clinical intimate personal care and chaperoning policy - NHS Scotland
clinical intimate personal care and chaperoning policy - NHS Scotland
clinical intimate personal care and chaperoning policy - NHS Scotland
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
CLINICAL<br />
INTIMATE PERSONAL CARE AND<br />
CHAPERONING POLICY<br />
Authors: Kathryn Bailey &<br />
Kevin Hurst<br />
Review Group:<br />
Last Updated: July 2009 Review Date: July 2011<br />
Document No: Issue No:<br />
UNCONTROLLED WHEN PRINTED<br />
Signed: Executive Lead<br />
Officer<br />
(Authorised Signatory)
CONTENTS<br />
Section Title Page Number<br />
1. PURPOSE AND SCOPE 3<br />
2. STATEMENT OF POLICY 3<br />
3. DEFINITIONS 3-4<br />
4. RESPONSIBILITIES AND ORGANISATIONAL 4-6<br />
ARRANGEMENTS<br />
5. FLOW CHART 7<br />
6. REFERENCES 8<br />
7. BIBLIOGRAPHY AND FURTHER READING 8<br />
8. RAPID IMPACT CHECKLIST 9-14<br />
9. POLICY APPROVAL CHECKLIST 11<br />
2
1. PURPOSE AND SCOPE<br />
The purpose of this <strong>policy</strong> is to set out the st<strong>and</strong>ards, which must be adhered to when providing<br />
<strong>intimate</strong> <strong>personal</strong> <strong>care</strong> <strong>and</strong> <strong>chaperoning</strong> to patients. Through this <strong>policy</strong> staff will be able to offer a<br />
co-ordinated service <strong>and</strong> approach, which acknowledges their responsibilities <strong>and</strong> protect the rights<br />
of everyone involved. This <strong>policy</strong> will enable the service to comply with; The Children (Scotl<strong>and</strong>) Act<br />
1995, Adults with Incapacity (Scotl<strong>and</strong>) Act 2000, <strong>and</strong> Human Rights Act 2000. It gives specific<br />
guidance regarding babies, children <strong>and</strong> individuals with special needs, adults at risk, <strong>and</strong> those<br />
whose first language is not English, <strong>and</strong> pre verbal infants. This <strong>policy</strong> also adheres to the human<br />
rights principles found in the Mental Health (Care <strong>and</strong> Treatment) (Scotl<strong>and</strong>) Act 2003.<br />
2. STATEMENT OF POLICY<br />
<strong>NHS</strong> Tayside attaches the highest importance to ensuring a culture that values the privacy <strong>and</strong><br />
dignity of all patients who are <strong>care</strong>d for within the organisation. Staff have a professional duty of <strong>care</strong>,<br />
<strong>and</strong> have responsibilities to act in the patients best interest <strong>and</strong> are accountable for their actions.<br />
Staff must be sensitive to differing expectations associated with race, ethnicity, age, gender,<br />
disability, religion/faith, <strong>and</strong> sexual orientation.<br />
The <strong>policy</strong> applies to the <strong>care</strong> of patients who require support of an <strong>intimate</strong> nature, including<br />
examinations, procedures <strong>and</strong> interventions. Intimate <strong>and</strong> <strong>personal</strong> <strong>care</strong> is an important area of an<br />
individual’s self image <strong>and</strong> respect. The apparent nature of many <strong>care</strong> interventions, if not practised<br />
in a sensitive <strong>and</strong> respectful manner, can lead to misinterpretation <strong>and</strong> occasionally allegations of<br />
abuse. Not underst<strong>and</strong>ing an individual’s specific needs can lead to confusion <strong>and</strong> misunderst<strong>and</strong>ing.<br />
It is therefore important that health<strong>care</strong> professionals are sensitive to these issues <strong>and</strong> alert to the<br />
potential for individuals, especially children, young people <strong>and</strong> other ‘at risk’ groups to become the<br />
victims of abuse.<br />
A relationship of trust is required to ensure that all patients receive the same degree of <strong>care</strong> <strong>and</strong><br />
support, (Children (Scotl<strong>and</strong>) Act, 1995; Adults with Incapacity (Scotl<strong>and</strong>) Act, 2000). A relationship<br />
of trust can be described as one in which one party is in a position of power or influence over the<br />
other by virtue of their work or the nature of their activity. Relationships developed by professions<br />
such as medicine, nursing <strong>and</strong> allied health professionals are all founded on trust (Home Office,<br />
1999).<br />
The Adult Support & Protection (Scotl<strong>and</strong>) Bill as passed, is intended to give greater protection to<br />
adults at risk of abuse. This includes those who are mentally unwell. The new Bill gives new powers<br />
<strong>and</strong> a statutory responsibility to local agencies to investigate any risk of harm or abuse to adults living<br />
in <strong>care</strong> homes or in the community. Part 1 of the Bill is concerned with adult protection. Within<br />
