Endoscopic Ultrasound–Guided Fine Needle Aspiration Cytology of ...
Endoscopic Ultrasound–Guided Fine Needle Aspiration Cytology of ...
Endoscopic Ultrasound–Guided Fine Needle Aspiration Cytology of ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
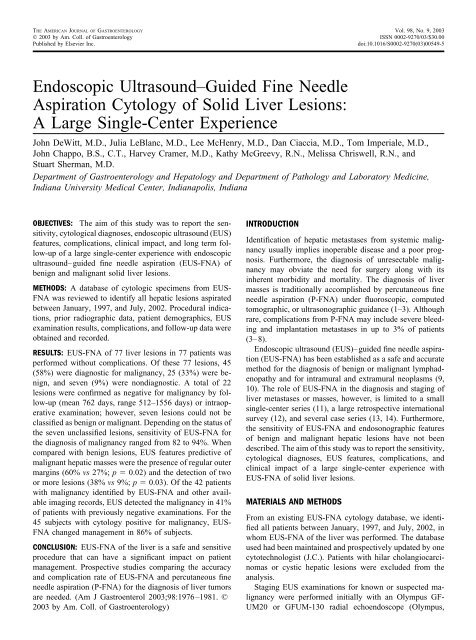
THE AMERICAN JOURNAL OF GASTROENTEROLOGY Vol. 98, No. 9, 2003<br />
© 2003 by Am. Coll. <strong>of</strong> Gastroenterology ISSN 0002-9270/03/$30.00<br />
Published by Elsevier Inc.<br />
doi:10.1016/S0002-9270(03)00549-5<br />
<strong>Endoscopic</strong> <strong>Ultrasound–Guided</strong> <strong>Fine</strong> <strong>Needle</strong><br />
<strong>Aspiration</strong> <strong>Cytology</strong> <strong>of</strong> Solid Liver Lesions:<br />
A Large Single-Center Experience<br />
John DeWitt, M.D., Julia LeBlanc, M.D., Lee McHenry, M.D., Dan Ciaccia, M.D., Tom Imperiale, M.D.,<br />
John Chappo, B.S., C.T., Harvey Cramer, M.D., Kathy McGreevy, R.N., Melissa Chriswell, R.N., and<br />
Stuart Sherman, M.D.<br />
Department <strong>of</strong> Gastroenterology and Hepatology and Department <strong>of</strong> Pathology and Laboratory Medicine,<br />
Indiana University Medical Center, Indianapolis, Indiana<br />
OBJECTIVES: The aim <strong>of</strong> this study was to report the sensitivity,<br />
cytological diagnoses, endoscopic ultrasound (EUS)<br />
features, complications, clinical impact, and long term follow-up<br />
<strong>of</strong> a large single-center experience with endoscopic<br />
ultrasound–guided fine needle aspiration (EUS-FNA) <strong>of</strong><br />
benign and malignant solid liver lesions.<br />
METHODS: A database <strong>of</strong> cytologic specimens from EUS-<br />
FNA was reviewed to identify all hepatic lesions aspirated<br />
between January, 1997, and July, 2002. Procedural indications,<br />
prior radiographic data, patient demographics, EUS<br />
examination results, complications, and follow-up data were<br />
obtained and recorded.<br />
RESULTS: EUS-FNA <strong>of</strong> 77 liver lesions in 77 patients was<br />
performed without complications. Of these 77 lesions, 45<br />
(58%) were diagnostic for malignancy, 25 (33%) were benign,<br />
and seven (9%) were nondiagnostic. A total <strong>of</strong> 22<br />
lesions were confirmed as negative for malignancy by follow-up<br />
(mean 762 days, range 512–1556 days) or intraoperative<br />
examination; however, seven lesions could not be<br />
classified as benign or malignant. Depending on the status <strong>of</strong><br />
the seven unclassified lesions, sensitivity <strong>of</strong> EUS-FNA for<br />
the diagnosis <strong>of</strong> malignancy ranged from 82 to 94%. When<br />
compared with benign lesions, EUS features predictive <strong>of</strong><br />
malignant hepatic masses were the presence <strong>of</strong> regular outer<br />
margins (60% vs 27%; p 0.02) and the detection <strong>of</strong> two<br />
or more lesions (38% vs 9%; p 0.03). Of the 42 patients<br />
with malignancy identified by EUS-FNA and other available<br />
imaging records, EUS detected the malignancy in 41%<br />
<strong>of</strong> patients with previously negative examinations. For the<br />
45 subjects with cytology positive for malignancy, EUS-<br />
FNA changed management in 86% <strong>of</strong> subjects.<br />
CONCLUSION: EUS-FNA <strong>of</strong> the liver is a safe and sensitive<br />
procedure that can have a significant impact on patient<br />
management. Prospective studies comparing the accuracy<br />
and complication rate <strong>of</strong> EUS-FNA and percutaneous fine<br />
needle aspiration (P-FNA) for the diagnosis <strong>of</strong> liver tumors<br />
are needed. (Am J Gastroenterol 2003;98:1976–1981. ©<br />
2003 by Am. Coll. <strong>of</strong> Gastroenterology)<br />
INTRODUCTION<br />
Identification <strong>of</strong> hepatic metastases from systemic malignancy<br />
usually implies inoperable disease and a poor prognosis.<br />
Furthermore, the diagnosis <strong>of</strong> unresectable malignancy<br />
may obviate the need for surgery along with its<br />
inherent morbidity and mortality. The diagnosis <strong>of</strong> liver<br />
masses is traditionally accomplished by percutaneous fine<br />
needle aspiration (P-FNA) under fluoroscopic, computed<br />
tomographic, or ultrasonographic guidance (1–3). Although<br />
rare, complications from P-FNA may include severe bleeding<br />
and implantation metastases in up to 3% <strong>of</strong> patients<br />
(3–8).<br />
<strong>Endoscopic</strong> ultrasound (EUS)–guided fine needle aspiration<br />
(EUS-FNA) has been established as a safe and accurate<br />
method for the diagnosis <strong>of</strong> benign or malignant lymphadenopathy<br />
and for intramural and extramural neoplasms (9,<br />
