the final maturation of follicular B2 cells.
Wiebke Hansen, Simone Reinwald, Astrid M. Westendorf, Carsten Wiethe, Jan Buer<br />
CD83 is involved in the immunosuppressive function of<br />
regulatory T cells<br />
The transmembrane protein CD83 has been initially described as maturation marker for<br />
dendritic cells (DCs). Moreover, there is increasing evidence that CD83 also regulates B<br />
cell function, thymic T cell maturation and peripheral T cell activation. Here, we show<br />
that CD83 plays also a pivotal role in regulatory T cells (Treg) biology. CD83 is upregulated<br />
in CD4 + CD25 + Treg cells of both murine and human origin in comparison to<br />
their naïve counterparts. Furthermore, stimulation in vitro leads to a further increase in<br />
CD83 protein expression on Treg cells. Transduction of naïve CD4 + CD25 - T cells with<br />
CD83 encoding retroviruses confers suppressive activity in vitro, which is accompanied<br />
by the induction of Foxp3 expression. Functional analysis of CD83-transduced T cells in<br />
vivo demonstrate that these CD83 + Foxp3 + T cells are able to interfere with the effector<br />
phase of a severe contact hypersensitivity reaction of the skin and prevent the paralysis<br />
associated with experimental autoimmune encephalomyelitis (EAE). In summary, our<br />
data demonstrate that CD83 seems to be involved in the immunosuppressive function<br />
of Treg cells and thereby might play a crucial role in the course of immune responses.
Birte Kretschmer, Katja Lüthje, Andreas H. Guse, Svenja Ehrlich, Friedrich Koch-<br />
Nolte, Friedrich Haag, Bernhard Fleischer, Minka Breloer<br />
CD83 modulates B cell function in vivo and in vitro<br />
The murine transmembrane glycoprotein CD83 is an important regulator of both:<br />
thymic T cell maturation and peripheral T cell responses. Here we provide evidence that<br />
CD83 is also involved in the regulation of B cell function. We therefore compared the<br />
function of CD83Tg B cells that overexpress CD83 and CD83 mutant (CD83mu) B cells<br />
that display a drastically reduced CD83 expression. Correlating with CD83 expression,<br />
the basic as well as the LPS induced expression of the activation markers CD86 and<br />
MHC-II was significantly increased on CD83Tg B cells and reciprocally decreased on<br />
CD83mu B cells. Wild-type B cells rapidly upregulate CD83 within three hours post BCR<br />
or TLR engagement. The forced premature expression of CD83 on CD83Tg B cells<br />
resulted in reduced calcium signaling, reduced Ig secretion and a reciprocally increased<br />
IL-10 production upon in vitro activation. This altered phenotype was mediated by CD83<br />
expressed on the B cells themselves, since it was observed in purified B cells and<br />
therefore in the absence of accessory cells. Although reduced CD83 expression on<br />
CD83mu B cells did not alter the response of whole spleen cell cultures to LPS<br />
stimulation in vitro, a slight reduction in IL-10 release together with a non-significant<br />
increase in Ig secretion was observed in purified CD83mu B cells.<br />
Employing a non-conditional transgenic model we cannot rule out the possibility that<br />
artificial CD83 expression on B cells during their maturation within the CD83Tg mice<br />
results in the generation of dysfunctional B cells. Nevertheless we were able to show<br />
that the treatment of non-Tg C57BL/6 mice with anti-CD83 mAb led to a dose<br />
dependent 10-fold increase in the antigen-specific IgG1 response to TI immunization<br />
thus demonstrating a genuine role for naturally induced CD83 in the regulation of<br />
peripheral B cell function. Although we still have to define the CD83-positive cell<br />
population(s) targeted by the anti-CD83 mAb in vivo, this finding already demonstrates<br />
a genuine role for naturally induced CD83 in the regulation of peripheral B cell function.
Thomas Bickert, Andrea Horst, Christoph Wagener, Bernhard Fleischer, Uwe Ritter<br />
CEACAM1 is crucial for lymphvasculogenesis during<br />
inflammatory immune responses<br />
Recently, it was shown that Carcinoembryonic antigen-related cell adhesion molecule 1<br />
(CEACAM1) plays an important role in angiogenesis. To investigate the possible impact<br />
of CEACAM1 in lymphvasculogenesis during a local inflammatory response, Ceacam1<br />
knock out (Ceacam1 -/- ) mice were infected subcutaneously with the obligate<br />
intracellular protozoan parasite Leishmania (L.) major. Ceacam1 -/- mice developed both<br />
humoral and cellular immunity against L. major. However, the lack of CEACAM1 resulted<br />
in delayed wound healing and oedema formation at the site of infection, indicating that<br />
formation of lymphatic vessels might be affected by the lack of CEACAM1 expression. To<br />
test this hypothesis, we analyzed the dermal infiltrate caused by the infection with L.<br />
major. These data revealed that CEACAM1 is highly expressed on infiltrating CD11b +<br />
cells, which in turn are known to be pivotal in lymphangiogenesis as recently shown in a<br />
transplantation model of mouse cornea. Furthermore, a subpopulation of these<br />
infiltrating myeloid CD11b + cells were positive for CEACAM1 and lymphatic vessel<br />
endothelial hyaluronic acid receptor (LYVE-1). Therefore, it is likely that CD11b + /<br />
CEACAM-1 + cells might be involved in formation of new lymphatic vessels. Detailed<br />
FACS analysis of bone marrow and blood exhibited that CD11b + monocytes were<br />
significantly reduced in Ceacam1 -/- mice leading to the assumption that a diminished<br />
precursor population was responsible for the failure in lymphvasculogenesis resulting in<br />
oedema formation. Interestingly, we could not detect reduced numbers of LYVE-1 + /<br />
CD11b + cells in the infected footpad of Ceacam1 -/- mice. However, histological staining<br />
of the inflamed footpad for LYVE-1 revealed striking differences. While LYVE-1 +<br />
lymphatic vessels were found within the inflammation in wild type mice, no<br />
incorporation of these cells into vessel-like structures was observed in Ceacam1 -/- mice.<br />
In conclusion, our results show that CEACAM1 is pivotal for the formation of functional<br />
cutaneous lymphatic vessels under inflammatory conditions caused by L. major.
Ulf Alexander Wenzel, Sonja Möller, Werner Solbach, Tamas Laskay, Ger van<br />
Zandbergen<br />
Cell death regulation controls Leishmania disease<br />
development<br />
An early marker for apoptosis is the exposure of phosphatidylserine (PS) on the outer<br />
leaflet of the cell membrane. PS can be detected using annexin A5 (AnxA5) and uptake<br />
of AnxA5 binding cells by professional phagocytes results in a silencing of the immune<br />
response. Leishmania major (L. major) is an obligate intracellular parasite elegantly<br />
misusing the apoptotic cell clearance system for disease development. This parasite<br />
enters polymorphonuclear neutrophil granulocytes (PMN) in its promastigote form.<br />
Hiding inside AnxA5-positive PMN the parasite transfers into macrophages (MF), where<br />
it multiplies in its amastigote form. We found that the presence of AnxA5-binding<br />
population of promastigotes is responsible for the survival and infectivity of viable<br />
promastigotes. It has been suggested that to silently infect MF, the amastigote form of<br />
the parasite uses PS-expression without subsequent cell death as a form of apoptotic<br />
mimicry.<br />
In this study we developed a novel in vitro method to culture the amastigote form of L.<br />
major. We compared cultured amastigotes with MF derived, as well as in vivo derived,<br />
amastigotes. AnxA5-binding and TUNEL-positivity were used as markers for apoptotic<br />
like death. Inside MF we found the presence of both TUNEL-positive and -negative<br />
amastigotes. In addition, we found that purified L. major amastigotes, taken from 8<br />
week infected BALB/c mice, contained both TUNEL-positive and -negative amastigote<br />
populations. Finally, we found that amastigote cultures contained an AnxA5-binding<br />
subpopulation. Moreover we could demonstrate that amastigote cultures contain a<br />
TUNEL-positive, non viable subpopulation. In contrast to the mimicry hypothesis, this<br />
data suggests that L. major parasites misuses an apoptotic like death system in at least<br />
three stages of the disease development. AnxA5-binding promastigotes help viable<br />
parasites to enter PMN, subsequently apoptotic PMN transfer the promastigote silently<br />
into MF. In MF the L. major amastigotes develop, again containing both a viable and an<br />
AnxA5-binding population that could help silencing the next host MF.
Norbert Koch, Alexander McLellan, Jürgen Neumann<br />
Chaperone Controlled Assembly and Matched Isotype Pairing<br />
of Major histocompatibility complex Class II Subunits<br />
The major histocompatibility complex class II (MHCII) region encodes highly<br />
polymorphic polypeptides, which form a heterodimeric peptide receptor. How is it<br />
achieved that the great variety of inherited allotype or isotype subunits of MHCII,<br />
combine to functional peptide receptors? Discovery of a novel molecular mechanism for<br />
MHCII subunit assembly revealed that pairing of alpha and beta polypeptides is<br />
controlled by expression of invariant chain (Ii). Assembly of MHCII is initiated by<br />
sequential binding of alpha and subsequent association of beta chain to Ii. Interaction of<br />
Ii to the highly conserved MHCII alpha chain may explain the promiscuous binding of Ii<br />
to the large cohort of polymorphic MHCII heterodimers. The various allo- and isotypic<br />
beta chains expressed in APC compete for binding to the alpha-Ii matrix, yielding<br />
isotype matched alpha-beta-Ii complexes. Moreover, Ii controls formation of the nonclassical<br />
MHCII molecule DM. HLA-DR and DM subunits form mixed complexes that are<br />
only dissolved when Ii is present. In Ii-gene deficient mice aberrant interaction of I-A<br />
and H2-M subunits impairs the function of H2-M. The catalytic activity of H2-M is<br />
rescued by expression of low amounts of Ii.
Johann Poetzl, Catherine Botteron, Daniela Maennel, Anja Lechner<br />
Characterisation of long-lived CCR6 expressing T H cells in the<br />
immune response<br />
The function of T cell subsets in vivo depends on their location. Chemokines are small<br />
chemotactic cytokines that guide leukocytes through the body. The chemokine CCL20 is<br />
expressed in mucosal and dermal tissues and its only known receptor is CCR6, which is<br />
a trait of effector and memory T cells. CCR6 positive T cells are associated with different<br />
autoimmune processes, i.e. psoriasis, atopic dermatitis and colitis. Yet, its function on T<br />
cells in infectious diseases seems to be elusive.<br />
In experimental murine leishmaniasis we could recently show that CCR6 deficiency is<br />
associated with impaired T helper (TH ) cell function. To further elucidate the function of<br />
CCR6 for the generation of antigen specific TH cells, we analysed the generation of<br />
CCR6 positive, activated TH cells after ovalbumin immunisation. Phenotypically, the<br />
population of CCR6 expressing TH cells does not alter significantly after immunisation.<br />
In mice, TH cells show co-expression of CCR6 with CD127 and a down-regulation of the<br />
lymph node homing adhesion molecule CD62L. In this regard the expression profile of<br />
such cells is characteristic for short-lived effector or long-lived effector memory T cells.<br />
To dissect these two possibilities we performed in vitro proliferation assays at different<br />
time points after immunisation. After antigen specific restimulation the population of<br />
proliferating T cells consisted mainly of CCR6 positive T cells. In addition, the preference<br />
of CCR6 positive T cells for antigen specific proliferation was obvious over the whole<br />
observation period from day 2 to day 28 compared to CCR6 negative T cells.<br />
From this data we conclude that CCR6 positive TH cells seem to represent a long lived,<br />
stable subset of effector memory TH cells, which are generated early in the immune<br />
response.
Bernhard Fleischer, Juliane Ladhoff, Elke Effenberger, Cornelia Doebis, Hans-Dieter<br />
Volk, Martina Seifert<br />
Characterisation of NK cell attacks towards MHC class I<br />
deficient rat aortic endothelial cells in vitro<br />
Background: MHC (major histocompatibility) class I deficient rat aortic endothelial cells<br />
(RAEC) have been generated in the past by expression of an anti-MHC class I-intrabody.<br />
The MHC-I-down regulation resulted in a reduced susceptibility of RAEC to humoral and<br />
CTL-mediated immune attacks. Those cells are interesting tools for generating vascular<br />
allografts. However, due to their MHC class I deficiency RAEC may become a target of<br />
Natural Killer (NK) cell lysis.<br />
Methods: Rat NK cells of the recipient rat strain were isolated from spleen by density<br />
gradient centrifugation combined with nylon wool adherence and MACS-separation<br />
technology using an anti-NKR-P1 antibody. Characterization of isolated NK cells was<br />
performed flow cytometrically. Rat NK cells were cultured for 2 days in IL-2 containing<br />
medium and then used as killer cells in a Calcein-based cytotoxicity assay. NK cell lysis<br />
was tested with syngeneic, allogeneic and allogeneic but MHC class I deficient cells. YAC-<br />
1 tumor cell line was used as a positive control for NK cell killing.<br />
Results: Rat NK cells could be isolated with a purity of 70-80 %, defined by the coexpression<br />
of ratNKR-P1 and ratNKp46 and the absence of CD3/T cell receptor (TCR)<br />
expression. In cytotoxicity assays wild type RAEC of syngeneic as well as allogeneic<br />
origin were killed to a low degree (10-40 %) by NK cells, whereas the YAC-1 cells were<br />
almost <strong>complete</strong>ly lysed. MHC class I deficient RAEC displayed comparable low specific<br />
lysis rates similar to that of wild type cells.<br />
Conclusion: Down regulation of surface MHC class I on RAEC does not increase<br />
susceptibility to NK cell mediated lysis. This immunological resistance of MHC I deficient<br />
RAEC would allow their use as an essential component for covering the luminal surface<br />
of vascular allografts.
Mirjam Peter, Klaus Heeg, Alexander Dalpke<br />
Characterization of a guanosine-rich suppressive<br />
oligodesoxynucleotide which inhibits Toll-like receptor-9<br />
signaling<br />
Bacterial DNA as well as synthetic oligonucleotides containing unmethylated CpG<br />
sequences (CpG-ODN) activate immune cells by stimulating Toll-like receptor 9 (TLR9).<br />
This activation leads to cytokine secretion and up-regulation of costimulatory molecules<br />
in macrophages and dendritic cells (DCs) as well as B-lymphocyte proliferation. Beside<br />
these physiological effects TLR9 activation is accused to be responsible for the onset<br />
and aggravation of autoimmune diseases. Recently, suppressive ODN have been<br />
described which inhibit TLR9 induced activation of immune cells. Here we describe a<br />
novel guanosine-rich, suppressive ODN (G-ODN) which inhibits CpG induced activation<br />
of TLR9 in murine macrophages and DCs as well as in human plasmacytoid DCs (pDCs).<br />
G-ODN blocked the secretion of TNFα and IL12p40 as well as up-regulation of<br />
costimulatory molecules. We observed an early block of signaling as activation of MAP-<br />
Kinases and NF-κB was inhibited but G-ODN did not inerfere with cellular uptake.<br />
Inhibition was TLR9 specific as it was not observed for stimulation of other TLRs. This<br />
was confirmed using a TLR9 specific transfection model. G-ODNs even inhibited in a<br />
molar ratio of 10:1 and were also inhibitory when given up to 6 hours after initial CpG<br />
stimulation. G-ODNs were also suppressive in an in vivo model of CpG-induced cytokine<br />
shock. Therefore this class of G-ODN could be of therapeutic use in clinical situations<br />
with increased TLR9 activation as suggested for certain autoimmune diseases.
Andrea Kiessling, Dagmar Riemann, Susanne Fuessel, Esther Kamphausen, Barbara<br />
Seliger<br />
Characterization of expression pattern and regulation of<br />
ISGylation system in tumors<br />
Following the identification of ubiquitin as central regulator of proteasomal degradation,<br />
a number of ubiquitin-like proteins have been identified. Interferon-stimulated gene 15<br />
(ISG15), a member of this family, was recently described to exert a dual function as<br />
intracellular modifier of proteins negatively regulating the polyubiquitination and as an<br />
extracellular cytokine-like modulator of innate immune responses.<br />
In this study, we analyzed the expression and regulation of ISG15 and of the enzymes<br />
involved in ISG15 conjugation to proteins (Ube1L, UbcH8, and Herc5) in human tumors.<br />
By quantitative PCR, all components of the ISGylation system were found in 16/17 renal<br />
cell carcinoma (RCC), 6/7 squamous cell carcinoma, 37/39 melanoma, and 2/2 prostate<br />
carcinoma cell lines. However, basal expression levels of the individual components did<br />
not strictly correlate with each other. The transcript quantification in paired malignant<br />
and non-malignant tissue samples from RCC patients revealed increased ISG15 and<br />
UbcH8 expression in the tumors in 9/9 and 6/9 tissue samples, respectively. In<br />
contrast, Ube1L and Herc5 were heterogeneously expressed in the tumors. In paired<br />
specimens from prostate cancer patients, ISG15 and UbcH8 were upregulated in 11/14<br />
tumors and 10/14 tumors, respectively. Furthermore, the tumor-associated expression<br />
of these genes was more prominent in advanced tumors.<br />
In order to determine the functional role of ISG15 in tumors, the regulation of<br />
ISGylation system by various stimuli was analyzed. The ISGylation system was highly<br />
upregulated by type I IFN in tumor cell lines of distinct origin and by type II IFN<br />
particularly in melanoma cell lines. According to the presence of several p53 sites in the<br />
ISG15 promoter, ISG15, but none of the other ISGylation components, was increased<br />
after exposure to UV light.<br />
Our results show that ISG15, in contrast to the other components of ISGylation, is<br />
upregulated in tumors, indicating (i) an IFN-independent, cell stress-mediated<br />
mechanism of regulation, and (ii) a role of ISG15 in tumors that is independent from its<br />
function as covalent modifier of proteins.
Christoph Treese, Franziska Lange, Nadja Hilger, Anja Mittag, Attila Tarnok, Andreas<br />
Lösche, Frank Emmerich, Ulrich Sack<br />
Characterization of fibroblasts eroding cartilage in arthritis<br />
INTRODUCTION: The pathology of rheumatoid arthritis (RA) is characterized by<br />
destruction of articular cartilage and bone. In this process, functionally altered<br />
fibroblasts play a key role as they secrete distinct patterns of matrix proteinases,<br />
cytokines, and express variable levels of costimulatory and adhesion molecules. We<br />
have compared a destructive and a non-destructive fibroblast cell line for functional and<br />
phenotypic differences. The purpose of this study was to gain a deeper understanding of<br />
cartilage destruction in arthritis.<br />
METHODS: The destructive fibroblast line LS48 and the non-destructive 3T3 cells were<br />
cultured and characterized by slide based and flow cytometry, using antibodies against<br />
several adhesion molecules, pro- and anti-inflammatory cell surface antigens, and line<br />
and progenitor specific cell markers.<br />
RESULTS: Invasive fibroblasts are characterized by significant higher expression of<br />
adhesion molecules such as CD51 (vitronectin receptor), CD61 (GPIIIa), CD44 (H-Cam),<br />
and CD147 (EMMPRIN) that are involved in attachment and invasion of these cells.<br />
Furthermore, destructive cells were shown to express more DR5 (TRAIL-R2), CD95<br />
(Fas), and CD40 (Bp50) that are responsible for apoptotic and inflammatory processes.<br />
Finally, CD90 (Thy-1) and CD34 were shown to be strongly depressed. Expression of<br />
further molecules such as Fc receptors could be induced by culture in the presence of<br />
added immunoglobulin preparations.<br />
CONCLUSION: Our results reveal different phenotypic and functional characteristics of<br />
invasive and non-invasive fibroblasts. The expression is regulated by mediators that are<br />
typically present in arthritic joints. These findings will help us to gain further knowledge<br />
about the role of fibroblast in the pathogenesis of RA.
Jan Leipe, Alla Skapenko, Hendrik Schulze-Koops<br />
Characterization of human Interleukin 17 (IL-17)-producing T<br />
helper cells (Th17 cells) in healthy individuals and in patients<br />
with rheumatoid arthritis<br />
Th17 cells have recently been described as a distinct pro-inflammatory CD4 T cell<br />
population that contributes to the development of several autoimmune disorders in<br />
murine disease models. Their role in human autoimmune diseases, however, is less<br />
clear as their phenotype and effector functions in humans has not been thoroughly<br />
delineated. We analyzed Th17 cells in healthy human individuals and in patients with<br />
the prototype autoimmune disease, rheumatoid arthritis. CD4 T cell-derived IL-17 was<br />
detected by ELISA in the culture supernatants of ex vivo activated freshly isolated<br />
mononuclear cells from the peripheral circulation of healthy individuals and RA patients<br />
indicating the presence of Th17 cells in the peripheral circulation of both, controls and<br />
patients. IL-17 was also produced by CD4 T cells from the synovial fluid of patients with<br />
RA. Expression of IL-17 could be induced from highly purified memory CD4 T cells by<br />
TCR stimulation with mAbs to CD3 and further enhanced by costimulation via CD28. Of<br />
interest, IL-17 production was not modulated by IL-6 or TGF-beta, both of which have<br />
been implicated in Th17 differentiation in mice. In contrast to memory T cells, naive<br />
cells did not produce IL-17, even in the presence of IL-23. Together, the data indicate<br />
the presence of IL-17-producing CD4 T cells in patients with rheumatoid arthritis but<br />
also in healthy individuals. The precise function of these cells in autoimmune diseases,<br />
therefore, remains to be shown.
Michael Mihlan, Mario Hebecker, Markus Huber-Lang, Peter F. Zipfel, Mihály Józsi<br />
Characterization of ligand binding of the human Factor Hrelated<br />
protein 4 (FHR-4) provides insight into function<br />
Factor H-related protein 4 (FHR-4) is a unique member of the factor H protein family, as<br />
two isoforms has been described. FHR-4A has nine short consensus repeat (SCR)<br />
domains and includes a duplicated region of four domains, where SCR1-4 and SCR5-8<br />
are closely related. FHR-4B is a short isoform and consists of five SCRs, corresponding<br />
to SCR1 and SCR6-9 of FHR-4A.<br />
In order to analyze the function of FHR-4, the two isoforms and fragments of FHR-4A,<br />
representing SCR1-3, SCR4-9, SCR5-7 and SCR8-9, were recombinantly expressed and<br />
their binding properties to the central complement component C3b and to the acute<br />
phase protein C-reactive protein (CRP) were analyzed. Both FHR-4 isoforms as well as<br />
SCR4-9 and SCR8-9 bound to C3b, suggesting a binding site in the two C-terminal<br />
domains. In fluid phase cofactor assay, both FHR-4 isoforms enhanced the cofactor<br />
activity of factor H for C3b cleavage, but the FHR-4 variants alone lacked cofactor<br />
activity.<br />
Both FHR-4A and FHR-4B bound to CRP in the presence of Ca2+, independent of ionic<br />
strength. SCR1-3 but not the other FHR-4A fragments bound to CRP, indicating that<br />
SCR1 is necessary for CRP binding. CRP-binding was confirmed by surface plasmon<br />
resonance analysis and by coimmunoprecipitation. In addition, complexes of FHR-4A<br />
and CRP were isolated from serum of sepsis patients by immunoprecipitation, thus<br />
demonstrating in vivo interaction between the two proteins.<br />
In summary, we identify complement C3b and CRP binding domains of FHR-4A. The<br />
binding characteristics of the protein fragments give further insight into the function of<br />
the FHR-4 proteins, as the separation of binding sites allows simultaneous binding of<br />
FHR-4A to C3b and CRP. Thus, our data indicate a role of FHR-4 in innate immune<br />
response and inflammation.
Sandra Klein, Cosima Kretz, Nina Oberle, Martin Hartmann, Alexander Enk, Peter H.<br />
Krammer, Elisabeth Suri-Payer, Annegret Kuhn<br />
Characterization of regulatory T cells in human autoimmune<br />
diseases with skin manifestations<br />
A dysfunction of CD4 + CD25 + regulatory T cells (Treg) is known to be involved in a<br />
variety of human autoimmune diseases. Recently, our group demonstrated that the<br />
number of Treg in skin lesions of patients with lupus erythematosus (LE) was<br />
significantly reduced compared to other chronic inflammatory skin diseases.<br />
Furthermore, a significant reduction in the number of peripheral Treg was only found in<br />
patients with an active flare of systemic organ manifestation of the disease. We also<br />
analyzed the frequency and phenotype of Treg in different forms of scleroderma,<br />
another complex autoimmune disease with skin and systemic organ involvement. Thus,<br />
the number of Treg in skin specimens of patients with scleroderma was investigated<br />
using anti-Foxp3 and anti-CD4 monoclonal antibodies for immunohistochemistry. In<br />
addition, characterization of peripheral Treg from patients with different forms of the<br />
disease was carried out by flow cytometry. Quantitative analysis of CD4 + T cells in skin<br />
lesions of patients with scleroderma revealed a significantly reduced number compared<br />
to LE and other chronic inflammatory skin diseases such as psoriasis and atopic<br />
dermatitis. Moreover, the frequency of Treg in the skin expressed as percentages of<br />
Foxp3 + cells from CD4 + cells in the inflammatory infiltrate of scleroderma was similar to<br />
the frequency found in LE but significantly reduced compared to the other control<br />
diseases. In peripheral blood, preliminary data show a higher number of total Foxp3 +<br />
Treg in patients with scleroderma compared to normal healthy donors while the number<br />
of CD4 + CD25 high Foxp3 + Treg seems to be normal. In conclusion, our results suggest a<br />
significant reduction of Treg in the skin of patients with different forms of scleroderma.<br />
Further investigations will evaluate if there is also a peripheral dysfunction of Treg in<br />
patients with this autoimmune disease.
Björn Kolbe, Ulrike Kolrep, Roland Wagner, Jürgen Schmitz, Ian C.D. Johnston<br />
Characterization of the natural ligand of the plasmacytoid<br />
dendritic cell-specific marker CD303<br />
CD303, the human Blood Dendritic Cell Antigen (BDCA)-2, belongs to the Type II C-<br />
Type Lectin family and is specifically expressed on Plasmacytoid Dendritic Cells (PDC).<br />
The Type I IFN secretion of PDC plays a major role in inflammatory autoimmune<br />
diseases such as Systemic Lupus Erythematosus. The natural ligand of CD303 may<br />
prove to be a key molecule in understanding these diseases, as it has been shown that<br />
cross linking of CD303 with the monoclonal antibody AC144 inhibits PDC IFN production.<br />
In order to identify the CD303 ligand (CD303L), we generated a CD303-Fc fusion<br />
protein containing the extracellular domain of CD303, an HA-tag and a human IgG1-Fc<br />
domain for purification and detection of the protein. CD303 protein purified by ProteinA<br />
chromatography can be detected by a panel of CD303 antibodies in ELISA studies and<br />
inhibits the staining of PDC with AC144 antibody. However, as high titers of protein<br />
were required in these assays, a second affinity purification step using AC144-coupled<br />
Sepharose was introduced. CD303 purified via this 2-step protocol showed an at least<br />
10x better binding to AC144 in ELISA than the ProteinA purified protein, indicating that<br />
only a fraction of the original protein was in fact correctly processed and fully functional.<br />
Many human and non-human cell lines express CD303L (determined by FACS analysis)<br />
and the highly purified CD303 also stained these cells 200x more effectively than only<br />
ProteinA purified protein. Therefore, high affinity binding of CD303 to AC144 correlates<br />
with binding to the natural CD303L.<br />
This protein will now be used to isolate the CD303L by immunoprecipitation from L+<br />
cells, and as lectins are known to recognize pathogen carbohydrate structures (eg. DC-<br />
SIGN), glycan binding studies will also be performed.
Stefanie Gross, Uwe Trefzer, Wolfram Sterry, Peter Walden<br />
Characterization of tumor-specific versus virus-specific tumorinfiltrating<br />
and peripheral blood T cells from melanoma<br />
patients<br />
Successful tumor immunotherapy depends on two aspects. First, the generation of<br />
sufficient numbers of tumor-specific T cells and, second, that these cells finally „do their<br />
job“. In numerous studies it has been shown, that the first part can be achieved now<br />
quite well. Following vaccination, vaccine-specific T cells can be monitored in the blood<br />
of the patients, but the clinical outcome still remains poor. In a few cases T cells have<br />
been monitored within the tumor as well. These cells are different in phenotype and<br />
functional capacity compared to those from the blood. The changes T cells are<br />
undergoing within the tumor microenvironment are still poorly understood, but remain<br />
one of the obstacles for successful immunotherapy.<br />
To address the question, whether or not, the changes T cells are undergoing within the<br />
tumor microenvironment depend on the specificity of the T cells, we evaluated the<br />
phenotypes of tumor-specific tumor-infiltrating T cells (TIL) and peripheral T cells in<br />
melanoma patients in comparison to T cells specific for immunodominant viral antigens.<br />
We used 12 color flow cytometry to analyze Dextramer stained cells ex vivo. In total 76<br />
samples (54 tumors and 22 PBMC) of 49 patiens and 3 healthy donors were analyzed.<br />
Tumor specific (Tyrosinase, Telomerase and gp100) Dextramer positive cells were<br />
compared to virus specific (CMV and EBV) Dextramer positive cells. These cells were<br />
phenotyped for the expression of markers that are indicators for activation,<br />
differentiation and negative regulation.<br />
In the tumor, we found both, tumor-specific and virus-specific T cells. The tumorspecific<br />
T cells are enriched in the tumor compared to the peripheral blood, but still it<br />
seems that non-tumor-specific T cells represent the majority of T cells within the tumor.<br />
However, the tumor specific T cells showed a different expression pattern for the<br />
activation markers CD25 and CD69 and for the negative regulatory markers PD-1 and<br />
CTLA-4 than the virus specific T cells.<br />
From our results it can be concluded that the infiltration of T cells into the tumor does<br />
not depend on their specificity. T cells which do not recognize tumor cells do enter the<br />
tumor and are affected by the tumor associated cytokine milieu.<br />
Nonetheless, some of the phenotypic changes T cells undergo within the tumor<br />
microenvironment seem to depend on the recognition of their cognate epitope on the<br />
tumor cells.
Marco Frentsch, Regina Starke, Sarah Meier, Gebhardt Friedemann, Dirk Busch,<br />
Chiara Romagnani, Andreas Thiel<br />
Characterization of versatile CD8 memory T-cells with potent<br />
APC helper function<br />
A classical paradigm in T-cell immunity is that CD8+ T-cells exert cytolytic cellular<br />
immunity while CD4+ T-cells provide helper and inducer functions for a variety of cells<br />
involved in the humoral as well as in cellular immune responses. Based on our recently<br />
established methods to assess antigen-induced CD40L (CD154) activated CD4+ T-cells<br />
we have identified a new subset of memory CD8+ T-cells in healthy humans capable of<br />
CD40L expression after activation.<br />
Most CD8+ TT40L-cells display a characteristic central memory T-cell phenotype<br />
expressing CD27, CD28, CD62L and CD127 but lacking surface markers characteristic<br />
for effector T-cells such as CD56. Upon activation CD8+ TT40L-cells secrete mainly IL-2,<br />
TNFα, MIP1β and partly IFNγ or IL-4 but lack expression of perforin or GranB. CD8+<br />
TT40L-cells express a chemokine receptor profile predisposing them to migrate to<br />
peripheral-epithelium and to recirculate through secondary lymphoid organs. In vitro<br />
CD8+ TT40L-cells exert potent helper function such as induction of dendritic cell<br />
maturation and B-cell activation.<br />
CD8+ TT40L-cells might represent essential cells in protective immunity particularly in<br />
situations when classical CD4+ Th-cells are absent or their appropriate function is<br />
altered. According to their unique functional CD8+ TT40L-cells may become potent<br />
candidate cells for qualitative immune monitoring and adoptive T-cell therapies in<br />
infection and cancer.
Shipra Gupta, Sebastian Rieder, Sylvia Escher, Aleksandra Heitland, Wolf-Georg<br />
Forssmann, Jörn Elsner, Ulf Forssmann<br />
Chemokine receptor-mediated intravascular inactivation of<br />
leukocytes by a non-glycosaminoglycan(GAG)-binding variant<br />
of NNY-CCL14.<br />
Chemokines play an important role in the selective recruitment of leukocytes during<br />
inflammation and immunosurveillance. Glycosaminoglycan (GAG) binding has been<br />
shown to be essential for the in vivo activity of certain chemokines. NNY-CCL14 has<br />
been proposed as a potential therapeutic compound acting as a CD26-resistant,<br />
agonistic inactivator of CCR1, CCR3 and CCR5. In this study, a non-GAG-binding variant<br />
of NNY-CCL14 was generated by mutating basic (B) amino acids to glycine or alanine<br />
within the identified 49BBXB52 GAG-binding motif. This variant, NNY-CCL14(G50,A51),<br />
does not bind to heparin in contrast to its precursor NNY-CCL14. Its biological activity<br />
was tested on CCR1, CCR3 and CCR5 using stably transfected cell lines or leukocytes in<br />
comparison with NNY-CCL14. NNY-CCL14(G50,A51) demonstrated a two-fold reduced<br />
ability to activate CCR1, but internalization of CCR1 was not affected. Surprisingly, the<br />
activity on human CCR3 was strongly reduced. The biological effects on human CCR5<br />
remained totally unaffected. There was a marked decrease in chemotaxis of eosinophils<br />
and monocytes in response to NNY-CCL14(G50,A51). In mice treated i.v. with NNY-<br />
CCL14(G50, A51), a sustained in vivo down-modulation of CCR5 was observed over a<br />
3h period.<br />
This non-GAG-binding mutant NNY-CCL14(G50,A51) retains the potential to induce<br />
receptor desensitization and internalization, but cannot be presented on the<br />
endothelium via heparin binding sites. Thus, after injection, it is available in the<br />
circulation distant from otherwise physiologically presented GAG-bound chemokines.<br />
These properties suggest that, when administered systemically, this receptor agonist is<br />
able to modulate leukocyte functions (i.e. receptor internalization) prior to their<br />
interaction with other endothelium-bound chemokines expressed under pathophysiological<br />
conditions such as allergic inflammation.<br />
Financial support: DFG grant FO77/10-1
Silvia Capellino, Peter Angele, Werner Falk, Maurizio Cutolo, Rainer H. Straub<br />
Chromaffin-like cells and catecholamine production: role on<br />
the inflammatory response in rheumatoid arthritis (RA)<br />
patients<br />
Introduction: It is well known that norepinephrine (NE) influence the immune response.<br />
We already demonstrated that in RA synovial tissue there is a loss of sympathetic nerve<br />
fibers compared to osteoarthritis (OA). However, there is no difference in NE release<br />
from synovial tissue in both groups.<br />
Aim: To identify cells positive for tyrosine hydroxylase (TH) and PGP9.5 (neuronal<br />
marker) and to understand the role of the local catecholamine production during the<br />
inflammatory response in RA patients.<br />
Materials and methods: Synovial samples were obtained from OA and RA patients who<br />
underwent knee joint replacement surgery. Tissue samples were frozen and than<br />
analyzed for TH, PGP9.5 and synovial cell markers by doublestain-immunofluorescence.<br />
From the same patients, synovial cells were isolated by tissue enzymatic digestion, and<br />
cultured with Reserpine (10 -6 to 10 -8 M) or medium (control) for 24 hours.<br />
Determination of TNFα, IL-10, IL-8 and IL-6 was performed by Luminex technique and<br />
ELISA.<br />
Results: Only in RA we found cells expressing PGP9.5. These cells did not doublestain<br />
with markers for fibroblasts, macrophages, T-cells and B-cells but also express TH. The<br />
blockade of catecholamine release by Reserpine 10 -6 M caused a reduction of TNFα by<br />
60% compared to control cells in RA patients. In OA there was a reduced TNFα<br />
production in Reserpine-treated cells, but the effects were lower than in RA. The<br />
production of IL -6 and IL -8 tended to be lower in Reserpine-treated RA cells, but not in<br />
OA.<br />
Conclusions: We hypothesize that chromaffin-like cells are present in RA synovial tissue,<br />
producing NE and other catecholamines, and acting on local inflammation. Our future<br />
goal is to investigate the effects of the different catecholamines on the inflammatory<br />
reaction.
Thomas Bollinger, Monika Bajtus, Annalena Bollinger, Stojan Dimitrov, Werner Solbach<br />
Circadian Rhythm of Regulatory T Cell distribution and<br />
function<br />
Vaccination is a powerful tool for the prevention of infectious diseases. Relatively little is<br />
known about the impact of the time point of vaccination on the ensuing immune<br />
response. Previous studies showed that vaccination in the afternoon compared to that<br />
applied in the morning hours caused a highly significant approx. fourfold higher mean<br />
antibody titer. No information is available on the underlying mechanisms. One<br />
possibility could be modulation of anti-vaccine immune responses by regulatory T cells<br />
(Treg). Thus, it seems reasonable that number and/or function of Treg might have a<br />
circadian rhythm. We investigated 12 healthy young men for 24 hours and monitored<br />
various parameters in the peripheral blood bi-hourly. We analysed the absolute<br />
numbers of Tregs by FACS using CD4-FITC- and CD25-PE-antibodies . Cosinor analysis<br />
revealed significant circadian rhythm in this population with highest levels during night<br />
time (approximately 95 Treg/µl blood) and lowest levels in the day (approximately 55<br />
Treg/µl blood) . In a second study we addressed the analysis of the functional circadian<br />
rhythm of Treg by performing proliferation and suppression assays for the measurement<br />
of the suppressive capacity of Treg at different time points during a 24 hour period. The<br />
first data provide evidence for circadian rhythm of regulatory T cell function with the<br />
lowest suppressive capacity of Treg at 7:00 am. At 3:00 pm for example we measured a<br />
significant higher suppressive capacity (p
Nicholas Schwab, Christoph Leder, Chi Wang Ip, Antje Kroner, Klaus-Armin Nave,<br />
Klaus Dornmair, Rudolf Martini, Heinz Wiendl<br />
Clonal expansions of pathogenic CD8+ effector T cells in the<br />
CNS of myelin mutant mice<br />
The causal interrelation of CNS degeneration and adaptive immunity is assumed as a<br />
critical pathogenic element influencing the clinical phenotype in neuroinflammatory as<br />
well as in neurodegenerative disorders. We have recently shown that primary<br />
oligodendrocytic damage (by overexpression of PLP) leads to a low-grade inflammatory<br />
reaction of high pathological impact in the CNS, probably reflecting pathogenic<br />
principles in some forms of multiple sclerosis. As a <strong>complete</strong>ly novel finding, these<br />
reactions were mediated by CD8+ T cells whereas CD4+ cells were not necessary for<br />
the pathological effects of the immune system.<br />
We here present a detailed immunological characterization of systemic and CNS-specific<br />
CD8+ T cell responses in PLP transgenic mice and aged wild type mice. We provide<br />
evidence that T effector cells are surveying the CNS of PLP transgenic and wild-type<br />
mice. These cells accumulate with age and show a higher level of activation in PLP<br />
transgenic mice. Exclusively in PLP transgenic mice, T cells show clonal expansions, as<br />
demonstrated by T cell receptor CDR3-spectratype analysis. Although we could not find<br />
specific CD8+ T cell responses against myelin-antigen-derived peptides, Vβ/Jβ<br />
similarities strongly suggest specificity against a common antigen.<br />
Our data thus demonstrate that a primary degenerative CNS disorder can be associated<br />
with secondary expansions of pathogenically relevant CD8+ T cells in the CNS. These<br />
findings have implications for our understanding of the role of secondary adaptive<br />
immune reactions in the context of neurodegenerative and neuroinflammatory diseases.
Andreas Grahnert, Steffi Richter, Sunna Hauschildt<br />
Cloning and characterization of an enzymatically active ADPribosyltransferase<br />
4 (ART4) from chicken<br />
ADP-ribosylation is a posttranslational protein modification, by which the ADP-ribose<br />
moiety of NAD + is transferred to an amino acid of the target protein. Enzymes<br />
catalyzing this reaction are called Mono-ADP-ribosyltransferases (ARTs). In mammals<br />
five ARTs have been identified. Except for human ART3 and ART4 their catalytic cleft<br />
contains an R-S-EXE motif and they are enzymatically active. By database searches a<br />
predicted chicken ART4 (chART4) gene was found. Using 5’ and 3’ RACE-PCR as<br />
molecular cloning procedures (based on the predicted nucleic acid sequence) we<br />
obtained the cDNA of this chART. Compared to the other human ARTs, the derived<br />
amino acids show the highest degree of identity with human ART4 (hART4, 42 %).<br />
Furthermore, the chART and the hART4 map to regions of conserved linkage synteny.<br />
Therefore the cloned chART could represent an ortholog of the human ART4. We<br />
detected the mRNA of this protein in bone marrow cells and yolk sack. In contrast to<br />
human and mouse ART4 the chART4 contains the R-S-EXE motif, characteristic for<br />
arginine-specific ARTs. In transfection experiments we could show, that the chART4 is<br />
indeed enzymatically active. We confirmed the arginine specificity and showed, that the<br />
chART4 is an about 40 kDa, GPI-linked and glycosylated protein. Like human ART4 the<br />
mRNA of chART4 was found in an erythroblast cell line. We would assume that the<br />
chART4 may also play a role in other cells originating from myeloid stem cells like<br />
human monocytes, in which we already detected ART4 mRNA.
Jens Wuerfel, Alina Smorodchenko, Elena Pohl, Johannes Vogt, Eva Tysiak, Robert<br />
Glumm, Sven Hendrix, Robert Nitsch, Frauke Zipp, Carmen Infante-Duarte<br />
CNS-irrelevant T cells enter the brain, cause blood-brain<br />
barrier disruption but no cellular neuropathology<br />
Invasion of autoreactive T cells and alterations of the blood-brain barrier (BBB)<br />
represent early pathological manifestations of multiple sclerosis (MS) and its animal<br />
model experimental autoimmune encephalomyelitis (EAE). Non-CNS-specific T cells are<br />
also capable of entering the CNS. But studies investigating the spatial pattern of BBB<br />
alterations as well as the exact localization and neuropathological consequences of<br />
transferred non-CNS-specific cells have been thus far lacking. Here, we used magnetic<br />
resonance imaging (MRI) and multiphoton microscopy (MPM) as well as histochemical<br />
and high-precision unbiased stereological analyses to compare T cell transmigration,<br />
persistence, relation to BBB disruption, and subsequent effects on CNS tissue in a model<br />
of T-cell transfer of ovalbumin (OVA)- and proteolipid protein (PLP)-specific T cells. BBB<br />
alterations were present in both EAE-mice and mice transferred with OVA-specific T<br />
cells. In the latter case, BBB alterations were less pronounced, but the pattern of initial<br />
cell migration into the CNS was similar for both PLP- and OVA-specific cells. Increased<br />
microglia density and astrogliosis were, however, observed exclusively in the brain of<br />
EAE mice. While mice transferred with non-neural-specific cells showed similar levels of<br />
rhodamine-dextran extravasation in susceptible brain regions, EAE mice presented huge<br />
BBB disruption in brain stem and moderate leakage in cerebellum. This suggests that<br />
antigen-specificity and not the absolute number of infiltrating cells determine the<br />
magnitude of BBB disruption and cellular pathology.
Maria Lawrenz, Alexander Visekruna, Thorsten Joeris, Nicole Schmidt, Anjo Kroesen,<br />
Stefan H.E. Kaufmann, Ulrich Steinhoff<br />
Coherence or Coincidence ? - ERK activation and<br />
Immunoproteasomes in Crohn Disease<br />
It is a common hypothesis, that Inflammatory Bowel Disease (IBD), namely Crohn<br />
Disease (CD) and Ulcerative Colitis (UC), results from inappropriate immune response<br />
to normal mucosal microflora. LPS signals via Toll Like Receptor 4 (TLR4) and activates<br />
the TPL2/ERK pathway, a MAPK pathway, that is linked to NF-kB and leads to<br />
production of proinflammatory signals. In this study, we investigated the role of ERK<br />
activation in IBD. Inflamed colonic mucosa from 25 patients with either CD or UC was<br />
analysed by immunohistochemistry and Western Blot. We observed highly activated<br />
ERK in the inflamed colon of patients with CD but not in patients with UC. Furthermore,<br />
in vitro experiments with macrophages from proteasome mutant LMP2 and LMP7 KO<br />
mice revealed a correlation between ERK activation and proteasomal activity. These<br />
findings demonstrate, that high amounts of immunoproteasomes present in inflamed<br />
mucosa of CD patients contribute to activation of the proinflammatory TPL2/ERK<br />
pathway. We suggest that blocking of the immunoproteasome activity by specific<br />
inhibitors is a promising therapeutic intervention strategy in treatment of CD patients.
Marcus Gereke, Jan Buer, Dunja Bruder<br />
Collaboration of the innate and adaptive immune system<br />
leads to immunological tolerance in the lung<br />
The lung with its exposed position has many tolerogenic properties to avoid an<br />
immunological collapse due to infection and inflammation. However, little is known<br />
about synergisms of innate and adaptive immunity in inducing peripheral tolerance in<br />
the lung. To get further immunological and molecular insights in the mechanisms<br />
underlying peripheral tolerance induction in the lung, CD4+ T cell reactivity to a lungspecific<br />
antigen was studied by transgenic expression of hemagglutinin (HA) in alveolar<br />
type II epithelial cells. Concomitant expression of HA and a MHC class II-restricted T cell<br />
receptor specific for HA in double transgenic mice resulted in a severe immunemediated<br />
interstitial lung disease. Despite aggressive and rapid progression of<br />
inflammation in lungs of young mice, pulmonary inflammation reached a plateau state<br />
in elder mice, suggesting the induction of peripheral tolerance mechanisms. Intensive<br />
characterization of self-reactive CD4+ T cells isolated from the inflamed lung suggested<br />
the induction of functional regulatory T cells at the site of inflammation. Epithelial cells<br />
represent a part of the innate immune system and play an important role supporting<br />
immune responses. Isolation of antigen-expressing alveolar type II epithelial cells (AEC<br />
II) enabled us to directly demonstrate that these particular cells are capable to induce<br />
antigen-specific T cell proliferation. Moreover, AEC II from diseased mice have a<br />
reduced capacity to stimulate naïve self-reactive CD4+ T cells and exhibit broad<br />
changes in their gene expression profile compared to AEC II derived from healthy<br />
control mice. Furthermore, AEC II from the inflamed lung secrete soluble factors that<br />
down modulate T cell proliferation. Data obtained by extensive functional and molecular<br />
characterization suggest an important role of alveolar type II epithelial cells for the<br />
induction of T cell tolerance and immune regulation in the lung and point at a close<br />
collaboration between the innate and adaptive immune system.
Jan Hendrik Niess, Frank Leithauser, Guido Adler, Jörg Reimann<br />
Commensal-driven local TH17 responses trigger inflammatory<br />
bowel disease<br />
The gastrointestinal immune system has evolved to respond to a vast array of stimuli<br />
for the innate and adaptive immune system derived from the enteric microflora. To<br />
determine if the development of TH17 cells in the colonic lamina propria (cLP) depends<br />
on the enteric microflora CD4 T cells that can be induced to secrete IL-17A were<br />
isolated from the lamina propria of B6 mice housed under standard pathogen free (SPF)<br />
or syngeneic (age- and sex-matched) germ-free (GF) mice. Increased numbers of CD4<br />
TH17 cells were found in the lamina propria of the ileum and colon but not the<br />
duodenum, jejunum, mesenteric lymph nodes, spleen or liver of SPF mice. In syngeneic<br />
(age- and sex-matched) GF mice, the absence of the commensal bacteria in the gut<br />
correlated with low numbers of cLP CD4 TH17 cells demonstrating that the microflora is<br />
required for the accumulation of IL-17-producing CD4 T cells in the cLP. Studies in<br />
genetically deficient, congenic SPF mice indicated that (type I and type II) interferons<br />
suppress but IL-4 and IL-12p40-containing cytokines support the accumulation of CD4<br />
TH17 cells in the cLP. cLP CD4 TH17 cells produce IL-17 but not IFNγ, IL-4 or IL-10.<br />
Colitis can be readily induced by adoptive CD4 T cell transfer into congenic,<br />
immunodeficient SPF hosts characterized by progressively increasing numbers of CD4<br />
TH17 cells that ‘spontaneously’ produce abundant amounts of IL-17 which can be<br />
further accelerated by transfer of IFNγ-deficient CD4 T cells into immunocompromised<br />
SPF recipients. In absence of the enteric flora naïve CD4 T cells failed to proliferate in<br />
transplanted GF but not in SPF hosts. Increased IL-17 levels were only found in sera of<br />
SPF but not GF hosts and thus immunocompromised GF recipients lacking the enteric<br />
flora are protected from the development of colitis. A deregulated, commensal bacteriadriven<br />
local expansion of CD4 TH17 cells is a key feature of the inflammatory bowel<br />
disease in this model and the increased numbers of TH17 cells in the cLP may restrict<br />
the potential harmful action of the enteric flora to the local microenvironment.
Maria Diedrichs-Möhring, Georges M.G.M. Verjans, Seerp G. Baarsma, Gerhild<br />
Wildner<br />
Comparison of antigen-specific cytokine secretion and<br />
proliferation of T lymphocytes in vitro<br />
Response of T lymphocytes following stimulation with antigen or mitogen can be<br />
determined either by proliferation or by secretion of distinct cytokines. Due to limited<br />
material it is often not possible to establish cultures for early and lately secreted<br />
cytokines as well as to detect proliferation. Therefore, we combined both methods.<br />
Lymphocytes were stimulated in 96-well-plates with different antigens or mitogen.<br />
Culture supernatants were collected after 24 h, 48 h, 72 h and 96 h and frozen until<br />
use. The remaining cultures were used to determine proliferation by 3H-thymidine<br />
uptake. Supernatants from the various time points were pooled to analyze the secreted<br />
cytokines by multiplex bead immunoassay. To verify this approach peripheral blood<br />
lymphocytes from two donors were stimulated in the same way and cytokine<br />
concentrations were determined from samples of single time points (24 h, 48 h, 72 h<br />
and 96 h) as well as from pooled supernatants.<br />
Using this approach we were able to detect early as well as lately secreted cytokines in<br />
the supernatants of stimulated T lymphocytes. Interestingly, the peak of distinct<br />
cytokine secretion in response to a certain antigen varied between different individuals.<br />
Comparing cytokine secretion and proliferation of T lymphocytes we found no<br />
correlation: high amounts of TNF-α and / or IFN-γ were found in weakly proliferating<br />
cultures and vice versa. These results indicate that cytokine secretion and proliferation<br />
are two different aspects of lymphocyte response following stimulation and these<br />
parameters are not replaceable by each other.<br />
Supported by Deutsche Forschungsgemeinschaft, SFB 571
Vera Jakobi, Swen Wagner, Michael Loos, Franz Petry<br />
Complement activation of Cryptosporidium parvum<br />
(Apicomplexa, Protozoa) via the classical and lectin pathways<br />
C. parvum causes self-limiting diarrhoea in the immunocompetent and chronic and lifethreatening<br />
disease in immunocompromised individuals. In order to overcome the<br />
infection a specific CD4+-T-cell response is essential. Infection is mainly restricted to<br />
the epithelium of the small intestine and no systemic infections have been reported. We<br />
investigated if complement contributes to the host defence against cryptosporidiosis.<br />
We could show that both, human and mouse C1q bind to the extracellular stages of C.<br />
parvum, the sporozoites and oocysts, independently of specific antibodies. Binding was<br />
demonstrated by incubation of the parasites with normal sera or C1q-deficient sera<br />
supplemented with purified C1q. After intensive washing parasites were lysed in SDS<br />
sample buffer, electrophoresed and blotted onto nitrocellulose. C1q was detected by<br />
immunoblotting. The binding of C1q was dependent on the ionic strength and<br />
temperature. Affinity of purified C1q to the parasite was higher than serum C1/C1q.<br />
Similar experiments were performed to demonstrate human and mouse MBL binding to<br />
C. parvum. MBL binding was Ca++ dependent and could be competed with mannose<br />
during incubation. Activation of complement was demonstrated by deposition of C3b/<br />
iC3b on oocysts in an immunofluorescence test. Despite the in vitro activation of the<br />
classical and lectin pathway mice deficient in C1q or MBL-A and MBL-C were not more<br />
susceptible to infection than wild type controls as judged by parasite shedding in the<br />
faeces. However, RT-PCR amplification of parasite mRNA from ilea of infected mice<br />
suggested slightly higher infection levels than C57BL/6 controls. From these data we<br />
conclude that the classical and lectin pathways may contribute to the restriction of the<br />
infection to epithelia of the host.
Feng Guo, Debra Weih, Elke Meier, Falk Weih<br />
Constitutive alternative NF-?B signaling promotes marginal<br />
zone B cell development but disrupts the marginal sinus and<br />
induces HEV-like structures in the spleen<br />
Nuclear factor (NF)-?B plays a crucial role in B cell and lymphoid organ development.<br />
Here, we studied the consequences of constitutive, signal-independent activation of the<br />
alternative NF-?B pathway for the splenic marginal zone (MZ). In contrast to nfkb2-/-<br />
mice, which lack both p100 and p52, mice that lack only the inhibitory p100 precursor<br />
(p100-/-), but still express the p52 subunit of NF-?B2, had markedly elevated MZ B cell<br />
numbers. Both cell intrinsic mechanisms and increased stromal expression of vascular<br />
cell adhesion molecule-1 (VCAM-1) contributed to the accumulation of MZ B cells in<br />
p100-/- spleen. While migration of p100-/- MZ B cells towards the lysophospholipid<br />
sphingosine-1 phosphate (S1P) was not affected, CXCL13-stimulated chemotaxis was<br />
impaired, correlating with reduced migration of MZ B cells into follicles in response to<br />
LPS. Strikingly, p100 deficiency resulted in the absence of a continuous marginal sinus<br />
but strongly induced expression of mucosal addressin cell adhesion molecule-1<br />
(MAdCAM-1) and glycosylated cell adhesion molecule-1 (GlyCAM-1) and the formation<br />
of ectopic high endothelial venule (HEV)-like structures in the splenic red pulp. Thus,<br />
constitutive activation of the alternative NF-?B pathway favors MZ B cell development<br />
and accumulation but leads to a disorganized microarchitecture of the splenic MZ.
Christian Koble, Jens Derbinski, Bruno Kyewski<br />
CONSTITUTIVE CROSS-PRESENTATION OF ENDOGENOUS<br />
SELF- ANTIGENS BY THYMIC DENDRITIC CELLS<br />
The role of central tolerance induction has recently been revised following the discovery<br />
of promiscuous expression of tissue-restricted self-antigens in the thymus. The extent<br />
of tissue representation afforded by this mechanism and its cellular and molecular<br />
regulation are barely defined. We have previously shown that medullary thymic<br />
epithelial cells (mTECs) are specialized to express a highly diverse set of genes<br />
representing essentially all tissues of the body thus mimicking the transcriptome of<br />
multiple peripheral tissues and maximizing the scope of central self-tolerance. It is,<br />
however, less clear whether mTECs and/or thymic dendritic cells (DCs) are responsible<br />
for presentation of these tissue-restricted self-antigens to developing thymocytes. Here,<br />
we analyzed ex vivo presentation of MHC class I- and II-restricted, endogenous selfantigens<br />
by purified mTECs and thymic DC. Although expression of all tested selfantigens<br />
at the RNA level was largely confined to mTECs, we consistently found crosspresentation<br />
by thymic DC. As a result of this constitutive cross-presentation within the<br />
thymic medulla, the frequency of APCs potentially tolerizing for a specific self-antigen is<br />
larger than previously estimated, when self-antigen expression had been detected at<br />
the mRNA or protein level [1, 2]. In conjunction with extensive scanning of medullary<br />
stromal cells by thymocytes, spreading of self-antigens from mTECs to hemopoietic<br />
APCs should enhance the efficacy of self-tolerance induction.<br />
[1] Klein, L. et al.: Sampling of complementing self-antigen pools by thymic stromal<br />
cells maximizes the scope of central T cell tolerance, Eur. J. Immunol. 2001 Aug; 31(8):<br />
2476-86<br />
[2] Derbinski, J. et al.: Promiscuous gene expression in medullary thymic epithelial cells<br />
mirrors the peripheral self, Nat. Immunol. 2001 Nov; 2(11): 1032-9
Katja Sabel, Oleg Krut, Martin Krönke, Alexander Klimka<br />
Construction of a recombinant intrabody library to select for<br />
inhibitors of intracellular pathogens<br />
Intracellular interactions between pathogen and host cell factors during infection are<br />
very complex and offer a wide range of therapeutic targets. Single chain fragment<br />
antibodies (scFv) can be functionally expressed inside the cell (intrabodies) and<br />
specifically bind cellular or pathogenic molecules thus inhibiting microbial pathogenicity.<br />
To reveal the anti-infectious potential of intrabodies experimentally, we have<br />
constructed a lentiviral scFv library which was stably expressed in mammalian target<br />
cells. To ensure that diversity of the scFv library was maintained during library cloning,<br />
randomized clones have been analysed by DNA fingerprint and sequencing and<br />
intrabody expressing cells were selected by negative selection using cytotoxic agents.<br />
As a proof of concept an HSV-1 thymidine kinase (TK) expressing cell line has been<br />
transduced with the intrabody library and subsequently treated with the cytotoxic base<br />
analog ganciclovir, which resulted in intrabody expressing, gancyclovir-resistant cell<br />
lines. As to the infection model, scFv-transduced HeLa cells were infected with the<br />
cytotoxic Staphylococcus aureus strain MW2. After four rounds of infection a significant<br />
reduction of pathogenicity was observed. Surviving HeLa cell clones are currently<br />
analysed to identify and characterize the specificity of intrabodies inhibiting S. aureus<br />
cytotoxicity. The findings of our study demonstrate the potential of intrabodies to both<br />
investigate and target eukaryotic as well as microbial factors determining host-pathogen<br />
interactions.
Vladimir Kocoski, Norbert Tautz, Eberhard Burkhardt<br />
CONSTRUCTION OF A STABLE TRANSFECTED, PERMANENTLY<br />
SECRETING BHK Tet-On CELL LINE CARRYING THE SINGLE-<br />
CHAIN CANINE IL-12 FOR APPLICATION IN THE TUMOR<br />
IMMUNOTHERAPY IN DOG<br />
INTRODUCTION: Besides being the most important tumor patient in veterinary<br />
medicine, the dog is a promising model for tumor immunotherapy in man. As one of the<br />
approaches in tumor immunotherapy, the cytokine stimulation of Natural Killer and<br />
cytotoxic T cells represents a promising way to specifically fight the tumor cells. Among<br />
the cytokines showing potent anti-tumor activities the heterodimeric interleukin-12 (IL-<br />
12) plays a significant role. However, in contrast to mice and human, detailed studies<br />
on this area in dogs are lacking. In order to provide reliable sources for future<br />
investigations on the field of tumor immunotherapy in dogs, we (1) constructed a singlechain<br />
canine IL-12 sequence, (2) stably transfected it into a baby hamster kidney (BHK)-<br />
Tet-On cell line, which would serve as a constant and inducible (Doxycycline) protein<br />
source and (3) demonstrated the biological activities of the constructed protein.<br />
METHODS: Both sequences coding for the canine IL-12, p35 and p40, were amplified by<br />
PCR, ligated as a single chain in a pTRE/luciferase vector and afterwards stably<br />
transfected into the BHK-Tet-On cell line. Using canine interferon-gamma (IFN-<br />
&gamma) ELISA and cytotoxicity test (Rose Bengal Assay), the bioactivity of the IL-12<br />
containing supernatants was investigated.<br />
RESULTS: Canine IL-2 blasts incubated with the supernatant from the transfected clone<br />
showed significantly increased IFN-&gamma production, which was <strong>complete</strong>ly blocked<br />
by an anti-canine IL-12 neutralizing antibody. The supernatant also showed increased<br />
cytolytic activity of the IL-2 blasts against the canine thyroid adenocarcinoma (CTAC)<br />
target cells at 50:1 ratio.<br />
CONCLUSIONS: The transfected clone produces the single-chain canine IL-12 in the<br />
supernatant, which shows the full bioactivity like the commercially available IL-12.<br />
Perspectively, this cell clone can be used for further investigation of the IL-12 induced<br />
anti-tumor effects of canine lymphocytes, especially NK cells. Moreover, the nucleotide<br />
sequence of the single-chain IL-12 could be used in gene delivery studies in dogs.
Alexey Popov, Julia Driesen, Zeinab Abdullah, Claudia Wickenhauser, Tomo Saric,<br />
Svenja Debey-Pascher, Trinad Chakraborty, Martin Krönke, Olaf Utermöhlen, Joachim L.<br />
Schultze<br />
Containment of pathogens and induction of the local immune<br />
privilege by IDO + denritic cells in granulomatous infections<br />
and its implication for human disease<br />
In the first decades following the discovery of the tryptophan-catabolizing enzyme<br />
indoleamine 2,3-dioxygenase (IDO), the molecule was thought to be mostly involved in<br />
the repression of bacterial and viral infections. Recently, however, evidence has<br />
emerged that this enzyme is also capable of promoting local immune privilege.<br />
However, these opposite activities of IDO could hardly be imagined within one<br />
pathological condition. Here, we attempted to link two converse sides of IDO inhibitory<br />
function – bacteriostasis and immune inhibition – in one in vivo situation. We could<br />
show for the first time in human <strong>list</strong>eriosis, but also in granulomatous infections, caused<br />
by other intracellular pathogens (i.e. tuberculosis or cat-scratch disease), that IDO +<br />
dendritic cells (DC) and macrophages prevent the spreading of the pathogens by<br />
formation of granuloma, which encapsulate the bacteria and “keep the bug at bay”. At<br />
the same time, massive enrichment of IDO-competent APC inhibits effector immune<br />
cells from entering the granulomas, thereby preventing these granulomas from<br />
destruction and avoiding pathogen dissemination, a dangerous situation detrimental to<br />
the host’s survival. Infection of human DC by Listeria monocytogenes in vitro results in<br />
significant induction of IDO both on transcriptional and protein levels. Moreover,<br />
enzymatic function of IDO in <strong>list</strong>eria-infected DC is tightly controlled by TNFα, which<br />
might explain exacerbation of granulomatous infections during anti-TNFα therapy.<br />
These findings clearly demonstrate that IDO can play a dual role during life-threatening<br />
infections, inducing local immune privilege and pathogen containment at the same time.<br />
It will be of great interest to map out if IDO plays a similar role in other infectious and<br />
non-infectious diseases.
Kathrin Westphal, Sara Leschner, Holger Loessner, Siegfried Weiss<br />
Containment of tumor colonizing bacteria by host neutrophils<br />
Systemic administration of several facultative anaerobic bacteria into tumor bearing<br />
mice leads to a preferential accumulation and proliferation of the microorganisms inside<br />
the solid tumor. Up to now, all known tumor-targeting bacteria show a poor<br />
dissemination inside solid tumors as they accumulate exclusively inside large necrotic<br />
areas and spare a rim of viable tumor cells. Interestingly, this bacteria-containing<br />
necrosis is separated from the viable tumor cells by a barrier of host neutrophils that<br />
have migrated into the tumor tissue. We report here that depletion of host neutrophils<br />
results in enhanced dissemination of tumor-targeting bacteria. Besides a noticeable<br />
higher total number of bacteria inside the tumor, we found an increase of the size of<br />
necrosis and a migration of bacteria into the vital tumor tissue. The border of host<br />
neutrophils that obviously trap the bacteria inside the necrosis had vanished and the<br />
few neutrophils left were bypassed by the bacteria. In addition, neutrophil-depletion<br />
might positively influence the therapeutic effects of tumor-colonizing bacteria. Thus,<br />
depletion of neutrophils should be considered as additional measure during bacterial<br />
tumor therapy.
Martin Schlee, Michael Bscheider, Veit Hornung, Andrea Ablasser, Stefan Endres,<br />
Gunther Hartmann<br />
Contrasting roles of p38 in TLR signaling<br />
Toll-like receptors 7 and 8 are activated by the synthetic compound Resiquimod (R848).<br />
According to previous studies, TLR7/8 stimulation involves NF?B, IRF and MAP kinase<br />
activation, which leads to secretion of proinflammatory cytokines in myeloid cells as well<br />
as type I IFN release in plasmacytoid dendritic cells (PDC).<br />
To further evaluate the role of different MAP kinases, we incubated peripheral blood<br />
mononuclear cells (PBMCs) or murine bone marrow-derived dendritic cells obtained<br />
from a Flt3-ligand (Flt3–L) culture with synthetic inhibitors and monitored cytokine<br />
secretion induced by TLR stimulation.<br />
Here we present data that suggest a negative influence of p38 MAP kinase on IL12<br />
secretion after stimulation with R848 but not LPS. Using the well-characterized selective<br />
chemical p38 inhibitor SB203580 from the family of the pyridinyl imidazoles, we could<br />
dose-dependently increase the amount of IL12 secreted by human monocytes. This<br />
increased cytokine secretion was independent of the Th1-inhibitory cytokine IL10. In<br />
contrast, inhibition of p38 almost <strong>complete</strong>ly abolished IFNa production after R848<br />
stimulation of PDCs. Similar results were gained regarding the signaling of murine<br />
myeloid bone marrow-derived dendritic cells (mDC) obtained from a Flt3–L culture. An<br />
increase of IL12 production in the presence of SB203580 after R848 and CpG<br />
stimulation was observed, while IFN alpha secretion by murine Flt3–L PDCs was<br />
strongly inhibited by SB203580. Surprisingly, IL12 secretion by murine Flt3–L PDCs was<br />
not increased but slightly decreased by SB203580, pointing towards a cell type-specific<br />
role of p38 in TLR signaling rather than a target gene-specific signaling.
Bishnudeo Roy, Oliver Pabst, Swati Shukla, Sandra Düber, Siegfried Weiss<br />
Contribution of B-1 cells to gut associated humoral immunity<br />
The relative contribution and repertoire of B-1 and B-2 cell derived IgA in the gut<br />
immune system is still a controversial issue. The lack of an exclusive B-1 cell marker<br />
has made it difficult to delineate the B-1 and B-2 cell derived IgA producing plasma<br />
cells. To circumvent these problems, we have used the L2 mouse line which is<br />
transgenic for λ2315 light chain and virtually consists of B-1 cells exclusively. A<br />
particular feature of these mice is the presence of a few B-1 cell derived specificities at<br />
dominating frequencies in the peritoneum. In this work, these specificities, detectable<br />
as VH sequences, were used as markers to investigate the participation of B-1 cells in<br />
IgA production at the intestinal mucosa.<br />
Analysis of IgM VH sequences derived from Peyer´s patches (PP) B cells of L2 mice<br />
showed that 10% of these IgM VH sequences were identical to IgM VH sequences<br />
derived from peritoneal cavity (PEC) B-1 cells of these mice. Also, some commonality<br />
amongst the IgM VH sequences derived from the lamina propria (LP) B cells, and PEC B-<br />
1 cell associated sequences from L2 mice could be observed.<br />
On the other hand, analysis of IgA VH sequences derived from the LP and PP B cells<br />
showed no match with B-1 cell associated Ig VH sequences. Additionally, IgA VH sequences derived from the LP associated plasma B cells was rather heterogeneous and<br />
showed N/P nucleotide addition in the CDR3 region and somatic hypermutation through<br />
out the VH chain. Histology done for the intestine showed a decreased number of IgA+<br />
plasma cells in the LP of L2 mice in comparison to NT control mice. Consistent with this,<br />
there was a decrease in the levels of secretory IgA in the intestinal lumen of L2 mice.<br />
In addition, IgA expressing B cells, majority of which was B-1 cells (IgA+CD43+) could<br />
be observed in the PEC of L2 as well as NT mice. Analysis of PEC B-1b cell derived IgA<br />
VH sequences of normal mice showed the presence of nucleotide exchanges through out<br />
the VH sequences at a high frequency.<br />
Altogether, these data suggest that IgA producing B cells might be a highly selected<br />
population and PEC B-1 cells might diversify due to antigen driven selection in the<br />
GALT.
Susanne Kirschnek, Robert Paul, Bianca Obermaier, Georg Häcker, Uwe Koedel<br />
Contribution of cell death in phagocytes and resident cells to<br />
the outcome of pneumococcal meningitis in mice<br />
Efficient uptake and elimination of bacteria by neutrophil granulocytes and macrophages<br />
is a crucial step in the defence against bacterial infections. We observed phagocytosisassociated<br />
apoptosis of macrophages and granulocytes after uptake and digestion of<br />
bacteria, which proceeds via the mitochondrial pathway and is at least in part<br />
dependent on the BH3-only protein Bim. To investigate the significance of bacteriainduced<br />
phagocyte apoptosis for infection, a mouse model of pneumococcal meningitis<br />
was used. Phagocyte and/or resident tissue apoptosis was inhibited by Bcl-2<br />
overexpression or Bim deficiency. In this model, neutrophil granulocyte function is<br />
known to be crucial for efficient defence against bacterial infection. Mice overexpressing<br />
Bcl-2 in the hematopoietic compartment had more severe symptoms and higher<br />
lethality than wild type littermates. We observed a similar recruitment of leukocytes into<br />
the brain at early time points during infection but a significantly higher leukocyte count<br />
in the cerebrospinal fluid at later stages. This was accompagnied by a loss of bloodbrain-barrier<br />
function and impaired clearance of bacteria in the blood in Bcl-2transgenic<br />
mice. In addition, more pronounced histopathological alterations, indicative<br />
of enhanced inflammation, were observed. Experiments with bim-/- mice further<br />
indicate that the loss of the pro-apoptotic Bcl-2 family protein Bim leads to a different<br />
phenotype where higher leukocyte counts in the cerebrospinal fluid are correlated with<br />
lower bacterial load in the brain and better maintenance of the blood-brain-barrier.<br />
Thus, in contrast to Bcl-2 overexpression (which was restricted to the hematopoetic<br />
compartment), Bim deficiency in all cell types conferred enhanced resistance to<br />
pneumococcal meningitis. These results indicate a physiological function for phagocyte<br />
apoptosis in the control of bacterial infections and suggest that cell death in nonhematopoetic<br />
cells contributes to the outcome of pneumococcal meningitis.
Gabriele Weintz, Michael Hammer, Ilona Moßbrugger, Leticia Quintanilla-Martinez,<br />
Christian Stemberger, Dirk H. Busch, Roland Lang<br />
Control of inflammation and host resistance during Listeria<br />
infection by the MAPK-Phosphatase DUSP1<br />
Innate immune cell activation via pattern recognition receptors induces the release of<br />
inflammatory cytokines, chemokines and mediators that are essential for the control<br />
and elimination of pathogens. To avoid excessive inflammation and tissue damage, the<br />
intensity and duration of this response are tightly regulated by multiple mechanisms.<br />
We and others have recently identified the MAPK phosphatase DUSP1 as an essential<br />
negative regulator of the inflammatory response to TLR activation. In the absence of<br />
DUSP1, LPS causes deregulated p38 activation in macrophages in vitro and high<br />
lethality in vivo due to excessive production of inflammatory cytokines. Infection with<br />
Listeria monocytogenes activates p38 MAPK and has been shown to induce expression<br />
of DUSP1 in macrophages. Here, we ask whether DUSP1 controls the type and intensity<br />
of the host response to Listeria infection, in terms of inflammation and control of<br />
bacterial replication. Our data show that DUSP1-deficient mice have reduced bacterial<br />
loads in the spleen on day 3 after intravenous infection compared to wildtype mice. At<br />
the histological level, the development of necrotic lesions in the spleen and liver<br />
appeared to be reduced. However, contrary to our expectation, the better protection<br />
against Listeria was not accompanied by enhanced cytokine production, neither 3 days<br />
nor 2 hours after infection, when bacterial loads were equal in DUSP1-deficient and<br />
wildtype mice. We are currently determining the efficiency of bacterial killing, the<br />
production of nitric oxide, and the kinetics of p38 MAPK activation of in vitro infected<br />
DUSP1-deficient macrophages to elucidate the mechanism(s) responsible for the<br />
increased resistance to Listeria infection.
Caspar Ohnmacht, Nico van Rooijen, David Voehringer<br />
Cooperation between innate and adaptive immunity during<br />
type 2 immune responses in vivo.<br />
Type 2 immune responses are associated with allergic diseases and parasite infections.<br />
They are mediated by IL-4/IL-13 expressing effector cells of the innate and adaptive<br />
immune system. Using sensitive IL-4/eGFP reporter mice (4get mice) we could identify<br />
eosinophils and basophils as the main IL-4 expressing cell types of the innate immune<br />
system recruited to the lung during infection with the helminth parasite Nippostrongylus<br />
brasiliensis or OVA-induced allergic inflammation. Reconstitution of T cell-deficient mice<br />
with IL-4/IL-13-deficient CD4+ T cells was sufficient to mediate parasite expulsion from<br />
the intestine and induction of effector cell recruitment and airway hyperreactivity in the<br />
lung. Therefore, innate IL-4/IL-13 expressing cells play a crucial role during the effector<br />
phase of type 2 immune responses.<br />
We analyzed development, migration and turnover of eosinophils and basophils in vivo.<br />
Both cell types could be identified in the fetal liver. Staining for the surface markers<br />
FIRE, CCR3, Siglec-F and CD62L revealed a gradual maturation process of eosinophils<br />
and enabled us to determine the activation status of eosinophils in different tissues.<br />
Eosinophils showed an activated phenotype in lymph nodes, thymus and Peyers’<br />
patches indicating that they had entered these tissues via the afferent lymph from sites<br />
of inflammation. In contrast to basophils, eosinophils actively migrated to the peritoneal<br />
cavity, where they survived for several days and from where they could recirculate to<br />
other organs.
Kathrin Schönberg, Gesine Kögler, Johannes Fischer, Markus Uhrberg<br />
Correlation of KIR expression and presence of HLA-C ligands<br />
in adult but not neonatal NK cells: transition from a naïve to<br />
an adult NK cell repertoire<br />
The functional repertoire of human natural killer (NK) cells is shaped by interaction of<br />
killer cell inhibitory receptors (KIR) and HLA class I ligands. It is so far unknown, how<br />
HLA class I-dependent education of NK cells is achieved. Here, a comparative analysis<br />
of NK cell repertoires was performed in peripheral blood (PB, n=154) and cord blood<br />
(CB, n=100) of a mainly Caucasoid cohort. A 6-color flow cytometric protocol was set<br />
up to differentiate between the four HLA class I-specific KIR encoded on group A<br />
haplotypes in combination with NKG2A. Similar to a recent study in a Japanese cohort,<br />
the presence of HLA-C ligands strongly correlated with an increased frequency of NK<br />
cells from PB expressing the respective cognate KIR. In contrast, no influence of HLA-C<br />
on the KIR repertoire was detected in NK cells from CB. Generally, significantly more<br />
KIR-expressing NK cells are present in PB than in CB. Nonetheless, the percentage of<br />
NK cells that are lacking inhibitory receptors for self-HLA class I is significantly lower in<br />
CB. This is due to a much higher frequency of NKG2A-expressing NK cells in CB. The<br />
data suggest that the NK cell repertoire goes through a transition from birth to<br />
adulthood, which is characterized by a marked decrease of NKG2A and an increase of<br />
self-HLA class I-specific KIR. The repertoire transition appears to be <strong>complete</strong>d at<br />
adulthood as no significant changes of NKG2A and KIR frequencies beyond age 20 were<br />
detectable in the cohort. The possible consequences regarding change in NK cell<br />
function and the clinical use of cord blood as stem cell source will be discussed.
Zoe Waibler, Martina Anzaghe, Abdo Konur, Shizuo Akira, Werner Müller, Ulrich Kalinke<br />
CpG 1668 treatment stimulates an anti-inflammatory<br />
environment that abrogates CpG 2216 induced type I IFN<br />
responses by pDC<br />
Upon incubation with a wide range of concentrations of the synthetic CpG<br />
oligodeoxynucleotide 2216 (CpG 2216), mouse bone marrow derived plasmacytoid<br />
dendritic cells (BM-pDC) are stimulated to produce interferon (IFN)-alpha, whereas only<br />
intermediate but not high doses of CpG 1668 induce IFN-alpha responses. To address<br />
why high dose CpG 1668 does not induce type I IFN, we co-incubated BM-pDC with high<br />
doses of CpG 2216 and CpG 1668 that resulted in the shut off of CpG 2216 induced IFNalpha<br />
responses. Incubation with supernatant of high dose CpG 1668 treated BM-pDC<br />
caused more than 90% inhibition of CpG 2216 induced IFN-alpha responses indicating<br />
that secreted inhibitor(s) plaid a major role. Among cytokines found in the inhibitory<br />
supernatant, IL-10 turned out to be one important negative regulator. In line with this,<br />
supernatant of IL-10 deficient BM-pDC stimulated with high dose CpG 1668 did not<br />
significantly inhibit IFN-alpha production, whereas addition of IL-10 neutralizing<br />
antibodies dramatically reduced the inhibitory capacities of wild-type supernatants.<br />
Moreover, recombinant IL-10 inhibited CpG 2216 induced IFN-alpha production.<br />
Interestingly, also IFN-alpha secretion upon stimulation with the DNA-encoded mouse<br />
cytomegalovirus (MCMV) was significantly diminished upon co-incubation with high dose<br />
CpG 1668. Thus, depending on the concentration used, CpG 1668 can be stimulatory or<br />
regulatory by inducing IL-10 that affects signaling by synthetic and/or natural Toll-like<br />
receptor (TLR) 9 ligands.<br />
Mechanisms described here probably reflect a physiological system to protect the<br />
organism from hyperactivation of dendritic cells that could lead to autoimmune<br />
reactions.
Viktor Kölzer, David Anz, Michaela Golic, Cornelia Wurzenberger, Stefan Endres,<br />
Carole Bourquin<br />
CpG Oligonucleotide Treatment Alters the Morphological<br />
Distribution and Phenotype of Regulatory T Cells<br />
Regulatory T cells (Treg) contribute to the maintenance of immunological homeostasis<br />
and limit autoimmune reactions. However, Treg also suppress anti-tumor immunity and<br />
may reduce the efficacy of cancer immunotherapy. Synthetic oligonucleotides containing<br />
immunostimulatory CpG motifs (CpG) that signal via Toll-like receptor 9 evoke Th1-type<br />
responses and pro-inflammatory cytokine production. They effectively induce anti-tumor<br />
immune responses in many experimental cancer models and are currently tested in<br />
phase III clinical studies. Despite this promising application in cancer therapy, little is<br />
known about their influence on Treg in vivo.<br />
In healthy, CpG-treated mice, we evaluated Foxp3-positive Treg populations in<br />
secondary lymphoid organs by flow cytometry and immunohistology. The influence of<br />
CpG-based cancer therapy on Treg was investigated in mice carrying subcutaneous<br />
tumors derived from a C26 colon carcinoma.<br />
We show that CpG treatment leads to a shift in the CD25low/CD25high Treg ratio in the<br />
spleen and lymph nodes, with an increase of CD25low expressing Treg phenotypes. Our<br />
analysis also demonstrates that regulatory T cells accumulate in the spleen during CpG<br />
treatment and display an altered morphological distribution. At the same time, CpG<br />
treatment decreases the fraction of CD25low-expressing Treg within PBMC and reduces<br />
the accumulation of Treg in peripheral blood of tumor-bearing mice. CpG application<br />
also slightly reduces the Treg population within tumor-draining lymph nodes.<br />
In summary, we show that CpG-based immunotherapy leads to a shift in the balance<br />
between CD25low and CD25high Treg phenotypes and to their accumulation in the<br />
spleen. We suggest that the described enhancement of anti-tumor immunity through<br />
CpG is unlikely to result from a general reduction of the Treg population. Instead, a<br />
redistribution of Treg during immunotherapy could support anti-tumor immune<br />
responses. Further investigation of the influence of immunotherapy on Treg may<br />
support the development of improved therapeutic regimens.
Wolfgang Kastenmüller, Georg Gasteiger, Ingo Drexler<br />
Cross-competition of CD8+ T cells shapes the<br />
immunodominance hierarchy during recall vaccination<br />
CD8+ T cell responses directed against multiple pathogen-derived epitopes are<br />
characterized by defined immunodominance hierarchy patterns. One possible<br />
explanation for this phenomenon is that CD8+ T cells of different specificities compete<br />
for the access to epitopes on antigen presenting cells and that the outcome of this so<br />
called cross-competition reflects the number of induced T cells. In our study using a<br />
vaccinia virus infection model, we found that T cell cross-competition is highly relevant<br />
during boost vaccination, thereby shaping the immunodominance hierarchy in the recall.<br />
We demonstrate that competition was of no importance during priming and unaffected<br />
by the applied route of immunization. It strongly depended on the timing of viral<br />
antigen expression in infected APC and was characterized by poor proliferation of T cells<br />
recognizing epitopes derived from late viral proteins. To our knowledge, this is the first<br />
demonstration of functional importance of T cell cross-competition during a viral<br />
infection. Our findings provide a basis for novel strategies of how boost vaccination to<br />
defined antigens can be selectively improved. They give important new insights into the<br />
design of more efficient pox-viral vectors for immunotherapy.
Nanette von Oppen, Linda Diehl, Rene Tolba, Percy Knolle<br />
CROSS-PRESENTING LIVER SINUSOIDAL ENDOTHELIAL CELLS<br />
ESTABLISH ANTIGEN-SPECIFIC ADHESION OF NAÏVE CD8 T<br />
CELLS LEADING TO T CELL TOLERANCE IN VIVO<br />
Presentation of antigen in the liver leads to induction of T cell tolerance rather than<br />
immunity. The ability of liver sinusoidal endothelial cells (LSEC) to cross-present<br />
exogenous antigens on MHC I molecules to naïve CD8 T cells and to induce CD8 T cell<br />
tolerance contributes to the hepatic immune regulatory function. However, the<br />
mechanisms underlying recruitment of naïve CD8 T cells to the liver remained unclear.<br />
We provide evidence that organ-resident cross-presenting liver sinusoidal endothelial<br />
cells recruit naïve CD8 T cells antigen-specifically to the liver. Antigen-specific hepatic<br />
recruitment of naïve CD8 T cells occurred rapidly within 4 hours after antigen-challenge<br />
and was exclusively observed in the liver but not in spleen, lymph nodes or lung.<br />
Expression of CD54 supported antigen-specific T cell adhesion but was not essential.<br />
Antigen-specific adhesion was accompanied by rapid stimulation of T cells, as shown by<br />
up-regulation of CD69, which was also predominantly observed in the liver. Experiments<br />
employing bone marrow chimeric mice unequivocally demonstrated that organ-resident<br />
but not myeloid APC were responsible for antigen-specific naïve T cell adhesion.<br />
Importantly adhesion of naïve CD8 T cells to cross-presenting LSEC in bone marrow<br />
chimeric mice resulted in tolerance of these cells. Our data attribute a novel function to<br />
LSEC, i.e. antigen-specific retention of naïve CD8 T cells, which is not observed for<br />
other organs. Delivery of a flow-stop signal by tolerogenic LSEC to passenger naïve CD8<br />
T cells in the hepatic circulation provides a mechanistic insight into the early steps of<br />
induction of CD8 T cell tolerance in the liver.
Heinke Conrad, Kerstin Gebhard, Julia Neudorfer, Christian Peschel, Helga Bernhard<br />
Cross-reactivity of HER2p369-377 reactive CTL clones against<br />
other HER family members<br />
Immunotherapies against tumor associated antigens are a promising field in oncology.<br />
Until now several vaccination studies against HER2 which is overamplified in about 25%<br />
of breast cancer were performed but the objective response rate achieved was only<br />
2.6%. The goal of our studies is the adoptive transfer of in vitro stimulated and<br />
expanded tumor-reactive, HER2-specific cytotoxic T cells (CTL) for patients with HER2overexpressing<br />
breast cancer.<br />
(1) CD8 T cells derived from an HLA-A2 donor were stimulated with autologous dendritic<br />
cells (DC) transfected with HER2-mRNA. (2) CD8 T cells isolated from an HLA-A2<br />
negative donor were stimulated with allogeneic HLA-A2 positive DC pulsed with the<br />
peptide HER2p369-377 known to be naturally presented with HLA-A2. HER2p369-377<br />
specific T cells were screened via ELISpot and FACS sorting, respectively, cloned and<br />
further tested in 51CRA and ELISA using HER3 and HER4 peptides corresponding to<br />
HER2p369-377 pulsed as well as HER2-, HER3- and HER4 overexpressing cell lines.<br />
Additionally, cell lines were transfected with either of the HER cDNA and a HER2 and<br />
HER3 overexpressing tumor cell line was transfected with the respective siRNA.<br />
The HER2-reactive CTL derived from both stimulation methods recognized the peptide<br />
HER2p369-377 and lysed the same panel of HLA-A2-matched, HER2-overexpressing cell<br />
lines as determined by lytic activity and cytokine secretion. Interestingly, the HER2p369-<br />
377 specific CTL clones were not only able to recognize the synthetic HER3 and/or HER4<br />
peptides corresponding to HER2p369-377 but also a cell line expressing either HER2,<br />
HER3 or HER4. Using downregulation of the respective HERs we could show that HER2<br />
and HER3 both contribute to the recognition by the CTL clones.<br />
As HER2 and HER3 both contribute to the malignant phenotype of HER2/HER3overexpressing<br />
breast cancer cells, the parallel targeting of HER2 and HER3 by crossspecific<br />
CTLs may inhibit the selective outgrowth of escape variants. These results will<br />
contribute to the design of T cell-based therapies for the treatment of breast cancer<br />
patients.
Mandy Pierau, Engelmann Swen, Thomas Drewes, Thabo Lapp, Dirk Reinhold,<br />
Burkhart Schraven, Ursula Bommhardt<br />
Cross-talk between PKB/Akt and TGFβ signalling in T cell<br />
activation<br />
The TGFβ family of cytokines are important regulators of cellular proliferation, apoptosis<br />
and differentiation. TGFβ is a key regulator of inflammatory responses and has been<br />
linked to the pathogenesis of experimental autoimmune encephalomyelitis (EAE).<br />
Binding of TGFβ to type II and type I serine-threonine kinase receptors leads to<br />
phosphorylation of the intracellular signal mediators, the Smad proteins. Activated<br />
Smad2 and Smad3 bind Smad4 and as heteromeric Smad complexes, once translocated<br />
to the nucleus, cooperate with other nuclear co-factors to induce the transcription of<br />
target genes. Several Smad regulatory proteins control the subcellular localization,<br />
phosphorylation and the binding of transcriptional partners of the Smads. Interestingly,<br />
a cross-talk between TGFβ signalling and the PI3K/PDK1/PKB pathway has been<br />
suggested from findings in cell lines that Smad proteins can physically interact with PKB<br />
or PDK1. We previously showed that T cells from transgenic (tg) mice expressing a<br />
constitutively active form of PKBα (myrPKB) are hyperreactive and show enhanced<br />
survival. Surprisingly, MOG-peptide induced EAE in myrPKB tg mice showed a milder<br />
disease progression compared to wild type mice. Since the amelioration of EAE<br />
pathology in myrPKB tg mice could be coupled to differences in TGFβ-mediated<br />
signalling events, we studied the response of T cells to TGFβ. In contrast to wild type<br />
CD4+ T cells TCR/CD3 induced proliferation of myrPKB tg T cells proceeded in the<br />
presence of TGFβ. Active PKB thus counteracts the inhibitory signals of TGFβ, although<br />
nuclear translocation of activated Smad2/3 proteins was normal. Data on candidate<br />
proteins that are affected by myrPKB and likely contribute to the "resistance" to TGFβ<br />
will be presented and discussed.
Sven Burgdorf, Christian Kurts<br />
Current models and mechanisms of antigen crosspresentation<br />
After internalization and processing of extracellular antigens, dendritic cells can induce<br />
an adaptive immune response by presenting antigenic epitopes on both MHC II<br />
molecules (to activate CD4+ T helper cells) and MHC I molecules (to activate CD8+<br />
cytotoxic T killer cells). The latter process has been termed cross-presentation.<br />
Increasing evidence supports an important role of cross-presentation in various<br />
biological processes. Nevertheless, the molecular mechanisms regulating intracellular<br />
processing of internalized antigens and loading of the derived peptides on MHC class I<br />
molecules remain largely unknown.<br />
At present, several models have been proposed to explain how endocytosed antigens<br />
might reach the MHC I presentation pathway. Most of them point out a decisive role of<br />
the ER associated degradation machinery (ERAD) and the cytoplasmic proteasome. Our<br />
recent findings support a further mechanism in which distinct endocytosis mechanisms<br />
selectively introduce soluble antigens into an organelle dedicated to cross-presentation<br />
and distinct from classical lysosomes. In this presentation, I will review the current cellbiological<br />
models of cross-presentation, focussing on their similarities and distinctions<br />
and on the unanswered questions pertaining to its molecular regulation.
Jörg Rossbacher, Frank Wilde, Gerd Müller, Martin Lipp<br />
CXCR5 as a therapeutic target in Non Hodgkin lymphomas<br />
and autoimmune disease<br />
Homeostatic chemokine receptors and their ligands control the trafficking of<br />
lymphocytes to and within secondary lymphoid organs. The receptor CXCR5 is<br />
expressed on mature recirculating B cells, a subset of memory T cells and follicular B<br />
helper cells (TFH). In cooperation with its ligand, CXCL13, which is expressed on<br />
stromal and follicular dendritic cells in the B cell follicle, CXCR5 is responsible for B/T<br />
separation in lymphoid tissues. It was shown that CXCR5 plays a major role in the<br />
development of secondary lymphoid structures like Peyers Patches and certain lymph<br />
nodes and therefore is suspected to be essential in ectopic follicle formation in chronic<br />
inflammatory diseases like Rheumatoid Arthritis, Sjogren's syndrome and Helicobacter<br />
pylori-induced chronic gastritis.Together with the fact that 90% of B cell non Hodgkin<br />
lymphomas (NHL) express significant levels of CXCR5 on their surface we propose that<br />
CXCR5 is a suitable therapeutic target in B cell NHL and chronic autoimmune disease.<br />
We therefore generated a hybrid hybridoma producing the trifunctional bispecific<br />
antibody bsCXCR5xCD3 to perform CXCR5 positive cell depletion. Bispecificity should<br />
enhance the lytic ability by bringing target and effector cells into close proximity and<br />
the intact Fc portion could attract FcR bearing effector cells or even initiate complement<br />
lysis. We tested the antibody on CXCR5 expressing NHL cell lines and observed<br />
increased cell lysis at various conditions and time points. In addition we tested primay B<br />
cells obtained from healthy human donors and observed efficient cell lysis at<br />
comparable concentrations and time points. These results show that the bispecific<br />
antibody is able to deplete target cells “in vitro”, no matter if they are cancer cell lines<br />
or primary human cells.
Sven Hartmann, Antje M. Wengner, Uta E. Hoepken, Peter K. Petrow, Uta Schurigt,<br />
Rolf Braeuer, Martin Lipp<br />
CXCR5- and CCR7-dependent lymphoid neo-genesis in a<br />
chronic model of antigen-induced arthritis (AIA)<br />
Rheumatoid arthritis (RA) is a common autoimmune disease affecting about 1% of the<br />
adult population and is mainly characterized by chronic, polyarticular, synovial<br />
inflammation, which can lead to long-term joint damage resulting in chronic pain and<br />
disability. The molecular and cellular pathogenic mechanisms, which lead to RA and<br />
maintain the chronicity of the disease, are still poorly understood. Characteristically for<br />
RA is the infiltration into the synovial tissue by granulocytes and large numbers of<br />
mononuclear cells, such as T and B lymphocytes, monocytes, neutrophils and<br />
macrophages. We have developed a novel model of antigen-induced arthritis in mice<br />
resembling the chronic phase of the human disease including frequent formation of<br />
ectopic follicular structures, a hallmark of human RA. In our model formation of ectopic<br />
follicles with segregated B and T cell areas can be regularly induced by intra-articular<br />
injection of mBSA into the knee joints of pre-immunized C57BL/6 and BALB/c mice. In<br />
CXCR5- and CCR7-deficient mice the formation and organization of these ectopic<br />
structures are severely impaired in proving that both chemokine receptors play an<br />
important role in lymphoid neo-organogenesis during chronic inflammatory conditions<br />
as in RA. Remarkably, most follicles show topologically segregated T and B cell areas<br />
with presence of CD8 and CD4 T cells, the formation of active germinal centers (GC)<br />
and generation of antigen-specific CD138+ plasma cells. Moreover, formation of ectopic<br />
follicles is entirely dependent on the presence of the chemokine receptors CXCR5 or<br />
CCR7. Our results suggest that continuous inflammatory stimuli, e.g. by autoantigens,<br />
are sufficient to induce lymphoid neo-organogenesis at extra-nodal sites, which in turn<br />
allows local antigen-dependent interaction of memory/effector B and T lymphocytes<br />
resulting in aberrant chronic autoreactive immune responses.
Tanja Nicole Hartmann, Bretton Summers, Valentin Grabovsky, Eilon Woolf, Ziv<br />
Shulman, Eike Buss, Tom Schall, Marcus Thelen, Ronen Alon<br />
CXCR7 blockage inhibits in human hematopoietic progenitor<br />
cells and T cells a CXCR4 subset specialized in integrin<br />
activation by CXCL12 under shear stress conditions<br />
CXCR7 (RDC1) is a novel CXCL12-binding chemokine receptor. Our earlier results<br />
suggested a crucial role for the major CXCL12 binding GPCR, CXCR4, in motility and<br />
integrin activation of human HPCs and T lymphocytes. We investigated the function of<br />
CXCR7 in CXCL12-mediated motility and integrin activation processes in these cells. We<br />
report that CXCR7 modulates the function of a small CXCR4 subset, which is specialized<br />
in CXCL12-stimulated integrin activation under shear flow. Inhibition of CXCR7 by<br />
blocking antibodies and a small molecular weight compound specifically interfered with<br />
CXCL12-dependent LFA-1 and VLA-4 activation and T cell adhesiveness to surfaceimmobilized<br />
anti-CXCR4 under shear flow. However, CXCR7 blockage did not interfere<br />
with CXCR4 surface expression nor with CXCL12-triggered T cell motility or chemotaxis<br />
in shear free and integrin independent assays, in contrast with previous reports.<br />
Strikingly, CXCR7 was not found on the surface at detectable amounts, but highly<br />
expressed in the cytoplasm. We suggest that both the inhibitory antibodies and the<br />
compound enter the cell via the small recycling pool and inhibit CXCR4-mediated<br />
integrin activation. This is a first demonstration that inhibition of an intracellular GPCR<br />
with undetectable expression on the cell surface can effectively interfere with a<br />
physiological key function of this GPCR.
Tobias Bopp, Christian Becker, Matthias Klein, Stefan Klein-Heßling, Alois<br />
Palmetshofer, Edgar Serfling, Marc Becker, Jan Kubach, Schmitt Steffen, Sabine Stoll,<br />
Hansjoerg Schild, Martin Staege, Michael Stassen, Helmut Jonuleit, Edgar Schmitt<br />
Cyclic AMP: The decicive component of naturally occuring<br />
regulatory T cell-mediated suppression<br />
Naturally occurring regulatory T cells (nTregs) are crucial for the maintenance of<br />
peripheral tolerance by suppressing auto-reactive T cells via cell contact-dependent<br />
mechanisms. Moreover, by limiting the magnitude of all adaptive immune responses,<br />
nTregs also play a pivotal role in adequately controlling immune pathologies. Although<br />
the underlying mechanisms of nTreg-mediated suppression are still elusive, a hallmark<br />
of this process is the inhibition of IL-2 production in the responder T cells. We found<br />
that nTregs harbour high levels of cyclic AMP (cAMP). This second messenger is known<br />
to be a potent inhibitor of IL-2 production and subsequent proliferation of conventional<br />
T cells. Upon co-culture with nTregs the cAMP content of the conventional T cells<br />
strongly increases. Furthermore, we demonstrate that nTregs and conventional T cells<br />
communicate via cell-contact dependent gap junction formation. The suppressive<br />
activity of nTregs is abolished by a cAMP-specific antagonist as well as by a gap junction<br />
inhibitor which blocks the cell contact-dependent transfer of cAMP to responder T cells.<br />
Hence, our results demonstrate that cAMP is crucial for nTreg-mediated cell contactdependent<br />
suppression by traversing membranes via gap junctions.
Bianca Paul, Linda Diehl, Alexander Knorre, Percy Knolle, Marc Beyer, Waldemar<br />
Kolanus<br />
Cytohesin-3 Links B7H1 mediated Shut-down of the PI3<br />
Kinase Pathway to the Repression of IL-2 Synthesis in<br />
Anergic T cells<br />
T cell anergy, defined by the repression of cytokine production in the presence of<br />
cognate antigen, is a hallmark of peripheral tolerance. This process is controlled by<br />
poorly defined signaling through co-inhibitory molecules, such as PD-1 on T cells and its<br />
ligand B7H1 on antigen presenting cells. Here we show that the guanine nucleotide<br />
exchange factor cytohesin-3 is an important, conserved repressor of IL-2 transcription<br />
in anergic T cells. B7H1-mediated inhibition of PI3-kinase activation in T cells results in<br />
a strong induction of cytohesin-3 expression. Furthermore, cytohesin-3, which lacks a<br />
carboxy-terminal serine phosphorylation site present in other cytohesins, is shown to<br />
mediate selective inhibition of NFkB- and ERK1/2-, but not of NFAT-dependent signal<br />
transduction pathways. We propose that cytohesin-3, an endogenous antagonist of<br />
phospho-cytohesin-1 signaling, is an essential component of a novel type of inhibitory<br />
circuitry leading to the attenuation of immune effector functions.
Sabrina Hoffmann, Michael Winkler, Marcus Gutscher, Helmut Fickenscher, Carsten<br />
Watzl<br />
Cytomegalovirus infected fibroblasts downregulate ligands<br />
for the Natural Cytotoxicity receptors NKp30 and NKp44<br />
Activation of Natural Killer (NK) cells is controlled by an elaborate system of activating<br />
and inhibiting receptors. The family of Natural Cytotoxicity Receptors (NCR) plays an<br />
important role in NK cell activation. The members of this family, including NKp30 and<br />
NKp44, have been shown to be involved for NK cell activation during tumor clearance<br />
and the lysis of virally infected cells. Although the cellular ligands to these receptors still<br />
remain elusive to date, we are able to detect these ligands using novel trimeric NCR<br />
fusion proteins.<br />
Human Cytomegalovirus (hCMV) is known to introduce a vast number of changes within<br />
the host cell machinery upon infection. Here we examine the role of NCR ligands during<br />
CMV infection of primary human foreskin fibroblasts (HFF). Non-infected fibroblasts<br />
readily express the ligands for NKp30 and NKp44 on their surface. Upon infection HFF<br />
show a clear decrease in staining intensity for both ligands. Killing of HFF by human NKcells<br />
is partly dependent on NKp30. Interestingly, the lysis of CMV infected HFF is no<br />
longer dependent on NKp30. UV-inactivation of viral particles and inhibition of<br />
expression of CMV early genes abrogates this effect suggesting that a specific CMV gene<br />
product is responsible. These results demonstrate that CMV infection causes a downmodulation<br />
of the ligands for NKp30 and NKp44, leading to reduced activation of NK<br />
cells. The down-regulation of NCR ligands might therefore constitute a new strategy of<br />
hCMV to escape the attac of NK cells.
Doris Urlaub, Sven Mesecke, Hauke Busch, Roland Eils, Carsten Watzl<br />
Decision making in NK cells<br />
The effector functions of NK cells are controlled by a balance of positive and negative<br />
signals that are transmitted via various kinds of surface receptors. To date our<br />
understanding about the integration of positive and negative signals and the decision<br />
making process inside NK cells remains poor.<br />
With the help of bioinformatic modelling we try to understand how NK cells first<br />
integrate antagonising signals and then compute a reliable killing decision. Gradual<br />
signal input through activating and inhibitory receptors is integrated to come to a "yes<br />
or no" decision by the NK cell to kill an attached target cell. Triggering of activating<br />
receptors leads to Src kinase activation and Vav-1 phosphorylation, whereas inhibitory<br />
receptors dephosphorylate Vav-1 via the phosphatase SHP-1. Therefore, we proposed in<br />
a first hypothesis, that Vav-1 is the decision making point in the signal transduction<br />
network. With this hypothesis we created a simplified model describing NK cell<br />
activation upon various stimuli and compared the results with experimental data. A<br />
Lattice Gas Monte Carlo Simulation showed that increased clustering of activating<br />
receptors already leads to a rapid switch-like increase in Src kinase phosphorylation. We<br />
confirmed this experimentally by showing that increasing the amount of activating<br />
receptor stimulation already behaves switch-like on the level of Vav-1 phosphorylation.<br />
Similarly, also the engagement of inhibitory receptors leads to a switch-like<br />
dephosphorylation of Vav-1.<br />
We are currently refining our mechanistic model and are testing predictions derived<br />
from this experimentally. This model of NK cell regulation enables a novel insight into<br />
the decision making process during lymphocyte activation.
Jochen Maul, Susanne Pförtner, Robert Geffers, Kerstin Kapp, Jan Buer, Martin Zeitz,<br />
Rainer Duchmann<br />
Decreased expression of CCR4 on CD4+CD25 high regulatory T<br />
cells as a possible mechanism for impaired migration to<br />
inflamed mucosa in Crohn´s disease<br />
Background: Regulatory T cells (Treg) prevent and treat established colitis in animal<br />
models. Although previous findings show that CD4+CD25 high FOXP3+ Treg from patients<br />
with Crohn´s disease (CD) display normal suppressive function to allogeneic antigens in<br />
vitro, Treg function may be impaired in vivo.<br />
Aims: To elucidate possible mechanisms for impaired Treg function in CD.<br />
Materials and Methods: Treg and naive T cells were isolated from peripheral blood of<br />
patients with active (aCD; n=3) and inactive CD (iCD; n=3) and healthy controls (HC;<br />
n=11) using MACS. Hybridisation to a self-developed microarray (Human TReg Chip)<br />
enabling simultaneous expression measurement of 350 genes selected for their<br />
potential implication in Treg biology was performed and differential expression was<br />
analysed by SAM. Regulation of candidate genes was confirmed by FACS analysis with a<br />
different group of HC (n=5) and CD patients (n=9).<br />
Results: 39 genes are significantly up-regulated when comparing Treg from HC to aCD<br />
and 25 genes comparing HC to iCD. In both groups, 10 genes were up-regulated more<br />
than 5fold. Transcripts for chemokine receptor 4 (CCR4) were among the strongest<br />
expressed. FACS analysis showed no significant difference in the percentage of CCR4+<br />
Treg comparing HC to CD (57.9±11.3 vs. 54.4±12.7), but comparison of normalized<br />
mean fluorescence intensity (nMFI; MFI CCR4+/MFI CCR4-) showed a significant<br />
decrease of nMFI in CD (15.8±3.7 vs 10.4±3.4; p=0.019).<br />
Conclusions: CCR4 is a possible target gene for Treg pathobiology in CD. Since the<br />
chemokines TARC and MDC – both ligands for CCR4 - are expressed in inflamed<br />
mucosa, the decreased expression of CCR4 points to an impaired mucosal Treg<br />
migration in CD.
Mahmoud Sadeghi, Gerhard Opelz, Volker Daniel, Cord Naujokat, Rainer<br />
Zimmermann, Angela Huth-Kühne, Caner Süsal<br />
Decreasing Soluble CD30 and Increasing IFN-γ Plasma Levels<br />
are Indicators of Effective Highly Active Antiretroviral<br />
Therapy.<br />
Abstract<br />
It was previously reported that, without highly active antiretroviral therapy (HAART),<br />
secretion of Th1 cytokines and antiviral IFN-γ in HIV-infected patients is decreased,<br />
whereas the production of Th2 cytokines, proinflammatory cytokines, and TNF-α is<br />
increased. We studied the effect of HAART on Th1-, Th2-, and monocyte-derived<br />
cytokines, and on the Th2-type immune response marker soluble (s)CD30 in HIV-1infected<br />
hemophilia patients. Viral Load (VL), CD4+ lymphocyte counts, and plasma<br />
levels of sIL-1RA, IL-2, sIL-2R, IL-3, IL-4, IL-6, sIL-6R, IL-7, IL-10, TNF-α, TGF-β2, IFNγ,<br />
and sCD30 were measured in 18 patients who received HAART. Nine patients were<br />
initially treatment-naïve and were monitored after the initiation of HAART. sCD30<br />
median levels were significantly higher in treatment-naïve patients than in patients who<br />
were on HAART (77 vs. 30U/ml, p=0.005). A strong association was observed between<br />
sCD30 and VL (r=0.85, p=0.004). After the initiation of HAART, sCD30 levels decreased<br />
and remained low (at 1 year: 38; at 2 years: 41U/ml; p=0.012 and p=0.021,<br />
respectively, as compared to baseline level) and this was accompanied by a decrease in<br />
VL and monocyte-derived IL-6 and an increase in CD4+ lymphocyte counts and Th1derived<br />
IFN-γ. One year after the initiation of HAART a strong inverse correlation was<br />
observed between IFN-γ and VL (r=-0.83, p=0.006). In contrast to sCD30 and IFN-γ,<br />
CD4 counts and plasma IL-6 did not correlate with VL at any time. Our data suggest<br />
that decreasing sCD30 and increasing IFN-γ plasma levels are indicators of effective<br />
HAART treatment and CD4 Th1 cell recovery in HIV-infected patients.
Nadine Voelxen, Sylvia Gutenberger, Hans-Hartmut Peter, Hermann Eibel, Klaus<br />
Warnatz<br />
Defective activation of B cells in persistent polyclonal B cell<br />
lymphocytosis (PPBL)?<br />
Persistent polyclonal B cell lymphocytosis (PPBL) is a disorder which mainly affects<br />
female smokers in their 4.-6. decade. The origin of this polyclonal lymphocytosis of<br />
atypical B cells often associated with a polyclonal rise of serum IgM is not understood.<br />
We therefore examined B cells of 6 PPBL patients (all female, age: 35-63 years)<br />
phenotypically by FACS as well as by activation in vitro.<br />
The characterization of the B cell subpopulations showed a polyclonal expansion of CD27<br />
+IgD+IgM+ memory type B cells up to 88.8% of CD19+ B cells (normal range: 7.8 –<br />
36%) as well as an increased number of CD21low B cells up to 30% of CD19+ B cells<br />
(normal range: 1.1-6.9%). There were no aberrations within the T cell compartment<br />
detectable.<br />
Functional analysis revealed a reduced proliferation especially after stimulation with anti-<br />
CD40, a decreased expression of CD86 on the surface of cells(17.98-70.43% with a<br />
mean of 37,91% compared to 53.54-73.76% with a mean of 62,59% in healthy donor),<br />
as well as enhanced apoptosis revealed by staining for annexin (21.69-55.81% with a<br />
mean of 39,76% versus 5.82-19.68% with a mean of 15,43% in healthy donor),<br />
despite an expansion of these cells in vivo.<br />
Based on our findings we currently investigate early and late signalling events<br />
downstream of CD40 and the B cell receptor in isolated B cells via western blotting and<br />
FACS to identify potential defects in these pathways.
Christine Skerka, Nadine Lauer, Claudia N Keilhauer, Lars Fritsche, Bernhard H.F.<br />
Weber, Peter F. Zipfel<br />
Defective Binding of Factor H (Y402H) and FHL-1 to CRP and<br />
Collagen in Age Related Macular Degeneration<br />
The common Y402H variant in the human complement Factor H (CFH) is linked to agerelated<br />
macular degeneration (AMD), a prevalent disorder leading to visual impairment<br />
and irreversible blindness in elderly patients. At present it is unclear how the variant of<br />
CFH contributes to the occurrence of drusen and the progression to AMD. In order to<br />
define a molecular role of CFH in AMD we purified CFH from plasma of genotyped AMD<br />
patients and control persons which are homozygous HH402, homozygous YY402 and<br />
heterozygous H/Y402. In addition we recombinantly expressed FHL-1, the alternative<br />
splice product of CFH, with the risk H402 and the protective Y402 variant. Functional<br />
tests were performed to compare these CFH and FHL-1 subtypes. The risk variants<br />
402H of both proteins CFH and FHL-1 showed reduced binding to C reactive protein<br />
(CRP). Using extracellular matrix protein array analysis reduced binding of the risk<br />
variants was identified to collagen 1, a major component of drusen. This reduced<br />
binding may cause inefficient complement regulation at the cell surface, particularly<br />
under conditions of inflammation, when CRP is recruited to injured sites and tissue. CFH<br />
and FHL-1 may act in concert and in the eye the reduced surface binding may result in<br />
inappropriate local complement control, which leads to inflammation, disturbance of<br />
local physiological homeostasis and progression to cell damage. As a consequence,<br />
these processes may lead to AMD pathogenesis.
Florian Börncke, Beatrix Pollok-Kopp, Mladen V. Tzvetkov, Martin Oppermann<br />
Defective Binding to C-Reactive Protein and Impaired<br />
Cofactor Activity of the Allotypic Y402H Variant of<br />
Complement Factor H<br />
Common polymorphisms in the human complement Factor H (FH) gene have been<br />
associated with either enhanced or reduced risk of developing age-related macular<br />
degeneration. Using FH preparations which were isolated from the sera of genotyped<br />
individuals we show that allotypic variation of two different amino acids (Y402H and<br />
I62V) affects binding of native FH to C-reactive protein (CRP), but not to C3b, heparin<br />
or retinal pigment epithelial cells. Variant-specific monoclonal antibodies which<br />
recognize distinct SCR7 epitopes showed that amino acid 402 not directly interacts with<br />
CRP, but probably indirectly affects SCR7 conformation. While both polymorphic FH<br />
forms showed similar cofactor activities for the Factor I-mediated C3b cleavage, the<br />
resulting iC3b fragment was much less efficiently converted to C3dg in the presence of<br />
the FH H402 risk variant compared to FH Y402. Reduced binding of FH H402 via CRP to<br />
cellular surfaces and sustained expression of iC3b, the major ligand for complement<br />
receptors CR3 and CR4 on macrophages, could result in enhanced inflammation in the<br />
subretinal space of AMD patients.
Frank Guenther, Gertud Maria Hänsch, Christof Wagner<br />
DEFENCE AGAINST BACTERIAL BIOFILMS: ROLE OF<br />
POLYMORPHONUCLEAR NEUTROPHILS (PMN)<br />
The formation of bacterial biofilms is increasingly recognised as the leading cause of<br />
chronic infections, particularly in patients with implanted devices, such as catheters,<br />
artificial heart valves or orthopaedic prostheses. It is generally assumed that the<br />
infection persists because bacteria organised as biofilms escape the host defence<br />
mechanisms. On the other hand we observed massive infiltration of leukocytes,<br />
predominantly of PMN, into the site of infection. To examine the question how PMN<br />
interact with bacterial biofilms, Staphylococcus aureus were cultivated under conditions<br />
allowing biofilm formation. The biofilms were then opsonised with normal human serum<br />
(NHS), immunoglobulin-depleted NHS, or complement-inactivated NHS and incubated<br />
with PMN derived from healthy donors. Interactions were observed by time lapse video<br />
microscopy, and by confocal laser scan microscopy. PMN adhered to, migrated on and<br />
into the biofilm. The PMN aggregated considerably, and eventually the formation of<br />
large cells clusters was observed. The clusters contained also extracellular PMN-derived<br />
DNA, consistent with the formation of neutrophil extracellular traps (NETs). Bacteriafree<br />
zones appeared around the PMN, and phagocytosis, apparent as uptake of bacteria<br />
into the PMN, was also observed. Depletion of bacteria and efficiency of phagocytosis<br />
depended on the opsonisation of the biofilm and of its maturation in vitro. Taken<br />
together, our data provide evidence that bacteria in biofilms are not entirely protected<br />
against host defence but that phagocytosis is still possible. Whether NET and cluster<br />
formation contributes to bacteria killing in biofilms cannot be decided as yet, but<br />
remains an attractive alternative.
Tobias Schulze, Katrin Räbel, Sven Golfier, Martin Lipp<br />
Deficiency in Sphingosine-1-phosphate receptor 4 (S1P4)<br />
results in deviated humoral immune responses<br />
The receptors S1P1 and S1P4 represent the major populations of Sphingosine-1phosphate<br />
receptors expressed on lymphocytes. Besides various functions in other cell<br />
types of the immune system, S1P1 is required for egress of lymphocytes from<br />
peripheral lymph nodes and thymus as well as B-cell positioning within the spleen. The<br />
role of S1P4 in lymphocyte homeostasis has not been well established yet. In order to<br />
assess the biological function of the later receptor, we have generated a murine S1P4-/model.<br />
Overall B and T cell distribution in secondary lymphoid organs were not significantly<br />
different in S1P4-/- and wild type (WT) mice. However, analysis of immunglobuline<br />
isotypes showed significant differences concerning IgG, IgA and IgE levels in the plasma<br />
and serum. Interestingly, IgA levels were similar in brocheal lavage fluids of S1P4-/-<br />
and WT mice. Epicutaneous challenge with FITC of previously sensitised mice revealed<br />
increased reactivity in the S1P4-/-mice. In contrast, the type IV hypersensitivity<br />
response were significantly decreased in S1P4-/- mice.<br />
Our findings in the S1P4-/- mice indicate that, although there are no imbalances in<br />
overall T- and B cell distribution, S1P4 is implicated in the polarisation of the immune<br />
response. Interestingly, it has been reported that S1P1 bias the immune response<br />
towards an TH2 phenotype. The possibility of a potential interaction between S1P1 and<br />
S1P4 in the polarisation of the immune response is currently assessed using lentiviral<br />
based shRNA mediated S1P1 knock down in S1P4-/- mice.
Anja Erika Hauser, Tobias Junt, Thorsten R. Mempel, Michael W. Sneddon, Steven H.<br />
Kleinstein, Sarah E. Henrickson, Ulrich H. von Andrian, Mark J. Shlomchik, Ann M.<br />
Haberman<br />
Definition of Germinal Center B Cell Migration In Vivo Reveals<br />
Predominant Intra-zonal Circulation Patterns<br />
The formation of germinal center (GC) derived high affinity memory B cells and plasma<br />
cells constitutes an important element of an effective adaptive immune response.<br />
Proliferation, mutation and selection in the GC are thought to occur in distinct<br />
microanatomical compartments—the dark zone (DZ) and the light zone (LZ). The DZ<br />
compartment is located more proximal to the T cell zone. It is primarily comprised of<br />
blasting B cells and represents the site where somatic hypermutation occurs. The LZ is<br />
characterized by the presence of follicular dendritic cells (FDCs), which are able to trap<br />
antigen (Ag) in the form of immune complexes on their surface. Affinity maturation has<br />
been posited to require frequent trafficking between zones: newly generated GC B cells<br />
have to migrate from the DZ to the LZ in order to test their BCR affinity against the Ag<br />
on the FDCs. After positive selection, they migrate back to the DZ for further<br />
proliferation.<br />
Here, we report the use of multi-photon in vivo microscopy to determine migration<br />
patterns of GC B cells. Analysis of time-resolved images revealed unexpected patterns<br />
of movement as well as GC B cell morphology. In contrast to an anticipated frequent<br />
movement between the DZ and LZ, few cells were observed to cross the DZ/LZ<br />
interface. Moreover, cell track trajectories indicated that cell movement in this region is<br />
predominantly parallel to the interface, suggesting that B cells circulate within individual<br />
LZ and DZ compartments. The results suggest a revision to our views of B cell<br />
circulation within the GC and the functional relationship of its two major compartments.
Christine Skerka, Mihály Józsi, Stefanie Strobel, Stefan Heinen, Matthew Edey, Svante<br />
L. H. Zipfel, Judith A Goodship, Timothy H.J. Goodship, Christoph Licht, Peter F. Zipfel<br />
Deletion of CFHR1 and CFHR3 correlates with presence of<br />
Factor H autoantibodies in hemolytic uremic syndrome<br />
Atypical Hemolytic Uremic Syndrome (aHUS) is a severe renal disease that is caused by<br />
defective complement regulation and multiple factors predispose to the disease. Disease<br />
associated mutations have been described in the genes encoding the complement<br />
regulators factor H (CFH), membrane cofactor protein (MCP), factor I (IF)) and factor B<br />
(FB). We showed in two independent cohorts of aHUS patients that a chromosomal<br />
deletion of 84 kb in the RCA gene cluster results in the loss of the genes coding for<br />
factor H related proteins CFHR1 and CFHR3 and increases the risk for aHUS. Here we<br />
identify in the same cohort of 121 aHUS patients 16 juvenile individuals (i.e. 13%) who<br />
are positive for CFH autoantibodies. Interestingly 13 of these individuals showed also<br />
homozygous CFHR1 and CFHR3 deficiency. Family studies showed a strong correlation<br />
of the presence of autoantibodies and CFHR1/CFHR3 deficiency with HUS and that the<br />
absence of CFHR1/CFHR3 alone represents a risk factor for HUS. Using a novel protein<br />
nanoarray with domain mapped Factor H monoclonal antibodies (mAb) the binding<br />
epitope of all analyzed autoantibodies was localized to the C-terminus of Factor H. This<br />
domain harbors the cell binding region of the complement inhibitor and represents a hot<br />
spot for HUS associated mutations. In hemolytic assays two C-terminally binding mAbs<br />
C02 and C18 which compete for autoantibody binding and serum from autoantibody<br />
positive patients showed enhanced lysis of unsensitized sheep erythrocytes. Thus we<br />
conclude that CFHR1/CFHR3 deficiency is a risk factor to develop Factor H<br />
autoantibodies that are associated with HUS.
Thorsten Feyerabend, Annette Tietz, Herve Luche, Freddy Radtke, Hans Joerg<br />
Fehling, Hans Reimer Rodewald<br />
DELETION OF NOTCH-1 IN KIT+ PRO-T CELLS BLOCKS T CELL<br />
DEVELOPMENT, BUT DOES NOT CONVERT T CELL<br />
PROGENITORS INTO THYMIC B CELLS<br />
Loss of Notch-1 in bone marrow cells, or interference in the thymus with Notch-1-Notch<br />
ligand interactions is associated with a block in T cell development in favor of aberrant B<br />
cell development. It is, therefore, widely accepted that Notch-1 signaling determines<br />
the developmental choice within single uncommitted progenitors between the two major<br />
lymphocyte lineages. To ‘fate map’ hematopoietic pathways in vivo, we have generated<br />
a Cre recombinase mouse (Mc-cpa Cre ) in which Cre expression is controlled by a<br />
myeloid gene locus (mast cell-carboxypeptidase A [Mc-cpa]). Surprisingly, when<br />
crossed to a Cre-dependent red fluorescent protein (Rosa-RFP flox ) indicator mouse, Mccpa<br />
Cre labels ~90% of T but only ~10% of B lineage cells. Labeling along the T cell<br />
pathway takes place very early in the thymus in a major fraction of Kit + pro-T cells. We<br />
have taken advantage of this unprecedented and T cell-biased onset of Cre-expression<br />
to delete Notch-1 in pro-T cells while simultaneously turning on RFP. Cre-mediated<br />
Notch-1 deletion recapitulates the thymic Notch-1 deficiency phenotype, i.e. a block in T<br />
cell development at the apparent expense of B cell development. However, the fraction<br />
of RFP-labeled thymic B cells is not increased under conditions of Notch-1 deletion in<br />
pro-T cells. We conclude that loss of Notch-1 in Kit + pro-T cells blocks T cell<br />
development but does not convert T cell progenitors into B cells. The abundant<br />
immature thymic B cells that arise under Notch-1 deficiency represent T-lineage<br />
independent B cells that might capitalize on the free niches in the thymus made<br />
available by fading Notch-1 -/- pro-T cells.
Carsten Wiethe, Alexander Steinkasserer, Manfred Lutz, Andre Gessner<br />
Dendritic cell differentiation state and their interaction with<br />
NKT cells determines Th1/Th2 differentiation in the murine<br />
model of Leishmania major infection<br />
Recent reports demonstrated that dendritic cells (DC) sense inflammatory and microbial<br />
signals differently, redefining their classical subdivision into an immature endocytotic<br />
and a mature antigen-presenting differentiation stage. While both signals induce DC<br />
maturation by upregulating MHC II and costimulatory molecules, only Toll-like receptor<br />
signals are able to trigger proinflammatory cytokine secretion by DC, including Th1polarising<br />
IL-12.<br />
Here, we explored the murine Leishmania major infection model to examine the CD4+ T<br />
cell response induced by differentially matured DC. Initial experiments showed that<br />
pulsing DC with L. major lysate did not affect DC maturation with TNF&alpha (TNF-DC)<br />
or LPS+anti-CD40 (LPS+CD40-DC). When partially matured TNF-DC were injected into<br />
Balb/c mice prior to L. major infection, the mice failed to control infection and<br />
developed a Th2 response which was dependent on IL-4R&alpha signaling. In contrast,<br />
injections of fully matured LPS+CD40-DC induced a Th1 response controlling the<br />
infection. Furthermore, when the expression of different Notch ligands on DC was<br />
analyzed, we found increased expression of Th2-promoting Jagged2 in TNF-DC whereas<br />
LPS+CD40-DC upregulated the Th1-inducing Delta4 and Jagged1 molecules. The Th2<br />
polarization induced by TNF-DC required interaction with CD1d-restricted NKT cells.<br />
However, NKT cell activation by L. major lysate-pulsed DC was not affected by blockade<br />
of the endogenous glycolipid suggesting exchange with exogenous parasite-derived CD1<br />
glycolipid antigen.<br />
In sum, the differentiation stage of DC as well as their interaction with NKT cell<br />
determines Th1/Th2 differentiation. These results have generic implications for the<br />
understanding of DC instructed Th cell responses and the development of improved DC<br />
vaccines against leishmaniasis.
Stefan A. Kaden, Juergen Schmitz, Gregor Winkels<br />
Dendritic Cell immuno-activating receptor 1 –<br />
Characterization of a novel member of the C-type Lectin family<br />
C-type lectins (CLECs) are involved in a variety of immune interactions, in which they<br />
have been shown to act as both, pathogen recognition as well as adhesion receptors.<br />
The recently described murine dendritic cell (DC) immuno-receptor (DCIR)/DC immunoactivating<br />
receptor (DCAR) family consists of six type II CLECs clustered on<br />
chromosome 6. Beside the already characterised mDCIR, mDCIR2 (33D1) and mDCAR,<br />
little is known about mDCAR1, mDCIR3 and mDCIR4.<br />
To study phenotype and function of these gene products, we generated monoclonal<br />
antibodies (mAbs) against mDCAR1. In contrast to the previously published gene<br />
expression profile of DCIR/DCAR family genes, in which mDCAR1 was found to be<br />
restricted to NK cells (NK), we identify the receptor in bone marrow on subsets of F4/80<br />
+ macrophages and Ly6G + granulocytes, but not on NK or DC. Noteworthy, in thymus,<br />
expression of mDCAR1 is restricted to CD11c high DC. mDCAR1 + thymocytes comprise a<br />
typical myeloid DC phenotype characterised by the expression of CD8α and CD205, as<br />
well as the absence of CD11b. These mature DC express high amounts of MHCII and<br />
the costimulatory molecules CD40, CD80, CD86. mDCAR1 + thymic DC are positive for<br />
CD54, CD90, the stem cell and progenitor markers Sca-1 and c-kit (CD117), as well as<br />
the thymic specific DC marker BP-1.<br />
The successful generation of mAbs allowed us to identify the expression of mDCAR1,<br />
being the first step to uncover a presumably interesting function of this representative<br />
of the CLEC receptor family in the immune system.
Marcin •yszkiewicz, Natalia Zi•tara, Manfred Rohde, Kurt Dittmar, Jadwiga<br />
Jab•o•ska, Siegfried Weiss<br />
Dendritic cell like function of ER-TR9 + marginal zone<br />
macrophages<br />
ER-RT9 + marginal zone macrophages (MZM)) are found in the spleen at a strategic<br />
position for capturing blood borne antigen and pathogens. They are located where the<br />
central arteriole opens into the splenic sinus and form a tight network by extending long<br />
dendroid like protrusions. This DC like property prompted us to investigate the antigen<br />
presenting capacity of such cells. ER-TR9 + MZM were able to present peptide and<br />
soluble antigen to naïve CD4 T cells in vitro. Interestingly, such cells were also able to<br />
efficiently present peptide to major histocompatibility complex MHC class I restricted<br />
naïve CD8 T cells. More importantly, ER-TR9+ MZM cells were able to efficiently<br />
processe native OVA and cross-present it to OT-I T cells in vitro while other splenic<br />
macrophages (MF), like metalophillic MF and red pulp MF were unable to do so. This<br />
cross-presenting ability of ER-TR9 + MZM was found for soluble OVA as well as for latex<br />
bead-associated OVA. ER-TR9 + MZM, in addition to CD8a + DC and plasmacytoid DC, are<br />
effective in phagocytosis of Listeria monocytogenes that invade the spleen. By ex-vivo<br />
studies, we could show that both ER-TR9+ MZM and CD8α + DC were able to efficiently<br />
cross-present antigen secreted by L. monocytogenes to CD8 T cells. Our data identified<br />
ER-TR9+ MZM as professional splenic APCs with DC like properties. They are able to<br />
cross-present antigen and to activate naïve CD4 and CD8 T cells.
Kristin Hochweller, Jörg Striegler, Günter J Hämmerling, Natalio Garbi<br />
Dendritic cells control awareness of T lymphocytes for antigen<br />
In the body, dendritic cells (DCs) are in continuous cointact with T lymphocytes. In<br />
order to investigate potential consequences of this contact, we generated genetically<br />
modified mice that allow long-term depletion of DC. In the respective BAC CD11c.DTR<br />
transgenic mice, designated CD11c.DOG, the human diphtheria toxin receptor (DTR) is<br />
expressed in CD11c-positive DC. Depletion with diphtheria toxin (DT) eliminated more<br />
than 90-95% of DC. However, the DCs were regenerated within 3-4 days so that for<br />
long-term ablation repetitive injections of DT were required.<br />
CD4 T cells isolated from mice lacking DC exhibited a drastic decline in basal TCR<br />
signalling as indicated by decreased phosphorylation of the TCR ζ chain. No differences<br />
were observed in CD4 or TCR β surface expression. The reduced DC - T cell contact had<br />
profound functional consequences for the response of T cells to antigen. Naive CD4 T<br />
cells from DT-treated CD11c.DOG x 2D2 mice, which harbour a transgenic TCR reactive<br />
against the Ab/MOG35-55 determinant, failed to respond to MOG35-55 peptide<br />
presented by irradiated splenocytes. Likewise, T cells from DC-deficient mice showed a<br />
drastically reduced response to SEA superantigen presented by functional DC.<br />
The dramatic effect of the absence of DC on basal T cell sensitivity adds another major<br />
role to the wide range of functions of DC. Thus, in addition to being crucial for the<br />
balance between T cell immunity and tolerance, DCs provide continuous stimulation for<br />
naive T cells, thereby keeping T cells in a state of awareness that allows them to<br />
effectively respond to foreign antigens.
Mathias Lucas, William Schachterle, Karin Oberle, Peter Aichele, Andreas Diefenbach<br />
Dendritic Cells Prime Natural Killer Cells<br />
by trans-Presenting Interleukin 15<br />
Natural killer (NK) cells are lymphocytes of the rapidly acting innate immune system<br />
that play an essential role in the recognition and eradication of virally infected cells and<br />
tumors. Recent in vitro data suggested that dendritic cells (DC)- or macrophage-derived<br />
cytokines are able to enhance NK cell functions. However, it is unknown if NK cell<br />
effector responses in vivo depend on the NK cells’ interaction with myeloid cells. Using a<br />
mouse model for the inducible ablation of DC, we show that the in vivo priming of NK<br />
cell responses to viral and bacterial pathogens depended on the presence of CD11c high<br />
DCs. After peripheral Toll-like receptor (TLR) stimulation, priming of NK cells required<br />
their recruitment to local lymph nodes and interaction with DCs resulting in the<br />
emergence of effector NK cells in the periphery. NK cell priming was dependent on the<br />
recognition of type I IFN signals by DCs and the subsequent production and transpresentation<br />
of IL-15 by DCs to resting NK cells. CD11c high DC-derived IL-15 was<br />
necessary and sufficient for the priming of NK cells. Our data define a unique in vivo<br />
role of DC for the priming of NK cells, revealing a striking and previously unappreciated<br />
homology to T lymphocytes of the adaptive immune system. These results have<br />
important implications for the development of immunotherapeutic strategies aiming to<br />
boost NK cell effector
Anja Saalbach, Claudia Klein, Ulf Anderegg, Jan C. Simon<br />
Dermal fibroblasts induce maturation of dendritic cells<br />
To trigger an effective T cell-mediated immune response in the skin, dendritic cells (DC)<br />
migrate into locally-draining lymph nodes where they present antigen to naive T cells.<br />
During their migration to secondary lymphoid organs, DC have to travel through the<br />
stromal microenvironment comprised of the extracellular matrix and stromal cells such<br />
as fibroblasts, macrophages and endothelial cells. Little is known about the interaction<br />
of DC with these various cellular microenvironments. Here, we show that DC are located<br />
in close proximity to stromal fibroblasts in inflamed skin. In accordance, a Thy-1- and<br />
ICAM-1-dependent adhesion of DC to fibroblast could be detected in vitro. Co-culture<br />
experiments demonstrate that fibroblasts are effective in inducing both phenotypic and<br />
functional maturation of DC in a TNF alpha dependent manner. The resulting fibroblastmatured<br />
DC are able to support T cell driven immune responses reflected by CD25<br />
expression and enhanced T cell proliferation [1]. Together these data demonstrate that<br />
dermal fibroblast which DC can encounter during their trafficking from skin to lymph<br />
node may act as potent regulators of DC differentiation and function, and thus may<br />
actively participate in the regulation and outcome of DC-driven cutaneous immune<br />
responses.<br />
[1]Saalbach et al.; J Immunol, 2007, 178: 4966–4974.
Elke Pogge von Strandmmann, Boris Böll, Daniel Re, Andreas Engert, Venkateswara<br />
Simhadri<br />
Detection of HLA-B associated transcript 3 (BAT3) in sera<br />
from Hodgkin Lymphoma patients and its release from<br />
Hodgkin lymphoma cells<br />
Major triggering NK cell receptors such as NKG2D and the Natural Cytotoxicity<br />
Receptors Nkp30, 44 and 46 are critically involved in tumor cell recognition and<br />
surveillance, since a decrease of the corresponding ligands on tumor cells correlates<br />
with impaired NK cell-dependent killing and tumor progression. However, sustained<br />
expression and the release of soluble ligands for the NKG2D receptor negatively<br />
imprints the local and systemic immune response and correlates with a poor prognosis<br />
for haematological and epithelial malignancies.<br />
Hodgkin Lymphoma (HL) patients have impaired NK cell activity in the peripheral blood<br />
and the level of NK anergy correlates with a bad prognosis. Since spleen derived NK<br />
cells exhibit normal or increased activity, a serum-derived factor is probably involved in<br />
NK cell inhibition. In order to asses the role of HLA-B-associated transcript 3 (BAT3), we<br />
screened the sera of healthy donors and early and late stage HL patients using a BAT3<br />
specific sandwich-ELISA. BAT3, recently characterized in our lab, is a tumor-released<br />
ligand, that engages the triggering Natural Cytotoxicity Receptor NKp30. The BAT3<br />
serum level was significantly elevated in HL patients in comparison to healthy donors<br />
(p=0.0002). Interestingly, the early stage patients had a more pronounced increase<br />
compared to the advanced stage patients (p=0.024). We next analyzed whether cellular<br />
stress signals, such as HDAC inhibition and proteasomes inhibition could modulate the<br />
expression/release of BAT3 from Hodkin lymphoma-derived cell lines. A panel of cell<br />
lines were incubated with subtoxic concentrations of valproate and bortezomib and the<br />
supernatants were collected for a BAT3-specific ELISA. A significant increase of BAT3 in<br />
response to both substances was detected, that was irrespective of the IkB-a mutation<br />
status of the cell lines. The analysis of released BAT3 using fractionation and Western<br />
blotting revealed that different BAT3 isoforms were secreted, that may exhibit distinct<br />
modulation of NK cell-activity.
Leander Grode, Hans-Heinrich Henneick v. Zepelin, Albrecht Laeufer, Bernd Eisele<br />
Developing a TB vaccine for human use<br />
Vakzine Projekt Management GmbH (VPM) acquires promising vaccine candidates from<br />
academia, develops them with a consortium of partners and commercializes the results.<br />
With this goal VPM acquired a Tuberculosis vaccine candidate (VPM1002) from Max-<br />
Planck Institute of Infection Biology and develops this candidate through all necessary<br />
stages onto clinical Phase I and II. The project is divided into the three parts technology<br />
transfer & production, preclinic & pharm/tox and clinical Phase I and II.<br />
VPM1002 is a recombinant bacterial vaccine candidate for the prevention of tuberculosis<br />
for residents in endemic areas and persons at risk in non-endemic areas.<br />
It is well known that the existing BCG vaccine offers only little, if any, protection against<br />
pulmonary tuberculosis in adults. VPM1002’s strength is its ability to induce a CD8 T cell<br />
response which is crucial in immunity to M. tuberculosis.<br />
Recombinant M. bovis BCG expressing Listeriolysin (Hly) is able to induce poreformation<br />
in the phagosomal membrane and to leave the mycobacterial phagosome.<br />
The lysis by the Hly can be further enhanced by lowering the pH. Therefore the urease<br />
activity was knocked out by destruction of the ureC gene. Hly promotes antigen<br />
translocation into the cytoplasm and apoptosis of infected target cells, thus promoting a<br />
more profound immune response comprising both antigen-specific CD4 and CD8 T cells.<br />
VPM1002 is manufactured by a novel submerse fermentation in minimal medium. The<br />
final product is a lyophilised cake of live bacteria. Establishment of a GMP process is<br />
<strong>complete</strong>d. The process has been designed to offer full scalability. The GLP<br />
pharmacology is ongoing. The clinical phase I is planned for 2007.
Stefan Porubsky, Anneliese O. Speak, Bruno Luckow, Vincenzo Cerundolo, Frances M.<br />
Platt, Hermann-Josef Gröne<br />
Development and function of invariant natural killer T cells in<br />
mice with isoglobotrihexosylceramide (iGb3) deficiency<br />
Invariant natural killer T (iNKT) cells represent a distinct lymphocyte population which<br />
co-express natural killer (NK) surface markers such as NK1.1 (CD161) and a T cell<br />
receptor (TCR), which is composed of an invariant TCR-chain encoded by Vα14-Jα18<br />
gene segments in mice and Vα24-Jα18 in humans. iNKT cells play an essential role in<br />
immunoregulatory processes, such as tolerance, host defense and tumor surveillance.<br />
iNKT cells are positively selected in the thymus by CD1d molecules expressed by CD4+/<br />
CD8+ cortical thymocytes, but the identity of the endogenous lipid(s) responsible for<br />
positive selection of iNKT cells remains unclear. One candidate lipid proposed to be<br />
responsible for the positive selection is isoglobotrihexosylceramide (iGb3). To directly<br />
investigate the role of iGb3 in iNKT cell selection, we have generated mice deficient in<br />
iGb3 synthase (iGb3S, also known as α1-3galactosyltransferase 2, A3galt2). These mice<br />
developed, grew and reproduced normally and exhibited no overt behavioral<br />
abnormalities. Consistent with the notion that iGb3 is only synthesized by iGb3S, we<br />
demonstrate the lack of iGb3 in iGb3S-/-, as compared to iGb3S+/- mice. iGb3S-/- mice<br />
showed normal numbers of iNKT cells in the thymus, spleen and liver with selected TCR<br />
Vβ chains identical to controls. Upon administration of α-galactosylceramide, activation<br />
of iNKT and dendritic cells was similar in iGb3S-/- and iGb3S+/- mice, as measured by<br />
up-regulation of CD69 as well as intracellular IL-4 and IFN-γ in iNKT cells, up-regulation<br />
of CD86 on dendritic cells and rise in serum concentrations of IL-4, IL-6, IL-10, IL-<br />
12p70, IFN-γ, TNF-α, Ccl2/MCP-1. Our results strongly suggest that iGb3 is unlikely to<br />
be an endogenous CD1d lipid ligand determining thymic iNKT selection.
Nina Wantia, Tanja Ertl, Christine Cirl, Nuria Rodriguez, Hermann Wagner, Thomas<br />
Miethke<br />
Development of a protein and CpG-based vaccination against<br />
Chlamydophila pneumoniae<br />
Chlamydophila pneumoniae induces a pneumonia in C57/BL6 mice after nasal<br />
application of 1,75x10 6 IFU (infectious units). Six days after infection the mice were<br />
sacrificed, and chlamydial burden was measured in cell culture and by real-time PCR.<br />
First we investigated whether protection is achievable, hence mice were low-dose<br />
(0,5x10 6 IFU) infected three weeks before standard infection with 1,75x10 6 IFU. They<br />
hardly lost weight and showed no clinical signs of infection. Chlamydial burden was<br />
reduced to 0,2% in these mice compared to control mice. When we examined lung T<br />
cells of these mice, we could show that after restimulation with infected dendritic cells<br />
17,2% of CD4 + cells were IFN-γ positive (mock-infected mice: 0,055%). IFN-γ<br />
producing T cells are known to be protective against chlamydial infection.<br />
To generate a protective immunity against Cp. pneumoniae we tested several different<br />
chlamydial proteins. Membrane proteins of Cp. pneumoniae are accessible to the<br />
immune system and polymorphic membrane proteins (PMP) have been of<br />
immunological interest recently. Although the exact function of this new protein family<br />
is still unknown, it is known that they are able to induce neutralizing antibodies in<br />
Chlamydia trachomatis and are promising candidates for vaccination, especially PMP21<br />
and PMP10 and 11 are auspicious for protective vaccination.<br />
Protein and CpG 1826 were injected subcutaneously, followed by the infectious<br />
challenge three weeks later. Vaccination with OMP2 reduced chlamyidal burden to<br />
10,0% compared to correspondig control mice. PMP21 could even decrease chlamydial<br />
burden to 4,6%, whereas weight loss and lung weight was just slightly decreased in<br />
both cases. To induce better protection including less weight loss and lung weight we<br />
trapped the proteins in a organic polymer of Poly-DL-lactide-co-glycolide. This polymer<br />
was shown to release the antigen slowly into the cell and induces robust T cell<br />
responses.
Augustin J Kerkdijk, Gerhard Held, Antje Mueller, Wolfgang L Gross, Michael<br />
Pfreundschuh, Jan Voswinkel<br />
Development of a System to Test for Specificity of B-cell<br />
Receptors found in Granulomatous Lesions of Wegeners<br />
Granulomatosis patients<br />
Central in the pathogenesis of Wegeners granulomatosis (WG) is the PR3-ANCA, an<br />
antibody with specificity against proteinase-3 (PR3), a serine protease which is<br />
expressed on primed neutrophilic granulocytes. The ANCA-antigen-interaction leads to<br />
vasculitis. The biphasic nature of WG starting with a localised granulomatous<br />
inflammation followed by systemic necrotising small-vessel vasculitis seems to have a<br />
pathophysiological background in that the granulomatous disease gives rise to the<br />
systemic vasculitis by ANCA-priming.<br />
The granulomatous lesions of WG patients have been examined and germ-like centers<br />
have been discovered with B-cells and plasma cells in the vicinity of PR3-protein. We<br />
hypothesized that these germinal-center-like structures function as a tertiary lymphoid<br />
structure in which the plasma cells which produce the PR3-ANCAs are formed and that<br />
PR3 might be the antigen upon which affinity maturation takes place. The goal of this<br />
study was to develop a system which allows us to investigate the specificity of the Bcells<br />
found in the granulomatous lesions of WG patients. We characterised the antibody<br />
coding DNA derived from individual B-cells found in the granulomatous lesions and<br />
cloned this DNA into a phagemid vector which allowed us to produce fab-fragments,<br />
which are antibodies lacking the Fc-fragment. These fab-fragments are analogous to the<br />
B-cell receptor from which the DNA was derived. In this way we investigated six B-cells<br />
from granulomatous lesions of WG patients for their specificity against PR3 using ELISAs<br />
and Western blots. Furthermore we panned the fab-fragments against a phage randompeptide<br />
library to find other possible epitopes. We could not find fab-fragment binding<br />
against PR3 in ELISA or western blot analysis and we could not characterize a currently<br />
known peptide as a target fo the fabs in the random peptide library. This might be due<br />
to conformational differences between B-cell receptors and fab-fragments which render<br />
the latter dysfunctional or to low affinity of ANCA- binding.
Nadja Hilger, Rico Hiemann, Jörg Michel, Ursula Anderer, Martin Weigert, Ulrich Sack<br />
Development of an <strong>complete</strong>ly automatized system for image<br />
aquisition and detection of HEp-2 immunofluorescence<br />
patterns<br />
The standard screening test for the diagnosis of autoimmune diseases is the detection<br />
of autoantibodies in serum of patients by indirect immunofluorescence (IIF) based on<br />
HEp-2 cells. Manual evaluation of this test is very subjective, slow and there are no<br />
objective parameters as guidelines available. Interlaboratory tests show occasionally<br />
large deviations in the test evaluation resulting in a high variance of results. The aim of<br />
this project is the fast, objective, safe and economical automatic analysis of HEp-2 IIF<br />
patterns. Images of IIF patterns were <strong>complete</strong>ly automatically captured by use of an<br />
inverse motorized fluorescence microscope. Thereby, device-specific parameters were<br />
controlled automatically, too. For fast analysis of IIF patterns new algorithms of image<br />
processing were developed. Artifacts were recognized and excluded from analysis by the<br />
developed software. Analysis of more than 80.000 images clearly demonstrated full<br />
automatization and fast processing of IIF patterns. Additionally serum-specific<br />
fluorescence could be easily distinguished from background. Even very weak but<br />
positive patterns can be recognized and used for diagnosis. A detailed separation into<br />
different basic patterns is possible.<br />
Objective, fast and disease-related economical analysis of HEp-2 immunofluorescence<br />
patterns is feasible. The implemented software algorithms allows a mathematically way<br />
of describing IIF patterns and can therefore be a useful tool for the needed<br />
standardisation process.
