Rush 09_online.indd - Rush University Medical Center
Rush 09_online.indd - Rush University Medical Center
Rush 09_online.indd - Rush University Medical Center
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
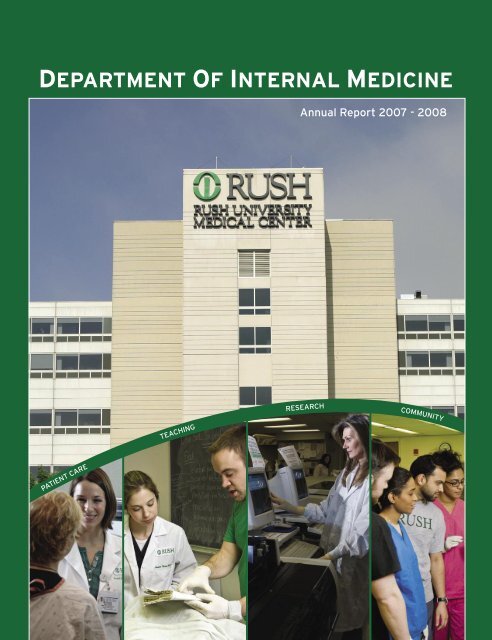
DEPARTMENT OF INTERNAL MEDICINE<br />
Annual Report 2007 - 2008<br />
PATIENT CARE TEACHING RESEARCH COMMUNITY
TABLE OF CONTENTS<br />
Comments from the Chair 2<br />
History of the Department 3<br />
Organizational Chart 4<br />
<strong>Medical</strong> Education Program 5<br />
Clinical Activities 10<br />
Research Activities 11<br />
Statistical Snapshot 12<br />
Section of Cardiology 16<br />
Section of Community Epidemiologic Research 18<br />
Division of Digestive Disease 20<br />
Section of Endocrinology 24<br />
Section of General Internal Medicine 27<br />
Section of Geriatric Medicine and Palliative Care 30<br />
Division of Pulmonary and Critical Care Medicine 34<br />
Section of <strong>Medical</strong> Informatics and Patient Safety Research 37<br />
Division of Hematology/Oncology/BMT 38<br />
Section of Infectious Disease 42<br />
Section of Pharmacy Practice 46<br />
Section of Rheumatology 48<br />
Division of Nephrology 54<br />
Mission<br />
The mission statement of <strong>Rush</strong> <strong>University</strong> <strong>Medical</strong><br />
<strong>Center</strong> is to provide the very best care for our<br />
patients. Our education and research endeavors,<br />
community service programs and relationships with<br />
other hospitals are dedicated to enhancing excellence<br />
in patient care for the diverse communities of the<br />
Chicago area, now and in the future.
COMMENTS FROM THE CHAIR<br />
2<br />
Stuart Levin, MD<br />
Chair, Department of<br />
Internal Medicine<br />
Dear Colleagues and Friends,<br />
I am particularly proud of the accomplishments of the Department of Internal Medicine<br />
during the fiscal and academic year of 2008. During this period, we continued to provide<br />
outstanding care, ground breaking research, superb teaching and strong outreach to<br />
our community.<br />
Patient Care - The Department implemented a number of programs and initiatives to<br />
improve the quality of care and increase patient satisfaction. There was a successful<br />
recruitment of experienced heart failure cardiologists to complement the heart transplant<br />
program. This has resulted in an increased volume of activities in both the medical and<br />
surgical aspects of the program. We opened the Coleman Foundation Comprehensive<br />
Clinic for Gastrointestinal Cancers, which allows patients access to a multidisciplinary<br />
team of experts to treat their cancer. Additionally, we implemented nocturnists as<br />
part of our hospitalists program to allow for 24/7 attending coverage for emergencies,<br />
instantaneous coverage for code situations, and support the cardio-thoracic program<br />
in surgery. The hospitalist system is matured and highly successful related to education<br />
and patient care. The Department also reorganized the leadership of the intensive care<br />
units to allow for implementation of quality improvement initiatives and to improve bed<br />
control management. Moreover, our Quality Assurance program, led by Dr. Robert Rosen,<br />
continues to be a success because of the collaboration between Chief Residents, faculty,<br />
nursing management and risk management.<br />
Research - The Department of Internal Medicine has continued to develop its research<br />
program with considerable success. Over the past year, the program, led by Dr. Ali<br />
Keshavarzian is expanding. The number of mentees has grown by 21% and over 17<br />
seminars were available for mentees and hospital staff on key topics related to research.<br />
Education - The medical residency program in the Department of Internal Medicine<br />
has enhanced its offerings to benefit both residents and faculty. The areas of<br />
concentration over the past year include evidence-based medicine, physical diagnosis and<br />
pathophysiology. The Department has an impressive track record of continuing to match<br />
in all of its residency and fellowships at 100%. The Internal Medicine Residency Program<br />
and all of the subspecialty fellowship programs received continued full accreditation<br />
following their RRC/ACGME site visits. Also, during this period, our residency, fellowship<br />
and clerkship programs implemented an electronic evaluation program.<br />
Community Outreach - <strong>Rush</strong> has continued to develop a strong relationship with J.H.<br />
Stroger Hospital of Cook County. Our partnership allows for physicians at Stroger to share<br />
great experiences and teach our first and second year medical students. Additionally, as<br />
partners, we are developing collaborative research programs in a variety of areas, such as<br />
infectious disease HIV studies. The Department also assisted with providing colonoscopies<br />
and endoscopies to patients at a time when Stroger hospital provided limited services.<br />
We hope that you will find this report informative and helpful to you.<br />
Stuart Levin, MD Chair, Department of Internal Medicine
The story of Department of Internal Medicine began in 1904. During<br />
its distinguished history, the department has been led by a number of<br />
renowned figures in American academic medicine among them Frank<br />
Billings and James Herrick.<br />
Frank Billings, MD, (1905-1923) played an important role in the<br />
development of Chicago as a leading medical center. He joined the<br />
<strong>Rush</strong> <strong>Medical</strong> College faculty in 1898 and served there as a professor<br />
of medicine and head of the Department of Internal Medicine. Under<br />
his leadership, the hospital rapidly developed as a center of better<br />
teaching, of better training for practitioners and as a better field of<br />
investigation. He researched the germ cause of disease, contributing<br />
the concept of focal infection, which helped explain at that time the<br />
cause of strange diseases of unknown origin.<br />
James Bryan Herrick, MD, (1923-1926) was selected to lead the<br />
department after Dr. Billings. Dr. Herrick discovered sickle cell<br />
anemia and the relationship between coronary thrombosis and heart<br />
attacks. He was one of the most important internists of his time. He<br />
was a graduate of <strong>Rush</strong> <strong>University</strong> <strong>Medical</strong> College, and made all of<br />
his most important discoveries while working on the campus. He<br />
was instrumental in establishing Internal Medicine as a specialty in<br />
Chicago and on an international level.<br />
OTHER LUMINARIES WHO HAVE LED THE DEPARTMENT INCLUDE:<br />
Robin T. Woodyatt, MD 1927-32<br />
George Dick, MD 1932-33<br />
Ernest E. Irons, MD 1933-42<br />
Ralph C. Brown, MD 1942-48<br />
S.Howard Armstrong Jr., MD 1948-52<br />
Thomas J. Coogan, MD 1952-54, 1956-59<br />
Howard Wakefield, MD 1954-56<br />
James A. Campbell, MD 1953-66<br />
John S. Graettinger, MD 1966-71<br />
Theodore B. Schwartz, MD 1970-82<br />
Robert W. Carton, MD 1982-84<br />
Roger C. Bone, MD 1984-91<br />
Stuart Levin, MD 1991-Present<br />
HISTORY OF THE DEPARTMENT<br />
Frank Billings, MD<br />
The First Chairman<br />
of the Department<br />
1905 - 1923<br />
3
INTERNAL MEDICINE ORGANIZATIONAL CHART<br />
4<br />
Residency<br />
Program<br />
Director<br />
Sr. Associate<br />
Residency<br />
Program<br />
Director<br />
Associate<br />
Residency<br />
Program<br />
Directors<br />
Vice Chairman,<br />
IM Academics<br />
Section of<br />
Nutrition and<br />
Epidemiology<br />
Section of<br />
Bone Marrow<br />
Transplant<br />
Student<br />
Program<br />
Director<br />
Vice Chairman,<br />
IM Research<br />
Section of<br />
Cardiology<br />
Division of<br />
Digestive<br />
Disease<br />
Section of<br />
Gastroenterology<br />
Division of<br />
Hematology/<br />
Oncology/BMT<br />
Section of<br />
Hematology<br />
Chairman, Department of<br />
Internal Medicine Stroger<br />
Sr. Assist.<br />
Chairman<br />
Chief<br />
Administrative<br />
Officer<br />
Section of<br />
Rheumatology<br />
Section of<br />
Hepatology<br />
Section of<br />
Oncology<br />
Section of<br />
Infectious<br />
Diseases<br />
DEAN, RMC<br />
Chairman,<br />
Department<br />
of Internal<br />
Medicine<br />
Sr.Associate<br />
Chariman<br />
Clinical Affairs<br />
Chief <strong>Medical</strong> Officer<br />
Section of<br />
Community<br />
Epidemiologic<br />
Research<br />
Section of<br />
Endocrionology<br />
Stroger<br />
Section of<br />
GIM Stroger<br />
Assist.<br />
Chariman<br />
Chief Financial<br />
Officer<br />
Division of<br />
Endocrinology<br />
Division of<br />
General Internal<br />
Medicine<br />
Section of<br />
Geriatric and<br />
Palliative Care<br />
Section of<br />
Endocrinology<br />
<strong>Rush</strong><br />
Section of<br />
GIM <strong>Rush</strong><br />
Associate<br />
Chair, Quality<br />
and Safety<br />
Section of<br />
Pharmacy<br />
Practice<br />
Section of<br />
Critical Care<br />
Medicine<br />
Section of<br />
Transplant<br />
Nephrology<br />
Director of<br />
Compliance<br />
Section of <strong>Medical</strong><br />
Informatics and<br />
Patient Safety<br />
Research<br />
Division of<br />
Pulmonary &<br />
Critical Care<br />
Division of<br />
Nephrology<br />
Section of<br />
Pulmonary<br />
Medicine<br />
Section of<br />
Nephrology
GRADUATE MEDICAL EDUCATION<br />
Internal Medicine Residency Training Program<br />
<strong>Rush</strong> <strong>Medical</strong> College, whose initial charter dates back to 1837, was one<br />
of the first medical schools west of the Allegheny Mountains. As the<br />
principal teaching hospital for <strong>Rush</strong> <strong>Medical</strong> College and <strong>Rush</strong> <strong>University</strong>,<br />
<strong>Rush</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong> serves as a primary care facility for the<br />
near west side of Chicago and as a referral center for the Chicago area and<br />
the entire Midwest. Our trainees benefit from the cultural, ethnic, racial,<br />
socioeconomic and religious diversity of this wonderful city.<br />
The Department of Medicine has two primary goals: to provide excellent<br />
patient care and to offer outstanding education for trainees in internal<br />
medicine. These goals are inextricably linked; the foundation for this linkage<br />
is open communication among all members of the health care team.<br />
Residents in the Department of Internal Medicine participate in a<br />
program that focuses on carefully balancing the appropriate amount of<br />
supervision and autonomy based on the level of training. Our program is<br />
markedly weighted in favor of education over service. To ensure an optimal<br />
educational experience for each patient they care for, residents obtain their<br />
own history and physical examination, formulate a differential diagnosis,<br />
recommend a diagnostic/therapeutic management plan, and review the<br />
plan with a senior supervisor. In many settings, the house officer, regardless<br />
of level of training, works directly with the attending in a one-on-one<br />
relationship, e.g. emergency room and ambulatory experiences. In other<br />
settings, residents work in teams, such as inpatient medical floors, consult<br />
services and intensive care units.<br />
Our curriculum is assessed and refined on a continuous basis. The<br />
Department of Internal Medicine Curriculum Committee meets regularly to<br />
review and improve our educational program. There is representation from<br />
faculty, chief residents, and housestaff on this committee. The core subject<br />
matter is repetitive on a two to three year basis so that all trainees will<br />
receive education in those areas deemed essential for the practice of internal<br />
medicine. Our subspecialty sections provide two types of curricula: a) the<br />
general information all residents need to learn irrespective of whether they<br />
rotate on that subspecialty service during the course of their residency; and<br />
b) a curriculum that is specific to the subspecialty rotation.<br />
Given the day to day supervisory responsibility of attending staff, we believe<br />
that substantive evaluation and feedback occurs on a daily basis based on<br />
interpersonal interaction. Nonetheless, our Department has in place an<br />
extensive, comprehensive, detailed and organized system of evaluation and<br />
feedback. In addition to structured evaluations, the Department of Internal<br />
Medicine leadership has an open door policy and residents are encouraged<br />
to discuss their concerns and request feedback as they deem necessary.<br />
MEDICAL EDUCATION PROGRAM<br />
Richard I. Abrams, MD<br />
Assistant Chairman,<br />
Residency Program<br />
Director<br />
Clerkship Director<br />
Elizabeth A. Baker, MD<br />
Associate Program<br />
Directors<br />
Alan A. Harris, MD<br />
Scott G. Hasler, MD<br />
Andem Ekpenyong, MD<br />
Stephanie C. Wang, MD<br />
Support Staff<br />
Sr. Residency Coordinators<br />
Sharon Rosentein<br />
Emelina Quintana<br />
Clerkship Coordinator<br />
Laurel A. Pawlak<br />
5
<strong>Medical</strong> Education Program<br />
6<br />
L to R row: Amy J. Tucker,MD, Sonali Khandelwal,MD, Carol Burke, MD, Prakash Balan, MD<br />
Our program has many strengths. The most important of these assets is our outstanding clinical<br />
training in a board range of clinical settings. Our patient experience occurs at the <strong>Medical</strong> <strong>Center</strong><br />
and throughout the metropolitan area. In addition to the parent hospital, there are affiliations<br />
with the John H. Stroger, Jr. Hospital of Cook County Hospital and <strong>Rush</strong> North Shore <strong>Medical</strong><br />
<strong>Center</strong>. These training affiliations provide unparalleled clinical breadth and depth and outstanding<br />
relationships between faculty and staff. These relationships lead to a friendly and collegial, yet<br />
academically challenging environment. The success of the hospital and all the training programs<br />
at <strong>Rush</strong> are directly related to our superior house officers.<br />
GRADUATE MEDICAL EDUCATION POSITIONS<br />
Medicine Residents 54<br />
Categorical 34<br />
Preliminary 14<br />
Chief Residents 6<br />
Medicine Fellows 77<br />
Cardiology 19<br />
Clinical Cardiac Electrophysiology 1<br />
Endocrinology 4<br />
Gastroenterology 10<br />
Geriatric 4<br />
Hematology/Oncology 6<br />
Infectious Disease 11<br />
Interventional Cardiology 2<br />
Nephorology 6<br />
Pulmonary/Critical Care 9<br />
Rheumatology 4<br />
Sleep Disorders& Research <strong>Center</strong> 1
UNDERGRADUATE MEDICAL EDUCATION<br />
Internal Medicine Clerkship and Subinternship<br />
The Internal Medicine Clerkship is a three month<br />
experience, with each student spending one<br />
month on an inpatient service at RUMC, one<br />
month on an inpatient service at the John H.<br />
Stroger Hospital of Cook County, and one month<br />
in a general internal medicine outpatient setting.<br />
Elizabeth Baker, MD directs the clerkship, with<br />
Jah-Won Koo, MD and Viju John, MD heading<br />
the ambulatory block and Sandra Frellsen, MD<br />
and Susan Glick, MD directing the Stroger block.<br />
Students are given the opportunity to evaluate and<br />
manage a wide variety of patients in our diverse<br />
settings, developing history taking, physical<br />
examination and diagnostic reasoning skills. A<br />
variety of teaching strategies are utilized including<br />
case studies, debates and student run conferences.<br />
Internal medicine clerkship faculty lead the <strong>Rush</strong><br />
<strong>Medical</strong> College effort to more fully integrate<br />
the clinical clerkships, leading plans for an<br />
interdisciplinary curriculum on finding and using<br />
quality information and for an interdisciplinary<br />
faculty development program.<br />
Over 80% of <strong>Rush</strong> <strong>Medical</strong> College students<br />
choose to complete a subinternship in internal<br />
medicine. Students function at an advanced level,<br />
completing histories and physical examinations,<br />
diagnostic evaluations, and initiating appropriate<br />
therapy under the close supervision of resident and<br />
attending staff. Michelle Sweet, MD and Viju John,<br />
MD direct this experience and provide didactic<br />
and interactive formal educational experiences for<br />
the students in addition to their clinical work.<br />
Introduction to Clinical Skills and<br />
Pathophysiology Courses<br />
<strong>Medical</strong> Education Program<br />
The Department of Internal Medicine is also<br />
responsible for the following clinical skills<br />
courses: M1 Introduction to the Patient and M2<br />
Introduction to Clinical Skills. The co-course<br />
directors are Andem Ekpenyong, MD and Kuenok<br />
Lee, MD. These courses provide students with<br />
basic history taking and physical examination<br />
skills. Drs. Ekpenyong and Lee also organize<br />
the M3 Clinical Skills Assessment (CSA) during<br />
which each M3 student participates in a 6-station<br />
Objective Structured Clinical Examination<br />
(OSCE).<br />
Pathophysiology is another important course,<br />
led by Syed H. Shah, MD, that runs in the<br />
second year of <strong>Rush</strong> <strong>Medical</strong> College. It has been<br />
designed to introduce the aberrations of Human<br />
Physiology that lead to a disease state. This<br />
course uses the patient case as the tool to outline<br />
Pathophysiological principles and develop<br />
clinical reasoning.<br />
The small group sessions are the primary avenue<br />
for learning in this course. With the guidance<br />
of a faculty facilitator, the students are expected<br />
to work through patient case presentations,<br />
identify questions, and then work collaboratively<br />
to answer those questions. Each group has 15-<br />
16 students and is led by facilitators who are<br />
clinician- educators (in the Department of Internal<br />
Medicine). There are a total of 29 two hour<br />
sessions over the course of the year for each group.<br />
7
<strong>Medical</strong> Education Program<br />
Scott G. Hasler, MD<br />
Senior Associate Residency<br />
Program Director<br />
Dr. Hasler, Senior Associate<br />
Program Director of the Internal<br />
Medicine Residency and General<br />
Internist, has been serving the<br />
Chicago metropolitan community<br />
for more than 10 years and received<br />
two “Department of Medicine<br />
Teaching and Service Award” and<br />
<strong>Rush</strong>’s “Intern of the Year.” His<br />
association with numerous medical<br />
safety committees has been vital<br />
to the university medical system.<br />
He has published his research on<br />
medical errors, diagnostic mistakes,<br />
and safety efforts in many journals<br />
including AHRQ, Lancet, and<br />
JAMA.<br />
8<br />
Alan A. Harris, MD, Senior Assistant<br />
Chairman, Vice Chairman of<br />
Academic Affairs, Associate Program<br />
Director for Subspecialty Programs<br />
Dr. Harris, professor of medicine and<br />
preventive medicine has been serving<br />
the Chicago medical community<br />
for 35 years. An infectious disease<br />
physician and epidemiologist, he has<br />
served as a Vice Chair of the State of<br />
Illinois Governor’s Panel of Public<br />
Health Advisors. He is a member of<br />
the Chicago Department of Health<br />
Advisory Groups on Communicable<br />
Disease and Bio-terrorism, the Chicago<br />
<strong>Medical</strong> Reserve Corps and a local<br />
consultant to the CDC. At <strong>Rush</strong>, he has<br />
chaired the medical school admissions<br />
committee, the committee on Medicare<br />
compliance, the task force on resident<br />
staffing, the Infectious Disease and<br />
Sepsis Control Committee, and the<br />
Antibiotic Review Subcommittee. He<br />
has the authored numerous journal<br />
articles, abstracts, and book chapters.<br />
He is the recipient of the Department of<br />
Medicine Award for Teaching, the John<br />
S. Graettinger, MD Award for Clinical<br />
Bedside Teaching, and the Stuart<br />
Levin, MD Excellence in Medicine<br />
Award. He is a member of the Mark<br />
H. Lepper, MD Society of Teachers.<br />
In 1999, Dr. Harris was awarded the<br />
Edwin S. Hamilton Interstate Teaching<br />
Award as the outstanding postgraduate<br />
medical educator in the tri-state area of<br />
Illinois, Iowa, and Wisconsin. Prior to<br />
becoming Vice Chairman of Academic<br />
Affairs, Dr. Harris was our residency<br />
program director for 16 years.<br />
Andem Ekpenyong, MD<br />
Associate Program<br />
Director for Curriculum<br />
Dr. Ekpenyong is an excellent<br />
educator who has been serving<br />
the <strong>Rush</strong> <strong>University</strong> for more than<br />
10 years. Raised in Nigeria and a<br />
native Chicagoan, she pursued the<br />
field of medicine and, yet, excelled<br />
in <strong>Medical</strong> Academia. She was<br />
one of two faculty who developed<br />
the <strong>Medical</strong> Student Clinical<br />
Skills Assessment (CSA) Program<br />
and is a Co-Course Director for<br />
two clinical skills courses for the<br />
<strong>Medical</strong> College. Through the<br />
Department of Internal Medicine,<br />
she has been recognized via three<br />
“Teaching and Service Awards”.<br />
Dr. Ekpenyong is the Chair of the<br />
Curriculum Committee for our<br />
residency program. She graduated<br />
from Stanford Faculty Development<br />
Clinical Teaching Program and<br />
currently disseminates this faculty<br />
development program here at <strong>Rush</strong>.
