Management of Skin and Soft Tissue Infections in
Management of Skin and Soft Tissue Infections in
Management of Skin and Soft Tissue Infections in
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
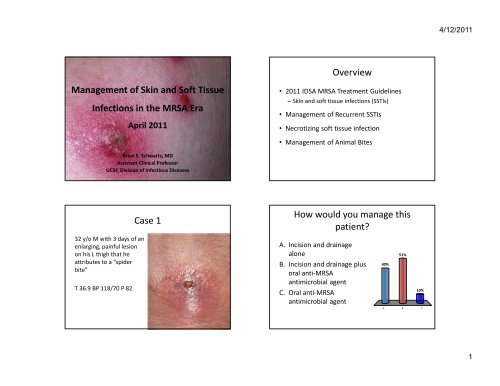
<strong>Management</strong> <strong>of</strong> <strong>Sk<strong>in</strong></strong> <strong>and</strong> S<strong>of</strong>t <strong>Tissue</strong><br />
<strong>Infections</strong> <strong>in</strong> the MRSA Era<br />
April 2011<br />
Brian S. Schwartz, MD<br />
Assistant Cl<strong>in</strong>ical Pr<strong>of</strong>essor<br />
UCSF, Division <strong>of</strong> Infectious Diseases<br />
32 y/o M with 3 days <strong>of</strong> an<br />
enlarg<strong>in</strong>g, pa<strong>in</strong>ful lesion<br />
on his L thigh that he<br />
attributes to a “spider<br />
bite”<br />
T 36.9 BP 118/70 P 82<br />
Case 1<br />
Overview<br />
• 2011 IDSA MRSA Treatment Guidel<strong>in</strong>es<br />
– <strong>Sk<strong>in</strong></strong> <strong>and</strong> s<strong>of</strong>t tissue <strong>in</strong>fections (SSTIs)<br />
• <strong>Management</strong> <strong>of</strong> Recurrent SSTIs<br />
• Necrotiz<strong>in</strong>g s<strong>of</strong>t tissue <strong>in</strong>fection<br />
• <strong>Management</strong> <strong>of</strong> Animal Bites<br />
How would you manage this<br />
patient?<br />
A. Incision <strong>and</strong> dra<strong>in</strong>age<br />
alone<br />
B. Incision <strong>and</strong> dra<strong>in</strong>age plus<br />
oral anti-MRSA<br />
antimicrobial agent<br />
C. Oral anti-MRSA<br />
antimicrobial agent<br />
40%<br />
51%<br />
10%<br />
A. B. C.<br />
4/12/2011<br />
1
Microbiology <strong>of</strong> Purulent SSTIs<br />
Moran NEJM 2006<br />
Is treatment failure the only<br />
important endpo<strong>in</strong>t? Recurrent SSTI?<br />
• Duong : 10 days<br />
– 9% TMP-SMX vs. 28% placebo , p = .02<br />
• Schmitz: 30 days<br />
– 13% TMP-SMX vs 26% placebo, p= .04<br />
Schmitz G Ann Emerg Med 2010; Duong Ann Emerg Med 2009<br />
% patients cured<br />
Abscesses: Do antibiotics provide<br />
benefit over I&D alone?<br />
100%<br />
80%<br />
60%<br />
40%<br />
20%<br />
0%<br />
p=.25 p=.12 p=.52<br />
Cephalex<strong>in</strong> TMP-SMX TMP-SMX<br />
Rajendran '07 Duong '09 Schmitz '10<br />
Placebo<br />
Antibiotic<br />
1 Rajendran AAC 2007; 2 Schmitz G Ann Emerg Med 2010; 3 Duong Ann Emerg Med 2009<br />
Antibiotic therapy is recommended<br />
for abscesses associated with:<br />
• Severe disease, rapidly progressive with<br />
associated cellulitis or septic phlebitis<br />
• Signs or symptoms <strong>of</strong> systemic illness<br />
• Associated comorbidities, immunosuppressed<br />
• Extremes <strong>of</strong> age<br />
• Difficult to dra<strong>in</strong> area (face, h<strong>and</strong>, genitalia)<br />
• Failure <strong>of</strong> prior I&D<br />
Liu C. Cl<strong>in</strong> Infect Dis. 2011<br />
4/12/2011<br />
2
When to culture a purulent SSTI?<br />
• Patients Rx with antibiotics<br />
• Patients with severe local <strong>in</strong>fections<br />
• Patients with signs <strong>of</strong> systemic illness<br />
• Patient has not responded to <strong>in</strong>itial Rx<br />
• Concern for outbreak or cluster<br />
28 y/o woman presents<br />
with erythema <strong>of</strong> her left<br />
foot over past 48 hrs<br />
No purulent dra<strong>in</strong>age,<br />
exudate , or fluctuance.<br />
T 37.0 BP 132/70 P 78<br />
