World Journal of Diabetes (World J Diabetes
World Journal of Diabetes (World J Diabetes
World Journal of Diabetes (World J Diabetes
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>World</strong> <strong>Journal</strong> <strong>of</strong><br />
<strong>Diabetes</strong><br />
<strong>World</strong> J <strong>Diabetes</strong> 2011 January 15; 2(1): 1-18<br />
P/D1 cells <strong>of</strong> fundus <strong>of</strong> the stomach Epsilon cells <strong>of</strong> the pancreas Hypothalamic arcuate nucleus<br />
Vagal afferent endings<br />
Ghrelin<br />
Leukocytes, Macrophages,<br />
T and B cells Cardiovascular system Respiratory system CNS<br />
↓ Immune response<br />
↓ TNF, IL-6, HMGB1<br />
↓ Inflammation and sepsis<br />
Akt/eNOS<br />
↓ Ischemia/reperfusion<br />
injury Atherosclerosis<br />
www.wjgnet.com<br />
↓ Immune response<br />
↓ TNF, IL-6, HMGB1<br />
↓ Sepsis-induced lung injury<br />
ISSN 1948-9358 (online)<br />
GH, Corticosteroids,<br />
dopamine, insulin,<br />
leptin, etc .<br />
↑ Appetite<br />
↓ Depression<br />
↑Learning<br />
and memory
Contents<br />
EDITORIAL<br />
ORIGINAL ARTICLES<br />
DREAM 2020<br />
1 Relationship between gut and sepsis: Role <strong>of</strong> ghrelin<br />
Das UN<br />
8 Excessive 5-year weight gain predicts metabolic syndrome development in<br />
healthy middle-aged adults<br />
Lin YC, Chen JD, Chen PC<br />
16 Continuous positive airway pressure to improve insulin resistance and glucose<br />
homeostasis in sleep apnea<br />
Steiropoulos P, Papanas N<br />
WJD|www.wjgnet.com I<br />
Monthly Volume 2 Number 1 January 15, 2011<br />
January 15, 2011|Volume 2|Issue 1|
Contents<br />
ACKNOWLEDGMENTS<br />
APPENDIX<br />
ABOUT COVER<br />
AIM AND SCOPE<br />
FLYLEAF<br />
EDITORS FOR<br />
THIS ISSUE<br />
NAME OF JOURNAL<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> <strong>Diabetes</strong><br />
LAUNCH DATE<br />
March 15, 2010<br />
SPONSOR<br />
Beijing Baishideng BioMed Scientific Co., Ltd.,<br />
Room 903, Building D, Ocean International Center,<br />
No. 62 Dongsihuan Zhonglu, Chaoyang District,<br />
Beijing 100025, China<br />
Telephone: 0086-10-8538-1892<br />
Fax: 0086-10-8538-1893<br />
E-mail: baishideng@wjgnet.com<br />
http://www.wjgnet.com<br />
EDITING<br />
Editorial Board <strong>of</strong> <strong>World</strong> <strong>Journal</strong> <strong>of</strong> <strong>Diabetes</strong>,<br />
Room 903, Building D, Ocean International Center,<br />
No. 62 Dongsihuan Zhonglu, Chaoyang District,<br />
Beijing 100025, China<br />
Telephone: 0086-10-5908-0038<br />
Fax: 0086-10-8538-1893<br />
E-mail: wjd@wjgnet.com<br />
http://www.wjgnet.com<br />
PUBLISHING<br />
Baishideng Publishing Group Co., Limited,<br />
Room 1701, 17/F, Henan Building,<br />
No.90 Jaffe Road, Wanchai,<br />
Hong Kong, China<br />
Fax: 00852-3115-8812<br />
Telephone: 00852-5804-2046<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> <strong>Diabetes</strong><br />
Volume 2 Number 1 January 15, 2011<br />
I Acknowledgments to reviewers <strong>of</strong> <strong>World</strong> <strong>Journal</strong> <strong>of</strong> <strong>Diabetes</strong><br />
I Meetings<br />
I-V Instructions to authors<br />
Das UN. Relationship between gut and sepsis: Role <strong>of</strong> ghrelin<br />
<strong>World</strong> J <strong>Diabetes</strong> 2011; 2(1): 1-8<br />
http://www.wjnet.com/1948-9358/full/v2/i1/1.htm<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> <strong>Diabetes</strong> (<strong>World</strong> J <strong>Diabetes</strong>, WJD, online ISSN 1948-9358, DOI: 10.4239),<br />
is a monthly, open-access, peer-reviewed journal supported by an editorial board <strong>of</strong> 323<br />
experts in diabetes mellitus research from 38 countries.<br />
The major task <strong>of</strong> WJD is to report rapidly the most recent results in basic and<br />
clinical research on diabetes including: metabolic syndrome, functions <strong>of</strong> α, β, δ and<br />
PP cells <strong>of</strong> the pancreatic islets, effect <strong>of</strong> insulin and insulin resistance, pancreatic islet<br />
transplantation, adipose cells and obesity, clinical trials, clinical diagnosis and treatment,<br />
rehabilitation, nursing and prevention. This covers epidemiology, etiology, immunology,<br />
pathology, genetics, genomics, proteomics, pharmacology, pharmacokinetics, pharmacogenetics,<br />
diagnosis and therapeutics. Reports on new techniques for treating diabetes<br />
are also welcome.<br />
I-III Editorial Board<br />
Responsible Assistant Editor: Na Liu Responsible Science Editor: Hai-Ning Zhang<br />
Responsible Electronic Editor: Na Liu Pro<strong>of</strong>ing Editorial Office Director: Hai-Ning Zhang<br />
Pro<strong>of</strong>ing Editor-in-Chief: Lian-Sheng Ma<br />
E-mail: baishideng@wjgnet.com<br />
http://www.wjgnet.com<br />
SUBSCRIPTION<br />
Beijing Baishideng BioMed Scientific Co., Ltd.,<br />
Room 903, Building D, Ocean International Center,<br />
No. 62 Dongsihuan Zhonglu, Chaoyang District,<br />
Beijing 100025, China<br />
Telephone: 0086-10-8538-1892<br />
Fax: 0086-10-8538-1893<br />
E-mail: baishideng@wjgnet.com<br />
http://www.wjgnet.com<br />
ONLINE SUBSCRIPTION<br />
One-Year Price 216.00 USD<br />
PUBLICATION DATE<br />
January 15, 2011<br />
CSSN<br />
ISSN 1948-9358 (online)<br />
PRESIDENT AND EDITOR-IN-CHIEF<br />
Lian-Sheng Ma, Beijing<br />
STRATEGY ASSOCIATE EDITORS-IN-CHIEF<br />
Undurti Narasimha Das, Ohio<br />
Min Du, Wyoming<br />
Gregory I Liou, Georgia<br />
Zhong-Cheng Luo, Quebec<br />
Demosthenes B Panagiotakos, Athens<br />
WJD|www.wjgnet.com II<br />
EDITORIAL OFFICE<br />
Hai-Ning Zhang, Director<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> <strong>Diabetes</strong><br />
Room 903, Building D, Ocean International Center,<br />
No. 62 Dongsihuan Zhonglu, Chaoyang District,<br />
Beijing 100025, China<br />
Telephone: 0086-10-5908-0038<br />
Fax: 0086-10-8538-1893<br />
E-mail: wjd@wjgnet.com<br />
http://www.wjgnet.com<br />
COPYRIGHT<br />
© 2011 Baishideng. All rights reserved; no part <strong>of</strong> this<br />
publication may be commercially reproduced, stored<br />
in a retrieval system, or transmitted in any form or<br />
by any means, electronic, mechanical, photocopying,<br />
recording, or otherwise without the prior permission<br />
<strong>of</strong> Baishideng. Authors are required to grant <strong>World</strong><br />
<strong>Journal</strong> <strong>of</strong> <strong>Diabetes</strong> an exclusive license to publish.<br />
SPECIAL STATEMENT<br />
All articles published in this journal represent the<br />
viewpoints <strong>of</strong> the authors except where indicated<br />
otherwise.<br />
INSTRUCTIONS TO AUTHORS<br />
Full instructions are available online at http://www.<br />
wjgnet.com/1948-9358/g_info_20100107165233.<br />
htm. If you do not have web access please contact<br />
the editorial <strong>of</strong>fice.<br />
ONLINE SUBMISSION<br />
http://www.wjgnet.com/1948-9358<strong>of</strong>fice<br />
January 15, 2011|Volume 2|Issue 1|
Online Submissions: http://www.wjgnet.com/1948-9358<strong>of</strong>fice<br />
wjd@wjgnet.com<br />
doi:10.4239/wjd.v2.i1.1<br />
Relationship between gut and sepsis: Role <strong>of</strong> ghrelin<br />
Undurti N Das<br />
Undurti N Das, Jawaharlal Nehru Technological University, Kakinada<br />
533003, India<br />
Undurti N Das, UND Life Sciences, Shaker Heights, OH 44120,<br />
United States<br />
Author contribution: Das UN contributed solely to this paper.<br />
Correspondence to: Undurti N Das, MD, FAMS, Jawaharlal<br />
Nehru Technological University, Kakinada 533003,<br />
India. Undurti@hotmail.com<br />
Telephone: +912162315548 Fax: +919288330316<br />
Received: September 19, 2010 Revised: December 22, 2010<br />
Accepted: December 29, 2010<br />
Published online: January 15, 2011<br />
Abstract<br />
Ghrelin is a growth hormone secretagogue produced<br />
by the gut, and is expressed in the hypothalamus<br />
and other tissues as well. Ghrelin not only plays an<br />
important role in the regulation <strong>of</strong> appetite, energy balance<br />
and glucose homeostasis, but also shows antibacterial<br />
activity, suppresses proinflammatory cytokine<br />
production and restores gut barrier function. In<br />
experimental animals, ghrelin has shown significant<br />
beneficial actions in preventing mortality from sepsis.<br />
In the critically ill, corticosteroid insufficiency as a result<br />
<strong>of</strong> dysfunction <strong>of</strong> the hypothalamicpituitaryadrenal<br />
axis is known to occur. It is therefore possible that both<br />
gut and hypothalamus play an important role in the<br />
pathogenesis <strong>of</strong> sepsis by virtue <strong>of</strong> their ability to produce<br />
ghrelin, which, in turn, could be a protective phenomenon<br />
to suppress inflammation. It remains to be<br />
seen whether ghrelin and its analogues are <strong>of</strong> benefit in<br />
treating patients with sepsis.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: Ghrelin; Sepsis; Cytokines; Inflammation;<br />
Critically ill; Insulin<br />
Peer reviewers: Vladimir N Uversky, Senior Research Pr<strong>of</strong>essor,<br />
Center for Computational Biology & Bioinformatics,<br />
Department <strong>of</strong> Biochemistry and Molecular Biology, Indiana<br />
University School <strong>of</strong> Medicine, Indianapolis, IN 46202, United<br />
States; Joseph Fomusi Ndisang, PharmD, PhD, Assistant Pro<br />
WJD|www.wjgnet.com<br />
<strong>World</strong> J <strong>Diabetes</strong> 2011 January 15; 2(1): 1-7<br />
ISSN 1948-9358 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
EDITORIAL<br />
fessor, College <strong>of</strong> Medicine, Epartment <strong>of</strong> Physiology, University<br />
<strong>of</strong> Saskatchewan, 107 Wiggins Road, Saskatoon, SK, Canada<br />
Das UN. Relationship between gut and sepsis: Role <strong>of</strong> ghrelin.<br />
<strong>World</strong> J <strong>Diabetes</strong> 2011; 2(1): 17 Available from: URL: http://<br />
www.wjgnet.com/19489358/full/v2/i1/1.htm DOI: http://dx.doi.<br />
org/10.4239/wjd.v2.i1.1<br />
INTRODUCTION<br />
Ghrelin, a peptide hormone that serves as the endogenous<br />
ligand <strong>of</strong> the growth hormone secretagogue receptor,<br />
is secreted mainly by P/D1 cells lining the fundus <strong>of</strong><br />
the human stomach, and the epsilon cells <strong>of</strong> the pancreas<br />
that stimulate hunger [1] . Ghrelin is also secreted from the<br />
small intestine and the colon. It is expressed in the hypothalamus,<br />
pituitary, and several peripheral tissues suggesting<br />
that it could have diverse physiological functions [25] .<br />
Ghrelin regulates growth hormone secretion, and plays an<br />
important role in the regulation <strong>of</strong> appetite, energy balance<br />
and glucose homeostasis. It regulates gastrointestinal,<br />
cardiovascular, and immune functions, and bone physiology<br />
[612] . Ghrelin levels increase before meals, decrease<br />
after meals, and serve as the counterpart <strong>of</strong> leptin, which<br />
induces satiation when present at higher levels. Bariatric<br />
procedures lead to a reduction in the amount <strong>of</strong> ghrelin<br />
produced, which causes the satiation that could explain<br />
the weight loss occurring after gastric bypass surgery.<br />
Receptors for ghrelin are expressed by the neurons in the<br />
arcuate nucleus and the ventromedial hypothalamus [13] that<br />
have a regulatory role in insulin secretion and participate<br />
in the pathophysiology <strong>of</strong> type 2 diabetes mellitus, thus<br />
implying that ghrelin has a role in insulin resistance. The<br />
ghrelin receptor is a G proteincoupled receptor. Ghrelin<br />
is essential for cognitive adaptation to changing environments<br />
and the process <strong>of</strong> learning [14] , and activates endothelial<br />
nitric oxide synthase (eNOS) [15,16] . Obestatin, which<br />
is derived from the same gene as ghrelin, has opposite ac<br />
tions to that <strong>of</strong> ghrelin on energy homeostasis and gastroin<br />
testinal function, thus adding complexity to the role <strong>of</strong> ghre<br />
lin in various physiological and pathological situations [17] .<br />
1 January 15, 2011|Volume 2|Issue 1|
positive result <strong>of</strong> intensive insulin therapy on the critically<br />
ill could be attributed to the prevention <strong>of</strong> sepsis, multiple<br />
organ failure and need for prolonged invasive organ<br />
support and intensive care. These results suggest that reduced<br />
stimulation <strong>of</strong> pituitary function seen in prolonged<br />
critically ill patients needs to be corrected to reverse the<br />
paradoxical ‘wasting syndrome’, and that maintenance <strong>of</strong><br />
strict normoglycemia with insulin is important to increase<br />
the chances <strong>of</strong> survival <strong>of</strong> these patients. It is now believed<br />
that, from an endocrinological point <strong>of</strong> view, the<br />
acute phase and the later phase <strong>of</strong> critical illness manifest<br />
themselves differently. When the disease process becomes<br />
prolonged, there is a uniformlyreduced pulsatile secretion<br />
<strong>of</strong> anterior pituitary hormones, with proportionally<br />
reduced concentrations <strong>of</strong> peripheral anabolic hormones.<br />
During critical illness, prolonged activation <strong>of</strong> the HPA<br />
axis can result in hypercortisolemia and hypocortisolemia;<br />
both can be detrimental to recovery from critical illness.<br />
Recognition <strong>of</strong> adrenal dysfunction in critically ill patients<br />
is difficult because a reliable history is not available, and<br />
laboratory results are difficult to interpret [43,44] . For instance,<br />
the acute phase <strong>of</strong> critical illness is characterized<br />
by an actively secreting pituitary, but the concentrations <strong>of</strong><br />
most peripheral effector hormones are low, partly due to<br />
the development <strong>of</strong> targetorgan resistance. In contrast,<br />
in prolonged critical illness, predominantly hypothalamic<br />
suppression <strong>of</strong> the (neuro)endocrine axes occurs, leading<br />
to the low serum levels <strong>of</strong> the respective targetorgan hormones.<br />
The adaptations in the acute phase are considered<br />
to be beneficial for shortterm survival. In the chronic<br />
phase, however, the observed (neuro)endocrine alterations<br />
contribute to the general wasting syndrome. With<br />
the exception <strong>of</strong> intensive insulin therapy, and perhaps<br />
hydrocortisone administration for a subgroup <strong>of</strong> patients,<br />
no hormonal intervention has proven to affect outcome<br />
beneficially [45] . In this context, the recently described beneficial<br />
actions <strong>of</strong> ghrelin in the critically ill may have important<br />
clinical implications.<br />
GHRELIN IN SEPSIS<br />
Experimental studies<br />
In the rat model <strong>of</strong> septic shock which was made by<br />
caecal ligation and perforation, infusion <strong>of</strong> ghrelin 10<br />
nmol/kg at the time <strong>of</strong> operation through the femoral<br />
vein, followed by a sc (subcutaneous) injection at 8 h after<br />
operation, revealed that, compared to that <strong>of</strong> the septic<br />
shock group, mean arterial blood pressure (MABP) <strong>of</strong> rats<br />
in the ghrelintreated group increased by 33 % (P < 0.01);<br />
the values <strong>of</strong> +LVdp/dtmax and LVdp/dtmax increased<br />
by 27 % and 33 %, respectively (P < 0.01), but LVEDP<br />
decreased by 33 % (P < 0.01). The plasma glucose concentration<br />
and myocardial ATP content increased by<br />
53% and 22 %, respectively, whereas plasma lactate concentration<br />
decreased by 40% in the ghrelintreated rats (P<br />
< 0.01). The plasma ghrelin level in rats with septic shock<br />
was 51% higher than that <strong>of</strong> rats in the sham group,<br />
and was negatively correlated with MABP and blood<br />
glucose concentration (r = 0.721 and 0.811, respectively,<br />
P < 0.01). The mortality rates were 47% (9/19) in rats<br />
WJD|www.wjgnet.com<br />
Das UN. Ghrelin and sepsis<br />
with septic shock and 25% (3/12) in rats <strong>of</strong> the ghrelintreated<br />
group, respectively, suggesting that treatment with<br />
ghrelin could at least partially correct the abnormalities <strong>of</strong><br />
hemodynamics and metabolic disturbance in septic shock<br />
<strong>of</strong> rats [46] .<br />
In an extension <strong>of</strong> these studies, it was noted that<br />
even endotoxininduced shock and mortality could be<br />
significantly decreased by ghrelin treatment in rats [47] .<br />
Early and late (12 h after lipopolysaccharide injection)<br />
treatment with ghrelin markedly increased the plasma<br />
glucose concentration, and decreased the plasma lactate<br />
concentration. This action on the part <strong>of</strong> ghrelin in increasing<br />
plasma glucose levels (resulting in hyperglycemia)<br />
may suggest that it could be harmful in the setting <strong>of</strong><br />
sepsis or critical illness, since hyperglycemia is believed to<br />
accentuate inflammation. In the initial stages <strong>of</strong> sepsis,<br />
hyperglycemia (reactive hyperglycemia) as a result <strong>of</strong><br />
the enhanced production <strong>of</strong> hypercortisolemia occurs,<br />
whereas in the later stages, hypoglycemia sets in, partly<br />
due to hypocortisolemia [48,49] . It was reported that during<br />
the early phase <strong>of</strong> sepsis, plasma glucose levels increased,<br />
whereas plasma insulin and glucagon levels remained<br />
unchanged, but corticosterone levels increased 2.5fold<br />
over control values. At later stages <strong>of</strong> sepsis, plasma<br />
glucose levels returned to normal, whereas insulin, glucagon,<br />
and corticosterone levels increased significantly i.e.<br />
40fold, 6.5fold, and 6fold respectively [48,49] . Therefore,<br />
the initial rise and subsequent decline in blood glucose<br />
correlated well with a corticosterone followed by an insulindependent<br />
phenomenon. Thus, blood glucose levels<br />
