Cervical Cancer Screening and Human Papillomavirus (HPV ... - KCE
Cervical Cancer Screening and Human Papillomavirus (HPV ... - KCE
Cervical Cancer Screening and Human Papillomavirus (HPV ... - KCE
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
16 <strong>Cervical</strong> cancer screening <strong>and</strong> <strong>HPV</strong> <strong>KCE</strong> reports vol.38<br />
defined at HSIL+ for an outcome of CIN2+ was 7% higher than for CP <strong>and</strong> this<br />
difference was significant (ratio: 1.07; CI: 1.03-1.12). For AutoCyte, the relative PPV<br />
was significantly higher than CP when the threshold was ASCUS+ for both outcomes:<br />
ratio of 1.26 (CI: 1.07-1.56) for CIN2+ <strong>and</strong> 1.22 (CI: 1.10-1.36) for CIN1+, but there<br />
was only one study that contributed data 52 . Repeating the meta-analysis of the testpositivity<br />
rate ratio, restricted to studies where the PPV for CIN2+ was sufficiently<br />
documented, showed: increased positivity rate for HSIL+ in ThinPrep <strong>and</strong><br />
AutoCyte/SurePath compared to CP (for ThinPrep: ratio: 1.52; CI: 1.10-2.12; for<br />
AutoCyte/SurePath: 1.53; 1.03-2.27) <strong>and</strong> an increased rate of LSIL in ThinPrep (ratio:<br />
1.79; CI: 1.05-3.06).<br />
2.4.2.3 Accuracy for histological confirmed CIN2+<br />
Test<br />
threshold<br />
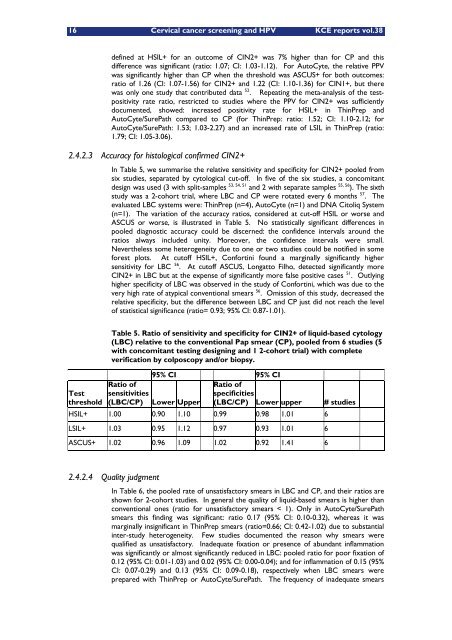
In Table 5, we summarise the relative sensitivity <strong>and</strong> specificity for CIN2+ pooled from<br />
six studies, separated by cytological cut-off. In five of the six studies, a concomitant<br />
design was used (3 with split-samples 53, 54, 51 <strong>and</strong> 2 with separate samples 55, 56 ). The sixth<br />
study was a 2-cohort trial, where LBC <strong>and</strong> CP were rotated every 6 months 57 . The<br />
evaluated LBC systems were: ThinPrep (n=4), AutoCyte (n=1) <strong>and</strong> DNA Citoliq System<br />
(n=1). The variation of the accuracy ratios, considered at cut-off HSIL or worse <strong>and</strong><br />
ASCUS or worse, is illustrated in Table 5. No statistically significant differences in<br />
pooled diagnostic accuracy could be discerned: the confidence intervals around the<br />
ratios always included unity. Moreover, the confidence intervals were small.<br />
Nevertheless some heterogeneity due to one or two studies could be notified in some<br />
forest plots. At cutoff HSIL+, Confortini found a marginally significantly higher<br />
sensitivity for LBC 56 . At cutoff ASCUS, Longatto Filho, detected significantly more<br />
CIN2+ in LBC but at the expense of significantly more false positive cases 51 . Outlying<br />
higher specificity of LBC was observed in the study of Confortini, which was due to the<br />
very high rate of atypical conventional smears 56 . Omission of this study, decreased the<br />
relative specificity, but the difference between LBC <strong>and</strong> CP just did not reach the level<br />
of statistical significance (ratio= 0.93; 95% CI: 0.87-1.01).<br />
Table 5. Ratio of sensitivity <strong>and</strong> specificity for CIN2+ of liquid-based cytology<br />
(LBC) relative to the conventional Pap smear (CP), pooled from 6 studies (5<br />
with concomitant testing designing <strong>and</strong> 1 2-cohort trial) with complete<br />
verification by colposcopy <strong>and</strong>/or biopsy.<br />
95% CI 95% CI<br />
Ratio of<br />
sensitivities<br />
(LBC/CP) Lower Upper<br />
Ratio of<br />
specificities<br />
(LBC/CP) Lower upper # studies<br />
HSIL+ 1.00 0.90 1.10 0.99 0.98 1.01 6<br />
LSIL+ 1.03 0.95 1.12 0.97 0.93 1.01 6<br />
ASCUS+ 1.02 0.96 1.09 1.02 0.92 1.41 6<br />
2.4.2.4 Quality judgment<br />
In Table 6, the pooled rate of unsatisfactory smears in LBC <strong>and</strong> CP, <strong>and</strong> their ratios are<br />
shown for 2-cohort studies. In general the quality of liquid-based smears is higher than<br />
conventional ones (ratio for unsatisfactory smears < 1). Only in AutoCyte/SurePath<br />
smears this finding was significant: ratio 0.17 (95% CI: 0.10-0.32), whereas it was<br />
marginally insignificant in ThinPrep smears (ratio=0.66; CI: 0.42-1.02) due to substantial<br />
inter-study heterogeneity. Few studies documented the reason why smears were<br />
qualified as unsatisfactory. Inadequate fixation or presence of abundant inflammation<br />
was significantly or almost significantly reduced in LBC: pooled ratio for poor fixation of<br />
0.12 (95% CI: 0.01-1.03) <strong>and</strong> 0.02 (95% CI: 0.00-0.04); <strong>and</strong> for inflammation of 0.15 (95%<br />
CI: 0.07-0.29) <strong>and</strong> 0.13 (95% CI: 0.09-0.18), respectively when LBC smears were<br />
prepared with ThinPrep or AutoCyte/SurePath. The frequency of inadequate smears