the use of tissue expansion in the treatment of burn sequelas – our ...
the use of tissue expansion in the treatment of burn sequelas – our ...
the use of tissue expansion in the treatment of burn sequelas – our ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
scar removal was done <strong>in</strong> a s<strong>in</strong>gle stage <strong>of</strong> <strong>expansion</strong>,<br />
<strong>in</strong> 13/106 patients <strong>the</strong>re were necessary 2 stages, 3/106<br />
patients needed 3 stages, and 2/106 patients needed 4<br />
stages <strong>of</strong> <strong>tissue</strong> <strong>expansion</strong>. There are 18/106 patients<br />
(16.98%) still <strong>in</strong> <strong>treatment</strong>. Some patients were treated<br />
by us<strong>in</strong>g 2 expanders simultaneously; <strong>in</strong> one patient we<br />
<strong>use</strong>d 4 expanders <strong>in</strong> <strong>the</strong> same time (one for cervical<br />
area, one for <strong>the</strong> anterior trunk and 2 for <strong>the</strong> lower<br />
limb). (Table 3)<br />
Table 3. Number <strong>of</strong> patients with def<strong>in</strong>itive scar excision and<br />
reconstruction versus those still <strong>in</strong> c<strong>our</strong>se <strong>of</strong> <strong>treatment</strong>, accord<strong>in</strong>g to <strong>the</strong><br />
<strong>expansion</strong> stage.<br />
Total number<br />
<strong>of</strong> patients <strong>in</strong><br />
<strong>the</strong> study:<br />
106 patients<br />
Patients with<br />
complete scar<br />
removal<br />
88 patients<br />
(83.01%)<br />
Patients <strong>in</strong><br />
c<strong>our</strong>se <strong>of</strong><br />
<strong>treatment</strong><br />
18 patients<br />
(16,98%)<br />
DISCUSSIONS<br />
1 st stage <strong>of</strong><br />
<strong>expansion</strong><br />
2 nd stage <strong>of</strong><br />
<strong>expansion</strong><br />
3 rd stage <strong>of</strong><br />
<strong>expansion</strong><br />
4 th stage <strong>of</strong><br />
<strong>expansion</strong><br />
1 st stage <strong>of</strong><br />
<strong>expansion</strong><br />
2 nd stage <strong>of</strong><br />
<strong>expansion</strong><br />
3 rd stage <strong>of</strong><br />
<strong>expansion</strong><br />
70 patients<br />
13 patients<br />
3 patients<br />
2 patients<br />
12 patients<br />
4 patients<br />
2 patients<br />
Spontaneous heal<strong>in</strong>g <strong>of</strong> <strong>in</strong>termediate deep <strong>burn</strong>s<br />
and sk<strong>in</strong> graft coverage <strong>of</strong> deep <strong>burn</strong>s leaves beh<strong>in</strong>d<br />
areas <strong>of</strong> postcombustional scars that raise o<strong>the</strong>r<br />
issues: <strong>the</strong>y tend to shr<strong>in</strong>k dur<strong>in</strong>g <strong>the</strong>ir evolution and<br />
frequently become unstable, thus hav<strong>in</strong>g a high risk <strong>of</strong><br />
ulceration, leav<strong>in</strong>g beh<strong>in</strong>d functional impairment and<br />
unpleasant appearance.<br />
In <strong>the</strong> past, <strong>the</strong> <strong>treatment</strong> <strong>of</strong> large area post<strong>burn</strong><br />
sequelae consisted ma<strong>in</strong>ly <strong>in</strong> <strong>in</strong>cision/excision<br />
followed by sk<strong>in</strong> grafts or transposition <strong>of</strong> local sk<strong>in</strong><br />
flaps. Frequently encountered problems were sk<strong>in</strong><br />
graft retraction with functional deficit and unpleasant<br />
