Support for Soldiers and Veterans You Gotta Have Heart The Joy of ...
Support for Soldiers and Veterans You Gotta Have Heart The Joy of ...
Support for Soldiers and Veterans You Gotta Have Heart The Joy of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
New St<strong>and</strong>ard<br />
Summer 2012 An employee publication <strong>of</strong> the North Shore-LIJ Health System<br />
<strong>Support</strong> <strong>for</strong><br />
<strong>Soldiers</strong> <strong>and</strong><br />
<strong>Veterans</strong><br />
<strong>You</strong> <strong>Gotta</strong><br />
<strong>Have</strong> <strong>Heart</strong><br />
<strong>The</strong> <strong>Joy</strong> <strong>of</strong><br />
[Healthy]<br />
Cooking
what’s INSIDE<br />
2 Summer 2012<br />
9On the Job at 30,000 Feet<br />
Two North Shore University Hospital nurses flying to<br />
Florida <strong>for</strong> some R&R respond to a medical emergency.<br />
22Zeroing In on Sepsis<br />
<strong>The</strong> health system’s new, more stringent criteria <strong>for</strong><br />
diagnosis will save lives.<br />
34New Discovery in Ovarian Cancer<br />
MicroRNA, a genetic marker, can help in choosing<br />
the best course <strong>of</strong> treatment.<br />
72 A First in New York State<br />
Percutaneous mitral valve replacement is per<strong>for</strong>med<br />
at Lenox Hill Hospital.<br />
88 Ambulance Tracker Launched at LIJ<br />
A new wireless system can collect patient data be<strong>for</strong>e<br />
they arrive at the ED.<br />
94 Remembering Spinney Hill<br />
A health system employee honors a historic African-<br />
American community in his documentary film.<br />
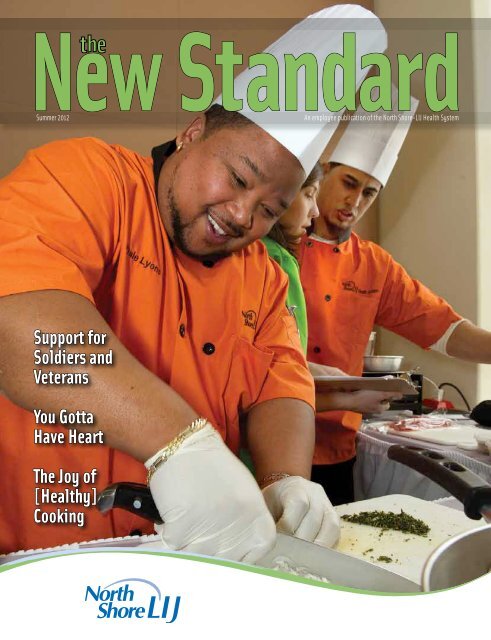
On the Cover<br />
Forest Hills Hospital chef Dale Lyons clearly loves his work – even<br />
chopping onions. He <strong>and</strong> fellow Forest Hills chef Gary DeFreitas,<br />
pictured in the background in the white chef’s toque, were winners<br />
<strong>of</strong> the health system’s Ultimate Chef Healthy Entrée Challenge.<br />
Summer 2012<br />
Editor in Chief<br />
Terry Lynam<br />
Director <strong>of</strong> Editorial Services<br />
Maria Con<strong>for</strong>ti<br />
Contributors<br />
Alex<strong>and</strong>ra Brovey<br />
Allison Bunin<br />
Lisa D’Ambruoso<br />
Gerri Ganz<br />
Marc Greene<br />
<strong>The</strong>resa Jacobellis<br />
Dana Klosner<br />
Susan Kreimer<br />
Kristen Longo<br />
Stacey Makely<br />
Erica Manney<br />
Barbara Mlawer<br />
Brian Mulligan<br />
Emily Ng<br />
Margarita Oksenkrug<br />
Betty Olt<br />
Barbara Osborn<br />
Terri Ann Parnell, RN, DNP<br />
Michelle Pinto<br />
Michelle Pipia-Stiles<br />
Kathleen Rohan<br />
Neil Rosen<br />
Arleen Ryback<br />
Ann Silverman<br />
Peter Spanos<br />
Jamie Talan<br />
Timothy Vassilakos<br />
Kathleen Waton<br />
<strong>The</strong>a Welch<br />
Elaine Wohl<br />
Photography<br />
North Shore-LIJ Studios,<br />
except as noted<br />
Graphic Design<br />
Gina Reduzzi/Reduzzi Design<br />
Comments/Suggestions? Contact:<br />
Public Relations Department<br />
125 Community Drive<br />
Great Neck, NY 11021<br />
(516) 465-2600
a MESSAGE from the PRESIDENT<br />
See more<br />
Walk to Paris<br />
photos on<br />
page 47.<br />
Building a Wellness Culture<br />
Just a few weeks removed from the conclusion <strong>of</strong> the Walk to Paris, I can say without hesitation<br />
that it was the most successful employee engagement we’ve ever done. <strong>You</strong> demonstrated your<br />
enthusiasm right from the start, with about 15,000 employees (1,493 teams <strong>of</strong> 10) enrolling in this<br />
first-ever fitness campaign <strong>and</strong> 914 teams (comprising 9,000+ employees) successfully completing<br />
the challenge, each team collectively walking 7.2 million steps – the approximate distance from New<br />
York to Paris.<br />
All told, participants walked over five million miles <strong>and</strong> took more than 10 billion steps.<br />
<strong>You</strong> lost an estimated 145,000 pounds – the equivalent <strong>of</strong> 764 adult males, 73 elephants or 66<br />
Honda Civics.<br />
We’re pleased to have recognized your ef<strong>for</strong>ts by raffling <strong>of</strong>f free trips to Paris to four<br />
teams (40 employees) <strong>and</strong> giving out some great consolation prizes to 10 additional teams (100<br />
employees), including choices<br />
<strong>of</strong> gym memberships, wellness<br />
retreats <strong>and</strong> massages.<br />
But as we all know, the<br />
Walk to Paris was about more<br />
than winning a trip to Paris –<br />
the overriding goal is to change<br />
our culture <strong>and</strong> help us make<br />
wellness part <strong>of</strong> our lifestyle. It<br />
has to be part <strong>of</strong> our DNA if we<br />
are going to change the health<br />
<strong>of</strong> our communities.<br />
We have already made some<br />
major progress. Several years<br />
ago, we became a tobacco-free<br />
organization, <strong>and</strong> through<br />
our free smoking cessation<br />
program, nearly 1,000<br />
employees have quit smoking.<br />
We started our “Weight<br />
Watchers At Work” program,<br />
enrolling thous<strong>and</strong>s <strong>of</strong><br />
Rosemarie Ennis celebrates when the team she captained, Twinkle Toes, was<br />
r<strong>and</strong>omly selected to go to Paris. Other Paris-bound teams were: Walka-<br />
Walka-Walka <strong>of</strong> Patient Financial Services in Westbury, Microbiologie Marche<br />
A’Paris <strong>of</strong> North Shore-LIJ Laboratories in Lake Success, <strong>and</strong> Champs-Elysees<br />
<strong>of</strong> LIJ Medical Center.<br />
employees across the health system. We also opened our own fitness facility, Vivo Health Fitness,<br />
<strong>and</strong> <strong>of</strong>fer various discounted gym memberships across the New York metro area.<br />
Perhaps most importantly, as part <strong>of</strong> our Know <strong>You</strong>r Numbers Program, more than 8,000<br />
employees participated in free onsite health screenings <strong>and</strong> another 5,000 saw their personal<br />
physicians to learn about their numbers <strong>and</strong> their risks <strong>for</strong> serious illness just this past winter.<br />
Going <strong>for</strong>ward, we’re planning another team-based competition <strong>and</strong> education program to<br />
help you <strong>and</strong> your families incorporate more fruits <strong>and</strong> vegetables (five servings a day) into your diet.<br />
Many <strong>of</strong> our cafeterias also are undergoing food <strong>and</strong> nutrition makeovers, <strong>and</strong> will be <strong>of</strong>fering more<br />
nutritious foods with more fruits <strong>and</strong> vegetables. We’re also looking to roll out fruit <strong>and</strong> vegetable<br />
carts at our hospitals, particularly during night shifts, where healthy eating is most challenging.<br />
So, welcome to the wellness revolution – <strong>and</strong> congratulations on an incredible achievement.<br />
<strong>The</strong> New St<strong>and</strong>ard<br />
3
For Craig Washington,<br />
serving overseas in the<br />
military meant missing<br />
family milestones, from the<br />
birth <strong>of</strong> his first niece to his<br />
cousin’s high school graduation.<br />
It also meant not being around<br />
<strong>for</strong> day-to-day chores, like<br />
helping his then-wife with yard<br />
work or fixing the television<br />
when it went out.<br />
“<strong>You</strong> feel very helpless<br />
because you’re over there<br />
<strong>and</strong> she’s over here,” said Mr.<br />
Washington, an Air Force<br />
veteran who completed two<br />
tours in Afghanistan. “Coming<br />
back, you have to overcome that<br />
— <strong>and</strong> it’s not always easy.”<br />
<strong>The</strong> transition process<br />
eventually led to the demise<br />
<strong>of</strong> his marriage, said Mr.<br />
Washington, who now works as<br />
the patient support manager at<br />
<strong>The</strong> Zucker Hillside Hospital.<br />
Hundreds <strong>of</strong> thous<strong>and</strong>s <strong>of</strong><br />
veterans like Mr. Washington<br />
have struggled with the<br />
transition from war back into<br />
civilian life. Almost 20 percent<br />
4 Summer 2012<br />
Partnership <strong>Support</strong>s<br />
<strong>Veterans</strong> <strong>and</strong> <strong>The</strong>ir Families<br />
By Stacey Makely<br />
<strong>of</strong> veterans who served in Iraq<br />
<strong>and</strong> Afghanistan reported<br />
symptoms <strong>of</strong> post-traumatic<br />
stress disorder or major<br />
depression in a 2008 study by<br />
the RAND Corporation.<br />
<strong>The</strong> Unified Behavioral<br />
Health Center <strong>for</strong> Military<br />
<strong>Veterans</strong> <strong>and</strong> <strong>The</strong>ir Families,<br />
scheduled to open later this<br />
year as a partnership between<br />
the US Department <strong>of</strong> <strong>Veterans</strong><br />
Affairs <strong>and</strong> Zucker Hillside,<br />
will help ease the strain <strong>of</strong> these<br />
<strong>and</strong> other issues that so <strong>of</strong>ten<br />
face veterans <strong>and</strong> their families.<br />
<strong>The</strong> 4,000-square-foot Bay<br />
Shore building will include a<br />
behavioral health center side<br />
by side with a VA healthcare<br />
facility. <strong>The</strong> pairing is the only<br />
one <strong>of</strong> its kind in New York<br />
State <strong>and</strong> will allow vets to<br />
receive medical care on one side<br />
<strong>of</strong> the building <strong>and</strong> behavioral<br />
healthcare on the other.<br />
“In a very unique way,<br />
the center will be able to treat<br />
veterans <strong>and</strong> their family<br />
members,” said Andrew<br />
Roberts, director <strong>of</strong> North<br />
Shore-LIJ’s Office <strong>of</strong> Military<br />
<strong>and</strong> <strong>Veterans</strong> Liaison Services.<br />
Mr. Roberts knows firsth<strong>and</strong><br />
just how important this<br />
kind <strong>of</strong> treatment can be: He<br />
served in Iraq from 2003<br />
to 2004 as an Army battery<br />
comm<strong>and</strong>er <strong>and</strong> returned with<br />
post-operational stress.<br />
But so many other soldiers<br />
never made it home from the<br />
war, <strong>and</strong> Mr. Roberts believes<br />
that veterans owe it to those<br />
soldiers to become reintegrated<br />
into society <strong>and</strong> live a full life —<br />
something that can be difficult<br />
without healing from the<br />
emotional wounds <strong>of</strong> war.<br />
“<strong>The</strong> stress that can come<br />
with a deployment to Iraq<br />
or Afghanistan can have a<br />
tremendous impact on not just<br />
the service member but also<br />
the family,” Mr. Roberts said.<br />
“Speaking as someone who<br />
suffered when I came back, it’s<br />
not always easy to realize or be<br />
aware that you’re struggling<br />
with something. Talking to a<br />
pr<strong>of</strong>essional who is trained<br />
in evidence-based therapies<br />
can really help you feel like<br />
yourself again.”<br />
Soldier Ride<br />
Join us on July 20 <strong>for</strong> a great ride <strong>for</strong> the<br />
Wounded Warrior Project.<br />
Soldier Ride is an inspiring opportunity<br />
<strong>for</strong> the public to participate in a cycling<br />
event that honors the men <strong>and</strong> women<br />
<strong>of</strong> our military who sacrificed so much.<br />
Soldier Ride raises awareness <strong>for</strong><br />
our nation’s wounded warriors who<br />
courageously battle the physical <strong>and</strong><br />
psychological damages <strong>of</strong> war,<br />
<strong>and</strong> <strong>of</strong>fers the public a chance to ride<br />
alongside as our nation’s wounded<br />
warriors promote their positive<br />
message <strong>of</strong> recovery!<br />
For further in<strong>for</strong>mation, call<br />
Lisa Finnegan at (631) 647-3825.
MANHASSET — Since Operation<br />
Iraqi Freedom began in<br />
2003, much has been written<br />
about the plight <strong>of</strong> returning<br />
military personnel. One member<br />
<strong>of</strong> the US Army Reserves,<br />
Michael Kentner, Platoon Sergeant,<br />
773rd Transportation<br />
Company, Fort Totten, who is<br />
also a New York City firefighter<br />
<strong>and</strong> a maintenance worker at<br />
the North Shore-LIJ Stern<br />
Center <strong>for</strong> Rehabilitation,<br />
knows how important it is <strong>for</strong><br />
reservists to have a supportive<br />
work environment.<br />
Last year, Sgt. Kentner<br />
found a Web site maintained<br />
by Employer <strong>Support</strong> <strong>of</strong> the<br />
Guard <strong>and</strong> Reserve, a US<br />
Department <strong>of</strong> Defense agency<br />
that sought Patriot Award<br />
nominations <strong>for</strong> employers<br />
that support military-reservist<br />
obligations. He wrote a letter<br />
extolling his immediate<br />
supervisor, Walter Oberman,<br />
the Stern Center’s assistant<br />
director <strong>of</strong> engineering, who<br />
“continues to support what I’m<br />
doing with a special sincerity<br />
that gives you chills. This guy<br />
embodies a certain intangible<br />
patriotism that simply cannot<br />
be articulated in words on<br />
paper.”<br />
At the recent ceremony to<br />
accept the Patriot Award, Mr.<br />
Oberman was surrounded by<br />
colleagues, veterans <strong>and</strong> active<br />
duty <strong>and</strong> reserve military<br />
personnel. He said he was<br />
<strong>The</strong> recipient <strong>of</strong> the Patriot Award, Walter Oberman (third from right), with: (from left) Andrew Roberts, Sergeant Major<br />
Vincent Mannion, Maureen McClusky, First Sergeant Kilsi Ciprian <strong>and</strong> Michael Kentner, platoon sergeant <strong>and</strong> Stern<br />
Center staff member.<br />
What It Means to Be<br />
a Patriotic Employer<br />
By Michelle Pinto<br />
both humbled <strong>and</strong> honored<br />
to work with his good friend,<br />
who, he added, “is clearly an<br />
American hero. How can you<br />
not want to help someone<br />
whose only thought is to help<br />
his country <strong>and</strong> his city?”<br />
Andrew Roberts, director<br />
<strong>of</strong> North Shore-LIJ’s Office <strong>of</strong><br />
Military <strong>and</strong> <strong>Veterans</strong> Liaison<br />
Services, led the ceremony.<br />
Mr. Roberts noted that the<br />
North Shore-LIJ Health System<br />
has recruited 100 veterans<br />
<strong>for</strong> various staff positions<br />
throughout health system<br />
facilities in the past year. He<br />
praised the health’s system<br />
practice <strong>of</strong> paying employees<br />
on military leave the difference<br />
between military pay <strong>and</strong> their<br />
regular salaries, ensuring that<br />
their service to our country does<br />
not create economic hardship.<br />
Also on h<strong>and</strong> to present<br />
the award was Sgt. Major<br />
Vincent Mannion, 301st<br />
In<strong>for</strong>mation Operations<br />
Battalion, Fort Totten.<br />
“<strong>The</strong>re are so many people<br />
who talk the talk but wind<br />
up complaining about<br />
the reservists’ military<br />
obligations,” he said,<br />
congratulating Maureen<br />
McClusky, executive director<br />
<strong>of</strong> the Stern Center, <strong>and</strong> staff<br />
members <strong>for</strong> providing true<br />
support <strong>and</strong> concern.<br />
<strong>The</strong> New St<strong>and</strong>ard<br />
5
LAKE SUCCESS —<br />
Normally, when you hear<br />
the word “PJs” you think<br />
<strong>of</strong> pajamas. But on a<br />
recent Friday afternoon,<br />
“PJs” took on an entirely<br />
different meaning. On this<br />
particular afternoon, a group<br />
<strong>of</strong> Pararescue Jumpers, aka<br />
PJs, from the 103rd Rescue<br />
Squadron <strong>of</strong> the New York Air<br />
National Guard/US Air Force<br />
from Westhampton Beach, came<br />
to the North Shore-LIJ Biokills<br />
Education Center in Lake<br />
Success <strong>for</strong> a special workshop<br />
on combat medical care.<br />
<strong>The</strong> pararescuers, some <strong>of</strong><br />
whom deployed to the Mideast<br />
within a week <strong>of</strong> their visit to<br />
the Bioskills Center, are the<br />
elite combat <strong>for</strong>ce specifically<br />
organized, trained <strong>and</strong> equipped<br />
to conduct both conventional<br />
<strong>and</strong> unconventional combat <strong>and</strong><br />
noncombat rescue operations.<br />
<strong>The</strong>y are the most highly<br />
trained <strong>and</strong> versatile personnel<br />
recovery specialists in the world.<br />
Because <strong>of</strong> their training, the<br />
pararescuers are called on to<br />
execute the most extreme rescue<br />
missions across the globe.<br />
In light <strong>of</strong> the<br />
pararescuers’ critical mission,<br />
the workshop — directed by<br />
Lieutenant Colonel Stephen<br />
Rush, MD, a pararescue flight<br />
surgeon, <strong>and</strong> Jason D’Amore,<br />
MD, director <strong>of</strong> the North<br />
Shore-LIJ Advanced Airway<br />
6 Summer 2012<br />
Special Forces Medics<br />
Trained at North Shore-LIJ<br />
By Marc Greene<br />
Training Center — focused on<br />
the advanced life-saving skills<br />
necessary when per<strong>for</strong>ming<br />
in severe environments.<br />
<strong>The</strong> operating room <strong>for</strong><br />
pararescuers is frequently in<br />
the back <strong>of</strong> a helicopter.<br />
While training at the<br />
Bioskills Education Center,<br />
part <strong>of</strong> North Shore-<br />
LIJ’s Center <strong>for</strong> Learning<br />
<strong>and</strong> Innovation (CLI),<br />
pararescuers learned critical<br />
techniques in such areas as<br />
advanced airway intubation,<br />
chest tube placement <strong>and</strong><br />
deep-wound packing, along<br />
with multiple suturing <strong>for</strong><br />
skin closure.<br />
“I can say without<br />
equivocation that the care that<br />
we are able to render to our<br />
military personnel in critical<br />
rescue situations is truly<br />
enhanced by our experience<br />
at the Bioskills Center,” said<br />
Colonel Rush. “We have<br />
been <strong>for</strong>tunate to have Dr.<br />
D’Amore as an enthusiastic<br />
<strong>and</strong> expert teacher.”<br />
Colonel Rush also<br />
thanked the North Shore-LIJ<br />
Health System <strong>for</strong> opening<br />
its doors to the military, <strong>and</strong><br />
Bioskills Education Center<br />
director Joseph Colaccico <strong>for</strong><br />
his logistical help <strong>and</strong> support.<br />
Colonel Rush said the<br />
103rd Rescue Squadron<br />
currently has three airmen<br />
deployed in the theater <strong>of</strong><br />
operation. “Not only were<br />
two lives saved because <strong>of</strong><br />
techniques that we practice <strong>and</strong><br />
honed in the Bioskills Labs,<br />
but also the patients were kept<br />
more com<strong>for</strong>table,” he said.<br />
North Shore-LIJ’s<br />
Biokills Education Center<br />
brings the latest operative<br />
techniques to physicians,<br />
medical students, nurses<br />
<strong>and</strong> surgical technologists.<br />
Coupled with the most<br />
advanced technologies in<br />
video <strong>and</strong> endoscopic surgical<br />
equipment, the center<br />
supports surgical training,<br />
continuing medical education<br />
<strong>and</strong> research.<br />
Watch the pararescuers<br />
in action at the Bioskills<br />
Education Center at<br />
http://bit.ly/zbMwNS.<br />
Above: Jason D’Amore, MD, center,<br />
trains pararescuers from the 103rd<br />
Rescue Squadron <strong>of</strong> the New York<br />
Air National Guard/US Air Force<br />
during a recent visit to the North<br />
Shore-LIJ Bioskills Education<br />
Center.
H<strong>of</strong>stra North Shore-LIJ School <strong>of</strong> Medicine<br />
Helps Vets With Unique Healthcare Needs<br />
<strong>The</strong> H<strong>of</strong>stra North Shore-LIJ School <strong>of</strong> Medicine has signed<br />
on with First Lady Michelle Obama’s Joining Forces initiative,<br />
which is committed to creating a new generation <strong>of</strong> doctors,<br />
medical schools <strong>and</strong> research facilities that will make sure our<br />
heroes receive the care worthy <strong>of</strong> their service. Recognizing<br />
Necessity Spurs Innovation<br />
When Jason D’Amore, MD, director <strong>of</strong> the North Shore-LIJ Advanced<br />
Airway Training Center, began conducting workshops on combat medical care<br />
with the Air National Guard pararescuers, he was surprised when he took a<br />
close look at one <strong>of</strong> the surgical medical kits <strong>for</strong> cricothyrotomy, commonly<br />
called a cric kit, used by the military in the field.<br />
“<strong>The</strong> kit was clearly designed by people who never went into the field to use<br />
it. <strong>The</strong>re were basic surgical tools that should’ve been included but weren’t, <strong>and</strong><br />
some <strong>of</strong> the tools that were needed were just too big to fit in the st<strong>and</strong>ard issue kit.”<br />
Necessity being the mother <strong>of</strong> invention <strong>and</strong> innovation, Dr. D’Amore teamed<br />
with medical device manufacturer Cook Medical to create a new cric kit that would<br />
not only have the appropriate surgical tools, but would also fit in a pararescuer’s<br />
fanny pack. “One <strong>of</strong> the pararescuemen showed me his own kit that he had literally<br />
taped together with surgical tools from an assortment <strong>of</strong> scavenged kits. I knew<br />
that we had a serious need that had to be addressed, but I also knew that we could<br />
put something together that would fit the bill — <strong>and</strong> the fanny pack.”<br />
This is the redesigned kit developed at North Shore-LIJ’s Bioskills Education<br />
Center with Cook Medical.<br />
veterans’ <strong>and</strong> their families’ sacrifice <strong>and</strong> commitment, H<strong>of</strong>stra<br />
North Shore-LIJ School <strong>of</strong> Medicine pledged to mobilize its<br />
integrated missions in education, research, <strong>and</strong> clinical care<br />
to train physicians to meet veterans’ <strong>and</strong> their families’ unique<br />
healthcare needs, including post-traumatic stress disorder (PTSD)<br />
<strong>and</strong> traumatic brain injury (TBI).<br />
“We are honored to participate in the White House<br />
Joining Forces initiative to address the healthcare needs <strong>of</strong><br />
military service members <strong>and</strong> veterans <strong>and</strong> their families,” said<br />
Lawrence Smith, MD, founding dean <strong>of</strong> the medical school.<br />
“Since 2006, North Shore-LIJ has served military personnel<br />
<strong>and</strong> their families, including young children, through its<br />
Rosen Family Wellness Center <strong>for</strong> Law En<strong>for</strong>cement <strong>and</strong><br />
Military Personnel <strong>and</strong> <strong>The</strong>ir Families, as well as other<br />
veterans-related services. As a result, the health system has<br />
extensive experience diagnosing <strong>and</strong> treating military service<br />
members <strong>and</strong> their families with behavioral health issues. This<br />
commitment to veterans carries over to our medical school<br />
<strong>and</strong> our curriculum.”<br />
<strong>The</strong> School <strong>of</strong> Medicine joins the Association <strong>of</strong><br />
American Medical Colleges (AAMC) <strong>and</strong> the American<br />
Association <strong>of</strong> Colleges <strong>of</strong> Osteopathic Medicine (AACOM)<br />
in the commitment to enrich medical education to ensure<br />
that physicians are aware <strong>of</strong> the unique clinical challenges <strong>and</strong><br />
best practices associated with caring <strong>for</strong> this group; to develop<br />
new research <strong>and</strong> clinical trials on PTSD <strong>and</strong> TBI to foster<br />
better underst<strong>and</strong>ing <strong>and</strong> treatment <strong>of</strong> these conditions; to<br />
share their in<strong>for</strong>mation <strong>and</strong> best practices with each other<br />
through a collaborative Web <strong>for</strong>um created by the AAMC;<br />
<strong>and</strong> to grow the body <strong>of</strong> knowledge leading to improvements<br />
in healthcare <strong>and</strong> wellness <strong>for</strong> our military service members,<br />
veterans <strong>and</strong> their families.<br />
First Lady Michelle Obama <strong>and</strong> Dr. Jill Biden created<br />
Joining Forces to bring Americans together to recognize, honor<br />
<strong>and</strong> take action to support veterans <strong>and</strong> military families as they<br />
serve our country <strong>and</strong> throughout their lives. <strong>The</strong> initiative<br />
aims to educate, challenge <strong>and</strong> spark action from all sectors<br />
<strong>of</strong> society to ensure veterans <strong>and</strong> military families have the<br />
support they have earned. <strong>The</strong> initiative focuses on key priority<br />
areas — employment, education <strong>and</strong> wellness — while raising<br />
awareness about the service, sacrifice <strong>and</strong> needs <strong>of</strong> America’s<br />
veterans <strong>and</strong> military families. More in<strong>for</strong>mation is available at:<br />
JoiningForces.gov <strong>and</strong> NorthShoreLIJ.com/rosen.<br />
<strong>The</strong> New St<strong>and</strong>ard<br />
7
in the SPOTLIGHT<br />
Members <strong>of</strong> the HealthPort team,<br />
pictured from left to rignt, are<br />
Christina Birrer, Devon Kelly,<br />
Jaclyn Kelly, Ron Sharpe,<br />
Fabrizio DiFazio, Cathlyn Fagan,<br />
Kai Chan <strong>and</strong> Jose Villamar.<br />
<strong>The</strong> HealthPort Team<br />
By Jamie Talan<br />
Less than a decade ago, an employee wanting to know what was going<br />
on in the ever-exp<strong>and</strong>ing North Shore-LIJ Health System could find a single<br />
page on the intranet. And it required a person to log in. Today, the virtual<br />
site <strong>for</strong> HealthPort is more like a city than a home. <strong>The</strong> renovation is nothing<br />
short <strong>of</strong>, well, BIG. It’s a community that serves the health system’s 43,000<br />
employees <strong>and</strong> allows them to navigate the entire l<strong>and</strong>scape <strong>of</strong> the health<br />
system’s infrastructure. <strong>The</strong>re are neighborhoods <strong>for</strong> nurses, doctors <strong>and</strong> other<br />
employees. Trustees even have their own key that provides them access to<br />
in<strong>for</strong>mation they can use to underst<strong>and</strong> the everyday operations <strong>of</strong> the system.<br />
It’s a city that has close to 40,000 unique visitors a month. Imagine a day<br />
when you had to hunt down a binder filled with hospital policies <strong>and</strong> procedures.<br />
If you needed to find a fellow employee, ha! It was virtually impossible. Now,<br />
it is virtually possible with one keystroke. PeopleFinder tells you where people<br />
work, how to find them <strong>and</strong> who they work <strong>for</strong>. People can sell cars <strong>and</strong> houses.<br />
<strong>The</strong>y can download any one <strong>of</strong> thous<strong>and</strong>s <strong>of</strong> <strong>for</strong>ms that once had been housed<br />
across the health system. And every day, HealthPort staff is creating even more<br />
customized features <strong>and</strong> is now designing an integrative social networking<br />
portal. People can now add their events themselves. HealthPort posts over 30<br />
new events a month.<br />
Training on the site is also saving time <strong>and</strong> money <strong>for</strong> the health system.<br />
Nurses can train at their desks with online nursing modules that have led to<br />
8 Summer 2012<br />
HealthPort has just won a 2012 LISA Award <strong>for</strong> Top S<strong>of</strong>tware Products<br />
from the Long Isl<strong>and</strong> S<strong>of</strong>tware & Technology Network (LISTnet). This puts<br />
North Shore-LIJ in the elite company <strong>of</strong> winners such as CA Technologies,<br />
Motorola, Northrop Grumman, PC Richard <strong>and</strong> Oracle. Congrats to the<br />
HealthPort team <strong>for</strong> the high-quality work you do!<br />
cost savings <strong>of</strong> almost $1 million, according to HealthPort manager Devon Kelly.<br />
Managers can now log on to the site <strong>and</strong> read <strong>and</strong> analyze financial score cards<br />
from every hospital in the health system. <strong>The</strong>y have access to daily census reports.<br />
And now doctors <strong>and</strong> other health practitioners have the tools at h<strong>and</strong> to read<br />
electronic medical records – <strong>and</strong> have x-rays <strong>and</strong> other scans uploaded to their<br />
desktop or phone, a private cyber-medical <strong>of</strong>fice.<br />
<strong>The</strong> HealthPort business team is powered by three full-time employees<br />
who work closely with the Web Services team. Last year, they implemented <strong>and</strong><br />
completed over 700 major projects <strong>for</strong> the site. “We are growing <strong>and</strong> creating<br />
a world where employees can find in<strong>for</strong>mation that will make their jobs easier,”<br />
said Devon Kelly, HealthPort manager. Employees also have remote access to<br />
HealthPort. <strong>The</strong>re are newsletters <strong>and</strong> events pages. Thous<strong>and</strong>s <strong>of</strong> people click<br />
in every day to the Employee Bulletin Board, where they can list items <strong>for</strong> sale<br />
or purchase them. <strong>The</strong> team has won 10 awards in the last few years. And they<br />
continue to talk to department heads about their specific needs so they can<br />
develop department-specific content <strong>for</strong> employees.<br />
“We see this as our home, our community,” said Ms. Kelly. And, “the virtual<br />
door is always open.”<br />
Users can contact the Help Desk at (516) 470-7272,<br />
HealthPortWebmaster@nshs.edu or Devon Kelly at (516) 465-3144.
A DAY in the LIFE<br />
Joanne Turnier<br />
Program Manager, Diversity,<br />
Inclusion <strong>and</strong> Health Literacy<br />
Q: What are your responsibilities?<br />
A: I promote health literacy, cultural diversity <strong>and</strong> inclusion throughout North<br />
Shore-LIJ. I also assess <strong>and</strong> implement strategies to improve the health literacy<br />
<strong>of</strong> our staff members, patients <strong>and</strong> their families. Along with Dr. Terri Parnell, I<br />
create health literacy programs <strong>for</strong> healthcare pr<strong>of</strong>essionals, cultural resources<br />
<strong>for</strong> employees <strong>and</strong> educational content <strong>for</strong> patient-room TVs across the system.<br />
I also teach <strong>and</strong> develop curricula <strong>for</strong> the Center <strong>for</strong> Learning <strong>and</strong> Innovation <strong>and</strong><br />
the Nursing Institute.<br />
Q: How did your career path lead to this role?<br />
A: I began my career in neonatal intensive care, <strong>and</strong> eventually transitioned to<br />
working with those who’ve experienced the sudden traumatic death <strong>of</strong> a loved<br />
one. Meanwhile, I worked as a nurse educator focusing on staff wellness <strong>and</strong><br />
end-<strong>of</strong>-life care. This experience in program development <strong>and</strong> exposure to<br />
diverse populations prepared me <strong>for</strong> my current position. I believe effective<br />
communication is essential in healthcare no matter the situation.<br />
Q: What initiatives are you working on?<br />
A: I am particularly focused on our Dignity <strong>and</strong> Respect = Inclusion campaign.<br />
This program educates employees about various cultures <strong>and</strong> how to overcome<br />
biases or lack <strong>of</strong> knowledge so misin<strong>for</strong>mation does not hinder the healthcare we<br />
provide. <strong>The</strong> Office <strong>of</strong> Diversity, Inclusion <strong>and</strong> Health Literacy is introducing the<br />
program through videos <strong>and</strong> live presentations. I’m also developing a number <strong>of</strong><br />
educational initiatives <strong>and</strong> staff resources that we will launch soon.<br />
Q: What is your #1 tip to those who want to promote diversity, inclusion <strong>and</strong><br />
health literacy?<br />
A: Approach patients <strong>and</strong> families with a compassionate heart <strong>and</strong> cultural<br />
humility. Be aware <strong>of</strong> your own biases; don’t be afraid to ask questions about<br />
your patients’ beliefs, traditions <strong>and</strong> culture.<br />
Take the pledge: NorthShoreLIJ.com/inclusionpledge.<br />
— By Erica Manney<br />
Duty Calls at 30,000 Feet<br />
For Two NSUH Nurses<br />
By <strong>The</strong>a Welch<br />
Debbie Smith, RN, <strong>and</strong> Connie Kwiatkowski, RN, were on a<br />
JetBlue flight to West Palm Beach in April, getting away <strong>for</strong> some<br />
R&R at Ms. Smith’s condo, when an announcement by the flight<br />
attendant made them realize that they weren’t on vacation quite yet.<br />
“She said, ‘Medical to the front, medical to the front,’” Ms.<br />
Smith recalled, “<strong>and</strong> then she said, ‘Any nurse or doctor, to the<br />
front.’ Connie <strong>and</strong> I looked at each other <strong>and</strong> she said to me, ‘I<br />
guess that’s us.’”<br />
So the nurses made their way to the front <strong>of</strong> the plane. <strong>The</strong>re<br />
they found an older woman on the floor, with a younger man<br />
kneeling beside her <strong>and</strong> supporting her head. “<strong>The</strong> first thing I<br />
said was, ‘Lay her down,’ Ms. Smith said. ‘Her blood needs to be<br />
flowing to her head.’ He didn’t respond. ‘Lay her down!’ I said,<br />
more <strong>for</strong>cefully. Finally he did. ‘I’m a nurse,’ he said. ‘We are,<br />
too,’ I said. I didn’t tell him that we have more than 50 years <strong>of</strong><br />
nursing experience between us, but I guess he felt the woman was<br />
in capable h<strong>and</strong>s, because he went back to his seat.”<br />
continued on page 69<br />
Connie Kwiatkowski (left) <strong>and</strong> Debbie Smith, nurses at NSUH, were pressed<br />
into service on a recent flight to Florida.<br />
<strong>The</strong> New St<strong>and</strong>ard<br />
9
LIJ, North Shore University Hospital<br />
Rank Tops <strong>for</strong> <strong>Heart</strong> Care in New York<br />
By Betty Olt<br />
NEW HYDE PARK — LIJ<br />
Medical Center <strong>and</strong> North<br />
Shore University Hospital provide<br />
some <strong>of</strong> New York State’s<br />
best outcomes <strong>for</strong> open-heart<br />
surgery <strong>and</strong> percutaneous coronary<br />
interventions, according<br />
to reports recently released by<br />
the state Department <strong>of</strong> Health.<br />
In fact, LIJ was the only hospital<br />
in the state with significantly<br />
better outcomes <strong>for</strong> both cardiac<br />
surgery <strong>and</strong> percutaneous<br />
coronary interventions.<br />
According to the Department<br />
<strong>of</strong> Health’s latest report<br />
on adult cardiac surgery (covering<br />
2007 to 2009), LIJ was<br />
one <strong>of</strong> only four hospitals in<br />
New York State — <strong>and</strong> the only<br />
one on Long Isl<strong>and</strong> — whose<br />
risk-adjusted mortality rates<br />
were significantly better than<br />
the statewide average <strong>for</strong> 676<br />
patients undergoing surgeries<br />
to repair or replace heart<br />
valves <strong>and</strong> <strong>for</strong> those in need<br />
<strong>of</strong> surgeries <strong>for</strong> both valve<br />
<strong>and</strong> coronary artery bypass<br />
graft (CABG) surgery. In a<br />
separate category analyzing<br />
outcomes <strong>for</strong> CABG, valve or<br />
valve/CABG, LIJ <strong>and</strong> North<br />
Shore University Hospital were<br />
among six hospitals in the state<br />
— <strong>and</strong> the only ones on Long<br />
Isl<strong>and</strong> — distinguished by low<br />
risk-adjusted mortality rates.<br />
Over the three-year period<br />
analyzed by the Department <strong>of</strong><br />
Health, the combined volume<br />
<strong>of</strong> cardiac surgeries at North<br />
Shore University Hospital <strong>and</strong><br />
LIJ Medical Center was 2,082<br />
— the most in the state.<br />
In addition to the<br />
10 Summer 2012<br />
hospitals’ top rankings, two<br />
LIJ heart surgeons, Robert<br />
Palazzo, MD, <strong>and</strong> S. Jacob<br />
Scheinerman, MD, <strong>and</strong> two<br />
North Shore University Hospital<br />
surgeons, Alan Hartman,<br />
MD, <strong>and</strong> Robert Kalimi,<br />
MD, were among 13 surgeons<br />
statewide to earn the Department<br />
<strong>of</strong> Health’s prestigious<br />
double asterisk <strong>for</strong> their<br />
extraordinarily low mortality<br />
rates — out <strong>of</strong> a total <strong>of</strong> about<br />
190 surgeons at 40 hospitals<br />
who per<strong>for</strong>med open-heart<br />
surgeries during that period.<br />
In fact, Dr. Palazzo per<strong>for</strong>med<br />
225 CABG surgeries over the<br />
three-year period covered in<br />
the Department <strong>of</strong> Health report<br />
without a single death.<br />
In a separate New York<br />
State Department <strong>of</strong> Health<br />
report on percutaneous<br />
coronary interventions, Lenox<br />
Hill Hospital had the lowest<br />
risk-adjusted mortality<br />
rate in the state in 2009 <strong>for</strong><br />
2,940 patients undergoing<br />
angioplasty (a procedure that<br />
clears blocked heart arteries<br />
to increase blood flow). Over<br />
the three years covered in the<br />
report (2007 to 2009), LIJ<br />
was one <strong>of</strong> six hospitals statewide<br />
with statistically superior<br />
outcomes <strong>for</strong> angioplasty. In<br />
addition, North Shore was one<br />
<strong>of</strong> only three hospitals in New<br />
York — <strong>and</strong> the only one on<br />
Long Isl<strong>and</strong> — with significantly<br />
better outcomes <strong>for</strong> 935<br />
emergency angioplasty patients.<br />
From an individual<br />
st<strong>and</strong>point, LIJ Medical<br />
Center’s Barry Kaplan, MD,<br />
<strong>and</strong> North Shore University<br />
Hospital’s Loukas Boutis, MD,<br />
<strong>and</strong> Donna Marchant, MD,<br />
were among only a h<strong>and</strong>ful<br />
<strong>of</strong> cardiologists in New York<br />
State — out <strong>of</strong> more than 300<br />
statewide — who were outliers<br />
<strong>for</strong> superior outcomes.<br />
Since 2000, the Department<br />
<strong>of</strong> Health has released<br />
eight reports <strong>for</strong> angioplasty.<br />
LIJ has received double-asterisk<br />
rankings <strong>for</strong> all cases in six <strong>of</strong><br />
those reports, which is more<br />
than any other hospital in the<br />
state, according to Dr. Kaplan,<br />
vice chair <strong>of</strong> cardiology <strong>for</strong> the<br />
North Shore-LIJ Health System.<br />
In addition to LIJ being<br />
the only hospital in New York<br />
to receive a double asterisk<br />
<strong>for</strong> both cardiac surgery <strong>and</strong><br />
angioplasty in the current<br />
Department <strong>of</strong> Health reports,<br />
North Shore was the only<br />
other hospital in the state to<br />
also have statistically superior<br />
outcomes in at least one<br />
category <strong>for</strong> both open-heart<br />
surgery <strong>and</strong> angioplasty.<br />
“<strong>The</strong> New York Department<br />
<strong>of</strong> Health’s analysis <strong>of</strong><br />
cardiac outcomes in hospitals<br />
across the state has contributed<br />
to continuous improvements<br />
in the care delivered to New<br />
Yorkers with heart disease,”<br />
said Stanley Katz, MD, senior<br />
vice president <strong>of</strong> cardiovascular<br />
services <strong>for</strong> North Shore-<br />
LIJ <strong>and</strong> chair <strong>of</strong> cardiology at<br />
North Shore University Hospital<br />
<strong>and</strong> LIJ Medical Center. He<br />
added that heart disease is the<br />
number one cause <strong>of</strong> death in<br />
this state <strong>and</strong> in this country.<br />
“<strong>The</strong> availability <strong>of</strong> these<br />
reports provides heart patients<br />
<strong>and</strong> their families with valuable<br />
in<strong>for</strong>mation <strong>for</strong> making<br />
in<strong>for</strong>med decisions about their<br />
cardiac care.”<br />
“Teamwork is at the heart<br />
<strong>of</strong> everything we do,” said Dr.<br />
Hartman, chair <strong>of</strong> cardiothoracic<br />
surgery at North Shore-LIJ.<br />
“Fortunately, the same <strong>for</strong>mula<br />
<strong>for</strong> success that has enabled us to<br />
consistently provide exceptional<br />
open-heart surgery at North<br />
Shore University Hospital <strong>and</strong><br />
LIJ Medical Center has been<br />
replicated at Southside Hospital.”<br />
Since the launch <strong>of</strong> Southside’s<br />
cardiothoracic program in<br />
February 2011, Dr. Hartman’s<br />
team has per<strong>for</strong>med 359 surgeries,<br />
ensuring that residents <strong>of</strong><br />
Suffolk County’s South Shore<br />
get the same access to state-<strong>of</strong>the-art<br />
heart care as the tens <strong>of</strong><br />
thous<strong>and</strong>s who have entrusted<br />
their lives to LIJ <strong>and</strong> North<br />
Shore University Hospital.<br />
Adult Cardiac Surgery<br />
http://www.health.ny.gov/statistics/diseases/cardiovascular/heart_disease/docs/2007-2009_adult_cardiac_surgery.pdf<br />
Angioplasty<br />
http://www.health.ny.gov/statistics/diseases/cardiovascular/docs/pci_2007-2009.pdf
Aesthetics, Smarts <strong>and</strong> Compassion Built into New LIJ Unit<br />
By Betty Olt<br />
NEW HYDE PARK — If not <strong>for</strong> the<br />
cutting-edge bedside technology,<br />
you might mistake a patient room<br />
in LIJ Medical Center’s new 30-bed<br />
Cardiovascular <strong>and</strong> Thoracic Unit <strong>for</strong><br />
a sleek hotel room. That’s because,<br />
when planning the new space,<br />
designers focused on delivering care<br />
that is not only state-<strong>of</strong>-the-art, but<br />
also compassionate. So each room is<br />
private <strong>and</strong> provides ample space <strong>for</strong><br />
loved ones at the bedside <strong>and</strong> if they<br />
choose to stay overnight.<br />
<strong>The</strong> Cardiovascular <strong>and</strong><br />
Thoracic Unit is dedicated to<br />
patients undergoing cardiothoracic<br />
surgery, cardiac catheterization<br />
<strong>and</strong> electrophysiology procedures.<br />
Telemetry technology equips each<br />
patient room, allowing remote<br />
monitoring <strong>of</strong> vital signs; bedside<br />
computers give clinicians access to<br />
patients’ electronic health records.<br />
Amenities <strong>of</strong> patient rooms<br />
within the 29,000-square-foot<br />
medical/surgical unit include a full<br />
bathroom <strong>and</strong> shower, a 42-inch flatscreen<br />
TV, mini-refrigerator, Internet<br />
access, a desk <strong>and</strong> a visiting area<br />
with a pullout loveseat. Rich wood<br />
floors <strong>and</strong> nature-inspired motifs <strong>and</strong><br />
artwork provide a warm, welcoming<br />
setting that accommodates patient<br />
needs <strong>and</strong> privacy. Carpeted corridors<br />
are not only visually appealing, but<br />
also help reduce noise. Extra-large<br />
windows in each patient room <strong>and</strong><br />
family lounges provide access to<br />
natural daylight <strong>and</strong> views.<br />
<strong>The</strong> cardiac suite opened to<br />
rave reviews from patients <strong>and</strong> staff<br />
alike, but the new facility is built<br />
on the reputation <strong>of</strong> LIJ’s cardiac<br />
services. “LIJ has consistently<br />
excelled in per<strong>for</strong>ming angioplasty<br />
<strong>and</strong> cardiac surgery, <strong>and</strong> has<br />
achieved outst<strong>and</strong>ing outcomes <strong>for</strong><br />
both procedures in New York State,”<br />
said Barry Kaplan, MD, vice chair <strong>of</strong><br />
cardiology <strong>for</strong> LIJ <strong>and</strong> North Shore<br />
University Hospital. (See related<br />
story at left.) “Now, with the new<br />
unit, we can practice in a world-class<br />
facility <strong>and</strong> provide the best possible<br />
care to patients in a beautiful <strong>and</strong><br />
healing environment.”<br />
By decentralizing nursing<br />
stations <strong>and</strong> locating supply closets<br />
adjacent to every patient room<br />
entrance, nurses’ spend less time<br />
walking the floor — <strong>and</strong> more time<br />
with patients. A pharmacy on the<br />
floor ensures timely, accurate<br />
delivery <strong>of</strong> medications. And the<br />
needs <strong>of</strong> special patient populations<br />
are addressed via two dedicated<br />
<strong>The</strong> hospitality industry inspired the design <strong>of</strong> the Cardiovascular <strong>and</strong> Thoracic Unit. <strong>The</strong> inpatient space is on the eighth<br />
floor in the Zuckerberg Pavilion, part <strong>of</strong> a $300 million, 10-story tower that also houses the Katz Women’s Hospital.<br />
Barry Kaplan, MD, vice chair <strong>of</strong><br />
cardiology <strong>for</strong> LIJ <strong>and</strong> North Shore<br />
University Hospital, <strong>and</strong> S. Jacob<br />
Scheinerman, MD, vice chair <strong>of</strong><br />
cardiothoracic surgery at LIJ,<br />
showcase LIJ’s new Cardiovascular<br />
<strong>and</strong> Thoracic Unit.<br />
isolation rooms with anterooms <strong>for</strong><br />
patient observation <strong>and</strong> a bariatric<br />
room equipped with overhead lifts<br />
<strong>for</strong> patient <strong>and</strong> staff safety.<br />
In addition to beauty <strong>and</strong><br />
efficiency, LIJ’s new Cardiovascular <strong>and</strong><br />
Thoracic Unit is ecologically kind, too.<br />
As part <strong>of</strong> the North Shore-LIJ Health<br />
System’s commitment to sustainable<br />
<strong>and</strong> environmentally responsible<br />
healthcare, the unit is registered<br />
with the Green Building Certification<br />
Institute <strong>and</strong> has been designed to<br />
achieve a Silver rating from LEED,<br />
the accepted industry benchmark <strong>for</strong><br />
sustainable design, green building<br />
materials <strong>and</strong> energy efficiency.<br />
Take a tour <strong>of</strong> the new space at<br />
http://www.northshorelij.com/NSLIJ/<br />
media-portal/homepage-videochannel/lij-cardiac-units.<br />
<strong>The</strong> New St<strong>and</strong>ard 11
Ann Pszybylski, 84, is the first patient on Long Isl<strong>and</strong> to receive the only FDA-approved nonsurgical heart valve<br />
replacement device. Members <strong>of</strong> LIJ’s cardiac team wished her well as she prepared to leave the hospital. Ms. Pszybylski<br />
is shown above with, from the left, Dr. Scheinerman; Dorothy Veron, RN, nurse manager <strong>of</strong> the catheterization lab; Dr.<br />
Jauhar; Annmarie Copertino, RN, nurse manager; <strong>and</strong> Robert Rodriguez, RN.<br />
New Nonsurgical <strong>Heart</strong> Procedure<br />
Gives Hope to Older Patients<br />
Ask 84-year-old Ann<br />
Pszybylski what it was like to<br />
take just a short walk down<br />
a hallway, fighting <strong>for</strong> each<br />
breath. She was in desperate<br />
need <strong>of</strong> a new heart valve,<br />
but her age <strong>and</strong> other medical<br />
problems made open heart<br />
surgery too risky.<br />
A new technical<br />
advance recently approved<br />
by the US Federal Drug<br />
Administration (FDA) – the<br />
Sapien transcatheter aortic<br />
12 Summer 2012<br />
valve replacement (TAVR) –<br />
is helping older people like<br />
Mrs. Pszybylski with severe<br />
aortic stenosis to breathe <strong>and</strong><br />
move about more easily, <strong>and</strong><br />
providing them with a new<br />
lease on life.<br />
“No more huffing <strong>and</strong><br />
puffing,” said Mrs. Pszybylski.<br />
<strong>The</strong> Hauppauge resident,<br />
who was not a c<strong>and</strong>idate <strong>for</strong><br />
the traditional heart valve<br />
replacement procedure, was<br />
the first patient at LIJ Medical<br />
By Betty Olt<br />
Center to receive the TAVR<br />
device. She is now on the<br />
move with her eight gr<strong>and</strong>-<br />
<strong>and</strong> great-gr<strong>and</strong>children.<br />
She said she wants to resume<br />
traveling, but mostly, she<br />
added, “I’m looking <strong>for</strong>ward<br />
to living longer.”<br />
Cardiologists <strong>and</strong><br />
cardiothoracic surgeons at<br />
LIJ are the first in Queens<br />
<strong>and</strong> Long Isl<strong>and</strong> to implant<br />
the new nonsurgical heart<br />
valve replacement device<br />
in patients with failing<br />
heart valves. “TAVR is a<br />
breakthrough because it <strong>of</strong>fers<br />
some patients who could not<br />
withst<strong>and</strong> the conventional<br />
surgery due to age or serious<br />
medical conditions a viable<br />
treatment option,” said S.<br />
Jacob Scheinerman, MD,<br />
vice chair <strong>of</strong> cardiothoracic<br />
surgery at LIJ. <strong>The</strong> TAVR is<br />
manufactured by Edwards<br />
Lifesciences in Irvine, CA.<br />
Similar to a technique<br />
to implant cardiac stents<br />
into clogged arteries, the<br />
TAVR procedure involves the<br />
physician guiding a catheter,<br />
or thin tube, attached to the<br />
Sapien valve through the<br />
patient’s femoral artery, in<br />
the thigh. <strong>The</strong> cardiac team<br />
uses transesophageal echo<br />
(TEE) <strong>and</strong> fluoroscopic<br />
imaging guidance <strong>for</strong> proper<br />
placement. <strong>The</strong> Sapien valve<br />
is exp<strong>and</strong>ed by a balloon in<br />
the delivery system (about<br />
the diameter <strong>of</strong> a quarter),<br />
pushing away the calcium to<br />
enlarge the opening <strong>of</strong> the<br />
valve. Once it is placed at<br />
the opening <strong>of</strong> the valve it is<br />
anchored inside the aorta <strong>and</strong><br />
blood flow is restored<br />
Approximately 250,000<br />
Americans suffer from<br />
severe aortic stenosis, <strong>of</strong>ten<br />
developing debilitating<br />
symptoms that can affect<br />
normal day-to-day activities<br />
such as walking short distances<br />
or climbing stairs. Generally,<br />
the condition affects people<br />
over 70. Aortic stenosis
occurs when the aortic valve<br />
does not properly open <strong>and</strong><br />
close, usually due to a buildup<br />
<strong>of</strong> calcium. <strong>The</strong> calcium<br />
build-up restricts blood flow<br />
from the heart to the rest<br />
<strong>of</strong> the body. This increases<br />
pressure within the heart,<br />
causing heart muscles to<br />
weaken. All <strong>of</strong> these events<br />
increase the risk <strong>of</strong> heart<br />
failure. Symptoms <strong>of</strong> the<br />
disease can include extreme<br />
fatigue, dizziness, chest pain<br />
or pressure, shortness <strong>of</strong><br />
breath during activity, rapid<br />
or irregular heartbeat <strong>and</strong><br />
fainting.<br />
“Patients who do not<br />
receive an aortic valve<br />
replacement have no effective,<br />
long-term treatment option<br />
to prevent or delay the<br />
progression <strong>of</strong> severe aortic<br />
stenosis <strong>and</strong> eventual death,”<br />
said Dr. Scheinerman, noting<br />
that approximately 50 percent<br />
<strong>of</strong> patients who are in their<br />
80s <strong>and</strong> have symptoms <strong>of</strong><br />
congestive heart failure with<br />
critical aortic stenosis will die<br />
in six months to a year without<br />
treatment. “For patients who<br />
were previously inoperable,<br />
the new TAVR gives hope <strong>for</strong><br />
extending <strong>and</strong> improving the<br />
quality <strong>of</strong> their lives.”<br />
Dr. Scheinerman, Barry<br />
Kaplan, MD, vice chair <strong>of</strong><br />
cardiology at LIJ <strong>and</strong> North<br />
Shore University Hospital<br />
<strong>and</strong> an interventional<br />
cardiologist, Rajiv Jauhar,<br />
MD, chief <strong>of</strong> cardiology<br />
<strong>and</strong> director <strong>of</strong> the cardiac<br />
catheterization laboratory <strong>and</strong><br />
interventional cardiology at<br />
LIJ, <strong>and</strong> Robert Palazzo, MD,<br />
a cardiothoracic surgeon,<br />
joined the multidisciplinary<br />
team to per<strong>for</strong>m the procedure<br />
on Mrs. Pszybylski. <strong>The</strong><br />
procedure was per<strong>for</strong>med in<br />
the new state-<strong>of</strong>-the art hybrid<br />
operating room built at LIJ.<br />
<strong>The</strong> $5 million surgical suite<br />
combines the latest surgical<br />
<strong>and</strong> cardiac catheterization,<br />
robotic technology <strong>and</strong><br />
three-dimensional radiologic<br />
imaging capabilities with realtime<br />
patient monitoring.<br />
“Having all the<br />
equipment <strong>and</strong> members <strong>of</strong><br />
the cardiac team in one OR<br />
saves time <strong>and</strong> eliminates<br />
the need <strong>for</strong> a patient to be<br />
moved from one room to<br />
another,” said Dr. Kaplan.<br />
“Interventional cardiologists<br />
<strong>and</strong> cardiac surgeons are able<br />
to collaborate closely during<br />
the procedure. Working<br />
in our new hybrid surgical<br />
suite allows us to be ready<br />
<strong>for</strong> any situation or potential<br />
emergency.”<br />
To watch a video featuring the<br />
cardiac team at LIJ who per<strong>for</strong>med<br />
the first TAVR procedures visit<br />
NorthShoreLIJ.com/NSLIJ/vitalityvideos,<br />
or use your smartphone<br />
to scan the QR code.<br />
Hybrid OR:<br />
Making Many Things Possible<br />
By Betty Marton<br />
Two new hybrid operating rooms — the first in Queens <strong>and</strong> Nassau<br />
County — are letting previously inoperable patients benefit from cutting-<br />
edge combination surgical, cardiac <strong>and</strong> vascular interventions, including<br />
a life-saving heart valve replacement procedure. Located at LIJ Medical<br />
Center <strong>and</strong> North Shore University Hospital, these interdisciplinary,<br />
multifunctional rooms allow cardiologists <strong>and</strong> cardiothoracic surgeons to<br />
per<strong>for</strong>m a range <strong>of</strong> open, minimally invasive, image-guided <strong>and</strong> catheter-<br />
based procedures in one operating suite.<br />
“It’s the ideal environment to bring interventional cardiologists <strong>and</strong><br />
cardiac surgeons together in a team approach that is relatively unusual <strong>and</strong><br />
unprecedented,” explained Barry Kaplan, MD, vice chair <strong>of</strong> cardiology at LIJ<br />
<strong>and</strong> North Shore University Hospital.<br />
<strong>The</strong> hybrid OR incorporates robotic technology <strong>and</strong> three-dimen-<br />
sional radiologic imaging capabilities with real-time patient monitoring<br />
that, when not needed, can easily be moved out <strong>of</strong> the way to support<br />
general surgical procedures. Maximizing room use <strong>and</strong> efficiency makes it<br />
possible to per<strong>for</strong>m such procedures as the Sapien® transcatheter aortic<br />
valve replacement (TAVR) on patients with severe aortic stenosis. TAVR is<br />
per<strong>for</strong>med via the femoral artery, which is similar to the approach used <strong>for</strong><br />
cardiac catheterization. <strong>The</strong> cardiac team then uses transesophageal echo<br />
(TEE) <strong>and</strong> fluoroscopic imaging guidance <strong>for</strong> proper placement.<br />
“TAVR only requires a two- or three-centimeter incision, which<br />
allows us to treat patients who were previously deemed inoperable due to<br />
age or serious medical conditions,” said S. Jacob Scheinerman, MD, vice<br />
chair <strong>of</strong> cardiothoracic surgery at LIJ.<br />
According to Robert Blenderman PA, director <strong>of</strong> cardiovascular <strong>and</strong><br />
thoracic surgery at North Shore University Hospital <strong>and</strong> LIJ, the $5 million<br />
hybrid surgical suites, built at a time when healthcare dollars are stretched<br />
thin, exemplify the North Shore-LIJ Health System’s commitment to<br />
providing the highest-quality treatment <strong>and</strong> care <strong>for</strong> its patients.<br />
“North Shore-LIJ has gone above <strong>and</strong> beyond in supporting this<br />
hybrid OR technology to meet the needs <strong>of</strong> future procedures,” he said.<br />
“It’s a beautiful thing to have the ability to <strong>of</strong>fer a quality treatment<br />
to those patients who previously had no other options. This is a<br />
groundbreaking development in cardiovascular surgery <strong>and</strong> shows our<br />
dedication to growing our discipline in a quality way.”<br />
<strong>The</strong> New St<strong>and</strong>ard 13
HealthGrades Rates LIJ, North Shore<br />
Among Best <strong>for</strong> Cardiovascular Care in US<br />
By Betty Olt<br />
LIJ Medical Center<br />
<strong>and</strong> North Shore University<br />
Hospital (NSUH) have been<br />
named among America’s 100<br />
Best Hospitals <strong>for</strong> cardiac care,<br />
cardiac surgery <strong>and</strong> coronary<br />
intervention, according to<br />
a recently released report by<br />
HealthGrades, an independent<br />
group that analyzes hospital<br />
quality outcomes. LIJ was also<br />
ranked number one in New<br />
York State <strong>for</strong> cardiac surgery<br />
<strong>for</strong> two consecutive years<br />
(2011 <strong>and</strong> 2012); <strong>and</strong> NSUH<br />
was ranked number two in<br />
the state <strong>for</strong> overall cardiac<br />
services, cardiology services <strong>and</strong><br />
coronary interventional (heart<br />
stent) procedures in 2012.<br />
HealthGrades analyzed<br />
Medicare patient outcome<br />
data from 5,000 hospitals<br />
nationwide from 2008 through<br />
2010, the most recent years<br />
<strong>for</strong> which data was available.<br />
It published per<strong>for</strong>mance<br />
outcomes <strong>for</strong> cardiac services in<br />
its 2011 Healthcare Consumerism <strong>and</strong><br />
Hospital Quality in America report. A<br />
quality comparison <strong>of</strong> doctors<br />
<strong>and</strong> hospitals in the New York<br />
area can be found online at<br />
HealthGrades.com.<br />
Among the achievements<br />
noted in the report, NSUH <strong>and</strong><br />
LIJ consistently received fivestar<br />
ratings, the highest possible<br />
hospital rating, in multiple<br />
cardiac service areas, which<br />
translates to a 73 percent lower<br />
chance <strong>of</strong> death compared to<br />
one-star hospitals, according to<br />
HealthGrades.<br />
“<strong>The</strong> North Shore-LIJ<br />
Health System is committed<br />
14 Summer 2012<br />
to providing the highestquality<br />
care to our patients,”<br />
said Stanley Katz, MD,<br />
senior vice president <strong>of</strong><br />
cardiovascular services<br />
<strong>and</strong> chair <strong>of</strong> cardiology at<br />
North Shore-LIJ. “Our<br />
cardiac physicians <strong>and</strong><br />
their teams at LIJ Medical<br />
Center <strong>and</strong> North Shore<br />
University Hospital are<br />
making major treatment<br />
breakthroughs in the field,<br />
improving the lives <strong>of</strong> our<br />
patients in our community.<br />
<strong>The</strong> HealthGrades ratings<br />
demonstrate our excellent<br />
outcomes in cardiac care, which<br />
are accessible to consumers<br />
online <strong>and</strong> are extremely useful<br />
<strong>for</strong> patients <strong>and</strong> loved ones<br />
making the important decision<br />
<strong>of</strong> choosing their cardiologists<br />
<strong>and</strong> hospitals.”<br />
LIJ Medical Center<br />
was also recognized <strong>for</strong> the<br />
following clinical achievements:<br />
LIJ Ranked Nationally<br />
Among the top 5 percent <strong>for</strong><br />
coronary interventional<br />
procedures (2008-2012)<br />
Among the top 5 percent <strong>for</strong><br />
cardiac surgery (2011-2012)<br />
Among the top 5 percent<br />
<strong>for</strong> overall cardiac services<br />
(2011-2012)<br />
LIJ Ranked in NY State<br />
Among the top 10 <strong>for</strong> coronary<br />
interventional procedures<br />
(2008-2012)<br />
Among the top 10 <strong>for</strong> cardiac<br />
surgery (2010-2012)<br />
Among the top 10 <strong>for</strong> overall<br />
cardiac services (2011-2012)<br />
NSUH received five-star ratings <strong>for</strong> the following clinical achievements:<br />
Overall cardiac services <strong>for</strong> five years in a row (2008-2012)<br />
Cardiac surgery <strong>for</strong> five years in a row (2008-2012)<br />
Cardiology services <strong>for</strong> two years in a row (2011-2012)<br />
Coronary bypass surgery in 2012<br />
Valve surgery <strong>for</strong> six years in a row (2007-2012)<br />
Coronary interventional procedures <strong>for</strong> 10 years in a row (2003-2012)<br />
Treatment <strong>of</strong> heart attack <strong>for</strong> seven years in a row (2006-2012)<br />
Treatment <strong>of</strong> heart failure in 2012<br />
LIJ received five-star recognition <strong>for</strong> the following clinical achievements:<br />
Overall cardiac services <strong>for</strong> two years in a row (2011-2012)<br />
Coronary interventional procedures <strong>for</strong> 10 years in a row (2003-2012)<br />
Cardiac surgery <strong>for</strong> three years in a row (2010-2012)<br />
Coronary bypass surgery <strong>for</strong> four years in a row (2009-2012)<br />
Valve surgery <strong>for</strong> two years in a row (2011-2012)<br />
In addition, North<br />
Shore University Hospital was<br />
recognized <strong>for</strong> the following<br />
clinical achievements:<br />
NSUH Ranked Nationally<br />
Among the top 5 percent <strong>for</strong><br />
coronary interventional<br />
procedures (2003-2012)<br />
Among the top 5 percent<br />
<strong>for</strong> overall cardiac services<br />
(2008-2012)<br />
Among the top 5 percent <strong>for</strong><br />
cardiac surgery in 2012<br />
Among the top 5 percent <strong>for</strong><br />
cardiology services in 2012<br />
NSUH Ranked in NY State<br />
Among the top 5 <strong>for</strong> coronary<br />
interventional procedures<br />
(2003-2012)<br />
Among the top 5 <strong>for</strong> cardiology<br />
services in 2012<br />
Among the top 10 <strong>for</strong> overall<br />
cardiac services (2005-2012)<br />
Among the top 10 <strong>for</strong> cardiac<br />
surgery (2007-2012)<br />
Key findings <strong>of</strong> the<br />
HealthGrades 2011 Healthcare<br />
Consumerism <strong>and</strong> Hospital Quality in<br />
America report include:<br />
q On average, patients had<br />
a 73 percent lower risk <strong>of</strong><br />
dying in a five-star-rated<br />
hospital compared to a<br />
one-star-rated hospital,<br />
<strong>and</strong> a 54 percent lower<br />
risk <strong>of</strong> dying in a five-starrated<br />
hospital compared to<br />
the national average.<br />
q If all Medicare patients<br />
from 2008 through 2010<br />
had been treated at fivestar<br />
hospitals, 240,040<br />
lives could have potentially<br />
been saved.<br />
q If all Medicare patients<br />
from 2008 through 2010<br />
had gone to five-star<br />
hospitals <strong>for</strong> their procedure,<br />
164,472 in-hospital<br />
complications could have<br />
potentially been avoided.