Tayside, there is a multi-agency protocol to guide <strong>and</strong> inform local inter-agency procedures &<br />
practice concerning the protection of vulnerable adults – Protecting Vulnerable Adults in Tayside.<br />
3. DEFINITIONS<br />
WHAT IS INTIMATE CARE?<br />
Intimate <strong>care</strong> covers all areas of <strong>personal</strong> <strong>care</strong> that most individuals learn to carry out independently<br />
as they grow <strong>and</strong> develop, but some are unable to do so because of impairment or<br />
disability/age/underst<strong>and</strong>ing due to communication difficulties. Individuals may require help with<br />
eating <strong>and</strong> drinking, washing <strong>and</strong> dressing <strong>and</strong> toileting. Help may also be required to change stoma<br />
bags, manage urinary catheters or administer rectal medication (Scottish Executive, 1999).<br />
Other procedures such as <strong>intimate</strong> examinations undertaken whilst an individual is in hospital also<br />
require the same degree of respect.<br />
3
WHAT IS A CHAPERONE?<br />
An individual who acts as an advocate for the patient during examination or procedure, providing<br />
explanation <strong>and</strong> reassuring the patient whilst safeguarding against unnecessary discomfort, pain,<br />
humiliation or intimidation (Royal College of Nursing, 2002).<br />
AT RISK GROUPS<br />
Any individuals dependent on others for <strong>care</strong> are vulnerable. Factors, which may increase this<br />
vulnerability, may include:<br />
• Reduced control over their lives or decisions due to their disability or lack of underst<strong>and</strong>ing<br />
• Lack of sex education which can lead to difficulty in children recognising abusive behaviour<br />
• Reduced communication skills to let someone know they are not happy<br />
• Multiple <strong>care</strong>rs due to hospital admissions or respite/residential <strong>care</strong><br />
• Differences in appearance or behaviour may be attributed to a child’s disability/age <strong>and</strong> not to the<br />
possibility that something may be wrong<br />
• Discrimination against children <strong>and</strong> adult with disabilities in society<br />
• Individuals whose first language is not English<br />
• Pre Verbal infants <strong>and</strong> children<br />
• Individuals suffering from a mental illness including people with dementia<br />
(Scottish Executive, 1999; Scottish Executive, 2000)<br />
From a child protection perspective, <strong>intimate</strong> <strong>personal</strong> <strong>care</strong> involves risks for both the child <strong>and</strong> the<br />
adult providing the <strong>care</strong> as it may involve the adult touching <strong>intimate</strong> parts of the child’s body. By<br />
addressing the issue we create an awareness of the importance of maximising safety for all<br />
concerned <strong>and</strong> promote the best interest of the child. This will not completely eliminate the risk but<br />
will minimise the potential of its occurrence.<br />
While this is an important issue when caring for children, the same risks are present when providing<br />
<strong>care</strong> to vulnerable adults. To ensure staff protect the rights of everyone involved, all staff providing<br />
<strong>care</strong> within <strong>NHS</strong> Tayside must comply with the following principles for practice.<br />
4. RESP0NSIBILITIES AND ORGANISATIONAL ARRANGEMENTS<br />
4.1 PRINCIPLES FOR PRACTICE<br />
All staff must ensure that they promote <strong>and</strong> enable each individual to be part of the decision making<br />
process in relation to their <strong>intimate</strong> <strong>and</strong> <strong>personal</strong> <strong>care</strong>, giving all relevant information, to ensure<br />
patient choice <strong>and</strong> that informed consent has been obtained, in adherence with <strong>NHS</strong> Tayside’s<br />
Informed Consent Policy. In the event that the patient does not have the capacity to consent to<br />
treatment, The Adults with Incapacity (Scotl<strong>and</strong>) Act 2000 provides a comprehensive framework to<br />
ensure equity of treatment <strong>and</strong> choice for adults with incapacity, <strong>and</strong> makes provision for decisions to<br />
be made on behalf of an adult, subject to safeguards <strong>and</strong> in specific <strong>and</strong> well-defined situations.<br />
Incapacity is defined within that Act as being incapable of: acting, making decisions, communicating<br />
decisions, underst<strong>and</strong>ing decisions or retaining the memory of decisions, by reason of mental<br />
disorder or of inability to communicate because of physical disability. If required, an incapacity<br />
certificate must be completed prior to any intervention or treatment. Independence must still be<br />
