Pollicization of the Index Finger
Pollicization of the Index Finger
Pollicization of the Index Finger
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
~s recorded a<br />
it.<br />
that <strong>the</strong>y have<br />
~o comments in<br />
~ne tumors in <strong>the</strong><br />
pie reported a car<br />
chondroblastoma<br />
¯ In my series <strong>of</strong><br />
¯ pal involvement.<br />
ladelphia. J. B. Lip<br />
: Surg., 35-A: S88-893~)<br />
Flynn, pp. 1027-103<br />
as, 1957.<br />
¯ 43-A: 861-864, Se<br />
:!roma <strong>of</strong> Bone. Arch.<br />
nts. pp. 169-195.<br />
s and Feet. Radiology~ ;’<br />
. A Case Report. Bull.<br />
9-148, 1937.<br />
scano, 1957.<br />
v <strong>of</strong> 110 Cases. J.<br />
AND JOINT SURGERY<br />
<strong>Pollicization</strong> <strong>of</strong> <strong>the</strong> <strong>Index</strong> <strong>Finger</strong><br />
METHOD ~’: AND RESULTS IN APLASIA AND HYPOPLASIA OF THE THUMB<br />
BY DIETER BUCK-GRAMCKO, M.D.’~, HAMBURG. GERMANY<br />
From <strong>the</strong> Department <strong>of</strong> Hand Surgery and Plastic Surgery,<br />
Berufsgenossenschaftliches Unfallkrankenhaus Hamburg<br />
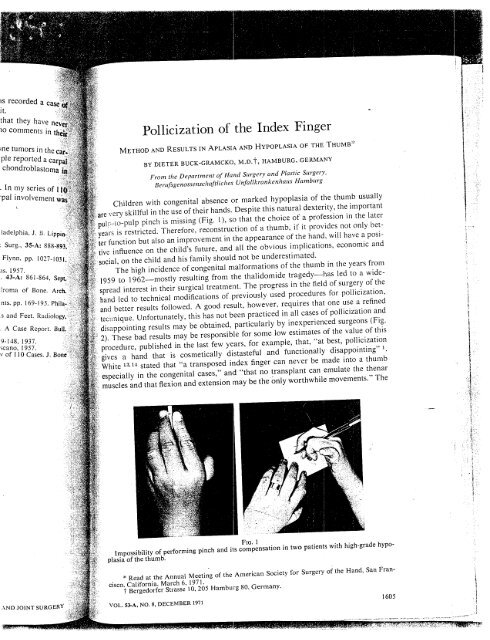
Children with congenital absence or marked hypoplasia <strong>of</strong> <strong>the</strong> thumb usually<br />
skillful in <strong>the</strong> use <strong>of</strong> <strong>the</strong>ir hands. Despite this natural dexterity, <strong>the</strong> important<br />
pul?
1606 DIETER BUCK-GRAMCKo<br />
FIG.<br />
Figs. :~ 2-A and 2-B: Disappointing result <strong>of</strong> a trial to pollicise <strong>the</strong> index finger performed else~<br />
where. An osteotomy <strong>of</strong> <strong>the</strong> metacarpal and resection <strong>of</strong> <strong>the</strong> proximal interphal~ngeal joints was<br />
done, but <strong>the</strong> essential features <strong>of</strong> shortening muscle stabilization, and adequate rotation were<br />
lacking. ,<br />
results presented in this paper show that <strong>the</strong>se statements are not correct if small but<br />
important details <strong>of</strong> technique are observed.<br />
The technique <strong>of</strong> pollicization in congenital cases is based on <strong>the</strong> procedure:<br />
evolved for <strong>the</strong> reconstruction <strong>of</strong> <strong>the</strong> thumb in traumatic amputations. From <strong>the</strong> fas<br />
cinating literature concerning this problem, I would emphasize <strong>the</strong> contributions in<br />
operative technique by Gosset, Hilgenfeldt, and Littler 10,11, who developed<br />
fundamental principles for pollicization in cases <strong>of</strong> aplasia and hypoplasia <strong>of</strong> <strong>the</strong><br />
thumb. O<strong>the</strong>r authors such as Harrison z, s and Riordan 12 also have made important<br />
contributions. ’<br />
From 1959 to <strong>the</strong> present I have performed 114 pollicization operations, and<br />
<strong>of</strong> this number 100 were in congenital cases. The experience with this large number<br />
<strong>of</strong> pollicizations has led to modifications in <strong>the</strong> operative technique with improvement<br />
<strong>of</strong> <strong>the</strong> results z,3,4. Twenty-one <strong>of</strong> <strong>the</strong> seventy-three patients had unilateral<br />
problems, with normal contralateral upper extremities. In sixteen <strong>the</strong>re were ot<br />
THE JOURNAL OF BONE AND JOINT suRGERY<br />
(Fig.<br />
vide!
