Developing Federally Qualified Health Centers into Community ...
Developing Federally Qualified Health Centers into Community ...
Developing Federally Qualified Health Centers into Community ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
percent), and finds that its work with <strong>Community</strong> <strong>Health</strong> Partners enables it to offer<br />
patients a variety of services that a small practice could not otherwise furnish.<br />
In addition to care management services, practices take part in quarterly medical<br />
management sessions on educational topics chosen by the provider community.<br />
LESSONS LEARNED AND CHALLENGES<br />
The North Carolina CCNC model has evolved over the past 13 years <strong>into</strong> a mature care<br />
coordination and support system. The grassroots development approach has resulted in a<br />
variety of different network structures, including an FQHC-based network, that operate<br />
using common principles.<br />
The success of the CCNC model has been documented in an independent report<br />
prepared by the Mercer Human Resources Consulting Group. 18 The report found that the<br />
CCNC program saved approximately $60 million in state fiscal year 2003, $124 million<br />
in state fiscal year 2004, and $231 million in state fiscal years 2005 and 2006, compared<br />
with the costs of the previous primary care case management model. Subsequent costeffectiveness<br />
analysis continues to show that CCNC is holding down costs for the North<br />
Carolina Medicaid program. In addition, health outcomes have improved, particularly for<br />
those with asthma and diabetes. 19 The <strong>Community</strong> <strong>Health</strong> Partners network has also<br />
observed promising changes in acute care utilization in recent years (Table 1).<br />
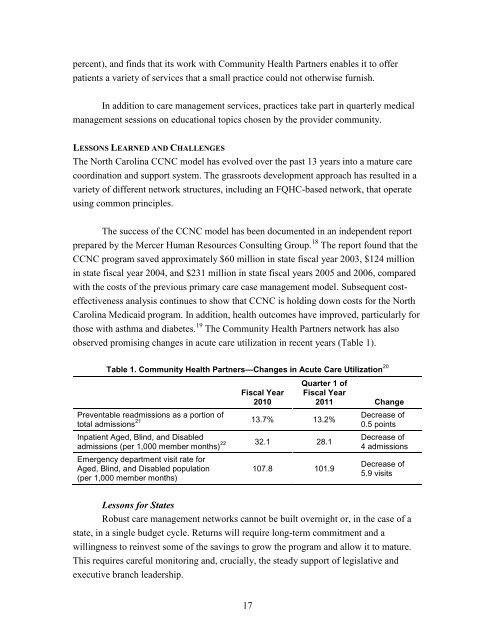
Table 1. <strong>Community</strong> <strong>Health</strong> Partners—Changes in Acute Care Utilization 20<br />
Preventable readmissions as a portion of<br />
total admissions 21<br />
Inpatient Aged, Blind, and Disabled<br />
admissions (per 1,000 member months) 22<br />
Emergency department visit rate for<br />
Aged, Blind, and Disabled population<br />
(per 1,000 member months)<br />
Fiscal Year<br />
2010<br />
17<br />
13.7% 13.2%<br />
32.1 28.1<br />
107.8 101.9<br />
Quarter 1 of<br />
Fiscal Year<br />
2011 Change<br />
Decrease of<br />
0.5 points<br />
Decrease of<br />
4 admissions<br />
Decrease of<br />
5.9 visits<br />
Lessons for States<br />
Robust care management networks cannot be built overnight or, in the case of a<br />
state, in a single budget cycle. Returns will require long-term commitment and a<br />
willingness to reinvest some of the savings to grow the program and allow it to mature.<br />
This requires careful monitoring and, crucially, the steady support of legislative and<br />
executive branch leadership.