promoted, <strong>and</strong> consideration given to additional needs, communication methods or tool that maybe<br />
required.<br />
Consent for a child can be given by a variety of individuals depending on the circumstances<br />
regarding their <strong>care</strong>. In most cases consent if given by the mother, father if married to the mother or<br />
has been or a legally appointed guardian. Staff should refer to the Children Scotl<strong>and</strong> Act 1995 for<br />
further guidance. Individuals working with children must also be aware that a person under the age<br />
of 16 years shall have a legal capacity to consent on his/her own behalf to any surgical, medical or<br />
dental procedure or treatment where, in the opinion of a qualified medical practitioner attending<br />
4
him/her, he/she is capable of underst<strong>and</strong>ing the nature <strong>and</strong> possible consequences of the procedure<br />
<strong>and</strong> treatment. (The Age of Legal Capacity, 1991)<br />
The following principles for good practice should assist in this matter:<br />
• Allow the individual to <strong>care</strong> for him/herself as far as possible<br />
• Allow an individual wherever possible to express a preference for his/her <strong>care</strong>r<br />
• Where the individual is unable to give consent, discussions must take place with themselves,<br />
their parent/<strong>care</strong>r or other legally appointed representative as to their preferences<br />
• Allow the individual a choice in the sequence of <strong>care</strong> they receive, where possible.<br />
• Ensure the privacy <strong>and</strong> dignity of the individual<br />
• Be aware of <strong>and</strong> responsive to the individual’s reactions<br />
• If carrying out <strong>intimate</strong> <strong>care</strong> away from the ward area/respite/residential facility/individuals home,<br />
ensure the privacy <strong>and</strong> safety of the individual.<br />
• Any individual carrying out <strong>intimate</strong> <strong>personal</strong> <strong>care</strong> to children <strong>and</strong> young people must have an<br />
enhanced disclosure Scotl<strong>and</strong> check undertaken<br />
All staff should be familiar with the following documents:<br />
The Age of Legal Capacity (Scotl<strong>and</strong>) Act, 1991<br />
Children (Scotl<strong>and</strong>) Act, HMSO, London, 1995<br />
Protecting Children A shared Responsibility, Scottish Executive, 2000<br />
Human Rights Act, The Home Office, 2000<br />
Adults with Incapacity (Scotl<strong>and</strong>) Act, 2000<br />
Mental Health (Care & Treatment) (Scotl<strong>and</strong>) Act 2003<br />
The Adult Support & Protection (Scotl<strong>and</strong>) Bill<br />
A Multi-Faith Resource for Health<strong>care</strong> Staff, <strong>NHS</strong> Education Scotl<strong>and</strong><br />
<strong>NHS</strong> Tayside Informed Consent Policy, 2007<br />
Protecting Vulnerable Adults in Tayside: A Multi-Agency Protocol<br />
4.2 PROVIDING INTIMATE CARE<br />
In the provision of health <strong>care</strong>, staff are in a position of trust <strong>and</strong> responsibility. This trust <strong>and</strong><br />
responsibility is heightened when providing <strong>intimate</strong> <strong>care</strong>. It is neither practical nor possible to<br />
eliminate the fact that <strong>intimate</strong> <strong>care</strong> may be provided by a member of staff of the opposite gender.<br />
However, in order to safeguard patients, staff must practice in accordance with the following<br />
statements: -<br />
4.2.1 If any <strong>personal</strong> <strong>care</strong> support is to be given by a member of the opposite sex, the individual<br />
must be offered the option of a chaperone. The chaperone must be wherever possible, the same sex<br />
as the individual receiving the <strong>care</strong> (RCN, 2002; GMC, 2006). The name of any chaperone must be<br />
documented in the individuals <strong>care</strong> plan (NMC, 2005). If a chaperone is not available <strong>and</strong> <strong>care</strong> is not<br />
urgent this must be explained to the patient to ascertain if they would prefer to proceed without a<br />
chaperone or offer to delay the <strong>care</strong> until such time as a chaperone is available (RCN, 2002).<br />
Nurses <strong>and</strong> other health <strong>care</strong> professionals should also consider being accompanied by a chaperone<br />
when undertaking <strong>intimate</strong> examinations <strong>and</strong> procedures to avoid misunderst<strong>and</strong>ing <strong>and</strong>, in rare<br />
cases, false accusations of abuse. If the patient prefers to undergo an examination/procedure<br />
without the presence of a chaperone, this should be respected (RCN, 2002).<br />
Wherever possible, a chaperone should be a health<strong>care</strong> professional, but it is recognised that in<br />