Elizabeth A. Baker, MD<br />
Director of <strong>Medical</strong> Student<br />
Programs, Clerkship Director,<br />
Associate Professor, and General<br />
Internist in the Department of<br />
Internal Medicine<br />
Dr. Baker has been serving <strong>Rush</strong><br />
<strong>University</strong> for over 20 years.<br />
She has been awarded with<br />
two “Department of Medicine<br />
Teaching and Service Awards”<br />
and was elected into the Mark H<br />
Lepper, MD Society of Teachers<br />
in 2004. She has developed myriad<br />
programs within the <strong>Rush</strong> <strong>Medical</strong><br />
College Internal Medicine Core<br />
Clerkship, Subinternship, and<br />
CRASH (Clinical Resources and<br />
Skills for the Hospital) courses.<br />
Her research interests in medical<br />
education are wide, with recent<br />
publications on struggling medical<br />
students and the relationship<br />
between medical students and<br />
the pharmaceutical industry. She<br />
currently serves as chair of <strong>Rush</strong><br />
<strong>Medical</strong> College’s Committee on<br />
Curriculum and Evaluation and<br />
is a member of <strong>Rush</strong> <strong>University</strong>’s<br />
Faculty Nomination Committee.<br />
She practices both outpatient<br />
general internal medicine and<br />
hospital medicine as part of <strong>Rush</strong><br />
<strong>University</strong> Internists.<br />
Stephanie C. Wang, MD<br />
Associate Program Director of<br />
Evaluation and Ambulatory Care<br />
Dr. Wang has been serving the<br />
<strong>Rush</strong> <strong>University</strong> and metropolitan<br />
Chicago area for more than<br />
10 years. Her achievement in<br />
medical academia has been<br />
outstanding. While serving her<br />
residency, she received numerous<br />
awards including Department of<br />
Medicine teaching and Service,<br />
Upjohn Achievement, outstanding<br />
intern, and outstanding resident<br />
award for RUMC. Not only that,<br />
she was inducted in 2006 as a<br />
recipient of the Lepper Award.<br />
Her involvement in various<br />
committees has been valuable<br />
to the university; she has been<br />
a member of faculty council,<br />
curriculum, and dean search<br />
committee for the <strong>University</strong>. As of<br />
now, she is instituting a project for<br />
International Healthcare Program<br />
relation and sending cross-specialty<br />
teams in remote area of Peralta,<br />
Dominican Republic.<br />
<strong>Medical</strong> Education Program<br />
Richard I. Abrams, MD<br />
Assistant Chairman, Program<br />
Director of the Internal Medicine<br />
Residency Training Program,<br />
Associate Section Head Section of<br />
General Internal Medicine, and<br />
Assistant Professor of Medicine<br />
Dr. Abrams has been serving<br />
<strong>Rush</strong> <strong>University</strong> for more than<br />
20 years. During this time he<br />
has received recognition for his<br />
teaching abilities including three<br />
Department of Medicine Teaching<br />
and Service Awards, an American<br />
College of Physicians Community<br />
Based Teaching’ Excellence in<br />
Teaching Award, the Stuart Levin<br />
Excellence in Medicine Award, and<br />
election to the Lepper Society of<br />
Teachers. He has been a member<br />
of great number institutional<br />
and departmental committees,<br />
currently serving on the Graduate<br />
<strong>Medical</strong> Education Committee,<br />
the Department of Medicine’s<br />
Quality Assurance Committee<br />
and Patient Safety Committee.<br />
He has publications in a number<br />
of prestigious journals including<br />
JAMA, Lancet, <strong>Medical</strong> Care,<br />
and the Journal of General Internal<br />
Medicine.<br />
9
CLINICAL ACTIVITIES<br />
10<br />
Robert L. Rosen, MD<br />
Associate Chair<br />
of Department of<br />
Internal Medicine<br />
The Department of Internal Medicine Quality Assurance (QA) is a<br />
comprehensive effort that focuses on providing high quality, safe care to<br />
our patients both in the inpatient and outpatient settings. The Chair of<br />
Department of Internal Medicine provides leadership to the department and<br />
all section heads are related to the importance of monitoring and improving<br />
patient care.<br />
The quality assurance and implementation functions of the Department of<br />
Internal Medicine center in a weekly forum, the <strong>Medical</strong> Advisory and Quality<br />
Implementation Committee, which is routinely attended by all involved in<br />
the patient care provided by the department. Attendees include the Internal<br />
Medicine’s administrative leadership, leadership of the residency program,<br />
chief medical residents, leadership of the <strong>Rush</strong> <strong>University</strong> Internist group<br />
that provides both inpatient care thru the hospitalists and outpatient care,<br />
leadership of both acute care and critical care nursing, nursing unit directors<br />
of the medical units, medical leadership of the critical care units, risk<br />
management, pharmacy, bed management, discharge planning, radiology, and<br />
laboratory services. This standing meeting provides a framework for discussing<br />
issues in real time and acting on them quickly since the participants are in<br />
positions where change can be effected.<br />
There are a number of ongoing areas of attention. Interactions and<br />
communication between physicians, nurses, ancillary services, and<br />
administration are constantly addressed in order to optimize the work<br />
environment of all. Patient and family concerns are discussed. Review of<br />
morbidities and unexpected mortalities takes place in this forum. The group<br />
addresses issues related to electronic applications used in medicine at <strong>Rush</strong><br />
with a special emphasis on new implementations of the electronic medical<br />
records and medical reconciliation.<br />
Specific departmental initiatives in patient safety are developed and<br />
implemented by the Section of Patient Safety Research based on issues raised<br />
in the Department of Internal Medicine Quality Implementation Committee.<br />
Current priority issues include safety checklists, pain management, avoidance<br />
of hypoglycemia, reduction of polypharmacy, medication reconciliation, and<br />
implementation of electronic applications in medicine.<br />
Many of the subspecialty sections are actively involved in patient safety efforts.<br />
The Division of Pulmonary and Critical Care has coordinated a combined<br />
morbidity and mortality meeting with the surgical departments in addition to<br />
a primary overview of quality and safety issues in the <strong>Medical</strong> Intensive Care<br />
Unit. Cardiology, Nephrology, and Digestive Diseases also have a systematic<br />
approach to monitoring procedures and care that they provide.
Over the past year, the Department<br />
of Internal Medicine has continued to<br />
develop its research program through the<br />
continued development of two objectives:<br />
1) to facilitate Interdepartmental<br />
Collaborative Research Projects; and<br />
2) to mentor junior faculty to become<br />
leading researchers through the<br />
Research Mentoring Program.<br />
Interdepartmental Collaborative<br />
Research Projects<br />
The Joint MetaBiome <strong>Center</strong>, a<br />
partnership with George Mason<br />
<strong>University</strong>, is an example of an<br />
interdepartmental collaborative<br />
research project within <strong>Rush</strong>. The<br />
focus of the center will be clinical<br />
applications of dysbiosis of the entire<br />
human microbiome that resides in the<br />
gut, mouth, urogenital, and respiratory<br />
tract and characterize the homeostatic<br />
interactions between the microbiome<br />
and human genome or homobiome.<br />
Another collaborative research project<br />
included the SCOR study or the Study<br />
of Orthotic Shoe Inserts for Controlling<br />
Osteoarthritic Knee Pain. This research,<br />
led by Dr. Joel Block in the Department of<br />
Rheumatology, included the Departments<br />
of Biochemistry and Orthopedics to<br />
evaluate the effectiveness of customized<br />
shoe insets in controlling and relieving<br />
the pain of knee osteoarthritis.<br />
Research Mentoring Program<br />
The Research Mentoring Program<br />
is designed to prepare junior faculty<br />
members in the Department of Medicine<br />
at <strong>Rush</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong> and<br />
Stroger Hospital of Cook County to<br />
lead funded programs of translational<br />
research that will have a direct impact<br />
on the health of the nation. To achieve<br />
its goal, the program relies on two<br />
primary mechanisms: good mentoring<br />
and resources. Mentees are paired with<br />
experienced and committed mentors<br />
who work very closely with the mentee<br />
on her/his research project. The program<br />
also provides a range of resources to<br />
mentees, including: data management,<br />
statistical analysis, professional grant<br />
writing and manuscript editing, support<br />
staff, and regular workshops and seminars<br />
on a variety of research-related and grantwriting<br />
topics.<br />
The program currently has 27 mentees<br />
and more than 30 mentors and consists of<br />
four translational research tracks: clinical<br />
(outcomes and behavioral interventions,<br />
decision-making, communication, and<br />
safety); population-based; genetic-based;<br />
and laboratory-based.<br />
Program Goals<br />
The Research Mentoring program has<br />
four program goals for the upcoming<br />
year:<br />
1. To improve our marketing of the<br />
program throughout the <strong>University</strong>;<br />
2. To continue to recruit new mentees<br />
and mentors across colleges;<br />
3. To hire a master’s level statistician; and<br />
4. To secure long-term funding for<br />
the program.<br />
RESEARCH ACTIVITIES<br />
Ali Keshavarzian,<br />
MD,<br />
- Vice Chairman<br />
of Medicine for<br />
Academic and<br />
Research Affairs<br />
- Director of Division<br />
of Digestive Disease<br />
11
STATISTICAL SNAPHOT OF<br />
DEPARTMENT OF INTERNAL MEDICINE<br />
John Rechner, MBA, CMPE<br />
Executive Administrator<br />
John Paulsen<br />
Director of Finance<br />
Kathryn Larsen<br />
Sr. Financial Analyst<br />
12<br />
60,000<br />
50,000<br />
40,000<br />
30,000<br />
20,000<br />
10,000<br />
0<br />
DEPARTMENT OF INTERNAL MEDICINE TOTAL WORK RVUs<br />
9,883 10,275<br />
51,458<br />
Inpatient Admissions Inpatient Patient Days<br />
2007 2008<br />
51,082<br />
CLINICAL (FY08)<br />
Inpatient Admissions 10,275<br />
Inpatient Patient Days 51,082<br />
Average Length of Stay 4.97<br />
Inpatient Discharges 10,384<br />
Outpatient Visits<br />
Senior Care 5,463<br />
Cardiology 15,061<br />
General Internal Medicine 57,223<br />
Endocrinology 7,167<br />
Pulmonary/Critical Care 4,832<br />
BMT/Hematology 14,455<br />
Oncology 25,389<br />
Hepatology 2,103<br />
Rheumatology 13,026<br />
Gastroenterology 15,720<br />
TOTAL 160,439<br />
WORK RVU<br />
500,000<br />
400,000<br />
300,000<br />
200,000<br />
100,000<br />
0<br />
355,157<br />
415,145<br />
476,831<br />
FY2007 FY2008 FY20<strong>09</strong>*
IN MILLIONS<br />
3.0<br />
2.5<br />
2.0<br />
1.5<br />
1.0<br />
0.5<br />
0.0<br />
0.9<br />
DEPARTMENT OF INTERNAL MEDICINE REVENUE PROFILE<br />
1.8<br />
1.9<br />
2.6<br />
1.8<br />
2.5<br />
70% - Other RUMC Patient Days<br />
2006 2007 2008<br />
Total Research Revenue Clinical Revenue Other Revenue<br />
2.1<br />
2<br />
Department of Internal Medicine<br />
30% - Internal Medicine Patient Days<br />
67% - Other RUMC Admission<br />
33% - Internal Medicine Admission<br />
2.2<br />
13
Department of Internal Medicine<br />
DEPARTMENT OF INTERNAL MEDICINE CLINICAL ACTIVITY<br />
Total Work RVUs % change Patient Revenues % change<br />
2007 2008 2007 to 2008 2007 2008 2007 to 2008<br />
Bone Marrow Transplant 7,691 11,526 50% 925,121 1,002,155 8%<br />
Endocrinology 14,747 16,930 15% 1,452,469 1,358,459 -6%<br />
Hematology 23,074 32,885 43% 3,379,472 4,073,420 21%<br />
Pulmonary/Critical Care 37,711 40,668 8% 1,951,364 2,029,341 4%<br />
General Internal Med. 119,385 150,437 26% 9,801,879 11,361,947 16%<br />
Senior Care 21,539 26,167 21% 1,641,487 1,858,264 13%<br />
Oncology 23,<strong>09</strong>4 28,6<strong>09</strong> 24% 6,414,745 6,936,525 8%<br />
Cardiology 80,664 79,646 -1% 7,117,324 6,713,885 -6%<br />
Gastroenterology 51,859 50,162 -3% 6,152,802 6,283,101 2%<br />
Rheumatology 22,785 20,463 -10% 7,660,157 7,492,084 -2%<br />
Total 402,549 457,493 14% 46,496,820 49,1<strong>09</strong>,181 6%<br />
Does not include Hepatology and Private Practices<br />
14<br />
DEPARTMENT OF INTERNAL MEDICINE BUDGETED RESEARCH TOTALS- $M<br />
FY06 FY07 FY08<br />
NIH & Gov Non-Gov Total NIH & Gov Non-Gov Total NIH & Gov Non-Gov Total<br />
Cancer 0.0 2.0 2.0 0 1.6 1.6 0.1 2.7 2.8<br />
Cardiology 0.4 0.5 0.9 0.0 1.0 1.0 0.0 1.3 1.3<br />
Endocrinology 0.0 0.0 0.0 0.0 0.2 0.2 0.0 0.2 0.2<br />
Epidemiology & Aging 3.8 0.0 3.8 3.9 0.3 4.2 5.7 0.2 5.9<br />
Geriatrics 0.1 0.0 0.1 0.1 0.1 0.2 0.0 0.2 0.2<br />
GI-DD 1.3 0.0 1.3 1.4 0.1 1.5 0.5 0.1 0.6<br />
Hepatology 0.1 0.4 0.5 0.0 0.1 0.1 0.0 0.1 0.1<br />
ID 1.3 0.1 1.4 1.1 0.6 1.7 1.0 0.5 1.5<br />
Nephrology 0.0 0.3 0.3 0.0 0.2 0.2 0.0 0.1 0.1<br />
Pulmonary 0.0 0.1 0.1 0.0 0.1 0.1 0.0 0.1 0.1<br />
Rheumatology 1.0 0.4 1.4 0.3 0.2 0.5 1.0 0.1 1.1<br />
Total 8.0 3.8 11.8 6.8 4.5 11.3 8.3 5.6 13.9
CHAIR ENDOWMENT PRINCIPAL BALANCES FY08 $M<br />
FACULTY APPOINTMENTS (FULL TIME)<br />
Department of Internal Medicine<br />
Cancer 14.6<br />
Cardiology 8.5<br />
Rheumatology 7.0<br />
Health & Aging 4.0<br />
Administration 4.3<br />
Nephrology 4.0<br />
Infectious Diseases 3.8<br />
Hepatology 3.7<br />
Gastroenterology 2.6<br />
Endocrinology 1.6<br />
Pulmonary 0.6<br />
TOTAL $54.7<br />
Professor 35<br />
Associate Professor 30<br />
Assistant Professor 129<br />
Instructor 35<br />
Lecturer 4<br />
TOTAL 233<br />
MANAGEMENT OVERSIGHT IN ANNUAL FY08 $M<br />
GME $3.4<br />
RMC $2.3<br />
MSPs/PBC $49.2<br />
Funded Research & Clinical Trials $13.9<br />
Endowed Chair Income $3.4<br />
TOTAL $72.2<br />
15
SECTION OF CARDIOLOGY<br />
1725 W. Harrison Street, 11th Floor<br />
(312) 563-3801<br />
16<br />
James E. Calvin, Jr.,MD, FACC<br />
Section Director<br />
James B. Herrick Professor<br />
of Medicine<br />
Faculty<br />
Professors:<br />
Gary L. Schaer, MD<br />
Philip R. Liebson, MD<br />
Richard G. Trohman, MD, FAHA,<br />
FACC, FHRS<br />
Steven B. Feinstein, MD, FACC<br />
Associate Professors:<br />
Annabelle S. Volgman, MD,<br />
FACC<br />
Barbara Pisan, MD<br />
Clifford J. Kavinsky, MD, PhD<br />
Lynn Braun, PhD, RN,ARNP<br />
Jeffrey S. Soble, MD<br />
R. Jeffrey Snell, MD<br />
Jose C. Mendez, MD<br />
Assistant Professors:<br />
Bosko Margeta, MD (Stroger)<br />
Carolina Karam-Demori, MD<br />
(0.2/0.8 Stroger)<br />
Claudia Gidea, MD<br />
Donald J. Tanis, MD<br />
Kousik Krishnan, MD, FACC<br />
Payman Sattar, MD, FACC<br />
(0.25/0.75 Stroger)<br />
Rami Doukky, MD, FACC<br />
Robert Creek, MD<br />
The Section of Cardiology at <strong>Rush</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong> and<br />
the <strong>Rush</strong> Heart and Vascular Institute are deeply committed to the<br />
three pillars of academic medicine: delivering the finest care to our<br />
patients with cardiovascular disease; educating the very best academic<br />
physicians who will become leaders in their field; and furthering<br />
medical knowledge through the pursuit of innovative research in<br />
cardiovascular disease.<br />
The Section of Cardiology has had a very successful year in all of its<br />
missions, education, research and clinical service. We maintain an<br />
outstanding fellowship program, a growing research program, have<br />
rebuilt the Heart Failure/Transplant program and have expanded the<br />
Structural Heart Disease/Adult Congenital Heart Disease program.<br />
The remainder of this report specifically addresses each mission.<br />
Education<br />
The section continues to support one of the largest cardiology<br />
fellowship programs in the Midwest: 18 general cardiology, two<br />
interventional and one electrophysiology fellow(s). The section receives<br />
close to 600 applications for the six first year slots each year and this<br />
year matched with our first six selections. For the past five years, we<br />
have conducted an annual in-service exam for all general cardiology<br />
fellows. Pass rates on the ABIM-cardiovascular medicine exam<br />
exceeds 85%.<br />
Post graduate teaching through the critical care unit and consultation<br />
team rounds is active with approximately 14 housestaff involved each<br />
week. Undergraduate lectures are organized for the cardiovascular<br />
block in second year. Fellows are currently engaged in individual<br />
faculty mentored research studies under the director of Dr. Philip<br />
Liebson. There are currently 17 projects being performed by cardiology<br />
fellows. We believe that our fellowship program has evolved into one<br />
of the finest and most comprehensive training programs available in<br />
cardiovascular medicine in the country.<br />
Research<br />
The Section of Cardiology has an active clinical research and preclinical<br />
research program. Areas of interest include treatment of<br />
heart failure and coronary artery disease, medical and non-medical<br />
management of cardiac arrhythmia, cardiac prevention and cardiac<br />
imaging. The Section has been awarded seven industry-based grants.<br />
The Section has authored or co-authored 60 peer review papers<br />
including 17 papers where the primary author was a cardiology fellow.