10). The role <strong>of</strong> EUS-FNA in the diagnosis and staging <strong>of</strong><br />
liver metastases or masses, however, is limited to a small<br />
single-center series (11), a large retrospective international<br />
survey (12), and several case series (13, 14). Furthermore,<br />
the sensitivity <strong>of</strong> EUS-FNA and endosonographic features<br />
<strong>of</strong> benign and malignant hepatic lesions have not been<br />
described. The aim <strong>of</strong> this study was to report the sensitivity,<br />
cytological diagnoses, EUS features, complications, and<br />
clinical impact <strong>of</strong> a large single-center experience with<br />
EUS-FNA <strong>of</strong> solid liver lesions.<br />
MATERIALS AND METHODS<br />
From an existing EUS-FNA cytology database, we identified<br />
all patients between January, 1997, and July, 2002, in<br />
whom EUS-FNA <strong>of</strong> the liver was performed. The database<br />
used had been maintained and prospectively updated by one<br />
cytotechnologist (J.C.). Patients with hilar cholangiocarcinomas<br />
or cystic hepatic lesions were excluded from the<br />
analysis.<br />
Staging EUS examinations for known or suspected malignancy<br />
were performed initially with an Olympus GF-<br />
UM20 or GFUM-130 radial echoendoscope (Olympus,
AJG – September, 2003<br />
EUS-FNA <strong>Cytology</strong> <strong>of</strong> Solid Liver Lesions<br />
1977<br />
Table 1. Indications for EUS Examinations by <strong>Cytology</strong> Results <strong>of</strong><br />
EUS-FNA <strong>of</strong> the Liver<br />
Melville NY). The right lobe <strong>of</strong> the liver was surveyed from<br />
the duodenum and distal stomach, whereas the left lobe was<br />
imaged from the proximal and mid-stomach. Endoscope<br />
rotation was used as necessary to visualize as much <strong>of</strong> the<br />
liver parenchyma as possible. EUS-FNA was performed<br />
using the Pentax 32-UA, Pentax 36-UX (Pentax Precision<br />
Instruments, Orangeburg, NY), Olympus GF-UC30P, or<br />
Olympus GF-UC140P curvilinear array echoendoscope.<br />
EUS-FNA was performed using a 22-gauge, 8-cm Wilson-<br />
Cook EUSN-1, EUSN-2, or EUSN-3 needle (Wilson-Cook<br />
Medical, Winston-Salem, NC) by one <strong>of</strong> four physicians<br />
(J.D., D.C., L.M., or J.L.). Doppler color angiography was<br />
used to ensure the absence <strong>of</strong> intervening vascular structures<br />
along the anticipated needle path. Depending on the amount<br />
<strong>of</strong> blood anticipated during tissue sampling, full, partial, or<br />
no suction was applied at the discretion <strong>of</strong> the endoscopist,<br />
cytotechnologist, or cytopathologist. A cytotechnologist or<br />
cytopathologist was available on-site for preliminary interpretations<br />
on all procedures. Samples aspirated were expressed<br />
onto a glass slide and two smear preparations were<br />
made. One slide was air-dried and stained with a modified<br />
Giemsa stain for rapid on-site interpretation. The other slide<br />
was alcohol-fixed and stained by the Papanicolaou method.<br />
EUS-FNA was repeated until a definitive diagnosis was<br />
made or the endoscopist believed that further sampling<br />
would not likely increase yield. Within several days <strong>of</strong> each<br />
EUS examination, a final cytological diagnosis was rendered<br />
by a staff cytopathologist.<br />
A true positive EUS-FNA for malignancy is defined as<br />
unequivocal cytological evidence <strong>of</strong> malignancy. A false<br />
negative aspirate is a nondiagnostic or benign specimen,<br />
which is subsequently found to be malignant by percutaneous<br />
FNA or intraoperative findings. A true negative EUS-<br />
FNA for malignancy is defined as benign or nondiagnostic<br />
samples that are either confirmed as benign by alternative<br />
sampling, intraoperative examination, or appropriate clinical<br />
follow-up. Specimens with benign hepatocytes without<br />
evidence <strong>of</strong> atypical cells are categorized as benign aspirates.<br />
Aspirates from EUS-FNA that are interpreted as nondiagnostic,<br />
highly suspicious, suspicious, or atypical for<br />
malignancy are considered as negative for malignancy.<br />
Medical records <strong>of</strong> enrolled subjects were reviewed and<br />
procedural indications, prior radiographic data, patient demographics,<br />
EUS test results, clinical outcomes, procedural<br />
complications, and follow-up data were abstracted. When<br />
multiple liver lesions were noted, the endosonographic description<br />
<strong>of</strong> only the aspirated lesion was recorded. When<br />
charts were incomplete, written informed consent was sent<br />
and follow-up telephone calls were made to the subject,<br />