Anne Brüstle, Sylvia Heink, Magdalena Huber, Christine Rosenplänter, Christine<br />
Stadelmann, Philipp Yu, Enrico Arpaia, Tak W. Mak, Thomas Kamradt, Michael Lohoff<br />
Development of inflammatory Th17 cells requires interferon<br />
regulatory factor 4<br />
The transcription factor IRF4 is essential for T helper 2 (Th2) development. We show<br />
here that IRF4 is also critical for generating Th17 cells, pro-inflammatory cytokineproducing<br />
cells associated with autoimmune diseases like experimental autoimmune<br />
encephalomyelitis (EAE). IRF4-deficient (IRF4-/-) mice did not develop EAE and IRF4-/-<br />
Th cells failed to differentiate into Th17 cells. Transfer of IRF4+/+ Th cells rendered<br />
IRF4-/- mice susceptible to EAE. IRF4-/- Th cells showed reduced expression of RORgt<br />
and increased expression of Foxp3, transcription factors important for Th17 and<br />
regulatory T cell differentiation, respectively. The dysregulation of both factors<br />
contributed to the phenotype of IRF4-/- Th cells . Our data position IRF4 at the center<br />
of Th development, influencing not only Th2 but also Th17 differentiation.
Christian Menge, Evelyn A. Nystrom<br />
Dexamethasone depletes γδT cells and alters the activation<br />
state and responsiveness of bovine peripheral blood<br />
lymphocyte subpopulations<br />
Administration of dexamethasone (DEX) to cattle is commonly used in models of stressinduced<br />
effects on the host defense. Even though the effects of DEX on the bovine<br />
adaptive immune are not fully elucidated yet. Previous studies showed that lymphocyte<br />
subsets are differentially affected by DEX. The objective of the present study was to<br />
characterize subsets of circulating lymphocytes in calves prior to and 48 h after the<br />
onset of parenteral DEX treatment. Treatment significantly reduced the overall<br />
percentage of circulating lymphocytes, and disproportionately depleted the population of<br />
γδTCR+/CD8α- cells. Analysis within the CD8α+ population of T cells further revealed<br />
that DEX treatment also reduced the CD8αlow subset of γδT cells coexpressing the<br />
activation marker ACT-2+. By contrast, DEX treatment did not affect the percentage of<br />
CD8αlow/CD25+ cells, indicating that cells with a special activation state were affected.<br />
Despite a sharp increase in the number of CD25+ PBMC from DEX-treated calves, only<br />
marginal differences were noted in the percentages and the proliferative capacity of the<br />
major lymphocyte subsets. Transcription of several Th-prototype cytokines (IL-2, IFN-γ,<br />
IL-4, TGF-β) was reduced in short term-PBMC cultures from DEX-treated calves, sparing<br />
il-10. The results of this study extend the evidence that DEX treatment does not<br />
generally suppress the bovine immune system but has a number of different effects on<br />
different lymphocyte subpopulations. This information must be considered when utilizing<br />
DEX treatment to improve bovine infection models.
Christian Menge, William C. Stoffregen, Joachim F.L. Pohlenz, Evelyn A. Nystrom<br />
Dexamethasone differentially down-regulates L-Selectin<br />
(CD62L) expression by bovine lymphocyte subsets in vivo and<br />
depletes the intestinal mucosa of intraepithelial γδT cells<br />
Intraepithelial lymphocytes (IEL) mainly are non-proliferating cells and less prone to the<br />
anti-proliferative effect of dexamethasone (DEX). Since DEX also alters the adhesion<br />
molecule expression, we hypothesized that DEX treatment of cattle affects IEL by<br />
interfering with lymphocyte homing. The objectives of the study were to investigate the<br />
effects of parenteral DEX treatment of calves (1) on the expression of CD62L - a<br />
prototype adhesion molecule - by peripheral lymphocyte subsets and (2) on the<br />
composition of intestinal IEL. Quantitation of CD62L on peripheral lymphocytes showed<br />
that DEX treatment down-regulated CD62L 48 h after first treatment. Consistent with a<br />
principal reduction of CD62L expression on γδT cells, the effect mainly pertained to CD4-<br />
and to CD8αlow cells. CD8αhigh lymphocytes were not affected. Analysis of IEL<br />
preparations from ileum, cecum, and distal colon 96 h after onset of treatment showed<br />
that DEX depleted intraepithelial γδT cells, some of which coexpressed CD8α. Variable<br />
effects of DEX treatment on other subsets and expression of activation markers by γδTCR<br />
+ and CD8α+ T cells were noted in ileum, colon, and cecum. Cytokine profiling (mRNA<br />
of mucosal tissue scrapings) showed that DEX treatment lowered the amounts of il-2<br />
and il-4 but increased il-8 and ifn-γ transcripts. Despite the variable effects of DEX<br />
treatment on IEL composition, changes in cytokine transcription were similar throughout<br />
the intestine. The study provides first evidence that differential effects of DEX on<br />
adhesion molecule expression by lymphocyte subsets alters the composition of intestinal<br />
IEL in cattle.
Eva Rieser, Monika Braun, Barbara Simm, Barbara Mosetter, Christine S. Falk<br />
Differences between cytotoxicity and cytokine expression are<br />
due to different phosphorylation patterns<br />
Introduction: The plasticity of human natural killer cells is reflected by the individual<br />
expression pattern of activating as well as inhibitory receptors. Besides this receptor<br />
expression, the amplitude of activity is determined by the intracellular signaling status.<br />
Previous studies have shown that NK cells expressing a similar receptor repertoire do<br />
not necessarily resemble identical activity regarding cytotoxicity and cytokine<br />
expression. Therefore, the differences in the intracellular signaling status of each NK cell<br />
may influence its reactivity to receptor-mediated triggering. Presuming that<br />
dysfunctions in different signaling cascades might explain the hyporeactivity of certain<br />
NK cells, we analyzed the intracellular phosphorylation patterns in response to various<br />
stimuli. We used several NK lines that differ in cytotoxicity and cytokine secretion,<br />
respectively.<br />
Materials and methods: Three NK lines were compared regarding cytotoxicity (CD107a<br />
degranulation) and cytokine secretion (multiplex technology). Phosphorylation patterns<br />
following PMA/ionomycin and receptor-mediated stimulation were determined by<br />
phosphoplex analysis quantifying total amounts of more than 10 kinases and their<br />
phosphorylated proportions.<br />
Results: Substantial differences were observed in their individual cytolytic activity and<br />
cytokine secretion pattern. In addition to these functional differences, the<br />
phophorylation status and the overall amount of signaling molecules also varied<br />
substantially between these NK lines. Our results implicate a correlation between low<br />
cytotoxic activity a special set of cytokine production and less phosphorylation for most<br />
of the tested signaling proteins. Therefore, receptor expression alone is not sufficient for<br />
NK function because the kinase compositions and the phosphorylation cascades<br />
determine the individual reactivity and, thus, plasticity of NK cells.
Marcel Andre Krüger, Kathrin Kopplin, Nadine Unterwalder, Christian Meisel, Hans-<br />
Dieter Volk, Gerald Grütz<br />
Differences in Lipopolysaccharide and Lipid A desensitisation<br />
Despite of great efforts, sepsis is still one of the major causes of death in intensive care<br />
units. It is characterised by an overproduction of pro-inflammatory cytokines in the<br />
early phase. This can lead to a systemic inflammatory response syndrome (SIRS). In<br />
prolonged sepsis the overproduction of anti-inflammatory cytokines is becoming more<br />
and more important due to a counter-regulation. This can develop into a compensatory<br />
anti-inflammatory response syndrome (CARS), also called immunoparalysis. During<br />
CARS the antigen-presentation and TNF-alpha production of monocytes is down<br />
regulated systemically, while the production of anti-inflammatory mediators like IL-10<br />
and IL-1RA is high. Due to this, the immune function is very low.<br />
A common in vitro model for CARS is LPS-desensitisation. For this, monocytes are<br />
incubated with LPS for 24 h. After rechallenge with LPS, the TNF-alpha-production of<br />
the cells is strongly decreased. This phenotype is similar to that of monocytes from<br />
patients with immunoparalysis.<br />
It is commonly believed, that Lipid A is the immunological relevant part of LPS, while<br />
the sugar residues only play a minor role. In contradiction to this common opinion, we<br />
demonstrate that desensitised monocytes that are restimulated with Lipid A behave<br />
different to monocytes restimulated with LPS, concerning TNF-alpha-production. We<br />
could show that in LPS-desensitisation IL-10 plays a major role when the cells are<br />
rechallenged with LPS, since desensitisation can be prevented by neutralising anti-IL-10antibodies.<br />
In contrast to this, neutralising anti-IL-10-antibodies have no effect when<br />
the cells are rechallenged with Lipid A.<br />
In summary our results raise new interesting questions on how LPS really interacts with<br />
its receptors on the surface of the cell.
Jan Diekmann, Olaf Beck, Georg Rauser, Hansjörg Schild, Hermann Einsele, Max S.<br />
Topp<br />
Different mechanisms contribute to the immune evasion of<br />
Epstein-Barr virus latent membrane protein 1<br />
Epstein-Barr virus (EBV) infection is associated with several pathogenic conditions such<br />
as nasopharyngeal carcinoma, NK and T cell lymphomas and Hodgkin`s disease, which<br />
all express latency type II proteins including the latent membrane proteins 1 and 2<br />
(LMP1/2). Both LMP1 and 2 have been suggested to represent targets for<br />
immunotherapy with antigen-specific CD8+ T cells. After generation of HLA-A*0201<br />
restricted CD8+ T cells specific for the YLLEMLWRL and CLGGLLTMV epitopes from the<br />
LMP1 and LMP2, respectively, we could show, that only the LMP2-specific CD8+ T cells<br />
were able to lyse antigen-expressing target cells.<br />
In order to investigate the mechanism responsible for the observed unresponsiveness of<br />
the LMP1-specific CD8+ T cells against LMP1-expressing target cells, the targets were<br />
treated with the proteasomal inhibitors MG132 and Epoxomicin. Both inhibitors could<br />
restore the immunogenicity of the target cells towards the LMP1-specific CD8+ T cells,<br />
suggesting, that blocking of the proteasome prevents destruction of the epitope and the<br />
same time enables processing through other proteases. Blocking of the proteasome by<br />
siRNA targeting of POMP greatly enhanced epitope-specific activation of the T cells<br />
emphasising, that prevention of proteasomal processing of LMP1 allows sufficient<br />
generation of viral epitopes.<br />
Alternatively, genetic truncation of the cytosolic part and the first four transmembrane<br />
regions of LMP1 could also restore good target recognition, stressing that LMP1 may<br />
contain sequences for selective inhibition of cytosolic proteases such as tripeptidyl<br />
peptidase II (TPPII) or thimet oligopeptidase (ThOP).<br />
These findings indicate, that the LMP1 epitope YLLEMLWRL is prevented from MHC-I<br />
presentation by distruction through the proteasome and inhibitory influences of the Nterminal<br />
transmembrane domains of the protein. We propose that this novel function<br />
may represent an additional immune evasion strategy employed by Epstein-Barr virus.
Diana Dudziak, Alice O'Kamphorst, Gordon F. Heidkamp, Veit R. Buchholz, Christine<br />
Trumpfheller, Chae Gyu Park, Ralph M. Steinman, Michel C. Nussenzweig<br />
Differential Antigen Processing and Presentation by Dendritic<br />
Cell Subsets in vivo<br />
Dendritic cells (DCs) process and present self and foreign antigens to induce tolerance<br />
or immunity. In vitro models suggest that induction of immunity is controlled by<br />
regulating the presentation of antigen, but little is known about how murine DCs control<br />
antigen presentation in vivo. To evaluate regulation of antigen processing and T cell<br />
activation by CD11c+/CD8+ and CD11c+CD8- DCs in vivo we delivered antigens to the<br />
DCs by using chimeric anti DEC205-Ova or 33D1-Ova antibodies. We could show that<br />
DCs targeted with anti DEC205-OVA or 33D1-OVA in vivo are distinct in their ability to<br />
present antigen on MHCI and MHCII, in that DEC205 expressing CD8+ DCs are<br />
specialized for cross-presentation on MHC class I, and CD8- DCs for presentation on<br />
MHC class II. By using transgenic mice that express human DEC205 under the CD11c<br />
promoter we could demonstrate that the difference in antigen processing is intrinsic to<br />
the DC subsets and independend of the receptor that was targeted. Moreover, we found<br />
an increased expression of proteins involved in MHC class I processing in CD11c+/CD8+<br />
DCs and in MHC class II processing in CD11c+CD8- DCs. This specialization may have<br />
important implications for understanding the initiation of T cell responses in vivo.<br />
This work was supported by the German Research Foundation (D.D., DU548/1-1)
Seray Cetin, Niels Kruse, Andrew Chan, Ralf Gold, Fred Lühder<br />
Differential expression of BDNF mRNA splice variants in<br />
mouse brain and immune cells<br />
Brain-derived neurotrophic factor (BDNF) is a member of the neurotrophin family and<br />
plays a key role in neuronal survival, differentiation and plasticity. Its neuroprotective<br />
character was pointed out by therapeutic application of BDNF. Neurons are the main<br />
cellular source of this neurotrophin, but it was also demonstrated that immune cells,<br />
namely T cells, B cells and monocytes express bioactive BDNF. The regulation of BDNF<br />
gene expression is not fully understood yet, but several mRNA splice variants of BDNF<br />
were recently described, each producing the same protein. In this study we analyzed<br />
the expression of mBDNF mRNA splice variants in cells of the immune system in<br />
comparison to cells of the central nervous system (CNS). We find that all splice variants<br />
are expressed in the CNS, whereas only mBDNF3 mRNA is expressed in lymphoid<br />
organs, immune cells and microglia. Activation of purified T cells lead to an increased<br />
expression of only mBDNF3, while activation of macrophages and microglia results in a<br />
decreased expression of this splice variant. These results show that mBDNF mRNA is<br />
differentially regulated in the CNS and the immune system by presumable different<br />
signalling networks. It additionally offers the chance to manipulate mBDNF expression<br />
in immune cells without affecting BDNF expression in the CNS.
Ildiko Boross, Christine Lux, Hans-Anton Lehr<br />
Differential expression of IL-17F and IL-17A in the lung of<br />
patients affected with bronchioalveolar cell carcinoma<br />
It is now widely accepted that IL-17 plays a pivotal role in mediating autoimmunity and<br />
inflammation however its role on the immuno-pathogenesis of tumor has not been<br />
clarified yet. The IL-17 cytokine family has many members, among them IL-17F and A<br />
have been shown the highest homology and functional properties. Different studies<br />
have been reported showing that both TGF-b and IL-6 are required for the<br />
differentiation of the TH17 clone producing both IL-17A and F. We thus first analysed<br />
the IL-17A and IL-17F expression in a group of normal subjects (n=9 ) as well as in<br />
patients with bronchioalveolar cell carcinoma (n=12). We found that although IL-17A<br />
expression did not differ between subjects with or without this lung tumor, IL-17F<br />
protein expression was downregulated in lung from patients affected by<br />
bronchioalveolar cell carcinoma as assessed both by western blot analysis and<br />
immunohistochemistry. We then investigated TGF-beta and IL-6 protein expression in<br />
these human lung samples. We found that both TGF-beta and IL-6 were upregulated in<br />
the lung samples fom subjects affected by bronchioalveolar cell carcinoma. Thus the<br />
defect we found in IL-17F production in the lung of patients with this tumour must map<br />
downstream of TGF-beta and IL-6.<br />
This work is funded by the Graduiertenkolleg 1043 and Immuno-intervention Cluster of<br />
Excellence (ICE, Mainz, Germany).
Markus Kleinewietfeld, Giovanna Borsellino, Adamo Diamantini, Alexander Sternjak,<br />
Luca Battistini, Olaf Rötzschke, Kirsten Falk<br />
Differential expression of VLA-4 by functional Treg and<br />
effector CD4+ T cells<br />
Migration and homing of lymphocytes is largely controlled by chemokine receptors and<br />
adhesion molecules. Since no chemokine receptor is expressed exclusively by Foxp3+<br />
CD25+ regulatory T cells (Treg), it remains the question how the trafficking of Treg can<br />
be selectively controlled. We therefore compared the expression of various integrins on<br />
human regulatory CD25high T cells and on CD25low effector CD4+ T cells. A striking<br />
difference was only observed for CD49d, the alpha-chain of the integrin VLA-4<br />
(alpha4beta1). The effect was evident only on effector/memory-like cells (CD45RO<br />
+CCR6+), where alpha4 was down-regulated on most of the Treg cells but up-regulated<br />
on the effector T cells. Loss of VLA-4 on Treg cells was compensated by the expression<br />
of CLA (cutaneous lymphocyte antigen), which is regulated in opposite to CD49d.<br />
Therefore, CCR6+ Treg cells are equipped to efficiently bind E-selectin via CLA, whereas<br />
CD4+ effector T cells preferentially adhere to the VLA-4 ligand VCAM-1. Notably, CD49d-<br />
CCR6+ Treg cells show the highest Foxp3 expression among all CD25high Treg and only<br />
these cells express the ectonucleotidase CD39 (ENTPD1), we have recently shown to be<br />
crucial for Treg mediated immune suppression. In line with the phenotype, the CD49d-<br />
CCR6+ Treg exhibit the strongest suppressive capacity among human Treg cells. Thus,<br />
the differential expression of VLA-4 and CLA provides a mechanism for the selective<br />
recruitment of either CCR6 expressing effector/memory-like Treg (TREM ) or ´<br />
conventional ´ effector/memory cells (TEM ). Moreover the absence of CD49d can be<br />
used together with CCR6 and CD39 as a key-marker to distinguish functional from other<br />
´ inactive ´ peripheral Treg cells in humans.
Florian Reißfelder, Jutta Schröder-Braunstein, Thomas Giese, Carolin Reiser, Stefan<br />
C. Meuer, Bernd Sido<br />
Differential inhibition of human intestinal lamina propria Tlymphocyte<br />
activation versus peripheral blood T cells by the<br />
gold-compound auranofin<br />
The oxidoreductase Thioredoxin (TRX) potentiates cytokine production in and<br />
proliferation of lymphocytes. Human intestinal lamina propria T-cells (LPT) constitutively<br />
contain high amounts of TRX, produce large quantities of cytokines and proliferate<br />
vigorously upon CD2 stimulation as compared to peripheral blood T-cells (PBT). To<br />
become immunologically active, oxidized TRX needs to be reduced by TRX reductase.<br />
We, therefore, aimed to inhibit the immune response of LPT in vitro through Auranofin<br />
(AF), a potent inhibitor of TRX reductase.<br />
Isolated LPT from fresh surgical specimens of normal colon mucosa and autologous PBT<br />
were stimulated via CD2 using a combination of mitogenic mAb. AF (0,5•M) inhibited<br />
proliferation of LPT to nearly background levels, whereas it was enhanced in PBT.<br />
Correspondingly, the vigorous cytokine mRNA expression in LPT following CD2<br />
stimulation (IL2, TNFα, TNFβ, IFNγ, GMCSF) was nearly <strong>complete</strong>ly abolished by AF in<br />
contrast to PBT, in which it was enhanced twofold. The CD2 immune response of LPT<br />
was paralleled by a high-level expression of the antioxidative fraction of TRX as<br />
determined by redox Western-blot analysis. This fraction was partly oxidized in LPT in<br />
the presence of AF, whereas it was further increased in PBT. The differential<br />
immunomodulatory activity of AF in LPT versus PBT was not due to differences in TRX<br />
reductase expression. However, Annexin V and Propidium Iodide staining revealed that<br />
LPT are constitutively more sensitive to spontaneous apoptosis than PBT, which is<br />
further enhanced by AF during CD2 stimulation. Inflammatory bowel disease (IBD) is<br />
characterized by hyperreactivity of LPT along with resistence to apoptosis as compared<br />
to LPT from normal gut. AF may, thus, represent an innovative immunomodulatory<br />
strategy in the therapy of IBD.
Svetlana Karakhanova, Karsten Mahnke, Alexander Enk<br />
Differential modulation of B7-H1 expression in pDCs and<br />
mDCs upon maturation of dendritic cells (DCs).<br />
Expression of regulatory molecules of the B7-H family by DCs plays an important role in<br />
the regulation of immune responses. However, their function(s) as well as regulation of<br />
their expression during DC maturation is not <strong>complete</strong>ly understood. To test how<br />
different types of DC maturation affect expression of these molecules, we stimulated in<br />
vitro prepared monocyte derived DCs (MoDCs) as well as genuine DCs, isolated from<br />
peripheral blood of healthy donors. Stimulation of MoDCs with a cytokine cocktail<br />
resulted in increased stimulatory capacity as well as increased expression of CD80,<br />
CD83, CD86 molecules. In parallel we observed upregulation of B7H1. Similar results<br />
were observed using genuine DCs. This means that cytokine cocktail maturated genuine<br />
DCs showed enhanced stimulatory capacity and upregulation of B7H1 expression. While<br />
MoDC represent a homogenous population of myeloid origin, genuine DCs consist of a<br />
mixed (mDC and pDCs) population with a different repertoire of TLR receptors. Total<br />
genuine DC populations were stimulated with various TLR ligands and assessed by FACS<br />
and functional assays to determine whether the surface expression of B7H1 molecules is<br />
affected. LPS as well as cytokines enhance expression of B7H1 preferentially in mDC,<br />
while Poly IC induced B7H1 expression in pDC. We furthermore show that stimulation<br />
activates the MAPK kinase pathway in MoDCs and blocking of ERK/MAPK<br />
phosphorylation with a specific inhibitor reduced increased B7H1 expression. This<br />
indicates that the expression of B7H1, at least in part, is regulated by the MAPK kinase<br />
pathway. Additional assays are going to be performed to identify supplementary<br />
signalling events responsible for B7H1 upregulation and to dissect the initial receptor/<br />
receptors responsible for activation.
Daniel Engel, Ulrich Dobrindt, Juliane Maurer, Frank Tacke, Christian Kurts<br />
Differential role of CCR2 on Gr1HI and Gr1LO monocyte<br />
migration in response to bacterial infection<br />
Monocytes are crucial immune effectors in bacterial infection, but the mechanisms<br />
governing their migration are not <strong>complete</strong>ly understood. The chemokine receptor 2<br />
(CCR2) regulates migration of monocytes, which is important for the defense against<br />
several pathogens. It has been shown recently that CCR2 is required for bone marrow<br />
(BM) emigration of monocyte precursors expressing high levels of the Gr1 (GR1HI)<br />
molecules. A differential effect of CCR2 on the migration of Gr1HI and Gr1LO monocytes<br />
in response to bacterial infection remains to be clarified.<br />
We have established a murine model of urinary tract infection (UTI) by injection of<br />
uropathogenic E.coli (UPEC) into the bladder of C57/BL6 mice. The numbers of<br />
macrophages in infected bladders of CCR2-deficient mice were reduced significantly.<br />
Using a recently published monocyte tracking method, we found that CCR2 was<br />
dispensable for immigration of both Gr1LO and Gr1HI monocytes into the infected<br />
bladder. Analysis of the blood of CCR2-deficient mice revealed a striking reduction of<br />
circulating monocytes, whereas no changes were seen in the BM. Mixed BM-chimeric<br />
mice, reconstituted with CD45.1 CCR2-competent and CD45.2 CCR2-deficient BM<br />
showed, that expression of CCR2 did not affect monocyte numbers in the BM, whereas<br />
the number of CD45.2 CCR2-deficient donor cells in the blood were severely decreased.<br />
These data indicated that CCR2 mediated emigration of monocyte precursors out of the<br />
BM, but neither immigration of mature monocytes into the BM, nor into the infected<br />
bladder in UTI.
Maik Moermann, Mareike Thederan, Christof Wagner, Inaam Nakchbandi, Gertrud<br />
Maria Hänsch<br />
Differentiation of the promonocytic cell-line U 937 to<br />
osteoclasts by bacterial lipopolysaccharides: a link between<br />
infection and pathological bone resorption.<br />
Bacterial biofilms formed on orthopaedic implants elicit persistent inflammation with<br />
massive tissue destruction and osteolysis. To establish a link between infection and<br />
osteolysis, we explored the possibility that bacterial infections promote the generation<br />
of bone resorbing osteoclasts. In that context, the effect of bacterial lipopolysaccharides<br />
(LPS) on the generation of osteoclasts was tested in vitro. Osteoclasts are derived from<br />
haematopoietic cells, and differentiate to osteoclasts under the influence of signals<br />
derived from stromal cells and/or T-lymphocytes. To exclude the effect of those cells,<br />
the promonocytic cell line U937 was used. U937 were differentiated to monocytes by<br />
use of phorbol ester, and then cultivated further with LPS. During culture U937 acquired<br />
the LPS receptor CD14. As the culture progressed, expression of numerous monocytetypical<br />
receptors, including CD11b, MHC class II, and CD 86 was induced, as were<br />
osteoclast specific proteins like the tartrate resistant acid phosphatase (TRAP) and<br />
cathepsin K. Furthermore, between days 4-6 by light microscopy a massive aggregation<br />
of the cells was observed followed by cell fusion. By day 15 multinuclear cells with the<br />
morphological characteristics of osteoclasts appeared. These cells were TRAP-positive<br />
and able to degrade calcium phosphate coated on cover slips and ivory as well. Thus,<br />
LPS as a single stimulus induces the differentiation of monocytes to cells with the<br />
phenotypical and functional characteristics of osteoclasts generated by established<br />
protocols. In conclusion, we propose that local bacterial infections could create a<br />
microenvironment that promotes the generation of bone resorbing cells, which, in turn,<br />
could contribute to the infection-associated osteolysis.
Kristine Kohl, Sylvia Schnautz, Elisabeth Klein, Thomas Bieber, Susanne Koch<br />
DIFFERENTIATION SIGNALS FOR HUMAN LANGERHANS CELL<br />
PRECURSORS IDENTIFIED BY SEQUENTIAL MIGRATION OF<br />
MONOCYTES<br />
Precursors of dendritic cells (DC) are myeloid cells transported via the blood stream,<br />
which migrate into tissues, where they differentiate to DC, most probably following<br />
locally released chemotactic signals. Using human peripheral blood monocytes, we<br />
investigated the impact of trans-endothelial migration on phenotype and function of<br />
Langerhans cell (LC) precursors, which are paradigmatic DC from the epithelial layer in<br />
the skin. On their way from the blood vessels to the epidermis, LC precursors need to<br />
cross the endothelial layers. They are guided by chemoattractants from dermal<br />
fibroblasts and from epidermal keratinocytes. In an in vitro transwell system,<br />
monocytes migrated towards medium conditioned by fibroblasts. Only CD14 low cells,<br />
which had migrated towards fibroblast conditioned medium, began to express CD1a,<br />
additionally a population of the CD14 low cells became CCR6 positive after migration and<br />
incubation. 14 hours later, in a second migration assay, only monocytes having<br />
migrated towards fibroblast-conditioned medium could migrate towards keratinocyteconditioned<br />
medium. Thus, trans-endothelial migration of human peripheral blood<br />
monocytes towards fibroblast-conditioned medium enabled them to subsequently<br />
migrate towards keratinocyte-conditioned medium. This would be a feature expected<br />
from LC precursors. The investigation of chemokine receptors of freshly isolated<br />
monocytes and after their various migration steps revealed that their trans-endothelial<br />
migration towards fibroblast-conditioned medium rescued the expression of chemokine<br />
receptor CCR2, which was otherwise rapidly down regulated. We therefore hypothesize<br />
that trans-endothelial migration of monocytes is a critical step for their differentiation to<br />
Langerhans cells.
Tim Meyer, Susann Beetz, Daniela Wesch, Ina Martens, Dieter Kabelitz<br />
Direct Costimulatory Effect of TLR3 Ligand Poly(I:C) on T cells<br />
We and others have recently shown that human αβ- as well as γδ- T lymphocytes<br />
express Toll-like receptor 3 (TLR3). As a classical pattern recognition receptor, TLR3<br />
binds double-stranded viral RNA and a synthetic analog, polyinosinic-polycytidylic acid<br />
[poly(I:C)]. Our earlier results indicated that poly(I:C) alone does not activate γδ- T<br />
cells but strongly increases the T cell receptor (TCR) stimulated interferon-γ secretion<br />
and expression of activation markers. Using primary human CD4+ αβ- T cells and Jurkat<br />
cells, we now also observed enhanced surface expression of CD69 and CD25 as well as<br />
IL-2 production in CD4+ αβ- T cells stimulated via the TCR in combination with poly(I:C)<br />
but not by poly(I:C) stimulation alone. To elicit the molecular basis of a potential crosstalk<br />
between TLR3 and TCR signalling, we performed luciferase assays. We observed<br />
that costimulation via TLR3 in comparison to TCR stimulation alone enhanced NF-κB but<br />
not NFAT activation. This tendency was underlined by the fact that the expression of the<br />
strictly NF-κB-dependent gene A20 was enhanced in Jurkat cells upon costimulation.<br />
These results indicate that TLR3 signalling modulates TCR-driven responses in different<br />
T cell populations.
Chiara Massa, Christiane Kellert, Esther Kamphausen, Barbara Seliger<br />
Disparate modulation of antigen processing components<br />
during maturation of the different human DC subsets.<br />
Dendritic cells (DC) are the most potent antigen presenting cells (APC) of the immune<br />
system and have thus been employed in the cell-based approach to tumor<br />
immunotherapy. After the modest successes obtained using DC pulsed with single<br />
tumor-derived epitopes, the latest strategies aim at broadening the repertoire of<br />
antigens provided by the vaccine in order to activate a more efficient immune response.<br />
To this purpose DC vaccines have been loaded with the entire tumor antigenic<br />
repertoire either in the form of RNA or proteins. In this therapeutic setting the final<br />
pattern of epitopes presented to the immune system is shaped by the antigen<br />
processing machinery of the DC and can thus be different from the one produced by the<br />
tumor itself. Indeed, some tumor epitopes can be destroyed by the immunoproteasome<br />
of professional APC. Aim of this study was to characterise the different subsets of<br />
human DC for the constitutive expression of the cyosolic and reticular peptidases<br />
involved in the antigen processing pathway and the modulation of these enzymes<br />
during the maturation process. To this purpose, myeloid CD1c+ and plasmacytoid<br />
BDCA4+DC were purified from the blood of healthy donors and stimulated with the<br />
appropriate TLR ligand. CD14+ monocytes were differentiated into DC either using the<br />
classical protocol of 7 days culture with GM-CSF and IL4 or the proposed amelioration<br />
using IL15 for the generation of Langerhans-like cells or a shorter 2 days protocol. The<br />
characterisation of the mRNA expression patterns of these enzymes revealed an<br />
opposite behaviour among DC types: a prevalent down-regulation in the expression<br />
pattern of peptidases was found in the plasmacytoid DC, whereas in myeloid DC the<br />
enzymes are up-regulated, in particularly in response to poly IC. Functional experiments<br />
will be performed to confirm whether the different expression patterns identified have<br />
any consequences on the epitope repertoire presented by the DC types, thus providing<br />
useful information for the establishment of DC-based vaccines that process tumor<br />
antigens in the most tumor-like fashion.
Andreas Hombach, Markus Chmielewski, Tobias Riet, Caroline Kopecky, Patrick Schmidt,<br />
Nadin Fein, Claudia Ederer, Anja Hombach, Heike Koehler, Hinrich Abken<br />
Dissecting and modulating a redirected anti-tumor T-cell<br />
response for adoptive immunotherapy: second generation of<br />
recombinant immunoreceptors.<br />
During the last years we have shown that naive T cells can be redirected towards<br />
defined target antigen by retroviral expression of a recombinant immunoreceptor that<br />
mediates both binding to antigen via an antibody domain and induction of cellular<br />
activation via the intracellular CD3z domain. The design of the immunoreceptor has a<br />
number of advantages: (i) the molecule is modularily composed allowing de novo<br />
composition of signaling and binding properties; (ii) receptor binding is independent of<br />
MHC presentation of antigen allowing T cell targeting towards unconvential T cell<br />
targets, i.e., carbohydrates or lipids; (iii) the receptor molecule triggers T cell effector<br />
functions upon binding. We demonstrated the feasibility of the concept using primary<br />
tumor cells and T cells from the same tumor patient in order to break tumor tolerance<br />
and to eliminate the autologous tumor cells, e.g primary melanoma cells, colon<br />
carcinoma cells or chronic lymphocytic leukemia cells. The concept, moreover, has the<br />
power to modulate the induced T cell response in a predictive way. By introducing<br />
costimulatory domains of the CD28 family, i.e., CD28, OX40 or 4-1-BB, we demonstrate<br />
that the anti-tumor response of T cells is specifically modulated with respect to induced<br />
secretion of IFN-g and IL-2, cytolytic activity and resistance to activation induced cell<br />
death. By introducing the CD28 costimulatory domain, moreover, T cells are rendered<br />
resistant to TGF-b mediated immune suppression as mediated by the tumor itself. By<br />
altering the epitope specificity and/or the binding affinity of the immunoreceptor, the<br />
efficacy of antigen-mediated T cell activation is dramatically modulated. By altering the<br />
structural prerequisites of the immunoreceptor molecule, interactions with the<br />
endogenous TCR of the engineered T cells are minimized in order to avoid generation of<br />
unwanted specificities. These newly identified parameters were integrated into a second<br />
generation of recombinant immunoreceptors which are expected to display an increased<br />
anti-tumor efficiency upon adoptive transfer.
Marc A. Blank, Olaf Utermohlen, Holger M. Reichardt, Marco J. Herold<br />
Dissecting the apoptotic pathways induced by Glucocorticoids<br />
in T-cells<br />
Glucocorticoids (GC) induce apoptosis in many cell types, but the mechanisms are not<br />
well understood. Recently it was reported that the proapoptotic Bcl-2 family member<br />
Bim and an upregulation of ceramides by a caspase-activated acidic sphingomye- linase<br />
(aSMase) play important roles. In order to study their involvement in GC- induced<br />
apoptosis we took advantage of the GC-sensitive murine T-cell lymphoma line WEHI<br />
7.15a. Overexpression of retrovirally expressed shRNAs against Bim or aSMase had no<br />
influence, whereas knockdown of the GC receptor (GR) itself rendered these cells<br />
resistant to Dexamethasone. In addition, various pharmacological inhibitors of ceramide<br />
production had no influence on GC-induced apoptosis. Moreover, thymocytes and<br />
peripheral T-cells from aSMase knockout mice were equally sensitive to GC induced<br />
apoptosis as wildtype cells. Furthermore, we confirmed the in vitro knock down results<br />
of Bim and the GR by introducing shRNAs into hematopoietic stem cells that were used<br />
to reconstitute lethally irradiated mice. While Bim inactivation did not impact ex vivo GCinduced<br />
apoptosis, loss of GR expression prevented cell death. Therefore we conclude<br />
that the involvement of Bim and aSMase is negligible in GC-induced apoptosis of T-cells.
Annelies Verbrugge, Adelheid Cerwenka<br />
Dissecting the molecular mechanisms involved in the synergy<br />
of TREM-1 with TLRs<br />
The innate immune system uses a broad spectrum of receptors to detect invading<br />
pathogens. A major class of these receptors are formed by the Toll-Like Receptor (TLR)<br />
s, which directly recognize pathogen-associated molecules and trigger the production of<br />
pro-inflammatory cytokines. In addition, several receptors can act together to enhance<br />
the immune response. One receptor that has been shown to cooperate with TLRs to<br />
induce cytokine production is Triggering Receptor Expressed on Myeloid cells (TREM)-1.<br />
TREM-1 is expressed on neutrophils and monocytes and is upregulated upon stimulation<br />
with LPS. Triggering of TREM-1 results in the production of pro-inflammatory cytokines,<br />
including TNFα. More importantly, TREM-1 synergizes with TLRs in cytokine production.<br />
The goal of our study is to dissect the molecular mechanisms leading to this synergy.<br />
Using quantitative RT-PCR, we found that LPS induced TNFα mRNA in primary human<br />
monocytes. Triggering of TREM-1 did not lead to detectable transcription of TNFα.<br />
However, when TREM-1 was triggered in the presence of LPS a substantial increase in<br />
TNFα mRNA was observed, compared to stimulation with LPS alone. The increase in<br />
TNFα mRNA occurred within the first two hours after stimulation, preceding LPS-induced<br />
upregulation of TREM-1 cell surface expression. Importantly, we found that preengagement<br />
of TREM-1 enhanced TNFα production upon subsequent stimulation with<br />
LPS. In current studies we aim to identify genes involved in the synergy of TREM-1 with<br />
TLRs using microarray-based gene expression profiling. Insight in the molecular<br />
mechanisms leading to synergy will enhance our understanding of the inflammatory<br />
response during sepsis.
Sven Burgdorf, Andreas Kautz, Volker Böhnert, Percy Knolle, Christian Kurts<br />
Distinct antigen uptake and intracellular routing mechanisms<br />
for activation of CD4+ and CD8+ T cells<br />
Adaptive immunity requires activation of T lymphocytes by antigen-presenting cells,<br />
which present the processed antigens on their MHC molecules. Intracellularly<br />
synthesised antigens, for example of viral or tumour origin, are presented by MHC I<br />
molecules and activate CD8+ cytotoxic T cells. Extracellular antigens can be presented<br />
on both MHC II molecules (to activate CD4+ T helper cells) and on MHC I molecules.<br />
The latter process has been termed cross-presentation. Current mechanistic models of<br />
cross-presentation assume that endocytosed antigens must be rescued from lysosomal<br />
degradation by diversion from a common pool of endosomes towards the cytoplasmic<br />
proteasome, but the underlying mechanisms remain unresolved and controversial. We<br />
investigated the influence of antigen uptake mechanisms on the intracellular routing<br />
and presentation on MHC I vs. MHC II molecules. We could show that if the model<br />
antigen, soluble ovalbumin, was taken up by pinocytosis or scavenger receptormediated<br />
endocytosis, it was targeted rapidly into lysosomes, where it was loaded<br />
selectively on MHC II molecules. Concurrently, ovalbumin was endocytosed by the<br />
mannose receptor into a distinct early-endosomal compartment, resulting in exclusive<br />
loading on MHC I molecules. We conclude that the endocytosis mechanism determines<br />
the intracellular destination of antigen, and thereby its processing and presentation to<br />
CD4+ or CD8+ T cells. Furthermore, this model implies that soluble antigen intended<br />
for cross-presentation does not have to be intracellularly diverted from lysosomes, but<br />
can enter a distinct endosomal compartment already during endocytosis. These findings<br />
pertain to our general understanding of antigen presentation and may provide a<br />
mechanistic basis for improving vaccination strategies.
Astrid Menning, Uta Hoepken, Kerstin Siegmund, Martin Lipp, Alf Hamann, Jochen<br />
Huehn<br />
Distinctive role of CCR7 in migration and functional activity of<br />
naïve- and effector/memory-like Treg subsets<br />
Foxp3+CD25+CD4+ Tregs play a fundamental role in the maintenance of self-tolerance<br />
and the control of inflammatory reactions. Previous data demonstrated a division of<br />
labor between naïve- and effector/memory-like Treg subsets, which is largely based on<br />
their lymph node-recirculating and inflammation-seeking migration behavior,<br />
respectively. The chemokine receptor CCR7 is expressed on both types of Treg subsets,<br />
albeit at different levels. Whether it fulfills similar or distinct roles in these subsets has<br />
not been studied so far. We here show that the recirculation of naïve-like Tregs through<br />
LNs and, to some extent, the gut is dependent on CCR7. Lack of CCR7 not only<br />
prevents recirculation but also almost <strong>complete</strong>ly abolishes the ability of naïve-like<br />
Tregs to control the priming phase of an immune response. In contrast, CCR7 deficiency<br />
in effector/memory-like Tregs promotes their accumulation in inflamed sites, compatible<br />
with a role of CCR7 for exit from the tissue. Local Treg accumulation was accompanied<br />
by an enhanced suppression of inflammation. Together, our findings provide conclusive<br />
evidence that CCR7 expression on Tregs differentially controls in vivo function of the<br />
naïve- and effector/memory-like subsets.
Julia Polansky, Jennifer Freyer, Stefan Floess, Karsten Kretschmer, Harald von<br />
Boehmer, Alf Hamann, Jochen Huehn<br />
DNA methylation controls foxp3 gene expression<br />
The forkhead box transcription factor Foxp3 is a key regulator for Treg function and<br />
lineage identity. To date, despite a recent initial characterization of the human FOXP3<br />
promoter, molecular mechanisms controlling and stabilizing Foxp3 expression are only<br />
poorly understood. Recently, we have described the Treg specific demethylated region<br />
(TSDR), an evolutionary conserved element upstream of exon -1 in the foxp3 locus that<br />
in Tregs showed a selectively demethylated state on all its numerous CpG motifs when<br />
compared to non-regulatory T cells subsets. However, murine Foxp3+ induced Tregs,<br />
which were generated in vitro from CD4+CD25-Foxp3- T cells by TCR-mediated<br />
stimulation in the presence of TGF-ß, displayed only weak and partial demethylation of<br />
TSDR. Upon restimulation in the absence of TGF-ß, most of these cells lost Foxp3<br />
expression, indicating that <strong>complete</strong> demethylation of TSDR might be critical for stable<br />
Foxp3 expression. Repetitive restimulation and TGF-ß signaling was not sufficient to<br />
stabilize expression of Foxp3 in induced Tregs. Yet, interference with the DNAmethylation<br />
status by treatment with 5-aza-2‘-deoxycytidine led to an induction of<br />
Foxp3 in CD4+CD25- T cells and stabilized Foxp3 expression in TGF-ß-induced Tregs.<br />
Hence, our data show that DNA methylation is critically involved in the maintenance of<br />
Foxp3 expression, suggesting that epigenetic modifications allow heritable and stable<br />
expression of this key transcription factor in Tregs.
Manije Sabet, Maja Frankuski, Anja Reutzel-Selke, Andreas Pascher, Peter Neuhaus,<br />
Johann Pratschke, Katja Kotsch<br />
Donor pretreatment with Simvastatin reduces graft<br />
immunogenicity following prolonged cold ischemia in an<br />
experimental model of kidney transplantation<br />
The protective effects of 3-Hydroxy-3-methylglutaryl coenzyme A reductase inhibitors<br />
(HMG-CoARIs, statins) have been demonstrated in numerous cerebral, cardiac and<br />
renal ischemia models. The inhibition of free radicals substantially contribute to the<br />
beneficial effects of statins, however the exact modulatory mechanisms remain unclear.<br />
Based on their anti-inflammatory and anti-oxidative properties, we investigated the<br />
potential beneficial effect of donor pretreatment with statins on ischemia/reperfusion<br />
injury in a rat model of kidney transplantation (Tx). F-344 donor rats were pretreated<br />
with Simvastatin for 3 days prior to transplantation (10 mg/kg/day). Kidneys were<br />
grafted into Lewis recipients following a prolonged cold ischemia of 24h. Grafts and<br />
spleens of recipients were harvested 24h and 14 days post transplantation (n=6/group).<br />
Frequencies of cell populations were analyzed by flow cytometry and the mRNA<br />
expression of relevant candidate genes (CD3, IL-12, MHC class II, CD80, CCR7, CCL19<br />
and CCL21) was evaluated by real-time RT-PCR. After 24h and 14 days post Tx number<br />
of CD4+ cells were slightly reduced in spleens of recipients following donor<br />
pretreatment with Simvastatin (Simvastatin vs. control, 24h: 43.9±2.3% vs. 49.2<br />
±3.7%, p=0.027; d14: 44.3±2.4% vs. 49.8±1.8%, p=0.07). Interestingly, the<br />
frequency of CD3-CD4+ monocytes was significantly reduced in the Simvastatin group<br />
(Simvastatin vs. control, 24h: 6.8±2.1% vs. 12.1±2.6%, p=0.007; d14: 20.3±2.9 vs.<br />
25.0±1.0%, p=0.018), whereas the number of CD3+CD4+ T cells was comparable in<br />
both groups. In the spleen reduced mRNA expression level of CD3 as a marker of T cell<br />
infiltration as well reduced mRNA expression of IL-12 and CD80 were detected.<br />
Furthermore the chemokine receptor CCR7 was markedly reduced in the spleen as well<br />
as its ligands CCL19 and CCL21 displayed enhanced mRNA expression in the graft.<br />
Additionally we revealed a notable decrease of MHC class II in both kidney and spleen.<br />
Our data suggest that donor pretreatment with Simvastatin following prolonged cold<br />
ischemia reduces graft immunogenicity by modulating potential antigen presenting cells<br />
and their homing to lymphoid organs. Donor pretreatment with Simvastatin may<br />
therefore represent an attractive tool to preserve renal function after ischemia/<br />
reperfusion injury.
Xiaoqian Wang, Luca Simeoni, Jonathan A. Lindquist, Julio Saez-Rodriguez, Ernst D.<br />
Gilles, Stefanie Kliche, Burkhart Schraven<br />
Dynamics of proximal signaling events after TCR/CD8mediated<br />
induction of<br />
proliferation or apoptosis in mature CD8+ T-cells<br />
Engagement of the T-cell antigen receptor (TCR) can induce different functional<br />
outcomes such as activation, proliferation, survival or apoptosis. How the TCR-mediated<br />
signaling cascades generating these distinct cellular responses are organized on the<br />
molecular level is so far not <strong>complete</strong>ly understood. To obtain insight into this question,<br />
we analysed TCR/CD8-mediated signaling events in mature OT-I TCR transgenic T-cells<br />
under conditions of stimulation that either lead to proliferation or to apoptosis. These<br />
experiments revealed major differences in the phosphorylation dynamics of ZAP-70, LAT<br />
and PLC-y1. Moreover, input signals leading to apoptosis induce a strong, but transient<br />
activation of ERK1/2 mainly at sites of TCR-engagement, whereas stimuli promoting<br />
survival/proliferation generate a low and sustained activation of ERK1/2 in distinct<br />
subcellular compartments. The transient activation of ERK1/2 under pro-apoptotic<br />
conditions of stimulation is at least partially due to the rapid poly-ubiquitination and<br />
subsequent degradation of ZAP-70 whereas the sustained activation of ERK1/2 under<br />
survival promoting conditions is paralleled by the induction/phosphorylation of antiapoptotic<br />
molecules such as PKB and Bcl-xL. Collectively, our data provide signaling<br />
signatures that are associated with proliferation or apoptosis of T-cells.
Börge Arndt, Burkhart Schraven, Luca Simeoni<br />
Dynamics of TCR signaling events leading to human T-cell<br />
proliferation<br />
The use of cross-linked soluble antibodies (xsAbs) directed against the TCR/CD3<br />
complex and costimulatory molecules is the standard procedure to study intracellular<br />
biochemical cascades during T-cell activation. Despite the fact that stimulation of T cells<br />
via xsAbs results in the activation of several signaling molecules downstream of the<br />
TCR, it does not result in T-cell proliferation. Instead, it appears that xsAbs induce other<br />
cellular outcomes like apoptosis or unresponsivness. To investigate the dynamics of the<br />
signaling events that lead to T-cell proliferation we developed a method to stimulate T<br />
cells with antibodies immobilized on small particles (iAbs) to mimic an antigen<br />
presenting cell. We though that under these experimental conditions T cells would<br />
receive a more physiological stimulation that ultimately would lead to proliferation.<br />
Indeed, we found that stimulation with CD3 and CD28 iAbs induced a strong<br />
proliferation of peripheral human T cells, whereas CD3 and CD28 xsAbs induced T-cell<br />
unresponsiveness. The analysis of TCR-mediated signalling pathways revealed that<br />
xsAbs induced a very strong, rapid and transient phosphorylation (less than 15<br />
minutes) of a variety of signalling molecules including ZAP-70, LAT and MAPKs.<br />
Conversely, stimulation with iAbs results in a very weak but sustained activation of TCR<br />
proximal signalling molecules (ie, ZAP70, LAT and PLCγ1). Surprisingly, we found that<br />
the activation of more downstream signalling molecules such as MAPKs or transcription<br />
factors was very strong and sustained for more than 2 hours in cells stimulated with<br />
iAbs. In summary, our data demonstrate that the dynamics of signalling pathways that<br />
lead to T-cell proliferation do not correlate with those induced by crosslinked soluble<br />
antibodies.
Stephan Meinke, Philipp Eissmann, Carsten Watzl<br />
Early events in NTB-A signaling<br />
The activating receptor NTB-A belongs to the family of SLAM-related receptors and is<br />
expressed on NK, T and B-cells. Engagement of NTB-A on human NK cells by homophilic<br />
interaction with NTB-A expressing target cells can trigger cytotoxicity, cytokine<br />
production and proliferation.<br />
The crystal structure of the NTB-A homodimer has been solved recently. To confirm the<br />
functional relevance of the interactions seen in the crystal, selected residues in the<br />
binding region have been mutated. Cells transfected with the mutated receptors have<br />
been used as targets of NK cells expressing wild type NTB-A in cytotoxicity assays.<br />
Preliminary data show that the mutation of Histidine 54 or Serine 90 to Alanine reduces<br />
the susceptibility to wt NTB-A mediated lysis, while changing Glutamine 88 to Alanine<br />
does not.<br />
Signal transduction via NTB-A is mediated by two immunoreceptor tyrosine-based<br />
switch motifs (ITSM) in its cytoplasmic tail, which can bind the adapter molecules SLAMassociated<br />
protein (SAP) and EWS-activated transcript 2 (EAT-2). To define the role of<br />
these adapters in NTB-A signaling a stable knock down of SAP has been established in<br />
NK cell lines. While 2B4 function was abolished in these cells, cytotoxicity against NTB-A<br />
expressing target cells was not impaired upon SAP knock down. In agreement with the<br />
functional data, western blotting experiments reveal no difference in NTB-A<br />
phosphorylation between SAP knock down and control cells before and after receptor<br />
engagement. These data suggest that the phosphorylation and function of NTB-A are<br />
independent of SAP expression and imply a novel role of EAT-2 in the signal<br />
transduction of NTB-A. To confirm these observations in a more physiological setting,<br />
we are currently knocking down SAP expression in primary human NK cells.
Claudia N. Detje, Hauke Schmidt, Thomas Meyer, Marco Prinz, Ulrich Kalinke<br />
Early type I interferon responses exclude nerotropic viruses<br />
from central nervous system<br />
Mice infected with vesicular stomatitis virus (VSV) mount a protective anti-viral immune<br />
response. It is generally believed that if clearance of the pathogen in the periphery fails,<br />
neurotropic virus can enter the central nervous system (CNS) to replicate and cause<br />
severe brain damage that ultimately leads to death. This concept is supported by the<br />
observation that type I interferon receptor deficient mice (IFNAR-/-) that usually<br />
succumb to VSV infection within 2-3 days are protected if they have been immunized<br />
with UV-inactivated VSV before challenge.<br />
To investigate whether in IFNAR-/- mice viral infection of the CNS was primarily<br />
associated with the failure of the peripheral immune system to control the virus or with<br />
the failure of the interferon system to protect neurons against virus infection, we are<br />
studying the pathogenesis of VSV infection in mice with a cell type-specific IFNAR<br />
deletion in neurons of the CNS (NesCre+/-IFNARflox/flox). In recent experiments we<br />
verified the specificity and efficiency of IFNAR deletion in NesCre+/-IFNARflox/flox mice.<br />
Unlike IFNAR-/- mice that died within 3 days after VSV infection, NesCre+/-IFNARflox/<br />
flox mice did not show signs of disease before 5-6 days after infection. Then, NesCre+/-<br />
IFNARflox/flox mice became hemiplegic, started to move around in circles and<br />
eventually died. In contrast, wild type mice did not show any sign of disease and<br />
survived VSV infection. The different courses of disease observed correlated with a<br />
severe infection of basically any type of tissue in IFNAR-/- mice, whereas in NesCre+/-<br />
IFNARflox/flox mice only CNS was infected. Terminally diseased NesCre+/-IFNARflox/<br />
flox mice showed approximately 10 to 100-fold higher virus loads in the brain than<br />
IFNAR-/- mice, whereas only very little or no virus was found in liver, kidney and<br />
spleen. In contrast IFNAR-/- mice showed high virus titers in all tissues analyzed.<br />
In conclusion, the data collected so far suggest that early type I interferon responses<br />
play a crucial role in excluding virus from CNS. It will be a matter of future research to<br />
determine whether early type I interferon crosses the blood brain barrier or whether it<br />
is produced within the CNS.
Andrey Bogdanov, Tatyana Rybakova, Anna Nizkorodova, Nikolay Belyaev<br />
Effect of alpha-fetoprotein-activated hematopoietic stem cells<br />
on monocytes functional activity<br />
I was shown, alpha-fetoprotein (AFP) disturbs certain function of monocytes in vitro and<br />
in vivo models. In our previous work, we discovered AFP as an inductor of mice bone<br />
marrow hematopoietic stem cells (HSCs) suppression activity in vitro. Whether<br />
possibility of AFP-activated HSCs modulates monocytes activity and amplifies direct<br />
effects of AFP is unknown. We investigated effect of AFP-activated mice bone marrow<br />
HSCs on monocytes functions. Our results show that AFP-activated HSCs suppressed<br />
the spontaneous expression as well as inhibited LPS-induced up-regulation of •••I, CR3,<br />
CR4, and especially CD80, CD86, ICAM-1, LFA-1 and •••II. AFP-activated HSCs almost<br />
<strong>complete</strong>ly suppressed synthesis of IL-1β, IL-6, IL-12, IL-18 and TNF-α from other site,<br />
they increased IL-10 and TGF-β1 production in monocytes. AFP-activated HSCs<br />
decreased their capacity to secret chemokines as IL-8 and MCP-1 as well as eicosanoids<br />
as leukotriene C4 and prostaglandin D2. However, some HSCs subpopulations increase<br />
prostaglandin E2 production. Analysis of monocytes effector functions presented<br />
number of considerable impairments. The first, HSCs-treated monocytes showed weak<br />
phagocytosis and NO production abilities. The second, both oxygen-dependent and<br />
oxygen-independent potentials of HSCs-treated monocytes were significantly<br />
suppressed. The third, HSCs-treated monocytes inhibited cytotoxic activity of naive NK<br />
cells and CTL, and were not able to stimulate IFN-γ and TNF-α production in them. The<br />
fourth, HSCs-treated monocytes had a weak antigen-presenting capacity for naive CD8<br />
+ T cells. In the end, HSCs-treatment monocytes induced differentiation of naive CD4+<br />
• cells and Th1 cells into Th2 cells. Thus, effect of AFP-activated HSCs on monocytes<br />
contributes to their immunosuppression profile.
Pablo Ariel Casalis, Martin Griebenow, Maria Laura Zenclussen, Ana Claudia<br />
Zenclussen, Hans-Dieter Volk, Christian Woiciechowsky, Ulrich-Wilhelm Thomale<br />
Effect of injury severity on the local and systemic cytokine<br />
expression in a rat model of traumatic brain injury<br />
Traumatic brain injury (TBI) is a major health problem worldwide, which is often<br />
associated with immunological complications. Previous works from our group showed<br />
that patients suffering from brain injury demonstrated a systemic anti-inflammatory<br />
response without preceding signs of systemic inflammation. The main aim of this work<br />
was to analyze whether there is a correlation between brain trauma severity and the<br />
generated local and systemic cytokine profiles. Different groups of two brain trauma<br />
severities and different endpoints after TBI (4h, 24h, 96h) as well as sham operated<br />
animals (rats subjected to all surgical procedures except brain injury) and unaffected<br />
control animals were included in the study. In those animals receiving trauma, a left<br />
cortical contusion was induced on the exposed brain using a controlled cortical impact<br />
injury model and trauma severity was adjusted by differing deformation depth of the<br />
impactor between 2 mm (moderate) and 2.5 mm (severe). The expression of cytokines<br />
was determined in liver and brain at the respective endpoints using real time RT PCR.<br />
Locally, augmented levels of IL-6, IL-1β, TNF-α and IL 12 were found 4h after TBI that<br />
then decreased to normal levels. Surprisingly, IL-10 was also locally augmented 4h<br />
after TBI. Additionally, immune cell infiltration into the contusion started already at 4h<br />
and was significantly augmented 24h after trauma, confirming a local inflammatory<br />
response. Interestingly, a systemic augmentation of the IL 10/TNF-α ratio was observed<br />
24h after TBI in both groups. Nevertheless, no significant differences between trauma<br />
severities were found, indicating that in this model if the trauma exceeds a moderate<br />
level there is no correlation between trauma severity and the intensity of the<br />
immunosuppression.
Michael Schramm, Ulrike Karow, Albert Haas, Martin Krönke, Olaf Utermöhlen<br />
Effects of Acid SphingoMyelinase on <strong>list</strong>eriocidal activiy of<br />
macrophages<br />
Deficiency in the enzyme acid sphingomyelinase (ASMase) impairs the capacity of<br />
macrophages to kill intracellular bacteria, e.g. Listeria monocytogenes. Here, we<br />
analyzed the impact of deficiency in ASMase on antibacterial effector mechanisms in<br />
macrophages.<br />
The classical antibacterial effector mechanisms, i.e. generation of antimicrobial reactive<br />
oxygen and nitrogen intermediates, was not altered in ASMase-deficient (ASMase -/- )<br />
compared to wild type macrophages. In contrast, maturation of phagosomes containing<br />
either vital Listeria monocytogenes or heat killed L. monocytogenes (HKLM) was<br />
significantly impaired as indicated by reduced colocalization of bacteria with the<br />
lysosomal marker protein lamp1 in ASMase -/- macrophages. Both vital L.<br />
monocytogenes and HKLM showed a significantly prolonged colocalization with the late<br />
phagosomal marker protein mannose-6-phosphate receptor. Thus, maturation of late<br />
phagosomes containing L. monocytogenes into bactericidal phagolysosomes is impaired<br />
in ASMase -/- macrophages. Consistently, the transfer of lysosomal fluid phase markers<br />
into phagosomes containing HKLM was significantly reduced in ASMase -/- macrophages.<br />
The transfer of lysosomal cargo of high molecluar weight was more impaired than that<br />
of low molecular weight. Transfer of cathepsin D, a lysosomal protease involved in<br />
bacterial degradation, from lysosomes to phagosomes containing L. monocytogenes was<br />
markedly reduced in ASMase -/- compared to wild type cells. The reduced transfer of<br />
lysosomal contents into phagosomes containing L. monocytogenes suggests that<br />
ASMase regulates the fusion of phagosomes with lysosomes which is essentially<br />
required for elimination of bacteria.
Markus Janke, Jens Poth, Thomas Giese, Gunther Hartmann<br />
Effects of immunostimulatory RNA on human granulocyte<br />
populations<br />
Immunostimulatory RNA (isRNA) is known to stimulate plasmacytoid dendritic cells<br />
(PDC) and other immune cells via TLR7 or TLR8, which then produce large amounts of<br />
type I interferon and other cytokines, followed by induction of immune responses of<br />
potential therapeutical relevance. The expression of TLR7 and TLR8 on granulocytes is<br />
not doubtlessly clarified and the response to isRNA is still unclear. In this study we<br />
analyzed the effect of isRNA 9.2s on neutrophils and eosinophils as the largest fraction<br />
of white blood cells.<br />
To analyze potential activation of neutrophils and eosinophils we studied upregulation of<br />
CD11b and downregulation of CD62L as granulocyte activation markers in whole blood<br />
assays after stimulation with isRNA 9.2s by FACS. TLR expression profile and direct<br />
effects were analyzed on highly purified neutrophils. Quantification of expressed<br />
cytokines and chemokines after stimulation was performed by cytometric bead array<br />
(CBA). For functional analysis of purified neutrophils we tested the impact of isRNA<br />
stimulation on degranulation and respiratory burst activity.<br />
We found that neutrophils but not eosinophils are activated after isRNA stimulation in<br />
human whole blood. This stimulatory effect of isRNA 9.2s was shown to be indirect and<br />
TLR7 dependent. The only ribonucleic acid recognizing TLR expressed on neutrophils<br />
was TLR8, which showed functional activity on purified cells. Thus direct neutrophil<br />
activation via isRNA 9.2s should be restricted to TLR8 but not TLR7 but purified<br />
neutrophils responded with cytokine and chemokine release, respiratory burst and<br />
degranulation only after stimulation with synthetic TLR-8 agonists. IsRNA 9.2s did not<br />
induce any direct effects.<br />
In conclusion this study clearly shows that neutrophils express only TLR8 but not TLR7<br />
for nucleic acid recognition. IsRNA 9.2s had no direct influence on neutrophil or<br />
eosinophil activation. Thus side effects that could emanate from direct activation of<br />
granulocytes seem to be improbable when isRNA 9.2s is used in prospective<br />
therapeutical approaches.
Özen Sercan, Günter J. Hämmerling, Bernd Arnold, Thomas Schüler<br />
EFFECTS OF INTERFERONγ ON CD8 + T CELL HOMEOSTASIS<br />
Interferon-γ (IFNγ) is an inflammatory cytokine, which contributes to host defenses<br />
against microbial infections. Besides its anti-microbial activity, IFNγ also regulates<br />
antigen specific CD8 + T cell homeostasis. However, whether cell types other than<br />
activated T cells contribute to this process has not been clarified. We addressed this<br />
question by adoptively transferring T cell receptor transgenic CD8 + T cells into IFNγ-<br />
and IFNγ receptor (IFNγ)- deficient mice. Our findings suggest that IFNγ promotes<br />
antigen specific CD8 + T cell expansion but also limits memory T cell formation via its<br />
actions on host cells. Furthermore, we showed, that in response to IFNγR signaling,<br />
CD11b + macrophage-like cells are sufficient to normalize expansion and memory<br />
formation of CD8 + T cells. Macrophage-derived nitric oxide, which suppresses T cell<br />
expansion in various experimental models, is not responsible for the suppression of T<br />
cell responses in our system. In conclusion, our experiments demonstrate that IFNγ is<br />
necessary for efficient T cell expansion and contributes to the regulation of memory T<br />
cell formation.
Besir Okur, Rainer Glauben, Arvind Batra, Thorsten Stroh, Inka Fedke, Jeannette<br />
Pietsch, Martin Zeitz, Britta Siegmund<br />
Effects of Leptin on T helper cell polarisation<br />
Leptin is an adipokine, initially described as regulator of food intake. Recent data<br />
suggest an additional regulatory function in the immune system, for instance<br />
stimulation of naïve T cells in the presence of leptin enhances polarisation to a Th1<br />
phenotype. Aim of the present study was to characterize the effect of leptin on T cell<br />
polarisation applying antigen-specific and unspecific systems. Naive CD4 + T cells from<br />
Balb/c, leptin-deficient ob/ob and ovalbumine-TCR transgenic DO11.10 mice were<br />
stimulated in vitro under polarising conditions either specifically in the presence of<br />
antigen presenting cells (APC) and the specific antigen or unspecifically via anti-CD3<br />
anti-CD28. As described previously stimulation of naive T-cells under non-polarising<br />
conditions in the presence of leptin did increase the amount of Th1 cells. Furthermore,<br />
under polarizing conditions in the antigen-unspecific system leptin not only increased<br />
the polarization of Th1 cells, but furthermore induced a significant decrease of the<br />
amount of Th2 cells. However, when applying the antigen-specific system under<br />
polarising conditions, effects of leptin were more diverse and varied depending on the<br />
antigen and APC chosen: In vitro stimulation of naive DO11.10 T-cells in the presence<br />
of leptin did not affect the amount of Th1 cells and restimulation even decreased the<br />
percentage of Th1 polarised cells. This effect was equally evident using WT or ob/ob<br />
APCs. Similarly, polarisation to Th2 cells was not affected by leptin and restimulation in<br />
the presence of WT APCs with ovalbumine resulted in increased, but restimulation with<br />
OVA-peptide led to decreased Th2 polarization. In summary, our data further provide<br />
strong evidence that the adipokine leptin does affect T helper cell polarisation. However,<br />
this effect strongly depends on the type of antigen chosen, suggesting that in vivo leptin<br />
effects might be far more intricately balanced than prior reports based on unspecific<br />
studies in vivo may have suggested.
Stephan Paxian, Markus P. Kummer, Lars Tatenhorst, Klaus Pfeffer, Frank Kirchhoff,<br />
Roland Schmid, Michael T. Heneka<br />
Effects of neuronal and microglial disrupted RelA(p65) in the<br />
CNS during neuroinflammatory disorders<br />
Proteins of the NF-κB/Rel family of transcription factors are ubiquitously expressed and<br />
play a key role in a variety of physiological processes as acute phase, stress- and<br />
immune response, cell cycle and apoptosis. In mammals, the NF-κB/Rel family<br />
comprises five members, RelA (p65), RelB, c-Rel, NF-κB1 (p105/p50) and NF-κB2<br />
(p100/p52). Its role in the immune system and host defence has been well defined over<br />
the last decades. In contrast, our understanding of the function of this transcription<br />
factors in the nervous system (NS) is only emerging. Recent reports decipher the<br />
diverse functions of NF-κB in NS development and activity, which range from the control<br />
of cell growth, survival and inflammatory response to synaptic plasticity, behavior and<br />
cognition. Particular attention is given to the specific roles of NF-κB in the various cells<br />
of the NS, e.g. neurons and glia as NF-κB participates to several neurodegenerative<br />
disorders, such as Alzheimer´s, Parkinson´s and Multiple Sklerosis. To determine the<br />
specific role of the NF-κB subunit RelA(p65) in the NS we generated conditional RelA<br />
knockout mice using the Cre/lox-system to bypass the embryonic letality of mice with a<br />
conventional inactivated RelA. Intercrossing these mouse line with mice expressing<br />
either a neuronal (NEXC) or microglial (F4/80) specific Cre generates mice exhibiting a<br />
specific deletion of RelA in the referring tissue. Current inspections determine the<br />
efficiacy of the Cre specified RelA deletion in the CNS. In addition, histological analysis<br />
show a clear tissue defined effect of a Cre induced RelA inactivation. Ongoing<br />
experiments allocate the specific expression profiles and protein patterns of NF-κB/RelA<br />
target genes of isolated primary neurons (NEXC) or microglia (F4/80) from mice with a<br />
disrupted RelA in these cells. In addition, mouse models of neuroinflammatory disorders<br />
as e.g. MPTP (Parkinson), intercrossed APP/PS1 mice (Alzheimer), EAE (experimental<br />
autoimmune encephalomyelitis) and stroke should be established, as well as behavioral<br />
and cognitive (Morris water maze, open field, active avoidance) changes in these mice.
Fanny Edele, Cindy Reinhold, Stefan F. Martin<br />
Efficiency of T cell defence against melanoma depends on the<br />
DC immunization route<br />
We have recently shown that different routes of DC immunization induce effector/<br />
memory CD8+ T cells expressing different arrays of tissue-specific homing receptors.<br />
This polarization is driven in vivo by tissue-specific DC. In our current study, we<br />
investigate the role of homing receptor polarization by DC vaccination for the efficiency<br />
of anti-tumor immunity in the mouse model of B16.F10 melanoma. We use the parental<br />
tumor as well as B16.F10GP33 that expresses a T cell epitope from the glycoprotein of<br />
lymphocytic choriomeningitis virus (LCMV).<br />
We examined the role of different DC immunization routes for the homing of T cell<br />
receptor transgenic P14 effector/memory T cells and wild type T cells that recognize<br />
GP33 and its correlation with the ability to control tumor growth.<br />
We adoptively transferred naive P14 T cells and activated them in vivo with GP33pulsed<br />
DC via the intracutaneous (i.c.), i.v. or i.p. route. After subcutaneous inoculation<br />
of B16.F10 or B16.F10GP33 melanoma cells into the left and right flanks of C57BL/6<br />
mice, respectively, tumor size was measured every 2 days. DC-GP33 prevented the<br />
growth of B16.F10GP33 tumor in all groups independent of the immunization route.<br />
Thus, induction of skin-specific homing receptors upon i.c. DC injection or the lack of a<br />
tissue-specific polarization or flexible reprogramming when DC are injected i.v. or i.p.,<br />
respectively, allow efficient tumor defence in this setting. However, a different outcome<br />
was observed in recipient mice when no P14 T cells were transferred. In this case, longterm<br />
protective immunity against B16.F10GP33 melanoma required the induction of<br />
skin-specific CD8+ T cells by immunization with DC-GP33 via the i.c. route. Thus, tissuetargeting<br />
of tumor antigen-specific effector T cells by the appropriate DC vaccination<br />
route determines the efficiency of the anti-tumor immune response.<br />
Our findings are relevant for the biological therapy of human cancers.
Prajeeth Chittappen Kandiyil, Thomas Ebensen, Carlos Guzmàn, Reinhold Schmidt,<br />
Georg Behrens<br />
Efficient cross-priming induced by the toll-like receptor 2/6<br />
agonist MALP-2<br />
Introduction: MALP-2, a synthetic derivative of a lipopeptide from Mycoplasma<br />
fermentas which acts via the TLR 2/6 heterodimer has been widely exploited as<br />
adjuvant. MALP-2 also binds to CD36, a selective sensor of microbial diacylglycerides,<br />
being this association partially essential for its TLR signalling. Given that CD36 is<br />
exclusively expressed on CD8 + DC we hypothesized that MALP-2 can also exert a potent<br />
adjuvant activity for cross-priming against co-administered antigens.<br />
Methods: DC subpopulations from the spleen were enriched for antigen presentation<br />
assays in vitro and in vivo using ovalbumin (OVA) as a model antigen. The efficacy of<br />
MALP-2 in generating effector CTLs by cross-priming was further tested by in vivo killing<br />
assays.<br />
Results: Systemic administration of MALP-2 to mice led to upregulation of MHC-II,<br />
CD80 and CD86 on CD8 + and CD8 - DC in the spleen. Cross-presentation of OVA was<br />
enhanced in mice receiving MALP-2, as determined by increased proliferation of OVAspecific<br />
CD8+ T-cells (OT-I) in vivo and in vitro. MALP-2 also increased the antigen<br />
presentation of spleen-derived CD4 + DC to OVA-specific CD4 + T-cells (OT-II) in vitro.<br />
Importantly, co-administration of MALP-2 and cellular OVA resulted in generation of an<br />
effective CTL response, as assessed by an in vivo killing assay. Further, the inability to<br />
induce effective CTL response in MHC class II deficient mice suggests that MALP-2 aided<br />
cross-priming is dependent on CD4 + T cell help. In contrast to other TLR ligands, preactivation<br />
of DC with MALP-2 neither inhibited antigen uptake nor antigen presentation.<br />
Conclusion: Our data provide evidence that MALP-2 is a potent stimulus to generate<br />
CTLs via cross-priming and this activity is CD4 + T cell help dependent. Therefore, MALP-<br />
2 represents a promising tool for the establishment of immune interventions.
Julius Hafalla, Ana Rodriguez, Fidel Zavala<br />
Efficient development of Plasmodium liver stage-specific<br />
memory CD8+ T cells during the course of blood stage<br />
malaria infection<br />
Immunity to Plasmodium liver stages in individuals in endemic areas is inextricably<br />
linked to concomitant blood stage parasitemia. While Plasmodium sporozoite infection<br />
induces measurable CD8+ T cell responses, memory T cell development during active<br />
erythrocytic infection remains uncharacterized. Using transgenic T cells, we assessed<br />
antigen-specific CD8+ T cell effector responses induced by normal (NorSpz) and<br />
radiation-attenuated (IrrSpz) P. yoelii sporozoites. The magnitude, phenotypic<br />
activation and differentiation pathway of CD8+ T cells were similarly induced by NorSpz<br />
and IrrSpz. Moreover, in normal mice, memory T cells elicited after priming with NorSpz<br />
and IrrSpz generated identical recall responses following a heterologous boost strategy.<br />
Furthermore, these recall responses exhibited comparable in vivo anti-parasite activity.<br />
Our results indicate that sporozoites which retain their infective capacity induce memory<br />
CD8+ T cells that are robustly recalled by secondary immunization. Thus, erythrocytic<br />
infection does not preclude establishment of memory CD8+ T cell responses to malaria<br />
liver stages.
Stefanie Hoyer, Katrin Birkholz, Verena Wellner, Ina Müller, Erwin Schultz, Gerold<br />
Schuler, Niels Schaft, Jan Dörrie<br />
Electroporation of TCR-encoding RNA into CD4+ T cells in<br />
order to provide T-cell help<br />
Cancer immunotherapy has mainly focused on CD8+ cytotoxic T cells, even though CD4<br />
+-mediated T-cell help is required for an efficient anti-tumor response. Therefore, it<br />
would be beneficial to provide tumor-specific CD4+ T cells either for transfer together<br />
with tumor-specific CTL or to support tumor vaccination. Up to now, efficient T-cellreceptor<br />
(TCR) transfer required stable retroviral transduction. However, this method<br />
includes many risks like insertional mutagenesis, further unwanted effects of viruses,<br />
and genetic alteration, which could result into long lasting autoimmunity. Thus, we used<br />
an optimized RNA transfection protocol, to transiently introduce T-cell-receptor (TCR)<br />
alpha and beta chains, with a known antigen/MHC-specificity. Electroporation of CD4+ T<br />
cells with EGFP-RNA resulted in a high transfection efficiency (>85%). Furthermore,<br />
electroporation of CD4+ T cells with RNA coding for either a MAGE-3/HLA-DP4-specific<br />
TCR or a gp100/HLA-A2-specific TCR resulted in antigen-specific pro-inflammatory<br />
cytokine production. After antigen-specific stimulation with peptide-loaded DC<br />
particularly the Th1 cytokines IL-2, TNF, and IFNgamma were produced, but also lower<br />
amounts of IL-4, IL-6 and IL-10. Moreover, surface-antigen-profiles on T cells and DC<br />
were determined by FACS. These experiments also showed effects in an antigendependent<br />
manner; i.e. an increase in CD25, CD80 and CD86 expression on DC and of<br />
CD25 on CD4+ T cell. These data indicate that TCR-transfected CD4+ T cells can induce<br />
DC maturation and can therefore be used to provide T-cell help. Accordingly, this<br />
method for transient TCR transfer using RNA electroporation into CD4+ T cells can form<br />
a new strategy to induce more efficient CD8+ T-cell responses for the immunotherapy<br />
of cancer.
Stefanie Helm, Patrick Pankert, Stefanie Eikelmeier, Edward Shang, Hans Ulrich<br />
Weltzien, Martina Schnoelzer, Hermann-Josef Thierse<br />
Elements of the innate immune barrier: Proteomic<br />
identification of allergen-protein interactions in the human<br />
epidermis<br />
Background:<br />
Innate and adaptive molecular events underlying the most common contact<br />
hypersensitivity towards heavy metal nickel (Ni) are still in<strong>complete</strong>ly understood.<br />
Aiming to identify primary allergen-protein interactions in the human epidermis, we<br />
have chosen a specific immunoproteomic approach. Keratinocyte derived Ni-interacting<br />
proteins were identified by mass spectrometric analysis and compared to previously<br />
generated data of human antigen presenting cells.<br />
Results:<br />
To investigate molecular effects of Ni ions on human keratinocytes immobilized metal<br />
ion affinity chromatography (IMAC) was used to isolate Ni-interacting proteins from<br />
primary cell lysates. After 2-dimensional gel electrophoresis (2D-PAGE), laser scanning<br />
of fluorescent protein gels (Fujifilm Europe, FLA 5100) followed by spot picking (Bruker<br />
Daltonics, Proteineer II), trypsin digestion and mass spectrometric analysis (Bruker<br />
Reflex II) more than 15 Ni-interacting epithelial proteins were identified in isolated<br />
human keratinocytes. Comparative analysis from previous studies revealed differential<br />
as well as similar Ni-interacting molecules in human B-cells, in-vitro generated DCs and<br />
primary human keratinocytes. Among others, several heat shock proteins were<br />
detected, which may be involved in initial cellular stress responses towards heavy metal<br />
Ni.<br />
Conclusion:<br />
Immunoproteomic identification of Ni-interacting proteins in primary keratinocytes is an<br />
important step in increasing the understanding of molecular mechanisms involved in the<br />
development and the pathophysiology of human nickel allergy. Results indicate a pivotal<br />
role for heat shock proteins and are discussed in light of Polly Matzinger's danger<br />
theory.<br />
(This work was supported in part by the Landesstiftung Baden-Wuerttemberg,<br />
Germany, Forschungsprogramm “Allergologie” by grant P-LS-AL/26, and the European<br />
Union, as part of the project Novel Testing Strategies for In Vitro Assessment of<br />
Allergens (Sens-it-iv), LSHB-CT-2005 – 018681, www.sens-it-iv.eu).
Benjamin Frey, Luis E. Munoz, Friederike Pausch, Ernst Pöschl, Klaus von der Mark,<br />
Martin Herrmann, Udo S. Gaipl<br />
Endogenous AnnexinA5 is Involved in the Immune Reaction<br />
Against Allogeneic Cells<br />
The exposition of phosphatidylserine (PS) on the outer leaflet of the cellular membrane<br />
is a hallmark of apoptotic cells. The high affinity binding of labelled annexinA5 (AxA5) is<br />
extensively used for the detection of apoptotic cells. In general, AxA5 is a highly specific<br />
ligand for PS. The latter provides a swift recognition and uptake of dying cells by<br />
professional phagocytes. Therefore AxA5 may interfere with the immunosuppressive<br />
effects of apoptotic cells.<br />
To study the effect of endogenous AxA5 on the immune reaction against allogeneic cells<br />
we are using AxA5-deficient mice. Interestingly, in contrast to WT mice, the AxA5deficient<br />
mice showed no reaction against allogeneic cells necrotized by mechanical<br />
stress. Furthermore, the delayed type hypersensitivity reaction in WT animals was<br />
significantly higher after immunization with late apoptotic cells. Additional,<br />
macrophages of AxA5-deficient animals bear a higher immunosuppressive potential. To<br />
further investigate immunomodulatory effects of AxA5 in the alloreaction, we<br />
subcutaneously injected viable, allogeneic tumour cells. In WT animals a significantly<br />
faster decline in size of the injected tumour cells was to be observed.<br />
As shown previously by us and others, a disturbed PS-dependent clearance by<br />
macrophages of apoptotic cells leads to the accumulation of the latter and to the<br />
occurrence of late apoptotic/secondary necrotic cells. This consequently leads to the<br />
release of danger signals and to a pro-inflammatory microenvironment. We conclude<br />
that the immunity against allogeneic cells is increased in the presence of endogenous<br />
AxA5.
Christina Hartwig, Miriam Mazzega, Thomas Tschernig, Detlef Neumann<br />
Endogenous IL-18 in experimentally induced asthma affects<br />
cytokine serum levels but is irrelevant for clinical symptoms<br />
T cells and T cell derived cytokines are involved in the complex pathogenesis of asthma.<br />
The role of the cytokine IL-18 however, is not clearly defined so far. On the one hand<br />
side IL-18 induces Th1-type cytokines and thereby might counter-regulate Th2mediated<br />
allergic asthma. On the other hand IL-18 also bears proinflammatory effects<br />
possibly enhancing experimental asthma. In order to elucidate the role of IL-18 in<br />
allergic pulmonary inflammation typical symptoms were compared after induction of<br />
experimental asthma in IL-18 -/- and in wt mice. Asthma was induced using ovalbumin<br />
(OVA) as allergen for sensitization and challenge. Sham sensitized and OVA challenged<br />
mice served as controls. BAL-fluid cytology, leukocyte infiltration in lung tissues, serum<br />
levels of OVA specific IgE and cytokines, and lung function were analyzed. Clear<br />
differences could be observed between control and asthma mice in wild type and IL-<br />
18 -/- animals. Surprisingly, no differences were found between asthmatic wild type and<br />
IL-18 -/- mice. Thus, in contrast to conflicting data in the literature IL-18 did not<br />
suppress or enhance the pulmonary allergic immune response in a murine experimental<br />
model of asthma.
Niklas Engels, Jürgen Wienands<br />
Enhanced signaling of the IgG-BCR is accomplished by<br />
tyrosine-phosphorylation of the cytoplasmic mIgG tail<br />
Depending on the developmental stage, B lymphocytes express on their cell surface<br />
distinct antigen receptor (BCR) classes, which are defined by the isotype of the<br />
immunoglobulin (Ig) subunit. All BCR classes utilize Ig-associated Igα and Igβ proteins<br />
as common signaling subunits. Yet, the BCR of the IgM class on naïve B cells triggers<br />
activation less potently than the IgG-BCR on class-switched memory B cells during<br />
secondary immune responses. We now demonstrate that increased signaling by the IgG-<br />
BCR is accomplished by inducible phosphorylation of an evolutionary conserved tyrosine<br />
residue in the cytoplasmic tail of the membrane-bound IgG (mIgG) heavy chain.<br />
Tyrosine-phosphorylated mIgG binds the adaptor molecule growth factor receptorbound<br />
protein 2 (Grb2) and triggers prolonged activation of protein tyrosine kinases as<br />
well as intracellular Ca 2+ mobilization. Hence, the Ig component of the IgG-BCR not<br />
only functions as antigen recognition device but actively improves the immune response<br />
of memory B cells, which is a fundamental requisite for successful vaccination against<br />
pathogens.
Fanny Edele, Rosalie Molenaar, Cindy Reinhold, Dominique Gütle, Jan C. Dudda, Reina<br />
Mebius, Mathias Hornef, Stefan F. Martin<br />
Environmental instruction of dendritic cells for T cell homing<br />
receptor imprinting<br />
Imprinting of tissue-specific homing receptors on T cells is induced by dendritic cells<br />
(DC) in lymph nodes draining e.g. the skin or the small intestine. However, it is yet<br />
unclear whether this process is governed by lymph node resident DC or rather by DC<br />
immigrating from the peripheral tissue. Our recent demonstration that Langerhans cells<br />
efficiently imprint skin homing receptors on T cells led us to the hypothesis that the<br />
peripheral tissue microenvironment licenses dendritic cells for homing receptor<br />
imprinting upon T cell priming in the draining lymph nodes. To analyse the role of nonhematopoietic<br />
cells in the microenvironment of the skin and the small intestine in the<br />
imprinting of the DC itself, we used co-cultures of bone marrow-derived (BM-) DC<br />
pulsed with the T cell epitope GP33 from the LCMV glycoprotein, TCR transgenic P14<br />
splenocytes and either dermal fibroblasts or small intestinal epithelial cells (SIEC). After<br />
co-culture of peptide pulsed BM-DC, P14 cells and dermal fibroblasts we observed an upregulation<br />
of the skin homing receptor E-selectin ligand on the CD8+ P14 T cells. In<br />
contrast, in co-cultures with SIEC, we observed an up-regulation of the gut homing<br />
receptors α4β7 integrin and CCR9 on the P14 T cells.<br />
DC re-isolated from co-culture with SIEC had only marginally up-regulated CD103 (αE<br />
integrin), but showed a clear expression of retinal dehydrogenases (RALDH). Thus, the<br />
BM-DC had acquired features of gut-specific DC.<br />
In summary, our results show that the peripheral tissue microenvironment induces<br />
tissue-specific characteristics in DC and endows them with the capacity to imprint the<br />
homing receptor profile specific for their tissue of origin on T cells in the draining lymph<br />
nodes.
Jana Zeitvogel, Thomas Werfel, Miriam Wittmann<br />
Epidermal stem cells differ in their response to IFN&gamma<br />
from other proliferative keratinocytes<br />
The epidermis has a pool of adult stem cells (ESC). Although the localisation of ESC is<br />
well described, we lack a clear understanding of their role in perturbed conditions such<br />
as inflammation. One of the most important mediators in inflammatory skin diseases<br />
acting on keratinocytes is IFN&gamma. The assumption that ESC might generate a<br />
protected niche prompted us to investigate their response to the pro-inflammatory<br />
cytokine IFN&gamma. In this study we isolated two populations of keratinocytes<br />
according to their adherence ability. ESC enriched by adherence showed a higher CD29<br />
and CD49f expression compared to other keratinocytes. Surprisingly, surface expression<br />
of CD54 was more inducible upon IFN&gamma stimulation in the ESC subpopulation. In<br />
contrary to that, a markedly lower induction of IL-18 and reduced basal production of<br />
CCL2 were observable in ESC. No differences in IFN&gamma induced IL-10, CXCL10,<br />
CCL22 or TGF&beta1 secretion was detectable between the two keratinocyte<br />
subpopulations. These results suggest that ESC respond to IFN&gamma with an<br />
"restricted" pattern of pro-inflammatory cytokines, and do not build up an antiinflammatory<br />
microenvironment by means of TGF&beta or IL-10. Activated ESC possess<br />
the capability to interact with infiltrating lymphocytes via CD54. In conclusion, the ESC<br />
compartment might actively contribute to the immunological properties of the skin<br />
organ.
Ellen Andresen, Joern Bullwinkel, Christoph Lange, Holger Heine<br />
Epigenetic regulation of defensin gene expression in lung<br />
epithelial cells and COPD<br />
Chronic obstructive pulmonary disease (COPD) includes emphysema and chronic<br />
bronchitis and is one of the most common diseases worldwide. Although inflammatory<br />
processes are thought to play an important role in the pathogenesis of COPD, the exact<br />
role of the innate immune system of the bronchial system and in particular the mode of<br />
action of epithelial cells in COPD remains poorly understood. Preliminary results of a<br />
recently started study with COPD patients of different clinical stages indicated an<br />
increased expression of human β-defensin (hBD)-1, but not hBD-2, compared with<br />
healthy controls. However, the mechanism by which the chronic inflammation of<br />
bronchial epithelial cells in COPD patients leads to a persisting overexpression of<br />
constitutively expressed antimicrobial peptides is not very well understood. Whereas<br />
active promoters generally contain histone H3/H4 hyperacetylation and tri-methylation<br />
at H3 lysine 4, the histone H3 lysine 9 methylation (H3K9me3) has been extensively<br />
correlated with repression. Our first results with lung epithelial cell lines show the<br />
absence of active histone modifications under non-induced conditions around the<br />
transcription start, while H3K9me3 is present throughout the hBD-1 and -2 loci. The<br />
modulation of defensin gene expression in COPD might be, in part, a consequence of<br />
epigenetic alternations in the chromatin structure of the defensin genes. The<br />
understanding of the basic mechanisms that mediate epigenetic regulation of defensin<br />
gene expression may lead to a better understanding of the pathogenesis of COPD, thus<br />
providing an unique platform for the development of new therapeutic strategies<br />
(supported by DFG, SFB617, project A23).
Anke Schütz, Hongqi Lue, Jürgen Bernhagen<br />
ERK1/2-MAPK signaling induced by macrophage migration<br />
inhibitory factor (MIF) is influenced by its CXXC motif<br />
MIF is a pleiotropic inflammatory cytokine that plays a pivotal role in a variety of acute<br />
and chronic inflammatory conditions such as septic shock, rheumatoid arthritis and<br />
atherosclerosis. MIF activates the canonical extracellular signal-regulated mitogenactivated<br />
protein kinase (ERK1/2-MAPK) pathway in a sustained fashion and MIFmediated<br />
ERK signaling has been suggested to contribute to the pro-inflammatory<br />
function of MIF in the above diseases. MIF-induced ERK signaling involves CD74, the<br />
cell surface form of invariant chain, and Src kinase activation, but the structure-function<br />
relationships of MIF underlying its ability to activate MAPK signaling have been<br />
unknown. We recently found that MIF activates transient ERK signaling and observed<br />
that the anti-apoptotic activity of MIF was dependent on its Cys-Ala-Leu-Cys (CXXC)<br />
redox sequence motif (Lue et al., Cell. Signal. 2006; Nguyen et al., J. Immunol. 2003).<br />
Here, we wished to examine the role of CXXC on MIF-mediated ERK1/2 signaling in<br />
fibroblasts. We first compared the effects of recombinant C60SMIF, a mutant in which<br />
the critical Cys60 residue of CXXC is mutated to serine, with the effect of wildtype MIF<br />
on ERK1/2 activity in immortalized and primary MIF -/- -mouse embryonic fibroblasts<br />
(MEFs). Surprisingly, C60SMIF was found to be a potent agonist of the MIF-stimulated<br />
ERK signaling effect. To confirm this observation and to test for autocrine effects,<br />
endogenous C60SMIF, which was derived from the supernatants of stimulated MEFs<br />
isolated from transgenic C60S/C60S-MIF mice (MIF cs/cs ), was analyzed. Compared to<br />
wtMEF supernatants, MIF cs/cs supernatants led to a marked upregulation of phospho-<br />
ERK1/2 levels, confirming the critical role that the CXXC motif appears to have for MIFstimulated<br />
ERK-MAPK signaling.
Winfried Barchet, Vera Wimmenauer, Leonid Gitlin, Susan Gilfillan, Marina Cella,<br />
Marco Colonna, Gunther Hartmann<br />
Essential Role of MDA-5 in Type I IFN Responses<br />
to Poly (I:C) and Encephalomyocarditis Picornavirus<br />
The cytosolic helicases RIG-I and MDA-5 detect conserved nu-<br />
cleic acid structures present during RNA virus replication. How-<br />
ever, the viral RNA ligand for MDA-5 is currently unknown. We<br />
generated MDA-5 deficient mice and have recently shown that<br />
MDA-5, not TLR3, is the dominant receptor mediating type I IFN<br />
secretion in response to the synthetic dsRNA analogue poly-<br />
riboinosinic:polyribocytidylic acid (poly I:C) in vitro and in vivo.<br />
Moreover, recognition of the encephalomyocarditis picornavirus<br />
was also entirely dependent on MDA-5. Consequently MDA-5<br />
deficient mice exhibit a selectively impaired antiviral response to<br />
this virus. We are currently evaluating whether a common MDA-<br />
5 stimulatory motif can be derived and incorporated into short<br />
RNA oligonucleotides. This would substantially widen the range<br />
of cell types receptive to immunostimulatory oligonucleotides, to<br />
include also non-immune cells.
Roman Karwot, Joachim Maxeiner, Steffen Schmitt, Petra Scholtes, Michael Hausding,<br />
Ildiko Boross, Hans Lehr, Susetta Finotto<br />
Essential role of NFATc2 in CD8+ cells in a murine model of<br />
allergic sensitization<br />
The development of allergic immune responses is mediated by CD4+ effector T cells<br />
producing T helper 2 cytokines. However the role of IFN-γ in asthma/allergy is not fully<br />
understood. We demonstrate that mice lacking nuclear factor of activated T cells-2<br />
(NFATc2) developed increased airway hyperresponsiveness. This AHR was associated<br />
both with activated, hyperproliferative lung CD4+ Th2 cells and with CD8+ T cells<br />
defective in IFN-γ production. Moreover, lung effector CD8+ T cells from NFATc2 (-/-)<br />
and IFN-γ (-/-) mice contained increased numbers of CD8+ CD122+ (IL-2Rβ chain)<br />
double positive T regulatory (Treg) cells resulting in increased interleukin-10 (IL-10)<br />
release. Adoptive transfer of ovalbumin (OVA) specific CD8+NFATc2 (-/-) T cells<br />
enhanced AHR generated by NFATc2 (-/-) CD4+T cells in immunodeficient mice.<br />
Interestingly, depletion of CD8+CD122+ cells abrogated the increased AHR present in<br />
CD8+NFATc2 (-/-) T cell-reconstituted SCID mice, by inducing IFN-γ in the airways.<br />
Thus, NFATc2 deficiency in CD8+ T cells results in IFN-γ downregulation and a<br />
concomitant increase in AHR. Taken together, our results identify NFATc2 as a key<br />
transcription factor that governs the function of CD8+ T cells in allergic asthma.<br />
This work is supportet by DFG FI-187.
Andre Tittel, Daniel Engel, Ulrich Dobrindt, Christian Kurts<br />
Establishing a murine model system to investigate the<br />
adaptive immune response against urinary tract infection<br />
Urinary tract infections (UTI), such as cystitis and pyelonephritis, are among the most<br />
common infection diseases worldwide. They are usually caused by uropathogenic gramnegative<br />
Escherichia coli bacteria (UPEC). The mechanisms underlying adaptive<br />
immunity against UPEC are unknown.<br />
To address this question, we established a murine model of UTI by inoculating UPEC of<br />
the E. coli strain 536, which had been isolated from a patient with chronic cystitis, into<br />
the bladders of C57/BL6 mice. This resulted in bladder infection of 20 % of the recipient<br />
mice, as detected by counting colony forming units arising from homogenized tissue on<br />
LB culture plates. In 10 % of the mice, bacterial ascension to the kidney was observed.<br />
Sporadically, death by urosepsis occurred. When mice were infected a second time after<br />
3 hours, the proportion of mice with UPEC ascending to the kidney increased to 90-100<br />
%, enabling studies also on pyelonephritis in our system.<br />
To study in vivo presentation of UPEC antigens, we transformed E. coli 536 with the<br />
pnir15ova plasmid containing the ovalbumin gene, and verified expression by western<br />
blot. In the next step, we injected mice with CFSE-labelled OT-I and/or OT-II cells as in<br />
vivo probes for presentation of bacterial antigen. After infecting mice with OVAtransfected<br />
UPEC, we observed specific proliferation of both OT-I and OT-II cells in the<br />
bladder and kidney draining LNs. Activation may have occurred by presentation of OVA<br />
associated with phagocytosed bacteria, or of OVA secreted from transfected UPEC.<br />
Future studies in this model will address the mechanisms of antigen transport from<br />
infected organs to draining LNs, the identity of the antigen presenting cell that activated<br />
T cells, and the immune effector functions resulting from such activation.
Marion Nonn, Shamsul A. Khan, Eva Distler, Ralf G. Meyer, Leonard D. Shultz, Rupert<br />
Handgretinger, Christoph Huber, Wolfgang Herr, Udo F. Hartwig<br />
Establishment of a NOD/SCID/IL2Rγc null hematopoietic stem<br />
cell transplantation model to study graft-vs-host and graft-vsleukemia<br />
immune responses of ex vivo modified human T<br />
lymphocyte grafts.<br />
Donor lymphocyte graft engineering to abrogate graft-vs-host (GVH) reactivity while<br />
improving graft-vs-leukemia (GVL) immunity is of key interest in allogeneic<br />
hematopoietic stem cell transplantation (HSCT). We established a HSCT model using<br />
NOD/SCID/IL2R common γ-chain null (γc null ) mice to evaluate GVH and GVL immunity of<br />
human leukemia-reactive T cell lines in vivo. These T cells were generated by in vitro<br />
stimulation of donor lymphocytes against primary acute myeloid leukemia (AML) blasts<br />
followed by CD137-mediated immunodepletion of alloreactivity using allogeneic<br />
fibroblasts (FB).>sup>1>/sup><br />
Firstly, GVH responses of T cell lines were tested by subcutaneously implanting skin<br />
substitutes composed of primary dermal or bone marrow stromal FB embedded in a<br />
collagen matrix into NOD/SCID/γc>sup>null mice. Following adoptive transfer of<br />
undepleted human haploidentical CD3 + T cells, up to 23% of alloreactive T cells<br />
specifically migrated into viable and vascularized substitutes explanted 21d post<br />
adoptive transfer. In addition, selected T cell subsets elicited xenoreactivity induced by<br />
residual murine antigen-presenting cells. In contrast, no allo- and xenoreactivity was<br />
observed upon transfer of donor T cells enriched for leukemia reactivity.<br />
Secondly, to study GVL immunity, we examined protection to engraftment of human<br />
primary AML blasts in NOD/SCID/γc null mice by AML-reactive cytotoxic T cells (CTL)<br />
expanded from CD8 + donor lymphocytes in short term cultures. After 24h coculture of<br />
anti-leukemia CTL with AML blasts in vitro, both T cells and leukemia were transferred<br />
into NOD/SCID/γc null recipients. In contrast to controls, AML-reactive CTL were capable<br />
of <strong>complete</strong>ly preventing AML engraftment in these mice.<br />
We conclude that the NOD/SCID/γc null HSCT model may be a valuable tool for<br />
evaluating GVH and GVL immunity in vivo following donor T lymphocyte graft<br />
modifications in vitro.<br />
1 Wehler T and Nonn M, et al. Blood 2007;109:365-373
Rainer Wurth, Angelika Bold, Thomas Keller, Ulrike Trahorsch, Peter Voigt, Stefan<br />
Schubert, Ulrich Sack<br />
Evaluation and validation of a manual low-cost assay for the<br />
monitoring of CD4 counts in HIV-infected individuals in non-<br />
OECD countries<br />
Background: The CD4+ T-cell count is considered to be the best surrogate marker for<br />
monitoring the clinical course of infection with HIV. Flow cytometry, as the standard<br />
reference method for the enumeration of CD4+ T-cells, requires expensive equipment<br />
and well-trained technicians, thus preventing its widespread use in developing<br />
countries.<br />
Objective: In order to make this important surrogate marker available to more patients<br />
in non-OECD countries, we have modified a commercially available density-based cell<br />
preparation assay to make it applicable for low-cost cell enumeration.<br />
Methods: 1.) For evaluation (step 1), whole venous blood taken from 25 HIV-patients<br />
as well as 29 healthy blood donors was incubated with a cocktail of bi-specific<br />
tetrameric antibody complexes which crosslink unwanted nucleated cells (NC) to red<br />
blood cells (RBC) by forming RBC rosettes around targeted NC. After the following<br />
gradient centrifugation over a density medium, the enriched CD4+ T-cells were<br />
harvested and then counted on a haemocytometre using a light optical microscope. In<br />
parallel, the CD4 count of each sample was assessed by flow cytometry. 2.) For<br />
validation (step 2), this method was performed in blind quintuplicates on 12 HIV+ blood<br />
samples according to the FDA guidelines ICH-Q2A and ICH-Q2B.<br />
Results: Association of the introduced method (modified negative selection, MNS) with<br />
the reference method (flow cytometry, FCM) is given by regression models for both<br />
steps:<br />
Step 1: slope = 1.091, intercept = -46.5; (95% confidence intervall [CI] = 0.948 to<br />
1.240). Step 2: slope = 1.074, intercept = -38.3 (CI = 0.971 to 1.200 (step 2). The<br />
imprecision of MNS assessed during step 2 was 21.2% (intra-serial) and 18.8% (interserial).<br />
The cost of the examination of one blood sample is $0.30 - $0.50 per sample.<br />
Conclusion: The results suggest that the MNS-method, at is capable of providing an<br />
approximate CD4 count. This would enable a physician attending to an HIV+ patient to<br />
decide whether or not to start HAART or OI prophylaxis. At a cost of $0.30 - $0.50, it is<br />
affordable to patients living in resource-restrained areas. The technique has the<br />
potential to deliver an accurate, precise, low-cost test to monitor the status of HIV+<br />
patients, especially in small laboratories in non-OECD countries.<br />
Keywords: CD4 count; HIV-infection; HIV-monitoring; RosetteSepTM; low-cost<br />
assay; non-OECD countries
Mathias Fousse, Robert Dinser, Urban Sester, Katinka Albrecht, Mahavir Singh, Hans<br />
Köhler, Ulf Müller-Ladner, Martina Sester<br />
Evaluation of latent tuberculosis infection in patients with<br />
inflammatory arthropathies before treatment with tumour<br />
necrosis factor-α blocking drugs using a novel flowcytometric<br />
interferon-γ release assay<br />
In this study, we compared the efficacy of the conventional skin test and a novel flow<br />
cytometric whole blood assay in the diagnosis of latent tuberculosis infection (LTBI) in<br />
patients with rheumatologic diseases evaluated for treatment with TNFα-blocking<br />
agents.<br />
97 patients were prospectively assessed for the presence of LTBI through clinical<br />
history, skin testing, and chest x-ray. In addition, T-cell reactivity towards tuberculin<br />
(PPD) and the M. tuberculosis specific proteins ESAT-6 and CFP-10 was determined ex<br />
vivo using a flow cytometric whole blood assay.<br />
After standard screening, 15% of patients receiving TNFα-blocking therapy were<br />
pretreated with isoniazide (INH), another 5% of patients did not receive TNFα-blocking<br />
therapy because of LTBI. PPD-reactivity in the skin was observed in 14% of patients<br />
compared to 39% with the whole blood test. Analysis of the M. tuberculosis specific<br />
response to ESAT-6 and CFP-10 revealed positive results in 16% of patients. Using a<br />
decision tree incorporating history, chest x-ray and either skin-test or ESAT-6/CFP-10<br />
results, 18 or 22% of patients, respectively, were classified as latently infected with M.<br />
tuberculosis. Four patients treated with INH because of a positive skin reaction did not<br />
show reactivity to ESAT-6/CFP-10 in the whole blood assay. Another six patients not<br />
pretreated with INH because of negative skin tests would have received INH, had the<br />
results of the whole blood assay been taken into account.<br />
In conclusion, the skin test has a low sensitivity and specificity for the diagnosis of LTBI<br />
in our cohort, resulting in both over- and undertreatment with prophylactic INH. The<br />
flow cytometric analysis of T-cell reactivity to proteins specific to M. tuberculosis is a<br />
promising approach for refining diagnostic testing.
Katherina Sewald, Maja Henjakovic, Simone Switalla, Norbert Krug, Armin Braun<br />
Ex vivo Immunomodulatory Testing using Precision Cut Lung<br />
Slices: Focus on Dendritic Cells<br />
Introduction: Precision cut lung slices (PCLS) offer the distinctive opportunity to gain<br />
insight into lung morphology and physiology under in vitro cell culture conditions.<br />
Objective of this work is the assessment of the immune modulating potency of<br />
substances on PCLS, especially on dendritic cells (DCs). DC activation and maturation<br />
are characterized by changes in cell surface marker expression (e.g. MHCII, CD86,<br />
CD40) and cytokine production.<br />
Methods: Extraction of lung tissue (mouse) was performed directly post mortem to<br />
conserve vitality of the tissue. Lungs were filled and cut with a special microtome. After<br />
preparation of PCLS with a thickness of approx. 220 µm slices were cultivated at 37 °C<br />
under cell culture conditions. Vitality of the lung slices was either controlled by<br />
measurement of LDH enzyme activity or live/dead staining with calcein AM/ethidium<br />
homodimer-1 using confocal laser scanning microscopy (CLSM). Cytokines and<br />
chemokines were detected with Luminex technology. Dendritic cell markers CD11c, MHC<br />
class II, CD40 and CD86 were investigated in living mouse PCLS in situ using CLSM.<br />
Results: Ex vivo incubation of PCLS with LPS induced both changes in cytokine profile<br />
and in expression of cell surface markers on DCs. LPS induced and dexamethasone<br />
prevented LPS induced release of cytokines and chemokines such as IL-5 (180 % for<br />
LPS to 0 % for LPS/dexamethasone), IL-1 (1550 % to 325 %), TNF-alpha (5340 % to<br />
470 %), IL-12 (723 % to 170 %) and Rantes (1060 % to 120 %) in PCLS. Expression of<br />
MHC class II, CD40 and CD11c but not CD86 could be observed in naive untreated<br />
PCLS. After incubation of PCLS with LPS exclusively a strong enhancement of MHC class<br />
II was found. In contrast, coculture of PCLS with ovalbumin-specific T-cells and<br />
activation with ovalbumine resulted in an upregulated expression of MHC class II and<br />
CD86 which was inhibited by dexamethasone. Thus, the method of PCLS might provide<br />
an in vitro technique to predict immune modulating potencies of inhaled substances on<br />
dendritic cells.
Ingo Irmler, Mieczyslaw Gajda, Rolf Bräuer<br />
Exacerbation of Antigen induced Arthritis in IFN-γ-deficient<br />
Mice as a Result of Unrestricted IL-17 Response<br />
In rheumatoid arthritis (RA), Th cells are supposed to be involved in induction and<br />
perpetuation of autoimmune disease with a dominance of the pro-inflammatory Th1<br />
response. However, the role of IFN-γ, the major cytokine produced by Th1 cells, is still<br />
in<strong>complete</strong>ly defined. We investigated antigen-induced arthritis, an animal model of RA,<br />
in IFN-γ-deficient and wild-type C57Bl/6.<br />
Inflammatory response in the acute stage was strikingly increased in IFN-γ-deficient<br />
mice, demonstrated by exacerbated joint swelling, DTH reaction and histopathological<br />
assessment of arthritis. Intraarticular administration of exogenous IFN-γ significantly<br />
suppressed inflammation in IFN-γ-deficient as well as in wild-type mice.<br />
Increased production of IL-2, IL-4, IL-5, IL-6 and in particular IL-17 upon stimulation of<br />
lymph node and spleen cells from IFN-γ-deficient mice was associated with a decreased<br />
humoral immune response with low serum levels of total and antigen specific<br />
immunoglobulins (IgG, IgG1, IgG2a, IgG2b, IgG3). The lack of endogenous IFN-γ<br />
resulted in large numbers of neutrophil granulocytes infiltrating acute inflamed knee<br />
joints. Monoclonal antibodies neutralising IL-17 diminished acute inflammation. In vitro,<br />
we found that Th cell expansion and production of IL-17 upon re-stimulation was<br />
effectively inhibited by IFN-γ in a dose-dependent manner. These results clearly<br />
demonstrate in vivo a dominance of anti-inflammatory properties of IFN-γ during the<br />
initial phase of AIA and suggest disease promoting effects of IFN-γ-deficiency acting via<br />
IL-17 modulated pathways.
Gasteiger Georg, Kastenmuller Wolfgang, Sutter Gerd, Drexler Ingo<br />
Exclusive cross-priming of cytotoxic T-cells dictates antigen<br />
requisites for MVA vector vaccines<br />
Viral vectors are evaluated as recombinant vaccines but little is known about the<br />
antigen-presentation pathways that are important to induce efficient T-cell immunity<br />
with these vectors. Many viruses can infect pAPCs resulting in direct presentation of<br />
antigenic determinants. MHC-I-restricted cross-presentation of exogenous antigen,<br />
however, can contribute to antiviral immunity. We confirm metabolic stability as a<br />
critical factor for access of antigenic substrates for antigen-presenting pathways. We<br />
analyzed vaccines based on the replication-deficient vaccinia virus MVA in two distinct<br />
mouse models. Infection with MVA expressing the model antigens tyrosinase or<br />
ovalbumin either targeted for rapid proteasomal degradation or expressed as minigenes<br />
enhanced MHC-class-I/peptide presentation on DC as well as non-pAPC in vitro and in<br />
vivo, but dramatically impaired CD8+ T-cell (TCD8+)priming. Similar results were<br />
obtained when antigen presentation was restricted to cross-presentation in vivo<br />
indicating that direct priming plays a minor role for TCD8+ induction. Additionally,<br />
downregulation of cross-presentation by CpG-induced maturation of DC prior to<br />
immunization abrogated TCD8+ priming, but did not affect infectivity rate, antigen<br />
processing or direct priming of TCD8+ in vivo.<br />
Our results show that MVA vaccines exclusively depend on TCD8+ cross-priming. This is<br />
surprising, as we show that MVA easily infects DC and allows strong antigen<br />
presentation by these pAPC in vivo. The data reveal new aspects concerning biological<br />
properties of antigens that can be selected to induce strong T-cell immunity. Moreover,<br />
we show that it is possible and necessary to adjust the target antigens to the intrinsic<br />
requirements of the delivering vector with direct implications for the design of optimized<br />
vaccines targeting TCD8+ responses in infectious disease and cancer. Recent clinical<br />
studies suggest that our findings might also apply to humans.
daomin gong<br />
Expression of human GITRL on myeloid dendritic cells<br />
enhances their immunostimulatory function but does not<br />
abrogate the suppressive effect of CD4+CD25+ regulatory T<br />
cells<br />
CD4(+)CD25(+) regulatory T cells (Treg) have been described as an important hurdle<br />
for immunotherapy. Engagement of glucocorticoid-induced TNF receptor-related protein<br />
(GITR) has emerged recently as an important mechanism to control the suppression of<br />
CD4(+)CD25(+) Treg. Furthermore, it has been documented extensively that GITR<br />
ligation is costimulatory for naive and activated T cells in the murine setting. However,<br />
little is known about the role of the human GITR ligand (huGITRL). We wanted to<br />
explore whether huGITRL could enhance antigen-specific T cell priming by dendritic cells<br />
(DC). First, we confirmed the endogenous expression of GITRL on HUVEC. We also<br />
detected GITRL expression on EBV-B cell lines, whereas no GITRL expression was<br />
observed on human monocyte-derived DC. Electroporation of GITRL mRNA in monocytederived<br />
DC resulted in a strong and long-lasting surface expression of GITRL. In<br />
contrast to data obtained in mice, no significant abrogation of Treg suppression by<br />
GITRL-expressing human DC was observed. Consistent with our mouse data, we<br />
showed that huGITRL is costimulatory for responder T cells. Furthermore, we found that<br />
GITRL-expressing DC primed increased numbers of Melan-A-specific CD8(+) T cells. We<br />
conclude that although huGITRL is not capable of alleviating Treg suppression of<br />
responder T cells, huGITRL overexpression on monocyte-derived DC enhances their<br />
capacity to induce antigen-specific T cell responses. Thus, GITRL incorporation in DC<br />
might improve the antitumor immune response after vaccination.
Katjana Klages, Anja Stirnweiss, Jörg Reimann, Hansjörg Hauser, Andrea Kröger<br />
EXPRESSION OF INTERFEON REGULATORY FACTOR-1 IN CT26<br />
COLON CARCINOMA CELLS INDUCES ANTI-TUMOR ACTIVITY<br />
The transcription factor Interferon regulatory factor-1 (IRF-1) was originally identified<br />
as a protein mediating the effects of the interferon system. Besides its regulatory<br />
functions of the cellular response in host defense, e.g. establishing the antiviral state,<br />
IRF-1 was found to be a tumor suppressor. To study the tumor suppressive effects of<br />
IRF-1 in vitro and in vivo the colon carcinoma cell line CT26 was transduced by lentiviral<br />
vectors to express the IRF-1 gene under control of the tetracycline inducible promoter.<br />
The tumor cells showed a significant growth arrest after induction of IRF-1. Furthermore<br />
the reversion of the transformed phenotype could be demonstrated by decrease of<br />
anchorage independent growth in soft agar assays. Upon expression of IRF-1 an<br />
increase of MHC class I expression was detected and these tumor cells showed a<br />
significantly higher recognition and elimination rate by specific cytotoxic T cells. In<br />
addition, the induction of chemokines like Cxcl10 or Ccl19 was shown and transwell<br />
assays indicated that IRF-1 expression in tumor cells leads to an increased attraction of<br />
lymphocytes. Besides these direct effects on tumor cells IRF-1 is capable of mediating<br />
its anti-tumor effects by inducing a tumor specific immune response in the host. To<br />
evaluate whether intrinsic IRF-1 effects are sufficient to reject tumors in vivo the tumor<br />
cells were subcutaneously injected in nude mice. Tumor growth was delayed in nude<br />
mice, but <strong>complete</strong> tumor rejection was observed in immune competent syngenic mice.<br />
Tumor specific cytotoxic T cells were detected in mice rejected the tumor upon IRF-1<br />
induction. Further experiments revealed that also established tumors were rejected<br />
upon IRF-1 expression. These results demonstrate that IRF-1 expression in tumor cells<br />
leads to an induction of a tumor specific immune response, which can be responsible for<br />
a <strong>complete</strong> tumor rejection.
Thorsten Stroh, Arvind Batra, Rainer Glauben, Inka Fedke, Stephen Girardin, Martin<br />
Zeitz, Britta Siegmund<br />
Expression of NOD2 but not NOD1 is modulated by proinflammatory<br />
cytokines in murine preadipocytes<br />
Preadipocytes are linked to the innate immune system indicated by their expression of<br />
functional Toll-like receptors (TLR) and ability to phagocytosis. Recent studies of our<br />
group revealed the expression of members of the nucleotide-binding site and leucinerich<br />
repeat (NBS-LRR) proteins. These proteins belong to the family of intracellular<br />
pattern recognition receptors which act as sensors for motifs found in the<br />
peptidoglycans (PG) from bacteria. NOD1 binds to Lactyl-Tetra-DAP a peptidoglycan<br />
motif mainly found in PG from Gram-negative bacteria, NOD2 detects muramyl<br />
dipeptide (MDP) a motif contained in PG derived from Gram-positive bacteria.<br />
This study aimed to investigate the expression of NOD1 and NOD2 and their<br />
functionality in murine preadipocytes. Changes in expression were analysed after ligandspecific<br />
stimulation and stimulation with pro-inflammatory cytokines using quantitative<br />
real-time RT-PCR. Functionality of these receptors was tested by ligand-specific<br />
stimulation, and the subsequent response was evaluated by IL-6 production and<br />
activation of the NF-κB pathway. Specificity of stimulation was confirmed by RNA<br />
interference (RNAi) strategies. NOD1 mRNA was detectable in all samples. The<br />
expression was not altered after ligand–specific stimulation or stimulation with the<br />
proinflammatory cytokines IL-1β and TNFα. In contrast, NOD2 was slightly increased by<br />
NOD1-specific stimulation but could significantly be upregulated by stimulation with IL-<br />
1β. The strongest upregulation was observed after stimulation with LPS but different<br />
from stimulation with IL-1β or TNFα, LPS-induced upregulation was only present after<br />
4h of stimulation. Specific stimulation of NOD1 by LT-DAP resulted in a strong activation<br />
of the NF-κB pathway and a significant IL-6 production could be observed.<br />
Our data provide evidence that functional NBS-LRR proteins are expressed in<br />
preadipocytes and that expression of NOD2 can be modulated by pro-inflammatory<br />
cytokines. Thus underlining the position of preadipocytes in the innate immune system.
Cemil Korcan Ayata, Cinthia Farina, Markus Krumbholz, Florian Weisel, Thomas<br />
Winkler, Andreas Rosenwald, Reinhard Hohlfeld, Edgar Meinl<br />
Expression of p75 neurotrophin receptor (p75NTR) and brain<br />
derived neurotrophic factor (BDNF) in germinal centers<br />
The neurotrophin receptor (p75NTR) is a pan receptor for all neurotrophins (NGF, BDNF,<br />
NT3, NT4/5). Neurotrophins have mainly been studied because of their effect on<br />
survival of neuronal populations. P75NTR is classified as a member of TNF receptors,<br />
but no TNF ligand and no function in the immune system has been identified so far.<br />
We report that full length transcripts of p75NTR were expressed in immune organs and<br />
some peripheral blood mononuclear cells. Adult CNS tissue and immune organs<br />
transcribed similar levels of p75NTR as seen by TaqMan PCR. A subset of B cells in<br />
adenoids/tonsils, but not in blood expressed p75NTR as seen by both FACS and TaqMan<br />
PCR. Double stainings showed p75NTR expression on follicular dendritic cells. A<br />
potential ligand of p75NTR, BDNF, was seen in germinal centers by immunostaining and<br />
confirmed by TaqMan PCR of LASER capture dissected material. P75NTR was also highly<br />
expressed in extranodal follicles in Hashimoto Thyroiditis and follicular B cell lymphoma.<br />
The abundant expression of p75NTR and one of it’s ligands in germinal centers in<br />
normal lymphatic tissue and in extranonal follicles suggests a role of this TNF receptor<br />
in Ig production and in immunopathology.
Matthias M Gaida, Frank Guenther, Martin Loos, Christof Wagner, Gertrud Maria<br />
Hänsch, Helmut Friess, Nathalia Giese, Wente Moritz<br />
Expression of the chemokine receptor CXCR6 on<br />
polymorphonuclear neutrophils (PMN) in pancreatic tumour<br />
specimen and in acute, localised bacterial infections<br />
The chemokine receptor (CXCR) 6 has been described on lymphoid cells, and is thought<br />
to participate in the homing of activated T-cells to non-lymphoid tissue. We now provide<br />
evidence that CXCR6 is also expressed by activated polymorphonuclear neutrophils<br />
(PMN) in vivo: Examination of biopsies derived from patients with pancreatic cancer by<br />
confocal laser scan microscopy revealed a massive infiltration of PMN that also<br />
expressed CXCR6. PMN of the peripheral blood of these patients, in contrast, did not. To<br />
answer the question whether CXCR6 expression is a property of infiltrated PMN,<br />
leukocytes were collected from patients with localised soft tissue infections in the course<br />
of the wound debridement. By cytofluorometry, the majority of these cells were<br />
identified as PMN. Up to 50 % of these PMN were also positive for CXCR6. Again, PMN<br />
from the peripheral blood of these patients were negative for CXCR6, as were PMN of<br />
healthy donors. In a series of in vitro experiments, up-regulation of CXCR6 on PMN of<br />
healthy donors by a variety of cytokines was tested. So far, a minor, although<br />
reproducible effect of tumour-necrosis factor α was seen: brief exposure of PMN to lowdoses<br />
of TNF α induced surface expression of CXCR6 on 18.5 ± 9 % of the PMN (mean<br />
± SD, n=6). In summary, our data provide evidence that CXCR6 is not constitutively<br />
expressed on PMN, but is up-regulated under inflammatory conditions.
Eric Keil, Nana Ueffing, Linda Clayton, Ellis Reinherz, Klaus Schulze-Osthoff, Ingo<br />
Schmitz<br />
Expression profiling identifies Gadd45β as a novel mediator of<br />
negative selection<br />
Apoptosis is essential for the development of multicellular organisms and its<br />
deregulation may lead to various diseases. In the immune system, reduced apoptosis<br />
results in the accumulation of autoreactive T cells leading to impaired tolerance and<br />
autoimmunity. Autoimmune diseases like type I diabetes or multiple sclerosis arise from<br />
defects in peripheral tolerance, while the autoimmune polyglandular syndrome type 1<br />
(APS-1 or APECED) is due to impaired central tolerance, i.e. negative selection. To get<br />
further insights into the process of negative selection we have analyzed gene induction<br />
during peptide-induced negative selection in vivo by oligonucleotide arrays. The most<br />
strongly induced gene was Gadd45β, which is implicated in differentiation and<br />
apoptosis. Upregulation of Gadd45β was verified on the mRNA and protein level by<br />
quantitative PCR and Western blotting, respectively. Importantly, Gadd45β-expression<br />
in vivo was stimulated by peptides inducing negative selection but not by those inducing<br />
positive selection. In situ hybridization supported a role for Gadd45β in negative<br />
selection as its mRNA was specifically expressed in the medulla. Finally, overexpression<br />
of Gadd45β induced apoptosis in CD4+CD8+ double positive T cells. Thus, Gadd45β<br />
may induce a yet unrecognized pathway for clonal deletion in the thymus next to the<br />
established once induced by Bim, Nur77 and FasL/CD95L.
Silke Meister, Kirsten Neubert, Kai Herrmann, Renate Burger, Martin Gramatzki,<br />
Sabine Hahn, Sandra Schreiber, Ulrich Schubert, Hans-Martin Jäck, Reinhard Voll<br />
Extensive immunoglobulin production sensitizes myeloma<br />
cells for proteasome inhibition<br />
Multiple myeloma (MM), an incurable plasma cell neoplasia, is characterized by<br />
overproduction of monoclonal immunoglobulins (Ig). The recently clinically approved<br />
proteasome inhibitor bortezomib (Bz) acts directly on MM cells to cause cell death,<br />
supposedly by blocking the antiapoptotic factor NF-κB. However, the exact mechanism<br />
by which Bz acts is still under investigation. Extensive synthesis of Ig in MM cells results<br />
also in defective ribosomal products (DRiPs) and unfolded proteins degraded by the<br />
proteasome. Therefore, we hypothesized that the proapoptotic effect of Bz is due to the<br />
accumulation of unfolded proteins and DRiPs along with inhibition of NF-κB. Using the<br />
human MM IgG-secreting cell line JK-6L and murine •H-chain-transfected Ag8.H<br />
myeloma cells, proteasome inhibitor treatment induced markedly more apoptotic cell<br />
death in subclones producing high compared to low amounts of Ig. Unexpectedly,<br />
bortezomib did not markedly alter NF-κB activity. In contrast, Ig positive MM cells<br />
showed a highly induced AP-1 DNA binding activity upon Bz treatment. Importantly, in<br />
Ig-high MM cells Bz triggered production of reactive oxygen species (ROS) as well as<br />
strong activation of endoplasmic reticulum (ER) stress components involved in apoptosis<br />
such as CHOP and caspases. Additionally, cells harbouring Ig showed enhanced<br />
expression of the proapoptotic factor Bax and reduced expression of the antiapoptotic<br />
protein Bcl-2 due to Bz treatment. Moreover, proteasome inhibition results in formation<br />
and accumulation of IgG-derived DRiPs. Hence, we conclude that proteasome inhibition<br />
preferentially affects cells producing high amounts of proteins. Bz-induced cell death in<br />
MM cells is most likely mediated by ER stress induced through accumulation of unfolded<br />
proteins/DRiPs.
Carina Klein, Anja Grahnert, Sunna Hauschildt<br />
Extracellular NAD+ triggers transient [Ca2+]i changes in LPSactivated<br />
human monocytes via P2Y receptors<br />
In previous studies we have shown, that stimulating freshly isolated human monocytes<br />
with NAD + rapidly causes a transient concentration-dependent elevation of [Ca2+ ] i . This<br />
increase seems to be performed by Ca2+ influx via ligand-gated P2X receptors. Since<br />
calcium signals play an important role in triggering monocyte functions such as<br />
chemotaxis, phagocytosis and cytokine production, NAD + can provide a powerful mean<br />
to interfere with such functions. Here we asked whether extracellular NAD + also affects<br />
the [Ca2+ ] i in LPS-activated monocytes. We found that cultivating the cells for 16h<br />
resulted in a <strong>complete</strong> loss of the calcium response but this lack of response was<br />
prevented when LPS was present during the 16h incubation time. The NAD + -induced<br />
LPS-dependent increase is composed of a release of Ca2+ from intracellular stores and a<br />
calcium release activated influx of Ca2+ from the extracellular medium. The Ca2+ release from intracellular stores suggests that NAD + seems to exert its effects by<br />
interacting with G-protein-coupled P2Y members of the P2 receptor family which<br />
mobilize stored Ca2+ via PLC-β activation and IP3 production. By the use of agonists<br />
and specific antagonists of P2Y receptor subtypes we identified the P2Y11 receptor as<br />
one of the main receptors to be involved in the calcium response.
Anja Grahnert, Erik Schilling, Carina Klein, Sunna Hauschildt<br />
Extracellular NAD + triggers transient [Ca 2+ ] i changes in<br />
human monocytes<br />
via P2X-receptors<br />
Recently extracellular NAD + has been identified as a stimulus capable of inducing a rise<br />
in [Ca 2+ ] i in different cell types by different mechanism. In this study we could show<br />
that NAD + leads to a transient increase in [Ca 2+ ] i in human monocytes mediated by an<br />
influx of [Ca 2+ ] i from the extracellular medium. As NAD + does not exert its effect by<br />
entering the cells and as ATP prevents the NAD + induced effect we investigated the<br />
involvement of ATP receptors in the Ca2+ -response. ATP receptors are P2 purinoceptors<br />
classified into ionotropic P2X and metabotropic, G-protein-coupled P2Y receptors. P2Y<br />
receptors can be excluded, because NAD + only leads to an influx of extracellular Ca2+ .<br />
Of the seven P2X receptors P2X1 , P2X4 , and P2X7 were found to be expressed on<br />
human monocytes. The involvement of P2X1 as a receptor subtype mediating the effect<br />
of NAD + is supported by the finding that the increase in [Ca2+ ] i is inhibited by the<br />
specific P2X1 antagonists NF449 and suramin. Furthermore P2X7 plays a role by the NAD<br />
+ -induced increase in [Ca2+ ]i . The P2X7 antagonist KN62 and an anti- P2X7-Ab block<br />
the NAD + effect.<br />
Surprisingly the binding of the P2X7 receptor did not lead to a pore formation. These<br />
data show for the first time that extracellular NAD + acts as a ligand at P2X receptors of<br />
human monocytes.
Kristin Hochweller, Jörg Striegler, Günter J Hämmerling, Natalio Garbi<br />
Feed-back control of dendritic cell homeostasis<br />
Dendritic cells (DCs) are pivotal coordinators of the immune system, governing the<br />
choice between T cell immunity and tolerance. Despite their importance, the<br />
mechanisms regulating the size of the DC compartment are largely unknown. In order<br />
to investigate DC homeostasis we have developed a BAC transgenic mouse strain in<br />
which CD11c+ DCs express the diphtheria toxin receptor (DTR). In this CD11c-DOG<br />
strain, about 95% of DCs are depleted by a single DT application. Due to their fast turnover,<br />
continuous DC depletion requires daily DT application.<br />
Here we show that a residual fraction of DC progenitors can be induced to repopulate<br />
the DC compartment using wild-type and CD11c-DOG mixed bone marrow chimeras in<br />
which most of the DCs derive from CD11c-DOG bone marrow and, thus, can be<br />
depleted by DT. These results indicate that there exist active homeostatic mechanisms<br />
controlling the DC pool size. To investigated whether DC progenitors respond to the size<br />
of the DC compartment by modulating their differentiation potential, we performed<br />
competitive cotransfers of splenic DC progenitors obtained from mice with normal or<br />
reduced DC numbers. About two thirds of the donor-derived DCs differentiated from<br />
progenitors obtained from DC-deficient mice, indicating that a reduced number of DCs<br />
leads to an increased activity of their precursors. The increased progenitor activity is<br />
likely due to an increased frequency of DC progenitors in the spleen of DC-deplete mice<br />
as suggested by colony forming assays in vitro in response to GM-CSF. Furthermore, a<br />
reduced DC number also appears to increase the differentiation activity of DC<br />
progenitors on a per-cell basis because the number of DCs recovered after transfer of<br />
splenic DC progenitors from untreated mice into DC-deficient mice is ten times higher<br />
than that obtained when the same precursors are transferred into mice with normal DC<br />
numbers.<br />
Thus, these results demonstrate that there are active homeostatic mechanisms<br />
controlling the size of the DC compartment via a feedback loop whereby the number of<br />
DCs controls the activity of their progenitors.
Karsten Kretschmer, Alexander Marson, Garrett M. Frampton, Julia Polansky, Richard<br />
A. Young, Harald von Boehmer<br />
Foxp3-dependent gene regulation requires T cell activation<br />
Foxp3-expressing CD4+CD25+ regulatory T cells play an essential role in the regulation<br />
of immune responses under physiological conditions. While the function of Foxp3 in Treg<br />
lineage specification has been firmly established, the molecular pathways involved in<br />
the Foxp3-specified developmental and suppressor program are still poorly understood.<br />
Here we report on new evidence that T cell receptor signaling strength greatly<br />
influences the induction of Foxp3 expression in initially naïve CD4+Foxp3- T cells.<br />
Consistent with in vivo experiments, lack of co-stimulation (e.g. via CD28) or inhibition<br />
of T cell receptor-emanating signals during the conversion process enhances TGF-beta<br />
dependent induction of Foxp3 expression in vitro. In addition, global gene expression<br />
profiling in conjunction with genome-wide DNA based location analysis (ChIP-on-Chip)<br />
using custom-spotted tiling arrays, which interrogated Foxp3 binding to 5’ promoters of<br />
approximately 16000 annotated mouse genes, indicated that Foxp3 had very little effect<br />
on gene expression in un-stimulated T cells. In contrast, stimulated Foxp3- and Foxp3+<br />
T cells exhibited significant differences in expression of almost 1% of mouse genes.<br />
Although we found that Foxp3 could also function to activate gene expression, the<br />
predominant effect of Foxp3 promoter occupancy was to suppress the NFAT-dependent<br />
activation of target genes upon T cell stimulation. Consistently, Foxp3-bound promoters<br />
were enriched for NFAT binding sites.
Thomas Quast, Barbara Tappertzhofen, Cora Schild, Waldemar Kolanus<br />
Function of CD81 in dendritic cell migration<br />
CD81 belongs to the Tetraspanin superfamily of evolutionary conserved membrane<br />
proteins. The most distinctive feature of the Tetraspanins is their ability to form lateral<br />
associations with one another and with numerous other molecules including integrins,<br />
cell surface receptors and signaling molecules, creating multi-molecular signaling<br />
complexes at the cell surface. Hence, Tetraspanins have been implicated in the<br />
coordination of signal transduction, antigen-presentation, activation, cell adhesion and<br />
migration, cell-cell interactions and cell fusion.<br />
Dendritic cells are the most important antigen presenting cells at the interface of innate<br />
and adaptive immunity. Upon capturing antigens in context of an inflammatory<br />
situation, dendritic cells undergo a phenotypic and functional maturation process, which<br />
includes the increase of cell motility. The capacity of dendritic cells to activate naive T<br />
cells depends on their ability to migrate to T-cell areas in the lymph nodes.<br />
Using siRNA techniques, we could show that comparable to Rac1-deficient cells CD81deficient<br />
human mature monocyte-derived dendritic cells show significantly reduced cell<br />
migration, which is accompanied with strong deficiencies in lamellipodia formation.<br />
Furthermore, CD81 is required for the phosphorylation of members of the ezrin/radixin/<br />
moesin (ERM) family of proteins, which function as cytoskeleton linkers that are<br />
involved in membrane protrusion formation and cell motility. As Tetraspanins recruit<br />
intracellular-signaling enzymes, including protein kinase C (PKC), and organize them in<br />
the “Tetraspanin-Web” and the phosphorylation of ERM proteins is thought to be<br />
downstream of PKC, we propose that CD81 is a crucial component in the signaling<br />
network coordinating dendritic cell migration.
Sebastian Dütting, Wolfgang Schuh, Kai Hermann, Christiane Lang, Hans-Martin Jäck,<br />
Dirk Mielenz<br />
Function of Swiprosin-2/EFhd1 during B cell development<br />
Functional peripheral B cell subsets are produced from hematopoietic stem cells. An<br />
important early checkpoint of this process is the transient expression of the pre-B cell<br />
receptor (pre-BCR) at the transition from the late progenitor B cell (pro-B) to the large<br />
precursor B cell (pre-B) stage. The pre-BCR consists of a membrane-anchored HC of the<br />
• isotype (•HC) associated with λ and VpreB, and drives pre B cells into a clonal<br />
expansion phase of two to five cell divisions.<br />
Swiprosin-2 (also: EFhd1/Mitocalcin) is a close homologue of Swiprosin-1/Efhd2, an<br />
adaptor protein we showed recently to be involved in proximal B cell receptor signaling.<br />
In contrast to Swiprosin-1 that was expressed in all murine B cell lines and primary B<br />
cells examined, albeit at different levels, Swiprosin-2 protein and mRNA were only<br />
expressed in a transformed pro-B-cell line (38B9) and in primary pro-B cells. We thus<br />
hypothesized that Swiprosin-2 is down-regulated by the pre-BCR. Using a transgenic tetoff<br />
system that allows inducible pre-BCR-expression in primary cells, we demonstrated<br />
pre-BCR-dependent down-regulation of Swiprosin-2 on mRNA and protein level. We<br />
corroborated this result with IL-7 dependent R5B pro-B cells and transformed 38B9 pro-<br />
B cells either lacking or expressing a functional surface pre-BCR. A dysfunctional,<br />
cytoplasmic •HC did not regulate Swiprosin-2 expression, demonstrating that only<br />
signals from the surface pre-BCR induce Swiprosin-2 down-regulation. We hypothesize<br />
that pre-BCR-induced down-regulation of murine Swiprosin-2 is required for pre-B cell<br />
differentiation and/or proliferation. To test this hypothesis we are currently infecting<br />
primary pro-B cells with a Swiprosin-2-encoding retrovirus that overcomes downregulation<br />
of Swiprosin-2. In the future, we want to identify the function of Swiprosin-2<br />
during B cell development and determine the mechanisms by which Swiprosin-2<br />
potentially affects B cell development.
Cornelia Rosner, Lutz Walter<br />
Functional analysis of MHC class I genes in the rhesus<br />
monkey (Macaca mulatta)<br />
The rhesus macaque represents a widely used animal model for the study of infectious<br />
diseases, organ transplantation, and in development of vaccines. Recently, the major<br />
histocompatibility complex (MHC) of the rhesus macaque (Mamu) was sequenced<br />
<strong>complete</strong>ly (Daza-Vamenta et al., 2004), revealing extensive duplications in the class I<br />
gene subregions. The sequenced haplotype displayed 2 and 19 loci, which show close<br />
relationship to HLA-A and HLA-B, respectively. The functional significance of this<br />
plethora of class I genes is, however, unknown so far.<br />
In order to study the function of particular class I molecules, we cloned representatives<br />
of Mamu-A and Mamu-B genes in an expression vector that contains AcGFP. These<br />
constructs were transfected in the MHC class I-negative cell line K562. Surface staining<br />
with the human MHC antibody W6/32 revealed variable expression patterns. Natural<br />
killer (NK) cell activity against different Mamu-A and Mamu-B expressing transfectants<br />
was tested by degranulation assays with freshly isolated rhesus monkey PBMCs. Some<br />
transfectants exhibit higher inhibitory capacity, as exemplified by lower cell surface<br />
expression of the CD107a molecule (degranulation marker). Currently, we are<br />
investigating the specific binding of KIRs and MHC class I ligands by biochemical means.<br />
Daza-Vamenta R, Glusman G, Rowen L, Guthrie B, Geraghty DE (2004) Genetic<br />
divergence of the rhesus macaque major histocompatibility complex. Genome Res 14:<br />
1501-1515
Simone Abel, Jan Buer, Wiebke Hansen<br />
Functional analysis of Neuropilin1 in regulatory T cells<br />
Recently, we could identify Neuropilin1 (Nrp1) as a useful surface marker molecule for<br />
regulatory T cells (Treg). Nrp1 has been initially described as semaphorin III and VEGF<br />
receptor, being essential for axonal guidance and vascularisation, but little is known<br />
about the function of Nrp1 in immune regulation. To gain further insights into the role of<br />
Nrp1 on Treg cells, we have constructed retroviral vectors encoding the full length Nrp1<br />
cDNA and have optimized the retroviral transduction protocol to overexpress Nrp1 in<br />
freshly isolated CD4 + CD25 - naïve T cells. Using this approach we are able to analyse<br />
the impact of Nrp1 on the proliferative and suppressive capacity of Treg cells.<br />
Furthermore, we will analyse the expression of the Treg specific transcriptional regulator<br />
Foxp3 and other molecules known to be involved in Treg cell function as well as the<br />
cytokine profile of Nrp1-transduced T cells in comparison to control vector transduced T<br />
cells. These results may contribute to a better understanding in the molecular<br />
mechanism of Treg cell function.
Gamze Kabalak, Torsten Matthias, Reinhold E. Schmidt, Torsten Witte<br />
FUNCTIONAL CHARACTERISATION OF ILT6 AS GENETIC RISK<br />
FACTOR FOR MULTIPLE SCLEROSOS AND SJÖGREN’S<br />
SYNDROME<br />
Introduction: Autoimmune diseases Multiple Sclerosis (MS) and Sjögren’s syndrome<br />
(SS) are polygenic disorders and appear to be triggered by EBV infection. Risk genes for<br />
Multiple sclerosis (MS) are localized on chromosome 6 and the chromosomal region<br />
19q13.4, the later harboring the genes of the Immunoglobulin-like transcripts (ILTs).<br />
ILTs are expressed on antigen presenting cells, T and NK cells and play a role in the<br />
tolerance induction of the immune system by interacting with regulatory T cells. A<br />
homozygous deficiency of ILT6 was shown to be associated with MS and SS. As ILT6 is<br />
lacking a transmembrane domain, it is likely to be secreted and may act as a soluble<br />
mediator. To address the question of the role of ILT6 the recombinant protein was<br />
expressed and functional studies were performed.<br />
Methods: Adhesion tests with MCF-7 cells and ILT6 were performed. These cells express<br />
MHC class I on there surface. Therefore T cell clones expressing either CD8 alpha or<br />
beta were incubated together with MCF-7 cells in the presence or absence of ILT6.<br />
Further mixed lymphocyte reaction (MLR) as well as cytotoxicity assays were performed<br />
with changing concentrations of ILT6.<br />
Results: These experiments revealed a concentration dependent blockade of the<br />
interaction of CD8 α and MHC I by ILT6. Furthermore the proliferation of T cells in the<br />
MLR was increased by addition of ILT6. On the other hand cytotoxicity assays showed<br />
no influence of ILT6 on NK cells.<br />
Conclusion: ILT6 may act as a natural immunomodulator with profound effect on T cells.<br />
Supported by Gemeinnuetzige Hertie Stiftung, Sicca-Forschungsfoerderung and BMBF<br />
KN Rheuma C2.12
Kathrin Gube, Inga Gebuhr, Katrin Vogt, Erik Kwidzinski, Christine Brandt, Hans-Dieter<br />
Volk, Birgit Sawitzki<br />
FUNCTIONAL CHARACTERISATION OF THE TOLERANCE<br />
ASSOCIATED GENE (TOAG-1)<br />
Backround: The tolerance associated gene 1 (TOAG-1) has been identified to be highly<br />
expressed in graft infiltrating cells of tolerance developing treated recipients in several<br />
experimental transplant models (Sawitzki et. al. AJT). TOAG-1 is highly expressed in<br />
DC’s and CD4+ T cells. The amino acid sequences of rat, mouse and human isoforms<br />
contain no homology to known proteins but they contain a cleavage site for<br />
mitochondrial presequences. Aim: Here we analysed the subcellular localisation of TOAG-<br />
1, its transcriptional regulation as well as effects of TOAG-1 over expression in murine<br />
CD4+ T cells. Methods and Results: Transfection of mouse fibroblast 3T3 cells with Nterminal<br />
fusion protein of TOAG-1 and EGFP lead to accumulation of green fluorescence<br />
in organelle like structures. Costaining of TOAG-1-EGFP transfectants with fluorescent<br />
probes or antibodies (e.g. anti-Hsp60) either accumulating within mitochondria<br />
(Mitotracker) or lysosomes (Lysotracker) revealed an exclusive expression of TOAG-1 in<br />
mitochondria. To analyse transcriptional regulation of TOAG-1, CD4+ T cells from naïve<br />
C57BL/6 mice were stimulated with allogeneic (BALB/c) splenocytes which resulted in a<br />
10 fold down regulation of TOAG-1 transcription. This down-regulation could be<br />
inhibited by a treatment with the non-depleting anti-CD4 antibody (YTS177) and<br />
<strong>complete</strong>ly prevented by Cyclosporin A. Overexpression of TOAG-1 in murine CD4+ T<br />
cells via retroviral gene transfer resulted in a lower mitochondrial membrane potential<br />
(FACS: TMRM) and a higher predisposition to undergo apoptosis (FACS: Annexin) after<br />
allo-activation in vitro. Conclusions: TOAG-1 is exclusively localised within mitochondria<br />
and its transcription tightly controlled after T cell activation in vitro and in vivo. By<br />
lowering the mitochondrial potential and predisposing T cells to apoptosis TOAG-1 may<br />
be involved in controlling and terminating T cell activation. Further studies clarifying its<br />
function are ongoing.
Susanne Stutte, Sabine Brauer, Irmgard Förster<br />
FUNCTIONAL ROLE OF CCL17 IN ALLERGIC IMMUNE<br />
REACTIONS OF THE SKIN<br />
Professional antigen presenting cells of the skin, namely Langerhans cells (LC) and<br />
dermal dendritic cells (DC), are continuously exposed to environmental stimuli and are<br />
crucial for the induction of different skin immune reactions via presentation of the<br />
antigen in draining lymph nodes (LN) and secretion of cytokines and chemokines. The<br />
chemokine CCL17, which binds to the receptor CCR4, mediates the attraction of<br />
activated/memory T cells to dendritic cells (DC). We generated CCL17/EGFP knockin<br />
mice that express the enhanced green fluorescent protein (EGFP) under the control of<br />
the endogenous ccl17 promoter. These mice can be used as heterozygous reporter mice<br />
with normal CCL17 production or as homozygous CCL17 knockout mice which also<br />
express the EGFP reporter. We demonstrated that the EGFP+ cells represent almost<br />
exclusively CD11c+ DC, including activated LC and dermal DC. Functionally, the<br />
deficiency of CCL17 leads to reduced contact hypersensitivity responses to the haptens<br />
DNFB and FITC. Presently, we analyze the role of CCL17 expressing DC in allergic<br />
reactions of the skin using a mouse model for atopic dermatitis (AD). Since CCL17 is<br />
consistently upregulated in the skin of AD patients, thus chemokine may play an<br />
important function in the pathogenesis of AD. First results indicate an essential role for<br />
CCL17 secreting DC in the induction of the humoral immune response during chronic<br />
skin sensitization, as CCL17 deficient mice show a decreased antigen specific IgE, IgG1<br />
and IgG2a production. Surprisingly, in the absence of CCL17 dermal DC and LC exhibit<br />
a reduced migratory behaviour to the skin draining LN. In addition, a lower number of<br />
IL-4 and IL-5 secreting CD4+ T cells could be detected in skin draining LN of CCL17<br />
knockout mice. Thus, CCL17 appears to be critically involved in the immunopathology of<br />
atopic dermatitis.
Daniel Reim, Kay Westenfelder, Simone Kaiser-Moore, Sylvia Schlautkötter, Bernhard<br />
Holzmann, Heike Weighardt<br />
Functional role of T cells during mixed bacterial peritonitis<br />
The general concept of immune defense against microbial pathogens supports the idea<br />
that early defense mechanisms are controlled by cells of the innate immune system,<br />
whereas the adaptive immune system is critically engaged in the immune response at<br />
later time points. During sepsis the innate immune system is crucial for the induction of<br />
immune reactions against the pathogen, but, in addition, lymphocytes are involved in<br />
the immune response early at the onset of septic peritonitis. Mice deficient for RAG-1,<br />
which lack mature B and T cells, show enhanced susceptibility to acute mixed bacterial<br />
peritonitis as compared to wildtype mice. Whereas B cell-deficient µMT mice show no<br />
significant difference in the survival rate after peritonitis induction, T cell-deficient nude<br />
mice (balb/c nu/nu) exhibit enhanced susceptibility to septic peritonitis as compared to<br />
controls.<br />
Analysis of cytokine production in either RAG-1-deficient or T cell-deficient nude mice<br />
indicated attenuated sepsis-induced IL-12 and IL-10 production both systemically and<br />
locally in spleens of septic mice as compared to wildtype controls. To further analyse<br />
the contribution of T cells to the immunopathology of severe sepsis we analysed the<br />
capacity of T cells to contribute to cytokine production during sepsis. Purified splenic T<br />
cells of septic mice were capable to produce IL-10 and IFNg. These results imply that T<br />
cells are not only important for adaptive immune processes but are also able to<br />
contribute to the immunopathology of severe infections via their ability to produce<br />
immune mediators.
