Gastric Cardia Lipoma
Gastric Cardia Lipoma
Gastric Cardia Lipoma
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
J Med Sci 2006;26(3):111-114<br />
http://jms.ndmctsgh.edu.tw/2603111.pdf<br />
Copyright © 2006 JMS<br />
Received: July 21, 2005; Revised: October 28, 2005;<br />
Accepted: November 15, 2005.<br />
* Corresponding author: Cheng-Jueng Chen, Division of<br />
General Surgery, Department of Surgery, Tri-Service General<br />
Hospital, 325, Cheng-Gong Road Section 2, Taipei 114,<br />
Taiwan, Republic of China. Tel: +886-2-87927191; Fax:<br />
+886-2-87927273; E-mail: doc20227@ndmctsgh.edu.tw<br />
<strong>Gastric</strong> <strong>Cardia</strong> <strong>Lipoma</strong><br />
Hao-Ming Chang 1 , Teng-Wei Chen 1 , Yi-Jen Peng 2 , Chung-Bao Hsieh 1 , De-Chuan Chan 1 ,<br />
Jyh-Cherng Yu 1 , Yao-Chi Liu 1 , Kuo-Liang Shen 1 , and Cheng-Jueng Chen 1*<br />
1 Division of General Surgery, Department of Surgery, 2 Department of Pathology,<br />
Tri-Service General Hospital, National Defense Medical Center,<br />
Taipei, Taiwan, Republic of China<br />
Hao-Ming Chang, et al.<br />
Here we present an extremely rare case of a gastric cardia lipoma. <strong>Lipoma</strong>s are rare in the gastrointestinal tract, are usually<br />
asymptomatic and often discovered incidentally. When a lipoma becomes larger than 4 cm, the most common indicator of<br />
clinical presence is upper gastrointestinal hemorrhage. A 73-year-old female patient presented with melena and dysphagia.<br />
Abdominal computed tomography revealed a gastric cardia lipoma. At laparotomy, a gastric cardia lipoma was found with<br />
ulceration that was causing esophageal obstruction. The lipoma was removed through a gastrotomy with incision of the<br />
mucosa and shelling out of the tumor. Recovery was uneventful.<br />
Key words: cardia, lipoma, stomach<br />
INTRODUCTION<br />
<strong>Gastric</strong> lipomas are rare benign tumors. However, 6%<br />
of all gastrointestinal tumors are classified as lipomas 1 .<br />
The stomach is rarely affected in most cases. When present,<br />
the most common site of involvement is the antrum (75%) 2 .<br />
The tumor location and size most often determines the<br />
symptomatology and the treatment methods for each case.<br />
The rarity of this condition prompts us to report a case of<br />
gastric cardia lipoma that was removed using a gastrotomy<br />
approach.<br />
CASE REPORT<br />
The patient was a 73-year-old female who presented<br />
with symptoms with dysphagia for solid foods and melena<br />
for one week. No body weight loss was noted and no<br />
abnormalities were found upon physical examination.<br />
Laboratory data revealed normocytic anemia. Blood chemistry<br />
profiles and coagulation studies were within normal<br />
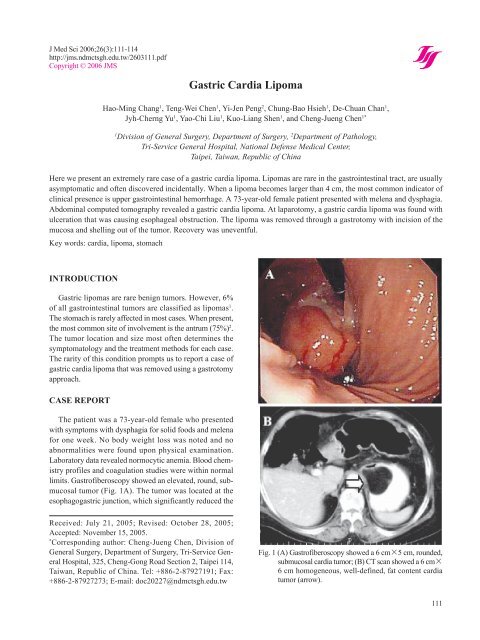
limits. Gastrofiberoscopy showed an elevated, round, submucosal<br />
tumor (Fig. 1A). The tumor was located at the<br />
esophagogastric junction, which significantly reduced the<br />
Fig. 1 (A) Gastrofiberoscopy showed a 6 cm×5 cm, rounded,<br />
submucosal cardia tumor; (B) CT scan showed a 6 cm×<br />
6 cm homogeneous, well-defined, fat content cardia<br />
tumor (arrow).<br />
111
<strong>Lipoma</strong><br />
lumen of the cardia. Gastrofiberoscopy showed the overlying<br />
mucosa was smooth, and the lesion was soft and<br />
compressible. Computed tomography (CT) revealed a<br />
smooth, round, homogeneous, and well-encapsulated fat<br />
tumor found over the cardia. The Hounsfield unit for this<br />
case was–82. (Fig. 1B). Barium studies revealed a welldefined<br />