closest relative <strong>of</strong> the deceased, or referring physician for<br />
clarification or any required further information. The potential<br />
clinical impact <strong>of</strong> EUS-FNA <strong>of</strong> a liver metastasis or<br />
malignancy is defined as results that met the following<br />
criteria: 1) avoided surgery (results precluded resectable<br />
malignancy); 2) made diagnosis (results provided initial<br />
diagnosis <strong>of</strong> malignancy); 3) upstaged tumor (results upstaged<br />
primary malignancy); 4) incurred no change in management<br />
(results did not change patient treatment). This<br />
study was approved by the Institutional Review Board at our<br />
institution.<br />
Statistical Analysis<br />
Assuming that the EUS-FNA diagnosis <strong>of</strong> malignancy is a<br />
true positive, sensitivity was calculated as the proportion <strong>of</strong><br />
patients with cancer in whom EUS-FNA was positive for<br />
malignancy. For analysis, continuous variables were described<br />
as means and standard deviations, and dichotomous<br />
variables were expressed as simple proportions with or<br />
without 95% confidence limits. Student’s t test and 2 or<br />
Fisher’s exact tests were used to test for differences in<br />
comparisons between continuous and dichotomous variables,<br />
respectively.<br />
RESULTS<br />
Indication<br />
All<br />
(n 77)<br />
<strong>Cytology</strong> Result<br />
Malignant<br />
(n 45)<br />
Benign/ND<br />
(n 32)<br />
Abnormal ERCP 21 (27) 11 (24) 10 (31)<br />
Pancreatic mass on CT 19 (25) 12 (27) 7 (22)<br />
Staging <strong>of</strong> known cancer 10 (13) 7 (16) 3 (9)<br />
Liver mass on CT 9 (12) 9 (20) 0 (0)<br />
Other abnormal CT findings 4 (5) 1 (2) 3 (9)<br />
Suspected recurrent cancer 2 (3) 1 (2) 1 (3)<br />
Chronic abdominal pain 2 (3) 0 (0) 2 (7)<br />
Other 10 (12) 4 (9) 6 (19)<br />
Total 77 45 32<br />
ND nondiagnostic<br />
In total, EUS-FNA was performed on 77 different liver<br />
lesions in 77 patients (42 male and 35 female, 69 white and<br />
eight African American, with a mean age <strong>of</strong> 63 11 yr).<br />
Follow-up was available in all patients.<br />
Indications for EUS Examinations<br />
The indications for the 77 EUS procedures are recorded in<br />
Table 1. The two most common indications were abnormal<br />
ERCP findings, the majority <strong>of</strong> which were strictures, and a<br />
pancreatic mass on CT scan, which accounted for 27% and<br />
25% <strong>of</strong> the procedures performed, respectively. Ten (13%)<br />
<strong>of</strong> 77 procedures were done for staging <strong>of</strong> a recently diagnosed<br />
malignancy (pancreas in five, esophageal in four, and<br />
lung in one). Of the 45 malignancies diagnosed by EUS-<br />
FNA, the most common indications for the EUS were a CT<br />
finding <strong>of</strong> a pancreatic mass (27%) and abnormal ERCP<br />
findings (24%).<br />
Characteristics <strong>of</strong> EUS Examination<br />
EUS-FNA was performed in 77 patients (mean 3.4 1.8<br />
passes, range 1–8) into the left lobe (n 66; 86%) and right<br />
lobe (n 11; 14%) <strong>of</strong> the liver without procedural compli-
1978 DeWitt et al. AJG – Vol. 98, No. 9, 2003<br />
Table 2. Characteristics <strong>of</strong> EUS Examination<br />
All*<br />
(n 77)<br />
Malignant†<br />
(n 48)<br />
Benign‡<br />
(n 22) p-value§<br />
Site <strong>of</strong> FNA<br />
Left lobe 66 (86) 41 (85) 20 (91) 0.57<br />
Right lobe 11 (14) 7 (15) 2 (9)<br />
No. <strong>of</strong> passes 3.4 1.8 3.5 1.5 3.2 1.5 0.44<br />
Range 1–8 1–8 1–8<br />
Echogenicity<br />
Hypoechoic 52 (68) 33 (69) 13 (59) 0.36<br />
Hyperechoic 23 (30) 13 (27) 9 (41)<br />
Both 2 (2) 2 (4) 0 (0)<br />
Margins<br />
Regular 39 (51) 29 (60) 6 (27) 0.02<br />
Irregular 38 (49) 19 (40) 16 (73)<br />
Size (mm) 16.0 10.8 15.6 7.7 16.7 12.0 0.70<br />
Range 3–40 3–35 4–40<br />
No. <strong>of</strong> lesions seen<br />
1 57 (74) 30 (62) 20 (91) 0.03<br />
1 20 (26) 18 (38) 2 (9)<br />
* Includes seven patients unable to be classified as benign or malignant.<br />
† Includes 45 positive and three false negative EUS-FNA results.<br />
‡ By follow-up or intraoperative findings.<br />
§ Between malignant and benign lesions.<br />
cations (upper 95% CI 4.7%; see Table 2). A total <strong>of</strong> 45<br />
(58%) aspirates were diagnostic for malignancy. Three false<br />
negatives were later discovered by intraoperative findings (n<br />
2) or P-FNA (n 1). One patient with pancreatic adenocarcinoma<br />
(as confirmed by EUS-FNA <strong>of</strong> the pancreas)<br />
had benign cytology <strong>of</strong> a 6-mm left lobe mass that intraoperatively<br />
was confirmed as metastatic adenocarcinoma. A<br />
second patient with pancreatic adenocarcinoma (as confirmed<br />
