Prenatal Screening for Fetal Aneuploidy in Singleton ... - SOGC
Prenatal Screening for Fetal Aneuploidy in Singleton ... - SOGC
Prenatal Screening for Fetal Aneuploidy in Singleton ... - SOGC
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
SCREENING FOR CHROMOSOMAL ANOMALIES<br />
Traditionally, <strong>in</strong> Canada, the option of <strong>in</strong>vasive test<strong>in</strong>g<br />
was recommended when a woman’s risk of hav<strong>in</strong>g a<br />
pregnancy with a chromosome anomaly was higher than<br />
the risks associated with the common <strong>in</strong>vasive procedures<br />
(amniocentesis or CVS). New developments <strong>in</strong> maternal<br />
serum and ultrasound screen<strong>in</strong>g have improved the ability to<br />
identify pregnancies at <strong>in</strong>creased risk <strong>for</strong> Down syndrome,<br />
trisomy 18, and other chromosomal abnormalities. This<br />
allows use of these screen<strong>in</strong>g tests to identify pregnancies<br />
at high enough risk to warrant <strong>in</strong>vasive diagnostic test<strong>in</strong>g,<br />
which has a risk of pregnancy loss.<br />
The most common chromosome conditions associated<br />
with advanced maternal age <strong>in</strong>volve the presence of an<br />
additional chromosome (21, 18, 13, or X). Down syndrome,<br />
trisomy 18, and trisomy 13 are associated with congenital<br />
anomalies and <strong>in</strong>tellectual disability. With ultrasound and<br />
maternal serum screen<strong>in</strong>g, pregnancies affected by these<br />
conditions can now be recognized with a significant<br />
degree of reliability. The practice of us<strong>in</strong>g solely maternal<br />
age at the estimated date of delivery to identify at-risk<br />
pregnancies should be abandoned. The maternal age-related<br />
risk should be modified by additional non-<strong>in</strong>vasive markers,<br />
which consist of maternal serum markers and ultrasound<br />
assessment. The approach to screen<strong>in</strong>g and diagnosis may<br />
vary between prov<strong>in</strong>ces. It is the responsibility of each<br />
health care provider to be aware of what is available to his<br />
or her patients so that appropriate counsell<strong>in</strong>g is provided.<br />
<strong>Prenatal</strong> <strong>Screen<strong>in</strong>g</strong> <strong>for</strong> <strong>Fetal</strong> <strong>Aneuploidy</strong> <strong>in</strong> S<strong>in</strong>gleton Pregnancies<br />
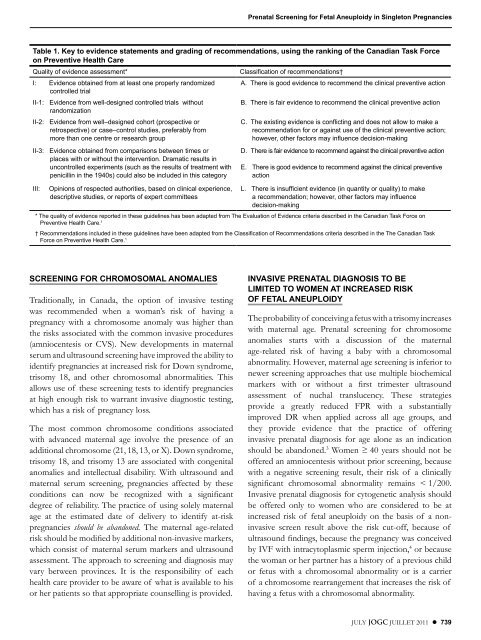
Table 1. Key to evidence statements and grad<strong>in</strong>g of recommendations, us<strong>in</strong>g the rank<strong>in</strong>g of the Canadian Task Force<br />
on Preventive Health Care<br />
Quality of evidence assessment* Classification of recommendations†<br />
I: Evidence obta<strong>in</strong>ed from at least one properly randomized A . There is good evidence to recommend the cl<strong>in</strong>ical preventive action<br />
controlled trial<br />
II-1: Evidence from well-designed controlled trials without<br />
B . There is fair evidence to recommend the cl<strong>in</strong>ical preventive action<br />
randomization<br />
II-2: Evidence from well–designed cohort (prospective or<br />
retrospective) or case–control studies, preferably from<br />
more than one centre or research group<br />
II-3: Evidence obta<strong>in</strong>ed from comparisons between times or<br />
places with or without the <strong>in</strong>tervention . Dramatic results <strong>in</strong><br />
uncontrolled experiments (such as the results of treatment with<br />
penicill<strong>in</strong> <strong>in</strong> the 1940s) could also be <strong>in</strong>cluded <strong>in</strong> this category<br />
