ACUTE BRONCHITIS - McGraw-Hill Professional
ACUTE BRONCHITIS - McGraw-Hill Professional
ACUTE BRONCHITIS - McGraw-Hill Professional
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
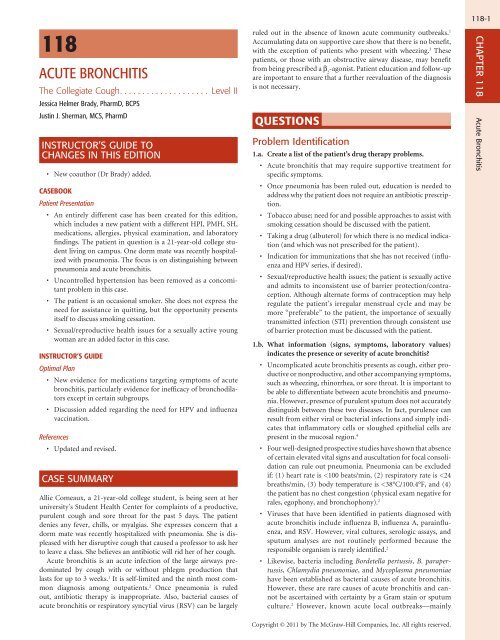
118<br />
<strong>ACUTE</strong> <strong>BRONCHITIS</strong><br />
The Collegiate Cough Level II<br />
Jessica Helmer Brady, PharmD, BCPS<br />
Justin J. Sherman, MCS, PharmD<br />
INSTRUCTOR’S GUIDE TO<br />
CHANGES IN THIS EDITION<br />
•<br />
New coauthor (Dr Brady) added.<br />
CASEBOOK<br />
Patient Presentation<br />
• An entirely different case has been created for this edition,<br />
which includes a new patient with a different HPI, PMH, SH,<br />
medications, allergies, physical examination, and laboratory<br />
findings. The patient in question is a 21-year-old college student<br />
living on campus. One dorm mate was recently hospitalized<br />
with pneumonia. The focus is on distinguishing between<br />
pneumonia and acute bronchitis.<br />
• Uncontrolled hypertension has been removed as a concomitant<br />
problem in this case.<br />
• The patient is an occasional smoker. She does not express the<br />
need for assistance in quitting, but the opportunity presents<br />
itself to discuss smoking cessation.<br />
• Sexual/reproductive health issues for a sexually active young<br />
woman are an added factor in this case.<br />
INSTRUCTOR’S GUIDE<br />
Optimal Plan<br />
• New evidence for medications targeting symptoms of acute<br />
bronchitis, particularly evidence for inefficacy of bronchodilators<br />
except in certain subgroups.<br />
• Discussion added regarding the need for HPV and influenza<br />
vaccination.<br />
References<br />
• Updated and revised.<br />
CASE SUMMARY<br />
Allie Comeaux, a 21-year-old college student, is being seen at her<br />
university’s Student Health Center for complaints of a productive,<br />
purulent cough and sore throat for the past 5 days. The patient<br />
denies any fever, chills, or myalgias. She expresses concern that a<br />
dorm mate was recently hospitalized with pneumonia. She is displeased<br />
with her disruptive cough that caused a professor to ask her<br />
to leave a class. She believes an antibiotic will rid her of her cough.<br />
Acute bronchitis is an acute infection of the large airways predominated<br />
by cough with or without phlegm production that<br />
lasts for up to 3 weeks. 1 It is self-limited and the ninth most common<br />
diagnosis among outpatients. 2 Once pneumonia is ruled<br />
out, antibiotic therapy is inappropriate. Also, bacterial causes of<br />
acute bronchitis or respiratory syncytial virus (RSV) can be largely<br />
ruled out in the absence of known acute community outbreaks. 1<br />
Accumulating data on supportive care show that there is no benefit,<br />
with the exception of patients who present with wheezing. 3 These<br />
patients, or those with an obstructive airway disease, may benefit<br />
from being prescribed a β 2 -agonist. Patient education and follow-up<br />
are important to ensure that a further reevaluation of the diagnosis<br />
is not necessary.<br />
QUESTIONS<br />
Problem Identification<br />
1.a. Create a list of the patient’s drug therapy problems.<br />
• Acute bronchitis that may require supportive treatment for<br />
specific symptoms.<br />
• Once pneumonia has been ruled out, education is needed to<br />
address why the patient does not require an antibiotic prescription.<br />
• Tobacco abuse; need for and possible approaches to assist with<br />
smoking cessation should be discussed with the patient.<br />
• Taking a drug (albuterol) for which there is no medical indication<br />
(and which was not prescribed for the patient).<br />
• Indication for immunizations that she has not received (influenza<br />
and HPV series, if desired).<br />
• Sexual/reproductive health issues; the patient is sexually active<br />
and admits to inconsistent use of barrier protection/contraception.<br />
Although alternate forms of contraception may help<br />
regulate the patient’s irregular menstrual cycle and may be<br />
more “preferable” to the patient, the importance of sexually<br />
transmitted infection (STI) prevention through consistent use<br />
of barrier protection must be discussed with the patient.<br />
1.b. What information (signs, symptoms, laboratory values)<br />
indicates the presence or severity of acute bronchitis?<br />
• Uncomplicated acute bronchitis presents as cough, either productive<br />
or nonproductive, and other accompanying symptoms,<br />