by EUS-FNA <strong>of</strong> the pancreas) had benign cytology<br />
<strong>of</strong> a 6-mm right lobe mass, which was later confirmed by<br />
percutaneous ultrasound-guided biopsy as metastatic adenocarcinoma.<br />
The third patient with a false negative EUS-FNA<br />
had a 29-mm left lobe mass that was benign by EUS-FNA.<br />
Intraoperative examination, however, confirmed hepatocellular<br />
carcinoma. Overall, 48 <strong>of</strong> 77 (62%) <strong>of</strong> the liver masses<br />
were malignant. Among the remaining 29 subjects with<br />
nonmalignant aspirates, in 22 (76%) the masses were considered<br />
benign by clinical follow-up (n 18; mean 762<br />
days; range: 512–1556 days) or intraoperative evaluation (n<br />
4). Seven (24%) <strong>of</strong> the subjects with nonmalignant<br />
masses with pancreatic adenocarcinoma (as confirmed by<br />
EUS-FNA <strong>of</strong> the pancreas; n 6) or lung cancer (n 1)<br />
died (mean 154 days, range 14–424 days) without follow-up<br />
imaging, biopsy <strong>of</strong> the liver, or autopsy and therefore<br />
cannot be classified as benign or malignant. The 45<br />
diagnostic aspirates for malignancy are considered true positives<br />
(Fig. 1). Assuming that the test results for these seven<br />
patients were all true negatives or all false negatives, the<br />
sensitivity <strong>of</strong> EUS-FNA for the diagnosis <strong>of</strong> malignancy<br />
would range from 82 to 94%.<br />
In comparison between benign and malignant lesions<br />
detected by EUS-FNA (Table 2), no statistically significant<br />
difference was found between the liver lobe aspirated (p <br />
0.57), number <strong>of</strong> passes (p 0.44), lesion size (p 0.70),<br />
Figure 1. Sensitivity <strong>of</strong> EUS-FNA <strong>of</strong> the liver for the diagnosis <strong>of</strong><br />
malignancy.<br />
or echotexture (p 0.36). Malignant masses, however,<br />
were more <strong>of</strong>ten accompanied by the presence <strong>of</strong> multiple<br />
hepatic lesions detected on EUS (38% vs 9%; p 0.03; 2<br />
analysis) and to have regular margins (60% vs 27%; p <br />
0.02; 2 analysis).<br />
Diagnoses from EUS-FNA <strong>of</strong> the Liver<br />
The final diagnoses for the 45 malignant liver aspirates are<br />
recorded in Table 3. Of these, 44 (98%) were metastatic and<br />
one (2%) was a hepatocellular carcinoma. The most common<br />
diagnosis was metastatic adenocarcinoma from the<br />
pancreas, which accounted for 34 <strong>of</strong> 45 (76%). The next<br />
most frequent diagnosis was metastatic neuroendocrine tumor<br />
from the pancreas (n 5; 11%). Of the 32 nonmalignant<br />
aspirates, 25 (33%) were cytologically benign and<br />
seven (9%) were nondiagnostic. One (4%) benign aspirate<br />
demonstrated cytological features consistent with an<br />
abscess.<br />
Previous Imaging <strong>of</strong> Malignancy Diagnosed by<br />
EUS-FNA<br />
Prior radiographic imaging reports were available for 42 <strong>of</strong><br />
45 (93%) malignant hepatic masses diagnosed by EUS-<br />
Table 3. Diagnoses <strong>of</strong> Malignant Aspirates <strong>of</strong> the Liver<br />
Diagnosis No. (%)<br />
Pancreatic adenocarcinoma 34 (76)<br />
Pancreatic neuroendocrine tumor 5 (11)<br />
Renal cell carcinoma 2 (5)<br />
Gallbladder adenocarcinoma 1 (2)<br />
Colon cancer 1 (2)<br />
Hepatocellular carcinoma 1 (2)<br />
Esophageal adenocarcinoma 1 (2)<br />
Total 45
AJG – September, 2003<br />
EUS-FNA <strong>Cytology</strong> <strong>of</strong> Solid Liver Lesions<br />
1979<br />
FNA. All imaging had been performed within 45 days <strong>of</strong> the<br />
EUS examination. Of these 42 lesions, EUS-FNA detected<br />
malignancy in 17 (41%) when prior imaging <strong>of</strong> the liver by<br />
CT alone (n 13), transabdominal ultrasound (US) alone (n<br />
1), or both (n 3) were normal. For the 32 patients in<br />
whom CT alone was performed, EUS-FNA initially detected<br />
a malignancy in 13 (41%). For the nine patients in<br />
whom CT and US were both performed, EUS-FNA initially<br />
detected malignancy in three (33%). The mean size <strong>of</strong> the 17<br />
malignant liver lesions detected initially by EUS-FNA was<br />
12.6 mm (range 3–26 mm). Of these 17, six (35%) were 1<br />
cm in diameter.<br />
Clinical Impact <strong>of</strong> EUS-FNA <strong>of</strong> the Liver<br />
For the 45 patients with malignant cytology, EUS-FNA had<br />
(by protocol definition) a clinical impact in all patients.<br />
EUS-FNA changed management, however, in only 38<br />
(84%) <strong>of</strong> these patients, because in seven cases (16%) tumor<br />
was upstaged but did not change overall patient management.<br />
EUS-FNA provided the initial diagnosis <strong>of</strong> malignancy<br />