Quick, Collaborative Cardiac Care Saves Patient<br />
“It felt like there was a dagger in my back,” said 47-year-old Noel Riley.<br />
<strong>The</strong> Valley Stream resident awakened with chest pain <strong>and</strong> intermittent searing<br />
pain across his back, <strong>and</strong> when the pain would not go away, he headed to Franklin<br />
Hospital, where Mollie Williams, MD, made a diagnosis that would save his life.<br />
Mr. Riley was experiencing an ascending (Type A) aortic dissection which, without<br />
treatment, kills 90 percent <strong>of</strong> patients within 48 hours.<br />
Aortic dissection happens when a tear inside the layered wall <strong>of</strong> the aorta<br />
(the largest artery <strong>of</strong> the body) causes<br />
bleeding into <strong>and</strong> along the wall,<br />
<strong>for</strong>cing the layers apart. Symptoms<br />
are varying <strong>and</strong> similar to those <strong>of</strong><br />
other heart problems — such as a<br />
severe ripping or tearing pain from the<br />
shoulder blades or back <strong>and</strong> extending<br />
to the chest, loss <strong>of</strong> consciousness,<br />
shortness <strong>of</strong> breath, sweating or<br />
overall weakness — which can make<br />
proper diagnosis difficult. Mr. Riley<br />
“did not have chronic hypertension,<br />
his EKG [electrocardiography] <strong>and</strong><br />
blood work were normal <strong>and</strong> he looked<br />
healthy,” said Dr. Williams, who<br />
treated him in Franklin’s Emergency<br />
Department. Considering his symptoms, she ordered a computed tomography<br />
(CT) scan, a test commonly used to diagnose aortic dissection, <strong>and</strong> discovered<br />
the severity <strong>of</strong> his condition.<br />
Mr. Riley required emergency surgery to prevent rupture <strong>and</strong> death — <strong>and</strong><br />
was transferred to LIJ Medical Center’s Department <strong>of</strong> Cardiothoracic Surgery.<br />
<strong>The</strong>re, a team <strong>of</strong> clinicians rushed him into surgery where S. Jacob Scheinerman,<br />
MD, associate chairman <strong>of</strong> the department, removed the damaged segments <strong>of</strong> the<br />
MANHASSET — For the second<br />
consecutive year, the American<br />
<strong>Heart</strong> Association (AHA) has<br />
awarded North Shore University<br />
Hospital its Platinum-Level<br />
Recognition <strong>for</strong> being a “Fit-<br />
Friendly” organization. <strong>The</strong> AHA’s<br />
Fit-Friendly Company Program<br />
recognizes employers who<br />
encourage the health <strong>of</strong> their<br />
employees <strong>and</strong> work to create a<br />
physically fit <strong>and</strong> healthy work<br />
environment.<br />
“We’re proud to achieve<br />
the American <strong>Heart</strong> Association’s<br />
‘Fit-Friendly’ designation <strong>for</strong> a<br />
second straight year,” said Susan<br />
Somerville, the hospital’s executive<br />
director. “We believe strongly that<br />
as members <strong>of</strong> a healthcare team,<br />
our employees have a responsibility<br />
to set a positive example <strong>for</strong> the<br />
patients they serve by maintaining a<br />
healthy lifestyle.”<br />
<strong>The</strong> AHA program honors<br />
companies in several ways. “Gold”<br />
ascending aorta, replaced the tissue with a graft <strong>and</strong>, along with Robert Palazzo,<br />
MD, repaired the damaged aortic valve. “Mr. Riley’s Type A dissection, which<br />
involves the root <strong>of</strong> the aorta, is the most dangerous type,” said Dr. Scheinerman.<br />
“<strong>The</strong> key to his survival was how quickly Franklin’s team made a diagnosis <strong>and</strong> got<br />
him to our operating room. Many people never even make it to the hospital.”<br />
<strong>The</strong> risk factors <strong>for</strong> aortic dissection include a history <strong>of</strong> uncontrolled<br />
hypertension, aortic aneurysm, a dilated aorta or congenital connective tissue<br />
disorders such as Marfan syndrome or Ehlers-Danlos<br />
syndrome, explained Dr. Scheinerman. Mr. Riley had<br />
none <strong>of</strong> these risk factors.<br />
As an orthotist (a specialist in the design <strong>of</strong><br />
orthopedic appliances), Mr. Riley was familiar with<br />
the condition, but was shocked by the diagnosis.<br />
“Dr. Williams’ ability to listen was pivotal to my<br />
survival,” said Mr. Riley. Her quick actions to explore<br />
all causes <strong>of</strong> his pain are the reason he made it<br />
to surgery in time, <strong>and</strong> the collaboration <strong>of</strong> the<br />
healthcare teams at Franklin Hospital <strong>and</strong> LIJ Medical<br />
Center saved his life.<br />
“Mr Riley’s case highlights the benefits<br />
patients receive from the collaboration <strong>of</strong> North<br />
Shore-LIJ hospitals,” said John Rohe, MD, director<br />
<strong>of</strong> emergency medicine at Franklin. “Our facilities<br />
truly work together to save lives.” Mr. Riley’s survival is also a testament to the<br />
health system’s cardiac care <strong>and</strong> each hospital’s access to that care, wellevidenced<br />
by Dr. Williams calling in the expertise <strong>of</strong> LIJ’s cardiac Emergency<br />
Medical Services transfer team <strong>and</strong> Aortic Surgery Center physicians.<br />
Mr. Riley has nothing but praise <strong>for</strong> the care he received at both Franklin<br />
Hospital <strong>and</strong> LIJ Medical Center. “It was nothing short <strong>of</strong> excellent,” he said. “<strong>The</strong>y<br />
saved my life.”<br />
American <strong>Heart</strong> Association Recognizes<br />
North Shore University Hospital as “Fit-Friendly”<br />
is the first tier <strong>of</strong> recognition <strong>and</strong><br />
“Platinum” is the advanced tier.<br />
Recognition is valid <strong>for</strong> one year<br />
<strong>and</strong> companies must renew annually<br />
by completing a renewal <strong>for</strong>m. <strong>The</strong><br />
AHA <strong>of</strong>fers employers numerous<br />
recommendations that enable them<br />
to achieve Fit-Friendly recognition,<br />
including: providing walking routes,<br />
promoting walking programs <strong>and</strong><br />
allowing staff to wear athletic shoes<br />
in the workplace on designated<br />
“sneaker days.”<br />
In addition to the Walk<br />
to Paris (see p. 3, p. 47), NSUH<br />
<strong>of</strong>fers on-site wellness programs<br />
such as Zumba <strong>and</strong> yoga fitness<br />
classes, individualized nutrition<br />
counseling <strong>and</strong> classes <strong>and</strong> wellattended<br />
multidisciplinary health<br />
<strong>and</strong> wellness fairs. <strong>The</strong> hospital<br />
is also making strides in helping<br />
employees select healthier food<br />
options, by programming vending<br />
machines to display selections’<br />
nutritional content.<br />
<strong>The</strong> New St<strong>and</strong>ard 15
around the system<br />
HUNTINGTON — Neither<br />
Peter Morley nor Tom O’Reilly<br />
works at Huntington Hospital<br />
or even in the healthcare field.<br />
But they serve side by side<br />
with hospital staff <strong>and</strong> board<br />
members on the hospital’s new<br />
Patient/Family Centered Care<br />
Partnership Council. Chaired by<br />
Amy Loeb, RN, nurse manager<br />
<strong>of</strong> 2SouthWest, the Council’s<br />
mission is “to create dynamic<br />
patient, family <strong>and</strong> caregiver<br />
partnerships that enhance<br />
the healthcare experience at<br />
Huntington Hospital.”<br />
<strong>The</strong> group aims to enhance<br />
the patient experience by encouraging open, twoway<br />
communication, articulating patients’ <strong>and</strong> family<br />
members’ needs <strong>and</strong> ensuring those needs are met.<br />
“We want community members to have a real<br />
partnership with the hospital to help enhance the<br />
patient experience,” Ms. Loeb said. “We want the<br />
patient <strong>and</strong> family perspective so we don’t have to<br />
assume we know what they want <strong>and</strong> need.”<br />
Huntington board member Carmela Anglim brings<br />
decades <strong>of</strong> experience to the partnership, including<br />
service as a hospital trustee, a hospital volunteer <strong>and</strong><br />
administrator <strong>of</strong> volunteer services <strong>for</strong> another Long Isl<strong>and</strong> hospital.<br />
“<strong>The</strong> hospital is the great equalizer,” she said. “Sooner or later<br />
we all get here. Patients can feel frightened <strong>and</strong> isolated <strong>and</strong> families<br />
may be reluctant to be involved. Our goal is to empower patients <strong>and</strong><br />
families <strong>and</strong> bring them into the circle <strong>of</strong> care.”<br />
<strong>The</strong> council will do more than enhance patient com<strong>for</strong>t.<br />
“This is a safety initiative too,” said Ms. Loeb. “By facilitating<br />
communication, when patients leave the hospital they will<br />
underst<strong>and</strong> why they were here <strong>and</strong> what they need to do to stay<br />
well in the future.”<br />
Ms. Loeb pointed to existing hospital programs that support the<br />
goals <strong>of</strong> the council. Weekly patient safety rounds bring department<br />
heads onto patient care units where direct care providers can discuss<br />
emerging concerns <strong>and</strong> issues. <strong>The</strong> Palliative Medicine Program is<br />
another avenue <strong>for</strong> patients <strong>and</strong> caregivers to set mutual goals.<br />
This collaborative approach is beginning to take root at hospitals<br />
16 Summer 2012<br />
Patient/Family/Caregiver<br />
Partnerships Include<br />
Community Members<br />
By <strong>The</strong>resa Jacobellis<br />
around the country. It began at Johns Hopkins in Baltimore following<br />
the tragic death <strong>of</strong> a child whose mother’s concerns were not taken<br />
seriously by her healthcare team. <strong>The</strong> Institute <strong>for</strong> Healthcare<br />
Improvement, the World Health Organization <strong>and</strong> other national <strong>and</strong><br />
international groups focused on healthcare quality endorse healthcare<br />
teams <strong>for</strong>mally including patient <strong>and</strong> family input.<br />
“Patients <strong>and</strong> their loved ones are our eyes <strong>and</strong> ears,” said Ms.<br />
Loeb. “We want to invite them to be our partners in caring because<br />
it benefits all <strong>of</strong> us.”<br />
“For me, this is not just another clinical initiative but a pathway<br />
to truly having a transparent organization,” said Deborah Feehan,<br />
RN, clinical nursing supervisor. “Through community input we can<br />
improve the care <strong>and</strong> experience our patients receive.”<br />
Pictured above are members <strong>of</strong> the new Patient/Family Centered Care<br />
Partnership Council.
Weight-Loss Surgery Study<br />
Combines Two Approaches<br />
By Kristen Longo<br />
SYOSSET — For patients considering weight-loss surgery, Syosset<br />
Hospital’s Center <strong>for</strong> Bariatric Surgical Specialties is participating<br />
in a national research study designed to evaluate the weight-loss<br />
results <strong>of</strong> b<strong>and</strong>ed gastric plication, an investigational procedure<br />
combining two common bariatric surgical methods under the<br />
hypothesis <strong>of</strong> earlier <strong>and</strong> more rapid weight loss with fewer<br />
risks. <strong>The</strong> research study has been reviewed <strong>and</strong> approved by an<br />
Institutional Review Board (IRB).<br />
B<strong>and</strong>ed gastric plication combines two minimally invasive<br />
procedures — adjustable gastric b<strong>and</strong>ing, which entails placing<br />
an adjustable silicone b<strong>and</strong> around the upper stomach, <strong>and</strong><br />
plication, a technique that uses sutures to fold the external wall <strong>of</strong><br />
the stomach, creating a sleeve-like contour to the lower part <strong>of</strong> the<br />
stomach below the b<strong>and</strong>. Both methods promote weight loss <strong>and</strong><br />
control hunger by reducing stomach size, limiting food intake <strong>and</strong><br />
increasing gastric emptying.<br />
Potential benefits <strong>of</strong> the procedure include reduced surgical<br />
risk, fewer gastric b<strong>and</strong> adjustments <strong>and</strong> significant short- <strong>and</strong> longterm<br />
weight loss. <strong>The</strong> process does not cut the stomach or reroute the<br />
intestines <strong>and</strong>, as a result, patients experience lower infection <strong>and</strong><br />
complication risks, faster recovery times <strong>and</strong> minimal post-operative<br />
pain <strong>and</strong> scarring as compared to more invasive bariatric methods<br />
like gastric bypass or sleeve gastrectomy. Potential risks are considered<br />
infrequent <strong>and</strong> are similar to those <strong>for</strong> medical or laparoscopic<br />
revision surgery. <strong>The</strong>se risks generally include gastric outlet<br />
obstruction (inability <strong>of</strong> food to pass from the stomach to the small<br />
intestine), bleeding from the stitched line, dilation (enlargement)<br />
<strong>of</strong> the plicated tissue over time <strong>and</strong> ischemic (restricted blood flow)<br />
complication at the surgery site.<br />
“Early studies have shown that b<strong>and</strong>ed gastric plication,<br />
compared to the gastric b<strong>and</strong> alone, may be a more durable<br />
surgical weight loss solution,” said Alan Geiss, MD, director <strong>of</strong><br />
the Center <strong>for</strong> Bariatric Surgical Specialties. “<strong>The</strong> early results are<br />
very encouraging.” As with any study, long-term data is still being<br />
compiled to support the long-term effectiveness <strong>of</strong> the procedure.<br />
Preliminary results showed evidence <strong>of</strong> a marked increase in the<br />
percent <strong>of</strong> excess weight loss over seven months’ to one-year followup.<br />
<strong>The</strong> procedure requires one <strong>and</strong> a half hours <strong>and</strong> patients stay in<br />
the hospital <strong>for</strong> one day.<br />
For more in<strong>for</strong>mation call (516) 496-2752.<br />
CCMC Diabetes Program Recognized <strong>for</strong> Superior-Quality Care<br />
NEW HYDE PARK — <strong>The</strong> Diabetes<br />
Program in the Division <strong>of</strong> Pediatric<br />
Endocrinology at the Steven <strong>and</strong><br />
Alex<strong>and</strong>ra Cohen Children’s Center<br />
<strong>of</strong> New York (CCMC) was recently<br />
certified by the National Commission<br />
<strong>for</strong> Quality Assurance (NCQA), a<br />
private, nonpr<strong>of</strong>it organization<br />
that is a widely recognized symbol<br />
<strong>of</strong> healthcare quality. <strong>The</strong> CCMC<br />
program had previously been<br />
recognized by the American Diabetes<br />
Association as a certified Pediatric<br />
Diabetes Education Center.<br />
NCQA’s Diabetes Recognition<br />
Program (DRP) is designed to<br />
recognize physicians <strong>and</strong> other<br />
clinicians who provide excellent care<br />
to their patients with diabetes using<br />
10 evidence-based measures, such<br />
as LDL (low-density lipoprotein) <strong>and</strong><br />
blood pressure control. Achieving<br />
DRP recognition means that the<br />
CCMC program is part <strong>of</strong> an elite<br />
group that provides the very highest<br />
level <strong>of</strong> diabetes care.<br />
Phyllis Speiser, MD, chief <strong>of</strong><br />
pediatric endocrinology at CCMC,<br />
along with Margaret Pellizzari, RN,<br />
assistant nurse manager, <strong>and</strong> their<br />
team <strong>of</strong> nurses, nutritionists, social<br />
workers <strong>and</strong> physicians cares <strong>for</strong><br />
about 800 children with diabetes<br />
every year. From the day they are<br />
diagnosed until they “graduate” from<br />
pediatric care, the staff is dedicated<br />
to helping them maintain good<br />
glycemic control aimed at prolonging<br />
life <strong>and</strong> preventing complications,<br />
<strong>and</strong> educating their parents so they<br />
can be their children’s advocates. Dr.<br />
Speiser’s group worked closely with<br />
Pranav Mehta, MD, vice president<br />
<strong>for</strong> ambulatory per<strong>for</strong>mance<br />
improvement <strong>for</strong> the North Shore-LIJ<br />
Health System, <strong>and</strong> his staff to<br />
achieve this prestigious recognition.<br />
“Future healthcare delivery <strong>and</strong><br />
reimbursement models rely heavily<br />
on documenting efficiency, cost<br />
savings <strong>and</strong> superior-quality care,”<br />
said Dr. Speiser. “We are proud to<br />
be in the <strong>for</strong>efront <strong>of</strong> these changes<br />
sweeping the medical l<strong>and</strong>scape,<br />
Phyllis Speiser, MD<br />
<strong>and</strong> honored to display this newest<br />
evidence <strong>of</strong> our successful ef<strong>for</strong>ts to<br />
deliver the best care to our children<br />
affected with diabetes.”<br />
<strong>The</strong> New St<strong>and</strong>ard 17
around the system<br />
Enhancing Safety in<br />
Behavioral Health Settings<br />
SYOSSET — A new protocol implemented on the Behavioral Health Unit at<br />
Syosset Hospital has dramatically reduced episodes <strong>of</strong> patient aggression.<br />
<strong>The</strong> plan includes:<br />
• a violence assessment screening during patient admission, after which<br />
patients at risk are identified <strong>and</strong> communicated about at daily briefs <strong>for</strong><br />
every shift;<br />
• personal alarms provided to each staff member;<br />
• crisis prevention training <strong>for</strong> all nurses <strong>and</strong> security staff;<br />
• an additional nurse practitioner staff position during <strong>of</strong>f-hours; <strong>and</strong><br />
• additional mental wellness programs <strong>for</strong> patients including activities<br />
during evenings <strong>and</strong> weekends, increased snacks <strong>and</strong> dietician<br />
evaluations, fresh air walks, family support groups, nicotine withdrawal<br />
assessments <strong>and</strong> games <strong>and</strong> exercise materials<br />
18 Summer 2012<br />
Plainview Hospital<br />
Serves Up Tastier,<br />
Healthier Meals<br />
Syosset Collaborative Care Council members Mercy Jaiswal, RN,<br />
left,<strong>and</strong> Debra Dyck<strong>of</strong>f, RN, nurse manager <strong>of</strong> the hospital’s<br />
Behavioral Health Unit, were invited to present their project,<br />
Prevention <strong>of</strong> Violence in Inpatient Behavioral Health, at the Eighth<br />
Annual Maryl<strong>and</strong> Patient Safety Conference this spring.<br />
PLAINVIEW — While showing a patient the newly revised<br />
Plainview Hospital menu (below), nutrition coordinator Nina Eng<br />
discusses the importance <strong>of</strong> nutritional in<strong>for</strong>mation to recovering<br />
<strong>and</strong> maintaining health. <strong>The</strong> latest Plainview menus feature<br />
nutritional in<strong>for</strong>mation, including amounts <strong>of</strong> calories, fat,<br />
sodium <strong>and</strong> carbohydrates, next to every item <strong>of</strong>fered. Patients can<br />
call ahead <strong>and</strong> substitute alternative hot or cold items, including<br />
treats like bacon, sausage <strong>and</strong> cheese pizza,<br />
in serving sizes that provide nutritional<br />
value without risky calory, fat <strong>and</strong> salt<br />
counts. “We’re giving patients the tools<br />
that they need to make in<strong>for</strong>med decisions<br />
about what they eat,” said Ms. Eng.<br />
<strong>The</strong>re are also modifications available<br />
<strong>for</strong> each type <strong>of</strong> diet, including calculated,<br />
diabetic, no concentrated sweets, cardiac,<br />
low sodium, no added salt <strong>and</strong> renal.<br />
“Being able to provide food that patients<br />
crave <strong>and</strong> enjoy is key to promoting<br />
recovery <strong>and</strong> health,” said Eric Sieden,<br />
director <strong>of</strong> food <strong>and</strong> nutritional services at<br />
Plainview. “To create the meals that people<br />
want to eat, we use only fresh, highquality<br />
ingredients from local vendors <strong>and</strong><br />
farmers in the community. We make sure<br />
that the items ordered arrive the way they<br />
are requested, so there’s always something<br />
they want to eat.”
National Recognition<br />
For Spine Program<br />
GLEN COVE — <strong>The</strong> Center <strong>for</strong> Spine Services at Glen Cove<br />
Hospital was recently recognized as an Aetna Institute <strong>of</strong> Quality<br />
<strong>for</strong> Spine Surgery, a designation that highlights the center’s<br />
expertise, excellent surgical outcomes <strong>and</strong> patient-focused care.<br />
“This accreditation is another layer <strong>of</strong> credibility. It tells the<br />
community that we not only per<strong>for</strong>m a large number <strong>of</strong> spinal<br />
procedures, but also, more importantly, we do them very well,”<br />
said Vincent Leone, MD, director <strong>of</strong> orthopedic spine surgery at<br />
Glen Cove Hospital.<br />
To qualify <strong>for</strong> the designation, Glen Cove underwent a<br />
rigorous review process, meeting strict criteria regarding the<br />
center’s use <strong>of</strong> evidence-based protocols, follow-up support <strong>of</strong><br />
patients, program breadth, education <strong>and</strong> training <strong>of</strong> the medical<br />
<strong>and</strong> nonmedical community <strong>and</strong> quality improvement.<br />
History Exhibit Honors<br />
Fallen Firefighter<br />
STATEN ISLAND — To wrap up the anniversary <strong>of</strong> its 150-year history, Staten<br />
Isl<strong>and</strong> University Hospital (SIUH) recently opened a history exhibit in honor<br />
<strong>of</strong> Fire Department <strong>of</strong> New York (FDNY) Assistant Chief Gerard Barbara, who<br />
gave his life on 9/11.<br />
“Part <strong>of</strong> his timeline is the timeline <strong>of</strong> the hospital,” said Monsignor<br />
John Delendick, FDNY chaplain. “He served his community <strong>and</strong> city well; he<br />
there<strong>for</strong>e served this hospital with the same passion.”<br />
<strong>The</strong> exhibit features a plaque honoring Mr. Barbara <strong>and</strong> a timeline <strong>of</strong><br />
the hospital’s history, augmented by antiques from the hospital’s past. Mr.<br />
Barbara’s wife, Joanne, unveiled the exhibit as her family <strong>and</strong> about 200 firefighters,<br />
hospital employees <strong>and</strong> others looked on at the Regina M. McGinn,<br />
MD, Education Center.<br />
“My inspiration <strong>for</strong> getting involved in a project at Staten Isl<strong>and</strong><br />
University Hospital is because Jerry was an advocate <strong>for</strong> continuing education<br />
– especially in fire safety. This center is an education center, <strong>and</strong> that’s what<br />
we wanted to promote,” Ms. Barbara said.<br />
“<strong>The</strong> wall unites the hospital’s detailed history while honoring one <strong>of</strong> our<br />
community’s biggest role models,” said Anthony Ferreri, president <strong>and</strong> CEO <strong>of</strong><br />
SIUH. “Jerry was a leader, <strong>and</strong> he deserves to be remembered as a hero in our<br />
area <strong>for</strong> eternity.”<br />
See the exhibit in the Regina M. McGinn, MD, Education Center at SIUH’s<br />
north campus, 475 Seaview Ave. in Staten Isl<strong>and</strong>.<br />
<strong>The</strong> recently opened history exhibit at Staten Isl<strong>and</strong> University Hospital’s Regina M.McGinn, MD, Education Center, dedicated to the memory <strong>of</strong> firefighter<br />
Gerard Barbara. who died on 9/11.<br />
<strong>The</strong> New St<strong>and</strong>ard 19
around the system<br />
Lenox Hill Hospital volunteer Vincent Foster<br />
<strong>and</strong> Auxilian Ellen Starr were honored at the<br />
United Hospital Fund’s 19th Annual Hospital<br />
Auxilian <strong>and</strong> Volunteer Achievement Awards<br />
ceremony, held this spring at the Waldorf-Astoria. Mr.<br />
Foster <strong>and</strong> Ms. Starr were part <strong>of</strong> an elite group <strong>of</strong> 89<br />
volunteers who were honored <strong>for</strong> providing exceptional<br />
service to hospitals throughout the five boroughs <strong>of</strong> New<br />
York City. Janice Huff, chief meteorologist <strong>of</strong> NBC4 New<br />
York, was the special guest at the event, which drew nearly<br />
800 attendees to the hotel’s Gr<strong>and</strong> Ballroom.<br />
Mr. Foster has been a volunteer at Lenox Hill<br />
Hospital <strong>for</strong> over eight years. He has volunteered<br />
in the Pharmacy Department <strong>and</strong> most recently as a<br />
receptionist in the Human Resources Department.<br />
Glenn Courounis, vice president <strong>of</strong> human resources,<br />
lauds Mr. Foster as a thorough <strong>and</strong> detail-oriented<br />
worker who is always punctual <strong>and</strong> reliable, someone who<br />
takes his responsibilities very seriously. Mr. Foster is a<br />
retired social studies teacher in the NYC Public School<br />
System <strong>and</strong> an accomplished trumpet player. He is also a<br />
minister at the Christadelphian Ecclesia Church.<br />
Ms. Starr has been a member <strong>of</strong> Lenox Hill<br />
Hospital’s Auxiliary <strong>for</strong> over 15 years. She has chaired<br />
several fundraising events, including the Auxiliary’s annual<br />
theater benefit, which raises funds to support programs<br />
<strong>and</strong> enhancements at the hospital, <strong>and</strong> has served on the<br />
Auxiliary’s Executive Committee. Ms. Starr has done<br />
a great deal <strong>for</strong> the morale <strong>of</strong> the Auxiliary by putting<br />
together various outings, such as museum tours <strong>and</strong><br />
benefits. Auxilian Colleen Pizzitola says that with these<br />
events that encourage a sense <strong>of</strong> camaraderie she is the<br />
“glue that holds us together.” Ms. Starr is a principal in an<br />
interior design firm <strong>and</strong> has brought her creative eye to<br />
many hospital events including the annual Autumn Ball.<br />
Mr. Foster <strong>and</strong> Ms. Starr were chosen from among<br />
50,000 New York City healthcare volunteers who give <strong>of</strong><br />
their time willingly <strong>and</strong> selflessly to improve healthcare<br />
in our city.<br />
<strong>The</strong> United Hospital Fund’s Hospital Auxilian <strong>and</strong><br />
Volunteer Achievement Awards are part <strong>of</strong> the United<br />
Hospital Fund’s ef<strong>for</strong>ts to mobilize the energies <strong>of</strong><br />
volunteers, recognize volunteer achievements <strong>and</strong> open<br />
new avenues <strong>for</strong> volunteer involvement in healthcare.<br />
20 Summer 2012<br />
Two Lenox Hill Hospital<br />
Volunteers Honored<br />
By Barbara Osborn<br />
Above: Honoree Vincent Foster, center, with, from left: Susan E. Brown, Carol Braverman,<br />
volunteer coordinator at the hospital, Elaine Rosenblum, senior associate executive director,<br />
<strong>and</strong> Evelyn Foster, his mother. Below: Honoree Ellen Starr, center, with her husb<strong>and</strong>, Michael<br />
Starr, MD, chief <strong>of</strong> corneal/external disease in the Department <strong>of</strong> Ophthalmology at Lenox<br />
Hill, <strong>and</strong> her daughter, Olivia, who works at the hospital in HR.
Nassau County Attorney<br />
Survives Sepsis<br />
By Kristen Longo<br />
VALLEY STREAM — Nassau<br />
County Attorney John<br />
Ciampoli showed up at<br />
Franklin Hospital mainly to<br />
ease the minds <strong>of</strong> family <strong>and</strong><br />
friends. He hadn’t been feeling<br />
well <strong>for</strong> over a week, <strong>and</strong> the<br />
antibiotics he was taking did<br />
not seem to be knocking out<br />
an infection. Yet he continued<br />
to put in long hours. When he<br />
arrived at the hospital, he was<br />
in a hurry to get back to work<br />
— but five hours later, he was<br />
on a ventilator.<br />
“Anywhere from two to<br />
four hours longer getting to<br />
the hospital, it would have<br />
been a one-way trip,” said Mr.<br />
Ciampoli. “When they asked,<br />
‘Did they take your temperature?<br />
What was it?’ I said,<br />
`Sure, they took my temperature,<br />
it was 250 degrees,’ <strong>and</strong><br />
my friend who was there with<br />
me said, ‘Listen, I know this<br />
guy, he has a sense <strong>of</strong> humor —<br />
that wasn’t his sense <strong>of</strong> humor.<br />
He’s losing it.’” That was<br />
Mr. Ciampoli’s last memory<br />
until he woke up a week later.<br />
Thanks to the expertise <strong>of</strong><br />
Southside Establishes Surgical Program<br />
<strong>for</strong> Complex Liver, Pancreas Diseases<br />
BAY SHORE — Patients with complex problems <strong>of</strong> the liver, bile<br />
ducts <strong>and</strong> pancreas can now find state-<strong>of</strong>-the-art surgical care at<br />
Southside Hospital’s new Hepatobiliary <strong>and</strong> Pancreatic Surgery<br />
Program. It is led by Juan Madariaga, MD, PhD, who was trained<br />
<strong>and</strong> practiced as a liver surgeon at the prestigious University <strong>of</strong><br />
Pittsburgh’s Thomas E. Starzl Transplantation Institute <strong>and</strong> subsequently<br />
at the University <strong>of</strong> Miami Transplant Center.<br />
Dr. Madariaga said patients with complex liver or biliary<br />
problems are <strong>of</strong>ten referred to the North Shore-LIJ Health System<br />
because <strong>of</strong> its “expertise <strong>and</strong> good patient outcomes.”<br />
No Need to Travel <strong>for</strong> Care<br />
“It’s great news <strong>for</strong> patients <strong>and</strong> their families that they don’t<br />
have to travel outside <strong>of</strong> their local community to find the highly<br />
specialized care they need,” said Christopher Nelson, assistant vice<br />
president <strong>of</strong> surgery. “<strong>The</strong> expansion <strong>of</strong> our hepatobiliary surgery<br />
program allows patients to stay in the community where they<br />
reside, closer to family <strong>and</strong> friends who play a crucial role in the<br />
recovery process.”<br />
clinicians at Franklin Hospital,<br />
he is alive to share his story.<br />
Mr. Ciampoli was suffering<br />
from sepsis, an overblown<br />
immune response that causes<br />
blood pressure to drop <strong>and</strong><br />
major organs to fail. “In the<br />
emergency departments across<br />
North Shore-LIJ, we have a<br />
very heightened awareness<br />
<strong>of</strong> sepsis,” said John Rohe,<br />
MD, director <strong>of</strong> emergency<br />
medicine at Franklin.“We<br />
have an evidence-based sepsis<br />
protocol, which has helped us<br />
reduce the number <strong>of</strong> deaths.”<br />
“<strong>The</strong> quicker we can<br />
recognize sepsis, the better<br />
patients respond clinically,” said<br />
Scott Horowitz, MD, acting<br />
chief <strong>of</strong> infectious disease at<br />
Franklin. Mr. Ciampoli is<br />
grateful that he went to Franklin<br />
<strong>for</strong> treatment. “<strong>The</strong> people<br />
there knew how to react, knew<br />
what to do, <strong>and</strong> they pulled me<br />
through,” he said.<br />
To see a video <strong>of</strong> Mr.<br />
Ciampoli’s story, visit http://<br />
bit.ly/nslijsurvivingsepsis<br />
Common conditions that hepatobiliary surgeons treat include<br />
liver, gallbladder or bile duct cancer; noncancerous liver tumors;<br />
narrowing or blockages <strong>of</strong> the bile ducts; <strong>and</strong> injury to the liver or<br />
bile ducts.<br />
<strong>The</strong> program employs a multidisciplinary team, including<br />
a hepatobiliary surgeon <strong>and</strong> a variety <strong>of</strong> specialists, who meet to<br />
review <strong>and</strong> discuss patients’ test results <strong>and</strong> develop individualized<br />
treatment plans.<br />
Minimally Invasive Procedures Available<br />
<strong>The</strong> surgeons in the program are skilled in open, laparoscopic<br />
<strong>and</strong> robotic methods <strong>of</strong> surgical treatment <strong>of</strong> disease. Because<br />
minimally invasive, cutting-edge surgery <strong>of</strong> the liver can mean<br />
faster patient recovery <strong>and</strong> less pain, surgeons opt <strong>for</strong> it whenever<br />
possible, Dr. Madariaga said. Patients also receive high-quality<br />
postoperative care from a highly skilled <strong>and</strong> experienced team to<br />
ensure a safe <strong>and</strong> speedy recovery. “With such a comprehensive<br />
<strong>and</strong> experienced team,” Dr. Madariaga said, “our patients can be<br />
assured <strong>of</strong> receiving the highest level <strong>of</strong> care.”<br />
<strong>The</strong> New St<strong>and</strong>ard 21
Shown conducting a “Code Sepsis” drill in the ED <strong>of</strong> Glen Cove Hospital, applying new, more stringent criteria <strong>for</strong> sepsis diagnosis, from left, are Patricia Davis, RN,<br />
John D’Angelo, MD, director <strong>of</strong> the ED, Lorraine Lehmann, PCA, Alfredo Benito, RN, <strong>and</strong> Evelyn Mulvaney, nurse manager.<br />
An elderly man presents<br />
at the Emergency<br />
Department (ED) <strong>of</strong><br />
a North Shore-LIJ hospital.<br />
He has a dry cough, a fever<br />
<strong>of</strong> 101 degrees <strong>and</strong> his heart<br />
rate is slightly elevated at 97.<br />
He doesn’t feel well, but his<br />
blood pressure is normal. He is<br />
undergoing chemotherapy <strong>for</strong><br />
colon cancer <strong>and</strong> his last chemo<br />
session was three weeks ago.<br />
A few years ago, that<br />
patient may have been triaged<br />
<strong>and</strong> treated as nonemergent,<br />
which means he may have<br />
taken his place in line behind<br />
cases that more clearly<br />
required emergent attention.<br />
All that has changed, however,<br />
thanks to the health system’s<br />
Surviving Sepsis Program that<br />
began in 2008.<br />
Sepsis is a lifethreatening<br />
condition<br />
that arises when a systemic<br />
22 Summer 2012<br />
Sepsis-Related Mortality<br />
Reduced by 35 Percent<br />
But the Work Is Just Beginning<br />
By <strong>The</strong>a Welch<br />
inflammatory response to<br />
infection or injury attacks<br />
the body’s own tissues<br />
<strong>and</strong> organs. Without<br />
diagnosis <strong>and</strong> treatment,<br />
it can proceed rapidly <strong>and</strong><br />
irrevocably to severe sepsis<br />
(sepsis complicated by organ<br />
dysfunction) <strong>and</strong> then septic<br />
shock (acute circulatory<br />
failure). In 2008, it was<br />
the single greatest cause<br />
<strong>of</strong> in-hospital mortality in<br />
the health system; further,<br />
North Shore-LIJ’s mortality<br />
rates were statistically higher<br />
than predicted, according to<br />
HealthGrades.<br />
As part <strong>of</strong> his no-tolerance<br />
approach to preventable death,<br />
North Shore-LIJ President<br />
<strong>and</strong> Chief Executive Officer<br />
Michael Dowling targeted sepsis<br />
as a major problem to address.<br />
That’s why, today, as soon<br />
as the patient hits the door<br />
to the ED, he is recognized<br />
as a possible sepsis patient,<br />
<strong>and</strong> everything speeds up. An<br />
established sepsis treatment<br />
algorithm is followed<br />
immediately, including<br />
drawing blood <strong>and</strong> ordering<br />
tests, such as serum lactate<br />
level (elevated serum lactate<br />
is associated with increased<br />
mortality in severe sepsis<br />
patients). <strong>The</strong> staff begins<br />
administering intravenous (IV)
fluids <strong>and</strong> antibiotics if there<br />
is any evidence <strong>of</strong> infection,<br />
<strong>and</strong> the patient’s vital signs<br />
are monitored continuously.<br />
Everyone in the ED is aware<br />
that with sepsis, as with trauma,<br />
a heart attack or a stroke,<br />
there is a “golden hour” — a<br />
critical period during which the<br />
progression <strong>of</strong> the illness must<br />
be halted.<br />
Since 2008, the lives <strong>of</strong><br />
hundreds <strong>of</strong> patients like our<br />
hypothetical patient have been<br />
saved. <strong>The</strong> health system’s<br />
mortality rate <strong>for</strong> severe sepsis<br />
<strong>and</strong> septic shock has declined to<br />
35 percent (as <strong>of</strong> August 2011)<br />
— a significant accomplishment,<br />
certainly. But the real work<br />
is just beginning, according<br />
to Martin Doerfler, MD, the<br />
health system’s vice president <strong>of</strong><br />
evidence-based clinical practice<br />
<strong>and</strong> co-chair <strong>of</strong> the North<br />
Shore-LIJ Sepsis Task Force,<br />
with John D’Angelo, MD,<br />
director <strong>of</strong> emergency medicine<br />
at Glen Cove Hospital, <strong>and</strong><br />
Darlene Parmentier, RN,<br />
manager <strong>for</strong> critical care at Glen<br />
Cove Hospital.<br />
“Over the last three years,<br />
we’ve laid the foundation<br />
<strong>for</strong> fighting sepsis,” said Dr.<br />
Doerfler. “<strong>The</strong>re is no question<br />
that we have made progress.<br />
But now, in collaboration with<br />
the Institute <strong>for</strong> Healthcare<br />
Improvement [IHI], we are<br />
rolling it out on a gr<strong>and</strong><br />
scale.” In addition to the sepsis<br />
initiative, the partnership<br />
with IHI has three other<br />
phases: improving the quality<br />
<strong>and</strong> accessibility <strong>of</strong> palliative<br />
care, preparing students <strong>and</strong><br />
pr<strong>of</strong>essionals to be outst<strong>and</strong>ing<br />
“improvers,” <strong>and</strong> improving<br />
the health system’s capacity to<br />
improve. <strong>The</strong> kick-<strong>of</strong>f event<br />
<strong>for</strong> the work phase <strong>of</strong> the<br />
sepsis initiative was a two-day<br />
workshop held the last week<br />
<strong>of</strong> February at the Swan Club<br />
in Roslyn, <strong>and</strong> attended by<br />
clinicians <strong>and</strong> administrators<br />
from the health system <strong>and</strong><br />
every hospital.<br />
“In the past we focused on<br />
the intensive care units. More<br />
recently we have focused on<br />
the EDs, where patients are<br />
<strong>of</strong>ten at the sicker end <strong>of</strong> the<br />
sepsis spectrum — low-hanging<br />
fruit,” said Dr. Doerfler.<br />
“Next, we want to move the<br />
focus upstream — to catch<br />
them on the floors <strong>and</strong> treat<br />
them be<strong>for</strong>e they progress<br />
to severe sepsis.” Over the<br />
next four years <strong>of</strong> the IHI<br />
partnership, Mr. Dowling has<br />
challenged the task <strong>for</strong>ce to cut<br />
the health system’s 35 percent<br />
mortality rate in half, which<br />
will put North Shore-LIJ in<br />
the company <strong>of</strong> the top 10<br />
percent <strong>of</strong> its peers <strong>for</strong> severe<br />
sepsis/septic shock mortality.<br />
“I commend emergency<br />
services personnel <strong>and</strong><br />
nursing leadership at the<br />
health system <strong>and</strong> hospital<br />
level <strong>for</strong> stepping up to the<br />
plate in an exemplary way,”<br />
said Dr. Doerfler. “So far, the<br />
work has fallen on them <strong>and</strong><br />
they have embraced it. <strong>The</strong>y<br />
have helped us take many steps<br />
<strong>for</strong>ward. In this next phase,<br />
many additional people in the<br />
health system will be involved,<br />
working with IHI teams on<br />
a weekly basis, at a much<br />
deeper level <strong>of</strong> engagement<br />
<strong>and</strong> underst<strong>and</strong>ing. We<br />
have some distance yet to<br />
cover, but I believe we have a<br />
reachable goal.”<br />
Jumping <strong>for</strong><br />
Good Health<br />
Over the past year, Cohen Children’s<br />
Medical Center (CCMC) <strong>and</strong> Kohl’s Cares<br />
<strong>for</strong> Kids have conducted an educational<br />
program with students at Jackson Main<br />
Elementary School in Hempstead. <strong>The</strong><br />
program was a health <strong>and</strong> wellness<br />
initiative aimed at educating students<br />
on proper nutrition, the importance <strong>of</strong><br />
exercise <strong>and</strong> how to stay fit at home.<br />
Teachers worked with a program called<br />
“Activity Works,” which urges youngsters<br />
to per<strong>for</strong>m 12 minutes a day <strong>of</strong> exercise<br />
in the classroom, <strong>and</strong> to report what<br />
they’ve learned to their parents <strong>and</strong><br />
siblings. Students worked so hard to<br />
meet their exercise goals that CCMC <strong>and</strong><br />
Kohl’s decided to surprise them with a<br />
visit <strong>and</strong> per<strong>for</strong>mance from the nationally<br />
recognized jump rope team, Lucie B.<br />
Jump N Fun Rocket Ropers. Afterwards,<br />
students joined in the fun.<br />
<strong>The</strong> New St<strong>and</strong>ard 23
nursing mission<br />
A Legacy <strong>of</strong> Nursing Excellence:<br />
Three Who Left <strong>The</strong>ir Mark<br />
HUNTINGTON — Phyllis<br />
Barlow, RN, began working at<br />
Huntington Hospital in 1958.<br />
Lola Goldman, RN, joined in<br />
1968. Myrna Myers-Laque,<br />
RN, who recently retired as<br />
vice president <strong>of</strong> nursing <strong>and</strong><br />
chief nursing <strong>of</strong>ficer, came<br />
in 1974. <strong>The</strong>se three nursing<br />
pr<strong>of</strong>essionals have witnessed<br />
tremendous progress in the<br />
field <strong>of</strong> medicine <strong>and</strong> the<br />
practice <strong>of</strong> nursing over the<br />
decades, <strong>and</strong> they have made<br />
enormous contributions to<br />
the high st<strong>and</strong>ard <strong>of</strong> nursing<br />
excellence that Huntington<br />
Hospital is known <strong>for</strong> today.<br />
“In 1958, the typical<br />
nurse was young. She wore a<br />
starched white uni<strong>for</strong>m, white<br />
shoes, white hose <strong>and</strong> a cap<br />
that indicated the school she<br />
graduated from,” recalled Ms.<br />
Barlow. Beyond the uni<strong>for</strong>m,<br />
1950s-era nurses adopted an<br />
attitude <strong>of</strong> subservience to<br />
physicians. “We stood when a<br />
doctor entered the room, <strong>and</strong><br />
we moved to the rear <strong>of</strong> the<br />
elevators when one got on.”<br />
In those days, licensed<br />
practical nurses (LPNs)<br />
worked alongside registered<br />
nurses. Eventually, LPNs were<br />
phased out, <strong>and</strong> registered<br />
nurses were encouraged to<br />
pursue advanced degrees as<br />
an increasing emphasis was<br />
placed on education.<br />
As director <strong>of</strong> nursing<br />
24 Summer 2012<br />
Phyllis Barlow<br />
<strong>and</strong> eventually vice president<br />
be<strong>for</strong>e retiring from the<br />
hospital in 1991, Ms. Barlow<br />
encouraged nurses to<br />
continue their education, as<br />
did Ms. Myers-Laque.<br />
One result was a shift<br />
in the relationship between<br />
nurses <strong>and</strong> physicians.<br />
“Relationships became more<br />
collaborative as a result <strong>of</strong> the<br />
increased pr<strong>of</strong>essionalism<br />
that came with additional<br />
education,” said Ms. Goldman.<br />
Today’s patients tend<br />
to be sicker than those 30<br />
years ago, Ms. Goldman<br />
noted. Thanks to advances in<br />
minimally invasive surgical<br />
techniques, patients require<br />
less time in the hospital <strong>and</strong><br />
spend more time recovering<br />
at home. Changing<br />
demographics have caused<br />
another shift in the patient<br />
pr<strong>of</strong>ile. Today’s hospital<br />
patients are <strong>of</strong>ten older <strong>and</strong><br />
frailer than their counterparts<br />
a generation or two ago.<br />
By <strong>The</strong>resa Jacobellis<br />
Myrna Myers-Laque, left, <strong>and</strong><br />
Lola Goldman<br />
“In this country, those<br />
over 85 are the fastest growing<br />
segment <strong>of</strong> the population,”<br />
said Ms. Myers-Laque.<br />
“Taking care <strong>of</strong> an 85-yearold<br />
is very different from<br />
taking care <strong>of</strong> a 45-year-old.”<br />
To help ensure that<br />
the needs <strong>of</strong> this exp<strong>and</strong>ing<br />
geriatric population are met,<br />
Ms. Myers-Laque challenged<br />
Huntington Hospital’s<br />
nursing staff to become<br />
certified in gerontological<br />
nursing, <strong>and</strong> more than 100<br />
nurses accepted.<br />
As with every aspect <strong>of</strong><br />
life, computerization has<br />
radically altered the practice<br />
<strong>of</strong> nursing. Be<strong>for</strong>e, “we did<br />
everything by h<strong>and</strong>,” Ms.<br />
Goldman said. Today, one<br />
glance at a central monitor in<br />
the Nursing Administration<br />
Department reveals the<br />
number <strong>and</strong> location <strong>of</strong><br />
available beds, <strong>and</strong> clinical<br />
in<strong>for</strong>mation can be accessed<br />
from any computer.<br />
As she steps away from her<br />
role as VP <strong>of</strong> nursing <strong>and</strong> takes<br />
on a new challenge as a nursing<br />
consultant, Ms. Myers-Laque<br />
looks toward the future.<br />
“<strong>The</strong> real issue in<br />
nursing is the need to<br />
trans<strong>for</strong>m the environment<br />
so nurses can spend more<br />
time at the bedside,” she said,<br />
citing a recent Robert Wood<br />
Johnson Foundation study<br />
that found that up to 60<br />
percent <strong>of</strong> a nurse’s time is<br />
spent on h<strong>and</strong>ling paperwork,<br />
hunting <strong>for</strong> supplies or<br />
transporting patients.<br />
Improved technology <strong>and</strong><br />
a redesign <strong>of</strong> patient care<br />
units will help with that<br />
trans<strong>for</strong>mation.<br />
One <strong>of</strong> the highlights<br />
<strong>of</strong> Ms. Myers-Laque’s 38year<br />
career at Huntington<br />
was the receipt <strong>of</strong> Magnet<br />
designation, conferred<br />
by the American Nurses<br />
Credentialing Center<br />
(ANCC). <strong>The</strong> program<br />
recognizes hospitals <strong>for</strong><br />
high st<strong>and</strong>ards <strong>of</strong> patient<br />
care, nursing excellence<br />
<strong>and</strong> innovations in nursing<br />
practice.<br />
According to the<br />
ANCC, Magnet hospitals<br />
report increased retention<br />
<strong>of</strong> nursing staff, a decreased<br />
nursing turnover rate <strong>and</strong><br />
higher job satisfaction among<br />
nurses. Additionally, Magnet<br />
facilities are associated with<br />
increased patient satisfaction,<br />
decreased mortality rates<br />
<strong>and</strong> improved patient<br />
safety. Ms. Myers-Laque<br />
is currently charged with<br />
helping Huntington prepare<br />
<strong>for</strong> its Magnet recertification<br />
scheduled <strong>for</strong> later this year.