in sepsis depend to a large extent on the balance between<br />
corticosterone and insulin levels, and the stage <strong>of</strong> sepsis [49] .<br />
Hence, the ability <strong>of</strong> ghrelin to enhance plasma glucose<br />
levels could, especially in the later stages <strong>of</strong> sepsis, prevent<br />
hypoglycemia that is detrimental and ghrelin may therefore<br />
be useful in later stages <strong>of</strong> sepsis. Furthermore, ghrelin<br />
and insulin seem to have both positive and negative feedback<br />
control over each other [5052] , suggesting that ghrelin<br />
may be involved in maintaining glucose homeostasis,<br />
under both normal conditions and sepsis.<br />
Early treatment with ghrelin significantly attenuated<br />
the deficiency in myocardial ATP content, but late treatment<br />
with ghrelin had no effect on myocardial ATP content.<br />
The plasma ghrelin level was significantly increased<br />
in the rats with endotoxin shock, and it increased further<br />
after ghrelin administration. Exposure <strong>of</strong> rat gastric mucosa<br />
in vitro to lipopolysaccharide (1.0 to 100 µg/mL) triggered<br />
the release <strong>of</strong> ghrelin from mucosa tissue in a dose<br />
and timedependent manner [47] . These results suggest that<br />
lipopolysaccharide directly stimulates gastric mucosa to<br />
synthesize and secrete ghrelin, that may result in a decrease<br />
in endotoxininduced target organ damage.<br />
Ghrelin suppresses production <strong>of</strong> pro-inflammatory<br />
cytokines<br />
Ghrelin-inhibited proinflammatory cytokine production,<br />
mononuclear cell binding, and nuclear factorkappaB<br />
activation in human endothelial cells in vitro, and endotoxininduced<br />
cytokine production in vivo, by interacting<br />
with growth hormone secretagogue receptors and thus,<br />
3 January 15, 2011|Volume 2|Issue 1|
Das UN. Ghrelin and sepsis<br />
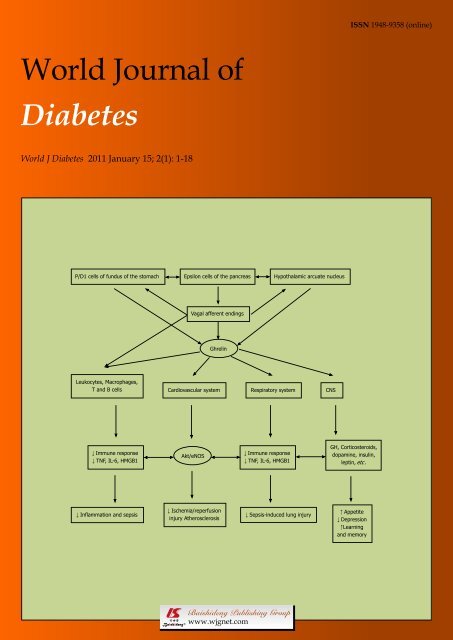
P/D1 cells <strong>of</strong> fundus <strong>of</strong> the stomach Epsilon cells <strong>of</strong> the pancreas Hypothalamic arcuate nucleus<br />
ghrelin behaves as an endogenous anti-inflammatory mo-<br />
lecule [53] . These anti-inflammatory actions <strong>of</strong> ghrelin may<br />
explain why it is able to improve cachexia in heart fai<br />
lure and cancer, and to ameliorate the hemodynamic and<br />
metabolic disturbances in septic shock (Figure 1). By<br />
virtue <strong>of</strong> its anti-inflammatory action, ghrelin could play<br />
a modulatory role in atherosclerosis as well, especially in<br />
obese patients, in whom ghrelin levels are reduced. In a rat<br />
model <strong>of</strong> polymicrobial sepsis induced by cecal ligation<br />
and puncture, though ghrelin levels decreased at early (at<br />
5 h after ligation and puncture) or late sepsis (20 h after<br />
ligation and cecal puncture) its receptor was markedly<br />
elevated in early sepsis. Moreover, ghrelininduced relaxation<br />
in resistance blood vessels <strong>of</strong> the isolated small<br />
intestine increased significantly during early sepsis, but<br />
was not altered in late sepsis. GHSR1a expression in<br />
smooth muscle cells was significantly increased at mRNA<br />
and protein levels with stimulation by LPS at 10 ng/mL,<br />
suggesting that GHSR1a expression is upregulated, and<br />
vascular sensitivity to ghrelin stimulation is increased in<br />
the hyperdynamic phase <strong>of</strong> sepsis [54] as a compensatory<br />
phenomenon to septic process. Furthermore, ghrelin improved<br />
tissue perfusion in severe sepsis by downregulating<br />
endothelin1 involving a NFkappaBdependent pathway<br />
[55] .<br />
These experimental results are supported by the report<br />
that during postoperative intraabdominal sepsis seen in<br />
WJD|www.wjgnet.com<br />
Vagal afferent endings<br />
Ghrelin<br />
Leukocytes, Macrophages,<br />
T and B cells Cardiovascular system Respiratory system CNS<br />
↓ Immune response<br />
↓ TNF, IL6, HMGB1<br />
↓ Inflammation and sepsis<br />
Akt/eNOS<br />
↓ Ischemia/reperfusion<br />
injury Atherosclerosis<br />
↓ Immune response<br />
↓ TNF, IL6, HMGB1<br />
↓ Sepsisinduced lung injury<br />
GH, Corticosteroids,<br />
dopamine, insulin,<br />
leptin, etc .<br />
↑ Appetite<br />
↓ Depression<br />
↑Learning<br />
and memory<br />
Figure 1 Scheme showing various actions <strong>of</strong> ghrelin and their possible clinical importance. Ghrelin seems to be <strong>of</strong> benefit in suppressing inflammation and<br />
sepsis; protects against ischemia/reperfusion-induced myocardial damage; protects lungs from sepsis-induced damage, enhances appetite, relieves depression and<br />
enhances learning and memory. GH: growth hormone; CNS: central nervous system.<br />
patients, both ghrelin and leptin plasma levels were elevated<br />
and positively correlated with both inflammatory cytokines<br />
(TNFα, IL-6) and CRP. However, this hormonal<br />
reaction does not seem to be specific to sepsis since a significant<br />
increase in both ghrelin and leptin was observed<br />
to occur during an uncomplicated postoperative response,<br />
although to a lesser extent than was shown in sepsis [56] .<br />
Ghrelin stimulates vagus nerve<br />
Ghrelin stimulates the vagus nerve. Since plasma levels <strong>of</strong><br />
ghrelin were significantly reduced in sepsis; and ghrelin<br />
administration improved organ perfusion and function, it<br />
was hypothesized that ghrelin decreases pro-inflammatory<br />
cytokines in sepsis by means <strong>of</strong> activation <strong>of</strong> the vagus<br />
nerve. This is so since the vagus mediator, acetylcholine,<br />
has potent antiinflammatory actions and suppresses<br />
TNFα, IL6 and HMGB1 production by stimulating the<br />
alpha7 subunitcontaining nicotinic acetylcholine receptor<br />
(alpha7nAChR) [57,58] . As predicted, experimental studies revealed<br />
that vagotomy prevented ghrelin’s downregulatory<br />
effect on TNFα and IL-6 production, thus confirming<br />
that ghrelin downregulates proinflammatory cytokines<br />
in sepsis through activation <strong>of</strong> the vagus nerve [59] . It was<br />
reported that ghrelin has sympathoinhibitory properties<br />
that are mediated by central ghrelin receptors, involving<br />
a NPY/Y1 receptordependent pathway [60] . Ghrelin also<br />
inhibited the production <strong>of</strong> HMGB1 by activated macro<br />
4 January 15, 2011|Volume 2|Issue 1|
Ghrelin<br />
Gut<br />
Disruption<br />
<strong>of</strong> gut<br />
barrier<br />
function<br />
phages, and also showed antibacterial activity [61] that may<br />
explain its beneficial action in sepsis and other inflammatory<br />
conditions [6264] . It is important to note that ghrelin<br />
ameliorated gut barrier dysfunction [65] , an abnormality that<br />
is seen in patients with sepsis.<br />
CONCLUSION<br />
Absorption<br />
<strong>of</strong><br />
endotoxin<br />
CRH, ACTH,<br />
corticosterone<br />
Melanocortins<br />
It is evident from the preceding discussion that ghrelin<br />
has anti-inflammatory, para-sympathetic stimulatory and<br />
sympathoinhibitory effects that may underlie its beneficial<br />
actions in sepsis and other inflammatory conditions.<br />
In addition, ghrelin seems to be <strong>of</strong> significant benefit<br />
in improving cachexia in heart failure and cancer, and<br />
the ameliorization <strong>of</strong> the hemodynamic and metabolic<br />
disturbances in septic shock (Figure 1). The ability <strong>of</strong><br />
ghrelin to suppress the synthesis and release <strong>of</strong> proinflammatory<br />
cytokines such as TNF-α, IL6 and HMGB1<br />
suggests that it may find its use in the management <strong>of</strong><br />
other inflammatory conditions such as atherosclerosis,<br />
lupus and rheumatoid arthritis, but this remains to be<br />
determined. The fact that ghrelin is capable <strong>of</strong> restoring<br />
gut barrier function and possess antimicrobial action suggests<br />
that it may be useful in the management <strong>of</strong> cirrhosis<br />
<strong>of</strong> the liver where gut barrier function is compromised,<br />
leading to endotoxin absorption into the circulation. Since<br />
failure <strong>of</strong> gut barrier function is also one <strong>of</strong> the initial<br />
abnormalities seen in sepsis, ghrelin is eminently suited<br />
to be employed in its therapy, either by itself, or in combination<br />
with other therapies. These actions <strong>of</strong> ghrelin<br />
WJD|www.wjgnet.com<br />
Infection/Injury/Surgery<br />
Activation <strong>of</strong> neutrophils,<br />
T cells and macrophages<br />
Elimination <strong>of</strong> invading pathogens<br />
Excess TNFα, IL6, MIF,<br />
HMGB1<br />
Excess free radicals,<br />
eicosanoids and nitric oxide<br />
Hypoglycemia, hypotension and<br />
decreased tissue perfusion<br />
Sepsis and septic shock<br />
Stimulation<br />
<strong>of</strong> gut<br />
Ghrelin<br />
Das UN. Ghrelin and sepsis<br />
↑ Vagal nerve<br />
stimulation and<br />
acetylcholine<br />
release<br />
Figure 2 Scheme showing the actions <strong>of</strong> ghrelin that are relevant to its potential benefit in sepsis. CRH: corticotropin-releasing hormone; ACTH:<br />
adrenocorticotropic hormone.<br />
suggest that ghrelin has the potential to be <strong>of</strong> significant<br />
benefit in sepsis and other critically ill patients (Figure<br />
2). Obviously, large scale human studies are need before<br />
ghrelin comes into the clinic in the management <strong>of</strong> sepsis.<br />
Ghrelin has been shown to have the ability to alter<br />
nerve cell connections and synaptic plasticity [66,67] in the<br />
melanocortin system, implying that ghrelin regulates me<br />
tabolic control by a central action. Melanocortins are kno<br />
wn to have anti-inflammatory actions [68,69] suggesting that<br />
modulation <strong>of</strong> the melanocortin system could be yet another<br />
means by which ghrelin could bring about its anti<br />
inflammatory action. It has, in fact, been reported that<br />
ghrelin inhibited POMC neurons [70] , and stimulated the<br />
hypothalamopituitaryadrenal (HPA) axis, resulting in<br />
the release <strong>of</strong> corticotropin-releasing hormone (CRH),<br />
adrenocorticotropic hormone (ACTH), and corticosterone,<br />
suggesting a hypothalamic site <strong>of</strong> action [71] . Thus,<br />
ghrelin could be producing its anti-inflammatory actions<br />
by inducing the release <strong>of</strong> CRH, ACTH and corticosterone.<br />
Ghrelin might also help prevent the stressinduced<br />
depression and anxiety [72,73] that is common in patients<br />
with sepsis and the critically ill. Ghrelin may thus be <strong>of</strong><br />
significant benefit in the management <strong>of</strong> sepsis and the<br />
critically ill, provided that clinical trials confirm the anticipated<br />
benefits.<br />
ACKNOWLEDGMENTS<br />
Dr UN Das was in receipt <strong>of</strong> the Ramalingaswami Fellow-<br />
5 January 15, 2011|Volume 2|Issue 1|
Das UN. Ghrelin and sepsis<br />
ship <strong>of</strong> the Department <strong>of</strong> Biotechnology, India, during<br />
the tenure <strong>of</strong> this study.<br />
REFERENCES<br />
1 Kojima M, Hosoda H, Date Y, Nakazato M, Matsuo H, Kangawa<br />
K. Ghrelin is a growth-hormone-releasing acylated peptide<br />
from stomach. Nature 1999; 402: 656-660<br />
2 Sato T, Fukue Y, Teranishi H, Yoshida Y, Kojima M. Molecular<br />
forms <strong>of</strong> hypothalamic ghrelin and its regulation by<br />
fasting and 2-deoxy-d-glucose administration. Endocrinology<br />
2005; 146: 2510-2516<br />
3 Iglesias MJ, Piñeiro R, Blanco M, Gallego R, Diéguez C,<br />
Gualillo O, González-Juanatey JR, Lago F. Growth hormone<br />
releasing peptide (ghrelin) is synthesized and secreted by<br />
cardiomyocytes. Cardiovasc Res 2004; 62: 481-488<br />
4 Volante M, Allìa E, Gugliotta P, Funaro A, Broglio F, Deghenghi<br />
R, Muccioli G, Ghigo E, Papotti M. Expression <strong>of</strong> ghrelin<br />
and <strong>of</strong> the GH secretagogue receptor by pancreatic islet<br />
cells and related endocrine tumors. J Clin Endocrinol Metab<br />
2002; 87: 1300-1308<br />
5 Ueberberg B, Unger N, Saeger W, Mann K, Petersenn S. Expression<br />
<strong>of</strong> ghrelin and its receptor in human tissues. Horm<br />
Metab Res 2009; 41: 814-821<br />
6 Wang DH, Hu YS, Du JJ, Hu YY, Zhong WD, Qin WJ. Ghrelin<br />
stimulates proliferation <strong>of</strong> human osteoblastic TE85 cells<br />
via NO/cGMP signaling pathway. Endocrine 2009; 35: 112-117<br />
7 Tesauro M, Schinzari F, Caramanti M, Lauro R, Cardillo C.<br />
Metabolic and cardiovascular effects <strong>of</strong> ghrelin. Int J Pept<br />
2010; 2010: 864342<br />
8 Zhang GG, Teng X, Liu Y, Cai Y, Zhou YB, Duan XH, Song<br />
JQ, Shi Y, Tang CS, Yin XH, Qi YF. Inhibition <strong>of</strong> endoplasm<br />
reticulum stress by ghrelin protects against ischemia/reperfusion<br />
injury in rat heart. Peptides 2009; 30: 1109-1116<br />
9 Schwenke DO, Tokudome T, Kishimoto I, Horio T, Shirai<br />
M, Cragg PA, Kangawa K. Early ghrelin treatment after<br />
myocardial infarction prevents an increase in cardiac sympathetic<br />
tone and reduces mortality. Endocrinology 2008; 149:<br />
5172-5176<br />
10 Himmerich H, Sheldrick AJ. TNF-alpha and ghrelin: opposite<br />
effects on immune system, metabolism and mental health.<br />
Protein Pept Lett 2010; 17: 186-196<br />
11 Dixit VD, Yang H, Cooper-Jenkins A, Giri BB, Patel K, Taub<br />
DD. Reduction <strong>of</strong> T cell-derived ghrelin enhances proinflammatory<br />
cytokine expression: implications for age-associated<br />
increases in inflammation. Blood 2009; 113: 5202-5205<br />
12 Hattori N. Expression, regulation and biological actions <strong>of</strong><br />
growth hormone (GH) and ghrelin in the immune system.<br />
Growth Horm IGF Res 2009; 19: 187-197<br />
13 Mondal MS, Date Y, Yamaguchi H, Toshinai K, Tsuruta T,<br />
Kangawa K, Nakazato M. Identification <strong>of</strong> ghrelin and its<br />
receptor in neurons <strong>of</strong> the rat arcuate nucleus. Regul Pept<br />
2005; 126: 55-59<br />
14 Atcha Z, Chen WS, Ong AB, Wong FK, Neo A, Browne ER,<br />
Witherington J, Pemberton DJ. Cognitive enhancing effects<br />
<strong>of</strong> ghrelin receptor agonists. Psychopharmacology (Berl) 2009;<br />
206: 415-427<br />
15 Xu X, Jhun BS, Ha CH, Jin ZG. Molecular mechanisms <strong>of</strong><br />
ghrelin-mediated endothelial nitric oxide synthase activation.<br />
Endocrinology 2008; 149: 4183-4192<br />
16 Shimizu Y, Nagaya N, Teranishi Y, Imazu M, Yamamoto H,<br />
Shokawa T, Kangawa K, Kohno N, Yoshizumi M. Ghrelin<br />
improves endothelial dysfunction through growth hormoneindependent<br />
mechanisms in rats. Biochem Biophys Res Commun<br />
2003; 310: 830-835<br />
17 Nogueiras R, Pfluger P, Tovar S, Arnold M, Mitchell S,<br />
Morris A, Perez-Tilve D, Vázquez MJ, Wiedmer P, Castañeda<br />
TR, DiMarchi R, Tschöp M, Schurmann A, Joost HG, Williams<br />
LM, Langhans W, Diéguez C. Effects <strong>of</strong> obestatin on<br />
energy balance and growth hormone secretion in rodents.<br />
Endocrinology 2007; 148: 21-26<br />
WJD|www.wjgnet.com<br />
18 Lall S, Tung LY, Ohlsson C, Jansson JO, Dickson SL. Growth<br />
hormone (GH)-independent stimulation <strong>of</strong> adiposity by<br />
GH secretagogues. Biochem Biophys Res Commun 2001; 280:<br />
132-138<br />
19 Tschöp M, Smiley DL, Heiman ML. Ghrelin induces adiposity<br />
in rodents. Nature 2000; 407: 908-913<br />
20 Hewson AK, Dickson SL. Systemic administration <strong>of</strong> ghrelin<br />
induces Fos and Egr-1 proteins in the hypothalamic arcuate<br />
nucleus <strong>of</strong> fasted and fed rats. J Neuroendocrinol 2000; 12:<br />
1047-1049<br />
21 Dickson SL, Leng G, Robinson ICAF. (1993). Systemic administration<br />
<strong>of</strong> growth hormone-releasing peptide activates<br />
hypothalamic arcuate neurons. Neuroscience 1993; 54: 303-306<br />
22 Dickson SL, Luckman SM. Induction <strong>of</strong> c-fos messenger ribonucleic<br />
acid in neuropeptide Y and growth hormone (GH)releasing<br />
factor neurons in the rat arcuate nucleus following<br />
systemic injection <strong>of</strong> the GH secretagogue, GH-releasing peptide-6.<br />
Endocrinology 1997; 138: 771-777<br />
23 Hewson AK, Tung LY, Connell DW, Tookman L, Dickson<br />
SL. The rat arcuate nucleus integrates peripheral signals provided<br />
by leptin, insulin, and a ghrelin mimetic. <strong>Diabetes</strong> 2002;<br />
51: 3412-3419<br />
24 Jerlhag E, Egecioglu, E, Dickson SL, Andersson M, Svensson<br />
L, Engel JA. Ghrelin Stimulates Locomotor Activity and Accumbal<br />
Dopamine-Overflow via Central Cholinergic Systems<br />
in Mice: Implications for its Involvement in Brain Reward.<br />
Addict Biol 2004; 11: 45-54.<br />
25 Jerlhag E, Egecioglu E, Dickson SL, Douhan A, Svensson<br />
L, Engel JA. Ghrelin administration into tegmental areas<br />
stimulates locomotor activity and increases extracellular concentration<br />
<strong>of</strong> dopamine in the nucleus accumbens. Addict Biol<br />
2007; 12: 6-16<br />
26 Hewson AK, Tung LY, Connell DW, Tookman L, Dickson<br />
SL. The rat arcuate nucleus integrates peripheral signals<br />
provided by leptin, insulin, and a ghrelin mimetic. <strong>Diabetes</strong><br />
2002; 51: 3412-3419<br />
27 Kobeissy FH, Jeung JA, Warren MW, Geier JE, Gold MS.<br />
Changes in leptin, ghrelin, growth hormone and neuropeptide-Y<br />
after an acute model <strong>of</strong> MDMA and methamphetamine<br />
exposure in rats. Addict Biol 2008; 13: 15-25<br />
28 Wurst FM, Rasmussen DD, Hillemacher T, Kraus T, Ramskogler<br />
K, Lesch O, Bayerlein K, Schanze A, Wilhelm J,<br />
Junghanns K, Schulte T, Dammann G, Pridzun L, Wiesbeck<br />
G, Kornhuber J, Bleich S. Alcoholism, craving, and hormones:<br />
the role <strong>of</strong> leptin, ghrelin, prolactin, and the pro-opiomelanocortin<br />
system in modulating ethanol intake. Alcohol Clin<br />
Exp Res 2007; 31: 1963-1967<br />
29 Santos M, Bastos P, Gonzaga S, Roriz JM, Baptista MJ, Nogueira-Silva<br />
C, Melo-Rocha G, Henriques-Coelho T, Roncon-<br />
Albuquerque R Jr, Leite-Moreira AF, De Krijger RR, Tibboel<br />
D, Rottier R, Correia-Pinto J. Ghrelin expression in human<br />
