Chapter 26 - McGraw-Hill Professional
Chapter 26 - McGraw-Hill Professional
Chapter 26 - McGraw-Hill Professional
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
485<br />
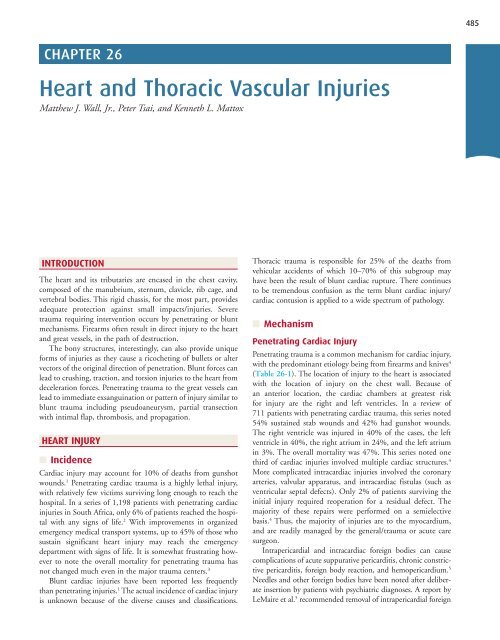
CHAPTER <strong>26</strong><br />
Heart and Thoracic Vascular Injuries<br />
Matthew J. Wall, Jr., Peter Tsai, and Kenneth L. Mattox<br />
INTRODUCTION<br />
The heart and its tributaries are encased in the chest cavity,<br />
composed of the manubrium, sternum, clavicle, rib cage, and<br />
vertebral bodies. This rigid chassis, for the most part, provides<br />
adequate protection against small impacts/injuries. Severe<br />
trauma requiring intervention occurs by penetrating or blunt<br />
mechanisms. Firearms often result in direct injury to the heart<br />
and great vessels, in the path of destruction.<br />
The bony structures, interestingly, can also provide unique<br />
forms of injuries as they cause a ricocheting of bullets or alter<br />
vectors of the original direction of penetration. Blunt forces can<br />
lead to crushing, traction, and torsion injuries to the heart from<br />
deceleration forces. Penetrating trauma to the great vessels can<br />
lead to immediate exsanguination or pattern of injury similar to<br />
blunt trauma including pseudoaneurysm, partial transection<br />
with intimal flap, thrombosis, and propagation.<br />
HEART INJURY<br />
■<br />
Incidence<br />
Cardiac injury may account for 10% of deaths from gunshot<br />
wounds. 1 Penetrating cardiac trauma is a highly lethal injury,<br />
with relatively few victims surviving long enough to reach the<br />
hospital. In a series of 1,198 patients with penetrating cardiac<br />
injuries in South Africa, only 6% of patients reached the hospital<br />
with any signs of life. 2 With improvements in organized<br />
emergency medical transport systems, up to 45% of those who<br />
sustain significant heart injury may reach the emergency<br />
department with signs of life. It is somewhat frustrating however<br />
to note the overall mortality for penetrating trauma has<br />
not changed much even in the major trauma centers. 3<br />
Blunt cardiac injuries have been reported less frequently<br />
than penetrating injuries. 1 The actual incidence of cardiac injury<br />
is unknown because of the diverse causes and classifications.<br />
Thoracic trauma is responsible for 25% of the deaths from<br />
vehicular accidents of which 10–70% of this subgroup may<br />
have been the result of blunt cardiac rupture. There continues<br />
to be tremendous confusion as the term blunt cardiac injury/<br />
cardiac contusion is applied to a wide spectrum of pathology.<br />
■<br />
Mechanism<br />
Penetrating Cardiac Injury<br />
Penetrating trauma is a common mechanism for cardiac injury,<br />
with the predominant etiology being from firearms and knives 4<br />
( Table <strong>26</strong>-1 ). The location of injury to the heart is associated<br />
with the location of injury on the chest wall. Because of<br />
an anterior location, the cardiac chambers at greatest risk<br />
for injury are the right and left ventricles. In a review of<br />
711 patients with penetrating cardiac trauma, this series noted<br />
54% sustained stab wounds and 42% had gunshot wounds.<br />
The right ventricle was injured in 40% of the cases, the left<br />
ventricle in 40%, the right atrium in 24%, and the left atrium<br />
in 3%. The overall mortality was 47%. This series noted one<br />
third of cardiac injuries involved multiple cardiac structures. 4<br />
More complicated intracardiac injuries involved the coronary<br />
arteries, valvular apparatus, and intracardiac fistulas (such as<br />
ventricular septal defects). Only 2% of patients surviving the<br />
initial injury required reoperation for a residual defect. The<br />
majority of these repairs were performed on a semielective<br />
basis. 4 Thus, the majority of injuries are to the myocardium,<br />
and are readily managed by the general/trauma or acute care<br />
surgeon.<br />
Intrapericardial and intracardiac foreign bodies can cause<br />
complications of acute suppurative pericarditis, chronic constrictive<br />
pericarditis, foreign body reaction, and hemopericardium. 5<br />
Needles and other foreign bodies have been noted after deliberate<br />
insertion by patients with psychiatric diagnoses. A report by<br />
LeMaire et al. 5 recommended removal of intrapericardial foreign
486 Management of Specific Injuries<br />
SECTION 3 X<br />
TABLE <strong>26</strong>-1 Etiology of Traumatic Heart Diseases<br />
I. Penetrating<br />
(A) Low entry<br />
1. Stab wounds—knives, swords, ice picks,<br />
fence posts, wire, sports<br />
(B) High entry<br />
2. Gunshot wounds—handguns, rifles, nail guns,<br />
lawnmower projectiles<br />
3. Shotgun wounds—close range versus distant<br />
4. Blast—fragments<br />
II. Nonpenetrating (blunt)<br />
(A) Motor vehicle accident<br />
(B) Vehicular–pedestrian accident<br />
(C) Falls from height<br />
(D) Crush—industrial accident<br />
(E) Blast—explosives, fragments, improvised<br />
explosive devices<br />
(F) Assault<br />
(G) Sternal or rib fractures<br />
(H) Recreational—sporting events, rodeo, baseball<br />
III. Iatrogenic<br />
(A) Catheter induced<br />
(B) Pericardiocentesis induced<br />
(C) Percutaneous interventions<br />
IV. Others<br />
(A) Electrical<br />
(B) Embolic—missiles<br />
(C) Factitious—needles, foreign bodies<br />
bodies that are greater than 1 cm in size, that are contaminated,<br />
or that produce symptoms.<br />
Intracardiac missiles are embedded in the myocardium,<br />
retained in the trabeculations of the endocardial surface, or free<br />
in a cardiac chamber. These result from direct penetrating thoracic<br />
injury or injury to a peripheral venous structure with<br />
embolization to the heart. Observation might be considered<br />
when the missile is small, right sided, embedded completely in<br />
the wall, contained within a fibrous covering, not contaminated,<br />
and producing no symptoms. Right-sided missiles can<br />
embolize to the pulmonary artery, where they can be removed<br />
if large. In rare cases they can embolize through a patent foramen<br />
ovale or atrial septal defect. Left-sided missiles can manifest<br />
as systemic embolization shortly after the initial injury.<br />
as a spectrum of free septal rupture, free wall rupture, coronary<br />
artery thrombosis, cardiac failure, complex and simple<br />
dysrhythmias, and rupture of chordae tendineae or papillary<br />
muscles. 5 The specific mechanisms include motor vehicle<br />
accidents, vehicular–pedestrian accidents, falls, crush injuries,<br />
blast/explosion, assaults, CPR, and recreational events. Blunt<br />
injury may be associated with sternal or rib fractures. In one<br />
report a fatal cardiac dysrhythmia occurred when the sternum<br />
was struck by a baseball, which may be a form of commotio<br />
cordis. 6<br />
True cardiac rupture carries a significant risk of mortality. The<br />
biomechanics of this injury include (1) direct transmission of<br />
increased intrathoracic pressure to the chambers of the heart; (2)<br />
a hydraulic effect from a large force applied to the abdominal or<br />
extremity veins, causing the force to be transmitted to the right<br />
atrium; (3) a decelerating force between fixed and mobile areas,<br />
explaining atriocaval tears; (4) a direct force causing myocardial<br />
contusion, necrosis, and delayed rupture; and (5) penetration<br />
from a broken rib or fractured sternum. 1 From autopsy data,<br />
blunt cardiac trauma with chamber rupture occurs most often to<br />
the left ventricle. In contrast, in patients who arrive alive to the<br />
hospital, right atrial disruption is more common. These are seen<br />
at the SVC–atrial junction, IVC–atrial junction, or the right atrial<br />
appendage. Blunt rupture of the cardiac septum occurs most frequently<br />
near the apex of the heart. Multiple ruptures as well as<br />
disruption of the conduction system have been reported. Injury<br />
to only the membranous portion of the septum is the least common<br />
blunt VSD. Traumatic rupture of the thoracic aorta is also<br />
associated with lethal cardiac rupture in almost 25% of cases.<br />
Pericardial tears secondary to increased intra-abdominal<br />
pressure or lateral decelerative forces can occur. These can occur<br />
on the left side, usually parallel to the phrenic nerve; to the<br />
right side of the pericardium; to the diaphragmatic surface of<br />
the pericardium; and finally to the mediastinum. Cardiac herniation<br />
with cardiac dysfunction can occur in conjunction with<br />
these tears. The heart may be displaced into either pleural cavity<br />
or even the abdomen depending on the tear. In the circumstance<br />
of right pericardial rupture, the heart can become<br />
twisted, leading to the surprising discovery of an “empty” pericardial<br />
cavity at resuscitative left anterolateral thoracotomy.<br />
With a left-sided cardiac herniation through a pericardial tear,<br />
a trapped apex of the heart prevents the heart from returning to<br />
the pericardium and the term strangulated heart has been<br />
applied. Unless the heart is returned to its normal position,<br />
hypotension and cardiac arrest can occur. 7 One clue to the presence<br />
of cardiac herniation in a patient with blunt thoracic<br />
injury is sudden loss of pulse when the patient is repositioned,<br />
such as when moved or placed on a stretcher.<br />
Blunt Cardiac Injury<br />
Blunt cardiac trauma has replaced the term “cardiac contusion”<br />
and describes injury ranging from insignificant bruises of the<br />
myocardium to cardiac rupture. Pathology can be caused by<br />
direct energy transfer to the heart or by a mechanism of compression<br />
of the heart between the sternum and the vertebral<br />
column at the time of the accident. Cardiac rupture during<br />
external cardiac massage as part of cardiopulmonary resuscitation<br />
(CPR) can occur. Blunt cardiac injuries can thus manifest<br />
Iatrogenic Cardiac Injury<br />
Iatrogenic cardiac injury can occur with central venous catheter<br />
insertion, cardiac catheterization procedures, endovascular<br />
interventions, and pericardiocentesis. Cardiac injuries caused by<br />
central venous catheter placement usually occur with insertion<br />
from either the left subclavian or the left internal jugular vein. 8<br />
Perforation causing tamponade has also been reported with a<br />
right internal jugular introducer sheath for transjugular intrahepatic<br />
portocaval shunts. Insertion of left-sided central lines,
Heart and Thoracic Vascular Injuries<br />
487<br />
especially during dilation of the line tract, can lead to SVC and<br />
atrial perforations. Even optimal technique carries a discrete<br />
rate of iatrogenic injury secondary to central venous catheterization.<br />
Common sites of injury include the superior vena caval–<br />
atrial junction and the superior vena cava–innominate vein<br />
junction. These small perforations sometimes lead to a compensated<br />
cardiac tamponade. Drainage by pericardiocentesis is<br />
often unsuccessful, and evacuation via subxiphoid pericardial<br />
window or full median sternotomy is sometimes required. At<br />
operation, when the pericardium is opened, the site of injury<br />
has sometimes sealed and may be difficult to find.<br />
Complications from coronary catheterization including<br />
perforation of the coronary arteries, cardiac perforation, and<br />
aortic dissection can be catastrophic and require emergency<br />
surgical intervention. 9<br />
Other iatrogenic potential causes of cardiac injury include<br />
external and internal cardiac massage, and right ventricular<br />
injury during pericardiocentesis, endovascular interventions,<br />
transthoracic percutaneous interventions, and intracardiac<br />
injections. 10<br />
Electrical Injury<br />
Cardiac complications after electrical injury include immediate<br />
cardiac arrest; acute myocardial necrosis with or without ventricular<br />
failure; myocardial ischemia; dysrhythmias; conduction<br />
abnormalities; acute hypertension with peripheral vasospasm;<br />
and asymptomatic, nonspecific abnormalities evident on an<br />
electrocardiogram (ECG). Damage from electrical injury is due<br />
to direct effects on the excitable tissues, heat generated from the<br />
electrical current, and accompanying associated injuries (e.g.,<br />
falls, explosions, fires). 11<br />
■<br />
Clinical Presentation<br />
Penetrating Cardiac Injury<br />
Wounds involving the epigastrium and precordium can raise<br />
clinical suspicion for cardiac injury. Patients with cardiac injury<br />
can present with a clinical spectrum from full cardiac arrest to<br />
asymptomatic with normal vital signs. Up to 80% of stab<br />
wounds that injure the heart eventually manifest tamponade.<br />
Rapid bleeding into the pericardium favors clotting rather than<br />
defibrination. 1 As pericardial fluid accumulates, a decrease in<br />
ventricular filling occurs, leading to a decrease in stroke volume.<br />
A compensatory rise in catecholamines leads to tachycardia and<br />
increased right heart filling pressures. The limits of right-sided<br />
distensibility are reached as the pericardium fills with blood, and<br />
the septum shifts toward the left side, further compromising left<br />
ventricular function. As little as 60–100 mL of blood in the<br />
pericardial sac can produce the clinical picture of tamponade. 1<br />
The rate of accumulation depends on the location of the<br />
wound. Because it has a thicker wall, wounds to the ventricle<br />
seal themselves more readily than wounds to the atrium.<br />
Patients with freely bleeding injuries to the coronary arteries<br />
present with rapid onset of tamponade combined with cardiac<br />
ischemia.<br />
The classic findings of Beck’s triad (muffled heart sounds,<br />
hypotension, and distended neck veins) are seen in a minority<br />
of acute trauma patients. Pulsus paradoxus (a substantial fall in<br />
systolic blood pressure during inspiration) and Kussmaul’s sign<br />
(increase in jugular venous distention on inspiration) may be<br />
present but are also not reliable signs. A more valuable and<br />
reproducible sign of pericardial tamponade is narrowing of the<br />
pulse pressure. An elevation of the central venous pressure often<br />
accompanies overaggressive cyclic hyperresuscitation with crystalloid<br />
solutions, but in such instances a widening of the pulse<br />
pressure occurs.<br />
Gunshot wounds to the heart are more frequently associated<br />
with hemorrhage than with tamponade. The kinetic energy is<br />
greater with firearms, and the wounds to the heart and pericardium<br />
are usually more extensive. Thus, these patients present<br />
with exsanguination into a pleural cavity more often.<br />
Blunt Cardiac Injury<br />
Clinically significant blunt cardiac injuries include cardiac rupture<br />
(ventricular or atrial), septal rupture, valvular dysfunction,<br />
coronary thrombosis, and caval avulsion. These injuries manifest<br />
as tamponade, hemorrhage, or severe cardiac dysfunction. Septal<br />
rupture and valvular dysfunction (leaflet tear, papillary muscle,<br />
or chordal rupture) can initially appear without symptoms but<br />