Jan Kubach, Petra Lutter, Tobias Bopp, Sabine Stoll, Christian Becker, Jürgen Knop,<br />
Stefan Müllner, John Wijdenes, Edgar Schmitt, Helmut Jonuleit<br />
Galectin-10, a previously unnoted protein essential for the<br />
functional activity of human CD4+CD25+ regulatory T cells<br />
CD4+CD25+Foxp3+ regulatory T cells (CD25+ Tregs) comprise a separate lineage of T<br />
cells that are essential for maintaining immunological tolerance to self. However, the<br />
molecules mediating the anergic state and regulatory function of CD25+ Tregs are still<br />
elusive.<br />
Here we report the identification and functional characterization of galectin-10, a protein<br />
found to be predominantly expressed by CD25+ Tregs, which is essential for the anergic<br />
phenotype and suppressive function of these cells. Using differential proteomics, we<br />
found three isoforms of a 16kDa protein, identified as galectin-10 being constitutively<br />
expressed in human CD25+ Tregs and nearly absent in conventional CD4+ T cells.<br />
Expression was up to 40 times higher in CD25+ Tregs and two of the isoforms were<br />
previously unknown. In contrast, other members of the galectin family like galectin-1<br />
showed only slight expression differences in this comparison or were upregulated in<br />
conventional T cells upon activation (e.g. galectin-8). So far, galectin-10 has only been<br />
described in granulocytes and its expression is restricted to humans. Predominant<br />
expression of galectin-10 in CD25+ Tregs was also confirmed on mRNA level. Single cell<br />
staining and flow cytometry showed a strictly intracellular expression of galectin-10 in<br />
CD25+ Tregs.<br />
Most notably, specific inhibition of galectin-10 restored the proliferative capacity of CD25<br />
+ Tregs and abrogated their suppressive function. Thus, expression of galectin-10 on<br />
mRNA and protein level seems to be essential for the functional activity of human CD25<br />
+ Tregs.
Kerstin Sarter, Connie Schulze, Sandra Franz, Benjamin Frey, Luis Munoz, Udo Gaipl,<br />
Martin Herrmann<br />
Galectins contribute to the recognition and clearance of<br />
apoptotic cells<br />
Galectins are _-galactoside-binding proteins. A characteristic of galectins is the<br />
presence of one or two carbohydrate recognition domains (CRD) of about 135 amino<br />
acids with an affinity for _-galactosides. Various functions were ascribed to Galectins,<br />
which have been detected in numerous cells and tissues. Galectins are present in T<br />
cells, B cells, macrophages, eosinophils, basophils, and thymic epithelial cells.<br />
Moreover, galectin expression is modulated by various inflammatory stimuli. Galectins<br />
display pleiotropic effects. Galectin-1 induces apoptosis of thymocytes and of activated<br />
T lymphocytes. Galectin-3 induces superoxide production of neutrophils, regulation of T<br />
cell apoptosis, and is involved in actin remodelations in macrophages during<br />
phagocytosis. Galectin-9 causes thymocyte apoptosis and serves as chemoattractant for<br />
eosinophils.<br />
We show that galectins serve as ligands for apoptotic and necrotic cells. Most<br />
importantly, in contrast to other ligands for dying or dead cells, galectins show a<br />
different binding to ageing apoptotic granulocytes and irradiated apoptotic lymphocytes,<br />
respectively. Furthermore, the binding of the several galectin family members differed<br />
considerably. In phagocytosis assays we observed that several Galectins significantly<br />
increase the phagocytic clearance of apoptotic lymphocytes. Furthermore, Galectins<br />
seem to influence the anti-inflammatory potency of apoptotic cells during phagocytosis<br />
as demonstrated by the release of TNF_ by macrophages during phagocytosis of e.g.<br />
Galectin-3,-4, and -5 -opsonised cells.<br />
We conclude that Galectins play an important role as opsonising molecules for apoptotic<br />
cells. Furthermore, they may serve as adaptor molecules during phagocytosis. They are<br />
therefore important molecules in the clearance synapse.
Nadja Hilger, Frank Emmrich, Ulrich Sack<br />
Gene expression in microdissected invasive fibroblast isolated<br />
from arthritic joints from patients with RA<br />
The etiology of Rheumatoid Arthritis remains in<strong>complete</strong>ly understood. Inflammatory<br />
fibroblasts (FB) are necessary for joint destruction and the propagation of inflammation<br />
while cytokines and their receptors play an important role in the pathogenesis, namely<br />
in the intercourse of FB with inflammatory and lymphoid cells and in the destruction of<br />
cartilage and bone.<br />
Studies of invasive FB isolated from homogenized synovial membrane failed to provide<br />
detailed insight into the characteristics of erosive FB at the site of cartilage and bone<br />
destruction. By modifying the latest microdissection technologies, we have analysed<br />
small cell groups from destructive regions in biopsies of patients and compared them<br />
with FB from non-arthritic regions. In this way, differential expression of cytokines and<br />
further candidate genes can be investigated. So we investigated to what extent an<br />
investigation of mRNA from few cells is possible and whether RNA amplification should<br />
be attached.<br />
Cells were isolated by laser capture microdissection. High laser intensity and specialized<br />
slides were found to be pre-requisites for successful isolation of small cellular units.<br />
After optimisation of the different methods, RNA of sequential cell numbers starting with<br />
1000 cells was isolated. One part was reverse transcribed and the other fraction was<br />
amplified. In order to examine differences, expression of different genes was examined<br />
and compared in both preparations.<br />
We were able to dissect small cell groups out of erosive sites and non-inflammed parts<br />
of synovial tissues from RA patients. We showed that RNA isolation from very small cell<br />
numbers with following expression analysis is possible. The house keeping gene and a<br />
FB-specific genes could be detected in all samples without amplification. The<br />
quantification of cytokine expression was limited.<br />
We could show that through our approach an optimized investigation of RNA from few<br />
cells derived from RA synovial tissue is possible. By identifying function-specific<br />
markers, erosive FB will be better accessible in future and can be investigated more<br />
easily.
Alexander Gerbaulet, Julia Scholten, Thomas Krieg, Karin Hartmann, Axel Roers<br />
Generation of a Mouse Model for Mastocytosis<br />
Mastocytosis is characterized by infiltration of abnormal numbers of mast cells into skin<br />
and internal organs. The clinical spectrum is broad ranging from mild increases in<br />
cutaneous mast cell numbers to severe forms of mast cell leukaemia. The disease is<br />
associated with activating somatic point mutations of the receptor tyrosine kinase Kit,<br />
however, the relevance of these mutations for the different forms of the disease is<br />
unclear. We generated a transgenic mouse model based on a 200 kb BAC containing the<br />
entire kit gene. Two modifications were introduced: 1) the activating point mutation<br />
D814V and 2) a floxed “stop” cassette, allowing Cre/LoxP-mediated control of transgene<br />
expression. The construct was pronucleus-injected and founder animals transmitted the<br />
transgene in the germline. Kit D814Vflox transgenic mice were bred to the hCMV (deleter)-<br />
Cre-line for ubiquitous deletion of the stop element, which should result in expression of<br />
the mutated kit under the control of the kit promotor elements contained in the<br />
transgene. Kit D814Vflox deleter-Cre double transgenic mice were born in numbers<br />
significantly lower than expected indicating a high frequency of lethality during<br />
gestation. The few animals born alive displayed a diverse spectrum of phenotypes.<br />
While some mice showed cutaneous mastocytosis of variable intensity, others<br />
developed various additional neoplasms including malignant mast cell tumors. We are<br />
presently investigating the cause of embryonic death in the majority of Kit D814Vflox<br />
deleter-Cre double transgenic embryos, the effect of Kit D814V expression in mature mast<br />
cells of Kit D814Vflox Mcpt5-Cre double transgenic mice and the induction of Kit D814V<br />
expression in adult Kit D814Vflox Mx-Cre double transgenic mice.
Dafne Müller, Bettina Meißburger, Katharina Frey, Anette Karle, Ines Höfig, Roland<br />
Stork, Roland E. Kontermann<br />
Generation of an improved recombinant bispecific antibody<br />
molecule and B7 fusion proteins for targeted cancer<br />
immunotherapy<br />
The recombinant bispecific antibody format single-chain diabody (scDb) has shown to<br />
be able to retarget T lymphocytes to tumor cells, leading to their destruction. However,<br />
therapeutic efficacy is hampered by the short serum half-life of this small molecule (55<br />
kDa). Thus, improvement of the pharmacokinetic properties of small bispecific antibody<br />
formats is required to enhance efficacy in vivo. We have generated a fusion protein of<br />
single chain diabody and human serum albumin (scDb-HSA) and analyzed this molecule<br />
for biological activity and pharmacokinetic properties. The scDb-HSA, which is directed<br />
against the tumor antigen carcinoembryonic antigen (CEA) and the T cell receptor<br />
complex molecule CD3, retained full binding capacity to both antigens and showed<br />
strong increase in circulation time compared to the unfused scDb molecule. In order to<br />
provide a tumor target specific costimulatory signal, fusion proteins of the extracellular<br />
domain of B7.2 (CD86) and single chain Fv or diabody against CEA were generated.<br />
This constructs showed specific binding to CEA and CD28/CTLA-4. Costimulatory<br />
properties were assayed in combination with the scDb (providing the first stimulatory<br />
signal) by monitoring IL-2 release after incubation with PBMCs. Here, B7-Db showed to<br />
be superior to B7-scFv. Thus, in combination with B7-Db an enhancement of tumor<br />
antigen-specific retargeting and activation of T cells could be achieved for scDb and<br />
scDb-HSA. In summary, combining recombinant bispecific antibodies with improved<br />
pharmacokinetic properties and tumor directed costimulatory fusion proteins might be a<br />
promising approach for efficient retargeting and activation of cytotoxic T lymphocytes in<br />
cancer immunotherapy.
Kathrin Hofer, Holger Kroenig, Heinke Conrad, Barbara Kast, Christian Peschel, Helga<br />
Bernhard<br />
Generation of Th1 lymphocyte clones against an<br />
immunodominant epitope of NY-ESO-1<br />
Since CD4+ T cells play a critical role in generating and maintaining antigen-specific<br />
cellular and humoral immune responses our current study focuses on the generation of<br />
T helper cells from healthy donors and multiple myeloma patients. Our approach is the<br />
isolation of high avidity tumor antigen specific class - II- restricted T cell receptors<br />
(TCRs) for an optimized T cell transfer strategy.<br />
The Cancer Testis (CT) antigen NY-ESO-1 is one of the most immunogenic cancer<br />
antigens eliciting strong humoral and cellular immune responses in tumor patients and<br />
is a promising candidate antigen for successful adoptive T cell transfer.<br />
We achieved to generate NY-ESO-1 specific T helper1 clones from HLA-DR1+ and HLA-<br />
DR4+ healthy donors by stimulation of CD4+ T cells with autologous dendritic cells (DC)<br />
pulsed with the NY-ESO-1 87-111 peptide known to be presented with HLA-DR1+ and<br />
HLA-DR4+. The specifity of CD4+ T helper cell clones was determined by proliferation<br />
assays and IFN gamma ELISPOT through screening with NY-ESO-187-111 peptide. By<br />
limiting dilution of the NY-ESO-1-specific T cell populations we succeeded to isolate T<br />
cell clones which recognized NY-ESO-1-pulsed target cells and DCs pulsed with NY-ESO-<br />
1 protein.<br />
The ability to isolate NY-ESO-1- specific T helper1 cells facilitates the development of T<br />
cell transfer regiments which are based on class-II-restricted TCR-transduced T cells for<br />
a treatment of patients with multiple myeloma.
Johannes Stephani, Ronald Naumann, Hermann Wagner, Tim Sparwasser<br />
Generation of TLR- „humanized“ Mice with Bacterial Artificial<br />
Chromosome-Technology<br />
”Humanized“ transgenic mice expressing human pattern recognition receptors<br />
specifically on DCs are urgently needed to develop small animal models for testing new<br />
vaccination strategies, since significant immunologic differences limit the interpretation<br />
of data obtained from mouse experiments. In comparison to mice, human Toll-like<br />
receptor 9 (TLR9) has a different ligand specificity and is expressed on different immune<br />
cells. In mice, TLR9 recognizes unmethylated CpG DNA and is expressed on<br />
conventional dendritic cells (cDCs), plasmacytoid dendritic cells (pDCs) and B cells. In<br />
humans, TLR9 is only detectable on pDCs and B cells and mediates immune cell<br />
activation by slightly different CpG sequences. We attempted to generate a mouse<br />
model mimicking human TLR9 expression by transgenesis of a Bacterial Artificial<br />
Chromosome (BAC) containing human TLR9 together with all its cis- and transregulatory<br />
regions. The purified and linearized BAC has been injected into pronuclei of<br />
fertilized C57BL/6 mouse eggs, and human BAC-transgenic mice were generated. Two<br />
BAC transgenic founder mice were obtained which are currently backcrossed to a<br />
murine TLR9 deficient background. First preliminary immunization data with “human”<br />
CpG sequences may suggest that the human promoter is functional in mice. Currently<br />
we are analyzing the expression level and specificity of human TLR9 in mice. This<br />
mouse model may provide us with new valuable tools to directly examine the role of<br />
human TLR9 on plasmacytoid DCs and B cells in vaccination studies and may allow us to<br />
test the therapeutical potential of CpG oligonucleotides in various diseases such as<br />
infection, allergy and tumor models.
Sandra Ehser, Jing-Jing Chuang, Lucian Jiga, Christian Kleist, Flavius Sandra-Petrescu,<br />
Gerhard Opelz, Peter Terness<br />
Generation of tolerogenic dendritic cells by treatment with<br />
Mitomycin C<br />
Dendritic cells (DCs) are the most potent antigen-presenting cells and play a central<br />
role in initiation of immunity or tolerance. Their controlling abilities offer possibilities for<br />
modulation of immune responses in an antigen-specific manner in organ transplantation<br />
or autoimmune diseases. To this end, either naturally suppressive DC subpopulations or<br />
ex vivo manipulated cells can be used. A series of pharmacological agents have been<br />
shown to alter the properties of DCs. We showed that after a short in vitro treatment<br />
with the akylating drug mitomycin c (MMC) DCs acquire tolerogenic properties. They<br />
irreversibly suppress allogeneic T cell responses in vitro and the treatment of recipients<br />
with MMC-incubated donor DCs strongly prolongs heart allograft survival in rats. In<br />
order to elucidate the mechanism of suppression we analyzed the supernatants of MMC-<br />
DCs. They did not mediate any suppressive effect. Therefore, the lacking T cell response<br />
could not be explained by secreted molecules. For this reason next we looked at the<br />
gene expression profile of MMC-treated cells. Over 47,000 transcripts and variants were<br />
analyzed by Affymetrix array, revealing 100 constantly modified gene expressions.<br />
Intriguingly, we found that one gene cluster was involved in apoptosis and another one<br />
– as shown in previous studies - in mediation of tolerance. It has been held that<br />
necrotic cells stimulate, whereas apoptotic cells sometimes inhibit the immune<br />
response. Our studies indicate that MMC induces apoptosis and upregulates tolerogenic<br />
molecules, thus, converting DCs into inhibitory cells. MMC-DCs might offer a therapeutic<br />
tool for antigen-specific suppression of unwanted immune reactions in clinical settings.
Ann-Kristin Mueller, Martina Deckert, Kirsten Heiss, Kristin Goetz, Kai Matuschewski,<br />
Dirk Schlüter<br />
Genetically Attenuated Plasmodium berghei Liver Stages<br />
Persist and Elicit Sterile Protection Primarily via CD8 T Cells<br />
Live-attenuated Plasmodium liver stages remain the only experimental model that<br />
confers <strong>complete</strong> sterile protection against malaria. Irradiation-attenuated Plasmodium<br />
parasites mediate protection primarily by CD8 T cells. In contrast, it is unknown how<br />
genetically attenuated liver-stage parasites provide protection. Here, we show that<br />
immunisation with uis3(-) sporozoites does not cause breakthrough infection in T and B<br />
cell-deficient rag1-/-and IFN γ-/- mice. However, protection was abolished in these<br />
animals, suggesting a crucial role for adaptive immune responses and interferon γ.<br />
Although uis3(-) immunisation induced Plasmodium-specific antibodies, B cell-deficient<br />
mice immunised with uis3(-) sporozoites were <strong>complete</strong>ly protected against wild-type<br />
sporozoite challenge infection. T-cell depletion experiments before parasite challenge<br />
showed that protection is primarily mediated by CD8 T cells. In good agreement,<br />
adoptive transfer of total spleen cells and enriched CD8 T cells from immunised animals<br />
conferred sterile protection against malaria transmission to recipient mice, whereas<br />
adoptive transfer of CD4 T cells was less protective. Importantly, primaquine treatment<br />
<strong>complete</strong>ly abolished the uis3(-)-mediated protection, indicating that persistence of uis3<br />
(-)-attenuated liver stages is crucial for their protective action.<br />
These findings establish the basic immune mechanisms underlying protection induced<br />
by genetically attenuated Plasmodium(-) parasites and substantiate their use as<br />
vaccines against malaria.
Marc Beyer, Sabine Classen, Daniela Eggle, Alexey Popov, Svenja Debey-Pascher,<br />
Elmar Endl, Percy A. Knolle, Jim Riley, Joachim L. Schultze<br />
Genomic screening reveals new proteins specifically<br />
expressed by human regulatory CD4+ CD25high FOXP3+<br />
CD127low T cells<br />
Natural regulatory T cells (Treg cells) in humans can be defined by the expression of<br />
FOXP3, low expression of CD127 and intermediate to high expression of CD25. While it<br />
has been clearly established that FOXP3 is an essential factor for differentiation and<br />
function of these cells, it is also apparent that additional yet unknown genes and their<br />
respective proteins must exist contributing to full regulatory function of these cells. To<br />
determine novel proteins involved in activation or function of human Treg cells we<br />
initiated a systems biology approach using genome-wide transcriptional profiles. A total<br />
of 192 individual experiments interrogating conventional and Treg cells from healthy<br />
donors and cancer patients in different states of activation were performed. The first<br />
surprising result was the identification of a rather small core transcriptome of Treg cells<br />
comprising of only 43 genes. As expected, genes previously associated with Treg cells<br />
such as FOXP3 or CD127 were within the specific Treg cell core transcriptome.<br />
Interestingly, the Treg cell specific genes within the core transcriptome are not enriched<br />
for cell membrane-associated proteins suggesting that Treg cell lineage is a function of<br />
fixed transcriptional regulation rather than modulation by extracellular signals. So far,<br />
only one newly identified transcript was predicted to encode a putative gene containing<br />
a transmembrane-domain. We first determined the full length transcript of this novel<br />
gene. Apparently no splice variants exist in humans. By expression cloning we<br />
established that the transcript is indeed encoding a 18 kDa protein. To study the cellular<br />
localization of the newly identified protein, we generated a GFP-tagged fusion construct,<br />
which was inserted into a lentiviral vector. Infection of Jurkat cells with this construct<br />
revealed that the protein is translated in Jurkat cells and does not exert toxic effects on<br />
the cells. Interestingly, initial studies to determine its cellular localization hint at an<br />
intracellular expression of the protein product. Taken together, genome-wide<br />
transcriptional analysis using the most recent array technology and novel bioinformatics<br />
approaches have revealed genes specifically expressed within Treg cells. Currently<br />
ongoing and future studies are focused on deciphering the biology of these novel<br />
proteins.
Charles Andrew Stewart, Thierry Walzer, Scott Hamilton Robbins, Bernard Malissen, Eric<br />
Vivier, Immo Prinz<br />
Germline and rearranged Tcrd transcription distinguish bona<br />
fide NK cells and NK-like γδ T cells<br />
NK cells and γδ T cells are distinct subsets of lymphocytes that contextually share<br />
multiple phenotypic and functional characteristics. However, the acquisition and the<br />
extent of these similarities remain poorly understood. Here, using Tcrd-H2BEGFP<br />
reporter mice, we show that germline transcription of Tcrd occurs in all maturing NK<br />
cells. We also describe a population of mouse NK-like cells that are indistinguishable<br />
from “bona fide” NK cells using standard protocols. Requirements for V(D)J<br />
recombination and a functional thymus, along with very low level expression of surface<br />
TCRγδ but high intracellular CD3 define these cells as γδ T cells. “NK-like γδ T cells” are<br />
CD127+, have a memory-activated phenotype, express multiple NK cell receptors and<br />
readily produce interferon-γ in response to IL-12/IL-18 stimulation. The close<br />
phenotypic resemblance between NK cells and NK-like γδ T cells is a source of<br />
experimental ambiguity in studies bridging NK and T cell biology, such as those on<br />
thymic NK cell development. Instead, it ascribes chronic TCRγδ engagement as a means<br />
of acquiring NK-like function.
Benjamin Wilde, Xin Cai, Sebastian Dolff, Andreas Kribben, Jan Dürig, Christof Specker,<br />
Thomas Philipp, Oliver Witzke<br />
GITR and CD134 expression on T-lymphoctyes is associated<br />
with disease activity in Wegener's Granulomatosis<br />
Aim/Background: In 2005 it has been reported by Marinaki et al. that the CD25<br />
expression is increased on CD4+ T-cells in patients suffering from ANCA-associated<br />
vasculitis. In this study CD4+CD25+ T-cell populations in patients with Wegener’s<br />
granulomatosis are further characterised.<br />
Methods: 12 Patients meeting the ACR’s criteria defining WG and 6 healthy controls<br />
were included in this study. The disease activity and extension were measured by<br />
common scores such as Birmingham Vasculitis Activity Score (BVAS) and Disease<br />
Extent Index (DEI). Lymphocytes were analysed by FACS for the expression levels of<br />
CD134, GITR, CD122, CD103, CD152 and CD80.<br />
Results: The percentage of patients’ CD25+ cells within the CD4+ T-cell population was<br />
increased in accordance to Marinaki et al. (27 ±3% vs. 13 ±1% p
Adjobimey Tomabu, Arndts Kathrin, Satoguina Judith, Hörauf Achim<br />
GITR-GITRL interactions regulate the IgG induction by<br />
regulatory T cells<br />
Regulatory T cells play a crucial role in maintaining control of effector lymphocytes in<br />
different immunological contexts. In chronic onchocerciasis for example, IL-10<br />
producing antigen specific regulatory T cells (Tr) could be cloned in high frequency, in<br />
particular from patients with high worm load and little pathology. Many mechanisms<br />
have been proposed to explain regulatory T cells immunosuppressive activities<br />
implicating IL-10, TGF-β , CTLA-4, GITR. It has recently been shown that IL-10<br />
produced by Tr cells induces B cells to secrete IgG4, a non-inflammatory antibody, in a<br />
cell-contact-dependent manner. The present study was aimed at understanding the<br />
mechanisms whereby Tr cells preferentially induce IgG4 by B cells. For this purpose, we<br />
generated FOXP3+GITR+IL10+ Tr clones from human PBMC, using vitamin D3,<br />
dexamethason and tetanus toxoid as antigen model. These Tr cells were co-cultured<br />
with autologous purified B Cells to induce IgG4. Using blocking antibodies, we found<br />
that neutralizing anti-GITR Abs selectively inhibited IgG4 production and increased IgG2<br />
production. Antibodies against GITRL, IL-10, CTLA-4 and against TGF-β also blocked<br />
IgG4 production, while anti-ICOS Abs had no effect on IgG4 production. Furthermore,<br />
the production of IL-10 by the co-cultured cells decreased in the presence of anti-GITR<br />
antibodies also, the inhibition of IgG4 induction by anti-GITR antibodies was reversed<br />
by the addition of excess recombinant IL-10 but not of recombinant TGF-β. These<br />
results indicate that GITR-GITRL interactions modulate IgG4 induction partially through<br />
induction of other factors chiefly IL10.
Matthias Krusch, Katrin Miriam Baltz, Tina Baessler, Helmut Rainer Salih<br />
Glucocorticoid-Induced TNF Related Protein (GITR) ligand is<br />
spontaneously released by tumor cells and diminishes antitumor<br />
reactivity of NK cells<br />
Members of the TNF/TNF receptor (TNFR) family mediate multiple cellular functions<br />
including proliferation, differentiation and cell death. Many TNF family members are<br />
released as soluble forms, which affects cell-cell interactions by reduction of ligand<br />
densities and distally modulates effector cells bearing the respective receptor. Here we<br />
report that human tumor cells spontaneously release a soluble form of Glucocorticoid-<br />
Induced TNF Related Protein (GITR) ligand (sGITRL), which inhibited cytotoxicity and<br />
IFN-γ production of GITR-expressing NK cells in a concentration dependent manner. NK<br />
cell functions were restored by neutralization of sGITRL by addition of a GITR-Ig fusion<br />
protein in coculture assays. While tumor-derived GITRL did not induce apoptosis, it<br />
diminished nuclear localized c-Rel and RelB in GITR-expressing NK cells indicating that<br />
sGITRL negatively modulates NK cell NF-κB activity. To determine whether release of<br />
GITRL was in fact relevant as an immune escape mechanism of human tumors in vivo<br />
we analyzed sGITRL levels in sera of cancer patients. While sera of the healthy<br />
volunteers contained no detectable sGITRL, sera of patients with rectum-, stomach-,<br />
lung-cancer and germ line tumors contained substantially elevated sGITRL levels. The<br />
strong correlation of tumor incidence and elevated sGITRL levels clearly suggests that<br />
sGITRL is released at significant amounts from tumor cells in vivo. Patient sera<br />
containing sGITRL reduced NK cell reactivity, which could again be restored by addition<br />
of a GITR-Ig fusion protein. Our data indicate that sGITRL released by tumor cells<br />
diminishes NK cell-mediated immunosurveillance, and GITRL-neutralization may be<br />
employed in therapeutic strategies like adoptive NK cell transfer.
Denise Tischner, Nora Müler, Jens van den Brandt, Andreas Weishaupt, Holger<br />
Reichardt<br />
Glucocorticoids exert distinct effects on Experimental<br />
Autoimmune Encephalomyelitis<br />
Multiple sclerosis (MS) and its animal model Experimental Autoimmune<br />
Encephalomyelitis (EAE) are chronic inflammatory diseases of the central nervous<br />
system (CNS) of presumed autoimmune origin. Acute relapses of MS are most<br />
commonly treated with high doses of glucocorticoids (GCs). However, severe adverse<br />
effects and in<strong>complete</strong> recovery accompany such therapies. Therefore a better<br />
understanding of the mechanisms of GC action in MS is urgently needed. To distinguish<br />
effects of GCs on pathogenic and conventional T cells we induced an AT-EAE by<br />
adoptive transfer of eGFP+ encephalitogenic T lymphocytes into Lewis rats followed by<br />
treatment with 20 mg/kg dexamethason three days after disease induction. This led to<br />
a rapid amelioration of the disease and a reduced infiltration of the spinal cord. We<br />
found that dexamethasone similarly induced apoptosis in pathogenic as well as<br />
conventional T cells, restored the integrity of the blood-brain barrier and downregulated<br />
ICAM-1 and IP-10 expression in the spinal cord. Accumulation of<br />
encephalitogenic T cells in the spleen supported the notion that impaired T cell<br />
migration to the CNS may contribute to therapeutic efficacy. While GCs did not alter the<br />
expression of integrins and the chemokine receptor CXCR-3, we identified cytoskeletal<br />
rearrangements accompanied by the loss of the migratory phenotype. We believe that<br />
this may partially underlie the reduced lymphocyte infiltration of the CNS. We hope that<br />
a better understanding of GC action in the treatment of MS helps to improve the<br />
available therapies.
Sabine Stegmaier, Christof Wagner, Gertrud Maria Hänsch<br />
Granzyme B expression in mature polymorphonuclear<br />
neutrophils (PMN) and in their precursor cells<br />
Polymorphonuclear neutrophils (PMN) are important effector cells of the innate immune<br />
response and are mainly appreciated for their phagocytic and bactericidal capacity.<br />
PMN, however, are also effector cells of the antibody-mediated cellular cytotoxicity<br />
(ADCC). Recently, we described that PMN also contained granzyme B and perforin, the<br />
major protagonists of cellular cytotoxicity of T cells or natural killer (NK) cells. In<br />
extension of our previous studies we now attempted to localise granzyme B in the PMN.<br />
Granules were fractionated using the established protocols. The majority of granzyme B<br />
was found in association with primary granules, a minor expression was seen in<br />
secondary granules, and the membrane fraction. According to the “targeting by timing”<br />
theory the presence in primary granules of granzyme B suggested that it is synthesised<br />
in a very early developmental state of the cell. Indeed, by cytofluorometry, we detected<br />
granzyme B in the myloid cell lines HL-60 and U937, and in bone-marrow derived CD34<br />
+ cells as well. Following in vitro differentiation of the CD34+ cells to PMN, granzyme B<br />
expression was preserved. In summary, our data provide evidence that PMN contain<br />
granzyme B, which on one hand enhances their cytotoxic potential, and on the other<br />
provides an additional means for degradation of extracellular matrices.
Praxedis Martin, Julian Pardo, Reinhard Wallich, Klaus Ebnet, Sandra Iden, Aynur<br />
Ekiciler, Arno Muellbacher, Michael Huber, Markus M. Simon<br />
Granzyme B is expressed in mouse mast cells in vivo and in<br />
vitro and causes delayed cell death independent of perforin<br />
The proteases granzyme (gzm) A and gzmB have been mainly linked to natural killer<br />
(NK) cells and cytotoxic T lymphocytes (CTL) and their lytic machinery so far. Together<br />
with perforin (perf) both gzms are released through exocytosis of NK/CTL secretory<br />
granule contents into a synapse formed between the killer cell and its target cell. After<br />
their access to the target cell cytosol they initiate alternative, but strictly perfdependent<br />
proteolytic pathways leading to apoptosis. However, in addition to these<br />
intracellular activities, secreted gzmA and gzmB may also function extracellularly by<br />
cleaving components of extracellular matrices and basal laminae, including fibronectin<br />
and vitronectin. These processes may result in cell detachment of susceptible targets<br />
and indirectly in their delayed death, termed anoikis. Recent evidence suggests that<br />
cells other than NK cells and CTL also express gzms, indicating their involvement in<br />
additional biological activities.<br />
Here we present evidence that skin-, but not lung-associated primary mouse mast cells<br />
as well as in vitro differentiated bone marrow derived mast cells (BMMC) express gzmB,<br />
but not gzmA or perf. GzmB is associated with cytoplasmic granules of mouse mast cells<br />
and secreted by BMMC upon Fcε-receptor mediated activation. BMMC from wild type but<br />
not gzmB-deficient mice cause cell death in susceptible adherent target cells indicating<br />
that the perf-independent cytotoxic potential of BMMC is executed by gzmB.<br />
Furthermore, purified recombinant gzmB induces a disorganization of endothelial cellcell<br />
contacts. The data suggest that activated mast cells contribute via secreted gzmB to<br />
cell death, increased vascular permeability, leukocyte extravasation and subsequent<br />
inflammatory processes in affected tissues.
Gerhard Wingender, Jonathan Braun, James Borneman, Mitchell Kronenberg<br />
Gut derived antigens trigger the final steps of Vα14 iNKT cell<br />
differentiation<br />
Invariant NKT (iNKT) cells carry a canonical Vα14 to Jα18 TCR rearrangement in mice,<br />
recognize glycolipids presented by CD1d and have been implicated in diverse immune<br />
reactions. Their constitutive activated/memory phenotype and their rapid initiation of<br />
effector functions after activation are indicative of previous antigen specific stimulation.<br />
However the nature of this stimulation is so far unresolved. Recently natural antigens<br />
for the majority of iNKT cells could be defined in the proteobacterium Sphingomonas<br />
spp. Here we show that Sphingomonas bacteria are commensals in the intestine of<br />
mice, and that a surplus of bacteria increases the expression levels of activation<br />
markers by iNKT cells. Furthermore we demonstrate that iNKT cells from germ free<br />
animals display a less mature phenotype and are hypo-responsive to activation with the<br />
model antigen α-galactosylceramide. Per-os reconstitution of the germ free animals with<br />
Sphingomonas bacteria, but not with E.coli, a bacterium lacking specific iNKT cell<br />
antigens, could recover full maturity of iNKT cells, phenotypically and functionally.<br />
These data indicate that bacterial iNKT cell antigens can be taken up from the intestine<br />
and are required for the final differentiation of iNKT cells.
Dagmar Quandt, Hubert Ludwiczak, Barbara Seliger<br />
Heterogeneous B7-H molecule expression and regulation in<br />
RCC and melanoma<br />
The successful fight of the immune system against cancer involves two distinct signals:<br />
the first is mediated through the interaction of tumor-associated antigens (TAA)<br />
presented by MHC class I molecules and the specific T cell receptor (TCR), whereas the<br />
second signal involves the binding of costimulatory partners on both cells. Costimulatory<br />
molecules are known to efficiently shape the effector immune response towards<br />
silencing or activation of immune cells. Tumors evade the elimination by T lymphocytes<br />
due to diverse escape mechanisms including the differential expression of activating or<br />
inhibitory costimulatory molecules. The newly identified members of the B7-H family<br />
(B7-H1-4) represent important players in this process. We analyzed a large series of<br />
melanoma and RCC cell lines for the mRNA and protein expression of the B7-H<br />
molecules. The results show a heterogeneous constitutive expression pattern for B7-H1,<br />
2 and 4 at the transcript and/or protein level. In addition, we identified for the first time<br />
an epigenetic silencing of the B7-H1 expression due to methylation of the promoter in<br />
melanoma cell lines, which could be reversed by the demethylating agent<br />
deoxyazacytidine.<br />
B7-H3 was homogenously expressed on all melanoma and RCC cell lines tested.<br />
Furthermore, 88% of primary RCC lesions exhibit B7-H3 expression, which significantly<br />
differed between the lesions. Strong B7-H3 expression correlated with a higher CD8 and<br />
inverse CD4 T cell infiltration when compared to lesions weakly expressing or lacking B7-<br />
H3 molecules. Moreover, a strong B7-H3 expression was significantly associated with a<br />
low pT value in the RCC patients. Immune effector assays to dissect the immunological<br />
role of the B7-H molecules on tumor cells are under investigation.
Christian Stemberger, Katharina Huster, Martina Koffler, Florian Anderl, Matthias<br />
Schiemann, Hermann Wagner, Dirk Busch<br />
Heterogeneous subset generation from a single naïve CD8+ T<br />
cell upon in vivo priming<br />
CD8+ T cells are crucial for protection against intracellular pathogens and some tumors.<br />
Upon first encounter with their cognate antigen, naïve T cells get activated (‘primed’),<br />
clonally expand, and can develop into very distinct subsets. These comprise short-living<br />
effector T cells that confer immediate protection by different types of effector functions,<br />
and memory T cell subsets such as effector- and central memory T cells. Because these<br />
subsets contribute differently to protective immunity and therefore have different<br />
implications for the development of vaccination strategies, it is of outstanding interest<br />
to understand how subset diversity is generated. However, so far it has only been<br />
possible to tackle questions regarding the origin of diversification via analysis of indirect<br />
parameters, such as TCR repertoires, and these experiments were limited to global<br />
analyses of clonotypic T cells.<br />
To improve analysis of T cell subset generation on a cellular level in vivo, we developed<br />
a novel adoptive transfer system that allows for the first time to trace the fate of a<br />
single antigen-specific naïve T cell in a normal (wild-type) recipient mouse. Upon<br />
immunization, clonal expansion and differentiation of single cell-derived daughter cells<br />
was monitored in a natural in vivo setting. Phenotypical and functional analyses of<br />
“single cell”-expanded populations demonstrated that a wide range of diversity can<br />
develop out of a single naïve precursor cell, including different types of effector cells<br />
and long-living memory T cell subsets. Most interestingly, we uncovered that subset<br />
diversification derived from a single cell strictly reflects the differentiation pattern found<br />
for the endogenous repertoire (in the same individual mouse). This finding indicate that<br />
the origin of subset diversification lies primarily in the intrinsic plasticity within clonal<br />
precursors, or in differences in the range of signals provided to their progeny at stages<br />
during expansion going far beyond the first cell division.
Wibke Bayer, Simone Schimmer, Dennis Hoffmann, Ulf Dittmer, Oliver Wildner<br />
Heterologous Prime-Boost Vaccination with Ad5 and Fiber<br />
Chimeric Adenoviral Vectors Enhances Immune Protection<br />
against Friend Virus<br />
In a vaccination study against the Friend virus we evaluated an Ad5-based vector and a<br />
fiber chimera expressing the fiber protein of Ad35 (Ad5F35). The Friend virus is an<br />
immunosuppressive retroviral complex of spleen focus forming virus and Friend murine<br />
leukemia virus (F-MuLV) that causes lethal erythroleukemia and splenomegaly in<br />
susceptible adult mice. The FV is regarded as a useful model to elucidate basic<br />
requirements for immune protection against retroviral infections.<br />
We vaccinated C57BL/6 and the highly susceptible CB6F1 hybrid mice with Ad5 or<br />
Ad5F35 vectors expressing F-MuLV env and gag proteins or with a prime-boost<br />
combination of the two. After challenge infection, viral load in the spleens of C57BL/6<br />
mice was reduced ~250-fold and was below the detection threshold in more than 50%<br />
of the mice. In CB6F1 mice, on day 10 p.i. all vaccinated animals showed significantly<br />
reduced viremia compared to unvaccinated control mice and the onset of disease was<br />
significantly delayed. The prime-boost combination of the two Ad vectors resulted in<br />
improved immune protection with significantly lower viremia compared to vaccination<br />
with the individual vectors.
Maren Mönkemeyer, Hans Heiken, Rachel Thomas, Reinhold E. Schmidt, Torsten Witte<br />
Higher risk of CMV reactivation in HIV-1 infected patients<br />
homozygous for MICA5.1<br />
Background:<br />
Infection with human cytomegalovirus (CMV) induces surface expression of MHC class I<br />
chain-related A (MICA), a ligand for the activating receptor NKG2D. This leads to<br />
improved recognition and elimination of infected cells by NK cells as well as CD8+ T<br />
cells. The MICA allele MICA5.1 codes for a truncated, dysfunctional protein.<br />
The aim of this study was to investigate the contribution of genetic ability to express<br />
functional MICA protein on the susceptibility to severe CMV reactivation in<br />
immunocompromised individuals. HCV and GBV-C coinfected HIV-1 infected patients<br />
were analysed as controls.<br />
Methods:<br />
The frequency of the MICA5.1 allele was assessed in 230 Caucasian HIV-1 infected<br />
patients as well as in 29 healthy controls. MICA5.1 allele was analysed by PCR. The<br />
association of MICA5.1 homozygosity and risk of CMV reactivation was calculated by<br />
Pearson Chi-Square.<br />
Results:<br />
Comparison of patients with and without a history of CMV disease manifestation<br />
revealed an enhanced susceptibility to reactivation of CMV for HIV-1 infected patients,<br />
homozygous for MICA5.1. The percentage of homozygous MICA5.1 individuals was<br />
similar in HIV-1 infected patients and healthy controls. In contrast, no evidence was<br />
found for a correlation between a homozygous MICA5.1 genotype and an increased risk<br />
of infection with GBV-C or HCV.<br />
Conclusions:<br />
This study is the first to evaluate in vivo the impact of a MICA polymorphism on risk of<br />
viral infections. A significant correlation between homozygous MICA5.1 genotype and<br />
susceptibility to CMV, but not to GBV-C or HCV coinfection, in immunocompromised<br />
individuals was demonstrated. The elimination of infected cells via NKG2D-expressing<br />
NK and T cells appears to be a more important immune reaction in CMV than HIV-1,<br />
GBV-C or HCV infection.<br />
Supported by BMBF KN Rheuma C2.12
Konrad Alexander Bode, Klaus Heeg, Alexander H. Dalpke<br />
Histone deacetylase inhibitor butyric acid of bacterial origin<br />
as mediator of tolerance in the intestinal mucosa<br />
Posttranslational modifications of histones by acetylation are a major mechanism to<br />
modify chromatin structure and gene expression in eukaryotic DNA. In a recent work we<br />
could show that histone HDAC inhibitors like trichostatin A or suberoylanilide<br />
hydroxamic acid (SAHA) in non-apoptotic concentrations strongly inhibit the TLRinduced<br />
cytokine expression of dendritic cells. In the present work we investigated<br />
whether the HDAC inhibitor butyric acid, a product of the metabolism of some anaerobe<br />
bacteria, is involved in the induction of tolerance towards the physiological bacterial<br />
flora in the mucosa of the intestine.<br />
We could show in bone marrow derived dendritic cells that butyric acid inhibits the<br />
expression of several TLR induced cytokines like IL-12p40, IFN&beta and TNF&alpha on<br />
protein (ELISA and FACS-analysis) and mRNA (real-time RT-PCR) level. Whereas TLR<br />
stimulation resulted in transient histone H4 acetylation at selected regions of the IL-<br />
12p40 promoter as shown by chromatin immunoprecipitation, butyric acid induced a<br />
hyperacetylation of the whole IL-12p40 locus for a prolonged period. HDAC inhibitors<br />
had no effects on upstream NF&kappaB activation and nuclear translocation as well as<br />
on MAP kinase signaling (immuno-blot and gel-shift) but the binding of selected<br />
transcription factors on the IL-12p40 promoter region were impaired in the presence of<br />
butyric acid.<br />
The results give evidence that butyric acid, a product of the metabolism of some<br />
anaerobe bacteria, affects intestinal immune cells by inhibiting HDACs.
Mareike Schmudde, André Braun, Ulrike Klier, Daniela Pende, Jürgen Sonnemann,<br />
Lorenzo Moretta, James F. Beck, Barbara M. Bröker<br />
Histone deacetylase inhibitors sensitize tumour cells for<br />
cytotoxic effects of natural killer cells<br />
Introduction: Histone deacetylase inhibitors (HDIs) are currently emerging as potent<br />
anti-tumour agents. By influencing the transcription of up to 22 % of genes, they induce<br />
cell cycle arrest, differentiation and/or apoptosis in tumour cells. Beside their direct antitumour<br />
activity, HDIs enhance the cytotoxic effects of ionizing radiation, chemotherapy<br />
and recombinant tumour necrosis factor-related apoptosis-inducing ligand (TRAIL). This<br />
raises the question, whether cytotoxic effector functions of natural killer (NK) or T cells<br />
are partially responsible for the anti-tumour effects of HDIs.<br />
Materials and Methods: HDI (SAHA, NaB)-treated tumour cell lines (prostate cancer<br />
PC3, medulloblastoma DAOY) were exposed to IL2-activated human PBMCs. Cell death<br />
was quantified by flow cytometric counting of surviving tumour cells and by 51 Cr-release<br />
assays. The involvement of activating NK receptors in tumour cell recognition was<br />
determined using masking antibodies in the 51Cr-release assays. Surface expression of<br />
NK receptor ligands on tumour cells was measured by flow cytometry.<br />
Results: Both HDIs and PBMCs induced tumour cell death in a dose-dependent manner.<br />
In combination, their effects were synergistic. Killing of tumour cells depended on the<br />
activating NK receptors NKG2D, DNAM-1 and the natural cytotoxicity receptors (NCRs).<br />
HDI-treatment did not result in the engagement of alternative activating NK receptors.<br />
However, it increased the redundancy of the involved receptors. Furthermore, HDIs<br />
increased the expression of the NKG2D ligands MICA and ULBP2.<br />
Conclusions: PBMCs and HDIs synergize in the induction of tumour cell death in vitro.<br />
This indicates that cytotoxic effector functions of the immune system may contribute to<br />
the therapeutic activity of HDIs in tumour patients. On a molecular level, this might be<br />
performed by NK cells, which are more efficiently activated due to increased expression<br />
of activating NK receptor ligands.
Vanessa Witte, Andreas Baur<br />
HIV-1 Nef enhances viral gene expression by linking<br />
transcriptional derepression and activation events<br />
HIV-associated disease is characterized by a successive dysregulation of the immune<br />
system due to massive CD4 + T cell depletion. Viral infection of these predominantly<br />
resting cells drives their activation. This facilitates viral replication but also causes cell<br />
death. Partly responsible is the Nef protein of HIV-1, which is required for the<br />
maintenance of high viral loads. Whether this is due to a direct effect of Nef on viral<br />
transcription remains a matter of debate.<br />
Luciferase reporter assays revealed a positive effect of Nef on HIV promoter activity,<br />
which was dependent on cotransfection of Tat and on the presence of the NFkB<br />
enhancer. Importantly, Nef expression did not initiate nuclear translocation of RelA/p65<br />
as shown by cellular fractionation experiments and immunofluorescence techniques.<br />
Instead, PMA- or CD3/CD28-mediated nuclear translocation of RelA/p65 was<br />
significantly prolonged in Nef-expressing cells. Surpisingly, chromatin<br />
immunoprecipitation (CHIP) analysis demonstrated that nuclear RelA/p65 only bound to<br />
the HIV promoter in Nef-expressing cells. Concomitantly, we found that Nef expression<br />
alone results in the specific Crm1-dependent removal of proteins from the nucleus, such<br />
as the Polycomb group (PcG) protein Eed, the NFkB kinase IKKalpha or NFkB2/p100,<br />
and that these proteins interact with histone deacetylases.<br />
In summary, these results may suggest, that in the absence of Nef, the HIV promoter is<br />
occupied by inhibitory histone deacetylase-containing protein complexes, which hinder<br />
HIV gene expression. Nef expression then leads to the removal of these inhibitory<br />
complexes thus allowing the binding of positive regulatory transcription factors such as<br />
NFkB. It is intriguing to speculate that by linking activation with derepression Nef finetunes<br />
HIV transcription thus facilitating gene expression in the presence of suboptimal<br />
activation stimuli.
Karsten Gülow, Marcin Kaminski, Peter H. Krammer<br />
HIV-Tat induced generation of Reactive Oxygen Species<br />
sensitizes T cells towards Activation-Induced Cell Death<br />
The elimination of activated T cells during the termination phase of an immune response<br />
is called Activation Induced Cell Death (AICD). AICD is induced via stimulation of the<br />
death receptor CD95 (APO-1, Fas) by its ligand CD95L. In AIDS patients, AICD is<br />
strongly enhanced. Here, we show that Reactive Oxygen Species (ROS) generated upon<br />
T cell activation function as crucial second messengers in activation-induced CD95L<br />
expression. The oxidative signal combined with simultaneous increase in intracellular<br />
Ca2+ constitutes for minimal requirement to induce CD95L expression. Either signal<br />
alone is insufficient. Further, we show that HIV-Tat induces ROS generation and<br />
depletion of reduced glutathione (GSH). The increase in ROS induced by HIV-Tat<br />
enhances T cell receptor (TCR) signalling. Thus, cells preincubated with Tat and<br />
stimulated via the TCR reveal a strong increase in the ROS signal leading to a significant<br />
increase in CD95L expression and AICD. Since CD4 stimulation can induce Ca2+ influx<br />
into the cytosol, ROS generation due to Tat treatment is sufficient to induce AICD.<br />
Therefore, our data provide a possible explanation for CD4+ T lymphocyte depletion<br />
during progression of AIDS.
Claudia Sievers, Kasia Nasilowska, Kerstin Wolk, Robert Sabat, Hans-Dieter Volk,<br />
Christian Meisel<br />
HO-1 inhibits constitutive and IFNg-induced HLA-DR<br />
expression on myeloid antigen-presenting cells via inhibition<br />
of IFNg receptor signalling and down-regulation of CIITA<br />
expression<br />
Strong and prolonged systemic immunodepression after surgery and major trauma,<br />
characterised by monocyte deactivation and T cell dysfunction, may predispose critically<br />
ill patients to infectious complications. The mechanisms that induce and sustain this<br />
condition are still in<strong>complete</strong>ly understood. Previous studies showed increased<br />
expression of heme oxygenase-1 (HO-1) in peripheral blood leukocytes in a subset of<br />
surgical patients who developed post-operative long-lasting immunodepression and<br />
infectious complications. HO-1 is a stress-inducible heat shock protein with potent antiinflammatory<br />
activities. We hypothesized that increased expression of HO-1 may play a<br />
role in the induction of long-lasting immunodepression. Here, we investigated the<br />
effects of HO-1 on APC and T cells function in vitro by using the specific HO-1 inducer<br />
cobalt protoporphyrin IX (CoPP). CoPP increased HO-1 expression in human monocytes<br />
and monocyte-derived dendritic cells, but not in lymphocytes. HO-1 induction resulted<br />
in diminished constitutive surface MHCII expression on myeloid APC, while MHCI<br />
expression was unaffected. HO-1 overexpression in monocytes resulted in decreased<br />
transcription of CIITA and other accessory genes essential for MHCII protein stability<br />
and peptide loading, including CD74, HLA-DM and Cathepsin S. Decreased STAT-1<br />
phosphorylation in response to IFNg in CoPP-treated monocytes suggests that HO-1<br />
impairs cytokine-induced up-regulation of HLA-DR expression also by interfering with<br />
cytokine-receptor signalling. Enhanced expression of HO-1 in APC resulted in diminished<br />
antigen-dependent T-cell cytokine production and proliferation. Taken together these<br />
data indicate that increased HO-1 activity may partake in the induction of<br />
immunodepression in critically ill patients.
Nadja Brachwitz, Maria Laura Zenclussen, Andre Sollwedel, Ritschel Stefanie, Hans-<br />
Dieter Volk, Ana Claudia Zenclussen<br />
HO-1 up-regulation increases the number of uNK at the fetalmaternal<br />
interface<br />
We previously suggested a protective function for HO-1 in pregnancy after observing<br />
diminished levels of HO-1 in human and murine miscarriage. Accordingly, up-regulation<br />
of HO-1 significantly diminished the abortion rate in mice. At the beginning of<br />
pregnancy uterine natural killer cells (uNK) start to invade the uterus. It is known that<br />
they are necessary for a successful pregnancy outcome. Due to the importance of both<br />
HO-1 and uNK at the fetal-maternal interface, we aimed to investigate whether HO-1<br />
acts by regulating the number of uNK invading the uterine tissue.<br />
The expression of perforin (a product of mature NK) and HO-1 was determined by qRT-<br />
PCR and by immunohistochemistry in uterus, placenta and decidua of normal pregnant<br />
(CBA/J x BALB/c) and abortion-prone mice (CBA/J x DBA/2J) at different time points of<br />
pregnancy. Additionally, uNK were quantified at the feto-maternal interface after<br />
visualization with DBA-lectin staining. Furthermore we performed in vivo studies by upregulating<br />
HO-1 by Co-PP application on gestation day (gd) 4 or by HO-1-adenoviral<br />
gene transfer on gd 5 to quantify the number of uNK cells. PBS, Zn-PP or GFP-Ad<br />
treated animals served as controls.<br />
An augmentation on HO-1 mRNA and protein levels as well as an increased number of<br />
uNK beginning on gd 8 could be observed at the feto-maternal interface in both mating<br />
combinations. Compared to the normal pregnant mice the uNK cell number and the<br />
perforin mRNA expression were reduced in abortion-prone mice. Up-regulation of HO-1<br />
prevented fetal rejection, which was accompanied by an enhanced uNK cell number.<br />
Our data confirm the hypothesis that HO-1 and uNK are relevant for the survival of the<br />
fetus within the maternal uterus. Furthermore, our results suggest that HO-1 has an<br />
influence on the migration of uNK at the feto-maternal interface and may be one of the<br />
mechanisms underlying its protective effect.
Jan C. Dudda, Nikole Perdue, Mary Beauchamp, Daniel J. Campbell<br />
Homing receptors CD62L and CD103 mark different subsets of<br />
development and function of Regulatory T cells for<br />
suppression of autoimmunity<br />
FoxP3+ regulatory T cells (Treg) control inflammation throughout life. Treg leave the<br />
thymus with “central” homing receptors (HR) such as CD62L, targeting them to<br />
lymphoid tissues. The induction of “effector/memory” Treg with “peripheral” HR takes<br />
place in the lymph nodes (LN), which includes downregulation of CD62L but expression<br />
of CD103, an integrin involved in epithelial localization. We here tested the impact of<br />
these HR on the homeostasis and function of Treg after transfer into the autoimmune<br />
scurfy mouse, which lacks all FoxP3-dependent Treg. CD62L expression and LN<br />
localization was essential for Treg survival in the neonate and a transfer of wildtype but<br />
not CD62L-/- Treg suppressed multi-organ autoimmunity. Furthermore, BM-chimeras of<br />
scurfy and CD62L-/- mice, in which all Treg emerged from the CD62L-/- donor,<br />
suggested that CD62L was not crucial for Treg survival in the adult, but important for<br />
the full control of autoimmune scurfy cells. Surprisingly, when we chose a more<br />
aggressive model transferring scurfy effector cells and CD62L-/- Treg into RAG-/- mice,<br />
CD62L-/- Treg could expand and control autoimmunity to some extend, after they had<br />
differentiated into CD103+ effector Treg. Interestingly, the transfer of CD103+ or<br />
negative Treg alone or in competition with each other into neonatal scurfy mice<br />
revealed, that CD103 is dynamically regulated and marks a subset of Treg, which is<br />
effectively suppressing autoimmunity. Thus, LN localization is important for activation of<br />
naïve-like Treg, whereas effector/memory Treg can home to LN and suppress<br />
autoimmunity in a largely CD62L independent manner. Additionally, our observation<br />
that autoimmune suppressors preferentially reside in the CD103+ subset may have<br />
implications for therapy of autoimmune diseases.
Otilia Postea, Christian Weber, Andreas Ludwig<br />
Homocysteine-induced adhesive and scavenger activity of<br />
endothelial cells involves upregulation of the transmembrane<br />
chemokine CXCL16 by a PPAR-gamma dependent mechanism<br />
Hyperhomocysteinemia induces endothelial dysfunction and promotes atherosclerotic<br />
vascular disease. Infiltrates of activated macrophages and T cells are observed in<br />
human and experimental atherosclerotic lesions. Enrollment of these cells to lesions is<br />
guided by endothelial-leukocyte adhesion molecules and chemoattractants. The CXCL16<br />
chemokine is playing a double role, acting as adhesion molecule by interacting with its<br />
receptor, CXCR6 and as scavenger for oxidized LDL (oxLDL). As the adhesion of<br />
leukocytes to activated endothelial cells (EC) and uptake of modified lipids are crucial<br />
stages for the development of atherosclerosis, we investigated the effect of<br />
homocysteine (Hcy) on the expression and function of CXCL16 chemokine on cultured<br />
EC (EA.hy 926 cells). Incubation of EC with different pathophysiological relevant<br />
concentrations of L-Hcy (50 to 200•M) dose-dependently increased T cell adhesion to<br />
EC as demonstrated in a static adhesion assay. In contrast, D-Hcy and L-cysteine have<br />
no significant effect. Furthermore, stimulation with L-Hcy increased binding of DiI-oxLDL<br />
to EC as detected by flow cytometry. L-Hcy-stimulated EC also show a significant<br />
increase in CXCL16 mRNA and surface expression. Pretreatment of EC with an anti-<br />
CXCL16 monoclonal antibody reduces T cell adhesion to Hcy-incubated EC and uptake of<br />
DiI-oxLDL, suggesting that Hcy may influence leukocyte-endothelial cell interaction and<br />
lipid uptake via the modulation of CXCL16 expression. Antioxidants (Tiron 2,5mM) and<br />
Pioglitazone (100 •M) significantly reduce Hcy´s stimulatory effect indicating that<br />
induction of CXCL16 by Hcy involves the disruption of the PPAR-gamma defense<br />
mechanism against oxidative stress. These data suggest that upregulation of CXCL16 in<br />
response to homocystemia promotes increased adhesion of CXCR6 expressing<br />
circulating T cells and scavenging of modified lipids, both events critically implicated in<br />
the formation and progression of atherosclerotic lesions.
Matthias von Herrath, Christophe Filippi<br />
How viral infections prevent type 1 diabetes by augmenting<br />
Treg function<br />
The most popular hypothesis circulating within the scientific community is that viral<br />
infections are good candidates for enhancing or eliciting autoimmune disorders such as<br />
type 1 diabetes (T1D), because they induce strong inflammation, can enhance antigen<br />
presentation and directly lyse target cells. However, mounting recent evidence shows<br />
that the opposite scenario, which is prevention or amelioration of T1D by viral infections<br />
might be at least as common or even a more common outcome. Two recent publications<br />
in J. Virol. clearly demonstrated that a multitude of Coxsackie B virus and rotavirus<br />
strains prevented T1D in the NOD mouse model for spontaneous diabetes, and our own<br />
previous work (Christen et al JCI 2004) showed that LCMV virus commonly prevents<br />
T1D in two animal models when encountered during the pre-diabetic phase. Thus, it is<br />
time to rethink this issue.<br />
A new discovery made by us strongly supports the concept that viral infections<br />
themselves might be potent enhancers of regulatory T cell (Treg) function: We observed<br />
that viral (LCMV) infection of NOD mice enhances CD25+FoxP3+ Treg function and<br />
prevents T1D and that such virally-enhanced Tregs can transfer protection upon<br />
adoptive transfer into naïve pre-diabetic NOD recipients. In addition, we found that Treg<br />
lines induced by lymphocytic choriomeningitis virus (LCMV) in vivo, or grown specific for<br />
the virus or viral epitopes in vitro, were capable to delay autoimmune diabetes in the<br />
RIP-LCMV model, but failed to significantly affect the anti-viral immune response.<br />
Thus, encounters with pathogens might be crucial for ‘tuning’ the immune system and<br />
maintain a sufficient degree of systemic immune regulation, in this way making the<br />
occurrence of autoimmunity less likely.
Stefan Welte, Kathrin Pietschmann, Lothar Marischen, Susann Beetz, Ina Martens,<br />
Daniela Wesch, Dieter Kabelitz<br />
Human γδ T lymphocytes express pattern recognition receptors<br />
Pattern recognition receptors such as Toll-like (TLR) and NOD-like receptors recognize<br />
conserved pathogen-associated molecular patterns which distinguish foreign/ dangerous<br />
organisms from the host cells. With respect to human blood derived γδ T lymphocytes,<br />
we found reproducible expression of TLR1, 2, 3, 5, 6, 7 and NOD2 mRNA. To analyze<br />
the functional relevance of the expression of these proteins in more detail, we<br />
stimulated freshly isolated, highly purified γδ T cells with TLR specific surrogate ligands,<br />
e.g. bacterial lipopeptides Pam2CSK4 and Pam3CSK4 for TLR2, poly(I:C) for TLR3,<br />
flagellin for TLR5, and with the NOD2 ligand MDP. In general, all used TLR ligands exert<br />
no or only limited effects by itself but increased the T cell receptor (TCR) stimulated IFNγ<br />
production of γδ T lymphocytes. Furthermore, incubation with TLR ligands enhanced<br />
secretion of TNF-α, RANTES and MIP-1α. MDP caused a small increase in IFN-γ<br />
production of TCR stimulated cells, also in combination with Pam2CSK4 and Pam3CSK4. Furthermore, we investigated freshly isolated Vδ1 and Vδ2 γδ T lymphocytes, the two<br />
major subpopulations in the human blood, separately. Both cell populations express a<br />
similar level of the pattern recognition receptors. In functional tests, Vδ1 γδ T cells<br />
produce only little IFN-γ upon stimulation, whereas Vδ2 γδ T cells are strong IFN-γ<br />
producers. The differential stimulation by the different TLR and NOD ligands is currently<br />
under investigation.<br />
This study was supported by DFG SPP 1110 “Innate Immunity” (Ka 502/8-3).
Susann Beetz, Tim Meyer, Ina Martens, Thomas Stempfl, Daniela Wesch, Dieter<br />
Kabelitz<br />
Human γδ T lymphocytes can initiate an anti-viral immune<br />
response to double-stranded RNA<br />
Human blood derived γ&delta T lymphocytes express Toll-like receptor (TLR) 3. After<br />
stimulation via the T cell receptor (TCR), highly purified γ&delta T lymphocytes can be<br />
costimulated by the surrogate TLR3-ligand poly(I:C). We performed cDNA microarray<br />
experiments to investigate differences in gene expression between γ&delta T cells<br />
stimulated via TCR in comparison to cells stimulated via TCR and with poly(I:C). By<br />
applying a 1.5fold cutoff, poly(I:C) treatment increased the transcription of 380 genes<br />
including CD38, CD86, CD274, IL-15Rα, Trail, Fas-Ligand, MHC class I-related molecule<br />
MICB, granzyme B, perforin and TLR3 itself. The most striking differences concerned<br />
genes involved in launching an intracellular antiviral response such as myxovirus<br />
resistance (Mx) proteins, OligoA synthetase, and adenosine deaminase acting on RNA<br />
(ADAR). Other upregulated genes belong to the immunity/inflammatory cluster and<br />
include genes for interferon-α, -β, and -γ, TNF-α, CXCL10, and IL-15. Furthermore, the<br />
production of interferon regulatory factor (IRF) 7 as well as TLR7 mRNAs was triggered.<br />
The data suggest that human γ&delta T lymphocytes are able to sense viral infection<br />
and then produce type I interferons and exhibit an enhanced cytotoxic activity. The<br />
microarray results of some selected genes were confirmed by real-time PCR and flow<br />
cytometry. In future functional assays the influence of poly(I:C) on the behaviour of<br />
γ&delta T cells such as cytotoxicity will be investigated.
Thi Thu Hoai Nguyen, Silva Holtfreter, Thi Thu Hong Le, Harald Kusch, Michael<br />
Hecker, Susanne Engelmann, Alex van Belkum, Uwe Völker, Heiman Wertheim, Barbara<br />
M. Bröker<br />
Human antibody response to experimental colonization with<br />
Staphylococcus aureus<br />
Thi Thu Hoai Nguyen1, Silva Holtfreter1, Thi Thu Hong Le2, Anne-Kathrin Ziebandt3,<br />
Harald Kusch3, Quoc Phong Truong2, Leif Steil2, Michael Hecker3, Susanne<br />
Engelmann3, Alex van Belkum4, Uwe Völker2, Heiman Wertheim4,5, Barbara M.<br />
Bröker1<br />
1) Department of Immunology, University of Greifswald, Germany<br />
2) Department of Functional Genomics, University of Greifswald, Germany<br />
3) Institute of Microbiology and Molecular Biology, University of Greifswald, Germany<br />
4) Department of Medical Microbiology and Infectious Diseases, University Medical<br />
Center, Rotterdam, The Netherlands<br />
5) Oxford University Clinical Research Unit National Institute of Infectious and Tropical<br />
Diseases Bach Mai Hospital, Hanoi, Vietnam<br />
Staphylococcus aureus (S. aureus) is the most common cause of nosocomial infections<br />
and it can cause a wide range of human diseases ranging from superficial abscesses and<br />
wound infections to systemic infections, such as osteomyelitis, infective endocarditis,<br />
and sepsis. At the same time, the microorganism is also a frequent colonizer among the<br />
normal human flora. In S. aureus carriers we found a strong neutralizing antibody<br />
response against superantigens secreted by their colonizing strain. It is not known how<br />
the adaptive immune response against S. aureus proteins is triggered. We colonized 16<br />
healthy volunteers with the S. aureus strain 8325-4, which was selected because of its<br />
low virulence, and obtained serum samples before and four weeks after colonization. To<br />
investigate whether colonization induces changes in the antibody profiles against S.<br />
aureus, we separated the secreted staphylococcal proteins by two-dimensional gel<br />
electrophoresis, transferred them onto a PVDF membrane and afterwards performed<br />
immunoblots with the human sera. The results show a large inter-individual variability<br />
in the antibody profiles against S. aureus 8325-4. Even before experimental<br />
colonization, healthy individuals harboured high titre antibodies directed against a broad<br />
range of extracellular S. aureus proteins. These antibodies are likely due to previous<br />
encounters with S. aureus. Only rarely we observed additional antibody signals or<br />
increased signal intensities after experimental colonization with S. aureus. Therefore,<br />
short term colonization per se does not appear to trigger strong antibody responses to<br />
S. aureus. We conclude that the high antibody titres seen in most healthy individuals, in<br />
particular in S. aureus carriers, require either long lasting contact with S. aureus or,<br />
most likely, minor infections as they commonly occur with this microorganism,<br />
especially with strains of higher invasive potential.
Anja Mayer, Holger Bartz, Fabian Fey, Alexander Dalpke<br />
Human bronchial epithelial cells modify function and<br />
phenotype of dendritic cells in inflammatory settings<br />
Bronchial epithelial cells (BEC) represent the first line of defence against invading<br />
microbial pathogens. Epithelial cells not only function as tight barrier but also actively<br />
contribute to immune recognition of invading pathogens. We can show that BECs<br />
functionally express various pattern recognition receptors. Moreover, gene array<br />
analyses show that BECs are able to induce a pathogen-adopted defence program.<br />
Despite activation of a pro-inflammatory program we noticed that also immunemodulatory<br />
and genes were induced which might influence professional immune cells.<br />
Dendritic cells (DCs) are present at the base of bronchial epithelium and serve as major<br />
antigen-presenting cells in the lung. To investigate the interplay of BECs with dendritic<br />
cells we performed co-incubation experiments. We observed that dendritic cells secreted<br />
less IL-12 and TNF-α when co-incubated with BEAS-2B monolayers. DCs also lost their<br />
ability to release IL-12 when they were cultured with supernatants from BEAS-2B or<br />
stimulated in a transwell-system. Furthermore, DC phenotype was modified in the<br />
presence of BEAS-2B supernatant with slight reduction of CD86 and enhanced<br />
phagocytotic activity. Finally, DC mediated mixed leukocyte reaction (MLR) was<br />
significantly reduced in the presence of BECs. Current work aims at the identification of<br />
BEC-secreted immuno-modulatory factors.<br />
The results indicate that the functional properties of DCs are markedly affected by<br />
surrounding bronchial epithel cells. Thus, immune homeostasis in the lung is influenced<br />
by both, epithelial as well as dendritic cells. Similar results within the intestine indicate<br />
that the microenvironment in general shapes the functional competence of DCs and<br />
influences microbial recognition processes.
Caroline Maas, Shenchu Jin, Oliver Germandi, Gerd Otto, Peter Galle, Dennis Strand,<br />
Susanne Strand<br />
Human Chorionic Gonadotropin protects against T cellmediated<br />
liver injury in mice by downregulating Bim and<br />
Puma<br />
Clinical symptoms of Th1 mediated autoimmune diseases regress in many patients<br />
during pregnancy. Human chorionic gonadotropin (HCG) plays a major role in early<br />
human development through a series of well recognized pregnancy-promoting actions<br />
that are exerted in various reproductive and gestational tissues. Recent research<br />
indicates that HCG can exert significant physiological actions via its cell surface receptor<br />
(LH/CG-receptor) in different nongonadal tissues. In our investigations we tested the<br />
effect of HCG in a mouse model of autoimmune hepatitis. HCG decreased the<br />
histological manifestations of the Concanavalin A induced cell-mediated<br />
immunoinflammatory hepatitis, decreased the number of apoptotic hepatocytes in the<br />
liver and profoundly lowered the increased transaminase levels in the serum. To explore<br />
the mechanisms underlying the inhibition of apoptosis after HCG treatment, we used<br />
primary mouse human hepatocytes. We show that HCG can decrease the nuclear<br />
localization of the transcription factor FOXO3a and concomitantly lower levels of the<br />
proapoptotic FOXO3a downstream targets, Bim and Puma.<br />
HCG might be a promising strategy for the clinical treatment of human autoimmune<br />
disease.
Clarissa Mindnich, Sonja Bonness, Kristine Kohl, Sylvia Schnautz, Dagmar von Bubnoff,<br />
Dagmar Wilsmann-Theis, Susanne Koch, Thomas Bieber<br />
HUMAN IN VITRO GENERATED DENDRITIC CELLS EXPRESS<br />
THE INDUCIBLE NITRIC OXIDE SYNTHASE (iNOS)<br />
iNOS is a P-450-type cytoplasmic protein that catalyzes the conversion of L-arginine to<br />
L-citrulline and nitric oxide (NO). NO has been shown to play a role in inflammatory and<br />
autoimmune tissue injury because of its cytotoxic and immunoregulatory properties.<br />
The inducible form of NOS is able to produce large amounts of NO and can be expressed<br />
in a number of mammalian cells after challenge with proinflammatory cytokines.<br />
Dendritic cells (DC) present antigenic peptides to T cells and thus initiate an adaptive<br />
immune response. We investigated, whether human in vitro derived DC express iNOS.<br />
Staining of cryo-fixed human monocyte-derived DC (MoDC) with an iNOS-specific<br />
monoclonal antibody visualized with phosphatase-coupled secondary reagents revealed<br />
discrete intracellular localizations of the enzyme. iNOS protein was found in the<br />
cytoplasm, in a perinuclear region and close to the plasma membrane. Interestingly, the<br />
magnitude of iNOS protein expression and its localization was influenced by MoDC<br />
stimulation with Staphylococcus aureus. Also, RT-PCR analysis of MoDC mRNA showed<br />
enhanced expression of the enzyme after Staphylococcus aureus treatment. As a means<br />
of measuring functional iNOS activity, we investigated the occurrence of NO in the<br />
supernatants from unstimulated and Staphylococcus aureus-stimulated MoDC. NO was<br />
detected in supernatants from Staphylococcus aureus-stimulated MoDC cultures from<br />
two out of 17 patients with psoriasis, but not in supernatants derived from MoDC from<br />
healthy controls. We conclude that iNOS mRNA and protein can be expressed by human<br />
in vitro generated MoDC. However, its functional activity requires additional so far<br />
unknown factor(s) active under certain pathological conditions.
Annette Paschen, Mostafa Jarahian, Antje Sucker, Sandra Striegel, Iris Moll, Dirk<br />
Schadendorf, Frank Momburg<br />
Human Natural Killer (NK) Cells Effectively Kill Autologous<br />
Melanoma Cells In Vitro but Limited NK Cell Infiltration into<br />
Tumor Metastasis might Interfere with an Effective Anti-<br />
Tumor Immunity In Vivo<br />
Malignant melanoma in its metastatic disease stage is known to down-regulate or even<br />
<strong>complete</strong>ly lose the surface presentation of human leukocyte antigen (HLA) class I<br />
molecules. Cells displaying an altered HLA class I expression should be eliminated by<br />
cytotoxic NK cells, as long as ligands of activating NK cell receptors are presented on<br />
the tumor cell surface. Therefore, we asked about the NK cell recognition of melanoma<br />
cells with different HLA class I phenotypes. Melanoma cell lines were established from<br />
HLA class I-positive and -negative metastatic tumor tissues of different patients. In<br />
general, HLA class I loss on tumor cells was due to mutations affecting the β2microglobulin<br />
gene. Irrespective of their HLA class I phenotype, tumor cells expressed<br />
ligands of the activating NK cell receptors NKG2D, DNAM-1 and NCR. Interestingly, in<br />
vitro activated, polyclonal NK cells isolated from the peripheral blood of a melanoma<br />
patient were capable of effectively killing autologous HLA class I-positive and -negative<br />
tumor cells, suggesting that activated NK cells might be exploited for melanoma<br />
immunotherapy. However, when metastatic tumor tissues were analysed for immune<br />
cell infiltration, CD56 + NK cells were hardly detectable in most cases, suggesting that<br />
an inefficient tumor infiltration might be a barrier for an effective NK-based<br />
immunotherapy of melanoma.
Anja A. Kuehl, Jürgen Westermann, Nina N. Pawlowski, Katja Grollich, Martin Zeitz,<br />
Jörg C. Hoffmann<br />
Human peripheral γδ T Cells posses regulatory Potential<br />
Background and Aim: In animal models of inflammatory bowel disease γδ T cells play<br />
a protective role by prolonging the survival and diminishing epithelial damage. For<br />
therapeutical use in inflammatory bowel disease, the regulatory properties of human γδ<br />
T cells have to be elucidated. Therefore, proliferation, suppression, and cytokine<br />
secretion of γδ T cells were determined in vitro.<br />
Methods and Material: Human peripheral γδ T cells were isolated from whole blood of<br />
healthy donors by MACS technology. The proliferative response was measured by 3 [H]-<br />
Thymidine incorporation and the cytokine profile of culture supernatants by ELISA as<br />
well as intracellularly by flow cytometry. Additionally, the suppressive capacity was<br />
determined by flow cytometry in coculture experiments.<br />
Results: Human γδ T cells showed in vitro anergic behaviour and suppressed the<br />
growth of CD4-positive T cells even at low cell ratios. Additionally, they secreted both<br />
anti- and proinflammatory cytokines. The regulatory properties of human γδ T cells were<br />
superior to other regulatory T cells (CD4CD25-positive) regarding their suppressive<br />
behavior and cytokine profile.<br />
Conclusions: Regulatory γδ T cells could be of therapeutical use in treatment of<br />
inflammatory bowel disease as they are anergic and act suppressive as well as secret<br />
protective cytokines. For application of human γδ T cells in therapy their expansion<br />
under maintenance of their regulatory properties should be elucidated.
Anja Saalbach, Jacqueline Lessig, Jan C Simon, Jürgen Arnhold, Ulf Anderegg<br />
Human Thy-1 induces secretion of matrix metalloproteinase-9<br />
and CXCL8 from neutrophils<br />
Neutrophils are the first cells at sites of inflammation. On their way from blood to the<br />
site of infection neutrophils have to adhere to endothelial cells (EC), to transverse the<br />
basement membrane and subsequently to travel through the interstitial matrix.<br />
Recently, we have shown that Thy-1 is an adhesion molecule on activated dermal EC<br />
and fibroblasts mediating the binding of neutrophils via Mac-1. Thus, human Thy-1 is an<br />
alternate EC receptor for the leukocyte integrin Mac-1 that contributes to leukocyte<br />
recruitment to sites of inflammation thus providing a new pathway for adhesion and<br />
transmigration of neutrophils.<br />
Here, we studied whether Thy-1 mediated adhesion of neutrophils mediates only the<br />
physical contact or further influences neutrophil functions. Since MMP-9 plays an<br />
important role for the migration of neutrophils through the basement membrane we<br />
analyzed secreted MMP-9 after interaction of neutrophils with Thy-1. Indeed, binding of<br />
neutrophils to recombinant Thy-1 stimulated secretion and activation of MMP-9 from<br />
neutrophils resulting in an enhanced migration through a collagen-IV barrier.<br />
Accordingly, blocking Thy-1 on activated dermal EC or fibroblasts decreased the MMP-9<br />
secretion from neutrophils in co-cultures.<br />
Next, we investigate whether the interaction of neutrophils with Thy-1 regulates the<br />
secretion of CXCL8 and thus might support the attraction of additional neutrophils at<br />
sites of inflammation. Binding of neutrophils to Thy-1 induced the release of CXCL8.<br />
Blocking of Thy-1 on activated dermal EC or fibroblasts in co-cultures with neutrophils<br />
decreased the CXCL8 secretion confirming the role of Thy-1 in regulation of CXCL8<br />
release.<br />
In summary, Thy-1 mediates not only the adhesion of neutrophils to activated dermal<br />
EC and fibroblasts but also regulates neutrophil function. These results support the<br />
general concept that the function of ‘adhesion molecules’ may not only be to provide<br />
mechanical support but might also be to regulate functions such as motility or release of<br />
chemotactic factors.
Sabrina Laing, Mareike Pilz, Michel Seman, Friedrich Koch-Nolte, Friedrich Haag<br />
Human TNF&alpha is a substrate for modification by ADPribosyltransferase-1<br />
(ART1)<br />
Mono-ADP-ribosyltransferases (ARTs) are GPI-anchored ectoenzymes that covalently<br />
modify cell surface or soluble target proteins by transferring ADP-ribose from NAD+ to<br />
arginine residues. In the mouse, ART2, expressed on resting T lymphocytes, plays an<br />
immunoregulatory role by ADP-ribosylating the P2X7 purinoreceptor, thereby initiating<br />
rapid apoptosis in T-cells. ART2 is shed from the cell surface in an enzymatically active<br />
form upon T-cell activation. However, ART2 is a pseudogene in man, and the question<br />
as to whether ADP-ribosylation plays an immunoregulatory role in the human immune<br />
system is open. We asked whether in humans the immunoregulatory function of ART2<br />
might be carried out by ART1. We identified ART1 transcripts in human peripheral blood<br />
leukocytes, as well as in heart and skeletal muscle, by RT-PCR analysis. We<br />
hypothesized that ART1, like ART2, might be released from cells and be present in the<br />
circulation in a soluble form. We thus asked whether soluble ART1 could modify small<br />
messenger proteins such as cytokines. Indeed, soluble ART1, released from the surface<br />
of transfected cells by PI-PLC, modified recombinant human TNF&alpha in vitro.<br />
Furthermore, co-transfection of HEK293 cells with ART1 and human TNF&alpha resulted<br />
in modification of TNF&alpha at at least 2 distinct sites, i.e. one within the domain shed<br />
from the cell surface by the action of the metalloproteinase TNF&alpha Converting<br />
Enzyme (TACE), and one on the stalk that remains connected with the cell membrane<br />
after cleavage by TACE. Experiments to investigate the functional consequences of ADPribosylation<br />
of TNF&alpha as well as to identify the ADP-ribosylation sites are currently<br />
in progress.
Petra Richl, Martin Albers, Henner Morbach, Stephanie Brändlein, H. Peter Vollmers,<br />
Hermann Girschick<br />
Humoral immunity against malignant gastric carcinoma cells:<br />
molecular characterization and age-related frequency of SC-1<br />
antibody positive B cells<br />
Objective: The human monoclonal IgM antibody SC-1 was isolated from splenic B cells<br />
of an adult patient with adenocarcinoma of the stomach. It detects an isoform of the<br />
DAF/CD55 receptor, expressed specific on gastric adenocarcinoma. Given that this<br />
antibody is considered to belong to the "natural" or "innate" immunity and is found in<br />
healthy individuals as well, molecular analysis (use of immunoglobulin genes) and<br />
analysis of age-related frequency of SC-1 producing B cells is of particular relevance for<br />
further understanding of natural anti-tumor immunity.<br />
Methods: By means of an anti-SC-1 antibody we were able to isolate and characterize<br />
(CD19, CD5, CD27, IgD) B cells from the peripheral blood by multi-color FACS staining.<br />
In order to uncover an age-related presence of SC-1 positive B cells, we analyzed<br />
PBMCs from cord blood, children, adults (30, 50 and 70 years old) and compared the<br />
findings with those from carcinoma patients. Molecular characterization of the B cell<br />
receptor was carried out by sequence analysis of lambda light chain genes on single cell<br />
level.<br />
Results: Across all ages the relative number of SC-1+ B cells was constant at 5%<br />
whereas the number doubled in carcinoma patients (10%). Combined analysis of<br />
different epitopes revealed age-related frequencies. Strikingly we revealed a statistically<br />
significant decrease of SC-1+IgD+ B cells in case of carcinoma and a concomitant<br />
change of the phenotype to SC-1+IgG+ B cells.<br />
In both healthy individuals and carcinoma patients SC-1+CD5+ B cells were isolated<br />
which predominantly carry the lambda light chain 3r (85%). Further analysis revealed a<br />
selection of short CDRIII regions (27 bp) and a selection of JL 2/3 in SC-1+CD5+ B cells<br />
of tumor patients.<br />
Conclusion: The comparative molecular characterization and phenotyping of B cells<br />
from healthy individuals of different age and carcinoma patients gives information about<br />
the natural immune-surveillance against tumors, the age-related presence and<br />
variability. Furthermore, this analysis provides an insight into the clonal expansion and<br />
differentiation of tumor-specific B cells.
Gordon Grochowy, Michelle Hermiston, Arthur Weiss, Michael Huber<br />
Hyperactivation of mast cells from CD45 E613R („wedge“)<br />
mice<br />
The transmembrane protein tyrosine phosphatase CD45 is involved in the activation of<br />
the Src kinase Lyn and thus in the antigen-triggered FcεR1-mediated activation of mast<br />
cells (MCs). Hence, CD45-deficient bone marrow-derived MCs (BMMCs) exhibit<br />
increased inhibitory Lyn phosphorylation and drastically reduced effector functions<br />
(degranulation and cytokine secretion). Due to a mutation at the tip of the so-called<br />
wedge-region, CD45 E613R is unable to dimerize and prone to hyper-activity.<br />
Correlating, CD45 E613R BMMCs show stronger effector functions after antigentriggering<br />
than wild-type BMMCs, however, inhibitory phosphorylation of Lyn is<br />
comparable to CD45-deficient BMMCs. This unexpected phenotype most likely is due to<br />
attenuated interaction between CD45 E613R and Lyn and a hyper-activation of the Fynregulated<br />
phosphatidylinositol-3-kinase pathway. Interestingly, depending on the<br />
addressed receptor systems CD45-deficient and CD45 E613R BMMCs are able to show<br />
uniform phenotypes as well. Proliferation of both cell types in response to IL-3 and/or<br />
SF is enhanced compared to wild-type BMMCs. In conclusion, we demonstrate that<br />
CD45 is required to fine-tune MC responses mediated by different ligand-receptor<br />
systems. This is reinforced by studying a CD45 inhibitor, which, depending on the<br />
concentration used, can augment or attenuate MC effector functions.
Ursula Ellinghaus, Rudolf Rupec, Oliver Pabst, Ralf Ignatius, Reinhold Förster, Bernd<br />
Dörken, Franziska Jundt<br />
IκBα is crucial for marginal zone B cell development<br />
Marginal zone B (MZB) cells constitute a distinct B cell lineage located in the splenic<br />
marginal zone that is specialized in the rapid response to blood-borne pathogens.<br />
Development of MZB cells depends on the strength of B cell receptor signaling, Notch2<br />
signaling and subunits of nuclear factor kappa B (NF-κB). The function of Notch2 is<br />
impressively illustrated by a <strong>complete</strong> loss of MZB cells in mice with a B-cell-specific<br />
Notch2-deletion. In contrast, the function of NF-κB remains to be fully elucidated.<br />
Analysis in mice lacking the NF-κB subunit p50 demonstrated an essential role of p50<br />
for MZB cell generation, whereas other subunits appear to contribute to a lower extent.<br />
We investigated the role of IκBα, the main inhibitor of NF-κB, for MZB cell development<br />
and function. To this aim we generated a B-cell-specific deletion of IκBα in mice<br />
resulting in a constitutive activation of NF-κB. This caused a 70 % reduction of MZB<br />
cells as well as putative MZB cell precursors. In contrast, follicular B and B1 cells<br />
remained unaltered. Interestingly, we observed decreased Notch2 signaling in IκBαdeficient<br />
splenic B cells, indicated by suppressed transcription of Notch2 and its target<br />
genes Hes1, deltex1 and Cd21. In contrast, the expression levels of the B-cell-specific<br />
transcription factors Pax5 and Ebf1 remained unaltered. In order to evaluate the<br />
functional relevance of a reduced MZB cell population we injected IκBα mice with<br />
Staphylococcus aureus as a model for infection with blood-borne pathogens.<br />
Interestingly, IκBα-deficient mice showed a decreased survival compared to wildtype<br />
mice. This suggests that a reduction of MZB cells in mice with the B-cell-specific<br />
deletion of IκBα results in an impaired clearence of blood-borne bacterial infection.
R. Riedl, J. Sommer, K. Prinz, A. Egyed, C. Schellack, A. von Gabain, E. Nagy, K.<br />
Lingnau<br />
IC31TM: a novel adjuvant that potently activates Type I<br />
immune responses<br />
The novel adjuvant IC31TM consists of a combination of a negatively-charged synthetic<br />
oligodeoxynucleotide and a positively-charged peptide. IC31TM is characterized by a<br />
broad mechanism of action, as well as an excellent safety profile. Detailed analyses<br />
showed that the immunostimulatory effect of IC31TM is mediated via the TLR9/MyD88dependent<br />
signaling pathway of the innate immune system. Additionally, both depot<br />
formation at the injection site as well as sustained activation of antigen presenting cells,<br />
followed by antigen uptake and processing, is likely responsible for the induction of the<br />
observed IC31TM-mediated antigen-specific immune responses. It could be shown in<br />
mice that IC31TM induces strong T cell responses activating both CD4+ helper T cells as<br />
well as CD8+ cytotoxic T cells. In addition, strong humoral immune responses with<br />
increased antibody titers are generated by IC31TM. Because of its activation of innate<br />
immune cell types, such as NK cells and DC, as well as its stimulation of Type I T cell<br />
responses, IC31TM may show broad applicability to the treatment of infectious diseases<br />
and tumors.
Alexandra Doerr, Carsten Watzl, Michael Kirschfink<br />
iC3b binding to Raji cells modulates Rituximab- induced<br />
antibody-dependent cellular cytotoxicity (ADCC)<br />
Malignant cells are protected against autologous complement by various mechanisms<br />
including the overexpression of membrane-associated complement regulators, and<br />
soluble complement inhibitors, secreted into the tumour microenvironment. This<br />
complement resistance represents a major barrier for successful anti-tumour<br />
immunotherapy. Conflicting results exist on the possible impact of complement on NK<br />
cell-mediated cytotoxicity.<br />
In the present study we investigated the ability of complement to increase antibodymediated<br />
NK cell cytotoxicity, induced by Rituximab, a chimeric anti-tumour antibody,<br />
which is directed against CD20 expressed on B-cells and successfully applied in<br />
immunotherapy of Non-Hodgkin-B-cell lymphomas.<br />
Raji cells were preincubated with C5 depleted human serum as source of complement<br />
before exposure to freshly isolated NK cells. Complement- and NK cell- mediated<br />
cytotoxicity was measured by 51 Cr release assay and binding of complement proteins to<br />
tumour cell surface by cytofluorometry.<br />
As Raji cells activate the alternative pathway of the complement cascade, a significant<br />
amount of iC3b was deposited on the tumour cell surface and complement-mediated<br />
tumour cell lysis (CDC) occured, even in the absence of Rituximab. Rituximab dosedependently<br />
induced ADCC, as well as CDC and the deposition of iC3b in the presence<br />
of normal human serum. Tumour-directed NK cell cytotoxicity increased after<br />
preexposure to serum complement even in the absence of antibody. If Raji cells were<br />
incubated with low concentrations of Rituximab in the presence of C5-depleted serum<br />
leading to binding of iC3b on targeted Raji cells, ADCC of the tumour cells was<br />
augmented. However, if Raji cells were exposed to higher concentrations of Rituximab<br />
in the presence of C5 depleted serum, higher amounts of iC3b exerted an inhibitory<br />
effect on NK cell lysis.<br />
This demonstrates that the amount of deposited iC3b on the target cell determines if<br />
complement has a positive or negative effect on NK cell-mediated ADCC.<br />
-->
Yvonne Burmeister, Timo Lischke, Anja C. Dahler, Hans-Werner Mages, Kong-Peng<br />
Lam, Anthony J. Coyle, Richard A. Kroczek, Andreas Hutloff<br />
ICOS controls the pool size of effector-memory and<br />
regulatory T cells<br />
Inducible co stimulator (ICOS) is an important regulator of T cell effector function. ICOSdeficient<br />
patients as well as knock-out mice show severe defects in T cell-dependent B<br />
cell responses. Several in vitro and in vivo studies attributed this phenomenon to<br />
impaired upregulation of cell surface communication molecules and cytokine synthesis<br />
by ICOS deficient T cells. However, we now could show in a murine adoptive transfer<br />
system with antigen specific T cells that signaling via ICOS does not significantly affect<br />
early T cell activation. Instead, ICOS substantially contributes to the expansion and<br />
survival of effector T cells upon local challenge with antigen and adjuvant. Importantly,<br />
the observed biological function of ICOS also extends to FoxP3+ regulatory T cells, as<br />
can be observed after systemic antigen delivery without adjuvant. In line with these<br />
findings, absence of ICOS under homeostatic conditions of non-immunized mice leads to<br />
reduced numbers of both effector-memory and FoxP3+ regulatory T cells. Based on<br />
these results, we propose a biological role for ICOS as a costimulatory, agonistic<br />
molecule for a variety of effector T cells with differing and partly opposing functional<br />
roles. This concept may reconcile a number of past in vivo studies with seemingly<br />
contradictory results on ICOS function.
Eva Nina Huter, Sabine Stoll, Julia Horn, Juergen Knop, Bodo Grimbacher, Helmut<br />
Jonuleit<br />
ICOS plays an essential role in the development of anergic<br />
and suppressive CD4+ T cells<br />
The type and maturation state of dendritic cells (DC) determines the differentiation of<br />
resting CD4+ T cells. While activated, mature myeloid DC support efficient clonal<br />
expansion of these lymphocytes and their differentiation into IFN-γ-producing effector<br />
cells, immature DC instead induce anergic, IL-10-producing T cells with suppressive<br />
properties. Since Inducible Costimulator (ICOS) is involved in the induction of IL-10 in T<br />
cells and expression of ICOS Ligand (ICOS-L) on mature plasmacytoid DC contributes to<br />
the induction of suppressive T cells in an inflammatory environment, we analyzed the<br />
functional role of ICOS in the differentiation of human CD4+ T cells upon their<br />
interaction with myeloid DC. We report that the induction of T cell anergy by immature<br />
DC is <strong>complete</strong>ly blocked after siRNA-mediated knockdown of ICOS expression.<br />
Furthermore, anergy induction was also abolished in CD4+ T cells from ICOS-deficient<br />
patients. In contrast to CD4+ T cells from healthy volunteers, ICOS-deficient CD4+ T<br />
cells showed strong proliferation in the presence of allogeneic immature DC and<br />
differentiated into effector T cells with increased IL-4 and reduced but still significant IL-<br />
10 production. Additionally, after priming and restimulation with allogeneic immature<br />
DC ICOS-deficient CD4+ T cells were not suppressive in contrast to T cells from healthy<br />
controls. Taken together, these results indicate a crucial role for ICOS in the induction<br />
of peripheral tolerance by immature DC.
Johann Röhrl, Thomas Hehlgans<br />
Identification and Biological Characterization of Mouse Beta<br />
Defensin 14 – an Ortholog of Human Beta Defensin 3<br />
Beta defensins are small antimicrobial polypeptides mainly expressed by epithelial cells<br />
which play an important role in the antimicrobial innate immune response.<br />
In addition to the direct microbicidal effects of these polypeptides it became evident<br />
that certain members of the beta-defensin family have the capacity to promote local<br />
innate inflammatory and systemic adaptive immune responses by interacting with the<br />
CC-chemokine receptor CCR6.<br />
We have identified mouse beta defensin 14 (mBD14 or DEFB114) as an ortholog of<br />
human beta defensin 3 (hBD3 or DEFB103). Based on primary structural analysis<br />
mBD14 demonstrates 68% homology to its human ortholog, containing three conserved<br />
cystein linkages, characteric for the beta defensin family. MBD14 is expressed in a wide<br />
variety of tissues including spleen, colon and tissues of the upper and lower respiratory<br />
tract. Interestingly, we detected mBD14 expression also in immature CD11c positive<br />
bone marrow derived dendritic cells. The expression of mBD14 can be induced by TLR<br />
agonists such as LPS and poly I:C and by pro-inflammatory stimuli e.g. TNF.<br />
Furthermore, expression of mBD14 seems to be regulated by activation of the<br />
intracellular pattern recognition receptor NOD2/CARD15 as revealed by reporter gene<br />
assays. A recombinant mBD14-fusionprotein demonstrated antimicrobial activity against<br />
E.coli (ATCC 25922) and S. aureus (ATCC 6538).<br />
In contrast to another recently described member of the mouse beta defensin family<br />
(mBD4) and its human ortholog human beta defensin 2 (hBD2), mBD14 does not seem<br />
to interact with the CC-chemokine receptor CCR6.
Laura Rivino, Federica Sallusto, Antonio Lanzavecchia, Jens Geginat<br />
Identification and characterization of human "contextdependent<br />
Tr1/memory" cells.<br />
Two types of regulatory T cells have been described: “natural” CD25+Foxp3+ Tregs and<br />
“adaptive” Tr1 cells with unknown phenotype. CCR6 expression on in vitro primed<br />
human T cells required TGF-beta and the absence of polarising cytokines. Circulating<br />
CCR6+CD25- T cells were Foxp3-, but produced IL-10 with autologous DC that<br />
suppressed auto-reactive T cell proliferation. Interestingly, T cells reacting with the selfantigen<br />
MelanA were exclusively CCR6+ in healthy individuals, but were predominantly<br />
CCR6- in Viltiligo autoimmune patients. CCR6+ T cells responded also to various recall<br />
antigens and we isolated T cell clones that suppressed responses to autologous DC via<br />
IL-10, but that produced IL-2 and proliferated with tetanus toxoid. We propose that<br />
CCR6 is expressed on context-dependent “Tr1/memory” cells that act as conventional<br />
memory cells in recall responses, but behave Tr1-like upon recognition of cross-reactive<br />
antigens under steady-state conditions.
Andrea Baetz, Christoph Koelsche, Alexander Dalpke<br />
Identification of a nuclear localization signal (NLS) in SOCS1<br />
Suppressor of cytokine signaling (SOCS) proteins are inducible feedback inhibitors of<br />
janus kinase (JAK) and signal transducer and activator of transcription (STAT) signaling<br />
pathways. Moreover, SOCS proteins act as part of an ECS-type ubiquitin ligase complex<br />
which extends the functional range of this protein family to a so far not <strong>complete</strong>ly<br />
understood level. We here analyzed temporal-spatial mechanisms of SOCS action by<br />
generating GFP-SOCS fusion proteins. To our surprise we observed that SOCS-1 but not<br />
further SOCS family members localized predominantly to the nucleus when expressed in<br />
HEK293 cells. Similar results were observed in further cell lines and with different tags.<br />
Sequence analysis revealed a putative bipartite nuclear localization signal (NLS) located<br />
between the SH2 and the SOCS-box domain. Deletion of this region, introduction of a<br />
series of R/A point mutations or substitution of this sequence with the respective region<br />
of SOCS-3 resulted in loss of nuclear and increasing cytoplasmic localization. Fusion of<br />
the SOCS-1-NLS to cytokine-inducible SH2 region containing protein (CIS) resulted in<br />
nuclear localization of this otherwise cytoplasmic protein. Although the generated<br />
mutants of SOCS-1 showed loss of nuclear localization they were still partly effective in<br />
suppressing IFN-α mediated STAT1 tyrosine phosphorylation and reporter gene activity.<br />
The results identify a NLS in SOCS-1; however the functional significance differs from<br />
the well known role in JAK/STAT inhibition.
Theresa Tretter, Ram Kumar Venigalla, Volker Eckstein, Hanns Martin Lorenz<br />
Identification of human B cells with immunoregulatory<br />
properties<br />
Introduction: B cells are well known as mediators of humoral immunity and as antigen<br />
presenting cells in generation of T cell mediated responses. However observations from<br />
certain mouse models for autoimmunity point also to a role for B cells in maintaining<br />
tolerance. So far little is known yet about their immunoregulatory properties,<br />
specifically in humans and the mechanisms behind.<br />
Methods: Highly purified CD19+B and CD4+T cells were separated from human PBMC<br />
by MACS. B cells were prestimulated with SAC, aIgM/IgG or aCD40, and set up in<br />
cocultures with autologous CD4+T cells under addition of aCD3 +IL-2 or aCD28. CD4+<br />
T cell proliferation was determined after 3-6d by 3H Thymidine incorporation and PKH-<br />
26; apoptosis by AnnexinV.<br />
Results: under optimal stimulatory conditions T cell proliferation was inhibited by more<br />
than 50% in presence of SAC-activated B cells and to a lesser extent by aIgM/IgG<br />
stimulated B cells. There was a strong correlation with activation status of the B cell<br />
since enrichment of the large SAC activated CD25+ B cell population by FACSsorting<br />
further enhanced suppression to more than 70%, while the small SAC activated CD25-<br />
B cell population had no significant effect. Separation of B and T cells by cell culture<br />
inserts abolished inhibition, suggesting a requirement for direct cell-contact. In addition,<br />
optimal stimulatory conditions were necessary for inhibitory effects since suppression<br />
was not observed in absence of CD28 or exogenous IL-2. In addition to growth<br />
inhibition, T cell specific cytokine production (IFN-gamma, IL-10) was downregulated,<br />
and a significant proportion of T cells went into apoptosis.<br />
Conclusions: B cells are able to inhibit T cell mediated responses depending on their<br />
mode of activation. Further experiments are dealing with the mechanisms of B cell<br />
mediated suppression and their pathophysiological impact also in autoimmune diseases.
Tereza Havlova, Anja Tessarz, Vaclav Horejsi, Adelheid Cerwenka<br />
Identification of Key-Players in TREM1/DAP12 Signaling<br />
Pathway<br />
Triggering Receptor Expressed on Myeloid cells (TREM-1) is a recently described<br />
receptor expressed by monocytes and neutrophils, which plays an important role during<br />
immune responses to microbial infection. The engagement of TREM-1 leads to the<br />
production of pro-inflammatory cytokines such as TNF-α and IL-8 and thereby<br />
contributes to inflammatory conditions. TREM-1 associates with the ITAM-containing<br />
adapter DNAX Activation Protein of 12 kDa (DAP12). In general, ITAM-mediated signals<br />
lead to cell activation, although DAP12 was recently implicated in inhibitory signaling in<br />
mouse macrophages and dendritic cells.<br />
So far, the downstream signaling pathways following receptor triggering have not been<br />
well characterized. Recently, we identified NTAL/LAB/LAT2 as an important gate-keeper<br />
of TREM-1/DAP12-induced signaling in myeloid cells. This transmembrane adaptor<br />
protein is phosphorylated upon TREM-1 ligation in a myelo-monocytic cell line and<br />
primary human granulocytes. Using siRNA mediated knock-down to decrease NTAL<br />
expression levels, we observed enhancement of ERK 1/2 phosphorylation, delay in Ca 2+<br />
mobilization and a substantial decrease in TNF-α and IL-8 production after TREM-1<br />
stimulation.<br />
We are currently focusing on the identification of proteins associated with NTAL in<br />
context of the TREM-1/DAP12 signaling pathway. In addition, we are analyzing proteins,<br />
which become phosphorylated upon TREM-1 triggering, via mass spectrometry to obtain<br />
new insights about the known and yet unknown key-players in this signaling pathway.<br />
The knowledge gained by this study could help to define novel therapeutic targets for<br />
the treatment of inflammatory diseases and sepsis.
Katja Kotsch, Vera Merck, Kristina Kunert, Anja Reutzel-Selke, Andreas Pascher, Hans-<br />
Dieter Volk, Peter Neuhaus, Johann Pratschke<br />
Identification of molecular candidate marker in zero kidney<br />
biopsies are indicative for graft quality<br />
In renal transplantation, allograft biopsies provide valuable diagnostic information.<br />
Consequently, several attempts have been made to predict the early graft outcome by<br />
histological and molecular analyses in zero-hour graft biopsies illustrating that subtle<br />
inflammation and immune activation detected in the intraoperative period are<br />
associated with adverse allograft outcome post transplantation. The clinical outcome is<br />
dependent upon various risk factors including donor brain death or prolonged cold<br />
ischemia (CI). However, current knowledge about the influence of brain death and CI is<br />
only restricted to a low number of genes and the molecular and cellular mechanisms are<br />
thus far unknown. Efficient strategies to prevent prolonged cold ischemia or brain death<br />
related complications require a better understanding of the molecular processes<br />
reflecting intragraft inflammation present intraoperatively at the zero-hour. We<br />
therefore studied mRNA gene expression of zero kidney biopsies derived from 63<br />
cadaveric donors (CAD) (CI=13,3 ± 3,6) and 27 living donors (LD) (CI=2,8 ± 0,7).<br />
Intraoperative biopsies were taken 30 min. after vascular reperfusion and were<br />
immediately snap-frozen. Messenger RNA was extracted and gene expression was<br />
measured by real-time RT-PCR. Recently it has been demonstrated that the induction of<br />
the T cell marker CD3 or the intercellular adhesion molecule (ICAM)-1 in zero biopsies<br />
are predictive of acute rejection (Avihingsanon et al. 2005). By comparing zero biopsies<br />
from CAD versus LD we observed a significant induction of CD3 (p
Katja Kotsch, Vera Merck, Kristina Kunert, Anja Reutzel-Selke, Andreas Pascher, Hans-<br />
Dieter Volk, Peter Neuhaus, Johann Pratschke<br />
Identification of molecular candidate marker in zero kidney<br />
biopsies are indicative for graft quality<br />
In renal transplantation, allograft biopsies provide valuable diagnostic information.<br />
Consequently, several attempts have been made to predict the early graft outcome by<br />
histological and molecular analyses in zero-hour graft biopsies illustrating that subtle<br />
inflammation and immune activation detected in the intraoperative period are<br />
associated with adverse allograft outcome post transplantation. The clinical outcome is<br />
dependent upon various risk factors including donor brain death or prolonged cold<br />
ischemia (CI). However, current knowledge about the influence of brain death and CI is<br />
only restricted to a low number of genes and the molecular and cellular mechanisms are<br />
thus far unknown. Efficient strategies to prevent prolonged cold ischemia or brain death<br />
related complications require a better understanding of the molecular processes<br />
reflecting intragraft inflammation present intraoperatively at the zero-hour. We<br />
therefore studied mRNA gene expression of zero kidney biopsies derived from 63<br />
cadaveric donors (CAD) (CI=13,3 ± 3,6) and 27 living donors (LD) (CI=2,8 ± 0,7).<br />
Intraoperative biopsies were taken 30 min. after vascular reperfusion and were<br />
immediately snap-frozen. Messenger RNA was extracted and gene expression was<br />
measured by real-time RT-PCR. Recently it has been demonstrated that the induction of<br />
the T cell marker CD3 or the intercellular adhesion molecule (ICAM)-1 in zero biopsies<br />
are predictive of acute rejection (Avihingsanon et al. 2005). By comparing zero biopsies<br />
from CAD versus LD we observed a significant induction of CD3 (p
Wolfram Osen, Mingxia Song, Sabine Soltek, Barbara Leuchs, Julia Steitz, Xuan Duc<br />
Ngyuen, Dirk Schadendorf, Annette Paschen<br />
Identification of novel CD4+ T cell epitopes from human<br />
tyrosinase related protein 2 (TRP-2) by a combinatorial<br />
approach based on the immunisation of HLA-transgenic mice<br />
with recombinant Adenovirus and antigen peptide library<br />
screening<br />
Melanoma differentiation antigen TRP-2 is a target of spontaneous cytotoxic CD8+ T cell<br />
(CTL) responses in tumor patients and can thus be considered as a melanoma<br />
associated tumor antigen (TA). Since induction and maintenance of tumor-specific CD8<br />
+ T cell responses depends on the activity of specific CD4+ T helper (Th) cells, we set<br />
out to identify novel TRP-2-specific Th epitopes that could be included in<br />
immunotherapy approaches against malignant melanoma. Using recombinant<br />
Adenovirus expressing human TRP-2 (Ad/TRP-2) as an immunogen followed by<br />
combinatorial peptide library screening in vitro we were able to identify novel<br />
DRB1*0301-restricted T cell epitopes in HLA-DRB1*0301 transgenic mice. Notably, the<br />
same epitope was found to be recognized by Th cells of DRB1*03+ donors on syngeneic<br />
Ad/TRP-2 infected DC, showing that the epitope identified in the HLA-DRB1*0301<br />
transgenic mouse system is also processed and presented by human DRB1*03+<br />
individuals.
Josip Zovko, Marco Herold, Christa Kraus, Andrea Peters, Ingolf Berberich<br />
Identification of proteins that influence stability and<br />
functionality of the anti-apoptotic Bcl-2 family member A1/<br />
Bfl-1<br />
Members of the Bcl-2 family control the integrity of mitochondria and thereby influence<br />
survival and death of cells. Most Bcl-2 family members can localize to intracellular<br />
membranes via hydrophobic sequences within their C-terminal portion.<br />
Murine A1 and its human homologue Bfl-1 are anti-apoptotic members of the Bcl-2<br />
family. A1 is expressed in small amounts in the bone marrow and immature B cells, but<br />
in high amounts in mature B cells. Thus the protein seems to be important for B cell<br />
maturation.<br />
We analyzed the function of the C-terminus of A1. Unless the C-terminal ends of other<br />
Bcl-2 proteins the tail of A1 does not function as a membrane anchor. Nevertheless, the<br />
last amino acids of A1 are important for the protein. In fact, the C-terminus of A1<br />
serves a dual function by being required for the instability and the anti-apoptotic<br />
potential of the protein. We show that A1 undergoes proteosomal degradation controlled<br />
by its C-terminus. Interestingly, binding to the pro-apoptotic Bcl-2 factor BimEL results<br />
in increased stability of A1. This is due to reduced ubiquitination of A1 after binding of<br />
BimEL. We conclude that the C-terminus of A1/Bfl-1 serves as a docking site for E3<br />
ubiquitin ligase(s) that control the stability of A1 by targeting the protein to the<br />
proteasomal pathway. Currently, we are trying to identify such proteins by affinity<br />
chromatography and mass spectrometry.
Susanne Berchtold, Edda Fahl, Mathias Hornef, Julia Geisel, Julia-Stefanie Frick, Erwin<br />
Bohn<br />
IFIT-2 – a putative novel negative regulator of<br />
proinflammatory responses<br />
Interferon-induced tetratricopeptide repeat protein (IFIT-) 2 is induced upon acute<br />
infection with Yersinia enterocolitica in CD11b-positive cells of the spleen of mice as well<br />
as in the colon of IL-2 deficient mice which develop inflammatory bowel disease. IFIT-2<br />
is induced by type II and type I interferons or indirectly by LPS in an IFN dependent<br />
manner. Recently it was reported that mouse IFIT2 (P54) affects protein synthesis by<br />
interaction with the translation initiation factor eIF3c. Therefore we speculated that this<br />
gene could represent a negative regulator of host responses by down regulating protein<br />
synthesis. To address the role of IFIT2, stably transfected RAW 264.7 macrophages<br />
were established overexpressing IFIT-2. These cells were viable and showed similar<br />
proliferation as control cells. IFIT-2 overexpression did not alter LPS triggered p38, ERK,<br />
JNK and IκB phosphorylation indicating that IFIT-2 does not affect LPS mediated signal<br />
transduction. Overexpression of IFIT-2 in RAW 264.7 macrophages reduced LPS induced<br />
protein expression in a selective manner at a posttranscriptional level. Thus, TNF-<br />
&alpha, IL-6 and MIP-2 secretion but not protein expression of IFIT-1 or early growth<br />
reponse 1 were affected by IFIT-2. IFIT-2 may thereforee represent a novel negative<br />
regulator of proinflammatory responses.
Uwe Müller, Werner Stenzel, Gabriele Köhler, Gesine Hansen, Nicole Schütze, Reinhard<br />
Straubinger, Manfred Blessing, Andrew McKenzie, Frank Brombacher, Gottfried Alber<br />
IL 13 induces disease promoting type 2 cytokines,<br />
alternatively activated macrophages and allergic<br />
inflammation during pulmonary infection of mice with<br />
Cryptococcus neoformans<br />
In the murine model of Cryptococcus neoformans (C. neoformans) infection Th1 (IL-12/<br />
IFN-&gamma) and Th17 responses (IL-23/IL-17) are associated with protection,<br />
whereas an IL-4-dependent Th2 response exacerbates disease. In order to investigate<br />
the role of the Th2 cytokine IL-13 during pulmonary infection with C. neoformans, IL-13transgenic<br />
(IL-13 T/+ ), IL-13-deficient (IL-13 -/- ), and wild-type (WT) mice were infected<br />
intranasally. Susceptibility to C. neoformans infection was found when IL-13 was<br />
induced in WT mice or over-produced in IL-13 T/+ mice. Infected IL-13 T/+ mice had a<br />
reduced survival time and higher pulmonary fungal load as compared to WT mice. In<br />
contrast, infected IL-13 -/- mice were resistant and 89% of these mice survived the<br />
entire period of the experiment. Antigen-specific production of IL-13 by susceptible WT<br />
and IL-13 T/+ mice was associated with a significant type 2 cytokine shift but only minor<br />
changes in IFN-&gamma production. Consistent with enhanced type 2 cytokine<br />
production, high levels of serum IgE and low ratios of serum IgG2a/IgG1 were detected<br />
in susceptible WT and IL-13 T/+ mice. Interestingly, expression of IL-13 by susceptible<br />
WT and IL-13 T/+ mice was associated with reduced IL-17 production. IL-13 was found<br />
to induce formation of alternatively activated macrophages (aaMph) expressing<br />
arginase-1, macrophage mannose receptor (CD206) and YM1. In addition, IL-13<br />
production led to lung eosinophilia, goblet cell metaplasia and elevated mucus<br />
production, and enhanced airway hyperreactivity. This indicates that IL-13 contributes<br />
to fatal allergic inflammation during C. neoformans infection.
Annette Erhardt, Markus Biburger, Gisa Tiegs<br />
IL-10 AND REGULATORY T CELLS – THE MAIN MEDIATORS OF<br />
IMMUNOLOGICAL TOLERANCE AGAINST CONCANAVALIN A<br />
Injection of the plant lectin Concanavalin A (ConA) induces pronounced T- and NKT-cell<br />
activation followed by the onset of acute liver injury. ConA hepatitis has often been<br />
described as a murine model for immune-mediated hepatitis in humans. Recently, we<br />
have shown that ConA pretreated mice developed tolerance against ConA rechallenge<br />
within 8 days. Suppression of liver damage upon ConA pretreatment was characterized<br />
by decreased plasma transaminase levels and an anti-inflammatory cytokine response<br />
with increased IL10 production. Tolerance was fully reversed in IL10 KO mice<br />
emphasizing the important role of IL10 during ConA tolerance.<br />
To confirm the relevance of IL10, neutralizing experiments with an anti-IL10R antibody<br />
were performed blocking the binding site of IL10. Antibody injection prior to ConA<br />
pretreatment, imitating IL10 KO mice, or prior to ConA restimulation largely reduced<br />
the tolerogenic effect, suggesting that IL10 participates in long-term differentiation<br />
processes but also acts as short-term immunosuppressive mediator in vivo.<br />
Depletion of regulatory T cells (Tregs) and Kupffer cells in vivo prior to ConA<br />
rechallenge significantly diminished IL10 production, revealing these cells as main<br />
sources of IL10. Accordingly, Tregs isolated from ConA tolerized mice exhibited<br />
significantly enhanced IL10 production after ex vivo restimulation in contrast to control<br />
Tregs. However, in vitro neutralization of IL10 in co-cultures of responder cells and<br />
Tregs failed to reverse the immunosuppressive effect of Tregs from control as well as<br />
from ConA tolerant mice.<br />
In an immuno-therapeutic approach Tregs isolated from tolerized WT mice conferred<br />
significant protection from ConA-induced liver damage in contrast to Tregs from<br />
tolerized IL10 KO mice.<br />
In summary, we demonstrated that ConA tolerance, characterized by both<br />
immunosuppression and protection from liver injury, is mediated by Kupffer cells, Tregs,<br />
and IL10. Hence, ConA tolerance appears to be an appropriate model for evaluation of<br />
therapeutic intervention strategies in complex immuno-regulatory systems.
Anne Schumacher, Paul Ojiambo Wafula, Ana Teles, Hideo Yagita, Hans-Dieter Volk,<br />
Ana Zenclussen<br />
IL-10 but not TGF-ß is essential for the suppressor function of<br />
Treg cells in murine pregnancy<br />
Problem<br />
The physiological state of pregnancy is characterised by the tolerance of the maternal<br />
immune system to paternal/fetal alloantigens. Regulatory T cells (Treg) were described<br />
to play an important role in the maintenance of this tolerance state and several<br />
mechanisms were proposed for their regulatory activity. In this context immune<br />
suppressive molecules such as IL-10 and TGF-ß seem to be essential for Treg function.<br />
Therefore we aimed to investigate whether the pregnancy-protective effect of Treg is<br />
mediated by IL-10 or TGF-ß.<br />
Methods of the study<br />
CBA/J females were mated with BALB/c males (normal pregnant). On day 14 of<br />
pregnancy Treg were isolated and transferred into DBA/2J-mated CBA/J females<br />
(abortion-prone). These animals were additionally treated with either anti IL-10, anti-<br />
TGF-ß or IgG (isotype control) antibodies on days 0 and 7 of pregnancy. Normal<br />
pregnant and untreated abortion-prone females were used as controls.<br />
Results<br />
Treg + IgG-treated animals had a similar abortion rate as the normal pregnant group.<br />
In contrast CBA/J females which received Treg and were additionally treated with anti-<br />
IL-10 presented an increased abortion rate, which was even higher than in the<br />
untreated abortion-prone group. The application of anti-TGF-ß did not substantially<br />
modify the abortion rate as compared to Treg + IgG-treated animals.<br />
Conclusion<br />
These results suggest that IL-10, but not TGF-ß is essential for the immune regulatory<br />
function of Treg during pregnancy. It further underlines the assumption that Treg<br />
mediate their suppressive activity against alloreactive maternal immune cells through<br />
the release of immune suppressive molecules in vivo, being IL-10 essential in this<br />
context.
Hyun-Dong Chang, Jun Dong, Andreas Thiel Thiel, Andreas Radbruch<br />
IL-10 Expression in Th lymphocytes is conditional<br />
T helper (Th) lymphocytes have the ability to memorize the expression of cytokines<br />
which they were instructed to express during the primary activation. Cytokine memory<br />
can thus contribute to the maintenance of chronic inflammation. Cytokine memory is<br />
accompanied by the stable upregulation of transcription factors and epigenetic<br />
imprinting of cytokine genes. Here we analyse the memory of Th lymphocytes for the<br />
reexpression of interleukin-10 (IL-10), critical in the regulation of immune responses<br />
and reduction of immunopathology. IL-10 is induced by IL-4 and IL-12 and remains<br />
conditional on the provision of the inducing cytokines. In addition, IL-10 expressing Th<br />
cells isolated ex vivo using the cytometric cytokine secretion assay do not memorize IL-<br />
10 expression upon repeated in vitro restimulations. Whereas repeated stimulation with<br />
IL-4 leads to the establishment of a stable IL-10 memory which goes along with GATA-3<br />
mediated epigenetic imprinting of the il10 gene, IL-12 induced IL-10 expression in Th1<br />
cells requires continued IL-12 signaling. In accordance, we could detect no epigenetic<br />
modifications in the il10 gene in ex vivo isolated and Th1 derived IL-10 expressing cells.<br />
The maintained dependency of IL-10 expression of Th1 lymphocytes suggests an<br />
unexpected anti-inflammatory potential of IL-12: In memory Th1 cells IL-10 expression<br />
remains dependent on IL-12, while reexpression of IFN-γ is independent of the original<br />
inducer IL-12. The exclusion of IL-10 from the functional memory of Th1 cells may<br />
reflect the requirement for conditional regulation of inflammatory immune responses.
Manuel N. D. M. Guerreiro, Anne Marie Asemissen, Gianna Schulz, Il-Kang Na, Jochen<br />
Hühn, Sandra Bauer, Eckhard Thiel, Ulrich Keilholz, Carmen Scheibenbogen<br />
IL-2 induces IL-10 producing regulatory CD3+ T cells in vitro<br />
and in vivo<br />
Purpose:<br />
IL-10-producing regulatory T cells have recently gained much interest as important<br />
players in immune regulation. In this study we have analyzed in melanoma patients the<br />
influence of IL-2 treatment and of in-vitro IL-2 exposure on IL-10-producing regulatory<br />
T cells.<br />
Materials and methods:<br />
PBMC from 6 melanoma patients who had been treated with IL-2 and from healthy<br />
subjects were analyzed ex vivo or after 72h incubation with IL-2 (50 U/ml) for IL-10<br />
producing capacity of T cells by intracellular cytokine staining. Further phenotypic and<br />
functional characterization was performed by flow cytometry.<br />
Results:<br />
Less than 1% of unprimed PB T cells produced IL-10 in response to PMA/Ionomycin<br />
(n=9 healthy subjects). IL-10-producing T cells could be primed by short-term<br />
incubation with IL-2. After 3 days median 6.29% (range 0.79 – 23.04) of CD4+ and<br />
10.64% (range 0.64 – 34.99) of CD8+ T cells produced IL-10 in response to PMA/Iono<br />
(n=9 healthy subjects). CFSE staining revealed that the capacity to produce IL-10 is<br />
due to priming by IL-2 and not due to expansion of this subset. In PBMCs cultured with<br />
IL-2 for longer periods further upregulation of IL-10 producing capacity was observed<br />
on day 7. We next studied IL-10-producing capacity in PBMC from 6 melanoma patients<br />
who had been treated with IL-2. In accordance with the in vitro studies less than 0.2%<br />
of unstimulated CD3+T cells produced IL-10 before, and after IL-2 therapy. Upon PMA/<br />
Ionomycin stimulation both CD3+CD4+ and CD8+T cells showed enhanced IL-10 but<br />
not IFN-g-producing capacity in samples obtained 5 days after IL-2 treatment as<br />
compared to pretreatment samples in 4 of 6 patients. Phenotypic characterization of IL-<br />
10-producing T cells showed lack of FOXP3 expression, failure to produce IL-4 and IFNg<br />
and lack of CD25. A major subset of IL-10+ T cells expressed the mucosal chemokine<br />
receptors CCR6 and/or CCR9, and approximately 30% the inflammatory chemokine<br />
receptor CXCR3. Interestingly, CD8+ IL-10+ T cells were not detectable in bone marrow<br />
suggesting that the IL-10+ T cells have a restricted migratory capacity. PBMC primed in<br />
the presence of IL-2 and stimulated by anti-CD2/-CD3/-CD28 were able to substantially<br />
inhibit the proliferation of stimulated PBMCs as assed by CFSE proliferation assay.<br />
Further we could demonstrate the in vitro generation of IL-10-producing influenzapeptide-specific<br />
T cells by IL-2 with a mean of 1.35 % influenza-specific CD8+IL-10+ T<br />
cells (range 0.14 – 3.33 %, n= 3) after 7 days. We also could generate MART-1 and<br />
Tyrosinase-peptide specific CD3+CD8+ IL-10 producing T cells in 4 of 6 melanoma<br />
patients (0.03-0.13%). The study of the single nucleotide polymorphism –1082 (G/A)<br />
located in the proximal promoter of the IL-10 gene from 8 healthy subjects did not<br />
correlate with the frequency of the IL-10+ T cells, suggesting a predominantely<br />
adaptive response. The effect of IL-7, IL-15, IL-21, also belonging to the gamma chain<br />
cytokines family, on IL-10-producing and secreting capacity were compared.<br />
Interestingly, IL-15 had similar IL-10 priming capability as IL-2, while IL-21 did not<br />
enhance IL-10 production.<br />
Conclusion<br />
IL-2 primes IL-10-producing T cells in vivo and in vitro. This finding has important<br />
implications for the use of IL-2 as vaccine adjuvant in cancer immunotherapy as well as<br />
for adoptive T cell therapy. Importantly, the gamma chain cytokine IL-21 does not<br />
enhance IL-10 production.
Kerstin Wolk, Ellen Witte, Ute Hoffmann, Wolf-Dietrich Döcke, Stefanie Endesfelder,<br />
Khusru Asadullah, Wolfram Sterry, Hans-Dieter Volk, Bianca Maria Wittig, Robert Sabat<br />
IL-22 Induces Lipopolysaccharide-Binding Protein in<br />
Hepatocytes: A Potential Systemic Role of IL-22 in Crohn's<br />
Disease<br />
Crohn's disease (CD) is a common, chronic, inflammatory bowel disease characterized<br />
by intestinal infiltration of activated immune cells and distortion of the intestinal<br />
architecture. In this study, we demonstrate that IL-22, a cytokine that is mainly<br />
produced by activated Th1 and Th17 cells, was present in high quantities in the blood of<br />
CD patients in contrast to IFN-γ and IL-17. In a mouse colitis model, IL-22 mRNA<br />
expression was elevated predominantly in the inflamed intestine but also in the<br />
mesenteric lymph nodes. IL-22BP, the soluble receptor for IL-22, demonstrated an<br />
affinity to IL-22 that was at least 4-fold higher than its membrane-bound receptor, and<br />
its strong constitutive expression in the intestine and lymph nodes was decreased in the<br />
inflamed intestine. To investigate the possible role of systemic IL-22 in CD, we then<br />
administered IL-22 to healthy mice and found an up-regulation of LPS-binding protein<br />
(LBP) blood levels reaching concentrations known to neutralize LPS. This systemic upregulation<br />
was associated with increased hepatic but not renal or pulmonary LBP mRNA<br />
levels. IL-22 also enhanced the secretion of LBP in human primary hepatocytes and<br />
HepG2 hepatoma cells in vitro. This increase was mainly transcriptionally regulated and<br />
synergistic with that of other LBP inducers. Finally, elevated LBP levels were detected in<br />
CD patients and the mouse colitis model. These data suggest that systemic IL-22 may<br />
contribute to the prevention of systemic inflammation provoked by LPS present in the<br />
blood of CD patients through its induction of hepatic LBP.
Daniel Hebenstreit, Elisabeth Maier, Jutta Horejs-Hoeck, Min Li-Weber, Albert Duschl<br />
IL-4 suppresses the Gene Expression of TCF-1 in T cells in a<br />
STAT6 dependent way<br />
The Wnt signalling pathway plays an important role in numerous developmental<br />
processes including T cell development. Yet, data on Wnt signalling in mature T cells are<br />
scarce. T cells have a key function in most immune responses and are also associated<br />
with a number of pathologic conditions, such as allergy. T cells involved in the latter are<br />
mainly of the Th2 lineage. Differentiation towards the Th2 type is induced by TCR<br />
engagement following IL-4 stimulation.<br />
The present study focuses on the influence of IL-4 signalling on the Wnt downstream<br />
effector T Cell Factor 1 (TCF-1). Realtime PCR studies on cDNAs from primary human<br />
and mouse T show a decrease of TCF-1 mRNA after stimulation with IL-4. In contrast,<br />
this effect does not occur in STAT6 knock out mice.<br />
By bioinformatics analyses, two STAT6 binding motifs highly conserved between mouse<br />
and human have been identified in the TCF-1 locus. As demonstrated in EMSA, one of<br />
these can bind to STAT6 present in nuclear extracts from IL-4 treated primary human T<br />
cells. To test its repressive effect, this STAT6 binding site was cloned into a plasmid that<br />
carries a highly IL-4 inducible promoter construct of eotaxin 3 and the luciferase<br />
reporter gene. Transfection experiments show that the STAT6 binding site from TCF-1<br />
reduces luciferase activity significantly, whereas a mutated version does not.<br />
Briefly, our current findings have identified STAT6 to be responsible for the IL-4 induced<br />
suppression of TCF-1.
Manuel Otte<br />
IL-4R – signaling through an alternative signal transduction<br />
pathway<br />
Manuel Otte, Mario Zaiss, Susanne Bürgis, Anja Thiel, Georg<br />
Schett and André Gessner<br />
Institute of Medical Microbiology, Immunology and Hygiene;<br />
University of Erlangen-Nuremberg<br />
Interleukin-4 (IL-4) is a pleiotropic cytokine that has different functions on various cell<br />
types. The IL-4 receptor (IL-4R) binds IL-4 and transduces the signal through the<br />
Insuline Receptor Substrate (IRS)- and Signal Transducer and Activator of Transcription<br />
6 (STAT6)- signaling pathways initiating proliferation and gene expression. We<br />
investigated IL-4 induced cell proliferation in a system of human TF1 cells stably<br />
transfected with different variants of murine IL-4R α-chains and observed IL-4 induced<br />
proliferation independent of the IRS- and STAT6-signaling pathways. Therefore we<br />
postulated that an alternative IL-4R signaling pathway must exist. Interaction studies<br />
with IL-4R Δ388, the shortest proliferation mediating IL-4R variant, leads to<br />
identification of p62, JAB1 and p39. These proteins could be possibly involved in<br />
alternative signaling pathways. Transgenic mice were generated that merely expressing<br />
the truncated IL-4R Δ388 in the absence of wild type IL-4R. Experiments with different<br />
cell types of the transgenic mice revealed that the IL-4R Δ388 is still able to promote<br />
proliferation and anti-apoptosis of CD4+ cells and inhibits osteoclast differentiation of<br />
bone marrow monocytes. In contrast differentiation of TH2 cells and IgE class switch of<br />
B cells were not induced via the truncated IL-4R. Thus, the newly established mouse<br />
model allows to discriminate IRS/STAT6- dependent and independent IL-4 functions.
Julia-Stefanie Frick, Julia Geisel, Frauke Kahl, Hermann Wagner, Carsten Kirschning,<br />
Ingo Autenrieth<br />
IL-6 and maturation govern TLR2 and TLR4 induced TLR<br />
agonist tolerance and cross-tolerance in dendritic cells<br />
Stimulation of murine bone-marrow-derived-dendritic-cells (DC) with lipopolysaccharide<br />
(LPS) or the synthetic lipopeptide N-Palmitoyl-S-[2,3bis(palmitoyloxy)-(2RS)-propyl]-<br />
[R]-cysteinyl-[S]-seryl-[S]-Lys4 x 3 HCl (P3CSK4) induces expression of TNF-a in a<br />
TLR4- and respectively TLR2-dependent fashion. Pre-treatment of DC with LPS results in<br />
hyporesponiveness to a subsequent LPS stimulation, termed LPS-tolerance and to<br />
subsequent P3CSK4 stimulus, termed cross-tolerance. Respectively treatment of DC<br />
with P3CSK4 resulted in homo-tolerance towards subsequent P3CSK4 stimulation as<br />
well as cross-tolerance towards subsequent LPS stimulation. Different mechanism seem<br />
to account for induction of tolerogenic DC. Pre-stimuation with low concentrations of<br />
LPS or P3CSK4 induced tolerogenic DC in an IL-6-dependent fashion and was neither<br />
related to activation and maturation of DC nor to downregulation of TLR2/4 expression.<br />
In contrast, induction of tolerogenic DC by treatment with high concentrations of LPS or<br />
P3CSK4 was independent of IL-6. In homo-tolerogenic DC degradation of IkB was<br />
inhibited, as well as in cross-tolerogenic DC pretreated with high concentration of LPS or<br />
P3CSK4. In contrast, cross-tolerance in DC pretreated with low concentrations of LPS or<br />
P3CSK4 was not related to inhibition of IkB degradation. The data indicate that in DC<br />
TLR4 and TLR2 stimulation results in homo- as well as cross-tolerance and that different<br />
mechanistic effects account for the reduced responsivness of DC.
Marsilius Mues, Marco Mank, Oliver Griesbeck, Hartmut Wekerle, Florian Kurschus<br />
Imaging Activation: FRET-based Calcium Biosensors in T-<br />
Lymphocytes<br />
Interaction between an antigen-presenting cell (APC) and a T-cell leads to the rapid<br />
formation of an immunological synapse. Upon recognition of the appropriate antigen, a<br />
swift rise of intracellular calcium is triggered within the T-cell which can be used to<br />
monitor the activation status of the lymphocyte. However, in vivo calcium imaging in Tcells<br />
still remains a major challenge as synthetic calcium indicators do not persist<br />
intracellularly for a sustained period. To overcome this problem we generated<br />
transgenic mice expressing a novel fluorescence resonance energy transfer (FRET)based<br />
calcium sensor under control of the T-cell specific human CD2 promoter. This<br />
sensor features spectrally optimized derivatives of the fluorescent proteins CFP and YFP<br />
linked by the calcium-sensitive domain Troponin C (Heim et al. 2007, Nature Methods<br />
4:127-129). Although it was originally designed for calcium imaging in neurons, the<br />
sensor is also capable of responding to modest alterations in lymphocyte intracellular<br />
calcium levels. This transgenic mouse will be used for in vivo imaging studies in<br />
experimental autoimmune encephalomyelitis (EAE). We plan to track the migration and<br />
activation of T-cells upon the encounter of APCs, e.g. during or after passing the bloodbrain<br />
barrier and while infiltrating the CNS. For this purpose various inducible, as well as<br />
spontaneous mouse models of EAE, are available in our lab thus providing the<br />
opportunity to investigate T-cell activation under different disease conditions.
Thomas G. Berger, Hendrik Schulze-Koops, Michaela Schäfer, Ester Müller, Manfred B.<br />
Lutz<br />
Immature and maturation-resistant human dendritic cells<br />
generated from bone marrow under GMP conditions induce<br />
allogeneic T cell anergy in vitro<br />
Immature dendritic cells (DC) have been shown to act tolerogenic. Therfore they<br />
represent potential clinical tools for tolerogenic cellular immunotherapy in<br />
transplantation or autoimmunity. A major drawback for their in vivo application is their<br />
potential to mature during infections or inflammations which would convert their<br />
tolerogenicity into immunogenicity. Here we extend our findings in the murine system<br />
and describe the generation of immature DC from human bone marrow (BM) or CD34+<br />
precursor cells by low doses of GM-CSF (LowGM) in the absence of IL-4 under GMP<br />
conditions which are also resistant to maturation by inflammatory cytokine cocktail,<br />
CD40 ligation or signals through Toll-like receptors (TLR) as detected by surface<br />
markers and primary stimulation of an allogeneic T cells. This could not be observed<br />
with BM-derived DC generated with high doses of GM-CSF plus IL-4 (HighGM/4). As<br />
tolerance mechanism T cell anergy was induced most prominently after two subsequent<br />
stimulations by both types of immature DC. Anergy induction was more profound with<br />
LowGM-DC due to their maturation resistance. Together, the generation of immature,<br />
maturation-resistant LowGM-DC offers the possibility of tolerance induction for clinical<br />
use.
Daniel Nickel, Sven Poppert, Tatjana Zelenski, Nicole Kästner, Heiko Bruns, Axel<br />
Schubert, Axel Spahr, Steffen Stenger<br />
Immune modulation mediated by Aggregatibacter<br />
actinomycetemcomitans as a possible mechanism for the<br />
development of periodontitis<br />
There are more than 200 different species of bacteria colonizing the human gingiva.<br />
About 5% - among them Aggregatibacter actinomycetemcomitans (Aa) - are frequently<br />
found in periodontal lesions. To mimic the site of oral inflammation we initially<br />
investigated the interaction between Aa and human peripheral blood mononuclear cells<br />
(PBMC). For determining the efficiency of infection we designed probes specific for Aa<br />
and performed fluorescence in situ hybridization (FISH). The majority of the bacteria<br />
were in the proximity of or adjacent to PBMC implying the possibility of immunological<br />
interaction. This finding prompted us to measure cytokine production (TNF, IFN-γ) and<br />
bacterial survival using a co-culture system of Aa and PBMC. By ELISA we measured<br />
1300 pg/ml TNF after 24 h and 540 pg/ml after 72 h. The results for IFN- γ were 290 pg/<br />
ml after 24 h and 1600 pg/ml after 72 h. Under these conditions (5% human serum) no<br />
viable bacteria were found after 24 h of incubation.<br />
We are currently trying to establish conditions that permit survival of both eukaryotic<br />
and prokaryotic cells. Ultimately we intend to identify immune deviations in patients<br />
with severe periodontitis that account for the hyper inflammation characteristic for this<br />
disease.
Jessica Butz, Cordula Fuchs, Barbara Kessler, Heiner Voigt, Daniel Wienhold, Mathias<br />
Buettner<br />
Immune reaction of swine after repeated intra-muscular (i.<br />
m.) immunization with avian influenza virus H5<br />
In swine there is little evidence of virus host inaction during the recent avian influenza<br />
virus (AIV) H5N1 epidemics in Asia and South East Asia. To induce and characterize an<br />
immune response in swine inactivated H5N1 (mallard/Bavaria/1/06)) was injected two<br />
times intra-muscular (i. m.) followed by a third i. m. injection of live low pathogenic<br />
H5N2 AIV subtype.<br />
In total ten animals were immunized, five without and five with parapoxvirus as an<br />
adjuvant.<br />
Only after the second and third application H5-specific antibodies were detected in<br />
swine sera with slightly higher titers in the sera of the adjuvant immunized animals. In<br />
vitro re-stimulation of peripheral blood mononuclear cells (PBMC) with various live AIV<br />
subtypes including the vaccine virus and swine pathogenic subtypes did not result in<br />
significant antigen mediated interferon gamma secretion as measured by ELISPOT. The<br />
PBMC from immunized animals also showed no or weak interferon alpha secretion after<br />
AIV stimulation in contrast to other control viral stimuli. Possible immune response<br />
counteracting activity of virulent avian influenza A subtypes will be investigated.
Marcin Wlodarski, Zachary Nearman, Alan Lichtin, Hans-Dieter Volk, Jaroslaw<br />
Maciejewski<br />
IMMUNODOMINANT CYTOTOXIC T LYMPHOCYTE EXPANSIONS<br />
IN PATIENTS WITH UNEXPLAINED NEUTROPENIA.<br />
Some cases of idiopathic neutropenia (IN) may result from a T cell-mediated immune<br />
attack directed against myeloid progenitors. Unlike in large granular lymphocyte<br />
leukemia (LGL) that is characterized by highly skewed chronic lymphoproliferation,<br />
cytotoxic T-cell (CTL) expansions in IN may not be discovered using traditional<br />
laboratory tools. We hypothesized that a precise T-cell receptor (TCR) repertoire<br />
analysis may uncover CTL expansions in IN that are pathophysiologicaly analogous to<br />
those seen in large granular lymphocyte leukemia (LGL) and thus can serve as markers<br />
for CTL mediated process.<br />
We previously established algorithms for TCR analysis and in-vivo tracking of CTL<br />
responses that include TCR variable beta (VB) phenotyping followed by subcloning of<br />
TCR-VB families and clonotypic sequencing, or multiplex VB-PCR and sequencing of the<br />
entire VB repertoire. For quantitative clonotype tracking we introduced a novel<br />
clonotypic Taqman-PCR that allows for a very precise detection of patient-specific TCR<br />
VB chains. Using this approach we studied patients with neutropenia: 12/20 displayed<br />
CTL expansions that were less dominant than those detectable in LGL but clearly<br />
distinguishable from subclinical CTL expansions in healthy controls. As a surrogate of<br />
cytotoxic activity, we found markedly increased production of interferon-G in most<br />
patients irrespective of the presence of immunodominant CTL clones.<br />
These results suggest that while CTL clonalities are detectable only in a proportion of<br />
patients, cytotoxic pathophysiology may be a general mechanism in idiopathic<br />
neutropenia and immunodominant expansions indicate an autoimmune process.<br />
Conversely, highly polarized responses in a subset of neutropenic LGL patients may<br />
represent the “extreme” end of the clonal continuum.
Doreen Haase, Anne Marie Asemissen, Carmen Scheibenbogen<br />
Immunogenic epitopes of the PAX2 transcription factor<br />
recognized by colon carcinoma patients<br />
PAX2 is a member of the highly conserved transcription factor family of paired box<br />
genes. It confers its major role in the embryonic development of the kidney and parts of<br />
the central nervous system. In the adult organism PAX2 expression is downregulated<br />
except for certain cells that are believed to be stem cells. This is in accordance with<br />
PAX2 being implicated in essential functions important for stem cells like proliferation,<br />
differentiation and migration. Interestingly, PAX2 expression is restored in a variety of<br />
solid tumors, including renal cell, prostate and colon carcinomas, as well as in<br />
lymphomas. Thus PAX2 would be an interesting target of novel therapeutic strategies<br />
against cancer.<br />
To identify PAX2 as a tumor rejection antigen, we searched for potential epitopes of the<br />
protein that are presented by HLA-A2. For prediction of candidate epitopes the<br />
SYFPEITHI algorithm (www.syfpeithi.de) was used which gives binding probabilities for<br />
each possible peptide of a given protein to the chosen HLA molecule. PAX2 nonamer<br />
and decamer epitopes with a high binding probability to HLA-A2 that were cleaved by<br />
the constitutive and immunoproteasome according to the PAProC database (www.<br />
paproc.de) were synthesized.<br />
Screening of the HLA-A2 restricted PAX2 candidate epitopes showed that 10 out of 20<br />
(50%) HLA-A2 positive colon carcinoma patients had interferon-gamma or TNF-alpha<br />
producing PAX2 specific CD8+ T cells. It is noteworthy that the epitopes with a positive<br />
T-cell response cluster in the unique region of PAX2 that shows no homology to other<br />
PAX family members. None of the 20 healthy donors presented reactivity towards any of<br />
the PAX2 peptides.<br />
Currently, different protocols for expansion of PAX2 specific cytotoxic T-cells (CTL) are<br />
compared. An efficient expansion will allow further characterization of these tumor<br />
specific CTLs including their ability to secrete cytokines like interferon-gamma and TNFalpha<br />
as well as their cytolytic activity towards PAX2 loaded cells and PAX2 expressing<br />
tumor cell lines.<br />
Taken together our data show the high immunogenicity of PAX2 in cancer patients<br />
whereas it is not immunogenic in healthy subjects. As a next step it will be important to<br />
analyse the therapeutic activity of PAX2-directed CTL in preclinical models in order to<br />
develop PAX2-based T-cell therapy.
Lukas Frenzel, Zeinab Abdullah, Anja Kriegeskorte, Rebecca Borsutzky, Manoj K.<br />
Gupta, Olaf Utermöhlen, Dirk H. Busch, Martin Krönke, Jürgen Hescheler, Tomo Saric<br />
Immunological properties of murine embryonic stem cellderived<br />
cardiomyocytes<br />
Embryonic stem (ES) cells are regarded as a very promising source of differentiated<br />
cells for tissue regeneration. ES cell-derived cardiomyocytes could functionally replace<br />
irreversibly lost cardiac tissue in various animal models of ischaemic heart disease.<br />
However, clinical application of this therapeutic approach will be hampered by<br />
immunological rejection of transplanted cells by histoincompatible recipients. To address<br />
the question of immunological properties of murine ES cell-derived cardiomyocytes we<br />
have utilized a transgenic murine ES cell line D3aPIG engineered to express GFP and<br />
antibiotic resistance specifically in ES cell-derived heart cells. This cell line enabled us to<br />
highly purify GFP-positive cardiac progenitor cells and to specifically address the<br />
question of their immunogenic properties. To this end, we have determined their<br />
immunophenotype by flow cytometry, assessed their response to the inflammatory<br />
cytokine interferon gamma, assayed their physical interaction with cytotoxic T<br />
lymphocytes (CTLs) and tested their susceptibility to lysis by activated NK cells and<br />
cytotoxic T cells. These studies have demonstrated that ES cell-derived cardiomyocytes<br />
constitutively express very low levels of MHC class I molecules on their cell surface,<br />
which were strongly upregulated by interferon gamma. Interestingly, the cytotoxicity<br />
experiments revealed that ES cell-derived cardiac cells were resistant to killing by poly I:<br />
C activated syngeneic and allogeneic NK cells as well as by allogeneic cytotoxic T cells.<br />
Even strong upregulation of MHC class I molecules on the surface of cardiac cells by<br />
interferon gamma did not render them sensitive to lysis by immune effector cells,<br />
indicating that transplanted ES cell-derived cardiomyocytes might be less susceptible to<br />
rejection as compared to whole organ transplants. Further studies are planned to<br />
elucidate the molecular basis of this resistance and to assess the engraftment capacity<br />
and immunogenicity of ES cell-derived cardiomyocytes in vivo upon allotransplantation.
Felix Heymann, Emma E. Hamilton-Williams, Isis Ludwig-Portugall, Susan Quaggin,<br />
Jürgen Floege, Hermann-Josef Gröne, Christian Kurts<br />
Immunopathology of T cell-mediated glomerulonephritis<br />
The different forms of immune-mediated glomerulonephritis (GN) represent a major<br />
cause of end stage kidney disease. The role of antibodies and immune-complexes has<br />
been extensively studied, whereas the ability of T cells to mediate glomerular damage<br />
has been proposed, but awaits experimental verification. We have generated transgenic<br />
mice expressing a fusion protein consisting of chicken ovalbumin and hen egg lysozyme<br />
as a model autoantigen in glomerular podocytes under the control of the nephrin<br />
promoter (NOH mice). Injection of transgenic OVA-specific T cells into NOH mice<br />
allowed to determine the type of renal immunopathology mediated by T cells specific for<br />
a glomerular autoantigen. OVA-specific CD8+ effector T cells (OT-I cells) were activated<br />
by cross-presentation and proliferated in the renal lymph nodes of NOH mice. Injection<br />
of activated OT-I cells increased cross-presentation in this node, presumably by<br />
cytotoxic release of antigen from the kidney. Renal immunopathology was only<br />
observed when with OT-I cells were co-injected with activated OVA-specific CD4+<br />
helper cells (OT-II cells). Surprisingly, the typical form of podocyte damage, namely<br />
foot process fusion, was not detected. Instead, immunopathology was dominated by<br />
periglomerular mononuclear infiltration, reminiscent of transplant glomerulitis or of<br />
rapid progressive forms of glomerulonephritis. Adjacent to this infiltrate, the parietal<br />
glomerular epithelial cells showed signs of injury. Repetitive injection of OT cells<br />
resulted in proteinuria, reduced creatinin-clearance and structural kidney damage<br />
accompagnied by massive periglomerular infiltartes. These infiltrates contained many<br />
dendritic cells expressing CD11c, CD11b, F4/80, and CD8, which showed signs of<br />
activation. Ablation of these DC resolved the inflammatory infiltrate, demonstrating a<br />
functional role of kidney DC in mediating kidney damage. In conclusion, we<br />
demonstrate that T cells can recruit kidney DCs to induce periglomerular infiltrates<br />
resulting in glomerular immunopathology.
Nadine Nippe, Katja Gutsche, Mechthild Jung, Gerald Grütz<br />
Immunoregulation of IL-10 induced Autotaxin<br />
Cytokines are regulators of host response to inflammation. Some cytokines have to be<br />
associated with the pathogenesis of diseases, whereas others serve to reduce<br />
inflammatory responses. The mediator of inflammation HMGB1 and IL-1ß are secreted<br />
by monocytes and macrophages through a non-classical pathway.<br />
High-mobility group protein 1(HMGB1), a non-histone nuclear protein, functions as a<br />
late mediator of inflammation. Passive immunization with anti-HMGB1 antibodies<br />
protects against endotoxin lethality in mice. Active secretion of HMGB1 by monocytes<br />
and macrophages occurs in response to LPS. We show that its release can also be<br />
triggered by LPC.<br />
Secretion of IL-1ß needs two distinct stimuli. An initial inflammatory stimulus, LPS,<br />
induces synthesis of pro-IL-1ß, processing and release of matured IL-1ß is inefficient. A<br />
secondary stimulus such as ATP can trigger rapid processing and massive release of IL-<br />
1ß.<br />
IL-10 is one of the major immunosuppressive cytokine. It strongly down-regulates the<br />
expression of proinflammatory cytokines. In order to identify genes which could mediate<br />
the IL-10 inhibition we analyzed the expression profile of IL-10 regulated genes in<br />
human monocytes by comparison of expression level of 12000 genes in IL-10<br />
stimulated monocytes and unstimulated cells. A possible candidate is Autotaxin. We<br />
show that Autotaxin is highly up regulated by IL-10 in human monocytes.<br />
Autotaxin is an ecto-enzyme with pyrophosphatase/phosphodiesterase-activity. But<br />
primarily functions as a lysophospholipase D, degrading lysophosphatidylcholine (LPC)<br />
into lysophosphatidic acid (LPA).<br />
Therefore, we hypothesized that Autotaxin could reduces HMGB1 and IL-1ß release by<br />
degradation of LPC and ATP. We would like to demonstrate first functional results.
