National Rural Health Mission - Amravati
National Rural Health Mission - Amravati
National Rural Health Mission - Amravati
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Progamme<br />
Implementation<br />
Plan<br />
201112<br />
<strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong><br />
<strong>Amravati</strong> District
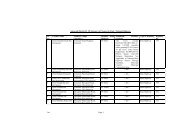
INDEX<br />
Sr.No. Particulars Page<br />
1 Executive Summery 1‐27<br />
2 Chapter 1 – Out come analysis of PIP 28‐32<br />
3<br />
Chapter 2 ‐ Policy and systemic reforms in<br />
strategic areas.<br />
33‐34<br />
4 Chapter 3 ‐ Conditionalities 35‐38<br />
5 Chapter 4 – Sheme/Programe 39‐77<br />
A RCH Flexi pool 78‐122<br />
B NRHM Flexi pool 123‐173<br />
C Immunization 174‐184<br />
D Disease Control Programme 185‐203<br />
E Inter Sectoral Covergence 204‐205<br />
6 Chapter 5 – Monitoring and Evaluation 206‐208<br />
7 Chapter 6 – Financial Management 209‐225<br />
8 Chapter 7 ‐ Resourses and other sources of<br />
funds for health sector<br />
226‐229<br />
9 Chapter 8 – Priority projects 230‐239
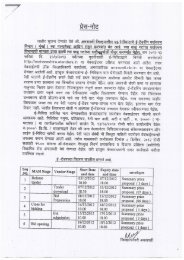
Foreword:<br />
<strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong> is implemented in District <strong>Amravati</strong> from year<br />
2006‐2007. The aims and objective of the mission is “<strong>Health</strong> for all by 2012” and reduced<br />
IMR, MMR, TFR. To achieved said goal of NRHM District implemented all the activity of<br />
NRHM. From year 2006‐07 to 2009‐10 by implementing various types of schemes for rural<br />
and urban area and specialy for Melghat tribal area. There are lot of difficulties district<br />
Administraton have been faced, it inclueds geographical, a traditional, factor and also non<br />
availability of specialist, doctors. There is huge disparity of specialists Doctors in the district<br />
specialy in Melghat area. Infant mortality rate and maternal mortality rate is still high in the<br />
tribal areas. There is low acceptance of family planning services and so TFR is high.<br />
By implementing Maternal releated activity and development of<br />
infrastructure in tribal area, Institutional delivery rate is improoved up to 42% as compare<br />
to initial rate of 2006‐07 of 7%. For imprving institutional delivery through NRHM following<br />
activity shall be taken by District health society.<br />
1) Infrastructute development<br />
2) Man power recruitment<br />
3) Involovement of non official<br />
4) Public private partnership<br />
5) NGO involvement<br />
6) Training & capacity building<br />
7) Monitoring activity<br />
8) Referal services<br />
High growth rate in population has imbalanced the infrastructure in the district. The clients<br />
are not satisfied with the Government <strong>Health</strong> Institutions because of non availability of minimum<br />
requirement i.e. sanitation, condition of equipments and instruments, regularity of human resources<br />
and inadequate medicines. But by implementing and by proper execution of above activity the<br />
situation has now been changed and satisfaction of client and poor rural patients will be seen by<br />
growth rate of OPD/IPD and improved percentage of institutional delivery.<br />
This plan will definitely improve availability, utilization and quality of <strong>Health</strong> Services<br />
to the community at all levels. We expect necessary support form the Sate Government for<br />
implementation of NRHM activities.<br />
Civil Surgeon District <strong>Health</strong> Officer, Chief Executive Officer,<br />
District Hospital <strong>Amravati</strong>. Zilla Parishad <strong>Amravati</strong> Zilla Parishad , <strong>Amravati</strong>.
Executive Summery:<br />
Sr. No. Items<br />
BACK GROUND AND CURRENT STATUS<br />
General Information of the District<br />
General Information‐ Amaravati<br />
1 Total Population (Cen. 2001) 26,07,160<br />
<strong>Rural</strong> (Source Census 2001) 1707581<br />
Urban (Source Census 2001) 899579<br />
Percentage of SC/ST 30.81%<br />
2 Total Tahsil 14<br />
3 Corporation 1<br />
4 Municipal councils 10<br />
5 Geographical Area ( Sq. K.M.) 12,212<br />
6 Land under forest 3,575<br />
7 Total Villages 1,547<br />
8 Ratio of Women's in thousand male 941<br />
9 Average Rain fall ( ml) 858<br />
Institutional Mechanisms<br />
INSTITUTIONAL MECANISUM<br />
Sr.No. Institute No.<br />
1 District Hospital 1<br />
2 Women Hospital 1<br />
3 SDH 4<br />
4 RH 9<br />
5 PHC 56<br />
6 Sub centre 333<br />
7 BLOCK 14<br />
8 Taluka <strong>Health</strong> Office 14<br />
9 Regional Referral Center 1<br />
10 T.B. Hospital 1<br />
Total… 434<br />
District Integrated <strong>Health</strong> & Family Welfare Society<br />
<strong>Amravati</strong> Districted had Programme wise District Society and Bank Accounts for funding<br />
procedures. In 2006 <strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong> was started and as per guidelines the district<br />
health programme societies i.e. district Malaria society, district T.B. Control Society, district<br />
Blindness control society, district leprosy control society these all are merged in District Integrated<br />
<strong>Health</strong> & Family Welfare Society and now funds are operated through this society since 2006. The<br />
society has been registered with Joint Society Registrar <strong>Amravati</strong>. The registration no is MAH/736/05
dated 20/09/2005 and Account is opened in ICICI Bank <strong>Amravati</strong> and No. is 042801000258 dated<br />
04/12/2007.<br />
The above society programme officers are the members of District Integrated <strong>Health</strong> &<br />
Family Welfare Society. But in 2006‐07 and 2007‐08 the programme society budget was not<br />
received to District Integrated <strong>Health</strong> & Family Welfare Society and was operated Independently by<br />
the programme officers. Only RCH, Immunization and NRHM budget was received to the District<br />
Integrated <strong>Health</strong> & Family Welfare Society <strong>Amravati</strong>.<br />
Fund Flow Systems<br />
In 2009‐10 funds from State Society received to District Integrated <strong>Health</strong> & Family Welfare<br />
Society form NRHM, RCH, IDW, Immunization and some budget for Training. The budget directly<br />
transferred from State to district account of the society. The district Society distributed budget to<br />
BPMU by Cheques as per norms according to the availability of funds. BPMU distributed budget to<br />
PHCs by Cheques as per norms according to the availability of funds. From PHC to sub centres the<br />
funds are distributed as per norms.<br />
Decentralization<br />
For health Institute management and planning RKS established for each Institute. Similarly at<br />
village level Village <strong>Health</strong> Sanitation and Nutrition Committee is established. The requirements are<br />
approved by these societies and funds are utilized for fulfillment of requirement. The Finanancial<br />
powers are delegated as per G.R. No. PHD/dated 30/12/2005 amendment dated 04/05/2006 and<br />
09/01/2007to the concerned officers and they are utilizing funds accordingly.<br />
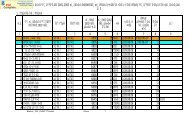
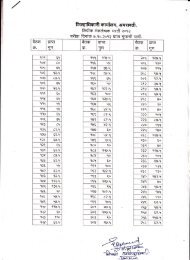
BLOCK WISE INFORMATION<br />
Sr.<br />
No.<br />
Name of Block <strong>Rural</strong><br />
Population<br />
No. of<br />
Villages<br />
Sex Ratio No. of PHCs No. of Sub<br />
Centres<br />
1 <strong>Amravati</strong> 127735 89 943 4 23<br />
2 Bhatkuli 108662 108 960 3 18<br />
3 Daryapur 130195 133 941 4 24<br />
4 Anjangaon 101438 101 945 3 16<br />
5 Achalpur 160928 127 919 3 23<br />
6 Chandur Bz 173803 114 934 4 25<br />
7 Morshi 141919 89 939 5 21<br />
8 Warud 151263 99 933 5 22<br />
9 Tiosa 109629 79 952 3 15<br />
10 Chandur Rly. 68287 70 948 2 13<br />
11 Dhamangaon Rly. 106049 83 927 4 18<br />
12 Nandgaon Kh. 127330 125 945 5 20<br />
13 Dharni 180958 171 945 6 54<br />
14 Chikhaldara 103566 159 968 5 41<br />
Total 1791762 1547 941 56 333
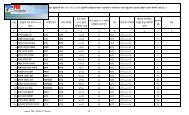
YEAR WISE COMPARISON OF VITAL RATES OF DISTRICT<br />
SURVEY OF CAUSES OF DEATH SCHEME (RURAL)<br />
YEAR WISE COMPARISON OF VITAL RATES OF AMRAVATI DISTRICT<br />
S.N. RATE 2005 2006 2007 2008 2009 2010<br />
A FERTILITY ANALYSIS<br />
1 Crude Birth Rate 15.61 15.57 15.0 14.56 14.3 14.37<br />
2 Still Birth Rate 9.06 7.55 7.20 23.49 16.21 15.27<br />
3 General Fertility Rate 60.43 57.91 60.00 53.88 53.12 52.79<br />
4 Total Fertility Rate 2.00 1.86 2.00 1.99 1.97 1.97<br />
5 Gross Reproductive Rate 0.98 0.90 0.97 0.95 0.94 0.94<br />
6 Age Specific Fertility Rate<br />
6(I) 15‐19 10.42 4.31 1.39 7.92 7.67 9.16<br />
6(II) 20‐24 254.39 243.54 251.11 226.06 223.64 251.32<br />
6(III) 25‐29 110.85 108.23 100.19 129.62 124.69 123.7<br />
6(IV) 30‐34 20.59 13.99 17.86 32.35 32.99 8.08<br />
6(V) 35‐39 3.48 2.08 0.73 3.26 4.39 1.91<br />
6(VI) 40‐44 0.00 0.00 0.70 0.00 0.00 0.18<br />
6(VII<br />
)<br />
45‐49 0.00 0.00 0.00 0.00 0.00 0<br />
7 Sex Ratio at Birth 96.44 94.13 97.80 92.30 91.81 91.44<br />
B MORTALITY ANALYSIS<br />
1 Crude Death Rate 7.22 7.50 8.26 6.96 6.31 6.65<br />
2 Perinatal Mortality 23.95 25.49 38.70 29.65 30.3 27.93<br />
3 Early Neonatal Mortality 15.11 18.13 15.85 17.08 14.59 13.09<br />
4 Late Neonatal Mortality 3.02 0 9.51 6.41 6.48 8.72<br />
5 Neonatal Mortality 18.13 18.13 25.36 23.49 21.06 21.81<br />
6 Post neonatal Mortality 10.57 1.51 12.68 11.74 9.73 7.63<br />
7 Infant Mortality ( 0‐1 ) 32.01 19.64 38.03 35.24 30.79 29.44<br />
8 Child Mortality Rate ( 0‐4 ) 8.14 7.24 9.16 7.9 5.43 7.33<br />
9 Sex Ratio at Death 65.76 60.3 66.01 85.68 73.46 78.36<br />
10<br />
Maternal Mortility Rate ( In<br />
Lakhs ) ( Year<br />
: March to April10)<br />
N.A. 76.93 134.73 102.36 150.37 120.26
Vital Indicators:<br />
Sr. Indicator<br />
As per MIS of<br />
the district<br />
1 Crude Birth Rate 15.40<br />
As per Sample<br />
survey of the<br />
district<br />
(SRS 2005)<br />
State – 19<br />
Dist ‐ 17.6<br />
SCD 2008<br />
Goal of<br />
achievement<br />
by 2012<br />
14.3 12<br />
2<br />
Crude Death<br />
Rate<br />
7.23 State 6.7 6.31 6<br />
3<br />
Neonatal<br />
Mortality Rate<br />
21.08 25 21.06 16<br />
4<br />
Infant Mortality<br />
Rate<br />
28.36<br />
State‐ 36<br />
Dist‐ 29.4<br />
30.79 25<br />
5<br />
U‐5 Mortality<br />
Rate<br />
9.84 9.10 5.43 7<br />
6<br />
Maternal<br />
Mortality Rate<br />
1.503 2.1 1.503 < 1<br />
8 Anemia 40 38 42 30<br />
9 NVBDCP ‐ ‐ - ‐<br />
10<br />
TB<br />
1) Cure Rate<br />
2) N.S.P. Case<br />
84%<br />
85%%<br />
Deflction<br />
Rate<br />
45%<br />
‐<br />
-<br />
70%<br />
11 Laprocy PR 0.89 ‐ - 0.50<br />
District <strong>Amravati</strong> has low Social economic profile with minimum Specialist services in the<br />
District. The districts have high IMR in tribal block and Nutritional problems. Some of the Villages are<br />
inaccessible in rainy season and hence there are difficulties in providing health services. Special<br />
premansoon drives are arranged to identify high risk group. It is also planned for availability of<br />
health personnel in such remote villages. The necessary supplies are given well in advance to all<br />
peripheral health institutes. The necessary support of ASHA, ANGANWADI is also taken to provide<br />
health services. PADA workers are appointed every year in these tribal areas. They also help in<br />
providing health services.<br />
The family planning performance in urban area and some of the blocks is below overall<br />
district performance is as per ELA. The NSV acceptance is still not satisfactory. The compensation<br />
rates for NSV are increased and hence in 2011‐12 the performance will definately improve.<br />
In tribal area utilization of services is not satisfactory the awareness activity will improve the<br />
utilization of RCH services. To reduce malnutrition problem ICDS department is taking efforts, the<br />
<strong>Health</strong> department will also support them for regular checkups and Immunization, Vit A and IFA<br />
supplementation. The Nutrition rehabilitation centres are started at rural hospitals. In Remote<br />
villages day care centres are established and malnourished children are admitted in these centres<br />
and given supplementary feeding. Maher scheme is proposed in tribal PHCs. in Dharni and<br />
Chilkhaldara Block. Special efforts are made to involve tradinational practitioners for delivery of the<br />
health services.
SITUATIONAL ANALYSIS<br />
Socio‐economic and Demographic features of Amaravati<br />
District Sex ratio<br />
<strong>Amravati</strong> district as a whole, there are 943 females per every 1000 males (source‐NFHS‐III).<br />
This is much higher than that of the State average of 913. But still Achalpur, Dhamangaon, Warud,<br />
Chandur Bz. and Morshi Block has low sex ratio than the district. Special efforts for awareness will be<br />
taken in these blocks.<br />
Literacy<br />
The literacy rate of Amaravati district in 2001 was 82.5 percent. For the district as a whole, the<br />
literacy rate for males is much higher than that of females. The literacy rate for males is 88.9 % against<br />
75.7 % for females. As compared to state the literacy rate is better but in tribal area Dharni and<br />
Chikhaldara it is less than in the district<br />
Economic features:<br />
The economy of the district is primarily agriculture based. But the fact that cultivators (21.53 %)<br />
and agricultural labourers (52.43 %) together constitute 73.96 % of total work force in the district. The<br />
agriculture sector has thus absorbed nearly three fourth of the total main workers in the district. This is<br />
so because there are few alternative employment opportunities available in the district. Remaining 25 %<br />
of workers are engaged in non‐agricultural activities such as trade, commerce, manufacturing and<br />
processing units. The district has very low Industrial setup and is not on the <strong>National</strong> Railway line. Hence<br />
economic growth is very slow. There by living slandered is not up to the mark which in term is<br />
responsible for poor health.<br />
Geographical situation<br />
<strong>Amravati</strong> is situated right in the centre of the northern border of Maharashtra state. It is bounded in the<br />
North by Madhya Pradesh State in the East by Nagpur and Wardha district and in the south by<br />
Yawatmal and Washim district & on west by Akola district. The district headquarter is located at<br />
Amaravati.<br />
The district has an area of 12210 sq. km. which constituted 0.04 % of the total area of the State.<br />
According to the 2001 census, the population of district is 26, 07,160 {2.79 % of the State} with 1345614<br />
males and 1261546 females. Out of the total population, 65.5 % are residing in rural area and the<br />
remaining 34.5 % are residing in urban area. It has 1996 villages out of which 1681 villages are inhabited<br />
and 315 are uninhabited. The urban population is distributed among 11 units of which one is Municipal<br />
Corporation and other ten are Municipal towns. It ranks eighth in terms of area and sixteenth in terms<br />
of population among the 33 districts in the State. The density of population is 214 persons per sq. km.<br />
The district may be broadly divided in to two geographic regions, the Melghat hilly and tribal area and<br />
the plain no tribal area Melghat is hilly and has steep slopes. There is also deep forest and scattered<br />
habitation. The forest animals are common in this area.<br />
The population of the district as recorded in the 2001 census, stand at 26, 07,160 as against<br />
2200057 in 1991 indicate net addition of 407113 persons during the decade.
The average growth rate for rural and urban areas of the district is 12.61 % and 31.70 %<br />
respectively. Census data indicate that scheduled tribes and scheduled castes, which form the most<br />
vulnerable section of the population, constitute 18.5 and 15 percent of the total population,<br />
respectively.<br />
The sex ratio at age 0‐6 has also declined from 950 in 1991 to 941 in 2001. The rising incidence<br />
of female foeticide appears to be mainly responsible for the decline in the juvenile sex ratio.<br />
In the district blocks like Achalpur, Dhamangaon, Warud, Chandur Bazar, Morshi are having<br />
sex ratio less than district average.<br />
In <strong>Amravati</strong> District, 49 PHCs had adequate physical infrastructure such as building, water<br />
and electricity supply, 49 PHCs have labour room facilities, All PHCs have Govt vehicles, 11 PHCs<br />
have Laboratory facilities, 46 PHCs have adequate staff in position, all PHCs have adequate vaccines<br />
and contraceptives, and have adequate equipment’s in function, such as weighing machine, BP<br />
instruments, autoclave.<br />
All the 56 PHCs have received sub‐centre kit for head quarter sub centre. The position of CHCs,<br />
FRUs, and district hospitals were somewhat better having better supplies. The staffs in position in CHCs<br />
(50%) and all FRUs was also far from adequate staff position. Only 15‐20 percent of them had adequate<br />
infrastructure, staff and supplies.<br />
It was also observed that around 80 % of medical and paramedical staff had received adequate<br />
in‐service training.<br />
<strong>Health</strong> Institutes<br />
1 Divisional Referral Hospital 1<br />
2 Private Medical College. ‐ PDMMC, <strong>Amravati</strong> 1<br />
3 Ayurvedic Medical Colleges 2<br />
4 Homeopathic Medical Colleges 2<br />
5 Dist. General Hospitals 1<br />
6 Dist. Women Hospitals 1<br />
7 Govt. T.B. Hospitals 1<br />
8 Sub‐Dist. Hospitals 4<br />
9 <strong>Rural</strong> Hospitals 9<br />
10 Primary <strong>Health</strong> Centres 56<br />
11 <strong>Health</strong> Sub‐Centres 333<br />
12 Allopathic Dispensaries 18<br />
13 Ayurvedic Dispensaries 65<br />
14 Primary <strong>Health</strong> Units 12<br />
15 Mobile <strong>Health</strong> Units 7<br />
16 Anganwadi Kendra 2022<br />
17 Grampanchayat 842<br />
18 Ashram School 53<br />
19 Literacy rate 82.5<br />
Blood banks, blood storage facility in the district<br />
- District Hospital <strong>Amravati</strong><br />
- SDH, Dharni<br />
- P.D.M.C. <strong>Amravati</strong>.<br />
- Dr.Varma Laboratory – Achalpur<br />
- Bhagwat Pvt. Laboratory – <strong>Amravati</strong><br />
- Dr.Dara Blood Bank – <strong>Amravati</strong>.
N.R.H.M. Progress<br />
“ASHA” are appointed in tribal as well as non trible area. Fourth Modules Training of ASHA is<br />
complited and in non‐trible area First modules training is started. Second A.N.M. for Sub centre has<br />
been appointed. Similarly additional man power at P.H.C. is also appointed. The infrastructure<br />
strengthening, skilled training, maintenance of buildings etc. are going on. The funds are distributed<br />
to peripheral health institutes and regular expenses are carried out. The V.H.Cs are established at<br />
village level and the R.KS. is established at all health institutes. B.P.M.U. and I.D.W. are established<br />
and functioning.<br />
Sr.<br />
No.<br />
Block/Distric<br />
Institutional Delivery<br />
2004‐05 2005‐206 2006‐07 2007‐08 2008‐09 2009‐10<br />
1 Chikhaldara 528 785 919 259 1034 1855<br />
2 Dharni 1056 1619 1948 611 2344 4163<br />
3 Non Tribal Block 8055 8834 9015 8652 8950 8807<br />
Total …… 9639 11238 11882 9522 12328 14825<br />
Efforts taken for Malnurished Children<br />
Sr. No. Block<br />
SAM/MAM Children in District<br />
Total<br />
Population<br />
0 to 6 year<br />
Children<br />
SAM Child MAM Child Normal<br />
1 <strong>Amravati</strong> 132400 11663 289 1003 10371<br />
2 Achalpur 154466 13662 154 534 12974<br />
3 Daryapur 130901 10180 119 456 9605<br />
4 Bhatkuli 105119 9075 144 677 8254<br />
5 Anjangaon Surji 100406 8689 82 250 8357<br />
6 Morshi 138998 12129 105 620 11404<br />
7 Nandgaon Kh. 125421 10258 333 1298 8627<br />
8 Tiosa 101665 8340 50 113 8177<br />
9 Chandur Bz. 176649 14701 289 1185 13227<br />
10 Chandur Rly. 72810 6238 119 576 5543<br />
11 Warud 149379 12908 137 641 12130<br />
12 Dhamangaon Rly 106862 8828 130 485 8213<br />
13 Dharni 176433 22570 1154 2228 19188<br />
14 Chikhaldara 108719 14422 233 791 13398
Sr.<br />
no<br />
Completed CTC in District<br />
block PHC<br />
NO.<br />
OF<br />
CTC/<br />
PHC<br />
Admitted children Improved Children<br />
SAM MAM total<br />
SAM<br />
to<br />
MAM<br />
SAM<br />
to<br />
Nor<br />
mal<br />
MAM<br />
to<br />
Normal<br />
1 <strong>Amravati</strong> 4 1 13 1 14 6 1 0 7 7 0 0<br />
2 Achalpur 3 2 2 10 12 32 0 0 0 0 0 0<br />
3 Bhatkuli 3 2 8 18 26 2 0 15 17 9 0 0<br />
4 Anjangoan S. 3 2<br />
5 Chandur bz 4 3 27 13 40 16 0 7 23 16 1 16<br />
6 Dharni 6 6 53 6 59 27 0 15 42 17 5 0<br />
7 Chikhaldara 5 5 23 24 47 7 4 24 35 8 4 0<br />
total 28 21 126 72 198 90 5 61 124 57 10 16<br />
Completed VCDC in District<br />
Sr. No. Block VCDC SAM MAM Total<br />
total<br />
Waig<br />
ht<br />
Gain<br />
Admitted Children Improved Children<br />
SAM to<br />
MAM<br />
MAM to<br />
Normal<br />
Waig<br />
ht<br />
not<br />
Gain<br />
Reffr<br />
al<br />
Not<br />
Improved<br />
Children<br />
1 Dharni 68 96 587 683 189 146 348<br />
2 Chikhaldara 53 118 325 443 70 253 120<br />
3 <strong>Amravati</strong> 21 27 190 217 15 178 24<br />
Total.. 142 241 1102 1343 274 577 492<br />
VCDC ‐ Dahendri<br />
VCDC – Malki
Infrastructure Development by NRHM<br />
In District to improve health care facility at health institution existing infrastructure become<br />
main hardals because of the old and shabey impression of the health facility prevent petiet to avail<br />
regular heatlh facility in Government hospital for that District Society decide to improve health<br />
institution through infrastructure development wing. Priority was given to IPHS institution and the<br />
institution were delivery took place. Also taking into consideration petent load and delivery load 8<br />
new sub center are constructed and handed over to villagers. Also Village <strong>Health</strong> sanitation and<br />
nutrition committee are established at village level. P.H.C., Block and district mission are formed and<br />
they are functioning. Regular meetings are conducted and monthly progress is reviewed. R.K.S. is<br />
established at all P.H.Cs and R.H. and functioning. District Hospital is functioning with I.P.H.S.<br />
standered.<br />
New Face to <strong>Health</strong> Institution
PHC – Dhamak, Block – Nandgaon Khandeshwar<br />
Before renovation<br />
After renovation
Repair Work Taken During Year 2008‐09 & 2009‐10<br />
PHC – Anjagaon Bari, Block – <strong>Amravati</strong>
New Construction Work Taken During Year 2008‐09 & 2009‐10<br />
SC‐ Chandikapur, PHC‐ Chandrapur, Block‐ Daryapur<br />
SC‐ Dhanora, PHC‐ Papal, Block‐ Nandgaon Kh.
PROCESS OF PIP PREPERATION<br />
Planning process:<br />
As directed by the State in State level workshop conducted on 23/12/2010 and attend by<br />
Noal Officer, Principal HFWTC, at District level workshop was organized on 27/12/2010 &<br />
28/12/2010 at <strong>Amravati</strong>. Nodal officer, DHO, CEO, CS, and All concerned Programme Officers, were<br />
called for this workshop. The information about preparation of DHAP 2011‐12 was given in details.<br />
Planning Phase :<br />
To prepare a comprehensive district plan. A district level planning & monitoring committee<br />
was formed under the chairmanship of Chief Executive Officer Zilla Parishad Amaravati. The planning<br />
committee has following members<br />
Core Team<br />
1. Mr. Omprakash bakoria, Chief Executive Officer, Zilla Parishad, <strong>Amravati</strong><br />
2. Smt. Dr. Sandhay Khadse Nodel Officer NRHM Mumbai.<br />
3. Dr. P.S. Dalu, Principal H.F.W.T.C., <strong>Amravati</strong><br />
4. Dr. S.K. Yelurkar, District <strong>Health</strong> Officer, <strong>Amravati</strong>.<br />
5. Dr. C.L. Sonkusre, Civil Surgeon, <strong>Amravati</strong>.<br />
6. Dr. Ramesh Bansod , District RCH Officer, <strong>Amravati</strong><br />
7. Mr. P.R. Jagtap, District Programme Manager (NRHM)<br />
8. Mr. R.S. Lanjewar, District Account Manager (NRHM)<br />
9. Mr. Praful Ridhore, M&E Officer (NRHM)<br />
Others<br />
1. Dr. C. U. Bendale, RMO, Outreach<br />
2. Dr. S. H. Nikam, A.O. DH, <strong>Amravati</strong><br />
3. Dr. Suresh Tarodekar, District Malaria Officer<br />
4. Dr. Sharad Patil, District T B officer & Additional Director <strong>Health</strong> Services (Leprosy)<br />
The above committee members met and the following steps were decided to undertake in preparing<br />
the DHAP for <strong>Amravati</strong> district.<br />
1. Orientation of planning team on NRHM initiatives<br />
2. Orientation of block level functionaries on NRHM and on Intersectoral convergence<br />
3. Planning team meeting to develop a plan of action<br />
4. Desk review by the planning team<br />
5. Block level consultations<br />
6. Collection of village information in Gramsabha.<br />
7. Preparation of Dispensary plan.<br />
8. Preparation of PHC plan.<br />
9. Preparation of Block level action plans<br />
10. District level Consultation from Senior Public Heath Experience person<br />
11. Preparation of PIPs for disease control programmes & other <strong>National</strong> <strong>Health</strong> Programme by<br />
respective Programme officers<br />
12. Preparation of District plan at HFWTC.<br />
13. Preparation of Action plan and Report writing<br />
14. Presentation of DHAP‐ during district level meeting<br />
15. Finalizing the draft and submission to GOVT Of MAHARASHTRA
Time Table of Organization Activities<br />
Date Activity Level<br />
23.12.2010<br />
27.12.2010<br />
28.12.2010<br />
28.10.2010<br />
29‐31 Dec<br />
2010<br />
29‐31 Dec<br />
2010<br />
4.1.2011<br />
5‐7 Jan<br />
2011<br />
6.1.2011<br />
7‐12 Jan<br />
2011<br />
13.1.2011<br />
14.1.2011<br />
Dissemination of<br />
guidelines to Districts<br />
District Level Workshop<br />
of Medical Officers PHC<br />
& Medical Supt<br />
PHC Level Meetings of<br />
PHC Staff.<br />
Hospital level meeting of<br />
RH/SDH/WH/GH staff<br />
Village level planning and<br />
approval of VHC and<br />
Gram Sabha<br />
SC level planning and<br />
approval of SC<br />
Monitoring Committee<br />
Approval of GB of RKS of<br />
concerned <strong>Health</strong><br />
Institutes<br />
Preparation of Block<br />
Level Plans<br />
Approval of Block Plans<br />
by Block <strong>Health</strong> <strong>Mission</strong><br />
Preparation of District<br />
Plans<br />
Approval of Executive<br />
Committee and<br />
Governing body<br />
Approval of District<br />
<strong>Health</strong> <strong>Mission</strong> and<br />
information to DPDC<br />
Responsible<br />
officer<br />
State SHS<br />
District<br />
Nodal Officer<br />
(RCH)/ DHO/CS<br />
Block THO/MO PHC<br />
Block<br />
Sub<br />
Center<br />
Sub<br />
Center<br />
Block &<br />
PHC<br />
Block<br />
Medial<br />
Superintendent/CS<br />
ANM/MPW<br />
ANM / MPW<br />
MO PHC/THO<br />
MS<br />
RH/SDH/WH/GH<br />
DHO/CS<br />
DPM<br />
DAM<br />
Block THO/MS<br />
District<br />
DHO/CS/DPM<br />
15.1.2011 Submission of PIP to SHS District DHO/CS/DPM<br />
Remarks<br />
Dissemination of guidelines to PHCs<br />
along with formats and required<br />
material<br />
Dissemination of guidelines along with<br />
formats and required material<br />
Use of Village health register for PIP<br />
preparation. PIP need to be approved<br />
by Gram Sabha. After approval,<br />
forward the copy of PIP to MO PHC.<br />
PIP to be prepared based on SC<br />
format. PIP approved by SC Monitoring<br />
Committee. PIP to be submitted to MO<br />
PHC on 31.12.2010<br />
Submission of Plans to EC and GB of<br />
RKS for sanctioning. Once the plans are<br />
approved by EC and GB, forward<br />
approved plans to THO for preparation<br />
of block plans.<br />
All the block plans are prepared at<br />
district HQ in district level workshop.<br />
DPM will be responsible for<br />
arrangement of workshop. Workshop<br />
will be attended by MS, THO, MO.<br />
There will be two sections of block<br />
plan. Section ‐ I of the block plan will<br />
consist of plan of all PHCs put together<br />
+ THO HQ plan.<br />
Section ‐ II of the plan will consist of<br />
plan of all the RH/SDH in block put<br />
together.<br />
Block plan (both sections) to be<br />
approved by Block <strong>Health</strong> <strong>Mission</strong>.<br />
District Plan will be prepared by<br />
addition of block plans, plans of<br />
District and regional level hospitals<br />
situated in district and District HQ<br />
plan.<br />
Workshop will be organised at<br />
HFWTCs for preparation of District<br />
PIPs during 10‐13 January 2011.<br />
District DHO/CS/DPM Approval of PIP by EC and GB.<br />
District DHO/CS/DPM Approval of PIP by DHM<br />
Submission of PIP to SHS after<br />
approval by District <strong>Health</strong> <strong>Mission</strong>
Village level Planning:<br />
Medical Officers oriented his staff and Anganwadi for village level planning<br />
Form no. 1 is translated in Marathi and given 10 forms to each ANM. Considering the<br />
manpower the support of MPW/Anganwadi is taken. The Gram sevaks were informed well in time by<br />
taluka health officer and most of them were present in Gram Sabha. The village health sanitation<br />
and nutrition committee members, Gram panchayat members, SHGs , Social leaders and other<br />
prominent peoples were present in the meeting at most of the places involvement of women was<br />
there. This activity was completed in one week’s time.<br />
Approval by Committees:<br />
Village level: The village plan form was discussed with village health sanitation and nutrition<br />
committee. There suggestions and comments were noted and included in block plan.<br />
PHC level: All village plans analysed at PHC level and also the form no. 2 of the institutes were filled<br />
in by concerned persons. Staff meeting was called at PHC and PHC plan was prepared in form no. 3.<br />
And included the suggestions made by the field staff.<br />
Block level: Taluka health officer arranged the workshop of medical officers of PHC and Medical<br />
Superintendent along with stake holder departments. Form no. 5 of Block plan was filled in with<br />
summation of form 3 and 4 including block THO demand. This block plan was prepared and<br />
discussed with DPM and DHO, Civil surgeon and finalized. Final Block plan is approved by block<br />
mission committee.<br />
District Level : All Block plans were collected and consolidated at HFWTC level in one week. The<br />
programme officer’s annual plan and civil surgeon’s hospital plan were collected and complete<br />
district plan for 2011‐12 is prepared, This district action plan is discussed with the collector and chief<br />
executive officer zilla parishad <strong>Amravati</strong>. The final plan is approved by district mission committee.
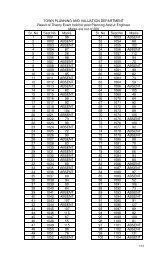
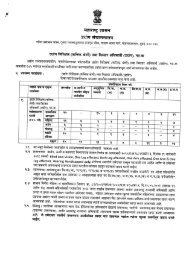
Budget Summery<br />
Sr No Main Heads Components Budget Amount<br />
(Rest in Lakh)<br />
1 Human Resources Contractual Remuneration for ANMs, Nurses, SNs, LHVs 426.55<br />
Contractual Remuneration for LTs,MPWs 0<br />
Contractual Remuneration of Specialists (Anesthetists,<br />
0<br />
Pediatricians, Ob/Gyn, Surgeons, Physicians, Dental<br />
Surgeons, Radiologist, Sonologist, Pathologist, Specialist for<br />
CHCs.)<br />
Medical Officers at CHCs / PHCs 0<br />
Contractual Remuneration of PHNs at CHC, PHC level 0<br />
Additional Allowances/ Incentives to M.O.s of PHCs and<br />
CHCs<br />
Payment to Others ‐ Computer Assistants/ BCC Co‐ordinator<br />
etc<br />
1.16<br />
Incentive/ Awards etc. to SN, ANMs etc. 0<br />
Human Resources Development (Other than above) 0<br />
Other Incentives Schemes (Please Specify) Hardship<br />
113.28<br />
Allwownce<br />
Strengthening of SHS /SPMU (Including HR, Management<br />
0<br />
Cost, Mobility Support, Field Visits)<br />
Strengthening of DHS/DPMU (Including HR, Management<br />
17.60<br />
Cost, Mobility Support, Field Visits )<br />
Strengthening of Block PMU (Including HR, Management<br />
81.48<br />
Cost, Mobility Support, Field Visits )<br />
Strengthening (Others) 0<br />
FMG 4.08<br />
RKS Coordinator 4.44<br />
IDW wing 17.88<br />
IPHS wing 7.32<br />
Other Programme Management Costs (Audit Fees,<br />
Concurrent Audit etc.)<br />
Mobility Support, Field Visits to BMO/MO/Others 27.11<br />
Payment to AYUSH M.O.s 30.80<br />
Payment to AYUSH Other Staffs 0<br />
2 Training Training under Maternal <strong>Health</strong> 0<br />
Training under Child <strong>Health</strong> 0<br />
Training under Family Planning Services 0<br />
Strengthening Training Institutions 0<br />
Development of training packages 0<br />
IMEP Trainings 0<br />
ARSH Training 0<br />
Programme Management Training 0<br />
Training (Nursing) 0<br />
Training (Other <strong>Health</strong> Personnel) 0<br />
0<br />
0
Sr No Main Heads Components Budget Amount<br />
(Rest in Lakh)<br />
Training for Cold Chain Handlers/refrigerator mechanics 0<br />
Training of M.O.s /Other Staffs on R.I. 0<br />
3 Infrastructure Up gradation of CHCs, PHCs, Dist. Hospitals to IPHS) 488.00<br />
Strengthening of District, Sub‐divisional Hospitals, CHCs,<br />
PHCs<br />
0<br />
New Constructions/ Renovation and Setting up CHCs, PHCs,<br />
HSCs,<br />
430.00<br />
Construction (Others) 0<br />
Minor civil works for operationalisation of FRUs 0<br />
Minor civil works for operationalisation of 24 hour services<br />
at PHCs<br />
106.50<br />
Civil Work under RNTCP 0<br />
Other Civil Works 0<br />
4 Procurement Procurement of Drugs & Supplies 0<br />
Procurement of Equipment 0<br />
Procurement of Others 30.40<br />
5 IEC/BCC Development of State BCC/IEC strategy 0<br />
Implementation of BCC/IEC strategy 0<br />
<strong>Health</strong> Mela 0<br />
Creating awareness on declining sex ratio issue 0<br />
Other activities (Kalapathk, Radeo Jingal, wall painting &<br />
hordings)<br />
7.80<br />
6 Untied funds Untied funds for,VHSC, SC CHC,PHC 234.75<br />
Annual Maintenance Grants for CHCs, PHCs 113.90<br />
Panchayati Raj Initiatives 0<br />
7 ASHA ASHA Payments under NRHM Additionalities 0<br />
Selection & Training of ASHA 0<br />
Procurement of ASHA Drug Kit 0<br />
Incentive to ASHAs under JSY 28.54<br />
Incentive under Family Planning Services 0<br />
Incentive under Child <strong>Health</strong> 0<br />
Incentive to ASHA's for motivating families for Sanitary<br />
Toilets/Other Incentives<br />
156.51<br />
Awards to ASHA's/Link workers 0<br />
ASHA Incentive under Immunisation 31.89<br />
ASHA Incentive under NLEP 0.91<br />
ASHA Incentive under NVBDCP 2.07<br />
ASHA Incentive under NBCP 6.54<br />
ASHA Incentive under RNTCP 0.88<br />
8 RKS Corpus grants to RKS 85.00<br />
9 JSY Home Deliveries 7.43<br />
Institutional Deliveries 91.65<br />
C‐Section 4.02<br />
Sanitory Napkin for delivery 14.86
Sr No Main Heads Components Budget Amount<br />
(Rest in Lakh)<br />
Adminstration cost 5.24<br />
10 Sterlisation Compensation for Male sterlisation 16.80<br />
Compensation for Female sterlisation 83.16<br />
NSV Camps 0.53<br />
Female Sterlisation Camps 0<br />
IUD workshop 4.20<br />
Social Marketing of contraceptives 0<br />
POL for Family Planning 11.20<br />
Repairs of Laparoscopes 2.00<br />
Other Expenses (Mini camps) 0.88<br />
11 Referral Transport Referral Transport 8.40<br />
12 Other RCH<br />
Activities<br />
ARSH 8.70<br />
Urban RCH 35.04<br />
Tribal RCH 33.06<br />
PCPNDT 5.15<br />
Maternal <strong>Health</strong> 20.97<br />
Child <strong>Health</strong> 159.79<br />
Infrastructure & human resourses 1.60<br />
13 Vulnerable Group Vulnerable Groups 2.40<br />
14 Other <strong>Mission</strong><br />
activities<br />
Research Studies, 0<br />
New Initiatives 0<br />
Support to other programmes 0<br />
District <strong>Health</strong> Action Plan 8.40<br />
Mainstreaming of AYUSH 0<br />
MMU 15.76<br />
SHSRC 0<br />
School <strong>Health</strong> Programme 139.54<br />
<strong>Health</strong> Insurance 0<br />
Planning , Implementation, Monitoring 12.24<br />
Telemedicine 7.35<br />
Strenthning of Nursing School 117.40<br />
Sickle cell Disease 41.52<br />
Coordination Cell DH 4.58<br />
Maher Scheme 16.40<br />
Volunteer to tribal PHC 12.96<br />
Diet facility for PHC 19.80<br />
15 PPP/NGO NGO activities, PPP under NRHM Additionalities 0<br />
Other NDCPs (RNTCP, NPCB etc) 6.86<br />
16 Operational Cost<br />
(NDCPs)<br />
Mobility, Review Meeting ,field visits,<br />
531.78<br />
formats & reports, Communication etc for<br />
NDCPs<br />
Lab consumables, AMC etc for NDCPs 0
Sr No Main Heads Components Budget Amount<br />
(Rest in Lakh)<br />
17 Financial aid/grant<br />
to Institutions<br />
(NDCPs)<br />
Financial Support to Medical colleges 0<br />
Financial Support to Referral Institutes 0<br />
Financial Support to Sentinel sites 0<br />
18 Immunization Other Immunization activity 22.97<br />
Grand Total 3930.03<br />
Sr. No. Name of Scheme 2010‐11<br />
Budget Abstract<br />
Expenditure<br />
(Nov 10)<br />
%<br />
2011‐2012<br />
Proposed<br />
Extra<br />
Budget<br />
Part A RCH 575.86 234.77 40.77 688.04 112.18<br />
Part B NRHM Additionalities 1880.68 593.69 31.57 2646.79 766.11<br />
Part C Routine<br />
Immunization<br />
49.70 26.39 53.10 54.86<br />
5.16<br />
Total … 2506.24 854.85 3389.69 883.45<br />
Part D<br />
DESEASE CONTROL<br />
PROGRAME<br />
1<br />
2<br />
3<br />
4<br />
5<br />
6<br />
7<br />
8<br />
<strong>National</strong> Vector Born<br />
Disease Control<br />
Programme<br />
Revised <strong>National</strong><br />
Tuberculosis Control<br />
Programme<br />
<strong>National</strong> Programme<br />
for Control of Blindness<br />
<strong>National</strong> Leprosy<br />
Elimination Programme<br />
Integrated Disease<br />
Surveillance<br />
Programme<br />
19.83 2.090 10.54 374.02 354.19<br />
35.75 17.780 49.73 73.41 37.66<br />
23.08 18.63 80.72 18.34 ‐4.74<br />
10.39 4.09 39.36 9.98 ‐0.41<br />
8.13 1.10 13.53 9.03 0.9<br />
District tobacco Control<br />
Programme<br />
0 0 0.00 12.16 12.16<br />
<strong>National</strong> Mental <strong>Health</strong><br />
Programme<br />
0 0 0.00 42.45 42.45<br />
<strong>National</strong> Deafness<br />
Control Programme<br />
3.25 0 0.00 9.65 6.4<br />
Total 100.43 43.69 193.888 549.04 448.61<br />
Grand Total 2606.67 898.54 193.888 3938.73 1332.06
ACTIVITY* Approved<br />
Budget<br />
PART –A<br />
RCH-II Budget Abstract<br />
2010-11 2011-12<br />
Physical<br />
Target<br />
Proposed<br />
Budget<br />
Proposed<br />
Physical<br />
Target<br />
Additional<br />
Budget<br />
Proposed for<br />
2011-12<br />
RCH Flexipool<br />
Maternal <strong>Health</strong> 13.46 40.05 26.59<br />
JSY 58.22 7339 151.76 14866 93.54<br />
Child <strong>Health</strong> 61.40 159.79 98.39<br />
Family Planning 95.51 11200 116.77 11200 21.26<br />
ARSH 5.70 8.70 3.00<br />
Urban RCH 32.38 31 35.04 35 2.66<br />
Tribal RCH 33.72 33.72 0.00<br />
Vulnerable Groups 1.80 2 2.40 2 0.60<br />
Innovations / PPP/ NGO 4.55 5.15 0.60<br />
Infrastructure & HR 103.02 107.66 4.64<br />
Institutional<br />
Strengthening<br />
8.65 1.60 0<br />
Training 0.00 0.00 0.00<br />
BCC/IEC 8.00 7.80 0<br />
Program Management 17.61 17.60 0<br />
Total… 444.02 18572 688.04<br />
Maternal <strong>Health</strong> ‐ Additional budget of Rs. 10.81 against last year sanction PIP is proposed<br />
for following activities.<br />
(1) Rs. 0.75 Lacs is demanded for refferal of 1400 EmOC cases @ Rs. 300/‐ per case. Against<br />
last year sanction budget for 1400 EmOC cases @ Rs. 300/‐ per case.<br />
(2) Rs. 2.16 Lacs is demanded for additional 108 highrisk ANC & gynic clinic camps at PHC<br />
level @ Rs. 2000/‐ per camp. Against last year sanction PIP.<br />
(3) Additional budget of Rs. 6.72 Lacs is demanded for 6720 benefieries @ Rs. 150/‐ per<br />
beneficiaries for fee diet allowance against last year sanction budget for 3360 beneficiaries<br />
@ Rs. 100/‐ per beneficiaries.<br />
(4) Additional budget of Rs. 1.18 Lacs is demanded for 2340 benefieries @ Rs. 150/‐ per<br />
beneficiaries for fee diet allowance against last year sanction budget for 2340 beneficiaries<br />
@ Rs. 100/‐ per beneficiaries.<br />
JSY ‐ In financial year 2010‐11 budget of Rs. 58.22 Lacs is sanction against expected number<br />
of 7339 benefiaries but actual number of expected number of benefiaries are higher than<br />
target. Hence in financial year 2011‐12 is proposed budget of Rs. 136.88 against 14866<br />
expected no. of JSY benefiaries.<br />
Child <strong>Health</strong> ‐ Additional budget of Rs. 10.81 against last year sanction PIP is proposed for<br />
following activities. Additional budget of Rs. 98.39 against last year sanction PIP is proposed<br />
for following activities.<br />
(1) Additional budget of Rs. 5.18 Lacs is demanded for 26 CTC for 10 Children per CTC @ Rs.
3360/‐ per children for 21 days at RH/SDH level against last year sanction budget for 13 CTC<br />
for 8 children for CTC @ Rs. 3360/‐ per children for 21 days.<br />
(2) Additional budget of Rs. 96 Lacs is demanded for VCDC at subcentre level for 15000 SAM<br />
& MAM Children @ Rs. 960 Lacs per children.<br />
(3) Rs. 0.60 Lacs is demanded for additional 30 Peadiatrician checkup camps at PHC level @<br />
Rs. 2000/‐ per camp. Against last year sanction PIP.<br />
Family Planning ‐ Additional budget of Rs. 21.26 Lacs against last year sanction PIP is<br />
proposed for following activities.<br />
(1) Additional budget of Rs. 1.12 Lacs is demanded for Transport of 11200 Family Planning<br />
cases @ Rs. 100/‐ per case against last year sanction budget for 10080 cases @ Rs. 100/‐<br />
(2) Additional of Rs. 0.06 Lacs is demanded for additional 2 camps @ Rs. 300/‐ per camp of<br />
Promotion of IUD 380A & EC Pills through sensitization of SHG.<br />
(3) Additional budget of Rs. 12.67 Lacs is demanded for Compensation of 10080 female<br />
sterilisation cases @ Rs. 825/‐ per case against last year sanction budget for 10640 cases @<br />
Rs. 662.50 per case.<br />
(4) Additional budget of Rs. 8.40 Lacs is demanded for Compensation for 1120 NSV<br />
Acceptance cases @ Rs. 1500 per case against last year sanction budget for 560 cases @ Rs.<br />
1500/‐ per case.<br />
ARSH ‐ In last year sanction PIP budget of Rs. 3.00 Lacs is sanction for Sensitization peer<br />
groups in villages through community based approach for 6 months only. Hence during the<br />
financial year additional budget of Rs. 3.00 Lacs is proposed for other 6 months.<br />
Urban RCH‐ Additional budget of Rs. 2.66 lacs is required for additional 4 ANM @ Rs. 5500/‐<br />
against last year sanction PIP.<br />
Vulnerable Groups‐ In last year sanction PIP 9 month salary of 2 counselor @ Rs. 10000/‐ is<br />
sanction. Against which additional budget of Rs. 0.60 lacs is required for 3 month salary of<br />
counselor.<br />
Innovations / PPP/ NGO ‐ In last year sanction PIP 9 month salary of 2 counselor @ Rs.<br />
10000/‐ is sanction. Against which additional budget of Rs. 0.60 lacs is required for 3 month<br />
salary of counselor.<br />
Infrastructure & HR‐ Additional budget of Rs. 4.64 Lacs is demanded for Repair and<br />
expantation of 30 sub center labour room @ Rs. 2.50 Lac per unit and 9 PHC labour room @<br />
Rs. 3.50 Lac per unit against last year sanction budget of Rs. 101.82 for 60 repair and<br />
expantation of labour rooms at sub center & PHC level.