later demonstrate the delayed sequela of heart failure. 1<br />
Blunt cardiac injury can also present as a dysrhythmia, most<br />
commonly premature ventricular contractions, the precise<br />
mechanism of which is unknown. Ventricular tachycardia, ventricular<br />
fibrillation, and supraventricular tachyarrhythmias can<br />
also occur. These symptoms usually occur within the first<br />
24–48 hours after injury.<br />
A major difficulty in managing blunt cardiac injury relates<br />
to definitions. “Cardiac contusion” is a nonspecific term, which<br />
should likely be abandoned. It is best to describe these injuries<br />
as “blunt cardiac trauma with”—followed by the clinical manifestation<br />
such as dysrhythmia or heart failure. 12<br />
Pericardial Injury<br />
Traumatic pericardial rupture is rare. Most patients with pericardial<br />
rupture do not survive transport to the hospital due to other<br />
associated injuries. The overall mortality of those who are<br />
treated at trauma centers with such injury remains as high as<br />
64%. 13 An overwhelming majority of these cases are diagnosed<br />
either intraoperatively or on autopsy. 7 The clinical presentation<br />
of pericardial rupture, with cardiac herniation, can mimic that<br />
of pericardial tamponade with low cardiac output due to<br />
impaired venous return. When the heart returns to its normal<br />
position in the pericardium, venous return resumes. Positional<br />
hypotension is the hallmark of cardiac herniation due to pericardial<br />
rupture, 7 whereas pericardial tamponade is associated with<br />
persistent hypotension until the pericardium is decompressed.<br />
Therefore, a high index of suspicion is helpful when evaluating<br />
polytrauma patients with unexplained positional hypotension.<br />
■<br />
Evaluation<br />
The diagnosis of heart injury requires a high index of suspicion.<br />
On initial presentation to the emergency center, airway, breathing,<br />
and circulation under the Advanced Trauma Life Support<br />
CHAPTER <strong>26</strong> X
488 Management of Specific Injuries<br />
SECTION 3 X<br />
protocol are evaluated and established. 14 Two large-bore intravenous<br />
catheters are inserted, and blood is typed and crossmatched.<br />
The patient can be examined for Beck’s triad of<br />
muffled heart sounds, hypotension, and distended neck veins,<br />
as well as for pulsus paradoxus and Kussmaul’s sign. These findings<br />
suggest cardiac injury but are present in only 10% of<br />
patients with cardiac tamponade. The patient undergoes<br />
focused assessment with sonography for trauma (FAST). If the<br />
FAST demonstrates pericardial fluid in an unstable patient<br />
(systemic blood pressure 90 mm Hg), transfer to the operating<br />
room can then occur.<br />
Patients in extremis can require emergency department thoracotomy<br />
for resuscitation. The clear indications for emergency<br />
department thoracotomy by surgical personnel include the<br />
following: 15<br />
fluid. 17 Ultrasonography in this setting is not intended to reach<br />
the precision of studies performed in the radiology or cardiology<br />
suite but is merely intended to determine the presence of<br />
abnormal fluid collections, which aids in surgical decision making.<br />
18 Ultrasonography is safe, portable, and expeditious and<br />
can be repeated as indicated. If performed by a trained surgeon,<br />
the FAST examination has a sensitivity of nearly 100% and a<br />
specificity of 97.3%. 17 As the use of FAST evolves, and highspeed<br />
abdominal CT scans are readily available, the most universally<br />
agreed-upon indication for its use is evaluation for<br />
pericardial blood.<br />
To evaluate more subtle findings of blunt cardiac injury,<br />
such as wall motion, valvular, or septal abnormalities in the<br />
stable patient, formal transthoracic echocardiography (TTE) or<br />
transesophageal echocardiography (TEE) can be obtained.<br />
1. Salvageable postinjury cardiac arrest (e.g., patients who<br />
have witnessed cardiac arrest with high likelihood of<br />
intrathoracic injury, particularly penetrating cardiac<br />
wounds)<br />
2. Severe postinjury hypotension (i.e., systolic blood pressure<br />
60 mm Hg) due to cardiac tamponade, air embolism, or<br />
thoracic hemorrhage<br />
If, after resuscitative thoracotomy, vital signs are regained,<br />
the patient is transferred to the operating room for definitive<br />
repair.<br />
Chest radiography is nonspecific, but can identify hemothorax<br />
or pneumothorax. Other potentially indicated examinations<br />
include computed tomography (CT) scan for trajectory<br />
and laparoscopy for diaphragm injury.<br />
Electrocardiography<br />
In cases of blunt cardiac injury, conduction disturbances can<br />
occur. Sinus tachycardia is the most common rhythm disturbance<br />
seen. Other common disturbances include T wave and<br />
ST segment changes, sinus bradycardia, first- and seconddegree<br />
atrioventricular block, right bundle branch block, right<br />
bundle branch block with hemiblock, third-degree block, atrial<br />
fibrillation, premature ventricular contractions, ventricular<br />
tachycardia, and ventricular fibrillation. Thus, a screening<br />
12-lead ECG can be helpful for evaluation.<br />
Cardiac Enzymes<br />
Much has been written about the use of cardiac enzyme determinations<br />
in evaluating blunt cardiac injury. However, no<br />
relationship among serum assays and identification and prognosis<br />
of injury has been demonstrated with blunt cardiac<br />
injury. 16 Therefore, cardiac enzyme assays are unhelpful unless<br />
one is evaluating concomitant coronary artery disease. 16<br />
Focused Assessment with<br />
Sonography for Trauma (FAST)<br />
Surgeons are increasingly performing ultrasonography for thoracic<br />
trauma. The FAST examination evaluates four anatomic<br />
windows for the presence of intra-abdominal or pericardial<br />
Echocardiography<br />
TTE can have a limited use in evaluating blunt cardiac trauma<br />
because most patients also have significant chest wall injury,<br />
thus rendering the test technically difficult to perform. Its<br />
major use is in diagnosing intrapericardial blood and tamponade<br />
physiology. In stable patients, TEE can be used to evaluate<br />
blunt cardiac injury. Cardiac septal defects and valvular insufficiency<br />
are readily diagnosed with TEE. Ventricular dysfunction<br />
can often mimic cardiac tamponade in its clinical<br />
presentation. Echocardiography is particularly useful in older<br />
patients with preexisting ventricular dysfunction. However,<br />
most blunt cardiac injuries identified by echocardiography<br />
rarely require acute treatment.<br />
Subxiphoid Pericardial Window<br />
Subxiphoid pericardial window has been performed both in the<br />
emergency department and in the operating room with the<br />
patient under either general or local anesthesia. In a prospective<br />
study, Meyer et al. 19 compared the subxiphoid pericardial window<br />
with echocardiography in cases of penetrating heart injury<br />
and reported that the sensitivity and specificity of subxiphoid<br />
pericardial window were 100% and 92%, respectively, compared<br />
with 56% and 93% with echocardiography. They suggested<br />
that the difference in sensitivity may have been due to<br />
the presence of hemothorax, which can be confused with pericardial<br />
blood, or due to the fact that the blood had drained into<br />
the pleura. 19 Although there has been significant controversy in<br />
the past with regard to the indication for subxiphoid pericardial<br />
window, recent enthusiasm for ultrasonographic evaluation has<br />
almost eliminated the role of subxiphoid pericardial window in<br />
the evaluation of cardiac trauma. It is almost never needed in<br />
the ED.<br />
Pericardiocentesis has had significant historical support,<br />
especially when the majority of penetrating cardiac wounds<br />
were produced by ice picks and the (surviving) patients arrived<br />
several hours and/or days after injury. In such instances there<br />
was a natural triage of the more severe cardiac injuries and the<br />
intrapericardial blood had become defibrinated and was easy to<br />
remove. Currently, many trauma surgeons discourage pericardiocentesis<br />
for acute trauma. 10
Heart and Thoracic Vascular Injuries<br />
489<br />
■<br />
Treatment<br />
FIGURE <strong>26</strong>-1 Transdiaphragmatic exploration of the pericardium<br />
during laparotomy. ( Copyright © Baylor College of Medicine. )<br />
There are probably more injuries from pericardiocentesis<br />
than diagnoses acutely.<br />
Indications for use of pericardiocentesis may apply in the<br />
case of iatrogenic injury caused by cardiac catheterization, at<br />
which time immediate decompression of the tamponade may<br />
be lifesaving, or in the trauma setting when a surgeon is not<br />
available. For the most part, as a diagnostic tool it has been<br />
replaced by the FAST examination. Pericardial exploration is<br />
sometimes used via a transdiaphragmatic route during laparotomy<br />
to evaluate the pericardium ( Fig. <strong>26</strong>-1 ).<br />
Penetrating Injury<br />
Only a small subset of patients with significant cardiac injury<br />
reaches the emergency department, and expeditious transport<br />
to an appropriate facility is important to survival. Transport<br />
times of less than 5 minutes and successful endotracheal intubation<br />
are positive factors for survival when the patient suffers<br />
a pulseless cardiac injury. 20<br />
Definitive treatment involves surgical exposure through an<br />
anterior thoracotomy ( Fig. <strong>26</strong>-2 ) or median sternotomy. The<br />
mainstays of treatment are relief of tamponade and hemorrhage<br />
control. Then reestablishment of effective coronary perfusion is<br />
pursued by appropriate resuscitation.<br />
Exposure of the heart is accomplished via a left anterolateral<br />
thoracotomy, which allows access to the pericardium and heart<br />
and exposure for aortic cross-clamping if necessary. This incision<br />
can be extended across the sternum to gain access to the<br />
right side of the chest and for better exposure of the right<br />
atrium. Manual access to the right hemithorax from the left<br />
side of the chest can be achieved via the anterior mediastinum<br />
by blunt dissection. This allows rapid evaluation of the right<br />
side of the chest for major injuries without transecting the<br />
sternum or placing a separate chest tube. Once the left pleural<br />
space is entered, the lung can be retracted to allow clamping of<br />
the descending thoracic aorta. The amount of blood present in<br />
the left chest suggests whether hemorrhage or tamponade is the<br />
primary issue. The pericardium anterior to the phrenic nerve is<br />
opened, injuries are identified, and repair is performed.<br />
In selected cases, particularly for small stab wounds to<br />
the precordium, median sternotomy can be used. This allows<br />
exposure of the anterior structures of the heart, but limits access<br />
CHAPTER <strong>26</strong> X<br />
FIGURE <strong>26</strong>-2 Left anterior thoracotomy (extension across the sternum if required). ( Copyright © Baylor College of Medicine, 2005. )
490 Management of Specific Injuries<br />
SECTION 3 X<br />
A<br />
B<br />
C<br />
D<br />
FIGURE <strong>26</strong>-3 Temporary techniques to control bleeding. (A) Finger occlusion; (B) partial occluding clamp; (C) Foley balloon catheter;<br />
(D) skin staples. ( Copyright © Baylor College of Medicine, 2005. )<br />
to the posterior mediastinal structures and descending thoracic<br />
aorta for cross-clamping.<br />
Cardiorrhaphy should be carefully performed. Poor technique<br />
can result in enlargement of the lacerations or injury to<br />
the coronary arteries. If the initial treating physician is uncomfortable<br />
with the suturing technique, digital pressure can be<br />
applied until an experienced surgeon arrives. Other techniques<br />
that have been described include the use of a Foley balloon<br />
catheter or a skin stapler ( Fig. <strong>26</strong>-3 ). Injuries adjacent to coronary<br />
arteries can be managed by placing the sutures deep to the<br />
artery ( Fig. <strong>26</strong>-4 ). Mechanical support or cardiopulmonary<br />
bypass is very uncommonly required in the acute setting. 4<br />
For multiple fragments in stable patients, diagnosis in<br />
the past was pursued with radiographs in two projections,<br />
fluoroscopy, angiography, or echocardiography. Recently, the<br />
multidetector CT scan can be used to diagnose and locate<br />
these fragments. The full-body topogram scan can identify all<br />
missiles, and then the cross-sectional images can be directed to<br />
precisely locate them. Trajectories can be ascertained. Treatment<br />
of retained missiles is individualized. Removal is recommended<br />
for intracardiac missiles that are left sided, larger than 1–2 cm,<br />
rough in shape, or that produce symptoms. Although a direct<br />
approach, either with or without cardiopulmonary bypass, has<br />
been advocated, a large percentage of right-sided foreign bodies<br />
can now be removed by endovascular techniques.<br />
Blunt Cardiac Injury<br />
Much debate and discussion has occurred about the clinical<br />
relevance of “cardiac contusion.” Most trauma surgeons suggest
Heart and Thoracic Vascular Injuries<br />
491<br />
FIGURE <strong>26</strong>-4 Injuries adjacent to coronary arteries can be<br />
addressed by placing sutures deep, avoiding injury to the artery.<br />
( Copyright © Baylor College of Medicine, 2005. )<br />
that this diagnosis should be eliminated because it does not<br />
affect treatment strategies. The majority of these patients seen<br />
are normotensive patients with normal initial ECG and suspected<br />
blunt cardiac injury. These cases are managed in observation<br />
units, with no expected clinical significance. Patients<br />
with an abnormal ECG are admitted for monitoring and<br />
treated accordingly. Patients who present in cardiogenic shock<br />
are evaluated for a structural injury, which is then addressed. 12<br />
■<br />
Results<br />
Many factors determine survival in patients with traumatic<br />
cardiac injury including mechanism of injury, location of<br />
injury, associated injuries, coronary artery and valvular involvement,<br />
presence of tamponade, length of prehospital transport,<br />
requirement for resuscitative thoracotomy, and experience of<br />
the trauma team. The overall hospital survival rate for patients<br />
with penetrating heart injuries ranges from 30% to 90%. The<br />
survival rate for patients with stab wounds is 70–80%, whereas<br />
survival after gunshot wounds ranges between 30% and 40%.<br />
Cardiac rupture has a worse prognosis than penetrating injuries<br />
to the heart, with a survival rate of approximately 20%.<br />
Complex Cardiac Injuries<br />
Complex cardiac injuries include coronary artery injury, valvular<br />
apparatus injury (annulus, papillary muscles, and chordae<br />
tendineae), intracardiac fistulas, and delayed tamponade. These<br />
delayed sequelae have been reported to have a broad incidence<br />