such as wheezing, rhinorrhea, or sore throat. It is important to<br />
be able to differentiate between acute bronchitis and pneumonia.<br />
However, presence of purulent sputum does not accurately<br />
distinguish between these two diseases. In fact, purulence can<br />
result from either viral or bacterial infections and simply indicates<br />
that inflammatory cells or sloughed epithelial cells are<br />
present in the mucosal region. 4<br />
• Four well-designed prospective studies have shown that absence<br />
of certain elevated vital signs and auscultation for focal consolidation<br />
can rule out pneumonia. Pneumonia can be excluded<br />
if: (1) heart rate is
118-2<br />
SECTION 16 Infectious Diseases<br />
documented on college campuses and on military bases—are<br />
associated with a higher incidence of a bacterial cause. 1<br />
• Another influenzalike illness that should be ruled out is severe<br />
acute respiratory syndrome, which is highly infectious and<br />
has spread worldwide since being first seen in China in 2002.<br />
Health care workers are at high risk of exposure with severe<br />
acute respiratory syndrome, and symptoms include a nonproductive<br />
cough, fever, myalgias, and dyspnea. 2 These, of course,<br />
are symptoms not found in this case.<br />
1.c. What additional information must be considered before<br />
deciding whether antimicrobial therapy is indicated?<br />
• As described previously (see question 1.b.), the absence of<br />
certain vital signs combined with a finding of no focal consolidation<br />
on auscultation greatly reduces the likelihood of pneumonia.<br />
In contrast, if any of the vital signs are elevated (i.e.,<br />
heart rate is >100 beats/min, respiratory rate is >24 breaths/<br />
min, or body temperature is >38°C/100.4°F), or if there is a<br />
high index of clinical suspicion or prolonged cough, a chest<br />
radiograph could be ordered to definitively rule out pneumonia<br />
with an absence of an infiltrate. 2<br />
Desired Outcome<br />
2. What are the goals of pharmacotherapy in this case?<br />
• Relieve the symptoms of uncomplicated acute bronchitis.<br />
• Although the patient would not be given an antibiotic, the<br />
patient should be counseled to explain why that particular<br />
expectation may not be met in this case.<br />
• Educate the patient about self-treatment—both over-the-counter<br />
(OTC) and nonmedication strategies that are available.<br />
• Educate the patient about the dangers of using medications for<br />
which there is no medical indication and which have been prescribed<br />
for someone other than the patient.<br />
• Offer appropriate pharmacotherapy for the most optimal<br />
chance to succeed during a current smoking cessation attempt<br />
(if needed/desired by the patient).<br />
• Consider appropriate patient-specific medications/immunizations<br />
to address her sexual/reproductive health issues.<br />
Therapeutic Alternatives<br />
3.a. What nondrug therapies might be useful for this patient?<br />
• Eliminating environmental cough triggers such as dust and dander<br />
and providing vaporized air treatments are low-cost and<br />
low-risk actions that can help attenuate severity of symptoms. 4<br />
Vaporized air treatments may be useful in environments that<br />
have low humidity (e.g., high-altitude climates). Expectoration<br />
can also be enhanced by increasing fluid intake. However, evidence<br />
for the degree of benefit provided with these measures has<br />
not been substantiated by randomized, controlled clinical trials. 4<br />
• The patient should be encouraged to discontinue cigarette<br />
smoking during the illness, with strong urging for continued<br />
total abstinence. Counseling the patient to stop smoking may<br />
be more effective if she is approached during this episode of<br />
acute bronchitis. 2 Advice should include that smoking cessation<br />
is the single most important action that the patient can<br />
take to protect her health now and in the future. Benefits should<br />
be discussed, including an incrementally decreased risk of lung<br />
cancer, stroke, heart attack, and chronic lung diseases with each<br />
year of smoking cessation.<br />
✓ An action plan should be discussed with the patient if<br />
she indicates a sincere desire to stop smoking. To give this<br />
Copyright © 2011 by The <strong>McGraw</strong>-<strong>Hill</strong> Companies, Inc. All rights reserved.<br />