in 35 patients (78%) and avoided surgery in 12<br />
(27%). Of the 35 patients in whom EUS-FNA made the<br />
initial diagnosis <strong>of</strong> malignancy, 34 (97%) had metastases<br />
and one (3%) had a hepatocellular carcinoma. In 25 patients<br />
(55%), the FNA provided both the primary diagnosis and<br />
upstaged the malignancy. In nine subjects (20%), EUS-FNA<br />
made the initial diagnosis, upstaged the tumor, and prevented<br />
surgery. Three EUS-FNAs (7%) were diagnostic in<br />
which previous CT-FNA was benign (two <strong>of</strong> three) or<br />
nondiagnostic (one <strong>of</strong> three). In three patients with nonmalignant<br />
EUS-FNA aspirates, malignancy was later confirmed<br />
by surgery (n 2) or percutaneous biopsy (n 1).<br />
Follow-Up After EUS-FNA<br />
Of the 45 patients with malignant cytology from EUS-FNA,<br />
40 have died, with a mean time to death after EUS-FNA <strong>of</strong><br />
135 days (range 7–754 days). The patient who died 7 days<br />
after EUS-FNA expired in his sleep outside the hospital<br />
without any apparent adverse consequence from EUS-FNA;<br />
however, no autopsy was performed. The patient who lived<br />
754 days had metastatic pancreatic cancer and enrolled in an<br />
experimental chemotherapy protocol at another institution.<br />
The longest survival otherwise was 298 days. Five patients<br />
remain alive with a mean follow-up <strong>of</strong> 64 days (range<br />
30–140 days). The mean time to death from metastatic<br />
pancreatic adenocarcinoma to the liver was 113 days (n <br />
31; range 7–754 days).<br />
DISCUSSION<br />
The results <strong>of</strong> this study demonstrate that EUS-guided FNA<br />
<strong>of</strong> solid hepatic masses is sensitive, safe, and has a significant<br />
impact on patient management when malignancy is<br />
diagnosed. In our series, the sensitivity <strong>of</strong> EUS-FNA for the<br />
diagnosis <strong>of</strong> malignancy ranged from 82% to 94%. Although<br />
it may be presumed that we obtained no false positive<br />
results when testing aspirates, the inability to histologically<br />
corroborate this does not allow for calculation <strong>of</strong><br />
specificity. A previous report <strong>of</strong> 14 patients that underwent<br />
EUS-FNA <strong>of</strong> liver metastases described a sensitivity and<br />
specificity <strong>of</strong> 100% and 100% for the diagnosis <strong>of</strong> malignancy<br />
(11). To our knowledge, however, our study is the<br />
first report <strong>of</strong> the test characteristics <strong>of</strong> EUS-FNA <strong>of</strong> the<br />
liver that includes both malignant and benign hepatic lesions.<br />
The sensitivity <strong>of</strong> the EUS-FNA <strong>of</strong> the liver we report<br />
is similar to previous series that describe the sensitivity <strong>of</strong><br />
EUS-FNA <strong>of</strong> pancreatic malignancy (9, 15–17) and P-FNA<br />
<strong>of</strong> liver tumors (2, 18–20). Despite the good sensitivity <strong>of</strong><br />
EUS-FNA <strong>of</strong> liver tumors, we obtained three false negative<br />
results. Therefore, follow-up percutaneous biopsy or intraoperative<br />
evaluation is warranted when the diagnosis <strong>of</strong><br />
malignancy in the liver is strongly suspected and would<br />
significantly affect patient management.<br />
The mean number <strong>of</strong> overall passes performed for the<br />
diagnosis <strong>of</strong> hepatic lesions (n 3.2; range 1–8) is slightly<br />
higher in our series than has been previously reported (11).<br />
The exact reason for this difference is not clear, although it<br />
is not significantly different from the number required for<br />
ultrasound-guided P-FNA <strong>of</strong> small hepatic masses (21). In a<br />
series <strong>of</strong> 14 patients with EUS-FNA <strong>of</strong> a malignant liver<br />
lesion, Nguyen et al. reported a mean <strong>of</strong> 2.0 (range 1–5)<br />
passes for the diagnosis <strong>of</strong> malignancy (11). The presence <strong>of</strong><br />
a cytopathologist on-site was implied, as interpretation <strong>of</strong><br />
specimens was performed before making repeated passes.<br />
We also have a cytotechnologist or cytopathologist available<br />
on site to assess the adequacy <strong>of</strong> obtained specimens.<br />
Because the diagnosis <strong>of</strong> metastatic disease is clinically<br />
relevant and initial air-dried preparations are sometimes<br />
difficult to interpret, we will <strong>of</strong>ten repeat another pass to<br />
ensure that cytology is sufficient to render a diagnosis if the<br />
adequacy <strong>of</strong> a specimen is initially interpreted as “suspicious”<br />