(4–56%), depending on the definition. Coronary artery injury<br />
is a rare injury, occurring in 5–9% of patients with cardiac<br />
injuries, with a 69% mortality rate. 4 A coronary artery injury is<br />
most often controlled by simple ligation, but bypass grafting<br />
using a saphenous vein may be required for proximal left anterior<br />
descending or right coronary artery injuries (with cardiopulmonary<br />
bypass). 4 Off-pump bypass can theoretically be used<br />
for cases of these injuries in the highly unlikely event that the<br />
patient is hemodynamically stable.<br />
Valvular apparatus injury is rare (0.2–9%) and can occur<br />
with both blunt and penetrating trauma. 4 ,5 The aortic valve is<br />
most frequently injured, followed by the mitral and tricuspid<br />
valves, though most victims of aortic valve injuries likely die at<br />
the scene. These injuries are usually identified postoperatively<br />
after the initial cardiorrhaphy and resuscitation have been performed.<br />
Timing of repair depends on the patient’s condition. If<br />
severe cardiac dysfunction exists at the time of the initial operation,<br />
and valvular injury is identified, immediate valve repair or<br />
replacement may be required; otherwise, delayed repair is more<br />
commonly advised. 8<br />
Intracardiac fistulas include ventricular septal defects, atrial<br />
septal defects, and atrioventricular fistulas, with an incidence of<br />
1.9% among cardiac injuries. The management depends on<br />
symptoms and degree of cardiac dysfunction, with only a<br />
minority of these patients requiring repair. 4 These injuries are<br />
also usually identified after primary repair is accomplished, and<br />
they can be repaired after the patient has recovered from the<br />
original and associated injuries. Echocardiography should be<br />
obtained before repair so that specific anatomic sites of injury<br />
and incision planning can be accomplished.<br />
Dysrhythmias can occur as a result of blunt injury, ischemia,<br />
or electrolyte abnormalities and are addressed according to the<br />
injury ( Table <strong>26</strong>-2 ). Delayed pericardial tamponade is rare. It<br />
can occur as early as 1 hour after initial operation and to days<br />
after the injury.<br />
TABLE <strong>26</strong>-2 Dysrhythmias Associated with Cardiac Injury<br />
Penetrating cardiac injury<br />
Sinus/supraventricular tachycardia<br />
ST segment changes associated with ischemia<br />
Supraventricular tachycardia<br />
Ventricular tachycardia/fibrillation<br />
Blunt cardiac injury<br />
Sinus tachycardia<br />
ST segment, T wave abnormalities<br />
Atrioventricular conduction defects, bradycardia<br />
Ventricular tachycardia/fibrillation<br />
Electrical injury<br />
Sinus tachycardia<br />
ST segment, T wave abnormalities<br />
Conduction/bundle branch delay<br />
Axis deviation<br />
Prolonged QT intervals<br />
Paroxysmal supraventricular tachycardia<br />
Atrial fibrillation<br />
Ventricular tachycardia, fibrillation<br />
Asystole (lightning strike)<br />
CHAPTER <strong>26</strong> X
492 Management of Specific Injuries<br />
SECTION 3 X<br />
■<br />
Follow-Up<br />
As discussed above, secondary sequelae in survivors of cardiac<br />
trauma include valvular abnormalities and intracardiac<br />
fistulas. 4 , 19 , 21 Early postoperative clinical examination and ECG<br />
findings are unreliable. 4 , 21 Thus, echocardiography is recommended<br />
during the initial hospitalization in all patients to<br />
identify occult injury and establish a baseline study. Because the<br />
incidence of late sequelae can be as high as 56%, follow-up<br />
echocardiography 3–4 weeks after injury has been recommended<br />
by<br />
19 , 21<br />
some.<br />
THORACIC GREAT VESSEL INJURY<br />
Injuries to the thoracic great vessels—the aorta and its brachiocephalic<br />
branches, the pulmonary arteries and veins, the superior<br />
and intrathoracic inferior vena cava, and the innominate<br />
and azygos veins—occur following both blunt and penetrating<br />
trauma. Exsanguinating hemorrhage, the primary acute manifestation,<br />
also occurs in the chronic setting when the injured<br />
great vessel forms a fistula involving an adjacent structure or<br />
when a post-traumatic pseudoaneurysm ruptures.<br />
Current knowledge regarding the treatment of injured thoracic<br />
great vessels has been derived primarily from experience<br />
with civilian injuries. Great vessel injuries have been repaired<br />
with increasing frequency, a phenomenon that has paralleled<br />
the development of techniques for elective surgery of the thoracic<br />
aorta and its major branches.<br />
A detailed understanding of normal and variant anatomy<br />
and structural relationships is important for the surgeon and<br />
any one who is a consultant to the surgeon in the evaluation of<br />
imaging studies. Venous anomalies are infrequent with the most<br />
common being absence of the left innominate vein and persistent<br />
left superior vena cava. Thoracic aortic arch anomalies are<br />
relatively common ( Table <strong>26</strong>-3 ). Knowledge of such anomalies<br />
is essential for both open and catheter-based therapies.<br />
TABLE <strong>26</strong>-3 Thoracic Aortic Anomalies<br />
Common origin of innominate and left carotid arteries<br />
(“bovine arch”)<br />
Ductus diverticulum<br />
Persistent left ductus arteriosus<br />
Aberrant takeoff of the right subclavian artery from the<br />
descending thoracic aorta<br />
Dextroposition of the thoracic aorta<br />
Coarctation of the thoracic aorta<br />
Origin of left vertebral artery off the aortic arch<br />
Pseudocoarction of the thoracic aorta (“kinked aorta”)<br />
Double aortic arch<br />
Right ductus arteriosus<br />
Persistent truncus arteriosus<br />
Cervical aortic arch (persistent complete third aortic<br />
arch)<br />
Absence of the internal carotid artery<br />
Cardio-aortic fistula<br />
ETIOLOGY AND PATHOPHYSIOLOGY<br />
More than 90% of thoracic great vessel injuries are due to penetrating<br />
trauma: gunshot, fragments, and stab wounds or therapeutic<br />
misadventures. 22 Iatrogenic lacerations of various thoracic<br />
great vessels, including the arch of the aorta, are reported complications<br />
of percutaneous central venous catheter placement.<br />
The percutaneous placement of “trocar” chest tubes has caused<br />
injuries to the intercostal arteries and major pulmonary and<br />
mediastinal vessels. Intra-aortic cardiac assist balloons can produce<br />
injury to the thoracic aorta. During emergency center<br />
resuscitative thoracotomy, the aorta may be injured during<br />
clamping if a crushing (nonvascular) clamp is used. Overinflation<br />
or migration of the Swan–Ganz balloon has produced iatrogenic<br />
injuries to pulmonary artery branches with resultant fatal<br />
hemoptysis; therefore, once a linear relationship has been established<br />
between the pulmonary artery diastolic pressure and the<br />
pulmonary capillary wedge pressure, further “wedging” may be<br />
unnecessary. Self-expanding metal stents have recently produced<br />
perforations of the aorta and innominate artery following<br />
placement into the esophagus and trachea, respectively. 23<br />
The great vessels particularly susceptible to injury from blunt<br />
trauma include the innominate artery origin, pulmonary veins,<br />
vena cava, and, most commonly, the descending thoracic aorta. 24<br />
Aortic injuries have caused or contributed to 10–15% of deaths<br />
following motor vehicle accidents for nearly 50 years. These<br />
injuries usually involve the proximal descending aorta (54–65%<br />
of cases), but often involve other segments—that is, the ascending<br />
aorta or transverse aortic arch (10–14%), the mid- or distal<br />
descending thoracic aorta (12%), or multiple sites (13–18%).<br />
The postulated mechanisms of blunt great vessel injury include<br />
(1) shear forces caused by relative mobility of a portion of the<br />
vessel adjacent to a fixed portion, (2) compression of the vessel<br />
between bony structures, and (3) profound intraluminal hypertension<br />
during the traumatic event. The atrial attachments of the<br />
pulmonary veins and vena cava and the fixation of the descending<br />
thoracic aorta at the ligamentum arteriosum and diaphragm<br />
enhance their susceptibility to blunt rupture by the first mechanism.<br />
At its origin, the innominate artery may be “pinched”<br />
between the sternum and the vertebrae during sternal impact.<br />
Blunt aortic injuries may be partial thickness—histologically<br />
similar to the intimal tear in aortic dissection—but most commonly<br />
are full thickness and therefore equivalent to a ruptured<br />
aortic aneurysm that is contained by surrounding tissues. The<br />
histopathological similarities between aortic injuries and nontraumatic<br />
aortic catastrophes suggest that similar therapeutic<br />
approaches be employed. Therefore, in hemodynamically stable<br />
patients with blunt aortic injuries, the concepts of permissive<br />
hypovolemia and minimization of arterial pressure impulse<br />
(d P /dT )—which are widely accepted in the treatment of aortic<br />
dissection and aneurysm rupture—should be considered. In<br />
opposition to patients with aortic intimal disease where the adventitia<br />
is the restraining barrier, with blunt injury to the descending<br />
thoracic aorta, it is the intact parietal pleura (not the adventitia)<br />
that contains the hematoma and prevents a massive hemothorax.<br />
True traumatic aortic dissection, with a longitudinal separation<br />
of the media extending along the length of the aorta, is<br />
extremely rare. 25 The use of the term “dissection” in the setting
Heart and Thoracic Vascular Injuries<br />
493<br />
TABLE <strong>26</strong>-4 Groups of Patients with Thoracic Aortic Injury<br />
Group Description Time to Diagnosis Location of Death Mortality (%) Cause of Death<br />
1<br />
2<br />
3<br />
Dead/dying at scene<br />
Unstable during<br />
transport<br />
Stable<br />
60 min<br />
1–6 h<br />
4–18 h<br />
Scene/EMS<br />
EMS/EC<br />
ICU<br />
100<br />
96<br />
5–30<br />
Bleeding<br />
Multisystem trauma<br />
CNS injury<br />
CHAPTER <strong>26</strong> X<br />
of aortic trauma should be equally rare, being used only in a few<br />
appropriate cases. Similarly, the terms “aortic transection” and<br />
“blunt aortic rupture” should be used only when describing<br />
specific injuries, that is, full-thickness lacerations involving<br />
either the entire or partial circumference, respectively.<br />
Increasingly, patients with thoracic great vessel injury have<br />
associated head, abdominal, and extremity injury. Often preexisting<br />
medical conditions are present, such as diabetes, hypertension,<br />
coronary artery disease, or cirrhosis. These patients are<br />
also on a large variety of medications, often aspirin, warfarin, or<br />
other platelet inhibitors. These interfere with the clotting<br />
mechanism and adaptations in treatment must be made.<br />
PATIENT CLASSIFICATION<br />
Three distinctly different groups of patients with thoracic aortic<br />
trauma exist ( Table <strong>26</strong>-4 ). The epidemiology of aortic<br />
injury is changing, due to rapid accident notification and<br />
emergency medical system (EMS) transport. The mortality<br />
statistics reveal that those whose cause of death is exsanguinating<br />
hemorrhage almost all die within the first 0–2 hours of<br />
injury. Those who die in the emergency department, operating<br />
room, or intensive care unit (ICU) within 2–4 hours of injury<br />
often have extensive multisystem injury with hemorrhage often<br />
being from sites other than the thoracic aorta. Hemodynamically<br />
stable patients who are subsequently found to have aortic<br />
injury but who die most often have central nervous system<br />
injury as the cause of their injury. It is this later group in whom<br />
the diagnosis is made by the trauma team, and therefore amenable<br />
to appropriate screening, diagnostic, and therapeutic<br />
considerations.<br />
INITIAL EVALUATION<br />
■<br />
Prehospital Management<br />
Interventions often performed by paramedics during transport<br />
include judicious intravenous fluid administration and endotracheal<br />
intubation when indicated. <strong>26</strong> Though seldom seen,<br />
pneumatic anti-shock garment (PAST) application in patients<br />
with thoracic great vessel injuries statistically increases the<br />
chance of death in both adult and pediatric populations. 27 The<br />
PAST elevate blood pressure by increasing afterload and are<br />
equivalent to placing a cross-clamp distal to the potential<br />
injury—a clearly counterproductive maneuver. Similarly, in<br />
patients with acute thoracic great vessel injuries, excessive fluid<br />
resuscitation with the goal of increasing blood pressure to<br />
normal or supernormal levels increases the incidence of mortality,<br />
ARDS, and other postoperative complications. 28<br />
■<br />
Emergency Center Evaluation<br />
History<br />
In cases of penetrating thoracic trauma, information regarding<br />
the length of a knife, the firearm type and number of rounds<br />
fired, and the patient’s distance from the firearm is sought from<br />
the patient or accompanying persons. Unfortunately, this is<br />
frequently unavailable and unreliable.<br />
Although the head-on motor vehicle collision is often considered<br />
the typical mechanism for blunt aortic injury, recent<br />
epidemiological data reveal that up to 50% of cases occur following<br />
side-impact collisions. Blunt aortic injuries have also<br />
been reported following equestrian accidents, blast injuries,<br />
auto-pedestrian accidents, crush injuries, and falls from heights<br />
of 30 ft or more. 29<br />
In addition to information involving the mechanism of<br />
injury, the emergency transport personnel can provide medical<br />
information important in evaluating the potential for a thoracic<br />
great vessel injury, such as the amount of hemorrhage at the<br />
scene, the extent and location of damage to the vehicle, any<br />
history of intermittent paralysis following the accident, and<br />
hemodynamic instability during transport.<br />
Physical Examination<br />
On arrival to the emergency center, each patient is given a rapid,<br />
thorough examination. External signs of penetrating or blunt<br />
trauma are noted. With an intrapericardial vascular injury, the<br />
classic signs of pericardial tamponade (distended neck veins,<br />
pulsus paradoxus, muffled heart sounds, elevated central venous<br />
pressure) may be present but not uniformly. Clinical findings<br />
associated with thoracic great vessel injury include:<br />
1. Hypotension<br />
2. Upper extremity hypertension<br />
3. Unequal blood pressures or pulses in the extremities (upper<br />
extremity from innominate or subclavian injury, or lower<br />
extremity from pseudocoarctation syndrome)<br />
4. External evidence of major chest trauma (e.g., steering<br />
wheel imprint on chest)<br />
5. Expanding hematoma at the thoracic outlet<br />
6. Intrascapular murmur<br />
7. Palpable fracture of the sternum<br />
8. Palpable fracture of the thoracic spine<br />
9. Left flail chest
494 Management of Specific Injuries<br />
