Developing Federally Qualified Health Centers into Community ...
Developing Federally Qualified Health Centers into Community ...
Developing Federally Qualified Health Centers into Community ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
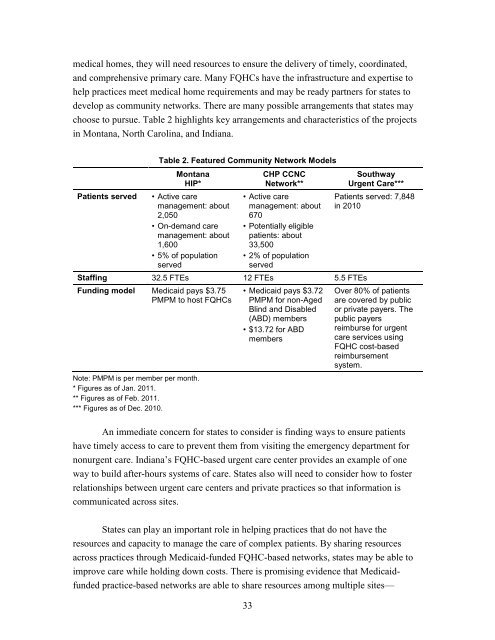
medical homes, they will need resources to ensure the delivery of timely, coordinated,<br />
and comprehensive primary care. Many FQHCs have the infrastructure and expertise to<br />
help practices meet medical home requirements and may be ready partners for states to<br />
develop as community networks. There are many possible arrangements that states may<br />
choose to pursue. Table 2 highlights key arrangements and characteristics of the projects<br />
in Montana, North Carolina, and Indiana.<br />
Table 2. Featured <strong>Community</strong> Network Models<br />
Montana<br />
HIP*<br />
Patients served • Active care<br />
management: about<br />
2,050<br />
• On-demand care<br />
management: about<br />
1,600<br />
• 5% of population<br />
served<br />
33<br />
CHP CCNC<br />
Network**<br />
• Active care<br />
management: about<br />
670<br />
• Potentially eligible<br />
patients: about<br />
33,500<br />
• 2% of population<br />
served<br />
Staffing 32.5 FTEs 12 FTEs 5.5 FTEs<br />
Funding model Medicaid pays $3.75<br />
PMPM to host FQHCs<br />
Note: PMPM is per member per month.<br />
* Figures as of Jan. 2011.<br />
** Figures as of Feb. 2011.<br />
*** Figures as of Dec. 2010.<br />
• Medicaid pays $3.72<br />
PMPM for non-Aged<br />
Blind and Disabled<br />
(ABD) members<br />
• $13.72 for ABD<br />
members<br />
Southway<br />
Urgent Care***<br />
Patients served: 7,848<br />
in 2010<br />
Over 80% of patients<br />
are covered by public<br />
or private payers. The<br />
public payers<br />
reimburse for urgent<br />
care services using<br />
FQHC cost-based<br />
reimbursement<br />
system.<br />
An immediate concern for states to consider is finding ways to ensure patients<br />
have timely access to care to prevent them from visiting the emergency department for<br />
nonurgent care. Indiana’s FQHC-based urgent care center provides an example of one<br />
way to build after-hours systems of care. States also will need to consider how to foster<br />
relationships between urgent care centers and private practices so that information is<br />
communicated across sites.<br />
States can play an important role in helping practices that do not have the<br />
resources and capacity to manage the care of complex patients. By sharing resources<br />
across practices through Medicaid-funded FQHC-based networks, states may be able to<br />
improve care while holding down costs. There is promising evidence that Medicaidfunded<br />
practice-based networks are able to share resources among multiple sites—