Sr.<br />
No.<br />
Initiative Number<br />
Proposed<br />
PART B<br />
<strong>Mission</strong> Flexipool<br />
Budget for 2011 – 12<br />
2010‐11 2011‐12 Difference<br />
Total<br />
Amount<br />
(in Lacs)<br />
Number<br />
Proposed<br />
Total<br />
Amount<br />
(in Lacs)<br />
Number<br />
Proposed<br />
Total<br />
Amount<br />
(in Lacs)<br />
1 ASHA 2068 91.73 2068 156.51 0 64.78 (+)<br />
2<br />
Addititinal ANM sub‐<br />
center<br />
285 296.28 333 331.08 48 34.80 (+)<br />
3 Staff Nurse at 24 x 7 PHCs 38 42.00 47 52.68 9 10.68 (+)<br />
4 Supervior in Nurse (LHV) 33 38.62 36 42.79 3 4.17 (+)<br />
5 VHSNWC 1547 154.70 1547 154.70 0 0.00<br />
6 Untied Fund for SC 333 33.30 333 33.30 0 0.00<br />
7 Untied Fund for PHU 83 20.75 103 25.75 20 5.00 (+)<br />
8 Untied Fund for PHC 56 14.00 56 14.00 0 0.00<br />
9<br />
Untied Fund for<br />
RH/SDH/WH<br />
14 7.00 14 7.00 0 0.00<br />
10 Rogi Kalyan Samiti‐DH 1 5.00 1 5.00 0 0.00<br />
11 Rogi Kalyan Samiti‐SDH 4 4.00 4 4.00 0 0.00<br />
12 Rogi Kalyan Samiti‐RH/WH 10 10.00 10 10.00 0 0.00<br />
13 Rogi Kalyan Samiti‐ PHC 56 56.00 56 56.00 0 0.00<br />
14 Rogi Kalyan Samiti‐ TB 1 5.00 1 5.00 0 0.00<br />
15 Rogi Kalyan Samiti‐ RRC 1 5.00 1 5.00 0 0.00<br />
16<br />
Annual Maintenance<br />
Grant‐DH<br />
1 5.00 1 5.00 0 0.00<br />
17<br />
Annual Maintenance<br />
Grant‐SDH/RH/WH<br />
14 14.00 14 14.00 0 0.00<br />
18<br />
Annual Maintenance<br />
Grant‐RRC<br />
1 5.00 1 5.00 0 0.00<br />
19<br />
Annual Maintenance<br />
Grant‐PHU<br />
62 31.00 62 31.00 0 0.00<br />
20<br />
Annual Maintenance<br />
Grant‐PHC<br />
48 24.00 48 24.00 0 0.00<br />
21<br />
Annual Maintenance<br />
Grant‐SC<br />
299 29.90 299 29.90 0 0.00<br />
22<br />
Annual Maintenance<br />
Grant TB<br />
1 5.00 1 5.00 0 0.00<br />
23<br />
Repairs and New<br />
Construction<br />
58 72.00 61 430.00 3 358.00 (+)<br />
24<br />
Ambulance services for<br />
PHC‐ Repairs<br />
56 18.45 56 18.45 0 0.00<br />
25<br />
Ambulance services for<br />
RH/SDH/WH<br />
14 1.68 14 7.00 0 5.32 (+)<br />
26<br />
Ambulance services for<br />
DH<br />
0 0.00 2 1.00 2 1.00 (+)<br />
27 IPHS up‐gradation SC 83 83.00 83 83.00 0 0.00<br />
(+)<br />
(-)
28 IPHS up‐gradation PHC 34 170.00 34 170.00 0 0.00<br />
29 IPHS up‐gradation RH 4 48.00 1 20.00 -3 -28.00 (-)<br />
30<br />
IPHS up‐gradation SDH‐<br />
100<br />
1 18.00 1 20.00 0 2.00 (+)<br />
31 IPHS up‐gradation SDH‐50 3 42.00 3 60.00 0 18.00 (+)<br />
32 IPHS up‐gradation WH 1 35.00 1 35.00 0 0.00<br />
33 IPHS up‐gradation DH 1 50.00 1 50.00 0 0.00<br />
34 IPHS – ISO Certification 10 34.07 10 50.00 0 15.93 (+)<br />
35 Telemedicine Center 1 3.67 3 7.35 2 3.68 (+)<br />
36<br />
Strengthening of Nursing<br />
Services<br />
2 137.40 2 117.40 0 -20.00 (-)<br />
37 School <strong>Health</strong> Programme 0 0.00 16 139.54 16 139.54 (+)<br />
38<br />
Sickle Cell Disease<br />
Programme<br />
1 33.10 1 41.52 0 8.42 (+)<br />
39 Procurement Plan 2 1.20 16 30.40 14 29.20 (+)<br />
40 Co‐ordination Cell DH 1 3.64 1 4.58 0 0.94 (+)<br />
41 Maher Scheme 6 10.50 9 16.40 3 5.90 (+)<br />
42 Volunteer to trible PHCs 11 4.40 34 12.96 23 8.56 (+)<br />
43 Diet facility for PHC 11 4.95 11 19.80 0 14.85 (+)<br />
44 AYUSH Cell 26 27.84 28 30.80 2 2.96 (+)<br />
45<br />
Hardship Allowances to<br />
Regular <strong>Health</strong> Staff<br />
2 58.56 14 113.28 12 54.72 (+)<br />
46 Mobile Medical Unit 1 10.18 1 15.76 0 5.58 (+)<br />
47 DHAP 14 8.40 14 8.40 0 0.00<br />
48 M & E Cell 4 9.84 4 12.24 0 2.40 (+)<br />
49 FMG 2 3.62 2 4.08 0 0.46 (+)<br />
50 RKS Coordinator 1 1.86 1 4.44 0 2.58 (+)<br />
51 IDW Wing 6 19.56 6 17.88 0 -1.68 (-)<br />
52 IPHS Wing 2 6.13 2 7.32 0 1.19 (+)<br />
53<br />
Block Program<br />
Management Unit<br />
14 66.36 14 81.48 0 15.12 (+)<br />
TOTAL 1880.69 5482 2646.79 5482 766.10 (+)<br />
Write up of extra budget proposed for the year 2011-12<br />
ASHAs ‐ in the year 2010-11 non tribal ASHAs selection procedure completed in the month<br />
of Dec 09. Hence performance incentive & meeting expenditure will be carried out from Jan<br />
10, and expenditure booked for 3 month. for proposed financial year budget required for 400<br />
tribal & 1668 non tribal ASHA throughout the year. additional budget of Rs. 81.22 lacs<br />
required for performance based incentive and meeting expenditure of ASHA.<br />
Additional ANM sub‐center ‐ in the year 2010-11 salary budget required for total 285 ANMs<br />
including 45 tribal ANM. But in year 2011-12 it is expected that all the vacancies are get<br />
fulfilled and hence budget required for 333 ANMs, i.e. Rs. 331.08 additional budget including<br />
fix PTA & cost of PTLA, compare to last year required Rs. 34.80 lacs.
Staff Nurse at 24 x 7 PHCs ‐ in the year 2010-11 salary budget required for 38 Staff Nurse of<br />
Rs. 42.00 lacs for year 2011-12 it is expected to appoint more 9 Staff Nurse. Hence budget of<br />
Rs. 10.68 lacs.<br />
Supervior in Nurse (LHV) ‐ In the year 2010-11 budget approved of Rs. 38.62 lacs for 33 LHV.<br />
But in year 2011-12 it is expected to appoint more 3 LHVs. for that budget of Rs. 4.17 lacs<br />
additional is required. Total budget Required of Rs. 42.79 lacs.<br />
Untied Fund for PHU ‐ In the year 2011-12 additional 20 PHUs proposed compare to last year<br />
for that budget of Rs. 5.00 lacs is required. Total budget required for Rs. 25.75 lacs.<br />
Repairs and New Construction ‐ In the year 2010-11 minor repair and new work of SC &<br />
PHCs are taken and for total 58 works budget shall approved of Rs. 72.00 lacs. For year<br />
2011-12 district is proposed new works of 13 SC of Rs. 130.00 lacs, spill over works of PHC<br />
for Rs.100.00 lacs and new work of 1PHCs for Rs. 120.00 repair of TB Hospitalof Rs. 5.00<br />
lacs. Hence total budget requird for all proposed works will be Rs. 355.00lacs. And compare<br />
to last year additional budge of Rs.283.00lacs is requied.<br />
Ambulance services for RH/SDH/WH ‐ In the year 2010-11 for 14 RH/SDH/WH budget of Rs.<br />
0.50 lacs per institute will be proposed. Hence 5.32 lacs additional budget required.<br />
Ambulance services for DH ‐ Budget required for Ambulance POL/Repair of DH Rs. 1.00 lacs<br />
for year 2011-12.<br />
IPHS up‐gradation RH ‐ As per state norms non avaibility of 3 specialist at RH Anjangaon<br />
Surji, Dhamangaon Rly. & Chandur Rly. It will delete for IPHS upgradation in current year.<br />
Only one RH Warud who will full fill above criteria is proposed for IPHS and budget of Rs.<br />
20.00 lacs will be required. Hence budget will be reduced of Rs. 28.00 lacs for year 2011-12.<br />
IPHS up‐gradation SDH‐100 For full filling requirement of specialist, man power & medicine<br />
additional budget of Rs. 2.00 lacs required for SDH Achalpur for year 2011-12.<br />
IPHS up‐gradation SDH‐50 ‐ In year 2010-11 budget of Rs. 14.00 lacs per institute are<br />
sanctioned for IPHS upgredation. Taking in to consideration additional man power, specialist<br />
avability & medicine budget of Rs. 20.00 lacs per SDH will be proposed. Hence additional<br />
budget of Rs. 18.00 lacs will be required.<br />
IPHS – ISO Certification ‐ Budget required for 10 IPHS institution @ 5.00 lacs per institute for<br />
ISO-Certification in the year 2011-12. Hence additional budget of Rs. 50.00 lacs is required.<br />
Telemedicine Center ‐ Budget required for 10 IPHS institution @ 5.00 lacs per institute for<br />
ISO-Certifiation in the year 2011-12. Hence additional budget of Rs. 50.00 lacs is required.<br />
School <strong>Health</strong> Programme ‐ School health programme is not included in <strong>Mission</strong> flexipool in<br />
year 2010-11. it will be included in <strong>Mission</strong> flexipool for year 2011-12. Hence additional<br />
budget of Rs. 151.46 is required.<br />
Sickle Cell Disease Programme ‐ Activity for card printing at PHC level proposed per PHC @<br />
0.60 lacs.and salary of lab technician at SDH/RH level. For that budget of Rs. 1.92 lacs<br />
required Hence additional budget or Rs.2.33 lacs is required.
Procurement Plan ‐ It is proposed to construct warehouse at DHO including equipment,<br />
furniture & contigency and repaire of ware house at DH, total budget of Rs. 29.20 lacs is<br />
required.<br />
Co‐ordination Cell DH ‐ Budget for Co-ordination Cell is proposed for 12 month. In sanction<br />
PIP year 2010-11, it is approved for 10 months. Hence difference amount of Rs. 0.94 lacs will<br />
be shown as additional budget.<br />
Maher Scheme ‐ New construction of Maher Ghar at PHC Katkumb & Salona @ 5.50 lacs per<br />
PHC will be proposed. And maintenance cost of SHG @ 400/- per delivery for 1350 deliveries<br />
in 9 Maher Ghar is proposed. Hence total budget of Rs. 16.40 lacs is required. Taking in to<br />
consideration additional two Maher Ghar budget of Rs. 5.90 lacs more is required.<br />
Volunteer to tribal PHCs ‐ In tribal there are 2 volunteers will be appointed per institute, for 14<br />
institute 28 counselors is working. For SDH Achalpur, DH & WH additional 2 volunteers will<br />
be appointed. Hence total 34 volunteers is posted at health institution. Budget required Rs.<br />
12.96 lacs as honorarium, additional budget of Rs. 8.56 lacs is required.<br />
Diet facility for PHC ‐ In last year PIP budget of Rs. 22500/- per PHC is sanction for 11 PHC<br />
of tribal. for year 2011-12 Diet facility @ Rs. 600/- per delivery for 4 days is proposed for<br />
1650 deliveries in tribal area, budget of Rs. 9.90 lacs for diat and Rs. 9.90 lacs for loss of<br />
wages is required. Total budget of Rs. 19.80 lacs is required. Hence additional budget of Rs.<br />
14.85 is required.<br />
AYUSH Cell ‐For AYUSH cell at district level, one data entry operator, office furniture,<br />
computer, printer & contingency additionally proposed for that additional budget of Rs. 2.96<br />
lacs is required compare to year 2010-11.<br />
Hardship Allowances to Regular <strong>Health</strong> Staff ‐ Hardship allowance to regular health staff in<br />
melghat area cover only MBBS Mos and paramedical staff of extreme difficult PHCs and<br />
Specialist Budget for year 2010-11 is Rs 58.56 lacs. But taking in to consideration total<br />
melghat area and discussion with the melghat health staff it is proposed to give incentive of<br />
hardship allowance to all health staff of melghat including BAMS MO, MOs of RH/SDH and all<br />
paramedical staff reside at melghat. Total budget of Rs. 113.28 lacs required. Hence<br />
additional budget or Rs. 54.72 lacs required as compare to year 2010-11.<br />
Mobile Medical Unit ‐ For year 2010-11 Mobile Medical Unit budget sanction for six month.<br />
For year 2011-12 it is proposed to sanction budget for 12 month so additional grant of Rs.<br />
5.58 lacs required for salary of staff of Mobile Medical Unit.<br />
M & E Cell ‐ For year 2011-12 increase salary of staff as per new norms will be given after<br />
approval from state level. The additional budget of Rs. 2.40 lacs will be required.<br />
FMG ‐ For year 2011-12 increase salary of staff as per new norms will be given after<br />
approval from state level. The additional budget of Rs. 0.46 lacs will be required.<br />
RKS Coordinator ‐ It is proposed to appoint one data entry operator for RKS Coordinator for<br />
year 2011-12 salary of data entry operator & TA/DA of RKS Coordinator will be proposed in<br />
addition. Hence additional budget of Rs. 2.58 lacs will be required.<br />
IPHS Wing ‐ For year 2011-12 increase salary of staff as per new norms will be given after<br />
approval from state level. The additional budget of Rs. 1.19 lacs will be required for additional<br />
salary, TA & contingency.
Block Program Management Unit ‐ For year 2011-12 increase salary of block level staff as<br />
per new norms will be given after approval from state level. The additional budget of Rs.<br />
15.12 lacs will be required for additional salary, TA & contingency for THO BPMU staff.<br />
ACTIVITY* Approved<br />
Budget<br />
Rountin<br />
Immunasation<br />
PART ‐ C<br />
RI Budget Abstract<br />
2010-11 2011-12<br />
49.70<br />
Physical<br />
Target<br />
Proposed<br />
Budget<br />
Proposed<br />
Physical<br />
Target<br />
Additional Budget<br />
Proposed for 2011-<br />
12<br />
Immunasation<br />
22176<br />
Session<br />
54.86 21262 Session 5.16<br />
Rountin Immunasation ‐ Additional budget of Rs. 5.16 against last year sanction PIP is<br />
proposed for following activities.<br />
(1) Additional budget of Rs. 0.03 Lacs is demanded for Mobility support for Supervision<br />
Supervisory visits by district level officers.<br />
(2) Additional budget of Rs. 0.06 Lacs is demanded for Cold Chain maintenance<br />
(3) Additional budget of Rs. 3.62 Lacs is demanded for Mobilization of children through<br />
ASHA/ mobilizers.<br />
(4) Additional budget of Rs. 0.70 Lacs is demanded for Alternative Vaccine Delivery.<br />
(5) Additional budget of Rs. 0.10 Lacs is demanded for Support for Computer Assistant<br />
(6) Additional budget of Rs. 0.21 Lacs is demanded for Quarterly Review meeting.<br />
(7) Additional budget of Rs. 0.24 Lacs is demanded for to develop sub-center and PHC.<br />
(8) Additional budget of Rs. 0.15 Lacs is demanded for Pol for Vaccine delivery.<br />
(9) Additional budget of Rs. 0.05 Lacs is demanded for One day refresher training.
Summery Budget :<br />
BUDGET ABSTRACT<br />
Sr. No. Name of Scheme 2011-2012<br />
Part A Reproductive and Child <strong>Health</strong> 679.34<br />
Part B NRHM Additionalities 2646.79<br />
Part C Routine Immunization 54.86<br />
Part D DESEASE CONTROL PROGRAME<br />
1 <strong>National</strong> Vector Born Disease Control Programme 374.02<br />
2 Revised <strong>National</strong> Tuberculosis Control Programme 73.41<br />
3 <strong>National</strong> Programme for Control of Blindness 18.34<br />
4 <strong>National</strong> Leprosy Elimination Programme 9.98<br />
5 Integrated Disease Surveillance Programme 9.03<br />
6 District tobacco Control Programme 12.16<br />
7 <strong>National</strong> Mental <strong>Health</strong> Programme 42.45<br />
8 <strong>National</strong> Deafness Control Programme 9.65<br />
Grand Total 3930.03
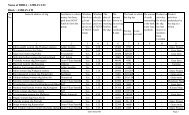
CHAPTER-1:<br />
OUTCOME ANALYSIS OF PIP OF 2009-10 AND 2010-11<br />
In this chapter physical and financial outcomes in respect of various parameters of the PIP of<br />
2009‐10 and 2010‐11 (30.09.2010) should be indicated. For this the sequence of activities given in<br />
the RoP should be followed and information should be provided in the following format:<br />
ACTIVITY*<br />
Financial Physical<br />
(Rs. in lakh)<br />
2009-10 2010-11 2009-10 2010-11<br />
Amount<br />
Approved<br />
Exp Amount<br />
Approved<br />
RCH Flexipool<br />
Maternal <strong>Health</strong> 11.92 3.62 13.46 4.60<br />
Exp Expected<br />
Output<br />
Achieve<br />
me nts<br />
Expected<br />
Output<br />
Achieve<br />
me nts<br />
JSY 84.33 104.19 58.22 74.26 10747 12303 7339 8192<br />
Child <strong>Health</strong> 23.71 16.30 193.24 56.95<br />
Family Planning 136.19 122.14 95.51 40.94 13161 11613 11200 4664<br />
ARSH 22.00 0.25 5.70 0.94<br />
Urban RCH 25.71 14.65 32.38 13.35 35 31 35 31<br />
Tribal RCH 14.58 23.26 33.73 5.44<br />
Vulnerable Groups 0.94 0 1.80 0.09<br />
Innovations / PPP/ NGO 2.38 7.40 4.55 0.45<br />
Infrastructure & HR 167.30 43.04 103.02 26.44<br />
Institutional Strengthening 1.88 0.34 8.65 0.22<br />
Training 0 0.61 0 0<br />
BCC/IEC 17.50 9.34 8.00 0.37<br />
Program Management 21.40 15.35 17.61 8.69 3 3 3 3<br />
<strong>Mission</strong> Flexible Pool<br />
ASHA Programme 93.07 38.53 91.73 43.45 2068 2062 2068 2064<br />
Untied Fund 229.75 163.41 229.75 57.87 2029 2029 2029 2029<br />
AMG 91.40 69.33 113.90 32.52 446 446 413 413<br />
Institutional Strengthening 326.36 223.16 376.90 175.37<br />
Construction /<br />
Upgradation<br />
157.60 138.02 72.00 40.55<br />
Rogi Kalyan Samiti 81.00 77.70 85.00 41.28 73 71 73 73<br />
DHAP 5.60 4.00 8.40 0 14 14 14 14<br />
Strengthening of Training<br />
Centres<br />
Swablamban Yojna<br />
90.57 80.15 137.40 10.42 2 2 2 2
<strong>Health</strong> Mela<br />
ACTIVITY*<br />
Mobility Support for<br />
Medical Officers<br />
Logistics<br />
Financial Physical<br />
2009-10 2010-11 2009-10 2010-11<br />
Amount<br />
Approved<br />
Exp Amount<br />
Approved<br />
Exp Expected<br />
Output<br />
Achieve<br />
me nts<br />
Expected<br />
Output<br />
Achieve<br />
me nts<br />
25.25 17.24 20.13 8.27 71 71 70 70<br />
Procurement 5.16 4.85 1.20 0.52 2 2 2 1<br />
Quality Assurance<br />
Difficult Area Allowance 22.80 14.77 58.56 0 24 21 63 0<br />
Upgradation of <strong>Health</strong><br />
Centers as per Indian<br />
Public <strong>Health</strong> Standards<br />
(IPHS)<br />
426.00 397.08 480.07 120.45 122 127<br />
MMU/EMRI 12.76 0 10.18 0 1 0 1 0<br />
Community Monitoring 9.33 16.99 9.84 3.56 5 5 4 4<br />
District Specific<br />
Interventions<br />
200.47 163.61 60.26 16.13<br />
Mainstreaming of AYUSH 0 0 27.84 14.37 0 0 25 22<br />
Management Cost 80.70 65.63 97.53 39.35<br />
Deafness Programme. 0 0 3.25 0<br />
Immunization<br />
Mobility support for<br />
Supervision and<br />
Monitoring at districts and<br />
state level.<br />
0.47 0.18 0.47 0.05<br />
Cold chain maintenance 0.45 0.01 0.44 0<br />
Alternate Vaccine<br />
Delivery to Session sites<br />
Focus on urban slum &<br />
underserved areas<br />
Social Mobilization by<br />
ASHA /Link workers<br />
Computer Assistants<br />
support at State/district<br />
level<br />
Printing and dissemination<br />
of immunization cards,<br />
tally sheets, charts,<br />
registers, receipt book,<br />
monitoring formats etc.<br />
11.55 11.15 11.92 6.75 19056 19594 22176 12488<br />
0 0 0 0<br />
28.58 27.36 28.28 16.92 19056 19594 22176 12488<br />
0.96 0.95 1.05 0.64 1 1 1 1
ACTIVITY*<br />
Quarterly review meeting<br />
at state/District/Block<br />
level<br />
District level Orientation<br />
for 2 days ANMs,<br />
MPHW,LHV Trainings<br />
To develop micro plan at<br />
sub-centre level and block<br />
level<br />
For consolidation of micro<br />
plan at PHC/CHC level<br />
POL for vaccine delivery<br />
from state to District and<br />
PHC/CHCs<br />
Consumables for computer<br />
including provision for<br />
internet access<br />
Red/Black/Zipper bags<br />
Bleach/Hypochlorite<br />
solution<br />
Twin Bucket<br />
Civil works<br />
Laboratory materials<br />
Honorarium<br />
IEC/ Publicity<br />
Equipment maintenance<br />
Training<br />
Vehicle maintenance<br />
Vehicle hiring<br />
NGO/PP support<br />
Financial Physical<br />
2009-10 2010-11 2009-10 2010-11<br />
Amount<br />
Approved<br />
Miscellaneous 2.54 0.79<br />
Contractual services<br />
Printing<br />
Medical Colleges<br />
Procurement -vehicles<br />
Procurement - equipment<br />
Exp Amount<br />
Approved<br />
1.32 0.66 6.39 1.40<br />
0.74 0.29 0.25 0.03<br />
0.85 0.77 0.85 0.60<br />
0.05 0.01 0.05 0<br />
Disease Control Program<br />
NVBDCP<br />
Exp Expected<br />
Output<br />
Achieve<br />
me nts<br />
Expected<br />
Output<br />
Achieve<br />
me nts
Malaria<br />
Filaria<br />
ACTIVITY*<br />
Dengue/Chikungunya<br />
Cash assistance for<br />
decentralized commodities<br />
Commodity support by<br />
GoI<br />
Surveillance preparedness,<br />
training & staff salary<br />
Financial Physical<br />
2009-10 2010-11 2009-10 2010-11<br />
Amount<br />
Approved<br />
Outbreak investigation 0 0<br />
Analysis & use of data 0 0<br />
Exp Amount<br />
Approved<br />
IDSP<br />
NPCB<br />
Grant in aid (for Cataract<br />
Operations) 18 629584 18<br />
Vision Centre<br />
(50X50,000)<br />
Exp Expected<br />
Output<br />
184239<br />
6<br />
Achieve<br />
me nts<br />
Expected<br />
Output<br />
Achieve<br />
me nts<br />
8500 8011 9000 3153<br />
0 0 0 0 0 0 0 0<br />
Medical Colleges (3X40) 0 0 0 0 0 0 0 0<br />
Strengthening of District<br />
Hospital / Sub District<br />
Hospital<br />
Eye Donation Centre (Non<br />
Recurring 3X1)<br />
Remuneration (SBCS) &<br />
Staff Salary/ Other<br />
Activities/Post<br />
Requirement<br />
IEC Activities (50X20<br />
Thousand + SBCS 1 Lacs)<br />
Proposal for Sutures /(Per<br />
Pieces 10.0) /Ophth.<br />
Equipments<br />
Establishment of IDD<br />
Control Cell<br />
Establishment of IDD<br />
Monitoring Lab<br />
a)<strong>Health</strong> Education and<br />
Publicity<br />
0 0 0 0<br />
As<br />
Above<br />
As Above As Above As Above<br />
0 0 0 0 100 24 40 16<br />
0.24 0.24 0.24 0.12 0 0 0 0<br />
0.18 0.18 0.18 0.09 0 0 0 0<br />
2 0 0 0 0 0 0 0<br />
NIDDCP
ACTIVITY*<br />
b) Salt Testing Kits<br />
supplies by GOI (3,84,000<br />
No)<br />
IDD surveys<br />
Financial Physical<br />
2009-10 2010-11 2009-10 2010-11<br />
Amount<br />
Approved<br />
Exp Amount<br />
Approved<br />
NLEP<br />
Exp Expected<br />
Output<br />
Achieve<br />
me nts<br />
Expected<br />
Output<br />
Achieve<br />
me nts<br />
Contractual Services 0.06 0.06 0.06 0.04 1 1 1 1<br />
Services through<br />
ASHA/USHA<br />
Office expenses &<br />
Consumables<br />
0.24 0.4 0.42 0.35 60 15 80 65<br />
0.32 0.32 0.33 0.16 1 1 1 1<br />
Capacity building 1.43 0.65 1.48 0.46 90 58 90 45<br />
Behavioural Change<br />
Communication<br />
POL/Vehicle operation &<br />
hiring<br />
0.19 0.19 0.25 0.23 0.18 0.18 0.80 0.73<br />
0.75 0.75 0.75 0.56 1 1 1 1<br />
DPMR 5.68 5.02 5.37 2.50 255 169 215 89<br />
Material & Supplies 0.27 0.27 0.27 0.27 96 96 89 89<br />
Urban Leprosy Control 0.85 0.85 1.01 0.016 280 280 280 280<br />
Supervision, Monitoring &<br />
Review<br />
0.15 0.15 0.21 0.12 300 391 300 205<br />
Cash assistance 0 0 0 0 0 0 0 0<br />
NIPPCD<br />
Training 0 0 0 0 0 0 0 0<br />
Capacity building<br />
PHCs/CHCs & District<br />
Hospitals<br />
Manpower at district level<br />
0 0 0 0 70 70 0 0<br />
0 0 0 0<br />
3 ENT<br />
Surgeon<br />
2 Audiolo<br />
gist<br />
0 0<br />
Screening Camps 0 0 0 0 4 4 12 1<br />
Hearing Aids 200 HI per<br />
district per year<br />
0 0 0 0 200 200 200 200<br />
Central Cell at state level 0 0 0 0 0 0 0 0<br />
The list of activity given above may vary from State to State. Therefore States should list the<br />
activities as per their RoP
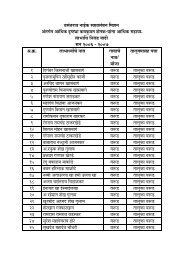
CHAPTER-2:<br />
POLICY AND SYSTEMIC REFORMS IN STRATEGIC AREAS<br />
Lack of systems approach may result in serious gaps that affect service delivery. For instance,<br />
investments in FRUs are to a large extent nullified if there is an irrational deployment of doctors<br />
trained in EMOC and LSAS and there is a sub optimal maximum utilisation of HR, equipments &<br />
facility upgradation. Similarly, the promise of free institutional deliveries remains un‐kept if drugs<br />
and consumables are not available.<br />
The experience so far tells us that the States have addressed these criticalities in an uneven<br />
manner and to a varying extent. In this Chapter, the States should clearly describe the policies and<br />
systems that the States have put in place (and proposed, if any, with timelines) in respect of at least<br />
the following 20 management imperatives:<br />
1. HR policies for Doctors,<br />
Nurses paramedical staff and<br />
programme management<br />
staff<br />
2. Accountability and<br />
Performance appraisal<br />
3. Policies on drugs,<br />
procurement system and<br />
Logistics management<br />
Minimizing vacancies, timely recruitment, transparent<br />
selection, career progression, professional development,<br />
rational deployment, skill utilization, stability of tenure<br />
Sustainability of HR under NRHM.<br />
Facility based monitoring; Incentive for both the HSP and<br />
the facility based on functioning.<br />
Performance appraisal against benchmarks, renewal of<br />
contracts based on performance.<br />
Incentives for performance above benchmark, special<br />
incentives for difficult areas.<br />
Articulation of policy on entitlements. E.g. free vs. charges<br />
drugs for OPD/IPD. Emergency patients, free vs. charged<br />
deliveries etc, rational prescriptions, timely procurement<br />
of drugs and consumables, smooth distribution to<br />
facilities from DH to SC, uninterrupted availability to<br />
patients, minimization of out‐of‐pocket expenses, quality<br />
assurance, prescription audits, EDL in public domain,<br />
computerized drugs and logistics MIS system.<br />
4. Equipments Availability of essential functional equipments in all<br />
facilities, regular needs assessment. Timely indenting and<br />
procurement and identification of unused/faulty<br />
5. Ambulance Services and<br />
Referral Transport<br />
6 Maintenance of buildings.<br />
Sanitation, Water, Electricity,<br />
laundry, kitchen<br />
equipment, regular maintenance and MIS.<br />
Availability of ambulances for critical patients; reliable,<br />
assured and affordable transport for pregnant women and<br />
newborn/infants<br />
Clear policy articulation on entitlements both for mother<br />
and newborn<br />
Establishing Control Rooms for timely response and<br />
provision of services.<br />
Drop back facility: from village to institution and from<br />
institution to village<br />
24 x 7 maintenance and round the clock plumbing,<br />
electrical, carpentry services, power backup, cleanliness<br />
and sanitation in PH facilities, upkeep of toilets, electricity,<br />
clean linen, diet for pregnant women.<br />
7 Diagnostics Rational prescription of diagnostic test, reliable and<br />
affordable availability to patients; partnerships with private<br />
service providers. Prescription audits.<br />
8 Patient's feedback and Feedback from patients, expeditious grievance redressal
grievance redressal Analysis of feedback for corrective action<br />
9 Private Public Partnership<br />
(PPP)<br />
Partnership with private providers to supplement<br />
governmental efforts in underserved and vulnerable areas<br />
for deliveries, family planning services and diagnostics etc.<br />
10 Intersect oral convergence Effective coordination with key departments to address<br />
health determinants viz. water, sanitation, hygiene,<br />
nutrition, IYCF, gender, education, women empowerment,<br />
convergence with SABLA, SSA, ICDS etc.<br />
11 Community mobilization Active community participation, strong VHSCs, social audit.<br />
Effective VHNDs<br />
12 IEC Comprehensive communication strategy with a strong BCC<br />
component in the IEC strategy, dissemination in villages/<br />
urban slums/ peri urban areas.<br />
13. Civil Registration System (CRS) 100% registration of births and deaths, capturing of births<br />
in private institutions, reliability to health data on<br />
institutional deliveries, sex ratio etc.<br />
14. Supportive Supervision Supervision of field activities/performance, handholding,<br />
strengthening of LHVS, DPHNOS, MPHS etc<br />
15. Monitoring and Review Regular, focused reviews at different levels viz CM/ <strong>Health</strong><br />
Minister/<strong>Health</strong> Secretary/ MD/DHS/officers at Block/ PHC<br />
16 Meetings of State <strong>Health</strong><br />
<strong>Mission</strong>/Society/District<br />
<strong>Health</strong> Society<br />
17 Medical Colleges (New<br />
Colleges and Upgradation of<br />
existing ones)<br />
level, use of the HMIS data for reviews<br />
Regular meetings for periodic review and future road map,<br />
clear agenda and follow‐up action<br />
Enhances supply of doctors, expansion of tertiary health<br />
care, use of medical colleges as resource centers for<br />
national health programmes.<br />
18 Nursing Schools Augmented supply of nurses, quality assurance, avenues for<br />
career progression of in‐service staff.<br />
19 Paramedical education Availability of quality paramedical staff, capacity building,<br />
avenues for career progression of in‐service staff.<br />
20 Capacity building Strengthening of SHIFE/DTC. Quality Assurance Availability<br />
of centralized training log Monitoring of post training<br />
outcomes Induction training for all key cadres Management<br />
training for clinicians
CHAPTER-3:<br />
CONDITIONALITIES<br />
a) Release of the first tranche of funds:<br />
The first tranche of funds would be released by GOI to States for PIPs 2011‐12 on fulfillment<br />
of the following conditions:<br />
• A full‐ time <strong>Mission</strong> Director for NRHM (for States having resource envelop of more than<br />
Rs 50 crores), other than the administrative Secretary. MD NRHM would not hold<br />
additional charge outside the <strong>Health</strong> Department.<br />
• A full‐ time Director/Joint Director/Deputy Director (Finance) (depending on resource<br />
envelop of State), not holding any additional charge outside the <strong>Health</strong> Department,<br />
from the State Finance Services<br />
• A commitment to increase State Plan Budget for 2011‐12 by at least 10% over and above<br />
the 15% State share under NRHM.<br />
b) Release of second tranche of funds:<br />
Action on the following issues would be looked at while considering the release of second<br />
tranche of funds:<br />
• HR POLICIES & SYSTEMS as mentioned at S.NO. 1 of the Management imperatives,<br />
measures should be initiated to ensure rational deployment with stability of tenure by<br />
way of a clear transfer policy and facility based monitoring for results.<br />
• DRUG POLICY & SYSTEMS, including a sound procurement and logistics mechanism as<br />
mentioned at S.NO. 3 of the management Imperatives, with the objective of minimizing<br />
out‐of‐pocket expenses.<br />
• The compliance status in respect of the 31 conditionalities mentioned below is provided<br />
for the year 2010‐11 in the prescribed format.<br />
S. No Conditionality<br />
Compliance<br />
Status<br />
1. All posts under NRHM are on contract and based on local criteria. The<br />
contract should be done by the Rogi Kalyan Samiti /District <strong>Health</strong> Society.<br />
The stay of person so contracted at place of posting is mandatory. All such<br />
contracts are for a particular institution and non transferable. The<br />
contracted person will not be attached for any purpose at any place.<br />
yes<br />
2. The state agrees to credit 15% of the State share to the account of the<br />
State <strong>Health</strong> Society in two installments. The State also aggresses to<br />
enhance the over‐all expenditure on health by the State Government by a<br />
minimum of 10 percent per year.<br />
State Releted<br />
3. Blended payments comprising of a base salary and a performance based<br />
component, should be encouraged.<br />
yes<br />
4. State Government must fill up its existing vacancies against sanctioned State Releted<br />
posts, preferably by contract. Top most priority in contractual<br />
5.<br />
recruitments should be for backward districts and for difficult, most<br />
difficult and inaccessible health facilities.<br />
Delegation of administrative and financial powers should be completed<br />
during the current financial year. If not already done.<br />
6. State shall set up a transparent and credible procurement and Supply<br />
chain management system and Procurement Management Information<br />
System (PROMIS) [on the lines of the Tamil Nadu Medical Services<br />
yes
S. No Conditionality<br />
Corporation]. State agrees to periodic procurement audit by third party to<br />
ascertain progress in this regard.<br />
Compliance<br />
Status<br />
7. The State shall undertake institution specific monitoring of performance of<br />
Sub Centre, PHCs, CHCs, DHs, etc.<br />
State Releted<br />
8. The State shall operationalise an on‐line HMIS in partnership with<br />
MOHFW.<br />
State Releted<br />
9. The State shall take up capacity building exercise of Village <strong>Health</strong> and<br />
Sanitation Committees, Rogi Kalyan Samiti and other community /PRI<br />
institutions at all levels.<br />
State Releted<br />
10. The State shall ensure regular meetings of all community Organizations<br />
/District /State <strong>Mission</strong> with public display of financial resources received<br />
by all health facilities.<br />
State Releted<br />
11. The State Govts. shall also make contributions to Rogi Kalyan Samiti and<br />
transfer responsibility for maintenance of health institutions to them.<br />
yes<br />
12. The State shall prepare Essential Drug lists of generic drugs and Standard<br />
treatment Protocols, and give it wide publicity.<br />
State Releted<br />
13. The State shall focus on the health entitlements of vulnerable social<br />
groups like SCs, STs, OBCs, Minorities, Women, migrants etc.<br />
yes<br />
14. The State shall ensure timely performance based payments to yes<br />
15.<br />
ASHAs/Community <strong>Health</strong> Workers.<br />
The State shall encourage in patient care and fixed day services for family<br />
planning.<br />
yes<br />
16. The State shall ensure effective and regular organization of Monthly<br />
<strong>Health</strong> and Nutrition Days and set up a mechanism to monitor them.<br />
yes<br />
17. All performance based payments/incentives should be under the<br />
supervision of Community Organizations (PRI)/RKS.<br />
yes<br />
18. The State agrees to follow all the financial management systems under<br />
operation under NRHM and shall submit Audit Reports, FMRs, Statement<br />
of Fund Position, as and when they are due. State also agrees to undertake<br />
Monthly District Audit and periodic assessment of the financial system.<br />
State Releted<br />
19. The State agrees to fast track physical infrastructure upgradation by<br />
crafting State specific implementation arrangements. State also agrees to<br />
external evaluation of its civil works programmes.<br />
State Releted<br />
20. The State Govt. agrees to co‐locate AYUSH in PHCs/CHCs, wherever<br />
feasible.<br />
State Releted<br />
21. The State agrees to focus on quality of services and accreditation of<br />
government facilities.<br />
State Releted<br />
22. The State/UT agrees to undertake community monitoring on pilot basis,<br />
wherever not tried out as yet, and scale up with suitable model wherever<br />
piloted earlier.<br />
State Releted<br />
23. The State/UT agrees to undertake continuing medical and continuing<br />
nursing education.<br />
State Releted<br />
24. The State agrees to make health facilities handling JSY, women and child<br />
friendly to ensure that women and new born children stay in the facility<br />
for 48 hours.<br />
yes<br />
25. The State Governments shall, within 45 days of the issue of the Record of<br />
proceedings, issue detailed District wise approvals and place them on their<br />
website for public information.<br />
State Releted<br />
26. The State agrees to return unspent balance against specific releases made<br />
in 2005‐06, if any.<br />
State Releted
S. No Conditionality<br />
27. The State is entitled to engage a second ANM to the extent that it provides<br />
for MPW (Male) or the contractual amount of 2 nd ANM be paid out of<br />
State Budget and Third functionary may be engaged from NRHM Fund.<br />
28. The State shall put in place a transparent and effective human resource<br />
policy so that difficult, most difficult and inaccessible areas attract human<br />
resources for health.<br />
29. The State agrees to fast track physical infrastructure up‐gradation by<br />
crafting State specific implementation arrangements. State also agrees to<br />
external evaluation of its civil works programmes. The State shall provide<br />
names of all facilities where civil works are undertaken and also certify<br />
that the location of these facilities is such that poor households can seek<br />
services from them. Prior approval of place of construction by GoI will be<br />
mandatory before taking up new construction under NRHM. Thrust must<br />
be on meeting infrastructure gap in backward districts and difficult, most<br />
difficult and inaccessible facilities.<br />
30. The State agrees that the provision for EMRI operational cost to States will<br />
be on declining basis. For first year operational cost will be 60%, 2 nd year<br />
40%, 3rd year 20% and nil thereafter.<br />
31. The State agrees to comply with the following over a period of six months:<br />
• System for assured and affordable referral transport for pregnant<br />
women and sick children/infants.<br />
• Facility upkeep(including maintenance of building ‐ sanitation, laundry,<br />
water, electricity, kitchen) and grievance redressal mechanisms.<br />
• Performance benchmarks for staff prior to renewal of contracts and<br />
incentives.<br />
• Availability of functional equipments at all facilities.<br />
Compliance<br />
Status<br />
State Releted<br />
State Releted<br />
State Releted<br />
State Releted<br />
State Releted<br />
d) Conditionalities for release of Disease Control Program funds for 2011‐12:<br />
In addition to the conditionalities mentioned in the proceeding section, States are required<br />
to comply with some conditionalities pertaining to disease control program which are<br />
enumerated below:<br />
I. NATIONAL VECTOR BORNE DISEASE CONTROL PROGRAMME:<br />
i. Mandatory<br />
• Regular and dedicated State and Districts Programme Officer (VBD) for all Vector Borne<br />
Disease.<br />
• Contractual positions under NVBDCP to be filled 100% wherever applicable.<br />
• Release of Grant ‐ in ‐Aid under NVBDCP from State <strong>Health</strong> Society to DistrictsSocieties<br />
within 30 days after receipt of Grant ‐in ‐ Aid from GOI.<br />
ii. Desirable<br />
• For Malaria, Annual Blood Examination Rate (ABER) should be more than 10% of<br />
population under surveillance‐State and District‐wise.<br />
• Minimum 30% of Pf. Cases should be detected through rapid Diagnostic Test (RDT) I<br />
identified malaria ‐ endemic districts.<br />
• Indoor Residual Spray (IRS) coverage should be minimum 80% of targeted population<br />
projected in PIP.
• For Dengue, Chikungunya and Japanese Encephalitis (JE), the identified sentinel<br />
surveillance hospitals (SSH) to be made functional (at least 80% of allotted SSH).<br />
• For Kala‐azar, achievement of cases less than 1 per 10,000 population at Block level<br />
(applicable only for State of Bihar, Jharkhand and West Bengal).<br />
• Zonal Entomological to be made functional. NOTE : 1. All non‐negotiable conditions are<br />
to be fulfilled.<br />
2. If desirable conditions are not fulfilled, those will be converted as non‐negotiable<br />
conditions for release of grant in next fiscal year.<br />
II. REVISED NATIONAL TUBERCULOSIS CONTROL PROGRAM<br />
i. Mandatory<br />
• All States and Districts should have regular, full time State and Districts Tuberculosis<br />
officers.<br />
• At least 70% of new sputum positive case detection rate should be achieved in all<br />
districts/States.<br />
• Default rate should not be more than 5% in any of the Districts /States.<br />
ii. Desirable<br />
• Establishment and accreditation of at least one intermediate reference laboratory for<br />
the diagnosis of Multi ‐ Drug Resistant Tuberculosis in the State as per the plan.<br />
• DOT PLUS programme for Multi‐ Drug Resistant Tuberculosis should be started as per<br />
plan.<br />
III. INTEGRATED DISEASE SURVEILLANCE PROGRAM(IDSP)<br />
i. Mandatory<br />
• Dedicated State Surveillance Officer.<br />
• Reporting of Surveillance data through portal.<br />
ii. Desirable<br />
• Recruited of contractual manpower<br />
• Dedicated District Surveillance Officer.<br />
IV. LEPROSY<br />
i. Mandatory<br />
• Dedicated State Level officer in each State /UT and District Level officers in 123 districts<br />
where PR is more than one per 10,000 populations.<br />
ii. Desirable<br />
• Recruitment of contractual manpower.<br />
e) Incentivizing Good Performance<br />
It is proposed to set up an incentive pool for rewarding robust performance under NRHM. For this<br />
purpose, guidelines would be issued separately. Cost effective innovations with potential for large<br />
impact and models of good governance and systems reforms would also attract bonus/incentive by<br />
way of enhanced resource allocation.
CHAPTER-4:<br />
SCHEME/PROGRAM UNDER NATIONAL RURAL<br />
HEALTH MISSION<br />
A. RCH FLEXIPOOL<br />
ANNEXTURE 3b<br />
ANNEXTURE 3d<br />
ANNEXTURE 3e
Writeup for RCH Activity<br />
1. MATERNAL HEALTH<br />
1.1.2.1 Prepare plan for operationalisation across districts<br />
Budget of Rs. 0.25 Lacs is proposed for decimation of RCH Activity guideline to Block<br />
by conducting workshop at District level.<br />
1.1.5.1 Prepare plan for operationalising services at sub‐centers.<br />
Budget of Rs. 0.70 Lacs is proposed for decimation of RCH Activity guideline to PHC<br />
by conducting workshop at Block level.<br />
1.2.1 Implementation by districts ‐ 25 EmOC cases per PHC per year will require referral<br />
@ Rs. 600/‐ per case .<br />
In emergency EmOC cases needs referral to higher centres. All the PHCs are having<br />
vehicles and they are instructed to refer an emergency cases in govt vehicle without<br />
charges for that purpose Budget of Rs. 4.20 Lacs is proposed for referral of 25 EmOC<br />
cases per PHC per year @ Rs.300 per case.<br />
1.3 Integrated outreach RCH services<br />
1.3.1 RCH Outreach Camps in un‐served/ under‐served areas (state should focus on<br />
facility based services and outreach camps to be restricted to areas without<br />
functional health facilities)<br />
Total budget required Rs. 0.90 lacs for the year<br />
1.4 JANANI SURKHSHA YOJANA<br />
1.4.2.1 Home deliveries<br />
In financial year 2011‐12 it is proposed to give benefit to 1486 JSY home deliveries.<br />
The budget of Rs. 7.43 is proposed for JSY benefit to home deliveries @ Rs. 500/‐ per<br />
deliveries.<br />
1.4.2.2.1 <strong>Rural</strong><br />
In financial year 2011‐12 it is proposed to give benefit to 11373 JSY <strong>Rural</strong><br />
institutional deliveries. The budget of Rs. 79.61 Lacs is proposed for JSY benefit to<br />
institutional deliveries @ Rs. 700/‐ per deliveries.
1.4.2.2.2 Urban<br />
In financial year 2011‐12 it is proposed to give benefit to 2007 JSY Urban<br />
institutional deliveries. The budget of Rs. 12.04 Lacs is proposed for JSY benefit to<br />
institutional deliveries @ Rs. 600/‐ per deliveries.<br />
1.4.2.2.3 C‐sections<br />
In financial year 2011‐12 it is proposed to give benefit to 268 C‐section cases. The<br />
budget of Rs. 4.02 Lacs is proposed for C‐ section deliveries @ Rs. 1500/‐ per<br />
deliveries.<br />
1.4.3 Other activites (JSY)<br />
Sanitari Napkin for Delivery petaent<br />
Provision for Sanitary Napkin for Delivery petient @ Rs.100/‐ per Petient as per<br />
actual target of JSY. Expetcted benefisaries 14866 and total budget requires Rs.<br />
14.86 for the year.<br />
1.4.3.1 ASHA Incentive<br />
In financial year 2011‐12 it is proposed to give Incentive to ASHA for brining JSY<br />
beneficiary to institution for delivery. For that expected tribal institutional delivery<br />
1448 @ Rs. 600/‐ per delivery and expected non tribal institutional delivery 9925 @<br />
Rs. 200/‐ Total budget of Rs. 28.54 Lacs is proposed.<br />
1.4.3.2 Admin Cost (5%)<br />
Administration cost for printing of JSY forms and other miscellanious expenditure @<br />
4% of Total budget. Hence budget of Rs. 5.24 Lacs is proposed.<br />
1.5.2 High Risk ANC & Gynac Clinic including screening for Ca Cx & treatment by<br />
Cryocautery.<br />
High Risk ANC & Gynac Clinic including screening for Ca Cx & treatment by<br />
Cryocautery – per Month at one PHC in 12 Non tribal block and each PHC in two<br />
tribal block. Total 276 Camps are to be arrange, budget of Rs.5.52 is proposed @ Rs.<br />
2000/‐ per camp for Mobility and specialist charges.<br />
1.5.3 Free diet allowance to Institutional delivery for 2 days for 10 Deliveries per month<br />
per PHC @ Rs. 75/‐ per day.<br />
It is proposed to give Free diet allowance to Urban Institutional delivery for 2 days<br />
for 10 Deliveries per month per PHC @ Rs. 75/‐ per day. Total budget of Rs. 10.08<br />
Lacs is proposed for 56 PHCs @ 18000/‐ per year per PHCs.
1.5.4 Free diet allowance to Institutional delivery for 2 days for 15 Deliveries per month<br />
per RH @ Rs. 75/‐ per day. Total amount per case Rs. 150/‐<br />
It is proposed to give Free diet allowance to <strong>Rural</strong> Institutional delivery for 2 days for<br />
15 Deliveries per month per RH/SDH @ Rs. 75/‐ per day. Total budget of Rs. 3.52<br />
Lacs is proposed for 9 RH & 4 SDH @ 27000/‐ per year per RH/SDH.<br />
2. CHILD HEALTH<br />
2.8.1 Maintenance of sick new born care unit at district hospital<br />
Budget of Rs. 0.20 Lacs is proposed for maintenance of sick new born care unit<br />
established at district hospital.<br />
2.8.2 Maintenance of New Born Care corners at FRUs<br />
Budget of Rs. 1.00 Lacs is proposed for maintenance of New Born Care corners<br />
established at FRUs.<br />
2.8.3 Maintenance of New born care corner at 24x7 PHC<br />
Budget of Rs. 5.60 Lacs is proposed for maintenance of New born care corner<br />
established at 24x7 PHC.<br />
2.8.4 Child Treatment Center at PHC<br />
At 56 PHCs it is proposed to take 2 CTC Camp for 900 Malnourished & Sick Children<br />
from non tribal & 220 children from Tribal. @ Rs. 160/‐ per child per day for 21 days.<br />
Total budget of Rs. 37.63 lacs is proposed for financial 2011‐12.<br />
2.8.5 Child Treatment Center at SDH / RH ( Rs. 3360/‐ per child for 21 days for 10<br />
children per SDH / RH)<br />
At 9 RH & 4 SDH it is proposed to take 2 CTC Camp for 260 Malnourished & Sick<br />
Children. @ Rs. 160/‐ per child per day for 21 days. Total budget of Rs. 8.74 lacs. is<br />
proposed for financial 2011‐12.<br />
2.8.6 Village Child Development Center (VCDC ) at SC level AWW<br />
It is proposed to arrange Village Child Development Center (VCDC ) at SC level. For<br />
333 sub center budget of Rs. 96.00 Lacs is proposed for expected 10000 SAM &<br />
MAM children @ Rs. 960/‐ per child for 30 days.<br />
2.8.7 Organizational cost for Implementation of ‐ Bi Annual Deworming & Vitamin A<br />
Supplementation & Iron Folic Acid Supplementation<br />
It is proposed to implement Bi Annual Deworming & Vitamin A & Iron Folic Acid<br />
Supplementation in District through PHC. The budget will be proposed for
Organizational cost for Implementation of ‐ Bi Annual Deworming & Vitamin A<br />
Supplementation & Iron Folic Acid Supplementation @ Rs. 2500/‐ per PHC for 56<br />
PHCs. The total budget of Rs. 2.80 Lacs will be proposed for financial year 2011‐12.<br />
2.8.8 Pediatrician services for examination, treatment and referral seek<br />
It is proposed to take Pediatrician services per Month at one PHC in 12 Non tribal<br />
block and each PHC in two tribal block. Total 276 Camps are to be arrange. The<br />
budget of Rs. 5.52 Lacs is proposed @ Rs. 2000/‐ per camp for Mobility and specilist<br />
charges.<br />
2.8.9 Referreal Transport for critical ill child<br />
For Referreal of critical ill child from PHC to RH/SDH/DH Refferreal Transport budget<br />
of Rs. 2.02 is proposed for @ Rs. 300 per child X 12 children per year per PHC.<br />
2.8.10 Child Death Audit<br />
It is proposed to done Child Death Audit in Districts. 70 deaths are expected per<br />
block per year (1 Tribal and 1 Non Tribal Block). Investigation will be done by THO/<br />
MO @ Rs.200 per case, in designed detailed 16 pages formats which is designed at<br />
State Level for Child Death Investigation. Total budget of Rs. 0.28 Lacs is expected.<br />
3. FAMILY PLANNING<br />
3.1.3.2 Organize NSV camps<br />
For achievement of target and for training of MBBS MOs, it is proposed to conduct<br />
NSV Camp of 100 cases each in District. There will be 1 camps proposed during the<br />
financial year 2011‐12. The budget of Rs. 0.53 Lacs is proposed for 1 camps @ Rs.<br />
53000/‐ per camp.<br />
3.1.3.3 Compensation for female sterilization<br />
For District it is proposed as per GOI guideline budget for female sterilization @ Rs.<br />
1000/‐ per case for BPL/SC/ST and 50% APL @ Rs. 650/‐. Average cost of Rs. 825/‐<br />
per case. Estimated female sterilization cases for 2011‐12 is 10080. The total budget<br />
of Rs. 83.16 Lacs is proposed for 10080 cases @ Rs. 825/‐ per case.<br />
3.1.3.4 Compensation for NSV Acceptance<br />
It is proposed to make provision for estimated 1120 NSV acceptance cases i.e. 10%<br />
of Total Sterilization Target @ Rs. 1500 /‐ per case. Total budget of Rs. 16.80 is<br />
proposed for 1120 cases @ Rs. 1500/‐ per case.
3.5.2 Provision for Transport of family planning Sterilization Cases & Surgeon<br />
It is proposed to provide transport facility for family planning sterilization cases and<br />
surgeon @ Rs. 100/‐ per case. Total estimated number of cases in District are 11200.<br />
The budget of Rs. 11.20 Lacs is proposed for 11200 cases @ Rs. 100/‐ per case.<br />
3.5.3 Organization of Mini Camps for Laproscopy/Minilap/NSV<br />
For laprosocopy/minilap/NSV mini camp, it is proposed to provide organization cost<br />
@ Rs.50/‐ per case for minimum 25 cases per camp. The budget of Rs. 0.88 Lacs is<br />
proposed for expected number of 50 camp @ Rs. 1250 per camp.<br />
3.5.4 Promotion of IUD 380A & EC Pills through sensitization of SHG<br />
It is proposed to take activity of promotion of IUD 380 A & EC pills through<br />
sensitization of private doctors, SHG etc. A workshop will be arranged twice in a year<br />
of private doctors and SHG members, organization cost of Rs. 3000 per workshop<br />
will be required. The budget of Rs. 4.20 Lacs is proposed for 140 workshop @ Rs.<br />
3000/‐ per workshop at 70 institutes (PHC, RH, SDH, WH).<br />
4. ARSH<br />
4.2.1 Strengthening of functioning establishing new ARSH Clinic at Women Hospital.<br />
It is proposed to implement ARSH activity by setting up of adolescent clinic at<br />
women hospital. Budget required for setup and other necessary activity Rs. 50000/‐<br />
4.2.2 Continuation of counselors on contractual basis at districts Hospitals already<br />
appointed at the respective AFHS clinics.<br />
The budget of Rs. 1.20 Lacs is proposed for counselors on contractual basis at<br />
districts Hospitals already appointed at the respective AFHS clinics. @ Rs. 10000/‐<br />
per month.<br />
4.2.3 Sensitization peer groups in villages through community based approach<br />
Sensitization of Peer Groups in villages through Community based approach, female<br />
Volunters shall be sensitized for menustrial hygine & sanitary napkins in District. 2<br />
Male & 2 Fmale Peer Volunters per village will be sensitized. Orientiation session<br />
shall be conducted by ANM / AWW /ASHA. 500 villages from 4 blocks. 4 peer<br />
volunteers @ Rs. 25/‐ per month. Total budget required Rs.6.00 lacs.<br />
4.2.4 Prevention /control of Nutritional Anemia in Adolescent Girls<br />
The budget of Rs. 1.00 Lacs is proposed for prevention /control of Nutritional<br />
Anemia in Adolescent Girls as Organizational cost.