patient an optimal chance for success, components of this<br />
action plan should include smoking cessation medication;<br />
behavioral, cognitive, and stress management therapy given<br />
either as a group or individually; and group and/or family<br />
support.<br />
✓ The STAR approach is one method of a quit plan, which<br />
includes:<br />
Set a quit date within 2 weeks.<br />
Tell family and friends about the quit attempt and request<br />
their support.<br />
Anticipate challenges to a planned quit attempt, including<br />
nicotine withdrawal symptoms.<br />
Remove tobacco products from the environment, and<br />
avoid smoking prior to the quit date in places where she<br />
spends much of her time.<br />
✓ Follow-up with the patient is essential after the quit date<br />
because the most intense withdrawal symptoms are experienced<br />
within 48 hours after the quit date. Ideally, follow-up<br />
should be in person; however, reaching the patient by telephone<br />
is also an effective method.<br />
• Examples of behavioral techniques include:<br />
✓ Because she admits to smoking during social situations,<br />
she should be encouraged to avoid the places/people with<br />
which she associates her smoking habits while actively trying<br />
to quit. She should be encouraged to ask friends who use<br />
tobacco to refrain around her while she is trying to quit.<br />
✓ Many smokers feel compelled to smoke within the first 30<br />
minutes of awakening. They should be encouraged to switch<br />
their morning routines at this time, such as showering or<br />
going for a walk first before making coffee, which is a technique<br />
sometimes called “scrambling.”<br />
✓ Since cigarettes often are smoked after a meal, smokers<br />
may subconsciously use this to signal the end of the meal.<br />
The patient should set an ending time prior to the meal,<br />
and then push away from the table and go for a walk at the<br />
designated time.<br />
✓ Smokers often miss the hand-to-mouth routine of smoking<br />
when they stop. They should be encouraged to substitute<br />
when they experience cravings, including the following: use<br />
hard, sugarless candy, suck on a straw, or have raw vegetables<br />
such as carrots to chew.<br />
• Examples of cognitive techniques include:<br />
✓ Avoid allowing a craving to lead to a slip by encouraging the<br />
patient to refocus her thoughts. The patient could be trained<br />
to think of the command “STOP!” or to snap a rubber band<br />
around the wrist whenever cravings begin.<br />
✓ Patients can use a visualization exercise to focus on something<br />
else rather than on the craving.<br />
• Consistent use of barrier contraceptives to prevent pregnancy<br />
and STIs.<br />
3.b. What feasible pharmacotherapeutic alternatives are available<br />
for treatment of uncomplicated acute bronchitis?<br />
• Antibiotics are inappropriate and ineffective for this patient<br />
because ≥90% of cases of uncomplicated acute bronchitis are<br />
attributed to nonbacterial causes. Several meta-analyses have<br />
reached the following conclusion: routine antibiotic treatment<br />
of acute bronchitis does not impact severity or duration of illness,<br />
time lost from work, limitation of activity, or the likelihood<br />
of developing pneumonia. Therefore, antibiotic use is not<br />
recommended. 2
• β -Adrenergic agonist bronchodilators have not consistently<br />
2<br />
shown benefit for patients with symptoms of acute bronchitis,<br />
per a recent Cochrane review. 3 Daily cough scores were<br />
not consistently diminished, nor were the number of patients<br />
coughing reduced after 7 days of treatment. However, a subgroup<br />
of patients who were wheezing or had airflow obstruction<br />
at presentation did benefit from a bronchodilator. Since<br />
this patient did not experience wheezing, she is not likely to<br />
benefit from bronchodilator use.<br />
• Anticholinergics have not been conclusively shown to be effective<br />
for relieving the symptoms of acute bronchitis. 2<br />
• Inhaled corticosteroids are not very effective for this indication<br />
because of the delay in onset of action. 2<br />
• Antitussives (e.g., codeine, dextromethorphan) are of uncertain<br />
benefit in uncomplicated acute bronchitis, since they have<br />
not been systematically studied in adequate trials. However,<br />
antitussives have been useful in reducing subjective cough<br />
scores and can be offered for short-term relief of symptoms. 2<br />