performed<br />
mgeal joints was<br />
.re rotation<br />
.~ct if small<br />
<strong>the</strong><br />
From <strong>the</strong><br />
retributions in<br />
developed<br />
oplasia <strong>of</strong><br />
ade important<br />
perations, and<br />
large number<br />
~vith improvehad<br />
unilateral<br />
~re were o<strong>the</strong>r<br />
JOINT sURGERy<br />
POLLICIZATION OF THE INDEX FINGER<br />
1607<br />
lformations <strong>of</strong> <strong>the</strong> o<strong>the</strong>r hand which did not require pollicizations with <strong>the</strong> excep<strong>of</strong><br />
nine in whom <strong>the</strong> procedure will soon be done. This leaves twenty-seven pa-<br />
..nts who had <strong>the</strong> procedure done bilaterally.<br />
Twelve <strong>of</strong> <strong>the</strong> patients who had pollicization also had a radial club hand on <strong>the</strong><br />
~ide operated on, and six <strong>of</strong> <strong>the</strong>m had <strong>the</strong> condition bilaterally; but I did not pollicize<br />
<strong>the</strong> index finger in any patient with bilateral involvement. However, I did perform<br />
a centralization procedure on <strong>the</strong> contra[ateral hand in two <strong>of</strong> <strong>the</strong> six patients<br />
ith bilateral involvement. In this procedure <strong>the</strong> hand was centralized over <strong>the</strong> end<br />
’ <strong>the</strong> ulna.<br />
Theoretical Concepts<br />
In creating a new thumb from <strong>the</strong> index finger with stability and optimum posi-<br />
.tion. <strong>the</strong> reduction <strong>of</strong> <strong>the</strong> length <strong>of</strong> <strong>the</strong> bones is important. For attaining <strong>the</strong> same<br />
nun:L)er <strong>of</strong> bones and joints as in a normal thumb a shortening <strong>of</strong> <strong>the</strong> over-all length<br />
<strong>of</strong> <strong>the</strong> ray is necessary: <strong>the</strong> second metacarpal is removed with <strong>the</strong> exception <strong>of</strong> its<br />
head which acts as <strong>the</strong> new trapezium. However, <strong>the</strong> metacarpal should not be allowed<br />
to continue to grow much; for this reason <strong>the</strong> epiphysis must be resected. The<br />
metacarpophalangeal joint will <strong>the</strong>n become <strong>the</strong> new carpometacarpal joint. The<br />
~roximal phalanx <strong>of</strong> <strong>the</strong> index will become <strong>the</strong> first metacarpal and <strong>the</strong> proximal interphalangeal<br />
joint <strong>the</strong> metacarpophalangeal joint <strong>of</strong> <strong>the</strong> new thumb, and so forth<br />
(Fig. 3).<br />
A rotation <strong>of</strong> <strong>the</strong> index finger on its longitudinal axis is also performed to provide<br />
proper axial alignment. Rotation <strong>of</strong> only 90 degrees, as is <strong>of</strong>ten done, will not<br />
giv.= good oppositio~.,:The result will be a type <strong>of</strong> key grip against <strong>the</strong> long finger.<br />
The index finger has to be initially rotated about 160 degrees during <strong>the</strong> operation<br />
so that it is opposite <strong>the</strong> pulp <strong>of</strong> <strong>the</strong> ring finger. This position changes somewhat<br />
during <strong>the</strong> suturing <strong>of</strong> <strong>the</strong> muscles and <strong>the</strong> skin, so that at <strong>the</strong> end <strong>of</strong> <strong>the</strong> operation<br />
<strong>the</strong>re is rotation <strong>of</strong> about 120 degrees.<br />
In addition to <strong>the</strong> shortening and rotation, an angulation <strong>of</strong> about 40 degrees <strong>of</strong><br />
palmar abduction should be obtained. In this way, <strong>the</strong> new thumb is <strong>the</strong>n well placed<br />
to later move in opposition as well as in adduction and-abduction-<br />
DIP<br />
Ext. ind.
1608 DIETER BUCK-GRAMCKO<br />
FIG. 4<br />
Photographs showing a long (left) and a short thumb (right) after pollicization <strong>of</strong> <strong>the</strong> index<br />
finger.<br />
Operative Technique<br />
For <strong>the</strong> pollicization operation <strong>the</strong>re are four basic principles <strong>of</strong> equal importance,<br />
relating to <strong>the</strong> following: (a) <strong>the</strong> neurovascular pedicle; (b) <strong>the</strong> skeletal<br />
readjustment with preservation <strong>of</strong> <strong>the</strong> metacarpophalangeal joint; (c) <strong>the</strong> muscular<br />
stabilization; (d) <strong>the</strong> skin incision.<br />
The first, <strong>the</strong> technique <strong>of</strong> fashioning <strong>the</strong> neurovascular pedicle, is now well<br />
known. The freeing-up <strong>of</strong> <strong>the</strong> neurovascular bundle between <strong>the</strong> index and <strong>the</strong> long<br />
finger is obtained by ligating <strong>the</strong> artery to <strong>the</strong> radial side <strong>of</strong> <strong>the</strong> long finger. The common<br />
digital nerve is <strong>the</strong>n carefully separated into its component parts for <strong>the</strong> two<br />
adjacent fingers. This ensures that no tension will be present after <strong>the</strong> index finger is<br />
rotated. Sometimes an anomalous neural ring is fot]nd around <strong>the</strong> artery 5. This ring<br />
Fro. 5<br />
Roentgenogram <strong>of</strong> a hyperextension<br />
deformity with dorsal subluxation <strong>of</strong>-<strong>the</strong><br />
former metacarpophalangeal joint.<br />
(Fig. 4). The metacarpal head is fixed<br />
is split very carefully so that angulation <strong>of</strong> <strong>the</strong><br />
artery after transposition <strong>of</strong> <strong>the</strong> finger will<br />
not occur. The radial digital artery to <strong>the</strong> index<br />
finger is occasionally absent. In such<br />
