Klinefelter Syndrome in Adolescence - The Journal of Clinical ...
Klinefelter Syndrome in Adolescence - The Journal of Clinical ...
Klinefelter Syndrome in Adolescence - The Journal of Clinical ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
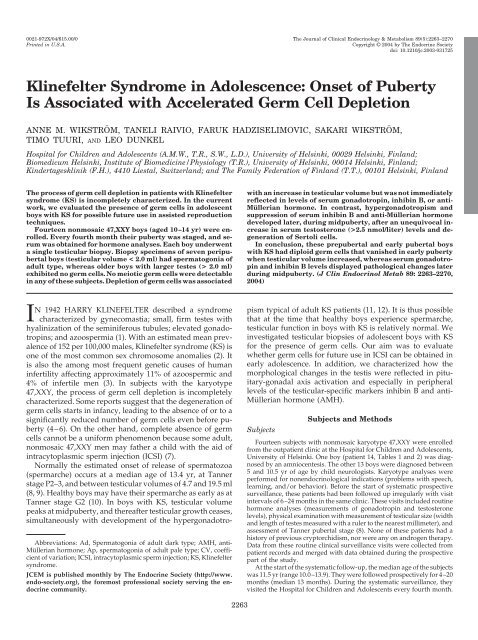
0021-972X/04/$15.00/0 <strong>The</strong> <strong>Journal</strong> <strong>of</strong> Cl<strong>in</strong>ical Endocr<strong>in</strong>ology & Metabolism 89(5):2263–2270<br />
Pr<strong>in</strong>ted <strong>in</strong> U.S.A. Copyright © 2004 by <strong>The</strong> Endocr<strong>in</strong>e Society<br />
doi: 10.1210/jc.2003-031725<br />
<strong>Kl<strong>in</strong>efelter</strong> <strong>Syndrome</strong> <strong>in</strong> <strong>Adolescence</strong>: Onset <strong>of</strong> Puberty<br />
Is Associated with Accelerated Germ Cell Depletion<br />
ANNE M. WIKSTRÖM, TANELI RAIVIO, FARUK HADZISELIMOVIC, SAKARI WIKSTRÖM,<br />
TIMO TUURI, AND LEO DUNKEL<br />
Hospital for Children and Adolescents (A.M.W., T.R., S.W., L.D.), University <strong>of</strong> Hels<strong>in</strong>ki, 00029 Hels<strong>in</strong>ki, F<strong>in</strong>land;<br />
Biomedicum Hels<strong>in</strong>ki, Institute <strong>of</strong> Biomedic<strong>in</strong>e/Physiology (T.R.), University <strong>of</strong> Hels<strong>in</strong>ki, 00014 Hels<strong>in</strong>ki, F<strong>in</strong>land;<br />
K<strong>in</strong>dertageskl<strong>in</strong>ik (F.H.), 4410 Liestal, Switzerland; and <strong>The</strong> Family Federation <strong>of</strong> F<strong>in</strong>land (T.T.), 00101 Hels<strong>in</strong>ki, F<strong>in</strong>land<br />
<strong>The</strong> process <strong>of</strong> germ cell depletion <strong>in</strong> patients with <strong>Kl<strong>in</strong>efelter</strong><br />
syndrome (KS) is <strong>in</strong>completely characterized. In the current<br />
work, we evaluated the presence <strong>of</strong> germ cells <strong>in</strong> adolescent<br />
boys with KS for possible future use <strong>in</strong> assisted reproduction<br />
techniques.<br />
Fourteen nonmosaic 47,XXY boys (aged 10–14 yr) were enrolled.<br />
Every fourth month their puberty was staged, and serum<br />
was obta<strong>in</strong>ed for hormone analyses. Each boy underwent<br />
a s<strong>in</strong>gle testicular biopsy. Biopsy specimens <strong>of</strong> seven peripubertal<br />
boys (testicular volume < 2.0 ml) had spermatogonia <strong>of</strong><br />
adult type, whereas older boys with larger testes (> 2.0 ml)<br />
exhibited no germ cells. No meiotic germ cells were detectable<br />
<strong>in</strong> any <strong>of</strong> these subjects. Depletion <strong>of</strong> germ cells was associated<br />
IN 1942 HARRY KLINEFELTER described a syndrome<br />
characterized by gynecomastia; small, firm testes with<br />
hyal<strong>in</strong>ization <strong>of</strong> the sem<strong>in</strong>iferous tubules; elevated gonadotrop<strong>in</strong>s;<br />
and azoospermia (1). With an estimated mean prevalence<br />
<strong>of</strong> 152 per 100,000 males, <strong>Kl<strong>in</strong>efelter</strong> syndrome (KS) is<br />
one <strong>of</strong> the most common sex chromosome anomalies (2). It<br />
is also the among most frequent genetic causes <strong>of</strong> human<br />
<strong>in</strong>fertility affect<strong>in</strong>g approximately 11% <strong>of</strong> azoospermic and<br />
4% <strong>of</strong> <strong>in</strong>fertile men (3). In subjects with the karyotype<br />
47,XXY, the process <strong>of</strong> germ cell depletion is <strong>in</strong>completely<br />
characterized. Some reports suggest that the degeneration <strong>of</strong><br />
germ cells starts <strong>in</strong> <strong>in</strong>fancy, lead<strong>in</strong>g to the absence <strong>of</strong> or to a<br />
significantly reduced number <strong>of</strong> germ cells even before puberty<br />
(4–6). On the other hand, complete absence <strong>of</strong> germ<br />
cells cannot be a uniform phenomenon because some adult,<br />
nonmosaic 47,XXY men may father a child with the aid <strong>of</strong><br />
<strong>in</strong>tracytoplasmic sperm <strong>in</strong>jection (ICSI) (7).<br />
Normally the estimated onset <strong>of</strong> release <strong>of</strong> spermatozoa<br />
(spermarche) occurs at a median age <strong>of</strong> 13.4 yr, at Tanner<br />
stage P2–3, and between testicular volumes <strong>of</strong> 4.7 and 19.5 ml<br />
(8, 9). Healthy boys may have their spermarche as early as at<br />
Tanner stage G2 (10). In boys with KS, testicular volume<br />
peaks at midpuberty, and thereafter testicular growth ceases,<br />
simultaneously with development <strong>of</strong> the hypergonadotro-<br />
Abbreviations: Ad, Spermatogonia <strong>of</strong> adult dark type; AMH, anti-<br />
Müllerian hormone; Ap, spermatogonia <strong>of</strong> adult pale type; CV, coefficient<br />
<strong>of</strong> variation; ICSI, <strong>in</strong>tracytoplasmic sperm <strong>in</strong>jection; KS, <strong>Kl<strong>in</strong>efelter</strong><br />
syndrome.<br />
JCEM is published monthly by <strong>The</strong> Endocr<strong>in</strong>e Society (http://www.<br />
endo-society.org), the foremost pr<strong>of</strong>essional society serv<strong>in</strong>g the endocr<strong>in</strong>e<br />
community.<br />
2263<br />
with an <strong>in</strong>crease <strong>in</strong> testicular volume but was not immediately<br />
reflected <strong>in</strong> levels <strong>of</strong> serum gonadotrop<strong>in</strong>, <strong>in</strong>hib<strong>in</strong> B, or anti-<br />
Müllerian hormone. In contrast, hypergonadotropism and<br />
suppression <strong>of</strong> serum <strong>in</strong>hib<strong>in</strong> B and anti-Müllerian hormone<br />
developed later, dur<strong>in</strong>g midpuberty, after an unequivocal <strong>in</strong>crease<br />
<strong>in</strong> serum testosterone (>2.5 nmol/liter) levels and degeneration<br />
<strong>of</strong> Sertoli cells.<br />
In conclusion, these prepubertal and early pubertal boys<br />
with KS had diploid germ cells that vanished <strong>in</strong> early puberty<br />
when testicular volume <strong>in</strong>creased, whereas serum gonadotrop<strong>in</strong><br />
and <strong>in</strong>hib<strong>in</strong> B levels displayed pathological changes later<br />
dur<strong>in</strong>g midpuberty. (J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 89: 2263–2270,<br />
2004)<br />
pism typical <strong>of</strong> adult KS patients (11, 12). It is thus possible<br />
that at the time that healthy boys experience spermarche,<br />
testicular function <strong>in</strong> boys with KS is relatively normal. We<br />
<strong>in</strong>vestigated testicular biopsies <strong>of</strong> adolescent boys with KS<br />
for the presence <strong>of</strong> germ cells. Our aim was to evaluate<br />
whether germ cells for future use <strong>in</strong> ICSI can be obta<strong>in</strong>ed <strong>in</strong><br />
early adolescence. In addition, we characterized how the<br />
morphological changes <strong>in</strong> the testis were reflected <strong>in</strong> pituitary-gonadal<br />