and rat fetal lungs and the effect <strong>of</strong> ghrelin administration in<br />
nitr<strong>of</strong>en-induced congenital diaphragmatic hernia. Pediatr Res<br />
2006; 59: 531-537<br />
30 Volante M, Fulcheri E, Allìa E, Cerrato M, Pucci A, Papotti M.<br />
Ghrelin expression in fetal, infant, and adult human lung. J<br />
Histochem Cytochem 2002; 50: 1013-1021<br />
31 Nunes S, Nogueira-Silva C, Dias E, Moura RS, Correia-Pinto<br />
J. Ghrelin and obestatin: different role in fetal lung development?<br />
Peptides 2008; 29: 2150-2158<br />
32 Ware LB, Matthay MA. The acute respiratory distress syndrome.<br />
N Engl J Med 2000; 342: 1334-1349<br />
33 Hotchkiss RS, Karl IE. The pathophysiology and treatment<br />
<strong>of</strong> sepsis. N Engl J Med 2003; 348: 138-150<br />
34 Heidecke CD, Hensler T, Weighardt H, Zantl N, Wagner H,<br />
Siewert JR, Holzmann B. Selective defects in T lymphocyte<br />
function in patients with lethal intraabdominal infection.<br />
Am J Surg 1999; 178: 288-292<br />
35 Wu R, Dong W, Zhou M, Zhang F, Marini CP, Ravikumar<br />
TS, Wang P. Ghrelin attenuates sepsis-induced acute lung<br />
injury and mortality in rats. Am J Respir Crit Care Med 2007;<br />
176: 805-813<br />
6 January 15, 2011|Volume 2|Issue 1|
36 Hassig A, Kremer H, Liang WX, Stampfli K. The role <strong>of</strong><br />
the Th-1 to Th-2 shift <strong>of</strong> the cytokine pr<strong>of</strong>iles <strong>of</strong> CD4 helper<br />
cells in the pathogenesis <strong>of</strong> autoimmune and hypercatabolic<br />
diseases. Med Hypotheses 1998; 51: 59-63<br />
37 Van den Berghe G. Endocrinology in intensive care medicine:<br />
new insights and therapeutic consequences. Verh K<br />
Acad Geneeskd Belg 2002; 64: 167-187; discussion 187-188<br />
38 van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx<br />
F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers<br />
P, Bouillon R. Intensive insulin therapy in the critically ill<br />
patients. N Engl J Med 2001; 345: 1359-1367<br />
39 Das UN. Is insulin an antiinflammatory molecule? Nutrition<br />
2001; 17: 409-413<br />
40 Das UN. Insulin and the critically ill. Crit Care 2002; 6: 262-263<br />
41 Das UN. Is insulin an endogenous cardioprotector? Critical<br />
Care 2002; 6: 389-393<br />
42 Das UN. Current advances in sepsis and septic shock with<br />
particular emphasis on the role <strong>of</strong> insulin. Med Sci Monit 2003;<br />
9: RA181-RA192<br />
43 Johnson KL, Rn CR. The hypothalamic-pituitary-adrenal<br />
axis in critical illness. AACN Clin Issues 2006; 17: 39-49<br />
44 Gauna C, van den Berghe GH, van der Lely AJ. Pituitary<br />
function during severe and life-threatening illnesses. Pituitary<br />
2005; 8: 213-217<br />
45 Vanhorebeek I, Langouche L, Van den Berghe G. Endocrine<br />
aspects <strong>of</strong> acute and prolonged critical illness. Nat Clin Pract<br />
Endocrinol Metab 2006; 2: 20-31<br />
46 Chang L, Du JB, Gao LR, Pang YZ, Tang CS. Effect <strong>of</strong><br />
ghrelin on septic shock in rats. Acta Pharmacol Sin 2003; 24:<br />
45-49<br />
47 Chang L, Zhao J, Yang J, Zhang Z, Tang C. Therapeutic<br />
effects <strong>of</strong> ghrelin on endotoxic shock in rats. Eur J Pharmacol<br />
2003; 473: 171-176<br />
48 Maitra SR, Wang S, Braithwaite CE, El-Maghrabi MR. Alterations<br />
in glucose-6-phophatase gene expression in sepsis. J<br />
Trauma 2000; 49: 38<br />
49 Li J, Zhang H, Wu F, Nan Y, Ma H, Guo W, Wang H, Ren J,<br />
Das UN, Gao F. Insulin inhibits tumor necrosis factor-alpha<br />
induction in myocardial ischemia/reperfusion: role <strong>of</strong> Akt<br />
and endothelial nitric oxide synthase phosphorylation. Crit<br />
Care Med 2008; 36: 1551-1558<br />
50 Saad MF, Bernaba B, Hwu CM, Jinagouda S, Fahmi S, Kogosov<br />
E, Boyadjian R. Insulin regulates plasma ghrelin concentration.<br />
J Clin Endocrinol Metab 2002; 87: 3997-4000<br />
51 Yada T, Dezaki K, Sone H, Koizumi M, Damdindorj B,<br />
Nakata M, Kakei M. Ghrelin regulates insulin release and<br />
glycemia: physiological role and therapeutic potential. Curr<br />
<strong>Diabetes</strong> Rev 2008; 4: 18-23<br />
52 Sun Y, Asnicar M, Smith RG. Central and peripheral roles <strong>of</strong><br />
ghrelin on glucose homeostasis. Neuroendocrinology 2007; 86:<br />
215-228<br />
53 Li WG, Gavrila D, Liu X, Wang L, Gunnlaugsson S, Stoll<br />
LL, McCormick ML, Sigmund CD, Tang C, Weintraub NL.<br />
Ghrelin inhibits proinflammatory responses and nuclear factor-kappaB<br />
activation in human endothelial cells. Circulation<br />
2004; 109: 2221-2226<br />
54 Wu R, Zhou M, Cui X, Simms HH, Wang P. Upregulation <strong>of</strong><br />
cardiovascular ghrelin receptor occurs in the hyperdynamic<br />
phase <strong>of</strong> sepsis. Am J Physiol Heart Circ Physiol 2004; 287:<br />
H1296-H302<br />
55 Wu R, Dong W, Zhou M, Cui X, Hank Simms H, Wang P.<br />
Ghrelin improves tissue perfusion in severe sepsis via downregulation<br />
<strong>of</strong> endothelin-1. Cardiovasc Res 2005; 68: 318-326<br />
56 Maruna P, Gürlich R, Frasko R, Rosicka M. Ghrelin and<br />
leptin elevation in postoperative intra-abdominal sepsis. Eur<br />
Surg Res 2005; 37: 354-359<br />
57 Parrish WR, Rosas-Ballina M, Gallowitsch-Puerta M, Ochani<br />
M, Ochani K, Yang LH, Hudson L, Lin X, Patel N, Johnson<br />
SM, Chavan S, Goldstein RS, Czura CJ, Miller EJ, Al-Abed Y,<br />
Tracey KJ, Pavlov VA. Modulation <strong>of</strong> TNF release by choline<br />
WJD|www.wjgnet.com<br />
Das UN. Ghrelin and sepsis<br />
requires alpha7 subunit nicotinic acetylcholine receptor-mediated<br />
signaling. Mol Med 2008; 14: 567-574<br />
58 Yoshikawa H, Kurokawa M, Ozaki N, Nara K, Atou K,<br />
Takada E, Kamochi H, Suzuki N. Nicotine inhibits the production<br />
<strong>of</strong> proinflammatory mediators in human monocytes<br />
by suppression <strong>of</strong> I-kappaB phosphorylation and nuclearkappaB<br />
transcriptional activity through nicotinic acetylcholine<br />
receptor alpha7. Clin Exp Immunol 2006; 145: 116-123<br />
59 Wu R, Dong W, Cui X, Zhou M, Simms HH, Ravikumar TS,<br />
Wang P. Ghrelin down-regulates proinflammatory cytokines<br />
in sepsis through activation <strong>of</strong> the vagus nerve. Ann Surg<br />
2007; 245: 480-486<br />
60 Wu R, Zhou M, Das P, Dong W, Ji Y, Yang D, Miksa M,<br />
Zhang F, Ravikumar TS, Wang P. Ghrelin inhibits sympathetic<br />
nervous activity in sepsis. Am J Physiol Endocrinol Metab<br />
2007; 293: E1697-E1702<br />
61 Chorny A, Anderson P, Gonzalez-Rey E, Delgado M. Ghrelin<br />
protects against experimental sepsis by inhibiting highmobility<br />
group box 1 release and by killing bacteria. J Immunol<br />
2008; 180: 8369-8377<br />
62 Wu R, Dong W, Zhou M, Zhang F, Marini CP, Ravikumar<br />
TS, Wang P. Ghrelin attenuates sepsis-induced acute lung<br />
injury and mortality in rats. Am J Respir Crit Care Med 2007;<br />
176: 805-813<br />
63 Wang W, Bansal S, Falk S, Ljubanovic D, Schrier R. Ghrelin<br />
protects mice against endotoxemia-induced acute kidney<br />
injury. Am J Physiol Renal Physiol 2009; 297: F1032- F1037<br />
64 Shah KG, Wu R, Jacob A, Blau SA, Ji Y, Dong W, Marini<br />
CP, Ravikumar TS, Coppa GF, Wang P. Human ghrelin ameliorates<br />
organ injury and improves survival after radiation<br />
injury combined with severe sepsis. Mol Med 2009; 15: 407-414<br />
65 Wu R, Dong W, Qiang X, Wang H, Blau SA, Ravikumar TS,<br />
Wang P. Orexigenic hormone ghrelin ameliorates gut barrier<br />
dysfunction in sepsis in rats. Crit Care Med 2009; 37: 2421-2426<br />
66 Carlini VP, Monzon ME, Varas MM, Cragnolini AB, Schioth<br />
HB, Scimonelli TN, de Barioglio SR. Ghrelin increases anxiety-like<br />
behavior and memory retention in rats. Biochem Biophys<br />
Res Commun 2002; 299: 739-743<br />
67 Diano S, Farr SA, Benoit SC, McNay EC, da Silva I, Horvath B,<br />
Gaskin FS, Nonaka N, Jaeger LB, Banks WA, Morley JE, Pinto<br />
S, Sherwin RS, Xu L, Yamada KA, Sleeman MW, Tschöp MH,<br />
Horvath TL. Ghrelin controls hippocampal spine synapse<br />
density and memory performance. Nat Neurosci 2006; 9:<br />
381-388<br />
68 Getting SJ, Gibbs L, Clark AJ, Flower RJ, Perretti M. POMC<br />
gene-derived peptides activate melanocortin type 3 receptor<br />
on murine macrophages, suppress cytokine release, and inhibit<br />
neutrophil migration in acute experimental inflammation.<br />
J Immunol 1999; 162: 7446-7453<br />
69 Ichiyama T, Zhao H, Catania A, Furukawa S, Lipton JM.<br />
alpha-melanocyte-stimulating hormone inhibits NF-kappaB<br />
activation and IkappaBalpha degradation in human glioma<br />
cells and in experimental brain inflammation. Exp Neurol<br />
1999; 157: 359-365<br />
70 Cowley MA, Smith RG, Diano S, Tschop M, Pronchuk N,<br />
Grove KL. The distribution and mechanism <strong>of</strong> action <strong>of</strong> ghrelin<br />
in the CNS demonstrates a novel hypothalamic circuit<br />
regulating energy homeostasis. Neuron 2003; 37: 649-661<br />
71 Wren AM, Small CJ, Fribbens CV, Neary NM, Ward HL, Seal<br />
LJ, Ghatei MA, Bloom SR. The hypothalamic mechanisms <strong>of</strong><br />
the hypophysiotropic action <strong>of</strong> ghrelin. Neuroendocrinology<br />
2002; 76: 316-324<br />
72 Lutter M, Sakata I, Osborne-Lawrence S, Rovinsky SA,<br />
Anderson JG, Jung S, Birnbaum S, Yanagisawa M, Elmquist<br />
JK, Nestler EJ, Zigman JM. The orexigenic hormone ghrelin<br />
defends against depressive symptoms <strong>of</strong> chronic stress. Nat<br />
Neurosci 2008; 11: 752-753<br />
73 Himmerich H, Sheldrick AJ. TNF-alpha and ghrelin: opposite<br />
effects on immune system, metabolism and mental health.<br />
Protein Pept Lett 2010; 17: 186-196<br />
S- Editor Zhang HN L- Editor Herholdt A E- Editor Liu N<br />
7 January 15, 2011|Volume 2|Issue 1|
Online Submissions: http://www.wjgnet.com/1948-9358<strong>of</strong>fice<br />
wjd@wjgnet.com<br />
doi:10.4239/wjd.v2.i1.8<br />
ORIGINAL ARTICLES<br />
Excessive 5-year weight gain predicts metabolic syndrome<br />
development in healthy middle-aged adults<br />
Yu-Cheng Lin, Jong-Dar Chen, Pau-Chung Chen<br />
Yu-Cheng Lin, The Department <strong>of</strong> Occupational Medicine, En<br />
Chu Kong Hospital, New Taipei City, 23742, Taiwan, China<br />
Yu-Cheng Lin, School <strong>of</strong> Medicine, Fu Jen Catholic University,<br />
New Taipei City 24205, Taiwan, China<br />
Jong-Dar Chen, Department <strong>of</strong> Family Medicine, Shin Kong<br />
Wu Ho-Su Memorial Hospital, Taipei 111, Taiwan, China<br />
Yu-Cheng Lin, Pau-Chung Chen, Institute <strong>of</strong> Occupational Medicine<br />
and Industrial Hygiene, College <strong>of</strong> Public Health, National<br />
Taiwan University, Taipei 100, Taiwan, China<br />
Author contributions: Lin YC collected and analyzed data; Lin<br />
YC and Chen JD interpreted data; Lin YC drafted the article;<br />
Chen JD revised critically for important intellectual content; and<br />
Chen PC finally approved the version to be published.<br />
Correspondence to: Pau-Chung Chen, Pr<strong>of</strong>essor, Institute <strong>of</strong><br />
Occupational Medicine and Industrial Hygiene, College <strong>of</strong> Public<br />
Health, National Taiwan University, No. 17, Xu-Zhou Road, Taipei<br />
10020, Taiwan, China. pchen@ntu.edu.tw<br />
Telephone: +886-02-3366-8088 Fax: +886-02-2341-8570<br />
Received: August 31, 2010 Revised: December 1, 2010<br />
Accepted: December 8, 2010<br />
Published online: January 15, 2011<br />
Abstract<br />
AIM: To quantitatively examine the impacts <strong>of</strong> an easyto-measure<br />
parameter - weight gain - on metabolic<br />
syndrome development among middle-aged adults.<br />
METHODS: We conducted a five-year interval observational<br />
study. A total <strong>of</strong> 1384 middle-aged adults not<br />
meeting metabolic syndrome (MetS) criteria at the initial<br />
screening were included in our analysis. Baseline data<br />
such as MetS-components and lifestyle factors were<br />
collected in 2002. Body weight and MetS-components<br />
were measured in both 2002 and 2007. Participants<br />
were classified according to proximal quartiles <strong>of</strong><br />
weight gain (WG) in percentages (%WG ≤ 1%, 1% <<br />
%WG ≤ 5%, 5% < %WG ≤ 10% and %WG > 10%,<br />
defined as: control, mild-WG, moderate-WG and severe-<br />
WG groups, respectively) at the end <strong>of</strong> the follow-up.<br />
Multivariate models were used to assess the association<br />
WJD|www.wjgnet.com<br />
<strong>World</strong> J <strong>Diabetes</strong> 2011 January 15; 2(1): 8-15<br />
ISSN 1948-9358 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
between MetS outcome and excessive WG in the total<br />
population, as well as in both genders.<br />
RESULTS: In total, 175 (12.6%) participants fulfilled<br />
MetS criteria within five years. In comparison to the control<br />
group, mild-WG adults had an insignificant risk for<br />
MetS development while adults having moderate-WG<br />
had a 3.0-fold increased risk for progression to MetS<br />
[95% confidence interval (CI), 1.8-5.1], and this risk<br />
was increased 5.4-fold (95% CI, 3.0-9.7) in subjects<br />
having severe-WG. For females having moderate- and<br />
severe-WG, the risk for developing MetS was 3.6 (95%<br />
CI, 1.03-12.4) and 5.5 (95% CI, 1.4-21.4), respectively.<br />
For males having moderate- and severe-WG, the odds<br />
ratio for MetS outcome was respectively 3.0 (95% CI,<br />
1.6-5.5) and 5.2 (95% CI, 2.6-10.2).<br />
CONCLUSION: For early-middle-aged healthy adults<br />
with a five-year weight gain over 5%, the severity <strong>of</strong><br />
weight gain is related to the risk for developing metabolic<br />
syndrome.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: Excess weight gain; Metabolic syndrome;<br />
Middle-aged adults; Follow-up; Worker population<br />
Peer reviewers: Yoshinari Uehara, MD, PhD, Department <strong>of</strong><br />
Cardiology, Fukuoka University Faculty <strong>of</strong> Medicine, 7-45-1<br />
Nanakuma, Jonan-ku, Fukuoka 814-0180 Japan; Mark A Sperling,<br />
MD, Pr<strong>of</strong>essor <strong>of</strong> Pediatrics, Children's Hospital <strong>of</strong> Pittsburgh<br />
<strong>of</strong> UPMC, 4401 Penn Avenue, Division <strong>of</strong> Endocrinology,<br />
Faculty Pavilion -8th Floor, Pittsburgh, PA 15224, United States;<br />
Narattaphol Charoenphandhu, MD, PhD, Department <strong>of</strong> Physiology,<br />
Faculty <strong>of</strong> Science, Mahidol University, Rama VI Road,<br />
Bangkok 10400, Thailand<br />
Lin YC, Chen JD, Chen PC. Excessive 5-year weight gain<br />
predicts metabolic syndrome development in healthy middleaged<br />
adults. <strong>World</strong> J <strong>Diabetes</strong> 2011; 2(1): 8-15 Available from:<br />
URL: http://www.wjgnet.com/1948-9358/full/v2/i1/8.htm DOI:<br />
http://dx.doi.org/10.4239/wjd.v2.i1.8<br />
8 January 15, 2011|Volume 2|Issue 1|
INTRODUCTION<br />
Measuring body weight is noninvasive, inexpensive and<br />
reliable both in terms <strong>of</strong> clinical and self-health monitoring<br />
[1] . Analyses from the general population have<br />
revealed excessive weight gain (WG) as an important risk<br />
factor for developing metabolic syndrome (MetS) [2,3] . MetS<br />
is also becoming an important concern in workplaces [4-6]<br />
for its impacts on both the health condition [7] and productivity<br />
[8] <strong>of</strong> employees. Excessive WG is common in<br />
the early-middle-aged population [9,10] who account for<br />
the majority <strong>of</strong> the workforce. However, there was a lack<br />
<strong>of</strong> a comprehensive follow-up survey for examining the<br />
possible quantitative association between WG severity<br />
and the risk for MetS development in the early-middleaged<br />
worker population. Improving our knowledge <strong>of</strong> the<br />
impacts <strong>of</strong> WG on MetS development is helpful to health<br />
promotion in workplaces. Since periodic routine health<br />
checkups are compulsory for employees at many worksites<br />
in Taiwan, we had an opportunity to conduct a workplacebased<br />
follow-up observation for MetS development. We<br />
used this approach to evaluate the impacts <strong>of</strong> excessive<br />
WG on MetS development among early-middle-aged employees.<br />
MATERIALS AND METHODS<br />
Participants<br />
A flowchart <strong>of</strong> the experimental protocol is shown below<br />
in the Figure 1. In 2002 and 2007, 1648 eligible employees<br />
<strong>of</strong> an electronic manufacturing company underwent compulsory<br />
health checkups in accordance with the Labor<br />
Health Protection Regulation <strong>of</strong> the Labor Safety and Health Act.<br />
The final analysis <strong>of</strong> this follow-up study only included<br />
subjects who did not fulfill MetS criteria in 2002. In total,<br />
256 employees were excluded from the study because they<br />
had been screened previously for MetS. Final records from<br />
a total <strong>of</strong> 1384 workers (338 female and 996 male workers,<br />
aged 18 to 58 years with a mean age <strong>of</strong> 32.3 years) made<br />
up the cohort for the study and for the endpoint analysis.<br />
Most <strong>of</strong> the employees <strong>of</strong> this electronics manufacturing<br />
company were residents <strong>of</strong> northern Taiwan.<br />
The health examination was open to all registered<br />
employees during every working day within a one-month<br />
period. All <strong>of</strong> the employees were recommended to avoid<br />
vigorous physical exercise for three days before their<br />
health examination. The subjects’ identities were anonymous<br />
and were not linked to the data. This analytical<br />
study, limited to health checkup records, followed the<br />
ethical criteria for human research and the study protocol<br />
(TYGH09702108) was reviewed and approved by the<br />
Ethics Committee <strong>of</strong> the Tao-Yuan General Hospital,<br />
Taiwan.<br />
Demographics, lifestyle data, and biological<br />
measurements<br />
In 2002, the examinees completed a questionnaire about<br />
their baseline personal history, including their lifestyle<br />
factors.<br />
WJD|www.wjgnet.com<br />
Lin YC et al . Excessive weight gain predicts metabolic syndrome<br />
