William M. Feinberg Award for Excellence in Clinical Stroke
William M. Feinberg Award for Excellence in Clinical Stroke
William M. Feinberg Award for Excellence in Clinical Stroke
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
■ PAST RECIPIENTS<br />
2012 Jeffrey L. Saver<br />
2011 Stephen Davis<br />
2010 Markku Kaste<br />
2009 Larry B. Goldste<strong>in</strong><br />
2008 S. Claiborne Johnston<br />
2007 Geoffrey Donnan<br />
2006 Ralph L. Sacco<br />
2005 John R. Marler<br />
2004 Philip B. Gorelick<br />
2003 Joseph P. Broderick<br />
2002 Julien Bogousslavsky<br />
2001 J. Donald Easton<br />
2000 Anthony J. Furlan<br />
1999 James C. Grotta<br />
1998 Werner Hacke<br />
1997 Thomas Brott<br />
1996 J. P. Mohr<br />
1995 Not <strong>Award</strong>ed<br />
1994 David G. Sherman<br />
1993 Harold P. Adams Jr.<br />
1992 Philip A. Wolf<br />
© 2013 American Heart Association.<br />
National Center<br />
7272 Greenville Avenue<br />
Dallas, Texas 75231-4596<br />
americanheart.org<br />
<strong>William</strong> M. <strong>Fe<strong>in</strong>berg</strong><br />
<strong>Award</strong> <strong>for</strong> <strong>Excellence</strong><br />
<strong>in</strong> Cl<strong>in</strong>ical <strong>Stroke</strong><br />
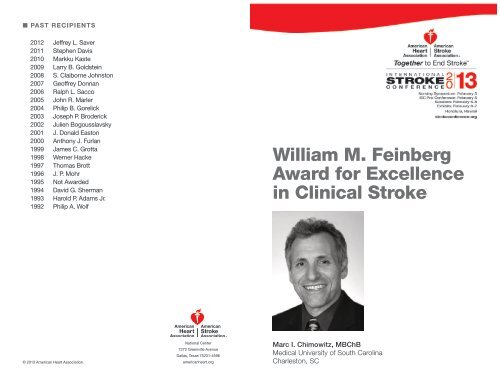
Marc I. Chimowitz, MBChB<br />
Medical University of South Carol<strong>in</strong>a<br />
Charleston, SC
■ WILLIAM M. FEINBERG AWARD FOR<br />
EXCELLENCE IN CLINICAL STROKE<br />
Marc I. Chimowitz, MBChB<br />
Dr. Chimowitz grew up <strong>in</strong> Zimbabwe and<br />
went to medical school at the University of<br />
Cape Town <strong>in</strong> South Africa. After mov<strong>in</strong>g<br />
to the United States, he completed a<br />
Neurology residency at Tufts — New<br />
England Medical Center and a <strong>Stroke</strong><br />
fellowship at the Cleveland Cl<strong>in</strong>ic. He has<br />
had faculty positions at the University<br />
of Michigan and Emory University, and<br />
is currently Professor of Neurology and Associate Dean of Faculty<br />
Development at the Medical University of South Carol<strong>in</strong>a <strong>in</strong> Charleston.<br />
His ma<strong>in</strong> career <strong>in</strong>terests are <strong>in</strong> improv<strong>in</strong>g treatments <strong>for</strong> patients with<br />
<strong>in</strong>tracranial arterial atherosclerotic stenosis and help<strong>in</strong>g to mentor the<br />
next generation of cl<strong>in</strong>ical and translational scientists. He has led three<br />
large consecutive NIH / NINDS funded multicenter cl<strong>in</strong>ical studies over<br />
the past 15 years (the WASID trial, the NIH W<strong>in</strong>gspan Stent registry,<br />
and the Stent<strong>in</strong>g and Aggressive Medical Management <strong>for</strong> Prevent<strong>in</strong>g<br />
Recurrent stroke <strong>in</strong> Intracranial Stenosis [SAMMPRIS] trial), which<br />
have led to new standards of care <strong>for</strong> the treatment of atherosclerotic<br />
<strong>in</strong>tracranial arterial stenosis. Additionally, he has extensive experience<br />
with mentor<strong>in</strong>g tra<strong>in</strong>ees and junior faculty and has been the recipient of<br />
a NIH K24 award <strong>for</strong> this purpose. He is on the editorial boards <strong>for</strong> the<br />