Case 2<br />
Liu C. Cl<strong>in</strong> Infect Dis. 2011<br />
Eels SJ et al Epidemiology <strong>and</strong> Infection 2010<br />
Empiric oral antibiotic Rx<br />
for uncomplicated purulent SSTI<br />
Drug Adult Dose<br />
TMP/SMX DS 1-2 BID<br />
Doxycycl<strong>in</strong>e, M<strong>in</strong>ocycl<strong>in</strong>e 100 BID<br />
Cl<strong>in</strong>damyc<strong>in</strong> 300-450 TID<br />
L<strong>in</strong>ezolid 600 BID<br />
*Rifamp<strong>in</strong> is NOT recommended for rout<strong>in</strong>e treatment <strong>of</strong> SSTIs<br />
How would you manage this<br />
patient?<br />
A. Cl<strong>in</strong>damyc<strong>in</strong> 300 mg TID<br />
B. Cephalex<strong>in</strong> 500 mg QID,<br />
monitor cl<strong>in</strong>ically with addition<br />
<strong>of</strong> TMP/SMX if no response<br />
C. Cephalex<strong>in</strong> 500 mg QID + TMP/<br />
SMX 2 DS BID<br />
21%<br />
54%<br />
25%<br />
A. B. C.<br />
4/12/2011<br />
3
Nonpurulent Cellulitis: pathogen?<br />
β-hemolytic strep vs. S. aureus?<br />
• Prospective study, hospitalized patients (N=248)<br />
Methods<br />
– Acute <strong>and</strong> convalescent titers (ASO <strong>and</strong> anti-DNaseB)<br />
– Rx with β -lactam antibiotics (cefazol<strong>in</strong>/oxacill<strong>in</strong>)<br />
Results<br />
– 73% due to β-hemolytic strep; 27% none identified<br />
– 96% response rate to β-lactam antibiotic<br />
Silj<strong>and</strong>er T. Cl<strong>in</strong> Infect Dis. 2008 Jeng A. Medic<strong>in</strong>e 2010. Elliott Pediatrics 2009<br />
Summary: empiric management <strong>of</strong> SSTIs<br />
Uncomplicated<br />
Complicated<br />
•I&D<br />
Purulent<br />
(MRSA)<br />
Consider addition <strong>of</strong> anti-MRSA<br />
antibiotic <strong>in</strong> select situations 1<br />
•I&D plus vancomyc<strong>in</strong> (or<br />
alternative) 2<br />
Non-purulent<br />
(β-hemolytic strep)<br />
• Cephalex<strong>in</strong> 500 QID<br />
• Dicloxacill<strong>in</strong> 500 QID<br />
Consider addition <strong>of</strong> MRSA active<br />
agent if no response 1<br />
•Vancomyc<strong>in</strong> (or<br />
alternative) 2<br />
1. Systemic illness, purulent cellulitis/wound <strong>in</strong>fection, comorbidities, extremes <strong>of</strong> age,<br />
abscess difficult to dra<strong>in</strong> or face/h<strong>and</strong>, septic phlebitis, lack <strong>of</strong> response <strong>of</strong> to I&D alone.<br />
PO antibiotic : TMP-SMX 1 DS BID, Cl<strong>in</strong>damyc<strong>in</strong> 300 mg TID, Doxycycl<strong>in</strong>e 100 PO BID<br />
2. Daptomyc<strong>in</strong>, l<strong>in</strong>ezolid, telavanc<strong>in</strong>, ceftarol<strong>in</strong>e<br />
Empiric treatment <strong>of</strong> uncomplicated<br />
nonpurulent cellulitis?<br />
• Anti-β-hemolytic strep antibiotic (+/- anti-MSSA)<br />
Drug Adult Dose<br />
Cephalex<strong>in</strong> 500 QID<br />
Dicloxacill<strong>in</strong> 500 QID<br />
Cl<strong>in</strong>damyc<strong>in</strong>* 300-450 TID<br />
L<strong>in</strong>ezolid* 600 BID<br />
*Have activity aga<strong>in</strong>st MRSA<br />
• If poor response, add anti-MRSA antibiotic<br />
Empiric antibiotics for complicated SSTI<br />
Antibiotic Adult Pediatric<br />
Vancomyc<strong>in</strong> 15-20 mg/kg IV Q8-12 15 mg/kg IV Q6<br />
L<strong>in</strong>ezolid 600 mg PO/ IV BID 10 mg/kg PO/IV Q8<br />
Daptomyc<strong>in</strong> 4 mg/kg IV QD Ongo<strong>in</strong>g study<br />