axis activation and especially <strong>in</strong> peripheral<br />
levels <strong>of</strong> the testicular-specific markers <strong>in</strong>hib<strong>in</strong> B and anti-<br />
Müllerian hormone (AMH).<br />
Subjects<br />
Subjects and Methods<br />
Fourteen subjects with nonmosaic karyotype 47,XXY were enrolled<br />
from the outpatient cl<strong>in</strong>ic at the Hospital for Children and Adolescents,<br />
University <strong>of</strong> Hels<strong>in</strong>ki. One boy (patient 14, Tables 1 and 2) was diagnosed<br />
by an amniocentesis. <strong>The</strong> other 13 boys were diagnosed between<br />
5 and 10.5 yr <strong>of</strong> age by child neurologists. Karyotype analyses were<br />
performed for nonendocr<strong>in</strong>ological <strong>in</strong>dications (problems with speech,<br />
learn<strong>in</strong>g, and/or behavior). Before the start <strong>of</strong> systematic prospective<br />
surveillance, these patients had been followed up irregularly with visit<br />
<strong>in</strong>tervals <strong>of</strong> 6–24 months <strong>in</strong> the same cl<strong>in</strong>ic. <strong>The</strong>se visits <strong>in</strong>cluded rout<strong>in</strong>e<br />
hormone analyses (measurements <strong>of</strong> gonadotrop<strong>in</strong> and testosterone<br />
levels), physical exam<strong>in</strong>ation with measurement <strong>of</strong> testicular size (width<br />
and length <strong>of</strong> testes measured with a ruler to the nearest millimeter), and<br />
assessment <strong>of</strong> Tanner pubertal stage (8). None <strong>of</strong> these patients had a<br />
history <strong>of</strong> previous cryptorchidism, nor were any on androgen therapy.<br />
Data from these rout<strong>in</strong>e cl<strong>in</strong>ical surveillance visits were collected from<br />
patient records and merged with data obta<strong>in</strong>ed dur<strong>in</strong>g the prospective<br />
part <strong>of</strong> the study.<br />
At the start <strong>of</strong> the systematic follow-up, the median age <strong>of</strong> the subjects<br />
was 11.5 yr (range 10.0–13.9). <strong>The</strong>y were followed prospectively for 4–20<br />
months (median 13 months). Dur<strong>in</strong>g the systematic surveillance, they<br />
visited the Hospital for Children and Adolescents every fourth month.
2264 J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab, May 2004, 89(5):2263–2270 Wikström et al. Testicular Degeneration <strong>in</strong> Adolescent KS Boys<br />
TABLE 1. Histomorphometric analyses <strong>of</strong> testicular biopsies <strong>of</strong> 14 boys with KS, with key characteristics at the time <strong>of</strong> the biopsy<br />
Patient<br />
no.<br />
At each visit, a physical exam<strong>in</strong>ation was carried out as previously<br />
described; testicular volume was calculated with the formula 0.52 <br />
length width (2), and converted to milliliters (13 and was expressed<br />
as the mean volume <strong>of</strong> the left and right testis. Once a year skeletal age<br />
was assessed accord<strong>in</strong>g to the atlas <strong>of</strong> Greulich and Pyle (14). Sera were<br />
obta<strong>in</strong>ed for FSH, LH, <strong>in</strong>hib<strong>in</strong> B, and AMH measurements every fourth<br />
month and for testosterone, SHBG, and estradiol measurements at least<br />
once a year.<br />
<strong>The</strong> parents <strong>of</strong> each boy gave their <strong>in</strong>formed consent for participation<br />
<strong>in</strong> this study that had been approved by the research ethics committee<br />
<strong>of</strong> the hospital.<br />
Assays<br />
Group<br />
no.<br />
Age<br />
(yr)<br />
Tanner<br />
stage<br />
Mean testicular<br />
volume (ml)<br />
Ap Ad<br />
spermatogonia/<br />
tubule<br />
<strong>The</strong> blood samples were drawn between 0830 and 1530 h. After<br />
clott<strong>in</strong>g, the serum was separated by centrifugation and stored at 20<br />
C until required. Serum FSH and LH levels were measured by ultrasensitive<br />
immun<strong>of</strong>luorometric assays, as previously described (15). FSH<br />
and LH concentrations <strong>of</strong> less than 0.1 IU/liter were treated as 0.1<br />
IU/liter. <strong>The</strong> <strong>in</strong>terassay coefficient <strong>of</strong> variation (CV) for FSH was less<br />
than 3.3% and for LH less than 4.4%. <strong>The</strong> <strong>in</strong>traassay CV for FSH was less<br />
than 4.4% and for LH less than 4.1%. Serum testosterone concentrations<br />
were measured by a RIA after separation <strong>of</strong> steroid fractions on Lipidx-<br />
5000 microcolumns (16, 17). <strong>The</strong> detection limit for testosterone was 0.1<br />
nmol/liter. <strong>The</strong> <strong>in</strong>terassay CV was less than 15% and the <strong>in</strong>traassay CV<br />
was less than 9%. Serum <strong>in</strong>hib<strong>in</strong> B (Serotec, Oxford, UK) and AMH<br />
Ad<br />
spermatogonia/<br />
tubule<br />
(Immunotech-Coulter, Marseille, France) levels were measured by commercially<br />
available immunoenzymometric assays accord<strong>in</strong>g to manufacturers’<br />
<strong>in</strong>structions. <strong>The</strong> detection limit for <strong>in</strong>hib<strong>in</strong> B was 15.6 pg/ml.<br />
<strong>The</strong> <strong>in</strong>terassay CV was less than 15% and the <strong>in</strong>traassay CV less than 5%.<br />
<strong>The</strong> detection limit for AMH was 5.5 pmol/liter, and the <strong>in</strong>terassay CV<br />
was 13.4%.<br />
Testicular biopsies<br />
Sertoli cells type<br />
Leydig cell<br />
hyperplasia<br />
Interstitium and<br />
peritubular<br />
connective tissue<br />
1 I 10.1 P1/G1 1.1 1.2 0.01 Sa/Sb fibr ()<br />
2 I 10.1 P1/G1 1.3 0.04 0 Sa/Sb fibr , hyal<strong>in</strong><br />
3 I 10.3 P1/G1 0.8 0.8 0.006 Sa/Sb fibr ()<br />
4 I 10.7 P1/G1 1.6 1.0 0.03 Sa/Sb fibr <br />
5 I 11.6 P1/G1 1.0 0.1 0.01 Sa/Sb, pale fibr <br />
6 I 11.9 P1/G1 1.8 1.2 0.01 Sa/Sb fibr , hyal<strong>in</strong><br />
7 I 12.5 P2/G2 1.7 1.2 0.03 Sa/Sb fibr , hyal<strong>in</strong><br />
8 IIA 11.7 P1/G2 2.0 0 0 Sa/Sb fibr ()<br />
9 IIA 11.9 P1/G2 2.5 0 0 Sa/Sb, degen fibr <br />
10 IIA 13.0 P1/G2 1.8 0 0 Sa/Sb, degen fibr , hyal<strong>in</strong><br />
11 IIB 11.8 P2/G2 3.9 0 0 Sa, pale, degen fibr , hyal<strong>in</strong><br />
12 IIB 13.7 P1/G2 3.4 0 0 pale, degen fibr <br />
13 IIB 14.0 P2/G2 3.2 0 0 pale, degen fibr , hyal<strong>in</strong><br />
14 IIB 14.0 P3/G4 3.1 0 0 pale, degen, hyal<strong>in</strong> fibr , hyal<strong>in</strong><br />
<strong>The</strong> patients are divided <strong>in</strong>to two groups accord<strong>in</strong>g to presence or absence <strong>of</strong> spermatogonia. Group II is divided <strong>in</strong>to subgroups A and B<br />
accord<strong>in</strong>g to presence or absence <strong>of</strong> hypergonadotropic hypogonadism (see Table 2). Puberty staged accord<strong>in</strong>g to Tanner (8). Ap and Ad<br />
spermatogonia counts per cross-section <strong>of</strong> sem<strong>in</strong>iferous tubule. Sertoli cells staged as Sa, Sb, pale, and degenerat<strong>in</strong>g. <strong>The</strong> degree <strong>of</strong> Leydig cell<br />