WOODBURY — Amy Resnick,<br />
RN, pictured here, primary<br />
nurse in the Hospice Care<br />
Network, makes a difference in<br />
her patients’ <strong>and</strong> families’ lives<br />
— in large <strong>and</strong> small ways.<br />
In addition to her clinical<br />
duties, she’s gone the extra<br />
mile to babysit a terminally ill<br />
baby <strong>and</strong> her sibling so their<br />
exhausted mother could nap.<br />
She’s encouraged a teenage<br />
mother, distracted by her ill<br />
son’s care, to remember to<br />
eat. Ms. Resnick has gained<br />
the trust <strong>and</strong> affection <strong>of</strong> a<br />
man with pancreatic cancer<br />
who said that his greatest wish<br />
be<strong>for</strong>e dying was to find her<br />
a husb<strong>and</strong> (preferably his<br />
“h<strong>and</strong>some son”).<br />
<strong>The</strong> connections <strong>and</strong><br />
impressions Ms. Resnick makes<br />
are lasting. She was the first to<br />
learn that the teenage mother<br />
(now 20) is having another<br />
baby <strong>and</strong> among the first to be<br />
invited to her wedding this year.<br />
“This is what I was put<br />
on this earth to do,” Ms.<br />
Resnick said. “It’s a very<br />
vulnerable time <strong>for</strong> [patients<br />
<strong>and</strong> families] <strong>and</strong> they trust<br />
me to help.” In addition to<br />
clinical assessments, symptom<br />
management <strong>and</strong> patient/<br />
Being Present as<br />
Time Winds Down<br />
By Kathleen Waton<br />
family education related to<br />
end-<strong>of</strong>-life care, it’s “being<br />
kind <strong>and</strong> present,” she said.<br />
<strong>The</strong> role <strong>of</strong> caring <strong>for</strong><br />
patients at the end <strong>of</strong> life comes<br />
naturally to Ms. Resnick.<br />
“[Death] is going to happen to<br />
everyone <strong>and</strong> I just want to do<br />
<strong>for</strong> others what I would want<br />
NPs Facilitate Care at Forest Hills<br />
By Kathleen Waton<br />
FOREST HILLS — Forest Hills Hospital, like other facilities across the North Shore-<br />
LIJ Health System, is employing more nurse practitioners (NPs) in various areas<br />
to make a difference in patient care. Advanced practice nurses facilitate care by<br />
“functioning to the limit <strong>of</strong> their licensure” as “we face a shortage <strong>of</strong> practitioners<br />
in the future,” said Rita Mercieca, RN, executive director.<br />
Last fall, NPs entered two areas in particular that dem<strong>and</strong> more ef<strong>for</strong>t:<br />
heart failure <strong>and</strong> pain management. “One <strong>of</strong> our major causes <strong>of</strong> readmission to<br />
the hospital within 30 days after discharge is heart failure,” Ms. Mercieca said.<br />
Hallie Bleau, NP, coordinates the care <strong>of</strong> heart failure patients in the<br />
community to prevent readmission. “We’re not going to be able to keep all<br />
<strong>of</strong> them out <strong>of</strong> the hospital,” she said, “because heart failure is a progressive<br />
disease <strong>and</strong> patients continue to get sicker.” But following up with patients<br />
after discharge <strong>and</strong> teaching simple steps like daily weighings to manage water<br />
retention <strong>and</strong> encouraging patients to visit their physicians within three to<br />
seven days after discharge help reduce readmission. Ms. Bleau’s role as NP also<br />
done <strong>for</strong> me,” she said.<br />
<strong>The</strong> work undoubtedly<br />
is very sad at times, she<br />
admitted, yet there are many<br />
happy moments. “Unless<br />
you do this work, it’s hard to<br />
underst<strong>and</strong> how much fun it<br />
can be. Patients’ guards are<br />
down <strong>and</strong> they welcome you<br />
into their family. It’s such an<br />
easy relationship.”<br />
When Ms. Resnick first<br />
meets patients <strong>and</strong> families,<br />
however, “they think it’s going<br />
to be gloom <strong>and</strong> doom, but it’s<br />
really talking about living until<br />
you are no longer living.”<br />
Ms. Resnick’s dedication<br />
to her patients makes an<br />
impression. “She is the ultimate<br />
in dedicated, bright <strong>and</strong><br />
compassionate staff,” said Nan<br />
Toelstedt, RN, executive vice<br />
president <strong>of</strong> the Hospice Care<br />
Network. “We are lucky to have<br />
her — <strong>and</strong> so are her patients.”<br />
involves nursing education, including making sure bedside nurses are attentive to<br />
weight gain <strong>and</strong> check low-sodium diets <strong>for</strong> heart failure patients.<br />
Jamina John, NP, manages patients’ pain <strong>and</strong> ensures patients with<br />
patient-controlled analgesia know how to use the PCA effectively. “It’s great<br />
that ordering medication is within my scope <strong>of</strong> practice,” Ms. John said, “so<br />
I can make changes to the order, transition from IV medication to pills or order<br />
changes to the device so patients get proper relief.” For major surgery like knee<br />
or hip replacements, new morphine epidurals provide continuous medication<br />
management <strong>for</strong> 48 hours after surgery, <strong>and</strong> allow Ms. John to tweak the dosage to<br />
manage pain.<br />
“Just having the time to sit in the room <strong>and</strong> talk makes the patient feel so<br />
much more com<strong>for</strong>table,” she said. “I’m so happy Forest Hills Hospital started<br />
this role <strong>and</strong> excited <strong>for</strong> the future. We’ve had so much positive feedback — from<br />
patients <strong>and</strong> staff.”<br />
<strong>The</strong> New St<strong>and</strong>ard 25<br />
Jeanne Morrison, LMSW
nursing mission<br />
NEW HYDE PARK — <strong>The</strong><br />
unique pro-education<br />
environment at the North<br />
Shore-LIJ Health System <strong>and</strong><br />
its nurses’ commitment to<br />
further their education were<br />
the focus <strong>of</strong> an article in the<br />
March issue <strong>of</strong> <strong>The</strong> Journal <strong>of</strong><br />
Continuing Education in Nursing. <strong>The</strong><br />
article, entitled “Continuing<br />
Nursing Education: A<br />
Partnership Between Learner<br />
<strong>and</strong> Teacher,” by Lena<br />
Garafalo, RN, North Shore-<br />
LIJ’s nursing education<br />
coordinator, highlights how<br />
health system nurses are<br />
26 Summer 2012<br />
Partnering <strong>for</strong><br />
Education<br />
By Kathleen Waton<br />
encouraged to continue their<br />
pr<strong>of</strong>essional development<br />
<strong>and</strong> provide input to improve<br />
programs.<br />
To be effective, Ms.<br />
Garafalo wrote, education<br />
should be interactive. Taking<br />
needs assessment/evaluation<br />
seriously guides the educator<br />
in ensuring timely, relevant<br />
educational activity <strong>and</strong> meets<br />
the “participants’ learning needs<br />
<strong>and</strong> career goals,” she said.<br />
Nursing feedback has led<br />
to more interactive breakout<br />
sessions <strong>and</strong> h<strong>and</strong>s-on<br />
experience with insulin pumps<br />
&<br />
<strong>and</strong> pens at a popular diabetes<br />
conference, <strong>and</strong> top certified<br />
wound <strong>and</strong> ostomy continence<br />
nurses leading a workshop<br />
on practical foot care <strong>for</strong><br />
nurses to apply in everyday<br />
practice. And a pediatric<br />
conference exp<strong>and</strong>ed into two<br />
separate learning tracks — one<br />
<strong>for</strong> critical care nurses <strong>and</strong><br />
another <strong>for</strong> med/surg nurses —<br />
based on input from nurses.<br />
To “share a common<br />
vision” <strong>for</strong> education, North<br />
Shore-LIJ executive nursing<br />
leadership <strong>and</strong> nursing educators<br />
meet monthly to roll up<br />
nursing input <strong>and</strong> share strategies<br />
<strong>for</strong> improvement, said<br />
Elaine Smith, RN, EdD, vice<br />
president <strong>for</strong> nursing education<br />
<strong>for</strong> the health system. “This is a<br />
wonderful benefit in an organization<br />
<strong>of</strong> this size,” she said.<br />
This ongoing<br />
communication has led to<br />
an all-day diabetes program<br />
Nursing Conferences<br />
Continuing Education Programs<br />
Enhance skills or build new ones with help from the North Shore-LIJ Institute <strong>for</strong> Nursing.<br />
July<br />
26<br />
Pediatric Conference<br />
Swan Club, Glenwood L<strong>and</strong>ing<br />
September<br />
12<br />
Critical Care/Emergency Conference<br />
Swan Club, Glenwood L<strong>and</strong>ing<br />
18<br />
Nursing Education Conference<br />
Swan Club, Glenwood L<strong>and</strong>ing<br />
27-28<br />
Oncology Nursing Society Chemo/<br />
Biotherapy Course<br />
Southside Hospital, Bay Shore<br />
<strong>The</strong> North Shore-LIJ Health System is an approved provider <strong>of</strong> continuing nursing education by the New York State Nurses<br />
Association, an accredited approver by the American Nurses Credentialing Center’s Commission on Accreditation. Conferences<br />
<strong>and</strong> programs are added regularly. For more in<strong>for</strong>mation, please call the Institute <strong>for</strong> Nursing at (718) 470-3890 or register at<br />
NorthShoreLIJ.com/NSLIJ/nurses.<br />
becoming an annual event; the<br />
addition <strong>of</strong> a full-day program<br />
<strong>for</strong> emergency department<br />
nurses <strong>and</strong> technicians;<br />
<strong>and</strong> the rebirth <strong>of</strong> a critical<br />
care conference <strong>for</strong> nurses.<br />
In 2012, new conferences<br />
are coming in nursing<br />
in<strong>for</strong>matics, urology <strong>and</strong> one<br />
just <strong>for</strong> nurse practitioners.<br />
Dr. Smith said Ms.<br />
Garafalo demonstrates<br />
“developing the pr<strong>of</strong>essional<br />
dimensions <strong>of</strong> her own role”<br />
by writing peer-reviewed<br />
articles <strong>and</strong> developing the<br />
“large number <strong>of</strong> programs<br />
to enhance pr<strong>of</strong>essional<br />
competence.”<br />
About 100 continuing<br />
education programs benefit<br />
more than 6,000 system<br />
nurses a year. “That’s above <strong>and</strong><br />
beyond the general education<br />
taking place at other local<br />
hospitals,” Dr. Smith said.<br />
Bedside or not, nurses<br />
must be accountable <strong>for</strong><br />
learning, Ms. Garafalo<br />
added: “That’s what makes<br />
our health system <strong>and</strong> our<br />
nursing pr<strong>of</strong>ession so strong<br />
— <strong>and</strong> why we can provide<br />
such a high level <strong>of</strong> care to our<br />
patients <strong>and</strong> their families.”
SYOSSET — Jeanine Norton,<br />
RN, had just finished her daily<br />
early-morning workout when<br />
she saved the life <strong>of</strong> a 44-yearold<br />
man.<br />
<strong>The</strong> Post-Anesthesia Care<br />
Unit nurse at Syosset Hospital<br />
was preparing to leave the gym<br />
at 6 a.m. when staff asked if<br />
she could help a man having<br />
“seizures.” With 13 years <strong>of</strong><br />
critical care experience, Ms.<br />
Norton ran to help. She<br />
recognized the man who had<br />
recently started exercising<br />
regularly at the gym <strong>and</strong> saw<br />
he had no pulse <strong>and</strong> wasn’t<br />
breathing.<br />
Ms. Norton made sure<br />
that 911 had been called<br />
<strong>and</strong> then per<strong>for</strong>med chest<br />
compressions on the man<br />
<strong>for</strong> almost half an hour,<br />
while two physicians at the<br />
gym helped “get breath into<br />
him.” She continued applying<br />
chest compressions after the<br />
ambulance arrived so the<br />
emergency medical technicians<br />
(EMTs) could intubate the<br />
man. After attempting an<br />
intravenous line <strong>and</strong> resorting<br />
to an interoscular device in the<br />
leg, the EMTs administered<br />
epinephrine <strong>and</strong> atropine <strong>for</strong><br />
cardiac arrest.<br />
<strong>The</strong> ambulance rushed<br />
him to nearby Syosset<br />
Hospital, where he was<br />
stabilized <strong>and</strong> later transferred<br />
to North Shore University<br />
Hospital. In their cardiac cath<br />
lab, North Shore University<br />
Hospital staff discovered the<br />
main vessel in his heart was<br />
blocked. “It’s also known as the<br />
‘widow maker,’” Ms. Norton<br />
said, “because most people<br />
don’t survive that.”<br />
Recovery<br />
Nurse<br />
Saves<br />
Life at<br />
Gym<br />
By Kathleen Waton<br />
<strong>The</strong> man lived <strong>and</strong> after<br />
2.5 weeks in the hospital, was<br />
discharged with a pacemaker<br />
defibrillator.<br />
After responding<br />
immediately to the emergency,<br />
Ms. Norton continues to be<br />
affected by the event. “I wasn’t<br />
sure if he was going to be brain<br />
dead <strong>and</strong> would be on life<br />
support <strong>for</strong> the rest <strong>of</strong> his life<br />
because he had been without<br />
oxygen <strong>for</strong> so long. His doctor<br />
says he doesn’t know how he<br />
survived, without a heartbeat<br />
<strong>for</strong> 30 minutes. When I see<br />
him at the gym now, tears<br />
come to my eyes, the rescue<br />
was so amazing.”<br />
Ms. Norton encourages<br />
others to overcome their fears<br />
<strong>and</strong> act in an emergency.<br />
“Reach out <strong>and</strong> try to help,” she<br />
said. “Even if you can’t do CPR,<br />
get help, do something. Don’t<br />
just walk by. Give someone a<br />
second chance at life.”<br />
Above: Jeanine Norton, RN<br />
Zuckerberg Awards<br />
Nurses from throughout the North Shore-LIJ System recently received<br />
the 2012 Zuckerberg Family Awards <strong>for</strong> Nursing Service Excellence. <strong>The</strong><br />
honorees were recognized <strong>for</strong> meeting or exceeding expectations in all criteria<br />
on per<strong>for</strong>mance evaluations, <strong>and</strong> exceeding expectations in quality <strong>of</strong> work,<br />
attitude, interpersonal relationships <strong>and</strong> attendance. Winners each received<br />
a certificate <strong>and</strong> $1,000. <strong>The</strong> awards program is supported by Roy Zuckerberg,<br />
<strong>for</strong>mer chairman <strong>of</strong> the health system’s Board <strong>of</strong> Trustees.<br />
Award recipients were:<br />
Mavis Barriteau, RN, BSN<br />
Franklin Hospital<br />
Pat Loccisano, RN<br />
Forest Hills Hospital<br />
Megan Burt, RN<br />
Glen Cove Hospital<br />
Camille Hertzel, RN<br />
Huntington Hospital<br />
Jennifer Thys-Rose, RN<br />
Lenox Hill Hospital<br />
Marybeth Grieser, RN<br />
Long Isl<strong>and</strong> Jewish Hospital<br />
Lisa Flick, RN<br />
Manhattan Eye, Ear & Throat<br />
Hospital<br />
Cindy Gomez, RN<br />
North Shore University Hospital<br />
Carol Carlson, RN<br />
Plainview Hospital<br />
Frances McCarthy, RN<br />
Staten Isl<strong>and</strong> University<br />
Hospital North<br />
Frederick Cappetta, RN<br />
Staten Isl<strong>and</strong> University<br />
Hospital South<br />
Charla Doherty, RN<br />
Steven <strong>and</strong> Alex<strong>and</strong>ra Cohen<br />
Children’s Medical Center <strong>of</strong><br />
New York<br />
Charlotte Maloney, RN<br />
Southside Hospital<br />
Stella Bacus, RN<br />
Syosset Hospital<br />
Elise Bailey, RN<br />
<strong>The</strong> Zucker Hillside Hospital<br />
<strong>The</strong> New St<strong>and</strong>ard 27
nursing mission<br />
Psychiatric Nursing<br />
Research Fills In the Gaps<br />
GLEN OAKS — Nurses at<br />
<strong>The</strong> Zucker Hillside Hospital<br />
(ZHH) are breaking new<br />
ground in psychiatric care<br />
research.<br />
At the beginning <strong>of</strong> the<br />
year, the nursing leadership<br />
team launched a pilot study to<br />
determine patient outcomes<br />
after a rapid response team<br />
(RRT) call in a psychiatric<br />
setting. An RRT is called when<br />
a patient’s clinical condition<br />
meets criteria requiring a team<br />
<strong>of</strong> providers to respond, assess<br />
<strong>and</strong> treat immediately.<br />
“We are conducting a<br />
collaborative Institutional<br />
Review Board [IRB]-<br />
28 Summer 2012<br />
approved research study<br />
between nursing <strong>and</strong> internal<br />
medicine to look at nurseinitiated<br />
RRT calls in a<br />
behavioral health setting,”<br />
said Marybeth McManus, RN,<br />
associate executive director <strong>of</strong><br />
patient care services. “<strong>The</strong>re<br />
is currently a lack <strong>of</strong> literature<br />
on medical rapid response<br />
teams in freest<strong>and</strong>ing<br />
psychiatric hospitals.”<br />
<strong>The</strong> nurses will review<br />
100 cases in the pilot study<br />
phase to collect data on such<br />
variables as the reason <strong>for</strong><br />
activating the call, shift/day<br />
<strong>of</strong> week distribution, staffing,<br />
location, psychiatric diagnoses<br />
By Kathleen Waton<br />
<strong>and</strong> follow-up care.<br />
“We’ll review patient<br />
outcomes,” Ms. McManus<br />
said, “such as whether patients<br />
require evaluation in an<br />
emergency department or are<br />
admitted to a medical unit.<br />
<strong>The</strong> goal is to ensure the<br />
provision <strong>of</strong> the appropriate<br />
level <strong>of</strong> medical care in an acute<br />
behavioral health hospital.”<br />
Once the pilot is completed,<br />
the data will be<br />
submitted to the IRB <strong>for</strong> acceptance<br />
as a <strong>for</strong>mal research<br />
study with Ms. McManus <strong>and</strong><br />
Peter Manu, MD, director <strong>of</strong><br />
medical services, as principal<br />
coinvestigators.<br />
Another study in the planning<br />
stages involves helping<br />
patients stop smoking on a<br />
long-term basis.<br />
Since ZHH is a smokefree<br />
environment, patients do<br />
not smoke <strong>for</strong> the two or three<br />
weeks they usually remain<br />
there. Nurses hope to capitalize<br />
on that smoke-free time<br />
to help patients stop smoking<br />
long term after discharge.<br />
<strong>The</strong> nurses will study the<br />
effectiveness <strong>of</strong> a technique<br />
called motivational interviewing,<br />
which involves at least<br />
three one-to-one nurse-<strong>and</strong>patient<br />
sessions that educate<br />
<strong>and</strong> encourage patients to<br />
remain smoke-free. Patients<br />
will be interviewed by phone at<br />
set intervals after discharge to<br />
assess their smoke-free status.<br />
“Nursing research is one<br />
<strong>of</strong> the best ways to study <strong>and</strong><br />
document organizational<br />
processes that improve patient<br />
outcomes <strong>and</strong> quality,” Ms.<br />
McManus said.<br />
Maureen White to Be Inducted into<br />
the American Academy <strong>of</strong> Nursing<br />
<strong>The</strong> American Academy <strong>of</strong> Nursing recently announced its 2012 Class <strong>of</strong><br />
Fellows, <strong>and</strong> in this group <strong>of</strong> 176 esteemed nurse leaders from all over the<br />
country is North Shore-LIJ Health System Chief Nurse Executive Maureen<br />
White, RN, MBA, NEA-BC. At the health system’s nursing retreat in May at<br />
the Swan Club in Roslyn, Ms. White was recognized <strong>for</strong> this honor, one <strong>of</strong><br />
the most prestigious in the field <strong>of</strong> nursing, by Michael Dowling, the health<br />
system’s president <strong>and</strong> chief executive <strong>of</strong>ficer, right, <strong>and</strong> Mark Solazzo,<br />
executive vice president <strong>and</strong> chief operating <strong>of</strong>ficer. Selection criteria include<br />
evidence <strong>of</strong> significant contributions to nursing <strong>and</strong> healthcare <strong>and</strong> the<br />
shaping <strong>of</strong> health policies. When she is inducted in October at the Academy’s<br />
39th Annual Meeting <strong>and</strong> Conference in Washington, DC, she will be in the<br />
elite company <strong>of</strong> about 1,800 nurse leaders in education, management,<br />
practice, policy <strong>and</strong> research, <strong>and</strong> she will be able to add FAAN (Fellowship <strong>of</strong><br />
the American Academy <strong>of</strong> Nursing) to her credentials.
Collaborative Care Councils<br />
Get Results<br />
By Kathleen Waton<br />
<strong>The</strong>odore J. (“T.J.”)<br />
Vlavianos, LMHC, <strong>and</strong> his<br />
fellow collaborative care council<br />
members streamlined the<br />
admissions process last year at<br />
<strong>The</strong> Zucker Hillside Hospital,<br />
improving orienting patients<br />
to the 33-bed adult acute care<br />
psychiatric unit, introducing<br />
treatment team members <strong>and</strong><br />
discharging patients. <strong>The</strong>y<br />
introduced addressing patient<br />
concerns twice a day. <strong>The</strong>ir<br />
success was reflected in higher<br />
continued on page 75<br />
Zucker Hillside Enhances Calming Environment<br />
By Kathleen Waton<br />
GLEN OAKS — A comprehensive<br />
program to reduce impulsive behavior<br />
in patients at <strong>The</strong> Zucker Hillside<br />
Hospital is moving the hospital closer<br />
to becoming restraint-free.<br />
<strong>The</strong> workhorse <strong>of</strong> the program<br />
is DASA (Dynamic Appraisal<br />
<strong>of</strong> Situational Aggression), a<br />
computerized assessment tool that<br />
predicts patients who are most likely<br />
to exhibit seven high-risk symptoms:<br />
negative attitudes, impulsivity,<br />
irritability, verbal threats, sensitivity<br />
to perceived provocation, being<br />
easily angered when requests are<br />
made <strong>and</strong> unwillingness to follow<br />
directions.<br />
Nurses <strong>and</strong> other clinicians<br />
score each patient on the criteria<br />
over a 24-hour period. “Anyone on<br />
the multidisciplinary team can check<br />
<strong>of</strong>f the seven points,” said Marybeth<br />
McManus, RN, associate executive<br />
director <strong>of</strong> patient care services.<br />
<strong>The</strong> night nurse enters the<br />
scores into the electronic health<br />
record. Each patient scoring three<br />
or more on the DASA is listed on a<br />
computerized report automatically<br />
sent each morning to nursing<br />
leaders <strong>and</strong> others who use it to<br />
guide staffing, admissions, care<br />
plans <strong>and</strong> other decisions.<br />
To ward <strong>of</strong>f high-risk episodes<br />
be<strong>for</strong>e they occur, patient engagement<br />
specialists (PES) — team members<br />
specially trained in deescalation<br />
<strong>and</strong> communication skills — are<br />
dispatched to the appropriate units.<br />
<strong>The</strong> PES team is the latest addition to<br />
the initiative. Under RN supervision,<br />
they engage patients in diversionary<br />
activities, such as talking <strong>and</strong><br />
walking with them, playing chess or<br />
listening to music to calm patients<br />
<strong>and</strong> redirect behavior.<br />
<strong>The</strong> user-friendly DASA has<br />
been in use approximately a year.<br />
It was piloted on a 20-bed adult<br />
inpatient unit <strong>for</strong> two months in<br />
the autumn <strong>of</strong> 2010, <strong>and</strong> then<br />
implemented on five other adult units<br />
<strong>and</strong> the hospital’s adolescent pavilion.<br />
<strong>The</strong> program has been very<br />
successful in keeping patients <strong>and</strong><br />
staff safe <strong>and</strong> creating a calmer<br />
atmosphere at Zucker Hillside. In<br />
2011, the hospital “decreased the use<br />
<strong>of</strong> restraints by almost 90 percent<br />
without increasing our seclusion<br />
rate,” Ms. McManus said. “That<br />
puts us well on our way to meeting<br />
our overarching goal <strong>of</strong> providing a<br />
therapeutic healing environment that<br />
is serene <strong>and</strong> calming.”<br />
Making a Vision<br />
Reality<br />
A decade ago, Maureen<br />
White, RN, senior vice president<br />
<strong>and</strong> chief nurse executive,<br />
pondered how to involve frontline<br />
staff more in decisionmaking,<br />
to meet patient needs<br />
<strong>and</strong> to help make the North<br />
Shore-LIJ Health System more<br />
agile in responding to change. “An<br />
empowering environment” was<br />
essential, Ms. White said, “one<br />
in which people feel com<strong>for</strong>table<br />
saying, ‘This doesn’t work,’ <strong>and</strong><br />
proposing solutions.”<br />
To support Ms. White’s<br />
vision, in 2007, Plainview<br />
Hospital piloted collaborative<br />
care councils, the same<br />
year Lily Thomas, PhD, RN,<br />
vice president, system<br />
nursing research, introduced<br />
TeamSTEPPS, an evidence-based<br />
communication tool.<br />
Devised by the Agency<br />
<strong>for</strong> Healthcare Research <strong>and</strong><br />
Quality (AHRQ), the tool fosters<br />
teamwork, “because teamwork is<br />
correlated with patient safety,” Dr.<br />
Thomas said. “It allows everyone<br />
to speak up in a way that puts the<br />
patient first.”<br />
Today, more than 30,000<br />
staff members are trained in<br />
TeamSTEPPS, <strong>and</strong> more than 300<br />
councils are active throughout<br />
the health system. <strong>The</strong>y are<br />
“still in early development,”<br />
according to Ms. White. “People<br />
are still getting used to the<br />
power <strong>of</strong> the councils <strong>and</strong> the<br />
differences they can make. But I<br />
feel the networking has improved<br />
communication <strong>and</strong> is bringing<br />
us closer to a work<strong>for</strong>ce that can<br />
turn on a dime. Healthcare is not<br />
known <strong>for</strong> rapid cycle change<br />
[but] in our fifth year we’re<br />
seeing dramatic changes.”<br />
<strong>The</strong> New St<strong>and</strong>ard 29
Evaluation <strong>of</strong> <strong>and</strong><br />
treatment <strong>for</strong> a rare<br />
birth defect that affects<br />
the brain are available right<br />
in your own backyard at the<br />
Hypothalamic Hamartoma<br />
Center (HHC), part <strong>of</strong><br />
North Shore-LIJ’s Cushing<br />
Neuroscience Institute (CNI).<br />
A hypothalamic<br />
hamartoma is a benign<br />
brain lesion found in the<br />
hypothalamus, a small<br />
but critical area located<br />
deep within the brain that<br />
is responsible <strong>for</strong> many<br />
automatic functions,<br />
including hunger, thirst, body<br />
temperature <strong>and</strong> hormone<br />
regulation. A hypothalamic<br />
hamartoma can cause seizures,<br />
premature puberty <strong>and</strong><br />
progressive deterioration<br />
<strong>of</strong> behavioral <strong>and</strong> cognitive<br />
function.<br />
30 Summer 2012<br />
New Center Takes On<br />
Rare Birth Defect<br />
By Michelle Pipia-Stiles<br />
“Hypothalamic<br />
hamartomas are debilitating,<br />
but the good news is that<br />
surgical removal <strong>of</strong> this birth<br />
defect can result in a normal<br />
or much improved life <strong>for</strong> the<br />
patient,” said neurosurgeon<br />
Harold Rekate, MD, director<br />
<strong>of</strong> CNI’s Hypothalamic<br />
Hamartoma Center. “Although<br />
several treatment options are<br />
available, the plan <strong>of</strong> clinical<br />
care must be strategically<br />
individualized because what<br />
may be appropriate <strong>for</strong><br />
one patient may not be <strong>for</strong><br />
another, depending on the<br />
anatomy <strong>of</strong> the lesion.”<br />
In addition to Dr. Rekate,<br />
the HHC is staffed with a<br />
multidisciplinary team <strong>of</strong><br />
experts. “Since our physicians<br />
<strong>and</strong> specialists are involved in all<br />
treatment plans <strong>and</strong> therapies,<br />
the Hypothalamic Hamartoma<br />
Center is a prime destination<br />
<strong>for</strong> those suffering from this<br />
rare condition,” said Dr. Rekate.<br />
Surgical removal <strong>of</strong><br />
hypothalamic hamartoma<br />
involves working within the<br />
center <strong>of</strong> the brain, while<br />
protecting the many vital<br />
structures that surround<br />
the mass, including all the<br />
arteries that supply the brain.<br />
In most cases, the hamartoma<br />
can be removed using an<br />
endoscope, through a very<br />
small hole in the skull, but<br />
some patients require more<br />
than one approach to remove<br />
the mass completely.<br />
Above: Two-year-old Mathewas<br />
Ephrem, who was successfully<br />
treated by Dr. Harold Rekate at the<br />
Cushing Neuroscience Institute’s<br />
Hypothalamic Hamartoma Center, is<br />
pictured with his grateful parents.
Staying<br />
Quit<br />
By Betty Marton<br />
Anthony DeGeorge <strong>and</strong> Geraldine<br />
Cruz-DeGeorge, both pack-a-day<br />
smokers, tried several times to quit.<br />
But it never stuck, so when they<br />
decided to marry, they realized they<br />
needed a different approach.<br />
“My main concern was that I’d be<br />
craving a cigarette during the wedding<br />
<strong>and</strong> the reception,” said Ms. Cruz-<br />
DeGeorge, a nurse on 6Monti at North<br />
Shore University Hospital. “I didn’t<br />
want that.”<br />
More than a year be<strong>for</strong>e their 2007<br />
wedding, the couple reached out to the<br />
North Shore-LIJ Center <strong>for</strong> Tobacco<br />
Control (CTC) <strong>for</strong> help withdrawing<br />
from cigarettes — the leading<br />
preventable cause <strong>of</strong> death <strong>and</strong> disease<br />
in the world. Based on guidelines from<br />
the Centers <strong>for</strong> Disease Control, the<br />
center’s quit-smoking program <strong>of</strong>fers<br />
employees <strong>and</strong> community members<br />
quitting <strong>and</strong> maintenance strategies<br />
plus individual <strong>and</strong> group support.<br />
Open 24/7, the CTC also educates<br />
healthcare providers throughout the<br />
metro New York region about how to help<br />
their patients.<br />
Approximately 4,000 people —<br />
including 630 employees — have taken<br />
advantage <strong>of</strong> the program’s counseling,<br />
nicotine replacement products <strong>and</strong><br />
medications between 1999 <strong>and</strong> 2010. And<br />
since the health system implemented a<br />
smoking ban on all properties in 2010,<br />
an additional 185 people have taken the<br />
challenge. According to Pat Folan, RN,<br />
director <strong>of</strong> the center, the numbers include<br />
repeat clients, because many people try many<br />
times be<strong>for</strong>e they’re successful.<br />
“We can get almost everyone to quit,”<br />
she explained. “It’s staying quit that’s<br />
difficult, so if one approach doesn’t work,<br />
we try different strategies.”<br />
<strong>The</strong> six-week program focuses on<br />
keeping people com<strong>for</strong>table while they break<br />
the habit. <strong>The</strong> DeGeorges first contacted<br />
the CTC in January 2006 <strong>and</strong> set a stopsmoking<br />
date <strong>of</strong> February 1. Whenever they<br />
felt their commitment waver, they met with<br />
or emailed Ms. Folan <strong>and</strong> other CTC staff<br />
members <strong>for</strong> support.<br />
“<strong>The</strong>y made sure they were always<br />
available <strong>for</strong> whatever we needed,”<br />
said Mr. DeGeorge, communications<br />
supervisor at Center <strong>for</strong> Emergency<br />
Medical Services.<br />
As an added incentive, as part <strong>of</strong> its<br />
health benefits program, North Shore-LIJ<br />
awards employees a $10 per paycheck credit<br />
to lower their health insurance premiums<br />
<strong>for</strong> those who pledge to be tobacco-free.<br />
And the DeGeorges have an additional<br />
incentive: plans to begin a family.<br />
“It’s good to look <strong>for</strong>ward to having<br />
children <strong>and</strong> not to have to worry about<br />
smoking,” Ms. Cruz-DeGeorge said.<br />
Get help kicking the habit at<br />
NorthShoreLIJ.com/stopsmoking or<br />
(516) 466-1980.<br />
Above: With their wedding on the horizon, the<br />
couple decided to get healthier beginning in 2006.<br />
<strong>The</strong> New St<strong>and</strong>ard 31
under the microscope<br />
MANHASSET — Adaptive radiotherapy (ART) can be beneficial<br />
with only one or two applications within a six-week treatment period,<br />
according to findings by researchers led by a senior investigator<br />
at the H<strong>of</strong>stra North Shore-LIJ School <strong>of</strong> Medicine <strong>and</strong> <strong>The</strong> Feinstein<br />
Institute <strong>for</strong> Medical Research. <strong>The</strong> National Cancer Institute<br />
sponsored the first-<strong>of</strong>-its-kind clinical trial, which focused on ART<br />
<strong>for</strong> head <strong>and</strong> neck cancer.<br />
Trial Examines Role<br />
<strong>of</strong> Radiotherapy in<br />
Head/Neck Cancer<br />
Physicians <strong>of</strong>ten use radiotherapy to treat head <strong>and</strong> neck cancer.<br />
A type <strong>of</strong> radiotherapy that is commonly used is intensity-modulated<br />
radiotherapy, or IMRT. IMRT allows physicians to “sculpt” radiation<br />
<strong>and</strong> have it bend around healthy tissue <strong>and</strong> target the tumor so the<br />
radiation adapts to the anatomy <strong>of</strong> each patient. Although IMRT<br />
is a preferred mode <strong>of</strong> cancer treatment, its Achilles heel is that<br />
it is based entirely on computed tomography (CT) or magnetic<br />
resonance imaging (MRI) per<strong>for</strong>med be<strong>for</strong>e a treatment period<br />
begins. Since typical radiation treatment periods <strong>for</strong> head <strong>and</strong> neck<br />
cancer take six to seven weeks, st<strong>and</strong>ard IMRT cannot compensate<br />
<strong>for</strong> common changes that occur in a patient’s body during treatment.<br />
Such changes could include weight loss, tumor shrinkage or gradual<br />
movement <strong>of</strong> normal tissues. By not compensating <strong>for</strong> these<br />
changes, there is increased risk <strong>of</strong><br />
toxicity or even missing the tumor.<br />
For the new trial, investigators<br />
started patients on st<strong>and</strong>ard IMRT.<br />
<strong>The</strong>n, they took CT scans while<br />
patients were lying in the radiation<br />
treatment room each day so they could<br />
monitor changes in tumor <strong>and</strong> normal<br />
tissues during the course <strong>of</strong> treatment<br />
(six weeks). Through computerized<br />
techniques, the investigators “adapted” David Schwartz, MD<br />
32 Summer 2012<br />
By Emily Ng<br />
(thus the name “adaptive radiotherapy”) according to significant<br />
tumor or body changes.<br />
“ART keeps radiation treatment tightly fitted to a patient’s body,<br />
almost as if it were being shrink-wrapped,” noted David Schwartz,<br />
MD, vice chair <strong>of</strong> radiation medicine at the North Shore-LIJ<br />
Health System <strong>and</strong> a senior investigator at the Feinstein. “It is as<br />
individualized as our current treatment can realistically be.”<br />
“What was most encouraging about the trial findings was that<br />
ART appears effective with only one or two additional replans. This<br />
means that ART does not have to be overly burdensome or expensive<br />
to make a difference. This is something that is feasible, <strong>and</strong> could<br />
eventually make a real-world difference in many clinics.”<br />
<strong>The</strong> findings <strong>of</strong> this trial were recently released online in<br />
advance <strong>of</strong> publication in the International Journal <strong>of</strong> Radiation Oncology<br />
*Biology* Physics.<br />
Above: Intensity-modulated radiotherapy, or IMRT, allows physicians to<br />
“sculpt” radiation <strong>and</strong> have it bend around healthy tissues <strong>and</strong> target a tumor.
MANHASSET — Two<br />
researchers at <strong>The</strong> Feinstein<br />
Institute <strong>for</strong> Medical Research<br />
have received novel research<br />
grants from the Lupus<br />
Research Institute (LRI) to<br />
study potential diagnostic <strong>and</strong><br />
therapeutic options <strong>for</strong> lupus<br />
<strong>and</strong> why the disease turns the<br />
body’s immune system against<br />
itself. A total <strong>of</strong> $3.6 million<br />
was committed to the novel<br />
research program by LRI.<br />
Meggan Mackay, MD, <strong>and</strong><br />
Thomas Rothstein, MD, PhD,<br />
received the grants.<br />
Dr. Mackay <strong>and</strong> her<br />
Feinstein colleagues will use<br />
brain imaging to investigate<br />
the relationship between<br />
certain autoantibodies<br />
(proteins made by the immune<br />
system that are directed against<br />
one or more <strong>of</strong> the individual’s<br />
own proteins) <strong>and</strong> brain<br />
dysfunction in lupus patients.<br />
Previous research in mice has<br />
shown that antibodies directed<br />
against the NMDA receptor in<br />
the brain alter the function <strong>of</strong><br />
brain cells, causing memory<br />
<strong>and</strong> behavioral problems.<br />
<strong>The</strong>y will use a new<br />
radiochemical tracer that<br />
binds to NMDA receptors in<br />
the brain so they can visualize<br />
receptor activity <strong>of</strong> lupus<br />
patients with <strong>and</strong> without the<br />
autoantibodies. If successful,<br />
the technology will be<br />
developed as a new method to<br />
evaluate brain involvement in<br />
lupus. <strong>The</strong> technology might<br />
also help monitor a patient’s<br />
response to treatment <strong>for</strong><br />
brain disease.<br />
Dr. Rothstein will study<br />
B1 cells. B1 cells are a small<br />
subpopulation <strong>of</strong> B cells,<br />
which are responsible <strong>for</strong><br />
producing natural antibodies<br />
that protect against infection<br />
<strong>and</strong> help dispose <strong>of</strong> cellular<br />
debris. Dr. Rothstein <strong>and</strong> his<br />
team were the first to identify<br />
B1 cells in humans, <strong>and</strong> they<br />
will continue to study whether<br />
B1 cells produce harmful<br />
autoantibodies in lupus. If<br />
B1 cells do produce harmful<br />
autoantibodies, Dr. Rothstein<br />
will explore if therapies could<br />
be developed that target B1<br />
cells without damaging healthy<br />
B cells, which are needed to<br />
respond to vaccination <strong>and</strong><br />
defend against many microbial<br />
pathogens (various species <strong>of</strong><br />
bacteria, viruses <strong>and</strong> protozoa).<br />
Meggan Mackay, MD, <strong>and</strong> Thomas Rothstein, MD, PhD<br />
Lupus Grant <strong>for</strong><br />
Feinstein Researchers<br />
By Emily Ng<br />
An Invitation to Participate in Discovery<br />
<strong>The</strong> Feinstein Institute <strong>for</strong> Medical Research’s new Recruitment Registry matches people who want to<br />
participate in clinical research with North Shore-LIJ researchers. Volunteers <strong>of</strong> any age, race, ethnicity or health<br />
status (including North Shore-LIJ staff) are invited. Participation ranges from<br />
a survey that you can do at home to a clinical trial that may<br />
involve a treatment on-site.<br />
One example <strong>of</strong> a current clinical trial is<br />
the Genotype <strong>and</strong> Phenotype (GaP) Research<br />
Registry Program. <strong>The</strong> GaP Registry allows<br />
scientists to study healthy individuals <strong>and</strong><br />
learn about the role <strong>of</strong> genes (or DNA) in<br />
many different illnesses. More than 4,000<br />
volunteers have enrolled; the long-term goal<br />
is to enroll 20,000 volunteers.<br />
Learn about promoting a healthier future by<br />
calling 1-877-GO-NSLIJ (1-877-466-7545) or visiting<br />
FeinsteinInstitute.org/Feinstein/Recruitment+Registry.<br />
<strong>The</strong> New St<strong>and</strong>ard 33
under the microscope<br />
Ovarian cancer patients’ blood samples can help<br />
determine their best treatment plan, according to a<br />
new discovery by researchers <strong>and</strong> physicians from the<br />
North Shore-LIJ Health System <strong>and</strong> <strong>The</strong> Feinstein<br />
Institute <strong>for</strong> Medical Research. More specifically, a genetic marker<br />
embedded in deoxyribonucleic acid (DNA), called microRNA,<br />
indicates whether an ovarian tumor is benign or malignant, <strong>and</strong><br />
whether the patient will benefit from chemotherapy after surgical<br />
removal <strong>of</strong> the tumor.<br />
<strong>The</strong>re will be approximately 22,280 new cases <strong>and</strong> 15,500<br />
deaths from ovarian cancer in the United States this year. Due to<br />
lack <strong>of</strong> adequate screening, the majority <strong>of</strong> patients with ovarian<br />
cancer are diagnosed at Stage III (the second-to-last <strong>and</strong> most<br />
devastating stage <strong>of</strong> cancer), when 70 percent <strong>of</strong> these patients will<br />
die within 5 years.<br />
“<strong>The</strong> discovery that microRNAs can help assess the best<br />
treatment plan <strong>for</strong> women with ovarian cancer — who are most<br />
likely at Stage III <strong>of</strong> the disease — <strong>of</strong>fers them enormous hope,” said<br />
Iuliana Shapira, MD, director <strong>of</strong> the Cancer Genetics Program at<br />
the Monter Cancer Center. “We can now in<strong>for</strong>m Stage III patients<br />
whether they will have success with chemotherapy following<br />
surgery, similar to patients who are at Stage I. This in<strong>for</strong>mation<br />
gives them hope that the disease is curable, despite being diagnosed<br />
at an ‘advanced stage.’ It also gives them the strength necessary to<br />
undergo chemotherapy.”<br />
Several microRNAs have been found to have links with various<br />
types <strong>of</strong> cancer. Researchers at the North Shore-LIJ Health System<br />
<strong>and</strong> <strong>The</strong> Feinstein Institute <strong>for</strong> Medical<br />
Research found that microRNA-195<br />
increased 40-fold during chemotherapy<br />
<strong>and</strong> microRNA-16 increased 80-fold<br />
during chemotherapy. <strong>The</strong>se changes may<br />
explain why some women experience side<br />
effects from ovarian cancer chemotherapy,<br />
others are cured by chemotherapy <strong>and</strong><br />
others need ongoing chemotherapy to<br />
continue living with the cancer.<br />
34 Summer 2012<br />
Discovery<br />
Helps Assess<br />
Best Treatment<br />
<strong>for</strong> Ovarian Cancer<br />
Patients<br />
By Emily Ng<br />
Iuliana Shapira, MD Annette Lee, PhD<br />
“Underst<strong>and</strong>ing the changes in microRNA throughout<br />
chemotherapy helps us better underst<strong>and</strong> ovarian cancer <strong>and</strong><br />
how best to treat patients with this disease,” said Annette Lee,<br />
PhD, associate investigator at the Feinstein. “<strong>The</strong> genetic markers<br />
we identified allow patients to individualize their own therapy<br />
in order to get maximum benefit <strong>and</strong> minimal side effects. In<br />
addition, this knowledge will help<br />
researchers develop new ovarian<br />
cancer treatments.”<br />
Dr. Shapira added, “We<br />
applied <strong>for</strong> a government grant <strong>and</strong><br />
hope to receive the funds needed to<br />
validate these markers that result in<br />
women receiving therapies that are<br />
more personalized <strong>and</strong> match their<br />
genetic makeup.”<br />
Thinkstock
Morbid Obesity Deters Potential Kidney Donors<br />
Morbidly obese patients<br />
are generally excluded as organ<br />
donors given their increased<br />
risk <strong>for</strong> complications during<br />
surgery <strong>and</strong> the development<br />
<strong>of</strong> chronic conditions linked<br />
to obesity (e.g., type 2<br />
diabetes, heart disease, etc.).<br />
Researchers at the H<strong>of</strong>stra<br />
North Shore-LIJ School <strong>of</strong><br />
Medicine <strong>and</strong> <strong>The</strong> Feinstein<br />
Institute <strong>for</strong> Medical Research<br />
conducted a retrospective<br />
analysis that found that <strong>of</strong> 104<br />
potential living kidney donors,<br />
Cushing<br />
Neuroscience<br />
Institute<br />
Microsite News<br />
<strong>The</strong> Cushing Neuroscience<br />
Institute (CNI) recently launched<br />
their new microsite, neurocni.<br />
com. <strong>The</strong> comprehensive site<br />
showcases the breadth <strong>of</strong> services<br />
<strong>of</strong>fered at CNI <strong>and</strong> features expert<br />
physicians <strong>and</strong> state-<strong>of</strong>-the-art<br />
technology. <strong>The</strong> new Web site<br />
has been designed to be more<br />
user friendly <strong>and</strong> interactive,<br />
<strong>and</strong> will grow <strong>and</strong> thrive with<br />
fresh, updated content, rotating<br />
banners <strong>and</strong> active links. Users<br />
have access to in<strong>for</strong>mation they<br />
need to make finding the right<br />
service, physician <strong>and</strong> location<br />
easier. <strong>The</strong>y will also be able to<br />
check out the latest news <strong>and</strong><br />
patient success stories, which will<br />
continually be updated.<br />
Visit neurocni.com today!<br />
23 (22 percent) were classified<br />
as morbidly obese, only three<br />
(13 percent) <strong>of</strong> whom were<br />
able to successfully lose weight<br />
<strong>and</strong> donate their kidney.<br />
According to Mala Sachdeva,<br />
MD, assistant pr<strong>of</strong>essor <strong>of</strong><br />
medicine at the H<strong>of</strong>stra North<br />
Shore-LIJ School <strong>of</strong> Medicine<br />
<strong>and</strong> the lead investigator, “As<br />
a next step, we must conduct<br />
larger studies that assess how<br />
vast a problem this is on a<br />
national level <strong>and</strong> how best to<br />
exp<strong>and</strong> our living donor pool<br />
<strong>for</strong> kidney transplantation.<br />
Perhaps potential donors who<br />
are excluded from donation<br />
due to their high BMI should<br />
participate in more stringent<br />
weight loss programs, check<br />
in much more regularly at<br />
their transplant center <strong>for</strong><br />
follow-ups <strong>and</strong> even join social<br />
support groups as a means <strong>of</strong><br />
motivation.” Dr. Sachdeva<br />
presented this data at the<br />
National Kidney Foundation<br />
(NKF) 2012 Spring Clinical<br />
Meetings.<br />
Mala Sachdeva, MD<br />
Science Camp Discounted 20 Percent<br />
LAKE SUCCESS — Children <strong>of</strong> North Shore-LIJ employees can get a 20 percent discount on summer science camp at the<br />
DNA Learning Center (DNALC) West. Kids entering sixth through 12th grades are eligible <strong>for</strong> the week-long camps at 5<br />
Delaware Drive, Suite 5, in the Lake Success Quadrangle.<br />
Camps include Fun with DNA (entering grade 6 or 7); World <strong>of</strong> Enzymes (entering grade 8 or Fun with DNA alumni<br />
entering grade 7); Forensic Detectives (entering grade 9 or World <strong>of</strong> Enzymes alumni entering grade 8); Green Genes<br />
(entering grade 9 or World <strong>of</strong> Enzymes alumni entering grade 8); Barcoding Biodiversity (Green Genes alumni); DNA<br />
Science (entering grades 10–12); Silencing Genomes (DNA Science alumni entering grades 10-12); Human Genomics<br />
(DNA Science alumni entering grade 11 or 12); <strong>and</strong> Plant Genomics (DNA Science alumni entering grade 11 or 12).<br />
Over the last decade, more than 28,000 students have attended DNALC West, with participants taking lab field<br />
trips including a tour <strong>of</strong> North Shore-LIJ’s Core Laboratory. <strong>The</strong> Core Lab/DNA Learning Center West partnership<br />
is designed to spark an early interest in<br />
medicine, expose students to healthcare<br />
careers, <strong>of</strong>fer career guidance, allow students<br />
to experience a laboratory environment <strong>and</strong><br />
learn from healthcare pr<strong>of</strong>essionals, according<br />
to Bob Stallone, vice president <strong>of</strong> laboratories<br />
<strong>for</strong> North Shore-LIJ.<br />
H<strong>and</strong>s-on experiences at DNALC West are<br />
supplemented by online resources at dnalc.<br />
org <strong>and</strong> the Gene Screen app, while a DNALC<br />
West internship gives students experience in<br />
molecular biology techniques by assisting in lab<br />
routines. Learn more at summercamps.dnalc.<br />
org; details about the staff discount at DNALC<br />
West appear under FAQ.<br />
<strong>The</strong> New St<strong>and</strong>ard 35
physician’s rounds<br />
Dolan Center Trains Residents<br />
from Glen Cove Family Practice<br />
By <strong>The</strong>resa Jacobellis<br />
HUNTINGTON — Pediatricians at<br />
Huntington Hospital’s Dolan Family<br />
Health Center are passing the flame<br />
<strong>of</strong> knowledge on to future physicians<br />
through a unique collaboration with Glen<br />
Cove Hospital’s Family Practice Program.<br />
Under the arrangement, second- <strong>and</strong><br />
third-year family practice residents,<br />
physicians who are undergoing<br />
post-graduate training, will spend<br />
two years rotating through the<br />
Dolan Center to gain experience<br />
in pediatric medicine.<br />
Family practitioners take care<br />
<strong>of</strong> patients <strong>of</strong> all ages, from infancy<br />
through geriatrics. While residents<br />
in Glen Cove’s Family Practice<br />
Program get first-h<strong>and</strong> experience<br />
in caring <strong>for</strong> adults, the number <strong>of</strong><br />
children treated there has declined<br />
over the years.<br />
“At Dolan, we take care <strong>of</strong> a<br />
large <strong>and</strong> diverse group <strong>of</strong> pediatric<br />
patients,” said William Gehrhardt,<br />
MD, pediatrician <strong>and</strong> medical<br />
director <strong>of</strong> the Dolan Center.<br />
“We are partnering with the<br />
Dolan Family Health Center because<br />
it is an exceptional outpatient<br />
facility with very capable staff <strong>and</strong><br />
physicians <strong>and</strong> a wonderfully diverse<br />
demographic mix <strong>of</strong> patients,” said<br />
William Bennett, MD, director<br />
<strong>of</strong> Glen Cove Hospital’s Family<br />
Practice Program. “This partnership<br />
is a tribute to the excellence <strong>of</strong> the<br />
Dolan facility.”<br />
Under the arrangement, a<br />
group <strong>of</strong> 10 to 12 residents spends<br />
half a day at the Dolan Center,<br />
working side-by-side with either<br />
Dr. Gehrhardt or pediatrician<br />
36 Summer 2012<br />
Roberto Bl<strong>and</strong>o, MD. Residents<br />
participate in taking patient histories,<br />
checking vital signs <strong>and</strong> making diagnoses<br />
as well as treatment recommendations.<br />
Eventually, they will learn to use the Dolan<br />
Center’s electronic medical record (EMR).<br />
<strong>The</strong> relatively new arrangement<br />
already shows signs <strong>of</strong> success, according<br />
What’s Up, Doc?<br />
Doctoring is North Shore-LIJ’s new physician-centric<br />
communications piece. Available <strong>for</strong> free as a print publication,<br />
monthly e-newsletter <strong>and</strong> interactive app, it furnishes intriguing<br />
content about the science <strong>and</strong> art <strong>of</strong> practicing medicine.<br />
Visit DoctoringMag.com to learn more.<br />
to Dr. Gehrhardt. “We have observed the<br />
residents to be a highly qualified, diligent,<br />
really good group <strong>of</strong> people,” he said.<br />
In the past, the center has been<br />
involved with training pediatric residents<br />
<strong>and</strong> nurse practitioners. H<strong>of</strong>stra North<br />
Shore-LIJ School <strong>of</strong> Medicine students<br />
will also participate in educational<br />
experiences at Dolan.<br />
Dr. Gehrhardt is<br />
proud <strong>of</strong> the contributions<br />
that the Dolan Center is<br />
making, ensuring that future<br />
generations <strong>of</strong> physicians are<br />
well-trained <strong>and</strong> prepared.<br />
“It is an honor to be asked to<br />
do this,” he said. “Teaching<br />
others is an indication <strong>of</strong><br />
excellence, <strong>and</strong> the presence<br />
<strong>of</strong> these residents enhances<br />
the care <strong>and</strong> education that<br />
we are able to provide to our<br />
patients.”<br />
Right: Glen Cove Hospital family<br />
practice resident Kapeel Kumar,<br />
MD, left, <strong>and</strong> Dolan Family Health<br />
Center pediatrician Roberto<br />
Bl<strong>and</strong>o, MD, examine six-monthold<br />
Stephenie Rivera Ochoa.<br />
Correction<br />
In the spring issue <strong>of</strong> <strong>The</strong> New<br />
St<strong>and</strong>ard, Ron Israeli, MD, was<br />
shown in a photo with his wife,<br />
Nancy Lippman-Israeli, MD, who<br />
was incorrectly identified as a<br />
patient.