Telavanc<strong>in</strong> 10 mg/kg IV QD *No data<br />
Ceftarol<strong>in</strong>e 600 mg IV Q12 *No data<br />
4/12/2011<br />
4
Classic impetigo<br />
Ecythema<br />
Impetigo<br />
Case 3<br />
Bullous impetigo<br />
• Patient presents with 4 th abscess <strong>in</strong> 4 months<br />
• Prior abscesses have been treated with I&D<br />
<strong>and</strong> antibiotics with resolution<br />
• He asks if there is anyth<strong>in</strong>g he can do to<br />
prevent recurrences<br />
Impetigo<br />
• Def<strong>in</strong>ition: superficial, <strong>in</strong>tra-epidermal <strong>in</strong>fection<br />
• Epi: Common <strong>in</strong> children, highly communicable<br />
• Pathogens: S. aureus, Group A strep<br />
• Treatment:<br />
– Few lesions (topical = systemic)<br />
• Mupiroc<strong>in</strong> or Retapamul<strong>in</strong> o<strong>in</strong>tment<br />
– Multiple lesions (systemic >> topical)<br />
• Pick agent(s) active aga<strong>in</strong>st CA-MRSA <strong>and</strong> Group A strep<br />
How would you manage this<br />
patient?<br />
A. Emphasize personal hygiene<br />
measures<br />
B. Decolonize with mupiroc<strong>in</strong> <strong>and</strong><br />
chlorhexid<strong>in</strong>e<br />
C. Decolonize with TMP-SMX <strong>and</strong><br />
rifamp<strong>in</strong><br />
D. All the above<br />
9%<br />
65%<br />
11%<br />
15%<br />
A. B. C. D.<br />
4/12/2011<br />
5
How to Manage Recurrent <strong>Sk<strong>in</strong></strong> <strong>and</strong><br />
S<strong>of</strong>t <strong>Tissue</strong> <strong>Infections</strong>?<br />
Host<br />
Environment Pathogen<br />
Decolonization strategies<br />
• Intranasal mupiroc<strong>in</strong><br />
• Chlorhexid<strong>in</strong>e washes<br />
• Suppressive oral antibiotics<br />
• Oral therapy with rifamyc<strong>in</strong>s<br />
What is the <strong>Management</strong> <strong>of</strong> Recurrent <strong>Sk<strong>in</strong></strong> <strong>and</strong><br />
S<strong>of</strong>t <strong>Tissue</strong> <strong>Infections</strong>?<br />
Environmental Hygiene (CIII)<br />
-Clean high-touch surfaces<br />
Personal Hygiene Hygiene/ Wound Care (AIII)<br />
Host<br />
Environment Pathogen<br />
-Cover dra<strong>in</strong><strong>in</strong>g wounds<br />
-H<strong>and</strong> hygiene<br />
-Avoid shar<strong>in</strong>g if active <strong>in</strong>fection<br />
Decolonization*<br />
Decolonization (CIII)<br />
Liu C. Cl<strong>in</strong> Infect Dis. 2011<br />
Intra-nasal mupiroc<strong>in</strong> to prevent<br />
recurrent MSSA SSTI?<br />
• Methods:<br />
– ≥ 3 SSTIs <strong>in</strong> 2 years plus S. aureus nasal carriage<br />
– R<strong>and</strong>omized study<br />
– Intervention: Nasal mupiroc<strong>in</strong> BID 1 wk/mo x 1 yr<br />
• Results: (N=40)<br />
– Primary endpo<strong>in</strong>t: recurrent SSTI<br />
– 6% (mupiroc<strong>in</strong>) vs. 47% (placebo); p < 0.02<br />
Raz R. Arch Int Med. 1996<br />
4/12/2011<br />
6
Intra-nasal mupiroc<strong>in</strong> to prevent<br />
CA-MRSA SSTI?<br />
• 1° prophylaxis (prospective RCT)<br />
– 134 soldiers with CA-MRSA nasal colonization<br />
– Mupiroc<strong>in</strong> (5d) vs. placebo<br />
– SSTI: 10.6% mupiroc<strong>in</strong> vs. 7.7% placebo<br />
• 2° prophylaxis (retrospective)<br />
– 38 HIV+ with CA-MRSA SSSI <strong>and</strong> nasal colonization<br />
– Mupiroc<strong>in</strong> vs. no treatment<br />
– Recurrent SSTI: 32% mupiroc<strong>in</strong> vs. 52% no treatment<br />