III: Op<strong>in</strong>ions of respected authorities, based on cl<strong>in</strong>ical experience,<br />
descriptive studies, or reports of expert committees<br />
C . The exist<strong>in</strong>g evidence is conflict<strong>in</strong>g and does not allow to make a<br />
recommendation <strong>for</strong> or aga<strong>in</strong>st use of the cl<strong>in</strong>ical preventive action;<br />
however, other factors may <strong>in</strong>fluence decision-mak<strong>in</strong>g<br />
D . There is fair evidence to recommend aga<strong>in</strong>st the cl<strong>in</strong>ical preventive action<br />
E . There is good evidence to recommend aga<strong>in</strong>st the cl<strong>in</strong>ical preventive<br />
action<br />
L . There is <strong>in</strong>sufficient evidence (<strong>in</strong> quantity or quality) to make<br />
a recommendation; however, other factors may <strong>in</strong>fluence<br />
decision-mak<strong>in</strong>g<br />
* The quality of evidence reported <strong>in</strong> these guidel<strong>in</strong>es has been adapted from The Evaluation of Evidence criteria described <strong>in</strong> the Canadian Task Force on<br />
Preventive Health Care . 1<br />
† Recommendations <strong>in</strong>cluded <strong>in</strong> these guidel<strong>in</strong>es have been adapted from the Classification of Recommendations criteria described <strong>in</strong> the The Canadian Task<br />
Force on Preventive Health Care . 1<br />
INVASIVE PRENATAL DIAGNOSIS TO BE<br />
LIMITED TO WOMEN AT INCREASED RISK<br />
OF FETAL ANEuPLOIDY<br />
The probability of conceiv<strong>in</strong>g a fetus with a trisomy <strong>in</strong>creases<br />
with maternal age. <strong>Prenatal</strong> screen<strong>in</strong>g <strong>for</strong> chromosome<br />
anomalies starts with a discussion of the maternal<br />
age-related risk of hav<strong>in</strong>g a baby with a chromosomal<br />
abnormality. However, maternal age screen<strong>in</strong>g is <strong>in</strong>ferior to<br />
newer screen<strong>in</strong>g approaches that use multiple biochemical<br />
markers with or without a first trimester ultrasound<br />
assessment of nuchal translucency. These strategies<br />
provide a greatly reduced FPR with a substantially<br />
improved DR when applied across all age groups, and<br />
they provide evidence that the practice of offer<strong>in</strong>g<br />
<strong>in</strong>vasive prenatal diagnosis <strong>for</strong> age alone as an <strong>in</strong>dication<br />
should be abandoned. 3 Women ≥ 40 years should not be<br />
offered an amniocentesis without prior screen<strong>in</strong>g, because<br />
with a negative screen<strong>in</strong>g result, their risk of a cl<strong>in</strong>ically<br />
significant chromosomal abnormality rema<strong>in</strong>s < 1/200.<br />
Invasive prenatal diagnosis <strong>for</strong> cytogenetic analysis should<br />
be offered only to women who are considered to be at<br />
<strong>in</strong>creased risk of fetal aneuploidy on the basis of a non<strong>in</strong>vasive<br />
screen result above the risk cut-off, because of<br />
ultrasound f<strong>in</strong>d<strong>in</strong>gs, because the pregnancy was conceived<br />
by IVF with <strong>in</strong>tracytoplasmic sperm <strong>in</strong>jection, 4 or because<br />
the woman or her partner has a history of a previous child<br />
or fetus with a chromosomal abnormality or is a carrier<br />
of a chromosome rearrangement that <strong>in</strong>creases the risk of<br />
hav<strong>in</strong>g a fetus with a chromosomal abnormality.<br />
JULY JOGC JUILLET 2011 l 739