Clinical Services<br />
Cardiac clinical service focus on the evaluation<br />
and non-surgical treatment of heart failure,<br />
coronary artery disease (acute and chronic),<br />
cardiac arrhythmias and cardiac prevention.<br />
Diagnostic services include echocardiography,<br />
electocardiography, diagnostic heart catheterization,<br />
stress testing (including nuclear), Holter monitoring<br />
and electrophysiology. Therapeutic interventions<br />
including medical therapy for all cardiac conditions,<br />
coronary intervention, structural heart disease<br />
intervention, cardiac arrhythmia ablation and<br />
pacemaker and defibrillator insertion. The following<br />
table summarizes the number of cardiac procedures<br />
and services provided by the Section of Cardiology<br />
during the past year.<br />
CLINICAL TRIALS AND INDUSTRY STUDIES<br />
Services Total Per FY 08<br />
Left Heart Cath 921<br />
Coronary Angios 921<br />
PCIs 257<br />
Echocardiogram 8,355<br />
Nuclear Stress 3,477<br />
Echo Stress 1,<strong>09</strong>5<br />
Clinic Visits 12,800<br />
Hospital Patient Days 1,582<br />
EP Tests 190<br />
Arrhythmia Ablations 168<br />
AICDs 156<br />
Pacemakers 76<br />
Holter Monitors 706<br />
Section of Cardiology<br />
Study Title Principal Investigator Award Amount ($)<br />
Atherosclerosis Disease Measured by Carotid<br />
Intima-Media Thickness<br />
Implant to Reduce Refractory Migraine<br />
Headache with Aura<br />
Prevention of Vascular Events for<br />
Elevated Acute Coronary Syndromes<br />
Heparin Study for Stable Coronary<br />
Artery Disease PCI<br />
Dell Delivery and Retension Helix in an<br />
Acute Preclinical Setting<br />
Carotid Revascularization Evolution<br />
Post Approval Study<br />
Acunav Peer Training<br />
Implant of SAPIEN Transcatheter<br />
Heart Valve in Pulmonic Position<br />
Heart Failure Adherence<br />
and Retention Trial<br />
Feinstein, Steven 99,840<br />
Kavinsky, Clifford 219,800<br />
Schaer, Gary 65,000<br />
Schaer, Gary 41,847<br />
Schaer, Gary 136,<strong>09</strong>8<br />
Snell, Jeffrey 112,000<br />
Hijazi, Ziyad 15,141<br />
Hijazi, Ziyad 83,535<br />
Calvin, James<br />
Powell, Lynda<br />
550,000<br />
17
SECTION OF COMMUNITY EPIDEMIOLOGIC RESEARCH<br />
1645 W. Jackson Blvd, Suite 675<br />
(312) 942-3350<br />
18<br />
Carlos F. Mendes de Leon, PhD<br />
Section Director<br />
Faculty<br />
Professors:<br />
Denis A. Evans, MD<br />
Carlos F. Mendes de Leon, PhD<br />
Associate Professors:<br />
Liesi Hebert, ScD<br />
Jeremiah Kelly, MD<br />
Assistant Professors:<br />
Xinqi Dong, MD<br />
Kimberly A. Skarupski, PhD<br />
Jennifer Weuve, ScD<br />
The primary mission of the Section of Community Epidemiologic<br />
Research is to conduct community-based epidemiologic research<br />
on common, aging-related chronic conditions and their functional<br />
consequences. The Section also participates in educational services<br />
within the Department of Internal Medicine and the <strong>Medical</strong> School more<br />
generally. The Section has historically consisted of faculty that represents<br />
several academic disciplines, including internal medicine, epidemiology,<br />
and biostatistics. The Section has developed extensive collaborations<br />
with other academic and clinical Departments at <strong>Rush</strong> <strong>University</strong> <strong>Medical</strong><br />
School, the <strong>Rush</strong> College of Nursing and Stroger Hospital of Cook<br />
County, as well as other academic institutions in Chicago and elsewhere<br />
in the US.<br />
In July of 2008, the Section underwent a transition in leadership. After<br />
many years of outstanding service, Dr. Evans has stepped down as Section<br />
Director and was succeeded by Dr. Mendes de Leon. The Section has<br />
also added a new faculty member, Dr. Jennifer Weuve, Assistant Professor<br />
of Internal Medicine (Epidemiology), who has joined the Section after<br />
completing her doctoral and post-doctoral training at the Harvard School<br />
of Public Health.<br />
Education<br />
The Section plays an active role in the Department of Internal Medicine<br />
Mentorship Program. Drs. Evans and Mendes de Leon serve on<br />
the Mentorship Program Steering Committee, and jointly lead the<br />
Population-Based Translational Track of this Program. They have<br />
mentored five faculty members of the Departments of Internal Medicine<br />
at <strong>Rush</strong> and Cook County. The Section has also offered biostatistical,<br />
data analysis and data management services to the Mentorship Program.<br />
Section members further contribute to the core course in epidemiology<br />
and biostatistics that is part of the 2nd year <strong>Medical</strong> School curriculum.<br />
Research<br />
As part of the core mission, the Section of Community Epidemiologic<br />
Research conducts several population-based research studies aimed at<br />
improving our understanding of the determinants and consequences of<br />
common, aging-related chronic conditions. The primary research study<br />
is the Chicago Health and Aging Project, which is a population-based,<br />
longitudinal study aimed at identifying risk factors for Alzheimer’s<br />
disease. The study takes place in a population of older Blacks and Whites<br />
who live in three community areas on the south side of Chicago. The<br />
study started in 1993 and is currently in its 15th year of operations. A<br />
number of other research projects have been built on this study, including<br />
studies of the influence of the physical and social environments on agingrelated<br />
health and disability, genetic risk factors for Alzheimer’s disease,
studies of care giving for patients with Alzheimer’s<br />
disease, clinical course of disease after diagnosis<br />
of Alzheimer’s disease, and secular changes in the<br />
prevalence of Alzheimer’s disease.<br />
The Section has begun to focus increasingly on<br />
aging-related health issues in disadvantaged<br />
populations. An important of this work focuses on<br />
elder abuse and neglect, which is a geriatric topic<br />
of substantial clinical importance but which has<br />
received very little attention in the medical literature.<br />
Other aspects involve more detailed studies of racial<br />
disparities in aging-relate health, with a focus on<br />
the social and biological pathways that lead to these<br />
disparities in older age.<br />
GRANTS<br />
Section of Epidemilogic Research<br />
The Section has also started to prepare for new<br />
studies related to aging-related health in diverse<br />
communities of older adults. One of the projects<br />
currently in development is a study that will<br />
investigate the role of health care trust in the health<br />
in several other populations in the city of Chicago,<br />
including the Chinese American community and<br />
the Latino community. Additional plans are being<br />
development for studies on health-related quality of<br />
life, end-of-life care, and the role of air pollution and<br />
other types of environmental exposures in causing<br />
late-life cognitive impairment and other health<br />
problems.<br />
Sponsor Principal Investigator Focus Yearly Funding<br />
Consequences of Self-Neglect in a<br />
NIH-K23 XinQi Dong, MD<br />
Biracial Population of Older People<br />
$92,559<br />
Partners in Research Program with<br />
NIH-R03 XinQi Dong, MD $37,407<br />
Chinese Community<br />
Risk Factors for Incident<br />
NIH-R01 Denis A. Evans, MD $1,829,375<br />
Alzheimer’s Disease<br />
Epidemiologic Study of Persons<br />
NIH-R01 Denis A. Evans, MD $639,424<br />
with Alzheimer’s Disease<br />
Genetic Epidemiology of Cognitive<br />
NIH-R01 Denis A. Evans, MD $611,861<br />
Decline in an Aging Population Sample<br />
Secular Changes in Alzheimer’s<br />
NIH-R03 Liesi E. Hebert, PhD $65,268<br />
Disease Risk<br />
NIH-R21 Jeremiah Kelly, MD<br />
Relationship Between AD<br />
Clinicopathological Changes and CNS<br />
Sex Steroid Hormones<br />
$153,750<br />
NIH-R01 Carlos Mendes de Leon, PhD Psychosocial Factors and Stroke Risk in $113,500<br />
Subcontract<br />
a Biracial Population<br />
NIH-R01 Carlos Mendes de Leon, PhD SES and Age-Related Disability in a<br />
Biracial Community<br />
$576,864<br />
NIH-R01 Carlos Mendes de Leon, PhD<br />
Early and Mid-Life Social<br />
Determinants of Racial Disparities in<br />
Late-Life Health<br />
$448,289<br />
19
DIVISION OF DIGESTIVE DISEASE<br />
1725 W. Harrison St, Suite 206<br />
(312) 942-5861<br />
20<br />
Ali Keshavarzian, MD<br />
Division Director<br />
Stanley M. Cohen, MD<br />
Director, Section of Hepatology<br />
Mark T. DeMeo, MD<br />
Director, Section of<br />
Gastroenterology & Nutrition<br />
Martha C. Morris, Sc.D<br />
Director, Section of Nutrition<br />
and Nutritional Epidemiology<br />
Faculty<br />
Professors:<br />
Martha C. Morris, Sc.D<br />
Nutrition and Nutritional<br />
Epidemiology<br />
Ali Keshavarzian, MD<br />
Gastroenterology<br />
The Division of Digestive Diseases<br />
consists of three sections:<br />
Section of Hepatology, Section of<br />
Gastroenterology & Nutrition, and the Section<br />
of Nutrition and Nutritional Epidemiology.<br />
Over the past year, the Division has expanded<br />
its clinical offerings and launched three<br />
subspecialty programs and clinics in the areas<br />
of Adult Celiac Disease, Inflammatory Bowel<br />
Disease and Gastrointestinal Cancer.<br />
The new Section of Nutrition and Nutritional<br />
Epidemiology, led by Martha C. Morris, PhD,<br />
which will focus on the nutrition related effects<br />
on chronic conditions and diseases associated<br />
with aging.<br />
The Adult Celiac Disease Program, launched<br />
in November 2007 by Mark DeMeo, MD<br />
has been a large success. The program offers<br />
patients access to weekly clinic, linkages to<br />
subspecialty physicians with celiac disease and<br />
access to a dietitian with expertise in glutenfree<br />
diets and a gastrointestinal psychologist.<br />
Additionally, the program hosts a number of<br />
Sohrab Mobarhan, MD<br />
Gastroenterology<br />
David Van Thiel, MD<br />
Hepatology<br />
Associate Professors:<br />
Michael D. Brown, MD<br />
Gastroenterology<br />
Keith Bruninga, MD<br />
Gastroenterology<br />
Stanley M. Cohen, MD<br />
Hepatology<br />
Mark T. DeMeo, MD<br />
Gastroenterology<br />
John Losurdo, MD<br />
Gastroenterology<br />
Ece Mutlu, MD<br />
Gastroenterology<br />
Carline Quander, MD<br />
Gastroenterology<br />
Nikunj Shah, MD<br />
Hepatology<br />
Assistant Professors:<br />
Joseph Ahn, MD<br />
Hepatology<br />
Ashkan Farhadi, MD<br />
Gastroenterology<br />
Garth Swanson, MD<br />
Gastroenterology<br />
patient education events throughout the year,<br />
including a gluten-free cooking seminar.<br />
The Inflammatory Bowel Disease Program,<br />
led by Ece Mutlu, MD, offers patients with<br />
ulcerative colitis and Crohn’s disease access to<br />
dedicated clinic, a monthly support group led<br />
by our Section’s gastrointestinal psychologist<br />
and access to numerous clinical trials.<br />
The Division also launched the Coleman<br />
Foundation Comprehensive Clinic for<br />
Gastrointestinal Cancers, led by Sohrab<br />
Mobarhan, MD. This multidisciplinary clinic<br />
consists of gastroenterologists, nutrition<br />
specialists, medical oncologists, pathologists,<br />
diagnostic radiologists, radiation oncologists,<br />
surgeons, nurses and staff who provide<br />
patients with preventive services and the latest<br />
diagnostic and treatment services for all types<br />
of gastrointestinal cancers.<br />
Education<br />
The Division of Digestive Disease fellowship at<br />
<strong>Rush</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong> is a three-year
program. Three positions are available each<br />
year. Currently, there are 10 individuals enrolled<br />
in the fellowship.<br />
The core curriculum includes rotations in outpatient<br />
and inpatient gastroenterology, hepatology and<br />
liver transplant inpatient services, endoscopy and<br />
interventional endoscopy rotations. Trainees, also<br />
participate in additional rotations such as pathology,<br />
radiology and nutrition. In addition to the <strong>Rush</strong> main<br />
campus, fellows participate in off-site rotations in<br />
general gastroenterology at <strong>Rush</strong> Oak Park and <strong>Rush</strong><br />
North Shore hospitals. Fellows also have access to<br />
an Immersion endoscopy simulator, which is used<br />
for training. Six months of the three-year program<br />
are dedicated to mentored research by Section<br />
attendings. Fellows are expected to submit and<br />
present abstracts at national meetings.<br />
Research<br />
The Division of Digestive Diseases has a vibrant<br />
translational medical research program which<br />
incorporates data from patient clinical studies,<br />
research using animal models of human diseases, and<br />
experiments on human cells grown in tissue culture.<br />
Division of Digestive Disease<br />
A major overall theme of the Division’s research is<br />
the role of the intestinal epithelium in health and<br />
disease, especially permeability of the epithelium<br />
to products in the intestine during inflammation.<br />
Abnormal intestinal permeability has been<br />
implicated in several human diseases including<br />
inflammatory bowel disease, alcoholic liver disease,<br />
Parkinson’s disease, and autism.<br />
The Division has several focus areas of research on<br />
this theme. One major area involves the effects of<br />
alcohol on the epithelium and the role of alcoholstimulated<br />
cell signaling in the intestinal epithelium<br />
in promoting alcoholic liver disease by making<br />
the intestine more ‘leaky’. Several independent<br />
but interrelated lines of investigation are currently<br />
examining how alcohol promotes abnormal signaling<br />
in intestinal cells. These include the roles of growth<br />
factor receptor signaling, especially the epidermal<br />
growth factor, the role of membrane lipid rafts in cell<br />
signaling, and the role of intestinal metalloproteases<br />
in cell signaling. The Division of Digestive Diseases<br />
Research Laboratory is committed to the <strong>Rush</strong> vision<br />
of promoting medical knowledge and excellence<br />
in patient care through cutting edge translational<br />
medical research.<br />
21
Division of Digestive Disease<br />
GRANTS<br />
Sponsor Principal Investigator Focus<br />
NIH-R01 Ali Keshavarzian, MD<br />
NIH-R21 Ali Keshavarzian, MD<br />
NIH-R21 Ece Mutlu, MD<br />
NIH-R21 Ece Mutlu, MD<br />
Dept of Defense Ece Mutlu, MD<br />
Gilead Stanley M. Cohen, MD<br />
Roche Stanley M. Cohen, MD<br />
Vertex Stanley M. Cohen, MD<br />
Bristol Myers Squibb Stanley M. Cohen, MD<br />
Abbott Ece Mutlu, MD<br />
Centocor Ece Mutlu, MD<br />
Centocor Ece Mutlu, MD<br />
22<br />
Alcohol, iNos upregulation, leaky gut and liver disease<br />
Mindfulness, stress and IBD Flare-Up<br />
Dietary Treatment of Crohn’s Disease<br />
Dysbiosis in Inflammatory Bowel Disease<br />
Impact of Colonic Microbiota on Breast Cancer<br />
Study Comparing Tenofovir Disoproxil Fumarate, Emtricitabine Plus<br />
Tenofovir Disoproxil Fumarate, and Entecavir in the Treatment of<br />
Chronic Hepatitis B Subjects with Decompensated Liver Disease and<br />
in the Prevention of Hepatitis B Recurrence Post-Transplantation.<br />
Study of 360 µcg Induction Dosing of Peg in Combination with<br />
Higher Copegus Doses in Tx-Naïve Pts w/ CHC Genotype 1 if High<br />
Viral Titer and Body Wt ≥ 85 kg.<br />
Study of Stopping Treatment at 24 Weeks or Continuing Treatment<br />
to 48 Weeks in Treatment-Naïve Subjects with Genotype 1 Chronic<br />
Hepatitis C who Achieve an Extended Rapid Viral Response (eRVR)<br />
While Receiving Telaprevir, Peginterferon Alfa2a (Pegasys®) and<br />
Ribavirin (Copegus®)<br />
Study of Entecavir to Assess Long-term Outcomes Associated<br />
with Nucleoside/Nucleotide Monotherapy for Patients with Chronic<br />
HBV Infection.<br />
Registry Study of HUMIRA® (Adalimumab)<br />
Effect of Gastric Electrical Stimulation System in the Treatment<br />
of Chronic Intractable Nausea and Vomiting Secondary to<br />
Gastroparesis of Diabetic or Idiopathic Etiology<br />
Study to Evaluate the Safety and Efficacy of Golimumab Maintenance<br />
Therapy with Moderately to Severely Active Ulcerative Colitis<br />
The Crohn’s Therapy, Resource Evaluation and Assessment<br />
Tool Registry
Sponsor Principal Investigator Focus<br />
Centocor Ece Mutlu, MD<br />
Bristol Myers Squibb Ece Mutlu, MD<br />
Bristol Myers Squibb Ece Mutlu, MD<br />
Protherics Sohrab Mobarhan, MD<br />
Novartis Nikunj Shah, MD<br />
GlaxoSmithKline David VanThiel, MD<br />
GlaxoSmithKline David VanThiel, MD<br />
Bristol Myers Squibb David VanThiel, MD<br />
Division of Digestive Disease<br />
Study to Evaluate the Safety and Efficacy of Golimumab Induction<br />
Therapy with Moderately to Severely Active Ulcerative Colitis<br />
Study to Evaluate the Clinical Efficacy and Safety of Induction<br />
and Maintenance Therapy with Abatacept in Subjects with Active<br />
Ulcerative Colitis<br />
Study to Evaluate the Clinical Efficacy and Safety of Induction<br />
and Maintenance Therapy with Abatacept in Subjects with Active<br />
Crohn’s Disease<br />
Study of the efficacy and safety of OncoGel treatment as an adjunctive<br />
therapy in subjects with localized or locoregional esophageal cancer<br />
Study of Tyzeka(telbivudine) in nucleos(t)ide-naïve subjects of Black/<br />
African American and/or Hispanic/Latino origin with compensated<br />
chronic hepatitis B virus infection.<br />
Study to assess the efficacy and safety of eltrombopag in<br />
thrombocytopenic subjects with Hepatitis C Virus infection who are<br />
otherwise eligible to initiate antiviral therapy (pegylated interferon plus<br />
ribavirin) ENABLE 1 (Eltrombopag to iNitate and Maintain Interferon<br />
Antiviral Treatment to Benefit Subjects with Hepatitis C related Liver<br />
DiseasE.<br />
Study to assess the efficacy and safety of eltrombopag in<br />
thrombocytopenic subjects with hepatitis C virus (HCV) infection<br />
who are otherwise eligible to initiate antiviral therapy (peginterferon<br />
alfa-2b plus ribavirin) ENABLE 2 (Eltrombopag to iNitiate and<br />
Maintain Interferon Antiviral Treatment to Benefit Subjects with<br />
Hepatitis C Related Liver DiseasE).<br />
Study to Describe the Antiviral Effect of Entecavir (ETV) in Blacks/<br />
African Americans and Hispanics with Chronic Hepatitis B Virus<br />
(HBV) who are Nucleoside/tide-Naïve.<br />
23
SECTION OF ENDOCRINOLOGY<br />
1725 W. Harrison St. Suite 250<br />
(312) 942-6163<br />
24<br />
David Baldwin, MD<br />
Section Director<br />
Faculty<br />
Associate Professor:<br />
David Baldwin, MD<br />
Leon Fogelfeld, MD<br />
Assistant Professors:<br />
Alexander Lurie, MD<br />
Rema Gupta, MD<br />
Chung-Kay Koh, MD<br />
Tiffany K. Hor, MD<br />
The Section of Endocrinology offers a full range of services in<br />
endocrinology, including outpatient provocative endocrine testing,<br />
thyroid biopsy and intensive diabetes management and education.<br />
Endocrinology focuses on glands that secrete hormones, which are<br />
chemical messengers that travel throughout the bloodstream to regulate<br />
different bodily functions. These glands include the thyroid, parathyroid<br />
pituitary gland, hypothalamus, pancreas, adrenal glands and gonads.<br />
Outpatient Clinical Activities<br />
We continue to be very busy in our care of patients with diabetes and<br />
other endocrine conditions. Each faculty member sees patients in<br />
our outpatient office for 4 hours each day. We offer expertise in the<br />
comprehensive management of patients with type 1 and type 2 diabetes.<br />
In 2007, all 4 faculty in the Section earned recognition from the National<br />
Committee for Quality Assurance (NCQA) for excellence in diabetes<br />
care in the Diabetes Physician Recognition Program. Our group is the<br />
only endocrinologists in the Chicago metropolitan area to have received<br />
this distinction. We also offer expert assistance to patients with insulin<br />
pumps and continuous glucose sensors in conjunction with our diabetes<br />
education program (vide infra). We maintain a close collaboration with<br />
our colleagues in the <strong>Rush</strong> Section of Transplantation. Dr. Baldwin is<br />
the transplant endocrinologist within the kidney-pancreas transplant<br />
program. Additionally all transplant patients who develop diabetes are<br />
followed by endocrinology providers both in the hospital and in the<br />
outpatient clinic. One of our nurse practitioners is bilingual and has a<br />
busy practice seeing Spanish-speaking patients, including many transplant<br />
recipients. Twenty to thirty percent of all transplant patients have<br />
diabetes, many are Spanish speaking, and the section makes important<br />
contributions to their care and to the success of the transplant programs.<br />
We also are busy seeing outpatients with thyroid disease. All patients<br />
receive a clinical evaluation frequently supplemented by our performance<br />
of thyroid ultrasound examination and ultrasound guided fine needle<br />
aspiration. Our expertise in this area is complimented by collaboration<br />
with <strong>Rush</strong> colleagues in general surgery, ENT surgery, pathology, and<br />
nuclear medicine.