<strong>The</strong> New St<strong>and</strong>ard<br />
37
physician’s rounds<br />
NASA Advisory Board Taps Harold Rekate, MD<br />
By Michelle Pipia-Stiles<br />
When the National Aeronautics<br />
<strong>and</strong> Space Administration<br />
(NASA) sought medical<br />
insight on how to protect astronauts’<br />
vision, they knew where to turn.<br />
Harold Rekate, MD, director <strong>of</strong><br />
the Chiari Institute at North Shore<br />
University Hospital, world-renowned<br />
<strong>for</strong> his research over the past 30 years<br />
relating to the causes <strong>and</strong> treatment<br />
<strong>of</strong> raised intracranial pressure,<br />
recently joined the agency’s advisory<br />
board <strong>for</strong> the Visual Impairment<br />
Intracranial Pressure (VIIP) Program.<br />
<strong>The</strong> program analyzes the<br />
physiological <strong>and</strong> anatomical changes<br />
in astronauts who participate in<br />
long-duration space missions, where<br />
intracranial pressure may cause<br />
long-term visual impairment. A study<br />
sponsored by NASA found that space<br />
flights lasting six months or more<br />
can cause a spectrum <strong>of</strong> changes in<br />
astronauts’ visual systems, including<br />
blurry vision <strong>and</strong> excess fluid around<br />
the optic nerve.<br />
CME Conferences<br />
<strong>The</strong> North Shore-LIJ Office <strong>of</strong> Continuing Medical Education has a full slate <strong>of</strong> continuing medical education (CME) conferences on tap this year.<br />
Sept<br />
Oct<br />
Nov<br />
38 Summer 2012<br />
“Be<strong>for</strong>e astronauts<br />
embark on space missions,<br />
we need to determine who<br />
is at risk <strong>of</strong> developing<br />
intracranial hypertension.<br />
When they return, we need<br />
to determine who has<br />
suffered visual impairment<br />
as a result <strong>of</strong> ICP <strong>and</strong><br />
decide how to best treat<br />
astronauts to prevent these<br />
problems,” said Dr. Rekate.<br />
“Intracranial hypertension<br />
can be measured with a<br />
spinal tap where a needle is<br />
inserted into the spinal canal<br />
in the lower part <strong>of</strong> the back<br />
to measure cerebrospinal<br />
fluid surrounding the brain<br />
<strong>and</strong> spinal cord. <strong>The</strong> advisory<br />
board is looking into other kinds<br />
<strong>of</strong> treatment that are less invasive,<br />
such as an ultrasound. <strong>The</strong> advisory<br />
board will first need to determine if<br />
the raised intracranial pressure is a<br />
result <strong>of</strong> an eye or brain problem.”<br />
21 Melanoma Conference H<strong>of</strong>stra North Shore-LIJ School <strong>of</strong> Medicine<br />
24 Current Topics in Pediatric <strong>and</strong> Adolescent Gynecology North Shore University Hospital<br />
2 Urology <strong>and</strong> Urogynecology Conference Feinstein Institute <strong>for</strong> Medical Research<br />
3 Wound Care Conference Long Isl<strong>and</strong> Marriott<br />
Infection-control training is available online any time at NorthShoreLIJ.edu/ict.<br />
In coming months, the VIIP<br />
advisory board will meet to enact<br />
protocols so astronauts can be<br />
screened be<strong>for</strong>e a space mission; to<br />
determine what astronauts can do to<br />
relieve ICP while in space; <strong>and</strong> upon<br />
their return, to measure ICP levels<br />
immediately <strong>and</strong> treat those with<br />
elevated levels.<br />
Above: Dr. Rekate exits the space<br />
shuttle astronaut training facility at<br />
NASA’s Johnson Space Center.<br />
Conference in<strong>for</strong>mation is updated weekly. To learn more, visit NorthShoreLIJ.edu/cme or call 516-465-3CME (516-465-3263). <strong>The</strong> North Shore-LIJ Health System<br />
is accredited by the Accreditation Council <strong>for</strong> Continuing Medical Education to provide continuing medical education <strong>for</strong> physicians.<br />
NASA
It’s in His Bones:<br />
Orthopedic Surgeon<br />
Pays It Forward<br />
By Margarita Oksenkrug<br />
Leon E. Popovitz, MD, orthopedic surgeon <strong>and</strong> sports<br />
medicine specialist at Lenox Hill Hospital, recently created the<br />
Efim <strong>and</strong> Mila Popovitz Scholarship <strong>for</strong> Exceptional Character at<br />
the Sophie Davis School <strong>of</strong> Biomedical Education, his alma mater.<br />
<strong>The</strong> scholarship, named in honor <strong>of</strong> Dr. Popovitz’s parents, will<br />
be <strong>of</strong>fered to one deserving student annually over the next five<br />
years. Each winner, who will be chosen based on exemplary moral<br />
character, will receive a $20,000 gift toward his or her medical<br />
education. “I stress the importance <strong>of</strong> ‘exceptional character’ in<br />
the scholarship because when it comes down to it, no matter our<br />
intelligence or accomplishments, it is our character that is the<br />
measure <strong>of</strong> what kind <strong>of</strong> people we are,” explained Dr. Popovitz.<br />
“That is particularly true <strong>of</strong> doctors.”<br />
Founded at City College in 1973, the Sophie Davis School <strong>of</strong><br />
Biomedical Education is far from a typical medical university. Its<br />
socially, economically <strong>and</strong> ethnically diverse base <strong>of</strong> students is<br />
recruited right out <strong>of</strong> high school; the students are committed to<br />
Residents <strong>and</strong> Fellows Plan<br />
More Community Involvement<br />
A relatively<br />
new initiative<br />
by the North<br />
Shore-LIJ Residents<br />
<strong>and</strong> Fellows Forum strives to<br />
increase staff involvement in<br />
volunteer <strong>and</strong> community<br />
services activities.<br />
<strong>The</strong> original mission <strong>of</strong> the<br />
Residents <strong>and</strong> Fellows Forum<br />
was to serve as a liaison with administration<br />
<strong>and</strong> hospital staff<br />
to address <strong>and</strong> resolve matters<br />
within North Shore-LIJ. But<br />
over the past several years, the<br />
mission has evolved to include<br />
a more patient-centered focus<br />
both within hospitals <strong>and</strong> now,<br />
the community.<br />
Since the North Shore-<br />
LIJ Health System already<br />
had strong community<br />
service involvement, several<br />
residents <strong>and</strong> fellows seized<br />
the opportunity to spearhead a<br />
program at CitiField. During<br />
the 2012 baseball season,<br />
members are spending time at<br />
the Health In<strong>for</strong>mation Team<br />
pursuing a career in medicine from a very young age. One <strong>of</strong> the<br />
school’s core principles, according to Dr. Popovitz, is ensuring<br />
that its alumni give back to communities that are underprivileged<br />
<strong>and</strong> underserved, similar to the ones they themselves have come<br />
from. That concept struck a resonant chord with the doctor,<br />
who immigrated to the US from the Soviet Union as a young<br />
boy <strong>and</strong> recalls that the first few years here were “arduous <strong>and</strong><br />
impoverished times,” as his parents struggled to create a better<br />
life <strong>for</strong> him <strong>and</strong> his brother.<br />
Inspired by the unwavering support, confidence <strong>and</strong><br />
encouragement from his parents to pursue his American dream,<br />
Dr. Popovitz created the scholarship to help a new generation<br />
<strong>of</strong> aspiring physicians turn their own fantasies into real<br />
success stories. “I established this scholarship because it is my<br />
responsibility as an alumnus<br />
to give support to those special<br />
people who are devoted to<br />
making somebody’s life better,”<br />
remarked Dr. Popovitz in the<br />
speech he made at the school’s<br />
recent white coat ceremony<br />
in which he announced the<br />
inception <strong>of</strong> the scholarship.<br />
<strong>The</strong> first recipient <strong>of</strong> the Efim<br />
<strong>and</strong> Mila Popovitz Scholarship<br />
<strong>for</strong> Exceptional Character will<br />
be selected this summer.<br />
Leon Popovitz, MD<br />
(HIT) booth sponsored by<br />
the North Shore-LIJ Health<br />
System <strong>and</strong> the Katz Institute<br />
<strong>for</strong> Women’s Health. Residents<br />
<strong>and</strong> fellows educate fans about<br />
health <strong>and</strong> wellness issues <strong>and</strong><br />
solutions be<strong>for</strong>e <strong>and</strong> during<br />
the game.<br />
What does the future<br />
hold <strong>for</strong> the health system’s<br />
residents <strong>and</strong> fellows? During<br />
the next year, the plan is to<br />
focus on undergraduate <strong>and</strong><br />
medical student mentorship<br />
programs, health literacy<br />
seminars in the community<br />
<strong>and</strong> child safety initiatives.<br />
Through these opportunities,<br />
the leadership <strong>of</strong> the Residents<br />
<strong>and</strong> Fellows Forum believes<br />
that together, the residents,<br />
fellows <strong>and</strong> the healthcare<br />
system can have a measurable<br />
impact on the community <strong>for</strong><br />
many years to come.<br />
<strong>The</strong> New St<strong>and</strong>ard 39
physician’s rounds<br />
North Shore University Hospital’s Palliative Care Program<br />
Receives Advanced Certification Status from the Joint Commission<br />
MANHASSET — <strong>The</strong> Palliative Care Program at North Shore University Hospital<br />
(NSUH) was recently awarded advanced certification status by the Joint<br />
Commission, which accredits <strong>and</strong> certifies more than 19,000 healthcare<br />
organizations <strong>and</strong> programs in the United States. NSUH is one <strong>of</strong> only six<br />
hospitals in the country to receive this honor from the Joint Commission, which<br />
signifies that NSUH has achieved a national level <strong>of</strong> excellence in patient- <strong>and</strong><br />
family-centered care.<br />
Palliative care is defined as specialized medical care <strong>for</strong> people with<br />
advanced illness. This type <strong>of</strong> care is focused on providing patients with relief<br />
from the symptoms, pain <strong>and</strong> stress <strong>of</strong> their disease. North Shore University<br />
Hospital has a dedicated 10-bed Palliative Care Unit, where care is provided by a<br />
team <strong>of</strong> doctors, nurses <strong>and</strong> other specialists who work with the patient’s team <strong>of</strong><br />
healthcare providers to produce an extra layer <strong>of</strong> support.<br />
“This national distinction was achieved through the visionary leadership <strong>of</strong><br />
Michael Dowling, the support <strong>of</strong> our hospital leaders <strong>and</strong> the specialized palliative<br />
Charles Schleien, MD, Appointed<br />
Chair <strong>of</strong> Pediatrics at CCMC<br />
Charles Schleien, MD, MBA, is the<br />
new chair <strong>of</strong> pediatrics at the Steven <strong>and</strong><br />
Alex<strong>and</strong>ra Cohen Children’s Medical<br />
Center <strong>of</strong> New York.<br />
Dr. Schleien was executive<br />
vice chairman in the<br />
Department <strong>of</strong> Pediatrics at the<br />
Columbia University College<br />
<strong>of</strong> Physicians & Surgeons,<br />
<strong>and</strong> pr<strong>of</strong>essor <strong>of</strong> pediatrics<br />
<strong>and</strong> anesthesiology at New York<br />
Presbyterian Hospital. He is past<br />
director <strong>of</strong> the Division <strong>of</strong> Pediatric<br />
Critical Care Medicine, which he founded<br />
upon his arrival at Columbia in 1999, <strong>and</strong><br />
served as medical director <strong>of</strong> the Pediatric<br />
Intensive Care Unit at the Morgan<br />
Stanley Children’s Hospital <strong>of</strong> Columbia<br />
University.<br />
Dr. Schleien previously served<br />
as director <strong>and</strong> fellowship director—<br />
40 Summer 2012<br />
pediatric critical care medicine in the<br />
Department <strong>of</strong> Pediatrics at the University<br />
<strong>of</strong> Miami/Jackson Memorial Medical<br />
Center; <strong>and</strong> pr<strong>of</strong>essor <strong>of</strong> pediatrics<br />
<strong>and</strong> anesthesiology at the<br />
University <strong>of</strong> Miami School <strong>of</strong><br />
Medicine.<br />
Dr. Schleien received<br />
a bachelor’s degree from<br />
the City University <strong>of</strong> New<br />
York’s (CUNY) Queens<br />
College <strong>and</strong> his medical degree<br />
from the Mount Sinai School <strong>of</strong><br />
Medicine. He completed a pediatric<br />
residency at Texas Children’s Hospital,<br />
Baylor University Affiliated Hospitals,<br />
Houston; an anesthesia residency at the<br />
Johns Hopkins Hospital, Baltimore; <strong>and</strong><br />
a fellowship in pediatric critical care<br />
medicine at the Johns Hopkins Hospital.<br />
care team who are committed to improving care <strong>for</strong> patients with serious illness<br />
<strong>and</strong> their families,” said Dana Lustbader, MD, section head <strong>of</strong> palliative medicine.<br />
“Our primary goal is to align treatments with patient preferences while relieving<br />
suffering. Research shows that patients with advanced illness who get palliative<br />
care live longer. Palliative care is appropriate at any age <strong>and</strong> at any stage in a<br />
serious illness, <strong>and</strong> can be provided together with curative treatment.”<br />
Jeremy Boal, MD, North Shore-LIJ’s chief medical <strong>of</strong>ficer, said education<br />
<strong>and</strong> improved communication are critical components in successful palliative<br />
care programs. “We need to underst<strong>and</strong> our patients’ preferences <strong>for</strong> care so that<br />
we can build the best approach to meeting those preferences <strong>and</strong> goals,” said<br />
Dr. Boal. “Many patients with advanced illness would choose care focused on<br />
maintaining com<strong>for</strong>t <strong>and</strong> dignity over more aggressive <strong>for</strong>ms <strong>of</strong> care if they were<br />
well in<strong>for</strong>med <strong>of</strong> the benefits <strong>and</strong> burdens <strong>of</strong> such care. Others would choose more<br />
aggressive care. In either case, our responsibility is to underst<strong>and</strong> their needs<br />
<strong>and</strong> goals <strong>and</strong> to meet them.”<br />
2011-2012<br />
Feinstein Report<br />
<strong>The</strong> recently published 2011-2012<br />
Annual Report <strong>of</strong> the North Shore-LIJ Health<br />
System’s Feinstein Institute <strong>for</strong> Medical<br />
Research provides an overview <strong>of</strong> how the<br />
Feinstein Institute succeeds at creating <strong>and</strong><br />
disseminating new knowledge, achieving<br />
medical advances, providing service to our<br />
community <strong>and</strong> beyond <strong>and</strong> constantly<br />
striving to cure disease by studying disease.<br />
See it at http://www.northshorelij.com/<br />
NSLIJ/NSLIJ+Annual+Reports.
New York Head <strong>and</strong> Neck Institute<br />
Names Ian Storper, MD, Director <strong>of</strong> Otology<br />
Ian S. Storper, MD, has been<br />
appointed director <strong>of</strong> the Otology Program<br />
<strong>for</strong> the New York Head <strong>and</strong> Neck Institute<br />
at Lenox Hill Hospital. He comes to Lenox<br />
Hill from Columbia University College<br />
<strong>of</strong> Physicians <strong>and</strong> Surgeons where he was<br />
director <strong>of</strong> neurotology. Dr. Storper,<br />
an internationally recognized otologist/<br />
neurotologist who specializes in the<br />
medical <strong>and</strong> surgical treatment <strong>of</strong> ear<br />
disease, has a special interest in hearing<br />
restoration surgery, including cochlear<br />
implant, stapedectomy <strong>and</strong> ossicular<br />
reconstruction. He has contributed<br />
innovative surgical techniques to the<br />
field in the areas <strong>of</strong> laser stapes surgery,<br />
implantable hearing aids <strong>and</strong> surgery<br />
<strong>for</strong> Meniere’s disease, cholesteatoma,<br />
tympanoplasty <strong>and</strong> mastoidectomy. Dr.<br />
Storper received his medical degree in<br />
1988 from the University <strong>of</strong> Pennsylvania.<br />
<strong>The</strong> North Shore-LIJ Department <strong>of</strong><br />
Medicine, in conjunction with the Krasn<strong>of</strong>f<br />
Quality Management Institute <strong>of</strong> the North<br />
Shore-LIJ Health System, has appointed<br />
Maria Torroella Carney, MD,<br />
to the position <strong>of</strong> director <strong>of</strong><br />
community-based geriatrics<br />
<strong>for</strong> the North Shore-LIJ<br />
Health System.<br />
Dr. Carney is also<br />
an assistant pr<strong>of</strong>essor <strong>of</strong><br />
medicine at the H<strong>of</strong>stra<br />
North Shore-LIJ School <strong>of</strong><br />
Medicine. Her primary role<br />
in the Department <strong>of</strong> Medicine is<br />
He completed both an internship in<br />
general surgery in 1990 <strong>and</strong> a residency<br />
in head <strong>and</strong> neck surgery in 1994 at<br />
UCLA Medical Center <strong>and</strong> fellowships<br />
in neuroscience in 1992 at UCLA School<br />
<strong>of</strong> Medicine <strong>and</strong> in otology/neurotology<br />
in 1995 at the Otology Group/<strong>The</strong> EAR<br />
Foundation in Nashville, TN. Dr. Storper<br />
received the Maxwell Abramson Teaching<br />
Award from Columbia University <strong>and</strong> the<br />
Malcolm Schvey Teaching Award from<br />
its Department <strong>of</strong> Otolaryngology/ Head<br />
<strong>and</strong> Neck Surgery <strong>and</strong> has instructed<br />
CME-accredited courses. He is the<br />
author <strong>of</strong> numerous book chapters <strong>and</strong><br />
publications in peer-reviewed journals,<br />
lectures frequently <strong>and</strong> is a fellow in the<br />
American Academy <strong>of</strong> Otolaryngology,<br />
the American College <strong>of</strong> Surgeons <strong>and</strong> the<br />
American Neurotology Society. He was<br />
senior investigator in studies on the use<br />
Maria Carney, MD, Former Nassau County<br />
Commissioner <strong>of</strong> Health, Joins North Shore-LIJ<br />
to work in partnership with the Krasn<strong>of</strong>f<br />
Quality Management Institute to utilize,<br />
assess <strong>and</strong> evaluate health system data to<br />
effect program change. She will assist in<br />
expansion <strong>of</strong> academics, research <strong>and</strong><br />
clinical outcome studies to improve<br />
education opportunities <strong>for</strong> medical<br />
students, residents <strong>and</strong> fellows in<br />
medical training.<br />
Dr. Carney received her MD<br />
at New York Medical College, <strong>and</strong><br />
carried out her residency training<br />
in internal medicine at New York<br />
Presbyterian Hospital - Weill/Cornell<br />
Medical Center. She went on to complete<br />
Ian Storper, MD<br />
<strong>of</strong> steroids <strong>and</strong> antivirals in the treatment<br />
<strong>of</strong> sudden hearing loss <strong>and</strong> in the use<br />
<strong>of</strong> glycopyrrolate in the treatment <strong>of</strong><br />
Meniere’s disease.<br />
a two-year clinical- <strong>and</strong> research-oriented<br />
fellowship in geriatric medicine at the<br />
Mount Sinai School <strong>of</strong> Medicine in New<br />
York City.<br />
Dr. Carney had been commissioner<br />
<strong>for</strong> the Nassau County Department <strong>of</strong><br />
Health, where she effectively addressed<br />
major challenges including the 2010<br />
H1N1 influenza response, <strong>for</strong> which<br />
she received the BOCES (Board <strong>of</strong><br />
Cooperative Education Services) Nassau<br />
County Council <strong>of</strong> Superintendents’<br />
Award, <strong>and</strong> New York State Association<br />
<strong>of</strong> County Health Officials’ Public Health<br />
Pr<strong>of</strong>essional <strong>of</strong> the Year Award.<br />
<strong>The</strong> New St<strong>and</strong>ard 41
hearts <strong>and</strong> h<strong>and</strong>s<br />
One afternoon, Susie Wong left quite<br />
an impression on a woman in the Stroke<br />
Unit at North Shore University Hospital.<br />
<strong>The</strong> patient’s family watched as Ms. Wong<br />
<strong>and</strong> her pet therapy dogs entered the room.<br />
“My very loving dog, Orion, gently<br />
laid his head on her chest <strong>and</strong> looked<br />
deep into her eyes,” Ms. Wong said <strong>of</strong> her<br />
Great Pyrenees, a large <strong>and</strong> fluffy breed<br />
with a gentle <strong>and</strong> caring nature. “It was at<br />
that moment, while Orion’s breath tickled<br />
her cheek, that I picked up her h<strong>and</strong> <strong>and</strong><br />
helped her stroke his head.”<br />
42 Summer 2012<br />
Pet <strong>The</strong>rapy Gives<br />
the Warm Fuzzies<br />
By Susan Kreimer<br />
<strong>The</strong> patient, in her 40s, had been<br />
paralyzed by the stroke, which struck during<br />
a family vacation. But soon, Ms. Wong<br />
recalls, “the attention <strong>of</strong> everyone in the<br />
room was captivated when she started to<br />
twitch her fingers in the h<strong>and</strong> stroking<br />
Orion. She regained eye movement <strong>and</strong><br />
smiled. <strong>The</strong>re wasn’t a dry eye in the room.”<br />
Research has shown that animals’<br />
unconditional love <strong>and</strong> acceptance provide<br />
medical <strong>and</strong> emotional benefits to people<br />
both young <strong>and</strong> old. That’s the rationale<br />
behind the work <strong>of</strong> pet therapy volunteers<br />
like Ms. Wong within the North Shore-LIJ<br />
Health System.<br />
“Our pet therapy visits take place at<br />
bedside or in the playroom, depending<br />
on patients’ needs. <strong>The</strong> dogs are there to<br />
help brighten the patients’ day, to help<br />
them take their minds <strong>of</strong>f their situations,<br />
if only <strong>for</strong> a moment,” said Maura Tully,<br />
pet therapy coordinator in the Child Life<br />
Department at Cohen Children’s Medical<br />
Center (CCMC) <strong>of</strong> New York.<br />
“Patients who were feeling down have<br />
smiled <strong>for</strong> the first time during a visit from<br />
a pet therapy dog,” Ms. Tully added. “I<br />
have had patients say that they <strong>for</strong>got about<br />
their pain while they were visiting with one<br />
<strong>of</strong> the dogs. <strong>The</strong> dogs also help motivate<br />
the patients. Those who wouldn’t get out <strong>of</strong><br />
bed or go to the playroom will do so <strong>for</strong> a<br />
pet therapy visit.”<br />
<strong>The</strong>re are currently six pet therapy dogs
Concierge Smooths Patients’ ED Experience<br />
By Susan Kreimer<br />
VALLEY STREAM — At the end <strong>of</strong> Arlene Veltri’s fourhour<br />
shift, the staff is sad to see her leave.<br />
“When I say I have to go home now, they say,<br />
‘No, not now.’ It’s a very helpful job,” the 81-yearold<br />
volunteer said. <strong>The</strong> time goes by fast. “I’m busy,<br />
but that’s a good thing.”<br />
Ms. Veltri, a retired special education aide,<br />
volunteers in Franklin Hospital’s Emergency Department<br />
Concierge Program, launched in the spring <strong>of</strong><br />
2009. She greets patients <strong>and</strong> directs them where<br />
to sign in.<br />
Concierge volunteers also bring wheelchairs to<br />
patients, help them on <strong>and</strong> <strong>of</strong>f with their coats, call a<br />
taxi afterward <strong>and</strong> give some TLC, said Myra Cohen,<br />
director <strong>of</strong> volunteer services at Franklin Hospital.<br />
“<strong>The</strong> concierges speak with patients <strong>and</strong> provide<br />
needed company,” Ms. Cohen said. “<strong>The</strong>y help<br />
take the anxiety out <strong>of</strong> the emergency room visit.”<br />
in the program at CCMC. Most visit patients<br />
twice a month with their owners, who are<br />
volunteers. <strong>The</strong> participants are a black<br />
Labrador retriever, yellow Lab, Maltese,<br />
Papillon, golden retriever <strong>and</strong> greyhound.<br />
All <strong>of</strong> them were certified by a therapy dog<br />
organization be<strong>for</strong>e consideration <strong>for</strong> the<br />
hospital. Certified dogs also participate in<br />
onsite behavioral screening.<br />
“<strong>The</strong>y must go through a series <strong>of</strong><br />
tests to see how they would react in the<br />
hospital environment,” said Ms. Tully,<br />
who evaluates each c<strong>and</strong>idate. She has also<br />
placed volunteers with pet therapy dogs at<br />
<strong>The</strong> Zucker Hillside Hospital. LIJ Medical<br />
Center <strong>of</strong>fers pet therapy too.<br />
“We test to see how they react to<br />
walkers, wheelchairs, crutches <strong>and</strong> IV<br />
poles,” she said. “We test to see how they<br />
would react to loud noises <strong>and</strong> strange<br />
behavior. We also test to see how they<br />
engage with our pediatric patients.”<br />
If a dog passes the behavioral<br />
screening, Ms. Tully asks to review its<br />
veterinary records. <strong>The</strong> h<strong>and</strong>ler must be a<br />
volunteer at the health system.<br />
“It is quite a commitment, <strong>and</strong> it takes<br />
Sometimes a patient who comes in later is<br />
treated be<strong>for</strong>e another who arrived earlier. “If<br />
anybody feels somebody went ahead,” Ms. Veltri<br />
explains, “you can assure them that the person is<br />
quite ill <strong>and</strong> has to be seen.”<br />
From 9 a.m. to 1 p.m. on Thursday, her volunteering<br />
helps reduce waiting times, <strong>and</strong> to patients,<br />
the process appears to proceed more quickly, even<br />
when it seems slow.<br />
“We try to appease them in whatever way that<br />
we can,” she said <strong>of</strong> the concierges’ duties. “Some<br />
patients are friendly <strong>and</strong> want to talk. And if they<br />
don’t, you don’t intrude on them at all.”<br />
Ms. Veltri escorts patients to the fast-track<br />
area if they have a minor ailment, such as a sore<br />
throat, <strong>and</strong> are likely to go home. If they have<br />
an illness or injury that may require hospitalization,<br />
she takes them to a different section <strong>of</strong> the<br />
a very dedicated h<strong>and</strong>ler to get through the<br />
whole process,” she said. “We only accept<br />
the best-trained dogs into our program.”<br />
Ms. Wong has volunteered with her<br />
dogs at North Shore University Hospital<br />
since June 2006. All <strong>of</strong> them are Great<br />
Pyrenees with champion status.<br />
“I bring at least two at a time,” said<br />
Ms. Wong, who has accumulated more<br />
than 500 volunteer hours. She takes as<br />
many as six or eight to the Stroke Club,<br />
with the help <strong>of</strong> her youngest child <strong>of</strong><br />
three, 15-year-old Michelle, who also has<br />
pet therapy licenses <strong>for</strong> each dog. Together<br />
they com<strong>for</strong>t <strong>and</strong> cheer up stroke survivors<br />
<strong>and</strong> their caretakers.<br />
In addition, her pooches interact with<br />
patients on various floors <strong>of</strong> the hospital,<br />
including the Child Life Program <strong>and</strong> the<br />
Palliative Care Unit. <strong>The</strong>y also visit the Stern<br />
Family Center <strong>for</strong> Rehabilitation. Wherever<br />
the dogs go, they wear custom-made outfits.<br />
Ms. Wong is one <strong>of</strong> eight volunteers<br />
who bring their dogs to North Shore<br />
University Hospital <strong>for</strong> pet therapy, said Lisa<br />
Breiman, director <strong>of</strong> volunteer services. “I<br />
see first-h<strong>and</strong> what a tremendous positive<br />
Emergency Department. This relieves the nurse <strong>of</strong><br />
that responsibility <strong>and</strong> speeds up registration <strong>for</strong><br />
other patients.<br />
“Arlene is a friendly, outgoing woman who is<br />
wonderfully helpful to patients, visitors <strong>and</strong> staff,”<br />
Ms. Cohen says. “She is perfect <strong>for</strong> this program.”<br />
A resident <strong>of</strong> Lawrence, Ms. Veltri began<br />
volunteering at Franklin Hospital in May 2009. She<br />
started in the Medical Records Department, assisting<br />
with filing <strong>and</strong> other requests. After taking some<br />
time <strong>of</strong>f due to health issues, Ms. Veltri became a<br />
concierge in last spring.<br />
Franklin Hospital staff members, including<br />
the nurses, registrars <strong>and</strong> security guards, are<br />
delightful, she said. “<strong>The</strong>y make you feel that you’re<br />
wanted <strong>and</strong> that you’re useful.”<br />
impact pet therapy has on our patients, their<br />
family members <strong>and</strong> also our staff, who look<br />
<strong>for</strong>ward to their visits,” Ms. Breiman says.<br />
Aside from volunteering, Ms. Wong<br />
works five overnight shifts per week as a<br />
technician’s <strong>and</strong> doctor’s assistant, as well<br />
as a receptionist, at Central Veterinary<br />
Associates’ 24-hour emergency hospital in<br />
Valley Stream. Henry Wong, her husb<strong>and</strong><br />
<strong>of</strong> 26 years, is a pharmacist at North Shore<br />
University Hospital.<br />
Ms. Wong, who lives in Woodmere <strong>and</strong><br />
also has two cats, lectures about pet therapy<br />
at various schools <strong>and</strong> colleges. Instead <strong>of</strong><br />
accepting compensation, she encourages<br />
her listeners to donate to North Shore<br />
University Hospital.<br />
“This is a passion,” she said, adding<br />
that it takes two hours to groom each dog<br />
the day prior to pet therapy visits, which<br />
she does one to three times per week. “It’s<br />
not something that I get paid <strong>for</strong>. But the<br />
reward is so much more than money.”<br />
Opposite: Ms. Wong with Delilah, left, <strong>and</strong> Orion.<br />
Custom outfits <strong>for</strong> her therapy dogs add even more<br />
cheer to patient visits.<br />
<strong>The</strong> New St<strong>and</strong>ard 43
hearts <strong>and</strong> h<strong>and</strong>s<br />
A Big-League Volunteer <strong>for</strong> Generations <strong>of</strong> Kids<br />
By Susan Kreimer<br />
NEW HYDE PARK — Mike Oshinsky attends<br />
religious services every morning. His Jewish faith<br />
has taught him the importance <strong>of</strong> visiting <strong>and</strong><br />
com<strong>for</strong>ting the sick.<br />
With that in mind, he started volunteering<br />
nearly 29 years ago at what’s now known as the<br />
Cohen Children’s Medical Center (CCMC). For full<br />
days on Tuesday <strong>and</strong> Thursday, he volunteers in the<br />
Hematology/Oncology Unit.<br />
“I had retired <strong>and</strong> I was looking <strong>for</strong> something<br />
to do,” said Mr. Oshinsky, 83, who lives in North<br />
Woodmere <strong>and</strong> is still involved in commercial<br />
real estate. “Friends <strong>of</strong> mine recommended that I<br />
volunteer at the hospital.”<br />
Believing that “young people keep you young,”<br />
he quickly aligned himself with helping pediatric<br />
patients. “Obviously, it went well. I’m still there.”<br />
A Child Life Program didn’t exist at the<br />
time. “It was up to the volunteers to do whatever<br />
they thought they should do to keep the children<br />
occupied <strong>and</strong> busy,” Mr. Oshinsky recalled. “And<br />
that’s what we did.”<br />
He supplied the playroom with a lot <strong>of</strong> fun<br />
stuff. Friends from various businesses donated<br />
baseball hats <strong>and</strong> sticker books. He obtained the<br />
stickers at wholesale prices. “What I couldn’t get<br />
donated,” Mr. Oshinsky said, “I bought.”<br />
CCMC’s Child Life Department now manages<br />
special events <strong>and</strong> donations <strong>for</strong> patients, said<br />
Maxine Legall, coordinator <strong>of</strong> volunteer services.<br />
Mr. Oshinsky also made contacts with the New<br />
York Isl<strong>and</strong>ers — a top hockey team in those days,<br />
having won four Stanley Cups. In September 1984,<br />
he brought one <strong>of</strong> the team’s core players, Bryan<br />
Trottier, <strong>for</strong> a visit.<br />
“<strong>The</strong> Isl<strong>and</strong>ers have been coming to the<br />
hospital ever since,” said Mr. Oshinsky, a sports<br />
enthusiast who plays racquetball <strong>and</strong> tennis. “It’s an<br />
Isl<strong>and</strong>er tradition to visit the hospital every year.”<br />
<strong>The</strong> New York Jets <strong>and</strong> the Mets have also com<strong>for</strong>ted<br />
children in the hospital.<br />
<strong>The</strong> benefits <strong>of</strong> aging well <strong>and</strong> giving back to<br />
the community complement each other. Marilyn<br />
Oshinsky, his wife <strong>of</strong> 62 years, volunteered in the<br />
hospital’s gift shop in the mid- to late 1980s.<br />
“<strong>You</strong> have to keep your mind active,” Mr.<br />
44 Summer 2012<br />
Oshinsky says. “<strong>You</strong> have to keep your body active.<br />
<strong>You</strong> have to keep your soul active. <strong>You</strong> do all three.”<br />
Danielle Davis, a certified Child Life specialist<br />
in hematology/oncology, is in awe <strong>of</strong> Mr. Oshinsky’s<br />
knack <strong>for</strong> connecting with youngsters.<br />
“Mike has this amazing ability to <strong>for</strong>m a<br />
relationship with a child <strong>of</strong> any age, gender or<br />
cultural background. He truly makes a lasting<br />
impression,” Ms. Davis says. “It’s clear how<br />
much <strong>of</strong> a difference he makes in the lives <strong>of</strong> our<br />
patients <strong>and</strong> families, when they continue to talk<br />
about him <strong>and</strong> remember him long after their<br />
treatment is finished.”<br />
Above: Volunteer Mike Oshinsky <strong>and</strong> a young<br />
patient are clearly connecting at the CCMC.
Huntington Auxiliary Giving Nears $200,000<br />
Kevin Lawlor, Huntington Hospital president <strong>and</strong> CEO, right, recently thanked Auxiliary members <strong>for</strong> their $198,465<br />
donation. From left: Thomas Rizzo, treasurer; Anita Rizzo, vice president/advocacy; <strong>and</strong> Edna Fetkowitz, president. <strong>The</strong><br />
gift represented proceeds <strong>of</strong> the Auxiliary’s 2011 fundraising ef<strong>for</strong>ts, which included lobby sales, telephone <strong>and</strong> TV rentals<br />
<strong>and</strong> special events.<br />
NEW HYDE PARK — For<br />
Barbara Raber, volunteering<br />
is a natural extension <strong>of</strong> her<br />
life’s calling. First a teacher,<br />
then a principal at Lakeville<br />
Elementary School in Great<br />
Neck <strong>for</strong> 26 years, she chose<br />
the North Shore-LIJ Health<br />
System <strong>for</strong> her community<br />
service endeavor.<br />
<strong>The</strong> summer be<strong>for</strong>e <strong>of</strong>ficially<br />
retiring on Sept. 1,<br />
2010, she trained with Denice<br />
Romero, director <strong>of</strong> volunteer<br />
services at LIJ Medical Center.<br />
This way, she would be ready<br />
to begin as soon as possible.<br />
“I adore children,” said<br />
Ms. Raber, 76. She started volunteering<br />
at Cohen Children’s<br />
Medical Center (CCMC),<br />
“supporting in whatever<br />
capacity I could. I would help<br />
a number <strong>of</strong> the older patients<br />
with homework.”<br />
At the hospital, she also<br />
played games <strong>and</strong> read books<br />
to the youngsters. She brought<br />
Former Educator<br />
Serves as LIJ<br />
Ambassador<br />
By Susan Kreimer<br />
arts <strong>and</strong> crafts to them. And<br />
when they couldn’t come to the<br />
playroom, she went to their<br />
rooms <strong>and</strong> engaged them in<br />
activities.<br />
Ms. Raber represents the<br />
new face <strong>of</strong> volunteers who<br />
want meaningful involvement<br />
in their golden chapters, after<br />
long <strong>and</strong> accomplished careers.<br />
“Years ago, the gift shop<br />
was a prime assignment,” Ms.<br />
Romero says. It was <strong>of</strong>ten run<br />
by stay-at-home moms, the<br />
wives <strong>of</strong> hospital physicians.<br />
“Now, our retirees want a con-<br />
tinuance <strong>of</strong> their pr<strong>of</strong>essional<br />
status.” She has trained a<br />
retired flight attendant, editor,<br />
teachers <strong>and</strong> administrators to<br />
serve as dedicated volunteers.<br />
Many doctors <strong>and</strong> other<br />
hospital staff members know<br />
Ms. Raber because she taught<br />
or supervised their children in<br />
school. Now, they’re surprised<br />
to see her in their workplace.<br />
“What are you doing here,<br />
Barbara?” is a common question<br />
they pose.<br />
“Barbara is able to engage<br />
people <strong>and</strong> provide all the<br />
needed in<strong>for</strong>mation effectively,”<br />
Ms. Romero says. “Her winning<br />
smile <strong>and</strong> overt caring are evident<br />
in each interaction.”<br />
In late January, upon<br />
the opening <strong>of</strong> LIJ Medical<br />
Center’s Katz Women’s Hospital<br />
<strong>and</strong> Zuckerberg Pavilion, she<br />
changed volunteering roles.<br />
“Denice asked whether I would<br />
consider switching to an ambassadorship,”<br />
Ms. Raber recalls.<br />
“And I said to her, ‘As long as I<br />
don’t have to leave the country, I<br />
would be happy to try it.’ ”<br />
Once a week, she assists at<br />
the new main entrance. With a<br />
friendly face, she guides visitors<br />
to where they need to go<br />
<strong>and</strong> helps melt away their anxiety<br />
over coming to a hospital,<br />
whether it’s to have surgery,<br />
give birth or undergo tests.<br />
Sometimes she escorts them<br />
personally in a wheelchair or<br />
on foot.<br />
“I really run <strong>for</strong> four<br />
hours bringing people all over<br />
the complex,” Ms. Raber says<br />
<strong>of</strong> her 9 a.m. to 1 p.m. shift on<br />
Tuesday. “It’s very active <strong>and</strong><br />
very busy.”<br />
Ms. Raber is multitalented.<br />
Aside from her hospital<br />
volunteer duties, she plays<br />
tennis in a women’s league.<br />
And as a young woman, she<br />
trained as a concert pianist.<br />
Rewards from volunteering<br />
come in the <strong>for</strong>m <strong>of</strong> smiles <strong>and</strong><br />
hugs. “We are helping people<br />
who, at the time <strong>of</strong> their illness,<br />
need some additional support,”<br />
Ms. Raber says. “Whatever little<br />
words <strong>of</strong> com<strong>for</strong>t you can <strong>of</strong>fer<br />
are so appreciated.”<br />
<strong>The</strong> New St<strong>and</strong>ard 45
hearts <strong>and</strong> h<strong>and</strong>s<br />
HUNTINGTON — On the calendar, Bill<br />
Segal is 79 years old, but “in my heart,<br />
I’ll always be 39,” he jokingly said. It’s no<br />
wonder he brings boundless energy to<br />
volunteering at Huntington Hospital.<br />
Mr. Segal, who turns 80 in August,<br />
has poured tons <strong>of</strong> passion into helping<br />
others. After retiring at age 66, “I decided<br />
I was too young to sit in a rocking chair,”<br />
said the <strong>for</strong>mer advertising <strong>and</strong> marketing<br />
executive. Seeking a rewarding outlet <strong>for</strong><br />
his spare time led him to Huntington<br />
Hospital. By the end <strong>of</strong> 2011, Mr. Segal<br />
had clocked 4,500 volunteer hours;<br />
this February, he celebrated his 12th<br />
anniversary.<br />
“Over the years, I’ve done everything<br />
from volunteering in the Post-Anesthesia<br />
Care Unit to the admissions desk,” he said.<br />
On Friday afternoons, he’s assigned to<br />
the pharmacy <strong>and</strong> delivers medications to<br />
nursing units. And on Monday afternoons,<br />
he discharges patients while escorting<br />
newcomers to the Emergency Department.<br />
He also delivers flowers <strong>and</strong> supervises the<br />
junior volunteers on that day.<br />
<strong>The</strong> juniors are high school students<br />
from the Huntington area. “<strong>The</strong>re are<br />
some kids who put in their hours <strong>and</strong><br />
then they disappear,” says Mr. Segal,<br />
who lives in Huntington Village <strong>and</strong> has<br />
likely supervised more than a thous<strong>and</strong><br />
junior volunteers over the years. “And<br />
then there are others who will put in<br />
several hundred hours because they get<br />
46 Summer 2012<br />
enthusiastic about the program.”<br />
That’s the kind <strong>of</strong> attitude Mr. Segal<br />
hopes to encourage in the youngsters<br />
he mentors. At least 75 hours per year<br />
are required to be considered a junior<br />
Huntington Volunteer<br />
Touts the Rewards <strong>of</strong><br />
Community Service<br />
By Susan Kreimer<br />
volunteer in good st<strong>and</strong>ing <strong>and</strong> at<br />
least 100 hours are needed to receive a<br />
recommendation letter from the hospital<br />
in applying to college.<br />
“A lot <strong>of</strong> them become involved<br />
because it looks good on a college<br />
application,” Mr. Segal says. “And I try<br />
to convince them that they will feel good<br />
about themselves <strong>for</strong> volunteering.”<br />
While it can be challenging, Mr.<br />
Segal enjoys showing teenagers the value<br />
<strong>of</strong> community service. On Christmas<br />
morning, he <strong>and</strong> a group <strong>of</strong> junior<br />
volunteers tour the hospital, singing<br />
carols to patients while Santa distributes<br />
presents provided by the Huntington<br />
Hospital Auxiliary.<br />
“I have to remind them every now<br />
<strong>and</strong> then that they’re volunteering in a<br />
hospital, <strong>and</strong> I want them to find this to be<br />
a rewarding experience,” Mr. Segal says.<br />
“Everything they do helps the nursing staff.”<br />
Gina Torchon, director <strong>of</strong> volunteer<br />
services at Huntington Hospital, admires<br />
his unwavering dedication. “Bill is a one<strong>of</strong>-a-kind<br />
volunteer,” she says. “He is very<br />
generous with his time <strong>and</strong> wisdom, <strong>and</strong> he<br />
is a role model <strong>for</strong> our junior volunteers.”<br />
Between 175 <strong>and</strong> 200 junior<br />
volunteers usually serve at the hospital<br />
during the same calendar year. <strong>The</strong>y stay<br />
anywhere from one to four years.<br />
Mr. Segal also takes on various<br />
other roles at hospital functions, from<br />
assisting with registration at public health<br />
screenings to attending retirement parties<br />
<strong>and</strong> Cancer Survivors’ Day.<br />
“He gets along with so many people<br />
<strong>and</strong> is so well-liked that he doesn’t want to<br />
miss anything,” Ms. Torchon says. “He is<br />
very involved.”<br />
NSUH Auxiliary Golf<br />
Classic To Honor<br />
Susan Somerville<br />
This is the 34th year that North<br />
Shore University Hospital has held a<br />
golf outing, <strong>and</strong> it is the first year that<br />
the event has had an honoree. Susan<br />
Somerville, RN, MA, has been chosen<br />
<strong>for</strong> this distinction; she is the hospital’s<br />
executive director. <strong>The</strong> 34th Annual Golf<br />
Classic will be held on Monday, July<br />
16, at the North Shore Country Club in<br />
Glen Head. Proceeds will benefit the<br />
development <strong>of</strong> the West Wing at NSUH.<br />
For further in<strong>for</strong>mation, please call the<br />
Volunteer-Auxiliary Office at<br />
(516) 562-4947.
Walk to Paris Winners Announced<br />
On Valentine’s Day, North Shore-LIJ announced a challenge <strong>for</strong> all<br />
employees: In teams <strong>of</strong> 10, walk the 7.2 million steps it would take to reach<br />
Paris from New York, in exchange <strong>for</strong> better health <strong>and</strong> the chance to win a<br />
free trip to Paris. An unprecedented 15,000 employees participated in the<br />
Walk to Paris – <strong>for</strong>ming teams, walking at least 8,000 steps every day <strong>and</strong><br />
having a great time doing it.<br />
<strong>The</strong> challenge ended in late June with a closing ceremony <strong>and</strong><br />
winners’drawing held at the Crest Hollow Country Club in Woodbury. North<br />
Shore-LIJ President <strong>and</strong> CEO Michael Dowling surprised everyone by drawing<br />
four gr<strong>and</strong> prize winners. Congratulations to the<br />
gr<strong>and</strong>-prize winning teams: Walka Walka Walka,<br />
Microbiologie Marche A’ Paris, Champs-Elysees<br />
<strong>and</strong> Twinkle Toes.<br />
In addition to the 40 employees now<br />
going to Paris, Mr. Dowling drew the names <strong>of</strong><br />
11 more teams to win the second-place prize:<br />
a wellness package, valued at $1,000, <strong>for</strong> each<br />
team member.<br />
“Walk to Paris is part <strong>of</strong> a much larger<br />
commitment that North Shore-LIJ is making to its<br />
employees,” Mr. Dowling said. “Our careers are<br />
based on helping others achieve wellness, <strong>and</strong><br />
we know that we have a tremendous opportunity<br />
to help our employee community reach their own<br />
personal wellness goals.”<br />
Mr. Dowling noted that wellness is part <strong>of</strong><br />
the health re<strong>for</strong>m movement. “This is part <strong>of</strong> the<br />
whole ef<strong>for</strong>t that the Supreme Court dealt with,”<br />
Mr. Dowling said. “Wellness is not going away<br />
<strong>and</strong> we are proud to be supporting our employees<br />
<strong>and</strong> leading the way <strong>for</strong> others.”<br />
Top Right: <strong>The</strong> Walk to Paris team wearing pink<br />
is Sistaz with Blistaz – one <strong>of</strong> the first five teams<br />
to cross the finish line. Bottom Right: <strong>The</strong> team in<br />
white is Lab Rats on the Run from North Shore-LIJ<br />
Laboratories.<br />
<strong>The</strong> New St<strong>and</strong>ard 47
mission possible<br />
While vacationing in Oaxaca, Mexico, last year, Matthew<br />
Kaufman, MD, walked into the local hospital <strong>and</strong> began<br />
introducing himself to the doctors. Still in vacation<br />
mode, the chief resident in LIJ Medical Center’s Emergency<br />
Department told them that he worked <strong>for</strong> an American healthcare<br />
system that helped other medical centers <strong>and</strong> asked where they<br />
needed support.<br />
Recounting the story <strong>of</strong> a recent mudslide, the Mexican<br />
physicians voiced their concerns about being unprepared in a<br />
major crisis or natural disaster.<br />
Impromptu Discussion<br />
Spurs Emergency<br />
Training Conference<br />
“It’s a very interesting thing to go into a different culture with<br />
different resources <strong>and</strong> see how they would h<strong>and</strong>le this,” he said. Dr.<br />
Kaufman immediately wanted to get involved. He had never gone on<br />
medical mission be<strong>for</strong>e, but envied his colleagues’ medical missions.<br />
When he returned home, Dr. Kaufman continued talking with<br />
doctors <strong>and</strong> the Red Cross in Oaxaca, <strong>and</strong><br />
began building a North Shore-LIJ team<br />
that could help the Mexican hospital better<br />
prepare <strong>for</strong> a major crisis. Luckily <strong>for</strong> all,<br />
LIJ is the site <strong>of</strong> an international emergency<br />
medicine fellowship <strong>and</strong> Dario Gonzalez,<br />
MD, the medical director <strong>for</strong> New York<br />
City’s Office <strong>for</strong> Emergency Management<br />
<strong>and</strong> associate medical director <strong>of</strong> the FDNY,<br />
is a faculty member. Led by Dr. Gonzalez’s<br />
expertise in disaster management, the<br />
team included Gino Farina, MD; Herberth<br />
Balsells, DO; <strong>and</strong> Kathryn Bailey, AB.<br />
This January, the group traveled to<br />
Oaxaca to conduct a needs assessment <strong>of</strong><br />
the hospitals that would be most vulnerable<br />
in a disaster. <strong>The</strong> team also presented<br />
an emergency management conference<br />
that attracted nearly 400 participants,<br />
including doctors, firefighters, emergency<br />
medical technicians, Red Cross workers,<br />
epidemiologists <strong>and</strong> military <strong>of</strong>ficials.<br />
48 Summer 2012<br />
“<strong>The</strong> conference itself was really an amazing event,” Dr.<br />
Kaufman said. “I think it allowed attendees to evaluate their<br />
own system in a critical way. I also see an opportunity <strong>for</strong> us to<br />
continue this process <strong>and</strong> help to facilitate these changes.” Most<br />
importantly, the event began a dialogue between agencies that had<br />
not previously convened.<br />
Emergency medicine specialists from North Shore-LIJ have<br />
worked with hospitals in India, Haiti <strong>and</strong> other underdeveloped<br />
countries that face such problems as poorly constructed facilities<br />
or lack <strong>of</strong> <strong>for</strong>mal training programs <strong>for</strong> doctors, said Mae Ward,<br />
RN, senior research director <strong>of</strong> emergency medicine at North<br />
Shore University Hospital. Sassan Naderi, MD, director <strong>of</strong> the<br />
international emergency medicine fellowship at LIJ, had previously<br />
arranged a three-year emergency medicine training program in<br />
Durgapur, India.<br />
This trip, however, was different because Oaxaca has the facilities<br />
<strong>and</strong> the doctors, but needed the communication tools <strong>and</strong><br />
organizational structure to respond to a crisis. <strong>The</strong> response in<br />
Oaxaca has been tremendous, Dr. Kaufman said, adding that medical<br />
<strong>of</strong>ficials there have already started making changes. <strong>The</strong> initial<br />
trip to Oaxaca was funded largely through a grant from Goldman<br />
Sachs Gives, a donor-advised fund that gives grants to nonpr<strong>of</strong>its.<br />
As the project continues, there will be more trips to Oaxaca with<br />
additional training exercises run by Dr. Kaufman <strong>and</strong> his team.<br />
“I certainly intend to make this kind <strong>of</strong> project an ongoing<br />
part <strong>of</strong> my career,” he said. “<strong>The</strong>se projects are really exciting <strong>and</strong><br />
meaningful, especially because you can make systematic changes.”<br />
North Shore-LIJ volunteers convened an emergency management conference in Oaxaca, Mexico.
<strong>The</strong> New St<strong>and</strong>ard<br />
49
PLAINVIEW — <strong>Veterans</strong> <strong>of</strong><br />
World War II, the Korean<br />
War <strong>and</strong> Vietnam who live in<br />
the Plainview-Old Bethpage<br />
neighborhood naturally occurring<br />
retirement community<br />
(NNORC) recently gave<br />
history lessons that Mepham<br />
High School in Bellmore<br />
students won’t soon <strong>for</strong>get.<br />
<strong>The</strong>ir videotaped interviews<br />
have been archived with the<br />
Library <strong>of</strong> Congress <strong>Veterans</strong><br />
History Project.<br />
“I listened to the story<br />
<strong>of</strong> one man’s journey from a<br />
young boy in Brooklyn to a<br />
50 Summer 2012<br />
Nurse Helps Plainview<br />
<strong>Veterans</strong> Give Real-Life<br />
History Lesson<br />
prisoner <strong>of</strong> war in Germany,<br />
<strong>and</strong> realized that I’d stumbled<br />
upon a reservoir <strong>of</strong> history on<br />
the verge <strong>of</strong> being lost,” said<br />
Kelly Soel, RN, a North Shore-<br />
LIJ community health nurse<br />
who works with a number <strong>of</strong><br />
veterans through the Plainview-<br />
Old Bethpage NNORC.<br />
Ms. Soel established a<br />
group among the NNORC<br />
members in which veterans<br />
could gather to share their<br />
experiences while promoting<br />
well-being <strong>and</strong> a deeper sense<br />
<strong>of</strong> community. In researching<br />
discussion topics, she found the<br />
By Kristen Longo<br />
Library <strong>of</strong> Congress <strong>Veterans</strong><br />
History Project <strong>and</strong> arranged<br />
<strong>for</strong> the veterans to share their<br />
war stories with a group <strong>of</strong><br />
Mepham High School students<br />
<strong>and</strong> answer their questions.<br />
Paul Zad<strong>of</strong>f, 90, told<br />
students about his World War<br />
II experience <strong>of</strong> serving on Iwo<br />
Jima. “<strong>You</strong> learn about the war<br />
through textbooks, but it was<br />
nothing like being there,” he<br />
said. “We went directly into<br />
combat <strong>and</strong> many <strong>of</strong> us expected<br />
to die — but I made it back <strong>and</strong><br />
have the real story to tell so it’s<br />
not <strong>for</strong>gotten.” Melvin Breshin,<br />
67, who served as an Army<br />
captain in South Korea during<br />
the Vietnam War, also emphasized<br />
to students the importance<br />
<strong>of</strong> learning what happened <strong>and</strong><br />
passing that knowledge to future<br />
generations.<br />
<strong>The</strong> veterans were more<br />
than happy to share their<br />
past. “<strong>The</strong>ir legacy will live on<br />
through the bright young minds<br />
<strong>of</strong> tomorrow,” said Ms. Soel.<br />
She feels a deep connection to<br />
the project through her work<br />
with the NNORC <strong>and</strong> hopes<br />
that some day her son, a second-class<br />
petty <strong>of</strong>ficer with the<br />
US Navy, will be able to teach<br />
the next generation first-h<strong>and</strong><br />
about the sacrifices <strong>and</strong> bravery<br />
<strong>of</strong> those serve our country.<br />
Above: Paul Zad<strong>of</strong>f shared maps <strong>and</strong><br />
photos with his first-h<strong>and</strong> account<br />
<strong>of</strong> his experience on the front lines<br />
on Iwo Jima with Kelly Soel, RN,<br />
community health nurse <strong>for</strong> the health<br />
system, <strong>and</strong> a group <strong>of</strong> Mepham High<br />
School students—who are the age that<br />
he was when he left <strong>for</strong> war.