but not diagnostic <strong>of</strong> malignancy. We found no<br />
statistically significant difference between the numbers <strong>of</strong><br />
passes required for the diagnosis <strong>of</strong> benign (n 3.2; range<br />
1–8) or malignant (n 3.5; range 1–8) lesions. In addition,<br />
no difference existed between the number <strong>of</strong> passes required<br />
during the first or second half <strong>of</strong> the study. This implies that<br />
increased experience with this technique may not decrease<br />
the number <strong>of</strong> passes needed to obtain an accurate cytological<br />
diagnosis.<br />
Despite the relatively higher number <strong>of</strong> passes performed<br />
in this study, we observed no complications after EUS-FNA<br />
<strong>of</strong> the liver. In a large international survey <strong>of</strong> 167 cases<br />
describing EUS-FNA <strong>of</strong> the liver, however, six complications<br />
(4%) were described (12). These complications included<br />
one death in a patient who underwent EUS-FNA <strong>of</strong><br />
the liver despite a suspected obstructed biliary stent. Other<br />
complications noted were bleeding, abdominal pain, and<br />
fever. Although it is standard practice for gastroenterologists<br />
to observe patients in the right lateral decubitus position<br />
for several hours after percutaneous biopsy <strong>of</strong> the liver,<br />
we discharge stable patients within 60–75 min after EUS-
1980 DeWitt et al. AJG – Vol. 98, No. 9, 2003<br />
FNA <strong>of</strong> the liver. Furthermore, we do not routinely place<br />
patients on their right side during recovery before discharge.<br />
A recent series (5) describing the use <strong>of</strong> P-FNA in the<br />
diagnosis <strong>of</strong> 216 liver tumors reported the occurrence <strong>of</strong><br />
implantation metastases in seven patients (3%) a median 4<br />
months (range 2–49 months) after P-FNA <strong>of</strong> liver masses<br />
from colorectal cancer (n 5), gallbladder carcinoma (n <br />
1), and a hepatoma (n 1). In addition, the implantation<br />
metastases caused major problems locally and were fatal in<br />
four patients. This complication has not been described after<br />
EUS-FNA <strong>of</strong> the liver. The true incidence <strong>of</strong> implantation<br />
metastases after EUS-FNA <strong>of</strong> the liver, however, is difficult<br />
to estimate, inasmuch as hepatic metastases from pancreatic<br />
malignancy (which comprise 87% <strong>of</strong> malignancies in our<br />
study) usually carry a dismal prognosis and are managed<br />
nonoperatively. Therefore, as the overwhelming majority <strong>of</strong><br />
patients diagnosed with <strong>of</strong> hepatic metastases after EUS-<br />
FNA <strong>of</strong> the liver do not undergo intended curative resection,<br />
the true incidence <strong>of</strong> this complication is not known. The<br />
most common malignancies diagnosed by P-FNA (colorectal<br />
metastases and primary hepatomas) are <strong>of</strong>ten managed<br />
surgically with curative intent. We believe that these fundamental<br />
differences partially explain the disparity in reported<br />
incidence <strong>of</strong> implantation metastases between EUS-<br />
FNA and P-FNA <strong>of</strong> liver masses. Studies comparing the<br />
diagnostic accuracy and complications EUS-FNA and P-<br />
FNA <strong>of</strong> all types <strong>of</strong> suspected liver tumors are needed to<br />
resolve these issues.<br />
The overall sensitivity <strong>of</strong> transabominal US for the detection<br />
<strong>of</strong> liver metastases is reportedly between 80% and<br />
90% (22, 23). Recent studies using helical CT and magnetic<br />
resonance imaging, however, show that noninvasive imaging<br />
is relatively insensitive for lesions 1 cm(24–26). By<br />
EUS and EUS-FNA, we detected 17 malignant hepatic<br />
lesions (mean 12.6 mm, range 3–26 mm) with a previously<br />
normal CT alone (n 13), CT and US (n 3), or US alone<br />
(n 1). Of these, six (35%) were 1 cm in diameter. These<br />
17 lesions were found in 41% <strong>of</strong> the 42 patients with<br />
available radiographic imaging information performed before<br />
EUS. Nguyen et al. (11) reported that CT performed<br />
before EUS-FNA <strong>of</strong> the liver failed to detect liver lesions in<br />
11 <strong>of</strong> 14 patients (79%). Collectively, these results demonstrate<br />
the utility <strong>of</strong> EUS-FNA for the detection <strong>of</strong> malignant<br />
liver lesions that have been missed by prior radiographic<br />
imaging. Further comparative studies are needed to determine<br />
whether other imaging modalities such as fluorine-18<br />