Inpatient Clinical Activities<br />
We maintain 4 inpatient consult services:<br />
1. Diabetes management all transplant/general<br />
surgery patients, 9N- 1 attending physician 4<br />
hours per day<br />
2. Diabetes management orthopedic/general<br />
surgery/neurology/rehabilitation patients, 9S, 9K,<br />
3K, 6N, 7S- 1 nurse practitioner 8 hours per day<br />
3. Diabetes management all cardiovascular surgery,<br />
vascular surgery, thoracic surgery, neurosurgery<br />
patients 8N, 8K- 1 attending physician 4 hours<br />
per day<br />
4. General endocrine consult service, all patients<br />
on any medical unit, all patients with diabetic<br />
ketoacidosis, all patients in the surgical ICU, and<br />
all non-diabetes consults elsewhere throughout<br />
the hospital- 1 attending physician supervising an<br />
endocrine fellow, medical residents, and medical<br />
students 4 hours per day.<br />
Education<br />
The section is involved in educational activities for<br />
both medical professionals and for patients.<br />
The section participates in a 2 year fellowship training<br />
program jointly based at <strong>Rush</strong> and at the John H.<br />
Stroger, Jr. Hospital of Cook County. The fellowship<br />
director is Dr. Leon Fogelfeld, the director of the<br />
Division of Endocrinology at Stroger Hospital and<br />
<strong>Rush</strong> <strong>University</strong>. Our total of four fellows spend<br />
three months per year at <strong>Rush</strong> on our inpatient<br />
consult service, three months per year on the Stroger<br />
inpatient consult service, three months per year in<br />
ambulatory rotations at Stroger and three months per<br />
year working on clinical research projects mentored<br />
by endocrine faculty from either <strong>Rush</strong> or Stroger. All<br />
endocrine faculty and fellows participate together in a<br />
clinical conference weekly, and in a journal club, in a<br />
Section of Endocrinology<br />
research conference, and in a basic science conference<br />
monthly. The fellows also have elective rotations in<br />
neurosurgery (pituitary) clinic, pediatric endocrine<br />
clinic, and high-risk obstetrics clinic.<br />
We have 2-4 medical residents and 0-2 medical<br />
students rotating on the <strong>Rush</strong> consult service each<br />
month. In conjunction with the endocrine attendings<br />
at Stroger and our fellows, we provide a 1 hour<br />
teaching session every morning for all of the residents<br />
and students who are rotating on the endocrine<br />
teams at Stroger and <strong>Rush</strong>. Each resident and student<br />
spends 4 hours per day seeing outpatients in our clinic<br />
supervised by endocrine faculty, and 4 hours seeing<br />
inpatient consults on the team with the fellow and<br />
supervising faculty. Thus all residents and students<br />
get a chance to work with the entire endocrine faculty<br />
during their rotation.<br />
The section faculty also conducts a 1-hour teaching<br />
session every day during the months of July-<br />
December aimed at teaching the first year house<br />
officers the essentials of insulin management. Each<br />
of the approximately 55 interns receives 4-6 hours of<br />
instruction in small ward based groups.<br />
Endocrine faculty continues to teach second year<br />
medical school pathophysiology and pharmacology<br />
lectures, as well as lectures for the <strong>Rush</strong> nurse<br />
practitioner program.<br />
In the area of patient education, the section runs<br />
an active center for the teaching of diabetes selfmanagement<br />
skills. A dietician-diabetes educator, a<br />
nurse-diabetes educator, and two nurse practitionerdiabetes<br />
educators all make important contributions<br />
to this program. Individual and group classes are<br />
conducted daily. The <strong>Rush</strong> Diabetes <strong>Center</strong> is the<br />
sole resource for diabetes education at the medical<br />
center and its staff sees 1,040 new patients and office<br />
consultations during the fiscal year. In 2008, the<br />
American Diabetes Association again awarded the<br />
25
Section of Endocrinology<br />
26<br />
<strong>Rush</strong> Diabetes <strong>Center</strong> with its three-year Certificate<br />
of Education Recognition. The Diabetes <strong>Center</strong><br />
maintains a computerized database on all of the<br />
patients who have gone through self-management<br />
training as well as all patients with diabetes followed<br />
by providers in the outpatient endocrinology clinics.<br />
Records of all important data relevant to the care of<br />
these patients with diabetes are maintained in this<br />
patient registry and are used for quality improvement<br />
and clinical research activities within the section.<br />
Research<br />
The Section continues to be involved in a number<br />
of clinical research activities. Most clinical trials<br />
have focused on the management of diabetes in<br />
the hospitalized patient. Many projects have had<br />
significant contributions from our endocrine fellows<br />
as well as from medical residents and medical<br />
students. In 2007-2008, we had 5 medical residents<br />
who worked on research projects mentored by<br />
CLINICAL TRIALS AND GRANTS<br />
endocrine faculty. During the year, we also had<br />
5 <strong>Rush</strong> medical students who made important<br />
contributions through the summer research<br />
fellowship program that the section funds<br />
and mentors.<br />
We completed a 2 year project at Saint Anthony<br />
Hospital in 2008 in which a nurse, a nurse<br />
practitioner, and an endocrine attending, all from the<br />
section, implemented modern protocols for diabetic<br />
management throughout the hospital. Negotiations<br />
are ongoing to reach out to another Chicago safetynet<br />
hospital with a similar project.<br />
We have completed or have ongoing 3 other<br />
investigator initiated clinical trials as listed below.<br />
2 additional trials are currently planned and grant<br />
applications are in preparation. 0.We have also just<br />
begun a 5 year clinical trial in collaboration with all<br />
of the other academic medical centers in Chicago of<br />
therapy to prevent nephropathy in patients with<br />
type 1 diabetes.<br />
Sponsor Investigator Areas of Focus Funding($)<br />
Fry Foundation D. Baldwin Saint Anthony Hospital 337,000<br />
NovoNordisk D. Baldwin Inpatient Insulin Trial 127,000<br />
NovoNordisk D. Baldwin ED- Inpt. Insulin Trial 115,000<br />
Sanofi-Aventis D. Baldwin Insulin in renal failure 134,000<br />
JDRF/NIH A. Lurie Nephropathy-type 1 DM 56,000
SECTION OF GENERAL INTERNAL MEDICINE<br />
The Section of General Internal Medicine is composed of a diverse group<br />
of dedicated physicians. These salaried and private-practice doctors see<br />
outpatients in a variety of offices, on and off the campus of the medical center.<br />
They also provide care to many hospitalized patients. General internists follow<br />
most patients admitted to the general medical services, and consult on and/or<br />
co-manage patients on non-medical services. General internists had almost<br />
6,300 inpatient admissions at <strong>Rush</strong> in academic year 2007/2008, with nearly<br />
27,000 inpatient hospital days.<br />
During the academic year, the Section of General Internal Medicine had<br />
32 salaried physicians who worked part or full-time in outpatient offices:<br />
24 physicians worked at <strong>Rush</strong> <strong>University</strong> Internists (RUI) on the north<br />
side of the Eisenhower Expressway in the Triangle Office Building, four<br />
physicians worked at <strong>Rush</strong> <strong>University</strong> Internal Medicine in the Chicago loop,<br />
two physicians worked in the Associates in Internal Medicine office in the<br />
Professional Office Building, two physicians worked with private practice<br />
physicians in the West Loop <strong>University</strong> Medicine office, and one physician<br />
worked with private practice physicians in the Palmer – Zavala, SC practice.<br />
Together these physicians had almost 62,000 outpatient visits during the year.<br />
The goal in all of the offices is to deliver high-quality, comprehensive, patientcentered<br />
primary care, with referral to <strong>Rush</strong> subspecialists when needed.<br />
In addition to the salaried physicians, over a dozen private internists see<br />
outpatients at the medical center in the Professional Office Building. An<br />
even larger group of private practice general internists have offices away from<br />
the medical center, but hospitalize patients at <strong>Rush</strong>. One on-campus private<br />
practice has its own hospitalist. Several on-campus practices have added new<br />
(salaried) physicians in their offices, as part of a RUMC strategic initiative<br />
to grow and develop primary care. In addition, two private physicians have<br />
established a “concierge” practice at the medical center; the practice has<br />
1,400 patients and a waiting list of patients who would like to join.<br />
<strong>Rush</strong> <strong>University</strong> Internists’ Hospital Medicine Service covers more hospitalized<br />
patients than any other group of physicians in the Department of Medicine,<br />
and provides the backbone for inpatient student and resident education in the<br />
department. RUI hospitalists cover over 80% of the patients on the general<br />
medical floors, and see 60-75 patients on non-medical services per day. The<br />
RUI Hospital Medicine Service had over 5,000 admissions in 2007/2008.<br />
The RUI Hospital Medicine Service is broken down into 8 general medical<br />
teams, each with an attending hospitalist; there are also has 2 consult<br />
physicians, 1 “short-stay” team physician, and 1 ICU physician on-service<br />
at any given time. In 2007/2008, the service was staffed by 11 full-time<br />
hospitalists, 2 “research hospitalists”, and 11 part-time hospitalists (including<br />
4 chief residents). Most subspecialty patients were admitted to the RUI<br />
hospitalist service, with the subspecialty services providing the expertise<br />
needed to diagnose and manage complex subspecialty problems. The patient<br />
1653 W Congress Parkway<br />
(312) -942-6600<br />
Margaret McLaughlin,<br />
MD Section Director<br />
27
Section of General Internal Medicine<br />
28<br />
care goals of the hospitalist service include improving<br />
patient safety, and expediting high-quality care via<br />
the immediate availability of attending physicians.<br />
In 2007/2008, the service added three nocturnists,<br />
thereby providing near 24-hour attending coverage<br />
for medical emergencies.<br />
Providing expanded medical coverage to patients on<br />
surgical services has become an important activity for<br />
general internists at <strong>Rush</strong>. Private practice physicians<br />
see many patients for pre-operative evaluation, and<br />
then follow these patients when they are admitted<br />
to the hospital. The RUI hospitalist service screens<br />
patients on the orthopedic surgery and rehabilitation<br />
services to ensure that patients needing to be comanaged<br />
by an internist are being actively followed.<br />
This screening activity has successfully reduced the<br />
number of patients needing emergency medical<br />
evaluations on non-medical services.<br />
Education<br />
The faculty from the Section of General Internal<br />
Medicine provide leadership for the internal<br />
medicine residency program, for which all four<br />
program directors (Drs. Richard Abrams, Scott<br />
Hasler, Andem Ekpenyong, and Stephanie Wang) are<br />
general internists. Undergraduate medical education<br />
is also led by general internists. Dr. Elizabeth Baker<br />
oversees the undergraduate medical education<br />
courses in the department, with the assistance of<br />
course directors from the section: Physical Diagnosis<br />
(Dr. Andem Ekpenyong), Pathophysiology (Dr. Syed<br />
Shah), the Internal Medicine Core Clerkship (Drs.<br />
Viju John, Jah-Won Koo, Jill Wener, and Shobha<br />
Rao), and the Internal Medicine Subinternship<br />
(Drs. Viju John and Michelle Sweet).<br />
RUI hospitalists are the principal educators of<br />
internal medicine residents on the general medical<br />
inpatient services. In addition, a resident is assigned<br />
to the General Medicine Consult service each month,<br />
on which he/she learns the fundamentals of pre<br />
and peri-operative care. In the outpatient setting,<br />
the core faculty in the <strong>Rush</strong> <strong>University</strong> Internists’<br />
outpatient office are responsible for the outpatient<br />
continuity training of approximately 100 internal<br />
medicine residents each year. The core faculty,<br />
under the guidance of Dr. Stephanie Wang, with the<br />
assistance of Dr. Andem Ekpenyong, oversee the<br />
resident outpatient continuity clinic. In 2007/2008,<br />
categorical internal medicine and medicine/<br />
psychiatry residents saw just over 11,000 patients<br />
at RUI. Drs. Wang and Ekpenyong have worked<br />
tirelessly with the core faculty and non-medical staff<br />
at RUI to improve residents’ outpatient experience<br />
and training, with substantial improvement in<br />
residents’ rating of their continuity experience<br />
over the past two years.<br />
Research<br />
Research in the Section of General Internal<br />
Medicine is focused in two main areas: patient<br />
safety (mainly evaluating inpatient care); and<br />
medical education. Several members of the section<br />
are on the department’s Patient Safety Committee.<br />
Two hospitalist members of the committee are<br />
participating in the department’s faculty mentoring<br />
program to further enhance their research training.<br />
In 2007/2008, the section had two one-year<br />
“research hospitalists,” each of whom worked on<br />
a research project, in addition to attending on the<br />
GIM inpatient services. One research hospitalist<br />
investigated anti-thrombotic therapy in patients<br />
with atrial fibrillation, and one looked for ways to<br />
reduce the number alerts firing for drug allergies<br />
in the electronic provider order entry system. Both<br />
physicians presented abstracts at the Chicago Patient<br />
Safety Forum. Dr. Richard Abrams participated in<br />
the national DEER (Diagnostic Error and Evaluation<br />
Research) project, and was a co-author on an<br />
abstract which resulted from this work.<br />
<strong>Medical</strong> education research produced publications<br />
during the year looking at medical students’ opinions<br />
toward the pharmaceutical industry, policies<br />
throughout the country for student performance in<br />
the internal medicine clerkship, medical student selfassessment<br />
of clinical skills, and simulator training of<br />
internal medicine residents to manage pain in<br />
cancer patients.