hyperplasia staged to . <strong>The</strong> degree <strong>of</strong> fibrosis <strong>of</strong> the <strong>in</strong>terstitium are staged to and presence <strong>of</strong> hyal<strong>in</strong>ization is marked hyal<strong>in</strong>.<br />
TABLE 2. Laboratory parameters <strong>of</strong> 14 boys with KS at the time <strong>of</strong> testicular biopsy<br />
Patient no. Group no.<br />
FSH<br />
(IU/liter)<br />
S-LH<br />
(IU/liter)<br />
Testosterone<br />
(nmol/liter)<br />
<strong>in</strong>hib<strong>in</strong> B<br />
(pg/ml)<br />
AMH<br />
(pmol/liter)<br />
1 I 0.1 0.1 0.3 103 503<br />
2 I 1.0 0.2 0.3 78 758<br />
3 I 1.5 0.1 0.3 66 345<br />
4 I 1.9 0.4 0.3 127 606<br />
5 I 1.0 0.3 0.8 68 1156<br />
6 I 1.5 0.5 0.8 75 803<br />
7 I 1.1 0.5 1.1 69 1062<br />
8 IIA 1.3 0.5 0.7 301 2658<br />
9 IIA 0.5 0.2 0.3 166 1251<br />
10 IIA 0.7 0.1 0.5 97 878<br />
11 IIB 7.5 1.2 2.3 15.6 81<br />
12 IIB 17.9 6.9 3.9 29 101<br />
13 IIB 33.2 9.7 15.7 15.6 96<br />
14 IIB 38.6 11.4 10.2 15.6 16<br />
Patients are divided <strong>in</strong>to two groups accord<strong>in</strong>g to presence or absence <strong>of</strong> spermatogonia (see Table 1). Group II is divided <strong>in</strong>to subgroups A<br />
and B accord<strong>in</strong>g to presence or absence <strong>of</strong> hypergonadotropic hypogonadism.<br />
An open-knife testicular biopsy was taken under general anesthesia<br />
from each subject. <strong>The</strong> major portion <strong>of</strong> the specimen was cryopreserved<br />
for possible further use <strong>in</strong> ICSI <strong>in</strong> adulthood (see below). A piece was<br />
fixed <strong>in</strong> glutaraldehyde and then further subdivided and embedded <strong>in</strong><br />
Epon, sectioned at 1.0 m, and sta<strong>in</strong>ed with toluid<strong>in</strong>e blue. Histomorphometric<br />
analysis was performed by light microscopy at a total magnification<br />
<strong>of</strong> 400. <strong>The</strong> Leydig cells were morphologically classed as<br />
fetal, juvenile, or adult types by the follow<strong>in</strong>g criteria: Leydig cells were<br />
regarded as fetal if they had an extr<strong>in</strong>sically located large nucleus with<br />
two or more nucleoli, juvenile if they had an irregular nucleus and dark<br />
cytoplasm, and adult if they were large cells with a round nucleus and<br />
a cytoplasm conta<strong>in</strong><strong>in</strong>g crystalloid and lipid droplets. <strong>The</strong> Sertoli cells<br />
were morphologically classed as Sa, Sb, and Sc types and were regarded<br />
as Sa type if they were round with scant cytoplasm and had a round<br />
nucleus, and Sb if they were oval and larger and had an irregular oval<br />
nucleus and cytoplasm with recognizable structures. <strong>The</strong>y were classi-
Wikström et al. Testicular Degeneration <strong>in</strong> Adolescent KS Boys J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab, May 2004, 89(5):2263–2270 2265<br />
fied as Sc or adult if they were large and had a nucleus display<strong>in</strong>g one<br />
or more deep <strong>in</strong>vag<strong>in</strong>ations (18, 19).<br />
For all specimens conta<strong>in</strong><strong>in</strong>g germ cells, germ cell counts (number <strong>of</strong><br />
adult type pale spermatogonia per sem<strong>in</strong>iferous tubule, Ap/tubule, and<br />
number <strong>of</strong> adult type dark spermatogonia, Ad/tubule) were calculated<br />
per cross-section <strong>of</strong> tubule. Spermatogonia were regarded as type A if<br />
they were <strong>of</strong> an irregular shape with a round nucleus. Furthermore, they<br />
were regarded as Ap type if the nucleus had one or two nucleoli and as<br />
Ad if the nucleus had one or two pale round areas (19). All tubules from<br />
an average <strong>of</strong> n<strong>in</strong>e sections (range 6–12) per biopsy specimen were<br />
studied. <strong>The</strong> average number <strong>of</strong> tubules studied per biopsy specimen<br />
was 130 (range 71–177).<br />
Germ cell numbers were quantitatively compared with those <strong>of</strong> available<br />
normal testicular biopsies. Eleven identically prepared testicular<br />
specimens <strong>of</strong> adolescent boys were analyzed (11 yr, n 5; 13 yr, n 4;<br />
15 yr, n 1; and 19 yr, n 1). Indications for these biopsies had been<br />
scrotal pa<strong>in</strong> (n 5), hydatid torsion (n 3), retractile testis (n 1), and<br />
paratesticular fibrosis (n 1); one specimen was taken postmortem<br />
(accidental death).<br />
For electron microscopy, one Epon-embedded specimen was sectioned<br />
at 50 nm with a Reichert E ultramicrotome (Reichert Jung, Vienna,<br />
Austria) and sta<strong>in</strong>ed with uranyl acetate and lead citrate. Observations<br />
were made with a JEOLJEM 1200 EX transmission electron microscope<br />
(JEOL, Tokyo, Japan).<br />
Cryopreservation <strong>of</strong> testicular tissue<br />
Testicular tissue was cut <strong>in</strong>to small pieces <strong>in</strong> <strong>in</strong> vitro fertilization-<br />
Universal medium (Medicult, Copenhagen, Denmark) and diluted<br />
slowly drop by drop with equal volume <strong>of</strong> freez<strong>in</strong>g medium (Irv<strong>in</strong>e<br />
Scientific, Santa Ana, CA). <strong>The</strong> samples were frozen <strong>in</strong> 0.5-ml straws by<br />
exposure <strong>of</strong> the straws first for 15 m<strong>in</strong> to 4 C, then 15 m<strong>in</strong> to 20 C,<br />
and for 45 m<strong>in</strong> <strong>in</strong> nitrogen vapor before plac<strong>in</strong>g them <strong>in</strong>to liquid nitrogen.<br />
Two to seven vials were created per patient.<br />
Statistical analyses<br />
Descriptive data are reported as medians and ranges or means. In<br />
those cases with no laboratory analyses at the time <strong>of</strong> testicular biopsy,<br />
values were <strong>in</strong>terpolated from data obta<strong>in</strong>ed before and after biopsy<br />
with the assumption that changes between the two time po<strong>in</strong>ts had been<br />
l<strong>in</strong>ear. <strong>The</strong> unpaired two-tailed Student’s t test was used for comparisons<br />
between groups; P 0.05 was considered significant.<br />
Results<br />
Results <strong>of</strong> histomorphometric analyses <strong>of</strong> the biopsy specimens,<br />
as well as the key characteristics <strong>of</strong> the 14 patients at<br />
the time <strong>of</strong> testicular biopsy are presented <strong>in</strong> Table 1. <strong>The</strong>se<br />
biopsies were obta<strong>in</strong>ed at a median age <strong>of</strong> 11.8 yr (range<br />
10.1–14.0). Representative specimens from five KS boys and<br />
one boy with a normal karyotype are shown <strong>in</strong> Fig. 1. <strong>The</strong><br />
subjects were divided <strong>in</strong>to two groups accord<strong>in</strong>g to the presence<br />
(group I) or absence (group II) <strong>of</strong> germ cells <strong>in</strong> the<br />
biopsies.<br />
Germ cells<br />
Spermatogonia <strong>of</strong> Ap type were found <strong>in</strong> seven <strong>of</strong> 14 and<br />