5. URBAN RCH<br />
5.2.1 <strong>Health</strong> Posts in urban areas<br />
The budget of Rs. 5.92 Lacs is proposed for <strong>Health</strong> Posts in Achalpur for Salary of the<br />
Contractual staff posted in <strong>Health</strong> Post and contingent items to run HP.<br />
5.2.2 Urban ANMs for M. Councils under RCH<br />
The budget of Rs. 23.12 Lacs is proposed for 35 Urban ANMs urban ANM salary @<br />
Rs. 5500/‐ per month.<br />
5.2.3 RCH PIP of M. Coucils<br />
The budget of Rs. 6.00 Lacs is proposed for RCH PIP of M. Coucils (> 1 Lakh popn.)‐<br />
Need based Technical activties for reducing MMR, IMR and TFR.<br />
6. TRIBAL RCH<br />
6.2.1 <strong>Health</strong> Checkup of Sick Children at Anganwadi<br />
It is necessary for MO to done checkup of Anganwadi children regularly for that it is<br />
proposed to make provision of monthly mobility support for 11 PHC of tribal block<br />
@ Rs. 500/‐ per month. Total budget of Rs. 0.66 lacs is proposed.<br />
6.2.2 Involvement of ASHA for implementation of essential new born care activity in all<br />
tribal blocks<br />
Involvement of ASHA for implementation of essential new born care activity in all<br />
tribal blocks. Dharni & Chikhaldara at rate Rs. 4000/‐ Per ASHA for 300 Asha. Total<br />
budget of Rs. 12.00 Lacs is proposed.<br />
6.2.3 Hardship Allowance to Medical Officers of Bharari Pathak in Tribal<br />
In tribal area of District there are 22 Bharari Pathak functioning, salary of MO is Rs.<br />
6000/‐ per month. It is proposed to give additional payment of Rs. 6000/‐ per month<br />
per MO through RCH. Total budget of Rs. 15.84 lacs is proposed.<br />
6.2.4 Operational Research in regarding Referral services<br />
The lumsum budget of Rs. 5.00 Lacs is proposed for Operational Research regarding<br />
Referral services.
6.2.5 Documentary Evidence of improvement in grades of Malnutrition in the form of<br />
photographs<br />
The budget of Rs. 0.22 Lacs is proposed for Documentary Evidence of improvement<br />
in grades of Malnutrition in the form of photographs. @ Rs.30/‐ per child for 3<br />
photographs. For 150 children per PHC in selected 5 tribal PHCs.<br />
7. VULNERABLE GROUPS<br />
7.2.1 Appointment of counselor at DH and WH for women victims of violence<br />
The budget of Rs. 2.40 Lacs is proposed for Salary of Counselors for women victims<br />
of violence at District & Women Hospital @ Rs. 10000/‐ per month.<br />
8. INNOVATIONS/ PPP/ NGO<br />
8.1.2 Orientation of programme managers and service providers on PC & PNDT Act<br />
It is proposed to conduct orientation workshop at District level for programme<br />
managers and service providers on PC & PNDT Act. The budget of Rs. 0.30 Lacs is<br />
proposed for organization cost for 3 workshop @ Rs. 10000/‐ per workshop.<br />
8.1.5 Support for sting operation under PCPNDT Act<br />
The lumsum budget of Rs. 0.50 Lacs is proposed for Support for sting operation<br />
under PCPNDT Act.<br />
8.1.6 Provision for Witness support participated in PCPNDT court cases<br />
The lumsum budget of Rs. 0.15 Lacs is proposed for Witness support participated in<br />
PCPNDT court cases.<br />
8.1.7 Support for teams at district level for inspection of sonography centers registered<br />
under PC PNDT Act<br />
It is necessary to have inspection of Sonography Center register under PCPNDT act in<br />
District by District level inspection team. For that the budget of Rs. 1.00 Lacs is<br />
proposed for mobility support @ Rs. 1000/‐ per person per center.<br />
8.1.8 Support for Scrutiny of Form‐F by the NGOs/MSW Students<br />
The budget of Rs. 0.50 Lacs is proposed for Scrutiny of Form‐F by the NGOs/MSW<br />
Students @ Rs. 5/‐ per form.<br />
8.1.9 Training for Centers for Online Data Entry of Filling Form ‐ F<br />
It is proposed to conduct training for Centers for Online Data Entry of Filling Form ‐<br />
F. The budget of Rs. 0.30 Lacs is proposed as a organization cost for training.
8.1.10 One counselor will be appointed at the each District Hospital & Women Hospital<br />
The budget of Rs. 2.40 Lacs is proposed for Salary of Counselors appointed at District<br />
& Women Hospital @ Rs. 10000/‐ per month.<br />
9. INFRASTRUCTURE AND HUMAN RESOURCES<br />
9.1.6 Incentive to Medical Officers<br />
The budget of Rs. 1.16 Lacs is proposed for Incentive to Medical Officer for EmOC &<br />
LSAS cases @ Rs. 1500/‐ & Rs. 750/‐ respectively.<br />
9.3.3 Infrastructure‐ MH: Maternity wards, labour rooms<br />
The total budget of Rs. 106.50 Lacs is proposed for minor Repair and expantation of<br />
30 sub center labour room @ Rs. 2.50 Lac per labour room and 9 PHC labour room<br />
@ Rs. 3.50 Lac per labour room.<br />
10. INSTITUTIONAL STRENGTHENING<br />
10.3.4 Provision for equipment at District Level<br />
The Budget of Rs. 1.00 Lac is proposed for annual AMC of Computer, purchase of<br />
Software & Hardware and Antivirus for system.<br />
10.3.5 Expenditure on monthly/ quarterly meetings at distric level<br />
The budget of Rs. 0.60 Lacs is proposed for monthly TMO/MO meeting @ Rs. 5000/‐<br />
per month at district level.<br />
11. TRAINING<br />
12. BCC / IEC<br />
12.4.1 Street Play & Kalapathak<br />
For effective publicity of <strong>Health</strong> activity in villages through Kalapathak at village level<br />
the budget of Rs. 2.40 Lacs is proposed for 120 programmes of Kalapathak @ Rs.<br />
2000/‐ per programme.<br />
12.4.2 Radio Jingles<br />
For effective publicity of activity through Radio Jingles upto village levels by All India<br />
Radio the budget of Rs. 2.40 Lacs is proposed for Radio Jingles.
12.4.3 Wall painting & Hoardings<br />
It is proposed to give message through wall painting & hoardings at prominent<br />
places in Melghat area. Provision are made for 100 places wall painting & 100 places<br />
for Hording addressing of <strong>Health</strong> Activities. The Budget of Rs. 3.00 Lacs is proposed<br />
for 100 places wall painting @ Rs. 2000/‐ per wall painting & for 150 places Hoarding<br />
@ Rs. 1000/‐ per hoarding.<br />
13. PROCUREMENT<br />
14. PROGRAMME MANAGEMENT<br />
14.2.1 Contractual Staff for DPMSU recruited and in position<br />
The budget of Rs. 17.60 Lacs is proposed for salary of DPM/DAM/DEO at revised rate<br />
by increasing 50% in current salary TA/DA, mobility support and contingent<br />
expenditure.
S.<br />
No.<br />
Area Indicator<br />
Planned<br />
(2005‐11)<br />
Number of facilities/HR<br />
Total<br />
Achievement<br />
(2005‐11, till<br />
November<br />
2010)<br />
Percentage<br />
(%)<br />
Achievement<br />
Plan for<br />
2011‐2012<br />
1 No. of FRUs Operationalised 10 5 50 5<br />
2<br />
3<br />
No. of 24x7 PHCs<br />
Operationalised<br />
No. of sub‐centres<br />
operationalised as delivery<br />
points<br />
42 28 67 6<br />
229 83 36.24 146<br />
Service utilisation* (average per month per<br />
facility/ trained provider)<br />
C‐sections<br />
MTPs<br />
Services<br />
Male sterilisations<br />
Female sterilisations<br />
Normal deliveries<br />
MTPs<br />
Male sterilisations<br />
Female sterilisations<br />
IUD insertions<br />
Normal deliveries<br />
IUD insertions<br />
4 No. of SNCUs operationalised 2 2 100 Newborns treated<br />
5<br />
Facility<br />
Operationalisation<br />
No. of NBSUs operationalised 14 5 35 11 Newborns treated<br />
14 Capacity Building EmOC training ‐ ‐ ‐ 3 C‐sections<br />
Based on<br />
performance<br />
during Apr‐<br />
Nov 2010<br />
15 LSAS training 8 4 ‐ 1 C‐sections 1 1<br />
16 SBA 652 150 ‐ 8 Deliveries conducted<br />
17 MTP 90 47 MTPs<br />
18 RTI/STI 277 54 ‐ 4<br />
19 IMNCI 3380 1902 ‐ 36<br />
20<br />
F‐IMNCI 32 35<br />
Children and infants<br />
treated<br />
Projection<br />
for<br />
2011‐12
S.<br />
No.<br />
Area Indicator<br />
21 NSSK<br />
Planned<br />
(2005‐11)<br />
Number of facilities/HR<br />
Total<br />
Achievement<br />
(2005‐11, till<br />
November<br />
2010)<br />
Percentage<br />
(%)<br />
Achievement<br />
Plan for<br />
2011‐2012<br />
Service utilisation* (average per month per<br />
facility/ trained provider)<br />
Services<br />
Newborns<br />
resuscitated<br />
22 Minilap 90 15 ‐ 6 Sterilisations<br />
23 NSV 40 25 ‐ 1 Sterilisations<br />
24 Laparoscopic sterilization Sterilisations<br />
25 IUD 526 79 ‐ 12 IUD insertions<br />
Based on<br />
performance<br />
during Apr‐<br />
Nov 2010<br />
Projection<br />
for<br />
2011‐12
A.2: MATERNAL HEALTH GUIDELINES AND FORMATS<br />
Generic comments for preparing PIP 2011‐12:<br />
• Any procurement should be done based on competitive bidding and by following<br />
Government protocols.<br />
• Procurement of equipment should be need based, linked with its utilization and availability<br />
of required manpower.<br />
• Hiring of additional staff should be avoided on generic basis beyond the approved norms and<br />
should be linked with case load and quality of service delivery.<br />
• Incentives should be on state specific situation and rationality for the same may be shared.<br />
• A table on incentives must be indicated giving details on RCH incentives being planned either<br />
in NRHM or in RCH.<br />
• Individual incentives should be minimum and need based.<br />
• Incentives to service providers may be given to a group of providers and linked with ensuring<br />
quality protocols of the service rendered.<br />
• RCH Drugs/Any other drugs should be budgeted under State head or under NRHM except for<br />
the states where World bank has approved their procurement procedure.<br />
• Monitoring visits should be comprehensive for all the programs and should be budgeted<br />
under separate headings of monitoring and supervision.<br />
• Platform of Quality Assurance cell at state and district level be utilized for such monitoring<br />
visits.<br />
• The state wise comments of MH Division will be shared with the states after receiving PIP for<br />
2011‐12 and planning of the activities in the PIP should be done accordingly.<br />
• In case of any difference of opinion due to local/state specific circumstances, the same may<br />
please be shared before implementation<br />
• Monitoring should also be conducted by State/District program officers.<br />
• Some of the states have put their RCH activities particularly related with Maternal <strong>Health</strong><br />
under NRHM, may be because of budget related issues. Such states must see and conform to<br />
the state wise comments given by MH division on all MH related activities whether booked<br />
under RCH or NRHM, during appraisal of the PIPs and plan accordingly.<br />
FRU Operationalisation:<br />
• Holistic planning for FRUs should be done linking HR, procurement, BSCs, logistics, manpower,<br />
training etc.<br />
• Facilities operationalized should be as per GOI Guidelines including establishment of<br />
BSCs.<br />
• Besides linking components of HR, infrastructure including BSC etc, preference to be given to<br />
those facilities for upgradation and operationalisation where delivery load is substantial.<br />
• Geographical mapping must be carried out to identify those facilities for Upgradation to FRUs,<br />
which are located in areas with no other functional facility nearby.<br />
• Funds for heads like equipments, infrastructure etc. should be budgeted under respective<br />
RCH II/ NRHM head.<br />
• Medical College strengthening is not the part of RCH and can be kept under NRHM Additionality.<br />
• Some state has budgeted DDK for FRUs/CEmOC services. They are requested that DDK should be<br />
used only in c/o out reach services.<br />
Operationalisation 24* 7 PHCs:
• Holistic planning for operationalisation of 24* 7 PHCs should be done and should be linked to<br />
infrastructure, procurement, drugs/medicines; state has also to plan for training of MOs esp. in<br />
Basic Obstetric Care and SNs/LHVs/ANMs in Skilled Birth Attendance.<br />
• Funds for heads like equipments, infrastructure etc. should be budgeted under respective<br />
RCH II/ NRHM head.<br />
• Facilities operationalized should be as per GOI Guidelines.<br />
• Besides linking components of HR, infrastructure including newborn care corners etc, preference<br />
to be given to those facilities for up‐gradation and operationalisation where delivery load is<br />
substantial.<br />
• Geographical mapping must be carried out to identify those facilities for upgradation to 24*7<br />
PHCs, which are located in areas with no other functional facility nearby.<br />
A. SERVICES:<br />
1. ANC, INC, PNC:<br />
• State is requested to ensure that post delivery mother should stay for at least 48 hours<br />
which is quite necessary to provide full range of care. Any infrastructure improvement plan if<br />
needed should be undertaken accordingly.<br />
• Monitoring during OR/VHNDs sessions should be strengthened so that quality of ANC<br />
including IFA tab etc, PNC is ensured.<br />
• Tracking of missed out and left out cases of ANC, PNC should be done.<br />
• State has to gear up to provide full ANC of good quality.<br />
• Comprehensive Monitoring plan for these activities should be developed and budgeted.<br />
2. Institutional Delivery including JSY:<br />
• Micro Birth Planning should be emphasized as a part of JSY.<br />
• 48 hr stay post delivery should be emphasized especially among JSY beneficiaries.<br />
• Benefits under JSY should be as per GoI norms.<br />
• Qualities of services being provided under JSY are poor, facilities are overcrowded and<br />
beneficiary are discharged before 48 hours, micro plan is not in place, as per JSY evaluation.<br />
There is a need for augmenting manpower and provision of beds in the health facilities.<br />
• JSY deliveries should be co‐linked with service provision and facility upgradation and<br />
budgeted accordingly.<br />
• Tertiary facilities are overloaded so micro plan should promote primary and secondary<br />
facilities for services.<br />
• Grievance‐redressal mechanism should be established.<br />
• Funds should also be kept for monitoring visits.<br />
• Guidelines on record up keeping (physical and financial) should be disseminated.<br />
• TBAs should not be promoted as primary provider of deliveries.<br />
• Support to MCs under JSY should not be budgeted under RCH.<br />
• JSY benefits to the clients delivering at accredited private health facilities can be provided<br />
either to the beneficiary or to the service provider from GoI funding, within the approved JSY<br />
limit. Any benefits beyond the approved limit needs prior approval<br />
from MoHFW.<br />
3. Safe Abortion Services:<br />
• State should plan for Comprehensive Abortion services as per GoI guidelines.<br />
• There should be focus on comprehensive abortion services (MVA, EVA, MA) upto FRU/CHC<br />
level and at least MA, MVA at 24*7 PHCs.<br />
• Funds for heads like equipments, infrastructure etc. should be budgeted under<br />
respective RCH II/ NRHM head.
• Accreditation of private health facilities also needs to be done to ensure wider availability of<br />
this service, through District Accreditation Committee as laid down in<br />
the MTP Act.<br />
• District level committee to accredit private sector for MTP services need to be activated and<br />
pending applications for accreditation should be processed on priority.<br />
• Physical progress on this may please be shared every quarter.<br />
• Funds should also be kept for monitoring the operationalisation of Safe Abortion Services.<br />
4. RTI/STI services:<br />
• Training should be as per the GoI guidelines on RTI/STIs.<br />
• Holistic Plan including training of staff, provision of drugs, lab investigations and convergence<br />
with the NACP (THROUGH SACS) is advised for comprehensive RTI/STI services.<br />
• Funds for strengthening of facilities for RTI/STI services have to be kept.<br />
• Funds for heads like equipments, infrastructure etc. should be budgeted under<br />
respective RCH II/ NRHM head.<br />
• Ensure privacy and full treatment as per <strong>National</strong> Guidelines on Prevention, Management<br />
and Control of RTI infections including STIs.<br />
• Ensure that Wet Mount is available for Diagnosis at health Facilities.<br />
• Funds should also be kept for monitoring the operationalisation of RTI/STI services.<br />
5. Maternal Death Review(MDR):<br />
• Facility based MDR: All health facilities should maintain meticulous records of maternal<br />
deaths with finer details including patient's particulars and probable cause of death. An audit<br />
is conducted at the facility level and subsequently the report is shared with the district CMO<br />
for further action. FBMDR should start initially at District Hospital and Medical Colleges and<br />
later on at block level and accredited private sector facilities should also be included within<br />
scope of these reviews.<br />
• Line listing of maternal deaths occurring at accredited private sector facilities should be done<br />
and the records of these deaths subjected to audit at District level.<br />
• Community based MDR: Line listing of maternal deaths should be done through the<br />
ANMs/ASHAs/ other community resource and the audit of such deaths should be done at the<br />
block/district level.<br />
• GoI is in the process of finalizing simple tools for conducting both the audits. However the<br />
states can continue the process of maternal death audits as before.<br />
• The tools of MDR may be shared with GoI and should be initially limited to 2‐3 districts as a<br />
pilot and cost involved in such pilots vis‐a‐vis benefits be analyzed before scaling up.<br />
6. VHNDs:<br />
• Since VHNDS is a platform all RCH activities, so state should ensure that all these activities<br />
should take place holistically. The efforts should be for providing all planned services like<br />
ANC, PNC, Immunization and Counseling services as per the GOI guidelines.<br />
• Too many types of the out reaches should be avoided and thrust should be on<br />
comprehensive VHNDs.<br />
• Wherever possible FGDs should be conducted for maternal deaths taking place.<br />
• Monitoring and ensuring quality in all VHNDs should be done.<br />
• Funds for monitoring of VHNDs session should be kept.<br />
• Stress should be also on missed/lost cases for ANC.<br />
• VHNDs should be linked with provision of facilities at institutions.<br />
• The focus should be on regular VHNDS and mobile units should be utilized only for those<br />
areas where VHNDs cannot be organized.<br />
• In RCH II focus is on Operationalising health facilities and as such camp/mobile mode is<br />
suggested for hard to reach areas.
7. Referral Transport:<br />
• Every state is advised to have a comprehensive referral policy with scope of flexibility and<br />
variations from district to district as per the local need and situations.<br />
• Tribal and hilly areas must have linkages like Palki or similar facilities for bringing the<br />
pregnant women upto the road head from where a referral transport can pick her. Such<br />
places can be linked with Birth waiting rooms at health facilities on Tamil Nadu pattern.<br />
• There is a need for assured referral linkage both from the beneficiary/community to the<br />
facilities and also between the facilities.<br />
• State needs to establish such system either through government mechanism or through<br />
outsourcing.<br />
• Norms for reimbursement to beneficiary should be as per JSY.<br />
• Outsourcing of referral transport can be preferred than the purchase of government vehicle<br />
and regular driver for providing Referral transport.<br />
• Outsourcing of referral transport should be through the process of competitive bidding.<br />
• Cost benefit analysis of referral transport mechanism should be done taking into<br />
consideration cost incurred per referral, no of pt being referred to pvt sector and no of lives<br />
saved in public sector.<br />
• EMRI model /call centers for referral should be evaluated in terms of cost & benefit before<br />
scaling up.<br />
• Payment for referral can be differential and may be linked with range of km travelled.<br />
8. RCH Camps:<br />
• State is organizing RCH Camps since RCH‐I but the benefits have not yet been analyzed.<br />
• In RCH II focus is on Operationalising health facilities and as such camp mode is suggested as<br />
time gap arrangement restricted for hard to reach areas. State should also indicate that how<br />
many health facilities have been operationalized in hard to reach areas till now.<br />
• RCH Camps should be organized and funded as per GoI norms.<br />
• Stress should be kept on organizing VHNDS regularly.<br />
• Inter‐sectoral co‐ordination should be emphasized while organizing these camps.<br />
• Such outreach camps have taken out the focus on operationalisation of facilities and this may<br />
be one of the reasons for decline in Maternal <strong>Health</strong> parameters in the state.<br />
• State is requested to analyze the functioning and benefits of Mobile Medical Unit along with<br />
the services rendered on pilot basis before scaling up. Such analysis may please be shared<br />
with GoI. Since MMU for RCH services is a type of outreach and various types of out reaches<br />
hampers the focused activities of ANC, PNC etc being undertaken at VHNDs.<br />
• While planning for such outreach activities it should be ensured that routine service<br />
delivery by MOs/ health workers at fixed health facilities (PHCS/CHCs/DHs etc)<br />
does not suffer.<br />
B. TRAININGS:<br />
1. Life Saving Anesthesia Training:<br />
• Target for LSAS training should be calculated after taking into account the no. of FRUs to be<br />
operationalized, CEmOC target and total no. of specialist to be appointed.<br />
• Target and Achievement of the MOs for 2010‐11 and Training plan for 2011‐12 should be<br />
shared with GoI by the State as per the enclosed formats<br />
• No of trained doctors posted at FRUs<br />
• Trainings should be conducted as per GoI norms.<br />
• Training institutes should be strengthened as per the GoI protocols. Funds can be kept under<br />
Training head.
• State should ensure that DHs should also be strengthened simultaneously for the practical<br />
part of the training. Scaling up can be planned as per GoI road map. Funds can be kept under<br />
Training head.<br />
• State should undertake regular monitoring both during and post training.<br />
• State should ensure that MOs are posted at Facilities which have been operationalized for<br />
CEmOC services.<br />
• Funds should be kept for monitoring during and after training.<br />
2. CEmOC Training:<br />
• Target for CEmOC training should be calculated after taken into account the no. of FRUs to<br />
be operationalised, LSAS target and total no. of specialist to be appointed.<br />
• State should ensure that MOs are posted at Facilities which have been operationalised for<br />
CEmOC services.<br />
• Target and Achievement of the MOs for 2010‐11 and Training plan for 2011‐12 should be<br />
shared with GoI by the State as per the enclosed formats<br />
• State should ensure that DHs should also be strengthened simultaneously for the practical<br />
part of the training. Scaling up can be planned as per GoI road map. Funds can be kept under<br />
Training head.<br />
• Trainings should be conducted as per GoI norms.<br />
• Training institutes should be strengthened as per the GoI protocols. Funds can be kept under<br />
Training head.<br />
• State should undertake regular monitoring both during and post training.<br />
• State should ensure that MOs are posted at Facilities which have been operationalised for<br />
CEmOC services.<br />
• Funds should be kept for monitoring of the training and post training follow‐up<br />
3. BEmOC Training:<br />
• BEmOC training is designed for MOs posted at PHCs. State should ensure that duplication<br />
should not take place by giving different names for this training.<br />
• Training should be as per GoI protocols of 10 days.<br />
• Training institutes should be strengthened as per the GoI protocols. Funds can be kept under<br />
Training head.<br />
• State should undertake regular monitoring both during and post training.<br />
• State should ensure that MOs are posted at Facilities which have been operationalised for<br />
BEmOC services.<br />
• Funds should be kept for monitoring of the training and post training follow‐up.<br />
4. Skilled Birth Attendant Training:<br />
• Training should be as per GoI norms. Kindly follow the GoI operational guidelines on the<br />
same for 3 week training.<br />
• State is requested to emphasize that training centres follow protocols of SBA training i.e.<br />
practice of partograph, AMTSL, ENBC etc. Funds for centre strengthening can be kept under<br />
Training head. Post training skill practise by the trained personnel should be ensured.<br />
• State where training is going on at a good pace, it is requested to evaluate the SBA training in<br />
the State.<br />
• State should undertake regular monitoring both during and post training.<br />
• Funds for monitoring of the training and post training follow up should be kept<br />
5. Blood Storage Training:<br />
• Blood Donation Camps are accessory activities but State should also emphasize<br />
establishing BSCs/ linkages to Blood bank at all the facilities providing CEmOC services.<br />
• Training should be as per GoI norms.
• Also the state is requested to avoid transfers of MOs/LTs who have been trained. If needed<br />
transfer should be from one FRU to other.<br />
• State should develop convergence with SACS for utilizing their resources in training.<br />
6. MTP Training:<br />
• State should follow Comprehensive Abortion Guidelines (will soon be disseminated by GoI)<br />
to operationalise its facilities for MTP services and to train MOs in same. MVA guidelines for<br />
training PHC MOs already exist.<br />
• Trainings should be conducted as per GoI norms.<br />
• Nurses and ANMs should be trained to provide assistance to the certified MTP provider and<br />
also counselling services to clients. It may be noted that nurses and ANMs are currently NOT<br />
permitted to be trained as primary service provider for<br />
MTP under the MTP Act and Rules.<br />
• D & C is not a recommended method for MTP.<br />
• State should also plan for training of MOs in Medical Abortion Services.<br />
• State is also requested to plan for training of MOs in 2nd trimester abortion services<br />
(currently approved methods), as these services should be made available at District<br />
Hospitals and FRUs. Also strengthening of facilities should be done for same.<br />
• Training institutes should be strengthened as per the GoI protocols. Funds for centre<br />
strengthening can be kept under Training head.<br />
• State should ensure that MOs are posted at Facilities which have been operationalised for<br />
MTP services.<br />
• Funds should be kept for monitoring of the training and post training follow up.<br />
7. RTI/STI Training:<br />
• State should plan to operationalise health facilities for RTI/STI services.<br />
• State is requested to plan for RTI/STI training, as per GoI norms.<br />
• Funds for the operationalisation and monitoring of RTI/STI services should be kept.<br />
• Training of sub district level health functionaries posted at FRUs/CHCs and PHCs may be done<br />
by utilizing the training resources (faculty, training material) of the NACP (through SACS). This<br />
is an agreed action under the convergence framework.<br />
C. Quality Assurance:<br />
• State is requested to enlarge the scope of QA cells for RCH services including FP services.<br />
• QA cell should be established both at the level of State and District for all MCH activities at State<br />
and District Level.<br />
• TORs of the QA cell communicated to the State should be followed.<br />
• QA cell should ensure quality and monitoring of all MCH activities which should also include<br />
monitoring of the training.<br />
• Budget has to be indicated for monitoring activities by QA Cell under MH or M & E.<br />
• State is accrediting its health facilities under NABH and NABL but before going for such expensive<br />
accreditations, it may evaluate the quality of services offered through its own mechanism of QA<br />
Cell.<br />
D. Miscellaneous:<br />
• Specific plan for those districts classified as poor performing in the NRHM should have a separate<br />
priority plan.<br />
• State may define difficult, most difficult and inaccessible areas as per geographical location or in<br />
terms of difficulty to find HR for these areas.<br />
• State should take measure to ensure continuity of contractual appointments and take steps to<br />
regularize them.
• Additional allowances should be for regular staff, so as to promote them to work in rural/hard<br />
areas.<br />
• Incentives for specialist and MOs for difficult areas and on performance basis should be defined<br />
clearly and tabulated. Hard to reach areas/ the places where specialist/MOs do not join can be<br />
identified and defined for difficult area allowance and should be restricted to a reasonable<br />
amount which can vary as per the cadre.<br />
• Incentives on 'per case basis' should be avoided, however the same can be given to a group of<br />
service providers i.e. doctor, staff nurses etc. if a particular protocol of the service is maintained<br />
for e.g. conducting normal delivery should be linked with 48 hrs stay, EBF and provision of PNC<br />
protocols to both the mother and child. Such incentives can be restricted to Rs 200/‐.<br />
• It is suggested that all incentive schemes, giving the details may be tabulated and may please be<br />
indicated and given comprehensively.<br />
• TBA/Dai should not be promoted as primary provider for deliveries but can be utilized for<br />
community based services. However the services of Dais should be well defined to avoid conflict<br />
of interest between link workers. Some of the suggested roles for TBAs are: birth preparedness,<br />
birth companion, assistance to ANM in A/N, I/N and P/N Care, home‐based new born care,<br />
arrange referral transport/escort the pregnant woman to the institution for delivery, as a depot<br />
holder for contraceptives, DOTs Provider, report births and deaths of neonates, infants and<br />
mothers. However, please ensure that TBAs should be utilized only where there is no ASHA,<br />
otherwise there will be conflict of interest.<br />
• Any incentives for Dais need approval so kindly indicate the details.<br />
• Unit cost of the Blood camp should be indicated and such camps should be linked with blood<br />
banks and NACO.<br />
• The accreditation guidelines for any of the RCH services should synchronize with GoI guidelines<br />
on accrediting private health facilities.<br />
• The focus of such accreditation scheme should be at sub‐district level.<br />
• Budget for different strategies like incentives/bed nets/supplementary food/IEC etc should be<br />
under respective heads.<br />
• New constructions are not permitted under RCH. So funds for new SCs construction should be<br />
reflected under NRHM and ID division.<br />
• State needs to look into the quality of the service provided by the NGOs running APHCs. Cost<br />
effectiveness of these outsourced PHCs needs to be evaluated before scaling up.<br />
• PPP for health facilities be preferably allotted on competitive bidding and service quality should<br />
be monitored closely.<br />
• PPP for skill based training should be encouraged as per GoI guidelines. Close monitoring in such<br />
cases should be undertaken to ensure skill practice by the trainees at such facilities.<br />
E. Additionalities under NRHM:<br />
• Remuneration to contractual staff should be as per RCH/NRHM norms.<br />
• Activities under NRHM need approval from NRHM Division.<br />
• ASHA incentive for any scheme should be budgeted under Training/NRHM and too many<br />
fragmentations should be avoided.<br />
• Hiring of additional staff should be avoided on generic basis beyond the approved norms and<br />
should be linked with case load and quality of service delivery.<br />
F. Budget:<br />
• Budgeting should be as per GoI criteria and norms, and should not be duplicated.<br />
• RCH Drugs/Any other drugs should be budgeted under State head or under NRHM except for<br />
those states whose procurement procedures are in accordance with World Bank Guidelines.<br />
• Budget head under each activity for previous years should include both allocation and<br />
expenditure.<br />
• JSY deliveries should be co‐linked with service provision and facility upgradation and budgeted<br />
accordingly.
• Adequate funds for monitoring of MH activities including trainings should be kept.<br />
• Final costing should be as per the competitive bidding and following procurement procedure.<br />
• Sub‐heads related to monitoring visits and should form part of comprehensive monitoring.<br />
• Funds from Untied grant to VHSCs should be budgeted under NRHM.<br />
• Rent for SC should be under Infrastructure.<br />
• Funding for BCC/IEC components should be the part of comprehensive BCC/IEC strategy.<br />
STATUS OF FACILITY OPERATIONALISATION *<br />
S. No. Facility Total No.<br />
Planned till<br />
2012<br />
(cumulative<br />
)<br />
Total No<br />
operationalised<br />
till 2010 (till<br />
Dec. 2010<br />
cumulative)<br />
Target for<br />
201011<br />
Achievement<br />
in 2010-11<br />
(till December,<br />
2010)<br />
Target<br />
for 201112<br />
1. FRUs 14 6 6 5 6<br />
2. 24x7 PHCs 34 28 6 28 6<br />
* Must fulfil GoI minimum criteria, including availability of Blood Storage centres (for FRUs)<br />
States to provide separate targets, quarter-wise, for 2012 for high focus districts<br />
(consolidated) and State total<br />
STATUS OF MCH CENTRES OPERATIONALISATION<br />
S. Facility Total identified Total No operationalised till Target for<br />
No.<br />
December 2010 (cumulative) 2011-12<br />
1. MCH Centre Level III 28 28 34<br />
2. MCH Centre Level II 9 5 14<br />
3. MCH Centre Level I 2 1 1<br />
* Must fulfill GoI minimum criteria, including availability of Blood Storage centers (for FRUs)<br />
States to provide separate targets, quarter-wise, for 2012 for high focus districts<br />
(consolidated) and State total<br />
PERFORMANCE BASED INCENTIVES<br />
Name of<br />
the<br />
Scheme/<br />
Activity<br />
Type of<br />
worker<br />
Type of<br />
work being<br />
incentives<br />
Level of<br />
Facility<br />
(CHCs/<br />
PHCs/<br />
Sub-<br />
Centers<br />
Amount<br />
of<br />
Incentive<br />
e<br />
ASHA ASHA JSY 200/‐<br />
JSY Tribal 600/‐<br />
F.F. Male 200/‐<br />
F.F. Female 150/‐<br />
RNTCP 250/‐<br />
Maleria B.S. 5/‐<br />
Maleria P.F. 20/‐<br />
Maleria 50/‐<br />
Performance<br />
Expected<br />
No of<br />
workers<br />
given<br />
incentive<br />
Quantifiable<br />
e Output
Name of<br />
the<br />
Scheme/<br />
Activity<br />
Type of<br />
worker<br />
Type of<br />
work being<br />
incentives<br />
P.V.<br />
Maleria<br />
Referal<br />
Level of<br />
Facility<br />
(CHCs/<br />
PHCs/<br />
Sub-<br />
Centers<br />
Amount<br />
of<br />
Incentive<br />
e<br />
50/‐<br />
NLEP N.P. 100/‐<br />
NLEP M.B. 400/‐<br />
NLEP P.B. 200/‐<br />
RI 90 500/‐<br />
RI 100 750/‐<br />
VHSC<br />
<strong>Mission</strong> P.<br />
150/‐<br />
I.<br />
25+100/‐<br />
<strong>Mission</strong> 25/‐<br />
<strong>Mission</strong> HIV 10/‐<br />
<strong>Mission</strong><br />
ANC HIV<br />
300/‐<br />
<strong>Mission</strong><br />
PPTCT<br />
500/‐<br />
NPCB 175/‐<br />
RCH VHND 150/‐<br />
VHSC 175/‐<br />
<strong>Mission</strong><br />
Birth Reg.<br />
10/‐<br />
<strong>Mission</strong><br />
Maternal<br />
Death<br />
500/‐<br />
<strong>Mission</strong><br />
Child death<br />
RCH<br />
50/‐<br />
Performance<br />
Expected<br />
No of<br />
workers<br />
given<br />
incentive<br />
Quantifiable<br />
e Output
CHILD HEALTH PROGRAMME IMPLEMENTATION FORMAT FOR THE YEAR 2011‐12<br />
DISTRICT ‐ <strong>Amravati</strong><br />
1. IMR (SRS 2008) 30.79<br />
2. Goal: Overall NRHM 2012 25<br />
3. Goal: Annual 2011‐2012 29<br />
2. SITUATION ANALYSIS:<br />
2.1 Mortality Indicators NFHS 2 NFHS 3 SRS 2007 SRS 2008 Trend Analysis<br />
Neo Natal Mortality Rate 23.35<br />
Infant Mortality Rate<br />
Under Five Mortality<br />
25.64<br />
50.58 43.96<br />
13.65 8.45<br />
PROCESS INDICATORS<br />
2.2 ANAEMIA NFHS 2 NFHS 3 Coverage<br />
Evaluation<br />
Survey (CES)<br />
2009<br />
% of children (under 5<br />
years) of age with anaemia<br />
2.3 INFANT & YOUNG<br />
CHILD FEEDING<br />
Children under 3 years<br />
breastfed within one hour<br />
of birth<br />
Children age 6 months and<br />
above exclusively breastfed<br />
Children age 6 ‐ 24 months<br />
received solid/semisolid<br />
foods and are still breast<br />
fed<br />
NFHS 2 NFHS 3 DLHS 2 DLHS 3<br />
‐ 64.60<br />
‐ 42.70<br />
‐ 93.30<br />
Trend Analysis<br />
Coverage<br />
Evaluation<br />
Survey (CES)<br />
2009<br />
Trend<br />
Analysis
DIARRHOEA & ARI NFHS 2 NFHS 3 DLHS 2 DLHS 3 Coverage<br />
Evaluation<br />
Survey (CES)<br />
2009<br />
Children with Diarrhoea<br />
in the last 2 weeks who<br />
received ORS<br />
Children with Diarrhoea<br />
in the last 2 weeks who<br />
were given treatment at<br />
facilities.<br />
Children with ARI or<br />
fever in the last 2 weeks<br />
who were given<br />
treatment at facilities.<br />
TRAINING UNDER CHILD HEALTH<br />
4.1 Progress till date ‐ no. of trainings conducted/<br />
health persons trained / districts covered<br />
• IMNCI<br />
- No. of trainings<br />
- No. of persons trained<br />
- No. of Districts implementing<br />
• Pre‐ Service IMNCI<br />
- No. of trainings<br />
- No. of persons trained<br />
- No. of Districts implementing<br />
• F‐IMNCI<br />
- No. of trainings<br />
- No. of persons trained<br />
- No. of Districts implemented<br />
37.90 44.60<br />
82.20 78.30<br />
174 367<br />
Planned<br />
For 2010‐11<br />
Trend Analysis<br />
Held/ Trained (til<br />
Nov / Dec 2010)
4.1 Progress till date ‐ no. of trainings conducted/<br />
health persons trained / districts covered<br />
• Navjaat Shishu Suraksha Karyakram (NSSK)<br />
- No. of trainings<br />
- No. of persons trained<br />
- No. of Districts implemented<br />
• Any other<br />
KEY CHILD HEALTH PERFORMANCE INDICATORS<br />
Progress on CH interventions<br />
• IYCF<br />
- No. of Newborn breastfed within one<br />
hour<br />
- No. of children 6 months and above<br />
exclusive breastfed<br />
• Mgmt of Acute Respiratory Infection<br />
- No. of children below (5 years) with<br />
ARI screened/detected<br />
- No. of children (below 5 years) with<br />
ARI treated at facilities.<br />
• Mgmt of Diarrhoea<br />
- No. of children below 5 years with<br />
Diarrhoea in the last 2 weeks who<br />
received ORS and Zinc.<br />
- No. of children with Diarrhoea in the<br />
last 2 weeks who were given<br />
treatment at facilities.<br />
• Iron Folic Acid supplementation<br />
- No. of children below 5 years provided<br />
IFA Syrup/Tablet<br />
Planned<br />
For 2010‐11<br />
Planned<br />
For 2010‐11<br />
35848<br />
35848<br />
13978<br />
1397<br />
1397<br />
139<br />
Held/ Trained (til<br />
Nov / Dec 2010)<br />
Held/ Trained (til<br />
Nov / Dec 2010)<br />
22313<br />
16432<br />
143<br />
72<br />
39<br />
0
Progress on CH interventions<br />
• Vit A supplementation<br />
- No. of children below 5 years provided<br />
Vitamin A Syrup<br />
• Mgmt of Malnutrition / Severe Acute<br />
Malnutrition<br />
- No. of children with SAM detected<br />
- No. of children referred to<br />
NRC/facilities for Mgmt.<br />
Key Programme indicators<br />
Home visits for newborn by IMNCI trained<br />
person<br />
No. of newborn children visited on 1 st Day/ 3 rd<br />
Day/ 7 th Day.<br />
Number of Low Birth Weight babies visited on<br />
14 th , 21 st & 28 th day.<br />
No. of Sick Children Screened/detected &<br />
managed at home.<br />
No. of Sick Newborn & Children treated at<br />
facilities for Sepsis, Asphyxia, Severe<br />
dehydration, Pneumonia etc.<br />
No. of NSSK trained person conducting<br />
deliveries at facilities.<br />
Planned<br />
For 2010‐11<br />
416<br />
67<br />
260<br />
28<br />
109794<br />
111889<br />
3338<br />
3338<br />
Held/ Trained (til<br />
Nov / Dec 2010)<br />
416<br />
67<br />
260<br />
28<br />
38756<br />
111404<br />
3338<br />
1888
5. Establishment of newborn and child care facilities at<br />
Maternal and Child <strong>Health</strong> (MCH) Centres<br />
Level III<br />
MCH Centre<br />
Level II<br />
MCH Centre<br />
Level I<br />
MCH Centre<br />
• Special Newborn Care Units<br />
(SNCU) at district hospitals<br />
• Newborn and child Stabilization<br />
Units at FRUs<br />
• Newborn Care Corner at 24x7<br />
PHCs<br />
• Nutritional Rehabilitation centres<br />
1<br />
6<br />
28<br />
2027<br />
6. Any other activities under Child <strong>Health</strong> which have been reflected in PIP<br />
<br />
<br />
<br />
7. IEC/BCC<br />
Provision for IEC material planned<br />
New born Care<br />
- Early initiation of Breastfeeding.<br />
- Protection from infection<br />
- Protection from Hypothermia<br />
Recognition of Danger signs<br />
BCC<br />
Other Activities<br />
8. Supplies & Stock position<br />
ORS<br />
Zinc<br />
Antibiotics (Cotrimoxazole)<br />
Received Quantity Utilization Balance<br />
in stock<br />
Nil<br />
Nil<br />
Nil<br />
Nil<br />
Nil<br />
Nil
Vitamin A<br />
Iron & Folic Acid<br />
Albendazole Tablet<br />
Nil<br />
Nil<br />
Nil<br />
152440<br />
Planning for the year 2011‐12 1 st Qtr<br />
9. IMNCI<br />
Number of districts<br />
planned for IMNCI<br />
implementation.<br />
Number of IMNCI training<br />
planned.<br />
Number of persons<br />
planned to be trained<br />
Target<br />
2 nd Qtr<br />
Target<br />
Nil<br />
Nil<br />
Nil<br />
3 rd Qtr<br />
Target<br />
151200<br />
4 th Qtr<br />
Target<br />
40<br />
Nil<br />
Nil<br />
Nil<br />
Total<br />
Target
Planning for the year 2011‐12 1 st Qtr<br />
10. F‐IMNCI<br />
Number of districts<br />
facilities planned for<br />
implementing F‐ IMNCI<br />
Number of persons<br />
(MO/SN) planned to be<br />
trained<br />
11. Navjaat Shishu Suraksha<br />
Karyakram (NSSK)<br />
Number of districts<br />
facilities planned for<br />
implementing NSSK<br />
Number of persons<br />
(MO/SN) planned to be<br />
trained in NSSK<br />
12. Pre‐ Service IMNCI Training<br />
Number of medical<br />
colleges/ nursing colleges<br />
planned for implementing<br />
Pre‐Service IMNCI<br />
Number of medical/nursing<br />
students planned to be<br />
trained<br />
13. Establishment of newborn and<br />
child care facilities at Maternal<br />
and Child <strong>Health</strong> (MCH) Centres<br />
Level III<br />
MCH Centre<br />
• Special<br />
Newborn Care<br />
Units (SNCU) at<br />
district<br />
hospitals<br />
1<br />
Target<br />
2 nd Qtr<br />
Target<br />
3 rd Qtr<br />
Target<br />
4 th Qtr<br />
Target<br />
‐ ‐ ‐ 1<br />
Total<br />
Target
Planning for the year 2011‐12 1 st Qtr<br />
Level II<br />
MCH Centre<br />
Level I<br />
MCH Centre<br />
• Newborn and<br />
child<br />
Stabilization<br />
Units at FRUs<br />
• Newborn Care<br />
Corner at 24x7<br />
PHCs<br />
• Nutritional<br />
Rehabilitation<br />
centres<br />
14. Community based initiatives<br />
Organization of VHNDs<br />
15. School <strong>Health</strong> Scheme<br />
Target<br />
2 nd Qtr<br />
Target<br />
Number of children screened for illness.<br />
Number of children provided IFA Tablet.<br />
Number of children provided Albendazole Tablets.<br />
15. Budget<br />
• Budget allotted (2010‐11)<br />
• Budget utilized (Dec 2010)<br />
16. Budget proposed for Child <strong>Health</strong> for the year 2011 – 12<br />
3 rd Qtr<br />
Target<br />
4 th Qtr<br />
Target<br />
6 ‐ ‐ ‐ 6<br />
28 ‐ ‐ ‐ 28<br />
Total<br />
Target<br />
2027 ‐ ‐ ‐ 2027<br />
45586 minor illness<br />
3132 reffer<br />
56000<br />
112000<br />
100.31<br />
59.28<br />
159.79
A.4: FAMILY PLANNING<br />
The following are the important issues that states can consider while strategizing and formulating<br />
the PIP (2010‐12) for Family Planning:<br />
STRATEGY / ACTIVITY Planned Achi<br />
eved<br />
1 FAMILY PLANNING MANAGEMENT<br />
1.1 Review meetings on Family Planning<br />
performance and initiatives at the<br />
state and district level (periodic)<br />
1.2 Monitoring and supervisory visits to<br />
districts/ facilities<br />
1.3 Orientation workshops on technical<br />
manuals of FP viz. standards, QA,<br />
FDS approach, SOP for camps,<br />
Insurance etc.<br />
WORK<br />
PLAN<br />
SCHEDUL<br />
ED/ Trg.<br />
LOAD<br />
2010‐11 2011‐12<br />
BUDGET (In<br />
lakhs)<br />
36 27 36 2.00<br />
70 70 70 5.00<br />
4 3 4 0.10<br />
2 TERMINAL/LIMITING METHODS (Providing sterlisation services in districts)<br />
2.1 Plan for facilities providing FEMALE<br />
sterilisation services on fixed days at<br />
health facilities in districts<br />
2.2 Plan for facilities providing NSV<br />
services on fixed days at health<br />
facilities in districts<br />
2.3 Number of FEMALE Sterilisation<br />
camps in districts.<br />
55 55 55<br />
55 55 55<br />
2640 1320 2640<br />
2.4 Number of NSV camps in districts. 1 1 1 0.53<br />
2.5 Compensation for sterilisation<br />
(female)<br />
2.6 Compensation for sterilisation NSV<br />
(male)<br />
10080 4088 10080 100.80<br />
1120 576 1120 17.00<br />
2.7 Mobility support to surgeon's team 4 4 4 5.00<br />
2.8 Accreditation of private<br />
centres/NGOs for sterilization<br />
services<br />
93 93<br />
2.9 Plan for post partum sterilisation 55 55 55
STRATEGY / ACTIVITY Planned Achi<br />
eved<br />
3 SPACING METHOD (Providing of IUD services by districts)<br />
3.1 Plan for providing IUD services at<br />
health facilities in districts<br />
WORK<br />
PLAN<br />
402 402 402<br />
3.2 No. of IUD camps in districts ‐ ‐ ‐<br />
3.3 Compensation for IUD ‐ ‐ ‐<br />
3.4 Compensation to ASHA for ensuring<br />
retention of IUD by clients<br />
4 SOCIAL MARKETING OF CONTRACEPTIVES<br />
4.1 Setting up CBD Outlets<br />
5 FAMILY PLANNING TRAINING<br />
5.1 Laparoscopic Sterilisation Training<br />
5.1<br />
.1<br />
‐ ‐ ‐<br />
TOT on laparoscopic sterilisation 1 1 1<br />
5.1 Laparoscopic sterilisation training<br />
for<br />
.2 service providers (gynaecologists<br />
/surgeons)<br />
5.2 Minilap Training for MOs/ MBBS<br />
5.2<br />
.1<br />
5.2<br />
.2<br />
TOT on Minilap<br />
Minilap training for service<br />
providers (medical officers)<br />
5.3 Non‐Scalpel Vasectomy (NSV)<br />
Training<br />
5.3<br />
.1<br />
5.3<br />
.2<br />
TOT on NSV<br />
NSV training for medical officers<br />
5.4 IUD Insertion training<br />
1 1 1<br />
1 1 1<br />
SCHEDUL<br />
ED/ Trg.<br />
LOAD<br />
BUDGET (In<br />
lakhs)
5.4<br />
.1<br />
5.4<br />
.2<br />
5.4<br />
.3<br />
5.4<br />
.4<br />
STRATEGY / ACTIVITY Planned Achi<br />
eved<br />
TOT for IUD insertion<br />
Training of Medical officers in IUD<br />
insertion<br />
Training of staff nurses in IUD<br />
insertion<br />
Training of ANMs / LHVs in IUD<br />
insertion<br />
5.5 No. of Contraceptive Update<br />
trainings for health providers in the<br />
districts<br />
5.7 Other FP trainings (please specify)<br />
6 BCC/IEC<br />
activities/campaigns/melas for<br />
family planning e.g. Funds<br />
earmarked for district and block<br />
level activities during 'World<br />
Population Day' celebration week<br />
7 PROCUREMENT of<br />
DRUGS/MATERIALS<br />
WORK<br />
PLAN<br />
7.1 NSV Kits 300<br />
7.2 IUD insertion Kits 402<br />
7.3 Minilap Set 69<br />
7.4 Procurement/ repair of<br />
laparoscopes<br />
7.5 Procurement of drugs & supplies for<br />
FP<br />
8 Innovatory schemes for promoting<br />
FP at state or district level<br />
9 Performance based rewards to<br />
institutions and providers for FP<br />
performance at state and district<br />
level<br />
4<br />
SCHEDUL<br />
ED/ Trg.<br />
LOAD<br />
BUDGET (In<br />
lakhs)
A.5: ARSH<br />
Adolescents constitute a vulnerable and large (22%) segment of the population in need of focused<br />
attention. Adolescent Reproductive & Sexual <strong>Health</strong> (ARSH) has been identified as one of the four<br />
strategies under RCH‐II and implementing context ‐ sensitive ARSH interventions is now over four<br />
years old. While preparing for the PIP 2011‐12 states are requested to make a holistic plan for ARSH<br />
interventions. This may include the following:<br />
1. List of districts where ARSH program has already been rolled out.<br />
2. List of districts where the state plans to roll out ARSH program 2011‐12.<br />
3. Parameters on the basis of which the state has decided to identify these districts.<br />
4. Plan of the state to address the ARSH needs of school/college/non‐school going children.<br />
5. Is there any existing community based ARSH programme which has increased facility<br />
utilization? Please provide details.<br />
6. IEC activities under taken on ARSH issues in the state.<br />
7. Innovations by the state if any.<br />
Please also provide details of the ARSH program as per the formats in Annexure II<br />
The districts to be selected for implementation of ARSH strategy in 2011‐12 could be selected based<br />
on following DLHS‐3 indicators:<br />
1. Sex Ratio in age 10‐19 years<br />
2. Female literacy rate in 10‐19 years<br />
3. Mean age at marriage of women in district<br />
4. Rate of deliveries in 15‐19 years age group.<br />
5. Women (age 15‐19) who heard of HIV/AIDS<br />
Check‐list for ARSH activities<br />
S. No. Activity Status as<br />
on<br />
01.04.2010<br />
1. 1‐day State<br />
Orientation<br />
Workshop for ARSH<br />
2. State level Training<br />
of Trainers (3 days)<br />
3. Printing of Training<br />
Modules<br />
Planned<br />
for 2010‐<br />
11<br />
Achievement<br />
against plan<br />
till<br />
31.12.2010<br />
Planning<br />
budget<br />
for 2011‐<br />
12<br />
0<br />
0<br />
0<br />
Remarks<br />
4. IEC for ARSH 1.00 GH, WH,<br />
<strong>Amravati</strong><br />
Achalpur,<br />
Dharni,<br />
Warud<br />
5. Helpline for ARSH 0.2 GH,
6. Convergence with<br />
other programmes /<br />
departments (WCD,<br />
SACS, MoYAS, HRD)<br />
7. Other activities<br />
(pls specify)<br />
A Strengthening of<br />
old/new clinic<br />
0<br />
0<br />
<strong>Amravati</strong><br />
2.00 GH, WH<br />
<strong>Amravati</strong>,<br />
Achalpur,<br />
Dharni,<br />
1.44<br />
B Salary of ARSH<br />
Counselor<br />
TA/DA 0.50 GH<br />
<strong>Amravati</strong><br />
C Peer Educator group<br />
4.00 <strong>Amravati</strong><br />
(CBA)<br />
Achalpur,<br />
Dharni,<br />
Warud<br />
8. Out reach activity 1.5 GH, WH<br />
<strong>Amravati</strong>,<br />
Achalpur,<br />
Dharni,<br />
Electronic goods<br />
1.00 GH,<br />
(computer printer<br />
etc)<br />
11.64<br />
Amravti<br />
States to provide separate targets, quarter-wise, for 2012 for high focus districts (consolidated) and State<br />
total<br />
Name of<br />
district<br />
Training Status as<br />
on 01.04.2010<br />
ARSH Training<br />
Training Planned<br />
for 2010‐11<br />
Achievement<br />
against plan till<br />
31.12.2010<br />
Planning for<br />
2011‐12<br />
MO ANM/LHV MO ANM/LHV MO ANM/LHV MO ANM/LHV<br />
<strong>Amravati</strong> 40 207 24 172 16 35
Total District Hospital: 1<br />
District hospital with AFHS clinic: 5<br />
Planned AFHS clinic in DH in 2011‐12: 1<br />
Name of<br />
district<br />
AFHS clinics<br />
Total PHC PHC with AFHS clinic<br />
as on 01.04.10<br />
AFHS clinics<br />
planned in<br />
2010<br />
Achievements<br />
till 31.12.2010<br />
AFHS clinics<br />
planned for<br />
2011‐12<br />
<strong>Amravati</strong> 56 0 0 0 18<br />
Any other AFHS clinic at CHC/SDH<br />
Name of<br />
district<br />
Amarav<br />
ati<br />
Number<br />
of AFHS<br />
clinics<br />
Adolescent<br />
attending<br />
AFHS clinics<br />
Utilization of Adolescent services in AFHS clinics<br />
RTI/ STI/<br />
HIV<br />
cases<br />
Anaemia/<br />
Under<br />
nutrition<br />
Pregnancy<br />
/ MTP<br />
Condom/<br />
OCP/ ECP<br />
Counselling<br />
provided<br />
Mental<br />
disorders/<br />
sexual abuse<br />
5 800 60 239 0 2 800 0<br />
Monitoring formats for scheme for promotion of menstrual hygiene at state and district level<br />
1. State level Formats:<br />
1a. State level Format: (data to be collected on an Annual basis)<br />
Name of<br />
district<br />
Total<br />
number<br />
of rural<br />
girls<br />
Total<br />
number of<br />
villages<br />
Number of<br />
girls to be<br />
reached<br />
Number of<br />
SN packs<br />
required<br />
Sourcing<br />
agency<br />
Quality<br />
Assurance<br />
agency<br />
Storage<br />
available<br />
or hired<br />
<strong>Amravati</strong> 1543 0 ‐ ‐ ‐ ‐ ‐<br />
Total<br />
Transport<br />
available<br />
or hired<br />
1b. State level Format: (data to be consolidated on a Monthly basis from the district records i.e.<br />
2b)<br />
Name of<br />
District<br />
Total<br />
Numb<br />
er of<br />
girls<br />
reache<br />
d per<br />
month<br />
Numbe<br />
r of SN<br />
packs<br />
sold/<br />
distribu<br />
ted<br />
Numbe<br />
r of<br />
monthl<br />
y<br />
meetin<br />
g held<br />
Amount of Incentive<br />
paid to ASHA<br />
Sale of Sunday<br />
napkins meetings<br />
Amount of<br />
funds<br />
recouped<br />
to the DHS<br />
Rental cost<br />
for storage<br />
arrangeme<br />
nts if any.<br />
Costs of<br />
transpo<br />
rtation
2. District level Formats:<br />
2a. Data to be collected on an annual basis<br />
- Number of girls to be reached ‐<br />
- Number of SN packs required<br />
- Transport systems to enable reach of SN to the blocks<br />
- Storage arrangements if required<br />
- Annual audit of accounts at district and block<br />
- Training: TOT held for trainers<br />
2b. Data to be collected on a monthly basis at district level<br />
Name<br />
of<br />
Block<br />
Total<br />
Number<br />
of girls<br />
reached<br />
per<br />
month<br />
Total<br />
number<br />
of<br />
villages<br />
in block<br />
3. Block level Formats:<br />
Number<br />
of SN<br />
packs<br />
sold/<br />
distribut<br />
ed<br />
Number<br />
of<br />
monthly<br />
meetings<br />
held<br />
3a. Data to be collected on an annual basis<br />
- Number of girls to be reached<br />
- Number of SN packs required<br />
Amount of<br />
Incentive paid to<br />
ASHA<br />
Sale of<br />
napkins<br />
- Number of SN packs procured from SHG last year<br />
Sunday<br />
meetings<br />
- Transport systems to enable reach of SN to the Sub Centre<br />
- Storage arrangements<br />
- Training:<br />
- Training of ASHA<br />
Name of<br />
block<br />
- Orientation of VHSC<br />
- Orientation of ANM<br />
Total<br />
number<br />
of ASHA<br />
Target for<br />
training<br />
ASHA in<br />
2011‐12<br />
Achievements in<br />
training 2011‐12<br />
Total<br />
number<br />
of ANM<br />
Amount<br />
of funds<br />
recouped<br />
to the<br />
DHS<br />
ANM<br />
oriented<br />
in 2011‐<br />
12<br />
Rental<br />
cost for<br />
storage<br />
arrangem<br />
ents if<br />
any.<br />
- - - - - - -<br />
- - - - - - -<br />
- - - - - - -<br />
Costs<br />
of<br />
transp<br />
ortatio<br />
n<br />
Total<br />
number<br />
of VHSC<br />
oriented
3b1. Data to be collected on a monthly basis at block level<br />
Name of<br />
Sub<br />
Centre<br />
Total<br />
3b.2<br />
Number<br />
of girls<br />
reached<br />
per<br />
month<br />
Name of sub<br />
centre<br />
Total<br />
Number<br />
of SN<br />
packs<br />
Received<br />
Total number of<br />
ASHA<br />
Number of<br />
SN packs<br />
Distributed<br />
Balance<br />
Packs<br />
Amount of Incentive<br />
paid to ASHA for SN<br />
packs<br />
Amount of<br />
Incentive<br />
paid to<br />
ASHA<br />
Amount of<br />
funds<br />
recouped<br />
to SC<br />
Amount of<br />
Incentive paid to<br />
ASHA for meeting<br />
4. Monthly Monitoring format/Register for Sub Centre<br />
a. Rental cost for storage arrangements (e.g. SC, rented godown)<br />
b. Costs of transportation<br />
Name of<br />
Village<br />
Total<br />
Name of<br />
ASHA<br />
Number of<br />
girls reached<br />
per month<br />
Number of<br />
SN packs<br />
Recd from<br />
block<br />
Number of<br />
SN packs<br />
sold<br />
Balance<br />
SN packs<br />
Rental cost<br />
for storage<br />
arrangemen<br />
ts, if any.<br />
Costs of<br />
transpo<br />
rtation<br />
Average<br />
attendance in<br />
monthly meeting<br />
Amount of<br />
Incentive paid to<br />
ASHA<br />
Sale of<br />
napkins<br />
Sunday<br />
meeting<br />
s<br />
Amoun<br />
t of<br />
funds<br />
recoup<br />
ed to<br />
SC<br />
5. The ASHA will maintain a tracking register (Format A) of the adolescent girls in her village and submit<br />
a monthly report to the ANM in the Format B.<br />
Format A<br />
Name<br />
of Girl<br />
Total<br />
number<br />
of SN<br />
packs<br />
sold<br />
Jan<br />
Sunday mtg.<br />
attendance<br />
number<br />
of SN<br />
packs<br />
sold<br />
Feb Mar Apr<br />
Sunday<br />
mtg.<br />
attendance<br />
number<br />
of SN<br />
packs<br />
sold<br />
Sunday mtg.<br />
attendance<br />
number<br />
of SN<br />
packs<br />
sold<br />
Sunday mtg.<br />
attendance
Format B – Monthly Report<br />
1. Name of ASHA:<br />
2. Name of village:<br />
3. Stock of SN packs at the beginning of the month:<br />
4. Stock of SN packs at the end of the month:<br />
5. Cost of transporting from SC to village:<br />
S.<br />
No.<br />
Total #<br />
of girls<br />
Sunday meetings held and attendance by<br />
category<br />
Date #. of<br />
girls<br />
# of VHSC<br />
members<br />
ANM AWW<br />
Number of SN<br />
packs sold<br />
The following are the important area states consider to strategies and formulate the PIP<br />
S.No. Name of cities<br />
identified for<br />
implementing UHPs.<br />
In the State PIPs.<br />
Under<br />
Urban RCH, so far<br />
Major urban<br />
health<br />
strategies/activitie<br />
s carried out<br />
under Urban RCH<br />
so far, city‐wise<br />
Information in respect of Special Schemes (for each city)<br />
Name of city ‐<br />
Sl. No. Govt. <strong>Health</strong> Facilities ‐<br />
under Grant‐in‐aid<br />
from GOI<br />
No. of <strong>Health</strong> Posts<br />
Type A<br />
Type B<br />
Type C<br />
Type D<br />
No. of Urban Family<br />
Welfare Centres<br />
Type I<br />
Type II<br />
Type III<br />
Controlling agency<br />
(SG/LB/VO/Ors.)<br />
Urban health<br />
strategies/activities<br />
as proposed now in<br />
the State PIP under<br />
Urban RCH, city‐<br />
wise<br />
Status<br />
(Functional/closed)<br />
Amount of<br />
incentive<br />
earned<br />
Brief on<br />
activities<br />
being<br />
supported by<br />
external<br />
agencies<br />
Brief<br />
summary of<br />
activities being<br />
carried out
A.6 URBAN HEALTH PROGRAMME PIP2011‐12<br />
The following are the important area states consider to strategies and formulate the PIP<br />
S.No. Name of cities identified<br />
for implementing UHPs.<br />
In the State PIPs. Under<br />
Urban RCH, so far<br />
Major urban health<br />
strategies/activitie s<br />
carried out under<br />
Urban RCH so far,<br />
city‐wise<br />
Urban health<br />
strategies/activities<br />
as proposed now in<br />
the State PIP under<br />
Urban RCH, city‐wise<br />
1 Achalpur <strong>Health</strong> post <strong>Health</strong> post<br />
Urban ANM<br />
Need base technical<br />
activity<br />
Information in respect of Special Schemes (for each city)<br />
Name of city ‐<br />
Sl. No. Govt. <strong>Health</strong> Facilities ‐<br />
under Grant‐in‐aid<br />
from GOI<br />
No. of <strong>Health</strong> Posts<br />
Type A<br />
Type B<br />
Type C<br />
Type D<br />
No. of Urban Family<br />
Welfare Centres<br />
Type I<br />
Type II<br />
Type III<br />
Controlling agency<br />
(SG/LB/VO/Ors.)<br />
Status<br />
(Functional/closed)<br />
Brief on<br />
activities<br />
being<br />
supported by<br />
external<br />
agencies<br />
Brief<br />
summary of<br />
activities being<br />
carried out
A.7 SOCIAL AND GENDER EQUITY<br />
CHECKLIST FOR INCLUSION OF SOCIAL AND GENDER EQUIT<br />
District Level<br />
CHECKLIST FOR INCLUSION OF SOCIAL AND GENDER EQUITY<br />
I Strengthened Institutional Mechanisms for Social and Gender Equity<br />
The key entry points identified for addressing social inclusion and gender equity ‐ a<br />
nodal gender and equity person, plans to train ANMs, ASHS, district level functionaries,<br />
use of MIS, BCC<br />
Has the plan been built on systematic mapping of underserved districts and vulnerable<br />
social groups 1 , including (but not limited to) the Tribal areas.<br />
II Improved Services for Disadvantaged Social Groups and Women as Clients<br />
Are specific strategies or mechanisms proposed to reach at a scale including budget<br />
allocations for 1) Under Served Districts 2. Social Group ‐ ANC, PNC, Nutrition and <strong>Health</strong>,<br />
Ambulance and Transport Facilities, Trained medical staff, hospitals, safe community<br />
friendly alternative systems<br />
Are there strategies specified to ensure quality of services from a woman’s perspective<br />
(e.g. through expansion of district Quality of Care Protocols, district teams). Are issues<br />
such as adequate, clean and separate toilets for women, privacy with the help of<br />
screens/ partitions, sufficient water, clean linen etc included as an aspect of quality?<br />
Is there a plan for adolescent friendly health services ‐ anemia treatment, delay<br />
marriages, delay pregnancy, etc (inclusion of adolescent boys/girls, married and<br />
unmarried, out‐of‐school and in‐school for SRH education and service provision).<br />
Are there strategies for development of capacity to provide counseling services at<br />
appropriate levels (e.g. for Family Planning, HIV prevention and testing, STI ‐partner<br />
management and Gender Based Violence) and integrate these in health services<br />
III Improved <strong>Health</strong> Financing<br />
Is there sufficient allocation of funds for emergency transport, emergency obstetric care,<br />
MTP services, maternal complications<br />
Is there adequate allocation of funds for health delivery strategy made for women and<br />
BPL, SC, ST, migrants, urban poor, minorities and locally vulnerable groups<br />
IV Training<br />
Do training plans include a focus on provision of MTP, management of RTI/STI, insertion<br />
of IUDs, vasectomies?<br />
VI Improved Community Involvement ‐ RCH ‐ NRHM<br />
Are there plans and funds for communication, networking and BCC activities through<br />
community and women’s groups for improved RCH outcomes (e.g. involvement of<br />
community volunteers, health messages through SHGs, strengthening of Mahila<br />
Swasthya Sanghs, health action groups and community health dialogues)<br />
Are there mechanism to ensure participation of socially marginalized groups and 50%<br />
women’s participation in RKS and VHSCs<br />
Are there mechanisms to involve Panchayati Raj Institutions/Self Help Groups in needs<br />
assessment and planning?<br />
VII Innovative approaches to make services and service environment client friendly<br />
Are there provision for innovative approaches to making services client –centered (e.g.<br />
24 hour help counters at district hospitals for assisted referrals, helplines for emergency<br />
1<br />
By vulnerable groups we mean SC, ST, minorities, urban Poor, women, adolescent girls and boys,<br />
occupation based groups, migrants, etc.