Wolfgang G Bessler, Karola Puce, Carsten Kirschning, Maria Huber<br />
Immunostimulating effects of the bacterial extract OM-89<br />
OM-89 (Urovaxom®) is a bacterial extract prepared from 18 uropathogenic Escherichia<br />
coli strains used for the treatment of recurrent infections of the urinary tract. We<br />
investigated in a mouse model the immunostimulating effects of the bacterial extract.<br />
After the oral administration of OM-89, we observed ex vivo the production of TNFalpha<br />
in supernatants of peritoneal cells. Leukocyte activation could also be shown by a<br />
chemiluminescence assay in blood and liver cells. After repeated oral administration of<br />
OM-89, an increased serum IgG and IgA response against the Escherichia coli strains<br />
used for the preparation of OM-89 was observed. We also could demonstrate defined<br />
adjuvant properties of the extract using ovalbumin as an antigen. Corresponding to our<br />
findings in the mouse system, preliminary in vitro assays in the human system showed<br />
an increase in TNF-alpha IL-6, IL-10, and IL-12 production after the stimulation of<br />
monocyte derived dendritic cells with OM-89. Activation is likely to be mediated via Toll<br />
like receptors: we could demonstrate the binding of components of the extract to TLR-4<br />
and marginally to TLTR-2.
Kerstin Annika Sauer, Joachim Heinrich Maxeiner, Petra Scholtes, Roman Karwot,<br />
Hans-Anton Lehr, Mark Birkenbach, Richard Steven Blumberg, Susetta Finotto<br />
Immunosurveillance of lung melanoma metastasis in EBI-3<br />
(-/-) mice by NK-DCs- induced CD8+ T cells<br />
Antigen presentation plays an important role in lung metastasis, although the<br />
immunological mechanisms are not <strong>complete</strong>ly understood. Epstein-Barr virus-induced<br />
gene 3 codes for a soluble type 1 receptor homologous to the p40 subunit of IL-12 that<br />
is expressed by antigen presenting cells following activation. Adoptive intravenous<br />
injection of the B16-F10 cell line resulted in a significant reduction of lung tumor<br />
metastasis in EBI-3 (-/-) recipient mice compared to wild type. Consistently, we found<br />
that EBI-3 (-/-) mice had decreased number of VCAM-1+ endothelial cells. The<br />
immunological finding accompanying this therapeutic effect was the orchestrate priming<br />
and activation of T cells by a newly described Dendritic Cell (DC) subset called Natural<br />
Killer Dendritic Cells (NK-DC). NK-DCs from EBI-3 (-/-) mice released increased<br />
amounts of IFN-gamma thereby inducing augmented CD8+ T cell responses in the lung.<br />
This in turn resulted in a TNF-alpha-TRAIL mediated programmed cell death of local<br />
metastatic tumor cells in the lung of EBI-3 deficient mice. Finally, adoptive transfer of<br />
EBI-3 (-/-) NK-DC primed CD8+ T cells into tumor bearing wild-type mice ameliorated<br />
the development of lung metastasis in recipient mice. Taken together, these data<br />
demonstrate that EBI-3 is a crucial regulator of anti-tumor CD8+ T cell responses in the<br />
lung by controlling NK-DC activity.<br />
This work is funded by the Graduiertenkolleg 1043 and Immuno-intervention Cluster of<br />
Excellence (ICE, Mainz, Germany).
Henoch Hong, Nupur Bhatnagar, Maren Mönkemeyer, Hans Heiken, Reinhold E.<br />
Schmidt, Dirk Meyer-Olson<br />
Impact of HIV-1 Vpr on type I and type II interferon<br />
secretion by plasmacytoid dendritic cells and natural killer<br />
cells<br />
Objectives: Type I and type II interferons (IFNs) can induce an antiviral state in target<br />
cells, which impairs virus replication. In humans, plasmacytoid dendritic cells (pDCs)<br />
are the most potent type I IFN producers whereas type II IFNs are released by<br />
activated T cells and natural killer (NK) cells. The molecular and cellular mechanism of<br />
HIV-induced impairment of IFN secretion is not yet fully understood. Here we addressed<br />
the question whether HIV-1 Vpr is able to disturb the interplay between NK cells and<br />
pDCs with regard to their IFN production.<br />
Methods: We sorted NK cells and pDCs from peripheral blood of healthy donors. Highly<br />
purified NK cells and pDCs were cultured in the presence or absence of synthetic HIV-1<br />
Vpr. In order to be able to evaluate the effects of Vpr, pDC/NK cocultures were also<br />
stimulated with CpG. NK phenotype was assessed by FACS analysis and functions by<br />
standard 51Cr release assay and IFN-γ ELISA. We analyzed direct effects of Vpr on IFNα<br />
secretion by pDCs.<br />
Results: As reported previously, CpG stimulated pDCs were able to activate NK cells as<br />
determined by higher CD69 expression, increased cytolytic activity and moderate IFN-γ<br />
release. Vpr did not impair pDC mediated upregulation of CD69 in NK cells and did not<br />
interfere with increased NK killing activity. However, we found that Vpr substantially<br />
decreased pDC induced IFN-γ secretion. Furthermore, Vpr significantly hampered IFN-α<br />
production by CpG activated pDCs.<br />
Conclusion: The data suggest that Vpr mediates a dysregulation of early IFN-γ<br />
expression by NK cells and IFN-α production by pDCs, which could be of considerable<br />
importance in the pathogenesis of HIV infection and deserves further studies.
Nadine Kämper, Claudia Wegscheid, Jörg Keßler, Norbert Koch<br />
Impact of HLA encoded BAT3 splice variants on MHC class I<br />
and class II expression<br />
Division of Immunobiology, Institute of Genetics, University of Bonn<br />
The BAT3 gene locates in the class III region of the HLA complex on chromosome 6.<br />
The gene is composed of 25 exons. By alternative splicing of the pre RNA numerous<br />
variants of BAT3 polypeptides can be generated. It was suggested that BAT3 proteins<br />
are involved in apoptosis, possibly by regulating proteasomal degradation. BAT3 is a<br />
proline-rich protein, which contains a zinc finger-like domain, a nuclear localization<br />
signal and a BAG domain. Aim of our study is to determine expression and subcellular<br />
distribution of BAT3 splice variants in human cells and their impact on the level of MHC<br />
class I and class II surface expression. While some BAT3 splice variants show nuclear<br />
expression other variants were detected in the cytoplasm. Since BAT3 exhibits a short<br />
half life, it is possible to determine its impact on regulation and induction of MHC genes.<br />
By transfection of cells with siRNA or with miRNA, the expression of BAT3 was strongly<br />
reduced. Inspection of MHC and of accessory molecules revealed that in transfected<br />
cells expression of the MHC class II associated invariant chain (Ii) was depleted. This<br />
result suggests that the gene regulation of Ii depends on BAT3 expression.
Diana Fleissner, Jan Buer, Astrid Westendorf<br />
Impact of intestinal dendritic cells for the induction of<br />
tolerance or pathology<br />
Several studies have suggested that chronic inflammatory bowel disease may be a<br />
consequence of antigen specific recognition by appropriate T cells which expand and<br />
induce immunopathology. To analyse the impact of intestinal dendritic cells (DCs) for<br />
the presentation of intestinal self-antigens and the induction of immunopathology or<br />
tolerance we used VILLIN-HA transgenic mice that show specific expression of<br />
hemagglutinin (HA) from influenza virus A exclusively in enterocytes of the intestinal<br />
epithelium. Adoptive transfer of naïve HA-specific CD8+ T cells into VILLIN-HA recipient<br />
mice leads to strong expansion of antigen-specific CD8+ T cells and the development of<br />
severe intestinal inflammation. In contrast, adoptive transfer of HA-specific CD4+ T<br />
cells into VILLIN-HA transgenic mice results in proliferation of HA-specific T cells but<br />
fails to induce intestinal inflammation. Interestingly, cotransfer of HA-specific CD4+ and<br />
CD8+ T cells further aggravates the pathology. Therefore, auto-reactive CD8+ T cells<br />
may come first before pathogenic CD4+ T cells ultimately drive disease. Based on these<br />
findings we analyzed the impact of intestinal DCs for the presentation of intestinal selfantigen.<br />
Comparison of DCs from the mesenteric lymphnode (MLN) versus lamina<br />
propria (LP) reveals a slight upregulation of MHC class II, CD80 and CD86 on DCs<br />
isolated from the LP. Furthermore, DCs isolated from the MLN of VILLIN-HA transgenic<br />
induce proliferation of HA-specific CD8+ and CD4+ T cells without adding of external HA<br />
peptide in vitro. These results demonstrate that DCs sample intestinal epithelial<br />
antigens in the lamina propria and migrate to the MLN where they present the antigen.<br />
In future experiments we want to characterize the phenotype of DC-stimulated CD8+<br />
and CD4+ T cells in more detail to dissect the pathologic and regulatory function of<br />
these cells. In conclusion, the gut-associated mucosal immune system develops certain<br />
mechanisms which lead either to immunity or tolerance.
Johannes Lutz, Werner Müller, Chander Raman, Hans-Martin Jäck<br />
Impaired B Cell Development in the Presence of a Non-Coding<br />
IgM mRNA<br />
To establish allelic exclusion (AE) at the Ig heavy chain (IgH) locus VDJ recombination<br />
of the second locus must be terminated once a productive VDJ rearrangement has been<br />
made. Many studies have demonstrated that the suppression of further VDJ<br />
rearrangements is mediated by the newly synthesized IgM heavy chain (•HC) through<br />
pre-B cell receptor (pre-BCR) signals. However, it is still unclear how rearrangement of<br />
the second IgH allele is prevented during the time required for the synthesis of the •HC<br />
and the initiation of pre-BCR signals. Here we present evidence that a stable •HC<br />
transcript, which reflects the presence of a productive rearrangement, can already exert<br />
a suppressive effect on VDJ recombination in the absence of a •HC signal. B cell<br />
development was impaired at the pro-B to pre-B cell transition with an increased<br />
frequency of •HC-negative pro-B cells in transgenic mice expressing a non-coding •HC<br />
transcript. This transcript contains a premature translational stop codon at position +3<br />
and resembles rather a stable productive than an extremely unstable non-productive<br />
•HC mRNA. Providing a productive transgenic •HC restored B cell development, which<br />
indicated that the non-coding •HC transcript interfered with no other processes than<br />
VDJ recombination at the IgH locus. These observations suggest a new role for •HC<br />
transcripts by indicating the presence of a productive VDJ rearrangement and<br />
temporarily suppressing VDJ recombination of the second IgH allele until the initiation of<br />
signals provided by a •HC.<br />
The work was supported in part by the project grant SFB466 and the research grant JA<br />
968/2 from the Deutsche Forschungsgemeinschaft (DFG) to H.-M. J.
Verena Moos, Kristina Allers, Thomas Schneider<br />
Impaired innate functions of monocytes and macrophages in<br />
Whipple`s disease<br />
Whipple`s disease is a rare chronic multisystemic infectious disease caused by the<br />
actinomycete Tropheryma whipplei. Symptoms are heterogenous, but arthropathy,<br />
weight loss, and diarrhea are present in most cases. Host factors like a reduced capacity<br />
of T. whipplei-specific Th1 reactivity are suspected to be responsible for the<br />
pathogenesis of Whipple`s disease. Monocytes and macrophages as important cells of<br />
the innate immune response have been shown to be involved in the pathogenesis of<br />
Whipple`s disease, but innate defense mechanism induced by T. whipplei were not<br />
ivestigated so far. Therefore, we studied phagocytosis and the induction of oxidative<br />
burst induced by T. whipplei in comparison to related and unrelated bacteria in fresh<br />
blood of patients with Whipple´s disease. Analysis included serum concentration of<br />
cyto- and chemokines indicative for macrophage activation, and the phenotypical<br />
characterization of peripheral and duodenal macrophages.<br />
T. whipplei is phagocytosed and induces a robust oxidative burst in monocytes of<br />
healthy controls. However, Whipple`s disease patients showed reduced phagocytosis<br />
and oxidative burst upon exposure to T. whipplei, whereas their capacity to react to<br />
other related and not related bacteria was not reduced compared to controls.<br />
Macrophages of Whipple´s disease patients reveal an alternatively activated phenotype<br />
in vivo and in situ indicated by the expression of CD163, and the cytokine pattern in the<br />
sera of Whipple´s disease patients. Hence, we conclude that ineffective innate defense<br />
mechanism may be responsible for an impaired clearance of T. whipplei and might<br />
initiate insufficient T. whipplei-specific T cell responses in Whipple`s disease patients.
Kittan Nicolai A., Bergua Antonio, Haupt Sabrina, Donhauser Norbert, Schuster Philipp,<br />
Korn Klaus, Harrer Thomas, Schmidt Barbara<br />
Impaired plasmacytoid dendritic cell (PDC) innate immune<br />
responses in patients with herpesvirus-associated severe<br />
acute retinal necrosis (ARN)<br />
Background: Plasmacytoid dendritic cells (PDC), the main producers of type I<br />
interferons (IFN) in the blood, are important for the recognition and control of viral and<br />
bacterial infections. Since several viruses are known to induce IFN-alpha production,<br />
severe courses of herpes virus infections in non-immunocompromised patients may be<br />
related to numerical or functional PDC deficits.<br />
Methods: To evaluate this hypothesis, peripheral blood mononuclear cells (PBMC) and<br />
PDC were repeatedly isolated from eight patients with a history of or an acute episode<br />
of acute retinal necrosis (ARN), caused by herpes simplex or varicella zoster virus, and<br />
18 age-matched healthy controls.<br />
Results: The patients experienced meningitis/encephalitis and frequent infections in<br />
childhood (n=2), recurrent herpes virus infections at unusual localizations (n=2), ocular<br />
surgery (n=1), infections and stress around ARN (n=6). The median percentage of<br />
isolated PDC was significantly lower in patients compared to controls, confirmed by<br />
FACS analysis using peripheral blood, and extremely low during acute disease. PDC<br />
counts dropped in five controls suffering from respiratory infections or diarrhea. IFNalpha<br />
production was significantly lower in patients than controls; anergy to these<br />
stimuli was observed on four occasions. Real-time analyses for interferon regulatory<br />
factor (IRF)-7 mRNA and evaluation of PDC surface markers revealed immune<br />
stimulation in patients compared to controls.<br />
Conclusion: These data support a model, in which numerical and functional deficits in<br />
PDC innate immune responses contribute to an impaired control of latent herpes virus<br />
infections and subsequent development of ARN. The role of CD8+ and natural killer cells<br />
will be discussed.
Daniela Wesch, Philine Wrobel, Hamed Shojaei, Hans-Heinrich Oberg, Monika Kunz,<br />
Dieter Kabelitz<br />
Implications for the design of γδ T cell-based cancer<br />
immunotherapy<br />
There is a substantial interest in γδ T cell-based cancer immunotherapy due to their<br />
potent MHC-nonrestricted cytotoxicity towards various tumor cells. We analyzed the<br />
susceptibility of a broad range of epithelial tumor cells to V9γVδ2 γδ T cell cytotoxicity.<br />
The involvement of T cell receptor (TCR) and NKG2D-dependent recognition in tumor<br />
cell recognition was characterized by antibody blockade. Our experiments revealed<br />
three patterns of inhibition, i.e. preferential inhibition by anti-TCR antibody or anti-<br />
NKG2D antibody, or the additive blockade by both antibodies. The extent of inhibition<br />
did not correlate directly with the level of NKG2D ligand expression on epithelial tumor<br />
cells. Further, our results indicate for the first time that the NKGD2 pathway is involved<br />
in the lysis of different melanomas, squameous cell carcinomas of the head and neck<br />
(SCCHN), lung carcinomas, and pancreatic adenocarcinomas. Lysis of poorly killed<br />
tumor cells was enhanced by the pre-treatment of γδ T cells with TCR-stimulating<br />
pyrophosphomonoesters or aminobisphosphonates. The enhancing effect by these<br />
stimuli was independent of the degree of HLA (mis)match between target and effector.<br />
Moreover, we currently investigate whether Toll-like receptor agonists, which are<br />
suggested as adjuvant therapy in clinical trials for different types of cancer including<br />
adenocarcinomas, have an influence on lysis of tumor cells by γδ T cells.<br />
Our results indicate that tumors recognized independently of the TCR might be less<br />
suited for γδ T cell immunotherapy with pyrophosphomonoesters or<br />
aminobisphosphonates.<br />
This study was supported by Werner and Klara Kreitz-Stiftung.
Inga Gebuhr, Kathrin Gube, Katrin Vogt, Christian Meisel, Sandra Naundorf, Hans-<br />
Dieter Volk, Birgit Sawitzki<br />
Importance of cell surface N-glycosylation for activation of T<br />
cell subpopulations<br />
Introduction: Recently, we demonstrated that infiltrating CD4+ T cells of tolerance<br />
developing kidney grafts recipients express high levels of alpha-1,2-Mannosidase, an<br />
important enzyme for the N-glycosylation of proteins. The impact of N-glycosylation of<br />
surface proteins such as costimulatory molecules on T cells for their activation is still<br />
poorly understood.<br />
Aim: Here we investigated the role of alpha-1,2-Mannosidase and cell surface Nglycosylation<br />
for the activation of different T cell subpopulations.<br />
Methods: Human CD4+, CD4+CD45RA naïve, and CD4+CD45RO memory T cells were<br />
purified using MACS separation. Cells were cultivated for 2 days in the presence or<br />
absence of the alpha-1,2-Mannosidase specific inhibitor Kifunensine. Preincubated T<br />
cells were stimulated with allogenic PBMCs. PHA binding was used to determine<br />
Mannosidase activity. CD69 expression, cytokine production and Mannosidase<br />
transcription was analysed.<br />
Results: The inhibition of Mannosidase activity in CD4+ T cells prior to stimulation<br />
resulted in a dramatic reduction of cell surface N-glycosylation levels. This reduction<br />
was accompanied by 2 to 3 fold increase in CD69 frequency, an earlier IL-2 production<br />
and transcription. This early increase in IL-2 production was due to faster activation of<br />
ERK. Interestingly, memory T cells displayed 5 fold higher transcription levels and 2 fold<br />
increased PHA binding capacities when compared to naïve T cells. During allostimulation<br />
mRNA transcription in memory T cells did not change whereas in naïve T<br />
cells transcription was transiently down-regulated followed by a 4 fold upregulation.<br />
Furthermore, naïve and memory T cells also differ in their susceptibility to Nglycosylation<br />
mediated regulation of T cell activation. Only in naïve T cell inhibition of Nglycosylation<br />
resulted in increased cytokine production.<br />
Conclusions: Our data show that N-glycosylation of cell surface proteins negatively<br />
regulates T cell activation. Furthermore the magnitude and impact of N-glycosylation is<br />
highly regulated among T cell subpopulations.
Lydia-Mareen Köper, Andrea Schulz, Hans-Jürgen Ahr, Hans-Werner Vohr<br />
In vitro Differentiation of Skin Sensitizers by Cell Signaling<br />
Pathways<br />
Introduction: Animal testing causes ethical problems and due to the EU-guideline<br />
(76/768/EEC, Feb. 2003), which prohibits the use of animals for the assessment of<br />
toxicological data for cosmetic ingredients as of 2009, the development of in vitro<br />
assays has become even more important. In this study, we investigated whether<br />
analyses of cell signaling pathways can provide a methodology for the detection of<br />
sensitizing compounds in vitro.<br />
Methods: Murine and human skin explants as well as reconstituted skin models<br />
(epidermal model EST-1000 and full-thickness model AST-2000) were exposed to<br />
sensitizing (Oxazolone and DNFB) or irritant compounds (SDS and TritonX-100).<br />
Phosphorylation of MAP-kinases (p38, ERK1/2 and JNK1/2), STAT1 and PLCγ were<br />
determined by cytometric bead array (CBA).<br />
Results: In skin explants, all three MAP-kinases were exclusively activated after<br />
exposure to sensitizing compounds. For the reconstituted skin models phosphorylations<br />
of p38 and JNK1/2 were obtained after stimulation with allergens, whereas treatments<br />
with irritant compounds lead to ERK1/2 activation.<br />
Conclusion: MAP-kinase activation provides a promising in vitro tool for the<br />
discrimination between sensitizers and irritants. The reconstituted skin models AST-<br />
2000 and especially the EST-1000 showed high induction levels of phospho-p38 specific<br />
for exposure to sensitizing compounds, comparable to those found in skin explants, i.e.<br />
complex immune competent tissues.
Sabine Ring, Karsten Mahnke, Alexander Enk<br />
In vivo activation of injected Tregs precedes the suppression<br />
of the elicitation phase of Contact hypersensitivity reactions<br />
independent from spleen and lymph nodes<br />
We previously demonstrated that adoptively transferred naïve CD4+CD25+ T cells<br />
(Treg) suppress the elicitation phase of allergic contact dermatitis (CHS), by inhibiting<br />
the endothelium-interaction and extravasation of effector CD8+ T cells.<br />
Since activation of Treg is necessary to generate this suppressive activity, we<br />
determined the activation status of isolated Tregs in the course of injection. Directly<br />
after isolation, the naïve CD4+CD25+ T cells displayed a non-activated phenotype as<br />
assessed by low expression of CD69 and CD44, and high expression of CD62L. 2h after<br />
injection and re-isolation of the dye-labelled Treg we detected significantly increased<br />
expression of the activation markers CD69, Foxp3 and CD44, whereas CD62L decreased<br />
in Treg in vivo after hapten application. This indicates that Treg become activated in<br />
vivo after injection and explains the comparable suppressive function of naïve and<br />
activated Treg in vivo. To further determine the importance of homing to lymphoid<br />
organs for Treg action, we splenektomised mice or injected CD62L- Treg. By this way<br />
we excluded the homing of Treg to spleen or lymph nodes, respectively. In these<br />
experiments the Treg were still able to suppress the elicitation phase of CHS, indicating<br />
that peripheral lymphoid organs are not essential for the activation and consequently<br />
for the suppressive capacity of injected naïve Treg in vivo.<br />
These data show that naïve Treg upregulate characteristic activation markers in vivo<br />
after hapten application which results in the suppression of the elicitation phase of CHS,<br />
independently of peripheral lymphoid organs. Therefore we can speculate that cellular<br />
interaction(s) in the blood or at the site of inflammation and/or soluble factors are<br />
involved in mediating suppressive function(s) of Treg in a CHS model.
Sonja Schallenberg, Sabine Ring, Tanja Bedke, Sabrina Schmitt, Kurt Schönfeld,<br />
Karsten Mahnke, Elisabeth Suri-Payer, Alexander H. Enk<br />
In vivo depletion of CD4+CD25+Foxp3+ regulatory T cells<br />
does not affect the growth of established B16 tumors<br />
Naturally occurring regulatory T cells (Treg) have been described to impede immune<br />
responses against several tumors, thus depletion of Treg before tumor challenge results<br />
in diminished tumor growth in several tumor models.<br />
In order to set up a therapeutical regimen and to improve anti-melanoma therapy we<br />
used a murine B16 melanoma model. We treated tumor-bearing mice with a<br />
combination of Treg depletion and stimulation of effector T cells (Teff) via immunization<br />
with tumor-antigen-loaded dendritic cells (DC). As expected injection of anti-CD25 mAb<br />
(PC61) before B16 tumor inoculation led to decreased tumor growth. However,<br />
depletion of CD25+ cells 5-10 days after tumor challenge resulted in enhanced tumor<br />
growth suggesting that PC61 mAb additionally depletes proliferating CD25+ Teff. To<br />
test this assumption, we injected CFSE-labeled OVA-specific TCR-transgenic CD4+ cells<br />
into mice, immunized them with OVA-loaded DC’s and at the same time injected PC61<br />
mAb. Five days later, draining lymph nodes were isolated and analyzed by flow<br />
cytometry. To our surprise, recovery, proliferation and IL-2 production of Teff was not<br />
diminished but rather enhanced compared to the control group without PC61. Next, we<br />
investigated the efficacy of the Treg depletion during tumor development in different<br />
organs. We found that Treg (CD25+Foxp3+ cells) in lymphoid organs were depleted,<br />
whereas they were still detectable inside the tumors.<br />
These results suggest that the injection of PC61 mAb did not influence Teff activity.<br />
Further, the tumor creates its own immunosuppressive environment where Treg cannot<br />
be depleted, either because the mAb does not penetrate well enough into the tumor, or<br />
because the tumor constantly generates new Treg.
Alla Skapenko, Joachim R. Kalden, Peter E. Lipsky, Hendrik Schulze-Koops<br />
In vivo function of IL-4-induced Tregs<br />
We have previously shown that injection of human peripheral blood mononuclear cells<br />
(PBMC) into the peritoneal cavity of NOD/SCID mice results in the development of a<br />
Th1-mediated immune response of human cells against murine tissue accompanied by<br />
an increase in the frequency of CD25+CD4+ T cells. Here, we used this model to<br />
analyze the role of interleukin (IL)-4 in the generation of human CD25+ regulatory T<br />
cells in an in vivo situation. NOD/SCID mice were injected intraperitoneally with human<br />
PBMC and treated with human IL-4 or a neutralizing antibody to human IL-4. IL-4treatment<br />
down-modulated systemic inflammation as assessed by a decrease of serum<br />
levels of the human inflammatory cytokines, TNF and IFN-gamma whereas<br />
neutralization of endogenous IL-4 resulted in an exaggeration of inflammation. Analysis<br />
of the frequencies of CD25+CD4+ T cells within the human cells recovered from the<br />
peritoneal cavity of the mice revealed that treatment with IL-4 augmented and IL-4<br />
neutralization diminished the increase of CD25+CD4+ T cells associated with the<br />
immune response. Examination of the immunosuppressive ability of recovered human T<br />
cells in vitro revealed an inhibititory capacity of CD25+, but not of CD25- T cells, for the<br />
proliferative response of autologous PBMC. Importantly, when injected into animals with<br />
an ongoing Th1-mediated immune reaction driven by syngeneic human PBMC, purified<br />
CD25+ T cells were able to reduce serum levels of human IFN-gamma and TNF,<br />
whereas injection of CD25- T cells resulted in increased levels of both cytokines. Thus,<br />
CD25+ Tregs that developed in vivo in the presence of IL-4 were functionally competent<br />
Tregs. This conclusion is supported by the fact that the frequency of CD25+CD4+ T<br />
cells recovered from the peritoneal cavity at the peak of the xenogeneic reaction in mice<br />
injected with human PBMC inversely correlated with serum concentrations of human<br />
IFN-gamma and TNF. Together, the data indicate that CD25+CD4+ T cells which<br />
accumulate during the Th1-mediated immune response of human cells in NOD/SCID<br />
mice possess an immunosuppressive phenotype in vivo. Moreover, the data further<br />
imply that IL-4 controls the generation of competent CD25+ Tregs during an immune<br />
response in vivo.
Marcus Gereke, Karsten Mahnke, Elmar Jäckel, Jan Buer, Dunja Bruder<br />
In vivo induction of tolerance via DEC-205 mediated antigen<br />
delivery – therapeutic safety in the context of infection<br />
Targeting of antigens to immature dendritic cells has been shown to result in antigenspecific<br />
T cell tolerance in vivo. In the INS-HA/TCR-HA transgenic mouse model for type<br />
I diabetes we tested the potential of the dendritic cell-specific monoclonal antibody DEC-<br />
205 conjugated to the HA antigen (DEC-HA) to prevent disease onset. Whereas<br />
untreated INS-HA/TCR-HA mice all develop insulitis and about 40 percent of these mice<br />
become diabetic, repeated injection of newborn mice with DEC-HA protects almost all<br />
mice from disease development. Histological examination of the pancreata revealed<br />
significant reduction of peri-islet infiltrations in DEC-HA treated mice and the islet<br />
structure remained intact. Moreover, HA-specific CD4+ T cells from anti-DEC-HA treated<br />
INS-HA/TCR-HA mice exhibited increased expression of Foxp3, CTLA-4 and the<br />
immunosuppressive cytokines IL-10 and TGF-β. These findings argue, that targeting of<br />
the HA antigen to immature DCs in vivo leads to the expansion of antigen-specific Foxp3<br />
+ regulatory T cells that suppress autoimmune tissue destruction.<br />
With respect to a possible application of such approach in human patients it must be<br />
excluded that DEC-205 mediated antigen delivery in the context of infection, i.e. under<br />
conditions that result in maturation of DC, would result in T cell activation and<br />
precipitation of autoimmunity. To address this issue we experimentally infected mice<br />
before, during or after treatment with antigen coupled to DEC-205 antibodies and<br />
assess the kinetics of diabetes induction. We demonstrated that treatment with DEC205-<br />
HA before, during and after infection with bacterial and viral pathogens did not<br />
precipitate in autoimmunity in diabetes prone mice. In addition we could demonstrate<br />
an unperturbed adaptive immune response against pathogen with preservation of the<br />
general immunocompetence. Together, we provide evidence that DEC-205 mediated<br />
antigen delivery in the context of infection does not result in uncontrolled T cell<br />
activation and autoimmune disease.
Andreas Wieland, Markus Denzel, Jörg Reimann, Reinhold Schirmbeck<br />
In vivo produced complexes of antigen with stress proteins<br />
are potent immunogens<br />
To facilitate priming of T cells, stress (or heat shock) proteins of the Hsp70/90 families<br />
have been incorporated into vaccine formulations (by loading antigenic peptides to Hsp,<br />
or constructing Hsp/antigen fusion proteins). We expressed a chimeric protein<br />
containing a Hsp-capturing, J-homologous domain and an antigen-encoding sequence to<br />
produce in situ Hsp/antigen complexes. DNA vaccines expressing antigens with this<br />
stress protein-capturing domain display enhanced immunogenicity for T and B cells.<br />
Complexes of antigen associated with constitutively expressed Hsp73 or stress induced<br />
Hsp70 accumulate to high steady state levels in transfected eukaryotic cells that<br />
produce these chimeric proteins. We designed a purification method to isolate from<br />
transfectants native Hsp/antigen complexes that efficiently elicit antigen-specific<br />
immune responses in mice. Similar to peptide-bound Hsps these complexes facilitate<br />
priming of CD8 T cells. The delivery of chaperone-associated antigen is thus an<br />
attractive strategy to elicit multispecific responses of different compartments of the<br />
immune system.
Undine Meusch, Manuela Rossol, Holm Häntzschel, Christoph Baerwald, Sunna<br />
Hauschildt, Ulf Wagner<br />
Increased Infliximab-induced monocyte apoptosis via reverse<br />
signalling of membrane TNF in patients with rheumatoid<br />
arthritis<br />
Treatment of inflammatory autoimmune diseases like rheumatoid arthritis (RA) with<br />
anti-TNF antibodies is a common way to neutralize soluble TNF alpha and reduce<br />
inflammation and bone destruction. In the last years another possible mechanism<br />
explaining the action of anti-TNF antibodies gets into focus. Anti-TNF antibodies are able<br />
to bind to membrane TNF which leads to signal transduction by a mechanism called<br />
reverse signalling. In the study presented here, we analyzed apoptosis due to reverse<br />
signalling in human monocytes of healthy donors and patients with RA. In vitro<br />
incubation of human monocytes with the anti-TNF antibody Infliximab led to a<br />
significant increase in apoptosis after 16 h. Interestingly, only one third of the healthy<br />
donors showed this response whereas 80% of the RA patients underwent apoptosis in<br />
this in vitro system. Considering only donors who responded with apoptosis, monocytes<br />
of RA patients underwent apoptosis with a higher rate than monocytes of healthy<br />
donors. In addition, apoptosis of monocytes of RA patients strongly correlated with the<br />
expression of membrane TNF. Infliximab-induced apoptosis was independent of caspase<br />
3, 8 and 9, therefore other pathways were evaluated. Reverse signalling of membrane<br />
TNF induced phosphorylation of the MAP kinase Erk after 16 h. Accordingly, inhibition of<br />
Erk activation led to a decreased Infliximab- induced apoptosis. Inhibition of casein<br />
kinase 1, the enzyme responsible for TNF phosphorylation, resulted in a diminished<br />
activation of Erk and a decreased apoptosis rate.<br />
In summary, reverse signalling of membrane TNF induces increased apoptosis in human<br />
monocytes of RA patients in comparison to healthy donors. Infliximab-induced apoptosis<br />
of RA monocytes requires cell surface expression of membrane TNF and an involvement<br />
of the MAP kinase Erk and casein kinase 1.
Joachim Heinrich Maxeiner, Kerstin Annika Sauer, Roman Karwot, Petra Scholtes,<br />
Rainer Wiewrodt, Hans-Anton Lehr, Susetta Finotto<br />
Increased lung tumor in NFATc2 (-/-) mice mediated by<br />
defective CD8+ T cells and increased CD4+CD25+ lung T cells<br />
Lung cancer, including bronchoalveolar adenocarcinoma is the major cause of death in<br />
the USA and Europe. The transcription factors nuclear factor of activated T cells (NFAT)s<br />
are critical in regulating early gene transcription in response to T cell receptor mediated<br />
signals in lymphocytes. Previous studies on mice lacking NFATc2, a NFAT family<br />
member, have demonstrated that these mice display hyperproliferation of T and B<br />
lymphocytes, however little is known about its role in CD8+ T cells.<br />
In the present study, we show that mice lacking nuclear factor of activated T cells-2<br />
(NFATc2) develop increased lung metastasis in a bronchoalveolar adenocarcinoma<br />
murine model twenty-one days after intravenous injection of the L1C2 adenocarcinoma<br />
cell line. Moreover, significant elevated TGF-beta protein in the airways was<br />
accompanied by increased number of CD4+CD25+ T cells in the lungs of L1C2 treated<br />
NFATc2 (-/-) mice. Furthermore, although dendritic cells isolated from the lungs of<br />
NFATc2 (-/-) mice were of more mature phenotype, they could not induce CD8+ T<br />
effector (Teff) cell responses as demonstrated by unchanged levels of CD8+CD25+ Teff<br />
cells and increased development of IL-15 dependent CD8+ T cells (CD8+CD122+) in<br />
the lung of NFATc2(-/-) mice bearing tumor. In addition, histologically, lung metastasis<br />
of NFATc2 (-/-) mice were characterized by decreased necrosis in tumor cells as<br />
compared to those developed in the lung of the wild type littermates. These results<br />
imply that immunotherapy based on adoptive transfer of dendritic cells might be<br />
unsuccessful in absence of NFATc2 expression in CD8+ T cells leading to lack of an<br />
effective CTL response into this tumor model.<br />
This work is supported by a DFG (FI-817) and SFB 548 grant.
Matthias Kresse, Ingo Uthe, Heike Weighardt, Irmgard Förster<br />
Inducible ablation of CCL17 positive DC in vivo<br />
CCL17 (TARC) is a CC chemokine which is expressed by a subpopulation of CD11bpositive<br />
dendritic cells (DC), in particular following maturation of these cells. CCL17<br />
expressing DC can be detected in thymus, lymph nodes, Peyer’s Patches, lung, and<br />
inflamed skin but not in spleen. CCL17 binds to CCR4 which is highly expressed on TH2<br />
cells but also on other activated T cells. To investigate the role of CCL17 in vivo we<br />
generated mice expressing a DTR-EGFP fusion protein under the control of the<br />
endogenous CCL17 promotor using a knockin approach (CCL17/DTR mice). These mice<br />
developed normally and expression of the DTR-EGFP fusion protein was detectable on<br />
DC following LPS stimulation. We could demonstrate that application of diphtheria toxin<br />
(DT) leads to the ablation of CCL17 expressing bone marrow derived DC in vitro. In<br />
addition, CCL17 expressing DC are efficiently deleted in vivo after application of DT to<br />
CCL17/DTR mice. To analyse the role of CCL17 expressing DC in TH1 versus TH2 driven<br />
immune responses we backcrossed CCL17/DTR mice to a C57Bl/6 or Balb/c<br />
background, respectively. Surprisingly, we observed a significantly reduced size of<br />
mesenteric lymph nodes and Peyer’s Patches in Balb/c CCL17/DTR mice compared to<br />
C57Bl/6 CCL17/DTR mice and littermate controls, presumably resulting from enhanced<br />
expression of the DTR-EGFP fusion protein in dendritic cells of Balb/c mice. The<br />
functional effects of CCL17 positive DC ablation in innate and adaptive immune<br />
responses are currently under investigation.
Katharina A. Remer, Calin Apetrei, Tobias Schwarz, Heidrun Moll<br />
Induction of a local Th1 response after plasmacytoid dendritic<br />
cell-based vaccination protects mice against infection with<br />
Leishmania major<br />
Protective immunity against the protozoan parasite Leishmania is attributed to the<br />
development of a Th1-type T-cell response, while a Th2-type response results in<br />
progressive disease cumulating in lethal visceral leishmaniasis. Since distinct DC<br />
subsets have been proposed to direct the predominant development of either Th1- or<br />
Th2 T-cell responses, we analyzed the capability of plasmacytoid DC (pDC) to induce<br />
protection and elicit a Th1 response against Leishmania major in susceptible mice.<br />
Pulsing with L. major lysate induced the activation and maturation of murine pDC that<br />
had been isolated from the spleen, as indicated by up-regulation of co-stimulatory<br />
molecules. Vaccination of susceptible mice with L. major lysate-loaded pDC induced<br />
highly effective immunity against a challenge infection with L. major parasites.<br />
Surprisingly, the protection was not accompanied by a polarized systemic Th1 cytokine<br />
profile, although protected mice had a lower ratio of Leishmania-specific IgG1 to IgG2a<br />
than mock-treated controls. In contrast, upon restimulation with L. major lysate, cells<br />
from lymph nodes draining the infected lesions showed a higher IFN-γ to IL-10 ratio<br />
than the mock-treated controls, indicating the compartmentalized induction of a local<br />
Th1-type response. The protective immune response induced by vaccination with<br />
antigen-loaded pDC is mediated by T cells, since adoptive transfer of T cells from<br />
protected mice confers <strong>complete</strong> protection against a challenge infection with L. major<br />
promastigotes to naïve susceptible mice. Again, a local Th1-biased response in the<br />
presence of a systemic mixed Th1/Th2 response was sufficient to protect susceptible<br />
animals against an otherwise lethal infection with L. major. These findings demonstrate<br />
that vaccination with antigen-loaded pDC is able to induce a protective immune<br />
response against a parasite disease that is mediated by T cells, but unexpectedly<br />
compartmentalized. Our study underlines that experimental leishmaniasis is a suitable<br />
model to elucidate the mechanisms underlying DC-based vaccination against infections.
Christine Warmbold, Arthur Ulmer, Thomas Roeder<br />
Induction of inflammatory signal transduction pathways in a<br />
Drosophila-derived cell line<br />
The innate immune system of Drosophila has been introduced as a system for analysing<br />
basic aspects of inflammation. This includes the discovery of two different signal<br />
transduction pathways, the Toll-pathway and the IMD-pathway. The Toll-pathway is<br />
said to response principally to infections with Gram-positive bacteria whereas the IMDpathway<br />
answers mainly to infection with Gram-negative bacteria. Well described<br />
ligands for these pathways are for example peptidoglycans and LPS. In vertebrates<br />
bacterial lipopeptides are well known ligands for the Tol-like receptor 2. Now we have<br />
investigated that these bacterial compounds are also recognized by the Drosophila<br />
immune system.<br />
For our analysis we use the cell line SL2 which is a macrophage-like, epithelial cell line<br />
isolated from emryos of the D.m. strain Oregon R.<br />
In this studies the lipopeptides Pam2C-SK4 and Pam3C-SK4 are discovered as new<br />
ligands for the two pathways (Toll and IMD). Our knowledge is based on luciferase<br />
reporter assays. Here, a Firefly-luciferase is under the control of promotors for<br />
antimicrobial peptides that are activated by one of these pathways, namely drosomycin<br />
by the Toll-pathway and diptericin by the IMD-pathway. The data are normalised by the<br />
constitutively expressed Renilla-luciferase.<br />
By using real-time PCR and RNAi-experiments we will confirm our current data and look<br />
for crosstalks between these two pathways.<br />
(supported by SFB TR 22, A7)
Julia Strebovsky, Claus Kaiser, Alexander Dalpke, Klaus Heeg, Holger Bartz<br />
Induction of regulatory T-cells by Toll-like receptor-ligand<br />
derived deviant dendritic cells<br />
Dendritic cells (DCs) are professional antigen-presenting cells (APCs) which are the<br />
most potent stimulators of T-cell (TC) responses. In vitro human CD14+ monocytes can<br />
be differentiated into DCs by stimulation with granulocyte- macrophage- colony-<br />
stimulating factor (GM-CSF) and Interleukin-4 (IL-4). Further maturation is achieved by<br />
subsequent TLR-stimulation (which mimics microbial encounter) or CD40 ligation.<br />
However, these DC precursor cells also express TLRs (Toll-like receptors), thus they are<br />
sensitive to TLR stimulation not only during the maturation but also during the<br />
differentiation period.<br />
Here we analyzed the effects of TLR stimulation during the process of GM-CSF-<br />
mediated in vitro generation of DCs from precursor cells. Precursor cells of DCs which<br />
encounter microbial TLR-dependent stimuli in an early developmental stage<br />
differentiated into deviant DCs. Those aberrantly generated DCs showed reduced<br />
expression of CD1a, modified co-stimulatory molecule and reduced cytokine expression.<br />
They induced less T-cell proliferation in an allogenic MLR. However, deviant DCs had an<br />
increased expression of PD-ligands suggesting a role in the induction of Tregs. Thus we<br />
focused on the characterization of TC-responses induced by deviant DCs and<br />
determined the induction of Tregs which are proven to hold a regulatory capacity.<br />
Moreover, this regulatory function is shown to be dependent on the presence of IL-2<br />
which in turn leads to the phosphorylation of STAT5 and the expression of FoxP3.In<br />
summary we show that early TLR stimulation results in deviant DCs which are shown to<br />
be potent inducers of Tregs. These findings suggest a model for down-regulation of<br />
adaptive immune responses by deviant DCs/Tregs in late-stage infection which will be<br />
presented.
Ria Baumgrass, Vladimir Pavlovic, Britta Lamottke, Maria Lexberg, Joachim Grün, Uwe<br />
Niesner, Andreas Radbruch<br />
Induction of Treg cells by manipulation of TCR signalling<br />
The molecular mechanisms regulating induction of Treg cells are unknown. Recent data<br />
show that peripheral Treg cells can be induced by concomitant stimulation of<br />
transforming growth factor beta (TGF-beta) and T cell receptors (TcR). We found the<br />
TGF-beta interacting factor (TGIF) to be a candidate modulator of this process. TGIF is<br />
expressed by TcR stimulation and acts as a transcriptional repressor of TGF-beta<br />
signalling. Impaired TcR signalling by low-dosed CsA leads to a low expression of TGIF<br />
and therefore to Treg cell induction even at very low concentrations of TGF-beta. The<br />
induced Treg cells are immunosuppressive both, in vitro and in vivo. TGIF knock-down<br />
by TGIF-siRNA induced Treg cells from naïve Th cells. Altogether our data provide<br />
evidence that TGIF acts as a regulator of TGF-beta dependent Treg cell induction.<br />
Therefore it is a potential novel target molecule for therapeutic manipulation toward<br />
Treg cell induction in autoimmune diseases.
Stephan Fricke, Nadja Hilger, Manuela Ackermann, Peter Ruschpler, Lutz Uharek,<br />
Guido Hildebrandt, Jan Matthias Braun, Frank Emmrich<br />
Induction of xenogenic acute graft versus host disease<br />
(aGvHD) in mice<br />
Introduction: Acute graft versus host disease (aGvHD) is one of the major causes of<br />
unsuccessful haematopoietic stem cell transplantation. aGvHD occurs approximately to<br />
40%-70% in all cases and is initiated by “supravital” donor T lymphocytes which<br />
recognize the minor or major histocompatibility antigens of a recipient. Until now, no<br />
standard therapy for steroid refractory aGvHD is available. The development of new<br />
therapeutic strategies (anti T cell antibodies or cellular therapeutics) and protocols<br />
presumes suitable animal models.<br />
Aims: The induction of graft versus host disease in a murine xenograft model by<br />
intravenous transfer of human peripheral blood mononuclear cells in human CD4+,<br />
murine CD4-, human DR+ triple transgenic and wild-type mice should be investigated.<br />
Methods: Induction and severity of aGvHD in wild-type (C57/Bl/6) and triple transgenic<br />
human CD4+, murine CD4- and human DR+ mice were investigated. Mice received<br />
chemotherapy (cyclophosphamide and treosulfan) on day -3 to -1 before intravenous<br />
transplantation of human PBMCs. All experimental groups were daily examined for<br />
GvHD symptoms (severe weight loss [>10%], hunched posture, ruffled fur, reduced<br />
mobility, tachypnoea). For determination of leucocytes by FACS and cytokines by CBA<br />
blood of all mice were weekly collected by retro orbital bleeding. Finally, histological<br />
examination of gut and spleen were added.<br />
Results: By using of the triple transgenic human CD4+, murine CD4-, human DR+ mice<br />
an acute xenogenic GvHD syndrome could be observed. In contrast, wild-type mice did<br />
not show a GvHD syndrome (clinical scoring and histology).<br />
Conclusion: Our results show the induction of xenogenic aGvHD in DR+ transgenic mice<br />
while MHC-wild-type mice did not develop GvHD. In terms of application of monoclonal<br />
antibodies as therapeutic potentiality should be considered that they have to be<br />
produced for specific human epitopes. Therefore, the used humanised triple transgenic<br />
mouse model is advantageously as interaction of human cell surface molecules could be<br />
simulated.
Uta Bussmeyer, Arup Sarkar, Kirsten Broszat, Ger van Zandbergen, Christian Bogdan,<br />
Werner Solbach, Friederike von Loewenich, Tamás Laskay<br />
Infection with Anaplasma phagocytophilum inhibits IFN-<br />
&gamma signaling in human neutrophils<br />
Anaplasma phagocytophilum (Ap) is a tick-borne obligate intracellular bacterium that<br />
survives and multiplies inside polymorphic neutrophilic granulocytes (PMN). Previous<br />
findings demonstrated that the bacterium actively subverts antimicrobial effector<br />
mechanisms of PMN including the oxidative burst after priming with IFN-&gamma. The<br />
present study aimed to investigate whether an infection with Ap leads to a more general<br />
impairment of IFN-&gamma signaling in PMN that enables intracellular survival of the<br />
bacterium.<br />
The capability of Ap to interfere with IFN-&gamma-mediated activation of PMN was<br />
assessed by measuring MIG and IP-10 secretion. Neutrophils secreted substantial levels<br />
of both chemokines when stimulated with IFN-&gamma for 18h. Infection of PMN with<br />
Ap markedly decreased the secretion of MIG and IP-10 by PMN. To obtain first insights<br />
into the molecular events leading to the diminished secretion of IFN-&gamma-induced<br />
chemokines, the phosphorylation of STAT1 was investigated. Western blot analysis<br />
revealed that IFN-&gamma-induced STAT1 phosphorylation was diminished in Apinfected<br />
PMN. In further experiments flow cytometry analyses showed a markedly<br />
decreased expression of the IFN-&gamma receptor alpha chain CD119 on the surface of<br />
Ap-infected PMN. Moreover, using quantitative RT-PCR a strong upregulation of the<br />
negative regulator SOCS3 was observed in infected cells.<br />
Taken together our data show that infection with Anaplasma phagocytophilum results in<br />
a decreased CD119 surface expression, diminished tyrosine phosphorylation of STAT1<br />
and augmented SOCS3 gene expression in infected cells and, consequently, results in<br />
compromised IFN-&gamma-responsiveness of infected PMN. Impaired IFN-&gamma<br />
signaling in infected cells is likely to contribute to intracellular survival of Ap in PMN.
Vilma Urbonaviciute, Barbara G. Fürnrohr, Silke Meister, Petra Heyder, Martin<br />
Herrmann, Joachim R. Kalden, Reinhard E. Voll<br />
Inflammation and immune activation by HMGB1-nucleosome<br />
complexes – implications for the etiopathogenesis of systemic<br />
lupus erythematosus<br />
Pathogenic autoantibodies against dsDNA and nucleosomes (NCs) represent a hallmark<br />
of systemic lupus erythematosus (SLE). However, the factors breaking the<br />
immunological tolerance are not fully identified. An important initial step in the<br />
immunopathogenesis may involve impaired phagocytosis of apoptotic cells with a<br />
consecutive release of nuclear antigens. The nuclear DNA-binding protein and<br />
proinflammatory cytokine high mobility group box protein 1 (HMGB1) gets tightly<br />
attached to chromatin of apoptotic cells and is not released, since apoptotic cells are<br />
immediately engulfed by phagocytes. We hypothesized, that in case of clearance<br />
deficiency ”endogenous adjuvant” HMGB1 in complex with NCs can be released and may<br />
foster an autoimmune response towards NCs, a crucial autoantigen in SLE.<br />
We found that HMGB1 remains bound to NCs released from apoptotic cells in vitro . Also<br />
in sera and plasma of some patients with SLE, but not in controls, complexes of HMGB1<br />
and NCs were detected. Importantly, HMGB1 containing NCs from apoptotic cells<br />
induced secretion of cytokines including IL-1β, IL-10, and TNFα as well as expression of<br />
costimulatory molecules on human macrophages and dendritic cells (DC), respectively.<br />
Neither HMGB1-free NCs from living cells nor from apoptotic HMGB1- or HMGB1/2deficient<br />
cells induced marked cytokine production or DC activation. Additionally,<br />
specific inhibition of HMGB1 activity by antagonistic A box domain significantly reduced<br />
capacity of “apoptotic “ NCs to induce TNFα and IL-10 release by macrophages.<br />
We conclude that HMGB1 in complex with NCs activate antigen presenting cells thereby<br />
contributing to breaking of the immunological tolerance against nuclesomes/dsDNA and,<br />
hence, to the immunopathogenesis of SLE.
Simone Vallbracht, Birthe Jessen, Sonja Mrusek, Anselm Enders, Peter L. Collins,<br />
Christine D. Krempl, Stephan Ehl<br />
Influence of a single viral epitope on T cell response and<br />
disease after infection of mice with respiratory syncytial virus<br />
Cytotoxic T cells (CTL) are important for virus clearance, but also contribute to<br />
immunopathology after infection of BALB/c mice with respiratory syncytial virus (RSV).<br />
The pulmonary immune response to RSV is dominated by a CTL population directed<br />
against the CTL epitope M2-1 82-90. Infection with a virus carrying a M2-1 N89A<br />
mutation introduced by reverse genetics failed to activate this immunodominant CTL<br />
population leading to a significant decrease in the overall antiviral CTL response. There<br />
was no compensatory increase in responses to the mutated neoepitope, to the<br />
subdominant epitope F 85-93 or to yet undefined minor epitopes in the N or the P<br />
protein. However, there was some increase in the response to the subdominant epitope<br />
M2-1 127-135 which is located in the same protein and presented by the same H-2Kd<br />
MHC molecule. Infection with the mutant virus reversed the oligoclonality of the T cell<br />
response elicited by the wild type virus. These changes in the pattern and composition<br />
of the antiviral CTL response only slightly impaired virus clearance, but significantly<br />
reduced RSV induced weight loss. These data illustrate how T cell epitope mutations can<br />
influence the virus-host relationship and determine disease after an acute respiratory<br />
virus infection.
Torsten Lowin, Rainer H. Straub, Olga Wiesner, Ulf Müller-Ladner, Jörg Schedel<br />
Influence of cortisol on the expression of integrins and<br />
intracellular signaling molecules in synovial fibroblasts in<br />
rheumatoid arthritis<br />
Purpose: In rheumatoid arthritis (RA) synovial fibroblasts (SF) are localized at sites of<br />
invasion of the hyperplastic synovial tissue into cartilage and bone, and are able to<br />
degrade the extracellular matrix (ECM). Integrins mediate adhesion of SF to ECM<br />
components and influence outside-in and inside-out signaling pathways. As cortisol<br />
levels are relatively low in chronic inflammation, we examined the influence of different<br />
cortisol concentrations on the expression of integrins in SF. Furthermore, we<br />
investigated if cortisol alters intracellular signaling pathways which could, in turn,<br />
influence the invasive behaviour of RA-SF.<br />
Methods: Synovial tissue samples from patients with RA and osteoarthritis (OA)<br />
obtained during arthroplastic surgery were examined using immunofluorescence (IF)<br />
with anti-alpha5, -alphaν, -alpha5beta1 and anti-beta1 integrin antibodies. To<br />
characterise the expression profile quantitatively, fluorescence intensity was analysed in<br />
pixels/cell at the site of invasion and the cartilage-remote region. Isolated RA- and OA-<br />
SF were incubated with decreasing cortisol concentrations ranging from 10-5 M to 10-9<br />
M. Integrin expression was evaluated 24 h after stimulation by FACS analysis and<br />
quantitative PCR (qPCR). To evaluate the specificity of cortisol on integrins,<br />
cycloheximide (10 µg/ml) and the glucocorticoid receptor antagonist mifepristone (10-5<br />
M) were used. The activation of intracellular signaling molecules was determined by a<br />
"cellular activation of signaling ELISA"(CASE).<br />
Results: IF showed enhanced expression of alpha5, -alphaν, -beta1 integrins at the site<br />
of invasion in RA synovial tissue compared to OA synovial tissue. The increase of<br />
integrin expression in RA was greater than in OA varying from 24 % up to 61 %<br />
Treatment of isolated RA- and OA-SF with cortisol resulted in a concentrationdependent<br />
upregulation of target integrins with the highest effect seen at 10-5 and 10-6<br />
M as demonstrated by FACS analysis and qPCR. The effect was abrogated when either<br />
10 µg/ml cycloheximide or the glucocorticoid receptor antagonist mifeprestone (10-5 M)<br />
were present. CASE showed an activation by phosphorylation of the intracellular<br />
signaling kinases ERK, Src, p38 and PI3K upon integrin crosslinking. The presence of 10-<br />
6M cortisol resulted in a 50 % reduction of kinase phosphorylation.<br />
Conclusions: In RA, integrins were expressed at the site of invasion to an enhanced<br />
extent when compared to OA samples. The expression pattern suggests a functional<br />
role of the investigated integrins in cartilage and bone invasion in RA. Cortisol upregulated<br />
alpha5 and beta1 integrin expression in a dose-dependent manner. This fact<br />
and the decreased phosphorylation of intracellular signaling molecules after cortisol<br />
treatment might lead to a less invasive phenotype of RA-SF.
Veronika Lukacs-Kornek, Verena Semmling, Christian Kurts<br />
Influence of Cross-Presentation via CCR7<br />
Cross-presentation of extracellular antigens plays an important role in inducing<br />
cytotoxic immune responses against bacteria and viruses, as well as in maintaining CD8<br />
T cell tolerance against self antigens. It requires cellular contact between several rare<br />
immune cells, such as specific CD8 T cells, specific CD4 T cells and cross-presenting<br />
dendritic cells. Such encounters are usually regulated by chemokines and their<br />
receptors. These mediators can guide immunocytes towards one destination, where<br />
their encounters become more likely or can affect cellular function important in cross<br />
priming. In the present study, we describe a role of a chemokine, CCL19, which signals<br />
through CCR7, in cross-presentation.<br />
Using CCR7-deficient mice we demonstrated that CCR7 decreased activation of CD8 T<br />
cells by cross priming of cell-associated and of soluble antigens in vivo. To identify the<br />
cells affected by CCR7 ligands during cross-presentation, we established an in vitro<br />
cross-presentation assay. We could show that addition of CCL19 to the culture resulted<br />
in increased cross-presentation, as evidenced by higher expression of early activation<br />
markers such as CD69 and CD25 and elevated amounts of IL-2 produced by specific<br />
CD8 T cells. CCR7 did not affect the antigen uptake capacity of dendritic cells (DC) in<br />
vitro. Furthermore, selective CCR7-deficiency in DC did not prevent the stimulatory<br />
effect of CCL19 on CD8 T cell activation. However, this effect was <strong>complete</strong>ly abolished<br />
when CCR7-/- CD8 T cells were used. Therefore the increased activation of CD8 T cells<br />
during cross-presentation was exclusively mediated by a direct effect of CCL19 on the<br />
CD8 T cells. Future efforts are aimed identifying the intracellular mechanisms employed<br />
by CCL19 to stimulate CD8 T cells.
Birgit Weinberger, Ilka Weiskirchner, Beatrix Grubeck-Loebenstein<br />
Influence of latent infection with Cytomegalovirus on Epstein-<br />
Barr viral parameters in healthy elderly individuals: possible<br />
interaction of different herpesviruses in immunosenescence<br />
Latent infection with CMV leads to acceleration and enhancement of age-related<br />
immunological changes. The influence of other herpesviruses like Epstein-Barr virus<br />
(EBV) on immunosenescence seems to be less pronounced. Presumably, there are also<br />
interactions between different herpesviruses and the corresponding immune responses<br />
in the elderly.<br />
Antibody titers and viral load in whole blood were analyzed for CMV and EBV in 233<br />
healthy elderly donors (>60 years) and EBV-parameters were compared in CMV-positive<br />
and CMV-negative individuals.<br />
We could show that EBV-DNA load in whole blood is significantly higher in CMV-positive<br />
elderly individuals and that slightly elevated DNA-levels are seen almost exclusively in<br />
CMV-positive persons. A positive correlation of titers of EBV-specific antibodies with EBV-<br />
DNA load was only observed in CMV-positive elderly donors. No such correlation was<br />
observed in the CMV-negative cohort.<br />
We conclude that EBV-infection is less controlled by the cellular immune response in<br />
elderly individuals with latent CMV-infection.
Sandra Martina Dittrich, Elfriede Noessner, Hans Demmelmair, Gernot Desoye, Dolores<br />
Schendel, Berthold Koletzko, Susanne Krauss-Etschmann<br />
Influence of n3/n6 polyunsaturated fatty acids on placental<br />
immune responses<br />
Introduction<br />
N3/n6-long chain polyunsaturated fatty acids (LC-PUFA) modulate immune responses.<br />
In addition, docosahexaenoic acid (n3, DHA) and arachidonic acid (n6, AA) are<br />
important for the neural development and selectively transported to the fetus. However,<br />
it is unknown how n3/n6-LC-PUFA affect placental immune responses.<br />
Material and methods<br />
Basal mRNA expression levels of IL-6, IL-8, IL-12, TGF-β, MCP-1 and RANTES were<br />
quantified in choriocarcinoma lines (ACH-3P, BeWo, JAR, JEG) and eight non-placental<br />
carcinoma lines by real time RT-PCR (iCycler, Fa. Biorad). Selected cell lines were<br />
incubated with 1•M, 10•M and 100•M DHA, eicosapentaenoic acid (EPA) and AA using<br />
monounsaturated oleic acid (OA) and saturated palmitic acid (PA) as controls. Cytokine<br />
expression patterns and the cell proliferation rate (cellscreen, Fa. Innovatis) were<br />
determined after 1h, 6h, 24h and 48h.<br />
Results<br />
Basal mRNA expression levels of IL-6, IL-8, TGF-β, MCP-1 and RANTES were<br />
comparable in JAR, ACH-3P, RCC 26 (renal cell carcinoma) and MCF-7 (mamma<br />
carcinoma). IL-12 mRNA was detectable only in BeWo, Du 145 (prostate carcinoma)<br />
and HEK 293 (human, adenovirally immortalised embryonic kidney cell line). PA<br />
increased the proliferation rate of JAR and MCF-7. EPA increased the proliferation rate of<br />
JAR. PA and OA slightly increased IL-6 and RANTES mRNA expression levels, while EPA<br />
decreased IL-6 mRNA expression levels in JAR. There was no effect of any fatty acid on<br />
RCC 26.<br />
Conclusion<br />
Choriocarcinoma lines had heterogeneous cytokine expression patterns. Even very<br />
related choricarcinoma lines showed clear differences. EPA, PA and OA modulated<br />
proliferation rates and cytokine expression levels. However, the changes were small and<br />
need further confirmation.
Stephan Sudowe, Karina Gisch, Nadine Gehrke, Matthias Bros, Christina Priesmeyer,<br />
Angelika B. Reske-Kunz<br />
Inhibition of allergic sensitization and suppression of Th2mediated<br />
airway inflammation by application of formalinfixed<br />
Staphylococcus aureus-particles<br />
Background: Bacterial infections are supposed to act counterregulatory to the<br />
development of allergen-specific Th2 immune responses. We analyzed whether<br />
administration of extracellular Staphylococcus aureus inhibited sensitization against<br />
allergens in a mouse model of type I allergy. Methods: BALB/c mice were immunized<br />
with alum-adsorbed ovalbumin (OVA) together with formalin-fixed Staphylococcus<br />
particles. OVA-specific antibody production and cytokine synthesis by spleen cells was<br />
analyzed. Airway reactivity and cellular infiltration into the airways was assessed after<br />
intranasal challenge of mice with OVA. In addition, the capacity of Staphylococcus<br />
particles to modulate cytokine production by bone marrow-derived dendritic cells was<br />
analyzed in vitro. Results: Simultaneous application of OVA and Staphylococcus<br />
particles very efficiently inhibited production of specific IgE and IgG1 as well as<br />
secretion of IL-4 and IL-5 by splenocytes, while enhancing IgG2a formation and<br />
production of IFN-γ, indicating a shift from a Th2 response towards a Th1-biased<br />
response. This effect was not dependent on the expression of protein A by<br />
Staphylococcus. Treatment of mice with Staphylococcus particles during the<br />
sensitization phase attenuated Th2-dependent inflammatory reactions in the lung<br />
(airway hyperreactivity, eosinophilia) after local challenge with OVA. Culture of bone<br />
marrow-derived dendritic cells with Staphylococcus particles induced IL-12p35 and p40<br />
mRNA expression as well as secretion of IL-12p70, and increased production of IL-10<br />
mRNA and protein. However, an enhanced frequency or activity of regulatory T cells<br />
after administration of Staphylococcus particles was not apparent. Conclusions:<br />
Application of formalin-fixed Staphylococcus particles induced Th1-biased immune<br />
responses and prevented allergic sensitization as well as symptoms of allergic airway<br />
inflammation.
Tobias Frankenberg, Susanne Kirschnek, Hans Häcker, Uwe Koedel, Georg Häcker<br />
Inhibition of apoptosis conserves neutrophil effector function<br />
and can contribute to inflammation in vivo<br />
Neutrophil granulocytes have essential functions during immune responses against<br />
pyogenic bacteria. Following pathogen clearance, neutrophils have to be removed from<br />
sites of infection, a process that may involve apoptosis. We have previously found that<br />
in a murine model of Streptococcus pneumonia-induced meningitis, overexpression of<br />
the anti-apoptotic protein Bcl-2 in the haematopoietic system aggravates inflammationinduced<br />
tissue damage. The continued presence of neutrophils in these mice despite<br />
clearance of bacteria suggested that the block of apoptosis caused sustained pleocytosis<br />
and contributed to the severity of the inflammation. To test this hypothesis, we<br />
compared in vitro apoptosis and effector function of wt and Bcl-2 overexpressing<br />
neutrophils derived from isolated bone-marrow progenitor cells retrovirally transduced<br />
with regulable Hoxb8. In its active state, Hoxb8 promotes progenitor expansion while<br />
upon inactivation permits cellular differentiation. This culture system thus provides the<br />
possibility to generate almost unlimited numbers of ‘near-primary’ neutrophils.<br />
Differentiated Hoxb8 neutrophils displayed the typical nuclear morphology, expressed<br />
Gr-1, and were phagocytosis-proficient. No obvious differences in terms of<br />
differentiation and effector functions were observed between wt and Bcl-2 neutrophils.<br />
Upon prolonged culture the vast majority of differentiated wt neutrophils underwent<br />
apoptosis. The overexpression of Bcl-2 efficiently protected neutrophils from cell death<br />
and, importantly, these ‘undead’ cells retained at least some of their effector functions.<br />
These data show that inhibition of apoptosis can prolong neutrophil lifespan and effector<br />
function, which very likely contributes to the more severe pathology in Streptococcus<br />
pneumonia-induced murine meningitis. This model therefore suggests that granulocyte<br />
apoptosis is an important event for the termination of the innate immune response.
Martin Raftery, Günther Schönrich<br />
Inhibition of CD1 Antigen Presentation by Human<br />
Cytomegalovirus<br />
The betaherpesvirus human cytomegalovirus (HCMV) encodes many molecules that<br />
block classical and nonclassical MHC molecules. No interaction has been reported,<br />
however, between HCMV and the only family of nonclassical MHC class I molecules, the<br />
CD1 family. The CD1 family is particularly interesting as they are present almost<br />
exclusively on professional antigen presenting cells such as dendritic cells (DC), which<br />
are in turn a major target for HCMV infection and latency. Furthermore a relationship<br />
between CD1 antigen presentation and antiviral immunity has recently been<br />
established. We have determined that HCMV encodes multiple blocking strategies<br />
targeting group 1 CD1 molecules. HCMV-encoded cmvIL-10 strongly downregulates CD1<br />
transcription, as does human and ebvIL-10. HCMV also blocks CD1 antigen presentation<br />
post-transcriptionally. This function is not encoded by a known HCMV MHC blocking<br />
molecule, and requires the cytoplasmic domain of the CD1 molecule. The HCMV block is<br />
particularly effective against CD1b, whereas in comparison HSV1-induced block is weak.<br />
This preferential block implies a role for CD1b in antiviral immunity.
Dorit Fabricius, Sue O’Dorisio, Sue Blackwell, Bernd Jahrsdörfer, Klaus-Michael Debatin<br />
Inhibition of IFN-α Secretion and Modulation of<br />
Immunophenotype and Stimulatory Capacity of Human<br />
Plasmacytoid Dendritic Cell by Vasoactive Intestinal Peptide<br />
Plasmacytoid dendritic cells (PDC) represent a central link between innate and adaptive<br />
immunity. The special feature of PDC compared to other DC subsets is that they not<br />
only are capable of antigen presentation but also unite the capacities of high IFN-α and<br />
Granzyme B production. The increased frequency in various tumor tissues and in sites<br />
of active autoimmune processes reflects an essential role of PDC both for tumor and<br />
auto-immunity. While the role of granzyme B secretion by PDC is still unclear, excessive<br />
IFN-α production seems to be a key factor in driving pathogenesis in certain<br />
autoimmune diseases, mainly systemic lupus erythematodes. A better understanding of<br />
PDC regulation is therefore crucial for more effective immunotherapeutic approaches to<br />
cancer and autoimmunity. We show here that the neuropeptide vasoactive intestinal<br />
peptide (VIP) significantly down-regulates IFN-α secretion by PDC and modulates PDC<br />
immunophenotype. Furthermore, VIP inhibits the potential of PDC to induce proliferation<br />
of allogeneic CD4+ T cells and VIP-treated PDC decrease the ratio of IFN-γ to IL-4<br />
secreted by CD4+ T cells. We also demonstrate that PDC actively secrete the cytotoxic<br />
molecule granzyme B, and that this process can be regulated by VIP and cytokines such<br />
as interleukin 21 (IL-21). We conclude that modulation of PDC by VIP may be one<br />
possible escape mechanism of malignancies that secrete this neuropeptide. In contrast,<br />
VIP may turn out to be an exciting new candidate for immunotherapeutic intervention in<br />
autoimmune diseases, since it suppresses the pathogenetically critical IFN-α secretion<br />
and the T cell-stimulatory capacity of PDC.
Rainer Glauben, Arvind Batra, Thorsten Stroh, Elena Sonnenberg, Inka Fedke, Hans<br />
Anton Lehr, Paolo Mascagni, Martin Zeitz, Britta Siegmund<br />
Inhibition of NF-κB by histone deacetylase inhibitors in<br />
models of inflammation-related tumorigenesis<br />
Histone deacetylase inhibitors (HDACi) have been described initially for their antiproliferative<br />
effect in cell lines as well as in models of experimental tumor growth. In<br />
addition, recent studies from our group provide evidence for an anti-inflammatory<br />
potency of HDACi by using various models of experimental colitis. To characterize the<br />
combined effect of the anti-inflammatory and anti-proliferative potency of HDACi in<br />
vivo, the AOM/DSS-model as well as the IL-10KO-model of inflammation-mediated<br />
colon carcinogenesis were applied. The HDACi SAHA and ITF2357 were administered<br />
throughout the entire experimental period via oral gavage and the progression of<br />
tumorigenesis was monitored by lower endoscopy. In both models, HDACi treatment<br />
resulted in a delay of tumor development as evaluated by endoscopy and histology. In<br />
addition, the absolute number of adenomas was significantly reduced in the HDACitreated<br />
groups when compared to vehicle-treated animals as determined by histology.<br />
Remarkably, the strongest suppression of tumorigenesis was observed in animals<br />
treated with ITF2357. Recently it was descibed that the transcription factor NF-κB acts<br />
as a key factor within the process of inflammation-linked carcinogenesis. Furthermore,<br />
several studies indicate that inhibition of HDAC affects the NF-κB pathway. To further<br />
explore the mechanistic effects of HDACi treatment in the employed models of<br />
tumorigenesis, nucleus extraction experiments from colon sections of the ITF2357<br />
treated as well as untreated AOM/DSS-exposed mice were performed. These<br />
experiments indicate, that the HDACi treatment inhibits the translocation of p65, a<br />
subunit of NF-κB, into the nucleus. Consequently, the inhibition of tumor development<br />
by HDACi is paralleled by a profoundly reduced activation of NF-κB at the site of<br />
inflammation. Since inflammatory bowel disease (IBD) in humans is associated with an<br />
increased risk of colorectal cancer, a pharmacological strategy exerting antiinflammatory<br />
as well as anti-proliferative properties would be highly intriguing for the<br />
long-term therapy in IBD.
Dirk Reinhold, Alexander Goihl, Bianca Guth, Uwe Lendeckel, Ute Bank, Michael Täger,<br />
Siegfried Ansorge, Jürgen Faust, Klaus Neubert, Stefan Brocke<br />
Inhibitors of dipeptidyl peptidase IV (DP IV, CD26)-like and<br />
of aminopeptidase N (APN, CD13) enzymatic activity suppress<br />
human T cell activation and IL-17 production in vitro and in<br />
vivo<br />
Peptidases like dipeptidyl peptidase IV (DP IV, CD26) and aminopeptidase N (APN,<br />
CD13) play a regulatory role in T cell activation and represent potential targets for the<br />
treatment of inflammatory disorders. Compelling evidence has recently demonstrated<br />
that IL-17-producing CD4 cells (Th17 cells) are a major contributor to the pathogenesis<br />
of autoimmune inflammation. Since we and others have previously shown that synthetic<br />
inhibitors of DP IV-like enzymatic activity and of APN suppress disease in models of<br />
autoimmunity, we tested the hypothesis that these inhibitors target the production of IL-<br />
17. Here, we demonstrate that the inhibitors of DP IV-like activity, Lys[Z(NO2 )]thiazolidide<br />
and Lys[Z(NO2 )]-pyrrolidide, as well as the APN inhibitor actinonin inhibit IL-<br />
17 production and IL-17 mRNA expression in human mitogen-stimulated T cells.<br />
Moreover, combining DP IV and APN inhibitors increases the suppressive effect on T cell<br />
proliferation and IL-17 production in vitro in comparison to a single peptidase inhibitor.<br />
In order to investigate the mechanism by which peptidase inhibitors limit autoimmune<br />
disease in vivo, we tested the effect of DP IV and APN inhibitors on IL-17 production in<br />
experimental autoimmune encephalomyelitis (EAE), an animal model of multiple<br />
sclerosis. Our results show that IL-17 plasma levels are decreased in EAE mice treated<br />
with combined peptidase inhibitors.<br />
Collectively, our data suggest that combined inhibition of DP IV-like and APN enzymatic<br />
activity in pathogenic T cells represents a novel and efficient therapeutic approach<br />
targeting IL-17 production in autoimmunity.
Simone Klöter, Max v. Holleben, Bernhard Reis, Klaus Pfeffer, Sandra Beer<br />
Interaction analysis of the adaptor protein SLy2<br />
Adaptive immunity is crucial for protective host defense and the development of<br />
immunological disorders. An increasing number of molecules with SH2 or SH3 domains<br />
involved in the T or B cell receptor signal transduction pathways have been discovered<br />
in the last years.<br />
SLy2 (SH3 domain protein expressed in lymphocytes 2) was recently identified as an<br />
SH3- and SAM-domain containing protein. In humans, the SLy2 gene is located on<br />
chromosome 21, in mice on chromosome 16. SLy2 is expressed in hematopoetic tissues<br />
as well as in brain, lung and pancreas. Additionally, SLy2 is up-regulated in activated<br />
human B cells treated with IL-4, CD40L and anti-IgM. Therefore, SLy2 might be a<br />
component of signalling cascades that lead to B cell activation and differentiation.<br />
To elucidate the function of SLy2 we screened for possible interaction partners of this<br />
adaptor protein. Considering the fact that SH3- and SAM-domains can mediate<br />
homodimerization of proteins we performed coimmunoprecipitations with differentially<br />
tagged SLy2 constructs. We were able to show the formation of SLy2 homodimers in<br />
293T cells via the SH3 domain.<br />
In order to identify further interaction partners of SLy2 a Yeast Two Hybrid Screen with<br />
a mouse T cell lymphoma library was carried out. This resulted in two putative<br />
interaction partners of SLy2: Sin3-associated polypeptide p30 (SAP30) and ribosomal<br />
protein L12 (rpL12). SAP30 is a component of the histone deacetylase complex<br />
including HDAC1, HDAC2, mSin3 as well as other proteins and consequently is capable<br />
of repressing the transcription of different genes. rpL12 is associated with the assembly<br />
of the 40S and 60S subunit of eukaryotic ribosomes. The interactions of SLy2 with both<br />
proteins were confirmed by coimmunoprecipitations with lysates from transiently<br />
transfected 293T cells. This interaction of SLy2 with SAP30 and rpL12 insinuates<br />
transcriptional and/or translational regulatory functions of SLy2.
Pia Herzberger, Corinna Siegel, Christine Skerka, Volker Fingerle, Ulrike Schulte-<br />
Spechtel, Bettina Wilske, Volker Brade, Reinhard Wallich, Peter F. Zipfel, Peter Kraiczy<br />
Interaction of immune regulators factor H and FHL-1 with the<br />
Lyme disease spirochete Borrelia spielmanii sp. nov. is<br />
mediated by a plasmid-encoded complement regulatoracquiring<br />
surface protein-1<br />
Borrelia spielmanii sp. nov., one of the etiological agents of Lyme disease found in<br />
Europe escapes complement-mediated killing by recruitment of immune regulators<br />
factor H and FHL-1 from human serum. Serum-resistant and intermediate serumresistant<br />
isolates express up to three distinct complement regulator-acquiring surface<br />
proteins (CRASPs) that bind to factor H and/or FHL-1. Here we report identification and<br />
functional characterization of BsCRASP-1, the dominant factor H and FHL-1 binding<br />
protein of B. spielmanii. BsCPASP-1 is a 27.7 kDa outer surface lipoprotein, which after<br />
processing is predicted to be 24.9 kDa. The gene encoding BsCRASP-1 is a single<br />
genetic locus that maps to a linear plasmid of approximately 55 kb. Ligand affinity blot<br />
techniques revealed that both, native and recombinant BsCRASP-1 from different<br />
isolates, bind to FHL-1 and weaker to factor H. Deletion mutants of BsCRASP-1 were<br />
generated and a high affinity binding site for factor H and FHL-1 was mapped to a 10<br />
amino acid residue domain at the C-terminus of BsCRASP-1. Similarly, the predominant<br />
binding site of factor H and FHL-1 was localized to short consensus repeats 5 to 7.<br />
Factor H and FHL-1 maintain their cofactor activity for factor I-mediated C3b<br />
inactivation when bound to full-length BsCRASP-1 but not to a deletion mutant lacking<br />
more than 10 amino acid residues at its C-terminus. In conclusion, BsCRASP-1 binds<br />
the host immune regulators factor H and FHL-1 with high affinity and is the key<br />
molecule of the spirochetes’ complement resistance. Thus, BsCRASP-1 most likely<br />
contributes to persistence of B. spielmanii and to pathogenesis of Lyme disease. This<br />
work was funded by the Deutsche Forschungsgemeinschaft DFG, Project Kr3383/1-1<br />
and Wa533/7-1.
Nikola Baschuk, Olaf Utermöhlen, Roland Gugel, Gabriele Warnecke, Ulrike Karow,<br />
Daniela Paulsen, Frank Brombacher, Martin Krönke, Wolfgang Deppert<br />
Interleukin-4 impairs granzyme-mediated cytotoxicity of<br />
Simian virus 40 large tumor antigen-specific CTL in Balb/c<br />
mice<br />
In this report we analysed the impact of interleukin-4 (IL-4) on tumor-associated simian<br />
virus 40 (SV40) large T-antigen (TAg)-specific CD8 + cytotoxic T cells during rejection of<br />
syngeneic SV40 transformed mKSA tumor cells in Balb/c mice.<br />
Strikingly, challenge of naive mice with low doses of mKSA tumor cells revealed a CD8 +<br />
T cell-dependent prolonged survival time of naive IL-4 -/- mice.<br />
In mice immunized with SV40 TAg we observed in IL-4 -/- mice, or in wild type mice<br />
treated with neutralizing anti-IL-4 monoclonal antibody, a strongly enhanced TAgspecific<br />
cytotoxicity of tumor associated CD8 + T cells. The enhanced cytotoxicity in IL-<br />
4 -/- mice was accompanied by a significant increase in the fraction of CD8 + tumor<br />
associated T-cells expressing the cytotoxic effector molecules granzyme A and B and in<br />
granzyme B-specific enzymatic activity.<br />
The data suggest that endogenous IL-4 can suppress the generation of CD8 + CTL<br />
expressing cytotoxic effector molecules especially when the antigen induces only a very<br />
weak CTL response.
Michael Meyer-Hermann, Marc Thilo Figge<br />
Interpreting two-photon lymphocyte motility data of the<br />
germinal centre: Predictions and analysis by mathematical<br />
models<br />
The germinal centre reaction is central to adaptive immunity. Recent progress in<br />
intravital imaging has provided the first movies of cell trafficking in secondary lymphoid<br />
follicles [1]. The results of these measurements confirm predictions from our<br />
mathematical models [2]. In particular, it was predicted and now measured that B<br />
lymphocytes do not actively move between the zones. However, this result is not<br />
possible to be deduced from multi-photon measurements alone. It is essential that the<br />
data are interpreted with mathematical methods.<br />
We show how mathematical modelling of germinal centre reactions is useful to<br />
interprete multi-photon intravital imaging data in two steps: At first the models that led<br />
to the prediction of the undirected motility of lymphocytes are presented. It is shown<br />
that no directed motility is needed in order to get a fully functional germinal centre<br />
reaction. In a second step it is shown which results would be expected in multi-photon<br />
imaging when either undirected motility or directed movement between the zones is<br />
assumed. This clearly shows that the recent imaging results do not exhibit any link to<br />
active movement between the zones.<br />
[1] Allen CD, Okada T, Tang HL, Cyster JG, Science 26 (2007) 528;<br />
Schwickert et al., Nature 446 (2007) 83;<br />
Hauser et al., Immunity 2007 in press.<br />
[2] Meyer-Hermann M, J. Theor. Biol. 216 (2002) 273;<br />
Meyer-Hermann M, Maini PK 174 (2005) 2489;<br />
Meyer-Hermann M, Figge MT 2007 in preparation.
Astrid M. Westendorf, Wiebke Hansen, Jan Buer<br />
Intestinal antigen display promotes the peripheral induction<br />
of antigen specific CD8 + Foxp3 + T cells<br />
Little data exist regarding mechanisms of mucosal T cell reactivity or tolerance against<br />
the variety of antigens in the intestine. In contrast to antigen specific CD4 + regulatory T<br />
cells, the generation and function of immunomodulatory antigen-specific CD8 + T cells is<br />
less well defined. To dissect the immunologic mechanisms of CD8 + T cell function in the<br />
mucosa, reactivity to a self-antigen expressed in intestinal epithelium of mice bearing a<br />
MHC class-I-restricted T-cell-receptor specific for this antigen was studied. Here, we<br />
demonstrate that intestinal self-antigen expression leads to peripheral induction of<br />
antigen-specific CD8 + Foxp3 + T cells rather than the induction of cytotoxic CD8 +<br />
effector T cells and intestinal pathology. This induction is restricted to the mesenteric<br />
lymphnode and the lamina propria. Antigen-experienced CD8 + T cells in this transgenic<br />
mouse model are characterized by significantly upregulation of CD103, CD83, GPR83<br />
and granzyme A/B expression, molecules also expressed on regulatory CD4 + T cell<br />
subsets. Despite the fact that naïve and antigen-experienced CD8 + T cell exhibit the<br />
same proliferative capacity in vitro, CD8 + T cells from this transgenic mouse model<br />
produce much less IFN-gamma and no TNF-alpha after in vitro stimulation in<br />
comparison to naïve CD8 + T cells. In addtion, whereas naïve CD8 + T cells further<br />
aggravate CD4 + T cells proliferation in an inhibition assay CD8 + T cells isolated from<br />
this transgenic mouse model slightly reduce antigen-specific CD4 + T cell proliferation in<br />
vitro. In summary, we demonstrate that self-antigen expression of intestinal epithelial<br />
cells is sufficient to induce CD8 + regulatory T cells which maintain intestinal<br />
homeostasis by down-modulating effector functions of T cells.
Ilka Knippertz, Andrea Hesse, Eckhart Kaempgen, Gerold Schuler, Alexander<br />
Steinkasserer, Dirk. M. Nettelbeck<br />
Intracellular expression of CD40L after adenoviral<br />
transduction in combination with IFN-gamma treatment<br />
generates human dendritic cells that both secrete IL-12 and<br />
have migratory functions<br />
In Dendritic cell (DC)- based vaccination trials often monocyte-derived DCs (moDCs)<br />
matured with a cocktail composed of IL-1ß, TNF-alpha, IL-6 and prostaglandine E2<br />
(PGE2) have been used. It has been shown that PGE2 is indispensable for DC-migration<br />
but it is also known to inhibit IL-12p70 expression. Moreover other labs reported that<br />
these two essential functions of DCs are frequently not linked. Here we describe a new<br />
and interesting method to overcome this problem and to generate mature moDC<br />
capable of both migrating and producing biologically active IL-12p70. This could be<br />
achieved by a combined treatment with recombinant human interferon gamma (rh-IFNgamma)<br />
and adenoviral gene transfer of the trimeric CD40L. Immature moDCs were<br />
infected with an adenovirus serotype 5 coding for the trimeric human CD40L<br />
(Ad5hCD40L) in an autologous monocyte-conditioned medium supplemented with GM-<br />
CSF, IL-4, IL-1ß, TNF-alpha, IL-6 and PGE2. Afterwards (1.5 hours later) rh-IFN-gamma<br />
was added to the infected cells. 24 hours later cells were checked for their migratory<br />
capacity, their IL-12 production as well as their CD40L expression and maturation<br />
status. Interestingly, moDCs infected with Ad5hCD40L and subsequently treated with rh-<br />
IFN-gamma fully matured, showed a high IL-12p70 secretion ( approx. 700 pg/ml ) as<br />
well as high migratory capacity. Even when the migrated cells were cultured for an<br />
additional time period of 24 hours they were still able to secrete notable amounts of IL-<br />
12p70 ( approx. 160 pg/ml). In summary, using this new maturation protocol, we could<br />
generate mature DCs which are able to both (i) migrate and (ii) secrete high levels of IL-<br />
12p70 providing a potentially new therapeutic tool for DC-based vaccination trials.
Silke Overbeck, Peter Uciechowski, M. Leigh Ackland, Dianne Ford, Lothar Rink<br />
Intracellular Zinc Homeostasis in Leukocyte Subsets is<br />
Regulated by Different Expression of Zinc Exporters ZnT-1 to<br />
ZnT-9<br />
Zinc is an essential trace element, which is a fundamental component of more than 300<br />
metalloenzymes and plays an important role in the immune system. Because zinc<br />
deficiency results in decreased immune functions, regulation of intracellular zinc<br />
homeostasis by zinc binding proteins and zinc transporters is crucial. In the present<br />
study, we quantified in a first global view the expression of all characterized human zinc<br />
exporters (hZnT-1-9) in different leukocyte subsets in response to zinc supplementation<br />
and depletion and analysed their influence on alterations in the intracellular zinc<br />
concentration. We found that hZnT-1 is the most regulated zinc exporter. Furthermore,<br />
we discovered that hZnT-4 is localised in the plasma membrane similar to hZnT-1. hZnT-<br />
4 is most highly expressed in T cells, up-regulated after treatment with PHA and is<br />
responsible for the measured decrease of intracellular zinc content after high zinc<br />
exposure. In addition, we found that hZnT-5, hZnT-6 and hZnT-7 in B cells as well as<br />
hZnT-6 and hZnT-7 in monocytes are up-regulated in response to cellular zinc<br />
depletion. Those zinc exporters are all localised in the Golgi network and this type of<br />
regulation explains the observed zinc increase in both cell types after up-regulation of<br />
their expression during zinc deficiency and, subsequently, high zinc exposure.<br />
Furthermore, we detected, for the first time, the expression of hZnT-8 in peripheral<br />
blood lymphocytes, which varied strongly between individuals. While hZnT-2 was not<br />
detectable, hZnT-3 and hZnT-9 were expressed at low levels. These data provide insight<br />
into the regulation of intracellular zinc homeostasis in cells of the immune system and<br />
may explain the variable effects of zinc deficiency on different leukocyte subsets.
Benedikt Fritzsching, Jürgen Haas, Fatima König, Eva Pauly, Johannes Pöschl, Peter<br />
Krammer, Wolfgang Brück, Elisabeth Suri-Payer, Brigitte Wildemann<br />
Intracerebral Human Regulatory T Cells: Analysis of CD4<br />
+CD25+FOXP3+ T Cells in Brain Lesions and Cerebrospinal<br />
Fluid of Multiple Sclerosis Patients<br />
Impaired suppressive capacity of CD4+CD25+FOXP3+ regulatory T cells (Treg) from<br />
peripheral blood of Multiple Sclerosis (MS) patients has been reported my multiple<br />
laboratories. However, it is unclear if Treg dysfunction in MS patients is limited to a<br />
reduced control of peripheral T cell activation since most studies analyzed only<br />
peripheral blood samples. Increasing evidence supports an anti-inflammatory role of<br />
Treg at the site of organ destruction during autoimmune diseases. To test if human Treg<br />
migrate into the CNS, we analyzed human tissue from active MS lesions by FOXP3<br />
immunohistochemistry in human brain biopsies. Similarly, we detected Treg from<br />
cerebrospinal fluid (CSF) of treatment-naïve MS patients by flow cytometry. Treg were<br />
detected in more than 50% of MS brain biopsies and in all CSF-samples from MS<br />
patients. However absolute numbers for FOXP3+ and CD4+ cells were rather low in MS<br />
lesions and Treg were not detectable in 30% of MS biopsies with CD4+ cell infiltrates.<br />
Given the high sensitivity of previously activated Treg (CD45ROhiCD95hi) towards<br />
CD95L-mediated apoptosis (*), we tested if CSF-derived lymphocytes contain a higher<br />
proportion of CD45ROhiCD95hi Treg than peripheral blood derived Treg from MS<br />
patients. Indeed, pairwise analysis of Treg in CSF and peripheral blood from the same<br />
MS patients clearly demonstrated an enhanced proportion of apoptosis-sensitive Treg in<br />
the CSF. We suggest, that intracerebral elimination of Treg by CD95L-mediated<br />
apoptosis could critically affect Treg numbers in the MS lesion.<br />
(*) Fritzsching et al., Cutting Edge, J. Immunology. 2005 Jul 1; 175(1):32-6
Sebastian Kreiter, Mustafa Diken, Abderraouf Selmi, Abdo Konur, Michael Koslowski,<br />
Christoph Huber, Özlem Türeci, Ugur Sahin<br />
Intranodal RNA immunisation – a potent method for the<br />
induction of immunity by selective transfection of DC<br />
We propose the usage of naked IVT-RNA given as intranodal (i.n.) injection as a new<br />
vaccination method. We could show by FACS analysis after i.n. injection of eGFP RNA<br />
into inguinal lymph nodes (LN) of BALB/c mice that DCs were transfected. Histological<br />
analysis of RNA uptake (Cy5-RNA) in LN showed a positive signal for CD11b+ DCs in<br />
the paracortical zone with sparing of B-cell follicles. By FACS analysis of similar treated<br />
LN we could show that a RNA signal was predominatly measurable in CD11c/CD11b+<br />
myeloid DCs. Using in vitro and in vivo test systems we proved that human and mouse<br />
DCs have a high capacity for uptake of RNA in comparison to other cell populations. To<br />
assess the translational efficacy we used the firefly luciferase system and in vivo<br />
luminescense. After i.n., i.d. or s.c. RNA injection we measured time kinetics. The<br />
results showed superior translational efficacy (factor 10-20) for i.n. application in<br />
comparison with other application modalities<br />
Using Influenza-HA specific CD4+ and CD8+ T-cells for adoptive transfer experiments<br />
we tested the ability of i.n. RNA vaccination to expand T-cells. Strong i.n. expansion<br />
followed by systemic distribution of T-cells was detected. They showed full effector<br />
functions as shown by IFNγ secretion and cytotoxicity. Priming in naïve mice was tested<br />
after i.n. immunisations with SIINFEKL RNA resulting in up to 29 % antigen-specific CD8<br />
+ T-cells. Furthermore we showed T-cell priming against Influenza-HA, hCMV pp65 and<br />
gp70. We could show superior T-cell expansion with i.n. RNA in comparison to i.d. or s.<br />
c. immunisation. In tumor protection assay using an A20 Influenza HA transfectant cell<br />
line all mice were long time protected after 4 i.n. RNA immunisations. 60% of BALB/c<br />
mice survived in therapeutic assay after 5 i.n. RNA immuniations.<br />
In summary we have shown that the usage of naked IVT-RNA for intranodal<br />
immunisation is feasible, preserves lymph node structure, confers selective transfection<br />
of DCs, leads to expansion of antigen-specific T-cells and allows the induction of antitumor<br />
immunity.
Stephanie Konrad, Linda Engling, Reinhold E. Schmidt, J. Engelbert Gessner<br />
INVERSE REGULATION OF THE MURINE FcγRIIB AND FcγRIII<br />
GENE EXPRESSION BY C5a IS MEDIATED THROUGH DISTINCT<br />
DNA-RESPONSE ELEMENTS<br />
The crucial role of Fcγ receptors (FcR) in antibody-mediated autoimmune diseases is<br />
reflected in gene deletion studies in mice. Like other immune regulatory receptor pairs,<br />
the FcR system is constituted by a balanced action of activating and inhibitory receptors<br />
that bind immune-complexed IgG with same affinity. Analyses of animal models have<br />
shown that the inhibitory FcγRIIB can suppress antibody-mediated autoimmunity,<br />
whereas activating FcR - FcγRIII promote disease development. Although in vivo<br />
analysis of alveolar and peritoneal macrophages in mice shown an indispensable role of<br />
the complement component C5a in the regulation of FcR and the sensing of FcRdependent<br />
effector cell responses but the molecular mechanism is still unclear. To<br />
understand the C5a-mediated regulatory mechanisms of FcR expression, we cloned<br />
both the murine FcγRIII and FcγRIIB genes and demonstrated that inverse gene<br />
regulation of FcγRIII and FcγRIIB is mediated by functionally distinct cis-active DNA<br />
promoter elements in their 5´-end regions, which show a similar sequence motive.<br />
Deletion analysis defined a contribution of the 48-bp(–808/–760) region of the FcγRIII<br />
promoter and the promoter-associated intronic 42-bp(+442/+484) region of FcγRIIB in<br />
confering C5a responsiveness of FcγRIII induction versus FcγRIIB suppression. The<br />
importance of Gi, PI3K and Akt signaling molecules in the C5aR activation pathway that<br />
differentially control FcR reporter gene activities was further established by<br />
pharmacological inhibition studies in transfected MH-S and RAW 264.7 macrophage cell<br />
lines. This study provides insight into the transcriptional regulation of FcR,<br />
demonstrating the importance of functional different DNA elements in the murine<br />
FcγRIIB and FcγRIII genes.<br />
Research supported by SFB587 to JE.G.
Luise Weigand, Xiaoling Liang, Florian Anderl, Judith van der Griendt, Ingrid Schuster,<br />
Andreas Moosmann, Bernhard Helga, Elfriede Nößner, Dirk Busch, Angela Krackhardt<br />
Investigation of allorestricted peptide-specific T cell<br />
responses against Her2/neu – implications for adoptive T cell<br />
therapy in solid cancer<br />
Complete remissions have been observed after adoptive T cell transfer in different solid<br />
cancers including metastatic breast cancer. As allorestricted peptide-specific T cells<br />
might be a source of specific high-avidity T cell responses against tumor cells, we aimed<br />
to generate allorestricted T cells with specificity for the model antigen Her2/neu.<br />
We used T2 cells pulsed with different peptide concentrations of the Her2/neu-derived<br />
peptide 369 for stimulation of HLA-A2-negative T cells. Peptide-specific T cells were<br />
isolated by tetramers and streptamers and cloned by limited dilution. Proliferating T cell<br />
clones were analyzed for their function and T cell receptor repertoire.<br />
Repeated T cell stimulation with low antigen dose and tetramer-sorting resulted in<br />
highly peptide-specific T cells. However, tumor reactivity was low. In contrast, one-time<br />
stimulation resulted in T cells with higher tumor reactivity but partially alloreactivity<br />
independent of peptide concentration. Interestingly, all CTL clones sorted by tetramers<br />
showed an intermediate avidity for peptide-pulsed target cells, independent of the<br />
antigen concentration they have been stimulated with. Sorting with streptamers<br />
resulted in T cells with high peptide-specificity and these T cells partially showed tumorreactivity.<br />
Specific T cell clones revealed an almost exclusive usage of the V beta 6.3<br />
family although different recombined CDR3 sequences have been identified. Finally,<br />
cocultivation of highly active allorestricted T cells with tumor cells resulted in increased<br />
IL-8 secretion which has been reported to play an important role in tumorigenesis and<br />
metastasis.<br />
In conclusion, allorestricted T cells with specificity for Her2/neu (peptide 369) may<br />
represent potent tools for targeting Her2/neu-overexpressing tumor cells. However,<br />
selective tumor-reactivity and potential alloreactivity of allorestricted peptide-specific T<br />
cell receptors needs to be further investigated by transfer studies. Moreover, the<br />
potential role of IL-8 in tumor escape in this setting needs to be explored.
Stefanie Margraf, Carsten Watzl<br />
Investigation of membrane microdomains surrounding<br />
Natural Killer cell receptors<br />
Natural killer (NK) cells play a central role in linking the adaptive and the acquired<br />
immune system. They represent the first lymphoid subpopulation in the defence against<br />
tumors and viral infection. The activity of NK cells is regulated by the interplay of<br />
activating and inhibitory surface receptors. The engagement of these receptors as well<br />
as the localization within different membrane areas is crucial for signalling. We have<br />
recently shown that the activating receptors 2B4 (CD244) and NKG2D are localized in<br />
so called ‘lipid rafts’ upon ligand binding or stimulation by mAbs. The localization in<br />
these specialized membrane domains is crucial for the function of these receptors. Lipid<br />
rafts are typically analyzed via cold non-ionic detergent lysis and sucrose density<br />
gradient centrifugation. However, this method has been criticized to result in artefacts.<br />
A limitation of this method is the isolation and examination of all lipid raft membrane<br />
fractions and their associated proteins within a cell. Here we use a new approach to<br />
isolate membrane fragments surrounding a specific surface receptor without destroying<br />
its natural composition. NK cell receptors are stimulated by antibodies coupled to<br />
magnetic beads. NK cells are then physically disrupted in a nitrogen-cavitation bomb<br />
and membrane fractions surrounding the stimulated receptor are immunoisolated by<br />
separating the magnetic beads. The protein composition of the purified membrane<br />
clusters is then analyzed via 2D-Gelelectrophoresis. Examination of the natural<br />
environment of activating and inhibitory NK cell receptors will give us a new insight into<br />
the structure and composition of lipid microdomains and will help us to understand their<br />
role in the regulation of NK cell activity.
Vivienne Engelschalt, J. Engelbert Gessner, Richard A. Kroczek<br />
Involvement of complement and Fc-receptors in the depletion<br />
of T cells in vivo<br />
Antibody-mediated depletion of specific cell populations is a promising tool in the<br />
therapy of cancer and autoimmune diseases. Although depletion of cell populations has<br />
been successfully performed in a number of systems in vivo, only very few studies have<br />
dealt with the involved mechanisms. We have chosen to analyze the depletion of CD4 +<br />
T cells in the mouse as an initial model system. The application of a single dose of 100<br />
µg of the anti-CD4 mAb YTS191.1 resulted in a 70-80% depletion of CD4 + T cells in the<br />
spleen and peripheral lymph nodes (popliteal, mandibular, mesenteric, axillary, Peyer’s<br />
patches) within 72 h, whereas no depletion was observed in the thymus. Significant<br />
depletion could be observed after 12 h, the maximal effect was achieved around 72 h;<br />
the kinetics of depletion were comparable in all lymphatic organs. Complement C3deficient<br />
mice gave the same results as wild-type animals, ruling out a major<br />
involvement of this factor. In contrast, a dramatic reduction of CD4 + T cell depletion<br />
was observed in animals lacking the γ-chain common to Fc-receptors, indicating a<br />
critical involvement of Fc-receptors in antibody-mediated cell depletion. In animals<br />
lacking only FcγRII, no change in the depletion pattern was observed. Mice lacking<br />
FcγRI, FcγRIII, or a combination thereof, showed a more discrete reduction in depletion,<br />
suggesting that the absence of individual Fc-receptors can be compensated by the<br />
remaining Fc-receptors. Our present investigations are aimed at determining the role of<br />
NK cells in CD4 + T cell depletion. Further, we will attempt to define the Fc-receptorbearing<br />
cell type(s) involved in the depletion process.
Alexander Fassold, Werner Falk, Rainer H. Straub<br />
Is neuropilin-2 a possible target for the treatment of arthritis?<br />
Background: Sympathetic neurotransmitters in high concentrations exert antiinflammatory<br />
effects via beta2-adrenergic receptors. Their loss in inflamed tissue<br />
probably aggravates inflammation. Semaphorin 3C and placental growth factor, which<br />
bind to neuropilin-2 (NPN-2), are probably involved in repulsion of sympathetic nerve<br />
fibers (SNF).<br />
Objectives: To study density of SNF using NPN-2 as the antigenic target. To neutralize<br />
ligands to NPN-2 with a self-manufactured NPN-2 Fc fusion construct and to investigate<br />
the effects of inhibition in vitro and in vivo.<br />
Methods: Immunohistochemistry was used to investigate presence of NPN-2 positive<br />
nerve fibers in synovial tissue of 10 patients with rheumatoid arthritis (RA) and 10 with<br />
osteoarthritis (OA). In order to be able to study the effect of the Fc fusion construct,<br />
sympathetic ganglia of mice were cultured and outgrowth speed analysed. The NPN-2<br />
Fc-fusion construct was tested in vivo in collagen type II-induced arthritis in DBA/1<br />
mice.<br />
Results: In patients with RA compared to OA, density of NPN-2– positive nerve fibers<br />
was decreased (p
Selina Christen, Edith Hintermann, Monika Bayer, Urs Christen<br />
JAM-C and its influence on the pathogenesis of type 1 diabetes<br />
Type 1 diabetes (T1D) results from the autoimmune destruction of insulin-producing<br />
beta-cells in the pancreas. Recruitment of inflammatory cells, such as T-cells, B-cells<br />
and dendritic cells is prerequisite to beta-cell-injury. Such a process includes several<br />
molecular interactions between circulating and endothelial cells. The junctional adhesion<br />
molecule (JAM) family proteins JAM-B and JAM–C, are expressed on endothelial cells of<br />
high endothelial vessels and appear to be involved in leukocyte rolling, firm adhesion<br />
and transmigration. It was recently demonstrated that after blocking of JAM-C ceruleininduced<br />
pancreatitis was efficiently attenuated in mice. Early intervention with a<br />
monoclonal antibody directed against JAM-C reduced cytokine production, leukocyte<br />
influx, and hence tissue damage.<br />
In order to investigate the influence of JAM-C on trafficking and transmigration of<br />
antigen-specific, autoaggressive T-cells we used the RIP-LCMV mice as a model system.<br />
These mice express the nucleoprotein (NP) of lymphocytic choriomeningitis virus<br />
(LCMV) as a target autoantigen specifically in the beta-cells of the islets of Langerhans<br />
and turn diabetic after LCMV infection. In such diabetic RIP-LCMV mice the expression<br />
of JAM-C is detectable around the vessels within the pancreas. Interestingly,<br />
immunohistological evaluation of pancreas sections revealed that JAM-C was expressed<br />
directly in between cellular infiltrations and beta-cells.<br />
Our data suggest that JAM-C might be involved in the final steps of trafficking and<br />
transmigration of antigen-specific autoaggressive T-cells to the islets of Langerhans and<br />
might therefore play an important role in the pathogenesis of T1D.
Nils Schoof, Frederike von Bonin, Lorenz Trümper, Dieter Kube<br />
Janus kinases are targets of tyrphostin AG17 and HSP90inhibitor<br />
17-AAG in classical Hodgkin Lymphoma<br />
Classical Hodgkin Lymphoma (cHL) is a malignancy originated of germinal center (GC) B<br />
cells. Defective immunoglobulin rearrangement should have destined these GC B cells<br />
for apoptosis. Multiple deregulated signaling pathways are associated with survival and<br />
proliferation of cHL cells. Chemotherapeutic regimens for cHL are associated with<br />
stagnant rates of secondary malignancies requiring the development of new therapeutic<br />
strategies.<br />
Recently, we and others have shown that permanently activated Signal Transducer and<br />
Activator of Transcription (STAT) molecules are essential for cHL cell proliferation, and<br />
inhibitors of the tyrphostin-class are capable of inhibiting STAT tyrosine<br />
phosphorylation. Here we focused on the Janus kinases (Jaks), the major components<br />
involved in signal transduction from cytokine receptors to the STAT transcription<br />
factors. In cHL cells we observed high levels of permanently tyrosine phosphorylated<br />
Jak1, Jak2, Jak3 and Tyk2. Tyrphostin AG17 reduced tyrosine phosphorylation of Jaks1-<br />
3 in cHL cell lines in vitro and decreased tumour formation of L428 cHL cells in<br />
chorioallantoic membrane assay in vivo. Since Jaks are thought to be stabilised by heat<br />
shock protein 90 (HSP90) and cHL cell proliferation is inhibited by HSP90-inhibitor 17-<br />
AAG, the effects of 17-AAG on Jak-STAT signaling in cHL cells were investigated. 17-<br />
AAG led to a <strong>complete</strong> inhibition of STAT1, -3, -5 and -6 activation. Moreover, 17-AAG<br />
treatment was accompanied by significant reduction of Jak protein expression. To<br />
further test the role of HSP90 in stabilisation of Jaks co-immunoprecipitations as well as<br />
RNAi against HSP90 were performed.<br />
Our results suggest that recently described effects of 17-AAG on cHL cell proliferation<br />
are due to inhibition of Jak-STAT signaling. Therapeutics comprising inhibition of Jaks<br />
either by dephosphorylation or downregulation, with tyrphostin AG17 and 17-AAG<br />
respectively, may be a promising strategy in cHL and other cancer entities associated<br />
with permanent STAT activation.
Eva Schlecker, Isabel Hartmann, Michael Ackmann, Elisabeth Weiss<br />
KIR2DS2 and interaction with DAP12<br />
The KIR locus is characterized by fluctuating gene content, which mainly depends on<br />
the presence or absence of activating KIRs, and allelic variation. Whereas the function<br />
and ligands of the inhibitory KIRs have been extensively studied, similar facts are<br />
lacking for the activating KIRs. Several studies have demonstrated that activating KIRs<br />
might be involved in the progression of autoimmune disease and also play a role in<br />
transplantation situations. For most of the activating receptors no ligands have been<br />
identified yet. We tried to establish a cell based read-out system to identify ligands for<br />
activating KIRs by coexpression of KIR2DS2 and DAP12 in Jurkat and HEK 293T cells in<br />
the presence of luciferase reporter vectors regulated by NFAT or a minimal IFNgamma<br />
promoter.<br />
In HEK293T cells DAP12 was higly expressed at the cell surface even in the absence of<br />
KIR2DS2. Thus, DAP12 cell surface transport does not need transmembrane partners or<br />
DAP12 associates with a yet unknown polypeptide in these cells. KIR2DS2 was only<br />
weakly detected at the cell surface in both transfectant cell types. It is possible that the<br />
GL183 antibody does not recognize KIR2DS2 efficiently. Cross-linking of KIR2DS2,<br />
DAP12 or KIR2DS2/DAP12 did not result in the activation of the luciferase reporter<br />
vectors. Moreover, no tyrosine phosphorylation of DAP12 was detected, whereas using<br />
antibody stimulation of cells expressing hybrid CD3zeta/CD94 and NKG2A molecules<br />
resulted in tyrosine phosphorylation of CD3zeta. We conclude that on the one hand the<br />
low binding of the GL183 antibody to KIR2DS2 might be responsible for the lack of<br />
activation, as several studies have shown that interactions between low-avidity ligands<br />
could induce an inhibitory signal by recruiting SHP1 to the signalling ITAM complex and<br />
that DAP12 can also inhibit cellular activation. On the other hand, the association of<br />
KIR2DS2 with DAP12 might also trigger a repressive state.
Gleb Turchinovich, Jan Kranich, Sonja Schmid, Jürgen Bachl, Jörg Kirberg<br />
Kruppel-like factor 3 (KLF3) affects marginal zone B cell<br />
differentiation<br />
We have demonstrated that the hypermutating Abelson-leukemia virus induced pre-B<br />
cell line 18-81 harbors a single provirus within the KLF3 locus, leading to constitutive<br />
KLF3 expression. To study functions of KLF3 in B cells we generated transgenic mice<br />
over-expressing KLF3 (CD19:KLF3).<br />
Surprisingly, marginal zone (MZ) B cells were increased 3-10 fold in CD19:KLF3 mice.<br />
To determine whether the increase is caused cell autonomously, competitive fetal liver<br />
chimaeras were generated. Here, KLF3 over-expression did not affect the maturation of<br />
FO B cells as these were derived from normal or CD19:KLF3 cells to the same extent as<br />
they contributed to immature B cells, respectively. In contrast, the MZ B cell<br />
compartment became almost exclusively dominated by CD19:KLF3 transgenic cells. To<br />
ascertain that this altered lineage commitment occurs independent to receptor<br />
specificity, CD19:KLF3 mice were crossed to B1-8H/3-83κ knock-in mice. Normally, B<br />
cells expressing the B1-8H/3-83κ combination are mostly in the FO, while cells<br />
expressing another light chain are enriched in the MZ. Strikingly, KLF3 over-expression<br />
drives B1-8H/3-83κ expressing cells to mature extensively into the MZ lineage. Thus,<br />
KLF3 activity alters MZ commitment independent of BCR receptor specificity. However,<br />
no evidence of increased Ca++ mobilization, tyrosine-phosphorylation, or receptor<br />
induced proliferation was detectable in KLF3 over-expressing B cells.<br />
The KLF3 homologous factor KLF2/LKLF regulates S1P-R expression in T cells affecting<br />
cell migration. We hypothesized that KLF3 over-expression in B cells similarly leads to<br />
constitutive S1P-R expression and consequently enhanced B cell migration into/or<br />
retention within the MZ. Normally, LPS stimulation leads to S1P-R down-regulation and<br />
MZ B cell migration into the follicle. In contrast to our expectation, the migration of MZ<br />
B cells into the follicle following LPS stimulation was unaffected in CD19:KLF3 transgenic<br />
mice indicating that S1P-R expression is still under physiological control.<br />
Thus, further experiments will focus on alternative pathway(s) known to modulate the<br />
maturation of MZ and FO B cells.
Dietmar Zehn, Michael J. Bevan<br />
Lack of peripheral control of low avidity self reactive T cells<br />
Autoimmune diseases develop despite the presence of numerous safeguards to<br />
eliminate or control T cells directed against self-antigens. This raises the question how<br />
disease-causing T cells escape elimination or inactivation. We have studied the<br />
repertoire of T cells directed against a pancreatic antigen that is also ectopically<br />
expressed in the thymus. T cells responding strongly to this antigen are efficiently<br />
eliminated. In contrast, central and peripheral tolerance routinely fail to eliminate cells<br />
that are weakly reactive with this organ specific self-antigen. These low avidity T cell<br />
cause autoimmunity upon activation via molecular mimicry. While in the periphery,<br />
these low avidity T cell continuously encounter tissue derived cognate self-antigen<br />
crosspresented by lymph node dendritic cells. We have analyzed how this chronic<br />
exposure impacts the low avidity T cells. Our data indicate that the low avidity cells can<br />
be detected throughout life and retain their disease causing potential as the mice age.<br />
Moreover, the ability to recruit low avidity T cells into autoimmune responses does not<br />
rely on the supply of recent thymic emigrants nor does the presence or absence of the<br />
cognate self-antigen in the periphery alter the reactivity of these low avidity T cells. In<br />
the model we study, low avidity self-reactive T cells are long lived populations that are<br />
not changed by peripheral antigen recognition. Thus, we conclude that cells like these<br />
are a normal part of the T-cell repertoire in healthy individuals. The constitutive<br />
presence of such cells requires mechanisms that prevent their activation. Unexpectedly,<br />
the selective elimination of Foxp3+ T cells did not enhance autoimmunity, but rather<br />
interfered with the ability of low avidity T cells to induce disease.
Gordon Wilke, Gretel Wittenburg, Claudia Berek<br />
Laser Capture Microdissection and Mircroarray: a<br />
Characterisation of Follicular Dendritic Cells<br />
Follicular dendritic cells (FDC) play a crucial role in B cell homeostasis and<br />
differentiation, nonetheless little is known about this cell type. In the primary follicle B<br />
cells are embedded into a network of FDC. When germinal centres are induced, FDC<br />
build the micro-environment where the affinity maturation of the immune response<br />
takes place. Their tight interaction with B cells and also their fragility make the study of<br />
FDC a challenging undertaking.<br />
To further understand the role of FDC within the follicle and their close interaction with<br />
B cells a new approach was taken. Tissue sections were prepared, stained with FDCspecific<br />
antibodies and FDC networks of primary follicle directly isolated by Laser<br />
Capture Microdissection. In addition, spleen suspensions were prepared and follicular B<br />
cells sorted by FACS. From both cell preparations RNA was extracted and amplified.<br />
Gene expression was analysed by hybridisation to Affymetrix microarrays.<br />
Gene expression in FDC networks and in B cells was compared and differentially<br />
expressed genes in the FDC network identified. The expression of genes characteristic<br />
for FDC such as CXCL13, VCAM-1 and BP3 demonstrates that this procedure is useful<br />
for the identification of novel FDC genes. A set of interesting genes was selected and<br />
their specific expression in FDC verified by immunohistology and in situ hybridisation.<br />
Murine knock-out models for novel FDC genes were used to demonstrate their effect on<br />
the development of primary follicles.<br />
In addition, the question of the origin of FDC was addressed by comparing the<br />
expression pattern of FDC and stromal cells of splenic follicle anlagen. Finding a high<br />
degree of accordance in gene expression supports the hypothesis that FDC develop<br />
from sessile stromal cells.
Katja Farhat, Sabine Riekenberg, Jennifer Debarry, Roland Lang, Jörg Mages, Günther<br />
Jung, Karl-Heinz Wiesmüller, Artur J. Ulmer<br />
LIGAND BINDING AND SIGNAL TRANSDUCTION INDUCED BY<br />
LIPOPEPTIDES<br />
Toll-like receptors (TLRs) are primary triggers of the innate immune system by<br />
recognizing various microorganisms through conserved pathogen-associated molecular<br />
patterns (PAMPs). Among all TLRs, TLR2 is the receptor for a functional recognition of<br />
bacterial lipopeptides (LPs) and is upregulated during various disorders like chronic<br />
obstructive pulmonary disease (COPD) and sepsis. This receptor is unique in its ability<br />
to form heteromers with either TLR1 or TLR6 to mediate intracellular signaling.<br />
According to the fatty acid pattern as well as the assembling of the polypeptide tail LPs<br />
can signal through TLR2 in a TLR1- or TLR6-dependent manner. As shown recently<br />
there are also di- and triacylated LPs which stimulate TLR2 independently of TLR1 and<br />
TLR6.<br />
In this study we investigate the signal transduction pathways activated by the different<br />
TLR2 dimers in murine bone marrow derived macrophages, using the synthetic LPs<br />
PamOct2C-(VPGVG)4VPGKG, FSL 1 and Pam2C-SK4 to specifically target TLR2/TLR1,<br />
TLR2/TLR6 and TLR2, respectively. Immunoblotting of MAP-kinases, usage of dominant<br />
negative forms of adaptor molecules as well as microarray analyzes indicate that all<br />
dimers use the same signaling cascade to activate transcription factors leading to an<br />
identical pattern of gene activation. In conclusion, LPs from mycoplasma, Gram-positive<br />
and Gram-negative bacteria, although they may use different TLR2 dimers, induce the<br />
same signal transduction pathway during infection.
Christian Draing, Christoph Rockel, Susanne Deininger, Stefanie Sigel, Oliver Dehus,<br />
Tamara Rupp, Artur Ulmer, Thomas Hartung, Corinna Hermann, Sonja von Aulock<br />
Lipoteichoic acid from a lipoprotein diacylglycerol transferase<br />
deletion mutant is a potent immunobiologically active<br />
compound<br />
Lipoteichoic acid (LTA) is a potent immunostimulatory surface component of Grampositive<br />
bacteria as shown by preparation of the full native structure by optimized<br />
isolation procedures in the absence of contaminations, e.g. lipopolysaccharide, and by<br />
chemical synthesis of a full structure based on the LTA of Staphylococcus aureus.<br />
This was recently challenged with an LTA preparation from a lipoprotein diacylglycerol<br />
transferase deletion (Δlgt) mutant, reported to lack palmitate-labeled lipoproteins and<br />
immunostimulation. In the present study, however, LTA from the mutant and LTA from<br />
the respective wild type SA 113 strain induced a comparable release of TNFα in<br />
incubations with human whole blood or peripheral blood mononuclear cells. In contrast,<br />
the LTA from the mutant strain was unable to induce cytokine release in the murine<br />
macrophage cell lines J774.1, MH-S or primary murine macrophage populations from<br />
the bone marrow or peritoneum. Likewise, the human monocytoid cell line THP-1 was<br />
unresponsive to the LTA of the mutant strain. The unresponsiveness of the human cell<br />
line was caused by an inhibitory effect of the FCS used as medium supplement; that of<br />
the murine cells by differences in the composition of fatty acids compared to LTA from<br />
the wild type strain and not by the lack of lipoproteins. Thus, LTA and not lipoproteins<br />
represent the main stimulus of Gram-positive bacteria in human leukocytes.
Anna Schurich, Silke Hegenbarth, Jan Böttcher, Sven Burgdorf, Andreas Dolf, Elmar<br />
Endl, Christian Kurts, Percy A. Knolle<br />
Liver sinusoidal endothelial cells are more efficient in crosspresentation<br />
than CD8alpha splenic dendritic cells expressing<br />
endocytic receptors devoted to cross-presentation<br />
Liver sinusoidal endothelial cells (LSEC) constitute a unique antigen presenting cell<br />
population. LSEC efficiently take up and cross-present antigen to naïve CD8 T-cells<br />
inducing T-cell tolerance. In order to unambiguously investigate and compare crosspresentation<br />
in LSEC to conventional APC such as DCs we developed a new isolation<br />
method that involves functional identification of LSEC in vivo via their extraordinary<br />
scavenger activity and fluorescence activated cell sorting. This method yielded highly<br />
pure cell populations (≥ 99.9 %) for functional analysis ex vivo. We compared the<br />
efficiency of isolated LSEC and splenic DCs for cross-presentation of ovalbumin to CD8<br />
T- cells ex vivo one hour after intravenous antigen injection. LSEC were more efficient<br />
in cross-presentation on a per cell basis than CD8α positive splenic DCs. However,<br />
antigen was not retained in LSEC in vivo, because 90% of antigen was lost after 24h<br />
and cross-presentation decreased correspondingly. In contrast less efficient crosspresentation<br />
by DCs was maintained over 24h. It was recently shown that crosspresentation<br />
of soluble exogenous ovalbumin in DCs is determined by the receptor used<br />
for endocytosis: the mannose receptor (MR) routing ovalbumin into cross-presentation<br />
and scavenger receptors into MHC II restricted presentation. We found that MR cell<br />
surface expression was higher in LSEC than in DCs. MR -/- LSEC, in contrast to DC, do<br />
not rely exclusively on the MR, but were still capable of cross-presenting ovalbumin<br />
indicating expression of another receptor involved in cross-presentation. Further<br />
experiments will characterise this receptor.<br />
Collectively our data show that LSEC are more efficient than CD8&alpha positive DC in<br />
cross-presentation of soluble exogenous ovalbumin, utilising endocytic receptors<br />
devoted to cross-presentation.
Matthias Hardtke-Wolenski, Nadja Saal, Konstantinos Iordanidis, Mark S Anderson,<br />
Michael P Manns, Elmar Jäckel<br />
Liver specific immune responses related to AIRE mutations<br />
The AIRE gene (autoimmune regulator) has been identified as an important mediator of<br />
central tolerance against ectopically expressed peripheral antigens. Mutatations of AIRE<br />
are responsible for autoimmune polyendocrinopathy syndrome type I (APSI) in human<br />
characterized by a multiorgan autoimmune disease. Autoimmune hepatitis (AIH) is part<br />
of the clinical spectrum in humans and mice. 19% of patients with AIRE mutations<br />
develop an autoimmune hepatitis which is characterized by autoantibodies against<br />
cytochrome P450 2A6 and 1A2.<br />
We investigated AIH in mouse models with various AIRE mutations on different genetic<br />
backgrounds. Initially we characterized the immunohistochemical staining pattern of<br />
sera from AIRE -/- mice on rat liver, kidney and stomach sections and on HepG2 cells. In<br />
parallel, sera analysis has been done on western-blots loaded with whole liver lysate.<br />
We could demonstrate that the the strength and broadness of the humoral immune<br />
response correlates well with disease activity of the AIH in AIRE deficient mice. We<br />
could show that AIH development is dependent on the genetic background used.<br />
Furthermore within the Balb/c background AIH development is dependent on the<br />
underlying AIRE mutation. Humoral immune responses in AIRE deficient mice are not<br />
directed against the antigens described for human AIH. We therefore set out to<br />
characterize the target antigens of the adaptive immune response in mice with AIH to<br />
study the defects in their immune tolerance. We therefore developed a column retention<br />
assay of for non-denatured liver antigens followed by a proteomics analysis with mass<br />
spectroscopy. With this approach we identified several potential new autoantigens of the<br />
humoral immune response.
Stephan Borte, Uwe Gerd Liebert, Michael Borte, Ulrich Sack<br />
Long-term cell-mediated immunity following vaccination with<br />
live, attenuated measles-mumps-rubella-vaccine in children<br />
with juvenile idiopathic arthritis under treatment with lowdose<br />
Methotrexate and/or tumour necrosis factor α receptor<br />
antagonist<br />
Juvenile idiopathic arthritis (JIA) represents a heterogeneous group of disorders<br />
characterized by chronic inflammatory arthritis and turns out to be the commonest<br />
rheumatic disease seen in childhood worldwide. The multidisciplinary management of<br />
JIA is founded on anti-inflammatory and immunomodulating drugs. However, infection<br />
is one of the leading causes of morbidity and mortality in JIA. The risks of serious<br />
adverse events following vaccination and the immunogenicity of vaccines at all have<br />
been a matter of controversy and there is some reluctance to vaccination that need to<br />
be enlightened. We intended to display the course of humoral and cell-mediated<br />
immunity to measles-mumps-rubella-vaccination (MMR) in healthy children and<br />
adolescents and to evaluate potential influences of low-dose Methotrexate therapy and<br />
Etanercept treatment in JIA on success of immunisation and maintenance of long-term<br />
immunity. Therefore, production of IFNγ by T memory cells upon in vitro stimulation<br />
with measles, mumps and rubella antigens and seroprevalence of virus-specific IgG<br />
antibodies were investigated in PBMC and plasma from 16 healthy children and 16<br />
children with JIA, being treated with low-dose Methotrexate or in combination with<br />
Etanercept. Our results indicate that MMR-vaccination induced immunity in childhood is<br />
characterized by steady decline of humoral immunity and development of long-term cellmediated<br />
immunity. Low-dose MTX therapy following <strong>complete</strong>d MMR-vaccination was<br />
proved not to hamper Th1-like cell-mediated immunity in vitro. Furthermore, neither<br />
low-dose MTX nor Etanercept treatment during the course of vaccination showed to<br />
markedly interfere with intended outcome of immunisation and generation of long-term<br />
cell-mediated immunity to MMR. No cases of serious adverse events following MMRvaccination<br />
were observed. In conclusion, these results argue for MMR-vaccination in<br />
children with JIA using live, attenuated vaccines to ensure protection from infection and<br />
to prevent morbidity and mortality related to this diseases.
Christian Pötschke, Mandy Busse, Annegret Dummer, Tobias Traeger, Wolfram<br />
Keßler, Erika Friebe, Marlene Mikulcak, Claus-Dieter Heidecke, Stefan Maier, Barbara<br />
Bröker<br />
Long-term effects of polymicrobial sepsis on the adaptive<br />
immune system<br />
Generalized polymicrobial infection leading to sepsis remains a common and life<br />
threatening condition. Following initial hyperinflammation, many patients experience a<br />
hypoinflammatory phase, for which there is no therapy. Furthermore long-time<br />
survivors have an increased mortality rate. Using colon ascendens stent peritonitis with<br />
intervention (CASP-I), a clinically relevant mouse model of diffuse peritonitis, we have<br />
investigated the long-term consequences of sepsis.<br />
After CASP-I inflammatory cytokines like TNFα, IL-6, IL-10 and MCP-1 were increased in<br />
the serum of C57BL/6 mice on the first day of sepsis, while IL-12 and IFNγ became<br />
measurable on day seven. In the thymic cortex a dramatic increase of apoptosis<br />
occurred, leading to the elimination of thymocytes by day three. On day 14 thymic<br />
architecture and thymocyte counts were reconstituted. In the spleen Foxp3-positive as<br />
well as Foxp3-negative T cells rapidly upregulaed CTLA-4. Later, we observed germinal<br />
centers and, in the red pulp, structures sharing features with germinal centres. This<br />
may be related to the strong increase of total IgM and IgG titers in the serum seven<br />
and 14 days after CASP-I, respectively.<br />
When a primary immune response to the model antigen TNP-KLH was induced following<br />
CASP-I, the ex vivo splenocyte proliferation in response to KLH decreased over time<br />
following sepsis. In contrast, the TNP-specific IgM and IgG concentrations increased.<br />
Surprisingly, a similar increase of TNP-reactive antibody titers was also observed after<br />
CASP-I in mice that had not been immunized.<br />
Our data indicate that generalized bacterial infection leads to the rapid activation of the<br />
adaptive immune system. The balance between regulatory and effector T cell<br />
subpopulations may decide about the outcome of sepsis. In pilot studies, the primary T<br />
cell response to a novel antigen appeared to be suppressed following sepsis. The<br />
presumed lack of T cell help for B cells in sepsis appeared to be compensated by a<br />
polyclonal B cell response. How these B cells are activated will be the focus of our future<br />
studies.
Zulema Cabail, Holger Hoff, Heike Hirseland, Steven Nadler, Gerd R. Burmester, Monika<br />
C. Brunner-Weinzierl<br />
Longevity of CD28null T Lymphocytes is abrogated by CTLA-<br />
4Ig treatment<br />
CTLA4Ig engages CD80 and CD86 on antigen-presenting cells, which are both ligands<br />
for CD28 and CD152 on T cells. CTLA4Ig-treatment has demonstrated efficacy in<br />
treating rheumatoid arthritis and psoriasis. The traditional view of the mechanism of the<br />
CTLA-4Ig treatment is inhibition of CD28-costimulation preventing activation of<br />
inflammatory T lymphocytes.<br />
In autoimmune diseases such as rheumatoid arthritis, CD28null T cells accumulate in<br />
the joint which show high IFN• production and longevity. In this study, we used<br />
CTLA4Ig (abatacept•) to investigate the CD80/CD86 costimulatory requirements of<br />
heterogeneous CD28null T cells. First we could show that despite the loss of CD28<br />
expression these cells are able to express intracellular CD152. Using a sensitive staining<br />
method, we demonstrate that they also express CD152 at their cell surface. In vitro<br />
activation of CD28null CD4 or CD8 T cells in the presence of CTLA4Ig leads to enhanced<br />
frequencies of AnnexinV+ T Lymphocytes: 10% for CD8 and 25% for CD4 T<br />
lymphocytes. IDO activation by CTLA-4Ig engagement of CD80 and CD86 was excluded.<br />
Their Fas -expression at the cell surface was upregulated independently of CTLA-4Ig<br />
treatment. Apoptosis induction was confirmed demonstrating enhanced Caspase<br />
activation in CD28null cells stimulated under CTLA-4Ig treatment. These results suggest<br />
that the efficacy of the CTLA4Ig treatment might be, at least in part, due to absent<br />
CD152 signalling in inflammatory lymphocytes inducing their elimination by apoptosis.
Anja Siepert, Birgit Sawitzki, H.M. Reichardt, Jochen van den Brandt, Markus Tiedge,<br />
Manfred Lehmann, Hans-Dieter Volk, Petra Reinke<br />
Low dose CNI treatment can control effector function of<br />
depletion resistant<br />
allo-specific memory T cells (financial support by Else-Kröner-<br />
Fresenius-Stiftung P14/06//A01/06)<br />
Donor-specific tolerance to transplanted tissues remains an elusive goal in clinical<br />
transplantation. Lymphocyte depletion is a commonly used approach in clinical renal<br />
transplantation as part of standard induction immunosuppressive therapy but also<br />
tolerance induction protocols. But preliminary studies in humans have shown that<br />
monotherapies with depleting antibodies can result in severe acute rejection episodes. A<br />
high pool of donor reactive memory T-cells in transplant recipients is considered to be<br />
the main reason for these rejection episodes.<br />
Here we developed an experimental transplant model with an increased allo-specific<br />
memory T cell pool and tested their influence on graft survival and responsiveness to<br />
different therapeutic approaches.<br />
For tolerance induction kidney grafted rats (DA to LEW) were treated with combination<br />
of the depleting mAbs Ox8 (anti-rat CD8; 4 x 1 mg/kg b.w.) and Ox38 (anti-rat CD4; 4<br />
x 10 mg/kg b.w.). Allo-specific memory-like T-cells (15 x 106 cells) were transferred 7<br />
days prior to transplantation. To determine the effect of CNI on memory-like T-cells rats<br />
were treated additionally with short time or permanent low dose CyA (3 mg/kg b.w. d 0-<br />
9 or d 0-150). Serum creatinine and survival of allografted rats were used as read-out<br />
parameters. Graft biopsies from days 5 and 150 pTx were evaluated by<br />
immunohistology.<br />
Long-term function of kidney grafts was maintained by perioperative T-cell depletion<br />
using mAbs Ox8 and Ox38 (MST >150 d). Additional application of allo-specific memory<br />
T-cells resulted in acute rejection in 5 out of 6 rats (MST >12,7 ± 11,8). Despite<br />
inducing strong T-lymphopenia, surviving transferred allo-specific memory T cells can<br />
affect the graft. Short time CyA-application led to prolongation of graft survival time<br />
with a declining transplant function, 4 out of 6 rats died (MST >51,3 ± 24,8). In<br />
contrast, permanent CyA therapy induced long-term acceptance of kidney grafts (MST<br />
> 80 d).<br />
Depletion of T-lymphocyte combined with low dose permanent CyA is sufficient to<br />
control effector function of depletion resistant allo-specific memory T cells.
Markus Kleinewietfeld, Mireille Starke, Thomas Blankenstein, Kirsten Falk, Olaf<br />
Rötzschke<br />
Low dose cyclophosphamide tumor rejection is independent<br />
of CD4+ CD25+ regulatory T cells (Treg)<br />
Cyclophosphamide (Cy) is a chemotherapeutic widely used in cancer treatment. It is an<br />
alkylating agent that in high dosage (>400 mg/kg) effects the proliferating tumor cells.<br />
More recently it was rediscovered as an immunomodulatory drug. At a concentration of<br />
200-400 mg/kg it seems to target preferentially the cycling Tregs, which leads to<br />
decreased cell numbers, alters the ratio between effector and regulatory T cells and<br />
inhibits the suppressive capability of Tregs. Moreover, in several experimental tumor<br />
models striking rejections of tumour cells were observed at concentrations as low as 15<br />
mg/kg.<br />
In this study we show that in low dose rejection of tumors by Cy is not driven by<br />
neutralizing regulatory T cells. In BALB/c mice injected with J558L tumour cells we<br />
observed tumor rejection of established tumors by a single low dose Cy treatment (15<br />
mg/kg). This effect was independent of CD25+ T cells, since a depletion with αCD25<br />
prior the Cy administration did not affect the kinetics of tumor rejection. CD25 depletion<br />
alone without Cy treatment also induced a delayed rejection. Although, in principle, the<br />
neutralization of Treg cells can trigger tumor rejection also in this model system, the<br />
rapid rejection observed after low-dose Cy administration is apparently not a result of<br />
selective inhibition of Tregs.<br />
We conclude that low dose cyclophosphamide treatment can trigger rejection of certain<br />
tumors but depletion or inactivation of CD4+CD25+ T cells is not the driving force of<br />
tumor rejection. Other mechanisms have to be considered and in particular the<br />
induction of innate immune responses by low dose cyclophosphamide treatment has to<br />
be further investigated.
Juliane Ladhoff, Michael Bader, Sabine Brösel, Elke Effenberger, Isabela Schmitt-<br />
Knosalla, Hans-Dieter Volk, Martina Seifert<br />
Low immunogenicity of rat embryonic stem cell derivatives<br />
Introduction: Embryonic stem cells are suggested to be immune-privileged, but they<br />
carry the risk of tumor development. With proceeding differentiation they lose their<br />
tumor forming capacity, but they become immunogenic expressing a normal set of<br />
Major Histocompatibility Complex (MHC) molecules. This immunogenicity might trigger<br />
rejection processes after application in regenerative therapies.<br />
Methods: Two cell lines of rat embryonic stem cell like cells (RESC) were driven towards<br />
the endothelial lineage and analyzed for their phenotype. MHC levels in response to<br />
interferon-γ (IFNγ) were determined flow cytometrically compared to primary rat aortic<br />
endothelial cells (EC). Allo-responses were analyzed in vitro by Calcein-based<br />
cytotoxicity assays, determination of allo-antibody/complement mediated lysis and<br />
CFSE-based proliferation assays with allogeneic CD4+ T cells. Immune reactions in vivo<br />
were measured by allo-antibody production.<br />
Results: RESC derivatives expressed only low levels of MHC class I and several<br />
endothelial markers, but they do not express MHC class II. In response to IFNγ they<br />
induced MHC class I, however MHC class II expression remained absent, due to a<br />
lacking induction of the MHC class II transactivator. RESC derivatives displayed a<br />
diminished sensitivity to allo-specific T cell attack, were resistant to allo-antibody/<br />
complement mediated lysis as opposed to high lysis rates of aortic EC. Furthermore, in<br />
vitro RESC derivatives exhibited a notably lower capacity to stimulate allogeneic CD4+ T<br />
cells. Allo-antibody production in vivo sustained these data.<br />
Conclusions: RESC derivatives elicit less allo-specific immune responses than their<br />
differentiated adult counterparts. Furthermore, they are resistant against humoral<br />
mechanisms of allorecognition and are partially protected against cellular immune<br />
attack. This opens up ways to use stem cell derived endothelium as a powerful tool in<br />
regenerative cell therapies.
Anette Brass, Shiyuan Hong, Nicole Schwarz, George Dubyak, Michel Seman, Friedrich<br />
Koch-Nolte, Friedrich Haag<br />
LPS and interferons induce surface expression and activity of<br />
ADP-ribosyltransferase ART2.1 on murine bone marrowderived<br />
macrophages<br />
Nicotinamide adenosine dinucleotide (NAD), a predominantly intracellular metabolite, is<br />
released into the extracellular compartment consequent to cell lysis or by regulated<br />
secretion. Extracellular NAD modulates immune and inflammatory responses by serving<br />
as a substrate for cell surface ADP-ribosyltransferases (ARTs) that transfer ADP-ribose<br />
from NAD to arginine residues on target proteins. In the murine immune system, the<br />
major sources of ART activity are the two ART2 isoforms ART2.1 and ART2.2, which so<br />
far have only been detected on T cells. On these cells, ADP-ribosylation of the P2X7<br />
purinoreceptor leads to activation of the receptor and rapid cell death. ART2.1 differs<br />
from ART2.2 in that it carries an extra disulfide bond, making its activity dependent on<br />
the presence of thiol reducing agents. We now report that bone marrow-derived<br />
macrophages (BMDM) from BALB/c mice up-regulate ART2.1, but not ART2.2, in<br />
response to multiple proinflammatory mediators including agonists for toll-like receptors<br />
(TLR) and type-1/2 interferons. Stimulation of BMDM with LPS, interferon-&Gamma<br />
(IFN-&Gamma) or interferon-&beta (IFN-&beta) induced high expression of ART2.1 as a<br />
GPI-anchored cell surface ecto-enzyme. The catalytic function of the induced cell<br />
surface ART2.1 was strictly dependent on the presence of extracellular thiol reducing<br />
cofactors, suggesting that in vivo activity of ART2.1-expressing macrophages may be<br />
potentiated in hypoxic or ischemic compartments. Consistent with the mutated Art2a<br />
gene in C57BL/6 mice, LPS- or IFN-stimulated BMDM from this strain lacked expression<br />
of cell surface ART2 activity in the presence or absence of extracellular thiol reductants.<br />
In transfection experiments, P2X7 was activated by ART2.1 in the presence of NAD and<br />
reducing agents. Collectively, these findings implicate NAD-dependent ADP-ribosylation<br />
as a potential immunoregulatory mechanism for inflammatory macrophages as well as<br />
for T cells.
Christian Schiller, John-Christian Eilert, Maximilian Nitschké, Alexander Seidl, Michael<br />
Schleicher, Dolores J. Schendel, Elisabeth H. Weiss<br />
LST1: a potential transmembrane adaptor protein that<br />
modulates cell morphology<br />
The MHC class IV region encodes numerous genes involved in inflammatory responses<br />
and harbours the LST1 gene which is strongly expressed in immune cells, especially<br />
monocytes and dendritic cells. LST1 undergoes extensive alternative splicing resulting in<br />
12 soluble or transmembrane isoforms. It has been proposed that LST1 plays an<br />
important role in both regulating the immune response and enabling cell-cell<br />
communication, but the exact mechanisms involved are yet to be elucidated.<br />
Overexpression of full lenght LST1 in a variety of cell lines results in the formation of<br />
numerous long and thin cellular extensions, we found these processes to have the same<br />
physical characteristics as tunneling nanotubes (TNT). However, in HeLa LST1<br />
transfectants microinjection experiments revealed that these did not enable transport of<br />
molecules between cells and were thus not functional.<br />
Membrane orientation of transmembrane LST1 proteins was determined by analyzing<br />
cell surface expression of FLAG-tagged LST1 isoforms transiently expressed in HEK<br />
293T cells. Our results show that LST1 encodes type-I transmembrane proteins with a<br />
short extracellular and a long cytoplasmic domain. Database analysis revealed several<br />
evolutionary conserved regions in the cytoplasmic domain including two tyrosine<br />
phosphorylation sites and one ITIM which displayed phosphorylation in pervanadate<br />
treated LST1 transfectants. We also found two conserved cysteines in the cytoplasmic<br />
domain to be required for the formation of LST1 homodimers and homotrimers. These<br />
results lead us to postulate that LST1 multimers may act as transmembrane adaptor<br />
proteins by transducing signals received from an associated coreceptor, which we are<br />
currently in the process of identifying.
Niklas Engels, Gökhan Yigit, Christoph Emmerich, Dirk Czesnik, Detlev Schild, Jürgen<br />
Wienands<br />
Lytic replication of Epstein-Barr virus can be induced by<br />
LMP2A<br />
The B-lymphotropic Epstein-Barr virus (EBV) encodes two integral membrane proteins,<br />
LMP1 and LMP2A, which can be expressed in infected B cells during difference stages of<br />
viral latency. LMP2A contains an immunoreceptor tyrosine-based activation motif<br />
(ITAM) in its N-terminal cytoplasmic tail that is thought to provide a maintenance signal<br />
for EBV-infected cells. However, no cellular systems are available to study LMP2A<br />
function independently of other virally encoded proteins. We have generated a Cre/LoxPbased<br />
system for inducible expression of LMP2A in the DT40 B cell line, which allows<br />
real time monitoring of LMP2A-induced signaling events. We can show that mere<br />
expression of LMP2A results in ligand-independent activation of protein tyrosine kinases<br />
and phospholipase-γ2 (PLC-γ2). Activated PLC-γ2 produces the second messengers IP3<br />
and DAG, which causes oscillatory cytosolic Ca2+ waves and activation of the Erk-MAP<br />
kinase pathway, respectively. The latter pathway turned out to be a mandatory positive<br />
feedback mechanism for LMP2A protein production itself. Eventually, LMP2A-activated<br />
signaling cascades culminate in expression of BZLF1, the key regulator of lytic EBVreplication.<br />
Hence, the physiologic function of LMP2A is not to support survival of<br />
latently infected cells but to act as positive regulator of lytic EBV replication.
Heiko Johnen, Tamara Kuffner, Andrew Cook, Emma Braine, Ben Wu, Roland Stocker,<br />
Samuel Norbert Breit<br />
Macrophage Inhibitory Cytokine 1(MIC-1) reduces disease<br />
severity in mouse models of arthritis and atherosclerosis<br />
Macrophage Inhibitory Cytokine 1 (MIC-1) is a member of the TGF-beta superfamily and<br />
is mainly expressed in the CNS, epithelial cells and macrophages. MIC-1 is upregulated<br />
in response to cellular stress, p53 activation, malignancy, injury and inflammation.<br />
Elevated serum MIC-1 levels were found in rheumatoid arthritis (RA) patients, and have<br />
been associated with an increased risk of developing cardiovascular diseases.<br />
Additionally, MIC1 has been detected in macrophages within human atherosclerotic<br />
lesions and in rheumatoid synovial tissue. These results suggest a role for MIC-1 in<br />
inflammatory or autoimmune diseases like atherosclerosis and RA.<br />
Methods:<br />
We created MIC-1 transgenic mice using the c-fms (macrophage specific) promoter. The<br />
effect of MIC-1 overexpression was analyzed by comparing disease progression in the<br />
ApoE KO mouse models of atherosclerosis, collagen induced arthritis (CIA), and the KRN<br />
model of serum transfer arthritis.<br />
Results:<br />
ApoE KO mice also overexpressing MIC-1 had smaller lesions in the aortic sinus and the<br />
thoracic aorta compared to ApoE KO mice, but unchanged serum levels of cholesterol,<br />
CRP, selected inflammatory mediators, and other serum markers of liver and renal<br />
function. In serum transfer arthritis and CIA, MIC-1 overexpression reduces disease<br />
severity. In CIA no difference in collagen specific T-cell proliferation or IgG production<br />
could be detected.<br />
Whilst the underlying mechanism is as yet not fully understood, the protection from<br />
disease in these 3 different animal models supports that MIC-1 acts as an antiinflammatory<br />
cytokine in vivo.
Katharina Kronenberg, Beate G. Exner, Christine Sattler, James A. Hutchinson,<br />
Gudrun E. Koehl, Stefan Farkas, Hans J. Schlitt, Fred Fändrich, Edward K. Geissler<br />
Macrophages Driven to a Novel State of Activation have Anti-<br />
Inflammatory Properties in Mice<br />
Recurrent episodes of inflammation underlie numerous pathologies, notably the<br />
inflammatory bowel diseases (IBD). Here, we describe a population of macrophagederived<br />
cells which mitigate autoimmune colitis in mice, leading to histological<br />
resolution of the affected intestinal mucosa. Cells were generated from murine<br />
mononuclear cells in the presence of M-CSF and subsequently stimulated with IFN-g to<br />
produce what we refer to as “IFN-g-stimulated monocyte-derived cells” (IFNg-MdCs).<br />
Cells were characterized by FACS and immunomodulation was examined by assays for<br />
cell death and T cell regulation. Therapeutic effects were assessed in mouse models of<br />
chronic colitis. IFNg-MdCs express markers including CD11b/c, CD14, CD86, CD123,<br />
and PD-L1; IFNg-MdCs only arise when macrophages are cultivated in the presence of<br />
CD4+ T cells, M-CSF and IFN-g. In vitro, IFNg-MdCs profoundly delete lymphocytes (by<br />
>60%) derived from mice with colitis by a cell-contact, cell activation, and caspasedependent<br />
mechanism. Intriguingly, lymphocytes surviving in IFNg-MdC cocultures are<br />
highly enriched for CD4+CD25+Foxp3+ cells, which show up-regulation of IL-10, and<br />
actively suppress T cell proliferation. CD11b+ cells within the IFNg-MdC population are<br />
responsible for lymphocyte depletion and CD4+CD25+Foxp3+ cell induction.<br />
Additionally, using knock-out mice, we show that signaling via IFN-gR and CD40 on<br />
IFNg-MdCs are necessary for the generation of T regulatory cells. Regarding potential<br />
therapeutic activity for IBD, IFNg-MdCs reduced established inflammation in two mouse<br />
models of chronic colitis. We conclude that IFNg-MdCs represent macrophages in a<br />
novel state of activation, possessing multiple T cell-suppressive effects with therapeutic<br />
potential to mitigate autoimmune inflammation.