<strong>of</strong> Ad type <strong>in</strong> six <strong>of</strong> 14 biopsy specimens (Table 1). In the<br />
specimens with germ cells present, the average number <strong>of</strong> Ap<br />
spermatogonia per sem<strong>in</strong>iferous tubule was reduced; mean<br />
number <strong>of</strong> Ap spermatogonia was 0.77 (range 0.04–1.17), and<br />
average number <strong>of</strong> Ad spermatogonia per tubule was 0.01,<br />
whereas all normal controls had consistently more than 0.46<br />
(mean 1.5) Ad spermatogonia per tubule (P 0.001). No<br />
meiotically divid<strong>in</strong>g germ cells (spermatocytes) or postmeiotic<br />
spermatids appeared <strong>in</strong> any <strong>of</strong> the biopsy specimens <strong>of</strong><br />
the KS subjects. Furthermore, at the time <strong>of</strong> cryopreservation<br />
<strong>of</strong> testicular tissue, no spermatozoa were seen <strong>in</strong> any <strong>of</strong> the<br />
specimens. <strong>The</strong> parents and the older boys have received this<br />
<strong>in</strong>formation, and we have thoroughly discussed these results<br />
with them.<br />
Sertoli cells, Leydig cells, and <strong>in</strong>terstitial tissue<br />
In the biopsy specimens <strong>of</strong> patients 1–10, the Sertoli cells<br />
were <strong>of</strong> Sa and Sb type and exhibited relatively normal appearance<br />
(Table 1, and Figs. 1, A and B, and 2). However,<br />
marked degeneration <strong>of</strong> Sertoli cells was evident <strong>in</strong> patients<br />
11–14 (Table 1, Fig. 1, C and D). Boys 1–10 had Leydig cells<br />
<strong>of</strong> juvenile type that showed none or only moderate hyperplasia,<br />
whereas the older subjects 11–14 had huge hyperplastic<br />
Leydig cells (Table 1, Fig. 1, C and D). Group II could<br />
thus be subdivided <strong>in</strong>to two groups based on absence (group<br />
IIA) or presence (group IIB) <strong>of</strong> Sertoli cell degeneration and<br />
Leydig cell hyperplasia. Fibrosis and hyal<strong>in</strong>ization <strong>of</strong> the<br />
<strong>in</strong>terstitium and peritubular connective tissue were visible <strong>in</strong><br />
all groups; <strong>in</strong> addition, these signs <strong>of</strong> degeneration <strong>in</strong>creased<br />
with age (Table 1). Figure 1, A–D, show the differ<strong>in</strong>g degrees<br />
<strong>of</strong> the degeneration process. <strong>The</strong> degeneration was not uniformly<br />
detectable throughout the relatively small biopsy<br />
specimens, whereas we found with<strong>in</strong> the same biopsies areas<br />
with marked degeneration and areas with only moderate<br />
changes (Fig. 1E).<br />
Testicular morphology reflected <strong>in</strong> hormone levels<br />
Patients <strong>in</strong> group I (n 7) (spermatogonia present <strong>in</strong><br />
biopsy specimen) showed no signs <strong>of</strong> hypergonadotropic<br />
hypogonadism (Table 2). <strong>The</strong>re occurred, however, an overlap<br />
<strong>in</strong> serum FSH, LH, testosterone, <strong>in</strong>hib<strong>in</strong> B, and AMH<br />
levels with group II (no spermatogonia <strong>in</strong> the specimen).<br />
Subjects <strong>in</strong> group IIA (n 3) ma<strong>in</strong>ta<strong>in</strong>ed normal gonadotrop<strong>in</strong>,<br />
<strong>in</strong>hib<strong>in</strong> B, and AMH levels, whereas those <strong>in</strong> more<br />
advanced puberty (group IIB, n 4) had clear hypergonadotropism<br />
and low levels <strong>of</strong> circulat<strong>in</strong>g Sertoli cell markers,<br />
<strong>in</strong>hib<strong>in</strong> B, and AMH (Table 2). Testicular volume was therefore<br />
the only statistically significant variable that could fully<br />
differentiate between groups I and II (Fig. 3A). Although<br />
differences <strong>in</strong> FSH and testosterone levels were not statistically<br />
significant between these two groups, levels were<br />
higher <strong>in</strong> group II (Fig. 3A and Table 2). Furthermore, all<br />
subjects with FSH and LH concentrations above 7 IU/liter<br />
showed depletion <strong>of</strong> germ cells and clear degeneration <strong>of</strong><br />
Sertoli cells (i.e. f<strong>in</strong>d<strong>in</strong>gs consistent with group IIB) (Tables<br />
1 and 2).<br />
Longitud<strong>in</strong>al changes <strong>in</strong> serum hormone levels<br />
Serum <strong>in</strong>hib<strong>in</strong> B <strong>in</strong>creased <strong>in</strong> early puberty, but this <strong>in</strong>itial<br />
rise was followed by a rapid suppression accompanied by a<br />
simultaneous <strong>in</strong>crease <strong>in</strong> serum testosterone (Figs. 4 and 5).<br />
A strong, <strong>in</strong>verse nonl<strong>in</strong>ear correlation existed between serum<br />
<strong>in</strong>hib<strong>in</strong> B and testosterone levels (Fig. 4B).<br />
Dur<strong>in</strong>g prepuberty and early puberty, serum AMH levels<br />
were high, but with advanc<strong>in</strong>g puberty, AMH was suppressed<br />
simultaneously with <strong>in</strong>hib<strong>in</strong> B (Figs. 4 and 5). <strong>The</strong>re<br />
also existed a strong, <strong>in</strong>verse nonl<strong>in</strong>ear relationship between<br />
serum AMH and testosterone levels (Figs. 4 and 5). Before
2266 J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab, May 2004, 89(5):2263–2270 Wikström et al. Testicular Degeneration <strong>in</strong> Adolescent KS Boys<br />
FIG. 1. Testicular biopsies <strong>of</strong> five adolescent boys with KS from list <strong>in</strong> Table 1 and one normal boy. Sta<strong>in</strong>, Toluid<strong>in</strong>e blue. A, Patient 4, two<br />
types <strong>of</strong> sem<strong>in</strong>iferous tubules identifiable: those with no spermatogonia on the right and those with spermatogonia <strong>of</strong> adult pale type (Ap) on<br />
the left. Ad, Spermatogonia <strong>of</strong> adult dark type. Sertoli cells, Sa and Sb type; Leydig cells, juvenile type, some hyperplasia; <strong>in</strong>terstitium, <strong>in</strong>creased<br />
fibrosis (magnification, 400). B, Patient 8, no spermatogonia. Sertoli cells, Sa and Sb type; Leydig cells, juvenile type. Interstitial compartment<br />
appears normal (magnification, 400). C, Patient 12, no spermatogonia. Sertoli cells, Sa and Sb type, pale and degenerative. Interstitial<br />
compartment has <strong>in</strong>creased volume, hyperplastic Leydig cells, and some fibrosis (magnification, 400). D, Patient 14, sem<strong>in</strong>iferous tubules<br />
completely hyal<strong>in</strong>ized. Interstitial compartment has hyperplastic Leydig cells and extensive fibrosis (magnification, 400). E, Patient 7,<br />
centrally sem<strong>in</strong>iferous tubules with Ap and/or Ad spermatogonia. This area is surrounded by tubules <strong>in</strong> which the degeneration process is<br />
evident: tubules with pale degenerative Sertoli cells and small tubules with dark small apoptotic cells (magnification, 200). F, Normal control,<br />
age 11 yr, testicular biopsy taken at surgical exploration because <strong>of</strong> scrotal pa<strong>in</strong> (magnification, 200).
