Gebruik van point-of care systemen bij patiënten met orale ... - KCE
Gebruik van point-of care systemen bij patiënten met orale ... - KCE
Gebruik van point-of care systemen bij patiënten met orale ... - KCE
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>KCE</strong> Reports 117 POC Anticoagulation 119<br />
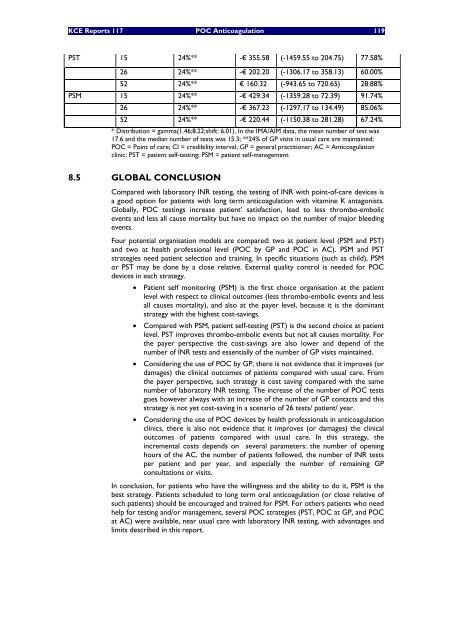
PST 15 24%** -€ 355.58 (-1459.55 to 204.75) 77.58%<br />
26 24%** -€ 202.20 (-1306.17 to 358.13) 60.00%<br />
52 24%** € 160.32 (-943.65 to 720.65) 28.88%<br />
PSM 15 24%** -€ 429.34 (-1359.28 to 72.39) 91.74%<br />
26 24%** -€ 367.23 (-1297.17 to 134.49) 85.06%<br />
52 24%** -€ 220.44 (-1150.38 to 281.28) 67.24%<br />
* Distribution = gamma(1.46;8.22;shift: 6.01). In the IMA/AIM data, the mean number <strong>of</strong> test was<br />
17.6 and the median number <strong>of</strong> tests was 15.3; **24% <strong>of</strong> GP visits in usual <strong>care</strong> are maintained;<br />
POC = Point <strong>of</strong> <strong>care</strong>; CI = credibility interval; GP = general practitioner; AC = Anticoagulation<br />
clinic; PST = patient self-testing; PSM = patient self-management<br />
8.5 GLOBAL CONCLUSION<br />
Compared with laboratory INR testing, the testing <strong>of</strong> INR with <strong>point</strong>-<strong>of</strong>-<strong>care</strong> devices is<br />
a good option for patients with long term anticoagulation with vitamine K antagonists.<br />
Globally, POC testings increase patient’ satisfaction, lead to less thrombo-embolic<br />
events and less all cause mortality but have no impact on the number <strong>of</strong> major bleeding<br />
events.<br />
Four potential organisation models are compared: two at patient level (PSM and PST)<br />
and two at health pr<strong>of</strong>essional level (POC by GP and POC in AC). PSM and PST<br />
strategies need patient selection and training. In specific situations (such as child), PSM<br />
or PST may be done by a close relative. External quality control is needed for POC<br />
devices in each strategy.<br />
• Patient self monitoring (PSM) is the first choice organisation at the patient<br />
level with respect to clinical outcomes (less thrombo-embolic events and less<br />
all causes mortality), and also at the payer level, because it is the dominant<br />
strategy with the highest cost-savings.<br />
• Compared with PSM, patient self-testing (PST) is the second choice at patient<br />
level. PST improves thrombo-embolic events but not all causes mortality. For<br />
the payer perspective the cost-savings are also lower and depend <strong>of</strong> the<br />
number <strong>of</strong> INR tests and essentially <strong>of</strong> the number <strong>of</strong> GP visits maintained.<br />
• Considering the use <strong>of</strong> POC by GP, there is not evidence that it improves (or<br />
damages) the clinical outcomes <strong>of</strong> patients compared with usual <strong>care</strong>. From<br />
the payer perspective, such strategy is cost saving compared with the same<br />
number <strong>of</strong> laboratory INR testing. The increase <strong>of</strong> the number <strong>of</strong> POC tests<br />
goes however always with an increase <strong>of</strong> the number <strong>of</strong> GP contacts and this<br />
strategy is not yet cost-saving in a scenario <strong>of</strong> 26 tests/ patient/ year.<br />
• Considering the use <strong>of</strong> POC devices by health pr<strong>of</strong>essionals in anticoagulation<br />
clinics, there is also not evidence that it improves (or damages) the clinical<br />
outcomes <strong>of</strong> patients compared with usual <strong>care</strong>. In this strategy, the<br />
incremental costs depends on several para<strong>met</strong>ers: the number <strong>of</strong> opening<br />
hours <strong>of</strong> the AC, the number <strong>of</strong> patients followed, the number <strong>of</strong> INR tests<br />
per patient and per year, and especially the number <strong>of</strong> remaining GP<br />
consultations or visits.<br />
In conclusion, for patients who have the willingness and the ability to do it, PSM is the<br />
best strategy. Patients scheduled to long term oral anticoagulation (or close relative <strong>of</strong><br />
such patients) should be encouraged and trained for PSM. For others patients who need<br />
help for testing and/or management, several POC strategies (PST, POC at GP, and POC<br />
at AC) were available, near usual <strong>care</strong> with laboratory INR testing, with ad<strong>van</strong>tages and<br />
limits described in this report.