Taking Steps to Protect<br />
<strong>You</strong>ng Athletes From<br />
Sexual Assault<br />
With the London<br />
Summer Olympics<br />
approaching <strong>and</strong><br />
young people across the<br />
country taking part in team<br />
sports, North Shore-LIJ,<br />
Nassau County Executive<br />
Ed Mangano <strong>and</strong> the Nassau<br />
County Sports Commission<br />
have joined together to<br />
identify ways <strong>of</strong> recognizing<br />
<strong>and</strong> preventing sexual abuse in<br />
youth sports.<br />
At a news conference<br />
held recently in Mineola,<br />
the keynote speaker was<br />
Katherine Starr, a member<br />
<strong>of</strong> the 1984 <strong>and</strong> 1988 Great<br />
Britain Olympic swim team,<br />
who had her athletic career<br />
destroyed after being sexually<br />
assaulted by her coach. Now<br />
the founder <strong>and</strong> president<br />
<strong>of</strong> a nonpr<strong>of</strong>it organization<br />
she named Safe4Athletes,<br />
Ms. Starr says, “Every athlete<br />
should be provided a safe <strong>and</strong><br />
positive environment free <strong>of</strong><br />
sexual abuse, bullying <strong>and</strong><br />
harassment.”<br />
“We are very proud to<br />
work with Nassau County <strong>and</strong><br />
the Sports Commission to<br />
find new ways to help young<br />
people who fall victim to<br />
these predators,” said Jamie<br />
H<strong>of</strong>fman-Rosenfeld, MD,<br />
chief <strong>of</strong> child advocacy <strong>and</strong><br />
protection services at Cohen<br />
Children’s Medical Center. “It<br />
is our responsibility to alert<br />
parents, teachers, educators<br />
<strong>and</strong> young people that we are<br />
here to listen to them.”<br />
County Executive<br />
Mangano said Nassau County<br />
supports this ongoing work.<br />
“We must do whatever we<br />
can to keep our children<br />
safe,” he said, “<strong>and</strong> eradicate<br />
predators from young<br />
people’s sporting activities.”<br />
<strong>The</strong> most heartfelt words<br />
came from Ms. Starr, who<br />
spoke about the devastation<br />
<strong>and</strong> loss associated with her<br />
personal tragedy. “When this<br />
happened to me, it destroyed<br />
my dreams,” she said. “<strong>The</strong>re<br />
was no one I could talk to,<br />
because I felt that I had no<br />
power. It’s my goal that no<br />
young athlete should ever have<br />
to be in this position again.”<br />
FOR your BENEFIT<br />
Planning <strong>for</strong> the Future<br />
Just Got Easier<br />
It’s never too early to plan <strong>and</strong> save <strong>for</strong> your future, but sometimes it can<br />
seem overwhelming or confusing. But a new Web site — NSLIJRetirementPlans.<br />
com — gives North Shore-LIJ Health System employees easy-to-underst<strong>and</strong> tools<br />
to maximize their retirement benefits <strong>and</strong> start saving.<br />
“We provide not only exceptional retirement benefits including retirement<br />
savings plans, but also resources to help employees become more proactive<br />
about financial planning,” said Joseph Cabral, Chief Human Resources Officer. “No<br />
one is born an expert at retirement planning, so North Shore-LIJ <strong>of</strong>fers these free<br />
services. We encourage employees to take full advantage <strong>of</strong> them.”<br />
In partnership with MetLife, North Shore-LIJ <strong>of</strong>fers many ways <strong>for</strong><br />
employees to get the in<strong>for</strong>mation they need — either through in-person<br />
classes held around the system, one-on-one planning sessions with a<br />
financial services representative or online videos <strong>and</strong> presentations. Log on to<br />
NSLIJRetirementPlans.com <strong>for</strong> in<strong>for</strong>mation about 403(b) <strong>and</strong> 401(k) retirement<br />
savings accounts, retirement calculators, registration <strong>for</strong> on-site seminars or to<br />
arrange <strong>for</strong> one-on-one sessions with a MetLife financial services representative.<br />
Shown at a recent news conference, from the left, are Brian Revello, executive director <strong>of</strong> the Nassau County Sports<br />
Commission, Nassau County Executive Ed Mangano, Dr. Jamie H<strong>of</strong>fman-Rosenfeld <strong>and</strong> Katherine Starr, <strong>for</strong>mer<br />
Olympian <strong>and</strong> founder <strong>of</strong> Safe4Athletes.<br />
<strong>The</strong> New St<strong>and</strong>ard 51
Story-telling is not something that is usually<br />
part <strong>of</strong> a hospital visit. But LIJ Medical<br />
Center <strong>and</strong> Hospice Care Network have<br />
partnered with StoryCorps Legacy, a pilot<br />
program that provides people with life-threatening<br />
conditions <strong>and</strong> their families the opportunity to<br />
record, preserve <strong>and</strong> share their stories. And our<br />
patients are sharing stories that will be h<strong>and</strong>ed<br />
down to their families <strong>and</strong> the community at large.<br />
StoryCorps works with a variety <strong>of</strong><br />
organizations including hospitals, palliative care<br />
departments <strong>and</strong> hospices to help them incorporate<br />
the reminiscence interview experience into their<br />
existing services. Legacy staff train <strong>and</strong> prepare<br />
partners to conduct <strong>and</strong> record interviews using<br />
pr<strong>of</strong>essional broadcast equipment on loan from<br />
StoryCorps. Participants receive a CD <strong>of</strong> the interview<br />
to share with friends <strong>and</strong> family, <strong>and</strong> another copy<br />
is archived at the American Folklife Center at the<br />
Library <strong>of</strong> Congress in Washington, DC.<br />
At the health system, StoryCorps Legacy is<br />
collaborating with LIJ’s Departments <strong>of</strong> Geriatric <strong>and</strong><br />
Palliative Medicine <strong>and</strong> Patient <strong>and</strong> Family Centered<br />
Care <strong>and</strong> the Hospice Care Network’s Complementary<br />
<strong>The</strong>rapy Program. <strong>The</strong> project runs through July <strong>and</strong><br />
both organizations expect to conduct a total <strong>of</strong> 60<br />
interviews. <strong>The</strong> program is funded by a grant from<br />
the Jordan Family Foundation.<br />
“<strong>The</strong> StoryCorps project is a natural extension<br />
<strong>of</strong> the conversations we share on a daily basis in<br />
caring <strong>for</strong> older patients with serious illnesses <strong>and</strong><br />
supporting their loved ones,” said Tanveer Mir, MD,<br />
associate chief <strong>of</strong> geriatric <strong>and</strong> palliative medicine at<br />
LIJ. “This project allows us to explore <strong>and</strong> celebrate<br />
people’s lives <strong>and</strong> document their stories <strong>for</strong><br />
generations to come.”<br />
Christina Lightbourne, a volunteer at LIJ<br />
<strong>for</strong> the last couple <strong>of</strong> years, became involved<br />
in the StoryCorps project because she said she<br />
enjoyed connecting <strong>and</strong> talking with older patients<br />
<strong>and</strong> it seemed like a “natural segue” given her<br />
activities at the hospital. In her first interview, Ms.<br />
Lightbourne arranged a conversation between her<br />
84-year-old aunt, Ruth Robinson, who has been<br />
treated at LIJ <strong>for</strong> cancer <strong>and</strong> other conditions, <strong>and</strong><br />
her husb<strong>and</strong>, Paul Lightbourne. “I was surprised<br />
at how much detail my aunt remembered about<br />
her childhood teacher Miss Green, who taught her<br />
how to read <strong>and</strong> write. My aunt was also excited<br />
to talk about her family, in more depth than at our<br />
reunions every two years.”<br />
“<strong>The</strong> StoryCorps program helps us capture the<br />
voices <strong>of</strong> patients <strong>and</strong> family members <strong>and</strong> helps<br />
us to look at the patient as a complete person,” said<br />
52 Summer 2012<br />
Partnership Gives Voices to Patients<br />
with Life-Threatening Illnesses<br />
By Betty Olt<br />
Kirby Veevers, coordinator <strong>of</strong> patient- <strong>and</strong> family-<br />
centered care at LIJ. “People have a big life be<strong>for</strong>e<br />
they become patients at the hospital <strong>and</strong> we want<br />
to honor that.”<br />
Eva Pendleton, LMT, director <strong>of</strong> complementary<br />
therapy at Hospice Care Network, said the StoryCorps<br />
program is “striking a chord” with volunteers <strong>and</strong><br />
staff members <strong>and</strong> there has been an overwhelming<br />
response to the project. “<strong>The</strong>re is a fundamental<br />
need <strong>for</strong> people to be heard. People love to tell a<br />
story <strong>and</strong> everyone has a story to tell,” she said.<br />
“In hospice care, life review <strong>and</strong> the<br />
conversations we have with patients are done in<br />
the spirit <strong>of</strong> the work we do every day,” explained<br />
Ms. Pendleton. “StoryCorps is important because it<br />
leaves a legacy <strong>for</strong> loved ones.”<br />
Since 2003, StoryCorps has collected <strong>and</strong><br />
archived more than 35,000 interviews from more than<br />
70,000 people. Some stories are shared during weekly<br />
National Public Radio broadcasts <strong>of</strong> the show Morning<br />
Edition. For more in<strong>for</strong>mation, visit StoryCorps.org<br />
Above: Volunteer Christina Lightbourne with<br />
her 84-year-old aunt, Ruth Robinson, who had<br />
stories to tell.
allied NATION<br />
In the past, general practitioners were expected to manage<br />
the majority <strong>of</strong> medical issues, from arthritis to high blood<br />
pressure, pneumonia to appendicitis. Today’s healthcare,<br />
however, trends toward exceptionally individualized <strong>and</strong><br />
specialized patient care cases, requiring the specialist — like the<br />
rheumatologist, internist, pulmonologist, <strong>and</strong> laparoscopic surgeon<br />
— to provide more expertise on each specific concern. While this<br />
trend builds, community hospitals must find ways to continue to<br />
meet all general healthcare needs <strong>and</strong> to provide a wide variety<br />
<strong>of</strong> services <strong>and</strong> care to keep up with every<br />
patient. At Forest Hills Hospital, physician<br />
assistants (PAs) help to achieve the level <strong>of</strong><br />
care necessary to provide all services <strong>for</strong> all<br />
patients. <strong>The</strong>y are the hospital staff who step<br />
in to coordinate timely, safe <strong>and</strong> efficient<br />
care <strong>for</strong> every patient. <strong>The</strong>y are the new<br />
generalists.<br />
PAs are highly trained healthcare<br />
pr<strong>of</strong>essionals who are licensed <strong>and</strong><br />
credentialed to practice medicine in<br />
physician-led teams. <strong>The</strong>y conduct physical<br />
exams <strong>and</strong> histories, diagnose <strong>and</strong> treat<br />
illnesses, order <strong>and</strong> interpret tests, counsel<br />
patients, make rounds, assist in surgery <strong>and</strong><br />
write prescriptions. <strong>The</strong>y are involved in<br />
day-to-day care <strong>and</strong> make medical-related<br />
decisions, turning to their supervising<br />
physicians when complicated cases require<br />
further medical expertise. PAs also h<strong>and</strong>le<br />
patient complaints <strong>and</strong> follow-up visits<br />
while providing a broad range <strong>of</strong> diagnostic,<br />
therapeutic, administrative, educational <strong>and</strong><br />
research services. According to the Bureau <strong>of</strong><br />
Labor Statistics, the PA pr<strong>of</strong>ession is among<br />
the fastest growing in the country.<br />
“Given the challenges ahead — such<br />
as regulatory compliance, pay-<strong>for</strong>per<strong>for</strong>mance<br />
<strong>and</strong> the increasing number<br />
<strong>of</strong> Baby Boomers entering the health<br />
system <strong>for</strong> care — the physician/PA team<br />
will help to keep waiting times low <strong>and</strong><br />
patient satisfaction high while filling in<br />
the gaps wherever there is a shortage <strong>of</strong><br />
physicians <strong>and</strong> residents,” said Martin Morales, corporate director<br />
<strong>of</strong> physician assistant services.<br />
At Forest Hills Hospital, PAs work closely with specialist<br />
surgeons in all departments —including general, vascular, thoracic,<br />
plastic, urological <strong>and</strong> bariatric surgeries — <strong>and</strong> coordinate the care<br />
<strong>of</strong> patients requiring any <strong>of</strong> these services. <strong>The</strong> plan <strong>of</strong> care <strong>for</strong> any<br />
patient is determined by his or her physician, but helping to develop<br />
that plan <strong>and</strong> ensuring it is properly followed <strong>and</strong> assigned the proper<br />
specialists is the role <strong>of</strong> the PA. <strong>The</strong>y also respond to emergencies,<br />
codes <strong>and</strong> rapid responses, are a resource <strong>for</strong> the nurses, manage<br />
patients in the Emergency Department <strong>and</strong> Intensive Care Unit <strong>and</strong><br />
provide expert surgical assistance in the Operating Room.<br />
On average, the PAs at Forest Hills have 11 years <strong>of</strong> experience<br />
in the medical field, more than twice the period <strong>of</strong> time it takes to<br />
train a board-eligible surgeon. <strong>The</strong>y practice in the Orthopedic,<br />
Radiology, Obstetrics <strong>and</strong> Gynecology <strong>and</strong> Surgery Departments —<br />
in fact, the 10-member surgery team assisted in almost 3,000<br />
<strong>The</strong> New Generalists<br />
Physician Assistants at Forest Hills Hospital<br />
Physician assistants Rupert Evans, left, Diane Marchiafava <strong>and</strong> Khaim Babayev are on the Forest Hills<br />
Hospital team that coordinates timely, safe <strong>and</strong> effective medical care.<br />
operative procedures during the last year alone. <strong>The</strong>ir competence<br />
in <strong>and</strong> underst<strong>and</strong>ing <strong>of</strong> each surgeon’s practice lead to enormous<br />
satisfaction among the surgeons, as well as the rest <strong>of</strong> the hospital<br />
staff <strong>and</strong> patients, which in turn motivates this proud North<br />
Shore-LIJ Health System team. Lead PA Diane Marchiafava,<br />
RPA-C, says, “<strong>The</strong> best part <strong>of</strong> our PA team is, we get to use all <strong>of</strong><br />
our skills <strong>and</strong> everyone benefits.”<br />
<strong>The</strong> New St<strong>and</strong>ard 53
GREEN solutions<br />
New Structure Meets<br />
Sustainability Benchmark<br />
By Neil Rosen<br />
<strong>The</strong> Katz Women’s Hospital<br />
at North Shore<br />
University Hospital<br />
recently was the first New<br />
York hospital to receive LEED<br />
platinum certification. <strong>The</strong><br />
Katz Women’s Hospital uses<br />
about 18.6 percent less energy<br />
<strong>and</strong> 51 percent less water. Furthermore,<br />
all <strong>of</strong> the electricity<br />
consumed in its first two years<br />
<strong>of</strong> operation will come from<br />
renewable energy generated by<br />
wind power in Texas.<br />
<strong>The</strong> recognized st<strong>and</strong>ard<br />
<strong>of</strong> the sustainable building<br />
54 Summer 2012<br />
movement, LEED st<strong>and</strong>s<br />
<strong>for</strong> Leadership in Energy<br />
<strong>and</strong> Environmental Design,<br />
a rating system <strong>for</strong> green<br />
buildings that was developed<br />
by the United States Green<br />
Building Council. Designed<br />
to encourage, st<strong>and</strong>ardize,<br />
<strong>and</strong> award sustainable building<br />
ef<strong>for</strong>ts, LEED provides a<br />
framework <strong>for</strong> identifying <strong>and</strong><br />
implementing practical <strong>and</strong><br />
quantifiable green building<br />
solutions.<br />
<strong>The</strong> LEED system outlines<br />
a number <strong>of</strong> credits <strong>and</strong> as-<br />
North Shore University Hospital Wins<br />
National Award <strong>for</strong> Eco-Friendly Practices<br />
Practice Greenhealth, a<br />
national organization <strong>for</strong> healthcare<br />
facilities committed to environmentally<br />
responsible operations,<br />
recently presented NSUH with the<br />
2012 Partner <strong>for</strong> Change Award. <strong>The</strong><br />
award is one <strong>of</strong> the organization’s<br />
Environmental Excellence Awards<br />
given each year to honor outst<strong>and</strong>ing<br />
environmental achievements in the<br />
healthcare sector.<br />
<strong>The</strong> Partner <strong>for</strong> Change Award<br />
recognizes healthcare facilities that<br />
continuously improve <strong>and</strong> exp<strong>and</strong><br />
upon their mercury elimination,<br />
waste reduction <strong>and</strong> source reduction<br />
programs. At a minimum, facilities<br />
applying <strong>for</strong> this award must be<br />
recycling 15 percent <strong>of</strong> their total<br />
waste, be well on the way to mercury<br />
elimination <strong>and</strong> have developed<br />
other successful pollution prevention<br />
programs in many different areas.<br />
“This award demonstrates<br />
North Shore University Hospital’s <strong>and</strong><br />
the North Shore-LIJ Health System’s<br />
commitment to our patients, staff<br />
members <strong>and</strong> the community to<br />
protect public health <strong>and</strong> preserve<br />
the environment,” said Maurice<br />
LaBonne, senior vice president <strong>of</strong><br />
facilities services at North Shore-LIJ.<br />
“North Shore-LIJ is truly demonstrating<br />
leadership <strong>for</strong> the future <strong>of</strong> health<br />
care <strong>and</strong> sustainability.”<br />
NSUH received the Partner <strong>for</strong><br />
Change Award <strong>for</strong> environmental<br />
per<strong>for</strong>mance in the following areas:<br />
recycling <strong>and</strong> waste reduction,<br />
participation in the health system’s<br />
green cleaning program, measures<br />
to reduce mercury in all medi-<br />
signs points to a project based<br />
on how many credits the<br />
project fulfills. Based on the<br />
number <strong>of</strong> points earned, a<br />
project can earn titles ranging<br />
from certified to silver, gold<br />
<strong>and</strong> platinum. Only the most<br />
sustainable projects achieve the<br />
platinum rating.<br />
<strong>The</strong>re are six major LEED<br />
categories: sustainable sites,<br />
water efficiency, energy <strong>and</strong><br />
atmosphere, materials <strong>and</strong><br />
resources, indoor environmental<br />
quality <strong>and</strong> innovation<br />
in design.<br />
cal procedures <strong>and</strong> nontoxic paint<br />
products. In addition, in February,<br />
the Katz Women’s Hospital third-floor<br />
renovation project achieved a LEED<br />
platinum certification, the industry’s<br />
highest rating <strong>for</strong> sustainable design,<br />
green building materials <strong>and</strong> energyefficient<br />
systems. <strong>The</strong> facility is the<br />
third hospital project worldwide to<br />
receive this distinction.<br />
“We are pleased to be<br />
recognized <strong>for</strong> this significant<br />
achievement,” said Neil Rosen,<br />
director <strong>of</strong> sustainable development<br />
at North Shore-LIJ. “We are proud<br />
to be a model <strong>of</strong> how hospitals can<br />
develop <strong>and</strong> implement eco-friendly<br />
programs <strong>and</strong> sustainable buildings<br />
to improve the health <strong>of</strong> people <strong>and</strong><br />
our planet.”<br />
North Shore-<br />
LIJ Launches<br />
Interactive TV<br />
Programming<br />
GREAT NECK — North<br />
Shore-LIJ Health TV,<br />
an interactive television<br />
service, recently premiered<br />
on iO TV channel 616.<br />
Presented by the North<br />
Shore-LIJ Health System<br />
<strong>and</strong> Cablevision, the videoon-dem<strong>and</strong><br />
channel <strong>of</strong>fers<br />
health <strong>and</strong> wellness in<strong>for</strong>mation<br />
to Cablevision’s<br />
nearly three million digital<br />
cable customers on Long<br />
Isl<strong>and</strong> <strong>and</strong> in the Bronx,<br />
Brooklyn, Westchester,<br />
Lower Hudson Valley, New<br />
Jersey <strong>and</strong> Connecticut.<br />
“<strong>The</strong> launch <strong>of</strong> North<br />
Shore-LIJ Health TV with<br />
Cablevision provides a<br />
groundbreaking experience<br />
that utilizes the strengths<br />
<strong>of</strong> both organizations to<br />
deliver health <strong>and</strong> wellness<br />
in<strong>for</strong>mation via video-ondem<strong>and</strong><br />
content from New<br />
York’s very best physicians<br />
<strong>and</strong> clinicians into living<br />
rooms,” said Michael<br />
Dowling, president <strong>and</strong><br />
CEO <strong>of</strong> the health system.<br />
<strong>The</strong> health system<br />
is the first New Yorkarea<br />
healthcare provider<br />
to establish its own TV<br />
channel. North Shore-<br />
LIJ Health TV provides<br />
access to a video library<br />
<strong>of</strong> health <strong>and</strong> wellness<br />
topics <strong>and</strong> in<strong>for</strong>mation on<br />
North Shore LIJ hospitals,<br />
<strong>and</strong> viewers can request<br />
additional in<strong>for</strong>mation on<br />
the health system’s services.
Over 2,400 Celebrate at<br />
NSUH-LIJ’s Sixth Combined<br />
Cancer Survivors’ Day<br />
More than 2,400 cancer<br />
survivors <strong>and</strong> their guests<br />
attended the invitation-only<br />
Cancer Survivors’ Day celebration,<br />
held at the North Shore-LIJ Health<br />
system’s Monter Cancer Center on<br />
June 2. <strong>The</strong> keynote speaker was<br />
Shannon Miller, Olympic gold medalwinning<br />
gymnast <strong>and</strong> US Olympic Hall<br />
<strong>of</strong> Famer, whose greatest win <strong>of</strong> all<br />
was against ovarian cancer.<br />
<strong>The</strong> large gathering watched<br />
monitors positioned throughout the<br />
340-foot-by-100-foot tent, where<br />
a brief video brought back memories<br />
<strong>of</strong> the determined little blonde girl’s<br />
per<strong>for</strong>mance on the balance beam at<br />
the 1996 Summer Olympics in Atlanta.<br />
<strong>The</strong> audience listened attentively as<br />
she recounted her thoughts on that<br />
stellar day 16 years ago; then she<br />
described how she felt in December<br />
2010, when at age 33 she received<br />
word from her doctors that she had<br />
a rare from <strong>of</strong> ovarian cancer: a<br />
baseball-size germ cell tumor.<br />
<strong>The</strong> malignant cyst was<br />
removed from her ovary <strong>and</strong> she went<br />
through nine weeks <strong>of</strong> chemotherapy.<br />
“On my last day <strong>of</strong> chemo I was so<br />
excited that it was over, but at the<br />
same time it hit me – is it going<br />
to come back? When will it come<br />
back?” Ms. Miller told the people in<br />
her audience, many <strong>of</strong> whom have<br />
felt the same uncertainty <strong>and</strong> fear.<br />
She decided to focus on “helping<br />
people, encouraging them to get<br />
regular screenings, because early<br />
detection does save lives. That has<br />
become a mantra <strong>for</strong> me.”<br />
<strong>The</strong> American Cancer<br />
Society estimates that there<br />
will be nearly 22,000 new cases<br />
<strong>of</strong> ovarian cancer this year <strong>and</strong><br />
more than 15,000 related deaths,<br />
making it the deadliest (in terms<br />
<strong>of</strong> percentages) gynecologic<br />
cancer. Ms. Miller is now<br />
dedicated to raising women’s<br />
awareness <strong>of</strong> this disease.<br />
At the end <strong>of</strong> her<br />
presentation, North Shore-<br />
LIJ Board Chairman Richard<br />
Goldstein <strong>and</strong> President <strong>and</strong><br />
Chief Executive Officer Michael<br />
Dowling presented Ms. Miller<br />
with a special white lab coat,<br />
embroidered with her name,<br />
making her an honorary member<br />
<strong>of</strong> the North Shore-LIJ faculty. Mr.<br />
Dowling also presented a special<br />
award <strong>of</strong> recognition to Ruthee-<br />
Lu Bayer, MD, director <strong>of</strong> the Don<br />
Monti Adult Hematopoietic Stem<br />
Cell Transplant Program at North<br />
Shore University Hospital, <strong>for</strong> her<br />
contributions to the care <strong>of</strong> her<br />
healthcare LITERACY<br />
Health Literacy<br />
Seminar Updates<br />
North Shore-LIJ’s health literacy <strong>and</strong> clear communication<br />
course, Can We Talk? features new components based on employee<br />
feedback. <strong>The</strong> program is available more frequently (six times this<br />
year) at the Center <strong>for</strong> Learning <strong>and</strong> Innovation <strong>and</strong> has been<br />
customized according to the participants’ scope <strong>of</strong> practice; new<br />
simulated scenarios add interactivity into the mix.<br />
To learn how to enhance written <strong>and</strong> oral communication,<br />
<strong>and</strong> how to create or choose patient-friendly written education<br />
materials, register <strong>for</strong> Can We Talk? at NorthShoreLIJ.com/cli.<br />
<strong>The</strong> Remaining 2012 course dates are:<br />
q Licensed/clinical pr<strong>of</strong>essionals — September 12<br />
q Ancillary/support staff members — July 18, November 14<br />
Call the Office <strong>of</strong> Diversity, Inclusion <strong>and</strong> Health Literacy at<br />
(516) 396-6373 <strong>for</strong> more in<strong>for</strong>mation.<br />
patients <strong>and</strong> to the unique research<br />
she is conducting to treat cancer.<br />
Earlier in the program, two<br />
local Long Isl<strong>and</strong> cancer survivors<br />
spoke eloquently about their<br />
personal battles <strong>and</strong> how they<br />
overcame the disease. <strong>The</strong>y were<br />
Judith Dowd, <strong>of</strong> Floral Park, an<br />
ovarian cancer survivor, <strong>and</strong> Lee<br />
Ielpi <strong>of</strong> Great Neck, a survivor <strong>of</strong><br />
Waldenstrom macroglobulinemia.<br />
From left are: Vincent Vinciguerra,<br />
MD, Judith Dowd, Lee Ielpi,<br />
Shannon Miller, Richard Goldstein<br />
<strong>and</strong> Michael Dowling.<br />
<strong>The</strong> New St<strong>and</strong>ard 55
NEW HYDE PARK — Samuel<br />
Kenan, MD, was always<br />
interested in fixing things, so<br />
it was no surprise that by his<br />
last year <strong>of</strong> medical school he<br />
decided to take a residency in<br />
orthopedics. But the chairman<br />
<strong>of</strong> the department at Hadassah<br />
University Medical Center,<br />
Mayer Makin, MD, had other<br />
things in mind <strong>for</strong> the young<br />
man. He recommended that he<br />
train in orthopedic oncology<br />
<strong>and</strong> spend a year working in<br />
bone pathology to underst<strong>and</strong><br />
everything he could about<br />
bone cancer.<br />
That was 1977 when<br />
fixing bone tumors meant<br />
amputation. But the chairman<br />
had hopes that Dr. Kenan<br />
would move the field into new<br />
directions that included limbsparing,<br />
life-saving surgeries.<br />
His mentor was right.<br />
Dr. Kenan finished his<br />
year-long stint at Hadassah’s<br />
pathology laboratory <strong>and</strong> completed<br />
six years <strong>of</strong> residency<br />
in orthopedic surgery at the<br />
Israeli health system be<strong>for</strong>e<br />
coming to New York <strong>for</strong> a fellowship<br />
with Michael Lewis,<br />
MD, at the Hospital <strong>for</strong> Joint<br />
Diseases. Dr. Lewis was doing<br />
precisely what the Hadassah<br />
chairman <strong>of</strong> orthopedics had<br />
envisioned: he was creating<br />
joint prosthetics made <strong>of</strong> metal<br />
<strong>and</strong> bone, <strong>and</strong> enabling pediatric<br />
cancer patients to walk<br />
out <strong>of</strong> surgery with their leg.<br />
<strong>The</strong> bone prosthetics<br />
were a major advance but the<br />
pediatric population brought<br />
new problems. Children<br />
grow, <strong>and</strong> Drs. Kenan, Lewis<br />
<strong>and</strong> others knew they had to<br />
figure out a way to get both<br />
legs to match. <strong>The</strong>y developed<br />
bone prosthetics that could<br />
56 Summer 2012<br />
Saving Lives <strong>and</strong> Limbs<br />
By Jamie Talan<br />
be exp<strong>and</strong>ed as their patients<br />
grew. It changed the field, <strong>and</strong><br />
Dr. Kenan became a fixer with<br />
a mission. “It’s hard enough<br />
that children have bone cancer,<br />
but then to tell them that they<br />
might lose a leg was just too<br />
much,” Dr. Kenan said.<br />
He began working on sparing<br />
the growth plate, even when<br />
tumors were precariously close<br />
to the plate. Saving the growth<br />
plate meant that the child’s limb<br />
would grow naturally to match<br />
the other leg.<br />
Dr. Kenan went on<br />
to head several orthopedic<br />
oncology programs, from the<br />
Hospital <strong>for</strong> Joint Diseases to<br />
Mount Sinai Medical Center<br />
<strong>and</strong> Hadassah. He was recently<br />
recruited by the North Shore-<br />
LIJ Health System to head<br />
an initiative in orthopedic<br />
oncology that <strong>of</strong>fers young<br />
patients access to a team <strong>of</strong><br />
health pr<strong>of</strong>essionals, starting<br />
from the initial suspicion that<br />
there may be something wrong,<br />
to chemotherapy, surgery <strong>and</strong><br />
lifelong care.<br />
In addition to his<br />
technical skill in the surgical<br />
suite cutting out diseased<br />
bone, crafting an implant <strong>and</strong><br />
setting the stage <strong>for</strong> healing,<br />
Dr. Kenan connects with his<br />
young patients in indelible<br />
ways. When 18-year-old<br />
Mariela Calderon <strong>of</strong> Port<br />
Washington showed up last<br />
October with osteosarcoma,<br />
Dr. Kenan called Nicole<br />
Lubin <strong>of</strong> Hempstead, a<br />
teenager who recently<br />
underwent surgery <strong>for</strong> bone<br />
cancer, <strong>and</strong> brought the girls<br />
together. While Mariela was<br />
in Cohen Children’s Medical<br />
Center (CCMC), Nicole<br />
came to visit. Watching Nicole<br />
walk ef<strong>for</strong>tlessly gave Mariela<br />
hope that someday soon her<br />
crutches would be a thing<br />
<strong>of</strong> the past, <strong>and</strong> her leg, like<br />
Mariela’s, would be spared.<br />
“Dr. Kenan is technically<br />
exceptional,” <strong>and</strong> it is the<br />
whole package <strong>of</strong> what he<br />
brings to the surgical table,<br />
said Jeffrey Lipton, MD, PhD,<br />
chief <strong>of</strong> pediatric hematology/<br />
oncology <strong>and</strong> stem cell<br />
transplantation at CCMC.<br />
“<strong>The</strong>se patients are complex,<br />
<strong>and</strong> we have teams <strong>of</strong> pr<strong>of</strong>essionals<br />
working with patients.”<br />
Dr. Kenan has per<strong>for</strong>med<br />
nearly 250 <strong>of</strong> these surgical<br />
cases in his career. And he<br />
keeps in touch with many <strong>of</strong><br />
the children, some <strong>of</strong> whom<br />
are now grown. He saves<br />
videos <strong>and</strong> photos <strong>of</strong> his young<br />
patients during all stages <strong>of</strong> the<br />
process. He pulls up a digital<br />
picture <strong>of</strong> John Browndorf,<br />
who is now 28 <strong>and</strong> taller than<br />
his doctor. Mr. Browndorf was<br />
six years old when he was diagnosed<br />
with Ewing Sarcoma.<br />
It was located in the proximal<br />
tibia. <strong>The</strong> first thought was<br />
that there would be no way<br />
to spare the growth plate; the<br />
tumor was too close. But his<br />
father, a golfer, wanted his son<br />
to walk – with both feet planted<br />
on the green – in his footsteps.<br />
“Do what you can to save<br />
the growth plate,” his father<br />
said. And Dr. Kenan listened,<br />
carrying <strong>of</strong>f the complicated<br />
surgery. Now, more than two<br />
decades later, Mr. Browndorf<br />
st<strong>and</strong>s tall. And plays golf.<br />
Mariela said that she wants<br />
to be a medical assistant when<br />
she grows up. And she looks<br />
<strong>for</strong>ward to the day when she<br />
can replace her crutches with a<br />
fancy pair <strong>of</strong> high heels.<br />
Above: Dr. Kenan with Mariela<br />
Calderon, left, <strong>and</strong> Nicole Lubin.
Parenting, Baby Care &CPR<br />
Classes<br />
Stay safe <strong>and</strong> healthy with<br />
the help <strong>of</strong> programs <strong>of</strong>fered<br />
by North Shore-LIJ’s Department<br />
<strong>of</strong> Public Health Education.<br />
To learn more, go to<br />
NorthShoreLIJ.com. Click on<br />
“Classes,” then “Community<br />
Wellness, Parenting or CPR,”<br />
or call 516-465-2500 <strong>for</strong> a<br />
brochure. Sorry, no phone<br />
registrations.<br />
LAMAZE CHILDBIRTH<br />
For expectant mothers <strong>and</strong><br />
their partners.<br />
Instruction in stages <strong>of</strong> labor,<br />
role <strong>of</strong> labor partner, relaxation<br />
<strong>and</strong> pushing techniques,<br />
hospital admission procedures,<br />
anesthesia/analgesic<br />
options, cesarean <strong>and</strong> vaginal<br />
birth after cesarean <strong>and</strong> postpartum<br />
expectations.<br />
Class includes a tour <strong>of</strong> postpartum<br />
<strong>and</strong> nursery units.<br />
Lamaze instruction must be<br />
completed two weeks prior to<br />
expected delivery date.<br />
$175 per couple<br />
Weekends: Saturday or Sunday<br />
(one session)<br />
9 a.m. to 5 p.m.<br />
Weekends: Saturday <strong>and</strong><br />
Sunday (two sessions)<br />
9:30 a.m. to 2:30 p.m.<br />
Weekdays (three sessions)<br />
7 to 10 p.m.<br />
BREAST-FEEDING I:<br />
THE BASICS<br />
Expectant mothers <strong>and</strong> their<br />
partners can learn about<br />
breast-feeding techniques,<br />
facts <strong>and</strong> myths. Bring a baby<br />
doll or stuffed animal.<br />
7 to 9:30 p.m.;<br />
$40 per person/$65 per couple<br />
BREAST-FEEDING II:<br />
BEYOND THE BASICS<br />
For expectant <strong>and</strong> new mothers<br />
<strong>and</strong> their partners. Covers<br />
bottle use, returning to work<br />
<strong>and</strong> breast pumping.<br />
7 to 9:30 p.m.; $40 per<br />
person/$65 per couple<br />
BABY CARE BASICS<br />
Expectant parents, gr<strong>and</strong>parents<br />
<strong>and</strong> childcare providers<br />
can learn about characteristics<br />
<strong>of</strong> the newborn, feeding,<br />
bathing, diapering, cord <strong>and</strong><br />
circumcision care, temperature<br />
taking, baby equipment,<br />
safety, sleep <strong>and</strong> immunization.<br />
Bring a baby doll.<br />
7 to 9:30 p.m.;<br />
$50 per person/$75 per<br />
couple<br />
BABY SAFE<br />
Topics include creating a safe<br />
home environment <strong>for</strong> baby,<br />
home emergencies <strong>and</strong> basic<br />
first aid <strong>for</strong> bleeding, burns,<br />
fractures, shock <strong>and</strong> poisoning.<br />
7 to 9 p.m.;<br />
$20 per person/$35 per couple<br />
CARDIOPULMONARY<br />
RESUSCITATION (CPR)<br />
Cardiopulmonary resuscitation<br />
(CPR ) is a technique that<br />
revives victims <strong>of</strong> cardiovascular<br />
emergencies by helping to<br />
maintain blood flow to the<br />
victim’s heart <strong>and</strong> brain.<br />
<strong>The</strong> North Shore-LIJ Health<br />
System’s awardwinning<br />
Department <strong>of</strong> Pr<strong>of</strong>essional <strong>and</strong><br />
Public Health Education <strong>of</strong>fers<br />
CPR courses tailored <strong>for</strong> babies,<br />
children <strong>and</strong> adults.<br />
Courses include instruction<br />
in CPR <strong>and</strong> <strong>for</strong>eign-body<br />
airway obstruction clearance<br />
techniques.<br />
Mets’ Murphy Visits Cohen<br />
INFANT CPR<br />
CPR <strong>for</strong> newborn to 1-yearold<br />
children.<br />
$45 per person/$75 per couple<br />
INFANT/CHILD CPR<br />
CPR <strong>for</strong> newborn to 8-yearold<br />
children.<br />
$45 per person/$75 per couple<br />
ADULT CPR<br />
Adult course includes a<br />
take-home kit with inflatable<br />
mannequin, practice DVD,<br />
American <strong>Heart</strong> Association<br />
booklet <strong>and</strong> accessories.<br />
$55 per person<br />
<strong>The</strong> Katz Womens’ Hospital<br />
in New Hyde Park <strong>of</strong>fers<br />
childbirth preparation classes,<br />
breast-feeding education, baby<br />
care programs <strong>and</strong> orientation<br />
tours <strong>of</strong> the Maternity Unit.<br />
For more in<strong>for</strong>mation, call the<br />
Parents’ Education Office at<br />
(718) 470-5134.<br />
New York Mets’ first baseman Daniel Murphy recently paid a visit to Cohen Children’s Medical Center <strong>of</strong> New<br />
York, putting a smile on the faces <strong>of</strong> children <strong>and</strong> family members as he signed baseballs <strong>and</strong> hats <strong>for</strong> Joseph<br />
Lacasse, left, <strong>and</strong> his father Joseph <strong>of</strong> Syosset, <strong>and</strong> Lucas Shannon <strong>of</strong> Williston, being held by his gr<strong>and</strong>mother.<br />
<strong>The</strong> 26-year-old Murphy hit .320 last year <strong>for</strong> the Mets, the second-highest batting average on the team.<br />
<strong>The</strong> New St<strong>and</strong>ard 57
kudos<br />
Mauricio Alarçon, analyst in the North Shore-LIJ Health<br />
System’s Office <strong>of</strong> the Chief In<strong>for</strong>mation Officer, was a member <strong>of</strong><br />
one <strong>of</strong> the winning teams, Team greatOne, which placed third in<br />
the popHealth Tool Development Challenge. <strong>The</strong> competition was<br />
launched in the fall <strong>of</strong> 2011 as part <strong>of</strong> the Office <strong>of</strong> the National<br />
Coordinator <strong>for</strong> Health In<strong>for</strong>mation Technology’s Investing in<br />
Innovation (i2) initiative.<br />
<strong>The</strong> title <strong>of</strong> Master <strong>of</strong> the American College <strong>of</strong> Physicians<br />
was bestowed on Jack Ansel, MD, chairman <strong>of</strong> the Department <strong>of</strong><br />
Medicine at Lenox Hill Hospital, in recognition <strong>of</strong> his outst<strong>and</strong>ing<br />
<strong>and</strong> extraordinary career accomplishments. He received the title at<br />
a convocation ceremony during the American College <strong>of</strong> Physicians’<br />
Annual Meeting, Internal Medicine 2012, held in New Orleans.<br />
Michael S. Aron<strong>of</strong>f, MD, a long-st<strong>and</strong>ing voluntary attending<br />
in the Department <strong>of</strong> Psychiatry at Lenox Hill Hospital <strong>and</strong> host<br />
<strong>of</strong> a two-hour interview <strong>and</strong> call-in program, <strong>The</strong> Psychiatry Show, on<br />
SiriusXM Doctor Radio, presented a paper titled “Terrorism: <strong>The</strong><br />
Ecstasy <strong>of</strong> Hatred” at the Annual Tristate American Academy <strong>of</strong><br />
Psychiatry <strong>and</strong> the Law (SSPL) Forensic Psychiatry Conference in<br />
San Juan, Puerto Rico, in December 2011.<br />
Louis-Jean Auguste, MD, a surgeon with privileges at North<br />
Shore University Hospital (NSUH) <strong>and</strong> LIJ, co-authored two<br />
abstracts accepted <strong>for</strong> publication at the Society <strong>of</strong> Surgical<br />
Oncology meeting in Orl<strong>and</strong>o, FL, this spring: “Gastric Cancer<br />
Surgery in a Low Volume Center – Are Long Term Outcomes<br />
Comparable?” <strong>and</strong> “<strong>Have</strong> Outcomes in Gastric Adenocarcinoma<br />
Improved over the Last Decade? A 20-Year Retrospective Review.”<br />
Patrick Basu, MD, chief <strong>of</strong> gastroenterology <strong>and</strong> gastrointestinal<br />
endoscopy at Forest Hills Hospital, <strong>and</strong> Sakina Farhat, MD, thirdyear<br />
medical resident, recently lectured on “Effect <strong>of</strong> Vitamin E<br />
<strong>and</strong> Alfa Lipoic Acid (ALA) in Non Alcoholic Fatty Liver Disease:<br />
A R<strong>and</strong>omized, Placebo Controlled Open Label Prospective<br />
Clinical Trial — VAIN Trial” at the Annual Scientific Meeting <strong>of</strong> the<br />
American College <strong>of</strong> Gastroenterology (ACG) in Washington, DC,<br />
<strong>and</strong> received the ACG Auxiliary Award <strong>for</strong> the best scientific paper<br />
by physicians in training or by a fellow/member <strong>of</strong> the ACG. <strong>The</strong>y<br />
also received the ACG 2011 Presidential Poster Award <strong>for</strong> “Single<br />
Use <strong>of</strong> Romilopostim Thrombopoietin Analogue (TPO) in Severe<br />
Thrombocytopenia <strong>for</strong> Outpatient Percutaneous Liver Biopsy in<br />
Patients with Chronic Liver<br />
Disease (CLD).”<br />
Catherine Blotiau,<br />
coordinator <strong>of</strong> the health system’s<br />
Department <strong>of</strong> Public Health<br />
Education <strong>and</strong> Nassau County’s<br />
58 Summer 2012<br />
Safe Kids coordinator, was one <strong>of</strong> the leaders <strong>of</strong> a “Train the<br />
Trainers” session held in Levittown in February. <strong>The</strong> trainees were<br />
16 Circle Kers, members <strong>of</strong> Circle K International, a Kiwanis<br />
service organization that is open to college <strong>and</strong> university students.<br />
<strong>The</strong> lessons included bike <strong>and</strong> helmet safety, fire safety, water safety,<br />
pedestrian safety <strong>and</strong> how to call 9-1-1.<br />
Leigh Briscoe-Dwyer, PharmD, RPh, chief pharmacy <strong>and</strong><br />
medical safety <strong>of</strong>ficer <strong>for</strong> the North Shore-LIJ Health System, has<br />
been named to the Executive Committee <strong>of</strong> the New York State<br />
Board <strong>of</strong> Pharmacy, which regulates the practice <strong>of</strong> pharmacy in<br />
the state. She is in line to chair the board in 2015.<br />
Alan Cooper, PhD, vice president <strong>of</strong> learning <strong>and</strong> innovation<br />
<strong>for</strong> the North Shore-LIJ Health System, associate dean <strong>for</strong><br />
knowledge management <strong>and</strong> associate pr<strong>of</strong>essor <strong>of</strong> science education<br />
<strong>and</strong> population health at the H<strong>of</strong>stra North Shore-LIJ School <strong>of</strong><br />
Medicine, has been named associate editor <strong>for</strong> the Leadership<br />
<strong>and</strong> Organizational Development (LOD) collection <strong>of</strong> the MedEd<br />
PORTAL <strong>of</strong> the Association <strong>of</strong> American Medical Colleges (AAMC).<br />
<strong>The</strong> LOD collection is an online repository <strong>of</strong> innovative materials<br />
pertaining to leadership development <strong>and</strong> its relationship to<br />
improved organizational per<strong>for</strong>mance.<br />
Nick Fitterman, MD, FACP, FHM, has been elected governor<br />
<strong>of</strong> the American College <strong>of</strong> Physicians (ACP) <strong>for</strong> the Long Isl<strong>and</strong><br />
Region. Dr. Fitterman, medical director <strong>of</strong> the newly established<br />
Group Health Management <strong>and</strong> <strong>for</strong>mer director <strong>of</strong> hospitalist<br />
services <strong>and</strong> chief <strong>of</strong> staff at Huntington Hospital, began a oneyear<br />
term as governor-elect in April, to be followed by a four-year<br />
term as governor.<br />
Steven Fishbane, MD, director <strong>of</strong> research in the Department<br />
<strong>of</strong> Medicine, North Shore University Hospital <strong>and</strong> LIJ Medical<br />
Center, <strong>and</strong> vice president <strong>of</strong> network dialysis services, North<br />
Shore-LIJ Health System, was elected to the Board <strong>of</strong> Directors<br />
<strong>of</strong> the Renal Physicians Association (RPA), an association <strong>of</strong><br />
5,000 nephrologists. He also serves on their Government Affairs,<br />
Anemia <strong>and</strong> Quality, Safety <strong>and</strong> Accountability Committees.<br />
Sajith Foustin, MD, <strong>and</strong> Lynn Ang, MD, medical residents<br />
at Forest Hills Hospital, presented three posters at the Annual<br />
Scientific Meeting <strong>of</strong> the ACG in Washington, DC. <strong>The</strong> posters<br />
were: “Effect <strong>of</strong> Interferon Alpha on Parathyroid Gl<strong>and</strong> in Chronic<br />
Hepatitis B <strong>and</strong> C”; “Serum Retinol<br />
Binding Protein 4 (RBP) Is a<br />
Unique Surrogate Marker <strong>of</strong> End<br />
Stage Liver Disease” <strong>and</strong> “Irritable<br />
Bladder Syndrome (IBS) Is a Part <strong>of</strong><br />
Functional Bowel Syndrome (FBS).”
Marianne Frieri, MD, PhD, attending physician in medicine<br />
<strong>and</strong> pediatrics <strong>for</strong> the North Shore-LIJ Health System, presented a<br />
symposium entitled “Update on Asthma Pathogenesis, Treatment<br />
<strong>and</strong> Airway Remodeling” at the 2012 Eastern Regional Meeting <strong>of</strong><br />
the American Federation <strong>for</strong> Medical Research in Washington, DC.<br />
Christine Ginocchio, PhD, chief <strong>of</strong> microbiology at the North<br />
Shore-LIJ Health System Core Laboratory, is pictured on the cover<br />
<strong>of</strong> the April 2012 issue <strong>of</strong> CAP Today, a publication <strong>of</strong> the College <strong>of</strong><br />
American Pathologists, <strong>and</strong> was interviewed <strong>for</strong> a feature article. She<br />
called this “an excellent time to be working in infectious diseases.”<br />
Ariel T. Goldman, MD, orthopedic traumatologist at NSUH<br />
<strong>and</strong> LIJ, was recently inducted as a fellow <strong>of</strong> the American Academy<br />
<strong>of</strong> Orthopaedic Surgeons.<br />
Gady Har-El, MD, chairman <strong>of</strong> the Department <strong>of</strong><br />
Otolaryngology-Head <strong>and</strong> Neck Surgery at Lenox Hill Hospital,<br />
was elected secretary <strong>of</strong> the American Laryngological Association<br />
(ALA), one <strong>of</strong> the oldest subspecialty organizations in the<br />
world. Dr. Har-El, who also served in the past as president <strong>of</strong><br />
the ALA’s sister society, the American Broncho-Esophagological<br />
Association, was elected during the recent ALA Annual Meeting<br />
in San Diego. He will serve a four-year term.<br />
Cynthia Harden, MD, chief <strong>of</strong> epilepsy <strong>and</strong><br />
electroencephalography at the Cushing Neuroscience Institute, has<br />
coauthored an article published in a recent issue <strong>of</strong> Neurology, the<br />
prestigious medical journal <strong>of</strong> the American Academy <strong>of</strong> Neurology<br />
(AAN). <strong>The</strong> article issues an updated guideline that recommends<br />
monitoring the spinal cord during spinal surgery <strong>and</strong> certain<br />
chest surgeries to help prevent paralysis or loss <strong>of</strong> muscle function<br />
related to the surgeries.<br />
Clarita Herrera, MD, received the 2012 Bertha Van Hoosen<br />
Award at the 97th annual meeting <strong>of</strong> the American Medical Women’s<br />
Association (AMWA) in Miami. <strong>The</strong> annual award honors a woman<br />
physician who has been an active member <strong>of</strong> the association <strong>for</strong> at<br />
least five years <strong>and</strong> who has demonstrated exceptional leadership<br />
<strong>and</strong> service to AMWA. <strong>The</strong> award is named in honor <strong>of</strong> Bertha Van<br />
Hoosen, MD, who founded AMWA in 1915.<br />
Warren Huberman, PhD, affiliate clinical psychologist<br />
in the Department <strong>of</strong> Psychiatry at Lenox Hill Hospital, has<br />
written a book titled Through Thick & Thin: <strong>The</strong> Emotional Journey <strong>of</strong><br />
Weight Loss Surgery.<br />
Employee Development Ef<strong>for</strong>ts Get Some Bling<br />
<strong>The</strong> North Shore-LIJ Health<br />
System’s investment in staff<br />
development recently received<br />
high praise from the Br<strong>and</strong>on Hall<br />
Group. <strong>The</strong> research <strong>and</strong> analysis<br />
organization recognized Corporate<br />
Human Resources’ High Potential<br />
Program with the Gold Award <strong>for</strong><br />
Excellence in Talent Management <strong>for</strong><br />
Leadership Training.<br />
In addition, the health system<br />
was designated a member <strong>of</strong> the<br />
program’s Elite 8 <strong>for</strong> superior<br />
demonstration <strong>of</strong> organizational<br />
leadership. It is the program’s highest<br />
recognition – <strong>and</strong> North Shore-LIJ<br />
was the only healthcare organization<br />
selected <strong>for</strong> it. <strong>The</strong> North Shore-LIJ<br />
High Potential Program began in 2008<br />
to identify, develop <strong>and</strong> fast-track the<br />
organization’s top per<strong>for</strong>mers. To date,<br />
the program has had 444 participants<br />
with a retention rate <strong>of</strong> 90 percent.<br />
Furthermore, North Shore-LIJ<br />
was recently named one <strong>of</strong> the 50<br />
Most Engaged Workplaces in the US<br />
by Achievers, a national organization<br />
dedicated to developing solutions<br />
to reward work<strong>for</strong>ce per<strong>for</strong>mance.<br />
<strong>The</strong> award recognizes employers that<br />
demonstrate superior leadership<br />
<strong>and</strong> innovation toward engaging<br />
employees <strong>and</strong> commitment to<br />
creating thriving work environments.<br />
Joseph Cabral, center, senior vice president <strong>and</strong> chief human resources (HR)<br />
<strong>of</strong>ficer <strong>for</strong> the health system, accepted the award at the 50 Most Engaged<br />
Workplaces Gala. Accompanying him were Lisa D’Ambruoso, left, senior specialist<br />
<strong>of</strong> HR project content; <strong>and</strong> Claudine Cangiano, senior director <strong>of</strong> HR.<br />
<strong>The</strong> New St<strong>and</strong>ard 59
kudos<br />
Andrew Jacono, MD, section head <strong>of</strong> facial plastic <strong>and</strong><br />
reconstructive surgery at NSUH, presented lectures at several<br />
national meetings, including “Minimal Access Deep Plane<br />
Extended Face Lift” <strong>and</strong> “Utilizing a New Classification <strong>of</strong><br />
Midfacial Aging to Direct Treatments in Midfacial Rejuvenation” at<br />
the American Academy <strong>of</strong> Facial Plastic <strong>and</strong> Reconstructive Surgery<br />
Nation Rejuvenation <strong>of</strong> the Aging Face Course in San Diego.<br />
Ramtin Kassir, MD, FACS, otolaryngologist <strong>and</strong> facial<br />
plastic <strong>and</strong> reconstructive surgeon at Lenox Hill Hospital, was<br />
the primary investigator <strong>for</strong> the original research report “Intense<br />
Pulsed Light <strong>for</strong> the Treatment <strong>of</strong> Rosacea <strong>and</strong> Telangiectasias,”<br />
which was recently published in the Journal <strong>of</strong> Cosmetic <strong>and</strong> Laser<br />
<strong>The</strong>rapy, as well as <strong>for</strong> “Extensive Necrosis After Injection<br />
<strong>of</strong> Hyaluronic Acid Filler: Case Report <strong>and</strong> Review <strong>of</strong> the<br />
Literature,” recently published in the Journal <strong>of</strong> Cosmetic Dermatology.<br />
In addition, in January 2012, Dr. Kassir received his third board<br />
certification, this one in sleep medicine.<br />
Seymour Katz, MD, an attending gastroenterologist at North<br />
Shore University Hospital <strong>and</strong> LIJ Medical Center, recently<br />
received the 2011 Distinguished Physician Lifetime Achievement<br />
Award from the Crohn’s <strong>and</strong> Colitis Foundation <strong>of</strong> America <strong>for</strong><br />
his contributions to the management <strong>of</strong> patients with inflamma-<br />
Elaine Smith Is National Finalist<br />
In Nursing Spectrum Competition<br />
At the Nursing Spectrum gala in Teaneck, NJ, in<br />
June, it was announced that Elaine Smith, RN, MSN,<br />
North Shore-LIJ’s vice president <strong>for</strong> nursing education,<br />
is a regional winner <strong>and</strong> has moved on to the national<br />
level in the 2012 Nursing Spectrum Nursing Excellence<br />
competition. <strong>The</strong> national winners will be announced in<br />
the fall. Ms. Smith was a regional finalist in the Education &<br />
Mentoring category; three other regional finalists representing the North<br />
Shore-LIJ Nursing Leadership team were Lily Thomas, RN, the health system’s<br />
vice president <strong>for</strong> nursing research <strong>and</strong> evidence-based practice, <strong>and</strong> Cari<br />
Quinn, RN, MSN, associate executive director <strong>for</strong> patient care services at<br />
Cohen Children’s Medical Center (CCMC), both in the Advancing & Leading<br />
the Pr<strong>of</strong>ession category, <strong>and</strong> Lory Tortelli, BSN, RN, director <strong>of</strong> patient<br />
care services at North Shore-LIJ’s Goldman Diagnostic Imaging Center, in<br />
Community & Ambulatory Care.<br />
60 Spring 2012<br />
tory bowel disease <strong>and</strong> the education <strong>of</strong> physicians on the subject.<br />
He also delivered the keynote address at the annual meeting <strong>of</strong> the<br />
American College <strong>of</strong> Gastroenterology <strong>and</strong> received the Edward J.<br />
Berk Distinguished Lecturer Award.<br />
Andrew Roberts, director <strong>of</strong> the North Shore-LIJ Health<br />
System’s Office <strong>of</strong> Military <strong>and</strong> <strong>Veterans</strong> Liaison Services,<br />
administrator <strong>of</strong> the Rosen Family Wellness Center <strong>and</strong> project<br />
director <strong>for</strong> the soon-to-be-opened Unified Family Behavioral<br />
Health Center, a joint endeavor with the US Department <strong>of</strong><br />
<strong>Veterans</strong> Affairs, has been appointed to the New York State<br />
Council on Returning <strong>Veterans</strong> <strong>and</strong> <strong>The</strong>ir Families. <strong>The</strong> Rosen<br />
Center has been providing no-cost behavioral healthcare to law<br />
en<strong>for</strong>cement, military, veterans <strong>and</strong> their families since 2006<br />
<strong>and</strong> the Unified Family Behavioral Health Center will provide<br />
collaborative services to veterans <strong>and</strong> their families. He has also<br />
been appointed to the New York Community Trust <strong>Veterans</strong> Fund<br />
Advisory Committee, comprising representatives from public<br />
agencies, nonpr<strong>of</strong>it organizations <strong>and</strong> veterans’ advocates, which<br />
assesses the status <strong>of</strong> veterans’ services, determines where private<br />
dollars can be most useful <strong>and</strong> develops grant strategies.<br />
José A. Rodriguez, MD, orthopedic surgeon <strong>and</strong> section chief <strong>of</strong><br />
adult reconstruction at Lenox Hill Hospital, recently cowrote “Long-<br />
Term Results <strong>of</strong> Arthroscopic Labral Debridement: Predictors <strong>of</strong><br />
Outcomes” <strong>for</strong> Orthopedics. He was also a podium co-presenter at the<br />
Eastern Orthopedic Association 2011 Annual Meeting in Kingsmill,<br />
VA. <strong>The</strong> topics included: “Fixation <strong>of</strong> Unstable Intertrochanteric<br />
Fractures in Internal Rotation: An Important Predictor <strong>of</strong> Fracture<br />
Union,” “Metaphyseal Sleeves in Revision TKA with Bone Loss –<br />
Does Cementation <strong>Have</strong> a Role?” <strong>and</strong> “Sexual Function Be<strong>for</strong>e <strong>and</strong><br />
After Primary Total Hip <strong>and</strong> Knee Arthroplasty.”<br />
Elise M. Ross, the Hospice Care Network’s vice president<br />
<strong>for</strong> human resources, received the Joseph C. Duffy Lifetime<br />
Achievement Award from the Society <strong>of</strong> Human Resource<br />
Management’s Long Isl<strong>and</strong> Chapter.<br />
Jesse Roth, MD, diabetes researcher at <strong>The</strong> Feinstein Institute<br />
<strong>for</strong> Medical Research, was presented with an honorary doctoral<br />
degree by Ben-Gurion University <strong>of</strong> the Negev at the 42nd Board<br />
<strong>of</strong> Governors Meeting held recently in Beer-Sheva, Israel. Dr.<br />
Roth is pr<strong>of</strong>essor <strong>of</strong> medicine at the H<strong>of</strong>stra North Shore-LIJ<br />
School <strong>of</strong> Medicine. He is also a pr<strong>of</strong>essor at the Elmezzi Graduate<br />
School <strong>of</strong> Molecular Medicine, <strong>and</strong> an investigator at the Laboratory<br />
<strong>of</strong> Diabetes & Metabolic Disorders, both <strong>of</strong> which operate in<br />
collaboration with the Feinstein.