transport)<br />
Are putting up patients rights charters, rate charts, timings, in local languages at all<br />
health centres, putting up complaints boxes and credible grievance redressal system<br />
being practiced?<br />
Are plans for linking hospitals with NGOs, Women’s groups, help lines to address gender<br />
based violence<br />
VIII Men as partners and clients<br />
Are there innovative plans and allocation to improve provision of STI services to men<br />
(e.g. through BCC, male health workers, partner notification and treatment)<br />
Are their plans and allocations for BCC and MPW training to improve men’s involvement<br />
in family planning including use of condoms and terminal methods<br />
IX Women <strong>Health</strong> Care Providers<br />
Are there mechanisms to report or address sexual harassment at work‐place at the<br />
district level?<br />
Are field level functioning of ANMs/ Frontline workers e.g. provision of mobile phones,<br />
provision of vehicles for easy transport<br />
X Better implementation of PCPNDT Act<br />
Are there plan and allocations for better implementation of the PNDT act to stop sex‐<br />
selection, specifically for<br />
‐support cells at district providing monitoring or legal help ‐<br />
‐ capacity‐building of Appropriate Authorities and other stakeholders including for<br />
monitoring visits
CONSOLIDATED BUDGET SHEET -RCH FLEXIBLE POOL<br />
Sl.No. Activity Unit<br />
Cost<br />
Physical<br />
Targets<br />
Required<br />
fund<br />
under RCH<br />
RCH Flexible Pool<br />
A.1 MATERNAL HEALTH 0<br />
A.1.1 Operationalise facilities (only dissemination,<br />
monitoring, and quality)<br />
0.25 1 0.25<br />
A.1.1.1 Operationalise FRUs 0<br />
A.1.1.2 Operationalise 24x7 PHCs 0<br />
A.1.1.3 MTP services at health facilities 0<br />
A.1.1.4 RTI/STI services at health facilities 0<br />
A.1.1.5 Operationalise Sub‐centres 0.05 14 0.70<br />
A.1.2 Referral Transport 0.006 1400 8.40<br />
A.1.3 Integrated outreach RCH services 0<br />
A.1.3.1 RCH Outreach Camps 0.15 6 0.90<br />
A.1.3.2 Monthly Village <strong>Health</strong> and Nutrition Days 0<br />
A.1.4 Janani Suraksha Yojana / JSY 0<br />
A.1.4.1 Home Deliveries 0.005 1486 7.43<br />
A.1.4.2 Institutional Deliveries 0.007 13380 91.65<br />
A.1.5 24 Hours Deliveries 0<br />
A1.6 Payment to Link Workers/AWW/AWS (other than 0.006/0. 11373 28.54<br />
ASHA)<br />
002<br />
A1.6.1 C‐sections 0.015 268 4.02<br />
A1.6.2 Sanitory Napkin for Delivery cases 0.001 14866 14.86<br />
A.1.6.3 Administration cost (5%) 1 5.24<br />
A.1.6.4 High risk ANC & Gynac clinic 0.02 267 5.52<br />
A.1.6.5 Free diet allowance to Institutional Delivery PHC 0.0015 6720 10.08<br />
A.1.6.6 Free diet allowance to Institutional Delivery RH 0.0015 2340 3.52<br />
A.1.7 Maternal Death Audit 0<br />
A.2 CHILD HEALTH 0<br />
A.2.1 IMNCI 0<br />
A.2.2 Facility Based Newborn Care/FBNC 0<br />
A.2.3 Home Based Newborn Care/HBNC 0<br />
A.2.4 School <strong>Health</strong> Programme 0<br />
A.2.5 Infant and Young Child Feeding/IYCF 0<br />
A.2.6 Care of Sick Children and Severe Malnutrition at<br />
PHC & RH/SDH<br />
0.672 138 46.37<br />
A.2.7 Management of Diarrohea, ARI and Micronutrient<br />
Malnutrition<br />
0<br />
A.2.8 Other strategies/activities 0<br />
A.2.8.1 Maintainance of sick new born care unit at district<br />
hospital<br />
0.20 1 0.20<br />
A.2.8.2 Maintainance of New Born Care corners at FRUs 0.20 5 1.00<br />
A.2.8.3 Maintainance of New born care corner at 24x7 PHC 0.20 28 5.60
Sl.No. Activity Unit<br />
Cost<br />
A.2.8.4 Village Child Development Center ( VCDC ) at SC<br />
level AWW ( Rs. 960/‐ per child for 30 days for 10<br />
children per SC)<br />
A.2.8.5 Organisational cost for Implementation of ‐ Bi<br />
Annual Deworming & Vitamin A Supplementation &<br />
Iron Folic Acid Supplementation<br />
A.2.8.6 Peadiatrician servicess for examination, treatment<br />
and referal seek children – Per month at 56 PHC on<br />
fixed day. Mobility + Incentive for Private<br />
Peadiatrician ‐ Rs.1500/‐honorarium + Rs.500/‐<br />
mobilit.<br />
A.2.8.7 Referreal Transport for critical ill child for Rs. 600<br />
per child X 12 children per year per PHC<br />
Physical<br />
Targets<br />
Required<br />
fund<br />
under RCH<br />
0.0096 10000 96.00<br />
0.025 112 2.80<br />
0.020 276 5.52<br />
0.006 672 2.02<br />
A.2.9 Infant Death Audit 0.002 140 0.28<br />
A.3 FAMILY PLANNING 0<br />
A.3.1 Terminal/Limiting Methods 0<br />
A.3.1.1 Dissemination of manuals on sterilisation standards<br />
0<br />
& quality assurance of sterilisation services<br />
A.3.1.2 Female Sterilisation 0.0825 10080 83.16<br />
A.3.1.2.1 Compansetion for NSV acceptance 0.0150 1120 16.80<br />
A.3.1.3 NSV camps 0.0530 1 0.53<br />
A.3.1.6 Accreditation of private providers for sterilisation<br />
0<br />
services<br />
A.3.2 Spacing Methods 0<br />
A.3.2.1 IUD camps 0<br />
A.3.2.2 IUD services at health facilities 0<br />
A.3.2.3 Accreditation of private providers for IUD insertion<br />
0<br />
services<br />
A.3.2.4 Social Marketing of contraceptives 0<br />
A.3.2.5 Contraceptive Update seminars 0<br />
A.3.3 POL for Family Planning 0.001 11200 11.20<br />
A.3.4 Repairs of Laparoscopes 2.00<br />
A.3.5 Other strategies/activities 0<br />
A.3.5.1 Orgnisation of mini camps for<br />
laproscopy/minilap/NSV<br />
0.01250 70 0.88<br />
A3.5.2 Promotion of IUD 380 & EC Pills through<br />
sensitization of SHG<br />
0.030 140 4.20<br />
A.4 ADOLESCENT REPRODUCTIVE AND SEXUAL HEALTH<br />
/ ARSH<br />
0<br />
A.4.1 Adolescent services at health facilities. 0<br />
A.4.2 Other strategies/activities 0<br />
A.4.2.1 Strengthening of functning establishing new ARSH<br />
Clinic at Women Hospital.<br />
0.50 1 0.50
Sl.No. Activity Unit<br />
Cost<br />
A.4.2.2 Continuation of counselors on contractual basis at<br />
districts Hospitals already appointed at the<br />
respective AFHS clinics.<br />
A.4.2.3 Sensitization peer groups in villages through<br />
community based approach<br />
A.4.2.4 Prevention /control of Nutritional Anemia in<br />
Adolescent Girls. Organizational cost Rs.1.00 lakhs<br />
per district .<br />
Physical<br />
Targets<br />
Required<br />
fund<br />
under RCH<br />
0.10 1 1.20<br />
1.50 4 6.00<br />
1.00 1 1.00<br />
A.5 URBAN RCH 0<br />
A.5.1 <strong>Health</strong> Posts in urban areas ‐ Salary of the<br />
Contractual staff posted in <strong>Health</strong> Post and<br />
contingent items to run HP<br />
5.92 1 5.92<br />
A.5.2 Urban ANMs for M. Councils under RCH 0.055 35 23.12<br />
A.5.3 RCH PIP of 15 M.Coucils(> 1 Lakh popn.)‐Need based<br />
Technical activties for reducing MMR, IMR and TFR<br />
6.00 1 6.00<br />
A.6 TRIBAL RCH 0<br />
A.6.1 <strong>Health</strong> Checkup of Sick Children at Anganwadi‐ 0.005<br />
Mobility Support @ Rs.500/‐ per PHC per month i.e<br />
Rs.6000/‐ per PHC per year.<br />
11 0.66<br />
A.6.2 Involvement of ASHA for implementation of<br />
essential new born care activity in all tribal blocks.<br />
At rate Rs. 4000/‐ Per ASHA based on performance<br />
A.6.3 Hardship Allowance to Medical Officers of Bharari<br />
Pathak in Tribal blocks @ Rs. 6000/‐ per month.<br />
A.6.4 Operational Resarch in regarding Referral services.<br />
Lump sum Budget is shown .<br />
A.6.5 Documentary Evidence of improvement in grades of<br />
Malnutrition in the form of photographs. @ Rs.30/‐<br />
per child for 3 photographs. For 150 children in<br />
selected 5 tribal PHCs.<br />
0.04<br />
0.06<br />
5.00<br />
300 12.00<br />
22 15.84<br />
1 5.00<br />
750 0.22<br />
A.7 VULNERABLE GROUPS 0<br />
A.7.1 Appointment of counselor at DH and WH for<br />
women victims of violence. This counselor will also<br />
act for PCPNDT<br />
0.10 2 2.40<br />
A.8 Other RCH Activities PC, PNDT & Sex ratio 0<br />
A.8.1 Orientation of programme managers and service<br />
providers on PC & PNDT Act<br />
0.10<br />
3 0.30<br />
A.8.2 Support for sting operation under PCPNDT Act 0.50 1 0.50<br />
A.8.3 Provision for Witness support participated in<br />
PCPNDT court cases<br />
A.8.4 Support for teams at district level for inspection of<br />
sonography centers registered under PC PNDT Act<br />
0.15<br />
1.00<br />
1 0.15<br />
1 1.00
Sl.No. Activity Unit<br />
Cost<br />
A.8.5 Support for Scrutiny of Form‐F by the NGOs/MSW<br />
Students<br />
A.8.6 Training for Centers for Online Data Entry of Filling<br />
Form ‐ F<br />
A.8.7 One counsellar will be appointed at the each District<br />
Hospital & Women Hospital<br />
0.30<br />
0.10<br />
Physical<br />
Targets<br />
Required<br />
fund<br />
under RCH<br />
10000 0.50<br />
1 0.30<br />
2 2.40<br />
A.9 INFRASTRUCTURE & HUMAN RESOURCES 0<br />
A.9.1 Contractual Staff & Services 0<br />
A.9.1.1 ANMs, Staff Nurses, 0<br />
A.9.1.2 Laboratory Technicians, ,MPWs 0<br />
A.9.1.3 Specialists (Anesthetists, Pediatricians, Ob/Gyn,<br />
Surgeons, Physicians, Dental Surgeons, radiologist,<br />
Sonologist, Pathologist,Specialist for CHC )<br />
0<br />
A.9.1.4 PHNs at CHC, PHC level 0<br />
A.9.1.5 Medical Officers at CHCs / PHCs 0<br />
A.9.1.6 Additional Allowances/ Incentives to M.O.s of PHCs 0.02350 52 1.16<br />
and CHCs<br />
A.9.1.7 Others ‐ Computer Assistants/ BCC Co‐ordinator etc 0<br />
A.9.1.8 Incentive/ Awards etc. to SN, ANMs etc. 0<br />
A.9.1.9 Human Resources Development (Other than above) 0<br />
A.9.1.10 Other Incentives Schemes (Pl.Specify) 0<br />
A.9.1.11 Staff/ Supervisory Nurses for PHCs,CHCs(for AYUSH) 0<br />
A.9.1.12 Medical Officers at CHCs/ PHCs (for AYUSH) 0<br />
A.9.2 Minor civil works 0<br />
A.9.2.1 Minor civil works for operationalisation of FRUs 0<br />
A.9.2.2 Minor civil works for operationalisation of 24 hour<br />
services at PHCs<br />
0<br />
A.9.2.2.1 Repair & expantion of maternity ward, labour room 3.00 39 106.50<br />
A.9.2.2.2 Provision for equipment at District Level 1.00 1 1.00<br />
A.9.2.2.3 Expenditure on monthly/ quarterly meetings at<br />
distric level<br />
0.05<br />
12 0.60<br />
A.10 TRAINING 0<br />
A.10.1 Strengthening of Training Institutions 0<br />
A.10.2 Development of training packages 0<br />
A.10.3 Maternal <strong>Health</strong> Training 0<br />
A.10.3.1 Skilled Birth Attendance / SBA 0<br />
A.10.3.2 EmOC Training 0<br />
A.10.3.3 Life saving Anesthesia skills training 0<br />
A.10.3.4 MTP training 0<br />
A.10.3.5 RTI / STI Training 0<br />
A.10.3.6 Dai Training 0<br />
A.10.3.7 Other MH Training (ISD Refresher ) 0<br />
A.10.4 IMEP Training 0<br />
A.10.5 Child <strong>Health</strong> Training 0<br />
A.10.5.1 IMNCI 0
Sl.No. Activity Unit<br />
Cost<br />
Physical<br />
Targets<br />
Required<br />
fund<br />
under RCH<br />
A.10.5.2 Facility Based Newborn Care 0<br />
A.10.5.3 Home Based Newborn Care 0<br />
A.10.5.4 Care of Sick Children and severe malnutrition 0<br />
A.10.5.5 Other CH Training (pl. specify) 0<br />
A.10.6 Family Planning Training 0<br />
A.10.6.1 Laparoscopic Sterilisation Training 0<br />
A.10.6.2 Minilap Training 0<br />
A.10.6.3 NSV Training 0<br />
A.10.6.4 IUD Insertion Training 0<br />
A.10.6.5 Contraceptive Update/ISD Training 0<br />
A.10.6.6 Other FP Training (pl. specify) 0<br />
A.10.7 ARSH Training 0<br />
A.10.8 Programme Management Training 0<br />
A.10.8.1 SPMU Training 0<br />
A.10.8.2 DPMU Training 0<br />
A.10.9 Other training (pl. specify) 0<br />
A.10.10 Training (Nursing) 0<br />
A.10.10.1 Strengthening of Existing Training Institutions /<br />
Nursing School<br />
0<br />
A.10.10.2 New Training Institutions/School 0<br />
A.10.11 Training (Other <strong>Health</strong> Personnel) 0<br />
A.10.11.1 Promotional Trg of health workers females to lady<br />
0<br />
health visitor etc.<br />
A.10.11.2 Training of AMNs, Staff nurses, AWW, AWS 0<br />
A.10.11.3 Other training and capacity building programmes 0<br />
A.11 PROGRAMME / NRHM MANAGEMENT COSTS 0<br />
A.11.1 Strengthening of SHS /SPMU (Including HR,<br />
Management Cost, Mobility Support, field visits )<br />
0<br />
A.11.2 Strengthening of DHS/DPMU (Including HR,<br />
Management Cost, Mobility Support, field visits )<br />
3 17.60<br />
A.11.3 Strengthening of Block PMU (Including HR,<br />
0<br />
Management Cost, Mobility Support, field visits )<br />
A.11.4 Strengthening (Others) 0<br />
A.11.4.1 Street Play & Kalapathak 0.02 120 2.40<br />
A.11.4.2 Radio Jingles 6 2.40<br />
A.11.4.3 Wall painting & Hordings 200 3.00<br />
A.11.5 Audit Fees 0<br />
A.11.6 Concurrent Audit 0<br />
A.11.7 Mobility Support to BMO/MO/Others 0<br />
679.34<br />
Note Reimbursable activities are shown in Green
B NRHM FLEXI POOL<br />
B.1 CORE ACTIVITIES<br />
B.1.1 Non Negotiable components:<br />
For certain components, the allocation of funds has to be made as per pre‐determined norms and<br />
the States cannot deviate from them. These non negotiable components are‐ Village <strong>Health</strong> and<br />
Sanitation Committee Funds, Untied Funds for different levels of facilities, Annual Maintenance<br />
Grants to health facilities, Rogi Kalyan Samiti Funds and ASHA training and durgkits. The norms for<br />
allocation of funds under non negotiable components are as under:<br />
❖ Facility level funds:<br />
Levels of facility Annual Maintenance Grant Untied Funds(UF) RKS Grants (RKS)<br />
Sub‐centre Rs. 10,000 Rs. 10,000 —<br />
PHC Rs. 50,000 Rs. 25,000 Rs. 1,00,000<br />
CHC/SDH Rs. 1,00,000 Rs. 50,000 Rs. 1,00,000<br />
DH — — Rs. 5,00,000<br />
Village <strong>Health</strong> and Sanitation Committee Funds: Rs 10,000 per year<br />
ASHA : Rs 10,000 per ASHA per year for training and drug kits<br />
B.1.2 ASHA: Following issues pertaining to ASHA have been highlighted in assessments and<br />
feedbacks:<br />
■ Streamlining delays in payment of performance incentives to ASHAs.<br />
■ Regular upgradation of skill / completion of training in all prescribed modules<br />
■ The timely and sustainable availability of drug kits<br />
■ Supervisory and supportive structure for ASHAs<br />
■ Attrition of ASHAs<br />
■ List of performance incentives with rates<br />
■ The required number of ASHAs for the entire State, based on rural population, and the number<br />
of ASHAs in place against this should be explicitly mentioned<br />
In the PIP of 2011‐12 details of strategies/activities to tackle above mentioned issues and other<br />
issues highlighted in assessment of ASHA initiative should be given.<br />
B.1.3 Village <strong>Health</strong> and Sanitation Committee: NRHM envisaged constitution of 100% VH&SC in<br />
over 6 lakhs villages and provision of untied grants to them by 2008. The issues pertaining to VH&SC<br />
which require a deeper look are:<br />
a. Constitution of the Village <strong>Health</strong> and Sanitation Committee<br />
b. Orientation for planning process and capacity building of community leaders/PRIs in<br />
Village Level Planning<br />
c. Utilization of the Untied fund for the VH&SC and large unspent balances
In the PIP details of strategies/activities to be undertaken tackle above mentioned issues and other<br />
issues which have been highlighted in the performance assessment of VH&SCs should be given.<br />
Progress made so far should be indicated in the following format:<br />
Activity Cumulative Achievements so far<br />
No. of Revenue Villages 1547<br />
Number of Village <strong>Health</strong> & Sanitation committees<br />
constituted<br />
1543<br />
No. of Joint Account opened 1543<br />
Total funds released to VHSCs (Rs in lakh) 1543<br />
Total amount spent by VHSCs so far 51.64<br />
Total unspent balance<br />
No of VHSCs members trained<br />
102.66<br />
B.1.4 Untied Funds: Pace of utilisation of untied fund at various levels of health facilities to be<br />
enumerated including major areas in which these funds have been utilized. Improvements made in<br />
the health facilities should be including innovative and best practices adopted should be described.<br />
Cumulative achievements so far should be indicated in the following format:<br />
Facility level Number of Total amount Total amount Unspent<br />
facilities released so far utilized balance<br />
Untied Fund for SCs 333 33.30 13.11 20.19<br />
Untied Fund for PHCs 56 14.00 7.99 6.01<br />
Untied Fund for CHCs 14 7.00 2.60 4.40<br />
Untied Fund for DH 1 ‐ ‐ ‐<br />
B.1.5 Annual Maintenance Grants: Proper maintenance of physical infrastructure is a must to<br />
ensure quality services in various health facilities. Annual Maintenance Grants given to the health<br />
facilities should be effectively utilized to improve the facilities continuously through regular<br />
maintenance and repair works. Requirement of funds should be indicated in the following format:<br />
Facility level Number of Total amount Total amount Unspent<br />
facilities released so far utilized balance<br />
AMG fund for SCs 296 14.80 10.06 4.74<br />
AMG fund for PHCs 48 24.00 14.15 9.85<br />
AMG fun for CHCs 16 24.00 7.12 16.88<br />
AMG fund for DH 1 5.00 4.00 1.00<br />
B.1.6 Rogi Kalyan Samitis: RKSs have contributed to local level leadership and need based decision<br />
making. The issues which now need to find a reflection in planning would interalia relate to:<br />
• Constitution of RKS in 100% facilities<br />
• Performance of RKS and pace of utilization of funds<br />
• Activities being under taken by RKS<br />
• Capacity building of RKS members<br />
• Sharing of success stories and best practices.
Details of status and activities to be undertaken on above mentioned issues should be given in the<br />
PIP. Information on cumulative amount released to Rogi Kalyan Samitis and amount utilized so far<br />
should be summarized in the following format:<br />
(Rs in lakh)<br />
Facility Number of Total amount Total amount Unspent<br />
RKS released so far utilized balance<br />
District Hospital 1 6.54 4.46 2.08<br />
Sub Divisional Hospital 4 4.86 2.60 2.26<br />
Community <strong>Health</strong> Centres 12 30.67 12.82 17.85<br />
Primary <strong>Health</strong> Centres<br />
Other health facilities (Please<br />
Specify)<br />
56 59.86 30.45 29.41<br />
B.2 HEALTH CARE INFRASTRUCTURE:<br />
B.2.1 Civil Constructions<br />
All infrastructure proposals both for new construction and expansion shall be based on both facility<br />
and area mapping exercise and not just a district wise allocation exercise. The need of the<br />
underserved areas has to be taken into consideration and strengthening of facilities in close<br />
contiguity needs to be discouraged unless justified by a heavy case load. Therefore the focus should<br />
be on consolidation and need based expansion supplemented with a HR plan. A bird's eye view of<br />
available infrastructure should be given in the following format:<br />
States' Requirement of Infrastructure DH SDH CHC PHC SHC<br />
Required as per population norms<br />
Existing Facilities<br />
Shortfall<br />
Mapping of facilities undertaken<br />
Requirement of new facilities after mapping exercise<br />
Requirement of facility up gradation after mapping<br />
exercise as per IPHS<br />
New construction proposed under NRHM after gap analysis<br />
for 2011‐12<br />
Facilities proposed for up gradation after gap analysis for<br />
2011‐12<br />
The infrastructure issues which have been highlighted from time to time include:<br />
• Infrastructure expansion without requisite human resource, equipments<br />
supplementation<br />
• Deployment of human resources not based on need. Suboptimal or over utilisation of the<br />
manpower<br />
• Consolidation of health facilities before further expansion feasibility of ensuring 24X 7<br />
services in all the extant PHCs‐ redefining the numbers as per evidence and need<br />
Quality of care being provided at all the health institutions.
Operational Blood storage units need to be ensured at CHC's and above level of health<br />
facilities.<br />
Performance parameters for service delivery and quality of care needs furtherimprovement<br />
and closer monitoring<br />
Limited managerial capacities to manage health facilities<br />
Limited capacity for supply chain management to ensure timely supply of drugs and<br />
diagnostics<br />
Limited referral and mobility arrangements Varied use of RKS , AMG and Untied Funds<br />
made available Non standardized treatment protocols leading to ad hoc in care Inadequate<br />
PPP arrangements with the private sector in the area<br />
These issues need closer deliberation in the Plans of 2011‐12. Full justification for expansion needs<br />
to be provided if consolidation of available infrastructure has not been achieved. Need based<br />
expansion clearly articulating the area of requirement needs to be highlighted with a clear human<br />
resource placement plan. Information should be provided on cumulative achievements so far (since<br />
launch of NRHM) in the following format:<br />
Activity<br />
Cumulative Achievements so far<br />
Physical Financial<br />
Sub‐Centres<br />
Construction of new sub‐centre buildings 7 77.07<br />
Renovation of sub‐centre buildings<br />
Setting up of new Sub‐centres<br />
Upgradation of sub‐centres<br />
New Construction of PHC building<br />
30<br />
PHC<br />
45.57<br />
Renovation of PHC buildings<br />
Setting up of new PHCs<br />
139 160.33<br />
Upgradation of PHCs<br />
Availability of 24x7 services<br />
New Construction of CHC building<br />
Renovation of CHC buildings<br />
Setting up of new CHCs<br />
Upgradation of CHCs<br />
Blood storage unit<br />
Strengthening of District & Sub divisional<br />
Hospitals<br />
Upgradation of SDH<br />
Renovation of SDH<br />
Renovation of DH<br />
42<br />
CHC<br />
SDH/DH<br />
88.23<br />
B.2.2 Mobile Medical Units/Emergency Referral Transport: State specific requirement of MMUs<br />
needs to be assessed realistically. Performance parameters which help in gauging performance of<br />
MMUs like, a)Frequency of Visit b)Following of Schedule c) Advance Intimation of Schedule d)<br />
Duration of Stay and Timing of MMU e)Doctors accompanying f)Availability of Medicine g)Cured of<br />
illness in last visit h)People satisfaction about skill and behaviour i)Location of MMU j)Average
distance travelled to MMU k)average time taken per patient l)Availability of diagnostics m) Follow<br />
up of Patients etc need to be reflected in the MMU plan. Information on cumulative achievements<br />
(since launch of NRHM) so far should be provided the following:<br />
Activity<br />
Mobile Medical Unit(MMU)<br />
Emergency & Referral Services (EMRI)<br />
Others<br />
B.3 MANPOWER<br />
Cumulative Achievements so far<br />
Physical financial<br />
NRHM has led to augmentation of considerable contractual human resources at all<br />
levels. Current status should be provided in the following format:<br />
State Requirement of HR Specialists Doctors Nurses ANMs Pharmacists Lab tech<br />
Required staff as per IPHS for<br />
the existing facilities<br />
120 179 670 236 103 97<br />
Sanctioned staff 71 115 300 234 61 54<br />
In Position<br />
Vacancy against sanctioned<br />
76 74 355 192 43 30<br />
Vacancy against IPHS<br />
Vacancies already filled up by<br />
the State<br />
Proposed filling up of<br />
vacancies by the State for<br />
2011‐12<br />
Contractual engagement so far<br />
through NRHM<br />
Additional contractual<br />
engagement proposed under<br />
NRHM for 2011‐12<br />
44 105 315 44 60 67<br />
Provision of human resource should be based on gap analysis with adequate/ incentivized provision<br />
for difficult and hard to reach areas. Following issues in provision of human resources continue to<br />
need attention:<br />
1. Capacity and skill development of the human resource both contractual and permanent.<br />
2. Filling up of existing vacancies by the State Government<br />
Efforts and roadmap to address these issues should be elaborated in the PIP. B.4<br />
TRAINING AND CAPACITY BUILDING:<br />
Training is one of the critical areas to provide services guaranteed under NRHM. States should give a<br />
training calendar and names of training institutions for various categories of manpower. The training<br />
budget should be given in the RCH Flexible Pool in stipulated format.
B.5 INNOVATIONS<br />
Some local problems that emerge as priority in the Block/District Action Plans may require<br />
innovative solutions. Such innovative measures may be supported under NRHM. States should<br />
provide the details of innovations and suggest cost as per need.<br />
B.6 FUNDS FOR IMPACT ASSESSMENT OF NRHM AND ASSESSMENT OF VARIOUS COMPONENTS:<br />
Continuous assessment and evaluation of the program is important to keep us focused and do the<br />
necessary course corrections swiftly. States must propose an amount from NRHM Flexipool for<br />
evaluation and assessment activities of NRHM and components like ASHA, VHSCs, RKS, etc. Reputed<br />
medical, Public <strong>Health</strong>, Management and Research Institutes should be identified for such<br />
evaluation/assessments and should be accredited with the Government of India. Only such<br />
accredited institutes may be allowed to take up the assessment work.<br />
B.7 ADDITIONAL FUNDS FOR COMMUNICABLE DISEASES:<br />
States should analyze and identify areas/ Districts that have a high burden of communicable<br />
diseases. The additional funds required to tackle the same should be budgeted for in the NRHM<br />
<strong>Mission</strong> Flexipool. Detailed information should be provided under the concerned disease control<br />
program. A summary of information should be provided under this section.<br />
B.8 ACTIVITIES TAKEN UP WITH SUPPORT UNDER OTHER PROGRAMMES:<br />
Activities taken up with support under other programmes such as Donor Partners, Minority<br />
Development, Finance Commission Award, Labour, DONER and any other scheme etc. to be clearly<br />
reflected in this section. Similarly details of PPP activities, <strong>Health</strong> Insurance scheme and any other<br />
district innovation funds being solicited, details need to be spelt out in this<br />
Part.<br />
B.10 DISTRICT PLANS<br />
This chapter should contain information pertaining to District health Action Plans and resources<br />
proposed and approved for each district.<br />
S. No. Name of<br />
Districts<br />
PIP<br />
prepared<br />
Yes/No<br />
Whether<br />
DPAP format<br />
followed<br />
Yes/No<br />
Resource<br />
envelop<br />
indicated by<br />
the State (Rs<br />
in Lakh)<br />
Amount<br />
Proposed by<br />
districts(Rs in<br />
Lakh)<br />
1 <strong>Amravati</strong> Yes Yes ‐ 3930.03<br />
Amount<br />
Approved to<br />
districts(Rs in<br />
Lakh)*<br />
*Note: As per the Conditionalities the State Governments shall, within 45 days of the issue of the<br />
Record of proceedings, issue detailed District wise approvals and places them on their website for<br />
public information.