<strong>Rush</strong> <strong>University</strong> Internists’ Hospitalists<br />
Faculty<br />
Associates in Internal Medicine<br />
– Pamela Strauss , MD<br />
– Vianka Legra-Delgado, MD<br />
Hyde Park Associates<br />
– Roberto Ramirez, MD<br />
– David Scheiner , MD<br />
– Stephanie Weaver, MD<br />
– David Wechter, MD<br />
Kehoe and Djordjevic, SC<br />
– William Kehoe, MD<br />
– Dragan Djodjevic, MD<br />
Oak Park Hospital Physicians<br />
– Louis Barnes, MD<br />
Palmer-Zavala, SC<br />
– Myriame Casimir, MD<br />
– Albene Kokocinski, MD<br />
– Scott Palmer, MD<br />
– Gilberto Zavala, MD<br />
Private Solo Practices<br />
– Michael Bice, MD<br />
– Jeffrey Dugas, MD<br />
– Rolanda Lara, MD<br />
– Henry Palmer, MD<br />
– Patricia Shipley, MD<br />
– Danny Sugimoto, MD<br />
– Gayathri Sundaresan, MD<br />
West Loop <strong>University</strong> Medicine<br />
– Michele Bailey, DO<br />
– David Buyer, MD<br />
– Joseph Hennessy, MD<br />
– Frank Kelly, MD<br />
– Jeffrey Nekomoto, DO<br />
– Laura Smiricky, MD<br />
<strong>Rush</strong> <strong>University</strong> Internal<br />
Medicine<br />
– John Brill, MD<br />
– Bruce Huck, MD<br />
– Michele Kannin, MD<br />
– Daniel Pohlman, MD<br />
<strong>Rush</strong> <strong>University</strong> Internists<br />
– Richard Abrams, MD<br />
– Mary Anderson, MD<br />
– David Ansell, MD<br />
– Elizabeth Baker, MD<br />
– Rohini Bhat, MD<br />
– Bezalel Dantz, MD<br />
– Suma Dasari, MD<br />
– Soni Dhanireddy, MD<br />
– Catherine Dimou, MD<br />
– Jennifer Earvolino, MD<br />
– Andem Ekpenyong, MD<br />
– Laura Fassari, MD<br />
– Roman Gimpelevich, MD<br />
– Ann Goh, MD<br />
– Scott Hasler, MD<br />
– Richard Huh, MD<br />
– Josune Iglesias, MD<br />
– Viju John, MD<br />
– Jisu Kim, MD<br />
– Suchita Kishore, MD<br />
– Jah-Won Koo, MD<br />
– Vance Lauderdale, MD<br />
– Jacqueline Leavitt, MD<br />
– Jeehyun Lee, MD<br />
– Cynthia Louie, MD<br />
– Geoffrey Lowrey, MD<br />
– Bradley Manning, MD<br />
– Margaret McLaughlin, MD<br />
– Catherine Park, MD<br />
– Umesh Patel, MD<br />
– Andrew Peng, MD<br />
– Ruby Pouw, MD<br />
– Jeffrey Rado, MD<br />
– Shobha Rao, MD<br />
– Meilyn Reyes, MD<br />
– Daniel Rosenthal, MD<br />
– Syed Shah, MD<br />
– Michelle Sweet, MD<br />
– Jennifer Towbin, MD<br />
– Stephanie Wang, MD<br />
– Jill Wener, MD<br />
29
SECTION OF GERIATRIC MEDICINE AND PALLIATIVE CARE<br />
428 Johnston R. Bowman <strong>Center</strong><br />
(312) 942-5321<br />
30<br />
Martin J. Gorbien, MD, FACP, AGSF<br />
- Section Director,<br />
- Associate Director, The Johnston R.<br />
Bowman Health <strong>Center</strong><br />
Faculty<br />
Assistant Professors:<br />
Maria Hansberry, MD<br />
Associate Section Director<br />
Xinqi Dong, MD<br />
<strong>Rush</strong> Institute for Healthy Aging<br />
Magda Houlberg, MD<br />
(Works half-time at Howard Brown<br />
Health <strong>Center</strong>)<br />
Michael Leiding, MD<br />
Associate Fellowship Program Director<br />
Daniel Maher, MS, GNP<br />
Jack Olson, MD<br />
Fellowship Program Director<br />
Anthony Perry, MD<br />
Director, Johnston R. Bowman <strong>Center</strong><br />
Mona Tareen, MD<br />
Director, Adult Palliative Care Services<br />
The Section of Geriatric Medicine and Palliative Care continue<br />
to expand and modify its clinical services. In the past two years,<br />
we have assumed responsibility for the medical center’s palliative<br />
care program. This involves in-patient consultation and daily<br />
care, out-patient consultation as well as a variety of associated<br />
educational and administrative activities. Four members of the<br />
Section participate in <strong>Rush</strong> CON’s grant which developed an<br />
elective course in palliative care for medical and nursing students.<br />
Dr. Tareen, Dr. Hansberry and others participate in institutional<br />
committee work led by the CMO. These collective activities<br />
promise serve the medial center through enhanced quality of care,<br />
improved safety, improved length of stay and decrease mortality<br />
rates through prompt and appropriate transfer to hospice. Dr.<br />
Tareen serves a medical director for Heartland Hospice.<br />
Outpatient activities continue to expand due to enhanced capacity<br />
for geriatric assessment. Our outpatient clinic, <strong>Rush</strong> Senior Care,<br />
continues to be a popular training site for third year medical<br />
students, residents from <strong>Rush</strong> and outside hospitals (Stroger and<br />
others) and our fellows. The Section of General Internal Medicine<br />
has worked with our Section in order to develop guidelines for<br />
appropriate geriatric medicine and palliative care consultation. The<br />
success of this initiative will ideally have clinical and educational<br />
benefits. Outpatient clinics are being developed with other<br />
Sections including Geriatric Gastroenterology and Palliative Care.<br />
Members of our Section have administrative responsibilities<br />
related to nursing home care. Dr. Gorbien is the corporate medical<br />
director for Boulevard Healthcare. Dr. Leiding is associate medical<br />
director for Warren Barr Nursing and Rehabilitation <strong>Center</strong>. Dr.<br />
Hansberry is associate medical director for Lakeview Nursing<br />
and Rehabilitation <strong>Center</strong>. The relationships between the nursing<br />
facilities and <strong>Rush</strong> allows our patients to enjoy high-quality posthospital,<br />
skilled care delivered by <strong>Rush</strong> doctors. This provides<br />
continuity and insures that <strong>Rush</strong> patients return to <strong>Rush</strong> when in<br />
need of hospitalization. Dr. Perry continues to direct the Johnston<br />
R. Bowman <strong>Center</strong>. Additionally, he spends half of his time<br />
working with hospital administration on behalf of the Office<br />
of Transformation.<br />
Education<br />
Our fellowship is the oldest in Illinois. Despite the very difficult<br />
nature of recruitment into primary care and geriatrics, <strong>Rush</strong><br />
continues to do well. We have trained 42 fellows since 1994. We<br />
enjoy having an internal medicine student each month while they
complete the ambulatory portion of their internal<br />
medicine core clerkship. <strong>Rush</strong> internal medicine<br />
residents spend time in our clinic as well as on our<br />
two in-patient services while they do their required<br />
geriatric medicine rotation. We have created a new<br />
relationship with Stroger Hospital and they typically<br />
send one resident per month to complete their<br />
geriatric medicine requirement. We have increasing<br />
numbers of residents from other hospitals requesting<br />
to complete rotations at <strong>Rush</strong>. Dr. Gorbien is in his<br />
eleventh years as the faculty sponsor of the <strong>Rush</strong><br />
<strong>University</strong> Geriatric Interest Group (GIG). This<br />
student organization enjoys community outreach,<br />
lunchtime presentations, movie night, health fairs<br />
and academic mentorship.<br />
Gerontology and Palliative Care Grand Rounds<br />
are now in their eleventh year. Twice monthly we<br />
convene to provide education in the field of aging.<br />
These lectures are intended for an interdisciplinary<br />
audience. Our lecturers cover a wide range of topics<br />
including subjects related to palliative care. This<br />
unique interdisciplinary educational activity has had<br />
sustained growth and interest over the last ten years.<br />
Dr. Magda Houlberg splits her time between <strong>Rush</strong><br />
and Howard Brown Health <strong>Center</strong>. There, she is<br />
working to develop a comprehensive outreach<br />
program for older adults in the gay, lesbian, bisexual,<br />
and transgendered population. <strong>Rush</strong> is one of three<br />
partner organizations working with Howard Brown<br />
to meet the needs of this disenfranchised populations<br />
of elders. Eventually, Howard Brown will serve as a<br />
training site for <strong>Rush</strong> medical students, residents and<br />
fellow. This is a ground breaking initiative and this<br />
program will be the first of this kind in the nation.<br />
Research<br />
Section of Geriatric Medicine and Palliative Care<br />
Although geriatric medicine at <strong>Rush</strong> has traditionally<br />
been known for excellence in clinical care, important<br />
advances have been made in our nascent research<br />
initiative. Under the mentorship of Dr. Denis Evans,<br />
Dr. XinQi Dong has been awarded a prestigious<br />
Beeson Grant. The Beeson is a very competitive<br />
grant and is a very high honor in the field of geriatric<br />
medicine. Drs. Gorbien and Dong continue to work<br />
with students and fellows on academic projects<br />
(abstracts, review papers etc).<br />
31
Section of Geriatric Medicine and Palliative Care<br />
32<br />
Research in the Section of Geriatric Medicine and<br />
Palliative Care at <strong>Rush</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong> are<br />
carried out by a variety of individuals with diverse<br />
interests. The major themes of the Section’s research<br />
are elder abuse and palliative care education.<br />
The Section Director, Dr. Martin Gorbien, has a<br />
well-published, ongoing interest in ethical and legal<br />
issues involved in the care of older adults, with<br />
particular interest in recognizing and reporting elder<br />
abuse. This same topic is the foundation of ongoing<br />
research by Section faculty in collaboration with the<br />
<strong>Rush</strong> Institute on Healthy Aging. Special interest<br />
is directed to studying determination of decisional<br />
capacity and medical implications of self neglect.<br />
Since the Section assumed responsibility for the<br />
medical center’s palliative care program, multiple<br />
Section members have participated in research<br />
efforts aimed at improving education of nursing<br />
and medical trainees in the principles and practice<br />
of palliative care. Collaborating with faculty of<br />
PEER REVIEWED GRANTS<br />
the college of nursing and with staff at off-site<br />
practice venues, Section faculty are developing<br />
and testing innovative education tools for trainees<br />
and practitioners to teach them clinical skills to<br />
thoughtfully approach the care of older patients,<br />
chronically ill patients, and patients near the end<br />
of life.<br />
Recently, the Section created a partnership with<br />
Howard Brown Health <strong>Center</strong>, where Section faculty<br />
research interest is directed to the study of aging<br />
in the gay, lesbian, bisexual, and transgendered<br />
population. Recognizing the current limits of<br />
information in this understudied population, an<br />
education program has been developed to train<br />
nursing staff in an expanded cultural competency.<br />
The research endeavors of the Section of Geriatric<br />
Medicine and Palliative Care reflect a commitment to<br />
increasing the body of knowledge about the special<br />
needs of a growing segment of the population as well<br />
as to trainee education to practice that knowledge.<br />
Martin Gorbien, MD<br />
a. Contract #: 1 D31 AH7 0<strong>09</strong>6-02 Morley (PI) 10/1/00 to 9/30/05<br />
HRSA: Geriatric Education <strong>Center</strong>, subcontractor to St. Louis <strong>University</strong>,<br />
Five year grant, $420,000.<br />
Role: Senior Co-Investigator, Martin J. Gorbien, MD<br />
b. Contract # 1239I 9/1/01 to 6/30/04<br />
Washington Square Health Foundation’s Geriatric Student Interest Group<br />
Project. 3 year grant*, $90,000. Mentor: Martin J. Gorbien, MD, Role: This<br />
project involved Dr. Gorbien in the role of the mentor to the Geriatric<br />
Students Interest Group and reviewer of its research ideas.<br />
*annual reapplications are required.<br />
c. Grant Number: 1 R25 CA114084-01 <strong>09</strong>/29/2005 - 8/31/2006 Project Period: <strong>09</strong>/29/2005 - 08/31/2010,<br />
Project Title: Interdisciplinary Palliative Care Education Program<br />
PI: Margaret E. Faut-Callahan, PhD, Role: Martin J. Gorbien, MD, Co-Investigator<br />
d. RRF Grant # 2006-235 Budget Period 4/01/07 – 03/30/<strong>09</strong><br />
Project Title: “Assessment of Capacity in Older Adults: A Growing Challenge<br />
for Physicians” This project represents a joint effort between <strong>Rush</strong> and the<br />
American Barr Association.<br />
Role: Co-Primary Investigator, Martin J. Gorbien, MD
XinQi Dong, MD<br />
a. <strong>University</strong> Research Committee, <strong>Rush</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong> 7/2007-6/2008<br />
Pilot Study of Elder Self-Neglect in a Biracial Population. The goal<br />
of this project is to preliminarily examine characteristics of elder self-neglect<br />
in a population-based epidemiological study of a biracial community.<br />
Role: Principle Investigator, XinQi Dong, MD.<br />
b. Retirement Research Foundation/Gorbien and Eisenstein (Co-PIs) 4/2007-3/20<strong>09</strong><br />
Assessment of Capacity in Older Adults: A Growing Challenge for Physicians.<br />
The aim of this project is to create an <strong>online</strong> curriculum for training physicians<br />
to understand clinical and legal concepts of capacity and to inform the<br />
healthcare community about capacity training.<br />
Role: Co-Investigator, XinQi Dong, MD.<br />
c. OVW-2006-1200 Gallagher (PI) 10/2006-10/20<strong>09</strong><br />
U.S. Department of Justice Elder Abuse Criminal Justice Training Program.<br />
The goal of this study is to perform multidisciplinary training to the judiciary<br />
system to improve the criminal justice system response to elder abuse<br />
victims in Chicago.<br />
Role: Co-Investigator, XinQi Dong, MD.<br />
d. Paul Beeson Physician Scholar in Aging Award 8/2008 – 8/2012<br />
The <strong>Medical</strong> Implications of Self-Neglect in the Elderly NIH- NIA- Hartford<br />
Foundation-Atlantic Philanthropies -Starr Foundation. $750,000<br />
Maria R. Hansberry, MD<br />
CFDA No. 93.250 10/2007 – 9/2010<br />
Geriatric Academic Career Award: HRSA-07-GACA, The goal of this project<br />
is to develop a teaching curriculum in palliative care and long-term care for<br />
medical students, medical residents and nursing home staff.<br />
Role: Maria R. Hansberry, MD, Primary Investigator<br />
Daniel Loiterstein, MD (left RUMC in June 2008)<br />
Grant #: 1 KO1 HP00167-01 2005 - 2006<br />
Geriatric Academic Career Award, Health Resources and Services Administration.<br />
The goal of this project is to improve and establish enhanced educational opportunities<br />
for trainees at <strong>Rush</strong> <strong>University</strong>, including a Geriatric Psychiatry Fellowship.<br />
Role: Daniel Loiterstein, M.D., Primary Investigator.<br />
Mona Tareen, MD<br />
Grant Number: 1 R25 CA114084-01 <strong>09</strong>/29/2005 - 08/31/2010<br />
Project Title: Interdisciplinary Palliative Care Education Program,<br />
PI: Margaret E. Faut-Callahan, PhD, Role: Martin J. Gorbien, MD,<br />
Co-Investigator, Mona Tareen, MD, Co-Investigator<br />
Magda Houlberg, MD<br />
Submitted 12/11/08 by Dr. Houlberg at Howard Brown Health <strong>Center</strong><br />
HRSA Comprehensive Geriatric Education Program, “Developing a Nursing<br />
Curriculum in Cultural Competency for LGBT Elders”, 20<strong>09</strong>-2012, $160,000,<br />
Magda Houlberg, Co-Investigator<br />
Section of Geriatric Medicine and Palliative Care<br />
33
DIVISION OF PULMONARY AND CRITICAL CARE MEDICINE<br />
1725 W. Harrison Street, Suite 054<br />
(312) 942-6744<br />
34<br />
Robert A. Balk, MD<br />
Division Director<br />
Faculty:<br />
Professors:<br />
David Gurka, MD, PhD<br />
Robert L. Rosen, MD<br />
Associate Professors:<br />
Larry Casey, MD, PhD<br />
Michael Silver, MD<br />
Assistant Professors:<br />
Omar Lateef, DO<br />
Richard Lenhardt, MD, MPH<br />
Rajive Tandon, MD<br />
Mark Yoder, MD<br />
The Division of Pulmonary and Critical Care medicine participates<br />
in clinical, educational, and research activities at <strong>Rush</strong> <strong>University</strong><br />
<strong>Medical</strong> <strong>Center</strong>. The Division is comprised of the Section of<br />
Pulmonary Medicine and the Section of Critical Care Medicine.<br />
Pulmonary medicine provides outpatient and inpatient evaluation and<br />
management for a wide variety of patients with lung disease at <strong>Rush</strong>.<br />
The Section of Critical Care Medicine provides inpatient critical care<br />
evaluation and management for patients in the medical intensive care<br />
unit and the surgical intensive care unit at <strong>Rush</strong>. The Division also<br />
runs a fellowship training program in pulmonary and critical care<br />
medicine. As part of the training program and the academic mission,<br />
the division also participates in basic and clinical research.<br />
Education<br />
The Division of Pulmonary and Critical Care Medicine has an<br />
ACGME approved 3 year fellowship training program that has<br />
just been accredited for 5 years. There are 3 fellows each year for<br />
a total of 9 trainees in the program. The program works with the<br />
John H. Stroger, Jr. Hospital of Cook County to offer combined core<br />
curriculum and clinical conferences as part of an affiliation agreement.<br />
The fellowship program has a good relationship with training<br />
programs in surgery (and the surgical sub-specialties), anesthesia,<br />
neurology, and sleep medicine to facilitate collaborative training<br />
experiences. The fellowship program has a full array of educational<br />
conferences, offers training in the experiences and procedures of<br />
pulmonary and critical care medicine, and has opportunities<br />
for research.<br />
Clinical Programs<br />
The Division of Pulmonary and Critical Care medicine provides<br />
pulmonary consultation and clinical patient management for<br />
inpatients and outpatients with pulmonary issues at <strong>Rush</strong> <strong>University</strong><br />
<strong>Medical</strong> <strong>Center</strong>. The outpatient program includes a general<br />
pulmonary clinic for consultation and clinical management. In<br />
addition, there are several sub-specialty clinics run by the division<br />
which cater to special populations of patients. These subspecialty<br />
clinics include an adult cystic fibrosis clinic, difficult to treat asthma<br />
clinic, interstitial lung disease clinic, pulmonary hypertension clinic,<br />
and oxygen clinic. The division outpatient office also contains the<br />
adult pulmonary function laboratory for the hospital. This laboratory<br />
is under the direction of Dr. Larry Casey and is capable of performing<br />
basic pulmonary function testing (spirometry, lung volumes,<br />
and diffusion capacity measurement), arterial blood gas analysis,<br />
methacholine bronchoprovocational testing, high-altitude simulation
testing, oxygen desaturation testing, oxygen<br />
prescription determination, impulse oscillometry<br />
determination of airways resistance, timed walk<br />
distance, and cardiopulmonary exercise testing.<br />
The division is also involved in the evaluation and<br />
management of critically ill patients admitted to the<br />
medical intensive care unit and the surgical intensive<br />
care unit. Dr. David Gurka is the director of the<br />
section of critical care medicine in the division and he<br />
also directs adult critical care for the institution. Dr.<br />
Omar Lateef is the medical director of the medical<br />
intensive care unit. Other administrative positions<br />
held by members of the division include, Dr. Larry<br />
Casey – <strong>Medical</strong> Director of Bronchoscopy and the<br />
Pulmonary Function Laboratory, Dr. Mark Yoder<br />
– <strong>Medical</strong> Director of Respiratory Care Services.<br />
PEER REVIEWED GRANTS<br />
Chiron; Michael Silver, MD P.I.<br />
Sanofi Aventis; David Gurka, MD, PhD P.I.<br />
Artisan Pharma; Robert Balk, MD P.I.<br />
Astellas Pharma; Robert Balk, MD P.I.<br />
Research<br />
Division of Pulmonary and Critical Care Medicine<br />
The Division of Pulmonary and Critical Care<br />
Medicine has an active research program. The<br />
majority of the projects are clinical, however, there<br />
are some basic investigations and opportunities for<br />
translational research through relationships with<br />
the Department of Allergy and Immunology and the<br />
Department of Pharmacology. Approximately 20<br />
research projects were conducted this past year or<br />
are currently in progress.<br />
A Phase 3, Multicenter, Randomized, Placebo-Controlled, Doubleblind,<br />
Three-Arm Study to Evaluate the Safety and Efficacy of Tifacogin<br />
(Recombinant Tissue Factor Pathway Inhibitor) Administration in<br />
Subjects with Severe Community-Acquired Pneumonia;<br />
(CAPTIVATE Study)<br />
An International, multicenter, randomized, double-blind, doubledummy,<br />
parallel group, study of 3-month or 6-month treatment with<br />
SSR126517E (3.0mg s.c. once weekly) versus oral INR-adjusted warfarin<br />
in the treatment of patients with symptomatic pulmonary embolism,<br />
with or without symptomatic deep venous thrombosis.<br />
CASSIOPEA Study)<br />
A Randomized, Double-Blind, Placebo-Controlled, Phase-2b Study<br />
to Assess the Safety and Efficacy Effects of ART-123 on Subjects with<br />
Sepsis and Disseminated Intravascular Coagulation; (Protocol# 2-001<br />
ART Study)<br />
A Phase IIIb, Randomized, Double-Blind, Parallel Group, Multi-<br />
<strong>Center</strong> Study to Assess the Efficacy and Safety of Multiple 30 Minute<br />
Infusions of Conivaptan in Subjects with Euvolemic or Hypervolemic<br />
Hyponatremia; (Protocol No: 087-CL-088)<br />
35
Division of Pulmonary and Critical Care Medicine<br />
36<br />
Agennix: Robert Balk, MD P.I.<br />
Bristol Myers Squibb; Robert Balk, MD P.I.<br />
Division funding; Rajive Tandon, MD P.I.<br />
Division funding; Richard Lenhardt, MD P.I.<br />
Division funding; Larry Casey, MD, PhD P.I.<br />
Stroger <strong>Rush</strong> funding; Rajive Tandon, MD P.I.<br />
Division funding; Omar Lateef, DO P.I.<br />
Division funding; Mark Pamer, DO & David<br />
Gurka, MD PhD Co-P.I.s<br />
Division funding; Mark Yoder, MD P.I.<br />
Division funding; Robert Balk, MD P.I.<br />
2007-2008, renewed 2008-20<strong>09</strong> Yoder M<br />
(PI), Ojielo C, Forsyth C. <strong>Rush</strong>/Stroger<br />
Research Affiliation Committee.<br />
IRB approval 2008. Yoder M (PI)<br />
IRB approval 2007. Pamer M, Yoder M<br />
(faculty supervisor)<br />
IRB approval 2007. Yoder M (PI)<br />
A Phase 2 Randomized, Double-blind, Placebo-controlled Study<br />
of the Safety and Efficacy of Talactoferrin Alfa in Patients with<br />
Severe Sepsis;<br />
A Phase 3, Randomized, Double-blind, Parallel-group, Multi-center<br />
Study of the Safety and Efficacy of Apixaban for Prophylaxis of<br />
Venous Thromboembolism in Acutely Ill <strong>Medical</strong> Subjects During<br />
and Following Hospitalization,Protocol: (CV185-03 Adopt Study)<br />
28 Day Mortality for patients w/ PAH admitted to MICU<br />
Survey of sepsis management in Illinois Eds and ICUs<br />
IOS v Methacholine Bronchoprovocational Study in the Diagnosis<br />
of Airflow Obstruction<br />
Pulmonary Hypertension in HIV patients With Dyspnea<br />
Enteral Nutrition in Critical Illness Outcomes<br />
Comparison of Upper and Lower Extremity Central Venous<br />
Oxygenation and Pressures in Critical Illness<br />
Relationship between physiological decline and mortality<br />
in Pulmonary Sarcoidosis Database for ILD Patients<br />
Vasopressor Choice and outcome in Septic Shock<br />
Relationship between FSP1 and matrix metalloproteinase levels and<br />
disease severity in collagen vascular disease-associated interstitial<br />
lung disease. Pilot study aimed at discovering biomarkers of disease<br />
progression in CVD-ILD.<br />
Lung cancer screening with low-dose chest computed tomography.<br />
Clinical trial within the context of the International Early Lung<br />
Cancer Action Program (I-ELCAP) with a substudy comparing<br />
outcomes between healthy subjects and those with lung disease.<br />
Database for ILD patients. Collecting longitudinal physiologic and<br />
radiographic data to assess responses of diverse disease subtypes to<br />
various treatments.<br />
Mast cell infiltration of airway smooth muscle in asthma and chronic<br />
obstructive pulmonary disease. Study assessing the relationship<br />
between mast cells and bronchoconstriction.<br />
The relationship between physiologic decline and mortality in<br />
pulmonary sarcoidosis. Study to determine the independent<br />
association between pulmonary function decline and mortality<br />
in sarcoidosis.