Antitussives should be instituted cautiously in this patient<br />
because her cough is productive. Suppression of cough may<br />
inhibit expectoration of mucus.<br />
• Antipyretics and analgesics (e.g., acetaminophen, aspirin, ibuprofen)<br />
may be effective for symptoms of lethargy, fever, and<br />
malaise. 1<br />
• Expectorants (e.g., guaifenesin) are of questionable clinical effectiveness<br />
for the symptoms of acute bronchitis but may be used<br />
to increase expectoration. 1<br />
TablE 118-1 Advantages and Disadvantages of Smoking Cessation Medications<br />
3.c. What are the most likely alternatives for smoking cessation?<br />
• Considerations for smoking cessation medications should<br />
include: (1) the degree of success during past attempts at cessation<br />
with a particular medication, (2) possible adverse effects<br />
or drug interactions, (3) whether the medication is available<br />
OTC or is prescription-only, and (4) other advantages or disadvantages<br />
as outlined in Table 118-1.<br />
3.d. What sexual/reproductive health considerations are applicable<br />
to this patient?<br />
• The instructor is referred to the textbook chapter for a complete<br />
discussion of therapeutic options. The patient reports<br />
inconsistent use of condoms as her means of birth control. In<br />
addition to the risk of pregnancy from inconsistent condom<br />
use, the patient is at risk for STIs, including HIV. She should<br />
be counseled regarding these risks and the need for consistent<br />
condom use, regardless of the use of other birth control<br />
methods.<br />
• HPV vaccination for the prevention of cervical cancer (and<br />
genital warts if HPV4 vaccine is administered).<br />
3.e. What psychosocial considerations are applicable to this<br />
patient?<br />
• Although clinicians may be aware that antibiotics are not indicated<br />
for uncomplicated acute bronchitis, they may perceive that<br />
the patient or caregiver expects a prescription. However, studies<br />
suggest that an office encounter concluding with receipt of<br />
antibiotic treatment does not necessarily correlate with increased<br />
Smoking Cessation<br />
Medication Advantages Disadvantages<br />
Nicotine patch Easy for patients to use Pruritus is relatively common<br />
Can be obtained OTC<br />
Nicotine levels more consistent<br />
Discontinue with “step-down” therapy<br />
Avoid in patients with certain dermatologic conditions<br />
Nicotine gum Adjustable use with specific schedule to follow Proper chewing technique must be used<br />
Can be obtained OTC Not appropriate for denture wearers<br />
Has been shown to delay weight gain for some patients Acidic beverages can decrease efficacy if used within 15 min before<br />
May be good for adjunct therapy with longer-acting medication using lozenge<br />
Nicotine lozenge No need to “chew and park” like gum Not appropriate for denture wearers<br />
Adjustable use with specific schedule to follow Acidic beverages can decrease efficacy if used within 15 min before<br />
Can be obtained OTC<br />
May be good for adjunct therapy with longer-acting medication<br />
chewing gum<br />
Nicotine inhaler Adjustable use with specific schedule to follow<br />
Great choice for patients needing “hand-to-mouth” routine<br />
Discontinue with “step-down” therapy<br />
Available by prescription only<br />
Patient dependence is possible<br />
Initial mouth or throat irritation<br />
Avoid in patients with severe reactive airway disease<br />
Acidic beverages can decrease efficacy<br />
Nicotine nasal spray Adjustable use with a specific schedule Available by prescription only<br />
Discontinue with “step-down” therapy Potential for mouth or throat irritation<br />
Avoid in patients with severe reactive airway disease<br />
Bupropion SR Oral medication, easy to use twice daily by mouth Available by prescription only<br />
May delay weight gain Timing is crucial (must begin at least 1 week prior to quit date)<br />
Can also be used for depression Avoid in patients with high seizure risk<br />
Multiple medication interactions<br />
Contraindicated in pregnancy<br />
Varenicline Oral medication, easy to use twice daily by mouth Available by prescription only<br />
No problems in patients with seizure risk Timing is crucial (must begin at least 1 week prior to quit date)<br />
No known medication interactions Pregnancy class C<br />
OTC, over-the-counter.<br />
Copyright © 2011 by The <strong>McGraw</strong>-<strong>Hill</strong> Companies, Inc. All rights reserved.<br />
118-3<br />