fluorodeoxyglucose positron emission tomography (27),<br />
magnetic resonance imaging (28), harmonic ultrasound imaging<br />
(29), or ultrasound contrast agents (30) <strong>of</strong>fer any<br />
advantages over EUS for detection <strong>of</strong> occult or subcentimeter<br />
liver metastases.<br />
When compared with benign lesions, we found that malignant<br />
lesions detected by EUS-FNA <strong>of</strong> the liver were more<br />
likely to have regular margins (60% vs 27%; p 0.02) and<br />
to be accompanied by at least one other lesion detected on<br />
EUS (38% vs 9%; p 0.03). Furthermore, no statistically<br />
significant difference was found with regard to site <strong>of</strong> biopsy<br />
(p 0.57), size (p 0.70), echogenicity (p 0.36), or<br />
number <strong>of</strong> passes performed (p 0.44) for these lesions.<br />
Although EUS features <strong>of</strong> malignant lymphadenopathy have<br />
been described (31), to our knowledge the endosonographic<br />
features for malignant liver lesions have not been previously<br />
reported. These findings may help to guide decision making<br />
and assessment <strong>of</strong> the risk/benefit ratio <strong>of</strong> EUS-FNA <strong>of</strong><br />
hepatic masses.<br />
In conclusion, the results <strong>of</strong> our study show that the<br />
sensitivity <strong>of</strong> EUS-FNA <strong>of</strong> the liver for the diagnosis <strong>of</strong><br />
malignancy ranges from 82% to 94% and that, contrary to<br />
previous reports, it is a safe procedure. When malignancy is<br />
diagnosed, EUS-FNA <strong>of</strong> the liver significantly affects patient<br />
management and implies a poor overall prognosis.<br />
EUS features predictive <strong>of</strong> malignant hepatic masses are the<br />
presence <strong>of</strong> regular outer margins and the detection <strong>of</strong> two<br />
or more lesions. In this series, EUS and EUS-FNA detected<br />
malignant liver tumors that were not seen by CT or US (or<br />
both) in 41% <strong>of</strong> subjects. Therefore, surveillance <strong>of</strong> the<br />
entire liver is indicated during evaluation <strong>of</strong> known or<br />
suspected malignancy. Prospective studies are needed to<br />
compare the accuracy and complication rate <strong>of</strong> EUS-FNA<br />
and P-FNA for the diagnosis <strong>of</strong> liver tumors.<br />
Reprint requests and correspondence: John M. DeWitt, M.D.,<br />
Department <strong>of</strong> Medicine, Division <strong>of</strong> Gastroenterology, Indiana<br />
University Medical Center, 550 N. University Boulevard, UH<br />
4100, Indianapolis, IN 46202-5121.<br />
Received Nov. 11, 2002; accepted Jan. 30, 2003.<br />
REFERENCES<br />
1. Tatsuta M, Yamamoto R, Kasugai H, et al. Cytohistologic<br />
diagnosis <strong>of</strong> neoplasms <strong>of</strong> the liver by ultrasonically guided<br />
fine-needle aspiration biopsy. Cancer 1984;54:1682–6.<br />
2. Buscarini L, Fornari F, Bolondi L, et al. Ultrasound-guided<br />
fine-needle biopsy <strong>of</strong> focal liver lesions: Techniques, diagnostic<br />
accuracy and complications. A retrospective study on 2091<br />
biopsies. J Hepatol 1990;11:344–8.<br />
3. Edoute Y, Ben-Haim S, Brenner B, et al. Fatal hemoperitoneum<br />
after fine-needle aspiration <strong>of</strong> a liver metastases. Am J<br />
Gastroenterol 1992;87:358–9.<br />
4. Kowdley KV, Aggarwal A, Sachs PB. Delayed hemorrhage<br />
after percutaneous liver biopsy: Role <strong>of</strong> therapeutic angiography.<br />
J Clin Gastroenterol 1994;19:50–3.<br />
5. Ohlsson B, Nilsson J, Stenram U. Percutaneous fine-needle<br />
aspiration cytology in the diagnosis and management <strong>of</strong> liver<br />
tumors. Br J Surg 2002;89:757–62.<br />
6. Goletti O, Chiarugi M, Buccianti P, et al. Subcutaneous implantation<br />
<strong>of</strong> liver metastasis after fine needle biopsy. Eur<br />
J Surg Oncol 1992;18:636–7.<br />
7. Scheele J, Alterndorf-H<strong>of</strong>mann A. Tumor implantation from<br />
needle biopsy <strong>of</strong> hepatic metastases. Hepato-Gastroenterology<br />
1990;37:335–7.<br />
8. Andersson R, Andren-Sanberg A, Lundstedt C, et al. Implantation<br />
metastases from gastrointestinal cancer after percutaneous<br />
puncture or biliary drainage. Eur J Surg 1996;162:551–4.<br />
9. Wiersema MJ, Vilmann P, Giovannini M, et al. Endosonography-guided<br />
fine needle aspiration biopsy: Diagnostic accu-
AJG – September, 2003<br />
EUS-FNA <strong>Cytology</strong> <strong>of</strong> Solid Liver Lesions<br />
1981<br />
racy and complication assessment. Gastroenterology 1997;<br />
112:1087–95.<br />
10. Gress FG, Savides TJ, Sandler A, et al. <strong>Endoscopic</strong> ultrasonography,<br />
fine-needle aspiration biopsy guided by endoscopic<br />