SECTION 3 X<br />
Chest Radiography<br />
On arrival, a supine anteroposterior 36-in chest radiograph<br />
should be performed, ideally in the emergency center and not<br />
in a distant radiologic suite. Emergency physicians, radiologists,<br />
and surgeons should develop diagnostic experience viewing<br />
supine portable chest x-rays as many trauma patients are hemodynamically<br />
unstable or have suspected spinal injuries, making<br />
an “upright” 72-in posterior–anterior chest radiograph unsafe<br />
to obtain. In many cases of great vessel injury, the radiologic<br />
findings are sufficient to warrant immediate arteriography or<br />
direct transport to the operating room.<br />
For penetrating injuries, it is helpful to place radiopaque<br />
markers to identify the entrance and exit sites. Radiographic findings<br />
that suggest penetrating thoracic great vessel injury include:<br />
1. Large hemothorax<br />
2. Foreign bodies (bullets or shrapnel) or their trajectories in<br />
proximity to the great vessels<br />
3. A foreign body out of focus with respect to the remaining<br />
radiograph, which may indicate its intracardiac location<br />
( Fig. <strong>26</strong>-5 )<br />
4. A trajectory with a confusing course, which may indicate a<br />
migrating intravascular bullet ( Fig. <strong>26</strong>-6 )<br />
5. “A missing” missile in a patient with a gunshot wound to<br />
the chest, suggesting distal embolization in the arterial tree<br />
Several radiographic findings have been associated with<br />
blunt injuries of the descending thoracic aorta ( Table <strong>26</strong>-5 ).<br />
The most reliable of these signs is the loss or “double shadowing”<br />
of the aortic knob contour, creating a “funny-looking<br />
mediastinum.” Mediastinal widening at the thoracic outlet and<br />
leftward tracheal deviation are suggestive of innominate artery<br />
injury. These signs are secondary to a mediastinal hematoma,<br />
which is an indirect sign of thoracic great vessel injury. The presence<br />
of any of these signs is a positive screening test and not a<br />
diagnosis.<br />
Missile wounds that appear to traverse the mediastinum create<br />
concern regarding injury to the heart, esophagus, trachea,<br />
spinal cord, or major vasculature. Should cardiac or vascular<br />
injury occur, tamponade or major hemorrhage is usually obvious.<br />
The newer multidetector CT is often used to demonstrate<br />
missile trajectory and aid the surgeon in a decision regarding<br />
directed thoracotomy or endoscopy.<br />
■<br />
Initial Treatment and Screening<br />
Emergency Center Thoracotomy<br />
Emergency center thoracotomy in patients presenting with<br />
signs of life and hemodynamic collapse may reveal injuries to<br />
major thoracic vessels. These injuries require temporizing<br />
maneuvers that gain rapid control of bleeding, allowing resuscitation,<br />
and subsequent transfer to the operating room for<br />
definitive repair. 30 Subclavian vessel injuries, for example, can<br />
be controlled by packing, clamping at the thoracic apex, or<br />
inserting intravascular balloon catheters. Major hemorrhage<br />
from the pulmonary hilum can be temporally managed by<br />
cross-clamping the entire hilum proximally or twisting the lung<br />
180° after releasing the inferior pulmonary ligament.<br />
Tube Thoracostomy<br />
When the chest radiograph indicates a significant hemothorax,<br />
the chest tube can be connected to a repository for autotransfusion.<br />
An initial “rush” of a large volume of blood (1,500 mL)<br />
or significant ongoing hemorrhage (200–250 mL/h) may<br />
indicate great vessel injury, and is considered an indication for<br />
urgent thoracotomy.<br />
FIGURE <strong>26</strong>-5 Lateral chest x-ray demonstrating an “out of focus”<br />
bullet over the cardiac silhouette. The bullet was lodged in the<br />
wall of the right ventricle.<br />
Intravenous Access and Fluid Administration<br />
Currently, unless a patient is in extremis, large-bore intravenous<br />
portals are obtained but high-volume resuscitation<br />
avoided, until the time of an operation. If a subclavian venous<br />
catheter is required in a patient with a suspected subclavian<br />
vascular injury, the contralateral side should be used for<br />
cannulation.<br />
The treatment of severe shock should include blood transfusion.<br />
However, rapid infusions of excessive volumes of either<br />
blood or crystalloid solutions prior to operation may increase<br />
the blood pressure to a point that a protective soft perivascular
Heart and Thoracic Vascular Injuries<br />
495<br />
CHAPTER <strong>26</strong> X<br />
FIGURE <strong>26</strong>-6 Series of x-rays demonstrating the entrance site of a bullet in the left groin. The bullet embolized to the right pulmonary<br />
artery, as confirmed by arteriography.<br />
TABLE <strong>26</strong>-5 Radiographic Clues that should Prompt<br />
Suspicion of a Thoracic Great Vessel Injury<br />
Fractures<br />
• Sternum<br />
• Scapula<br />
• Multiple left ribs<br />
• Clavicle in multisystem injured patients<br />
• (?) First ribs<br />
Mediastinal clues<br />
• Obliteration/double shadow of aortic knob contour<br />
• Widening of the mediastinum 8 cm<br />
• Depression of the left mainstem bronchus 140°<br />
from trachea<br />
• Loss of perivertebral pleural stripe<br />
• Calcium layering at aortic knob<br />
• “Funny-looking” mediastinum<br />
• Deviation of nasogastric tube in the esophagus<br />
• Lateral displacement of the trachea<br />
Lateral chest x-ray<br />
• Anterior displacement of the trachea<br />
• Loss of the aortic/pulmonary window<br />
Other findings<br />
• Apical pleural hematoma<br />
• Massive left hemothorax<br />
• Obvious blunt injury to the diaphragm<br />
clot is “blown out” and fatal exsanguinating hemorrhage<br />
ensues. The principles of permitting moderate hypotension<br />
(systolic blood pressure of 60–90 mm Hg) and limiting fluid<br />
administration until achieving operative control of bleeding<br />
are cornerstones in the management of rupturing abdominal<br />
aortic aneurysms and equally apply to acute thoracic great vessel<br />
injury. Aggressive preoperative fluid resuscitation increases<br />
postoperative respiratory complications and may contribute to<br />
an increased mortality when compared to fluid restriction. 28<br />
With both penetrating and blunt chest trauma, associated<br />
pulmonary contusions are common and provide an additional<br />
rationale for limiting the infusion of preoperative crystalloid<br />
solutions.<br />
Impulse Therapy/Beta-Blockade<br />
The pharmacological reduction of d P /d T has remained a critical<br />
component of the treatment of aortic dissection since its<br />
original description by Wheat et al. in 1965. 31 Based on the<br />
similarity between aortic dissection and blunt aortic injury, this<br />
principle was first applied to d P /d T reduction to patients with<br />
blunt aortic injury in 1970. Subsequent reports have described<br />
using beta-blockers in hemodynamically stable patients who<br />
had proven blunt aortic injuries but required a delay in definitive<br />
operative treatment. 32 Some centers routinely begin betablockade<br />
therapy as soon as an aortic injury is suspected—prior<br />
to obtaining diagnostic studies as an attempt to reduce the risk<br />
of fatal rupture during the interval between presentation<br />
and confirmation of the diagnosis. While retrospective studies
496 Management of Specific Injuries<br />
suggest that it is safe, no prospective studies have demonstrated<br />
either the safety or efficacy of such treatment.<br />
SECTION 3 X<br />
Screening/Planning CT Scan<br />
for Thoracic Vascular Injury<br />
Multidetector CT scan of the chest is recommended by many<br />
radiologists as a screening test for mediastinal hematoma usually<br />
associated with aortic injury. 33 In addition, various other<br />
aortic wall and intraluminal findings suggest aortic injury on<br />
the CT scan. Very often, the initial chest x-ray has already<br />
demonstrated findings suggestive of mediastinal hematoma.<br />
Some clinicians require the additional screening CT scan to<br />
substantiate a request for a diagnostic arteriogram. Although<br />
an increasing number of surgeons and radiologists have developed<br />
a “skill” and comfort level in performing an operation<br />
based on the CT findings alone, many surgeons use the arteriographic<br />
roadmap to determine the specific injury and any<br />
unexpected vascular anomalies. This also occurs when a confirmatory<br />
aortogram is obtained prior to thoracic endograft<br />
deployment. It is interesting to thus note in a 2008 report by<br />
Demetriades et al. of a multicenter study on blunt aorta injuries<br />
that CT was used as the primary “diagnostic” modality in<br />
93% of patients, but as the majority of patients underwent<br />
endograft repair an aortogram was usually obtained. 34 As resolution<br />
and experience in using CT to plan operations increases,<br />
it is important to assure that the same information regarding<br />
extent of injury, anatomy, and aberrant branches, as well as<br />
location of injury, is obtainable. Even when radiologists and<br />
surgeons have utilized CT scans as a diagnostic test, this test<br />
has primarily been used for injuries of the proximal descending<br />
thoracic aorta. Motion artifact in the proximal ascending aorta<br />
can be difficult to interpret on CT. CT scan gated to cardiac<br />
motion may better delineate the ascending aorta and provide<br />
increased resolution. 35<br />
The diagnostic controversy regarding CT for thoracic injuries<br />
may lie in the technology. CT scan technology has evolved<br />
at a very rapid rate. It is important to understand that a<br />
4-channel 16-detector machine has different capabilities than a<br />
64-channel/detector machine. With increasing technical complexity,<br />
the protocols for obtaining the CT examination such as<br />
number and spacing of detectors, channels, pitch, slice thickness,<br />
contrast injection, and timing can significantly alter the<br />
information obtained.<br />
The raw CT data are then manipulated in a “postprocessing”<br />
function to deliver the final images. The previous static<br />
CT film images are now read on digital displays where a<br />
knowledgeable observer can further manipulate the image.<br />
Three-dimensional reconstructions, while impressive to view,<br />
take a lot of processing resources and have not added a lot to<br />
the evaluation of blunt aortic injuries ( Fig. <strong>26</strong>-7 ). Multiplanar<br />
reformatting is a postprocessing mode where the CT slice can<br />
be angled and positioned to best display the pathology. This<br />
is most useful for the evaluation of blunt aortic injury when<br />
the CT slice/virtual gantry is aligned with the curvature of<br />
the ascending/arch/descending thoracic aorta and the slices<br />
can traverse through the aorta ( Fig. <strong>26</strong>-8 ). This is very helpful<br />
not only for diagnosis but also for planning, selecting device,<br />
FIGURE <strong>26</strong>-7 A three-dimensional reconstruction of the CT in a<br />
patient with an injury to the aortic isthmus showing the thoracic<br />
endograft deployed.<br />
and evaluating landing/seal zones for the device. Centerline<br />
flow analysis displays the aorta as a straight line along its<br />
center allowing precise measurements of diameter and accurate<br />
measurements of seal zones/landing zones for planning<br />
( Fig. <strong>26</strong>-9 ). It is our observation and a local postulate that as<br />
FIGURE <strong>26</strong>-8 Multiplanar reformatting display of a typical injury<br />
through the descending thoracic aorta distal to the left subclavian<br />
artery. This allows the viewer to align the slice along the axis of<br />
the aorta. The small cube in the lower right corner represents the<br />
orientation.
Heart and Thoracic Vascular Injuries<br />
497<br />
CHAPTER <strong>26</strong> X<br />
FIGURE <strong>26</strong>-9 Centerline flow analysis of a patient with injury at the aortic isthmus. This view electronically straightens the aorta along<br />
the centerline axis of flow allowing accurate measurements regarding landing zones/seal areas and the device length to the determined.<br />
This analysis shows that by covering the left subclavian artery, a 15- to 16-mm proximal seal area is available and a 35-mm area will<br />
need to be covered. This display also shows the average aortic diameter to be 19 mm. This can be useful to plan difficult cases for which<br />
the landing zones/seal areas are difficult to precisely determine.<br />
the technology progresses, if the clinician directly caring for<br />
the patient cannot manipulate and interpret the images himself<br />
or herself, much useful information as well as artifacts<br />
may not be appreciated. This may explain a lot of the confusion<br />
regarding multiple conflicting reports and opinions on<br />
the utility of CT for screening or diagnosis. With appropriate<br />
scanners, protocols, processing, display, and experience,<br />
CT potentially could yield more information than catheter<br />
angiography.<br />
If a mediastinal hematoma is visualized on CT, formal aortography<br />
is usually obtained to specifically determine the site(s)<br />
of the injury(s) and to identify any vascular anomalies that<br />
require modifications in the operative approach. This is also<br />
uniformly done as part of the process immediately prior to placing<br />
an aortic endograft. Decision trees can be constructed to aid<br />
the surgeon in reaching a diagnosis and treating a patient with<br />
aortic injury ( Fig. <strong>26</strong>-10 ). As experience is developed with<br />
catheter-based methods, however, the CT scan is also helpful for
498 Management of Specific Injuries<br />
A<br />
Major Thoracic Injury<br />
Potential Thoracic Vascular Injury<br />
SECTION 3 X<br />
Screening Techniques<br />
(History, Physical Examination, Chest X-Ray, FAST, Chest CT)<br />
Patient in<br />
Extremis<br />
Hypotensive<br />
(Unstable)<br />
Normotensive<br />
(Stable)<br />
Diagnostic Techniques<br />
(Tube thoracostomy, FAST, Arteriogram)<br />
Hemopericardium<br />
Immediate<br />
Thoracotomy<br />
Massive<br />
Hemothorax<br />
Plan Therapy<br />
Vascular<br />
Injury<br />
Endovascular<br />
Plan position, access,<br />
imaging, control and devices<br />
Open<br />
Procedure<br />
Plan Position<br />
& Incision<br />
Reconstruct<br />
B<br />
Blunt Chest Injury<br />
Potential for Thoracic Aortic Injury<br />
Suggestive History or Physical Examination<br />
Afterload reduction<br />
(unless low BP or patient “unstable”)<br />
SCREENING Chest X-Ray/CT<br />
with appropriate protocol<br />
Strongly Suggestive/Equivocal<br />
“Normal”<br />
Treat Other Injuries<br />
AORTOGRAPHY<br />
Positive Negative Trivial<br />
Treatment<br />
Treat<br />
Other<br />
Injuries<br />
Timely<br />
Repeated<br />
Studies<br />
Immediate<br />
Delayed<br />
Open<br />
Endovascular<br />
FIGURE <strong>26</strong>-10 (A) Algorithm for an approach to patients with suspected thoracic vascular injury. (B) Algorithm for the evaluation and<br />
treatment of a patient suspected of having a blunt injury to the thoracic aorta.