cosmetic aspects, or <strong>in</strong>sufficient local res<strong>our</strong>ces for<br />
cover<strong>in</strong>g <strong>the</strong> rema<strong>in</strong><strong>in</strong>g sk<strong>in</strong> defects after scar excision.<br />
Use <strong>of</strong> free <strong>tissue</strong> transfer is a tedious procedure,<br />
with more or less donor site availability and morbidity<br />
and higher risk <strong>of</strong> flap necrosis. In <strong>the</strong> last years, <strong>tissue</strong><br />
<strong>expansion</strong> technique has improved <strong>the</strong> postoperative<br />
results <strong>in</strong> <strong>the</strong>se cases.<br />
One <strong>of</strong> <strong>the</strong> ma<strong>in</strong> advantages <strong>of</strong> <strong>tissue</strong> <strong>expansion</strong> is<br />
that it allows full <strong>use</strong> <strong>of</strong> <strong>the</strong> tegument <strong>of</strong> any region. 4<br />
A<br />
B<br />
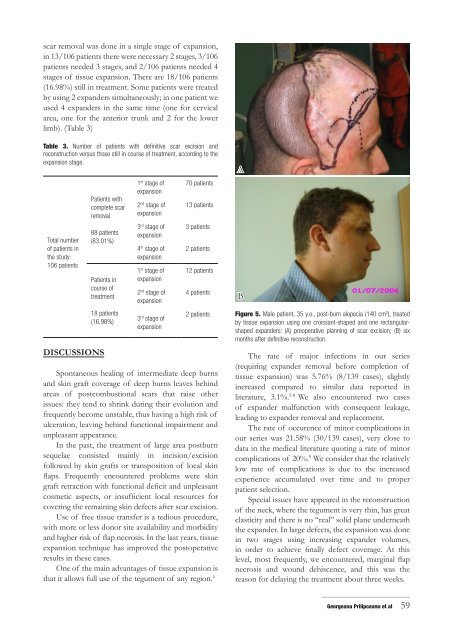
Figure 5. Male patient, 35 y.o., post-<strong>burn</strong> alopecia (140 cm 2 ), treated<br />
by <strong>tissue</strong> <strong>expansion</strong> us<strong>in</strong>g one croissant-shaped and one rectangularshaped<br />
expanders: (A) preoperative plann<strong>in</strong>g <strong>of</strong> scar excision; (B) six<br />
months after def<strong>in</strong>itive reconstruction.<br />
The rate <strong>of</strong> major <strong>in</strong>fections <strong>in</strong> <strong>our</strong> series<br />
(requir<strong>in</strong>g expander removal before completion <strong>of</strong><br />
<strong>tissue</strong> <strong>expansion</strong>) was 5.76% (8/139 cases), slightly<br />
<strong>in</strong>creased compared to similar data reported <strong>in</strong><br />
literature, 3.1%. 5-8 We also encountered two cases<br />
<strong>of</strong> expander malfunction with consequent leakage,<br />
lead<strong>in</strong>g to expander removal and replacement.<br />
The rate <strong>of</strong> occurence <strong>of</strong> m<strong>in</strong>or complications <strong>in</strong><br />
<strong>our</strong> series was 21.58% (30/139 cases), very close to<br />
data <strong>in</strong> <strong>the</strong> medical literature quot<strong>in</strong>g a rate <strong>of</strong> m<strong>in</strong>or<br />
complications <strong>of</strong> 20%. 9 We consider that <strong>the</strong> relatively<br />
low rate <strong>of</strong> complications is due to <strong>the</strong> <strong>in</strong>creased<br />
experience accumulated over time and to proper<br />
patient selection.<br />
Special issues have appeared <strong>in</strong> <strong>the</strong> reconstruction<br />
<strong>of</strong> <strong>the</strong> neck, where <strong>the</strong> tegument is very th<strong>in</strong>, has great<br />
elasticity and <strong>the</strong>re is no “real” solid plane underneath<br />
<strong>the</strong> expander. In large defects, <strong>the</strong> <strong>expansion</strong> was done<br />
<strong>in</strong> two stages us<strong>in</strong>g <strong>in</strong>creas<strong>in</strong>g expander volumes,<br />
<strong>in</strong> order to achieve f<strong>in</strong>ally defect coverage. At this<br />
level, most frequently, we encountered, marg<strong>in</strong>al flap<br />
necrosis and wound dehiscence, and this was <strong>the</strong><br />
reason for delay<strong>in</strong>g <strong>the</strong> <strong>treatment</strong> about three weeks.<br />
_____________________________<br />
Georgeana Prilipceanu et al 59