cases it is possible to perform <strong>the</strong><br />
tion on a vascular pedicle <strong>of</strong> only one<br />
On <strong>the</strong> dorsal side at least one <strong>of</strong> <strong>the</strong> great<br />
veins must be preserved. ~.<br />
For skeletal fixation after bone readjustment,<br />
<strong>the</strong> length <strong>of</strong> <strong>the</strong> index finger is <strong>of</strong> considerable<br />
importance. If <strong>the</strong> phalanges are<br />
relatively short, <strong>the</strong> base <strong>of</strong> <strong>the</strong> metacarpal<br />
must be retained in order to obtain <strong>the</strong> right<br />
length <strong>of</strong> <strong>the</strong> new thumb. The metacarpal<br />
head is fixed to its base by means <strong>of</strong> one or<br />
two Kirschner wires. If <strong>the</strong> phalanges are<br />
normal length, <strong>the</strong> whole metacarpal is resected<br />
with <strong>the</strong> exception <strong>of</strong> its head. A<br />
short thumb is desirable , as it is functionally<br />
and es<strong>the</strong>tically better than a long one, which<br />
bears too close a resemblance to a finger<br />
by sutures to <strong>the</strong> joint capsule and <strong>the</strong> carpal<br />
THE JOURNAL OF BONE AND JOINT SURGERY<br />
Diagram <strong>of</strong> reduc<br />
<strong>the</strong> metacarpal head<br />
be,~es, which in ,.<br />
not essential. Fit:<br />
good function.<br />
The physiol~<br />
especially in <strong>the</strong><br />
my earlier cases /<br />
deformity is now<br />
so that its palma<br />
phalanx is broug<br />
head. The norma<br />
Sl~0n is possible.<br />
creased <strong>the</strong> stabil<br />
observed.<br />
For muscle<br />
trinsic mechanis~<br />
intrinsic muscles<br />
for <strong>the</strong> mobility,<br />
than mobility fo~<br />
necessary to sho~<br />
months to <strong>the</strong> sh:<br />
degree. One <strong>of</strong> t:.<br />
is severed at thc<br />
metacarpal resec<br />
first metacarpal)<br />
proprius tendon<br />
The ~ intero.<br />
<strong>of</strong> <strong>the</strong> thumb, q<br />
lateral bands <strong>of</strong><br />
partially strippc<br />
necessity.<br />
VOL. 53-A, NO. 8, D1
:ation <strong>of</strong> <strong>the</strong> ind,<br />
es <strong>of</strong> equal<br />
(b) <strong>the</strong> skeletal<br />
c) <strong>the</strong> muscular,<br />
:.le, is now well<br />
iex and <strong>the</strong> long(<br />
inger. The comz<br />
arts for <strong>the</strong> two<br />
e index finger<br />
tery 5. This rin<br />
mgulatic<br />
¯ <strong>the</strong> finger wil<br />
artery to <strong>the</strong> in’<br />
~bsent. In such<br />
,’n <strong>the</strong><br />
only one<br />
,ne <strong>of</strong> <strong>the</strong><br />
ljus<br />
finger is <strong>of</strong><br />
phalanges<br />
<strong>the</strong> metacarpal<br />
obtain <strong>the</strong> ri<br />
7he<br />
~eans <strong>of</strong> one<br />
halanges are<br />
~tacarpal is re-<br />
)f its he~id.<br />
:is functionally<br />
ong one, which<br />
Ice to a<br />
: and <strong>the</strong> carpal)<br />
POLLICIZATION OF THE INDEX FINGER<br />
1609<br />
Fta. 6<br />
Diagram <strong>of</strong> reduction, rotation, and angulation <strong>of</strong> <strong>the</strong> index finger: in <strong>the</strong> circle <strong>the</strong> turning <strong>of</strong><br />
<strong>the</strong> metacarpal head for prevention <strong>of</strong> <strong>the</strong> hyperextension deformity is shown.<br />
bones, which in young children can be pierced with a sharp needle. Bone union is<br />
not essential. Fibrous fixation <strong>of</strong> <strong>the</strong> head to its new surroundings is sufficient for<br />
good function.<br />
The physiologically wide range <strong>of</strong> movement <strong>of</strong> <strong>the</strong> metacarpophalangeal joint,<br />
~ecially in <strong>the</strong> child, was <strong>the</strong> reason that hyperextension deformity developed in<br />
my earlier cases (Fig. 5). It was more disturbing es<strong>the</strong>tically than functionally. This<br />
deformity is now prevented by turning <strong>the</strong> metacarpal head about 70 to 80 degrees<br />
so that its palmar side becomes proximal (Fig. 6)."In o<strong>the</strong>r words, <strong>the</strong> proximal<br />
~halanx is brought into a position <strong>of</strong> hyperextension in relation to <strong>the</strong> metacarpal<br />
head. The normal joint looseness is markedly reduced and hardly any fur<strong>the</strong>r extenis<br />
possible. This procedure, combined with <strong>the</strong> new muscle attachments has inicreased<br />
<strong>the</strong> stability <strong>of</strong> <strong>the</strong> thumb. No fur<strong>the</strong>r tendency to hyperexten~ion has been<br />
:i bbserved.<br />
For muscle stabilization, <strong>the</strong> adjustment <strong>of</strong> <strong>the</strong> extensor tendons and <strong>the</strong> inmechanism<br />
is one <strong>of</strong> <strong>the</strong> most important steps <strong>of</strong> <strong>the</strong> operation (Fig. 7). The<br />
muscles and <strong>the</strong> long extensor and flexor tendons are responsible not only<br />
for <strong>the</strong> mobility, but also for <strong>the</strong> stability <strong>of</strong> <strong>the</strong> digit. Stability is more important<br />
than mobility for good function <strong>of</strong> <strong>the</strong> thumb. Experience has shown that it is not<br />
to shorten <strong>the</strong> flexor tendons. They adapt <strong>the</strong>mselves in <strong>the</strong> course <strong>of</strong> a few<br />
months to <strong>the</strong> shortening <strong>of</strong> <strong>the</strong> ray and will <strong>the</strong>n flex <strong>the</strong> new thumb to <strong>the</strong> required<br />
’ee. One <strong>of</strong> <strong>the</strong> two extensor tendons, that <strong>of</strong> <strong>the</strong> extensor digitorum communis,<br />