ultrasonography, and computed tomography in the preoperative<br />
staging <strong>of</strong> non-small cell lung cancer: A comparison<br />
study. Ann Intern Med 1997;127:604–12.<br />
11. Nguyen P, Feng JC, Chang KJ. <strong>Endoscopic</strong> ultrasound (EUS)<br />
and EUS-guided fine-needle aspiration (FNA) <strong>of</strong> liver lesions.<br />
Gastrointest Endosc 1999;50:357–61.<br />
12. tenBerge J, H<strong>of</strong>fman BJ, Hawes RH, et al. EUS-guided fine<br />
needle aspiration <strong>of</strong> the liver. indications, yield, and safety<br />
based on an international survey <strong>of</strong> 167 cases. Gastrointest<br />
Endosc 2002;55:859–62.<br />
13. Bentz J, Kochmann M, Faigel D, et al. <strong>Endoscopic</strong> ultrasoundguided<br />
real-time fine-needle aspiration: Clinicopathologic features<br />
<strong>of</strong> 60 patients. Diagn Cytopathol 1998;18:98–100.<br />
14. Fritscher-Ravens A, Schirror L, Atay Z, et al. Endosonographically<br />
controlled fine needle aspiration-cytology-indications<br />
and results in routine diagnosis. Z Gastroenterol 1999;<br />
37:343–51.<br />
15. Williams DB, Sahai AV, Aabakken L, et al. <strong>Endoscopic</strong> ultrasound<br />
guided fine needle aspiration biopsy: A large single<br />
center experience. Gut 1999;44:720–6.<br />
16. Hunerbein M, Dohmoto M, Haensch W, et al. Endosonography-guided<br />
biopsy <strong>of</strong> mediastinal and pancreatic tumors. Endoscopy<br />
1998;30:32–6.<br />
17. DeWitt J, Devereaux B, Ciaccia D, et al. Prospective evaluation<br />
<strong>of</strong> endoscopic ultrasound fine-needle aspiration (EUS-<br />
FNA) for the diagnosis <strong>of</strong> suspected pancreatic malignancy.<br />
Gastrointest Endosc 2002;55:AB246.<br />
18. Montali G, Solbati L, Croce F, et al. <strong>Fine</strong>-needle aspiration<br />
biopsy <strong>of</strong> liver focal lesions ultrasonically guided with a realtime<br />
probe. Report on 126 cases. Br J Radiol 1982;55:717–23.<br />
19. Bru C, Maroto A, Bruix J, et al. Diagnostic accuracy <strong>of</strong><br />
fine-needle aspiration biopsy in patients with hepatocellular<br />
carcinoma. Dig Dis Sci 1989;34:1765–9.<br />
20. Bognel C, Rougier P, Leclere J, et al. <strong>Fine</strong> needle aspiration <strong>of</strong><br />
the liver and pancreas with ultrasound guidance. Acta Cytol<br />
1988;32:22–6.<br />
21. Middleton W, Hiskes SK, Teffey SA, et al. Small (1.5 cm or<br />
less) liver metastases: US-guided biopsy. Radiology 1997;<br />
205:729–32.<br />
22. Gore RM, Levine MS, Laufer I. Textbook <strong>of</strong> gastrointestinal<br />
radiology. Philadelphia: WB Saunders, 1994:1935.<br />
23. Grainger RG, Allison DJ. Diagnostic radiology: A textbook <strong>of</strong><br />
medical imaging, 3rd ed. New York: Churchill Livingstone,<br />
1998:1162.<br />
24. Ward J, Naid KS, Guthrie JA, et al. Hepatic lesion detection:<br />
Comparison <strong>of</strong> MR imaging after the administration <strong>of</strong> superparamagnetic<br />
iron oxide with dual-phase CT by using alternative-free<br />
response receiver operating characteristic analysis.<br />
Radiology 1999;210:459–66.<br />
25. Hagspiel KD, Neidl KFW, Eichenberger AC, et al. Detection<br />
<strong>of</strong> liver metastases: Comparison <strong>of</strong> superparamagnetic iron<br />
oxide-enhanced and unenhanced MR imaging at 1.5 T with<br />
dynamic CT, intraoperative US and percutaneous US. Radiology<br />
1995;196:471–8.<br />
26. Kuszyk BS, Bluemke DA, Urban BA, et al. Portal-phase<br />
contrast-enhanced helical CT for the detection <strong>of</strong> malignant<br />
hepatic tumors: Sensitivity based on intraoperative and pathologic<br />
findings. Am J Roentgenol 1996;166:91–5.<br />
27. Nakamoto Y, Higashi T, Sakahara H, et al. Contribution <strong>of</strong><br />
PET in the detection <strong>of</strong> liver metastases from pancreatic tumors.<br />
Clin Radiol 1999;54:248–52.<br />
28. Schima W, Fugger R, Schober E, et al. Diagnosis and staging<br />
<strong>of</strong> pancreatic cancer: Comparison <strong>of</strong> mangafodipir trisodiumenhanced<br />
MR imaging and contrast-enhanced helical hydro-<br />
CT. Am J Roentgenol 2002;179:717–24.<br />
29. Strobel D, Hahn EG, Becker D. Harmonic imaging for improving<br />
diagnosis <strong>of</strong> liver tumors—a preliminary report. Z<br />
Gastroenterol 2001;39:292–4.<br />
30. Harvey CJ, Blomley MJ, Eckersley RJ, et al. Pulse-inversion<br />
mode imaging <strong>of</strong> liver specific microbubbles: Improved detection<br />
<strong>of</strong> subcentimetre metastases. Lancet 2000;355:807–8.<br />
31. Catalano MF, Sivak MJ, Rice T, et al. Endosonographic features<br />
predictive <strong>of</strong> lymph node metastasis. Gastrointest Endosc<br />
1994;40:442–6.