Wikström et al. Testicular Degeneration <strong>in</strong> Adolescent KS Boys J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab, May 2004, 89(5):2263–2270 2267<br />
FIG. 2. Patient 2, group I (Table 1). Electron micrograph <strong>of</strong> testicular<br />
biopsy <strong>of</strong> boy with KS at age 10.1 yr and Tanner stage P1G1. Undifferentiated<br />
Sertoli cells resembl<strong>in</strong>g Sa type with a round nucleus with<br />
a small nucleolus lack<strong>in</strong>g lamellar body and with crystalloids from<br />
Charcot-Bötscher. In the center, one degenerat<strong>in</strong>g Sertoli cell<br />
(magnification, 2500).<br />
testosterone had reached 2.5 nmol/liter, a marked drop <strong>in</strong><br />
serum AMH had already occurred (Fig. 4B).<br />
Discussion<br />
With the aid <strong>of</strong> modern <strong>in</strong>fertility treatment technologies<br />
such as ICSI, some men with KS may father children. However,<br />
<strong>in</strong> adulthood, when these treatments come <strong>in</strong>to consideration,<br />
the testes <strong>of</strong> most KS men are completely atrophied.<br />
In the current work we <strong>in</strong>vestigated whether<br />
adolescent patients with KS have germ cells and evaluated<br />
whether early puberty is the optimal period for retriev<strong>in</strong>g<br />
germ cells for further use <strong>in</strong> ICSI. Although this concept has<br />
ga<strong>in</strong>ed further actuality with the recent report <strong>of</strong> a successful<br />
extraction <strong>of</strong> sperm-conta<strong>in</strong><strong>in</strong>g tissue from a 15-yr-old boy<br />
with KS (20), it has not been previously <strong>in</strong>vestigated<br />
systematically.<br />
We found, surpris<strong>in</strong>gly, that <strong>in</strong> early adolescence as many<br />
as 50% <strong>of</strong> the boys with KS had germ cells <strong>in</strong> their testes and<br />
that the depletion <strong>of</strong> these cells accelerated at the onset <strong>of</strong><br />
puberty. This presence <strong>of</strong> germ cells dur<strong>in</strong>g peripuberty contrasts<br />
with results <strong>of</strong> a report by Müller et al. (5), <strong>in</strong> which no<br />
germ cells were detectable <strong>in</strong> KS boys beyond the age <strong>of</strong> 2 yr.<br />
A probable explanation is that all boys <strong>in</strong> Müller’s publication<br />
were cryptorchid, whereas none <strong>in</strong> our group had any<br />
history <strong>of</strong> testicular maldescendent. Cryptorchidism is<br />
known to cause marked decrease <strong>in</strong> germ cell numbers also<br />
<strong>in</strong> boys with a normal karyotype (21, 22).<br />
Ad spermatogonia that develop postnatally from fetal<br />
spermatogonia under gonadotrop<strong>in</strong> and testosterone stimulation<br />
are <strong>of</strong> fundamental importance for the development<br />
<strong>of</strong> male fertility (23). In the boys with KS, the fact that the<br />
number <strong>of</strong> these cells was markedly reduced <strong>in</strong>dicates a<br />
severely impaired fertility potential even <strong>in</strong> early puberty.<br />
Furthermore, we observed only type A spermatogonia <strong>in</strong> our<br />
boys with KS, which suggests an arrest <strong>in</strong> germ cell development<br />
at the stage <strong>of</strong> A spermatogonia. Normally, type A<br />
spermatogonia transform <strong>in</strong>to type B spermatogonia and<br />
further to the first primary spermatocytes at the age <strong>of</strong> 5 yr<br />
(18, 24). At present, whether this defect <strong>in</strong> spermatogenesis<br />
<strong>in</strong> the XXY testis is <strong>in</strong>tr<strong>in</strong>sic to germ cells or due to the<br />
<strong>in</strong>ability <strong>of</strong> the Sertoli cells to support normal germ cell<br />
development is unknown. A defect <strong>in</strong> Sertoli and germ cell<br />
communication <strong>in</strong> the differentiat<strong>in</strong>g XXY testis has been<br />
suggested (25).<br />
Activation <strong>of</strong> the hypothalamic pituitary testicular axis<br />
was associated with depletion <strong>of</strong> germ cells. A strong correlation<br />
appeared between an <strong>in</strong>creas<strong>in</strong>g testosterone level<br />
and suppression <strong>of</strong> the Sertoli cell markers <strong>in</strong>hib<strong>in</strong> B and<br />
AMH. It is possible that the molecular mechanisms <strong>in</strong>duced<br />
by the altered dosage <strong>of</strong> X-encoded genes <strong>in</strong> testicular cells<br />
may accelerate loss <strong>of</strong> germ cells. For example, the androgen<br />
receptor gene is located on the X chromosome (26).<br />
<strong>The</strong> testicular volume <strong>of</strong> KS boys is already below normal<br />
dur<strong>in</strong>g childhood (1.0–1.5 ml; normally 1.8 ml) (27, 28). Dur<strong>in</strong>g<br />
puberty their testes grow (11, 12), which was also observed<br />
<strong>in</strong> the current work (Figs. 3 and 5). In healthy boys,<br />
the proliferation <strong>of</strong> germ cells is predom<strong>in</strong>antly responsible<br />
for the pubertal growth <strong>of</strong> the testes (29, 30). Because we<br />
could detect no spermatogenesis beyond the development <strong>of</strong><br />
type A spermatogonia and the number <strong>of</strong> these cells was low,<br />
the pubertal testicular growth <strong>in</strong> KS boys was due almost<br />
solely to the proliferation <strong>of</strong> Sertoli cells and <strong>in</strong>terstitial cells.<br />
This might suggest that the immature Sertoli cells <strong>of</strong> boys<br />
with KS are respond<strong>in</strong>g to the pubertal <strong>in</strong>crease <strong>in</strong> FSH<br />
stimulation, as seen <strong>in</strong> boys with a normal karyotype. On the<br />
other hand, the prepubertal Sa and Sb cells were not capable<br />
<strong>of</strong> transform<strong>in</strong>g <strong>in</strong>to the adult Sc cell type, and the degeneration<br />
<strong>of</strong> Sertoli cells <strong>in</strong>creased markedly dur<strong>in</strong>g puberty. It<br />
is therefore tempt<strong>in</strong>g to hypothesize that the regression <strong>of</strong> the<br />
testes <strong>in</strong> KS <strong>in</strong>cludes Sertoli cell degeneration. Consistently,<br />
electron microscopy revealed degenerat<strong>in</strong>g Sertoli cells, a<br />
rare f<strong>in</strong>d<strong>in</strong>g <strong>in</strong> testes <strong>of</strong> healthy early pubertal boys.<br />
<strong>The</strong> concept <strong>of</strong> Sertoli cells <strong>in</strong> boys with KS regress<strong>in</strong>g after<br />
the <strong>in</strong>itial phase <strong>of</strong> Sertoli cell proliferation dur<strong>in</strong>g early<br />
puberty is <strong>in</strong> agreement with changes observed <strong>in</strong> serum<br />
levels <strong>of</strong> <strong>in</strong>hib<strong>in</strong> B (31). This glycoprote<strong>in</strong> is thought to reflect<br />
Sertoli cell function dur<strong>in</strong>g prepuberty and become germ cell<br />
dependent dur<strong>in</strong>g midpuberty (32). In our cohort <strong>of</strong> boys<br />
with KS, serum <strong>in</strong>hib<strong>in</strong> B levels dur<strong>in</strong>g prepuberty and early<br />
puberty were normal (33–35), and measurable <strong>in</strong>hib<strong>in</strong> B levels<br />
did not fully correlate with the presence <strong>of</strong> germ cells <strong>in</strong><br />
the testes. This suggests that dur<strong>in</strong>g early puberty, serum<br />
<strong>in</strong>hib<strong>in</strong> B levels <strong>in</strong> boys with KS reflect the <strong>in</strong>tegrity or number<br />
<strong>of</strong> Sertoli cells or both. A normal <strong>in</strong>hib<strong>in</strong> B level and a low<br />
testosterone level were also shown to be <strong>in</strong>consistent with the<br />
presence <strong>of</strong> spermatogonia (group IIA <strong>in</strong> Tables 1 and 2 and<br />
Fig. 4A).<br />
AMH or Müllerian-<strong>in</strong>hibit<strong>in</strong>g substance, a glycoprote<strong>in</strong><br />
dimer <strong>of</strong> the TGF family, is expressed <strong>in</strong> prepubertal but not<br />
adult Sertoli cells (36). Serum AMH levels rema<strong>in</strong> high
2268 J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab, May 2004, 89(5):2263–2270 Wikström et al. Testicular Degeneration <strong>in</strong> Adolescent KS Boys<br />
FIG. 3. A, Testicular volumes and serum FSH,<br />
testosterone, <strong>in</strong>hib<strong>in</strong> B, and AMH levels <strong>in</strong> 14<br />
boys with KS with spermatogonia present or<br />
absent <strong>in</strong> the biopsy specimen (n 7, both<br />
groups). Horizontal l<strong>in</strong>es, 10th, 25th, 50th,<br />
75th, and 90th percentiles, and extreme values<br />
are shown separately. B, Longitud<strong>in</strong>al changes<br />
<strong>in</strong> <strong>in</strong>dividual testis volumes. Black circles,<br />
group I, white circles, group II (see Table 1).<br />
FIG. 4. A, Longitud<strong>in</strong>al changes <strong>in</strong> <strong>in</strong>hib<strong>in</strong><br />
B, testosterone, and AMH concentrations<br />
<strong>in</strong> 14 boys with KS. B, Correlations between<br />
<strong>in</strong>hib<strong>in</strong> B and testosterone and AMH<br />
and testosterone. Dashed l<strong>in</strong>es, serum testosterone<br />
2.5 nmol/liter. Black circles,<br />
group I; white circles, group II (see Table 1).
