Procedure for tracheal bronchial suctioning in adults.pdf
Procedure for tracheal bronchial suctioning in adults.pdf
Procedure for tracheal bronchial suctioning in adults.pdf
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Volume 8<br />
Patient Care<br />
ASHFORD AND ST PETER’S HOSPITALS NHS TRUST<br />
PROCEDURE FOR TRACHEAL BRONCHIAL SUCTIONING<br />
See also: Tracheostomy care pictorial guide<br />
Tracheostomy care observation chart<br />
Tracheostomy care competency<br />
Tracheostomy Care Plan<br />
<strong>Procedure</strong> <strong>for</strong> removal of <strong>in</strong>ner cannula of a tracheostomy tube<br />
1.0 DEFINITION<br />
Tracheal <strong>bronchial</strong> <strong>suction<strong>in</strong>g</strong> is the removal of sputum via placement of a sterile suction catheter <strong>in</strong>to<br />
a tracheostomy tube us<strong>in</strong>g a sterile non-touch technique.<br />
2.0 AIMS<br />
Tracheal <strong>bronchial</strong> <strong>suction<strong>in</strong>g</strong> aims to effectively remove the maximum amount of secretions with<br />
m<strong>in</strong>imal risk of complications to the patient.<br />
3.0 INDICATIONS FOR PROCEDURE<br />
3.1 A tracheostomy provides a patient with a patent airway. If the patient is unable to clear<br />
secretions from the airway <strong>in</strong>dependently, <strong>suction<strong>in</strong>g</strong> is <strong>in</strong>dicated<br />
3.2 Frequency <strong>for</strong> <strong>tracheal</strong> suction is determ<strong>in</strong>ed by <strong>in</strong>dividual cl<strong>in</strong>ical assessment of patient need<br />
and should not be considered as a rout<strong>in</strong>e procedure. The follow<strong>in</strong>g are recognised <strong>in</strong>dications<br />
<strong>for</strong> <strong>tracheal</strong> suction and <strong>in</strong>clude:-<br />
• Patient request of <strong>in</strong>ability to cough up secretion<br />
• Increased cough<strong>in</strong>g of patient<br />
• Audible secretions <strong>in</strong> chest by listen<strong>in</strong>g or chest auscultation<br />
• Secretions felt on chest by resonance on chest wall<br />
• Increased work of breath<strong>in</strong>g and/ or use of accessory muscles<br />
• Tachypnoea / <strong>in</strong>crease <strong>in</strong> respiratory rate<br />
• Change <strong>in</strong> sk<strong>in</strong> colour or peripheral desaturation <strong>in</strong>dicated by a significant reduction <strong>in</strong><br />
SpO2 from basel<strong>in</strong>e<br />
• Reduction <strong>in</strong> anticipated ventilatory parameter (if patient receiv<strong>in</strong>g non-<strong>in</strong>vasive positive<br />
pressure ventilation)<br />
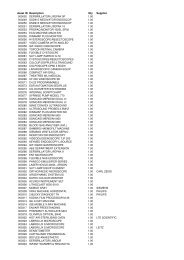
4.0 EQUIPMENT/ PREPARATION REQUIRED<br />
• Emergency equipment, ambu bag -valve mask, Tracheostomy Emergency Box<br />
• A functional suction unit 13.5 – 20 Kpa (Glass & Graz, 1995 Regan, 1998)<br />
• Correct size sterile catheters (Formula Tracheostomy tube size –2 x2 i.e. size 8 tube : 8 – 2 = 6<br />
x2 = 12)<br />
• Yankeur suction catheter<br />
• Disposable sterile gloves<br />
• Latex universal gloves<br />
• Protective eye wear<br />
• Apron<br />
Ratified<br />
May 2006<br />
Reviewed Issue 1 Page 2 of 8