some areas or situations an additional health<strong>care</strong> professional may not be available. If this occurs,<br />
<strong>and</strong> if the examination/procedure cannot be safely postponed, then the patient must be offered to<br />
invite a relative, <strong>care</strong>r or friend to be present. If this is not possible, then a non-<strong>clinical</strong> member of<br />
staff from the health<strong>care</strong> team may be asked to undertake the role of chaperone. The patient must be<br />
made aware of the fact that the chaperone is a non-<strong>clinical</strong> member of staff <strong>and</strong> again given the<br />
opportunity to refuse or delay the procedure. All non-<strong>clinical</strong> members of staff undertaking this<br />
5
esponsibility such as administration <strong>and</strong> clerical staff, will have undergone chaperone training <strong>and</strong><br />
are aware of the role expected of them, how to raise concerns <strong>and</strong> also their contractual obligations<br />
regarding issues of confidentiality.<br />
Staff must record discussions <strong>and</strong> outcomes of any of the above in the individuals <strong>care</strong> plan (GMC,<br />
2001; NMC, 2005).<br />
4.2.2 In areas where <strong>intimate</strong> <strong>personal</strong> <strong>care</strong> may be given on a regular basis by members of the<br />
opposite sex, information must be given <strong>and</strong> where possible discussion <strong>and</strong> agreement should take<br />
place with the individual, parent/<strong>care</strong>r, their family or where appropriate legally appointed<br />
representative. This information must be recorded in the individual’s <strong>care</strong> plan (NMC, 2005).<br />
4.2.3 When a chaperone has been required <strong>and</strong> a member of staff of the same gender has been<br />
requested but not available this must be brought to the attention of the nurse/midwife in charge. In<br />
addition a brief note should be made in the individual’s notes for each occasion <strong>and</strong> must include:<br />
Date/Time/Care given/Immediate necessity that led to opposite sex <strong>personal</strong> <strong>care</strong><br />
being given or details of what <strong>care</strong> was omitted or delayed plus reason why member of<br />
same gender was not available.<br />
It is the responsibility of staff, through record keeping to monitor the frequency of same gender staff<br />
not being available for <strong>intimate</strong> <strong>personal</strong> <strong>care</strong> needs.<br />
4.2.4 Religious views of families must be taken into account. It may be the case that males can only<br />
have <strong>intimate</strong> <strong>care</strong> provided by another male, therefore involvement of the family in the <strong>care</strong> of the<br />
individual is important.<br />
<strong>NHS</strong> Education for Scotl<strong>and</strong> (NES) has produced a booklet called Spiritual Care: A Multi-Faith<br />
Resource for Health<strong>care</strong> Staff through its Health<strong>care</strong> Chaplaincy Training <strong>and</strong> Development Unit in<br />
consultation with a multi-faith group which represents the main faith <strong>and</strong> belief groups in Scotl<strong>and</strong>.<br />
Although it cannot cover every group, this booklet contains information for most of the smaller faith<br />
communities on issues such as:<br />
• Attitudes to health<strong>care</strong> staff <strong>and</strong> illness<br />
• Washing <strong>and</strong> toilet<br />
• Ideas of modesty <strong>and</strong> dress<br />
Each ward or department has a hard copy of this booklet or it can be found on staffnet under Spiritual<br />
<strong>care</strong> or Diversity <strong>and</strong> Equality or online at http://www.nes.scot.nhs.uk/publications.<br />
The Department of Spiritual Care can contact any faith community if you require further information.<br />
4.2.5 Apart from in emergency situations, staff must get to know the child/ vulnerable adult before<br />
being involved in any <strong>intimate</strong> or <strong>personal</strong> <strong>care</strong>. They must also reach agreement with the child <strong>and</strong><br />
family/vulnerable adult <strong>and</strong> <strong>care</strong>r/family on the names used for <strong>intimate</strong> body parts.<br />
4.2.6 Whilst children must be protected from receiving inappropriate touches, it is important that<br />
touch is not withdrawn completely from infants <strong>and</strong> children with profound disabilities for whom it will<br />
always be essential for providing reassurance <strong>and</strong> <strong>personal</strong> <strong>and</strong> social development. Massage is<br />
commonly used to develop sensory <strong>and</strong> body awareness for infants <strong>and</strong> children with complex needs<br />
