Effects of Dehydroepiandrosterone Therapy on Pubic Hair Growth ...
Effects of Dehydroepiandrosterone Therapy on Pubic Hair Growth ...
Effects of Dehydroepiandrosterone Therapy on Pubic Hair Growth ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
1184 Binder et al. DHEA Replacement in Young Females J Clin Endocrinol Metab, April 2009, 94(4):1182–1190<br />
99.5%/aerosol 0.5%. For the assessment <str<strong>on</strong>g>of</str<strong>on</strong>g> compliance, unused capsules<br />
were counted at each visit.<br />
Efficacy assessment<br />
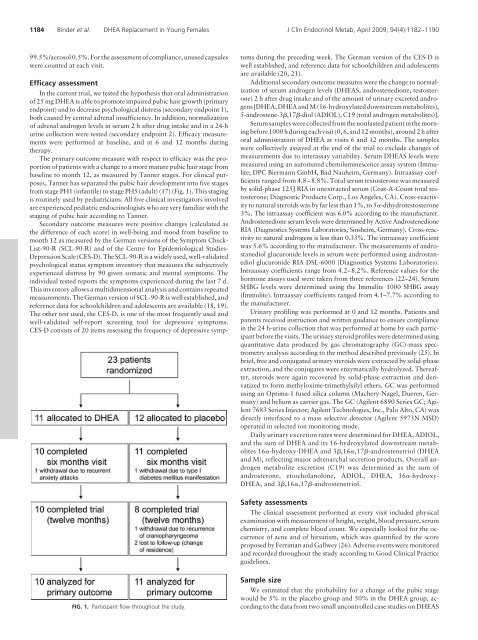
In the current trial, we tested the hypothesis that oral administrati<strong>on</strong><br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> 25 mg DHEA is able to promote impaired pubic hair growth (primary<br />
endpoint) and to decrease psychological distress (sec<strong>on</strong>dary endpoint 1),<br />
both caused by central adrenal insufficiency. In additi<strong>on</strong>, normalizati<strong>on</strong><br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> adrenal androgen levels in serum 2 h after drug intake and in a 24-h<br />
urine collecti<strong>on</strong> were tested (sec<strong>on</strong>dary endpoint 2). Efficacy measurements<br />
were performed at baseline, and at 6 and 12 m<strong>on</strong>ths during<br />
therapy.<br />
The primary outcome measure with respect to efficacy was the proporti<strong>on</strong><br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> patients with a change to a more mature pubic hair stage from<br />
baseline to m<strong>on</strong>th 12, as measured by Tanner stages. For clinical purposes,<br />
Tanner has separated the pubic hair development into five stages<br />
from stage PH1 (infantile) to stage PH5 (adult) (17) (Fig. 1). This staging<br />
is routinely used by pediatricians. All five clinical investigators involved<br />
are experienced pediatric endocrinologists who are very familiar with the<br />
staging <str<strong>on</strong>g>of</str<strong>on</strong>g> pubic hair according to Tanner.<br />
Sec<strong>on</strong>dary outcome measures were positive changes (calculated as<br />
the difference <str<strong>on</strong>g>of</str<strong>on</strong>g> each score) in well-being and mood from baseline to<br />
m<strong>on</strong>th 12 as measured by the German versi<strong>on</strong>s <str<strong>on</strong>g>of</str<strong>on</strong>g> the Symptom Check-<br />
List-90-R (SCL-90-R) and <str<strong>on</strong>g>of</str<strong>on</strong>g> the Centre for Epidemiological Studies-<br />
Depressi<strong>on</strong> Scale (CES-D). The SCL-90-R is a widely used, well-validated<br />
psychological status symptom inventory that measures the subjectively<br />
experienced distress by 90 given somatic and mental symptoms. The<br />
individual tested reports the symptoms experienced during the last 7 d.<br />
This inventory allows a multidimensi<strong>on</strong>al analysis and c<strong>on</strong>tains repeated<br />
measurements. The German versi<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> SCL-90-R is well established, and<br />
reference data for schoolchildren and adolescents are available (18, 19).<br />
The other test used, the CES-D, is <strong>on</strong>e <str<strong>on</strong>g>of</str<strong>on</strong>g> the most frequently used and<br />
well-validated self-report screening tool for depressive symptoms.<br />
CES-D c<strong>on</strong>sists <str<strong>on</strong>g>of</str<strong>on</strong>g> 20 items assessing the frequency <str<strong>on</strong>g>of</str<strong>on</strong>g> depressive symp-<br />
FIG. 1. Participant flow throughout the study.<br />
toms during the preceding week. The German versi<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> the CES-D is<br />
well established, and reference data for schoolchildren and adolescents<br />
are available (20, 21).<br />
Additi<strong>on</strong>al sec<strong>on</strong>dary outcome measures were the change to normalizati<strong>on</strong><br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> serum androgen levels (DHEAS, androstenedi<strong>on</strong>e, testoster<strong>on</strong>e)<br />
2 h after drug intake and <str<strong>on</strong>g>of</str<strong>on</strong>g> the amount <str<strong>on</strong>g>of</str<strong>on</strong>g> urinary excreted androgens<br />
[DHEA, DHEA and M (16-hydroxylated downstream metabolites),<br />
5-androstene-3,17-diol (ADIOL), C19 (total androgen metabolites)].<br />
Serum samples were collected from the n<strong>on</strong>fasted patient in the morning<br />
before 1000 h during each visit (0, 6, and 12 m<strong>on</strong>ths), around 2 h after<br />