is severed at <strong>the</strong> metacarpophalangeal level; its proximal end is sutured, after <strong>the</strong><br />
metacarpal resection, to <strong>the</strong> base <strong>of</strong> <strong>the</strong> former proximal phalanx (now acting as<br />
first metacarpal), to become <strong>the</strong> new abductor pollicis longus. The extensor indicis<br />
proprius tendon is shortened and <strong>the</strong>n resutured by end-to-end anastomosis.<br />
The interosseus muscles <strong>of</strong> <strong>the</strong> inde, x finger are also important for stabilization<br />
<strong>of</strong> <strong>the</strong> thumb. They should first be detached from <strong>the</strong> proximal phalanx and <strong>the</strong><br />
lateral bands <strong>of</strong> <strong>the</strong> dorsal apone-urosis. Their origins from <strong>the</strong> metacarpal bone are<br />
partially stripped subperiosteally. Careful preservation <strong>of</strong> nerves and vessels is a<br />
necessity.<br />
VOL. 53-A, NO. 8, DECEMBER 1971
1610 DIETER BUCK-GRAMCKO<br />
FtG. 7<br />
Diagram <strong>of</strong> <strong>the</strong> muscle stabilization by <strong>the</strong> two interossei resutured to <strong>the</strong> separated<br />
bands <strong>of</strong> <strong>the</strong> dorsal aponeurosis. The extensor communis tendon is fixed to <strong>the</strong> base <strong>of</strong> <strong>the</strong> new:¯<br />
metacarpal as an abductor polticis longus; <strong>the</strong> extensor indicis proprius tendon is shortened.<br />
After osteotomy and resection <strong>of</strong> <strong>the</strong> second metacarpal, <strong>the</strong> head <strong>of</strong> <strong>the</strong> second<br />
metacarpal must be set in <strong>the</strong> aforementioned position between <strong>the</strong> muscles in<br />
a way that <strong>the</strong>y hold <strong>the</strong> bone well. The stabilization <strong>of</strong> <strong>the</strong> ray will be ensured<br />
resuturing <strong>the</strong> tendinous insertions <strong>of</strong> <strong>the</strong> two interossei to <strong>the</strong> lateral bands <strong>of</strong> <strong>the</strong><br />
dorsal aponeurosis. These lateral slips will have been separated from <strong>the</strong> middle;<br />
band <strong>the</strong> entire length <strong>of</strong> <strong>the</strong> proximal phalanx. The slips are woven through<br />
distal parts <strong>of</strong> <strong>the</strong> muscles and turned back to form a loop. In this way, <strong>the</strong><br />
palmar interosseus will become an adductor pollicis, and <strong>the</strong> first dorsal<br />
an abductor brevis.<br />
The new way <strong>of</strong> attaching <strong>the</strong> muscles is accompanied by a fur<strong>the</strong>r change<br />
<strong>the</strong> skin incision. Previously, an S-shaped incision was made on <strong>the</strong> radial side<br />
<strong>the</strong> hand with an oval incision at <strong>the</strong> base <strong>of</strong> <strong>the</strong> index finger. Now, since <strong>the</strong><br />
terossei are reattached in <strong>the</strong> neighborhood <strong>of</strong> <strong>the</strong> proximal interphalangeal joint,<br />
additional dorsal longitudinal incision over <strong>the</strong> proximal phalanx is needed.<br />
<strong>the</strong> volume <strong>of</strong> <strong>the</strong> space comprising <strong>the</strong> proximal phalanx has been increased<br />
muscle and tendon transfers, direct closure is not possible. A dorsal skin flap<br />
to close this defect.<br />
In order to obtain this flap, <strong>the</strong> incision is made more palmarly than<br />
It also continues as far as <strong>the</strong> middle <strong>of</strong> <strong>the</strong> phalanx (Fig. 8). The distal end<br />
flap is excised.<br />
Follow-up<br />
Each patient was seen routinely during <strong>the</strong> first year after operation, and<br />
after at two years, four years, and six to eight years. Depending on <strong>the</strong> year in<br />
<strong>the</strong> operation was done, follow-up was as follows: twelve years, one patient;<br />
eight years, seven patients; four to six years, twenty patients; tWO to four<br />
twenty-five patients; one to two years, seven patients, and less than one year,<br />
patients. Many <strong>of</strong> <strong>the</strong> patients had bilateral involvement: this accounts for <strong>the</strong><br />
THE JOURNAL OF BONE AND JOINT<br />
ons (100).<br />
betwc<br />
The main<br />
on took<br />
tee weeks <strong>of</strong><br />
uld move ju~"<br />
dren gained th~<br />
:and some coul~<br />
<strong>the</strong> sixth to<br />
!<strong>the</strong> operation.<br />
There<br />
Diagram <strong>of</strong> <strong>the</strong><br />
facilitate<br />
VOL. 53-A NO. 8, D
ted lateral<br />
<strong>of</strong> <strong>the</strong> new<br />
.’ned.<br />
le second<br />
s in such<br />
~sured by<br />
ds <strong>of</strong> <strong>the</strong><br />
ough<br />
<strong>the</strong> first<br />
terosseus"::~:<br />
:hange in i<br />
~.1 side<br />
:e <strong>the</strong><br />
joint,<br />
ed. Since’::<br />
radially.<br />
ad <strong>of</strong> this<br />
in<br />
nt; six<br />
ur<br />
., thirteen<br />
r <strong>the</strong><br />
POLLICIZATION OF THE INDEX FINGER<br />
crepancy between <strong>the</strong> number <strong>of</strong> patients (seventy-three) and <strong>the</strong> number <strong>of</strong> pollicizations<br />
(100).<br />
Results<br />
1 61 1<br />
The main change in <strong>the</strong> range <strong>of</strong> motion and in <strong>the</strong> dexterity <strong>of</strong> <strong>the</strong> hand operated<br />
on took place during <strong>the</strong> first two years after <strong>the</strong> operation. At <strong>the</strong> end <strong>of</strong> <strong>the</strong><br />
three weeks <strong>of</strong> immobilization after operation, <strong>the</strong> joints <strong>of</strong> <strong>the</strong> pollicized index finger<br />