as well as a means of relaxation.<br />
6
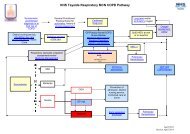
5. INTIMATE PERSONAL CARE AND CHAPERONING FLOW CHART<br />
When <strong>intimate</strong> <strong>and</strong> <strong>personal</strong> <strong>care</strong> is required, assessment must take place as to who is the most appropriate person to undertake this <strong>care</strong>, taking<br />
cognisance of the patients wishes.<br />
Same sex individual is available to undertake <strong>care</strong><br />
YES NO<br />
Undertake <strong>care</strong> as required<br />
Provide <strong>care</strong> with chaperone present.<br />
Document the full name of the<br />
chaperone in the patient <strong>care</strong> plan<br />
Chaperone available<br />
YES NO<br />
Explain the required procedure to patient <strong>and</strong> its<br />
urgency. If the patient continues to refuse consent<br />
to the procedure without a chaperone, <strong>and</strong> the<br />
treatment is necessary to preserve life, <strong>care</strong> may<br />
be provided<br />
Chaperone to be offered to the<br />
patient<br />
Patient refuses chaperone<br />
Ascertain if the <strong>care</strong> is urgent<br />
YES NO<br />
Document clearly in the <strong>care</strong> plan the patient’s<br />
decision not to have a chaperone present. Undertake<br />
<strong>care</strong> as required<br />
Explain to the patient the lack of an appropriate<br />
chaperone <strong>and</strong> discuss the options of: (a)<br />
undertaking <strong>care</strong> without a chaperone present, or<br />
(b) delaying the <strong>care</strong> until later in the day.<br />
Option A preferred by patient Option B preferred by patient<br />
Document in the patients <strong>care</strong> plan an agreed time to<br />
undertake the <strong>care</strong> with chaperone present
6. REFERENCES<br />
Adults with incapacity (Scotl<strong>and</strong>) Act, The stationery Office, Edinburgh, 2000<br />
Caring for Young People <strong>and</strong> the Vulnerable, Home Office, 1999<br />
Chaperoning: The role of the nurse <strong>and</strong> the rights of patients, RCN, 2002<br />
Children (Scotl<strong>and</strong>) Act, HMSO, London, 1995<br />
Good Medical Practice – Maintaining Boundaries, General Medical Council 2006<br />
Guidelines for records <strong>and</strong> record keeping, Nursing & Midwifery Council, 2005<br />
Guidelines for staff who provide <strong>intimate</strong> <strong>care</strong> for children <strong>and</strong> young people with disabilities, Scottish<br />
Executive 1999<br />
Human Rights Act, The Home Office, 2000<br />
Mental Health (Care <strong>and</strong> Treatment) (Scotl<strong>and</strong>) Act 2003<br />
<strong>NHS</strong> Tayside Informed Consent Policy, 2007<br />
Protecting Children A shared Responsibility, Scottish Executive, 2000<br />
Spiritual Care: A Multi-Faith Resource for Health<strong>care</strong> Staff, <strong>NHS</strong> Education for Scotl<strong>and</strong> 2007<br />
The Adult Support & protection (Scotl<strong>and</strong>) Bill, Scottish Executive<br />
The Age of Legal Capacity (Scotl<strong>and</strong>) Act, HMSO, 1991<br />
7. BIBLIOGRAPHY AND FURTHER READING<br />
Illness <strong>and</strong> disability in Children <strong>and</strong> Young People, Action for Sick Children, 1996<br />
Practitioner-client relationships <strong>and</strong> the prevention of abuse, Nursing & Midwifery Council, London, 2002<br />
Protection of nurses working with children <strong>and</strong> young people: Guidance for nursing staff, RCN 2001<br />
The essence of Care, Department of Health, London, 2001<br />
The Code: St<strong>and</strong>ards of Conduct, Performance <strong>and</strong> Ethics for Nurses <strong>and</strong> Midwives, Nursing & Midwifery<br />
Council, London, 2008<br />
The Same As You, Scottish Executive, 2001<br />
8
Name of Function/Policy/Strategy<br />
EQUALITY AND DIVERSITY RAPID IMPACT ASSESSMENT<br />
Intimate Personal Care & Chaperoning Policy<br />
Workstream<br />
Clinical<br />
Location of Function/Policy/Strategy<br />
What are the main aims of your function/<strong>policy</strong>/strategy<br />
To provide clear guidance with regard to the requirement to provide patients with informed choices<br />
regarding their <strong>intimate</strong> <strong>personal</strong> <strong>care</strong> & <strong>chaperoning</strong>, & therefore provide a framework to ensure that<br />
patient’s dignity, privacy & respect is maintained at all time.<br />
Is this a new/existing <strong>policy</strong>/function/strategy?<br />
New<br />
What are the intended outcomes from the proposed function/<strong>policy</strong>/strategy?<br />
To enhance & improve the patients experience of health<strong>care</strong> within <strong>NHS</strong>T.<br />
Priority: state whether high/low?<br />
High<br />
