Clinical Laboratory News - American Association for Clinical ...
Clinical Laboratory News - American Association for Clinical ...
Clinical Laboratory News - American Association for Clinical ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
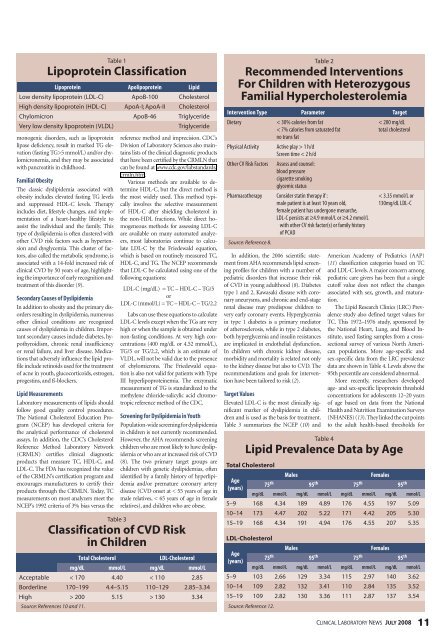
table 1<br />
lipoprotein classification<br />
Lipoprotein Apolipoprotein Lipid<br />
low density lipoprotein (ldl-C) apob-100 Cholesterol<br />
High density lipoprotein (Hdl-C) apoa-i; apoa-ii Cholesterol<br />
Chylomicron apob-46 triglyceride<br />
Very low density lipoprotein (Vldl) triglyceride<br />
monogenic disorders, such as lipoprotein<br />
lipase deficiency, result in marked TG elevation<br />
(fasting TG>5 mmol/L) and/or chylomicronemia,<br />
and they may be associated<br />
with pancreatitis in childhood.<br />
Familial Obesity<br />
The classic dyslipidemia associated with<br />
obesity includes elevated fasting TG levels<br />
and suppressed HDL-C levels. Therapy<br />
includes diet, lifestyle changes, and implementation<br />
of a heart-healthy lifestyle to<br />
assist the individual and the family. This<br />
type of dyslipidemia is often clustered with<br />
other CVD risk factors such as hypertension<br />
and dysglycemia. This cluster of factors,<br />
also called the metabolic syndrome, is<br />
associated with a 14-fold increased risk of<br />
clinical CVD by 50 years of age, highlighting<br />
the importance of early recognition and<br />
treatment of this disorder (9).<br />
Secondary Causes of Dyslipidemia<br />
In addition to obesity and the primary disorders<br />
resulting in dyslipidemia, numerous<br />
other clinical conditions are recognized<br />
causes of dyslipidemia in children. Important<br />
secondary causes include diabetes, hypothyroidism,<br />
chronic renal insufficiency<br />
or renal failure, and liver disease. Medications<br />
that adversely influence the lipid profile<br />
include retinoids used <strong>for</strong> the treatment<br />
of acne in youth, glucocorticoids, estrogen,<br />
progestins, and ß-blockers.<br />
Lipid Measurements<br />
<strong>Laboratory</strong> measurements of lipids should<br />
follow good quality control procedures.<br />
The National Cholesterol Education Program<br />
(NCEP) has developed criteria <strong>for</strong><br />
the analytical per<strong>for</strong>mance of cholesterol<br />
assays. In addition, the CDC’s Cholesterol<br />
Reference Method <strong>Laboratory</strong> Network<br />
(CRMLN) certifies clinical diagnostic<br />
products that measure TC, HDL-C, and<br />
LDL-C. The FDA has recognized the value<br />
of the CRMLN’s certification program and<br />
encourages manufacturers to certify their<br />
products through the CRMLN. Today, TC<br />
measurements on most analyzers meet the<br />
NCEP’s 1992 criteria of 3% bias versus the<br />
reference method and imprecision. CDC’s<br />
Division of <strong>Laboratory</strong> Sciences also maintains<br />
lists of the clinical diagnostic products<br />
that have been certified by the CRMLN that<br />
can be found at www.cdc.gov/labstandards/<br />
crmln.htm.<br />
Various methods are available to determine<br />
HDL-C, but the direct method is<br />
the most widely used. This method typically<br />
involves the selective measurement<br />
of HDL-C after shielding cholesterol in<br />
the non-HDL fractions. While direct homogeneous<br />
methods <strong>for</strong> assessing LDL-C<br />
are available on many automated analyzers,<br />
most laboratories continue to calculate<br />
LDL-C by the Friedewald equation,<br />
which is based on routinely measured TC,<br />
HDL-C, and TG. The NCEP recommends<br />
that LDL-C be calculated using one of the<br />
following equations:<br />
LDL-C (mg/dL) = TC – HDL-C – TG/5<br />
or<br />
LDL-C (mmol/L) = TC – HDL-C – TG/2.2<br />
Labs can use these equations to calculate<br />
LDL-C levels except when the TGs are very<br />
high or when the sample is obtained under<br />
non-fasting conditions. At very high concentrations<br />
(400 mg/dL or 4.52 mmol/L),<br />
TG/5 or TG/2.2, which is an estimate of<br />
VLDL, will not be valid due to the presence<br />
of chylomicrons. The Friedewald equation<br />
is also not valid <strong>for</strong> patients with Type<br />
III hyperlipoproteinemia. The enzymatic<br />
measurement of TG is standardized to the<br />
methylene chloride-salicylic acid chromotropic<br />
reference method of the CDC.<br />
Screening <strong>for</strong> Dyslipidemia in Youth<br />
Population-wide screening <strong>for</strong> dyslipidemia<br />