mass-like filling defect over the posterior right<br />
lateral aspect of the gastric cardia region.<br />
On laparotomy, through an upper midline incision and<br />
gastrotomy approach, a soft yellowish mass with small<br />
ulceration in the center was identified over the posterior<br />
aspect of the cardia (Fig. 2A). The lipoma was easily<br />
enucleated after incision of the mucosa without damage to<br />
the muscle layer. The mucosa was closed. Frozen section<br />
and histopathological examination confirmed the diagnosis<br />
of submucosal lipoma (Fig. 2B). The patient’s recovery<br />
was uneventful.<br />
DISCUSSION<br />
<strong>Lipoma</strong>s are rare in the gastrointestinal tract, where they<br />
represent 6% of all gastrointestinal tumors classified 1 . The<br />
most common site is the colon, followed by the small<br />
intestine 3 , with the stomach rarely being affected 4,5 . The<br />
etiology of gastric lipoma is unknown. The common view<br />
favors embryologically sequestered adipose tissue 6 . <strong>Lipoma</strong>s<br />
are usually asymptomatic and often discovered incidentally.<br />
It is when the lipomas become larger that they can be<br />
manifest clinically. Symptoms are most often related to<br />
size and location 4,7 . The most common clinical presence<br />
(50%) is upper gastrointestinal hemorrhage caused by<br />
pressure necrosis and ulceration of the overlying mucosa 6 .<br />
Obstructive symptoms are also frequent (42%) and antral<br />
lipomas may cause gastroduodenal intussu-sception 8 .<br />
Barium studies typically reveal a smooth submucosal<br />
mass, normal wall contractility, and changes in shape with<br />
peristalsis 9,10 . The most reliable diagnostic tool is considered<br />
to be a CT scan 11 , which provides more accurate data<br />
about mass shape and structure. <strong>Lipoma</strong>s are usually<br />
homogenous and have a typical fat density ranging from–<br />
80 to–120 Hounsfield unit. A CT scan allows a differential<br />
diagnosis with liposarcoma, which appears either as a<br />
heterogeneous mass containing septum, or as large areas<br />
that appear to have variable tissue density 12 . <strong>Gastric</strong> lipomas<br />
can be definitively diagnosed with CT in most cases,<br />
and unnecessary endoscopy or surgery can be avoided.<br />
Surgery is presently indicated only when malignancy<br />
cannot be ruled out or in symptomatic patients. The choice<br />
of treatment is based on the tumor size and location.<br />
Endoscopic therapy is based on snare removal of small<br />
112<br />
Fig. 2 (A) The excised specimen showed a 7 cm×6 cm<br />
submucosal yellowish tumor with ulceration (arrows);<br />
(B) The micrography illustrates the area of esophageal<br />
– gastric junction. Notice the transition of glandularsquamous<br />
mucosa and esophageal submucosal glands.<br />
The muscularis mucosa was fragmental, and the lipoma<br />
composed of mature adipose tissue located in the submucosal<br />
layer (hematoxylin and eosin; magnification,<br />
×40).<br />
lesions less than 3 cm 13 . Although excision with simple<br />
closure is recommended, gastrotomy with incision of the<br />
mucosa and shelling out of the tumor may be resorted to<br />
when it is very large or near the cardia, as wedge resection<br />
here will destroy the esophagogastric angle and promote<br />
reflux 14 . In emergency situations, such as massive hematemesis,<br />
gastric resection is indicated because a diagnosis<br />
cannot usually be confirmed. Importantly, utilizing intraoperative<br />