A total 1648 eligible employees completed a questionnaire about their<br />
baseline personal, occupational and lifestyle history; received physical<br />
checkups including Mets components and body weight, in 2002<br />
1384 workers not fulfilling Mets criteria in 2002 were<br />
followed up for Mets components and body weight, in 2007<br />
175 workers fulfilled Mets<br />
criteria in 2007<br />
Figure 1 Flowchart <strong>of</strong> experimental protocol.<br />
256 workers were excluded<br />
from the study because being<br />
screened Mets in 2002<br />
1209 workers did not fulfill<br />
Mets criteria in 2007<br />
Physical examinations and blood tests were performed<br />
on all participants in both 2002 and 2007. The participants<br />
arrived at the health care unit <strong>of</strong> the factory in the morning,<br />
between 07:30 and 09:30 h, after an overnight 8<br />
h fast. The physical examination records included measurements<br />
<strong>of</strong> waist circumference, weight, height and<br />
blood pressure. All the measuring apparatuses were rou<br />
tinely calibrated. Waist circumference was measured midway<br />
between the lowest rib and the superior border <strong>of</strong><br />
the iliac crest. After being seated for 5 min, sitting blood<br />
pressure was measured with the dominant arm using digital<br />
automatic sphygmomanometers (model HEM 907,<br />
Omron, Japan) two times with a 5 min interval; the mean<br />
<strong>of</strong> these readings was used in the data analysis. After the<br />
physical examination, participants were placed in a reclined<br />
position, and venous blood (20 mL) was taken from an<br />
antecubital vein <strong>of</strong> the arm for subsequent tests. Blood<br />
specimens were centrifuged immediately thereafter, and<br />
were frozen and shipped on dry ice to a central clinical<br />
laboratory in the Tao-Yuan General Hospital (certified<br />
by ISO 15189 and ISO 17025). Glucose, triglyceride and<br />
high-density lipoprotein (HDL) cholesterol analyses were<br />
conducted by a Hitachi autoanalyzer model 7150 (Hitachi,<br />
Tokyo, Japan).<br />
Weight gain evaluation<br />
Weight gain (WG) was calculated as a percentage by the<br />
formula: [(body weight 2007 - body weight 2002)/body weight<br />
2002] and was represented as %WG. Participants were classified<br />
into four subgroups according to their proximal<br />
quartiles <strong>of</strong> increased weight gain (%WG ≤ 1%, 1% <<br />
%WG ≤ 5%, 5% < %WG ≤ 10% and 10% > %WG,<br />
defined as: control, mild-WG, moderate-WG and severe-<br />
WG groups, respectively) at end <strong>of</strong> the follow-up examination.<br />
Metabolic syndrome<br />
The MetS designation was made if three or more <strong>of</strong> the<br />
following five criteria were fulfilled: central obesity (waist<br />
9 January 15, 2011|Volume 2|Issue 1|
the two genders. Also, as shown at the bottom <strong>of</strong> Table<br />
1, 12.6 % <strong>of</strong> total population developed MetS within five<br />
years; this value was 8.8% for female and was significantly<br />
higher for male workers, at 14.2%.<br />
Among the four WG subgroups (Table 2), the baseline<br />
measurements <strong>of</strong> body weight, body mass index, waist circumstance<br />
and most lifestyle factors were not significantly<br />
different, except that workers who had moderate and<br />
severe weight gain tended to snack before sleeping. The<br />
mean age <strong>of</strong> the severe-WG subgroup was lower than<br />
that <strong>of</strong> the other subgroups and the severe-WG subgroup<br />
was healthier than other subgroups at beginning <strong>of</strong> the<br />
experiment in terms <strong>of</strong> the baseline MetS-component<br />
measures. Table 2 also shows that the five-year occurrence<br />
rates <strong>of</strong> MetS were significantly higher in the moderate-<br />
and severe-WG subgroups.<br />
Since the baseline measurements were significantly<br />
different between the two genders, Table 3 presents the<br />
baseline data for the MetS-components according to the<br />
severity <strong>of</strong> weight gain for both genders. For the earlymiddle-aged<br />
females, the subjects showing severe-WG<br />
were younger than those in other WG groups. Although<br />
the majority <strong>of</strong> baseline characteristics were similar, females<br />
who gained a moderate or severe amount <strong>of</strong> weight<br />
tended to snack between meals and before sleeping (Table<br />
3). In our male adults, the severe WG group was the youngest<br />
and had better MetS-component baseline data than<br />
the other subgroups. Males who gained a moderate or<br />
severe amount <strong>of</strong> weight were inclined to snack before<br />
sleeping.<br />
Table 4 presents the changes <strong>of</strong> MetS-component<br />
factors and the occurrence <strong>of</strong> MetS among four WG<br />
WJD|www.wjgnet.com<br />
Lin YC et al . Excessive weight gain predicts metabolic syndrome<br />
Table 2 Summary <strong>of</strong> baseline characteristics <strong>of</strong> variables for the total population and five-year occurrence rates <strong>of</strong> metabolic<br />
syndrome according to the severity <strong>of</strong> weight gain (N = 1384)<br />
Baseline data WG within 5 years<br />
Control Mild Moderate Severe<br />
%WG ≤ 1% 1% < %WG ≤ 5% 5% < %WG ≤ 10% %WG > 10%<br />
n = 341 n =337 n =387 n =391<br />
Measurements; mean (standard deviation)<br />
Age (year) b<br />
33.5 (6.8) 33.3 (6.4) 32.4 (6.4) 29.7 (5.7)<br />
Body weight (kg) 64.4 (10.5) 63.9 (11.8) 63.6 (11.0) 62.9 (10.3)<br />
Body mass index (kg/m 2 ) 23.3 (2.8) 23.1 (3.0) 23.0 (3.2) 22.6 (2.9)<br />
Waist (cm) 76.0 (8.2) 75.8 (8.9) 75.8 (9.1) 74.5 (8.0)<br />
Systolic blood pressure (mmHg) a<br />
118.9 (14.5) 116.4 (14.4) 117.0 (15.0) 115.7 (13.3)<br />
Diastolic blood pressure (mmHg) b<br />
73.3 (9.4) 71.7 (9.3) 71.5 (9.8) 70.2 (7.8)<br />
Fasting blood glucose (mg/dL) a<br />
95.8 (15.1) 94.5 (7.9) 93.9 (7.4) 92.8 (19.5)<br />
Triglycerides (mg/dL) b<br />
115.4 (118.8) 105.5 (65.0) 98.8 (55.9) 89.9 (52.2)<br />
HDL cholesterol (mg/dL)<br />
Prevalent rates (%)<br />
Lifestyle factors<br />
49.2 (11.0) 50.6 (12.7) 50.8 (12.6) 51.6 (10.7)<br />
Physical exercise; > 3 times a week 34.90% 30.90% 31.30% 31.30%<br />
Habitual drinker 6.20% 7.10% 8.50% 3.90%<br />
Having snacks before sleeping (≥ third a week) b<br />
34.00% 35.90% 44.20% 43.30%<br />
Having snacks between meals (≥ third a week) 46.60% 43.60% 47.00% 48.90%<br />
Ever been a smoker (yes vs no) 31.10% 29.70% 33.10% 34.80%<br />
MetS development within 5 years 9.10% b<br />
9.50% b<br />
15.80% b<br />
16.00% b<br />
a P < 0.05; b P < 0.01; An ANOVA was conducted, adjusting for age, using a Tukey’s test. A trend test was conducted for categorical variables. WG: weight<br />
gain; HDL: high density lipoprotein cholesterol.<br />
subgroups for each gender. For our early-middle-aged<br />
females, the changes in the factors for central obesity<br />
and in Low-HDL levels were significantly less favorable<br />
in workers who gained moderate or severe amounts <strong>of</strong><br />
weight and the development <strong>of</strong> MetS was found to be<br />
significantly higher in these subgroups than in others. For<br />
the male adults in our study, the moderate- and severs-<br />
WG subgroups showed significantly more unfavorable<br />
changes in nearly all MetS-components and had higher<br />
rates <strong>of</strong> MetS within five years than mild-WG and control<br />
subgroups.<br />
After controlling for the confounding factors <strong>of</strong> initial<br />
age, MetS-components and lifestyle factors, a multivariate<br />
analysis was conducted and the results are shown in Table<br />
5. The risk <strong>of</strong> developing MetS in subjects with moderate-<br />
and severe-WG was 3.0-times [95% confidence interval<br />
(CI), 1.8-5.1] and 5.4-times (95% CI, 3.0-9.7) greater<br />
than with the control group. For female workers with<br />
moderate- and severe-WG, the risk <strong>of</strong> developing MetS<br />
was 3.6-times (95% CI, 1.03-12.4) and 5.5-times (95%<br />
CI, 1.4-21.4) higher than the control group. Females who<br />
had been smokers had an increased risk (6.7 times higher,<br />
95% CI, 1.2-36.7) <strong>of</strong> developing MetS than those who<br />
had never smoked. The risk <strong>of</strong> developing MetS in male<br />
adults with moderate- and severe-WG was 3.0-times [95%<br />
confidence interval (CI), 1.6-5.5] and 5.2-times (95% CI,<br />
2.6-10.2) greater than the control group.<br />
DISCUSSION<br />
In this five-year interval follow up, approximately half<br />
<strong>of</strong> healthy middle-aged adults had a WG <strong>of</strong> over 5%,<br />
11 January 15, 2011|Volume 2|Issue 1|
Lin YC et al . Excessive weight gain predicts metabolic syndrome<br />
Table 3 Summary <strong>of</strong> baseline characteristics <strong>of</strong> variables for female and male adults according to the severity <strong>of</strong> weight gain<br />
and a quarter <strong>of</strong> the overall sample had a WG <strong>of</strong> more<br />
than 10%. Major clinical manifestations in adults, such<br />
as cardiovascular complications and diabetes, have been<br />
associated with excess WG [10,15] . In a preventive sense, our<br />
analyses show that the development <strong>of</strong> MetS, a precursor<br />
<strong>of</strong> diabetes [16,17] , is significantly quantitatively associated<br />
with a five-year WG exceeding 5% in healthy early-middleaged<br />
adults <strong>of</strong> both genders (Table 5).<br />
Waist circumference is an important factor for MetS.<br />
It is likely that weight gain contributes to increases in<br />
waist circumference. However, for the general population,<br />
the body weight measurement is less rigorous than waist<br />
measurement which has a specific anatomic definitions [18]<br />
and ,therefore, present study investigated changes in<br />
WJD|www.wjgnet.com<br />
Female N = 388<br />
Baseline data WG within 5 years<br />
Control Mild Moderate Severe<br />
%WG ≤ 1% 1% < %WG ≤ 5% 5% < %WG ≤ 10% %WG >10%<br />
n = 105 n = 100 n = 99 n = 84<br />
Measurements; mean (standard deviation)<br />
Age (year) 33.6 (8.7) 33.0 (7.4) 33.1 (8.1) 31.1 (7.0)<br />
Body weight (kg) 55.3 (7.3) 53.0 (7.5) 53.5 (8.3) 55.3 (8.8)<br />
Body mass index (kg/m 2 ) b<br />
23.9 (2.7) 23.8 (2.8) 23.3 (3.0) 22.6 (2.8)<br />
Waist (cm) 68.8 (5.9) 67.8 (6.4) 68.1 (7.9) 69.5 (7.2)<br />
Systolic blood pressure (mmHg) 112.2 (13.8) 109.7 (12.1) 113.2 (14.6) 110.6 (12.9)<br />
Diastolic blood pressure (mmHg) 68.9 (9.0) 67.7 (8.8) 69.8 (9.6) 67.7 (8.1)<br />
Fasting blood glucose (mg/dL) 94.0 (9.1) 94.7 (8.6) 94.2 (7.0) 91.9 (7.4)<br />
Triglycerides (mg/dL) 79.4 (38.3) 73.4 (33.6) 74.0 (33.1) 73.2 (51.9)<br />
HDL cholesterol (mg/dL)<br />
Prevalent rates (%)<br />
Lifestyle factors<br />
53.2 (11.6) 57.1 (12.9) 56.4 (14.4) 55.6 (10.2)<br />
Physical exercise; ≥ 3 times a week 25.70% 26.00% 23.20% 27.40%<br />
Habitual drinker 1.00% 0.00% 0.00% 0.00%<br />
Having snacks before sleeping (≥ third a week) 28.60% 26.00% 44.40% 27.40%<br />
Having snacks between meals (≥ third a week) 59.00% 55.00% 74.70% 54.80%<br />
Ever been a smoker (yes vs no) 6.70% 3.00% 4.00% 7.10%<br />
Male N = 996<br />
Baseline data WG within 5 years<br />
Control Mild Moderate Severe<br />
%WG ≤ 1% 1% < %WG ≤ 5% 5% < %WG ≤ 10% %WG > 10%<br />
n = 236 n = 237 n = 288 n = 235<br />
Measurements; mean (standard deviation)<br />
Age (year) b<br />
33.4 (5.7) 33.5 (6.0) 32.2 (5.7) 29.2 (5.0)<br />
Body weight (kg) b<br />
68.5 (9.0) 68.6 (10.1) 67.1 (9.6) 65.6 (9.5)<br />
Body mass index (kg/m 2 ) 22.2 (2.8) 21.6 (2.8) 21.8 (3.5) 22.4 (3.1)<br />
Waist (cm) b<br />
79.3 (7.0) 79.2 (7.5) 78.4 (7.9) 76.3 (7.5)<br />
Systolic blood pressure (mmHg) b<br />
121.8 (13.8) 119.2 (14.3) 118.2 (14.9) 117.6 (13.0)<br />
Diastolic blood pressure (mmHg) b<br />
75.2 (8.9) 73.4 (8.9) 72.0 (9.8) 71.1 (7.6)<br />
Fasting blood glucose (mg/dL) 96.6 (17.1) 94.4 (7.6) 93.8 (7.5) 93.2 (22.3)<br />
Triglycerides (mg/dL) b<br />
131.5 (137.6) 119.1 (70.2) 107.3 (59.5) 95.9 (51.1)<br />
HDL cholesterol (mg/dL) a<br />
Prevalent rates (%)<br />
Lifestyle factors<br />
47.4 (10.3) 47.9 (11.5) 48.8 (11.3) 50.1 (10.5)<br />
Physical exercise; ≥ 3 times a week 39.00% 32.90% 34.00% 32.80%<br />
Habitual drinker 8.50% 10.10% 11.50% 9.40%<br />
Having snacks before sleeping (≥ third a week) a 36.40% 40.10% 44.10% 48.90%<br />
Having snacks between meals (≥ third a week) 41.10% 38.80% 37.50% 46.80%<br />
Ever been a smoker (yes vs no) 41.90% 40.90% 43.10% 44.70%<br />
a P < 0.05, b P < 0.01, An ANOVA was conducted, adjusting for age, using a Tukey’s test. A trend test was conducted for categorical variables; WG: weight<br />
gain; HDL: high density lipoprotein cholesterol.<br />
weight. Nevertheless, we treated waist circumference as a<br />
confounder in the multivariate analysis (Table 5) because<br />
it has a decisive influence on the development <strong>of</strong> metabolic<br />
syndrome. On the other hand, occupational and<br />
lifestyle factors naturally affect dietary behaviors and thus<br />
affect body weight changes [19] and other factors <strong>of</strong> atherosclerosis<br />
which are important in MetS development,<br />
including total cholesterol, low density lipoprotein cholesterol,<br />
uric acid and insulin. Our present study focused<br />
on body weight changes, and although we controlled<br />
some occupational, lifestyle and baseline metabolic factors<br />
(not shown in tables), the detailed impact <strong>of</strong> these factors<br />
needs to be clarified by other investigations.<br />
Findings from both our study (Table 4) and other<br />
12 January 15, 2011|Volume 2|Issue 1|
follow-up observations [20] indicate that the adults without<br />
excess WG have stable or improved serum levels <strong>of</strong><br />
HDL and glucose, while the adults gaining excess weight<br />
over several years have dramatically greater changes in<br />
triglyceride levels than other groups. HDL levels demonstrated<br />
improving trends in our middle aged sample population.<br />
This dissimilar to earlier findings in an elderly<br />
population [21] , but similar to what was shown in other<br />
follow-up observations for healthy Asian adults [22] . Discussing<br />
these findings in an earlier article [12] ; we suggested<br />
that our relative young healthy workers might not yet<br />
have reached their HDL concentration plateau so had the<br />
potential to increase their HDL concentration within our<br />
WJD|www.wjgnet.com<br />
Lin YC et al . Excessive weight gain predicts metabolic syndrome<br />
Table 4 Summary <strong>of</strong> five-year changes in metabolic syndrome-components for female and male adults and the occurrence rates <strong>of</strong><br />
metabolic syndrome according to the severity <strong>of</strong> weight gain<br />
Female N = 388<br />
Follow-up changes (%) WG within 5 years<br />
Control Mild Moderate Severe<br />
%WG ≤ 1% 1% < %WG ≤ 5% 5% < %WG ≤ 10% %WG > 10%<br />
n = 105 n = 100 n = 99 n = 84<br />
△Central obesity b<br />
8.50% 16.00% 22.60% 32.80%<br />
△High blood pressure 22.90% 28.70% 28.50% 37.00%<br />
△Hyperglycemia -3.40% -4.20% -3.10% 1.30%<br />
△Hypertriglyceridemia b<br />
-0.40% 8.00% 15.60% 24.30%<br />
△Low-HDL cholesterol b<br />
-14.40% -17.70% -5.90% -6.00%<br />
MetS Development within 5 years b<br />
5.70% 3.00% 14.10% 13.10%<br />
Male N = 996<br />
Follow-up changes (%) WG within 5 years<br />
Control Mild Moderate Severe<br />
%WG ≤ 1% 1% < %WG ≤ 5% 5% < %WG ≤ 10% %WG > 10%<br />
n = 236 n = 237 n = 288 n = 235<br />
△Central obesity b<br />
10.00% 3.00% 21.20% 40.50%<br />
△High blood pressure a<br />
21.00% 20.00% 21.20% 19.00%<br />
△Hyperglycemia -8.00% -11.00% -5.10% -2.40%<br />
△Hypertriglyceridemia b<br />
2.00% 2.00% 8.10% 11.90%<br />
△Low-HDL cholesterol b<br />
-34.00% -24.00% -24.20% -7.10%<br />
MetS development within 5 years 10.60% 12.20% 16.30% 17.00%<br />
a b<br />
P < 0.05; P < 0.01; An ANOVA was conducted, adjusting for age, using Tukey’s test. Δ: Differences between 2007 and 2002; minus indicates decreasing<br />
trend within follow-up; WG: weight gain; HDL: high density lipoprotein cholesterol.<br />
Table 5 The adjusted risks for development <strong>of</strong> metabolic<br />
syndrome<br />
WG severities Odd ratio 95% CI<br />
Total population<br />
Mild WG (1% < %WG < 5%) 1.2 0.70 - 2.2<br />
Moderate WG (5% < %WG < 10%) b<br />
3.0 1.80 - 5.1<br />
Severe WG (%WG > 10%) b<br />
Female<br />
5.4 3.00 - 9.7<br />
Mild WG (1% < %WG < 5%) 0.9 0.20 - 4.5<br />
Moderate WG (5% < %WG < 10%) a<br />
3.6 1.03 - 12.4<br />
Severe WG (%WG > 10%) b<br />
Male<br />
5.5 1.40 - 21.4<br />
Mild WG (1% < %WG < 5%) 1.4 0.70 - 2.7<br />
Moderate WG (5% < %WG < 10%) b<br />
3/0 1.60 - 5.5<br />
Severe WG (%WG > 10%) b<br />
5.2 2.60 - 10.2<br />
a b<br />
P < 0.05; P < 0.01; Adjusted variables were age, metabolic syndrome<br />
components and lifestyle and occupational factors; WG: weight gain.<br />
follow-up. Significantly, moderate or severe weight gainers<br />
had much lower capacity for increasing their HDL levels<br />
than those free from significant weight gain (Table 4).<br />
In addition, as presented in Tables 3 and 4, although the<br />
severe-WG subgroups were the youngest (mean aged 31<br />
years) at the outset, after five years they showed the worst<br />
changes in all MetS-components and the highest MetS<br />
occurrence rate among the workers examined. We found<br />
that the glucose and lipid metabolism capabilities in our<br />
young workers with excessive WG became significantly<br />
worse than in older subjects without excessive WG. This<br />
phenomenon supports, in terms <strong>of</strong> nutritional metabolism,<br />
the hypothesis that rapidly becoming obese can<br />
speed up the aging process in adults [23] . Experts have sug-<br />
gested that public health efforts need to tackle rapid WG<br />
in adolescents [24] and our findings indicate that these efforts<br />
should be extended to early-middle-aged workers.<br />
Since “yo-yo” effects [25] have appeared in many trials for<br />
weight reduction, body weight monitoring and preventing<br />
excess WG is an important strategy for maintaining heal-<br />