in children is not currently recommended.<br />
However, the AHA recommends screening<br />
children who are most likely to have dyslipidemia<br />
or who are at increased risk of CVD<br />
(8). The two primary target groups are<br />
children with genetic dyslipidemias, often<br />
identified by a family history of hyperlipidemia<br />
and/or premature coronary artery<br />
disease (CVD onset at < 55 years of age in<br />
male relatives, < 65 years of age in female<br />
relatives), and children who are obese.<br />
table 3<br />
classification of cvd risk<br />
in children<br />
Total Cholesterol LDL-Cholesterol<br />
mg/dL mmol/L mg/dL mmol/L<br />
acceptable < 170 4.40 < 110 2.85<br />
borderline 170–199 4.4–5.15 110–129 2.85–3.34<br />
High > 200 5.15 > 130 3.34<br />
Source: References 10 and 11.<br />
table 2<br />
recommended interventions<br />
<strong>for</strong> children with heterozygous<br />
familial hypercholesterolemia<br />
Intervention Type Parameter Target<br />
Dietary < 30% calories from fat<br />
< 7% calories from saturated fat<br />
no trans fat<br />
Physical Activity Active play > 1 h/d<br />
Screen time < 2 h/d<br />
Other CV Risk Factors Assess and counsel:<br />
blood pressure<br />
cigarette smoking<br />
glycemic status<br />
Pharmacotherapy Consider statin therapy if :<br />
male patient is at least 10 years old,<br />
female patient has undergone menarche,<br />
LDL-C persists at ≥4.9 mmol/L or ≥4.2 mmol/L<br />
with other CV risk factor(s) or family history<br />
of PCAD<br />
Source: Reference 8.<br />
In addition, the 2006 scientific statement<br />
from AHA recommends lipid screening<br />
profiles <strong>for</strong> children with a number of<br />
pediatric disorders that increase their risk<br />
of CVD in young adulthood (8). Diabetes<br />
type 1 and 2, Kawasaki disease with coronary<br />
aneurysms, and chronic and end-stage<br />
renal disease may predispose children to<br />
very early coronary events. Hyperglycemia<br />
in type 1 diabetes is a primary mediator<br />
of atherosclerosis, while in type 2 diabetes,<br />
both hyperglycemia and insulin resistances<br />
are implicated in endothelial dysfunction.<br />
In children with chronic kidney disease,<br />
morbidity and mortality is related not only<br />
to the kidney disease but also to CVD. The<br />
recommendations and goals <strong>for</strong> intervention<br />
have been tailored to risk (2).<br />
Target Values<br />
Elevated LDL-C is the most clinically significant<br />
marker of dyslipidemia in children<br />
and is used as the basis <strong>for</strong> treatment.<br />
Table 3 summarizes the NCEP (10) and<br />
< 200 mg/dL<br />
total cholesterol<br />
< 3.35 mmol/L or<br />
130mg/dL LDL-C<br />
<strong>American</strong> Academy of Pediatrics (AAP)<br />
(11) classification categories based on TC<br />
and LDL-C levels. A major concern among<br />
pediatric care givers has been that a single<br />
cutoff value does not reflect the changes<br />
associated with sex, growth, and maturation.<br />
The Lipid Research Clinics (LRC) Prevalence<br />
study also defined target values <strong>for</strong><br />
TC. This 1972–1976 study, sponsored by<br />
the National Heart, Lung, and Blood Institute,<br />
used fasting samples from a cross-<br />
sectional survey of various North <strong>American</strong><br />
populations. More age-specific and<br />
sex-specific data from the LRC prevalence<br />
data are shown in Table 4. Levels above the<br />
95th percentile are considered abnormal.<br />
More recently, researchers developed<br />
age- and sex-specific lipoprotein threshold<br />
concentrations <strong>for</strong> adolescents 12–20 years<br />
of age based on data from the National<br />
Health and Nutrition Examination Surveys<br />
(NHANES) (13). They linked the cut points<br />
to the adult health-based thresholds <strong>for</strong><br />
table 4<br />
lipid prevalence data by age<br />
Total cholesterol<br />
Age<br />
(years)<br />
Males Females<br />
75 th 95 th 75 th 95 th<br />
mg/dL mmol/L mg/dL mmol/L mg/dL mmol/L mg/dL mmol/L<br />
5–9 168 4.34 189 4.89 176 4.55 197 5.09<br />
10–14 173 4.47 202 5.22 171 4.42 205 5.30<br />
15–19 168 4.34 191 4.94 176 4.55 207 5.35<br />
ldl-cholesterol<br />
Age<br />
(years)<br />
Males Females<br />
75 th 95 th 75 th 95 th<br />
mg/dL mmol/L mg/dL mmol/L mg/dL mmol/L mg/dL mmol/L<br />
5–9 103 2.66 129 3.34 115 2.97 140 3.62<br />
10–14 109 2.82 132 3.41 110 2.84 135 3.52<br />
15–19 109 2.82 130 3.36 111 2.87 137 3.54<br />
Source: Reference 12.<br />
CliniCal laboratory news JuLy 2008 11