Günes Esendagli, Kirsten Bruderek, Torsten Goldmann, Andreas Busche, Detlev<br />
Branscheid, Ekkehard Vollmer, Sven Brandau<br />
Malignant and non-malignant lung tissue areas are<br />
differentially populated by natural killer cells and regulatory T<br />
cells in non-small cell lung cancer<br />
Even though the lung represents a special immune compartment with the capacity of a<br />
high inflammatory response, ineffective anti-tumor immunity is common in lungassociated<br />
malignancies. We asked whether a differential composition of the immune<br />
cell infiltrate in malignant (MLTAs) and non-malignant lung tissue areas (N-MLTAs)<br />
exists and might potentially contribute to this effect. We performed a comparative<br />
analysis of immune cells residing in MLTAs and N-MLTAs of non-small cell lung cancer<br />
(NSCLC) patients. To this end, we used immunophenotyping and functional analyses on<br />
directly isolated immune cells and tissue arrays on archived paraffin-embedded<br />
specimens. A strong T cell infiltration was prominent in both tissue compartments<br />
whereas CD4+CD25+CD127- T regulatory cells were present in MLTAs only.<br />
Nonetheless, concurrent functional ex vivo T cell analyses revealed no<br />
significant difference between T cells of MLTA and N-MLTA, suggesting that<br />
tumor-infiltrating T cells were not functionally impaired. Interestingly, T cell infiltration<br />
was less pronounced in specimens with a high neutrophilic infiltrate. NK cell infiltration<br />
was strikingly heterogenous between MLTA and N-MLTA. While NK cells were almost<br />
absent in the malignant tissue regions, non-malignant counterparts were selectively<br />
populated by NK cells and those NK cells showed strong cytotoxic activity ex vivo. We<br />
report that malignant and non-malignant tissue areas in NSCLC are selectively<br />
infiltrated by certain immune cell types with NK cells being displaced from the tumor<br />
tissue. These phenomena have important implications for tumor immunology of NSCLC<br />
and should be considered for the development of future immunologic intervention<br />
therapies.
Christina Janko, Udo S. Gaipl, Sandra Franz, Nina Ebel, Eberhard Schlücker, Roland<br />
Meyer-Pittroff, Martin Herrmann, Benjamin Frey<br />
Mammalian cells under pressure – Cell death pathways and<br />
immunogenicity of dying cells<br />
Today, various forms of cancer cause the death of every forth human world wide. The<br />
classical therapies for solid cancer have limitations in prolonging the live span of the<br />
patients. Therefore, treatment of cancer requires new therapeutic strategies. Recently<br />
described therapeutic approaches are based on the vaccination of cancer patients with<br />
autologous, inactivated tumour cells. The master requirements of cell based,<br />
therapeutic tumour vaccines are (I) the <strong>complete</strong> inactivation, (II) the preservation of<br />
their immunogenicity, and (III) the accordance with statutory provisions. Currently,<br />
physical treatments (e.g. X-ray, freeze-thaw) and chemotherapeutics are used to<br />
inactivate tumour cells for vaccination, but all procedures have methodological,<br />
therapeutical, or legal restrictions. For this reason, we are involved with high<br />
hydrostatic pressure (p > 50 MPa) for inactivation of tumour cells.<br />
When tumour cells treated with pressure up to 100 MPa they interrupted proliferation<br />
but the treatment did only marginally affect cells’ viability. A treatment with pressure<br />
above 200 MPa, however, resulted in cell death without survivors even in long-term<br />
culture. We analyzed the matter of cell death and detected, that cells pressurized with<br />
200 MPa died in consecutive cultures by apoptosis with preservation of the ion<br />
selectivity of the plasma membrane, phosphatidylserine exposure, and morphological<br />
alterations typical for apoptosis. In contrast, the cells treated with pressure above 300<br />
MPa necrotize during treatment. Most importantly, both pressurized apoptotic and<br />
necrotic cells largely retained their immunogenicity. In contrast to alternative methods<br />
for the induction of necrosis (heat, detergent, oxidative stress), the nuclei of HHP<br />
treated cells were efficiently degraded by a Ca2+-dependent DNase within a few hours<br />
in culture. Furthermore, the viscosity of the cytoplasm increased dramatically.<br />
Therefore, soluble constituents of the cells are retained within the jellified cytoplasm.<br />
These features favour HHP as a powerful technique for the inactivation of tumour cells<br />
employed in whole cell-based vaccination trials.
Christoph Lauer, Michael Basler, Susan D. Demo, Marcus Groettrup<br />
Manipulation of MHC class I antigen presentation by a LMP7specific<br />
inhibitor<br />
The proteasome is responsible for the generation of most epitopes presented on MHC<br />
class I molecules. Treatment of cells with interferon-? leads to the replacement of the<br />
constitutive catalytic subunits ?1, ?2 and ?5 by the inducible subunits LMP2 (?1i), MECL-<br />
1 (?2i) and LMP7 (?5i). The incorporation of these subunits seems to be required for the<br />
production of several MHC class I restricted T cell epitopes. In this study, we<br />
investigated the effect of a novel LMP7-specific inhibitor on antigen presentation.<br />
Fluorogenic assays with substrates specific for the chymotrypsin-like activity<br />
demonstrated that the inhibitor acts specifically on LMP7 in a concentration range of<br />
100-300nM. Furthermore, experiments with immunoproteasome deficent mice revealed<br />
that the generation of the male HY-derived Uty246-254 epitope is not only LMP7dependent,<br />
as previously reported, but also dependent on LMP2. Treatment of male<br />
splenocytes with the LMP7-specific inhibitor reduced the Uty246-254 presentation to<br />
background levels. Flow cytometric analysis of inhibitor treated splenocytes showed a<br />
reduction of MHC-I expression on wild type, but not on LMP7-deficient cells. Moreover,<br />
inhibition of LMP7 in cells infected with lymphocytic choriomenengitis virus (LCMV), led<br />
to decreased presentation of the LCMV-derived GP33-41 epitope. Taken together, we<br />
were able to show for the first time, that a specific inhibition of the ifn-? inducible<br />
immunoproteasome subunit LMP7 leads to a reduced presentation of several MHC class<br />
I restricted epitopes.
Lisa Bruns, Oliver Frey, Christiane Landgraf, Rudolf Volkmer, Thomas Kamradt<br />
Mapping of T cell epitopes in Glucose-6-Phosphate-Isomerase<br />
induced arthritis<br />
Immunization of certain non-transgenic mouse strains with recombinant human Glucose-<br />
6-Phosphate-Isomerase (huG6PI) leads to the development of polysymmetric arthritis,<br />
an animal model for Rheumatoid arthritis. We found that DBA/1 mice as well as SJL<br />
mice are susceptible for G6PI-induced arthritis. We have already demonstrated that CD4<br />
+ T cells are crucial both in the induction and effector phase of the disease. Therefore<br />
we used pools of overlapping huG6PI peptides to determine T cell epitopes that are<br />
relevant for G6PI-induced arthritis. We figured out two potential T cell epitopes:<br />
huG6PI85-99 and huG6PI469-483. Interestingly, we discovered the same epitopes both<br />
in DBA/1 and SJL mice. After immunization of DBA/1 mice with huG6PI85-99 and<br />
huG6PI469-483, the mice developed a mild arthritis with lower incidence. The time<br />
course of disease of peptide immunized mice differed from mice immunized with<br />
<strong>complete</strong> protein. Additionally we found huG6PI-specific antibodies not only in huG6PI<br />
immunized mice but also in peptide immunized mice. Thus, we conclude that huG6PI85-<br />
99 and huG6PI469-483 are important T cell epitopes in G6PI-induced arthritis.
Peter Kramer, Frank Siebenhaar, Marcus Maurer, Sven Hendrix<br />
Mast cell deficient mice display increased brain inflammation,<br />
neurodegeneration and astrogliosis<br />
Mast cells (MCs) play a key role in the development and severity of multiple sclerosis<br />
and its animal model, experimental autoimmune encephalomyelitis. However, the role<br />
of mast cells in the wound healing response after traumatic brain injury is unknown.<br />
Here, we compared mast cell-deficient W/Wv-mice and wildtype controls after<br />
mechanical brain injury. We used the well-studied entorhinal cortex lesion (ECL) model<br />
to analyze the immunoreactivity patterns of glial fibrillary acidic protein (GFAP,<br />
astrocyte activation), neurofilament 200 (neurons), isolectin B4 (IB-4, microglia), Ki67<br />
(proliferation) and FluoroJade B (neurodegeneration) after injury. GFAP<br />
immunoreactivity and astrocyte proliferation around the lesion was two times higher in<br />
mast cell-deficient mice compared to controls, while neurofilament 200 expression at<br />
the lesion site was substantially reduced. Mast cell-deficient mice showed a significantly<br />
higher number of IB-4-positive cells including a high number of proliferating cells in the<br />
lesion area compared to controls. Finally, at day 4 after lesion there is a significantly<br />
higher number of FluoroJade B positive neurons in mast cell-deficient mice. These data<br />
suggest that MCs protect from brain inflammation, neurodegeneration and astrogliosis.
Yves Montier, Axel Lorentz, Sigrid Krämer, Stephan C Bischoff<br />
Mast cell mediators stimulate fibroblasts to produce IL-6 that<br />
vice versa supports mast cell survival<br />
Background: Human intestinal mast cells (MC) are key effector cells in allergic reactions<br />
but also involved in host defense and tissue remodeling processes such as wound<br />
healing, angiogenesis, and fibrogenesis. We have shown previously that human<br />
intestinal fibroblasts (FB) suppress apoptosis in human intestinal MC independent of the<br />
mast cell growth factor stem cell factor (SCF) as well as IL-3, IL-4 and NGF. Here, we<br />
show that IL-6 is the missing factor. Methods: Human intestinal MC and FB were<br />
isolated from surgical tissue specimens using a four-step enzymatic dispersion method.<br />
Following overnight culture, MC were separated from adherent FB and purified using<br />
MACS-technique. Results We found that intestinal FB are capable of producing IL-6<br />
provided that they were stimulated directly by MC in co-culture or by MC mediators<br />
such as TNF-α, IL-1β, tryptase or histamine. In order to investigate the role of IL-6 for<br />
the survival of intestinal MC, MC were incubated with different concentrations of IL-6. 2<br />
ng IL-6/ml or higher concentrations of IL-6 supported MC survival until 12-16 d of<br />
culture. But, in contrast to treatment with SCF, all MC incubated with IL-6 died after 20-<br />
24 d of culture. Interestingly, culture of MC with supernatants of FB stimulated with TNF-<br />
• or IL-1• gave the same result: MC survived 12-16 d of culture, but they died after 20-<br />
24 d. MC survival in response to treatment with FB supernatant could be blocked using<br />
an anti-IL-6 Ab. Conclusion: Our findings suggest that MC mediators (TNF-α, IL-1β,<br />
histamine and tryptase) stimulate FB to produce IL-6 that vice versa supports MC<br />
survival.
Julia Scholten, Alexander Gerbaulet, Giuseppe Testa, Thomas Krieg, Karin Hartmann,<br />
Axel Roers<br />
Mast cell-specific Cre/loxP-mediated mutagenesis in vivo<br />
Mast cells are important effector cells in type I allergy, but were recently also shown to<br />
play key roles in host defence against pathogens. In addition, mast cells were<br />
implicated in tissue remodeling, wound healing and transplant tolerance. Investigation<br />
of this important cell type, however, was severely hampered by the scarcity of mast<br />
cells in the various tissues and the lack of protocols for ex vivo culture of mast cells.<br />
Until today, in vivo analysis of mast cell-specific functions of individual genes relied on<br />
the reconstitution of genetically mast cell-deficient mice with mast cells differentiated in<br />
vitro from bone marrow of mice deficient for the gene of interest. This system yielded<br />
important information in the past, but suffers severe limitations. Herein, we use the Cre/<br />
loxP recombination system for conditional mast cell-specific mutagenesis in vivo. In a<br />
bacterial artificial chromosome (BAC) containing the entire mouse mast cell protease 5<br />
(Mcpt5) locus, the coding region of exon 1 was replaced by a Cre cassette. The BAC<br />
insert was purified and micro-injected into pronuclei of fertilized C57BL/6 oocytes to<br />
obtain transgenic mice. In order to demonstrate mast cell-specific Cre-mediated<br />
recombination, six Mcpt5-Cre founder lines were crossed to a Rosa26-EYFP Cre-excision<br />
reporter line and cell suspensions of various tissues were analysed by flow cytometry.<br />
Two of the transgenic lines showed highly efficient Cre-mediated induction of the<br />
fluorescent reporter protein in mast cells, but not in other cell types. The new Cretransgenic<br />
mouse lines will be useful tools in the elucidation of mast cell biology.
ERIETTA STELEKATI, ZANE ORINSKA, ANNALENA BOLLINGER, SILVIA BULFONE-PAUS<br />
Mast cells modulate CD8+ T cell responses.<br />
Mast cells are considered to contribute dominantly to the establishment of an innate<br />
immune response. However, mast cells can also act as important participants of the<br />
adaptive immune response, by regulating the phenotype and function of the adaptive<br />
immunity players (B cells, dendritic cells and T cells). T cells represent a cutting edge<br />
for the induction of adaptive immunity and CD8+ T cells have been reported to be<br />
recruited in vivo by mast cells. Therefore, this study was focused on the crosstalk<br />
between mast cells and CD8+ T cells. The potential of mast cells to induce antigenspecific<br />
CD8+ immune responses was investigated. We could demonstrate that bone<br />
marrow derived mouse mast cells (BMMCs) labelled with OVA-derived OT-I peptide were<br />
able to induce activation, cytokine production and proliferation of transgenic, OT-I<br />
specific CD8+ T cells. Moreover, blocking of cytokine synthesis in BMMCs by mitomycin<br />
C treatment and, to a higher extent, fixation of BMMCs by paraformaldeyde treatment,<br />
decreased their ability to specifically activate CD8+ T cells, thus demonstrating that the<br />
specific activation of CD8+ by BMMCs is dependent both on membrane-bound peptides<br />
and on soluble factors produced by BMMCs. Furthermore, Toll like receptor – specific<br />
pre-priming of BMMCs increased their ability to induce antigen specific CD8+ responses.<br />
Finally, BMMCs were able to induce antigen specific proliferation of naïve primary CD8+<br />
T cells in vivo, as measured by CFSE staining. Taken together, these data demonstrate<br />
that mast cells can potently induce antigen specific CD8+ responses. This function of<br />
mast cells can be modulated by Toll like receptor signals. Thus, it is suggested that<br />
mast cells play a key regulatory role at the cross-roads of innate and adaptive immunity.
Milan Popovic, Ana Teles, Catharina Thuere, Anne Schumacher, Paul Ojiambo Wafula,<br />
Hans-Dieter Volk, Ana Claudia Zenclussen<br />
Mast-cell-associated genes Thp1, Mcpt1 and Mcpt5 are upregulated<br />
after Treg-induced tolerance at the fetal-maternal<br />
interface: new role for mast cells in pregnancy-induced<br />
tolerance?<br />
Objective - CD4+ CD25+ foxp3+ regulatory T cells (Treg) are known to play an<br />
important role in murine pregnancy outcome by inducing tolerance towards the<br />
semiallogenic fetus. Mast cells (MC) are known as primary responders in allergic<br />
reactions. Furthermore, it has been shown that activated MC produce a broad spectrum<br />
of pro- and anti-inflammatory mediators having very important role in immune<br />
response to foreign antigens. Recent studies revealed a novel role for MC in the Tregdependent<br />
allograft tolerance by secreting interleukin-9 (IL)-9. Here, we investigated<br />
whether MC may be also involved in Treg- mediated tolerance towards the<br />
semiallogenic fetus.<br />
Methods – We employed a well characterized murine combination for spontaneous<br />
abortion (DBA/2J-mated CBA/J females) to identify and quantify MC and their related<br />
molecules. BALB/c-mated CBA/J females served as controls for normal pregnancy.<br />
Furthermore, a further group was included, which consisted of animals rescued from<br />
abortion after transfer of antigen-specific Treg. Localization of MC at the fetal-maternal<br />
interface was verified by Giemsa staining. The mRNA expression of MC-associated genes<br />
(tryptophan hydorxylase (Tph)-1 as well as mast cell protease (Mcpt)-1 and Mcpt-5 in<br />
normal pregnant (NP) mice, abortion-prone (AP) and abortion-prone mice treated with<br />
Treg (AP+Treg) was analyzed in placental and decidual samples from normal pregnant<br />
(NP), abortion-prone (AP) and AP mice transferred with Treg by real-time RT-PCR.<br />
Results and conclusions – Mast cells were localized preferentially in decidua according to<br />
their granulary morphology, while very few MC could be detected in the placenta. The<br />
transcript levels of Tph1, Mcpt-1 and Mcpt-5 were comparable during the all pregnancy<br />
stages (days: 8, 10, 12 and 14) between NP and AP mice. However,treatment with Treg<br />
on day 14 markedly up-regulated their levels in both, decidua and placenta to the levels<br />
observed in NP mice. Our results indicate that as already observed in transplantationassociated<br />
tolerance, MC might contribute to the Treg-induced tolerance at the fetalmaternal<br />
interface.
Kristina Wiege, Syed Raza Ali, Stephanie Konrad, Roland Piekorz, Bernd Nürnberg,<br />
Reinhold E Schmidt, J Engelbert Gessner<br />
MECHANISM OF CELL AND ISOTYPE SPECIFIC Gαi DEPENDENT<br />
SIGNALING IN IMMUNE EFFECTOR CELLS<br />
G-protein- coupled receptor (GPCR) signal transduction contributes to the course of<br />
inflammation processes. In the context of immune complex (IC) mediated lung<br />
inflammation the GPCR, the complement 5a receptor (C5aR) is significantly involved in<br />
lung pathology. Previous experimental data verified pertussis toxin sensitive FcRγ<br />
regulation by C5aR suggesting for Gαi -dependent signal transduction mechanism. From<br />
the three known isoforms of inhibitory Gαi proteins, Gαi2 and Gαi3 but not Gαi1 are<br />
expressed on alveolar leukocytes, including macrophages (AM) and neutrophils with the<br />
exception of a splice variant of Gαi2 (sGαi2 ) which appearance is restricted to AM. Mainly<br />
Gαi2 appears to be involved in the regulation IC mediated inflammation. Genetic<br />
deletion of Gαi2 resulted in reduced lung inflammation whereas it was unaffected in<br />
mice lacking Gαi3 . On AM from Gαi2 deficient mice C5aR expression was reduced; this<br />
was not seen for neutrophils, suggesting cell and isotype specific functions of (s)Gαi2 /<br />
Gαi3 . To verify the role of the different isotypes we are using the RNA-Interference<br />
technique. We could demonstrate that the knock down of Gαi2 mRNA leads to the<br />
reduced expression of C5aR on peritoneal macrophage cell line. This effect could be<br />
rescued by the overexpression of Gαi2 . Future work comprises the analysis of sGαi2 and<br />
Gαi3 overexpression in Gαi2 knock down cells to clarify the role of the specific isoforms<br />
on the trafficking and functioning of the C5aR.<br />
Part of the work was supported to K.W. by graduate program (GRK705) of the Deutsche<br />
Forschungsgemeinschaft
Marco Wendel, Elisabeth Suri-Payer, Adelheid Cerwenka<br />
Mechanisms of NK cell migration in response to tumors<br />
Natural Killer (NK) cells are among the first immune cells to enter and eradicate<br />
growing tumors, in particular tumors with deficiency in MHC class I expression. In<br />
several studies high numbers of tumor infiltrating NK cells correlated with a good<br />
prognosis for cancer patients. However, only little is known about the factors regulating<br />
NK cell migration during anti-tumor immune responses. Our study aimed at identifying<br />
these factors in the model of subcutaneously growing MHC class I deficient lymphoma<br />
RMA-S. We observed that IFN-γ was absolutely required for NK cells to accumulate<br />
within the tumor tissue. Much fewer NK cells were infiltrating the tumors in IFN-γR KO<br />
mice or when IFN-γ was neutralized and exogenous application of IFN-γ further<br />
increased NK cell infiltration. We also observed that the depletion of regulatory T cells<br />
led to increased numbers of NK cells in the tumors, which was also dependent on the<br />
presence of IFN-γ. Since it has been reported that IFN-γ regulates the expression of the<br />
chemokine IP-10 and its receptor CXCR3, we determined their contribution to NK cell<br />
migration in our model. Tumor infiltrating NK cells were significantly decreased in<br />
CXCR3 -/- mice and the migratory capacity of adoptively transferred CXCR3 -/- NK cells in<br />
wt mice was impaired. Accordingly, intratumoral injection of IP-10 resulted in locally<br />
increased NK cell numbers and IP-10 transduced RMA-S cells were rejected in wt mice<br />
in a NK dependent manner. These data identify the expression of the chemokine<br />
receptor CXCR3 as a major prerequisite for NK cell migration towards the tumor.<br />
Exploitation of strategies to augment NK cell accumulation in the tumor tissue might<br />
prove beneficial in developing more powerful anti-tumor therapies.
Barbara C. Rütgen, Wilhelm Gerner, Armin Saalmüller, Sabine E. Hammer<br />
MHC typing in swine: The SLA-haplotype repertoire of<br />
Austrian Large White, Landrace, and Pietrain breeding stocks<br />
MHC (major histocompatibility complex) genes encode cell surface glycoproteins which<br />
bind and present antigenic peptides to T cells. The genes within this complex are highly<br />
polymorphic, suggesting that diversity in MHC genes is a good measure of population<br />
fitness. Resource herds of swine leukocyte antigen (SLA)-characterized pigs are<br />
valuable large animal models for biomedical research in terms of immune responses,<br />
disease resistance, and production traits. This study represents the initial<br />
characterization of founder haplotypes of commercial pigs in Austria which are F2<br />
descendants of purebred Large White, Landrace, and Pietrain populations. The<br />
respective founder SLA-haplotypes were detected by a reverse transcription-polymerase<br />
chain reaction (RT-PCR)-based SLA typing method to clone and DNA sequence the<br />
putative alleles at four SLA class Ia loci, designated as SLA-1, SLA-2, SLA-3, and SLA-6<br />
and four SLA class II loci, SLA-DQA1, SLA-DQB1, SLA-DRA1, and SLA-DRB1. The data<br />
obtained so far indicate that the Large White, Landrace, and Pietrain pigs have at least<br />
four SLA class Ia founder haplotypes (4a.0, 4b.0, 13.0, 5.0) and three SLA class II<br />
founder haplotypes (0.4, 0.2, 0.9). Furthermore, the analyzed specimen point toward<br />
the occurrence of at least three novel SLA class Ia haplotypes. The newly generated<br />
sequences will be used to design allele-specific primers for establishing a rapid SLA<br />
typing assay to discriminate each allele using PCR with sequence-specific primers (PCR-<br />
SSP). To check the PCR screening approach for false negatives, positive control primers<br />
were also designed to amplify a portion of the alpha-actin gene and multiplexed with<br />
the allele-specific primers. By applying a combination of SLA typing by cloning and DNA<br />
sequencing together with PCR-SSP, we will be able to characterize the entire Large<br />
White, Landrace, and Pietrain breeding stocks and to identify the SLA haplotype<br />
distribution present in the respective breeds.
J. Albrecht, T. J. Boeld, K. Doser, R. Eder, J. Stahl, R. Andreesen, J. Ermann, M.<br />
Edinger, P. Hoffmann<br />
MHC-compatibility between conventional and regulatory T<br />
cells is required for suppression of allospecific T cell responses<br />
Natural CD4+CD25+ regulatory T cells (Treg) contribute to tolerance induction after<br />
transplantation. We, and others, previously showed that the adoptive transfer of donorderived<br />
Treg cells prevents lethal graft-versus-host disease (GVHD) after allogeneic<br />
bone marrow transplantation (BMT) in mice. In contrast, host-type Treg cells failed to<br />
protect when co-transplanted under identical conditions. This raises the question<br />
whether MHC compatibility with CD25-CD4+ and CD8+ T cells (Tconv) is a general<br />
prerequisite for the suppression of alloresponses by Treg cells, or whether merely<br />
elimination of host-type Treg by allo-aggressive Tconv cells occurred. To address this<br />
issue, mixed lymphocyte cultures were performed in which CFSE-labelled responder T<br />
cells (Tresp), Treg cells and antigen presenting cells (APC) were systematically varied<br />
with regard to their MHC haplotype. When C57BL/6 Tresp cells were stimulated with<br />
irradiated CB6F1 (BALB/c x C57BL/6) APC, 16.9 + 1.5% of the CD4+ cells and 81.5 +<br />
2.5% of the CD8+ cells had gone through at least one cell cycle after 6 d. In the<br />
presence of syngeneic C57BL/6 Treg cells, proliferation of CD4+ and CD8+ Tresp cells<br />
was decreased to 5.2 + 2% and 26.5 + 3.5%, respectively. In contrast, in cultures with<br />
allogeneic BALB/c Treg cells, proliferation remained at 10.3 + 0.3% and 89.9 + 0.9%<br />
for CD4+ and CD8+ Tresp cells, respectively. Stimulation with either mixed C57BL/6<br />
and BALB/c APC or third party APC (DBA/1) led to comparable results. Lack of<br />
suppression cannot be explained by early elimination of allogeneic Treg cells, since they<br />
were still detectable on d6 in co-cultures with MHC mismatched Tresp cells. In<br />
corresponding in vivo studies, CB6F1 recipients were only protected from lethal GVHD<br />
when both donor T cell populations were MHC-identical, but not when Tconv and Treg<br />
cells were derived from the two separate parental strains. These data indicate that MHCidentity<br />
between Tresp and Treg cells is required for maximum suppression of an<br />
alloresponse and that Treg cells isolated from a third party donor might not be suited<br />
for the prevention of GVHD after allogeneic BMT.
Romney Haylett, Lothar Rink<br />
MHC-II Signaling Directs the Activation of NFAT but not NF-κB<br />
in B Cells<br />
For over a decade major histocompatibility complex class II (MHC-II) molecules have<br />
been acknowledged as signaling receptors although their mode of signaling and exact<br />
signaling pathways have yet been fully clarified. In this study, the MAP kinase pathway<br />
leading to ERK1/2 activation was explored for all three HLA isotypes (HLA-DR, -DP, -<br />
DQ) in the B cell lines BJAB and Raji. Not only could ERK1/2 activity be observed after<br />
signaling through all three isotypes, but the activation of c-Fos, a well-described<br />
component of the AP-1 transcription factor known to be phosphorylated by ERK1/2, was<br />
also established. This led to further studies pertaining to transcription factor activation<br />
where ligation of MHC-II molecules ultimately led to NFAT1 activation but not NF-κB<br />
activation in B cells. Future investigations should elucidate whether or not the entire AP-<br />
1 complex interacts with NFAT in B cells after MHC-II ligation. Although NFAT1<br />
activation has been described in B cells, relatively few work has been conducted in this<br />
field. With the novel discovery of MHC-II molecules capable of inducing NFAT activation,<br />
the understanding of MHC-II signaling and NFAT activation in B cells can be<br />
tremendously greatened.
Karina Stein, Jennifer Debarry, Anna Hanuszkiewicz, Otto Holst, Jörg Mages, Roland<br />
Lang, Holger Heine<br />
Microarray analysis of human dendritic cells stimulated with<br />
four different bacterial strains with focus on allergyprotecting<br />
mechanisms<br />
The incidence of allergic diseases is increasing, especially in industrialized regions. A<br />
growing number of publications indicate that farming environment in early childhood<br />
reduces the occurrence of allergic reactions later in life. Recently, we showed that the<br />
cowshed isolates Lactococcus lactis G121 and Acinetobacter lwoffii F78 prevent allergic<br />
immune responses in a mouse asthma model. However, the molecular mechanisms<br />
modulating allergic reactions in humans are only poorly understood. Thus, we<br />
stimulated human dendritic cells (DC) with these bacteria and two other reference<br />
strains, E. coli F1111 9-41 and B. subtilis DSM618, and prepared microarray analysis<br />
after 3, 6 and 12 hrs. A total number of 3623 probe sets in L. lactis-, 4254 sets in A.<br />
lwoffii- and 4625 sets in E. coli-treated DCs was regulated at least three-fold but only<br />
1939 probe sets in B. subtilis-treated DCs. Scatterplot analysis revealed that the<br />
induced expression pattern of E. coli and A. lwoffii stimulated DCs is comparable, with<br />
already a high number of regulated genes after 3 hrs. In contrast, nearly no genes were<br />
regulated in L. lactis-treated DCs after 3 or 6 hrs and only a moderate number after<br />
stimulation with B. subtilis. However, after 12 hrs of stimulation, L. lactis-treated DCs<br />
showed an expression pattern similar to that induced by A. lwoffii and E. coli whereas<br />
DCs treated with B. subtilis differed clearly. Cluster analysis confirmed a close relation<br />
between A. lwoffii-, E. coli- and L. lactis-treated DCs after 12 hrs whereas B. subti<strong>list</strong>reated<br />
DCs formed a separate cluster. Overall, the analysis of cowshed bacteriainduced<br />
gene expression patterns leads to a better understanding of the molecular<br />
mechanism preventing allergic immune responses (supported by DFG, SFB/TR22,<br />
project A2).
Kristina Allers, Désirée Kunkel, Verena Moos, Martin Eisenblätter, Christiane Stahl-<br />
Hennig, Annette Schrod, Ralf Ignatius, Franz-Josef Kaup, Thomas Schneider<br />
Migration patterns of activated versus non-activated nonhuman<br />
primate T lymphocytes: preferential homing of<br />
activated autologous CD8+ T cells in the rectal mucosa<br />
Background: Adoptive cell transfer (ACT) is a promising approach to induce antitumour<br />
immune responses in cancer patients. However, crucial for successful therapy is the<br />
access of the transferred cells to the tumours. Little is known about the migration<br />
patterns of in vitro activated primate T cells and their persistence in different anatomical<br />
compartments after ACT. Here, we describe a model, which enables the long-term<br />
tracking of T cells in the peripheral blood, secondary lymphoid tissues, or<br />
gastrointestinal mucosa after re-infusion of autologous peripheral lymphocytes into<br />
rhesus macaques.<br />
Methods: PBMC from 4 or 3 rhesus macaques were activated with aCD3/aCD28 or not,<br />
stained with CFSE and autologously re-injected. Blood samples, lymph node (LN) as<br />
well as mucosal biopsies (duodenum, rectum) were collected at various time points over<br />
28 days and analysed for the presence of labeled CD4+ and CD4- T cells using flow<br />
cytometry.<br />
Results: On d1 post transfer of activated cells the frequency of labeled cells was 0.2,<br />
3.8 and 4.6% of total CD4+ T cells in blood, duodenum and rectum, respectively.<br />
Within the CD4- T cells the frequency of labeled cells was 0.2% in blood and 6.7% in<br />
the duodenum but as high as 27.5% in the rectal mucosa. 7 days post transfer of<br />
activated cells 0.3, 0.6, 0.5 and 0.4% labeled CD4+ T cells were present in the blood,<br />
LN, duodenum and rectum, respectively. Within the CD4- T cells the frequency of<br />
labeled cells was 0.03% in the blood, 0.3% in LN and 2.9% in the duodenum. In the<br />
rectal mucosa labeled cells constituted 29.6% of the total CD4- T cells indicating<br />
persistence of activated CD8+ T cells in the rectal mucosa.<br />
Conclusions: Injection of CFSE-labeled, autologous T cells into rhesus macaques allows<br />
the tracking of lymphocyte migration to various anatomical compartments and thus<br />
representing a pre-clinical model for the evaluation of T cell-based immunotherapy. Nonspecificly<br />
activated CD8+ T cells preferentially migrate to and persist in the rectal<br />
mucosa whereas activated CD4+ T cells are found in much less numbers at this site but<br />
also in other compartments.
Stefan Wiehr, Thomas Herrmann<br />
Milk-derived immune cells may serve as Trojan Horses in<br />
Toxoplasma gondii transmission<br />
Beside vertical transmission of T. gondii from acutely infected mothers in utero,<br />
transmission of T. gondii via the maternal milk has also been reported. To further<br />
analyze the lactogenic route of infection our study focused on parameters of humoral<br />
and cellular immune responses in congenitally versus milk infected rats. F344 rats were<br />
inoculated i.p. with 1x10e6 NTE or Prugneaud beta-gal tachyzoites at day 14 of<br />
gestation and blood and milk were taken every second day after delivery. Cells were<br />
isolated from the milk by density gradient centrifugation and analyzed by FACS and<br />
confocal microscopy. By using a human foreskin fibroblasts bioassay T. gondii positive<br />
milk samples could be detected until day 22 p.i.<br />
T. gondii tachyzoites could be observed inside cells whereas the non-cellular milk<br />
fraction was predominantly T. gondii negative, suggesting that T. gondii infected cells<br />
might serve as a vehicle for oral transmission to neonates. Strikingly, a strong antibody<br />
response was found in milk of infected rats. Moreover, the cellular fraction of the milk of<br />
infected rats showed a highly elevated number of CD45 positive cells consisting of all<br />
major alpha-beta and gamma-delta T cell and of granulocytes. To investigate whether<br />
the presence of tachyzoites in the milk correlated with transmission of T. gondii to<br />
uninfected offspring, we performed criss-cross experiments. Two months after birth,<br />
one out of 24 offspring fed with T. gondii positive milk showed a sustained increase of<br />
T. gondii antigen specific IgG2b as well as antigen specific proliferation with secretion of<br />
IFN-gamma by mesenteric lymph node cells and splenocytes. Six out of 44 offspring by<br />
which the parasite was transmitted in utero and 6 of 41 born from infected mothers<br />
exhibited the same type of immune response.<br />
These results indicate that T. gondii infected cells found in maternal milk may serve as a<br />
vehicle for parasite transmission and that both diaplacental and lactogenic infection<br />
induces a TH1 dominated immune response in the offspring of infected mothers.<br />
herrmann-t@vim.uni-wuerzburg.de
Marcin Kaminski, Peter H. Krammer, Karsten Gülow<br />
Mitochondria function as oxidative signalling organelles in<br />
activation-induced apoptosis of T cells.<br />
Reactive oxygen species (ROS) generated upon T cell activation are crucial for induction<br />
of CD95L expression and, consequently, for apoptosis of activated T cells (Activation<br />
Induced T cell Death - AICD). The molecular source and the signalling steps leading to<br />
activation-induced ROS production are still unclear.<br />
Our data show that the proximal T cell receptor (TCR) signalling machinery, consisting<br />
of ZAP70, LAT, SLP76, PLCγ1 and PKCθ, is crucial for ROS production. Upon activation,<br />
PKCθ translocates to the mitochondria. The depletion of mitochondrial DNA led to<br />
identification of mitochondria as source of activation-induced ROS. Pharmacological<br />
inhibition of the mitochondrial respiratory chain complex I (NADH-quinone<br />
oxidoreductase) or siRNA-mediated knockdown of the complex I assembly factor<br />
chaperone NDUFAF1 resulted in blocking of ROS production. Upregulation of MnSOD, a<br />
crucial mitochondrial antioxidative enzyme, converts ROS released by complex I into a<br />
hydrogen peroxide signal (H2O2). Since this signal is essential for CD95L expression,<br />
inhibition of complex I assembly by NDUFAF1-specific siRNA prevents AICD.<br />
Interestingly, application of metformin, an antidiabetic drug and mild, non-toxic<br />
complex I inhibitor, also led to decrease in activation-induced ROS production, CD95L<br />
expression and AICD.<br />
Therefore, PKC θ-dependent ROS release by mitochondrial complex I constitutes a<br />
crucial signalling event leading to AICD of T cells.
Martina Anzaghe, Zoe Waibler, Holger Ludwig, Shizuo Akira, Siegfried Weiss, Gerd<br />
Sutter, Ulrich Kalinke<br />
Modified vaccinia virus Ankara induces Toll-like receptor<br />
independent type I interferon responses<br />
Modified vaccinia virus Ankara (MVA) is a highly attenuated vaccinia virus strain<br />
undergoing clinical evaluation as a replication-deficient vaccine vector against various<br />
infections and tumor diseases. To analyze the basis of its high immunogenicity, we<br />
investigated the mechanism of how DNA encoded MVA induces type I interferon (IFN)<br />
responses. MVA stimulation of bone marrow derived dendritic cells (DC) showed that<br />
plasmacytoid DC were main IFN-alpha producers that were triggered independently of<br />
productive infection, viral replication, or intermediate and late viral gene expression.<br />
Increased IFN-alpha levels were induced upon treatment with mildly UV irradiated MVA<br />
suggesting that virus encoded immune-modulator(s) interfered with the host cytokine<br />
response. Mice devoid of Toll-like receptor (TLR) 9, the receptor for double stranded<br />
DNA, mounted normal IFN-alpha responses upon MVA treatment. Furthermore, mice<br />
devoid of adaptors of TLR signaling, MyD88 or TRIF, and mice deficient of protein kinase<br />
R (PKR) showed IFN-alpha responses that were only slightly reduced when compared to<br />
wild-type mice. MVA induced IFN-alpha responses were critically dependent on<br />
autocrine/paracrine triggering of the IFN-alpha/beta receptor (IFNAR) and were<br />
independent of IFN-beta, thus involving “half” a positive feedback-loop. In conclusion,<br />
MVA mediated type I IFN secretion was primarily triggered by non-TLR molecules, was<br />
independent of virus propagation and critically involved IFN-feedback stimulation. These<br />
data provide the basis to further improve MVA as a vaccine vector.
Christian Jacobi, Jürgen Roemisch, Stefan Meuer, Thomas Giese<br />
Modulation of gene expression by IVIG in healthy donors and<br />
multiple sclerosis patients<br />
Intravenous immunoglobulin G (IVIG) has become an established first- and second-line<br />
line treatment in a number of immune mediated diseases during recent years. IVIG is<br />
now proposed to modulate a wide range of molecules (e.g. bacterial/viral antigens,<br />
toxins, Fc receptors, complement, autoantibodies), to act on different cell types (e.g. B<br />
cells, T cells, macrophages, dendritic cells, endothelial cells), and to modulate various<br />
immunological pathways at both the humoral and cellular levels including inflammation,<br />
antigen presentation, cell growth and apoptosis. Using a variety of specific assays many<br />
distinct effects of IVIG have been demonstrated in vitro. To provide further insight into<br />
the mechanisms involved in IVIG-dependent immunmodulation under physiological<br />
conditions, we have established a human whole blood gene expression assay in vitro.<br />
There, we analyzed the effect of IVIG on CD2-, CD3-, LPS- and PMA/Ionomycin<br />
stimulated leukocytes in whole blood of 20 healthy donors, 15 untreated MS patients<br />
and two MS patients during relapse. IVIG induces among others the expression and<br />
release of Interferon-gamma, MCP1 and IP10. Interestingly, IVIG reduces the MCP1 and<br />
IP10 expression and release upon LPS stimulation, whereas Interferon-gamma<br />
expression is further enhanced. Since both chemokines are physiologically induced by<br />
Interferon, this effect of IVIG is unanticipated and deserves further investigation for its<br />
possible role in anti-inflammatory properties of IVIG. No significant differences in the<br />
IVIG induced expression profile between healthy donors and MS patients could be<br />
observed.
Anastasia Schneider, Tatiana Binder, Rodica Bernatowicz, Anke Zobywalski, Christine<br />
Falk, Anton Hartmann, Dolores Schendel, Susanne Krauss-Etschmann<br />
MODULATION OF HUMAN DENDRITIC CELLS BY SIX<br />
DIFFERENT PROBIOTIC BACTERIAL STRAINS<br />
Background<br />
Lactobacilli (Lb) and bifidobacteria (Bb) are probiotic bacteria and have been suggested<br />
to protect against allergic diseases. Since the underlying immune mechanisms are<br />
unclear at present, we tested whether six different probiotic strains polarize the<br />
maturation of human monocyte-derived dendritic cells (moDC).<br />
Methods<br />
UV-inactivated and live Lb rhamnosus GG (LGG, Valio Ltd, Finland), Bf. species 420<br />
(Bifidobacterium lactis, Danisco Deutschland GmbH), Lb acidophilus LA-5, Lb paracasei<br />
subsp. paracasei LC-01, Bb animalis BB-12 and Bb longum BB-46 (Chr.Hansen GmbH,<br />
Denmark) or LPS were co-cultured with moDC at ratios of 1-100 bacteria per one DC for<br />
24 h. UV-inactivated bacteria were counted visually after DAPI-staining. Viability of live<br />
bacteria was more than 90% as evaluated with a live/dead-staining kit (Invitrogen<br />
GmbH). Surface expression of costimulatory molecules on DC was analyzed by flow<br />
cytometry. Cytokines (IL-1beta, -6, -10, -12, TNF-alpha, IFN-gamma) and chemokines<br />
(IL-8, MIP-1alpha, MIP-1beta) were quantified in culture supernatants by multiplex<br />
assay (Bio-Rad Laboratories GmbH). Results are expressed as percentage of LPS<br />
stimulation.<br />
Results<br />
Priming with UV-inactivated BB-12 induced the highest synthesis of IL-6, -8, -10, -12,<br />
TNF-alpha and MIP-1alpha by moDC, while UV-inactivated LA-5 induced the highest<br />
synthesis of IL-1beta, IFN-gamma and MIP-1beta. In preliminary experiments, UVinactivated<br />
or live probiotics induced similar expression of costimulatory molecules on<br />
moDC.<br />
Conclusions<br />
The response of human moDC to UV-inactivated probiotics depends on the bacterial<br />
strain. UV-inactivated and live probiotics lead to similar expression profiles of<br />
costimulatory molecules on moDC. The analysis of the cytokine production of DC will<br />
show, whether this extends to soluble signals.
Irene Wittmman, Diana Aichele, Gerhard Groer, André Gessner, Markus Schnare<br />
Modulation of innate immune responses by recombinant<br />
murine bactericidal permeability / increasing protein through<br />
neutralizaton of LPS and Gram-negative bacteria<br />
Rationale: Recognition of LPS by TLR4 initiates inflammatory responses inducing potent<br />
anti-microbial immunity. However, uncontrolled inflammatory responses can be<br />
detrimental. In order to prevent the development of septic shock during an infection<br />
with Gram-negative bacteria the immune system has developed regulatory mechanisms<br />
to neutralize LPS by specialized proteins. Here we report the recombinant expression<br />
and functional characterization of the mouse homolog of human bactericidal<br />
permeability / increasing protein (BPI).<br />
Methods: Mouse BPI was stably expressed and highly purified by affinity<br />
chromatography. RAW 267.4 cells as well as bone marrow derived dendritic cells were<br />
stimulated with various TLR-ligands in the presence or absence of recombinant mouse<br />
BPI (rmBPI). Activation of the cells was determined by ELISA (TNF, IL-12), NO-assay as<br />
well as flow cytometry (CD86). In addition RAW macrophages expressing a NFκBreporter<br />
construct were stimulated with UV-treated Gram-negative (E. coli, S.<br />
typhimurium, N. meningitis, P. aeruginosa) as well as Gram-positive (Staph. aureus, L.<br />
monocytogenes, group B Streptococcus) bacteria in the presence or absence of rmBPI.<br />
The cellular activation was determined by TNF-ELISA and NFκB activity. Finally<br />
replicating E. coli were cultured with RAW macrophages in the presence or absence of<br />
rmBPI. The bacterial numbers as well as the cell activation was analyzed.<br />
Results: Purified rmBPI is a 60kD protein that was able to specifically neutralize LPSmediated<br />
activation of macrophages and to block LPS-dependent maturation of dendritic<br />
cells. Importantly, rmBPI neutralized the capacity of UV-irradiated and live Gramnegative<br />
bacteria to activate immune cells but it did not influence the stimulatory<br />
properties of Gram-positive bacteria. Finally rmBPI did not influence the bacterial<br />
growth.<br />
Conclusion: Together these data demonstrate that murine BPI is a potent LPS<br />
neutralizing protein that may play an important role as a negative modulator of innate<br />
immune responses during Gram-negative infections.
Stephan Schierer, Andrea Hesse, Ina Mueller, Eckhart Kaempgen, David T. Curiel,<br />
Gerold Schuler, Alexander Steinkasserer, Dirk M. Nettelbeck<br />
Modulation of viability and maturation of human monocytederived<br />
dentritic cells by oncolytic adenoviruses<br />
In spite of intensive efforts to modify oncolytic adenovirus (ads) for improved specificity<br />
and efficacy of cancer cell lysis, it is becoming increasingly clear that the killing of noninfected<br />
cancer cells in parallel to viral cell lysis will be crucial for oncolytic ads to be<br />
effective in the clinic. An attractive scenario towards this goal is the induction of<br />
systemic anti-tumor immunity by adenoviral oncolysis. In order to establish the basis<br />
for the development of adenoviral oncolytic vaccination we examined the effects of<br />
oncolytic ads on the biology of human dendritic cells (DCs). DCs are the most potent<br />
antigen presenting cells, key regulators of immune induction and have been intensively<br />
exploited for various vaccination protocols. The prime objective of this study was to<br />
investigate how optimized, melanoma-targeted oncolytic ads affect the viability and<br />
maturation of human monocyte-derived DC and the potency of such DCs to activate T<br />
cells.<br />
Both immature DCs (iDCs) and mature DCs (mDCs) were transducible with luciferase<br />
encoding ads at high titers. Fiber chimeric ads with an ad serotype 3 derived knob<br />
domain (5/3fiber) showed an improved transduction efficacy compared with an ad with<br />
serotype 5 (5fiber) fiber. After infection of iDC and mDC with oncolytic ads (5 or<br />
5/3fiber) at high titers (5000vp/cell), no significant toxicity was observed. Oncolytic ads<br />
showed no or strongly attenuated DNA replication in human DCs, thus confirming their<br />
replication specificity. As determined by staining of cell surface maturation markers of<br />
DCs two to three days post infection with oncolytic ads (5 or 5/3fiber), we observed,<br />
dependent on the donor, no or a partial DC maturation. With respect to the maturability<br />
of DCs with cytokines and/or LPS, no negative influence of infection with oncolytic<br />
adenovirus was documented. However, we did find an increase in the IL-12 secretion of<br />
LPS resp. LPS/IFNg matured DCs after infection with oncolytic ads. Finally DCs, infected<br />
with oncolytic ads for 3 days, matured and then loaded with peptide were still able to<br />
prime and stimulate specifically CD-8 T-cells with similar or superior efficacy compared<br />
to uninfected DCs, dependent on the donor.<br />
In conclusion, oncolytic ads do not harm viability and maturability of monocyte derived<br />
DCs, but also do not induce <strong>complete</strong> maturation of these cells. Therefore, oncolytic ads<br />
might represent a promising tool for oncolysis-induced anti-tumor immune activation,<br />
however, this strategy might require additional maturation signals for DCs, for example<br />
by expression of immunostimulatory genes inserted into the genome of oncolytic ads.
Philip Kruse, Cornelia Rosner, Lutz Walter<br />
Molecular characterisation of the killer cell immunoglobulinlike<br />
receptors (KIR) of the rhesus macaque (Macaca mulatta)<br />
The killer cell immunoglobulin-like receptors (KIR) belong to the immunoglobulin<br />
superfamily and are expressed mainly on the surface of natural killer (NK) cells. These<br />
receptors interact with the major histocompatibility complex (MHC) class I molecules<br />
and can mediate either an activating or an inhibitory signal to the NK cell. In contrast to<br />
the activating receptors almost all ligands of the inhibitory receptors are known in<br />
humans.<br />
We have started to analyse KIR genes and their function in the rhesus macaque<br />
(Macaca mulatta), a frequently used primate model for the study of infection diseases,<br />
organ transplantation and in development of vaccines. A cDNA library of enriched NK<br />
cells from 30 rhesus macaques has been established. Up to now, more then 15 new KIR<br />
cDNA clones could be isolated. Phylogenetic analysis with already known rhesus<br />
macaque KIR sequences confirms rapid evolution of KIR genes in primates. Further<br />
analyses indicate the occurrence of two different activating KIR gene lineages in rhesus<br />
macaques, which have developed independently from each other and both differ from<br />
the lineage of human activating KIR genes.<br />
The main differences of the rhesus macaque activating KIRs and the KIRs in hominoid<br />
primates can be found in the transmembran region. Rhesus macaque activating KIRs<br />
contain an arginin instead of a lysine in humans in the transmembran region. Usually,<br />
this lysine residue interacts with the DAP12 adaptor molecule, which mediates<br />
activating signals to the NK cell. Therefore, it is still open which adaptor molecule<br />
interact with the activating KIRs of the rhesus macaque. Currently we are investigating<br />
whether these activating KIRs do interact with adaptor molecules other than DAP12.
Cary Mac Millan, Alexander Hann, Peter Bannas, Wolfgang Koestner, Friedrich Buck,<br />
Friedrich Haag, Friedrich Nolte<br />
Molecular characterization of ADP-ribosylated T cell<br />
membrane proteins<br />
NAD-dependent ADP-ribosylation is a posttranslational protein modification catalyzed by<br />
ADP-ribosyltransferases (ARTs). ART2.2 is a GPI-anchored ecto-enzyme expressed on<br />
murine T cells, Tregs, IELs, and NKT cells. Exposure of T cells to the ART substrate,<br />
NAD, results in ADP-ribosylation of cell surface proteins, affecting important T cell<br />
effector functions, including Calcium signalling, clustering of the T cell receptor,<br />
adhesion to target cells, and apoptosis by as yet unknown mechanisms. ART2 is a<br />
promiscuous enzyme which can ADP-ribosylate different proteins in vitro. On the T cell<br />
surface, the specificity of ART2 is restricted by its association with lipid rafts, which<br />
focuses ART2 onto specific target proteins (1). Some of the known targets for ADPribosylation<br />
on T cells (P2X7, LFA-1, and CD45) are involved in T cell activation and<br />
associate with lipid rafts in an activation dependent manner. In order to identify further<br />
functionally interesting ART target-proteins we used the NAD analogue etheno-NAD as<br />
substrate to etheno-ADP-ribosylate cells surface proteins on lymphoma cells (2). Etheno-<br />
ADP-ribosylated targets were purified from cell lysates by affinity chromatography on a<br />
monoclonal antibody specific for etheno-adenosine and were analyzed by mass<br />
spectrometry. The results revealed a number of interesting proteins, including CD25,<br />
CD205, and CD229, as candidates for further functional studies.<br />
(1) Bannas, et al. Blood, 105: 3663-70 (2005)<br />
(2) Krebs, et al. Anal. Biochem 314:108-15 (2003)
Viet Bui, Andreas Diefenbach<br />
Molecular cloning and functional characterization of a novel<br />
stimulatory immunoreceptor expressed by myeloid cells<br />
Innate immune cells express stimulatory receptors to recognize diseased cells or<br />
pathogens. We have identified and cloned a novel stimulatory immunoreceptor<br />
expressed in mice. This novel receptor contains a single Ig-V domain and is a member<br />
of the Ig-superfamily. A charged residue in the transmembrane domain indicated<br />
association with a signaling adaptor molecule. Indeed, the receptor could not be<br />
expressed in cell lines lacking signaling adaptor molecules. Our studies demonstrated a<br />
requirement of the signaling adapter KARAP/DAP12 for surface expression and<br />
signaling. We have generated a monoclonal antibody specific for this receptor.<br />
Preliminary experiments revealed the receptor to be expressed by myeloid cells such as<br />
dendritic cells, macrophages, and neutrophils while being absent from T, B, NK, and<br />
NKT cells. Interestingly, we identified another gene within the same locus encoding<br />
another immune receptor sharing 87% identity in the extracellular domain. These data<br />
suggest that both receptors may recognize the same cognate ligand. In contrast to the<br />
stimulatory receptor, this second receptor possesses a consensus ITIM motif in its<br />
cytoplasmic tail region suggesting it to be an inhibitory receptor. This inhibitory receptor<br />
shares the same expression pattern as the stimulatory receptor. Whereas stimulation of<br />
myeloid cells leads to the down-regulation of the stimulatory receptor, its inhibitory<br />
counterpart seems to be up-regulated. Based on these initial findings, we hypothesize<br />
that these two receptors are paired stimulatory/inhibitory receptors expressed by<br />
myeloid cells that likely recognize the same cognate antigen. The inverse nature of their<br />
expression would suggest that this receptor pair is an important molecular switch<br />
regulating the function of myeloid cells.
Susan M Schlenner, Lars A Schneider, Thorsten B Feyerabend, Markus Wunderlin,<br />
Hans-Reimer Rodewald<br />
Molecular mechanism of mast cell-mediated innate defense<br />
against endothelin and snake venom sarafotoxin<br />
Mast cells are protective against snake venom sarafotoxins that belong to the<br />
endothelin peptide family. The molecular mechanism underlying this recently recognized<br />
innate defense pathway is unknown but secretory granule proteases have been invoked.<br />
To specifically disrupt a single protease function without affecting expression of other<br />
proteases, we have generated a mouse mutant lacking selectively mast cell<br />
carboxypeptidase A (Mc-cpa) activity. Using this mutant, we have now identified Mc-cpa<br />
as the essential protective mast cell enzyme. Mass spectrometry of peptide substrates<br />
after cleavage by normal or mutant mast cells showed that removal of a single amino<br />
acid, the C-terminal tryptophan, from endothelin and sarafotoxin by Mc-cpa is the<br />
principle molecular mechanism underlying this very rapid mast cell response. Mast cell<br />
proteases can also cleave endothelin and sarafotoxin internally but such ‘nicking’ is not<br />
protective since intra-molecular disulfide bridges maintain peptide function. We<br />
conclude that mast cells attack endothelin and sarafotoxin exactly at the structure<br />
required for toxicity, and hence sarafotoxins could not ‘evade’ Mc-cpa’s substrate<br />
specificity without loss of toxicity.
Jennifer Debarry, Anna Hanuszkiewicz, Otto Holst, Holger Heine<br />
Molecular mechanisms of human dendritic cell stimulation by<br />
the Allergy-protective Lactococcus lactis strain G121<br />
Exposure to farming environment during early childhood strongly influences the<br />
development of allergic reactions later in life (“hygiene hypothesis”). As the first year of<br />
life is important for the establishment of the THelper cell balance, environmental<br />
influences such as increased exposure to certain bacteria might play a pivotal role in<br />
adjusting this balance by promoting TH1 responses and thereby inhibiting TH2 responses<br />
which are associated with allergies and asthma. The Gram-positive bacterium<br />
Lactococcus lactis strain G121 was isolated from a cowshed and could be shown to<br />
reduce allergic reactions in a mouse allergy model. Furthermore, we were able to show<br />
a TH1 polarizing effect of L. lactis G121 in human dendritic cells (DCs) which might be<br />
the underlying mechanism of the allergy-protective properties. Activation of DCs is<br />
mainly mediated through NOD2 and the TH1 polarization by L. lactis G121 is impaired<br />
after blocking the access to intracellular receptors via inhibition of phagocytosis. With<br />
respect to the involved signal transduction pathways we next analyzed the NF-κB<br />
pathway. In contrast to stimulation with E. coli we were unable to detect any substantial<br />
translocation of p65 into the nucleus, even when the cells were monitored for up to 3<br />
hrs. However, translocation of the c-Rel subunit into the nucleus was strongly<br />
detectable within 120 min of stimulation. C-Rel is essential for the induction of TH1 polarizing cytokines since it controls IL12p35 and IL23p19 gene expression. In addition,<br />
we detected a sustained activation of DCs for up to 48 hrs with respect to the TH1 polarizing IL12p35 and IL12p40 gene expression. This could be an important<br />
mechanism for a prolonged triggering of an anti-allergic immune response (supported<br />
by DFG, SFB/TR22, project A2).
Malte Bachmann, Jens Paulukat, Josef Pfeilschifter, Heiko Mühl<br />
MOLECULAR MECHANISMS OF IFNγ-INDUCED IL-18 BINDING<br />
PROTEIN PROMOTER ACTIVATION AS DETECTED IN HUMAN<br />
DLD-1 COLON CARCINOMA CELLS<br />
Due to its prominent activity as IFNγ inducing factor, IL-18 has been introduced as a<br />
pivotal mediator of inflammation. Accordingly, IL-18 bioactivity is strongly associated<br />
with the pathogenesis of acute and chronic inflammatory diseases, among others,<br />
sepsis, rheumatoid arthritis, and Crohn`s disease. IL-18 Binding Protein (IL-18BP) is a<br />
naturally occurring inhibitor that counteracts IL-18 bioactivity. We and others could<br />
previously demonstrate that IL-18BP is strongly induced by IFNγ, resulting in a negative<br />
feedback mechanism that has been recognized in cell culture and in vivo. Here we<br />
sought to investigate in DLD-1 colon carcinoma cells molecular mechanisms that direct<br />
IL-18BP expression under the influence of IFNγ. The capability of IFNγ to induce IL-18BP<br />
was confirmed on the promoter level by performing luciferase reporter studies. Those<br />
experiments revealed that a proximal GAS element (gamma-activated sequence;-24bp<br />
to -32bp) plays a pivotal role in IL-18BP expression by IFNγ activated DLD-1 cells. IL-<br />
18BP was dependent on STAT1 activation as shown by siRNA technology. Indeed, EMSA<br />
and ChIP analysis proved STAT1 binding to the GAS element at the proximal IL-18BP<br />
promoter position. Full induction of IL-18BP by IFNγ was in part dependent on de novo<br />
protein synthesis. In fact, induction of IRF-1 by IFNγ and the presence of an IRF-1<br />
binding site close to the GAS element under investigation suggests a role for IRF-1 in<br />
IFNγ induced IL-18BP. Altogether, data on DLD-1 colon carcinoma cells presented herein<br />
indicate that direct action of STAT1 on the proximal GAS element of the IL-18BP<br />
promoter is key to IFNγ induction of this most relevant immunoregulatory cytokine<br />
antagonist.
Maria Papatriantafyllou, Thilo Oelert, Günter Hämmerling, Bernd Arnold<br />
MOLECULAR MECHANISMS OF PERIPHERAL CD8 T CELL<br />
TOLERANCE<br />
Clarifying the mechanisms of immunological tolerance is essential for the development<br />
of effective therapies against cancer and autoimmunity. Central tolerance is achieved by<br />
clonal deletion or the intrathymic induction of regulatory T cells. However, not all<br />
autoreactive T cells are eliminated in the thymus and self-tolerance is further assured<br />
by rendering autoreactive T cells that escape negative selection, tolerant in the<br />
periphery. In our model a regulatory CD8 + CD25 - T cell population mediates peripheral<br />
tolerance against self antigen. In neonates CD8 T cells pass through the endothelium<br />
and have access to tissues (e.g. liver, skin). Those that have specific T cell receptor<br />
(TCR) for autoantigens are rendered tolerant and suppress immune response against<br />
self during the adult phase. In detail, transgenic mice express anti-Kb TCR (Des-TCR) in<br />
CD8 T cells and the Kb molecule under the control of the 2,4Ker-IV promoter in the skin<br />
but not in the thymus (DesTCRxKerKb mice). As a result, the CD8 T cells recognize the<br />
antigen in the periphery during the neonatal phase, become tolerant and suppress the<br />
immune response against Kb self antigen. This model is being used to investigate the<br />
gene expression pattern of tolerant CD8 T cells and clarify the molecular mechanisms of<br />
peripheral CD8 T cell tolerance. Either naïve, activated or tolerant CD8 T cells are sorted<br />
from the spleen of DesTCR mice or Des-TCRxKerKb mice respectively and their gene<br />
expression profile is determined with the oligonucleotide microarrays from Affymetrix.<br />
According to the microarray data genes that are involved in the suppression of the<br />
immune response are upregulated in tolerant CD8 T cells, such as components of the<br />
TGF-β1 and Notch pathways. The most prominent candidates are under investigation<br />
and their contribution to CD8 T cell tolerance will be discussed.
Tobias Schwerd, Johannes C. Hellmuth, Andreas Schmidt, Hendrik Poeck, Michael<br />
Wenzel, Stefan Endres, Simon Rothenfusser<br />
Molecular mechanisms of virus recognition by Rig-I-like<br />
helicases<br />
Viral infections are a constant threat to the integrity of human beings. Survival of the<br />
host organism depends on the rapid induction of innate immune responses including the<br />
production of interferon type I. The newly described family of cytoplasmic Rig-I-like<br />
helicases sense viral infection via the recognition of viral RNA, and trigger a potent<br />
antiviral defense. This family comprises Retinoic acid-inducible gene I (RIG-I) and<br />
melanoma differentiation associated gene 5 (MDA-5) two non-redundant signalling<br />
receptors and the regulatory protein Lgp-2.Rig-I was recently shown to bind and detect<br />
RNA of negative stranded RNA viruses, via a virus-specific 5’-triphosphate modification<br />
absent in normal cytoplasmic RNAs. This provided a structural basis for the distinction<br />
of self- and non-self RNA. We are interested in the molecular details leading from ligandbinding<br />
by these helicases to the activation of anti-viral signalling processes.<br />
Classically, helicases are known to unwind double-stranded (ds)RNA in an ATPdependent<br />
fashion. Using an in vitro assay we demonstrate, that the ATPase activity of<br />
RIG-I is triggered in the presence of dsRNA. Interestingly, RIG-I-dependent ATP<br />
hydrolysis can also be activated by in vitro transcribed but not synthetic single-stranded<br />
(ss)RNA. In both settings activation of RIG-I’s ATPase activity is independent of 5’-end<br />
modifications. To investigate the correlation between helicase activity and signalling we<br />
tested a similar set of ligands in IFN-beta luciferase reporter assays. Our experiments<br />
indicated that helicase activity triggered by dsRNA is required but not sufficient for IFN<br />
promoter activation. In addition, pull-down assays show that an intact ATP-binding<br />
motif is not needed for ligand binding.<br />
In conclusion, we propose that double-strandedness is an important molecular feature<br />
for recognition and downstream signaling of viral RNA by Rig-I. This may facilitate the<br />
development of new therapeutic molecules in tumor immunology and viral infection.
Petra Riedl, Kurt Reifenberg, Joerg Reimann, Reinhold Schirmbeck<br />
Mono-specific, hepatic CD8 T cell responses primed by<br />
cationic peptide/oligonucleotide complexes suppress viral<br />
replication in HBV transgenic mice<br />
Preclinical mouse models are informative to explore the possibilities for specific immune<br />
interventions in chronic viral infection. We describe a novel Hepatitis B Virus (HBV)specific<br />
transgenic (tg) mouse model (1.4HBV-Smut mice). Due to a point mutation in<br />
the translational start codon of the small HBV surface protein (HBs), no infectious viral<br />
particles can be assembled.<br />
We tested if hepatic CD8 T cell responses can be elicited by a peptide-based vaccination<br />
strategy in which an antigenic, Kb-restricted HBs peptide (S190-197; VWLSVIWM) is<br />
fused to a cationic HIV-tat derived peptide (RKKRRQRRR). Positively charged fusion<br />
peptides are quantitatively complexed with negatively charged immunostimulating<br />
oligonucleotides (ODN). In non-transgenic mice, HBs-encoding plasmid DNA- and<br />
peptide- based vaccination protocols efficiently primed Kb/S190-197-specific CD8 T cell<br />
responses. In contrast, only the peptide/oligonucleotide vaccine (but not the pCI/S DNA<br />
vaccine) elicited Kb/S190-197 specific CD8 T cell responses in 1.4HBV-Smut mice. CD8<br />
T cells accumulate in the livers of tg mice and efficiently inhibit HBV replication. Thus,<br />
minimal cationic peptide/ODN vaccines are attractive tools that elucidate cellular and<br />
molecular events that lead to a monospecific, therapeutic CD8 T cell response in the<br />
HBV expressing liver.
Sonja Schmucker, Mario Assenmacher, Anne Richter<br />
Monocytes and myeloid dendritic cells are both able to induce<br />
primary activation of naïve MART-1-specific CD8 + T cells in<br />
vitro<br />
Adoptive T cell therapy for cancer and viral infections in immuno-compromised patients<br />
is hampered by the lack of reliable protocols for primary activation and expansion of<br />
naïve tumor or virus-specific T cells.<br />
In this study we examined the capacity of monocytes and myeloid dendritic cells (MDC)<br />
to in vitro prime naïve MART-1-specific CD8 + T cells.<br />
Therefore we magnetically isolated CD14 + monocytes, CD1c + myeloid dendritic cells<br />
(MDC), and naïve CD8 + CD25- CD45RO- CD45RA + CD62L + T cells from peripheral blood<br />
mononuclear cells (PBMC) of healthy HLA-A2-positive donors. Naïve T cells were<br />
stimulated with either autologous MART-126-35 peptide-pulsed CD14 + monocytes or<br />
CD1c + MDC in the presence of CD28 antibodies, IL-7 and IL-15. For further expansion<br />
IL-2 was added subsequently from day three on. At day eight to ten the frequency, the<br />
degree of expansion, and the expression of CD45RA, CD45RO and CD62L of HLA-A2/<br />
MART-1-Tetramer + CD8 + T cells was determined. Additionally, production of IFN-? by<br />
the expanded T cells was analysed after restimulation with MART-1-pulsed monocytes.<br />
In PBMC of healthy donors naïve HLA-A2/MART-1-Tetramer + CD8 + T cells are<br />
detectable at frequencies of around 0.07% of the CD8 + T cell population. Eight to ten<br />
days after in vitro primary activation the frequencies of HLA-A2/MART-1-Tetramer + CD8<br />
+ T cells increased to 0.3% - 5.7%, irrespective of whether monocytes or MDC were<br />
used as antigen presenting cells (APC). We found a 90-fold expansion of MART-1specific<br />
T cells, which showed a CD45RA + CD45RO-/+ CD62L- effector/effector memory<br />
phenotype. Restimulation of the activated and expanded CD8 + T cells with MART-126-35 peptide- but not irrelevant peptide-pulsed monocytes led to IFN-? production in up to<br />
70% of the HLA-A2/MART-1-Tetramer + CD8 + T cells, confirming antigen specificity and<br />
indicating functionality of the cells.<br />
In conclusion we established an in vitro protocol for priming and expansion of MART-1specific<br />
CD8 + T cells based on the use of peptide-pulsed monocytes or MDC as APC
Beatrice Jahn-Schmid, Gottfried Fischer, Gabriele Gadermaier, Matthias Egger,<br />
Fatima Ferreira, Christof Ebner, Barbara Bohle<br />
Mugwort pollen allergy as a unique model for the<br />
investigation of allergen-specific CD4+T cells using HLA<br />
classII/peptide tetramers<br />
Mugwort pollen allergens represent the main cause of pollinosis in late summer in<br />
Europe. Ninety-five percent of mugwort–allergic patients are sensitized to the major<br />
allergen Art v 1. In contrast to other common pollen allergens which contain multiple T<br />
cell epitopes, Art v 1 contains only one single immunodominant T cell epitope (Art v<br />
125•36). We characterized the minimal epitope of Art v 125-36 in detail and<br />
investigated a possible association of Art v 1-reactivity with HLA class II-phenotypes. In<br />
addition, the potential use of HLA-classII tetramers was evaluated.<br />
Art v 1-specific T cell lines (TCL) and clones (TCC) were established from 51 patients<br />
with clinically defined mugwort pollen allergy and IgE specific for Art v 1. In 96% of the<br />
patients a cellular response to Art v 125-36 was obtained and a core region of 5-10<br />
amino acids containing 3-5 amino acids essential for T cell reactivity was defined by<br />
using truncated and single-substitution analog peptides for T cell stimulation. The<br />
frequency of HLA-DRB1*01 in patients recognizing Art v 125-36 was significantly<br />
increased as compared to healthy controls (69% vs. 21%; odds ratio: 8,45; p
Andreas Junker, Jana Ivanidze, Joachim Malotka, Ingrid Eiglmeier, Hans Lassmann,<br />
Hartmut Wekerle, Edgar Meinl, Reinhard Hohlfeld, Klaus Dornmair<br />
Multiple Sclerosis: T cell receptor transcriptome in distinct<br />
brain regions<br />
We investigated the T cell receptor repertoire in distinct lesions and normal appearing<br />
white matter (NAWM) of multiple sclerosis patients. To this end we analyzed 19 lesions<br />
(inactive demyelinated, 15; slowly expanding chronic, 3;active lesions, 1) and five<br />
NAWM regions from postmortem brains of four MS patients by CDR3 spectratyping. For<br />
each anatomical site 325 semi-nested PCR reactions were performed. About 800 V_-<br />
NDN-J_ combinations were sequenced.<br />
We identified several distinct T cell clones at different anatomical sites in all patients.<br />
Some clones were present in all investigated lesions, and additionally, even in NAWM. A<br />
single clone was detected in nine different sites in one patient. None of the clones was<br />
shared among different patients. Analysis of the hypervariable NDN region revealed<br />
silent nucleotide exchanges.<br />
Individual CD8+ T cells were isolated from cryosections by laser microdissection and<br />
characterized by single-cell PCR. We found at least some of the pervasive T cell clones<br />
belonged to the CD8+ compartment.<br />
This study shows that pervasive T cell clones exist in distinct regions of MS brain which<br />
are not restricted to lesions, but are also present in NAWM. All clones are<br />
"private" (unique) to individual patients. Several silent nucleotide exchanges suggest<br />
that the corresponding T cell clones were stimulated by particular antigens. Some of the<br />
highly pervasive clones were CD8+, supporting the pathogenic relevance of this T cell<br />
subset.
Felix C. Popp, Elke Eggenhofer, Prezemyslaw Slowik, Philipp Renner, Katharina<br />
Kronenberg, Hans J. Schlitt, Pompiliu Piso, Marc H. Dahlke<br />
MULTIPOTENT MESENCHYMAL STROMAL CELLS INDUCE LONG-<br />
TERM ALLOGRAFT ACCEPTANCE MEDIATED THROUGH IDO<br />
Multipotent mesenchymal stromal (MS) cells isolated from adult bone marrow inhibit the<br />
T cell response in mixed lymphocyte cultures. Modulating the immune system through<br />
MS cells may play an important role in organ transplantation since new concepts of cell<br />
based immunosuppression are urgently needed.<br />
Here we applied MS cells four days in advance of performing a <strong>complete</strong>ly MHC<br />
mismatched heart transplantation followed by a seven day course of mycophenolate<br />
mofetil (MMF). The median survival of the transplanted grafts was greater than 100<br />
days as compared with 15 days when applying MMF alone.<br />
After applying 1-methyl tryptophan, a potent inhibitor of IDO, animals rejected heart<br />
graft early. However, real time PCR for IDO mRNA levels produced no significant<br />
differences. Presumably MS cells induce tolerance during a narrow time window after<br />
transplantation. This assumption is supported by the fact that the timing of MS cell<br />
application is crucial for achieving long term allograft acceptance.<br />
In conclusion, MS cells induced long-term graft acceptance in our heart transplantation<br />
model. Blocking IDO resulted in rejection, indicating a central role of IDO in MS cell<br />
mediated graft acceptance. To further elucidate the mechanism behind MS cell mediated<br />
tolerance, animals need to be analyzed at time points closer to the heart<br />
transplantation.
Verena Besche, Christina Glowacki, Nadine Wiechmann, Andrea Renzing, Ngoc-Anh<br />
Dang, Stephan Sudowe, Jürgen Knop, Angelika B. Reske-Kunz, Matthias Bros<br />
Murine dendritic cells exert tolerogenic function at their<br />
immature state and upon differentiation in the presence of<br />
dexamethasone<br />
Under homeostatic conditions, dendritic cells (DC) are involved in the maintainance of<br />
peripheral tolerance against self as well as harmless environmental antigens by inducing<br />
antigen-specific regulatory T cells. Upon inflammation glucocorticoids are generated<br />
endogenously as a negative feedback regulatory mechanism by cells of the adrenal<br />
cortex. Due to their potent anti-inflammatory effects, glucocorticoids are frequently<br />
prescribed in the treatment of severe allergic diseases. Here we show that addition of<br />
the synthetic glucocorticoid dexamethasone (DEX) to murine bone marrow derived DC<br />
(BM-DC) cultures resulted in reduced expression of costimulatory molecules and<br />
accessory molecules involved in DC-T cell interaction as compared with untreated<br />
immature BM-DC. Moreover, DEX largely prevented upregulation of these molecules<br />
upon stimulation with lipopolysaccharide (LPS). DEX upregulated expression of<br />
glucocorticoid-responsive genes shown to exert anti-inflammatory activities like FcgRIIB<br />
and IL1RA. Functionally, DEX-treatment prevented the acquisition of potent T cell<br />
stimulatory capacity upon stimulation with LPS. Both immature BM-DC and DEX-treated<br />
cells exerted tolerogenic function, since prestimulated alloreactive T cells were<br />
refractory to restimulation and suppressed proliferation of naive T cells upon allogeneic<br />
stimulation.
Ulrich Salzer, Chiara Bacchelli, Stephanie Jennings, Allesandro Plebani, Helen Chapel,<br />
Hans D Ochs, Simon Urschel, Bernd H Belohradsky, H Bobby Gaspar, Bodo Grimbacher<br />
Mutations in TACI/TNFRSF13b in patients with CVID – a<br />
genetic, immunological and clinical study in a large patient<br />
cohort<br />
Background: TACI (TNFRSF13b) is an important regulator of B cell responses and<br />
differentiation. We recently showed that TACI sequence variants are associated with<br />
common variable immunodeficiency (CVID) and that some of these variants are present<br />
in the general population at lower frequencies.<br />
Results: We studied a cohort of 570 new CVID patients. 54 patients (9.5%) showed at<br />
least one mutated TACI allele. 12 patients (22%) showed homozygous or compound<br />
heterozygous (c.h.) mutations in TNFRSF13b, while most of the patients (n=42; 78%)<br />
were heterozygous. 16 different mutations were identified, of which 13 have not been<br />
described. TACI-C104R and A181E were the most frequent alleles (n=39; 72%), being<br />
present also in about 2% of healthy controls, whereas their combined frequencies in<br />
CVID were about 7%. Importantly, all of the variants seen in controls were<br />
heterozygous and did not include frameshift or nonsense changes, which were exclusive<br />
to the CVID population. Homozygous or c.h. mutated receptors did not bind the ligand<br />
APRIL. Functional analysis of heterozygous TACI mutants implied that these may act<br />
differently or are being compensated by the redundant system of BAFF/APRIL receptors.<br />
Analysis of B cells in 31 TACI-deficient patients did not show a distinct B cell phenotype.<br />
The patients presented with the full clinical spectrum of CVID. Autoimmunity was seen<br />
in 11 of 39 patients (28%) and clinical signs of lymphoproliferation were present in 23<br />
of 41 patients (56%).<br />
Conclusions: TACI is a highly polymorphic gene, shows a complex pattern of sequence<br />
variants and is mutated in 10% of CVID patients. While B cells with homozygous or c.h.<br />
mutated TACI receptors showed specific functional defects, the role and significance of<br />
heterozygous mutations is still unclear. In addition, the occurrence of heterozygous<br />
TACI-C104R and A181E alleles in normal controls suggests that these variants act more<br />
as disease modifiers rather than being disease causing in CVID. However, the<br />
immunological and clinical phenotype of TACI-deficient patients was indistinguishable<br />
from that of other CVID patients.<br />
Supported by DFG SFB620/C2; NIH/NIAID: USIDnet grant # NO1-A1-30070 (B. G.),<br />
the Primary Immunodeficiency Association and the Medical Research Council, UK (C.B.).
Max Bastian, Tobias Braun, Heiko Bruns, Martin Röllinghoff, Steffen Stenger<br />
Mycobacterial Lipopeptides Elicit CD4+ Cytolytic T<br />
Lymphocytes in Mycobacterium tuberculosis Infected Humans<br />
An ex vivo model was developed to study frequency, phenotype and effector functions<br />
of human T lymphocytes recognizing hydrophobic antigens of Mycobacterium<br />
tuberculosis (M.Tb). To obtain unbiased results we chose to characterize T-lymphocytes<br />
responding to a chloroform methanol extract (M.Tb-CME) containing the whole<br />
spectrum of mycobacterial glycolipids and lipopeptides. A significant proportion (290<br />
IFN-g+ T cells/ 10EE5 PBMCs) of T lymphocytes recognized M.Tb-CME and developed to<br />
effector memory cells as determined by the expression of CD45RO and the chemokine<br />
receptors CXCR3 and CCR5. Antigen-specifically expanded lymphocytes were isolated<br />
and further analyzed for their potential to provide protection against M.Tb. Purified cells<br />
fulfilled all criteria required for an efficient immune response against tuberculosis: i)<br />
release of macrophage-activating Th1 cytokines and chemokines required for the spatial<br />
organization of local immune responses ii) cytolytic activity against antigen-pulsed<br />
macrophages and iii) recognition of M.Tb-infected macrophages resulting in killing of<br />
intracellular bacteria. Phenotypically, M.Tb-CME expanded cells were CD4+, challenging<br />
current concepts that cytotoxic and antimicrobial effector cells are restricted to the CD8<br />
+ T-cell compartment. The T cell responses to the hydrophobic M.Tb-CME preparation<br />
were MHC class II restricted. Pretreatment of M.Tb-CME with proteinase or delipidation<br />
by alkaline hydrolysis abolished the stimulatory capacity. This indicates that lipidated<br />
peptides of M.Tb induce CD4+ cytolytic and antimicrobial T-lymphocytes that recognize<br />
their epitope on infected macrophages. Our data support the emerging concept that T<br />
cells specific for hydrophobic antigens play an important role in the immune defense<br />
against microbial pathogens and may extend the scope of immunogenic compounds that<br />
should be included in novel vaccine formulations against tuberculosis.
Peter Reichardt, Bastian Dornbach, Song Rong, Stefan Beissert, Faikah Güler, Karin<br />
Loser, Matthias Gunzer<br />
Naive B cells generate regulatory T cells in the presence of a<br />
mature immunological synapse<br />
Naïve B cells are ineffective antigen presenting cells and considered unable to activate<br />
naïve Tcells. However, antigen specific encounter of these cells leads to stable cell pairs<br />
that remain associated over hours in lymph nodes in vivo. The mechanism of signalling<br />
and the physiological outcome of such pairs has not been evaluated. We show here that<br />
antigen specific conjugates between naïve B cells and naïve T cells display a mature<br />
immunological synapse (mIS) as signalling device in the contact zone which is absent in<br />
specific T cell-dendritic cells (DC) pairs. Thereby, B cells induce substantial proliferation<br />
but contrary to DC no loss of L-Selectin in T cells. Surprisingly, while DC-triggered T<br />
cells develop into normal effector cells, B cell stimulation over 72 hours induces<br />
regulatory T cells that inhibit de novo priming of fresh T cells in a contact dependent<br />
manner in vitro. Due to their high levels of L-selectin these cells home to lymph nodes<br />
where they also potently inhibit T cell priming in vivo. Such, immune responses in an<br />
hypersensitivity model and rejection of organ grafts was prevented. Thus, presentation<br />
of specific antigen by naive B cells drives naïve T cells into a regulatory phenotype. This<br />
might explain old findings on tolerance induction by B cells, identifies the mIS as a<br />
central functional module of this process and may represent a powerful approach for<br />
therapeutic intervention.
Nils Kruse, Arnhild Schrage, Katrin Neumann, Katharina Eulenburg, Friderike<br />
Blumenthal-Barby, Simon Fillatreau, Percy A. Knolle, Martin Zeitz, Alf Hamann, Katja<br />
Klugewitz<br />
Naive CD4+ T cells primed by Liver Sinusoidal Endothelial<br />
Cells (LSEC) do not differentiate into cytokine producing<br />
effector cells and fail to induce a delayed type<br />
hypersensitivity reaction (DTH)<br />
The liver, which is known to have immunomodulatory functions, favours the induction of<br />
tolerance rather than immunity. For example LSEC, one population of hepatic nonprofessional<br />
antigen presenting cells (APC) prime CD8 + T cells leading to anergy or<br />
deletion. But it is controversial if LSEC can prime naive CD4 + T cells. Whereas LSEC<br />
isolated by counterflow elutriation primed naive CD4 + T cells, others have reported that<br />
LSEC isolated by depletion of CD45 + cells were not sufficient to induce proliferation of<br />
naive CD4 + T cells.<br />
In our study we investigated if naïve CD4 + T cells can be primed by LSEC alone by<br />
using a novel experimental approach. To exclude the influence of professional APC, we<br />
immunomagnetically purified LSEC from bone marrow chimeric mice that express MHC<br />
class II exclusively on non-hematopoietic cells. We analyzed the phenotype and the<br />
functional properties of the LSEC primed CD4 + T cells.<br />
We demonstrated that LSEC alone can prime naive CD4 + T cells in vitro, determined by<br />
proliferation. However the LSEC were weak presenters, as high antigen concentrations<br />
were required. The CD4 + T cells neither differentiated into IFNγ expressing Th1 cells nor<br />
produced IL-4 or IL-10. In an in vitro suppression assay this T cell population<br />
suppressed the proliferation of naive CD4 + T cells. But markers characteristic for<br />
regulatory T cells (CD25, Foxp3 and αE) were negligible. Concerning their<br />
proinflammatory capacity LSEC primed CD4 + T cells did not induce a DTH reaction in<br />
contrast to CD4 + T cells primed by professional APC. Determining the stability of their<br />
phenotype in vivo we observed that the cells did not express IFNγ after transfer into<br />
syngeneic mice, even in the presence of the specific antigen.<br />
Taken together CD4 + T cells can be primed by LSEC and acquire an anergic phenotype.<br />
This modulation might be involved in establishing and maintaining hepatic tolerance not<br />
only for CD8 + T cells but also for CD4 + T cells.
Benedikt Fritzsching, Eva Pauly, Nina Oberle, Navina Kuss, Katrin Hartmann, Peter<br />
Ruf, Johannes Pöschl, Peter Krammer, Elisabeth Suri-Payer<br />
Naive regulatory T cells: activation and apoptosis<br />
sensitization of this novel Treg subpopulation during the<br />
human neonatal period<br />
CD4+CD25+FOXP3+ regulatory T cells (Treg) are potent immunosuppressive T cells.<br />
Reduction of peripheral blood Treg numbers or function have been reported to be<br />
associated with human autoimmune disease. However, the mechanisms responsible for<br />
Treg -reduction are not clear. We have recently reported high sensitivity of the majority<br />
of Treg towards CD95L-mediated apoptosis*. However, a Treg subpopulation remains<br />
consistently apoptosis-resistant. Gene micro array and 6-color flow cytometry analysis<br />
including FOXP3 revealed that naïve Treg constitute this so far neglected apoptosis<br />
resistant Treg population. Naïve Treg show a phenotype similar to naïve conventional T<br />
cells (CD45RA+, CD45RO-, partly CD31+, CCR6-, CD95-). Whereas naïve Treg<br />
represent only a minority of Treg in adults, almost all cord blood Treg show such a<br />
naïve phenotype. Here, we analyzed the postnatal activation status of Treg during the<br />
first 28 days of healthy newborn infants. Whereas most conventional T cells showed a<br />
naïve phenotype, Treg rapidly acquired an activated phenotype. Similar to adult Treg<br />
these in vivo activated neonatal Treg showed an enhanced apoptosis sensitivity. Treg<br />
activation and apoptosis sensitization occurred during the early postnatal expansion<br />
phase of lymphocytes. This observation might reflect an important tolerance mechanism<br />
for the control of the proliferating T cell compartment in the first weeks of a newborn´s<br />
life.<br />
Benedikt.Fritzsching@med.uni-heidelberg.de<br />
* Fritzsching et al., Cutting Edge, Journal of Immunology l. 2005 Jul 1; 175(1):32-6
Manoj Kumar, Norman Putzki, Hans Christoph Diener, Hans Grosse-Wilde, Ernst<br />
Kreuzfelder<br />
Natalizumab seems to effect mainly B lymphocytes in patients<br />
with Multiple Sclerosis<br />
Multiple Sclerosis (MS) is an autoimmune disease of the central nervous system which is<br />
characterized by inflammation, demyelination, gliosis and axonal damage. Natalizumab<br />
[anti-very late antigen-4 (VLA-4) antibody] is approved as monotherapy for the<br />
treatments of relapsing remitting MS. It exerts its immunologic effects by targeting the<br />
VLA-4, alpha4 integrin receptor, the site responsible for the migration of leukocytes<br />
from the blood into inflamed tissue.<br />
Twenty-four patients with relapsing remitting course of MS were included in our study.<br />
To investigate the influence of natalizumab therapy on the counts of leukocytes and<br />
their subpopulations as well as VLA-4 expression in B lymphocytes in whole blood, we<br />
used flow cytometry before treatment initiation (baseline) and during follow up to 6<br />
months.<br />
Relative (%) and absolute counts (cells/microL) of lymphocytes were significantly (p <<br />
0.05. Kruskal-Wallis test) increased following treatment (e.g. 6 months: 42 %, 3081<br />
cells/ microL) with natalizumab compared with baseline values (26%, 1815 cells/<br />
microL). Within lymphocytes, there is increase in relative and absolute counts of B cells<br />
(e.g. 6 months: 22%, 720 cells/ microL) compared with baseline (17%, 307 cells/<br />
microL) but T lymphocytes and natural killer cells were not significantly different during<br />
ongoing treatment. We measured VLA-4 expression in B lymphocytes and found that<br />
there is significant decrease in percentage as well as mean fluorescence intensity (MFI)<br />
of VLA-4 positive B cells during therapy (e.g. 6 months; percentage: 86 %, MFI; 739<br />
channels) compared with baseline (percentage: 39%, MFI: 706 channels).<br />
Therefore natalizumab may increase counts of lymphocytes. This seems due to<br />
increased B cell counts. Increase in B lymphocytes counts may be explained by<br />
suppression of transmigration because percentage of VLA-4 positive B cells and VLA-4<br />
expression decreased during therapy.
Stephanie Joachim, Martin Wax, Daniela Kraft, Norbert Pfeiffer, Franz Grus<br />
Neurodegeneration of the optic nerve and changes in<br />
antibody profiles after immunization with heat shock protein<br />
27<br />
In previous studies complex antibody profiles against retinal antigens were found in<br />
patients with glaucoma. Antibodies against heat shock protein 27 (HSP27) have been<br />
identified in these studies in sera of glaucoma patients. The aim of this study was to<br />
analyze, if immunization with HSP27 can cause retinal ganglion cell loss in rats similar<br />
to the loss found in glaucoma patients.<br />
Lewis rats were immunized with 100 mg HSP27 (plus Freund’s adjuvant and pertussis<br />
toxin) and divided into three groups: group 1 was euthanized after 4 weeks (n=6),<br />
group 2 after 5 weeks (n=6), and group 3 after 6 weeks (n=9). Control animals that<br />
received no immunization were euthanized after 6 weeks (n=10, group 4). Intraocular<br />
pressure was measured during the course of the study and blood was collected at<br />
several time points. Serum was used to detect IgG antibody patterns against retina via<br />
Western blotting and Protein G bead techniques. The antibody patterns were analyzed<br />
by multivariate statistical techniques. Eyes were harvested the day the animals were<br />
euthanized and were fixed and flatmounts were stained with Brn-3a, which detects the<br />
retinal ganglion cell (RGC) nuclei. We used a computer assisted quantitation of RGC<br />
density.<br />
No significant changes in intraocular pressure were observed during the course of the<br />
study. The animals immunized with HSP27 showed a lower number of RGCs in<br />
comparison to controls (P
Barbara Daller, Michaela Jungbeck, Klaus Pfeffer, Daniela N. Männel, Thomas Hehlgans<br />
Neutralization of LIGHT ameliorates DSS-induced intestinal<br />
inflammation<br />
Activation of the lymphotoxin-b receptor (LTbR) is essential for the development,<br />
maturation and maintenance of secondary lymphoid organs. Recent studies identified<br />
LTbR activation as a critical signaling pathway in the gut and highly relevant to<br />
intestinal inflammation. In order to investigate the role of the LTbR ligand LIGHT<br />
(lymphotoxin-like inducible protein that competes with glycoprotein D for binding to<br />
herpesvirus entry mediator on T cells) in the pathology of colitis, we used LIGHTdeficient<br />
mice in a model of acute colitis induced by oral administration of dextran<br />
sulfate sodium (DSS).<br />
LIGHT-deficient mice developed almost no intestinal inflammation according to<br />
histological score, weight loss, and colonic myeloperoxidase activity. Therefore, mouse<br />
anti-mouse LIGHT monoclonal antibodies were generated by immunization of LIGHTdeficient<br />
mice and standard hybridoma techniques. ELISA and Western blot analysis<br />
demonstrated specific binding of the monoclonal antibodies to mouse LIGHT protein.<br />
Furthermore, two of the monoclonal antibodies neutralized mouse LIGHT in vitro and in<br />
vivo. This was demonstrated by a significantly reduced intestinal inflammation of<br />
C57BL/6 mice treated with anti-mouse LIGHT antibodies during the induction of acute<br />
DSS-colitis.<br />
LIGHT serum levels in patients with Crohn´s disease and ulcerative colitis were found to<br />
be significantly elevated. Thus, the present study clearly demonstrates a role for LIGHT<br />
in enhancing intestinal inflammation and also indicates that neutralization of LIGHT<br />
might be beneficial in treatment of acute inflammatory diseases.
Katrin Birkholz, Niels Schaft, Jan Dörrie, Michael Schwenkert, Christian Kellner, Georg<br />
Fey, Gerold Schuler<br />
New strategies for antigen loading of human monocytederived<br />
DC<br />
Although responses in dendritic cell (DC)-based vaccination of melanoma and renal cell<br />
carcinoma patients are encouraging, further improvement of the efficiency of these<br />
vaccines is needed. A comparison of different methods, such as electroporation of<br />
defined tumor-antigen RNA or total tumor RNA, phagocytosis of tumor cells, direct<br />
peptide loading, or the use of antibody-antigen constructs, is necessary to optimize DC<br />
antigen loading. To examine this, we chose MAGE-A3, a cancer-testis antigen expressed<br />
in malignant melanoma, multiple myeloma, and many other tumors, as a model<br />
antigen. As a read-out for antigen-presentation efficiency, CD4 and CD8 T cells,<br />
transfected with RNA encoding TCR recognizing MHC-presented MAGE-A3 epitopes were<br />
used. As one possible loading strategy, we cloned antibody-antigen constructs,<br />
consisting of a single-chain Fragment variable (scFv) directed against DEC205, an<br />
endocytosis receptor expressed on the surface of DC, genetically linked to different<br />
parts of MAGE-A3. After receptor-mediated endocytosis, the MAGE-A3 antigen should<br />
be delivered into the DC, and subsequently presented on MHC class II molecules. The<br />
expressed and purified fusion proteins were detected in western blot analysis and<br />
displayed specific binding to mature (m)DC and DEC205-transfected CHO cells. In<br />
another loading strategy, MAGE-A3-DCLAMP RNA was used. The DCLAMP sequence<br />
targets the antigen to lysosomes, which leads to MHC class II presentation. Indeed,<br />
electroporation of mDC with MAGE-A3-DCLAMP RNA resulted in HLA-DP4-restricted<br />
presentation of the MAGE-A3 peptide KKLLTQHFVQENYLEY. Taken together, we have<br />
established tools to optimize loading of DC with tumor antigen which might lead to<br />
better anti-tumor DC vaccines.
Timo Herrmann, Nousheen Zaidi, Hubert Kalbacher<br />
New strategies for the analysis of processed antigens in<br />
dendritic cells<br />
During antigen processing, protein antigens are taken up by antigen presenting cells<br />
(APCs) like dendritic cells (DCs) and subequently proteolytically processed by different<br />
proteases. Antigenic peptides are then displaced on MHC class II molecules and<br />
presented to T-helper cells to modulate immune response. Understanding how foreign<br />
antigens are proteolysed to antigenic peptides is therefore key to understanding both<br />
the normal and abnormal function of the immune system. However the analysis of<br />
processed protein antigens in antigen presenting cells is still difficult because of the very<br />
low concentration of internalized species but moreover because of the very high<br />
complexity of processed self proteins in a given cell.<br />
For this reason, new strategies have been developed in our lab, based on specifially<br />
labeled proteins and antibody-based affinity capturing with biomagnetizable beads in<br />
combination with high resolution mass spectrometry. Recombinant proteins, e.g. myelin<br />
basic protein (MBP) or myelin oligodendrocyte glycoprotein (MOG) and large peptide<br />
fragments of known epitopes were labeled with fluorescein labels (FITC) or biotin and<br />
used for pulse chase experiments in DCs. FACS analysis was used to control the<br />
internalization. The DCs were then subjected for subcellular fractionation allowing to<br />
analyze organelles relevant to antigen processing (endosomes/lysosomes) by western<br />
blot analysis and high sensitive RP-HPLC with fluorescence detection. Finally in a key<br />
step, capturing of the labelled antigens was achieved by Ab-coated magnetic beads. The<br />
antibodies were generated in our lab, carefully purified and characterized and then<br />
covalently coupled to activated beads. The captured-peptides were eluted in a one-stepprocedure<br />
directly onto a MALDI-target and characterized.<br />
This approach allows the exclusive analysis of pulsed antigen fragments and even more<br />
to analyze processed ligands associated to MHC class II molecules.<br />
It could be used as a readout for functional studies of antigen processing, e.g. knockout<br />
systems, si-RNA-studies or specific cell-penetrating inhibitors, regarding processing<br />
relevant proteases.
Hamid Kashkar, Anke Deggerich, Jens-Michael Seeger, Benjamin Yazdanpanah, Katja<br />
Wiegmann, Dirk Haubert, Carola Pongratz, Martin Krönke<br />
NF-kappaB independent down-regulation of XIAP by<br />
bortezomib sensitizes Hodgkin Lymphoma B-cells against<br />
cytotoxic drugs<br />
The proteasome inhibitor, bortezomib, has been shown to possess promising anti-tumor<br />
activity and significant efficacy against a variety of malignancies. Different studies<br />
demonstrated that bortezomib breaks the chemoresistance in different tumor cells<br />
basically by altering nuclear factor-kappaB (NF-kappaB) activity. NF-kappaB has been<br />
shown to be constitutively active in the vast majority of primary Hodgkin-Reed-<br />
Sternberg (H-RS) cells in lymph node sections and in Hodgkin’s lymphoma (HL) cell<br />
lines and was suggested to be a central molecular switch in apoptosis resistance in HL.<br />
Here we report a bimodal effect of bortezomib in HL cells. Whereas high-dose<br />
bortezomib induced direct cytotoxicity which correlated with decreased NF-kappaB<br />
activity, low-dose bortezomib sensitized HL cells against a variety of cytotoxic drugs<br />
without altering NF-kappaB action. Strikingly, bortezomib induced marked XIAP downregulation<br />
at the post-translational level which was independent of the NF-kappaB<br />
status. Similarly, RNA interference (RNAi)-mediated XIAP down-regulation generated<br />
susceptibility to cytostatic agents. The results identify XIAP as an NF-kappaB<br />
independent target of bortezomib action that controls the chemoresistant phenotype of<br />
HL cells.
Michael Kiessling, Peter H. Krammer, Karsten Gülow<br />
NF-kB suppression sensitizes cells towards ROS-induced<br />
apoptosis<br />
Various types of cancer show resistance towards apoptosis induction. One reason for<br />
the resistance is constitutive activation of the nuclear factor-kappa B (NF-kB) pathway.<br />
Selective inhibition of NF-kB by overexpression of the super-repressor form of IkBα led<br />
to increased apoptosis in Jurkat T-cells. However, the mechanism of this enhanced cell<br />
death remained unclear.<br />
Here, we show that higher levels of reactive-oxygen-species, whose accumulation is<br />
increased in IkB&alpha overexpressing cells, promote c-jun N-terminal kinase (JNK)<br />
phosphorylation. Treatment of cells with antioxidants such as N-acetyl cysteine (NAC)<br />
abrogated PMA-induced ROS formation, JNK activity and thus, apoptosis. Further,<br />
downregulation of JNK by siRNA resulted in reduced apoptosis. One putative target for<br />
ROS may be MAPK phosphatases (MKP), whose catalytic cysteine residue is oxidized by<br />
ROS and therefore inactivated.
Maren Claus, Sabine Wingert, Carsten Watzl<br />
NK cell activity is regulated by CD48 - 2B4 (CD244)<br />
interaction in cis and in trans<br />
Function of human NK cells is regulated by a variety of different cell surface receptors.<br />
SLAM-related receptors (SRR) are important modulators of NK cell activity. Most SRR<br />
are activated by homophilic interaction. Thus, SRR do not only function as activating NK<br />
cell receptors, but also as activating NK cell ligands. 2B4 (CD244) is the only SRR that is<br />
activated by binding to a distinct ligand: CD48 is a GPI-anchored surface molecule that<br />
is widely expressed on hematopoietic cells. Recent work demonstrated that, like other<br />
SRR, 2B4 expressing target cells can also induce NK cell cytotoxicity by interacting with<br />
NK cell expressed CD48. These findings suggest an additional function of the 2B4-ligand<br />
CD48 as an activating receptor on NK cells.<br />
In the present study, we show that 2B4 does not only bind in trans to CD48 on<br />
neighboring cells, but can also interact in cis with CD48 molecules on the same NK cell,<br />
thereby modulating NK cell activity. The expression level of CD48 on NK cells is about<br />
20fold higher than that of 2B4. Using soluble CD48-ILZ fusion proteins, we demonstrate<br />
that removal of endogenous CD48 from the cell surface by phosphatidylinositol-specific<br />
phospholipase C (PI-PLC) increases the binding of soluble CD48 to NK cell 2B4. This<br />
suggests that the interaction between CD48 and 2B4 in cis prevents the 2B4 receptor<br />
from recognizing CD48 in trans. To test if this also has functional consequences we<br />
decreased the density of CD48 on the cell surface of NK92 cells by PI-PLC treatment.<br />
This significantly increased 2B4-mediated cytotoxicity against CD48 expressing target<br />
cells. Taken together, our findings provide evidence for the modulation of NK cell<br />
activity by the density of 2B4 and CD48 on both the NK cell and the potential target<br />
cell. Further, the present data suggest functional consequences of an in cis interaction<br />
between 2B4 and CD48 for NK cell activity.
Matthias Krusch, Sorin Armeanu, Ulrich Martin Lauer, Alexander Steinle, Michael<br />
Bitzer, Helmut Rainer Salih<br />
NK cell lysis of hepatoma cells following specific induction of<br />
NKG2D ligands by the proteasome inhibitor Bortezomib<br />
Natural killer (NK) cells as components of the innate immunity substantially contribute<br />
to anti-tumor immune responses. However, the tumor-associated ligands engaging<br />
activating NK cell receptors are largely unknown. An exception are the MHC class-I<br />
chain-related molecules MICA and MICB and the UL16-binding proteins (ULBP) which<br />
bind to the activating immunoreceptor NKG2D expressed on cytotoxic lymphocytes and<br />
potently stimulate anti-tumor immune responses. Here we report that treatment of<br />
human hepatocellular carcinoma (HCC) cells with the proteasome inhibitor Bortezomib<br />
stimulates recognition of cancer cells by cytotoxic lymphocytes via NKG2D. Bortezomib<br />
treatment induced transcription of MICA and MICB in the HCC cell lines PLC, HUH-7 and<br />
Hep3B leading to increased total and cell surface MIC protein expression. The induction<br />
of MIC molecules increased lysis of HCC cells by NK cells, which was abolished by<br />
blocking NKG2D-NKG2D ligand interaction using anti-MIC F(ab’)2 fragments.<br />
Importantly, Bortezomib treatment did not induce MIC protein expression in primary<br />
human hepatocytes and did also not alter NK cell viability and effector functions. Taken<br />
together, our data demonstrate that Bortezomib mediates specific priming of malignant<br />
cells for NK cell effector mechanisms. These results suggest the clinical evaluation of<br />
Bortezomib in solid tumors such as HCC, especially in combination with immunotherapy<br />
approaches like adoptive NK cell transfer.
Marion Schneider, Xuefang Ren, Ying Wang<br />
NK cell targeting of phagocytic dendritic cells<br />
NK dysfunction appears to be responsible for i)massive hemophagocytosis and ii)<br />
exceedingly high concentrations of interferon-g in a disease called hemophagocytic<br />
lymphohistiocytosis (HLH). Genetic NK deficiency is either due to mutations of the<br />
perforin gene, vesicular trafficking molecules such as Munc13-4 or syntaxin11. In<br />
addition, transient NK dysfunction may occur in infectious diseases such as EBV,<br />
leishmaniosis and also in autoimmune diseases. Using in vitro cultures supplemented<br />
with high dose IL-2 (10 3 IU/ml), NK function can be reconstituted in vitro. In the<br />
current study, hemophagocytes were enriched from patients with HLH and phenotyped<br />
by flow cytometry. Phagocytes were then tested as targets in cellular cytotoxicity<br />
assays using IL-2 activated effectors of these patients.<br />
Results: HLH derived phagocytes exhibited a dendritic cell phenotype expressing low<br />
CD80 and CCR7, but high densities of CD40, CD86, CD11c, CD63, CD64, and HLA-DR.<br />
CD209 was variably positive as well as BDCA4, CD1a, CD178 (FAS-Ligand) as well as<br />
TRAIL (tumor necrosis factor related apoptosis inducing ligand) receptor DR4.<br />
Phagocytes often lacked polarization and ultrastructural studies demonstrated even<br />
distribution of Golgi stacks in the cell. cells were derived from patients with HLH as well<br />
as from healthy donors. NK cytolysis by IL-2 acitvated killer effectors (derived from<br />
patients as well as healthy donors) was positive against 51chromium labeled cultured<br />
phagocytes as well as against K562 target cells and against allogeneic, EBV-transformed<br />
B cells. Lytic function was in a large portion independent of calcium and granule release.<br />
In defined effector target combinations, phagocytes were totally resistant to NK<br />
cytolysis. In the presence of TRAIL blocking antibodies, we found that DR4 positive<br />
phagocytes were killed by IL-2 activated receptors but DR4 negative phagocytes were<br />
not killed. We conclude that TRAIL and Trail Receptor DR4 play an important role in NK<br />
control of hemophagocytic cells overactivated in HLH. This context opens new aspects of<br />
treatment and cure.
Cédric VONARBOURG, Andreas DIEFENBACH<br />
NK CELLS EXPRESSING CLASS II MHC MOLECULES: SEPARATE<br />
LINEAGE OR JUST NK CELLS ?<br />
NKG2D is a stimulatory immunoreceptor constitutively expressed by all NK cells, a<br />
subset of NKT cells and the gd T cells of the skin. NKG2D interacts with a group of class<br />
I MHC-like molecules (NKG2D ligands, NKG2DL) that are upregulated on stressed cells<br />
whereas normal cells do not express these molecules. The NKG2D receptor/ligand<br />
system functions as a sentinel system to alert the immune system to endogenous<br />
cellular stress. Recent data from our lab indicated that vaccination of mice with NKG2DL<br />
+ tumor cells (but not with the parental NKG2DL- cells) leads to enhanced priming of<br />
tumor antigen-specific CD8 T cell responses. We wanted to investigate the molecular<br />
mechanism of how NKG2D-mediated innate immune activation leads to the<br />
enhancement of adaptive immunity. We hypothesized that NKG2D could regulate the<br />
function of antigen presenting cells (APC). During these studies, we identified a<br />
population of NKG2D+ cells co-expressing class II MHC which resides in the lymph<br />
nodes (ca. 30-40% of all NK cells) whereas this population was rather small in the<br />
spleen (
Petra Prinz, Ainhoa-Marie Figel, Judith Hosse, Peter J Nelson, Julia S Schleypen, Nicole<br />
Baur, Dolores J Schendel, Christine S Falk, Elfriede Noessner<br />
NK cells with distinct phenotypic and functional profile in the<br />
context of myeloid infiltration and renal cell carcinoma milieu<br />
Renal cell carcinoma (RCC) harbor high numbers of infiltrating lymphocytes with<br />
apparent limited efficacy in tumor control. Two groups of clear cell RCC were identified,<br />
one containing high (>20% of the lymphocyte population, n=14), the other low (
Rachel Thomas, Maren Mönkemeyer, Gamze Kabalak, Reinhold E. Schmidt, Torsten<br />
Witte<br />
NKG2D polymorphism associated with reactivation of CMV in<br />
HIV-1 infected patients<br />
Background<br />
NKG2D is an activating C-type lectin-like receptor expressed on NK cells and cytotoxic T<br />
lymphocytes. Upon ligand binding (ligands: stress-inducible MICA/B, ULBPs) NKG2D<br />
signals via the associated DAP10 adaptor protein, inducing cytotoxicity in NK cells and<br />
co-stimulation of the TCR.<br />
The two alleles of NKG2D differ by one nucleotide, guanine (G) or adenine (A), which<br />
results in an amino acid residue substitution in the transmembrane region at the<br />
binding site to DAP10. One of these alleles may be less functionally efficient in costimulating<br />
the TCR, and is associated with SLE, Sjögren`s syndrome and scleroderma.<br />
The aim of this study is to investigate any association of these alleles with HIV and<br />
CMV.<br />
Methods<br />
PCR and RFLP analyses were used to determine the allelic distribution of NKG2D in 240<br />
HIV patients and 239 healthy controls (all Caucasian). Fisher’s exact test was used to<br />
calculate the significance of the association.<br />
Results<br />
The A allele of NKG2D was found to be associated with HIV (with a frequency of 36% in<br />
HIV patients, 27% in healthy controls), as well as with CMV reactivation in HIV patients<br />
(48%). Associations with other co-infections (including GBV-C and HCV) have yet to be<br />
determined.<br />
Conclusions<br />
This study is investigating the importance of NKG2D signalling in HIV and CMV<br />
infections. The NKG2D-mediated control of CMV infection in HIV co-infected patients<br />
appears to play an important role, as the functionally less efficient allele is correlated<br />
with CMV reactivation.<br />
Supported by BMBF KN Rheuma C2.12
Benjamin Stoelcker, Kirsten Krätzel, Günther Eissner, Michael Pfeifer, Christian Schulz<br />
NKG2D-triggered effector function of bronchial epithelial cell<br />
activated alloreactive CD8+ T cells<br />
Allogeneic hematopoietic stem cell transplantation (SCT) has emerged as a curative<br />
therapeutic option still holding severe side effects including pulmonary toxicity. The<br />
exact role of GvHD for the lung injury after SCT has still to be determined. Induction of<br />
GvHD is considered to depend upon interactions between donor T cells and host APCs,<br />
but it has recently been shown that non-haematopoetic allograft cells can directly<br />
activate host CD8+ T cells. This prompted us to investigate in vitro the potential of<br />
bronchial epithelial cells to activate allogeneic CD8+ T cells and to study the induced<br />
cytotoxic effector functions.<br />
The bronchial epithelial cell line BEAS-2B was shown to express MHC I, MIC A and B,<br />
ULBP-2 and -3, ICAM1, CD70, B7-H1,-H2,-H3, but no or only very low levels of CD80<br />
and CD86. Purified allogeneic CD3+ CD8+ CD4- CD16/56- T cells cocultured with<br />
irradiated BEAS-2B in the presence of low dose IL-2 produced significant amounts of<br />
IFNγ, upregulated alloantigen activation markers CD69 and HLA-DR and showed high<br />
proliferation as compared to IL-2 alone stimulated T cells. Cytotoxicity assays<br />
demonstrated that specific, Granzyme B-mediated cytolytic activity against BEAS-2B<br />
was induced in the alloactivated CD8+ T cells. They showed increased expression of<br />
NKG2D and their cytolytic activity was inhibited using a blocking anti-NKG2D antibody,<br />
but not by blocking MHC I with antibody W6/32. IL-15, which has been shown to be<br />
able to contribute to TCR-independent CTL effector function could not be detected in the<br />
supernatants of the BEAS-2B/CD8+ T cell cocultures. This, together with the low dose<br />
IL-2 used argues against the induction of LAK cells. Cold target inhibition assays with<br />
K562 cells revealed that cytotoxicity was not the result of contaminating NK or NKT<br />
cells.<br />
Our in vitro data let us speculate that bronchial epithelial cell triggered NKG2Dsignalling<br />
contributes to a MHC-unrestricted CTL effector function in lung-directed<br />
alloreaction. This might be of clinical relevance for the course of GvHD after SCT.
Hansjörg Thude, Kathrin Rebstock, Bärbel Lutz, Jörg Blume, Dagmar Barz<br />
No association of the CD45 C77G gene polymorphism with<br />
inflammatory bowel disease in German patients<br />
Background: Inflammatory bowel diseases (IBD) like the Crohn`s disease (CD) and the<br />
ulcerative colitis (UC) are related with environmental, genetic, and immunological<br />
factors. Many aspects of the pathophysiology and the interactions are still unknown. In<br />
the present study we investigated whether C into G transversion at position 77 of exon<br />
A of the CD45 gene contributes to IBD. It has been described that this transversion<br />
prevents splicing of exon A of the CD45 gene and leads to a variant expression pattern<br />
of CD45RA on leucocytes. Material and methods: In a first step we analysed CD45RA/<br />
CD45RO expression patterns on lymphocytes from patients with CD (n=178), UC<br />
(n=122), and healthy control individuals (n=360) by flow cytometric analysis.<br />
Subsequently all members of the study were genotyped for CD45 C77G polymorphism<br />
by polymerase chain reaction-allele specific restriction enzyme analysis. Results: Two<br />
patients with CD, six patients with UC, and eight control individuals displayed the<br />
variant CD45RA expression pattern. All identified individuals with variant CD45RA<br />
expression carried the C into G transversion in a heterozygous form. No homozygous<br />
individual was detected. The corresponding allele frequency of G was 0.55% in patients<br />
with CD, 2.45% in patients with UC, and 1.11% in control individuals demonstrating no<br />
significant difference (P=0.375 for CD vs controls and P=0.125 for UC vs controls) in<br />
the distribution of the 77G allele. Conclusion: These data shows that the C77G<br />
transversion is unlikely to be involved in IBD susceptibility in a German population.
Sascha Rutz, Marko Janke, Manuela Krueger, Alexander Scheffold<br />
Notch induces interleukin-10 production by T helper 1 cells<br />
T helper 1 (Th1) cells direct pro-inflammatory reactions and enable cellular immune<br />
responses against intracellular pathogens. If not properly controlled, Th1 cells may also<br />
cause immunopathology. IL-10 is a potent regulator of Th1 responses. Recently, IL-10<br />
production by Th1 cells has been identified as a critical self-limiting mechanism during<br />
infection.<br />
We identify Notch as a potent inducer of IL-10 in developing and established Th1 cells.<br />
Notch-modified Th1 cells still produce high levels of interferon-γ, but <strong>complete</strong>ly lose<br />
their pro-inflammatory capacity and instead potently suppress Th1-mediated responses.<br />
IL-10 induction is strictly dependent on IL 12/STAT4, and can be triggered by Delta-like<br />
Notch-ligands.<br />
We show that Notch/Dll interactions directly modify the inflammatory potential of Th1<br />
cells via the induction of IL-10, which may be part of a Th1-intrinsic self-limiting<br />
mechanism. These data suggest that triggering the Notch pathway facilitates a<br />
conversion of pro-inflammatory effector cells into regulatory cells; a finding of great<br />
interest regarding new therapeutic strategies in Th1-mediated chronic inflammatory<br />
diseases.
Anne Endmann, Dirk Bumann, Susanne zur Lage, Marcin Lyszkiewicz, Siegfried Weiss,<br />
Holger Lößner<br />
Novel Salmonella vaccine strains with in vivo amplifiable<br />
antigen expression plasmids<br />
Live attenuated Salmonella enterica serovars are explored as mucosal vectors for the<br />
delivery of heterologous antigens or DNA vaccines. Conventional expression systems<br />
are based on maintenance of the expression plasmids at multi-copy numbers<br />
representing a high metabolic burden for the bacteria. We have developed a novel<br />
Salmonella vaccine strain with amplifiable expression plasmids bearing two replication<br />
origins. The first replicon derived from the F factor or plasmid pSC101 ensures the<br />
minimal-copy number state. A second medium-copy replicon derived from plasmid RK2<br />
is responsible for conditional amplification of the expression plasmids under control of<br />
Salmonella-specific in vivo inducible promoters. This replicon mediated strong<br />
amplification of the plasmid copy number up to 50-100 copies. Consequently, enhanced<br />
expression of plasmid-encoded antigen was observed in vitro and in vivo. Furthermore,<br />
the expression level of the antigen could be further increased and tightly controlled in<br />
vivo by regulating its transcription via in vivo inducible promoters at the same time. The<br />
novel Salmonella vaccine strains were assessed regarding their colonization properties<br />
after oral administration and their immunogenicity in an adoptive transfer model.<br />
Intravenous immunization with such novel strains resulted in substantial ovalbuminspecific<br />
CD4+ T cell responses.
Britta Schneider, Jeannette Gerspach, Sabine Münkel, Harald Wajant, Peter Scheurich,<br />
Klaus Pfizenmaier<br />
Novel TRAIL fusion proteins as promising candidates for<br />
cancer therapy<br />
Homotrimeric soluble TRAIL is currently been clinically exploited as cancer therapeutic,<br />
but shows little antitumoral activity in monotherapy. In an attempt to further improve<br />
TRAIL’s tumour selective activity we generated new TRAIL fusion proteins comprising an<br />
antibody fragment (scFv) for targeting ErbB2. Further, a variant was designed, where<br />
TRAIL is expressed as a single polypeptide chain (scTRAIL). Apoptotic activity of<br />
scTRAIL is equivalent to a homotrimeric TRAIL molecule. We compared tumour<br />
targeting and apoptosis induction of scTRAIL based and of conventional, homotrimeric<br />
TRAIL fusion proteins with nontargeted TRAIL. Interestingly, among the tested TRAIL<br />
molecules, the tumour antigen targeted scTRAIL fusion protein showed highest<br />
apoptotic activity in vitro. The underlying mechanisms of this difference in apoptotic<br />
activity will be discussed. Superior apoptosis induction of targeted TRAIL molecules<br />
represent a promising strategy to improve TRAIL’s anti-tumoral action and minimizes<br />
potential non-targeted actions on normal tissues.
Verena Susanne Meyer, Dagmar Sigurdardottir, Wolfgang Kastenmüller, Georg<br />
Gasteiger, Ingo Drexler, Stefan Stevanovic<br />
Novel vaccinia virus T-cell epitopes identified by mass<br />
spectrometry of HLA ligands<br />
Modified vaccinia virus Ankara (MVA) is currently under consideration as a third<br />
generation vaccine against smallpox as well as tested as recombinant viral vector<br />
vaccine for immunotherapy of infectious diseases and cancer. CD8 T-cell responses<br />
against MVA are well documented, but only a few vaccinia virus T-cell epitopes are well<br />
characterized.<br />
In this study, we describe a novel approach to identify vaccinia virus-derived MHC class<br />
I peptide ligands. Peptides isolated from HLA molecules of MVA-infected and noninfected<br />
B-cells were differentially labeled by chemical modification, separated by HPLC<br />
and sequenced using ESI mass spectrometry. Using this approach, we identified several<br />
MVA-specific HLA-A*0201 and HLA-B*0702 ligands. The majority of these peptide<br />
determinants were derived from early viral proteins. Only one ligand corresponded to a<br />
late gene product. Importantly, we confirmed the presence and functionality of CD8 Tcells<br />
recognizing these ligands in PBMCs derived from MVA-vaccinated donors. Two of<br />
the 6 epitopes were identical to recently published determinants found to be reactive in<br />
Dryvax vaccinees. The data will help to further characterize and to evaluate the<br />
immunogenicity of vaccines based on orthopoxviruses.
Kurt Schönfeld, Sabine Ring, Tanja Bedke, Sonja Schallenberg, Karsten Mahnke,<br />
Alexander H. Enk<br />
Nucleofection is an effective method to transduce regulatory<br />
T cells with different homing receptors.<br />
Regulatory T cells (Tregs) are a well described subset of CD4 T cells. They are<br />
characterized by the expression of CD4, CD25 and the transcription factor FoxP3, as<br />
well as by their ability to suppress the proliferation of CD4 T cells.<br />
We have recently shown that in a murine contact hypersensitivity (CHS) model, injected<br />
Tregs are able to suppress the contact allergen induced ear swelling reaction through<br />
inhibition of the CD8 cells. So far it is not clear as to how Tregs suppress CD8 cells and<br />
whether homing to the skin and or to the skin draining lymph nodes is mandatory for<br />
their function. Thus, to investigate whether homing of Tregs to different tissue sites<br />
affects their ability to suppress CHS reactions, we set out to clone the cDNA of the<br />
murine homing receptors CCR7, CCR9, CCR10, Itgae and PSGL-1 and to transfect<br />
Tregs.<br />
Using EL-4 T cell line as well as expanded and freshly isolated Tregs we were able to<br />
establish reliable transfection of Tregs with the respective plasmids using the Amaxa<br />
nucleofection method. Using this method we yielded transfection rates of 50%, (EL-4)<br />
20% (freshly isolated and stimulated Tregs) and 10% (expanded Tregs), respectively.<br />
In further experiments we plan to inject these cells into mice and to analyse their<br />
migration pattern as well as their suppressive function in the CHS model. These<br />
experiments will clarify as to how different adhesion molecules guide Treg homing in<br />
vivo and whether differential homing affects the suppressive activity of the Tregs.
Sabrina Schmitt, Karsten Mahnke, Kurt Schönfeld, Svetlana Karakhanova, Alexander<br />
H. Enk<br />
Number and function of regulatory T cells in GvHD increase by<br />
Extracorporeal Photopheresis<br />
Extracorporeal Photopheresis (ECP) is a procedure commonly used to reduce transplant<br />
rejection. It is also applied in diseases like GvHD, cutaneous T cell lymphoma and other<br />
medical conditions involving overboarding immune reactions.<br />
The mechanism by which ECP exerts its immunosuppressive properties remains elusive.<br />
However, since regulatory T cells (Treg) are a major cellular component that contributes<br />
to immunosuppressive mechanisms, we set out to investigate whether ECP affects Treg<br />
function.<br />
For this end we analysed peripheral blood of patients with GvHD after bone marrow<br />
transplantation who received ECP-treatment. The patients were ECP treated on 2<br />
consecutive days and blood samples were taken before and after each session. First, we<br />
prepared PBMC and compared the respective amounts of various cell types within the<br />
peripheral blood of the patients before and after treatment via FACS analysis. Here we<br />
observed an increase of CD4+ CD25+ FoxP3+ Treg directly after each ECP cycle and<br />
also in the general course of treatment (6 cycles, over 3 months analysed).<br />
Moreover, to study functional properties of this distinct population we analysed the<br />
suppressive effect of MACS-bead isolated Treg before and after ECP using conventional<br />
suppression assays. As controls Treg were isolated from untreated healthy volunteers.<br />
These assays revealed that Treg before ECP showed a significantly reduced suppression<br />
of T cell proliferation, whereas after ECP, Treg equalled Treg isolated from healthy<br />
volunteers in their suppressive capacity.<br />
In conclusion ECP may exert its immunosuppressive functions by upregulating the<br />
number and the suppressive capacity of regulatory T cells and may thus be an<br />
appropriate therapy to prevent over-reactions of the immune system after stem cell<br />
transplantations.
Martin Kolev, Marieta Ruseva, Steffen Thiel, Frederik Hansen, Jens Jensenius<br />
On the role of MBL in a murine model of oral infection with<br />
Salmonella typhimurium<br />
Salmonella enterica is a gram-negative intracellular microorganism, which grows in the<br />
mononuclear phagocytic system of the host and causes disease. The complex<br />
interaction between the both host and the bacterium is still unknown. Multiple humoral<br />
and cellular effector mechanisms, implicated in host resistance to Salmonella infections<br />
have been described.•<br />
Complement plays a major role in host defense against bacteria and fungi. •<br />
MBL (mannan binding lectin)-a plasma protein belonging to a family of proteins known<br />
as collectins. It interacts with a wide array of microorganisms, including Salmonella spp. •<br />
Mice and calf models have been used to study the mechanism of Salmonella infection in<br />
vivo. •<br />
The model we used relies on pretreating mice with Streptomycin, which kills the normal<br />
gut flora and allows for subsequent infection with Salmonella.•<br />
We infected them with Salmonella enterica serovar Typhimurium SL1344 - a naturally<br />
occurring strain that is streptomycin resistant.•<br />
We followed the course of Salmonella infection for 3 days in wild-type (WT) female<br />
C57BL/6 mice and compared disease severity with female MBL double knock-out (DKO)<br />
mice (both MBL-A and MBL-C deleted). We observed about 100 fold increased bacterial<br />
loads of the cecum in MBL DKO compared to wild-type animals. These results were also<br />
confirmed by H&E staining of ceca cryosections. There was also an about 10-fold<br />
increase in bacterial loads in fecal pellets of MBL DKO mice, when compared with WT.<br />
However, no difference in liver loads between WT and DKO was observed. The latter<br />
suggests that the infection after 3 or 4 days is systemic. The greater severity in DKO<br />
was also reflected by rapid weight loss. •<br />
The results suggest an important role of MBL in the immune response to systemic<br />
Salmonella infection.
Monika Braun, Christine Sers, Ruprecht Kuner, Barbara Simm, Barbara Mosetter,<br />
Dolores Schendel, Christine Falk<br />
Oncogenic KRAS-signalling and DNMT activity are involved in<br />
immune escape of tumor cells<br />
The transformation process of cancer cells is often accompanied by an accumulation of<br />
genetic and epigenetic abnormalities that lead to indefinite proliferation and evasion of<br />
immune recognition by immune effector cells such as CTL and NK cells. The impact of<br />
these malignant alterations on immune evasion strategies by tumor cells is still poorly<br />
understood. HCT116 colon carcinoma cell lines were selected with respect to mutated Ki-<br />
Ras that is associated with oncogenic constitutive MEK/ERK signalling. In addition,<br />
variants of this cell line with aberrant DNA-methylation due to deletion of DNAmethyltransferase<br />
DNMT1 and/or 3b were available.<br />
These cells were treated with a MEK/ERK pathway inhibitor (U0126) and analysed for<br />
mRNA expression profiles by microarray-analysis and RT-PCR, for promoter-methylation<br />
patterns by bisulphite sequencing and for surface expression by FACS analysis. The<br />
functional relevance for immune recognition was tested using HLA class I-restricted CTL<br />
and allogeneic NK cells. In addition, the effect of IFN-α versus IFN-γ treatment in<br />
combination with Ras-signalling inhibition and DNMT-deficiency was analysed with<br />
respect to sensitivity to lysis by CTL and NK cells.<br />
The analysis revealed that some immune genes are co-regulated via DNMT and MEK/<br />
ERK signalling. HLA-A and NKG2D-ligand ULBP2 surface expression was up-regulated by<br />
inhibition of MEK/ERK signalling and/or deletion of DNMT, with highest expression levels<br />
in those cells where both systems were blocked. Using an HLA-A2-restricted CTL clone<br />
as effector cell, these changes in the density of HLA-A could be sensed and led to<br />
enhanced tumor lysis. In addition, treatment with IFN-γ could further enhance CTL lysis,<br />
but diminished NK-mediated killing. In contrast, IFN-α treatment could increase CTL<br />
lysis without decreasing the NK cell response. Taken together, our data indicate that<br />
both, oncogenic Ras-signalling and DNMT activity contribute to the immune escape<br />
against CTL recognition. Importantly, this escape could be reversed by IFN-α but not<br />
IFN-γ with respect to both, CTL and NK recognition.
Varsha Kumar, Jens Stein<br />
Optical ProjectionTomography as a tool for studying the threedimensional<br />
structure of Seconday Lymphoid Organs*<br />
The internal organization of complex organs, such as secondary lymphoid organs (SLO),<br />
is essential to understand their function. So far, most information regarding SLO<br />
organization and restructuring during inflammation has been obtained using traditional<br />
two-dimensional (2D) sectioning of tissue followed by immunofluorescent or<br />
immunohistologic labeling. However, differences obtained due to the plane of cutting of<br />
the specimen and the lack of a three-dimensional (3D) context makes interpretation of<br />
2D sections not always reliable. Optical Projection Tomography (OPT) is a recently<br />
developed imaging technique ideally suited to examine internal 3D structures of wholemount-labeled<br />
specimen (0.5 to 15 mm diameter), which elies on the reconstruction of<br />
high-resoulution virtual sections using computer-based back-projection algorithms. Our<br />
first whole-mount staining of B cell follicles in LN and spleen for OPT provided us with<br />
high resolution, qualitative 3D overviews of B cell follicle structure. To the best of our<br />
knowledge, these images covering entire LNs and extensive spleen sections constitute<br />
the first 3D overviews over these important microcompartments. This allowed us to<br />
identify the polarized localization of B cell follicles in LN and previously unnoticed “B cell<br />
bridges” between subsets of individual follicles, which would have been difficult to<br />
assess in 2D sections. More importantly, we quantitatively analyzed B cell follicle<br />
number, volume, and relative distances, with image analysis software (Imaris, Bitplane,<br />
Switzerland) and showed that number and volume of B cell follicles to the total volume<br />
of LN remains constant in any given LN. Furthermore, we have also established staining<br />
techniques to label vascular network which will allow us to examine, by OPT, the 3D<br />
relationship between various microcompartments before and after inflammation. Thus,<br />
our studies not only aim to characterize the 3D anatomy of murine SLO, but also to<br />
form a more objective basis to model changes during inflammatory processes.
Mathias Fousse, Ulrich Mack, Tobias Hodapp, Urban Sester, Gerhard W. Sybrecht,<br />
Hans Köhler, Martina Sester<br />
OPTIMIZED DIAGNOSIS OF LATENT TUBERCULOSIS<br />
INFECTION BY ANALYSIS OF ESAT-6 AND CFP-10 SPECIFIC T-<br />
CELL REACTIVITY USING A RAPID FLOW-CYTOMETRIC ASSAY<br />
We have recently shown that a flow-cytometric whole blood assay based on tuberculin<br />
(PPD) and the M. tuberculosis specific proteins ESAT-6 and CFP-10 may be superior in<br />
diagnosing a latent tuberculosis infection as compared to the established skin test. This<br />
study was carried out to establish a clinically relevant threshold of PPD reactivity<br />
including cytokine profiles and T-cell reactivity towards ESAT-6 and CFP-10.<br />
Whole blood from 439 patients was stimulated in vitro with PPD, ESAT-6 and CFP-10.<br />
After 6 h, the number and cytokine pattern (IFNγ, IL-2) of T cells as potential marker for<br />
disease activity was determined using flow-cytometry. In 310 patients, skin-testing and<br />
flow-cytometry was compared using ROC analysis.<br />
Skin test induration and PPD reactive T-cell frequencies showed a significant correlation<br />
(r=0,60, p
Gudrun Szalay, Martina Sauter, Carmen Ruoff, Reinhard Kandolf, Karin Klingel<br />
Osteopontin is not involved in antiviral immunity but in<br />
cardiac fibrosis during chronic enterovirus myocarditis<br />
Osteopontin (OPN) is a pleiotropic cytokine involved in tissue remodeling, chemotaxis<br />
and cell-mediated immunity. OPN is expressed by different cell-types like macrophages,<br />
T-cells, epithelial cells and smooth muscle cells, and expression is strongly up-regulated<br />
in inflamed tissues. After coxsackievirus B3 (CVB3) infection, OPN was detected as one<br />
of the highest regulated genes in murine hearts by microarray analysis. Therefore, we<br />
wanted to elucidate whether OPN plays a role in heart remodeling and/or in cellmediated<br />
immunity to enterovirus infection.<br />
We used quantitative RT-PCR to examine cardiac OPN expression in CVB3-infected mice<br />
at different time points post infection (pi). Mice, susceptible for chronic myocarditis,<br />
showed a higher OPN expression during acute and chronic myocarditis with a maximum<br />
at day 8 pi, than mice resistant to chronic myocarditis. OPN gene deficient (OPN-ko)<br />
mice revealed a course of myocarditis with viral titers, IFNγ and IL-10 secretion patterns<br />
and no chronic inflammation, which is typical for resistant mice. By in situ hybridization<br />
and immunohistochemistry we detected macrophages as producers of OPN within<br />
inflammatory lesions in the heart. Transcript levels for matrixmetalloproteinase-3,<br />
tissue inhibitor of metalloproteinase-1, urokinase-plasminogen activator and procollagen<br />
I – all molecules involved in cardiac remodeling – were high in susceptible mice,<br />
whereas in resistent mice and OPN-ko mice only minimal levels were detected. In<br />
addition, morphometric analysis demonstrates a more distinct myocardial fibrosis in<br />
susceptible mice than in resistent mice and OPN-ko mice only had minimal fibrosis.<br />
OPN is not involved in the cell-mediated immunity against CVB3. However, OPN<br />
expression induces the expression of proteins responsible for remodeling thereby<br />
leading to pronounced myocardial fibrosis.
Stefan Ehlers, Sahar Aly, Klaus Wagner, Sven Malm, Tamas Laskay, Jörg Mages,<br />
Roland Lang, Ian Orme, Franz Bange<br />
Oxygen Status of Lung Granulomas in M. tuberculosis-<br />
Infected Mice and Guinea Pigs and Causal Involvement of<br />
CXCR3-targeted Chemokines in Granuloma Necrosis<br />
It is often assumed that Mycobacterium tuberculosis (Mtb) -induced granulomatous<br />
lesions, particularly those undergoing central caseation, are anoxic, and that the<br />
survival of Mtb in these lesions requires the integrity of its non-oxidative respiratory<br />
pathways. Using the hypoxia marker pimonidazole we provide immunohistochemical<br />
evidence that in the most frequently used animal model system of inbred mice, Mtbinduced<br />
granulomas, even after more than one year of aerogenic infection, are not<br />
severely hypoxic. Direct measurements of oxygen tension with a flexible microelectrode<br />
in mouse lungs chronically infected with Mtb revealed a wide range of oxygen partial<br />
pressures in different parts of the lungs which, however, rarely approached the anoxic<br />
conditions consistently found in necrotizing tumors. We further show that a Mtb mutant<br />
defective in nitrate reductase (narG) necessary for survival under anaerobic conditions<br />
in vitro, can persist in the lungs of chronically infected mice to a similar extent as wild<br />
type Mtb. In contrast, necrotizing granulomas in guinea pig lungs and lymph nodes<br />
infected by aerosol with Mtb consistently showed staining patterns indicative of severe<br />
hypoxia, when examined with pimonidazole immunohistochemistry. Interestingly,<br />
necrotizing granulomas in mice aerogenically infected with Mycobacterium avium<br />
TMC724 also had hypoxic zones immediately adjacent to their caseating centers.<br />
Granuloma vascularization was significantly decreased in central, but not peripheral,<br />
areas of granulomas of infected wild-type (WT) compared to IFN-gamma knock-out<br />
(GKO) mice infected with M. avium TMC724. This was associated with a reduced mRNA<br />
expression of angiostatic chemokines, such as CXCL9-11, in GKO mice.<br />
Histomorphology in CXCR3-KO mice, however, showed similar caseating granulomas as<br />
WT mice 16 weeks after TMC724 infection.<br />
Conclusion: The combined evidence of microbiological, immunohistological, and<br />
biophysical approaches strongly supports the conclusion that Mtb-induced granulomas<br />
are not anoxic in mice. This is in contrast to Mtb-induced lesions in guinea pigs which<br />
appear to be severely hypoxic. Therefore, the in vivo validation of metabolic pathways<br />
that are induced in Mtb under severely reduced oxygen tension in vitro may not<br />
unequivocally be performed in the mouse model of tuberculosis and may need to resort<br />
to other experimental model systems, for example the guinea pig.<br />
Using the M. avium model of lung immunopathology, we demonstrate that, while IFNgamma<br />
causes a dysbalance between angiostatic and angiogenic mediators and a<br />
concomitant reduction in granuloma vascularization, CXCR3-targeted chemokines are<br />
not sufficient to induce granuloma necrosis.<br />
This work was supported in part by grants to SE (SFB367-C9, NGFN2/NIE-S05T22), TL<br />
(SFB367-B10, La1267/1), RL (NGFN2/NIE-S31T29) and to IMO (NIH/AI054697).
Michal Smida, Anita Posevitz-Fejfar, Burkhart Schraven, Jonathan A. Lindquist<br />
PAG downregulation results in increased proximal signaling<br />
but reduced functional outcomes in primary T cells<br />
PAG (the phosphoprotein associated with glycosphingolipid-enriched microdomains) is a<br />
transmembrane adaptor protein that recruits Csk (C-terminal Src kinase) to the plasma<br />
membrane, where it then phosphorylates inhibitory tyrosines within Src kinases.<br />
Recently, we have also shown that PAG negatively regulates Ras activation by recruiting<br />
RasGAP. Thus, PAG functions as a negative regulator of both Src kinases and Ras. Since<br />
PAG knockout mice possess no apparent phenotype, the importance of PAG as a<br />
negative regulator has been questioned. Therefore we investigated PAG function in<br />
primary human T cells and in Jurkat T cells using RNA interference.<br />
Suppression of PAG expression leads to an enhancement of kinase activity in both Fyn<br />
and Lck, which is reflected by increased phosphorylation of their activatory tyrosines. As<br />
a consequence, we detect enhanced basal tyrosine phosphorylation in resting cells,<br />
which is also more sustained upon TCR stimulation. Additionally, we have investigated<br />
specific proteins involved in the proximal signaling. We observed an enhanced activation<br />
of ZAP70 and PLC gamma and a 5-fold increase in Ras activation. However, IL-2<br />
promotor activity appears to be decreased and also the proliferation of PAG deficient<br />
cells was reduced, as measured by both CFSE labeling and thymidine incorporation.<br />
Thus, although the removal of a negative regulator leads to enhanced proximal<br />
signaling, this does not necessarily lead to an increase in proliferation or IL-2<br />
production, but rather may potentiate other outcomes of T-cell activation, e.g. cell<br />
death.
Gurumoorthy Krishnamoorthy, Florian C. Kurschus, Klaus Dornmair, Reinhard<br />
Mentele, Hans Lassmann, Hartmut Wekerle<br />
Paradoxical autoimmunity: Molecular self mimicry initiates<br />
spontaneous autoimmunity in myelin-specific T cell receptor<br />
transgenic mice deficient of cognate self antigen<br />
We describe here the identification of neurofilament medium (NF-M), a neuron-specific<br />
cytoskeletal intermediate filament protein, as a cross-reactive autoantigen for a myelin<br />
oligodendrocyte glycoprotein (MOG)-specific T cell receptor (TCR). Studying the<br />
mechanisms of spontaneous autoimmunity in MOG-specific TCR transgenic mice (2D2),<br />
we bred the TCR transgene into MOG deficient (MOG-/-) mice of appropriate C57BL/6<br />
background. Surprisingly, MOG-deficient 2D2 TCR transgenic mice (2D2 x MOG-/-)<br />
developed experimental autoimmune encephalomyelitis (EAE) with frequency and<br />
symptoms undistinguishable from single transgenic MOG+/+ 2D2 mice. About 10 - 20%<br />
of the 2D2 and 2D2 x MOG-/- mice developed spontaneous EAE at around 5-8 weeks of<br />
age. The T cells isolated from the inflamed central nervous system (CNS) predominantly<br />
contained transgenic T cell populations ruling out any endogenous T cells might be<br />
responsible for autoimmunity. The clinical and histological features of the EAE were<br />
similar between these two strains.<br />
Having excluded failed gene ablation in our MOG-/- strain, we scanned MOG-/- CNS<br />
tissue for 2D2 T cell activating activity. We identified one fraction which induced a<br />
strong proliferative response of 2D2 T cells. Mass spectrometry analysis identified<br />
neurofilament proteins as major components. Sequence alignment of NF-M and MOG<br />
revealed a motif shared by the MOG 35-55 peptide and a segment of NF-M. We<br />
confirmed cross-reactivity between MOG and NF-M on the level of recombinant proteins<br />
and synthetic peptides.<br />
This is the first report of a pathogenic, myelin specific T cell clone cross-reacting with<br />
another CNS self-protein which can serve as target of an autoimmune attack.
Hanna Erdmann, Paul Crocker, Bernhard Fleischer, Thomas Jacobs<br />
Pathogenic Trypanosoma cruzi interacts with the immune<br />
modulatory molecule mouse Siglec-E (sialic acid-binding Iglike<br />
lectin-E)<br />
The protozoan parasite Trypanosoma cruzi is the causative agent of Chagas disease, a<br />
chronic infection, in which a strong suppression of the immune response leads to a lifelong<br />
persistence of parasites in host cells. The trypanosomal trans-sialidase is described<br />
to be a major virulence factor. This enzyme allows the parasite to acquire sialic acids<br />
from its environment by cleavage from host glycoconjugates and direct transfer to GPIanchored<br />
mucin-like molecules on its own cell surface. In the current investigation we<br />
provide evidence that the murine molecule Siglec-E directly interacts with sialylated<br />
ligands on the surface of T. cruzi. Siglecs are sialic acid-binding Ig-like lectins that are<br />
expressed on most cell types of the immune system. They have been shown to act as<br />
inhibitory receptors, ascribed to the presence of conserved immunoreceptor tyrosinebased<br />
inhibition motifs (ITIMs) in their cytoplasmic regions. The murine Siglec-E is<br />
expressed on phagocytic cells as well as on NK cells. Using Siglec-E transfected CHOcells<br />
and a Siglec-E-Fc fusion molecule we demonstrate that Siglec-E binds with high<br />
affinity to both extracellular trypomastigotic and intracellular amastigotic parasites of<br />
the pathogenic T. cruzi Tulahuen strain. In contrast, we can detect only a weak binding<br />
of Siglec-E to extracellular trypomastigotic parasites of the apathogenic T. cruzi<br />
Tehuantepec strain, whereas the binding of Siglec-E to intracellular amastigotic<br />
parasites of this apathogenic strain is <strong>complete</strong>ly absent.<br />
These results raise the possibility that the pathogenic parasite dampens immune<br />
responses via binding to the inhibitory receptor Siglec-E, allowing the parasite to persist<br />
and to establish a chronic infection.
Jan Dirks, Urban Sester, Daniela Presser, Heinrike Wilkens, Hans Köhler, Martina Sester<br />
PD-1 expression on CMV specific CD4 T cells is associated<br />
with viremia and reversible functional anergy in patients after<br />
organ transplantation<br />
Recently, chronic infections with LCMV, HIV or HCV were shown to be associated with<br />
anergic T cells characterised by high expression of PD-1. We have previously shown that<br />
uncontrolled CMV replication after transplantation correlates with a drop in CMV specific<br />
T cells. This study was extended to analyse whether functional anergy of specific T cells<br />
in individuals with and without CMV viremia may affect control of CMV replication.<br />
CMV specific CD4 T cells from 12 controls, 25 hemodialysis patients, 43 renal and 14<br />
lung-transplant patients were quantified using flow cytometry and analysed for their<br />
expression of PD-1 and cytokines IFNγ and IL2. Specific proliferation was analysed by<br />
CFDA-SE dilution. CMV-DNA was quantified using PCR.<br />
In viremic patients, a significantly higher proportion of CMV specific CD4 T cells were PD-<br />
1 positive (median 42.3%) as compared to non-viremic patients (7.4%), hemodialysis<br />
patients (8.8%) or controls (3.1%, p=0.001). In line with functional impairment, PD-1<br />
positive T cells produced significantly less IFNγ as compared to PD-1 negative cells (MFI<br />
101 vs. 210, p
Hiroaki Azukizawa, Nobuo Kanazawa, Manfred B. Lutz<br />
Peripheral de novo induction of CD4+ CD25+ Foxp3+<br />
regulatory T cells by steady state migratory dendritic cells<br />
Transport of microbial antigens from infection sites to the draining lymph nodes by<br />
dendritic cells (DC) is well established. Accumulating evidence suggests that DC<br />
migration also occurs under steady state conditions resulting in tolerance induction to<br />
peripheral self antigens. However, the precise migratory DC phenotype and the CD4+ T<br />
cell tolerance mechanism induced by such migratory DC remain unclear. We show that<br />
steady state migration of skin DC depends on CCR7 but not on inflammation or<br />
microbial stimuli, since skin-derived DC are present in peripheral lymph nodes of germfree<br />
mice and mice deficient for in CD40L, TNFR1/2 or MyD88. At their surface<br />
migratory DC express elevated levels of MHC II and costimulatory molecules but they<br />
do not produce cytokines, thus representing a semi-mature state. Only migratory DC<br />
within draining lymph nodes contained peripheral self antigens as apoptotic cells. In<br />
transgenic mice expressing OVA as cell-associated neo-self antigen in the skin (K5mOVA),<br />
or mice subcutaneously implanted with OVA-secreting osmotic pumps, only<br />
migratory skin-derived DC but not immature lymph node-resident DC were able to<br />
present OVA in vitro or in the peripheral lymph nodes to adoptively transferred OVAspecific<br />
CD4+ T cells (OT-2), as evaluated by the use of K5-mOVA x CCR7-/- mice,<br />
lacking migratory DC. In both models of antigen transport, adoptively transfered OT-2 x<br />
RAG-/- T cells, which are devoid of natural Tregs, became activated in the peripheral<br />
lymph nodes and developed into CD4+ CD25+ Foxp3+ regulatory T cells within 2<br />
weeks. Together, our data indicate that semi-mature, steady state migratory DC induce<br />
Treg against soluble and cell-associated self-antigens in peripheral lymph nodes under<br />
steady state conditions.
Fabien Agenes, Jean-Pierre Dangy, Jörg Kirberg<br />
Peripheral inter-clonal competitiveness requires T cell<br />
receptor contact to restricting MHC molecules<br />
In the adult, peripheral lymphocyte numbers are relatively constant, indicating that<br />
there are homeostatic control mechanisms. Known requirements for peripheral T cell<br />
survival, as well as homeostatic proliferation, are the TCR interaction with restricting<br />
self-MHC molecules and the availability of lymphokines, such as IL-7. It is possible that<br />
by competition towards these factors T cells reach a constant steady state number;<br />
however, the mechanisms by which these restrains interrelate are not <strong>complete</strong>ly<br />
understood.<br />
It has been noted that upon adoptive transfer, homeostatic proliferation of donor T cells<br />
can occur even in the full complement of host cells, provided the latter express a<br />
different TCR. In other combinations, however, donor T cells are blocked by the<br />
preformed presence of unrelated T cells. Thus there might be a “hierarchicalcompetitiveness”.<br />
We find such hierarchical-competitiveness in the order OT-1 TCR ><br />
P14-TCR > F5-TCR. As the OT-1 TCR is restricted to Kb, and the others are to Db, it<br />
was possible to remove the OT-1 TCR ligand exclusively. Using various Kb-mutant mice<br />
we demonstrate that proliferation of OT-1 T cells in hosts harboring P14-TCR expressing<br />
cells, and, likewise, the competence of OT-1 T cells to block proliferation of P14-TCR<br />
expressing cells, requires OT-1 TCR binding to Kb. Detecting no functional crossreactivity<br />
of the OT-1 TCR, this excludes that direct competition for MHC molecules<br />
causes hierarchical-competitiveness. Furthermore, parabiosis experiments with Kbmutant<br />
mice exclude that the hierarchical-competitiveness is caused by competition for<br />
direct cellular contact to, or modulation of, the restricting MHC-bearing cells. Thus, it is<br />
the apparent avidity of the TCR to restricting MHC molecules that defines a relative<br />
competence to compete, secondarily, for a trophic resource available in limited supply<br />
and not bound to the APC. Such mechanism would allow for a localized competitiveness<br />
operating beyond a T cells’ specificity.