could move just a few degrees, usually; but in <strong>the</strong> next three to six weeks, all children<br />
gained <strong>the</strong> ability to perform pinch between <strong>the</strong> new thumb and <strong>the</strong> long finger,<br />
and some could even touch <strong>the</strong> thumb to <strong>the</strong> ring finger. Most children could do this<br />
by <strong>the</strong> sixth to eighth week, and could touch <strong>the</strong> little finger four to five months after<br />
<strong>the</strong> operation.<br />
There was no significant difference in <strong>the</strong> rate <strong>of</strong> improvement with different<br />
Fro. 8<br />
Diagram <strong>of</strong> <strong>the</strong> new incision (above) and suture line at <strong>the</strong> end <strong>of</strong> <strong>the</strong> operation (below).<br />
letters facilitate <strong>the</strong> orientation for shifting <strong>of</strong> <strong>the</strong> different skin flaps.<br />
VOL. 53-A, NO. 8, DECEMBER 1971
1612 DIETER BUCK-GRAMCKO<br />
ages, except for infants under <strong>the</strong> age <strong>of</strong> fifteen months, who could not cooperate to<br />
demonstrate pinch, but even <strong>the</strong>se infants were able to use <strong>the</strong> hand operated on in a<br />
natural way and were gripping objects between <strong>the</strong> new thumb and fingers or between<br />
<strong>the</strong> new thumb and <strong>the</strong> long finger. Active flexion <strong>of</strong> <strong>the</strong> pollicized finger sometimes<br />
began in <strong>the</strong> fourth week, but in <strong>the</strong> majority not before <strong>the</strong> third month. The<br />
motion increased slowly but steadily during <strong>the</strong> first year because <strong>of</strong> slow adaptive<br />
shortening <strong>of</strong> <strong>the</strong> flexor tendons, not shortened surgically.<br />
The motion and strength <strong>of</strong> radial abduction was <strong>the</strong> greatest variable in <strong>the</strong><br />
group <strong>of</strong> patients. They depended not only on <strong>the</strong> strength <strong>of</strong> <strong>the</strong> extensor muscle,<br />
and on <strong>the</strong> position <strong>of</strong> fixation <strong>of</strong> <strong>the</strong> metacarpal head relative to <strong>the</strong> remains <strong>of</strong> its<br />
base on <strong>the</strong> carpal bones, but also on <strong>the</strong> active use, and on <strong>the</strong> presence <strong>of</strong> o<strong>the</strong>r<br />
anomalies in <strong>the</strong> extremity. For instance, in <strong>the</strong> radial club hand, <strong>the</strong>re usually was<br />
little active motion in <strong>the</strong> interphalangeal joints <strong>of</strong> <strong>the</strong> index and long fingers, and.<br />
<strong>the</strong>refore, after pollicization, little motion existed in <strong>the</strong> former metacarpophalangeal<br />
joint and none in <strong>the</strong> interphalangeal joints. In this case, <strong>the</strong>refore, <strong>the</strong> digit had to<br />
be fixed in less radial abduction and act more as a post for <strong>the</strong> function <strong>of</strong> pinch.<br />
All <strong>of</strong> <strong>the</strong> children used <strong>the</strong>ir new thumbs naturally except those with radial<br />
club hand, who frequently used <strong>the</strong> side-to-side grip <strong>of</strong> ring and long fingers for<br />
smaller objects. One o<strong>the</strong>r exception was a child with a "five fingered" hand, who<br />
used this method for pinch preoperatively and continued to do so because <strong>of</strong> insufficient<br />
power in <strong>the</strong> intrinsic muscles. None <strong>of</strong> <strong>the</strong> new thumbs showed sensory or<br />
vascular deficiency with one exception a hand in which <strong>the</strong>re was anomalous absence<br />
<strong>of</strong> <strong>the</strong> pahnar arteries and postoperative thrombosis <strong>of</strong> <strong>the</strong> metacarpal artery<br />
with necrosis and subsequent loss <strong>of</strong> <strong>the</strong> thumb.<br />
It was necessary to add skin grafts in six operations, in three <strong>of</strong> which scars<br />
from previous operations were <strong>the</strong> reason. In <strong>the</strong> o<strong>the</strong>r three a small lull thickness<br />
graft was used from <strong>the</strong> excess skin on <strong>the</strong> dorsum <strong>of</strong> <strong>the</strong> finger. In <strong>the</strong>se <strong>the</strong> reason<br />
was retention <strong>of</strong> much <strong>of</strong> <strong>the</strong> second metacarpal because <strong>of</strong> <strong>the</strong> shortness <strong>of</strong> <strong>the</strong><br />
phalanges.<br />
The reattached intrinsic muscles were important for <strong>the</strong> appearance as well as<br />
for <strong>the</strong> function <strong>of</strong> <strong>the</strong> thumb. They gave to <strong>the</strong> transposed index finger <strong>the</strong> appearance<br />
<strong>of</strong> a thumb. They also produced a real <strong>the</strong>nar eminence, and, after a period<br />
<strong>of</strong> training, led to relatively normal mobility <strong>of</strong> <strong>the</strong> thumb (Fig. 9).<br />
Fro. 9<br />
Normal opposition and radial abduction <strong>of</strong> a pollicised index finger with a real <strong>the</strong>nar eminence<br />
by <strong>the</strong> described muscle transfer.<br />
THE JOURNAL OF BONE AND JOINT SURGERY<br />
Hyg<br />
years<br />
on th<br />
were<br />
were<br />
rotat~<br />
biliz~:<br />
perf~<br />
radi:<br />
<strong>the</strong> ,<br />
ring<br />
pop<br />
vOI
could not cooperate<br />
’. hand operated on in<br />
mb and fingers or<br />
pollicized finger SOme-<br />
~ <strong>the</strong> third month. The<br />
:ause <strong>of</strong> slow adaptive<br />