CONSOLIDATED BUDGET SHEET FOR MISSION FLEXIBLE POOL<br />
Sl. No. Activity Unit Cost Physical<br />
Targets<br />
<strong>Mission</strong> Flexipool<br />
Required fund<br />
under NRHM<br />
B1 ASHA 0<br />
B1.1 Selection & Training of ASHA 0<br />
B1.2 Procurement of ASHA Drug Kit 0<br />
B1.3 Incentive to ASHAs under JSY 0<br />
B1.4 Incentive under Family<br />
Planning Services<br />
B1.5 Incentive under Child <strong>Health</strong> 0<br />
B1.6 Other Incentives to ASHAs 2068 156.51<br />
B1.7 Awards to ASHA's/Link<br />
workers<br />
0<br />
B2 Untied Funds 0<br />
B2.1 Untied Fund for CHCs<br />
(RH/SDH/WH)<br />
0.50 14 7.00<br />
B2.2 Untied Fund for PHCs 0.25 56 14.00<br />
B2.3 Untied Fund for Sub Centers 0.10 333 33.30<br />
B2.4 Untied fund for VHSC 0.10 1547 154.70<br />
B2.5 Untied fund for PHU 0.25 103 25.75<br />
B.3 Annual Maintenance Grants 0<br />
B4.1 CHCs (RH/SDH/WH) 1.00 14 14.00<br />
B4.2 PHCs 0.50 48 24.00<br />
B4.3 Sub Centers 0.10 299 29.90<br />
B4.1.3 PHUs 0.50 62 31.00<br />
B4.1.4 DH/TB/RRC 5.00 3 15.00<br />
B4.1.5 Others 0<br />
B.4 Hospital Strengthening 0<br />
B.4.4 Upgredation of CHCs, PHCs,<br />
DH to (IPHS)<br />
0<br />
B.4.1.1 Distirct Hospital 50.00 1 50.00<br />
B.4.1.2 Women Hospital 35.00 1 35.00<br />
B.4.1.3 CHC (RH/SDH) 20.00 5 100.00<br />
B.4.1.4 PHCs 5.00 34 170.00<br />
B.4.1.5 Sub Center 1.00 83 83.00<br />
B.4.1.6 Other – (ISO Certification) 50.00 1 50.00<br />
B 4.2 Strengthening of District, Su‐<br />
divisional Hospitals, CHCs,<br />
PHCs<br />
0<br />
B.4.3 Sub Centre Rent and<br />
Contingencies<br />
0<br />
B.4.4 Logistics management/<br />
improvement<br />
0<br />
0
Sl. No. Activity Unit Cost Physical Required fund<br />
Targets under NRHM<br />
B5 New Constructions/<br />
Renovation and Setting up<br />
0<br />
B5.1 CHCs (TB Hospital) 5.00 1 5.00<br />
B5.2 PHCs 18 275.00<br />
B5.3 SHCs/Sub Centers 13 150.00<br />
B5.4 Setting up Infrastructure wing<br />
for Civil works<br />
0<br />
B5.5 Govt. Dispensaries/ others<br />
renovations<br />
0<br />
B5.6 Construction of BHO, Facility<br />
improvement, civil work,<br />
BemOC and CemOC centers<br />
0<br />
B.5.7 Major civil works for<br />
operationalisation of FRUS<br />
0<br />
B.5.8 Major civil works for<br />
operationalisation of 24 hour<br />
services at PHCs<br />
0<br />
B.5.9 Civil Works for Operationalise<br />
Infection Management &<br />
Environment Plan at health<br />
facilities<br />
0<br />
B.6 Corpus Grants to HMS/RKS 0<br />
B6.1 District Hospitals 5.00 1 5.00<br />
B6.2 CHCs (RH/SDH/WH) 1.00 14 14.00<br />
B6.3 PHCs 1.00 56 56.00<br />
B6.4 Other – TB/RRC 5.00 2 10.00<br />
B7 District Action Plans<br />
(Including Block, Village)<br />
0.56 15 8.40<br />
B8 Panchayati Raj Initiative 0<br />
B8.1 Constitution and Orientation<br />
of Community leader & of<br />
VHSC,SHC,PHC,CHC etc<br />
B8.2 Orientation Workshops,<br />
Trainings and capacity building<br />
of PRI at State/Dist. <strong>Health</strong><br />
Societies, CHC,PHC<br />
B8.3 Others 0<br />
B9 Mainstreaming of AYUSH 28 30.80<br />
B9.1 Activities other than HR 0<br />
B10 IEC‐BCC NRHM 0<br />
B.10 Strengthening of BCC/IEC<br />
Bureaus (state and district<br />
levels)<br />
B.10.1 Development of State<br />
BCC/IEC strategy<br />
B.10.2 Implementation of BCC/IEC<br />
strategy<br />
0<br />
0<br />
0<br />
0<br />
0
Sl. No. Activity Unit Cost Physical Required fund<br />
Targets under NRHM<br />
B.10.2.1 BCC/IEC activities for MH 0<br />
B.10.2.2 BCC/IEC activities for CH 0<br />
B.10.2.3 BCC/IEC activities for FP 0<br />
B.10.2.4 BCC/IEC activities for ARSH 0<br />
B.10.2.5 Other activities (please<br />
specify)<br />
0<br />
B.10.4 <strong>Health</strong> Mela 0<br />
B.10.5 Creating awareness on<br />
declining sex ratio issue<br />
0<br />
B.10.6 Other activities 0<br />
B11 Mobile Medical Units<br />
(Including recurring<br />
expenditures)<br />
1 15.76<br />
B12 Referral Transport 0<br />
B12.1 Ambulance/ EMRI 0<br />
B12.2 Operating Cost (POL) 72 26.45<br />
B13 School <strong>Health</strong> Programme 16 139.54<br />
B14 PPP/ NGOs 0<br />
B14.1 Non governmental providers<br />
of health care RMPs/TBAs<br />
0<br />
B14.2 PNDT and Sex Ratio 0<br />
B14.3 Public Private Partnerships 0<br />
B14.4 NGO Programme/ Grant in Aid<br />
to NGO<br />
0<br />
B14.5 Other innovations( if any) 0<br />
B15 Planning, Implementation and<br />
Monitoring<br />
0<br />
B15.1 Community Monitoring<br />
(Visioning workshops at state,<br />
Dist, Block level)<br />
0<br />
B15.1.1 State level 0<br />
B15.1.2 District level 0<br />
B15.1.3 Block level 0<br />
B15.1.4 Other 0<br />
B15.2 Quality Assurance 0<br />
B15.3 Monitoring and Evaluation 0<br />
B15.3.1 Monitoring & Evaluation /<br />
HMIS<br />
0<br />
B15.3.2 Computerization HMIS and e‐<br />
governance, e‐health<br />
0<br />
B15.3.3 Other M & E 4 12.24<br />
B.16 PROCUREMENT 0<br />
B16.1 Procurement of Equipment 0<br />
B16.1.1 Procurement of equipment:<br />
MH<br />
0
Sl. No. Activity Unit Cost Physical Required fund<br />
Targets under NRHM<br />
B16.1.2 Procurement of equipment:<br />
CH<br />
0<br />
B16.1.3 Procurement of equipment: FP 0<br />
B16.1.4 Procurement of equipment:<br />
IMEP<br />
0<br />
B16.1.5 Procurement of Others 0<br />
B.16.2 Procurement of Drugs and<br />
supplies<br />
0<br />
B.16.2.1 Drugs & supplies for MH 0<br />
B.16.2.2 Drugs & supplies for CH 0<br />
B.16.2.3 Drugs & supplies for FP 0<br />
B.16.2.4 Supplies for IMEP 0<br />
B.16.2.5 General drugs & supplies for<br />
health facilities<br />
0<br />
B.17 PNDT Activities 0<br />
B.18 Regional drugs warehouses 0<br />
B.18.1 Procurment plant 2 30.40<br />
B.19 New Initiatives/ Strategic<br />
Interventions (As per State<br />
health policy)/ Innovation/<br />
Projects (Telemedicine,<br />
Hepatitis, Mental <strong>Health</strong>,<br />
Nutition Programme for<br />
Pregnant Women, Neonatal)<br />
NRHM Helpline) as per need<br />
(Block/ District Action Plans)<br />
3 7.35<br />
B.20 <strong>Health</strong> Insurance Scheme 0<br />
B.21 Research, Studies, Analysis 0<br />
B.22 State level health resources<br />
center(SHSRC)<br />
0<br />
B23 Support Services 0<br />
B23.1 Support Strengthening NPCB 0<br />
B23.2 Support Strengthening<br />
Midwifery Services under<br />
medical services<br />
B23.3 Support Strengthening<br />
NVBDCP<br />
2 117.40<br />
B23.4 Support Strengthening RNTCP 0<br />
B23.5 Contingency support to Govt.<br />
dispensaries<br />
B23.6 Other NDCP Support<br />
Programmes<br />
B.24 Other Expenditures 0<br />
B.24.1 Contractural ANM/LHV/Staff<br />
Nurse<br />
416 426.55<br />
B.24.2 Sickle Cell Disease 1 41.52<br />
0<br />
0<br />
0
Sl. No. Activity Unit Cost Physical Required fund<br />
Targets under NRHM<br />
B.24.3 Co‐ordination Cell DH 1 4.58<br />
B.24.4 Maher Scheme 9 16.40<br />
B.24.5 Volunteer to tribal PHC 34 12.96<br />
B.24.6 Diet facility for PHC 11 19.80<br />
B.24.7 Hardship Allowance to<br />
regular<strong>Health</strong> Staff<br />
146 113.28<br />
B.24.8 FMG 2 4.08<br />
B.24.9 RKS Coordinator 1 4.44<br />
B.24.10 IDW Wing 6 17.88<br />
B.24.11 IPHS Wing 2 7.32<br />
B.24.12 BPMU 14 81.48<br />
Total.. 2646.79
PART B<br />
NRHM ADDITIONALITIES<br />
Budget 2011 – 12<br />
NATIONAL RURAL HEALTH MISSION<br />
Budget Format for NRHM <strong>Mission</strong> Flexipool Part ‘B’.<br />
Sr. No. Initiative<br />
2011‐12<br />
Number Proposed Total Amount (in Lacs)<br />
1 ASHA 2068 156.51<br />
2 Addititinal ANM sub‐center 333 331.08<br />
3 Staff Nurse at 24 x 7 PHCs 47 52.68<br />
4 Supervior in Nurse (LHV) 36 42.79<br />
5 VHSNWC 1547 154.70<br />
6 Untied Fund for SC 333 33.30<br />
7 Untied Fund for PHU 103 25.75<br />
8 Untied Fund for PHC 56 14.00<br />
9 Untied Fund for RH/SDH/WH 14 7.00<br />
10 Rogi Kalyan Samiti‐DH 1 5.00<br />
11 Rogi Kalyan Samiti‐SDH 4 4.00<br />
12 Rogi Kalyan Samiti‐RH/WH 10 10.00<br />
13 Rogi Kalyan Samiti‐ PHC 56 56.00<br />
14 Rogi Kalyan Samiti‐ TB 1 5.00<br />
15 Rogi Kalyan Samiti‐ RRC 1 5.00<br />
16 Annual Maintenance Grant‐DH 1 5.00<br />
17 Annual Maintenance Grant‐SDH/RH/WH 14 14.00<br />
18 Annual Maintenance Grant‐RRC 1 5.00<br />
19 Annual Maintenance Grant‐PHU 62 31.00<br />
20 Annual Maintenance Grant‐PHC 48 24.00<br />
21 Annual Maintenance Grant‐SC 299 29.90<br />
22 Annual Maintenance Grant TB 1 5.00<br />
23 Repairs and New Construction 61 430.00<br />
24 Ambulance services for PHC‐ Repairs 56 18.45<br />
25 Ambulance services for RH/SDH/WH 14 7.00<br />
26 Ambulance services for DH 2 1.00<br />
27 IPHS up‐gradation SC 83 83.00<br />
28 IPHS up‐gradation PHC 34 170.00<br />
29 IPHS up‐gradation RH 1 20.00<br />
30 IPHS up‐gradation SDH‐100 1 20.00<br />
31 IPHS up‐gradation SDH‐50 3 60.00<br />
32 IPHS up‐gradation WH 1 35.00<br />
33 IPHS up‐gradation DH 1 50.00<br />
34 IPHS – ISO Certification 10 50.00<br />
35 Telemedicine Center 3 7.35
Sr. No. Initiative<br />
2011‐12<br />
Number Proposed Total Amount (in Lacs)<br />
36 Strengthening of Nursing Services 2 117.40<br />
37 School <strong>Health</strong> Programme 16 139.54<br />
38 Sickle Cell Disease Programme 1 41.52<br />
39 Procurement Plan 16 30.40<br />
40 Co‐ordination Cell DH 1 4.58<br />
41 Maher Scheme 9 16.40<br />
42 Volunteer to trible PHCs 34 12.96<br />
43 Diet facility for PHC 11 19.80<br />
44 AYUSH Cell 28 30.80<br />
45 Hardship Allowances to Regular <strong>Health</strong> Staff 14 113.28<br />
46 Mobile Medical Unit 1 15.76<br />
47 DHAP 14 8.40<br />
48 M & E Cell 4 12.24<br />
49 FMG 2 4.08<br />
50 RKS Coordinator 1 4.44<br />
51 IDW Wing 6 17.88<br />
52 IPHS Wing 2 7.32<br />
53 Block Program Management Unit 14 81.48<br />
TOTAL 5482 2646.79<br />
<strong>National</strong> rural health mission has been launched with a view to bringing about<br />
dramatic improvement in health system and health status of people, especially those who live in<br />
rural areas of the country. The mission seeks to provide universal access to equitable, affordable and<br />
quality health care which is accountable and at the same time responsive to the needs of people,<br />
reduction in child and maternal deaths as well as population stabilisation and gender and<br />
demographic balance.<br />
Key features in order to achieve the goals of the <strong>Mission</strong> include making the public<br />
health delivery system fully functional and accountable to the community, human resource<br />
management, community involvement, decentralisation, rigorous monitoring and evaluation against<br />
standards, convergence of health and related programs from village level upwards, innovations and<br />
flexible financing and also interventions for improving health indicators.<br />
To facilitate fund release and monitoring, the NRHM plan is divided in following components:
A. ASHA<br />
Selection of ASHA<br />
Sr Area<br />
Target for<br />
selection<br />
No. selected<br />
during 2010‐11<br />
Proposed to be<br />
selected during<br />
2011‐12<br />
Total selection<br />
1 Tribal areas 400 400 0 400<br />
2 Non‐tribal areas 1668 1668 0 1668<br />
Total 2068 2068 0 2068<br />
Training of ASHA during 2011‐12<br />
Number to be trained during 2011‐12<br />
Sr Module<br />
Tribal Non‐tribal Total<br />
Budget<br />
required for<br />
training<br />
Likely date<br />
of<br />
completion<br />
of training<br />
1 Module – I 40 165 205 4.95 Dec 2011<br />
2 Module – II 40 165 205 2.98 Dec 2011<br />
3 Module – III 40 165 205 2.98 Jan 2012<br />
4 Module – VI 40 1668 1708 21.63 Jun 2011<br />
5 Module – V 40 1668 1708 21.63 Aug 2011<br />
6<br />
Module –VI<br />
Phase 1<br />
‐ 1668 1668 38.19 Dec 2011<br />
7<br />
8<br />
9<br />
Module – VI<br />
Phase 2<br />
400 1668 2068 46.09<br />
Tribal<br />
Mar 2011<br />
Non Tribal<br />
Mar 2012<br />
Module –VII<br />
Phase 3<br />
400 ‐ 400 92.19 Apr 2011<br />
Module –VII<br />
Phase 4<br />
400 ‐ 400 92.19 June 2011<br />
Total 1200 7167 8567 322.83<br />
Training of Block Faciliator during 2011‐12<br />
Number to be trained during 2011‐12<br />
Sr Module<br />
Tribal Non‐tribal Total<br />
Budget<br />
required for<br />
training<br />
Likely date<br />
of<br />
completion<br />
of training<br />
1 Genral Module 40 45 85 2.77 Apr 2011<br />
2<br />
Module VI<br />
Phase 1<br />
40 45 85 2.77 June 2011<br />
3<br />
Module VI<br />
Phase 2<br />
40 45 85 2.08 Aug 2011<br />
4<br />
Module VII<br />
Phase 3<br />
40 45 85 2.08 Oct 2011<br />
5<br />
Module<br />
VII Phase 4<br />
40 45 85 2.08 Dec 2011<br />
Total 200 225 425 11.78
Training of ASHA TOT during 2011‐12<br />
Sr Module<br />
Number to be trained during 2011‐12<br />
Tribal Non‐tribal Total<br />
Budget<br />
required for<br />
training<br />
Likely date<br />
of<br />
completion<br />
of training<br />
1 Module I 0 0 0 0 ‐<br />
2 Module II 0 0 0 0 ‐<br />
3 Module III 0 120 120 HFWTC Feb 2011<br />
4 Module IV 0 120 120 HFWTC Apr 2011<br />
5 Module V 0 120 120 HFWTC Jul 2011<br />
6<br />
7<br />
8<br />
Medicine Kit<br />
Module VI & VII<br />
Phase 1 (14 days)<br />
Module VI & VII<br />
Phase 2 (8 days)<br />
Module VI & VII<br />
Phase 3<br />
13 0 13 State Level State level<br />
13 0 13 State Level State level<br />
13 0 13 State Level State level<br />
39 360 399<br />
Requirement of ASHA medicines kits during year 2011‐12 : 2070<br />
Performance based compensation :<br />
Sr Program<br />
Budget required<br />
for tribal areas<br />
Budget required<br />
for non‐tribal<br />
areas<br />
Total budget<br />
required<br />
1 RCH – Family planning cases 0.80 1.35 2.15<br />
2 RCH – JSY 8.69 19.85 28.54<br />
3 <strong>Mission</strong> Flexi‐pool (Additional<br />
ties)<br />
13.70 46.75 60.45<br />
4 NVBDCP 0.82 1.25 2.07<br />
5 RNTCP 0.38 0.50 0.88<br />
6 NLEP 0.12 0.79 0.91<br />
7 NPCB 0.70 5.84 6.54<br />
8 Other (VHSC) 14.92 54.75 69.67<br />
Total 171.21
Addition of new activity for performance compensation to ASHA for year 2011‐12<br />
Sr.No. Activity Proposed compensation Justification<br />
1 ANC Registration & 5 Time<br />
Checkup<br />
2 Motivate to Water<br />
Conservation or kitchen<br />
gardening<br />
3 Motivate to Malnourished<br />
Children in VCDC/CTC<br />
4 Registration to Newly<br />
Margie Couple<br />
5 0 to 28 days new born baby<br />
Care<br />
6 Promote to STI/RTI Checkup<br />
for 13 to 49 age Ladies<br />
Rs .20/‐ per checkup After registration ANC , it is<br />
proposed to give incentive of<br />
Rs. 20/‐ per checkup to ASHA<br />
for further 5 checkup<br />
Rs. 75/‐ Per activity It is proposed to give incentive<br />
of Rs. 75/‐ for motivating for<br />
water conservation or prepare<br />
of kitchen garden in her field<br />
area.<br />
Rs. 10/‐ Per Child For motivating children for<br />
admit in VCDC/CTC and for<br />
prepare a list of SAM/MAM<br />
children. and to look after their<br />
progress and maintain record in<br />
PHC Rs. 10/‐ Per Child will be<br />
proposed as a incentive<br />
Rs. 25/‐ Per Registration for motivating newly married<br />
couple for marriage registration<br />
and maintained early age<br />
married couple record<br />
,counseling spacing material<br />
etc. incentive of rs25/‐ per<br />
registration will be proposed.<br />
Rs. 25/‐ Per Child Registered to new born baby,<br />
and look after 0 to 7 days daily<br />
with 2 visits , 8 to 28 days after<br />
one days visit to home and to<br />
take record progress of<br />
children, inform to PHC/SC, in<br />
critical situation Referred to<br />
nearest health institute. For<br />
that rs 25/‐ per child incentive<br />
will be proposed.<br />
Rs. 25/‐ Per chekup To get help to 13 to 49 age<br />
ladies for STI/RTI Checkup in<br />
PHC/RH and motivate to<br />
propertreatment,and mentain<br />
the RTI/STI record in PHC level.<br />
Rs 25/‐ per checkup will be<br />
proposed as a incentive.
ASHA Support services<br />
Request budget for following activities<br />
Sr Particulars<br />
1<br />
2<br />
District Level<br />
Salary TA/DA of Community<br />
Mobiliser (Rs. 12000/PM)<br />
Salary of Data Assistant (Rs.<br />
10000/PM)<br />
Budge<br />
required<br />
/ unit<br />
Tribal areas Non tribal areas<br />
Total<br />
Units<br />
Budget<br />
required<br />
Total<br />
Units<br />
Budget<br />
required<br />
Total<br />
budget<br />
required<br />
2 1 1.44 1 1.44 2.88<br />
1 0 0 1 1.20 1.20<br />
3 Contingency 0.30 0 0.30 0 0 0.30<br />
District Total 1.74 2.64 4.38<br />
Block level<br />
1 Salary & TA/DA BCM 2 2 2.40 0 0 2.40<br />
2 Contingency 0.5 2 0.10 12 0.60 0.70<br />
Block total 2.50 0.60 3.10<br />
PHC Level<br />
1 Block Facilitator (1/PHC) 0.04 40 19.20 45 21.60 40.80<br />
2 ASHA meeting 150 400 7.20 1668 30.024 37.224<br />
3 Block Facilitator Meeting 150 40 0.72 45 0.81 1.53<br />
3<br />
Honorarium to MO for<br />
reorientation<br />
150 11 0.20 45 0.81 1.01<br />
4<br />
Honorarium to LHV for<br />
reorientation<br />
500 11 0.66 45 2.70 3.36<br />
5 Contingency 5000 11 0.55 45 2.25 2.80<br />
PHC Total 28.53 58.19 86.72<br />
Grand Total 32.77 61.43 94.20<br />
ASHA mentoring group<br />
NRHM has instructed to establish ASHA mentoring groups at district and block level. These groups<br />
will require budget for meetings as follows:<br />
Tribal areas Non‐tribal areas Total<br />
Sr Level Unit cost No. of<br />
units<br />
Budget<br />
required<br />
No. of<br />
units<br />
Budget<br />
required<br />
Budget<br />
required<br />
1 District Level 0.045 4 0.18 0.18<br />
2 Block level 0.03 8 0.24 48 1.44 1.68<br />
Total 0.42 1.44 1.86
ADDITIONAL ANM AT SUB‐CENTRE<br />
Appointment of additional ANM (contractual)<br />
Sr Area of Sub‐Center<br />
No. in place during 2010‐<br />
11 (currently filled in and<br />
expected to be appointed<br />
up to 31.3.2011)<br />
Expected to be<br />
appointed during<br />
2011‐12<br />
Total ANMs at<br />
end of 2011‐12<br />
1 Non‐tribal areas 230 8 238<br />
2 Tribal areas 95 0 95<br />
3 Naxalite affected areas 0 0 0<br />
Total 325 8 333<br />
Budget requirement<br />
Salary, travel allowances and honorarium to Part Time Lady Attendant (PTLA) of regular ANM is<br />
borne though regular funds. Similar to regular ANM, additional ANM will require budget for salary,<br />
daily allowances during travel and honorarium for PTLA. Accordingly, budget required to for<br />
additional ANM is as follows:<br />
Budget required for Additional ANMs at Sub‐Centres<br />
Sr. Place of<br />
posting<br />
No.<br />
expected<br />
in 2011‐<br />
12<br />
Unit<br />
cost<br />
(month)<br />
Salary Fixed PTA PTLA<br />
Budget<br />
required<br />
Unit<br />
cost<br />
(month)<br />
Budget<br />
required<br />
Unit<br />
cost<br />
(month)<br />
Budget<br />
required<br />
Rs. In Lakhs<br />
Total<br />
budget<br />
required<br />
1 Non‐<br />
trible SC<br />
238 0.07 199.92 0.005 14.28 0.005 14.28 228.48<br />
2 Trble SC 95 0.08 91.20 0.005 5.70 0.005 5.70 102.60<br />
Total 331.08<br />
Staff Nurses in 24 x 7 and IPHS PHCs<br />
Action to be taken to fill up vacant posts<br />
It has been difficult to fill the position of Staff Nurses position in the 24X7 PHC because of non<br />
availability of candidates. The eligibility criteria that candidate should have registered with<br />
Maharashtra Nursing council should be relaxed and authorisation should be given to the district to<br />
hire candidates from any state and private universities.<br />
A. STAFF NURSE IN 24HRS AND IPHS PHCs<br />
Sr Area of PHC No. in place during 2010‐11 Expected to be Total Staff Nurses<br />
(currently filled in and expected appointed at end of 2011‐12<br />
to be appointed up to<br />
31.3.2011)<br />
during 2011‐12<br />
1 Non‐tribal areas 24 07 31<br />
2 Tribal areas 3 13 16<br />
3 Naxalite affected<br />
areas<br />
0 0 0<br />
Total 27 20 47
Budget requirement<br />
Budget requirement for support to contractual Staff Nurse is for salary. As these staff nurses are not<br />
supposed to travel, budget for travel charges and PTLA need not be requested.<br />
Budget required for Staff Nurses at PHC Rs. In Lakhs<br />
Sr Particulars Monthly Already appointed To be appointed Total<br />
amount nurses<br />
nurses<br />
No. Budget No. Budget No. Budget<br />
required<br />
required<br />
required<br />
1 Non‐tribal<br />
areas<br />
0.09 24 25.92 7 7.56 31 33.48<br />
2 Tribal areas 0.10 3 3.60 13 15.60 16 19.20<br />
Total 52.68<br />
SUPERVISARY NURSES (LHV) TO ALL PHCs<br />
After appointment of additional ANM at sub center level, supervisory work‐load has increased in<br />
PHC. As per GOI recommendation, district shall appoint one supervisory nurse in each PHC.<br />
Accordingly, the district shall appoint one supervisory nurse in 56 PHC.<br />
B. SUPERVISORY NURSE IN ALL PHCs (LHV)<br />
Sr Area of PHC No. in place during 2010‐ Expected to be Total LHVs at<br />
11(currently filled in and appointed end of 2011‐12<br />
expected to be appointed<br />
up to 31.3.2011)<br />
during 2011‐12<br />
1 Non‐tribal areas 16 09 36<br />
2 Tribal areas 0 11 11<br />
3 Naxalite affected areas<br />
Total 16 20 47<br />
Budget requirement<br />
Table – A: ‐ For Non‐tribal and Non‐naxalite areas @ Rs. 9000/‐ PM<br />
Rs. In Lakhs<br />
Sr Particulars Monthly Already appointed To be appointed Total<br />
amount nurses<br />
nurses<br />
No. Budget No. Budget No. Budget<br />
required required required<br />
1 Monthly salary 0.09 16 17.28 9 9.72 25 27.00<br />
2 Fixed PTA 0.006 16 1.15 9 0.65 25 1.80<br />
Total 28.80
Table ‐ B : ‐ For Tribal areas – Rs. 10000/‐ PM<br />
Rs. In Lakhs<br />
Sr Particulars Monthly Already appointed To be appointed Total<br />
amount nurses<br />
nurses<br />
No. Budget No. Budget No. Budget<br />
required required<br />
required<br />
1 Monthly salary 0.10 0 0 11 13.20 11 13.20<br />
2 Fixed PTA 0.006 0 0 11 0.79 11 0.79<br />
Total 13.99<br />
Table ‐ C : Total budget required<br />
Sr Particulars Already appointed To be appointed Total<br />
nurses<br />
nurses<br />
No. Budget No. Budget No. Budget<br />
required<br />
required<br />
required<br />
1 Monthly salary 16 17.28 20 22.92 36 40.20<br />
2 Fixed PTA 16 1.15 20 1.44 36 2.59<br />
Total 42.79
VILLAGE HEALTH SANITATION WATER SUPPLY AND NUTRITION COMMITTEE<br />
No. of villages in district : 1547<br />
No. of villages requreing untied fund in district : 1547<br />
UNTIED FUND TO SC, PHC & RH/SDH<br />
Sr Type of hospital No. of institutions<br />
Unit rate<br />
Budget required<br />
Total budget<br />
required<br />
1 Sub‐Centre 333 0.10 33.30<br />
2 PHU 103 0.25 25.75<br />
3 PHC 56 0.25 14.00<br />
4 RH/SDH/WH 14 0.50 7.00<br />
5 VHNSC 1547 0.10 154.70<br />
Total 234.75<br />
RUGNA KALYAN SAMITEE<br />
Sr Type of hospital<br />
No. of Total budget required<br />
institutions Unit rate Budget required<br />
1 PHC 56 1.0 56.00<br />
2 RH/SDH/WH/GH 14 1.0 14.00<br />
3 Leprosy Hospitals 0 1.0 0.00<br />
4 Mental Hospitals 0 1.0 0.00<br />
5 TB Hospital 1 5.0 5.00<br />
3 District Hospitals 1 5.0 5.00<br />
4 RRC 1 5.0 5.00<br />
Total 73 85.00
STRENGTHENING OF PHYSICAL INFRASTRUCTURE<br />
ANNUAL MAINTENANCE GRANTS<br />
Annual Maintenance Grants are distributed for maintenance of health institutions.<br />
Do not provide AMG to institutions which are in ranted building or are working from PHC, PHU or<br />
any other government building which is already getting AMG.<br />
Request the AMG grants as mentioned in table below:<br />
Sr Type of health institution<br />
No. of<br />
institutions<br />
in district<br />
Institutes<br />
eligible for<br />
AMG<br />
Unit rate<br />
AMG<br />
Budget<br />
required<br />
1 Sub‐Centre 333 299 0.10 29.90<br />
2 Primary dispensaries 103 62 0.50 31.00<br />
2 PHC 56 48 0.50 24.00<br />
3 RH/SDH/WH 14 14 1.0 14.00<br />
4 DH 1 1 5.0 5.00<br />
5 RRC 1 1 5.0 5.00<br />
6 TB Hospital 1 1 5.00 5.00<br />
Civil Works<br />
Total 509 426 113.90<br />
Spillover (works which will start before 1.4.2011, continue during 2011‐12 and need payment to<br />
be done during 2011‐12)<br />
Repairs and maintenance New construction Total<br />
Sr Type of institute No. of Budget No. of Budget budget<br />
works required works required required<br />
1 SC 0 0 8 60.00 60.00<br />
2 PHU 0 0 0 0 0<br />
3 PHC 0 0 1 80.00 80.00<br />
4 RH/SDH/GH 0 0 0 0 0<br />
5 WH 0 0 0 0 0<br />
6 DH 0 0 0 0 0<br />
7 Mental Hosp. /<br />
Leprosy Hosp / TB<br />
Hosp<br />
0 0 0 0 0<br />
Total 0 0 9 140.00 140.00
New works proposed during 2011‐12<br />
Sr Type of institute No. of<br />
works<br />
Repairs and maintenance New construction<br />
Budget<br />
required<br />
No. of<br />
works<br />
Budget<br />
required<br />
Total<br />
budget<br />
required<br />
1 SC 0 0 5 90.00 90.00<br />
2 PHC 11 35.00 6 160.00 195.00<br />
3 RH/SDH/GH 0 0 0 0 0<br />
4 WH 0 0 0 0 0<br />
5 DH 0 0 0 0 0<br />
6 Mental Hosp. /<br />
Leprosy Hosp / TB<br />
Hosp/ other<br />
1 5.00 0 0 5.00<br />
Total 18 40.00 11 250.00 290.00<br />
Summary of budget required<br />
Spillover of 2010‐11 New works during 2011‐12 Total<br />
Sr Type of institute No. of Budget No. of Budget budget<br />
works required works required required<br />
1 SC 8 60.00 5 90.00 150.00<br />
3 PHC 1 80.00 17 195 275.00<br />
4 RH/SDH/GH 0 0 0 0 0<br />
5 WH 0 0 0 0 0<br />
6 DH<br />
Mental Hosp. /<br />
0 0 0 0 0<br />
7 Leprosy Hosp / TB<br />
Hosp<br />
0 0 1 5.00 5.00<br />
Total 9 140.00 23 290.00 430.00<br />
PROVISION OF IMPORTANT FACILITIES FOR HEALTH INSTITUTIONS<br />
MOBILITY SUPPORT<br />
POL & Repairs of existing ambulances<br />
Sr Type of institute<br />
No. of ambulance<br />
available<br />
No. requiring repairs<br />
including purchase of<br />
tyres, batries, etc<br />
Budget required<br />
for repairs<br />
1 PHC – Non tribal 45 0.30 13.50<br />
PHC ‐ Tribal 11 0.45 4.95<br />
2 RH/SDH/WH 14 0.50 7.00<br />
3 DH 2 0.50 1.00<br />
Total 72 26.45
Primary <strong>Health</strong> Unit in District<br />
Sr. No. Name of Block Name of PHC Name of PHU<br />
Nimdari<br />
Dhamangaon Gadhi Chamak Bu.<br />
Kavita Bu.<br />
Kustha Bu.<br />
1 Achalpur<br />
Pathrot<br />
Kakda<br />
Shindhi Bu.<br />
Kolha<br />
Yesurna<br />
Anjangaon Bari<br />
Wadani Khu.<br />
Asatpur<br />
Rasegaon<br />
Mahuli JH<br />
Nandgaon Peth<br />
Salora<br />
2 <strong>Amravati</strong><br />
Rohankheda<br />
Shirala(<strong>Amravati</strong>) Antora<br />
Yavali Sh.<br />
Walgaon<br />
Kapustalni<br />
Nandure<br />
3 Anjangaon Suraji<br />
Kokarda<br />
Sategaon<br />
Kasabegavan<br />
Bhandaraj<br />
Chincholi Bu.<br />
Rama<br />
Aashti<br />
Takarkheda<br />
Sahur<br />
Haturna<br />
4 Bhatkuli<br />
Bhatkuli<br />
Sayat<br />
Kavatha Bu.<br />
Asara<br />
Dhamori<br />
Kholapur<br />
Virshi<br />
Wathoda Shu.<br />
Asegaon Purna<br />
Rajana Purna<br />
Hirulpurna<br />
Bramhanwada Thadi<br />
Sonori<br />
Devurwada<br />
Karanja Bahiram<br />
5 Chandur Bazar<br />
Karjgaon<br />
Thugaon Pimpari<br />
Kurha Deshmukh<br />
Shirajgaon K.<br />
Kharpi<br />
Borala<br />
Talwel<br />
Kuralpurna<br />
Belora<br />
6 Chandur Railway Amla V
7 Chikhaldara<br />
8 Daryapur<br />
9 Dhamangaon Rly<br />
10 Dharani<br />
11 Morshi<br />
12 Nandgaon Kh<br />
Palaskhed<br />
Jawala Dhotara<br />
Malkhed<br />
Hataru Ektai<br />
Katkumbh<br />
Katkumbh<br />
khari<br />
chunkade<br />
Selona Gaolkheda Ba.<br />
Semadoh Raypur<br />
Akhi<br />
Tembhursonda Gullarghat<br />
Vastapur<br />
Mahuli Dhande<br />
Chandrapur<br />
Uprai<br />
Jasapur<br />
Kanholi<br />
Amla E Amla E<br />
Ramtirtha<br />
Tonglabad<br />
Adula bazar<br />
Vadalgavan<br />
Yewada<br />
Warud Bu.<br />
Wadnergangai<br />
Anjansingi Verul Ronghe<br />
Mangrul Dast Kavali Vasad<br />
Nimboli<br />
Talegaon Das<br />
Zadgaon<br />
Bairaghad<br />
Chatvabod<br />
Ragubali<br />
Bijudhawdi Mogarda<br />
Dhulghat Railway Ranigaon<br />
Harisal Bod<br />
Kalamkhar Chakarda<br />
Hirabambai<br />
Sadrawadi<br />
Susarda<br />
Titamba<br />
Ambada<br />
Hiwarkhed<br />
Pimpalkhuta<br />
Khed<br />
Udaykhed<br />
Riddhapur<br />
Nerpingalai<br />
Rajurwadi<br />
Shirkhed<br />
Vichori<br />
Dhamak<br />
Adgaon<br />
Dhamangaon Ka.<br />
Wadura<br />
Loni Takli<br />
Hiwara Bu.<br />
Dhanora Farshi<br />
Mangrul Chavla Mahuli Chor
13 Tiosa<br />
14 Warud<br />
Alopathic<br />
Displiancy<br />
Mangrul Chavala<br />
Wadhona<br />
Papal<br />
Palasmandal<br />
Pimpalgaon Ni.<br />
Yerangaon<br />
Satergaon<br />
Majari Masla<br />
Murtizapur<br />
Kurha<br />
Warha<br />
Pimpalkhuta<br />
Mardi (Tiwasa)<br />
Salora Bz.<br />
Talegaon Thakur Varkhed<br />
Amaner Ekdara<br />
Benoda<br />
Loni warud<br />
Karajgaon G.<br />
Mangruli peth<br />
Pusala<br />
Pavani<br />
Rajura Bazar<br />
Jarud<br />
Shendurjanaghat Temburkheda<br />
Primary <strong>Health</strong> Unit Abstract<br />
Ayurvedic<br />
Displiancy<br />
Primary <strong>Health</strong><br />
Unit<br />
Mobile<br />
Squade<br />
Total<br />
18 65 12 8 103
Sr.<br />
No.<br />
UP GRADATION OF HEALTH INSTITUTIONS FOR QUALITY SERVICES<br />
UP GRADATION OF HEALTH INSTITUTIONS TO INDIAN PUBLIC HEALTH STANDARDS<br />
Criteria for selection of hospitals for IPHS<br />
District Hospitals : District hospital should be included only if it is with Public <strong>Health</strong> Department and<br />
not attached to Government Medical College<br />
Women Hospitals : Continue all last years hospitals + any new WH if established during 2011‐12<br />
SDH/GH : Continue all the 50 to 200 bedded hospitals in district + any new hospital established or<br />
upgraded from RH to SDH/GH<br />
<strong>Rural</strong> Hospitals : Do not add new RH unless the RH has regular medical superintendent, own building<br />
and possibility of getting all five specialist either from regular or on contractual basis.<br />
PHC : We have to include maximum PHCs. Add PHCs with two MOs, 2 Staff nurses and own building.<br />
Sub‐Center : Include 50% SC with priority to building and two nurses are available<br />
Make list of institutes to be selected and provide information as mentioned below Information<br />
regarding budget should be based on facility survey of the institute.<br />
IPHS SC<br />
Sub ‐ Center PHC Taluka<br />
Own<br />
building<br />
2 ANM<br />
available<br />
(one egular<br />
and one<br />
contractual)<br />
Total budget<br />
requirement<br />
as per<br />
External<br />
Facility<br />
survey<br />
Budget<br />
demand<br />
for year<br />
2010‐11<br />
1 Bhankheda Kh Anjangaon Bari <strong>Amravati</strong> Yes 2 1.00 1.00<br />
2 Pardi Yes 2 1.00 1.00<br />
3 Reosa Walgaon Yes 2 1.00 1.00<br />
4 Devra Shirala Yes 2 1.00 1.00<br />
5 Yawali Shahid Yes 2 1.00 1.00<br />
6 Nandgaon Peth Mahuli J. Yes 2 1.00 1.00<br />
7 Ganoja Devi Bhatkuli Bhatkuli Yes 2 1.00 1.00<br />
8 Uttamsara Yes 2 1.00 1.00<br />
9 Aasra Yes 2 1.00 1.00<br />
10 Wathoda<br />
Shukleshwar<br />
Kholapur<br />
Yes<br />
2<br />
1.00 1.00<br />
11 Khartalegaon Yes 2 1.00 1.00<br />
12 Karatkhed Ramtirth Daryapur Yes 2 1.00 1.00<br />
13 Pimplod Yeoda Yes 2 1.00 1.00<br />
14 Nanded Bk Amala (A) Yes 2 1.00 1.00<br />
15 Shignapur Chandrpur Yes 2 1.00 1.00
Sr.<br />
No.<br />
Sub ‐ Center PHC Taluka<br />
Own<br />
building<br />
2 ANM<br />
available<br />
(one egular<br />
and one<br />
contractual)<br />
Total budget<br />
requirement<br />
as per<br />
External<br />
Facility<br />
survey<br />
Budget<br />
demand<br />
for year<br />
2010‐11<br />
16 Mahimapur Yes 2 1.00 1.00<br />
17 Dhanegaon Kokarda<br />
Anjangaon<br />
Surji Yes<br />
2<br />
1.00 1.00<br />
18 Kamalpur Taroda Yes 2 1.00 1.00<br />
19 Bhandaraj Sategaon Yes 2 1.00 1.00<br />
20 Gavandgaon Yes 2 1.00 1.00<br />
21 Sindhi Pathrot Achalpur Yes 2 1.00 1.00<br />
22 Wadgaon<br />
Fattepur<br />
Yes<br />
2<br />
1.00 1.00<br />
23 Rasegaon Yesuran Yes 2 1.00 1.00<br />
24 Asadpur Yes 2 1.00 1.00<br />
25 Naigaon<br />
Dhamangaon<br />
Ghadi<br />
Yes<br />
2<br />
1.00 1.00<br />
26 Gaurkheda Yes 2 1.00 1.00<br />
27 Kurha Karajgaon Chandur Bazar Yes 2 1.00 1.00<br />
28 Shirajgaon Yes 2 1.00 1.00<br />
29 Kalhodi Yes 2 1.00 1.00<br />
30 Kajali B. Thadi Yes 2 1.00 1.00<br />
31 Vani Yes 2 1.00 1.00<br />
32 Talegaon Mohana Asegaon P. Yes 2 1.00 1.00<br />
33 Pala Hiwarkhed Morshi Yes 2 1.00 1.00<br />
34 Pimpalkhuta Big Ambada Yes 2 1.00 1.00<br />
35 Rajurwadi Nerpinglai Yes 2 1.00 1.00<br />
36 Adgaon Vichori Yes 2 1.00 1.00<br />
37 Ridhpur Khed Yes 2 1.00 1.00<br />
38 Ekdara Amner Warud Yes 2 1.00 1.00<br />
39 Jarud‐1 Rajura Bz. Yes 2 1.00 1.00<br />
40 Haturna Yes 2 1.00 1.00<br />
41 Mangruli Peth Loni Yes 2 1.00 1.00<br />
42 Tembhurkheda She. Ghat Yes 2 1.00 1.00<br />
43 Shirajgaon Mozari Mardi Tiosa Yes 2 1.00 1.00<br />
44 Shivangaon Yes 2 1.00 1.00<br />
45 Talegaon Thakur Talegaon T. Yes 2 1.00 1.00<br />
46 Marda Kurha Yes 2 1.00 1.00<br />
47 Ashok Nagar Anjansingi<br />
Dhamangaon<br />
Rly Yes<br />
2<br />
1.00 1.00
Sr.<br />
No.<br />
48<br />
Sub ‐ Center PHC Taluka<br />
Juna<br />
Dhamangaon<br />
Own<br />
building<br />
Yes<br />
2 ANM<br />
available<br />
(one egular<br />
and one<br />
contractual)<br />
2<br />
Total budget<br />
requirement<br />
as per<br />
External<br />
Facility<br />
survey<br />
Budget<br />
demand<br />
for year<br />
2010‐11<br />
1.00 1.00<br />
Virul Ronghe Yes 2 1.00 1.00<br />
Jhadgaon Nimboli Yes 2 1.00 1.00<br />
Kawli Mangrul Dast. Yes 2 1.00 1.00<br />
Ghuikhed Amala V. Chandur Rly Yes 2 1.00 1.00<br />
Rajura Palskhed Yes 2 1.00 1.00<br />
Satefal Yes 2 1.00 1.00<br />
Dhanora Fasi Loni T. Nandgaon KH. Yes 2 1.00 1.00<br />
Wadhona<br />
Ramnath<br />
Papal<br />
Yes<br />
2<br />
1.00 1.00<br />
Sultanpur Dhamak Yes 2 1.00 1.00<br />
Mahuli Chor Mungrul C. Yes 2 1.00 1.00<br />
Pimpalgaon<br />
Nipani<br />
Papal<br />
Yes<br />
2<br />
1.00 1.00<br />
Motha Salona Chikhaldara Yes 2 1.00 1.00<br />
Bhulori Yes 2 1.00 1.00<br />
Bihali Yes 2 1.00 1.00<br />
Borala Yes 2 1.00 1.00<br />
Makhla semadoh Yes 2 1.00 1.00<br />
Raipur Yes 2 1.00 1.00<br />
Tarubandha Yes 2 1.00 1.00<br />
Ambapati Tembursonda Yes 2 1.00 1.00<br />
Khatkali Yes 2 1.00 1.00<br />
Jarida Katkumbh Yes 2 1.00 1.00<br />
Awagadh Yes 2 1.00 1.00<br />
Kharya Tembhru Kalamkhar Dharani Yes 2 1.00 1.00<br />
Karda Yes 2 1.00 1.00<br />
Berdabharu Yes 2 1.00 1.00<br />
Rehtyakheda Sadrawadi Yes 2 1.00 1.00<br />
Dhodhra Yes 2 1.00 1.00<br />
Berdabarda Harisal Yes 2 1.00 1.00<br />
Nanduri Yes 2 1.00 1.00<br />
Chipoli Yes 2 1.00 1.00<br />
Dhakana B. Dhawadi Yes 2 1.00 1.00<br />
Jutpani Yes 2 1.00 1.00
Sr.<br />
No.<br />
Sub ‐ Center PHC Taluka<br />
Own<br />
building<br />
2 ANM<br />
available<br />
(one egular<br />
and one<br />
contractual)<br />
Total budget<br />
requirement<br />
as per<br />
External<br />
Facility<br />
survey<br />
Budget<br />
demand<br />
for year<br />
2010‐11<br />
Kutanga Bairagad Yes 2 1.00 1.00<br />
Khamda Yes 2 1.00 1.00<br />
Baratanda Dhulghat Rly Yes 2 1.00 1.00<br />
IPHS PHC<br />
Sr Name of the<br />
PHC<br />
Total.. 166 83.00 83.00<br />
Block Number of<br />
MO<br />
available<br />
No. of nurses at<br />
HQ (ANM, LHV<br />
and contractual<br />
staff nurse)<br />
Own<br />
building<br />
(Yes/No)<br />
Total budget<br />
requirement as<br />
per External<br />
Facility survey<br />
Budget<br />
demand<br />
for year<br />
2010‐11<br />
1 Walgaon <strong>Amravati</strong> 1 2 Yes 5.00 5.00<br />
2 Anjangaon<br />
Bari<br />
2<br />
2 Yes 5.00 5.00<br />
3 Pathrot Achalpur 2 2 Yes 5.00 5.00<br />
4 Dhamangaon<br />
Ghadi<br />
2<br />
2 Yes 5.00 5.00<br />
5 Amala V. Chandur Rly 2 2 Yes 5.00 5.00<br />
6 Palskhed 2 2 Yes 5.00 5.00<br />
7<br />
Talegaon D.<br />
Dhamangaon<br />
Rly 2<br />
2 Yes 5.00 5.00<br />
8 Anjansingi 1 2 Yes 5.00 5.00<br />
9 Rajura Bz. Warud 2 2 Yes 5.00 5.00<br />
10 Loni (w) 2 2 Yes 5.00 5.00<br />
11 Pusala 2 2 Yes 5.00 5.00<br />
12<br />
Loni T.<br />
Nandgaon<br />
KH. 2<br />
2 Yes 5.00 5.00<br />
13 Papal 2 2 Yes 5.00 5.00<br />
14 Chandrpur Daryapur 2 2 Yes 5.00 5.00<br />
15 Yeoda 2 2 Yes 5.00 5.00<br />
16 Amala Emali 2 2 Yes 5.00 5.00<br />
17 Bhatkuli Bhatkuli 2 2 Yes 5.00 5.00<br />
18 Kholapur 2 2 Yes 5.00 5.00<br />
19 Semadoh Chikhaldara 1 2 Yes 5.00 5.00<br />
20 Tembursonda 2 2 Yes 5.00 5.00<br />
21 Katkumbh 2 2 Yes 5.00 5.00<br />
22 Salona 2 2 Yes 5.00 5.00<br />
23 Harisal Dharni 2 2 Yes 5.00 5.00
24 Sadrawadi 2 2 Yes 5.00 5.00<br />
25 Bijudhawadi 2 2 Yes 5.00 5.00<br />
26 Bairagad 1 2 Yes 5.00 5.00<br />
27 Kurha Tiosa 2 2 Yes 5.00 5.00<br />
28 Mardi 2 2 Yes 5.00 5.00<br />
29 Nerpinglai Morshi 2 2 Yes 5.00 5.00<br />
30 Hiwarkhed 2 2 Yes 5.00 5.00<br />
31<br />
Karajgaon<br />
RH/SDH/GH/WH/GH/DH<br />
Sr Name of the<br />
Hospital<br />
Type<br />
(RH/SDH/GH/<br />
WH/DH)<br />
No. of beds Total budget<br />
requirement as<br />
per External<br />
Facility survey<br />
Budget<br />
demand for<br />
year 2010‐11<br />
1 District Hospital DH 379 50.00 50.00<br />
2 Women Hospital WH 200 35.00 35.00<br />
3 Achalpur SDH SDH 100 20.00 20.00<br />
4 Dharni SDH SDH 50 20.00 20.00<br />
5 Morshi SDH SDH 50 20.00 20.00<br />
6 Daryapur SDH DH 50 20.00 20.00<br />
7 Warud RH 30 20.00 20.00<br />
Total 185.00<br />
Total budget required<br />
Chandur<br />
Bazar 2<br />
2 Yes 5.00 5.00<br />
32 Asegaon P. 1 2 Yes 5.00 5.00<br />
33 Kokarda Anjangaon 1 2 Yes 5.00 5.00<br />
34 Sategaon 1 2 Yes 5.00 5.00<br />
61 68 170.00 170.00<br />
Provide information on budget requirement for IPHS. Use the institute wise format for this purpose.<br />
Request for the budget as per table given below:<br />
Sr Institute Total no. in district No. selected for<br />
IPHS<br />
Budget requirement<br />
1 Sub‐Center 333 83 83.00<br />
2 PHC 56 34 170.00<br />
3 RH 9 1 20.00<br />
4 SDH – 50 3 3 60.00<br />
5 SDH – 100 1 1 20.00<br />
6 GH – 200 1 1 0<br />
7 WH 1 1 35.00<br />
8 DH 1 1 50.00<br />
9 ISO Certification for<br />
IPHS Institute<br />
71 10 50.00<br />
Total 488.00
TELEMEDICINE CENTER<br />
One telemedicine center at District Hospital and one at SDH are being established in District.<br />
Sr Particulars<br />
1<br />
2<br />
3<br />
4<br />
Honorarium to Doctors – Patient<br />
node<br />
Honorarium to Doctors‐Specialist<br />
node<br />
Salary of Facility Manager (Rs.<br />
15000/PM)<br />
Travel and daily allowances to Facility<br />
Manager (Rs. 500/PM)<br />
Unit<br />
cost<br />
District Hospital SDH<br />
No. of<br />
units<br />
Budget<br />
required<br />
No. of<br />
units<br />
Budget<br />
required<br />
0.001 500 0.50 500 0.50<br />
0.003 250 0.75 250 0.75<br />
0.15 1 1.80 1 1.80<br />
0.005 1 0.60 1 0.60<br />
5 Construction of telemedicine room 0 0.00<br />
6<br />
Installation and commissioning of<br />
equipment<br />
0 0.50<br />
7 Contingency 0.50 0.50<br />
Total 4.15 4.65<br />
Telemedicine Communication (Broad Band budget) for 2011‐12<br />
Sr. No Name Amount<br />
1 DH <strong>Amravati</strong> 0.90<br />
2 SDH Dharni 0.90<br />
3 RH Chikhaldara 0.90<br />
Total 2.70
STRENGTHENING OF NURSING SERVICES<br />
Nursing services are backbone of the health system. Skilled nurses in sufficient number are required<br />
at all health institutions from SC to District Hospitals for services.<br />
In additionalities, nursing services are to be strengthened, all the required facilities are to be<br />
provided as per MNC norms.<br />
Provide information about nursing services as follows:<br />
Sr Particulars Unit price<br />
1<br />
2<br />
Hiring of support staff at Nursing Schools<br />
(service wise separate row)<br />
Hiring of teaching staff (cadre wise separate<br />
row)<br />
No. of<br />
units<br />
required<br />
Total budget<br />
required<br />
5.00 2 10.00<br />
4.00 2 8.00<br />
3 Strengthening of Annex building 10.00 1 10.00<br />
4 New construction of annex building 0 0 0<br />
5<br />
Repairs and new construction of nursing<br />
school main building<br />
15.00 2 30.00<br />
6 Repairs and new construction of hostel 10.00 2 20.00<br />
7 Hiring of vehicle for nursing school 0 0 0<br />
8<br />
9<br />
10<br />
11<br />
12<br />
13<br />
Computer stationery, other expenses,<br />
contingency<br />
Meeting MNC requirements (indicator wise<br />
information)<br />
Stipend to nurses (additional capacity) as per<br />
government rates – ANM students<br />
Stipend to nurses (additional capacity) as per<br />
government rates – GNM students<br />
Stipend to nurses (additional capacity) as per<br />
government rates – LHV students<br />
Stipend to nurses (additional capacity) as per<br />
government rates – PHN students<br />
1.20 2 2.40<br />
6.00 2 12.00<br />
5.00 1 5.00<br />
5.00 1 5.00<br />
0 0 0<br />
0 0 0<br />
14 PPP‐Stipend to ANM students 0 0 0<br />
15 PPP – Stipend to GNM students 0.05 50 2.50<br />
16 PPP – Fees on loan basis to students 0.25 50 12.50<br />
17 Block PHN TA 0 0 0<br />
Total 61.50 117.40
SCHOOL HEALTH PROGRAM<br />
Planning of this program is to be done by Civil Surgeon.<br />
This program includes examination of all the school children in rural areas between 1 st to 10 th<br />
standard.<br />
Furnish following program related information:<br />
Sr.<br />
No<br />
Activities Available in<br />
district<br />
Expected<br />
achievement<br />
(Nov 2010)<br />
1 No. of Schools to be covered 2256 1709<br />
2 No. of Students to be covered 368952 245628<br />
3 Treatment of minor ailments by SH team ‐ 34456<br />
4 Specialist care<br />
5 Major – tertiary care<br />
School <strong>Health</strong> Programme<br />
Salary, Daily Allowances (DA) and Travel Allowances (TA)<br />
Sr Particulars Monthly<br />
budget<br />
requirement<br />
Rs. In Lakhs<br />
No. Budget required<br />
for 2011‐12<br />
1 Salary of SHP Coordinator 0.13 1 1.56<br />
2 Salary of DEO 0.10 1 1.20<br />
3 Contingency (stationary, internet,<br />
office maintenance, photocopying,<br />
AMC of office equipment, etc)<br />
0.02 0.24<br />
4 Travel to SHP Coordinator 0.10 1 1.20<br />
5 Printing of cards 1 0.20<br />
6 Communication District 0.10 1 0.10<br />
7 Over head District 0.06 1 0.06<br />
Total 4.56
Total budget requirement<br />
(Propose total budget required under PMU including SHP wing, etc.)<br />
You can add any other component for budget requirement with due explanation<br />
Sr Particulars Monthly budget<br />
requirement<br />
Budget required<br />
for 2011‐12<br />
Remarks<br />
1 Salary of contractual staff 5.32 63.84 It is proposed to<br />
Salary of SHP MO<br />
@ Rs. 15000/‐<br />
per month, &<br />
Pharmasist @ Rs.<br />
8000/‐ Per Month<br />
2 Salary of contractual staff<br />
(Tribal)<br />
0.88 10.56 It is proposed to<br />
Salary of Tribal<br />
SHP MO @ Rs.<br />
18000/‐ per<br />
month, &<br />
Pharmasist @ Rs.<br />
8000/‐ Per Month<br />
3 Hiring of one vehicle 3.20 38.40 @ Rs. 0.20 per<br />
month<br />
4 Contingency Distict (stationary,<br />
internet, office maintenance,<br />
photocopying, AMC of office<br />
equipment, etc)<br />
5 Contingency Block (stationary,<br />
internet, office maintenance,<br />
photocopying, AMC of office<br />
equipment, etc)<br />
6 Referral Services and<br />
investigation<br />
0.08 0.08<br />
0.10 1.60<br />
8.50<br />
7 SHP Medicine 12.00<br />
Total 134.98
SCHEMES FOR TRIBAL AND LEFTIST EXTREMISM AFFECTED AREAS<br />
PREVENTION OF SICKLE CELL DISEASE<br />
Under this program, budget is provided for testing to health institutions and IEC and counseling to<br />
ASHA through PHC.<br />
Physical target for district :<br />
No. of solubility tests to be performed in district during 2010‐11 ‐ 5916<br />
No. of electrophoresis tests to be performed during 2011‐12 ‐ 37<br />
Budget for health institutions:<br />
Sr Particulars<br />
1<br />
2<br />
3<br />
Unit<br />
cost<br />
First phase districts Second phase districts<br />
No. of<br />
units<br />
Budget<br />
required<br />
Unit<br />
cost<br />
No. of<br />
units<br />
Budget<br />
required<br />
Total<br />
budget<br />
required<br />
PHC‐Laboratory<br />
consumables/<br />
Contingency/ Card<br />
printing<br />
RH/SDH – Lab<br />
0.60 11 6.60 0 0 0 6.60<br />
consumables/<br />
Contingency<br />
Celebration of Sickle<br />
0.84 3 2.52 0 0 0 2.52<br />
Cell Week at<br />
PHC/RH/SDH<br />
0.20 14 2.80 0 0 0 2.80<br />
Total 11.92<br />
District level budget requirement:<br />
First phase districts Second phase districts Total<br />
Sr Particulars<br />
Unit<br />
cost<br />
No. of<br />
units<br />
Budget<br />
required<br />
Unit<br />
cost<br />
No. of<br />
units<br />
Budget<br />
required<br />
budget<br />
required<br />
1 SCD Coordinator 0.15 1 1.80 1.80<br />
2<br />
Contingency to District<br />
including TA/DA<br />
0.10 1 1.20 1.20<br />
3<br />
Budget for Solubility<br />
Test<br />
0.10 11 1.10 1.10<br />
4<br />
Budget for<br />
Electrophoresis test<br />
0.84 3 2.52 2.52<br />
5 Support to DH 5.00 1 5.00 5.00<br />
6 IEC of Sickle Cell week 0.05 14 0.70 0.70<br />
7 Salary of Lab Tech. 0.08 2 1.92 1.92<br />
Total 14.24
Incentive to ASHA :‐<br />
In tribal area sickle cell disease programme will be run through Government staff. In this programme<br />
main focus is on ASHA Volunteers who will going to support for achieving target of Solubulity test of<br />
villagers age group 1 to 30 years.and also main stress on married couple.<br />
For that it is proposed to give performance based incentive to ASHA for motivating people and<br />
couple for solubility test at PHC.<br />
Expected budget required Rs. 15.36 lacs for 2011‐12.<br />
Sr.<br />
No.<br />
1.<br />
2.<br />
3.<br />
4.<br />
5.<br />
6.<br />
Activity<br />
Awareness of people for<br />
Solubility test and<br />
counseling.<br />
Supervision to Block<br />
Facilitator on Solubility<br />
Test and Counseling ASHA<br />
Solubility positive person<br />
promote to<br />
Electrophoresis test.<br />
Sickle Cell Diseases Control Programme<br />
Rate<br />
Per<br />
Unit<br />
No of<br />
Unit<br />
Total<br />
Budget<br />
15 56130 841950<br />
100 40 4000<br />
50 1793 89650<br />
Collect the village wise list<br />
for the Sickle Cell effected<br />
patient and give the<br />
home visit to counseling<br />
and referral services for<br />
the treatment.<br />
Meeting on Sickle Cell<br />
programme in Residential<br />
75 664 49800<br />
School/ Anganwadi<br />
centre/other School<br />
(Quarterly Meeting)<br />
Monthly Meeting in PHC<br />
150 3540 531000<br />
for ASHA worker, Block<br />
facilitator, ANM, LHV and<br />
Lab. Technician<br />
150 132 19800<br />
Total … 540 62299 1536200<br />
Justification<br />
Total population in Melghat are<br />
282227 in between 1 to 30 year target<br />
population are 84668 and 30 to 49 age<br />
group Mother are 5003 total<br />
beneficiary 89671 last two year 33541<br />
solubility test completed. In financial<br />
target achieve 100%. There for 56130<br />
this year. ASHA worker promoted<br />
Solubility test and give the incentive Rs.<br />
15/‐ per test.<br />
Total block facilitator in Melghat 40<br />
give the Rs. 100/‐ for Solubility Test<br />
and Counseling ASHA<br />
Total covered beneficiary 2% Solubility<br />
positive rate and covered 25%<br />
Solubility positive promoted to<br />
Electrophoresis test by ASHA worker<br />
and give the incentive Rs. 50/‐ per test.<br />
Give referral services and village wise<br />
list for Sickle Cell patient, give the<br />
incentive Rs. 75/‐ per patient by ASHA<br />
worker.<br />
Take the Meeting for Residential<br />
School and Anganwadi centre and<br />
other School to conduct Lab.<br />
Technician and MO School <strong>Health</strong>.<br />
Review Meeting PHC level conduct by<br />
PHC MO.
