Transapical neochord implantation - Multimedia Manual Cardio ...
Transapical neochord implantation - Multimedia Manual Cardio ...
Transapical neochord implantation - Multimedia Manual Cardio ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
doi:10.1510/mmcts.2010.004606<br />
<strong>Transapical</strong> <strong>neochord</strong> <strong>implantation</strong><br />
Joerg Seeburger*, Michael Winkfein, Michael Hoebartner, Thilo Noack, Philipp Kiefer,<br />
Marcel Vollroth, Sergej Leontjev, Friedrich Wilhelm Mohr<br />
Heart Center, Leipzig University, Struempelstrasse 39, 04289 Leipzig, Germany<br />
The NeoChord procedure has recently been introduced to facilitate chordal replacement for<br />
mitral valve repair using a transapical beating heart off-pump approach. We herein elucidate<br />
on the concept, the technique, the operative approach and the procedure in a ‘how-to-doit’<br />
manner.<br />
Keywords: Beating heart; Chordal replacement; Mitral valve repair; <strong>Transapical</strong><br />
Introduction<br />
Degenerative mitral valve (MV) disease may lead to<br />
chordae rupture with subsequent leaflet prolapse and<br />
mitral regurgitation (MR) w1, 2x. Current standard of<br />
care for MV prolapse with severe MR is surgical MV<br />
repair w1, 2x. Implantation of neo-chordae with the use<br />
of expanded polytetrafluoroethylene (ePTFE) sutures<br />
(Gore Associates, Flagstaff, AZ, USA) has since its<br />
introduction into clinical practice by Frater et al. proven<br />
to be a valuable technique for contemporary MV<br />
repair w3–6x. Chordal replacement enables preservation<br />
of native valve anatomy, physiological leaflet<br />
motion and creation of large mitral orifice area w6, 7x.<br />
Furthermore, it has contributed to the reparability<br />
independent of valve complexity w4, 8x.<br />
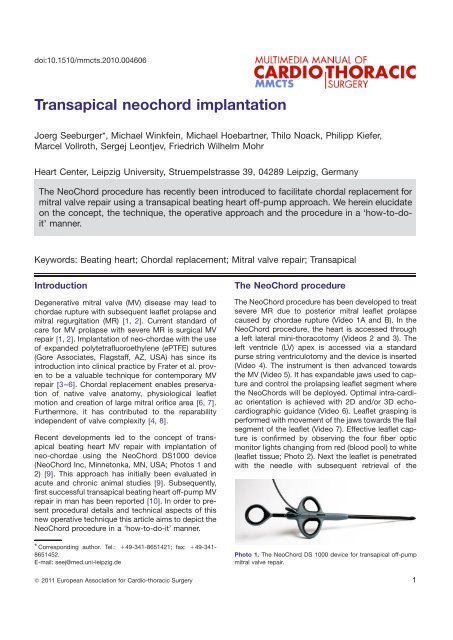
Recent developments led to the concept of transapical<br />
beating heart MV repair with <strong>implantation</strong> of<br />
neo-chordae using the NeoChord DS1000 device<br />
(NeoChord Inc, Minnetonka, MN, USA; Photos 1 and<br />
2) w9x. This approach has initially been evaluated in<br />
acute and chronic animal studies w9x. Subsequently,<br />
first successful transapical beating heart off-pump MV<br />
repair in man has been reported w10x. In order to present<br />
procedural details and technical aspects of this<br />
new operative technique this article aims to depict the<br />
NeoChord procedure in a ‘how-to-do-it’ manner.<br />
* Corresponding author. Tel.: q49-341-8651421; fax: q49-341-<br />
8651452.<br />
E-mail: seej@med.uni-leipzig.de<br />
� 2011 European Association for <strong>Cardio</strong>-thoracic Surgery<br />
The NeoChord procedure<br />
The NeoChord procedure has been developed to treat<br />
severe MR due to posterior mitral leaflet prolapse<br />
caused by chordae rupture (Video 1A and B). In the<br />
NeoChord procedure, the heart is accessed through<br />
a left lateral mini-thoracotomy (Videos 2 and 3). The<br />
left ventricle (LV) apex is accessed via a standard<br />
purse string ventriculotomy and the device is inserted<br />
(Video 4). The instrument is then advanced towards<br />
the MV (Video 5). It has expandable jaws used to capture<br />
and control the prolapsing leaflet segment where<br />
the NeoChords will be deployed. Optimal intra-cardiac<br />
orientation is achieved with 2D and/or 3D echocardiographic<br />
guidance (Video 6). Leaflet grasping is<br />
performed with movement of the jaws towards the flail<br />
segment of the leaflet (Video 7). Effective leaflet capture<br />
is confirmed by observing the four fiber optic<br />
monitor lights changing from red (blood pool) to white<br />
(leaflet tissue; Photo 2). Next the leaflet is penetrated<br />
with the needle with subsequent retrieval of the<br />
Photo 1. The NeoChord DS 1000 device for transapical off-pump<br />
mitral valve repair.<br />
1
2<br />