CHAPTER 118<br />
Acute Bronchitis
118-4<br />
SECTION 16 Infectious Diseases<br />
patient satisfaction. Rather, the time spent interacting with the<br />
patient explaining the condition and the treatment plan is more<br />
conducive to increasing satisfaction. 2 Furthermore, one study<br />
suggests that when a patient is told their diagnosis is “bronchitis,”<br />
they are more dissatisfied with not receiving an antibiotic than<br />
when the terms “chest cold” or “viral infection” are used. 5 Thus,<br />
more benign-sounding labels for the patient may improve satisfaction<br />
with not being prescribed an antibiotic. Therefore, taking<br />
time to counsel the patient and considering what terminology to<br />
use are important for alleviating potential patient dissatisfaction<br />
with not receiving an antibiotic.<br />
Optimal Plan<br />
4.a. What drugs, dosage form, dose, schedule, and duration of<br />
therapy are best to alleviate this patient’s symptoms of acute<br />
bronchitis?<br />
• For this patient, symptomatic treatment is the most appropriate<br />
approach.<br />
• Antibiotics have no role in the management of this patient<br />
because they are not useful for treating uncomplicated acute<br />
bronchitis. The patient does not present with abnormal vital<br />
signs and chest congestion, so treatment for possible pneumonia<br />
with antibiotics is not appropriate.<br />
• Treatment should include attempts to enhance expectoration<br />
by increasing fluid intake and using air humidifiers.<br />
• Since this patient did not have wheezing at presentation, cough<br />
relief would not likely be achieved through the use of a bronchodilator,<br />
such as inhaled albuterol. Also, the inappropriate<br />
use of a medication that was not prescribed for the patient<br />
should be addressed.<br />
• Dextromethorphan could be considered for supplemental use<br />
for cough, along with guaifenesin to help increase expectoration.<br />
Combination dextromethorphan/guaifenesin products<br />
may be given (e.g., Robitussin DM or generic equivalent two<br />
teaspoonfuls Q 4 h), or the drugs may be given separately (e.g.,<br />
long-acting Delsym Suspension two teaspoonfuls Q 12 h or<br />
Humibid one to two tablets Q 12 h).<br />
• Acetaminophen 650 mg Q 4–6 h can be given for pain relief as<br />
needed.<br />
4.b. What medication and dosage should be recommended for<br />
this patient’s smoking cessation plan?<br />
• At this time, the patient is not interested in smoking cessation<br />
but should be encouraged to seek the help of a health care professional<br />
for any future cessation attempts. Smoking cessation<br />
should be addressed at any and all follow-up visits. Table 118-1<br />
illustrates various smoking cessation options for this patient.<br />
Outcome Evaluation<br />
5. What clinical and laboratory parameters are necessary to evaluate<br />
the therapy for achievement of the desired outcome and to<br />
detect or prevent adverse effects?<br />
• Uncomplicated acute bronchitis is usually self-limited, and this<br />
patient does not have a history of chronic bronchitis. Therefore,<br />
this presentation is not likely to be an acute exacerbation of<br />
chronic bronchitis. However, if the cough persists, the clinician<br />
should consider a possible change in diagnosis. For example,<br />
an emerging case of chronic bronchitis should be considered<br />
if patients have cough and sputum production on most days<br />
of the month for at least 3 months of the year during 2 consecutive<br />
years. 6 In such patients, there would be a progressive<br />
worsening of symptoms and air flow.<br />
Copyright © 2011 by The <strong>McGraw</strong>-<strong>Hill</strong> Companies, Inc. All rights reserved.<br />
• Also, if the cough persists for >3 weeks, the patient’s diagnosis<br />
should be reevaluated. Other diagnoses that should be considered<br />
at that time would be postinfectious cough, upper respiratory<br />
cough syndrome due to several rhinosinus conditions,<br />
asthma, and gastroesophageal reflux disease. 7<br />
Patient Education<br />
6. What information should be provided to the patient to enhance<br />
adherence, ensure successful therapy, and minimize adverse<br />
effects?<br />
General information:<br />
• You have what is known as acute bronchitis. This disorder is<br />
usually caused by a virus that we cannot specifically identify.<br />
Because antibiotics are effective only against bacteria, they will<br />