Carlos E. Ruiz, MD, PhD, director <strong>of</strong> the structural<br />
<strong>and</strong> congenital heart disease program <strong>of</strong> the Department <strong>of</strong><br />
Interventional Cardiology at Lenox Hill Hospital, recently wrote<br />
“Optimizing Transcatheter Aortic Valve Sizing <strong>and</strong> Minimizing<br />
Vascular Complications,” <strong>and</strong> cowrote “Percutaneous Closure<br />
<strong>of</strong> Periprosthetic Paravalvular Leaks,” “Clinical Outcomes in<br />
Patients Undergoing Percutaneous Closure <strong>of</strong> Periprosthetic<br />
Paravalvular Leaks” <strong>and</strong> “Clinical Experience with Percutaneous<br />
Left Ventricular Transapical Access <strong>for</strong> Interventions in Structural<br />
<strong>Heart</strong> Defects: A Safe Access <strong>and</strong> Secure Exit” <strong>for</strong> the Journal <strong>of</strong> the<br />
American College <strong>of</strong> Cardiology. In addition, he coauthored “Vacuum<br />
Thrombectomy <strong>of</strong> Large Right Atrial Thrombus” <strong>for</strong> Catheterization<br />
Cardiovascular Interventions, “Percutaneous Mitral Valve Treatment” <strong>for</strong><br />
Minerva Cardiologica, <strong>and</strong> “Use <strong>of</strong> Multi-Modality Imaging in a Patient<br />
with a Persistent Left Superior Vena Cava, Partial Anomalous<br />
Pulmonary Venous Connection, <strong>and</strong> Sinus Venosus-Type Atrial<br />
Septal Defect” <strong>for</strong> the European <strong>Heart</strong> Journal.<br />
Neil Sanghvi, MD, cardiologist <strong>and</strong> cardiac electrophysiologist<br />
at Lenox Hill Hospital, recently wrote “Mechanisms <strong>and</strong> Application<br />
<strong>of</strong> Cardiac Cryoablation” <strong>for</strong> EP Lab Digest.<br />
Giles R. Scuderi, MD, vice president <strong>of</strong> orthopedic services<br />
<strong>for</strong> the North Shore-LIJ Health System, coauthored several<br />
chapters <strong>of</strong> the 2012 edition <strong>of</strong> the textbook Surgery <strong>of</strong> the Knee.<br />
<strong>The</strong>se include “Surgical Approaches in Total Knee Arthroplasty,”<br />
“Posterior Cruciate Ligament Substituting Total Knee Arthroplasty,”<br />
“Complications <strong>of</strong> Total Knee Arthroplasty” <strong>and</strong> “Revision <strong>of</strong><br />
Aseptic Failed Total Knee Arthroplasty.” Dr. Scuderi <strong>and</strong><br />
Nicholas A. Sgaglione, MD, chair <strong>of</strong> orthopedic surgery at<br />
NSUH <strong>and</strong> LIJ, were recently named to the “125 Outst<strong>and</strong>ing<br />
Knee Surgeons” list published by Becker’s Orthopedic, Spine & Pain<br />
Management Review.<br />
Michael Setzen, MD, FACS, FAAP, chief <strong>of</strong> rhinology at NSUH,<br />
recently served as program organizer <strong>and</strong> scientific chairman <strong>for</strong><br />
the December 2011 meeting <strong>of</strong> the American College <strong>of</strong> Surgeons,<br />
co-sponsored by the Nassau Surgical Society <strong>and</strong> the Brooklyn<br />
Long Isl<strong>and</strong> Chapter. <strong>The</strong> keynote speaker was Mike Francesa <strong>of</strong><br />
WFAN’s “Mike <strong>and</strong> the Mad Dog” <strong>and</strong> “Miked Up” programs. This<br />
year’s attendance set a record <strong>of</strong><br />
510 surgeons, many from the<br />
North Shore-LIJ Health System.<br />
Terence Smith, administrator<br />
<strong>of</strong> Huntington Hospital’s<br />
Dolan Family Health Center, was<br />
Kanti Rai, MD,<br />
Receives ASCO Award<br />
Kanti R. Rai, MD, BS, one <strong>of</strong> the Special Awards<br />
Honorees <strong>of</strong> the American Society <strong>for</strong> Clinical Oncology, is the<br />
recipient <strong>of</strong> the 2012 David A. Karn<strong>of</strong>sky Memorial Award <strong>and</strong><br />
Lecture <strong>for</strong> his outst<strong>and</strong>ing achievements in<br />
cancer research <strong>and</strong> <strong>for</strong> his influence on the<br />
treatment <strong>of</strong> patients with cancer. Dr. Rai is<br />
chief <strong>of</strong> the North Shore-LIJ Health System’s<br />
Chronic Lymphocytic Leukemia Research <strong>and</strong><br />
Treatment Program <strong>and</strong> the Joel Finkelstein<br />
Cancer Foundation Pr<strong>of</strong>essor <strong>of</strong> Medicine at<br />
the H<strong>of</strong>stra North Shore-LIJ School <strong>of</strong> Medicine, where he<br />
also holds the title <strong>of</strong> pr<strong>of</strong>essor <strong>of</strong> molecular medicine. As an<br />
investigator with <strong>The</strong> Feinstein Institute <strong>for</strong> Medical Research,<br />
Dr. Rai is known <strong>for</strong> establishing the Rai clinical staging system<br />
<strong>for</strong> chronic lymphocytic leukemia (CLL), which is based on an<br />
analysis <strong>of</strong> how the body is affected by the abnormal lymphocytes.<br />
Giles Scuderi, MD,<br />
Knee Society President<br />
Giles R. Scuderi, MD, vice president <strong>of</strong> orthopedic<br />
services <strong>for</strong> the North Shore-LIJ Health System <strong>and</strong> an<br />
attending at Franklin <strong>and</strong> Lenox Hill Hospitals, was recently<br />
appointed president <strong>of</strong> <strong>The</strong> Knee Society at its Open Meeting<br />
in San Francisco. <strong>The</strong> Knee Society, founded<br />
in 1983, is a closed-membership organization<br />
<strong>of</strong> orthopedic surgeons specializing in<br />
treatment <strong>of</strong> the knee joint. Dr. Scuderi has<br />
served on the society’s executive board <strong>for</strong> the<br />
last decade in numerous leadership positions.<br />
He also chaired the Society’s Research<br />
Committee <strong>and</strong> plays an instrumental role in the development<br />
<strong>and</strong> worldwide distribution <strong>of</strong> <strong>The</strong> 2011 Knee Society Scoring<br />
System © , a universally recognized outcomes measurement tool.<br />
one <strong>of</strong> the honorees at the Leadership Huntington gala <strong>and</strong> graduation<br />
<strong>of</strong> the class <strong>of</strong> 2012 in April, receiving the Community Leadership<br />
Award. He is described by Leadership Huntington as a “passionate<br />
advocate <strong>for</strong> af<strong>for</strong>dable community healthcare.” <strong>The</strong> Dolan<br />
Family Health Center opened its doors in October 1995 as Long<br />
Isl<strong>and</strong>’s only privately owned, charitably supported, free-st<strong>and</strong>ing<br />
facility dedicated to providing primary <strong>and</strong> preventive healthcare to<br />
uninsured <strong>and</strong> underinsured families.<br />
<strong>The</strong> New St<strong>and</strong>ard 61
kudos<br />
Donald Tanenbaum, DDS, section head <strong>of</strong> the Division <strong>of</strong><br />
Or<strong>of</strong>acial Pain/TMD/Dental Sleep Medicine in the Department<br />
<strong>of</strong> Dental Medicine at LIJ <strong>and</strong> clinical assistant pr<strong>of</strong>essor at the<br />
H<strong>of</strong>stra North Shore-LIJ School <strong>of</strong> Medicine, has written a new<br />
book, Doctor, Why Does My Face Still Ache?, which provides in<strong>for</strong>mation<br />
<strong>and</strong> solutions <strong>for</strong> the 75 million Americans suffering intense ear,<br />
teeth <strong>and</strong> jaw pain, which can also cause severe headaches, loud<br />
snoring <strong>and</strong> sleep problems.<br />
A research study led by Lily Thomas, RN, North Shore-LIJ<br />
vice president <strong>for</strong> nursing research <strong>and</strong> evidence-based practice,<br />
which was conducted at NSUH, is the basis <strong>for</strong> an article that<br />
appeared recently in the American Journal <strong>of</strong> Hospice <strong>and</strong> Palliative Care<br />
Nursing. Kathy Trombley, RN, <strong>and</strong> Mary Brennan, RN, <strong>of</strong> NSUH,<br />
brought to Ms. Thomas’s attention their observations that patients<br />
in the Palliative Care Unit developed what appeared to be pressure<br />
injuries within hours or days <strong>of</strong> their death, <strong>and</strong> she helped<br />
them design the study. Discovery <strong>of</strong> what has been named the<br />
Trombley-Brennan pressure injury is a major breakthrough in<br />
underst<strong>and</strong>ing pressure injuries.<br />
Kevin J. Tracey, MD, president <strong>of</strong> <strong>The</strong> Feinstein Institute <strong>for</strong><br />
Medical Research, was inducted into the Long Isl<strong>and</strong> Technology<br />
Hall <strong>of</strong> Fame (LITHF) in May. He was selected <strong>for</strong> his personal<br />
accomplishments <strong>and</strong> the accomplishments <strong>of</strong> researchers at the<br />
Feinstein Institute. “I’m honored to be inducted into the Long<br />
Isl<strong>and</strong> Technology Hall <strong>of</strong> Fame <strong>and</strong> am proud <strong>of</strong> the research<br />
conducted at the Feinstein Institute,” said Dr. Tracey. “We work<br />
every day at the Feinstein to study disease so that we can cure<br />
disease, <strong>and</strong> this kind <strong>of</strong> recognition is very much appreciated.”<br />
Sung K. Min, chair <strong>of</strong> the board <strong>of</strong> directors <strong>of</strong> the Korean-<br />
American Association <strong>of</strong> Greater New York (KAAGNY), recently<br />
presented Mark Solazzo, executive vice president <strong>and</strong> chief operating<br />
<strong>of</strong>ficer <strong>of</strong> the North Shore-LIJ Health System, with an appreciation<br />
award in recognition <strong>of</strong> the health system’s support <strong>of</strong> KAAGNY’s<br />
recent gala celebrating its 52nd anniversary. In addition, KAAGNY<br />
presented Emily Kao, RPh, associate executive director at North<br />
Shore University Hospital, with its Person <strong>of</strong> the Year Award.<br />
Adrianna Vlachos, MD, a pediatric oncologist/hematologist<br />
at Cohen Children’s Medical Center (CCMC), <strong>and</strong> Jeffrey M.<br />
Lipton, MD, PhD, chief <strong>of</strong> hematology/oncology at CCMC <strong>and</strong><br />
head <strong>of</strong> the Feinstein Institute’s Susan & Herman Merin<strong>of</strong>f Center<br />
<strong>for</strong> Patient-Oriented Research, were among the coauthors <strong>of</strong><br />
“Cancer Surveillance Defines Diamond Blackfan Anemia (DBA)<br />
62 Summer 2012<br />
As a Cancer Predisposition Syndrome,” which received the award<br />
<strong>for</strong> best abstract in the general category <strong>of</strong> epidemiology at the 2nd<br />
National Conference on Blood Disorders in Public Health held in<br />
March in Atlanta.<br />
Robert Waldbaum, MD, has received a 50-year citation from<br />
the Nassau County Medical Society. Dr. Waldbaum is chairman<br />
emeritus <strong>of</strong> urology at North Shore University Hospital, where he<br />
was the hospital’s first chairman <strong>of</strong> urology <strong>and</strong> served as director<br />
<strong>of</strong> urology <strong>for</strong> more than 30 years.<br />
Bruce Zagelbaum, MD, FACS, has co-authored a book chapter<br />
in the ophthalmology textbook series Duane’s Clinical Ophthalmology,<br />
published by Lippincott Williams & Wilkins. <strong>The</strong> chapter is<br />
titled “Surgical Management<br />
<strong>of</strong> Anterior Segment Trauma.”<br />
Another book coauthored by<br />
Dr. Zagelbaum, Ophthalmic Surgical<br />
Procedures, was recently published<br />
in a Portuguese language<br />
translation.<br />
Eli Cometh<br />
Super Bowl champion New York Giants’ quarterback Eli Manning was the<br />
keynote speaker at North Shore University Hospital’s Medical Staff Society<br />
Annual Meeting May 14 at the Garden City Hotel. Among those welcoming him<br />
were Carole Moodhe, MD, right, the medical staff society’s president. State<br />
Health Commissioner Nirav Shah, MD, also addressed the packed house.
Project Sunshine<br />
Honors Michael Dowling<br />
Michael Dowling, president <strong>and</strong> CEO <strong>of</strong> the North Shore-LIJ Health System (left),<br />
was the honoree at the recent benefit celebration <strong>of</strong> Project Sunshine, held at<br />
Cipriani Wall Street in Manhattan. Project Sunshine is a nonpr<strong>of</strong>it organization<br />
that provides free educational, recreational <strong>and</strong> social programs to children <strong>and</strong><br />
families living with medical challenges. Pictured with Mr. Dowling is Bernard<br />
Ros<strong>of</strong>, MD, chair <strong>of</strong> the Board <strong>of</strong> Directors <strong>of</strong> Huntington Hospital <strong>and</strong> a member <strong>of</strong><br />
the Executive Committee <strong>of</strong> the North Shore-LIJ Health System Board <strong>of</strong> Trustees.<br />
NEW HYDE PARK — For<br />
the sixth consecutive year, the<br />
Steven <strong>and</strong> Alex<strong>and</strong>ra Cohen<br />
Children’s Medical Center <strong>of</strong><br />
New York (CCMC) has been<br />
ranked among the best children’s<br />
hospitals in the nation in US<br />
News & World Report’s 2012-13<br />
“America’s Best Children’s<br />
Hospitals” survey.<br />
CCMC placed among<br />
the top 50 hospitals in seven<br />
different pediatric specialty<br />
areas surveyed in the magazine’s<br />
annual rankings, specifically:<br />
cancer, diabetes <strong>and</strong><br />
endocrinology; neonatalogy;<br />
nephrology; neurology <strong>and</strong><br />
neurosurgery; pulmonology<br />
<strong>and</strong> urology. <strong>The</strong> hospital was<br />
ranked 16th in the nation <strong>for</strong><br />
pediatric urology, its highest<br />
placement in the survey.<br />
<strong>The</strong> U.S. News Rankings<br />
are based on a hospital’s<br />
reputation, medical outcomes<br />
such as death <strong>and</strong> infection<br />
rates, <strong>and</strong> care-related<br />
New MPH Program<br />
at H<strong>of</strong>stra<br />
HEMPSTEAD — In collaboration with the North Shore-LIJ Health System <strong>and</strong> the<br />
H<strong>of</strong>stra-North Shore LIJ School <strong>of</strong> Medicine, H<strong>of</strong>stra University has created a<br />
Master <strong>of</strong> Public Health (MPH) program scheduled to begin September 4.<br />
H<strong>of</strong>stra is accepting applications <strong>and</strong> enrolling students through mid-<br />
August. <strong>The</strong> MPH program <strong>of</strong>fers an innovative, interdisciplinary curriculum <strong>and</strong><br />
advanced training <strong>for</strong> the next generation <strong>of</strong> health pr<strong>of</strong>essionals. <strong>The</strong> faculty<br />
includes clinicians, practitioners, researchers, policymakers <strong>and</strong> policy analysts<br />
from H<strong>of</strong>stra’s programs in health pr<strong>of</strong>essions, the North Shore-LIJ Health<br />
System <strong>and</strong> the medical school. <strong>The</strong>ir combined decades <strong>of</strong> experience provide<br />
students with a strong academic foundation <strong>and</strong> the practical preparation<br />
necessary to meet the challenges <strong>of</strong> increasingly complex <strong>and</strong> changing health<br />
care policy re<strong>for</strong>ms.<br />
Advanced training in public health enables healthcare pr<strong>of</strong>essionals to<br />
identify risks to health <strong>and</strong> prevention strategies <strong>and</strong> interventions earlier in<br />
the disease process, leading to a more efficient <strong>and</strong> effective health system.<br />
<strong>The</strong> program is designed to accommodate full-time pr<strong>of</strong>essionals, <strong>and</strong> can be<br />
completed on a part-time basis in less than three years. For more in<strong>for</strong>mation<br />
about this dynamic new program go to www.h<strong>of</strong>stra.edu/publichealth or contact<br />
H<strong>of</strong>stra University’s Office <strong>of</strong> Graduate Admissions at www.h<strong>of</strong>stra.edu/graduate<br />
or 1-866 -GRADHOF.<br />
US News Ranks Cohen Among America’s Best<br />
Children’s Hospitals <strong>for</strong> Sixth Straight Year<br />
indicators such as patient<br />
volume, nurse staffing <strong>and</strong><br />
availability <strong>of</strong> specialized<br />
programs. <strong>The</strong> magazine’s<br />
“Best Children’s Hospitals”<br />
edition is accessible online<br />
at www.usnews.com/<br />
childrenshospitals.<br />
“<strong>The</strong> US News & World Report<br />
rankings provide unparalleled,<br />
quality-related in<strong>for</strong>mation<br />
<strong>and</strong> serve as an invaluable<br />
guide <strong>for</strong> parents looking<br />
to make decisions regarding<br />
high quality healthcare <strong>for</strong><br />
their children,” said Kevin<br />
McGeachy, CCMC’s executive<br />
director. “Being ranked <strong>for</strong><br />
six straight years as one <strong>of</strong><br />
the nation’s best pediatric<br />
hospitals is testament to the<br />
excellent care provided by our<br />
physicians <strong>and</strong> nurses. It is<br />
one <strong>of</strong> the reasons the Cohen<br />
Children’s Medical Center<br />
is a destination hospital <strong>for</strong><br />
children from around the<br />
world.”<br />
<strong>The</strong> New St<strong>and</strong>ard 63
Franklin to Exp<strong>and</strong> Care to JFK<br />
VALLEY STREAM — Franklin Hospital<br />
is providing additional around-theclock<br />
healthcare services <strong>for</strong> JFK<br />
International Airport staff <strong>and</strong> patrons,<br />
as part <strong>of</strong> a new clinical affiliation<br />
agreement with Airport Medical Offices<br />
(AMO). <strong>The</strong> agreement enhances the<br />
services provided by AMO by <strong>of</strong>fering<br />
airport employees <strong>and</strong> patrons an<br />
additional treatment site <strong>and</strong> greater<br />
access to care — including inpatient,<br />
outpatient <strong>and</strong> emergency services —<br />
at Franklin Hospital, a short distance<br />
from the airport.<br />
In case patients require<br />
specialized treatment, they will<br />
now have 24/7 access to the full<br />
Photo courtesy <strong>of</strong> NYRR<br />
64 Summer 2012<br />
range <strong>of</strong> services <strong>of</strong>fered by<br />
Franklin Hospital <strong>and</strong> the North<br />
Shore LIJ Health System, including:<br />
cancer care, cardiology, wound<br />
care, neurology, orthopedics, pain<br />
management, psychiatry, radiology,<br />
rehabilitation <strong>and</strong> surgery. Franklin<br />
<strong>and</strong> AMO will also partner to provide<br />
preventive care, health <strong>and</strong> wellness<br />
in<strong>for</strong>mation <strong>and</strong> screenings at the<br />
airport <strong>and</strong> local venues. “We are<br />
pleased to partner with AMO to bring<br />
a comprehensive array <strong>of</strong> specialty<br />
care to those who work <strong>and</strong> live in<br />
<strong>and</strong> around our shared communities,”<br />
said Catherine Hottendorf, RN,<br />
new executive director <strong>of</strong> Franklin<br />
Hospital. “Our physicians, nurses<br />
<strong>and</strong> clinical <strong>and</strong> administrative staff<br />
are looking <strong>for</strong>ward to providing<br />
high-quality, compassionate care to<br />
AMO patients.”<br />
AMO caters to the healthcare<br />
needs <strong>of</strong> employees, travelers <strong>and</strong><br />
those that reside in the surrounding<br />
communities. <strong>The</strong> program provides<br />
a full range <strong>of</strong> healthcare services,<br />
including all aspects <strong>of</strong> occupational<br />
health <strong>and</strong> medical treatment <strong>for</strong><br />
accidents, injuries <strong>and</strong> illnesses<br />
in the workplace, primary care,<br />
internal medicine, family practice<br />
<strong>and</strong> urgent care, <strong>and</strong> AMO clinicians<br />
will also become credentialed to care<br />
Health System<br />
Helps Kick Off<br />
City Parks Event<br />
Staff from Lenox Hill Hospital, the<br />
Manhattan Eye, Ear <strong>and</strong> Throat<br />
Hospital (MEETH) <strong>and</strong> the North<br />
Shore-LIJ Health System were out<br />
in <strong>for</strong>ce in April during the City<br />
Parks Foundation’s annual Run<br />
<strong>for</strong> the Parks in Central Park. <strong>The</strong><br />
four-mile race, sponsored by North<br />
Shore-LIJ, which kicked <strong>of</strong>f the<br />
running season in New York City,<br />
has the distinction <strong>of</strong> being the<br />
largest one-day running event in<br />
Central Park. <strong>The</strong>re was also a kids’<br />
race (top). Lenox Hill <strong>and</strong> MEETH<br />
staff provided free blood pressure<br />
screenings <strong>and</strong> pocket-sized<br />
sunscreen to the more than 7,000<br />
runners who turned out <strong>and</strong> other<br />
participants. In the bottom photo,<br />
Jennifer Mieres, MD, left, senior<br />
vice president <strong>of</strong> North Shore-LIJ’s<br />
Office <strong>of</strong> Community <strong>and</strong> Public<br />
Health, greeted the race’s overall<br />
winner, Ro Crispin, <strong>of</strong> Clifton,<br />
NJ, who burned up the course in<br />
20:26 – a 5:07 pace.<br />
<strong>for</strong> patients at Franklin Hospital.<br />
Patients are welcome 24 hours a<br />
day, seven days a week <strong>and</strong> Airport<br />
Medical participates with most major<br />
insurance plans.<br />
“<strong>The</strong> affiliation with Franklin<br />
Hospital provides our patients<br />
with access to the highest levels <strong>of</strong><br />
specialty care available,” said Thomas<br />
D. Kelliher, Esq., executive director<br />
<strong>of</strong> AMO. “We are proud to work with<br />
such a top-notch team <strong>of</strong> healthcare<br />
pr<strong>of</strong>essionals <strong>and</strong> happy to advance<br />
our mission to provide timely access<br />
to exceptional healthcare, coupled<br />
with extraordinary convenience, to<br />
our patients.”
life SAVER<br />
Employee<br />
Blood Drives<br />
7/10 Franklin Hospital<br />
7/11 Glen Cove Hospital<br />
7/11 SIUH South<br />
7/12 Plainview Hospital<br />
7/17 NSUH<br />
7/17 SIUH North<br />
7/18 NSUH<br />
JULY<br />
7/19 Center <strong>for</strong> Advanced Medicine<br />
(CFAM)<br />
7/19 Administrative Offices-<br />
Westbury<br />
7/25 SIUH Pouch<br />
7/27 Corporate Offices-<br />
Lake Success<br />
8/8 SIUH North<br />
8/15 Physician <strong>and</strong> Ambulatory<br />
AUGUST<br />
Network Services (PAANS)<br />
8/15 SIUH South<br />
8/23 Southside Hospital<br />
8/24 Forest Hills Hospital<br />
Lenox Hill Auxiliary Hosts Luncheon<br />
Holly Phillips, MD, <strong>of</strong> CBS “This Morning,” was the moderator at Lenox Hill Hospital’s annual A Healthy Give &<br />
Take luncheon, held in April at the New York Historical Society <strong>and</strong> hosted by the hospital’s Auxiliary. Now in<br />
its fourteenth year, the luncheon was attended by over 225 people; this year’s theme was “Stents, Statins <strong>and</strong><br />
Supplements…Oh My.” <strong>The</strong> program focused on advances being made in cardiac <strong>and</strong> vascular medicine, with an<br />
expert panel <strong>of</strong> hospital physicians discussing steps we can take to promote good health. Above, from left, are<br />
panel members Maja Zaric, MD, Tara Narula, MD, <strong>and</strong> Lara Oboler, MD, with moderator Holly Phillips.<br />
North Shore-LIJ: A Great Place to Work<br />
Becker’s Hospital Review <strong>and</strong> Becker’s ASC Review have again selected the North Shore-LIJ Health<br />
System as one <strong>of</strong> the 100 Great Places to Work in Healthcare. Making the list <strong>for</strong> the second<br />
consecutive year, North Shore-LIJ was chosen <strong>for</strong> its “demonstrated excellence in providing<br />
robust benefits, wellness initiatives, pr<strong>of</strong>essional development opportunities <strong>and</strong> atmospheres<br />
<strong>of</strong> employee unity <strong>and</strong> satisfaction.”<br />
Several factors earned North Shore-LIJ a spot on the list, including:<br />
o the opening <strong>of</strong> the new H<strong>of</strong>stra North Shore-LIJ School <strong>of</strong> Medicine;<br />
o pr<strong>of</strong>essional development courses <strong>of</strong>fered through the health system’s Center <strong>for</strong><br />
Learning <strong>and</strong> Innovation;<br />
o extensive tuition reimbursement <strong>for</strong> advanced college degrees, including a master’s<br />
program in healthcare or quality management at H<strong>of</strong>stra University, as well as a nursing<br />
doctorate program;<br />
o programs to identify, develop <strong>and</strong> fast-track its top per<strong>for</strong>mers;<br />
o a wellness program that <strong>of</strong>fers Zumba, yoga, guided imagery, meditation, nutrition <strong>and</strong><br />
other fitness classes to employees; <strong>and</strong><br />
o the introduction <strong>of</strong> a new “CEO Chat” in which President <strong>and</strong> CEO Michael Dowling<br />
addresses the work<strong>for</strong>ce.<br />
To see a full list, go to: www.beckershospitalreview.com <strong>and</strong> type “best workplaces” in the search.<br />
<strong>The</strong> New St<strong>and</strong>ard 65
Hospital <strong>and</strong> Clinical Leadership Changes<br />
North Shore-LIJ President <strong>and</strong> Chief Executive Officer Michael<br />
Dowling <strong>and</strong> Chief Operating Officer Mark Solazzo recently<br />
announced the following changes to the health system’s hospital<br />
<strong>and</strong> clinical leadership teams:<br />
Winifred Mack, RN, BSN, has been<br />
named regional executive director <strong>for</strong> the<br />
health system’s Eastern Region, which<br />
includes Franklin, Huntington, Plainview,<br />
Southside <strong>and</strong> Syosset Hospitals. Ms.<br />
Mack’s responsibilities include coordinating<br />
activities within the region to focus on<br />
building physician partnerships <strong>and</strong> looking<br />
<strong>for</strong> new opportunities <strong>for</strong> growth <strong>and</strong> investment.<br />
She succeeds Deborah Tascone, RN, who resigned in March <strong>for</strong><br />
health reasons.<br />
Donna Moravick, NP, succeeds Winnie Mack<br />
as executive director <strong>of</strong> Southside Hospital.<br />
She is responsible <strong>for</strong> oversight <strong>of</strong> the hospital<br />
<strong>and</strong> works closely with members <strong>of</strong> Southside’s<br />
management team <strong>and</strong> Ms. Mack as the<br />
regional executive director.<br />
William O’Connell, RN, succeeds Donna<br />
Moravick as vice president <strong>for</strong> North Shore-<br />
LIJ’s cardiac service line, with oversight <strong>for</strong><br />
daily operations <strong>of</strong> cardiac services at our<br />
tertiary hospitals, community hospitals <strong>and</strong><br />
ambulatory sites. Mr. O’Connell is also<br />
responsible <strong>for</strong> the service line’s financial<br />
<strong>and</strong> operational per<strong>for</strong>mance, <strong>and</strong> works with<br />
senior administrators <strong>and</strong> physicians developing<br />
strategic business plans <strong>and</strong> new programs.<br />
Joseph Manopella has been named vice<br />
president <strong>of</strong> Physician <strong>and</strong> Ambulatory<br />
Network Services (PAANS) regional strategy<br />
<strong>and</strong> business development. He is responsible<br />
<strong>for</strong> creating regional physician strategy,<br />
working with Deborah Schiff, PAANS’ vice<br />
president <strong>of</strong> strategy <strong>and</strong> business development.<br />
Catherine Hottendorf, RN, succeeds<br />
Joe Manopella as executive director <strong>of</strong><br />
Franklin Hospital. She oversees day-today<br />
administration <strong>of</strong> the hospital <strong>and</strong> is<br />
responsible <strong>for</strong> finance, operations, quality,<br />
patient satisfaction <strong>and</strong> staff per<strong>for</strong>mance.<br />
66 Summer 2012<br />
Patricia Farrell, RN, succeeds Cathy<br />
Hottendorf as associate executive director<br />
<strong>of</strong> patient care services at Southside. As<br />
the hospital’s chief nursing <strong>of</strong>ficer, she has<br />
oversight <strong>for</strong> all nursing services, including<br />
strategic planning, budget management <strong>and</strong><br />
regulatory compliance.<br />
Eileen Lovett, currently the vice president<br />
<strong>of</strong> ambulatory services at PAANS at Lenox<br />
Hill Hospital, has been named vice<br />
president <strong>of</strong> physician administration at<br />
Staten Isl<strong>and</strong> University Hospital. She has<br />
oversight <strong>for</strong> SIUH physician relations.<br />
Joseph Baglio, currently the deputy<br />
executive director at Plainview Hospital, has<br />
been appointed assistant vice president <strong>of</strong><br />
physician administration at Lenox Hill<br />
Hospital, succeeding Eileen Lovett. He<br />
is responsible <strong>for</strong> managing day-to-day<br />
physician partnerships <strong>and</strong> relationships<br />
with the hospital’s faculty.<br />
Ann Roderick, RN, currently the assistant<br />
director <strong>of</strong> cardiology services at LIJ Medical<br />
Center, has been appointed director <strong>of</strong><br />
cardiac services at LIJ Medical Center,<br />
succeeding Pat Farrell. In this role, she<br />
is responsible <strong>for</strong> patient care, business<br />
development, clinical management, finance<br />
<strong>and</strong> quality management <strong>for</strong> the hospital’s<br />
cardiac services.<br />
Cathy Devlin, RN, currently the associate executive director<br />
at Southside, has been named assistant vice president <strong>of</strong><br />
perioperative services <strong>for</strong> the health system. She assists in the<br />
development, coordination <strong>and</strong> administration <strong>of</strong> perioperative<br />
services; has oversight <strong>for</strong> related in<strong>for</strong>mation systems <strong>and</strong><br />
technology; <strong>and</strong> facilitates quality improvement initiatives.<br />
Please join us in congratulating these individuals <strong>and</strong> wishing<br />
them success in their new positions.
PAANS Exp<strong>and</strong>s to Meet Community Needs<br />
MANHASSET — As the North Shore-LIJ Health System adapts to meet the future<br />
needs <strong>of</strong> the communities it serves throughout the metropolitan area, there<br />
has been a major focus on the evolution <strong>of</strong> our clinical <strong>and</strong> business models.<br />
Physician <strong>and</strong> Ambulatory Network Services (PAANS) continues to play a major<br />
role in this realignment as the paradigm shifts from providing care in the<br />
traditional hospital setting to an even greater focus on the care provided outside<br />
<strong>of</strong> the hospital.<br />
In the four years since PAANS was established, its network has grown from<br />
a budget <strong>of</strong> $450 million to $1.1 billion this year. During this same period, PAANS<br />
has grown from 3,200 employees to more than 4,700, with a 34 percent increase<br />
in employed physicians. <strong>The</strong> health system now has more than 2,400 full-time<br />
physicians geographically dispersed over nearly 250 inpatient <strong>and</strong> ambulatory<br />
facilities – <strong>and</strong> those numbers continue to grow. In a recent issue <strong>of</strong> Modern<br />
Healthcare magazine, the North Shore-LIJ Medical Group was ranked as the<br />
nation’s sixth-largest group practice, larger than the Mayo Clinic <strong>and</strong> numerous<br />
other nationally recognized providers.<br />
“We would like to acknowledge <strong>and</strong> express our appreciation <strong>for</strong> the<br />
work <strong>and</strong> ef<strong>for</strong>ts <strong>of</strong> the clinical leadership <strong>of</strong> the Medical Group in guiding <strong>and</strong><br />
developing this rapid growth in size <strong>and</strong> scope <strong>of</strong> services,” said Dennis Dowling,<br />
regional executive director <strong>of</strong> PAANS.<br />
PAANS’ expansion requires the health system to work differently to ensure<br />
that it meets the needs <strong>of</strong> its integrated network <strong>of</strong> employed physicians,<br />
ambulatory care centers, state-<strong>of</strong>-the-art tertiary care facilities, premier local<br />
community hospitals, nationally ranked specialty care hospitals <strong>and</strong>, most<br />
importantly, its patients. To support those ef<strong>for</strong>ts, PAANS is adding talent <strong>and</strong><br />
building the infrastructure needed to position it <strong>for</strong> continued success.<br />
<strong>The</strong> following individuals were recently appointed to work with PAANS’<br />
leadership — Dennis Dowling, Deborah Schiff, Sharon <strong>Joy</strong>, Kim Schneider,<br />
Rosalie Long <strong>and</strong> Andrew Sama, MD, chair <strong>of</strong> the North Shore-LIJ Medical Group’s<br />
Executive Committee — to help lead the trans<strong>for</strong>mation <strong>and</strong> continued growth:<br />
Joseph Moscola, PA-C, MBA, has been promoted to<br />
vice president <strong>of</strong> ambulatory services. He joins PAANS<br />
from his previous role as director <strong>of</strong> corporate services<br />
system operations. In his new role, he oversees the<br />
development, integration <strong>and</strong> coordination <strong>of</strong> ambulatory<br />
operations, affiliated relationships, marketing,<br />
communications <strong>and</strong> operational responsibilities. <strong>The</strong>se<br />
include both financial <strong>and</strong> strategic planning activities.<br />
Mr. Moscola reports to Mr. Dowling.<br />
Susan Browning, BA, MPH, has been named vice<br />
president <strong>of</strong> ambulatory services. Her previous role<br />
was at Staten Isl<strong>and</strong> University Hospital as senior<br />
vice president <strong>of</strong> business development <strong>and</strong> practice<br />
management. In her new role, she oversees the<br />
day-to-day program development <strong>of</strong> the ambulatory<br />
sites established throughout the health system, with a<br />
focus on capital <strong>and</strong> facilities. Ms. Browning reports to<br />
Deborah Schiff, PAANS’ vice president <strong>of</strong> strategy <strong>and</strong><br />
business development.<br />
Anne Arthur, BS, MBA, has been promoted to<br />
assistant vice president <strong>of</strong> ambulatory services. She<br />
joins PAANS from Southside Hospital, where she was<br />
director <strong>of</strong> access management <strong>and</strong> patient throughput.<br />
In her new position, she is working on the coordination<br />
<strong>of</strong> ambulatory services <strong>for</strong> PAANS. She is responsible <strong>for</strong><br />
the oversight <strong>of</strong> the financial integration <strong>of</strong> our multispecialty<br />
centers, as well as directing the development,<br />
coordination <strong>and</strong> administration <strong>of</strong> daily practice <strong>and</strong><br />
ambulatory operations. She reports to Mr. Moscola.<br />
Lenny Nartowicz, BS, MBA, has been appointed<br />
assistant vice president <strong>of</strong> finance business plan<br />
modeling. In his previous role, he was associate<br />
executive director <strong>of</strong> finance at <strong>The</strong> Zucker Hillside<br />
Hospital. He is overseeing the daily financial<br />
operations <strong>of</strong> PAANS, including budget preparation,<br />
business plan modeling <strong>and</strong> the integrity <strong>of</strong> financial<br />
statements. Mr. Nartowicz reports to Sharon <strong>Joy</strong>,<br />
PAANS’ vice president <strong>of</strong> finance.<br />
R<strong>and</strong>i Mednick, BS, MHA, has been promoted to<br />
assistant vice president <strong>of</strong> the obstetrics/gynecology<br />
service line. She was previously senior director <strong>of</strong><br />
business development <strong>for</strong> post-acute services <strong>and</strong><br />
director <strong>of</strong> the health system’s cardiovascular service<br />
line. Her new responsibilities focus on building an<br />
infrastructure <strong>for</strong> the ob/gyn service line, including:<br />
oversight <strong>of</strong> existing operations, strategic development<br />
<strong>and</strong> implementation <strong>of</strong> new practices <strong>and</strong> helping our<br />
hospitals integrate new opportunities. Ms. Mednick reports to Adiel Fleischer,<br />
MD, the health system’s chair <strong>of</strong> ob/gyn.<br />
Patricia Dillman, RN, has been appointed assistant vice president <strong>of</strong><br />
ambulatory services. She joins PAANS from Columbia University Medical Center,<br />
where she was director <strong>of</strong> clinical operations <strong>of</strong> the hospital’s faculty practice<br />
organization. In her new role, Ms. Dillman will be a key member <strong>of</strong> the PAANS<br />
trans<strong>for</strong>mation team, preparing practices to meet the challenges <strong>for</strong> delivering<br />
<strong>and</strong> coordinating care within the ambulatory setting. She reports to Rosalie Long,<br />
PAANS’ vice president <strong>of</strong> ambulatory services.<br />
<strong>The</strong> New St<strong>and</strong>ard 67
Executive Appointments<br />
Barbara Felker has been named vice president <strong>of</strong> community<br />
<strong>and</strong> external affairs, reporting to Jennifer Mieres, MD, in the<br />
North Shore-LIJ Health System’s Office <strong>of</strong> Community<br />
<strong>and</strong> Public Health. Prior to this appointment,<br />
Ms. Felker served as the vice president <strong>for</strong><br />
corporate human resources, overseeing talent<br />
management <strong>and</strong> talent acquisition.<br />
In her new role, Ms. Felker will develop <strong>and</strong><br />
implement community engagement strategies<br />
to enhance the healthcare needs <strong>and</strong> wellness <strong>of</strong><br />
communities served by North Shore-LIJ. As part <strong>of</strong><br />
the health system’s diversity, inclusion <strong>and</strong> health literacy strategy,<br />
Ms. Felker will also develop <strong>and</strong> implement affinity-based employee<br />
resource groups to create business plans that drive employee<br />
engagement, increase talent retention <strong>and</strong> serve as ambassadors to<br />
internal <strong>and</strong> external communities.<br />
Be<strong>for</strong>e joining North Shore-LIJ, Ms. Felker held various<br />
leadership positions at companies including New York<br />
Presbyterian’s Morgan Stanley Children’s Hospital <strong>and</strong> HR<br />
Dynamics Consulting, Inc., <strong>and</strong> served as the legislative director<br />
<strong>for</strong> the New York State Senate.<br />
Catherine Galla has been promoted to assistant vice president<br />
<strong>for</strong> nursing initiatives at the North Shore-LIJ Institute <strong>for</strong> Nursing.<br />
Ms. Galla has been with the North Shore-LIJ Health System since<br />
1981 in a variety <strong>of</strong> clinical staff <strong>and</strong> leadership<br />
positions. In 1999, she transitioned into a project<br />
management position in the Office <strong>of</strong> the Chief<br />
Nurse Executive, where she coordinated projects<br />
related to st<strong>and</strong>ardizing nursing practice across<br />
the health system.<br />
During the past 12 years, Ms. Galla’s role<br />
has exp<strong>and</strong>ed to include leadership <strong>of</strong> large-scale,<br />
patient-care-related process <strong>and</strong> practice changes<br />
across the system, including the design <strong>and</strong> implementation <strong>of</strong> the<br />
clinical in<strong>for</strong>mation system, IV pump product selection, rollout<br />
<strong>of</strong> the collaborative care model <strong>and</strong> the cross-country vendor<br />
management agreement.<br />
Susan Knoepffler, RN, has been named vice<br />
president <strong>of</strong> nursing <strong>and</strong> chief nursing <strong>of</strong>ficer<br />
at Huntington Hospital. Ms. Knoepffler joins<br />
Huntington from LIJ Medical Center, where she<br />
served as senior administrative director <strong>of</strong> the<br />
Emergency Department. Ms. Knoepffler began<br />
her 30-year career as a staff nurse in the Neonatal<br />
Intensive Care Unit at North Shore University<br />
Hospital. Career highlights include leadership roles<br />
as administrative supervisor <strong>and</strong> nursing care coordinator at<br />
St. Francis Hospital be<strong>for</strong>e joining LIJ in 2008. In her new<br />
68 Summer 2012<br />
role, Ms. Knoepffler’s top priorities are to enhance the patient<br />
experience, work toward achieving Magnet redesignation <strong>and</strong><br />
focus on employee engagement.<br />
Ms. Knoepffler earned a bachelor <strong>of</strong> science in nursing<br />
from the University <strong>of</strong> Delaware, <strong>and</strong> a master’s in public health<br />
administration from Long Isl<strong>and</strong> University — CW Post. She<br />
is a certified nurse executive <strong>and</strong> is a member <strong>of</strong> the American<br />
Organization <strong>of</strong> Nurse Executives.<br />
Joseph Molloy has been appointed vice president <strong>of</strong> managed<br />
care benefits <strong>and</strong> direct contracting with the North Shore-LIJ<br />
Health System. In this role, he will develop relationships to deliver<br />
North Shore-LIJ’s healthcare services directly<br />
to employers, Taft-Hartley Health Funds <strong>and</strong><br />
partnerships with insurance carriers <strong>and</strong> thirdparty<br />
administrators.<br />
<strong>The</strong> dem<strong>and</strong> <strong>for</strong> this position comes as the<br />
health system’s model <strong>of</strong> care continues to evolve<br />
to focus more specifically on preventing <strong>and</strong><br />
managing disease, as well as promoting wellness<br />
<strong>and</strong> healthy lifestyles. Mr. Molloy will work to deliver<br />
quality, evidence-based care to develop products <strong>and</strong> services <strong>for</strong><br />
employers, union funds <strong>and</strong> insurance carriers.<br />
Prior to this position, Mr. Molloy served as the health system’s<br />
vice president <strong>of</strong> benefits <strong>and</strong> human resources services, overseeing<br />
nearly $1 billion <strong>of</strong> annual benefits, including the redesign <strong>of</strong> the<br />
health plan to incentivize the use <strong>of</strong> system facilities, hospitals <strong>and</strong><br />
CIIPA network.<br />
Ms. Diaz Named PA Director<br />
Elizabeth Diaz, PA, has<br />
been appointed director <strong>of</strong><br />
physician assistants at North<br />
Shore University Hospital. She<br />
had been supervising PA in the<br />
Department <strong>of</strong> Surgery <strong>for</strong> a<br />
year <strong>and</strong> a half. Ms. Diaz joined<br />
the hospital from St. Vincent’s<br />
Medical Center in Manhattan,<br />
where she served as supervising<br />
PA <strong>for</strong> four years. She graduated<br />
in 2001 from the Saint Vincent’s<br />
Catholic Medical Center’s PA<br />
Program <strong>and</strong> holds an MPA<br />
from New York University’s<br />
Robert F. Wagner School <strong>of</strong><br />
Public Service.
George Richardson has been named vice president <strong>of</strong><br />
development at Huntington Hospital. Most recently, Mr.<br />
Richardson served as executive director <strong>of</strong> development <strong>and</strong> alumni<br />
relations at St. John’s University School <strong>of</strong> Law.<br />
He began his career as an administrator at Mercy<br />
Medical Center, where he was director <strong>of</strong><br />
external affairs, <strong>and</strong> held various fundraising<br />
positions at H<strong>of</strong>stra University.<br />
Mr. Richardson is a graduate <strong>of</strong> Fairfield<br />
University <strong>and</strong> holds an MBA from H<strong>of</strong>stra.<br />
He is a <strong>for</strong>mer <strong>and</strong> current board member <strong>of</strong> the<br />
Association <strong>of</strong> Fundraising Pr<strong>of</strong>essionals/Long Isl<strong>and</strong><br />
Chapter. For the past two years, he has served as a Eucharistic<br />
minister at Huntington Hospital.<br />
GROUP HEALTH MANAGEMENT<br />
North Shore-LIJ has established a new entity called Group<br />
Health Management to work with clinical <strong>and</strong> administrative<br />
leadership to develop a comprehensive strategy <strong>for</strong><br />
addressing the needs <strong>of</strong> the chronically ill.<br />
This will help the health system transition<br />
to a new value-based Medicare/Medicaid<br />
reimbursement system that rewards wellness<br />
promotion <strong>and</strong> disease prevention.<br />
Nick Fitterman, MD, is the medical director <strong>of</strong><br />
the new entity, <strong>and</strong> Irina Mitzner, RN, has been<br />
named vice president <strong>of</strong> clinical operations.<br />
A team <strong>of</strong> case managers, nurse practitioners, educators <strong>and</strong><br />
other health pr<strong>of</strong>essionals led by Dr. Fitterman <strong>and</strong> Ms. Mitzner<br />
will identify health system patients who are the largest users <strong>of</strong> our<br />
services. <strong>The</strong>y will work with their physicians <strong>and</strong> other caregivers<br />
to pursue better ways <strong>of</strong> caring <strong>for</strong> them, beyond traditional<br />
approaches that not only have proven to be inefficient <strong>and</strong> costly,<br />
but do not produce the clinical outcomes we hope to achieve.<br />
Dr. Fitterman previously served as chief <strong>of</strong> staff <strong>and</strong> medical<br />
director <strong>of</strong> hospitalist services at Huntington Hospital, <strong>and</strong><br />
Ms. Mitzner’s <strong>for</strong>mer position was as vice president <strong>of</strong> clinical<br />
operations at the North Shore-LIJ Home Care Network. In their<br />
new roles with Group Health Management, Dr. Fitterman <strong>and</strong><br />
Ms. Mitzner will work with Merryl Siegel, executive director <strong>of</strong><br />
post-acute services <strong>for</strong> the health system, <strong>and</strong> Howard Gold, the<br />
health system’s senior vice president <strong>of</strong> revenue <strong>and</strong> business<br />
development, to establish a groundbreaking model <strong>for</strong> managing<br />
the care. As medical director <strong>of</strong> this new entity, Dr. Fitterman will<br />
also coordinate activities with Jeremy Boal, MD, the health system’s<br />
chief medical <strong>of</strong>ficer.<br />
Duty Calls at 30,000 Feet<br />
For Two NSUH Nurses<br />
from page 9<br />
<strong>The</strong> flight attendant supplied a portable external<br />
defibrillator, which wasn’t needed because the woman had<br />
a pulse, although she was semi-conscious. <strong>The</strong> nurses took<br />
her pulse <strong>and</strong> her blood pressure, which were normal, <strong>and</strong> as<br />
she seemed to revive a bit lying flat, they asked her some key<br />
questions: Are you a diabetic? Do you have a heart condition?<br />
Any allergies? Are you on medication? Do you have chest pains?<br />
When did you last have something to eat? Something to drink?<br />
“We also did some neurochecks,” said Ms. Kwiatkowski, “like<br />
what’s called A&O (<strong>for</strong> aware <strong>and</strong> oriented) times 4: What’s your<br />
name? Where are you? What time is it? What’s happening? She<br />
knew the answers. If it was a stroke, the plane would have had to<br />
divert to the nearest airport, but we ruled that out.”<br />
“She was on an antibiotic <strong>for</strong> a minor illness, but she said<br />
she hadn’t had anything to eat or drink in a while,” Ms. Smith said.<br />
“I had a hunch that she was dehydrated. <strong>The</strong> flight attendant<br />
brought us three bottles <strong>of</strong> water, <strong>and</strong> the woman drank two<br />
<strong>of</strong> them <strong>and</strong> then said she was feeling much, much better. She<br />
got up <strong>and</strong> sat down, <strong>and</strong> Connie sat with her <strong>and</strong> her husb<strong>and</strong><br />
until we l<strong>and</strong>ed. <strong>The</strong>re was only room <strong>for</strong> one <strong>of</strong> us, so I went<br />
back to my seat.”<br />
“Her poor husb<strong>and</strong> was an absolute wreck,” said Ms.<br />
Kwiatkowski. “<strong>The</strong>y had been married <strong>for</strong> more than 50 years,<br />
<strong>and</strong> he was so afraid <strong>for</strong> her. In situations like that, you have two<br />
patients: the one who is sick <strong>and</strong> the one who is about to collapse<br />
with anxiety.<br />
But his wife <strong>and</strong> I were able to reassure him.”<br />
When the plane l<strong>and</strong>ed, the pilot <strong>and</strong> the co-pilot came out<br />
<strong>of</strong> the cabin to shake their h<strong>and</strong>s. <strong>The</strong> pilot arranged <strong>for</strong> each<br />
<strong>of</strong> them to get a $100 credit from JetBlue. And a man who was<br />
sitting behind the couple asked the nurses where they worked.<br />
When they told him they worked at North Shore University<br />
Hospital, he beamed. He introduced himself as Mark Claster,<br />
vice president <strong>of</strong> the North Shore-LIJ Board <strong>of</strong> Trustees, <strong>and</strong><br />
he told them how proud he was <strong>of</strong> them. “Michael Dowling’s<br />
going to hear about this,” he said.<br />
And Michael Dowling did. In the letter that Mr. Claster sent<br />
to the president <strong>and</strong> CEO <strong>of</strong> the North Shore-LIJ Health System,<br />
he wrote, “<strong>The</strong> two nurses couldn’t have been more caring,<br />
skillful <strong>and</strong> unflappable in a very stressful situation. <strong>The</strong>y deserve<br />
recognition. <strong>The</strong>y were everything we would hope <strong>for</strong> as nurses<br />
in our health system <strong>and</strong> as human beings.”<br />
In his letters to the nurses, Michael Dowling expressed<br />
his sincere appreciation <strong>for</strong> their “willingness to provide care<br />
without hesitation.” He wrote, “<strong>You</strong> exemplify the values <strong>of</strong><br />
caring <strong>and</strong> putting patients first that we are most proud <strong>of</strong> here at<br />
the North Shore-LIJ Health System.”<br />
<strong>The</strong> New St<strong>and</strong>ard 69
Healthcare Challenges Seen as Opportunities<br />
at National Meeting Hosted by North Shore-LIJ<br />
By <strong>The</strong>a Welch<br />
MANHASSET — Healthcare<br />
may be in crisis in the US,<br />
but a spirit <strong>of</strong> excitement <strong>and</strong><br />
even optimism prevailed at<br />
the recent 2012 Corporate<br />
Member Meeting <strong>of</strong> the<br />
Commission on Accreditation<br />
<strong>of</strong> Healthcare Management<br />
Education (CAHME), hosted<br />
by the North Shore-LIJ Health<br />
System, a CAHME corporate<br />
member. Entitled “Healthcare<br />
Re<strong>for</strong>m: Positioning Graduate<br />
Healthcare Management<br />
Education <strong>for</strong> the Future,”<br />
the meeting was held at <strong>The</strong><br />
Feinstein Institute <strong>for</strong> Medical<br />
Research.<br />
“<strong>The</strong>re are huge<br />
challenges in healthcare<br />
today, but there are also<br />
huge opportunities,” said<br />
keynote speaker Richard J.<br />
Umbdenstock, president <strong>and</strong><br />
chief executive <strong>of</strong>ficer <strong>of</strong> the<br />
American Hospital Association<br />
(AHA). “I believe we are closer<br />
70 Summer 2012<br />
than ever to getting it right.”<br />
His optimism was echoed<br />
by North Shore-LIJ President<br />
<strong>and</strong> CEO Michael Dowling,<br />
who welcomed the 66<br />
CAHME corporate member<br />
representatives in attendance,<br />
including CEOs <strong>of</strong> some<br />
<strong>of</strong> the nation’s largest <strong>and</strong><br />
most highly respected health<br />
systems. “For those who aren’t<br />
afraid to embrace change, the<br />
future looks fantastic,” he said.<br />
Mr. Umbdenstock <strong>and</strong> Mr.<br />
Dowling, both national leaders<br />
in healthcare themselves, agreed<br />
that educating to a new kind <strong>of</strong><br />
leadership is vitally important.<br />
“Team-based healthcare delivery<br />
is like a new sport,” said Mr.<br />
Umbdenstock, “<strong>and</strong> the new<br />
leader must be less the captain<br />
<strong>of</strong> the ship <strong>and</strong> more the leader<br />
<strong>of</strong> the team.” In keeping with<br />
that theme, Mr. Dowling<br />
said, “We shouldn’t confuse<br />
leadership with management.<br />
2011 Annual Report<br />
North Shore-LIJ President <strong>and</strong> CEO Michael Dowling, right, with Richard<br />
Umbdenstock, left, president <strong>and</strong> CEO <strong>of</strong> the American Hospital Association,<br />
<strong>and</strong> David Fine, president <strong>and</strong> CEO <strong>of</strong> St. Luke’s Episcopal Health System in<br />
Houston, TX, <strong>and</strong> chair <strong>of</strong> the Commission on Accreditation <strong>of</strong> Healthcare<br />
Management Education, which held a board meeting at <strong>The</strong> Feinstein<br />
Institute <strong>for</strong> Medical Research.<br />
Both are necessary, but while<br />
managers create order, leaders<br />
create the future.”<br />
In regards to concerns<br />
about shrinking reimbursements,<br />
Mr. Umbdenstock said,<br />
<strong>The</strong> North Shore-LIJ Health System’s recently published<br />
2011 Annual Report, Partners in Health, recognizes our<br />
relationships with individuals, organizations <strong>and</strong> the<br />
community at large; every one plays a vital role in helping us<br />
fulfill our mission. See it at http://www.northshorelij.com/<br />
NSLIJ/NSLIJ+Annual+Reports.<br />
“We will never be better paid<br />
than we are today. <strong>The</strong>re is<br />
no new money. <strong>The</strong> old<br />
approach has been, ‘Well,<br />
we’ll do more with less.’ I say<br />
the new approach should be,<br />
‘Let’s do less with less — <strong>and</strong><br />
get better outcomes.’”<br />
In small breakout sessions,<br />
meeting attendees tackled<br />
tough <strong>and</strong> timely healthcare<br />
topics led by experts such as<br />
Robert Henkel, president <strong>and</strong><br />
CEO <strong>of</strong> Ascension Health,<br />
headquartered in St. Louis,<br />
MO; Chris Van Gorder,<br />
president <strong>and</strong> CEO <strong>of</strong> San<br />
Diego, CA-based Scripps<br />
Health; <strong>and</strong> Kathleen Gallo,<br />
PhD, RN, North Shore-LIJ’s<br />
senior vice president <strong>and</strong> chief<br />
learning <strong>of</strong>ficer.
Kids Give Tobacco the Kiss-Off<br />
<strong>You</strong>ngsters from the Cross Isl<strong>and</strong> YMCA in Bellerose learned about the dangers <strong>of</strong> smoking at an educational workshop led by Nancy Copperman, RD, director <strong>of</strong> public<br />
health initiatives at North Shore-LIJ. <strong>The</strong> event was part <strong>of</strong> National Kick Butts Day, which focuses attention on community activism by boys <strong>and</strong> girls to take a st<strong>and</strong><br />
against tobacco. <strong>The</strong> children created posters with antismoking messages <strong>and</strong> per<strong>for</strong>med a short rap song pledging not to smoke. <strong>The</strong> Y also announced its new<br />
smoke-free outdoor air policy to protect children <strong>and</strong> the community from the hazards <strong>of</strong> smoking <strong>and</strong> second-h<strong>and</strong> smoke. <strong>The</strong> project was funded by a grant from<br />
the Queens Smoke-Free Partnership, with help from the North Shore-LIJ Health System. Back row, from left: Deanna Bitetti, chief <strong>of</strong> staff <strong>for</strong> Assemblyman David<br />
Weprin, Jamé Krauter <strong>of</strong> the Cross Isl<strong>and</strong> YMCA, Ms. Copperman, <strong>and</strong> Tina Stinson-Lewis, also <strong>of</strong> the Cross Isl<strong>and</strong> Y.<br />
North Shore-LIJ Epilepsy Center Is First on LI<br />
to Offer New Device to Stimulate Vagus Nerve<br />
<strong>The</strong> Comprehensive<br />
Epilepsy Care Center at<br />
North Shore-LIJ’s Cushing<br />
Neuroscience Institute (CNI)<br />
is the first center on Long<br />
Isl<strong>and</strong> to <strong>of</strong>fer the new version<br />
<strong>of</strong> vagus nerve stimulation<br />
(VNS) therapy, implanting an<br />
AspireHC generator into<br />
a 23-year-old female patient<br />
from Hicksville with refractory<br />
epilepsy this spring.<br />
Asesh Mehta, MD, director<br />
<strong>of</strong> epilepsy surgery at the<br />
Comprehensive Epilepsy Care<br />
Center, said, “VNS <strong>The</strong>rapy<br />
is an effective, safe option <strong>for</strong><br />
epilepsy patients who are not<br />
achieving satisfactory seizure<br />
control from medications.<br />
Because this newest model<br />
<strong>of</strong> the vagus nerve stimulator<br />
has the longest battery life<br />
<strong>of</strong> any VNS therapy device,<br />
replacement <strong>of</strong> the generator<br />
can take place less frequently<br />
<strong>for</strong> patients who are on<br />
higher doses <strong>of</strong> stimulation.<br />
In addition, the AspireHC,<br />
which is about the size <strong>of</strong> a<br />
small pocket watch, will provide<br />
improved quality <strong>of</strong> life benefits<br />
<strong>for</strong> VNS therapy patients.”<br />
Dr. Mehta explained that<br />
implantation is a short outpatient<br />
procedure lasting one<br />
to two hours. <strong>The</strong> stimulator<br />
is implanted in the patient’s<br />
left chest area, where a thin<br />
flexible wire (lead) sends mild<br />
stimulation to the left vagus<br />
nerve in the neck automatically<br />
at regular intervals.<br />
<strong>The</strong> Comprehensive<br />
Epilepsy Care Center is a truly<br />
integrated <strong>and</strong> multidisciplinary<br />
endeavor, with epilepsy<br />
doctors, nurses, pharmacists,<br />
neurosurgeons, neuropsychologists,<br />
social workers, technical<br />
staff <strong>and</strong> an administrative<br />
team all working together<br />
to provide care <strong>and</strong> support<br />
<strong>for</strong> both adult <strong>and</strong> pediatric<br />
epilepsy patients. It is the largest<br />
<strong>and</strong> most comprehensive<br />
program on Long Isl<strong>and</strong> <strong>for</strong><br />
the evaluation <strong>and</strong> medical <strong>and</strong><br />
surgical treatment <strong>of</strong> epilepsy<br />
in children <strong>and</strong> adults.<br />
<strong>The</strong> New St<strong>and</strong>ard 71
Lenox Hill Hospital First in New York State to<br />
Per<strong>for</strong>m Minimally Invasive Mitral Valve Replacement<br />
NEW YORK — A 76-yearold<br />
woman from Flushing,<br />
Queens, was the first patient<br />
in New York <strong>and</strong> only the<br />
second in the entire country<br />
to undergo a percutaneously<br />
implanted mitral valve<br />
replacement.<br />
<strong>The</strong> procedure,<br />
per<strong>for</strong>med in February, was<br />
executed conjointly by Lenox<br />
Hill Hospital’s Carlos Ruiz,<br />
MD, director <strong>of</strong> the Structural<br />
<strong>and</strong> Congenital <strong>Heart</strong> Disease<br />
Program <strong>of</strong> the Department<br />
<strong>of</strong> Interventional Cardiology,<br />
<strong>and</strong> Gregory P. Fontana, MD,<br />
chairman <strong>of</strong> the Department <strong>of</strong><br />
Cardiothoracic Surgery. This<br />
minimally invasive procedure<br />
is used to repair a blocked or<br />
leaky mitral heart valve that<br />
had previously been replaced.<br />
<strong>The</strong> replacement valve is<br />
inserted percutaneously<br />
through a vein in the groin<br />
<strong>and</strong> positioned within the<br />
72 Summer 2012<br />
mitral valve. It is an option <strong>for</strong><br />
individuals who are at high risk<br />
<strong>for</strong> undergoing a second openheart<br />
surgery given their age or<br />
current medical condition.<br />
“Transcatheter valve<br />
replacement is a major<br />
breakthrough in the treatment<br />
<strong>of</strong> heart disease <strong>and</strong> is part<br />
<strong>of</strong> an important trend in<br />
which minimally invasive<br />
procedures are used in place <strong>of</strong><br />
traditionally invasive surgical<br />
procedures,” noted Dr. Ruiz.<br />
“What is unique at Lenox<br />
Hill Hospital is the close<br />
collaboration between the<br />
interventional cardiologists<br />
<strong>and</strong> the heart surgeons. <strong>The</strong><br />
doctors <strong>of</strong>ten review <strong>and</strong><br />
discuss all available test results<br />
to <strong>of</strong>fer a joint opinion to<br />
ensure that each patient<br />
receives the best treatment <strong>for</strong><br />
his or her particular problem.”<br />
“It is a true<br />
multidisciplinary ef<strong>for</strong>t,”<br />
added Dr. Fontana.<br />
“Cardiologists, cardiac<br />
surgeons <strong>and</strong> vascular surgeons<br />
all work together in a single<br />
setting with a single goal:<br />
to provide extraordinary,<br />
minimally invasive, efficient<br />
heart care to patients suffering<br />
from all <strong>for</strong>ms <strong>of</strong> heart disease<br />
<strong>and</strong> vascular disease.”<br />
Girl Scouts Find a<br />
Few Good Babies<br />
It’s never too early to recruit new<br />
members, which is why the Girl Scouts<br />
<strong>of</strong> Nassau County came to LIJ’s Katz<br />
Women’s Hospital this spring to present<br />
honorary memberships to all baby<br />
girls born on March 12, 2012, the 100th<br />
anniversary <strong>of</strong> Girl Scouting in America.<br />
Pictured are four new recruits with<br />
their mothers, members <strong>of</strong> Girl Scouts<br />
<strong>of</strong> Nassau County <strong>and</strong> the leadership <strong>of</strong><br />
Katz Women’s Hospital.