Wikström et al. Testicular Degeneration <strong>in</strong> Adolescent KS Boys J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab, May 2004, 89(5):2263–2270 2269<br />
FIG. 5. Distributions <strong>of</strong> serum FSH,<br />
LH, testosterone, <strong>in</strong>hib<strong>in</strong> B, and AMH<br />
concentrations and testicular volume <strong>in</strong><br />
14 boys with KS followed up dur<strong>in</strong>g puberty.<br />
Tanner G stages. <strong>The</strong>re were<br />
22–32 observations at stage G1, 13–21<br />
observations at G2, 14–16 observations<br />
at G3, and five to six observations at G4.<br />
Horizontal l<strong>in</strong>es, 10th, 25th, 50th, 75th,<br />
and 90th percentiles, and extreme values<br />
are shown separately (white circles).<br />
throughout childhood and wane at puberty (37). We observed<br />
high AMH values <strong>in</strong> KS boys dur<strong>in</strong>g prepuberty and<br />
early puberty, followed by a decl<strong>in</strong>e as serum testosterone<br />
<strong>in</strong>creased: the tim<strong>in</strong>g and magnitude <strong>of</strong> this decrease was<br />
similar to that <strong>in</strong> normal boys (37, 38) and <strong>in</strong> agreement with<br />
the <strong>in</strong>verse correlation between serum AMH and testosterone<br />
dur<strong>in</strong>g normal puberty (38). It has been proposed that the<br />
dramatic suppression <strong>of</strong> AMH production requires meiotic<br />
entry <strong>in</strong> spermatogenesis (39). Rajpert-De Myets et al. (40) <strong>in</strong><br />
their 1999 study noted, however, that the switch <strong>in</strong> AMH<br />
expression occurred also <strong>in</strong> adolescent boys without germ<br />
cells. Our observations, be<strong>in</strong>g consistent with these f<strong>in</strong>d<strong>in</strong>gs,<br />
suggest that meiotic activity is unnecessary for down regulation<br />
<strong>of</strong> AMH expression (Table 2). <strong>The</strong> decrease <strong>in</strong> serum<br />
AMH levels thus cannot serve as an <strong>in</strong>dicator <strong>of</strong> spermatogenetic<br />
activity <strong>in</strong> KS boys because the biopsy specimens <strong>of</strong><br />
the boys with low AMH values showed no spermatocytes<br />
(group IIB, Tables 1 and 2).<br />
We obta<strong>in</strong>ed only a s<strong>in</strong>gle biopsy from each subject, but<br />
even <strong>in</strong> these very small specimens, we could demonstrate<br />
the focal nature <strong>of</strong> the sem<strong>in</strong>iferous epithelium degeneration<br />
(Fig. 1E), perhaps expla<strong>in</strong><strong>in</strong>g the fact that some adult men<br />
with KS display areas <strong>of</strong> spermatogenesis. It is possible that<br />
<strong>in</strong> our work such areas or their predecessors may have escaped<br />
detection. In adult subjects with KS, the success rate<br />
for obta<strong>in</strong><strong>in</strong>g spermatozoa with sperm-conta<strong>in</strong><strong>in</strong>g tissue is<br />
currently at least 50% (41), but multiple testicular biopsies are<br />
always required for successful sperm recovery (42). We<br />
therefore hypothesize that if several biopsies had been performed,<br />
more germ cells would have been found <strong>in</strong> our<br />
subjects. <strong>The</strong> diagnosis <strong>of</strong> <strong>in</strong>fertility <strong>in</strong> KS boys cannot be<br />
made on the basis <strong>of</strong> only one biopsy. <strong>The</strong>se issues were<br />
thoroughly discussed with the boys and their parents.<br />
Only a m<strong>in</strong>ority <strong>of</strong> subjects with KS is diagnosed before<br />
puberty (2). Later the condition may come to attention dur<strong>in</strong>g<br />
evaluation <strong>of</strong> hypogonadism and <strong>in</strong>fertility. In the current<br />
work, all boys were diagnosed prepubertally, and 13 <strong>of</strong> 14<br />
patients <strong>in</strong>itially presented with language and behavioral<br />
problems. We cannot formally exclude the possibility that<br />
these boys differ from other KS subjects <strong>in</strong> terms <strong>of</strong> fertility<br />
prognosis. However, to our knowledge there is no evidence<br />
<strong>in</strong> the literature <strong>in</strong>dicat<strong>in</strong>g that early neurological problems<br />
<strong>in</strong> KS are related to testicular function.<br />
<strong>The</strong> possible future use <strong>of</strong> the cryopreserved testicular<br />
samples <strong>of</strong> KS patients <strong>in</strong> <strong>in</strong>fertility treatments most probably<br />
requires <strong>in</strong> vitro maturation <strong>of</strong> spermatogonia <strong>in</strong>to mature<br />
spermatozoa or at least <strong>in</strong>to late/elongated spermatids. Recent<br />
studies (43, 44) <strong>in</strong>dicate that human testicular tissue can<br />
be cultured for at least up to 3 wk without essential loss <strong>of</strong><br />
spermatogonia. Early results also suggest that meiosis and<br />
spermatogenesis may resume under culture conditions,<br />
yield<strong>in</strong>g normal spermatids with some fertiliz<strong>in</strong>g potential<br />
(44).<br />
In conclusion, we <strong>in</strong>vestigated whether early adolescence<br />
is a suitable time period <strong>in</strong> life for obta<strong>in</strong><strong>in</strong>g germ cells for<br />
future <strong>in</strong>fertility treatment <strong>in</strong> subjects with KS. Our results<br />
show that early adolescent boys with KS have testicular germ<br />
cells that display a maturational arrest at the level <strong>of</strong> type A<br />
spermatogonia. No meiotic cells were detected <strong>in</strong> any <strong>of</strong> the<br />
biopsy specimens, and onset <strong>of</strong> puberty was associated with<br />
depletion <strong>of</strong> spermatogonia. Based on these results, it seems<br />
that early puberty does not provide an unique w<strong>in</strong>dow <strong>of</strong><br />
opportunity to <strong>in</strong>crease fertility potential <strong>of</strong> subjects with KS.<br />
Future research is thus required to elucidate the mechanisms<br />
activated at puberty that ultimately lead to hypogonadism<br />
characteristic for the syndrome.<br />
Acknowledgments<br />
Received October 3, 2003. Accepted February 10, 2004.<br />
Address all correspondence and requests for repr<strong>in</strong>ts to: Leo Dunkel,<br />