reatest variable in <strong>the</strong><br />
f <strong>the</strong> extensor muscle,<br />
e to <strong>the</strong> remains <strong>of</strong> its<br />
<strong>the</strong> presence <strong>of</strong> o<strong>the</strong>r<br />
and, <strong>the</strong>re usually was<br />
and l~ng fingers, and,<br />
metacarpophalangeal<br />
efore, <strong>the</strong> digit had to<br />
function <strong>of</strong> pinch.<br />
:ept those with radial<br />
and long fingers for<br />
fingered" hand, who<br />
~ so because <strong>of</strong> insuf-<br />
Os showed sensory or<br />
"e was anomalous ab<strong>the</strong><br />
metacarpal artery :’<br />
three <strong>of</strong> which scars<br />
a small full thickness<br />
r. In <strong>the</strong>se <strong>the</strong><br />
<strong>the</strong> shortness <strong>of</strong><br />
ppearance as well as<br />
index finger <strong>the</strong> a<br />
e, and, after a period<br />
9).<br />
ith a real <strong>the</strong>nar emi-<br />
AND JOINT SURGERY<br />
POLLICIZATION OF THE INDEX FINGER 1613<br />
Fro. 10<br />
Hypoplastic thumb in <strong>the</strong> left hand in a boy <strong>of</strong> <strong>the</strong> age <strong>of</strong> five; result <strong>of</strong> pollicization three<br />
years later.<br />
The quality <strong>of</strong> <strong>the</strong> results depended on <strong>the</strong> preoperative state <strong>of</strong> <strong>the</strong> hand, and<br />
<strong>the</strong> additional anomalies on muscles, tendons, bones, and .joints. The best results<br />
were in hands with a hypoplastic thumb (Fig. 10). The bones <strong>of</strong> <strong>the</strong> hypoplasfic digit<br />
were removed, but <strong>the</strong> intrinsic muscles were left to provide intrinsic power .for <strong>the</strong><br />
rotated index finger. These muscles gave <strong>the</strong> ne_w thumb normal balance ~ind stabilization,<br />
which are <strong>the</strong> prior conditions for good mobility, as well as <strong>the</strong> ability to<br />
pinch and normal prehension (Fig. 1 1).<br />
In cases <strong>of</strong> radial club hand, usually <strong>the</strong>re were several additional anomalies<br />
: and bad mobility <strong>of</strong> <strong>the</strong> radial fingers; <strong>the</strong> postoperative results in <strong>the</strong>se cases were<br />
! not as good as those previously described, but <strong>the</strong> operation did provide an increase<br />
in function and usefulness <strong>of</strong> <strong>the</strong> hand. The correction<strong>of</strong> <strong>the</strong> club hand by centralization<br />
<strong>of</strong> <strong>the</strong> hand with removal <strong>of</strong> <strong>the</strong> lunate and capitate bones and tendon transfers<br />
performed at <strong>the</strong> first operation, <strong>the</strong> pollicization at <strong>the</strong> second (Fig. 12).<br />
In <strong>the</strong> case <strong>of</strong> <strong>the</strong> so-called five-fingers-hand <strong>the</strong> decision whe<strong>the</strong>r or not <strong>the</strong><br />
radial finger was to be removed or used for pollicization sometimes was difficult. If<br />
<strong>the</strong> radial finger was <strong>of</strong> about <strong>the</strong> equal size <strong>of</strong> a normal finger, pollicization <strong>of</strong> this<br />
finger gave a very satisfactory result (Fig. 13). If <strong>the</strong> finger was too small and hypoplastic,<br />
it was better to remove it and pollicise <strong>the</strong> index finger.<br />
Finally, <strong>the</strong> optimum age for performance <strong>of</strong> <strong>the</strong> operation was <strong>the</strong> first year <strong>of</strong><br />
VOL. 53-A, NO. 8, DECEMBER 1971
1614 DIETER BUCK-GRAMCKO<br />
Result three years after pollicization; normal position in writing and crochet-work.<br />
life. At <strong>the</strong> beginning, I considered’that <strong>the</strong> age <strong>of</strong> two and a half years was most appropriate.<br />
However, in <strong>the</strong> last few years I have operated upon several infants, <strong>the</strong><br />
youngest being eleven weeks old, and now I think that <strong>the</strong> first year <strong>of</strong> life is <strong>the</strong> best<br />
age for pollicization and, incidentally, for some o<strong>the</strong>r operations in congenital m-a-l-:<br />
formations <strong>of</strong> <strong>the</strong> hand. There are two decisive factors here: The first is that it is<br />
from <strong>the</strong> age <strong>of</strong> about six months onward that <strong>the</strong> so-called thumb feeling is sup-<br />
FIG. 12<br />
Result in radial club hand with centralization <strong>of</strong> <strong>the</strong> hand and pollicization <strong>of</strong> <strong>the</strong> index finger.<br />
THE JOURNAL OF BONE AND JOINT SURGERY
and crochet-work.<br />
xlf years was most ap-<br />
~n several infants <strong>the</strong><br />
year <strong>of</strong> life is <strong>the</strong><br />
~ns in congenital real;<br />
The first is that it is<br />
thumb feeling is<br />
Lion <strong>of</strong> <strong>the</strong> index finger.<br />
~E AND JOINT SURGERY<br />
POLLICIZATION OF THE INDEX FINGER<br />
FIG. 13<br />
"Five-fingers-hand" before and after pollicization <strong>of</strong> <strong>the</strong> radial finger.<br />
1615<br />
posed to develop, and, <strong>the</strong>refore, <strong>the</strong> new thumb will be felt as being a normal one.<br />
The second is <strong>the</strong> fact that <strong>the</strong> transposed index finger will have <strong>the</strong> longest period<br />
possible for growth under <strong>the</strong> influence <strong>of</strong> its function as a thumb. Several years after<br />
pollicization we have been able to demonstrate a slow transformation <strong>of</strong> <strong>the</strong> structures<br />
<strong>of</strong> <strong>the</strong> pollicized index finger in <strong>the</strong> direction <strong>of</strong> a normal thumb. Not only do<br />