PROCUREMENT PLAN<br />
Warehouse (Medicine Store) information of district<br />
Sr Place of<br />
warehouse<br />
(medicine store)<br />
Repairs New<br />
Construction<br />
Budget requirement<br />
Equipment<br />
and furniture<br />
Contingency<br />
Total<br />
budget<br />
required<br />
1 DHO Warehouse 0 15.00 7.00 1.50 23.50<br />
2 Civil Surgeon<br />
Warehouse<br />
3 Salary of<br />
Pharmacist<br />
DHO/CS<br />
3.00 0 0 1.50 4.50<br />
0 0 0 0 2.40<br />
Total 3.00 15.00 7.00 3.00 30.40
INNOVATIVE SCHEMES<br />
CO‐ORDINATION CELL AT DISTRICT HOSPITAL :‐<br />
Peripheral health institutions (SCs, PHCs, CHCs, etc.) have to refer patients to District Hospitals in<br />
emergency. District Hospitals have different sections for registration, laboratory checkup, X‐ray,<br />
medicines, blood bank, etc. Tribal patients do not have orientation of hospital and also cannot<br />
understand the language and there is delay in getting all the formalities done. Because of such<br />
environment, tribal patients are not willing to stay in hospital and many of the times insist for<br />
discharge even if the condition of patient is critical. To avoid this, one Coordination cell for patients<br />
referred from PHCs/CHCs in district will be established in each of 6 tribal district hospitals of state.<br />
The coordination cell will be established in District Hospital.<br />
Geographical distribution<br />
Districts Hospitals included are : Thane, Nashik, Nandurbar, Amarawati, Gondia and Gadchiroli.<br />
Structure of Coordination cell<br />
The cell will be structured as follows:<br />
1. There will be one Supervisor and 4 Coordinators in the Cell.<br />
2. Supervisor should be at least 12 th standard pass and Coordinators should be at least 10 th<br />
pass.<br />
3. Two coordinators will be males and two will be females. This can be changed as per need by<br />
districts.<br />
4. Coordinator and Supervisor must be from tribal community and able to speak local tribal<br />
language prevalent in district or in patients coming to DH.<br />
5. One desk should be given to Cell in ODD and Casualty of the hospital at prominent place<br />
with signboard.<br />
Appointment of Coordination cell staff<br />
Coordination cell staff will be appointed by Selection committee constituted under Chairmanship of<br />
Chairman EC RKS. Selection should be by advertisement in newspaper. It is important that the<br />
Supervisor and Coordinators should be from tribal community and should understand tribal<br />
language and should be good in communication skills.<br />
Functions of Coordination Cell<br />
One person should be available either in OPD or Casualty from coordination cell to help the serious<br />
tribal patients. Following will be the functions of Tribal cell :<br />
• Informing all the Sub‐Centers, PHCs and Hospitals about tribal cell and telephone and mobile<br />
numbers of the Cell Staff.<br />
• Receiving the serious / referred patients from health facilities in tribal areas, helping them in<br />
formalities for check‐up, admission and investigations.<br />
• Requesting the Medical Officers or specialists to attend to patients if required<br />
• Admitting the patient in hospital
• Daily visit to patient to solve any problem till discharge.<br />
• Coordinating with welfare agencies and donors for any special service required to tribal<br />
patients and their relatives.<br />
• Making arrangements for transport after discharge.<br />
Instructions to Civil Surgeon<br />
• Do not give any other work to Coordination Cell staff. Do not engage them with duty of<br />
regular patients or VIP patients.<br />
• Do not send the Coordination Cell staff on tour to other places.<br />
• Duty of the Supervisor and Coordinators should be in such a way that one person is always<br />
available in either OPD or Casualty.<br />
Budget requirement<br />
Budget is provided for following purposes:<br />
Salary of Supervisor<br />
Supervisor is paid Rs. 6000/PM. He/She will be in charge of the Coordination Cell. Budget is provided<br />
for 10 months salary of Supervisor (Rs. 0.6 Lakh). If necessary, the EC RKS can increase the salary of<br />
Supervisor up to Rs. 8000/PM within the budget provided to the activity.<br />
Salary of Coordinator<br />
There will be four Coordinators in Cell. Salary of Coordinator is Rs. 4000/PM. Budget is provided for<br />
10 months salary of Coordinator (Rs. 0.4 Lakh per person – total Rs. 1.60 L). If necessary, the EC RKS<br />
can increase the salary of Coordinator up to Rs. 6000/PM within the budget provided to the activity.<br />
a. Furniture and Renovation of Help Desk<br />
Coordination Cell Help desk will be made available at OPD and Casualty. Rs. 0.5 Lakh is provided for<br />
furniture of help desk. Procure furniture and required partition from this grant for sitting<br />
arrangement of the Coordination staff.<br />
b. Communication (Telephone and Mobile charges)<br />
Budget for telephone line and mobile is provided for Coordination cell. If required install one<br />
telephone line to the Coordination Cell, otherwise provide mobile handsets to Cell staff from this<br />
grant. Rs. 10000/‐ is provided for mobile charges to Cell staff. Mobile charges maximum up to Rs.<br />
400/PM for Coordinator and Rs. 500/PM for Supervisor are permissible. If budget is not sufficient<br />
then savings of Telephone line or contingency should be used for this purpose.<br />
c. Overheads<br />
Grant of Rs. 60000/‐ is provided as overheads to Coordination Cell. This grant can be used for<br />
stationary and other minor expenses of cell and also for any activity mentioned above if the allotted<br />
grant is not sufficient.
Budget requirement for Coordination Cell during the year 2011‐12<br />
Rs. In Lakhs<br />
Sr Particulars Monthly budget No. of Unit Budget required<br />
requirement<br />
for 2011‐12<br />
1 Salary of Supervisor 0.06 1 0.72<br />
2 Salary Coordinator 0.04 4 1.92<br />
3 Furniture & renovation of Help<br />
desk<br />
0.50 1 0.50<br />
4 Telephone facility to Help desk 0.02 12 0.24<br />
5 Mobile Charges to all Members 0.01 5 0.60<br />
6 Over heads 0.60 1 0.60<br />
Total 4.58<br />
MAHER SCHEME<br />
Maher scheme<br />
Melghat have hilly terrain and many of the tribal padas do not have pukka roads. Even if<br />
pukka roads are available, there is no reliable transportation system for transferring pregnant<br />
women in labour to nearby PHC. This is the one of the important cause of high maternal and<br />
neonatal mortality and morbidity.<br />
Since accurate predication cannot be made on the time of delivery, hence it puts the mother<br />
in danger if she develops complicacies and does not find transportation facilities. Hence Maher<br />
scheme is implemented in Melghat area in which one room is build in PHC premises where pregnant<br />
woman will get admitted one week before her due date. She can be daily checked by Doctor of PHC<br />
and can be transported to suitable referral centre if any complications are detected during waiting<br />
period or during labour.<br />
Following facilities are proposed in ‘Maher’<br />
• One room of 5×5 meters<br />
• One sanitary block (Toilet and bathroom)<br />
• One kitchen ota with smokeless chulha<br />
• One solar water heater system on roof of the room<br />
‘Maher’ will be maintained by local Self Help Group. When mother is admitted, mother, her young<br />
child and one relative will be provided food three times a day. It is proposed to provide Rs. 400/‐ per<br />
delivery. In 2008‐10, 9 PHCs Maher room constructions get completed. Hence remaining 2 PHCs in<br />
Melghat areas will be proposed under this scheme.<br />
Melghat PHC : 1) Katkumbh<br />
2) Salona
Budget requirement for Maher Scheme<br />
Sr Particulars Unit cost No. of units<br />
Rs. In Lakhs<br />
Budget required<br />
1 One room construction 5.50 L/PHC 2 11.00<br />
2 Maintenance cost to SHG Rs. 400/‐ per delivery 1350 5.40<br />
Total 16.40<br />
VOLUNTEER TO TRIBAL PHCS<br />
Tribal population do not accept the health services from institutions as expected. The cause<br />
of non acceptance are manifold, one of which is their communication with the PHC staffs who are<br />
normally out of the tribal areas. Besides the staffs belong to different culture and different<br />
understanding about various diseases. Considering this, it is proposed that two local volunteers, who<br />
knows the local language and can understand the concept of positive health, can be appointed as<br />
Volunteer in tribal PHC. This volunteer will counsel the patients, direct them for case papers, and<br />
inform them about the instructions given by doctor and nurses and give simple public health<br />
messages. Hence there is a need of appointing 28 volunteers in Melghat area and 6 volunteers are<br />
appointed at DH/WH/SDH Achalpur.<br />
Budget requirement for Volunteer to tribal PHCs<br />
Sr Particulars Unit cost No. of units<br />
Rs. In Lakhs<br />
Budget required<br />
1 Honorarium to volunteer<br />
PHC/RH/SDH<br />
Rs. 0.03 L/Vol/PM 30 10.80<br />
2 Honorarium to volunteer<br />
DH/WH/SDH<br />
Rs. 0.045 L/Vol/PM 4 2.16<br />
Total 12.96<br />
Diet Facility for PHC and RH/SDH level:‐<br />
Budget requirement for Diet & Loss of wages to deliveries<br />
Rs. In Lakhs<br />
Sr Particulars Unit cost No. of units Budget required<br />
1 Diet @ Rs. 600/‐ Per<br />
Delivery (4 days)<br />
2 Loss of Wages @ Rs.<br />
600/‐ per Delivery<br />
(4 Days)<br />
Rs. 600/‐ per delivery 1650 9.90<br />
Rs.600/‐ per delivery 1650 9.90<br />
Total 19.80
AYUSH MAINSTREAMING<br />
AYUSH facility is being provided to selected health institutions. Under this scheme, doctors from<br />
Ayurved, Homeopathy and unani faculties are being appointed in hospitals. Budget will be required<br />
for salary of these medical offices and medicines.<br />
Mainstreaming means provision of AYUSH services in allopathic hospital so that patient has choice to<br />
choose between all the available types of treatment.<br />
Following are broad guidelines for implementation of AYUSH program in districts<br />
i. AYUSH facility should be started in PHCs where regular Ayurved Medical Officers are posted. No<br />
contractual doctor is allowed to be appointed at PHC level.<br />
ii. Selected RH/SDH in state will have all the three AYUSH faculties – Ayurved, Unani and<br />
Homeopathy. Out of these, Ayurved doctors will be full time and Homeopathy and Unani<br />
doctors will be part time. Names of such doctors is already communicated.<br />
iii. At DH all the three pathies along with Yoga – Naturopathy will be available. All the doctors here<br />
are full time. Indoor facility for AYURVED will also be available in DH. In DH, one post of<br />
pharmacist and one post of masagist is also sanctioned.<br />
iv. All these doctors will be provided medicine kits through AYUSH department of GoI. Till we get<br />
the medicines from AYUSH department, medicines can be purchased from IPHS funds only at<br />
places where AYUSH contractual doctors are appointed. Guidelines issued for AYUSH medicine<br />
purchase and IPHS purchase should be followed for this purpose.<br />
v. Guidelines issued by SHS should be followed for appointment and medicine and equipment<br />
purchase in AYUSH facilities.<br />
District AYUSH Cell<br />
Ayush cell is established in all the districts. Extension officer (Ayurved) will be in charge of the cell. If<br />
the Extension Officer is not available in district, one Ayurvedic postgraduate doctor can be appointed<br />
on contract basis for cell. Alternatively, one Ayurvedic Graduate Medical Officer can be taken on<br />
deputation and contractual MO can be posted at his/her place. Budget provision for the AYUSH cell<br />
is as follows:<br />
a. Salary of contractual MO : If EO (Ayurved) is not available in district, one postgraduate<br />
ayurvedic doctor should be appointed. Salary of the doctor will be Rs. 16000/PM. Budget if<br />
provided to pay the salary of contractual MO. Alternately one interested Ayurvedic Graduate<br />
regular MO can be appointed for this post and the contractual MO can be appointed in place<br />
of the regular MO.<br />
b. Contingency : Contingency @ Rs. 5000/‐ is provided this year. Stationary, Annual<br />
Maintenance of equipment and other office expenses should be made through this grant.
Budget requirement for AYUSH Cell during the year 2011‐12<br />
Sr Particulars Monthly budget<br />
requirement<br />
1 AYUSH Center in RH/SDH<br />
Rs. In Lakhs<br />
No. Budget required<br />
for 2011‐12<br />
a MO (AYUR) Full time 0.12 6 8.64<br />
b MO (HOMEO) Part time 0.08 6 5.76<br />
c MO (UNANI) Part time 0.08 6 5.76<br />
2 AYUSH Center in DH 0<br />
a MO (AYUR) Full time 0.12 1 1.44<br />
b MO (HOMEO) Full time 0.12 1 1.44<br />
c MO (UNANI) Full time 0.12 1 1.44<br />
d Pharmacist 0.07 1 0.84<br />
e Yoga Teacher 0.06 1 0.72<br />
f Mussagist cum Attendant<br />
(Male/Female)<br />
0.05 2 1.20<br />
District AYUSH Cell 0<br />
a Data Entry Operator 0.08 1 0.96<br />
b Office Furniture / Computer &<br />
Printer<br />
2.00 1 2.00<br />
c Contingency 0.05 1 0.60<br />
Total 30.80
Hardship allowance to régular staff working in extremly difficult health facilities<br />
In tribal and LEA areas, there are few RHs, PHCs and Sub‐Centers where regular staff do not join<br />
even if appointed. Such health institutions cannot provide services to community. Besides, large<br />
investments of government also remain unutilized. These areas are also having very high IMR and<br />
MMR and are in need of critical staff. Regular nurses, doctors and specialists will be provided<br />
allowances over and above their salary.<br />
This scheme is for extremely difficult tribal and/or leftist extremism affected areas of Thane, Nashik,<br />
Dhule, Nandurbar, Nanded, Amarawati, Yawatmal, Gondia, Chandrapur and Gadchiroli districts.<br />
Important instructions in this regard are as follows:<br />
• Regular nurses, MBBS doctors and specialists in RH will get his/her regular pay and tribal /<br />
naxalite area allowances as usual from Zilla Parishad / treasury. The hardship allowance<br />
provided by NRHM is over and above this salary. This should be paid by cheque to these staff<br />
by THO/MS or Civil Surgeon.<br />
• The health institutions to be included in this scheme should be decided by District <strong>Health</strong><br />
Society. Such institutions should have record of non‐availability of nurses (SC/PHC) MBBS<br />
doctors (PHC/RH) and specialists (RH) for long time.<br />
• Hardship allowances to be provided to all ANMs, LHVs and Staff Nurses working in notified<br />
Sub‐Centers, PHCs and RH/SDH.<br />
• Hardship allowances to be provided to MBBS doctors working in PHCs or RH/SDH and<br />
specialists of only five specialties (Medicine, Surgery, OBGY, Pediatrics and Anesthesia) and<br />
Medical Superintendent of RH (any speciality).<br />
• Specialist allowances can be paid to MBBS doctors who have undergone multi‐skill training<br />
and are providing specialty care.<br />
• It is mandatory to stay at HQ for the staff to be eligible for the scheme.<br />
• If government servant is on leave for more than one week, then allowance should be<br />
proportionately reduced for that month.<br />
Budget utilization<br />
a. Allowances to ANM : Regular ANM if staying at HQ and providing services such as delivery<br />
should be paid Rs. 4000/PM over and above her regular salary from NRHM funds. ANM<br />
include ANM posted at notified Sub‐Centre and also the notified PHC in the district.<br />
b. Allowances to LHV/Staff Nurse/NM : She should be paid Rs. 6000/PM over and above salary<br />
provided she is actively involved in RCH activities including ANC checkup, delivery and<br />
immunization and providing services by staying at HQ. The LHV/staff nurse /NM include<br />
nurses working in notified PHC as well as notified <strong>Rural</strong> Hospital.<br />
c. Allowances to MO PHC : Regular MO with MBBS degree if staying at HQ and providing all<br />
the services is eligible for hardship allowance. Hardship allowance for MO PHC is Rs.<br />
12000/PM over and above regular salary.
d. Allowances to RH doctors : Medical Superintendent and regular medical officers of<br />
specialties mentioned above should be paid hardship allowances @ Rs. 18000/PM. MBBS<br />
doctors trained in cesarean section, anesthesia and neonatal/child care should also be paid<br />
specialist hardship allowances @ Rs. 18000/PM if they provide specialist services.<br />
Sometimes MBBS doctors are posted at identified RH as there is no specialist available.<br />
These doctors should also be paid hardship allowance. However rate of hardship allowance<br />
should be 12000/PM.<br />
Budget requirement for Hardship allowance during the year 2011‐12<br />
Rs. In Lakhs<br />
Sr Particulars Monthly budget No. Budget required<br />
requirement<br />
for 2011‐12<br />
1 ANM 0.04 95 45.60<br />
2 NM/LHV‐ PHC/RH/SDH 0.06 17 12.24<br />
3 MO PHC/RH/SDH 0.12 25 36.00<br />
4 Specialist 0.18 9 19.44<br />
Total 113.28<br />
MOBILE MEDICAL UNITS<br />
<strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong>, Framework for Implementation (2007‐12) has mentioned support to<br />
Mobile Medical Units in rural areas of the state. Objective of providing these units is to take health<br />
care to the doorstep of the public in the rural areas, especially in under‐served areas. The GOI has<br />
suggested establishing one Mobile Medical Unit (MMU) per district, however it has advised states to<br />
consider diversity and ensure the adoption of most dutiable and sustainable model for the MMU to<br />
suit their local requirements. States are also required to plan for long‐term sustainability of the<br />
intervention.<br />
Budget requirement for Mobile Medical Unit during the year 2011‐12<br />
Rs. In Lakhs<br />
Sr Particulars Monthly budget No. Budget required<br />
requirement<br />
for 2011‐12<br />
1 Salary of Staff of Mobile<br />
a<br />
Medical Unit<br />
Project Manager 0.10 1 1.20<br />
b Accountant 0.06 1 0.72<br />
c MO – I 0.16 1 1.92<br />
d MO‐ II 0.15 1 1.80<br />
e Staff Nurse 0.08 1 0.96<br />
f Lab Technician 0.07 1 0.84<br />
g Pharmacist 0.07 1 0.84<br />
h Support Staff 0.06 1 0.72<br />
i Driver 0.06 2 1.44<br />
2 Recurring<br />
Salary<br />
Cost other than
a Vehicle repair & POl 0.20 1 2.40<br />
b Equipment maintenance 0.20<br />
c Consumable 0.50<br />
d Medicine 0.36<br />
e Other Expenses 0.36<br />
f Overheads 1.00<br />
3 Initial support to NGO 0.50<br />
Total 15.76<br />
PREPARATION OF DISTRICT HEALTH ACTION PLAN (DHAP)<br />
In order to make NRHM fully accountable, the district health action plan will be the principal<br />
instrument for planning, implementation and monitoring, formulated through a participatory and<br />
bottom up planning process. District <strong>Health</strong> <strong>Mission</strong> constituted as per guideline is responsible for<br />
the planning of district.<br />
Considering the bottom up approach being used by Maharashtra, grant is released to districts @ Rs.<br />
0.6 Lakh per block for preparation of PIP of year 2011‐12.<br />
Guidelines for preparation of PIP and utilization of PIP funds will be provided in third quarter.<br />
Budget requirement for DHAP during the year 2011‐12<br />
Rs. In Lakhs<br />
Sr Particulars Budget per unit No. of unit Budget required<br />
for 2011‐12<br />
1 Preparation of DHAP 0.60 14 8.40
MONITORING AND EVALUTION CELL<br />
Monitoring is a periodic collection and analysis of selected indicators of the Program to enable<br />
health managers to determine whether key activities are being carried out as per the action plan. It<br />
is carried out at both the services delivery unit through direct contact with health workers and at the<br />
managing office by examining periodic reports. Monitoring provides feedback to project manager in<br />
order to improve the operation plan and to take mid course corrective measures if necessary.<br />
Evaluation of a program or of a component helps to assess the tracking/success/failure of any<br />
program and also the reasons for the above. It is also necessary task at regular interval for ongoing<br />
projects and at end of the pilot projects/initiatives and also before up scaling any program initiative.<br />
Budget requirement for M & E Cell during the year 2010‐11<br />
Sr Particulars Monthly budget No. Budget required<br />
requirement<br />
for 2011‐12<br />
1 Salary of M & E Officer 0. 27 1 3.24<br />
2 Salary of DEO 0.15 3 5.40<br />
3 Contingency (stationary,<br />
internet, office maintenance,<br />
photocopying, AMC of office<br />
equipment, etc)<br />
0.10 1.20<br />
4 Travel to statistical officer 0.10 1 1.20<br />
5 T.A. & D.A. of M & E officer 0.10 1 1.20<br />
Total 0.35 12.24<br />
FINANCIAL MANAGEMENT GROUP<br />
Budget requirement for F.M.G. during the year 2011‐12<br />
Sr Particulars Monthly budget No. Budget required<br />
requirement<br />
for 2011‐2012<br />
1 Salary of Accountant 0.12 2 2.88<br />
2 T.A. & D.A. of Accountant 0.02 2 0.48<br />
3 Contigency 0.06 1 0.72<br />
Total 4.08<br />
Budget requirement for RKS Coordinator during the year 2010‐11<br />
Sr Particulars Monthly budget No. of unit Budget required<br />
requirement<br />
for 2011‐12<br />
1 Salary of RKS Coordinator 0.15 1 1.80<br />
2 Salary of Proposed DEO 0.12 1 1.44<br />
3 Contingency (stationary,<br />
internet, office maintenance,<br />
photocopying, AMC of office<br />
equipment, etc)<br />
0.05 1 0.60<br />
4 T.A. & D.A. of RKS Coordinator 0.05 1 0.60<br />
Total 0.47 4.44
INFRASTRUCTURE DEVELOPMENT WING (IDW)<br />
IDW is established in your district as a construction wing of DPMU. IDW staff should be<br />
accommodated at the place where DPMU is situated.<br />
As budget required for functioning of IDW is to be shown under construction, it is shown separately<br />
from the DPMU budget. The heads of particulars are same except the vehicle hiring.<br />
Propose the IDW HQ budget in following tables. You can add any other component if required for<br />
budget. Prepare this table in coordination with Deputy Engineer<br />
Salary, Daily Allowances (DA) and Travel Allowances (TA) to HQ staff of IDW<br />
Sr Particulars<br />
No. of<br />
persons<br />
Monthly<br />
salary<br />
No. of<br />
expected<br />
tour days<br />
Rate<br />
DA<br />
Monthly<br />
budget<br />
TA ‐<br />
Monthly<br />
budget<br />
required<br />
1 Deputy Engineer 1 0.24 10 200.00 0.02 0.10<br />
2<br />
Junior Engineer<br />
(Block level)<br />
4 0.72 20 100.00 0.08 0.16<br />
3 Data Entry Operator 1 0.12<br />
Total 1.08 0.10 0.26<br />
Budget required for IDW HQ<br />
Sr Particulars<br />
Monthly budget<br />
requirement<br />
Budget required<br />
for 2011‐12<br />
1 Salary of IDW staff 1.08 12.96<br />
2 DA to IDW staff 0.10 1.20<br />
3 TA to IDW staff<br />
Contingency (stationary,<br />
0.26 3.12<br />
4<br />
internet, office maintenance,<br />
photocopying, AMC of office<br />
equipment, etc)<br />
0.05 0.60<br />
Total 1.49 17.88<br />
Remarks
IPHS MONITORING UNIT<br />
It has been decided to include 30% Sub‐Centers, 30% PHCs 30% SDH/RH and all District Hospitals to<br />
upgrade as IPHS standard hospitals. As this will be major task requiring large budget and continuous<br />
monitoring, it is proposed to establish one IPHS monitoring unit under each civil surgeon. This unit<br />
will work under RMO (O) on day to day basis.<br />
Civil Surgeon should provide sufficient space to the IPHS unit.<br />
Budget required for IPHS monitoring unit will be as follows:<br />
Salary, Daily Allowances (DA) and Travel Allowances (TA)<br />
Sr Designation<br />
No. of<br />
persons<br />
Monthly<br />
salary<br />
No. of<br />
expected<br />
tour days<br />
Rate<br />
DA<br />
Monthly<br />
budget<br />
TA ‐<br />
Monthly<br />
budget<br />
required<br />
1 IPHS Coordinator 1 0.27 10 200.00 0.02 0.10<br />
2 DEO 1 0.12<br />
Total 0.39 0.02 0.10<br />
Total budget requirement<br />
(Propose total budget required under PMU including IDW, IPHS wing, etc.)<br />
You can add any other component for budget requirement with due explanation<br />
Sr Particulars Monthly budget Budget required<br />
requirement for 2011‐12<br />
1 Salary of contractual staff 0.39 4.68<br />
2 Daily allowances to contractual<br />
staff<br />
0.02 0.24<br />
3 Travel Allowances to<br />
contractual staff<br />
0.10 1.20<br />
4 Contingency (stationary,<br />
internet, office maintenance,<br />
photocopying, AMC of office<br />
equipment, etc)<br />
0.10 1.20<br />
Total 0.61 7.32<br />
Remarks
BLOCK PROJECT MANAGEMENT UNIT<br />
BPMU is established in all blocks of your district. The BPMU will require sufficient office space to<br />
function efficiently. BPMU should be located at taluka HQ, preferably in old PHC building or SDH/RH<br />
building.<br />
Describe the number of BPMU in district, present places of BPMU, place is sufficient in how many<br />
blocks and not sufficient in how many blocks.<br />
Request for budget for salary, travel expenses and daily allowances to contractual staff, minor<br />
repairs, furniture and contingency.<br />
Propose the budget in following tables<br />
Salary, Daily Allowances (DA) and Travel Allowances (TA)<br />
Sr Designation<br />
No. of<br />
persons<br />
(one per<br />
block)<br />
Monthly<br />
salary<br />
No. of<br />
expected<br />
tour days<br />
Rate<br />
DA<br />
Monthly<br />
budget<br />
TA ‐<br />
Monthly<br />
budget<br />
required<br />
1 THO 14 10 1.40<br />
2 Accountant 14 1.68 10 150 0.21 0.28<br />
3 DEO 14 1.26 10 150 0.21 0.14<br />
4<br />
Total 2.94 0.42 1.82<br />
Note : As THO is government officer, his/her DA should not be proposed from NRHM funds<br />
Total budget required for BPMU<br />
Sr Particulars Monthly budget Budget required<br />
requirement for 2011‐12<br />
1 Salary of contractual staff 2.94 35.28<br />
2 Daily allowances to contractual<br />
staff<br />
0.42 5.04<br />
3 Travel Allowances to THO and<br />
contractual staff<br />
1.82 21.84<br />
4 Contingency (stationary,<br />
internet, office maintenance,<br />
photocopying, AMC of office<br />
equipment, etc)<br />
1.40 16.80<br />
5 Honorarium to Block PHN 0.21 2.52<br />
Total 6.79 81.48<br />
Remarks
IMMUNIZATION<br />
PIP 2011-12
C. IMMUNISATION<br />
C.1: Situation analysis of the DistrictImmunization Program<br />
1. Current scenario of implementation of immunization program<br />
a. State level coverage as per District Level Household Survey‐3, Coverage Evaluation<br />
Survey 2009 & Reported coverage for 2009‐10, 2010‐11 till Dec'10.<br />
b. District wise coverage levels of all antigens for 2009‐10, 2010‐11 till Dec'10<br />
(including Hepatitis B & JE wherever applicable).<br />
c. Reasons for Shortfall in coverage<br />
d. Reporting and incidence of VPDs for 2010‐11 till Dec'10.<br />
e. Reporting and Response to Outbreaks and AEFIs for, 2009‐10 till Dec'10.<br />
2. Strategies for further improving Routine Immunization<br />
a. What is the target of immunization coverage for this year?<br />
b. To improve the accessibility of routine immunization services (reflected by BCG and<br />
DPT‐1 coverage); identify the districts with poor access and reasons thereof.<br />
c. To reduce dropouts (reflected by DPT3 coverage); reasons for dropout and specify<br />
Steps taken for this.<br />
d. To create community demand for routine immunization;(write specific steps taken)<br />
e. Any other innovation started for strengthening of routine immunization in the state.<br />
3. Status of micro planning‐ Number of districts where RI micro‐plans have been updated in 2010‐<br />
11. (Provide details in the format enclosed).<br />
4. What are the roles & responsibilities pertaining to immunization of 1 st ANM, 2 nd ANM,<br />
and HW (Male) ?<br />
5. What is the mechanism of coordination & convergence between AWW and ASHA?<br />
6. Alternate Vaccine Delivery System‐ what system is in place, whether it is working and what are<br />
issues faced?<br />
7. Supervision and Monitoring‐Status of Routine Immunization cell, Supportive Supervision<br />
Structure in field, Review meetings and data analysis and action taken at all levels etc).<br />
8. Status of RIMS implementation for monitoring (details of districts uploading data regularly,<br />
issues with other districts and proposed support required).<br />
9. Co‐ordination with Partners (ICDS, Public Private Partnerships, Other agencies).<br />
10. Component‐wise receipt & expenditure of funds received from 2009‐10 onwards (format<br />
attached).<br />
11. Status of Cold Chain Equipment‐<br />
i.) ILRs, DF, Voltage stabilizers
a) Plan for replacement of all condemned or non service able equipment which is beyond<br />
repair.<br />
b) Expansion: ‐ Need based depending on the setting up of New PHC/ cold chain points.<br />
c) All CFC equipments supplied till 1992 has been replaced with Non CFC equipment. The<br />
expansion plan should include replacement of remaining CFC equipments supplied<br />
during the period of 93‐98<br />
ii.) Cold boxes, Vaccine carriers ‐ replacement plan for expansion or replacement of<br />
condemn equipment.<br />
iii.) Insulated/Non Insulated vaccine van: Plan for supply of insulated vaccine vans against<br />
condemned vehicles and expansion plan for supply of vaccine van for newly created<br />
district.<br />
iv.) Mechanism for cold chain maintenance and repairs‐ HR structure, AMC(if any) etc.<br />
12. Status of implementation of Procurement Management Information System (ProMIS).<br />
13. IEC plan for strengthening UIP; however the budget for IEC is to be provisioned under RCH.<br />
14. Infrastructural and manpower requirements that are essential for implementation of UIP but<br />
not admissible under Part C (Immunization) may be provisioned under the NRHM/RCH heads.<br />
(eg; Refrigerator mechanics, renovation of stores etc.) This should include district level need for<br />
go‐down for vaccine/logistics.<br />
15. Additional support required to improve Routine Immunization; for any state specific need please<br />
provide a separate write‐up on objective, strategy, expected output and budgetary basis for the<br />
activities.<br />
A. Basic information of the State/UT related to Immunization Programme<br />
Programme implementation Plan (PIP) for Immunization Programme Year 2011‐2012<br />
District / Corp. Name‐ <strong>Amravati</strong><br />
A‐1 Basic information of the District / Corp.related to Immunization Programme<br />
Position Name Contact No./Email<br />
District <strong>Health</strong> Officer / MOH Dr S. K. Yelurkar 0721/2662591<br />
dhozpamt@gmail.com<br />
Civil Surgeon Dr. C.L. Sonkusre 0721/2663337,38<br />
cs_amaravati@rediffmail.com<br />
District Immunization Officers (DIO) / Dr. R. Bansod (Addi 0721/2550183<br />
Immunization Officers<br />
Charge)<br />
modtt.amravati@gmail.com<br />
RMO Outreach Dr. Bandale 0721/2663337,38<br />
(Addi Charge) cs_amaravati@rediffmail.com<br />
Cold chain Technician Shri Qurishi 0721/2662591<br />
District Level Data Assistant Shri V.P. Badge<br />
dhozpamt@gmail.com<br />
0721/2662591<br />
dhozpamt@gmail.com
A‐2<br />
S.No Beneficiaries<br />
Target<br />
2009‐10 2010‐11 2011‐12<br />
1. Pregnant women 35702 34059 35150<br />
2. 0 to 1 yr infants 31321 32165 32575<br />
3. 1‐2 yr 34123 31321 30321<br />
4. 2‐5 yr 123161 97251 97145<br />
5. 5 yr 44138 51485 51220<br />
6. 10 yr 44138 51485 51220<br />
7. 16 yr 46812 45927 44325<br />
A‐3<br />
The following information is to be filled based on the RI micro‐plans. Please provide the details of<br />
held sessions for 2009‐10 & 10‐11, while for 2011‐12 the number of planned sessions is to be<br />
provided: Please submit information correctly so that budget can be proposed accordingly.<br />
S.No Routine Immunization Sessions 2009‐10<br />
2010‐11 Up to<br />
nov<br />
2011‐12<br />
1. Total Sessions planned (<strong>Rural</strong> +Urban ) (3+4) 22133 14014 21262<br />
2. Total Sessions Held (<strong>Rural</strong> +Urban ) 22092 13991 21262<br />
3. No. of Outreach Sessions (<strong>Rural</strong> +Urban ) (7+8) 19635 12498 18987s<br />
4.<br />
No. of Fixed site (Inst.) Sessions (<strong>Rural</strong> +Urban )<br />
(5+6) 2498 1516 2275<br />
5. No. of Fixed site (Inst.) Sessions (<strong>Rural</strong> ) 1970 11586 1763<br />
6. No. of Fixed site (Inst.) Sessions (Urban ) 528 912 512<br />
7. No. of Outreach Sessions (<strong>Rural</strong>) 18267 1180 17619<br />
8. No. of Outreach Sessions (Urban )<br />
No. of Outreach sessions in hard to reach (Hilly<br />
1368 336 1368<br />
9. )areas(<strong>Rural</strong>) out of No.7<br />
No. of Outreach sessions in hard to reach (Hilly<br />
3982 3982 3982<br />
10. )areas(Urban ) out of No.8<br />
No. of Outreach sessions in hard to reach (Hilly<br />
0 0 0<br />
11. )areas(R+U) out of No.3<br />
No. of session with hired vaccinators* only in<br />
3982 3982 3982<br />
12. urban slum & Corp. ‐‐ ‐‐ ‐‐<br />
13. No. of hired vaccinators* ‐‐ ‐‐ ‐‐<br />
14. No. of villages where sessions are held monthly<br />
No. of villages (smaller) where sessions are held<br />
1338 1338 1338<br />
15. on alternate months 100 100 100<br />
16. No. of villages where sessions are held quarterly 120 120 120
B. Existing Support to the District/ Corp.<br />
C.<br />
Sl<br />
N<br />
o<br />
Item<br />
Stock (functional) as<br />
on 31st Dec'10 2009‐10<br />
Requirement<br />
2010‐11 2011‐12<br />
1 Cold Chain Equipments ‐<br />
a) WIC<br />
b) WIF<br />
c) ILR 140, 54 20 20 12<br />
c) ILR 300 4 2<br />
1<br />
2 2<br />
d) DF 140 69 15 15 10<br />
d) DF 300 7 2<br />
1<br />
2 2<br />
e) Cold Boxes 197 10 10 20<br />
f) Vaccine Carrier 2470 300 350 800<br />
g) Ice Pack 20000 350 350 5000<br />
h) Vaccine Van Not Functional 1 1 1<br />
2<br />
Vaccine stock and requirement (including 25% wastage and 25%<br />
buffer)<br />
a) TT 21000 21600 21700 260000<br />
b) BCG 6700 48000 50000 52000<br />
c) OPV 28000 180000 260000 265000<br />
d) DPT* 29000 168000 260000 290000<br />
e) Measles 5000 48000 50000 52000<br />
f) Hep B 0 168000 141000 170000<br />
g) JE (Routine) 0 48000 52000 54000<br />
3 Syringes including wastage of 10% and 25 % buffer<br />
a) 0.1 ml 200 30000 50000 53000<br />
b) 0.5 ml 12000 406000 489480 510500<br />
c)<br />
Reconstitution<br />
Syringes 600<br />
70000<br />
130700 140000<br />
4 Hub Cutters 0 500 500 500<br />
*Note: DPT is to be given instead of DT at 5 yrs once the current stock of DT Vaccine<br />
is exhausted<br />
Remar<br />
ks
D. Additional Support required by the District/ Corp.<br />
Service Delivery: ‐ Norms*<br />
Mobility support for supervision @Rs.50,000 per District for district level officers<br />
(this includes POL and maintenance) per year<br />
Supervisory visits by state and district level<br />
officers for monitoring and supervision of RI By state level officers @ Rs.100,000 /year<br />
Cold Chain maintenance<br />
Focus on slum & underserved areas in<br />
urban areas:<br />
@ Rs 500 per PHC/CHC per year District Rs 10,000<br />
per year<br />
Hiring an ANM @Rs.300/session for four<br />
sessions/month/slum of 10000 population and<br />
Rs.200/‐ per month as contingency per slum of i.e.<br />
total expense of Rs. 1400/‐ per month per slum of<br />
10000 population.<br />
Expenditure<br />
2009‐10<br />
Achievement<br />
Expenditure & Achievement Remarks<br />
2010‐11(till<br />
Nov )<br />
2011‐12<br />
Expenditure<br />
Achievement<br />
Funds<br />
requirement<br />
0.18 0.05 0.5<br />
Target<br />
0.01 1.11% 0 0% 0.5 100%<br />
0 0 0 0
Service Delivery: ‐ Norms*<br />
Mobilization of children through ASHA/<br />
mobilizers<br />
Alternative Vaccine Delivery:<br />
Expen<br />
diture<br />
2009‐10<br />
Achiev<br />
ement<br />
Expenditure & Achievement Remarks<br />
2010‐11(till<br />
Nov )<br />
2011‐12<br />
Expen<br />
diture<br />
Achiev<br />
ement<br />
Funds<br />
requirement<br />
Target<br />
@ Rs 150/session (for all states/UT.s) 27.36 19594 16.92 12488 31.89 21262<br />
Geographically hard to reach areas (eg. Session<br />
site>30 kms from vaccine delivery point, river<br />
0 0<br />
0<br />
crossing etc.) @ Rs 100 per RI session<br />
11.15<br />
6.75<br />
0<br />
NE States and Hilly terrains @100 per RI session 4107 1958 3.98 3982<br />
For RI session in other areas @ Rs.50 per session.<br />
15487<br />
10530 8.64 17280<br />
State @Rs 12,000‐ 15,000 p.m.<br />
Support for Computer Assistant for RI<br />
reporting (with annual increment of 10%<br />
w.e.f. from 2010‐11) Districts @ Rs 8000‐ 10,000 p.m 0.95<br />
Printing and dissemination of<br />
immunization cards, tally sheets,<br />
monitoring forms, etc.<br />
1 1 1<br />
@ Rs 5 per beneficiary ‐‐‐‐‐‐‐‐ ‐‐‐‐‐‐‐ ‐‐‐‐‐‐‐ ‐‐‐‐‐‐‐ ‐‐‐‐‐‐‐ ‐‐‐‐‐‐‐ ‐‐‐‐‐‐‐<br />
Yes<br />
0.64<br />
Yes<br />
1.16
Service Delivery: ‐ Norms*<br />
Review Meetings<br />
Trainings<br />
District level orientation training for 2 days<br />
ANM, Multi Purpose <strong>Health</strong> Worker<br />
(Male), LHV, <strong>Health</strong> Assistant (Male /<br />
Female), Nurse Mid Wives, BEEs & other<br />
specialist (as per RCH norms)<br />
Quarterly Review & feedback meeting for<br />
exclusive for RI at district level with one<br />
Block MO.s, ICDS CDPO and other<br />
stakeholders@ Rs 100/‐ per participant<br />
for meeting expenses (lunch,<br />
organizational expenses)<br />
Quarterly review meeting exclusive for RI<br />
at Block level @Rs 50/‐pp as honorarium<br />
for ASHAs (travel) and Rs 25 per person at<br />
the disposal of MO‐I/C for meeting<br />
expenses(refreshments, stationery and<br />
misc. expenses)<br />
As per revised norms for trainings under<br />
RCH<br />
Expenditure<br />
Expenditure & Achievement Remarks<br />
2009‐10 2010‐11(till Nov ) 2011‐12<br />
Achievement<br />
Expenditure<br />
Achievement<br />
Funds<br />
requirement<br />
Target<br />
0.04 1 0.00 0 0.40 5<br />
0.62 8 1.4 28 6.2 56<br />
0<br />
No of<br />
persons<br />
trained<br />
0<br />
0<br />
No of<br />
persons<br />
trained<br />
0<br />
0<br />
No of<br />
persons<br />
trained<br />
0
Service Delivery: ‐ Norms*<br />
Three day training of Medical Officers on RI<br />
using revised MO training module<br />
One day refresher training of District RI<br />
Computer Assistants on RIMS/HMIS and<br />
Immunization formats under NRHM<br />
One day Cold Chain handlers training for<br />
block level cold chain handlers by State and<br />
District Cold Chain Officers and DIO for a<br />
batch of 15‐20 trainees and three trainers<br />
One day Training of block level data<br />
handlers by DIO and District Cold chain<br />
Officer to train about the reporting formats<br />
of Immunization and NRHM<br />
As per revised norms for trainings under<br />
RCH<br />
As per revised norms for trainings under<br />
RCH<br />
As per revised norms for trainings under<br />
RCH<br />
As per revised norms for trainings under<br />
RCH<br />
Expen<br />
diture<br />
Expenditure & Achievement Remarks<br />
2009‐10 2010‐11(till Nov ) 2011‐12<br />
Achiev<br />
ement<br />
No of<br />
persons<br />
trained<br />
Expen<br />
diture<br />
Achiev<br />
ement<br />
No of<br />
persons<br />
trained<br />
Funds<br />
requirement<br />
Target<br />
No of<br />
persons<br />
trained<br />
0 0 0 0 0.05 1<br />
No of<br />
persons<br />
trained<br />
No of<br />
persons<br />
trained<br />
No of<br />
persons<br />
trained<br />
No of<br />
persons<br />
trained<br />
No of<br />
persons<br />
trained<br />
No of<br />
persons<br />
trained
Service Delivery: ‐ Norms<br />
Microplanning<br />
To develop sub‐center and PHC microplans using bottom up<br />
planning with participation of ANM, ASHA, AWW<br />
POL for vaccine delivery from State to District and from<br />
district to PHC/CHCs<br />
Consumables for computer including provision for internet<br />
access for RIMS<br />
Injection Safety<br />
@ Rs 100/‐ per subcentre (meeting at<br />
block level, logistic)<br />
For consolidation of microplan at<br />
PHC/CHC level @ Rs 1000/‐ block & at<br />
district level @ Rs 2000/‐ per district<br />
Rs100,000/ district/year<br />
Red/Black Plastic bags etc @ Rs 2/bags/session<br />
Bleach/Hypochlorite solution @ Rs 500 per PHC/CHC per year<br />
Twin bucket @ Rs 400 per PHC/CHC per year<br />
Any District / Corp Specific Need with justification (Please<br />
provide a separate write‐up on objective, strategy,<br />
expected output and outcomes, basis for cost estimates<br />
etc.)<br />
Expen<br />
diture<br />
2009‐10<br />
Achiev<br />
ement<br />
Expenditure & Achievement Remarks<br />
2010‐11(till Nov<br />
)<br />
2011‐12<br />
Expen<br />
diture<br />
Achiev<br />
ement<br />
Funds<br />
requirement<br />
0.29 0 0.03 0 0.33<br />
0 0 0<br />
Yes<br />
0.16<br />
Target<br />
348<br />
0.77 90.59% 0.60 70.59% 1.0 100%<br />
@ 400/ ‐ month/ district 0.01 0 0 0.05<br />
0<br />
% funds<br />
used<br />
0<br />
% Funds<br />
used<br />
Total Budget 41.38 26.39 54.86<br />
% Funds<br />
used<br />
At State<br />
Level
Form D ‐ Name of District/ Corp –wise Coverage reports (in numbers)<br />
S. No<br />
S. No<br />
Name of<br />
District / Corp<br />
Yearly Target<br />
(2010‐11)<br />
Infants Pregnant<br />
Women<br />
BCG Coverage<br />
(in Numbers)<br />
OPV ‐ 1st Dose<br />
Coverage<br />
(in Numbers)<br />
OPV ‐ 3rd Dose<br />
Coverage<br />
(in Numbers)<br />
DPT ‐ 1st Dose<br />
Coverage<br />
(in Numbers)<br />
DPT ‐ 3rd Dose<br />
Coverage (in Numbers)<br />
2009‐10 2010‐11* 2009‐10 2010‐11* 2009‐10 2010‐11* 2009‐10 2010‐11* 2009‐10 2010‐11*<br />
32165 34059 32951 21734 33928 21943 32794 20805 33596 22018 32736 20805<br />
TOTAL 32165 34059 32951 21734 33928 21943 32794 20805 33596 22018 32736 20805<br />
Name of District<br />
/ Corp<br />
TOTAL<br />
# Coverage for 2010‐11 till Dec’10<br />
Measles Coverage<br />
District / –wise VPD reports in 2010‐11 (in numbers)<br />
S.<br />
No<br />
TT2+Booster Coverage<br />
Hep B ‐ Birth Dose<br />
Coverage (Wherever<br />
applicable)<br />
Hep B ‐ 1st Dose<br />
Coverage (Wherever<br />
applicable)<br />
Hep B ‐ 3rd Dose<br />
Coverage (Wherever<br />
applicable)<br />
2009‐10 2010‐11* 2009‐10 2010‐11* 2009‐10 2010‐11* 2009‐10 2010‐11* 2009‐10 2010‐11* 2009‐10<br />
32670 20715 36849 22768 0 2971 24698 22004 21134 20660 14231<br />
32670 20715 36849 22768 0 2971 24698 22004 21134 20660 14231<br />
JE‐routine<br />
(Wherever applicable)<br />
Name Diphtheria Whooping Cough Neonatal Tetanus a Measles Polio AES<br />
of the<br />
District/<br />
Cases Deaths<br />
Corp Cases Deaths Cases Deaths Cases Deaths Cases Deaths Cases Deaths Cases Deaths<br />
0 0 0 0 0 0 0 0 2 0 0 0 0 0<br />
TOTAL 0 0 0 0 0 0 0 0 2 0 0 0 0 0<br />
2010‐11*<br />
3828<br />
3828
C.6 Consolidated Budget of Routine Immunisation<br />
Sl. No. Activity Unit Cost Physical<br />
Targets<br />
C IMMUNISATION<br />
Routine Immunization<br />
C.1 RI strengthening project (Review meeting,<br />
Mobility support, Outreach services etc)<br />
Required fund<br />
under NRHM<br />
0 21262 53.15<br />
C.2 Salary of Contractual Staffs 0.09.06 1 1.16<br />
C.3 Training under Immunisation 0.05 0 0.05<br />
C.4 Cold chain maintenance 0.50 70 0.50<br />
C.5 Pulse Polio operating costs 0 0 0<br />
Total.. 54.86
OTHER DISEASE<br />
PROGRAMME
<strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong><br />
<strong>National</strong> Vector Born Disease<br />
Control Programme<br />
PIP 2011‐12
Disease Cash<br />
assistance<br />
from GoI<br />
Malaria<br />
a. DBS<br />
b. World Bank for<br />
project states<br />
c. GFATM for project<br />
states<br />
EXECUTIVE SUMMARY<br />
In the state Maharashtra vector borne diseases are major<br />
public health problem.<br />
Malaria is endemic in districts viz; Amaravati.<br />
Filaria is endemic in ‐‐‐ districts viz; Amaravati.<br />
Kala azar is endemic in ‐‐‐ districts viz; Nil .<br />
AES including JE is endemic in ‐‐‐ districts viz; Nil .<br />
Dengue is endemic in ‐‐‐ districts viz; Amaravati.<br />
Chikungunya is endemic in ‐‐‐ districts viz; Amaravati.<br />
The requirement for programme implementation has been indicated<br />
in detail and the summary is indicated below :<br />
0<br />
0<br />
0<br />
0<br />
Balance<br />
from<br />
previous<br />
years<br />
0<br />
0<br />
0<br />
0<br />
Committed<br />
expenditure<br />
32809210<br />
0<br />
0<br />
0<br />
Net<br />
requirement<br />
32809210<br />
0<br />
0<br />
0<br />
State<br />
resources<br />
Maharashtra<br />
0<br />
0<br />
Filaria 0 0 4218000 4218000 Maharashtra<br />
Kala‐azar 0 0 0 0 0<br />
Kala‐azar World Bank<br />
Project assistance<br />
0 0 0 0 0<br />
AES including JE 0 0 0 0 0<br />
Dengue<br />
Chikungunya<br />
0 0 375000 375000 Maharashtra<br />
Total 0 0 37402210 37402210 Maharashtra<br />
District Malaria Officer<br />
Amaravati<br />
0
Malaria<br />
DBS<br />
Expenditure ( Financial Performance)‐ Budget Proposal<br />
2010‐11<br />
Up to Oct<br />
2010<br />
2011‐12<br />
(Proposed)*<br />
MPW (Salary for Contractual) 144000 288000<br />
ASHA 80000 160000<br />
Operational Cost including spray wages<br />
NAMMIS 0 66000<br />
IEC<br />
,BCC<br />
&PPP<br />
Training (MPW)<br />
ASHA<br />
Spray worker<br />
Additional support under World Bank (if<br />
applicable)<br />
Human Resource<br />
LT<br />
26000<br />
0<br />
0<br />
0<br />
0<br />
0<br />
0<br />
200000<br />
66000<br />
200000<br />
164610<br />
618000<br />
42600<br />
100000<br />
Capacity building in project areas 0 500000<br />
Mobility support<br />
DMO Vehicle TATA SUMO<br />
ADMO Vehicle TATA SUMO<br />
Office Truck<br />
Taluka Superviser Vihicle<br />
POL<br />
Additional support under GFATM (if applicable)<br />
0<br />
0<br />
0<br />
0<br />
20000<br />
700000<br />
700000<br />
1000000<br />
150000<br />
120000<br />
Capacity Building 0 0<br />
Establishment State Society 0 0<br />
Human Resource 0 0<br />
Monitoring & Evaluation 0 0<br />
BCC/<br />
PPP/<br />
Soc.Mkt. (BS Back lock)<br />
Drugs<br />
Chloroquine phosphate tablets 0 200000<br />
Primaquine tablets 0 50000<br />
Quinine sulphate tablets 0 500000<br />
0<br />
0<br />
0<br />
0<br />
0<br />
0<br />
(Rs. in lakhs)<br />
Support to be met<br />
from NVBDCP/GoI<br />
or state resources<br />
or NRHM flexi fund
2010‐11<br />
Up to Oct<br />
2010<br />
2011‐12<br />
(Proposed)*<br />
Quinine Injections 0 20000<br />
Sulphadoxine + Pyremethamine tablets 0 50000<br />
Diagnostics<br />
RDT ASHA 2059 X 60 \30 X 3000 0 12354000<br />
IRS<br />
SFW Pay<br />
FW Pay<br />
0<br />
0<br />
360000<br />
1440000<br />
Wages 0 0<br />
Human resource 0 0<br />
Monitoring & Evaluation 0 50000<br />
Bednet<br />
Impregnated mosquito nets 150000 Population 0 5000000<br />
LLIN 150000 Population 0 5000000<br />
Insecticides 0 0<br />
DDT 50% wdp 0 0<br />
Synthetic Pyrethroid 5% WP 5625 Kg 0 765000<br />
Malathion 25%/Technical 0 25000<br />
UMS – Larvicides 0 0<br />
For polluted water Abate 0 100000<br />
For non‐polluted water 0 100000<br />
Pyrethrum extract 2% 0 100000<br />
Urban Malaria Scheme Corporation AMT<br />
(Slide Box, Insectiside, Hatch Rich, etc) 0 100000<br />
Other (Innovation) 0 152000<br />
Total Malaria 270000 32809210<br />
Filaria<br />
Drugs (by GoI) 0 0<br />
Training 0 880000<br />
BCC 0 240000<br />
Preparatory activity (may be shown activity‐wise<br />
including hydrocelectomy) 0 258000<br />
Drug distributor’s including ASHA and<br />
supervisors honorarium 0 890000<br />
FO Officer TATA SUMO Vehicle (Purchase New<br />
Vehicle)<br />
AFO Officer TATA SUME Vehicle (Purchase New<br />
Vehicle)<br />
POL (for 2 Vehicles)<br />
0<br />
0<br />
0<br />
700000<br />
700000<br />
400000<br />
Morbidity Management Kit 0 50000<br />
Night Clinic & Ragular Survey 0 50000<br />
Support to be met<br />
from NVBDCP/GoI<br />
or state resources<br />
or NRHM flexi fund
2010‐11<br />
Up to Oct<br />
2010<br />
2011‐12<br />
(Proposed)*<br />
Tarch, Slide Box etc 0 50000<br />
Total (Filaria) 0 4218000<br />
Dengue/Chikungunya<br />
Grant in respect of Dengue and Chikungunya<br />
Strengthening surveillance (As per GOI approval)<br />
Apex Referral Labs recurrent @ Rs/ 1.00 lakh<br />
Sentinel surveillance Hospital recurrent @<br />
Rs.0.50 lakhs<br />
Test kits (Nos.) to be supplied by GoI<br />
Monitoring/Supervision and Rapid Response 0 100000<br />
Epidemic Preparedness<br />
IEC/BCC/Social Mobilization<br />
0 50000<br />
0 25000<br />
Training/Workshop 0 200000<br />
Total Dengue/Chikungunya 0 375000<br />
AES/JE 0 0<br />
Diagnostics and Management 0 0<br />
Elisa Kits 0 0<br />
IEC/BCC 0 0<br />
Training 0 0<br />
Monitoring and Supervision 0 0<br />
Technical Malathion 0 0<br />
Total AES/JE 0 0<br />
Kala‐azar (only for 4 states) 0 0<br />
DDT 50% 0 0<br />
Amphotericin‐B 0 0<br />
Miltefosine 0 0<br />
RDK for Kala‐azar 0 0<br />
Case search 0 0<br />
Spray Pumps 0 0<br />
Operational cost for spray including spray wages 0 0<br />
Mobility/POL 0 0<br />
Training for spraying 0 0<br />
BCC/IEC 0 0<br />
Monitoring & Evaluation 0 0<br />
Kala‐azar Sub‐Total (DBS) 0 0<br />
Kala‐azar World Bank Project assistance 0 0<br />
Support to be met<br />
from NVBDCP/GoI<br />
or state resources<br />
or NRHM flexi fund
2010‐11<br />
Up to Oct<br />
2010<br />
2011‐12<br />
(Proposed)*<br />
Human resource 0 0<br />
Capacity building 0 0<br />
Mobility 0 0<br />
Kala‐azar Sub‐total (World Bank Project<br />
assistance) 0 0<br />
Kala‐azar Total 0 0<br />
Grand Total 270000 37402210<br />
Any activity not listed and if required may be shown in separate row.<br />
Outstanding balance Nil (as on previous month of submission of PIP).<br />
Committed expenditure Nil (till March, 2011).<br />
Balance expected Nil (on 1.04.2011).<br />
Support to be met<br />
from NVBDCP/GoI<br />
or state resources<br />
or NRHM flexi fund<br />
This is most important as cash releases are based on the funds availability with state in totality<br />
and not head wise.
<strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong><br />
<strong>National</strong> Leprosy Elimination<br />
Programme<br />
PIP 2011‐12
Sr<br />
No<br />
Total budjet provision praposed for <strong>Amravati</strong> distt<br />
Format for Submitting budget Praposal<br />
Activity Praposed Amount<br />
Praposed<br />
1 Contractual Services Distt 6000<br />
2 Office Expensences 35000<br />
3 Consumable 20000<br />
3b Services through AHSA/USHA(Insentive _ Sensetidation) 62000<br />
4 Capacity Building(Training)<br />
4 days training of Newly appointed MO's(<strong>Rural</strong>,Urban) 188430<br />
3 days training of Newly appointed HW,HA,Hs 192150<br />
2 days refresher training of MO's 63310<br />
5 days training of newly appointed Lab.Tech 7800<br />
5 Behavioural Change Communication(IEC)<br />
Mass Media,Out door media,<strong>Rural</strong> Media & Adocacy 35000<br />
6 DPMR<br />
MCR Footwear, 200000<br />
Aids & appliance,,(goggles,Splint & Self Care kits etc) 77000<br />
Welfare allowance to BPL pts for RCS 150000<br />
Estblishment of new Referal Center(Dryapur,Morshi,Warud) 315000<br />
Screening Camp for RCS Pts. at GH & SDH 15000<br />
7 Urban lep.control<br />
Township,medium city‐1,medium city‐2, Megh cities ‐ 145000<br />
8 Material & Supplies<br />
Supprtative drug 32000<br />
Equipment , (Computer, Printer etc) 145000<br />
9 Supervision & monitoring of DNT team 36000<br />
10 Pol/Vehicale opretion & highring‐2 vehicle at State level &<br />
one at Distt level<br />
100000<br />
Total 1,824,690.00<br />
Remarks
<strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong><br />
Revised <strong>National</strong> Tuberculosis<br />
Control Programme<br />
PIP 2011‐12
RNTCP<br />
Section D: Summary of proposed budget for the district –<br />
Budget estimate for the coming FY 2011‐ 12<br />
S.No. Category of Expenditure (To be based on the planned activities and<br />
expenditure in Section C)<br />
1 Civil works 135300<br />
2 Laboratory materials 212573<br />
3 Honorarium 641907<br />
4 IEC/ Publicity 140994<br />
5 Equipment maintenance 78000<br />
6 Training 629406<br />
7 Vehicle maintenance 300000<br />
8 Vehicle hiring 441000<br />
9 NGO/PP support 286000<br />
10 Miscellaneous 668128<br />
11 Contractual services 3185800<br />
12 Printing 81845<br />
13 Research and studies 0<br />
14 Medical Colleges 0<br />
15 Procurement –vehicles 0<br />
16 Procurement – equipment 0<br />
TOTAL 6800953<br />
** Only if authorized in writing by the Central TB Division<br />
• Additionality Funds from NRHM‐Details of the activities for which Additionality Funds<br />
are proposed to be sought.<br />
Proposed activities and Budget for RNTCP under NRHM Additionalties<br />
for the Year 2011‐2012<br />
Sr.No Category of Expenditure<br />
Budget for<br />
NRHM<br />
Additionalties<br />
FY 2011 ‐ 2012<br />
1 Wall paintings for each PHI (56 PHC + 14 RH) 1,05,000<br />
2<br />
Travel cost of MDR TB suspect to DTC for examination and sending the<br />
sample (500 suspect x Rs 200 per person public transport cost x 2 person)<br />
200000<br />
3 Special Investigations for MDR T.B. Patient (25X800)<br />
For Tribal Area Only<br />
20000<br />
4 Travel Cost for Patients & 1 attendant for X‐ray Examination (Expected<br />
200 NSN Patient likely X‐ray done 400X 300)<br />
120000<br />
5 Travel Cost for T.B. Patient Referred for HIV Testing (ICTC) Expected<br />
patient 466X150<br />
70000<br />
6 Travel Cost for T.B. /HIV Co‐infected Patient to ART Centre (50X500) 25000<br />
Grand Total 540000
<strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong><br />
<strong>National</strong> Programme for<br />
Control of Blindness<br />
PIP 2011-12
<strong>National</strong> Programme for Control of Blindness<br />
PIP for the year 2011‐12 – Maharashtra State <strong>Amravati</strong><br />
Trachoma Control Programme was launched in 1972‐73 in the state, and then it was<br />
reformed as <strong>National</strong> Programme for Control of Blindness in the year 1976 as 100 % centrally<br />
sponsored scheme with the goal of reducing the prevalence of blindness to 0.3% by 2020. Rapid<br />
survey on avoidable blindness conducted under NPCB during 2006 ‐07 showed reduction in the<br />
prevalence rate of blindness from 1.1% (2001 – 02) to 1% (2006‐07).<br />
The target for the 11 th five year plan is to reduce the prevalence rate of blindness to the level<br />
of 0.8% till 2012.<br />
The main objectives of the programme are :<br />
a. To reduce the backlog of the blindness through identification & treatment of blind<br />
b. To develop comprehensive eye care facilities in every district<br />
c. To develop human resources for providing eye care services<br />
d. To improve quality of service delivery<br />
e. To secure participation of voluntary organization / private practitioner in eye care<br />
f. To enhance community awareness of eye care<br />
To implement the Programme successfully, State <strong>Health</strong> Society Maharashra (Blindness<br />
Division) & District Integrated <strong>Health</strong> & Family Welfare Societies (Blindness Division) are establish in<br />
all the Districts of Maharashtra State including Bruhanmumbai Municipal Corporation as per the<br />
guidelines from Govt of India.<br />
The Programme was oriented mainly for Blind Survey, Cataract Surgeries & Screening of<br />
School Children with provision of Spectacles to the students having refractive errors. However,<br />
management of cases of Diabetic Retinopathy, Glaucoma Management, Corneal Transplantation,<br />
Vitreoretinal Surgery, and Treatment of Childhood Blindness is included for financial assistance in<br />
11 th Five Year Plan.<br />
General Information ‐<br />
Total Population of <strong>Amravati</strong> :‐ 630705<br />
Urban population :‐ 409823<br />
<strong>Rural</strong> Population :‐ 1770492<br />
Total No of Districts Population :‐ 2811020<br />
Similarly, following <strong>Health</strong> Institutional infrastructure available in Maharahstra State to implement<br />
the NPCB in Maharashtra state for management of Eye Care.
Infrastructure in Maharashtra State<br />
Sr. No. Name of Institute No<br />
1 Medical College (private) 2<br />
2 Super Specialty Hospitals 1<br />
3 District Hospitals 1<br />
4 Women Hospital 1<br />
5 General Hospital 1<br />
6 Sub District Hospital 4<br />
7 <strong>Rural</strong> Hospital 9<br />
8 Primary <strong>Health</strong> Centers 56<br />
Infrastructure under NPCB<br />
Sr. No. Name of Institute No<br />
1 Catops Centers 4<br />
2 <strong>Health</strong> Institutes having Dedicated 20 Beded Eye Ward 1<br />
3 District Mobile Units 1<br />
4 PMOOs working in Primary <strong>Health</strong> Centers 11<br />
5 PMOOs working in Sub District / <strong>Rural</strong> Hospital 12<br />
6 PMOOs working in District Hospital 3<br />
7 No of NGO’s Registered under NPCB for GIA 2<br />
Govt Eye Banks 1<br />
8 Eye Banks – 2<br />
Corporation Eye Bank 0<br />
NGO Eye Banks 0<br />
Private Eye Bank 1<br />
9 Vision Centers 1<br />
Manpower available under NPCB<br />
1<br />
Ophthalmic Surgeon ‐ Class I<br />
2 Available Ophthalmic Surgeons<br />
3<br />
Para Medical Ophthalmic Officers<br />
Performance of cataract Surgeries(GOVT)<br />
Sanctioned 2<br />
Filled in 0<br />
Vacant 2<br />
Govt.(oprating) 3<br />
NGO 2<br />
Sactioned 25<br />
Filled in 23<br />
Vancant 2<br />
Year<br />
Annual<br />
Target<br />
Achiev.<br />
%<br />
Achiev<br />
2007‐08 8000 8051 101<br />
2008‐09 9000 9285 103<br />
2009‐10 8500 8011 94<br />
2010 – 11 ( DEC 10) 9000 3426 38
Screening of School Children<br />
Year<br />
Students Screened Students with Free spects<br />
Target Achivement refractive errors provided<br />
2007‐08 55872 50837 1273 975<br />
2008‐09 55872 41673 1290 957<br />
2009‐10 55872 35335 2724 1118<br />
2010 – 11 (DEC 10) 55872 33534 1650 256<br />
Performance of Eye Donation & Keratoplasties<br />
Year<br />
Target<br />
Eye Balls collected<br />
Achievement %<br />
No. of<br />
Keratoplasties<br />
Surgery<br />
%<br />
2007‐08 40 0 0 0 0<br />
2008‐09 100 20 20 0 0<br />
2009‐10 100 18 18 0 0<br />
2010 – 11 ( NOV<br />
10)<br />
40 16 40 0 0<br />
1) Proposal for Non Recurring Assistance as per guidelines from GOI ‐<br />
1) The Non Recurring GIA for Strengthening & Upgradation of Medical Colleges on the lines<br />
of Shankara Hospital Chennai for treatment of Other Eye Diseases like ROP – Rs. 40.00<br />
lakhs per College<br />
There are 14 Govt Medical Colleges, 4 Corporation Medical Collage & 1 Armed Forces<br />
Medical Collage in the State. All these medical collages are provided with funds for up<br />
gradation in the year 2008 – 09.<br />
It is proposed to develop Ophthalmic Dept of GMC Latur, & GMC Akola on the lines of<br />
Shnakara Hosptial Chennai for treatment of Other Eye Diseases. The Ophthalmic Surgeons of<br />
these medical colleges will be trained at Shankara Hospital Chennai & equipment,<br />
instruments will be provided.<br />
The total fund requirement is Rs. 80.00 Lakhs<br />
2) The Non Recurring GIA for Upgradation & Strengthening of District Hospital ‐‐ Rs. 20.00<br />
Lakhs per Hospital<br />
Following Districts are proposed for upgradation & strengthening of District Hospitals<br />
Sr.No. District Amount Justification<br />
1 District Hospital Gadchiroli 20.00 lakhs<br />
2 District Hospital Gondia 20.00 lakhs<br />
3 District Hospital Chandrapur 20.00 lakhs<br />
4 District Hospital Sindhudurg 20.00 Lakhs<br />
5 District Hospital Jalgoan 20.00 Lakhs<br />
6 District Hospital Buldhana 20.00 Lakhs<br />
7 District Hospital Satara 20.00 Lakhs<br />
Total 140.00 Lakhs<br />
The district is tribal & remote<br />
district. No other major hospitals<br />
working for ophthalmology in the<br />
district<br />
Needs Strengthening
Out of 23 District Hospitals 2 District Hospitals namely DH Bhandara, & DH Nadurbar are<br />
sanctioned in 2010 – 11, remaining 21 DH will be upgraded in phased manner taking 7 DH<br />
each year in next 3 years. Funds required ‐ Rs. 140.00 Lakhs.<br />
3) The Non Recurring GIA for Upgradation & Strengthening of Eye Banks in NGO & Govt<br />
Sector – Rs. 15.00 lakhs per Eye Banks<br />
The following Eye Banks in Govt. Sector are proposed for upgradation & strengthening of<br />
Eye banks.<br />
Sr.No. District Amount Justification<br />
1 District Hospital AMARAVATI 20.00 lakhs The district is tribal & remote.<br />
No other major hospitals<br />
working for ophthalmology in<br />
the district<br />
Need strengthening.<br />
Total 20.00 lakhs<br />
It is proposed to strengthen Eye Banks DH in a phased manner and will be upgraded in 3<br />
years (i.e. 2011 – 12 –> 8, ; 2012‐13 –> 8; 2013‐14 –> 7). Funds Required ‐ Rs. 20.00 Lakhs.<br />
4) The Non Recurring GIA for Upgredation & Expansion of Eye Care Units of NGO – GIA to the<br />
tune of Rs. 30.00 Lakhs per NGO<br />
The NGO from Beed has submitted proposal for upgradation & Expansion.<br />
S.No. Name of Eye Care Unit Amount Justification<br />
1 Leprossy <strong>Mission</strong> Trust Hospital<br />
& Reseearch Center, Kothara<br />
Distt.<strong>Amravati</strong><br />
30.00 Lakhs The performance of Eye Care Unit is<br />
very good in the last 5 years. The<br />
proposal form the Eye Care Unit is<br />
received.<br />
2 Mahalaxmi Netralaya & 10.00 Lakhs The performance of Eye Care Unit is<br />
Reseearch Center,<br />
very good in the last 2 years. The<br />
Distt.<strong>Amravati</strong><br />
proposal form the Eye Care Unit is<br />
received.<br />
Total 40.00 Lakhs<br />
Funds required ‐ Rs. 40.00 Lakhs.<br />
5) Estd of Vision Center in NGO & Govt Sector Rs. 0.50 lakhs Only –<br />
All DHs have vision centers 16 SDH & 18 RH require vision centers those are proposed for<br />
inclusion in PIP 2011 – 12.<br />
Funds required for 16 SDH Rs. 8.00 Lakhs ( Rs. 0.50 Lakhs per center)<br />
Fuds required for 18 RH Rs. 9.00 Lakhs (Rs. 0.50 Lakkhs per center)<br />
Total Funds required for 2Vision Centers Rs. 1.0 Lakhs
6) The Non Recurring GIA for Upgredation & Strengthening of Sub District Hospital – GIA to<br />
the tune of Rs.5.00 Lakhs per SDH<br />
Sr.No. District Amount Justification<br />
1<br />
2<br />
3<br />
4<br />
SDH Achalpur Tq.Disrict<br />
<strong>Amravati</strong><br />
5.00 lakhs<br />
It is 100 beded hospital, where class I<br />
Ophthalmic Surgeon is working as a M.S.. &<br />
located in Tribal area.<br />
SDH Morshi<br />
<strong>Amravati</strong><br />
Tq.District<br />
5.00 Lakhs It is 50 beded hospitals<br />
SDH Dharni<br />
<strong>Amravati</strong><br />
Tq.District<br />
5.00 Lakhs<br />
It is 50 beded hospital, located in Tribal<br />
area<br />
SDH Daryapur<br />
<strong>Amravati</strong><br />
Tq.District<br />
5.00 Lakhs It is 50 beded hospital,<br />
Total 20.00 Lakhs<br />
Funds required ‐ Rs. 20.00 Lakhs.<br />
7) The Non Recurring GIA for Upgredation & Strengthening of Eye Donation Center (Govt /<br />
NGO Sector) – GIA to the tune of Rs.1.00 Lakhs per EDC<br />
Sr.No. District Amount Justification<br />
1 SDH Achalpur 1.00 lakhs<br />
2 SDH Morshi 1.00 lakhs<br />
3 SDH Dharni 1.00 lakhs<br />
4 SDH Daryapur 1.00 Lakhs<br />
Funds required Rs. 4.00 Lakhs. .<br />
B) Proposal for Recurring Assistance as per guidelines from GOI‐<br />
The district is tribal & remote. No other major<br />
hospitals working for ophthalmology in the<br />
district<br />
1) GIA for Cataract Operations – .<br />
The total expected Cataract Surgeries in the <strong>Amravati</strong> during 2011‐12 are 9000 The average<br />
performance of catops in Govt. & NGO Hospitals 9000. The expected number of catops<br />
during 2011‐12 in Govt. & NGOs will be 9000 surgeries.<br />
Expected Catops in Govt. Assistance per catops Total funds required<br />
Hospital & Registered NGOs<br />
9000 Rs. 750.00 Rs. 9750.00 lakhs<br />
Funds required GIA for Cataract operation is only Rs. 9750.00 Lakhs<br />
2) GIA for Other Eye Diseases – Rs. 16.00 Lakhs.<br />
The total expected other Eye Disease detection in the State during 2011‐12 are 32000.<br />
Roughly 50% of these surgeries will be performed in Govt. Hospitals & Registered NGO for<br />
getting GIA. It is proposed to sanction GIA for other Eye Diseases as mentioned in following<br />
table.
Expected Other Eye Diseases in Govt.<br />
Hospital & Registered NGOs<br />
Assistance per Surgery Total funds required<br />
500 Rs. 16.00 lakhs<br />
Less : unspent of 2010 – 11 Rs. 1000.00<br />
Rs. 10.00 Lakhs<br />
Total Funds required<br />
Rs. 26.00 Lakhs<br />
This year a balance of about Rs. 100.00 Lakhs is expected because this programme was<br />
launched in this year only and next year we expect greater momentum to this activity. Funds<br />
required ‐ GIA for Other Eye Diseases is Rs.2 6.00 Lakhs.<br />
3) GIA for free spectacles distribution to poor students having refractive error –<br />
The target for screening of school children for the year 2010‐11 is 1800. The same number of<br />
school children will be screened during 2011‐12. As per rough estimation 3 ‐ 4% of the<br />
students have refractive error. So the total number of students having refractive error will<br />
be 1.40 lakhs. Approximately 30% of students are poor so approximately 42000 students will<br />
require free spectacles.<br />
Eastimaed number of poor Students to whom<br />
free spects are distributed<br />
Cost of per pair<br />
spectacles<br />
Total funds required<br />
1800 Rs.200.00 per pair Rs. 3.60 Lakhs<br />
This year (2010 – 11) since spectacles to poor students are provided from Sarva Shiksha<br />
Abhiyan a balance of equivalent funds is likely therefore no additional funds are required.<br />
4) GIA for Eye Ball Collection ‐ Rs. 1.00 Lakhs.<br />
The maximum Eye Ball Collection in the <strong>Amravati</strong> in last five years is 40 . The estimated Eye<br />
Ball Collection during year 2011‐12 will be 20 So GIA required for this activity as under<br />
Estimated Eye Ball Collection GIA per Eye Ball Total funds required<br />
20 Rs.750.00 per Eye Ball Rs. 15000.00<br />
Funds required GIA for free Eye ball collection is Rs. 15000<br />
5) Training Activities –<br />
For training of Medical Officers, Paramedical Staff, ASHA, ICDS functionaries and District<br />
level Programme Management Staff funds required will be Rs. 4 lakhs.<br />
6) IEC Activities –<br />
For various IEC activities in the State as well as in the districts the funds required are as<br />
follows –<br />
Sr.<br />
No<br />
1<br />
IEC for ‐ Manpower IEC Material Amount<br />
Awareness creation about<br />
Other Eye Diseases i.e.<br />
Glaucoma, Dibetic Retinopathy,<br />
ROP, Laser Technique, Iritis,<br />
Iridocyclitis, Childhood<br />
Blindness, Squint etc<br />
Awareness will be<br />
created with the<br />
help of ASHA,<br />
AWW, <strong>Health</strong><br />
Worker & PMOOs<br />
etc<br />
Handbills<br />
Posters<br />
Rallies<br />
Meetings with NGO’s<br />
& Pvt practitioners<br />
TV Spots<br />
Radio Jingles<br />
Print Media<br />
Rs. 01.00<br />
Lakhs
2 Eye Donation<br />
10 th Std Students as<br />
Eye Donation<br />
Volunteers, PMOOs<br />
Total funds required for IEC activity – Rs.2.00 Lakhs<br />
Handbills<br />
Posters<br />
Rallies<br />
TV Spots<br />
Radio Jingles<br />
Print Media<br />
I Cards to volunteers<br />
Rs. 01.00<br />
Lakhs<br />
7) Remuneration to SPO/ DPM –<br />
The funds required for DPM of <strong>Amravati</strong> districts will be Rs.24000 (Rs.2000 X 12 months)<br />
8) Wages to Assistants – The funds required for Assistants of <strong>Amravati</strong> districts will be Rs.<br />
18000 (Rs.1500X12 months)<br />
9) Salaries for the contractual Staff ‐<br />
a) Paramedical Ophthalmic Assstants – The appointment of 2 PMOOs is sanctioned in year<br />
2010‐ 11. Trained PMOOs are now available in the state and will be appointed soon. For the<br />
year 2011 – 12 no need to be appointed on contractual basis. So the total funds required<br />
will be Rs192000 (Rs. 8000X12months)<br />
a) Eye Donation Counselor – One Eye Donation counselor needs to be appointed per district.<br />
Districts. The appointment of 1 Eye Donation Counselors was sanctioned in the year 2010‐<br />
11. During that year 1 appointment was done, from the balance grants this year (2010 – 11)<br />
1 Counselors are appointed.<br />
Total funds required will be Rs. 1200000 (Rs. 10000X12months)<br />
10) Maintenance of Ophthalmic Instruments & Equipments ‐ Most of the major equipments<br />
are old & are not in working condition. Maintainance & repairs of these equipments is<br />
essential. The funds required is Rs. 50000<br />
11) Funds for Ophth. Equipment – Purchase of Ophth. Equipments for District Hospitals Rs.<br />
200000 lakhs as per norms.<br />
12) Funds for SBCS – For Office Maintainace, POL, Vehicles Maintainace , TA / DA, of officers &<br />
Staffs etc. The funds required will be Rs. 1800000 lakhs as per norms.<br />
Sr no perticular Praposed Budget<br />
1 NGO 400000 likh<br />
2 Slari ophthalmic Assistants 192000 likh<br />
3 Eye Donetion Counselor 1200000 likh<br />
4 Remuneration to DPM 24,000 /‐<br />
5 Remuneration To Assistants 18,000/‐<br />
TOTAL 1834000 Likh
<strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong><br />
Integrated Disease Surveillance<br />
Programme<br />
PIP 2011‐12
IDSP PIP Activity Sheet of year 2011-12<br />
Activity Sub‐activity<br />
1. Training One day training of Hospital<br />
Doctors<br />
One day training of Hospital<br />
Pharmacist / Nurses<br />
2. Human<br />
Resources<br />
One day training of Medical<br />
College Doctors<br />
cost<br />
as per NRHM guidelines<br />
as per NRHM guidelines<br />
as per NRHM guidelines<br />
One day training Data entry and as per NRHM guidelines<br />
analysis training for Block <strong>Health</strong><br />
Team<br />
One day training of DM & DEO as per NRHM guidelines<br />
No of<br />
units<br />
Proposed<br />
Budget for 2011‐<br />
12<br />
4 0.4<br />
1 0.1<br />
0 0<br />
1 0.02<br />
SUB TOTAL 6 0.52<br />
Remuneration *<br />
district Epidemiologists<br />
( 1 each at district HQs ‐ DSUs)<br />
State/ district Microbiologists (1<br />
each at identified district priority<br />
labs:‐ beed & Nashik )<br />
Data Managers (1 each at district<br />
HQs ‐ DSUs)<br />
1 3.6<br />
1 2.5<br />
Data Entry Operators (1 each at<br />
district HQs ‐ DSUs and 1 at<br />
identified Medical Colleges<br />
identified under IDSP (there are<br />
19 medical colleges<br />
inMaharashtra..only those<br />
districts should mention the<br />
funds for DEO) 1 1.8<br />
SUB TOTAL 3 7.9<br />
Operational Costs<br />
Transport<br />
Office Expenses, Broadband<br />
Expenses,collection and<br />
transportation of samples and<br />
other misc.expenses (to be<br />
0 0.25<br />
specified)<br />
Community based surveillance<br />
including evaluation. (Only in<br />
0 0.36<br />
Nandurbar) 0 0<br />
SUB TOTAL 0 0.61
3. Laboratory<br />
support<br />
SUB TOTAL (Human Resources =<br />
Remuneration + Operational<br />
costs) 3 8.51<br />
Consumables and kits for Priority<br />
district labs<br />
culture‐media & reagents<br />
diagnostic kits<br />
glass ware<br />
miscellanious required items<br />
Referral lab network services (In<br />
World Bank funded States)<br />
Reimbursement‐based payments<br />
for tests (10 categories of<br />
tests.With each category priced<br />
individually)Cost of test to be<br />
reimbursed to be decided by the<br />
State<br />
Serological tests for typhoid<br />
ELISA /rapid test for leptospirosis<br />
ELISA for Dengue<br />
ELISA for Viral Hepatitis<br />
ELISA for Measles<br />
Rapid test for Meningococci<br />
Blood culture for Typhoid<br />
Diptheria culture<br />
Cholera culture<br />
other (state specific diseases)<br />
Minor laboratory operating<br />
expenses (consumables,<br />
reagents, kits, office expenses,<br />
part‐time staff costs, transport<br />
costs, minor repairs, etc)<br />
Rs 2,00,000/‐ per priority<br />
district lab per annum<br />
(Identified No. of District<br />
priority labs Maharashtra‐<br />
2 Beed , Nasik)only Beed &<br />
Nasik should mention<br />
funds in this column<br />
Not more than Rs<br />
3,00,000/‐per referral lab<br />
per annum (Identified<br />
No. of labs in States are as<br />
follows:Maharashtra‐10)<br />
not more than<br />
Rs.2,00,000/‐ (Referal<br />
laboratories of medical<br />
colleges :‐ Only those<br />
districts of which medical<br />
colleges are assigned MoU<br />
with SSU,Pune should<br />
mention referal lab funds<br />
in this column<br />
Total 9.03
<strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong><br />
District Tobacco Control Programme<br />
PIP 2011‐12
Sr.<br />
No.<br />
Proposed Budget for District Tobacco Control Programme (2011‐12)<br />
General Hospital <strong>Amravati</strong><br />
Components Calculation UNR Total INR<br />
1 Salaries<br />
1) Psychologist :‐ Rs 15000/‐<br />
2) Social Workar :‐ Rs. 10000/‐<br />
10000x12<br />
8000x12<br />
216000<br />
2 Training 200000 200000<br />
3 IEC Activity 200000 200000<br />
4 School Activity 400000 400000<br />
5 Monitoring of Tabacco Control Lows &<br />
Reporting<br />
100000 100000<br />
6 Contingency 100000 100000<br />
Total 1216000
<strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong><br />
<strong>National</strong> Mental <strong>Health</strong> Programme<br />
PIP 2011‐12
Activity Recuring /<br />
Manpower<br />
(Cleark,Psylogist<br />
Peun) & other<br />
Staff in regular<br />
from DHS<br />
NATIONAL MENTAL HELTH PROGRAMME<br />
Non Recuring<br />
GENERAL HOSPITAL AMRAVATI (DMHP)<br />
PIP 2011‐2012<br />
Fund available Fund needed 11‐<br />
12<br />
(Approx.)<br />
Expendule<br />
Recuring 8,70,000/‐ 2,70,000/‐ Process<br />
Complet<br />
Medicines Recuring 3,00,000/‐ 7,00,000/‐ Under Process<br />
Disel / Oil Recuring 50,000/‐ 75,000/‐ Under Process<br />
Stationery Recuring 50,000/‐ 50,000/‐ Under Process<br />
Machinary/<br />
Reparing<br />
Recuring 50,000/‐ 50,000/‐ Under Process<br />
Instruments Non Recuring 6,00,000/‐ ‐ Under Process<br />
Training Recuring 5,00,000/‐ ‐ Under Process<br />
IEC Recuring 2,00,000/‐ 3,00,000/‐ ‐<br />
Vehicle Required on rent<br />
base (25x12<br />
Month )<br />
3,00,000/‐ Not Avilable<br />
Building Fund Non Recuring 25,00,000/‐ Not Avilable
<strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong><br />
<strong>National</strong> Deafness Control Programme<br />
PIP 2011‐12
Following Equipments Required for Surgery<br />
<strong>National</strong> Deafness Control Programme<br />
PIP 2011‐12<br />
General Hospital <strong>Amravati</strong><br />
Sr.No. Name of Equipments Company Price Remark<br />
1 Nasal Endoscope 0‐ one Karl –storz 80000<br />
2 Nasal Endoscope 30 –one Karl –storz 80000<br />
3 Nasal Endoscope 90 –one Karl –storz 80000<br />
4 Light source with fiberoptic Cable<br />
one<br />
5 Oto Micro scope (for ear Surgery‐<br />
one<br />
6 Micro ear surgery instrument 2<br />
sets<br />
25000<br />
Zeiss 700000<br />
kalelkar<br />
Total 965000
E. INTER SECTORAL CONVERGENCE E.1<br />
Mainstreaming of AYUSH<br />
The budget requested from NRHM for Ayush manpower and other activities should be reflected in<br />
the concerned budget sheet under RCH Flexipool and NRHM Flexipool. Information related to<br />
number of Government AYUSH hospitals, number of beds, AYUSH dispensaries, co‐location of<br />
AYUSH facilities in PHC/CHCs/DH and AYUSH manpower deployed in district hospitals should be<br />
included in the quarterly MIS reports. In the PIP of 2011‐12, , States may give an overview of AYUSH<br />
activities, their plans to mainstream and strengthen AYUSH hospitals, dispensaries and manpower<br />
with full justification. Information regarding requirement of funds and targets should be provided in<br />
the following format:<br />
AYUSH Manpower<br />
Component Continuing from<br />
previous year<br />
(2010‐11)<br />
New proposed during<br />
2011‐12<br />
Manpower Institution Number Amount<br />
(Rs in<br />
Lakhs)<br />
Cumulative for 2011‐12<br />
Number Financial (Rs<br />
in Lakhs)<br />
AYUSH Doctors PHCs 0 0 0<br />
CHCs 18 0 0 18 20.16<br />
DHs 3 0 0 3 4.32<br />
Paramedical Staff<br />
(AYUSH)<br />
PHCs 0 0 0 0 0<br />
CHCs 0 0 0 0 0<br />
DHs 4 0 0 4 2.76<br />
Training of AYUSH Manpower<br />
IEC/BCC under NRHM for Mainstreaming of AYUSH<br />
S. NO Name of Activities Cost per units Number of<br />
Units<br />
Support from Department of AYUSH for PIP 2011‐<br />
12: Co‐location under NRHM<br />
Financial (in Lakhs)<br />
S. No. Centre One time assistance Recurring assistance Total Amount<br />
PHC<br />
CHC<br />
DH<br />
Total<br />
No. of<br />
Units<br />
Amount New Units Old<br />
Units<br />
Cumulativ<br />
e Amount
Upgradation of AYUSH Hospitals<br />
S.<br />
No.<br />
S.<br />
No.<br />
Centre One time assistance Recurring assistance Total Amount<br />
No. of<br />
Units<br />
Up gradation of AYUSH Dispensaries<br />
Amount New Units Old Units Cumulative<br />
Amount<br />
Centre One time<br />
assistance<br />
Recurring assistance Total Amount<br />
No. of Amount New Units Old Cumulative<br />
Units<br />
Units Amount<br />
i) Establishment of Programme Management Unit (Ayush) HMIS<br />
S. No. State One time<br />
assistance<br />
Recurring<br />
assistance<br />
ii) Procurment of essential drugs for AYUSH Hospital and Dispensaries<br />
S. No. Unit Stream Recurring<br />
assistance<br />
E.2: Intersectoral Convergence activities with line Departments:<br />
Total<br />
Amount<br />
Total<br />
Amount<br />
Inter‐sectoral Convergence activities with line Departments to be specified in this part of PIP<br />
including:<br />
• PRI,<br />
• ICDS<br />
• <strong>Rural</strong> Development<br />
• PHED<br />
• Education<br />
• Labour
CHAPTER‐5:<br />
MONITORING AND EVALUATION<br />
The physical and financial progress of NRHM is periodically assessed through monitoring and<br />
evaluation activities like HMIS, Surveys and Evaluation Studies. Some of the developments for<br />
improving the M&E interventions and strengthening the reporting systems are listed below. The<br />
States may ensure that the data reported through the HMIS Portal remains the single source for all<br />
reports to be sent to MoHFW.<br />
(i) For HMIS Portal:<br />
• Block level/Facility based reporting for physical performance (HMIS). All States are to shift to<br />
Facility based reporting during 2011‐12. States may also take steps to get data from the private<br />
sector health facilities.<br />
• The MIS for the <strong>National</strong> Disease Control Programmes has been integrated on the HMIS Portal<br />
and all States are to report their progress from the District level.<br />
• The FMRs, infrastructure details, facility survey reports are also integrated on the HMIS portal<br />
and all States need to ensure that it is regularly uploaded.<br />
• Inbuilt features are provided on the HMIS portal to check the consistency and validity of data<br />
which may be used for improving the quality of data.<br />
(ii) For MCH Tracking system (MCTS)<br />
• NIC has developed the software for data capturing and reporting. All State Nodal Officers and<br />
NIC Officers have been trained on the software.<br />
• States to ensure timely reporting of data on the MCTS software, which is available, both in the<br />
online and offline versions.<br />
(iii) A Core Team comprising faculty of PRCs, officers of Regional Directors (MoHFW) and<br />
SIHFWs has been constituted to continuously support States in checking the validity and<br />
reliability of data. States need to constitute similar teams at the State and District level<br />
involving the State Demographer and District Statistical Officer/Assistant and<br />
institutionalize a mechanism for reviewing the HMIS data in regular review meetings. It<br />
may also be ensured that the health interventions included in the State and District PIPs are<br />
supported with HMIS and survey data.<br />
To exploit the full benefits of the HMIS Portal, States may require augmenting its IT infrastructure<br />
and human resources including their training at various levels. Such initiatives may be backed by a<br />
comprehensive strategy for strengthening Monitoring & Evaluation in the State and detailed in the<br />
PIP with the associated budget head. This strategy may include the following components:<br />
(a) Integration of Monitoring & Evaluation activities across programmes: States need to integrate<br />
their Monitoring & Evaluation activities across health programmes to avoid duplication in the<br />
available resources like manpower, IT infrastructure, finances etc. Augmentation of these<br />
resources at any level should be need based. The Quality Assurance protocols may also be scaled<br />
up under this head. Surveys and Studies should be undertaken by States in areas not already<br />
covered through the DLHS‐III, Concurrent Evaluation of NRHM and Annual <strong>Health</strong> Survey.
(b) M&E Action Plan: The PIP should have a detailed M&E Action Plan for strengthening<br />
HMIS and MCH tracking. The Action Plan is to include the current status of HMIS and<br />
MCH tracking in the state and the districts and the plan of action propo<br />
(c) sed (with activities and budget‐line) for data capturing at the Sub District level including<br />
training plans. This should also include integration issues with the national HMIS and<br />
MCH tracking initiatives.<br />
(d) Ensuring Nodal M&E Officers are available at the State, District and Sub District levels<br />
for all health related information, HMIS, MCTS and for sending feedback to the lower<br />
formations. Adequate mobility provision may be kept for their supervisory visits. The PIP<br />
should include details on the status of notification of Nodal M&E Officers up to the block<br />
level. If different Nodal M&E Officers are designated for HMIS and MCH tracking, details<br />
should be clearly spelled out.<br />
Officers for HMIS and MCH tracking<br />
Level Nos. Required Nos. Present Remarks<br />
State<br />
Districts 1 1<br />
Blocks 14 14<br />
The letter of AS&MD (NRHM) dated 3 rd March, 2008 may kindly be referred in this regard and States<br />
may issue necessary notifications, if not already done, with a copy endorsed to MoHFW.<br />
(d) Strengthening IT infrastructure at appropriate levels: The IT infrastructure available across<br />
various programmes needs to be integrated to facilitate capturing physical and financial<br />
performance across programmes through the HMIS Portal. All efforts should first be made to<br />
utilize the resources available with other programmes including the Common Service Centres<br />
(CSCs) of the Department of Information Technology, GOI. Appropriate budgetary provisions<br />
may be made with timelines.<br />
(e) Training Strategy for M&E: Each State may put in place a strategy for training of human<br />
resources in monitoring and evaluation activities. This would include identification of nodal<br />
institutions like the SIHFWs, RHFWTCs etc. that could impart regular training courses on use of<br />
information for decision making in the <strong>Health</strong> Sector and creating capacities in these institutes.<br />
Appropriate budget along with the training plans, training load and timelines may be provided.<br />
(f) Strengthening Mother and Child Tracking System (MCTS): The States have been advised to<br />
expedite the name based tracking of pregnant women for ANC/PNCs and children for<br />
immunisation using the MCTS software prepared by NIC. The States may make adequate<br />
provision for strengthening of the IT infrastructure, as required, to ensure smooth<br />
implementation of the MCTS in all districts with timelines (if not already implemented).<br />
An integrated section giving the M&E strategy with budget lines for HMIS, Mother and Child<br />
Tracking System (MCTS), Quality Assurance, etc. across programmes may be provided, clearly<br />
mentioning the source of funding, that is, whether from NRHM, RCH, NVBDCP funds etc.
Budget Allocation: The budget for M&E in the State PIPs may be provided in the following format<br />
Major Head Minor Head Budget in<br />
Rs<br />
1.Strengthening of<br />
M&E/HMIS/ MCH<br />
Tracking<br />
2. Procurement of<br />
HW/SW and other<br />
equipments<br />
3.Operationalising<br />
HMIS at Sub<br />
District level<br />
4.Operationalising<br />
MCH tracking<br />
Salaries of M&E, MIS & Data<br />
Entry Consultants<br />
Details<br />
(including cost<br />
per unit)<br />
1.1 9.84 M&E @ Rs.<br />
0.27 Per<br />
Month DEO<br />
Rs.@ 0.15,<br />
PHS @Rs. 0.32<br />
Mobility for M & E Officers 1.2 1.20 M&E @<br />
Rs.0.10<br />
Workshops/Training on M & E 1.3 0.50<br />
M&E Studies 1.4 0.20<br />
Others (specify) 1.5 1.20 SO @ Rs. 0.10<br />
Hardware/ S oftware<br />
Procurement<br />
Remarks<br />
2.1 0.50 Give<br />
deploymen t<br />
details<br />
Internet connectivity 2.2 0.24 @ Rs. 0.02<br />
Annual Maintenance 2.3 0.12 @ Rs. 0.01<br />
Operational Costs<br />
(consumables etc)<br />
2.4 0.12 @ Rs. 0.01<br />
Others (Specify) 2.5 0<br />
Review of existing registers ‐to<br />
make them compatible with<br />
<strong>National</strong> HMIS<br />
3.1 0<br />
Printing of new<br />
registers/Forms<br />
3.2 1.20 HMIS for<br />
Training of staff 3.3 0.50 HA/HV/DEO<br />
Printing and reproducing 4.1 1.20 Register/<br />
Registers/ Forms<br />
form<br />
Capacity building of teams 4.2 0.50 Daily<br />
orientation<br />
Ongoing review of MCH tracking 4.3 0.12 @ 0.01<br />
activities<br />
monthly<br />
meeting<br />
Monitoring data collection and 4.4 0.25 Monthly<br />
data quality<br />
monitoring<br />
DLS<br />
Others (Specify) 4.5 0<br />
Total… 17.69
CHAPTER‐6:<br />
FINANCIAL MANAGEMENT<br />
The States are expected to provide detailed information on the present status and the proposals on<br />
various important issues of financial management and implementation of finance, accounts, audit,<br />
fund flow and other financial guidelines issued by the MoHFW. A separate chapter on Financial<br />
Management under NRHM may be incorporated in the PIP, providing information on the following<br />
key issues to bring about effective financial management and ensure timely and proper utilisation of<br />
funds to achieve the objectives of NRHM:<br />
1. Budgeting for various Activities<br />
The budgeting for various programmes/activities under NRHM should be proposed strictly in<br />
accordance with Financial Monitoring Report (FMR) Format so as to facilitate proper analysis of<br />
the progressive utilisation of funds and taking remedial measures. Indicate whether the Program<br />
Management cost has been kept within the ceiling of 6% and whether the proposals for<br />
construction works are within the ceiling of 33% for high focus states and 25% for non‐high focus<br />
states as per norms.<br />
2. Financial Management Staff:<br />
Status of Financial Management personnel whether Director (F&A), SFM, SAM, Accountants and<br />
Data Assistants are in position at State/District/Block levels may be indicated. If not, the action<br />
plan to fill up vacant positions may be given. It may also be stated whether the remuneration of<br />
the PMU staff including NDCPs has been revised and suitable incentive scheme worked out<br />
considering local conditions.<br />
3. Statutory Audit<br />
Whether Statutory Audit Report and UCs for 2009‐10 have been submitted and deficiencies<br />
intimated/feedback given by FMG has been complied with. Any problem being faced regarding<br />
the audit process may also be highlighted.<br />
4. Concurrent Audit<br />
Whether Concurrent Audit has been implemented at the State and all Districts and quarterly<br />
summary reports sent to MoHFW. If not reasons therefore. Status of Concurrent Auditor<br />
appointment for 201112 and action plan therefore may be incorporated.<br />
5. Implementation of Tally<br />
Whether Tally has been procured, training initiated and made operational at State and district<br />
level. If not, reasons therefore and the action plan for ensuring that this is done may be<br />
indicated.<br />
6. Mode of Fund Transfer<br />
Whether funds are being released electronically to all districts and blocks? If not reasons<br />
therefore and the expected time frame for achievement of e‐transfer may be indicated.
7. Uploading of FMRs on HMIS Portal<br />
Present district wise status may be indicated. If the data is not being uploaded, the reasons<br />
therefor along with the action plan for implementation of the same may be given.<br />
8. Financial reporting under NRHM<br />
9. MIS<br />
FMRs are not timely and accurate which leads to non‐ availability of reliable data. The State and<br />
District level FMGs shall monitor the release and utilization of funds for all programmes under<br />
NRHM including NDCPs and send a consolidated FMR for all programmes under NRHM<br />
including NDCPs. Mention whether FMR upto 31.12.10 has been submitted and deficiencies<br />
complied with.<br />
The submission of monthly MIS/FSP and quarterly MIS along with head wise and age wise<br />
details of advances upto 31.12.2010 may be indicated.<br />
10. Statutory Audit<br />
The audit reports for the accounts of 1009‐10 including all NDCPs and covering 100 per cent of<br />
the DHS and 40% of the blocks should have been submitted to the FMG by 31 December 2010.<br />
This may be confirmed. Release of funds in the second tranche is dependent on submission of<br />
the audit reports.<br />
11. RCH‐I Unspent Balance<br />
Indicate whether Unspent Balance of RCH‐I has been refunded and utilisation certificates or<br />
refunds the activity specific releases by individual program divisions during 2005‐06 and 2006‐<br />
07 have been sent.<br />
12. Key Areas for Priority during 2011‐12<br />
A clear Action Plan for identified backward districts on special interventions for identified high<br />
focus districts/backward areas such as difficult, left wing affected, minority, tribal, SC/ST,<br />
gender etc. for special incentives to medicos and para‐medicos for performing duties in such<br />
difficult areas may be incorporated with appropriate financial and other incentives scheme for<br />
attracting qualified human resource in may be worked out and proposed in the PIP with time‐<br />
bound targets for addressing the key issues and optimum utilization of funds to ensure<br />
effective implementation of NRHM.<br />
13. Committed and Uncommitted Unspent balances<br />
The programme‐wise committed unspent balances for the activities approved during the last<br />
years which are under implementation may be indicated, showing the amount already utilised<br />
and the timeframe for utilisation of the remaining amount with time frame for completion of<br />
the activities. Similarly, the details of uncommitted balances for the activities approved during<br />
previous years but not yet taken may also be given programme‐wise along with reasons for<br />
non‐start of such activities and whether the same are proposed to be implemented during<br />
2011‐12.
Conditions to be fulfilled to ensure smooth release of funds to the States<br />
a. The State shall not make any change in the allocation among different components/activities<br />
without<br />
approval of GOI. Any proposal for reappropriation between activities/functional heads within<br />
activities should be submitted to MoHFW in advance and should reflect realignment of activities<br />
in<br />
accordance with priority to high focus districts/involvement of NGOs. etc.<br />
b. The State shall ensure that 15% of its share, based on release of funds by MoHFW is credited to<br />
the<br />
account of the SHS within one month of issue of the release order. The overall expenditure on<br />
health<br />
by the State should also go up by a minimum of 10% each year.<br />
c. The State shall ensure complete delegation of administrative and financial powers at state,<br />
district andblock levels to ensure smooth fund flow at all levels.<br />
d. The State shall ensure timely submission of the Quarterly and Monthly MIS reports in the<br />
prescribed<br />
format including the statement of funds position and the age‐wise and head‐wise details of<br />
advances<br />
given to various implementing agencies.<br />
e. The State shall also intimate the interest amount earned on unspent balances which could be<br />
utilised<br />
against activities already approved and will also count towards the central share.