Review Team: who is assessing or considering the assessment?<br />
Nursing & Patient Services<br />
Names <strong>and</strong> titles of team members<br />
Kevin Hurst – Senior Nurse Practice Development<br />
Role of assessment team<br />
To impact assess the <strong>policy</strong><br />
When completed please this form to be emailed to ……………………………………<br />
9
Item<br />
No<br />
Considerations Detail Impact <strong>and</strong> Identify<br />
Groups Affected<br />
1. Which groups of the population will be affected<br />
by the function/<strong>policy</strong>?<br />
1.1 Will it impact on the whole population? Yes<br />
1.2 If not which groups of the population do you think will<br />
be affected by this function/<strong>policy</strong>?<br />
Item<br />
No<br />
• Minority ethnic population (including<br />
refugees, asylum seekers&<br />
gypsies/travellers)<br />
• Women <strong>and</strong> men<br />
• People in religious/faiths groups<br />
• Disabled people<br />
• Older people, children <strong>and</strong> young people<br />
• Lesbian, gay, bisexual <strong>and</strong> transgender<br />
people<br />
• People with mental health problems<br />
• Homeless people<br />
• People involved in criminal justice system<br />
• Staff<br />
All groups will be affected, as<br />
the six equality str<strong>and</strong>s apply to<br />
all patients admitted to <strong>NHS</strong><br />
Tayside<br />
Considerations Detail Impact <strong>and</strong> Identify<br />
Groups Affected<br />
2. What impact will the function/<strong>policy</strong> have on<br />
lifestyles?<br />
For example will the changes affect:<br />
• Diet & nutrition<br />
• Exercise & physical activity<br />
• Substance use: tobacco, alcohol or drugs<br />
Whilst the Policy should have<br />
no impact on lifestyle, the <strong>policy</strong><br />
will promote informed choices<br />
for patients in relation to their<br />
<strong>intimate</strong> & <strong>personal</strong> <strong>care</strong>. The<br />
<strong>policy</strong> will also provide a<br />
framework for the promotion of<br />
the patient’s rights to privacy,<br />
dignity & respect.<br />
Document the<br />
Evidence/Research<br />
Performance Through Inclusion<br />
documentation.<br />
Fair For All<br />
Document the<br />
Evidence/Research<br />
Actions Taken/To be Taken<br />
Awareness of the Policy will<br />
need raising with staff, & will be<br />
achieved through the<br />
implementation plan<br />
Actions Taken/To be Taken<br />
Review implementation plan<br />
10
Item<br />
No<br />
• Risk taking behaviours<br />
• Education & learning or skills<br />
• Other<br />
Considerations Detail Impact <strong>and</strong> Identify<br />
Groups Affected<br />
3. Does your function/<strong>policy</strong> consider the impact on<br />
the social environment?<br />
Item<br />
No<br />
Things that might be affected include:<br />
• Social status<br />
• Employment (paid/unpaid)<br />
• Social/family support<br />
• Stress<br />
• Income<br />
The Policy does consider the<br />
impact on the social<br />
environment. Wellbeing is<br />
increasingly being recognised<br />
as central to health <strong>and</strong><br />
therefore in-patients who feel<br />
comfortable within their<br />
environment will have a better<br />
sense of wellbeing <strong>and</strong><br />
therefore better <strong>clinical</strong> outcome<br />
when privacy <strong>and</strong> dignity are<br />
respected.<br />
Patient’s wishes must be<br />
respected when <strong>intimate</strong> <strong>care</strong> is<br />
being carried out or during<br />
examination, procedures &<br />
interventions of a <strong>personal</strong><br />
nature.<br />
Considerations Detail Impact <strong>and</strong> Identify<br />
Groups Affected<br />
4. Will the proposal have any impact on:<br />
5.<br />
• Discrimination<br />
• Equality of opportunity<br />
• Relations between groups<br />
• Other<br />
Will the function/<strong>policy</strong> have an impact on the<br />
physical environment?<br />
Adherence with the Policy will<br />
have a positive impact on<br />
privacy, dignity <strong>and</strong> respect<br />
therefore improving the patient<br />
experience.<br />
No<br />
Document the<br />
Evidence/Research<br />
Better Together SGHD Patient<br />
Experience Programme<br />
Chaperoning: The role of the<br />
nurse & the rights if the<br />
patients, RCN 2002<br />
Document the<br />
Evidence/Research<br />
Actions Taken/To be Taken<br />
Actions Taken/To be Taken<br />
11
Item<br />
No<br />
For example will there be impacts on:<br />
• Living conditions<br />
• Working conditions<br />
• Pollution or climate change<br />
• Accidental injuries/public safety<br />
• Transmission of infectious diseases<br />
• Other<br />
Considerations Detail Impact <strong>and</strong> Identify<br />
Groups Affected<br />