th: muscles become stronger, but also <strong>the</strong> bones. Especially <strong>the</strong> new first metacarpal<br />
becomes larger than <strong>the</strong> first phalanx <strong>of</strong> <strong>the</strong> long finger, to which it was equal in size<br />
preoperatively (Fig. 14).<br />
The operation was not done in <strong>the</strong> mildest cases <strong>of</strong> hypoplasia <strong>of</strong> <strong>the</strong> thumb,<br />
in which <strong>the</strong>re was only absence <strong>of</strong> <strong>the</strong>nar muscles and a slight adduction contracture.<br />
In all o<strong>the</strong>r cases <strong>of</strong> hypoplasia, in which <strong>the</strong>re were not enough good intrinsic muscles<br />
and long flexor and extensor tendons for good function, <strong>the</strong> dysplastic thumb was<br />
removed, and <strong>the</strong> index finger was pollicized. The operation also was not done in<br />
radial club hands where centralization <strong>of</strong> <strong>the</strong> hand over <strong>the</strong> ulna was not possible be-<br />
<strong>of</strong> restriction <strong>of</strong> elbow motion.<br />
Fro. 14<br />
Roentgenograms <strong>of</strong> a hand with pollicized index finger four years after operation. Note <strong>the</strong><br />
broadening <strong>of</strong> <strong>the</strong> base <strong>of</strong> <strong>the</strong> new first metacarpal in contrast to <strong>the</strong> base <strong>of</strong> <strong>the</strong> long finger.<br />
VOL. 53-A, NO. 8, DECEMBER 1971
1616 DIETER BUCK-GRAMCKO<br />
Su mmary -<br />
The experiences with 100 operations <strong>of</strong> pollicization <strong>of</strong> <strong>the</strong> index finger in congenital<br />
deformities <strong>of</strong> <strong>the</strong> thumb in seventy-three patients are reported on. The operation<br />
is indicated in aplasia and in hypoplasia if <strong>the</strong>re is no stable metacarpopha_<br />
langeal joint and <strong>the</strong>re are adduction contracture and poor mobility due to abnormal_<br />
ities <strong>of</strong> aluscles and tendons. The operative technique was improved by <strong>the</strong> experiences<br />
in twelve years <strong>of</strong> use. Most important are <strong>the</strong> bone fixation and <strong>the</strong> muscle<br />
stabilization. In transformation <strong>of</strong> an index finger into a thumb it is necessary to<br />
shorten <strong>the</strong> ray, to rotate it sufficiently, and to give it <strong>the</strong> right angle <strong>of</strong> abduction.<br />
The shortening takes place in <strong>the</strong> metacarpal bone with preservation <strong>of</strong> its head:<br />
<strong>the</strong> metacarpophalangeal joint becomes now <strong>the</strong> carpometacarpal joint and <strong>the</strong> metacarpal<br />
head <strong>the</strong> new trapezium. For preventing a hyperextension deformity it is<br />
necessary to rotate <strong>the</strong> metacarpal head For good muscle stabilization and good<br />
mobility <strong>the</strong> two interossei <strong>of</strong> <strong>the</strong> index finger have to be detached and to be fixed in<br />
<strong>the</strong> shortened position on both sides <strong>of</strong> <strong>the</strong> new thumb to <strong>the</strong> mobilized lateral slips<br />
<strong>of</strong> <strong>the</strong> dorsal aponeurosis. This new manner <strong>of</strong> muscle fixation gives a very good<br />
<strong>the</strong>nar eminence not only in respect to appearance but also in function with full or<br />
nearly full opposition and abduction. It requires a new skin incision with a dorsoradial<br />
skin flap for covering <strong>the</strong> gap between <strong>the</strong> wound edges <strong>of</strong> <strong>the</strong> former proximal<br />
phalanx broadened by <strong>the</strong> muscle masses. The excellent results show a surprising ....<br />
adaptation <strong>of</strong> bones and s<strong>of</strong>t tissues due to function and growth--a reason for an<br />
earl), performance <strong>of</strong> <strong>the</strong> operation. :.<br />
References<br />
1. BROOKS, DONAL: In Rehabilitation <strong>of</strong> <strong>the</strong> Hand. Ed. 2, pp. 336-348. Edited by C. B. Wynn<br />
Parry. London, Butterworths, 1966.<br />
2. BUCK-GRAMCKO, DIETER: Operative Behandlung einer Spiegelbild-Deformit~t der Hand.<br />
Ann. Chir. Plast., 9; 180-183, 1964.<br />
3. BUcK-GRAMCKO, DIETER: Daumenrekonstruktion bei Aplasie und Hypoplasie. Kiln. Med.,<br />
21; 325-329, 1966.<br />
4. BUCK-GRAMCKO, DIETER: Indikation und Technik der Daumenbildung bei Aplasie und<br />
Hypoplasie. Chit. Plast. Reconstr., 5:46-51. 1968.<br />
5. EDGERTON, M. T.: SNYDER, G. B.; and WEB~, W. L.: Surgical Treatment <strong>of</strong> Congenital<br />
Thumb Deformities (Including Psychological Impact <strong>of</strong> Correction). J. Bone and Joint<br />
Surg., 47-A-" 1453-1474, Dec. 1965.<br />
6. GOSSET, J.: La poIIicisation de l’index (Technique chirurgicale). J. Chir., 65:403-411, 1949.<br />
7. HARRISON, S. H.: Restoration <strong>of</strong> Muscle Balance in <strong>Pollicization</strong>. Plast. Reconstr. Surg., 34;<br />
236-240, 1964.<br />
8. HARRISOr~, S. H.: Pollicisation in Cases <strong>of</strong> Radial Club Hand. British J. Plast. Surg., 23~<br />
192-200, 1970.<br />
9. HILGENFELDT, OTTO: Operativer Daumenersatz und Beseitigung v0n Greifst6rungen bei<br />
<strong>Finger</strong>verlusten. Stuttgart, Ferdinand Enke Verlag, 1950.<br />
10. LITTER, J. W.: The Neurovascular Pedicle Method <strong>of</strong> Digital Transposition for Reconstruction<br />
<strong>of</strong> <strong>the</strong> Thumb. Plast. Reconstr. Surg., 12:303-319, 1953.<br />
11. LITTLER, J. W.: Digital Transposition. In Current Practice in Orthopaedic Surgery, Vol. 3,<br />
pp. 157-172. St. Louis, The C. V. Mosby Co., 1966.<br />