Ellis et al, AAC ’07. Rahima<strong>in</strong> et al, ICHE ’07<br />
Daily cl<strong>in</strong>damyc<strong>in</strong> to prevent<br />
recurrent SSTI?<br />
• Subjects: ≥3 abscesses <strong>in</strong> prior 6 months<br />
• Rx: cl<strong>in</strong>damyc<strong>in</strong> 150 mg QD vs. placebo<br />
• Results: Abscess dur<strong>in</strong>g Rx period<br />
– 33% (cl<strong>in</strong>da) vs. 81% (placebo); p=0.04<br />
– High recurrence rate after stopp<strong>in</strong>g cl<strong>in</strong>damyc<strong>in</strong><br />
Klempner MS. JAMA 1988.<br />
Chlorhexid<strong>in</strong>e to prevent SA SSTI<br />
• RCT <strong>of</strong> military recruits to prevent SSTI<br />
• Chlorhexid<strong>in</strong>e wipes vs. placebo 3 x/week<br />
• Results: SSTI rate at 6 weeks<br />
•<br />
% S. aureus carriage<br />
– 9.4% (chlorhexid<strong>in</strong>e) vs. 7.1% (placebo); p=0.13<br />
• Results: S. aureus colonization (45% basel<strong>in</strong>e)<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
– 52.6% (chlorhexid<strong>in</strong>e) vs. 67% (placebo)<br />
Whitman TJ. Infect Control Hosp Epidemiol. 2010<br />
Rifamp<strong>in</strong> for eradication <strong>of</strong><br />
S. aureus colonization?<br />
Rx period<br />
Control<br />
Rifamp<strong>in</strong><br />
Cloxacill<strong>in</strong><br />
Rifamp<strong>in</strong> <strong>and</strong> Cloxacill<strong>in</strong><br />
0 0.5 1 2 3 4 5 6 7 8 9 10 11 12<br />
Weeks<br />
Wheat J. JID. 1981.<br />
4/12/2011<br />
7
Case 4<br />
• 34 y/o M comes <strong>in</strong> with<br />
arm pa<strong>in</strong>, fever<br />
• Temp 38.9, HR 105, SBP<br />
100, RR 20<br />
• Appears ill <strong>and</strong> <strong>in</strong> more<br />
pa<strong>in</strong> than what you<br />
would expect for<br />
cellulitis<br />
Necrotiz<strong>in</strong>g sk<strong>in</strong> <strong>and</strong> sk<strong>in</strong> structure<br />
<strong>in</strong>fections<br />
• Def<strong>in</strong>ition: <strong>in</strong>fections <strong>of</strong> any layer with<strong>in</strong> the s<strong>of</strong>t<br />
tissue compartment that are associated with<br />
necrotiz<strong>in</strong>g changes<br />
• Monomicrobial<br />
– associated w/ m<strong>in</strong>or <strong>in</strong>juries<br />
• Polymicrobial<br />
– associated w/ abdom<strong>in</strong>al surgery, decub ulcers,<br />
IVDU, spread from GI tract<br />
What would your empiric therapy<br />
be <strong>in</strong> this case?<br />
A. Cephalex<strong>in</strong> plus TMP-SMX, send<br />
home<br />
B. Cl<strong>in</strong>damyc<strong>in</strong>, piperacill<strong>in</strong>tazobactam,<br />
<strong>and</strong> vancomyc<strong>in</strong><br />
C. Call surgery, vancomyc<strong>in</strong> <strong>and</strong><br />
ceftriaxone<br />
D. Call surgery, cl<strong>in</strong>damyc<strong>in</strong>,<br />
piperacill<strong>in</strong>-tazobactam, <strong>and</strong><br />
vancomyc<strong>in</strong><br />
0%<br />
13%<br />
40%<br />
47%<br />
A. B. C. D.<br />
Necrotiz<strong>in</strong>g s<strong>of</strong>t tissue <strong>in</strong>fections:<br />
risk factors<br />
• IVDU<br />
• Diabetes<br />
• Obesity<br />
• Chronic immune suppression<br />
Anaya DA. Cl<strong>in</strong> Infect Dis. 2007<br />
4/12/2011<br />
8
Why is early diagnosis so important?<br />
Wong CH. Jour <strong>of</strong> Bone <strong>and</strong> Jo<strong>in</strong>t Surg. 2003<br />