Kristina Streyl, Mikhail Nosov, Vijay Kumar Ulaganathan, Hartmut Wekerle, Alexander<br />
Flügel<br />
Peripheral milieus license autoaggressive effector T cells to<br />
invade their target organ<br />
Using a transfer model of experimental autoimmune encephalomyelitis (tEAE) we<br />
explore the question why the paralytic disease occurs only after an obligatory prodromal<br />
phase of several days after transfer of the autoaggressive T cells. Traditionally CNS<br />
invasion during EAE is believed to follow a biphasic course. The first infiltration wave<br />
occurs hours after T cell transfer. These “pioneer” cells are thought to prime the<br />
immune privileged CNS tissue and thus, pave the way for a second inflammatory wave,<br />
which occurs at the onset of clinical disease. Using retrovirally labeled green fluorescent<br />
protein expressing encephalitogenic T cells (T GFP cells) we now found that the<br />
numbers of pioneer T cells in the preclinical CNS parenchyma analyzed by<br />
cytofluorometry and microscopically were negligible low (
Sebastian Bunk, Iuliana Suznea, Jan Rupp, Matthias Maass, Michael Przybylski, Albrecht<br />
Wendel, Corinna Hermann<br />
Persisting Chlamydia pneumoniae infections are associated<br />
with differential immune responses<br />
The respiratory pathogen Chlamydia pneumoniae can disseminate from the lung via<br />
infected phagocytes and persist in the host tissue for years. A reliable diagnosis, which<br />
allows discrimination between past and persistent infection is a prerequisite to study its<br />
association with chronic inflammatory diseases. Our project aimed to investigate<br />
whether persistent C. pneumoniae infections are associated with specific antibody<br />
response patterns.<br />
Therefore, C. pneumonia proteins were prepared from elementary bodies, separated by<br />
2D-gel electrophoresis and blotted to nitrocellulose membranes. The membranes were<br />
incubated with 39 human sera and bound IgG antibodies were quantitatively analysed<br />
by a LAS-3000 imaging system. Nineteen of the 39 sera revealed evidence for<br />
persisting C. pneumoniae infections as determined by PCR analysis of monocytes or<br />
vasculatory samples. Using high resolution MALDI-FTICR-MS, we identified 38<br />
Chlamydia proteins originating from 33 genes which were frequently recognized among<br />
the 39 sera. About half of the proteins, including some with high antigenic potential,<br />
represent Chlamydia antigens not described before. Comparison of antibody response<br />
pattern between sera from subjects with and without evidence for persisting C.<br />
pneumoniae, resulted in differential reactivity of the two groups of sera towards twelve<br />
proteins. While the reactivity of sera from PCR-positive donors was increased for eight<br />
proteins, reactivity was decreased for four proteins, thereby reflecting altered protein<br />
expression patterns of in vitro models of C. pneumoniae persistence. Taken together,<br />
these results provide first evidence for serological differences associated with the status<br />
of C. pneumoniae infections.
Nirmal Robinson, Tom Li Stephen, Sonja Meemboor, Wiltrud M. Kalka-Moll, Georg Plum<br />
Phagosomal and endosomal trafficking studies by adenoviral<br />
Rab-GFP fusion proteins in primary cells<br />
Antigen presentation by major histocompatibility complex (MHC) class II on antigen<br />
presenting cells (APCs) is facilitated after a sequence of events that starts with a<br />
phagocytic process, followed by phagosomal processing of the antigen, phagolysosomal<br />
degradation of the phagocytosed material and loading of antigenic peptides onto MHC<br />
molecules. A detailed picture of this process termed phagosome maturation is beginning<br />
to emerge, involving regulators of membrane trafficking in mammalian cells and<br />
phagosomal interactions with endosomal organelles and the trans-Golgi network. So far,<br />
cell biology studies of antigen presentation can be performed in primary cells after<br />
fixation and permeabilization for staining with specific antibodies or probes for other<br />
endosomal pathway . Investigation in live cells is solely possible in cell lines after<br />
transfection with expression vectors for GFP-tagged endosomal marker proteins. In an<br />
effort to open up ways to elucidate the phagosomal processing events after antigen<br />
uptake in live primary antigen presenting cells of murine and human origin we have<br />
developed a set of adenoviral Rab-GFP fusion protein expression vectors that allow<br />
observation and tracking individual phagosomes. Transfection with the early endosomal<br />
marker Rab5-GFP, late endosomal marker Rab7-GFP, and transferrin receptor recycling<br />
marker Rab11-GFP was achieved in 92% to 93% of the mouse dendritic cells, in 89% to<br />
94% of human macrophages, and in 70% to 82% of mouse macrophages. Rab-GFP<br />
fusion proteins were readily expressed in these primary cells using these highly efficient<br />
adenoviral constructs allowing phagosome and endosome trafficking by fluorescently<br />
labeled fluid phase marker. Our data show that the intracellular endocytic trafficking<br />
events preceeding antigen presentation in primary APCs can be effectively studied in<br />
live cells by using our adenoviral expression systems.
Thomas Giese, Claudia Sommerer, Martin Zeier, Stefan Meuer<br />
Pharmacodynamic controlled tapering of Cyclosporine A – a<br />
new step towards individualized immunosuppressive therapy<br />
in transplanted patients<br />
Background. At present it is unclear which dose of Cyclosporine A (CsA) is optimal with<br />
respect to immunosuppressive efficacy and drug specific side effects at the level of the<br />
individual patient. Recently we proposed the quantitative assessment of NFAT regulated<br />
gene expression in peripheral lymphocytes as a new tool to measure the individual<br />
degree of immunosuppression by CsA and demonstrated that a significant correlation<br />
exists between suppression of NFAT-regulated genes and clinical complications such as<br />
infections and malignancies. The reduction of CsA dosage under close pharmacodynamic<br />
monitoring may lead to reduced drug specific side effects while maintaining optimal<br />
graft protection.<br />
Methods. Eight stable renal transplant recipients were enrolled and longitudinally<br />
followed for 27 (12-44) months. Median CsA dose was 1.83 mg/kg/day at the time of<br />
enrolment and was tapered to 1.19 mg/kg/day. NFAT-regulated gene expression was<br />
measured in peripheral blood lymphocytes stimulated with PMA and ionomycin ex vivo.<br />
All patients had an ultrasound guided allograft biopsy.<br />
Results. The stepwise reduction of CsA was inversely correlated to the residual NFATregulated<br />
gene expression. In seven patients there were no signs of acute rejection in<br />
the whole study period. One patient had a BANFF Ia rejection. In this patient the mean<br />
residual NFAT-regulated gene expression had increased up to 47% in the 6 month prior<br />
to rejection. All patients without rejection had a median NFAT-regulated gene<br />
expression of 25%.<br />
Conclusion. The measurement of residual NFAT-related gene expression is a helpful<br />
and reliable tool in individualizing the immunosuppressive therapy in long-term allograft<br />
recipients.
Carmen Scheibenbogen, Anne Letsch, Antonia Busse, Sandra Bauer, Alexander<br />
Schmittel, Wolf-Karsten Hofmann, Lutz Uharek, Eckhard Thiel, Ulrich Keilholz<br />
Phase II trial of vaccination with WT1 peptide, GM-CSF, and<br />
KLH in patients with acute myeloid leukemia: immunological,<br />
molecular, and clinical results<br />
Purpose: The transcription factor Wilms tumor protein (WT) 1 belongs to a new<br />
generation of tumor antigens, which are essential for tumor cell proliferation. A phase II<br />
trial of vaccination with an HLA-A2-restricted peptide was performed in patients (pts)<br />
with acute myeloid leukemia.<br />
Methods: Pts received repeated vaccinations with 0.2 mg WT1.126-134 peptide (day 3),<br />
62.5 mcg GM-CSF (days 1-4) as DC-stimulant and 1 mg KLH (day 3) as T helper<br />
protein. WT1-specific T cell responses were analysed by tetramer and cytokine flow<br />
cytometry. WT1 levels were assessed by qRT-PCR.<br />
Results:<br />
Of 29 pts enrolled 26 were evaluable for clinical and 25 for immunological outcome. One<br />
<strong>complete</strong> remission (514 days) and 13 stable diseases (99 to 339 days) were observed,<br />
5 with >50% blast reduction and 3 with hematological improvement. The median time<br />
to treatment failure (TTF) was 143 days. WT1 mRNA-levels as molecular marker of<br />
leukemia load decreased in 52% (2 to>50-fold). There was a significant association<br />
between decrease in WT1 mRNA levels and TTF (p=0.026).<br />
WT1 tetramer+ CD8+ T cells were found in 7 out of 25 pts before vaccination. At week<br />
10 a >2-fold-increase was observed in 13 of the 18 pts without a preexisting WT1<br />
specific T cell response in PB, whereas in the 7 pts with preexisting responses these<br />
could not be boosted. In 19 out of 25 pts T cell responses could be analysed in parallel<br />
in bone marrow at week 18, showing similar frequencies of WT1 tetramer+ CD8+ T<br />
cells in bone marrow (0.36%) and in PB (0.26%). WT1 specific cytokine producing T<br />
cells were found in 13 out of 25 pts at week 10 with 7 pts producing IFNg, 11 TNFa, and<br />
5 IL-2. In selected pts WT1-specific T cells were characterized as both effector and<br />
memory T cells and demonstrated cytotoxic and proliferative capacity and specific<br />
cytokine production in response to autologous leukemic blasts.<br />
Conclusion: This study proves immunological and clinical efficacy of WT1 peptide<br />
vaccination in AML. Two ongoing studies investigate WT1 vaccination in WT1 expressing<br />
carcinomas and as adjuvant therapy in high-risk AML.
Kai Schledzewski, Klein Diana, Martin Falkowski, Gerhard Moldenhauer, Jo van<br />
Ginderachter, Julia Kzhyshkowska, Lou de Leij, Gernot Geginat, Bernd Arnold, Sergij<br />
Goerdt<br />
Phenotype analysis, cytokine induction and gene expression<br />
profiling identify LYVE-1+ tumour associated macrophages to<br />
be a specialized subset of M2 macrophages<br />
Tumor-associated macrophages (TAMs) significantly contribute to regulation of tumor<br />
growth and metastasis. When analysing murine tumors immunohistochemically<br />
regarding lymphangiogenesis, we unexpectedly found a significant percentage of TAMs<br />
to express the lymphatic endothelium-specific hyaluronan receptor LYVE-1. Further<br />
analysis of these special TAMs in B16F1 melanoma and TS/A mammary carcinoma<br />
revealed that LYVE-1 expression occurred in a subset of CD11b+, F4/80+ tissue<br />
macrophages that preferentially co-expressed the sinusoidal endothelial scavenger<br />
receptor stabilin-1. In vitro, LYVE-1 expression was induced in 25-40% of murine bone<br />
marrow-derived macrophages upon exposure to B16F1 melanoma-conditioned medium<br />
and IL-4/dexamethasone. By FACS analysis, 11.5% of bone marrow-derived<br />
macrophages were LYVE-1+, stabilin-1+ double-positive, while 9.9% were LYVE-1+,<br />
stabilin-1- and 33.5% were LYVE-1-, stabilin-1+. As both LYVE-1 and stabilin-1 are thus<br />
shared endothelial-macrophage receptors, we further analyzed the molecular repertoire<br />
of these special LYVE-1+ macrophages by gene profiling. By comparing LYVE-1+ versus<br />
LYVE-1- bone marrow-derived macrophage populations using Affymetrix mouse genome<br />
MOE430 2.0 array chips, we identified a set of 121 genes highly overexpressed in the<br />
LYVE-1+ macrophage population. In addition to well known markers of alternatively<br />
activated (M2) macrophages such as arginase, CD163, and fibronectin, novel molecules<br />
including Mgl2 were identified demonstrating that LYVE-1+ macrophages are a<br />
specialized subset of M2 macrophages. This specialized M2 profile was confirmed by RT-<br />
PCR analysis of LYVE-1+ TAMS isolated ex vivo from TS/A tumors. To identify the<br />
factors necessary to induce LYVE-1+ macrophages in vitro, we tested a broad array of<br />
Th1- and Th2-associated factors. We could show that a mixture of Th2 cytokines<br />
administered sequentially mimicked the effects of the B16F1 conditioned medium. In<br />
order to further test the functions of LYVE-1+ M2 TAMs in vivo, bone marrow chimeras<br />
with bone marrow-specific cytokine receptor knock out as well as LYVE-1 and stabilin-1<br />
single and double knock out mice will be analyzed in the LYVE-1+ TAM-rich TS/A tumor<br />
model.
Tobias Käser, Wilhelm Gerner, Sabine Hammer, Martina Patzl, Armin Saalmüller<br />
Phenotypic and functional characterisation of porcine CD4<br />
+ CD25 high regulatory T cells<br />
Over the last years regulatory T cells (Tregs) were defined as CD4 + CD25 + T<br />
lymphocytes expressing the transcription factor Foxp3 (Forkhead Box P3) with the<br />
ability to down regulate various immune responses. In swine the existence of CD4 + CD25<br />
+ T-lymphocytes was described before but nothing is known about the function of this<br />
minor cell population to date. Therefore we studied porcine CD4 + CD25 + T cells with<br />
regard to major attributes of murine and human Tregs: their phenotype concerning the<br />
expression of several Treg-relevant antigens, including Foxp3, their IL-10 production<br />
and their suppressive capacity. Our results revealed that porcine CD4 + CD25 + T cells<br />
with high CD25 expression count for about 2 to 9% of the CD4 + T cell subset. They<br />
demonstrate a strong Foxp3 expression and a heterogeneous CD45RC-, CD8?- and MHC-<br />
II-defined phenotype. Additionally they show an enhanced IL-10 production. Cocultivation<br />
of increasing numbers of CD4 + CD25 high T cells with a constant number of<br />
CD4 + CD25 - responder-T cells caused a decrease in proliferation of the entire culture.<br />
This demonstrates the suppressive capacity of the CD4 + CD25 high T cell subset and-<br />
together with their Foxp3 expression- the existence of porcine Tregs.
Stefan Maßen, Dirk Jäger, Inka Seil, Barbara Mosetter, Christine Falk<br />
Phenotypic and functional characterization of KIR-expressing<br />
cytotoxic T cells<br />
Introduction: Expression of NK receptors of the KIR (Killer-Ig-like-receptor) family is<br />
mainly observed on NK cells. However, some cytotoxic T cells (CTL) have been shown to<br />
express KIR following allogeneic or tumorspecific stimulation, they have also been<br />
detected in peripheral blood of patients with autoimmune diseases like rheumathoid<br />
arthritis.<br />
Materials and Methods: We generated cytotoxic T cell lines by stimulating isolated<br />
CD8 positive T cells with peptides derived from the tumor associated antigens Rab38<br />
and NY-BR-1 that are mainly expressed by melanoma and breast cancer cells,<br />
respectively. The phenotypic characterization with respect to KIR and NK receptor<br />
expression was determined by multicolour flow cytometry. The specificities of the CTL<br />
lines were examined in chromium-release assays and CD107a-degranulation assays<br />
targeting Rab38- or NY-BR-1-loaded T2-cells. Cytokine secretion patterns were<br />
quantified by multiplex-analyses (Luminex).<br />
Results: Through an extensive phenotypic analysis, the CTL showed a broad expression<br />
of KIR receptors in addition to the activating receptors NKG2D and 2B4. The<br />
functionality of these receptors and their activating and inhibitory potential, tested in<br />
redirected-degranulation experiments, demonstrated that the cytotoxicity of the CTL<br />
lines was clearly dependent on the TCR complex. Activating as well as inhibitory KIR<br />
receptors have only a minor regulatory potential, even though the activating NK<br />
receptor, NKG2D, displayed some co-stimulatory effect. All CTL lines showed de novo<br />
secretion of GM-CSF, IFN-γ and TNF-α as a result of the TCR-complex-stimulation. In<br />
addition, the constitutive secretion of MIP-1β was significantly increased upon TCR<br />
triggering.<br />
Taken together, these data indicate that even in an autologous peptide-specific<br />
stimulation, some CTL maintain their KIR expression, although these KIR may be<br />
functionally dissociated from the TCR signaling cascade. In addition, these KIR-positive<br />
CTL displayed mixed cytokine/chemokine patterns distinct from classical TH1/TH2<br />
patterns.
Esther Wilk, Tibor Horvath, Katy Kalippke, Nadine Wilke, Reinhold E. Schmidt, Roland<br />
Jacobs<br />
Phenotypical and functional characteristics of CD20 + T cells<br />
In humans a small percentage (3-4%) of T cells coexpress CD20, which is commonly<br />
considered a marker of mature B cells. In order to characterize these cells in more<br />
detail, their function and phenotype were analyzed. The study revealed that CD3 + CD20<br />
+ cells are present in different compartments including blood, spleen and liver. The cells<br />
comprise a heterogenous T cell population with 60% coexpressing CD8 and 40%<br />
expressing CD4. Constitutive production of cytokines (i.e. IFNγ, IL-2, TNFα) and strong<br />
expression of CD95 indicate a high activation state of the cells and susceptibility to FasLmediated<br />
apoptosis. Together with their low proliferative capacity in response to various<br />
stimuli (e.g. PHA and CD3 crosslinking) our findings suggest that CD20 + T cells<br />
represent a terminally differentiated cell type with immune regulatory capacity. In<br />
summary, we present new phenotypical and functional characteristics of CD20 + T cells,<br />
providing a basis to further study the in vivo role of this T cell subset. This might be of<br />
particular interest in patients undergoing rituximab treatment since this antibody<br />
targets CD20 + cells and effectively depletes all CD3 + CD20 + T cells along with the<br />
intended B cells.
Bernhard Reis, Roland Piekorz, Bernd Nürnberg, Klaus Pfeffer, Sandra Beer<br />
PI3Kγ and δ play combined roles in B cell development<br />
Class I phosphoinositide 3-kinases are a family of intracellular signalling molecules<br />
which regulate cell differentiation, survival, proliferation, and migration through central<br />
downstream targets including Akt. The specific roles of the PI3K catalytic subunits p110γ<br />
and p110δ in lymphocyte development and function were demonstrated by generating<br />
gene-deficient mice. It was shown that in the thymus combined activities of PI3Kγ and<br />
PI3Kδ during positive and negative selection are essential for T cell differentiation and<br />
survival. Here, we extent the functional analysis of these PI3K isoforms in B cell<br />
differentiation and function. We show that peripheral B cell numbers are dramatically<br />
reduced in PI3Kγ/δ double deficient mice due to a developmental block at the pro-B cell<br />
stage. Moreover, upon antigen receptor triggering or LPS stimulation double deficient B<br />
cells failed to proliferate properly. Importantly, on a molecular level, the cells showed<br />
an impaired upregulation of key regulators of cell cycle progression and survival<br />
including D-type cyclins and bclx. Thus, both PI3Kγ and PI3Kδ display Isotype-specific<br />
and -redundant roles in B cell development and function.
Kerstin Schilling, Bin Hu, Karine Missy, Klaus-Dieter Fischer<br />
Pix proteins in B cell Signalling<br />
alphaPIX is a multi-domain signaling protein with a RhoGEF domain that activates Rac<br />
and CDC42. AlphaPix associates with proteins involved in cytoskeletal-membrane<br />
complexes and cell migration. It has been shown that PIX proteins play roles in some<br />
immune cells, including neutrophils and T cells. We have generated alphaPIX knockout<br />
mice and analyzed their immune system. alphaPIX protein was specifically expressed in<br />
immune cells, unlike its homolog betaPIX, which was expressed in immune cells and in<br />
a wide range of other cells. Although mice lacking alphaPIX had reduced numbers of<br />
mature lymphocytes and defective immune responses, the number of marginal zone B<br />
cells was inceased. In addition, basal migration of B cells and other lymphocytes was<br />
enhanced. Antigen receptor-directed proliferation of alphaPIX - T and B cells was also<br />
reduced, were as LPS induced proliferation of B cells was normal, suggesting for the<br />
first time that alphaPIX is important for B cell receptor (BCR) signaling. In addition,<br />
alphaPIX - B cells showed multiple molecular defects, including increased overall<br />
tyrosine phosphorylation and activation of ERK kinase, and reduced phosphorylation of<br />
PAK kinase following antigen receptor stimulation. These results reveal specific roles for<br />
alphaPIX in the immune system and suggest that alphaPIX is an important signaling<br />
intermediate downstream of the B cell receptor.
Katrin Moser, Oliver Winter, Nicole Haupt, Martin Szyska, Bimba F. Hoyer, Andreas<br />
Radbruch, Falk Hiepe, Rudolf A. Manz<br />
Plasma cell longevity in NZB/W mice<br />
Through the production of autoantibodies, plasma cells contribute to the pathogenesis<br />
of Systemic lupus erythematosus (SLE). In non-autoimmune individuals, long-term<br />
plasma cell survival occurs mainly in the bone marrow where lifetime can reach several<br />
months to years. The longevity of these cells depends on factors like IL-6 and SDF-1,<br />
produced by accessory cells. In NZB/W mice, a model for SLE, high numbers of plasma<br />
cells also survive in the spleen. We here address the question whether this abnormal<br />
plasma cell survival in spleens of NZB/W mice is due to an increased potential of this<br />
tissue to support plasma cell longevity and/or due to an enhanced intrinsic survival<br />
capacity of NZB/W plasma cells. To analyse the intrinsic survival capacities of plasma<br />
cells from different genetic backgrounds we performed in-vitro cultures with isolated<br />
plasma cells. Without addition of survival factors nearly all plasma cells died within 3<br />
days of culture. Addition of IL-6 resulted in an increase in surviving plasma cells which<br />
was much more pronounced with plasma cells derived from autoimmune NZB/W and<br />
NZB mice compared to plasma cells from non-autoimmune Bl6 and NZW mice.<br />
However, plasma cells of BALB/c origin showed the same survival capacity as NZB/W<br />
derived ones. Possibly indicating that higher sensitivity for IL-6 mediated survival can<br />
contribute, but is not sufficient to explain the increased plasma cell survival in NZB/W<br />
spleens. Therefore we also tested the microenvironment of plasma cells in the spleen of<br />
NZB/W mice in tissue sections for the presence of increased production of plasma cell<br />
survival factors. SDF-1 signals were found in close proximity to some, but not all<br />
plasma cells. Increased numbers of a subset of myeloid related cells located in close<br />
proximity to plasma cells and expressing multiple cytokines known to stimulate plasma<br />
cell survival were detected in NZB/W spleens. This finding stresses a main impact of the<br />
splenic microenvironment for the increased survival rate in NZB/W spleens.
Oliver Winter, Katrin Moser, Nicole Haupt, Martin Szyska, Andreas Radbruch, Rudolf A.<br />
Manz<br />
PLASMA CELL SURVIVAL AND DEVELOPMENT IN THE BONE<br />
MARROW<br />
Plasma cells secrete antibodies which are a key factor for the adaptive immune defence.<br />
Bone marrow is the major site where long-lived plasma-cells reside. Survival of these<br />
cells in specific microenvironments (niche) depends on survival factors supplied by<br />
proximate cells, including APRIL, IL-6, TNF-a. SDF-1+ reticular stromal cells found in<br />
association with plasma cells are likely to contribute to this niche.<br />
To further characterize these niches, we immunized B6 and Balb/c mice with the<br />
antigen ovalbumin, sacrificed them at several time points during the immune response<br />
and tracked ovalbumin specific plasma cells via confocal microscopy. Stromal cells<br />
found in close association with plasma cells were considered to contribute potentially to<br />
niches. These cells were further characterised by flow cytometry.<br />
Plasma cells enter the bone marrow via the vascular niche. Here, they are found during<br />
the first days following their immigration into the bone marrow in contact with B78+<br />
cells of the endothelial linage, possibly including mature endothelial cells and endothelial<br />
precursor cells. These plasma cells also make contact to Gr1 high cells, likely<br />
resembling mature granulocytes emigrating from the bone marrow.<br />
Later, at about 7 days after entering the bone marrow, plasma cells are found more<br />
distant from B78+ cells. They now are localized adjacent to VCAM-1+ reticular stromal<br />
cells where they also specifically bind to a particular type of myeloid related cells that<br />
produce multiple important plasma cell survival factors, including Il-6, TNF-a and APRIL.<br />
Our data suggest that following immigration of plasma cells via the vascular niche, longterm<br />
plasma cell survival later is supported in a second niche. Here, VCAM+ reticular<br />
stromal cells seem to provide a meeting point for long-lived plasma cells with myeloid<br />
related cells that support plasma cell survival through the production of multiple<br />
important plasma cell survival signals.
Julian Pardo, Christin Urban, Arno Müllbacher, Reinhard Wallich, Christoph Borner,<br />
Markus M Simon<br />
Pleiotropism of granzyme B-induced cell death; A means of<br />
the host to counter pathogens evasion strategies of CTLmediated<br />
recovery<br />
Granzyme B (gzmB) of cytotoxic lymphocytes is essential for recovery from intracellular<br />
pathogens, but the molecular basis is still unresolved. Here, we analyzed gzmBmediated<br />
death pathways under more physiological conditions using ex vivo virusimmune<br />
CTL that express perf and gzmB, but not gzmA (gzmB+CTL). We show that<br />
gzmB+CTL kill targets independent of caspases and mitochondrial signaling. In addition<br />
the data reveal that gzmB+CTL independently induce pro-apoptotic processes either via<br />
caspases 3/-7, leading to plasma membrane perturbance and ROS production, or via<br />
Bid/Bak/Bax, resulting in cytochrome c release and that both pathways elicit ??m<br />
suppression. Our data provide evidence for a pleiotropic pro-apoptotic function of gzmB<br />
suitable to counteract evasion strategies of pathogens and to control tumors.
Mario Fabri, Alessandra Zingarelli, Eva Flenner, Martina Bessler, Helena Hafke, Wiltrud<br />
Maria Kalka-Moll<br />
Polysaccharide modulates CD8+ T cell responses by<br />
enhancing TCR cross-linking<br />
Polysaccharides have been classically considered T cell-independent antigens. In<br />
contrast, zwitterionic capsular polysaccharids (ZPS) from bacteria such as Bacteroides<br />
fragilis and Streptococcus pneumoniae elicit potent CD4+ T cell responses in a MHC<br />
class II-dependent manner. ZPSs, which are characterized by having both positively and<br />
negatively charged substitutans on each repeating unit of a highly repetitive structure,<br />
induce CD4+ T cell-dependent formation of intraabdominal abscesses. Previous<br />
investigations on ZPS-induced intraabdominal abscesses have exclusively focused on<br />
the role of CD4+ T cells. Herein, we sought to elucidate the immune response of CD8+<br />
T cells to ZPSs. We characterize the function of CD8+CD28- T cells in a experimental<br />
model of ZPS-induced abscess formation in vivo and in vitro. Moreover, we provide<br />
evidence that ZPSs modulate CD8+ T cell activation by a previously unknown<br />
mechanism implying enhanced cross-linking of TCRs on CD8+ T cells. These data<br />
provide substantial new insights in the unique functions of ZPSs to induce and regulate<br />
T cell-dependent immune responses of both CD4+ an CD8+ T cells.
Hans-Willi Mittrücker, Steinhoff Ulrich, Stefan H. E. Kaufmann<br />
Poor correlation between BCG vaccination-induced T cell<br />
responses and protection against tuberculosis<br />
Mycobacterium bovis bacille Calmette-Guérin (BCG) is the most widely used live<br />
bacterial vaccine. However, limited information is available correlating route and dose of<br />
vaccination and induction of specific T cell responses with protection against<br />
tuberculosis. We compared efficacy of oral and systemic vaccination and correlated<br />
vaccine-induced T-cell responses with protection in experimental tuberculosis of mice.<br />
Following oral and systemic vaccination, we observed profound differences in<br />
persistence and dissemination of BCG, and frequencies and location of specific IFN-γsecreting<br />
CD4+ and CD8+ T cells. Yet, both vaccination routes caused comparable<br />
levels of protection against aerosol challenge with M. tuberculosis. Protection correlated<br />
best with rapid accumulation of specific CD8+ T cells in infected tissues of challenged<br />
mice. In contrast, specific IFN-γ production by CD4+ T cells reflected the load of M.<br />
tuberculosis rather than the strength of protection. Our data question the measurement<br />
of IFN-γ secretion by CD4+ T cells and emphasize the need for new biomarkers for<br />
evaluation of tuberculosis vaccine efficacies.
Michael Probst-Kepper, Andrea Kroeger, Robert Geffers, Christian Erck, Miguel<br />
Godinho, Vitor Martins dos Santos, Hansjörg Hauser, Jan Buer, Rudi Balling, Siegfried<br />
Weiss<br />
POSITIVE FEEDBACK-CONTROL BETWEEN GARP AND FOXP3<br />
IN REGULATORY T CELLS<br />
CD4 + CD25 hi regulatory T cells (Treg) have emerged as a unique population of<br />
suppressor T cells that critically depend on the transcription factor FOXP3 for their<br />
development and function. Therefore, FOXP3-transduction was suggested to generate<br />
antigen-specific Treg cells. However, this approach is insufficient for human effector CD4<br />
+ T cells (Th). Most likely this is due to the inadequate induction of the Treg-specific<br />
receptor GARP (glycoprotein-A repetitions predominant). We identified GARP as master<br />
switch receptor for Treg cells, since retroviral over-expression of GARP in antigenspecific<br />
Th cells was sufficient to induce sustained high levels of FOXP3, regulatory<br />
function, and an extended Treg/FOXP3-signature. Conversely, down-regulation of GARP<br />
in Treg cells by short-interfering RNA reduced FOXP3 expression and suppressor<br />
functions and vice versa, down-regulation of FOXP3 reduced GARP expression and<br />
suppressor functions. Thus, a positive feedback-loop was established. Two minor<br />
constituents of this regulatory circuit were identified, the endopeptidase legumain and<br />
the β-galactoside binding protein LGALS3. Both up-regulated FOXP3 although not<br />
reaching the levels induced by GARP. Whereas casein-kinase I phosphorylation at<br />
position-6 of LGALS3 was essential for FOXP3 induction, the kruppel-like factor 2<br />
(KLF2), involved in the regulation of T cell quiescence, was induced independent of this<br />
phosphorylation. A preliminary computational model based on a hybrid functional Petri<br />
net was developed to describe the main regulatory interactions. Thus, GARP represents<br />
a promising tool for stable conversion of antigen-specific Th towards regulatory T cells,<br />
the characterization of the underling regulatory network will be pivotal for an<br />
understanding of the regulatory program.
Nasr Hemdan, Frank Emmrich, Joerg Lehmann, Ulrich Sack<br />
Possible induction or exacerbation of autoimmune diseases<br />
by heavy metals through changing cytokine profiles<br />
The development of autoimmune diseases involves a combination of appropriate genetic<br />
predisposition and encounter with environmental risk factors such as immunotoxic<br />
agents. Because of their immunomodulative potency, some heavy metals have been<br />
implicated in the induction and exacerbation of autoimmune diseases. We aimed at<br />
testing the association of exposure to heavy metals and the possible roles of different<br />
cytokines in autoimmune disorders. BALB/c mice were exposed intraperitoneally to<br />
cadmium (Cd) acetate or mercuric (Hg) chloride, and following different exposure<br />
regimes, mice were killed and levels of Th1/Th2 and the pro-inflammatory cytokines<br />
were assessed. Our results show that, in response to heavy metal exposure, a<br />
significant increase in IL-2, IL-4, IL-5 measured after 5 weeks of exposure to Hg, and<br />
accompanied by decrease in IFN-γ release indicating possible proliferation of Th2 rather<br />
than Th1 subsets. However, the increase in Th2 cytokines was not significant in the 3week<br />
exposure group, and was accompanied by an increase in IFN-γ release. This<br />
indicates changing of cytokine profiles along different exposure periods, and thereby<br />
possible distinct roles of different cytokines in different phases of autoimmune diseases.<br />
The proinflammatory cytokines TNF-α and IL-6 show insignificant increase in<br />
comparison to control mice. In case of Cd-exposure, 5-week exposure lead to<br />
stimulation of IFN-γ release which was prominent following long exposure accompanied<br />
by increase in the Th2 cytokine IL-5. These results also indicate differences in response<br />
to heavy metals depending on the metal ion itself as well as duration of exposure, and<br />
highlights the dependence on T cells, or at least specific cytokines, for example IFN-γ, in<br />
different phases of autoimmune diseases.
Anja Dahten, Dennis Ernst, Dana Hoser, Margitta Worm<br />
PPARγ-ligation improves development of allergen-induced<br />
skin inflammation in a murine model of dermatitis<br />
Background: Recent studies point to the pathophysiological role of the nuclear receptor<br />
PPARγ in the inflammatory immune response. We have previously shown that a specific<br />
ligand of PPARγ attenuates the systemic immune response via regulation of humoral<br />
immunity and inhibition of T cell-derived inflammatory cytokine production. The<br />
objective of this study was to investigate the impact of PPARγ-ligand treatment on the<br />
local immune response in a murine dermatitis model. Methods: We established a murine<br />
model with reproducible, OVA-induced skin inflammation. In this model PPARγ-ligand<br />
was applied at different time points via intraperitoneal or epicutaneous routes. Skin and<br />
blood samples were obtained for analysis respectively. Affected skin areas were<br />
assessed by a standardised clinical skin score (CSS), histological and<br />
immunohistochemical analysis. OVA-specific IgE, IgG1 and IgG2a levels were measured<br />
by ELISA on different time points (day 1, 21, 35 and 70). Results: Systemic application<br />
of PPARγ-ligand reduced the severity of OVA-induced eczematous skin lesions up to<br />
70%. These observations were confirmed by histological examinations of skin biopsies,<br />
showing decreased thickness of dermis and epidermis (p < 0.001) accompanied by<br />
significantly reduced infiltration of CD4 and CD8 positive lymphocytes and mast cells.<br />
OVA-specific IgE and IgG1 responses were significantly inhibited on days 21/35, but<br />
IgG2a synthesis was not affected. Conclusion: Our results demonstrate PPARγ-ligand<br />
treatment inhibits the development of allergen-mediated dermatitis by local and<br />
systemic mechanisms. These findings are important for the development of novel<br />
therapeutic strategies involving a PPARγ-ligand based treatment in allergic diseases.
Luisa Klotz, Indra Dani, Linda Diehl, Ari Waisman, Thomas Klockgether, Percy Knolle<br />
PPARgamma ablation in CD4+ T cells augments T cell<br />
responses resulting in enhanced T cell infiltration of the CNS<br />
and increased disease severity during experimental<br />
autoimmune encephalomyelitis<br />
The peroxisome proliferator-activated receptor gamma (PPARgamma) belongs to a<br />
group of ligand-activated transcription factors involved in the regulation of metabolism<br />
and inflammation. PPARgamma is expressed in cells of the peripheral immune<br />
compartment like lymphocytes and dendritic cells, but also within the CNS, mainly in<br />
microglial cells and in neurons. Interestingly, oral administration of PPARgamma<br />
agonists ameliorates the clinical course and histopathological features in experimental<br />
autoimmune encephalomyelitis (EAE), an animal model for multiple sclerosis. However,<br />
it is still unclear which cell type is primarily involved in PPARgamma-mediated<br />
suppression of (auto)-immunity. Therefore, we generated mice with a T cell specific<br />
knock-out of PPARgamma employing a Cre-recombinase mediated ablation of<br />
PPARgamma which is limited to CD4+ cells. In these mice (CD4-PPARg-ko) and their<br />
Cre negative wild-type littermates, we investigated both disease course and T cell<br />
responses during actively induced MOG-EAE.<br />
CD4-PPARg-ko mice exhibited both an earlier disease onset and a signficantly increased<br />
disease severity during the induction phase of EAE when compared to wild-type mice.<br />
Accordingly, T cell infiltration of the CNS was significantly increased in CD4-PPARg-ko<br />
mice. Moreover, both priming of naïve CD4-PPARg-ko T cells in vitro as well as<br />
restimulation of CD4-PPARg-ko T cells primed in vivo yielded significantly augmented T<br />
cell responses characterized by an increase in T cell proliferation as well as production<br />
of proinflammatory cytokines.<br />
These data demonstrate that ablation of PPARgamma enhances T cell reactivity both in<br />
vitro and in vivo, resulting in pronounced T cell responses and consecutively increased<br />
disease severity in a model of CD4+ T cell mediated autoimmunity. Selective activation<br />
of PPARgamma in T cells therefore represents a promising future target for control of T<br />
cell mediated autoimmunity.
Jürgen Haas, Benedikt Fritzsching, Petra Truebswetter, Peter Krammer, Elisabeth Suri-<br />
Payer, Brigitte Wildemann<br />
Prevalence of Newly Generated Naïve Regulatory T-Cells is<br />
Critical for Treg Suppressive Function and Determines Treg<br />
Dysfunction in Multiple Sclerosis<br />
Suppressive function of CD4+CD25highFoxP3+ regulatory T-cells (Treg) is impaired in<br />
patients with relapsing remitting multiple sclerosis (MS). The mechanism underlying the<br />
Treg functional defect is unknown. Treg mature in the thymus and the majority of cells<br />
circulating in the periphery rapidly adopts a memory phenotype. Since our own previous<br />
findings suggest that the thymic output of T-cells is impaired in MS patients we<br />
hypothesized that an altered Treg generation may contribute to the suppressive<br />
deficiency associated with MS. We therefore determined the role of Treg which enter the<br />
circulation as recent thymic emigrants (RTEs) and, unlike their CD45RO+ memory<br />
counterparts, express CD31 as a typical surface marker.<br />
We show that numbers of CD31+ co-expressing CD4+CD45RA+CD45RO-Foxp3+Treg<br />
(RTE-Treg) within peripheral blood decline in dependence of age and are significantly<br />
reduced in MS patients, whereas the entire Treg population is equally distributed as<br />
compared to healthy control donors. Depletion of CD31+ cells from total Treg<br />
neutralizes the difference in inhibitory potencies of patient and donor Treg detectable<br />
when using total Treg in the co-culture experiments. Furthermore, patient derived Treg<br />
but not healthy Treg exhibit a contracted TCR V-beta repertoire.<br />
These observations suggest that a shift in the homeostatic composition of Treg subsets<br />
related to a reduced thymic-dependent de novo generation of Treg with compensatory<br />
expansion of less suppressive memory Treg may contribute to the Treg defect<br />
associated with MS.<br />
Supported by Hertie-Stiftung (1.01.1/04/003), Deutsche Forschungsgemeinschaft (SFB<br />
405, 5H, and SFB 571, B7), the Young Investigator Award from the Faculty of Medicine,<br />
University of Heidelberg to BF, and Serono GmbH Deutschland.
Reinhard Maier, Rita De Giuli, Veronika Nindl, Simone Miller, Volker Thiel, Roland<br />
Züst, Ari Waisman, Birgit Ledermann, Burkhard Ludewig<br />
Preventing autoimmune myocarditis through cardiac myosinspecific<br />
tolerance<br />
Virus-induced myocarditis might broaden the pathogen-specific immune response<br />
towards heart antigens such as the abundantly expressed myosin heavy chain alpha<br />
(myhca). The chronic immune response against cardiac self-antigens may lead to<br />
dilative cardiomyopathy (DCM), which represents a prevalent cause of human heart<br />
disease and heart failure. Immunization of BALB/c mice with the myhca-derived peptide<br />
(amino acids 614-629) elicits myocarditis induced by peptide-specific CD4 T cell<br />
responses, and therefore uncouples the chronic autoimmune phase from putative viral<br />
infections. In order to further characterize the mechanisms and effector molecules<br />
involved in autoimmune myocarditis and to evaluate therapeutic strategies, we have<br />
generated a novel transgenic mouse model. In this model (Rosa-IM mouse), the<br />
expression of the myhca peptide is directed to the MHC class II pathway through a<br />
chimeric invariant chain (Ii-myhca) in which the CLIP peptide sequence is replaced by<br />
the myhca614-629 peptide. The construct is designed in such a way that the expression<br />
is only achieved in the presence of Cre-recombinase. The ubiquitous expression of<br />
myhca in all MHC class II positive cells induced specific immune tolerance and as a<br />
consequence mice were protected from myocarditis. The Rosa-IM mouse represents<br />
therefore a versatile tool to dissect the basic mechanisms in autoimmune myocarditis,<br />
to delineate the decision making process between activation and tolerization of heartspecific<br />
CD4 T cells and to study the participation of different antigen presenting cells<br />
like dendritic cells, B cells and macrophages in the disease process.
Patrick Vollmar, Stefan Nessler, Bianca Wolff, Sudhakar Reddy Kalluri, Hans-Peter<br />
Hartung, Bernhard Hemmer<br />
Preventive and therapeutic effects of the antidepressant<br />
venlafaxine on murine experimental autoimmune<br />
encephalomyelitis<br />
Antidepressants, which are in use for the treatment of major depression, are known to<br />
impact on the immune system. In this study, we examined the immunomodulatory<br />
properties of venlafaxine, a selective serotonin-/norepinephrine reuptake inhibitor, in<br />
murine experimental autoimmune encephalomyelitis (EAE), a Th1-mediated central<br />
nervous system demyelinating disease model of multiple sclerosis. EAE was induced in<br />
SJL mice by adoptive transfer of PLP-specific T-cells. Mice received different doses of<br />
venlafaxine before transfer and after onset of disease. Sustained oral treatment with<br />
6mg and 60mg/kg per day significantly ameliorated the clinical course of disease<br />
compared to vehicle during both preventive and therapeutic intervention. The<br />
ameliorating effect was more pronounced in the high dose group with respect to the<br />
suppression of relapses in the chronic phase of disease. Continuous drug delivery for 14<br />
days was sufficient to delay the onset and peak of disease significantly. However,<br />
ameliorating effects were more pronounced in the sustained treatment experiments.<br />
Disease modifying effects are mediated by venlafaxine’s potential to reduce the<br />
secretion of the Th1 cytokines TNF-alpha and IFN-gamma in encephalitogenic T cell<br />
clones and lines. It further suppressed significantly the mRNA gene expression of<br />
proinflammatory cytokines IFN-gamma, TNF-alpha and the chemokine RANTES in the<br />
spinal cord of EAE mice. These findings demonstrate the strong immunomodulatory<br />
property of the antidepressant venlafaxine and pioneer further studies to clarify whether<br />
venlafaxine may exert similar effects in MS.
Ivan Bogeski, Valentin Mirceski, Markus Hoth<br />
Probing the redox activity of T-lymphocytes deposited at<br />
electrode surfaces with voltammetric methods<br />
Reactive oxygen species and redox signaling in general have a very important,<br />
physiological role in the regulation of the immune response. In addition, increased<br />
redox signaling is an attribute to many cancer cells thus having a pathological effect.<br />
The detection and the evaluation of these signaling events are very often accompanied<br />
with difficulties. Here, we describe a novel electrochemically-based technique for<br />
monitoring the T-lymphocyte redox state.<br />
T-lymphocytes were attached on the surface of a working electrode, which was<br />
previously modified with 2-Palmitoylhydroquinone as a redox mediator. Using cyclic<br />
voltammetry, we were able to indirectly (via the redox mediator) monitor an electron<br />
transport from the cells towards the working electrode, which enabled us to precisely<br />
evaluate the redox state and the redox potential of the cells. This new technique is<br />
rather simple and sensitive and may be used in the future as a valid diagnostic<br />
procedure in various branches of bio-medical science.
Lars-Oliver Tykocinski, Anna Sinemus, Esmail Rezavandy, Bruno Kyewski<br />
Promiscuous gene expression in the thymus - is epigenetic<br />
regulation the key?<br />
The scope of central tolerance is to a large extent dictated by expression of tissuerestricted<br />
antigens (TRA) by medullary thymic epithelial cells (mTECs), a process known<br />
as promiscuous gene expression (pGE). While increasing insight into the tolerance<br />
modes linked to pGE has been gained in the last years, the molecular mechanisms<br />
involved in the regulation of pGE in mTECs remain largely obscure. Promiscuously<br />
expressed genes tend to co-localize in clusters in the genome and imprinting of the<br />
insulin-like growth factor 2 gene is selectively lost in mTECs. Thus, apart from the<br />
involvement of the transcriptional regulator Autoimmune Regulator (Aire), epigenetic<br />
mechanisms may have an important contribution in the regulation of pGE in mTECs. To<br />
assess the role of epigenetic modifications in the regulation of pGE, we compared<br />
histone modifications and the DNA methylation status in a cluster of TRA genes in<br />
mTECs and the respective tissue cells. Our current results document a close correlation<br />
between promiscuous gene transcription and a permissive chromatin configuration at<br />
the single gene level in mTECs but not locus-wide chromatin alterations as observed in<br />
the tissue cells.
Thorsten Joeris, Petra Krienke, Ulrike Kuckelkorn, S.H.E. Kaufmann, Ulrich Steinhoff<br />
Proteasome assembly: Competitive integration of constitutive<br />
and IFNγ inducible catalytic subunits<br />
Proteasomes are multicatalytic protease complexes responsible for non-lysosomal<br />
degradation of proteins. In vertebrates 20S proteasomes occur in two major forms:<br />
constitutive proteasomes (c20S) and the IFNγ inducible immunoproteasomes (i20S).<br />
The two forms differ in their catalytically active subunits and consequently in their<br />
overall specificity and activity. Due to the diverse effects of proteasome composition on<br />
multiple cellular processes, it is of interest to understand the basic mechanisms of c20S<br />
and i20S formation. So far, formation of i20S is believed to be a result of cooperative<br />
integration of the IFNγ inducible subunits β1i, β2i and β5i. According to this concept β5i<br />
is necessary for processing of β1i and β2i precursor subunits during proteasome<br />
assembly. Here, we analyse the formation of 20S proteasomes during infection of WT<br />
and β5i deficient (lmp7 -/- ) mice with Listeria monocytogens. In lmp7 -/- mice β5 can<br />
easily process β1i and β2i resulting in the formation of mixed proteasomes (m20S). The<br />
observed accumulation of unprocessed β1i and β2i in precursor proteasomes is caused<br />
by a lack of β5 subunits and not by its inability to pair with β1i and β2i. As β5 is not<br />
upregulated by infection, it can not compensate the absence of β5i in lmp7 -/- mice. Our<br />
in vivo data question the current model of cooperative i20S formation. Instead, we<br />
provide evidence that the mechanism underlying i20S formation is substantially<br />
regulated by simultaneous overexpression of IFNγ inducible subunits, which enables<br />
them to outcompete the constitutive subunits at protein level during proteasome<br />
assembly.
Kirsten Neubert, Silke Meister, Damian Maseda, Kerstin Amann, Reinhard Voll<br />
Proteasome inhibition ameliorates lupus symptomes in NZB/<br />
W mice<br />
Systemic lupus erythematosus (SLE) is an autoimmune disease which is characterized<br />
by circulating IgG autoantibodies predominantly directed towards nuclear antigens. The<br />
proteasome inhibitor bortezomib (Bz) is used for the treatment of multiple myeloma, a<br />
malignant plasma cell neoplasia. One mechanism of Bz might be the blockade of the key<br />
transcription factor NF-κB, which is also important for survival of B lymphocytes<br />
especially mature B cells. Therefore, we investigated the effects of NF-κB inhibiting<br />
agents such as Bz in a mouse model for SLE.<br />
To address this question, we treated NZB/W mice with Bz twice weekly over 10 months.<br />
Bz-treated mice have significantly prolonged survival time and decreased proteinuria<br />
compared to the control mice. Histologically, there were no or only minor signs of<br />
glomerulonephritis in Bz-treated mice. The IgG anti-dsDNA and anti-Histone antibodies<br />
were strongly reduced during the whole treatment. The IgG concentrations in sera were<br />
significantly decreased during the first months of treatment, respectively. After the first<br />
month of treatment the IgG serum concentrations increased again and reached the<br />
levels of control mice.<br />
Flow cytometric analyses of the splenic lymphocyte compartment from NZB/W mice,<br />
which were Bz-treated over 8 weeks, revealed a strong reduction of T and B cell<br />
numbers. Interestingly, Bz had no significant effect on the B cell numbers in the bone<br />
marrow.<br />
These data indicate that Bz prolongs the survival and ameliorates the clinical<br />
parameters of lupus-like disease in NZB/W mice. We suggest that both T and B<br />
lymphocyte subsets are affected by Bz, potentially due to inhibition of NF-κB activation<br />
along with induction of terminal endoplasmic reticulum stress leading to apoptotic cell<br />
death of lymphocytes.
K. Doser, J. Albrecht, T. J. Boeld, R. Eder, J. Stahl, R. Andreesen, P. Hoffmann, M.<br />
Edinger<br />
Protection from graft-versus-host disease by donor CD4+CD25<br />
+ regulatory T cells improves B lymphocyte reconstitution<br />
after allogeneic bone marrow transplantation<br />
Allogeneic bone marrow transplantation (BMT) is a well-established therapy for<br />
hematologic malignancies. However, graft-versus-host disease (GVHD) caused by cotransplanted<br />
mature donor T cells, remains a significant problem. The major target<br />
organs of GVHD are skin, liver and intestines, but also lymphoid organs, thereby<br />
impairing immune reconstitution and increasing the susceptibility to opportunistic<br />
infections. We, and others, previously demonstrated that the adoptive transfer of donor<br />
CD4+CD25+ regulatory T (Treg) cells prevents GVHD. We now investigated how their<br />
suppressive activity influences immune reconstitution after allogeneic BMT by examining<br />
the regeneration of the B cell compartment. For this purpose, lethally irradiated BALB/c<br />
recipients were transplanted with either 5 x 106 T cell-depleted bone marrow cells (TCD<br />
BM) from C57BL/6 donors alone, or TCD BM plus 5 x 105 CD4+CD25- donor T cells<br />
(Tconv) with or without equal numbers of donor Treg cells. As expected, mice that<br />
received only TCD BM did not develop GVHD and reconstituted their B cell compartment<br />
from transplanted BM within 20-40 d, whereas those that received additional Tconv cells<br />
developed severe GVHD and lacked donor as well as host B lymphocytes in peripheral<br />
blood (PB) until their early death or sacrifice by d 100. In contrast, most animals that<br />
received Tconv and Treg cells at a 1:1 ratio were protected from GVHD and showed a<br />
<strong>complete</strong>, yet delayed reconstitution of their B cell compartment, with appox. 50%<br />
reconstitution by d45-60 and 100% by d100. Comparative analyses of BM, PB and<br />
spleen revealed that GVHD interferes with B cell reconstitution not solely by destroying<br />
peripheral lymphoid organs, but also by eliminating early B cell precursors in the BM.<br />
We thus speculate that the dysregulated production of pro-inflammatory cytokines<br />
during GVHD is toxic for early B cell precursors and/or that the alloresponse destroys<br />
the BM niche for developing B cells. Importantly, co-transplanted donor Treg cells<br />
prevent this pathology and therefore improve rather than impair immune reconstitution<br />
after allogeneic BMT.
Aleksandar Backovic, Nikolaus Wick, Georg Wick<br />
PROTEIN SIGNATURES ON SILICONE SURFACE AS<br />
BIOMARKERS FOR IMMUNOLOGIC-FIBROTIC SIDE EFFECTS<br />
TO IMPLANTS<br />
An inflammatory response with subsequent fibrotic reactions are the most common side<br />
effects of medical silicones. However, although there is a growing number of medical<br />
interventions that require long term active or passive silicone implants, there has been<br />
surprisingly little effort to understand the molecular mechanisms behind the adverse<br />
effects they might induce. In the present study we focused our attention onto proteins<br />
adhering to the surface of medical silicones, as they have been identified as the key<br />
activators of the host defense mechanisms that precede fibrotic changes in the tissue<br />
surrounding the implant. Interestingly, abundant mononuclear cells, including dendritic<br />
cells and macrophages can be found in the fibrotic tissue surrounding silicone implants.<br />
In the discovery phase, a proteomics approach was used to identify proteins adsorbed<br />
from the serum of silicone mammary implant (SMI) carriers to the surface of silicone in<br />
vitro. Out of the 184 proteins which adsorbed to silicone, 14 showed differences in the<br />
adhesion pattern between the non-symptomatic SMI carriers compared to the group of<br />
patients developing a fibrotic reaction (peri-SMI fibrotic capsule) to silicone. In the<br />
subsequent development phase, a simple silicone linked immuno-sorbent assay<br />
(SILISA) was developed that can simultaneously detect the signature of the 14<br />
differentially adhered proteins in a high throughput fashion. In a cohort study of 100<br />
SMI carriers the SILISA successfully discriminated patients with adverse reactions to<br />
silicone implants. Furthermore, the same test can be used to assess various silicone<br />
types for the development of fibrotic side effects, and in such way tailor the choice of<br />
implants to the test results of individual patient. Both, large scale prospective and<br />
retrospective blinded studies are being conducted to validate these preliminary results,<br />
and to determine accuracy, precision, linearity, range, and the robustness of the test<br />
system.<br />
The project has been supported by the Competence Center Medicine Tirol (KMT) and the<br />
Lore and Udo Saldow Foundation.
Bettina Tosetti, Eva Glowalla, Martin Krönke, Oleg Krut<br />
Proteomics Based Identification of Cell Wall-associated<br />
Proteins as Protective Vaccine Candidates against<br />
Staphylococcus aureus<br />
S. aureus is an important human pathogen with an increasing clinical impact due to the<br />
extensive spread of antibiotic resistant strains. Therefore the development of a<br />
protective polyvalent vaccine is of great clinical importance. We employed an<br />
intravenous immunoglobulin (IVIG) preparation as a source of antibodies directed<br />
against S. aureus surface proteins for the identification of novel vaccine protein<br />
candidates. IVIG induced a strong opsonophagocytic activity of human neutrophils for<br />
S. aureus. In order to identify proteins that are targeted by IVIG, subtractive proteome<br />
analysis (SUPRA) of S. aureus surface proteins was performed. Proteins solely reacting<br />
with IVIG, but not with IVIG depleted of S. aureus-specific opsonising antibodies<br />
(dSaIVIG), were predicted to serve as vaccine candidates. Nearly 40 promising vaccine<br />
candidates were identified by this preselection method using MALDI-TOF analysis. Three<br />
of these candidates, enolase (Eno), oxoacyl reductase (Oxo) and a hypothetical protein<br />
(hp2160), were expressed as GST-fusion proteins, purified and used for the enrichment<br />
of corresponding IgGs from IVIG by affinity chromatography. Affinity purified anti-Eno,<br />
anti-Oxo and anti-hp2160 antibodies showed significant opsonising activity enabling<br />
uptake and killing of S. aureus by human neutrophils. Significant antibody responses<br />
were elicited in mice immunised with recombinant antigens. After challenge with S.<br />
aureus, reduced staphylococcal spread was detected in immunised mice by an in vivo<br />
imaging system. The recovery of S. aureus CFUs from organs of immunised mice was<br />
diminished by 10-100-fold. Furthermore, immunisation with hp2160 led to an<br />
remarkably improved survival rate compared to control mice. The results of this study<br />
suggest our approach to be a valuable tool for the identification of novel vaccine<br />
candidates and therapeutic antibodies.
Dirk Haubert, Nina Gharib, Francisco Rivero, Katja Wiegmann, Marianna Hösel, Martin<br />
Krönke, Hamid Kashkar<br />
PtdIns(4,5)P-restricted plasma membrane localization of FAN<br />
is involved in TNF-induced actin reorganization<br />
The WD repeat protein FAN is a member of the family of TNF receptor adaptor proteins<br />
that are coupled to specific signaling cascades. However, the precise functional<br />
involvement of FAN in specific cellular TNF responses remained unclear. Here we report<br />
the involvement of FAN in TNF-induced actin reorganization and filopodia formation<br />
mediated by activation of Cdc42. We show that the PH domain of FAN specifically binds<br />
to phosphatidylinositol-4,5-bisphosphate (PtdIns(4,5)P) which targets FAN to the<br />
plasma membrane. Site-specific mutagenesis revealed that the ability of FAN to mediate<br />
filopodia formation was blunted either by the destruction of the PtdIns(4,5)P binding<br />
motif, or by the disruption of intramolecular interactions between the PH domain and<br />
the adjacent BEACH domain. Using pull-down experiments, FAN was shown to interact<br />
with the actin cytoskeleton machinery in TNF-stimulated cells. The results of this study<br />
suggest that PH-mediated plasma membrane targeting of FAN is critically involved in<br />
TNF-induced Cdc42 activation and cytoskeleton reorganization. Furthermore, in vivo<br />
analysis of FAN-deficient mice revealed impaired TNF-induced dendritic cell migration<br />
pointing to a role of FAN in TNF-dependent dendritic cell motility.
Carina Conrads, Ramona Siemer, Mario Assenmacher, Claudia Niemand<br />
Quality assessment of enriched CD4+CD25+ regulatory T cells<br />
Many publications during the last years have reported naturally occurring CD4+CD25+<br />
regulatory T cells to play an important role in autoimmunity, transplantation tolerance<br />
and tumor immunity. Intracellular FoxP3 staining is an important method for the<br />
analysis of regulatory T cells. In addition functional capacity of regulatory T cells is often<br />
assessed by in vitro suppression assays.<br />
We have developed a ready-to-use, well-defined, and robust method using<br />
MACSiBeadTM Particles for in vitro suppression assays. MACSiBeadTM Particles loaded<br />
with CD2, CD3 and CD28 antibodies act as artificial APCs and are simply added in a 1:1<br />
bead to cell ratio to the cell culture.<br />
Human CD4+CD25+ regulatory T cells were isolated from peripheral white blood cells<br />
using the MACS technology (n=9) with a mean purity of 87.8% (range 76.5-93.6%).<br />
More than 95% of isolated cells were CD4+, of which 78.5% were positive for FoxP3<br />
(range 63.8-88.5%).<br />
Isolated CD4+CD25+ regulatory T cells and autologous CD4+CD25- responder T cells<br />
were polyclonally stimulated with CD2, CD3 and CD28 antibody loaded MACSiBeadTM<br />
Particles (“Treg Suppression Inspector”) for 4 days and proliferation was analyzed by<br />
3H-thymidine incorporation for 16 hours. Isolated regulatory CD4+CD25+ T cells<br />
showed a mean suppression rate of 67.6% (range 38-92%) at a 1:1 ratio of regulatory<br />
T cells to responder T cells.<br />
We show that quality assessment of enriched CD4+CD25+ regulatory T cells is possible<br />
by staining for FoxP3 and using MACSiBeadTM Particles.
Tatiana Binder, Rodica Bernatowicz, Michael Rothballer, Michael Schmid, Susanne<br />
Krauss-Etschmann, Dolores J. Schendel, Anton Hartmann<br />
QUANTITATION OF LIVE VERSUS DEAD PROBIOTIC BACTERIA<br />
Background: The effect of probiotic bacteria on the immune system is subject of<br />
intensive research. However, live probiotic bacteria might induce different signals<br />
versus dead probiotic bacteria in bioassays, e.g. using dendritic cells. Therefore, we<br />
asked how standard culture affects the viability of different probiotic bacteria.<br />
Methods: Lactobacillus rhamnosus GG (LGG, Valio Ltd, Finland), Lactobacillus reuteri<br />
ATCC 55730 (BioGaia AB, Sweden), Bifidobacterium sp. 420 (Bifidobacterium lactis,<br />
Danisco Germany GmbH), Lactobacillus acidophilus LA-2, Lactobacillus acidophilus LA-5,<br />
Lactobacillus paracasei subsp. paracasei LC-01, Bifidobacterium animalis BB-12 and<br />
Bifidobacterium longum BB-46 (Chr. Hansen GmbH, Denmark) were cultured in MRSbroth<br />
(Merck KGaA) under anaerobic conditions for 24 hours. After cultivation the<br />
bacterial cells were stained with a LIVE/DEAD staining kit (Invitrogen GmbH). The<br />
percentage of dead bacteria within the total population of bacterial cells was counted<br />
visually via fluorescence microscopy.<br />
Results: The viability of LGG, B. lactis, LA-2, LA-5, LC-01, BB-12 and BB-46 ranged<br />
between 94%-99%. In contrast L. reuteri yielded only around 80% live bacteria after 24<br />
hours of cultivation.<br />
Conclusions: Our data show that viability of different probiotic strains can vary<br />
considerably under standard culture conditions. Therefore, the precise assessment of<br />
the viability of bacteria is important for functional immune assays. Currently, there are<br />
no straightforward bioassays at the single cell level available to distinguish among<br />
active, inactive or stressed live bacterial cells.
Guido Wabnitz, Urban Sester, Henning Kirchgessner, Yvonne Samstag<br />
Ras/PI3Kinase/cofilin independent activation of human<br />
CD45RA+ and CD45RO+ T-cells by superagonistic CD28<br />
stimulation<br />
T-cell activation requires costimulation of TCR/CD3 plus accessory receptors (e.g.<br />
CD28). A hallmark of costimulation driven T-cell activation is the dynamic<br />
reorganization of the actin cytoskeleton important for receptor polarization in the<br />
immunological synapse. The classical model of T-cell costimulation was challenged by<br />
detection of superagonistic CD28 antibodies. These antibodies induce T-cell proliferation<br />
and - as demonstrated here - production of IFN-γ, CD25 and CD69 even in the absence<br />
of TCR/CD3 triggering.<br />
Here we analyzed whether superagonistic CD28 stimulation induces costimulatory<br />
signaling events. Costimulation leads to phosphorylation of the actin bundling protein Lplastin<br />
and dephosphorylation of the actin reorganizing protein cofilin. Interaction of<br />
cofilin with actin is crucial for receptor polarization. Dephosphorylation of cofilin requires<br />
activation of Ras and PI3Kinase. Interestingly, superagonistic CD28 stimulation<br />
activates human peripheral blood T-cells (PBT) independently of Ras and PI3Kinase.<br />
Accordingly, it does not lead to cofilin dephosphorylation and receptor polarization.<br />
Likewise, L-plastin is not phosphorylated. Thus, superagonistic CD28 stimulation does<br />
not mimic costimulation. Instead, it leads to a Ras/PI3Kinase/cofilin independent state<br />
of "unpolarized T-cell activation". Finally, we demonstrate that superagonistic activation<br />
of human PBT requires calcium flux and activation of Src-kinases as well as PKC, Raf-1<br />
and Erk1/2.
Rebekka Wehner, Bärbel Löbel, Martin Bornhäuser, Ernst Peter Rieber, Marc Schmitz<br />
Reciprocal activating interaction between native human blood<br />
dendritic cells and NK cells in antitumor immunity<br />
Dendritic cells (DCs) are characterized by their unique capacity to induce primary T cell<br />
responses, providing the opportunity of DC-based cancer vaccination strategies.<br />
Additional findings reveal that DCs may also play a crucial role for the activation of<br />
innate antitumor immunity. Recently, we defined 6-sulfo LacNAc (slan) DCs (formerly<br />
termed M-DC8+ DCs) as a major subpopulation of human blood DCs which are capable<br />
of activating tumor-reactive cytotoxic T cells and of mediating tumor-directed<br />
cytotoxicity (Immunity 2002;17:289-301; Blood 2002;100:1502-1504, Immunity<br />
2006;24:767-777). Here, we investigated the reciprocal interaction between slanDCs<br />
and NK cells and the underlying mechanisms.<br />
To determine whether slanDCs promote NK cell activation, DCs were<br />
immunomagnetically purified from the blood of healthy donors and cultured for 6 h in<br />
the absence of exogeneous cytokines to allow spontaneous maturation. Subsequently,<br />
DCs were coincubated with NK cells in the presence of lipopolysaccharide (LPS). We<br />
found that LPS-stimulated slanDCs strongly stimulate proliferation and IFN-gamma<br />
secretion of NK cells. Furthermore, slanDCs markedly augmented the expression of the<br />
activating NK cell receptors NKp46 and NKp44. In addition, NK cell-mediated<br />
cytotoxicity against K-562 tumor cells and freshly prepared acute myeloid leukemia<br />
blasts was significantly improved by slanDCs which is dependent on interleukin (IL)-12.<br />
Further studies revealed that fresh NK cells efficiently enhance the secretion of the<br />
immunomodulatory cytokine IL-12 by slanDCs via IFN-gamma. In addition, the ability of<br />
slanDCs to produce the immunosuppressive cytokine IL-10 was markedly reduced by<br />
NK cells.<br />
In conclusion, we found that slanDCs strongly promote proliferation, IFN-gamma<br />
secretion, and tumor-directed cytotoxicity of NK cells. Reciprocally, NK cells efficiently<br />
modulate the production of IL-12 and IL-10 by slanDCs. These results indicate that the<br />
bidirectional cross-talk between native human DCs and NK cells may play a pivotal role<br />
in the regulation of antitumor immunity.
Andra Schromm, Jörg Howe, Artur Ulmer, Karl-Heinz Wiesmüller, Tobias Seyberth,<br />
Günther Jung, Manfred Rössle, Michel H.J. Koch, Klaus Brandenburg<br />
Recognition of bacterial lipopeptides by human macrophages<br />
is critically determined by physico-chemical parameters<br />
The importance of lipoproteins from the cell wall of Gram-positive and Gram-negative<br />
bacteria for the initiation of an innate immune defense is being increasingly recognized.<br />
It is well-established that lipoproteins are potent stimulants of the human innate<br />
immune system and elicit a variety of proinflammatory immune responses. However, in<br />
contrast to endotoxins (lipopolysaccharide, LPS), which are the main amphiphilic<br />
component of the outer membrane of Gram-negative bacteria, the molecular principles<br />
underling the immune stimulatory activity of lipopeptides are only partially understood.<br />
Investigations of synthetic lipopeptides corresponding to N-terminal partial structures of<br />
bacterial lipoproteins defined the chemical prerequisites for their biological activity and<br />
in particular the number and length of acyl chains and sequence of the peptide part.<br />
Here we present experimental data on the biophysical mechanisms underlying<br />
lipopeptide bioactivity. Investigation of selected synthetic diacylated and triacylated<br />
lipopeptides revealed, that the geometry of these molecules (i.e. the molecular<br />
conformations and supramolecular aggregate structures) and the preference for<br />
membrane intercalation provide an explanation for the biological activities of the<br />
different lipopeptides. This refers in particular to the agonistic or antagonistic activity (i.<br />
e., their ability to induce cytokines in mononuclear cells or to block this activity,<br />
respectively).<br />
The analytical data show that our concept of ‘endotoxic conformation’, originally<br />
developed for LPS, can be applied also to the investigated lipopeptides, and suggest<br />
that the molecular mechanisms of cell activation by amphiphilic molecules are governed<br />
by a general principle.
Ram Kumar Chowdary Venigalla, Theresa Tretter, Stefan Krienke, Regina Max,<br />
Norbert Blank, Volker Eckstein, Anthony D Ho, Hannes Martin Lorenz<br />
Reduced CD4+CD25- T Cell sensitivity to the suppressive<br />
function of CD4+CD25highCD127-/low Regulatory T Cells in<br />
active SLE Patients<br />
Introduction:<br />
SLE is a systemic autoimmune disease with an inflammatory phenotype, accompanied<br />
by high numbers of activated T cells (CD4+CD25+) in peripheral blood, which can lead<br />
to contamination of the nTreg population (CD4+CD25++) and discrepancies regarding<br />
their numbers and function. To overcome this problem, we have chosen low expression<br />
of CD127 along with CD4+CD25++ as a marker of true nTregs for cell sorting. This<br />
allowed us to gain highly purified nTregs and to study their role in patients with SLE.<br />
Methods:<br />
CD4+CD25++CD127-/low nTregs and CD4+CD25- T responder cells, (Tresp) were<br />
separated by FACSsorting. Proliferation was quantified by 3H Thymidine incorporation<br />
and Immunophenotype by FACScan.<br />
Results:<br />
We observed a slight but significant increase in the percentage of CD4+CD25highfoxp3<br />
+ T cells in active SLE patients (2.65 ± 0.4%) (SLEDAI >3, n = 13), and only marginal<br />
increase in inactive SLE patients (2.0 ± 0.4%) (SLEDAI ≤3, n = 11) compared with<br />
normal donors (1.75 ± 0.1%, n =19), correlating well with numbers of CD4+CD25+<br />
+CD127-/low nTreg. Proliferation of nTregs from patients sorted for CD4+CD25++ vs<br />
CD4+CD25++CD127-/low significantly decreased from 9704±1775 cpm to 2585±495<br />
cpm, (ND:2028±548 cpm to 1291±388 cpm), confirming reduced effector cell<br />
contamination. In suppressor assays Tresp of normal donors were regulated to a<br />
comparable extent by Tregs from normal donors (81 ± 2%) and active SLE patients (73<br />
±3%; p = 0.01), while Tresp from active SLE were less suppressed, regardless if Treg<br />
from healthy donors (54 ± 7%; p = 0.0009) or SLE patients (53 ± 6%, p = 0.0001)<br />
were present. This Tresp cell resistance showed a direct correlation to disease activity,<br />
with inactive SLE patients showing the lowest Tresp resistance.<br />
Conclusions:<br />
Highly purified nTreg from SLE patients show no defect in suppressor function compared<br />
to normal donors. However CD4+CD25-Tresp cells from active SLE patients overcome<br />
suppressive function of normal and SLE-Treg, which might contribute to pathogenesis of<br />
SLE.<br />
.
Annegret Plege, Katja Borns, Reinhard Schwinzer<br />
Reduction of human anti-pig T cell responses by transgenic<br />
expression of human PD-L1 on pig cells<br />
Objective: Antibody-mediated blocking of receptor-ligand interactions providing<br />
positive costimulatory signals (e.g. CD28/B7) is one approach to inhibit T cell mediated<br />
graft rejection after transplantation. Furthermore, promoting the interactions of cell<br />
surface molecules which deliver negative signals (e.g. PD-1/PD-L1) might also decrease<br />
T cell reactivity. To test this concept we asked whether human anti-pig T cell reactivity<br />
can be modulated by overexpression of the human negative costimulatory molecule PD-<br />
L1 on porcine cells.<br />
Methods: The pig B cell line L23 was transfected with the pIRES-AcGFP vector<br />
containing human PD-L1. Stable transfectants (L23-hPD-L1 cells) were established,<br />
phenotypically characterized and used for in vitro stimulation of purified human CD4+ T<br />
cells and as targets for cytotoxic effector T cells.<br />
Results: Wild-type L23 cells as well as mock transfected controls triggered strong<br />
proliferative responses in human CD4+ T cells. However, when L23-hPD-L1<br />
transfectants were used as stimulators, T cell proliferation was significantly reduced (30-<br />
50%). The decreased stimulatory capacity of PD-L1 transfectants could be reversed by<br />
treatment of the cells with monoclonal antibodies to PD-L1 or PD-1 suggesting that the<br />
inhibitory effects are mediated by the interaction of the PD-L1 transgene with PD-1 on T<br />
cells. L23 cells were highly sensitive to lysis by human cytotoxic effector T cells. In L23hPD-L1<br />
cells, however, the intensity of cell mediated cytotoxicity was significantly<br />
reduced.<br />
Conclusion: These data indicate that in human T cells activated by PD-L1 transfectants<br />
the balance between positive and negative costimulation is shifted towards negative<br />
signals thereby diminishing the intensity of the response. Transgenic expression of<br />
human PD-L1 in pig cells and tissues could be an approach to prevent T cell reactivity<br />
after pig to human xenotransplantation.
Niko Föger, Andrew Chan<br />
Redundant versus unique roles of the actin regulatory<br />
proteins coronin-1 and coronin-2 in the immune system<br />
The integrity of the actin cytoskeletal network is critical for many biological processes.<br />
Coronins constitute an evolutionary conserved family of proteins implicated in the<br />
regulation of actin cytoskeletal dynamics. Focusing on the physiologic function of<br />
coronin-1, a coronin family protein preferentially expressed in immune cells, we have<br />
demostrated a requirement for coronin-1 in maintaining the cellular steady-state F-actin<br />
content, chemokine-mediated functions in T cells and, most surprisingly, maintaining<br />
normal cellular survival. Coronin-2 is closely related to coronin-1 and the two genes are<br />
co-expressed in hematopoietic cells. In a genetic approach to address the question of<br />
functional redundancy in vivo, we have generated coronin-2 deficient mice and crossed<br />
them with coronin-1 deficient mice to obtain coronin-1_coronin-2 double deficient mice.<br />
Analysis of the T cell compartment in coronin-1_coronin-2 double deficient mice<br />
indicates a significantly exacerbated phenotype as compared to the respective single<br />
knock-outs. Further phenotypical and functional analysis of lymphocytes from these<br />
different coronin knock-out strains will define the relative roles of coronin-1 and coronin-<br />
2 in regulating actin cytoskeletal dynamics in lymphocytes and reveal the degree of<br />
potentially unique versus redundant functions of these proteins in the immune system.
Manuela Ahrendt, Reinhard Pabst, Ulrike Bode<br />
Regeneration of transplanted lymph node fragments in the<br />
mesentery to study effects of the gut lymph on lymph node<br />
cytokines and chemokines<br />
The mesenteric lymph nodes (mLN) are important for immune responses and<br />
acquisition of oral tolerance. However, the influence of the gut in forming and regulating<br />
the microenvironment of mLN and mediating immune responses is only partly known.<br />
To study this, rat and mouse mLNs were removed and either fragments of mesenteric<br />
(mLNtx) or peripheral lymph nodes (pLNtx) were transplanted into this region. Two, 4,<br />
6, 8 and 10 weeks after transplantation the lymph node tissue was excised and different<br />
cytokines and also chemokines were analysed by real-time PCR. The regeneration of the<br />
transplants was documented by a re-established flow of lymph from the gut wall to the<br />
lymph node tissue and by immunohistology of typical lymph node compartments.<br />
IL-10 and CCL8 mRNA were expressed at a similar level to mLN in normal untreated<br />
animals, whereas IL-4 regenerated <strong>complete</strong>ly after re-construction of the regenerated<br />
lymph nodes. Interestingly, IL-2 was expressed in the pLNtx comparable to the pLN<br />
control. In accordance with this expression pattern, CCR9 expression of the mLNtx was<br />
similar to that of the mLN control, whereas in the pLNtx CCR9 expression was<br />
comparable to that of the pLN control.<br />
On the one hand mLNtx and pLNtx expressed cytokines, e.g. IL-4 and CCL8, in a similar<br />
way after transplantation, suggesting that IL-4 and IL-10 were recruited from the<br />
draining gut wall. On the other hand IL-2 and CCR9 mRNA were expressed comparable<br />
to the control lymph nodes, indicating that these molecules were produced by the<br />
surviving cells.<br />
The regeneration of transplanted LN fragments in the mesentery is a useful technique to<br />
define the role of the gut wall for protein levels of different cytokines and chemokines in<br />
the mLN in inducing immune responses and oral tolerance in the gut immune system.
Michael Andrzejewski, Nicole Schwarz, Christian Weber, Andreas Ludwig<br />
Regulated shedding of transmembrane chemokines by the<br />
metalloproteinase ADAM10 facilitates detachment of adherent<br />
leukocytes<br />
CX3CL1 (fractalkine) and CXCL16 are unique members of the chemokine family since<br />
they occur not only as soluble but also as membrane-bound molecules. Expressed as<br />
type I transmembrane proteins, the ectodomain of both chemokines can be<br />
proteolytically cleaved from the cell surface, a process known as shedding. Our previous<br />
studies showed that the disintegrin and metalloproteinase 10 (ADAM10) mediates the<br />
largest proportion of constitutive CX3CL1 and CXCL16 shedding but is not involved in<br />
the phorbolester-induced release of the soluble chemokines (inducible shedding). Here<br />
we introduce the calcium-ionophore ionomycin as a novel, very rapid and efficient<br />
inducer of CX3CL1 and CXCL16 shedding. By transfection experiments in Cos-7 cells<br />
and ADAM10-deficient murine embryonic fibroblasts combined with the use of selective<br />
metalloproteinase inhibitors we demonstrate that the inducible generation of soluble<br />
forms of these chemokines is dependent on ADAM10 activity. Analysis of the C-terminal<br />
cleavage fragments remaining in the cell membrane reveals multiple cleavage sites<br />
used by ADAM10, one of which is preferentially used upon stimulation with ionomycin.<br />
Addressing the functional consequences of induced shedding we demonstrate that<br />
ionomycin-induced CX3CL1 shedding via ADAM10 can lead to the detachment of<br />
monocytic cells from their cellular substrate, pointing towards a release mechanism<br />
potentially important for leukocyte diapedesis.
Dirk Brenner, Alexander Golks, Mareike Becker, Christian R. Frey, Rostislav Novak,<br />
Friedemann Kiefer, Peter H. Krammer, Rüdiger Arnold<br />
Regulation of Activation-induced Cell Death by T Cell<br />
Receptor-Proximal Signalling<br />
Lymphocyte homeostasis is strictly controlled to maintain physiological levels.<br />
Activation-induced cell death (AICD) is one mechanism to delete superfluous and<br />
autoreactive lymphocytes by restimulation of their immunoreceptors. So far<br />
Immunoreceptor-proximal mechanisms leading to AICD are elusive. Here we<br />
characterize Hematopoietic Progenitor Kinase 1 (HPK1) as a differentially regulated TCRproximal<br />
signalling protein involved in AICD of primary T cells.<br />
We show that HPK1 is a functional component of the endogenous I-κB kinase (IKK)<br />
complex and prove HPK1 to be essential for TCR-mediated IKK and NF-κB activation.<br />
We demonstrate proteolytic processing of HPK1 into HPK1-C specifically in AICDsensitive<br />
primary T cells. The cleavage product HPK1-C sequesters the inactive IKK<br />
complex and suppresses NF-κB upon TCR restimulation. T cells of HPK1-C transgenic<br />
mice are sensitized towards TCR-mediated AICD. While it is well established that AICD<br />
of T cells partially depends on the CD95/CD95L system we show T and B lymphocytes<br />
from HPK1-C transgenic mice undergo AICD independently of CD95/CD95L. We show<br />
that CD95L-dependent and HPK1/HPK1-C-mediated cell death pathways complement<br />
each other in AICD of primary human T cells. Our results define HPK1 as a novel<br />
regulator of AICD in lymphocytes.
Christina Hartwig, Miriam Mazzega, Hanne Constabel, Georg Behrens, J. Engelbert<br />
Gessner, Thomas Tschernig<br />
Regulation of allergic inflammation in a murine asthma<br />
model: Antigen uptake via Fcγ-receptors by DC-subsets,<br />
impact on tolerance and immunity<br />
Murine Fcγ-receptors (FcγRI-IV) are expressed on many inflammatory cell types. The<br />
role of these receptors in the initiation or maintenance of allergic inflammation has not<br />
yet been well defined. To identify the impact of FcγR on the antigen uptake and antigen<br />
presentation of dendritic cells (DC), FcγR-deficient (γ-chain [γ -/-], FcγRII -/-) and<br />
control mice were sensitized and challenged with OVA or PBS. Relevant asthma markers<br />
such as IgE and IgG titre in serum, the number of eosinophils in BAL, the cytokine<br />
spectrum in serum and BAL-fluid as well as a possible pulmonary hyperresponsiveness<br />
were analysed. The numbers of eosinophils were significantly reduced in γ -/- mice after<br />
OVA treatment, whereas the levels of IgE and IgG were comparable with control mice.<br />
FcγRII -/- developed a strong inflammatory response, characterized by an eosinophil<br />
and neutrophil influx and an increased IgE level.<br />
Furthermore, the impact of FcγR on antigen presentation and T cell proliferation was<br />
determined in vitro and in vivo. In vitro, T cell proliferation was more strongly<br />
stimulated by OVA/ α-OVA immune complexes than by soluble OVA in C57Bl/6 wt and<br />
FcγRII -/- mice. In contrast the γ -/- mice show a greatly reduced T cell proliferation and<br />
no differences between soluble OVA or OVA/ α-OVA treated cells. To clarify the role of<br />
specific DC subsets CD8+, CD4+ and CD4/8 – spleen DCs were measured separately.<br />
To analyse the antigen uptake via immune complexes, T cell proliferation were also<br />
determined in vivo. OVA exposed C57Bl/6 wt mice and γ -/- mice show similar<br />
responses to those in vitro. Surprisingly, not only the T cell proliferation in γ -/- mice<br />
but also the proliferation in FcγRII -/- was reduced.<br />
These results demonstrate that FcγR are involved in the pathogenesis of experimental<br />
asthma, most probably by facilitating enhanced uptake of immune complexes by DCs.<br />
SFB 587, B5, B10 German Research Foundation
Daniela Sánchez, Sigrid Krämer, Yves Montier, Herbert Schmidt, Stephan C Bischoff<br />
Regulation of human intestinal fibroblasts by Endotoxins and<br />
Shiga toxins<br />
Introduction: Previous in vitro studies demonstrated activation of colonic fibroblasts by<br />
bacterial products indicating a role of fibroblasts in innate immunity. In this study, we<br />
investigated the expression of different cytokines, collagens and metalloproteinases<br />
(MMP) by human intestinal fibroblast after stimulation with the bacterial cell wall<br />
polymers LPS, LTA or Shiga toxin-containing bacterial supernatants respectively.<br />
Methods: Fibroblasts were isolated from surgical tissue specimens and cultured for 1-2<br />
weeks until they formed a subconfluent layer. Fibroblasts were challenged with different<br />
concentrations of LPS and LTA or with supernatants from E. coli bacteria expressing<br />
Shiga toxin 1 or Shiga toxin 2. Results: Stimulation of intestinal fibroblasts with LPS and<br />
LTA enhance the expression and release of proinflammatory cytokines (TNF-alpha, IL-8,<br />
IL-6); however, expression of collagen 3 and 13, as well as MMP3 was not affected.<br />
Furthermore, supernatants of Shiga toxin-releasing E. coli strains also significantly<br />
enhanced the mRNA-expression of TNF-alpha, IL-8 and IL-6. Conclusion: Human<br />
intestinal fibroblasts are capable of expressing different cytokines upon stimulation with<br />
LPS, LTA and supernatants of Shiga toxin-releasing E. coli strains. This data supports<br />
the concept that human intestinal fibroblasts have a role in innate immune response<br />
and act as a pro-inflammatory and immune regulatory but not profibrotic cell in<br />
bacterial infections.
Norbert Hüser, Annette Fasan, Monika Semmrich, Bernhard Holzmann, Melanie<br />
Laschinger<br />
Regulation of LFA-1 activity: Importance for leukocyte<br />
recruitment and alloantigenic T cell activation in cardiac<br />
allograft rejection<br />
The leukocyte-specific integrin LFA-1 is considered to be important for immune<br />
responses leading to organ transplant rejection. Regulating the affinity of LFA-1 for its<br />
ligand ICAM-1 is known to be crucial for its function. However, the importance for deactivating<br />
LFA-1 remains largely unknown. Using a mutant mouse that locks LFA-1 in an<br />
active state (LFA-1 d/d ) we investigated the function of LFA-1 de-activation and deadhesion<br />
in a model of heterotopic cardiac transplantation.<br />
Defect in LFA-1 de-activation ameliorates graft survival in LFA-1 d/d recipient mice. A key<br />
event in graft rejection is its infiltration by allogen-primed T cells. Constitutively active<br />
LFA-1 hinders activation and proliferation of allo-reactive T cells. We found expression<br />
of the chemokines CXCL10/IP-10 and CCL5/RANTES to be markedly reduced in grafts of<br />
LFA-1 d/d recipients. This defect translates into a low number of CD4 and CD8 T cells<br />
detected in the transplanted heart. Furthermore, major leukocytes initiating the<br />
inflammation at early stages of graft rejection are not efficiently recruited into cardiac<br />
allografts of LFA-1 d/d hosts. The reduced amount of TNFα and IFNγ in the allograft<br />
seems to account for this defect. We conclude that controlling LFA-1 de-activation is<br />
required for the generation of immune responses that are vital for allograft rejection.
Jens Derbinski, Sheena Pinto, Stefanie Rösch, Klaus Hexel, Bruno Kyewski<br />
Regulation of promiscuous gene expression within defined<br />
chromosomal regions<br />
Promiscuous expression of tissue-restricted auto-antigens in medullary thymic epithelial<br />
cells (mTECs) imposes central T cell tolerance and is essential for protection from organspecific<br />
autoimmune diseases. The molecular regulation of this unusual gene expression<br />
is not well characterized and its delineation from cell lineage-specific gene expression<br />
control remains unclear.<br />
Two alternative models have been postulated (i) emulation of cell-lineage specific gene<br />
signatures or (ii) loss of gene repression resulting in an apparently stochastic gene<br />
expression pattern. Each model predicts different gene expression patterns at the single<br />
cell level.<br />
In previous experiments using pooled mTECs we observed contiguous promiscuous<br />
gene transcription in the casein locus. Here, we compared the expression profile of the<br />
casein gene locus in mTECs and mammary gland epithelial cells by single cell PCR.<br />
Mammary gland cells showed highly correlated intra- and inter-chromosomal coexpression<br />
of milk proteins and one of its control elements (i.e. the casein genes,<br />
lactalbumin, WAP and Elf5). In contrast, at the single cell level we did not observe<br />
contiguous expression of the casein gene locus in mature CD80hi mTECs and the<br />
expression of these genes was not correlated and did not reveal discernible patterns.<br />
The apparent stochastic expression pattern within the casein locus in mTECs clearly<br />
delineates the molecular mechanism(s) of promiscuous gene expression from cell<br />
lineage-specific gene control.
Katja Thümmler, Andreas Ramming, Alla Skapenko, Hendrik Schulze-Koops<br />
Regulation of specific immunity by homotypic T cell/T cell<br />
interaction<br />
Specialized T cells with a regulatory phenotype are most important in controlling specific<br />
immunity to self-antigens and, thus, in maintaining peripheral tolerance. Different T cell<br />
subsets with a regulatory phenotype have been described that may develop in the<br />
periphery in response to T cell stimulation. Differentiation of T cells, in turn, is regulated<br />
by cytokines and a variety of cell surface receptors, for which activated effector T cells<br />
express the appropriate ligands. Here, we tested the hypothesis, that homotypic T cell<br />
interactions may permit the induction of T cells with a regulatory phenotype. CD4 T cells<br />
were isolated from the peripheral blood of healthy donors and activated under Th1 or<br />
Th2 conditions. The resulting effector cells were fixed with paraformaldehyd and<br />
cocultured together with syngeneic freshly isolated resting CD4 memory or naive T cells<br />
but in the absence of specific T cell stimulatory factors such as mAbs to T cell surface<br />
molecules, antigens or mitogens. After five days of coculture, the phenotype and<br />
function of the resulting cells were analyzed by assessing their production of cytokines<br />
by ELISA, flow cytometric analysis of cytoplasmic cytokines and realtime PCR and by<br />
determining their ability to prevent the proliferation of autologous responder T cells. T<br />
cells that had been generated in the presence of fixed Th2 effector cells produced IL-4,<br />
but little IFN-γ. In contrast, Th1 effector cells promoted the development of IL-10 and<br />
IFN-γ double-producing T cells. Of interest, both T cell populations that were generated<br />
by homotypic T-T cell interactions strongly inhibited the proliferation of CD25 negative<br />
responder T cells in a dose dependent manner. Although T-T cell-generated effector<br />
cells did not express Foxp3 their regulatory capacity was comparable to that of<br />
conventional CD25 positive Tregs. The results indicate that homotypic T-T cell<br />
interaction induces the generation of Th1-like or Th2-like effector T cells with a<br />
regulatory phenotyp, providing a novel potential negative feedback mechanism to<br />
control sustained T cell driven immunity.
Carl Friedrich Classen<br />
Regulation of the granzyme B inhibitor proteinase inhibitor 9<br />
(PI-9) in monocytes: Immunomodulating effects of<br />
cotrimoxazole<br />
Proteinase inhibitor 9 (PI-9) - the only known endogeneous natural antagonist of the<br />
lymphocyte protease granzyme B (GrB) - is an intracellular serpin expressed in<br />
lymphocytes and monocyte-derived cells. By intracellular flow cytometry, we have<br />
previously shown that ex-vivo stimulation by lipopolysaccharides leads to upregulation<br />
of PI-9 within 24 hours in the monocyte, but not the lymphocyte fraction; this can be<br />
inhibited by the NF-kappaB inhibitor pyrrolidin dithiocarbamate (PTDC). Co-trimoxazole<br />
- the combination of sulfamethoxazole and trimethoprim - is widely used as antibiotic<br />
for bacterial and pneumocystis infections. Since other sulfonamide metabolites like<br />
sulfasalazine have been described to exert immunomodulatory effects, we now asked<br />
whether co-trimoxazole might influence expression of PI-9 in monocytes and<br />
lymphocytes. A 24 hours incubation assay was done using heparinized full blood of<br />
healthy volonteers, and PI-9 expression was analysed by intracellular flow cytometry.<br />
We found that co-trimoxazole leads to PI-9 upregulation in monocytes at therapeutical<br />
concentrations (800 µM resp. 140 µM sulfamethoxazol/trimethoprim), similar to the<br />
upregulation induced by lipopolysaccharides. Combination of co-trimoxazole with<br />
lipopolysaccharides did not further enhance PI-9 expression. In lymphocytes, no<br />
alteration of PI-9 expression was induced. Since it has been shown that PI-9 overexpression<br />
in antigen presenting cells, e.g. dendritic cells, leads to an enhanced<br />
immune response, our finding may be relevant for specific immune regulation.<br />
Pharmacological modification of PI-9 expression may represent an interesting tool, both<br />
for the study of immune regulatory mechanisms or, even, for therapeutical<br />
interventions in immune diseases.
Jennifer Freyer, Stefan Floess, Alf Hamann, Jochen Huehn<br />
REGULATION OF THE MURINE TRANSCRIPTION FACTOR<br />
FOXP3<br />
The transcription factor Foxp3 is specifically expressed in natural CD4+ regulatory T<br />
cells and critically involved in their development and suppressive function. Although a<br />
lot of knowledge has been accumulated regarding the function of Foxp3, relatively little<br />
is known about the molecular regulation of Foxp3 expression. We have recently<br />
identified an evolutionarily conserved region within the foxp3 locus upstream of the<br />
translational start site, containing numerous CpG motifs, which in Tregs were selectively<br />
demethylated compared to non-regulatory T cells. This conserved region, which we<br />
named TSDR (Treg specific demethylated region), turned out to be associated with<br />
acetylated and trimethylated histones specifically in Tregs, indicating an open chromatin<br />
structure. Luciferase assays showed that the TSDR encompasses transcriptional activity,<br />
which was affected by in vitro methylation. Currently, we are generating deletion<br />
mutants of the TSDR to more precisely identify the critical elements involved in the<br />
molecular control of Foxp3 expression.
Janine Wehrhahn, Robert Kraft, Sunna Hauschildt<br />
Regulation of TRPM2 channels in human monocytes and<br />
macrophages<br />
TRPM2 belongs to the superfamily of transient receptor potential (TRP) proteins and<br />
functions as a calcium-permeable, nonselective cation channel. TRPM2 is specifically<br />
activated by intracellular ADP-ribose and can be opened during oxidant stress.<br />
Here we show for the first time the occurrence of TRPM2 in human monocytes and<br />
monocyte-derived macrophages on mRNA-, protein- and functional level. We studied<br />
freshly isolated monocytes and macrophages in comparison with 16 h cultivated<br />
unstimulated and LPS-stimulated (100ng/ml) cells.<br />
Besides the total TRPM2-mRNA we could detect the splice variants TRPM2-S and TRPM2-<br />
ΔC in both monocytes and macrophages. The splice variant TRPM2-ΔN was absent.<br />
Using semi-quantitative real time PCR we found that in monocytes TRPM2-mRNA was<br />
significantly down-regulated after 16 h cultivation in the absence but not in the<br />
presence of LPS. In human macrophages the TRPM2-mRNA-level was not affected by<br />
different incubation conditions.<br />
Western blot analyses showed that in human monocytes TRPM2 protein expression<br />
follows the same pattern as the mRNA-expression. In macrophages however the TRPM2<br />
protein-level does not exactly mirror the mRNA-level.<br />
Whole-cell patch clamp recordings using ADP-ribose in the pipette solution consistently<br />
revealed TRPM2-like cation currents in both monocytes and macrophages. The<br />
functional activity of TRPM2 correlated with the mRNA and protein data in monocytes<br />
and the mRNA data in macrophages.<br />
The expression and functionality of the cation channel TRPM2 in human monocytes and<br />
macrophages provide a potent mean to regulate intracellular calcium levels and<br />
biological answers. The inhibition of the TRPM2 channel will help to clarify its exact<br />
function in human monocytic cells.
Christian Erbel, Roland Klingenberg, Sultan Celik, Benjamin Funke, Hardy<br />
Schumacher, Nadine Wambsganss, Thomas Dengler<br />
Regulatorische T Zellen und Signalkaskaden über IL-17 und<br />
IL-10 als atheroprotektive Komponenten in<br />
atherosklerotischen Läsionen<br />
Atherosklerotische Läsionen enthalten typischerweise ein Infiltrat aus Makrophagen und<br />
T Zellen. Ziel dieser Studie ist der Nachweis regulatorischer T Zellen (Treg) als potentiell<br />
atheroprotektiver Komponente in atherosklerotischen Läsionen.<br />
Plaquegewebe aus den Karotiden von 47 Patienten, die sich einer TEA unterzogen,<br />
wurden gesammelt. Mit Hilfe der quantitativen PCR und der Immunohistochemie wurden<br />
die Immunzellen in dem Gewebe typisiert. Klinische Daten der Patienten wurden<br />
ausgewertet. Die Plaques wurden nach der Symptomatik der Patienten in eine<br />
symptomatische und eine asymptomatische Gruppe eingeteilt. Die Patientendaten<br />
wurden nach Vorhandensein einer Statin- und/oder Aspirintherapie unterteilt.<br />
Die Analyse aller Plaques zeigte lymphozytäre Infiltrate, insbesondere Tregs in fast allen<br />
Proben. Treg waren signifikant häufiger in Plaques von asymptomatischen Patienten im<br />
Vergleich zu Karotidenproben von symptomatischen Patienten (p=0,006) vorhanden.<br />
Zudem scheinen Treg unter einer Statintherapie oder ohne Aspirintherapie deutlich<br />
häufiger vertreten zu sein. Weiterhin war in Treg-positiven Karotisplaques eine erhöhte<br />
Expression des antiinflammatorischen Zytokines IL10 nachweisbar, welche u.a. von<br />
Treg produziert wird. Zudem zeigte sich ein signifikanter Unterschied in der Expresison<br />
von IL-17, vermehrt exprimiert im asymptomatischen Patientenkollektiv (p=0,03) und<br />
häufiger bei Patienten mit einer Statin- (p=0,02) oder Marcumar/Clopidogreltherapie.<br />
Die vorliegende Studie weißt Treg als mögliche atheroprotektive Komponente im<br />
immunzellulären Infiltrat von atherosklerotischen Läsionen nach und gibt somit einen<br />
Anhalt für eine mögliche Bedeutung von Treg für die Plaquegenese und Symptomatik,<br />
insbesondere aufgrund der Assoziation mit erhöhten Spiegeln von IL-10 in Treg-haltigen<br />
Plaques und der vermehrt auftretenden Treg in Patienten mit einer Statintherapie.<br />
Erstmals wird die Anwesenheit von IL-17 nachgewiesen, vornehmlich in<br />
asymptomatischen sowie bei Patienten mit einer Statintherapie.
Sabine Riekenberg, Katja Farhat, Jennifer Debarry, Holger Heine, Karl-Heinz<br />
Wiesmueller, Roland Lang, Artur J. Ulmer<br />
Regulators of G-protein signaling are modulated by bacterial<br />
lipopeptides and lipopolysaccharide<br />
Regulators of G-protein signaling (RGS) accelerate the GTPase activity of G&alpha<br />
subunits, thus driving G-proteins in their inactive GDP-bound form. This property<br />
defines them as GTPase activating proteins (GAPs). In our study we analyzed the effect<br />
of different Toll-like receptor (TLR) agonists on RGS1 and RGS2 expression in murine<br />
bone marrow-derived macrophages (BMDM) and J774 cells.<br />
To identify different signal transduction pathways and patterns of gene expression we<br />
stimulated BMDM cells for 2 and 6 h with different lipopeptides like PamOct2C(VPGVG)4-<br />
VPGKG, FSL-1 and Pam2C-SK4 to activate signal transduction through TLR2 in a TLR1-,<br />
TLR6-, or TLR1 & 6 independent manner and for 3 h with LPS to activate TLR4 signaling,<br />
respectively. Affimetrix micro array analyses showed a strong down-regulation of RGS1<br />
and RGS2 at 2 h and 6 h of stimulation with the different TLR2 ligands. Furthermore, we<br />
detected an up regulation of RGS1 as early as 15 min after stimulation. We confirmed<br />
these data by real-time PCR, flow cytometry and fluorescence microscopy. In addition<br />
we found a strong up regulation of both, RGS1 and RGS2 mRNA, after stimulation with<br />
LPS in MyD88-/- mice, indicating that a MyD88-independent pathway of TLR4 signaling<br />
is responsible for this up regulation. The application of poly I:C, a TLR3 ligand, and the<br />
usage of Trif-/- mice confirmed this conclusion.<br />
We suggest that modulating of RGS1 and RGS2 by TLR2 and TLR4 ligands play an<br />
important role during inflammatory and immunological reactions.<br />
(Supported by Deutsche Forschungsgemeinschaft UL68/3-2)
Arthur Liesz, Elisabeth Suri-Payer, Claudia Veltkamp, Henrike Dörr, Clemens Sommer,<br />
Thomas Giese, Roland Veltkamp<br />
Regulatory T Cells (Treg) are Important Cerebroprotective<br />
Immunomodulators in Acute Experimental Stroke by an<br />
Interleukin-10 Dependent Pathway.<br />
Inflammatory cascades contribute substantially to secondary infarct growth after<br />
ischemic brain damage. Because CD4+CD25+Foxp3+ Treg are important negative<br />
immunomodulators in various inflammatory diseases, we studied the role of Treg in<br />
experimental stroke and the involved immunosuppressive mechanisms.<br />
Permanent focal cerebral ischemia was induced by middle cerebral artery occlusion<br />
(MCAO) in C57BL/6 mice and Treg were eliminated in one group of mice by preischemic<br />
anti-CD25 mAb injection. While no difference was detectable between groups at 24h,<br />
infarct volumes became significantly larger between 3-7d after MCAO in Treg depleted<br />
mice. Correspondingly, transfer of only CD4+CD25- T cells into RAG-/- mice resulted in<br />
larger infarcts than transfer of total CD4+ cells. Treg started to invade the brain 3d<br />
after MCAO (shown by FACS and immunohistology). The lack of Treg resulted in<br />
significantly higher microglial activation (Iba1+ cells) 24h after MCAO. Further, levels of<br />
proinflammatory cytokines (RT-PCR and ELISA) were significantly more elevated in the<br />
ischemic brain hemisphere and the serum of Treg depleted mice at various time points<br />
after MCAO compared to control mice. The intraventricular injection of IL-10 prevented<br />
the secondary infarct growth in Treg depleted mice. Finally, RAG-/- mice receiving<br />
wildtype CD4+CD25- T cells plus Treg with impaired IL-10 secretion had significantly<br />
larger infarcts than mice receiving additional wildtype Treg.<br />
In conclusion, we show that Treg are physiological master anti-inflammatory modulators<br />
in ischemic stroke which substantially reduce secondary infarct progression. This effect<br />
is mainly mediated by early IL-10 signalling, inhibition of microglial activation and<br />
cytokine expression as well as delayed Treg invasion.
Paula Kolar, Holger Hoff, Karin Knieke, Kolja Hegel, Dagmar Quandt, Monika Brunner-<br />
Weinzierl<br />
Regulatory T cells require costimulation by CTLA-4 (CD152)<br />
Unwanted T cell responses in the periphery are suppressed by regulatory CD4+CD25+ T<br />
cells (Treg). Here we show that Treg cells strongly co-express Foxp3 and intracellular<br />
CTLA-4, a major inhibitory molecule of T cell responses. Additionally, we could show<br />
that Treg cells are the only population of T helper cells which express surface CTLA-4 ex<br />
vivo implying a constant or immediate need for CTLA-4 signaling. This assumption is<br />
extended using serological blockade of CTLA-4 during in vitro inhibition of inflammatory<br />
effector T cells by Tregs cells leading to reduced inhibitory capacity. Interestingly,<br />
blocking of CTLA-4 on Treg cells during in vitro stimulation in the absence of CD25-<br />
target cells rescues their proliferation, but not their cytokine production. Strikingly,<br />
serological blockade of CTLA-4 during activation of Treg cells leads to enhanced AICD.<br />
We could show that CTLA-4 induced signaling interferes with CD95/CD95L mediated<br />
activation of caspases. Our results suggest that the surface expression of CTLA-4 on<br />
Treg cells serves Treg cells´ basic needs to preserve the stringency of their anergic<br />
status and their survival under non/low-inflammatory conditions.
Ioanna Galani, Marco Wendel, Carola Schellack, Elisabeth Suri-Payer, Adelheid<br />
Cerwenka<br />
REGULATORY T CELLS SUPPRESS IFN-γ DEPENDENT<br />
LEUKOCYTE ACCUMULATION AND MACROPHAGE ACTIVATION<br />
IN LYMPHOMA<br />
Regulatory T cells (Treg) have been shown to suppress immune responses of tumorspecific<br />
T cells; yet, little is known about the impact of Treg on innate immune cells in<br />
tumor models. Since many tumors lose expression of MHC class I, our study aimed at<br />
defining strategies to strengthen immune responses against a high tumor burden of the<br />
MHC class I-deficient lymphoma RMA-S. We demonstrate that Treg depletion led to<br />
tumor rejection and generation of immunological memory. This tumor rejection was<br />
associated with a substantial, IFN-γ dependent increase in numbers of tumor-infiltrating<br />
leukocytes, including macrophages. Tumor-infiltrating macrophages from Treg depleted<br />
mice expressed increased amounts of MHC class II, produced enhanced levels of<br />
inflammatory cytokines and inhibited tumor cell proliferation. Our study reveals that in<br />
an in vivo tumor model, numbers and activity of macrophages are controlled by Treg.<br />
These data identify macrophages as novel targets for Treg mediated immune<br />
suppression in cancer.
Mario Zaiss, Jochen Zwerina, Karin Polzer, Eva Gückel, Alla Skapenko, Hendrick<br />
Schulze-Koops, Nikki Horwood, Andrew Cope, Georg Schett<br />
Regulatory T cells suppress osteoclast formation- a new link<br />
between the immune system and bone<br />
Objective.<br />
To investigate whether regulatory T cells can suppress osteoclast differentiation<br />
and to define a new potential link between the immune system and the skeleton.<br />
Methods.<br />
Regulatory CD4+CD25+foxp3+ T cells were isolated and purified from the spleen and<br />
co-cultured with CD11b+ osteoclast precursor cells isolated from the bone marrow.<br />
Osteoclastogenesis and bone erosion was assessed by TRAP staining and pit resorption<br />
assay, respectively. In addition, trans-well experiments and cytokine blocking<br />
experiments were performed to define the mechanisms of interaction between<br />
regulatory T cells and osteoclasts.<br />
Results.<br />
CD4+CD25+foxp3+ T cells dose dependently inhibited MCSF- and RANKL dependent<br />
osteoclast formation in contrast to CD4+CD25- T cells. Also pit formation was inhibited<br />
by up to 80%. The blockade of osteoclast formation was not based on an alteration of<br />
RANKL/OPG balance but essentially dependent on direct cell-cell contact via CTLA-4.<br />
Regulatory T cell-mediated expression of TGF-β, IL-4 and IL-10 contributed to the<br />
inhibitory effect on osteoclastogenesis, but was not essential.<br />
Conclusion.<br />
These data show that CD4+CD25+foxp3+ regulatory T cells suppress osteoclast<br />
formation. These data provide a new link between the immune system and bone and<br />
extend our knowledge on the regulation of bone homeostasis by the immune system.
Florian Eberle, Mehtap Sirin, Klaus Heeg, Alexander Dalpke<br />
Relevance of RNA-mediated immunostimulation for RNA-<br />
Interference (RNAi)<br />
Double-stranded RNAs can regulate endogenous messenger RNA stability which is<br />
referred to as RNA interference (RNAi). This process can be mimicked by small synthetic<br />
RNA, so called small inhibitory RNA (siRNA). In addition to the newly identified role of<br />
RNA in gene-silencing, it is known that RNA is also a target for immune recognition<br />
principles. Even more, siRNA can induce activation of some cell-types of the innate<br />
immune system thus mediating off-target effects. Immune-recognition of RNA is<br />
mediated by three members of the Toll-like-receptor family (TLR 3,7 and 8) as well as<br />
by the cytosolic RNA-binding proteins RIG-I and MDA5. Additional, there are evidences<br />
that RNA recognition occurs in a cell-type specific manner.<br />
We aimed to identify RNA motives, which determine the immunostimulatory potential of<br />
RNA and RNA oligonuclotides, such as siRNAs. We show that functional siRNAs were<br />
immunostimulatory on several cell-types of the innate immune system. By introducing<br />
uridine modifications, immunostimulation could be reduced significantly, whereas<br />
modifications of other nucleotides showed only marginal effects. We further show that<br />
bacterial RNA preparations were immunostimulatory not only on cells of the immune<br />
system but also were able to stimulate normal tissue cells. We can also show that<br />
recognition of bacterial RNA differs significantly from recognition of RNA<br />
oligonucleotides.
Christian Hofmann, Thomas Harrer, Kathrin Eismann, Silke Bergmann, Matthias Schmitt-<br />
Haendle, Gerold Schuler, Jan Dörrie, Niels Schaft<br />
REPROGRAMMING T CELLS WITH A HIV-1-SPECIFICTY BY<br />
ELECTROPORATION OF TCR-ENCODING RNA<br />
HIV-1 establishes a persistent infection in humans and destroys the patient’s CD4+<br />
immune cells, which ultimately leads to paralysis of the immune system. However, high<br />
levels and a broad specificity of anti-HIV-1 CD8+ cytotoxic T lymphocytes (CTL),<br />
especially against conserved epitopes, are considered to be critical for long-term control<br />
of HIV-1 replication. Unfortunately, most HIV-infected patients are unable to generate<br />
such a powerful immune response. A possible immunotherapy is the adoptive transfer<br />
of T cells, which were reprogrammed by introduction of an HIV-specific T cell receptor<br />
(TCR). Until now, these HIV-specific CTL were generated by retroviral transduction of<br />
TCR encoding cDNA. However, this strategy harbors the threat of stable genetic<br />
alteration of autologous cells. Therefore, we studied TCR transfer by RNA<br />
electroporation into CD8+ T cells. An HIVpol-specific TCR, which recognizes the HLA-A2<br />
restricted peptide ILKEPVHGV, was used. These reprogrammed T cells produced the proinflammatory<br />
cytokines IL-2, TNF, and IFNgamma after stimulation with peptide-loaded<br />
target cells, and efficiently and specifically killed these targets, even after<br />
cryopreservation. The cytolytic function of the reprogrammed T cells persisted for at<br />
least 72 h after transfection. Peptide-titration studies revealed that the lytic avidity of<br />
the TCR-RNA-electroporated CD8+ T cells was in the same range as that of the parental<br />
CTL clone. Taken together, we show here for the first time that functional transfer of<br />
virus-specific TCR by RNA electroporation is feasible. This technology represents an<br />
innovative, secure, and easy method to produce virus-specific T cells, and may<br />
represent a new tool in the fight against HIV infection.
Esther Wilk, Katy Kalippke, Sabine Buyny, Reinhold E Schmidt, Roland Jacobs<br />
Response of CD56 dim and CD56 bright NK cells to Interleukin 21<br />
IL-21 is a cytokine with pleiotropic effects on various cell types including DC, B, T, and<br />
NK cells. In order to evaluate the effects of IL-21 on human NK cell subpopulations<br />
functional studies were <strong>complete</strong>d on CD56 dim and CD56 bright NK cells, both bearing IL-<br />
21 receptors at identical densities. Stimulation with IL-21 strongly induced proliferation<br />
of CD56 bright NK cells. Cytotoxicity against K562 target cells was preferentially<br />
augmented in CD56 dim whereas the expression of granzyme K increased mainly in<br />
CD56 bright NK cells. Intracellular analysis of STAT proteins revealed IL-21 induced<br />
phosphorylation of STAT1 and STAT3 in CD56 dim NK cells, and to an even higher degree<br />
in CD56 bright NK cells. In the CD56 bright NK cell population, IL-2 led to a slight<br />
phosphorylation of STAT1 and 3, which was synergistically increased when cells were<br />
treated with IL-2 and IL-21 in combination. STAT5 was strongly phosphorylated in<br />
CD56 bright NK cells by low dose IL-2, while IL-21 did not affect STAT5. Our data<br />
indicates that the NK cell directed cytokines IL-2 and IL-21 not only differently affect<br />
functions in NK cell subpopulations but can also act in a synergistic fashion.<br />
Supported by DFG Priority Program SPP1110, project Ja1058.
Elke Scandella, Evelyn Lattmann, Sanjiv Luther, Simone Miller, Tobias Junt, Burkhard<br />
Ludewig<br />
Role for lymphoid tissue inducer-like cells in the restoration<br />
of immunopathological destruction of the lymphoid stroma<br />
cell network<br />
Many viral infections, including human Hepatitis B and C or immunodeficiency viruses<br />
(HIV) are associated with an immunopathological damage of secondary lymphoid<br />
organs leading to immunosupression. Similarly, infection of mice with the lymphocytic<br />
choriomengitis virus (LCMV) leads to destruction of secondary lymphoid organ structure<br />
which is mediated by virus-specific cytotoxic T cells (CTL). In this study we show that<br />
the destruction also affects follicular dendritic cells and gp38+ T zone stroma cells which<br />
are the major producers of the constitutive chemokines CXCL13, CCL19 and CCL21b<br />
and are therefore essential for the maintenance of lymphoid structures. Furthermore,<br />
LCMV infected gp38+ stroma cells were lysed by activated virus-specific CTL. The loss<br />
of stroma cell network is corroborated by a transient reduction of constitutive<br />
chemokines. A gene-array analysis revealed that genes which are crucial for the<br />
development of lymphoid organs, e.g. lymphotoxin-b, IL-7Ra or VCAM-1, were upregulated<br />
concomitantly, thus indicating the immediate initiation of a transcriptional<br />
'reorganization program'. Moreover, we found accumulation and proliferation of CD3-<br />
CD4+IL7-Ralpha+ positive cells, which phenotypically resemble lymphoid tissue inducer<br />
(LTi) cells and are required for lymphoid organ development. In addition, mice lacking<br />
LTi cells display a delay in the re-expression of CCL19, CCL21 and CXCL13 following<br />
LCMV infection.
Adan Chari Jirmo, Claus-Henning Nagel, Beate Sodeik, Reinhold E Schmidt, Georg<br />
Behrens<br />
Role of direct versus cross-presentation after acquisition of<br />
HSV-1 by murine DC for generating antiviral immunity<br />
Background:Phenotypically, murine splenic dendritic cells (DC) can be divided into at<br />
least three subsets. Differences in surface markers appear to correlate with functional<br />
differences including antigen acquisition, processing, and presentation. Using HSV-1 as<br />
an infectious model we aimed to explore the contribution of direct and indirect antigen<br />
preseantion to generate cytotoxic T lymphocytes (CTL).<br />
Methods: Spleen DC from C57BL/6 mice were sorted into different subsets their ability<br />
to present various forms of HSV-1 to HSVgB-specific TCR-transgenic T cells (gBT-1) was<br />
analysed. Using infected target cells and viral mutagenesis we established conditions to<br />
assess direct infection vs cross-presentation. In addition, we determined influence of<br />
TLR ligands and blocking phagocytosis on the ability of cross-presenting CD8+ DC to<br />
stimulate Ag-specific CD8+ T cells.<br />
Results: Although all splenic DC subsets express HSV-1 entry mediating receptors,<br />
produce late HSV-1 antigens, and effectively presented HSV-1 antigen to CTL upon<br />
direct infection in vitro, only the CD8+ DC subpopulation were capable of presenting<br />
cellular viral and non-viral antigen in the context of MHC class I (cross-presentation).<br />
However, this ability by CD8+ DC to cross-present is not due to the fact that they are<br />
the only subsets that are capable of taking up cellular antigen both in vitro and in vivo.<br />
Using gB- or gH-deficient HSV-1 (“single round virus”) we were unable to detect any<br />
contribution of direct presentation to the overall CTL generation in vitro after acquisition<br />
of virus from infected target cells. In addition, we observed almost <strong>complete</strong> diminished<br />
antigen presentation of cellular Ag after inhibition of DC phagocytosis.<br />
Conclusion: We conclude that cross-presentation is an intrinsic ability of CD8+ DC and<br />
the dominating antigen presentation pathway for generation of an effective CTL<br />
response in HSV-1 infection.
Katharina König, Linda Diehl, Carsten Golletz, Thomas Quast, Waldemar Kolanus,<br />
Percy Knolle, Reinhard Büttner, Lukas C Heukamp<br />
ROLE OF FHL2 IN THE REGULATION OF DENDRITIC CELL<br />
MIGRATION<br />
Regulation of cell migration is a hallmark of dendritic cells function and plays a central<br />
role in the initiation and regulation of immune responses. Under steady state conditions<br />
immature dendritic cells continuously acquire antigen in the periphery and migrate to<br />
draining lymph nodes, where they present exogenous antigens to T cells.<br />
Furthermore, cell migration is likely to be modulated in important pathological situations<br />
such as cell invasion and in tumor progression. Cellular motion through complex<br />
substrates is only partially understood. There is a large body of evidence suggesting<br />
that integrin-mediated force generation is required for cell locomotion on twodimensional<br />
(2D) substrates, but translocation of cells within (3D)-tissues can<br />
apparently resort to other mechanisms, in which selective involvement of the Rho<br />
GTPases RhoA and Rac1 has been proposed to play a major role. We have discovered<br />
that migration of murine, bone-marrow derived dendritic cells is differentially regulated<br />
in 2D and 3D-assay conditions. Furthermore, we found that the RhoA-regulated Fourand-a-half-Lim-Domain<br />
protein FHL2 plays important and so far unappreciated roles in<br />
these processes.<br />
FHL2 deficient bone marrow derived dendritic cells show a significantly increased<br />
migratory speed, a morphologically mature phenotype and altered expression of α and<br />
ß-integrins.
Kerstin Juelke, Andreas Thiel, Chiara Romagnani<br />
Role of inflammatory cytokines in modulating NK cell<br />
competence and maturation<br />
The role of NK cells in several protective responses has been extensively elucidated,<br />
while their contribution in self tolerance maintenance is still unclear. Recently it has<br />
been shown that self tolerance of NK cells can occur independently of MHC-mediated<br />
inhibition and hyporesponsiveness plays a role in self-tolerance of NK cells as it has<br />
been proposed for B and T cells.<br />
The comparative analysis of resting human CD56dim NK cells sorted according to the<br />
presence or lack of expression of KIR and NKG2A revealed that, although KIR- NKG2A-<br />
NK cells are hyporesponsive in response to MHC class I target cells, once stimulated<br />
with inflammatory cytokines, their cytotoxic hyporesponsiveness is reverted. Moreover,<br />
we showed that KIR- NKG2A- NK cells are at least as good as KIR+ NKG2A+ in<br />
proliferating and producing IFN-gamma in response to cytokines and that these<br />
functions are not related to NK cell competence but rather to NK cell maturation. In<br />
addition, we demonstrated that KIR- NKG2A- NK cells can acquire expression of KIR and<br />
NKG2A upon cytokine stimulation. These findings suggest that although NK cell<br />
hyporesponsiveness represents a mechanism of self tolerance maintenance in steady<br />
state conditions, during an immune response KIR- NKG2A- NK cells can produce IFNgamma,<br />
proliferate and acquire the expression of new inhibitory receptors which might<br />
allow them to regain competence. Thus, we propose a revised concept of NK cell self<br />
tolerance as a rather dynamic process in which NK cells might contextually change their<br />
competence properties during inflammation. These findings might have important<br />
implications in the pathogenesis of autoimmunity.
Romy Laugks, Patricia Schmidbauer, Bernhard Holzmann, Melanie Laschinger<br />
ROLE OF LFA-1 ACTIVITY REGULATION IN CELL CYCLE<br />
CONTROL OF PROLIFERATING T LYMPHOCYTES<br />
The leukocyte specific integrin LFA-1 (αLβ2) is crutial in the interaction between T<br />
lymphocytes and antigen-presenting cells. It is well established that LFA-1 needs to be<br />
activated in order to bind ligands. However, the function of LFA-1 de-activation is not<br />
<strong>complete</strong>ly understood. By the deletion of the cytoplasmic GFFKR motif of the αL<br />
subunit in mouse germ line we previously generated a mouse mutant that locks LFA-1<br />
in an inactive state (LFA-1d/d). The defect of LFA-1 de-activation leads to an impaired<br />
de-adhesion from its ligand ICAM-1 on endothelial cells reflected in a reduced migration.<br />
We found the antigen-specific proliferation of LFA-1d/d T cells to be dramatically<br />
reduced. The analysis of interaction between LFA-1d/d T cells and antigen-presenting<br />
dendritic cells exhibits the disability of T cells expressing LFA-1 in a constitutively active<br />
state to de-adhere from dendritic cells. Furthermore, we observed a different cell cycle<br />
profile of LFA-1d/d T cells compared to wildtype cells suggesting an influence of LFA-1<br />
in early cell cycle control.<br />
These data imply that LFA-1 de-activation is essential for cell cycle control during<br />
antigen-specific proliferation and clonal expansion of naïve T lymphocytes.
Chiara Cordiglieri, Werner Dammermann, Bo Zhang, Barry Potter, Andreas Guse,<br />
Alexander Flügel<br />
Role of NAADP-mediated Ca 2+ signalling in encephalitogenic<br />
CD4 + T cells<br />
Nicotinic acid adenine dinucleotide phosphate (NAADP) was recently discovered as a<br />
novel second messenger involved in the initiation and propagation of Ca 2+ signalling in<br />
T cells, but its impact on T cell function is still unknown.<br />
We developed small molecular antagonists based upon nicotinic acid that specifically<br />
block Ca 2+ mobilization by NAADP. These compounds suppressed antigen-driven<br />
proliferation and cytokine release in primary human and rat CD4 + T cells.<br />
To better address the importance of NAADP-mediated Ca 2+ signalling in the functions<br />
of CD4 + T cells, we used these antagonists in vivo, in a rat model of experimental<br />
autoimmune encephalomyelitis (EAE), the classical T cell mediated autoimmune model<br />
for Multiple Sclerosis.<br />
NAADP antagonists ameliorated the clinical courses of both active and adoptive transfer<br />
EAE. Molecular analyses and live two photon imaging of retrovirally-tagged fluorescent T<br />
cells revealed that NAADP antagonists mainly acted in the effector phase of EAE, where<br />
CNS inflammation is initiated by encephalitogenic autoaggressive T cells. NAADP<br />
antagonists interfered with the migration of the T cells to their target organ and with<br />
their efficient activation, thus ameliorating CNS inflammation and paralytic disease.<br />
These results show that the NAADP/Ca 2+ signaling pathway is crucial for the<br />
pathogenic potential of autoaggressive T cells and thus qualifies as novel target for the<br />
treatment of T cell-mediated autoimmune diseases.
Annette I. Garbe, Taras Kreslavsky, Harald von Boehmer<br />
Role of Notch in survival, proliferation and differentiation of<br />
alpha beta T cell precursors<br />
Notch signaling can synergize with both the pre-TCR and the gamma delta TCR to<br />
determine alpha beta lineage commitment. In case of gamma delta TCR expressing<br />
precursors the selected cells terminate gamma delta TCR expression and undergo Tcra<br />
rearrangement. Under physiological conditions gamma delta TCR expressing precursors<br />
have a competitive disadvantage to pre-TCR expressing cells. In recent studies we could<br />
show that precursors with a gamma delta TCR compete poorly for Notch ligands<br />
because they compete better with pre-TCR expressing cells when offered an excess of<br />
soluble ligands. Overexpression of intracellular Notch abolishes the competitive<br />
advantage entirely. Our results indicate that Notch signaling is not only essential for<br />
survival of DN3 precursors of alpha beta lineage cells but is essentially required for<br />
proliferation of DN3 and DN4 cells. The synergy of TCR and Notch signals becomes<br />
visible in increased CD5 expression that can be diminished by specifically interfering<br />
with Notch signaling. Preliminary data indicate that Notch signaling does not only<br />
contribute to alpha beta lineage choice by helping survival and proliferation of precursor<br />
cells: The differentiation into CD4+CD8+ alpha beta lineage cells of DN3 precursors<br />
with increased survival because of Bcl-2 overexpression still requires Notch signaling<br />
indicating that Notch contributes to survival, proliferation as well as differentiation of<br />
alpha beta lineage precursors.
Varsha Pattu, Bin Qu, Eva.C Schwarz, Tanja Mayer, Carolin Bick, Reiko Trautmann,<br />
Markus Hoth, Jens Rettig<br />
Role of SNARE proteins in vesicle fusion at the Immunological<br />
Synapse of Cytotoxic T lymphocytes.<br />
Cytotoxic T lymphocytes(CTLs), kill target cells through secretion of lytic vesicles<br />
containing cytotoxic components such as perforin and granzymes. Fusion of these<br />
vesicles occurs at the contact zone between the target cell and CTL, the immunological<br />
synapse(IS). We are interested in the molecular mechanism behind this fusion event.<br />
The specific Soluble NSF attachment receptor (SNARE) protein isoforms are well known<br />
to be required for vesicle fusion in neuronal synapses, but a potential function in CTLs<br />
remains unkown. We have established an efficient method of focal stimulation of human<br />
primary CD8 T lymphocytes by anti-CD3/anti-CD28 antibody coated beads. The effector<br />
status of these cells was confirmed by staining with specific markers such as CD25 and<br />
CD62L. We analysed the expression patterns of different SNARE proteins by reverse<br />
transcriptase PCR and found several candidates that are upregulated upon stimulation.<br />
Immunocytochemistry with isoform specific antibodies was used to further narrow down<br />
our candidates based on co-localisation with lytic vesicle markers. Functional studies<br />
like capacitance measurements and cytotoxicty assays were established to gain further<br />
insight into the field.
Stefano Majocchi, Natalio Garbi, Günter J Hämmerling<br />
Role of Tapasin-ERp57 heterodimers in the generation of MHC<br />
class I/peptide complexes<br />
Antigen presentation by MHC class I molecules is necessary for CD8 T cell activation.<br />
Optimal peptide loading onto MHC-I molecules occurs mainly in the peptide-loading<br />
complex in the endoplasmic reticulum. The loading complex is a multimeric structure<br />
that consists of MHC-I heavy chain, β2-microglobulin, the MHC-I-specialised chaperone<br />
tapasin (Tpn), the thiol oxidoreductase ERp57, the lectin binding chaperon calreticulin<br />
and the peptide transporters associated with antigen processing TAP1 and TAP2.<br />
The generation of peptide-receptive MHC-I molecules and their association into the<br />
peptide loading complex is relatively well understood. Recently we have shown that<br />
ERp57 has a critical structural role in the loading complex by increasing the affinity of<br />
Tpn for MHC-I molecules. This is achieved via a covalent association between Tpn and<br />
ERp57 mediated by a disulfide bond between C95 and C57, respectively. This<br />
association is believed to be stable, although ERp57 C60 can mediate the release of<br />
ERp57 from tapasin under certain conditions in vitro. In contrast, very little is known<br />
about the release of MHC-I/peptide complexes from the loading complex. In order to<br />
investigate whether dissociation of Tpn and ERp57 is required for the release of MHC-I/<br />
peptide from the loading complex, we have reconstituted ERp57 KO cells with wt or<br />
mutant forms of ERp57 that stabilise the Tpn-ERp57 covalent association. Results on<br />
the association of peptide-receptive MHC-I to the loading complex and release of MHC-I/<br />
peptide from the loading complex in the ERp57 mutant cell lines will be presented.
Carolin Konermann, Daniel Degrandi, Cornelia Beuter-Gunia, Sandra Beer, Klaus<br />
Pfeffer<br />
Role of the IFN-γ inducible 65kDa GTPases in pathogen<br />
defense<br />
IFN-γ induces a number of cellular programs functional in innate and adaptive resistance<br />
to infectious pathogens. Microarray expression studies of IFN-γ stimulated macrophages<br />
displayed a new family of murine GTPases, the 47kDa and 65kDa guanylate-binding<br />
proteins (GBPs), whose expression was highly upregulated. The members of the GBP<br />
family are structurally characterized by the canonical G(X)4GKS and D(X)2G motifs.<br />
Some GTPases carry a CAAX site for isoprenoid modification which regulates<br />
intracellular localization. Several studies revealed a pathogen specific protective<br />
function of members of the 47kDa family in mice. However, the role of 65kDa mGBPs<br />
during infection remains ill-defined.<br />
Via qRT-PCR and Western Blot analyses we confirmed the microarray data and analyzed<br />
the expression levels of the 65kDa GBPs mGBP1 to 5 in macrophage cultures stimulated<br />
with several cytokines and TLR ligands. Especially upon IFN-γ stimulation the mGBPs<br />
were strongly upregulated. Induction of these GTPases was STAT1 dependent, shown by<br />
the absence of mGBP expression in stimulated STAT1-/- fibroblasts. Furthermore, the<br />
GBPs were strongly induced in vivo in several organs of mice infected with L.<br />
monocytogenes or T. gondii. The degree of GBP induction after infection was different<br />
for each GTPase, indicating a non-redundant, pathogen specific role of these proteins.<br />
Fusion-proteins as well as intracellular staining of endogenous GTPases displayed<br />
localization in intracellular vesicle-like structures. After stimulation with IFN-γ and<br />
infection of macrophages or fibroblasts with T. gondii mGBP1, 2 and 3 migrated to the<br />
parasitophorous vacuole (PV) whereas mGBP5 did not recruit to the PV. The ability to<br />
accumulate at the PV was dependent on the isoprenylation but not GTP-binding or<br />
hydrolysation as shown with mutated fusion-proteins.<br />
These results demonstrate that the mGBPs belong to a novel class of GTPases<br />
specifically induced by the immunomodulatory and pro-inflammatory cytokine IFN-γ and<br />
therefore could be effectors of immunity in the defense against intracellular pathogens.
Christiane Habich, Volker Burkart<br />
Role of Toll-like receptor 4 (TLR4) in heat shock protein 60<br />
(hsp60)-mediated beta cell-directed immune reactivity in nonobese<br />
diabetic (NOD) mice<br />
Hsp60 expressed in beta cells is one of the putative autoantigens in the development of<br />
type 1 diabetes. Hsp60 shows receptor-mediated binding to macrophages and induces<br />
the release of beta cell damaging, inflammatory mediators (TNFα, IL6) from<br />
macrophages of NOD mice, a model of type 1 diabetes. The present study was designed<br />
to characterize the pro-inflammatory hsp60 signaling in macrophages and to analyze<br />
the role of TLR4 in these processes by the use of TLR4-deficient NOD mice. We<br />
investigated the activation of signaling proteins (NFkB, p42/p44, p38, JNKp46/p54)<br />
after hsp60 stimulation of macrophages from prediabetic and diabetic NOD/TLR4+/+,<br />
NOD/TLR4+/- and NOD/TLR4-/- mice. Hsp60 stimulated all investigated signaling<br />
proteins in prediabetic and diabetic NOD/TLR4+/+ mice. In NOD/TLR4+/- mice p38<br />
activation was weakly reduced (23-44%), whereas p42/p44 activation was strongly<br />
reduced (74-81%) independent of the diabetes stage. NFkB activation was continuously<br />
reduced with diabetes progression (38-99%). JNKp54 activation showed constant strong<br />
reduction (>90%), whereas JNKp46 was strongly reduced only in prediabetic mice<br />
(77%), but not in diabetic NOD/TLR4+/- mice (14%). In NOD/TLR4-/- mice activation<br />
of all investigated signaling proteins was constantly strongly reduced (NFkB >80%, p42/<br />
p44 >90%, p38 77-87%, JNKp46/p54 77-96%). By the use of specific inhibitors, we<br />
analyzed the role of these signaling proteins in the production of beta cell damaging<br />
mediators TNFα and IL6 by macrophages from NOD/TLR4+/+ mice. Independent of<br />
diabetes progression, JNKp46/p54 and NFkB were found to be involved in hsp60mediated<br />
IL6 production. Furthermore, we could show that hsp60-mediated TNFα<br />
production from NOD/TLR4+/+ macrophages is regulated by p42/p44, p38 and NFkB.<br />
We conclude, that differential activation of TLR4-dependent signaling pathways by<br />
hsp60 may contribute to increased beta cell-directed immune reactivity observed at the<br />
time of diabetes manifestation.
Bernadette Pöllinger, Gurumoorthy Krishnamoorthy, Michael Bösl, Hans Lassmann,<br />
Andeas Holz, Hartmut Wekerle, Florian C. Kurschus*<br />
RR Mouse: Spontaneous relapsing remitting EAE in SJL/J mice<br />
expressing a MOG responsive T cell receptor<br />
Myelin oligodendrocyte glycoprotein (MOG) is regarded as major autoantigen in Multiple<br />
Sclerosis (MS) and its animal model • experimental autoimmune encephalomyelitis<br />
(EAE). Its anatomic localization on the outermost layer on central nervous system<br />
(CNS) myelin sheets suites it perfectly as target for auto-antibodies. We recently<br />
described a double transgenic C57BL/6 (H-2b ) mouse strain carrying a MOG specific T<br />
cell receptor along with a MOG specific immunoglobulin H chain (Krishnamoorthy G. et<br />
al., J Clin Invest. 2006;116:2385-2392). These mice develop spontaneous autoimmune<br />
disease affecting spinal cord and optic nerve, but sparing brain and cerebellum, thus<br />
resembling human opticospinal myelitis (Devic disease).<br />
In order to explore the possible effect of genetic factors on disease expression, we now<br />
report about new similar transgenic mouse lines, but on SJL/J (H-2s ) background. We<br />
created three T cell receptor (TCR) transgenic lines bearing CD4 cells specific for MOG92- 106 presented by I-AS . These lines differ in their penetrance of transgene expression on<br />
CD4 cells (TCR1640 , 70%; TCR1639 , 20%; TCR1586 , 5%). In contrast to the Devic model,<br />
single (TCR-) transgenic SJL/J mice spontaneously develop EAE at high frequency.<br />
Disease occurs in more than 75 % of TCR1640 but only in about 15 % of TCR1586 mice,<br />
if bred on SJL/J, but not on the B10.S background. Spontaneous EAE in many cases<br />
takes a relapsing-remitting course, with individual disease bouts affecting distinct CNS<br />
parts (cerebellum vs. spinal cord). Intriguingly TCR1640 and diseased TCR1586 SJL/J<br />
mice select and activate endogenous MOG-specific B cells to produce MOG reactive IgG1<br />
and IgG2ab autoantibodies. This new form of autoimmune B cell recruitment does not<br />
occur on the MOG knockout -or B10.S background and may therefore involve MOG<br />
exposure to the immune system during preclinical EAE lesions.<br />
The RR mouse is the animal model most faithfully recapitulating the most frequently<br />
occurring human MS variant. It will be of use studying issues including relapse<br />
generation, autoimmune T-B cell cooperation, and drug discovery.
Elisa Monzón-Casanova, Christian Söllner, Nico Westphal, Ingolf Berberich, Tohru<br />
Miyoshi-Akiyama, Takehiko Uchiyama, Ingrid Müller, Lutz* Walter, Thomas* Herrmann<br />
RT1Db2: Identification and first functional analysis of a new<br />
non-polymorphic MHC class II molecule<br />
The <strong>complete</strong> sequence of the rat MHC allowed the identification of a duplicated class II<br />
beta chain gene locus RT1-Db (RT1D: rat homologue of H2-E and HLA-DR). The<br />
duplicated gene is designated RT1-Db2, maps between the RT1-Db1 and RT1-Da genes<br />
and encompasses about 20 kb. RT1-Db2 had not been noticed and characterized so far<br />
and shows some interesting features. Compared to RT1-Db1, the exons that code for<br />
the cytoplasmic region are deleted (exon 5) and inactivated (exon 6). Yet, RT1-Db2<br />
shows a <strong>complete</strong>ly novel exon, which codes for the <strong>complete</strong> cytoplasmic region. Upon<br />
sequencing of several inbred rat strains, RT1-Db2 turned out to be monomorphic in the<br />
(usually) polymorphic exon 2. According to RT-PCR, RT1-Db2 is expressed in rat<br />
lymphocytes and ConA-stimulated lymphoblasts. To compare functional features of RT1-<br />
Db and RT1-Db2, RT-PCR products were cloned and co-expressed with RT1-Da in class<br />
II molecules negative mouse cells. Staining with the Da specific mAb OX-17 revealed<br />
surface expression for both Da comprising molecules, but expression of DaDb1 was<br />
consistently higher than of DaDb2. DaDb1-EYFP and DaDb2-EYFP fusion proteins<br />
differed in their intracellular localization and DaDb2 failed to form SDS-stable dimers,<br />
which may indicate a function for DaDb2 distinct from that of a restriction element in Tcell<br />
antigen recognition. Nevertheless, DaDb1 and DaDb2 presented the bacterial<br />
superantigens SEB and MAS similarly efficient. Interestingly, DaDb2 presented YPM<br />
(Yersinia pseudotuberculosis mitogen) at least 1000 fold better than the “classical“<br />
RT1D (DaDb1). An analysis of Db1/Db2 chimeras allowed a preliminary localization of<br />
the regions of the Db2 molecule involved in high affinity-binding to YPM and decreased<br />
cell surface expression.<br />
*Shared senior authorship of TH and LW.<br />
Correspondence should be adressed to TH (herrmann-t@vim.uni-wuerzburg.de)
Julia Kzhyshkowska, Alexei Gratchev, Liis Krusell, Srinivas Mamidi, Gail Workman, E.<br />
Helene Sage, Sergij Goerdt<br />
Scavenger receptor stabilin-1 links endocytosis and<br />
intracellular sorting in alternatively activated macrophages<br />
The multifunctional scavenger receptor stabilin-1 is expressed on macrophages on<br />
placenta and adult tissues as well as on sinusoidal endothelial cells and macrophages in<br />
lymph nodes. In vitro induction of stabilin-1 on macrophages requires IL-4 and<br />
glucocorticoids. We showed that stabilin-1 mediates endocytosis of extracellular ligands<br />
acLDL, regulator of ECM-remodelling and cell adhesion SPARC, and hormone placental<br />
lactogen (PL). Both SPARC and acLDL are targeted via stabilin-1 for the degradation in<br />
lysosomes. In contrast, a portion of PL escapes degradation and is delivered into novel<br />
storage vesicles. These vesicles do not belong to classical endosomal/lysosomal system.<br />
However these vesicles communicate with trans-Golgi network (TGN). Stored PL can be<br />
secreted back to the extracellular space. Next, we found that stabilin-1 shuttles<br />
between TGN and endosomes. This trafficking pathway is mediated by GGAs, clathrin<br />
adaptors that interact with the DDSLL motif in the cytoplasmic tail of stabilin-1. Here<br />
stabilin-1 is involved in delivery of the novel chitinase-like protein SI-CLP from TGN to<br />
the endosomal/lysosomal compartment.<br />
SI-CLP was identified by us as a binding partner for stabilin-1 in yeast two-hybrid<br />
screening. SI-CLP contains a conservative lectin-type Glyco_18 domain, which lacks<br />
enzymatic activity, similarly to YKL-40 and Ym1/Ym2. YKL-40 and Ym1/Ym2 are<br />
secreted by macrophages, possess cytokine activity and are associated with Th2-type<br />
inflammations and allergies. We demonstrated that endogenous SI-CLP is<br />
overexpressed in human macrophages stimulated with IL-4 and dexamethasone and is<br />
transported via stabilin-1 from biosynthetic to the secretory pathway. High levels of SI-<br />
CLP were detected in bronchoalveolar lavage samples from patients with chronic<br />
bronchitis.<br />
We propose that alternatively-activated macrophages use stabilin-1 1) to coordinate<br />
ECM remodeling, angiogenesis, and tissue turnover via endocytosis and degradation of<br />
SPARC; 2) to regulate extracellular concentration of PL in placenta; 3) to regulate<br />
delivery of chitinase-like protein SI-CLP into the secretory pathway.
Tim Sparwasser, Andrea Hartl, Katharina Lahl, Heinz Fehrenbach, Holger Garn, Harald<br />
Renz, Hermann Wagner<br />
Selective depletion of Foxp3+ cells in DEREG mice allows<br />
functional analysis of regulatory T cells during experimental<br />
allergic airway inflammation<br />
Naturally occurring CD25+CD4+ regulatory T cells (Tregs) are currently intensively<br />
characterized because of their major importance in inhibiting the development of<br />
autoimmunity and allergy. Originally, CD4+ Tregs were identified exclusively by the<br />
constitutive expression of CD25, and many in vivo experiments have been performed<br />
using depleting antibodies directed against CD25. However, both the existence of CD25-<br />
Tregs, especially within peripheral tissues, as well as the expression of CD25 on<br />
activated conventional T cells, limits the interpretation of data obtained by the use of<br />
anti-CD25 depleting antibodies. The most specific Treg marker is the forkhead box<br />
transcription factor Foxp3, which has been shown to be expressed specifically in murine<br />
CD4+ Tregs. To address the question of the in vivo role of Tregs in asthma<br />
pathogenesis, we have generated bacterial artificial chromosome (BAC)-transgenic mice<br />
named DEREG (depletion of regulatory T cells), expressing a diphtheria toxin receptor<br />
(DTR) eGFP fusion protein under the control of the foxp3 locus allowing both detection<br />
and inducible depletion of Foxp3+ Tregs. Similar frequencies and total numbers of CD25<br />
+CD4+ Tregs, and comparable Foxp3 levels and suppressor function were observed<br />
between DEREG and WT mice. Histological and flow cytometry analysis of spleen, lymph<br />
node, and thymus revealed that the DTR-eGFP BAC transgene is specifically expressed<br />
in Foxp3+CD4+ T cells. The injection of diphtheria toxin led to at least 90% depletion of<br />
Foxp3+ Tregs and dramatically increased immune responses (DTH, OVA-immunization).<br />
Using a model of acute ovalbumin (OVA)-induced allergic airway inflammation we can<br />
demonstrate that depletion of Tregs during sensitization causes dramatically increased<br />
Th2 pathology. Since our model for the first time allows specific depletion of Tregs<br />
during acute immune responses without affecting activated effector T cells, our data<br />
obtained in DEREG mice will shed light on the key cellular players involved in the<br />
suppression of allergic airway inflammation.
Ulrike Schleicher, Jan Liese, Claudia Kurzmann, Christian Bogdan<br />
Selective requirement of Toll-like receptor 9 for the activation<br />
of natural killer cells in cutaneous and visceral leishmaniasis<br />
NK cells contribute to the control of intracellular parasites including Leishmania. In vitro<br />
studies suggested that the activation of NK cells depends on their interaction with<br />
plasmacytoid (pDC) or myeloid dendritic cells (mDC) that sense the pathogen and<br />
generate NK cell-stimulatory signals. Here, we investigated the cell types, pattern<br />
recognition receptors and cytokines that are required for NK cell activation during<br />
Leishmania infections in vivo.<br />
Toll-like receptor (TLR) 9 was indispensable for NK cell IFN-gamma production and<br />
cytotoxicity in both cutaneous (L. major) and visceral leishmaniasis (L. infantum). In<br />
vitro, plasmacytoid dendritic cells (pDCs) released both interferon (IFN)-alpha/beta and<br />
interleukin (IL)-12 in response to Leishmania promastigotes in a TLR9-dependent<br />
manner, although they did not internalize the parasites. In contrast, myeloid dendritic<br />
cells (mDCs) phagocytosed the parasites and produced high amounts of IL-12, but not<br />
IFN-alpha/beta, in the presence of TLR9. Studies with IL-12- or IFN-alpha/beta receptor<br />
(IFNAR)-knockout mice revealed that IFNAR-deficiency only slightly reduced the L.<br />
infantum-induced IFN-gamma production by NK cells, whereas NK cell cytotoxicity and<br />
IFN-gamma secretion was abolished in IL-12-deficient mice. The latter phenotype was<br />
also observed in mDC-depleted mice, whereas NK cell activation in response to L.<br />
infantum was maintained after depletion of pDCs. Intracellular cytokine staining showed<br />
that mDCs represent the source of IL-12 during the early phase of Leishmania infection.<br />
TLR9-deficient mice lacked IL-12 expression by mDCs after infection with L. major or L.<br />
infantum. Thus, NK cell priming in vivo in response to Leishmania parasites is strictly<br />
dependent on mDCs, which sense the pathogen via TLR9 and subsequently secrete IL-<br />
12 to stimulate the NK cells.