thy lipid and sugar metabolism in early-middle-aged workers.<br />
Weight gain <strong>of</strong> more than 5% within a five-year<br />
period should be avoided in order to prevent the development<br />
<strong>of</strong> MetS. On the other hand, limited weight gain was<br />
previously found not to be a risk factor for diabetes [15] and<br />
in the present analysis, five-year mild-WG (< 5% WG)<br />
appeared to be tolerable in terms <strong>of</strong> progression to MetS<br />
(Table 5).<br />
For both genders, there were differences in dietary<br />
habits among our four WG subgroups: the moderate- and<br />
severe- weight gainers were significantly more likely to<br />
snack between meals or before sleep (Table 3). The major<br />
13 January 15, 2011|Volume 2|Issue 1|
Lin YC et al . Excessive weight gain predicts metabolic syndrome<br />
weight-related behaviors in late-adolescence are snack-<br />
ing and late-night eating [26] .Further more, a study on twins<br />
showed that night-time eating was significantly more com-<br />
mon in obese subjects than in subjects with normal weight<br />
[27] . Because awareness <strong>of</strong> weight control is itself bene-<br />
ficial for the prevention <strong>of</strong> MetS [28] and our workers who<br />
gained excessive weight tended to snack in addition to<br />
regular meals, education and reminders <strong>of</strong> healthy dietary<br />
behaviors for employees are essential for MetS mana-<br />
gement in workplaces. Dietary behavior is an important<br />
but complex issue in surveys concerning MetS development<br />
[29,30] . However, there is a lack <strong>of</strong> precise data regarding<br />
caloric intake and dietary contents in the current<br />
analysis, and this might explain why our multivariate analysis<br />
involving dietary behaviors did not reach a statistical<br />
significance for MetS outcome. Future surveys for MetS<br />
in workplaces should focus on the details <strong>of</strong> dietary behaviors<br />
among employees.<br />
The present observational approach demonstrated a<br />
significant association between severity <strong>of</strong> weight gain<br />
and MetS outcome. However, there are several research<br />
limitations should be addressed. Because National Health<br />
Insurance in Taiwan provides convenient medical care<br />
for subjects with MetS traits, it was difficult to avoid<br />
confounding protective effects from the correction efforts<br />
for MetS components [31] during the period <strong>of</strong> our follow<br />
up. At the same time, our conclusions were drawn from<br />
the relatively healthy employees by excluding the data <strong>of</strong><br />
the workers who fulfilled the MetS criteria at baseline<br />
and, thus “healthy-worker effects [32] ” might be involved.<br />
Given the conditions mentioned above, it is possible<br />
that we might have underestimated the risk for MetS outcome.<br />
Finally, our findings were obtained from a five- year<br />
interval approach and thus the possible impacts on MetS<br />
outcomes <strong>of</strong> body weight changes over a shorter time<br />
period require further study. In conclusion, for early-middle-aged<br />
healthy adults with a five-year weight gain over<br />
5%, severity <strong>of</strong> weight gain is quantitatively associated<br />
with the risk for metabolic syndrome development. We<br />
suggest prioritizing the optimization <strong>of</strong> body weight and<br />
modifications in dietary behaviors for the prevention <strong>of</strong><br />
metabolic syndrome among early-middle-aged workers.<br />
ACKNOWLEDGMENTS<br />
The authors would like to thank the personnel <strong>of</strong> the<br />
Department <strong>of</strong> Family Medicine, Center <strong>of</strong> Health Management<br />
in the Tao-Yuan General Hospital for their support<br />
and generous assistance.<br />
COMMENTS<br />
Background<br />
Measuring body weight is noninvasive, inexpensive and reliable both in terms<br />
<strong>of</strong> clinical and self-health monitoring. Analyses from the general population<br />
have revealed excessive weight gain (WG) as an important risk factor for<br />
developing metabolic syndrome (MetS), which is becoming an important<br />
concern in workplaces for its impacts on both health conditions and productivity<br />
<strong>of</strong> employees. Excessive WG is common in the early-middle-aged population<br />
WJD|www.wjgnet.com<br />
who account for the majority <strong>of</strong> the workforce. However, there was a lack <strong>of</strong><br />
a comprehensive follow-up survey for examining the quantitative association<br />
between WG severity and the risk for MetS development in the early-middle-aged<br />
worker population.<br />
Research frontiers<br />
Improving our knowledge <strong>of</strong> the impacts <strong>of</strong> WG on MetS development is helpful to<br />
health promotion in workplaces. Periodic routine health checkups are compulsorily<br />
for employees at many worksites in Taiwan, thus we had an opportunity to<br />
conduct a workplace-based follow-up observation <strong>of</strong> MetS development. We used<br />
this approach to evaluate the impacts <strong>of</strong> excessive WG on MetS development<br />
among early-middle-aged employees.<br />
Innovations and breakthroughs<br />
In comparison to the control group, mild-WG adults had an insignificant risk for<br />
MetS development, while adults having moderate-WG had a 3.0-fold increased<br />
risk for progression to MetS [95% confidence interval (CI), 1.8-5.1], and this risk<br />
was increased 5.4-fold (95% CI, 3.0-9.7) in subjects having severe-WG. For<br />
females having moderate- and severe-WG, the risk for developing MetS was 3.6<br />
(95% CI, 1.03-12.4) and 5.5 (95% CI, 1.4-21.4), respectively. For males having<br />
moderate- and severe-WG, the odds ratio for MetS outcome was respectively 3.0<br />
(95% CI, 1.6-5.5) and 5.2 (95% CI, 2.6-10.2).<br />
Applications<br />
For early-middle-aged healthy adults with a five-year weight gain over 5%, severity<br />
<strong>of</strong> weight gain is related to the risk for developing metabolic syndrome. We<br />
suggest prioritizing body weight optimization and modifications in dietary behaviors<br />
for the prevention <strong>of</strong> metabolic syndrome among early-middle-aged workers.<br />
Terminology<br />
A designation <strong>of</strong> Metabolic Syndrome was made if three or more <strong>of</strong> the following<br />
five criteria were fulfilled: central obesity (waist circumference > 90 cm for males<br />
and > 80 cm for females based on Taiwanese criteria); High blood pressure<br />
(systolic blood pressure ≥ 130 mmHg or diastolic blood pressure ≥ 85 mmHg);<br />
hyperglycemia (fasting sugar ≥ 100 mg/dL); hypertriglyceridemia (triglycerides<br />
≥ 150 mg/dL); and low-HDL-cholesterolemia (high density lipoprotein cholesterol<br />
(HDL) < 40 mg/dL for males, < 50 for females).<br />
Peer reviews<br />
The major finding <strong>of</strong> the study is that weight gain, especially in the higher centiles<br />
is more likely to be associated with the development <strong>of</strong> the metabolic syndrome.<br />
Overall, this is a timely paper that could lead to public health measures<br />
encouraging exercise and care in the calorie consumption <strong>of</strong> workers in large<br />
plants. The benefits to the involved individuals, the companies they work for and<br />
society at large could be significant.<br />
REFERENCES<br />
1 Seagle HM, Strain GW, Makris A, Reeves RS. Position <strong>of</strong> the<br />
American Dietetic Association: weight management. J Am<br />
Diet Assoc 2009; 109: 330-346<br />
2 Zabetian A, Hadaegh F, Sarbakhsh P, Azizi F. Weight change<br />
and incident metabolic syndrome in Iranian men and women;<br />
a 3 year follow-up study. BMC Public Health 2009; 9: 138<br />
3 Hillier TA, Fagot-Campagna A, Eschwège E, Vol S, Cailleau<br />
M, Balkau B. Weight change and changes in the metabolic<br />
syndrome as the French population moves towards overweight:<br />
the D.E.S.I.R. cohort. Int J Epidemiol 2006; 35: 190-196<br />
4 Yoo HL, Eisenmann JC, Franke WD. Independent and combined<br />
influence <strong>of</strong> physical activity and perceived stress on<br />
the metabolic syndrome in male law enforcement <strong>of</strong>ficers. J<br />
Occup Environ Med 2009; 51: 46-53<br />
5 Sánchez-Chaparro MA, Calvo-Bonacho E, González-Quintela<br />
A, Fernández-Labandera C, Cabrera M, Sáinz JC, Fernández-<br />
Meseguer A, Banegas JR, Ruilope LM, Valdivielso P, Román-<br />
García J. Occupation-related differences in the prevalence <strong>of</strong><br />
metabolic syndrome. <strong>Diabetes</strong> Care 2008; 31: 1884-1885<br />
6 Oberlinner C, Humpert PM, Nawroth PP, Zober A, Morcos<br />
M. Metabolic syndrome in a large chemical company: prevalence<br />
in a screened worksite sample. Acta Diabetol 2008; 45:<br />
31-35<br />
7 León Latre M, Andrés EM, Cordero A, Pascual I, Vispe C,<br />
Laclaustra M, Luengo E, Casasnovas JA. Relationship be-<br />
14 January 15, 2011|Volume 2|Issue 1|
tween metabolic syndrome and ischemic heart disease mortality<br />
in Spain. Rev Esp Cardiol 2009; 62: 1469-1472<br />
8 Burton WN, Chen CY, Schultz AB, Edington DW. The prevalence<br />
<strong>of</strong> metabolic syndrome in an employed population and<br />
the impact on health and productivity. J Occup Environ Med<br />
2008; 50: 1139-1148<br />
9 Garrido RA, Semeraro MB, Temesgen SM, Simi MR. Metabolic<br />
syndrome and obesity among workers at Kanye Seventh-Day<br />
Adventist Hospital, Botswana. S Afr Med J 2009; 99:<br />
331-334<br />
10 Yamada J, Tomiyama H, Matsumoto C, Yoshida M, Koji Y,<br />
Shiina K, Nagata M, Yamashina A. Overweight body mass index<br />
classification modifies arterial stiffening associated with<br />
weight gain in healthy middle-aged Japanese men. Hypertens<br />
Res 2008; 31: 1087-1092<br />
11 Hsu PF, Chuang SY, Cheng HM, Tsai ST, Chou P, Chen CH.<br />
Clinical significance <strong>of</strong> the metabolic syndrome in the absence<br />
<strong>of</strong> established hypertension and diabetes: A communitybased<br />
study. <strong>Diabetes</strong> Res Clin Pract 2008; 79: 461-467<br />
12 Lin YC, Hsiao TJ, Chen PC. Persistent rotating shift-work<br />
exposure accelerates development <strong>of</strong> metabolic syndrome<br />
among middle-aged female employees: a five-year followup.<br />
Chronobiol Int 2009; 26: 740-755<br />
13 Tan CE, Ma S, Wai D, Chew SK, Tai ES. Can we apply the National<br />
Cholesterol Education Program Adult Treatment Panel<br />
definition <strong>of</strong> the metabolic syndrome to Asians? <strong>Diabetes</strong> Care<br />
2004; 27: 1182-1186<br />
14 Alkerwi A, Boutsen M, Vaillant M, Barre J, Lair ML, Albert<br />
A, Guillaume M, Dramaix M. Alcohol consumption and the<br />
prevalence <strong>of</strong> metabolic syndrome: a meta-analysis <strong>of</strong> observational<br />
studies. Atherosclerosis 2009; 204: 624-635<br />
15 Rurik I, Sandholzer H, Kalabay L. Does the dynamicity <strong>of</strong><br />
weight gain predict elements <strong>of</strong> metabolic syndrome? Differences<br />
in weight gain <strong>of</strong> hypertensive, diabetic, and obese<br />
elderly patients: a pilot study in primary care. Med Sci Monit<br />
2009; 15: CR40-CR44<br />
16 Ley SH, Harris SB, Mamakeesick M, Noon T, Fiddler E,<br />
Gittelsohn J, Wolever TM, Connelly PW, Hegele RA, Zinman<br />
B, Hanley AJ. Metabolic syndrome and its components as predictors<br />
<strong>of</strong> incident type 2 diabetes mellitus in an Aboriginal<br />
community. CMAJ 2009; 180: 617-624<br />
17 Mukai N, Doi Y, Ninomiya T, Hata J, Yonemoto K, Iwase M,<br />
Iida M, Kiyohara Y. Impact <strong>of</strong> metabolic syndrome compared<br />
with impaired fasting glucose on the development <strong>of</strong> type<br />
2 diabetes in a general Japanese population: the Hisayama<br />
study. <strong>Diabetes</strong> Care 2009; 32: 2288-2293<br />
18 Weaver TW, Kushi LH, McGovern PG, Potter JD, Rich SS,<br />
King RA, Whitbeck J, Greenstein J, Sellers TA. Validation<br />
study <strong>of</strong> self-reported measures <strong>of</strong> fat distribution. Int J Obes<br />
Relat Metab Disord 1996; 20: 644-650<br />
19 Lin YC, Hsiao TJ, Chen PC. Shift work aggravates metabolic<br />
WJD|www.wjgnet.com<br />
Lin YC et al . Excessive weight gain predicts metabolic syndrome<br />
syndrome development among early-middle-aged males<br />
with elevated ALT. <strong>World</strong> J Gastroenterol 2009; 15: 5654-5661<br />
20 Truesdale KP, Stevens J, Lewis CE, Schreiner PJ, Loria CM,<br />
Cai J. Changes in risk factors for cardiovascular disease by<br />
baseline weight status in young adults who maintain or gain<br />
weight over 15 years: the CARDIA study. Int J Obes (Lond)<br />
2006; 30: 1397-1407<br />
21 Wilson PW, Anderson KM, Harris T, Kannel WB, Castelli<br />
WP. Determinants <strong>of</strong> change in total cholesterol and HDL-C<br />
with age: the Framingham Study. J Gerontol 1994; 49: M2<br />
52-M257<br />
22 Park YW, Chang Y, Sung KC, Ryu S, Sung E, Kim WS. The sequential<br />
changes in the fasting plasma glucose levels within<br />
normoglycemic range predict type 2 diabetes in healthy,<br />
young men. <strong>Diabetes</strong> Res Clin Pract 2006; 73: 329-335<br />
23 Kim S, Parks CG, DeRoo LA, Chen H, Taylor JA, Cawthon<br />
RM, Sandler DP. Obesity and weight gain in adulthood and<br />
telomere length. Cancer Epidemiol Biomarkers Prev 2009; 18:<br />
816-820<br />
24 Nazmi A, Gonzalez DC, Oliveira IO, Horta BL, Gigante DP,<br />
Victora CG. Life course weight gain and C-reactive protein<br />
levels in young adults: findings from a Brazilian birth cohort.<br />
Am J Hum Biol 2009; 21: 192-199<br />
25 Goldbeter A. A model for the dynamics <strong>of</strong> human weight<br />
cycling. J Biosci 2006; 31: 129-136<br />
26 Nelson MC, Kocos R, Lytle LA, Perry CL. Understanding the<br />
perceived determinants <strong>of</strong> weight-related behaviors in late<br />
adolescence: a qualitative analysis among college youth. J<br />
Nutr Educ Behav 2009; 41: 287-292<br />
27 Tholin S, Lindroos A, Tynelius P, Akerstedt T, Stunkard AJ,<br />
Bulik CM, Rasmussen F. Prevalence <strong>of</strong> night eating in obese<br />
and nonobese twins. Obesity (Silver Spring) 2009; 17: 1050-1055<br />
28 La Londe MA, Graffagnino CL, Falko JM, Snow RJ, Spencer<br />
K, Caulin-Glaser T. Effect <strong>of</strong> a weight management program<br />
on the determinants and prevalence <strong>of</strong> metabolic syndrome.<br />
Obesity (Silver Spring) 2008; 16: 637-642<br />
29 Babio N, Bulló M, Salas-Salvadó J. Mediterranean diet and<br />
metabolic syndrome: the evidence. Public Health Nutr 2009;<br />
12: 1607-1617<br />
30 Lopez-Alvarenga JC, Ebbesson SO, Ebbesson LO, Tejero ME,<br />
Voruganti VS, Comuzzie AG. Polyunsaturated fatty acids<br />
effect on serum triglycerides concentration in the presence <strong>of</strong><br />
metabolic syndrome components. The Alaska-Siberia Project.<br />
Metabolism 2010; 59: 86-92<br />
31 Allen P, Thompson JL, Herman CJ, Whyte AN, Wolfe VK,<br />
Qualls C, Helitzer DL. Impact <strong>of</strong> periodic follow-up testing<br />
among urban American Indian women with impaired fasting<br />
glucose. Prev Chronic Dis 2008; 5: A76<br />
32 Nagaya T, Yoshida H, Takahashi H, Kawai M. Markers <strong>of</strong><br />
insulin resistance in day and shift workers aged 30-59 years.<br />
Int Arch Occup Environ Health 2002; 75: 562-568<br />
S- Editor Zhang HN L- Editor Hughes D E- Editor Liu N<br />
15 January 15, 2011|Volume 2|Issue 1|
ness and quality <strong>of</strong> life [5,6] . CPAP is commonly used to<br />
treat OSAS by delivering a constant pressure throughout<br />
inspiration and expiration to maintain upper airway patency<br />
during sleep. It consists <strong>of</strong> a flow generator that delivers<br />
airflow at a constant pressure to the patient through a<br />
mask via a tubing system. CPAP technology has improved<br />
considerably over the years. This technological progress<br />
notwithstanding, patient adherence to CPAP treatment<br />
remains suboptimal and its use during sleep time shows<br />
substantial variation between patients [7] .<br />
CONTINUOUS POSITIVE AIRWAY<br />
PRESSURE: ITS ROLE IN GLUCOSE<br />
HOMEOSTASIS<br />
Not only is CPAP the established treatment for OSAS,<br />
it may also have a favorable effect on insulin resistance<br />
and glucose metabolism in such patients. It has been postulated<br />
that CPAP can ameliorate intermittent hypoxia<br />
and sympathetic overactivation, both pathophysiological<br />
mechanisms responsible for the impaired glucose metabolism<br />
in OSAS patients. This additional therapeutic benefit<br />
conferred by CPAP is now attracting considerable interest<br />
but is still an issue <strong>of</strong> ongoing debate [8] . Indeed, findings<br />
from numerous studies on the effect <strong>of</strong> CPAP treatment<br />
on glucose metabolism, both in diabetic and non-diabetic<br />
populations, have been rather conflicting. This can be<br />
attributed to differences between the studied populations<br />
(i.e. diabetic, non-diabetic, obese or non-obese patients),<br />
the primary outcomes, the method <strong>of</strong> assessment <strong>of</strong> glucose<br />
metabolism (i.e. fasting glucose, glycated hemoglobin,<br />
hyperinsulinemic euglycemic clamp etc.), the period<br />
<strong>of</strong> CPAP application (ranging between 1 night and 2.9<br />
years) [8] and the patient’s adherence to CPAP use [9] . Unfortunately,<br />
only three randomised control studies have so<br />
far examined the effect <strong>of</strong> CPAP on different parameters<br />
<strong>of</strong> glucose metabolism [10-12] and only one, the most recent,<br />
has shown a favorable effect.<br />
The latter [10] demonstrated an increase in insulin sen-<br />
sitivity among the 31 patients with moderate/severe OS<br />
AS who received CPAP treatment, as opposed to no improvement<br />
among the 30 controls receiving sham CPAP.<br />
An additional improvement was also recorded after 12<br />
wk <strong>of</strong> CPAP use in subjects with body mass index exceeding<br />
25 kg/m 2[10] . The authors have used the short<br />