Mortality rate: > 30%<br />
Necrotiz<strong>in</strong>g s<strong>of</strong>t tissue <strong>in</strong>fections:<br />
radiographic techniques<br />
• Pla<strong>in</strong> films<br />
– Low sensitivity<br />
– Helpful if gas present<br />
• CT <strong>and</strong> ultrasound<br />
– May identify other Dx (abscess)<br />
• MRI<br />
– Enhanced sensitivity, low specificity<br />
% <strong>of</strong> patients<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Necrotiz<strong>in</strong>g s<strong>of</strong>t tissue <strong>in</strong>fections:<br />
cl<strong>in</strong>ical clues<br />
Wong CH. Jour <strong>of</strong> Bone <strong>and</strong> Jo<strong>in</strong>t Surg. 2003<br />
Late f<strong>in</strong>d<strong>in</strong>gs<br />
Necrotiz<strong>in</strong>g <strong>Sk<strong>in</strong></strong> <strong>and</strong> S<strong>of</strong>t <strong>Tissue</strong> Infection:<br />
Pathogens<br />
Monomicrobial Polymicrobial<br />
Group A strep<br />
Staphylococcus aureus<br />
Clostridia sp<br />
Gram negatives<br />
Vibrio vulnificus<br />
Aerobic gram +/gram -<br />
PLUS<br />
.<br />
Anaerobes<br />
Wong CH. J Bone <strong>and</strong> Jo<strong>in</strong>t Surg. 2003<br />
4/12/2011<br />
9
Empiric treatment <strong>of</strong> necrotiz<strong>in</strong>g s<strong>of</strong>t<br />
tissue <strong>in</strong>fections<br />
• Early surgical <strong>in</strong>tervention<br />
• Antimicrobial therapy<br />
– Piperacill<strong>in</strong>/tazobactam or carbapenem<br />
(anaerobes, GNR, streptococci)<br />
plus<br />
– Vancomyc<strong>in</strong> (MRSA)<br />
plus<br />
– Cl<strong>in</strong>damyc<strong>in</strong> (GAS)<br />
*Consider IVIG <strong>in</strong> severe<br />
cases <strong>of</strong> streptococcal<br />
toxic shock syndrome<br />
Which antibiotic regimen would be most<br />
appropriate for this patient ?<br />
A. Amoxicill<strong>in</strong>/clavulanic acid<br />
B. Cephalex<strong>in</strong><br />
C. Cl<strong>in</strong>damyc<strong>in</strong><br />
D. Metronidazole<br />
E. No antibiotics needed<br />
73%<br />
7%<br />
16%<br />
2%<br />
2%<br />
A. B. C. D. E.<br />
37 y/o male presents<br />
to cl<strong>in</strong>ic 4 days after<br />
receiv<strong>in</strong>g a dog bite to<br />
his forearm. He<br />
compla<strong>in</strong>s <strong>of</strong> pa<strong>in</strong>,<br />
some purulent<br />
dra<strong>in</strong>age.<br />
Case 5<br />
Animal Bites<br />
• 50% <strong>of</strong> Americans are bit by animals<br />
• 20% require medical attention<br />
• Animal bites account for 1% <strong>of</strong> ER visits<br />
• Bites result <strong>in</strong> 10,000 <strong>in</strong>pt admits/year<br />
4/12/2011<br />
10
Animal bites: bacteriology<br />
What’s <strong>in</strong> their mouth <strong>and</strong> on your sk<strong>in</strong><br />
• Average 5 organisms (range 0-16) per wound<br />
Dogs Cats<br />
Pasturella sp 50% 75%<br />
Streptococcus sp. 46% 46%<br />
Staphylococcus aureus 20% 4%<br />
Anaerobes mixed w/ aerobes 48% 63%<br />
Anaerobes alone 1% 0%<br />
Animal bites<br />
• Empiric treatment regimens<br />
Talan DA. NEJM. 1999<br />
– Amoxicill<strong>in</strong>/clavulanic acid +/- MRSA agent<br />
– Pen allergy: cipro + cl<strong>in</strong>damyc<strong>in</strong> or moxifloxac<strong>in</strong><br />
• Prophylaxis?<br />
– Moderate-severe bites or on face/h<strong>and</strong>s<br />
– Immunocompromised (splenectomized)<br />
– Cat bites<br />