SECTION OF MEDICAL INFORMATICS AND<br />
PATIENT SAFETY RESEARCH<br />
The Section of <strong>Medical</strong> Informatics and Patient Safety Research is dedicated to<br />
advancing quality of care and safety supported by information technology. The<br />
section is a sub-committee under the Department of Internal Medicine’s Quality<br />
Assurance (QA). The section utilizes our Quality Improvement, Education, and<br />
Clinical Practice Committees, as well as our Department’s financial staff, to work<br />
together to improve quality measures. A full time data manager, Richard Odwanzy,<br />
assists with data collection, project management and statistics. Brian Harting,<br />
MD is responsible for infection safety issues in the Department and co-director of<br />
Quality and Safety Research in the Department’s research mentoring program.<br />
The main purposes of the section are:<br />
1. Review reports of patients suffering adverse events and develop interventions<br />
to reduce those adverse events.<br />
Reports of adverse events are first discussed in QA and further evaluated<br />
by the Section to determine core problems in the delivery of safe care.<br />
Intervention ideas are proposed to the QA committee.<br />
2. Conduct research to prove the value of proposed changes.<br />
We conduct improvement projects based on our and the Department’s QA<br />
committee assessments of the root cause of adverse events. We use a “generic”<br />
project implementation sequence:<br />
– We present the case of a patient with an adverse event and the literature<br />
pertinent to the case to our residents during a “safety morbidity and<br />
mortality review”.<br />
– We send “email safety alerts” that highlight specific points about how to<br />
improve decision making or systems of care for the presented case.<br />
– We distribute to residents - either via “Chairman’s Rounds” or by decision<br />
alerts using our electronic medical record system - guidelines, constraints, or<br />
directed care orders aimed to reduce the chance of adverse events occurring.<br />
Projects have focused on reducing adverse events associated with delays in care,<br />
excess testing/overuse leading to missed signals of unsafe care, and the use of<br />
dangerous medications (such as potassium supplements, NSAIDs, PPIs, narcotic<br />
agents, or sliding scale insulin regimens).<br />
These projects have resulted in over 30 publications, 4 grants, a safety hospitalist<br />
program, and a research mentoring track for quality of care and safety research.<br />
The Otho S.A. Sprague Memorial Institute has awarded the Section a $124,633<br />
grant to support a first-of-its-kind patient-safety project that will pilot a program<br />
with <strong>Rush</strong>’s mediation team to develop interventions to avoid or modify activities<br />
and procedures that may lead to medical malpractice claims. This innovative<br />
program has the potential to serve as a model for similar mediation programs.<br />
Future projects will target adverse events caused by poor communication, excess<br />
end-of-life care, lack of appropriate informed consent, and use of dangerous<br />
medication combinations.<br />
Robert A. McNutt, MD<br />
- Professor of Medicine<br />
- Assistant Chairman<br />
- Chief of the Section of<br />
<strong>Medical</strong> Informatics<br />
and Patient Safety<br />
Research<br />
Assistant Proffesor:<br />
Brian P. Harting, MD<br />
37
DIVISION OF HEMATOLOGY/ONCOLOGY/BMT<br />
1725 W. Harrison St, Suite 8<strong>09</strong><br />
(312) 942-5904<br />
38<br />
Philip Bonomi, MD<br />
Division Director<br />
Faculty<br />
Professors:<br />
Melody Cobleigh, MD<br />
Henry C. Fung, MD<br />
Sefer Gezer, MD<br />
Stephanie A. Gregory, MD<br />
Janet Plate, PhD<br />
Parameswaran Venugopal, MD<br />
Janet Wolter, MD<br />
Associate Professors:<br />
John L. Showel, MD<br />
Margaret C. Telfer, MD, FACP<br />
Assistant Professors:<br />
Marta Batus, MD<br />
Lisa N. Boggio, MD, MS<br />
Gerry Bohac, MD<br />
Kent W. Christopherson II, PhD<br />
Mary Jo Fidler, MD<br />
Melissa L. Larson, MD<br />
William T. Leslie, MD<br />
Sarah T. Lincoln, MD<br />
John J. Maciejewski, MD, PhD<br />
Sunita Nathan, MD<br />
Ruta D. Rao, MD<br />
Jamile Shammo, MD<br />
Hande Tuncer, MD<br />
Lydia Usha, MD<br />
The Division of Hematology/Oncology at <strong>Rush</strong> <strong>University</strong> <strong>Medical</strong><br />
<strong>Center</strong> consists of three sections: oncology, hematology and bone<br />
marrow transplant which provide state-of-the-art care for individuals<br />
with all forms of hematological and oncological diseases.<br />
Clinical Services<br />
We offer patients access to seven comprehensive clinics for the following<br />
cancers: breast, gastrointestinal, head and neck, multiple myeloma, chest<br />
tumor, pigmented lesion and genitourinary. Funded by the Coleman<br />
Foundation, these are comprehensive and multidisciplinary clinics which<br />
offer patients the opportunity to be seen by leading specialists in the<br />
field, from medical oncology, radiation oncology, surgery, psychosocial<br />
oncologists and other relevant specialties in a single visit. The medical<br />
team for the clinic meets with patients and their families to discuss the<br />
diagnosis and develop personalized treatment plans.<br />
The Division places an emphasis on cancer screening and prevention,<br />
genetic counseling and testing and cancer support programs. We<br />
are committed to helping patients and their families cope with the<br />
psychological, emotional and spiritual effects of cancer. In partnership<br />
with the American Cancer Society, <strong>Rush</strong> offers a patient navigator<br />
who meets with patients and their family members to assess individual<br />
needs and provide vital support. Additionally, through the Cancer<br />
Integrative Medicine Program at <strong>Rush</strong>, patients have access to therapies<br />
that complement their medical treatments, such as acupuncture,<br />
biofeedback, massage, yoga, and nutritional and herbal counseling.<br />
Over the past 3 years, the Division has seen an increase in the number<br />
of new patient being seeing which is projected to be 4,500 for FY<strong>09</strong>.<br />
This is due to the increase in new faculties that have joined the Division<br />
over the past several years which has helped further grow each diseasespecific<br />
program.<br />
5000<br />
4000<br />
3000<br />
2000<br />
1000<br />
0<br />
NEW PATIENT VISITS (FY20<strong>09</strong> Annualized)<br />
3,903<br />
4,465<br />
FY2007 FY2008<br />
4,500<br />
FY20<strong>09</strong>*
Education<br />
The hematology/oncology fellowship program at<br />
<strong>Rush</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong> is a three-year<br />
program. Two positions are available each year<br />
for a total of six fellows. The program provides<br />
advanced clinical and research training under the<br />
supervision of specialists offering unique educational<br />
opportunities and diverse training experiences. Ours<br />
is a balanced program that strives to be outstanding<br />
in both the clinical and the investigative arenas.<br />
Fellows participate in rotations in hematology<br />
service, the bone marrow transplant unit and<br />
preceptorships with individual medical oncology<br />
faculty members. Fellows also take required rotations<br />
in blood banking, coagulation, hematopathology and<br />
chemotherapy/venous access devices. Additionally,<br />
fellows take electives in other programs including<br />
radiation oncology, gynecologic oncology, pathology<br />
and psychosocial oncology. All fellows participate<br />
in research during the program. There are weekly<br />
conferences at which fellows present and/or discuss<br />
patients currently being followed and two teaching<br />
conferences. Other weekly conferences include the<br />
Tumor Board, <strong>Rush</strong> Cancer Institute Lecture Series<br />
and Lymphoma Conference.<br />
The Division of Hematology/Oncology at the <strong>Rush</strong><br />
<strong>University</strong> <strong>Medical</strong> <strong>Center</strong> offers postdoctoral<br />
training leading to American Board of Internal<br />
Medicine (ABIM) board eligibility in hematology and<br />
medical oncology. The overall goal of the fellowship<br />
is to provide broad training in the disciplines of<br />
NUMBER OF PATIENTS<br />
150<br />
120<br />
90<br />
60<br />
30<br />
0<br />
TREATMENT ACCRUALS SINCE JANUARY 2006 CUMULATIVE BY MONTH<br />
Division of Hematology and Oncology<br />
hematology and oncology, focusing on the general<br />
competencies put forth by the American Council for<br />
Graduate <strong>Medical</strong> Education (ACGME).<br />
Research<br />
The Division of Hematology/Oncology oversees a<br />
number of clinical trials and works in collaboration<br />
with other Departments in the <strong>Medical</strong> <strong>Center</strong><br />
to promote awareness of cancer clinical trials,<br />
facilitate accrual to active protocols, and participate<br />
in education and training regarding Good Clinical<br />
Practices for the execution of trials. Our physicians<br />
are active investigators in trials utilizing novel<br />
therapies, both as partners with the pharmaceutical<br />
industry, and in their own investigator initiated trials.<br />
The Division is a long standing, productive<br />
contributor to National Cancer Institute cooperative<br />
group protocols through the National Surgical<br />
Adjuvant Breast and Bowel Project, Eastern<br />
Cooperative Oncology Group, Radiation Therapy<br />
Oncology Group, Gynecological Oncology Group,<br />
intergroup trials with Cancer and Leukemia Group<br />
B, Southwestern Oncology Group, and trials available<br />
through the Clinical Trials Support Unit.<br />
Currently, the Division has 82 active clinical trials<br />
and 321 patients have been enrolled to nontreatment<br />
studies and 194 patients have been<br />
enrolled to treatment studies since July 2007. The<br />
below illustrates the number of treatment accruals<br />
in clinical trials since January 2006.<br />
JAN FEB MAR APR MAY JUNE JULY AUG SEPT OCT NOV DEC<br />
2006 2007 2008<br />
39
Division of Hematology and Oncology<br />
40<br />
The Division also has two basic science researchers<br />
in Dr. Janet Plate and Dr. Kent Christopherson. Dr.<br />
Janet Plate’s research interests are in the regulation<br />
of immune cell differentiation including the role that<br />
cell surface molecules play in transmitting signals<br />
that initiate molecular steps in the differentiation<br />
pathway. The manner in which alterations in normal<br />
signaling pathways contribute to disease states are<br />
being investigated . Dr. Plate’s laboratory investigates<br />
two main diseases: Chronic Lymphocytic Leukemia<br />
(CLL), the most common adult leukemic disease<br />
of B-lymphocytes, and, pancreatic cancer - the<br />
fourth leading cause of cancer deaths. A variety of<br />
molecular and cellular biological approaches are<br />
being used in these studies.<br />
ACTIVE FUNDING -KENT W. CHRISTOPHERSON II, PH.D<br />
Dr. Christopherson joined <strong>Rush</strong> in September of<br />
2003 as an Assistant Professor in the Sections of<br />
Hematology and Stem Cell Transplantation, Division<br />
of Hematology/Oncology, Department of Medicine<br />
with a conjoint appointment in the Department<br />
of Immunology/ Microbiology at <strong>Rush</strong> <strong>University</strong><br />
<strong>Medical</strong> <strong>Center</strong>. Dr. Christopherson’s laboratory<br />
leads translational research from the laboratory<br />
bench to the clinical patient bedside for the Sections<br />
of Hematology and Stem Cell Transplantation. Dr.<br />
Christopherson’s primary research interests are<br />
directed at novel methods of increasing stem cell<br />
transplant efficiency. As one component of this<br />
project, the lab studies, collection, banking, and<br />
transplantation of umbilical cord blood stem cells<br />
for clinical and research purposes.<br />
07-10-19-CHRI (Kent W. Christopherson II, Ph.D.) 7/1/07-6/30/<strong>09</strong><br />
Agency: American Association for Cancer Research Role: PI<br />
“Umbilical Cord Wharton’s Jelly Mesenchymal Stem Cell Transplant Therapies”<br />
The major goals are to evaluate the ability of Mesenchymal Stem Cells<br />
derived from the Wharton’s Jelly of umbilical cord segments to support<br />
the ex vivo expansion of cord blood Hematopoietic Stem and Progenitor Cells.<br />
6044-08 (Kent W. Christopherson II, Ph.D.) 10/1/07-9/30/11<br />
Agency: Leukemia & Lymphoma Society Role: PI<br />
“Improvements in Hematopoietic Stem Cell Transplant Efficiency<br />
through Modulation of the Mechanisms Governing Hematopoietic<br />
Stem Cell Trafficking”<br />
The major goals are to test the effects of CD26 inhibition on human<br />
HSC/HPC functions important for transplantation in vitro and homing<br />
and engraftment in vivo in immunodeficient mice in order to generate<br />
data needed to propose a Phase I clinical trial.
1R21DK074892-01A2 (Kent W. Christopherson II, Ph.D.) 3/01/08-2/29/10<br />
Agency: NIH/NIDDK Role: PI<br />
“Cytokine Induced CD26 Modulation of Adult Hematopoietic Stem Cell Trafficking”<br />
The major goals are to test the effects of G-CSF, GM-CSF, and SCF<br />
treatment of umbilical Cord Blood on Hematopoietic Stem Cell<br />
Transplant efficiency and the involvement of CD26 mechanistically.<br />
1 T32 AR052272-01A2 (D. Rick Sumner, PhD) 8/1/07-7/31/12<br />
Sponsor: NIH/NIAMSD Role: NIH Training Grant Mentor<br />
The purpose of this program is to provide education, training and<br />
research opportunities to doctoral students, postdoctoral fellows and<br />
medical students interested in academic careers in skeletal biology<br />
Kent W. Christopherson II, Ph.D. (PI) 1/1/08-12/31/08<br />
Industry Sponsor: America Stem Cell Inc. Role: PI<br />
“America Stem Cell Pre-Clinical Dosing Study – 01”<br />
Kent W. Christopherson II, Ph.D. (PI) 2/7/08-12/31/08<br />
Industry Sponsor: Baxter Healthcare Inc. Role: PI<br />
“ISOLEX CD34+ Stem Cell Study - 01”<br />
Kent W. Christopherson II, Ph.D. (PI) 1/1/07-12/31/<strong>09</strong><br />
Agency: private philanthropy Role: PI<br />
“Hematologic Malignancy Research Fund”<br />
Stephanie A. Gregory, MD (PI) 1/1/07-12/31/<strong>09</strong><br />
Agency: private philanthropy Role: co-PI<br />
“Chronic Lymphocytic Leukemia Fund”<br />
The major goals are to develop an understanding of the mechanisms<br />
governing defects in hematopoiesis and innate immunity that exist in<br />
CLL patients and test novel therapeutic strategies with minimal toxicity.<br />
Stephanie A. Gregory, MD (PI) 7/1/06-6/30/<strong>09</strong><br />
Agency: private philanthropy Role: co-PI<br />
“Second Chance Fund”<br />
The major goals are to develop novel therapeutic strategies<br />
for Multiple Myeloma.<br />
Division of Hematology and Oncology<br />
41
SECTION OF INFECTIOUS DISEASE<br />
600 S. Paulina St., Ste. 140-143<br />
(312) 942-5865<br />
42<br />
Gordon M. Trenholme, MD<br />
Section Director and Fellowship<br />
Program Director<br />
Faculty<br />
Professors:<br />
Gordon M. Trenholme, MD<br />
Harold Kessler, MD<br />
John Segreti. MD<br />
Alan A. Harris, MD<br />
Associate Professors:<br />
Mary Hayden, MD<br />
Laurie Proia, MD<br />
David M. Simon, MD, PhD<br />
Beverly Sha, MD<br />
Kamaljit Singh, MD<br />
Kimberly Smith, MD, MPH<br />
Assistant Professors:<br />
Allan Tenorio, MD<br />
Michael Lin, MD<br />
Brian P. Harting, MD<br />
On Thursday, September 11th, 2008, Gordon M. Trenholme, MD<br />
was honored as the inaugural recipient of the INSIDER Award (IN<br />
Support of Infectious Disease Education and OutReach) given in<br />
partnership by The Metro Foundation and <strong>Rush</strong> <strong>University</strong> <strong>Medical</strong><br />
<strong>Center</strong>. The newly created award will be given annually to honor an<br />
individual affiliated with the infectious disease community for their<br />
lifetime professional and personal accomplishments.<br />
Travel Medicine<br />
The Section of Infectious Diseases has expanded its Travel Medicine<br />
and Immunization Clinic in the past year. Travel patients are seen 2<br />
days a week by appointment. The clinic offers comprehensive services<br />
for travelers, from immunizations and counseling before the trip to<br />
follow-up and after care. The Travel Medicine and Immunization<br />
Clinic staff includes two nurses who administer immunizations and<br />
medications and are directed by Kamaljit Singh, MD, an infectious<br />
diseases specialist who has extensive experience in travel medicine.<br />
In addition, the staff offers their unique expertise to the traveler with<br />
special needs, such as travelers who are pregnant or who have special<br />
concerns because of a pre-existing condition or complication, like<br />
HIV or transplant patients. Other members of the travel medicine<br />
team include Gordon Trenholme, MD, and James McAuley, MD,<br />
who specializes in pediatric infectious diseases.<br />
Education<br />
The infectious disease fellowship program is a joint program between<br />
<strong>Rush</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong> and Stroger Hospital of Cook County.<br />
<strong>Rush</strong>/Stroger Hospital Infectious Diseases (ID) Fellowship Training<br />
Program utilizes the resources of <strong>Rush</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong>, the<br />
CORE <strong>Center</strong> and Stroger Hospital of Cook County to provide a wellrounded<br />
and diverse educational experience in the clinical, didactic,<br />
and research training of ID fellows. Five positions are available each<br />
year. At present, the program requires a mandatory two year training<br />
period with an option to complete a third year for those fellows who<br />
wish more extensive training in research activities in preparation for<br />