WJD|www.wjgnet.com<br />
Steiropoulos P et al . CPAP in sleep apnea<br />
Table 1 Summary <strong>of</strong> the 3 randomised controlled trials which examined the role <strong>of</strong> continuous positive airway pressure on glucose<br />
homeostasis<br />
Author Patients Duration Methods Results<br />
Lam et al [10]<br />
West et al [11]<br />
Coughlin et al [12]<br />
61 1 wk Short insulin tolerance test Increase in insulin sensitivity after 1 wk <strong>of</strong> CPAP use. Further improvement<br />
after 12 wk in subjects with BMI < 25 kg/m 2<br />
12 wk<br />
42 3 mo Hyperinsulinemic euglycemic clamp,<br />
HOMA index, HbA1C<br />
No difference after 3 mo <strong>of</strong> APAP use<br />
24 6 wk Fasting glucose, insulin, HOMA index No difference<br />
CPAP: continuous positive airway pressure; APAP: automatic positive airway pressure; BMI: body mass index; HbA1c: haemoglobin A1c.<br />
insulin tolerance test, a rapid and simple test that has<br />
been validated against clamp studies [13] and whose short<br />
duration inhibits interference from counter regulatory<br />
hormones [14] . Additional strengths <strong>of</strong> the study include<br />
good CPAP adherence and exclusion <strong>of</strong> OSA patients<br />
with comorbidities, a fact that allows a clear delineation <strong>of</strong><br />
the impact <strong>of</strong> OSA per se on glucose metabolism.<br />
Conversely, two further randomised control studies<br />
indicate that CPAP treatment does not improve glucose<br />
metabolism. The first one by West et al [11] compared 20<br />
OSAS patients receiving automatic positive airway pressure<br />
(APAP) therapy with 22 OSAS patients receiving<br />
sham therapy for 3 mo (Table 1). All patients were male<br />
with established type 2 diabetes mellitus. There was no sig-<br />
nificant change in haemoglobin A1C (HbA1c), insulin sen-<br />
sitivity assessed by euglycemic clamp and HOMA in<br />
either group [11] . Even after excluding 8 patients with poor<br />
compliance, changes remained insignificant [11] . The other<br />
study by Coughlin et al [12] was a randomised placebocontrolled<br />
blinded cross-over trial, comparing 6 wk <strong>of</strong><br />
therapeutic and sham CPAP in 34 obese OSAS patients.<br />
No change occurred in fasting glucose and insulin levels<br />
or insulin resistance, as assessed by HOMA [12] . Nonetheless,<br />
it should be borne in mind that the study period<br />
was rather short. Indeed, the authors themselves queried<br />
whether a prolonged longer study period would be necessary<br />
to reveal significant changes [12] .<br />
Clearly, the role <strong>of</strong> CPAP in the improvement <strong>of</strong> glu-<br />
cose metabolism and insulin sensitivity has not been defined<br />
yet [8] . Results are conflicting which may be explained<br />
by the differences in recruited populations (diabetic or<br />
non-diabetic), adherence to CPAP use, as well as in study<br />
design (duration <strong>of</strong> follow-up) and endpoints (different<br />
parameters <strong>of</strong> insulin resistance and glucose homeostasis)<br />
[8] . In addition, other issues such as the role <strong>of</strong> diet and<br />
exercise should always be addressed.<br />
CONCLUSIONS AND FUTURE<br />
DIRECTIONS<br />
In the light <strong>of</strong> current knowledge, further research therefore<br />
needs to revisit the effect <strong>of</strong> CPAP on glucose homeostasis<br />
[8] . It is important to define which patients stand<br />
to benefit and how long the treatment takes to produce<br />
favorable changes. Moreover, the magnitude <strong>of</strong> the effect<br />
needs to be re-evaluated in terms <strong>of</strong> quantifying the<br />
17 January 15, 2011|Volume 2|Issue 1|
Steiropoulos P et al . CPAP in sleep apnea<br />
changes in insulin sensitivity, fasting and post-prandial glucose<br />
levels and HbA1c. These issues should be addressed<br />
by large-scale, long-term, randomised controlled trials.<br />
In the authors’ opinion, the accumulating evidence for a<br />
positive effect <strong>of</strong> CPAP on glycemic control is very promising<br />
and warrants careful attention. It has recently been<br />
realised that OSAS aggravates glycemic control, even at<br />
the earliest stages <strong>of</strong> glucose intolerance [15] , opening rich<br />
perspectives for application <strong>of</strong> CPAP. Patient health care<br />
is anticipated to have improved by 2020 and physicians<br />
will be able to make better and more individualised use <strong>of</strong><br />
CPAP to affect favorable changes in glucose homeostasis,<br />
targeting both hypoxia and hyperglycemia.<br />
REFERENCES<br />
1 Punjabi NM. The epidemiology <strong>of</strong> adult obstructive sleep<br />
apnea. Proc Am Thorac Soc 2008; 5: 136-143<br />
2 Lévy P, Bonsignore MR, Eckel J. Sleep, sleep-disordered<br />
breathing and metabolic consequences. Eur Respir J 2009; 34:<br />
243-260<br />
3 Spiegel K, Tasali E, Leproult R, Van Cauter E. Effects <strong>of</strong> poor<br />
and short sleep on glucose metabolism and obesity risk. Nat<br />
Rev Endocrinol 2009; 5: 253-261<br />
4 Malhotra A, Ayas NT, Epstein LJ. The art and science <strong>of</strong> continuous<br />
positive airway pressure therapy in obstructive sleep<br />
apnea. Curr Opin Pulm Med 2000; 6: 490-495<br />
5 Giles TL, Lasserson TJ, Smith BH, White J, Wright J, Cates<br />
CJ. Continuous positive airways pressure for obstructive<br />
sleep apnoea in adults. Cochrane Database Syst Rev 2006; 3:<br />
CD001106<br />
6 Gordon P, Sanders MH. Sleep.7: positive airway pressure<br />
WJD|www.wjgnet.com<br />
therapy for obstructive sleep apnoea/hypopnoea syndrome.<br />
Thorax 2005; 60: 68-75<br />
7 Weaver TE, Kribbs NB, Pack AI, Kline LR, Chugh DK, Maislin<br />
G, Smith PL, Schwartz AR, Schubert NM, Gillen KA,<br />
Dinges DF. Night-to-night variability in CPAP use over the<br />
first three months <strong>of</strong> treatment. Sleep 1997; 20: 278-283<br />
8 Steiropoulos P, Papanas N, Nena E, Maltezos E, Bouros D.<br />
Continuous positive airway pressure treatment in patients<br />
with sleep apnoea: does it really improve glucose metabolism?<br />
Curr <strong>Diabetes</strong> Rev 2010; 6: 156-166<br />
9 Steiropoulos P, Papanas N, Maltezos E, Bouros D. Is there<br />
a metabolic effect <strong>of</strong> continuous positive airway pressure in<br />
sleep apnoea? Adherence should not be underestimated. Eur<br />
Respir J 2009; 34: 1209-1210; author reply 1210-1211<br />
10 Lam JC, Lam B, Yao TJ, Lai AY, Ooi CG, Tam S, Lam KS, Ip<br />
MS. A randomised controlled trial <strong>of</strong> nasal continuous positive<br />
airway pressure on insulin sensitivity in obstructive<br />
sleep apnoea. Eur Respir J 2010; 35: 138-145<br />
11 West SD, Nicoll DJ, Wallace TM, Matthews DR, Stradling JR.<br />
Effect <strong>of</strong> CPAP on insulin resistance and HbA1c in men with<br />
obstructive sleep apnoea and type 2 diabetes. Thorax 2007; 62:<br />
969-974<br />
12 Coughlin SR, Mawdsley L, Mugarza JA, Wilding JP, Calverley<br />
PM. Cardiovascular and metabolic effects <strong>of</strong> CPAP in<br />
obese males with OSA. Eur Respir J 2007; 29: 720-727<br />
13 Bonora E, Moghetti P, Zancanaro C, Cigolini M, Querena M,<br />
Cacciatori V, Corgnati A, Muggeo M. Estimates <strong>of</strong> in vivo<br />
insulin action in man: comparison <strong>of</strong> insulin tolerance tests<br />
with euglycemic and hyperglycemic glucose clamp studies. J<br />
Clin Endocrinol Metab 1989; 68: 374-378<br />
14 Wallace TM, Matthews DR. The assessment <strong>of</strong> insulin resistance<br />
in man. Diabet Med 2002; 19: 527-534<br />
15 Steiropoulos P, Papanas N, Bouros D, Maltezos E. Obstructive<br />
sleep apnea aggravates glycemic control across the continuum<br />
<strong>of</strong> glucose homeostasis. Am J Respir Crit Care Med<br />
2010; 182: 286<br />
S- Editor Zhang HN L- Editor Roemmele A E- Editor Liu N<br />
18 January 15, 2011|Volume 2|Issue 1|
Online Submissions: http://www.wjgnet.com/1948-9358<strong>of</strong>fice<br />
wjd@wjgnet.com<br />
www.wjgnet.com<br />
ACKNOWLEDGMENTS<br />
Acknowledgments to reviewers <strong>of</strong> <strong>World</strong> <strong>Journal</strong> <strong>of</strong><br />
<strong>Diabetes</strong><br />
Many reviewers have contributed their expertise and<br />
time to the peer review, a critical process to ensure the<br />
quality <strong>of</strong> <strong>World</strong> <strong>Journal</strong> <strong>of</strong> <strong>Diabetes</strong>. The editors and<br />
authors <strong>of</strong> the articles submitted to the journal are<br />
grateful to the following reviewers for evaluating the<br />
articles (including those published in this issue and those<br />
rejected for this issue) during the last editing time period.<br />
Marcin Baranowski, PhD, Department <strong>of</strong> Physiology, Medical<br />
University <strong>of</strong> Bialystok, Mickiewicza 2c, Bialystok 15-222, Poland<br />
Narattaphol Charoenphandhu, MD, PhD, Department <strong>of</strong> Physiology,<br />
Faculty <strong>of</strong> Science, Mahidol University, Rama VI Road,<br />
Bangkok 10400, Thailand<br />
Nigel Irwin, PhD, School <strong>of</strong> Biomedical Sciences, University <strong>of</strong><br />
Ulster, Coleraine, Northern Ireland, BT52 1SA, United Kingdom<br />
Arulmozhi D Kandasamy, PhD, Cardiovascular Research Centre,<br />
4-62 Heritage Medical Research Centre, University <strong>of</strong> Alberta, Edmonton<br />
T6G 2S2, Alberta, Canada<br />
Reema Mody, PhD, MBA, Principal Scientist, Global Health<br />
Economic and Outcomes Research, Takeda Pharmaceuticals International,<br />
Inc., 33976 Wooded Glen Dr. Grayslake, IL 60030, United<br />
States<br />
Joseph Fomusi Ndisang, PharmD, PhD, Assistant Pr<strong>of</strong>essor,<br />
College <strong>of</strong> Medicine, Epartment <strong>of</strong> Physiology, University <strong>of</strong> Saskatchewan,<br />
107 Wiggins Road, Saskatoon, SK, Canada<br />
WJD|www.wjgnet.com I<br />
<strong>World</strong> J <strong>Diabetes</strong> 2011 January 15; 2(1): I<br />
ISSN 1948-9358 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
Craig S Nunemaker, PhD, University <strong>of</strong> Virginia, Charlottesville,<br />
VA 22901, United States<br />
Luciano Pirola, PhD, Epigenetics in Human Health and Disease<br />
Laboratory, Baker IDI Heart and <strong>Diabetes</strong> Institute, 75 Commercial<br />
Road, Melbourne, VIC 3004, Australia<br />
Cristina Rabadán-Diehl, PhD, MPH, Program Director, Division<br />
<strong>of</strong> Cardiovascular Diseases, National Heart, Lung, and Blood<br />
Institute/NIH, Rockledge II, Suite 8156, 6701 Rockledge Drive,<br />
Bethesda, MD 20892-7956, United States<br />
Mark A Sperling, MD, Pr<strong>of</strong>essor <strong>of</strong> Pediatrics, Children's Hospital<br />
<strong>of</strong> Pittsburgh <strong>of</strong> UPMC, 4401 Penn Avenue, Division <strong>of</strong> Endocrinology,<br />
Faculty Pavilion -8th Floor, Pittsburgh, PA 15224, United<br />
States<br />
Greg Tesch, PhD, Department <strong>of</strong> Nephrology, Monash Medical<br />
Centre, 246 Clayton Road, Clayton, Victoria 3168, Australia<br />
Yoshinari Uehara, MD, PhD, Department <strong>of</strong> Cardiology, Fukuoka<br />
University Faculty <strong>of</strong> Medicine, 7-45-1 Nanakuma, Jonan-ku,<br />
Fukuoka 814-0180 Japan<br />
Vladimir N Uversky, Senior Research Pr<strong>of</strong>essor, Center for<br />
Computational Biology & Bioinformatics, Department <strong>of</strong> Biochemistry<br />
and Molecular Biology, Indiana University School <strong>of</strong> Medicine,<br />
Indianapolis, IN 46202, United States<br />
Kevin CJ Yuen, MBChB, MRCP, CCST, MD, Department <strong>of</strong><br />
Endocrinology, Oregon Health and Science University, 3181 SW<br />
Sam Jackson Park Road, Mailcode L607, Portland, OR 97239,<br />
United States<br />
January 15, 2011|Volume 2|Issue 1|
Online Submissions: http://www.wjgnet.com/1948-9358<strong>of</strong>fice<br />
wjd@wjgnet.com<br />
www.wjgnet.com<br />
Meetings<br />
Events Calendar 2011<br />
January 14-15, 2011<br />
AGA Clinical Congress <strong>of</strong><br />
Gastroenterology and Hepatology:<br />
Best Practices in 2011 Miami<br />
FL, United States<br />
January 28, 2011<br />
<strong>Diabetes</strong> UK and External<br />
Conferences<br />
<strong>Diabetes</strong> Awareness Training<br />
London, United Kingdom<br />
January 28-29, 2011<br />
9. Gastro Forum München<br />
Munich, Germany<br />
February 13-27, 2011<br />
Gastroenterology: New Zealand<br />
CME Cruise Conference<br />
Sydney, NSW, Australia<br />
February 16-19, 2011<br />
The 4th International Conference on<br />
Advance Technologies & Treatments<br />
for <strong>Diabetes</strong><br />
London, United Kingdom<br />
February 24-26, 2011<br />
2nd International Congress on<br />
Abdominal Obesity<br />
Buenos Aires, Brazil<br />
February 26-March 1, 2011<br />
Canadian Digestive Diseases Week,<br />
Westin Bayshore, Vancouver<br />
British Columbia, Canada<br />
February 28-March 1, 2011<br />
Childhood & Adolescent Obesity: A<br />
Whole-system Strategic Approach<br />
Abu Dhabi, United Arab Emirates<br />
March 3-5, 2011<br />
42nd Annual Topics in Internal<br />
Medicine<br />
Gainesville, FL, United States<br />
March 14-17, 2011<br />
British Society <strong>of</strong> Gastroenterology<br />
Annual Meeting 2011, Birmingham<br />
England, United Kingdom<br />
March 17-20, 2011<br />
Mayo Clinic Gastroenterology &<br />
Hepatology<br />
Jacksonville, FL , United States<br />
March 18, 2011<br />
UC Davis Health Informatics:<br />
Change Management and Health<br />
Informatics, The Keys to Health<br />
Reform<br />
Sacramento, CA, United States<br />
March 25-27, 2011<br />
MedicReS IC 2011 Good Medical<br />
Research<br />
Istanbul, Turkey<br />
March 28–30, 2011<br />
The Second <strong>World</strong> Congress on<br />
Interventional Therapies for Type 2<br />
<strong>Diabetes</strong><br />
New York, United States<br />
April 25-27, 2011<br />
The Second International Conference<br />
<strong>of</strong> the Saudi Society <strong>of</strong> Pediatric<br />
Gastroenterology, Hepatology &<br />
Nutrition<br />
Riyadh, Saudi Arabia<br />
May 7-10, 2011<br />
Digestive Disease Week<br />
Chicago, IL, United States<br />
WJD|www.wjgnet.com I<br />
June 2-5, 2011<br />
The 1st Asia Pacific Congress on<br />
Controversies to Consensus in<br />
<strong>Diabetes</strong>, Obesity and Hypertension<br />
Shanghai, China<br />
June 11-12, 2011<br />
The International Digestive Disease<br />
Forum 2011<br />
Hong Kong, China<br />
June 22-25, 2011<br />
ESMO Conference: 13th <strong>World</strong><br />
Congress on Gastrointestinal Cancer<br />
Barcelona, Spain<br />
August 3-6, 2011<br />
AADE 38th Annual Meeting<br />
Las Vegas, United States<br />
October 16-18, 2011<br />
ISPAD Science School for Health<br />
Pr<strong>of</strong>essionals<br />
Miami, Unites States<br />
October 19-22, 2011<br />
ISPAD 36th Annual Meeting<br />
Miami, United States<br />
October 22-26, 2011<br />
19th United European<br />
Gastroenterology Week<br />
Stockholm, Sweden<br />
October 26-29, 2011<br />
CDA/CSEM Pr<strong>of</strong>essional<br />
Conference and Annual Meetings<br />
Toronto, Ontario, Canada<br />
October 28-November 2, 2011<br />
ACG Annual Scientific Meeting &<br />
Postgraduate Course<br />
Washington, DC, United States<br />
November 10-12, 2011<br />
The Second International <strong>Diabetes</strong> &<br />
Obesity Forum<br />
Istanbul, Turkey<br />
<strong>World</strong> J <strong>Diabetes</strong> 2011 January 15; 2(1): I<br />
ISSN 1948-9358 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
January 15, 2011|Volume 2|Issue 1|
Online Submissions: http://www.wjgnet.com/1948-9358<strong>of</strong>fice<br />
wjd@wjgnet.com<br />
www.wjgnet.com<br />
Instructions to authors<br />
GENERAL INFORMATION<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> <strong>Diabetes</strong> (<strong>World</strong> J <strong>Diabetes</strong>, WJD, online ISSN<br />
1948-9358, DOI: 10.4239), is a monthly, open-access (OA), pe<br />
er-reviewed journal supported by an editorial board <strong>of</strong> 323 experts<br />
in diabetes mellitus research from 38 countries.<br />
The biggest advantage <strong>of</strong> the OA model is that it provides<br />
free, full-text articles in PDF and other formats for experts and<br />
the public without registration, which eliminates the obstacle that<br />
traditional journals possess and usually delays the speed <strong>of</strong> the<br />
propagation and communication <strong>of</strong> scientific research results.<br />
Maximization <strong>of</strong> personal benefits<br />
The role <strong>of</strong> academic journals is to exhibit the scientific levels <strong>of</strong><br />
a country, a university, a center, a department, and even a scientist,<br />
and build an important bridge for communication between<br />
scientists and the public. As we all know, the significance <strong>of</strong> the<br />
publication <strong>of</strong> scientific articles lies not only in disseminating<br />
and communicating innovative scientific achievements and academic<br />
views, as well as promoting the application <strong>of</strong> scientific<br />
achievements, but also in formally recognizing the “priority” and<br />
“copyright” <strong>of</strong> innovative achievements published, as well as<br />
evaluating research performance and academic levels. So, to realize<br />
these desired attributes <strong>of</strong> WJD and create a well-recognized<br />
journal, the following four types <strong>of</strong> personal benefits should be<br />
maximized. The maximization <strong>of</strong> personal benefits refers to the<br />
pursuit <strong>of</strong> the maximum personal benefits in a well-considered<br />
optimal manner without violation <strong>of</strong> the laws, ethical rules and the<br />
benefits <strong>of</strong> others. (1) Maximization <strong>of</strong> the benefits <strong>of</strong> editorial<br />
board members: The primary task <strong>of</strong> editorial board members<br />
is to give a peer review <strong>of</strong> an unpublished scientific article via<br />
online <strong>of</strong>fice system to evaluate its innovativeness, scientific and<br />