6. Will the function/<strong>policy</strong> affect access to <strong>and</strong><br />
experience of services?<br />
For example:<br />
• Health<strong>care</strong><br />
• Social services<br />
• Education<br />
• Transport<br />
• Housing<br />
7. Consultation<br />
1) What existing consultation data do we have<br />
or need?<br />
• Existing consultation sources<br />
• Original consultations<br />
• Key learning<br />
2) What new consultation, if any, do you need<br />
to undertake?<br />
The Policy will improve patient’s<br />
experience of health<strong>care</strong>,<br />
through assuring privacy,<br />
dignity <strong>and</strong> respect, in addition<br />
to providing informed choices to<br />
patients regarding their <strong>care</strong>.<br />
The following groups have been<br />
consulted with <strong>and</strong> advice<br />
incorporated into the<br />
development of the Policy:<br />
• Public Partnership (Health)<br />
Group<br />
• <strong>NHS</strong>T staff from a range of<br />
professional backgrounds<br />
including medical,<br />
NMAHPs, A&C staff groups<br />
• Dept of Spiritual Care<br />
Document the<br />
Evidence/Research<br />
Better Together – SGHD<br />
Patient Experience Programme<br />
<strong>NHS</strong>T Informed Consent Policy<br />
Chaperoning: The role of the<br />
nurse & the rights if the<br />
patients, RCN 2002<br />
Performance Through Inclusion<br />
documentation.<br />
Fair For All<br />
Better Together – SGHD<br />
Patient Experience Programme<br />
<strong>NHS</strong>T Informed Consent Policy<br />
Human Rights Act 2000<br />
Actions Taken/To be Taken<br />
12
Item<br />
No<br />
Considerations Detail Impact <strong>and</strong> Identify<br />
Groups Affected<br />
8. In relation to the groups identified:<br />
Item<br />
No<br />
• What are the potential impacts on health?<br />
• Will the function/<strong>policy</strong> impact on access to<br />
health <strong>care</strong>? If yes – in what way?<br />
• Will the function/<strong>policy</strong> impact on the<br />
experience of health <strong>care</strong>? If yes – in what<br />
way?<br />
The Policy will improve patient’s<br />
experience of health<strong>care</strong>,<br />
through assuring privacy,<br />
dignity <strong>and</strong> respect, in addition<br />
to providing informed choices to<br />
patients regarding their <strong>care</strong>.<br />
Considerations Detail Impact <strong>and</strong> Identify<br />
Groups Affected<br />
9. Have any potential negative impacts been<br />
identified?<br />
• If so, what action has been proposed to<br />
counteract the negative impacts? (if yes state<br />
how)<br />
For example:<br />
• Is there any unlawful discrimination?<br />
• Could any community get an adverse<br />
outcome?<br />
• Could any group be excluded from the<br />
benefits of the function/<strong>policy</strong>? (consider<br />
groups outlined in item 3)<br />
• Does it reinforce negative stereotypes? (For<br />
example, are any of the groups identified at<br />
item 3 being disadvantaged due to<br />
perception rather than factual information?)<br />
The impact of patients refusing<br />
urgent treatment, examinations<br />
& interventions when a same<br />
sex chaperone has been<br />
requested but not available has<br />
been considered.<br />
Document the<br />
Evidence/Research<br />
Better Together – SGHD<br />
Patient Experience Programme<br />
Document the<br />
Evidence/Research<br />
Chaperoning: The role of the<br />
nurse & the rights if the<br />
patients, RCN 2002<br />
Actions Taken/To be Taken<br />
Actions Taken/To be Taken<br />
13
Item<br />
No<br />
Considerations Detail Impact <strong>and</strong> Identify<br />
Groups Affected<br />
10. Data & Research<br />
11. Monitoring<br />
• Is there need to gather further<br />
evidence/data?<br />
• Are there any apparent gaps in<br />
knowledge/skills?<br />
• How will the outcomes be monitored?<br />
• Who will monitor?<br />
• What criteria will you use to measure<br />
progress towards the outcomes?<br />
12. Recommendations<br />
Item<br />
No<br />
(This should include any actions required to address<br />
negative impacts identified)<br />
No<br />
If non-<strong>clinical</strong> staff are required<br />
to act as a chaperone, training<br />
is required. Training is not<br />
currently available for this<br />
Outcomes will be monitored<br />
locally & any issue that gives<br />
cause for concern will be acted<br />
on<br />
Complaints that result from<br />
patients regarding <strong>intimate</strong><br />
<strong>personal</strong> <strong>care</strong> & <strong>chaperoning</strong><br />
will be monitored, as the<br />
anticipated outcome of<br />
implementation of this <strong>policy</strong> will<br />
lead to a reduction in the<br />
number of these<br />
Considerations Detail Impact <strong>and</strong> Identify<br />
Groups Affected<br />