12. RIORDhN, D. C.: Congenital Absence <strong>of</strong> <strong>the</strong> Radius. J. Bone and Joint Surg., 37-A:<br />
1140, Dec. 1955.<br />
13. WroTE, W. F.: Pollicisation for <strong>the</strong> Missing Thumb, Traumatic or Congenital. The Hand,<br />
1: 23-26, 1969.<br />
14. WHITE, W. F.: Fundamental Priorities in <strong>Pollicization</strong>. J. Bone and Joint Surg., 52-B: 438-<br />
443, Aug. 1970.<br />
DISCUSSION<br />
.DR. J. W. LITTLER, NEW YORK, N. Y.: Through a tragic pharmacological mishap<br />
Buck-Gramcko has ga<strong>the</strong>red this unprecedented series (100 cases) <strong>of</strong> thumb aplasia. His paper<br />
a splendid one and <strong>the</strong>refore a pleasure to discuss: its clarity is refreshing, <strong>the</strong> surgical approach<br />
is exact, and <strong>the</strong> functional reward for <strong>the</strong>se little patients is superior. His outstanding contribution<br />
gives great authority to this particular procedure.<br />
Several points, however, deserve emphasis. First: <strong>the</strong> surgical timing. For many years I<br />
have resisted transposing <strong>the</strong> radial digit into thumb position during infancy, believing that <strong>the</strong><br />
THE JOURNAL OF BONE AND JOINT SURGERY
function with full or<br />
cision with a dorso-<br />
<strong>the</strong> former proximal<br />
:s show a surprising<br />
th--a reason for an<br />
Edited by C. B. Wynn<br />
Deformit/it der Hand.<br />
ypoplasie. Klin. Med.,<br />
POLLICIZATION OF THE INDEX FINGER<br />
ically unmolested child, possibly with ano<strong>the</strong>r anomaly, would better tolerate <strong>the</strong> operation<br />
i later. Never, however, have I hesitated to encourage <strong>the</strong> removal, relatively early, <strong>of</strong> any rudie<br />
index finger in con-<br />
:eported on. The o<br />
;table metacarpopha_<br />
~. i:;!~:!~;.i rnentary, functionally and hopelessly blighted first pre-axial digit.<br />
It is acknowledged that <strong>the</strong> thumbless child will endeavor to force his independent index<br />
finger as an opponent <strong>of</strong> <strong>the</strong> o<strong>the</strong>r digits. What we attempt with our surgery is to complete that<br />
!!~:!l(i ~ endeavor. Both Dr. Buck-Gramcko and Dr. Riordan now firmly believe that <strong>the</strong> digital transpotity<br />
due to abnormal, sition should be done during infancy. This may or may not be true for <strong>the</strong> best result. It is my<br />
,roved by <strong>the</strong> experi_, !i!i~, opinion that a non-existing thumb has no special cortical representation; any oppositional functtiorl<br />
and <strong>the</strong> muscle tion resides in <strong>the</strong> next most independent digit, regardless <strong>of</strong> <strong>the</strong> time <strong>of</strong> any transposition.<br />
nb it is necessary to<br />
Heret<strong>of</strong>ore, I have awaited <strong>the</strong> age <strong>of</strong> from two to four, but perhaps my approach is too cau-<br />
¯ angle <strong>of</strong> abductiot<br />
tious, despite parental pressure.<br />
Certain technical aspects are most important and <strong>of</strong> <strong>the</strong>se <strong>the</strong> incision is <strong>of</strong> primary con-<br />
:rvation <strong>of</strong> its head:<br />
cern, for finally <strong>the</strong> closure must have allowed <strong>the</strong> digit to be shifted into proper position, pro-<br />
11 joint and <strong>the</strong> meta- viding an adequate cleft and a sufficient proximal phalangeal skin envelope to house <strong>the</strong> bulk <strong>of</strong><br />
~sion~deformity it is<br />
<strong>the</strong> intrinsic muscles advanced to encompass <strong>the</strong> recessed proximal phalanx (now acting as <strong>the</strong><br />
~bilization and<br />
ed and to be fixSd in<br />
metacarpal).<br />
Though it is not carefully documented in this paper, <strong>the</strong> head <strong>of</strong> <strong>the</strong> epipyseal-arrested<br />
metacarpal fails to develop, but as shown in some <strong>of</strong> <strong>the</strong> illustrations, <strong>the</strong> hypertrophic proximal<br />
.obilized lateral slips<br />
phalanx has taken on <strong>the</strong> characteristics <strong>of</strong> a thumb metacarpal. It also shows good projection<br />
n gives a very good<br />
(despite an incomplete carpal arch) and has a firm fibrous base to meet <strong>the</strong> oppositional de-<br />
:tung bei Aplasie und<br />
,atme~it <strong>of</strong> Congenital<br />
~). J. Bone and Joint<br />
:.. 6~: 403-411, 1949. :21 ?~<br />
st. Reconstr. Surg., 34:<br />
;sh J. Plast. Surg., 23:<br />
m Greifst6rungen bei<br />
nsposition for<br />
~aedic Surgery, Vol. 3,<br />
int Surg., 37-A:<br />
7ongenital. The Hand,<br />
;0int Surg., 52-B:<br />
~cological mishap Dr.<br />
,b aplasia. His paper "<br />
. <strong>the</strong> surgical approach<br />
; outstanding contribu-<br />
ncy believing that <strong>the</strong><br />
1 617<br />
mands. In <strong>the</strong> words <strong>of</strong> Sir Charles Bell:<br />
"On <strong>the</strong> length, strength, free lateral motion and perfect mobility <strong>of</strong> <strong>the</strong> thumb, depends<br />
<strong>the</strong>power <strong>of</strong> <strong>the</strong> human hand. The thumb is called Pollex because <strong>of</strong> its strength; and that<br />
strength is necessary to <strong>the</strong> power <strong>of</strong> <strong>the</strong> hand, being equal to that <strong>of</strong> all <strong>the</strong> fingers."<br />
It must be admitted that to bring <strong>the</strong> thumb-deprived primitive hand into a more advanced<br />
state, <strong>the</strong> pre-axial finger can be substituted through careful surgery and that ~vith time and use,<br />
though imperfect, its appearance and function will approach quite nearly that prime digit which<br />
faiied to develop.<br />
: AND JOINT SURGERY ~ ~i~,~ VOL. 53-A, NO. 8, DECEMBER 1971