Antibiotic coverage for Pasturella<br />
• What you want to use but won’t work…<br />
– 1 st generation cephalospor<strong>in</strong><br />
– anti-staphylococcal penicill<strong>in</strong>s<br />
– cl<strong>in</strong>damyc<strong>in</strong><br />
• What works…<br />
–amoxicill<strong>in</strong><br />
–doxycycl<strong>in</strong>e<br />
–fluoroqu<strong>in</strong>olone<br />
• Bacteriology<br />
Human bites<br />
– Mixed <strong>in</strong>fection with streptococci, anaerobes <strong>and</strong><br />
gram negatives (Haemophilus sp., Eik<strong>in</strong>ella sp.)<br />
– High rates <strong>of</strong> <strong>in</strong>fection<br />
• Treatment<br />
– Same as animal bites<br />
• Prophylaxis – everyone, same as animal bites<br />
4/12/2011<br />
11
Rabies – what type <strong>of</strong> bites are high risk?<br />
Animal Type<br />
Dog, cats, ferrets<br />
Skunk, raccoons,<br />
foxes, bats<br />
Livestock, small<br />
rodents, rabbits,<br />
large rodents<br />
Evaluation <strong>and</strong><br />
disposure <strong>of</strong> animal<br />
Suspected/confirmed rabid<br />
Healthy<br />
Animal lost<br />
Regarded as rabid unless<br />
proven negative by lab test<br />
Consider <strong>in</strong>dividually<br />
Post-exposure<br />
prophylaxis<br />
Prophylaxis<br />
10 days observation/test<br />
Contact DPH<br />
Immediate prophylaxis<br />
Almost never require<br />
prophylaxis<br />
http://www.cdc.gov/rabies/resources/contacts.html<br />
45 y/o man presents<br />
with several weeks <strong>of</strong><br />
progressive pa<strong>in</strong>ful<br />
“bumps” spread<strong>in</strong>g up<br />
his left forearm.<br />
Case 6<br />
Rabies - Post-exposure prophylaxis<br />
• Wound cleans<strong>in</strong>g: virucidal agent (iod<strong>in</strong>e)<br />
• Rabies Immune Globul<strong>in</strong><br />
– 20 IU/kg body weight<br />
– Infiltrated full dose around the wound(s) <strong>and</strong><br />
rema<strong>in</strong><strong>in</strong>g volume IM at site distant from vacc<strong>in</strong>e<br />
• Vacc<strong>in</strong>ate: Days 0,3,7, <strong>and</strong> 14<br />
http://www.cdc.gov/mmwr/preview/mmwrhtml/rr57e507a1.htm,<br />
http://www.cdc.gov/mmwr/pdf/rr/rr5902.pdf<br />
Which <strong>of</strong> these questions<br />
should you ask?<br />
A. Do you have a fish tank?<br />
B. Have you been around a sick rabbit?<br />
C. Do you garden?<br />
D. Have you been travel<strong>in</strong>g <strong>in</strong> S.<br />
America?<br />
E. All <strong>of</strong> the above<br />
5%<br />
1%<br />
25%<br />
21%<br />
48%<br />
A. B. C. D. E.<br />
4/12/2011<br />
12
Nodular lymphangitis:<br />
management?<br />
• Take a good history<br />
• Obta<strong>in</strong> biopsy<br />
– Pathology: sta<strong>in</strong> for fungi <strong>and</strong> mycobacteria<br />
– Cultures: bacterial, fungal, <strong>and</strong> mycobacterial<br />
• Consider empiric therapy based on severity <strong>of</strong><br />
disease <strong>and</strong> history prior to biopsy results<br />
Nodular Lymphangitis: DDx<br />
• Short <strong>in</strong>cubation (days)<br />
– Francisella tularensis (rabbits, ticks)<br />
• Medium <strong>in</strong>cubation (2-4 weeks)<br />
– Nocardia (brasiliensis >> asteroides) (soil)<br />
• Long <strong>in</strong>cubation (weeks-months)<br />
– Mycobacterium mar<strong>in</strong>um (fish tanks)<br />
– Sporothrix schenkii (vegetation)<br />
– Leishmania sps (s<strong>and</strong>fly)<br />
4/12/2011<br />
13