Hospital for Children and Adolescents, University <strong>of</strong> Hels<strong>in</strong>ki, P.O. Box<br />
281, 00029 Hels<strong>in</strong>ki, F<strong>in</strong>land. E-mail: leo.dunkel@hus.fi.<br />
This work was supported by grants from the Medical Society <strong>of</strong><br />
F<strong>in</strong>land (F<strong>in</strong>ska Läkaresällskapet) (to A.M.W.), the Mjölbolsta Founda-
2270 J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab, May 2004, 89(5):2263–2270 Wikström et al. Testicular Degeneration <strong>in</strong> Adolescent KS Boys<br />
tion (to A.M.W.), the Foundation for Pediatric Research (to T.R.), and<br />
Hels<strong>in</strong>ki University Central Hospital.<br />
References<br />
1. <strong>Kl<strong>in</strong>efelter</strong> HF, Reifenste<strong>in</strong> EC, Albright F 1942 <strong>Syndrome</strong> characterized by<br />
gynecomastia, aspermatogenesis without a-Leydigism, and <strong>in</strong>creased excretion<br />
<strong>of</strong> follicle-stimulat<strong>in</strong>g hormone. J Cl<strong>in</strong> Endocr<strong>in</strong>ol 2:615–627<br />
2. Bojesen A, Juul S, Gravholt CH 2003 Prenatal and postnatal prevalence <strong>of</strong><br />
<strong>Kl<strong>in</strong>efelter</strong> syndrome: a national registry study. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 88:<br />
622–626<br />
3. Van Assche E, Bonduelle M, Tournaye H, Joris H, Verheyen G, Devroey P,<br />
Van Steirteghem A, Liebaers I 1996 Cytogenetics <strong>of</strong> <strong>in</strong>fertile men. Hum<br />
Reprod 11(Suppl 4):1–24; discussion 25–26<br />
4. Mikamo K, Aguercif M, Hazeghi P, Mart<strong>in</strong>-Du Pan R 1968 Chromat<strong>in</strong>positive<br />
<strong>Kl<strong>in</strong>efelter</strong>’s syndrome. A quantitative analysis <strong>of</strong> spermatogonial<br />
deficiency at 3, 4, and 12 months <strong>of</strong> age. Fertil Steril 19:731–739<br />
5. Muller J, Skakkebaek NE, Ratcliffe SG 1995 Quantified testicular histology<br />
<strong>in</strong> boys with sex chromosome abnormalities. Int J Androl 18:57–62<br />
6. Ferguson-Smith MA 1959 <strong>The</strong> prepubertal testicular lesion <strong>in</strong> chromat<strong>in</strong>positive<br />
<strong>Kl<strong>in</strong>efelter</strong>’s syndrome (primary micro-orchidism) as seen <strong>in</strong> mentally<br />
handicapped children. Lancet i:219–222<br />
7. Tachdjian G, Frydman N, Morichon-Delvallez N, Du AL, Fanch<strong>in</strong> R, Vekemans<br />
M, Frydman R 2003 Reproductive genetic counsell<strong>in</strong>g <strong>in</strong> non-mosaic<br />
47,XXY patients: implications for preimplantation or prenatal diagnosis: case<br />
report and review. Hum Reprod 18:271–275<br />
8. Tanner JM 1962 Growth at adolescence. 2nd ed. Oxford, UK: Blackwell<br />
9. Nielsen CT, Skakkebaek NE, Richardson DW, Darl<strong>in</strong>g JA, Hunter WM,<br />
Jorgensen M, Nielsen A, Ingerslev O, Keid<strong>in</strong>g N, Muller J 1986 Onset <strong>of</strong> the<br />
release <strong>of</strong> spermatozoa (spermarche) <strong>in</strong> boys <strong>in</strong> relation to age, testicular<br />
growth, pubic hair, and height. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 62:532–535<br />
10. Hirsch M, Lunenfeld B, Modan M, Ovadia J, Shemesh J 1985 Spermarche—<br />
the age <strong>of</strong> onset <strong>of</strong> sperm emission. J Adolesc Health Care 6:35–39<br />
11. Topper E, Dickerman Z, Prager-Lew<strong>in</strong> R, Kaufman H, Maimon Z, Laron Z<br />
1982 Puberty <strong>in</strong> 24 patients with <strong>Kl<strong>in</strong>efelter</strong> syndrome. Eur J Pediatr 139:8–12<br />
12. Salbenblatt JA, Bender BG, Puck MH, Rob<strong>in</strong>son A, Faiman C, W<strong>in</strong>ter JS 1985<br />
Pituitary-gonadal function <strong>in</strong> <strong>Kl<strong>in</strong>efelter</strong> syndrome before and dur<strong>in</strong>g puberty.<br />
Pediatr Res 19:82–86<br />
13. Hansen PF, With TK 1952 Cl<strong>in</strong>ical measurements <strong>of</strong> testes <strong>in</strong> boys and men.<br />
Acta Med Scand Suppl 206:457–465<br />
14. Greulich WW, Pyle SL 1959 Atlas <strong>of</strong> skeletal development <strong>of</strong> the hand and<br />
wrist. 2nd ed. Stanford, CA: Stanford University Press<br />
15. Dunkel L, Alfthan H, Stenman UH, Perheentupa J 1990 Gonadal control <strong>of</strong><br />
pulsatile secretion <strong>of</strong> lute<strong>in</strong>iz<strong>in</strong>g hormone and follicle-stimulat<strong>in</strong>g hormone <strong>in</strong><br />
prepubertal boys evaluated by ultrasensitive time-resolved immun<strong>of</strong>luorometric<br />
assays. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 70:107–114<br />
16. Apter D, Janne O, Karvonen P, Vihko R 1976 Simultaneous determ<strong>in</strong>ation <strong>of</strong><br />
five sex hormones <strong>in</strong> human serum by radioimmunoassay after chromatography<br />
on Lipidex-5000. Cl<strong>in</strong> Chem 22:32–38<br />
17. Janne O, Apter D, Vihko R 1974 Assay <strong>of</strong> testosterone, progesterone and<br />
17-hydroxyprogesterone <strong>in</strong> human plasma by radioimmunoassay after separation<br />
on hydroxyalkoxypropyl sephadex. J Steroid Biochem 5:155–162<br />
18. Seguchi H, Hadziselimovic F 1974 Ultramikroskopische untersuchungen am<br />
tubulus sem<strong>in</strong>iferus bei k<strong>in</strong>dern von der geburt bis zur pubertät. I spermatogonienentwicklung.<br />
Verh Anat Ges 68:133–148<br />
19. Hadziselimovic F, Herzog B 1990 Hodenerkrankungen im k<strong>in</strong>desalter. Stuttgart,<br />
Germany: Hippokrates Verlag<br />
20. Damani MN, Mittal R, Oates RD 2001 Testicular tissue extraction <strong>in</strong> a young<br />
male with 47,XXY <strong>Kl<strong>in</strong>efelter</strong>’s syndrome: potential strategy for preservation<br />
<strong>of</strong> fertility. Fertil Steril 76:1054–1056<br />
21. Hed<strong>in</strong>ger C 1971 Über den frühest erkennbarer hodenveränderungen beim<br />
kryptorchismus des kle<strong>in</strong>k<strong>in</strong>des. Verh Dtsch Ges Pathol 55:172–175<br />
22. Hadziselimovic F, Herzog B, Seguchi H 1975 Surgical correction <strong>of</strong> cryptorchism<br />
at 2 years: electron microscopic and morphometric <strong>in</strong>vestigations.<br />
J Pediatr Surg 10:19–26<br />
23. Hadziselimovic F, Herzog B 2001 <strong>The</strong> importance <strong>of</strong> both an early orchidopexy<br />