not be helpful to you in this situation. Also, using antibiotics<br />
without a clear indication may increase the chance of your<br />
becoming infected with resistant bacteria. An epidemic of antibiotic<br />
resistance exists, and this is caused when antibiotics are<br />
prescribed for conditions without clear benefit.<br />
• The cough may last for 10–14 days after this clinic visit. We<br />
can give you some medicine to help relieve the cough, but do<br />
not expect it to go away entirely very quickly. Although most<br />
symptoms should resolve on their own, the cough will need to<br />
be reevaluated if it lasts for longer than 3 weeks.<br />
• If your symptoms of cough and sore throat do not decrease<br />
within the next 2 weeks, please make a follow-up appointment<br />
at the clinic to be examined again by a physician.<br />
• The onset of new symptoms such as shortness of breath and<br />
new fever may indicate a bacterial infection; also, if fluid comes<br />
up with coughing, this could be a sign of reflux; please let us<br />
know if any of these new symptoms occur.<br />
Dextromethorphan/guaifenesin:<br />
• This medicine can be used to help decrease your cough and<br />
loosen the phlegm or mucus in your lungs. Take two teaspoonfuls<br />
every 4 hours if needed to help control your cough.<br />
• If your cough continues for more than 3 weeks, do not continue<br />
using this product. Instead, contact your physician for<br />
continued treatment advice. A persistent cough could be a sign<br />
of a serious condition.<br />
• Do not take more than six doses in a 24-hour period.<br />
Acetaminophen extra-strength tablets:<br />
• Acetaminophen can be used to help treat minor aches or pains<br />
or relieve fever.<br />
• Take two tablets by mouth every 4–6 hours as needed. Do not<br />
take more than eight tablets per day.<br />
• Do not take this for pain for more than 10 days or for fever<br />
more than 3 days without consulting your physician.<br />
• Do not drink alcohol while you are taking this medication.<br />
m FOLLOW-UP QUESTION<br />
1. What vaccinations should this patient receive?<br />
• The patient should receive the influenza vaccine each fall prior<br />
to the start of flu season.<br />
• The patient is also eligible to receive the HPV vaccination series if<br />
she so chooses. HPV vaccination is recommended by the Advisory<br />
Committee on Immunization Practices (ACIP) at age 11 or 12<br />
years with catch-up vaccination at ages 13–26 years. Ideally, the<br />
vaccine should be administered before potential exposure to
HPV through sexual activity; however, females who are sexually<br />
active should still be vaccinated consistent with age-based recommendations.<br />
Sexually active females who have not been infected<br />
with any of the four HPV types (types 6, 11, 16, 18 that HPV4<br />
[Gardasil] prevents) or any of the two HPV types (types 16, 18<br />
that HPV2 [Cervarix] prevents) receive the full benefit of the<br />
vaccination. Vaccination is less beneficial for females who have<br />
already been infected with one or more of the HPV types. 8<br />
REFERENCES<br />
1. Braman SS. Chronic cough due to acute bronchitis: ACCP evidencebased<br />
clinical practice guidelines. Chest 2006;129:95S–103S.<br />
2. Wenzel RP, Fowler AA. Acute bronchitis. N Engl J Med 2006;355:<br />
2125–2130.<br />
3. Smucny J, Flynn C, Becker L, Glazier R. β 2 -agonists for acute bronchitis.<br />
Cochrane Database Syst Rev 2006;(4).<br />
4. Gonzales R, Bartlett JG, Besser RE, et al. Principles of appropriate<br />
antibiotic use for treatment of uncomplicated acute bronchitis: background.<br />
Ann Intern Med 2001;134:521–529.<br />
5. Phillips TG, Hickner J. Calling acute bronchitis a chest cold may<br />
improve patient satisfaction with appropriate antibiotic use. J Am<br />
Board Fam Pract 2005;18:459–463.<br />
6. Brunton S, Carmichael BP, Colgan R, et al. Acute exacerbation of<br />
chronic bronchitis: a primary care consensus guideline. Am J Manag<br />
Care 2004;10:689–696.<br />
7. Irwin RS, Baumann MH, Boulet L, et al. Diagnosis and management<br />
of cough executive summary: ACCP evidence-based clinical practice<br />
guidelines. Chest 2006;129:1S–23S.<br />
8. Centers for Disease Control and Prevention. Recommended adult<br />
immunization schedule—United States, 2010. MMWR 2010;<br />
59(1):1–4.<br />
Copyright © 2011 by The <strong>McGraw</strong>-<strong>Hill</strong> Companies, Inc. All rights reserved.<br />
118-5<br />
CHAPTER 118<br />
Acute Bronchitis