Ulrich Salzer, Jennifer Birmelin, Chiara Bacchelli, Torsten Witte, Ulrike Buchegger-<br />
Podbielski, Rita Rzepka, H Bobby Gaspar, Reinhold E Schmidt, Inga Melchers§, Bodo<br />
Grimbacher§<br />
Sequence analysis of TNFRSF13b/TACI in patients with<br />
Systemic Lupus Erythematosus<br />
Background: BAFF and APRIL and their receptors BAFFR, BCMA and TACI are involved in<br />
the regulation of B cell homeostasis and differentiation. BAFF overexpression leads to<br />
systemic lupus erythematosus (SLE) like symptoms in mice and elevated BAFF levels<br />
have been observed in human SLE and mouse models for SLE. Furthermore, genetic<br />
inactivation of TACI in mice results in a SLE-like phenotype.<br />
Methods/Results: Based on our recent finding that TACI is mutated in patients with<br />
common variable immunodeficiency, of whom more than 30% suffer from autoimmune<br />
conditions, we analyzed TACI by heteroduplex analysis and subsequent sequencing in<br />
humans with SLE.<br />
Sequence analysis of TNFRSF13b/TACI in 119 unrelated SLE patients revealed four<br />
variants: R20C in exon 1, R72H in exon3, the silent variation c.327 G>A in exon 3, and<br />
A181E in exon 4.<br />
Conclusions: No significant association with any of these variants was found, when<br />
compared to the frequencies of the variants in a healthy control cohort. Furthermore the<br />
mutated alleles R20C and R72H did not segregate with the SLE phenotype in familial<br />
cases of SLE. Thus, our evaluation of the coding region of TNFRSF13b/TACI did not<br />
reveal any deleterious or disease associated mutations.<br />
Supported by EU SP23-CT-2005-006411; NIH/NIAID: USIDnet grant # NO1-A1-30070<br />
(B. G.), BMBF KN Rheuma C2.12 (T.W. and R.E.S), the BMBF KN Rheumatism 01 GI<br />
9949/C2.13 (I. M.).<br />
§contributed equally
Zeinab Abdullah, Tomo Saric, Hamid Kashkar, Nikola Baschuk, Benjamin<br />
Yazdanpanah, Bernd K. Fleischmann, Jürgen Hescheler, Martin Krönke, Olaf Utermöhlen<br />
Serpin-6 expression protects embryonic stem cells from lysis<br />
by antigen-specific CTL<br />
The immune response to embryonic stem (ES) cells is still poorly understood. In this<br />
study, we addressed the adaptive cellular immune response to undifferentiated and<br />
differentiated ES cells infected with lymphocytic choriomeningitis virus (LCMV), a<br />
vertically transmitted pathogen in mice and humans. In contrast to the prevailing view,<br />
we found that undifferentiated and differentiated murine ES cells express MHC class I<br />
molecules, although at low levels. When cocultured with LCMV-infected ES cells,<br />
syngeneic but not allogeneic LCMV-specific CTL secrete IFN-gamma. Strikingly, LCMVspecific<br />
CTL do not efficiently kill LCMV-infected ES cells. ES cells showed high-level<br />
expression of the serine protease inhibitor 6, an endogenous inhibitor of the CTLderived<br />
cytotoxic effector molecule granzyme B. Down-regulation of serpin-6 by RNA<br />
interference sensitized ES cells for CTL-induced cell death. The results of this study<br />
suggest that LCMV-infected murine ES cells present viral Ags and are recognized by<br />
LCMV-specific CTL in a MHC class I-restricted manner, yet resist CTL-mediated lysis<br />
through high-level expression of serine protease inhibitor 6
Michael Conzelmann, Michael Rieger, Michael Hess, Ulrich Strohhaecker, Axel Benner,<br />
Ute Hegenbart, Anthony D. Ho, Peter Dreger, Thomas Luft<br />
Serum cytokeratin-18 fragments as sensitive marker of<br />
epithelial apoptosis in intestinal and hepatic graft-versushost<br />
disease<br />
Graft-versus-host disease (GvHD) is a heterogenous group of syndromes with<br />
autoimmune-like characteristics that represents the main complication of allogeneic<br />
stem cell transplantation (SCT). However, diagnosis of GvHD and evaluation of response<br />
to immunosuppressive treatment is sometimes difficult. Since apoptosis is the<br />
histopathological hallmark in GvHD, we investigated whether the caspase-cleaved neoepitope<br />
of cytokeratin 18 fragments (CK18F) might be a serum marker for ongoing<br />
GvHD-induced target organ destruction.<br />
Serum CK18F kinetics was monitored by M30 antibody-based ELISA in 50 patients who<br />
fulfilled histopathological and/or clinical criteria diagnostic for GvHD. Both intestinal and<br />
hepatic GvHD were consistently associated with significant elevations of CK18F levels<br />
over baseline. Responses of GvHD to immunosuppressive therapy were paralleled by<br />
CK18F decreases, whereas resistant GvHD was characterized by persistent CK18F rises.<br />
In contrast, markers of T cell activation such as sCD25 responded to steroid therapy<br />
irrespective of clinical responses.<br />
Clinical conditions that might represent relevant differential diagnoses, such as toxic<br />
mucositis, non-complicated, infection-related diarrhea and veno-occlusive disease were<br />
not associated with CK18F elevations.<br />
In conclusion, CK18F monitoring provides a biomarker for quantitative assessment of<br />
GvHD-associated apoptotic activity in intestinal and hepatic GvHD which may help to<br />
distinguish active GvHD from GvHD-unrelated conditions with similar symptoms, and to<br />
monitor response to immunosuppressive treatment. Prospective studies are warranted<br />
to evaluate how CK18F may assist in diagnosis, grading, and treatment guidance of<br />
GvHD.
Pia Herzberger, Corinna Siegel, Christine Skerka, Volker Fingerle, Ulrike Schulte-<br />
Spechtel, Bettina Wilske, Volker Brade, Reinhard Wallich, Peter F. Zipfel, Peter Kraiczy<br />
Serum resistance of human pathogenic Borrelia spielmanii sp.<br />
nov. correlates with binding of complement regulators factor<br />
H and FHL-1<br />
B. spielmanii sp. nov. has recently been identified as a novel human pathogenic<br />
genospecies that cause Lyme disease in Europe. In order to elucidate immune evasion<br />
mechanisms of B. spielmanii as a means of evading the innate immune system we have<br />
compared the ability of isolates obtained from Lyme disease patients and tick isolate PC-<br />
Eq17 to escape from complement-mediated bacteriolysis. Applying a growth inhibition<br />
assay, we show that four B. spielmanii isolates, including PC-Eq17, are serum-resistant<br />
whereas a single isolate, PMew, was more sensitive to complement-mediated lysis. All<br />
isolates activate complement in vitro as demonstrated by covalent attachment of C3 ,<br />
however, deposition of later activation products C6 and C5b-9 was restricted to the<br />
moderately serum-resistant isolate PMew and serum-sensitive B. garinii isolate G1.<br />
Furthermore, serum adsorption experiments revealed that all B. spielmanii isolates<br />
acquire the host alternative pathway regulators factor H and FHL-1 from human serum.<br />
Both complement regulators retain their factor I-mediated C3b inactivation activity<br />
when bound to spirochetes. In addition, two distinct factor H and FHL-1 binding<br />
proteins, BsCRASP-1 and BsCRASP-2, were identified that are approximately 23 to 25<br />
kDa in size. A further factor H-binding protein, BsCRASP-3, was exclusively found in the<br />
tick isolate PC-Eq17. In conclusion, this is the first report describing an immune evasion<br />
mechanism utilized by B. spielmanii sp. nov. and demonstrates capture of human<br />
immune regulators to resist complement-mediated killing. This work was funded by the<br />
Deutsche Forschungsgemeinschaft DFG, Project Kr3383/1-1 and Wa533/7-1.
Anette J. Bauer, Katharina M. Huster, Verena Labi, Roland M. Schmid, Dirk H. Busch,<br />
Andreas Villunger, Georg Häcker<br />
Several members of the mitochondrial apoptosis pathway<br />
control activated T cell death to terminate the T cell immune<br />
response<br />
Stimulation of APC by adjuvants is an important step in development of an effective<br />
immune response through the upregulation of costimulatory molecules and the release<br />
of cytokines. Previous work has shown that stimulation of dendritic cells by adjuvant<br />
can reduce cell death of activated T cells at the end of the response. Furthermore, it has<br />
been shown that this cell death requires the pro-apoptotic protein Bim and is blocked by<br />
Bcl-2 expression in T cells. In this study we investigated the interrelations of proteins<br />
implicated in the regulation of this activated T cell death. TLR ligands present during<br />
stimulation of spleen cell populations or in vivo prolonged the survival of activated T<br />
cells, an activity that was mimicked by DC-derived factors or the presence of IL-1, IL-7<br />
or IL-15. Bcl-2-transgenic T cells showed better survival than bim-/--cells, and DCderived<br />
factors increased the survival of bim-/--T cells, indicating a Bim-independent<br />
pathway. This pathway was found largely to be regulated by the pro-apoptotic Bcl-2<br />
protein Puma, possibly with a marginal contribution from Noxa. The NF-kappa B<br />
regulator Bcl-3 was involved upstream of the activity of Bim and had an anti-apoptotic<br />
effect. Bim and Puma appeared to be regulated by similar molecular activation<br />
pathways as DC-derived cytokines were able to delay the activation of both. Expression<br />
analysis showed a strong divergence of Bim expression and –activity, strongly<br />
suggesting post-translational regulation of Bim. Additional experiments examining<br />
function of antigen specific Bcl-2 transgenic T cells during Listeria infection in vivo show<br />
that Bcl-2 not only blocks death but also conserves function of T cells at the end of the<br />
immune reaction. Thus, apoptosis of activated T cells at the end of an acute immune<br />
response is a process regulated by members of the mitochondrial apoptosis pathway<br />
that is instrumental in switching off the immune response.
Jessica Prüßmeyer, Rory Koenen, Line Fraemohs, Christian Weber, Andreas Ludwig<br />
SHEDDING OF THE JUNCTIONAL ADHESION MOLECULE JAM-A<br />
BY THE DISINTEGRIN AND METALLOPROTEINASE ADAM17<br />
REGULATES NEUTROPHIL TRANSMIGRATION<br />
Junctional Adhesion Molecule-A (JAM-A) is a transmembrane adhesive protein of the<br />
IgG superfamily expressed at endothelial and epithelial junctions and on leukocytes.<br />
JAM-A participates in the organization of tight junctions and has been implicated in<br />
adhesion and transendothelial migration of neutrophils or mononuclear cells. Here we<br />
demonstrate that cultured endothelial cells as well as the cell lines HEK293 and ECV304<br />
release considerable amounts of soluble JAM-A ectodomain detectable as 35 kDa protein<br />
by Western Blotting. This release is enhanced by treatment with the phorbolester PMA<br />
and suppressed by metalloproteinase inhibitors. Both, enhancement or inhibition of<br />
release are associated with the downregulation or accumulation of surface expressed<br />
JAM-A, respectively, as demonstrated by FACS analysis. Specific inhibitors allowing to<br />
distinguish the disintgrin-like metalloproteinases ADAM10 and ADAM17 suggest that<br />
constitutive and PMA-induced release are preferentially mediated by proteolytic<br />
shedding via the activity of ADAM17. These findings were corroborated in loss of<br />
function and gain of function experiments by downregulation or overexpression of this<br />
protease. Functionally, treatment of endothelial cells with PMA or ADAM10/17 inhibitors<br />
was associated with suppressed IL-8-induced neutrophil transmigration. Pretreatment of<br />
neutrophils with soluble JAM-A considerably reduced transmigration, whereas<br />
pretreatment of endothelial cells or ECV304 cells slightly enhanced neutrophil<br />
transmigration. These data suggest a dual role of ADAM17-mediated JAM-A shedding:<br />
at the endothelial cell surface shedding would release a soluble antagonist interacting<br />
with adhesion molecules on neutrophils and thereby downregulate transmigration,<br />
whereas within the endothelial junctions shedding may be required to facilitate<br />
transmigration of neutrophils.
Oliver Frey, Lisa Bruns, Andreas Reichel, Lars Morawietz, Thomas Kamradt<br />
Short-term depletion of regulatory T cells converts selflimiting<br />
arthritis into a chronic disease<br />
We have established a new arthritis model, induced by systemic immunization of nontransgenic<br />
mice with the ubiquitous autoantigen glucose-6-phosphate isomerase. The<br />
disease is dependent on B and T cells and is normally self limiting, leading to resolution<br />
of inflammation between day 30-40 after disease induction. We hypothesized that<br />
naturally occurring regulatory T cell (Treg) might be important for the resolution of the<br />
disease and therefore investigated their role.<br />
Treg cells were depleted by intraperitoneal injection of an anti-CD25-antibody. Arthritis<br />
was induced by immunization of mice with recombinant G6PI. The severity of the<br />
disease was assessed clinically on 0-3 point score for each limb and by histology at the<br />
end of the experiments. The degree of Treg-depletion (FoxP3 staining) and cytokine<br />
production was assessed by flow cytometry.<br />
Injection of anti-CD25 antibody on days –11 and –8 before immunization resulted in a<br />
transient reduction of Treg, which returned to base-line levels on the clinical peak of the<br />
disease (d 12-15 after disease induction). This transient depletion profoundly affected<br />
the disease course, resulting in chronic-destructive arthritis over the whole follow-up<br />
period (80 days) with active inflammation and joint destruction, as evidenced by<br />
histological examination. This exacerbated arthritis was accompanied by increased<br />
numbers of IL-17-producing T cells and T cell proliferation.<br />
We conclude from our experiments that Treg do not actively participate in the resolution<br />
of arthritis, since the disease is still chronifies, when Treg cell number are fully<br />
normalized. Our data show that they act rather in early stages of disease development<br />
by controlling the extent of T cell activation.
Wenhan Li, Stefan Schultz, Nicolas Geis, Michael Kirschfink<br />
shRNA-mediated knockdown of CD59 sensitises tumour cells<br />
to complement attack and inhibits proliferation<br />
Complement-resistance of neoplastic cells, often caused by overexpression of one or<br />
more membrane complement regulatory proteins (mCRPs) is considered a main<br />
hindrance for an effective antibody-based immunotherapy of cancer. We have<br />
previously reported that inhibition or transient down-regulation of mCRPs sensitises<br />
tumour cells for complement-mediated cytotoxicity (CDC).<br />
We here describe the effect of stable knockdown of CD59 expression in prostate<br />
carcinoma cells. Du145 and PC-3 cells were transfected with a pSilencer 4.1CMV neo<br />
vector encoding hairpin siRNA targeting CD59 for stable down-regulation of CD59<br />
expression. After 4 weeks selection with geneticin, real-time PCR indicated that mRNA<br />
levels of CD59 were significantly reduced, going along with decreased CD59 protein<br />
levels on transfected cells. CD59 deficient prostate tumor cells became sensitive to<br />
complement-mediated cytolysis. Unexpectedly, we also observed a marked inhibition of<br />
proliferation of transfected tumor cells if compared to control shRNA-transfected cells .<br />
It appears that long-term down-regulation of CD59 expression by siRNA not only<br />
increases the sensitivity of prostate carcinoma cells to complement attack but may also<br />
exert a therapeutically relevant effect on cancer cell proliferation.<br />
-->
David Frommhold, Andreas Ludwig, M. Gabi Bixel, Alexander Zarbock, Annette G.<br />
Beck-Sickinger, Alma Zernecke, Christian Weber, Dietmar Vestweber, Klaus Ley, Markus<br />
Sperandio<br />
Sialyltransferase ST3Gal-IV interferes with chemokinedependent<br />
leukocyte adhesion during inflammation<br />
Recent in-vitro findings have demonstrated a role of sialylation for chemokine receptor<br />
binding to its ligand. This prompted us to investigate chemokine-induced leukocyte<br />
adhesion in inflamed post-capillary cremaster muscle venules of α2,3 sialyltransferase<br />
(ST3Gal-IV)-deficient mice. We found a marked reduction of leukocyte adhesion in<br />
unstimulated cremaster muscle venules upon injection of keratinocyte-derived<br />
chemokine (KC), which interacts with chemokine receptor CXCR2. In TNF-α-treated<br />
cremaster muscle venules where leukocyte adhesion depends on the overlapping<br />
function of CXCR2 and E-selectin, leukocyte adhesion was significantly decreased in<br />
ST3Gal-IV-/- mice in those experiments where E-selectin function was blocked.<br />
Additional in vitro assays revealed that KC-binding to CXCR-2 on isolated ST3Gal-IV-/-<br />
neutrophils was markedly reduced. Furthermore, KC-mediated adhesion of ST3Gal-IV-/-<br />
leukocytes at physiological flow conditions was significantly reduced as well as<br />
transendothelial migration of ST3Gal-IV-/- leukocytes in response to KC. In human<br />
neutrophils, enzymatic desialylation led to decreased binding of CXCR-2 ligands to<br />
CXCR-2 and diminished neutrophil degranulation in response to these chemokines.<br />
Taken together, our results provide substantial evidence that sialylation by ST3Gal-IV<br />
significantly contributes to CXCR2-mediated leukocyte functions and is required for<br />
leukocyte arrest and extravasation during inflammation in vivo.
Andrea Kießling, Juliane Ladhoff, Mir Farzin Mashreghi, Sabine Brösel, Elke<br />
Effenberger, Hans-Dieter Volk, Martina Seifert<br />
Silencing of IFNγ-receptor by siRNA inhibits MHC class II<br />
upregulation on endothelial cells<br />
Introduction: Immunogenicity of allogeneic endothelial cells (EC) is determined by their<br />
constitutive expression of Major Histocompatibility Complex (MHC) class I. In the<br />
setting of transplantation the proinflammatory cytokine interferon-γ (IFNγ) plays a<br />
pivotal role as a mediator of the rejection process by enhancing MHC class I and<br />
inducing MHC class II expression on EC. Silencing of IFNγ-receptor chain 1 (IFNγ-R1) by<br />
short interfering RNA (siRNA) might reduce the IFNγ-mediated MHC upregulation on the<br />
cellular graft, thereby diminishing allorecognition mechanisms.<br />
Methods: Primary rat aortic EC were transfected in vitro with own designed siRNA (1-<br />
100 nM) directed against rat IFNγ-R1 mRNA. Subsequently, cells were stimulated with<br />
10 ng/ml IFNγ for 24 hours. Expression levels of IFNγ-R1 and IFNγ-R2 mRNA were<br />
determined by quantitative RT-PCR. Surface expression patterns (e.g. MHC I, MHC II,<br />
VCAM-1) were analyzed flow cytometrically in comparison to control siRNA- and nontransfected<br />
cells.<br />
Results: IFNγ-R1 siRNA was capable to decrease mRNA expression level of IFNγ-R1, but<br />
had no effect on IFNγ-R2 expression. In particular, specific IFNγ-R1 siRNA treatment<br />
effectively reduced MHC class II induction after IFNγ stimulation to approximately 50 %,<br />
whereas control siRNA or non-transfected cells displayed high MHC class II levels.<br />
Application of 5 nM siRNA resulted in optimal inhibitory effects and simultaneously<br />
lowered activation of EC by the transfection process itself.<br />
Conclusions: Silencing of IFNγ-R1 by siRNA is a suitable tool to knock down the MHC<br />
class II expression on EC under IFNγ exposure. This might be a useful application for<br />
cell therapeutic treatment in an allogeneic transplantation setting.
Verena Boschert, Anja Krippner-Heidenreich, Ingo Grunwald, Marie Kühnle, Klaus<br />
Pfizenmaier, Peter Scheurich<br />
Single chain TNF, a covalently stabilized TNF derivate<br />
The cytokine tumor necrosis factor has a potential as an antitumoral therapeutic agent.<br />
Bioactive TNF forms a homotrimer which, at low concentrations, dissociates into nonfunctional<br />
monomers. The idea of single chain TNF (scTNF) is to covalently stabilize the<br />
trimer with two short linker peptides. This leads to a protein with a 6 fold higher affinity<br />
to its receptors (TNFR1 and TNFR2), full bioactivity and a higher stability in vitro and in<br />
vivo when compared to soluble TNF. Therefore, single chain TNF represents an<br />
interesting molecule for drug design.<br />
We have generated scTNFs selective for TNFR1 (scTNF[R1]3) and TNFR2 (scTNF[R2]3)<br />
by insertion of mutations at the receptor binding sites. Because of the covalent linkage<br />
of the TNF monomers it is also possible to produce scTNF derivates with mixed<br />
selectivities (scTNF R1[R2]2 and scTNF [R1]2R2). We are currently using these<br />
derivates to investigate the stoichiometry of ligand/receptor interaction.
Friedrich Koch-Nolte, Jan Reyelt, Janusz Wesolowski, Kristina Burkert, Nicole<br />
Schwarz, Felix Scheuplein, Friedrich Haag, Vanina Alzogaray, Fernando Goldbaum<br />
Single domain antibodies from llama effectively and<br />
specifically block an immunoregulatory T cell surface enzyme<br />
in vivo<br />
T cells express a flurry of ecto-enzymes that have their active sites exposed in the<br />
extracellular environment. These enzymes play important roles in cell trafficking,<br />
inflammation and apoptosis (1). The goal of our study was to develop a tool for blocking<br />
the function of a specific T cell ecto-enzyme in vivo. ART2.2 is a toxin-related ectoenzyme<br />
that transfers the ADP-ribose moiety from NAD onto other cell surface proteins.<br />
ART2.2 induces T cell death by activating the cytolytic P2X7 purinoceptor via ADPribosylation<br />
(2). We successfully generated ART2.2-blocking single domain antibodies<br />
from an immunized llama (3). The variable domain of heavy-chain antibodies (VHH<br />
domain) represents the smallest known antigen-binding unit generated by adaptive<br />
immune responses. Their long CDR3 endows VHH domains with the extraordinary<br />
capacity to extend into and block molecular clefts. Following intravenous injection, the<br />
ART2.2-specific VHH domainss effectively shut-off the enzymatic and cytotoxic activities<br />
of ART2.2 in lymphatic organs. This blockade was highly specific (blocking ART2.2 but<br />
not the related enzymes ART1 or ART2.1), rapid (within 15 minutes after injection) and<br />
reversible (24 hours after injection). Our findings constitute a proof of principle that<br />
opens up a new avenue for targeting T cell ecto-enymes in vivo.<br />
1) Salmi & Jalkanen Nat Rev Immunol 5: 760-771 (2005)<br />
2) Seman, et al. Immunity 19: 571-82 (2003)<br />
3) Koch-Nolte, et al. FASEB J in press (2007)
Andrej Mantei, Sascha Rutz, Ioanna Andreou, Martin Weber, Alexander Scheffold<br />
siRNA-mediated gene knock-down in primary mouse T cells<br />
RNA interference (RNAi)-mediated knock-down of target genes represents a powerful<br />
approach for functional genomics as well as therapeutic applications. However, for T<br />
lymphocytes, central regulators of immunity and immunopathologies, the application of<br />
RNAi is limited since both, the RNAi machinery itself as well as the transfection<br />
technologies to introduce siRNA into primary lymphocytes are inefficient.<br />
Using modified electroporation (Nucleofection), we established siRNA transfection of<br />
primary murine T lymphocytes reaching about 90-100% transfection and knock-down<br />
efficiency with minimal impairment of cellular function. However, gene knockdown is<br />
only short-lived (24-48 hours) with conventional siRNA whereas persisting for up to 2<br />
weeks with chemically stabilized siRNA. Our data demonstrate that RNAi is fully<br />
functional in primary T lymphocytes but critically depends on siRNA stability within the<br />
cells. Targeting CD4 and the transcription factor GATA3 we show that this new approach<br />
allows functional gene analysis in primary T lymphocyte activation and differentiation in<br />
vitro as well as in vivo.
Uwe Koelsch, Burkhart Schraven, Luca Simeoni<br />
SIT and TRIM determine T-cell fate in the thymus<br />
Thymic selection is a tightly regulated developmental process essential for establishing<br />
central tolerance. Based upon experimental evidence, the intensity of TCR-mediated<br />
signaling is a key factor for determining cell fate in the thymus. It is widely accepted<br />
that low-intensity signals result in positive selection, whereas high-intensity signals turn<br />
on the negative selection program. Transmembrane adaptor proteins (TRAPs) have<br />
been demonstrated to be important regulators of T-cell activation. However, little is<br />
known on their role during T-cell development. We have previously shown that the<br />
transmembrane adaptor SIT regulates positive selection, whereas mice lacking the Tcell<br />
receptor interacting molecule (TRIM) showed normal T-cell development. As SIT<br />
and TRIM represent two related TRAPs strongly expressed in thymocytes, we have<br />
explored the possibility that they may share redundant functions during thymocyte<br />
selection. We found that SIT and TRIM cooperatively regulate TCR signaling potential,<br />
thus in turn influencing the outcomes of selection. Indeed, loss of both SIT and TRIM<br />
resulted in the upregulation of CD5, CD69 and TCRbeta expression, strong MAPK<br />
activation and enhanced positive selection. Moreover, by crossing SIT/TRIM doubledeficient<br />
mice onto transgenic mice carrying TCRs with different avidity/affinity, we<br />
found profound alterations of T-cell development. Unexpectedly, loss of SIT and TRIM<br />
resulted in a shift from non selection to positive selection whereas positive selection was<br />
converted to negative selection. In summary, we have demonstrated that SIT and TRIM<br />
have the striking ability to regulate cell fate of developing thymocytes, thus identifying<br />
TRAPs as essential regulators of central tolerance.
Anja Hänsel, Michael Meurer, Ernst Peter Rieber, Knut Schäkel<br />
Slan-dendritic cells (6-Sulfo LacNAc-expressing dendritic<br />
cells) in contrast to CD1c+ dendritic cells express high levels<br />
of functional TLR7- and TLR8- receptors<br />
The family of Toll like receptors (TLR) enables the recognition of specific microbial<br />
components widely expressed in bacteria, fungi, protozoa and viruses. Individual<br />
dendritic cell (DC) subtypes largely differ in their repertoire of expressed TLR which<br />
critically determines their functional role during the initiation of specific immune<br />
responses against individual pathogens. We previously described a highly<br />
proinflammatory type of myeloid DC called slanDC (6-Sulfo LacNAc-expressing dendritic<br />
cells) that produced particularly high levels of TNF-a as well as IL-12 in response to<br />
stimulation by the bacterial TLR4-ligand lipopolysaccharide. However, the exact<br />
expression pattern of TLR by slanDC remained unknown. Here we demonstrate that<br />
slanDC express high mRNA encoding for TLR2, 4, -5, -6, -7 and -8 as revealed by<br />
qualitative and quantitative RT-PCR. In contrast, CD1c+ myeloid DC express TLR3, but<br />
failed to express significant levels of TLR2, -4, -6 and -8, and plasmacytoid DC (pDC)<br />
expressed preferentially TLR7 and -9. In our functional studies we focussed on the<br />
relevance of the TLR7 and -8 expression by slanDC, whose natural ligands are single<br />
stranded viral DNA. When slanDC were stimulated with R848, a ligand of TLR7 and TLR8<br />
we observed a by far higher IL-12p40 and IL-12p70 production among slanDC<br />
compared to CD1c+ DC and pDC. Specific ligation of TLR7 (3M-001) and TLR8 (3M-002)<br />
revealed that slanDC, but not other DC subsets, can respond to both ligands with a<br />
strong production of IL-12 as well as TNF-a. The expression of functional TLR7 and TLR8<br />
by slanDC uncovered in this study may have practical implications when designing<br />
therapeutic vaccinations to induce prominent Th1-responses specific for tumor antigens.
Abudula Abulizi, Annika Grabbe, Markus Brechmann, Christian Polaschegg, Nadine<br />
Herrmann, Ingo Goldbeck, Kai Dittmann, Jürgen Wienands<br />
SLP-65 signal transduction requires SH2-mediated membrane<br />
anchoring and a kinase-independent adaptor function of Syk<br />
The SH2 domain-containing leukocyte adaptor protein of 65 kDa (SLP-65) is a substrate<br />
of activated tyrosine kinase Syk downstream of the B cell antigen receptor (BCR). A<br />
main function of SLP-65 is to orchestrate the assembly of Ca 2+ -mobilizing enzymes at<br />
the inner leaflet of the plasma membrane. However, the mechanism of SLP-65<br />
membrane anchoring remains an enigma. We now employed two genetic reconstitution<br />
systems to unravel structural requirements of SLP-65 for BCR-induced Ca 2+<br />
mobilization and subsequent nuclear responses. First, mutational analysis of SLP-65 in<br />
DT40 B cells revealed that its C-terminal SH2 domain controls efficient tyrosine<br />
phosphorylation by the kinase Syk, plasma membrane recruitment, Ca 2+ flux as well as<br />
subsequent NFAT activation for the initiation of gene transcription. Second, restoring<br />
the Ca 2+ response in Jurkat T cell mutants with B cell signaling proteins uncovered a<br />
kinase-independent adaptor function of Syk that is required for linking phosphorylated<br />
SLP-65 to Ca 2+ mobilization. Hence, Syk is upstream as well as downstream of SLP-65.<br />
Moreover, the mechanism by which SLP-65 translocates the Ca 2+ initiation complex to<br />
the plasma membrane in B cells turned out to be fundamentally different to that utilized<br />
by the closely related SLP-76 adaptor in activated T cells.
Bernhard Reis, Tanja Scheikl, Norbert Huser, Bernhard Holzmann, Klaus Pfeffer,<br />
Sandra Beer<br />
SLy-an Orphan Adaptor Protein Displaying a Nonredundant<br />
Role in Lymphocyte Development and Activation<br />
Lymphocyte activation by antigen receptor triggering is an essential step in adaptive<br />
immunity which must be tightly regulated to mount an immune response towards a<br />
pathogen and to avoid autoimmune disorders. Major players in this complex network<br />
are adapter proteins containing characteristic SH2 or SH3 domains which are known to<br />
mediate protein protein interactions.<br />
SH3 and SAM domain containing protein expressed in lymphocytes (SLy) is a member<br />
of a distinct family of putative adapter and/or scaffold proteins highly conserved in<br />
mammals. SLy is exclusively expressed in lymphocytes and has been shown to be<br />
phosphorylated specifically upon antigen receptor engagement.<br />
To investigate the physiological functions of SLy, sly-mutant mice expressing a<br />
truncated protein lacking the nuclear localisation signal and the phosphorylation site<br />
(SLYD/D) have been generated by our group. SlyD/D mice exhibit reduced lymphoid<br />
organ sizes, diminished marginal zone B cell numbers and severely impaired antibody<br />
responses against T-dependent and -independent antigens. B and T cell proliferation is<br />
attenuated and T cell cytokine production is severely reduced. In vivo, survival of semiidentical<br />
cardiac allografts was substantially prolonged in Sly1D/D mice. However,<br />
global tyrosine and MAP Kinase phosphorylation, Ca2+ flux and transcription factor<br />
activation are normal. We show that SLy wild-type protein specifically shuttles in<br />
between nucleus and cytoplasm after antigen receptor activation. In contrast, SLymutant<br />
protein shuttling is impaired. The signal transduction pathway leading to the<br />
induced translocation of SLy protein and the role of the phosphorylation status and the<br />
nuclear localisation signal are further dissected.<br />
To further characterize the importance of SLy protein and to determine if the truncated<br />
form acts in a dominant negative way, we recently generated full knockout mice<br />
(SLy-/-). Preliminary data will be presented comparing the related phenotype of SLy-/-<br />
mice and SlyD/D mice, respectively.
Max von Holleben, Simone Klöter, Bernhard Reis, Klaus Pfeffer, Sandra Beer<br />
SLy2 represents a new member of a recently identified family<br />
of adapter proteins<br />
A novel putative adapter protein, SH3-lymphocyte protein 2 (SLy2), was found by virtue<br />
of its homology to the previously identified SLy1. The two proteins share over 80%<br />
sequence identity and contain three characteristic domains: an N-terminal nuclear<br />
localization signal (NLS), an SH3 domain, and a C-terminal SAM domain. SH3 and SAM<br />
domains are known to be involved in protein-protein interactions, which in addition to<br />
the absence of an enzymatically active domain, indicates an adapter function for both<br />
SLy1 and SLy2.<br />
Using a polyclonal serum against the N-terminal part we could demonstrate SLy2<br />
expression by western blotting in a broad range of tissues, including bone marrow,<br />
thymus, spleen, lung, brain, liver and ovary. Western Blot analysis of primary murine<br />
lymphocytes indicates an upregulation of SLy2 expression in B lymphocytes, after<br />
stimulation with maturation-/differentiation-, and proliferation-inducing agents, such as<br />
•CD-40, LPS, and IL-4. The high basal level of SLy2 in T lymphocytes did not increase<br />
upon stimulation by •CD3/•CD28.<br />
Preliminary expression-analyses have revealed an increased expression of SLy2 in<br />
human colon-carcinomas, which is in line with previous findings of Claudio and<br />
coworkers, reporting elevated expression-levels of SLy2 (HACS1) in different human<br />
myeloma cell-lines. In marked contrast to its potentially oncogenic role, SLy2<br />
overexpressing Jurkat or SVEC cells exhibit a defect in proliferation.<br />
Interestingly, several reports suggest a connection between an expressional<br />
deregulation of SLy2 in the brain and the appearance of Alzheimer’s disease in human<br />
patients.<br />
With the aim to unravel the impact of SLy2 function for murine development, immune<br />
responses and its role in the emergence of different malignancies, we are currently<br />
generating a SLy2 deficient mouse strain.
Bin Qu, Varsha Pattu, Eva C. Schwarz, Tanja Mayer, Jens Rettig, Markus Hoth<br />
SNARE proteins are involed in cytotoxic granule secretion at<br />
the immunological synapse.<br />
Cytotoxic T lymphocytes (CTLs) exert their cytotoxic activity through the polarized<br />
secretion of cytotoxic granules at the immunological synapse (IS). Soluble NSF<br />
attachment receptor (SNARE) proteins are well-known as the critical effectors of<br />
exocytosis of synaptic granules in neuronal cells. However, the function of SNARE<br />
proteins in exocytosis of cytotoxic granules in CTLs still remains unclear. To address this<br />
question, we established a method to generate human primary CTLs, which is based on<br />
the stimulation of isolated CD8+ T cells with anti-CD3/anti-CD28 antibody coated<br />
beads. The activation state of the CTLs was checked by the expression level of either<br />
CD25 (Interleukin-2 receptor) or CD62L (L-selectin). The cytotoxic capacity of the CTLs<br />
was confirmed by a cytotoxicity assay either on 96-well plates or on single cell level. In<br />
addition, we analyzed the expression pattern of SNARE proteins by conventional RT-<br />
PCR. We found that the expression profile of SNARE proteins is regulated upon CTL<br />
maturation. As we investigated by immunohistochemistry, some but not all SNARE<br />
proteins co-localized with cytotoxic granules at the IS. These results implicate that<br />
SNARE proteins are likely to play important roles in cytotoxic granules serection at the<br />
IS. Our data provide not only a defined method to generate human primary CTLs, but<br />
also an overview of the expression of SNARE proteins in CTLs, which will facilitate the<br />
analysis SNARE protein function in the immune system.
Simon Frank, Leif Sander, Stephan Bischoff, Axel Lorentz<br />
SNARE proteins in mature primary human mast cells<br />
Rationale: Mediator release of mast cells is a key process in allergic reactions. The<br />
events facilitating the fusion of granule and plasma membrane in the course of mast cell<br />
degranulation are not clear. SNARE (Soluble NSF Attachment Protein Receptors)<br />
proteins have been demonstrated to be involved in fusion of opposing membrane layers<br />
during exocytosis. Here, we analyzed expression of SNARE isoforms in human mast<br />
cells and which of them might be crucial for mast cell degranulation. Methods: Human<br />
mast cells were isolated and purified from surgical specimen of intestinal mucosa, using<br />
enzymatic digestion and MACS-technique. SNARE-protein expression was demonstrated<br />
employing RT-PCR and Western blot. Interaction of SNAREs was analyzed by<br />
immunofluorescence and immunoprecipitation. Results: Mature primary human mast<br />
cells express the tSNAREs (=target SNAREs) Stx-1B, Stx-2, Stx-3, Stx-4 and SNAP-23,<br />
but not SNAP-25, and the vSNAREs (=vesicular SNAREs) VAMP-3, VAMP-7, and VAMP-<br />
8. VAMP-2, which has been demonstrated to play a key role in eosinophil exocytosis,<br />
was only expressed at very low levels. SNAP-23 formed complexes with VAMP-7 and<br />
Syntaxin-4. Fluorescence microscopy revealed translocation of both VAMP-7 and VAMP-<br />
8 to the plasma membrane upon stimulation of the cells using 10-6 M iono/PMA.<br />
Conclusion: Human mast cells express a specific pattern of SNARE isoforms which are<br />
able to form stable complexes. SNAREs might play a major role in human mast cell<br />
exocytosis; inhibition of which could represent a novel therapeutical approach in<br />
treatment of allergic disorders.
Manfred Hönig, Ansgar Schulz, Catharina Schütz, Paul Fisch, Tatjana Kersten, Ulrich<br />
Pannicke, Markus Rojewski, Wilhelm Friedrich, Klaus Schwarz<br />
Somatic reversion of lymphocyte subpopulations after HSCT<br />
in a patient with JAK3 deficiency -Evidence for independent<br />
αβ- and γδ- T-lineage stem cells<br />
Spontaneous somatic reversions are reported for various immunodeficiencies (e.g.<br />
IL2RG, ADA, WAS, RAG1, Artemis, LAD1). We report on a 14 year old girl with SCID<br />
due to JAK3 deficiency, who was treated in infancy by HLA-haploidentical<br />
haematopoietic stem cell transplantation (HSCT) without conditioning. A functional<br />
donor T cell system was established. 10 years after HSCT, a small amount (10%) of<br />
autologous T cells was noted in addition to donor T cells in routine chimerism analysis.<br />
Reversions of both compound heterozygous point mutations (NM_000215: c.424C>T,<br />
c.1351C>T leading to NM_00026: p.[Arg142Cys]+[Arg451X] ) to wild type (wt) -<br />
sequence were found in this autologous T-cell population: &alpha&beta-TCR positive T<br />
cells (and NK cells) are reverted to wt-sequence in Exon4, whereas &gamma&delta-TCR<br />
positive T cells are reverted in the other affected allele (Exon9). The TCR-repertoires of<br />
these T-cell populations are oligoclonal. The reversions thus must have occurred before<br />
TCR-rearrangement but after the determination of an &alpha&beta- or &gamma&delta-<br />
T-cell fate. These findings strongly support a non-instructive model for this decision in Tcell<br />
development.
Kevin Thurley, Dorothea Busse, Thomas Höfer<br />
Spatiotemporal Cytokine Dynamics in T-Cell Regulation -<br />
A Mathematical Model of IL-2• •Diffusion and Regulatory T-<br />
Cells• (•Treg•)<br />
Cytokine signalling is crucial for understanding the immune system.• •Up to now,•<br />
•most knowledge has been based on ELISA studies,• •indicating extremely low•<br />
(•picomolar•) •concentrations of cytokines.• •A classic calculation from diffusion-limited<br />
reaction theory• (•Berg and Purcell,• •1972•) •shows that under such conditions,• •a<br />
signal would take hours to occur.• •This raises the question how,• •nevertheless,•<br />
•sensitive cytokine signalling in a noisy environment can be achieved.•<br />
A two-dimensional reaction-diffusion model brings new insights to this question.• •We<br />
consider a well-studied and physiologically important sample system:• •Activation of Thcells<br />
via Interleukin(IL•)•-2• •and immunosuppression by Treg.• •The model reflects<br />
experimentally proven features like autoactivation of Th-cells and low IL-2•<br />
•concentrations in the bulk phase.• •Three major• •results have been obtained so far:•<br />
•Firstly,• •the model predicts high local IL-2• •concentrations at secretion sites,•<br />
•which can possibly be verified experimentally with quantitative secretion assays.•<br />
•Thus,• •this property may serve to justify the model just as to explain effective signals<br />
at low cytokine concentrations.• •Secondly,• •we can show a paracrine signal over<br />
several cell diameters,• •confirming recent experimental results which suggest<br />
paracrine rather than autocrine signalling in T-cell activation (Long and Adler,•<br />
•2006•)•.• •And finally,• •immunosuppression by Treg may be explained by<br />
competitive IL-2• •uptake.•<br />
With the spatiotemporal modeling approach,• •we are able to predict the range of a<br />
cytokine signal in dependence of important system parameters.• •Apparently,•<br />
•inhomogeneities in the cytokine distribution are necessary to explain basic properties<br />
of the complex cytokine network.•
Ariel H. Achtman, Sven Golfier, Martin Lipp<br />
SPHINGOSINE-1-PHOSPHATE RECEPTOR-4 IS MAINLY<br />
EXPRESSED BY LYMPHOID CELLS<br />
Sphingosine-1-phosphate is a bioactive lipid involved in cell migration, survival and<br />
differentiation. It binds to a panel of receptors, called S1P1 to S1P5 , which differ in their<br />
expression patterns. At the mRNA level, it has been shown that S1P4 expression is<br />
restricted to lymphocyte-containing tissues. However, determining protein expression<br />
patterns for S1P4 has been hampered by the lack of sufficiently sensitive antibodies.<br />
Therefore, a reporter gene mouse was generated, in which the S1P4 gene is replaced by<br />
lacZ. The insertion and correct orientation of the gene were confirmed by Southern Blot<br />
and PCR. Back crossing onto the C57BL/6 background was initiated. Expression levels of<br />
the reporter protein β-galactosidase were low but detectable by luminometric analysis. β-<br />
Galactosidase expression was detected in the spleen, bone marrow, lymph nodes,<br />
thymus, peripheral blood and Peyer’s plaques. No expression was seen in the lung,<br />
brain, liver or heart. Further analysis revealed that S1P4 is expressed on white blood<br />
cells but not erythrocytes. In sorted cell populations, B cells and CD4 + and CD8 + T cells<br />
were the main cell populations carrying the gene. More detailed analysis of changes in<br />
S1P 4 expression during active immune responses is currently underway.
Shin-Young Na, Heike Eujen, Catherine Toben, Yi Cao, Anneliese Schimpl, Ralf Gold,<br />
Thomas Hünig<br />
Spontaneous development of CD8-mediated EAE in a new<br />
transgeneic mouse model<br />
Experimental autoimmune encephalomyelitis (EAE) is a T cell-mediated central nervous<br />
system (CNS) autoimmune disease which widely used as an animal model of multiple<br />
sclerosis (MS). Previous studies have used immunization of rodents with myelin<br />
antigens in adjuvants to induce EAE, thereby focussing on pathogenic CD4 cells of the<br />
Th1 and Th17 types. More recently, however, also CD8 T-cells are increasingly receiving<br />
attention as major mediators of autoimmune attack in the human disease itself.<br />
We generated transgenic mice which express the model antigen ovalbumin (OVA) under<br />
an oligodendrocyte (ODC-)-specific MBP promoter. When we crossed these ODC-OVA<br />
transgenic mouse with either OT2 or OT1 transgenic mouse which express transgenic<br />
OVA-specific T-cell receptors (TCR) on CD4 and CD8 cells, respectively, we observed<br />
CD4 T cells are ignorant of OVA in ODC-OVA transgenic mice whereas OT1/ODC-OVA<br />
double transgenic mice develop fulminant EAE. Spontaneous development of severe EAE<br />
affected cerebellum, brainstem, optical nerve and spinal cord. Our initial data suggest<br />
that in this system, initial priming of OT-1 cells occurs within the brain, possibly by the<br />
OVA-expressing oligondenrocytes themselves.<br />
We also tested the ability of a mAb which recognises the OVA-8 peptide bound to the<br />
murine class I molecule H-2Kb (25-D1.16), for its ability to interfere with disease<br />
development and found that at high doses (>200µg/mouse), it was able to prevent<br />
spontaneous EAE development in OT1/ODC-OVA double transgenic mice.
Melinda Czéh, Gerald Willimsky, Thomas Kammertöns, Jehad Charo, Thomas<br />
Blankenstein<br />
Sporadic immunogenic cancer induces cytotoxic T lymphocyte<br />
unresponsiveness against MHC-mismatched targets<br />
Tumor-induced cytotoxic T lymphocyte (CTL) unresponsiveness against unrelated<br />
antigens has been described, but full MHC-mismatched CTL responses have not been<br />
found to be impaired. In a transgenic model of sporadic immunogenic cancer (LoxP-Tag<br />
mice) we investigated CTL responses against foreign peptide antigens and MHCallogeneic<br />
targets. Sporadic tumors in LoxP-Tag mice that express a strong tumorspecific<br />
transplantation rejection antigen (SV40 Tag) rapidly induce CTL tolerance,<br />
which is associated with enhanced serum TGF-β1 concentration and expansion of<br />
immature myeloid cells (Willimsky et al., manuscript in preparation). We show by in<br />
vivo kill assays that tumor bearing mice fail to develop LCMV-gp33-specific CTL<br />
responses. Furthermore, the tumors in H-2b LoxP-Tag mice induced <strong>complete</strong> CTL<br />
unresponsiveness against allogeneic H-2d antigens. Paradoxically, in most tumorbearing<br />
LoxP-Tag mice gp33-expressing or H2-d allogeneic tumor cells did not grew<br />
despite the CTL-unresponsiveness. The reason for this surprising discrepancy is<br />
currently being analyzed. Additionally, data on the function of NK cells in tumor-bearing<br />
LoxP-Tag mice will be presented.
Cornelia Beuter-Gunia, Daniel Degrandi, Sandra Beer, Klaus Pfeffer<br />
SSPII, a new IFN gamma upregulated secretory protein<br />
IFN gamma is a key regulator of a broad range of genes involved in innate immunity.<br />
By analyzing the transcriptome with Affymetrix Array Technology in IFNgamma/<br />
TNFalpha stimulated Ana-1 macrophages a set of uncharacterized transcripts could be<br />
identified.<br />
One IFN gamma induced gene encodes for a 78 aa long protein. Sequence analysis of<br />
the transcript suggests that it contains an N-terminal leader sequence responsible for<br />
targeting to the secretory pathway. In accordance with this observation we could<br />
demonstrate that the His-tagged fusion protein is readily secreted into the cell culture<br />
supernatant after transfection of a His tagged cDNA expression construct in 293T cells.<br />
Real time PCR studies in primary IFN gamma stimulated bone marrow derived<br />
macrophage cells (BMDMO) showed induction of this gene transcript comparable to<br />
classic IFN gamma induced genes such as mGBP2 or iNOS. Moreover, stimulation of<br />
BMDMOs from IFNgR-/- mice indicated that this gene transcript can be directly<br />
upregulated by TLR ligands and IFN type I. Thus, we would suggest to call this protein<br />
sspii, i.e. short secreted protein induced by interferons.<br />
Further in vivo studies revealed that in organs of Listeria monocytogenes and<br />
Toxoplasma gondii infected mice sspii mRNA was upregulated following infection, which<br />
let us to the hypothesis, that sspii contributes to the immune defense against<br />
pathogens.<br />
Sspii is encoded on chromosome 19 of the mouse genome within 3 exons. Gene<br />
targeted ES cells carrying an inactivation of sspii could already be established.<br />
Further in vitro and in vivo experiments as well as the characterisation of a sspii knock<br />
out mouse line will hopefully contribute to the understanding of interferon mediated<br />
immune responses.
Maria Lexberg, Hyun-Dong Chang, Andreas Radbruch<br />
Stability and plasticity of IL-17 producing T cells<br />
Maria Lexberg, Hyun-Dong Chang, Andreas Radbruch<br />
Deutsches Rheumaforschungszentrum, Berlin<br />
Chariteplatz 1<br />
10117 Berlin<br />
Germany<br />
Tel +49-30-28460-600/667<br />
radbruch@drfz.de<br />
lexberg@drfz.de<br />
Classically, effector memory CD4 T cells are divided into distinct lineages on the basis of<br />
their cytokine production profile and the resulting effector function. Recently, a novel<br />
lineage of CD4 T cells has been described which is characterised by the production of IL-<br />
17. These cells have been termed Th17 cells. In several reports, this lineage has been<br />
allocated a role in autoimmune inflammation, therefore it is of importance to determine<br />
the stability of its expression and how it could be modulated to attenuate disease<br />
symptoms.<br />
Our aim is to analyse the induction and maintenance of a functional cytokine memory of<br />
Th17 cells. We are investigating the plasticity and stability of IL-17 memory expression<br />
in relation to the cytokine memory expression of the other lineages.<br />
Both Th1 and Th2 cells proved refractory to IL-17 induction and maintained their<br />
phenotype when stimulated under Th17 inducing conditions in the presence of TGF-beta<br />
and IL-6. To test the stability and plasticity of Th17 cells, we cultured Th17 cells under<br />
Th1 and Th2 inducing conditions and measured cytokine expression. The frequency of<br />
IL-17 expressing cells observed in one or four week old Th17 cells was reduced when<br />
restimulated for just one week in the presence of IL-12 or IL-4, although the<br />
reexpression of IL-17 was increasingly stabilized depending on the duration of<br />
polarization. The plastic nature of IL-17 expression in Th cells reveals that Th17 cells<br />
may need a certain environment in vivo to maintain IL-17 expression and are prone to<br />
regulation by both Th1 and Th2 cells.
Anita Correll, Andrea Tuettenberg, Christian Becker, Jürgen Knop, Helmut Jonuleit<br />
Stage-dependent quantification of regulatory T cells and<br />
antigen-specific T cell responses in melanoma patients<br />
Naturally occurring CD4 + CD25 + regulatory T cells (nTregs) are key players in the<br />
tolerance network. As immunosuppression seems to be one important way by which<br />
tumors succeed in immune escape, nTregs are assumed to play a crucial role in<br />
mechanisms contributing to the development and progression of cancer.<br />
Unlike the murine system, human nTregs cannot be distinguished from conventional T<br />
helper cells easily by markers like CD25 or Foxp3 since both are also expressed by CD4<br />
+ T helper cells upon activation. In this study, we used different marker combinations<br />
for nTreg phenotyping (CD4, CD25, CD127, Foxp3, HLA-DR) for quantitative analysis of<br />
human nTregs in the peripheral blood of stage II-IV melanoma patients. Using this<br />
experimental setting, we observed increased ratios of CD4 + CD25 + Foxp3 + HLA-DR<br />
+ CD127 low Tregs in peripheral blood of melanoma patients compared to healthy<br />
volunteers. Moreover, the relative ratios of nTregs increased with the progression of<br />
disease. Additionally, accumulation of nTregs in progressed melanoma patients also<br />
correlated with a general reduction of T cell responsiveness not only to different tumorassociated<br />
antigens but also to various recall antigens. These observations, the<br />
suppressed T cell reactivity in combination with increased nTreg ratios in patients with<br />
progressive melanoma possibly explain the disappointing success of immunotherapies in<br />
the patients.
Christiane Siewert, Sascha Cording, Markus M. Heimesaat, Oliver Liesenfeld, Stefan<br />
Bereswill, Christoph Loddenkemper, Gunnar Loh, Michael Blaut, Alf Hamann, Jochen<br />
Huehn<br />
Stay with friends: commensal microflora drives expansion of<br />
Foxp3+ Tregs in gut-associated lymphoid tissue<br />
Colitis models have provided compelling evidence for a protective role of Foxp3+CD25<br />
+CD4+ regulatory T cells (Treg) in intestinal homeostasis. Foxp3+ Tregs have been<br />
described as thymus-derived cells, however, more recent studies demonstrate a<br />
significant peripheral turnover. Here we investigated the proliferation of Foxp3+ Tregs<br />
in gut-associated lymphoid tissues (GALT) and whether this process is driven by<br />
commensal microflora.<br />
Germ-free and antibiotics-treated mice were analyzed for frequencies and numbers of<br />
Foxp3+CD4+ T cells. In addition, in vivo proliferation of Foxp3+ Tregs in different<br />
lymphoid compartments was determined by BrdU-incorporation.<br />
In germ-free mice we observed a decreased number of Foxp3+CD4+ T cells in the<br />
GALT. Similarly, depletion of the commensal microflora by antibiotic treatment led to a<br />
reduction of CD4+Foxp3+ cell numbers in the GALT, and, moreover, in spleen and<br />
peripheral lymph nodes. A significantly reduced frequency of cycling BrdU+Foxp3+<br />
Tregs was found in the GALT. Interestingly, homeostatic proliferation was not<br />
compromised in mice deficient for TLR2, the main Toll-like receptor of Tregs.<br />
Stimuli from the commensal microflora of the gut contribute to the generation or<br />
maintenance of Tregs in the mucosal compartments and affect Treg numbers<br />
systemically. Lack of TLR2-mediated effects suggests that other signals, such as<br />
stimulation of Tregs by bacterial antigens, are driving Treg expansion in the mucosal<br />
system. These data show that microbial stimuli critically influence homeostasis of<br />
naturally occurring Foxp3+CD25+CD4+ Tregs and that these cells, which protect<br />
against intestinal inflammation, might not exclusively consist of self-reactive T cells.
Svetlana Karakhanova, Markus Schneider, Johannes Schenkel, Markus Munder<br />
Steroids modulate the T effector cell / TREG / dendritic cell<br />
balance during treatment of Graft-versus-Host Disease.<br />
Allogeneic stem-cell transplantation (allo-SCT) is a potentially curative treatment for<br />
various hematological malignancies. CD4+CD25++ regulatory T cells (TREG) regulate<br />
immune responses and Graft-versus Host Disease (GvHD) after allo-SCT. We have<br />
shown that the initial phase of GvHD correlates with a significant reduction of TREG in<br />
the peripheral blood, while at later stages and especially during intensified<br />
immunosuppressive therapy with steroids increased numbers of TREG appear in the<br />
peripheral blood. We also found a change in phenotype of highly purified, in vitro<br />
expanded CD4+CD25++ cells of patients during steroid medication. In contrast to<br />
expanded TREG from healthy donors or GvHD patients without steroid medication, CD4<br />
+CD25++ sorted cells from steroid-treated patients loose their TREG phenotype and<br />
function in expansion cultures. During in vitro activation, steroids induce an increased<br />
frequency of the CD4+CD25++ population in PBMC from healthy donors and lead to the<br />
acquisition of a TREG like phenotype in CD4+CD25- T cells. Also, CD4+CD25++ cells<br />
are less sensitive to steroid-induced cell death in comparison with conventional T cells.<br />
Finally, dexamethason treatment of different dendritic cell populations leads to the<br />
blockade of cytokine-induced maturation and consecutively to an impaired ability of the<br />
dendritic cells to prime immune responses in CD4+ cells. Our findings suggest that<br />
steroids can influence three major compartments of the immune response (T effector<br />
cells, TREG cells and dendritic cells) simultaneously. This has implications for the<br />
steroid-based treatment of GvHD after SCT.
Marcin Wlodarski, Lukasz Gondek, Zachary Nearman, Sandra Zwinger, Hans-Dieter<br />
Volk, Jaroslaw Maciejewski<br />
Strategies for quantitation and in-vivo tracking of clonal<br />
cytotoxic T-cell responses.<br />
Immune mechanisms are involved in the pathophysiology bone marrow failure<br />
syndromes. Hematopoietic inhibition can result from cytotoxic T cell (CTL) attack<br />
against normal hematopoiesis or reflect immune surveillance reaction directed against<br />
the dysplastic myeloid cell. We used clonally unique T-cell receptor (TCR) variable bchain<br />
(VB) CDR3 regions as markers of pathogenic CTL responses and show that while<br />
marrow failure syndromes are characterized by polyclonal expansions, overexpanded<br />
clones exist in these diseases and can be utilized in investigative setting. To test the<br />
applicability of clonotypic assays, we developed rational molecular methods for the<br />
detection of immunodominant clonotypes in blood and in historic marrow biopsies of 35<br />
aplastic anemia (AA), 37 myelodysplasia (MDS), and 21 paroxysmal nocturnal<br />
hemoglobinuria (PNH) patients, in whom specific CDR3 sequences and clonal sizes were<br />
determined. CTL expansions were detected in 81% and 97% of AA and MDS patients,<br />
respectively. In total, 81 immunodominant signature clonotypes were identified. Based<br />
on the sequence of immunodominant CDR3 clonotypes, we designed quantitative assays<br />
for monitoring corresponding clones, including clonotypic Taqman polymerase chain<br />
reaction (PCR)and clonotype-specific sequencing. No correlation was found between<br />
clonality and disease severity but in patients treated with immunosuppression, truly<br />
pathogenic clones were identified based on the decline that paralleled hematologic<br />
response. We conclude that immunodominant clonotypes associated with marrow failure<br />
may be used to monitor immunosuppressive therapy
Volker Teichgräber*, Surojit Sarkar*, Vandana Kalia, David Masopust, Laurie<br />
Harrington, Antonio Polley, Rafi Ahmed, E. John Wherry<br />
Strength of stimulus and clonal competition impact the rate of<br />
memory CD8 T cell differentiation<br />
The developmental pathways of long-lived memory CD8 T cells and the lineage<br />
relationship between memory T cell subsets remains controversial. While some<br />
studies indicate the two major memory T cell subsets, central memory (TCM) and<br />
effector memory (TEM), are related lineages others suggest that these subsets<br />
arise and are maintained independently of one another. In this study we have<br />
investigated this issue and examined the differentiation of memory CD8 T cell<br />
subsets by tracking the lineage relationships of both endogenous and TCR<br />
transgenic CD8 T cell responses after acute infection. Our data indicates that<br />
TCR transgenic as well as non-transgenic TEM differentiate into TCM in the<br />
absence of antigen. Moreover, the rate of memory CD8 T cell differentiation from<br />
TEM into the self-renewing and long-lived pool of TCM is influenced by signals<br />
received during priming including antigen levels, clonal competition and/or the<br />
duration of infection. While some TEM appear to not progress to TCM, the vast<br />
majority of TCM are derived from TEM. Thus, long-lasting, antigen-independent<br />
CD8 T cell memory results from progressive differentiation of memory CD8 T<br />
cells and the rate of memory T cell differentiation is governed by events occurring<br />
early during T cell priming.<br />
*These authors contributed equally
Sonja Meemboor, Eva Flenner, Alessandra Zingarelli, Martina Bessler, Wiltrud Kalka-<br />
Moll<br />
Streptococcus pneumoniae capsular polysaccharide-mediated<br />
CD4+ T cell-dependent immune response requires IL-6<br />
Abscess formation associated with intra-abdominal sepsis causes severe morbidity and<br />
can be fatal. Induction of abscesses requires the presence of CD4 + T cells. Zwitterionic<br />
polysaccharides (ZPS) represent a novel class of immunomodulatory bacterial antigens<br />
that stimulate CD4 + T cells in a MHC class II-dependent manner. The capsular<br />
polysaccharide Sp1 of Streptococcus pneumoniae serotype 1 is a ZPS model antigen<br />
and possesses a zwitterionic charge motif with free amino and carboxyl groups and<br />
promotes T cell-dependent intraperitoneal abscesses in an experimental murine model.<br />
Mice are administered Sp1 with sterile cecal content adjuvant (SCCA) which reflects the<br />
spillage of colonic contents that occurs during the onset of intra-abdominal sepsis in<br />
humans and aids the pro-inflammatory response. SCCA alone does not induce abscess<br />
formation. In this study we address the role of the pro- and anti-inflammatory acting<br />
cytokine IL-6 during Sp1-induced abscess formation. Macrophages are the most<br />
prevalent antigen-presenting cells in intraperitoneal lavage after intraperitoneal Sp1<br />
challenge and secrete significant amounts of IL-6 as shown by intracellular cytokine<br />
staining. Immunohistochemical analysis of the Sp1-induced abscesses reveal that IL-6<br />
secreting macrophages are incorporated in the abscess capsule. IL-6 induces a dosedependent<br />
CD4 + T lymphocytes migration as demonstrated in migration assays. We<br />
show that mice deficient of IL-6 fail to attract CD4 + T cells into the peritoneal cavity<br />
after Sp1 challenge and to hence develop abscesses. In addition, administration of a<br />
neutralizing Ab specific for IL-6 prevents abscess formation following Sp1 challenge.<br />
These data delineate the requirement of activation of antigen-presenting cells by ZPS<br />
and underscore the essential role of IL-6 in this disease process.
Daniel Schaefer, Anja Janysek, Jürgen Neumann, Norbert Koch<br />
Strong impact of invariant chain on surface expression of HLA-<br />
DQ<br />
Daniel Schaefer, Anja Janysek, Jürgen Neumann and Norbert Koch<br />
Division of Immunobiology, Institute of Genetics, University of Bonn<br />
MHC class II molecules are peptide receptors presenting peptides from extra cellular<br />
antigens on the cell surface of antigen-presenting cells. The peptide receptors are<br />
composed of alpha and beta subunits, which assemble in the ER with invariant chain<br />
(Ii). The HLA class II region encodes alpha and beta subunits of three different isotypes:<br />
DP, DQ and DR. In this study we examined the impact of Ii on intracellular transport<br />
and surface expression of HLA class II isotypes. We inspected various combinations of<br />
alpha and beta chain isotypes for transport and surface expression by employing<br />
western blotting, immunofluorescent staining and FACS-analysis. In contrast to DR and<br />
DP isotypes, surface expression of DQ heterodimers strictly depends on Ii.
Nana Ueffing, Eric Keil, Christian Freund, Ronald Kühne, Klaus Schulze-Osthoff, Ingo<br />
Schmitz<br />
Structural and mutational analyses of c-FLIP R reveal<br />
requirements for DISC-recruitment<br />
c-FLIP proteins are known as potent inhibitors of death receptor-mediated apoptosis by<br />
interfering with caspase-8 activation at the death-inducing signaling complex (DISC).<br />
Among the three human isoforms, c-FLIPlong (55 kDa), c-FLIPshort (26 kDa) and c-FLIPR (25 kDa), the latter one is only poorly characterized. Similar to procaspase-8 and -10<br />
and the viral FLIP protein MC159, FLIP proteins contain two rigidly associated death<br />
effector domains (DEDs) at their N-terminus that are thought to be important for DISC<br />
recruitment. However the precise molecular requirements for DISC formation are<br />
currently unknown. To further investigate the role of c-FLIPR in the regulation of death<br />
receptor pathways, we cloned mouse c-FLIPR from thymus by RT-PCR and found that it<br />
is the only short c-FLIP isoform expressed in mice. Molecular modeling showed that<br />
similar to FADD and MC159, c-FLIPR contains two prominent surface features in each<br />
DED important for protein-protein interactions, namely a hydrophobic patch and a<br />
charge triad (also called RxDL-motif). Interestingly, despite a high structural similarity<br />
of MC159 and c-FLIPR , point mutations in the charge triad, which abolish the antiapoptotic<br />
function of MC159, did not abrogate apoptosis inhibition by c-FLIPR . Instead,<br />
we show here that the hydrophobic patch in DED2 is critical for recruitment of c-FLIPR into the DISC. Thus, the DEDs of viral and cellular FLIPs interfere with apoptosis by<br />
divergent mechanisms, suggesting a surprisingly functional diversity of the DED motif.<br />
By the generation of different c-FLIPR deletion mutants we can show, however, that<br />
neither of the DEDs alone nor coexpression of both DEDs is sufficient to interact with<br />
the DISC or to protect from CD95-mediated apoptosis. Thus, also intra-molecular<br />
linkage and the tight package of both DEDs in c-FLIPR are essential for its anti-apoptotic<br />
capacities.
Björn Linke, Heiko Weyd, Lucie Dörner, Andrea Mahr, Peter H. Krammer<br />
Structural Requirements for Annexin 1 Mediated Suppression<br />
of Dendritic Cells<br />
Peripheral tolerance comprises several mechanisms to prevent autoimmune disease. To<br />
better understand molecular mechanisms of self-tolerance and nonresponsiveness<br />
against apoptotic “self” cells we generated monoclonal antibodies against apoptotic<br />
cells. We identified one monoclonal antibody which determined Annexin 1 as a new<br />
signalling molecule on the surface of human apoptotic cells. Coculture experiments of<br />
dendritic and apoptotic cells as well as incubation of dendritic cells with recombinant<br />
Annexin 1 lead to inhibition of DC maturation.<br />
The mechanism by which Annexin 1 mediates this effect remains to be studied further.<br />
In an attempt to identify the active site of Annexin 1 we generated different deletion<br />
constructs and mutants of Annexin 1. These proteins are analyzed for their capability to<br />
modulate maturation of DCs. Their effect on cytokine secretion and expression of DC<br />
surface markers including MHC and costimulatory molecules e.g. CD80 and CD86 and<br />
their influence on T cell proliferation in DC-T cell cocultures are studied.<br />
Furthermore, transwell experiments in our lab have shown that a direct cell contact<br />
between apoptotic and dendritic cells is required for the inhibition of DC maturation. By<br />
using photocrosslinking and immunoprecipitation we study the Annexin 1 receptor on<br />
the surface of DCs.
Nina Oberle, Nadine Eberhardt, Christine S Falk, Peter H Krammer, Elisabeth Suri-<br />
Payer<br />
Suppression Mechanisms of cytokine transcription in human<br />
CD4+CD25- T cells upon interaction with CD4+Foxp3+<br />
regulatory T cells<br />
CD4+CD25highFoxp3+ regulatory T cells (Treg) are critical mediators of peripheral self<br />
tolerance and immune homeostasis. Treg suppress proliferation and cytokine production<br />
by conventional T cells (Tcon). The exact mechanism of suppression, however, is still<br />
unknown. To gain a better understanding of Treg function, we investigated the kinetics<br />
of cytokine suppression in Tcon re-isolated from cocultures with pre-activated human<br />
Treg. Treg inhibited induction of Th1 cytokine mRNA as early as 1 hour after<br />
stimulation, whereas induction/suppression of Th2 cytokines was delayed to 10-15<br />
hours. We show that immediate cytokine mRNA suppression in Tcon was neither<br />
dependent on TGF-β / IL-10 or IL-2 consumption, nor on induction of the transcriptionalrepressor<br />
FOXP3 or other anergy-related genes (e.g. GRAIL, TOB, FOXJ1, ROG, ICER).<br />
In contrast, LAG-3, SOCS1 and SOCS3 mRNA were strongly upregulated in Tcon in the<br />
presence of Treg. However, protein analysis did not confirm a role for these proteins in<br />
early suppression. Thus, the identification of a fast inhibitory mechanism in Tcon<br />
induced by Treg constitutes an important step for future efforts to unravel the entire<br />
elusive suppressive mechanism.
Beatrix Schumak, Gerhard Wingender, Schwandt Timo, Frank Juengerkes, Thomas<br />
Tueting, Percy Knolle, Bernhard Holzmann, Andreas Limmer<br />
SUPPRESSION OF ADAPTIVE IMMUNE RESPONSES BY TOLL-<br />
LIKE RECEPTOR LIGANDS<br />
As bacterial infections are known to induce strong immune responses, immune<br />
activation by TLR-ligands demands effective control by the immune system;<br />
dysregulation can elicit extensive inflammatory reactions, causing immune damage, but<br />
also immune suppression. We observed that - in contrast to local application -systemic<br />
application of bacteria or bacterial CpG-rich DNA (CpG-ODN) in high concentrations<br />
inhibited the induction of adaptive immune responses. The suppressive effect was<br />
characterized by diminished CD8 T cell proliferation and reduced cytotoxicity in the<br />
spleen as well as a lack of CD4 mediated IgG antibody response. Experiments<br />
performed in splenectomized mice show that this CpG-mediated suppression is<br />
regulated in the spleen and several mechanisms are involved. Systemic CpG-ODN<br />
application leads in the spleen to induction of the enzyme indoleamine 2,3 dioxygenase<br />
(IDO), which depletes tryptophan that is necessary for T-cell proliferation. Furthermore,<br />
the production of interleukin 12 (IL-12) by CD8a positive dendritic cells in the spleen is<br />
also affected. These DCs are immune paralysed, as they are diminished in cell numbers<br />
and produce less IL-12, when they are re-stimulated in vivo. This phenomenon could<br />
have important implications in septic patients who suffer from long-term immune<br />
suppression and exhibit reduced levels of IL-12. This hypothesis is substantiated by<br />
CASP (colon ascendens stent peritonitis), a murine sepsis model. CASP performed<br />
before infection with adenovirus expressing ovalbumin (AdOVA) resulted also in<br />
suppressed adaptive immune responses against OVA. Analysis of bioluminescent<br />
luciferase expression (IVIS®200) as well as classical microbiological methods revealed<br />
that bacteria reached besides liver and lung the spleen in high numbers, where they<br />
induced IL-12 suppression and expression of IDO. This corresponded to subsequent<br />
induction of immune suppression.
Christiane A. Opitz, Tobias Lanz, Christian Lutz, Wolfgang Wick, Michael Platten<br />
Suppression of antigen-specific T cell immunity by<br />
mesenchymal stem cells: implications for stem cell therapy of<br />
autoimmune diseases.<br />
Mesenchymal stem cells (MSC) represent an attractive vehicle for the treatment of<br />
conditions associated with harmful T cell responses such as multiple sclerosis, as they<br />
not only home to sites of inflammation but also display unique suppressive properties<br />
on T cell immunity. Here we show that immunosuppression mediated by human MSC<br />
(hMSC) can be augmented by ligation of Toll-like receptors (TLR) expressed on hMSC.<br />
Activation of TLR3 and TLR4 on human MSC caused an upregulation of the tryptophandegrading<br />
enzyme indoleamine-2,3-dioxygenase (IDO). The upregulation of IDO by<br />
TLR3 activation was mediated in part by interferon-β (IFN-β) since IDO mRNA and<br />
kynurenine release were induced in response to IFN-β and since TLR3-mediated IDO<br />
upregulation and subsequent kynurenine release were suppressed by inhibition of the<br />
toll/IL-1 receptor domain-containing adapter inducing IFN-β (TRIF). Inhibition of IDO<br />
mitigated the immunosuppressive effect of TLR-activated MSC indicating that<br />
tryptophan catabolism is responsible for the immunosuppression induced by TLR<br />
activation. To evaluate the use of mesenchymal stem cells to suppress pathogenic<br />
antigen-specific T cell responses during autoimmune diseases we coincubated<br />
autologous MSC with T cells from mice carrying a transgenic T cell receptor that<br />
recognizes the immunodominant epitope of the myelin oligodendrocyte protein (MOG).<br />
MSC suppressed the proliferation of myelin-specific T cells after antigen-specific<br />
activation indicating that MSC may be active in suppressing pathogenic antigen-specific<br />
T cells responses during autoimmunity. Our data imply that MSC may be a novel<br />
immunomodulating approach to treat autoimmune disease such as multiple sclerosis.
Andrea Mahr<br />
Suppression of Dendritic Cell Activation by Annexin 1<br />
on the Surface of Apoptotic Cells<br />
Dendritic cells (DCs) are phagocytic cells that discriminate “non-self” from “self”<br />
structures, and consequently initiate immunity or tolerance. Pathogenic components,<br />
like bacteria-derived lipopolysaccharide (LPS), are recognized by Toll-Like Receptors<br />
(TLRs) on the surface of DCs, leading to DC activation and secretion of proinflammatory<br />
cytokines. This process can be inhibited by the uptake of apoptotic cells, the biggest<br />
source of “self”-material. Inhibition is probably mediated by tolerogenic signals on the<br />
surface of apoptotic cells, but the molecules relevant for this process are not yet well<br />
defined. A candidate protein is annexin 1, which is externalized by early apoptotic cells.<br />
In this study, it has been found that pre-incubation of DCs with apoptotic cells or<br />
purified recombinant annexin 1 before TLR stimulation could reduce the transcriptional<br />
upregulation and secretion of proinflammatory cytokines.<br />
Correspondingly, annexin 1 led to a substantial decrease of LPS-induced TLR signal<br />
transduction.<br />
The detailed analysis of annexin 1 function may lead to a more advanced understanding<br />
of the regulation of TLR signaling, and would give valuable insight into a potential<br />
mechanism of peripheral non-responsiveness.
Jens Haenig, Manfred B. Lutz<br />
Suppression of mature dendritic cell function by regulatory T<br />
cells in vivo is abrogated by CD40 licensing<br />
The priming of CD4+ effector T cells (Teff) in vivo is induced by mature dendritic cells<br />
(DC) and controlled by CD4+ CD25+ Foxp3+ regulatory T cells (Treg). It remains<br />
unclear however, how Teff priming versus Treg suppression are regulated during<br />
antigen presentation by DC in secondary lymphoid organs at the simultaneous presence<br />
of Teff and Treg. Here, we used an peptide-specific DO11.10 TCR-transgenic adoptive<br />
transfer model to follow the Teff priming kinetics and the mechanisms of suppression by<br />
Treg. Treg could not influence the early Teff expansion but limited and terminated the<br />
Teff response. DC-Treg cell contacts remained unaltered during suppression by Treg<br />
and led to a downregulation of the costimulatory molecules CD80, CD86, PD-L1 and PD-<br />
L2, but not MHC II, CD40, ICOS-L or CD70 from the mature DC surface. This effect was<br />
observed only after TNF or LPS maturation of DC but not after combined LPS-CD40<br />
stimulation. Together, our data indicate that Treg suppression against non-self antigens<br />
in vivo occurs delayed as compared to the Teff response, is mediated mainly through<br />
DC modulation, but is controlled by the type DC maturation.
Yu-Hwa Huang, Eva Tolosa, Heinz Wiendl<br />
Suppressive action of HLA-G-expressing T cells, a novel<br />
population of natural regulatory cells, is independent of<br />
antigen-presenting cell, facilitated by TCR-engagement,<br />
involves HLA-G-ILT-2 ligation and IL-10<br />
Regulatory T cells suppress harmful immune responses against foreign and self-antigens<br />
and play a key role in the mechanisms of autoimmunity. We recently identified a novel<br />
regulatory T cell population characterized by the expression of the immune-tolerogenic<br />
molecule HLA-G (Feger et al., 2007, Blood). “HLA-G T-regulatory cells” (HLA-G Tregs)<br />
exist in small, but sizeable quantities in peripheral blood under physiological conditions<br />
(0.1 to 4% of T cells). Our initial phenotypcial and functional characterization revealed<br />
that HLA-G Tregs are hypoproliferative, negative for FOXP3 and suppress autologous T<br />
cells in a non-contact-dependent manner.<br />
We here provide further data clarifying the mechanisms of suppression between HLA-G<br />
Tregs and CD4 T effector cells. CD4 HLA-G Tregs suppress proliferation of autologous<br />
polyclonal effector cells in the absence of antigen-presenting cells (APC), suggesting<br />
non-antigenic specifically suppression. This was demonstrated in an APC-free<br />
suppression system utilizing anti-CD3/28-beads as the stimulus for responder cells.<br />
Suppression was depending on the effector-responder ratio but independent from cellcell<br />
contact. Using a transwell system we could demonstrate that (i) TCR engagement<br />
facilitates CD4 HLA-G pos Treg - mediated suppression through the production of<br />
soluble HLA-G; (ii) Neutralization the engagement of HLA-G-ILT2 significantly reversed<br />
suppression; (iii) CD4 HLA-Gpos Treg produced IL-10 upon TCR stimulation; (iv)<br />
Blockage of the IL-10 receptor partially reversed suppression. In conclusion, CD4 HLA-G<br />
pos Treg exert suppression via a non-cell-cell contact dependent mechanism that<br />
involves HLA-G-ILT2 interaction as well as IL-10.
Kathrin Held, Elke Dauber, Michael Loos, Franz Petry<br />
Susceptibility of complement deficient mouse strains to<br />
systemic infection with Candida albicans<br />
C. albicans can activate all three pathways of the complement system leading to<br />
opsonization of the yeast cells, enhanced complement receptor mediated phagocytosis<br />
and infiltration of neutrophils due to C5a chemotactic activity. The aim of this study was<br />
to investigate the susceptibility to C. albicans infection in different complement deficient<br />
mouse strains. We compared mice with targeted disruption of the C1qa gene (C1q-/-)<br />
and a double knockout strain that lacks factor B and C2 (Bf/C2-/-). Mice were infected i.<br />
p. with 10 8 yeast cells of C. albicans SC5314 and monitored for mortality. Bf/C2-/- mice<br />
showed high mortality (90%) within the study period of 4 weeks. In contrast, mortality<br />
in C1q-/- mice was below 20% and all C57BL/6 control mice survived. Preliminary<br />
analysis of MBL-A and MBL-C double knockout mice suggest that they are more<br />
susceptible to infection than C1qa-/- mice but definitely more resistant than Bf/C2-/-<br />
mice. Kidneys of deceased mice were homogenized and the yeast load was estimated<br />
by culture. C.f.u. counts were approximately one log higher in Bf/C2-/- mice compared<br />
to C1qa-/- mice. PAS staining of kidney sections of Bf/C2-/- mice showed widespread<br />
germ tube formation confirming the high c.f.u. counts from cultured tissue<br />
homogenates. In C1qa-/- and MBL-A/C-/- mice germ tube formation was limited in size<br />
and number. In vitro binding studies demonstrated low efficiency of C1q binding but<br />
substantial binding of MBL-A and MBL-C. These results support the idea that total lack<br />
of complement activation in Bf/C2 double knock-out mice leads to uncontrolled tissue<br />
infection. Deficiency of classical pathway activation has only a low impact on host<br />
defence against C. albicans whereas the lectin pathway might contribute to the host<br />
defence against candidosis.
Liangping Li, Gerald Willimsky, Susanne Seitz, Yaxin Xu, Yongping Li, Lope Estevez<br />
Schwarz, Peter Schlag, Thomas Blankenstein<br />
SV40 LT-immortalized human primary normal and cancerous<br />
mammary epithelial cells are phenotypically similar but can<br />
be distinguished in selection medium and 3D culture<br />
Cellular immortalization is considered a hallmark of malignancy. Normal human<br />
mammary epithelial cells (NMECs) have two major in vitro growth restrictions,<br />
senescence and crisis. However, cancerous mammary epithelial cells (CMECs) that are<br />
thought to have passed growth barriers in vivo usually cannot be established long-term<br />
in vitro. Here we show that CMECs deprived of their natural environment and grown in<br />
conventional <strong>complete</strong> medium behave similar to NMECs, e.g. they stop producing<br />
telomerase and become senescent. Like NMECs, CMECs are rescued by SV40 large T<br />
(LT) from senescence but not from crisis. The telomere length of both NMEC-LT (N-LT)<br />
and CMEC-LT (C-LT) cells first shortens but later partially recovers after telomerase<br />
activation. Both cell types upregulate ErbB2 expression, acquire genetic changes,<br />
remain long-term dependent on LT and ErbB2 and are non-tumorigenic. Thus, CMECs<br />
are under a comparable in vitro selective pressure as NMECs despite their malignancy in<br />
vivo. This data demonstrate that most primary breast cancer cells are still unable to<br />
overcome the in vitro growth restrictions. Despite these similarities, N-LTs and C-LT<br />
cells cultured in selection medium show different growth in 2D/3D culture and in vivo.
Carmen Kroczek, Athanasia Avramidou, Stephan Feller, Christiane Lang, Hans-Martin<br />
Jäck, Dirk Mielenz<br />
Swiprosin-1 - molecular switch in B cell receptor signaling?<br />
B cell receptor (BCR) signals are essential for B cell differentiation, homeostasis and<br />
negative selection, which are regulated by strength and quality of BCR signals.<br />
Recently, we identified a novel adaptor protein, Swiprosin-1/EFhd2, in lipid rafts of B<br />
cell lines that undergo apoptosis after BCR stimulation. During murine B cell<br />
development, Swiprosin-1 exhibited highest expression in immature B cells of the bone<br />
marrow. Overexpression of Swiprosin-1 in the immature murine B cell line WEHI231<br />
enhanced spontaneous as well as BCR-induced apoptosis by lowering the BCR signal<br />
threshold. In contrast, shRNA-mediated down-regulation of Swiprosin-1 impaired<br />
specifically spontaneous and BCR-elicited apoptosis, but not BCR-induced G1 cell cycle<br />
arrest. Furthermore, Swiprosin-1 downregulation in WEHI231 cells led to increased IκBα<br />
phosphorylation and degradation after BCR stimulation whereas Erk phosphorylation<br />
was unchanged. Accordingly, Swiprosin-1 levels regulated net cell growth of WEHI231<br />
cell populations through reciprocal regulation of Bcl-xL-, but not Bim-levels, thereby<br />
controlling spontaneous apoptosis. Moreover Swiprosin-1 levels regulate proximal BCR<br />
signals: Downregulation of Swiprosin-1 prolonged total tyrosine phosphorylation,<br />
specifically tyrosine phosphorylation of a ~130 kDa protein, and diminished BCR<br />
induced calcium flux. We also observed co-clustering of a Swiprosin-1-EGFP fusion<br />
protein with the B-cell receptor in WEHI231 cells. Our data suggest that Swiprosin-1<br />
levels adjust BCR signaling thresholds in immature B cells. Hence, Swiprosin-1 may<br />
regulate life span and BCR signals in immature B cells by influencing the proximal BCR<br />
signaling pathway through as yet unidentified mechanisms.
Anke Osterloh, Ulrich Kalinke, Siegfried Weiß, Bernhard Fleischer, Minka Breloer<br />
SYNERGISTIC AND DIFFERENTIAL MODULATION OF IMMUNE<br />
RESPONSES BY HSP60 AND LPS<br />
Activation of professional antigen-presenting cells (APC) is a crucial step in the initiation<br />
of an efficient immune response. In this study we show that Hsp60 mediates immune<br />
stimulation by different mechanisms, dependent and independent of LPS. We have<br />
demonstrated earlier that both, Hsp60 and LPS, increase antigen-specific IFNgamma<br />
release in T cells. Here we show that in contrast to LPS Hsp60 induces IFNalpha<br />
production in professional APC. Neutralization of IFNalpha as well as the absence of<br />
functional IFNalpha/beta receptor on APC and T cells interfered with Hsp60-mediated<br />
IFNgamma secretion in antigen-dependent T cell activation, strongly suggesting that<br />
IFNalpha represents one factor contributing to Hsp60-specific immune stimulation. On<br />
the other hand, we show that Hsp60 bound to the cell surface of APC colocalizes with<br />
the LPS co-receptor CD14 and LPS binding sites. Hsp60 specifically binds bacterial LPS<br />
and both molecules synergistically enhanced IL-12p40 production in APC and<br />
IFNgamma release in antigen-dependent T cell activation. This effect was Hsp60-specific<br />
and dependent on LPS-binding by Hsp60. Furthermore, we show that Hsp60 exclusively<br />
binds to macrophages and DC but not to T or B lymphocytes and that both, T cell<br />
stimulation by Hsp60 as well as Hsp60/LPS complexes, strictly depends on the presence<br />
of professional APC and is not mediated by B cells.<br />
Taken together, our data support an extension of the concept of Hsp60 as an<br />
endogenous danger signal: Besides its function as a classical danger signal indicating<br />
unplanned tissue destruction to the innate immune system, in the incident of bacterial<br />
infection extracellular Hsp60 may bind LPS and facilitate microbe recognition by<br />
lowering the threshold of PAMP detection and enhancing TLR signaling.
Nousheen Zaidi, Timo Burster, Vinod Sommandas, Timo Herrmann, Bernhard O.<br />
Boehm, Wolfgang Voelter, Hubert Kalbacher<br />
Synthesis of novel cell penetrating aspartic proteases<br />
inhibitors as the targeted inhibitors of antigen processing<br />
Selective inhibition of enzymes involved in antigen processing such as cathepsin E and<br />
cathepsin D is a valuable tool for investigating the roles of these enzymes in the<br />
processing pathway. However, the aspartic protease inhibitors including the highly<br />
potent pepstatin A (PepA) are inefficiently transported across the cell membrane thus<br />
have a limited access to antigen processing compartments. Previously described<br />
mannose-pepstatin conjugates were efficiently taken up by the cells via receptor<br />
mediated uptake. But the cells that do not carry mannose receptors are not able to take<br />
up these conjugates efficiently. The aim of the present study was to synthesize new cell<br />
permeable aspartic protease inhibitors by conjugating pepstatin A with well-known cell<br />
penetrating peptides (CPPs). To achieve this the most frequently used CPPs namely, Tat<br />
(49-60), pAntp(43-58) (Penetratin) and 9-mer of L-arginine (R9), were synthesized on<br />
a trityl resin followed by coupling pepstatin A to the peptides as a <strong>complete</strong> molecule to<br />
the N-terminal amino group. The enzyme inhibition properties of these bioconjugates<br />
and their cellular uptake into dendritic cells, Boleths (EBV-transformed B cell line) and<br />
MCF7 (human breast cancer cell line) was studied. We found that the bioconjugate PepA-<br />
Penetratin (PepA-P) was the most efficient cell-permeable aspartic protease inhibitor in<br />
comparison to PepA. Moreover, we found that PepA-P efficiently inhibited the antigen<br />
processing in PMBCs (peripheral mononuclear blood cells), primary DCs (dendritic cells)<br />
and in primary B cells. Therefore, PepA-P can be used in studying the role of<br />
intracellular aspartic proteases in the MHC class II antigen processing pathway.
Edith Jasny, Martin Eisenblaetter, Tamara Visekruna, Klara Tenner-Racz, Christiane<br />
Stahl-Hennig, Andres Salazar, Ralph M. Steinman, Klaus Ueberla, Mariagrazia<br />
Uguccioni, Ralf Ignatius<br />
Synthetic double-stranded RNA, Poly ICLC, enhances the<br />
induction of cellular immune responses against protein<br />
antigens in rhesus macaques<br />
Background: Ligands for Toll-like receptors (TLRs) are promising adjuvants for the<br />
induction of humoral and cellular immune responses, as in the design of AIDS vaccines.<br />
Poly ICLC is a synthetic double-stranded RNA that should bind to TLR3 and has been<br />
stabilized against serum nucleases, which are present in the plasma of primates.<br />
Objectives: To study the effects of Poly ICLC on protein-specific immune responses of<br />
rhesus macaques in vivo and assess its effects on leukocyte subsets in vitro.<br />
Methods: Monkeys were immunized s.c. with keyhole limpet hemocyanin (KLH) together<br />
with or without Poly ICLC. Draining lymph nodes were removed after 18 h, and cellular<br />
and humoral immune responses were determined at several time points in standard<br />
assays.<br />
In vitro, human and monkey PBMCs or selected leukocyte subsets were incubated with<br />
Poly ICLC +/- Lipofectamine and cellular activation and cytokine secretion were<br />
monitored.<br />
Results: The application of Poly ICLC led to elevated serum levels of CXCL9 and<br />
CXCL10; both chemokines were also detected in draining lymph nodes by in situ<br />
hybridization. KLH-specific cellular immune responses were stronger in Poly ICLC coinjected<br />
animals than in controls and highest responses were observed in animals<br />
injected with 0.5 mg/kg Poly ICLC. Humoral immune responses to KLH were enhanced<br />
also by lower doses of Poly ICLC. The effect of Poly ICLC may not have been due to<br />
direct activation of dendritic cells (DCs) because rhesus macaque monocyte-derived DCs<br />
expressed little TLR3 as shown by flow cytometry. Likewise, we neither detected<br />
increased numbers of mature DCs in the draining lymph nodes following Poly ICLC<br />
injection nor could primary myeloid monkey DCs be activated by Poly ICLC in vitro.<br />
Instead, Poly ICLC did activate NK cells in PBMCs, as indicated by CD69 upregulation. In<br />
addition, Poly ICLC stimulated PBMCs secreted enhanced levels of CXCL9 and CXCL10.<br />
Conclusion: Poly ICLC has activity as an adjuvant for the induction of protein-specific<br />
cellular immune responses in monkeys.
Stefanie Frey, Christine D. Krempl, Stephan Ehl<br />
T cell dependent and T cell independent disease after<br />
infection with pneumonia virus of mice<br />
Infection of mice with pneumonia virus of mice (PVM) has been proposed as an<br />
excellent model to study the pathogenesis of human infection with the closely related<br />
respiratory syncytial virus (RSV). So far this model allowed interesting observations on<br />
pulmonary cytokine and chemokine responses, but poor lymphocyte recruitment, failure<br />
to detect dominant CTL epitopes and evidence for CTL suppression suggested that T<br />
cells play a minor role. We show that control of a sublethal infection with PVM strain 15<br />
in C57BL/6 mice was accompanied by a 100-fold increase in pulmonary CTL, 20% of<br />
which were specific for PVM. T cell deficient mice failed to eliminate PVM and became<br />
carriers in the absence of weight loss. CTL mediated virus control and weight loss were<br />
independent of IFN-γ or perforin. Mice with limited numbers of T cells could not achieve<br />
virus control without weight loss, indicating a tight balance between beneficial and<br />
detrimental effects of T cell responses to PVM. T cell deficiency slightly delayed but did<br />
not prevent mortality after high dose infection. These data demonstrate that both T cell<br />
dependent and T cell independent pathways contribute to PVM disease in a viral dosedependent<br />
fashion.
Annette I. Garbe, Jerome P. Jayasekera, Michael C. Carroll, Harald von Boehmer<br />
T cell vaccination with DEC-205-influenza hemagglutinin<br />
fusion antibodies<br />
Current influenza vaccines are known to induce antibodies to hemagglutinin (HA) and<br />
neuraminidase but less is known about their ability to induce cytolytic CD8 T cells to HA<br />
determinants. In the present study we have compared UV-inactivated influenza virus<br />
and HA delivered to dendritic cells by DEC-205 fusion antibodies in their ability to<br />
induce T cell memory. When analysing the generation of CD8 memory cells with a<br />
transgenic receptor for HA the DEC-205-HA fusion antibodies were found to be<br />
somewhat superior to UV-influenza virus. Moreover in wt BALB/c mice the fusion<br />
antibodies induced long term CD8 memory cells that developed into potent effector cells<br />
exhibiting cytolytic activity and IFN-gamma secretion after rechallenge with UVinactivated<br />
virus. On the other hand a single shot of DEC-205-HA fusion antibodies did<br />
not induce HA-specific antibodies whereas UV-inactivated virus did. Nevertheless the<br />
fusion-antibody vaccination increased HA-specific IgG2a, IgG2b and IgG1 antibodies if<br />
given prior to challenge with inactivated virus. Finally, in preliminary experiments a<br />
single dose of DEC-205-HA elicited protection against A/PR/8 virus. The results show<br />
that the HA-fusion antibody induces effective CD4 and CD8 T cell memory against<br />
influenza. This approach should be very useful for inducing T cell memory to cellinternal<br />
viral proteins of which only peptides are presented on the cell surface of<br />
infected cells and which are not subject to high mutation rates.
Christof Iking-Konert, Tim Vogl, Matthias Schneider, Konrad Andrassy, Gertrud Maria<br />
Hansch<br />
T-lymphocytes in patients with primary vasculitides:<br />
Expression of CD11b identifies activated T cells with the<br />
propensity to stimulate polymorphonuclear neutrophils<br />
Objetive<br />
To gain insight into the immune pathogenesis of primary, ANCA-associated vasculitides<br />
(AAV) T-lymphocytes of patients were analysed with regard to the expression of<br />
molecules indicative for current or previous activation. T-lymphocytes of patients with<br />
Wegener's granulomatosis (WG; n= 47), or microscopic polyangiitis (MPA; n=33) in<br />
remission were phenotypically and functionally analysed, and compared to Tlymphocytes<br />
of patients with active disease (n=10), and to cells of healthy donors. In<br />
vitro, T-cells of a similar phenotype were generated, and their interaction with<br />
polymorphonuclear neutrophils (PMN) was assessed.<br />
Results<br />
During active disease, a small, but conspicuous population of CD8+CD28+CD11b+ was<br />
found, which produced gamma interferon.Under immunosuppressive therapy, CD11b<br />
was exclusively seen on CD8+CD28- cells, the latter being more frequent in patients<br />
with long-lasting or severe disease. In vitro experiments confirmed that CD11b is upregulated<br />
by activated T-cells, concomitantly with synthesis of gamma interferon.<br />
During prolonged culture, CD11b remains on the surface, even when CD28 is lost,<br />
compatible with the notion that CD8+CD28+CD11b+ represent a transient phenotype in<br />
the course of T-cell activation. In vitro, the gamma interferon-producing T cells<br />
activated PMN to express CD64 and MHC class II molecules, thus generating the same<br />
PMN-phenotype as it is seen in patients with active ANCA-associated vasculitis. Of note<br />
is that a similar phenotype could be generated by supernatants of activated T-cells, or<br />
by gamma interferon alone, but not by antibodies to proteinase 3.<br />
In conclusion, CD11b expression identifies activation of a small population of CD8+Tcells<br />
during active primary vasculitis. By producing gamma interferon, these T-cells<br />
could activate PMN by a “cross talk” between PMN and T-cells, thus generating a longliving<br />
and potentially destructive PMN phenotpye.
Sven Meuth, Stefan Bittner, Ole Simon, Heinz Wiendl<br />
Tandem pore domain potassium channels TWIK-related acidsensitive<br />
K+ channel 1 (TASK1) and TASK3 modulate effector<br />
functions of T lymphocytes: a novel therapeutic target for Tcell<br />
mediated autoimmune diseases<br />
One decade ago, two-pore domain K+ channels (K2P), a new family of potassium<br />
channels was described and has since then attracted much attention due to their unique<br />
physiological properties. These potassium channels contribute to the resting membrane<br />
potential and a rising diversity of regulatory mechanisms (e.g. pH drop or O2<br />
deprivation) has been revealed. To date, little is known about their role on non-neuronal<br />
cells and under pathological conditions.<br />
We here investigate the role of the TWIK-related acid-sensitive potassium channels 1<br />
(TASK1) and TASK3 on human T lymphocytes for T cell functions in vitro as well as their<br />
pathogenic role in a model of multiple sclerosis (adoptive transfer experimental<br />
autoimmune encephalomyelitis, AT-EAE). TASK1 and TASK3 are expressed on human T<br />
lymphocytes as indicated by immunocytochemistry and western blotting procedures.<br />
Pharmacological treatment (bupivacaine, anandamide, spermine and ruthenium red) of<br />
isolated human CD3+ T cells revealed a dose dependent (~ 40%) reduction of an<br />
outward current in whole-cell patch-clamp recordings indicative of TASK channels.<br />
However, the same channel modulators significantly reduced IFNg production and<br />
decreased proliferation rate of T cells after CD3/CD28 bead stimulation. Kv1.3, an<br />
established potassium channel for T cell function, was used as control.<br />
In the next step we addressed the question whether the importance of TASK channels<br />
for T cell functions could as well be transferred into an in vivo model to demonstrate<br />
their pathogenetic relevance. AT-EAE was evoked by MBP-specific T lymphocytes and<br />
application of TASK channel inhibitors resulted in a delayed disease onset, milder<br />
disease course and earlier recovery.<br />
Taken together our data describe TASK channels as important mediators of T cell<br />
function in vitro and in a model of multiple sclerosis in vivo underlining their potential<br />
for immunotherapeutic strategies.
Kai Dittmann, Anja Uhmann, Ralf Dressel, Heidi Hahn, Jürgen Wienands<br />
Targeted inactivation of the Hh receptor Ptch abrogates<br />
lymphocyte development in mice<br />
The Hh/Ptch signaling system is known to control the development and neoplastic<br />
transformation of several cell types. However, the role of Hh/Ptch for the differentiation<br />
of B and T lymphocytes from hematopoietic stem cells (HSC) has not been assessed so<br />
far. To analyze the function of Hh/Ptch for lymphopoiesis in vivo, we have employed a<br />
genetically engineered mouse mutant in which the Ptch gene can be conditionally<br />
inactivated by virtue of the Cre/loxP recombination system. We show that targeted<br />
disruption of Ptch in the adult organism results in a dramatic specification and<br />
differentiation defect of the lymphoid lineage leading to rapid disappearance of newly<br />
generated B and T lymphocytes from peripheral lymphoid organs. The developmental<br />
block occurs at the level of the common lymphoid progenitor cell (CLP), which defines<br />
an early branching point of HSC differentiation and lineage commitment. In contrast to<br />
the lymphoid lineage, development of cell types of the myeloid lineage from common<br />
myeloid progenitors (CMP) appears normal. Our data identify Hh/Ptch-induced signaling<br />
as a key regulator for proper development of immunocompetent lymphocytes. Hence,<br />
the progression of tumors, which are initiated upon oncogenic Hh/Ptch mutations, may<br />
be further promoted due to impaired tumor surveillance by a compromised immune<br />
system.
Andreas Goldwich, Sabine Hahn, Sandra Schreiber, Ralf Wagner, Manfred Lutz,<br />
Eckhardt Kämpgen, Ulrich Schubert<br />
Targeting HIV-1 Gag into the DRiP-Pathway results in<br />
enhanced CD8 T cell activation<br />
The main source of peptides presented by the MHC-I pathway are proteins degraded via<br />
the ubiquitin proteasome pathway. Different protein substrate pools can be<br />
distinguished: first, short-lived defective ribosomal products (DRiPs) which are<br />
degraded in concert with or shortly after their synthesis, and second, functional proteins<br />
which are entering the standard protein live cycle.<br />
To analyze the contribution of these substrates to the generation of MHC- I-presented<br />
peptides, we established murine cell lines which express HIV-1 Gag variants harboring<br />
degron signals and the murine OVA-derived MHC-I model epitope SIINFEKL (SL).<br />
Although an HIV-1 Gag variant harboring an N-end degron (UbRGag) displayed wt half<br />
life, its inherent DRiP-rate was increased, resulting in enhanced MHC-I Ag presentation.<br />
Additionally, this increased presentation causes a better T cell stimulation of SL-specific<br />
B3Z hybridoma cells in vitro and adoptively transferred OT-1 T cells in vivo.<br />
Futhermore, enhanced numbers of SL-specific T cells in vivo were detected by IFN-γ<br />
ELISPOT after vaccination of naïve C57Bl6 mice in the case of the UbRGag variant.<br />
These results point out the importance of the DRiP-pathway in adaptive immunity and<br />
may be relevant for further vaccination studies against tumors or intracellular<br />
pathogens.
Stephan Schlickeiser, Katharina Tschimmel, Andreas Meisel, Christian Meisel, Inga<br />
Gebuhr, Uwe Pleyer, Hans-Dieter Volk, Birgit Sawitzki<br />
TARGETING N-GLYCOSYLATION AFFECTS APC FUNCTION IN<br />
VITRO AND IN VIVO<br />
Introduction: Transfer of tolerogenic DCs has become an attractive treatment<br />
alternative in transplantation and autoimmunity. Although distinct glycosylation patterns<br />
on tolerogenic immature DCs have been described, the impact of post-translational<br />
protein modification on DC function is still unexplored. Here we analyzed the effect of<br />
hypo-N-glycosylation on DC maturation and allo-stimulatory capacity in vitro and in<br />
vivo.<br />
Methods: BALB/c bone marrow-derived DCs were treated with the specific alpha-1,2mannosidase<br />
inhibitor kifunensine. After 24 h, DCs were matured with LPS, TNFa or anti-<br />
CD40mAb. DC N-glycosylation state (PHA binding), expression of MHCII and CD86 were<br />
analyzed by flow cytometry. Allo-stimulatory capacity of DCs was determined by<br />
analyzing the proliferation of co-cultured allogeneic T cells from naïve C57BL/6 mice.<br />
Capacity of hypo-N-glycosylated endogenous APC to elicit an effective anti-bacterial<br />
response was tested by injecting kifunensine in a mouse model of stroke (MCAO).<br />
Results: We detected a significantly enhanced PHA binding capacity in response to<br />
maturation stimuli. Hypo-N-glycosylation was accompanied by diminished surface<br />
expression of MHCII and CD86 prior and after maturation. LPS-induced activation of<br />
hypo-N-glycosylated DCs dramatically diminished their allo-stimulatory capacity as<br />
proliferation of co-cultured allogeneic T cells was <strong>complete</strong>ly abrogated. Control animals<br />
subjected to MCAO developed spontaneous systemic bacterial infections due to stroke<br />
induced immunodepression. Interestingly, injection of kifunensine dramatically<br />
enhanced APC deactivation, increased bacteremia and reduced overall survival rate<br />
from 75 to 37.5 %. In contrast Sham operated mice receiving kifunensine were not<br />
affected.<br />
Conclusions: Our results indicate that, depending on their maturation state, differences<br />
in protein N-glycosylation levels condition DCs to either stimulate or deactivate T cells.<br />
Thus, interference with APC N-glycosylation has high potential for tolerance induction in<br />
transplantation and autoimmune models.
Sebastian Temme, Anna Maria Eis-Hübinger, Peter Kuckenberg<br />
Targeting of the major histocompatibility complex class II<br />
pathway by herpes simplex virus type-1 glycoprotein B<br />
The HSV-1 encoded envelope protein gB mediates contact of the virus with the cell<br />
surface and initiates fusion with the plasma membrane. We discovered that gB is<br />
involved in an immune evasion strategy of HSV-1, targeting the MHC class II processing<br />
pathway, presumably to prevent presentation of viral peptides. Recently, we co-isolated<br />
complexes of HSV-1gB and MHC class II molecules from HSV-1 infected cells. In further<br />
studies the intracellular encounter of gB and MHC class II and their subcellular<br />
localisation was investigated. In transfected cells, invariant chain competes with gB for<br />
binding to MHC II subunits within the ER and largely prevents association of gB to MHC<br />
class II molecules. However, in the absence of invariant chain, gB and MHC class II<br />
subunits form aggregates that are retained in the ER. Despite the large excess of<br />
invariant chain, in gB-transfected cells some gB is found in association with MHC class<br />
II. Furthermore, the MHC II/gB complexes were not dectected on the cell surface. We<br />
conclude, that gB and MHC class II are transported separately and encounter after<br />
dissociation of invariant chain from MHC class II heterodimers, probably in endosomal<br />
compartments. Targeting of MHC II heterodimers by gB upon HSV-1 infection may<br />
silence a CD4+ T cell response.
Theron Johnson, Karsten Mahnke, Dirk Nettelbeck, Volker Storn, Alexander H. Enk<br />
Targeting of Tumor antigens to dendritic cells (DCs) using a<br />
novel single chain fragment variable<br />
DEC205 is a prototype receptor for antigen uptake, which is expressed specifically by<br />
DCs and increases antigen presentation by 500-fold over other presentation pathways<br />
such as pinocytosis. To utilize the antigen receptor to load DCs in vivo, we created novel<br />
single chain fragment variables (ScFv) specific for DEC205, using RT-PCR with<br />
degenerative primers on total RNA from a hybridoma cell line (HB290). The isolated<br />
variable heavy, and variable light regions were subcloned into an expression vector,<br />
fused to a His tag and c-myc tag, then expressed as a native protein in E. coli. The<br />
inclusion of the two tags allows for the isolation of the protein via a nickel-NTA column<br />
(His) and immunohistochemical detection (c-myc) via anti c-myc antibodies. In<br />
addition, we have created a ScFv anti-murine DEC205 fused to the melanoma tumor<br />
associated antigen gp100. In C57/Bl6 mice, initial immunohistochemical staining of<br />
CD11c+ lymph node cells showed positive staining of ScFv comparable to the mAb anti-<br />
DEC205. In further experiments, C57/Bl6 mice were vaccinated with the DEC205 ScFv<br />
in the footpad or left untreated. After 8 to 16 hours, lymph nodes were isolated and<br />
examined for DEC staining. Here, the ScFv vaccinated mice showed more c-myc<br />
positively stained cells in comparison to the untreated controls. The staining pattern is<br />
similar to immunohistochemical staining seen in mice injected with the mAb anti-<br />
DEC205. Thus, we can demonstrate that murine ScFv DEC205 can target to CD11c+<br />
DCs in vivo. Further experiments using the ScFv DEC205-gp100 will show whether this<br />
targeting can result in induction of GP100 specific CD8+ T cells and therefore, may be a<br />
useful tool for the induction of an anti-melanoma response.
Tobias Seibel, Florian Schuetz, Christoph Domschke, Mariana Bucur, Christoph Sohn,<br />
Philipp Beckhove<br />
TGFβ and IFN-α regulate Type 1 T-Cell Responses in Primary<br />
Breast Carcinomas<br />
INTRODUCTION:<br />
App. 60% of breast cancer patients spontaneously develop tumor-reactive memory T<br />
cells in their bone marrow and immune infiltrates have been detected frequently in<br />
breast cancer lesions. We hypothesized that the local cytokine environment in the tumor<br />
may regulate antigen specific systemic immunity by influences on immature DCs (iDCs)<br />
during antigen uptake.<br />
METHODS:<br />
We assessed the presence of tumor antigen-reactive T cells in the bone marrow of 123<br />
primary operated breast cancer patients using ex vivo short term interferon-γ (IFN-γ)<br />
Elispot assay. Cytokine contents of TGFß1, IL-10, IL-4, PGE2, IFN-α and IL-12 in tumor<br />
lysates were analyzed using high sensitivity ELISA. Cytokine expression in the tumor<br />
tissue was visualized by immunfluorescence. The influence of tumor-derived cytokines<br />
on the capacity of iDCs to prime tumor specific T cell responses was analyzed by IFN-γ<br />
Elispot-assay after 7 days coculture in vitro of separated naïve T cells from breast<br />
cancer patients with tumor antigen pulsed autologous DCs pretreated with respective<br />
cytokines at concentrations present in tumor tissues.<br />
RESULTS:<br />
Tumor-specific T cell responses were detected in 45% of patients. These correlated with<br />
low amounts of TGFβ1 and elevated levels of IFN-α in corresponding tumor tissues. The<br />
majority (60%) of TGFß1 positive cells in the tumors belonged to a population of<br />
CD90low stroma fibroblast cells located at the interface between stroma and tumor<br />
cells. In vitro, pretreatment of iDCs with TGFß1 inhibited, and with IFN-α supported the<br />
priming of tumor-specific T cells.<br />
CONCLUSION:<br />
These results suggest that TGFβ and IFN-α in primary breast cancer tissue regulate the<br />
induction of systemic anti-tumor T cell responses by influencing functional properties of<br />
immature dendritic cells at the site of antigen encounter in the tumor tissue.
Guido Wabnitz, Philipp Lohneis, Yvonne Samstag<br />
The actin bundling protein L-plastin is important for LFA-1<br />
accumulation in the pSMAC of the immunological synapse<br />
Recognition of antigen on professional antigen-presenting cells (APC) by T-cells leads to<br />
a tremendous reorganisation of the actin cytoskeleton resulting in an ordered<br />
accumulation of activation and adhesion molecules at the interface between T-cells and<br />
APCs, termed the immunological synapse (IS). These processes are strongly dependent<br />
on costimulation. One possible candidate for linking costimulation to the reorganisation<br />
of the actin cytoskeleton is L-plastin. This actin-bundling protein is phosphorylated<br />
within 5 to 15 minutes after costimulation, but not following TCR engagement alone.<br />
Phosphorylation occurs exclusively on Ser-5. It is important for the appearance of the T<br />
cell activation molecules CD69 on the cell surface of costimulated PBT.<br />
Here we show that L-plastin enriches at the IS between untransformed human<br />
peripheral blood T-cells (PBT) and superantigen loaded APCs. There, it colocalizes with Factin.<br />
Time-lapse-video microscopy revealed that the relocalization of L-plastin occurs<br />
within the first seconds of T-cell/APC contact formation. Thus, it is faster than the<br />
phosphorylation of L-plastin. Given that a non-phosphorylatable L-plastin mutant (5A-<br />
LPL) similarly enriches at the IS as wildtype L-plastin, these data show that<br />
phosphorylation is not required for relocalization of L-plastin to the IS. In contrast,<br />
deletion of the actin binding sites of L-plastin abrogates its relocation to the IS. The<br />
same holds true if cells are preincubated with the F-actin destabilizing agent<br />
cytochalasin D at concentrations which do not drastically diminish the number of cellcell<br />
contacts. From these data we conclude that L-plastin relocalizes to the IS in an actin<br />
dependent - but phosphorylation independent - manner. The relevance of L-plastin for<br />
the IS was analyzed employing an siRNA approach. These experiments revealed that Lplastin<br />
is crucial for the accumulation of LFA-1 in the IS. Thus, L-plastin contributes to<br />
the maturation of the IS by enabling the formation of the pSMAC.
Anne Sappok, Anna S. Wenning, Melodie-Jo Wolfs, Tanja Mayer, Bettina Strauß,<br />
Markus Hoth, Eva C. Schwarz<br />
The activation and proliferation of primary human CD4+ Tcells<br />
following focal stimulation<br />
The immunological synapse (IS) is a highly ordered complex of molecules at the contact<br />
area between a T-cell and an antigen presenting cell (APC). The formation of the IS is a<br />
prerequisite for an efficient T-cell immune response. The interaction of T-cell receptor<br />
(TCR)/CD3 complexes with the major histocompatibility complex (MHC) on APC is<br />
central to IS formation. The activation of T-cells is characterized by a sustained Ca2+<br />
influx through Ca2+ release activated Ca2+ (CRAC)/ORAI1 channels. To focally<br />
stimulate primary human CD4+ T-cells, we used anti-CD3- and anti-CD28-antibodies<br />
coated beads. To test if our antibody-coated bead-stimulation mimics the physiological<br />
stimulation with APC, we analyzed the effector status of our bead-stimulated CD4+ Tcells<br />
by the expression pattern of two surface proteins CD25 (interleukin-2 receptor)<br />
and CD62L (L-selectin). We observed up-regulation of CD25 and down-regulation of<br />
CD62L over two days, indicating T-cell activation. In addition, we observed a reorganization<br />
of the actin-cytoskeleton at the contact zone between the CD4+ T-cells<br />
and the antibody-coated beads, which is typical for the formation of an IS between a Tcell<br />
and an APC. We further analyzed IL-2 secretion and proliferation and their Ca2+dependence<br />
following bead-stimulation. To determine the doubling rate of the CD4+ Tcells<br />
under these conditions, we counted the cells over 13 days. Proliferation of CD4+ Tcells<br />
was preceded by an increase of the cells’ volume. From day 9 on, cell number<br />
decreased again, probably because apoptosis and necrosis exceeded proliferation.<br />
SiRNA technology (using Amaxa nucleofector) was established to down regulate several<br />
membrane proteins (e.g. TRPC3 and STIM1) in bead-stimulated CD4+ T-cells. Our<br />
results show that bead stimulation of primary human CD4+ T-cells together with siRNA<br />
technology can be used to analyze physiological functions of membrane proteins during<br />
T-cell activation.
Stefanie Kliche, Gael Menasche, Dennis Breitling, Mauro Togni, Xiaoqian Wang, Rico<br />
Pusch, Ana Kasirer-Friede, Theresia E. B. Stradal, Gary A. Koretzky, Burkhart Schraven<br />
THE ADAP/SKAP-55 SIGNALING MODULE REGULATES TCR-<br />
MEDIATED INTEGRIN ACTIVATION THROUGH PLASMA<br />
MEMBRANE TARGETING OF RIAM/RAP1<br />
Integrins, such as VLA-4 or LFA-1 (beta-1 or beta-2-integrins), play an important role<br />
during T-cell adhesion to the endothelium and also establishes and strengthens the<br />
contact between T-cells and APCs. However, on resting T-cells integrins are not<br />
constitutively adhesive. Rather, external stimuli (e.g. binding of antigen/MHC to the<br />
TCR) trigger the activation of LFA-1 or VLA-4 and enhance their avidity for their ligands<br />
ICAM-1, VCAM, or fibronectin (inside-out-signaling). The molecular basis for inside-outsignalling<br />
is not yet <strong>complete</strong>ly understood. Previously, it has been shown that two<br />
cytosolic adapter proteins, SKAP-55 (Src kinase-associated Phosphoprotein of 55 kDa)<br />
and ADAP (Adhesion and Degranulating promoting Adapter Protein), are critically<br />
involved in inside-out-signaling mechanism leading to activation of both LFA-1 and VLA-<br />
4. Moreover, we have shown that ADAP and SKAP-55 constitutively interact with each<br />
other and form a functional unit (the ADAP/SKAP-55 module) in T-cells. Structurefunction<br />
analysis further revealed that either the SH3 domain of SKAP-55 or the central<br />
proline-rich region of ADAP is absolutely mandatory to facilitate activation of integrins.<br />
We also show that Rap1-mediated activation of LFA-1 or VLA-4 is impaired in cells in<br />
which the interaction between ADAP and SKAP-55 has been interrupted. However, this<br />
is not due to an alteration of Rap1 GTPase activity but rather due to displacement of<br />
Rap1 from the plasma membrane (Kliche et al., 2006 MCB 26:7130-44). Recently, we<br />
identified RIAM (Rap1-GTP interacting adaptor molecule), a Rap1 effector protein, as a<br />
key component linking the ADAP/SKAP-55 module to the small GTPase Rap1 facilitating<br />
TCR-mediated integrin activation. We show that RIAM constitutively interacts with ADAP/<br />
SKAP-55 module in Jurkat T-cells and primary T-cells. Collectively, our data suggest<br />
that the ADAP/SKAP-55/RIAM complex is required to target activated Rap1 to the<br />
plasma membrane facilitating TCR-mediated integrin activation (Menasche et al., MCB<br />
in press).
Stephanie Joachim, Joachim Storf, Norbert Pfeiffer, Franz Grus<br />
The Analysis of Antibody Patterns in Glaucoma Patients<br />
Purpose: In previous studies changes in antibody profiles against ocular antigens have<br />
been shown in sera of glaucoma patients. These findings suggest an autoimmune<br />
involvement in the pathogenesis of glaucoma at least in some patients. All studies could<br />
consistently demonstrate up- and down-regulations in immunoreactivities in glaucoma<br />
patients compared to healthy control subjects. However, all these studies have in<br />
common that they used crude protein extracts from retina or optic nerve. Therefore, it<br />
was the aim of this study to analyze the immunoreactivities in sera of glaucoma<br />
patients against the most important purified antigens identified in previous studies by<br />
customized protein micro-arrays.<br />
Methods: Sera of patients with primary open-angle glaucoma (n=50) and healthy<br />
controls (n=50) were included in this study. The protein arrays were prepared by<br />
spotting commercial available antigens onto special nitrocellulose-coated slides. Up to<br />
80 different antigens were used in each customized protein micro-array. The arrays<br />
were incubated with sera of patients (1:25, overnight) and the antibody-antigenreactions<br />
were visualized by chloronaphthol staining. After digitizing, the spot intensities<br />
were compared and analyzed by multivariate statistical techniques.<br />
Results: Using protein micro-arrays, we were able to detect immunoreactivities in sera<br />
of patients and healthy controls against purified antigens like heat shock protein 27, 60,<br />
and 70, and glial fibrillary acidic protein, glutathione-S-transferase, α-fodrin, and αcrystallin.<br />
The statistical analysis revealed a significant difference (P
Bettina Jux, Markus Frericks, Charlotte Esser<br />
The arylhydrocarbon receptor is a critical regulator of<br />
Langerhans cell maturation<br />
Langerhans cells (LC) are the professional antigen-processing cells of the epidermis.<br />
The transcription factor arylhydrocarbon receptor (AHR) controls expression of the<br />
xenobiotic metabolizing enzymes which degrade many low molecular weight chemicals<br />
(LMWC) present in the natural environment. Metabolic transformation of LMWC may<br />
result in their covalent protein-binding and use as haptens, and eventually allergic<br />
reactions, including contact dermatitis. We studied whether and how LC have strategies<br />
to avoid this risk.<br />
We found that the AHR is abundantly expressed in LC, but its signalling is impeded, as<br />
treatment with a known strong AHR ligand (2,3,7,8 tetrachlorodibenzo-dioxin) does not<br />
lead to gene induction. The concomitant high constitutive expression of the AHRrepressor<br />
in LC might explain this finding, and points to a relevant tolerogenic strategy<br />
of LC. We therefore investigated LC maturation and function in AHR-deficient mice. We<br />
found that (i) their LC express the AHR-repressor only weakly, (ii) AHR ko LC were<br />
arrested in maturation, i.e. they remained smaller and less granular, and did not<br />
upregulate expression of co-stimulatory molecules CD40, CD80, and CD24 after in vitro<br />
maturation, and (iii) their phagocytic capacity was affected. GM-CSF, a potential inducer<br />
of co-stimulatory molecules, is secreted in significantly lower amounts by AHR-ko<br />
epidermal cells (i.e. keratinocytes and LC). Our data suggest that the AHR has a critical<br />
role in maturation of LC and is part of their risk strategy against unwanted immune<br />
activation by potential skin allergens.
Sonja Ortler, Christoph Leder, Michel Mittelbronn, Alla Zozulya, Lieping Chen, Antje<br />
Kroner, Heinz Wiendl<br />
The B7-homologue 1 (B7-H1/PD-L1) contributes to<br />
confinement of immunopathological CNS damage:<br />
implications for Multiple sclerosis<br />
The coinhibitory B7-H1 critically influences adaptive immune responses both in the<br />
initiation and the effector phases of experimental autoimmune encephalomyelitis (EAE),<br />
an animal model of multiple sclerosis. To further understand the role of B7-H1/PD1<br />
pathway in the CNS autoinflammation, we analyzed the kinetics of adaptive and<br />
regulatory immune responses in MOG 35-55 induced EAE using B7-H1 -/- mice. Here, we<br />
show that B7-H1 -/- mice exhibit an accelerated disease onset and significantly<br />
exacerbated EAE severity following MOG immunization. This disease pattern was<br />
followed by significantly different kinetic of IFNγ secretion suggesting an involvement of<br />
this molecule in maintaining the survival of antigen-specific T cells during EAE. In<br />
accordance with EAE data, the numbers of T cells in the CNS were increased in B7-H1 -/-<br />
mice with significantly elevated frequency of infiltrating neuroantigen-reactive T cells.<br />
Additionally, we demonstrate that MOG-specific T cell presence in B7-H1 -/- mice are<br />
exclusively restricted to the CNS depending on the stage of the disease. B7-H1<br />
specifically expressed by antigen presenting cells (APC) had an inhibitory effect on MOGreactive<br />
T cells. Although B7-H1 had no influence on B cell responses, the absence of<br />
B7-H1 was associated with lower numbers of CD8 + CD28 - regulatory T cells. We also<br />
describe a strong upregulation of B7-H1 with highest immunoreactivity in areas of<br />
severe inflammation in human brain lesions during MS.<br />
Our findings demonstrate the critical importance of B7-H1 as an immune-inhibitory<br />
molecule capable of downregulating encephalitogenic T cell activation and expansion in<br />
the CNS thus contributing to the confinement of immunopathological damage.
Thomas Ebensen, Kai Schulze, Peggy Riese, Michael Morr, Carlos A. Guzmán<br />
The bacterial second messenger cdiGMP exhibits promising<br />
activity as mucosal adjuvant<br />
The development of mucosal adjuvants is still a critical need in vaccinology. In the<br />
present work we show that bis-(3′,5′)-cyclic dimeric guanosine monophosphate<br />
(cdiGMP), a second messenger that modulates cell surface properties of several microorganisms,<br />
exerts potent activity both as mucosal adjuvant. BALB/c mice were<br />
immunized by intranasal route with the model antigen beta-Galactosidase (beta-Gal) coadministered<br />
with cdiGMP. Animals receiving cdiGMP as adjuvant showed significantly<br />
higher anti-beta-Gal immunoglobulin G (IgG) titers in sera than controls (i.e. 512-fold;<br />
p
Martin Klemke, Elisabeth Kramer, Guido Wabnitz, Mathias Konstandin, Yvonne<br />
Samstag<br />
The chemokine SDF-1α induces dephosphorylation of the actin<br />
remodelling protein cofilin via a Gi/Ras/MEK pathway in<br />
primary human T cells<br />
The homeostatic and inflammatory migration of T cells is mediated via several<br />
chemokines which act on different G protein-coupled receptors (GPCR). CXCR4, the<br />
receptor for the chemokine SDF-1α, is expressed by most human T cell subpopulations.<br />
SDF-1α treatment activates multiple downstream signaling pathways, e.g. the MEK- and<br />
PI3K-pathways, which finally leads to reorganization of the actin cytoskeleton. However,<br />
the exact molecular mechanisms of CXCR4-mediated actin reorganization in primary<br />
human T cells are still unclear. The actin-binding protein cofilin is a central regulator of<br />
actin dynamics through its actin depolymerizing and severing activity. In resting human<br />
T cells, most of the cofilin molecules are inactivated through phosphorylation at Ser3.<br />
Here we show, that cofilin is dephosphorylated/activated upon treatment of primary<br />
human T cells with SDF-1α. This dephosphorylation is mediated via a Gi/Ras/MEK<br />
pathway, whereas the PI3K pathway is not involved. Interference with the cofilin<br />
dephosphorylation pathway by inhibition of MEK results in enhanced SDF-1α-induced<br />
actin polymerization and reduced velocity during SDF-1α mediated cell migration. These<br />
data imply that dephosphorylation/activation of cofilin through a Gi/Ras/MEK signaling<br />
pathway is necessary for the proper reorganization of the actin cytoskeleton during SDF-<br />
1α mediated migration of primary human T cells.
Birgit C Viertlboeck, Sonja Schweinsberg, Matthias A Hanczaruk, Ramona Schmitt,<br />
Louis du Pasquier, Friedrich W Herberg, Thomas W Göbel<br />
The chicken leukocyte receptor complex encodes a<br />
primordial, activating, high affinity IgY Fc receptor.<br />
Fc receptors are key players of the immune system that link the fine specificity of<br />
immunoglobulins and innate effector responses. Here we describe the first nonmammalian<br />
Fc gamma receptor, CHIR-AB1, a member of the leukocyte receptor<br />
complex, that binds IgY with high affinity with its single Ig domain. It is expressed on<br />
immature and mature B-lymphocytes, monocytes, macrophages and natural killer cells<br />
and harbours motifs of activating and inhibitory Fc receptors. In the absence of the<br />
common gamma chain, CHIR-AB1 can be expressed on B cells, but crosslinking does<br />
not induce intracellular calcium release. In contrast, cells expressing CHIR-AB1 and<br />
common gamma chain are triggered to release intracellular calcium upon stimulation<br />
with heat-aggregated IgY. CHIR-AB1 thus represents a novel primordial Fc receptor that<br />
combines features of different mammalian counterparts.
Matthias A. Hanczaruk, Thomas W. Göbel, Birgit C. Viertlboeck<br />
THE CHICKEN TRIGGERING RECEPTOR EXPRESSED ON<br />
MYELOID CELLS (TREM)<br />
Triggering receptors expressed on myeloid cells (TREM) represent a multigene family on<br />
human chromosome 6 with numerous members. TREM homologues have recently been<br />
identified on chicken chromosome 26 as members of the Immunoglobulin-like receptor<br />
family including activating and inhibitory receptors. In contrast to human TREMs, in<br />
chicken there is only one activating member, TREM-A1, characterized by one<br />
extracellular Ig domain and a positively charged transmembrane residue. There are two<br />
inhibitory members, TREM-B1 and TREM-B2, displaying cytoplasmatic ITIMs. Three<br />
different splice variants of TREM-B2 have been identified, one variant with only one Ig<br />
domain, one with two and one with four Ig domains, whereas there’s only one variant of<br />
TREMB-1 containing two Ig domains, apparently.<br />
Gene expression pattern for the various chicken TREM were analyzed by real-time RT-<br />
PCR and normalized on the housekeeping gene 18S RNA. By employing real-time RT-<br />
PCR with primers spanning Ig domain and transmembrane region of TREM-A1, we<br />
showed that TREM-A1 mRNA is highly expressed in brain, bone marrow and<br />
macrophages. We also found a variant of TREM-A1, mainly occurring in thrombocytes,<br />
by using primers specific for the single Ig-domain of TREM-A1 in real-time RT-PCR,<br />
indicating that there is a real splice-variant. High mRNA levels of TREM-B1 were<br />
detected in thrombocytes and bone marrow. The splice variant of TREM-B2 containing<br />
four Ig domains is highly expressed in macrophages and bone marrow, too. After<br />
stimulation of macrophages with LPS, APEC LPS, IFNγ and bacterial DNA the mRNAexpression<br />
of all three members, especially of TREM-A1, is downregulated.<br />
TREM-A1 shows high homology with human TREM2, whereas TREM-B1 is more similar<br />
to human TLT-1. Apparently there is no mammalian homologue for TREM-B2.<br />
We have recently generated a monoclonal antibody against TREM-A1, too, which<br />
stained virtually macrophages by flow cytometry, which will be used for further<br />
investigations.<br />
In summary some of the chicken TREMs share mammalian homologues implicating a<br />
conserved TREM system in the chicken, whereas others might be unique to the chicken.
Barbara Simm, Matthias Witt, Monika Braun, Barbara Mosetter, Rudolf Gruber, Dolores<br />
Schendel, Christine Falk<br />
The correlation of CD6 expression with infiltration of NK cells<br />
into synovial fluid of Arthritis patients.<br />
The repertoire of infiltrating NK cells into synovia of patients with inflammatory arthritis<br />
has been shown to be reversed with respect to the major NK subpopulations that are<br />
defined as CD16 + CD56 dim and CD16 - CD56 bright NK cells. We analyzed 14 paired<br />
samples of synovial fluid and peripheral blood from patients with various rheumatic<br />
diseases regarding the phenotypical and functional characteristics of the infiltrating NK<br />
cells. Therefore, we focussed on possible correlations of various NK markers with<br />
infiltration, on the cytotoxic capacitiy and on the recognition of ULBP4, a ligand for the<br />
activating NK receptor NKG2D.<br />
The phenotype of the synovial and peripheral lymphocytes was analysed by screening<br />
>20 markers. HLA and KIR typing was performed using the Luminex SSO-Typing<br />
Method. For the determination of the cytokine profiles, we applied Multiplex Bead Arrays<br />
of 50 analytes. The function of synovial NK cells was defined by CD107a-degranulation<br />
assays. ULBP4-transfectants of C1R were utilized to discriminate differences in NKG2Dmediated<br />
activation between peripheral and synovial NK cells.<br />
Our results confirmed the predominance of the CD56 bright CD16 - NK subpopulation in<br />
the synovial fluid. Amongst all 20 markers tested, CD6 showed the strongest correlation<br />
with this NK cell infiltration. In the periphery, CD6 expression on NK cells strongly<br />
correlates with CD16 + CD56 dim subgroup. Remarkably, almost all NK cells in the CD16 -<br />
subset infiltrating into the joints also are CD6 negative. Our results indicate that CD6 is<br />
differentially expressed on NK cell subsets and presents a novel NK cell marker for<br />
infiltration into synovial tissue. These infiltrating CD56 bright CD6 - NK cells display<br />
cytotoxic capacity and were additionally activated by ULBP4. The cytokine pattern of<br />
synovial fluid showed an increase of proinflammatory cytokines and chemokines that<br />
may contribute to the attraction of these CD6 - NK cells into tissues, in general.
Edgar Serfling, Rene Rost, Wen Chen, Sergei Chuvpilo, Eisaku Kondo<br />
The Crosstalk between NF-kB and NFATc1/aA, the Inducible<br />
Short Isoform of NFATc1, Protects B-Lymphocytes against<br />
Apoptosis<br />
Among the NFATc proteins NFATc1, c2 and c3 which are expressed in lymphocytes, the<br />
synthesis of NFATc1 is strongly induced upon immunoreceptor and co-receptor<br />
stimulation. This concerns mainly NFATc1/alphaA, a short isoform of NFATc1 which<br />
differs in both its N- and C-terminal peptides from other NFATc proteins. Whereas<br />
NFATc2 and c3 exert a pro-apoptotic activity, we show here that (i) inactivation of the<br />
Nfatc1 gene in chicken DT40 B cells results in a marked increase of B cell receptor and<br />
Ca++- induced apoptosis, whereas (ii) re-expression of NFATc1/alphaA in these cells<br />
leads to a delay in apoptosis induction which can be rescued by low doses of cyclosporin<br />
A. In addition to the induction of Bcl-6 and BAG-2 (Bcl-2 associated anthanogene 2),<br />
this is due to the NFATc1/alpphaA-mediated increase in PKC-theta• levels and further<br />
proteins controling NF-kappaB induction. Our data show that by enhancing NF-kappaB<br />
levels, NFATc1/alphaA renders lymphocytes resistant to apoptosis when it is expressed<br />
at high concentrations.
Martin Holdener, Edith Hintermann, Eric F. Johnson, Michael P. Manns, Matthias G.<br />
von Herrath, Urs Christen<br />
The CYP450 mouse model for autoimmune hepatitis: Breaking<br />
of self-tolerance in transgenic CYP2D6 and wildtype FVB-mice<br />
by viral infection<br />
The etiology of autoimmune hepatitis (AIH) is poorly understood although the major<br />
autoantigen, cytochrome P450 2D6 (CYP2D6), has been identified and immunodominant<br />
epitopes mapped. Therefore, we generated an animal model for human AIH using the<br />
natural autoantigen CYP2D6. We infected transgenic mice expressing human CYP2D6 in<br />
the liver (CYP-2D6 mice) with an Adenovirus-CYP2D6 vector (Ad-2D6) to break selftolerance.<br />
Surprisingly, upon infection with Ad-2D6 not only transgenic CYP2D6 mice<br />
but also wildtype FVB mice showed several persistent features characteristic for liver<br />
damage associated with AIH. These features included massive hepatic fibrosis, ‘fused’<br />
liver lobules, disorganized architecture, cellular infiltrations and focal to confluent<br />
necrosis. Further, all Ad-2D6-infected mice generated high titers of anti-CYP2D6<br />
antibodies. Epitope mapping revealed that such anti-CYP2D6 antibodies predominantly<br />
recognized the core peptide sequence AQPPRD (CYP2D6 aa265-270), which is the<br />
immunodominant linear epitope recognized by LKM-1 antibodies from AIH patients. In<br />
contrast, mice infected with a control Adenovirus did neither develop liver damage nor<br />
generated anti-CYP2D6 antibodies. Interestingly the kinetics and severity of liver<br />
damage as well as antibody formation was enhanced in wildtype FVB mice compared to<br />
transgenic CYP2D6 mice. Our data indicate that the liver damage was reduced and<br />
delayed in transgenic CYP2D6 mice due to a certain degree of tolerance towards human<br />
CYP2D6 compared to wildtype FVBs, which do not express the human version of the<br />
2D6 isoenzyme. In wildtype FVB mice, due to the homology of the mouse isoenzymes of<br />
the CYP superfamily to human CYP2D6, autoimmune liver damage by Ad-2D6-infection<br />
was possibly induced via true ‘molecular mimicry’.
Tarvo Rajasalu, Wolfram Karges, Andreas Spyrantis, Andreas Wieland, Bernhard<br />
Böhm, Reinhold Schirmbeck<br />
The diabetogenic, insulin-specific CD8 T cell response primed<br />
in the experimental autoimmune diabetes model in RIP-B7.1<br />
mice<br />
Type 1 diabetes mellitus can result from the specific destruction of pancreatic beta cells<br />
by autoreactive T cells. As shown here, experimental autoimmune diabetes (EAD) is<br />
efficiently induced in RIP-B7.1 mice by preproinsulin (ppins)-encoding DNA vaccines.<br />
EAD develops in RIP-B7.1 mice within 3-4 weeks after a single immunization with ppinsencoding<br />
plasmid DNA. RIP-B7.1 mice develop insulitis, insulin deficiency and<br />
hyperglycemia after vaccination with plasmids encoding either murine ppins-I, murine<br />
ppins-II, or human hu-ppins. EAD induction critically depends on CD8 T cells and was<br />
independent of CD4 T cells. To be diabetogenic, ppins-specific CD8 T cells had to<br />
express IFNgamma. Neither expression of perforin, nor signaling through the type I<br />
interferon receptor are essential components of this pathogenic CD8 T cell phenotype.<br />
Using plasmids encoding truncated ppins variants, we show that EAD is only induced by<br />
DNA vaccines encoding the insulin A-chain. Diabetogenic CD8 T cells specifically<br />
recognize the Kb-restricted A12-21 epitope of the insulin A-chain. The RIP-B7.1 model<br />
hence represents an attractive model for the characterization of cellular and molecular<br />
events involved in the CD8 T cell- mediated immune pathogenesis of diabetes.
Stephan Thurau, Maria Diedrichs-Möhring, Christiane Hoffmann, Gerhild Wildner<br />
The distribution of uveitogenic GFP+ T cells in a rat model of<br />
uveitis<br />
Uveitis is an inflammatory autoimmune disease of the eye, mediated by CD4+ T cells<br />
specific for ocular antigens. In Lewis rats experimental autoimmune uveitis (EAU) can<br />
be induced by adoptive transfer of retina specific CD4+ T cells. In order to investigate<br />
the fate of uveitogenic T cells after ocular inflammation, during spontaneous relapses as<br />
well as during experimental reinduction of disease and after extended remission we<br />
injected GFP-transduced CD4+ T cell lines specific for the IRBP-peptide R14 in rats that<br />
developed uveitis 5-6 days later. At day 27 these rats were immunized with peptide R14<br />
in CFA and developed a uveitis relapse around day 35. In another experiment GFP+ CD4<br />
+ T cells specific for Ovalbumin (OVA) were adoptively transferred to Lewis rats. Nine<br />
days later rats were immunized with retinal peptide PDSAg in CFA to induce uveitis.<br />
Eyes, lymph nodes and spleens were collected at different time points. Six weeks after<br />
transfer GFP+ T cells of either specificity were observed in the retinas. In eyes with<br />
uveitis - either after spontaneous or induced relapse - the numbers of intraocular GFP+<br />
cells increased slightly. Clusters of retina-specific GFP+ T cells were detectable,<br />
suggesting clonal expansion or focal attraction of new GFP+ cells invading from the<br />
periphery, whereas in clinically quiet eyes single GFP+ cells were distributed within the<br />
retina. OVA-specific T cells also migrated into the retina independently of EAU<br />
development, but never formed clusters in either active inflammation or quiescent<br />
stage. GFP+ cells were also found in peripheral lymph nodes (inguinal, mesenteric) and<br />
spleens more than 5 weeks after adoptive transfer. GFP+ cells were seen in the T cell<br />
areas of the spleen and in lymph nodes at any time during the observation period.<br />
Activated T cells of any specificity can invade the ocular tissues and remain viable within<br />
the eyes and lymphoid tissues for an extended time period without undergoing<br />
apoptosis. They are recruited to the eye from the periphery during a secondary disease<br />
course, but may also clonally expand in situ after antigen-specific stimulation.
Tobias Haas, Jochen Metzger, Frank Schmitz, Antje Heit, Eicke Latz, Hermann Wagner<br />
The DNA sugar backbone 2-deoxyribose determines Toll-like<br />
receptor 9 activation<br />
Toll-like receptor 9 (TLR9) is believed to represent a pattern recognition receptor<br />
specific for pathogen derived DNA, equipped with competence for “foreign-self”<br />
discrimination. CpG-dinucleotides, abundant in microbial DNA yet largely absent from<br />
mammalian DNA, are considered important attributes of “foreign”. Based on<br />
experiments using phosphorothioate (PS)-modified oligodeoxynucleotides (ODN) to<br />
obviate DNase-sensitivity and inefficient uptake of natural phosphodiester (PD) ODN,<br />
TLR9 has been found to require such CpG-motifs within ss PS ODN to become activated.<br />
We show that different rules apply for TLR9-mediated recognition of unmodified, natural<br />
DNA: PD ODN devoid of CpG, unlike PS ODN, activate TLR9 when translocated into<br />
TLR9-containing endosomes of immune cells. Determinant of this CpG-motif<br />
independent recognition is the PD 2-deoxyribose sugar backbone, which, as base-free<br />
homopolymer, binds to and basally activates TLR9. Random bases add to the<br />
stimulatory potential, even atypical bases like uracil are tolerated. Substitution of the 2deoxyribose<br />
sugar backbone with ribose, however, abrogates TLR9-binding and<br />
stimulation. In contrast, homopolymeric, base-free PS 2-deoxyribose is bound by TLR9<br />
with 100fold higher affinity than PD 2-deoxyribose and, surprisingly, has a potent<br />
competitive-inhibitory effect on ligand induced TLR9 activation, both in vitro and in vivo.<br />
Adding random bases does not alter this dominant negative effect, whereas adding CpGmotifs<br />
reverses it and thus results in the well-known, robust TLR9-stimulatory activity<br />
of PS CpG ODN. These data show that the sugar backbone 2-deoxyribose determines<br />
TLR9-activation and explain the current misconception that CpG-motifs {interpreted as<br />
pathogen associated molecular patterns (PAMPs)} are crucial for DNA-recognition by<br />
TLR9. We propose that TLR9 is a receptor for natural DNA with no inherent ability to<br />
discriminate “foreign” from “self”. Expressed within endosomes, TLR9 is not exposed to<br />
extracellular “self”-DNA yet poised to recognise DNA from pathogenic invaders.
Dieter Kube, Diana Pinkert, Nils Schoof, Frederike von Bonin, Jennifer Theiss, Fred<br />
Schaper, Johannes Bode, Martina Vockerodt<br />
The EBV oncoprotein Latent Membrane Protein 1 affects the<br />
expression of suppressors of cytokine signaling (SOCS) in<br />
transformed B lymphocytes<br />
Constitutive activation of signal transducer and activator of transcription 1 and 3<br />
(STAT1, STAT3) is a distinctive feature of Epstein-Barr virus (EBV) infected B cells<br />
characterized by the latency program III. The expression of STAT1 and the activation of<br />
STAT3 in these cells can be modulated by the latent membrane protein 1 (LMP1), a<br />
protein with known oncogenic properties. The mechanism of activation and the<br />
functional responses are still unclear. The expression of full length LMP1 is responsible<br />
for an enhanced STAT1 protein expression in Burkitt lymphoma cells (BL). STAT3 is<br />
tyrosine phosphorylated without changes in STAT3 protein levels. A specific pattern of<br />
Janus kinases (Jak) is activated by EBV, in part by LMP1 mediated activation of<br />
respective cytokines. In LMP1 expressing BL cells suppressor of cytokine signaling<br />
(SOCS) 3 mRNA is expressed involving transcriptional and posttranscriptional<br />
mechanisms. The SOCS3 mRNA half life is regulated by LMP1 mediated p38/SAPK2<br />
activation. Jak3 is involved in SOCS3 expression in BL cells as shown by specific<br />
inhibitors. LMP1 activates SOCS3 promoter elements. Overexpression of SOCS3<br />
prevents to a defined extend the activation of STAT3 by cytokines. SOCS1 mRNA is<br />
expressed in all analysed cells independent from EBV. Our results support the role of<br />
LMP1 in modulating cytokine signaling (supported by DFG Ku 954/7-2 and the<br />
Graduiertenkolleg 1034).
Dong Wang, Melanie Drenker, Thomas Werfel, Miriam Wittmann<br />
The epidermal inflammatory response in lupus erythematosus<br />
shows an autocrine amplification loop. Major role of<br />
TNF&alpha and IL-18.<br />
Cutaneous manifestations belong to the most common clinical features of lupus<br />
erythematosus (LE). Tissue resident cells are increasingly being recognised as active<br />
cells in the pathophysiology of various autoimmune diseases. Evidence is accumulating<br />
that keratinocytes play an important role in regulating and maintaining the pathology in<br />
cutaneous LE. It was the aim of this study to analyse differences in the inflammatory<br />
response of keratinocytes from patients suffering from LE as compared to healthy<br />
controls. We analysed keratinocytes outgrown from epidermal stem cells from the outer<br />
root sheet of the hair follicle and could determine marked differences of keratinocytes in<br />
response to proinflamatory mediators. Main findings by flow cytometry and ELISA<br />
include that keratinocytes from LE patients express higher IL-18R on their cell surface in<br />
response to TNF&alpha or IFN&gamma stimulation. Furthermore in response to IL-18<br />
these cells produced large amounts of TNF&alpha but failed to express the cellprotective<br />
IL-12p40. IL-12 has been shown to protect keratinocytes from UV induced<br />
apoptosis. We found that keratinocytes derived from LE patients are as well protected<br />
as normal keratinocytes by IL-12 but not IL-18. In contrary, keratinocytes from LE<br />
patients were more prone to die upon exposure to IL-18. Our results demonstrate an<br />
intrinsic difference in the inflammatory response of keratinocytes and suggest an<br />
autocrine positive feedback loop involving TNF&alpha, IL-18 and IL-12 family members.<br />
These results point to a potential benefit of a local anti-TNF&alpha or anti-IL-18 therapy<br />
for cutaneous lupus manifestations.
Andreas Vilcinskas, Boran Altincicek<br />
The greater wax moth Galleria mellonella as a mini-host<br />
model for human pathogens and as a reservoir for novel<br />
peptide antibiotics<br />
Insects attract increasing attention as mini-host models for human pathogens to<br />
analyse infection and immunity at cellular and molecular level. Lacking adaptive<br />
immunity, insects are particularly suitable models to elucidate interaction between<br />
virulence factors and the innate immune system. Particularly one lepidopteran, the<br />
greater wax moth Galleria mellonella, has recently been emerged as a powerful model<br />
to study pathogenesis of prominent bacteria and yeasts causing severe diseases in<br />
humans (Chamilos et al. 2007, Lancet Infect Dis.7, 42-55). G. mellonella larvae provide<br />
a number of advantages, for example, they can be reared at temperatures to which<br />
human pathogens are adapted and which are essential for the synthesis of their<br />
virulence factors among which thermolysin-like metalloproteinases play a predominant<br />
role. The latter were discovered to mediate sensing of infection and activation of innate<br />
immune responses in G. mellonella in the sense of the danger model introduced by Poly<br />
Matzinger (Altincicek et al. 2007, Infect Immun 75, 175-183).<br />
In addition, combined transcriptomic and proteomic analyses of innate immunity in G.<br />
mellonella led to the identification of a diverse array of antimicrobial peptides among<br />
which the first and to date only inhibitor of microbial metalloproteinases from animals<br />
was discovered. This insect metalloproteinase inhibitor (IMPI) specifically inhibits toxic<br />
enzymes which are responsible for a broad spectrum of pathological symptoms during<br />
infectious diseases in humans, and which have been recognized as promising targets for<br />
the rational design of second generation antibiotics (Wedde et al. 2007, Biol Chem 388,<br />
119-127). Presently, we investigate the 3D-structure of the IMPI as a template for the<br />
design of novel peptide antibiotics.
Leslie Elsner, Vijayakumar Muppala, Mathias Gehrmann, Jingky Lozano, Heike<br />
Bickeböller, Thomas Herrmann, Lutz Walter, Frauke Alves, Gabriele Multhoff, Ralf<br />
Dressel<br />
The heat shock protein HSP70 promotes NK cell activity<br />
against tumors which express inducible NKG2D ligands<br />
The stress-inducible heat shock protein (HSP) 70 is known to function as an endogenous<br />
danger signal which can increase the immunogenicity of tumors and induce CTL<br />
responses. We show here that HSP70 also activates NK cells which recognize stressinducible<br />
NKG2D ligands on tumor cells.<br />
Tumor size and the rate of metastases derived from HSP70-overexpressing human<br />
melanoma cells were found to be reduced in T and B cell-deficient SCID mice, but not in<br />
SCID/beige mice which lack additionally functional NK cells. NK cells derived from SCID<br />
mice with HSP70-overexpressing tumors showed in vitro an augmented cytotoxicity<br />
against cells which expressed NKG2D ligands, such as MHC class I chain-related (MIC) A<br />
and B molecules. MICA/B expression was found to be induced in the tumors.<br />
Interestingly, a counter selection was observed against the expression of MICA/B in the<br />
HSP70-overexpressing melanomas compared to control melanomas in SCID, but not in<br />
SCID/beige mice. In accordance with these observations, HSP70-containing exosomes<br />
from HSP70-overexpressing tumor cells in contrast to HSP70-negative exosomes from<br />
control tumor cells were able to activate mouse NK cells in vitro to kill YAC-1 cells which<br />
express NKG2D ligands or human melanoma cells in which MICA/B expression was<br />
induced by pharmacological means. Recombinant HSP70 had similar effects on the NK<br />
cells as tumor cell-derived HSP70-positive exosomes.<br />
The synergistic activity of two stress-inducible danger signals, HSP70 and MICA/B,<br />
apparently leads in this model to enhanced activation of NK cells and results in a<br />
reduced tumor growth and <strong>complete</strong>ly suppresses metastatic disease.<br />
This work was supported by grants from the DFG (DR 394/2, GRK 1034) and the EU<br />
(MRTN-CT-2004-512253; TRANS-NET).