and germ cell maturation for fertility. Lancet 358:1156–1157<br />
24. Nistal M, Paniagua R 1984 Occurrence <strong>of</strong> primary spermatocytes <strong>in</strong> the <strong>in</strong>fant<br />
and child testis. Andrologia 16:532–536<br />
25. Hunt PA, Worthman C, Lev<strong>in</strong>son H, Stall<strong>in</strong>gs J, LeMaire R, Mroz K, Park<br />
C, Handel MA 1998 Germ cell loss <strong>in</strong> the XXY male mouse: altered X-chromosome<br />
dosage affects prenatal development. Mol Reprod Dev 49:101–111<br />
26. Quigley CA, De Bellis A, Marschke KB, el-Awady MK, Wilson EM, French<br />
FS 1995 Androgen receptor defects: historical, cl<strong>in</strong>ical, and molecular perspectives.<br />
Endocr Rev 16:271–321<br />
27. Laron Z, Hochman IH 1971 Small testes <strong>in</strong> prepubetal boys with <strong>Kl<strong>in</strong>efelter</strong>’s<br />
syndrome. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 32:671–672<br />
28. Rob<strong>in</strong>son A, Bender BG, Borelli JB, Puck MH, Salbenblatt JA, W<strong>in</strong>ter JS 1986<br />
Sex chromosomal aneuploidy: prospective and longitud<strong>in</strong>al studies. Birth<br />
Defects Orig Artic Ser 22:23–71<br />
29. Cortes D, Muller J, Skakkebaek NE 1987 Proliferation <strong>of</strong> Sertoli cells dur<strong>in</strong>g<br />
development <strong>of</strong> the human testis assessed by stereological methods. Int J<br />
Androl 10:589–596<br />
30. Muller J, Skakkebaek NE 1983 Quantification <strong>of</strong> germ cells and sem<strong>in</strong>iferous<br />
tubules by stereological exam<strong>in</strong>ation <strong>of</strong> testicles from 50 boys who suffered<br />
from sudden death. Int J Androl 6:143–156<br />
31. Christiansen P, Andersson AM, Skakkebaek NE 2003 Longitud<strong>in</strong>al studies<br />
<strong>of</strong> <strong>in</strong>hib<strong>in</strong> B levels <strong>in</strong> boys and young adults with <strong>Kl<strong>in</strong>efelter</strong> syndrome. J Cl<strong>in</strong><br />
Endocr<strong>in</strong>ol Metab 88:888–891<br />
32. Andersson AM, Muller J, Skakkebaek NE 1998 Different roles <strong>of</strong> prepubertal<br />
and postpubertal germ cells and Sertoli cells <strong>in</strong> the regulation <strong>of</strong> serum <strong>in</strong>hib<strong>in</strong><br />
B levels. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 83:4451–4458<br />
33. Raivio T, Perheentupa A, McNeilly AS, Groome NP, Anttila R, Siimes MA,<br />
Dunkel L 1998 Biphasic <strong>in</strong>crease <strong>in</strong> serum <strong>in</strong>hib<strong>in</strong> B dur<strong>in</strong>g puberty: a longitud<strong>in</strong>al<br />
study <strong>of</strong> healthy F<strong>in</strong>nish boys. Pediatr Res 44:552–556<br />
34. Andersson AM, Juul A, Petersen JH, Muller J, Groome NP, Skakkebaek NE<br />
1997 Serum <strong>in</strong>hib<strong>in</strong> B <strong>in</strong> healthy pubertal and adolescent boys: relation to age,<br />
stage <strong>of</strong> puberty, and follicle-stimulat<strong>in</strong>g hormone, lute<strong>in</strong>iz<strong>in</strong>g hormone, testosterone,<br />
and estradiol levels. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 82:3976–3981<br />
35. Cr<strong>of</strong>ton PM, Evans AE, Groome NP, Taylor MR, Holland CV, Kelnar CJ 2002<br />
Inhib<strong>in</strong> B <strong>in</strong> boys from birth to adulthood: relationship with age, pubertal stage,<br />
FSH and testosterone. Cl<strong>in</strong> Endocr<strong>in</strong>ol (Oxf) 56:215–221<br />
36. Lee MM, Donahoe PK 1993 Mullerian <strong>in</strong>hibit<strong>in</strong>g substance: a gonadal hormone<br />
with multiple functions. Endocr Rev 14:152–164<br />
37. Lee MM, Donahoe PK, Hasegawa T, Silverman B, Crist GB, Best S, Hasegawa<br />
Y, Noto RA, Schoenfeld D, MacLaughl<strong>in</strong> DT 1996 Mullerian <strong>in</strong>hibit<strong>in</strong>g<br />
substance <strong>in</strong> humans: normal levels from <strong>in</strong>fancy to adulthood. J Cl<strong>in</strong> Endocr<strong>in</strong>ol<br />
Metab 81:571–576<br />
38. Rey R, Lordereau-Richard I, Carel JC, Barbet P, Cate RL, Roger M, Chaussa<strong>in</strong><br />
JL, Josso N 1993 Anti-Mullerian hormone and testosterone serum levels are<br />
<strong>in</strong>versely dur<strong>in</strong>g normal and precocious pubertal development. J Cl<strong>in</strong> Endocr<strong>in</strong>ol<br />
Metab 77:1220–1226<br />
39. Al-Attar L, Noel K, Dutertre M, Belville C, Forest MG, Burgoyne PS, Josso<br />
N, Rey R 1997 Hormonal and cellular regulation <strong>of</strong> Sertoli cell anti-Mullerian<br />
hormone production <strong>in</strong> the postnatal mouse. J Cl<strong>in</strong> Invest 100:1335–1343<br />
40. Rajpert-De Meyts E, Jorgensen N, Graem N, Muller J, Cate RL, Skakkebaek<br />
NE 1999 Expression <strong>of</strong> anti-Mullerian hormone dur<strong>in</strong>g normal and pathological<br />
gonadal development: association with differentiation <strong>of</strong> Sertoli and granulosa<br />
cells. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 84:3836–3844<br />
41. Ron-El R, Raziel A, Strassburger D, Schachter M, Bern O, Friedler S 2000<br />
Birth <strong>of</strong> healthy male tw<strong>in</strong>s after <strong>in</strong>tracytoplasmic sperm <strong>in</strong>jection <strong>of</strong> frozenthawed<br />
testicular spermatozoa from a patient with nonmosaic <strong>Kl<strong>in</strong>efelter</strong><br />
syndrome. Fertil Steril 74:832–833<br />
42. Tournaye H, Staessen C, Liebaers I, Van Assche E, Devroey P, Bonduelle M,<br />
Van Steirteghem A 1996 Testicular sperm recovery <strong>in</strong> n<strong>in</strong>e 47,XXY <strong>Kl<strong>in</strong>efelter</strong><br />
patients. Hum Reprod 11:1644–1649<br />
43. Larsen HP, Thorup J, Skovgaard LT, Cortes D, Byskov AG 2002 Long-term<br />
cultures <strong>of</strong> testicular biopsies from boys with cryptorchidism: effect <strong>of</strong> FSH and<br />
LH on the number <strong>of</strong> germ cells. Hum Reprod 17:383–389<br />
44. Sousa M, Cremades N, Alves C, Silva J, Barros A 2002 Developmental potential<br />
<strong>of</strong> human spermatogenic cells cocultured with Sertoli cells. Hum Reprod<br />
17:161–172<br />
JCEM is published monthly by <strong>The</strong> Endocr<strong>in</strong>e Society (http://www.endo-society.org), the foremost pr<strong>of</strong>essional society serv<strong>in</strong>g the<br />
endocr<strong>in</strong>e community.