<strong>The</strong> North Shore-LIJ Health<br />
System recently <strong>for</strong>med a Lions<br />
Club International chapter,<br />
the Manhasset North Shore-<br />
LIJ Lions, with the mission to provide<br />
resources <strong>and</strong> support <strong>for</strong> the prevention<br />
<strong>and</strong> treatment <strong>of</strong> diabetes in Long Isl<strong>and</strong><br />
communities.<br />
Approximately 26 million people in<br />
the United States have diabetes <strong>and</strong> one in<br />
four is unaware. Estimates range as high as<br />
79 million who have pre-diabetes <strong>and</strong> are<br />
at a high risk <strong>for</strong> developing the disease.<br />
“Without prevention <strong>and</strong> treatment, the<br />
numbers will continue to rise,” said Tracy<br />
Breen, MD, director <strong>of</strong> diabetes care <strong>for</strong><br />
North Shore-LIJ. “Many Americans live<br />
with undiagnosed diabetes <strong>and</strong> don’t even<br />
know it. Routine checkups <strong>and</strong> blood work<br />
are the best prevention methods, <strong>and</strong><br />
access to that care is essential.”<br />
“As a major healthcare provider,<br />
it is our responsibility to provide<br />
multidisciplinary diabetes care <strong>and</strong><br />
prevention services to our communities,”<br />
said Susan Somerville, executive director<br />
<strong>of</strong> North Shore University Hospital.<br />
“Awareness is essential <strong>and</strong> our Lions<br />
Club’s charter is another step to helping<br />
make each community aware <strong>of</strong> the<br />
diabetes services available. With the<br />
additional support <strong>of</strong> dedicated Lions<br />
members <strong>and</strong> volunteers, we have the<br />
ability to make a difference <strong>for</strong> thous<strong>and</strong>s<br />
<strong>of</strong> at-risk New Yorkers.”<br />
Research shows that patients with<br />
diabetes or pre-diabetes, who are not<br />
carefully managed, experience poorer<br />
outcomes such as blindness, kidney failure<br />
<strong>and</strong> damage to the heart <strong>and</strong> circulatory<br />
system. <strong>The</strong> health system’s diabetes<br />
task <strong>for</strong>ce combines the expertise <strong>of</strong><br />
the departments <strong>of</strong> nursing, nutrition,<br />
medicine, surgery, pharmacy, social work,<br />
laboratory <strong>and</strong> quality management to<br />
Shown from left: Pat Webb McNally, guiding Lion, Rockville Centre Lions Club; Stephen Dean, district<br />
governor; Marie Frazzitta; <strong>and</strong> Wing-Kun Tam, Lions Clubs International President.<br />
Manhasset North Shore-LIJ<br />
Lions Club Receives Charter<br />
<strong>for</strong> Chapter to Address Diabetes<br />
reduce the incidence <strong>of</strong> diabetes <strong>and</strong><br />
coordinate patient care. “<strong>The</strong> best way<br />
to treat diabetes is to prevent it,” said<br />
Marie Frazzitta, director <strong>of</strong> diabetes<br />
education <strong>for</strong> North Shore-LIJ, president<br />
<strong>of</strong> the Manhasset North Shore-LIJ Lions<br />
Club <strong>and</strong> co-chair <strong>of</strong> the health system’s<br />
diabetes task <strong>for</strong>ce. “Our new Lions<br />
Club is committed to helping provide the<br />
screening <strong>and</strong> educational resources <strong>and</strong><br />
services to begin battling diabetes be<strong>for</strong>e<br />
it strikes, <strong>and</strong> to keep those diagnosed as<br />
healthy as possible.”<br />
<strong>The</strong> New St<strong>and</strong>ard 73
WOMEN’S corner<br />
North Shore-LIJ Physicians, Researcher<br />
Honored at Women’s Health Conference<br />
While hosting more than 600 attendees at its fifth women’s health conference on May 2,<br />
the North Shore-LIJ Health System took time out <strong>of</strong> a busy, day-long schedule <strong>of</strong> seminars<br />
to honor four physicians <strong>and</strong> a researcher <strong>for</strong> their contributions to their pr<strong>of</strong>essions <strong>and</strong><br />
the health system. <strong>The</strong> following individuals received awards named in honor <strong>of</strong> long-time<br />
donors <strong>and</strong> trustees whose support contributed greatly to North Shore-LIJ’s success:<br />
74 Summer 2012<br />
Lorinda De Roulet Award <strong>for</strong> Excellence in Research<br />
Christine Metz, PhD<br />
Investigator<br />
<strong>The</strong> Feinstein Institute <strong>for</strong> Medical Research<br />
Center <strong>for</strong> Immunology <strong>and</strong> Inflammation<br />
Center <strong>for</strong> Patient-Oriented Research<br />
Tita Monti Award <strong>for</strong> Outst<strong>and</strong>ing Community Education<br />
Dana Lustbader, MD<br />
Section Head, Palliative Medicine<br />
Intensivist, Critical Care Medicine<br />
North Shore University Hospital<br />
Ann Gottlieb Award <strong>for</strong> Excellence in<br />
Teaching<br />
Miriam Ann Smith, MD<br />
Chairman, Department <strong>of</strong> Medicine<br />
Residency Program Director<br />
Forest Hills Hospital<br />
S<strong>and</strong>ra Atlas Bass Award <strong>for</strong> Clinical<br />
Excellence<br />
Carmel Foley, MD<br />
Director <strong>of</strong> Consultation-Liaison Psychiatry<br />
Steven <strong>and</strong> Alex<strong>and</strong>ra Cohen Children’s<br />
Medical Center<br />
Sharon <strong>Joy</strong>ce Schlanger Award <strong>for</strong><br />
Outst<strong>and</strong>ing Community Service<br />
Jacqueline Moline, MD<br />
Vice President, Population Health<br />
North Shore-LIJ Health System<br />
Chair, Department <strong>of</strong> Population Health<br />
North Shore University Hospital <strong>and</strong><br />
H<strong>of</strong>stra North Shore-LIJ School <strong>of</strong> Medicine<br />
Dr. Nancy Snyderman at<br />
Women’s Health Conference<br />
“Celebrating a New Era in Women’s Health: In<strong>for</strong>mation/Innovation/<br />
Wellness” was the theme <strong>of</strong> the fifth North Shore-LIJ women’s health<br />
conference, held at the Long Isl<strong>and</strong> Marriott Hotel in Uniondale. Nancy<br />
Snyderman, MD, chief medical editor <strong>for</strong> NBC News, shared her medical<br />
insights <strong>and</strong> personal history with the 600 attendees. She is pictured with<br />
Michael Dowling, president <strong>and</strong> chief executive <strong>of</strong>ficer <strong>of</strong> the health system,<br />
left, <strong>and</strong> Richard Goldstein, chairman <strong>of</strong> the board. “If you feel that your<br />
doctor is not listening to you, it’s probably a good time to ask <strong>for</strong> your<br />
medical records <strong>and</strong> find another physician who does listen,” Dr. Snyderman<br />
said. “Women must take care <strong>of</strong> themselves first.”
nursing mission<br />
Collaborative Care Council<br />
Gets Results<br />
from page 29<br />
Press Ganey scores.<br />
Nelson Martinez,<br />
environmental aide at<br />
Plainview Hospital, co-chaired<br />
a council that was able to<br />
decrease bed turnaround<br />
time from 70 minutes to 62<br />
minutes. Danielle Green at<br />
Plainview co-chaired a food<br />
<strong>and</strong> nutrition council, <strong>and</strong><br />
the ratings <strong>for</strong> food service<br />
courtesy, overall meals <strong>and</strong><br />
meal quality all improved.<br />
At Franklin Hospital,<br />
a council on a med/surg<br />
oncology unit reduced the<br />
length <strong>of</strong> stay from 8.07<br />
days in January to 6.84 in<br />
November <strong>of</strong> 2011. “We<br />
focused on what we needed to<br />
do to get patients safely <strong>and</strong><br />
quickly through their hospital<br />
stay,” said Kathy Bradfield,<br />
LMSW, director <strong>of</strong> social work.<br />
At Long Isl<strong>and</strong> Jewish<br />
Medical Center, a council<br />
redesigned a surgical waiting<br />
room, provided more<br />
privacy <strong>for</strong> consultations <strong>and</strong><br />
improved communication<br />
between clinicians <strong>and</strong><br />
waiting families <strong>and</strong> patients<br />
in recovery, according to<br />
Agnes Barden, DNP, RN.<br />
Another council created a<br />
pre- <strong>and</strong> post-op surgical<br />
education class <strong>for</strong> patients<br />
<strong>and</strong> family, obtained a<br />
grant <strong>for</strong> DVD education<br />
<strong>and</strong> worked to collaborate<br />
more effectively with the<br />
cardiothoracic ICU on<br />
patient transfers. Automating<br />
physician orders on 7 South<br />
freed the unit receptionist,<br />
Patricia Rodriguez, to<br />
per<strong>for</strong>m a concierge role,<br />
keeping everyone in<strong>for</strong>med,<br />
helping solve problems<br />
<strong>and</strong> coordinating tests.<br />
Rachel Neuman, PT, who<br />
participated in the council<br />
with Ms. Rodriguez <strong>and</strong><br />
others, said the concierge<br />
position “changes the attitude<br />
<strong>of</strong> the whole team.”<br />
This is just a sampling<br />
<strong>of</strong> how more than 300<br />
collaborative care councils at<br />
North Shore-LIJ Health System<br />
are gaining measurable results.<br />
Collaborative ef<strong>for</strong>ts<br />
between facilities are reaping<br />
results, too. Collaborative<br />
care councils at North<br />
Shore University Hospital<br />
<strong>and</strong> Stern Family Center<br />
<strong>for</strong> Rehabilitation worked<br />
together to share more<br />
comprehensive <strong>and</strong> accurate<br />
patient in<strong>for</strong>mation on the<br />
clinical in<strong>for</strong>mation system<br />
to ensure better h<strong>and</strong><strong>of</strong>fs.<br />
As a result, “We were more<br />
prepared to admit patients<br />
when they came to us,” said<br />
Carole Clement, RN, Stern<br />
Family Center nurse manager.<br />
Press Ganey “likelihood to<br />
recommend” scores at the<br />
long-term care facility jumped<br />
from 77.1 in June 2011 to 92.9<br />
in November last year.<br />
Lynn Johnson, NP,<br />
manager, nursing initiatives,<br />
Institute <strong>for</strong> Nursing, who<br />
President’s Awards<br />
Keep an eye out <strong>for</strong> a special supplement on North Shore-LIJ’s President’s<br />
Award program featuring this year’s nominees <strong>and</strong> winners, including<br />
Sylvester Wallace <strong>of</strong> Cohen Children’s Medical Center <strong>of</strong> New York.<br />
facilitated both collaborative<br />
care councils, also helped<br />
roll out councils at Lenox<br />
Hill Hospital. Over 3,300<br />
employees learned about the<br />
collaborative care model last<br />
summer, <strong>and</strong> Lenox Hill<br />
is already gaining results.<br />
A council chaired by James<br />
Richter, MD, chief <strong>of</strong><br />
anesthesiology, succeeded<br />
at decreasing turnover time<br />
between OR cases, in part<br />
thanks to more realistic<br />
scheduling. “If there is ever<br />
going to be a mechanism<br />
<strong>for</strong> reducing turnover, the<br />
councils are it,” he said. Arlex<br />
Matulac, associate executive<br />
director, perioperative<br />
services, said, “We started with<br />
turnover at 51 minutes last<br />
fall <strong>and</strong> were at 48 minutes<br />
in February. Our goal is 45<br />
minutes <strong>and</strong> our stretch goal is<br />
30 minutes.”<br />
Linda DiCarlo, RN,<br />
director, nursing in<strong>for</strong>matics,<br />
Lenox Hill, attributes the<br />
success <strong>of</strong> collaborative care<br />
councils to “all the disciplines<br />
participating <strong>and</strong> everyone<br />
talking the same language,”<br />
but admits that it takes time to<br />
achieve full results.<br />
Catherine Galla, RN,<br />
assistant vice president,<br />
nursing initiatives, Institute<br />
<strong>for</strong> Nursing, concurs.<br />
“Trans<strong>for</strong>mational change<br />
never happens immediately,<br />
but we have a structure<br />
that supports incremental<br />
changes <strong>and</strong> staff working<br />
in interdisciplinary teams to<br />
improve the care we deliver.”<br />
<strong>The</strong> New St<strong>and</strong>ard 75
center <strong>for</strong> learning <strong>and</strong> innovation<br />
Center <strong>for</strong> Learning <strong>and</strong> Innovation<br />
Celebrates 10th Anniversary<br />
LAKE SUCCESS — <strong>The</strong> adage “if you build it, they will come”<br />
characterizes the 10 years that the Center <strong>for</strong> Learning <strong>and</strong><br />
Innovation has existed. <strong>The</strong> corporate university <strong>for</strong> the North<br />
Shore-LIJ Health System celebrated its tenth anniversary on January<br />
16, 2012. From its humble beginnings in a rented single classroom<br />
at the Dale Carnegie Institute in Woodbury, CLI has grown <strong>and</strong><br />
flourished, impacting employees from all levels <strong>and</strong> areas <strong>and</strong> now<br />
occupying a state-<strong>of</strong>-the-art facility in Lake Success. Through the<br />
end <strong>of</strong> 2011, CLI has taught 163,384 people <strong>and</strong> it has no plans to<br />
slow down. “Since it opened in 2002, CLI has become the largest<br />
corporate university in the healthcare industry, setting the st<strong>and</strong>ard<br />
<strong>for</strong> educational excellence <strong>and</strong> demonstrating the highest level <strong>of</strong><br />
innovation,” said Michael Dowling, president <strong>and</strong> CEO <strong>of</strong> the North<br />
Shore-LIJ Health System.<br />
A New Place to Play<br />
Officials from Smith <strong>Have</strong>n Mall in Lake Grove <strong>and</strong> Cohen Children’s Medical Center (CCMC) <strong>of</strong> New York<br />
recently celebrated the opening <strong>of</strong> the shopping center’s new children’s play area. Sponsored by the North<br />
Shore-LIJ Health System, the play space is located in the mall’s Sears Court. Among those at the opening were,<br />
from left: Cynthia Ruf, corporate director <strong>of</strong> marketing <strong>for</strong> the health system; Kevin Carraccio, CCMC’s vice<br />
president <strong>of</strong> philanthropy; Debora Riccardi, CCMC’s director <strong>of</strong> community outreach; Paul Fiore, Simon Property<br />
Group’s northeast regional director <strong>of</strong> business development; Sharon Ritterb<strong>and</strong>, Simon Property group’s<br />
area director <strong>of</strong> business development; <strong>and</strong> James Lundgren, Smith <strong>Have</strong>n Mall’s general manager.<br />
76 Summer 2012<br />
Based on Michael Dowling’s original white paper on the<br />
development <strong>of</strong> a leadership institute, CLI began 10 years ago with<br />
educational <strong>of</strong>ferings limited to Core Management <strong>and</strong> Six Sigma,<br />
which had instructors traveling to hospitals <strong>and</strong> using a rented<br />
classroom to <strong>of</strong>fer the education to employees. It was not until a year<br />
later, when CLI moved to its first location, that the education was<br />
centralized <strong>and</strong> the amount <strong>of</strong> programs that the corporate university<br />
was able to <strong>of</strong>fer began to grow. Over the years, CLI developed<br />
additional programs such as the administrative <strong>and</strong> physician high<br />
potential programs, as well as the scholar pipeline <strong>and</strong> administrative<br />
fellowships. In 2012, over 80 different enrichment courses are<br />
scheduled, with additional courses being developed due to the high<br />
dem<strong>and</strong> <strong>of</strong> learners <strong>and</strong> the continued growth <strong>of</strong> the health system.<br />
One <strong>of</strong> CLI’s innovations was the establishment <strong>of</strong> the<br />
Patient Safety Institute (PSI) in<br />
2006 to focus on preventable<br />
medical errors, teamwork <strong>and</strong><br />
communication. PSI provided<br />
the clinical aspect <strong>of</strong> education<br />
that was in high dem<strong>and</strong> <strong>for</strong> the<br />
organization’s team members who<br />
were directly involved in patient<br />
care. In 2011 alone, CLI <strong>and</strong> PSI<br />
conducted over 950 individual<br />
educational programs.<br />
Outside organizations<br />
repeatedly take notice <strong>of</strong> the<br />
work that is done by CLI. <strong>The</strong><br />
International Association <strong>for</strong><br />
Continuing Education <strong>and</strong> Training<br />
(IACET), which accredits CLI to<br />
<strong>of</strong>fer continuing education units,<br />
awarded the corporate university the<br />
2011 Exemplar Award <strong>for</strong> Internal<br />
Training. <strong>The</strong> Center <strong>for</strong> Learning<br />
<strong>and</strong> Innovation also received a<br />
Silver Award <strong>for</strong> Best Leadership<br />
Training Program. Most recently,<br />
Chief Learning Officer Magazine named<br />
CLI a 2012 Learning Elite Finalist.<br />
“We’re proud <strong>of</strong> CLI’s<br />
success <strong>and</strong> confident that its<br />
future achievements will enable<br />
us to reach even greater heights<br />
as a ‘learning organization,’” said<br />
Mr. Dowling.
Simulation Lab Creates Real-Life<br />
Scenarios <strong>for</strong> New Med Students<br />
H<strong>of</strong>stra North Shore-LIJ School <strong>of</strong> Medicine Students Benefit<br />
from Simulation Training at Center <strong>for</strong> Learning <strong>and</strong> Innovation<br />
Students in the inaugural class at the H<strong>of</strong>stra North Shore-<br />
LIJ School <strong>of</strong> Medicine have completed only one year <strong>of</strong><br />
study <strong>and</strong> already they have per<strong>for</strong>med physical exams on<br />
patients, cleared an obstructed airway <strong>and</strong> even assisted in<br />
the birth <strong>of</strong> a baby at the CLI’s Patient Safety Institute. While none<br />
<strong>of</strong> these procedures were carried out on real people, they certainly<br />
had the look <strong>and</strong> feel <strong>of</strong> true-to-life situations.<br />
“<strong>The</strong> exposure to simulation exercises, at one <strong>of</strong> the largest<br />
institutes <strong>of</strong> its kind in the country, certainly gives our students a<br />
wonderful opportunity to learn <strong>and</strong> strengthen their clinical skills<br />
at an early stage in their education,” said Lawrence Smith, MD,<br />
dean <strong>of</strong> the School <strong>of</strong> Medicine.<br />
Simulation education is a bridge between classroom learning<br />
<strong>and</strong> real-life clinical experience. CLI’s advanced learning facility<br />
features state-<strong>of</strong>-the-art human-simulation laboratories with<br />
digitally enhanced <strong>and</strong> controlled mannequins <strong>and</strong> partial-<br />
<strong>and</strong> full-body task trainers, st<strong>and</strong>ardized patient rooms, <strong>and</strong><br />
endovascular simulators <strong>for</strong> interventionalists. CLI helps<br />
students manage hypothetical patient cases as members <strong>of</strong> a<br />
multidisciplinary healthcare team. <strong>The</strong> exercises are followed by<br />
a debriefing with the med school faculty <strong>and</strong> the CLI staff, which<br />
comprises a multitude <strong>of</strong> complementary health pr<strong>of</strong>essions.<br />
“Our students are exposed to these simulation exercises much<br />
earlier than at most medical schools, which would normally cover<br />
this material in the third year. This gives our students a great advan-<br />
tage,” said Thomas Kwiatkowski, MD, assistant dean <strong>of</strong> education/<br />
simulation <strong>and</strong> course director <strong>for</strong> CPR at the School <strong>of</strong> Medicine.<br />
<strong>The</strong> high-tech, computerized mannequins at CLI are able to<br />
mimic real patients <strong>and</strong> are able to talk <strong>and</strong> respond to the medical<br />
students, who take vital signs <strong>and</strong> per<strong>for</strong>m emergency procedures,<br />
such as intravenous line insertion, breathing tube insertion<br />
<strong>and</strong> medication administration. <strong>The</strong> mannequin patients are<br />
controlled remotely by instructors at CLI, who can make them cry<br />
out in pain, move about <strong>and</strong> even react to a student’s touch.<br />
First-year medical student Niki Sheth called the CLI simulations<br />
“very realistic” <strong>and</strong> the detailed debriefings very helpful.<br />
“<strong>The</strong> debriefing was a great way <strong>of</strong> getting feedback,” she said.<br />
“It also helps you reason out <strong>and</strong> explain why you took certain<br />
actions during the exercise.”<br />
According to Dr. Kwiatkowski, lessons taught in a realistic<br />
simulation are retained better, due to the required active learning<br />
<strong>and</strong> focused concentration, the experience’s emotional investment<br />
<strong>and</strong> the direct association with the real world.<br />
Medical students also train at the world-renowned Feinstein<br />
Institute <strong>for</strong> Medical Research, the research arm <strong>of</strong> the health system.<br />
To see a video <strong>of</strong> this story, go to: www.northshorelij.com/<br />
NSLIJ/media-portal/homepage-video-channel/sim-lab.<br />
Above: Margaret Delaney, a nurse educator at North Shore-LIJ’s Patient Safety<br />
Institute, works with medical student Robert Metzler.<br />
<strong>The</strong> New St<strong>and</strong>ard 77
center <strong>for</strong> learning <strong>and</strong> innovation<br />
LAKE SUCCESS — <strong>The</strong><br />
Center <strong>for</strong> Learning <strong>and</strong><br />
Innovation (CLI) has established<br />
a Quality Academy to<br />
further improve per<strong>for</strong>mance<br />
in healthcare delivery at North<br />
Shore-LIJ facilities. <strong>The</strong> initiative<br />
builds on more than a<br />
decade <strong>of</strong> work<strong>for</strong>ce development<br />
programs to improve<br />
patient safety <strong>and</strong> quality care<br />
throughout the North Shore-<br />
LIJ Health System.<br />
<strong>The</strong> Quality Academy is<br />
grounded in staff members’<br />
need to keep pace with rapid<br />
changes in the healthcare field.<br />
At the same time, the science<br />
<strong>of</strong> improvement in healthcare<br />
has gotten more sophisticated<br />
<strong>and</strong> is constantly evolving.<br />
<strong>The</strong> academy addresses these<br />
challenges with a comprehensive,<br />
multitiered program to<br />
advance the knowledge base <strong>of</strong><br />
the work<strong>for</strong>ce to further enable<br />
staff members at every level to<br />
anticipate, recognize <strong>and</strong> solve<br />
problems to improve per<strong>for</strong>mance<br />
<strong>and</strong> to provide “perfect”<br />
care to patients <strong>and</strong> families.<br />
“<strong>The</strong> Quality Academy<br />
will allow the health system to<br />
combine <strong>and</strong> st<strong>and</strong>ardize all<br />
quality improvement education<br />
<strong>and</strong> training programs<br />
under one ro<strong>of</strong>,” said Jeremy<br />
Boal, MD, senior vice president<br />
<strong>and</strong> chief medical <strong>of</strong>ficer<br />
at North Shore-LIJ. “This<br />
78 Summer 2012<br />
allows us to <strong>for</strong>malize per<strong>for</strong>mance<br />
improvement initiatives,<br />
using the same measurement<br />
tools <strong>and</strong> metrics across<br />
the board in order to replicate<br />
high-quality outcomes in our<br />
patient care processes.” Dr.<br />
Boal added that front-line staff<br />
members are <strong>of</strong>ten in the best<br />
position to underst<strong>and</strong> <strong>and</strong><br />
improve their work environments<br />
to optimize patient care<br />
<strong>and</strong> outcomes.<br />
“Education programs<br />
at the academy will increase<br />
awareness about quality issues<br />
<strong>and</strong> further empower all<br />
employees to identify problems<br />
<strong>and</strong> take an active role in quality<br />
improvement, regardless <strong>of</strong><br />
job title,” said Alan Cooper,<br />
PhD, vice president <strong>of</strong> learning<br />
<strong>and</strong> innovation at North Shore-<br />
LIJ. For example, if nurses<br />
notice a delay in responding to<br />
patient call bells, they are in the<br />
best position to recognize ways<br />
to increase response time <strong>and</strong><br />
enhance patient satisfaction.<br />
Through proper education in<br />
improvement sciences, they can<br />
study the problem <strong>and</strong> engineer<br />
ways to improve workflow.<br />
“This not only creates a safer<br />
environment <strong>for</strong> patients, but<br />
also has the benefit <strong>of</strong> creating a<br />
more efficient workplace,” said<br />
Dr. Cooper.<br />
At the academy, quality<br />
improvement training <strong>and</strong><br />
education are being developed<br />
collaboratively with health<br />
system departments <strong>and</strong> business<br />
units, which will provide<br />
educational opportunities <strong>for</strong><br />
all North Shore-LIJ staff. For<br />
example, the Quality Academy<br />
will incorporate a section on<br />
quality improvement in Beginnings,<br />
the program geared toward<br />
new employees, <strong>and</strong> reach<br />
out to train other staff members.<br />
<strong>The</strong> Quality Academy is<br />
New Quality Academy Focuses<br />
on Improving Per<strong>for</strong>mance<br />
By Betty Olt<br />
also developing an online video<br />
introduction to the importance<br />
<strong>of</strong> everyone’s role in improving<br />
per<strong>for</strong>mance throughout the<br />
health system.<br />
Ultimately, programming<br />
will target all managers, directors<br />
<strong>and</strong> senior staff members;<br />
all chiefs, chairs <strong>and</strong> medical<br />
directors; all staff members<br />
hired in quality roles; <strong>and</strong> the<br />
highest level, or expert level,<br />
which will be designated <strong>for</strong><br />
staff including quality pr<strong>of</strong>essionals,<br />
administrators, managers,<br />
physicians <strong>and</strong> other<br />
Stay Connected, Get Inspired<br />
clinicians involved in multidepartmental,<br />
facility-wide or<br />
system-wide improvements.<br />
Learning will incorporate<br />
in-class training <strong>and</strong> online<br />
modules with group exercises.<br />
Already, all health system associate<br />
executive directors have<br />
attended the Quality Academy’s<br />
first course, “Quality,<br />
Safety <strong>and</strong> Improvement Sciences,”<br />
which is part <strong>of</strong> CLI’s<br />
new leadership development<br />
program, ALEAD – Applied<br />
Leadership Effectiveness <strong>and</strong><br />
Development.<br />
Fiona Levy, chief quality<br />
<strong>of</strong>ficer <strong>for</strong> the Cohen Children’s<br />
Medical Center <strong>of</strong> New<br />
York, leads <strong>and</strong> facilitates the<br />
Quality Academy development<br />
team. In addition to Drs. Boal,<br />
Cooper <strong>and</strong> Levy, the team<br />
includes Yosef Dlugacz, PhD,<br />
senior vice president <strong>and</strong> chief<br />
<strong>of</strong> clinical quality, education<br />
<strong>and</strong> research at the Krasn<strong>of</strong>f<br />
Quality Management Institute;<br />
Mark Jarrett, MD, vice president<br />
<strong>and</strong> health system chief<br />
quality <strong>of</strong>ficer; Marc Napp,<br />
MD, vice president <strong>of</strong> medical<br />
affairs; Karen Nelson, RN,<br />
vice president, clinical excellence<br />
<strong>and</strong> quality; <strong>and</strong> Elaine<br />
Smith, EdD, RN, vice president<br />
<strong>for</strong> nursing education.<br />
For more details about the<br />
Quality Academy, call CLI at<br />
(516) 396-6150.<br />
Inspiration is just a click away.<strong>The</strong> North Shore-LIJ Foundation<br />
supports health system services by sponsoring neighborhood events, walks,<br />
concerts, luncheons, sporting events <strong>and</strong> so much more. Stay in touch with all<br />
the North Shore-LIJ Foundation is doing by connecting with us at Facebook.<br />
com/NorthShoreLIJFoundation <strong>and</strong> on Twitter at Twitter.com/nslijfoundation.
According to the<br />
US Institute<br />
<strong>of</strong> Medicine<br />
(2000, 2001),<br />
the widespread incidence <strong>of</strong><br />
preventable errors in our<br />
nation’s hospitals revealed<br />
that how care is delivered is<br />
as important as what care is<br />
delivered. <strong>The</strong>se l<strong>and</strong>mark<br />
reports noted that developing<br />
effective clinical teams is essential to delivering care that is patientcentered,<br />
safer, timelier <strong>and</strong> more effective, efficient <strong>and</strong> equitable.<br />
To achieve those goals, the Center <strong>for</strong> Learning <strong>and</strong> Innovation<br />
(CLI) is exp<strong>and</strong>ing its ef<strong>for</strong>ts to “train in teams those that work<br />
in teams” in order to build interpr<strong>of</strong>essional teamwork <strong>and</strong><br />
collaboration. To that end, Barbara DeVoe, DNP, FNP-BC, has<br />
been promoted to vice president <strong>for</strong> interpr<strong>of</strong>essional learning <strong>and</strong><br />
education, a role in which she will enhance the strategic importance<br />
<strong>of</strong> interpr<strong>of</strong>essional learning <strong>and</strong> education throughout the health<br />
system. She will also continue her day-to-day responsibilities<br />
at CLI’s Patient Safety Institute (PSI). Barbara was recruited to<br />
CLI six years ago to develop the Critical Care Nurse Fellowship<br />
Program, <strong>for</strong> which we established our first simulation program.<br />
Her clinical background is critical care <strong>and</strong> emergency nursing. She<br />
is also a board-certified family nurse practitioner <strong>and</strong> has worked<br />
collaboratively in two physician practices. Barbara received her<br />
doctorate in nursing practice from Case Western Reserve University<br />
in 2009. Her areas <strong>of</strong> interests are patient safety, teamwork <strong>and</strong><br />
communication <strong>and</strong> human factors.<br />
Interpr<strong>of</strong>essional Education<br />
Fosters Clinical Teamwork,<br />
Increases Patient Safety<br />
Interpr<strong>of</strong>essional<br />
education (IPE) has been<br />
defined as: “when two or<br />
more pr<strong>of</strong>essionals learn with,<br />
from <strong>and</strong> about each other to<br />
improve collaboration <strong>and</strong><br />
the quality <strong>of</strong> care.” While<br />
this activity commonly occurs<br />
among clinical teams at PSI,<br />
it is incumbent upon us to<br />
exp<strong>and</strong> IPE even further,<br />
Barbara DeVoe<br />
considering its proven success<br />
in improving patient safety.<br />
Similar to CLI, PSI has grown rapidly, not only in reputation<br />
but also in programs, size <strong>and</strong> resources. What began as an idea<br />
<strong>and</strong> one simulator in 2006 has become an infrastructure that is<br />
strategically important to the health system as well as the H<strong>of</strong>stra<br />
North Shore-LIJ School <strong>of</strong> Medicine. CLI <strong>and</strong> PSI will continue to<br />
evolve as the needs <strong>of</strong> the health system change.<br />
Dowling<br />
at Dowling<br />
North Shore-LIJ President <strong>and</strong> CEO<br />
Michael Dowling spoke to more<br />
than 200 high school students from<br />
throughout Long Isl<strong>and</strong> during a<br />
Long Isl<strong>and</strong> <strong>You</strong>th Summit hosted<br />
last spring at Dowling College in<br />
Oakdale. <strong>The</strong> purpose <strong>of</strong> the Summit<br />
was to work with the brightest <strong>and</strong><br />
most active high school students in<br />
order to make them aware <strong>of</strong> the<br />
socioeconomic, environmental <strong>and</strong><br />
sociomedical issues affecting Long<br />
Isl<strong>and</strong> <strong>and</strong> to recommend solutions.<br />
<strong>The</strong> New St<strong>and</strong>ard 79
Hospital Chefs<br />
Compete in<br />
Healthy Cooking<br />
Challenge<br />
By Betty Olt<br />
GLEN COVE — Hospital food<br />
usually gets a bad rap, but<br />
chefs from 11 North Shore-LIJ<br />
hospitals recently competed in<br />
the health system’s first-ever<br />
cooking challenge to prove<br />
that hospital chefs can serve<br />
up gourmet restaurant-quality<br />
meals, but without high fat,<br />
calories or sodium.<br />
Coinciding with National<br />
Nutrition Month, culinary<br />
teams from Queens, Nassau,<br />
Suffolk, Manhattan <strong>and</strong> Staten<br />
Isl<strong>and</strong> faced <strong>of</strong>f at Glen Cove<br />
Hospital’s Pratt Auditorium,<br />
which was trans<strong>for</strong>med into a<br />
giant kitchen equipped with<br />
stove-top burners, a pantry<br />
<strong>and</strong> farmers’ market <strong>for</strong> the<br />
Ultimate Chef Healthy Entrée<br />
Challenge. Each team had<br />
one hour to create a delicious,<br />
attractive <strong>and</strong> nutritious meal.<br />
Three celebrity chef judges<br />
awarded Forest Hills Hospital’s<br />
chefs with the top prize <strong>for</strong><br />
their original dish <strong>of</strong> spinachstuffed<br />
pork tenderloin with<br />
cranberry wild rice. Lenox<br />
80 Summer 2012<br />
Hill Hospital<br />
received second<br />
place <strong>and</strong><br />
Syosset Hospital<br />
came in third.<br />
Michael<br />
Kiley, director<br />
<strong>of</strong> nutrition <strong>and</strong><br />
food services<br />
at Glen Cove<br />
Hospital, who<br />
also helps<br />
coordinate North Shore-LIJ’s<br />
chef committee, organized<br />
the cook-<strong>of</strong>f. “Patients <strong>of</strong>ten<br />
compare hospital food to<br />
restaurants, <strong>and</strong> this event<br />
showcases that hospital chefs<br />
can prepare appealing food<br />
that tastes really good <strong>and</strong> is<br />
nutritious,” said Mr. Kiley.<br />
Judges rated all entrees <strong>and</strong><br />
side dishes prepared during<br />
the competition based on taste,<br />
nutrition, originality <strong>and</strong><br />
presentation. Each hospital<br />
culinary team was paired with<br />
a registered dietician from<br />
a North Shore-LIJ hospital<br />
to ensure that each dish<br />
contained no more than 500<br />
calories, 15 grams <strong>of</strong> fat <strong>and</strong><br />
600 milligrams <strong>of</strong> sodium.<br />
Teams worked with a “surprise<br />
protein” — such as halibut,<br />
shrimp, chicken <strong>and</strong> pork<br />
tenderloin — to build a creative<br />
meal around the item.<br />
Winning chefs Gary<br />
DeFreitas <strong>and</strong> Dale Lyons from<br />
Forest Hills Hospital said they<br />
are used to preparing meals <strong>for</strong><br />
600 to 700 patients each day.<br />
After the awards ceremony, Mr.<br />
Lyons said, “This event gives us<br />
the opportunity to show what<br />
we can do in the kitchen.…<br />
It’s a dream come true.” Mr.<br />
DeFreitas, who has been<br />
cooking since he was 19 years<br />
old, said it was a “great honor”<br />
to receive first prize in the<br />
competition but pointed out<br />
that “love is the most important<br />
ingredient in cooking, <strong>and</strong> it<br />
always comes out in the dish.”<br />
Above: Chefs from Forest Hills<br />
Hospital won North Shore-LIJ’s<br />
Ultimate Chef Challenge cook-<strong>of</strong>f.<br />
Dale Lyons chops an onion <strong>for</strong> the<br />
winning dish — spinach-stuffed<br />
pork tenderloin with cranberry wild<br />
rice — while Gary DeFreitas consults<br />
with Malgorazata Rokoszak, RD, <strong>of</strong><br />
Staten Isl<strong>and</strong> University Hospital.
Ultimate Chef Healthy Entrée 1st Place Recipe<br />
Spinach-Stuffed Pork Tenderloin with Cranberry Wild Rice<br />
By: Gary DeFreitas <strong>and</strong> Dale Lyons<br />
Serving Size: 6 oz Stuffed Pork, 1/3 cup Wild Rice Preparation time: 30 minutes<br />
Servings: 4 Cooking time: 30 minutes<br />
Ingredients:<br />
Pork Tenderloin<br />
1 pound Pork Tenderloin, silver skin removed<br />
1 tablespoon Balsamic Vinegar<br />
½ tablespoon Dijon Mustard<br />
1/8 teaspoon Garlic Powder<br />
1/8 teaspoon Rosemary, fresh, chopped<br />
Stuffing<br />
1 tablespoon Canola Oil<br />
4 oz Fresh Baby Spinach<br />
2 oz Snap Peas<br />
2 oz Dried Figs, minced<br />
1 oz Pistachio Nuts, shelled <strong>and</strong> roughly chopped<br />
½ tablespoon Rosemary, fresh, chopped<br />
½ tablespoon Shallots, peeled <strong>and</strong> chopped<br />
1 ½ teaspoons Garlic, fresh, chopped<br />
Directions:<br />
1. Pork Tenderloin: Cut the pork<br />
tenderloin into 4 equal 4oz portions.<br />
Place each piece <strong>of</strong> pork onto a large piece<br />
<strong>of</strong> plastic wrap <strong>and</strong> cover it with another<br />
piece <strong>of</strong> plastic wrap. Pound each portion<br />
with a meat mallet or the bottom <strong>of</strong> a flat<br />
frying pan until it is thin: about a 4” x 6”<br />
piece <strong>of</strong> meat.<br />
2. Mix together the balsamic vinegar,<br />
mustard, garlic powder <strong>and</strong> rosemary.<br />
Drizzle or smear the mixture onto both<br />
sides <strong>of</strong> each pork cutlet. Reserve seasoned<br />
pork cutlets until ready to stuff.<br />
3. Spinach Stuffing: Preheat a sauté<br />
pan over medium-high heat. Add the<br />
canola oil <strong>and</strong> garlic to the hot pan. Cook<br />
garlic until golden, <strong>and</strong> then add the<br />
spinach, snap peas, dried figs, pistachio<br />
nuts, rosemary, shallots <strong>and</strong> garlic. Sauté<br />
the mixture <strong>for</strong> about 5 minutes until<br />
the spinach wilts <strong>and</strong> the flavors have<br />
developed.<br />
4. Lay each seasoned piece <strong>of</strong> pork<br />
Wild Rice<br />
½ cup Wild Rice<br />
½ cup Celery, minced<br />
¼ cup Onion, minced<br />
½ tablespoon Garlic, minced<br />
1 ½ teaspoons Canola Oil<br />
1 oz Dried Cranberries<br />
1 cup Water<br />
Pan Sauce<br />
1 ½ oz White Wine, dry<br />
1 ½ teaspoons Dijon Mustard<br />
4 leaves Radicchio <strong>for</strong> garnish<br />
tenderloin onto a flat surface like a cutting<br />
board. Place ¼ <strong>of</strong> the spinach mixture<br />
onto each <strong>of</strong> the 4 pieces <strong>of</strong> flattened <strong>and</strong><br />
seasoned pork tenderloin. Pat the spinach<br />
mixture down to cover the pork tenderloin<br />
cutlet. On the longest side <strong>of</strong> the cutlet,<br />
fold the pork over onto the spinach tightly.<br />
Continue to roll in a jelly roll fashion until<br />
you have a tight roulade.<br />
5. Wild Rice: Sauté wild rice in ½<br />
tablespoon <strong>of</strong> canola oil <strong>for</strong> one minute.<br />
Add the fresh chopped garlic, chopped<br />
celery <strong>and</strong> minced onion to the rice <strong>and</strong><br />
continue to cook <strong>for</strong> about 3-5 minutes.<br />
Add 1 cup water to the saucepan <strong>and</strong> bring<br />
the mixture to a boil. Cover <strong>and</strong> reduce<br />
heat to a simmer. Cook <strong>for</strong> 20 – 25<br />
minutes until the rice is tender <strong>and</strong> the<br />
water has been absorbed into the rice.<br />
6. While the rice is cooking, heat a<br />
frying pan over medium-high heat: Add 1<br />
teaspoon <strong>of</strong> canola oil to the pan <strong>and</strong> then<br />
add the four roulades. Position the stuffed<br />
pork pieces so that they are not touching<br />
each other. Cook the pork all around the<br />
roulades until the internal temperature<br />
reaches 140ºF. Take the pork out <strong>of</strong> the<br />
pan <strong>and</strong> place it onto a plate to rest.<br />
7. Sauce: Pour white wine <strong>and</strong> Dijon<br />
mustard into the frying pan <strong>and</strong> deglaze<br />
the pan. Simmer the wine mixture until it<br />
reduces slightly.<br />
8. Plating: After the rice is cooked<br />
add the dried cranberries <strong>and</strong> stir. With<br />
a sharp knife, slice each roulade into 1”<br />
pinwheel slices on the bias. Place 1/3<br />
cup <strong>of</strong> rice mixture into the center <strong>of</strong> a<br />
dinner plate using a cup as a mold. Place<br />
1 radicchio leaf into the rice so that it<br />
st<strong>and</strong>s up. Place the slices <strong>of</strong> the roulade<br />
around the rice. Drizzle the pan sauce<br />
around the plate <strong>and</strong> serve.<br />
Nutritional In<strong>for</strong>mation: 228 Calories, 8g Fat,<br />
26g Protein, 10g Carbohydrate, 62mg Cholesterol, 1g<br />
Fiber, 121mg Sodium, 570mg Potassium.<br />
<strong>The</strong> New St<strong>and</strong>ard 81
Miracle Foundation Palliative Care Center:<br />
It’s All About Quality <strong>of</strong> Life<br />
Patients living with a<br />
serious illness can find<br />
pain relief <strong>and</strong> address<br />
symptom management<br />
at home, in the company <strong>of</strong><br />
their loved ones, courtesy <strong>of</strong> the<br />
Miracle Foundation Palliative<br />
Care Center.<br />
“<strong>The</strong> Miracle Foundation<br />
Palliative Care Center dialogues<br />
with patients <strong>and</strong> families<br />
living with advanced illnesses<br />
about treatment options,<br />
<strong>of</strong>fers emotional support <strong>and</strong><br />
makes them as com<strong>for</strong>table<br />
as possible,” said Maureen<br />
Hinkelman, chief executive<br />
<strong>of</strong>ficer <strong>of</strong> the Hospice Care<br />
Network, part <strong>of</strong> the North<br />
Shore-LIJ Health System.<br />
Palliative care is<br />
comprehensive, individualized<br />
medical treatment that<br />
complements curative<br />
therapies <strong>for</strong> patients with<br />
life-threatening illness. In<br />
February <strong>and</strong> April 2011,<br />
Governor Cuomo passed two<br />
important pieces <strong>of</strong> legislation<br />
to address it. <strong>The</strong> Palliative<br />
Care In<strong>for</strong>mation Act requires<br />
that attending physicians<br />
<strong>and</strong> nurse practitioners<br />
<strong>of</strong>fer terminally ill patients<br />
in<strong>for</strong>mation <strong>and</strong> counseling<br />
concerning palliative care<br />
<strong>and</strong> appropriate end-<strong>of</strong>-life<br />
options. According to the<br />
New York State Department <strong>of</strong><br />
Health, the law helps to ensure<br />
that patients are fully in<strong>for</strong>med<br />
<strong>of</strong> their options when they face<br />
a terminal illness or condition.<br />
82 Summer 2012<br />
Jim Kennedy<br />
<strong>The</strong> second law, the<br />
Palliative Care Access<br />
Act, requires hospitals,<br />
nursing homes, home care<br />
agencies <strong>and</strong> assisted living<br />
residences to provide access to<br />
in<strong>for</strong>mation <strong>and</strong> counseling<br />
about palliative care to<br />
patients with advanced,<br />
life-limiting conditions <strong>and</strong><br />
illnesses. <strong>The</strong>se providers<br />
must also facilitate access to<br />
palliative care consultation<br />
<strong>and</strong> services that are<br />
consistent with the patient’s<br />
needs <strong>and</strong> preferences.<br />
“We are always looking <strong>for</strong><br />
better ways to serve the patients<br />
<strong>and</strong> families in our community.<br />
Many families have told us that<br />
they wished they had known<br />
sooner about palliative care <strong>and</strong><br />
hospice service options. <strong>The</strong><br />
Miracle Foundation Palliative<br />
Care Center addresses this<br />
concern by providing a useful<br />
venue to help physicians attend<br />
to the new requirements,” said<br />
Ms. Hinkelman.<br />
This unique center<br />
is generously funded by a<br />
$500,000 grant from the<br />
Miracle Foundation, an<br />
organization founded by<br />
Patti <strong>and</strong> Michael Tenaglia<br />
<strong>and</strong> dedicated to improving<br />
the lives <strong>of</strong> those diagnosed<br />
with cancer <strong>and</strong> other lifethreatening<br />
diseases.<br />
Above: With a live-in aide <strong>and</strong><br />
regular visits from palliative care<br />
nurse Laurie Alonso, NP, left,<br />
102-year-old George Wittmer is<br />
able to remain in his home.
Club TLC Benefits Families <strong>of</strong> “NICU Babies”<br />
A night <strong>of</strong> dancing, cocktails, light bites <strong>and</strong> socializing at the Maximus Spa & Salon in Mineola was also a fundraiser <strong>for</strong> the Tender<br />
Loving Care (TLC) Foundation, which raises funds <strong>for</strong> support programs geared toward families <strong>of</strong> newborns treated in the Neonatal<br />
Intensive Care Units (NICU) at the North Shore-LIJ Health System’s Steven <strong>and</strong> Alex<strong>and</strong>ra Cohen Children’s Medical Center <strong>of</strong> New York<br />
in New Hyde Park <strong>and</strong> Manhasset. Sick <strong>and</strong> critically ill newborns <strong>of</strong>ten spend weeks or months in the NICUs receiving highly specialized<br />
care, putting an enormous<br />
strain on families.<br />
Proceeds from this event<br />
<strong>and</strong> those in 2010 <strong>and</strong> 2011<br />
have helped or will help<br />
provide funding <strong>for</strong> muchneeded<br />
medical equipment<br />
such as a Transport Isolette<br />
<strong>and</strong> Retscan Retina Scanning<br />
Unit, as well as support <strong>for</strong> the<br />
music therapy program, family<br />
support groups, monthly<br />
dinners in the NICU <strong>and</strong><br />
sibling outreach.<br />
Shown at Club TLC, from left: David Goldberg, TLC chairman, his wife, Franessa, <strong>and</strong> <strong>Joy</strong>ce <strong>and</strong> Richard Calcasola, who<br />
generously hosted the event.<br />
Multispecialty<br />
Facility<br />
Ribbon-Cutting<br />
North Shore-LIJ <strong>of</strong>ficials<br />
gathered to celebrate the<br />
opening <strong>of</strong> a single destination<br />
<strong>for</strong> orthopedic, neuroscience<br />
<strong>and</strong> imaging services at 611<br />
Northern Boulevard in Great<br />
Neck. <strong>The</strong> new facility brings<br />
together the experience<br />
<strong>and</strong> resources <strong>of</strong> University<br />
Orthopedic Associates, the<br />
Cushing Neuroscience Institute<br />
<strong>and</strong> North Shore-LIJ Imaging.<br />
<strong>The</strong> New St<strong>and</strong>ard 83
Patients at North<br />
Shore-LIJ hospitals<br />
<strong>and</strong> facilities may now<br />
see visitors any time,<br />
thanks to a new visitation policy.<br />
Only occasional limitations may<br />
be needed <strong>for</strong> health reasons or<br />
certain situations.<br />
Active involvement <strong>of</strong><br />
patients <strong>and</strong> families in their<br />
healthcare helps improve the<br />
safety <strong>and</strong> overall quality <strong>of</strong><br />
care, according to the American<br />
Association <strong>of</strong> Critical Care<br />
Nurses. This is especially<br />
true in intensive care units,<br />
where patients <strong>of</strong>ten have<br />
breathing tubes inserted <strong>and</strong><br />
North Shore-LIJ Nursing Homes Among<br />
Best, says US News & World Report<br />
By Betty Olt<br />
<strong>The</strong> Stern Family Center <strong>for</strong> Rehabilitation in Manhasset <strong>and</strong> the Orzac Center <strong>for</strong> Rehabilitation in Valley Stream recently<br />
earned the top five-star overall quality ranking in US News & World Report’s 2012 Best Nursing Homes report. <strong>The</strong> report also<br />
recognized four health system affiliates: A. Holly Patterson Extended Care Facility in Uniondale; Amsterdam Nursing Home in<br />
Manhattan; Queens Boulevard Extended Care Facility in Woodside; <strong>and</strong> Fairview Nursing Care Center in Forest Hills.<br />
US News’ Best Nursing Homes recognizes top-rated facilities in all 50 states <strong>and</strong> <strong>of</strong>fers important guidance to families<br />
<strong>and</strong> healthcare providers caring <strong>for</strong> people who need a nursing home.<br />
<strong>The</strong> publication’s evaluation is based on data from Nursing Home Compare, the US Centers <strong>for</strong> Medicare <strong>and</strong><br />
Medicaid Services’ consumer Web site. <strong>The</strong> government agency sets <strong>and</strong> en<strong>for</strong>ces st<strong>and</strong>ards <strong>for</strong> nursing homes (defined<br />
as facilities or portions <strong>of</strong> facilities enrolled in Medicare or Medicaid that provide 24-hour nursing care <strong>and</strong> other<br />
medical services). Facilities earn an overall rating <strong>of</strong> one to five stars, as well as up to five stars in health inspections,<br />
nurse staffing <strong>and</strong> quality <strong>of</strong> care.<br />
Of more than 15,500 nursing homes rated <strong>and</strong> pr<strong>of</strong>iled on the US News Web site, North Shore-LIJ’s Stern <strong>and</strong> Orzac<br />
centers <strong>and</strong> its four affiliate nursing homes were among the fewer than one in eight that received a five-star overall quality<br />
rating in all four quarters <strong>of</strong> 2011. View Best Nursing Homes 2012 at USNews.com/nursinghomes.<br />
According to US News, more than three million Americans will spend part <strong>of</strong> this year in a nursing home. “Nursing<br />
homes in New York <strong>and</strong> across the country vary in quality <strong>of</strong> care <strong>and</strong> the healthcare services they provide to residents,” said<br />
Maureen McClusky, executive director <strong>of</strong> the Stern <strong>and</strong> Orzac facilities. “Earning US News’ five-star quality ranking <strong>for</strong> our<br />
facilities is a top honor, thanks to the dedication <strong>of</strong> our clinical teams <strong>and</strong> our entire staff. <strong>The</strong> report also gives concrete<br />
quality measures consumers can access online to help them select the best nursing home.”<br />
84 Summer 2012<br />
can’t speak <strong>for</strong> themselves.<br />
<strong>The</strong> association also pointed<br />
out that unrestricted visitation<br />
<strong>of</strong> a support person or<br />
family member can improve<br />
communication <strong>and</strong> help<br />
convey a better underst<strong>and</strong>ing<br />
<strong>of</strong> the patient.<br />
“<strong>The</strong> health system has<br />
created an environment where<br />
the patient’s voice is heard<br />
<strong>and</strong> where we value the<br />
benefit <strong>and</strong> support <strong>of</strong> family<br />
members <strong>and</strong> others involved<br />
in their loved ones’ care,” said<br />
Elaine Smith, EdD, RN, vice<br />
president <strong>for</strong> nursing education<br />
at North Shore-LIJ <strong>and</strong> co-<br />
chair <strong>of</strong> the newly <strong>for</strong>med<br />
Patient Rights Task Force.<br />
<strong>The</strong> task <strong>for</strong>ce focuses on<br />
reviewing <strong>and</strong> establishing a<br />
safe, open visitation process<br />
that protects all patients’<br />
privacy. James Romagnoli, the<br />
health system’s vice president<br />
Family-Friendly Visitation<br />
Puts Patients First<br />
By Betty Olt<br />
<strong>of</strong> protective services, also cochairs<br />
the interpr<strong>of</strong>essional<br />
task <strong>for</strong>ce, which combines<br />
the expertise <strong>of</strong> nurses,<br />
physicians, in<strong>for</strong>mation<br />
technology specialists,<br />
attorneys, staff educators,<br />
health literacy pr<strong>of</strong>essionals,<br />
hospital executive directors,<br />
clinical excellence <strong>and</strong> quality<br />
staff <strong>and</strong> security personnel.<br />
<strong>The</strong> visitation policy allows<br />
patients to designate a support<br />
person to carry out their wishes<br />
about who can visit <strong>and</strong> manage<br />
the flow <strong>of</strong> visitors to the<br />
hospital room. Children who<br />
are supervised by an adult are<br />
welcome to visit.<br />
Piloted at North Shore<br />
University Hospital (NSUH),<br />
the policy puts structure around<br />
visitation <strong>and</strong> supports families,<br />
patients <strong>and</strong> staff, according<br />
to task <strong>for</strong>ce member Joanne<br />
Bentson, RN, DNP, associate<br />
executive director at NSUH.<br />
“We know that having family<br />
members or significant others at<br />
the bedside is in the best interest<br />
<strong>of</strong> patients <strong>and</strong> promotes<br />
healing,” said Dr. Bentson.<br />
“Our policy puts patients first,<br />
while ensuring simple guidelines<br />
<strong>for</strong> safe, respectful visitation <strong>for</strong><br />
all patients.”<br />
Going<br />
Abroad?<br />
Protect your health when you<br />
travel overseas. Contact the North<br />
Shore-LI J Travel Immunization<br />
Center be<strong>for</strong>e your getaway. Call<br />
(516) 562-4280 to learn more.<br />
Thinkstock/Stockbyte
It’s three diamonds<br />
down, only two to go <strong>for</strong> Long<br />
Isl<strong>and</strong> Jewish Medical Center’s<br />
Satellite Dialysis Facility in<br />
Queens Village, led by John D.<br />
Wagner, MD, medical director.<br />
Yol<strong>and</strong>a A. Malone, RN,<br />
nurse manager, was recently<br />
in<strong>for</strong>med by the New York<br />
State ESRD (End Stage Renal<br />
Disease) Network that the<br />
facility had taken the measures<br />
necessary to achieve the third<br />
diamond in the 5-Diamond<br />
Patient Safety Program <strong>and</strong> will<br />
be recognized in the network<br />
newsletter. Sponsored by<br />
the CMS-contracted Quality<br />
Improvement Organization,<br />
a subsidiary <strong>of</strong> IPRO, the<br />
program is dedicated to assisting<br />
dialysis facilities in improving<br />
both staff <strong>and</strong> patient awareness<br />
<strong>of</strong> specific patient safety areas,<br />
promoting patient safety values<br />
<strong>and</strong> building a culture <strong>of</strong> patient<br />
safety in every dialysis facility.<br />
“<strong>The</strong> first module<br />
we completed was Patient<br />
LIJ Dialysis Facility Achieves<br />
Third Diamond in ESRD Program<br />
Safety Principles,” said Ms.<br />
Malone. “This m<strong>and</strong>atory<br />
module, representing the<br />
first diamond, teaches basic<br />
concepts <strong>of</strong> patient safety<br />
<strong>and</strong> the appropriate steps to<br />
prevent errors. <strong>The</strong> second<br />
module was Medication<br />
Reconciliation; it stresses<br />
the importance to both<br />
patients <strong>and</strong> staff <strong>of</strong> avoiding<br />
medication errors. Third<br />
was H<strong>and</strong> Hygiene. Next is<br />
Slips, Trips <strong>and</strong> Falls, <strong>and</strong> the<br />
module we will tackle last will<br />
be Emergency Preparation.”<br />
Following in the footsteps<br />
<strong>of</strong> the Queens Village facility<br />
is the pediatric chronic<br />
dialysis unit, located within<br />
the inpatient unit at LIJ,<br />
where Ms. Malone is also<br />
nurse manager; they hope<br />
soon to achieve their first<br />
diamond. Joanne Seylar, RN,<br />
Marlyn Batan, RN, <strong>and</strong> the<br />
entire nursing leadership join<br />
together in commending the<br />
staffs <strong>of</strong> both facilities <strong>for</strong><br />
their enthusiastic participation<br />
in the program, undergoing<br />
training <strong>and</strong> bringing the<br />
lessons learned down to the<br />
patient level.<br />
“We have a great team,”<br />
said Ms. Malone. “Everyone<br />
pitched in <strong>and</strong> helped, from<br />
leadership, especially Dr.<br />
Wagner, our educator, Nicole<br />
Lemoine, RN, on down. With<br />
that level <strong>of</strong> multidisciplinary<br />
collaboration, by the end <strong>of</strong><br />
2012, we expect that both units<br />
will be 5-Diamond facilities.”<br />
“<strong>The</strong> 5-Diamond<br />
program <strong>for</strong>mally measures<br />
<strong>and</strong> acknowledges our facility’s<br />
ef<strong>for</strong>ts in the areas cited, but<br />
our per<strong>for</strong>mance improvement<br />
program has always focused on<br />
these areas,” said Dr. Wagner.<br />
“Participating in the program<br />
confirms that we are on the<br />
right track, <strong>and</strong> it also applauds<br />
our achievements. I could<br />
not be prouder <strong>of</strong> the highly<br />
talented team <strong>of</strong> nurses, patient<br />
care technicians, dietitians,<br />
social workers <strong>and</strong> support<br />
staff who took the initiative to<br />
engage in this program.”<br />
Above: Shown in the pediatric<br />
chronic dialysis unit with a young<br />
patient are Yol<strong>and</strong>a Malone, RN,<br />
left, <strong>and</strong> Vera Benn, RN.<br />
<strong>The</strong> New St<strong>and</strong>ard 85
LAKE SUCCESS — <strong>The</strong>re<br />
was a surprise visitor this<br />
spring when North Shore-<br />
LIJ Laboratories hosted a<br />
reception to celebrate the<br />
10th anniversary <strong>of</strong> the DNA<br />
Learning Center West: none<br />
other than Nobel Laureate<br />
James Watson, PhD.<br />
<strong>The</strong> DNA Learning<br />
Center, a joint collaboration<br />
<strong>of</strong> North Shore-LIJ <strong>and</strong> Cold<br />
Spring Harbor Laboratory<br />
(CSHL), has provided<br />
education in genetics to more<br />
than 30,000 middle <strong>and</strong> high<br />
school students from across<br />
Long Isl<strong>and</strong>, New York City<br />
<strong>and</strong> the entire tri-state area<br />
since opening in June 2002.<br />
Within the 2,200-squarefoot<br />
education center, located<br />
adjacent to North Shore-LIJ<br />
Laboratories’ headquarters<br />
at 10 Nevada Drive in Lake<br />
Success, are a genetic/<br />
biochemistry lab, a prep lab,<br />
a lunchroom <strong>and</strong> an <strong>of</strong>fice.<br />
North Shore-LIJ Laboratories<br />
86 Summer 2012<br />
Nobel Laureate Helps<br />
DNA Learning Center West<br />
Celebrate 10th Anniversary<br />
underwrites the $250,000<br />
annual cost <strong>of</strong> the leased space.<br />
“For many <strong>of</strong> these<br />
students, the experience<br />
they’ve gained at the DNA<br />
Learning Center West has<br />
opened their eyes to careers<br />
in medicine, science <strong>and</strong><br />
other healthcare fields,”<br />
said Robert Stallone, vice<br />
president <strong>of</strong> North Shore-LIJ<br />
Laboratories. He said some<br />
<strong>for</strong>mer students now work as<br />
medical technologists <strong>and</strong> in<br />
other related jobs at North<br />
Shore-LIJ Laboratories, a<br />
fully automated, 60,000-<br />
square-foot facility that<br />
<strong>of</strong>fers a range <strong>of</strong> specialty<br />
lab testing to physician<br />
practices, hospitals, nursing<br />
homes <strong>and</strong> the biomedical<br />
industry. <strong>The</strong> lab’s business<br />
has doubled in the past four<br />
years, underscoring the career<br />
opportunities available <strong>for</strong><br />
young people in this field.<br />
<strong>The</strong> three-to-fourhour<br />
daily tours <strong>of</strong> the DNA<br />
Learning Center West <strong>and</strong><br />
North Shore-LIJ Laboratories<br />
are so popular that schools must<br />
book a year in advance, said<br />
center instructor Tedi Setton.<br />
In addition to the school tours,<br />
the DNA Learning Center hosts<br />
about 300 students during<br />
its annual summer program.<br />
Curriculum is developed <strong>and</strong><br />
taught by CSHL staff.<br />
Among the highlights<br />
<strong>of</strong> the center’s curriculum,<br />
students are able to view their<br />
own DNA, utilizing the center’s<br />
fingerprinting <strong>and</strong> human<br />
mitochondrial sequencing<br />
labs. <strong>The</strong> center’s interactive<br />
approach links the process<br />
<strong>of</strong> discovery to learning, said<br />
James Craw<strong>for</strong>d, MD, North<br />
Shore-LIJ’s chair <strong>of</strong> pathology.<br />
“Every time I come by the Lab,<br />
I’m looking <strong>for</strong> those bright<br />
eyes <strong>of</strong> students <strong>and</strong> they’re<br />
here five days a week, yearround,”<br />
said Dr. Craw<strong>for</strong>d.<br />
To learn more about the<br />
DNA Learning Center West,<br />
go to: www.dnalc.org/about/<br />
locations/aboutdnalcwest.html<br />
Among those celebrating the DNA<br />
Learning Center West’s 10th<br />
anniversary were, from left: Robert<br />
Stallone, vice president <strong>of</strong> North<br />
Shore-LIJ Laboratories; Dr. James<br />
Watson, chancellor emeritus at<br />
Cold Spring Harbor Laboratory<br />
(CSHL); David Micklos, founder<br />
<strong>and</strong> executive director <strong>of</strong> the DNA<br />
Learning Center; <strong>and</strong> Dr. James<br />
Craw<strong>for</strong>d, North Shore-LIJ’s chair<br />
<strong>of</strong> pathology.