Aysefa Doganci, Petra Scholtes, Joachim Maxeiner, Roman Karwot, Edgar Schmitt,<br />
Hans A. Lehr, I.Cheng Ho, Susetta Finotto<br />
The IL-2R alpha and IL-2R beta chains differentially regulated<br />
allergic airway inflammation in an experimental in vivo model<br />
To assess the role of IL-2 signal transduction in experimental asthma, we compared the<br />
effect of intranasal blockade of the IL-2Rα or β-chains. In our studies, local blockade of<br />
the IL-2Rβ-chain, led to an amelioration of airway resistance and inflammation in OVA<br />
sensitized and challenged mice. Moreover, both treatements led to a marked reduction<br />
of Th2 type cytokines IL-4, IL-5 while IL-13 was inhibited specifically by the blockade of<br />
the IL-2Rβ-chain. Consistent with these findings, blockade of the IL-2Rβ-chain, as<br />
opposed to blockade of the IL-2Rα chain, led to a suppression of CD4+ T cells<br />
proliferation in the local draining lymph nodes where immunosuppressive CD4+CD25+<br />
T regulatory cells were downregulated specifically only by the IL-2Rα blockade. Taken<br />
together these results suggest that local blockade of the IL-2Rβ-chain during the<br />
antigen challenge phase could be a successful therapy in allergic disease by rescuing<br />
the T regulatory cells in the local draining lymph nodes where they regulate the<br />
development of pathogenic Th2 cells in this experimental model of asthma.<br />
This work is supported by SFB 548 Grand.
Christine S. Falk, Dominik ter Meer, Iris Bigalke, Alexander Buchner, Barbara<br />
Mosetter, Barbara Simm, Monika Braun, Dusan Prevalsek, Dolores Schendel, Hans-<br />
Jochem Kolb<br />
The Impact of HLA-C and KIR Genetics on Survival of AML<br />
versus ALL Patients following Haploidentical Bone Marrow /<br />
Stem Cell Transplantation.<br />
Introduction: Recent evidence suggests that alloreactive NK cells in haploidentical BMT/<br />
SCT may provide graft-versus-leukemia (GVL) effects. In particular, the constellation of<br />
KIR-positive donor NK cells in absence of inhibitory HLA-C ligands in the patient may<br />
provide advantages for AML patients. Currently, clinical protocols attempt to benefit<br />
from NK alloreactivity by selecting KIR/HLA-C incompatible donors. Materials and<br />
Methods: Since 1996, more than 100 patients with leukemic malignancies have been<br />
transplanted with haploidentical bone marrow at day 0 followed by G-CSF-mobilized T<br />
cell-depleted peripheral blood stem cells (PBSC) at day 6 under immune suppression<br />
(ATG, MTX, CyA). PBSC derived from 37 donors were characterized with respect to NK<br />
and T cell subpopulations prior to and after T cell depletion. Functionality was<br />
determined by cell CD107a degranulation and cytokine secretion against K562 and<br />
some haploidentical recipient cells. HLA-C and KIR genes of 80 patient/donor<br />
combinations were typed by the Luminex-based SSO method. Results and Conclusions:<br />
Although <strong>complete</strong> haploidentical bone marrow was transplanted at day 0, no<br />
enhancement of acute GVHD compared to HLA-identical matched unrelated BMT was<br />
observed in 98 haploidentical transplanted patients – independently from HLA-C or KIR<br />
constellations. Complete chimerism was established early post transplantation. In<br />
general, T cell-depleted PBSC contained more NK cells than CD34+ stem cells<br />
demonstrating that high numbers of alloreactive NK cells do not correlate with aGVHD.<br />
Functional analyses of NK subpopulations in PBSC prior to and after T cell depletion<br />
revealed i) differences in cytokine secretion among particular donor/recipient<br />
constellations, ii) weak cytotoxic activity against K562, iii) changes in the composition of<br />
KIR-positive and KIR-negative NK subpopulations, vi.) Most importantly, the<br />
combination of HLA-C and KIR haplotypes revealed different constellations for AML vs.<br />
ALL patients that correlate with significantly increased propability of survival.
Kristina Kunert, Constanze Schönemann, Hans-Dieter Volk, Ruth Neuhaus, Andreas<br />
Pascher, Claudia Wenzel, Peter Neuhaus, Johann Pratschke, Katja Kotsch<br />
The impact of KIR/HLA ligand incompatibility on acute<br />
rejection episodes after orthotopic liver transplantation<br />
Killer-cell immunoglobulin-like receptors (KIRs) are expressed on natural killer cells<br />
(NK) and subpopulations of T cells of the memory phenotype. They encode both,<br />
inhibitory and activating receptors within the leukocyte receptor complex (LRC) located<br />
on chromosome 19. Several studies reported that incompatibility between donor KIR<br />
receptors and their corresponding HLA ligands in the recipient thus leading to<br />
alloreactivity of NK cells reduces the extent of Graft versus Host Disease (GvHD) and<br />
minimizes the risk of relapse following bone marrow transplantation. Our own studies<br />
demonstrated the influence of KIR/HLA-ligand incompatibility on the development of<br />
acute cellular rejection following renal transplantation. Recently it has been shown that<br />
particularly HLA-C epitope disparity between donors and recipients influences<br />
posttransplant liver outcome (Bishara et al., Human Immunol 2005). Because NK cells<br />
infiltrate liver allografts very early after transplantation (Obara et al., Am J Transplant,<br />
2005), we examined the relevance of KIR/HLA-ligand incompatibility in acute rejection<br />
following orthotopic liver transplantation. Analysis considered respective matches and<br />
mismatches between KIR receptors of the recipients and corresponding ligands of donor<br />
grafts. 28 patients of the collective showed one or more biopsy proven acute rejection<br />
episodes within the first week following liver transplantation. The control group included<br />
57 patients with stable graft function. By analyzing the HLA genotype of the donor we<br />
observed a significant higher percentage of patients rejecting their allograft who<br />
received a donor graft positive for the Bw4 epitope (p=0.006), the ligand for the<br />
inhibitory receptor KIR3DL1. Furthermore we detected significantly more recipients who<br />
received grafts displaying additional MHC molecules which are not recognized as “self”<br />
by the patient in the rejection group (p=0.015). In contrast to our initial hypothesis to<br />
uncover a higher percentage of KIR/HLA ligand incompatibilities within the rejection<br />
group, frequencies of disparities were reduced in patients suffering from acute rejection,<br />
especially in the case for the inhibitory receptors KIR2DL2, KIR3DL1 and the activating<br />
receptors KIR2DS1 and KIR2DS2. In summary a more comprehensive receptor-ligand<br />
interaction is necessary to understand how KIR-HLA genotypes contribute to transplant<br />
outcome but our data suggest an impact of KIR/HLA-ligand compatibility on graft<br />
rejection in the early period after liver transplantation.
Mauro Togni, Dirk Reinhold, Burkhart Schraven, Aneegret Reinhold<br />
The importance of adhesion and migration of dendritic cells<br />
during the induction of immune reaction: A role for the<br />
adaptor protein SKAP-HOM<br />
SKAP55 (Scr kinase-associated phosphoprotein of 55 kD) and the related protein SKAP-<br />
HOM are adaptor molecules involved in inside-out signalling. In contrast to SKAP55,<br />
which is exclusively expressed in T cells, SKAP-HOM is an ubiquitous adaptor protein.<br />
Previous studies have shown that in the absence of SKAP-HOM antigen receptor<br />
triggered integrin-mediated adhesion is severely impaired in B cells but not in T cells. In<br />
vivo, the loss of SKAP-HOM results in a less severe clinical course of experimental<br />
autoimmune encephalomyelitis (EAE) following immunization of mice with the<br />
encephalitogenic peptide of MOG (Myelin Oligodendrocyte Glycoprotein). Since SKAP-<br />
HOM is highly expressed also in dendritic cell (DC), this prompted us to study its role in<br />
DC biology. Here we show that the absence of SKAP-HOM does not affect the generation<br />
of DCs in the steady state as well as the organ colonization by DCs. In addition, the in<br />
vivo and in vitro maturation of DC is normal. In contrast, in FITC painting experiments,<br />
migration of DC from the skin to the draining lymph nodes is enhanced in the absence<br />
of SKAP-HOM. In vitro, the spontaneous and the CCL19-induced chemotaxis are also<br />
increased in DC lacking SKAP-HOM. Moreover, adhesion of mature DCs to extracellular<br />
matrix (fibronectin) was found to be reduced in the absence of SKAP-HOM.<br />
Furthermore, the conjugate formation in vitro between peptide-loaded DC and antigenspecific<br />
T cells was delayed. As a possible consequence, the in vivo activation of specific<br />
T cells after adoptive transfer experiments resulted to be reduced. In conclusion, our<br />
data suggest that SKAP-HOM plays a role in modulating the adhesion of different cell<br />
types upon activation.
Rachid Marhaba, Mario Vitacolonna, Dagmar Hildebrand, Michal Baniyash, Pia<br />
Freyschmidt-Paul, Margot Zöller<br />
The importance of myeloid suppressor cells in the regulation<br />
of autoimmune effector cells by a chronic allergic eczema<br />
Induction of a chronic allergic eczema is a most efficient therapeutic for alopecia areata<br />
(AA). We had noted a reduction in regulatory T cells (Treg) during AA induction and<br />
wondered, whether Treg may become recruited or expand during repeated skin<br />
sensitization or whether additional regulatory cells account for hair regrowth.<br />
AA could not be cured by the transfer of CD4 + CD25 high from mice repeatedly treated<br />
with a contact sensitizer. This obviously is a consequence of a dominance of freshly<br />
activated as compared to regulatory CD4 + CD25 + T cells. Instead, a population of Gr-1<br />
+ CD11b + cells was significantly increased in skin and spleen of AA mice repeatedly<br />
treated with a contact sensitizer. Gr-1 + CD11b + spleen cells mostly expressed CD31.<br />
Expression of several proinflammatory cytokines, the IFNγR and the TNFRI was<br />
increased. Particularly in the skin, Gr-1 + cells expressed several chemokines and CCR8<br />
at an high level. Gr-1 + CD11b + cells most potently suppressed AA effector cell<br />
proliferation. When co-cultured with CD4 + or CD8 + cells from AA mice, the Gr-1 + CD11b<br />
+ cells secreted high levels of NO. However, possibly due to high level Bcl-2 protein<br />
expression in AA T cells, apoptosis induction remained unaltered. Instead, ζ chain<br />
expression was strongly downregulated, which was accompanied by a decrease in<br />
ZAP70 and ERK1/2 phosphorylation.<br />
Thus, a chronic allergic eczema supports expansion and activation of myeloid<br />
suppressor cells that, via ζ-chain downregulation contribute to autoreactive T cell<br />
silencing.
Michal Smida, Sabine Lindquist, Anita Posevitz-Fejfar, Diana Karitkina, Ramnik Xavier,<br />
Brian Seed, Burkhart Schraven, Jonathan A. Lindquist<br />
The importance of PAG in regulating proximal signaling<br />
The phosphoprotein associated with glycosphingolipid-enriched microdomains (PAG) is a<br />
transmembrane adaptor protein that negatively regulates the activity of Src family<br />
kinases by recruiting the cytosolic C-terminal Src kinase (Csk) to the plasma<br />
membrane. Csk phosphorylates the negative regulatory tyrosine conserved within the Cterminus<br />
of all Src family kinases. Thus, given the potentially important role of PAG as a<br />
negative regulatory molecule, it was predicted that PAG-deficiency should have severe<br />
effects; a simple knock-out was expected to be embryonic lethal and deletion in early<br />
thymocytes was predicted to lead to TCR-independent T-cell development and<br />
autoimmunity, as had previously been shown for Csk. However, PAG/Cbp-deficient mice<br />
were recently published and appear to be perfectly normal; our investigation of PAGdeficient<br />
mice clearly shows that Src kinase activity is enhanced in newborn mice, as<br />
one would expect, and that a compensatory mechanism has developed by 3 months of<br />
age. Therefore, it appears that a redundant mechanism exists to ensure the Src kinases<br />
do not go unregulated and that a simple knock-out is not the best strategy to<br />
investigate PAG function.<br />
In addition to negatively regulating Src kinase activity, we have identified PAG as a<br />
negative regulator of Ras via its ability to recruit RasGAP. Additionally, we have shown<br />
that the displacement of PAG from the lipid rafts enhances both Src kinase activation<br />
and chemokine-induced migration. Since both the Src and Ras families are important for<br />
regulating cellular activation and oncogenesis, alterations in PAG expression or<br />
localization could be a contributing factor in cancer and autoimmunity.
Lilli Podola, Hans Jürgen Ahr, Hans-Werner Vohr<br />
THE INDUCTION PHASE OF ALLERGIC ASTHMA INVESTIGATED<br />
BY A SHORT-TERM MODEL IN BROWN NORWAY RATS<br />
Dermal and bronchial sensitization represents an increasing clinical problem. Particularly<br />
low-molecular weight molecules like isocyanides contribute to the development of<br />
occupational respiratory lung disease.<br />
Today pre-clinical studies for hazard identification of respiratory sensitisation are<br />
performed by long lasting and labour extensive inhalation studies which are currently<br />
based on biphasic study protocols, induction and challenge. As there are no validated<br />
protocols up to now exposure time and quantity vary in respect to the experimental<br />
design.<br />
The goal of our studies is to tap initiating mechanisms from short-term treatments as a<br />
tool for hazard identification. Therefore, our investigations concentrated upon the<br />
induction period of experimental asthma. Female Brown Norway rats were used after<br />
intra-tracheal application of test substances like TMA in a 4 day model. After application<br />
on two consecutive days evaluation of different parameters in the lung and draining<br />
lymph nodes were performed. To avoid pronounced influence by unspecific inflammation<br />
concentrations of applicants were used at the threshold level of irritation as measured<br />
by cytotoxic reactions in the lung. We focussed on cellular events and their regulatory<br />
mechanisms rather than the critical analysis of breathing pattern, i.e. functional activity.<br />
Surprisingly, cell counts of eosinophils, one end point very simple to determine in BALF,<br />
turned out to be a reliable end point. This holds true for the detection of asthmato-genic<br />
substances as well as the irritant SDS. However from the data obtained so far different<br />
kinetics of parameters seem to indicate distinct disease pattern.<br />
To further analyse specific activation special emphasis was put on the regulation of T<br />
cell responses in the draining lymph nodes and lungs followed by in vitro studies of<br />
specific cell proliferation and multiplex cytokine pattern.<br />
It should be possible to use this model to investigate the influence of routes of<br />
administration on the development of allergic asthma.
Lucie Dörner, Heiko Weyd, Andrea Mahr, Björn Linke, Dagmar Riess, Christine S. Falk,<br />
Peter H. Krammer<br />
The influence of apoptotic cells and annexin 1 on peripheral<br />
tolerance<br />
Peripheral tolerance comprises several mechanisms that ensure the elimination or<br />
silencing of potentially auto-reactive T cells that have escaped thymic selection.<br />
Peripheral T cells are silenced when they encounter self-antigen presented by dendritic<br />
cells (DC). One important source of auto-antigens are apoptotic cells that have been<br />
engulfed by DC. It has, however, not been fully understood which signals on apoptotic<br />
cells determine the non-reactivity against self. Analysing the surface of apoptotic cells<br />
we identified the cytosolic protein annexin 1 as an potential signal recognized by DC.<br />
In order to investigate the role of annexin 1, we established an ex vivo coculture system<br />
of primary murine DC and apoptotic spleen cells or recombinant annexin 1. DC that<br />
were cultured in the presence of apoptotic spleen cells or recombinant annexin 1,<br />
respectively, showed a reduced LPS-induced secretion of the pro-inflammatory<br />
cytokines TNF, IL-1β and IL-12. The secretion of other cytokines was not altered.<br />
Furthermore, recombinant annexin 1 reduced the LPS-induced surface expression of the<br />
costimulatory molecules CD86 and CD40 while the expression of MHC-II remained<br />
constant. Adding syngeneic OT-II-T cells, we observed a reduced T-cell stimulation as<br />
measured by IFN-γ secretion. Taken together, the data suggest that annexin 1 acts as<br />
an anti-inflammatory signal on the surface of apoptotic cells and might contribute to<br />
peripheral tolerance.
Shafaqat Ali, Michael Huber, Christian Kollewe, Werner Falk, Michael U. Martin<br />
The Interleukin-1 Receptor Accessory Protein is essential for<br />
Interleukin-33 induced activation of T cells and mast cells<br />
Interleukin-33 (IL-33) is a novel member of the IL-1 family of cytokines. It binds to the<br />
IL-33 receptor alpha chain, formerly known as ST2/T1, which is a member of the IL-1<br />
receptor family (Schmitz et al. Immunity 2005, 23, 479-490). Here we show that lack of<br />
the Interleukin-1 receptor accessory protein (IL-1RAcP) abrogates responses to IL-33 in<br />
the mouse thymoma clone EL-4 D6/76. Reconstitution with full length IL-1RAcP, but not<br />
with a C-terminally truncated version lacking the TIR-domain, is sufficient to restore<br />
responsiveness to IL-33. Blocking of murine IL-1RAcP with the neutralizing antibody<br />
4C5 inhibits response of mouse thymoma cells and bone marrow-derived mouse mast<br />
cells to IL-33 with respect to cytokine production. IL-33 activates IL-1 receptor<br />
associated kinase (IRAK-1), the stress kinases p38 and c-Jun N-terminal kinase, and<br />
the NF-kappaB pathway in an IL-1RAcP dependent manner. IL-33 is able to induce the<br />
production and release of pro-inflammatory cytokines in transiently transfected cells<br />
and bone marrow-derived mast cells, indicating that IL-33 may have a proinflammatory<br />
potential (in the innate response) like its relatives IL-1 and IL-18 besides<br />
of its Th2-skewing properties in the adaptive response described previously. The<br />
interaction of IL-1RAcP and IL-33Ralpha-chain is dependent on IL-33 as demonstrated<br />
in co-immunoprecipitation assays.<br />
We conclude that IL-1RAcP is required as co-receptor in the signalling IL-33 receptor<br />
complex. Thus IL-1RAcP is utilized by more than one beta-chain of the IL-1 receptor<br />
family and may resemble a common beta-chain of the IL-1 receptor family.
Manuela Hessmann, Dominik Rueckerl, Toshiyuki Takai, Stefan Ehlers, Christoph<br />
Hoelscher<br />
The ITAM-bearing adapter protein DAP12 modulates<br />
inflammatory immune responses after Mycobacterium<br />
tuberculosis infection<br />
Activation of the innate immune system leads to the release of pro-inflammatory<br />
cytokines and is considered to be a prerequisite for driving a protective adaptive<br />
immune response after infection. However, inflammatory immune responses may also<br />
lead to tissue destruction and regulatory mechanisms are necessary to prevent<br />
uncontrolled inflammation. Hence, activating and inhibitory host factors are required in<br />
order to balance protection and immunopathology. When associated with different<br />
receptors, the ITAM-containing signalling adaptor DAP12 (DNAX activating protein of 12<br />
kDa) has been shown to affect inflammatory immune responses.<br />
To analyse the influence of DAP12 on cell-mediated immune responses during<br />
mycobacterial infection we infected DAP12-deficient (KO) mice with Mycobacterium<br />
tuberculosis. In contrast to wildtype mice, infection of DAP12 KO animals resulted in<br />
increased inflammatory immune response. In the absence of DAP12, the expansion of<br />
activated T cells was enhanced accompanied with elevated antigen-specific effector<br />
functions. On the cellular level, we could show that DAP12 KO macrophages<br />
overproduce pro-inflammatory cytokines in response to M. tuberculosis infection.<br />
In summary, we assume DAP12-dependent pathways in macrophages to modulate<br />
inflammatory immune responses during mycobacterial infection. These signalling<br />
pathway may represent novel target in order to mitigate chronic inflammation in human<br />
tuberculosis.
Veronika Lukacs-Kornek, Sven Burgdorf, Sabine Specht, Miroslaw Kornek, Christian<br />
Kurts<br />
The kidney – renal LN system contributes to cross-tolerance<br />
against innocuous soluble antigen<br />
Soluble antigens devoid of inflammatory stimuli, derived for example from self-serum or<br />
food proteins, induce T cell tolerance in the spleen. Here we describe an additional role<br />
of the kidney – rLN system in tolerogenic presentation of such circulating antigens.<br />
Protein below albumin molecular weight constitutively passed the kidney glomerular<br />
filter and was concentrated in the tubular compartment. Enriched filtrated antigen was<br />
endocytosed by kidney dendritic cells (kDC). Simultaneously, it was transported cellindependently<br />
within two minutes to DC resident in rLNs. These DC phenotypically<br />
differed from kDC carrying filtrated antigen, and used a different mechanism, MRmediated<br />
endocytosis, to internalize antigen. They activated specific CD8+ T cells,<br />
which subsequently proliferated without producing effector cytokines or developing<br />
cytotoxic activity, and showed a curtailed life-span. Such tolerogenic T cell activation<br />
was independent of steady-state migratory kidney DC because nephrectomy after<br />
antigen injection did not change the T cell response. These findings demonstrate that<br />
the kidney dispatches concentrated blood-borne antigens to the rLNs, where they can<br />
be captured by resident DC, resulting in tolerogenic CD8+ T cell activation. This<br />
mechanism may contribute to T cell cross-tolerance against innocuous circulating<br />
protein antigens.
Gennadiy Zelinskyy, Sandra Balkow, Simone Schimmer, Tanja Werner, Markus M.<br />
Simon, Ulf Dittmer<br />
The level of Friend retrovirus replication determines the<br />
cytolytic pathway of CD8+ T cell-mediated pathogen control<br />
Cytotoxic T-cells (CTL) play a central role in the control of viral infections. Their antiviral<br />
activity can be mediated by at least two cytotoxic pathways namely the granule<br />
exocytosis pathway, involving perforin and granzymes, and the Fas-FasL pathway.<br />
However, the viral factor(s) that influence the selection of one or the other pathway for<br />
pathogen control are elusive. Here we investigate the role of viral replication levels on<br />
the induction and activation of CTL, including their effector potential, during acute<br />
Friend Murine Leukemia Virus (F-MuLV) infection. F-MuLV inoculation results in a lowlevel<br />
infection of adult C57BL/6 mice that is enhanced about 500-fold upon co-infection<br />
with the Spleen Focus Forming Virus (SFFV). Both the low- and high-level F-MuLV<br />
infection generated CD8+ effector T cells that were essential for the control of viral<br />
replication. However, the low-level infection induced CD8+ T cells expressing solely<br />
FasL but not the cytotoxic molecules granzyme A and B, whereas the high-level<br />
infection resulted in induction of CD8+ effector T cells secreting molecules of the<br />
granule exocytosis pathway. By using knockout mouse strains deficient in one or the<br />
other cytotoxic pathway we found that low-level viral replication was controlled by CTL<br />
that expressed FasL but control of high-level viral replication required perforin and<br />
granzymes. Additional studies, in which F-MuLV replication was enhanced<br />
experimentally in the absence of SFFV co-infection supported the notion that only the<br />
replication level of F-MuLV was the critical factor that determined the differential<br />
expression of cytotoxic molecules by CD8+ T cells and the pathway of CTL cytotoxicity.
Iryna Prots, Alla Skapenko, Jörg Wendler, Stefan Mattyasovszky, Clarisse Yone´,<br />
Bernd Spriewald, Harald Burkhard, Joachim R Kalden, Peter E Lipsky, Hendrik Schulze-<br />
Koops<br />
The loss-of-function IL4R single nucleotide polymorphism<br />
I50V is associated with early erosive rheumatoid arthritis<br />
IL4 and its receptor, IL4R, are major regulators of T helper cell differentiation and are<br />
believed to play an important role in the pathogenesis of rheumatoid arthritis (RA),<br />
which is characterized by unbalanced Th1-mediated inflammation. To evaluate the role<br />
of IL4R single nucleotide polymorphisms (SNPs) in RA pathogenesis, we analyzed the<br />
association of two IL4R SNPs, I50V and Q551R in the IL-4-binding and STAT6-binding<br />
domains, respectively with RA susceptibility and severity. A well-characterized cohort of<br />
471 RA patients and 371 age and sex matched healthy controls were genotyped by<br />
sequence specific PCR for their alleles at I50V and Q551R SNPs. The patients were<br />
stratified according to radiological outcome at two years disease duration into an<br />
erosive and a non-erosive group to assess disease progression as early bone erosions<br />
and joint destructions are most characteristic for severe RA. Allele frequencies,<br />
genotype frequencies and haplotype frequencies defined by the two IL4R SNPs were<br />
similar between RA patients and healthy controls. In marked contrast, significant<br />
differences between the erosive and the non-erosive group of patients were observed in<br />
the distribution of I50V genotypes. The V50 allele was strongly associated with early<br />
aggressive erosive disease, as 68.1% of the V50 homozygous patients compared to<br />
only 37% of the I50 homozygous patients had developed bone erosions two years after<br />
disease onset (OR 3.86, p < 0.0001). To delinate a possible mechanism by which IL-4R<br />
SNPs might modulate disease progression in RA, we analyzed the effect of IL-4 on the<br />
function of T cells of healthy individuals expressing different IL-4R I50V alleles. The V50<br />
allele significantly reduced the response of CD4 T cells to IL-4, as assessed by STAT6<br />
phosphorylation, GATA3 expression and downmodulation of the IL-12 receptor ?2 chain.<br />
Furthermore, the IL-4-mediated inhibition of Th1 and increase of Th2 cell differentiation<br />
was significantly diminished in V50 homozygous CD4 T cells. Our data identify the lossof-function<br />
I50V IL4R SNP as a novel genetic marker in RA with high predictive value for<br />
early joint destruction. Moreover, the data also provide a first intriguing molecular<br />
mechanism of an altered immune response that results in increased tissue destruction<br />
in a human autoimmune disease.
Petra Hoffmann, Tina J. Boeld, Ruediger Eder, Jochen Huehn, Stefan Floess, Udo<br />
Baron, Sven Olek, Reinhard Andreesen, Matthias Edinger<br />
The Naive CD45RA+, But Not The CD127- Subpopulation of<br />
Human CD4+CD25high T Cells Homogeneously Maintains<br />
Regulatory T Cell Characteristics Upon In Vitro Expansion<br />
The adoptive transfer of CD4+CD25high regulatory T (Treg) cells is envisaged as a<br />
promising strategy for the treatment of autoimmune diseases and the promotion of<br />
immunological tolerance after allogeneic organ or stem cell transplantation. For such<br />
clinical applications, efficient in vitro expansion protocols for Treg cells are required. We<br />
previously demonstrated that strong co-stimulation provided by cross-linked CD3 and<br />
CD28 antibodies together with high-dose IL-2 resulted in a more than 3-log polyclonal<br />
expansion of highly suppressive Treg cells (Blood 104:895; 2004). To avoid the<br />
outgrowth of potentially auto- or alloreactive effector T cells in such cultures, isolation<br />
of highly purified Treg cells from human PBMC is of crucial importance. Lack of IL-7<br />
receptor (CD127) expression has recently been proposed as a useful tool for the<br />
discrimination of Treg cells from activated conventional T cells. Here we analyzed FACSpurified<br />
CD127low/neg CD4+CD25+ T cells after 2 to 3 weeks of in vitro expansion. For<br />
all phenotypic and functional characteristics examined, such as CD25, CCR7, CD62L,<br />
CTLA-4 and FOXP3 expression, production of pro- and anti-inflammatory cytokines or<br />
methylation status of the foxp3 gene locus, CD127low/neg cells displayed a<br />
heterogeneous profile after in vitro expansion. This was mainly due to the presence of<br />
CD45RO+FOXP3+ memory type Treg cells in the starting population, as further purified<br />
CD45RA+CD127low/negCD4+CD25+ T cells developed into a homogeneous population<br />
that retained all characteristics of natural Treg cells after in vitro expansion. Similar<br />
results were obtained by us before with naive CD4+CD25high T cells isolated without<br />
consideration of CD127 as a separate sort criterion (Blood 108:4260; 2006). Based on<br />
these findings, we suggest that isolation of CD127low/neg CD4+CD25+ T cells is<br />
insufficient for the generation of pure Treg cell products, but that isolation and<br />
expansion of CD45RA+ naive CD4+CD25high T cells represents a promising strategy for<br />
adoptive cell therapies.
Sandra Düber, Martin Hafner, Elias Hobeika, Michael Reth, Ari Waisman, Karsten<br />
Kretschmer, Siegfried Weiss<br />
The origin of B-1a cells: Analysis in mice with inducible B cell<br />
development<br />
The origin of B-1a cells, which are suggested to act as a ‘first line of defense’ against<br />
mucosal and systemic pathogens, is still controversially discussed. It is unclear, whether<br />
these cells are only generated during fetal and neonatal life, or whether the adult bone<br />
marrow can also give rise to such B cells. Most of the previous results leading to the<br />
controversy were derived from transgenic mice or adoptive transfer experiments. But<br />
now we are able to investigate the origin of B-1a cells under more physiological<br />
conditions. For this we have generated mice with inducible B cell development.<br />
Switching on B cell development in adult mice should definitively answer the question<br />
about the involvement of the adult bone marrow in the generation of B-1a cells.<br />
To make B cell development inducible the recombination activating gene 1 (Rag1) was<br />
chosen as target. The coding sequence of Rag1 was initially inverted for gene<br />
inactivation resulting in a block of B (as well as T) cell development. Flanking this region<br />
with loxP sites in opposite orientation made it possible to revert it by expression of Cre<br />
recombinase resulting in restoration of the transcription unit. The temporal control of<br />
Cre expression was realized by crossing-in the MerCreMer mouse. These mice express<br />
the tamoxifen-inducible MerCreMer recombinase under the control of the B cell specific<br />
mb-1 promoter.<br />
Oral administration of tamoxifen to the mice leads to a wave of newly generated B cells<br />
and allows their analysis in the periphery. Experiments in which the mice were induced<br />
at an age of 8 weeks clearly show that B-1a cells are present in the peritoneum. Also if<br />
older mice were used for the induction (5 months old) B-1a cells can be detected in<br />
similar numbers. A certain proportion of these cells shows phosphatidyl choline (PtC)specificity,<br />
a typical property of B-1a cells.
Ulrich Steinhoff, Alexander Visekruna, Anjo Kroesen<br />
The proteasome controls NF-κB-mediated inflammation in IBD<br />
patients<br />
Proteasomes are the central proteolytic machinery of cells involved in degradation of<br />
proteins and generation of MHC class I epitopes. Additionally they play a central role in<br />
regulation of inflammatory processes mediated by NF-κB. We analyzed the structure<br />
and function of 20S proteasomes in normal and inflamed intestinal tissues from Crohn’s<br />
disease (CD)and ulcerative colitis (UC) patients.<br />
Our results show tissue-specific differences in proteasome composition as previously<br />
reported in mice.<br />
However, we found marked differences in proteasome composition between CD and UC<br />
patients. Inflammation affected the proteasome composition only in CD patients with<br />
strong expression of immunosubunits in the inflamed tissues.<br />
Immunoproteasomes isolated from CD patients degraded IκBα and processed p105<br />
much faster than constitutive proteasomes from UC patients. Immunohistochemical<br />
analysis confirmed that the amount of activated NF-κB correlated with the expression of<br />
immunoprotesasomes.<br />
This demonstrates that the mechanism of inflammation differs between UC and CD<br />
patients and that proteasomes are crucially involved in Th1-mediated inflammation.
Sandra Kraemer, Regina Krohn, Hongqi Lue, Manfred Dewor, Christian Weber, Jürgen<br />
Bernhagen<br />
The pseudo-ELR motif of MIF is required for its functions as<br />
CXC arrest chemokine<br />
Macrophage migration inhibitory factor (MIF) is a pleiotropic inflammatory cytokine that<br />
plays a pivotal role in acute and chronic inflammatory diseases such as septic shock,<br />
and atherosclerosis. We have recently demonstrated that MIF, contrary to its historic<br />
and eponymous name, is a non-cognate ligand of the chemokine receptor CXCR2. MIF<br />
binds to CXCR2 with nanomolar affinity and induces leukocyte arrest and chemotaxis<br />
through this receptor (Bernhagen et al., Nat. Med. 13, 2007). CXCR2 signaling induced<br />
by cognate ligands, such as IL-8, requires an N-terminal Glu-Leu-Arg (ELR) motif. The<br />
MIF monomer not only displays a striking architectural homology to the IL-8 dimer, but<br />
we also noticed that MIF has an ELR-like 3D motif, which we tentatively term pseudo-<br />
ELR motif. It is formed by the two non-adjacent residues Arg11 (R11) and Asp44 (D44),<br />
which reside in an ELR-like spacing in exposed neighboring loops, imitating the ELRmotif.<br />
While it is tempting to speculate that the pseudo-ELR motif conveys binding and<br />
activity specificity comparable to what is observed for classical ELR+ CXC chemokines,<br />
no functional data has been available. We have thus generated MIF mutants with<br />
residues R11 and D44 mutated to address the question whether the pseudo-ELR motif is<br />
functionally required for an interaction with CXCR2 and for MIF’s chemokine-like<br />
activities. We have cloned the mutants R11A-MIF, D44A-MIF, and the double mutant<br />
R11A-D44A-MIF. Although mutagenesis involved alterations in charge and isoelectric<br />
point, the mutants were expressed and purified by an almost identical procedure as that<br />
established for wildtype MIF. Spectroscopic analysis by far-UV circular dichroism<br />
confirmed that the mutants exhibited an overall structural integrity. However, R11A-MIF<br />
showed an increase in β-sheet structure, indicating that the pseudo-ELR site constitutes<br />
a sensitive conformational region of the molecule. We will report on the functional<br />
relevance of this motif for the leukocyte recruitment activity of MIF. Intriguingly, initial<br />
experiments suggest that mutating R11/D44 markedly interferes with CXCR2dependent<br />
monocyte arrest on human aortic endothelial cells in flow induced by MIF.
Nicole Dietrich, Nelson Gekara, Siegfried Weiss<br />
The regulatory mechanisms inviolved in iNOS, TNF-&alpha,<br />
and IL-6 induction during host defence<br />
One of the most important hallmarks of pathogen recognition by host cells is the<br />
secretion of inflammatory mediators. Depending on several factors, like the site of<br />
secretion and their relative concentrations, such mediators play two distinct roles in the<br />
disease state, one protective and the other injurious. Toll-like receptors (TLRs) play a<br />
central role in the inflammatory responses triggered by various pathogens. But even<br />
after an area of intense research focus, the signalling pathways via which the various<br />
TLRs induce different inflammatory responses are still not fully understood. TNF-&alpha,<br />
IL-6, and nitric oxide (NO) play critical roles in many of the anti-microbial defenses as<br />
well as in harmful disease such as septic shock and other injurious chronic inflammatory<br />
conditions. The present study was carried out with the aim to ellucidate the downstream<br />
signalling pathways via which TLR2, TLR3 and TLR4 agonists (MALP-2, Poly IC and LPS<br />
respectively) induce TNF-&alpha, IL-6 and NO responses. Using various pharmacological<br />
inhibitors for p38, JNK, ERK, PI3K, PKC and NF-kB signalling pathways (SB203580,<br />
SP600125, PD098059, LY294002, staurosporine and BAY11-7085 respectively), we<br />
show that the induction of these mediators involves overlapping as well as distinct<br />
signalling events. We show that all the tested inhibitors could block the induction of TNF-<br />
&alpha by the above agonists, but only the PI3K, PKC and JNK inhibitors could block IL-<br />
6 and NO responses. Interestingly the p38 pathway had an enhancing effect on IL-6 and<br />
NO production. Further analysis of macrophages deficient in IFNAR (Type I interferon<br />
receptor) suggest a role for Type I interferons in the induction of NO and IL-6 but not<br />
TNF-&alpha.
Uwe Kolsch, Christina Weber, Caroline Ritter, Anna Viehbahn, Thomas Brune<br />
THE REPRODUCTIVITY OF MICE IS INDEPENDENT OF A MHC-I<br />
HAPLOTYPE MISMATCH BETWEEN THE MOTHER AND THE<br />
FETUS<br />
Introduction: Recent investigations have shown fetal survival depending upon<br />
maternal TH2-switch and existence of regulatory T-cells. Up to now it is unclear if fetal<br />
survival depends on maternal TH1/TH2 basal immune responses and on MHC-recognition<br />
and MHC-haplotyp, factors influencing MHC - T cell interaction. Methods: To address<br />
the question whether different types of basal immune responses influence<br />
reproductivity, inbred mouse strains with different TH1/TH2-reactivities and different<br />
MHC haplotypes (CBA, Balb/C, C57BL/6, DBA1) were crossed to F3 generation. TH1/TH2 imbalances were measured by CD69-upregulation in mixed lymphocyte cultures (MLC)<br />
from parental animals. Results: CD8+-lymphocytes from TH1 reacting strains are<br />
activated to a higher extent when compared to lymphocytes of TH2 reacting strains. In<br />
contrast immune responses between MHC I-haplotype homozygous F2 and F3-animals<br />
are balanced. Numbers of progeny were significantly reduced when male TH2-reacting mice were crossed with female TH1-reacting mice compared to breedings from female<br />
TH2-reacting mice crossed with male TH1-reacting mice. The latter was comparable to<br />
F1-hybrid breeding pairs and breeding pairs of MHC I-haplotype homozygous F2 mice.<br />
There was no difference in progeny numbers when MHC I-haplotype homozygous F2<br />
mice with total or no MHC mismatch were crossed. Discussion: TH2 reactivity is<br />
advantageous for pregnancy outcome but TH2 switching is independent of MHC Ihaplotype.<br />
Breeding of genetically non identical mice positively influences pregnancy<br />
outcome independently of the MHC I-haplotype.
Andrey Bogdanov, Tatyana Rybakova, Nikolay Belyaev<br />
The role of alpha-fetoprotein in induction of immunological<br />
tolerance to tumor growth: direct and indirect breaking of<br />
tumor immunosurveillance<br />
It was shown, alpha-fetoprotein (AFP) is immunoregulatory agent provided the<br />
immunologic tolerance development during pregnancy. AFP induced disorders of certain<br />
cell-mediated immunity effector reactions in vitro and immunosuppression in AFPoverproducing<br />
transgenic mice. We investigated implication of AFP in down regulation of<br />
immunological resistance to cancerous tumor. Our results demonstrated that AFP<br />
preexposure promotes more intensive (almost in three times) growth of primary tumor<br />
nodule and dissemination of tumor. The latent periods of appearance of primary tumor<br />
nodule as well as first metastatic protuberances were shorter that in control animals.<br />
Study of cell-mediated immunity presented number of considerable impairments.<br />
Spontaneous and IL-12-induced productions of IFN-γ and TNF-α from NK cells and •D8+<br />
T cells, as well secretion of IFN-γ from NKT cells and TNF-β from •D8+ T cells were<br />
extensively inhibited as compared with control animals at the same period. Similar<br />
situation observed during cytolytic activity study of NK-, NKT- and •D8+ T cells as well<br />
as PHA-induced proliferation of NKT- and •D8+ T cells. Isolated dendritic cells from AFPinjected<br />
animals showed weaker antigen-presenting ability and secretion of IL-12, IL-<br />
15, IL-18 and IL-23. Investigation of effector •D4+ T cells demonstrated higher Th2<br />
cells prevalence on Th1 cells in AFP-injected animals that control animals at the same<br />
period or tumor development. In conclusion, numbers of functionally active Th3- and<br />
Treg1 cells as well as suppressor activity and numbers of TGF-β1- and IL-10-produced<br />
hematopoietic stem sells were higher in spleen of AFP-injected animals. All these<br />
immunological disorders were found at very early stages of tumor growth in AFPinjected<br />
animals only. Moreover, discovered changes of cell-mediated immunity<br />
displayed before appearance of palpable primary tumor nodule in AFP-injected animals.<br />
Thus, AFP induced both direct and/or indirect editing of cell-mediated immunity that<br />
lead to suppression of immune attack against tumor and in the end to extensive tumor<br />
invasion.
Filiz Demircik, Ari Waisman<br />
The role of B cells and other antigen presenting cells in<br />
infections<br />
To clarify the role of B cells in infection models like Leishmania major, murine<br />
Cytomegalovirus (MCMV) and influenza, we are using three different mouse strains. The<br />
JHT mice are B cells deficient; the IgG1i strain has B cells producing and secreting IgG1<br />
antibodies but no other antibody isotypes; and the IgMi mice, which can produce IgM as<br />
the B cell receptor but have no antibodies in the sera. In these mouse strains we are<br />
looking for differences in the T cell repertoire that is established upon infection.<br />
Furthermore we want to deplete B cells and thereby look at their role in infection. To<br />
deplete B cells at distinct time points during, before or after clearing of the infection, we<br />
will establish a CD19-Cre x iDTR mouse. In this developed novel iDTR system, the<br />
diphtheria toxin receptor (DTR) can be expressed on the surface of cells following a Cremediated<br />
deletion of a STOP cassette. In the iDTR mice, lineage ablation is achieved by<br />
injecting diphtheria toxin (DT) into mice expressing the iDTR as well as a tissue specific<br />
Cre transgene. Finally we plan to create a new mouse with the DTR downstream of the<br />
CD11b promoter and then together with lineage specific Cre mouse strains we will be<br />
able to achieve a more specific ablation, especially for antigen presenting cells and be<br />
able, for example, to specifically delete cells that express CD11b and CD11c or CD11b<br />
and LysM. This system will allow us to specifically ablate sub-populations of dendritic<br />
cells, macrophages or B cells (B-1 cells) and study their role in different infectious<br />
systems.
Sonja Reißig, Ari Waisman<br />
The Role of CYLD in T cell Development and Regulation<br />
CYLD is a tumour suppressor gene known to play an important role in NF-kappa B<br />
signaling.<br />
To analyse the function of CYLD in vivo we used the CYLD ex7/8 mouse strain, which is<br />
characterized by loss of the full-length transcript and overexpression of a short splice<br />
variant of the cyld gene. Here we show the role of CYLD in T cell development and T cell<br />
regulation by analysing CYLD ex7/8 mice and comparing them to wildtype mice.<br />
In CYLD ex7/8 mice the overexpression of the small transcript of CYLD resulted in<br />
splenomegaly and lymphadenopathy. Additionally, the B cell population in spleen and<br />
lymphnodes is increased at the expense of T cells.<br />
Analysis of T cell development in CYLD ex7/8 mice revealed a reduction of total numbers<br />
of thymocytes compared to control mice. Additionally, a partial developmental block at<br />
the DN1 stage was observed. In order to investigate the contribution of CYLD in positive<br />
and negative selection in the thymus in vivo, the HY-TCR transgene (HYtg) was crossed<br />
to CYLD ex7/8 mice. The analysis of CYLD ex7/8 HYtg males revealed an increase in CD4<br />
+ CD8 + DP as well as in CD8 SP thymocytes, suggesting a less pronounced negative<br />
selection in CYLD mutant mice compared to HYtg control mice. The analysis of<br />
CYLD ex7/8 HYtg females indicated a role of CYLD also in positive selection, since a<br />
developmental block in the transition of CD4 low CD8 + TCR high to CD4 + CD8 + DP<br />
thymocytes was observed. The investigation of peripheral lymphoid T cell populations in<br />
CYLD ex7/8 mice indicated an increased CD4 population at the expense of CD8 T cells. In<br />
addition, an increase in number and proportion of Tregs in CYLD ex7/8 mice was<br />
observed, most likely responsible for the perceived increase in CD4 T cells.<br />
The analysis of CYLD in NF-kappa B signaling demonstrated an increased activation of<br />
the NF-kappa B pathway in stimulated CYLD ex7/8 T cells. In addition, the expression of<br />
important tumour related genes in CYLD ex7/8 T cells was investigated and revealed an<br />
upregulation of different tumour promoting genes.<br />
Taken together, these results indicated an important role of the alternatively spliced<br />
transcript of CYLD ex7/8 in T cell development as well as in NF-kappa B signaling of T<br />
cells.
Fabia T.L. Rocha, Rüdiger Arnold, Renate Rutz, Michael Kirschfink<br />
The role of FLIP Long in C5a-modulated spontaneous apoptosis<br />
of neutrophils<br />
Neutrophils (PMN) are the most abundant type of immune cell in the circulation, and<br />
one of their key characteristics is their short life span (8-20 hours). In the absence of<br />
survival factors they undergo spontaneous apoptosis, a process critical to resolution of<br />
inflammation. The exact influence of the complement system in neutrophil apoptosis is<br />
still obscure. C5a has been described to delay PMN apoptosis through the Bad-mediated<br />
signaling pathway in mitochondria (intrinsic pathway), however, its possible impact on<br />
the extrinsic death receptor pathway in PMN apoptosis is still unknown.<br />
A possible involvement of C5a in the modulation of spontaneous PMN apoptosis was<br />
investigated by analysis of the extrinsic pathway regulator cellular FLIPLong (c-FLIPL ).<br />
Neutrophils were isolated from 20 healthy adult donors. FACS analysis of annexin V<br />
binding was carried out to evaluate apoptosis. Activity of caspases 9, 8, and 3 was<br />
measured by substrate cleavage using AFC fluorescence. c-FLIPL and β-actin were<br />
quantified using LightCycler-RT-PCR. For all experiments, neutrophils were analysed<br />
after 1 hour or 21 hours of incubation with or without C5a. After 21 hours of incubation<br />
we observed a significant delay in spontaneous apoptosis upon C5a treatment, however<br />
only in a subgroup of donors (10/20, p < 0.005). Delay in spontaneous PMN apoptosis<br />
of these individuals went along with a significant up regulation of the regulator c-FLIPL (p < 0,05), but not with reduced caspase 8 activity.<br />
These findings suggest that - in contrast to previous reports - C5a acts as a PMN<br />
survival factor only under certain conditions, which appear to involve the regulatory<br />
activity of c-FLIP. In our study we demonstrated for the first time the expression of<br />
FLIPL in neutrophils and its upregulation in cases where C5a delayed neutrophil<br />
apoptosis.<br />
-->
Denise Bogdanski, Thomas M. Frangen, Christian Schinkel, Gert Muhr, Manfred Köller<br />
The role of IL-17 in the post traumatic phase of polytrauma<br />
patients.<br />
Interleukin-17 (IL-17) is produced by a T-cell subpopulation (Th17/Th17). IL-17 as a<br />
central mediator in inflammatory processes connects T-cell stimulation with neutrophil<br />
mobilization. The role of IL-17 in the immune dysfunction after servere injuries is not<br />
clarified. In a study with 71 patients (55 men, 16 women) systemic IL-17 and IL-6<br />
concentrations of polytraumatized patients were daily analyzed by ELISA. The majority<br />
of the patients (94%) showed no systemic IL-17 or the IL-17 concentrations were in the<br />
range of healthy volunteers. Only in 6% of the patients was an increase in systemic IL-<br />
17 values detected. To identify the possible role of IL-17 in the post traumatic phase<br />
the patients were divided in two groups. Group A (47 men, 15 women) consists of<br />
patients with IL-17 concentrations in the range of healthy volunteers and group B (8<br />
men, 1 woman) consists of patients with elevated IL-17 concentrations. In group B<br />
systemic IL-6 (median 41 pg/ml, range 3-709 pg/ml) correlated with systemic IL-17 (75<br />
pg/ml, range 0.1-1822 pg/ml, r=0.258, p≤0.01). The patients in group B showed no<br />
conformity in injury patterns, ISS, age, outcome, intensive care periode or clinical<br />
complications.<br />
After a period of four years we were able to obtain a blood sample from a now<br />
recovered patient who formerly belonged to the high IL-17 group. Now, the systemic IL-<br />
17 level was below the detection limit, but stimulation of PBMCs obtained from this<br />
patient showed elevated numbers of IL-17 producing cells as determined by ELISpot<br />
and flow cytometry. It has to be proven by further studies whether highly increased<br />
systemic IL-17 concentrations detected in distinct patients were related to a genetic<br />
predisposition of these subjects.
Inna Lavrik, Alexander Golks, Dirk Brenner, Julia Hoffmann, Carina Pforr, Peter<br />
Krammer<br />
The role of new c-FLIP proteins in life and death of the T cell.<br />
C-FLIP, also known as FLAME-1/I-FLICE/CASPER/CASH/MRIT/CLARP/Usurpin, is a welldescribed<br />
inhibitor of death receptor-mediated apoptosis. Until present only two<br />
isoforms of c-FLIP: c-FLIPL and c-FLIPS, were found to be expressed at the protein<br />
level. In our studies, we found two new protein products of c–FLIP: p25-FLIP, which<br />
turned out to be the third c-FLIP isoform, c-FLIPR; and p22-FLIP, which was shown to<br />
be a c-FLIP N-terminal cleavage product. Both new c-FLIP proteins block caspase-8<br />
activation at the DISC and death receptor-induced apoptosis. In addition, p22-FLIP was<br />
shown to play a prominent role in NF-kappa B activation via interaction with the IKK<br />
complex. Recently, we developed new insight into the mechanism of c-FLIP-mediated<br />
NF-kappa B induction. Our new findings and the role of c-FLIP proteins in life and death<br />
of T cells are going to be discussed.
Eva Gueckel, Silke Meister, Mario Zaiss, Sankar Ghosh, Reinhard E. Voll<br />
The role of NF-κB for the development and function of<br />
naturally occurring regulatory T cells<br />
Naturally occurring CD4+CD25+Foxp3+ regulatory T cells (nTregs) develop in the<br />
thymus and represent a mature T cell subpopulation capable of inhibiting the<br />
proliferation and cytokine release of effector T cells. nTregs are involved in preventing<br />
autoimmune diseases and graft rejection; however, they may also prevent<br />
immunological tumour killing. Deletion of different components in the NF-κB signalling<br />
pathway using knockout-mouse models showed a strong decrease in the nTreg cell<br />
number. However, it is still unclear if NF-κB is important for the development and<br />
differentiation or survival of nTregs. In addition, the role of NF-κB for the<br />
immunoregulatory effector functions of nTregs is not yet clearly understood. To address<br />
these questions we used thymocyte-specific expression of either an inhibitor of NF-κB<br />
(IκBα-Tg) or a constitutively active mutant of IKKβ (IKKβ-Tg) in transgenic mice.<br />
Thymocytes from 4-/6-week-old IκBα transgenic mice showed a significant decrease in<br />
the relative and absolute numbers of nTregs. Unexpectedly, the analysis of thymocytes<br />
from IKKβ Tg mice, displaying increased NF-κB activity, also showed a trend towards<br />
decreased nTreg cell numbers. In the periphery the absolute numbers of nTregs did not<br />
show any marked differences in both transgenic mouse lines. Finally, sorted nTregs<br />
from IKKβ Tg mice were less potent in suppressing the proliferation of effector T cells<br />
than those from C57BL/6 mice. These data indicate that the NF-κB activity modulates<br />
nTreg cell development as well as their function. These findings have important<br />
implications for new therapeutical strategies targeting autoimmune diseases, allergies<br />
and chronic infections.
Zoran V. Popovic, Roger Sandhoff, Tjeerd P. Sijmonsma, Eva Kiss, Sylvia Kaden, Edgar<br />
Tone, Hermann-Josef Gröne<br />
The role of sulfatide SM4s in apoptotic cell uptake and<br />
macrophage phenotype alteration<br />
Sulfoglycolipids are present on the surface of a variety of cells. Sulfatide (SM4s) is<br />
increased in renal, colon, lung, and ovarian cancer and is a hallmark of adverse<br />
prognosis. Macrophages significantly contribute to the inflammatory infiltrate in<br />
malignancies. We postulated that SM4s can modulate macrophage function through an<br />
influence on apoptotic cell clearance at the cancer site. The effect of SM4s on the<br />
uptake of apoptotic particles by macrophages, macrophage cytokine profile and receptor<br />
expression were investigated. Murine peritoneal macrophages were incubated with<br />
either SM4s-loaded or SM4s-free Colon26 (murine colon cancer) or Renca (murine renal<br />
cancer) apoptotic cells. Presence of SM4s on apoptotic cells was confirmed by<br />
immunocytochemistry and transmission electron microscopy. Phagocytosis and receptor<br />
expression were analyzed by FACS. Uptake of apoptotic cells was confirmed by confocal<br />
and electron microscopy. Cytokines were measured by ELISA. Presence of SM4s in<br />
apoptotic cell membrane increased the number of apoptotic cells in the macrophage<br />
phagosomal compartment up to 3 fold. Scavenger receptors and the sulfate group of<br />
SM4s were the key factors for the increase in apoptotic cell clearance. Enhanced uptake<br />
of SM4-covered apoptotic cells led to an increase in P-selectin expression by<br />
macrophages (up to 40%, p
Marko Janke, Michael Peine, Thordis Hohnstein, Lars Morawietz, Alexander Scheffold<br />
THE ROLE OF TH1 AND TH17 T CELLS IN INFLAMMATORY<br />
REACTIONS IN VIVO<br />
Introduction:<br />
The role of Interferon-γ (IFN-γ) produced by Th1 cells in vivo is controversially<br />
discussed. While Th1 cells can induce inflammatory reactions, like delayed type<br />
hypersensitivity (DTH), neutralisation of the prototypic Th1 cytokine IFN-γ leads to an<br />
even more pronounced DTH or a more severe inflammatory arthritis. Recently, IL-17<br />
produced by Th17 cells was shown to act highly pro-inflammatory in inflammatory<br />
autoimmune diseases, like collagen-induced arthritis. Therefore, our aim was to analyse<br />
the role of Th1 vs Th17 cells in inflammatory reactions using DTH or the ovalbumininduced<br />
arthritis model (OIA). In this model, arthritis is induced by intra-articular (i.a.)<br />
injection of ovalbumin into Ova-immunised mice.<br />
Results:<br />
We show that IFN-γ as well as IL-17 is produced to equal amounts by ex vivo isolated<br />
antigen-specific CD4+ T cells taken from arthritic mice. Interestingly, in anti-IL-17<br />
treated mice arthritis was significantly ameliorated. In contrast, the transfer of in vitro<br />
generated Th17 cells did not enhance arthritis symptoms, while Th1 cells did enhance<br />
arthritis. Similarly, Th17 cells only evoked a mild DTH reaction in sharp contrast to Th1<br />
cells, which induced strong and long-lasting DTH. This difference was probably caused<br />
by different migratory capacity into inflammatory sites, since Th1 but not Th17 cells<br />
migrated into the inflammatory foot and the draining lymph node.<br />
Conclusion:<br />
In vitro generated Th1 cells exert the expected pro-inflammatory function in vivo. In<br />
contrast, while IL-17 seems to increase OIA severity, in vitro generated Th17 cells failed<br />
to enhance or evoke inflammatory reactions, like arthritis or DTH. Thus, IL-17<br />
producing cells generated by currently described in vitro protocols do not possess the<br />
full functional potential of there in vivo counterparts. It will be important to determine<br />
the missing parameters required for full Th17 functional activity, in addition to secretion<br />
of IL-17.
Jan Liese, Ulrike Schleicher, Christian Bogdan<br />
The role of TLR9 signalling in murine cutaneous leishmaniasis<br />
In most strains of mice subcutaneous infections with Leishmania (L.) major lead to selfhealing<br />
skin lesions. A prominent CD4+ T-helper cell (Th)-based interferon (IFN)gamma<br />
response is associated with the ultimate resolution of the disease. The innate<br />
immune respose against the pathogen is characterised by the expression of inducible<br />
nitric oxide synthase (iNOS) and by the rapid induction of NK cell cytotoxicity and IFNgamma<br />
production in the draining lymph node (LN). Mice deficient for the adaptor<br />
molecule MyD88 are unable to control Leishmania parasites in vivo, indicating the<br />
requirement of Toll-like receptor signalling for a protective immune reponse. TLR9,<br />
which uses MyD88 for signalling, is located in the endosome, where it might interact<br />
with intracellular L. major. Therefore, we investigated the immune response against<br />
Leishmania in TLR9 deficient (TLR9-/-) C57BL/6 mice.<br />
In the LN of L. major-infected TLR9-/- mice NK cell IFN-gamma expression and<br />
cytotoxicity were strongly reduced as compared to wild type controls. In vitro, L. major<br />
promastigotes as well as L. major DNA induced interleukin (IL)-12 in bone-marrow<br />
derived myeloid dendritic cells (DCs) in a TLR9-dependent manner. IL-12p35-/- mice<br />
were deficient for NK cell activation after L. major infection, suggesting that L. major<br />
induces IL-12 via TLR9 in DCs which in turn triggers early NK cell activity in the LN.<br />
TLR9-/- mice exhibited more severe dermal lesions during the acute phase of the<br />
infection compared to wild type mice, but ultimately controlled the infection. TLR9-/-<br />
and wild type mice showed no difference of the mRNA levels of IFN-gamma, IL-12p35,<br />
IL-12p40 or iNOS in the skin or LN. However, TLR9-/- mice transiently expressed higher<br />
levels of IL-4, IL-13, and arginase 1 mRNA, indicating an enhanced Th2 cytokine<br />
production.<br />
Thus, TLR9-/- mice have a deficient innate immune response to L. major, which is<br />
associated with an aggravated clinical course of infection, but does not influence the<br />
ultimate outcome of infection.
Paul Gutwein, Anja Schramme, Liliana Schäfer, Hermann-Josef Gröne, Mohamed<br />
Sadek, Ingeborg Hauser, Josef Pfeilschifter<br />
The role of transmembrane and released CXCL16 during<br />
inflammatory processes in the kidney<br />
Inflammatory cell infiltrates are a hallmark of chronic kidney diseases (CKDs).<br />
Understanding the molecular mechanism that regulate renal leukocyte recruitment<br />
suggest chemokines and chemokine receptors as new targets for specific<br />
pharmacological intervention. In vitro we have analyzed the expression, localization and<br />
cleavage of CXCL16 in human renal mesangial cells. We can show that CXCL16<br />
expression is found in the nucleus, in lysosomes and in the endoplasmatic reticulum<br />
whereas no colocalization of CXCL16 with the Golgi stacks could be observed.<br />
Interestingly, when we stimulated the cells with INF-g, IL1b or LPS we could induce the<br />
expression of CXCL16. Additionally the application of IFN-g resulted in increased<br />
amounts of soluble CXCL16 in the supernatant of the cells. By using RNA interference<br />
we could inhibit ADAM10 and ADAM17 very efficiently and we clearly can show that both<br />
metalloproteinases are involved in the constitutive as well as in the inducible release of<br />
CXCL16 from mesangial cells. Interestingly the expression of endogenous CXCL16 was<br />
not influenced by the knockdown of ADAM10 or ADAM17 suggesting that both<br />
metalloproteinases may play important function in the transport of CXCL16.<br />
In vivo we found CXCL16 expression in the healthy kidney mainly in podocytes and<br />
distal tubular cells. Furthermore increased amounts of CXCL16 were found in the<br />
glomerulus of kidney transplanted patients. Importantly CXCR6 expressing immune<br />
cells were found in high numbers in the inflamed kidney of transplanted patients.<br />
Analyzing urine samples of patients with inflammatory kidney diseases, we found<br />
increased amounts of soluble CXCL16 compared to healthy volunteers. Taken together<br />
this data suggest an important participation of the chemokine CXCL16 and its receptor<br />
CXCR6 in the recruitment of leukocytes into the kidney during inflammatory processes.
Kai Schulze, Thomas Ebensen, Karina Watzke, Michael Morr, Carlos Guzman<br />
The second messenger 5′GMP is a promising adjuvant for<br />
vaccine development<br />
Vaccination by the mucosal route usually requires the use of specific adjuvants in order<br />
to stimulate efficient immune responses. Unfortunately, there are only a few molecules<br />
exhibiting this property, and, up to now, there is no candidate licensed for human use.<br />
Thus, there is an urgent need to develop new adjuvants. In the present work we<br />
demonstrate that 5′ guanosine monophosphate (5´GMP), a second messenger which<br />
modulates the cell surface properties of several microorganisms, acts as a potent<br />
mucosal adjuvant. Co-administration of 5´GMP with the model antigen ß-galactosidase<br />
(β-gal) to BALB/c mice by intranasal route resulted in 2,300-fold increased ß-galspecific<br />
serum IgG titers respect to what observed in animals immunized with β-gal<br />
alone. Strong antigen-specific secretory IgA responses were also measured in lung<br />
lavages (p=0.003). The analysis of both the major antigen-specific IgG isotypes in sera<br />
and the cytokines secreted by splenocytes restimulated ex vivo with β-gal suggested<br />
that a mixed Th1/Th2-response pattern was promoted in vaccinated mice. The obtained<br />
results suggest that 5´GMP constitutes a promising candidate adjuvant for the<br />
establishment of immune prophylactic interventions.
Matthias Eberl, David Vermijlen, Francesco Dieli, Nadia Caccamo, Serena Meraviglia,<br />
Giuseppe Cicero, Andrew Roberts, Bernhard Moser, Hassan Jomaa, Adrian Hayday<br />
The unexpected functional plasticity of human γδ T cells:<br />
implications for immunotherapy and beyond<br />
Human peripheral blood Vγ9/Vδ2 T cells expand extensively in many infections, in<br />
reaction toward the microbial metabolite HMB-PP. This 'transitional' response of γδ T<br />
cells, occurring temporally between the rapid innate and slower adaptive response, is<br />
widely viewed as pro-inflammatory and/or cytolytic. However, under the influence of an<br />
appropriate microenvironment, Vγ9/Vδ2 T cells readily assume features conventionally<br />
associated with Th1 (IFN-γ, TNF-α), Th2 (IL-4, GATA3), and follicular B helper TFH cells<br />
(CXCL13, IL-21R), respectively, as well as with professional antigen-presenting cells<br />
(HLA-DR, CD86). Such broad plasticity emphasizes the capacity of human γδ T cells to<br />
influence profoundly the nature of the immune response to different challenges, and is<br />
of relevance for ongoing clinical applications. Among the molecular signatures identified,<br />
tumour necrosis factor-related apoptosis-inducing ligand (TRAIL), for instance, was only<br />
expressed by pro-inflammatory, Th1-like, but not by Th2-like or TFH-like Vγ9/Vδ2 T<br />
cells. This could be directly corroborated in vivo in a phase I trial to promote non-MHCrestricted<br />
anti-tumour efficacy in metastatic hormone-refractory prostate cancer, using<br />
the Vγ9/Vδ2 T cell agonist zoledronate. Most patients treated with zoledronate in<br />
combination with low-dose IL-2, but conversely only 2 out of 9 treated with zoledronate<br />
alone, displayed a long-term shift of γδ T cells toward an activated effector/memory-like<br />
state (TEM ), producing IFN-γ and perforin. These patients also maintained serum TRAIL<br />
levels. Most importantly, γδ TEM cell numbers showed a correlation with declining<br />
prostate-specific antigen levels and objective clinical outcomes. γδ T cell phenotypes and<br />
serum TRAIL may thus constitute novel biomarkers of prognosis in metastatic cancer<br />
immunotherapy. On a final note, our data also imply that while co-delivery of IL-2<br />
appears crucial for optimal cytotoxicity, the considered use of other cytokines such as IL-<br />
21 in carcinoma trials might potentially lead to an (unwanted or wanted) diversion of<br />
the immune system away from a pro-inflammatory response.
Rebekka Geiger, Antonio Lanzavecchia, Federica Sallusto<br />
THE “T CELL AMPLIFICATION METHOD” AS A NEW TOOL TO<br />
ANALYZE THE REPERTOIRE OF HUMAN T CELLS<br />
By using T cell receptor (TCR) gene amplification and subsequent sequencing it was<br />
shown that circulating human T cells contain 2.5x107 distinct TCRs in the naïve pool<br />
and 2x105 TCRs in the memory pool. These molecular approaches, while showing TCR<br />
heterogeneity, cannot establish a direct relationship between TCR sequence and antigenspecificity.<br />
We are developing a new method to analyze the antigen-specific repertoire<br />
of human T cells. Highly pure naïve CD4+ T cells were sorted from peripheral blood<br />
mononuclear cells (PBMC’s) of several healthy donors on the basis of CD45RA and CCR7<br />
expression and stimulated polyclonally in limiting dilution (1,000 cells/well) by PHA,<br />
irradiated feeder cells and IL-2. For comparison, memory T cells (CD45RA-) were also<br />
isolated from the same donors and stimulated in limiting dilution (400 cells/wells) under<br />
the same conditions. After a ~1000-5000-fold amplification, each line was stimulated<br />
with autologous monocytes and a panel of naïve and recall antigens. Proliferation was<br />
measured using 3H-Thymidine incorporation as read-out. Using this method we<br />
assessed frequencies of T cells specific for different antigens, e.g. KLH, Anthrax PA, TT,<br />
DerpI and PPD. The data obtained so far indicate that frequencies of antigen-specific T<br />
cells in the naïve pool are much higher than previously thought, whereas the<br />
frequencies of antigen-specific T cells in the memory pool vary with the antigenic<br />
experience of the individual.
Stefanie Thiele, Andreas Pahl<br />
Therapy of chronic airway diseases with nucleic acids<br />
Asthma is a chronic inflammatory disease of the airways characterized by airway<br />
obstruction, epithelial damage and airway hyperresponsiveness. Inflammatory cells like<br />
eosinophils, macrophages and neutrophils are capable of releasing cytokines, proteases,<br />
reactive oxygen species and lipid mediators that contributes to the pathogenesis of<br />
asthma. Chronic obstructive pulmonary disease (COPD) is a disease state characterized<br />
by a progressive, irreversible limitation of airflow associated with an abnormal<br />
inflammatory response to noxious particles or gases.<br />
Aim of the project is the development of a nucleic acid based therapy for these kinds of<br />
chronic airway diseases. First different knock-down strategies will be evaluated in vitro.<br />
In parallel the optimal route of application and in vivo delivery method is investigated.<br />
To this end transgenic GFP-mice will be used. This allows the monitoring of cell specific<br />
knock-down effects. Finally genes relevant for chronic airway diseases will be knocked<br />
down in vivo. Various animal models of chronic airway diseases are established in the<br />
laboratory. The effect of the gene specific knock-down will be analysed for various<br />
pathological features in these animal models.
Arvind Batra, Markus M. Heimesaat, Stefan Bereswill, Jeannette Pietsch, Thorsten<br />
Stroh, Rainer Glauben, Inka Fedke, Martin Zeitz, Britta Siegmund<br />
TLR – expression in cells from adipose tissue – a contribution<br />
to chronic inflammation?<br />
Hypertrophy of mesenteric fat is a characteristic finding in Crohn’s disease. However,<br />
the underlying mechanisms and the contribution to the disease itself are still unknown.<br />
In addition to its endocrine role, adipose tissue is the producer of various proinflammatory<br />
mediators like leptin, IL-6 and TNF-α. We recently demonstrated leptindependent<br />
expression and function of Toll-like receptors (TLR) in murine preadipocytes<br />
and adipocytes (Batra et al., Am J Pathol, in press). To transfer these findings to<br />
humans TLR1 to -10 expression and function was analyzed in preadipocyte cell lines,<br />
established from human mesenteric fat, by RT-PCR and TLR-specific stimulation with<br />
subsequent evaluation of cytokine production. To further determine whether in vivo a<br />
direct interaction of cells from adipose tissue and bacterial TLR-ligands can occur,<br />
bacterial translocation was monitored in acute and chronic DSS-induced colitis in WT<br />
and MyD88 +/- mice by analysis for the presence of life bacteria via culture.<br />
In concordance with the murine system, in human preadipocyte cell lines TLR mRNA is<br />
expressed and cells respond to TLR-specific stimulation as evaluated by IL-6 production.<br />
In acute DSS-induced colitis no bacterial translocation was observed. In chronic DSSinduced<br />
colitis bacterial translocation into various abdominal tissues including fat<br />
occurred. Interestingly, bacterial translocation was more common in the MyD88 +/- mice<br />
with alterations in TLR-signaling. Our data provide strong evidence that functional TLR<br />
are expressed in preadipocytes and adipocytes across species. Suggesting that bacteria<br />
translocating to the mesenteric fat during intestinal inflammations such as Crohn’s<br />
disease can directly activate preadipocytes and adipocytes and thus might contribute to<br />
the mesenteric hypertrophy observed.
Linda Diehl, Anna Schurich, Regina Grochtmann, Silke Hegenbarth, Lieping Chen,<br />
Percy Knolle<br />
Tolerogenic maturation of LSEC after cognate T cell<br />
interaction promotes<br />
B7-H1-dependent CD8 + T cell tolerance<br />
Liver sinusoidal endothelial cells are unique organ-resident antigen presenting cells<br />
capable of cross-presentation and subsequent tolerisation of naive CD8 + T cells. Here,<br />
we investigated the molecular mechanisms underlying this tolerance induction in naive<br />
CD8 + T cells. MHC class I-restricted antigen-presentation by LSEC led to initial<br />
stimulation of naive CD8 + T cells, which upregulated CD69, CD25, CD44 and PD-1 and<br />
proliferated similar to dendritic cell activated CD8 + T cells. Importantly, cognate<br />
interaction with naive CD8 + T cells triggered increased expression of co-inhibitory B7-<br />
H1 but not co-stimulatory CD80/86 molecules exclusively on LSEC but not DC. This<br />
matured phenotype of B7-H1 high CD80/86 low was critical for induction of CD8 + T cell<br />
tolerance by LSEC: B7-H1 deficient LSEC, that failed to interact with PD-1 on stimulated<br />
T cells, were incapable of inducing CD8 + T cell tolerance. Moreover, increased<br />
costimulation via CD28 interfered with tolerance induction, indicating that the noninducible<br />
low expression levels of CD80/86 on LSEC supported B7-H1-dependent<br />
tolerance induction. LSEC-tolerized CD8 + T cells had a distinctive phenotype from naive<br />
and activated T cells with CD25 low , CD44 high , CD62L high . They also expressed the<br />
homeostatic cytokine receptors CD127, CD122 and high levels of Bcl-2, indicating<br />
survival rather than deletion of tolerant CD8 + T cells. Importantly, upon adoptive<br />
transfer into congenic animals tolerized CD8 + T cells failed to show specific cytotoxicity<br />
in vivo. Conclusion: Cognate interaction of LSEC with nave CD8 + T cells elicits a unique<br />
tolerogenic maturation of LSEC and permissiveness of T cells for tolerogenic signals<br />
demonstrating that LSEC-induced tolerance is an active and dynamic process.
Elke Gülden, Seiji Imamura, Masaru Ihira, Christiane Habich, Hubert Kolb, Volker<br />
Burkart<br />
Toll-like receptor 4: A key regulator of beta-cell directed<br />
autoimmunity in a mouse model of type 1 diabetes.<br />
Type 1 (insulin-dependent) diabetes (T1D) is caused by the destruction of autologous<br />
insulin producing pancreatic beta cells by innate and adaptive immune mechanisms.<br />
Recent investigations implicate that the progression of autoimmune reactivity is<br />
controlled by Toll-like receptor 4 (tlr4), originally described as the mammalian receptor<br />
for lipopolysaccharide (LPS). To investigate the role of tlr4 in the pathogenesis of insulindeficiency<br />
diabetes, we backcrossed the tlr4 defect of the C57BL/10ScCr mouse on the<br />
background of the non-obese diabetic (NOD) mouse, a model of human T1D. We found<br />
that female NOD mice with a homozygous tlr4 defect (tlr4-/-), showed a significant<br />
acceleration of diabetes development (p
Marina Scheler, Manuela Brenk, Helene Wilms, Thomas Bieber, Dagmar von Bubnoff<br />
Toll-like receptor ligands, and not T cell signals, are strong<br />
inducers for Indoleamine-2,3-dioxygenase (IDO),and lead to<br />
T cell suppression<br />
Immature dendritic cells (DCs) express receptors for inflammatory chemokines and<br />
migrate to sites of inflammation. Inflammatory cytokines as well as classes of microbial<br />
molecules (pathogen-associated molecular patterns, PAMP) trigger maturation and drive<br />
migration of DCs into the T cell areas of the draining lymph nodes. Stimuli derived from<br />
activated T cells such as IFN-γ and CD40L further impact on DC activation and survival.<br />
The outcome of the DC-T cell interaction can be productive priming or tolerance.<br />
Indoleamine 2,3-dioxygenase (IDO) is an enzyme that degrades the essential aminoacid<br />
tryptophan from the environment and leads to T cell tolerance. IDO can be induced<br />
in antigen-presenting cells upon inflammatory stimuli. IDO is thought to be important to<br />
prevent autoimmunity and allergy, but IDO can also facilitate chronic inflammation<br />
through induction of pathogen persistence. Using quantitative assays to monitor IDO<br />
expression and enzyme activity, we show that DC maturation renders these cells<br />
putatively capable of inducing tolerance via IDO. The strongest IDO activity was not<br />
seen in DCs stimulated with the best-established IDO-inducing protocol (i.e. with IFN-γ),<br />
but during stimulation by strongly maturing TLR ligands such as highly purified LPS<br />
(TLR4 ligand) or poly I:C (TLR3 ligand), suggesting T cell independent and autonomous<br />
IDO induction through pathogens in the innate immune system. Further, we show a<br />
strong upregulation of IDO in human DCs in skin ulcera associated with severe<br />
pathogen load. Together, these results can be viewed as an immediate and T-cell<br />
independent mechanism to ensure control of immune effector functions aiming to<br />
counter-regulate the adaptive T cell response.
Hans-Heinrich Oberg, Jan Lenke, Susann Beetz, Norbert Reiling, Dieter Kabelitz,<br />
Daniela Wesch<br />
Toll-like receptor-2 ligands act on Treg to abolish suppression<br />
of CD4 + CD25 - responder T cell proliferation and IL-2<br />
production<br />
CD4 + CD25 high regulatory T cells (Treg) control cellular immune responses and maintain<br />
peripheral tolerance. Treg suppress proliferation of CD4 + CD25 - responder T cells, which<br />
can be overcome indirectly by stimulation of Toll-like receptors (TLR) on antigenpresenting<br />
cells. Thus, TLRs function as molecular sensors that guide innate immune<br />
responses and are also involved in the regulation of adaptive immune responses. We<br />
and others have recently shown that TLRs are also expressed in human T lymphocytes.<br />
In this study we investigated whether TLR2 ligands have a similarly crucial role in<br />
regulating human Treg as has been described for TLR5 and TLR8 ligands. We used a<br />
feeder cell-free suppression assay to examine the influence of TLR ligands in the<br />
absence of antigen-presenting cells. We observed that TLR2 ligands such as bacterial<br />
lipopeptides Pam2CSK4, Pam3CSK4 and FSL-1 did not exert any effect by themselves<br />
but enhanced the anti-CD3/anti-CD28-stimulated proliferation of CD4 + CD25 - T cells,<br />
whereas proliferation of Tregs was not affected. Moreover, lipopeptide-induced reversal<br />
of Treg suppression did not seem to be due to a costimulatory effect on CD4 + CD25 - T<br />
cells because only the preincubation of Treg but not of CD4 + CD25 - T cells with either<br />
Pam2CSK4, Pam3CSK4 or FSL-1 nearly <strong>complete</strong>ly restored the suppression. The IL-2<br />
content in supernatant of stimulated CD4 + CD25 - T cells was diminished in the presence<br />
of Treg and was restored when Treg were preincubated with TLR2 ligands. In ongoing<br />
investigations we examine the influence of TLR2 ligands on p27 kip as a marker for cell<br />
cycle arrest. Our results provide the first evidence that lipopeptides are able to<br />
antagonize human Treg activity and thus could play a critical role in regulating Treg and<br />
T cells activation.<br />
This work was supported by the DFG (SFB415, project A15)
Elena Babich, Ata-Ur Rasheed, Hans-Peter Rahn, Martin Lipp, Gerd Müller<br />
Tracking follicular B helper T cell differentiation and function<br />
by gene expression analysis<br />
T cell-dependent immune responses are associated with the development of germinal<br />
centers in which antigen-specific B cells differentiate into memory B cells and highaffinity<br />
antibody-secreting plasma cells. The germinal center reaction critically depends<br />
on the presence of follicular B helper T (TFH) cells, a specialized subset of CD4 T cells<br />
providing B cell help. TFH cells have been initially identified by expression of the<br />
chemokine receptor CXCR5, which guides these cells into follicles, and their ability to<br />
efficiently induce immunoglobulin secretion by germinal center B cells. In addition, TFH<br />
cells control affinity maturation and isotype switching of germinal center B cells. We<br />
have recently shown that the differential expression of CXCR5 and the co-stimulatory<br />
molecule ICOS defines subsets of tonsillar CD4 T cells that differ in their stimulatory<br />
capacity, proliferative capacity and susceptibility to apoptosis. Our results suggest that<br />
in humans follicular B helper T cell activity is confined to CXCR5(hi)ICOS(hi) CD4 T<br />
cells. To more precisely define the differentiation pathway and molecular mechanisms<br />
mediating essential physiological and pathophysiological functions of TFH cells we have<br />
now extended our gene expression analysis and functional characterization of CD4 T cell<br />
subsets. In this connection we are particularly interested in better understanding the<br />
relationship of CXCR5 expressing CD4 T cells in the periphery and in lymphoid tissues as<br />
well as the role of TFH cells in the pathophysiology of chronic inflammatory and<br />
autoimmune diseases.
Ana Teles, Catharina Thuere, Milan Popovic, Anne Schumacher, Paul Wafula, Hans-<br />
Dieter Volk, Ana Zenclussen<br />
Trafficking of regulatory T cells during pregnancy: Expression<br />
profile of Treg-related chemokine and chemokine receptor at<br />
the maternal-fetal interface.<br />
Regulatory T cells (Treg) are shown to have an important role in the maintenance of<br />
fetus tolerance along pregnancy. The mechanisms leading to the recruitment of these<br />
cells at the fetal-maternal interface are still unknown, but like in other systems,<br />
chemokines are likely to be involved.<br />
Given the existent concordance between the expression of chemokines in the uterus/<br />
placenta and their receptors in Treg, we selected several receptor-ligand pairs that may<br />
be involved in the recruitment of these cells into the fetal-maternal tissues along<br />
pregnancy. By real time RT-PCR we investigated the expression patterns of the selected<br />
chemokine ligands in different phases of pregnancy (day 0, 2, 5, 8, 10 or 12 of<br />
pregnancy) in uterus, decidua and placenta from normal pregnant C57/BL6-mated BALB/<br />
c mice. Levels of Treg were analyzed by flow cytometry and by quantifying foxp3<br />
mRNA.<br />
Pregnant animals showed a gradual increase in the % of Treg in blood, spleen and<br />
decidua along pregnancy as well as increased foxp3 mRNA levels at the fetal-maternal<br />
interface. Regarding chemokines, our data suggest differential patterns of expression at<br />
different time points. We observed a gradual up-regulation of CXCL12 in placenta<br />
beginning on day 12 and of CCL21 in decidua beginning on day 10 of pregnancy.<br />
CXCL12 was further found to be increased in decidual tissue with a peak on the 5th day<br />
of pregnancy (implantation). For the chemokines CXCL13 and CCL20 no specific pattern<br />
of expression could be found.<br />
These results suggest different chemokines being responsible for the trafficking of Treg<br />
at different pregnancy stages.
Katharina Gropp, Michael Reuter, Gerhard D. Wieland, Christine Skerka, Peter F. Zipfel<br />
Transcription factors EGR-2 and NFkappaB induce chemokine<br />
synthesis in macrophages challenged with the human<br />
pathogenic yeast Candida albicans<br />
Candida albicans is the major human opportunistic fungal pathogen that can cause lifethreatening<br />
systemic infections. Macrophages represent the first cellular level for<br />
recognition of this human pathogenic yeast and recognize yeast cells by Toll Like<br />
Receptors (TLRs) and induce immune response by synthesis of cytokines.<br />
Recently we described that EGRs (early growth response protein) interact with the<br />
nuclear factor NFkappaB and strongly activate cytokine gene expression. To investigate<br />
whether Candida albicans induces in macrophages the EGR and NFkappaB transcription<br />
factors we determined the induction and also the transcriptional function of EGR and<br />
NFkappaB in macrophages triggered by Candida albicans. RT-RNA analysis revealed<br />
strong induction of EGR-2 and NFkappaB in macrophages exposed to the yeast- and<br />
hyphae-form of Candida albicans. However, whereas the yeast-form of Candida albicans<br />
induces the synthesis of pro-inflammatory cytokines like MIP-1alpha and MIP-1beta, the<br />
hyphae-form leads to the induction of anti-inflammatory cytokines like IL-10. The use of<br />
defined signal transduction inhibitors (PD 98059 and BAY 11-7082) showed that the<br />
induction of cytokines MIP-1alpha and MIP-1beta in response to Candida albicans is<br />
transmitted via the ERK- und NFkappaB-pathway. With transfection assays and confocal<br />
microscopy we demonstrate that the synthesis of chemokines MIP-1alpha and MIP-<br />
1beta in macrophages in response to Candida albicans is mediated by synergistic<br />
activity of EGR-2 and NFkappaB.
Yuriy Shebzukhov, Sergei Grivennikov, Andrey Kruglov, Chang-Yi Cui, Ina Wagner,<br />
Anna Litvin, Hans-Joachim Mollenkopf, David Schlessinger, Dmitry Kuprash, Sergei<br />
Nedospasov<br />
Transcriptional analysis of lymphoid organs from mice with<br />
conditional inactivation of TNF and LT<br />
Tumor necrosis factor (TNF) alpha and lymphotoxins (LT) are important cytokines<br />
involved in development of immune system, autoimmunity and host defense against<br />
infections. Using mice with conditional inactivation of TNF-alpha or LT-alpha in T cells, B<br />
cells and macrophages/neutrophils we are dissecting physiological role of these<br />
cytokines produced by different types of leukocytes. To investigate underlying molecular<br />
mechanisms and signaling pathways we perform gene array analysis followed by<br />
Northern blotting and/or quantitative RT-PCR. We found that in lymphoid organs TNFalpha<br />
derived from different cell types can activate distinct sets of genes, including<br />
chemokines and adhesion molecules. Overall T and B cell derived TNF-alpha control<br />
distinct subsets of genes in the spleen and lymph nodes. Some of TNF-alpha dependent<br />
genes are controlled solely by B cells derived cytokine.<br />
Earlier we found that different in vivo functions of TNF-alpha and LT-alpha are mediated<br />
by distinct types of leukocytes, now we demonstrated that these functions might be<br />
controlled by different downstream genes.
Monika Lindemann, Alexandra Schumann, Melanie Fiedler, Camino Valentin-Gamazo,<br />
Dietmar Knop, Christoph E. Broelsch, Michael Roggendorf, Hans Grosse-Wilde<br />
Transfer of adoptive immunity to hepatitis B virus by liver<br />
transplantation*<br />
Liver transplantation is often the ultimate option of therapy for chronically hepatitis B<br />
virus (HBV) infected patients. Despite antiviral therapy reinfection is still a problem.<br />
Adoptive transfer of HBV immunity with the liver after vaccination of living liver donors<br />
could be a new approach to prevent reinfection in the recipients. The period in which to<br />
achieve HBV immunity in donors is usually short (1-2 months). In this study we<br />
vaccinated living liver donors in a short time immunization protocol (4 injections in two<br />
weeks intervals) using Hepimmune (Berna Biotech), a recombinant vaccine that<br />
contains the PreS1, PreS2, and S proteins of HBV. Humoral (anti-HBs titer) and cellular<br />
(proliferation assay) immune responses were examined prior to each immunization, pre<br />
and post transplantation. So far 14 patients received a liver from an immunized living<br />
donor. In 4 recipients adoptive immune transfer was observed. One HBV naive recipient<br />
developed humoral and cellular immune responses post transplantation (anti-HBs of<br />
1800 IU/l and stimulation index of 4.9). Two further naive recipients showed cellular<br />
immune responses (stimulation indices of 2.7 and 7.1) and in one chronically HBV<br />
infected recipient specific immune responses were measurable at day 5 (anti-HBs of 120<br />
IU/l) and vigorously increased thereafter (anti-HBs of 58000 IU/l and stimulation index<br />
of 3.1). This finding most likely reflects the boosting of HBV specific immunity by HBs<br />
antigen persisting in the host. Taken together, we were able to show that HBV specific<br />
humoral and cellular immunity can be transferred to recipients with the liver graft.<br />
Thereby, the reinfection in chronically HBV infected recipients could be prevented.<br />
*This study was partially supported by the DFG (KFO 117).
Annette Busch, Thomas Quast, Waldemar Kolanus, Percy Knolle, Andreas Limmer<br />
Transfer of T cell surface molecules to Dendritic cells upon T<br />
cell priming involving two distinct mechanisms differing in<br />
quality and time<br />
The adaptive immune response is initiated in secondary lymphoid organs by contact<br />
between antigen-presenting cells (APCs) and antigen-specific CD4+ T cells. This<br />
activation is characterized by multiple antigen recognition events that comprise the<br />
interaction of both cell types through various molecules. In addition to the exchange of<br />
costimulatory signals and cytokines the cells transfer cell surface molecules. To date<br />
this is reported only as a unidirectional process of transfer from APC surface molecules<br />
to the T cell. Here we describe for the first time the transfer of human and murine T cell<br />
surface receptors to the APC. This transfer occurs in two phases that differ in quality<br />
and time. The first set of molecules is transferred rapidly after T–APC contact, is cell–<br />
cell contact-dependent, bound in an acid wash-resistant form to the cell surface and<br />
resembles a mechanism described as trogocytosis, whereupon the APC actively gnaws<br />
membrane fragments from the T cell membrane. The second set of T cell molecules is<br />
exchanged after T cell activation (>16h), is non-covalently bound (acid wash sensitive)<br />
and is transferred in a cell–cell contact-independent mode, resembling molecule<br />
exchange via exosomes. The transferred molecules may have an important role in APC<br />
conditioning and immunoregulation since they include the T cell receptor (TCR), CD3<br />
and costimulatory molecules. Murine dendritic cells (DCs) loaded with T cell surface<br />
molecules from ovalbumin (OVA)-specific CD4+ T cells by antigen-specific interaction<br />
were less efficient in priming naïve CD4+ T cells of the same specificity. The great<br />
amount of transgenic TCR on the DC surface may be responsible for the reduced<br />
activation of the T cells by masking the antigen-bearing MHC molecules for access of<br />
following antigen-specific CD4+ T cells. These findings may indicate an important role of<br />
transferred T cell molecules to APC in the intraclonal competition of T cells for APC<br />
access.
Jacqueline Moebius, Michael Basler, Marcus Groettrup<br />
TRANSGENIC MICE REVEAL A NOVEL ROLE FOR LMP7 IN TCR<br />
TRIGGERED EXPANSION OF T CELLS<br />
During an ongoing immune response three cytokine-inducible proteasome-subunits,<br />
LMP2 (β1i), LMP7 (β5i) and Mecl-1 (β2i), are incorporated into newly synthesized<br />
proteasomes instead of their corresponding constitutive subunits Delta (β1), MB1 (β5)<br />
and MC14 (β2) to provide the cells with a more diverse antigen processing machinery.<br />
Accumulating evidences point to an additional, so far uncharacterised role of<br />
immunoproteasome subunits: In adoptive transfer experiments immunoproteasome<br />
deficient T cells are unable to compete against wild-type T cells of the recipient during<br />
an antiviral immune response. After ruling out rejection phenomena being responsible<br />
for these observations we are currently investigating how immunoproteasomes can<br />
control T cell expansion in terms of influencing homing, proliferation or apoptosis of<br />
cells.<br />
In a first approach we wanted to determine the fate of the virus-specific T cells in these<br />
experiments and therefore crossed LMP7 gene targeted mice with P14 mice (T cell<br />
receptor transgenic for the Lymphocytic Choriomeningitis Virus epitope GP33). Again,<br />
40 hours after transfer we found about ten times less LMP7 -/- /P14 T cells in the spleens<br />
of recipient mice than P14 T cells in the control animals. In vitro stimulation of these<br />
cells with their appropriate peptide (GP33), presented on gamma-irradiated spleen cells,<br />
leads to a profound hyper proliferation of the LMP7 -/- /P14 T cells compared with the P14<br />
wild-type cells. Currently, we are testing the propensity of LMP7 -/- T cells to undergo<br />
apoptosis after TCR triggering and we compare T cell differentiation markers of LMP7<br />
deficient and proficient T cells. We hypothesize that immunoproteasomes serve a<br />
function e.g. in the processing of a factor needed for antigen driven T cell expansion<br />
that can not be fulfilled by constitutive proteasomes.
Volker Storn, Karsten Mahnke, Sonja Schallenberg, Theron S. Johnson, Tanja Bedke,<br />
Natalio Garbi, Bernd Arnold, Günter J. Hämmerling, Alexander H. Enk<br />
Treatment of established RMA-Tag tumors via DC directed<br />
targeting of tumor antigens is further improved by depletion<br />
of regulatory T cells.<br />
Tumor antigens, chemically coupled to the antiDEC205 antibody, can target dendritic<br />
cells in vivo and were successfully applied in murine preventive tumor vaccination<br />
studies. In this study our aim was to test whether antiDEC205-protein conjugates have<br />
the potential to reduce the tumor growth of already established tumors. For this end we<br />
coupled the tumor antigen Tag to antiDEC205 and treated RMA-Tag tumor-bearing mice<br />
with these conjugates. When the tumors had reached an average diameter of 5 mm the<br />
mice were injected with antiDEC205-Tag conjugate or Tag protein, plus adjuvants in 5day<br />
intervals. Although tumor growth was initially slowed down after injection of the<br />
antiDEC205-Tag conjugates as compared to Tag-treated mice, it resumed two to three<br />
weeks after the first vaccination. Analysis of the immune response initially revealed a<br />
strong induction of tumor specific CD8+ T-cells in antiDEC205-Tag treated mice.<br />
However, when tumor growth resumed increased numbers of CD4+CD25+FoxP3+<br />
regulatory T cells (Tregs) in the tumor draining lymph node were noticeable. Thus, to<br />
assess the suppressive effects of Tregs during tumor therapy, anti-CD25 antibodies<br />
were used to deplete Tregs from tumor bearing animals during anti-tumor treatment.<br />
By concomitant injection of antiDEC205-Tag conjugates we could cure up to 40% of the<br />
tumor bearing mice and tumors were rejected. Furthermore, the survival of tumor<br />
bearing mice of the autochthonous tumor model RIP-Tag5 could be prolonged for up to<br />
ten weeks after treatment with antiDEC205-Tag conjugates compared to untreated, or<br />
Tag-treated mice respectively. In aggregate our data indicate that depletion of CD25+<br />
Treg during cancer therapy bolsters the effectiveness of DC based anti-tumor therapies<br />
and that antiDEC205 targeted vaccination improves treatment of autochthonous<br />
tumors.
German Salamov, Rupert Holms, Wolfgang G. Bessler, Ravshan Ataullakhanov<br />
Treatment of Hepatitis C Virus Infection with Human Ezrin<br />
Peptide One (HEP1) in HIV Infected Patients<br />
This report shows the therapeutic benefit of HEP1 (Human Ezrin Peptide 324-337;<br />
TEKKRRETVEREKE) monotherapy of HCV infection in HIV infected patients in 2 clinical<br />
studies. In the Pilot Study I, 16 of 18 patients responded well to the treatment with<br />
significant reductions of HCV viral load and a normalization of serum liver enzymes. In 8<br />
of 18 patients, HCV RNA became undetectable, and 3 of 8 interferon/ribavirin treatment<br />
failure patients showed undetectable HCV load following HEP1 treatment. In the second<br />
study, 8 of 10 patients responded well to the treatment with a pronounced reduction of<br />
the HCV viral load and a normalization of serum liver enzymes. 3 of 15 patients (20%)<br />
showed an undetectable viral load 30 days after the end of a 30 day course of HEP1<br />
treatment. In both studies, all genotypes of HCV were sensitive to HEP1 treatment.<br />
Analysis of the combined data from both studies showed the overall efficacy of HEP1<br />
therapy: in 37 HCV+HIV patients, HEP1 therapy gave the following results: 10 of 37<br />
(27%) HCV+HIV patients showed a reduction of viral load between -7 log (-<br />
10,000,000x) and -3 log (-1,000x); 4 of 37 (11%) a reduction of -3 log (-1,000x); 6 of<br />
37 (16%) a reduction of -2 log (-100x); 11 of 37 (30%) a reduction of -1 log (-10x); 6<br />
of 37 (16%) a reduction of less than -1 log (-10x); 0 of 37 (0%) had an increase in viral<br />
load, and the average reduction in viral load for all 37 patients was -2 log (-100x). No<br />
adverse reactions or side effects were detected and the improving CD4/CD8 ratio<br />
showed that the therapy had no negative impact on the immunological status. Thus,<br />
oral HEP1 therapy matches the efficacy results for injectable peginterferon/oral ribavirin<br />
therapy with the advantages of more rapid action and less side effects. HEP1 therapy<br />
should be used in patients where either peginterferon/ribavirin therapy fails or is<br />
contraindicated.
Claudia Stühler, Sarah Lurati, Manik Chatterjee, Ralf C. Bargou, Hermann Einsele, Max<br />
S. Topp<br />
Treatment of T lymphocytes with Hsp90 inhibitors selectively<br />
kills activated cells while preserving viability and<br />
functionality of resting cells<br />
Graft-versus-host disease (GvHD) is a major cause of morbidity and mortality in<br />
patients with hematological malignancies undergoing allogeneic hematopoietic stem cell<br />
transplantation (HSCT). Current treatment of GvHD utilizes immunosuppressive<br />
regimens which put the patient at a high risk of opportunistic infections. Therefore<br />
selective approaches for specific eradication of GvHD-specific T-cells are highly<br />
warranted. Inhibition of heat shock protein 90 (Hsp90) could be one approach, as<br />
Hsp90 aids in the maturation and stabilization of a wide variety of client proteins, some<br />
of which are integral components of signal transduction pathways of activated T-cells.<br />
In the first set of experiments selective upregulation of both Hsp90 subunits in activated<br />
primary T-cells was confirmed and shown to be impeded by application of the Hsp90<br />
inhibitors Geldanamycin and 17-DMAG as well as with siRNA. Addition of Hsp90 inhibitor<br />
to either mitogen-activated T-cells or T-cells activated by allogeneic stimulator cells lead<br />
to preferential eradication of activated cell populations. The preferential killing of only<br />
activated cells could be shown by stimulation of 17-DMAG pretreated mixed lymphocyte<br />
cultures with either autologous APC presenting viral antigens or rechallenge with the<br />
same allogeneic dendritic cells. Whereas virus-specific T-cells could readily be activated,<br />
no activation could be detected in 17-DMAG pretreated T-cell cultures exposed for a<br />
second time to the allogeneic stimulators. Untreated cultures on the other hand<br />
responded to both stimuli. To verify which crucial signalling pathways of activated Tcells<br />
are abrogated in the presence of Hsp90 inhibitors further western blot experiments<br />
were performed.<br />
This experimental data demonstrate that Hsp90 inhibitors can selectively remove<br />
alloreactive T lymphocytes upon activation without compromising the viability and<br />
functionality of the remaining lymphocyte populations including the virus-specific<br />
immune response.
Kai Zanzinger, Carola Schellack, Gernot Geginat, Adelheid Cerwenka<br />
TREM-1 in infection and cancer<br />
Cells of the innate immune system play an important role in the first line of defense<br />
against bacteria and viruses. Their activation is controlled by different receptor families<br />
including the Ig superfamily with both inhibitory and activating isoforms. Activating<br />
isoforms deliver stimulatory signals by their association with transmembrane adapter<br />
proteins bearing Immunoreceptor Tyrosine-based Activation Motifs (ITAM). DAP12 is<br />
such an adapter protein that associates with several receptor molecules such as the<br />
Triggering Receptor Expressed on Myeloid cells-1 (TREM-1).<br />
In human and mice, TREM-1 is highly expressed on granulocytes. However, little is<br />
known about the modulation of its expression on monocyte subpopulations in mice.<br />
Blood of naïve mice comprises two subsets of monocytes: ‘resident’ (F4/80 + Gr-1 - CD62L -<br />
CX3CR1 hi ) and ‘inflammatory’ monocytes (F4/80 + Gr-1 + CD62L + CX3CR1 lo ). In our study,<br />
we analyzed TREM-1 expression on these monocyte subsets upon stimulation with Tolllike<br />
receptor ligands, infection with L. monocytogenes and in different cancer models.<br />
We show that in naïve mice TREM-1 is only detectable on ‘resident’ but not on<br />
‘inflammatory’ monocytes. In contrast, TREM-1 is upregulated on the F4/80 + Gr-1 +<br />
‘inflammatory’ monocyte subpopulation upon application of Toll-like receptor ligands<br />
and in L. monocytogenes infection. In addition, also in different tumor models the<br />
‘inflammatory’ monocyte subpopulation upregulates TREM-1. Interestingly, this<br />
population in tumor-bearing mice is phenotypical and functionally identical to recently<br />
described myeloid-derived suppressor cells (MDSC).<br />
The future objectives of this project are to identify the factors that regulate TREM-1 on<br />
this monocyte subpopulation in cancer.
Anna-Maria Herr, Olivia Sövegjarto, Lutz Walter<br />
TRIM proteins: Novel candidates for HIV resistance?<br />
Evolutionary processes of host-pathogen interaction considerably shape the genomes of<br />
both organisms, favouring the development of resistance genes (host) and of immune<br />
escape mechanisms (pathogen). Notably, retroviruses impact the evolution of the<br />
vertebrate immune system. Retroviruses encounter dominant postentry restrictions in<br />
cells of particular species. Human immunodeficiency virus (HIV)-1 for example is<br />
blocked by TRIM5α, a tripartite motif (TRIM) protein, in cells of Old World monkeys.<br />
Rhesus monkey TRIM5α more potently blocks HIV-1 infection than human TRIM5α.<br />
Recently, dozens of novel TRIM proteins have been identified. Although most of their<br />
physiological roles are not yet clear, preliminary evidence suggests a rapid evolution<br />
and adaptation to antiviral activity of some of the TRIM proteins.<br />
In this work, the evolution of the TRIM genes is studied in the primate lineage. We<br />
focused on TRIM genes with comparable domain-structure as TRIM5α (RING, B-box 2,<br />
coiled coil and B30.2 domain). By comparing the rates of synonymous (dS) and<br />
nonsynonymous (dN) substitutions between human and rhesus macaque TRIM genes<br />
we found differentially conserved TRIM genes. In contrast to the more conserved<br />
TRIM10 with only a few nonsynonymous substitutions between human and rhesus<br />
macaque, TRIM22 shows signs of positive selection. Rhesus TRIM22 is 91% identical to<br />
human TRIM22 in amino acid sequence. Interestingly we found the B30.2 of TRIM22<br />
less conserved (dN/dS=1,24) than the tripartite motif (dN/dS=0,61). Stremlau et al.<br />
(2004) showed, that the B30.2 domain of TRIM5α is responsible for restriction of HIV in<br />
rhesus macaques. With respect to these findings our data suggest that TRIM22 and<br />
other TRIM genes could also be involved in evolutionary processes of host-pathogen<br />
interaction and may open up novel perspectives in antiviral therapies.
Christiane Desel, Stefan H.E. Kaufmann<br />
Tuberculosis: Efficacy of DNA vaccines encoding dormancyassociated<br />
antigens<br />
It is estimated that one third of the world’s population is latently infected with<br />
Mycobacterium tuberculosis, the causative agent of tuberculosis. Of those 2 billion<br />
people 5-10% will develop active disease during their lifetime. The infection claims 2<br />
million lives every year and 9 million new cases are reported annually.<br />
M. tuberculosis has a striking capacity to evade the host’s immune system and to<br />
prevent its elimination. As a response to stress caused by a vigorous immune response<br />
the bacteria induce a dormancy programme enabling survival within host macrophages.<br />
But as soon as the immune surveillance fails, the dormant bacteria will be resuscitated<br />
leading to active tuberculosis. The only available vaccine against tuberculosis is<br />
Mycobacterium bovis BCG, one of the safest live vaccines known. However its protective<br />
effect against pulmonary tuberculosis in adults is debatable and protection wanes with<br />
time. Not only better pre-exposure vaccines to prevent infection in the first place but<br />
also post-exposure vaccines for those individuals harbouring dormant bacteria are<br />
urgently needed.<br />
It is known that mycobacteria express different antigens during the dormant state as<br />
compared to actively replicating ones and also the immune mechanisms to control<br />
primary and latent infection differ. Post-exposure vaccines will have to be designed<br />
based on antigens upregulated or solely expressed during dormancy. Dormancy is<br />
linked to hypoxic conditions within the granuloma and surrounding tissue and the<br />
dormancy survival regulator DosR has been identified as the primary factor which<br />
mediates the genetic response to reduced oxygen levels as well as exposure to nitric<br />
oxide. Here we examine the immunogenicity and efficacy of DNA vaccines based on<br />
DosR-regulated antigens in murine models of persistent and latent Mycobacterium<br />
tuberculosis infection.
Jenny Pahne, Subramanya Hegde, Nadine Schröer, Sigrun Smola-Hess<br />
Tumor cell-derived interleukin-6 skews myeloid dendritic<br />
cells from an immunostimulatory to a pro-tumorigenic<br />
phenotype<br />
Persistent infection with human papillomaviruses can lead to cervical intraepithelial<br />
neoplasia, which after years may further progress to cancer. Development of malignant<br />
disease is not the direct consequence of infection but the result of a complex interplay<br />
between the transformed cells and their microenvironment. During progression to<br />
malignancy a pronounced shift from TH1 to TH2 cytokines is observed. As a<br />
consequence, cytotoxic T cell responses necessary to eliminate the tumor are impaired.<br />
Currently, the mechanism, how cervical neoplastic cells contribute to this immunological<br />
shift is not known.<br />
Here we show that supernatants of cervical carcinoma cells suppress up-regulation of<br />
CCR7 and production of interleukin-12 (IL-12) in myeloid dendritic cells, which is<br />
important for mounting a TH1 response. Signalling pathways regulating CCR7 and IL-12<br />
expression were investigated. Supernatants of neoplastic cells strongly inhibited nuclear<br />
factor-kappaB (NF-kappaB) binding activity in dendritic cells, which is central to their<br />
immunostimulatory function. Corresponding to the expression pattern in vivo, cervical<br />
carcinoma cells did not produce IL-10 in vitro, but the pro-inflammatory cytokine IL-6.<br />
Neutralization of IL-6 in cervical cancer cell supernatants restored IL-12 production and<br />
NF-kappaB binding activity in dendritic cells. Of note, not all functions of dendritic cells<br />
were suppressed by the neoplastic cells. Despite inhibition of NF-kappaB binding<br />
activity, tumor cell-derived IL-6 up-regulated the pro-angiogenic and pro-tumorigenic<br />
matrix-metalloproteinase MMP-9 in dendritic cells.<br />
In summary, our data demonstrate that tumor cell-derived IL-6 skews dendritic cells<br />
from an immunostimulatory to a pro-tumorigenic phenotype.
Gerald Willimsky, Melinda Czéh, Christoph Loddenkemper, Johanna Gellermann,<br />
Harald Stein, Peter Wust, Thomas Blankenstein<br />
Tumor immunogenicity, not tumor burden is the primary<br />
cause of general cytotoxic T lymphocyte unresponsiveness<br />
Cancer is sporadic in nature, characterized by an initial clonal oncogenic event and a<br />
usually long latency. When and how sporadic cancer subverts the immune system is<br />
unknown. Here we show in a model of sporadic immunogenic cancer that tumor-specific<br />
tolerance closely coincides with first tumor antigen recognition by B cells. During the<br />
subsequent long latency period until tumors progress the mice develop general<br />
cytotoxic T lymphocyte (CTL) unresponsiveness, which is associated with high TGF-<br />
&beta1 levels and expansion of immature myeloid cells (iMC). In contrast, in mice with<br />
large non-immunogenic tumors, unrelated CTL responses are undiminished.<br />
Interestingly in these tumor-bearing mice iMCs are most dramatically expanded, but<br />
TGF-&beta1 serum levels are normal. We conclude that premalignant immunogenic<br />
lesions induce tolerance and therefore tumor latency is unlikely caused by CTL control.<br />
A persistent immunogenic tumor antigen causes general CTL unresponsiveness but<br />
tumor burden and iMC per se do not mediate immune suppression.
Christoph D. Brenner, Susan King, Imke Wolters, Georg Bornkamm, Martin Röcken,<br />
Ralph Mocikat<br />
Tumour control by natural killer cells in a spontaneous mouse<br />
lymphoma model<br />
We have previously shown that downregulation of MHC class I provides a “danger”<br />
signal that alerts the immune system resulting in target cell rejection and T-cell<br />
memory. Injection of MHC class I-low target cells activated natural killer (NK) cells<br />
thereby instructing dendritic cells to express IL-12 and to prime cytotoxic T<br />
lymphocytes (CTL). This “cross-priming” could explain the rapid induction of T-cell<br />
responses against viruses but left unanswered the question as to why this NK-cell help<br />
is apparently not effective enough to convey protective CTL responses against MHC<br />
class I-modulated autochthonous tumours. In the present study we used c-myctransgenic<br />
mice, which spontaneously develop B-cell lymphomas by the age of 12<br />
weeks, and studied the impact of tumour progression on the tumour reactivity of NK<br />
cells. Activation markers of NK cells were elevated after onset of tumour growth and<br />
clearly correlated with MHC class I downregulation of the developing tumours.<br />
Nonetheless, NK cells isolated from tumour-bearing animals were not capable of lysing<br />
tumour cells in vitro, and this was associated with reduced expression of several surface<br />
markers such as CD49b. Most interestingly, tumour growth could be delayed if NK cells<br />
received additional stimuli in vivo by treating mice with NK-cell-activating reagents. This<br />
indicates that NK cells indeed play a role in controlling growth of spontaneous<br />
lymphoma.
Nicolas Sabarth, Louise Chamberlain, John Tite, Sara Brett, Craigen Jenny<br />
Two-sided effect of T cell help in tolerance breaking and<br />
immunodominance<br />
To develop a successful cancer vaccine it is necessary to break immunological tolerance<br />
to self-antigens expressed on tumour cells. Broken immunological tolerance results in a<br />
functional CD8 T cell response, the development of which is known to be dependent on<br />
provision of CD4 help. In the transgenic RIP OVALOW mouse model which is<br />
hyporesponsive, ergo immunological tolerant, to ovalbumin, DNA vaccination with<br />
ovalbumin in combination with GM-CSF and the TLR7 agonist Imiquimod provided a<br />
strong synergistic adjuvant effect on CD4 cells resulting in broken tolerance in both the<br />
CD4 and CD8 compartments. Compared to wildtype mice RIP OVALOW mice had CD8 T<br />
cells of lower avidity, but functional CD8 T cell responses were evident by induction of<br />
tumour protection and correlating autoimmunity which served as a surrogate of efficient<br />
target cell killing. Heterologous CD4 help has been shown to improve functional CD8<br />
responses and we confirmed that inclusion of the T helper epitope PADRE enhanced CD8<br />
responses compared to self antigen alone both in RIP OVALOW mice and their wildtype<br />
counterpart although no autoimmunity was induced. Addition of GM-CSF and Imiquimod<br />
however resulted in dominance of the PADRE response over the ovalbumin specific CD4<br />
responses in both mouse strains. The effect of the PADRE on the CD8 T cell response<br />
was depended on the state of tolerance of the animals: PADRE specific CD4 help<br />
compensated for the lack of ovalbumin specific CD4 help and the CD8 T cell response<br />
was little affected in wildtype mice. In contrast, in tolerant RIP OVALOW mice the<br />
combination of PADRE and GM-CSF & Imiquimod decreased ovalbumin specific CD8<br />
numbers and function, abrogating diabetes development. Only the limited use of PADRE<br />
together with adjuvant enhanced DNA immunisation provided some benefit evident by<br />
accelerated autoimmunity in RIP OVALOW mice, i.e. target cell killing.<br />
Hence, Imiquimod/GM-CSF enhanced DNA immunisation has good potential as<br />
therapeutic cancer vaccine but the use of heterologous T cell help has to be handled<br />
with care and needs further investigation.
Christian Wahl, Petra Bochtler, Reinhold Schirmbeck, Jörg Reimann<br />
Type I IFN-producing CD4 Valpha14i NKT cells facilitate<br />
priming of IL-10-producing CD8 T cells by hepatocytes<br />
Upon entering the liver CD8 T cells encounter large numbers of NKT cells patrolling the<br />
hepatocyte (HC) surface facing the perisinusoidal space. We asked whether hepatic NKT<br />
cells modulate the priming of CD8 T cells by HC. Hepatic (alpha-galactosyl-ceramideloaded<br />
CD1d dimer binding) NKT cells produce predominantly IL-4 when stimulated with<br />
glycolipid-presenting HC but predominantly IFN-gamma when stimulated with glycolipidpresenting<br />
dendritic cells. These NKT cells prime naive CD8 T cells to a (K(b)-presented)<br />
peptide ligand if they simultaneously recognize a CD1d-binding glycolipid presented to<br />
them on the surface of the responding CD8 T cells that they prime. No IL-10-producing<br />
CD8 T cells are detected if these T cells are primed by either HC or NKT cells. In<br />
contrast, IL-10 is produced by HC-primed CD8 T cells if IFN-beta-producing NKT cells<br />
are coactivated by the same HC presenting a glycolipid (in the context of CD1d) and an<br />
antigenic peptide (in the context of K(b)). Hence, IL-10-producing CD8 T cells are<br />
generated in a type I IFN-dependent manner if the three cell types (CD8 T cells, NKT<br />
cells, and ligand-presenting HC) specifically and closely interact. IL-10-producing CD8 T<br />
cells generated under these conditions down-modulate IL-2 (and proliferative)<br />
responses of naive CD4 or CD8 T cells primed by DC. If in close proximity, NKT cells can<br />
thus locally modulate the phenotype of CD8 T cells during their priming by HC thereby<br />
limiting the local activation of proinflammatory immune effector cells and protecting the<br />
liver against immune injury.
Markus Krumbholz, Hans Faber, Florian Steinmeyer, Lisa-Ann Hoffmann, Hannah<br />
Pellkofer, Tania Kümpfel, Tobias Derfuß, Camelia Ionescu, Michaela Starck, Thomas<br />
Giese, Gunther Hartmann, Christian Hafner, Reinhard Hohlfeld, Edgar Meinl<br />
Type I interferon therapy increases systemic BAFF expression<br />
Type I interferons (IFN-I) play a key role both in the physiological immune response<br />
after e.g. viral infection and in autoimmune diseases like SLE. Besides effects on T cells,<br />
effects on the B cell system are increasingly recognized. We asked whether IFN-I<br />
regulate the BAFF/APRIL system, which is crucial for the normal B cell physiology, and<br />
may also drive autoimmune diseases and malignancies.<br />
We report that systemic BAFF expression was elevated in MS patients treated with IFN-<br />
&beta, but not in untreated patients. BAFF transcription in vivo in monocytes and<br />
granulocytes correlated with that of MxA, a typical IFN-&beta regulated gene. Further in<br />
vitro analysis confirmed that IFN-&beta concentrations reached in vivo in treated MS<br />
patients induce BAFF in these immune cell subsets and also in tissue resident cells<br />
(fibroblasts and astrocytes). In contrast to BAFF, APRIL was only slightly induced by IFN-<br />
&beta. The hybrid transcript TWE-PRIL was expressed several orders of magnitude<br />
lower in vivo. The receptors BCMA, TACI, BARF-R were not regulated by IFN-&beta.<br />
The systemic induction of BAFF by type I IFNs shed light on a mechanism for the<br />
physiological interplay of innate and adaptive immunity at the level of B cells, on<br />
complex immunomodulatory effects of IFN-&beta treatment in MS patients, on how type<br />
I IFN therapy may lead to the known induction of autoantibodies or even clinical<br />
autoimmunity as a side effect, and on how type I IFNs may aggrevate autoimmunity in<br />
e.g. SLE.
Susanne Rauchmann, Karin Knieke, Marion Rudolph, Holger Hoff, Monika Brunner-<br />
Weinzierl<br />
Ubiquitin-ligases in co-stimulation of T-lymphocytes<br />
Many aspects of cellular function are regulated by ubiquitination. One aspect of Tlymphocyte<br />
function for which the contribution of ubiquitin-mediated regulation is not<br />
fully investigated is T cell activation mediated by co-stimulatory receptors. While it has<br />
been shown that CD28 mediated co-stimulatory signals down-regulate the activity of<br />
the ubiquitin-ligase Cbl-b the role of the closely related receptor CD152 (CTLA-4) in the<br />
regulation of ubiquitination is not known. Here we can show that in CD152 deficient Thelper<br />
cells the expression levels of several ubiquitin-ligases are drastically decreased.<br />
The diminished activity of the RING-domain containing ubiquitin-ligases c-Cbl and Cbl-b,<br />
the HECT-type ligases NEDD4 and Itch as well as Grail could explain the hyperactive<br />
phenotype displayed by CD152 deficient CD4+ T cells. This phenotype is less severe in<br />
TCR-transgenic CD152 deficient T-helper cells that corresponds with less drastic<br />
differences in the expression of ubiquitin-ligases. Different expression levels of c-Cbl,<br />
Cbl-b and Itch before onset as well as at late time-points after stimulation might point<br />
at an important role of ubiquitin-ligases for the induction of a resting phenotype. Future<br />
work will be necessary to analyse the different contribution of positive and negative costimulatory<br />
receptors for the induction of ubiquitin-ligase activity.
Christine Wolff, Peter Härle, Johannes Wildmann, Hugo O. Besedovsky, Rainer H.<br />
Straub, Adriana del Rey<br />
Uncoupling of the HPA axis and the sympathetic nervous<br />
system in rheumatoid arthritis is linked to marked changes of<br />
norepinephrine levels in the hypothalamus<br />
Introduction:<br />
Uncoupling of the hypothalamic-piuitary-adrenal (HPA) axis and the sympathetic<br />
nervous system (SNS) has been demonstrated in rheumatoid arthritis. This is evident<br />
by an overactivity of the SNS and a relative low activity of the HPA axis. However, the<br />
reasons for this phenomenon and the consequences for the inflammatory disease are<br />
not known.<br />
Aim of the study:<br />
To study the time course of norepinephrine content in the hypothalamus during the<br />
course of collagen type II – induced arthritis in the rat.<br />
Material and methods:<br />
Female Dark Agouti (DA) rats were immunized with type II collagen to induce arthritis.<br />
Animals were killed and samples were taken on day 5, 14, 28, 40 and 55.<br />
Measurements of norepinephrine (NE) of brain samples (hypothalamus, pons, medulla<br />
oblongata) were done via HPLC. To measure plasma NE and corticosterone we applied<br />
radioimmunoassay.<br />
Results:<br />
We could not find any significant differences in the neurotransmitter levels in the<br />
medulla oblongata and in the pons between controls and arthritic animals. Importantly,<br />
on day 5, the levels of NE in the hypothalamus of rats with arthritis were lower than in<br />
controls . Levels of NE subsequently increased and were significantly higher in arthritic<br />
animals on day 40 and 55. Blood levels of NE in rats with arthritis were significantly<br />
higher than in controls already at beginning of symptomatic arthritis. Furthermore, we<br />
found a significant increase of plasma corticosterone in arthritic animals on day 5<br />
followed by a reduction to baseline levels from day 14 onwards.<br />
Conclusion:<br />
For the first time, this study demonstrated uncoupling of the HPA axis and the SNS in<br />
animal model of arthritis. Future experiments are designed to modulate hypothalamic<br />
NE content in order to modulate peripheral inflammation.
Sonja Textor, Rosita Accardi, Matthias Dürst, Massimo Tommasino, Lutz Gissmann,<br />
Adelheid Cerwenka<br />
Up-regulated expression of activating NK cell receptor ligands<br />
in human cervical cancer<br />
NK cell activation is mediated by a delicate balance of signals received by activating and<br />
inhibiting receptors. Certain activating receptors recognize ligands, which are induced<br />
upon cellular stress like transformation or viral infection. Inhibitory signals are delivered<br />
to NK cells through interaction with self MHC class I or related molecules. Expression of<br />
these ligands is modulated by certain viruses and on tumors rendering the infected or<br />
transformed cells more or less susceptible to NK cell attack.<br />
The aim of our study was to evaluate the impact of the two major transforming<br />
oncogenes of Human Papilloma Viruses (HPV), E6 and E7, on the regulation of NK cell<br />
receptor ligand expression. First, we analysed the expression of NK cell receptor ligands<br />
on keratinocytes after transduction with a retroviral vector system carrying HPV16-E6<br />
and/or -E7 by flow cytometry. Comparing HPV16-E6E7 expressing keratinocytes with<br />
the corresponding parental cells, we detected up-regulation of MICA, a ligand for the<br />
activating NK cell receptor NKG2D. Expression of other ligands, like CD155, a ligand for<br />
the activating NK cell receptor DNAM-1, remained unchanged.<br />
Since high-risk HPVs, like HPV16, are the etiological agents of cervical cancer (CxCa),<br />
biopsies of CxCa and prelesions were stained for NK cell receptor ligands and NK cells<br />
by immuno-histochemistry in situ. Tumor-infiltrating NK cells (CD56+) were found in all<br />
cervical cancer stages. High expression of the activating NK cell receptor ligands, MICA<br />
and CD155, was only observed in CxCa specimens, whereas precursor lesions showed<br />
no MICA expression und moderate CD155 expression. Some CxCa biopsies showed low<br />
MHC class I expression in combination with high expression of activating NK cell<br />
receptor ligands, making CxCa an appealing target for NK cell- based immunotherapy.
Felix Lasitschka, Jutta Schröder-Braunstein, Thomas Giese, Carolin Reiser, Bernd<br />
Sido, Stefan C. Meuer<br />
Uptake of Cystine in T-Lymphocytes following CD2 and CD3<br />
stimulation<br />
Background:<br />
Glutathione (GSH) is the most abundant nonprotein thiol involved in the maintenance of<br />
the cellular redox state. In this capacity it influences T-Lymphocyte responsiveness to<br />
various stimuli and is a prerequisite for cell cycle progression following CD2 and CD3<br />
stimulation.<br />
While it is known that macrophages can provide T-Lymphocytes with cysteine, the<br />
limiting substrate for GSH synthesis, by intracellularly reducing cystine to cysteine, we<br />
now investigated the possibility of the direct uptake of cystine by T-Lymphocytes after<br />
stimulation.<br />
Methods:<br />
Uptake of radiolabelled cystine in cultured T-Lymphocytes following CD2 and CD3<br />
stimulation over the timecourse of 72 hours was measured in the presence or absence<br />
of different inhibitors of system xc-, a spe¬cific transporter for cystine. Proliferation was<br />
measured via uptake of [3H]-Thymidine , viability of cells was investigated through PI/<br />
Annexin V staining. xCT expression on T-Lymphocytes was analysed by flow cytometry .<br />
Results:<br />
T-Lymphocytes show a markedly increased uptake of cystine over the timecourse of 72<br />
hours following CD2 and CD3 stimulation. Inhibitors of system xc-, Glutamate,<br />
Quisqualate and Homocysteate, reduced the uptake of cystine and the prolifera¬tive<br />
potential of stimulated cells without affecting their viability. The percentage of xCT<br />
posi¬tive cells as determined by flow cytometry increased over time as well.<br />
Conclusion:<br />
CD2 and CD3 stimulation of T-Lymphocytes induces a hitherto unknown uptake of<br />
cystine, which can be reduced by specific inhibitors of system xc-. Thus, system xc-<br />
contributes in part to the redox regulated reactivity towards CD2 and CD3.<br />
Further investigations regarding cystine uptake in human lamina propria T-Lymphocytes<br />
(LPT) after stimulation, which show a lower response towards CD3 stimulation, but a<br />
preserved CD2 proliferation compared to autologuos peripheral blood T-Lymphocytes<br />
are required to test, whether the uptake of cystine by LPT plays a role in mucosal redox<br />
regulation.
Meike Winter, Roel Schins, Irmgard Förster<br />
Uptake of nanoparticles in the food by gut-associated<br />
dendritic cells<br />
Nanoparticles are defined as particles with a diameter smaller than 0.1µm. They are<br />
constituents of many foods including dairy creamers, ketchup and chewing gum. The<br />
regular intake of inorganic particles by humans is estimated as 10 12 particles per day.<br />
Since nanoparticles are already known to induce severe inflammatory reactions and<br />
cancer in the lung, and contribute to the establishment of cardiovascular diseases, there<br />
is an urgent need for further studies on the toxic potential of nanoparticles in the<br />
intestine. It has been suggested that a low nanoparticle diet might be associated with a<br />
better prognosis of inflammatory bowel disease (IBD), even though contradicting data<br />
exist. In ex vivo studies an amplifying effect of ultrafine titanium dioxide on LPSinduced<br />
gut inflammation could be demonstrated. We are presently analysing the<br />
uptake of orally administered nanoparticles in cells of the gut associated immune<br />
system, especially in dendritic cells, which are potent inducers of immunoreactions and<br />
thought to be involved in the pathology of IBD. In in vitro studies we could already<br />
show that murine bone marrow derived dendritic cells display differentiation defects if<br />
generated in the presence of nanoparticles. Differentiation was less efficient and a<br />
reduction of cell size could be observed in the presence of ultrafine titanium dioxide.<br />
When generated in the presence of ultrafine carbon black the effects were even more<br />
pronounced. Thus, the number of dendritic cells was reduced, cells were smaller and the<br />
density of MHC- and costimulatory molecules on the cell surface was reduced. If<br />
ultrafine carbon black was added to immature dendritic cells, MHC-class-II was<br />
upregulated, suggesting a stimulatory effect of ultrafine carbon black on dendritic cell<br />
maturation.<br />
In the future we aim to investigate the effect of nanoparticles on the manifestation of<br />
disease in different mouse models for acute and chronic IBD.
Sascha Barabas, Tanja Bauer, Regina Gary, Petra Lindner, Juha Lindner, Wolfgang<br />
Jilg, Hans Wolf, Ludwig Deml<br />
Urea-mediated cross-presentation of soluble Epstein-Barr<br />
Virus BZLF1<br />
Soluble extracellular polypeptides are almost exclusively delivered to the exogenous<br />
MHC class II presentation pathway of antigen-presenting cells (APC), thus diminishing<br />
their capacity to stimulate CD8+ cytotoxic T lymphocytes (CTL). Here, we describe the<br />
urea-mediated translocation of soluble Epstein-Barr virus (EBV) immediate early protein<br />
BZLF1 to the endogenous cytosolic pathway of MHC I-dependent polypeptide<br />
presentation.<br />
APC pulsed with urea-treated BZLF1 (uBZLF1) efficiently reactivate BZLF1-specific CTL<br />
and T helper cells from HLA-matched EBV-seropositive donors. uBZLF1 shows strong<br />
attachment to the cell membrane before uptake by clathrin-mediated endocytosis and<br />
degradation at the proteasome for cross-presentation. Dendritic cells, monocytes but<br />
also B cells are able to mediate MHC I-restricted epitope presentation from uBZLF1. This<br />
strategy considerably promotes reactivation and propagation of protein-specific CTL.<br />
The procedure described here has potential for use in evolving improved strategies for<br />
protein-specific monitoring and immunotherapy of viral infections.
Emmanuel Prodhomme, Claude Muller<br />
Vaccination against Tobacco Specific N-nitrosamines:<br />
Synthesis of a new NNK hapten for the induction of specific<br />
antibodies.<br />
4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) is one of the most abundant<br />
and potent pro-carcinogens in tobacco smoke. In order to induce a strong and<br />
substained antibody response against NNK we developed a functionalized derivative that<br />
closely mimicked its structural features in particular the pyridyloxobutyl moiety, the<br />
adjacent ketone and the N-nitrosamino-group. This hapten was conjugated via a linker<br />
to the highly immunogenic diphteria toxoid licensed as a vaccine in humans to induce<br />
polyclonal and monoclonal antibodies.<br />
Both monoclonal and polyclonal antibodies reacted strongly with NNK and NNAL and to<br />
a lesser extend with some of the metabolites of NNK. Interestingly, the mAbs did not<br />
react with the metabolites of the detoxification pathways such as NNK-N-Oxide and<br />
NNAL-N-Oxide. Therefore such antibodies detect NNK and NNAL and may have the<br />
potential to modulate their redistribution in vivo, perhaps reducing some detrimental<br />
effects of smoking.
Carsten Alt, Travis Harrison, Akihiro Matsukawa, Charles Litterst, Jon Mirsalis, Annalisa<br />
D'Andrea<br />
Vaginal cytokine production as a biomarker for the safety<br />
evaluation of microbicide-induced vaginal irritation<br />
Vaginal microbicides may help to reduce the risk of infection with HIV or other sexually<br />
transmitted diseases. For safety evaluation of novel vaginal microbicides, vaginal<br />
irritation is generally assessed in rabbits by histopathologic analysis of the gastrouterine<br />
organs after 10 days of treatment. This evaluation requires the sacrifice of the animals.<br />
Minimally invasive approaches to measure the vaginal irritation caused by novel<br />
microbicides would offer a more desirable alternative.<br />
We measured the vaginal irritation caused by the spermicides benzalkonium chloride<br />
(BZK) and nonoxynol-9 (N-9). We assessed not only the histopathological changes, but<br />
also: (a) the cytokine amounts in vaginal tissue lysates and in cotton swab samples<br />
collected from the vaginal surface, and (b) the inflammatory cells in cytobrush samples<br />
collected from the vaginal surface.<br />
After 6 days of treatment with N-9, a significant increase in histopathological changes<br />
was observed. This effect was transient, being no longer detectable after 10 days of<br />
treatment with N-9. Simultaneously processed vaginal tissues contained significantly<br />
increased amounts of IL-8 and IL-1β, but only after 10 days of treatment with BZK.<br />
Swab samples from the vaginal surface contained significantly elevated levels of MCP-1,<br />
IL-8, and IL-1β, in some cases as early as 3 days after treatment began. Increased<br />
numbers of inflammatory cells were detectable, possibly attracted by increased<br />
amounts of the inflammatory chemokines MCP-1 and IL-8 on the vaginal surface.<br />
These results suggest that measurement of IL-8, IL-1β, MCP-1, and inflammatory cells<br />
on the vaginal surface may offer a noninvasive method to assist in developing novel<br />
vaginal microbicides.
Beatrice Bolinger, Philippe Krebs, Engeler Daniel, Ying Hua Tian, Elke Scandella,<br />
Simone Miller, Nicola P. Restifo, Pierre-Alain Clavien, Burkhard Ludewig<br />
Vascular endothelial cells presenting minor histocompatibility<br />
antigen do neither activate nor tolerize CD8+ T cells<br />
Endothelial cells (EC) are located at a unique position between circulating lymphocytes<br />
and peripheral tissues and thereby participate in the recruitment of T lymphocytes from<br />
the bloodstream to the sites of infection and inflammation. After transplantation of<br />
vascularized allogeneic tissues, allopresentation by EC may contribute to allograft<br />
rejection. However, the interaction between T cells and EC presenting a minor<br />
histocompatibility antigen is still not fully understood. Using a transgenic mouse model<br />
with β-galactosidase (βgal) expression confined to the vascular endothelium (Tie2-LacZ<br />
mice) and mice with CD8+ T cells expressing a βgal-specific T cell receptor (Bg1 mice),<br />
the role of EC during cognate interaction with CD8+ T cells was assessed in vivo.<br />
Adoptive transfer of TCR transgenic Bg1 cells into naïve Tie2-LacZ recipients lead to<br />
activation and proliferation of Bg1 CD8+ T cells. Generation of bone marrow chimeric<br />
mice using mice which exhibit a mutated H2-Kb-molecule (bm1 mice) and impaired<br />
presentation of Kb-restricted peptides, revealed that activation of βgal-specific CD8+ T<br />
cells in Tie2-LacZ mice is mediated by bone marrow derived cells. In vivo depletion of<br />
dendritic cells (DC) revealed that activation of CD8+ T cells in this setting depended<br />
exclusively on cross-presentation by DC. Likewise, tolerization of TCR tg Bg1 cells was<br />
not dependent on Ag presentation by vascular EC. The finding that the βgal antigen<br />
expressed by vascular EC remains immunologically ignored by CTL in Tie2-LacZ mice<br />
could be reproduced using heterotopic heart and orthotopic liver transplantation of Tie2-<br />
LacZ organs into naïve C57BL/6 mice.Taken together, our results suggest that<br />
presentation of a minor histocompatibility antigen by vascular EC leads neither to<br />
activation nor to proliferation of specific CD8+ T cells.
Michaela Kern, Kai Scholz, Ulrich Kalinke, Joachim Schultze, Ulrich Koszinowski,<br />
Gunther Hartmann, Percy A. Knolle<br />
Viral infection but not pattern recognition induces functional<br />
maturation of tolerogenic liver endothelial cells leading to<br />
induction of effector CD8 T cells<br />
Liver sinusoidal endothelial cells (LSEC) contribute to the tolerogenic function of the<br />
liver by mediating CD4 and CD8 T cell tolerance towards soluble antigens. Here, we<br />
address the question whether tolerogenic LSEC also have sentinel function and are<br />
susceptible to functional maturation similar to dendritic cells that gain immunogenic<br />
properties upon appropriate maturation stimuli. LSEC constitutively expressed Toll like<br />
receptors 2, 3, 4, 7, 9 and were stimulated by ligands to membrane-bound TLRs as well<br />
as cytoplasmic helicases. Neither TLR nor helicase-mediated stimulation, however,<br />
changed the tolerogenic LSEC function revealing a fundamental difference to dendritic<br />
cells that undergo functional maturation upon similar stimuli. LSEC were susceptible to<br />
infection with murine cytomegalovirus (MCMV), but controlled viral immune escape and<br />
replication through early type I IFN expression. Importantly, infection of LSEC with<br />
recombinant MCMV-OVA prevented induction of CD8 T cell tolerance and led to<br />
generation of OVA-specific effector CD8 T cells. Virus-induced functional maturation of<br />
LSEC occurred in a cell-autonomous fashion, i.e. the tolerogenic phenotype of<br />
uninfected LSEC was not altered in coculture with infected LSEC. No single mechanism<br />
was identified that caused functional maturation. However, expression profiling of virusinfected<br />
vs TLR-stimulated LSEC revealed a complex gene expression signature. Our<br />
study demonstrates that ligation of PRR in itself is not sufficient to achieve functional<br />
maturation in organ resident APC. Unraveling the mechanisms responsible for such<br />
maturation will be important for our understanding of local immune regulation.
Dennis Lindau, Dagmar Sigurdardottir, Evelyna Derhovanessian, Thomas Leyhe,<br />
Graham Pawelec, Stefan Stevanovic, Lars Stoltze<br />
Visualizing Abeta-specific cytotoxic T cells with HLA tetramers<br />
Brains of individuals with Alzheimer´s disease (AD) are characterized by the formation<br />
of neurofibrillary tangels in neurons, the accumulation of amyloid-beta (Abeta) into<br />
senile plaques and a prominent activation of local inflammation. Because genetic<br />
approaches point to Abeta as a major pathologic mediator in AD, reducing its levels in<br />
the brain is seen as a promising disease-modifying therapy. However, a clinical trial of<br />
Abeta immunization in AD patients led to meningoencephalitis in 6 % of treated<br />
individuals and was discontinued. These side effects were most likely induced by CNSinfiltrating<br />
lymphocytes. In contrast new therapeutic interventions showed a decrease in<br />
the amyloid plaque burden of an AD mouse model after immunization with glatiramer<br />
acetate, which most likely is T cell mediated. To this end we have identified three<br />
different Abeta-derived epitopes recognized by human cytotoxic T cells (CTL) in the<br />
context of HLA-A*0201. In vitro expanded Abeta-specific CTLs are functional in terms of<br />
cytoxicity, showing high specifity without cross-reactivity and normal peptide avidity.<br />
Combining cell surface phenotyping by HLA tetramers with functional assays, we have<br />
obtained a detailed picture of Abeta-specific CTLs in healthy young and elderly donors<br />
as well as AD patients. The frequent detection in peripheral blood especially in the<br />
elderly groups of this auto-antigen-specific lymphocyte population will be discussed in<br />
relation to disease course and possible clinical use.
Patricia Bach, Elisabeth Kamphuis, Bernhard Odermatt, Gerd Sutter, Christian J.<br />
Buchholz, Ulrich Kalinke<br />
VSV-G Displaying Retrovirus-Like Particles Induce a Type I<br />
IFN Receptor Dependent Switch to Neutralizing IgG Antibodies<br />
Vesicular stomatitis virus (VSV) infection rapidly induces IFN-α/β that confers initial<br />
survival, whereas long-term protection is mediated by neutralizing IgG responses. Since<br />
co-administration of IFN-α/β can enhance antibody responses against soluble antigens,<br />
we addressed whether virus-induced IFN-α/β also had an impact on the induction of<br />
neutralizing antibody responses. To this end, we generated apathogenic retrovirus-like<br />
particles (VLP) displaying the VSV glycoprotein (VLP-VSV). Reminiscent of live VSV, VLP-<br />
VSV induced VSV neutralizing IgM responses that switched to IgG in a T help-dependent<br />
manner. In type I IFN receptor deficient (IFNAR-/-) mice, VLP-VSV injection elicited<br />
neutralizing IgM, whereas the IgG switch was absent. The lack of subclass switch was<br />
associated with a reduced germinal center reaction. Conditional knockout mice with a<br />
lymphocyte-specific IFNAR ablation showed normal antibody responses against VLP-<br />
VSV, as well as against live VSV. Thus, IFNAR triggering critically promoted the T helpdependent<br />
subclass switch of virus neutralizing antibody responses against VLP-VSV.<br />
Interestingly, in the context of VLP-VSV as well as VSV immunization, IFNAR triggering<br />
of B lymphocytes did not play a critical role.
Jessica Nickel, Birgit Löer, Reinhard Bauer, Roland Bornheim, Elisabeth Kremmer,<br />
Michael Hoch, Waldemar Kolanus<br />
Wech, a novel intracellular regulator of integrin-dependent<br />
cell adhesion<br />
Wech is a member of the RBCC/TRIM family of cytoplasmic multidomain proteins, which<br />
bears conserved protein motifs such as a BBox zinc-finger domain, a coiled coil domain<br />
and a carboxyterminal NHL domain. It was very recently linked to integrin-mediated<br />
adhesion regulation in Drosophila. Embryos deficient for wech have very similar<br />
phenotypes to integrin and talin null embryos, including muscle detachment from the<br />
body wall. It has been shown that wech is essential for the link between integrins and<br />
the cytoskeleton in the Drosophila epidermal muscle attachment site, by connecting ILK<br />
and talin to the integrin. Single copy genes of wech orthologs (also named LIN41) are<br />
found in mice and humans. We generated an antibody against human and murine wech<br />
and found that the murine wech protein is expressed in z-discs of adult muscles, where<br />
wech colocalizes with ILK and talin. We also detected a partial colocalization with β1integrins.<br />
SiRNA mediated knockdown of wech in the human keratinocyte line HaCat<br />
and in Hela cells results in a strong loss of productive anchorage and subsequent<br />
detachment of the cells. This indicates that wech is a positive regulator of cell adhesion<br />
in these cells. As already shown for ILK and talin, wech is essential for directional<br />
migration, as shown by wound healing experiments. We went on to analyze wech<br />
functions in immune cells and surprisingly found that wech is a negative regulator of cell<br />
adhesion in Jurkat E6 cells. SiRNA-mediated knock-down of wech resulted in a marked<br />
increase of Jurkat adhesion to ICAM-1. These results suggest a differential function of<br />
the wech protein in regulating β1- or β2-integrins. Together, our studies provide<br />
evidence that wech is a novel regulator of integrin-dependent cell adhesion in multiple<br />
cell types.
Hamid Kashkar, Jens Michael Seeger, Andreas Hombach, Anke Deggerich, Benjamin<br />
Yazdanpanah, Olaf Utermöhlen, Gerd Heimlich, Hinrich Abken, Martin Krönke<br />
XIAP targeting sensitizes Hodgkin Lymphoma cells for<br />
cytolytic T cell attack<br />
The immunosurveillance of Hodgkin's Lymphoma (HL) by cytotoxic T lymphocytes (CTL)<br />
is insufficient and the clinical experience with adoptive transfer of CTLs is limited. We<br />
have previously reported that defects in mitochondrial apoptotic pathways and elevated<br />
XIAP-expression confer resistance to different apoptotic stimuli in HL cells. Here we<br />
aimed to develop molecular strategies to overcome the resistance of HL cells against<br />
CTL-mediated killing via granzyme B (grzB). In HL cells grzB-induced mitochondrial<br />
release of pro-apoptotic Smac is blocked, which results in <strong>complete</strong> abrogation of<br />
cytotoxicity mediated by CTLs. Cytosolic expression of recombinant mature Smac<br />
enhanced caspase activity induced by grzB and restored the apoptotic response of HL<br />
cells. Similarly, down-regulation of XIAP by RNA interference markedly enhanced the<br />
susceptibility of HL cells for CTL-mediated cytotoxicity. XIAP gene knock-down<br />
sensitized HL cells for killing by antigen-specific CTLs redirected by grafting with a<br />
chimeric anti-CD30scFv-CD3zeta immunoreceptor. The results suggest that XIAP<br />
targeting by Smac agonists or XIAP-siRNA can be used as a synergistic strategy for<br />
cellular immunotherapy of Hodgkin´s lymphoma.
Isabel Koch, Reinhard Hoffmann<br />
Yersinia virulence protein YopP inhibits NK cell cytokine<br />
production by blocking host cell IL-12 signaling.<br />
Yersinia enterocolitica causes acute gastrointestinal disease and evades the host´s<br />
immune response by injecting, via a type III protein secretion system, anti host effector<br />
proteins into the host cell’s cytoplasm. These effector proteins (Yersinia outer proteins,<br />
Yops) interfere with host cell signal transduction; in particular, YopP inhibits NFκB and<br />
MAPK pathways.<br />
NK cells are an important early source of IFN-γ before the onset of adaptive immunity.<br />
To evaluate whether Y. enterocolitica could directly modulate NK cell function, we<br />
isolated 2B4 positive NK cells from spleens of C57BL/6 mice, infected them with highly<br />
virulent Y. enterocolitica in vitro, and evaluated NK cell IFN-γ production. Infection with<br />
wild-type Y. enterocolitica (translocating all six Yop effector proteins) markedly reduced<br />
IFN-γ production induced by IL-12, IL-12+IL-18, and agonistic α-NKG2D antibody in<br />
both naïve and IL-2 stimulatied NK cells. Evaluation of mutant Yersinia strains identified<br />
YopP as an important mediator of NK cell disarmament: YopP not only inhibited<br />
phosphorylation of p38 in response to stimulation with IL-12+IL-18, but also in<br />
response to IL-12 alone. Strikingly, YopP, which has not previously been shown to<br />
interfere with JAK-STAT signal transduction, inhibits tyrosine phosphorylation of STAT-4<br />
in response to IL-12 or IL-12+IL-18 stimulation.<br />
To demonstrate the relevance of these results in vivo, we isolated NK cells from mice<br />
infected with wild-type or YopP deficient Y. enterocolitica. We could show that NK cells<br />
from wild-type infected mice produce lower amounts of IFN-γ protein after restimulation<br />
with IL-12+IL-18. To the best of our knowledge, this is the first report of a<br />
bacterial pathogen directly targeting NK cells for the suppression of an effective immune<br />
response.
Hajo Haase, Lothar Rink<br />
Zinc ions act as a signal in leukocyte activation<br />
Cytosolic alterations of calcium ion concentrations are an integral part of intracellular<br />
signal transduction. Similar functions have been hypothesized for other metal ions, in<br />
particular zinc ions (Zn2+), but this still awaits experimental verification. Zn2+ is<br />
important for a range of cellular functions, especially in the immune system. Among<br />
other modulatory effects, it influences the formation and secretion of pro-inflammatory<br />
cytokines, including tumor necrosis factor (TNF)-alpha. However, it remains to be<br />
shown that these effects are due to a physiological intracellular signaling system<br />
involving Zn2+, rather than being coincidental. Here we demonstrate that an increase<br />
of intracellular zinc ion concentration occurs upon stimulation of human leukocytes, and<br />
that this increase is required for signal transduction. Treatment of whole blood with<br />
Escherichia coli, lipopolysaccharide, or Pam3CSK4, which trigger so-called pattern<br />
recognition receptors, led to an increase in intracellular Zn2+, predominantly in<br />
monocytes. Chelation of Zn2+ with the membrane permeable zinc-specific chelator<br />
TPEN (N,N,N’,N’-tetrakis-(2-pyridyl-methyl)ethylenediamine) <strong>complete</strong>ly blocked the<br />
increase and the E. coli-induced activation of p38 MAPK and Erk1/2, and abrogated the<br />
release of TNF-alpha, demonstrating that intracellular labile Zn2+ involved in signaling.<br />
This function of Zn2+ might not be limited to the immune system and pattern<br />
recognition receptors, but might be a generalized second signaling system based on<br />
intracellular fluctuations of metal ion concentrations, acting parallel to Ca2+.
Laura Kahmann, Sabine Warmuth, Birgit Plümäkers, Axel M. Gressner, Marco Malavolta,<br />
Eugenio Mocchegiani, Lothar Rink, Peter Uciechowski<br />
Zinc supplementation in the elderly reduces spontaneous<br />
inflammatory cytokine release and restores T cell functions<br />
Advanced aging is accompanied by low grade inflammatory activity that includes<br />
increased levels of pro-inflammatory cytokines. On the other hand, aging is also<br />
associated with mild zinc deficiency. Both conditions contribute to decreased immune<br />
functions resulting in increased susceptibility to autoimmune diseases, infections and<br />
malignancies. The aim of this study was to give more insight into what extent low grade<br />
inflammation is caused by zinc deficient status. Here we report the effect of improved<br />
intracellular zinc status on low grade inflammatory activity in 19 healthy elderly<br />
subjects. Our experiments show that adjustment of labile zinc by moderate zinc<br />
supplementation reduces spontaneous cytokine release such as IL-6 and defects in<br />
termination of inflammatory activity. Zinc supplementation results in reduced amounts<br />
of unspecific pre-activated T cells and leads to improved T cell response upon mitogenic<br />
stimulation shown by significantly increased IFN-γ, TNF-α and IL-10 release. Therefore,<br />
besides other anti-inflammatory drugs, zinc does not suppress, but improves immune<br />
reaction upon pathogen invasion. These results suggest that mild zinc deficient healthy<br />
elderly subjects might benefit from moderate zinc supplementation due to improved<br />
immune responses leading to reduced incidences of infections and autoimmune diseases.