practical values and determine whether it should be published or<br />
not. During peer review, editorial board members can also obtain<br />
cutting-edge information in that field at first hand. As leaders in<br />
their field, they have priority to be invited to write articles and<br />
publish commentary articles. We will put peer reviewers’ names<br />
and affiliations along with the article they reviewed in the journal to<br />
acknowledge their contribution; (2) Maximization <strong>of</strong> the benefits<br />
<strong>of</strong> authors: Since WJD is an open-access journal, readers around<br />
the world can immediately download and read, free <strong>of</strong> charge, highquality,<br />
peer-reviewed articles from WJD <strong>of</strong>ficial website, thereby<br />
realizing the goals and significance <strong>of</strong> the communication between<br />
authors and peers as well as public reading; (3) Maximization <strong>of</strong><br />
the benefits <strong>of</strong> readers: Readers can read or use, free <strong>of</strong> charge,<br />
high-quality peer-reviewed articles without any limits, and cite<br />
the arguments, viewpoints, concepts, theories, methods, results,<br />
conclusion or facts and data <strong>of</strong> pertinent literature so as to validate<br />
the innovativeness, scientific and practical values <strong>of</strong> their own<br />
research achievements, thus ensuring that their articles have novel<br />
arguments or viewpoints, solid evidence and correct conclusion;<br />
and (4) Maximization <strong>of</strong> the benefits <strong>of</strong> employees: It is an<br />
iron law that a first-class journal is unable to exist without firstclass<br />
editors, and only first-class editors can create a first-class<br />
academic journal. We insist on strengthening our team cultivation<br />
and construction so that every employee, in an open, fair and<br />
transparent environment, could contribute their wisdom to edit<br />
and publish high-quality articles, thereby realizing the maximization<br />
<strong>of</strong> the personal benefits <strong>of</strong> editorial board members, authors and<br />
readers, and yielding the greatest social and economic benefits.<br />
WJD|www.wjgnet.com<br />
I<br />
<strong>World</strong> J <strong>Diabetes</strong> 2011 January 15; 2(1): I-V<br />
ISSN 1948-9358 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
Aims and scope<br />
The major task <strong>of</strong> WJD is to report rapidly the most recent results<br />
in basic and clinical research on diabetes including: metabolic syndrome,<br />
functions <strong>of</strong> α, β, δ and PP cells <strong>of</strong> the pancreatic islets,<br />
effect <strong>of</strong> insulin and insulin resistance, pancreatic islet transplantation,<br />
adipose cells and obesity, clinical trials, clinical diagnosis and<br />
treatment, rehabilitation, nursing and prevention. This covers epidemiology,<br />
etiology, immunology, pathology, genetics, genomics,<br />
proteomics, pharmacology, pharmacokinetics, pharmacogenetics,<br />
diagnosis and therapeutics. Reports on new techniques for treating<br />
diabetes are also welcome.<br />
Columns<br />
The columns in the issues <strong>of</strong> WJD will include: (1) Editorial: To<br />
introduce and comment on major advances and developments<br />
in the field; (2) Frontier: To review representative achievements,<br />
comment on the state <strong>of</strong> current research, and propose directions<br />
for future research; (3) Topic Highlight: This column consists <strong>of</strong><br />
three formats, including (A) 10 invited review articles on a hot<br />
topic, (B) a commentary on common issues <strong>of</strong> this hot topic, and<br />
(C) a commentary on the 10 individual articles; (4) Observation:<br />
To update the development <strong>of</strong> old and new questions, highlight<br />
unsolved problems, and provide strategies on how to solve the<br />
questions; (5) Guidelines for Basic Research: To provide guidelines<br />
for basic research; (6) Guidelines for Clinical Practice: To provide<br />
guidelines for clinical diagnosis and treatment; (7) Review: To<br />
review systemically progress and unresolved problems in the field,<br />
comment on the state <strong>of</strong> current research, and make suggestions<br />
for future work; (8) Original Article: To report innovative and<br />
original findings in diabetes; (9) Brief Article: To briefly report<br />
the novel and innovative findings in diabetes research; (10) Case<br />
Report: To report a rare or typical case; (11) Letters to the Editor:<br />
To discuss and make reply to the contributions published in WJD,<br />
or to introduce and comment on a controversial issue <strong>of</strong> general<br />
interest; (12) Book Reviews: To introduce and comment on quality<br />
monographs <strong>of</strong> diabetes mellitus; and (13) Guidelines: To introduce<br />
consensuses and guidelines reached by international and national<br />
academic authorities worldwide on basic research and clinical<br />
practice in diabetes mellitus.<br />
Name <strong>of</strong> journal<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> <strong>Diabetes</strong><br />
CSSN<br />
ISSN 1948-9358 (online)<br />
Indexing/abstracting<br />
PubMed Central,PubMed<br />
Published by<br />
Baishideng Publishing Group Co., Limited<br />
SPECIAL STATEMENT<br />
All articles published in this journal represent the viewpoints <strong>of</strong> the<br />
authors except where indicated otherwise.<br />
Biostatistical editing<br />
Statisital review is performed after peer review. We invite an expert<br />
in Biomedical Statistics from to evaluate the statistical method used<br />
in the paper, including t-test (group or paired comparisons), chisquared<br />
test, Ridit, probit, logit, regression (linear, curvilinear, or<br />
January 15, 2011|Volume 2|Issue 1|
Instructions to authors<br />
stepwise), correlation, analysis <strong>of</strong> variance, analysis <strong>of</strong> covariance,<br />
etc. The reviewing points include: (1) Statistical methods should be<br />
described when they are used to verify the results; (2) Whether the<br />
statistical techniques are suitable or correct; (3) Only homogeneous<br />
data can be averaged. Standard deviations are preferred to standard<br />
errors. Give the number <strong>of</strong> observations and subjects (n). Losses<br />
in observations, such as drop-outs from the study should be reported;<br />
(4) Values such as ED50, LD50, IC50 should have their<br />
95% confidence limits calculated and compared by weighted probit<br />
analysis (Bliss and Finney); and (5) The word ‘significantly’ should<br />
be replaced by its synonyms (if it indicates extent) or the P value (if<br />
it indicates statistical significance).<br />
Conflict-<strong>of</strong>-interest statement<br />
In the interests <strong>of</strong> transparency and to help reviewersassess any<br />
potential bias, WJD requires authors <strong>of</strong> all papers to declare any<br />
competing commercial, personal, political, intellectual, or religious<br />
interests in relation to the submitted work. Referees are also asked<br />
to indicate any potential conflict they might have reviewing a<br />
particular paper. Before submitting, authors are suggested to read<br />
“Uniform Requirements for Manuscripts Submitted to Biomedical<br />
<strong>Journal</strong>s: Ethical Considerations in the Conduct and Reporting <strong>of</strong><br />
Research: Conflicts <strong>of</strong> Interest” from International Committee <strong>of</strong><br />
Medical <strong>Journal</strong> Editors (ICMJE), which is available at: http://www.<br />
icmje.org/ethical_4conflicts.html.<br />
Sample wording: [Name <strong>of</strong> individual] has received fees for<br />
serving as a speaker, a consultant and an advisory board member for<br />
[names <strong>of</strong> organizations], and has received research funding from<br />
[names <strong>of</strong> organization]. [Name <strong>of</strong> individual] is an employee <strong>of</strong><br />
[name <strong>of</strong> organization]. [Name <strong>of</strong> individual] owns stocks and shares<br />
in [name <strong>of</strong> organization]. [Name <strong>of</strong> individual] owns patent [patent<br />
identification and brief description].<br />
Statement <strong>of</strong> informed consent<br />
Manuscripts should contain a statement to the effect that all human<br />
studies have been reviewed by the appropriate ethics committee<br />
or it should be stated clearly in the text that all persons gave their<br />
informed consent prior to their inclusion in the study. Details that<br />
might disclose the identity <strong>of</strong> the subjects under study should be<br />
omitted. Authors should also draw attention to the Code <strong>of</strong> Ethics<br />
<strong>of</strong> the <strong>World</strong> Medical Association (Declaration <strong>of</strong> Helsinki, 1964,<br />
as revised in 2004).<br />
Statement <strong>of</strong> human and animal rights<br />
When reporting the results from experiments, authors should<br />
follow the highest standards and the trial should comform to Good<br />
Clinical Practice (for example, US Food and Drug Administration<br />
Good Clinical Practice in FDA-Regulated Clinical Trials; UK<br />
Medicines Research Council Guidelines for Good Clinical Practice<br />
in Clinical Trials) and/or the <strong>World</strong> Medical Association Declaration<br />
<strong>of</strong> Helsinki. Generally, we suggest authors follow the lead investigator’s<br />
national standard. If doubt exists whether the research<br />
was conducted in accordance with the above standards, the authors<br />
must explain the rationale for their approach and demonstrate<br />
that the institutional review body explicitly approved the doubtful<br />
aspects <strong>of</strong> the study.<br />
Before submitting, authors should make their study approved<br />
by the relevant research ethics committee or institutional review<br />
board. If human participants were involved, manuscripts must be<br />
accompanied by a statement that the experiments were undertaken<br />
with the understanding and appropriate informed consent <strong>of</strong> each.<br />
Any personal item or information will not be published without<br />
explicit consents from the involved patients. If experimental animals<br />
were used, the materials and methods (experimental procedures)<br />
section must clearly indicate that appropriate measures were taken to<br />
minimize pain or discomfort, and details <strong>of</strong> animal care should be<br />
provided.<br />
SUBMISSION OF MANUSCRIPTS<br />
Manuscripts should be typed in 1.5 line spacing and 12 pt. Book<br />
WJD|www.wjgnet.com II<br />
Antiqua with ample margins. Number all pages consecutively, and<br />
start each <strong>of</strong> the following sections on a new page: Title Page, Abstract,<br />
Introduction, Materials and Methods, Results, Discussion,<br />
Acknowledgements, References, Tables, Figures, and Figure Legends.<br />
Neither the editors nor the publisher are responsible for the<br />
opinions expressed by contributors. Manuscripts formally accepted<br />
for publication become the permanent property <strong>of</strong> Baishideng<br />
Publishing Group Co., Limited, and may not be reproduced by any<br />
means, in whole or in part, without the written permission <strong>of</strong> both<br />
the authors and the publisher. We reserve the right to copy-edit and<br />
put onto our website accepted manuscripts. Authors should follow<br />
the relevant guidelines for the care and use <strong>of</strong> laboratory animals<br />
<strong>of</strong> their institution or national animal welfare committee. For the<br />
sake <strong>of</strong> transparency in regard to the performance and reporting<br />
<strong>of</strong> clinical trials, we endorse the policy <strong>of</strong> the International Committee<br />
<strong>of</strong> Medical <strong>Journal</strong> Editors to refuse to publish papers<br />
on clinical trial results if the trial was not recorded in a publiclyaccessible<br />
registry at its outset. The only register now available,<br />
to our knowledge, is http://www. clinicaltrials.gov sponsored by<br />
the United States National Library <strong>of</strong> Medicine and we encourage<br />
all potential contributors to register with it. However, in the case<br />
that other registers become available you will be duly notified. A<br />
letter <strong>of</strong> recommendation from each author’s organization should<br />
be provided with the contributed article to ensure the privacy and<br />
secrecy <strong>of</strong> research is protected.<br />
Authors should retain one copy <strong>of</strong> the text, tables, photographs<br />
and illustrations because rejected manuscripts will not be returned<br />
to the author(s) and the editors will not be responsible for loss or<br />
damage to photographs and illustrations sustained during mailing.<br />
Online submissions<br />
Manuscripts should be submitted through the Online Submission<br />
System at: http://www.wjgnet.com/1948-9358<strong>of</strong>fice. Authors are<br />
highly recommended to consult the ONLINE INSTRUCTIONS<br />
TO AUTHORS (http://www.wjgnet.com/1948-9358/<br />
g_info_20100107165233.htm) before attempting to submit online.<br />
For assistance, authors encountering problems with the Online<br />
Submission System may send an email describing the problem<br />
to wjd@wjgnet.com, or by telephone: +86-10-59080038. If you<br />
submit your manuscript online, do not make a postal contribution.<br />
Repeated online submission for the same manuscript is strictly<br />
prohibited.<br />
MANUSCRIPT PREPARATION<br />
All contributions should be written in English. All articles must be<br />
submitted using word-processing s<strong>of</strong>tware. All submissions must<br />
be typed in 1.5 line spacing and 12 pt. Book Antiqua with ample<br />
margins. Style should conform to our house format. Required<br />
information for each <strong>of</strong> the manuscript sections is as follows:<br />
Title page<br />
Title: Title should be less than 12 words.<br />
Running title: A short running title <strong>of</strong> less than 6 words should<br />
be provided.<br />
Authorship: Authorship credit should be in accordance with the<br />
standard proposed by International Committee <strong>of</strong> Medical <strong>Journal</strong><br />
Editors, based on (1) substantial contributions to conception and<br />
design, acquisition <strong>of</strong> data, or analysis and interpretation <strong>of</strong> data; (2)<br />
drafting the article or revising it critically for important intellectual<br />
content; and (3) final approval <strong>of</strong> the version to be published. Authors<br />
should meet conditions 1, 2, and 3.<br />
Institution: Author names should be given first, then the complete<br />
name <strong>of</strong> institution, city, province and postcode. For example, Xu-<br />
Chen Zhang, Li-Xin Mei, Department <strong>of</strong> Pathology, Chengde<br />
Medical College, Chengde 067000, Hebei Province, China. One<br />
author may be represented from two institutions, for example, George<br />
Sgourakis, Department <strong>of</strong> General, Visceral, and Transplan-<br />
January 15, 2011|Volume 2|Issue 1|
tation Surgery, Essen 45122, Germany; George Sgourakis, 2nd<br />
Surgical Department, Korgialenio-Benakio Red Cross Hospital,<br />
Athens 15451, Greece<br />
Author contributions: The format <strong>of</strong> this section should be:<br />
Author contributions: Wang CL and Liang L contributed equally<br />
to this work; Wang CL, Liang L, Fu JF, Zou CC, Hong F and Wu<br />
XM designed the research; Wang CL, Zou CC, Hong F and Wu<br />
XM performed the research; Xue JZ and Lu JR contributed new<br />
reagents/analytic tools; Wang CL, Liang L and Fu JF analyzed the<br />
data; and Wang CL, Liang L and Fu JF wrote the paper.<br />
Supportive foundations: The complete name and number <strong>of</strong><br />
supportive foundations should be provided, e.g., Supported by<br />
National Natural Science Foundation <strong>of</strong> China, No. 30224801<br />
Correspondence to: Only one corresponding address should<br />
be provided. Author names should be given first, then author<br />
title, affiliation, the complete name <strong>of</strong> institution, city, postcode,<br />
province, country, and email. All the letters in the email should be<br />
in lower case. A space interval should be inserted between country<br />
name and email address. For example, Montgomery Bissell, MD,<br />
Pr<strong>of</strong>essor <strong>of</strong> Medicine, Chief, Liver Center, Gastroenterology<br />
Division, University <strong>of</strong> California, Box 0538, San Francisco, CA<br />
94143, United States. montgomery.bissell@ucsf.edu<br />
Telephone and fax: Telephone and fax should consist <strong>of</strong> +,<br />
country number, district number and telephone or fax number, e.g.,<br />
Telephone: +86-10-59080039 Fax: +86-10-85381893<br />
Peer reviewers: All articles received are subject to peer review.<br />
Normally, three experts are invited for each article. Decision for<br />
acceptance is made only when at least two experts recommend<br />
an article for publication. Reviewers for accepted manuscripts are<br />
acknowledged in each manuscript, and reviewers <strong>of</strong> articles which<br />
were not accepted will be acknowledged at the end <strong>of</strong> each issue.<br />
To ensure the quality <strong>of</strong> the articles published in WJD, reviewers<br />
<strong>of</strong> accepted manuscripts will be announced by publishing the<br />
name, title/position and institution <strong>of</strong> the reviewer in the footnote<br />
accompanying the printed article. For example, reviewers: Pr<strong>of</strong>essor<br />
Jing-Yuan Fang, Shanghai Institute <strong>of</strong> Digestive Disease, Shanghai,<br />
Affiliated Renji Hospital, Medical Faculty, Shanghai Jiaotong<br />
University, Shanghai, China; Pr<strong>of</strong>essor Xin-Wei Han, Department<br />
<strong>of</strong> Radiology, The First Affiliated Hospital, Zhengzhou University,<br />