13. Is a more detailed assessment needed?<br />
• If so, for what reason?<br />
14. Completed function/<strong>policy</strong><br />
15.<br />
• Who will sign this off?<br />
• When?<br />
Publication<br />
No<br />
Medical Director<br />
August2009<br />
Staffnet<br />
Document the<br />
Evidence/Research<br />
Document the<br />
Evidence/Research<br />
Actions Taken/To be Taken<br />
Identify any sources of training<br />
available, & develop training if<br />
required.<br />
Complaints are monitored by<br />
the organisation.<br />
Actions Taken/To be Taken<br />
14
9. <strong>NHS</strong> TAYSIDE - POLICY APPROVAL CHECKLIST<br />
This checklist must be completed <strong>and</strong> forwarded with <strong>policy</strong> to the appropriate<br />
forum/committee for approval: the Delivery Unit Executive Management Team <strong>and</strong> the<br />
Improvement <strong>and</strong> Quality Committee.<br />
POLICY AREA: Clinical<br />
POLICY TITLE: Intimate Personal Care & Chaperoning Policy<br />
LEAD OFFICER: Andrew Russell<br />
Why has this <strong>policy</strong> been developed?<br />
Has the <strong>policy</strong> been developed in<br />
accordance with or related to<br />
legislation? – Please give details of<br />
applicable legislation.<br />
Has a risk control plan been<br />
developed? Who is the owner of the<br />
risk?<br />
Who has been involved/consulted in<br />
the development of the <strong>policy</strong>?<br />
Has The <strong>policy</strong> been assessed for<br />
Equality <strong>and</strong> diversity in relation to:-<br />
Race/Ethnicity<br />
Gender<br />
Age<br />
Religion/Faith<br />
Disability<br />
Sexual<br />
orientation<br />
Yes<br />
Yes<br />
Yes<br />
Yes<br />
Yes<br />
Yes<br />
Does the <strong>policy</strong> contain evidence of<br />
the Equality & Diversity Impact<br />
Assessment Process?<br />
There is no existing <strong>policy</strong>. This <strong>policy</strong> will ensure<br />
that health professionals are able to comply with<br />
Legislation & recommendations from National<br />
Bodies.<br />
Adults with Incapacity (Scotl<strong>and</strong>) Act 2000<br />
Age of Legal Capacity (Scotl<strong>and</strong>) Act 1991<br />
The Children (Scotl<strong>and</strong>) Act 1995<br />
Mental Health (Care <strong>and</strong> Treatment) (Scotl<strong>and</strong>) Act<br />
2003<br />
Human Rights Act, 2000<br />
The Adult Support & Protection (Scotl<strong>and</strong>) Bill<br />
<strong>NHS</strong> Tayside Informed Consent Policy 2007<br />
Protecting Vulnerable Adults in Tayside: A Multi-<br />
Agency Protocol<br />
A Multi-Faith Resource for Health<strong>care</strong> Staff, <strong>NHS</strong><br />
Education Scotl<strong>and</strong><br />
Yes, Dr Andrew Russell<br />
Various groups of health <strong>care</strong> staff within <strong>NHS</strong>T,<br />
including patient & public groups.<br />
Has the <strong>policy</strong> been assessed For Equality <strong>and</strong><br />
Diversity not to disadvantage the following<br />
groups:-<br />
Minority Ethnic<br />
Communities<br />
(includes<br />
Gypsy/Travellers,<br />
Refugees & Asylum<br />
Seekers)<br />
Women <strong>and</strong> Men<br />
Religious & Faith Groups<br />
Disabled People<br />
Children <strong>and</strong> Young<br />
People<br />
Lesbian, Gay, Bisexual &<br />
Transgender Community<br />
YES<br />
Yes<br />
Yes<br />
Yes<br />
Yes<br />
Yes<br />
Yes<br />
Yes<br />
Yes
Is there an implementation plan? YES<br />
Which officers are responsible for<br />
implementation?<br />
The Medical Director is ultimately responsible<br />
but delegated responsibility lies with General<br />
Managers <strong>and</strong> CHP Managers.<br />
When will the <strong>policy</strong> take effect? Immediately following approval<br />
Who must comply with the <strong>policy</strong>? All health <strong>care</strong> practitioners who undertake any form<br />
of treatment, intervention or therapy<br />
How will they be informed of their The <strong>policy</strong> will be widely disseminated <strong>and</strong><br />
responsibilities?<br />
discussed within <strong>clinical</strong> governance forums,<br />
management meetings <strong>and</strong> be available on staffnet<br />
Is any training required? No<br />
If yes, has any been arranged? YES<br />
Are there any cost implications? NO<br />
If yes, please detail costs <strong>and</strong> note<br />
source of funding<br />
Who is responsible for auditing the<br />
implementation of the <strong>policy</strong>?<br />
What is the audit interval?<br />
Who will receive the audit reports?<br />
When will the <strong>policy</strong> be reviewed <strong>and</strong><br />
by whom? (please give designation)<br />
Annual<br />
Medical Director<br />
Two years (July 2011) by the Medical Director<br />
Name: _____________________________ Date: __________________<br />
16