Details of budget as per the functional heads should be provided in the following format:<br />
Sl.No. Activity Unit Cost Physical<br />
Targets<br />
Required<br />
fund under<br />
NRHM<br />
Human Resources<br />
A RCH<br />
1 Contractual Staff & Services<br />
1 Contractual Staff & Services(Excluding AYUSH)<br />
A.9.1 ANMs,Supervisory Nurses, LHVs, 416 526.55<br />
A.9.1.1 Laboratory Technicians,MPWs 0<br />
A.9.1.2 Specialists (Anesthetists, Pediatricians, Ob/Gyn,<br />
Surgeons, Physicians, Dental Surgeons,<br />
Radiologist, Sonologist, Pathologist,Specialist for<br />
CHC )<br />
0<br />
A.9.1.3 PHNs at CHC, PHC level 0<br />
A.9.1.4 Medical Officers at CHCs / PHCs 0<br />
A.9.1.5 Additional Allowances/ Incentives to M.O.s of<br />
PHCs and CHCs<br />
0.0223 52 1.16<br />
A.9.1.6 Others ‐ Computer Assistants/ BCC Coordinator<br />
etc<br />
0<br />
A.9.1.7 Incentive/ Awards etc. to SN, ANMs etc. 0<br />
A.9.1.8 Human Resources Development (Other than<br />
above)<br />
0<br />
A.9.1.9 Other Incentives Schemes (Pl.Specify) H.A. 146 113.28<br />
A.11 PROGRAMME / NRHM MANAGEMENT COSTS<br />
A.11.1 Strengthening of SHS /SPMU (Including HR,<br />
Management Cost, Mobility Support, Field Visits )<br />
A.11.2 Strengthening of DHS/DPMU (Including HR,<br />
Management Cost, Mobilty Support, Field Visits )<br />
3 17.60<br />
A.11.3 Strengthening of Block PMU (Including HR,<br />
Management Cost, Mobilty Support, Field Visits )<br />
14 81.48<br />
A.11.4 Strengthening (others)<br />
A.11.4.1 FMG 2 4.08<br />
A.11.4.2 RKS Coordinator 2 4.44<br />
A.11.4.3 IDW wing 6 17.88<br />
A.11.4.3 IPHS wing 2 7.32<br />
A.11.5 Audit Fees<br />
A.11.6 Concurrent Audit<br />
A.11.7 Mobility Support , Field Visits to<br />
BMO/MO/Others<br />
82 27.11<br />
B NRHM Additionalities<br />
B.9 Contractual Staff & Services(Only AYUSH)<br />
B.9.1 Staff/ Supervisory Nurses /Other Staffs for<br />
PHCs,CHCs<br />
B9.2 Medical Officers at CHCs/ PHCs 28 30.80<br />
C Routine Immunisation<br />
C.2 A) Computer Assistants Salary 1 1.16<br />
C.2 B) Other HR Personnels (Technicians, Cold Chain
Sl.No. Activity Unit Cost Physical<br />
Targets<br />
Required<br />
fund under<br />
NRHM<br />
Mechanic)<br />
Other <strong>National</strong> Disease Control Programme<br />
D NVBDCP<br />
a) Remuneration to Contractual MPWs 2.88<br />
b) Contractual LTs 6 1.00<br />
E NLEP<br />
a) Contractual Services (State SMO, BFO cum AO,<br />
Admn. Assistant, DEO)<br />
b) State Driver<br />
c) District Drivers<br />
0.005 1 0.06<br />
F NBCP<br />
a) Ophthalmic Surgeon<br />
b) Ophthalmic Assistant 0.08 2 1.92<br />
c) Eye Donation Counsellor 12.00<br />
G) RNTCP<br />
a) Honarium to DOT Providers<br />
b) Contractual Staff Payments 20 31.86<br />
H) IDSP<br />
a) Remuneration of Epidemiologists 0.30 1 3.60<br />
b) Remuneration of Microbiologists<br />
c) Remuneration of Entomologists<br />
d) Consultant‐Finance<br />
e) Consultant‐Training<br />
f) Data Managers 1 2.50<br />
g) Data Entry Operators 1 1.80<br />
I) NIDDCP<br />
IDD Control Cell‐<br />
(i) Technical Officer<br />
(ii) Statistical Assistant<br />
(iii) LDC Typist<br />
IDD Monitoring Lab‐<br />
(i) Lab Technician<br />
(ii) Lab. Assistant<br />
Training<br />
I RCH Flexible Pool<br />
A.10 TRAINING<br />
A.10.1 Strengthening of Training Institutions<br />
A.10.2 Development of training packages<br />
A.10.3 Maternal <strong>Health</strong> Training<br />
A.10.3.1 Skilled Birth Attendance / SBA<br />
A.10.3.2 EmOC Training
Sl.No. Activity Unit Cost Physical<br />
Targets<br />
A.10.3.3 Life saving Anesthesia skills training<br />
A.10.3.4 MTP training<br />
A.10.3.5 RTI / STI Training<br />
A.10.3.6 Dai Training<br />
A.10.3.7 Other MH Training (ISD Refresher )<br />
A.10.4 IMEP Training<br />
A.10.5 Child <strong>Health</strong> Training<br />
A.10.5.1 IMNCI<br />
A.10.5.2<br />
A.10.5.3<br />
A.10.5.4<br />
A.10.5.5<br />
Facility Based Newborn Care<br />
Home Based Newborn Care<br />
Care of Sick Children and severe malnutrition<br />
Other CH Training (pl. specify)<br />
Required<br />
fund under<br />
NRHM<br />
A.10.6 Family Planning Training<br />
A.10.6.1 Laparoscopic Sterilisation Training<br />
A.10.6.2 Minilap Training<br />
A.10.6.3 NSV Training<br />
A.10.6.4 IUD Insertion Training<br />
A.10.6.5 Contraceptive Update/ISD Training<br />
A.10.6.6 Other FP Training (pl. specify)<br />
A.10.7 ARSH Training<br />
A.10.8 Programme Management Training<br />
A.10.8.1 SPMU Training<br />
A.10.8.2 DPMU Training<br />
A.10.9 Other training (pl. specify)<br />
A.10.10 Training (Nurshing)<br />
A.10.10.1 Strengthening of Existing Training<br />
Institutions/Nursing School<br />
A.10.10.2 New Training Institutions/School<br />
A.10.11 Training (Other <strong>Health</strong> Pesonnels)<br />
A.10.11.1 Promotional Trg of health workers females to<br />
lady health visitor etc.<br />
A.10.11.2 Training of AMNs,Staff nurses,AWW,AWS<br />
A.10.11.3 Other training and capacity building<br />
programmes<br />
2 Routine Immunisation<br />
2.1 Training for Cold Chain Handlers/refrigerator<br />
mechanics<br />
2.2 Training of M.O.s /Other Staffs on R.I. 0.25 1 0.25<br />
2.3 Training of MOs/other staff on RI.<br />
Other <strong>National</strong> Disease Control Programme<br />
3 NVBDCP<br />
3.1 Training of MPWs 1.65
Sl.No. Activity Unit Cost Physical<br />
Targets<br />
Required<br />
fund under<br />
NRHM<br />
3.2 Training of ASHAs 2068 6.18<br />
3.3 Training of Supervisor 0.42<br />
3.4 Training of Para‐medical for MDA<br />
3.5 Other training & capacity building programme<br />
4 NLEP<br />
4.1 Training for Newly appointed medical and para<br />
medical staffs<br />
4.2 Training for existing medical and para medical<br />
staffs<br />
4.3 Other Training & Capacity building<br />
programmes<br />
140 2.52<br />
155 2.00<br />
5 NBCP<br />
5.1 Training /Capacity Building for <strong>Health</strong> personnels<br />
5.2 Training of Teachers & Others<br />
6 RNTCP<br />
6.1 Induction Training 906 6.26<br />
7 IDSP<br />
7.1 Training for M.O.s,Nurses, Data Managers and DEO 6 0.52<br />
8 NIDDCP<br />
Note: FMR Codes of NDCP' has not been given<br />
Civil Work<br />
B NRHM Additionalities<br />
B.4 Hospital Strengthening<br />
B.4.1 Upgradation of CHCs, PHCs, Dist. Hospitals to<br />
IPHS)<br />
B4.1.1 District Hospitals 50.00 1 50.00<br />
B4.1.2 CHCs RH/SDH 20.00 5 100.00<br />
B4.1.3 PHCs 5.00 34 170.00<br />
B4.1.4 Sub Centers 1.00 83 83.00<br />
B4.1.5 Others<br />
B4.1.5.1 WH 35.00 1 35.00<br />
B4.1.5.2 ISO 10 50.00<br />
B 4.2 Strengthening of District,Su‐divisional<br />
Hospitals,CHCs, PHCs<br />
B.4.3 Sub Centre Rent and Contingencies
Sl.No. Activity Unit Cost Physical<br />
Targets<br />
B.4.4 Construction (Others)<br />
Required<br />
fund under<br />
NRHM<br />
B5 New Constructions/ Renovation and<br />
Settingup<br />
B5.1 CHCs 5.00 1 5.00<br />
B5.2 PHCs 18 275.00<br />
B5.3 SHCs/Sub Centers 13 150.00<br />
B5.4 Setting up Infrastructure wing for Civil works<br />
B5.6 Construction of BHO, Facility improvement, civil<br />
work, BemOC and CemOC centers<br />
B.5.7 Major civil works for operationalisation of FRUS<br />
B.5.8 Major civil works for operationalisation of 24<br />
hour services at PHCs<br />
B.5.9 Civil Works for Operationalise Infection<br />
Management & Environment Plan at health<br />
facilities<br />
B6 Minor Civil Works<br />
B6.1 Minor civil works for operationalisation of FRUs<br />
B6.2 Minor civil works for operationalisation of 24<br />
hour services at PHCs<br />
E RNTCP<br />
39 106.50<br />
a) Civil Works 3 1.35<br />
F IDSP<br />
a) Civil Works<br />
Note: FMR Codes of NDCP' has not been given<br />
Procurements‐Drugs & Supplies<br />
B NRHM Additionalities<br />
B.16.2 Procurement of Drugs and supplies<br />
B.16.2.1 Drugs & supplies for MH<br />
B.16.2.2 Drugs & supplies for CH<br />
B.16.2.3 Drugs & supplies for FP<br />
B.16.2.4 Supplies for IMEP
Sl.No. Activity Unit Cost Physical<br />
Targets<br />
B.16.2.5 General drugs & supplies for health<br />
facilities<br />
C Routine Immunisation<br />
Procurement ‐Equipments (e.g.ADS, Bags,<br />
Buckets)<br />
Other <strong>National</strong> Disease Control Programme<br />
D NVBDCP<br />
a) Procurement ‐Kits (e.g. Elisa Kit, Chikengunia Kits<br />
)<br />
E NLEP<br />
a) Procurement of Equipments (Equipments related<br />
to RCS). Printing forms<br />
b) Other Procurements<br />
F NBCP<br />
a) Procurement of Equipments‐Opthalmic<br />
Microscopes, Flash Auto claves etc.<br />
G RNTCP<br />
a) Procurement of Equipments<br />
b) Procurement of Two wheelers<br />
H IDSP<br />
a) Procurement of Equipements for Strengthening<br />
of Survillance Unit.<br />
b) Other Procurements<br />
I NIDDCP<br />
Procurement of Kits (Salt Testing Kits)<br />
Note: In RNTCP, commodity grant for anti TB Drugs<br />
has been approved from Central Level<br />
procurements and specific Laboratory<br />
Equipments<br />
Procurements‐Equipment<br />
B NRHM Additionalities<br />
B16.1.1 Procurement under Maternal <strong>Health</strong><br />
B16.1.2 Procurement under Child <strong>Health</strong><br />
B16.1.3 Procurement under Family Planning Services<br />
B16.1.4 Procurement under IMEP<br />
B16.1.5 Procurement Others<br />
C Routine Immunisation<br />
Procurement ‐Equipments (e.g.ADS, Bags,<br />
Buckets)<br />
Other <strong>National</strong> Disease Control Programme<br />
D NVBDCP<br />
Required<br />
fund under<br />
NRHM<br />
8.20<br />
2.97
Sl.No. Activity Unit Cost Physical<br />
Targets<br />
a) Procurement ‐Kits (e.g. Elisa Kit, Chikengunia Kits<br />
)<br />
E NLEP<br />
a) Procurement of Equipments (Equipments related<br />
to RCS). Printing forms<br />
b) Other Procurements<br />
F NBCP<br />
a) Procurement of Equipments‐Opthalmic<br />
Microscopes, Flash Auto claves etc.<br />
G RNTCP<br />
a) Procurement of Equipments<br />
b) Procurement of Two wheelers<br />
Required<br />
fund under<br />
NRHM<br />
H IDSP<br />
a) Procurement of Equipements for<br />
Strengthening of Survillance Unit.<br />
b) Other Procurements<br />
I NIDDCP<br />
Procurement of Kits (Salt Testing Kits) 9.65<br />
IEC/BCC Works<br />
B10 IEC‐BCC NRHM<br />
B.10 Strengthening of BCC/IEC Bureaus (state and<br />
district levels)<br />
B.10.1 Development of State BCC/IEC strategy<br />
B.10.2 Implementation of BCC/IEC strategy<br />
B.10.2.1 BCC/IEC activities for MH<br />
B.10.2.2 BCC/IEC activities for CH<br />
B.10.2.3 BCC/IEC activities for FP<br />
B.10.2.4 BCC/IEC activities for ARSH<br />
B.10.2.5 Other activities (please specify)<br />
B.10.4 <strong>Health</strong> Mela<br />
B.10.5 Creating awareness on declining sex ratio issue<br />
B.10.6 Other activities 7.80<br />
Other NDCPs<br />
c) Routine Immunisation<br />
IEC‐BCC Activities<br />
D NVBDCP<br />
IEC‐BCC Activities 4.66<br />
E NLEP<br />
IEC‐BCC Activities<br />
F NBCP<br />
IEC‐BCC Activities<br />
a) Cataract Operations
Sl.No. Activity Unit Cost Physical<br />
Targets<br />
b) Eye Donation Camps<br />
c) Other Activities<br />
Required<br />
fund under<br />
NRHM<br />
G RNTCP<br />
IEC/Publicity 2.14<br />
H IDSP<br />
IEC‐BCC Activites<br />
I NIDDCP<br />
Untied Funds<br />
B NRHM Additionalities<br />
B.2 Untied Funds<br />
B2.1 Untied Fund for CHCs 0.50 14 7.00<br />
B2.2 Untied Fund for PHCs 0.25 56 14.00<br />
B2.3 Untied Fund for Sub Centers 0.10 333 33.30<br />
B2.4 Untied fund for VHSC 0.10 1547 154.70<br />
B2.5 Untied fund for PHU 0.25 103 25.75<br />
B.3 Annual Maintenance Grants<br />
B4.1 CHCs 1.00 14 14.00<br />
B4.2 PHCs 0.50 48 24.00<br />
B4.3 Sub Centres 0.10 299 29.90<br />
B4.4 PHU 0.50 62 31.00<br />
B8 Panchayti Raj Initiative<br />
B8.1 Constitution and Orientation of Community<br />
leader & of VHSC,SHC,PHC,CHC etc (DH/RRC/TB)<br />
5.00 3 15.00<br />
B8.2 Orientation Workshops, Trainings and capacity<br />
building of PRI at State/Dist.<br />
<strong>Health</strong> Societies, CHC,PHC<br />
B8.3 Others<br />
ASHAs<br />
B NRHM Additionalities<br />
B1 ASHA<br />
B1.1 Selection & Training of ASHA<br />
B1.2 Procurement of ASHA Drug Kit<br />
B1.3 Incentive to ASHAs under JSY 11373 28.54<br />
B1.4 Incentive under Family Planning Services<br />
B1.5 Incentive under Child <strong>Health</strong><br />
B1.6 Incentive to ASHA's for motivating families for<br />
Sanitary Toilets/Other Incentives<br />
2068 156.51<br />
B1.7 Awards to ASHA's/Link workers<br />
C Routine Immunisation<br />
a) Special ASHA Incentive under<br />
Immunisation
Sl.No. Activity Unit Cost Physical<br />
Targets<br />
Required<br />
fund under<br />
NRHM<br />
b) Social Mobilization by ASHA / Link 31.89<br />
Workers<br />
c) ASHA Incentive on PPI Day (may be considered<br />
with the cost of PPI)<br />
D NVBDCP<br />
a) Incentive to ASHAs 2.07<br />
E NLEP<br />
a) Services through ASHAs<br />
b) Honorium to ASHAs, Sensitization through ASHAs<br />
0.91<br />
F NBCP<br />
a) ASHA Incentive<br />
G RNTCP<br />
ASHA Incentive for DOTs 0.88<br />
1.1 RCH<br />
RKS/HMS<br />
1.2 NRHM Additionalities<br />
(i) Corpus Grants to HMS/RKS<br />
B6.1 District Hospitals 5.00 1 5.00<br />
B6.2 CHCs 1.00 14 14.00<br />
B6.3 PHCs 1.00 56 56.00<br />
B6.4 TB/RRC 5.00 2 10.00<br />
JSY<br />
a)<br />
1.1 RCH<br />
Maternal <strong>Health</strong><br />
Janani Suraksha Yojana / JSY<br />
Home Deliveries 0.005 1486 7.43<br />
b) Institutional Deliveries 13380 91.65<br />
c) 24 Hours Deliveries/ Others Operational<br />
15134 24.12<br />
Expenses C‐section & sanitary napkin<br />
d) Payment to Other Link Workers/AWW/AWS<br />
(Other than ASHA's)<br />
Incentive for Sterilization<br />
1 RCH<br />
A.3 FAMILY PLANNING<br />
A.3.1 Terminal/Limiting Methods<br />
A.3.1.1 Dissemination of manuals on sterilisation<br />
standards & quality assurance of sterilisation<br />
services<br />
A.3.1.2 Female Sterilisation camps
Sl.No. Activity Unit Cost Physical<br />
Targets<br />
Required<br />
fund under<br />
NRHM<br />
A.3.1.3 NSV camps 0.53 1 0.53<br />
A.3.1.4 Compensation for female sterilisation 0.008 10080 83.16<br />
A.3.1.5 Compensation for male sterilisation 0.015 1120 16.80<br />
A.3.1.6 Accreditation of private providers for sterilisation<br />
services<br />
A.3.2.1 IUD camps 0.03 140 4.20<br />
A.3.2.2 IUD services at health facilities<br />
A.3.2.3 Accreditation of private providers for IUD<br />
insertion services<br />
A.3.2.4 Social Marketing of contraceptives<br />
A.3.2.5 Contraceptive Update seminars<br />
A.3.3 POL for Family Planning 0.001 11200 11.20<br />
A.3.4 Repairs of Laparoscopes 2.00<br />
Referral Transport<br />
1.1 RCH<br />
Referral Transport<br />
a) Maternal <strong>Health</strong> 0.006 1400 8.40<br />
b) Other Programmes<br />
1.2 NRHM Additionalities<br />
Referral Transport<br />
a) Ambulance /EMRI<br />
b) Operating Cost (POL) /EMRI<br />
1.3 Routine Immunisation<br />
1.4 NVBDCP<br />
Referral Services<br />
1.5 NLEP<br />
1.6 NBCP<br />
1.7 RNTCP<br />
1.8 IDSP<br />
1.9 NIDDCP<br />
Other RCH Activities<br />
1 RCH<br />
1.1 Maternal <strong>Health</strong> 20.97<br />
1.1.2 Operationalise facilities (only<br />
dissemination, monitoring, and quality)<br />
(i) Operationalise FRUs<br />
(ii) Operationalise 24x7 PHCs 0.25 1 0.25<br />
(ii) MTP services at health facilities<br />
(iv) RTI/STI services at health facilities<br />
(v) Operationalise Sub‐centres 0.05 14 0.70<br />
1.1.3 Integrated outreach RCH services<br />
(i) RCH Outreach Camps 0.15 6 0.90<br />
(ii) Monthly Village <strong>Health</strong> and Nutrition Days
Sl.No. Activity Unit Cost Physical<br />
Targets<br />
Required<br />
fund under<br />
NRHM<br />
1.1.4 CHILD HEALTH 156.79<br />
(i) IMNCI<br />
(ii) Facility Based Newborn Care/FBNC<br />
(ii) Home Based Newborn Care/HBNC<br />
(iv) School <strong>Health</strong> Programme<br />
(v) Infant and Young Child Feeding/IYCF<br />
(vi) Care of Sick Children and Severe<br />
Malnutrition<br />
(vii) Management of Diarrohea, ARI and<br />
Micronutrient Malnutrition<br />
(viii) Other strategies/activities<br />
1.1.5 URBAN RCH<br />
a) Establishment of New Urban Centres<br />
b) Urban RCH Services 35 35.04<br />
1.1.6 ADOLESCENT REPRODUCTIVE AND SEXUAL<br />
HEALTH / ARSH<br />
a) Adolescent services at health facilities.<br />
b) Other strategies/activities 8.70<br />
Vulnerable Groups<br />
A RCH<br />
A.6 TRIBAL RCH<br />
a) Organise Tribal Camps<br />
b) Other Tribal Activities 33.06<br />
A.7 VULNERABLE GROUPS 2.40<br />
A.7.1 Infrastructure & Human resources 1.60<br />
A.7.2 Innovation/PPP/NGO 5.15<br />
Other <strong>Mission</strong> Flexible Pool Activities<br />
B NRHM Additionalities<br />
Other MFP activities<br />
B7 District <strong>Health</strong> Action Plans (Including Block,<br />
Village)<br />
B9 Mainstreaming of AYUSH<br />
B10 Mobile Medical Units (Including recurring<br />
expenditures)<br />
0.56 15 8.40<br />
1 15.76<br />
B13 School <strong>Health</strong> Programme 16 139.54<br />
B15 Planning, Implementation and Monitoring<br />
B15.1 Community Monitoring (Visioning<br />
workshops at state, Dist, Block level)<br />
B15.1.1 State level<br />
B15.1.2 District level<br />
B15.1.3 Block level<br />
B15.1.4 Other<br />
B15.2 Quality Assurance<br />
B15.3 Monitoring and Evaluation<br />
B15.3.1 Monitoring & Evaluation / HMIS<br />
B15.3.2 Computerization HMIS and e‐governance, e‐<br />
health<br />
B15.3.3 Other M & E 4 12.24
Sl.No. Activity Unit Cost Physical<br />
Targets<br />
Required<br />
fund under<br />
NRHM<br />
B.20 <strong>Health</strong> Insurance Scheme<br />
B21 Research, Studies, Analysis<br />
B.22 State level health resources<br />
center(SHSRC)<br />
B23 Support Services<br />
B23.1 Support Strengthening NPCB<br />
B23.2 Support Strengthening Midwifery Services under<br />
medical services<br />
B23.3 Support Strengthening NVBDCP<br />
B23.4 Support Strengthening RNTCP<br />
B23.5 Contingency support to Govt. dispensaries<br />
B23.6 Other NDCP Support Programmes<br />
B.24 Other Expenditures<br />
B.24.1 Telemedicine 3 7.35<br />
B.24.2 Strengthning of Nursing school 2 117.40<br />
B.24.3 Sickle cell disease 15 41.52<br />
B.24.4 Coordination cell DH 1 4.58<br />
B.24.5 Maher Scheme 11 16.40<br />
B.24.6 Volunteer to tribal PHC 34 12.96<br />
B.24.7 Diet facility for PHC 14 19.80<br />
INNOVATIONS/ PPP/ NGO<br />
B NRHM Additionalities<br />
B14 PPP/ NGOs<br />
B14.1 Non governmental providers of health care<br />
RMPs/TBAs<br />
B14.2 PNDT and Sex Ratio<br />
B14.3 Public Private Partnerships<br />
B14.4 NGO Programme/ Grant in Aid to NGO<br />
B14.5 Other innovations( if any)<br />
C Routine Immunization 21262 21.76<br />
1.4 NVBDCP<br />
D NLEP<br />
NGO Services<br />
a) NGOs<br />
b) Pvt. Sector<br />
E NBCP<br />
Cataract Performance<br />
a) NGOs 4.00<br />
b) Pvt. Sector<br />
F RNTCP<br />
NGO/PPP Support<br />
G IDSP
Sl.No. Activity Unit Cost Physical<br />
Targets<br />
H NIDDCP<br />
Required<br />
fund under<br />
NRHM<br />
Operational Cost<br />
E<br />
Other NDCPs<br />
NVBDCP<br />
Mobility Support<br />
Lab Consumables/ Materials<br />
Review Meetings<br />
Field Visits<br />
Formats and Reports<br />
Communication facility to Staffs<br />
Repair of Laparoscopes<br />
26.70<br />
Others 320.26<br />
F NLEP<br />
Mobility Support<br />
Lab Consumables<br />
Review Meetings<br />
Field Visits<br />
Office Expenditures, Formats and Reports 8.23<br />
G NBCP<br />
Mobility Support<br />
Lab Consumables<br />
Review Meetings<br />
Field Visits<br />
Formats and Reports<br />
Others 0.42<br />
H RNTCP<br />
Mobility Support<br />
Lab Consumables<br />
Review Meetings<br />
Field Visits<br />
3.00<br />
Formats and Reports 0.82<br />
Others 27.10<br />
I IDSP<br />
Mobility Support<br />
Lab Consumables<br />
Review Meetings<br />
Field Visits<br />
Formats and Reports<br />
0.25<br />
Others 0.36<br />
I NIDDCP<br />
Mobility Support<br />
Lab Consumables<br />
Review Meetings
Sl.No. Activity Unit Cost Physical<br />
Targets<br />
Required<br />
fund under<br />
NRHM<br />
Field Visits<br />
Formats and Reports<br />
DMHP 42.45<br />
DTCP 12.16<br />
Financial Aid /Grant to Institutions<br />
For all NDCP's—<br />
i) Financial Aid /Grant to Medical Collages<br />
ii) Financial Aid /Grant to Referral Institutions<br />
iii) Financial Aid /Grant to Sentinel Sites<br />
iv) Financial Aid /Grant to Medical Hopitals<br />
Financial Aid /Grant to Others (Pl. Specify)<br />
Total.. 3930.03
Sr.<br />
No.<br />
Chapter – 7<br />
Resources and other sources of fund for health sector<br />
Activities<br />
District Expenditure At a Glance<br />
RCH FLEXIPOOL<br />
District - <strong>Amravati</strong><br />
Allocation As<br />
Per PIP 2010-<br />
2011<br />
A RCH Flexipool<br />
1 Maternal <strong>Health</strong><br />
Expenditure Upto<br />
30 Nov. 2010<br />
(Rs. In Lakhs)<br />
Per. %<br />
(Progressive)<br />
a JSY 58.22 74.26 127.55<br />
b Others 13.46 4.60 34.18<br />
Sub Total 71.68 78.86 110.02<br />
2 Child <strong>Health</strong> 193.23 56.95 29.47<br />
3 Family planning -<br />
4<br />
Sterlisation Compensation 78.89 37.18 47.13<br />
NSV Camp 0.53 0.10 18.87<br />
Others 16.09 3.66 22.75<br />
Sub Total 95.51 40.94 42.86<br />
Adolscent Reproductive & Sexual<br />
<strong>Health</strong><br />
5.70 0.94 16.49<br />
5 Urban RCH 32.38 13.35<br />
6 Tribal RCH 33.73 5.44 16.13<br />
7 Vulnerable Group, including NRC 1.80 0.09 5.00<br />
8 Innovation / PPP/ NGO 4.55 0.45 9.89<br />
9 Infrastructure & Human Resources 103.02 26.44 25.66<br />
10 Institutional Strengthening 8.65 0.22 2.54<br />
11 Training - -<br />
12 BCC/IEC 8.00 0.37 4.63<br />
13 Procurement - -<br />
14 Programme Management 17.61 8.69 49.35<br />
Others - R 14 Register Printing 2.03<br />
TOTAL 575.86 232.74 40.42
Sr.<br />
No.<br />
Activities<br />
District Expenditure At a Glance<br />
NRHM Additionalities<br />
District - <strong>Amravati</strong><br />
Allocation As<br />
Per PIP 2009-<br />
2010<br />
B NRHM Additionalities<br />
Expenditure<br />
Upto 30 Nov.<br />
2010<br />
(Rs. In Lakhs)<br />
Per. %<br />
(Progressive)<br />
1 Asha 91.73 43.45 47.37<br />
2 Contractual Staff Payment<br />
a 24 x 7 Nurses . 42.00 12.35 29.40<br />
b LHV/ Supervisor 36.24 9.24 25.50<br />
c ANM Staff 248.40 143.92 57.94<br />
d Fixed TA To ANM / LHV 19.48 9.86 50.63<br />
e Monthly Remuneration To PTLA 30.78 - -<br />
3 Village <strong>Health</strong> Sanitation Committee 154.70 35.65 23.04<br />
4 Untied Fund<br />
a Sub Centre 33.30 10.62 31.89<br />
b PHU 20.75 3.21 15.47<br />
c PHC 14.00 6.20 44.29<br />
d RH 4.50 1.62 36.00<br />
e SDH 2.00 0.44 22.00<br />
f WH 0.50 0.13 26.00<br />
5 RKS<br />
a RKS at DH 5.00 3.38 67.60<br />
b RKS at PHC 56.00 23.61 42.16<br />
c RKS at RH 9.00 7.80 86.67<br />
d RKS at SDH 4.00 2.60 65.00<br />
e RKS at WH 1.00 0.84 84.00<br />
f RKS at TB Hosital 5.00 - -<br />
g RKS at RR Centre 5.00 3.05 61.00<br />
6 Annual Maintainance<br />
a SC 29.90 8.12 27.16<br />
b PHC 24.00 10.97 45.71<br />
c RH 9.00 3.19 35.44<br />
d DH 5.00 3.46 69.20<br />
e SDH 4.00 2.15 53.75<br />
f WH 1.00 0.07 7.00
g PHU 31.00 3.09 -<br />
h RR Centre 5.00 1.47 29.40<br />
i TB Hospital 5.00 - -<br />
7 Repairs and New Construction<br />
a Spill Over Works 72.00 40.55 56.32<br />
8 Ambulance Service Repair -PHC 18.45 7.51 40.70<br />
9 IPHS<br />
Ambulance Service Repair-RH/SDH 1.68 0.76 45.24<br />
a IPHS at SC 83 83.00 5.74 6.92<br />
b IPHS at PHC 34 170.00 29.28 17.22<br />
c IPHS at RH 4 48.00 21.57 44.94<br />
d IPHS at SDH 4 60.00 27.73 46.22<br />
e IPHS at WH 1 35.00 12.56 35.89<br />
f IPHS at DH 1 50.00 23.57 47.14<br />
10 ISO Certification Of IPHS Institutions 34.07 - -<br />
11 Ayush<br />
a Ayush Center in RH / SDH / WH 20.16 10.59 52.53<br />
b Ayush Center in DH 7.08 3.78 53.39<br />
c District Ayush Cell 0.60 - -<br />
12 Telemedicine - Existing Centre 2.20 1.08 49.09<br />
New Telemedicine Node IN SDH 1.47 - -<br />
13 Strengthening of Nursing School 122.40 10.42 8.51<br />
Public Private partnership 15.00 - -<br />
14 Mobile Medical Unit 10.18 - -<br />
15<br />
Hardship Allowance to Regular<br />
<strong>Health</strong> Staff<br />
58.56 - -<br />
16 Coordination Cell In Tribal Areas 3.64 0.45 12.36<br />
17 Sickle Cell 33.10 1.20 3.63<br />
18 Maher Scheme 10.50 0.84 8.00<br />
19 Honorarium To Volunteer 4.40 1.65 37.50<br />
20 Monitoring & Evalution 9.84 3.56 36.18<br />
21 District <strong>Health</strong> Action Plan 8.40 - -<br />
22<br />
Streamlining The Procurement<br />
( Repair / New Construction of Dist<br />
Warehouse)<br />
1.20 0.52 43.33<br />
23 Salary for Infrastruture Cell 19.56 6.31 32.26
24<br />
IPHS Wing - Salary IPHS<br />
Coordinator/ Deo / Contingency<br />
6.13 1.60 26.10<br />
25 FMG 3.62 1.11 30.66<br />
26 Institutional Fund Monitoring Unit 1.86 0.09 4.84<br />
27<br />
28<br />
Sr.<br />
No.<br />
Block PMU- Salary / TA /<br />
Contingency<br />
Diet & Loss Of Wages to Deliveries<br />
IN Tribal PHCs<br />
66.36 30.24 45.57<br />
4.95 0.49 9.90<br />
TOTAL 1,880.68 593.69 31.57<br />
Activities<br />
District Expenditure At a Glance<br />
Immunization<br />
District - <strong>Amravati</strong><br />
Allocation As Per PIP<br />
2010-2011<br />
Expenditure<br />
Upto 30 Nov.<br />
2010<br />
(Rs. In Lakhs)<br />
Per. %<br />
(Progressive)<br />
C Immunisation<br />
1 Routine Immunisation 49.70 26.39 53.10<br />
TOTAL 49.70 26.39 53.10
<strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong><br />
Additional Activity Suggested by<br />
District<br />
PIP 2011‐12
PART‐ A RCH – II Flexipool<br />
1) Child <strong>Health</strong><br />
Chapter 8<br />
Additional activities suggested by District for year 2011‐12<br />
1) Loss of daily wages for mother stay at VCDC for Melghat mothers<br />
It is proposed to give Loss of daily wages to mother staying at VCDC with child in Melghat<br />
area. It is proposed to give loss of daily wages for 30 days @ Rs. 60 per day. Total budget of<br />
Rs. 72.00 Lacs is proposed for expected 4000 mothers @ Rs. 60/‐ per day per mother for 30<br />
days.<br />
2) Family Planning<br />
1) Incentive for delaying first pregnancy for three year after marriage<br />
It is proposed to introduced incentive based scheme for the couple keeping spacing for 3<br />
years. Incentive of Rs. 10000/‐ per couple who’s married after 01/04/2008. Estimated couple<br />
will be 45. Total budget of Rs. 4.50 Lacs is proposed for 45 couples @ 10000/‐ per couple.<br />
2) Free diet allowance for Family planning cases 11200<br />
It is proposed to give Free diet allowance to Family Planning cases for 2 days @ Rs. 75/‐ per<br />
day. Total budget of Rs. 11.20 Lacs is proposed for 11200 cases @ Rs. 150/‐ per case.<br />
3) Tribal RCH<br />
1) Provision of MO, ANM, Pharmacist, Driver, POL & maintenance for two Mobile Van.<br />
It is proposed to provide team of MO, LMO, ANM, Pharmacist with Driver for two Mobile<br />
Van. Salary of two MOs at Rs. 15000/‐ per month , Pharmacist and ANM @ Rs. 6000/‐ per<br />
month, Driver & Attendant @ Rs. 5000/‐ & 4000/‐ Res. per month. and POL & maintenance<br />
for each Mobile Van Rs. 10000/‐ per month. The Budget of Rs. 14.64 is proposed for salary of<br />
MO, ANM, Pharmacist, Driver, Attendance and POL & Maintenance of Mobile Van.<br />
2) Helpline in Tribal Block (Dharni and Chikhaldara)<br />
The budget of Rs. 4.32 Lacs is demanded for Emergency Referral Services related to Mother<br />
and child in tribal block through 24 hours call attending system at block level for that office<br />
expenditure, rented vehicle and honorarium of attendance is proposed.
Budget Head<br />
3) Provision for Monitoring & Evaluation activity in Melghat through monthly, quarterly<br />
meeting and field visit.<br />
The provision is proposed for expected 24 meeting at Semadoh and quarterly 8 meeting at<br />
block level Dharni & Chikhaldara. The Budget of Rs. 3.00 Lacs is proposed for meeting and<br />
time to time visit of stae level authority.<br />
CHILD HEALTH<br />
Loss of daily wages for<br />
mother stay at VCDC<br />
for Melghat mothers<br />
FAMILY PLANNING<br />
Insentive for delaying<br />
first pregnancy for<br />
three year after<br />
marriage<br />
Free diet allowance for<br />
Family planning cases<br />
11200<br />
TRIBAL RCH<br />
Provision of MO, ANM,<br />
Pharmasist,Driver, POL<br />
& maintainance for two<br />
Mobile Van.<br />
Helpline in Tribal Block<br />
(Dharni and<br />
Chikhaldara)<br />
Unit of<br />
Measu<br />
re<br />
Mothe<br />
r<br />
Budget of Additional Activity RCH-II<br />
PHYSICAL TARGET (where applicable) BUDGET (RS. LAKHS)<br />
Q I<br />
Q II<br />
Q II<br />
Q IV<br />
Total Annual<br />
Rate<br />
(Rs./Unit)<br />
Q I<br />
Q II<br />
Q II<br />
Q IV<br />
Total Annual<br />
Budget<br />
(Rs. Lakhs)<br />
1000 1000 1000 1000 4000 0.018 18.00 18.00 18.00 18.00 72.00<br />
Couple 15 15 15 0 45 0.010 1.50 1.50 1.50 0.00 4.50<br />
Cases 2800 2800 2800 2800 11200<br />
0.001<br />
5<br />
4.20 4.20 4.20 4.20 16.80<br />
Blocks 2 2 2 2 2 1.220 3.66 3.66 3.66 3.66 14.64<br />
Block 2 2 2 2 2 1.08 1.08 1.08 1.08 4.32<br />
Provision for monthly<br />
meeting at Semadoh<br />
and quartorly meeting<br />
at block level Dharni &<br />
Chikhaldara<br />
Block 8 8 8 8 32 0.02 0.16 0.16 0.16 0.16 0.64<br />
Total.. 3827 3827 3827 3812 15281 1 29 29 30 28 112.90
PART – B <strong>Mission</strong> Felxipool<br />
1) Proposal for Rest house at Chikhaldara, Tq. Chikhaldara,<br />
Requirement / Necessity :<br />
Many of the <strong>Health</strong> Schemes are implemented by state & central Government in tribal region.<br />
Melghat with primitive development does not suffice to the requirement of rest house and lodging<br />
for the Visitors, <strong>Health</strong> Officers & dignitaries from State & District Level<br />
Site location :<br />
The site is located at hill station in the premises of Primary <strong>Health</strong> Center, Chikhaldara. Chikhaldara<br />
Hill Station is 87 Km away from <strong>Amravati</strong> & the site is easily approachable by road.<br />
Area :<br />
The area available at site is 3 acras (Approximately) surrounded by Hillock and natural beauty.<br />
Details of Proposal :<br />
The rest house proposed in a area 72665 sq. Feet. The facility proposed at rest house includes the<br />
following. :<br />
• Entrance foyer with receptionist counter.<br />
• Managers office block.<br />
• Waiting area about 300 Sq. Feet.<br />
• V.I.P. Suite 4 Nos & regular suites 5 Nos.<br />
• Recreation Hall 1 No.<br />
• Conference hall having sitting arrangement of 30 to 35 Persons.<br />
• Dining hall 2 Nos. VIP Dining hall & Dining Hall<br />
• Dormitories 2 Nos<br />
• Rooms 10 Nos.<br />
• Garden Space with fountains.<br />
• Security officer and guard room.<br />
• Kitchen with store room.<br />
• Quarters for labour staff.<br />
• Parking space for 30 four wheeler.<br />
Estimate Cost :<br />
The estimated cost of Project amount to Rs. 175.00 lakhs which includes Civil work, interior<br />
designing work, electrification of building, installation of security system, water supply and<br />
sanitation<br />
2) THO Office Counstruction ‐<br />
Due to un avaibility of addiquate space from THO Office in District they have to face many<br />
problems and because of non avability of well furnished infrastructure for regular working of THO
Office. The bare necessity of THO Office has been occurred and new construction for THO Office<br />
within available place at either Panchyat Sameeti or SDH/RH premises.<br />
Within Distirct there are 14 blocks which required construction of THO Office hence it is<br />
suggested that to construct well furnished building for THO. Approximetly budget of Rs. 9.00 lacs<br />
per block required, hence total budget of Rs. 126.00 lacs required.<br />
3) New Construction for Sub Center<br />
District proposed new sub center construction of 10 building were existing building of SC is<br />
not available and requirement of SC is needed.<br />
4) Repair of Existing quarter at RH Churni<br />
In Melghat area RH Churni is located at remote place, the distance of hospital is above 140<br />
k.m. from distirict head quarter. There is no alternative arrangement available for residence for<br />
staffs. Hence it is proposed to renovate existing quarters for residential perpose of staff. There is 9<br />
quarter available and all required repairs. Total budget required Rs. 22.00 lacs.<br />
5) Converstion of old PHC building at Churni as residential quarter.<br />
There is old PHC prmises at Churni, which is presentaly of no use. Hence it is proposed to<br />
renove it old building as quarter, for that budget of Rs. 10.00 lacs is required.<br />
6) Construction of compound wall for IPHS Sub Center<br />
In district it is proposed to construct compound wall for IPHS Sub Center, approximetly<br />
budget required for per sub center Rs. 3.60 lacs for 20 IPHS Sub Center. Total budget of Rs. 72.00<br />
lacs required.<br />
7) Concret road for PHC<br />
For IPHS PHC In district infracture development of premises ids done but from entrance to<br />
PHC building there is need of internal concret road. It is proposed to construct concret road for IPHS<br />
PHCs approximetly budget required for per PHC Rs. .75 lacs. And total budget required for 34 IPHS<br />
PHCs is RS 25.50 lacs..<br />
New works proposed during 2011‐12<br />
Sr Type of institute New construction Total budget required<br />
1 Rest House at Chikhaldara 1 175.00 175.00<br />
2 THO Office Construction 14 126.00 126.00<br />
3 Sub Center 10 180.00 180.00<br />
4 Repari of RH Churni Quarter 9 22.00 22.00<br />
5 Converstion of old PHC as residential quarter 1 10.00 10.00<br />
6 Compund wall for SC 20 72.00 72.00<br />
7 Concreat road for PHC 34 25.50 25.50<br />
Total 89 610.50 610.50
Additional Requirement for District Hospital, <strong>Amravati</strong><br />
1) Equipment‐ Color Doppler with Echo probe‐ Rs.16 lacs.<br />
Distt.Hospital has old sonograpy machine with limited functions and less accuracy. Hence<br />
new advanced color Doppler with echo probe is essential.<br />
2) Central Oxigination and suction‐ Rs.20 lacs.<br />
Distt.Hospital has well equipped ICU, but without central oxigination and suction. It creates<br />
many problem during treatment of the patient, so cenrral oxigination and suction is<br />
essential.<br />
3) Intercom‐ Rs. 10 lacs.<br />
Distt hospital has old manually operated intercom system with limited lines. So there are<br />
connections to limited wards, it creates day to day problems to communicate with the staff<br />
and follow up of the patients by the authority. It is essential to have new automatic intercom<br />
system with increase lines.<br />
4) C.C. TV‐ Rs. 5 lacs.<br />
After terrorist attack on the hospital in Gujrat, the local police authority has advised to have<br />
CC TV at all places in the hospital campus. Recently in Women hospital one female patient<br />
was absconded and was found dead in the campus.Police are investigating the matter and<br />
again the police commissioner has advised to set CC TV in govt.hospital. CC TV will help to<br />
control the anti social element and will also assist the authority to monitor the services.<br />
5) Biometric machine‐ Rs.2 lacs<br />
To monitor the attendance and regularity of the hospital staff it is essential.<br />
6) Building repair & coloring‐ Rs. 93 lacs.<br />
Distt hospital was established in 1928, so the building is very old and it requires repair at<br />
many places and coloring of the building. Local B & C deptt.has given an estimate of Rs.93<br />
lacs for the said work, hence it is essential.<br />
Total budget required for the above activities ‐ Rs.1,52 lacs.
Sickle Cell Disease Project in Morshi Taluka<br />
1 Information about sickle cell disease ‐<br />
It is a crippling disease caused by sickling of red blood cell because of hypoxia.<br />
It lowers average age of death and make life miserable for the patient.<br />
2 Project in Short ‐<br />
a) Screening of all population from 0 to 30 yrs age in Morshi Taluka for sickle cell<br />
disease by solubility test and confirmation by electrophoresis of those who found<br />
positive in solubility test. Screening will start from tribal villages in Morshi Taluka<br />
and step by step whole population of Morshi Taluka from 0 to 30 yrs will be covered.<br />
b) Treatment of sickle cell disease patients at government health facilities.<br />
c) <strong>Health</strong> education through IEC<br />
d) Counseling before marriage by trained counselor.<br />
3 Objective of the Project ‐<br />
1) To reduce mortality of Sickle Cell Disease patients.<br />
2) To reduce prevalence Sickle Cell Disease by doing pre marriage counseling.<br />
4 Implementation of Project ‐<br />
Step 1 ‐ To create awareness in the society about Sickle Cell Disease through IEC.<br />
Step 2 ‐ Mass screening will be done by ASHA. They will refer the client to the PHC, SDH<br />
for Solubility Test. ASHA will be paid Rs.10 per client for motivation. If it is found positive<br />
in solubility test then he will be refer for electrophoresis by ASHA and she will be paid<br />
Rs. 25 per patient.<br />
Step 3 ‐ Counseling of the Sickle Cell Disease patient by trained counselor including<br />
premarriage counseling .<br />
Step 4 ‐ Treatment of Sickle Cell Disease patients at PHC and SDH level including Blood<br />
Transfusion facility at SDH level.<br />
5 Manpower & Material requirement ‐<br />
1) Lab Technician ‐ 1 SDH<br />
Total 6<br />
2) Supervisor ‐ 1<br />
3) Date Entry Operator ‐ 1<br />
4) Counselor ‐ 1<br />
5 PHC
6 Estimated Cost of Project ‐<br />
1) Supervisor ‐ Rs 6000/month x 12 month = Rs. 72000.00<br />
2) Lab Tech ‐ (Rs 6000/monthx 6 person) x 12 month = Rs. 432000.00<br />
3) DEO ‐ Rs 6000/month x 12 month = Rs. 72000.00<br />
4) Counselor ‐ Rs 6000/month x 12 month = Rs. 72000.00<br />
5) TA to Counselor ‐Rs 1000/month x 12 month = Rs. 12000.00<br />
6) TA to Supervisor ‐Rs 1000/month x 12 month = Rs. 12000.00<br />
7) Office expenses ‐Rs 8000/month x 12 month = Rs. 96000.00<br />
8) IEC ‐Rs 1000/month x 12 month = Rs. 12000.00<br />
9) Insturment & Equipment = Rs. 500000.00<br />
10) Incentive to ASHA<br />
Total Population – 176864<br />
Population under screening – 63670 x Rs. 10 = Rs. 636700.00<br />
Population for electrophoresis – 12734 x Rs. 25 = Rs. 318350.00<br />
Total Rs. 2235050.00
Additional activity suggested for Melghat region<br />
1) Taluka Training Center :‐<br />
Justification :‐ The distance of District Training center from Melghat is about 100‐150 km.<br />
aprox. Travel facility between these two destination is not so frequent so the health<br />
personnel suffer from physical as well as mental stress and looking behind faulty technical<br />
training facility. So to save the time and avoid long journey to workers. So taluka training<br />
center is essential.<br />
Budget Required :‐<br />
Building ‐ 5000000/‐<br />
Manpower ‐ 500000 /‐<br />
Contigency ‐ 100000 /‐<br />
Equipments ‐ 400000 /‐<br />
Total 6000000/‐<br />
2) Two wheeler facility at PHC level :‐<br />
Justification :‐ As our taluka is tribal and villages are in remote places where the roads and<br />
transport facility is so poor. At the many villages there is difficulty in reaching by four<br />
wheelers.<br />
Also to implement many national programmes properly and timely with proper information<br />
and communication. Like immunization session in every month.<br />
Tracking sporadic cases first information to phc. There is a need of at least 4 two wheelers<br />
for supervisors with fuel facility.<br />
Budget Required for 11 PHC for Melghat:‐<br />
Vehicle Price ‐ 220000 /‐<br />
Fuel for year ‐ 48000 /‐<br />
Total Budget ‐ 268000/‐<br />
3) Strengthening of Bharari Pathak Yojana :‐<br />
Justification :‐ As there are 22 Medical officer working in 22 Bharari Pathak in very remote<br />
places where residence facility for Doctors are not available so many Doctors are not<br />
interested to give there best services. So there is a urgent need of residensial 1 BHK quarter<br />
at head quarter place of Bharari Pathak.<br />
Budget Required :‐ Per Quarter ‐ 1000000/‐<br />
5) Strengthening of <strong>Health</strong> workers, by providing residential quarters :‐<br />
Justification :‐<strong>Health</strong> workers in melghat are giving there services in so many remote places<br />
where the residence facility is not available for them.<br />
Only permanent ANMs lives in subcenter building but other contractual ANM and<br />
MPW are not provided with residence facility. So to improve ground level health services for
door to door facility residential quarters for MPW & Contractual ANM are required at each<br />
subcenter.<br />
6) OT Extension :‐<br />
Justification :‐ The already constructed OT’s in all PHC’s are of inadequate space so for<br />
adequate spacing and operative services OT extension is needed at each PHC level. Budget<br />
required of per PHC @ Rs. 5.00 lacs.<br />
7) Deep Burial Pit facility with sharp pit at each subcenter level :‐<br />
Justification :‐To dispose the biomedical waste (placenta) as well as chemical & sharp waste<br />
the deep burial pit with sharp pit is required at each subcenter. Budget required for 95 sub<br />
center @ Rs. 0.35 lacs per SC.<br />
8) Solar water heating facility at each subcenter level :‐<br />
Justification :‐To improve institutional deliveries at subcenter level warm water is required<br />
for patients so solar water heating system is needed at each subcenter level. Budget<br />
required @ Rs. 0.50 lacs per SC.<br />
9) Express feeder at each PHC’s :‐<br />
Justification :‐ PHC Services consist of immunization vaccines OT services, delivery services,<br />
emergency health services all needs 24 hour electricity. So there is a need of express feeder<br />
at each PHC’s in Dharni Taluka.<br />
10) Regular Workshop for Bhumka/Padiyal :‐<br />
Justification :‐In tribal melghat the impact of bhumka/padiyal is highly influenced on the<br />
mindset of villagers so the believe on them first of all to come out of there sufferings than<br />
health services and ultimately it results in increased child mortality and maternal mortality in<br />
tribal area. So to tackle the situation there is a need to organize regular training workshop<br />
for bhumka/padiyal in tribal region at block villages, PHC’s to change the killers to healer<br />
situation.<br />
11) Strengthening of MHU :‐<br />
Justification :‐ At Present there is a sanctioned mobile health vehicle but no staff and fuel as<br />
per previous year PIP. So there is a need of fulfillment of staff consisting of medical officer‐1,<br />
health worker (M/F)‐2, attendant‐1 & Driver‐1 for this mobile health unit to improve the IEC<br />
as well as campaign facility at remote villages.<br />
Budget Required :‐<br />
Employees Salary ‐ 360000 / year<br />
Vehicle maintenance & Fuel ‐ 75000 / year<br />
Total 435000 / year
12) Ideal awards for health employees :‐<br />
Justification :‐ <strong>Health</strong> employees are giving health services at very remote villages with their<br />
devotion & dedication. To encouraged them, an awards should be given for hard working &<br />
best working health employees.<br />
1) For best health assistant – Male & Female<br />
2) For best health worker – Male & Female<br />
3) For best Medical officer<br />
4) For best Honorary Medical Officer<br />
13) <strong>Health</strong>y baby competition at each village per quarter :‐<br />
Justification :‐To enhance the community participation and effective reduction in protein<br />
energy malnutrition status of children at each villages. There is urgent need to give special<br />
prizes to health babies.<br />
1) <strong>Health</strong>y baby at 6 month age<br />
2) <strong>Health</strong>y baby at 12 month age<br />
3) <strong>Health</strong>y baby at 36 month age<br />
4) <strong>Health</strong>y baby at 5 year age<br />
So that the parents/ relative on their own try to feed their babies take care, give health<br />
facility and ultimately the health babies in the community.<br />
14) Additional quarters at PHC’s :‐<br />
Justification :‐The health staff/employees give health services at PHC level where there is<br />
difficulty in getting the residence facility in villages. So to enhance the capacity of employees<br />
& better quality health services there is a need for additional residential quarters to<br />
1) For Lab Technician<br />
2) For <strong>Health</strong> Assistant Male<br />
3) For additional Medical Officer on deputation/specialist<br />
4) For <strong>Health</strong> worker Male<br />
15) Kitchen facility at PHC’s level :‐<br />
Justification :‐ At Present the diet tenders are given to personnel who resides out of PHC<br />
campus & not fully able to fulfill the quality diet needs of indoor patients. Hence there need<br />
to provide kitchen facility/canteen at each PHC consisting of cook & cooking experts &<br />
Kitchen room.