Heart and Thoracic Vascular Injuries<br />
499<br />
preoperative planning for stent graft repair and evaluation for<br />
access. TEE has added little in the screening or diagnosis of<br />
thoracic aortic injury. Magnetic resonance angiography (MRI)<br />
can generate similarly detailed information; however, its application<br />
in these potentially unstable trauma patients is not currently<br />
practical.<br />
■<br />
Diagnostic Studies<br />
Catheter Arteriography<br />
In penetrating thoracic trauma, catheter angiography is indicated<br />
for suspected aortic, innominate, carotid, or subclavian<br />
arterial injuries. Different thoracic incisions are required for<br />
proximal and distal control of each of these vessels. Arteriography,<br />
therefore, is essential for localizing the injury and planning the<br />
appropriate incision. Proximity of a missile trajectory to the<br />
brachiocephalic vessels, even without any physical findings of<br />
vascular injury, can be an indication for arteriography. Although<br />
aortography may also be useful in hemodynamically stable<br />
patients with suspected penetrating aortic injuries, its limitations<br />
in this setting must be recognized. A “negative” aortogram<br />
may convey a false sense of security if the laceration has temporarily<br />
“sealed off” or if the column of aortic contrast overlies a<br />
small area of extravasation ( Fig. <strong>26</strong>-11 ). Therefore, an effort<br />
must be made to obtain views tangential to possible injuries<br />
( Figs. <strong>26</strong>-12 and <strong>26</strong>-13 ).<br />
CHAPTER <strong>26</strong> X<br />
E<br />
A<br />
C<br />
B<br />
D<br />
FIGURE <strong>26</strong>-11 Misdiagnosis by aortography.<br />
(A) Chest radiograph of a patient with a tiny<br />
puncture wound from a Philips screwdriver<br />
at the left sternal border in the second<br />
intercostal space. The patient arrived in the<br />
emergency room 30 minutes after being<br />
wounded and had stable vital signs for the<br />
following 48 hours. (B) Anteroposterior<br />
projection of the aortogram was interpreted<br />
as showing no injury. (C) Left anterior<br />
oblique projection of the aortogram was<br />
also interpreted as showing no injury. (D)<br />
Near-lateral projection of the aortogram<br />
was also read as normal by staff radiologist.<br />
(E) Subtraction aortography in the lateral<br />
projection demonstrates tiny outpouching of<br />
the thoracic aorta anteriorly at the base of<br />
the innominate artery and posteriorly on the<br />
undersurface of the transverse aortic arch<br />
(arrows). Penetrating injury of the transverse<br />
aortic arch was confirmed intraoperatively.<br />
( Reproduced with permission from Mattox KL.<br />
Approaches to trauma involving the major<br />
vessels of the thorax. Surg Clin North Am.<br />
1989;69:83. © Elsevier. )
500 Management of Specific Injuries<br />
SECTION 3 X<br />
seemingly innocuous mechanisms—including low-speed automobile<br />
crashes (10 mph) with airbag deployment and intrascapular<br />
back blows used to dislodge an esophageal foreign<br />
body—have been reported. Additionally, 50% of patients with<br />
thoracic vascular injuries from blunt trauma present without any<br />
external physical signs of injury, and 7% of patients with blunt<br />
injury to the aorta and brachiocephalic arteries have a normalappearing<br />
mediastinum on admission chest radiography.<br />
TREATMENT OPTIONS<br />
■<br />
Nonoperative Management<br />
Nonoperative management of blunt aortic injuries should be<br />
considered in patients who are unlikely to benefit from an<br />
immediate repair:<br />
FIGURE <strong>26</strong>-12 Plain chest x-ray of a patient with a penetrating<br />
wound of the ascending aorta.<br />
Following blunt trauma, the potential for thoracic great<br />
vessel injury—and, therefore, the need to proceed with aortography—is<br />
determined based on (1) the mechanism of injury,<br />
(2) physical examination, (3) the standard chest radiograph, or<br />
(4) a screening CT scan.<br />
As each of these factors has inherent limitations, all must<br />
be considered in concert. Traumatic aortic ruptures following<br />
1. Severe head injury<br />
2. Risk factors for infection:<br />
• Major burns<br />
• Sepsis<br />
• Heavily contaminated wounds<br />
3. Severe multisystem trauma with hemodynamic instability<br />
and/or poor physiologic reserve<br />
In such instances, nonoperative management is actually a<br />
purposeful delay in operation that attempts to achieve physiologic<br />
optimization and improve the outcome of repair.<br />
Nonoperative management has also been used successfully in<br />
cases of “nonthreatening” aortic lesions, for example, minor<br />
intimal defects and small pseudoaneurysms. Close observation<br />
without operation is similarly reasonable for small intimal flaps<br />
involving the brachiocephalic arteries in asymptomatic patients,<br />
as many such lesions will heal spontaneously.<br />
With the increased use of endograft repair, as well as patients<br />
with increasing number of associated injuries, blunt aortic injuries<br />
are often definitively repaired greater than 24 hours after<br />
presentation when the patient is optimized. In a report by<br />
Demetriades et al. of a multicenter study, delayed repair<br />
(24 hours) of stable blunt thoracic aortic injury was associated<br />
with improved survival, but also a longer length of ICU<br />
stay and a higher complication rate. 32<br />
Although apparent minor vascular injuries may resolve or<br />
stabilize, their long-term natural history remains uncertain.<br />
Life-threatening complications of great vessel injuries—including<br />
rupture and fistulization with severe hemorrhage—occurring<br />
more than 20 years after injury are not uncommon. 29<br />
Therefore, careful follow-up, including serial imaging studies, is<br />
a critical component of nonoperative management. Avoiding<br />
hypertension and the use of impulse control agents are also<br />
recommended when patients with aortic injuries are treated<br />
nonoperatively.<br />
FIGURE <strong>26</strong>-13 Aortogram of the patient in Fig. <strong>26</strong>-9<br />
demonstrating no apparent injury in the anteroposterior<br />
projection, but revealing a defect in the anterior aortic wall on the<br />
left anterior oblique projection (arrows).<br />
■<br />
Endograft Repair<br />
From a technical standpoint, a chronic post-traumatic false<br />
aneurysm of the descending thoracic aorta should be a logical<br />
indication for placement of an aortic endograft. Beginning in<br />
the late 1990s, single case reports and small series of thoracic
Heart and Thoracic Vascular Injuries<br />
501<br />
endografting for acute transections of the proximal descending<br />
thoracic aorta were reported. These were often custom devices<br />
using aortic or iliac artery extenders. 36 Not infrequently the left<br />
subclavian artery was occluded by the endograft, with subsequent<br />
left carotid–subclavian bypass in some cases. Iatrogenic<br />
injury to the access site of the femoral or iliac artery was occasionally<br />
reported. No reports exist for repair of thoracic ascending/arch/aortic<br />
injury and have focused on the proximal<br />
descending thoracic aorta.<br />
In the United States three commercial devices have been<br />
approved by the Food and Drug Administration for thoracic<br />
aortic aneurysms by the end of 2008. These devices are FDA<br />
approved for the treatment of thoracic aneurysms and are used<br />
off-label in patients with traumatic injuries to the descending<br />
thoracic aorta. The average diameter of the thoracic aorta<br />
among patients with aortic tears is 19.3 cm. The manufacturers<br />
recommend 15–20% oversizing. Thus, these thoracic devices<br />
need an aorta diameter of greater than 18 mm. Smaller aortas<br />
treated with endografts require custom or off-label abdominal<br />
devices. With greater oversizing, compression and infolding<br />
have been reported and infolding has resulted in a devastating<br />
thrombosis of the aorta. Over 85% of descending thoracic<br />
aortic tears are less than 1 cm from the orifice of the subclavian<br />
artery. A sealing distance on either side of the pathology of<br />
2 cm is recommended. Additionally a young patient’s aorta has<br />
significant angulation in the potential proximal seal zone that<br />
can cause leading edge “beaking” and infolding. Thus, consideration<br />
for covering the left subclavian orifice occurs and can<br />
be influenced by the intracerebral and spinal circulation.<br />
Engineering challenges still exist regarding the existing approved<br />
thoracic aortic endografts when used in young trauma<br />
patients.<br />
Preoperative planning involves a carefully protocolized CT<br />
angiogram of chest/abdomen and pelvis, and delineating the<br />
size, tortuosity, and angulation of arterial vessels for determination<br />
of appropriateness or feasibility of introducer sheaths and<br />
devices capable of covering the aortic injury.<br />
Access can often be a problem in young patients, especially<br />
females, with small iliac/femoral arteries that prohibit safe introducer<br />
sheath placement due to small size mismatch. Currently<br />
the smallest commercially available thoracic endografts require<br />
a 7- to 8-mm external iliac artery. Direct introduction or sewing<br />
of an extra-anatomic graft to the common iliac artery or<br />
aorta to allow deployment of endovascular stent grafts may be<br />
necessary in such difficult cases. It should be noted that the<br />
majority of morbidity/mortality from thoracic endograft repair<br />
is from disruption of iliac vessels during endograft placement.<br />
In a composite report using a variety of approved and<br />
customized endografts, 239 patients have been reported to<br />
have been treated for blunt injury to the proximal descending<br />
thoracic aorta ( Table <strong>26</strong>-6 ). 37 Many other small series or single<br />
case reports exist. Among the 239 cases there were 9 deaths<br />
(3.8%), and 1 paraplegia (0.5%). Even with potential selection<br />
bias, the lower mortality and almost nonexistent paraplegia<br />
rate make consideration for endovascular repair very<br />
compelling. 38 The current trend in trauma is to favor delayed<br />
repair of stable patients. 32 , 34 , 39 Yet to be answered are the engineering<br />
challenges of graft compression and infolding as well<br />
TABLE <strong>26</strong>-6 Comparison of Open Versus Endovascular<br />
Treatment of Blunt Thoracic Aortic Injury<br />
Mortality (%)<br />
Average<br />
mortality<br />
(%)<br />
Paraplegia (%)<br />
Average<br />
paraplegia<br />
Complications<br />
as available smaller sizes, conformation of the endograft to the<br />
curvature of the arch, tailored/branched grafts, and improved<br />
delivery systems. The short-term and midterm follow-up have<br />
seemed favorable for endovascular stenting. 40 However, the<br />
long-term fate of the endograft as the aorta dilates with age is<br />
yet unanswered. With massive changes in the presenting<br />
patient population, technology related to diagnosis and imaging,<br />
and engineering improvements in endograft technology,<br />
the timing, diagnosis, and management of blunt aortic injuries<br />
have been dynamic. The report of Demetriades et al. of the<br />
AAST multicenter study with its two follow-up manuscripts<br />
documented a shift in original diagnostic modality to CT and<br />
a shift to endovascular repair with a decrease in mortality and<br />
paraplegia but an increase in device-related and access complications<br />
and concern for long-term sequelae. 32 , 34 , 39 These reports<br />
have been the most comprehensive to date, and are a template<br />
to track results as the technology evolves. Studies documenting<br />
the rate of aortic dilation after endograft repair are being<br />
reported 41 and will be important for assessing the long-term<br />
durability of endograft repair. The technology continues to<br />
evolve and improve on addressing the above-mentioned anatomic<br />
size challenges and capabilities of endografts available to<br />
treat acute injuries to the thoracic aorta.<br />
It is clear that the treatment for a specific patient will continue<br />
to be individualized, and multiple approaches (nonoperative/delayed/open/endograft)<br />
will continue to be<br />
32 , 34 , 39<br />
needed.<br />
■<br />
Surgical Repair<br />
Open<br />
Operations<br />
0–55<br />
13<br />
0–20<br />
10%<br />
ARDS<br />
CNS problems<br />
Neurologic<br />
Endograft<br />
Repair<br />
0–12<br />
3.8<br />
1<br />
1 out of 239 cases<br />
LSCA occlusion<br />
Graft compression<br />
Entry site problems<br />
ARDS, adult respiratory distress syndrome; CNS, central<br />
nervous system; LSCA, left subclavian artery.<br />
Indications for urgent transfer to the operating room for thoracotomy<br />
include hemodynamic instability, significant hemorrhage<br />
from chest tubes, and radiographic evidence of a rapidly<br />
expanding mediastinal hematoma ( Fig. <strong>26</strong>-14 ).<br />
In the preoperative phase, whenever possible, patients and<br />
their families should be made aware of the potential for neurologic<br />
complications—paraplegia, stroke, and brachial plexus<br />
injuries—following surgical reconstruction of thoracic great<br />
CHAPTER <strong>26</strong> X
502 Management of Specific Injuries<br />
SECTION 3 X<br />
FIGURE <strong>26</strong>-14 Plain chest x-ray in a patient with a blunt injury<br />
to the descending thoracic aorta. Note the rightward deviation of<br />
both the trachea and nasogastric tube in the esophagus.<br />
vessel injuries, as adequate exposure is important for proximal<br />
and distal control. Prepping and draping of the patient should<br />
provide access from the neck to the knees to allow management<br />
of all contingencies. For the hypotensive patient with an undiagnosed<br />
injury, the mainstay of thoracic trauma surgery is the<br />
left anterolateral thoracotomy with the patient in the supine<br />
position. In stable patients, preoperative arteriography may<br />
dictate an operative approach by another incision.<br />
Appropriate graft materials should be available. While the<br />
failure mode of an infected prosthetic graft is a pseudoaneurysm,<br />
a saphenous vein graft is a devitalized collagen tube susceptible<br />
to bacterial collagenase, which may cause graft<br />
dissolution with acute rupture and uncontrolled hemorrhage.<br />
Therefore, for vessels larger than 5 mm, a prosthetic graft is the<br />
conduit of choice, especially in potentially contaminated<br />
wounds. However, due to patency considerations, a saphenous<br />
vein graft may need to be used when smaller grafts are required.<br />
For fragile vessels, such as the subclavian artery and the aorta in<br />
young people, a soft knitted Dacron graft is useful.<br />