journals <strong>Stroke</strong> and Neurosurgery.<br />
■ TREATMENT OF INTRACRANIAL ATHEROSCLEROSIS:<br />
LEARNING FROM THE PAST AND PLANNING FOR<br />
THE FUTURE<br />
Intracranial atherosclerosis is one of the most common causes of<br />
stroke world-wide and is associated with a particularly high risk of<br />
recurrent stroke. Over the past decade, new therapeutic strategies<br />
have emerged <strong>for</strong> treat<strong>in</strong>g this high-risk disease. These <strong>in</strong>clude dual<br />
antiplatelet treatment, <strong>in</strong>tensive management of risk factors, and<br />
endovascular therapy.<br />
The early results of the SAMMPRIS trial showed that aggressive<br />
medical management (aspir<strong>in</strong> and clopidogrel <strong>for</strong> 90 days followed<br />
by aspir<strong>in</strong> alone, <strong>in</strong>tensive management of risk factors, and a<br />
lifestyle program) is superior to angioplasty and stent<strong>in</strong>g with the<br />
W<strong>in</strong>gspan stent system because of the high risk of early stroke<br />
after stent<strong>in</strong>g and lower than expected risk of stroke on aggressive<br />
medical therapy. While the current SAMMPRIS results suggest a<br />
much lower rate of the primary endpo<strong>in</strong>t (any stroke or death with<strong>in</strong><br />
30 days of enrollment or stroke <strong>in</strong> the territory beyond 30 days) <strong>in</strong><br />
patients treated with aggressive medical management compared<br />
with similar patients treated with usual medical management <strong>in</strong> the<br />
WASID trial (12.2% at 1 year <strong>in</strong> SAMMPRIS vs. 25% at 1 year <strong>in</strong><br />
WASID), the 1-year stroke rate <strong>in</strong> SAMMPRIS suggests that there<br />
are still subgroups of patients who are at very high risk of stroke<br />
despite aggressive medical therapy.<br />
To improve the treatment and outcome <strong>for</strong> these high-risk patients,<br />
further research is needed to identify these patients reliably and to<br />
develop more effective treatments. The mechanisms of stroke <strong>in</strong><br />
these high-risk patients <strong>in</strong>clude hypoperfusion, distal embolism,<br />
and local branch or per<strong>for</strong>ator occlusive disease. Non-<strong>in</strong>vasive<br />
vascular imag<strong>in</strong>g that could identify patients with impaired distal<br />
perfusion <strong>in</strong>clude fractional flow on MRA, quantitative MRA,<br />
and MR and CT perfusion, whereas high resolution MRI could<br />
identify patients with atherosclerotic plaque features (<strong>in</strong>traplaque<br />
hemorrhage, large lipid core, ruptured fibrous cap) that may<br />
<strong>in</strong>crease the risk of distal embolism or local branch and per<strong>for</strong>ator<br />
occlusion. Depend<strong>in</strong>g on the targeted mechanism of stroke,<br />
preventive therapies that may be considered <strong>for</strong> future cl<strong>in</strong>ical trials<br />
<strong>in</strong>clude angioplasty alone, <strong>in</strong>direct revascularization techniques,<br />
such as encephaloduroarteriosynangiosis, upper limb ischemic<br />
precondition<strong>in</strong>g, PCSK9 <strong>in</strong>hibitors, and direct thromb<strong>in</strong> or Xa<br />
<strong>in</strong>hibitors.