oral administrati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> DHEA at visits 6 and 12 m<strong>on</strong>ths. The samples<br />
were collectively assayed at the end <str<strong>on</strong>g>of</str<strong>on</strong>g> the trial to exclude changes <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
measurements due to interassay variability. Serum DHEAS levels were<br />
measured using an automated chemiluminescence assay system (Immulite;<br />
DPC Biermann GmbH, Bad Nauheim, Germany). Intraassay coefficients<br />
ranged from 4.8–8.8%. Total serum testoster<strong>on</strong>e was measured<br />
by solid-phase 125J RIA in unextracted serum (Coat-A-Count total testoster<strong>on</strong>e;<br />
Diagnostic Products Corp., Los Angeles, CA). Cross-reactivity<br />
to natural steroids was by far less than 1%, to 5-dihydrotestoster<strong>on</strong>e<br />
3%. The intraassay coefficient was 6.0% according to the manufacturer.<br />
Androstenedi<strong>on</strong>e serum levels were determined by Active Androstenedi<strong>on</strong>e<br />
RIA (Diagnostics Systems Laboratories, Sinsheim, Germany). Cross-reactivity<br />
to natural androgens is less than 0.33%. The intraassay coefficient<br />
was 5.6% according to the manufacturer. The measurements <str<strong>on</strong>g>of</str<strong>on</strong>g> androstanediol<br />
glucur<strong>on</strong>ide levels in serum were performed using androstanediol<br />
glucur<strong>on</strong>ide RIA DSL-6000 (Diagnostics Systems Laboratories).<br />
Intraassay coefficients range from 4.2–8.2%. Reference values for the<br />
horm<strong>on</strong>e assays used were taken from three references (22–24). Serum<br />
SHBG levels were determined using the Immulite 1000 SHBG assay<br />
(Immulite). Intraassay coefficients ranged from 4.1–7.7% according to<br />
the manufacturer.<br />
Urinary pr<str<strong>on</strong>g>of</str<strong>on</strong>g>iling was performed at 0 and 12 m<strong>on</strong>ths. Patients and<br />
parents received instructi<strong>on</strong> and written guidance to ensure compliance<br />
in the 24 h-urine collecti<strong>on</strong> that was performed at home by each participant<br />
before the visits. The urinary steroid pr<str<strong>on</strong>g>of</str<strong>on</strong>g>iles were determined using<br />
quantitative data produced by gas chromatography (GC)-mass spectrometry<br />
analysis according to the method described previously (25). In<br />
brief, free and c<strong>on</strong>jugated urinary steroids were extracted by solid-phase<br />
extracti<strong>on</strong>, and the c<strong>on</strong>jugates were enzymatically hydrolyzed. Thereafter,<br />
steroids were again recovered by solid-phase extracti<strong>on</strong> and derivatized<br />
to form methyloxime-trimethylsilyl ethers. GC was performed<br />
using an Optima-1 fused silica column (Machery-Nagel, Dueren, Germany)<br />
and helium as carrier gas. The GC (Agilent 6890 Series GC; Agilent<br />
7683 Series Injector; Agilent Technologies, Inc., Palo Alto, CA) was<br />
directly interfaced to a mass selective detector (Agilent 5973N MSD)<br />
operated in selected i<strong>on</strong> m<strong>on</strong>itoring mode.<br />
Daily urinary excreti<strong>on</strong> rates were determined for DHEA, ADIOL,<br />
and the sum <str<strong>on</strong>g>of</str<strong>on</strong>g> DHEA and its 16-hydroxylated downstream metabolites<br />
16-hydroxy-DHEA and 3,16,17-androstenetriol (DHEA<br />
and M), reflecting major adrenarchal secreti<strong>on</strong> products. Overall androgen<br />
metabolite excreti<strong>on</strong> (C19) was determined as the sum <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
androster<strong>on</strong>e, etiocholanol<strong>on</strong>e, ADIOL, DHEA, 16-hydroxy-<br />
DHEA, and 3,16,17-androstenetriol.<br />
Safety assessments<br />
The clinical assessment performed at every visit included physical<br />
examinati<strong>on</strong> with measurement <str<strong>on</strong>g>of</str<strong>on</strong>g> height, weight, blood pressure, serum<br />
chemistry, and complete blood count. We especially looked for the occurrence<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> acne and <str<strong>on</strong>g>of</str<strong>on</strong>g> hirsutism, which was quantified by the score<br />
proposed by Ferriman and Gallwey (26). Adverse events were m<strong>on</strong>itored<br />
and recorded throughout the study according to Good Clinical Practice<br />
guidelines.<br />
Sample size<br />
We estimated that the probability for a change <str<strong>on</strong>g>of</str<strong>on</strong>g> the pubic stage<br />
would be 5% in the placebo group and 50% in the DHEA group, according<br />
to the data from two small unc<strong>on</strong>trolled case studies <strong>on</strong> DHEAS