Verslag – Rapport – Bericht – Report - GSKE - FMRE
Verslag – Rapport – Bericht – Report - GSKE - FMRE
Verslag – Rapport – Bericht – Report - GSKE - FMRE
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
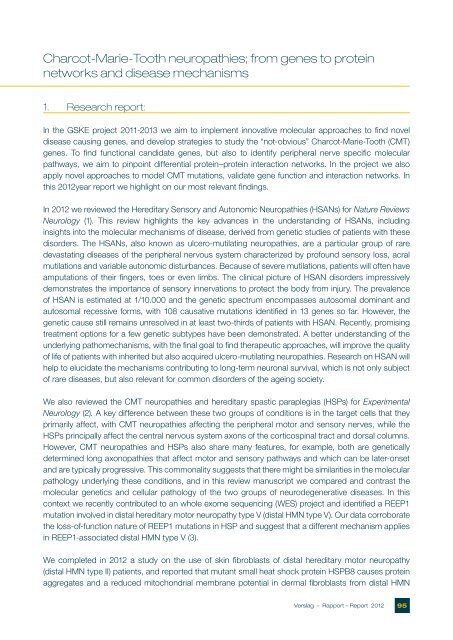
Charcot-Marie-Tooth neuropathies; from genes to protein<br />
networks and disease mechanisms<br />
1. Research report:<br />
In the <strong>GSKE</strong> project 2011-2013 we aim to implement innovative molecular approaches to find novel<br />
disease causing genes, and develop strategies to study the “not-obvious” Charcot-Marie-Tooth (CMT)<br />
genes. To find functional candidate genes, but also to identify peripheral nerve specific molecular<br />
pathways, we aim to pinpoint differential protein<strong>–</strong>protein interaction networks. In the project we also<br />
apply novel approaches to model CMT mutations, validate gene function and interaction networks. In<br />
this 2012year report we highlight on our most relevant findings.<br />
In 2012 we reviewed the Hereditary Sensory and Autonomic Neuropathies (HSANs) for Nature Reviews<br />
Neurology (1). This review highlights the key advances in the understanding of HSANs, including<br />
insights into the molecular mechanisms of disease, derived from genetic studies of patients with these<br />
disorders. The HSANs, also known as ulcero-mutilating neuropathies, are a particular group of rare<br />
devastating diseases of the peripheral nervous system characterized by profound sensory loss, acral<br />
mutilations and variable autonomic disturbances. Because of severe mutilations, patients will often have<br />
amputations of their fingers, toes or even limbs. The clinical picture of HSAN disorders impressively<br />
demonstrates the importance of sensory innervations to protect the body from injury. The prevalence<br />
of HSAN is estimated at 1/10.000 and the genetic spectrum encompasses autosomal dominant and<br />
autosomal recessive forms, with 108 causative mutations identified in 13 genes so far. However, the<br />
genetic cause still remains unresolved in at least two-thirds of patients with HSAN. Recently, promising<br />
treatment options for a few genetic subtypes have been demonstrated. A better understanding of the<br />
underlying pathomechanisms, with the final goal to find therapeutic approaches, will improve the quality<br />
of life of patients with inherited but also acquired ulcero-mutilating neuropathies. Research on HSAN will<br />
help to elucidate the mechanisms contributing to long-term neuronal survival, which is not only subject<br />
of rare diseases, but also relevant for common disorders of the ageing society.<br />
We also reviewed the CMT neuropathies and hereditary spastic paraplegias (HSPs) for Experimental<br />
Neurology (2). A key difference between these two groups of conditions is in the target cells that they<br />
primarily affect, with CMT neuropathies affecting the peripheral motor and sensory nerves, while the<br />
HSPs principally affect the central nervous system axons of the corticospinal tract and dorsal columns.<br />
However, CMT neuropathies and HSPs also share many features, for example, both are genetically<br />
determined long axonopathies that affect motor and sensory pathways and which can be later-onset<br />
and are typically progressive. This commonality suggests that there might be similarities in the molecular<br />
pathology underlying these conditions, and in this review manuscript we compared and contrast the<br />
molecular genetics and cellular pathology of the two groups of neurodegenerative diseases. In this<br />
context we recently contributed to an whole exome sequencing (WES) project and identified a REEP1<br />
mutation involved in distal hereditary motor neuropathy type V (distal HMN type V). Our data corroborate<br />
the loss-of-function nature of REEP1 mutations in HSP and suggest that a different mechanism applies<br />
in REEP1-associated distal HMN type V (3).<br />
We completed in 2012 a study on the use of skin fibroblasts of distal hereditary motor neuropathy<br />
(distal HMN type II) patients, and reported that mutant small heat shock protein HSPB8 causes protein<br />
aggregates and a reduced mitochondrial membrane potential in dermal fibroblasts from distal HMN<br />
<strong>Verslag</strong> <strong>–</strong> <strong>Rapport</strong> <strong>–</strong> <strong>Report</strong> 2012 95