Zhengzhou, Henan Province, China; and Pr<strong>of</strong>essor Anren Kuang,<br />
Department <strong>of</strong> Nuclear Medicine, Huaxi Hospital, Sichuan University,<br />
Chengdu, Sichuan Province, China.<br />
Abstract<br />
There are unstructured abstracts (no more than 256 words) and<br />
structured abstracts (no more than 480). The specific requirements<br />
for structured abstracts are as follows:<br />
An informative, structured abstracts <strong>of</strong> no more than 480<br />
words should accompany each manuscript. Abstracts for original<br />
contributions should be structured into the following sections. AIM<br />
(no more than 20 words): Only the purpose should be included.<br />
Please write the aim as the form <strong>of</strong> “To investigate/study/…;<br />
MATERIALS AND METHODS (no more than 140 words);<br />
RESULTS (no more than 294 words): You should present P values<br />
where appropriate and must provide relevant data to illustrate<br />
how they were obtained, e.g. 6.92 ± 3.86 vs 3.61 ± 1.67, P < 0.001;<br />
CONCLUSION (no more than 26 words).<br />
Key words<br />
Please list 5-10 key words, selected mainly from Index Medicus, which<br />
reflect the content <strong>of</strong> the study.<br />
Text<br />
For articles <strong>of</strong> these sections, original articles, rapid communication<br />
and case reports, the main text should be structured into<br />
the following sections: INTRODUCTION, MATERIALS AND<br />
WJD|www.wjgnet.com III<br />
Instructions to authors<br />
METHODS, RESULTS and DISCUSSION, and should include<br />
appropriate Figures and Tables. Data should be presented in the<br />
main text or in Figures and Tables, but not in both. The main<br />
text format <strong>of</strong> these sections, editorial, topic highlight, case<br />
report, letters to the editors, can be found at: http://www.wjgnet.<br />
com/1948-9358/g_info_20100107165233.htm.<br />
Illustrations<br />
Figures should be numbered as 1, 2, 3, etc., and mentioned clearly<br />
in the main text. Provide a brief title for each figure on a separate<br />
page. Detailed legends should not be provided under the figures.<br />
This part should be added into the text where the figures are<br />
applicable. Figures should be either Photoshop or Illustrator<br />
files (in tiff, eps, jpeg formats) at high-resolution. Examples can<br />
be found at: http://www.wjgnet.com/1007-9327/13/4520.<br />
pdf; http://www.wjgnet.com/1007-9327/13/4554.pdf;<br />
http://www.wjgnet.com/1007-9327/13/4891.pdf; http://<br />
www.wjgnet.com/1007-9327/13/4986.pdf; http://www.<br />
wjgnet.com/1007-9327/13/4498.pdf. Keeping all elements<br />
compiled is necessary in line-art image. Scale bars should be<br />
used rather than magnification factors, with the length <strong>of</strong> the bar<br />
defined in the legend rather than on the bar itself. File names should<br />
identify the figure and panel. Avoid layering type directly over<br />
shaded or textured areas. Please use uniform legends for the<br />
same subjects. For example: Figure 1 Pathological changes in<br />
atrophic gastritis after treatment. A: ...; B: ...; C: ...; D: ...; E: ...; F: ...;<br />
G: …etc. It is our principle to publish high resolution-figures for the<br />
printed and E-versions.<br />
Tables<br />
Three-line tables should be numbered 1, 2, 3, etc., and mentioned<br />
clearly in the main text. Provide a brief title for each table.<br />
Detailed legends should not be included under tables, but rather<br />
added into the text where applicable. The information should<br />
complement, but not duplicate the text. Use one horizontal line<br />
under the title, a second under column heads, and a third below<br />
the Table, above any footnotes. Vertical and italic lines should be<br />
omitted.<br />
Notes in tables and illustrations<br />
Data that are not statistically significant should not be noted. a P <<br />
0.05, b P < 0.01 should be noted (P > 0.05 should not be noted). If<br />
there are other series <strong>of</strong> P values, c P < 0.05 and d P < 0.01 are used.<br />
A third series <strong>of</strong> P values can be expressed as e P < 0.05 and f P < 0.01.<br />
Other notes in tables or under illustrations should be expressed as<br />
1 F, 2 F, 3 F; or sometimes as other symbols with a superscript (Arabic<br />
numerals) in the upper left corner. In a multi-curve illustration, each<br />
curve should be labeled with ●, ○, ■, □, ▲, △, etc., in a certain<br />
sequence.<br />
Acknowledgments<br />
Brief acknowledgments <strong>of</strong> persons who have made genuine contributions<br />
to the manuscript and who endorse the data and conclusions<br />
should be included. Authors are responsible for obtaining<br />
written permission to use any copyrighted text and/or illustrations.<br />
REFERENCES<br />
Coding system<br />
The author should number the references in Arabic numerals<br />
according to the citation order in the text. Put reference numbers<br />
in square brackets in superscript at the end <strong>of</strong> citation content or<br />
after the cited author’s name. For citation content which is part <strong>of</strong><br />
the narration, the coding number and square brackets should be<br />
typeset normally. For example, “Crohn’s disease (CD) is associated<br />
with increased intestinal permeability [1,2] ”. If references are cited<br />
directly in the text, they should be put together within the text, for<br />
example, “From references [19,22-24] , we know that...”<br />
When the authors write the references, please ensure that<br />
the order in text is the same as in the references section, and also<br />
ensure the spelling accuracy <strong>of</strong> the first author’s name. Do not list<br />
the same citation twice.<br />
January 15, 2011|Volume 2|Issue 1|
Instructions to authors<br />
PMID and DOI<br />
Pleased provide PubMed citation numbers to the reference list,<br />
e.g. PMID and DOI, which can be found at http://www.ncbi.<br />
nlm.nih.gov/sites/entrez?db=pubmed and http://www.crossref.<br />
org/SimpleTextQuery/, respectively. The numbers will be used in<br />
E-version <strong>of</strong> this journal.<br />
Style for journal references<br />
Authors: the name <strong>of</strong> the first author should be typed in boldfaced<br />
letters. The family name <strong>of</strong> all authors should be typed with<br />
the initial letter capitalized, followed by their abbreviated first<br />
and middle initials. (For example, Lian-Sheng Ma is abbreviated<br />
as Ma LS, Bo-Rong Pan as Pan BR). The title <strong>of</strong> the cited article<br />
and italicized journal title (journal title should be in its abbreviated<br />
form as shown in PubMed), publication date, volume number<br />
(in black), start page, and end page [PMID: 11819634 DOI:<br />
10.3748/wjg.13.5396].<br />
Style for book references<br />
Authors: the name <strong>of</strong> the first author should be typed in bold-faced<br />
letters. The surname <strong>of</strong> all authors should be typed with the initial<br />
letter capitalized, followed by their abbreviated middle and first<br />
initials. (For example, Lian-Sheng Ma is abbreviated as Ma LS, Bo-<br />
Rong Pan as Pan BR) Book title. Publication number. Publication<br />
place: Publication press, Year: start page and end page.<br />
Format<br />
<strong>Journal</strong>s<br />
English journal article (list all authors and include the PMID where<br />
applicable)<br />
1 Jung EM, Clevert DA, Schreyer AG, Schmitt S, Rennert J,<br />
Kubale R, Feuerbach S, Jung F. Evaluation <strong>of</strong> quantitative<br />
contrast harmonic imaging to assess malignancy <strong>of</strong> liver<br />
tumors: A prospective controlled two-center study. <strong>World</strong> J<br />
Gastroenterol 2007; 13: 6356-6364 [PMID: 18081224 DOI:<br />
10.3748/wjg.13.6356]<br />
Chinese journal article (list all authors and include the PMID where<br />
applicable)<br />
2 Lin GZ, Wang XZ, Wang P, Lin J, Yang FD. Immunologic<br />
effect <strong>of</strong> Jianpi Yishen decoction in treatment <strong>of</strong> Pixudiarrhoea.<br />
Shijie Huaren Xiaohua Zazhi 1999; 7: 285-287<br />
In press<br />
3 Tian D, Araki H, Stahl E, Bergelson J, Kreitman M. Signature<br />
<strong>of</strong> balancing selection in Arabidopsis. Proc Natl Acad Sci USA<br />
2006; In press<br />
Organization as author<br />
4 <strong>Diabetes</strong> Prevention Program Research Group. Hypertension,<br />
insulin, and proinsulin in participants with impaired<br />
glucose tolerance. Hypertension 2002; 40: 679-686 [PMID:<br />
12411462 PMCID:2516377 DOI:10.1161/01.HYP.00000<br />
35706.28494.09]<br />
Both personal authors and an organization as author<br />
5 Vallancien G, Emberton M, Harving N, van Moorselaar RJ;<br />
Alf-One Study Group. Sexual dysfunction in 1, 274 European<br />
men suffering from lower urinary tract symptoms. J Urol<br />
2003; 169: 2257-2261 [PMID: 12771764 DOI:10.1097/01.<br />
ju.0000067940.76090.73]<br />
No author given<br />
6 21st century heart solution may have a sting in the tail.<br />
BMJ 2002; 325: 184 [PMID: 12142303 DOI:10.1136/<br />
bmj.325.7357.184]<br />
Volume with supplement<br />
7 Geraud G, Spierings EL, Keywood C. Tolerability and safety<br />
<strong>of</strong> frovatriptan with short- and long-term use for treatment<br />
<strong>of</strong> migraine and in comparison with sumatriptan. Headache<br />
2002; 42 Suppl 2: S93-99 [PMID: 12028325 DOI:10.1046/<br />
j.1526-4610.42.s2.7.x]<br />
Issue with no volume<br />
8 Banit DM, Kaufer H, Hartford JM. Intraoperative frozen<br />
section analysis in revision total joint arthroplasty. Clin Orthop<br />
WJD|www.wjgnet.com IV<br />
Relat Res 2002; (401): 230-238 [PMID: 12151900 DOI:10.109<br />
7/00003086-200208000-00026]<br />
No volume or issue<br />
9 Outreach: Bringing HIV-positive individuals into care. HRSA<br />
Careaction 2002; 1-6 [PMID: 12154804]<br />
Books<br />
Personal author(s)<br />
10 Sherlock S, Dooley J. Diseases <strong>of</strong> the liver and billiary system.<br />
9th ed. Oxford: Blackwell Sci Pub, 1993: 258-296<br />
Chapter in a book (list all authors)<br />
11 Lam SK. Academic investigator’s perspectives <strong>of</strong> medical<br />
treatment for peptic ulcer. In: Swabb EA, Azabo S. Ulcer<br />
disease: investigation and basis for therapy. New York: Marcel<br />
Dekker, 1991: 431-450<br />
Author(s) and editor(s)<br />
12 Breedlove GK, Schorfheide AM. Adolescent pregnancy. 2nd<br />
ed. Wieczorek RR, editor. White Plains (NY): March <strong>of</strong> Dimes<br />
Education Services, 2001: 20-34<br />
Conference proceedings<br />
13 Harnden P, J<strong>of</strong>fe JK, Jones WG, editors. Germ cell tumours V.<br />
Proceedings <strong>of</strong> the 5th Germ cell tumours Conference; 2001<br />
Sep 13-15; Leeds, UK. New York: Springer, 2002: 30-56<br />
Conference paper<br />
14 Christensen S, Oppacher F. An analysis <strong>of</strong> Koza's computational<br />
effort statistic for genetic programming. In: Foster<br />
JA, Lutton E, Miller J, Ryan C, Tettamanzi AG, editors.<br />
Genetic programming. EuroGP 2002: Proceedings <strong>of</strong> the 5th<br />
European Conference on Genetic Programming; 2002 Apr<br />
3-5; Kinsdale, Ireland. Berlin: Springer, 2002: 182-191<br />
Electronic journal (list all authors)<br />
15 Morse SS. Factors in the emergence <strong>of</strong> infectious diseases.<br />
Emerg Infect Dis serial online, 1995-01-03, cited 1996-06-05;<br />
1(1): 24 screens. Available from: URL: http://www.cdc.gov/<br />
ncidod/eid/index.htm<br />
Patent (list all authors)<br />
16 Pagedas AC, inventor; Ancel Surgical R&D Inc., assignee.<br />
Flexible endoscopic grasping and cutting device and<br />
positioning tool assembly. United States patent US 200201<br />
03498. 2002 Aug 1<br />
Statistical data<br />
Write as mean ± SD or mean ± SE.<br />
Statistical expression<br />
Express t test as t (in italics), F test as F (in italics), chi square test as<br />
χ 2 (in Greek), related coefficient as r (in italics), degree <strong>of</strong> freedom<br />
as υ (in Greek), sample number as n (in italics), and probability as P (in<br />
italics).<br />
Units<br />
Use SI units. For example: body mass, m (B) = 78 kg; blood<br />
pressure, p (B) = 16.2/12.3 kPa; incubation time, t (incubation) =<br />
96 h, blood glucose concentration, c (glucose) 6.4 ± 2.1 mmol/L;<br />
blood CEA mass concentration, p (CEA) = 8.6 24.5 mg/L; CO 2<br />
volume fraction, 50 mL/L CO 2, not 5% CO 2; likewise for 40 g/L<br />
formaldehyde, not 10% formalin; and mass fraction, 8 ng/g, etc.<br />
Arabic numerals such as 23, 243, 641 should be read 23 243 641.<br />
The format for how to accurately write common units and<br />
quantums can be found at: http://www.wjgnet.com/1948-9358/<br />
g_info_20100107145507.htm.<br />
Abbreviations<br />
Standard abbreviations should be defined in the abstract and on first<br />
mention in the text. In general, terms should not be abbreviated<br />
unless they are used repeatedly and the abbreviation is helpful to<br />
the reader. Permissible abbreviations are listed in Units, Symbols<br />
and Abbreviations: A Guide for Biological and Medical Editors and<br />
Authors (Ed. Baron DN, 1988) published by The Royal Society <strong>of</strong><br />
Medicine, London. Certain commonly used abbreviations, such as<br />
DNA, RNA, HIV, LD50, PCR, HBV, ECG, WBC, RBC, CT, ESR,<br />
January 15, 2011|Volume 2|Issue 1|
CSF, IgG, ELISA, PBS, ATP, EDTA, mAb, can be used directly<br />
without further explanation.<br />
Italics<br />
Quantities: t time or temperature, c concentration, A area, l length,<br />
m mass, V volume.<br />
Genotypes: gyrA, arg 1, c myc, c fos, etc.<br />
Restriction enzymes: EcoRI, HindI, BamHI, Kbo I, Kpn I, etc.<br />
Biology: H. pylori, E coli, etc.<br />
Examples for paper writing<br />
Editorial: http://www.wjgnet.com/1948-9358/g_info_20100316<br />
080002.htm<br />
Frontier: http://www.wjgnet.com/1948-9358/g_info_20100316<br />
091946.htm<br />
Topic highlight: http://www.wjgnet.com/1948-9358/g_info_<br />
20100316080004.htm<br />
Observation: http://www.wjgnet.com/1948-9358/g_info_<br />
20100107142558.htm<br />
Guidelines for basic research: http://www.wjgnet.com/1948-9358/<br />
g_info_20100316092358.htm<br />
Guidelines for clinical practice: http://www.wjgnet.com/1948-<br />
9358/g_info_20100316092508.htm<br />
Review: http://www.wjgnet.com/1948-9358/g_info_2010<br />
0107142809.htm<br />
Original articles: http://www.wjgnet.com/1948-9358/g_info_<br />
20100107143306.htm<br />
Brief articles: http://www.wjgnet.com/1948-9358/g_info_2010<br />
0316093137.htm<br />
Case report: http://www.wjgnet.com/1948-9358/g_info_2010010<br />
7143856.htm<br />
Letters to the editor: http://www.wjgnet.com/1948-9358/<br />
g_info_20100107144156.htm<br />
Book reviews: http://www.wjgnet.com/1948-9358/g_info_2010<br />
0316093525.htm<br />
Guidelines: http://www.wjgnet.com/1948-9358/g_info_2010<br />
0316093551.htm<br />
SUBMISSION OF THE REVISED MANUSCRIPTS AFTER<br />
ACCEPTED<br />
Please revise your article according to the revision policies<br />
<strong>of</strong> WJD. The revised version including manuscript and highresolution<br />
image figures (if any) should be copied on a floppy or<br />
compact disk. The author should send the revised manuscript,<br />
along with printed high-resolution color or black and white<br />
WJD|www.wjgnet.com V<br />
Instructions to authors<br />
photos, copyright transfer letter, and responses to the reviewers<br />
by courier (such as EMS/DHL).<br />
Editorial Office<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> <strong>Diabetes</strong><br />
Editorial Department: Room 903, Building D,<br />
Ocean International Center,<br />
No. 62 Dongsihuan Zhonglu,<br />
Chaoyang District, Beijing 100025, China<br />
E-mail: wjd@wjgnet.com<br />
http://www.wjgnet.com<br />
Telephone: +86-10-59080038<br />
Fax: +86-10-85381893<br />
Language evaluation<br />
The language <strong>of</strong> a manuscript will be graded before it is sent for<br />
revision. (1) Grade A: priority publishing; (2) Grade B: minor<br />
language polishing; (3) Grade C: a great deal <strong>of</strong> language polishing<br />
needed; and (4) Grade D: rejected. Revised articles should reach<br />
Grade A or B.<br />
Copyright assignment form<br />
Please download a Copyright assignment form from http://www.<br />
wjgnet.com/1948-9358/g_info_20100107144846.htm.<br />
Responses to reviewers<br />
Please revise your article according to the comments/suggestions<br />
provided by the reviewers. The format for responses to the<br />
reviewers’ comments can be found at: http://www.wjgnet.<br />
com/1948-9358/g_info_20100107170340.htm.<br />
Pro<strong>of</strong> <strong>of</strong> financial support<br />
For paper supported by a foundation, authors should provide a<br />
copy <strong>of</strong> the document and serial number <strong>of</strong> the foundation.<br />
Links to documents related to the manuscript<br />
WJD will be initiating a platform to promote dynamic interactions<br />
between the editors, peer reviewers, readers and authors. After a<br />
manuscript is published online, links to the PDF version <strong>of</strong> the<br />
submitted manuscript, the peer-reviewers’ report and the revised<br />
manuscript will be put on-line. Readers can make comments on<br />
the peer reviewer’s report, authors’ responses to peer reviewers,<br />
and the revised manuscript. We hope that authors will benefit from<br />
this feedback and be able to revise the manuscript accordingly in a<br />
timely manner.<br />
Science news releases<br />
Authors <strong>of</strong> accepted manuscripts are suggested to write a science<br />
news item to promote their articles. The news will be released<br />
rapidly at EurekAlert/AAAS (http://www.eurekalert.org). The<br />
title for news items should be less than 90 characters; the summary<br />
should be less than 75 words; and main body less than 500 words.<br />
Science news items should be lawful, ethical, and strictly based on<br />
your original content with an attractive title and interesting pictures.<br />
Publication fee<br />
Authors <strong>of</strong> accepted articles must pay a publication fee.<br />
EDITORIAL, TOPIC HIGHLIGHTS, BOOK REVIEWS and<br />
LETTERS TO THE EDITOR are published free <strong>of</strong> charge.<br />
January 15, 2011|Volume 2|Issue 1|