J. Seeburger et al. / <strong>Multimedia</strong> <strong>Manual</strong> of <strong>Cardio</strong>thoracic Surgery / doi:10.1510/mmcts.2010.004606<br />
Photo 2. The NeoChord device monitor for confirmation of successful<br />
(poor) mitral valve leaflet grasp.<br />
Video 1. Mitral regurgitation.<br />
Severe mitral regurgitation due to chordae rupture and posterior<br />
mitral leaflet prolapse assessed with chest-wall (Video 1A) and<br />
three-dimensional transesophageal echocardiography (Video 1B).<br />
Video 2. Principle of the NeoChord procedure.<br />
Schematics of the NeoChord procedure are depicted in an animation<br />
video (with courtesy from NeoChord Inc, Minnetonka, MN,<br />
USA).<br />
NeoChord ePTFE suture (Video 8). Once the suture is<br />
retrieved and fully accessed free of the instrument<br />
after complete retraction of the NeoChord device (Video<br />
9), a girth hitch knot is secured to the leaflet (Video<br />
10). In case of insufficient result the NeoChord can be<br />
retrieved using an additional retraction suture. Then<br />
the procedure as shown in Videos 3–9 is repeatedly<br />
performed to re-suspend the complete prolapsing<br />
segment if necessary. After <strong>implantation</strong> of the necessary<br />
number of NeoChords final assessment of the<br />
operative result is achieved using echocardiography<br />
Video 3. Surgical access.<br />
A standard transapical access is used to expose the left ventricle<br />
of the heart via a small left lateral mini-thoracotomy.<br />
Video 4. <strong>Transapical</strong> introduction of the NeoChord device.<br />
Two purse string sutures with felt pledgets are sewn on the apex.<br />
A wire is inserted into the left ventricle and the access is dilated<br />
(Video 4A). This pre-dilated access is used to advance the Neo-<br />
Chord device into the left ventricle (Video 4B).<br />
Video 5. Advancing the NeoChord device to the mitral valve.<br />
Under constant echocardiographic guidance the device is further<br />
advanced through the mitral valve into the left atrium.<br />
Video 6. 3D echo guidance.<br />
Three-dimensional echocardiography allows for optimal orientation<br />
with regards to the prolapsing segment of the posterior leaflet.<br />
While performing the procedure the surgeon has to follow the echocardiography<br />
image to ‘find’ the prolapse – not vice versa.<br />
(Video 11). The final step of the procedure is to manually<br />
secure the properly tensioned NeoChords to the<br />
LV apex using a French-eye needle, additional felt<br />
pledgets and simple knots (Video 12). The operative<br />
result with elimination of MV prolapse and no evidence<br />
of MR is assessed with transesophageal echocardiography<br />
(Video 13A). At discharge of the patient
J. Seeburger et al. / <strong>Multimedia</strong> <strong>Manual</strong> of <strong>Cardio</strong>thoracic Surgery / doi:10.1510/mmcts.2010.004606<br />
Video 7. Leaflet grasping.<br />
When appropriate positioning has been achieved the two jaws on<br />
the tip of the device are opened facing towards the prolapsing segment.<br />
In practice the lower jaw can be used to ‘upload’ the posterior<br />
leaflet and thus minimize leaflet motion. For final grasping the surgeon<br />
needs to close the jaws while actively retracting the upper jaw<br />
(Video 7A and B). Confirmation of sufficient tissue grasp is derived<br />
from the numbers and color of the fiber optics on the device leaflet<br />
capture display (Photo 2).<br />
Video 8. Deployment of NeoChord.<br />
After successful grasping and confirmation the needle is fully<br />
advanced to puncture the leaflet segment and to ‘hook on’ to the<br />
ePTFE suture which is pre-loaded within the device. The needle is<br />
then completely retracted and the loop of the ePTFE suture is pulled<br />
outside the device. The needle is then put aside.<br />
Video 9. Retraction of the device.<br />
Once the NeoChord has been pulled through the tissue of the prolapsing<br />