MANHASSET — North<br />
Shore University Hospital has<br />
been designated an Academic<br />
Center <strong>of</strong> Excellence <strong>for</strong><br />
minimally invasive surgery<br />
in gynecologic oncology <strong>and</strong><br />
gynecology by the American<br />
Institute <strong>of</strong> Minimally Invasive<br />
Surgery (AIMIS), joining LIJ<br />
Medical Center as one <strong>of</strong> only<br />
28 Centers <strong>of</strong> Excellence in<br />
the country to achieve this<br />
designation <strong>and</strong> only one <strong>of</strong><br />
four centers in New York State.<br />
“This prestigious<br />
accreditation from AIMIS<br />
shows that we have a deep<br />
commitment to providing only<br />
the highest quality <strong>of</strong> care to<br />
all our female patients with<br />
state-<strong>of</strong>-the-art, minimally<br />
invasive <strong>and</strong> robotic surgical<br />
gynecologic expertise,” said<br />
Susan Somerville, executive<br />
director <strong>of</strong> the hospital. “This<br />
is an occasion to take pride<br />
in our work <strong>and</strong> to rededicate<br />
ourselves to continue at this<br />
same high level in the future.”<br />
AIMIS is the nation’s<br />
preeminent educator <strong>of</strong><br />
advanced surgical techniques<br />
<strong>for</strong> women’s health specialists<br />
<strong>and</strong> recognizes hospitals <strong>and</strong><br />
clinics that excel <strong>and</strong> provide<br />
leadership in leading-edge<br />
surgical techniques. A hospital<br />
or surgical center can be<br />
recognized as a Center <strong>of</strong><br />
Excellence once it has combined<br />
ef<strong>for</strong>ts with an accredited<br />
AIMIS surgeon <strong>and</strong> meets<br />
AIMIS st<strong>and</strong>ards. Recognized<br />
institutions have made<br />
minimally invasive surgery a<br />
priority, which helps minimize<br />
recovery times <strong>and</strong> provide<br />
better patient outcomes.<br />
“We have always taken<br />
great pride in our ability to<br />
North Shore Recognized <strong>for</strong><br />
Gynecological Surgery Expertise<br />
provide our patients with the<br />
latest that technology <strong>of</strong>fers<br />
in a safe, caring, pr<strong>of</strong>essional<br />
environment,” said Michael<br />
Nimar<strong>of</strong>f, MD, vice chair <strong>and</strong><br />
chief <strong>of</strong> gynecology at North<br />
Shore University Hospital. “We<br />
are fully committed to <strong>of</strong>fering<br />
our patients the full range<br />
<strong>of</strong> minimally invasive <strong>and</strong><br />
robotic surgical options that<br />
successfully treat a wide range<br />
<strong>of</strong> both benign conditions <strong>and</strong><br />
gynecological cancers.”<br />
North Shore University<br />
Hospital’s Division <strong>of</strong><br />
Gynecology per<strong>for</strong>med more<br />
gynecologic surgery procedures<br />
than any other hospital in<br />
New York State — a total<br />
<strong>of</strong> 3,935 cases in 2011. “It<br />
is because <strong>of</strong> our team <strong>of</strong><br />
highly trained gynecologists,<br />
urogynecologists, reproductive<br />
surgeons <strong>and</strong> gynecological<br />
oncologists that we have<br />
established a proven track<br />
record <strong>of</strong> positive surgical<br />
outcomes <strong>for</strong> women. We<br />
thank AIMIS <strong>for</strong> recognizing<br />
North Shore University<br />
Hospital with this highly<br />
sought-after accreditation,”<br />
said Dr. Nimar<strong>of</strong>f.<br />
Minimally invasive<br />
surgery, whether laparoscopic<br />
or robotically assisted, is<br />
advancing healthcare <strong>for</strong><br />
women by providing doctors<br />
new tools to accomplish the<br />
same goals as they would with<br />
traditional open surgery.<br />
Most patients undergoing<br />
minimally invasive procedures<br />
experience less pain <strong>and</strong> blood<br />
loss, decreased scarring, fewer<br />
complications, faster recovery<br />
<strong>and</strong> a decreased length <strong>of</strong><br />
hospital stay.<br />
AIMIS teaches <strong>and</strong><br />
supports minimally<br />
invasive gynecological <strong>and</strong><br />
urogynecological surgical<br />
methods while improving<br />
patient outcomes through<br />
advanced surgical techniques.<br />
<strong>The</strong> organization brings<br />
together hospitals, surgeons,<br />
clinics, medical technology<br />
companies, the insurance<br />
industry <strong>and</strong> patients by<br />
providing a plat<strong>for</strong>m to deliver<br />
advanced surgical procedures<br />
that improve healthcare <strong>for</strong><br />
women <strong>of</strong> all ages.<br />
Above: North Shore University<br />
Hospital’s minimally invasive <strong>and</strong><br />
robotic surgery team, pictured<br />
from left: Kelly Cifu, RN, associate<br />
executive director, peri-op services<br />
at NSUH; Chris Ciampa, quality<br />
management; Pat Moleski, RN,<br />
director, peri-op services; Adiel<br />
Fleischer, MD, North Shore-LIJ’s<br />
chair <strong>of</strong> obstetrics <strong>and</strong> gynecology;<br />
Emily Kao, RPh, associate executive<br />
director, NSUH; Robert Barnett,<br />
MD, AIMIS representative; Michael<br />
Nimar<strong>of</strong>f, MD, vice chair <strong>of</strong><br />
obstetrics <strong>and</strong> gynecology <strong>and</strong> chief<br />
<strong>of</strong> gynecology at NSUH; Cindy<br />
Girdusky, RN, nurse manager, periop<br />
services; <strong>and</strong> Andrea Restifo, RN,<br />
associate executive director, quality<br />
management.<br />
<strong>The</strong> New St<strong>and</strong>ard 87
Ambulance Tracking Tool<br />
Launched at LIJ<br />
By Betty Olt<br />
NEW HYDE PARK — North<br />
Shore-LIJ’s Center <strong>for</strong><br />
Emergency Medical Services<br />
(CEMS) has installed a new<br />
wireless tracking system to<br />
better predict ambulance<br />
arrivals <strong>and</strong> collect critical<br />
health data in real time be<strong>for</strong>e<br />
patients arrive at the Emergency<br />
Department (ED). <strong>The</strong> new<br />
technology was recently rolled<br />
out at LIJ, the first hospital on<br />
Long Isl<strong>and</strong> <strong>and</strong> Queens to use<br />
the s<strong>of</strong>tware.<br />
Responding to 911 calls,<br />
paramedics <strong>and</strong> emergency<br />
medical technicians (EMTs)<br />
begin their assessment<br />
<strong>and</strong> gather critical patient<br />
in<strong>for</strong>mation. Using a laptop<br />
computer, emergency medical<br />
workers transmit patients’<br />
age, gender, vital signs <strong>and</strong><br />
brief comments about their<br />
condition — <strong>for</strong> example,<br />
“dizziness, seizure, fainting.”<br />
In<strong>for</strong>mation is displayed on a<br />
40-inch monitor on the wall<br />
facing the entrance <strong>of</strong> LIJ’s<br />
ambulance bay (names are<br />
not used to protect patient<br />
privacy). Triage nurses or<br />
physicians can get a quick visual<br />
picture about the number <strong>of</strong><br />
ambulances en route to the<br />
88 Summer 2012<br />
hospital <strong>and</strong> the severity <strong>of</strong><br />
patients’ conditions, which<br />
allow staff to better prepare<br />
<strong>for</strong> patients <strong>and</strong> manage care.<br />
Physicians <strong>and</strong> nurses can also<br />
access patient in<strong>for</strong>mation on<br />
computers in the ED.<br />
“<strong>The</strong> ED is an<br />
unpredictable place,” said<br />
Salvatore Pardo, MD,<br />
associate chairman <strong>of</strong><br />
emergency medicine at LIJ.<br />
“<strong>The</strong> technology is a great<br />
tool because it gives the ED<br />
team in<strong>for</strong>mation at a glance<br />
to better plan <strong>for</strong> incoming<br />
patients.” From several yards<br />
away staff can see incoming<br />
cases blinking on the monitor,<br />
with trauma cases in black<br />
or cardiac arrests in orange,<br />
<strong>for</strong> example. Previously, Dr.<br />
Pardo said the ED would get<br />
a phone call from emergency<br />
medical staff in the ambulance<br />
<strong>and</strong> it was nearly impossible<br />
to capture all details <strong>of</strong> a<br />
patient’s condition. (EMTs<br />
will likely still call ahead to the<br />
ED to alert staff to heart attack<br />
or major trauma patients.)<br />
“<strong>The</strong> tracking system<br />
eliminates paperwork <strong>and</strong><br />
gets patients registered be<strong>for</strong>e<br />
they arrive, making treatment<br />
<strong>and</strong> the entire process more<br />
effective,” he added.<br />
<strong>The</strong> new tracking system,<br />
known as XChangER, was<br />
developed by the Duluth,<br />
MN-based company Sansio.<br />
Currently, North Shore-LIJ<br />
EMS <strong>and</strong> the SeniorCare EMS<br />
are using the system at LIJ.<br />
CEMS, the largest hospitalbased<br />
ambulance service in<br />
the New York metropolitan<br />
area <strong>and</strong> one <strong>of</strong> the largest<br />
in the country, plans to<br />
introduce the technology at<br />
other health system hospitals<br />
in the coming months.<br />
“<strong>The</strong> tracking technology<br />
provides a continuum <strong>of</strong><br />
care <strong>for</strong> patients, integrating<br />
in<strong>for</strong>mation taken at the<br />
emergency site <strong>and</strong> in the<br />
ambulance prior to arrival at<br />
the hospital <strong>for</strong> treatment,”<br />
said Alan Schwalberg, CEMS<br />
vice president. “Combining<br />
the technology <strong>of</strong> electronic<br />
medical records <strong>and</strong> this new<br />
tracking s<strong>of</strong>tware, we are<br />
providing accurate, up-to-the<br />
minute health in<strong>for</strong>mation<br />
about patients so ED staff can<br />
prepare <strong>and</strong> coordinate the<br />
best possible medical care.”<br />
In the past year, LIJ’s<br />
ED saw a 36 percent increase<br />
in patient visits, partially<br />
attributable to recent hospital<br />
closures in Queens, according<br />
to Patricia Farrell, RN, senior<br />
administrative director <strong>of</strong><br />
patient care services at LIJ.<br />
Each month, LIJ’s ED receives<br />
about 1,400 ambulances<br />
via 911 calls; it receives
approximately 80,000 patient<br />
visits annually.<br />
“We know that seconds<br />
count in a 911 call <strong>for</strong> a<br />
medical emergency,” said Ms.<br />
Farrell. “<strong>The</strong> tracking system<br />
jump-starts care <strong>and</strong> we are<br />
able to triage patients be<strong>for</strong>e<br />
they come through the door.”<br />
Ms. Farrell explained that<br />
the pre-hospital electronic<br />
records technology also helps<br />
the ED staff to better manage<br />
incoming ambulance traffic.<br />
Through CEMS, they have the<br />
ability to divert an ambulance<br />
to a nearby hospital, if<br />
necessary, improving<br />
“hospital throughput.”<br />
“If we see an increased<br />
volume <strong>of</strong> patients in the ED<br />
<strong>and</strong> we know their condition,<br />
we can notify the operating<br />
room or other hospital<br />
departments, <strong>for</strong> example,<strong>of</strong> a<br />
need <strong>for</strong> more beds,” she said.<br />
“This way, we have a game plan<br />
that not only enhances patient<br />
care <strong>and</strong> service, but makes the<br />
workflow more efficient.”<br />
Above: LIJ’s new tracking s<strong>of</strong>tware<br />
gives emergency medicine staff a<br />
snapshot <strong>of</strong> incoming ambulances<br />
<strong>and</strong> patients, which optimizes care.<br />
ER nurse Debbie Sutton-Williams,<br />
RN, left, discusses a patient’s case<br />
with North Shore-LIJ paramedics.<br />
<strong>The</strong> New St<strong>and</strong>ard 89
Make a Gift Now<br />
<strong>and</strong> Receive<br />
Payments<br />
<strong>for</strong> Life!<br />
It sounds too good to be true!<br />
Make a gift <strong>and</strong> gain an income<br />
stream <strong>for</strong> life.<br />
<strong>You</strong> can do just that — support<br />
yourself, <strong>and</strong> then support North<br />
Shore-LIJ. A charitable gift annuity<br />
enables you (or you <strong>and</strong> a spouse)<br />
to make a gift <strong>of</strong> $10,000+ <strong>and</strong> gain<br />
a fixed income stream <strong>for</strong> your life.<br />
Any remaining amount will be used<br />
by North Shore-LIJ to fulfill our mission<br />
<strong>of</strong> caring <strong>for</strong> our community.<br />
Here are some representative<br />
one-life rates:<br />
ONE LIFE<br />
Age Rate<br />
60 4.9%<br />
65 5.2%<br />
70 5.6%<br />
75 6.3%<br />
80 7.3%<br />
85 8.3%<br />
Example: Anna, age 78, donates<br />
$10,000. She would receive $690/<br />
year ($566 tax-free <strong>for</strong> 10.5 years)<br />
<strong>and</strong> may be eligible to claim a $4,052<br />
income tax deduction.<br />
For more in<strong>for</strong>mation <strong>and</strong><br />
a no-obligation personalized<br />
illustration <strong>of</strong> benefits, contact<br />
Alex<strong>and</strong>ra Brovey, senior director <strong>of</strong><br />
gift planning, at (516) 465-2610 or<br />
abrovey@nshs.edu.<br />
Rates are subject to change. Please<br />
contact us to discuss your rate, tax-free<br />
income <strong>and</strong> charitable deduction.<br />
90 Summer 2012<br />
North Shore-LIJ Integration Garners Praise<br />
GREAT NECK — <strong>The</strong> North Shore-LIJ Health System continues to rank among the top 100 integrated healthcare networks<br />
(IHNs) in the US, according to IMS Health. North Shore-LIJ ranked 31st out <strong>of</strong> 100 IHNs. A provider <strong>of</strong> in<strong>for</strong>mation services<br />
to the healthcare field, IMS Health rates each network’s per<strong>for</strong>mance <strong>and</strong> degree <strong>of</strong> integration.<br />
Rankings are determined by coming up with a system’s total score based on measurements <strong>of</strong> 33 attributes in<br />
weighted per<strong>for</strong>mance categories. Specifically, networks are rated on:<br />
w Hospital utilization: use <strong>of</strong> medical services, procedures <strong>and</strong> facilities (includes data on measures such as<br />
length <strong>of</strong> stay, tests <strong>and</strong> procedures, discharges, etc.).<br />
w Financial stability: network operating <strong>and</strong> pr<strong>of</strong>it margins, long-term debt-to-capitalization ratio <strong>and</strong><br />
financial results.<br />
w Physician participation: the size <strong>and</strong> scope <strong>of</strong> physicians in the network.<br />
w Services <strong>and</strong> access: the availability <strong>of</strong> specific services, network size <strong>and</strong> hospital accreditation.<br />
w Contractual capabilities: the ability to manage costs in the purchasing <strong>and</strong> managed care markets.<br />
w Outpatient utilization: patient care, continuum <strong>of</strong> care <strong>and</strong> effects <strong>of</strong> diversification.<br />
w Integration: coordination <strong>of</strong> administrative <strong>and</strong> clinical functions <strong>and</strong> procedures throughout the network.<br />
w Integrated technology: integration <strong>of</strong> the network’s technical systems, including the level <strong>of</strong> seamless<br />
communication <strong>and</strong> in<strong>for</strong>mation systems.<br />
Last year, North Shore-LIJ ranked 34th among the top 100 IHNs. <strong>The</strong> improved score reflects collaborative ef<strong>for</strong>ts<br />
throughout the health system to work effectively <strong>and</strong> efficiently.<br />
“Every Woman Matters” 5k Walk Attracts 5,000+<br />
<strong>The</strong> North Shore-LIJ Health<br />
System’s third annual Every Woman<br />
Matters Walk: A Walk <strong>for</strong> Women <strong>and</strong><br />
<strong>The</strong>ir Families at Jones Beach State<br />
Park brought together families, friends<br />
<strong>and</strong> the whole community to celebrate<br />
women’s health <strong>and</strong> wellness, <strong>and</strong><br />
support an initiative that promises<br />
to trans<strong>for</strong>m women’s healthcare<br />
throughout the region: North Shore-<br />
LIJ’s Katz Institute <strong>for</strong> Women’s Health<br />
<strong>and</strong> Katz Women’s Hospitals.<br />
Highlights <strong>of</strong> the day included<br />
demonstrations <strong>of</strong> the da Vinci robot,<br />
the state-<strong>of</strong>-the-art instrument that<br />
allows surgeons to remotely per<strong>for</strong>m<br />
minimally invasive surgeries, an<br />
early-morning yoga class, the Katz<br />
Institute <strong>of</strong> Women’s Health showcase<br />
tent <strong>and</strong> many giveaways from<br />
event sponsors. Many participants<br />
registered online, enticed by the<br />
incentive <strong>of</strong> receiving two tickets to<br />
an upcoming New York Mets game,<br />
donated by Saul Katz, president <strong>of</strong> the<br />
Mets <strong>and</strong> long-time North Shore-LIJ<br />
trustee <strong>and</strong> <strong>for</strong>mer chairman.<br />
Since the inception <strong>of</strong> the 5k<br />
walk in 2010, more than $1.5 million<br />
has been raised to support the Katz<br />
Women’s Hospitals.<br />
Above: <strong>The</strong> Third Every Woman<br />
Matters Walk
Mets Present “Every Woman Matters”<br />
Award to Dr. Michael Nimar<strong>of</strong>f<br />
Michael Nimar<strong>of</strong>f, MD, vice chair <strong>and</strong> chief <strong>of</strong> gynecology at the North Shore<br />
University Hospital (NSUH) Department <strong>of</strong> Obstetrics <strong>and</strong> Gynecology, was<br />
presented with the “Every Woman Matters” Award this spring at the New York<br />
Mets’ Welcome Home Dinner. <strong>The</strong> award is presented annually to an individual<br />
associated with North Shore-LIJ’s Katz Institute <strong>for</strong> Women’s Health <strong>and</strong><br />
the Katz Women’s Hospitals who exemplifies outst<strong>and</strong>ing care, compassion<br />
<strong>and</strong> achievement in the care <strong>of</strong> women. Dr. Nimar<strong>of</strong>f has been a pioneer in<br />
introducing minimally invasive surgical techniques, including robotic <strong>and</strong><br />
single-incision procedures designed to help women return to their normal lives<br />
as quickly as possible. He dedicates much <strong>of</strong> his time to training practitioners<br />
in the latest gynecologic surgical techniques. He established NSUH’s Minimally<br />
Invasive <strong>and</strong> Robotic Gynecologic Fellowship program in 2009. From left are:<br />
ob/gyn Daniel Kuo , MD; North Shore-LIJ Trustee <strong>and</strong> Mets President Saul B.<br />
Katz; Adiel Fleischer, MD, North Shore-LIJ’s chair <strong>of</strong> ob/gyn; Neeta Shah, MD, the<br />
health system’s vice president <strong>of</strong> women’s health; NSUH medical director Vicki<br />
LoPachin, MD; Dr. Nimar<strong>of</strong>f; <strong>and</strong> ob/gyns Helen Greco, MD, <strong>and</strong> Allen Toles, MD.<br />
MANHASSET — A US Food<br />
<strong>and</strong> Drug Administrationapproved<br />
revascularization<br />
device is now available to<br />
North Shore University<br />
Hospital patients suffering<br />
from acute ischemic stroke.<br />
Jeffrey Katz, MD, chief<br />
<strong>of</strong> vascular neurology <strong>and</strong><br />
director <strong>of</strong> the NSUH Stroke<br />
Center, recently used the<br />
Solitaire Flow Restoration<br />
(FR) device in 47-year-old<br />
Richard Hasselberger from<br />
Manhasset, who presented<br />
with a spontaneous carotid<br />
dissection <strong>and</strong> ischemic stroke.<br />
“<strong>The</strong> Solitaire device is<br />
relatively easy to use compared<br />
to the older technology we<br />
have been accustomed to <strong>and</strong><br />
has the potential to open<br />
blood vessels more rapidly<br />
than previous devices,” said<br />
Dr. Katz. “This is important<br />
because ‘time is brain’ when<br />
SIUH Receives<br />
Cancer Care Award<br />
<strong>The</strong> Commission on Cancer (CoC) <strong>of</strong> the American<br />
College <strong>of</strong> Surgeons has granted an Outst<strong>and</strong>ing Achievement<br />
Award (OAA) to Staten Isl<strong>and</strong> University Hospital. This<br />
puts the hospital in the distinguished company <strong>of</strong> 106 cancer<br />
programs nationwide being recognized <strong>for</strong> striving <strong>for</strong> excellence<br />
in providing quality care to cancer patients. <strong>The</strong> facilities so<br />
honored demonstrate a Commendation level <strong>of</strong> compliance<br />
in six areas <strong>of</strong> cancer program activity: cancer committee<br />
leadership, cancer data management, clinical management,<br />
research, community outreach <strong>and</strong> quality improvement.<br />
“As the primary deliverer <strong>of</strong> cancer care in our community,<br />
we are happy to service our patients. None <strong>of</strong> the staff seeks<br />
out praise <strong>for</strong> what they do, but it is always nice to be singled<br />
out by a national organization as a center <strong>of</strong> excellence,” said<br />
Dr. Frank Forte, program director <strong>of</strong> oncology/hematology/<br />
palliative care at SIUH. “Thank you to the entire pr<strong>of</strong>essional,<br />
administrative <strong>and</strong> support staff <strong>for</strong> a job well done.”<br />
Established in 1922 by the American College <strong>of</strong> Surgeons,<br />
the Commission on Cancer is a consortium <strong>of</strong> pr<strong>of</strong>essional<br />
organizations dedicated to improving patient outcomes <strong>and</strong><br />
quality <strong>of</strong> life <strong>for</strong> cancer patients through st<strong>and</strong>ard-setting,<br />
prevention, research, education <strong>and</strong> the monitoring <strong>of</strong><br />
comprehensive quality care.<br />
NSUH Stroke Center Offers New Treatment<br />
treating stroke patients. In the<br />
r<strong>and</strong>omized trial comparing<br />
the new Solitaire device to the<br />
Merci retriever, patients treated<br />
with Solitaire had excellent<br />
clinical outcomes, which is what<br />
we have seen in the first two<br />
patients we treated.”<br />
<strong>The</strong> Solitaire FR is a selfexp<strong>and</strong>ing,<br />
columnar metal<br />
cage device combining the<br />
ability to restore blood flow to<br />
the brain, administer medical<br />
therapy <strong>and</strong> retrieve the blood<br />
clot. Treatment with Solitaire<br />
allows the interventional<br />
neurologist to reopen target<br />
arteries in a much more<br />
effective <strong>and</strong> efficient way,<br />
resulting in less symptomatic<br />
intracranial hemorrhage <strong>and</strong><br />
better neurologic outcomes by<br />
three months after the stroke.<br />
<strong>The</strong> New St<strong>and</strong>ard 91
To help facilitate the<br />
commercialization<br />
<strong>of</strong> discoveries at <strong>The</strong><br />
Feinstein Institute<br />
<strong>for</strong> Medical Research <strong>and</strong><br />
pursue other opportunities<br />
across the the health system,<br />
North Shore-LIJ entered into<br />
an alliance this spring with the<br />
world-renowned Clevel<strong>and</strong><br />
Clinic’s venture arm, Clevel<strong>and</strong><br />
Clinic Innovations.<br />
“Our scientists are leaders<br />
in their fields, <strong>and</strong> we believe<br />
that the North Shore-LIJ/<br />
Clevel<strong>and</strong> Clinic alliance will<br />
help us translate discoveries<br />
made in our labs into<br />
significant patient benefits,”<br />
said Kevin Tracey, MD, the<br />
Feinstein’s president <strong>and</strong> chief<br />
executive <strong>of</strong>ficer. Considering<br />
that it typically takes years<br />
<strong>and</strong> costs millions <strong>of</strong> dollars<br />
to move research advances<br />
to market, the partnership<br />
is significant because <strong>of</strong><br />
Clevel<strong>and</strong> Clinic Innovations’<br />
solid track record <strong>of</strong> advancing<br />
fledgling research <strong>and</strong><br />
promising clinical discoveries.<br />
With 55 research<br />
laboratories organized into<br />
11 Centers <strong>of</strong> Excellence, the<br />
Feinstein has more than 1,500<br />
employees engaged in basic <strong>and</strong><br />
clinical research, working to<br />
move discoveries from the lab<br />
to the bedside. <strong>The</strong> Feinstein<br />
already receives about $60<br />
million annually in research<br />
grants, including about $45<br />
million from the National<br />
Institutes <strong>of</strong> Health (NIH).<br />
<strong>The</strong> Bayh-Dole Act <strong>of</strong><br />
1980 authorizes universities<br />
<strong>and</strong> research institutions to<br />
control <strong>and</strong> commercialize<br />
the patent rights arising<br />
from their research that is<br />
supported by federal grants.<br />
92 Summer 2012<br />
Generally, this is accomplished<br />
by licensing Feinstein patent<br />
rights, either to outside<br />
companies or to new ventures<br />
started by its entrepreneurial<br />
faculty members, which can<br />
support the high cost <strong>of</strong><br />
developing <strong>and</strong> validating new<br />
clinical products. Since the<br />
Feinstein’s founding in 1999,<br />
breakthroughs have led to the<br />
creation <strong>of</strong> a dozen startup<br />
companies <strong>and</strong> more than<br />
70 licensing opportunities,<br />
according to Kirk Manogue,<br />
PhD, vice president <strong>and</strong><br />
director <strong>of</strong> the Feinstein’s<br />
Office <strong>of</strong> Technology Transfer.<br />
Below are some <strong>of</strong> those<br />
companies <strong>and</strong> the promising<br />
technologies they are<br />
developing <strong>for</strong> clinical use.<br />
Established in 1998,<br />
Angion Biomedica Corp. has<br />
licensed Feinstein patent rights<br />
<strong>and</strong> is developing products<br />
relating to renal transplant<br />
<strong>and</strong> myocardial infarction.<br />
Since 2005, Angion has<br />
received more than $40<br />
million in NIH Small Business<br />
Innovation Research (SBIR)<br />
funding. Angion scientists at<br />
its multidisciplinary research<br />
<strong>and</strong> development facility in<br />
Uniondale are advancing<br />
several <strong>of</strong> its products to Phase<br />
I <strong>and</strong> Phase 2 clinical trials.<br />
In 2008, Critical<br />
<strong>The</strong>rapeutics, Inc., c<strong>of</strong>ounded<br />
in 2001 by Dr.<br />
Tracey, with colleagues<br />
from the Massachusetts<br />
General Hospital <strong>and</strong> the<br />
University <strong>of</strong> Pittsburgh,<br />
merged with Cornerstone<br />
Biopharma Holdings to create<br />
Cornerstone <strong>The</strong>rapeutics,<br />
Inc. Cornerstone holds<br />
licensed rights to autoimmune,<br />
inflammatory disease <strong>and</strong><br />
critical care treatments that<br />
are based on discoveries made<br />
in Dr. Tracey’s Laboratory <strong>of</strong><br />
Biomedical Sciences.<br />
SetPoint Medical,<br />
another faculty startup, is<br />
developing an implantable<br />
neuromodulator under<br />
license from the Feinstein.<br />
This computerized vagus<br />
nerve stimulator is based<br />
on discoveries made in Dr.<br />
Tracey’s laboratory <strong>and</strong> is<br />
presently in Phase 2 clinical<br />
trials in rheumatoid arthritis.<br />
Under license from the<br />
Feinstein <strong>and</strong> Cornerstone,<br />
Targacept, Inc. is developing<br />
a drug that acts through<br />
neuronal nicotinic receptors<br />
(NNRs), which are key<br />
regulators <strong>of</strong> the nervous<br />
system, to treat asthma <strong>and</strong><br />
type 2 diabetes. Phase 2<br />
clinical trials are ongoing.<br />
<strong>The</strong> drug is also based on<br />
discoveries made in Dr.<br />
Tracey’s laboratory.<br />
TissueGenesis, Inc.,<br />
founded in 1998 by Daniel<br />
Gr<strong>and</strong>e, PhD, has licensed the<br />
rights to develop products that<br />
enhance bone <strong>and</strong> cartilage<br />
repair through gene-enhanced<br />
tissue engineering. <strong>The</strong>se<br />
orthopedic implants are based<br />
on research conducted in<br />
Dr. Gr<strong>and</strong>e’s Laboratory <strong>of</strong><br />
Orthopedic Research.<br />
Clevel<strong>and</strong> Clinic Alliance to<br />
Enhance Feinstein Institute’s<br />
Commercial Success<br />
<strong>The</strong>raSource LLC is a<br />
faculty startup that has licensed<br />
patent rights to develop novel<br />
medicines <strong>for</strong> the treatment <strong>of</strong><br />
sepsis, ischemia/reperfusion<br />
injury <strong>and</strong> hemorrhagic<br />
shock. <strong>The</strong>raSource was<br />
founded by Ping Wang, MD,<br />
who leads the Laboratory <strong>of</strong><br />
Surgical Research, the source<br />
<strong>of</strong> discoveries that are now<br />
licensed to <strong>The</strong>raSource <strong>for</strong><br />
product development.<br />
T3 <strong>The</strong>rapeutics is<br />
under license to develop<br />
an experimental thyroid<br />
medication based on<br />
discoveries made at the<br />
Feinstein.
Eleven North Shore-LIJ Hospitals<br />
Recognized <strong>for</strong> Superior Stroke Care<br />
<strong>The</strong> American <strong>Heart</strong> Association/<br />
American Stroke Association’s Get With <strong>The</strong><br />
Guidelines®-Stroke Quality Achievement<br />
Award has been awarded to 11 North Shore-<br />
LIJ Health System hospitals, recognizing<br />
the facilities’ successes in implementing<br />
excellent care <strong>for</strong> stroke patients, according<br />
to evidence-based guidelines.<br />
To receive the Get With <strong>The</strong><br />
Guidelines®-Stroke Gold Plus or Gold<br />
Quality Achievement Award, each hospital<br />
achieved 24 consecutive months <strong>of</strong> 85<br />
percent or higher adherence to all stroke<br />
per<strong>for</strong>mance achievement indicators. <strong>The</strong>se<br />
measures include aggressive use <strong>of</strong> medications,<br />
such as tissue plasminogen activator<br />
(or tPA, a clot-busting drug); interventions<br />
to prevent blood clots; administration <strong>of</strong><br />
cholesterol-reducing drugs; <strong>and</strong> review <strong>of</strong><br />
smoking cessation techniques with patients.<br />
All the protocols are designed to reduce<br />
mortality <strong>and</strong> disability rates, <strong>and</strong> improve<br />
the lives <strong>of</strong> stroke patients. Gold Plus<br />
indicates hospitals that have met the Gold<br />
requirements AND have shown adherence<br />
to several additional quality measures.<br />
North Shore-LIJ hospitals received<br />
the following awards:<br />
Gold Plus Quality Achievement Award<br />
Forest Hills Hospital<br />
Franklin Hospital<br />
Glen Cove Hospital<br />
Huntington Hospital<br />
Long Isl<strong>and</strong> Jewish Medical Center<br />
North Shore University Hospital<br />
Plainview Hospital<br />
Southside Hospital<br />
Staten Isl<strong>and</strong> University Hospital<br />
Syosset Hospital<br />
Gold Achievement Award<br />
Lenox Hill Hospital<br />
In addition, Forest Hills Hospital <strong>and</strong><br />
Lenox Hill Hospital achieved Target: Stroke<br />
honor roll status, an additional campaign<br />
to improve outcomes <strong>for</strong> ischemic stroke<br />
patients, indicating the achievement <strong>of</strong><br />
door-to-needle (DTN) times <strong>of</strong> 60 minutes<br />
or less in at least 50 percent <strong>of</strong> stroke cases<br />
<strong>for</strong> at least one year. Shorter DTN times<br />
have been proven to improve outcomes <strong>and</strong>,<br />
through Target: Stroke, hospital teams can<br />
work toward eliminating delays <strong>and</strong> reducing<br />
long-term disability in stroke patients.<br />
“With a stroke, time lost is brain<br />
lost,” said Richard Libman, MD, chair <strong>of</strong><br />
North Shore-LIJ’s stroke task <strong>for</strong>ce <strong>and</strong> chief<br />
<strong>of</strong> vascular neurology at LIJ Medical Center.<br />
“<strong>The</strong> Get With <strong>The</strong> Guidelines®-Stroke<br />
Quality Achievement Awards demonstrate<br />
that our highly trained physicians <strong>and</strong><br />
nurses are committed to providing care that<br />
has been clinically proven to quickly <strong>and</strong><br />
efficiently treat stroke patients <strong>and</strong> save lives.”<br />
As New York State-designated stroke centers,<br />
all 11 hospitals have multidisciplinary stroke<br />
teams available 24 hours a day to assess <strong>and</strong><br />
treat stroke patients.<br />
North Shore-LIJ<br />
Goes to Harvard<br />
Twenty-four staff from throughout<br />
the North Shore-LIJ Health System,<br />
pictured at left, participated in<br />
the Harvard Project Management<br />
Program, a specialized training<br />
program designed <strong>for</strong> healthcare<br />
pr<strong>of</strong>essionals in both clinical <strong>and</strong><br />
operational roles that focuses<br />
on improving cost, quality <strong>and</strong><br />
delivery through management<br />
<strong>of</strong> both people <strong>and</strong> processes.<br />
Participants attended the five<br />
2-day modules over 10 months.<br />
<strong>The</strong> program enables participants<br />
to develop management skills to<br />
deliver projects on time, within<br />
budget <strong>and</strong> to specification.<br />
<strong>The</strong> New St<strong>and</strong>ard 93
MANHASSET — If you’ve<br />
driven north on Community<br />
Drive toward North Shore<br />
University Hospital, as many<br />
North Shore-LIJ Health System<br />
employees have, on your left<br />
you may have spotted a tiny<br />
white clapboard church. In the<br />
crush <strong>of</strong> fast-moving traffic, you<br />
may have caught a glimpse <strong>of</strong> a<br />
graveyard behind the church.<br />
Surrounded by modern medical<br />
facilities, they are clearly relics<br />
<strong>of</strong> another time <strong>and</strong> place. That<br />
time was the first half <strong>of</strong> the<br />
20th century, <strong>and</strong> the place was<br />
the vibrant African-American<br />
community called Spinney<br />
Hill that once spread over<br />
several acres <strong>of</strong> Great Neck <strong>and</strong><br />
Manhasset.<br />
Dedrick Johnson,<br />
coordinator <strong>of</strong> medical<br />
records at North Shore<br />
University Hospital, grew<br />
up in Spinney Hill, or more<br />
accurately, what remained <strong>of</strong><br />
Spinney Hill, in the seventies<br />
<strong>and</strong> eighties. (He still lives<br />
in the neighborhood, <strong>and</strong><br />
can walk to work.) A sense <strong>of</strong><br />
nostalgia, along with an urge<br />
to tell the story be<strong>for</strong>e it is lost<br />
in the past, led Mr. Johnson<br />
<strong>and</strong> his boyhood friend,<br />
Lloyd Means, now a s<strong>of</strong>tware<br />
engineer with Cablevision,<br />
to make a documentary about<br />
Spinney Hill.<br />
Sunday services are still<br />
conducted at the Lakeville<br />
AME Zion Church on<br />
Community Drive, which<br />
was founded by freed slaves<br />
in the 1820s. But the African<br />
American-owned businesses<br />
that once lined Northern<br />
Boulevard are gone. “<strong>The</strong>re<br />
was a barber shop, a beauty<br />
salon, a nightclub called<br />
Gibson’s, Hotel James,” said<br />
Mr. Johnson. “On what is now<br />
the golf course, black farmers<br />
grew asparagus. <strong>The</strong> hospital<br />
94 Summer 2012<br />
grounds were all fields, too, <strong>of</strong><br />
potatoes, probably, <strong>and</strong> corn.”<br />
Spinney Hill’s settlers<br />
were part <strong>of</strong> what is called the<br />
Great Migration <strong>of</strong> African-<br />
Americans, mostly from<br />
the tobacco fields <strong>of</strong> South<br />
Carolina, from about 1910 to<br />
1930. New York City’s rich<br />
<strong>and</strong> famous – the Astors, the<br />
V<strong>and</strong>erbilts – were building<br />
lavish mansions along Long<br />
Documentary<br />
Brings Forgotten<br />
African-American<br />
Community to Life<br />
By <strong>The</strong>a Welch<br />
Isl<strong>and</strong>’s Gold Coast, <strong>and</strong><br />
the new residents took jobs<br />
as cooks, yard men, maids,<br />
housekeepers, chauffeurs.<br />
Many became entrepreneurs.<br />
If they didn’t live on the gr<strong>and</strong><br />
estates, their homes were in<br />
Spinney Hill. In the fifties,<br />
legendary pro football player<br />
Jim Brown, who lived on<br />
Lee Avenue in Spinney Hill,<br />
graduated from Manhasset<br />
High School, having earned 17<br />
letters in a variety <strong>of</strong> sports. In<br />
the sixties, Dr. Martin Luther<br />
King, Jr., visited synagogues in<br />
Great Neck to raise money <strong>for</strong><br />
the cause <strong>of</strong> civil rights.<br />
Mr. Johnson <strong>and</strong> his friend<br />
enjoyed what he describes as a<br />
“Norman Rockwell childhood,”<br />
building <strong>for</strong>ts in the woods<br />
<strong>and</strong> skating on Whitney Pond.<br />
But the post-war Baby Boom<br />
<strong>and</strong> the suburbanization <strong>of</strong><br />
Long Isl<strong>and</strong> were eating away<br />
at Spinney Hill. <strong>The</strong> final<br />
blow was an urban renewal<br />
project in the mid-1980s, with<br />
medical <strong>and</strong> <strong>of</strong>fice buildings<br />
replacing most <strong>of</strong> the original<br />
establishments.<br />
For Mssrs. Johnson <strong>and</strong><br />
Means, the work is ongoing.<br />
<strong>The</strong>y are still collecting<br />
photographs <strong>and</strong> interviewing<br />
<strong>for</strong>mer residents about their<br />
memories — <strong>and</strong> they are<br />
making another film. “Two<br />
men we interviewed <strong>for</strong> the<br />
first film, William Singletary<br />
<strong>and</strong> Joe Oliphant, who both<br />
sang at Hotel James, died<br />
be<strong>for</strong>e the film was finished,”<br />
Mr. Johnson said. “We regret<br />
that they didn’t live to see it.<br />
We want the old-timers to<br />
know that Spinney Hill <strong>and</strong><br />
they are not <strong>for</strong>gotten.”<br />
Left: Dedrick Johnson st<strong>and</strong>s outside<br />
the tiny church, founded in the<br />
1820s by freed slaves.
Department <strong>of</strong> Medicine Presents Scherr Awards<br />
It’s a rite <strong>of</strong> spring at North Shore University Hospital (NSUH): the presentation<br />
<strong>of</strong> awards to interns, residents <strong>and</strong> fellows who have put <strong>for</strong>th significant time<br />
<strong>and</strong> ef<strong>for</strong>t in the pursuit <strong>of</strong> knowledge. <strong>The</strong> awards have been presented <strong>for</strong> 24<br />
years, but <strong>for</strong> the last five years they have been named in honor <strong>of</strong> Lawrence<br />
Scherr, MD, MACP, NSUH’s <strong>for</strong>mer chair <strong>of</strong> medicine <strong>and</strong> the North Shore-LIJ<br />
Health System’s academic dean emeritus <strong>and</strong> historian. <strong>The</strong> Lawrence Scherr,<br />
MD, MACP, Scholarly Activity Awards were presented May 3 at NSUH’s Rust<br />
Auditorium. From left are: Andrew Yacht, MD, associate dean <strong>for</strong> general medical<br />
education at Lenox Hill Hospital; Amgad Makaryus, MD, chair <strong>of</strong> the Scherr<br />
Awards Committee <strong>and</strong> director <strong>of</strong> echocardiography, cardiac CT <strong>and</strong> MRI in the<br />
North Shore-LIJ Laboratories<br />
Per<strong>for</strong>ms C-Reactive Protein Tests<br />
Live on “Dr. Oz Show”<br />
Eight New York State licensed medical technologists were chosen from<br />
North Shore-LIJ Laboratories <strong>and</strong> the Monter Cancer Center Laboratory<br />
to per<strong>for</strong>m129 fingerstick high-sensitivity CRP tests on members <strong>of</strong><br />
the studio audience. <strong>The</strong> testing <strong>of</strong> Dr. Oz himself was executed by<br />
Rosemary Frederick, manager <strong>of</strong> point <strong>of</strong> care testing, pictured here<br />
with the doctor. North Shore-LIJ Labs’ dedicated, knowledgeable<br />
<strong>and</strong> well-prepared team per<strong>for</strong>med a valuable service in terms <strong>of</strong><br />
increasing awareness <strong>of</strong> this test, not just <strong>for</strong> the studio audience but<br />
<strong>for</strong> the thous<strong>and</strong>s <strong>of</strong> people watching at home.<br />
Department <strong>of</strong> Cardiology; John Makaryus, MD, house staff awardee in the case<br />
reports category; Robert Sporter, MD, house staff co-awardee in the abstract<br />
category; Nishtha Sareen, MD, house staff co-awardee in the paper category;<br />
Sameer Khanjio, MD, house staff co-awardee in the paper category; Saima<br />
Chaudhry, MD, residency program director <strong>and</strong> associate chair <strong>of</strong> graduate<br />
medical education <strong>for</strong> the Department <strong>of</strong> Medicine; Thomas McGinn, MD, chair<br />
<strong>of</strong> the Department <strong>of</strong> Medicine; Elizabeth Forde, residency liaison <strong>for</strong> the Office<br />
<strong>of</strong> Graduate Medical Education; <strong>and</strong> David Battinelli, MD, North Shore-LIJ’s chief<br />
academic <strong>of</strong>ficer. (<strong>The</strong> house staff co-awardee in the abstract category, Shalin<br />
Desai, MD, was unable to be present at the ceremony.)<br />
<strong>The</strong> New St<strong>and</strong>ard 95
Drug “Take Back”<br />
Collection Hits<br />
New High<br />
<strong>The</strong> fourth drug “Take Back” event, held<br />
on Saturday, April 28, was the best yet, with<br />
all participating North Shore-LIJ facilities<br />
combined collecting 481 pounds <strong>of</strong> prescription<br />
drugs. That total represents 9 percent <strong>of</strong> what<br />
was collected on Long Isl<strong>and</strong>, <strong>and</strong> 8 percent <strong>of</strong><br />
what was collected in New York City.<br />
Each year, the rate <strong>of</strong> prescription drug<br />
abuse increases in the US, as does the number<br />
<strong>of</strong> accidental poisonings <strong>and</strong> overdoses. Studies<br />
show that a majority <strong>of</strong> abused prescription<br />
drugs are obtained from family <strong>and</strong> friends,<br />
including from home medicine cabinets.<br />
In addition, many Americans do not know<br />
how to properly dispose <strong>of</strong> their unused<br />
medicines, <strong>of</strong>ten flushing them down the<br />
toilet or throwing them away – both potential<br />
safety <strong>and</strong> health hazards. <strong>The</strong> “Take Back”<br />
initiative, conducted by the North Shore-LIJ<br />
Health System in partnership with the US<br />
Drug En<strong>for</strong>cement Administration (DEA)<br />
<strong>and</strong> other government, community, public<br />
health <strong>and</strong> law en<strong>for</strong>cement organizations,<br />
seeks to prevent increased pill abuse <strong>and</strong> theft<br />
by collecting potentially dangerous expired,<br />
unused <strong>and</strong> unwanted prescription drugs at<br />
system hospitals <strong>and</strong> disposing <strong>of</strong> them safely.<br />
“Each time we participate in this event<br />
our numbers increase, which I think is a<br />
reflection <strong>of</strong> all <strong>of</strong> the work you all do in<br />
getting the word out, as well as the ongoing<br />
need in our communities,” said Lisa Burch,<br />
MPH, system director <strong>of</strong> community <strong>and</strong><br />
public health. “To illustrate how the initiative<br />
has grown, in October 2011 we collected<br />
319 pounds, in April 2011 we collected 305<br />
pounds <strong>and</strong> in September 2010 we collected<br />
239 pounds. Once again, thank you <strong>for</strong> your<br />
participation <strong>and</strong> thank you <strong>for</strong> helping to<br />
keep our communities safe.”<br />
<strong>The</strong> DEA is already planning another<br />
“Take Back” event be<strong>for</strong>e the end <strong>of</strong> the year; it<br />
will be publicized when the date is set.<br />
96 Summer 2012<br />
COMPLIANCE corner
Spiritual Inspiration<br />
Among the features <strong>of</strong> LIJ Medical Center’s<br />
newly opened Katz Women’s Hospital <strong>and</strong><br />
Zuckerberg Pavilion is the Judy <strong>and</strong> Fred<br />
Wilpon Family Foundation Meditation<br />
Center. Open around-the-clock, the center<br />
is surrounded on three sides by a reflecting<br />
pool. Soon after the tower opened, LIJ<br />
administrators greeted priests, rabbis,<br />
ministers, an Imam, a nun <strong>and</strong> other clergy in<br />
the meditation center, which <strong>of</strong>fers various<br />
religious services throughout the week. Mr.<br />
Wilpon <strong>and</strong> North Shore-LIJ trustee Saul Katz<br />
are owners <strong>of</strong> the New York Mets.<br />
<strong>The</strong> New St<strong>and</strong>ard 97
98 Summer 2012
ORIGINS<br />
photo credit<br />
<strong>The</strong> First Miss North Shore Hospital<br />
In 1950, students in local high schools were invited to participate in a contest to raise money <strong>and</strong><br />
awareness <strong>of</strong> the need <strong>for</strong> a community hospital in Manhasset. <strong>The</strong> young women who entered wore<br />
nurse’s uni<strong>for</strong>ms (a “bathing beauty” contest was deemed inappropriate) <strong>and</strong> delivered one-minute<br />
speeches stating why the hospital should be built. <strong>The</strong> winner, pictured here, the first Miss North Shore<br />
Hospital, was 16-year-old Glorian Devereux, a senior at Manhasset High School (where football legend<br />
Jim Brown was a sophomore). With her is a young <strong>and</strong> h<strong>and</strong>some Perry Como, who was from Port<br />
Washington. He per<strong>for</strong>med at the event, held at Roosevelt Raceway, as did Frank Sinatra (although<br />
he was from New Jersey). “<strong>The</strong> prize was an all-expenses-paid trip to Bermuda, with a boyfriend <strong>and</strong><br />
a chaperone,” Mrs. Dorsey (her married name) recalled. “I think I received a set <strong>of</strong> luggage, too. <strong>The</strong><br />
chaperone was the high school gym teacher, who was only 22 herself, <strong>and</strong> the three <strong>of</strong> us rode bikes –<br />
not motor bikes – all over the isl<strong>and</strong>. We had a wonderful time.”<br />
New TV Star<br />
at PAANS<br />
Adrian Ashby, administrative<br />
support associate with the Physician<br />
<strong>and</strong> Ambulatory Network Services<br />
(PAANS), was selected to compete on<br />
the Food Network’s Chopped cooking<br />
competition program. Mr. Ashby,<br />
whose favorite hobby is cooking <strong>and</strong><br />
baking, stood out because <strong>of</strong> his<br />
extensive experience in throughout<br />
New York City’s competition circuit<br />
<strong>and</strong> <strong>for</strong> doing well during his screen<br />
test. Look <strong>for</strong> the program to air by<br />
the end <strong>of</strong> the year.<br />
<strong>The</strong> New St<strong>and</strong>ard 99
125 Community Drive<br />
Great Neck, NY 11021<br />
100 Summer 2012<br />
NON PROFIT<br />
U.S. POSTAGE<br />
PAID<br />
NSLIJHS