an academic career in infectious diseases. We currently have 1 3rd<br />
year fellow, 5 second year fellows, and 5 first year fellows.<br />
Both inpatient and outpatient clinical experiences and didactic<br />
training (lectures, conferences) for fellows are equally divided between<br />
the two hospitals and clinical and laboratory research projects may be<br />
undertaken at either institution. Performance of research is expected<br />
of all fellows, regardless of background or career interests, unless<br />
the fellowship is a purely clinical, one-year position. Participation in<br />
at least one “major’ project requiring one year or more to complete
is encouraged. Over the past few years, many of<br />
our fellows participated in research which led to<br />
publications and presentations at major conferences<br />
during the past academic year, including five journal<br />
articles, nine abstracts, 1 book chapter and one<br />
manuscript.<br />
Research<br />
The <strong>Rush</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong> Section of<br />
Infectious Diseases is doing federally supported<br />
research in a number of areas: HIV therapy,<br />
women with HIV, HIV immunology, HIV solid<br />
organ transplant, and Healthcare Epidemiology.<br />
Infectious diseases attending physicians are currently<br />
the principal investigators on 45 active research<br />
protocols.<br />
The Section of Infectious Diseases’ AIDS Clinical<br />
Trials Unit (ACTU) performs research in<br />
conjunction with a variety of sponsors. The <strong>Rush</strong><br />
ACTU is a site for the AIDS Clinical Trials Group,<br />
the largest and oldest HIV/AIDS research group, and<br />
for the Women’s HIV Interagency Study consortium.<br />
Dr. Beverly Sha is the site’s principal investigator for<br />
both the ACTG and WIHS.<br />
GRANTS<br />
Sponsor Focus<br />
Beverly Sha, MD - Principal Investigator<br />
NIH<br />
NIH<br />
Schering-Plough<br />
Abbott<br />
Sections of Infectious Disease<br />
Kimberly Smith, MD, MPH was appointed to the<br />
Executive Committee of the ACTG as of June 1,<br />
2008. She is also Chair of the Underrepresented<br />
Populations Committee of the ACTG. Over the<br />
past year, Dr. Smith was instrumental in setting up<br />
and mentoring an additional clinical research site to<br />
expand the research opportunities to communities<br />
of color.<br />
David Simon, MD, PhD is the principal<br />
investigator at <strong>Rush</strong> for the multi-site Solid Organ<br />
Transplantation in HIV protocol, studying the<br />
effects of kidney and liver transplants in patients<br />
with HIV/AIDS.<br />
All of the ID physicians who are active in HIV<br />
research meet periodically with the Chicago area<br />
Community Advisory Board (CAB) to provide<br />
educational updates to the community and to discuss<br />
the community members’ concerns related to HIV<br />
treatment and research with them.<br />
AIDS Clinical Trials Group; under this consortium Dr. Sha is PI of 8 HIV treatment protocols:<br />
A5241: A study of optimized treatment that includes or omits NRTIs using the cPSS to select<br />
effective regimen A5223: A comparison of PK in women and minority HIV+ patients. A5240:A study<br />
to evaluate the immugenicity of the HPV vaccine in HIV+ females. A5197: A treatment interruption<br />
trial of the antiretroviral effect of the MRK Ad5 HIV-1 GAG vaccine in HIV+ patients. A5244: An<br />
HIV treatment intensification trial using Raltegravir. A5247: Varicella vaccine trial in HIV+ patients.<br />
A5220: Improving Immune Response to Hepatitis B Vaccine in HIV+ patients using GM-CSF as a<br />
vaccine adjuvant. A5211: An HIV treatment study using Vicriviroc for patients failing therapy, now in<br />
long term follow up.<br />
Women’s Interagency HIV Study (WIHS): A long term study focused on the natural history of<br />
HIV in women.<br />
PO4100: Long term follow-up of A5211 patients<br />
M06-802 Comparing once daily vs. twie daily dosing of Kaletra in treatment experienced HIV patients.<br />
43
Sections of Infectious Disease<br />
GRANTS<br />
Sponsor Focus<br />
John Segreti, MD - Principal Investigator<br />
Cubist<br />
David Simon, MD, PhD - Principal Investigator<br />
NIH<br />
Roche<br />
Roche<br />
Merck<br />
Harold Kessler, MD - Principal Investigator<br />
Merck<br />
Thera<br />
Gilead<br />
Kimberly Smith, MD, MPH - Principal Investigator<br />
Tibotec<br />
Tibotec<br />
Tibotec<br />
Chiron<br />
ACTG<br />
Merck<br />
Allan Tenorio, MD - Principal Investigator<br />
Abbott<br />
Gilead<br />
ACTG<br />
ACTG<br />
ACTG<br />
44<br />
A comparison of Daptomycin at 2 doses vs.Vancomycin or Teicoplanin in the Treatment of Subjects<br />
Undergoing Surgical SOC for Osteomyelitis<br />
Solid Organ Transplantation in HIV: A multi-site study<br />
NV20234: A trial to evaluate the use of oseltamivir I(Tamiflu) n the treatment of<br />
immunocompromised patients.<br />
NV20235: A double-blind, randomized, placebo-controlled, multicenter trial of oseltamivir for the<br />
seasonal prophylaxis of influenza in immunocompromised subjects.<br />
Antibiotic Utilization in Critical Care; Merck substudy of Candidemia associated Septic Shock<br />
Merck-004: A probe study to evaluate the HIV-1 GAG DNA vaccine in HIV-1 infected individuals.<br />
A study of a designer growth hormone releasing factor analogue to reduce HIV related lipodystrophy.<br />
SPHERE Grant to run Rapid HIV Testing in ER<br />
TMC125-C216: A study of 2 experimental antiretroviral drugs given simultaneously for patients with<br />
limited treatment options.<br />
TMC114HIV3004 GRACE:An open-label, multi-center trial to compare the efficacy, safety, and<br />
tolerability of Prezizta/r by gender and race.<br />
TMC125-C217: A follow up protocol for TMC125-C216 patients<br />
SILCAAT: A study o f the efficacy of subcutaneous recombinant human IL-2 in HIV patients with low<br />
CD4+ counts under active ART.<br />
A5202: An open- label treatment trial powered to identify racial differences in treatment-naïve<br />
HIV+ patients<br />
Merck-023-00: Integrase (MK-0518) An Expanded Access Trial<br />
ICE-001: Investigator initiated study comparing 2 HAART regimens in ART naïve subjects with<br />
advanced HIV disease.<br />
Effect of Tenofovir on Innate Immunity.<br />
A5176: Dermavir. A Phase I/II Randomized, Double-Blind Study to Evaluate the Safety, Tolerability,<br />
and Immunogenicity of LC002, a Dermavir (transdermal)Vaccine in HIV-1 Infected Subjects Currently<br />
receiving HAART.<br />
A5217:A randomized study of the effect of immediate treatment with potent ART vs. observation with<br />
treatment as indicated in newly HIV-1 infected subjects: Does early therapy alter the virologic setpoint?<br />
A5229: A phase II/III randomized, double-blind placebo controlled trial of uridine supplementation in<br />
HIV Lipoatrophy
Sponsor Focus<br />
ACTG<br />
ACTG<br />
ACTG<br />
ACTG<br />
ACTG<br />
ACTG<br />
ACTG<br />
ACTG<br />
ACTG<br />
ACTG<br />
Stephanie Black, MD - Principal Investigator<br />
ACTG<br />
ACTG<br />
HRSA<br />
Laurie Proia, MD - Principal Investigator<br />
HRSA<br />
HRSA<br />
HRSA<br />
HRSA<br />
HRSA<br />
Kamaljit Singh, MD - Principal Investigator<br />
HRSA<br />
HRSA<br />
HRSA<br />
HRSA<br />
A5214: Phase I, randomized, placebo-controlled, double-blind study evaluating the safety of subcutaneous<br />
single dose Interleukin-7 in HIV-1 infected subjects who are receiving ART.<br />
52<strong>09</strong>: A pilot study of the safety, efficacy and tolerability of Ezetimibe (Zetia) in combination with statin<br />
therapy for the treatment of elevated LDL cholesterol in HIV-1 infected subjects.<br />
A5212: A double-blind, phase II study of multiple doses of palmifermin (rHuKGF) for the treatment of<br />
inadequate CD4+lymphocyte recovery in subjects on potent antiretroviral therapy with plasma HIV-1<br />
RNA levels less than or equal to 200 .<br />
A study of the effect of HIV on natural killer cell function.<br />
Changes in mucosal lymphocyte and innate immune cell populations in HIV-1 infected compared to<br />
uninfected patients.<br />
The role of T-regulatory cells in the response to influenza vaccination in HIV-1 infected individuals.<br />
Changes in lymph node lymphocyte and innate immune cell populations in HIV-1 infected patients<br />
The phenotype and function of hepatic natural killer cells<br />
Mucosal immunology of HIV infected patients with inflammatory bowel disease-a prospective study<br />
Risk Mucosal immunology of HIV infected patients with inflammatory bowel disease-a retrospective study<br />
Factors for Ventilator Associated<br />
Pneumonia in the PICU<br />
<strong>Rush</strong> <strong>Center</strong> of Excellence (COE) in Bioterrorism Preparedness<br />
Bioterrorism Training & Curriculum Preparedness<br />
Blastomycosis pyomyositis case series<br />
Linezolid Lock Retrospective Chart Review<br />
Vertebral Coccidiodomycosis: A case Series and Liturature Review<br />
A review of central nervous system Blastomycosis<br />
Histoplasmosis and blastomycosis following solid organ transplantation<br />
Use of Luminex multiplex RT-PCR for the detection of respiratory viruses<br />
Rapid identification of Staphylococcus spp. Directly from blood cultures using BBL CHROMager.<br />
Use of piperacillin/tazobactam for treatment of Pseudomonas Aeruginosa infection.<br />
Environmental contamination and body colonization with MRSA and the epidemic of<br />
community- acquired MRSA.<br />
Sections of Infectious Disease<br />
45
SECTION OF PHARMACY PRACTICE<br />
1653 W. Congress Parkway 0036 SB Atrium<br />
(312) 942-2108<br />
46<br />
Nora Flint, Pharm.D,<br />
FASHP, BCPS Section Head<br />
Faculty<br />
Instructors:<br />
Peggy Choye, Pharm.D.<br />
Chris Crank, Pharm.D., BCPS<br />
Nora Flint, Pharm.D., FASHP, BCPS<br />
Amy Green, Pharm.D., BCPS<br />
Ann Jankiewicz, Pharm.D, BCPS<br />
Julie Jun, Pharm.D.<br />
Mimi Lo, Pharm.D.<br />
Mira Loh-Trivedi, Pharm.D.<br />
Gourang Patel, Pharm.D.,MSc., BCPS<br />
Jeri Rothman, RPh, MBA<br />
Gail Ruderman, RPh.<br />
Beth Shields, Pharm.D.,<br />
Nina Sivanawin, Pharm.D.<br />
New Faculty<br />
(yet to be given<br />
academic appointments)<br />
Nicole Alvey, Pharm.D.<br />
Brian McBride, Pharm.D.<br />
Shane Scott, Pharm.D., BCOP<br />
The section of Pharmacy Practice expanded this past year with<br />
the addition of four members. Mira Loh-Trivedi, Pharm.D.was<br />
an employee of the Department of Anesthesia and transferred<br />
to the Department of Pharmacy. She rounds in the Surgical<br />
ICU. Nicole Alvey, Pharm.D., filled a long vacant position in the<br />
Department of Pharmacy in solid organ transplant, starting in<br />
August of this year.<br />
Two visiting faculty from Midwestern <strong>University</strong>’s Chicago<br />
College of Pharmacy began providing the service component<br />
of their positions at <strong>Rush</strong> this past year. Shane Scott, Pharm.<br />
D., BCOP is rounding with Dr. Showel in Oncology and Brian<br />
McBride, Pharm.D., is rounding in the Coronary Care Unit.<br />
Education<br />
The Department of Pharmacy continues to recruit 4 talented<br />
individuals into our Post Graduate Year 1 (PGY1) Pharmacy<br />
Residency Program each year. This residency program has been<br />
in existence at <strong>Rush</strong> for over 25 years. In addition, July 2008 is<br />
the beginning of our second year of providing a Post Graduate<br />
Year 2 (PGY2) Pharmacy Residency Program in Infectious<br />
Disease. This PGY2 residency program is funded through<br />
Midwestern <strong>University</strong>, but the primary service site is <strong>Rush</strong>.<br />
Dr. Chris Crank is the Residency Director of this program.<br />
In addition to the PGY2 in Infectious Disease, Midwestern<br />
<strong>University</strong> initiated a Pharmacy Fellowship in Infectious Disease<br />
through Midwestern <strong>University</strong>. The fellow started in July of<br />
this year and will complete the 2 year program with academic<br />
responsibilities at Chicago College of Pharmacy and service<br />
responsibilities both at <strong>Rush</strong> and at Northwestern<br />
Memorial Hospital.<br />
Accomplishments in 2007-2008<br />
Gourang Patel, Pharm.D. completed his Masters in Clinical<br />
Research from <strong>Rush</strong> <strong>University</strong>. His thesis was addressed the<br />
Efficacy and Safety of Dopamine versus Norepinephrine in the<br />
Management of Septic Shock.<br />
Chris Crank, Pharm.D. continues his curriculum in <strong>Rush</strong>’s<br />
Health Systems Management (HSM) program. He is due to<br />
complete this in summer of 20<strong>09</strong>.
Through her responsibilities in rounding with the<br />
NSICU, Amy Green, Pharm.D. contributed in a<br />
significant way to the development of a stroke<br />
program at <strong>Rush</strong> so that the medical center could<br />
be certified by The Joint Commission as a primary<br />
stroke center.<br />
Julie Jun, Pharm.D., and Peggy Choye, Pharm.D.<br />
have initiated a pilot program with RUI attending<br />
physicians to assess anticoagulation therapy and<br />
counsel patients prior to discharge. This is done on a<br />
consultation basis, whenever Drs. Jun or Choye are<br />
paged by a RUI attending.<br />
Nicole Alvey has contributed in a major way to<br />
the successful meeting of CMS requirements for a<br />
pharmacist to be part of the team that care for solid<br />
organ transplantation patients. She will be rounding<br />
with the liver, kidney and heart transplant teams<br />
and performing discharge consultations on this<br />
patient population, as part of the CMS accreditation<br />
requirements.<br />
Nina Sivanawin, Pharm.D., whose responsibility is to<br />
oversee the anticoagulation therapy for orthopedic<br />
Sections of Pharmacy Practice<br />
surgery on 9S Atrium has expanded her service from<br />
two orthopedic physicians to three. In addition, she<br />
has successfully developed a Home Health Care<br />
(HHC) protocol so that HHC nurses are able to<br />
manage the monitoring and dosing of warfarin on<br />
outpatients to complete the required three weeks<br />
of anticoagulant therapy for post-joint replacement<br />
patients.<br />
Beth Shields, Pharm.D. continues to work in the<br />
area of pediatrics to improve medication safety.<br />
She successfully worked with pediatric oncologists<br />
and nursing staff this past year to develop a process<br />
to have pediatric chemotherapy orders written<br />
and reviewed thoroughly prior to preparation and<br />
dispensing to patients. This project was required<br />
after the departure of two nurse practitioners in<br />
oncology from <strong>Rush</strong>.<br />
Nora Flint, Pharm.D. initiated a pilot project to place<br />
pharmacists on nursing units approving medication<br />
orders instead of from inside a pharmacy satellite.<br />
This was piloted on 9N, 9S and 9K. There is hope of<br />
expansion to other nursing units in the coming year.<br />
47
SECTION OF RHEUMATOLOGY<br />
1725 W Harrison Street, Suite 1017<br />
(312)-942-8268<br />
48<br />
Joel A. Block, MD<br />
The Willard L. Wood, MD<br />
- Professor of Rheumatology<br />
- Professor of Medicine and<br />
Biochemistry<br />
- Director, Section of<br />
Rheumatology<br />
Faculty<br />
Professors:<br />
Alison Finnegan, PhD<br />
Lawrence Layfer, MD<br />
Anna Plaas, PhD<br />
Winston Sequeira, MD<br />
Associate Professors:<br />
Paul B. Glickman, MD<br />
Charlotte A. Harris, MD<br />
Najia Shakoor, MD<br />
Assistant Professors:<br />
Sarah Everakes, MD<br />
Meenakshi Jolly, MD<br />
David Mael, MD<br />
Augustine M. Manadan, MD<br />
Carla R. Scanzello, MD, PhD<br />
Con-joint Faculty:<br />
Susan Chubinskaya, PhD<br />
Tibor Glant, MD, PhD<br />
Hee-Jeong Im-Sampen, PhD<br />
Eugene Thonar, PhD<br />
Laura Thorp, PhD<br />
Markus Wimmer, PhD<br />
James Williams, PhD<br />
The Section of Rheumatology is a dynamic and growing enterprise<br />
of approximately twenty five including faculty, co-joint faculty and<br />
fellows who are committed to providing outstanding state-of-the-art<br />
patient care and training the next generation of physicians.<br />
Patient care services are provided by physicians in two<br />
private practices, Rheumatology Associates and <strong>University</strong><br />
Rheumatologists. Services include:<br />
– Consultative care for patients with complex autoimmune<br />
connective tissue diseases, including lupus and rheumatoid<br />
arthritis<br />
– Primary management of musculoskeletal disorders, such as<br />
osteoarthritis, bursitis and tendonitis<br />
– Evaluation and treatment for osteoporosis<br />
In addition to providing comprehensive, compassionate patient<br />
care, section faculty members are involved in a number of research<br />
projects searching for the causes of arthritis and other rheumatic<br />
diseases.<br />
Rheumatologists at <strong>Rush</strong> provide treatment for arthritis, Lyme<br />
disease, lupus and other rheumatic diseases. The section also<br />
supports a center for the diagnosis and treatment of osteoporosis.<br />
In addition to its patient care services and research activities, the<br />
Section of Rheumatology also offers outstanding training in both<br />
the clinical and research aspects of rheumatic diseases.<br />
The Osteoporosis Treatment <strong>Center</strong> at <strong>Rush</strong> is dedicated to<br />
osteoporosis treatment, education and research. Our physicians<br />
specialize in osteoporosis, bone metabolism and other disorders of<br />
the musculoskeletal system. Through medical evaluations and bone<br />
mineral density testing, our skilled physicians and staff can help<br />
determine patients risk for developing osteoporosis. In addition,<br />
we use dual energy x-ray absorptiometry (DEXA) to measure bone<br />
mineral density. This is a painless, noninvasive procedure similar to<br />
an x-ray: A moveable arm is passed over the area to be tested. The<br />
test is completed in a matter of minutes and radiation exposure<br />
is minimal.