vessels. Careful documentation of preoperative neurologic status<br />
is important. With any suspicion of vascular injury, prophylactic<br />
antibiotics are administered preoperatively. In hemodynamically<br />
stable patients, fluid administration is limited until vascular<br />
control is achieved in the operating room. An autotransfusion<br />
device should be available. During the induction of anesthesia,<br />
wide swings in blood pressure should be avoided; while profound<br />
hypotension is clearly undesirable, hypertensive episodes<br />
can have equally catastrophic consequences.<br />
The operative approach to great vessel injury depends on<br />
both the overall patient assessment and the specific injury. The<br />
initial steps of patient positioning and incision selection<br />
( Table <strong>26</strong>-7 ) are particularly important in surgery for great<br />
Damage Control<br />
Patients with severely compromised physiologic reserve often<br />
require damage control injury management to achieve survival.<br />
The two approaches to thoracic damage control are (1) definitive<br />
repair of injuries using quick and simple techniques that restore<br />
survivable physiology during a single operation and less commonly<br />
(2) abbreviated thoracotomy that restores survivable<br />
physiology and requires a planned reoperation for definitive<br />
repairs. 30 Severe hilar vascular injuries can be quickly controlled<br />
by performing a pneumonectomy using stapling devices.<br />
Temporary vessel ligation or placement of intravascular shunts<br />
can control bleeding until the subsequent correction of acidosis,<br />
hypothermia, and coagulopathy allows the patient to be returned<br />
TABLE <strong>26</strong>-7 Recommended Incisions for Thoracic Great Vessel Injuries<br />
Injured Vessel<br />
Uncertain injury (hemodynamically unstable)<br />
Ascending aorta<br />
Transverse aortic arch<br />
Descending thoracic aorta<br />
Innominate artery<br />
Right subclavian artery or vein<br />
Left common carotid artery<br />
Left subclavian artery or vein<br />
Pulmonary artery<br />
Main/intrapericardial<br />
Right or left hilar<br />
Pulmonary vein<br />
Innominate vein<br />
Intrathoracic vena cava<br />
Incision<br />
Left anterolateral thoracotomy<br />
Transverse sternotomy<br />
Right anterolateral thoracotomy (clamshell)<br />
Median sternotomy<br />
Median sternotomy<br />
Neck extension<br />
Left posterolateral thoracotomy (fourth intercostal space)<br />
Median sternotomy with right cervical extension<br />
Median sternotomy with right cervical extension<br />
Median sternotomy with left cervical extension<br />
Left anterolateral thoracotomy (third or fourth intercostal space)<br />
with separate left supraclavicular incision connecting vertical<br />
sternotomy (“book” thoracotomy)<br />
Median sternotomy<br />
Ipsilateral posterolateral thoracotomy<br />
Ipsilateral posterolateral thoracotomy<br />
Median sternotomy<br />
Median sternotomy
Heart and Thoracic Vascular Injuries<br />
503<br />
to the operating room. En masse closure of a thoracotomy is<br />
more hemostatic than towel-clip closure. A “Bogotá bag” closure<br />
or “Vac Pack closure” can be used as a temporary closure of a<br />
median sternotomy in cases with associated cardiac dysfunction.<br />
ARTERIAL INJURIES<br />
Ascending Aorta<br />
Patients with blunt ascending aortic injuries rarely survive<br />
transportation to the hospital. Operative repair usually requires<br />
use of total cardiopulmonary bypass and insertion of a Dacron<br />
graft. If the sinuses or valves are involved, aortic root replacement<br />
with reimplantation of the coronary ostia may be<br />
required. 35<br />
Penetrating injuries involving the ascending aorta are<br />
uncommon ( Figs. <strong>26</strong>-12 and <strong>26</strong>-13 ). Survival rates approach<br />
50% for patients having stable vital signs on arrival at a trauma<br />
center. 42 Although primary repair of anterior lacerations can be<br />
accomplished without adjuncts, cardiopulmonary bypass may<br />
be required if there is an additional posterior injury. The possibility<br />
of a peripheral bullet embolus must be considered in<br />
these patients.<br />
CHAPTER <strong>26</strong> X<br />
Transverse Aortic Arch<br />
When approaching an injury to the transverse aortic arch,<br />
extension of the median sternotomy to the neck is necessary to<br />
obtain exposure of the arch and brachiocephalic branches. If<br />
necessary, exposure can be further enhanced by division of the<br />
innominate vein. When hemorrhage limits exposure, the use of<br />
balloon tamponade is useful as a temporary measure. Simple<br />
lacerations may be repaired by lateral aortorrhaphy. With difficult<br />
lesions, such as posterior lacerations or those with concomitant<br />
pulmonary artery injuries, cardiopulmonary bypass<br />
can be used. As with injuries to the ascending thoracic aorta,<br />
survival rates approaching 50% are possible. 42<br />
Innominate Artery<br />
Median sternotomy is employed for access to innominate artery<br />
injuries. A right cervical extension can be used when necessary.<br />
Blunt injuries typically involve the proximal innominate artery<br />
( Figs. <strong>26</strong>-15 and <strong>26</strong>-16 ) and therefore actually represent aortic<br />
injuries and require obtaining proximal control at the transverse<br />
aortic arch. In contrast, penetrating injuries of the<br />
innominate artery may occur throughout its course. Exposure<br />
is enhanced by division of the innominate vein.<br />
In selected patients with penetrating injuries, a running<br />
lateral arteriorrhaphy using 4-0 polypropylene suture is occasionally<br />
possible. More often, injuries to the innominate<br />
artery require repair via the bypass exclusion technique<br />
( Fig. <strong>26</strong>-17 ). 43 Bypass grafting is performed from the ascending<br />
aorta to the distal innominate artery (immediately proximal<br />
to the bifurcation of the subclavian and right carotid<br />
arteries) using a Dacron tube graft. The area of injury is<br />
avoided until the areas for bypass insertion are exposed. A<br />
vascular clamp is placed proximal to the bifurcation of the<br />
innominate artery to allow collateral flow to the brain via the<br />
FIGURE <strong>26</strong>-15 Plain chest x-ray of a patient with a blunt injury of<br />
the innominate artery. Note that the hematoma is at the thoracic<br />
outlet rather than the aortic isthmus.<br />
right subclavian and carotid arteries. Hypothermia, systemic<br />
anticoagulation, or shunting is not required. After the bypass<br />
is completed, the area of hematoma is entered, and the injury<br />
controlled with a partial occluding clamp (usually at the origin<br />
of the innominate artery) and oversewn. If concomitantly<br />
FIGURE <strong>26</strong>-16 Aortogram of the patient in Fig. <strong>26</strong>-12<br />
demonstrating the tear involving the proximal innominate artery.
504 Management of Specific Injuries<br />
SECTION 3 X<br />
A<br />
C<br />
FIGURE <strong>26</strong>-17 (A–C) Drawing depicting the bypass exclusion<br />
technique employed in patients with innominate artery injuries.<br />
( Copyright © Baylor College of Medicine, 1981. )<br />
B<br />
hospital alive, the majority of blunt aortic injuries are located at<br />
the isthmus ( Fig. <strong>26</strong>-18 ). Patients presenting with an injury in<br />
the mid-descending thoracic aorta or distally, near the diaphragm,<br />
are far less common ( Fig. <strong>26</strong>-19 ). Multiple blunt<br />
aortic injuries are rare, but may occur.<br />
Injury to the descending thoracic aorta is often accompanied<br />
by other organ injuries. If the patient has a stable thoracic<br />
hematoma and concomitant abdominal injury, laparotomy<br />
should be the initial procedure. For the patient with a rapidly<br />
expanding hematoma, however, repair of the thoracic injury<br />
should be the primary therapeutic goal. Sequencing is driven by<br />
the lesion that is most likely to cause exsanguination.<br />
The current standard technique of repair involves clamping<br />
and direct reconstruction ( Table <strong>26</strong>-8 ). Three commonly<br />
employed adjuncts to this approach are (1) pharmacological<br />
agents, (2) temporary, passive bypass shunts, and (3) pumpassisted<br />
atriofemoral bypass or cardiopulmonary bypass. In the<br />
latter approach, two options exist: traditional pump bypass,<br />
which requires heparin, and use of centrifugal (heparinless)<br />
pump circuits. All three of these adjunctive approaches to the<br />
clamp and repair principle should be in the armamentarium of<br />
the surgeon, who must choose the approach most appropriate<br />
to the specific clinical situation.<br />
Injury to the descending thoracic aorta is approached via a<br />
posterolateral thoracotomy through the fourth intercostal<br />
space. The injury usually originates at the medial aspect of the<br />
injured or previously divided, the innominate vein may be<br />
ligated with impunity. If the vein remains intact, a pedicled<br />
pericardial flap can be positioned between the vein and overlying<br />
graft to prevent erosion.<br />
The treatment of an iatrogenic tracheal-innominate artery<br />
fistula deserves special consideration. These fistulae are usually<br />
caused by the concave surface of a low riding tracheostomy<br />
tube eroding into the innominate artery. Sentinel bleeding<br />
through or around the tracheostomy tube should not be misinterpreted<br />
as “tracheitis.” Arteriography during a “stable<br />
interval” is generally not helpful in making a precise diagnosis;<br />
instead, the possibility of a tracheal-innominate fistula should<br />
be evaluated via bronchoscopy in the operating room. With<br />
massive bleeding, control is achieved by performing orotracheal<br />
intubation, removing the tracheostomy tube, and<br />
directly tamponading the bleeding digitally through the tracheotomy<br />
during transport to the operating room. Through a<br />
median sternotomy with a right neck extension, the innominate<br />
artery is ligated at its origin from the aorta and distally<br />
just before the division into the carotid and subclavian arteries.<br />
Despite a greater than 25% chance of neurologic complications,<br />
no attempt should be made at revascularization, since<br />
delayed graft infection with its dreaded complications inevitably<br />
occurs.<br />
Descending Thoracic Aorta<br />
Prehospital mortality is 85% for patients with blunt injury to<br />
the descending thoracic aorta. 44 In patients who arrive at the<br />
FIGURE <strong>26</strong>-18 Aortogram demonstrating the classic intimal tear<br />
and traumatic pseudoaneurysm of the descending thoracic aorta.
Heart and Thoracic Vascular Injuries<br />
505<br />
FIGURE <strong>26</strong>-19 Aortogram in a patient with blunt chest trauma<br />
demonstrating an intimal tear of the descending thoracic aorta at<br />
the diaphragm.<br />
aorta at the level of the ligamentum arteriosum; however, one<br />
must take care to avoid missing a second injury (usually at the<br />
level of the diaphragm).<br />
The initial objective is proximal control; therefore, the<br />
transverse aortic arch is exposed, and umbilical tapes are<br />
passed around the arch between the left carotid and subclavian<br />
arteries. Similarly, the subclavian artery is encircled with<br />
umbilical tape. Care should be taken to avoid injuring the left<br />
recurrent laryngeal nerve though this is often difficult to visualize<br />
in the hematoma. If it is suspected that the tear extends<br />
to the aortic arch or ascending aorta, cardiopulmonary bypass<br />
should be available in the operating room. If the patient has<br />
had previous coronary artery bypass surgery with use of the<br />
left internal mammary artery as a conduit, repair may require<br />
cardiopulmonary bypass perhaps with profound hypothermic<br />
circulatory arrest to eliminate the need to clamp the left subclavian<br />
artery.<br />
TABLE <strong>26</strong>-8 Current Therapeutic Approaches to the<br />
Management of Thoracic Aortic Injuries<br />
1. Surgical (clamp and direct reconstruction with or<br />
without an interposition graft)<br />
(a) Pharmacological control of proximal hypertension<br />
(b) Passive bypass shunts<br />
(c) Pump-assisted bypass<br />
• Traditional cardiopulmonary bypass (with<br />
total-body heparinization)<br />
• Atriofemoral bypass using centrifugal pump<br />
(with/without heparinization)<br />
2. Nonoperative and/or purposeful delay of operation<br />
(with pharmacological treatment and close radiologic<br />
surveillance)<br />
3. Endograft repair<br />
Vascular clamps are applied to three locations: proximal<br />
aorta, distal aorta, and left subclavian artery. Close communication<br />
between anesthesiologist and surgeon is essential to maintain<br />
stability of hemodynamic parameters before, during, and<br />
after clamping. The use of vasodilators prevents cardiac strain<br />
during clamping. The hematoma is entered and back-bleeding<br />
from intercostal arteries is controlled. Care is taken to avoid<br />
indiscriminate ligation of intercostal vessels; only those required<br />
for adequate repair of the aorta should be ligated. The proximal<br />
and distal ends of the aorta are completely transected and dissected<br />
away from the esophagus; this maneuver allows fullthickness<br />
suturing while minimizing the risk of a secondary<br />
aortoesophageal fistula. The injury is then repaired by either<br />
end-to-end anastomosis or graft interposition. Graft interposition<br />
is utilized in more than 85% of reported cases. Prior to<br />
clamp removal, volumes of fluid (blood and crystalloid) may<br />
need to be administered to avoid clamp release hypotension.<br />
For patients undergoing repair of blunt descending thoracic<br />
aortic injury, the reported mortality ranges from 0% to 55%<br />
(average 13%). 37 , 45 As expected in these victims of major blunt<br />
trauma, the mortality is primarily associated with multisystem<br />
trauma, and is ultimately due to head injury, infection, respiratory<br />
insufficiency, and renal insufficiency.<br />
The most feared complication of great vessel injury is paraplegia.<br />
Utilization of protective adjuncts when repairing<br />
descending thoracic aortic injuries remains a topic of considerable<br />
debate. There have been proponents of the use of passive<br />
shunts and cardiopulmonary bypass, with and without heparinization.<br />
The mortality rate with the use of routine cardiopulmonary<br />
bypass is probably secondary to the massive cerebral,<br />
abdominal, or fracture site hemorrhage that occurs in these<br />
victims of multisystem trauma. Recent experience using centrifugal<br />
pumps for left heart bypass without heparinization has<br />