segment and retracted, the grasping mechanism is relaxed<br />
to relief the leaflet. The device is then fully retracted and pulled<br />
outside the apex of the heart. The purse string sutures are then<br />
tightened to prevent loss of blood.<br />
chest wall echocardiography confirms no prolapse<br />
and no MR (Video 13B).<br />
Comment<br />
Chordal replacement for MV repair with the use of<br />
ePTFE sutures has shown to reach excellent results<br />
in large clinical series w4–8x. Over the last decade, it<br />
has gained a high-popularity even comparable to the<br />
classical technique of leaflet resection w6, 7, 11x. The<br />
rational of the NeoChord procedure, however, is to re-<br />
Video 10. Girth hitch knot.<br />
In this state of the procedure the loop of the ePTFE suture as well<br />
as both ends of the suture are outside of the chest while the ePTFE<br />
is led through the prolapsing segment of the leaflet. A girth hitch<br />
knot is tied by leading the two ends through the free loop of the<br />
suture. Subsequently, the knot is moved upwards to the mitral leaflet<br />
by gently pulling on both ends of the suture. Confirmation of this<br />
step is derived from reduction of leaflet motion and mitral regurgitation<br />
using echocardiography.<br />
Video 11. NeoChord in place.<br />
As previously indicated the NeoChord is easily visible on echocardiography<br />
and assessment of functionality can be achieved by pulling<br />
or relaxing on the NeoChord. In case of too much tension<br />
restriction of the posterior leaflet with induction of mitral regurgitation<br />
occurs. Depending on the operative result after <strong>implantation</strong> of<br />
the first NeoChord additional NeoChords are implanted by repeating<br />
the procedure as illustrated in Videos 4–10.<br />
Video 12. Fixation to apex.<br />
After completion of NeoChord <strong>implantation</strong> to the prolapsing segment<br />
a critical valve analysis using echocardiography is performed.<br />
Proper tensioning as well as proper distribution of NeoChords on<br />
the prolapsing segment with complete elimination of both prolapse<br />
and MR has to be achieved. If adequate, the NeoChords have to<br />
be anchored to the apex of the heart while securing perfect length<br />
and proper tensioning. Therefore, a French eye needle is used to<br />
lead the remaining two ends of the ePTFE suture through the myocardium<br />
exteriorly from the apical access and is finally fixed over<br />
an additional felt pledget (Video 12A and Photo 3). This step is<br />
repeated for each NeoChord separately (Photo 3). Under constant<br />
echocardiographic guidance and functional assessment the Neo-<br />
Chords are secured on the apex of the heart to achieve the final<br />
result (Video 12B).<br />
suspend the prolapsing leaflet segment while abandoning<br />
cardiopulmonary bypass and cardiac arrest.<br />
This in combination with the transapical direct access<br />
3
4<br />
J. Seeburger et al. / <strong>Multimedia</strong> <strong>Manual</strong> of <strong>Cardio</strong>thoracic Surgery / doi:10.1510/mmcts.2010.004606<br />
Photo 3. Schematics for apical fixation of NeoChords over additional<br />
felt pledgets.<br />
Video 13. Final result.<br />
After completion of the procedure, complete elimination of the mitral<br />
valve prolapse and mitral regurgitation is achieved (Video 13A). At<br />
discharge chest wall echocardiography control shows the Neo-<br />
Chord in place with no evidence of prolapse and no mitral regurgitation<br />
(Video 13B).<br />
to the MV is the main characteristic as well as apparent<br />
uniqueness of the NeoChord procedure. Since the<br />
NeoChord procedure represents a completely new<br />
operative technique it has yet to prove repeat clinical<br />
applicability. Nevertheless, feasibility of the procedure<br />
with first successful in man application has been<br />
demonstrated: complete elimination of MV prolapse<br />