Education<br />
The mission of the rheumatology fellowship training<br />
program is to produce physicians that<br />
1) are clinically superb in the field of rheumatology,<br />
2) are capable of working in a variety of settings,<br />
3) possess habits of life-long learning to build upon<br />
their knowledge, skills and professionalism, and<br />
4) contribute to the community by expanding<br />
knowledge and awareness of rheumatic diseases.<br />
The specific goals of our training program are<br />
derived from the Mission Statement:<br />
1) clinical competence,<br />
2) capable of working in a variety of settings,<br />
3) a life-long learner, and<br />
4) a contributor to the knowledge and awareness of<br />
rheumatic diseases.<br />
Our Section offers outstanding training in both<br />
the clinical and research aspects of rheumatic<br />
diseases. Our faculty members provide fellows<br />
with a broad range of expertise in basic sciences<br />
and clinical rheumatology. The Rheumatology<br />
Fellowship is a two-year program, with an optional<br />
third year available. It is offered to physicians who<br />
have completed two to three years of postgraduate<br />
training in Internal Medicine.<br />
Fellows work under the supervision of faculty<br />
members in a clinically oriented program at the<br />
office-based private rheumatology practice at<br />
<strong>Rush</strong>, developing assessment skills of patients with<br />
musculoskeletal and connective tissue diseases,<br />
and formulating diagnoses and care plans. In<br />
addition, fellows provide consultation to other<br />
inpatient services at <strong>Rush</strong> and at John H. Stroger, Jr.,<br />
Hospital of Cook County; fellows provide outpatient<br />
consultation services at <strong>Rush</strong>, John H. Stroger, Jr.,<br />
Hospital of Cook County and other outpatient<br />
clinics in the community.<br />
Research<br />
Section of Rheumatology<br />
The faculty in Rheumatology includes clinical<br />
investigators with primary interests in osteoarthritis,<br />
the role of biomechanics in the rheumatic diseases,<br />
systemic lupus, and scleroderma. Basic science<br />
interests include animal models of inflammatory<br />
arthritis, mechanisms of degeneration of articular<br />
cartilage, biomarkers, and basic cartilage biology. In<br />
addition, the Section of Rheumatology maintains<br />
strong research affiliations with the Departments of<br />
Biochemistry, Anatomy and Cell Biology, Orthopedic<br />
Surgery, and Immunology.<br />
Finally, we are researching causes and treatments for<br />
osteoporosis. Our physicians conduct clinical trials<br />
of the newest osteoporosis medications, and our own<br />
departmental studies evaluate the effects of certain<br />
medications on bone density. The result of these<br />
studies may provide future treatment options for<br />
patients and others.<br />
49
Section of Rheumatology<br />
CLINICAL TRIALS, INDUSTRY STUDIES AND GRANTS<br />
Sponsor Title<br />
Joel A. Block, MD<br />
NIH/NIAMS<br />
Knoll Pharmaceutical Company<br />
Centocor, Inc.<br />
Forest Research Institute<br />
Abbott Laboratories<br />
Jazz Pharmaceuticals, Inc.<br />
Wyeth Consumer Healthcare<br />
Anika Therapeutics, Inc.<br />
Abbott Laboratories<br />
Wyeth Research<br />
Novartis<br />
Novartis<br />
Anesiva, Inc.<br />
Eli Lilly and Company<br />
Hoffmann-LaRoche AG<br />
Hoffman-LaRoche AG<br />
Wyeth Research<br />
50<br />
“Clinical effects of altered biomechanics in knee OA.”<br />
“Specialized <strong>Center</strong> of Research in Osteoarthritis” (SCOR–OA), Administrative Core (co-P.I.). A Multi-<br />
<strong>Center</strong> Continuation Study of the Human Anti-TNF Antibody D2E7 Administered as a Subcutaneous<br />
Injection in Patients with Rheumatoid, Knoll Pharmaceutical Company.<br />
A Multi-<strong>Center</strong> Continuation Study of the Human Anti-TNF Antibody D2E7 Administered as a<br />
Subcutaneous Injection in Patients with Rheumatoid.<br />
A Multicenter International Observational Study of the Long-Term Safety of Infliximab (Remicade)<br />
Results: Remicade Safety Under Long-Term Study.<br />
A Phase III, Multicenter, Open-Label, Flexible-Dosing Study of Milnacipran for the Treatment of<br />
Fibromyalgia.<br />
A Multicenter, Randomized, Double-Period, Double-Blind Study to Determine the Optimal Protocol for<br />
Treatment Initiation with Methotrexate and Adalimumab Combination Therapy in Patients with Early<br />
Rheumatoid Arthritis<br />
A Long-Term, Open-Label Safety and Efficacy Study of Xyrem® (sodium oxybate) in Subjects with<br />
Fibromyalgia.<br />
The Efficacy and Safety of TDS-943 in the Treatment of Osteoarthritis of the Knee: Pivotal Study 1 (with<br />
PK Assessments).<br />
A Randomized, Double-Blind, Placebo Controlled, Multi-<strong>Center</strong> Study of a Single Injection Cross-<br />
Linked Sodium Hyaluronate (HA) to Provide Symptomatic Relief of Osteoarthritis of the Knee.<br />
A Multi-<strong>Center</strong>, Randomized, Double-Blind, Placebo-Controlled Study Comparing 780 mg of<br />
Adalimumab with Placebo and Demonstrating the Non-Inferiority of Monthly 80 mg Adalimumab<br />
Dosing Compared with 40 mg Adalimumab Every Other Week Dosing.<br />
A Randomized, Parallel, Double-Blind, Placebo-Controlled Dose Regimen Finding Study to Evaluate the<br />
Safety and Efficacy of TRU-015 in Subjects With Active Seropositive Rheumatoid Arthritis on a Stable<br />
Background of Methotrexate.<br />
3 Part Multicenter Study with a Randomized, Double-Blind Placebo Controlled, Withdrawal Design in<br />
Part II to Assess Efficacy, Safety and Tolerability of ACZ885 in Patients with Muckle-Wells Syndrome.<br />
An Open-Label, Long-Term Safety and Efficacy Study of ACZ885 for at least 6 Months in Patients with<br />
the Following Cryopyrin-Associated Periodic Syndromes.<br />
A Multicenter, Randomized, Double-Blind, Placebo-Controlled, Parallel-Group Study to Evaluate the<br />
Duration of Analgesic Efficacy, Safety and Tolerability of a Regimen of Intraarticular Injections of 4975 in<br />
Patients with Chronic Moderate to Severe Pain of the Knee Associated with Osteoarthritis.<br />
A Phase 2 Study of Multiple Intravenous Doses of LY2127399, an Anti-BAFF Human Antibody, in<br />
Patients with Rheumatoid Arthritis on Concomitant Methotrexate and an Inadequate Response to TNFa<br />
Inhibitor Therapy.<br />
A Randomized, Double-Blind, Parallel Group Study of the Safety and Prevention of Structural Joint<br />
Damage During Treatment with MRA Versus Placebo, in Combination with Methotrexate, in Patients<br />
with Moderate to Severe Active Rheumatoid Arthritis.<br />
Roche Sample Repository Research Project
Sponsor Title<br />
Wyeth Research<br />
Genentech<br />
ACR/REF<br />
Arthritis Foundation<br />
<strong>Rush</strong>/Cook County Consortium<br />
NIH/NIAMS<br />
NIH/NIAMS<br />
Susan Chubinskaya, PhD<br />
NIH/NIAMS<br />
NIH/NIAMS<br />
NIH/NIAMS<br />
Project One<br />
Core B<br />
NIH/NIAD<br />
Alternatives Grant<br />
Research programs<br />
Arthrex<br />
Zimmer, Inc<br />
Anesiva, Inc.<br />
Fundacion Mapfre<br />
Anesiva, Inc.<br />
Regentis, Inc<br />
Joint Restoration Foundation<br />
Alternatives Research &<br />
Development Foundation<br />
A Multicenter, Randomized, Double-Blind, Placebo-Controlled, Parallel-Group, Adaptive-Design,<br />
Efficacy, Safety and Tolerability Study of 4 Fixed Oral Doses of DVS SR in Adult Outpatients with<br />
Fibromyalgia Syndrome.<br />
A 6-Month Open-Label Extension Study of the Long-Term Safety of DVS SR in Outpatients with<br />
Fibromyalgia Syndrome.<br />
A Long-Term Study of the Safety of Rituxan® in Patients with Rheumatoid Arthritis After an Inadequate<br />
Response to Previous Anti-TNF Therapy<br />
American College of Rheumatology Research and Education Foundation Health Professional New<br />
Investigator Award: “An Analysis of the Effects of Exercise on a Biomechanical Risk Factor for Knee OA.”<br />
P.I.: L Thorp, PhD. Mentor.<br />
Arthritis Foundation Chicago Chapter Young Investigator Award 2008-2010<br />
“A Biomechanical Approach to Modify Risk Factors for Knee OA.” P.I.: L. Thorp, PhD. Role: Co-I, 5%<br />
Investigation of Genetic Variability at the Aggrecan Locus in African American Osteoarthritis Patients. “<br />
P.I.: D.M. Franks, PhD. Role: Co-I 3% Effort<br />
K23 AR049748 “Factors influencing the evolution of knee osteoarthritis.” P.I.: N. Shakoor, M.D. Role:<br />
Mentor 5% Effort.<br />
“Proprioception and strength in lower extremity osteoarthritis.” P.I.: N. Shakoor, M.D. Role: Supervisor.<br />
RO1 grant “Mineral Matrix Relations in Calcifying Tissues”, Collaborator (10%); W. Landis, Ph.D. – P.I.<br />
(Neoucom, Rootstown, OH)<br />
RO1 “Hyaluronan-Cell interactions in cartilage”, Co-investigator (5%); C Knudson, Ph.D. – P.I.<br />
SCOR grant “Osteoarthritis: A continuum (SCOR)”. K. Kuettner: Program Dir.<br />
“Mechanisms Involved in the Formation of a Cartilage Tissue by Osteoarthritic Cells” E. Thonar, P.I.; S.<br />
Chubinskaya, Collaborator, 3%<br />
“Biological Research Core”; C. Knudson, P.I., Co-Investigator, 3%.<br />
“Protein targets of ovarian and oocyte autoantibodies” J Luborsky PI (Consult).<br />
“Damaged Human Cartilage Proposal”. M. Wimmer (P.I.),Co-Investigator, 5%.<br />
Study “Differences in supraspinatus tendon biomechanics, histology, and ultrastructure that may<br />
affect the quality of single vs double row rotator cuff repair” B. Cole, MD, Principal Investigator.<br />
Co-Investigator (3% effort /.36 mo)<br />
M.Wimmer, PhD, Prinicipal Investigator; Co-Investigator (10%)<br />
“Rabbit GH Chondrolysis/Rotator Cuff Healing”. B. Cole, MD, PI; Co-Investigator (10%).<br />
Cartilage degradation in acute trauma model” PI; Cecilia Pascual, MD, postdoctoral fellow Becas<br />
Larramendi 2007, Spain.<br />
“Rabbit GH Chondrolysis/Rotator Cuff Healing”. B Cole, MD, PI; Co-Investigator (10%)<br />
Section of Rheumatology<br />
“Biochemical, histological, and structural analysis of newly formed cartilage in the model of<br />
osteochondral defects in goats” Principal Investigator (20%).<br />
51
Section of Rheumatology<br />
Sponsor Title<br />
Alison Finnegan, PhD<br />
NIH-NIAMS<br />
NIH-NIAMS<br />
NIH/NIAMS<br />
Tibor Glant, MD, PhD<br />
NIH/NIAMS<br />
Zimmer Research Foundation<br />
Grainger Foundation<br />
Hee-Jeong Im-Sampen, PhD<br />
NIH/NIAMS<br />
Arthritis Foundation<br />
Chicago Chapter<br />
Arthritis National<br />
Research Foundation<br />
Samsung Biomedical<br />
Research Institute Grant<br />
Zimmer Spine Research<br />
NIH/NIAMS<br />
NIH/NIAMS<br />
NIH/NIAMS<br />
Meenakshi Jolly, MD<br />
Cook County and <strong>Rush</strong><br />
Anna Plaas, PhD<br />
Seikagaku Inc.<br />
Glycosciences Inc<br />
52<br />
“Effect of catabolic mediators and biomechanical load on osteochondral allograft cartilage”. Principal<br />
Investigator (25%).<br />
“Response of Damaged Human Cartilage to Articular Motion – A Study Utilizing an Acute Trauma Model<br />
on Human Ankles”. M. Wimmer, PhD, Principal Investigator; S. Chubinskaya, Co-Investigator (5%).<br />
“Autoimmune Arthritis: Genetics and Cellular Regulation” Project #2 “Cytokine Regulation in<br />
Experimental Arthritis”<br />
“B cell Function in Autoimmune Arthritis”<br />
“Systemic Implication of Total Joint Replacement”<br />
“Autoimmune Arthritis: Genetics and Cellular regulation” (Program director Tibor Glant, M.D., Ph.D.)<br />
(PI: of Project 1 and Administrative Core B). Project 1: “Mapping of Arthritis Susceptible Gene” (PI)<br />
“Study of Autoimmune Progressive Polyarthritis”PI. Mechanisms of Arthritis Suppression by TSG-6<br />
(Tnfip6)” Mechanisms of Arthritis Suppression by TSG-6 (Tnfip6)” “B-cell Function in Autoimmune<br />
Arthritis”. PI: Finnegan, Co-investigator: Glant) Aggrecan-hG1 and LP Transgenic Mice as Models of OA<br />
PI: TT Glant.<br />
“Periprosthetic Osteolysis and Bone Remodeling” Funded at <strong>Rush</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong>, (PI: Glant)<br />
Project 1 Year 4<br />
Novel Diagnostic Tools for Rheumatoid Arthritis and Myeloid Leukemia” PIs: TT. Glant and K. Mikecz,<br />
“Pathological Role of bFGF in Human Adult Articular Cartilage” Role: PI<br />
“Molecular Mechanisms of Anti-Smad Pathway by bFGF in Cartilage” Role: PI<br />
“IL-1_-altered SUMO pathway in the pathogenesis of Osteoarthritis” Role: PI<br />
“Inhibitory Effect of Resveratrol on Intervertebral Disc Degeneration in Rabbit Model” Role: Co-PI<br />
PI: Dr. Howard S. An Role: Co-Investigator<br />
(Program Project Director: Dr. T. Oegema) “Osteoarthritis: A Continuum (SCOR) (multi-project<br />
program) Project One: “Mechanism Involved in the Formation of a Cartilage Tissue by Osteoarthritic<br />
Cells” Role: Co-Investigator<br />
Percentile: 9.4 “An Interdisciplinary and Integrative Study of Tendinopathy” Role: Consultant<br />
“Molecular mechanisms of exercise-modulated anti-inflammation in tendons” Cook County and <strong>Rush</strong><br />
<strong>University</strong> Collaborative grant. Serum markers for detecting lupus flares. Co-PI<br />
<strong>University</strong> Collaborative Grant
Sponsor Title<br />
Smith & Nephew Inc<br />
Pfizer Inc.<br />
Najia Shakoor, MD<br />
NIH<br />
Eugene Thonar, PhD<br />
NIH/ NIAMS<br />
Serum markers for detecting lupus flares. Co-PI.<br />
“Nanoparticle targeted treatment of Synovial Joint lining” PI<br />
“Effect of High Molecular Weight Hyaluronan on Synovial Inflammation in Osteoarthritis” PI<br />
“Oral HA oligosaccharides and Chondroprotection in Murine OsteoArthritis” PI<br />
Section of Rheumatology<br />
Strategic Alliance Support Grant “Effect of DMOADs of Tissue Degradative and Reparative Pathways in<br />
a Murine Model of OA”<br />
(PENDING) Altering biomechanics in knee osteoarthritis, PI: U01 (PENDING) PI: M Nevitt,<br />
<strong>University</strong> of California, Consultant. Factors influencing the evolution of knee osteoarthritis PI:<br />
70% Effort<br />
Spine Program Project Grant Project 3 Masuda (PI): Autocrine and Paracrine Control of Homeostasis<br />
of the Intervertebral Disc Role.<br />
53
DIVISION OF NEPHROLOGY<br />
1426 W. Washington Blvd.<br />
(312)850-8434<br />
54<br />
Stephen M. Korbet, MD<br />
Division Chief, Nephrology<br />
Edmund J. Lewis, MD<br />
Section Director, Nephrology<br />
Samuel N. Saltzberg, MD<br />
Section Director, Transplant<br />
Nephrology<br />
Faculty:<br />
Professors:<br />
Stephen M. Korbet, MD<br />
Edmund J. Lewis, MD<br />
Associate Professor:<br />
Roger A. Rodby, MD<br />
Assistant Professors:<br />
Samuel N. Saltzberg, MD<br />
Marvin V. Sinsakul, MD<br />
William L. Whittier, MD<br />
Instructor:<br />
Casey N. Gashti, MD<br />
The Division of Nephrology, comprised of the Section of Nephrology<br />
and Section of Transplant Nephrology, is an internationally recognized<br />
nephrology practice. The Division has been ranked as one of the top 25<br />
Kidney Disease Programs in the United States by U.S.News & World<br />
Report for the past several years. For over two decades, our physicians<br />
have been committed to the prevention and treatment of kidney disease<br />
and kidney failure.<br />
The nephrologists in our division are responsible for cutting-edge<br />
investigations which have changed the standards of medical practice<br />
worldwide. For over 30 years, Dr. Lewis has headed up the Collaborative<br />
Study Group (CSG), a research group representing 200 clinics in 20<br />
different countries. Studies conducted by the CSG demonstrated the<br />
use of angiotensin converting enzyme inhibitors in patients with Type<br />
1 diabetic nephropathy and the use of angiotensin receptor blockers<br />
in patients with Type 2 diabetic nephropathy slowed the progression<br />
of renal disease. These findings lead to changes in the management of<br />
diabetic nephropathy which have benefited millions of patients with<br />
diabetic renal disease.<br />
Other major advances pioneered within the practice include the<br />
classification and therapy of lupus nephritis and focal segmental<br />
glomerulonephritis. They have also been involved in studies which<br />
helped define the use of recombinant human erythropoietin in chronic<br />
dialysis patients, and we have been very involved in providing insight<br />
into the use of innovated forms of chronic dialysis such as peritoneal<br />
dialysis and daily home hemodialysis to patients with end-stage renal<br />
disease. In the area of acute dialysis, the Section of Nephrology was one<br />
of the first to provide continuous dialysis therapy using an innovative<br />
machine designed by NxStage which works on the principle of clearance<br />
by ultrafiltration.<br />
Education<br />
The nephrology faculty is actively involved in teaching medical students,<br />
resident and fellows. Additionally, many of our faculty members serve<br />
on editorial boards of peer reviewed journals and are actively involved<br />
with nephrology societies such as the American Society of Nephrology<br />
(ASN), International Society of Nephrology (ISN) and the National<br />
Kidney Foundation (NKF). The involvement in these societies includes<br />
serving on the program committees for annual meetings as well as<br />
moderating and lecturing at the annual meetings.<br />
The nephrology fellowship program at <strong>Rush</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong><br />
is committed to providing the finest subspecialty training in Nephrology<br />
available anywhere in the country. Our comprehensive program focuses<br />
on clinical nephrology and clinical research and prepares the trainee for<br />
all aspects of a career in clinical nephrology. The fellowship is a two-
year program, with three fellows at each level. The<br />
primary teaching institution for the subspecialty<br />
program is <strong>Rush</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong>, a<br />
1,000-bed tertiary care teaching hospital where the<br />
subspecialty fellows participate in rotations on the<br />
in-patient nephrology consult service, in-patient<br />
nephrology transplant service, renal pathology<br />
rotation, and pediatric nephrology. Fellows also<br />
rotate through the out-patient hemodialysis unit,<br />
outpatient peritoneal dialysis clinics and outpatient<br />
nephrology continuity clinics located about one<br />
quarter mile from the medical center at 1426 W.<br />
Washington Blvd.<br />
Research<br />
Division of Nephrology<br />
The Section of Nephrology at <strong>Rush</strong> <strong>University</strong><br />
<strong>Medical</strong> <strong>Center</strong> has a long tradition of research<br />
in glomerular pathology and treatment. The<br />
Nephrology Section Head is Dr. Edmund Lewis,<br />
the Principal Investigator of the Collaborative<br />
Study Group. Studies done by the Collaborative<br />
Study Group have defined the standard of care for<br />
lupus nephritis and both type 1 and type 2 diabetic<br />
nephropathy.<br />
55
56<br />
Ongoing Research<br />
E. J. Lewis, M.D. and M. Sinsakul, MD: A Randomized, Double-Blind,<br />
Placebo-Controlled, Multi-<strong>Center</strong>, Phase 2b Study to Evaluate the<br />
Safety and Efficacy of Pyridorin (pyridoxamine dihydrochloride) in<br />
Patients with Nephropathy Due to Type 2 Diabetes.<br />
S. M. Korbet, M.D. and M. Sinsakul, MD: A Safety and Tolerability<br />
Study of Zerenex (ferric citrate) in Patients with End-Stage Renal<br />
Disease (ESRD).<br />
M. Sinsakul, MD: Following Rehabilitation, Economics and Everyday<br />
Dialysis Outcome Measurements Study (FREEDOM).<br />
M. Sinsakul, MD and W. Whittier, MD: Comparison of Nocturnal<br />
Hemodialysis (NHD) and Short Daily Hemodialysis (DHD) with the<br />
NxStage System One.<br />
S. Saltzberg, MD: An open-label, concentration-controlled,<br />
randomized, 12-month study of prograf + rapamune + corticosteroids<br />
compared to cyclosporine USP (modified) + rapamune +<br />
corticosteroids in high risk renal allograft recipients (incorporating<br />
protocol amendment 2)<br />
S. Saltzberg, MD: A one-year, multicenter, partially blinded, doubledummy,<br />
randomized study to evaluate the efficacy and safety of<br />
FTY720 combined with reduced-dose or full-dose Neoral® and<br />
corticosteroids versus mycophenolate mofetil (MMF, CellCept)<br />
combined with full-dose Neoral® and corticosteroids, in de novo adult<br />
renal transplant recipients.<br />
S. Saltzberg, MD: A phase III, open-label, comparative, multi-center<br />
study to assess the safety and efficacy of prograf (tacrolimus)/MMF,<br />
modified release (MR) tacrolimus/MMF and Neoral (cyclosporine)/<br />
MMF in de novo kidney transplant recipients re: Protocol 02-0-158<br />
S. Saltzberg, MD: A randomized, open-label study to compare the<br />
safety and efficacy of two different sirolimus regimens to a tacrolimus +<br />
mycophenolate mofetil regimen in de novo renal allograft recipients.<br />
S. Saltzberg, MD: A prospective, randomized, open label, twenty-six<br />
week study of the efficacy and safety of converting kidney and liver<br />
transplant recipients with tacrolimus-associated abnormal glucose<br />
metabolism to Neoral® with C2 .<br />
W. Whittier, MD: Rapid Assessment of Vascular Graft Patency. NIH<br />
funded grant to noninvasively evaluate permanent dialysis accesses in<br />
patients with chronic renal failure.<br />
Sponsor<br />
NephroGenex Inc. Protocol Number<br />
PYR-210<br />
Keryx Biopharmaceuticals Inc.<br />
Protocol KRX-0502<br />
NxStage <strong>Medical</strong> CP00<strong>09</strong><br />
NxStage <strong>Medical</strong> CP0010.<br />
Wyeth-Ayerst-164<br />
Novartis CFTY720 0125, Protocol<br />
Amendment 4<br />
Fujisawa MR/Prograf/Neoral<br />
Wyeth-Ayerst (Orion) 497, Protocol<br />
No. 0468H1-101497<br />
Novartis (US06), Protocol No:<br />
COLO400A US06<br />
NIH No: R44 DK059685
The Department of Internal Medicine<br />
gratefully acknowledges Tulay Nalbant,<br />
project manager, for her superb work to<br />
create this Annual Report.