provided an attractive alternative for those who wish to use<br />
controlled flow bypass without systemic anticoagulation. This<br />
also allows unloading of the left heart during clamping, which<br />
can be helpful in patients with cardiac disease. The use of<br />
bypass systems, however, is not without complications. In the<br />
trauma patient, difficulty inserting cannulae may occur due to<br />
patient position, the presence of periaortic hematoma, and time<br />
constraints imposed by an expanding, pulsatile, uncontrolled<br />
hematoma. Intraoperative and postoperative complications<br />
include bleeding at the cannulation sites and false aneurysm<br />
formation.<br />
Use of simple clamp and repair for injuries to the descending<br />
thoracic aorta (without the use of systemic anticoagulation<br />
or shunts) is a technique that continues to be used with excellent<br />
results. Sweeney in 1992 reported using simple clamp and<br />
repair in 75 patients, only 1 of whom developed postoperative<br />
paraplegia.<br />
Ultimately, the determinants of postoperative paraplegia are<br />
multifactorial ( Table <strong>26</strong>-9 ); therefore, the precise causes cannot<br />
be precisely identified in an individual patient. Paraplegia has<br />
been associated with perioperative hypotension, injury or ligation<br />
of the intercostal arteries, and duration of clamp occlusion<br />
during repair. 46 However, there are reports of patients surviving<br />
surgery without paraplegia despite having long segments of aorta<br />
replaced and ligation of multiple intercostal arteries. The length<br />
CHAPTER <strong>26</strong> X
506 Management of Specific Injuries<br />
TABLE <strong>26</strong>-9 Possible Contributing Factors Related to the Multifactorial Development of Paraplegia Following<br />
Operations for Thoracic Great Vessel Injury<br />
SECTION 3 X<br />
Injury factors Direct segmental artery injury<br />
Direct radicular artery injury<br />
Direct spinal artery injury<br />
Spinal cord contusion/concussion<br />
Spinal canal compartment syndrome<br />
Severity of aortic injury<br />
Specific anatomic location of aortic injury<br />
Patient factors Location of arteri radicularis magna(?)<br />
Continuity of anterior spinal artery<br />
Caliber of individual segmental radicular arteries<br />
Congenital narrowing of spinal canal<br />
(?) Increased blood alcohol levels<br />
Total perispinal collateral blood supply<br />
Operative factors Required occlusion of segmental arteries<br />
Pharmacological agents required<br />
(?) Declamping hypotension<br />
(?) Required cross-clamp times (in combination with anatomic and injury factors<br />
cited in this table); length of required interposition grafting or required exclusion<br />
(?) Level of systolic (or mean) proximal aortic blood pressure<br />
(?) Level of distal aortic mean blood pressure<br />
(?) “Flow” in the aorta distal to clamp<br />
Postoperative factors Progressive swelling of the spinal cord<br />
Spinal canal compartment syndrome<br />
Delayed or secondary occlusion of injured or contused segmental, radicular, or<br />
spinal arteries<br />
Pharmacological induced spasm of spinal cord nutrient arteries<br />
of cross-clamp time does not directly correlate with occurrence of<br />
paraplegia. A cross-clamp time under 30 minutes has been<br />
argued to provide a safe margin against paraplegia, and shunting<br />
techniques have been recommended when longer cross-clamp<br />
times are necessary. 46 The use of a shunt, however, does not offer<br />
protection for the area of the spinal cord supplied by the arteries<br />
between the clamps. Furthermore, patients requiring longer<br />
clamp time or interposition grafts have more extensive injuries<br />
than those requiring shorter clamp times or end-to-end anastomoses.<br />
Thus, it is likely that an increased incidence of paraplegia<br />
associated with longer clamp times is secondary to more<br />
extensive disruption of intercostal arteries and other flow to the<br />
anterior spinal artery caused by the original injury.<br />
Various monitoring techniques are available to assess the<br />
effect of aortic occlusion on the spinal cord, including the measurement<br />
of somatosensory- and motor-evoked potentials.<br />
Although correlation appears to exist between loss of somatosensory-evoked<br />
potentials, duration of loss of conduction,<br />
and postoperative paraplegia, the use of this modality is not<br />
common to all trauma centers, the interpretation of results is<br />
still being debated, and actual positive applicability requires<br />
further delineation.<br />
Regardless of the technique used, paraplegia occurs in<br />
approximately 10% of these patients (range 0–22%). 37 , 45 No<br />
prospective, randomized trial has identified the superiority of<br />
any single method. Therefore, the choice of operative technique<br />
does not infer legal liability when paraplegia occurs.<br />
Even with potential selection bias in favor of endografts, the<br />
low mortality and almost nonexistent paraplegia rate make the<br />
use of endografting very compelling. The reported complications<br />
of graft migration, enfolding, compression, occlusion of<br />
the subclavian artery, and problems at the entry site are all<br />
technical and engineering challenges that may potentially be<br />
solved by new commercial devices.<br />
Subclavian Artery<br />
Subclavian vascular injuries can involve any combination of the<br />
following regions: intrathoracic, thoracic outlet, cervical (zone 1),<br />
and upper extremity. Preoperative arteriography allows for<br />
planning appropriate incision(s) to obtain adequate exposure<br />
and control.<br />
A cervical extension of the median sternotomy is employed<br />
for exposure of right-sided subclavian injuries. For left subclavian<br />
artery injuries, proximal control is obtained through an<br />
anterolateral thoracotomy (above the nipple, second or third<br />
intercostal space), while a separate supraclavicular incision provides<br />
distal control. Although these incisions can be connected
Heart and Thoracic Vascular Injuries<br />
507<br />
to create a formal “book” thoracotomy, this results in a high<br />
incidence of postoperative “causalgia”-type neurologic complications<br />
and its use should be limited to highly selected leftsided<br />
subclavian artery injuries.<br />
In obtaining exposure, it is important to avoid injuring the<br />
phrenic nerve (anterior to the scalenus anticus muscle). In subclavian<br />
vascular trauma, a high associated rate of brachial plexus<br />
injury is seen; thus, documentation of preoperative neurologic<br />
status is important. Intraoperative iatrogenic injury to the<br />
brachial plexus should also be avoided.<br />
In most instances, repair requires either lateral arteriorrhaphy<br />
or graft interposition. It is unusual that an end-to-end<br />
anastomosis can be employed. Associated injuries to the lung<br />
should be managed with stapled wedge resection or pulmonary<br />
tractotomy. 47 One pitfall in subclavian injuries is failure to<br />
anticipate the exposure necessary for proximal control. When<br />
approaching the subclavian artery via the deltopectoral groove<br />
without proximal control, exsanguination may occur. Resection<br />
of the clavicle may aid in proximal control. A combination of<br />
supraclavicular and infraclavicular incisions may be used to<br />
avoid the morbidity of clavicular resection. A mortality rate of<br />
4.7% for patients with subclavian artery injuries has been<br />
reported, but death is often due to associated injuries.<br />
With the density of vascular structures in the thoracic outlet,<br />
and the morbidity of the thoracic incisions needed for proximal<br />
control, it would seem that endovascular techniques to address<br />
subclavian artery injuries would be advantageous. There are<br />
increasing reports of endovascular approaches to the subclavian<br />
artery in both stable and unstable patients. 48 If diagnostic arteriography<br />
is performed in the OR, a balloon catheter can be left<br />
in the proximal left subclavian artery for proximal control.<br />
This is most applicable in centers where acute vascular imaging<br />
for trauma is available in the operating room and arteriography/covered<br />
stent placement can be performed by the<br />
trauma/cardiovascular surgeon. With a vascular imaging capable<br />
bed, a C-arm with vascular capability, and a simplified set<br />
of endovascular tools, even an unstable trauma patient can be<br />
brought to the operating room where he or she can be resuscitated,<br />
imaged/diagnosed, and bleeding controlled with both<br />
open and endovascular techniques.<br />
Left Carotid Artery<br />
The operative approach for injuries of the left carotid artery<br />
mirrors that used for an innominate artery injury: a median<br />
sternotomy with a left cervical extension added when necessary.<br />
As with other great vessel injuries, neither shunts nor pumps are<br />
employed. With transection at the left carotid origin, bypass<br />
graft repair is preferred over end-to-end anastomosis. Intraoperatively,<br />
a carotid shunt can be used to temporize these until<br />
resources/assistants can be gathered in the OR.<br />
Pulmonary Artery<br />
The intrapericardial pulmonary arteries are approached via<br />
median sternotomy. Minimal dissection is needed to expose the<br />
main and proximal left pulmonary arteries. 49 Exposure of the<br />
intrapericardial right pulmonary artery is achieved by dissecting<br />
between the superior vena cava and ascending aorta. Although<br />
anterior injuries can be repaired primarily without adjuncts,<br />
repair of a posterior injury usually requires cardiopulmonary<br />
bypass. Mortality rates for injury to the central pulmonary<br />
arteries or veins are greater than 70%. 22<br />
Distal pulmonary artery injuries present with massive<br />
hemothorax and are repaired through an ipsilateral posterolateral<br />
thoracotomy. When there is a major hilar injury, rapid<br />
pneumonectomy may be a lifesaving maneuver. The use of a<br />
large tamponading balloon catheter may control exsanguinating<br />
hemorrhage.<br />
Internal Mammary Artery<br />
The internal mammary artery in a young patient is capable of<br />
flows in excess of 300 mL/min. Injuries to this artery can produce<br />
extensive hemothorax or even pericardial tamponade,<br />
simulating a cardiac injury. Such injuries are usually serendipitously<br />
discovered at the time of thoracotomy for suspected great<br />
vessel or heart injury.<br />
Intercostal Arteries<br />
Persistent hemothorax can be caused by simple lacerations of<br />
the intercostal arteries. Because of difficulty in exposure, precise<br />
ligature can be difficult. At times, control must be achieved by<br />
circumferential ligatures around the rib on either side of the<br />
intercostal vessel injury.<br />
■<br />
Venous Injuries<br />
Thoracic Vena Cava<br />
Isolated injury to the suprahepatic inferior or superior vena<br />
cava is infrequently reported. Injury at either location has a<br />
high incidence of associated organ trauma and carries a mortality<br />
rate greater than 60%. Intrathoracic inferior vena cava<br />
injury produces hemopericardium and cardiac tamponade.<br />
Exposure of the thoracic inferior vena cava is extremely difficult<br />
unless the patient is placed on total cardiopulmonary<br />
bypass with the inferior cannula inserted via the groin in the<br />
abdominal inferior vena cava. Repair is exposed by a right<br />
atriotomy and intracaval balloon occlusion to prevent air<br />
entering the cannula and massive blood return to the heart<br />
except via the hepatic veins. Repair is achieved from inside the<br />
cava via the right atrium. Superior vena cava injuries are<br />
repaired by lateral venorrhaphy. At times, an intracaval shunt<br />
is necessary. 50 For complex injuries a PTFE patch or Dacron<br />
interposition tube graft can be used and is more expedient<br />
than the time-consuming construction of saphenous vein<br />
panel grafts.<br />
Pulmonary Veins<br />
Injury to the pulmonary veins is difficult to manage through<br />
an anterior incision. With major hemorrhage, temporary<br />
occlusion of the entire hilum may be necessary. If a pulmonary<br />
vein must be ligated, the appropriate lobe needs to be<br />
resected. Pulmonary vein injuries are often associated with<br />
concomitant injuries to the heart, pulmonary artery, aorta,<br />
and esophagus.<br />
CHAPTER <strong>26</strong> X
508 Management of Specific Injuries<br />
SECTION 3 X<br />
Subclavian Veins<br />
The operative exposure of the subclavian veins parallels that<br />
described for subclavian artery injuries: median sternotomy<br />
with cervical extension for right-sided injuries and left anterolateral<br />
thoracotomy with a separate supraclavicular incision for<br />
left-sided injuries. In most instances, repair requires either lateral<br />
venorrhaphy or ligation.<br />
Azygos Vein<br />
The azygos vein is not usually classified as a thoracic great vessel,<br />
but because of its size and high flow, azygos vein injuries<br />
must be considered potentially fatal. Penetrating wounds of the<br />
thoracic outlet can produce combinations of injuries involving<br />
the azygos vein, innominate artery, trachea or bronchus, and<br />
superior vena cava. These complex injuries have a very high<br />
mortality rate, and are particularly difficult to control if<br />
approached through a median sternotomy. Combined incisions<br />
and approaches are frequently needed for successful repair.<br />
When injured, the azygous vein is best managed by suture ligature<br />
of both sides of the injury ( Fig. <strong>26</strong>-20 ). Concomitant<br />
injury to the esophagus and bronchus should be considered and<br />
ruled out. 51<br />
structures, mandatory exploration has been advocated in the<br />
past. The evaluation of stable patients using less invasive<br />
means—combined aortography, bronchoscopy, echocardiography,<br />
and esophagoscopy—has been described. A thoracic CT<br />
scan will often show the bullet trajectory and guide a need for<br />
surgery or additional diagnostic tests.<br />
Thoracic Duct Injury<br />
Injuries to the thoracic great vessels may be complicated by<br />
concomitant thoracic duct injury, which, if unrecognized, may<br />
produce devastating morbidity due to marked nutritional<br />
depletion. 52 Diagnosed by chylous material draining from the<br />
chest tube, this condition is usually treated medically.<br />
Continued chest tube drainage, coupled with a diet devoid of<br />
long-chain fatty acids, usually results in spontaneous closure<br />
in less than 1 month. Prolonged hyperalimentation beyond<br />
3 weeks has not consistently resulted in spontaneous closure of<br />
thoracic duct fistula. If thoracotomy is required, a fatty meal or<br />