frozen section can avoid unnecessary gastric<br />
resections. Laparoscopic resection has been recommended<br />
for lipomas less than 6 cm in diameter. Although submu-
cosal tumors can be shelled out endoscopically, a combined<br />
laparoscopic and endoscopic approach is recommended<br />
because the danger of bleeding and small perforations<br />
can occur when endoscopy alone is used 15 .<br />
In this case, CT was the main diagnostic tool and<br />
allowed a differential diagnosis with liposarcoma, gastrointestinal<br />
stroma tumor, angiolipoma, and lymphoma<br />
by identifying a homogenous mass with a typical fat<br />
density of –80 to –120 Hounsfield unit. We consider<br />
that gastrotomy with incision of the mucosa and shelling<br />
out of the cardia lipoma can avoid injury of the esophagogastric<br />
angle and prevent reflux esophagitis.<br />
REFERENCES<br />
1. Johnson DC, DeGennaro VA, Pizzi WF, Nealon TF Jr.<br />
<strong>Gastric</strong> lipomas: A rare cause of massive upper gastrointestinal<br />
bleeding. Am J Gastroenterol 1981;75:<br />
299-301.<br />
2. Turkington RW. <strong>Gastric</strong> lipoma. Report of a case and<br />
review of the literature. Am J Dig Dis 1965;10:719-<br />
726.<br />
3. Kang JY, Chan-Wilde C, Wee A, Chew R, Ti TK. Role<br />
of computed tomography and endoscopy in the management<br />
of alimentary tract lipomas. Gut 1990;31:<br />
550-553.<br />
4. Regge D, Lo Bello G, Martincich L, Bianchi G, Cuomo<br />
G, Suriani R, Cavuoto F. A case of bleeding gastric<br />
lipoma: US, CT and MR findings. Eur Radiol 1999;9:<br />
256-258.<br />
5. Myint M, Atten MJ, Attar BM, Nadimpalli V. <strong>Gastric</strong><br />
lipoma with severe hemorrhage. Am J Gastroenterol<br />
1996;91:811-812.<br />
6. Chu AG, Clifton JA. <strong>Gastric</strong> lipoma presenting as<br />
peptic ulcer: Case report and review of the literature.<br />
Am J Gastroenterol 1983;78:615-618.<br />
Hao-Ming Chang, et al.<br />
7. Lacy AM, Tabet J, Grande L, Garcia-Valdecasas JC,<br />
Fuster J, Delgado S, Visa J. Laparoscopic-assisted<br />
resection of a gastric lipoma. Surg Endosc 1995;9:995-<br />
997.<br />
8. Lin F, Setya V, Signor W. Gastroduodenal intussusception<br />
secondary to a gastric lipoma. A case report<br />
and review of the literature. Am Surg 1992;58:772-<br />
774.<br />
9. Taylor AJ, Stewart ET, Dodds WJ. Gastrointestinal<br />
lipomas: A radiologic and pathologic review. Am J<br />
Roentgenol 1990;55:1205-1210.<br />
10. Winants D, Arnault G. Le lipome gastrique. J Radiol<br />
1989;70:633-636.<br />
11. Heiken JP, Forde KA, Gold RP. Computerized tomography<br />
as a definite method for diagnosing gastrointestinal<br />
lipomas. Radiology 1982;142:409-414.<br />
12. Megibow AJ, Redmond PE, Bosniak MA, Horowitz L.<br />
Diagnosis of gastrointestinal lipomas by CT. Am J<br />
Roentgenol 1979;133:743-745.<br />
13. Nakamura S, Iida M, Suekane H, Matsui T, Yao T,<br />
Fujishima M. Endoscopic removal of gastric lipoma:<br />
diagnostic value of endoscopic ultrasonography. Am J<br />
Gastroenterol 1991;86:619-621.<br />
14. Maderal F, Hunter F, Fuselier G, Gonzales-Rogue P,<br />
Torres O. <strong>Gastric</strong> lipomas: An update of clinical<br />
presentation, diagnosis and treatment. Am J<br />
Gastroenterol 1984;79:964-967.<br />
15. Treska V, Pesek M, Kreuzberg B, Chudacek Z,<br />
Ludvikova M, Topolcan O. <strong>Gastric</strong> lipoma presenting<br />
as upper gastrointestinal obstruction. J Gastroenterol<br />
1998;33:716-719.<br />
113
<strong>Lipoma</strong><br />
114