and MR was achieved in a patient with severe MR due<br />
to chordae rupture w10x. The NeoChord procedure is<br />
currently being investigated in the multicenter clinical<br />
TransApical Chordae Tendinae (TACT) trial with<br />
regards to safety and efficacy. Therefore, the presented<br />
clinical experience is very preliminary and the<br />
procedure is still considered to be experimental.<br />
Despite the simplicity of the NeoChord concept and<br />
its applicability as illustrated in this article the Neo-<br />
Chord procedure includes several crucial steps which<br />
need to be conducted with a high accuracy. Those<br />
are: (1) sufficient leaflet grasp of the prolapsing segment;<br />
(2) secure fixation of NeoChords to the MV leaflet<br />
edge; (3) sufficient distribution of NeoChords over<br />
the complete prolapsing segment; (4) proper tensioning<br />
and length adjustment of NeoChords; (5) assessment<br />
of functional result using echocardiography; and<br />
(6) echocardiographic guidance throughout the complete<br />
procedure.<br />
Conclusion<br />
In conclusion transapical beating heart off-pump <strong>implantation</strong><br />
of neo-chordae for MV repair is feasible.<br />
Further clinical experience, however, is inevitable.<br />
References<br />
w1x Adams DH, Rosenhek R, Falk V. Degenerative<br />
mitral valve regurgitation: best practice revolution.<br />
Eur Heart J 2010;31:1958–1966.<br />
w2x Enriquez-Sarano M, Akins CW, Vahanian A. Mitral<br />
regurgitation. Lancet 2009;373:1382–1394.<br />
w3x Frater RW, Vetter HO, Zussa C, Dahm M. Chordal<br />
replacement in mitral valve repair. Circulation 1990;<br />
82(5 Suppl):IV125–IV130.<br />
w4x David TE, Ivanov J, Armstrong S, Christie D,<br />
Rakowski H. A comparison of outcomes of mitral<br />
valve repair for degenerative disease with posterior,<br />
anterior, and bileaflet prolapse. J Thorac<br />
<strong>Cardio</strong>vasc Surg 2005;130:1242–1249.<br />
w5x Perier P, Hohenberger W, Lakew F, Batz G, Urbanski<br />
P, Zacher M, Diegeler A. Toward a new paradigm<br />
for the reconstruction of posterior leaflet<br />
prolapse: midterm results of the ‘‘respect rather<br />
than resect’’ approach. Ann Thorac Surg 2008;<br />
86:718–725.<br />
w6x Seeburger J, Falk V, Borger MA, Passage J,<br />
Walther T, Doll N, Mohr FW. Chordae replacement<br />
versus resection for repair of isolated posterior<br />
mitral leaflet prolapse: à ègalité. Ann Thorac Surg<br />
2009;87:1715–1720.<br />
w7x Falk V, Seeburger J, Czesla M, Borger MA, Willige<br />
J, Kuntze T, Doll N, Borger F, Perrier P, Mohr FW.<br />
How does the use of polytetrafluoroethylene <strong>neochord</strong>ae<br />
for posterior mitral valve prolapse (loop<br />
technique) compare with leaflet resection? A<br />
prospective randomized trial. J Thorac <strong>Cardio</strong>vasc<br />
Surg 2008;136:1205; discussion 1205–<br />
1206.<br />
w8x Seeburger J, Borger MA, Doll N, Walther T,<br />
Passage J, Falk V, Mohr FW. Comparison of outcomes<br />
of minimally invasive mitral valve surgery
J. Seeburger et al. / <strong>Multimedia</strong> <strong>Manual</strong> of <strong>Cardio</strong>thoracic Surgery / doi:10.1510/mmcts.2010.004606<br />
for posterior, anterior, and bileaflet prolapse. Eur<br />
J <strong>Cardio</strong>thorac Surg 2009;36:532–538.<br />
w9x Bajona P, Katz WE, Daly RC, Zehr KJ, Speziali G.<br />
Beating-heart, off-pump mitral valve repair by<br />
<strong>implantation</strong> of artificial chordae tendineae: an<br />
acute in vivo animal study. J Thorac <strong>Cardio</strong>vasc<br />
Surg 2009;137:188–193.<br />
w10x Seeburger J, Borger MA, Tschernich H, Leontjev<br />
S, Holzhey D, Noack T, Ender J, Mohr FW. <strong>Transapical</strong><br />
beating heart mitral valve repair. Circ<br />
<strong>Cardio</strong>vasc Interv 2010;3:611–612.<br />
w11x Carpentier A. Cardiac valve surgery – the ‘‘French<br />
correction’’. J Thorac <strong>Cardio</strong>vasc Surg 1983;86:<br />
323–337.<br />
5