heavy cream to increase the chylous flow and facilitate identification<br />
of the fistula is given to the patient a few hours before<br />
surgery. The fistula is simply ligated with fine monofilament<br />
suture (6-0).<br />
■<br />
Special Problems<br />
Mediastinal Traverse Injuries<br />
Because injuries from both stab and gunshot wounds that traverse<br />
the mediastinum are classically felt to have a high probability<br />
of injury to the thoracic great vessels and other critical<br />
Systemic Air Embolism<br />
A fistula between a pulmonary vein and bronchiole due to a<br />
penetrating lung injury results in systemic air embolism. The<br />
fistula allows air bubbles to enter the left heart and embolize to<br />
the systemic circulation, including the coronary and cerebral<br />
arteries ( Fig. <strong>26</strong>-21 ). Intrabronchial pressure above 60 torr<br />
increases the incidence of this complication. 53 Manifestations<br />
©2005 Baylor College of Medicine<br />
FIGURE <strong>26</strong>-20 Injury to the azygos vein with control with lateral repair, ligation, division, and oversewing. ( Copyright © Baylor College<br />
of Medicine, 2005. )
Heart and Thoracic Vascular Injuries<br />
509<br />
CHAPTER <strong>26</strong> X<br />
Venule<br />
Bronchiole<br />
©Baylor College of Medicine 1979<br />
100 mm<br />
Hg<br />
Alveolus<br />
FIGURE <strong>26</strong>-21 Drawing depicting the mechanism of systemic air embolism following a penetrating lung injury. ( Copyright © Baylor<br />
College of Medicine, 1979. )<br />
include seizures and cardiac arrest. Resuscitation requires thoracotomy,<br />
clamping of the pulmonary hilum to prevent further<br />
air embolization, and aspiration of air from the left ventricle<br />
and ascending aorta. Cardiopulmonary bypass can be considered;<br />
however, very few survivors have been reported.<br />
Foreign Body Embolism<br />
Because of their central location, the thoracic great vessels may<br />
serve as both an entry site and final resting place for intravascular<br />
bullet emboli. 54 These migratory foreign bodies present a<br />
diagnostic and therapeutic dilemma. As the result of intravascular<br />
embolization, bullets may produce infection, ischemia, or<br />
injury to organs distant from the site of trauma.<br />
Bullets and catheters can embolize to the pulmonary vasculature;<br />
25% of migratory bullets finally lodge in the pulmonary<br />
arteries ( Fig. <strong>26</strong>-6 ). 54 Although small fragments, such as those<br />
the size of a BB, can probably be left in place without causing<br />
problems, catheter emboli and larger bullet emboli should be<br />
removed to prevent pulmonary thrombosis, sepsis, or other<br />
complications. Percutaneous retrieval of the foreign body using<br />
transvenous catheters and fluoroscopic guidance may obviate<br />
the need for thoracotomy.<br />
■<br />
Postoperative Management<br />
A significant portion of the in-hospital mortality asso ciated<br />
with great vessel injury is secondary to the nature of the<br />
multisystem trauma in this group of patients. The operating<br />
surgeon is best qualified to direct the patient’s postoperative<br />
management. Careful hemodynamic monitoring,<br />
with avoidance of both hypertension and hypotension, is<br />
critical. While urinary output is a generally a good indicator<br />
of cardiac function, for the patient with massive injuries,<br />
Swan–Ganz monitoring is often necessary to optimize<br />
hemodynamic parameters and manage fluids, pressors, and<br />
vasodilators.<br />
Various pulmonary problems—including atelectasis, respiratory<br />
insufficiency, pneumonia, and adult respiratory dis tress<br />
syndrome—represent the primary postoperative complications<br />
in this group of patients. The presence of pulmonary<br />
contusions and the potential for development of adult respiratory<br />
distress syndrome mandate that fluid administration be<br />
carefully monitored. Ventilatory strategies to address potential<br />
complications of these lung injuries can be used. Patient mobility<br />
is important, and adequate medication for pain relief results in<br />
fewer pulmonary complications. For the management of pain<br />
related to a thoracotomy or multiple rib fractures, postoperative<br />
thoracic epidural anesthesia can be considered in stable patients<br />
without spinal injuries; alternatively, intercostal nerve blocks<br />
can be performed intraoperatively and repeated in the ICU.<br />
Postoperative hemorrhage may be due to a technical<br />
problem, but is often the result of coagulopathy related to<br />
hypothermia, acidosis, and massive blood transfusion. Coagulation<br />
studies can be carefully monitored and corrected with
510 Management of Specific Injuries<br />
SECTION 3 X<br />
administration of appropriate blood products. Blood draining<br />
via chest tubes can be collected and autotransfused.<br />
The presence of a prosthetic vascular graft requires special<br />
attention aimed at avoiding bacteremia. During the initial<br />
resuscitation of these critically injured patients, various intravascular<br />
lines are often rapidly placed at the expense of strict<br />
sterile technique; all such lines should be replaced after the<br />
patient has stabilized in the ICU. Antibiotic therapy should be<br />
continued into the postoperative period until potential sources<br />
of infection are eliminated. Patients are counseled regarding the<br />
necessity of antibiotic prophylaxis during invasive procedures,<br />
including dental manipulations.<br />
Most late complications are related to infections or sequelae<br />
from other injuries. Long-term complications specifically<br />
related to the vascular repair—including stenosis, thrombosis,<br />
arteriovenous fistula, graft infection, and pseudoaneurysm<br />
formation—are uncommon.<br />
REFERENCES<br />
1. Ivatury RR. Injury to the heart. In: Moore EE, Feliciano DV, Mattox KL,<br />
eds. Trauma . 5th ed. New York: <strong>McGraw</strong>-<strong>Hill</strong>; 2004.<br />
2. Campbell NC, Thomsen SR, Murkart DJ, et al. Review of 1198 cases of<br />
penetrating cardiac trauma. Br J Surg. 1997;84:1737.<br />
3. Thourani VH, Feliciano DV, Cooper WA, et al. Penetrating cardiac<br />
trauma at an urban trauma center: a 22 year perspective. Am Surg. 1999;<br />
65:811.<br />
4. Wall MJ Jr, Mattox KL, Chen CD, Baldwin JC. Acute management of<br />
complex cardiac injuries. J Trauma. 1997;42:905.<br />
5. LeMaire SA, Wall MJ Jr, Mattox KL. Needle embolus causing cardiac<br />
puncture and chronic constrictive pericarditis. Ann Thorac Surg. 1998;<br />
65:1786.<br />
6. Maron BJ, Link MS, Wang PJ, et al. Clinical profile of commotio cordis:<br />
an underappreciated cause of sudden death in young during sports and<br />
other activities. J Cardiovasc Electrophysiol. 1999;10:114.<br />
7. Wall MJ Jr, Mattox KL, Wolf DA. The cardiac pendulum—blunt rupture<br />
of the pericardium with strangulation of the heart. J Trauma. 2005;<br />
59:136.<br />
8. Baumgartner FJ, Rayhanabad J, Bongard FS, et al. Central venous injuries<br />
of the subclavian–jugular and innominate–caval confluences. Tex Heart<br />
Inst J. 1999;<strong>26</strong>:177.<br />
9. Medizinische Klinik IV. Perforation und Ruptur Koronaryarterien. Herz.<br />
1998;23:311.<br />
10. Ivatury RR, Simon RJ, Rohman M. Cardiac complications. In: Mattox<br />
KL, ed. Complications of Trauma . New York: Churchill Livingstone;<br />
1994:409–428.<br />
11. Lee RC. Injury by electrical forces: pathophysiology, manifestations, and<br />
therapy. Curr Probl Surg. 1997;34:677.<br />
12. Mattox KL, Flint LM, Carrico CJ, et al. Blunt cardiac injury (formerly<br />
termed “myocardial contusion”) [editorial]. J Trauma. 1992;31:653.<br />
13. Galindo Gallego M, Lopez-Cambra MJ, Fernandez-Acenero MJ, et al.<br />
Traumatic rupture of the pericardium. Case report and literature review.<br />
J Cardiovasc Surg (Torino). 1996;37:187.<br />
14. American College of Surgeons, Committee on Trauma. Advanced Trauma<br />
Life Support . Chicago: American College of Surgeons; 2008.<br />
15. Biffl WD, Moore EE, Johnson JL. Emergency department thoracotomy.<br />
In: Moore EE, Feliciano DV, Mattox KL, eds. Trauma . 5th ed. New York:<br />
<strong>McGraw</strong>-<strong>Hill</strong>; 2004.<br />
16. Bertinchant JP, Polge A, Mohty D, et al. Evaluation of incidence, clinical<br />
significance and prognostic value of circulating cardiac troponin I and T<br />
elevation in hemodynamically stable patients with suspected myocardial<br />
contusion after blunt chest trauma. J Trauma. 2000;48:924.<br />
17. Rozycki GS, Schmidt JA, Oschner MG, et al. The role of surgeonperformed<br />
ultrasound in patients with possible penetrating wounds: a<br />
prospective multicenter study. J Trauma. 1998;45:190.<br />
18. Mattox KL, Wall MJ Jr. Newer diagnostic measures and emergency<br />
management. Chest Surg Clin N Am. 1997;7:214.<br />
19. Meyer DM, Jessen ME, Grayburn PA. Use of echocardiography to detect<br />
occult cardiac injury after penetrating thoracic trauma: a prospective<br />
study. J Trauma. 1995; 39:902.<br />
20. Durham LA, Richardson R, Wall MJ, et al. Emergency center thoracotomy:<br />
impact of prehospital resuscitation. J Trauma. 1992;32:779.<br />
21. Mattox KL, Limacher MC, Feliciano DV, et al. Cardiac evaluation<br />
following heart injury. J Trauma. 1985;25:758.<br />
22. Matttox KL, Feliciano DV, Beall AC Jr, et al. Five thousand seven<br />
hundred sixty cardiovascular injuries in 4459 patients. Epidemiologic<br />
evolution 1958–1988. Ann Surg. 1989;209:698.<br />
23. Alfaro J, Varela G, De-Miguel E, de Nicilas M. Successful management of<br />
a tracheo-innominate artery fistula following placement of a wire selfexpandable<br />
tracheal Gianturco stent. Eur J Cardiothorac Surg. 1993;<br />
7:615.<br />
24. Horton TG, Cohn SM, Heid MP, et al. Identification of trauma patients<br />
at risk of thoracic aortic tear by mechanism of injury. J Trauma.<br />
2000;48:1008.<br />
25. Rogers FB, Osler TM, Shackford SR. Aortic dissection after trauma: case<br />
report and review of the literature. J Trauma. 1996;41:906.<br />
<strong>26</strong>. Mattox KL. Prehospital management of thoracic injury. Surg Clin North<br />
Am. 1989;69:21.<br />
27. Mattox KL, Bickell W, Pepe P, et al. Prospective MAST study in 911<br />
patients. J Trauma. 1989;29:1104.<br />
28. Bickell WH, Wall MJ, Pepe PE, et al. Immediate versus delayed fluid<br />
resuscitation for hypotensive patients with penetrating torso injuries.<br />
N Engl J Med. 1994;331:1105.<br />
29. McCollum CH, Graham JM, Noon GP, et al. Chronic traumatic<br />
aneurysms of the thoracic aorta: an analysis of 50 patients. J Trauma.<br />
1979;19:248.<br />
30. Wall MJ Jr, Soltero E. Damage control for thoracic injuries. Surg Clin<br />
North Am. 1997;77:863.<br />
31. Wheat MW Jr, Palmer RF, Bartley TD, et al. Treatment of dissecting<br />
aneurysm of the aorta without surgery. J Thorac Cardiovasc Surg.<br />
1965;50:364.<br />
32. Demetriades D, Velmahos GC, Scalea TM, et al. Blunt traumatic thoracic<br />
aorta injuries: early or delayed repair—results of an American Association<br />
for the Surgery of Trauma prospective study. J Trauma. 2009;66:967–973.<br />
33. Dyer DS, Moore EE, Ilke DN, et al. Thoracic aortic injury: how<br />
predictive is mechanism and is chest computed tomography a reliable<br />
screening tool? A prospective study in 1561 patients. J Trauma. 2000;<br />
48:673.<br />
34. Demetriades D, Velmahos GC, Scalea TM, et al. Diagnosis and treatment<br />
of blunt thoracic blunt thoracic aortic injuries: changing perspectives.<br />
J Trauma. 2008;64:1415–1419.<br />
35. Wall MJ Jr, Tsai PI, Gilani R, et al. Challenges in the diagnosis of unusual<br />
presentations of blunt injury to the ascending aorta and aortic sinuses.<br />
J Surg Res. 2010;163:176–178 [Epub ahead of print].<br />
36. Tehrani HY, Peterson BG, Katariya K, et al. Endovascular repair of<br />
thoracic aortic tears. Ann Thorac Surg. 2006;82:873.<br />
37. Mattox KL, Whigham C, Fisher RG, et al. Blunt trauma to the thoracic<br />
aorta: current challenges. In: Lumsden AB, Lin PH, Chen C, Parodi JC,<br />
eds. Advanced Endovascular Therapy of Aortic Disease . London: Blackwell<br />
Publishing; 2007.<br />
38. Patel HJ, Williams DM, Upchruch GR, et al. A comparative analysis of<br />
open and endovascular repair for the ruptured descending thoracic aorta.<br />
J Vasc Surg. 2009;50:1<strong>26</strong>5–1270.<br />
39. Demetriades D, Velmahos GC, Scalea TM, et al. Operative repair or<br />
endovascular stent graft in blunt traumatic thoracic aortic injuries: results<br />
of an American Association for the Surgery of Trauma multicenter study.<br />
J Trauma. 2008;64:561–571.<br />
40. Fernandez V, Mestres G, Maeso J, et al. Endovascular treatment of<br />
traumatic thoracic aortic injuries: short- and medium-term follow-up.<br />
Ann Vasc Surg. 2010;24:160–166.<br />
41. Forbes TL, Harris JR, Lawlor K, et al. Aortic dilation after endovascular<br />
repair of blunt traumatic thoracic aortic injuries. J Vasc Surg. 2010;52:<br />
45–48.<br />
42. Pate JW, Cole FH, Walker WA, et al. Penetrating injuries of the aortic<br />
arch and its branches. Ann Thorac Surg. 1993;55:586.<br />
43. Johnston RH Jr, Wall MJ, Mattox KL. Innominate artery trauma: a thirtyyear<br />
experience. J Vasc Surg. 1993;17:134.<br />
44. Parmley LF, Mattingly TW, Marian WC, et al. Nonpenetrating traumatic<br />
injury of the aorta. Circulation. 1958;17:1086.<br />
45. von Oppell UO, Dunne TT, De Groot MK, et al. Traumatic aortic<br />
rupture: twenty-year metaanalysis of mortality and risk of paraplegia.<br />
Ann Thorac Surg. 1994;58:585.<br />
46. Mattox KL. Fact and fiction about management of aortic transection<br />
[editorial]. Ann Thorac Surg. 1989;48:1.<br />
47. Wall MJ, Hirshberg A, Mattox KL. Pulmonary tractotomy with selective<br />
vascular ligation for penetrating injuries to the lung. Am J Surg.<br />
1994;168:1.
Heart and Thoracic Vascular Injuries<br />
511<br />
48. Gilani R, Tsai P, Wall JR, Mattox KL, Lin P. Endovascular management of<br />
complex subclavian artery injuries. J Trauma . 2012 (in press).<br />
49. Clements RH, Wagmeister LS, Carraway RP. Blunt intrapericardial<br />
rupture of the pulmonary artery in a surviving patient. Ann Thorac Surg.<br />
1997;64:258.<br />
50. DeBakey ME, Simeone FA. Battle injuries of arteries in World War II: an<br />
analysis of 2,471 cases. Ann Surg. 1946;123:534.<br />
51. Wall MJ Jr, Mattox KL, DeBakey ME. Injuries to the azygous venous<br />
system. J Trauma. 2006;60:357.<br />
52. Dulchavsky SA, Ledgerwood AM, Lucas CE. Management of chylothorax<br />
after blunt chest trauma. J Trauma. 1988;28:1400.<br />
53. Graham JM, Beall AC Jr, Mattox KL, et al. Systemic air embolism<br />
following penetrating trauma to the lung. Chest. 1977;72:449.<br />
54. Mattox KL, Beall AC Jr, Ennix CL, et al. Intravascular migratory bullets.<br />
Am J Surg. 1979;137:192.<br />
CHAPTER <strong>26</strong> X